Validating Cancer Biomarkers with Real-Time PCR: Protocols, Optimization, and Clinical Translation
This article provides a comprehensive guide for researchers and drug development professionals on implementing real-time quantitative PCR (qPCR) for robust cancer biomarker validation.
Validating Cancer Biomarkers with Real-Time PCR: Protocols, Optimization, and Clinical Translation
Abstract
This article provides a comprehensive guide for researchers and drug development professionals on implementing real-time quantitative PCR (qPCR) for robust cancer biomarker validation. It covers foundational principles, from biomarker definitions and assay design to advanced applications in minimal residual disease (MRD) detection and liquid biopsies. The content delivers actionable methodologies for troubleshooting common pitfalls, optimizing assay performance, and conducting rigorous analytical and clinical validation. A comparative analysis of qPCR against emerging technologies like digital PCR and next-generation sequencing is also presented, offering a complete framework for integrating qPCR into precision oncology workflows.
Laying the Groundwork: Core Principles of Biomarkers and qPCR in Oncology
Defining Predictive and Prognostic Biomarkers in Precision Oncology
Precision oncology represents a paradigm shift in cancer care, moving from a one-size-fits-all approach to tailored therapeutic strategies based on the unique molecular characteristics of individual tumors. Central to this approach are biomarkers—measurable biological indicators that provide critical information about disease state, trajectory, and therapeutic responsiveness. Predictive biomarkers identify patients who are likely to respond to a specific treatment, enabling therapy selection based on molecular profiling. In contrast, prognostic biomarkers provide information about overall clinical outcomes, such as disease recurrence or progression, independent of the therapy received [1]. The clinical implementation of these biomarkers, particularly through molecular techniques like real-time PCR (qPCR), requires rigorous validation to ensure analytical and clinical utility within well-defined contexts of use [2].
The evolving landscape of cancer biomarker research now integrates multiple technological approaches, from genomic and epigenomic analyses to proteomic and multiplexed assays. DNA methylation biomarkers, for instance, have emerged as particularly promising tools due to their stability, cancer-specific patterns, and early emergence in tumorigenesis [3]. Meanwhile, technological advances in digital PCR (dPCR) offer enhanced sensitivity for detecting rare mutations in liquid biopsies, facilitating minimal residual disease monitoring and therapy response assessment [4]. This document provides a comprehensive framework for the validation and application of predictive and prognostic biomarkers within precision oncology, with particular emphasis on protocols for real-time PCR-based biomarker validation in cancer research.
Biomarker Classification and Clinical Applications
Defined Biomarker Categories and Their Clinical Utility
Table 1: Classification and Clinical Utility of Key Cancer Biomarkers
| Biomarker Category | Definition | Primary Clinical Utility | Examples |
|---|---|---|---|
| Predictive | Identifies patients likely to respond to a specific treatment | Guides therapy selection; predicts treatment efficacy or resistance | PD-L1, MSI-H/dMMR, HER2, TMB, NTRK fusions [1] [5] |
| Prognostic | Provides information about cancer outcomes independent of treatment | Informs about natural disease history; assesses recurrence risk | TIMP1 in colorectal cancer, LDH, S100B in melanoma [1] [6] |
| Diagnostic | Confirms the presence or type of cancer | Aids in initial disease identification and classification | DNA methylation patterns in liquid biopsies [3] |
| Pharmacodynamic | Measures biological response to therapeutic intervention | Assesses target engagement and biological activity of treatment | ctDNA dynamics during therapy [1] |
Clinically Validated Predictive Biomarkers
Several predictive biomarkers have achieved clinical validation and are now standard in oncology practice. Programmed Death-Ligand 1 (PD-L1) expression is a key biomarker in non-small cell lung cancer (NSCLC), where patients with PD-L1 expression ≥50% experience significantly improved outcomes with pembrolizumab versus chemotherapy (median overall survival: 30 months versus 14.2 months) [1]. However, limitations exist, including assay variability and tumor heterogeneity, as evidenced by the CheckMate-026 trial where nivolumab failed to show similar survival advantages despite PD-L1 testing [1].
Microsatellite instability-high (MSI-H) and mismatch repair deficiency (dMMR) reflect defects in DNA repair pathways, resulting in high mutational burden and neoantigen formation. The FDA granted tissue-agnostic approval to pembrolizumab in 2017 based on trials showing MSI-H tumors had a 39.6% overall response rate with durable responses in 78% of cases [1]. MSI-H/dMMR testing is now recommended in guidelines by the American Society of Clinical Oncology (ASCO) and National Comprehensive Cancer Network (NCCN) [1].
Tumor mutational burden (TMB), defined as the number of somatic mutations per megabase, reflects neoantigen load and immunogenicity. Pembrolizumab was approved for TMB ≥10 mutations/Mb based on KEYNOTE-158, which showed a 29% objective response rate versus 6% in low-TMB tumors [1]. Gandara et al. reported that TMB ≥20 mutations/Mb was associated with improved survival across cancers (HR: 0.52; 95% CI: 0.47-0.58) [1].
Emerging Biomarker Approaches
Beyond single-analyte biomarkers, multi-omics approaches integrate genomic, transcriptomic, and proteomic data to improve biomarker precision. Bourbonne et al. demonstrated a ~15% improvement in predictive accuracy using multi-omics with machine learning models [1]. Li et al. identified gene clusters associated with durable response to PD-1 blockade [1]. In the Lung-MAP S1400I trial, high CD8⁺GZB⁺ T-cell infiltration predicted better response to nivolumab, while IL-6 and CXCL13 levels were linked to resistance [1].
Machine learning frameworks like MarkerPredict have been developed to identify predictive biomarkers by integrating network motifs and protein disorder features. This tool uses literature evidence-based training sets with Random Forest and XGBoost machine learning models on signaling networks, classifying target-neighbor pairs with 0.7-0.96 leave-one-out-cross-validation accuracy [7]. The resulting Biomarker Probability Score (BPS) helps rank potential predictive biomarkers for targeted cancer therapeutics [7].
Biomarker Validation Framework and Methodologies
Analytical Validation Requirements
The transition of biomarkers from research tools to clinical applications requires rigorous analytical validation. According to consensus guidelines, analytical validation must establish several key performance characteristics [2]:
- Analytical specificity: The ability of a test to distinguish the target from nontarget analytes
- Analytical sensitivity: The ability to detect the analyte, typically defined as the limit of detection (LOD)
- Analytical precision: The closeness of measurements to each other, including repeatability and reproducibility
- Analytical trueness: The closeness of measured values to true values
These validation parameters must be established within a fit-for-purpose framework, where the level of validation is sufficient to support the specific context of use [2]. For clinical research assays, this represents an intermediate level of validation between research use only (RUO) and fully regulated in vitro diagnostics (IVD) [2].
Clinical Validation and Utility Assessment
Beyond analytical performance, biomarkers must demonstrate clinical validity and utility. Clinical sensitivity reflects the true positive rate (correct identification of subjects with the disease), while clinical specificity reflects the true negative rate (correct identification of subjects without disease) [2]. Positive predictive value (PPV) and negative predictive value (NPV) are particularly important for clinical implementation, though these are dependent on disease prevalence [2].
The context of use (COU) elements provide a structured framework for defining a biomarker's utility, including: (1) what aspect of the biomarker is measured and in what form, (2) the clinical purpose of the measurements, and (3) the interpretation and decision/action based on the measurements [2]. For biomarkers supporting clinical decision-making, formal qualification concludes that a biomarker allows specific interpretation and application according to its COU in clinical product development [2].
PCR-Based Methodologies for Biomarker Analysis
Quantitative Real-Time PCR (qRT-PCR)
qRT-PCR remains a cornerstone technology for biomarker validation due to its sensitivity, specificity, and quantitative capabilities. The technique monitors amplification in real-time using fluorescent dyes or target-specific probes, allowing quantification of initial target concentration based on the cycle threshold (Ct) value [8].
Table 2: Essential Reagents for qRT-PCR Biomarker Assay Validation
| Reagent/Category | Specific Examples | Function in Assay | Quality Control Considerations |
|---|---|---|---|
| Nucleic Acid Purification | QIAamp Viral RNA Mini Kit [8] | Isolation of high-quality RNA/DNA from specimens | Yield, purity (A260/280 ratio), integrity (RIN) |
| Reverse Transcription | AgPath-ID one-step RT-PCR reagents [8] | cDNA synthesis from RNA templates | Efficiency, inhibition testing |
| Amplification Master Mix | Applied Biosystems reagents [8] | Provides enzymes, dNTPs, buffers for PCR | Lot-to-lot consistency, reaction efficiency |
| Sequence-Specific Primers | WHO-recommended SARS-CoV-2 primers [8] | Target-specific amplification | Specificity testing, primer-dimer formation |
| Fluorescent Probes | TaqMan probes with ROX reference [8] | Sequence-specific detection, normalization | Probe stability, fluorescence quenching |
| Reference Genes | GAPDH, ACTB, HPRT1 [2] | RNA quality and loading control | Stable expression across sample types |
Digital PCR (dPCR) for Enhanced Sensitivity
Digital PCR represents a significant advancement for detecting rare mutations and analyzing liquid biopsies. dPCR works by partitioning a PCR mixture into thousands of individual reactions, so that each partition contains 0, 1, or a few nucleic acid targets according to a Poisson distribution [4]. Following PCR amplification, the fraction of positive partitions is used to compute the absolute target concentration without need for calibration curves [4].
The BEAMing (Beads, Emulsion, Amplification, and Magnetics) technology, developed by Vogelstein et al., simplified compartmentalization by utilizing water-in-oil droplets to parallelize PCR [4]. This method involves encapsulating individual DNA molecules with magnetic beads coated with primers, permitting PCR amplification within the droplet. Modern dPCR platforms include droplet-based systems (ddPCR) and microchamber-based approaches (QIAcuity, QuantStudio, Digital LightCycler) [4].
dPCR offers particular advantages for liquid biopsy applications, including exceptional sensitivity for detecting rare mutations, absolute quantification without standard curves, and high precision despite low input DNA quantities [4]. These characteristics make it invaluable for monitoring treatment response, detecting minimal residual disease, and analyzing samples with limited tumor DNA content.
DNA Methylation Analysis Techniques
DNA methylation biomarkers are particularly promising for liquid biopsy applications due to their stability, cancer-specific patterns, and early emergence in tumorigenesis [3]. Various methods exist for methylation analysis, each with distinct advantages:
- Whole-genome bisulfite sequencing (WGBS) and reduced representation bisulfite sequencing (RRBS) provide broad methylome coverage through bisulfite-based chemical conversion [3]
- Enzymatic methyl-sequencing (EM-seq) and emerging third-generation sequencing technologies offer comprehensive profiling without chemical conversion, thereby better preserving DNA integrity [3]
- Targeted methods, including quantitative MSP and digital PCR assays, enable highly sensitive, locus-specific analysis ideal for clinical validation studies [3]
The inherent stability of methylated DNA fragments within the cell-free DNA pool, due to nucleosome interactions that protect them from nuclease degradation, makes them particularly suitable for liquid biopsy applications where sample integrity may be variable [3].
Experimental Protocols for Biomarker Validation
Protocol 1: qRT-PCR Assay Validation for RNA Biomarkers
This protocol outlines the validation of a qRT-PCR assay for detecting RNA biomarkers in clinical samples, based on consensus guidelines [2].
Sample Preparation and RNA Extraction
- Sample Collection: Collect samples (blood, tissue, etc.) in appropriate stabilization buffers to preserve RNA integrity. For blood samples, use PAXgene Blood RNA tubes for immediate stabilization.
- RNA Extraction: Isolate total RNA using silica-membrane based purification kits (e.g., QIAamp Viral RNA Mini Kit). Include DNase treatment to remove genomic DNA contamination.
- Quality Assessment: Determine RNA concentration and purity by spectrophotometry (A260/280 ratio ~2.0). Assess RNA integrity using automated electrophoresis (RIN >7 for high-quality samples).
Reverse Transcription
- cDNA Synthesis: Use 100-500 ng total RNA in a 20 μL reaction with reverse transcriptase, random hexamers, and dNTPs. Include no-reverse transcription controls (NRT) to detect genomic DNA contamination.
- Reaction Conditions: Incubate at 25°C for 10 min (primer annealing), 50°C for 30 min (reverse transcription), 85°C for 5 min (enzyme inactivation).
qPCR Assay Validation
- Primer/Probe Design: Design primers and TaqMan probes using bioinformatics tools. Ensure amplicons span exon-exon junctions to avoid genomic DNA amplification.
- Standard Curve Preparation: Create a 5-point, 10-fold serial dilution of synthetic oligonucleotide standards or validated positive control material.
- PCR Amplification: Perform reactions in triplicate using 2X TaqMan Master Mix, primers, probe, and cDNA template. Use the following cycling conditions: 50°C for 2 min, 95°C for 10 min, followed by 40 cycles of 95°C for 15 sec and 60°C for 1 min.
- Validation Parameters:
- Linearity: Assess through standard curve with R² > 0.98
- Amplification Efficiency: Calculate from slope of standard curve (90-110%)
- Limit of Detection (LOD): Determine as the lowest concentration detected in 95% of replicates
- Precision: Evaluate intra-assay and inter-assay CV (<5%)
Protocol 2: DNA Methylation Analysis via Bisulfite Conversion
This protocol describes the detection of DNA methylation biomarkers through bisulfite conversion and qPCR analysis.
Bisulfite Conversion
- DNA Treatment: Treat 500 ng genomic DNA with sodium bisulfite using commercial kits (e.g., EZ DNA Methylation Kit). This converts unmethylated cytosines to uracils while leaving methylated cytosines unchanged.
- Conversion Conditions: Denature DNA (95°C, 30 sec), incubate with conversion reagent (50°C, 12-16 hours), desalt, and desulfonate (room temperature, 15 min).
- Purification: Purify converted DNA using column-based purification and elute in 20 μL elution buffer.
Methylation-Specific PCR
- Primer Design: Design two primer sets—one specific for methylated sequences (binding to CpG-containing sequences after conversion) and one for unmethylated sequences (binding to TpG-containing sequences after conversion).
- PCR Amplification: Set up separate reactions for methylated and unmethylated assays using hot-start DNA polymerase. Include positive controls (fully methylated DNA) and negative controls (unmethylated DNA).
- qPCR Conditions: 95°C for 10 min, 40 cycles of 95°C for 15 sec, specific annealing temperature (optimized for each primer set) for 30 sec, and 72°C for 30 sec.
- Data Analysis: Calculate methylation percentage using the ΔΔCt method or standard curve approach with methylated standards.
Protocol 3: Liquid Biopsy Analysis Using dPCR
This protocol outlines the detection of rare mutations in cell-free DNA from plasma samples using dPCR.
Plasma Processing and DNA Extraction
- Blood Collection: Collect blood in EDTA or Streck Cell-Free DNA BCT tubes. Process within 4 hours of collection.
- Plasma Separation: Centrifuge at 800-1600 × g for 10 min at 4°C. Transfer supernatant to a fresh tube and centrifuge at 16,000 × g for 10 min to remove residual cells.
- cfDNA Extraction: Extract cell-free DNA using silica-membrane kits (e.g., QIAamp Circulating Nucleic Acid Kit). Elute in 20-50 μL elution buffer.
Droplet Digital PCR
- Reaction Setup: Prepare 20 μL reaction mixture containing ddPCR Supermix, target-specific primers/FAM probe, reference primers/HEX probe, and 5-10 μL cfDNA.
- Droplet Generation: Generate droplets using automated droplet generator according to manufacturer's instructions. Typically, 20,000 droplets per sample are generated.
- PCR Amplification: Transfer droplets to 96-well plate and amplify using the following conditions: 95°C for 10 min, 40 cycles of 94°C for 30 sec and 60°C for 1 min, 98°C for 10 min (enzyme deactivation).
- Droplet Reading: Analyze droplets using droplet reader that measures fluorescence in each droplet.
- Data Analysis: Use Poisson statistics to calculate absolute concentration of mutant and wild-type alleles. Report mutant allele frequency as percentage.
Visualizing Biomarker Workflows and Signaling Pathways
Biomarker Development and Validation Workflow
Biomarker Development Pipeline This diagram illustrates the sequential phases from biomarker discovery through clinical implementation, highlighting key transition points requiring rigorous validation.
Predictive Biomarker Signaling Network
Biomarker Signaling Context This network diagram illustrates how predictive biomarkers (blue diamond) function within signaling pathways and relate to molecular drug targets (red octagon).
Clinical Implementation Considerations
Regulatory and Reimbursement Framework
The implementation of biomarker tests in clinical practice requires careful consideration of regulatory and reimbursement frameworks. According to Carelon Medical Benefits Management guidelines, somatic genomic testing is considered medically necessary when several criteria are met [5]:
- The test has established analytical and clinical validity (FDA-approved when available) and is performed in a certified laboratory
- The test has established clinical utility such that results will meaningfully impact clinical management
- There are biomarker-linked therapies approved by the FDA for the specific cancer scenario
- Clinical decision-making incorporates the known impact of genomic alterations on protein function and published efficacy data
For tissue-agnostic testing in metastatic or advanced solid tumors, multi-gene panel testing is medically necessary when specific criteria are satisfied, including the presence of FDA-approved genomic biomarker-linked therapies and lack of satisfactory standard therapies [5]. Approved tissue-agnostic biomarkers include mismatch repair deficiency (dMMR), microsatellite instability (MSI), tumor mutational burden (TMB ≥10 mutations/megabase), and NTRK/RET fusions [5].
Challenges and Future Directions
Despite promising advances, several challenges remain in precision oncology implementation. Currently, only a minority of patients benefit from genomics-guided precision cancer medicine, as many tumors lack actionable mutations and treatment resistance remains common [9]. There is a concerning overemphasis on genomic biomarkers at the expense of other biomarker types, including proteomic, pharmacodynamic, and microenvironmental factors [9].
The field must also address semantic challenges—the distinction between "precision cancer medicine" (more accurately described as "stratified medicine" at present) and true "personalized cancer medicine" which would integrate multiple biomarker layers for truly individualized treatment selection [9]. Future development should incorporate additional biomarker layers, including pharmacokinetics, pharmacogenomics, imaging, histopathology, nutrition, comorbidity, and concomitant medications [9].
Clinical trial design must evolve beyond tumor-agnostic, single-drug approaches to include appropriate controls and more selective patient recruitment based on comprehensive biology. While synthetic controls and real-world data offer promising alternatives, some form of randomized trial design remains necessary to definitively establish clinical benefit [9].
The validation and implementation of predictive and prognostic biomarkers represent a cornerstone of precision oncology. PCR-based methodologies, from qRT-PCR to digital PCR, provide robust platforms for biomarker analysis with the sensitivity and specificity required for clinical application. Successful implementation requires rigorous analytical validation, demonstration of clinical utility, and navigation of regulatory frameworks. Future progress will depend on expanding beyond purely genomic biomarkers to integrate multiple data types, improving clinical trial designs to establish true clinical benefit, and ensuring equitable access to biomarker-guided therapies across diverse patient populations. As these advancements unfold, PCR-based biomarker validation will continue to play an essential role in translating molecular discoveries into improved cancer care.
Quantitative PCR (qPCR) remains a cornerstone technology in the molecular diagnostics pipeline, playing a critical role in the development and validation of cancer biomarkers. Its exceptional sensitivity, specificity, and reproducibility make it indispensable for translating potential biomarker candidates from discovery platforms into clinically applicable assays. In cancer research, qPCR serves as a vital bridge between high-throughput discovery methods like next-generation sequencing (NGS) and routine clinical implementation, enabling researchers to verify biomarker candidates with precise, quantitative measurements across patient cohorts.
The utility of qPCR spans the entire biomarker development workflow. As noted by Dr. Christopher Mason of Weill Cornell Medicine, "We use RNA sequencing extensively... however, qPCR is the most sensitive method we use to validate gene fusion events, expression changes, or isoform variations. I still consider qPCR the high bar for validation" [10]. This endorsement underscores qPCR's established position as the gold standard for confirmation of biomarker candidates identified through discovery-phase omics technologies. The technique's robustness, relatively low cost, and compatibility with various sample types—from tissue specimens to liquid biopsy sources like blood and urine—make it ideally suited for the rigorous validation requirements of clinical translation.
qPCR Across the Biomarker Development Workflow
The Biomarker Development Pipeline
The journey of a biomarker from initial discovery to clinical application follows a structured pathway with distinct stages, each with specific technical requirements and validation milestones. qPCR contributes uniquely to each phase of this pipeline, providing increasing levels of evidence for biomarker analytical and clinical validity.
Table 1: qPCR Applications Across Biomarker Development Stages
| Development Stage | Primary qPCR Application | Key Technical Considerations | Output Metrics |
|---|---|---|---|
| Discovery & Candidate Identification | Verification of candidates from NGS, microarrays, or bioinformatic analyses | High-throughput capability, multi-gene panels, preliminary assay design | Fold-change expression, p-values, differential expression confirmation |
| Assay Development & Optimization | Primer/probe design, reaction condition optimization, controls establishment | Specificity, efficiency, dynamic range, reproducibility | Amplification efficiency, R² values, CV%, LOD, LOQ |
| Analytical Validation | Establishing assay performance characteristics | Sensitivity, specificity, precision, robustness across operators/instruments | AUC, sensitivity %, specificity %, CV% |
| Clinical Validation | Testing in well-defined clinical cohorts | Blinded analysis, standardized protocols, multi-site reproducibility | Clinical sensitivity/specificity, PPV, NPV, odds ratios |
| Clinical Implementation | Deployment in clinical laboratory settings | SOPs, quality control, regulatory compliance | Turnaround time, success rate, clinical utility metrics |
The following workflow diagram illustrates how qPCR integrates into the complete biomarker development pipeline:
Candidate Verification Following Discovery
The initial stage of biomarker development involves identifying potential candidates through high-throughput discovery approaches. Whole transcriptome analysis through RNA sequencing and bioinformatic mining of public datasets represent powerful discovery tools. For example, one study leveraged The Cancer Genome Atlas (TCGA) and Genotype-Tissue Expression (GTEx) databases to identify mRNA biomarkers for colorectal cancer, subsequently validating the top candidates using qPCR [11]. This pattern of using qPCR to verify discoveries is consistent across biomarker types, including DNA methylation markers and various RNA species.
qPCR excels in this verification role due to its quantitative nature, which provides precise measurement of expression differences between case and control samples. When research identified a novel five-gene transcriptomic signature for pancreatic cancer through machine learning analysis of 14 public datasets, qPCR validation in peripheral blood samples confirmed the diagnostic potential with an AUC of 0.83 [12]. This demonstrates qPCR's crucial function in confirming that computationally identified biomarkers show measurable differential expression in clinically relevant samples.
qPCR Experimental Protocols for Biomarker Validation
Standard qPCR Protocol for mRNA Biomarker Validation
This protocol details the validation of mRNA biomarkers from peripheral blood samples, adapted from established methodologies in recent literature [12].
Sample Collection and RNA Extraction
- Collect peripheral blood (5 mL) in EDTA tubes under standardized conditions (early morning, fasting participants)
- Process samples within 2 hours of collection to preserve RNA integrity
- Extract total RNA using TRIzol LS reagent following manufacturer's protocol
- Assess RNA quality and quantity using NanoDrop spectrophotometer and Agilent 2100 Bioanalyzer
- Quality Threshold: Use only samples with RNA integrity number (RIN) >7 for subsequent analysis
cDNA Synthesis
- Use 1 μg of total RNA as input for first-strand cDNA synthesis
- Employ SuperScript III First-Strand Synthesis System with oligo(dT) primers
- Incubate at 65°C for 5 minutes, then place on ice for 1 minute
- Add reaction mix (5X First-Strand Buffer, 0.1 M DTT, RNaseOUT Recombinant RNase Inhibitor, SuperScript III Reverse Transcriptase)
- Incubate at 50°C for 50 minutes, followed by enzyme inactivation at 85°C for 5 minutes
- Dilute cDNA 1:5 with nuclease-free water before qPCR analysis
Quantitative PCR Setup
- Prepare reactions using SYBR Green Master Mix on 96-well or 384-well plates
- Use primer concentrations of 200-400 nM each in final reaction volume of 10-20 μL
- Include triplicate technical replicates for each sample
- Always include no-template controls (NTC) and positive controls
- Thermal Cycling Conditions:
- Initial denaturation: 95°C for 10 minutes
- 40 cycles of:
- Denaturation: 95°C for 15 seconds
- Annealing/Extension: 60°C for 1 minute
- Melt curve analysis: 60°C to 95°C with 0.5°C increments
Data Analysis
- Determine cycle threshold (Ct) values using instrument software
- Normalize target gene expression to reference genes (GAPDH, ACTB, or panel of housekeeping genes)
- Calculate relative expression using the 2-ΔΔCt method
- Perform statistical analysis using appropriate tests (t-tests, ANOVA, ROC analysis)
Advanced Protocol: Folate Ligand-Targeted qPCR for Circulating Tumor Cell Detection
This specialized protocol demonstrates the adaptation of qPCR for detecting folate receptor-positive circulating tumor cells (FR+ CTCs) in gastric cancer, showcasing the technology's versatility [13].
Folate-Oligonucleotide Conjugate Design
- Design a 30-nucleotide sequence with 5' folate moiety conjugation
- Incorporate iSp9 (Triethylene glycol PEG) spacer between folate ligand and oligonucleotide
- Add phosphorothioate bond at 3' end for nuclease resistance
- Purify conjugated probe using High-Performance Liquid Chromatography (HPLC)
Stem-Loop Primer Design
- Design stem-loop RT primer with:
- 5' linear sequence portion (overhung)
- Double-stranded stem region with complementary base pairing
- Single-stranded loop region at 3' end for specific target recognition
- Optimize using RNAfold web server to achieve Gibbs free energy (ΔG) of approximately -23.40 kcal/mol
- Validate through in silico simulations for hybridization capability
CTC Enrichment and Detection
- Enrich CTCs from blood samples by negative depletion of leukocytes
- Label enriched CTCs with folate-oligonucleotide conjugate
- Perform two-step process:
- Step 1: Complementary DNA synthesis when folate-oligonucleotide binds to overhung of stem-loop primer
- Step 2: PCR amplification using forward primer targeting folate oligo and universal reverse primer targeting stem-loop primer
- Optimize annealing temperature for stem-loop primer (40-45°C established as optimal)
Assay Performance Validation
- Establish standard curve using spiked HeLa cells in healthy donor blood
- Validate amplification efficiency (104% achieved in optimized assay)
- Confirm linearity (R² = 0.9970) between Ct values and logarithmic CTC concentrations
- Verify specificity through melt curve analysis and gel electrophoresis
Quantitative Performance Data
qPCR Performance in Validation Studies
Table 2: qPCR Performance Metrics Across Cancer Biomarker Studies
| Cancer Type | Biomarker Class | Sample Type | qPCR Performance | Reference |
|---|---|---|---|---|
| Pancreatic Cancer | 5-gene mRNA signature (LAMC2, TSPAN1, MYO1E, MYOF, SULF1) | Peripheral Blood | AUC: 0.83 (Validation cohort) | [12] |
| Gastric Cancer | Folate receptor-positive CTCs | Blood | Linearity: R² = 0.9970, Efficiency: 104% | [13] |
| Colorectal Cancer | 20-gene mRNA panel | Stool | AUC: 0.94 (CRC), 0.83 (Advanced Adenoma) | [11] |
| Various Cancers | Gene fusions, expression changes | Tissue, Blood | "High bar for validation" vs. NGS | [10] |
| Various Cancers | DNA methylation markers | Liquid Biopsies | High sensitivity after bisulfite conversion | [3] |
Comparison with Alternative Technologies
Table 3: qPCR vs. Other Biomarker Validation Technologies
| Parameter | qPCR | Digital PCR | RNA Sequencing | Microarrays |
|---|---|---|---|---|
| Sensitivity | High (detects <10 copies) | Very High (single molecule) | Moderate | Moderate |
| Throughput | Medium (96-384 wells) | Low-Medium | High | High |
| Cost per Sample | Low | Medium | High | Medium |
| Quantitative Accuracy | High | Very High | Moderate | Moderate |
| Multiplexing Capability | Low-Medium | Low | High | High |
| Ease of Implementation | High | Medium | Low | Medium |
| Best Application | Targeted validation, clinical assays | Rare target detection, absolute quantification | Discovery, novel biomarker identification | Large-scale screening |
The choice between qPCR and digital PCR depends on the specific application requirements. According to Dr. Mason, "We've used both qPCR and digital PCR for MRD. The choice depends on validated panels and known targets. qPCR is favored for its long-standing reliability and general robustness while digital PCR is effective for detecting rarer targets" [10].
The Scientist's Toolkit: Essential Reagents and Materials
Table 4: Essential Research Reagent Solutions for qPCR Biomarker Validation
| Reagent Category | Specific Product Examples | Function & Importance | Quality Control Parameters |
|---|---|---|---|
| RNA Extraction Kits | TRIzol LS, column-based kits | Maintain RNA integrity, remove inhibitors | RNA Integrity Number (RIN) >7, A260/A280 ~2.0 |
| Reverse Transcriptase Kits | SuperScript III, High-Capacity cDNA | Efficient cDNA synthesis, minimal bias | Efficiency >90%, high yield |
| qPCR Master Mixes | SYBR Green, TaqMan assays | Sensitive detection, robust amplification | Efficiency: 90-110%, R² >0.98 |
| Primers/Probes | Custom-designed, validated sequences | Target-specific amplification | Specificity, no primer-dimer |
| Reference Genes | GAPDH, ACTB, 18S rRNA, PPIA | Normalization, data standardization | Stable expression across samples |
| Quality Control Standards | Synthetic oligonucleotides, reference RNA | Inter-assay comparison, QC monitoring | Consistent Ct values, low CV% |
Implementation in Clinical Workflows
qPCR's transition from research tool to clinical application requires careful consideration of several factors. The technique has demonstrated particular utility in minimal residual disease (MRD) monitoring, where its sensitivity enables tracking of mutation levels in patient blood after therapy. As Dr. Mason notes, "qPCR, with its high sensitivity, will fundamentally change how we look at cancer. We will not just treat your cancer; we'll monitor it, look for variations of it, and search for new mutations that arise" [10].
The implementation of qPCR-based tests in clinical settings must address several critical aspects:
Standardization and Reproducibility
- Development of standardized operating procedures (SOPs)
- Implementation of quality control measures across multiple sites
- Establishment of reference materials and calibration standards
- Validation of assay performance in intended-use populations
Regulatory Considerations
- Analytical validation following regulatory guidelines (CLIA, FDA)
- Demonstration of clinical validity and utility
- Documentation of assay reproducibility and reliability
- Establishment of appropriate cut-offs for clinical decision-making
Integration with Clinical Practice
- Determination of clinical scenarios where the test provides actionable information
- Establishment of turnaround times compatible with clinical needs
- Education of clinicians on test interpretation and limitations
- Development of reporting formats that facilitate clinical decision-making
Workflow Visualization: qPCR Experimental Process
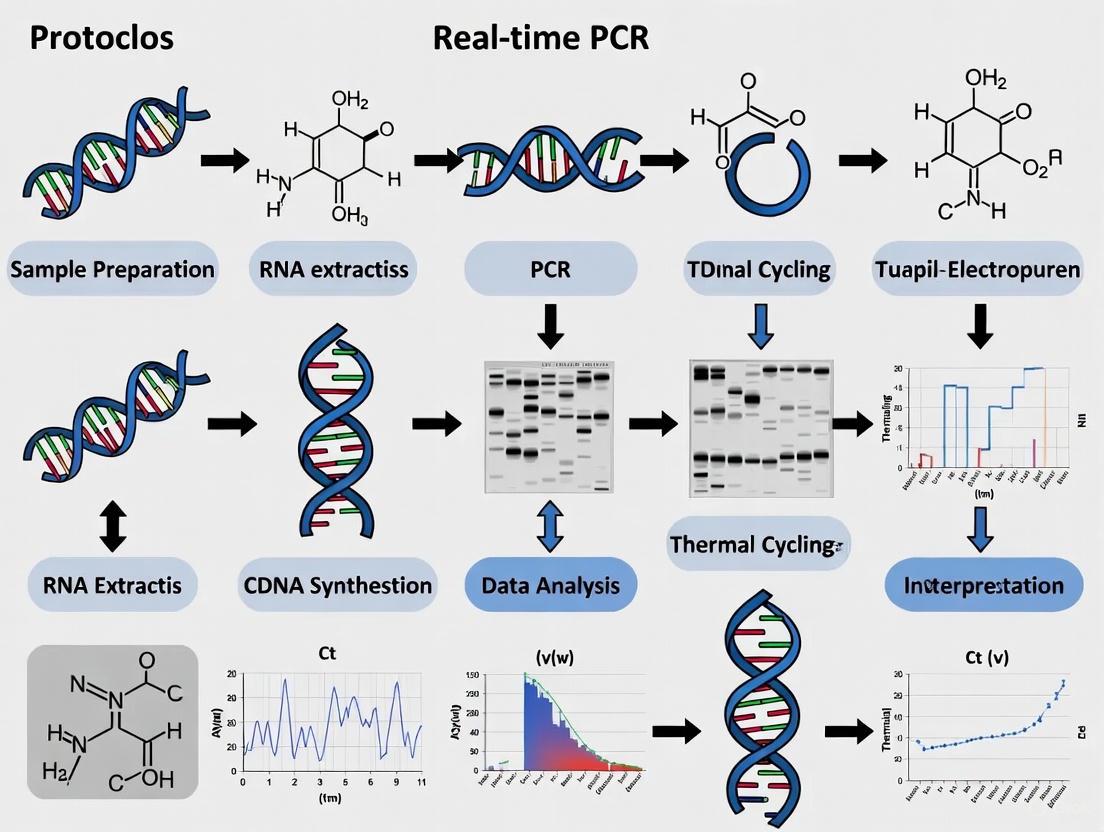
The following diagram illustrates the complete qPCR experimental workflow for biomarker validation, from sample collection to data analysis:
qPCR maintains a fundamental position in the biomarker development pipeline, serving as an essential technology for translating potential biomarker candidates from discovery to clinical application. Its robust quantitative capabilities, sensitivity, and reproducibility make it ideally suited for the rigorous validation requirements of clinical translation. As biomarker research evolves toward liquid biopsy applications and multi-analyte panels, qPCR methodologies continue to adapt, with innovations such as ligand-targeted approaches expanding its utility. While emerging technologies like digital PCR and next-generation sequencing offer complementary capabilities, qPCR remains the workhorse for targeted biomarker validation, striking an optimal balance between performance, practicality, and cost-effectiveness for both research and clinical implementation.
