Validating Computational Models for Cancer Target Identification: From AI Algorithms to Clinical Translation
This article provides a comprehensive overview of the methodologies, applications, and validation frameworks for computational models in cancer target identification.
Validating Computational Models for Cancer Target Identification: From AI Algorithms to Clinical Translation
Abstract
This article provides a comprehensive overview of the methodologies, applications, and validation frameworks for computational models in cancer target identification. Aimed at researchers and drug development professionals, it explores the foundational principles of AI and machine learning in oncology, details cutting-edge tools and their practical applications, addresses key challenges and optimization strategies, and establishes rigorous standards for model validation and benchmarking. By synthesizing recent advances and real-world case studies, this resource aims to bridge the gap between computational prediction and robust biological validation, ultimately accelerating the development of novel cancer therapeutics.
The New Frontier: How AI and Computational Biology are Revolutionizing Cancer Target Discovery
The Critical Need for Novel Target Identification in Oncology
The identification of novel therapeutic targets is a cornerstone of advancing oncology care. However, current targeted therapies face significant drawbacks, including a limited number of druggable targets, ineffective population coverage, and inadequate responses to drug resistance [1]. Approximately 90% of clinical drug development fails, with nearly half of these failures attributed to a lack of clinical efficacy, highlighting fundamental issues in target validation and selection [2]. Cancer progression is an evolutionary process where tumor cells behave as complex, self-organizing systems that adapt to microenvironmental proliferation barriers [3]. This complexity arises from intricate interactions between genes and their products, which traditional hypothesis-driven experimental approaches often fail to capture comprehensively [1].
Computational biology has emerged as a transformative approach to address these challenges. By employing artificial intelligence (AI) and mathematical modeling, researchers can now process biological network data to preserve and quantify interactions between cellular system components [1]. These computational models serve as virtual laboratories, allowing for hypothesis testing and therapeutic exploration without the constraints of traditional experimentation [3]. The integration of multi-omics technologies—including epigenetics, genomics, proteomics, and metabolomics—provides the essential data foundation for these computational approaches [1]. When effectively validated and implemented, computational models offer unprecedented insights into carcinogenesis and present powerful tools for identifying novel anticancer targets with improved therapeutic potential.
Computational Approaches for Target Identification
Network-Based Biology Analysis
Network-based algorithms analyze biological systems as interconnected networks where nodes represent biological entities (genes, proteins, mRNAs, metabolites) and edges represent associations or interactions between them (gene co-expression, signaling transduction, physical interactions) [1]. This approach provides a quantitative framework to study the relationship between network characteristics and cancer pathogenesis [1].
Key Methodologies and Applications:
- Shortest Path Analysis: Identifies the most direct connections between biological components, potentially revealing critical pathways in disease progression [1].
- Module Detection: Discovers densely connected subnetworks (modules) that often correspond to functional units or disease-related pathways [1].
- Network Centrality: Measures node importance based on its position within the network, helping identify hub genes/proteins critical for network stability and function [1].
- Network Controllability Analysis: Applies control theory principles to identify "indispensable" proteins that affect network controllability. Analysis of 1,547 cancer patients revealed 56 indispensable genes across nine cancers, 46 of which were newly associated with cancer, demonstrating this method's potential for novel disease gene discovery [1].
Machine Learning-Based Biology Analysis
Machine learning (ML) approaches efficiently handle high-throughput, heterogeneous molecular data to mine features and relationships within biological networks [1]. These methods are particularly valuable for pattern recognition in complex datasets and predictive modeling of drug responses.
Applications in Oncology Target Identification:
- Multi-Omics Integration: ML algorithms integrate genomic, transcriptomic, proteomic, and clinical data to identify molecular drivers of cancer growth and potential therapeutic targets [4].
- Patient Stratification: By combining genomic information with clinical data, ML models identify patient subgroups more likely to respond to specific therapies, enabling precision oncology approaches [4].
- Drug Response Prediction: ML models trained on historical patient data, including genetic information and drug response patterns, can forecast individual patient responses to treatments [4].
- Resistance Mechanism Analysis: ML tools track mutations in real-time by analyzing genomic data from tumor biopsies taken before and after treatment, identifying alterations that drive therapeutic resistance [4].
Structure-Based Computational Approaches
Structure-based methods leverage computational techniques to identify potential drug targets based on molecular structure information.
Inverse Virtual Screening (IVS) has emerged as a promising structure-based approach that decipher protein targets of bioactive compounds. This method can rationalize observed side effects and open new therapeutic strategies by identifying previously unknown target interactions [5].
Troubleshooting Guide: Validating Computational Predictions
Common Validation Challenges and Solutions
| Challenge | Potential Cause | Solution |
|---|---|---|
| Inaccurate Target Predictions | Noisy or incomplete biological data [6]; Model oversimplification [7] | Implement rigorous data cleaning and validation protocols [6]; Use ensemble modeling approaches that combine multiple algorithms [1] |
| Poor Translational Performance | Discrepancy between in silico models and human biology [2]; Omitting critical biological mechanisms [7] | Incorporate human-derived data (organoids, PDX models) [4]; Enhance models with tumor microenvironment components [7] |
| Inability to Recapitulate Disease Complexity | Lack of multi-scale dynamics [7]; Failure to capture emergent behaviors [7] | Develop multiscale models integrating molecular, cellular, and tissue levels [7]; Implement agent-based models to capture spatial heterogeneity [7] |
| Overhyped AI Expectations | Excessive promise without realistic assessment of limitations [8] | Maintain culture of realism about AI capabilities [8]; Set appropriate expectations about development timelines [8] |
| Resistance Mechanism Oversight | Failure to account for tumor evolutionary dynamics [3] | Incorporate evolutionary principles into models [3]; Analyze pre- and post-treatment biopsies to identify resistance patterns [4] |
Experimental Validation Workflow
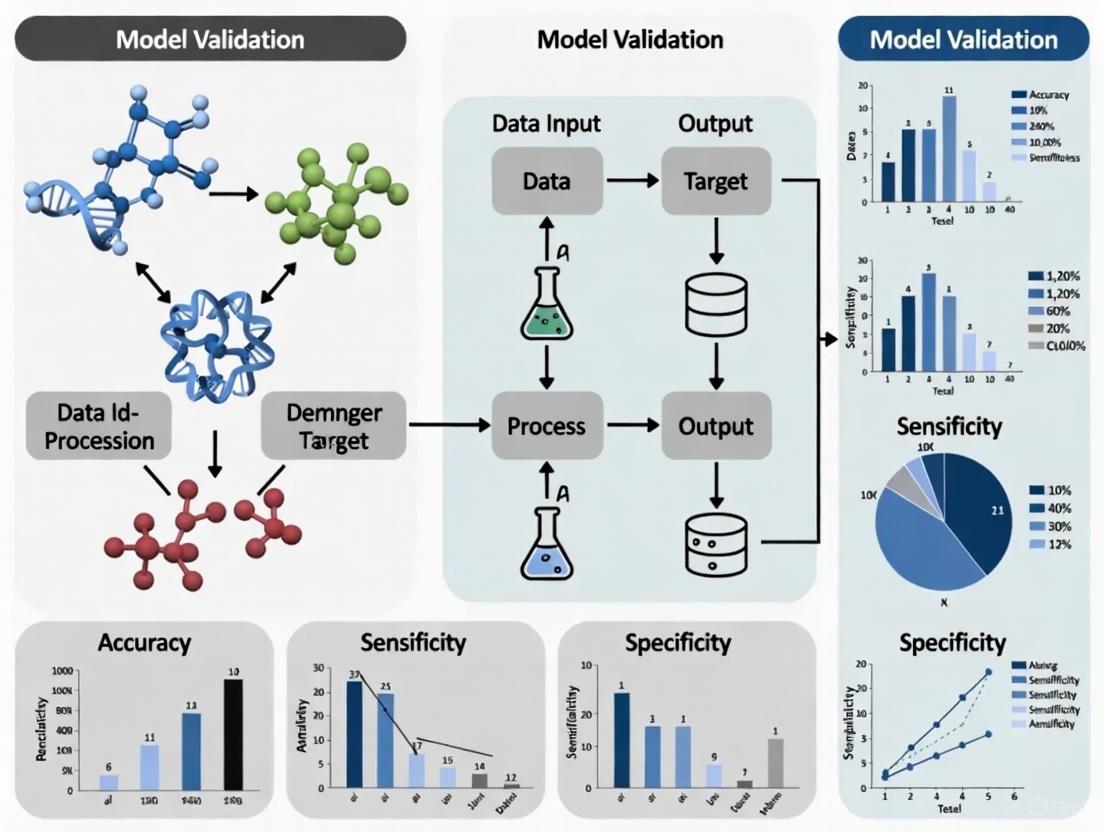
The following diagram illustrates a robust workflow for transitioning from computational predictions to experimentally validated targets:
Data Quality Assessment Protocol
Objective: Ensure biological data quality before computational analysis.
Procedure:
- Data Auditing: Perform comprehensive assessment of data sources for completeness, consistency, and potential biases [6].
- Noise Reduction: Apply appropriate filtering algorithms to remove technical artifacts while preserving biological signals [6].
- Batch Effect Correction: Implement statistical methods to minimize non-biological variations introduced by different experimental batches [6].
- Cross-Validation: Split datasets into training, validation, and test sets to evaluate model performance and prevent overfitting [4].
- Benchmarking: Compare computational predictions against known gold-standard targets to assess predictive accuracy [5].
Frequently Asked Questions (FAQs)
Q1: Why does approximately 90% of clinical drug development fail in oncology, and how can better target identification address this?
A1: Clinical drug development fails due to lack of efficacy (40-50%), unmanageable toxicity (30%), poor drug-like properties (10-15%), and insufficient commercial planning (10%) [2]. Improved target identification addresses these failures by: 1) Enhancing efficacy through better validation of target-disease relationships; 2) Reducing toxicity by identifying targets with better therapeutic windows; 3) Incorporating drug-like property considerations early in target selection; and 4) Ensuring targets have clear clinical and commercial pathways [2] [4].
Q2: What are the most significant limitations of current computational models in cancer target identification?
A2: Key limitations include: 1) Data challenges - handling gigantic datasets, ensuring data accuracy, and integrating different data types [6]; 2) Model complexity - balancing biological realism with computational feasibility [7]; 3) Validation barriers - scarcity of high-quality longitudinal datasets for parameter calibration [7]; 4) Technical expertise - shortage of professionals skilled in both biology and computation [6]; and 5) Standardization issues - lack of uniform databases, software tools, and coding practices across research groups [6].
Q3: How can researchers effectively bridge the gap between computational predictions and experimental validation?
A3: Successful integration requires: 1) Iterative refinement - using experimental results to improve computational models in a continuous cycle [9]; 2) Advanced model systems - employing patient-derived xenografts (PDXs) and organoids that better recapitulate human tumors [4]; 3) Multi-disciplinary collaboration - fostering teamwork between computational biologists, experimentalists, and clinicians [7]; and 4) AI-mediated integration - using artificial intelligence to prioritize the most promising predictions for experimental testing [9].
Q4: What role does the tumor microenvironment (TME) play in computational modeling for target identification?
A4: The TME is critical because: 1) Therapeutic resistance - TME interactions can promote drug resistance independent of cancer cell mutations [7]; 2) Spatial heterogeneity - nutrient and oxygen gradients create distinct cellular subpopulations with different target expression [3]; 3) Immune modulation - immune cell interactions influence tumor progression and treatment response [7]; and 4) Emergent behaviors - cell-cell interactions within the TME can produce unexpected phenomena not predictable from isolated cell studies [7]. Agent-based models (ABMs) are particularly useful for capturing these spatial and dynamic TME interactions [7].
Q5: How can the "overhyping" of AI in drug discovery negatively impact the field?
A5: Overhyping AI creates several problems: 1) Unrealistic expectations - promising rapid breakthroughs that don't materialize, leading to disillusionment [8]; 2) Resource misallocation - investments based on fear of missing out rather than scientific merit [8]; 3) Reduced creativity - overly conservative AI applications that stick too closely to known chemical space [8]; and 4) Long-term setbacks - if AI doesn't deliver promised results, it could "put the field back quite a long way when people stop thinking it can work" [8].
Research Reagent Solutions for Experimental Validation
The following table details essential materials and their applications in validating computationally predicted targets:
| Research Reagent | Function in Target Validation | Key Applications |
|---|---|---|
| Patient-Derived Xenografts (PDXs) | Maintain tumor heterogeneity and microenvironment of original tumors [4] | Preclinical efficacy testing; Biomarker discovery; Drug response prediction [4] |
| Organoids & 3D Culture Systems | Provide physiologically relevant models that recapitulate human tumors [4] | High-throughput drug screening; Personalized therapy testing; Tumor biology studies [4] |
| Fluorescent Ubiquitination-Based Cell Cycle Indicator (FUCCI) | Visualize cell cycle progression in live cells [3] | Study cell cycle dynamics; Drug mechanism studies; Cell division imaging [3] |
| Multi-Omics Datasets | Provide comprehensive molecular profiling of tumors [1] | Target identification; Biomarker discovery; Patient stratification [1] [4] |
| CRISPR/Cas9 Systems | Enable precise genome editing for functional validation [4] | Gene knockout studies; Functional genomics; Target validation [4] |
Quantitative Data Framework for Target Assessment
Key Parameters for Evaluating Potential Targets
| Assessment Category | Specific Metrics | Optimal Range/Values |
|---|---|---|
| Genetic Evidence | Mutation frequency in cancer cohorts; Germline association with cancer risk; Somatic signature | Recurrent mutations across independent cohorts; Significant GWAS associations [1] |
| Functional Impact | Network centrality scores; Essentiality scores (CRISPR screens); Pathway enrichment | High betweenness centrality; Essential in multiple cancer cell lines [1] |
| Druggability | Binding pocket characteristics; Similarity to known drug targets; Chemical tractability | Defined hydrophobic pockets; Similar to successful targets [2] |
| Therapeutic Window | Tissue expression specificity; Essentiality in normal cells; Phenotype of inhibition | High disease-tissue/normal-tissue ratio; Non-essential in vital tissues [2] |
| Clinical Correlation | Expression association with prognosis; Predictive biomarker potential; Resistance association | Significant survival correlation; Predictive of drug response [4] |
STAR Framework for Drug Candidate Classification
The Structure-Tissue Exposure/Selectivity-Activity Relationship (STAR) provides a systematic approach to classify drug candidates based on critical properties [2]:
The critical need for novel target identification in oncology demands a sophisticated approach that leverages computational power while maintaining rigorous experimental validation. Successful target discovery requires seamlessly integrating network biology, machine learning, and structural computational methods with physiologically relevant model systems and comprehensive data integration. The framework presented here—encompassing troubleshooting guidance, standardized protocols, and systematic assessment criteria—provides a pathway for researchers to navigate the complexities of cancer target validation.
Future advances will depend on overcoming key challenges in data quality, model refinement, and interdisciplinary collaboration. The emergence of AI for Science (AI4S) represents a transformative paradigm that integrates data-driven modeling with prior knowledge, enabling more autonomous and intelligent experimentation [10]. As these technologies evolve, the development of patient-specific 'digital twins'—virtual replicas that simulate disease progression and treatment response—may further accelerate target validation and therapeutic optimization [7]. By adopting these integrated approaches and maintaining realistic expectations about technological capabilities, the research community can significantly improve the efficiency and success of oncology drug development.
The validation of computational models is a critical step in cancer target identification research. This technical support center provides troubleshooting guides and FAQs to help researchers address specific issues encountered during experiments that utilize core AI technologies: Machine Learning (ML), Deep Learning (DL), and Natural Language Processing (NLP). The following sections are structured to directly support scientists in developing robust, reproducible, and clinically relevant computational findings.
Frequently Asked Questions (FAQs)
FAQ 1: What are the primary applications of ML, DL, and NLP in cancer target identification?
- Machine Learning (ML) is often used with structured data. Applications include survival prediction, therapy response forecasting, and identifying molecular subtypes from genomic biomarkers and lab values [11]. For example, ensemble methods can analyze genomic data from sources like The Cancer Genome Atlas (TCGA) to uncover novel therapeutic vulnerabilities [12].
- Deep Learning (DL), particularly architectures like Convolutional Neural Networks (CNNs), excels with image-based data. It is used for tumor detection, segmentation, and grading from histopathology slides and radiology scans [11] [13]. Recurrent Neural Networks (RNNs) and transformers are applied to sequential data like genomic sequences for biomarker discovery [11].
- Natural Language Processing (NLP) is key for knowledge extraction from unstructured text. It mines biomedical literature, clinical notes, and medical guidelines to identify relationships between entities, accelerating hypothesis generation [14] [15]. Large Language Models (LLMs) can preprocess clinical notes to improve the extraction of biomedical concepts, which is vital for curating datasets for other models [15].
FAQ 2: My DL model for histopathology image analysis is overfitting. What are the first steps to troubleshoot this?
Overfitting is a common challenge. Begin with the following steps:
- Data Augmentation: Artificially expand your training dataset using techniques like rotation, flipping, and color jittering on your digitized tissue slides.
- Regularization Techniques: Implement methods such as Dropout or L2 regularization within your network architecture to prevent complex co-adaptations to the training data.
- Review Dataset Size and Splitting: Ensure your dataset is large enough and that there is no data leakage between your training and validation sets. A model trained on a small dataset is prone to overfitting [12].
- Simplify the Model: Reduce the complexity of your network (e.g., number of layers or parameters) if your dataset is limited.
FAQ 3: How can I use NLP to generate a testable biological hypothesis for a new cancer target?
A validated approach involves using a foundation model to perform a virtual screen. A recent study provides a protocol:
- Task Formulation: Define a specific biological question. For example, "Find a drug that acts as a conditional amplifier of antigen presentation only in a specific immune-context-positive environment" [16].
- Dual-Context Virtual Screen: Simulate the effect of thousands of drugs across two computational contexts: a disease-relevant environment (e.g., patient samples with tumor-immune interactions) and a neutral control environment (e.g., isolated cell lines) [16].
- Prediction and Filtering: The model predicts candidate drugs that show the desired effect only in the disease-relevant context. This "context split" highlights the most promising and novel hypotheses [16].
- Experimental Validation: The top predictions, such as a specific kinase inhibitor, must be confirmed through in vitro lab experiments to verify the predicted biological effect [16].
FAQ 4: What are the key considerations for preparing multi-omics data for ML models?
- Data Modality Matching: Ensure your data modalities (e.g., genomics, transcriptomics, clinical records) are correctly aligned per patient sample.
- Structured Data Conversion: Convert genomic sequences and other complex data into structured formats that ML models can process [11].
- Handling Missing Data: Develop a robust strategy for dealing with missing values, such as imputation or removal, to prevent bias in your model's predictions [12].
- Feature Extraction: Use techniques like radiomics to extract quantitative features from standard medical scans, which can then be used as input for ML models to predict therapy response [13].
FAQ 5: My model's predictions lack interpretability, creating a barrier for clinical adoption. What can I do?
The "black box" nature of some complex AI models is a significant hurdle.
- Leverage Interpretability Tools: For DL models on images, use saliency maps that highlight which regions of a medical image (e.g., a mammogram or pathology slide) most influenced the prediction [11] [17].
- Incorporate Explainable AI (XAI) Methods: Integrate techniques like SHAP (SHapley Additive exPlanations) or LIME (Local Interpretable Model-agnostic Explanations) to explain the output of any model [12].
- Use Transparent Models Where Possible: For critical decisions where interpretability is paramount, consider using more interpretable classical ML models (e.g., logistic regression, decision trees) if they provide sufficient performance [11].
Troubleshooting Guides
Issue 1: Poor Generalization of a Prognostic Model to External Patient Cohorts
Problem: A prognostic model developed using an ML-driven approach performs well on internal validation but fails on an external cohort from a different clinical site [18].
Solution:
- Check 1: Data Heterogeneity. Investigate differences in data acquisition protocols, patient demographics, and cancer subtypes between the internal and external cohorts. These variations are a common source of performance drop.
- Check 2: Preprocessing Pipeline. Ensure the exact same preprocessing steps (e.g., normalization, gene scaling) used on the training data are applied to the external cohort data. Inconsistency here is a frequent error.
- Action 1: Algorithmic Adjustment. Employ training techniques that explicitly improve generalization, such as domain adaptation or federated learning, which can help models perform better across diverse datasets without sharing raw data [12].
- Action 2: Recalibration. Recalibrate the model's output on a small, representative sample from the external cohort before full deployment.
Issue 2: Failure in Experimental Validation of an AI-Predicted Drug Target
Problem: A small molecule or target identified through a virtual AI screen fails to show efficacy in wet-lab experiments [12] [19].
Solution:
- Check 1: Training Data Fidelity. Scrutinize the quality and biological relevance of the data used to train the AI model. Was it trained on data that accurately represents the disease context? Biased or noisy data leads to flawed predictions [12].
- Check 2: Contextual Mismatch. A leading cause of failure is a mismatch between the in silico context of the model and the in vitro/in vivo experimental conditions. Revisit the biological assumptions built into the AI screen [16].
- Action 1: Focus on Novel, Validated Hits. Prioritize candidates where the AI model has made a novel prediction that was subsequently confirmed in the lab, as this demonstrates true discovery power. For example, the Gemma model identified the CK2 inhibitor silmitasertib as a conditional amplifier of antigen presentation, which was then confirmed in human cell models [16].
- Action 2: Iterative Refinement. Use the experimental results to refine the AI model. Failed predictions are valuable data points that can be used to retrain and improve the next iteration of the model.
Issue 3: Inefficient Mining of Biomedical Literature for Target Discovery
Problem: An NLP pipeline is failing to efficiently extract meaningful relationships between genes, diseases, and drugs from large volumes of scientific literature [15].
Solution:
- Check 1: NLP Task Pipeline. Ensure your pipeline correctly sequences core NLP tasks: Tokenization, Named Entity Recognition (NER) to identify key concepts (e.g., gene names, diseases), and Relation Extraction to understand how these entities are connected in the text [20].
- Check 2: Domain-Specific Tuning. General-purpose NLP models may perform poorly on biomedical text full of specialized jargon. Use or fine-tune models that have been pre-trained on biomedical corpora (e.g., BioBERT, models from resources like LitCOVID) [14] [15].
- Action 1: LLM Preprocessing. Use Large Language Models (LLMs) to preprocess raw text from clinical notes or literature. They can correct spelling, expand acronyms, and standardize terminology, which significantly improves the performance of downstream relation extraction tools [15].
- Action 2: Hybrid Approach. Combine rule-based systems (for well-established relationships) with statistical or deep learning models (for discovering novel associations) to balance precision and recall [20].
Data Presentation
Table 1: Performance Metrics of AI Models in Cancer Detection
This table summarizes the quantitative performance of select AI systems as reported in recent studies, providing a benchmark for model validation [11].
| Cancer Type | Modality | AI System | Key Metric | Performance | Evidence Level |
|---|---|---|---|---|---|
| Colorectal Cancer | Colonoscopy | CRCNet | Sensitivity | 91.3% vs. Human 83.8% (p<0.001) | Retrospective multicohort [11] |
| Breast Cancer | 2D Mammography | Ensemble of 3 DL models | Specificity | +5.7% vs. Radiologists (p<0.001) | Diagnostic case-control [11] |
| Breast Cancer | 2D/3D Mammography | Progressively trained RetinaNet | AUC | 0.94 (Reader Study) | Diagnostic case-control [11] |
| Colorectal Polyps | Histopathology | Real-time image recognition | Accuracy (Neoplastic) | 95.9% Sensitivity, 93.3% Specificity | Prospective diagnostic [11] |
Table 2: Computational Requirements and Output of AI Techniques
This table helps researchers select the appropriate AI technology based on their computational resources and project goals [11] [12] [19].
| AI Technology | Typical Input Data | Example Tasks in Oncology | Key Algorithms/Models | Computational Intensity |
|---|---|---|---|---|
| Machine Learning (ML) | Structured data (genomic biomarkers, lab values) [11] | Survival prediction, therapy response, molecular subtyping [11] [18] | Logistic Regression, Random Forests, SVMs [19] | Low to Medium |
| Deep Learning (DL) | Imaging (histopathology, radiology), genomic sequences [11] | Tumor detection & segmentation, de novo drug design [11] [19] | CNNs, RNNs, GANs, VAEs [11] [19] | High (requires specialized hardware) |
| Natural Language Processing (NLP) | Unstructured text (literature, clinical notes) [15] | Named Entity Recognition, Relation Extraction, Literature-based discovery [14] [15] | Transformers, LLMs (e.g., GPT, BioBERT) [15] [20] | Medium to Very High (for large models) |
Experimental Protocols
Protocol 1: ML-Driven Workflow for Tumor Prognosis and Target Discovery
This protocol details a machine learning-driven approach for prognostic model development, molecular stratification, and drug target discovery, as adapted from a recent standardized research protocol [18].
Summary: The procedure involves using transcriptome data to develop a robust prognostic signature, identify molecular subtypes, and prioritize druggable transcription factors through drug sensitivity analysis.
Step-by-Step Instructions:
- Data Preprocessing and Feature Selection: Process RNA-seq data (e.g., from TCGA). Normalize read counts and filter for genes with significant variance. Perform robust gene signature prioritization using co-expression network analysis or similar methods [18].
- Prognostic Model Development: Divide the cohort into training and test sets. Using the training set, train a survival prediction model (e.g., Cox Proportional Hazards model with LASSO regularization) based on the prioritized gene signature. Validate the model's performance on the held-out test set using concordance index (C-index) [18].
- Molecular Subtyping: On the entire dataset, perform unsupervised clustering (e.g., k-means, consensus clustering) on the expression data of the key signature genes to identify distinct molecular subtypes. Train a supervised classifier (e.g., Random Forest) to assign new samples to these subtypes [18].