Quantitative real-time PCR (qPCR) is a foundational tool in molecular biology and oncology research, providing the sensitivity, specificity, and broad quantification range necessary for detecting and validating cancer biomarkers [14] [15]. The reliability of qPCR results depends significantly on the choice of detection chemistry, which fundamentally influences assay specificity, sensitivity, and applicability to different research scenarios. In the context of cancer biomarker validation, selecting the appropriate chemistry is critical for accurately identifying genomic alterations, quantifying gene expression changes, and detecting low-frequency mutations in challenging sample types like liquid biopsies [15] [16].
Two primary detection chemistries dominate the qPCR landscape: the DNA-binding dye SYBR Green and sequence-specific fluorogenic probes, most commonly represented by TaqMan chemistry [17]. SYBR Green provides a flexible and cost-effective detection system that binds indiscriminately to double-stranded DNA, while probe-based methods utilize target-specific oligonucleotides with reporter and quencher molecules for highly specific detection [17] [18]. Each approach offers distinct advantages and limitations that researchers must consider when designing experiments for cancer biomarker validation, particularly when working with precious clinical samples where material may be limited and false positives could lead to incorrect conclusions.
This application note provides a comprehensive comparison of these essential qPCR chemistries, detailing their mechanisms, optimal applications, and detailed protocols tailored specifically for cancer research. By understanding the fundamental principles and practical considerations of each system, researchers can make informed decisions that enhance the reliability and translational potential of their biomarker validation workflows.
Core Principles and Mechanisms
SYBR Green Chemistry
SYBR Green-based detection utilizes a fluorescent dye that binds non-specifically to the minor groove of double-stranded DNA (dsDNA) [17] [18]. The mechanism relies on the dramatic fluorescence enhancement that occurs when the dye intercalates with dsDNA—typically a 20- to 100-fold increase in fluorescence compared to the unbound state [18]. This property allows researchers to monitor PCR product accumulation in real time without the need for target-specific probes.
The step-by-step process begins with the free SYBR Green dye present in the reaction mixture exhibiting minimal fluorescence due to its unbound state. As amplification progresses during thermal cycling, the DNA polymerase synthesizes new DNA strands, creating dsDNA products. SYBR Green molecules then bind to these newly formed dsDNA amplicons, resulting in a significant increase in fluorescence intensity that is directly proportional to the amount of PCR product generated [17]. This fluorescence is detected by the qPCR instrument at the end of each amplification cycle, providing the characteristic amplification plot.
A critical requirement for SYBR Green assays is post-amplification melt curve analysis to verify reaction specificity [17]. Since the dye binds to any dsDNA present in the reaction, including non-specific products and primer-dimers, the melt curve analysis serves as an essential quality control step. This analysis involves gradually increasing the temperature after amplification while monitoring fluorescence, resulting in a characteristic dissociation curve where specific amplicons display a distinct melting temperature (Tm) based on their length, GC content, and sequence composition. The presence of a single peak in the melt curve typically indicates a specific amplification product, while multiple peaks suggest non-specific amplification or primer-dimer formation that could compromise quantification accuracy, particularly in cancer biomarker applications where false positives must be avoided.
Probe-Based Chemistry (TaqMan)
Probe-based qPCR chemistry employs target-specific oligonucleotide probes labeled with fluorescent reporter and quencher molecules, with TaqMan being the most widely used format [17]. These probes provide significantly higher specificity than SYBR Green because fluorescence generation requires not only successful amplification but also specific hybridization between the probe and its complementary target sequence [17] [18].
The fundamental mechanism relies on Fluorescence Resonance Energy Transfer (FRET) and the 5'→3' exonuclease activity of Taq DNA polymerase [17] [18]. A typical TaqMan probe consists of an oligonucleotide complementary to the target sequence, with a fluorescent reporter dye attached to the 5' end and a quencher molecule at the 3' end. When the probe is intact, the proximity of the quencher to the reporter dye prevents fluorescence emission through FRET. During the amplification process, when the probe is bound to its target sequence, the advancing Taq DNA polymerase cleaves the probe due to its inherent 5'→3' exonuclease activity. This cleavage separates the reporter dye from the quencher, allowing the reporter to emit fluorescence that is detected by the qPCR instrument [18].
The process occurs during each amplification cycle: first, the forward and reverse primers anneal to their complementary sequences on the denatured DNA template. Next, the TaqMan probe specifically hybridizes to its target sequence between the primer binding sites. As Taq DNA polymerase extends the primer, it eventually reaches and cleaves the bound probe, releasing the reporter dye and generating a fluorescent signal. With each subsequent cycle, additional reporter dye molecules are cleaved from their probes, resulting in a cumulative increase in fluorescence intensity directly proportional to the amount of amplified target [17]. This mechanism ensures that fluorescence is generated only when the specific target sequence is amplified, eliminating signals from non-specific amplification products and providing superior specificity for discriminating closely related sequences—a critical advantage when detecting cancer-associated mutations or single nucleotide polymorphisms (SNPs).
Advanced probe variants include TaqMan MGB (Minor Groove Binder) probes, which incorporate a minor groove binder molecule at the 3' end that increases the probe's melting temperature (Tm) [17]. This allows the use of shorter probes while maintaining high specificity, particularly beneficial for discriminating single-base differences in SNP genotyping and mutation detection assays common in cancer biomarker research [17].
Comparative Analysis: Probe-Based vs. SYBR Green Detection
Selecting the appropriate qPCR chemistry requires careful consideration of multiple performance parameters, cost factors, and application requirements. The following comparative analysis provides a structured framework for decision-making in cancer biomarker validation research.
Table 1: Performance Comparison of SYBR Green vs. Probe-Based qPCR Chemistry
| Parameter | SYBR Green | Probe-Based (TaqMan) |
|---|---|---|
| Specificity | Lower* (Depends on primer specificity and melt curve analysis) | Higher (Requires specific hybridization between probe and target) [17] |
| Sensitivity | Variable* (1-10 copies, depends on template quality and primer design) | High (Consistently detects 1-10 copies) [17] |
| Reproducibility | Medium* (More susceptible to reaction condition variations) | High (Superior consistency across replicates) [17] |
| Multiplexing Capability | No (Single-plex only) | Yes (Simultaneous detection of multiple targets using different reporter dyes) [17] |
| Assay Design & Optimization | Requires extensive primer validation and optimization | Predesigned assays available; minimal optimization required [17] |
| Cost Considerations | Lower setup cost (Only primers required) | Higher setup cost (Probes add significant expense) [17] |
| Primary Applications | Mycoplasma detection, NGS library quantification, telomere length analysis, gene expression with limited targets [17] | Gene expression analysis, miRNA quantification, pathogen detection, copy number variation, SNP genotyping, clinical research [17] |
*Performance highly dependent on template quality and primer design optimization [17].
The specificity advantage of probe-based chemistry stems from its requirement for three specific binding events (forward primer, reverse primer, and probe) compared to only two with SYBR Green, significantly reducing the risk of detecting non-specific amplification products [17]. This is particularly valuable when working with complex samples or closely related gene families. For multiplexing applications, probe-based systems support detection of multiple targets in a single reaction through use of differentially labeled probes, while SYBR Green is limited to single-target detection [17].
From a practical implementation perspective, SYBR Green offers advantages in flexibility and initial cost, as it can be applied to any gene target with appropriately designed primers and requires only standard primer synthesis. Probe-based assays, while more expensive initially, provide predesigned assay options and require less optimization time, potentially offsetting their higher upfront costs in high-throughput settings [17]. For cancer biomarker validation where reproducibility across experiments and laboratories is essential, the superior consistency of probe-based detection often justifies the additional investment.
Applications in Cancer Biomarker Research
SNP Genotyping and Mutation Detection
Probe-based qPCR excels in single nucleotide polymorphism (SNP) genotyping and mutation detection, crucial for identifying cancer-associated genetic variations [18]. The technology enables precise discrimination of single-base differences through allele-specific probes labeled with different fluorescent reporters. For example, a FAM-labeled probe can target the wild-type allele while a VIC-labeled probe targets the mutant allele, allowing simultaneous detection in a single reaction [18].
The assay relies on the principle that Taq DNA polymerase's 5'→3' exonuclease activity requires perfect complementarity at the 3' end of the probe. When a mismatch occurs between the probe and template DNA at the SNP position, hybridization is unstable, preventing probe cleavage and fluorescence emission [18]. This precise discrimination makes probe-based qPCR invaluable for profiling oncogenic mutations in genes like EGFR, KRAS, and BRAF, where treatment decisions depend on accurate mutation identification [15]. Multiplexed qPCR panels can simultaneously assess alterations in multiple clinically relevant genes, delivering results faster and using less input material than sequential testing approaches—a significant advantage when working with limited liquid biopsy samples [15].
Gene Expression Profiling
Both SYBR Green and probe-based chemistries are widely employed in gene expression analysis for cancer biomarker discovery, though with different considerations for assay robustness. Gene expression quantification typically follows the ΔΔCT method or the more efficiency-adjusted Pfaffl method, with normalization to appropriate reference genes [14].
Probe-based assays offer superior specificity for distinguishing between homologous genes or splice variants, which is particularly important when measuring expression of cancer-related gene families with high sequence similarity. The R package "rtpcr" provides comprehensive analysis capabilities for qPCR data, accommodating amplification efficiency values and supporting statistical analysis through t-tests, ANOVA, or ANCOVA depending on experimental design [14]. For clinical validation studies where reproducibility across multiple sites is essential, probe-based assays provide more consistent results due to their reduced susceptibility to reaction condition variations.
DNA Methylation Analysis
Epigenetic alterations, particularly DNA methylation changes, represent promising cancer biomarkers for early detection and prognosis. Probe-based qPCR enables targeted methylation analysis of specific CpG islands using bisulfite-converted DNA [18]. The process involves sodium bisulfite treatment, which converts unmethylated cytosines to uracils while leaving methylated cytosines unchanged, followed by qPCR with primers and probes specifically designed to distinguish methylated from unmethylated sequences [18].
TaqMan probes in methylation assays are designed to complement either the methylated or unmethylated sequence after bisulfite conversion. When the probe perfectly matches the methylated allele, it binds efficiently and generates fluorescence during amplification. Conversely, mismatches with the unconverted unmethylated allele prevent stable hybridization and fluorescence emission [18]. This targeted approach provides a quantitative alternative to genome-wide methylation analysis for validating specific epigenetic biomarkers identified through discovery-phase experiments.
Copy Number Variation (CNA) Analysis
Both chemistries can be applied to copy number variation analysis, which is increasingly recognized as clinically significant in oncology. A 2025 comparative study of real-time PCR and nCounter NanoString techniques for validating copy number alterations in oral cancer demonstrated qPCR's robustness for detecting genomic biomarkers [19]. The study analyzed 24 genes in 119 oral cancer samples and found moderate to substantial agreement between the techniques, with Spearman's rank correlation ranging from r = 0.188 to 0.517 [19].
For CNA analysis, the relative quantification method is typically employed, comparing target gene CT values to a reference gene with known copy number in a diploid genome. Probe-based assays generally provide more reproducible results for copy number determination due to their reduced variability and higher specificity, particularly when analyzing formalin-fixed paraffin-embedded (FFPE) samples where DNA quality may be compromised.
Detailed Experimental Protocols
Protocol 1: SYBR Green-Based Gene Expression Analysis
Principle: This protocol utilizes SYBR Green I dye to detect accumulated double-stranded DNA during PCR amplification, with post-amplification melt curve analysis to verify specificity [17].
Reagents and Materials:
- SYBR Green Master Mix (2× concentration)
- Forward and reverse primers (10 μM working concentration)
- RNA-free DNase/RNase-free water
- cDNA template (diluted to appropriate concentration)
- 96-well or 384-well optical reaction plates
- Optical adhesive seals
Procedure:
- Reaction Setup:
- Prepare master mix on ice: 10 μL SYBR Green Master Mix (2×), 1 μL forward primer (10 μM), 1 μL reverse primer (10 μM), 4 μL nuclease-free water per reaction.
- Aliquot 16 μL master mix into each well of optical plate.
- Add 4 μL cDNA template (20-100 ng total) to each well for final reaction volume of 20 μL.
- Include no-template controls (NTC) replacing cDNA with nuclease-free water.
qPCR Program:
- Stage 1: Enzyme activation - 95°C for 2 minutes (1 cycle)
- Stage 2: Amplification - 95°C for 15 seconds (denaturation) followed by 60°C for 1 minute (annealing/extension) for 40 cycles
- Stage 3: Melt curve analysis - 95°C for 15 seconds, 60°C for 1 minute, then gradual increase to 95°C with continuous fluorescence measurement (0.3°C increments)
Data Analysis:
Troubleshooting Notes:
- Multiple peaks in melt curve indicate primer-dimer formation or non-specific amplification—redesign primers or optimize annealing temperature.
- High NTC signals suggest contamination—prepare fresh reagents and use dedicated workspace.
- Poor efficiency (outside 90-110%) requires primer revalidation or concentration optimization.
Protocol 2: Probe-Based SNP Genotyping
Principle: This protocol uses allele-specific TaqMan probes with different fluorescent reporters to discriminate single nucleotide polymorphisms through differential probe hybridization and cleavage [18].
Reagents and Materials:
- TaqMan Genotyping Master Mix (2×)
- TaqMan SNP Genotyping Assay (20×) containing sequence-specific forward and reverse primers plus two allele-specific probes
- DNA template (5-20 ng/μL)
- Nuclease-free water
- Optical reaction plates and seals
Procedure:
- Reaction Setup:
- Prepare master mix: 5 μL TaqMan Genotyping Master Mix (2×), 0.5 μL TaqMan SNP Genotyping Assay (20×), 2.5 μL nuclease-free water per reaction.
- Aliquot 8 μL master mix into each well.
- Add 2 μL DNA template (10-40 ng total) per well for 10 μL final volume.
- Include positive controls for both homozygous and heterozygous genotypes if available.
qPCR Program:
- Stage 1: Enzyme activation - 95°C for 10 minutes (1 cycle)
- Stage 2: Amplification - 95°C for 15 seconds followed by 60°C for 1 minute for 40-50 cycles
- Note: No melt curve analysis required for probe-based genotyping
Endpoint Genotyping Analysis:
- Use the allelic discrimination plot feature in qPCR analysis software.
- FAM and VIC fluorescence measurements at endpoint define three distinct clusters: homozygous allele 1, homozygous allele 2, and heterozygous.
- Manual threshold setting may be required for optimal cluster separation.
Troubleshooting Notes:
- Poor cluster separation indicates suboptimal probe design or PCR efficiency—try TaqMan MGB probes for better discrimination [17].
- Failed reactions (no amplification) suggest poor DNA quality or inhibitor presence—purify DNA or dilute template.
- Atypical clustering patterns may indicate rare variants or tri-allelic SNPs—confirm by sequencing.
The Scientist's Toolkit: Essential Research Reagent Solutions
Table 2: Essential Reagents and Materials for qPCR Cancer Biomarker Research
| Reagent/Material | Function/Purpose | Application Notes |
|---|---|---|
| SYBR Green Master Mix | Provides DNA polymerase, buffer, dNTPs, and SYBR Green dye for detection | Ideal for initial screening and expression analysis of multiple targets; requires melt curve analysis [17] |
| TaqMan Universal Master Mix | Optimized for probe-based assays; contains AmpliTaq Gold DNA Polymerase, buffers, dNTPs | Delivers robust performance across diverse sample types; compatible with various probe chemistries [17] |
| TaqMan MGB Probes | Minor Groove Binder probes with non-fluorescent quencher for enhanced specificity | Superior SNP discrimination; shorter probe length improves mismatch discrimination [17] |
| Inhibitor-Resistant Polymerases | Engineered enzymes tolerant to PCR inhibitors in clinical samples | Essential for direct analysis of blood, FFPE, and other complex matrices without extensive purification [15] |
| Ambient-Stable Master Mixes | Lyophilized or chemically stabilized ready-to-use formulations | Enables decentralized testing; reduces cold chain dependence for resource-limited settings [15] |
| Multiplex PCR Master Mix | Specialized formulation supporting simultaneous amplification of multiple targets | Required for multi-gene panels; minimizes competition between amplifications [15] |
| Reference Gene Assays | Validated control assays for normalization | Essential for reliable quantification; should be stable across experimental conditions [14] |
Data Analysis and Interpretation
Quantitative Analysis Methods
Accurate data analysis is paramount for reliable cancer biomarker validation. The two primary mathematical approaches for qPCR data analysis are the Livak (2^(-ΔΔCT)) and Pfaffl methods [14]. The Livak method assumes ideal amplification efficiency (100%) for both target and reference genes, while the Pfaffl method incorporates actual amplification efficiencies for more precise quantification, particularly when efficiencies differ from 100% [14].
The Pfaffl method calculates fold change using the formula: FC = [Etarget^(ΔCTtarget)] / [Eref^(ΔCTref)] Where E represents amplification efficiency (typically 1.8-2.0) and ΔCT is the difference in CT values between treatment and control groups [14].
For copy number variation analysis, the comparative CT method (ΔΔCT) is employed relative to a diploid reference gene, with the formula: Copy Number = 2 × 2^(-ΔΔCT)
Statistical analysis of qPCR data typically employs t-tests for two-group comparisons or ANOVA for multi-group experiments, with appropriate multiple testing corrections for high-dimensional biomarker panels [14]. The R package "rtpcr" provides comprehensive analysis capabilities, including calculation of standard errors and confidence intervals according to established methodologies [14].
Quality Control Considerations
Robust quality control measures are essential for reliable biomarker validation:
- Amplification Efficiency: Should fall within 90-110% (3.6 > slope > 3.1) for reliable quantification.
- Standard Curves: Required for absolute quantification; R² > 0.98 indicates linearity.
- Replicate Consistency: Technical replicates should show minimal variation (CT standard deviation < 0.3 cycles).
- Reference Gene Stability: Must be validated across experimental conditions using algorithms like geNorm or NormFinder.
- NTC Monitoring: Should show no amplification or significantly delayed amplification (CT values > 5 cycles than sample wells).
Automated analysis tools like Auto-qPCR can streamline data processing, providing standardized workflows for amplification efficiency calculation, normalization, and statistical analysis while minimizing manual intervention errors [20].
The selection between SYBR Green and probe-based qPCR chemistries represents a critical methodological decision in cancer biomarker validation research. SYBR Green offers flexibility and cost-effectiveness for applications with lower specificity demands, while probe-based systems provide superior specificity, reproducibility, and multiplexing capabilities essential for clinical translation.
In oncology applications, probe-based qPCR continues to demonstrate particular value for its ability to detect clinically actionable biomarkers at low concentrations, support broader mutational profiling, and deliver rapid results in time-sensitive clinical scenarios [15]. The technology's compatibility with standardized formats, automation-friendly workflows, and established regulatory frameworks further enhances its utility in both research and clinical settings.
As cancer diagnostics evolve toward earlier detection, molecular stratification, and personalized therapy, both chemistries will maintain important roles in the biomarker validation pipeline. Understanding their complementary strengths and limitations enables researchers to implement the most appropriate detection system for their specific application, ultimately advancing more effective cancer diagnostics and therapeutic monitoring tools.
Cancer biomarkers are biological molecules, genes, or characteristics that provide crucial information about the presence, behavior, and potential treatment of cancer. These biomarkers encompass a broad category that includes genes, gene mutations, proteins, or other substances that can be measured in blood, tumor tissue, or other body fluids [21]. They serve as objective indicators of the molecular characteristics of cancer, enabling early diagnosis, prognosis prediction, treatment selection, and monitoring of disease recurrence [22]. The evolution from traditional tumor markers to sophisticated molecular biomarkers represents a fundamental shift in oncology, moving away from one-size-fits-all treatments toward precision medicine approaches tailored to the individual molecular profile of each patient's cancer [21] [23].
The clinical utility of biomarkers spans the entire cancer care continuum, from risk assessment and early detection to monitoring treatment response and guiding survivorship care [23]. Biomarker testing can be used at many stages—diagnosis, treatment, monitoring response, and survivorship—making it a dynamic process essential throughout the patient journey [23]. Progress in improving cancer outcomes increasingly involves precision medicine, with biomarker testing serving as a critical gateway to accessing targeted therapies that can lead to improved survivorship and better quality of life [24].
Classes of Molecular Biomarkers
Genetic Biomarkers
Genetic biomarkers consist of specific mutations, rearrangements, or variations in the DNA sequence that drive oncogenesis or influence treatment response. These include somatic mutations acquired in tumor cells and germline mutations inherited through familial lines. Key examples include EGFR mutations in non-small cell lung cancer, BRCA1/2 mutations in ovarian, breast, pancreatic, and prostate cancers, and the BCR-ABL fusion gene in leukemia and lymphomas [22] [21]. These biomarkers provide critical information for diagnosis, prognostication, treatment determination, and response monitoring [22].
Next-generation sequencing (NGS) technologies have revolutionized the detection of genetic biomarkers, allowing clinicians to sequence a tumor's DNA and identify targetable mutations [21]. As one oncology expert explained, "Checking the genetic signatures and profiling with next-generation sequencing tells you what type of mutations are present in the tumor. This is essential to determine what treatment options are unique to the tumor" [21]. This molecular profiling enables the matching of patients with precision therapies most likely to work for their specific disease, moving beyond the indiscriminate approach of traditional chemotherapy [21] [23].
Epigenetic Biomarkers
Epigenetic biomarkers involve modifications that regulate gene expression without altering the underlying DNA sequence, with DNA methylation being the most extensively studied. DNA methylation refers to the addition of a methyl group to the 5' position of cytosine, typically at CpG dinucleotides, resulting in 5-methylcytosine [3]. In cancer, DNA methylation patterns are frequently altered, with tumors typically displaying both genome-wide hypomethylation and hypermethylation of CpG-rich gene promoters [3]. Promoter hypermethylation of key tumor suppressor genes is commonly associated with gene silencing, while global hypomethylation can induce chromosomal instability, collectively disrupting normal growth pathways and driving malignant transformation [3].
The clinical appeal of DNA methylation biomarkers stems from several unique properties: these alterations often emerge early in tumorigenesis and remain stable throughout tumor evolution, making them ideal for early detection [3]. The inherent stability of DNA methylation patterns and the relative enrichment of methylated DNA fragments within the cell-free DNA pool also enhance their detectability in liquid biopsies [3]. Research presented at the Molecular Analysis for Precision Oncology Congress 2025 highlights how epigenetic changes represent critical events in cancer initiation, and molecular interrogation techniques combined with machine learning can harness this epigenetic information to enhance diagnosis and patient care [25].
Transcriptomic Biomarkers
Transcriptomic biomarkers encompass changes in RNA expression patterns, alternative splicing events, and non-coding RNAs that reflect the functional state of cancer cells. These biomarkers provide a dynamic view of gene expression activity, capturing the molecular mechanisms driving cancer progression. Recent advances in transcriptomic analysis have revealed robust cancer- and subtype-specific alternative splicing biomarkers that serve as critical regulators in cancer progression [26].
In lung cancer, for example, comprehensive transcriptomic analysis has identified alternative splicing biomarkers that are consistently effective in both tissue samples and cancer cell lines [26]. Regulatory network analysis has revealed RNA-binding proteins such as QKI and SR proteins as key splicing factors, with QKI modulating the splicing of PLEKHA1 exon 15 and SRSF1 regulating the splicing of MKNK2 exon 14 [26]. These splicing events represent potential therapeutic targets and diagnostic tools, providing valuable insights into the key alternative splicing events and their regulatory mechanisms in cancer [26].
Table 1: Major Biomarker Classes and Their Characteristics
| Biomarker Class | Molecular Basis | Key Technologies for Detection | Clinical Applications |
|---|---|---|---|
| Genetic | DNA sequence variations (mutations, rearrangements, copy number changes) | Next-generation sequencing, PCR, FISH | Diagnosis, prognosis, treatment selection, monitoring |
| Epigenetic | DNA methylation, histone modifications, chromatin remodeling | Bisulfite sequencing, methylation arrays, EM-seq | Early detection, prognosis, monitoring, screening |
| Transcriptomic | Gene expression patterns, alternative splicing, non-coding RNAs | RNA sequencing, microarrays, qRT-PCR | Subtyping, prognosis, therapeutic targeting |
Current Applications in Cancer Management
Diagnostic and Early Detection Applications
The application of biomarkers for early cancer detection represents one of the most promising areas in oncology, with the potential to significantly improve patient outcomes by enabling intervention when treatments are most effective. Early detection aims to identify carcinogenic changes at the earliest stage, when therapeutic intervention can result in improved survival rates and reduced morbidity [22]. Studies have demonstrated that early detection leads to a median overall survival of 38 months compared to 14 months with delayed diagnosis, while also improving quality of life scores from 55 to 75 and reducing severe treatment-related side effects from 18 to 45% [22].
Liquid biopsies have emerged as a particularly promising approach for early detection, offering a minimally invasive source for detecting a broad range of cancer biomarkers [3] [22]. These tests analyze tumor material shed into body fluids, including circulating tumor DNA (ctDNA), circulating tumor cells (CTCs), and exosomes [3]. Compared to tissue biopsies, liquid biopsies reflect the entire tumor burden and molecular cancer heterogeneity, are less invasive, and enable repeated sampling for monitoring treatment response and cancer progression [3]. DNA methylation biomarkers in liquid biopsies offer special advantages for early detection because methylation alterations often emerge early in tumorigenesis and remain stable throughout tumor evolution [3].
Prognostic and Predictive Applications
Beyond detection, biomarkers play crucial roles in predicting disease course and treatment response. Prognostic biomarkers provide information about the likely natural history of the cancer, while predictive biomarkers help identify patients who are most likely to respond to specific treatments. For example, in colorectal cancer, a robust five-gene prognostic signature (TIMP1, PCOLCE2, MEIS2, HDC, CXCL13) has been established through bioinformatics analysis and experimental validation [6]. High expression of TIMP1 in this signature is associated with poor prognosis, and functional experiments demonstrated that TIMP1 knockdown significantly inhibited CRC cell proliferation, metastasis, and promoted apoptosis [6].
The evolution of biomarker testing is reflected in the changing landscape of cancer care. As one breast cancer survivor diagnosed in 1994 noted, "Back then, all you got was ER and PR—HER2 hadn't been discovered yet. There wasn't even an internet when I was diagnosed" [21]. Thirty years later, patients need to understand the subtype of their cancer and their biomarker profile to access appropriate targeted drugs [21]. This shift toward precision oncology means that testing for biomarkers allows clinicians to match patients with precision therapies most likely to work for their specific disease [23].
Emerging Applications and Technologies
Innovative approaches are expanding the applications of biomarkers in clinical oncology. Machine learning and artificial intelligence are being applied to analyze complex biomarker data, enhancing predictive accuracy and enabling the integration of multiple data types for improved clinical decision-making [27]. For example, one study used nine different machine learning algorithms to analyze the relationship between 30 epigenetic biomarkers and the risk of diabetes and cancer, finding that epigenetic age acceleration was strongly associated with cancer risk [27].
Single-cell analyses are also providing unprecedented insights into tumor heterogeneity and microenvironment interactions. In high-grade serous ovarian cancer (HGSOC), characterized by significant intra-tumor heterogeneity, single-cell RNA-sequencing and single-cell epigenomics have identified 13 recurrent tumor transcriptomic phenotypes from over 200,000 malignant cells [25]. Longitudinal analyses revealed that chemotherapy enriched for cells possessing mesenchymal and inflammatory features while reducing cells displaying proliferative, hypoxic, and interferon-associated states [25]. Such detailed characterization of tumor heterogeneity represents a step toward personalized therapy for these patients.
Table 2: Clinically Validated Biomarkers Across Cancer Types
| Cancer Type | Validated Genetic Biomarkers | Validated Epigenetic Biomarkers | Associated Targeted Therapies |
|---|---|---|---|
| Colorectal Cancer | KRAS, NRAS, BRAF mutations, MSI-H | MLH1 promoter hypermethylation | Anti-EGFR therapies, Immune checkpoint inhibitors |
| Breast Cancer | BRCA1/2, HER2, PIK3CA mutations | - | PARP inhibitors, HER2-targeted therapies |
| Lung Cancer | EGFR, ALK, ROS1, BRAF mutations | - | EGFR inhibitors, ALK/ROS1 inhibitors |
| Leukemia/Lymphoma | BCR-ABL fusion gene | - | Tyrosine kinase inhibitors |
Experimental Protocols for Biomarker Analysis
Bioinformatics Workflow for Biomarker Discovery
The identification of novel biomarker signatures typically begins with comprehensive bioinformatics analysis of multi-omics data. A standard workflow for biomarker discovery involves several key stages, starting with data acquisition from public repositories such as The Cancer Genome Atlas (TCGA) and Gene Expression Omnibus (GEO) [6]. Differential expression analysis is performed using tools like the "DESeq2" package in R to identify genes that are significantly upregulated or downregulated in cancer tissues compared to normal controls [6].
Weighted gene co-expression network analysis (WGCNA) can then be applied to identify gene modules with comparable expression patterns and examine the relationship between these modules and specific clinical traits [6]. The "WGCNA" R package is used to construct a gene co-expression network, with a minimum number of genes per module typically set at 30 [6]. Functional enrichment analysis using Gene Ontology (GO) and Kyoto Encyclopedia of Genes and Genomes (KEGG) pathways helps identify biological processes and signaling pathways significantly associated with the candidate biomarker genes [6]. Protein-protein interaction (PPI) networks can be constructed using the STRING database and visualized in Cytoscape to identify hub genes within the biomarker network [6].
Diagram Title: Bioinformatics Biomarker Discovery Workflow
DNA Methylation Analysis Protocol
The analysis of DNA methylation biomarkers involves specific methodological considerations due to the chemical nature of this epigenetic modification. Various methods exist for DNA methylation analysis, broadly categorized into genome-wide discovery approaches and targeted validation methods [3]. Whole-genome bisulfite sequencing (WGBS) and reduced representation bisulfite sequencing (RRBS) are widely used for biomarker discovery, providing broad methylome coverage through bisulfite-based chemical conversion that converts unmethylated cytosines to uracils while leaving methylated cytosines unchanged [3].
Enzymatic methyl-sequencing (EM-seq), along with emerging third-generation sequencing technologies such as nanopore and single-molecule real-time sequencing, offers comprehensive methylation profiling without chemical conversion, thereby better preserving DNA integrity [3]. This is particularly advantageous for liquid biopsy analyses where DNA quantity is often limited. For clinical validation, targeted methods such as quantitative real-time PCR (qPCR) and digital PCR (dPCR) offer highly sensitive, locus-specific analysis, making them suitable for routine clinical use [3]. The selection of appropriate control groups and sufficient independent validation in large-scale clinical studies are critical factors for successful clinical translation of DNA methylation biomarkers [3].
Transcriptomic Analysis of Alternative Splicing
The identification of alternative splicing biomarkers requires specialized transcriptomic approaches. A standard protocol begins with RNA sequencing of patient samples and cancer cell lines, followed by comprehensive analysis of the transcriptomic landscape with a focus on alternative splicing events [26]. Bioinformatics tools are used to identify robust cancer- and subtype-specific alternative splicing biomarkers that are consistently effective across different sample types [26].
Regulatory network analysis with a focus on RNA-binding proteins can reveal key splicing factors such as QKI and SR proteins that modulate specific splicing events [26]. For example, studies have shown that QKI modulates the splicing of PLEKHA1 exon 15, a cancer-specific alternative splicing biomarker, while SRSF1 regulates the splicing of MKNK2 exon 14, a subtype-specific biomarker [26]. Experimental validation of these regulatory relationships typically involves modulation of the identified RNA-binding proteins (overexpression or knockdown) followed by analysis of the resulting splicing changes using RT-PCR or nanoscale liquid chromatography coupled to tandem mass spectrometry.
Research Reagent Solutions
The experimental workflows described require specialized reagents and kits optimized for specific applications. The following table outlines essential research reagent solutions for biomarker discovery and validation studies.
Table 3: Essential Research Reagents for Biomarker Studies
| Reagent Category | Specific Products/Kits | Application Note | Key Considerations |
|---|---|---|---|
| Nucleic Acid Extraction | Plasma cfDNA extraction kits, FFPE RNA extraction kits | Maintain integrity of degraded samples from liquid biopsies or archived tissues | For cfDNA: optimize for fragment length <200bp; For FFPE: include DNase/RNase treatment |
| Bisulfite Conversion | EZ DNA Methylation kits, Premium Bisulfite kits | Complete conversion of unmethylated cytosine to uracil | DNA damage minimization; conversion efficiency validation with controls |
| Library Preparation | TruSeq Methyl Capture EPIC, SMARTer Stranded RNA-Seq | Target enrichment for methylation or transcriptome | Input amount requirements; compatibility with downstream sequencing platforms |
| qPCR/dPCR Reagents | ddPCR Mutation Detection assays, MethyLight reagents | Absolute quantification of rare variants or methylation | Probe design for CpG sites; optimization of annealing temperatures |
| Antibodies | Anti-5-methylcytosine, Histone modification-specific antibodies | Immunoprecipitation-based enrichment | Specificity validation; application in MeDIP-seq or ChIP-seq protocols |
Regulatory and Implementation Considerations
The successful translation of biomarkers from research discoveries to clinical applications requires careful attention to regulatory and implementation challenges. Despite the identification of numerous potential biomarkers in research settings, only a limited number have achieved routine clinical adoption [3]. Searching PubMed with the MeSH terms "Biomarkers" and "DNA Methylation" together with "cancer" returns 6,191 publications since 1996, yet this vast amount of research is not reflected in the number of DNA methylation biomarkers in clinical use [3].
Several factors affect the successful clinical implementation of biomarkers, including the choice of liquid biopsy source, selection of appropriate control groups in both discovery and validation phases, sufficient independent validation, and large-scale clinical studies to demonstrate clinical utility [3]. The variability in overall cell-free DNA among patients with the same cancer type is often larger than the variability between different cancer types, while the fraction of circulating tumor DNA tends to differ more consistently between cancer types and stages—a crucial consideration for diagnostic sensitivity, particularly in early-stage disease [3].
Efforts to expand access to biomarker testing are underway through policy initiatives and educational programs. The American Cancer Society Cancer Action Network (ACS CAN) is working to expand insurance coverage of comprehensive biomarker testing, with biomarker testing coverage for state-regulated plans already established in multiple states including Arizona, California, New York, and Texas [24]. Educational initiatives like the Maine Cancer Genomics Initiative (MCGI) are working to bridge knowledge gaps by teaching healthcare providers how to interpret genomic testing and use cancer biomarkers to guide treatment, ensuring that precision oncology treatments aren't limited to major research hospitals [23]. Studies have shown that patients who receive genome-matched treatment based on biomarker testing are 31% less likely to die within one year compared to those who do not receive matched treatment [23].
The field of cancer biomarkers has evolved dramatically from simple protein-based tests to sophisticated multi-omics approaches that integrate genetic, epigenetic, and transcriptomic information. This evolution has transformed cancer care, enabling more precise diagnosis, prognosis, and treatment selection. The optimal selection of molecular targets requires careful consideration of the biological context, technological capabilities, and clinical utility, with validation workflows that progress from bioinformatics discovery to experimental verification and clinical correlation.
As the field advances, several key trends are shaping the future of cancer biomarkers: the increasing use of liquid biopsies for minimally invasive monitoring, the integration of multi-omics data through advanced computational approaches, the development of complex biomarker signatures rather than single biomarkers, and the implementation of educational initiatives to ensure equitable access to precision oncology [23]. While significant challenges remain in standardizing methodologies, demonstrating clinical utility, and expanding access, the continued refinement of biomarkers promises to further personalize cancer care and improve outcomes for patients across the cancer journey.
From Theory to Practice: Implementing qPCR Assays for Cancer Biomarkers
Circulating tumor DNA (ctDNA), a subset of cell-free DNA (cfDNA) released into the bloodstream by apoptotic and necrotic tumor cells, has emerged as a transformative, minimally invasive biomarker in oncology [28] [29]. Its clinical applications span early diagnosis, therapeutic target identification, treatment response monitoring, prognosis evaluation, and minimal residual disease (MRD) detection [28]. The successful validation of ctDNA-based biomarkers for real-time PCR and other downstream analyses is critically dependent on the integrity of the pre-analytical phase [30]. This document provides detailed, standardized protocols for the collection, processing, and storage of blood, tissue, and ctDNA samples, framed within the context of cancer biomarker validation research.
Pre-Analytical Procedures for Blood Collection and Plasma Preparation
The reliability of ctDNA analysis is profoundly influenced by pre-analytical variables. Standardized protocols are essential to prevent the introduction of biases that can lead to false-negative results or inaccurate quantification [28].
Timing of Blood Sampling
The timing of blood collection is crucial and should be strategically aligned with the clinical objective of the ctDNA test [28].
- For Molecular Alteration Identification: Blood should be collected before surgery, initiation of radiotherapy, or a new line of chemotherapy to baseline the tumor's genomic landscape [28].
- For Monitoring Minimal Residual Disease (MRD): Blood collection should not be performed immediately after treatment. Tissue injury from surgery or chemotherapy can increase background cfDNA levels, potentially diluting the ctDNA fraction below the assay's limit of detection. It is recommended to wait at least 1–2 weeks after surgery before sampling for MRD analysis [28].
Blood Collection, Transport, and Storage
The choice of collection tubes and handling conditions directly impacts cfDNA quality and quantity.
Table 1: Comparison of Blood Collection Tubes for ctDNA Analysis
| Tube Type | Anticoagulant | Maximum Time to Plasma Separation | Storage Temperature Before Processing | Key Considerations |
|---|---|---|---|---|
| K2/K3 EDTA | K2- or K3-EDTA | 4-6 hours [28] | Room temperature (18–25°C) or 4°C [28] | Plasma separation must be prompt to prevent leukocyte lysis and contamination from genomic DNA [28]. |
| Cell Stabilization Tubes | Proprietary additives | 5-7 days [28] | Room temperature (18–25°C) [28] | Extends processing window; must be inverted 8-10 times post-collection and handled per manufacturer's instructions [28]. |
- Optimal Sample Type: Plasma is recommended over serum for ctDNA analysis. The clotting process during serum preparation causes leukocyte degradation, releasing genomic DNA and thereby diluting the ctDNA fraction and reducing detection sensitivity [28].
- Blood Volume: The input plasma volume is directly proportional to the quantity of obtained cfDNA, which correlates with assay sensitivity. For high-sensitivity applications like MRD detection, drawing additional blood tubes is recommended to increase the plasma yield [28].
- Blood Transport: During transport, avoid agitation and extreme temperature fluctuations to prevent hemolysis and cellular damage [28].
Plasma Preparation and Quality Control
A two-step centrifugation protocol is critical to obtain cell-free plasma and remove residual cells and debris.
- Centrifugation Protocol for EDTA Tubes:
- First Spin: 800–1,600×g at 4°C for 10 minutes. This step separates plasma from blood cells. When transferring the supernatant, caution must be taken to avoid disturbing the buffy coat layer [28].
- Second Spin: 14,000–16,000×g at 4°C for 10 minutes. This high-speed centrifugation removes any remaining cells and platelets [28].
- Plasma Quality Control (QC): Visually inspect the plasma after separation. Red or orange coloring indicates hemolysis, which can interfere with analysis. Icteric (yellow-green) or opaque/lipemic plasma may yield lower cfDNA concentrations [28].
- Plasma Storage: To minimize nuclease activity and cfDNA degradation, extract DNA immediately after plasma separation. For short-term storage (up to 3 hours), plasma can be held at 4°C. For longer storage, freeze at -20°C. For long-term storage, plasma should be stored at -80°C [28].
The following workflow summarizes the key steps from blood draw to ctDNA analysis:
The Scientist's Toolkit: Essential Research Reagent Solutions
The following table details key reagents and materials required for experiments involving ctDNA analysis and cancer biomarker validation.
Table 2: Essential Research Reagent Solutions for ctDNA and Biomarker Research
| Reagent/Material | Function/Application | Key Considerations |
|---|---|---|
| Cell-Free DNA Blood Collection Tubes | Stabilizes nucleated blood cells for up to 7 days, preventing genomic DNA contamination [28]. | Essential for multi-center trials; allows for ambient temperature transport. |
| Nucleic Acid Extraction Kits | Isolate high-purity cfDNA/ctDNA from plasma samples. | Select kits optimized for short-fragment cfDNA to maximize yield. |
| PCR Master Mixes | Provide enzymes, dNTPs, and buffers for qPCR/dPCR amplification [31] [10]. | Includes hot-start Taq polymerases for specificity; choose mixes compatible with hydrolysis probes. |
| Sequence-Specific Primers & Probes | Enable specific amplification and detection of target mutations (e.g., in KRAS, EGFR, PIK3CA) [29]. | Meticulous in silico design and validation are required to avoid off-target amplification. |
| Reference Gene Assays | Amplify constitutively expressed genes (e.g., GAPDH) for data normalization in qPCR [10]. | Stability of reference genes must be verified across the sample set, as expression can vary [10]. |
| Digital PCR Reagents & Chips | Facilitate absolute quantification of target molecules by partitioning a sample into thousands of reactions [31]. | Includes droplet generator oil, supermixes, and microchamber chips for platforms like QIAcuity. |
Integration with PCR-Based Biomarker Validation
The pre-analytical protocols described above are foundational for robust biomarker validation using PCR technologies.
- Biomarker Workflow: The process begins with biomarker discovery, often using high-throughput sequencing, followed by assay development and analytical validation before clinical implementation [30] [32]. Careful study design and avoidance of "samples of convenience" are critical to successful translation [30].
- qPCR and dPCR in Validation: Quantitative PCR (qPCR) is widely regarded as a high-sensitivity method for validating gene fusions, expression changes, and mutations identified through next-generation sequencing (NGS) [10]. Digital PCR (dPCR), the third generation of PCR technology, offers absolute quantification without a standard curve and excels in detecting rare mutations, making it ideal for applications like MRD monitoring and liquid biopsy [31] [29].
- Application in MRD and Treatment Monitoring: The high sensitivity of qPCR and dPCR allows for tracking specific mutations (e.g., EGFR) in a patient's blood over time. A decrease in mutant allele concentration indicates treatment response, while its re-emergence can signal recurrence, enabling therapy adjustments [10]. The choice between qPCR and dPCR often depends on the availability of validated assays and the required sensitivity for the specific clinical question [10].
Standardized protocols for sample processing are not merely procedural guidelines but are fundamental to the integrity and success of cancer biomarker validation research. The meticulous attention to detail in the timing of blood draws, the selection of appropriate collection tubes, adherence to centrifugation protocols, and proper sample storage directly influences the quality of the extracted ctDNA and the reliability of subsequent real-time PCR analyses. By implementing these detailed application notes and protocols, researchers and drug development professionals can ensure the generation of robust, reproducible, and clinically meaningful data, thereby accelerating the translation of ctDNA biomarkers into precision oncology tools.
The detection of patient-specific genetic targets represents a cornerstone of precision medicine, enabling applications from minimal residual disease (MRD) monitoring in leukemia to liquid biopsy analysis in solid tumors. Achieving maximum specificity in these assays is paramount, as they must distinguish minute quantities of target sequences amidst a vast excess of wild-type genetic material. This protocol details the systematic design and validation of primer and probe systems for patient-specific real-time PCR assays, framed within the broader context of cancer biomarker validation research. We focus specifically on allele-specific oligonucleotide (ASO) real-time quantitative PCR (RQ-PCR) methodologies that target clonally rearranged immune genes or somatic mutations, providing a framework that balances analytical sensitivity with practical implementability across diverse laboratory settings.
Core Principles of Patient-Specific Assay Design
Fundamental Design Challenges
Patient-specific assays face unique challenges not encountered in conventional PCR design. Each assay requires custom-designed reagents tailored to individual genetic fingerprints, precluding batch validation approaches. The primary targets—such as immunoglobulin (IG) and T-cell receptor (TR) gene junctional regions or cancer-specific mutations—exist within complex genetic backgrounds and often at exceptionally low abundances (10⁻⁴ to 10⁻⁶) in clinical samples [33]. This demands exceptional specificity to avoid false positives from non-specific amplification.
Design considerations must account for the sequence context surrounding the patient-specific region. For rearrangement-based targets, this includes flanking conserved gene segments. For mutation-based targets, the wild-type sequence presents the primary challenge for discrimination. Both scenarios require strategic primer placement and stringent validation of specificity [34] [33].
Genomic Location and Target Selection
The genomic location of primer and probe binding sites critically influences assay performance. Suboptimal genomic placement can dramatically reduce clinical utility, as evidenced by studies of DNA methylation biomarkers where assay location variability hindered inter-study comparability [34]. For patient-specific mutation detection, primers should span the mutation site at the 3' end to enable allele-specific amplification, with careful consideration of the local sequence composition to minimize secondary structure formation.
Table 1: Technical Considerations for Target Region Selection
| Consideration | Impact on Specificity | Validation Approach |
|---|---|---|
| Sequence Uniqueness | Ensures amplification is specific to the intended target | BLAST analysis against relevant genomes [35] |
| Flanking Sequence Conservation | Affects primer binding efficiency in multiplex arrangements | Melting temperature (Tm) consistency analysis |
| Local GC Content | Influences secondary structure and primer annealing | Thermodynamic modeling using SantaLucia parameters [35] |
| Variant Allele Frequency | Determines required detection sensitivity | Dilution studies with synthetic controls |
Experimental Protocols
Primer and Probe Design Workflow
The following protocol outlines a systematic approach for designing patient-specific primers and probes, with an emphasis on achieving maximum specificity.
Input Sequence Preparation and Analysis
- Step 1: Obtain the patient-specific target sequence (e.g., CDR3 region from IG/TR sequencing or mutant allele sequence from tumor profiling).
- Step 2: Identify the patient-specific junction or mutation site as the core of the assay target.
- Step 3: Extract 150-200 base pairs of flanking sequence on each side of the specific region to accommodate primer placement.
- Step 4: Analyze the sequence for GC content, secondary structures, and repetitive elements using tools like NCBI's Primer-BLAST [35].
Allele-Specific Primer Design
- Step 5: Design the forward allele-specific primer with the 3' terminal base complementary to the patient-specific nucleotide. For rearrangement targets, position the 3' end within the junctional region.
- Step 6: Incorporate deliberate mismatches at the second or third position from the 3' end to enhance discriminatory power against similar sequences.
- Step 7: Design the reverse primer to bind to a conserved region 80-150 bp downstream from the forward primer site.
- Step 8: Maintain primer lengths of 18-25 nucleotides with Tm values of 58-62°C, with a maximum 2°C difference between forward and reverse primers.
Probe Selection and Design
- Step 9: Design hydrolysis probes (e.g., TaqMan) to bind immediately adjacent to the patient-specific region, with the 5' end located 1-3 bases away from the discriminatory primer site.
- Step 10: Select a probe Tm 8-10°C higher than the primer Tm to ensure probe hybridization prior to primer extension.
- Step 11: Avoid G at the 5' end of the probe, and keep probe length between 20-30 nucleotides.
- Step 12: Incorporate appropriate fluorophore-quencher pairs based on available detection channels and multiplexing requirements.
In Silico Specificity Validation
Before laboratory testing, comprehensive computational validation is essential:
- Step 13: Use Primer-BLAST with the following parameters [35]:
- Database: RefSeq mRNA or genome of target species
- Specificity check: Enabled with organism specified
- Primer Tm: SantaLucia 1998 thermodynamic parameters
- Exon junction span: Required for RNA targets
- Maximum product size: 150 bp
- Step 14: Verify that primer pairs do not generate significant off-target amplicons, with at least 3 mismatches to non-target sequences, particularly at the 3' end [35].
- Step 15: Check for potential primer-dimer and hairpin structures using tools like OligoAnalyzer.
Figure 1: Patient-specific assay design and validation workflow. The process begins with target sequence analysis and proceeds through iterative design and validation steps to ensure maximum specificity.
Validation Methodologies
Analytical Validation Framework
Robust validation is particularly challenging for patient-specific assays as each requires individual characterization. The following fit-for-purpose validation approach provides adequate evidence of analytical performance without being prohibitively resource-intensive.
Specificity Testing
- Step 16: Test each patient-specific assay against DNA from healthy donor peripheral blood mononuclear cells (PBMCs) to establish background signal levels.
- Step 17: For mutation detection, evaluate cross-reactivity with wild-type sequences using synthetic oligonucleotides or confirmed wild-type samples.
- Step 18: Assess potential interference from related sequences by testing against samples with similar but distinct targets (e.g., stereotyped B-cell receptor sequences in CLL) [33].
Sensitivity and Limit of Detection
- Step 19: Prepare dilution series of patient-specific positive control material (e.g., patient diagnostic DNA) in wild-type DNA to establish the quantitative range.
- Step 20: For MRD detection, demonstrate reliable detection at the clinical decision point (typically 10⁻⁴ to 10⁻⁶) through replicate testing (n ≥ 5) at each dilution level.
- Step 21: Calculate the limit of detection (LOD) using probit analysis, with 95% detection probability as the criterion [33].
Table 2: Performance Characteristics of Validated Patient-Specific ASO-PCR Assays
| Performance Parameter | CLL Assays | B-ALL Assays | T-ALL Assays | Validation Approach |
|---|---|---|---|---|
| Linearity Range | 10⁻¹ to 10⁻⁵ (92% of assays) | 10⁻¹ to 10⁻⁵ (89% of assays) | 10⁻¹ to 10⁻⁵ (87% of assays) | Dilution series in wild-type DNA [33] |
| Detection Limit (Cells) | 2.1-4.8 per 10⁵ leukocytes | 1.8-4.2 per 10⁵ leukocytes | 2.0-4.5 per 10⁵ leukocytes | Probit analysis of dilution replicates |
| Accuracy at Clinical Cut-off | 92% agreement with orthogonal methods | 89% agreement with orthogonal methods | 91% agreement with orthogonal methods | Comparison to flow cytometry/NGS [33] |
| Non-Specific Amplification Rate | 8.4% (technical replicates) | 6.2% (technical replicates) | 7.1% (technical replicates) | Testing with non-patient-specific assays [33] |
Controls and Standardization
Appropriate controls are critical for interpreting patient-specific assay results:
- Step 22: Include a positive control for the patient-specific target in each run, ideally diluted to the clinical decision point.
- Step 23: Implement a control gene assay (e.g., albumin, GAPDH, ABL1) to quantify input DNA and assess sample quality.
- Step 24: Validate housekeeping genes for each application, as commonly used references like GAPDH may be unsuitable in certain contexts [36] [37].
- Step 25: Establish a negative control pool from multiple healthy donors to identify non-specific amplification.
Implementation in Cancer Biomarker Research
Integration with Biomarker Validation Pipelines
Patient-specific assays serve critical functions throughout the biomarker development pipeline, from initial discovery to clinical application. The technical validation described here corresponds to the "clinical research assay" stage, bridging the gap between research use only and fully regulated in vitro diagnostics [2].
For comprehensive biomarker validation, patient-specific PCR assays should demonstrate:
- Analytical precision: <25% coefficient of variation at the clinical decision point
- Inter-laboratory reproducibility: >90% concordance between trained laboratories
- Sample type applicability: Consistent performance across relevant matrices (e.g., whole blood, bone marrow, FFPE tissue)
Figure 2: Integration of patient-specific assays within the broader biomarker validation pipeline, highlighting key analytical parameters at each development stage.
Comparison to Alternative Technologies
While patient-specific PCR assays provide exceptional sensitivity for targeted applications, understanding their position relative to alternative technologies informs appropriate implementation decisions.
Table 3: Platform Comparison for Patient-Specific Target Detection
| Technology | Analytical Sensitivity | Multiplexing Capacity | Turnaround Time | Best Application Context |
|---|---|---|---|---|
| ASO RQ-PCR | 0.001%-0.0001% [33] | Low (1-3 targets) | 4-6 hours | MRD monitoring, low variant frequency detection |
| Digital PCR | 0.01%-0.001% [38] | Medium (3-5 targets) | 6-8 hours | Absolute quantification, rare mutation detection |
| Ultrasensitive Real-time PCR | 0.001%-0.0001% [38] | Low (1-3 targets) | 4-6 hours | Liquid biopsy applications, low-cost alternative |
| Next-Generation Sequencing | 1%-0.1% (standard); 0.1%-0.01% (enhanced) [39] | High (hundreds to thousands of targets) | 3-7 days | Comprehensive profiling, novel target discovery |
The Scientist's Toolkit
Successful implementation of patient-specific PCR assays requires both specialized reagents and methodological rigor. The following reagents and resources constitute essential components of the experimental toolkit.
Table 4: Essential Research Reagent Solutions for Patient-Specific PCR
| Reagent/Resource | Function | Implementation Notes |
|---|---|---|
| High-Quality DNA Polymerase | Catalyzes DNA amplification with high fidelity | Select inhibitor-resistant formulations for clinical samples; ensure consistent performance across batches [15] |
| dNTP Mixture | Building blocks for DNA synthesis | Use quality-controlled, nuclease-free preparations to prevent degradation |
| Fluorescent Probes | Target sequence detection | Hydrolysis (TaqMan) or hybridization formats; validate quenching efficiency |
| Primer Design Software | In silico assay optimization | NCBI Primer-BLAST for specificity analysis; commercial tools for complex parameters [35] |
| Positive Control Templates | Assay performance monitoring | Synthetic oligonucleotides or cell line DNA with known target sequences |
| Standardized Master Mixes | Reaction consistency | Pre-formulated mixes with optimized buffer conditions; ambient-stable options for decentralized testing [15] |
Patient-specific PCR assays represent a powerful methodology for precision oncology applications requiring exceptional specificity. The primer and probe design strategies outlined here, coupled with rigorous validation frameworks, enable reliable detection of rare genetic targets amid complex biological backgrounds. By emphasizing genomic context, thoughtful primer placement, and comprehensive specificity testing, researchers can develop robust assays that support critical decisions in cancer biomarker research and patient management. The standardized approaches described bridge the gap between research use and clinical application, facilitating the translation of molecular discoveries into clinically actionable tools.
Measurable Residual Disease (MRD) refers to the small number of cancer cells that remain in a patient during or after treatment, undetectable by conventional microscopy. In lymphoid leukemias, MRD assessment has emerged as the most powerful independent prognostic factor, guiding risk stratification and therapeutic decisions [40]. Among the various methodologies, real-time quantitative PCR (RQ-PCR) analysis of clonal immunoglobulin (IG) and T-cell receptor (TR) gene rearrangements represents a gold standard in precision medicine [41] [42]. This patient-specific approach enables highly sensitive tracking of leukemic clones, allowing clinicians to detect treatment failure earlier and with greater reliability than traditional complete remission assessment.
The clinical significance of MRD negativity is profound. Meta-analyses involving over 13,000 patients with Acute Lymphoblastic Leukemia (ALL) demonstrate that MRD negativity is consistently associated with significantly improved event-free survival and overall survival [40]. Similarly, in Chronic Lymphocytic Leukemia (CLL), achieving undetectable MRD translates to a 72% reduction in the risk of progression or death [40]. This case study examines the implementation, validation, and clinical application of IG/TR-based RQ-PCR protocols within the context of cancer biomarker validation research.
Principles of IG/TR-Based MRD Detection
Biological Basis
Lymphoid leukemias originate from clonal expansions of B- or T-cell precursors. During normal lymphocyte development, IG and TR genes undergo somatic rearrangement to generate immense diversity in antigen receptors. Each leukemic clone possesses a unique DNA sequence in the complementarity-determining regions (CDRs) of these rearranged genes, serving as a unique, patient- and tumor-specific molecular fingerprint [42]. These patient-specific clonally rearranged immune receptor genes provide ideal targets for monitoring MRD with high specificity, as they can distinguish malignant cells from normal lymphocytes.
The IG/TR-based MRD approach involves identifying the specific rearrangement(s) in a patient's diagnostic sample and designing allele-specific oligonucleotide (ASO) primers for RQ-PCR. These patient-specific primers are then used to track the leukemic clone with high sensitivity in follow-up bone marrow samples during and after treatment [41]. The quantitative capability of RQ-PCR allows for precise measurement of MRD levels, typically expressed as a ratio of leukemic cells to normal cells (e.g., 10⁻⁴ represents 1 leukemic cell in 10,000 normal cells).
Experimental Protocols
Patient-Specific Assay Development
Objective: To identify clonal IG/TR gene rearrangements and design patient-specific RQ-PCR assays for MRD monitoring.
Materials:
- High-quality DNA extracted from diagnostic bone marrow sample (≥100 ng/µL)
- PCR reagents for BIOMED-2/EuroMRD approved multiplex PCR protocols
- Capillary electrophoresis equipment for fragment analysis
- Sanger sequencing or next-generation sequencing platforms
- Primer design software adhering to IMGT nomenclature guidelines
Procedure:
- DNA Quality Control: Verify DNA concentration and purity using spectrophotometry (e.g., NanoDrop). Confirm DNA integrity via control gene RQ-PCR (e.g., Albumin) [42].
- Clonality Screening: Perform multiplex PCR amplification of IG/TR gene rearrangements (IGH, IGK, TRB, TRG, TRD) using BIOMED-2/EuroMRD approved primer sets.
- Fragment Analysis: Separate PCR products by capillary electrophoresis to identify dominant clonal peaks against a polyclonal background.
- Sequence Identification: Purify clonal PCR products and perform Sanger sequencing to obtain the nucleotide sequence of the CDR3 region.
- Assay Design: Design allele-specific oligonucleotide (ASO) primers and probes targeting the unique CDR3 sequence, following EuroMRD guidelines for optimal positioning and specificity [42].
- Standard Curve Preparation: Prepare serial dilutions (10⁻¹ to 10⁻⁵) of diagnostic DNA in polyclonal donor DNA to establish quantitative range.
RQ-PCR MRD Analysis
Objective: To quantitatively measure MRD levels in follow-up patient samples using patient-specific RQ-PCR assays.
Materials:
- Patient DNA samples from follow-up time points (100 ng/µL concentration)
- Patient-specific ASO primers and dual-labeled hydrolysis probes (FAM/TAMRA)
- RQ-PCR master mix (e.g., TaqMan-based chemistry)
- Real-time PCR instrument with compatible software
- Control gene assay (e.g., Albumin) for DNA quality/quantity control
Procedure:
- Sample Preparation: Use follow-up DNA samples as supplied without concentration adjustment. Include negative controls (polyclonal DNA) and positive controls (serial dilutions of diagnostic DNA) in each run [42].
- Reaction Setup: Prepare reactions in triplicate containing:
- 100 ng DNA (1 µL of 100 ng/µL stock)
- 1X TaqMan Universal Master Mix
- Patient-specific ASO primers and probe at optimized concentrations
- Control gene primers and probe (different fluorophore, e.g., VIC)
- PCR Amplification: Run RQ-PCR using standardized cycling conditions:
- Initial denaturation: 95°C for 10 minutes
- 50 cycles of: 95°C for 15 seconds, 60°C for 60 seconds
- Data Collection: Monitor fluorescence accumulation in real-time during the annealing/extension step of each cycle.
- Threshold Setting: Set fluorescence threshold in the exponential phase of amplification, sufficiently above baseline but within the linear range of detection [43].
Data Interpretation and Quality Assurance
Objective: To accurately interpret RQ-PCR data according to international guidelines and ensure result reproducibility.
Materials:
- EuroMRD guidelines for data interpretation
- Quality assessment (QA) program materials
- Standardized data reporting forms
Procedure:
- Ct Determination: Record quantification cycle (Ct) values for each reaction. The Ct represents the intersection between an amplification curve and the threshold line, providing a relative measure of target concentration [43].
- Quantification: Calculate MRD levels using the standard curve method, comparing target gene Ct values to control gene Ct values to account for DNA quality variations.
- Result Classification: Categorize results according to EuroMRD guidelines:
- Quantifiable MRD: Results within the quantitative range (QR)
- MRD Low Positive, Below Quantitative Range: Detected but below QR
- MRD of Uncertain Significance: Very low positive signals requiring clinical correlation
- MRD Negative: No detectable leukemia-specific signal [42]
- QA Participation: Engage in regular external quality assessment rounds through the EuroMRD Consortium, which includes evaluation of data interpretation (Task 1) and wet lab performance (Tasks 2/3) [42].
Performance Specifications and Validation
Analytical Performance
Comprehensive validation of the IG/TR RQ-PCR methodology demonstrates robust performance characteristics suitable for clinical decision-making [41].
Table 1: Analytical Performance of IG/TR RQ-PCR MRD Assessment
| Performance Parameter | Specification | Validation Outcome |
|---|---|---|
| Linear Range | 10⁻¹ to 10⁻⁵ dilution | Linear for 90% of all assays |
| Detection Limit | Sensitivity threshold | 1.8-4.8 cells/100,000 leukocytes |
| Quantitative Range | Reliable quantification range | Typically 10⁻³ to 10⁻⁵ |
| Precision | Inter-laboratory reproducibility | High concordance across labs |
| Accuracy | Comparison to orthogonal methods | ~90% agreement with flow cytometry and NGS |
| PCR Efficiency | Assay performance threshold | 85-110% acceptable range [43] |
Clinical Cut-offs and Interpretation
The clinical utility of MRD monitoring depends on appropriate interpretation of quantitative results at specific treatment time points.
Table 2: MRD Result Classification and Clinical Significance
| Result Category | Definition | Clinical Implications |
|---|---|---|
| Quantifiable MRD | Results within established quantitative range | High relapse risk; may indicate need for treatment intensification |
| MRD Low Positive, Below Quantitative Range | Detected but below reliable quantification | Intermediate relapse risk; requires monitoring |
| MRD of Uncertain Significance | Very low positive signals | Clinical correlation needed; may represent residual disease or technical artifact |
| MRD Negative | No detectable leukemia-specific signal | Favorable prognosis; may allow for treatment de-escalation |
Quality Assurance Framework
The EuroMRD Consortium has established a comprehensive quality assessment scheme to ensure comparable, high-quality MRD diagnostics across participating laboratories [42]. This framework includes:
Membership Criteria: Laboratories must demonstrate extensive knowledge of IG/TR gene rearrangements, substantial experience with MRD detection, adequate laboratory size, and minimum annual patient intake [42].
Quality Assessment Rounds:
- Task 1: Paper-based data interpretation of 10 clinical cases
- Task 2: Complete marker identification and MRD analysis
- Task 3: MRD analysis of pre-tested samples only
Standardized Guidelines: Regularly updated interpretation guidelines based on collective experience and experimental data, ensuring uniform application across centers [42].
The Scientist's Toolkit: Research Reagent Solutions
Successful implementation of IG/TR-based MRD assessment requires specific reagents and materials standardized according to international guidelines.
Table 3: Essential Research Reagents for IG/TR MRD Analysis
| Reagent/Material | Function | Specifications |
|---|---|---|
| DNA Extraction Kits | Isolation of high-quality genomic DNA from patient samples | Minimum yield: 100 ng/µL; A260/A280 ratio: 1.8-2.0 |
| BIOMED-2 Primer Sets | Multiplex PCR amplification of IG/TR gene rearrangements | EuroMRD-approved; covers IGH, IGK, TRB, TRG, TRD |
| TaqMan Master Mix | RQ-PCR amplification with fluorescence detection | Optimized for allele-specific PCR; minimal batch variation |
| Allele-Specific Primers & Probes | Patient-specific detection of leukemic clones | HPLC-purified; designed according to IMGT nomenclature |
| Control Gene Assay | Quality control of DNA quantity/quality | Albumin or other single-copy gene; different fluorophore |
| Polyclonal Donor DNA | Diluent for standard curves and negative controls | Pooled from multiple healthy donors; confirmed polyclonality |
IG/TR-based RQ-PCR remains a gold standard for MRD assessment in lymphoid leukemias, with validated analytical performance and established clinical utility. The method's robustness stems from extensive standardization efforts led by the EuroMRD Consortium, which ensures reproducible and accurate MRD data across international centers. The patient-specific nature of this approach exemplifies precision medicine in oncology, enabling highly sensitive detection of residual disease that would otherwise remain undetectable by conventional methods. As MRD technologies continue to evolve, the foundational principles and quality frameworks established for IG/TR RQ-PCR will inform the development and validation of emerging platforms, including digital PCR and next-generation sequencing applications.