- Regulatory Network and Master Regulator Analysis: For each molecular subtype, infer a subtype-specific regulatory network. Use master regulator analysis (e.g., using the Algorithm for the Reconstruction of Accurate Cellular Networks, ARACNe) to identify key transcription factors that drive the subtype's gene expression profile [18].
- Drug Sensitivity Analysis and Repurposing: Correlate the expression of master regulators with publicly available drug sensitivity databases (e.g., GDSC, CTRP). Prioritize existing drugs or compounds that are predicted to be effective against a specific molecular subtype, thereby repurposing therapeutic candidates [18].
Protocol 2: Validating AI-Discovered Targets with Experimental Assays
This protocol outlines the critical steps for transitioning from an AI-generated hypothesis to experimental validation, a cornerstone of credible computational research [16].
Summary: After an AI model identifies a potential therapeutic target or drug candidate, this protocol guides the initial in vitro validation to confirm the predicted biological mechanism.
Step-by-Step Instructions:
- Hypothesis Definition from AI Output: Clearly state the AI-generated prediction. Example: "The CK2 inhibitor silmitasertib will synergistically enhance antigen presentation (MHC-I expression) only in the presence of low-dose interferon-gamma (IFN-γ)" [16].
- Cell Model Selection: Choose a relevant human cell model for the cancer type. Using a cell type that was not part of the AI model's training data strengthens the validation [16].
- Design Experimental Arms: Establish at least four treatment conditions:
- Arm A: Vehicle control (DMSO).
- Arm B: AI-predicted drug alone (e.g., silmitasertib).
- Arm C: Contextual signal alone (e.g., low-dose IFN-γ).
- Arm D: Combination (e.g., silmitasertib + low-dose IFN-γ) [16].
- Execute and Measure: Treat cells according to the experimental design. Use a standardized assay (e.g., flow cytometry) to quantitatively measure the relevant outcome (e.g., surface MHC-I expression). Perform multiple biological replicates.
- Analyze for Synergy: Statistically compare the results across all arms. A successful validation is indicated by a significant increase in the outcome measure only in Arm D (the combination), confirming the AI's prediction of a conditional or synergistic effect [16].
Signaling Pathways, Workflows, and Logical Diagrams
Multi-Omics AI Integration Workflow
Diagram 1: A high-level workflow for integrating multi-omics data using AI for cancer target identification.
PD-L1/IDO1 Signaling and AI Modulation
Diagram 2: Key immune checkpoint pathways (PD-L1/IDO1) and their modulation by AI-predicted small molecules.
The Scientist's Toolkit
Table 3: Research Reagent Solutions for Validation Experiments
This table lists essential materials and tools used in the AI-driven cancer research pipeline, from computational analysis to experimental validation [18] [16].
| Item Name | Function/Application | Example Use Case |
|---|---|---|
| Transcriptomic Data (e.g., TCGA) | Provides standardized RNA-seq data from thousands of tumor and normal samples for initial model training and discovery. | Developing a prognostic gene signature for gastric tumors [18]. |
| CK2 Inhibitor (e.g., Silmitasertib/CX-4945) | A small molecule kinase inhibitor used to experimentally test AI-generated hypotheses about modulating antigen presentation. | Validating the synergistic effect with low-dose interferon-gamma in neuroendocrine cell models [16]. |
| Digital Pathology Slide Scanner | Converts glass histopathology slides into high-resolution digital images for analysis by Deep Learning models (CNNs). | Enabling AI-powered detection of HRD characteristics (DeepHRD) from standard biopsy slides [17]. |
| Flow Cytometry Assay | A core laboratory technique for quantifying protein expression on the surface (e.g., MHC-I) or inside single cells. | Measuring the increase in antigen presentation on tumor cells after drug treatment [16]. |
| Biomedical NLP Toolkit (e.g., BioBERT) | A pre-trained language model designed to understand biomedical text, improving tasks like Named Entity Recognition. | Extracting relationships between genes, diseases, and drugs from scientific literature at scale [15]. |
Troubleshooting Guide: Data Access and Quality Control
- A1: Access issues often stem from browser, tool, or authentication problems. Follow these steps:
- Verify Data Availability: Confirm the file exists in the latest GDC Data Release. The GDC portal and announcements detail available data types and releases [21].
- Clear Browser Cache: Outdated cache can cause portal errors. Clear it and try again.
- Check GDC Status: Check the GDC website for scheduled maintenance or system outage announcements [21].
- Update Data Transfer Tool: Ensure you use the latest GDC Data Transfer Tool (DTT) client. Older versions may have compatibility issues [21].
- Review Access Authority: Controlled-access data requires dbGaP authorization. Verify your approval for the specific dataset.
Q2: After acquiring multi-omics data, what are the first critical steps to ensure data quality before integration?
- A2: Initial quality control (QC) is paramount to avoid propagating technical artifacts.
- Conduct Platform-Specific QC: For each data type (e.g., WGS, RNA-Seq, proteomics), use established pipelines to assess metrics like sequencing depth, mapping rates, and sample-level correlations [22].
- Perform Batch Effect Detection: Use Principal Component Analysis (PCA) or other methods to visualize data and check for groupings by processing date, sequencing lane, or other technical factors [22] [23].
- Apply Batch Correction: If batch effects are detected, apply correction algorithms like ComBat to remove technical variance without affecting biological signal [22].
- Address Missing Data: Develop a strategy for missing values, which may involve imputation using matrix factorization or deep learning methods, or removal of features with excessive missingness [23].
Troubleshooting Guide: Multi-Omics Data Integration
Q3: When integrating high-dimensional multi-omics data for model training, my models are overfitting. How can I improve generalizability?
- A3: Overfitting in multi-omics is common due to high feature-to-sample ratios.
- Employ Dimensionality Reduction: Use feature selection (e.g., based on variance) or extraction techniques (e.g., autoencoders) before model training to reduce noise [23].
- Utilize Regularization: Apply L1 (Lasso) or L2 (Ridge) regularization within your models to penalize complex, overfit solutions [23].
- Implement Rigorous Validation: Always use held-out test sets and cross-validation. Consider federated learning approaches, which train models across multiple institutions without sharing raw data, to enhance robustness and generalizability [22] [23].
- Incorporate Biological Networks: Use prior knowledge (e.g., protein-protein interaction networks) with Graph Neural Networks (GNNs) for more biologically meaningful integration than simple data concatenation [23].
Q4: How can I handle the challenge of missing data from one or more omics layers in a subset of my patient samples?
- A4: The choice of method depends on the extent and mechanism of missingness.
- For Small-Scale Missingness: Use imputation methods like multivariate imputation by chained equations (MICE) or k-nearest neighbors (KNN).
- For Large-Scale or Complex Missingness: Leverage generative deep learning models, such as Variational Autoencoders (VAEs) or Generative Adversarial Networks (GANs), which are particularly effective at synthesizing plausible multi-omics data to address missingness and class imbalance [23].
Troubleshooting Guide: High-Throughput Screens and Validation
Q5: My high-throughput drug screen results show high variability and poor reproducibility. What factors should I investigate?
- A5: Technical and biological noise can compromise screen quality.
- Audit Laboratory Protocols: Ensure consistent cell culture conditions, passage numbers, and reagent quality across all assay plates.
- Normalize Plate Effects: Use within-plate positive and negative controls to normalize for edge effects, evaporation, or dispenser errors.
- Employ Robust Statistical Scoring: Use metrics like Z'-factor to assess assay quality and quantify the separation between positive and negative controls.
- Integrate Multi-Omics Data: Correlate drug response with baseline multi-omics data (e.g., mutation status, gene expression) to identify molecular predictors of sensitivity, which can validate screen findings biologically [22] [11].
Q6: How can I validate a target identified computationally from TCGA data using experimental biology?
- A6: Computational findings require rigorous experimental confirmation.
- In Vitro Functional Studies: Use siRNA or CRISPR-Cas9 to knock down/out the target gene in relevant cancer cell lines and assay for changes in proliferation, invasion, or apoptosis.
- Ex Vivo Validation: Correlate target expression or mutation status with patient outcomes (e.g., survival, treatment response) in independent clinical cohorts or patient-derived organoids.
- Leverage Multi-Omics for Context: Integrate proteomic or phosphoproteomic data to understand the target's functional role within signaling networks and identify potential resistance mechanisms [22].
Experimental Protocols for Model Validation
Protocol 1: Multi-Omics Data Preprocessing and Integration for Classifier Development
This protocol outlines a workflow for processing diverse omics data from the GDC to build a robust molecular subtype classifier [22].
- Data Acquisition: Download harmonized Level 3 or 4 data (e.g., gene expression counts, somatic mutations, copy number variations) for your cancer of interest from the GDC Data Portal [21].
- Quality Control (QC):
- Genomics/Transcriptomics: Filter out genes with near-zero counts or variants with low allele frequency. Check for outlier samples using PCA.
- Proteomics: Remove proteins with many missing values. Impute remaining missing values using a method like KNN.
- Data Normalization:
- Apply platform-specific normalization (e.g., DESeq2 for RNA-Seq data, quantile normalization for proteomics data) [22].
- Feature Selection:
- Reduce dimensionality by selecting top variable features or those with known biological relevance to the cancer type.
- Data Integration and Model Training:
- Concatenate selected features from different omics layers into a unified matrix.
- Train a classifier (e.g., Random Forest, Support Vector Machine) using a cross-validated framework to predict known molecular subtypes.
- Model Interpretation:
Protocol 2: Cross-Platform Validation of a Transcriptomic Signature
This protocol ensures a gene expression signature derived from one platform (e.g., RNA-Seq) is valid and actionable on another (e.g., NanoString or RT-qPCR).
- Signature Definition: Define your gene signature from the discovery cohort (e.g., TCGA RNA-Seq data).
- Independent Cohort Selection: Identify a validation cohort with matching clinical data from a public repository (e.g., GEO) or an in-house dataset.
- Data Harmonization:
- Map the signature genes to their counterparts in the validation dataset.
- Apply the same normalization and scaling procedures used in the discovery phase to the validation data.
- Score Calculation: Calculate the signature score for each sample in the validation cohort using the same method (e.g., single-sample GSEA, mean of Z-scores).
- Statistical Validation:
- Test the association between the signature score and the clinical endpoint (e.g., overall survival using a Cox model, or response to therapy using a t-test) in the validation cohort.
- A statistically significant result in the independent cohort strengthens the validity of your computational model.
Table 1: Key NCI Genomic Data Commons (GDC) Data Releases and Content
This table summarizes recent data releases from the GDC, a primary source for TCGA and other multi-omics data [21].
| Data Release | Key Highlights and New Data Projects |
|---|---|
| Data Release 44 | New projects, new cases from existing projects. |
| Data Release 43 | New and updated data sets. |
| Data Release 42 | Release of 8,000+ new whole genome sequencing (WGS) variant calls. |
| Data Release 41 | New data sets for NCI-MATCH Trial arms, whole slide images. |
| Data Release 40 | Additional TCGA WGS alignments and variant calls, WXS and RNA-Seq data for new NCI-MATCH Trial arms. |
| Data Release 39 | New TCGA WGS variants, additional higher coverage alignments, five new projects from NCI’s MATCH program. |
Table 2: AI Model Applications in Oncology Data Analysis
This table categorizes artificial intelligence models by their primary application in processing complex oncology data [11].
| AI Model Type | Primary Data Modalities | Example Applications in Oncology |
|---|---|---|
| Classical Machine Learning (ML) | Structured data: genomic biomarkers, lab values [11]. | Survival prediction, therapy response [11]. |
| Convolutional Neural Networks (CNNs) | Imaging data: histopathology, radiology [11]. | Tumor detection, segmentation, and grading; automatic quantification of IHC staining [22] [11]. |
| Transformers / Recurrent Neural Networks (RNNs) | Sequential/text data: genomic sequences, clinical notes [11]. | Biomarker discovery, electronic health record (EHR) mining [11]. |
| Graph Neural Networks (GNNs) | Biological networks, multi-omics data [22]. | Modeling protein-protein interaction networks to prioritize druggable hubs [22]. |
Workflow and Signaling Pathway Diagrams
Multi-Omics AI Integration Workflow
Cancer Target Identification & Validation
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Research Reagents for Computational Oncology Validation
| Reagent / Material | Function in Experimental Validation |
|---|---|
| siRNA / shRNA Libraries | Gene knockdown to assess the functional necessity of a computationally identified target on cellular phenotypes (e.g., proliferation, apoptosis). |
| CRISPR-Cas9 Knockout Kits | Complete gene knockout for definitive functional validation of a candidate cancer target. |
| Patient-Derived Organoid (PDO) Cultures | Ex vivo models that retain tumor heterogeneity and microenvironment, used for high-throughput drug testing and validating target relevance. |
| Multiplex Immunohistochemistry (mIHC) Kits | Simultaneous detection of multiple protein biomarkers on a single tissue section to validate protein-level expression and spatial relationships predicted by multi-omics models. |
| Circulating Tumor DNA (ctDNA) Assay Kits | For non-invasive monitoring of tumor dynamics and resistance mutations during treatment, validating predictive models of therapy response [22]. |
The traditional single-target paradigm in cancer drug discovery, often guided by serendipitous findings, is increasingly giving way to a more systematic, network-based approach. This shift is driven by the critical challenge of drug resistance, where cancer cells bypass inhibited single targets by activating alternative pathways [24]. Furthermore, analysis of clinical trials reveals a "drug discovery winter," with over 96% of trials focusing on previously tested drug targets and only 12% of the human interactome being targeted [25]. If current patterns persist, it would take an estimated 170 years to target all druggable proteins [25].
Network-based approaches address these limitations by modeling the complex interactions within cancer systems, moving beyond the "tunnel vision" of single-target strategies to a more holistic view of drug mechanisms [26]. These methods leverage computational tools to identify optimal target combinations that can counteract resistance mechanisms by simultaneously targeting multiple nodes in cancer signaling networks [24].
Key Computational Tools and Methodologies
Network Analysis and Target Identification Tools
Table 1: Computational Tools for Network-Based Target Identification
| Tool Name | Primary Function | Key Features | Validation/Performance |
|---|---|---|---|
| DeepTarget [26] | Predicts primary & secondary targets of small-molecule agents | Integrates drug/genetic knockdown viability screens & omics data; open-source | Outperformed RoseTTAFold All-Atom & Chai-1 in 7/8 drug-target test pairs |
| Network-Informed Signaling-Based Approach [24] | Discovers optimal drug target combinations to counter resistance | Uses PPI networks & shortest paths (PathLinker algorithm) | Validated in patient-derived breast & colorectal cancers; resulted in tumor diminishment |
| Graph Convolutional Network (GCN) [24] | Optimizes drug combination prioritization | Semantic relationships between drug and disease; pathway crosstalk analysis | Identified rare, contingent drug synergies in cancer cell lines |
| Multi-dimensional Bioinformatic Analysis [27] | Identifies key therapeutic targets through integrative genomics | Combines Mendelian randomization, WGCNA, PPI networks, and eQTL/pQTL analyses | Identified and validated EGLN1 as a core causal protective target in high BMI-associated CRC |
Table 2: Essential Data Resources for Network-Based Cancer Research
| Resource Name | Data Type | Application in Network Modeling | Access Information |
|---|---|---|---|
| The Cancer Genome Atlas (TCGA) [28] [24] | Multi-omics data (genomics, transcriptomics, etc.) | Provides molecular profiles for 11,000+ tumor samples; identifies shared oncogenic drivers | Publicly available |
| HIPPIE PPI Database [24] | Protein-protein interactions | High-confidence human interactome for network path calculations | Publicly available |
| UCSC Genome Browser [28] | Multi-omics data integration | Copy number variations, methylation profiles, gene/protein expression | Publicly available |
| Gene Expression Omnibus (GEO) [28] | Gene expression data | Microarray and RNA-Seq data for cross-cancer pattern analysis | Publicly available |
| ClinicalTrials.gov [25] | Clinical trial metadata | Analysis of drug exploration patterns and target selection trends | Publicly available |
Frequently Asked Questions (FAQs)
Q1: What are the fundamental limitations of single-target approaches that network methods address? Single-target therapies frequently succumb to resistance because cancer cells activate alternative pathways (bypass mechanisms) [24]. Network analysis reveals that this resistance occurs through "local network effects" - when inhibition of one node simply shifts signaling to interacting proteins in the same network neighborhood [25]. Additionally, clinical trial data shows that the current drug discovery paradigm is stuck in a cycle of repeatedly targeting the same proteins, leaving most of the druggable genome unexplored [25].
Q2: How do we select the most relevant protein-protein interaction network for our specific cancer type? Network selection should be guided by confidence scores and biological relevance. The HIPPIE database provides a high-confidence, scored human interactome that has been successfully applied to breast and colorectal cancers [24]. For specific cancer contexts, integrate your own omics data (e.g., from TCGA) to filter networks to cancer-relevant interactions. Always validate that your proteins of interest are represented in the chosen network.
Q3: What computational workflow can we use to identify key bridge nodes in signaling networks? The following diagram illustrates a validated workflow for identifying critical bridge nodes in cancer networks:
Q4: How can we validate that computationally predicted network targets have real biological relevance? Validation requires a multi-step approach: First, use functional enrichment analysis (GO/KEGG) to confirm pathways are cancer-relevant [27]. Second, correlate target expression with patient outcomes using TCGA data. Third, perform experimental validation in relevant models - for example, testing alpelisib + LJM716 combinations in breast cancer PDXs or using in vitro assays to confirm that compounds like Cianidanol inhibit proliferation and invasion in CRC cells [24] [27].
Q5: What are the key metrics for evaluating the performance of network-based target prediction tools? Benchmark computational tools against established methods using metrics like prediction accuracy across diverse datasets, performance in real-world case studies (e.g., drug repurposing predictions), and experimental validation success rates [26]. For example, DeepTarget was benchmarked against RoseTTAFold and Chai-1 across eight drug-target test pairs [26].
Troubleshooting Common Experimental Challenges
Network Construction and Analysis Issues
Problem: Incomplete or low-quality PPI networks leading to inaccurate paths
- Solution: Use integrated, confidence-scored databases like HIPPIE [24]. Filter interactions by confidence score threshold (typically >0.7). Cross-reference with cancer-specific interaction databases to ensure biological relevance.
- Prevention Strategy: Perform sensitivity analysis by comparing results across different PPI resources. Validate that known interactions in your pathway of interest are present.
Problem: Too many potential bridge nodes identified, making prioritization difficult
- Solution: Implement multi-parameter filtering: (1) Calculate betweenness centrality, (2) Check druggability using databases like DrugBank, (3) Verify differential expression in cancer vs. normal tissue, (4) Check association with patient survival [24] [27].
- Prevention Strategy: Define clear criteria for bridge nodes upfront based on network topology measures and biological constraints.
Validation and Experimental Translation Challenges
Problem: Computational predictions fail to validate in cellular models
- Solution: This often indicates poor model specificity. Return to network analysis and: (1) Check if identified paths are active in your specific cell line using expression data, (2) Analyze potential compensatory mechanisms, (3) Consider combination targeting rather than single nodes [24].
- Prevention Strategy: Use cell line-specific omics data to filter networks before analysis. Implement multi-omics integration to ensure identified paths are transcriptionally active.
Problem: Drug combinations show unexpected toxicity despite computational prediction
- Solution: Network models might miss tissue-specific effects. (1) Analyze target expression in healthy tissues, (2) Check for pathway enrichment in essential processes, (3) Use more selective inhibitors or adjusted dosing schedules [24].
- Prevention Strategy: Incorporate tissue-specific networks where available. Perform differential pathway analysis between tumor and normal tissues.
Table 3: Key Research Reagent Solutions for Network-Based Target Validation
| Reagent/Resource | Function/Application | Example Use Case | Considerations |
|---|---|---|---|
| PathLinker Algorithm [24] | Identifies k-shortest paths in PPI networks | Finding signaling paths between proteins with co-existing mutations | Default k=200 provides balance between coverage and computational cost |
| Alpelisib (PIK3CA inhibitor) [24] | PI3K/AKT/mTOR pathway inhibition | Combination therapy in PIK3CA-mutated breast cancers | Resistance common via alternative pathways; requires combination targeting |
| Cianidanol [27] | EGLN1 modulator; natural compound | Targeting high BMI-associated colorectal cancer | Binding affinity: -11.24 kcal/mol; inhibits proliferation, migration, invasion |
| Patient-Derived Xenografts (PDXs) [24] | Preclinical validation of target combinations | Testing network-predicted combinations in physiologically relevant models | Maintains tumor heterogeneity and microenvironment interactions |
| Single-cell RNA Sequencing [27] | Cell-type specific target validation | Identifying EGLN1 enrichment in T cells and intestinal epithelial cells | Reveals tumor microenvironment context of targets |
| LJM716 (Anti-ERBB3 antibody) [24] | ERBB3/herceptin resistance inhibition | Combination with alpelisib in breast cancer targets | Targets resistance mechanism to PI3K inhibition |
Advanced Methodologies: Experimental Protocols for Network Target Validation
Protocol: Network-Based Combination Target Identification
Based on: Szalai B. et al. "Discovering anticancer drug target combinations via network-informed signaling-based approach" [24]
Workflow Diagram:
Step-by-Step Procedure:
- Data Collection: Obtain somatic mutation data from TCGA and/or AACR GENIE databases. Focus on primary tumor samples and remove low-confidence variants [24].
- Identify Co-existing Mutations: Perform pairwise analysis across proteins to find statistically significant mutation co-occurrences using Fisher's Exact Test with multiple testing correction [24].
- Network Construction: Download high-confidence human PPI network from HIPPIE. Filter interactions by confidence score threshold.
- Path Calculation: Use PathLinker algorithm (k=200) to compute shortest paths between proteins harboring co-existing mutations [24].
- Bridge Node Identification: Extract all nodes from calculated paths. Calculate betweenness centrality to identify critical bridge nodes.
- Target Selection: Prioritize bridge nodes that connect alternative signaling pathways to prevent bypass resistance.
- Experimental Validation: Test predicted target combinations in patient-derived xenograft models measuring tumor growth inhibition [24].
Protocol: Multi-dimensional Target Validation for Context-Specific Therapies
Based on: Yu X. et al. "Identification and validation of EGLN1 as a key target" [27]
Workflow Diagram:
Step-by-Step Procedure:
- Causal Inference: Perform two-sample Mendelian randomization to establish causal relationships between risk factors (e.g., high BMI) and cancer outcomes [27].
- Multi-omics Integration: Analyze differentially expressed genes and construct weighted gene co-expression networks (WGCNA) from transcriptomic data.
- Network Analysis: Build protein-protein interaction networks from intersecting gene sets and identify hub genes using topological analysis [27].
- Molecular QTL Integration: Perform eQTL and pQTL analyses to identify causal targets, followed by phenome-wide association studies to assess pleiotropy.
- Mechanistic Elucidation: Conduct single-gene GSEA and single-cell RNA sequencing to understand target function across cell types. Perform gut microbiota mediation analysis if relevant [27].
- Compound Screening: Computational screening of compound libraries followed by molecular docking to identify potential therapeutics.
- Functional Validation: In vitro assays measuring cell proliferation, migration, invasion, and target protein expression changes [27].
Troubleshooting Guide: Common Experimental Issues
Q: My computational model shows high accuracy in validation but fails in biological assays. What could be wrong? A: This often indicates overfitting or a failure to account for biological context. Key troubleshooting steps include:
- Verify Feature Biological Relevance: Ensure the input features (e.g., gene mutations, expression levels) have a documented causal relationship with the cancer phenotype, not just correlation.
- Check Data Leakage: Confirm that no information from your test set (e.g., patient outcomes) was used during the training phase of the model.
- Assay Translation Fidelity: Validate that your in vitro or in vivo assay system accurately recapitulates the human tumor microenvironment relevant to your target.
Q: How can I determine if my model's prediction is statistically significant and not due to chance? A: Implement robust statistical testing.
- Perform Permutation Testing: Randomly shuffle your outcome labels (e.g., "sensitive" vs. "resistant") and re-run your model multiple times (e.g., 1000 permutations). The p-value is the proportion of permutations where the model performance meets or exceeds the performance with the true labels.
- Apply Multiple Hypothesis Correction: If testing multiple hypotheses (e.g., many potential drug targets), use corrections like Bonferroni or Benjamini-Hochberg to control the false discovery rate (FDR).
Q: My visualization diagram has poor readability. How can I improve color contrast for nodes and text? A: Adhere to established color contrast rules.
- For Node Text: Explicitly set the
fontcolorattribute to ensure high contrast against the node'sfillcolor. The Web Content Accessibility Guidelines (WCAG) recommend a contrast ratio of at least 4.5:1 [29] [30]. - For Diagram Elements: Avoid using similar colors for foreground elements (like arrows or symbols) and the background. Use a color contrast checker to verify ratios [31].
Frequently Asked Questions (FAQs)
Q: What are the minimum validation steps required before a computational prediction can be considered for wet-lab experimentation? A: At a minimum, validation should include:
- Internal Validation: Use cross-validation on the training dataset to assess model stability.
- External Validation: Test the model's performance on a completely independent dataset, preferably from a different source or institution.
- Benchmarking: Compare your model's performance against established baseline methods or random predictors.
Q: Which statistical metrics are most informative for validating a classification model in this context? A: Rely on a suite of metrics, as no single metric tells the whole story.
- AUC-ROC (Area Under the Receiver Operating Characteristic Curve): Assesses the model's ability to distinguish between classes across all thresholds.
- Precision and Recall: Crucial when dealing with imbalanced datasets (e.g., few true positives among many candidates).
- F1-Score: The harmonic mean of precision and recall, providing a single balanced metric.
Q: How can I visually represent my experimental workflow and prediction logic clearly? A: Use Graphviz to create standardized diagrams. The DOT language allows you to define nodes, edges, and their properties systematically, ensuring consistency and clarity in your visual communications [32].
Quantitative Validation Criteria Table
The following table outlines key quantitative thresholds for model validation.
| Validation Metric | Minimum Threshold for Consideration | Target for Clinical Actionability | Technical Notes |
|---|---|---|---|
| AUC-ROC | > 0.70 | > 0.85 | Area Under the Curve; robust to class imbalance [31]. |
| Precision | > 0.80 | > 0.95 | Measures the fraction of true positives among all positive predictions. |
| Recall (Sensitivity) | > 0.70 | > 0.85 | Measures the fraction of actual positives correctly identified. |
| F1-Score | > 0.75 | > 0.90 | Harmonic mean of precision and recall. |
| p-value (vs. Random) | < 0.05 | < 0.01 | Derived from permutation testing. |
| False Discovery Rate (FDR) | < 0.10 | < 0.05 | Adjusted p-value for multiple comparisons. |
Experimental Protocol:In VitroValidation of a Predicted Cancer Target
Objective: To experimentally validate a computationally predicted cancer gene target for essentiality in a specific cell line.
Methodology: CRISPR-Cas9 Knockout and Viability Assay
sgRNA Design:
- Design 4-6 single-guide RNAs (sgRNAs) targeting the exon of the predicted gene.
- Design non-targeting control sgRNAs.
Lentiviral Transduction:
- Clone sgRNAs into a lentiviral vector (e.g., lentiCRISPRv2).
- Produce lentiviral particles in HEK293T cells.
- Transduce the target cancer cell line at a low MOI (Multiplicity of Infection) to ensure single copy integration.
- Select transduced cells with puromycin (2 µg/mL) for 72 hours.
Cell Viability Measurement:
- Seed selected cells in 96-well plates.
- Monitor cell viability for 5-7 days using a CellTiter-Glo Luminescent Cell Viability Assay.
- Measure luminescence daily.
Data Analysis:
- Normalize luminescence readings to the day of selection (Day 0).
- Compare the growth curve of cells with the target gene knocked out to those with non-targeting control sgRNAs.
- A statistically significant reduction in viability for the target knockout group validates the prediction.
Visualization Diagrams
Model Validation Workflow
This diagram outlines the logical flow from computational prediction to experimental validation.
Signaling Pathway Impact
This diagram illustrates how a predicted target hypothetically impacts a core cancer signaling pathway.
The Scientist's Toolkit: Research Reagent Solutions
| Reagent / Material | Function in Validation |
|---|---|
| lentiCRISPRv2 Plasmid | A lentiviral vector for the stable delivery of the CRISPR-Cas9 system and sgRNA for gene knockout studies. |
| Puromycin | A selection antibiotic used to eliminate non-transduced cells and create a pure population of CRISPR-edited cells. |
| CellTiter-Glo Assay | A luminescent assay that measures ATP levels as a proxy for metabolically active, viable cells in culture. |
| HEK293T Cell Line | A highly transfectable cell line commonly used for the production of lentiviral particles. |
| Non-Targeting Control sgRNA | A critical control sgRNA that does not target any genomic sequence, used to account for non-specific effects of the CRISPR system. |
Tools of the Trade: A Deep Dive into Cutting-Edge Computational Frameworks and Their Real-World Applications
Core Concepts and Workflow
What is DeepTarget and what is its primary function?
DeepTarget is a computational tool that predicts the mechanisms of action (MOA) driving a drug's anti-cancer efficacy. It integrates large-scale drug viability screens, genetic knockdown viability screens (specifically CRISPR-Cas9 knockout), and omics data (gene expression and mutation) from matched cancer cell lines to identify both primary and secondary drug targets, as well as mutation-specificity preferences [33] [34] [35]. Unlike structure-based methods that predict direct binding, DeepTarget captures both direct and indirect, context-dependent mechanisms driving drug efficacy in living cells [34].
What is the fundamental hypothesis behind DeepTarget's approach?
DeepTarget operates on the principle that CRISPR-Cas9 knockout (CRISPR-KO) of a drug’s target gene mimics the drug’s inhibitory effects across a panel of cancer cell lines. Therefore, identifying genes whose deletion induces similar viability patterns to drug treatment can reveal the drug's potential targets [34].
The following diagram illustrates the core three-step prediction pipeline of DeepTarget.
Performance and Validation Data
DeepTarget's performance was rigorously benchmarked against state-of-the-art tools across eight high-confidence, gold-standard datasets of cancer drug-target pairs [34] [26]. The following table summarizes its key quantitative performance metrics.
| Validation Metric | Performance Result | Comparative Performance (vs. RosettaFold & Chai-1) |
|---|---|---|
| Primary Target Prediction (Mean AUC across 8 datasets) | AUC 0.73 [34] [26] | Outperformed in 7 out of 8 datasets [34] [35] |
| Secondary Target Prediction | AUC 0.92 (vs. known multi-target drugs) [34] [36] | Not directly compared |
| Mutation-Specificity Prediction | AUC 0.78 (distinguishing mutant-specific inhibitors) [36] | Not directly compared |
| Dataset Scale | Predictions for 1,500 cancer-related drugs and 33,000 natural product extracts [33] [26] | N/A |
Frequently Asked Questions (FAQs) & Troubleshooting
Data Input and Preprocessing
Q: What are the specific data requirements to run DeepTarget? A: DeepTarget requires three types of data across a panel of cancer cell lines [34]:
- Drug Response Profiles: Viability data for the drug of interest. The source study used data for 1,450 drugs across 371 cancer cell lines from the DepMap repository.
- Genetic Knockdown Viability Profiles: Genome-wide CRISPR-KO viability profiles. The tool uses Chronos-processed CRISPR dependency scores to account for technical confounders.
- Omics Data: Corresponding gene expression and mutation data for the same cell lines.
Q: My gene of interest is not a known direct binding partner, yet it appears as a high-ranking prediction. Is this an error? A: Not necessarily. DeepTarget's predictions can include both direct binding targets and other genes in the drug’s mechanism of action pathway [34]. To distinguish between these, use the provided post-filtering steps (e.g., restricting to kinase proteins for kinase inhibitors) and pathway enrichment analysis to gain a systems-level view [34].
Interpretation of Results
Q: What does the Drug-KO Similarity (DKS) Score represent? A: The DKS score is a Pearson correlation quantifying the similarity between a drug's response profile and the viability profile resulting from knocking out a specific gene [34]. A higher score indicates stronger evidence that the gene is involved in the drug's mechanism of action.
Q: How does DeepTarget define and identify secondary targets? A: The tool identifies two types of context-specific secondary targets [34]:
- Type A: Those contributing to efficacy even when primary targets are present, identified via de novo decomposition of drug response.
- Type B: Those mediating responses specifically when primary targets are not expressed, identified by computing Secondary DKS Scores in cell lines lacking primary target expression.
Q: The tool seems to perform poorly for my drug targeting a GPCR. Why? A: This is a known current limitation. DeepTarget struggles on certain target classes like GPCRs, nuclear receptors, and ion channels [36]. For these, structure-based tools may currently be preferred if high-resolution structural data is available.
Experimental Validation Protocols
A key strength of DeepTarget is the experimental validation of its predictions. Below are detailed protocols for the case study that validated a secondary target.
Protocol: Validating a Predicted Secondary Target (Ibrutinib-EGFR)
Background: DeepTarget predicted that Ibrutinib, a drug whose primary target is BTK, kills lung cancer cells by acting on a secondary target, mutant EGFR, specifically the T790-mutated form [35] [37].
Objective: To experimentally validate that cancer cells harboring the mutant EGFR T790 are more sensitive to Ibrutinib.
Materials:
- Cell Lines: Lung cancer cell lines isogenic for the EGFR T790 mutation (with and without the mutation) [35] [37].
- Drug: Ibrutinib (FDA-approved BTK inhibitor).
- Equipment: Cell culture facility, equipment for measuring cell viability (e.g., plate reader for MTT or CellTiter-Glo assays).
Methodology:
- Cell Culture: Maintain the paired cell lines in standard conditions.
- Drug Treatment: Treat cells with a range of Ibrutinib concentrations.
- Viability Assay: Measure cellular viability after a predetermined incubation period (e.g., 72 hours) using a standard assay.
- Data Analysis: Calculate the half-maximal inhibitory concentration (IC50) for Ibrutinib in both cell lines. A statistically significant lower IC50 in the mutant EGFR T790 cell line compared to the wild-type control confirms higher sensitivity and validates EGFR as a functional secondary target [35] [37].
Expected Outcome: Cells with the EGFR T790 mutation will show significantly greater sensitivity (lower IC50) to Ibrutinib, confirming the prediction.
This experimental workflow for secondary target validation is summarized in the diagram below.
The Scientist's Toolkit: Research Reagent Solutions
The following table details key reagents and resources used in the development and validation of DeepTarget.
| Reagent / Resource | Function in DeepTarget Workflow | Source / Example |
|---|---|---|
| DepMap Data | Provides the foundational drug response, CRISPR knockout, and omics data across hundreds of cancer cell lines. | Dependency Map (DepMap) Consortium [34] [37] |
| Chronos-Processed CRISPR Scores | Provides corrected, high-quality genetic dependency scores, accounting for sgRNA efficacy, copy number effects, and other confounders. | DepMap/Chronos Algorithm [34] |
| Gold-Standard Datasets | Used for benchmarking and validating prediction accuracy against known, high-confidence drug-target interactions. | COSMIC, oncoKB, DrugBank, SelleckChem [34] |
| Open-Source Code | Allows researchers to run the DeepTarget algorithm on their own data. | GitHub Repository (CBIIT-CGBB/DeepTarget) [33] [34] |
| Predicted Target Profiles | Pre-computed predictions for thousands of compounds, enabling immediate hypothesis generation. | Provided for 1,500 drugs & 33,000 natural extracts [33] [26] |
Frequently Asked Questions (FAQs)
Q1: What is the primary purpose of the DrugAppy workflow? DrugAppy is an end-to-end deep learning framework designed for computational drug discovery. Its primary purpose is to identify druggable oncogenic vulnerabilities and design novel chemical entities against them, significantly accelerating the inhibitor discovery and optimization process. It uses a hybrid model that combines Artificial Intelligence (AI) algorithms with computational and medicinal chemistry methodologies. [38]
Q2: Which specific case studies have validated the DrugAppy workflow? The framework has been successfully validated through two key case studies:
- PARP1 Inhibitors: DrugAppy identified two molecules with activity comparable to the reference inhibitor olaparib. [38]
- TEAD4 Inhibitors: The workflow discovered a compound that outperforms the activity of IK-930, the reference inhibitor for this target. [38]
Q3: What computational tools are integrated into the DrugAppy workflow? DrugAppy is built on an imbrication of several specialized computational tools, each with a specific function [38]:
- SMINA & GNINA: Used for High Throughput Virtual Screening (HTVS) to rapidly evaluate compound binding.
- GROMACS: Employed for Molecular Dynamics (MD) simulations to study the dynamic behavior and stability of protein-ligand complexes.
- Proprietary AI Models: Trained on public datasets to predict key parameters like drug pharmacokinetics, selectivity, and potential activity.
Q4: My virtual screening results in an unmanageably high number of hits. How can I refine them? A high number of hits is common. The DrugAppy workflow addresses this by employing a multi-stage filtering process [38]. After the initial HTVS, hits are progressed to more rigorous molecular dynamics simulations using tools like GROMACS to assess binding stability. Furthermore, key parameters such as ADMET (Absorption, Distribution, Metabolism, Excretion, Toxicity) properties are predicted using AI models to prioritize candidates with desirable drug-like properties early in the process.
Q5: How can I characterize covalent inhibitors, which pose unique experimental challenges? Characterizing covalent inhibitors requires specific protocols. An enzyme activity-based workflow is recommended, which uses continuous assays to monitor time-dependent inhibition. This method streamlines the evaluation of these inhibitors by focusing on their functional impact on enzyme activity, enhancing the reliability and reproducibility of their assessment. [39]
Q6: The AI model's predictions for my novel target seem unreliable. What could be wrong? Unreliable predictions can often be traced to data quality or model applicability. Ensure that the training data used by the model is of high quality and relevant to your specific target. For novel targets with limited data, fine-tuning the model on a high-dimensional, target-specific dataset may be necessary to improve accuracy and generalizability. [40]
Troubleshooting Guides
Issue: Poor Binding Affinity Predictions during Virtual Screening
Problem: The binding affinity scores (e.g., from SMINA/GNINA) for your top hits are weak or do not correlate with subsequent experimental results.
Solution:
- Check Input Structures: Verify the protonation states and tautomeric forms of both the ligand and the protein binding site residues. Incorrect states can severely impact scoring.
- Refine Scoring Functions: Do not rely on a single scoring function. Use consensus scoring from multiple functions or consider re-scoring top hits with more computationally intensive, but potentially more accurate, methods.
- Progress to Dynamics: Move promising but weak hits to molecular dynamics (MD) simulations. MD can reveal stabilizing interactions that static docking misses and provide a more realistic assessment of binding stability and affinity over time. [38]
Issue: Inefficient Hyperparameter Tuning in AI Models
Problem: The deep learning models used for activity prediction are slow to train and converge to suboptimal performance.
Solution: Implement an advanced optimization framework like optSAE + HSAPSO (Hierarchically Self-Adaptive Particle Swarm Optimization). This hybrid approach integrates a stacked autoencoder for robust feature extraction with an adaptive PSO algorithm for hyperparameter tuning. This method has been shown to achieve high accuracy (95.52%) and significantly reduced computational complexity (0.010 seconds per sample). [40]
Issue: High Computational Cost of Molecular Dynamics Simulations
Problem: MD simulations with GROMACS for a large number of hits are prohibitively time-consuming and resource-intensive.
Solution:
- Strategic Sampling: Use the results from HTVS to create a highly focused subset of compounds for MD. Prioritize compounds with diverse chemotypes and strong binding scores.
- Active Learning Workflow: Implement an active learning pipeline that uses machine learning to select the most informative compounds for MD simulation, thereby reducing the total number of simulations required. This approach has been shown to get information from calculations 20 times faster than a brute-force approach. [41]
- Leverage HPC Resources: Utilize high-performance computing (HPC) environments, such as those offered by national supercomputing centers, to run multiple simulations in parallel. [41]
Key Experimental Data and Protocols
The following table summarizes the quantitative results from the case studies used to validate the DrugAppy workflow.
Table 1: DrugAppy Performance in Case Study Validation [38]
| Target | Reference Inhibitor | DrugAppy Discovery | Performance Outcome |
|---|---|---|---|
| PARP1 | Olaparib | Compound 1 | Activity comparable to Olaparib |
| PARP1 | Olaparib | Compound 2 | Activity comparable to Olaparib |
| TEAD4 | IK-930 | Novel Compound | Activity surpasses IK-930 |
Workflow for Covalent Inhibitor Characterization
This protocol outlines a robust, enzyme activity-based method for characterizing covalent inhibitors, which is crucial for assessing their unique mechanism of action. [39]
Principle: The protocol uses a continuous enzyme activity assay to monitor the time-dependent inhibition that is characteristic of covalent modifiers. The gradual, irreversible (or slowly reversible) inactivation of the enzyme results in a change in the assay signal over time.
Materials:
- Purified target enzyme
- Putative covalent inhibitor compounds
- Enzyme substrate and necessary cofactors
- Assay buffer
- Microplate reader capable of kinetic measurements
Procedure:
- Pre-incubation: In a microplate, prepare a mixture of the enzyme and varying concentrations of the inhibitor in an appropriate buffer. Do not add the substrate yet.
- Time-Course Measurement: Initiate the reaction by adding the substrate to the enzyme-inhibitor mixture.
- Data Acquisition: Immediately place the plate in the reader and continuously monitor the product formation (e.g., by absorbance or fluorescence) over a sufficient period (e.g., 30-60 minutes).
- Data Analysis:
- Plot the reaction velocity (signal slope) versus time for each inhibitor concentration.
- For a covalent inhibitor, you will observe a decrease in velocity over time, as more enzyme molecules become irreversibly inhibited.
- Fit the data to an appropriate model for time-dependent inhibition to determine the inhibition rate constant (k~inact~) and the inhibitor concentration that gives half-maximal rate of inactivation (K~I~).
Workflow and Pathway Visualizations
DrugAppy End-to-End Workflow
Covalent Inhibitor Assay Logic
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Computational Tools and Databases for the DrugAppy Workflow
| Item Name | Function / Purpose | Key Feature / Note |
|---|---|---|
| SMINA & GNINA [38] | High Throughput Virtual Screening (HTVS) for rapid docking of large compound libraries. | Specialized for robust and configurable docking simulations. |
| GROMACS [38] | Molecular Dynamics (MD) simulation software to study protein-ligand complex stability and dynamics. | Provides atomic-level insights into binding modes and stability over time. |
| OncoKB [42] | Precision oncology database providing curated information on oncogenic mutations and treatment implications. | Used to validate the clinical relevance of identified targets and inhibitors. |
| DrugBank / Swiss-Prot [40] | Public databases containing comprehensive drug, target, and protein sequence/functional information. | Serves as a primary data source for model training and validation. |
| AI/ML Models (e.g., SAE) [40] | Stacked Autoencoders for robust feature extraction from complex pharmaceutical data. | Achieves high accuracy in classification tasks (e.g., 95.52%). |
| HSAPSO Algorithm [40] | Hierarchically Self-Adaptive Particle Swarm Optimization for tuning AI model hyperparameters. | Enhances model performance, convergence speed, and stability. |
Troubleshooting Guide: Common Issues and Solutions
Users implementing the ABF-CatBoost framework for multi-target discovery in colon cancer may encounter several technical challenges. The table below outlines common issues and their solutions.
| Problem Scenario | Root Cause | Solution Steps | Expected Outcome |
|---|---|---|---|
| High-dimensional data causing model overfitting [43] | Noisy biomarkers and redundant features from gene expression data [43] | 1. Apply ABF optimization for rigorous feature selection [43]2. Implement cross-validation during training [43]3. Use regularization parameters within CatBoost | Improved model generalizability on external validation datasets |
| Poor generalization to external patient cohorts | Dataset-specific biases and insufficient molecular diversity [43] | 1. Integrate data from TCGA and GEO databases [43]2. Utilize external validation datasets for assessment [43]3. Analyze mutation patterns and resistance mechanisms [43] | Robust predictive accuracy across diverse populations |
| Suboptimal ABF parameter configuration | Non-adaptive search parameters limiting biomarker discovery [43] | 1. Refine ABF search parameters to maximize predictive accuracy [43]2. Use optimization to navigate high-dimensional search space effectively | Maximized accuracy, specificity, and sensitivity |
| Class imbalance in patient response data | Uneven distribution of drug responders vs. non-responders [43] | 1. Leverage CatBoost's built-in handling of imbalanced data2. Apply appropriate sampling techniques or class weighting | Balanced high sensitivity (0.979) and specificity (0.984) [43] |
Frequently Asked Questions (FAQs)
Model Performance and Interpretation
Q1: What performance metrics should I prioritize when validating the ABF-CatBoost model for colon cancer target discovery?
For a comprehensive validation of the ABF-CatBoost model, you should report a suite of metrics. The primary model achieved an accuracy of 98.6%, with complementary metrics including a sensitivity (recall) of 0.979, specificity of 0.984, and an F1-score of 0.978 [43]. These metrics collectively ensure the model is effective at identifying true positives (sensitivity) and true negatives (specificity), which is crucial for both patient classification and predicting drug response profiles [43].
Q2: The model performs well on training data but poorly on new validation sets. What could be the cause?
This is a classic sign of overfitting, a common challenge with high-dimensional molecular data [43]. To address this:
- Ensure the Adaptive Bacterial Foraging (ABF) optimization is actively refining the search parameters to select the most biologically relevant biomarkers, not just noisy features [43].
- Validate the model's generalizability using external datasets from repositories like TCGA and GEO [43].
- Verify that the integration of multiple data types (gene expression, mutation data, protein interaction networks) is done with proper normalization to reduce technical batch effects [43].
Data Integration and Biological Relevance
Q3: How does the ABF-CatBoost framework integrate multi-omics data to identify viable drug targets?
The framework integrates biomarker signatures from high-dimensional gene expression, mutation data, and protein-protein interaction (PPI) networks [43]. The ABF optimization algorithm sifts through this complex data to identify essential genes and pathways. Subsequently, CatBoost uses these refined features to classify patients and predict drug responses. This integrated approach allows for a multi-targeted strategy that can address complex drug resistance mechanisms by analyzing mutation patterns, adaptive resistance, and conserved binding sites [43].
Q4: What are the key signaling pathways implicated by this model in colon cancer?
The model's biomarker discovery often enriches pathways critical to colon cancer progression. Key pathways identified in related computational studies include the HIF-1 signaling pathway, PPAR signaling pathway, and processes related to lipid metabolism [27]. Furthermore, the framework can identify key hub genes such as KLF4 and MAPK3 from PPI networks, which are potential candidates for multi-targeted therapy [27].
Operationalization and Scaling
Q5: Can this computational framework be adapted for other cancer types?
Yes. The authors specify that by altering the biomarker selection and pathway analysis components, this computational framework can be modified for application to other cancers. This expands its impact significantly in the field of personalized cancer treatment [43].
Q6: What are the computational resource requirements for implementing such a model?
While the search results do not specify exact hardware requirements, working with high-dimensional molecular data (e.g., from microarrays and NGS) and complex optimization algorithms like ABF is computationally intensive [43]. Best practices from machine learning suggest ensuring sufficient memory (RAM) to handle large datasets and powerful processors (CPUs/GPUs) to manage the computational load of training ensemble models like CatBoost and running optimization algorithms in a reasonable time frame.
Experimental Protocol: ABF-CatBoost Workflow for Target Discovery
The following section details the methodology for implementing the ABF-CatBoost framework, from data curation to validation.
Data Acquisition and Pre-processing
- Data Sources: Acquire high-dimensional molecular data from public repositories such as The Cancer Genome Atlas (TCGA) and Gene Expression Omnibus (GEO). Essential data types include RNA-seq gene expression data, somatic mutation data, and protein-protein interaction networks [43].
- Pre-processing:
- Perform standard normalization and log-transformation on gene expression data.
- Handle missing values using appropriate imputation methods.
- Annotate data with clinical information, including patient outcomes and drug responses where available.
Feature Selection using Adaptive Bacterial Foraging (ABF)
- Objective: To identify the most predictive biomarkers from the high-dimensional input space [43].
- Procedure:
- Initialize a population of bacteria (candidate solutions), where each bacterium represents a subset of potential biomarkers (genes/features).
- Evaluate each bacterium's fitness based on its ability to improve predictive accuracy in a preliminary model.
- Chemotaxis: Simulate the movement and foraging behavior of bacteria. Each bacterium can take a step to a new location (a new subset of features) and evaluate the new fitness.
- Reproduction: The healthiest bacteria (best-performing feature subsets) split into two identical copies, replacing the least healthy ones.
- Elimination and Dispersal: With a low probability, random bacteria are eliminated and dispersed to a new random location in the feature space to avoid local optima.
- Adaptation: The run-length unit (step size) is adaptively tuned throughout the optimization process to balance exploration and exploitation [43].
- Terminate after a fixed number of iterations or upon convergence. The final population contains the optimized set of biomarker signatures.
Model Training with CatBoost
- Objective: To build a classifier that predicts patient groups or drug responses using the selected biomarkers [43].
- Procedure:
- Input: Use the refined feature set obtained from the ABF optimization step.
- Split Data: Partition the data into training, validation, and test sets (e.g., 70/15/15).
- Train Model: Utilize the CatBoost algorithm, a gradient boosting library that effectively handles categorical features and is robust to overfitting.
- Use default or cross-validated parameters as a starting point, paying attention to depth, learning rate, and number of iterations.
- Validate: Monitor performance on the validation set to prevent overfitting.
Model Validation and Interpretation
- Performance Metrics: Calculate accuracy, sensitivity, specificity, and F1-score on the held-out test set [43].
- External Validation: Assess the predictive accuracy and generalizability of the model on one or more completely independent external validation datasets [43].
- Biological Interpretation:
- Perform pathway enrichment analysis (e.g., GO, KEGG) on the top-ranked features from the model.
- Construct Protein-Protein Interaction (PPI) networks to identify hub genes among the selected biomarkers [43].
- The model can also be used to predict toxicity risks and drug efficacy profiles for safer treatment strategies [43].
The Scientist's Toolkit: Research Reagent Solutions
The table below catalogues essential computational and biomolecular reagents for replicating this research.
| Reagent / Resource | Type/Source | Function in the Experiment |
|---|---|---|
| TCGA-COAD Database | Public Genomic Database | Provides primary gene expression, mutation, and clinical data for colon adenocarcinoma patients for model training and testing [44]. |
| GEO (Gene Expression Omnibus) | Public Repository | Source of independent validation datasets to assess model generalizability and prevent overfitting [43]. |
| CatBoost Algorithm | Machine Learning Library | A gradient boosting algorithm that efficiently classifies patients based on molecular profiles and predicts drug responses [43]. |
| Cytoscape | Network Analysis Software | Used for constructing and visualizing Protein-Protein Interaction (PPI) networks to identify hub genes from the selected biomarkers [43]. |
| Molecular Docking Software (e.g., AutoDock) | Computational Tool | Used for in-silico validation of predicted drug-target interactions, such as assessing the binding affinity of compounds like Cianidanol to targets like EGLN1 [27]. |
| HCT116 Cell Line | Biological Model | A human colon cancer cell line used for in vitro functional validation of predicted targets and therapies (e.g., proliferation, migration assays) [27]. |
Model Performance Benchmarking
The ABF-CatBoost model was rigorously benchmarked against other established machine learning algorithms. The table below summarizes its superior performance.
| Model | Accuracy (%) | Sensitivity | Specificity | F1-Score |
|---|---|---|---|---|
| ABF-CatBoost (Proposed) | 98.6 [43] | 0.979 [43] | 0.984 [43] | 0.978 [43] |
| Random Forest | Not Explicitly Stated | Not Explicitly Stated | Not Explicitly Stated | Lower than proposed model [43] |
| Support Vector Machine (SVM) | Not Explicitly Stated | Not Explicitly Stated | Not Explicitly Stated | Lower than proposed model [43] |
Workflow and Pathway Diagrams
ABF-CatBoost Integrated Workflow
High BMI-Associated CRC Target Discovery
Key Signaling Pathways in Colon Cancer
Troubleshooting Guides and FAQs
Section 1: Target Identification and Validation
Q1: Our computational model identified a novel tumor-associated antigen, but our antibody-based imaging shows high background in normal tissues. What could be the issue?