Lung cancer remains a leading cause of cancer-related mortality worldwide, with survival outcomes strongly dependent on early detection [44]. In the era of precision oncology, liquid biopsies—the analysis of tumor-derived material in blood or other bodily fluids—offer a minimally invasive approach for cancer detection and monitoring [3] [45]. Among the various biomarkers detectable in liquid biopsies, DNA methylation has emerged as a particularly promising target due to its stability, cancer-specific pattern, and early occurrence in tumorigenesis [46] [3].
DNA methylation involves the addition of a methyl group to the cytosine base in CpG dinucleotides, typically leading to gene silencing when it occurs in promoter regions [46]. In cancer cells, tumor suppressor genes often undergo hypermethylation, while oncogenes may experience hypomethylation, making these patterns ideal biomarkers for detection [46] [3]. Methylation-specific quantitative PCR (qPCR) enables highly sensitive detection of these cancer-specific epigenetic signatures in circulating cell-free DNA (cfDNA), presenting a valuable tool for researchers and clinicians alike [46] [44].
This case study examines the application of methylation-specific qPCR for lung cancer detection in liquid biopsies, providing detailed protocols and performance data to support its implementation in cancer biomarker validation research.
Methylation Markers for Lung Cancer Detection
Key Methylation Biomarkers in Lung Cancer
Several DNA methylation markers have demonstrated clinical utility for lung cancer detection. The selection of appropriate markers is critical for assay sensitivity and specificity.
Table 1: Key Methylation Biomarkers for Lung Cancer Detection
| Gene Marker | Methylation Status in Cancer | Biological Function | Performance Characteristics |
|---|---|---|---|
| SHOX2 | Hypermethylated | Transcriptional regulator | 92.8% sensitivity in combined detection [47] |
| RASSF1A | Hypermethylated | Tumor suppressor | 94.7% specificity in combined detection [47] |
| HOXA9 | Hypermethylated | Developmental regulator | Included in ddPCR multiplex panels [44] |
The combination of multiple markers significantly improves detection rates compared to single-marker approaches. In one study, a five-marker ddPCR multiplex assay demonstrated ctDNA-positive rates of 38.7-46.8% in non-metastatic disease and 70.2-83.0% in metastatic lung cancer [44]. Higher sensitivities were observed for small cell lung cancer and squamous cell carcinoma compared to adenocarcinoma [44].
Biological Basis of Methylation Biomarkers
The biological stability of DNA methylation patterns makes them particularly suitable for liquid biopsy applications. Methylation changes often occur early in tumorigenesis and remain relatively stable throughout tumor evolution [3]. Furthermore, methylated DNA fragments demonstrate enhanced resistance to degradation during sample processing due to nucleosome interactions that protect methylated DNA from nuclease degradation [3]. The short half-life of circulating tumor DNA (ctDNA)—estimated from minutes to a few hours—enables real-time monitoring of tumor dynamics and treatment response [3] [45].
Experimental Workflow and Methodologies
Complete Experimental Workflow
The following diagram illustrates the comprehensive workflow for methylation-specific qPCR analysis of liquid biopsy samples, from sample collection to data interpretation:
Sample Collection and Processing Protocol
Materials Required:
- EDTA blood collection tubes (9 mL)
- Refrigerated centrifuge capable of 2,000 × g
- Plasma storage tubes (-80°C compatible)
- Pipettes and sterile tips
Procedure:
- Collect whole blood using EDTA tubes to prevent coagulation
- Process samples within 4 hours of collection
- Centrifuge at 2,000 × g for 10 minutes at room temperature to separate plasma from blood cells
- Carefully transfer the supernatant plasma to a fresh tube without disturbing the buffy coat
- Perform a second centrifugation at 10,000 × g for 10 minutes to remove residual cells [44]
- Aliquot plasma into cryovials and store at -80°C until cfDNA extraction
Technical Notes:
- Plasma is preferred over serum as it contains less genomic DNA contamination from lysed cells [3]
- Avoid repeated freeze-thaw cycles to preserve DNA integrity
- Record sample processing times consistently
cfDNA Extraction and Quality Control
Materials Required:
- Commercial cfDNA extraction kit (e.g., QIAsymphony DSP Circulating DNA Kit)
- Centrifugal filter units (e.g., Amicon Ultra-0.5)
- Qubit fluorometer or similar DNA quantification system
- ddPCR or qPCR reagents for quality assessment
Procedure:
- Extract cfDNA from 4 mL plasma using manufacturer's protocols
- Elute DNA in an appropriate buffer (typically 60 μL)
- Concentrate DNA using centrifugal filters if necessary [44]
- Quantify DNA concentration using fluorometric methods
- Assess DNA quality using multi-amplicon approaches:
- Amplify short (65 bp) and long (250 bp) regions of a reference gene (e.g., EMC7)
- Calculate the ratio to assess fragmentation level [44]
- Include an exogenous spike-in control (e.g., CPP1) to monitor extraction efficiency [44]
Quality Parameters:
- DNA concentration should be measurable, with qualification rates typically >98% [47]
- Fragmentation pattern should show enrichment for ~160-200 bp fragments (nucleosome-protected)
- Extraction efficiency should be >70% based on spike-in recovery
Bisulfite Conversion Protocol
Materials Required:
- Commercial bisulfite conversion kit (e.g., EZ DNA Methylation-Lightning Kit)
- Thermal cycler
- Nuclease-free water
Procedure:
- Use 100 ng cfDNA for conversion, concentrating if necessary [47]
- Follow manufacturer's protocol for denaturation and bisulfite conversion
- Typically involves:
- Denaturation at 98°C for 5-10 minutes
- Incubation with bisulfite reagent at 64°C for 30-45 minutes
- Desulfonation at room temperature for 15-20 minutes
- Elute converted DNA in 15-20 μL elution buffer
- Store converted DNA at -20°C if not used immediately
Technical Notes:
- Bisulfite conversion deaminates unmethylated cytosines to uracils, while methylated cytosines remain unchanged [46]
- The process is harsh and causes DNA fragmentation; handle samples gently
- Include unmethylated and methylated controls in each conversion batch
- Converted DNA should be used within a few weeks for optimal results
Primer and Probe Design for Methylation-Specific qPCR
Design Principles:
- Target CpG-rich regions (CpG islands) in gene promoters
- Ensure primers encompass multiple CpG sites for specificity
- Design primers to complement the bisulfite-converted sequence
- Place the 3' end of at least one primer over a CpG site to enhance methylation specificity [34]
Example Sequences for Lung Cancer Markers:
Table 2: Primer and Probe Sequences for Key Methylation Markers
| Gene | Primer/Probe | Sequence (5' to 3') | Application |
|---|---|---|---|
| SHOX2 | Forward Primer | TTGTTTTTGGGTTCGGGTT | Detection [47] |
| SHOX2 | Reverse Primer | CATAACGTAAACGCCTATACTCG | Detection [47] |
| SHOX2 | Probe | VIC-ATCGAACAAACGAAACGAAAATTACC | Detection [47] |
| RASSF1A | Forward Primer | CGGGGTTCGTTTTGTGGTTTC | Detection [47] |
| RASSF1A | Reverse Primer | CCGATTAAATCCGTACTTCGC | Detection [47] |
| RASSF1A | Probe | FAM-TCGCGTTTGTTAGCGTTTAAAGT | Detection [47] |
| β-ACTB | Forward Primer | AAGATAGTGGTGTGGGTGTAGGT | Internal control [47] |
| β-ACTB | Reverse Primer | CCTACTTAATACACACTCCAAAAC | Internal control [47] |
| β-ACTB | Probe | CY5-ACACCAACCTCATAACCTTATCACAC | Internal control [47] |
Validation Steps:
- Test primer specificity using in silico PCR with bisulfite-converted genome sequences
- Optimize annealing temperature through gradient PCR
- Verify amplification efficiency (90-110%) using standard curves
- Confirm methylation specificity with controls
Methylation-Specific qPCR Protocol
Reaction Setup:
- Total volume: 40 μL
- 5 μL bisulfite-converted DNA template
- 250 μM dNTPs
- 0.8 μL each primer (10 μM)
- 1.5-3 mM MgCl₂
- 20 μL 2× Taq buffer
- 13.4 μL nuclease-free water
- Appropriate probes (e.g., 85 nM) [47]
Thermal Cycling Conditions:
- Initial denaturation: 95°C for 10 minutes
- 45 cycles of:
- Denaturation: 95°C for 30 seconds
- Annealing/Extension: 58°C for 35 seconds, 72°C for 30 seconds [47]
- Final extension: 72°C for 8 minutes
Controls to Include:
- No-template control (nuclease-free water)
- Methylated positive control (commercial or plasmid-based)
- Unmethylated positive control (normal leukocyte DNA)
- Internal reference gene (e.g., β-ACTB) to quantify input DNA
Data Analysis and Interpretation
Calculation Methods
ΔCt Method:
- Calculate ΔCt = Ct[target gene] - Ct[reference gene]
- Establish cut-off values for positivity:
- For multi-gene panels, consider any positive gene as overall positive
Quantitative Approaches:
- Generate standard curves using synthetic methylated standards
- Calculate percentage methylation relative to standards
- Normalize to input DNA quantity
Performance Metrics in Validation Studies
Table 3: Performance Characteristics of Methylation-Specific qPCR in Lung Cancer Detection
| Parameter | SHOX2/RASSF1A Combined | Five-Marker ddPCR Multiplex | With Morphological Pathology |
|---|---|---|---|
| Sensitivity | 92.8% [47] | 38.7-83.0% (by stage) [44] | 96.0% [47] |
| Specificity | 94.7% [47] | Not specified | 94.7% [47] |
| AUC | Not specified | Not specified | Not specified |
| Early Stage (I-II) Detection | Not specified | 38.7-46.8% [44] | Not specified |
| Advanced Stage (IV) Detection | Not specified | 70.2-83.0% [44] | Not specified |
The Scientist's Toolkit: Essential Research Reagents
Table 4: Essential Research Reagents for Methylation-Specific qPCR
| Reagent Category | Specific Examples | Function | Technical Considerations |
|---|---|---|---|
| Blood Collection Tubes | EDTA tubes (9 mL) | Prevents coagulation and preserves cell-free DNA | Process within 4 hours; avoid heparin tubes [44] |
| cfDNA Extraction Kit | QIAsymphony DSP Circulating DNA Kit | Isolves cell-free DNA from plasma | Elution volume affects concentration; use 60 μL [44] |
| Bisulfite Conversion Kit | EZ DNA Methylation-Lightning Kit | Converts unmethylated cytosines to uracils | Causes DNA fragmentation; handle gently [44] |
| qPCR Master Mix | TaqMan Gene Expression Master Mix | Provides enzymes for amplification | Optimize MgCl₂ concentration for each assay [47] |
| Methylation-Specific Primers/Probes | SHOX2, RASSF1A assays | Detect methylated alleles | Design spanning multiple CpG sites [34] [47] |
| Quality Control Assays | EMC7 65bp/250bp, exogenous spike-in | Assess DNA quality and quantity | Ratio of long/short amplicons indicates fragmentation [44] |
| Reference DNA | Methylated and unmethylated controls | Assay validation and standardization | Use commercially available controls or characterized cell lines |
Troubleshooting and Technical Considerations
Common Technical Challenges
Low DNA Yield:
- Increase starting plasma volume (up to 4-10 mL)
- Concentrate eluted DNA using centrifugal filters
- Verify extraction efficiency with spike-in controls
Poor Amplification:
- Check bisulfite conversion efficiency
- Optimize primer annealing temperatures
- Verify DNA quality and fragmentation
- Ensure appropriate MgCl₂ concentration (1.5-3 mM) [47]
Inconsistent Results:
- Standardize sample processing times
- Implement batch testing with controls
- Ensure consistent DNA input (e.g., 100 ng for conversion) [47]
Assay Validation Guidelines
For robust biomarker validation, consider these key aspects:
- Analytical Sensitivity: Determine limit of detection using serial dilutions of methylated DNA
- Analytical Specificity: Test against unmethylated DNA and other cancer types
- Reproducibility: Assess inter- and intra-assay coefficients of variation
- Pre-analytical Factors: Standardize sample collection, processing, and storage conditions
Methylation-specific qPCR represents a powerful methodology for lung cancer detection in liquid biopsies, offering researchers a sensitive, specific, and relatively accessible approach for biomarker validation studies. The technique's ability to detect early-stage disease and monitor treatment response makes it particularly valuable in the context of precision oncology.
When implementing this technology, careful attention to pre-analytical variables, assay design, and validation parameters is essential for generating reliable, reproducible data. The protocols and considerations outlined in this case study provide a foundation for researchers developing methylation-based biomarkers for lung cancer and other malignancies.
As the field advances, integration of multiple methylation markers and combination with other genomic and fragmentomic approaches will likely enhance the sensitivity and clinical utility of liquid biopsy-based lung cancer detection.
Multiplex qPCR Strategies for Simultaneous Multi-Biomarker Analysis
The simultaneous quantification of diverse biomarker classes is pivotal for advancing precision diagnostics, particularly in oncology. Traditional methods for analyzing multiple molecular targets, such as mRNAs and proteins, are often constrained by low multiplexing capacity, separate instrumentation requirements, and inconsistent signal readouts, which hinder integrated data analysis and increase sample volume requirements [48]. Multiplex quantitative PCR (qPCR) strategies overcome these limitations by enabling the parallel measurement of several biomarkers from a single, minimal sample volume. This approach is increasingly vital for cancer biomarker validation, where analyte scarcity and tumor heterogeneity demand highly sensitive and comprehensive profiling techniques [3] [49]. This document outlines detailed application notes and protocols for implementing multiplex qPCR strategies in cancer research, providing a framework for robust, reproducible biomarker analysis.
Multiplex qPCR has evolved significantly, moving beyond simple multi-target amplification to sophisticated platforms capable of detecting diverse analyte classes. The FluoMag-dCoDe platform exemplifies this advancement, converting various analytes into distinct fluorescence-coded DNA templates for multiplexed quantification in a single digital PCR (dPCR) reaction using a universal primer and TaqMan probe set [48]. This unified approach allows researchers to co-measure, for instance, eight mRNA and three protein immune-response biomarkers in a two-color dPCR format, demonstrating strong concordance with single-plex RT-qPCR for mRNAs and superior analytical sensitivity to ELISA for proteins [48].
In clinical diagnostics, syndromic multiplex PCR panels have revolutionized the detection of gastrointestinal infections, allowing rapid, simultaneous identification of multiple pathogens with superior analytic sensitivity compared to conventional methods like bacterial culture or antigen tests [50]. The application of these principles to oncology enables researchers to address critical challenges such as early cancer detection, assessment of prognosis, and monitoring treatment response through liquid biopsies [3].
Table 1: Commercially Available Multiplex PCR Panels for Pathogen Detection
| Platform Name | Manufacturer | Key Targets | Clinical Utility |
|---|---|---|---|
| BioFire FilmArray GIP | BioFire Diagnostics | Campylobacter, Salmonella, Shigella/EIEC, STEC, Norovirus, Rotavirus, Cryptosporidium | Comprehensive gastrointestinal pathogen detection |
| xTAG GPP | Luminex | Similar to BioFire with slightly different target menu | Multiplex detection of common enteric pathogens |
| QIAstat-Dx GIP | QIAGEN | Extensive bacterial, viral, and parasitic targets | Syndromic testing for gastroenteritis |
| Verigene EP | Luminex | Campylobacter, Salmonella, Shigella, Vibrio, Norovirus, Rotavirus | Focused enteric pathogen detection |
Detailed Experimental Protocols
FluoMag-dCoDe for Multi-Analyte Detection
The FluoMag-dCoDe platform enables simultaneous quantification of mRNA and protein biomarkers from low blood volumes (~35 µL), making it particularly suitable for liquid biopsy applications where sample material is limited [48].
Workflow Overview:
- Sample Preparation: Collect blood via fingerstick and separate plasma within 2 hours. Isolate total RNA and protein fractions using commercial extraction kits. For proteins, use antibody-conjugated magnetic beads for target capture.
- Target Conversion: Convert mRNA targets to cDNA using reverse transcriptase. For protein targets, use DNA-barcoded detection antibodies to create surrogate DNA templates.
- Probe Hybridization: Combine all DNA templates (from both mRNA and protein targets) with fluorescence-coded universal TaqMan probes.
- Partitioning and Amplification: Perform digital PCR using a two-color detection system. Partition the reaction mixture into approximately 20,000 droplets for absolute quantification.
- Signal Detection and Analysis: Analyze fluorescence endpoints to determine the absolute copy number of each target using Poisson statistics.
Critical Optimization Steps:
- Maintain a 1:1 molar ratio of capture to detection antibodies for protein targets to minimize hook effects.
- Use blocking reagents (e.g., tRNA, salmon sperm DNA) to reduce non-specific binding of detection probes.
- Validate assay specificity for each target using positive and negative controls in the multiplex format.
Figure 1: FluoMag-dCoDe Workflow for Simultaneous mRNA and Protein Biomarker Detection
Multi-STEM MePCR for DNA Methylation Analysis
DNA methylation biomarkers are particularly valuable in oncology due to their early emergence in tumorigenesis and stability in circulating cell-free DNA [3]. The Multi-STEM MePCR system provides a bisulfite-free, highly sensitive method for multiplexed methylation detection.
Principle and Workflow:
- MDRE Digestion: Digest methylated DNA templates with a methylation-dependent restriction endonuclease (MDRE) to produce specific 5'-end products while leaving unmethylated templates intact.
- Tailored Foldable Primer (TFP) Binding: Hybridize TFPs to the digested products and extend with Taq DNA polymerase. The extension terminates precisely at cutting sites for methylated targets but continues nonspecifically for unmethylated templates.
- Intramolecular Folding: The extension products self-fold to form complete hairpin structures (HP2) through intramolecular binding—a step that only occurs successfully with properly digested methylated targets.
- Multiplexed Amplification: Use a combination of universal primers (UP) and terminal-specific primers (TSPs) to exponentially amplify the HP2 structures, enabling multiplexed detection of multiple methylated targets.
Key Advantages:
- Bisulfite-free approach avoids DNA degradation and false signals from incomplete conversion
- High sensitivity down to 0.1% methylated alleles in a background of unmethylated DNA
- Minimized cross-reactivity between targets through strategic primer design
- Effective discrimination of sites with significant variations in methylation abundance [49]
Figure 2: Multi-STEM MePCR Workflow for Bisulfite-Free DNA Methylation Analysis
The Scientist's Toolkit: Essential Research Reagents
Table 2: Key Research Reagent Solutions for Multiplex qPCR
| Reagent/Material | Function | Application Notes |
|---|---|---|
| Universal TaqMan Probes | Fluorescence-coded detection of multiple DNA templates | Enables unified readout for diverse analytes; critical for FluoMag-dCoDe [48] |
| Methylation-Dependent Restriction Endonucleases (MDRE) | Selective digestion of methylated DNA templates | Core component of bisulfite-free methylation detection; enables Multi-STEM MePCR [49] |
| Tailored Foldable Primers (TFPs) | Target-specific priming with self-folding capability | Forms stem-loop structures for specific amplification; minimizes cross-reactivity [49] |
| Antibody-Conjugated Magnetic Beads | Target capture and separation | Used for protein biomarker isolation in multi-analyte platforms [48] |
| Stem-Loop Primers | Enhanced specificity for cDNA synthesis | Particularly useful for low-abundance targets; employed in Folate-LT qPCR [51] |
Performance Metrics and Validation
Rigorous validation is essential for establishing reliable multiplex qPCR assays. Adherence to the MIQE (Minimum Information for Publication of Quantitative Real-Time PCR Experiments) guidelines ensures experimental reproducibility and data credibility [52] [53]. The recently updated MIQE 2.0 guidelines provide enhanced guidance for sample handling, assay design, validation, and data analysis.
Key Performance Parameters:
- Amplification Efficiency: Should be between 90-110% with R² values >0.990 for standard curves
- Limit of Detection (LOD): Multi-STEM MePCR demonstrates sensitivity to 10 copies per reaction and 0.1% detection against unmethylated background [49]
- Dynamic Range: FluoMag-dCoDe shows strong linearity across clinically relevant concentrations [48]
- Specificity: Minimal cross-interference between targets in multiplex reactions
Table 3: Quantitative Performance Metrics of Featured Platforms
| Platform | Sensitivity | Dynamic Range | Multiplexing Capacity | Sample Volume |
|---|---|---|---|---|
| FluoMag-dCoDe | Reliable TRAIL detection where ELISA failed | Strong linear concordance with single-plex methods | 11-plex (8 mRNA + 3 protein) | ~35 µL blood |
| Multi-STEM MePCR | 0.1% methylated alleles; 10 copies/reaction | Broad linear dynamic range | 3-plex demonstrated; scalable | Compatible with low-input liquid biopsies |
| Folate-LT qPCR | 104% amplification efficiency | R² = 0.9970 in standard curve | Single-plex with potential for multiplexing | Minimal blood volume |
Applications in Cancer Biomarker Validation
Multiplex qPCR strategies are particularly transformative for cancer biomarker validation research. The ability to simultaneously analyze multiple biomarker classes from limited samples addresses key challenges in translational oncology:
Liquid Biopsy Applications: DNA methylation biomarkers in liquid biopsies offer a minimally invasive solution for cancer management. Multiplex qPCR enables sensitive detection of these biomarkers in circulating tumor DNA (ctDNA), which reflects the entire tumor burden of a patient and captures molecular cancer heterogeneity more comprehensively than single-site tissue biopsies [3]. The stability of DNA methylation patterns and their early emergence in tumorigenesis make them ideal targets for multiplex qPCR approaches.
Therapeutic Monitoring: The Folate-LT qPCR method demonstrates application in detecting folate receptor-positive circulating tumor cells (CTCs) in gastric cancer, combining negative depletion with specific ligand targeting to overcome limitations of size-based or epithelial marker-dependent approaches [51]. This strategy shows promise for early cancer detection, disease progression monitoring, and treatment response assessment.
Troubleshooting and Technical Considerations
Assay Design Challenges: Multiplexing requires careful design to avoid primer-dimer formation and cross-reactions among different targets. For a reaction with 'n' targets, 3n primers are needed, creating significant design complexity [54] [49]. Computational tools and careful validation are essential to ensure specificity.
Sample Quality Considerations: Nucleic acid quality significantly impacts qPCR results. The MIQE guidelines emphasize proper assessment of RNA/DNA quality and integrity, which is particularly important for liquid biopsy samples where target abundance is low [53]. Implementing rigorous quality control measures at each processing step is critical for reliable results.
Data Interpretation: Quantitative claims based on small fold-changes (e.g., 1.2- to 1.5-fold) require careful validation with assessment of measurement uncertainty and technical variance [53]. Proper normalization using validated reference genes and calculation of actual PCR efficiencies rather than assumed values are essential for accurate data interpretation.
Quantitative PCR (qPCR) is an indispensable tool in cancer biomarker validation research, enabling the precise quantification of nucleic acids to assess gene expression, detect somatic mutations, and monitor minimal residual disease. The accurate interpretation of qPCR data hinges on understanding three fundamental concepts: the threshold cycle (Ct), amplification efficiency, and the quantitative models that transform raw fluorescence data into biologically meaningful information. In clinical cancer research, the rigor applied to these analyses directly impacts the reliability of biomarkers used for diagnosis, prognosis, and therapeutic monitoring.
Understanding the Threshold Cycle (Ct) and Its Significance
Definition and Theoretical Basis
The Threshold Cycle (Ct), also known as the Quantification Cycle (Cq), is defined as the PCR cycle number at which the fluorescence signal of a reaction crosses a predetermined threshold, indicating detectable amplification of the target sequence [55] [56]. This value represents the point during amplification where target accumulation first becomes statistically significant above background fluorescence. The Ct value has an inverse logarithmic relationship with the starting quantity of the target nucleic acid; each single-cycle difference in Ct represents an approximate two-fold difference in initial template concentration [57].
Mathematically, this relationship is expressed as:
[ Ct = -m \cdot \log{10}(X_0) + b ]
Where (X_0) is the initial template quantity, (m) is the slope of the standard curve, and (b) is the y-intercept [57].
Establishing Threshold and Baseline Parameters
Proper setting of the baseline and threshold is critical for accurate Ct determination:
- Baseline: Typically defined as the initial PCR cycles (usually cycles 3-15) where fluorescence remains relatively stable and no significant product accumulation occurs [57]. This represents the background fluorescence signal of the reaction before exponential amplification begins.
- Threshold: Generally set at 10 times the standard deviation of the baseline fluorescence or within the exponential phase of amplification, clearly above baseline variation but well before the reaction plateau [57]. The threshold must be consistent across all samples in an experiment to enable valid comparisons.
Table 1: Interpretation of Ct Values in Experimental Context
| Ct Value Range | Template Abundance | Technical Considerations | Application in Cancer Research |
|---|---|---|---|
| < 29 cycles | High abundance | Optimal for detection; minimal impact of technical variation | Reference genes; highly expressed oncogenes |
| 30-35 cycles | Medium abundance | Reliable detection with good precision | Medium-expression biomarkers; drug targets |
| 36-38 cycles | Low abundance | Increased variability; requires replication | Low-expression transcripts; rare splice variants |
| > 38 cycles | Very low abundance | High variability; potential false negatives | Circulating tumor DNA; minimal residual disease |
Experimental Protocol: Absolute Quantification for Cancer Biomarker Analysis
Principle and Applications
Absolute quantification determines the exact copy number of a target sequence in a sample by comparing Ct values to a standard curve of known concentrations [58] [56]. This method is particularly valuable in cancer research for applications such as quantifying viral load in virus-associated cancers, determining gene copy number variations, measuring circulating tumor DNA levels for monitoring therapeutic response, and quantifying microRNA expression patterns as diagnostic biomarkers [59].
Materials and Reagents
Research Reagent Solutions for qPCR in Cancer Biomarker Studies:
| Reagent Category | Specific Examples | Function in qPCR | Considerations for Cancer Biomarker Work |
|---|---|---|---|
| Nucleic Acid Isolation Kits | MolPure Cell/Tissue RNA Kit, TRIeasy Total RNA Extraction Reagent | High-quality RNA/DNA extraction from diverse sample types | Optimized for FFPE tissue, liquid biopsies, and rare cells |
| Reverse Transcription Reagents | Hifair AdvanceFast 1st Strand cDNA Synthesis Kit | cDNA synthesis from RNA templates | Maintains expression ratios; critical for gene signature validation |
| qPCR Master Mixes | Hieff UNICON Universal Blue qPCR SYBR Master Mix | Provides enzymes, dNTPs, buffers, and detection chemistry | Optimized for inhibitor-resistant amplification from clinical samples |
| Standard Curve Templates | Purified PCR products, synthetic oligonucleotides, plasmid DNA | Quantification reference standards | Should match target sequence length and composition |
| Quality Control Assays | RNA integrity tests, DNA contamination checks | Verify sample quality | Essential for degraded clinical specimens |
Step-by-Step Protocol
Standard Preparation:
- Generate a serial dilution series (typically 5-10-fold dilutions) of the standard template with known concentration [58].
- Use a minimum of five data points covering the expected concentration range of experimental samples.
- Include negative controls (no template control) with each run to detect contamination.
Sample Preparation:
- Extract nucleic acids from cancer specimens (tissue, blood, cytology samples) using appropriate methods.
- Treat samples with DNase if performing RNA analysis to eliminate genomic DNA contamination.
- Quantify nucleic acid concentration and quality using spectrophotometry or fluorometry.
qPCR Reaction Setup:
- Prepare master mix containing: 10 μL 2× qPCR master mix, 0.4 μL each forward and reverse primer (10 μM), 2 μL template (standard, sample, or control), and nuclease-free water to 20 μL total volume.
- Include triplicate reactions for each standard point and unknown sample to assess technical variability.
- Use a thermal cycling protocol appropriate for the polymerase chemistry and assay design.
Data Collection:
- Run qPCR program with fluorescence acquisition at the end of each extension phase.
- Ensure the run includes sufficient cycles (typically 40-45) to detect low-abundance targets common in cancer biomarker studies.
Standard Curve Analysis:
- Plot the log of the starting template quantity of each standard against its mean Ct value.
- Generate a linear regression line with the equation: ( y = mx + b ), where y = Ct, m = slope, x = log10(starting quantity) [58].
- Calculate amplification efficiency using the formula: ( E = 10^{(-1/slope)} - 1 ) [57].
Experimental Protocol: Relative Quantification for Gene Expression Analysis in Cancer
Principle and Applications
Relative quantification determines changes in gene expression between experimental samples relative to a reference group (e.g., normal tissue vs. tumor tissue) [56]. This approach is widely used in cancer research for profiling gene expression patterns, validating transcriptional biomarkers, assessing pathway activation in response to therapy, and identifying molecular subtypes based on gene signatures. The comparative Ct method (ΔΔCt) is commonly employed as it does not require a standard curve, though it depends on validation of equivalent amplification efficiencies between target and reference genes [56].
Protocol: Comparative Ct (ΔΔCt) Method
Reference Gene Selection:
- Select and validate appropriate endogenous control genes (e.g., GAPDH, ACTB, B2M) that show stable expression across all experimental conditions [60].
- In cancer studies, reference genes should be validated in the specific tissue type and experimental context, as expression stability can vary in malignant versus normal tissues.
Experimental Design:
- Include appropriate control samples (e.g., normal adjacent tissue, untreated cells) as calibrators.
- Randomize sample placement on qPCR plates to minimize positional effects.
- Include no-template controls and reverse transcription controls.
qPCR Execution:
- Amplify target genes and reference genes in separate wells for all samples.
- Use identical reaction conditions and master mixes for both target and reference amplifications.
- Ensure technical replicates (minimum of three) for each sample-gene combination.
Data Analysis:
- Calculate ΔCt for each sample: ( ΔCt = Ct{\text{target}} - Ct{\text{reference}} ) [56].
- Calculate ΔΔCt: ( ΔΔCt = ΔCt{\text{test}} - ΔCt{\text{calibrator}} ).
- Compute the fold change: ( \text{Fold Change} = 2^{-ΔΔCt} ).
Assessing Amplification Efficiency and Data Quality
Calculating Amplification Efficiency
Amplification efficiency (E) represents the proportion of template molecules that are duplicated in each PCR cycle. Ideal efficiency is 100%, meaning the template quantity doubles every cycle (E = 1) [57]. Efficiency can be calculated from the standard curve slope:
[ \text{Efficiency} (E) = 10^{(-1/\text{slope})} - 1 ] [ \text{Percentage Efficiency} = (E - 1) \times 100\% ]
For ideal amplification with a slope of -3.32, efficiency equals 100% [57].
Quality Control Parameters
Table 2: qPCR Validation Parameters for Cancer Biomarker Assays
| Parameter | Optimal Value | Acceptable Range | Calculation Method | Impact on Data Interpretation |
|---|---|---|---|---|
| Amplification Efficiency | 100% | 90-110% | From standard curve slope | Affects accuracy of quantification; requires correction outside 90-110% range |
| Standard Curve R² | >0.999 | >0.990 | Linear regression fit | Measures assay precision and dynamic range |
| Intra-assay CV (Ct) | <0.5% | <1.5% | (SD/mean Ct) × 100 | Assesses technical repeatability within a run |
| Inter-assay CV (Ct) | <1.5% | <2.5% | (SD/mean Ct) × 100 | Evaluates consistency between different runs |
| Slope of Standard Curve | -3.32 | -3.1 to -3.6 | Linear regression | Directly related to amplification efficiency |
Troubleshooting Suboptimal Efficiency
- Low Efficiency (<90%): Can result from inhibitor carryover, suboptimal primer design, inadequate reaction components, or improper thermal cycling conditions [57]. In cancer studies, this is particularly common when analyzing difficult samples like formalin-fixed paraffin-embedded (FFPE) tissues.
- High Efficiency (>110%): Typically indicates non-specific amplification, primer-dimer formation, or poor standard curve dilution accuracy [57].