This problem often stems from inadequate target antigen qualification. An ideal target should have high and homogeneous expression on malignant cells with minimal presence in normal tissues [45] [46].
Troubleshooting Steps:
- Verify Expression Patterns: Use multiple independent datasets (GTEx, TCGA) to confirm minimal expression in critical normal tissues.
- Check Antigen Shedding: Investigate if your target is a secreted antigen, which can cause circulating ADC binding and reduced tumor targeting [46].
- Assess Internalization Capacity: Ensure your target antigen efficiently internalizes upon antibody binding for proper ADC function [45].
Experimental Protocol for Internalization Validation:
- Label antibodies with pH-sensitive fluorescent dyes (e.g., pHrodo)
- Incubate with target-positive cells for 30-120 minutes at 37°C
- Monitor internalization via flow cytometry or confocal microscopy
- Compare internalization rates across cell lines with varying antigen density
Q2: We're exploring Fibroblast Activation Protein (FAP) as a target, but small molecule inhibitors show short tumor retention. What alternative targeting approaches should we consider?
FAP is characterized by high expression in cancer-associated fibroblasts (CAFs) and near absence in adult normal tissues, making it an excellent biomarker [47]. However, the short retention time of small molecule FAP inhibitors (FAPIs) limits therapeutic potential.
Recommended Solutions:
- Switch to Antibody-Based Formats: Antibodies and peptides have longer half-lives in vivo and extend tumor retention time [47].
- Consider Sibrotuzumab Approach: This humanized anti-FAP antibody demonstrated specific tumor localization in clinical studies, though renal clearance remained a consideration [47].
- Explore Peptide-Based Radiopharmaceuticals: FAP-targeted peptides combine good tissue permeability with longer retention compared to small molecules [47].
Table: Comparison of FAP-Targeting Modalities
| Modality | Tumor Retention | Tissue Permeability | Development Stage | Key Considerations |
|---|---|---|---|---|
| Small Molecule FAPIs | Short (hours) | High | Clinical | Rapid clearance limits therapy |
| Antibodies (e.g., Sibrotuzumab) | Prolonged (days) | Moderate | Clinical trials | Slow kidney clearance, optimal imaging at 3-5 days |
| FAP-Targeted Peptides | Intermediate | Good | Preclinical/Clinical | Balanced profile, easier tumor penetration |
Section 2: Computational Model Validation
Q3: Our pMHC-I presentation model performs well on training data but fails to predict true immunogenic peptides. How can we improve model generalizability?
This common issue often relates to false negative overfitting and inadequate allele representation.
Troubleshooting Steps:
- Implement Negative Set Switching: Sample new exclusive negative sets after each training epoch to prevent overfitting to falsely presumed negatives [48].
- Increase Allelic Diversity: Ensure training data covers rare alleles from underrepresented ancestries to improve pan-allelic generalization [48].
- Incorporate Protein Language Models: Add gene-level presentation-relevant features from protein language models to reduce dependency on gene expression measurements [48].
Experimental Protocol for Immunogenicity Validation:
- Transfer HLApollo predictions to peptide-MHC binding assays
- Confirm binding with surface plasmon resonance (SPR)
- Validate T-cell activation using interferon-γ ELISpot assays
- Use 8-14 amino acid peptides covering predicted neoantigens
Q4: When transforming peptides to small molecules, we lose target specificity. What strategies can preserve binding characteristics?
Peptide-to-small molecule conversion requires careful optimization to maintain the advantages of peptides while overcoming their limitations [49].
Recommended Strategies:
- Structural Mimicry: Use the peptide's bioactive conformation as a template for small molecule design.
- Pharmacophore Mapping: Identify critical interaction points between the peptide and target for incorporation.
- Stepwise Optimization: Gradually replace peptide segments with small molecule scaffolds while monitoring binding affinity.
Table: Advantages and Challenges of Therapeutic Modalities
| Modality | Advantages | Challenges | Ideal Use Cases |
|---|---|---|---|
| Small Molecules | Oral bioavailability, good membrane penetration, low cost [50] | Difficult to inhibit large protein-protein interactions [50] | Intracellular targets, chronic treatments |
| Therapeutic Peptides | High specificity, potent PPI inhibition, low immunogenicity [50] | Poor membrane permeability, low stability in vivo [50] | Extracellular targets, hormone receptors |
| Antibodies | High specificity, long half-life, effector functions [51] | Poor tumor penetration, immunogenicity, high cost [46] | Cell surface targets, oncology, immunotherapy |
| Antibody-Drug Conjugates | Targeted cytotoxicity, improved therapeutic window [51] [45] | Linker instability, premature payload release [51] | Oncology, targeted delivery of potent cytotoxics |
Section 3: Experimental Optimization
Q5: Our ADC shows excellent in vitro potency but has significant off-target toxicity in vivo. What linker strategies can improve the therapeutic index?
Linker instability is a common cause of ADC toxicity, leading to premature payload release in circulation [51] [45].
Advanced Linker Solutions:
- Protease-Cleavable Linkers: Use dipeptide substrates (e.g., Val-Cit) that are selectively cleaved by cathepsins in lysosomes [45].
- pH-Sensitive Linkers: Employ hydrazone or carbonate linkers that stabilize at neutral blood pH but hydrolyze in acidic endosomes.
- Site-Specific Conjugation: Implement engineered cysteine residues or unnatural amino acids for homogeneous DAR (drug-to-antibody ratio) [45].
Experimental Protocol for Linker Stability Assessment:
- Incubate ADC in human plasma at 37°C
- Sample at 0, 24, 48, and 72 hours
- Analyze payload release via LC-MS
- Compare stability across linker chemistries
Q6: Our anticancer peptides (ACPs) show potent cytotoxicity but also hemolytic activity. How can we improve selectivity for cancer cells?
This challenge requires optimizing the therapeutic window of ACPs by enhancing their selectivity for cancer cell membranes [52].
Design Strategies:
- Amphipathic Optimization: Balance hydrophobic and cationic residues to preferentially interact with negatively charged cancer cell membranes [52].
- Sequence Modulation: Replace strongly hemolytic residues (e.g., tryptophan) with alternatives that maintain anticancer activity.
- Peptide Templating: Use natural ACPs with known selectivity (e.g., LTX-315) as templates for engineering novel variants [52].
The Scientist's Toolkit: Essential Research Reagents
Table: Key Research Reagents for Antibody and Peptide Target Prediction
| Reagent/Category | Function | Example Applications | Key Considerations |
|---|---|---|---|
| Computational Tools | |||
| HLApollo | pMHC-I presentation prediction [48] | Neoantigen identification, cancer vaccine design | Transformer-based, handles multi-allelic data |
| NetMHC Suite | MHC binding prediction [48] | Epitope mapping, immunogenicity assessment | Established benchmark, multiple versions available |
| Protein Language Models | Protein feature extraction [48] | Presentation-relevant feature generation | Reduces need for gene expression data |
| Experimental Assays | |||
| Immunopeptidomics | Direct identification of presented peptides [48] | Ligandome characterization, model training | Requires LC-MS/MS expertise, specialized instrumentation |
| Surface Plasmon Resonance (SPR) | Binding affinity quantification [48] | Antibody-antigen kinetics, peptide-MHC binding | Label-free, real-time interaction data |
| pH-Sensitive Fluorophores | Internalization tracking [45] | ADC antigen internalization studies | Mimics lysosomal environment, quantitative |
| Biological Resources | |||
| Mono-allelic Cell Lines | Single HLA allele expression [48] | Clean training data for pMHC models | Engineered cell lines, reduced complexity |
| Patient-Derived Xenografts | In vivo target validation [47] | Translational target assessment, imaging studies | Preserves tumor microenvironment |
Pathway Diagrams
Target Prediction and Validation Workflow
Antibody-Drug Conjugate Mechanism
Anticancer Peptide Mechanisms of Action
Frequently Asked Questions
What is the core hypothesis of this case study? The core hypothesis is that pyrimethamine, an anti-parasitic drug, exerts anti-cancer effects by modulating mitochondrial function, specifically the oxidative phosphorylation (OXPHOS) pathway, rather than solely through its known inhibition of dihydrofolate reductase (DHFR) [53].
How was this new mechanism identified? This mechanism was computationally predicted by DeepTarget, a tool that integrates large-scale drug sensitivity and CRISPR genetic knockout screens. It identifies a drug's mechanism of action (MOA) by finding genes whose knockout mimics the drug's viability profile across hundreds of cancer cell lines [53].
Why is it important to validate a computationally predicted target? Validation bridges the gap between an in silico prediction and a biologically relevant mechanism. It confirms the prediction's accuracy, provides confidence for downstream drug development or repurposing efforts, and identifies potential biomarkers for patient stratification [53].
What are the major challenges in validating mitochondrial modulation? Key challenges include:
- Distinguishing Primary vs. Secondary Effects: Determining if mitochondrial dysfunction is a direct cause of cell death or a downstream consequence of other stress.
- Cellular Heterogeneity: Accounting for varying mitochondrial function and reliance across different cell lines.
- Technical Variability: Ensuring consistent and accurate measurements of mitochondrial parameters like oxygen consumption rate (OCR).
Troubleshooting Common Experimental Issues
This section addresses specific problems you might encounter during experimental validation.
| Problem | Possible Cause | Solution |
|---|---|---|
| High variability in mitochondrial respiration (Seahorse) assays. | Inconsistent cell seeding, improper cell counting, or inaccurate drug dilution. | Standardize seeding density using an automated cell counter. Create a master mix of the drug for all replicates and perform serial dilutions accurately. |
| No significant change in OCR after pyrimethamine treatment. | The cell line used may not be dependent on OXPHOS, the dose is too low, or the treatment duration is too short. | Select a cell line predicted by DeepTarget to be sensitive. Perform a dose-response curve (e.g., 1-100 µM) and a time-course experiment (e.g., 6-72 hours). |
| Inconsistent results in ATP level measurements. | Lysis is incomplete, or the assay is not performed on an equal number of live cells. | Normalize results to total protein concentration. Ensure complete lysis and use a validated ATP assay kit. |
| Failure to observe pyrimethamine binding to mitochondrial complexes in follow-up assays. | The interaction may be indirect, or the binding affinity may be weak. | Investigate downstream consequences, such as changes in complex I or IV protein levels via western blot, or analyze alterations in the mitochondrial membrane potential. |
Experimental Protocols for Validation
This section provides detailed methodologies for key validation experiments cited in the case study.
Mitochondrial Respiration Analysis using Seahorse XF Analyzer
Objective: To measure the effect of pyrimethamine on mitochondrial oxidative phosphorylation in live cells by monitoring the Oxygen Consumption Rate (OCR).
Workflow:
Key Reagents:
- Seahorse XFp/XFe96 Analyzer (Agilent)
- XF Base Medium (Agilent, #103335-100)
- Oligomycin (Complex V inhibitor, #S1478)
- FCCP (Uncoupler, #C2920)
- Rotenone & Antimycin A (Complex I & III inhibitors, #R8875 & #A8674)
Procedure:
- Cell Seeding: Seed 10,000-20,000 cells per well in a Seahorse XFp/XFe96 cell culture plate 24 hours before the assay.
- Drug Treatment: Treat cells with pyrimethamine (e.g., at IC50 concentration, or a range from 10-50 µM based on sensitivity) for the desired duration (e.g., 24-48 hours).
- Prepare Assay Medium: On the day of the assay, replace the growth medium with XF Base Medium supplemented with 1 mM pyruvate, 2 mM glutamine, and 10 mM glucose (pH 7.4). Incubate for 1 hour at 37°C in a non-CO2 incubator.
- Load Inhibitors: Load the Seahorse cartridge with the mitochondrial stress test compounds:
- Port A: Oligomycin (1.5 µM final concentration)
- Port B: FCCP (1.0 µM final concentration)
- Port C: Rotenone/Antimycin A (0.5 µM final concentration each)
- Run Assay: Calibrate the cartridge and run the standard Mitochondrial Stress Test program on the Seahorse Analyzer.
- Normalize Data: Normalize the OCR data to total protein content per well (using a BCA or Bradford assay).
Intracellular ATP Measurement
Objective: To quantify the cellular ATP levels following pyrimethamine treatment as a direct readout of energetic stress.
Workflow:
Key Reagents:
- ATP Determination Kit (e.g., Thermo Fisher Scientific, #A22066)
- Luminometer or Plate Reader capable of reading luminescence.
- Cell Lysis Buffer (provided in the kit or compatible RIPA buffer).
Procedure:
- Treatment: Seed and treat cells with pyrimethamine in a 96-well white-walled plate.
- Lysis: At the endpoint, remove the medium and lyse cells with the provided lysis buffer according to the manufacturer's instructions.
- Reaction Setup: Mix a volume of cell lysate with the standard reaction solution containing luciferin and firefly luciferase.
- Measurement: Measure luminescence immediately using a luminometer.
- Normalization: Generate an ATP standard curve. Normalize the luminescence readings of samples to the ATP standard curve and then to the total protein concentration of the lysate.
Data Presentation and Analysis
The following table summarizes the expected quantitative outcomes from the validation experiments based on the DeepTarget case study and mitochondrial biology [53] [54].
| Parameter | Assay | Expected Outcome with Pyrimethamine (vs. Control) | Biological Interpretation |
|---|---|---|---|
| Basal Respiration | Seahorse OCR | Decrease | Reduced overall mitochondrial oxygen consumption. |
| ATP Production | Seahorse OCR / ATP Assay | Decrease | Impaired capacity to generate ATP via OXPHOS. |
| Maximal Respiration | Seahorse OCR | Decrease | Reduced respiratory capacity under stress. |
| Proton Leak | Seahorse OCR | Variable | May increase if membrane integrity is compromised. |
| Glycolytic Rate (ECAR) | Seahorse ECAR | Increase | Compensatory upregulation of glycolysis. |
| Mitochondrial Membrane Potential (ΔΨm) | JC-1 / TMRM staining | Decrease | Loss of proton gradient, indicating dysfunction. |
| Cell Viability (IC50) | Cell Titer-Glo / CTG | Decrease (in sensitive lines) | Concentration-dependent cell killing. |
Mitochondrial Signaling Pathway Modulation
The diagram below illustrates the proposed signaling pathway through which pyrimethamine is hypothesized to modulate mitochondrial function and impact cancer cell survival, integrating the computational prediction with the experimental validation plan [53] [54] [55].
The Scientist's Toolkit: Research Reagent Solutions
This table details essential materials and reagents required to perform the validation experiments described in this case study.
| Item | Function / Application in Validation | Example Product / Catalog # |
|---|---|---|
| Pyrimethamine | Small molecule inhibitor; the compound under investigation for its mitochondrial modulatory effects. | Selleckchem, #S4675; Sigma-Aldrich, #46705 |
| Cancer Cell Lines | In vitro model system. Use lines predicted by DeepTarget to be sensitive (e.g., certain solid tumor lines). | ATCC (e.g., NCI-H1299, MIA PaCa-2) |
| Seahorse XFp/XFe96 Analyzer | Platform for real-time measurement of mitochondrial respiration (OCR) and glycolysis (ECAR) in live cells. | Agilent Technologies |
| Seahorse XF Mito Stress Test Kit | Contains optimized concentrations of oligomycin, FCCP, and rotenone/antimycin A for mitochondrial function profiling. | Agilent, #103010-100 |
| ATP Determination Kit | Provides reagents for sensitive luminescent quantification of intracellular ATP levels. | Thermo Fisher Scientific, #A22066 |
| JC-1 Dye | Fluorescent probe for assessing mitochondrial membrane potential (ΔΨm) by flow cytometry or microscopy. | Thermo Fisher Scientific, #T3168 |
| Antibodies for OXPHOS | For western blot analysis of electron transport chain complex protein levels (e.g., Total OXPHOS Rodent WB Antibody Cocktail). | Abcam, #ab110413 |
| Cell Titer-Glo Luminescent Cell Viability Assay | Homogeneous method to determine the number of viable cells in culture based on quantitation of ATP. | Promega, #G7570 |
Troubleshooting Guides
Issue: Poor Ibrutinib Efficacy in H1975 Xenograft Models
Problem: Despite strong in vitro activity, ibrutinib shows only moderate tumor growth inhibition in H1975 (EGFR L858R/T790M) xenograft models, slowing but not halting tumor progression [56].
Explanation & Solution: Ibrutinib exhibits a less efficient irreversible binding mode compared to canonical EGFR inhibitors. Washing-out experiments show EGFR phosphorylation recovers within 8 hours after drug removal, unlike WZ4002 which maintains suppression for 24+ hours [57]. This requires sustained drug exposure for maximal effect.
Recommended Actions:
- Optimize dosing schedule: Consider more frequent administration to maintain effective plasma concentrations
- Monitor target engagement: Use pharmacodynamic markers like EGFR Y1068 phosphorylation to verify pathway suppression
- Explore combination therapy: Preclinical data shows MEK inhibitor GSK1120212 potentiates ibrutinib against EGFR L858R/T790M in vitro [56]
Issue: Inconsistent DeepTarget Predictions for Off-Target Effects
Problem: DeepTarget predictions suggest context-specific secondary targets, but experimental validation yields variable results across cell lines.
Explanation & Solution: DeepTarget identifies secondary targets through two mechanisms: de novo decomposition of drug response and secondary DKS scores in primary target-deficient contexts [34]. Variability arises from cellular context dependencies.
Recommended Actions:
- Verify cellular context: Ensure cell lines lack primary target expression when testing secondary mechanisms
- Use Chronos-processed data: Account for sgRNA efficacy, screen quality, copy number effects, and growth rate variation [34]
- Leverage mutation-specificity scores: Compare DKS scores in mutant vs. wild-type contexts using DeepTarget's built-in analysis [34]
Frequently Asked Questions (FAQs)
Q: How does DeepTarget outperform structure-based methods for predicting ibrutinib-EGFR interactions?
A: Unlike structure-based tools (RosettaFold, Chai-1) that predict static binding affinities, DeepTarget integrates functional genomic data with drug response profiles to capture cellular context. It achieved mean AUC of 0.73 across eight gold-standard datasets versus 0.58 for RosettaFold and 0.53 for Chai-1 [34] [26]. DeepTarget identified EGFR T790M as mediating ibrutinib response in BTK-negative solid tumors by analyzing drug-KO similarity scores across 371 cancer cell lines [34].
Q: Why does ibrutinib show selectivity for mutant EGFR over wild-type?
A: Ibrutinib selectively inhibits EGFR-mutant NSCLC cells (H3255, PC-9, HCC827) with GI~50~ values of 0.05-0.11 μM while showing no activity against wild-type EGFR cells (GI~50~ >10 μM) [56]. This selectivity stems from its unique DFG-in/C-helix-out binding conformation to EGFR T790M kinase, demonstrated via X-ray crystallography [57]. The reversible analog PCI-R loses most activity, confirming covalent binding to Cys797 is essential [56].
Q: What key biochemical properties explain ibrutinib's distinct EGFR inhibition profile?
A: The following table summarizes critical biochemical parameters:
Table 1: Key Biochemical Properties of Ibrutinib's EGFR Inhibition
| Parameter | Value | Experimental Context | Significance |
|---|---|---|---|
| Biochemical IC~50~ | 9 nM | EGFR L858R/T790M kinase [56] | High potency in purified systems |
| Cellular Binding K~d~ | 0.18 μM | EGFR L858R/T790M [57] | Less efficient than WZ4002 (K~d~ 0.074 μM) |
| Covalent Binding Efficiency | Low | Washing-out experiments [57] | Requires sustained exposure for maximal effect |
| Structural Conformation | DFG-in/C-helix-out | X-ray crystallography [57] | Distinct from typical EGFR inhibitors |
Q: What experimental protocols validate DeepTarget predictions for ibrutinib-EGFR interactions?
A: The core methodology involves:
Drug-KO Similarity (DKS) Score Calculation:
- Obtain drug response profiles and Chronos-processed CRISPR dependency scores across 371 cancer cell lines from DepMap [34]
- Compute Pearson correlation between drug response and gene knockout viability patterns
- Apply linear regression to correct for screen confounding factors
- Generate DKS scores - higher scores indicate stronger target evidence [34]
Mutation-Specificity Validation:
- Compare DKS scores in cell lines with mutant vs. wild-type EGFR
- Calculate mutant-specificity score (positive values indicate mutant preference)
- For ibrutinib, this confirmed T790-mutated EGFR mediates response in BTK-negative tumors [34]
Experimental Follow-up:
- Test anti-proliferation in isogenic BaF3 cell lines expressing EGFR variants [57]
- Perform washing-out experiments to assess irreversible binding efficiency [57]
- Conduct colony formation assays in NSCLC cell lines (PC-9, H1975, HCC827) [56]
Experimental Protocols
DeepTarget Prediction Validation Workflow
The following diagram illustrates the computational and experimental workflow for validating DeepTarget predictions, integrating both bioinformatic and functional validation steps:
Ibrutinib-EGFR Binding Mechanism
This diagram illustrates ibrutinib's unique binding mode to EGFR T790M and the subsequent signaling effects:
Research Reagent Solutions
Table 2: Essential Research Reagents for Ibrutinib-EGFR Studies
| Reagent/Resource | Function/Application | Key Details | Source/Reference |
|---|---|---|---|
| DeepTarget Algorithm | Predicts drug MOA from genetic screens | Open-source; uses DKS scores; analyzes 1,500+ cancer drugs | GitHub: CBIIT-CGBB/DeepTarget [34] |
| Isogenic BaF3 Cell Lines | Engineered EGFR variants in consistent background | Express TEL-EGFR or full-length EGFR with defined mutations [57] | Available in academic research |
| H1975 Cell Line | NSCLC with EGFR L858R/T790M | Model for T790M gatekeeper mutation resistance studies [56] | ATCC CRL-5908 |
| PCI-R Compound | Reversible ibrutinib analog | Control for covalent binding effects (acrylamide → propionamide) [56] | Chemical synthesis required |
| Chronos-Processed Data | CRISPR dependency scores | Corrects for confounders in genetic screens [34] | DepMap database |
| ADP-Glo Kinase Assay | Biochemical kinase inhibition profiling | Measures IC~50~ values for EGFR variants [56] | Promega Corporation |
Navigating Pitfalls: Strategies to Overcome Data, Model, and Translational Challenges
Conquering Data Heterogeneity in Multi-Omics Integration
Troubleshooting Guide: Common Multi-Omics Integration Challenges
Table 1: Troubleshooting Common Data Heterogeneity Issues
| Challenge Category | Specific Problem | Potential Causes | Solution & Best Practices |
|---|---|---|---|
| Data Input & Quality | Incompatible data formats and scales [58] | Different omics technologies have unique measurement units and output structures [59]. | Standardize and harmonize data: Normalize for sample size/concentration, convert to common scale, remove technical biases [58]. |
| High technical noise and batch effects [59] | Different sequencing platforms, mass spectrometry configurations, or processing dates [59]. | Apply batch effect correction tools (e.g., ComBat) and rigorous quality control pipelines [59]. | |
| Integration & Analysis | "The curse of dimensionality" – far more features than samples [59] | Integrating millions of genetic variants with thousands of metabolites and proteins [59]. | Employ feature reduction techniques and AI models designed for high-dimensional spaces [1] [59]. |
| Poor model generalizability across populations [60] | Limited diversity in training cohorts and underlying biological differences [60]. | Prioritize multi-modal data fusion and validate models on independent, diverse cohorts [60]. | |
| Difficulty integrating matched vs. unmatched data [61] | Unclear strategy for data from the same cell (matched) vs. different cells/samples (unmatched) [61]. | Match the tool to the data: Use vertical integration (e.g., Seurat, MOFA+) for matched data; use diagonal integration (e.g., GLUE, LIGER) for unmatched data [61]. | |
| Interpretation & Translation | Model outputs are "black boxes" with limited clinical trust [59] | Complex AI/ML models lack inherent interpretability for biologists and clinicians [59]. | Leverage Explainable AI (XAI) techniques like SHAP to interpret feature contributions to predictions [59]. |
| Missing data across omics layers [59] | Technical limitations (e.g., undetectable low-abundance proteins) or biological constraints [59]. | Use advanced imputation strategies (e.g., matrix factorization, deep learning-based reconstruction) [59]. |
Frequently Asked Questions (FAQs)
Q1: Our multi-omics data comes from different platforms and has different scales. What is the most critical first step before integration?
A: The most critical first step is standardization and harmonization [58]. This process ensures data from different omics technologies are compatible. Key actions include:
- Normalization: Account for differences in sample size or concentration.
- Scale Conversion: Convert all data to a common scale or unit of measurement.
- Bias Removal: Filter out technical biases, artifacts, and low-quality data points [58]. It is also good practice to store and provide access to the raw data to ensure full reproducibility [58].
Q2: What is the practical difference between "matched" and "unmatched" multi-omics integration, and why does it matter?
A: The distinction is fundamental and dictates your choice of computational tool [61].
- Matched Integration: Data from different omics modalities (e.g., RNA and protein) are profiled from the same single cell. The cell itself is used as an anchor for integration. Use tools like Seurat v4, MOFA+, or totalVI for this purpose [61].
- Unmatched Integration: Data from different modalities are collected from different cells or different samples. This requires more complex methods that project cells into a shared space to find commonality. For this, use tools like GLUE, LIGER, or Pamona [61]. Selecting the wrong tool for your data type is a common pitfall that will lead to failed integration.
Q3: How can we address the "black box" problem of complex AI models to build trust in our identified cancer targets?