- Correcting for Efficiency Variations: When target and reference genes have different efficiencies, use efficiency-corrected calculations in relative quantification:
[ \text{Fold Change} = \frac{(E{\text{target}})^{-\Delta Ct{\text{target}}}}{(E{\text{reference}})^{-\Delta Ct{\text{reference}}}} ]
Advanced Applications in Cancer Biomarker Research
High-Sensitivity Detection Technologies
Emerging technologies are enhancing qPCR applications in cancer biomarker detection. Inhibition Probe Displacement Amplification (BDA) technology, developed by NuProbe, enables the detection of ultra-low frequency mutations by enriching mutant sequences 1000-fold over wild-type background [61] [62]. This technology significantly improves the sensitivity of qPCR platforms for detecting cancer-associated mutations in liquid biopsies and monitoring minimal residual disease with variant allele frequencies as low as 0.05% [61].
Case Study: microRNA Quantification in Lung Adenocarcinoma
In a recent study investigating miR-2110 as a potential tumor suppressor in lung adenocarcinoma, researchers employed stem-loop RT-qPCR methodology [59]. The protocol included:
- RNA Extraction: Using TRIeasy Total RNA Extraction Reagent from A549 cells and clinical tissue specimens.
- miRNA-Specific Reverse Transcription: Employing the Hifair miRNA 1st Strand cDNA Synthesis Kit with stem-loop primers for miR-2110 and U6 snRNA as an endogenous control.
- qPCR Amplification: Using miRNA-specific forward primers, universal reverse primers, and Hieff miRNA Universal qPCR SYBR Master Mix.
- Data Analysis: Applying the ΔΔCt method with U6 for normalization, revealing significantly decreased miR-2110 expression in lung adenocarcinoma tissues compared to normal controls (P<0.05) [59].
This approach demonstrated how precise qPCR methodology can identify and validate novel cancer biomarkers with potential clinical utility.
Robust calculation of Ct values, accurate determination of amplification efficiency, and appropriate selection of quantification models form the foundation of reliable qPCR data analysis in cancer biomarker research. The standardized protocols outlined in this document provide a framework for generating clinically relevant data with the precision required for translational cancer research. As qPCR technologies continue to evolve with enhanced sensitivity through methods like BDA technology [61] [62], the application of these fundamental principles will remain essential for validating molecular biomarkers that can guide cancer diagnosis, prognosis, and treatment selection.
Enhancing Assay Performance: Troubleshooting and Optimization Strategies
The validation of cancer biomarkers using real-time PCR (qPCR) is a cornerstone of modern molecular diagnostics and therapeutic development [3]. However, the path to robust, clinically applicable data is often obstructed by technical challenges that can compromise assay sensitivity, specificity, and reproducibility. These issues are particularly acute when analyzing precious clinical samples like liquid biopsies, where target molecules may be scarce and embedded in a complex background of inhibitors [3] [63]. This application note provides detailed protocols and strategic frameworks for overcoming three ubiquitous hurdles in qPCR-based cancer biomarker research: PCR inhibitors, low template DNA, and non-specific amplification. By integrating optimized experimental protocols with structured troubleshooting guides, we aim to enhance the reliability of qPCR data in translational cancer research.
The Challenge of PCR Inhibitors
PCR inhibitors are substances that co-purify with nucleic acids and impede the amplification reaction, leading to reduced sensitivity, false negatives, and inaccurate quantification [64]. Common inhibitors encountered in cancer research include heparin from blood collection tubes, hemoglobin from hemolyzed samples, ionic detergents, and various proteins [64].
- Blood-Derived Samples (Plasma/Serum): Heparin, hemoglobin, and immunoglobulin G (IgG) are frequent inhibitors in liquid biopsies. Heparin can inhibit DNA polymerase by binding to it, while hemoglobin may interfere with the hybridization process [64] [3].
- Formalin-Fixed Paraffin-Embedded (FFPE) Tissues: Formalin cross-linking and the presence of porphyrins from heme can significantly inhibit PCR [64].
- Complex Matrices: Stool, bile, and other bodily fluids used in local liquid biopsies contain complex polysaccharides and bile salts that are potent inhibitors [65] [3].
Strategies for Overcoming Inhibition
1. Optimized Nucleic Acid Extraction: The choice of extraction method is critical. Kit-based systems designed for specific sample types, such as the PowerSoil Pro Kit or PrepFiler BTA Forensic DNA Extraction Kit, are formulated to remove common inhibitors effectively [66] [67]. Silica-membrane columns can remove many impurities, while manual methods like chloroform extraction and ethanol precipitation offer alternatives for difficult samples [64].
2. Dilution of Nucleic Acid Eluate: A simple and effective strategy is to dilute the DNA template. This reduces the concentration of the inhibitor relative to the template, though it may also dilute the target of interest, which is a significant concern for low-abundance targets like circulating tumor DNA (ctDNA) [65].
3. Use of Inhibitor-Resistant Polymerase Master Mixes: Specialized master mixes contain engineered polymerases and buffer components that confer resistance to a wide range of inhibitors. These can be particularly valuable when the inhibitor cannot be completely removed or when the sample volume is too small for dilution [65].
4. Incorporation of Internal Controls: Process controls are essential for detecting inhibition. An exogenous internal control (e.g., a synthetic DNA sequence or a virus like MS2) can be spiked into the sample during lysis. Failure to amplify this control indicates the presence of inhibitors in the reaction [65] [68].
Table 1: Common PCR Inhibitors and Mitigation Strategies
| Inhibitor Source | Common Inhibitors | Impact on PCR | Recommended Mitigation Strategy |
|---|---|---|---|
| Blood/Plasma | Heparin, Hemoglobin, IgG | Binds to DNA polymerase, interferes with hybridization | Use of inhibitor-resistant polymerases; optimized plasma-based extraction kits [64] [3] |
| FFPE Tissues | Formalin, Porphyrins | Nucleic acid cross-linking, polymerase inhibition | Dedicated FFPE DNA/RNA kits; increased proteinase K digestion; sample dilution [64] |
| Stool/Bile | Polysaccharides, Bile Salts | Disrupt enzyme activity, precipitate DNA | Specific kits for complex matrices (e.g., PowerSoil Pro); extensive washing steps; dilution [66] [65] [3] |
| Phenol/EDTA | Phenol, EDTA | Denatures enzymes, chelates Mg²⁺ | Ensure complete removal during extraction (e.g., dialysis, chloroform extraction); avoid carryover [64] |
Protocol: Detection and Assessment of PCR Inhibition
Objective: To confirm the absence of inhibitors in a nucleic acid extract using a spike-in control. Materials: Test DNA samples, No Template Control (NTC) water, exogenous control template (e.g., non-human synthetic DNA), primer/probe set for the exogenous control, qPCR master mix.
- Preparation of Control Reaction: Create a control qPCR reaction containing the exogenous control template at a known, low concentration (e.g., 50 copies/µL) in NTC water.
- Preparation of Test Reactions: Spike the same amount of exogenous control template into a dilution of each test DNA sample.
- qPCR Run: Amplify all reactions using the primers/probes for the exogenous control.
- Data Analysis: Compare the Cq values of the control reaction (NTC water + control template) with the test reactions (sample DNA + control template).
- Interpretation: A delay in Cq (ΔCq > 0.5-1.0) in the test reaction compared to the control indicates the presence of PCR inhibitors in the sample DNA [68].
The Challenge of Low Template DNA
The analysis of samples with low concentrations of DNA (less than 100 pg/µL) is a common challenge in cancer research, especially when working with liquid biopsies like plasma, fine-needle aspirates, or single cells [3] [67]. In these low template DNA (LTDNA) samples, stochastic effects can lead to allelic dropout, increased data variability, and false negatives [67].
Consequences of Low Template DNA
- Allelic Dropout: The failure to detect one of two alleles in a heterozygous sample due to the stochastic sampling of a very small number of DNA molecules [67].
- Reduced Reproducibility: Amplification efficiency can vary significantly between replicates due to random sampling effects [67] [63].
- Inaccurate Quantification: Cq values become less reliable for absolute quantification as stochastic effects dominate [64] [67].
Strategies for Enhancing Sensitivity and Reliability
1. Reduced Amplification Volume: Scaling down the total PCR reaction volume from a standard 25 µL to 12 µL, 6 µL, or even 3 µL, while maintaining the concentration of reagents, can improve sensitivity by increasing the effective concentration of the template. Studies have shown that complete genetic profiles can be obtained from low template samples in reduced volumes [67]. The limiting factor is the absolute amount of DNA, not the reaction volume.
2. Increased Amplification Cycles: Raising the number of PCR cycles from 40 to 45-50 can enhance the detection of very rare targets by allowing more rounds of replication. However, this approach also increases the risk of amplifying background noise and non-specific products and is more susceptible to stochastic effects [67].
3. Multiplex Pre-Amplification: A short, multiplexed pre-amplification PCR using a pool of all target gene primers can be performed to generate a higher quantity of template for subsequent, individual qPCR assays. This is particularly useful for analyzing multiple biomarkers from a single, limited sample [63].
4. Digital PCR (dPCR) for Absolute Quantification: For absolute quantification of low-abundance targets, dPCR is often superior to qPCR. By partitioning a sample into thousands of individual reactions, dPCR mitigates the effects of template competition and allows for precise counting of target molecules without the need for a standard curve, making it ideal for analyzing rare mutations in ctDNA [3].
Table 2: Techniques for Low Template DNA (LTDNA) Analysis
| Technique | Principle | Advantages | Limitations |
|---|---|---|---|
| Reduced Volume PCR | Scaling down total reaction volume to increase effective template concentration. | Increased signal intensity; cost-saving on reagents [67]. | Requires precise pipetting; risk of increased dropouts if volume is too low [67]. |
| Increased Cycle Number | Performing additional amplification cycles (e.g., >45) to detect rare targets. | Enhanced sensitivity for very low-copy targets [67]. | Higher risk of non-specific amplification and primer-dimer artifacts [64] [67]. |
| Multiplex Pre-Amplification | A short, targeted pre-PCR to amplify multiple targets simultaneously before qPCR. | Enables analysis of multiple targets from minimal sample [63]. | Requires careful optimization to ensure balanced amplification of all targets. |
| Digital PCR (dPCR) | Absolute quantification via end-point PCR of partitioned samples. | High precision for low-abundance targets; resistant to PCR efficiency variations [3]. | Higher cost per sample; limited dynamic range compared to qPCR. |
Protocol: Optimized qPCR for Low Template DNA Samples
Objective: To reliably detect and quantify target genes in LTDNA samples using a reduced volume approach. Materials: LTDNA samples (e.g., <0.1 ng/µL), validated primer/probe sets, qPCR master mix (e.g., TaqMan), optical plates and seals, real-time PCR instrument.
- Sample and Reagent Preparation: Thaw all reagents and mix gently. Prepare a master mix containing all components except the DNA template. Centrifuge briefly.
- Reaction Assembly: Aliquot the master mix into the wells of an optical plate. For a 6 µL total reaction volume, a typical setup might be: 3 µL of 2x master mix, 0.6 µL of 10x primer/probe mix, and 1.4 µL of DNA template. Include positive controls (with known template) and NTCs.
- qPCR Cycling Conditions: Use standard cycling conditions as recommended by the master mix manufacturer. Do not reduce cycle times despite the smaller volume, as this can affect efficiency.
- Data Analysis and Interpretation: Analyze the amplification curves and Cq values. A significant increase in Cq variability between replicates or allelic dropout is indicative of stochastic effects from LTDNA. Results should be interpreted with caution, and technical replicates are essential [67].
The Challenge of Non-Specific Amplification
Non-specific amplification occurs when primers bind to non-target sequences, leading to the generation of unintended PCR products such as primer-dimers or amplification of homologous genes. This consumes reagents, competes with the target of interest, and results in overestimation of the target quantity and high background fluorescence [64] [69].
- Suboptimal Primer Design: Primers with low melting temperatures (Tm), high self-complementarity, or that span regions with high sequence similarity to homologous genes are a primary cause [69].
- Excessive Primer Concentration: High primer concentrations can promote off-target binding and primer-dimer formation [69].
- Low Annealing Temperature: An annealing temperature that is too low allows primers to bind to sequences with partial complementarity [64] [69].
Strategies for Ensuring Specific Amplification
1. Meticulous, Sequence-Specific Primer Design: For genes with homologs (e.g., in plant or complex cancer genomes), design primers based on single-nucleotide polymorphisms (SNPs) unique to the target sequence. This requires aligning all homologous sequences and placing the 3' end of a primer on a discriminating SNP to ensure specificity [69].
2. Optimization of Annealing Temperature: Perform a temperature gradient qPCR (e.g., from 55°C to 72°C) to determine the highest possible annealing temperature that still yields efficient target amplification. This minimizes off-target binding [64] [69].
3. Optimization of Primer and Template Concentration: Titrate primer concentrations (typically between 50-900 nM) to find the lowest concentration that gives a robust Cq value without non-specific products. Similarly, test a range of cDNA/DNA concentrations to ensure the reaction is within a linear dynamic range [69].
4. Use of Probe-Based Detection: Hydrolysis probes (TaqMan), Molecular Beacons, or Locked Nucleic Acid (LNA) probes add a second layer of specificity beyond the primers. The requirement for both primer binding and probe hybridization dramatically reduces false-positive signals from non-specific amplification or primer-dimers [68].
5. Validation of Amplification Curves and Products: Always analyze the melt curve when using intercalating dyes like SYBR Green. A single, sharp peak indicates a specific product, while multiple peaks suggest primer-dimers or non-specific amplification. Gel electrophoresis can also be used for confirmation [68].
Table 3: Research Reagent Solutions for qPCR Optimization
| Reagent / Kit | Function / Feature | Application Context |
|---|---|---|
| PowerSoil Pro Kit (Qiagen) | DNA extraction optimized for difficult, inhibitor-rich matrices. | Ideal for complex samples like stool or environmental samples used in microbiome-cancer studies [66]. |
| Inhibitor-Resistant Polymerase Mixes | Master mixes with engineered enzymes tolerant to common PCR inhibitors. | Essential for direct analysis of body fluids (e.g., blood, bile) without extensive cleanup [65]. |
| Hydrolysis Probes (TaqMan) | Sequence-specific probes that increase assay specificity and enable multiplexing. | Gold standard for validating specific cancer biomarkers and copy number variations in complex backgrounds [68] [63]. |
| SYBR Green Dye | Fluorescent dye that intercalates non-specifically into double-stranded DNA. | A cost-effective choice for initial assay development and optimization, requiring subsequent melt curve analysis [68]. |
Protocol: Stepwise Optimization of qPCR Assay Specificity
Objective: To develop a specific and efficient qPCR assay for a target cancer biomarker gene. Materials: cDNA or DNA template, designed primer pairs, qPCR master mix (SYBR Green or probe-based), real-time PCR instrument with gradient functionality.
- In Silico Primer Validation: Before testing, use tools like Primer-BLAST to check for off-target binding sites in the relevant genome [69].
- Annealing Temperature Optimization:
- Set up identical qPCR reactions with a single primer pair and template.
- Use the thermal cycler's gradient function to run annealing temperatures across a range (e.g., 58°C to 68°C).
- Select the temperature that yields the lowest Cq with no non-specific amplification (confirmed by melt curve or probe signal).
- Primer Concentration Titration:
- Using the optimal annealing temperature, test a range of primer concentrations (e.g., 100 nM, 300 nM, 500 nM).
- Select the concentration that gives the lowest Cq without increasing background fluorescence or creating primer-dimer peaks in the melt curve.
- Efficiency and Dynamic Range Validation:
Integrated Workflow for Cancer Biomarker Validation
The following workflow integrates the solutions for the discussed challenges into a cohesive protocol for validating DNA methylation biomarkers from liquid biopsies, a key application in cancer research [3].
Successfully navigating the challenges of inhibitors, low template DNA, and non-specific amplification is not merely a technical exercise but a fundamental requirement for generating reliable and clinically actionable data in cancer biomarker research. A systematic approach—incorporating rigorous sample preparation, validated and optimized assay conditions, and appropriate controls—is paramount. By adopting the detailed protocols and strategies outlined in this application note, researchers can significantly enhance the robustness, reproducibility, and translational potential of their qPCR-based findings, ultimately accelerating the development of next-generation cancer diagnostics and therapies.
The validation of cancer biomarkers through real-time PCR (qPCR) demands rigorous optimization of reaction components to ensure data accuracy, reproducibility, and sensitivity. This application note provides a detailed protocol for systematically optimizing three critical parameters: magnesium concentration, primer titration, and master mix selection. Designed within the context of cancer biomarker research, such as DNA methylation analysis and gene expression profiling, this guide aims to equip researchers and drug development professionals with standardized methodologies to enhance the reliability of their qPCR assays in oncology applications.
The accuracy of real-time PCR (qPCR) in cancer biomarker validation is highly dependent on the precise optimization of reaction components. In oncology research, where samples often include challenging templates such as bisulfite-converted DNA for methylation studies or low-abundance transcripts from liquid biopsies, suboptimal reaction conditions can lead to false negatives, reduced sensitivity, and inaccurate quantification. Key components requiring optimization include magnesium ion (Mg²⁺) concentration, a critical cofactor for DNA polymerase activity; primer concentration, which directly influences amplification efficiency and specificity; and the master mix composition, which provides the core enzymatic and buffer system for amplification. This document outlines a stepwise, data-driven approach to optimizing these parameters, providing foundational protocols for research in cancer diagnostics and therapeutic development.
Optimization of Magnesium Chloride Concentration
Background and Role in qPCR
Magnesium chloride (MgCl₂) is an essential cofactor for Taq DNA polymerase activity. Its concentration directly influences enzyme fidelity, primer-template binding stability, PCR efficiency, and DNA melting temperature. In the context of cancer genomics, Mg²⁺ concentration is particularly crucial for amplifying GC-rich promoter regions or bisulfite-converted DNA, where template secondary structure and thermodynamics are altered.
Experimental Protocol for MgCl₂ Titration
Materials:
- Template DNA: Use a standardized, well-characterized DNA sample relevant to your cancer biomarker (e.g., a plasmid control, cell line DNA, or a characterized patient sample).
- Primers: A pre-validated primer set for a control gene (e.g., ACTB).
- MgCl₂ Stock Solution: A sterile, nuclease-free MgCl₂ solution (typically 25 mM or 50 mM).
- 2x Master Mix: Use a master mix that does not contain MgCl₂ or where its concentration can be adjusted.
- Nuclease-free water.
- Real-time PCR instrument.
Method:
- Prepare a MgCl₂ Dilution Series: Create a series of MgCl₂ concentrations. A recommended range is 1.0 mM to 5.0 mM in 0.5 mM increments [70].
- Set Up Reactions: For each MgCl₂ concentration to be tested, prepare a 25 µL reaction mix as follows:
- 12.5 µL of 2x Master Mix (without MgCl₂)
- X µL of MgCl₂ stock solution (variable volume to achieve desired final concentration)
- Forward and Reverse Primer (final concentration 0.2 µM each for initial test)
- Template DNA (e.g., 10-50 ng of genomic DNA)
- Nuclease-free water to 25 µL
- Run qPCR Program: Use a standard cycling protocol, for example:
- Initial Denaturation: 95°C for 10 min
- 40-45 Cycles: 95°C for 15 sec, 60°C for 60 sec (with fluorescence acquisition)
- Melt Curve Analysis: 60°C to 95°C (if using SYBR Green chemistry)
- Replication: Perform all reactions in triplicate to ensure statistical robustness.
Data Analysis and Interpretation
The optimal MgCl₂ concentration is identified by evaluating two key parameters: the lowest Cq value (indicating highest efficiency) and the highest fluorescence amplitude (indicating high yield). Analysis of the melt curve is critical for SYBR Green assays to ensure a single, specific amplicon without primer-dimers.
Table 1: Example Data from MgCl₂ Titration for a GC-Rich Oncogene Amplification
| MgCl₂ Concentration (mM) | Mean Cq | ΔRFU (Fluorescence) | Melt Curve Peak | Remarks |
|---|---|---|---|---|
| 1.5 | 28.5 | 450 | Single, sharp | Low fluorescence |
| 2.0 | 25.1 | 1250 | Single, sharp | Optimal |
| 2.5 | 24.9 | 1200 | Single, sharp | Near optimal |
| 3.0 | 25.0 | 1150 | Single, sharp | Acceptable |
| 3.5 | 25.3 | 1050 | Minor shoulder | Slight non-specificity |
| 4.0 | 26.0 | 800 | Multiple peaks | Significant non-specificity |
Meta-analyses have demonstrated a logarithmic relationship between MgCl₂ concentration and DNA melting temperature, with increments of 0.5 mM consistently raising the melting temperature and impacting reaction efficiency, particularly within the 1.5–3.0 mM range [70].
Primer Titration for Specific Amplification
Background and Principles
Optimal primer concentration is paramount for specific and efficient amplification, minimizing the formation of primer-dimers and non-specific products. This is especially critical in multiplex qPCR assays for cancer gene expression panels or when detecting low-frequency mutations against a high wild-type background.
Experimental Protocol for Primer Titration
Materials:
- Optimized MgCl₂ concentration (as determined in Section 2).
- Template DNA (same as used in MgCl₂ optimization).
- Primer pair(s) of interest.
- 2x Master Mix (with optimized Mg²⁺).
- Nuclease-free water.
Method:
- Design Primer Pairs: For cancer biomarker research, primer design must account for homologous gene sequences. Design primers based on single-nucleotide polymorphisms (SNPs) unique to the target gene to ensure specificity against homologous sequences [69]. For DNA methylation analysis (e.g., qMSP), primers must be designed for the bisulfite-converted sequence.
- Prepare Primer Concentration Matrix: Test a matrix of forward and reverse primer concentrations. A common starting range is 50 nM to 900 nM.
- Example Setup: Test forward/reverse combinations: 50/50 nM, 50/300 nM, 300/50 nM, 300/300 nM, 300/900 nM, 900/300 nM, 900/900 nM.
- Set Up Reactions: For each primer combination, prepare a 25 µL reaction mix:
- 12.5 µL of 2x Master Mix (with optimized Mg²⁺)
- X µL of Forward Primer (variable concentration)
- Y µL of Reverse Primer (variable concentration)
- Template DNA
- Nuclease-free water to 25 µL
- Run qPCR Program: Use the same cycling protocol and melt curve analysis as in Section 2.2.
- Replication: Perform all reactions in triplicate.
Data Analysis and Interpretation
The optimal primer concentration combination yields the lowest Cq with the highest fluorescence (ΔRFU) and a single, sharp peak in the melt curve. A significant imbalance between forward and reverse primer concentrations can be tolerated and may sometimes improve specificity for difficult amplicons.
Table 2: Example Data from Primer Titration for a Tumor Suppressor Gene
| Forward Primer (nM) | Reverse Primer (nM) | Mean Cq | ΔRFU | Melt Curve Peak | Efficiency (R²) | Remarks |
|---|---|---|---|---|---|---|
| 50 | 50 | 27.5 | 800 | Single | 0.985 | Good efficiency, low yield |
| 50 | 300 | 26.8 | 950 | Single | 0.990 | Improved |
| 300 | 50 | 26.9 | 930 | Single | 0.988 | Improved |
| 300 | 300 | 25.2 | 1500 | Single | 0.998 | Optimal |
| 300 | 900 | 25.1 | 1450 | Single | 0.995 | Near optimal |
| 900 | 900 | 25.3 | 1400 | Minor shoulder | 0.980 | Slight non-specificity |
The goal is to achieve an amplification efficiency (E) of 100% ± 5% (corresponding to a slope of -3.1 to -3.6 in a standard curve) with an R² value ≥ 0.9999 for the most precise quantitative work [69].
Master Mix Selection and Validation
Background and Components
The master mix is the pre-mixed solution containing the core components for qPCR, including buffer, dNTPs, DNA polymerase, and often MgCl₂. Selection depends on the detection chemistry (e.g., SYBR Green, TaqMan, etc.), template type, and required sensitivity, especially for detecting rare mutations or low-level methylation in liquid biopsy samples.
Key Selection Criteria
- Polymerase Type: Hot-start Taq polymerase is essential to prevent non-specific amplification and primer-dimer formation during reaction setup by inhibiting polymerase activity at room temperature [71].
- MgCl₂ Provision: Determine if the master mix contains a pre-optimized, fixed concentration of MgCl₂ (e.g., 3.5 mM final is common) or if it is supplied separately for user optimization [71].
- Detection Chemistry Compatibility: Ensure the master mix is formulated for your chosen chemistry.
- SYBR Green: Contains a fluorescent DNA-intercalating dye.
- TaqMan/Probe-Based: Must be compatible with hydrolysis probes. Some master mixes are optimized for this use with additives that enhance probe cleavage efficiency.
- Inhibitor Resistance: For clinical samples like FFPE tissues or plasma-derived DNA, select master mixes that include additives to enhance resistance to common PCR inhibitors.
- Dye and Reference Standard: The mix should contain a passive reference dye (like ROX) if required by the real-time PCR instrument for signal normalization [71].
Protocol for Master Mix Comparison
Method:
- Select Candidate Master Mixes: Choose 2-3 different master mixes from leading manufacturers for comparison. Include one that is specifically marketed as "hot-start" and one optimized for probe-based detection if applicable.
- Standardize Reaction Conditions: Using the optimized MgCl₂ concentration and optimized primer concentrations determined in previous sections, set up identical qPCR reactions differing only in the master mix used.
- Run qPCR and Analyze: Use the standard cycling protocol. Evaluate the mixes based on:
- Amplification Efficiency (from a standard curve).
- Sensitivity (Cq value for a low-copy-number template).
- Specificity (melt curve for SYBR Green, or ΔRn for probes).
- Reproducibility (standard deviation of Cq across replicates).
Table 3: Comparison of Master Mix Performance for Methylated SHOX2 Detection [72]
| Master Mix Feature | Mix A (Standard SYBR) | Mix B (Hot-Start Probe) | Mix C (Inhibitor Resistant) |
|---|---|---|---|
| Polymerase Type | Standard Taq | Antibody-mediated Hot-Start | Chemically modified Hot-Start |
| MgCl₂ (Final) | 3.5 mM (fixed) | Provided separately | 4.0 mM (fixed) |
| Cq at LOD (0.01%) | Not Detected | 34.5 | 35.1 |
| Amplification Efficiency | N/A | 98% | 95% |
| Remarks | Failed at low target | Optimal sensitivity | Good sensitivity |
Integrated Workflow for Cancer Biomarker Assay Development
The following workflow integrates the optimization steps into a coherent pipeline for developing a qPCR assay, for example, to detect a methylated DNA cancer biomarker in plasma.
The Scientist's Toolkit: Research Reagent Solutions
Table 4: Essential Reagents for qPCR Optimization in Cancer Biomarker Research
| Reagent / Tool | Function / Principle | Application Note |
|---|---|---|
| Hot-Start Taq DNA Polymerase | Remains inactive until high temperature is applied, preventing non-specific amplification and primer-dimer formation during reaction setup [71]. | Critical for sensitive detection of low-abundance targets in a background of wild-type DNA, such as in liquid biopsy analysis. |
| dNTPs (with dUTP) | Deoxyribonucleotide triphosphates (dATP, dCTP, dGTP, dTTP) are the building blocks for DNA synthesis. Using dUTP in place of dTTP allows subsequent UNG treatment to degrade carryover contamination [71]. | Standard in pre-mixed master mixes. Essential for high-throughput clinical labs to prevent false positives. |
| Bisulfite Conversion Kit | Chemically converts unmethylated cytosine to uracil, while leaving methylated cytosine unchanged, enabling methylation-specific PCR (qMSP) [73] [72]. | Foundational for analyzing DNA methylation biomarkers in cancer (e.g., SHOX2 in lung cancer [72]). Column-based and magnetic bead-based kits are available. |
| TaqMan Mutation Detection Assays | Allele-specific PCR assays that use a primer and a MGB blocker oligonucleotide to suppress wild-type amplification, enabling highly specific detection of somatic mutations [74]. | Validated for use with gDNA from FFPE tissues, fresh frozen tissues, and cell lines. Ideal for detecting known oncogenic mutations (e.g., in KRAS, EGFR). |
| Internal Positive Control (IPC) Reagents | An exogenous DNA sequence and corresponding primers/probes that can be multiplexed with the target assay to distinguish true target negatives from PCR failure due to inhibition [74]. | Crucial for validating negative results in clinical sample testing, especially when sample quality is variable (e.g., FFPE DNA). |
| Standard DNA Calibrators | Synthetic DNA fragments of known concentration and methylation status (methylated vs. unmethylated) used to generate standard curves and determine the limit of detection (LOD) [72]. | Vital for absolute quantification and for validating the sensitivity of assays designed to detect rare alleles or low levels of methylation. |
In the field of cancer biomarker validation research, the precision of real-time PCR (qPCR) and digital PCR (dPCR) outcomes is fundamentally constrained by the quality of the DNA template. The reliability of these results directly influences critical decisions in diagnostic, prognostic, and therapeutic development. For liquid biopsies—a minimally invasive source of circulating tumor DNA (ctDNA)—this challenge is particularly acute. The rapid clearance of cell-free DNA (cfDNA), with half-lives ranging from minutes to a few hours, and the exceptionally low concentration of tumor-derived material against a background of normal DNA create an environment where template integrity and purity are paramount [3]. Even the most meticulously designed PCR assay cannot compensate for a degraded or contaminated sample. This document outlines essential protocols and application notes for the rigorous assessment of DNA quality, ensuring that downstream qPCR and dPCR analyses for cancer biomarker validation yield reliable, reproducible, and clinically actionable data.
Quantitative Assessment of DNA Quality
The initial quantification and qualification of DNA are critical first steps in evaluating template quality. The following parameters provide a comprehensive snapshot of nucleic acid integrity and purity, which are predictive of PCR performance.
Table 1: Key Metrics for DNA Quality Assessment
| Metric | Description | Ideal Value/Ratio | Measurement Technology | Implication for PCR |
|---|---|---|---|---|
| Concentration | Amount of DNA per unit volume. | Varies by application | Fluorometry (e.g., Qubit) | Ensures optimal template input; prevents inhibition or poor yield [75]. |
| A260/A280 Ratio | Purity assessment for protein contamination. | ~1.8 for pure DNA | UV Spectrophotometry (e.g., NanoDrop) | Ratios significantly lower than 1.8 may indicate protein contamination that can inhibit polymerase [66]. |
| A260/A230 Ratio | Purity assessment for salt or solvent contamination. | >2.0 | UV Spectrophotometry | Low ratios suggest chaotropic salt or phenol carryover from extraction, which can severely inhibit PCR [66]. |
| Fragment Size | Integrity and degree of degradation. | Distinct high-molecular-weight band. | Capillary Electrophoresis (e.g., Bioanalyzer, TapeStation) | Degraded DNA (smear on electropherogram) leads to preferential amplification of shorter fragments and biased quantification [3]. |
For liquid biopsy analysis, the Fragment Size metric is especially crucial. Research indicates that methylated DNA fragments, often the target of epigenetic cancer biomarker assays, exhibit relative enrichment in the cfDNA pool due to nucleosome interactions that protect them from nuclease degradation [3]. Therefore, assessing the fragment size distribution is not merely a quality check but a potential source of biological information.
Experimental Protocols for DNA Quality Control
Protocol: Integrity Analysis of Genomic DNA via Agarose Gel Electrophoresis
This protocol provides a rapid, cost-effective method for visualizing the integrity of high-quality genomic DNA, such as that extracted from formalin-fixed paraffin-embedded (FFPE) tissue sections or cell lines used in model system development.
Materials:
- DNA sample
- High Molecular Weight DNA Standard (e.g., Lambda DNA-Hind III digest)
- Agarose (Molecular Biology Grade)
- 1X TAE Buffer (Tris-acetate-EDTA)
- DNA Gel Stain (e.g., SYBR Safe, Ethidium Bromide)
- Gel Loading Dye (6X)
- Electrophoresis chamber and power supply
- UV Transilluminator or Gel Documentation System
Method:
- Prepare a 0.8-1.0% agarose gel by dissolving the agarose in 1X TAE buffer. Microwave until completely dissolved. Cool to approximately 55°C, add the DNA stain, and pour into a gel casting tray with a comb.
- Allow the gel to solidify completely at room temperature for at least 30 minutes.
- Prepare DNA samples by mixing 1 µL of 6X loading dye with 5 µL of DNA (50-100 ng). Include a well for the DNA standard.
- Load the samples and standard into the wells. Run the gel at 5-8 V/cm distance between electrodes until the dye front has migrated 70-80% of the gel length.
- Visualize the gel using a UV transilluminator. Intact genomic DNA should appear as a single, tight high-molecular-weight band with minimal smearing downward. A visible smear indicates degradation.
Protocol: Quality Control for Liquid Biopsy-Derived cfDNA
This protocol is tailored for the low-concentration, fragmented nature of cfDNA from plasma, urine, or other bodily fluids, utilizing high-sensitivity instrumentation.
Materials:
- Eluted cfDNA sample (typically 5-20 µL)
- High Sensitivity DNA Kit (e.g., Agilent Bioanalyzer HS DNA Kit or equivalent for Fragment Analyzer/TapeStation)
- Nuclease-Free Water
Method:
- Follow the manufacturer's instructions for the high-sensitivity DNA assay precisely. This typically involves priming the chip or plate, loading gel-dye mix, and loading samples and standards.