A: To build clinical and biological trust, employ Explainable AI (XAI) techniques. These methods help interpret how complex models make decisions. A prominent example is SHapley Additive exPlanations (SHAP), which can clarify how specific genomic variants or proteomic features contribute to a model's prediction, such as chemotherapy toxicity risk or drug sensitivity [59]. Integrating XAI into your workflow is essential for translating computational findings into actionable biological hypotheses.
Q4: Our multi-omics analysis has identified a promising novel cancer target. What are the next steps for experimental validation?
A: Transitioning from a computational finding to a validated target requires building a robust biological validation package. A structured approach, as used by specialized centers, includes [62]:
- In Silico Assessment: Evaluate target tractability, including 3D structure analysis and ligandability.
- Functional Genomics: Use CRISPR-based genome editing (e.g., "prime editing" with small degron tags) to degrade the endogenous target protein and study the phenotypic consequence.
- Developing a Therapeutic Hypothesis: Use multi-omics patient data to define which patient population (e.g., those with a specific synthetic lethality) is most likely to respond to targeting the gene. This process generates the high-quality, robust data required to empower drug discovery decision-making [62].
Experimental Protocols for Key Methodologies
Protocol 1: A Framework for Multi-Omics Data Preprocessing and Harmonization
Objective: To transform raw, heterogeneous omics data from diverse sources (genomics, transcriptomics, proteomics) into a standardized, analysis-ready format [58] [59].
Workflow Overview:
Steps:
- Quality Control & Filtering: Remove low-quality data points, outliers, and genes/proteins with excessive missing values. This step is platform-specific (e.g., for NGS, check sequencing depth and quality scores) [58] [59].
- Normalization: Adjust data to account for technical variations (e.g., differences in sequencing depth, sample concentration). Use methods like DESeq2 for RNA-seq data or quantile normalization for proteomics data [59].
- Batch Effect Correction: Identify and remove non-biological variations introduced by different processing batches, dates, or platforms. Apply tools like ComBat to align distributions across batches [59].
- Format Standardization: Convert all datasets into a unified format, typically an
n-by-ksamples-by-features matrix, ensuring compatibility with downstream machine learning and statistical analysis tools [58].
Protocol 2: Integrating Matched Single-Cell Multi-Omics Data Using Seurat
Objective: To integrate paired measurements of two modalities (e.g., gene expression and chromatin accessibility) from the same set of cells to define a unified cellular state [61] [63].
Workflow Overview:
Steps:
- Modality-Specific Preprocessing: Independently preprocess each modality. For RNA (scRNA-seq), this includes normalization and identification of highly variable genes. For ATAC (scATAC-seq), this includes term frequency-inverse document frequency (TF-IDF) normalization [61] [63].
- Find Weighted Nearest Neighbors (WNN): The core of Seurat's integration. The algorithm automatically learns the relative utility of each data type and constructs a WNN graph that defines the cellular neighbors based on a weighted combination of both modalities [61].
- Construct a UMAP Embedding: Use the WNN graph to generate a unified low-dimensional embedding (e.g., UMAP) where the proximity of cells reflects their similarity across both omics layers [61].
- Joint Cell Clustering and Analysis: Perform downstream analysis like clustering, differential expression, and marker identification on the integrated object. This allows for the identification of cell types and states informed by both gene expression and regulatory landscapes [61].
The Scientist's Toolkit: Essential Research Reagents & Solutions
Table 2: Key Computational Tools and Their Applications in Multi-Omics Integration
| Tool Name | Category | Primary Function | Ideal Use Case |
|---|---|---|---|
| Seurat (v4/v5) [61] | Matched / Unmatched Integration | Weighted nearest-neighbor analysis for integrating multiple modalities. | Integrating paired CITE-seq (RNA + protein) or 10x Multiome (RNA + ATAC) data. Bridge integration of datasets with only partial feature overlap [61]. |
| MOFA+ [61] | Matched Integration | Factor analysis model to disentangle the variation across multiple omics layers. | Identifying latent factors (sources of variation) that drive heterogeneity across genomics, epigenomics, and transcriptomics in the same samples [61]. |
| GLUE [61] | Unmatched Integration | Graph-linked unified embedding using variational autoencoders guided by prior knowledge. | Integrating multi-omics data from different cells (unmatched), especially for triple-omic integration (e.g., chromatin accessibility, DNA methylation, mRNA) [61]. |
| ION TORRENT PGM Dx / Illumina NGS [64] | Data Acquisition - Genomics | High-throughput sequencing for genomic, transcriptomic, and epigenomic profiling. | Comprehensive profiling of genetic variants, gene expression, and methylation status. Using molecular barcodes to reduce errors and detect rare mutations in ctDNA [64]. |
| TaqMan dPCR / qPCR [64] | Data Acquisition / Validation | Highly sensitive and absolute quantification of nucleic acids. | Validating specific variants discovered by NGS. Detecting low-frequency mutations in liquid biopsy samples due to superior sensitivity and specificity [64]. |
| ComBat [59] | Preprocessing | Empirical Bayes framework for batch effect correction. | Harmonizing data from multiple sequencing runs, different labs, or across diverse patient cohorts to remove non-biological technical artifacts [59]. |
Frequently Asked Questions
Q1: What are the most effective techniques to interpret predictions from a complex model for cancer target prioritization? Techniques from Explainable AI (XAI), such as SHAP (SHapley Additive exPlanations), are highly effective for interpreting complex model predictions. For instance, in a framework designed for cancer therapeutic target prioritization, GradientSHAP analysis was used to quantify the contribution of individual input features (like network centrality measures) to the model's final prediction. This allows researchers to see not just which genes are predicted as essential, but also why, by revealing that features like degree centrality were most influential [65]. This approach provides mechanistic transparency, turning a black-box prediction into an interpretable result.
Q2: Our model achieves high accuracy but the biological rationale is unclear. How can we resolve this? Integrating biologically meaningful features directly into the model architecture can resolve this. A proven method is to build models using features derived from protein-protein interaction (PPI) networks. You can compute established network centrality metrics (e.g., degree, betweenness, closeness) and generate Node2Vec embeddings to capture latent network topology. When these features are used to train a classifier, the model's high accuracy is grounded in known biological principles. Subsequent XAI analysis can then validate that the model is leveraging biologically plausible features for its predictions, thereby clarifying the rationale [65].
Q3: How can we ensure our computational findings are trusted and adopted by translational researchers and clinicians? To build trust with translational audiences, it is crucial to combine high performance with explainability. Develop a framework that not only reports accuracy metrics but also includes intuitive explanations for each prediction. For example, one study employed an XAI-assisted web application that allows users to upload data and receive a portable PDF report containing predictions alongside easy-to-understand explanations for the causal relationships identified [66]. Providing clear, context-specific explanations bridges the gap between computational output and clinical decision-making.
Q4: What is a practical way to create a robust gene prioritization list from my model's output? You can implement a blended scoring approach. This method goes beyond simply using the model's output probability. It combines the prediction probability with the magnitude of SHAP feature attributions. This creates a more robust ranking that considers both the model's confidence and the strength of evidence behind the prediction, helping to prioritize targets where the model is both confident and its reasoning is clear [65].
Troubleshooting Guides
Problem: Model Predictions Lack Biological Plausibility
- Symptoms: The model identifies potential cancer genes that are not supported by existing biological knowledge or known pathways.
- Possible Causes and Solutions:
| Cause | Solution | Verification |
|---|---|---|
| The input features are not biologically relevant to gene essentiality. | Integrate features with established biological foundations. Compute network centrality measures (Degree, Betweenness, Closeness, Eigenvector) from a high-confidence PPI network. These measures quantify a gene's topological importance, which often correlates with essentiality [65]. | Check the top features identified by SHAP analysis. A high contribution from known biological metrics is a good sign. |
| The model is learning from artifacts or biases in the data rather than true biological signals. | Incorporate latent network features using algorithms like Node2Vec. These embeddings capture complex topological patterns beyond first-order centrality measures, providing a richer biological context [65]. | Use XAI to identify which features are driving predictions for implausible genes. If non-biological features are dominant, revisit your feature set. |
Problem: Difficulty Reproducing a Published Computational Workflow
- Symptoms: Inability to replicate the performance or results of a previously published model for cancer target identification.
- Possible Causes and Solutions:
| Cause | Solution | Verification |
|---|---|---|
| Inconsistent data sources or pre-processing steps. | Meticulously document and replicate the data construction protocol. For a PPI network, this means using the same source (e.g., STRING database), species ID (e.g., 9606 for human), and applying the same confidence threshold (e.g., ≥700) as the original study [65]. | Compare the basic statistics of your processed dataset (e.g., number of nodes and edges) with those reported in the original paper. |
| Differences in the calculation of key features. | Precisely re-implement feature generation. For network centralities, use the same algorithms and software libraries. For ground truth labels, ensure you are using the same essentiality data source (e.g., DepMap CRISPR screens) and the same processing method (e.g., using median essentiality scores across cell lines) [65]. | Compare the distribution of a few key features (e.g., degree centrality) in your dataset with the original publication's reported distributions. |
Problem: Clinical Collaborators Find the AI Model Too Opaque to Trust
- Symptoms: Resistance to adopting model-derived insights for guiding experimental validation or patient stratification.
- Possible Causes and Solutions:
| Cause | Solution | Verification |
|---|---|---|
| The model is a "black box" with no insight into its decision-making process. | Integrate Explainable AI (XAI) techniques directly into the output. Use SHAP plots to show which features contributed to a specific prediction for a specific gene. This provides a quantitative, gene-specific rationale for the prediction [65]. | Present the model's output for a known essential gene (e.g., a ribosomal protein like RPS27A) alongside its SHAP explanation to a domain expert. The explanation should align with their biological knowledge. |
| The model's output is not presented in a clinically intuitive format. | Develop a user-friendly application that provides clear, actionable reports. As demonstrated in other studies, an XAI-assisted web app can generate portable PDF reports that summarize predictions and the reasoning behind them, making the information accessible to non-computationalists [66]. | Test the application and report format with a clinical collaborator and incorporate their feedback to improve clarity and relevance. |
Experimental Protocols & Data
Protocol: Constructing a High-Confidence PPI Network for Feature Extraction
This protocol details the construction of a protein-protein interaction network from the STRING database, a common first step in building a biologically-grounded model [65].
- Data Retrieval: Download protein-protein interaction data for Homo sapiens (species ID: 9606) from the STRING database (version 12.0 or later).
- Confidence Filtering: Apply a stringent combined confidence score threshold of ≥700 to retain only high-confidence interactions.
- Identifier Mapping: Map all STRING protein identifiers to official gene symbols using the database's provided metadata files.
- Network Pruning: Remove any interactions where either partner cannot be mapped to a recognized gene symbol.
- Component Extraction: For computational tractability, extract the largest connected component of the resulting network. The final network should comprise nodes (genes) and edges (high-confidence interactions).
Quantitative Performance of an Explainable DL Framework
The following table summarizes the performance metrics achieved by an explainable deep learning framework that integrated PPI network features, as reported in the literature [65].
| Metric | Value | Description |
|---|---|---|
| AUROC | 0.930 | Area Under the Receiver Operating Characteristic Curve. Measures the model's ability to distinguish between essential and non-essential genes. |
| AUPRC | 0.656 | Area Under the Precision-Recall Curve. More informative than AUROC for imbalanced datasets where essential genes are a minority class. |
| Essential Gene Correlation (ρ) | -0.357 | Spearman's correlation coefficient between degree centrality and gene essentiality scores (more negative DepMap scores indicate higher essentiality). |
Key Network Centrality Measures for Gene Essentiality
The table below lists key network centrality metrics that can be computed and have been shown to correlate with gene essentiality in cancer research [65].
| Centrality Measure | Function | Biological Interpretation |
|---|---|---|
| Degree | Measures the number of direct interactions a gene has. | Indicates local connectivity; hubs are often essential. |
| Strength | Weighted degree, summing confidence scores of interactions. | Measures the robustness of a gene's local connections. |
| Betweenness | Measures how often a gene lies on the shortest path between others. | Identifies bottleneck genes that control information flow. |
| Closeness | Measures the average shortest path distance to all other genes. | Indicates how quickly a gene can influence the network. |
| Eigenvector | Measures a gene's connection to other well-connected genes. | Identifies genes that are part of influential, interconnected modules. |
The Scientist's Toolkit: Research Reagent Solutions
| Item | Function in the Context of Cancer Target Identification |
|---|---|
| STRING Database | A comprehensive resource of known and predicted Protein-Protein Interactions (PPIs) used to construct biological networks for feature extraction [65]. |
| DepMap CRISPR Data | A gold-standard dataset providing gene essentiality scores from genome-wide CRISPR-Cas9 knockout screens across hundreds of cancer cell lines, used as ground truth for model training and validation [65]. |
| Node2Vec Algorithm | A graph embedding algorithm that generates latent vector representations of genes based on their network topology, capturing complex structural patterns beyond simple centrality [65]. |
| SHAP (SHapley Additive exPlanations) | An Explainable AI (XAI) method used to interpret the output of complex machine learning models by quantifying the contribution of each input feature to a specific prediction [65]. |
| cBioPortal for Cancer Genomics | An open-access resource for visualization and analysis of multidimensional cancer genomics data, useful for validating computational findings in patient cohorts [67]. |
Workflow and System Diagrams
XAI Cancer Target Framework
Model Interpretability with SHAP
Addressing Overfitting and Ensuring Generalizability Across Cancer Types
Frequently Asked Questions (FAQs)
1. What is overfitting and how can I detect it in my cancer prediction model? Overfitting occurs when a model performs well on training data but generalizes poorly to new, unseen data because it has learned the noise and specific patterns in the training set too closely [68] [69]. You can detect it by observing a high accuracy or performance on your training dataset alongside a significantly lower performance on your validation or test dataset [70] [71]. For example, a model with 99.9% training accuracy but only 45% test accuracy is clearly overfitted [70].
2. What are the most effective techniques to prevent overfitting? Several proven techniques can help prevent overfitting:
- Use more data: A larger and clean training dataset helps the model learn generalizable patterns rather than memorizing noise [70] [72].
- Apply regularization: Techniques like L1 (Lasso) and L2 (Ridge) regularization penalize model complexity to prevent overfitting [68] [72].
- Implement early stopping: Halt the training process before the model starts to learn the noise in the training data [69] [72].
- Use cross-validation: Methods like k-fold cross-validation provide a more robust estimate of model performance on unseen data [69] [70].
- Simplify the model: Reduce the number of model layers or neurons to decrease complexity [72] [71].
- Apply dropout: Randomly ignoring a subset of network units during training reduces interdependent learning among neurons [68] [72].
3. How can I ensure my model generalizes well across different cancer types? Generalizability across cancer types is a significant challenge due to histological differences [73]. Key strategies include:
- Using foundation models: Pre-training models on massive, diverse datasets of histopathological images from many cancer types (e.g., from The Cancer Genome Atlas) can help the model learn robust, generalizable features [73].
- Leveraging self-supervised learning (SSL): SSL methods, like masked image modeling (MIM), can learn meaningful representations from vast amounts of unlabeled data, reducing reliance on scarce expert annotations and improving adaptability to new tasks and cancer subtypes [73].
4. My model isn't performing well on any data. What is happening? This is likely underfitting, where the model is too simple to capture the underlying trends in the data [68] [71]. To address this, you can try training the model for more epochs, increasing model complexity (e.g., adding more layers or neurons), or reducing the strength of your regularization techniques [71].
Troubleshooting Guides
Guide 1: Diagnosing and Remedying Overfitting
Problem: The model's performance on the test set is significantly worse than on the training set.
Diagnosis Steps:
- Monitor Performance Metrics: During training, plot the loss and accuracy (or AUC) for both training and validation sets over time (epochs). A growing gap between the training and validation curves is a classic sign of overfitting [68] [71].
- Use Cross-Validation: Implement k-fold cross-validation. If the model performance varies greatly across different folds or is consistently much lower on the validation folds, overfitting is likely occurring [69] [70].
- Check Model Complexity: Evaluate if your model has more parameters than needed for the complexity of your task. Overly complex models are more prone to overfitting [72] [71].
Solutions:
- Immediate Action: Apply stronger L2 regularization or increase the dropout rate to constrain the model [68] [72].
- Data-Centric Solution: If possible, collect more training data or use data augmentation to artificially increase your dataset size and diversity [69] [72].
- Algorithmic Tuning: Systematically tune your hyperparameters using a grid search. Focus on parameters known to significantly impact overfitting, such as learning rate, batch size, and decay [68].
Guide 2: Improving Generalizability Across Cancer Subtypes
Problem: A model trained on one cancer type (e.g., breast cancer) performs poorly when applied to another (e.g., lung cancer).
Diagnosis Steps:
- Analyze Data Bias: Check if your training data lacks sufficient diversity in terms of cancer types, imaging protocols, or patient demographics. A model trained on a narrow dataset will not generalize well [69] [73].
- Test on External Datasets: Validate your model on a completely independent dataset sourced from a different institution or cohort to test its real-world robustness [73].
Solutions:
- Leverage Transfer Learning: Initialize your model with weights pre-trained on a large, diverse dataset of natural images (e.g., ImageNet) or, even better, on a foundation model pre-trained on massive histopathological image datasets like TCGA [73].
- Employ Multi-Task Learning: Design your model to simultaneously learn related tasks (e.g., classification of multiple cancer subtypes and survival prediction). This can force the model to learn more generalized features [73].
- Adopt a Foundation Model: Use or adapt a existing foundation model like BEPH, which was pre-trained on 11 million patches from 32 cancer types. Fine-tuning such a model on your specific task requires less data and often yields better generalizability [73].
Quantitative Data on Hyperparameter Impact
The following table summarizes findings from an empirical study on feedforward neural networks for breast cancer metastasis prediction, showing how various hyperparameters correlate with overfitting [68] [74].
Table 1: Hyperparameter Correlation with Overfitting and Performance
| Hyperparameter | Correlation with Overfitting | Impact on Prediction Performance | Notes and Practical Guidance |
|---|---|---|---|
| Learning Rate | Negative correlation | Significant positive impact | A higher learning rate can reduce overfitting and improve performance. Tune this parameter carefully [68]. |
| Decay | Negative correlation | Significant positive impact | Iteration-based decay helps reduce overfitting and is a key hyperparameter [68]. |
| Batch Size | Negative correlation | Significant positive impact | A larger batch size was associated with less overfitting in this study [68]. |
| L2 Regularization | Negative correlation | Positive impact | Weight decay penalty effectively constrains model complexity [68] [72]. |
| Momentum | Positive correlation | Context-dependent | Can increase overfitting, especially when combined with a large learning rate [68]. |
| Epochs | Positive correlation | Positive impact (to a point) | Training for too many epochs directly leads to overfitting. Use early stopping [68] [71]. |
| L1 Regularization | Positive correlation | Context-dependent | Its sparsity-inducing nature may surprisingly correlate with increased overfitting in this specific context [68]. |
| Dropout Rate | Not a top factor | Positive impact | Designed to reduce overfitting, but was less impactful than learning rate, decay, and batch size in this study [68]. |
Table 2: Key Experimental Results from the BEPH Foundation Model [73]
| Task | Dataset | Cancer Types / Subtypes | Performance (Accuracy / AUC) | Comparative Advantage |
|---|---|---|---|---|
| Patch-Level Classification | BreakHis | Benign vs. Malignant | 94.05% (Patient Level) | 5-10% higher than standard CNN models [73]. |
| Patch-Level Classification | LC25000 | Lung Subtypes | 99.99% | Outperformed multiple deep learning models [73]. |
| WSI-Level Classification | TCGA (RCC) | PRCC, CRCC, CCRCC | AUC: 0.994 | Superior performance in cancer subtyping [73]. |
| WSI-Level Classification | TCGA (BRCA) | IDC, ILC | AUC: 0.946 | Effective for WSI-level diagnosis [73]. |
| WSI-Level Classification | TCGA (NSCLC) | LUAD, LUSC | AUC: 0.970 | Demonstrates strong generalizability [73]. |
Detailed Experimental Protocols
Protocol 1: Grid Search for Hyperparameter Tuning to Mitigate Overfitting [68]
This protocol is designed to systematically find hyperparameters that minimize overfitting.
- Define Hyperparameter Space: Identify the hyperparameters to tune and their value ranges. Based on empirical evidence, prioritize:
- Learning Rate (e.g., 0.1, 0.01, 0.001)
- Decay (e.g., 0.1, 0.01, 0.001)
- Batch Size (e.g., 32, 64, 128)
- L2 Regularization (e.g., 0.01, 0.001, 0.0001)
- Set Up Grid Search: Use a framework (e.g., scikit-learn, Automated ML in Azure [70]) to iterate over all combinations of the defined hyperparameters.
- Implement Cross-Validation: For each hyperparameter set, perform k-fold cross-validation (e.g., k=5 or 10) on the training data. This ensures the performance estimate is robust and not dependent on a single train-test split [70].
- Evaluate and Select: Train a model for each hyperparameter set and evaluate it on the validation folds. Select the set of hyperparameters that yields the highest average performance on the validation sets, indicating better generalization.
- Final Evaluation: Train a final model with the selected optimal hyperparameters on the entire training set and evaluate it on a held-out test set that was not used during the tuning process.
Protocol 2: Fine-Tuning a Foundation Model for a New Cancer Task [73]
This protocol leverages pre-trained foundation models for tasks with limited data.
- Select a Foundation Model: Choose a model pre-trained on a large corpus of histopathological images, such as the BEPH model, which is based on BEiTv2 and pre-trained on 11.77 million patches from TCGA [73].
- Prepare Downstream Data: Collect and annotate your target dataset for a specific task (e.g., survival prediction for a new cancer subtype). The required data size can be small compared to pre-training.
- Modify Model Head: Replace the pre-training head (e.g., the masked image modeling head) with a new task-specific head (e.g., a classifier or regressor).
- Fine-Tune: Train the model on your downstream task data. It is common practice to use a lower learning rate for fine-tuning to adapt the pre-trained weights without destroying the useful features already learned.
- Validate Performance: Evaluate the fine-tuned model on an independent test set to assess its performance and generalizability for the new task.
Workflow and Methodology Visualizations
Diagram: Overfitting Diagnosis and Prevention Workflow
Diagram: Foundation Model for Generalizable Cancer Diagnosis
The Scientist's Toolkit: Key Research Reagents & Solutions
Table 3: Essential Materials and Computational Tools for Robust Cancer Modeling
| Item / Solution | Function / Purpose | Example / Note |
|---|---|---|
| The Cancer Genome Atlas (TCGA) | A public repository of cancer genomics and histopathological images from thousands of patients across dozens of cancer types. Serves as an essential data source for pre-training and benchmarking [73]. | Used to pre-train the BEPH foundation model with images from 32 cancer types [73]. |
| Foundation Models (e.g., BEPH) | A large model pre-trained on vast, diverse datasets that can be efficiently adapted (fine-tuned) to various downstream tasks with minimal task-specific data, enhancing generalizability [73]. | Based on BEiTv2 architecture; uses Masked Image Modeling (MIM) for self-supervised learning [73]. |
| Automated Machine Learning (AutoML) | Platforms that automate the process of applying machine learning, including hyperparameter tuning and cross-validation, to help identify and prevent overfitting without manual intervention [70]. | Azure Automated ML can automatically detect overfitting and stop training early [70]. |
| L1 & L2 Regularization | Mathematical techniques that add a penalty to the loss function to discourage model complexity, thereby reducing overfitting [68] [72]. | L2 regularization was found to negatively correlate with overfitting in empirical studies [68]. |
| Cross-Validation (k-Fold) | A resampling procedure used to evaluate a model on limited data. It provides a more reliable estimate of model performance and generalizability than a single train-test split [69] [70]. | Typically, a value of k=5 or k=10 is used as a good balance between computational cost and estimate accuracy [71]. |
| Dropout | A regularization technique for neural networks where randomly selected neurons are ignored during training, preventing complex co-adaptations and reducing overfitting [68] [72]. | Requires more epochs to converge but improves model robustness [72]. |
Frequently Asked Questions (FAQs)
FAQ 1: How do I select the most accurate force field for my specific biological system? Force field accuracy is not universal; it depends heavily on the system being modeled. A force field that performs well for proteins might be inadequate for ether-based liquid membranes or other specific components. It is essential to validate the force field against key experimental properties relevant to your research, such as density, shear viscosity, and partition coefficients, before committing to large-scale production simulations [75].
FAQ 2: My simulation crashes with "Atom index in position_restraints out of bounds." What does this mean?
This is a common error in GROMACS related to the incorrect ordering of position restraint files in your topology. The position restraint file for a specific molecule must be included immediately after the corresponding [ moleculetype ] directive for that molecule in your top file. Mixing the order will cause this error [76].
FAQ 3: Why do I get slightly different results when I run the same simulation on different machines or with a different number of processors? This is typically not a bug but expected behavior. Slight numerical round-off differences due to different domain decompositions, CPU architectures, or compiler optimizations can cause molecular dynamics trajectories to diverge after several hundred timesteps. The statistical properties (e.g., average energy) should remain consistent, even if the exact atomic paths differ [77].
FAQ 4: What is the number one cause of a simulation "blowing up" with unrealistic energy values? The most common cause is invalid physics or numerics in the simulation setup. This can include choosing a timestep that is too large, specifying incorrect force field coefficients, or having atoms placed too close together (steric clashes) in the initial configuration. Always monitor your thermodynamic output frequently to catch these issues early [77].
Troubleshooting Guides
Issue 1: Force Field Selection and Validation
Selecting an inappropriate force field is a primary source of error, leading to inaccurate physical properties and unreliable scientific conclusions.
- Problem: Your simulated system exhibits incorrect density, viscosity, or solvation properties.
- Solution: Conduct a preliminary validation against available experimental data.
- Protocol: The following methodology, adapted from force field comparison studies, provides a robust validation workflow [75]:
- Identify Key Properties: Determine the critical physical properties for your study (e.g., density, shear viscosity, interfacial tension, partition coefficients).