- Pipette 1 µL of the provided DNA ladder into the designated well.
- Pipette 1 µL of each cfDNA sample into separate sample wells.
- Place the chip or plate on the appropriate vortexer and run the analysis program on the instrument.
- Interpret the results. A high-quality plasma cfDNA sample from a healthy individual will show a dominant peak at approximately 167 bp, corresponding to mononucleosomal DNA. Deviations, such as a shift to longer fragments or a "ladder" pattern, can indicate cellular contamination or specific disease states like cancer [3]. The DV200 value (percentage of fragments >200 bp) is a useful quantitative metric for integrity.
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Reagents for DNA Quality Control and qPCR
| Item | Function | Key Consideration |
|---|---|---|
| Fluorometric DNA Quantitation Kits (e.g., Qubit dsDNA HS) | Highly specific, dye-based quantitation of double-stranded DNA. | Superior to spectrophotometry for low-concentration samples; ignores RNA and nucleotides [66]. |
| High-Sensitivity DNA Analysis Kits (e.g., Bioanalyzer HS) | Capillary electrophoresis for sizing and quantifying fragmented DNA. | Essential for analyzing cfDNA from liquid biopsies; provides critical fragment size data [3]. |
| Silica-Membrane Spin Columns (e.g., in many commercial kits) | Purification of DNA from complex matrices (tissue, biofluids). | Efficiently removes PCR inhibitors like salts and proteins; ensures high A260/A280 ratios [66]. |
| Magnetic Bead-Based Kits | Scalable, automatable nucleic acid purification. | Ideal for high-throughput settings; effective for a wide variety of sample inputs. |
| Probe-Based qPCR Master Mix (e.g., TaqMan Universal MM II) | Provides reagents for robust, specific amplification in qPCR. | Contains DNA polymerase, dNTPs, and optimized buffer. Probe-based chemistry offers superior specificity over intercalating dyes for complex samples [75]. |
| DNA Integrity-Specific qPCR Assays | Multi-copy gene assays that amplify long and short targets. | A ratio of long/short amplicon quantities (DIN-like metric) provides a functional measure of DNA integrity. |
Workflow and Impact of Template Quality
The process from sample collection to data interpretation is a chain where template quality is a foundational link. The following diagram illustrates the critical steps and decision points.
As shown, the failure to meet quality standards leads directly to unreliable data. In the context of cancer biomarkers, this can manifest as:
- False Negatives: Degraded DNA or the presence of PCR inhibitors can prevent the detection of low-abundance ctDNA targets, leading to incorrect assessments of minimal residual disease or treatment response [3].
- Quantitative Bias: Degraded DNA samples can cause preferential amplification of shorter fragments, skewing the quantification of biomarker copy numbers and leading to inaccurate estimates of tumor burden [75] [3].
In cancer biomarker research, the adage "garbage in, garbage out" holds profound significance. The validation of biomarkers using qPCR and dPCR is an exercise in detecting a faint signal against a noisy background. The quality of the DNA template is the primary factor that determines the signal-to-noise ratio. By implementing the rigorous quality assessment protocols and utilizing the recommended tools outlined in this document, researchers can safeguard the integrity of their data. A disciplined focus on DNA quality control is not merely a preliminary step but a continuous and non-negotiable practice that underpins the entire workflow, from the liquid biopsy tube to the final amplification plot, ensuring that research findings are robust, reproducible, and ultimately, translatable to clinical impact.
The accurate validation of cancer biomarkers using real-time quantitative PCR (qPCR) is frequently challenged by the complex nature of clinical samples. These challenges are particularly evident when working with difficult DNA templates derived from liquid biopsies, formalin-fixed paraffin-embedded (FFPE) tissues, or samples with low tumor cellularity. Such templates often exhibit high GC-content, secondary structures, and the presence of PCR inhibitors, which collectively promote nonspecific amplification, reduce target yield, and compromise assay reproducibility. For biomarker research requiring high precision—such as minimal residual disease (MRD) detection in leukemia or quantification of low-abundance transcripts from circulating tumor cells—these limitations present significant barriers to reliable data generation.
Hot-start PCR technology and strategic use of PCR additives represent powerful approaches to overcome these challenges. Hot-start methods prevent DNA polymerase activity during reaction setup, thereby reducing primer-dimer formation and nonspecific amplification that can deplete reagents and generate false-positive signals. When combined with optimized concentrations of additives like dimethyl sulfoxide (DMSO) and bovine serum albumin (BSA), researchers can achieve significantly improved amplification efficiency, specificity, and sensitivity for even the most challenging templates encountered in cancer biomarker validation.
Hot-Start PCR: Mechanisms and Implementation
Principles and Benefits of Hot-Start Technology
In conventional PCR, DNA polymerases exhibit residual activity at room temperature, allowing primers to bind nonspecifically to DNA templates or to each other during reaction setup. This leads to the extension of misprimed sequences and the formation of primer-dimers, which consume reaction components and compete with amplification of the desired target. The consequences are particularly detrimental in quantitative applications, where such artifacts can drastically reduce the yield of specific amplicons, lower detection sensitivity, and produce unreliable results that compromise downstream analysis.
Hot-start PCR addresses these limitations by employing various mechanisms to inhibit DNA polymerase activity at lower temperatures, preventing amplification until the reaction reaches stringent conditions during the initial denaturation step. This simple yet powerful modification offers several critical benefits for cancer biomarker research:
- Prevents mispriming by blocking extension of primers bound to template sequences with low homology
- Reduces primer-dimer formation during reaction setup on the bench or automated platforms
- Increases sensitivity and yield of target fragments, crucial for detecting low-abundance biomarkers
- Enables room-temperature setup without compromising specificity, facilitating high-throughput applications [76]
Comparison of Hot-Start Activation Methods
Various hot-start activation methods have been developed, each with distinct mechanisms, advantages, and considerations for research use. The selection of an appropriate hot-start method depends on experimental requirements, including target length, detection sensitivity, and compatibility with downstream applications. The table below summarizes the key characteristics of the most common hot-start technologies:
Table 1: Comparison of Major Hot-Start PCR Technologies
| Hot-Start Technology | Mechanism of Action | Activation Requirements | Key Benefits | Potential Limitations |
|---|---|---|---|---|
| Antibody-based | Antibody binds polymerase active site | Initial denaturation (95°C, 2-10 min) | Short activation time; full enzyme activity restored; features similar to native polymerase | Animal-origin components; higher exogenous protein content [76] |
| Chemical modification | Covalent chemical groups block activity | Extended activation (95°C, 10-12 min) | Stringent inhibition; free of animal-origin components | Longer activation time; may affect long targets (>3 kb) [76] |
| Affibody-based | Alpha-helical peptides block active site | Initial denaturation (95°C, 2-10 min) | Less exogenous protein; animal-origin free; short activation | Potentially less stringent; limited benchtop stability [76] |
| Aptamer-based | Oligonucleotides bind polymerase | Initial denaturation (95°C, 2-10 min) | Short activation; animal-origin free | May be less stringent; reversible activation; not ideal for low-Tm primers [76] |
| Primer-based | Thermolabile groups block primer extension | Elevated temperatures | Targeted inhibition; flexible design | Requires modified primer synthesis [77] |
| Physical separation | Wax barriers separate components | Wax melting (~70°C) | Compatible with various polymerases; simple formulation | Less convenient for high-throughput setups [78] |
Implementation Guidelines for Hot-Start PCR
Successful implementation of hot-start PCR in biomarker validation requires attention to several technical considerations. The following workflow illustrates the decision process for selecting and optimizing hot-start methods:
Protocol: Standard Hot-Start PCR Setup for Biomarker Assays
Reaction Setup:
- Prepare master mix on ice with the following components:
- 1X PCR Buffer (provided with enzyme)
- 0.2 mM each dNTP
- 0.3-1.0 µM forward and reverse primers
- 1-2 units hot-start DNA polymerase
- 5-50 ng template DNA (adjust based on template complexity)
- Nuclease-free water to final volume
Add template DNA last to minimize potential contamination.
If using antibody-based, Affibody-based, or aptamer-based hot-start enzymes, proceed directly to thermal cycling. For chemically modified enzymes, extend initial activation time.
Thermal Cycling Parameters:
- Initial activation: 95°C for 2-10 minutes (duration depends on hot-start method)
- Denaturation: 95°C for 15-30 seconds
- Annealing: Primer-specific temperature (55-68°C) for 15-30 seconds
- Extension: 72°C for 30-60 seconds per kb
- Number of cycles: 35-40
- Final extension: 72°C for 5-10 minutes
Critical Considerations:
- Maintain reactions on ice until thermal cycling begins
- Avoid prolonged benchtop incubation, especially with Affibody or aptamer-based methods
- For high-throughput applications, validate room temperature stability
- For long targets (>3 kb), prefer antibody-based over chemically modified hot-start methods [76]
PCR Additives for Difficult Templates
Mechanism of Action and Synergistic Effects
PCR additives enhance amplification of difficult templates through diverse biochemical mechanisms. DMSO reduces secondary structure formation in GC-rich regions by interfering with hydrogen bonding and lowering the melting temperature of DNA, facilitating strand separation during denaturation steps. Formamide further destabilizes DNA duplexes through similar mechanisms, though with a narrower effective concentration range. BSA functions as a stabilizer that binds inhibitors potentially present in clinical samples while also enhancing polymerase thermal stability.
Recent research has revealed that BSA acts as a powerful co-enhancer when used in combination with organic solvents. Studies demonstrate that BSA significantly increases PCR amplification yields of GC-rich DNA targets ranging from 0.4 kb to 7.1 kb when used as a co-additive along with DMSO or formamide. The enhancing effects of BSA occur primarily in the initial PCR cycles, with BSA additions producing no detrimental impact on PCR yield or specificity [79].
Optimization Strategies for Additive Combinations
The synergistic effect between BSA and organic solvents enables researchers to achieve high PCR yields while reducing the concentration of solvent required. This is particularly beneficial for sensitive downstream applications such as sequencing or cloning, where high organic solvent concentrations may have negative effects. The table below provides optimized concentration ranges for individual and combined additives:
Table 2: Optimization Guide for PCR Additives with Difficult Templates
| Additive | Common Working Concentration | Effective Range | Template Applications | Considerations |
|---|---|---|---|---|
| DMSO | 5% (v/v) | 1.25-10% | GC-rich targets (>60% GC); long amplicons | Can decrease specificity at high concentrations; reduces Taq activity by ~50% at 10% |
| Formamide | 2.5% (v/v) | 1.25-5% | GC-rich targets up to ~2.5 kb | Narrow effective range; effectiveness drops above 5% |
| BSA | 0.2-0.5 µg/µL | 0.1-1.0 µg/µL | Inhibitor-containing samples; GC-rich templates | Enhances effects of organic solvents; higher concentrations needed for longer fragments |
| BSA + DMSO | 0.5 µg/µL + 5% | BSA: 0.1-1.0 µg/µLDMSO: 2.5-7.5% | Broad size range GC-rich templates; complex clinical samples | Synergistic effect allows lower DMSO concentrations; improves yield in early cycles |
| BSA + Formamide | 0.5 µg/µL + 2.5% | BSA: 0.1-1.0 µg/µLFormamide: 1.25-5% | GC-rich templates <2.5 kb | Broadens effective formamide range; improves yield |
Protocol: Systematic Optimization of Additives for Challenging Templates
This protocol employs a strategic approach to optimize additive combinations for difficult templates, particularly relevant to GC-rich cancer biomarker targets:
Step 1: Initial Assessment
- Set up a base reaction without additives using optimal primer design and cycling conditions.
- If amplification is inefficient or nonspecific, proceed with additive optimization.
Step 2: Single Additive Screening
- Prepare separate reaction series with varying concentrations of individual additives:
- DMSO: 0%, 1.25%, 2.5%, 5%, 7.5%, 10%
- Formamide: 0%, 1.25%, 2.5%, 5%
- BSA: 0, 0.1, 0.2, 0.5, 1.0 µg/µL
- Assess amplification efficiency and specificity for each condition.
Step 3: Combination Optimization
- Based on single additive results, test synergistic combinations:
- BSA (0.5 µg/µL) + DMSO (2.5%, 5%, 7.5%)
- BSA (0.5 µg/µL) + formamide (1.25%, 2.5%)
- Include a control with organic solvent alone for comparison.
Step 4: Validation with Clinical Samples
- Test optimal additive conditions with clinical samples (e.g., FFPE-derived DNA, liquid biopsy samples).
- Verify that enhancement occurs in initial PCR cycles, as BSA's effects are most pronounced early in amplification [79].
Technical Notes:
- BSA enhancing effects increase with DNA fragment size up to a maximum concentration of 1.0 µg/µL
- For templates >2.5 kb, prefer DMSO over formamide as the organic solvent component
- BSA may become denatured over multiple cycles; for exceptionally long amplifications, consider supplementing with fresh BSA after 10 cycles
Integrated Workflow for Cancer Biomarker Validation
Application to Real-Time PCR in Cancer Research
The combination of hot-start PCR and optimized additives provides particular value in cancer biomarker validation, where reproducibility and sensitivity are paramount. In minimal residual disease (MRD) detection using patient-specific allele-specific oligonucleotide real-time quantitative PCR (ASO-qPCR), assay sensitivity reaching 1.8-4.8 tumor cells among 100,000 leukocytes has been demonstrated through rigorous standardization [33]. Such exceptional sensitivity demands minimization of nonspecific amplification, making integrated PCR enhancement essential.
For liquid biopsy applications utilizing circulating tumor DNA (ctDNA), template quality and quantity present additional challenges. ctDNA is highly fragmented and typically represents a small fraction (<1%) of total cell-free DNA in early-stage cancers. The workflow below illustrates how hot-start methods and additives can be integrated into a comprehensive biomarker validation pipeline:
Research Reagent Solutions for PCR Enhancement
Successful implementation of these advanced PCR techniques requires access to high-quality reagents specifically designed to address challenges in cancer biomarker research. The following table catalogues essential reagent solutions:
Table 3: Research Reagent Solutions for Enhanced PCR in Biomarker Validation
| Reagent Category | Specific Product Examples | Primary Function | Application Context |
|---|---|---|---|
| Hot-Start DNA Polymerases | Platinum Taq DNA Polymerase, DreamTaq Hot Start DNA Polymerase [76] | Antibody-mediated inhibition; rapid activation | Standard biomarker assays; high-throughput applications |
| Enhanced Specificity Enzymes | Phire Hot Start II DNA Polymerase, Platinum SuperFi II DNA Polymerase [76] | Affibody/antibody inhibition; high fidelity | Complex templates; cloning applications |
| Chemical Hot-Start Enzymes | AmpliTaq Gold DNA Polymerase [76] | Chemical modification; stringent inhibition | Applications requiring minimal pre-amplification activity |
| PCR Additives | Molecular biology-grade DMSO, acetylated BSA [79] | Secondary structure reduction; inhibitor binding | GC-rich templates; inhibitor-containing clinical samples |
| Specialized dNTPs | dUTP (with UDG treatment) [80] | Carryover contamination prevention | High-sensitivity clinical assays; regulated environments |
| Optimized Buffer Systems | Commercial PCR buffers with MgCl₂ | Cofactor provision; reaction stabilization | Standardized assay conditions; kit development |
The integration of hot-start PCR methodologies with strategically optimized additive combinations represents a powerful approach for overcoming the formidable challenges associated with difficult templates in cancer biomarker research. The implementation guidelines and protocols presented here provide researchers with a systematic framework for enhancing assay specificity, sensitivity, and reproducibility—critical factors in the translation of PCR-based biomarkers from research tools to clinical applications. As precision medicine continues to evolve, with increasing reliance on liquid biopsies and complex clinical samples, these advanced PCR techniques will play an indispensable role in unlocking the full potential of molecular biomarkers for cancer diagnosis, prognosis, and therapeutic monitoring.
The reliability of real-time quantitative PCR (qPCR) and reverse transcription qPCR (RT-qPCR) data is paramount in cancer biomarker validation research, where findings directly influence diagnostic assays and therapeutic target identification. In the context of liquid biopsies for cancer detection—a rapidly advancing field—DNA methylation biomarkers and gene expression signatures show significant promise [3] [6]. However, the successful translation of these discoveries from research to clinical practice is often hampered by a lack of rigorous, standardized quality control (QC) practices. This document details the essential QC procedures of incorporating controls and standard curves, which serve as the foundation for generating accurate, reproducible, and reliable quantification data in real-time PCR experiments, specifically framed within a cancer research setting.
The Critical Role of Standard Curves
Purpose and Importance
The standard curve is a cornerstone of quantitative PCR, enabling the conversion of the Cycle threshold (Ct) value into a meaningful quantitative measure, such as copy number or concentration. It is vital for assessing the efficiency (E) of the amplification reaction, a critical parameter indicating the rate at which a PCR amplicon is generated during each cycle [81]. In cancer biomarker studies, for instance when validating a prognostic gene signature, an accurate standard curve ensures that observed expression differences in genes like TIMP1 in colorectal cancer are biologically relevant and not artifacts of an inefficient assay [6].
Construction and Workflow
A standard curve is generated by performing qPCR on a series of serial dilutions of a target molecule of known concentration [81]. The workflow involves:
- Preparation of Standard Dilutions: A stock solution with a known concentration (e.g., copy number/µL) is serially diluted, typically in 10-fold increments, to create a concentration gradient.
- qPCR Amplification: The diluted standards are amplified in the qPCR instrument, ideally using three technical replicates per dilution to account for technical variability.
- Data Plotting and Analysis: The average Ct value for each standard is plotted against the logarithm of its initial concentration. A linear regression line is fitted to the data points, characterized by its slope and correlation coefficient (R²).
The following diagram illustrates the experimental workflow for creating and using a standard curve.
Key Quantitative Parameters from Standard Curves
The linear regression of the standard curve provides two key parameters essential for QC.
- Slope: The slope of the line is used to calculate the PCR efficiency using the formula: Efficiency (%) = (10^(-1/slope) - 1) × 100 [81].
- R² (Coefficient of Determination): This value indicates how well the data points fit the linear regression line. An R² value ≥ 0.99 is generally considered excellent, demonstrating high reproducibility across the dilution series [81].
The table below summarizes the interpretation of these key parameters:
Table 1: Interpretation of Standard Curve Parameters
| Parameter | Ideal Value | Acceptable Range | Interpretation |
|---|---|---|---|
| Amplification Efficiency (E) | 100% | 90–110% [81] | Reaction is optimal. Lower values indicate inhibition; higher values may suggest pipetting errors or inhibitor presence. |
| Slope | -3.32 | -3.1 to -3.6 [81] | Directly correlates with efficiency. A slope of -3.32 equals 100% efficiency. |
| R² | 1.000 | ≥ 0.990 [81] | Indicates high precision and linearity across the dynamic range. |
Addressing Variability in Standard Curves
Recent studies underscore the necessity of including a standard curve in every experimental run to ensure data accuracy. Research on virus quantification found significant inter-assay variability in standard curve efficiency and slope, even when using the same synthetic RNA standards and protocols [82]. For example, one study observed efficiency rates above 90% but noted heterogeneity between different viral targets; norovirus GII showed high inter-assay variability, while a SARS-CoV-2 target (N2 gene) showed the largest variability in Ct values (CV 4.38–4.99%) and the lowest efficiency (90.97%) [82]. This variability can be attributed to factors like the reverse transcription step, reagent quality, and pipetting inconsistencies. Consequently, relying on a single, historical standard curve or a "master curve" for subsequent experiments is not recommended, as it can compromise the reliability of quantitative results [82].
Essential Experimental Controls
Beyond standard curves, incorporating appropriate controls is non-negotiable for robust QC. They are critical for controlling the analytical specificity of assays designed to detect cancer-specific mutations or methylation patterns [3].
Types of Controls and Their Functions
Table 2: Types of Essential qPCR Controls
| Control Type | Function | Required For | Interpretation of Result |
|---|---|---|---|
| No-Template Control (NTC) | Detects contamination in reagents or environmental carryover. | Every run, every assay. | Amplification in NTC indicates contamination. |
| Positive Amplification Control | Verifies that all reagents are functioning correctly and the reaction conditions support amplification. | Every run. | Failure indicates issues with reagents, cycling conditions, or instrument. |
| Negative Biological Control | (e.g., healthy donor sample, non-target tissue). Establishes the baseline for non-specific signal or background noise. | Assay development and validation. | Amplification suggests lack of assay specificity. |
| Endogenous Control | A consistently expressed reference gene for RNA/DNA input normalization. | Every sample in gene expression or DNA quantification studies. | Ensures quantification is not biased by variations in sample quality or loading. |
Statistical Analysis for Robust Quantification
Proper statistical treatment of qPCR data is required to derive confident biological conclusions, especially when differentiating between patient groups in cancer studies.
Relative Quantification: The ΔΔCt Method
For most gene expression studies in cancer research (e.g., comparing tumor vs. normal tissue), relative quantification is sufficient. The Livak method (2^(-ΔΔCt)) is a widely used approach that relies on a stable endogenous control gene for normalization [83] [81]. This method assumes the amplification efficiencies of the target and reference genes are approximately equal and close to 100% [81].
The workflow for this method is as follows:
Advanced Statistical Models
For situations where PCR efficiency is not optimal or precisely known, more complex models are recommended. Multiple regression and Analysis of Covariance (ANCOVA) models have been developed which treat Ct as the dependent variable and can directly account for the effects of experimental factors like treatment group and cDNA concentration, providing confidence intervals and statistical significance for expression ratios [83].
Instrument Calibration and Quality Control
The qPCR instrument itself is a source of technical variance that must be controlled. Regular calibration is crucial because factors like edge effects (temperature and optical inhomogeneity across the sample block) can exponentially amplify small well-to-well differences, adversely affecting Ct values and melting curve analysis [84].
Physical Calibration Devices
Traditional calibration relies on biochemical standard substances, which are subject to degradation and pipetting errors. Emerging solutions involve integrated physics-based calibration devices that use temperature acquisition modules and calibrated LEDs to simulate the entire qPCR amplification process [84]. These devices can simulate standard curves by outputting fluorescence signals in response to temperature changes, allowing for comprehensive calibration of temperature and optical parameters without the variability of wet reagents [84]. This provides a more reliable and traceable method for the periodic quality control of qPCR instruments, ensuring data integrity in longitudinal cancer studies.
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Reagents and Kits for qPCR QC
| Item | Function/Benefit | Example Application |
|---|---|---|
| One-Step RT-qPCR Kits | Combine reverse transcription and PCR in a single tube, reducing hands-on time and cross-contamination risk. | High-throughput screening of candidate biomarkers. |
| Two-Step RT-qPCR Reagents | Separate RT and PCR steps; allow archiving of cDNA for multiple downstream targets. | Detailed validation of multiple genes from a single, precious RNA sample. |
| TaqMan Probe Master Mix | Ready-to-use mix for hydrolysis probe assays; offers high specificity and multiplexing capability. | Discriminating between mutant and wild-type alleles in cancer genes. |
| SYBR Green/BRYT Green Master Mix | Cost-effective dye-based detection; requires post-amplification melt curve analysis for specificity. | Initial screening of gene expression and biomarker discovery. |
| Commercial Synthetic RNA/DNA Standards | Provide a known, consistent template for generating standard curves. | Absolute quantification of viral load or gene copy number in a sample. |
| Nuclease-Free Water | A critical reagent for preparing dilutions and controls; ensures no enzymatic degradation of samples. | Preparation of all reagent mixes, standards, and controls. |
Ensuring Rigor: Analytical Validation and Comparative Technology Assessment
In the field of cancer biomarker validation research, robust analytical methods are fundamental for generating reliable and reproducible data. The development and validation of protocols for techniques like real-time PCR are critical for accurately detecting and quantifying biomarkers, such as those based on DNA methylation, which show great promise in liquid biopsies for cancer management [3]. These analytical procedures must undergo rigorous validation to ensure they are fit for their intended purpose, whether it is for drug development, clinical diagnostics, or translational research. This document outlines detailed guidelines and protocols for assessing the core analytical validation parameters—Sensitivity, Specificity, Precision, and Linearity—within the context of a real-time PCR workflow for cancer biomarker research. The principles described herein are aligned with the International Council for Harmonisation (ICH) Q2(R2) guideline on the validation of analytical procedures [85] [86].
Core Principles of Analytical Validation
Analytical method validation provides assurance that a specific method will consistently yield results that accurately reflect the quality of the material being tested. For real-time PCR assays targeting cancer biomarkers, this is paramount due to the often low abundance of targets like circulating tumor DNA (ctDNA) in liquid biopsies [3]. The following core parameters form the foundation of the validation process.
- Specificity is the ability of the assay to unequivocally assess the analyte in the presence of other components, such as impurities, matrix components, or normal genomic DNA. In real-time PCR for DNA methylation biomarkers, this confirms that the signal is generated only from the bisulfite-converted, methylated target sequence [86].
- Sensitivity encompasses both the Limit of Detection (LOD), the lowest amount of analyte that can be detected but not necessarily quantified, and the Limit of Quantification (LOQ), the lowest amount that can be quantified with acceptable accuracy and precision. This is particularly crucial for detecting low-frequency ctDNA in a high background of normal cell-free DNA [3] [86].
- Precision expresses the closeness of agreement between a series of measurements obtained from multiple sampling of the same homogeneous sample under prescribed conditions. It is typically investigated at three levels: repeatability (same operating conditions over a short interval), intermediate precision (different days, analysts, equipment), and reproducibility (between laboratories) [86].
- Linearity is the ability of the method to obtain test results that are directly proportional to the concentration of analyte within a given range. The range is the interval between the upper and lower concentrations for which suitability has been demonstrated [86].
Experimental Protocols for Validation
This section provides detailed, step-by-step protocols for conducting experiments to validate the key parameters of a real-time PCR assay for a cancer biomarker.
Protocol for Assessing Specificity
Objective: To demonstrate that the real-time PCR assay detects only the intended methylated target and does not cross-react with unrelated sequences, unmethylated alleles, or closely related gene family members.
Materials:
- Research Reagent Solutions:
- Bisulfite-Converted DNA Templates: Test samples (methylated target, unmethylated genomic DNA, and DNA with known sequence variants).
- Real-Time PCR Master Mix: Contains DNA polymerase, dNTPs, and optimized buffer.
- Sequence-Specific Primers and Probes: Designed for the methylated CpG island of interest.
- Nuclease-Free Water: To adjust reaction volume.
Methodology:
- Prepare Reaction Mix: On ice, prepare a master mix for the number of reactions plus 10% excess. Each 20 µL reaction should contain: 1X Real-Time PCR Master Mix, 300 nM forward and reverse primers, 200 nM probe, and nuclease-free water.
- Plate Setup: Aliquot 18 µL of the master mix into each well of a real-time PCR plate.
- Template Addition: Add 2 µL of each template DNA (50 ng/µL post-concentration) to the respective wells, including:
- Well 1-3: Methylated target control (synthetic oligo or methylated DNA).
- Well 4-6: Unmethylated genomic DNA (from healthy donor leukocytes).
- Well 7-9: No-template control (Nuclease-free water).
- Well 10-12: DNA with potential cross-reactive sequences.
- Run Real-Time PCR: Seal the plate, centrifuge briefly, and run on the real-time PCR instrument using the following cycling conditions:
- Initial Denaturation: 95°C for 2 minutes.
- 45 Cycles:
- Denature: 95°C for 15 seconds.
- Anneal/Extend: 60°C for 1 minute (with fluorescence acquisition).
- Data Analysis: Analyze the amplification curves and Cq (Quantification Cycle) values. The assay is considered specific if:
- Robust amplification is observed only in wells with the methylated target control.
- No amplification (Cq > 40 or undetermined) occurs in wells with unmethylated DNA, no-template controls, and cross-reactive sequences.
Protocol for Determining Sensitivity (LOD and LOQ)
Objective: To establish the lowest concentration of the methylated biomarker that can be reliably detected and quantified by the real-time PCR assay.
Materials:
- Research Reagent Solutions:
- Methylated Target Standard: A synthetic DNA fragment or cell line DNA with known methylation status, serially diluted in a background of unmethylated genomic DNA (e.g., 1%, 0.1%, 0.01%) to mimic clinical samples [3].
Methodology:
- Prepare Dilution Series: Create a serial dilution of the methylated target standard in a constant background of unmethylated DNA (e.g., 50 ng/µL). The dilution series should cover a range from an easily detectable concentration down to concentrations expected to be near the detection limit.
- Run Real-Time PCR: In replicate (n≥6), run the real-time PCR assay for each dilution level in the series, including a no-template control.
- Calculate LOD: The LOD is the lowest concentration at which ≥95% of the replicates show positive amplification (Cq value below a predetermined threshold). It can be determined statistically using probit analysis or based on the concentration where 95% of replicates are detected.
- Calculate LOQ: The LOQ is the lowest concentration that can be quantified with acceptable precision (e.g., %RSD ≤ 25%) and accuracy (e.g., 80-120% recovery). It is determined by identifying the lowest dilution level where the %RSD of the measured concentration for the replicates is within the predefined acceptance criteria.
Protocol for Evaluating Precision
Objective: To determine the variability of the real-time PCR assay under different conditions, including repeatability and intermediate precision.
Materials:
- Research Reagent Solutions:
- Quality Control (QC) Samples: Three levels of methylated DNA (low, medium, high) representing the expected range of the assay.
Methodology:
- Repeatability: A single analyst prepares and runs the three QC samples in six replicates each, within a single run on one day.
- Intermediate Precision: A second analyst repeats the experiment on a different day, using a different real-time PCR instrument and possibly different reagent lots.
- Data Analysis: For each QC level and each experiment, calculate the mean Cq value, standard deviation (SD), and percent relative standard deviation (%RSD).
- %RSD = (Standard Deviation / Mean) × 100%
- Interpretation: The precision is considered acceptable if the %RSD for all QC levels is within the predefined limits (e.g., ≤ 25% for the LOQ level and ≤ 15% for other levels) for both repeatability and intermediate precision [86].
Protocol for Establishing Linearity and Range
Objective: To demonstrate that the real-time PCR assay produces results directly proportional to the concentration of the methylated biomarker across the specified range.
Materials:
- Research Reagent Solutions:
- Calibrators: A series of at least five concentrations of the methylated target standard, spanning the entire expected range from the LOQ to the upper limit of quantification.
Methodology:
- Run Calibrators: Run the real-time PCR assay in duplicate or triplicate for each calibrator concentration.
- Plot Standard Curve: Plot the mean Cq value (y-axis) against the logarithm of the known template concentration (x-axis).
- Perform Regression Analysis: Perform linear regression analysis on the data to determine the correlation coefficient (R²), slope, and y-intercept.
- Assess Acceptance Criteria: The linearity is acceptable if the R² value is ≥ 0.98 and the back-calculated concentrations of the calibrators fall within ±20% of the nominal value (±25% at the LOQ) [86]. The range is validated from the lowest to the highest concentration that meets these criteria.
Data Presentation and Analysis
Table 1: Core Analytical Validation Parameters and Acceptance Criteria for a Real-Time PCR Assay
| Validation Parameter | Experimental Design | Key Outcome Measures | Typical Acceptance Criteria |
|---|---|---|---|
| Specificity | Amplification of target vs. non-target sequences (unmethylated DNA, NTC). | Presence/Absence of amplification; Cq values. | No amplification in non-target wells. |
| Sensitivity - LOD | Testing serial dilutions of methylated target in unmethylated DNA background (n≥6). | Proportion of positive replicates at each concentration. | ≥95% detection rate at LOD. |
| Sensitivity - LOQ | Testing serial dilutions (n≥6) with quantification. | %RSD and % Accuracy of measured concentration. | %RSD ≤ 25%; Accuracy 80-120%. |
| Precision - Repeatability | Multiple replicates (n=6) of QC samples within one run. | %RSD of Cq or concentration. | %RSD ≤ 15-25% (depending on level). |
| Precision - Intermediate Precision | Multiple replicates of QC samples across different days/analysts. | Overall %RSD combining within-run and between-run variability. | %RSD meets or exceeds repeatability criteria. |
| Linearity & Range | Testing a series of calibrators (≥5 points) across the intended range. | Correlation coefficient (R²); Accuracy of back-calculated values. | R² ≥ 0.98; Accuracy within ±15-20%. |
Table 2: Example of a Precision Study Results Table for a Hypothetical Methylation Biomarker Assay
| QC Level | Theoretical Concentration | Within-Run (Repeatability) | Between-Run (Intermediate Precision) | ||
|---|---|---|---|---|---|
| Mean Cq (SD) | %RSD | Mean Cq (SD) | %RSD | ||
| Low | 0.1% | 35.2 (0.5) | 1.4% | 35.4 (0.7) | 2.0% |
| Medium | 1% | 31.5 (0.3) | 1.0% | 31.6 (0.4) | 1.3% |
| High | 10% | 28.1 (0.2) | 0.7% | 28.2 (0.3) | 1.1% |
The Scientist's Toolkit: Essential Research Reagent Solutions
Table 3: Key Research Reagent Solutions for Real-Time PCR-Based Biomarker Validation
| Reagent/Material | Function and Importance in Validation |
|---|---|
| Bisulfite Conversion Kit | Chemically converts unmethylated cytosines to uracils, while leaving methylated cytosines unchanged, enabling the detection of methylation differences. Critical for assay specificity. |
| Methylated & Unmethylated DNA Controls | Serve as positive and negative controls for assay development and validation. Used to establish sensitivity, specificity, and as calibrators for linearity studies. |
| Real-Time PCR Master Mix | A optimized pre-mixed solution containing a thermostable DNA polymerase, dNTPs, MgCl₂, and stabilizers in a suitable buffer. Ensures robust and efficient amplification. |
| Sequence-Specific Primers and Probes | Oligonucleotides designed to bind exclusively to the bisulfite-converted, methylated DNA sequence. The probe (e.g., TaqMan) provides the fluorescent signal for detection and quantification. |
| Normal Human Genomic DNA | Used as a diluent for creating standard curves in a complex matrix and for assessing specificity by testing for off-target amplification. |
Workflow and Pathway Visualizations
Analytical Method Validation Workflow
Real-Time PCR Wet-Lab Experimental Pathway
Adherence to structured guidelines for analytical validation is non-negotiable in cancer biomarker research. By systematically assessing sensitivity, specificity, precision, and linearity as detailed in this document, researchers can ensure that their real-time PCR assays are robust, reliable, and capable of producing high-quality data. This rigor is essential for the successful translation of promising biomarkers, such as DNA methylation signatures in liquid biopsies, from the research bench to clinical applications, ultimately supporting advancements in cancer diagnostics and personalized medicine [3] [85] [86].