- Select Candidate Force Fields: Choose 2-3 modern, all-atom force fields parameterized for your class of molecules (e.g., CHARMM36, GAFF, OPLS-AA).
- Run Benchmark Simulations: Create small, representative systems and calculate the target properties.
- Compare with Experiment: Quantitatively compare the results with experimental data to identify the most accurate force field.
The table below summarizes a real-world comparison for Diisopropyl Ether (DIPE), demonstrating how force field performance can vary significantly [75].
| Force Field | Density Deviation from Experiment | Viscosity Deviation from Experiment | Recommended for Liquid Membranes? |
|---|---|---|---|
| GAFF | ~+3% to +5% | ~+60% to +130% | No |
| OPLS-AA/CM1A | ~+3% to +5% | ~+60% to +130% | No |
| COMPASS | Accurate | Accurate | Yes |
| CHARMM36 | Accurate | Accurate | Yes (Best) |
Issue 2: Parameter Optimization for Stability and Performance
Incorrect simulation parameters can lead to instability, integration errors, and physically meaningless results.
- Problem: Simulation crashes, reports "bonds stretching too far," or produces NaN (Not a Number) values.
- Solution: Systematically optimize critical parameters, including the integration time step and cutoffs, based on physical and numerical constraints [78].
- Protocol: A reliable parameter selection process involves:
- Time Step Selection: Use the cumulative error theory and bond-distance dynamics to determine a stable integration time step. For many systems, a time step between 1-2 femtoseconds (fs) is common, but studies on copper have shown that a rational range can be 4-12 fs [78].
- Cutoff and Non-bonded Interactions: Ensure your real-space cutoff for van der Waals and electrostatic interactions is appropriate for the force field. Use the Particle Mesh Ewald (PME) method for long-range electrostatics [79].
- Minimization and Equilibration: Always perform energy minimization to remove steric clashes and follow a careful equilibration protocol in the NVT and NPT ensembles before starting production runs.
Issue 3: Managing Computational Cost and Scalability
Large-scale biological simulations, such as those involving chromatin or multi-protein complexes, can require billions of atoms, pushing the limits of computational resources [79].
- Problem: Simulations are too slow, run out of memory, or cannot scale efficiently to a large number of processor cores.
- Solution: Utilize specialized MD software and optimize its configuration for large systems.
- Protocol: To enhance performance and enable large-scale simulations:
- Use Optimized Software: Employ MD packages like GENESIS, which are specifically designed for large-scale simulations on supercomputers. GENESIS uses advanced domain decomposition and FFT parallelization to scale beyond 100,000 processor cores [79].
- Optimize Decomposition: Adjust the spatial domain decomposition to balance the load between processors.
- Manage Memory: For analysis, reduce the number of atoms selected or the trajectory length to avoid "Out of memory" errors [76].
Issue 4: Resolving Common Software Errors
Even with a perfect model, simple configuration mistakes can halt simulations.
- Problem: GROMACS fails with "Residue 'XXX' not found in residue topology database."
- Solution: The force field you selected does not contain a definition for the residue 'XXX'. You can:
- Rename the residue in your coordinate file to match a known entry in the database.
- Use the
-ignhflag to letpdb2gmxignore existing hydrogens and add correct ones. - Manually create a topology for the residue and include it in your system [76].
- Problem: LAMMPS terminates with "Expected integer parameter instead of '1.0'."
- Solution: LAMMPS has strict typing. You provided a floating-point number '1.0' where an integer is required. Change the value to '1' [77].
The Scientist's Toolkit: Research Reagent Solutions
| Item | Function | Application Context |
|---|---|---|
| GENESIS MD Software | An MD package optimized for large-scale simulations on supercomputers, featuring efficient domain decomposition and FFT parallelization. | Enables billion-atom simulations of large biomolecular complexes like chromatin [79]. |
| CHARMM36 Force Field | An all-atom force field for biological macromolecules. Validated for accurate density and viscosity in complex systems like liquid membranes [75]. | simulating proteins, lipids, and ether-based systems in cancer target environments. |
| OPLS-AA Force Field | An all-atom force field parameterized for a wide range of organic liquids and biomolecules. | Commonly used for organic solvents and small molecules; requires validation for specific properties [80] [75]. |
| GAFF (General Amber Force Field) | A force field designed for drug-like small molecules. | Often used for ligands in protein-ligand binding studies; performance should be verified [75]. |
| LAMMPS MD Package | A highly versatile and widely-used open-source MD simulator. | Suitable for a vast range of materials and soft matter systems; strong community support [77]. |
| GROMACS MD Package | A high-performance MD software package primarily for biomolecular systems. | Known for its speed and efficiency in simulating proteins, nucleic acids, and lipids [76]. |
| PME (Particle Mesh Ewald) | An algorithm for efficiently calculating long-range electrostatic interactions in periodic systems. | Essential for obtaining accurate forces and energies in aqueous and charged biological systems [79]. |
| SPC/E Water Model | A rigid, three-site water model that explicitly treats hydrogen atoms. | Used in simulations of biomolecules in aqueous solution to model solvation and hydration effects [80]. |
Technical Support Center: Troubleshooting Computational Oncology Models
This technical support center provides practical solutions for researchers navigating the "Valley of Death" between preclinical discovery and clinical application in cancer research, with a specific focus on validating computational models for cancer target identification [81].
Frequently Asked Questions (FAQs)
Q1: Why do my computational predictions from preclinical models fail to translate to human clinical trials?
The primary reasons involve poor biological relevance of models and insufficient validation. Key factors include:
- Biological Irrelevance: Preclinical models often use younger animals for diseases of aging (e.g., Alzheimer's, osteoarthritis), mismatching human pathophysiology [82].
- Inadequate Validation: Many computational models are developed without proper analytical validation or demonstration of robustness [83].
- Sample Size Issues: Preclinical studies typically use much smaller sample sizes than clinical trials, limiting statistical power and generalizability [82].
- Technical Limitations: Many publications use research assays without demonstrating robustness, making clinical application unreliable [83].
Q2: What strategies can improve the translatability of my computational target identification workflow?
Implement these evidence-based approaches:
- Multi-Omics Integration: Combine epigenetics, genomics, proteomics, and metabolomics data in network structures to provide systems-level understanding [1].
- Human Tissue Validation: Use biospecimens to evaluate safety and identify potential "off-target" effects relevant to humans [82].
- Compound Library Screening: Utilize clinical trials in a dish (CTiD) techniques to test therapies on human cells from specific populations [82].
- Network-Based Analysis: Apply algorithms like shortest path, module detection, and network centrality to identify indispensable proteins in biological networks [1].
Q3: How can I better validate my computational predictions before proceeding to clinical development?
Employ this multi-layered validation framework:
- Experimental Validation: Use 3D organoids for swift drug screening and validation [82].
- Cross-Species Verification: Test predictions across multiple validated animal models that mimic human disease conditions [82].
- Multi-Model Approach: Combine different computational approaches (agent-based, continuum, hybrid) to capture different aspects of cancer biology [84].
- Clinical Data Correlation: Compare predictions with existing human tissue data and clinical outcomes where available [82].
Troubleshooting Guides
Problem: Poor reproducibility between computational predictions and experimental results
Table: Troubleshooting Poor Reproducibility
| Issue | Potential Causes | Solutions | Validation Experiments |
|---|---|---|---|
| Biological relevance gaps | Animal model doesn't mimic human pathophysiology; Limited understanding of tumor biology | Use human tissue organoids; Implement multi-omics integration; Focus on predictive accuracy over complete mechanistic understanding [82] [83] | Validate with 3D organoid systems; Test in multiple model systems; Compare with human tissue data [82] |
| Technical variability | Inconsistent data preprocessing; Poor quality control procedures; Algorithm parameter sensitivity | Standardize data processing pipelines; Implement rigorous quality control metrics; Use parameter optimization frameworks [83] | Conduct reproducibility studies; Perform cross-validation; Use independent validation datasets [83] |
| Insufficient model validation | Single validation method; Lack of external validation datasets; No clinical correlation | Implement multi-level validation; Use independent external datasets; Correlate with clinical outcomes where possible [83] | External dataset testing; Clinical outcome correlation; Multi-site validation studies [83] |
Experimental Protocol: Multi-Omics Network Validation for Target Identification
Materials Required:
- High-quality multi-omics datasets (genomics, transcriptomics, proteomics)
- Network analysis software/platform
- Validation models (3D organoids, multiple animal models)
- Analytical validation tools
Procedure:
- Data Integration and Network Construction
Computational Target Prioritization
Experimental Validation
Clinical Correlation
- Compare findings with existing human tissue databases
- Analyze correlation with clinical outcomes where data exists
- Refine models based on clinical feedback
Model Validation Workflow
Problem: Inadequate predictive power for clinical outcomes
Table: Quantitative Performance Metrics for Model Validation
| Validation Metric | Target Threshold | Measurement Method | Clinical Relevance |
|---|---|---|---|
| Area Under Curve (AUC) | >0.80 | Receiver Operating Characteristic analysis | Diagnostic accuracy for target identification [1] |
| Network Controllability | Identify indispensable nodes | Control theory analysis of biological networks [1] | Predicts essential targets for therapeutic intervention [1] |
| Cross-species Concordance | >70% conservation | Comparative analysis across model organisms | Predicts translatability to human biology [82] |
| Multi-omics Integration | Significant p-value (<0.05) | Statistical integration of epigenomic, genomic, proteomic data [1] | Comprehensive biological relevance [1] |
Experimental Protocol: Clinical Predictive Power Enhancement
Materials Required:
- Clinical outcome datasets
- Digital twin platforms (e.g., caiSC framework) [84]
- Multi-scale modeling tools
- Validation cohorts
Procedure:
- Clinical Data Integration
Predictive Model Enhancement
Validation and Refinement
- Test predictions against independent clinical datasets
- Use adaptive therapy frameworks to preemptively address resistance [84]
- Continuously refine models based on clinical feedback
Predictive Modeling Architecture
The Scientist's Toolkit: Research Reagent Solutions
Table: Essential Research Materials for Computational Model Validation
| Reagent/Resource | Function | Application in Validation |
|---|---|---|
| 3D Organoid Systems | Mimics human tissue architecture and pathophysiology [82] | Replacement for traditional animal models; High-throughput drug screening [82] |
| Human Tissue Biospecimens | Provides human-relevant biological context [82] | Target validation; Toxicity assessment; Off-target effect identification [82] |
| Multi-omics Datasets | Comprehensive molecular profiling (genomics, proteomics, metabolomics) [1] | Network construction; Target identification; Biomarker discovery [1] |
| Compound Libraries | Collections of chemical compounds for screening [82] | Drug repurposing; High-throughput screening; Combination therapy identification [82] |
| Digital Twin Platforms | Computational counterparts to living systems [84] | Individualized simulations for diagnosis and treatment planning [84] |
| Validated Animal Models | Genetically engineered models mimicking human cancers [82] | Therapeutic index evaluation; Resistance mechanism studies [82] |
Advanced Methodologies
Integrative Multi-Omics Analysis Protocol
Materials Required:
- Epigenetic modification data (histone modifications, DNA methylation)
- Genomic sequencing data
- Proteomic interaction data
- Metabolic profiling data
- Network analysis tools
Procedure:
- Data Collection and Preprocessing
- Collect epigenomic data including histone lysine demethylation patterns [1]
- Integrate genomic data to identify associations between genotype and phenotype [1]
- Incorporate proteomic data focusing on protein-protein interactions [1]
- Include metabolomic data for biomarker discovery and pathway analysis [1]
Network-Based Integration
Target Identification and Validation
This technical support framework provides actionable solutions to overcome the most significant challenges in translational computational oncology, helping researchers bridge the gap between preclinical discovery and clinical application.
Beyond Prediction: Establishing Rigorous Benchmarks and Validation Pipelines for Clinical Confidence
For researchers in oncology drug development, accurately identifying a drug's mechanism of action (MOA) is a critical but formidable challenge. Drugs often engage multiple targets with varying affinities across different cellular contexts, and systematically mapping these interactions has remained elusive [34]. While structure-based tools like RoseTTAFold All-Atom and Chai-1 predict direct protein-small molecule binding with high accuracy, their static, structure-first approach lacks the cellular context that dictates real-world drug efficacy [34] [85].
This technical guide explores the benchmarking and application of DeepTarget, a computational tool that represents a paradigm shift. Unlike its predecessors, DeepTarget bypasses structural prediction to instead integrate large-scale functional genomic data—including drug viability screens, CRISPR-Cas9 knockout viability profiles, and omics data from matched cell lines—to predict the primary and secondary targets driving a drug's anti-cancer effects [34] [35]. By mirroring the complex cellular environment where pathway-level effects are crucial, DeepTarget has demonstrated superior performance in real-world scenarios, offering a powerful, complementary approach to accelerate your drug discovery and repurposing pipelines [26] [86].
Benchmarking Data: Quantitative Performance Comparison
The performance of DeepTarget was rigorously evaluated against RoseTTAFold All-Atom and Chai-1 across eight gold-standard datasets of high-confidence cancer drug-target pairs [34]. The table below summarizes the key quantitative results.
Table 1: Benchmarking Performance on Primary Target Identification
| Benchmark Dataset | DeepTarget Mean AUC | RoseTTAFold All-Atom Mean AUC | Chai-1 Mean AUC |
|---|---|---|---|
| Overall Performance (Mean across 8 datasets) | 0.73 [34] | 0.58 [34] | 0.53 (without MSA) [34] |
| COSMIC Resistance (N=16 pairs) [34] | Included in overall mean | Included in overall mean | Included in overall mean |
| OncoKB Resistance (N=28 pairs) [34] | Included in overall mean | Included in overall mean | Included in overall mean |
| FDA Mutation-Approval (N=86 pairs) [34] | Included in overall mean | Included in overall mean | Included in overall mean |
| DrugBank Active Inhibitors (N=90 pairs) [34] | Included in overall mean | Included in overall mean | Included in overall mean |
| SelleckChem Selective Inhibitors (N=142 pairs) [34] | Included in overall mean | Included in overall mean | Included in overall mean |
DeepTarget's performance superiority was consistent, outperforming the other models in seven out of the eight tested datasets [34] [86] [35]. This strong predictive ability extends beyond primary target identification.
Table 2: Performance on Secondary and Mutation-Specific Tasks
| Prediction Task | DeepTarget Performance | Application Note |
|---|---|---|
| Secondary Target Identification | AUC of 0.92 against known data on 64 cancer drugs with multiple targets [34] [87] | Identifies context-specific targets active when primary targets are absent [34]. |
| Mutation Specificity | Average AUC of 0.78 distinguishing mutant-specific inhibitors [34] | Critical for patient stratification and drug positioning [34]. |
| Clinical Success Correlation | Predicted high-specificity kinase inhibitors showed increased clinical trial progression [34] [26] | Aids in prioritizing drug candidates with a higher likelihood of success [34]. |
Experimental Protocols: Validating DeepTarget's Predictions
Protocol 1: Primary Target Identification Workflow
This protocol outlines the core methodology for identifying a drug's primary protein target[scitation:1].
Principle: CRISPR-Cas9 knockout (CRISPR-KO) of a drug’s target gene is hypothesized to mimic the drug’s inhibitory effects across a panel of cancer cell lines [34].
Methodology:
- Data Acquisition: Obtain the three required data types for a panel of matched cancer cell lines (e.g., from the DepMap repository). The dataset used in the founding study included 1,450 drugs across 371 cancer cell lines [34] [87].
- Drug Response Profiles: Viability measurements after drug treatment.
- CRISPR-KO Viability Profiles: Genome-wide dependency scores (use Chronos-processed data to account for confounders like sgRNA efficacy and copy number effects) [34].
- Omics Data: Gene expression and mutation data for the same cell lines.
- Compute Drug-KO Similarity (DKS) Score: For the input drug, calculate the Pearson correlation between its viability profile and the viability profile resulting from the knockout of every gene across the cell line panel. This generates a DKS score for each drug-gene pair [34].
- Identification & Validation: Genes with high DKS scores are prioritized as potential primary targets. Validation includes checking if known drugs cluster by MOA in a UMAP projection based on DKS scores [34].
Protocol 2: Experimental Validation of a Secondary Target
This protocol details the wet-lab validation of a context-specific secondary target prediction, using the case study of Ibrutinib and EGFR [86] [87].
Background: Ibrutinib, a BTK inhibitor for blood cancer, was clinically observed to treat lung cancer, though its primary target (BTK) is not present in lung tumors. DeepTarget predicted mutant EGFR as a context-specific secondary target in BTK-negative solid tumors [86] [87].
Methodology:
- Cell Line Preparation: Select appropriate cancer cell lines that lack the primary target (BTK) but differ in the status of the predicted secondary target (EGFR). The validation study used solid tumor cell lines with and without the cancerous mutant EGFR (T790 mutation) [86] [87].
- Drug Treatment: Treat the prepared cell lines with a range of concentrations of the drug (Ibrutinib).
- Viability Assay: Measure cellular viability after treatment (e.g., using ATP-based assays).
- Data Analysis: Compare the dose-response curves and IC50 values between the cell lines. Validation is achieved if cells harboring the mutant EGFR show significantly higher sensitivity (lower IC50) to Ibrutinib, confirming the predicted target [86] [87].
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Resources for Implementing DeepTarget Methodology
| Resource / Reagent | Function in the Workflow | Key Details |
|---|---|---|
| DepMap (Dependency Map) Portal | Primary source for the three required data types: drug response, genetic dependency, and omics data from cancer cell lines [34] [87]. | The foundational study used data for 1,450 drugs across 371 cancer cell lines [34]. |
| CRISPR-KO Viability Data (Chronos) | Provides gene-effect scores from genome-wide knockout screens, essential for DKS score calculation [34]. | Use Chronos-processed data to correct for technical confounders like sgRNA efficacy and copy number effects [34]. |
| DeepTarget Open-Source Tool | The core computational pipeline for predicting MOAs. | Available on GitHub; includes pre-computed target profiles for 1,500 cancer-related drugs [34] [26]. |
| Cancer Cell Line Panel | Essential for experimental validation of predictions. | Should include lines with varying genetic backgrounds (e.g., different mutations, tissue origins) to test context-specificity [86]. |
Frequently Asked Questions (FAQs)
Q1: When should I use DeepTarget over a structure-based tool like RoseTTAFold or Chai-1?
A: The choice depends on your research question.
- Use DeepTarget when your goal is to understand the functional mechanism of action driving cancer cell death in a biologically complex, cellular context. It is superior for identifying both primary and context-specific secondary targets, predicting mutation-specificity, and drug repurposing [34] [35] [36].
- Use structure-based tools like RoseTTAFold All-Atom or Chai-1 when you need high-resolution, atomic-level structural models of a direct binding interaction between a drug and a well-characterized protein target, particularly for lead optimization [34] [88]. DeepTarget complements, rather than replaces, these structural methods.
Q2: My research involves targets like GPCRs or ion channels. Are there any limitations?
A: Yes. The developers note that DeepTarget's performance can be lower for certain target classes, including GPCRs, nuclear receptors, and ion channels [36]. This is likely because the functional genomic data it relies on (CRISPR viability screens) may not fully capture the complex biology and dependencies of these target types. For these proteins, structure-based methods or other specialized approaches may currently be more suitable.
Q3: What are the most common technical issues when calculating the DKS score?
A: A critical step is ensuring the quality and compatibility of your input data.
- Data Source: Always source CRISPR-KO data that has been processed with a tool like Chronos. This corrects for screen-quality confounders, sgRNA efficacy variation, and copy number effects, which is essential for generating reliable DKS scores [34].
- Cell Line Matching: The drug response profiles and genetic profiles must be from a panel of matched cell lines. Using data from different or misaligned cellular contexts will lead to inaccurate correlations and failed predictions.
Q4: The tool predicted a target, but my experimental validation did not support it. What could have gone wrong?
A: Several factors could explain a discrepancy:
- Context Discrepancy: The cellular context used in your validation experiment (e.g., cell type, growth conditions) may differ significantly from the context in which the prediction was made. DeepTarget's predictions are highly context-dependent [34].
- Phenotypic Focus: DeepTarget is trained to predict mechanisms affecting cell viability. If your validation assay measures a different phenotype (e.g., migration, differentiation), the prediction may not hold [36].
- Indirect Effects: The prediction may identify a gene in the drug's pathway rather than a direct binding target. Use the recommended post-filtering (e.g., restricting to kinase proteins for a kinase inhibitor) and pathway enrichment analysis to distinguish direct from indirect mechanisms [34].
FAQs and Troubleshooting Guides
CRISPR Experimental Validation
Q: My CRISPR-edited cell line shows efficient guide RNA cutting but no phenotypic change. What should I investigate?
A: This common issue requires systematic troubleshooting. First, confirm functional knockout at the protein level via western blot, not just genomic DNA cleavage. Second, investigate genetic compensation or redundancy; consider combinatorial knockout of paralogous genes. Third, assess clonal selection; a heterogeneous cell population can mask phenotypic effects—perform single-cell cloning and validate multiple clones. Always include a positive control guide RNA targeting a known essential gene to verify your experimental system is working.
Q: How can I minimize off-target effects in CRISPR screens?
A: Employ these validated strategies: 1) Use high-fidelity Cas9 variants (e.g., HiFi Cas9) to reduce off-target cleavage, 2) Implement computational prediction tools to select guides with minimal off-target potential, 3) Utilize dual-guRNA approaches requiring two guides for functional knockout, 4) Include multiple guide RNAs per gene and focus on genes with concordant phenotypes across guides, 5) For CRISPRi/a screens, titrate dCas9-effector expression to minimize nonspecific effects. Always validate screening hits with orthogonal approaches like RNAi or small-molecule inhibitors.
Q: My CRISPR-edited mouse embryos are not developing to term. How can I troubleshoot earlier?
A: Implement a cleavage assay (CA) to detect mutants efficiently before embryo transfer. This method is based on the inability of the RNP complex to recognize the target sequence after successful CRISPR-mediated editing due to target locus modification. This allows confirmation of gene editing in preimplantation embryos, saving time and animal usage compared to extensive Sanger sequencing. Validate your gRNA efficiency in cell lines before moving to embryos, and consider using fluorescently labeled gRNA to confirm RNP complex delivery.
Peptide Inhibitor Validation
Q: My designed peptide inhibitor shows good binding affinity in simulations but poor cellular activity. What could be wrong?
A: This disconnect between computational predictions and cellular efficacy typically stems from delivery or stability issues. First, assess peptide stability in cellular media—incorporate modifications like D-amino acids, N-methylation, or cyclization to enhance proteolytic resistance. Second, evaluate cellular uptake; consider conjugating to cell-penetrating peptides (e.g., TAT, penetratin) or using nanoparticle encapsulation. Third, verify target engagement in cells using techniques like fluorescence polarization, BRET, or cellular thermal shift assays. Finally, ensure your peptide is reaching the correct subcellular compartment—nuclear localization sequences may be needed for intracellular targets.
Q: How can I improve the binding affinity of my peptide inhibitor?
A: Employ iterative optimization strategies: 1) Use alanine scanning to identify critical residues, 2) Implement backbone cyclization or stapling to stabilize bioactive conformations, 3) Incorporate non-natural amino acids to enhance interactions, 4) Utilize phage display or mRNA display libraries for affinity maturation, 5) Apply computational approaches like molecular dynamics simulations to identify regions for optimization. For survivin-targeting peptides, research has shown that single-point mutations can significantly enhance binding affinities, with specific variants (P2, P3) demonstrating superior binding in both docking studies and molecular dynamics simulations [89].
Small Molecule Development
Q: My AI-predicted small molecule shows promising on-target activity but unexpected cytotoxicity. How should I proceed?
A: Begin by distinguishing on-target from off-target toxicity. First, generate and test structurally similar but inactive analogs—if toxicity remains, it's likely off-target. Second, use CRISPR-based target identification screens (e.g., using DeepTarget tool) to identify potential off-target interactions [26]. Third, evaluate cytotoxicity across multiple cell lines, including non-disease relevant models, to identify cell-type specific effects. Fourth, check for known structural alerts (e.g., pan-assay interference compounds, PAINS) and assess mitochondrial toxicity specifically. Finally, use computational ADMET prediction tools early in the optimization process to flag potential toxicity liabilities.
Q: How reliable are AI-based predictions for small molecule immunomodulators?
A: AI predictions require careful experimental validation. While AI excels at virtual screening and de novo design, establishing a rigorous validation pipeline is essential: 1) Always test AI-predicted compounds alongside known active and inactive controls, 2) Verify binding using biophysical methods (SPR, ITC) in addition to cellular assays, 3) Assess target engagement and functional effects in multiple assay formats, 4) Evaluate selectivity against related targets to confirm specificity, 5) Use AI as a prioritization tool rather than a definitive predictor—experimental confirmation remains essential. AI-designed molecules like DSP-1181 have achieved unprecedented development timelines, but still require thorough experimental validation [19].