In the field of cancer biomarker validation research, precise and sensitive molecular techniques are fundamental for reliable data generation. Quantitative real-time PCR (qPCR) and digital PCR (dPCR) are cornerstone technologies for quantifying nucleic acid biomarkers from various sources, including liquid biopsies [2] [87]. The analytical sensitivity and reliability of these assays are formally characterized by two critical performance parameters: the Limit of Detection (LOD) and the Limit of Quantification (LOQ) [88] [89]. Proper determination of LOD and LOQ is not merely a technical exercise; it is a fundamental prerequisite for ensuring that biomarker data used in clinical decision-making, such as diagnosis, prognosis, and monitoring therapeutic response, is analytically sound and fit-for-purpose [2]. This document provides detailed application notes and protocols for determining LOD and LOQ for PCR assays within the context of cancer biomarker validation.
Fundamental Concepts and Definitions
A clear understanding of the terminology is essential for implementing the correct validation procedures. The following definitions are based on standards from organizations such as the Clinical Laboratory Standards Institute (CLSI) [88].
- Limit of Detection (LOD): The lowest amount of analyte in a sample that can be detected with a stated probability. It indicates the presence of the target but does not imply that it can be accurately quantified [88] [90]. In diagnostic applications, LOD is sometimes referred to as "analytical sensitivity" [88].
- Limit of Quantification (LOQ): The lowest amount of measurand in a sample that can be quantitatively determined with stated acceptable precision and stated acceptable accuracy [88]. Results at or above the LOQ are considered reliably quantifiable.
- Limit of Blank (LoB): A related parameter, the LoB is the highest apparent analyte concentration expected to be found when replicates of a blank sample (containing no analyte) are tested. It is calculated as
LoB = mean_blank + 1.645 * SD_blank(assuming 95% confidence) [88].
The relationship between these parameters is foundational. In an ideal assay, the LoB is established first, followed by the LOD, which must be a concentration higher than the LoB. The LOQ is then determined at a higher concentration still, where acceptable precision and accuracy are achieved [88].
Statistical Frameworks and Calculation Methods
Determining LOD and LOQ for qPCR assays requires specialized statistical approaches because the data (quantification cycle, Cq) has a logarithmic relationship with the starting concentration and is not normally distributed in a linear scale [88]. Two primary methods are widely used.
The Probabilistic Method (Based on Replicate Analysis)
This method is based on the detection rate of a target across a dilution series with a high number of replicates at each concentration.
- Experimental Protocol:
- Prepare a serial dilution of the target nucleic acid (e.g., synthetic oligo, cell-free DNA, recombinant plasmid) in a matrix that mimics the clinical sample (e.g., plasma, buffer with background nucleic acids).
- Analyze a high number of replicates (e.g., n=20-64) for each dilution level, especially at the low concentrations near the expected limit [88] [89].
- Run the qPCR assay and record the Cq value for each reaction. A reaction is typically considered "detected" if its Cq value is below a predefined cut-off (e.g., 35 or 40 cycles) [88].
- Data Analysis:
- For each concentration, calculate the proportion of positive replicates (detection rate).
- Fit a logistic regression model to the data, with concentration (log-transformed) as the independent variable and detection rate as the dependent variable [88].
- The LOD is defined as the concentration at which 95% of the replicates test positive [88]. This is derived from the fitted logistic curve.
- The LOQ can be determined as the lowest concentration where the coefficient of variation (CV) for the measured concentration falls below an acceptable threshold, typically 20-25% for low-level quantification [89]. The CV must be calculated from the measured concentrations, not the Cq values, acknowledging the log-normal distribution of qPCR data [88].
The ROC Curve Method
The Receiver Operating Characteristic (ROC) curve analysis, commonly used in diagnostic test evaluation, can be adapted to determine LOD and LOQ in qPCR [90]. This method is particularly powerful as it leverages the relationship between sensitivity and specificity.
- Experimental Protocol:
- Assay a set of samples with a known true status ("positive" or "negative"). This can be achieved by using a "gold standard" method (e.g., melting curve analysis, sequencing) or by analyzing a spiked matrix with known concentrations [90].
- The qPCR Cq values for these known samples form the dataset for analysis.
- Data Analysis:
- For every possible Cq value that could serve as a cut-off, calculate the assay's sensitivity (true positive rate) and 1-specificity (false positive rate).
- Plot the ROC curve (sensitivity vs. 1-specificity).
- The Youden Index (J = sensitivity + specificity - 1) is used to identify the optimal cut-off Cq value that maximizes both sensitivity and specificity [90].
- The LOQ is defined as the amount of target DNA that corresponds to this optimal Cq cut-off value [90].
- The LOD can be defined as the lowest amount of target DNA that is amplified with a false-negative rate below a pre-defined acceptable threshold (e.g., 5%) [90].
The following diagram illustrates the logical workflow for determining LOD and LOQ using these two primary methods.
Experimental Protocols for LOD/LOQ Determination
Sample Preparation and Dilution Scheme
A key to success is a well-prepared dilution series in the appropriate matrix.
- Standard Material: Use a well-characterized nucleic acid standard, such as a synthetic gBlock gene fragment, a plasmid containing the target sequence, or genomic DNA calibrated against a reference standard like NIST SRM 2372 [88].
- Matrix: Dilutions must be made in a solution that mimics the clinical sample. For plasma cfDNA assays, this involves using pathogen-free human plasma or a suitable surrogate [89]. This controls for the effects of PCR inhibitors.
- Dilution Scheme: Create a serial dilution (e.g., 2-fold or 5-fold) covering a broad range, ensuring several concentration points are below the expected LOQ. The exact concentrations should be known and recorded.
qPCR Setup and Data Acquisition
- Reaction Composition: The master mix should be prepared according to the assay specifications. The use of probe-based chemistry (e.g., TaqMan) is recommended for superior specificity in validated assays [91].
- Replicates: A minimum of 6-8 technical replicates per concentration is recommended for a robust estimation. For the final LOD/LOQ validation, higher replicate numbers (e.g., 20) at the lowest concentrations are essential [88] [89].
- Thermal Cycling: Run the qPCR for a sufficient number of cycles (e.g., 50-55 cycles) to ensure low-abundance targets have the opportunity to amplify [92] [89].
- Data Collection: Record the Cq value for each well. Any reaction that does not amplify should be assigned a Cq value at the maximum cycle number for data analysis purposes.
A Practical Example: Validating a cfDNA Assay
A 2021 study validated a direct qPCR assay for cell-free DNA (cfDNA) in SLE patients, providing a clear application of these principles [89].
- Target: Abundant genomic repeats (LINE1 elements).
- Matrix: Human blood plasma, diluted 1:10.
- Replicates: All samples were measured in triplicates.
- Precision: Repeatability and intermediate precision were assessed, with CVs ≤ 12.1%.
- Results: The study established an ultra-low LOQ of 0.47 ng/mL for a 90 bp assay and 0.69 ng/mL for a 222 bp assay, demonstrating the method's applicability in a clinical cancer screening context [89].
Performance Criteria and Data Interpretation
The table below summarizes the key performance metrics and their acceptance criteria for a validated qPCR assay in a regulated research context [2] [88] [89].
Table 1: Key Performance Metrics for qPCR Assay Validation
| Parameter | Definition | Typical Acceptance Criteria | Example from Literature |
|---|---|---|---|
| Limit of Blank (LoB) | Highest measurement result of a blank sample. | Establish baseline noise. | N/A |
| Limit of Detection (LOD) | Lowest concentration detected with 95% probability. | ≥95% detection rate at that concentration. | Probabilistic method: 95% detection rate from logistic model [88]. |
| Limit of Quantification (LOQ) | Lowest concentration quantified with acceptable precision and accuracy. | CV ≤ 20-25% at that concentration [89]. | cfDNA assay: LOQ of 0.47 ng/mL with CV ≤ 12.1% [89]. \nddPCR miRNA assay: LoQ=13.45 copies/μL [92]. |
| Precision (Repeatability) | Closeness of agreement between results under identical conditions (intra-run). | CV ≤ 20-25% across replicates [89]. | Intra-batch CV of 2.31-21.63% for a ddPCR miRNA assay [92]. |
| Precision (Intermediate Precision) | Closeness of agreement under varied conditions (inter-run, different operators/days). | CV ≤ 25-30% across runs. | Intermediate precision ≤ 12.1% for cfDNA assay [89]. Inter-batch CV of 17.54% for ddPCR assay [92]. |
| Linearity | The ability of the assay to obtain results directly proportional to the analyte concentration. | R² ≥ 0.98 over the stated range. | A validated ddPCR assay showed R²=0.9965 over a wide range [92]. |
The Scientist's Toolkit: Essential Reagents and Materials
The following table lists critical reagents required for the development and validation of PCR assays for cancer biomarkers, as discussed in the cited literature.
Table 2: Key Research Reagent Solutions for PCR Assay Validation
| Reagent/Material | Function/Purpose | Example from Literature |
|---|---|---|
| Nucleic Acid Standard | Provides a known quantity of the target sequence for generating a standard curve and dilution series for LOD/LOQ. | Human genomic DNA calibrated against NIST SRM 2372 [88]. Custom-made plasmid or gene fragment (e.g., L1PA2) [89]. |
| Probe-Based Master Mix | Provides the enzymes, dNTPs, and buffer for efficient and specific amplification. Hydrolysis probes (e.g., TaqMan) enhance specificity. | TATAA Probe GrandMaster Mix [88]. Use of LNA-modified probes to enhance hybridization and signal [92]. |
| Biologically Relevant Matrix | The substance used for dilution to account for the effects of inhibitors and other components found in real samples. | Pathogen-free human plasma for cfDNA assays [89]. Naïve host tissue gDNA or total RNA for specificity testing [91]. |
| Primers & Probes | Specifically designed oligonucleotides that define the target amplicon. Critical for assay specificity and sensitivity. | Designed using software (e.g., Primer3, Primer-BLAST) and empirically screened [91]. Target exon-exon junctions for RNA, or vector-specific junctions for transgenes [91]. |
The rigorous determination of LOD and LOQ is a non-negotiable component of assay validation in cancer biomarker research. By adhering to the statistical frameworks and experimental protocols outlined in this document—whether the probabilistic method using logistic regression or the ROC curve analysis employing the Youden index—researchers can ensure their qPCR and dPCR assays are capable of reliably detecting and quantifying low-abundance targets. This reliability is the foundation upon which robust, reproducible, and clinically translatable cancer biomarker data is built, ultimately supporting critical decisions in drug development and patient management [2].
Inter-laboratory Reproducibility and Standardization Frameworks (e.g., EuroMRD Consortium)
The EuroMRD Consortium is a global network of over 65 molecular diagnostics laboratories dedicated to standardizing minimal/measurable residual disease (MRD) assessment using real-time quantitative PCR (RQ-PCR) [93] [94]. Established in 2001 and now an independent foundation, EuroMRD addresses the critical need for reproducible, high-quality MRD diagnostics in lymphoid malignancies, particularly acute lymphoblastic leukemia (ALL) [94]. The consortium's three pillars are Quality (organizing external quality assessment programs), Education (continuous member training), and Innovation (developing new MRD strategies and guidelines) [94]. For precision medicine applications, particularly in cancer biomarker validation, consistent MRD data is essential for appropriate risk-group classification and reliable inter-protocol comparisons across clinical trials [94] [33].
The EuroMRD Quality Assurance Scheme
The EuroMRD quality assurance (QA) scheme is a comprehensive system designed to ensure comparable, high-quality MRD diagnostics across all participating laboratories [94].
Membership Criteria and Laboratory Requirements
EuroMRD maintains strict membership criteria to ensure participating laboratories possess the necessary expertise. Requirements include extensive knowledge of immunoglobulin and T-cell receptor gene rearrangements, substantial experience with MRD detection at the DNA level, and adequate laboratory staffing with a minimum annual intake of new patients [94]. This selective participation ensures that all members are proficient in the complex ASO-PCR technology required for patient-specific MRD assessment [33].
Structure of the QA Program
The QA scheme consists of multiple tasks conducted biannually to continuously assess and improve laboratory performance [94].
Table: EuroMRD Quality Assurance Tasks and Structure [94]
| Task Number | Frequency per Year | Description |
|---|---|---|
| Task 1 | 2× | Paper-based interpretation of RQ-PCR data from 10 ALL cases analyzed by IG/TR gene rearrangements |
| Task 2 | 1× | Wet-lab task: IG/TR target detection, sequence analysis, and MRD quantification in artificial follow-up samples |
| Task 3 | 1× | Wet-lab task: Analysis of provided IG/TR sequences and RQ-PCR-based MRD quantification |
Sample Selection and Reference Data Establishment
Samples for QA tasks originate from leftover patient materials obtained during routine care with appropriate patient consent [94]. For wet-lab tasks, DNA is extracted from bone marrow samples with known ALL infiltration, and serial dilutions in polyclonal DNA create artificial MRD samples with predefined MRD values [94]. All samples are standardized to a concentration of 100 ng/μL, with concentration confirmation via both spectrophotometer measurement and control gene RQ-PCR [94]. Reference data are established by consensus among five experienced reference laboratories, ensuring objectively determined correct interpretations [94].
Updated EuroMRD Guidelines for MRD Data Interpretation
The EuroMRD consortium has developed and regularly updates guidelines for interpreting RQ-PCR MRD data, with the latest 2024 revisions introducing more precise categories for low-level MRD detection [94] [95].
Key Interpretation Categories
The updated guidelines provide a refined framework for classifying MRD results based on quantitative and qualitative data analysis [94].
Table: EuroMRD MRD Data Interpretation Categories [94]
| Category | Definition | Clinical Significance |
|---|---|---|
| Quantifiable MRD | MRD level within the quantitative range of the assay | Result is reliable and can be used for risk stratification |
| MRD Low Positive, Below Quantitative Range | MRD detected below the quantitative range but above the sensitivity threshold | Presence of MRD is certain, but level cannot be precisely quantified |
| MRD of Uncertain Significance | MRD detected at the very limit of assay sensitivity | Result should be interpreted with caution; clinical context critical |
| MRD Negative | No MRD detected above the sensitivity threshold | No evidence of residual disease at tested sensitivity level |
Parameters for MRD Assay Validation
The EuroMRD guidelines specify critical performance parameters that must be validated for each patient-specific ASO-PCR assay [33]:
- Quantitative Range (QR): The range over which quantitative results can be reliably reported, typically from 10⁻¹ to 10⁻⁵ for 90% of assays [33]
- Sensitivity: The minimal number of leukemic cells detectable among normal cells, with current standardized approaches achieving detection between 1.8 and 4.8 cells per 100,000 leukocytes [33]
- Specificity: The ability to distinguish the patient-specific clonal sequence from background polyclonal lymphocytes [33]
Experimental Protocol for IG/TR-Based MRD Assessment
This protocol outlines the standardized procedure for patient-specific MRD assessment following EuroMRD guidelines.
Sample Preparation and DNA Extraction
- Sample Collection: Bone marrow or peripheral blood samples should be collected in EDTA or heparin tubes and processed within 24-48 hours [94] [33]
- DNA Extraction: Extract DNA using validated methods (e.g., column-based or magnetic bead extraction). Quantify DNA using both spectrophotometric (e.g., NanoDrop) and fluorometric methods. Verify DNA quality via control gene RQ-PCR (e.g., Albumin gene) [94] [33]
- DNA Concentration: Adjust all samples to a standard concentration of 100 ng/μL without further dilution or concentration [94]
Patient-Specific Assay Design and Validation
- Target Identification: At diagnosis, identify clonal immunoglobulin (IG) and/or T-cell receptor (TR) gene rearrangements using multiplex PCR and sequencing [33]
- ASO Primer Design: Design allele-specific oligonucleotide (ASO) primers complementary to the unique junctional regions of the clonal rearrangement [33]
- Assay Validation: Validate each patient-specific assay for:
- Specificity: Test against polyclonal control DNA to ensure no cross-reactivity [33]
- Sensitivity: Determine the detection limit using dilution series of diagnostic DNA in polyclonal DNA [33]
- Efficiency: Ensure amplification efficiency between 90-110% [96]
- Quantitative Range: Establish the range over which reliable quantification occurs (typically 10⁻¹ to 10⁻⁵) [33]
RQ-PCR Setup and Reaction Conditions
- Reaction Master Mix: Use commercial master mixes (e.g., LightCycler 480 Probe Master, QPCR Mastermix Plus) with final reaction volumes of 20-25 μL [33]
- DNA Input: Use 300-500 ng DNA per reaction [33]
- Thermocycling Conditions:
- Initial denaturation: 95°C for 10 minutes
- 45-50 cycles of:
- Denaturation: 95°C for 15 seconds
- Annealing: 60°C for 30-60 seconds
- Extension: 72°C for 30 seconds
- Control Genes: Include control gene reactions (e.g., Albumin) in duplex or separate singleplex reactions to quantify DNA input [33]
Data Analysis and Interpretation
- Standard Curve Method: For absolute quantification, use dilution series of diagnostic DNA with known tumor percentage [33]
- ΔΔCT Method: For relative quantification, use the comparative CT method when absolute standards are unavailable [96]
- Quality Thresholds: Apply EuroMRD interpretation guidelines to categorize results as quantifiable, positive below quantitative range, uncertain significance, or negative [94]
The Scientist's Toolkit: Essential Reagents and Materials
Table: Essential Research Reagents for EuroMRD-Compliant MRD Analysis [94] [33] [96]
| Reagent/Material | Function | Specifications/Quality Controls |
|---|---|---|
| DNA Extraction Kits | Isolation of high-quality genomic DNA from patient samples | Validated for yield and purity; DNA quality confirmed by control gene PCR |
| RQ-PCR Master Mix | Provides optimal buffer conditions, enzymes, and dNTPs for amplification | Commercial master mixes (e.g., LightCycler 480 Probe Master) |
| Allele-Specific Oligonucleotide Primers | Patient-specific amplification of clonal IG/TR rearrangements | HPLC-purified; designed against unique junctional sequences |
| Control Gene Primers/Probes | Quantification of input DNA and sample quality assessment | Pre-validated assays for single-copy genes (e.g., Albumin) |
| Fluorescent Probes | Detection of accumulating PCR product in real-time | FAM-labeled for target genes; VIC-labeled for control genes |
| Standard Curve Materials | Quantification of MRD levels | Serial dilutions of diagnostic DNA with known tumor content |
Impact on Clinical Research and Clinical Trial Contexts
The standardized framework established by EuroMRD has significantly improved the reliability of MRD data supporting clinical trials and treatment decisions [94] [33].
Analytical Performance Validation
Comprehensive validation studies demonstrate that ASO-PCR following EuroMRD guidelines generates robust, reproducible data [33]:
- Accuracy: At the clinically significant MRD cutoff of 10⁻⁴, ASO-PCR shows high accuracy with minimal false positives or negatives [33]
- Precision: Inter-laboratory comparisons show consistent results across different facilities when following standardized protocols [33]
- Orthogonal Method Correlation: Approximately 90% overall agreement with flow cytometry and next-generation sequencing methods [33]
Application in Precision Medicine
The patient-specific nature of IG/TR-based MRD assessment makes it ideally suited for precision medicine approaches in oncology [33]. The high sensitivity and reproducibility of standardized RQ-PCR enable detection of early treatment failure or impending relapse, allowing for timely therapeutic adjustments [94] [33]. Furthermore, the quantitative nature of the data supports response-adapted treatment strategies, where therapy intensity is modulated based on MRD levels [94].
The validation of cancer biomarkers demands analytical techniques capable of detecting minute molecular changes with exceptional precision. Among these techniques, quantitative PCR (qPCR) has long been the gold standard for nucleic acid quantification. However, the emergence of digital PCR (dPCR) represents a paradigm shift in detection capabilities, particularly for challenging applications such as rare allele detection in circulating tumor DNA (ctDNA) and minimal residual disease (MRD) monitoring [4] [97]. This application note provides a structured comparison of the sensitivity and precision of qPCR versus dPCR methodologies, contextualized within cancer biomarker validation research. We present definitive quantitative data, detailed experimental protocols, and analytical workflows to guide researchers in selecting and implementing the optimal PCR strategy for their specific research requirements in oncology and drug development.
Fundamental Technological Principles
Quantitative PCR (qPCR)
qPCR, also known as real-time PCR, monitors the amplification of DNA during each PCR cycle via fluorescence detection [98] [99]. The key quantitative measurement is the Cycle Threshold (Ct), which represents the PCR cycle number at which the fluorescence signal crosses a predetermined threshold. The Ct value is inversely proportional to the initial amount of target nucleic acid [99]. Quantification requires comparison to a standard curve generated from samples of known concentration, providing relative quantification of the target sequence [98] [100].
Digital PCR (dPCR)
dPCR employs a fundamentally different approach by partitioning a single PCR reaction into thousands to millions of individual nanoliter-scale reactions [4] [98]. Following endpoint amplification, each partition is analyzed for fluorescence to determine if it contains the target sequence (positive) or not (negative). The absolute concentration of the target molecule in the original sample is then calculated using Poisson statistics based on the ratio of positive to negative partitions, eliminating the need for standard curves [4] [97] [99].
Quantitative Performance Comparison
Sensitivity and Precision Metrics
Table 1: Direct Performance Comparison of qPCR vs. dPCR
| Parameter | qPCR | dPCR | Experimental Evidence |
|---|---|---|---|
| Quantification Approach | Relative (requires standard curve) [98] [100] | Absolute (Poisson statistics) [4] [97] | Fundamental methodological difference |
| Detection Sensitivity | Moderate (limited by background and efficiency) [98] | High (partitioning enriches rare targets) [98] [97] | dPCR detected KRAS mutations at <0.2% VAF in pancreatic cancer [97] |
| Precision (Copy Number Variation) | 60% concordance with PFGE gold standard [101] | 95% concordance with PFGE gold standard [101] | Copy number measurement in DEFA1A3 gene locus [101] |
| Dynamic Range | Large (≥5 logs) [98] | Limited by partition count [98] | qPCR suitable for large expression differences; dPCR may require sample titration [98] |
| Tolerance to Inhibitors | Moderate (affects amplification efficiency and Ct) [98] | High (dilution effect during partitioning) [98] [99] | Partitioning reduces inhibitor concentration in positive partitions [98] |
| Rare Allele Detection | Limited by wild-type background [98] | Excellent; can detect rare mutants in excess wild-type [98] [97] | Critical for ctDNA analysis in liquid biopsies [97] [29] |
Application-Specific Performance in Cancer Research
Table 2: Performance in Key Cancer Biomarker Applications
| Research Application | qPCR Performance | dPCR Performance | Supporting Data |
|---|---|---|---|
| Liquid Biopsy / ctDNA Analysis | Limited sensitivity for early-stage or low-shedding tumors [29] | Detects molecular recurrence months before radiologic relapse [97] | Longitudinal ctDNA monitoring in breast cancer [97] |
| Minimal Residual Disease (MRD) | Standard for diseases like CML, but limited sensitivity threshold [97] | Ultra-sensitive MRD detection; informs treatment-free remission decisions [97] | BCR-ABL1 quantification in CML [97] |
| Copy Number Variation (CNV) | Weak correlation (r=0.57) with PFGE; tends to underestimate copy number [101] | Strong correlation (r=0.90) with PFGE; accurate across CNV range [101] | DEFA1A3 CNV analysis [101] |
| DNA Methylation Biomarkers | Applicable but with limited multiplexing capability [102] | High-sensitivity multiplex detection; 95% accuracy for 8 cancer types [102] | Multi-cancer detection using 3 methylation targets [102] |
| Rare Mutation Detection | Challenging below 1% variant allele frequency (VAF) [98] | Reliable detection down to 0.1% VAF or lower [98] [97] | KRAS mutation genotyping in pancreatic cancer [97] |
Experimental Protocols
Protocol A: Droplet Digital PCR for Rare Mutation Detection in ctDNA
Application: Detection of KRAS mutations in pancreatic cancer patient plasma [97]
Materials and Reagents:
- ddPCR Supermix for Probes (commercial formulation)
- KRAS Mutation-Specific Assays (FAM-labeled)
- Wild-Type KRAS Reference Assay (HEX/VIC-labeled)
- Droplet Generation Oil
- DG8 Cartridges and Gaskets
- Restriction Enzyme (optional, for complex genomes)
- CtDNA samples (20-100 ng input recommended)
- Microcentrifuge Tubes (PCR-grade)
Methodology:
- Reaction Setup:
- Prepare 20 μL reaction mix containing: 10 μL ddPCR Supermix, 1 μL KRAS mutation assay (FAM), 1 μL reference assay (HEX), 8 μL ctDNA sample (adjust volume based on concentration).
- Vortex gently and centrifuge to collect contents.
Droplet Generation:
- Transfer 20 μL reaction mix to DG8 cartridge well.
- Add 70 μL droplet generation oil to appropriate well.
- Place gasket and process in droplet generator.
- Carefully transfer generated droplets to a 96-well PCR plate.
PCR Amplification:
- Seal plate with foil heat seal.
- Perform thermal cycling: 95°C for 10 min (enzyme activation), then 40 cycles of 94°C for 30 sec (denaturation) and 55-60°C for 60 sec (annealing/extension), followed by 98°C for 10 min (enzyme deactivation) and 4°C hold.
- Ramp rate: 2°C/sec standard.
Droplet Reading and Analysis:
- Transfer plate to droplet reader.
- Analyze using companion software with threshold setting based on negative controls.
- Calculate variant allele frequency (VAF) using Poisson correction.
Technical Notes:
- Include no-template controls (NTC) and wild-type controls in each run.
- Optimal results achieved with 10,000-20,000 droplets per sample.
- For samples with very low ctDNA concentration, increase input volume but do not exceed 50% of reaction volume.
Protocol B: Quantitative PCR for Gene Expression Analysis in Tumor Tissue
Application: Gene expression profiling in breast cancer tissue samples
Materials and Reagents:
- qPCR Master Mix with UNG (uracil-N-glycosylase)
- Gene-Specific TaqMan Assays
- Reference Gene Assays (GAPDH, β-actin recommended)
- Nuclease-Free Water
- RNA Extraction Kit
- cDNA Synthesis Kit
- Multi-Well Plate or Strips
- Optical Adhesive Covers
Methodology:
- Sample Preparation:
- Extract RNA from tumor tissue using standardized protocol.
- Quantify RNA concentration and quality (A260/A280 ratio ~2.0).
- Synthesize cDNA using reverse transcriptase with oligo(dT) and/or random primers.
Reaction Setup:
- Prepare 20 μL reactions containing: 10 μL qPCR Master Mix, 1 μL TaqMan assay, 4 μL cDNA template (diluted 1:10), 5 μL nuclease-free water.
- Include serial dilutions of reference standard for standard curve generation.
- Perform triplicate technical replicates for each sample.
PCR Amplification and Data Collection:
- Seal plate and centrifuge briefly.
- Run on real-time PCR instrument with cycling conditions: 50°C for 2 min (UNG incubation), 95°C for 10 min, then 40 cycles of 95°C for 15 sec and 60°C for 60 sec.
- Set fluorescence acquisition during annealing/extension phase.
Data Analysis:
- Determine Ct values for all samples using instrument software.
- Generate standard curve from reference dilutions.
- Calculate relative gene expression using ΔΔCt method with normalization to reference genes.
Technical Notes:
- Optimize primer concentrations during assay validation.
- Ensure PCR efficiency between 90-110% with R² > 0.98 for standard curve.
- Include no-reverse transcription and no-template controls.
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Reagent Solutions for PCR-Based Cancer Biomarker Research
| Reagent/Category | Function | Application Notes |
|---|---|---|
| Hydrolysis Probes (TaqMan) | Sequence-specific detection with fluorescent reporter and quencher [99] | Essential for multiplex dPCR; FAM/HEX common for 2-plex; additional channels available |
| DNA Binding Dyes (SYBR Green) | Binds double-stranded DNA; less specific but more flexible [99] | Cost-effective for single-plex; requires melt curve analysis for specificity verification |
| Digital PCR Supermix | Optimized polymerase/buffer for partition-based amplification [97] | Formulated with high surfactant concentration for droplet stability |
| Droplet Generation Oil | Creates water-in-oil emulsion for droplet separation [4] | Must be compatible with instrument and contain appropriate surfactants |
| Bisulfite Conversion Kit | Converts unmethylated cytosine to uracil for methylation analysis [102] | Critical for DNA methylation biomarker studies; optimized protocols reduce DNA degradation |
| Unique Molecular Identifiers | Molecular barcodes for error correction in NGS [29] | Not typically used in dPCR but essential for sequencing-based ctDNA assays |
Technology Selection Framework
The choice between qPCR and dPCR for rare allele detection in cancer biomarker research depends fundamentally on the specific analytical requirements of the application. qPCR remains the superior choice for high-throughput screening applications where relative quantification suffices and targets are not extremely rare [98] [100]. In contrast, dPCR provides unequivocal advantages for detecting low-frequency mutations, precise copy number variation analysis, and absolute quantification without standard curves [97] [101]. The emerging applications in liquid biopsy, MRD monitoring, and multi-cancer methylation detection demonstrate how dPCR's partitioning principle and statistical approach enable research questions that were previously technically challenging [97] [102]. As both technologies continue to evolve, their complementary strengths will further empower researchers in cancer biomarker validation and precision oncology development.
Within precision oncology, the accurate validation of cancer biomarkers is fundamental for guiding targeted therapies and improving patient outcomes. The selection of an appropriate molecular diagnostic platform is a critical strategic decision for research and drug development professionals. This Application Note provides a detailed comparison between two cornerstone technologies—quantitative PCR (qPCR) and Next-Generation Sequencing (NGS)—framed within the context of protocols for real-time PCR in cancer biomarker validation research. We assess throughput, cost, and targeted sensitivity to offer clear, actionable guidance for developing robust experimental workflows. The expanding compendium of clinically actionable genomic alterations, such as those cataloged in the ESMO Scale for Clinical Actionability of molecular Targets (ESCAT), necessitates testing strategies that are not only accurate but also comprehensive and efficient [103].
Fundamental Principles and Distinguishing Features
- Quantitative PCR (qPCR): Also known as real-time PCR, this technology relies on the fluorescent detection of DNA amplification during PCR cycles to quantify specific, known nucleic acid sequences. It is a targeted, amplification-based method ideal for detecting predefined mutations or measuring gene expression levels of a limited number of genes [104] [105].
- Next-Generation Sequencing (NGS): This high-throughput technology enables the parallel sequencing of millions of DNA fragments, providing comprehensive genomic profiles. Unlike qPCR, NGS is a hypothesis-free approach that can identify both known and novel variants—including single nucleotide variants (SNVs), insertions/deletions (indels), copy number variations (CNVs), and gene fusions—without requiring prior knowledge of the sequence [106] [104].
The core distinction lies in discovery power. While qPCR is highly sensitive for detecting known sequences, NGS offers unparalleled breadth by interrogating thousands of genomic regions simultaneously, enabling novel biomarker discovery [106].
Comparative Performance and Economic Metrics
The following tables summarize the quantitative and economic differences between qPCR and NGS, critical for assay selection in cancer research.