Quantitative Data Tables
Table 1: CRISPR Screening Validation Parameters and Benchmarks
| Parameter | Optimal Range | Validation Method | Acceptance Criteria | Troubleshooting Tips |
|---|---|---|---|---|
| Guide RNA Efficiency | >70% indel frequency | T7E1 assay or NGS | Significant depletion in positive selection screens | Use algorithm-designed guides with high on-target scores |
| Library Coverage | >500x per guide | Sequencing library representation | >90% of guides detected in pre-screen sample | Amplify library with sufficient PCR cycles |
| Screen Quality | SSMD >2 | Redundant siRNA activity (RSA) analysis | Strong separation between essential and non-essential genes | Include positive and negative control guides |
| Off-Target Rate | <5% of total hits | Comparison with non-targeting guides | Minimal overlap with non-targeting control phenotype | Use multiple guides per gene; confirm with orthogonal validation |
| Hit Validation Rate | >30% in secondary assays | Secondary CRISPR, RNAi, or rescue | Phenotype reproducible in alternative system | Prioritize genes with multiple effective guides |
Table 2: Peptide Inhibitor Characterization Data
| Parameter | Experimental Method | Target Values | Interpretation Guidelines |
|---|---|---|---|
| Binding Affinity (KD) | Surface Plasmon Resonance (SPR), ITC | <10 µM for initial hits; <100 nM for optimized leads | Correlate with cellular activity; consider stoichiometry |
| Proteolytic Stability | Incubation in serum/lysate with LC-MS quantification | >4 hours half-life in relevant biological fluid | <2 hours may require formulation or stabilization |
| Cellular Permeability | Caco-2 assay, intracellular concentration measurement | Papp >1 × 10⁻⁶ cm/s for good permeability | Low permeability requires delivery strategy |
| Target Engagement (Cellular) | Cellular thermal shift assay (CETSA), BRET | Significant shift at relevant concentrations | Confirms compound reaches and engages intracellular target |
| Anticancer Activity | Cell viability assays (MTT, CellTiter-Glo) | IC50 <10 µM in target-positive lines | Compare to target-negative lines for specificity assessment |
Experimental Protocols
Purpose: To validate CRISPR/Cas9-mediated gene editing in preimplantation mouse embryos before embryo transfer, reducing animal usage and sequencing costs.
Materials:
- Mouse zygotes (C57BL/6 × CBA/H F1)
- CRISPR/Cas9 components: crRNA, tracrRNA, NLS-Cas9 protein
- Electroporation system (Genome Editor electroporator with LF501PT1-10 electrode)
- Embryo culture media: M2 and KSOM media
- Hyaluronidase solution (150 IU/ml M2)
Methodology:
- gRNA Production: Prepare gRNA by mixing 0.6 µl (100 µM) crRNA and 0.6 µl (100 µM) tracrRNA with 1.8 µl Nuclease-Free Duplex Buffer. Incubate at 95°C for 3 min and cool slowly for 30 min.
- RNP Complex Formation: Combine 0.96 µl of NLS-Cas9 (61 µM) and 6.04 µl of Opti-MEM I with annealed gRNA.
- Zygote Preparation: Superovulate donor females with PMSG and hCG, mate with males, and collect zygotes 20-24 hours post-hCG.
- Electroporation: Wash zygotes with Opti-MEM I, place in electrode gap with RNP complex solution (5 µl total volume). Electroporate at 30 V (3 ms ON + 97 ms OFF) with 10 pulses.
- Post-Electroporation Processing: Immediately collect zygotes, wash 4× with M2 medium and 3× with KSOM medium.
- Culture and Assessment: Culture in KSOM at 37°C, 5% CO2 to blastocyst stage. The cleavage assay is based on the inability of the RNP complex to recognize successfully modified target sequences.
Troubleshooting:
- Poor embryo survival: Optimize electroporation parameters; ensure proper media osmolarity.
- Low editing efficiency: Verify gRNA quality and concentration; test multiple gRNAs.
- Inconsistent results: Include positive control gRNA targeting a non-essential locus.
Purpose: To computationally validate peptide binding stability and interaction mechanisms with target proteins before experimental testing.
Materials:
- GROMACS software package or equivalent MD simulation platform
- Peptide and protein structures (from docking or homology modeling)
- High-performance computing cluster
- Visualization software (PyMOL, VMD)
Methodology:
- System Preparation:
- Obtain protein-peptide complex structure from molecular docking.
- Solvate the complex in appropriate water model (TIP3P) in a simulation box.
- Add ions to neutralize system charge and achieve physiological salt concentration.
Energy Minimization:
- Perform steepest descent energy minimization (maximum 50,000 steps) until maximum force <1000 kJ/mol/nm.
- Apply position restraints on protein and peptide heavy atoms.
Equilibration Phases:
- NVT equilibration: 100 ps with position restraints, gradually heating system to 300K.
- NPT equilibration: 100 ps with position restraints, maintaining constant pressure (1 bar).
Production MD Run:
- Run unrestrained simulation for 50-100 ns with 2 fs time step.
- Save coordinates every 10 ps for analysis.
Analysis Parameters:
- RMSD: Calculate for protein backbone and peptide heavy atoms to assess stability.
- Radius of Gyration (Rg): Measure structural compactness throughout simulation.
- Interaction Energy: Compute protein-ligand interaction energy using GROMACS.
- H-bond Analysis: Identify persistent hydrogen bonds between peptide and protein.
Validation Metrics:
- Stable RMSD values (<0.2-0.3 nm fluctuation) after initial equilibration period.
- Consistent radius of gyration indicating maintained structural integrity.
- Persistent interaction energy values throughout simulation timeframe.
- Reproduction of known binding motifs and interactions from experimental data.
Pathway and Workflow Visualizations
CRISPR Target Validation Workflow
Peptide Inhibitor Development Pathway
AI-Driven Small Molecule Discovery
Research Reagent Solutions
Table 3: Essential Research Reagents for Target Validation
| Reagent/Category | Specific Examples | Function/Application | Key Considerations |
|---|---|---|---|
| CRISPR Systems | Cas9, Cas12a, dCas9-effectors | Gene knockout, activation, interference | Choose based on editing efficiency, PAM requirements, and size constraints |
| sgRNA Libraries | Genome-wide, focused custom libraries | High-throughput functional genomics screens | Ensure high coverage (>500x), include non-targeting controls |
| Delivery Methods | Lentivirus, electroporation, LNPs | Introducing editing components into cells | Optimize for cell type; consider toxicity and efficiency trade-offs |
| Peptide Synthesis | Solid-phase, cell-free ribosomal systems | Production of designed peptide inhibitors | Incorporate modifications for stability (cyclization, D-amino acids) |
| Validation Assays | Western blot, flow cytometry, NGS | Confirming target modulation and phenotypic effects | Use orthogonal methods to avoid platform-specific artifacts |
| Cell Models | hiPS cells, organoids, primary cells | Physiologically relevant screening platforms | Consider genetic background, differentiation status, and culture requirements |
| Bioinformatics Tools | DeepTarget, CRISPR-GPT, MD software | Data analysis, target prediction, and prioritization | Validate computational predictions experimentally |
Frequently Asked Questions
Q: Our model shows high accuracy but poor clinical relevance. What could be the cause? A: High accuracy with low clinical relevance often indicates a problem with the dataset or the evaluation metrics. The model might be highly accurate at predicting targets that are not clinically "druggable" or it may be trained on data that does not adequately represent the biological heterogeneity of real-world patient populations. Re-evaluate your training data for biases and ensure your key performance indicators (KPIs) include clinical translatability measures.
Q: What is the best way to handle high Specificity but low Sensitivity in our target identification model? A: A model with high specificity but low sensitivity is conservative; it correctly rejects false targets but misses many true ones. This is often due to an imbalanced dataset or a classification threshold that is set too high. To troubleshoot, you can adjust the decision threshold of your model and employ techniques like SMOTE to address class imbalance in your training data. Furthermore, validate the model on an independent, well-characterized cell line or patient-derived dataset.
Q: How can we effectively validate a computational model without a large, independent clinical dataset? A: In the absence of a large clinical dataset, a tiered validation approach is recommended. Begin with rigorous internal validation using hold-out test sets and resampling methods like bootstrapping. Next, use existing public genomic databases (e.g., TCGA, DepMap) for external computational validation. Finally, design a small-scale wet-lab experiment to test the top-ranking model predictions, which provides crucial, direct biological evidence.
Experimental Protocols & Data Presentation
Quantitative Metrics for Model Validation
The following table summarizes the core quantitative metrics used for computational model validation in this context.
| Metric | Calculation Formula | Interpretation in Cancer Target Identification |
|---|---|---|
| Accuracy | (True Positives + True Negatives) / Total Predictions | Measures overall correctness. Can be misleading if the class of "viable targets" is rare. |
| Sensitivity (Recall) | True Positives / (True Positives + False Negatives) | The model's ability to identify all true therapeutic targets. Missed targets (false negatives) are critical failures. |
| Specificity | True Negatives / (True Negatives + False Positives) | The model's ability to correctly rule out non-targets. High specificity minimizes wasted resources on false leads. |
| Precision | True Positives / (True Positives + False Positives) | The proportion of predicted targets that are true targets. Directly relates to experimental efficiency. |
| Area Under the Curve (AUC) | Area under the ROC curve | Evaluates the model's overall ability to discriminate between targets and non-targets across all classification thresholds. |
Detailed Methodology: In Vitro Validation of Predicted Targets
This protocol provides a direct experimental validation for computationally predicted cancer targets.
- Cell Line Selection: Choose relevant cancer cell lines (e.g., from NCI-60 or patient-derived organoids) and appropriate normal control cells.
- Gene Knockdown/Out: Using siRNA, shRNA, or CRISPR-Cas9, perturb the expression of the top-ranked genes identified by your computational model.
- Phenotypic Assays:
- Viability: Measure cell viability 72-96 hours post-perturbation using assays like ATP-based luminescence (e.g., CellTiter-Glo).
- Proliferation: Perform clonogenic survival assays or use live-cell imaging to track proliferation over time.
- Apoptosis: Quantify apoptosis via flow cytometry using Annexin V/propidium iodide staining.
- Data Analysis: Compare phenotypic effects in test groups against non-targeting controls (e.g., scramble siRNA). A significant reduction in viability or increase in apoptosis in cancer cells, with minimal effect on normal cells, provides strong evidence for the model's prediction.
The Scientist's Toolkit: Research Reagent Solutions
| Reagent / Material | Function in Experimental Validation |
|---|---|
| siRNA/shRNA Libraries | Used for transient or stable gene knockdown to assess the functional importance of a predicted target on cell phenotype. |
| CRISPR-Cas9 Knockout Kits | Enables complete gene knockout to study the essentiality of a predicted target with high potency and specificity. |
| Cell Viability Assay Kits (e.g., MTT, CellTiter-Glo) | Provide a quantitative, luminescent or colorimetric readout of cell health and proliferation after target perturbation. |
| Annexin V Apoptosis Detection Kits | Allow for the precise quantification of programmed cell death, a key mechanistic endpoint for many cancer therapeutics. |
| Patient-Derived Xenograft (PDX) Models | Offer a clinically relevant in vivo model system for validating that a target drives tumor growth in a complex microenvironment. |
Model Validation and Target Prioritization Workflow
Key Metric Relationships in Model Evaluation
Troubleshooting Guides
Guide: Addressing Misleading High Accuracy in Imbalanced Cancer Datasets
Problem Statement Your model for detecting rare cancer subtypes achieves 95% accuracy, yet fails to identify most actual positive cases. This creates a false sense of performance security and compromises research validity. [90] [91]
Root Cause Analysis This phenomenon, known as the "Accuracy Paradox," occurs primarily in imbalanced datasets where one class significantly outnumbers another. [91] In cancer research, this happens when healthy samples far outnumber cancerous ones. A model can achieve high accuracy by simply always predicting the majority class, while completely failing on the critical minority class (e.g., cancerous cells). [91]
Diagnostic Steps
- Generate a Confusion Matrix: Calculate True Positives (TP), False Positives (FP), True Negatives (TN), and False Negatives (FN). [92] [93]
- Calculate Class Distribution: Determine the ratio between your majority and minority classes.
- Check Metric Discrepancies: Note if accuracy remains high while recall or F1-score are low.
Resolution Steps
- Switch Evaluation Metrics: Immediately move beyond accuracy to balanced metrics:
- Implement Resampling Techniques: Apply SMOTE for oversampling or controlled undersampling of majority classes.
- Adjust Classification Thresholds: Lower the prediction threshold to identify more positive cases when high recall is critical. [92]
Verification of Fix
- Confusion matrix shows improved minority class identification
- F1-score increases significantly while accuracy may decrease slightly
- Recall metric meets the minimum required for your clinical application
Guide: Resolving Precision-Recall Trade-offs in Cancer Target Identification
Problem Statement While optimizing your model for one metric (e.g., high recall to find all potential cancer targets), the complementary metric suffers (e.g., low precision yields too many false leads), making experimental validation inefficient and costly. [94]
Root Cause Analysis The precision-recall trade-off is fundamental in classification. Increasing recall (catching more true positives) typically decreases precision (more false positives), and vice versa. [94] In cancer target identification, this manifests when casting a wide net for potential targets also captures numerous non-relevant genes/proteins.
Diagnostic Steps
- Plot Precision-Recall Curves: Visualize the trade-off across different classification thresholds. [91]
- Quantify Cost of Errors: Determine the practical cost of false positives (wasted validation resources) versus false negatives (missed therapeutic targets) in your research context. [94]
- Analyze Business Impact: For drug development, missing a viable target (false negative) may be more costly than preliminary investigation of a non-viable one (false positive). [94]
Resolution Steps
- Apply the Fβ-Score: Use the Fβ-Score which allows weighting recall β-times more important than precision when missing targets is particularly costly. [92]
- Formula: Fβ = (1 + β²) × (Precision × Recall) / (β² × Precision + Recall)
- Threshold Optimization: Systematically test classification thresholds to find the optimal balance for your specific research goals.
- Ensemble Methods: Combine models optimized for different metrics to create a more balanced final prediction.
Verification of Fix
- F1-score or Fβ-score meets target threshold for your application
- Precision and recall values are both above minimum acceptable levels
- Downstream experimental validation shows improved hit rates
Frequently Asked Questions (FAQs)
Metric Selection & Interpretation
Q1: When should I use F1-Score instead of Accuracy in cancer research? Use F1-Score when:
- Working with imbalanced datasets (common in cancer vs. normal tissue samples) [94] [91]
- Both false positives and false negatives are important (typical in target identification) [94]
- You need a single metric that balances precision and recall [93]
Use Accuracy when:
- Classes are perfectly balanced
- All types of errors have equal cost
- You need a simple, intuitive metric for stakeholders [93]
Q2: What constitutes a "good" F1-Score in cancer diagnostic models? A "good" F1-Score is context-dependent: [94]
Table: F1-Score Benchmarks in Cancer Research Applications
| Research Context | Minimum Acceptable F1-Score | Good F1-Score | Excellent F1-Score |
|---|---|---|---|
| Initial Target Screening | 0.60+ | 0.70+ | 0.80+ |
| Diagnostic Assistance | 0.70+ | 0.80+ | 0.90+ |
| Patient Stratification | 0.75+ | 0.85+ | 0.92+ |
| Clinical Grade Diagnostics | 0.85+ | 0.90+ | 0.95+ |
Q3: How do I choose between optimizing for Precision vs. Recall? The choice depends on the consequences of each error type in your specific research phase: [94]
Optimize for RECALL when:
- Missing a true cancer target is more costly than validating a false lead
- In early discovery phases where comprehensive target identification is critical
- False negatives have serious downstream consequences
Optimize for PRECISION when:
- Experimental validation resources are extremely limited and expensive
- You need high confidence in selected targets before proceeding
- False positives would derail research directions
Technical Implementation
Q4: How do I calculate F1-Score and related metrics from a confusion matrix? Given a confusion matrix with True Positives (TP), False Positives (FP), True Negatives (TN), and False Negatives (FN): [92] [94] [93]
- Precision = TP / (TP + FP) - Measures prediction quality
- Recall (Sensitivity) = TP / (TP + FN) - Measures coverage of actual positives
- F1-Score = 2 × (Precision × Recall) / (Precision + Recall) - Harmonic mean
Table: Example Calculation from Sample Confusion Matrix
| Metric | Calculation | Example Values | Result |
|---|---|---|---|
| Precision | TP/(TP+FP) | 80/(80+20) | 0.80 |
| Recall | TP/(TP+FN) | 80/(80+40) | 0.67 |
| F1-Score | 2×(Precision×Recall)/(Precision+Recall) | 2×(0.80×0.67)/(0.80+0.67) | 0.73 |
Q5: What are the essential evaluation metrics beyond Accuracy and F1-Score? A comprehensive evaluation should include multiple perspectives: [92] [93] [91]
Table: Comprehensive ML Evaluation Metrics for Cancer Research
| Metric Category | Specific Metrics | Research Context |
|---|---|---|
| Threshold-Based | Accuracy, Precision, Recall, F1-Score | Binary classification tasks |
| Probability-Based | AUC-ROC, Logarithmic Loss | Model confidence assessment |
| Rank-Based | Lift Charts, Kolmogorov-Smirnov Chart | Candidate prioritization |
| Clinical Utility | Sensitivity, Specificity | Diagnostic applications |
Experimental Protocols & Methodologies
Standardized Model Evaluation Protocol
Purpose To ensure consistent, comparable evaluation of machine learning models across cancer target identification studies.
Materials
- Trained classification model
- Held-out test dataset (representative of real-world distribution)
- Computing environment with Python/R and necessary libraries (scikit-learn, pandas, numpy)
- Validation framework supporting multiple metrics
Procedure
- Data Preparation
- Partition data into training/validation/test sets (recommended: 60/20/20 split)
- Ensure test set remains completely unseen during model development
- Maintain class distributions across splits where appropriate
Prediction Generation
- Generate model predictions on test set
- Export both class predictions and probability estimates
- Record all predictions with ground truth labels
Metric Computation
- Calculate confusion matrix: TP, FP, TN, FN
- Compute primary metrics: Accuracy, Precision, Recall, F1-Score
- Compute secondary metrics: AUC-ROC, Specificity, NPV
- Generate visualization: ROC curve, Precision-Recall curve, Confusion Matrix heatmap
Statistical Validation
- Perform cross-validation (minimum 5-fold)
- Calculate confidence intervals for key metrics
- Conduct significance testing when comparing multiple models
Expected Outcomes
- Comprehensive performance assessment across multiple metrics
- Understanding of performance trade-offs (precision vs. recall)
- Statistical confidence in model capabilities
Workflow Visualization
The Scientist's Toolkit: Research Reagent Solutions
Table: Essential Computational Tools for ML Model Evaluation in Cancer Research
| Tool/Resource | Function/Purpose | Implementation Example |
|---|---|---|
| Scikit-learn Metrics Module | Comprehensive metric calculation | from sklearn.metrics import precision_score, recall_score, f1_score |
| Confusion Matrix Visualization | Visual performance analysis | sklearn.metrics.ConfusionMatrixDisplay |
| ROC-AUC Calculation | Model discrimination ability | sklearn.metrics.roc_auc_score |
| Cross-Validation Framework | Robust performance estimation | sklearn.model_selection.StratifiedKFold |
| Statistical Testing | Significance validation | scipy.stats.ttest_rel for paired tests |
| Imbalanced-learn Library | Handling class imbalance | imblearn.over_sampling.SMOTE |
Metric Relationships Visualization
Frequently Asked Questions (FAQs)
FAQ 1: What are the primary causes of unstable protein-ligand complexes during Molecular Dynamics (MD) simulations, and how can I fix them?
Instability in MD simulations often manifests as high Root Mean Square Deviation (RMSD) and can be caused by several factors. The table below summarizes common issues and their solutions.
| Issue | Symptom | Solution |
|---|---|---|
| Inadequate System Equilibration | Drifting RMSD, high energy | Extend equilibration phases (NVT, NPT) until system properties (temp, pressure, density) stabilize. [95] |
| Incorrect Force Field Parameters | Unphysical bond stretching/angles, ligand distortion | Use tools like CGenFF or ACPYPE to generate accurate parameters for non-standard residues or small molecules. |
| Structural Bias from Initial Guess | Artificially maintained structure, low conformational exploration | Use a random initial molecular conformation instead of a periodic or highly structured guess to avoid bias. [95] |
| Poorly Chosen Simulation Box | Artifacts from frontier effects, uneven density | Use a larger, cubic simulation box (e.g., 50×50×50 nm) to minimize boundary effects. [95] |
FAQ 2: My molecular docking results show good binding affinity, but biological assays show no activity. What could be wrong?
This common discrepancy can arise from issues in both the docking and post-docking analysis stages.
- Overlooking Protein Flexibility: Docking often uses a single, rigid protein conformation. If the binding site undergoes significant conformational change upon ligand binding, the docking pose may be incorrect. Solution: Use ensemble docking against multiple protein crystal structures or conformations extracted from an MD simulation. [96]
- Ignoring Solvation Effects: The scoring functions in docking programs may not accurately model water molecules that are crucial for binding. A pose that seems favorable in a vacuum might be unstable in a solvated environment. Solution: Rescore docking poses using more rigorous, explicit solvent methods like Molecular Mechanics/Poisson-Boltzmann Surface Area (MM/PBSA). [97] [98]
- Insufficient Validation: A good docking score alone is not a reliable indicator of binding. Solution: Always subject your top docking hits to MD simulations to assess the stability of the complex over time. A stable complex with consistent low RMSD and preserved key interactions is a more reliable predictor of true activity. [97] [99] [98]
FAQ 3: How long should my MD simulation be to ensure reliable results for protein-ligand binding?
There is no universal answer, as the required simulation time depends on the system and the biological process of interest. [96]
- For Binding Pose Stability: Simulations of 100 to 300 nanoseconds are often sufficient to confirm whether a docked pose is stable or if the ligand undergoes significant movement or dissociation. [98]
- For Studying Binding/Unbinding Events: Observing spontaneous dissociation or association in conventional MD is often not feasible for strong binders, as these events can occur on microsecond to millisecond timescales. Solution: If studying kinetics, employ enhanced sampling methods (e.g., GaMD, metadynamics) or build Markov State Models (MSMs) from many shorter simulations to access longer timescales. [96]
- General Rule: The simulation should be long enough for the system to reach a steady state, indicated by a plateau in the RMSD. Always run simulations in multiple replicas (typically 3) with different initial velocities to ensure your results are reproducible and not due to chance.
FAQ 4: What are the key parameters to check after an MD simulation to validate the stability of my complex?
A valid MD simulation requires checking the stability of both the protein and the complex. The table below outlines the key parameters to analyze.
| Parameter | What It Measures | Interpretation of a Stable Complex |
|---|---|---|
| RMSD (Backbone) | Deviation from initial structure | Plateaus after equilibration (typically < 2.0-3.0 Å). [99] |
| RMSF (Residues) | Flexibility of individual residues | Binding site residues should show reduced flexibility upon stable ligand binding. |
| Radius of Gyration (Rg) | Compactness of the protein | Remains stable, indicating no major unfolding or compaction. |
| Intermolecular H-bonds | Specific protein-ligand interactions | Key interactions (e.g., with catalytic residues) are maintained throughout the simulation. |
| MM/PBSA Binding Free Energy | Theoretical binding affinity | A consistently high negative value indicates strong, favorable binding. [98] |
Troubleshooting Guides
Guide 1: Troubleshooting Unstable Molecular Dynamics Simulations
Symptoms: The simulation crashes, or the RMSD of the protein backbone or ligand does not plateau and continues to increase indefinitely.
Step-by-Step Diagnostic Procedure:
- Check the Simulation Log Files: Look for error messages related to "Bond too long," "Velocity," or "LINCS warning," which often point to high energy states or parameter issues.
- Visualize the Trajectory: Use a tool like VMD or PyMol to watch the simulation. Look for:
- The ligand drifting away from the binding site.
- Unphysical distortion of the protein or ligand.
- Water molecules or ions entering forbidden areas.
- Plot Basic Stability Metrics: Generate time-series plots for RMSD, Rg, and potential energy. A stable simulation should show fluctuations around a mean value after an initial equilibration period.
Common Solutions:
- Problem: Incomplete or Rushed Equilibration.
- Solution: Re-run the simulation with longer NVT and NPT equilibration phases. Ensure temperature and pressure have fully stabilized before starting the production run.
- Problem: Incorrect Ligand Parameters.
- Solution: Re-generate the ligand's topology and parameters using a reliable force field. Pay special attention to partial charges, bond orders, and atom types.
- Problem: Bad Starting Structure.
- Solution: Avoid using a periodic starting structure for complex systems, as it can introduce bias. Use a random initial conformation for a more realistic setup. [95]
Guide 2: Troubleshooting Poor Molecular Docking Outcomes
Symptoms: All docked compounds show similar, non-discriminatory binding scores; predicted poses clash with the protein or are clearly incorrect upon visual inspection.
Step-by-Step Diagnostic Procedure:
- Validate Your Docking Protocol: Re-dock a known native ligand (co-crystallized with your protein) back into its binding site.
- A successful protocol should reproduce the experimental binding pose with a low ligand RMSD (typically < 2.0 Å).
- Check the Binding Site Definition: Ensure the grid box or search space is correctly centered on the binding site and is large enough to allow the ligand to rotate freely.
- Inspect the Protonation States: The protonation states of key protein residues (e.g., His, Asp, Glu) and the ligand at the simulation pH can drastically affect binding. Use tools like
PROPKAto determine correct states.
Common Solutions:
- Problem: The re-docked native ligand does not reproduce the experimental pose.
- Solution: Your protocol is flawed. Adjust the docking parameters (exhaustiveness, scoring function) or consider using a different docking software. Using a structure refined with homology modeling can also improve results if an experimental structure is unavailable. [97]
- Problem: Docking poses are nonsensical or clash with the protein.
- Solution: Account for protein flexibility. If possible, use an "induced fit" docking approach or perform ensemble docking against multiple protein structures. [96]
- Problem: Good docking poses do not hold up in simulation.
Experimental Protocols & Workflows
Detailed Protocol: Integrated Docking and MD Simulation for Cancer Target Validation
This protocol outlines a comprehensive structure-based drug discovery pipeline, as used in recent studies to identify natural inhibitors against cancer targets like the βIII-tubulin isotype and Jervine as a dual inhibitor of AURKB and CDK1. [97] [98]
1. System Preparation
- Protein Preparation:
- Obtain the 3D structure of the target protein (e.g., βIII-tubulin, AURKB) from the PDB.
- Remove heteroatoms (water, original ligands) except crucial cofactors.
- Add missing hydrogen atoms and assign protonation states using tools like
PDB2PQRorMolProbity.
- Ligand Library Preparation:
- Retrieve a library of compounds (e.g., from ZINC, IMPPAT databases).
- Generate 3D structures and convert them to a dockable format (e.g., PDBQT) using
Open Babel. - Minimize ligand energy and calculate partial charges. [97]
2. High-Throughput Virtual Screening
- Define the binding site (e.g., the 'Taxol site' on βIII-tubulin) using coordinates from a known ligand or literature. [97]
- Perform molecular docking against the entire library using a tool like
AutoDock VinaorCovDock(for covalent inhibitors). [97] [99] - Select top hits based on binding energy (e.g., the best 1000 compounds) for further filtering. [97]
3. Advanced Filtering and Machine Learning
- Filter hits based on drug-likeness (Lipinski's Rule of Five), PAINS filters, and predicted ADMET properties. [97] [99] [98]
- Use a machine learning classifier trained on known active/inactive compounds to further prioritize candidates with a high probability of being active. [97]
4. Molecular Dynamics Simulation
- System Setup: Solvate the top protein-ligand complexes in a cubic water box (e.g., TIP3P water model) and add ions to neutralize the system's charge.
- Energy Minimization and Equilibration:
- Minimize the system energy to remove steric clashes.
- Equilibrate first with position restraints on the protein and ligand (NVT ensemble, 100 ps), then without restraints (NPT ensemble, 100 ps) to stabilize temperature and pressure.
- Production Run: Run an unrestrained MD simulation for a sufficient duration (e.g., 100-300 ns). Use a temperature of 310 K and a pressure of 1 bar. [98]
- Replica Simulations: Run 3 independent replicas with different initial velocities to ensure result robustness.
5. Trajectory Analysis
- Calculate and plot RMSD, RMSF, Rg, and SASA using
GROMACStools. - Analyze hydrogen bonds and specific protein-ligand interactions over time.
- Calculate theoretical binding free energy using the MM/PBSA method. [98]
6. Experimental Validation
- The top computational hits, demonstrating stable binding in MD simulations and favorable MM/PBSA scores, should be forwarded for in vitro biological evaluation (e.g., testing on MCF-7 breast cancer cells) to confirm anti-cancer activity. [100] [98]
Workflow Diagram: Integrated Validation Pipeline
The following diagram illustrates the sequential steps of the integrated docking and MD validation protocol.
The Scientist's Toolkit: Essential Research Reagents & Software
This table details key computational tools and resources used in the featured protocols for cancer target validation. [97] [100] [99]
| Category | Item/Solution | Function in Research |
|---|---|---|
| Software & Tools | AutoDock Vina / CovDock | Performs molecular docking to predict ligand binding poses and affinities. [97] [99] |
| GROMACS | A versatile package for performing molecular dynamics simulations and trajectory analysis. [100] [99] | |
| PyMOL / VMD | Used for 3D visualization of protein structures, docking poses, and MD trajectories. [97] [99] | |
| AlphaFold 3 | Predicts the 3D structure of proteins and their complexes with ligands, nucleic acids, and more. [101] | |
| Databases | RCSB Protein Data Bank (PDB) | Primary repository for experimentally determined 3D structures of biological macromolecules. [98] |
| ZINC / IMPPAT / PubChem | Public databases containing millions of commercially available and natural compounds for virtual screening. [97] [98] | |
| SwissTargetPrediction | Predicts the most probable protein targets of small molecules based on similarity. [100] | |
| Methodologies | MM/PBSA | A method to calculate binding free energies from MD trajectories, providing a theoretical affinity score. [98] |
| Enhanced Sampling (GaMD, etc.) | Advanced MD techniques to accelerate the sampling of rare events like ligand binding/unbinding. [96] | |
| Machine Learning Classifiers | Used to distinguish active from inactive compounds based on chemical descriptor properties. [97] |
FAQs: Computational Model Validation & Translation
What constitutes a "validated" computational model for target identification in cancer research?
A validated computational model is one that has undergone a rigorous, multi-layered evidence-building process to ensure its predictions are reliable and biologically relevant for a specific Context of Use (COU). This process, often structured around a framework like the V3 Framework (Verification, Analytical Validation, and Clinical Validation) adapted for preclinical research, ensures the model is fit-for-purpose [102].
- Verification confirms that the software and algorithms used to build the model perform as intended without technical errors.
- Analytical Validation assesses the model's precision, accuracy, and reliability in generating its output (e.g., a target priority score or a binding affinity prediction). It ensures the model is robust and reproducible.
- Clinical Validation (or Biological Validation in this context) confirms that the model's output accurately predicts a meaningful biological state or therapeutic response in animal models relevant to human cancer [102].
Ultimately, validation is not a binary status but a continuum of confidence that must align with the model's intended application, from early-stage prioritization to serving as primary evidence for regulatory submissions [103] [104].
How can I troubleshoot a high rate of false-positive targets from my AI/ML model?
A high false-positive rate often stems from biases or limitations in the training data and a lack of mechanistic understanding. The table below outlines common issues and corrective actions.
Table: Troubleshooting False Positives in AI/ML Target Identification
| Issue | Diagnostic Check | Corrective Action |
|---|---|---|
| Biased Training Data | Audit training sets for overrepresentation of certain protein families (e.g., kinases, GPCRs) and underrepresentation of novel target classes [105]. | Curate diverse, balanced training data. Incorporate negative examples (non-targets) and use data augmentation techniques. |
| Lack of Genetic Evidence | Check if candidate targets have supporting human genetic data (e.g., from GWAS). | Prioritize targets where genetic evidence suggests a causal role in disease; this can increase clinical success odds by up to 80% [105]. |
| Over-reliance on Single Data Modalities | Evaluate if the model uses only one data type (e.g., genomics). | Integrate multi-omics data (proteomics, transcriptomics) and literature knowledge to build a more holistic, systems-level view [106]. |
| Poor Generalizability | Test model performance on a held-out validation set from a different source. | Implement cross-validation with diverse datasets. Use ensemble modeling and prioritize explainable AI (XAI) techniques to understand prediction drivers [103] [106]. |
What are the key considerations for validating a Digital Twin model for patient stratification?
Digital twins—virtual replicas of individual patients' physiology—require stringent validation to be used for stratifying patients into clinical cohorts.
- Multi-Omics Integration: The digital twin must accurately integrate genomic, proteomic, and clinical data to create a faithful virtual representation. In oncology, this has been used to simulate tumor growth and response to immunotherapy [103].
- Prospective Predictive Accuracy: The model must be validated by comparing its simulated predictions of therapeutic response to the actual outcomes observed in a clinical or preclinical trial setting.
- Regulatory-Grade Validation: For use in regulatory submissions, the digital twin platform must be developed within a standardized framework akin to Good Clinical Practice, with transparent algorithms and defined performance benchmarks [103]. The FDA has begun accepting such in silico evidence in model-informed drug development programs [103].
Our in vivo results do not match in silico predictions. What are the first steps in troubleshooting this disconnect?
This common challenge, often due to biological complexity or pharmacokinetic (PK) factors, requires a systematic investigation.
- Revisit the Model's Context of Use: Was the model designed and validated for the specific biological context (e.g., cancer type, genetic background) you are testing? A model trained on one cancer type may not translate to another.
- Interrogate the In Vivo Conditions:
- Confirm Target Engagement: Use pharmacodynamic (PD) biomarkers to verify that the drug is indeed engaging the intended target in the live animal.
- Assess Exposure at the Site of Action: A critical but often overlooked factor. Measure drug concentrations in the tumor tissue, not just in plasma. The formulation and route of administration can dramatically impact exposure [107]. For central nervous system targets, confirm the drug crosses the blood-brain barrier [107].
- Evaluate the Disease Model: The animal model (e.g., cell-line-derived xenograft, patient-derived xenograft) may not fully recapitulate the human tumor microenvironment, leading to divergent results.
Diagram: Systematic Troubleshooting for In Silico/In Vivo Disconnect
Experimental Protocols for Key Validation Steps
Protocol 1: High-Throughput In Vitro Screening for Target Prioritization
This protocol is used to functionally validate computationally-predicted targets or compound hits from large-scale in silico screens [104] [108].
- Assay Design: Develop a cell-based or biochemical assay targeting a specific molecular initiating event (e.g., receptor binding, enzyme inhibition). The assay should be scalable to a 384-well or 1536-well plate format.
- Reference Compounds: Include a set of well-characterized reference compounds (both positive and negative controls) in each run to demonstrate assay reliability and relevance [104].
- Concentration-Response: Test each compound or genetic perturbation (e.g., siRNA, CRISPR) in a concentration-response format (typically 8-12 point dilutions) to generate potency (IC50/EC50) data.
- Cytotoxicity Counter-Screen: Run a parallel cytotoxicity assay (e.g., measuring ATP levels) to de-prioritize hits that act through general cell killing [104].
- Data Analysis: Fit concentration-response curves to calculate potency and efficacy. Use the Z'-factor > 0.5 to confirm robust assay performance. Hits are prioritized based on potency, efficacy, and lack of cytotoxicity.
Protocol 2: Integrating Multi-Omics for Target Validation
This methodology leverages multiple data layers to build confidence in a target's role in cancer pathogenesis [106].
- Data Acquisition:
- Genomics: Perform Whole Genome Sequencing (WGS) or Whole Exome Sequencing (WES) on patient tumors to identify mutations and copy number variations in the candidate target [106].
- Transcriptomics: Conduct RNA-seq to analyze gene expression patterns and alternatively spliced isoforms.
- Proteomics: Use mass spectrometry to quantify protein expression and post-translational modifications.
- Data Integration & Bioinformatics Analysis: Use bioinformatics pipelines and network pharmacology approaches to integrate the multi-omics datasets. Identify differentially expressed genes/proteins and map them onto biological pathways (e.g., using KEGG, Reactome) to understand the target's functional context [106].
- Experimental Corroboration: Validate key findings using orthogonal methods:
Diagram: Multi-Omics Integration Workflow for Target Validation
The Scientist's Toolkit: Research Reagent Solutions
Table: Essential Tools for Building Target Validation Data Packages
| Category / Tool | Function in Validation | Example Use Case |
|---|---|---|
| AI/ML Platforms | Predict drug-target interactions, protein structures, and prioritize candidate targets. | Using AlphaFold for high-quality protein structure prediction to enable structure-based drug design [105]. |
| Toxicity Prediction Suites (e.g., ProTox-3.0, DeepTox) | In silico assessment of compound toxicity, absorption, distribution, metabolism, excretion (ADME) and potential off-target effects [103]. | Screening a virtual compound library to eliminate molecules with predicted hepatotoxicity early in the pipeline. |
| Network Pharmacology Tools | Construct and analyze drug-target-disease networks to identify mechanisms and multi-target therapy opportunities [106]. | Identifying synergistic drug combinations for oncology by modeling effects on interconnected signaling pathways. |
| Molecular Dynamics Simulation | Examine atomic-level interactions between a drug candidate and its target protein over time, informing on binding stability and energy [106]. | Calculating binding free energy (e.g., via MM/PBSA) to optimize the structure of a tankyrase inhibitor for cancer therapy. |
| High-Throughput Screening Assays | Rapidly test thousands of compounds or genetic perturbations for functional activity against a target in vitro [104] [108]. | Validating hits from an in silico screen in a cell-based assay measuring pathway activation or cell viability. |
| Digital Twin Technology | Create virtual patient models to simulate disease progression and therapeutic response across diverse populations [103]. | Personalizing cancer treatment strategies by simulating a patient's tumor response to different immunotherapy regimens. |
Conclusion
The validation of computational models for cancer target identification represents a paradigm shift in oncology drug discovery, moving the field from a focus on single targets to a holistic, systems-level understanding of drug mechanisms. The synergy between AI-driven prediction and rigorous experimental validation, as demonstrated by tools like DeepTarget and frameworks like the Centre for Target Validation, is crucial for building confidence in novel targets and accelerating their journey into the drug development pipeline. Future progress hinges on overcoming data quality and model interpretability challenges, fostering interdisciplinary collaboration, and developing standardized validation platforms. By continuing to refine these computational approaches and strengthening their integration with biological experimentation, the vision of precision oncology—delivering safer, more effective, and personalized cancer therapies—will become an increasingly attainable reality.
References
- 1. Artificial intelligence in cancer target identification and drug ... [https://www.nature.com/articles/s41392-022-00994-0]
- 2. Why 90% of clinical drug development fails and how to ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9293739/]
- 3. A comprehensive review of computational cell cycle models in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11226463/]
- 4. Transforming Oncology Drug Discovery with Data Science [https://blog.crownbio.com/data-integration-bioinformatics-oncology-drug-discovery]
- 5. Target identification by structure-based computational ... [https://www.sciencedirect.com/science/article/pii/S0960894X23000495]
- 6. 7 Emerging Challenges Computational Biology Students ... [https://www.mantechpublications.com/blog/computational-biology/]
- 7. Challenges and opportunities for the next generation of ... [https://journals.plos.org/plosbiology/article?id=10.1371/journal.pbio.3003269]
- 8. Five potential problems with overhyping AI in drug discovery [https://www.ddw-online.com/five-potential-problems-with-overhyping-ai-in-drug-discovery-34511-202504/]
- 9. Bridging the Gap Between Computational Biology and ... [https://www.linkedin.com/pulse/bridging-gap-between-computational-biology-validation-ahmed-elhadi-bafnc]
- 10. AI for Science 2025 [https://www.nature.com/articles/d42473-025-00161-3]
- 11. Artificial intelligence in cancer: applications, challenges, and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12574039/]
- 12. Artificial Intelligence in Cancer Drug Discovery in 2025 [https://oncodaily.com/oncolibrary/artificial-intelligence-in-cancer-drug-discovery]
- 13. How Artificial Intelligence Is Transforming Cancer Care in ... [https://oncodaily.com/oncolibrary/artificial-intelligence-ai]
- 14. Biomedical text mining for knowledge extraction @ ISMB 2025 [https://ai4biomed.org/ismb2025tutorial/]
- 15. Biomedical Natural Language Processing and Text Mining [https://www.mdpi.com/journal/information/special_issues/O18C9UE6D1]
- 16. Google's Gemma AI model helps discover new potential ... [https://blog.google/technology/ai/google-gemma-ai-cancer-therapy-discovery/]
- 17. Top Oncology Innovations That Shaped the First Half of 2025 [https://binaytara.org/cancernews/article/top-oncology-innovations-that-shaped-the-first-half-of-2025]
- 18. Protocol for tumor prognostic prediction, molecular ... [https://www.sciencedirect.com/science/article/pii/S2666166725005362]
- 19. Integrating artificial intelligence into small molecule ... [https://www.nature.com/articles/s44386-025-00029-y]
- 20. Natural Language Processing vs. Text Mining: The Difference [https://www.coherentsolutions.com/insights/natural-language-processing-vs-text-mining-key-differences]
- 21. News and Announcement Page | NCI Genomic Data Commons [https://gdc.cancer.gov/news-and-announcements]
- 22. AI-driven multi-omics integration in precision oncology [https://pmc.ncbi.nlm.nih.gov/articles/PMC12634751/]
- 23. Challenges in AI-driven multi-omics data analysis for ... [https://www.sciencedirect.com/science/article/pii/S2352914825000681]
- 24. Discovering anticancer drug target combinations via ... [https://www.nature.com/articles/s43856-025-01150-9]
- 25. The clinical trials puzzle: How network effects limit drug ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10749231/]
- 26. New Computational Tool Shows Strong Accuracy in ... [https://ascopost.com/news/november-2025/new-computational-tool-shows-strong-accuracy-in-predicting-cancer-drug-targets]
- 27. identification and validation of EGLN1 as a key target [https://pubmed.ncbi.nlm.nih.gov/41191606/]
- 28. Computational models for pan-cancer classification based on ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12599994/]
- 29. Text has enhanced contrast | ACT Rule | WAI [https://www.w3.org/WAI/standards-guidelines/act/rules/09o5cg/]
- 30. Text color must provide high contrast with its background [https://docs.acquia.com/web-governance/text-color-must-provide-high-contrast-its-background]
- 31. Contrast requirements for WCAG 2.2 Level AA [https://www.makethingsaccessible.com/guides/contrast-requirements-for-wcag-2-2-level-aa/]
- 32. Node Shapes [https://graphviz.org/doc/info/shapes.html]
- 33. DeepTarget predicts anti-cancer mechanisms of action ... [https://pubmed.ncbi.nlm.nih.gov/41193619/]
- 34. DeepTarget predicts anti-cancer mechanisms of action ... [https://www.nature.com/articles/s41698-025-01111-4]
- 35. Anti-Cancer Mechanisms of Small Molecule Drugs ... [https://www.genengnews.com/topics/drug-discovery/anti-cancer-mechanisms-of-small-molecule-drugs-predicted-by-deeptarget/]
- 36. Predicting Anti-Cancer Mechanisms of Action with DeepTarget ... [https://decodingbio.substack.com/p/biobyte-140-predicting-anti-cancer?utm_source=substack&utm_medium=email&utm_content=share&action=share]
- 37. Computational deep dive surfaces unexplored world of ... [https://www.eurekalert.org/news-releases/1106119]
- 38. DrugAppy - An end-to-end deep learning framework for ... [https://pubmed.ncbi.nlm.nih.gov/41110298/?utm_source=FeedFetcher&utm_medium=rss&utm_campaign=None&utm_content=0Ph-jmRVLdsuGJtcq0obeg9EU4bNT3NMuBSIlbkwUEY&fc=None&ff=20251031073824&v=2.18.0.post22+67771e2]
- 39. An enzyme activity-based workflow for the identification ... [https://pubmed.ncbi.nlm.nih.gov/40684945/]
- 40. Automated drug design for druggable target identification ... [https://www.nature.com/articles/s41598-025-18091-x]
- 41. Researchers Develop Active Learning Workflow to ... [https://www.cmu.edu/mcs/news-events/2023/0630-gutkin-gusev-journal]
- 42. Development and validation of an autonomous artificial ... [https://www.nature.com/articles/s43018-025-00991-6]
- 43. Machine learning-driven multi-targeted drug discovery in ... [https://www.nature.com/articles/s41698-025-01058-6]
- 44. New Biomarkers, Drug Targets Identified for Colorectal ... [https://www.ajmc.com/view/new-biomarkers-drug-targets-identified-for-colorectal-cancer]
- 45. Antibody–drug conjugates in cancer therapy [https://molecular-cancer.biomedcentral.com/articles/10.1186/s12943-025-02489-2]
- 46. Antibody drug conjugate: the “biological missile” ... - Nature [https://www.nature.com/articles/s41392-022-00947-7]
- 47. Beyond Small Molecules: Antibodies and Peptides for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10974899/]
- 48. Towards designing improved cancer immunotherapy ... [https://www.nature.com/articles/s41467-024-54887-7]
- 49. Transformation of peptides to small molecules in medicinal ... [https://www.sciencedirect.com/science/article/pii/S2211383524002508]
- 50. Therapeutic peptides: current applications and future ... [https://www.nature.com/articles/s41392-022-00904-4]
- 51. Antibody–Drug Conjugates (ADCs): current and future ... [https://jhoonline.biomedcentral.com/articles/10.1186/s13045-025-01704-3]
- 52. Biological Activity of Natural and Synthetic Peptides as ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11242495/]
- 53. DeepTarget predicts anti-cancer mechanisms of action ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12589559/]
- 54. Mitochondrial metabolism and cancer therapeutic innovation [https://www.nature.com/articles/s41392-025-02311-x]
- 55. A Review of Advances in Mitochondrial Research in Cancer [https://pmc.ncbi.nlm.nih.gov/articles/PMC11531673/]
- 56. Ibrutinib selectively and irreversibly targets EGFR (L858R ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4741607/]
- 57. Ibrutinib targets mutant-EGFR kinase with a distinct binding ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5342513/]
- 58. Ten quick tips for avoiding pitfalls in multi-omics data ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10325053/]
- 59. AI-driven multi - omics in precision oncology: bridging the... integration [https://link.springer.com/article/10.1007/s10238-025-01965-9]
- 60. Applications and challenges of biomarker-based predictive models in... [https://pubmed.ncbi.nlm.nih.gov/40900695/]
- 61. A Guide to Multi-omics Integration Strategies [https://frontlinegenomics.com/a-guide-to-multi-omics-integration-strategies/]
- 62. Centre for Target Validation [https://www.icr.ac.uk/research-and-discoveries/centres-and-strategic-collaborations/centre-for-target-validation]
- 63. Quantification of tumor heterogeneity: from data acquisition ... [https://www.sciencedirect.com/science/article/pii/S0167779921002675]
- 64. Cancer Heterogeneity and Liquid Biopsy [https://www.thermofisher.com/blog/behindthebench/precision-medicine-cancer-heterogeneity-liquid-biopsy/]
- 65. Explainable deep learning framework for cancer ... [https://arxiv.org/html/2511.12463v1]
- 66. An explainable AI-assisted web application in cancer drug ... [https://www.sciencedirect.com/science/article/pii/S221501612400150X]
- 67. FAQ [https://www.the-ici-fund.org/faq]
- 68. Empirical Study of Overfitting in Deep Learning for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10093528/]
- 69. Overfitting in Machine Learning Explained [https://aws.amazon.com/what-is/overfitting/]
- 70. Prevent overfitting and imbalanced data with Automated ML [https://learn.microsoft.com/en-us/azure/machine-learning/concept-manage-ml-pitfalls?view=azureml-api-2]
- 71. Model Validation: Problem Areas and Solutions [https://rocketloop.de/en/blog/model-validation-overfitting-underfitting/]
- 72. 8 Simple Techniques to Prevent Overfitting [https://towardsdatascience.com/8-simple-techniques-to-prevent-overfitting-4d443da2ef7d/]
- 73. A foundation model for generalizable cancer diagnosis and ... [https://www.nature.com/articles/s41467-025-57587-y]
- 74. Empirical Study of Overfitting in Deep FNN Prediction ... [https://arxiv.org/abs/2208.02150]
- 75. Force field comparison for molecular dynamics simulations ... [https://www.sciencedirect.com/science/article/abs/pii/S0167732224024061]
- 76. Common errors when using GROMACS [https://manual.gromacs.org/2024.4/user-guide/run-time-errors.html]
- 77. 7.1. Common issues that are often regarded as bugs [https://docs.lammps.org/Errors_common.html]
- 78. Some critical issues for a reliable molecular dynamics ... [https://www.sciencedirect.com/science/article/abs/pii/S0927025614002249]
- 79. Scaling Molecular Dynamics Beyond 100000 Processor ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7153361/]
- 80. Simulations of Subnanometer Scale Image Contrast in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10208375/]
- 81. Lost in translation: the valley of death across preclinical and ... [https://transmedcomms.biomedcentral.com/articles/10.1186/s41231-019-0050-7]
- 82. Bridging the gap between preclinical and clinical research [https://pmc.ncbi.nlm.nih.gov/articles/PMC10043823/]
- 83. Lost in Translation Problems and Pitfalls ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC2646591/]
- 84. Computational modeling and simulation in oncology - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC12411925/]
- 85. Challenges and limitations in computational prediction of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10796696/]
- 86. DeepTarget tool helps identify secondary cancer drug targets [https://www.drugtargetreview.com/news/190717/deeptarget-tool-helps-identify-secondary-cancer-drug-targets/]
- 87. DeepTarget tool uncovers primary and secondary drug ... [https://www.news-medical.net/news/20251118/DeepTarget-tool-uncovers-primary-and-secondary-drug-targets-across-cancer-types.aspx]
- 88. Chai-1 [https://biolm.ai/models/chai1/]
- 89. Computational and experimental discovery of peptide ... [https://www.nature.com/articles/s41598-025-13110-3]
- 90. 4 Powerful Metrics For Testing AI Model Performance [2025] [https://medium.com/demohub-tutorials/accuracy-vs-precision-what-they-really-mean-in-ai-53d6036efb07]
- 91. How to Check the Accuracy of Your Machine Learning ... [https://www.deepchecks.com/how-to-check-the-accuracy-of-your-machine-learning-model/]
- 92. 12 Important Model Evaluation Metrics for Machine ... [https://www.analyticsvidhya.com/blog/2019/08/11-important-model-evaluation-error-metrics/]
- 93. Evaluation Metrics in Machine Learning [https://www.geeksforgeeks.org/machine-learning/metrics-for-machine-learning-model/]
- 94. F1 Score in Machine Learning: Formula, Range & ... [https://futurense.com/blog/f1-score-in-machine-learning]
- 95. 2.2. Validation of the Computational Protocol [https://bio-protocol.org/exchange/minidetail?id=5472668&type=30]
- 96. Challenges and frontiers of computational modelling of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10299731/]
- 97. Structure based drug design and machine learning ... [https://www.nature.com/articles/s41598-025-17708-5]
- 98. Structure-based identification of Jervine as a potent dual ... [https://www.frontiersin.org/journals/pharmacology/articles/10.3389/fphar.2025.1662556/full]
- 99. Identification and Validation of Key Covalent Inhibitors ... [https://www.sciencedirect.com/science/article/abs/pii/S0006291X25016894]
- 100. Target screening and optimization of candidate ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12098522/]
- 101. Accurate structure prediction of biomolecular interactions ... [https://www.nature.com/articles/s41586-024-07487-w]
- 102. Validation framework for in vivo digital measures - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC11751004/]
- 103. In Silico Research Is Rewriting the Rules of Drug Development [https://pmc.ncbi.nlm.nih.gov/articles/PMC12070237/]
- 104. Perspectives on Validation of High-Throughput Assays ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3934015/]
- 105. AI approaches for the discovery and validation of drug targets [https://pmc.ncbi.nlm.nih.gov/articles/PMC11383977/]
- 106. Strategies for the drug development of cancer therapeutics [https://pmc.ncbi.nlm.nih.gov/articles/PMC12518319/]
- 107. In Vivo Research Strategies that Reduce Risk of Failure ... [https://www.criver.com/eureka/vivo-research-strategies-reduce-risk-failure-clinic]
- 108. In Vitro Pharmacology, Bioassay Development, and HTS ... [https://www.rti.org/solution/vitro-pharmacology-bioassay-development-and-high-throughput-screening-hts]