Table 1: Direct comparison of qPCR and NGS technical capabilities
| Parameter | qPCR | NGS |
|---|---|---|
| Discovery Power | Detects only known sequences [106] | Detects known and novel variants [106] |
| Quantitative Nature | Relative quantification (Cq/Ct values) [104] | Absolute quantification via read counts [106] [107] |
| Typical Targets per Run | 1 to 5 (with multiplexing) [104] | 1 to >10,000 [104] |
| Mutation Resolution | Limited to predefined variants [106] | Single-base resolution to large rearrangements [106] |
| Analytical Sensitivity | High for known targets [108] | High; can detect variants at allelic frequencies <5% [107] |
| Dynamic Range | Sufficient for most applications [109] | Wider dynamic range [106] |
Table 2: Economic and operational comparison in a clinical research context
| Aspect | qPCR | NGS |
|---|---|---|
| Cost per Sample | Low for a few targets [106] [110] | Higher per-sample cost; cost-effective for multiple targets [106] [110] |
| Equipment & Accessibility | Accessible; instruments in most labs [106] [109] | Higher initial investment; requires specialized infrastructure [110] |
| Sample-to-Answer Time | Rapid (1-3 hours) [104] | Slower; library prep and sequencing take hours to days [104] |
| Data Complexity | Simple, manageable datasets [110] | Complex; requires advanced bioinformatics [110] |
| *Cost in mNSCLC Testing | ~$18,246 per patient (including costs of delayed care) [111] | ~$8,866 per patient (more rapid, appropriate treatment) [111] |
Data from a cost model in metastatic non-small cell lung cancer (mNSCLC) including testing, delayed care, and suboptimal treatment costs [111].
Experimental Protocols for Cancer Biomarker Analysis
Protocol 1: Validating Known EGFR Mutations in NSCLC via qPCR
This protocol uses the IVD-certified cobas EGFR Mutation Test v2 (Roche Diagnostics) as a model for detecting classic activating mutations (e.g., exon 19 deletions, L858R) in formalin-fixed, paraffin-embedded (FFPE) tissue samples from non-small cell lung cancer (NSCLC) patients [107].
- Step 1: Nucleic Acid Extraction
- Isolate DNA from macro-dissected or micro-dissected FFPE tissue sections (5–10 μm) using a dedicated FFPE DNA extraction kit to maximize yield and minimize inhibitors. Quantify DNA using a fluorometric method.
- Step 2: Reaction Setup
- Prepare reactions according to the manufacturer's instructions. The test is a multiplexed assay with specific primers and probes for major EGFR mutations and a reference control. Use 50–100 ng of input DNA per reaction.
- Step 3: qPCR Amplification and Detection
- Run the plate on a compatible real-time PCR instrument using the following cycling conditions, or as specified by the kit:
- Hold Step: 95°C for 10 minutes (1 cycle)
- Amplification: 95°C for 30 seconds, 60°C for 60 seconds (45–50 cycles)
- Run the plate on a compatible real-time PCR instrument using the following cycling conditions, or as specified by the kit:
- Step 4: Data Analysis
- The instrument software automatically analyzes amplification curves and assigns a mutation status (positive/negative) for each target based on the presence of a fluorescent signal crossing a predefined threshold. Results are typically available in about 3 hours from sample setup.
Protocol 2: Comprehensive Profiling of Actionable Mutations via Targeted NGS
This protocol outlines a targeted NGS approach using the TruSight Tumor 15 assay (Illumina) to sequence key cancer genes, including EGFR, KRAS, BRAF, and TP53, from NSCLC FFPE samples [107].
- Step 1: DNA Extraction and QC
- Extract DNA from FFPE tissue as in Protocol 1. Assess DNA quality and fragmentation, e.g., via TapeStation or Bioanalyzer. Input requirement is 40 ng of DNA.
- Step 2: Library Preparation
- A. Target Enrichment: Amplify 250 target amplicons across 15 genes via a multiplexed PCR reaction using the TST15 panel-specific primers.
- B. Indexing and Clean-up: Attach dual indices (barcodes) and sequencing adapters to the amplified products via a second PCR. Purify the final library using magnetic beads to remove primers and enzymes.
- Step 3: Library Quantification and Pooling
- Quantify the final libraries using a fluorometric method. Normalize libraries to equimolar concentrations and pool them for multiplexed sequencing.
- Step 4: Sequencing
- Denature and dilute the pooled library according to the MiSeq System (Illumina) guide. Load onto a MiSeq flow cell for cluster generation and sequencing (2x 150 bp paired-end run).
- Step 5: Bioinformatic Analysis
- Primary Analysis: Convert raw images to FASTQ files (base calling).
- Secondary Analysis: Align sequences to a reference genome (e.g., hg19). Identify and annotate variants (SNVs, indels) and calculate variant allele frequencies (VAF). The reported median coverage should exceed 6,000x to reliably detect low-VAF variants [107].
Workflow Visualization and Decision Pathways
The following diagrams illustrate the experimental workflow for NGS and the decision-making process for selecting the appropriate technology.
Diagram 1: Targeted NGS workflow for cancer biomarker profiling from FFPE tissue.
Diagram 2: A decision pathway for selecting between qPCR and NGS based on project goals.
Research Reagent Solutions
The successful implementation of qPCR and NGS protocols relies on specific, high-quality reagents. The following table details essential materials and their functions.
Table 3: Key research reagents for qPCR and NGS workflows in biomarker validation
| Item | Function | Example Product(s) |
|---|---|---|
| FFPE DNA Extraction Kit | Isolates high-quality, amplifiable DNA from archived tissue specimens, removing formalin-induced crosslinks and inhibitors. | QIAamp DNA FFPE Tissue Kit (Qiagen) |
| qPCR Master Mix | A ready-to-use solution containing DNA polymerase, dNTPs, buffers, and fluorescent dye or probe for sensitive, specific real-time PCR detection. | TaqMan Gene Expression Master Mix [109] |
| Targeted NGS Panel | A predesigned set of probes or primers for enriching a defined set of cancer-related genes prior to sequencing. | TruSight Tumor 15 (Illumina) [107] |
| NGS Library Prep Kit | Reagents for fragmenting DNA, attaching universal adapters and sample-specific barcodes (indexes) for multiplexed sequencing. | Illumina DNA Prep Kit |
| NGS Polymerase | A high-fidelity, thermostable enzyme for accurate amplification during NGS library construction. | Meridian Bioscience Glycerol-Free Enzymes [105] |
Application in Cancer Research: Key Evidence
Clinical Concordance and Superior Detection with NGS
A 2024 study directly compared an NGS assay (TruSight Tumor 15) with the cobas EGFR Mutation Test v2 (qPCR) in 59 NSCLC clinical specimens. While both showed high sensitivity, the overall concordance was 76.14%, with several discordant results identified as false-positive calls for EGFR exon 20 insertions by the qPCR assay [107]. NGS provided exact variant identification and accurate VAF calculation, which is crucial for assessing tumor heterogeneity and clonal evolution. Furthermore, NGS simultaneously identified co-mutations in genes like TP53, offering a more comprehensive genomic profile from the same sample [107].
Economic Advantages in Metastatic NSCLC
Beyond technical performance, the economic impact of test choice is significant. A 2024 cost-analysis model for metastatic NSCLC found that the mean per-patient costs—incorporating testing, delayed care, and costs of suboptimal treatment—were substantially lower for NGS ($8,866) compared to PCR-based strategies ($18,246) [111]. This cost saving was driven by NGS providing more rapid results (2.1 vs. 5.2 weeks to appropriate therapy), minimizing the use of ineffective treatments and associated toxicities [111]. Another study introducing the "cost per correctly identified patient" (CCIP) metric demonstrated that NGS was more cost-effective than sequential single-gene testing in most solid tumors, including NSCLC, colorectal, and gastric cancers [103].
qPCR and NGS are not mutually exclusive but are complementary technologies in the cancer biomarker validation toolkit. qPCR remains the gold standard for rapid, sensitive, and cost-effective detection of a limited number of known biomarkers, making it ideal for high-throughput screening or validation studies [109] [105]. In contrast, NGS is the superior choice for discovery-oriented research, comprehensive genomic profiling, and clinical scenarios where the genetic landscape is complex and requires simultaneous assessment of numerous targets with high resolution [106] [107].
The emerging economic evidence strongly supports the use of NGS as a first-line testing strategy in cancers like metastatic NSCLC, where faster, more comprehensive results lead to better patient outcomes and lower overall healthcare costs [111] [103]. Therefore, research and drug development professionals should base their platform selection on a clear understanding of their study's goals, the number of targets, the need for discovery, and the total cost of the testing pathway, not just the price of an individual test.
Navigating Regulatory Pathways for Clinical Assay Approval
The development and approval of clinical assays, particularly those based on real-time PCR (qPCR) for cancer biomarker validation, require careful navigation of evolving regulatory frameworks. For researchers and drug development professionals, understanding these pathways is crucial for successfully translating molecular discoveries into clinically validated diagnostic tools. The regulatory environment is dynamic, with agencies like the U.S. Food and Drug Administration (FDA) providing specific pathways that balance rigorous evaluation with timely access to innovative technologies.
The emergence of precision medicine has increased reliance on biomarker-based assays that guide therapeutic decisions. These include predictive biomarkers that forecast response to specific therapies, prognostic biomarkers that inform about likely disease course, and diagnostic biomarkers that identify the presence of a disease condition [30]. The validation of these assays demands robust scientific evidence of analytical and clinical validity, with regulatory requirements varying based on the intended use and context of the test [112].
Essential Regulatory Pathways and Frameworks
FDA Regulatory Pathways for Clinical Assays
The FDA provides several distinct pathways for assay approval, each with specific requirements and appropriate use cases:
Traditional Premarket Approval (PMA) requires substantial evidence of effectiveness from adequate and well-controlled studies, typically demanding robust pre-market data from randomized controlled trials. This pathway remains the gold standard for establishing confidence in assay performance but may be impractical for rare diseases or highly specialized assays [113].
Accelerated Approval allows the FDA to approve therapies and their companion diagnostics based on surrogate endpoints reasonably likely to predict clinical benefit. This pathway requires post-market confirmatory trials to verify the anticipated clinical benefit. For assays, this might mean initial approval based on analytical validation and correlation with established biomarkers, with ongoing clinical validation required after approval [113].
The新兴 Plausible Mechanism (PM) Pathway represents a significant shift in regulatory philosophy, particularly relevant for ultra-rare diseases or highly individualized therapies where traditional trials are impractical. This pathway emphasizes biological plausibility, target engagement, and meaningful clinical improvement in small patient cohorts, coupled with rigorous post-market evidence collection. For biomarker assays, this pathway may accept validation based on strong mechanistic rationale and demonstrated technical robustness in limited populations [113].
Performance Standards and Documentation Requirements
For assays integral to clinical trials, the National Cancer Institute (NCI) expects compliance with specific performance standards. Integral assays—those that must be performed for a trial to proceed—require supporting information comparable to what would be needed for FDA clearance or approval. These assays must be performed in CLIA-certified laboratories at minimum, ensuring analytical validity throughout the trial process [112].
Supporting documentation should comprehensively address pre-analytical, analytical, and post-analytical phases of testing. This includes detailed protocols for specimen collection, processing, and storage; analytical validation data demonstrating accuracy, precision, sensitivity, and specificity; and established procedures for result interpretation and reporting. For qPCR-based assays, this extends to nucleic acid extraction methods, instrumentation specifications, and data analysis algorithms [112] [114].
Analytical Validation of qPCR Assays: Key Parameters and Protocols
Fundamental Validation Parameters for qPCR Assays
Robust validation of qPCR assays requires systematic assessment of multiple performance characteristics. The following parameters form the foundation of analytical validation for cancer biomarker assays:
Table 1: Essential Validation Parameters for qPCR-Based Clinical Assays
| Validation Parameter | Experimental Approach | Acceptance Criteria |
|---|---|---|
| Accuracy | Comparison with reference method or spike-recovery studies | Overall agreement of 90% compared to orthogonal methods [33] |
| Precision | Repeated testing of identical samples across different conditions | CV < 25% for copy number variation at the limit of quantification |
| Specificity | Testing against non-target sequences and closely related homologs | Minimal non-specific amplification in negative controls [33] |
| Sensitivity | Limit of Detection (LOD) and Limit of Quantification (LOQ) determination | LOD: 1.8-4.8 cells among 100,000 leukocytes for MRD assays [33] |
| Linearity & Range | Serial dilutions of target across expected concentration range | Linear between 10-1 and 10-5 for 90% of assays [33] |
| Reproducibility | Inter-laboratory studies using standardized protocols | Consistent results across laboratories with standardized protocols [33] |
Experimental Protocol for qPCR Assay Validation
The following protocol provides a detailed methodology for validating qPCR assays for cancer biomarker applications:
Protocol: Analytical Validation of qPCR Assays for Cancer Biomarkers
Step 1: Assay Design and Optimization
- Design sequence-specific primers and probes targeting the biomarker of interest
- Test at least three uniquely designed sets of primers and probes to ensure specificity and sensitivity
- Prefer TaqMan probe-based chemistry over SYBR Green for superior specificity in clinical samples
- Optimize primer concentrations (typically 50-900 nM) and annealing temperatures [75]
Step 2: Standard Curve Generation and Efficiency Determination
- Prepare serial dilutions of reference standard DNA (typically 101-108 copies)
- Include matrix DNA (genomic DNA from naive tissues) in standards to mimic patient samples
- Run standards in triplicate on each qPCR plate
- Calculate PCR efficiency using the formula: Efficiency (E) = 10-1/slope - 1
- Acceptable efficiency ranges from 90% to 110% (slope of -3.6 to -3.1) [75]
Step 3: Determination of Limit of Detection (LOD) and Limit of Quantification (LOQ)
- Prepare dilutions of target nucleic acid approaching expected detection limits
- Test each concentration with at least 12 replicates
- LOD: Lowest concentration detected in ≥95% of replicates
- LOQ: Lowest concentration quantified with acceptable precision (CV < 25%) [33]
Step 4: Precision Assessment
- Test intra-assay precision using replicates within the same run
- Test inter-assay precision across different days, operators, and instruments
- Include samples at critical decision points (e.g., clinical cut-offs)
- Calculate coefficient of variation (CV) for copy number determinations [33]
Step 5: Specificity Testing
- Test against non-target sequences, including closely related genetic elements
- Evaluate potential interference from co-amplification of homologous sequences
- Test in appropriate biological matrices (e.g., blood, tissue extracts)
- Verify minimal non-specific amplification in negative controls [33]
Step 6: Sample Stability Studies
- Evaluate pre-analytical variables affecting sample integrity
- Test different storage conditions and durations
- Assess freeze-thaw cycle effects on nucleic acid stability and assay performance
- Establish acceptable sample handling protocols [33]
Regulatory Strategy and Implementation Framework
Quality Management and Documentation Systems
Comprehensive documentation forms the foundation of regulatory compliance for clinical assays. The following dot language diagram illustrates the key components of an effective quality management system for clinical assay development:
Regulatory Documentation Framework
For compliance with the European In Vitro Diagnostic Regulation (IVDR), technical documentation must include specific elements demonstrating analytical and clinical performance. Technical files should comprehensively describe the assay design, intended use, and manufacturing processes. Validation reports must provide evidence of analytical performance including accuracy, precision, sensitivity, and specificity. Risk management documentation should follow ISO 14971 standards, identifying potential hazards and implementing appropriate control measures. Performance evaluation plans must outline the strategy for establishing clinical validity, including the use of retrospective specimens or clinical trial data [114].
The Scientist's Toolkit: Essential Research Reagent Solutions
Table 2: Key Research Reagent Solutions for qPCR Assay Development
| Reagent/Category | Function/Purpose | Examples/Specifications |
|---|---|---|
| Master Mixes | Provides optimized buffer, enzymes, and dNTPs for efficient amplification | TaqMan Universal Master Mix II, LightCycler 480 Probe Master [33] |
| Primers & Probes | Sequence-specific recognition and amplification of target biomarkers | HPLC-purified primers, FAM/TAMRA-labeled TaqMan probes [75] |
| Reference Standards | Calibration and quantification of target nucleic acids | Serially diluted plasmid DNA or synthetic oligonucleotides [75] |
| Control Materials | Monitoring assay performance and detecting contamination | Positive, negative, and internal controls (e.g., albumin gene) [33] |
| Nucleic Acid Extraction Kits | Isolation of high-quality DNA/RNA from clinical specimens | Silica-column or magnetic bead-based systems with DNase treatment [33] |
| Inhibition Relief Additives | Counteract PCR inhibitors in complex biological samples | BSA, T4 gene 32 protein, or commercial inhibition relief reagents [75] |
Case Studies and Applications in Cancer Biomarker Validation
Minimal Residual Disease (MRD) Detection in Leukemia
The validation of patient-specific qPCR assays for minimal residual disease (MRD) detection in lymphoid leukemia provides an exemplary model for personalized clinical assays. These assays target the unique junctional regions of rearranged immunoglobulin and T-cell receptor genes, serving as clone-specific fingerprints for malignant cells. Despite requiring custom reagents for each patient, standardized validation approaches have demonstrated robust performance across laboratories [33].
Key validation parameters for MRD assays include:
- Analytical specificity ensured through careful primer design targeting unique CDR3 sequences
- Linearity across a concentration range of 10-1 to 10-5 in 90% of assays
- Detection limit between 1.8 and 4.8 malignant cells among 100,000 leukocytes
- Reproducibility with approximately 90% overall agreement to orthogonal methods like flow cytometry and next-generation sequencing [33]
The international EuroMRD consortium has established standardized protocols, quality assessment programs, and data interpretation guidelines that facilitate regulatory compliance across multiple jurisdictions. This approach demonstrates how personalized assays can meet rigorous regulatory standards through methodological standardization and collaborative validation [33].
Advanced Multiplexing Strategies
The Multicolor Combinatorial Probe Coding (MCPC) strategy significantly expands the multiplexing capacity of real-time PCR platforms. This approach uses a limited number of fluorophores in various combinations to label multiple probes, enabling detection of numerous targets in a single reaction. With n different fluorophores, MCPC can theoretically distinguish 2n-1 different targets, dramatically increasing the information obtainable from limited sample material [115].
For cancer biomarker applications, MCPC facilitates:
- Comprehensive profiling of multiple biomarker signatures from small biopsy specimens
- Simultaneous detection of various cancer-associated pathogens (e.g., HPV typing)
- Identification of one potential target from multiple candidates in a single reaction
- Integration with the Homo-Tag Assisted Non-Dimer system to maintain sensitivity in multiplex reactions [115]
This strategy is particularly valuable for tumor classification, where detecting a specific genetic signature from multiple possibilities can guide therapeutic decisions without exhausting precious clinical samples.
Successfully navigating regulatory pathways for clinical assay approval requires a strategic, systematic approach that begins early in assay development. Researchers should clearly define the intended use context and regulatory classification during the design phase, as this determines the validation evidence required. Engagement with regulatory agencies through pre-submission meetings can provide valuable guidance and prevent costly missteps in development strategy.
The evolving regulatory landscape, including emerging pathways like the Plausible Mechanism Pathway, offers opportunities for efficient translation of innovative biomarkers into clinical practice. By implementing robust quality management systems, conducting comprehensive analytical validation, and maintaining thorough documentation, researchers can successfully navigate these pathways to deliver reliable diagnostic tools that advance precision oncology and improve patient care.
Conclusion
Real-time PCR remains a cornerstone technology for the precise and reliable validation of cancer biomarkers, playing a critical role in minimal residual disease monitoring, liquid biopsy applications, and companion diagnostic development. Success hinges on rigorous assay design, systematic optimization, and comprehensive analytical validation to meet regulatory standards. As the field advances, the integration of qPCR with emerging technologies like digital PCR and multi-omics platforms, coupled with standardized international protocols, will further enhance its utility. Future efforts should focus on developing novel biomarkers, improving the sensitivity for ultra-rare targets, and streamlining workflows to fully realize the promise of precision medicine in oncology.
References
- 1. Predictive Biomarkers in Cancer Immunotherapy [https://pmc.ncbi.nlm.nih.gov/articles/PMC12289453/]
- 2. Consensus guidelines for the validation of qRT-PCR ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8792405/]
- 3. a roadmap for DNA methylation biomarkers in liquid biopsies [https://www.nature.com/articles/s41388-025-03624-5]
- 4. Digital PCR: from early developments to its future application ... [https://pubs.rsc.org/en/content/articlehtml/2025/lc/d5lc00055f]
- 5. Somatic Tumor Testing 2024-11-17 updated 2025-01-01 [for ... [https://guidelines.carelonmedicalbenefitsmanagement.com/somatic-tumor-testing-2024-11-17-updated-2025-01-01/]
- 6. Bioinformatics mining and experimental validation of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12373585/]
- 7. MarkerPredict: predicting clinically relevant ... [https://www.nature.com/articles/s41540-025-00603-0]
- 8. Validation of real-time RT-PCR for detection of SARS-CoV- ... [https://www.nature.com/articles/s41598-021-94196-3]
- 9. Precision cancer medicine 2025: some concerns - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC12439214/]
- 10. Cancer Research to Microbes: Harnessing the Power of ... [https://www.thermofisher.com/blog/behindthebench/harnessing-the-power-of-qpcr/]
- 11. Bioinformatic screen with clinical validation for the ... [https://www.nature.com/articles/s41598-025-13074-4]
- 12. Integrating traditional machine learning with qPCR ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11754184/]
- 13. Optimization and Validation of a Folate Ligand-Targeted ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12530657/]
- 14. rtpcr: a package for statistical analysis and graphical ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12530193/]
- 15. qPCR in Early Cancer Detection: Why It Still Leads the Pack [https://www.meridianbioscience.com/lifescience-blog/why-qpcr-still-leads-in-oncology/]
- 16. Emerging biomarkers for early cancer detection and diagnosis [https://eurjmedres.biomedcentral.com/articles/10.1186/s40001-025-03003-6]
- 17. TaqMan vs. SYBR Chemistry for Real-Time PCR [https://www.thermofisher.com/us/en/home/life-science/pcr/real-time-pcr/real-time-pcr-learning-center/real-time-pcr-basics/taqman-vs-sybr-chemistry-real-time-pcr.html]
- 18. All About Probe-Based Real-Time qPCR Assays [https://www.goldbio.com/blogs/articles/all-about-probe-based-qpcr?srsltid=AfmBOoqAgdsmeCCgPmEOVudQB2-EqDFCbAaLRyRvv_QMLQC02LJ5P4TC]
- 19. Comparison of real-time PCR and nCounter NanoString ... [https://pubmed.ncbi.nlm.nih.gov/40595185/]
- 20. Auto-qPCR; a python-based web app for automated and ... [https://www.nature.com/articles/s41598-021-99727-6]
- 21. Biomarkers, tumor markers and tumor boards [https://www.fredhutch.org/en/news/center-news/2025/08/biomarkers-tumor-markers-what-cancer-patients-need-to-know.html]
- 22. Emerging biomarkers for early cancer detection and diagnosis [https://pmc.ncbi.nlm.nih.gov/articles/PMC12359849/]
- 23. Connecting the dots for cancer biomarkers and precision ... [https://www.jax.org/news-and-insights/2025/november/connecting-the-dots-for-cancer-biomarkers-and-precision-oncology]
- 24. Access to Biomarker Testing [https://www.fightcancer.org/what-we-do/access-biomarker-testing]
- 25. Epigenetic biomarkers for cancer diagnosis and prognosis [https://dailyreporter.esmo.org/molecular-analysis-for-precision-oncology-congress-map-2025/epigenetic-information-could-harbour-biomarkers-of-diagnosis-and-prognosis]
- 26. Transcriptomic analysis reveals lung cancer and subtype ... [https://pubmed.ncbi.nlm.nih.gov/40917894/]
- 27. The relationship between epigenetic biomarkers and ... [https://www.frontiersin.org/journals/public-health/articles/10.3389/fpubh.2025.1509458/full]
- 28. Clinical Practice Guideline for Blood-based Circulating Tumor ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10813828/]
- 29. Circulating tumor DNA to monitor treatment response in ... [https://www.nature.com/articles/s41698-025-00876-y]
- 30. Cancer biomarker discovery and validation - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC4511498/]
- 31. Digital PCR: from early developments to its future application ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12278255/]
- 32. Cancer biomarker discovery and validation - Goossens [https://tcr.amegroups.org/article/view/4536/html]
- 33. Patient specific real-time PCR in precision medicine [https://www.frontiersin.org/journals/oncology/articles/10.3389/fonc.2022.1111209/full]
- 34. Technical considerations in PCR-based assay design for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9047347/]
- 35. Primer designing tool - NCBI - NIH [https://www.ncbi.nlm.nih.gov/tools/primer-blast/]
- 36. Selecting Optimal Housekeeping Genes for RT-qPCR in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12429465/]
- 37. Selection and validation of reference genes for RT-qPCR ... [https://www.nature.com/articles/s41598-025-02951-7]
- 38. Direct comparison of an ultrasensitive real-time PCR assay ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11659196/]
- 39. Feasibility of high-throughput sequencing in clinical routine ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7383956/]
- 40. Measurable residual disease in hematologic malignancies [https://pmc.ncbi.nlm.nih.gov/articles/PMC12257026/]
- 41. Patient specific real-time PCR in precision medicine [https://pubmed.ncbi.nlm.nih.gov/36727082/]
- 42. Analysis of measurable residual disease by IG/TR gene ... [https://www.nature.com/articles/s41375-024-02272-0]
- 43. How To Interpret RT-qPCR Results [https://www.goldbio.com/blogs/articles/how-to-interpret-rt-qpcr-results?srsltid=AfmBOoq08sZQM2RhGReEdmiNMBk3UpC2v62L27R8ywrGWYFLPg5kN7cS]
- 44. Development and validation of a methylation-specific ... [https://www.nature.com/articles/s41598-025-15228-w]
- 45. Liquid biopsy in cancer: current status, challenges and ... [https://www.nature.com/articles/s41392-024-02021-w]
- 46. Methylation Analyses in Liquid Biopsy of Lung Cancer Patients [https://pmc.ncbi.nlm.nih.gov/articles/PMC12468824/]
- 47. Methylation detection in percutaneous lung biopsy ... [https://www.frontiersin.org/journals/oncology/articles/10.3389/fonc.2025.1611244/full]
- 48. A Unified Multiplex Digital PCR-based Platform for Multi ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12425032/]
- 49. Multi-STEM MePCR: a bisulfite-free, multiplex, highly sensitive ... [https://pubs.rsc.org/en/content/articlehtml/2025/sc/d5sc01429h]
- 50. Multiplex Polymerase Chain Reaction Panels for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12541719/]
- 51. Optimization and Validation of a Folate Ligand-Targeted ... [https://pubmed.ncbi.nlm.nih.gov/40729092/]
- 52. MIQE Guidelines | Thermo Fisher Scientific - US [https://www.thermofisher.com/us/en/home/life-science/pcr/real-time-pcr/real-time-pcr-assays/why-choose-taqman-assays/publish-real-time-pcr-results.html]
- 53. MIQE 2.0 and the Urgent Need to Rethink qPCR Standards [https://www.mdpi.com/1422-0067/26/11/4975]
- 54. Multiplex PCR Assay Market CAGR, Segments and ... [https://www.towardshealthcare.com/insights/multiplex-pcr-assay-market-sizing]
- 55. 浅谈定量PCR实验中的Ct值与Cq 值 [https://www.bioalpha2008.com/articles/qtdlpc.html]
- 56. 实时荧光定量PCR原理及基础知识 - 赛默飞 [https://www.thermofisher.cn/cn/zh/home/life-science/pcr/real-time-pcr/real-time-pcr-learning-center/real-time-pcr-basics/essentials-real-time-pcr.html]
- 57. qPCR(荧光定量PCR)的Ct值原创 [https://blog.csdn.net/qq_52813185/article/details/134605609]
- 58. 实时荧光定量PCR系列4-PCR技术的定量方法(绝对定量法) [https://shiyanjia.com/knowledge-articleinfo-3309.html]
- 59. miR-2110通过调节CDT1影响肺腺癌的生物学行为- PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC11536258/]
- 60. 涨知识|qPCR专场五:如何分析荧光定量数据? [https://www.yeasen.com/h5/solutiondetail/3442]
- 61. 阅尔基因与Bio-Rad签订独家许可协议,共同推动肿瘤数字PCR ... [https://caivd-org.cn/article.asp?id=14386]
- 62. 阅尔基因与全球数字PCR巨头Bio-Rad签订独家许可和产品 ... [https://news.sina.cn/sx/2022-11-11/detail-imqmmthc4174366.d.html]
- 63. Comparison of real-time PCR and nCounter NanoString ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12217074/]
- 64. Polymerase Chain Reaction (PCR) - StatPearls - NCBI - NIH [https://www.ncbi.nlm.nih.gov/books/NBK589663/]
- 65. Development of an in-house, one-step RT-qPCR mix and ... [https://www.sciencedirect.com/science/article/pii/S2215016125005473]
- 66. Development of real-time PCR methods for quality control ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12058689/]
- 67. Preliminary Results of Reduced Polymerase Chain ... [https://www.mdpi.com/2673-8856/5/1/2]
- 68. Insights into qPCR: Protocol, Detection Methods, and Analysis [https://www.the-scientist.com/insights-into-qpcr-protocol-detection-methods-and-analysis-71478]
- 69. An optimized protocol for stepwise optimization of real-time ... [https://www.nature.com/articles/s41438-021-00616-w]
- 70. Investigating concentration effects on reaction efficiency ... [https://www.sciencedirect.com/science/article/abs/pii/S0003269725001472]
- 71. Universal SYBR Green qPCR Protocol [https://www.sigmaaldrich.com/US/en/technical-documents/protocol/genomics/qpcr/sybr-green-qpcr?srsltid=AfmBOormVNpP9wLVlNSjXYjzfQpluua8ZHD7yHt5A6r7J5WpYC1uMoCf]
- 72. Novel Semi-Nested Real-Time PCR Assay Leveraging ... [https://www.mdpi.com/2218-273X/14/6/729]
- 73. Primer-Probe Innovation for Low-Concentration Clinical ... [https://www.medrxiv.org/content/10.1101/2025.08.25.25334047v1.full-text]
- 74. Mutation Detection With Real-Time PCR [https://www.thermofisher.com/sa/en/home/life-science/pcr/real-time-pcr/real-time-pcr-applications/mutation-detection-with-real-time-pcr.html]
- 75. qPCR and qRT-PCR analysis: Regulatory points to ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7786041/]
- 76. How is Hot-Start Technology Beneficial For Your PCR [https://www.thermofisher.com/us/en/home/brands/thermo-scientific/molecular-biology/molecular-biology-learning-center/molecular-biology-resource-library/spotlight-articles/hot-start-technology-benefits-PCR.html]
- 77. Hot Start PCR with heat-activatable primers [https://pmc.ncbi.nlm.nih.gov/articles/PMC2582603/]
- 78. Hot start PCR [https://en.wikipedia.org/wiki/Hot_start_PCR]
- 79. Bovine serum albumin further enhances the effects of organic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3466135/]
- 80. PCR Setup—Six Critical Components to Consider [https://www.thermofisher.com/us/en/home/life-science/cloning/cloning-learning-center/invitrogen-school-of-molecular-biology/pcr-education/pcr-reagents-enzymes/pcr-component-considerations.html]
- 81. How To Interpret RT-qPCR Results [https://www.goldbio.com/blogs/articles/how-to-interpret-rt-qpcr-results?srsltid=AfmBOoqAHCcnsrZMgYixuhKTzZd8OIx3toI1p2wfy4s-Mc975Xpec7gu]
- 82. The Impact of the Variability of RT-qPCR Standard Curves ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12029521/]
- 83. Statistical analysis of real-time PCR data - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC1395339/]
- 84. Physical Simulation-Based Calibration for Quantitative ... [https://www.mdpi.com/2076-3417/14/12/5031]
- 85. ICH Q2(R2) Validation of analytical procedures [https://www.ema.europa.eu/en/ich-q2r2-validation-analytical-procedures-scientific-guideline]
- 86. ICH Guidelines for Analytical Method Validation Explained [https://amsbiopharma.com/ich-guidelines-analytical-method/]
- 87. 基于液体活检技术的多癌种联合筛查专家共识(2025版) [http://www.cjco.cn/article/doi/10.12354/j.issn.1000-8179.2025.20250754]
- 88. Methods to determine limit of detection and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5496743/]
- 89. Validating quantitative PCR assays for cfDNA detection ... [https://www.nature.com/articles/s41598-021-92826-4]
- 90. Determination of the LOQ in real-time PCR by receiver ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3132422/]
- 91. Recommendations for Method Development and ... [https://link.springer.com/article/10.1208/s12248-023-00880-9]
- 92. A robust ddPCR assay for the absolute quantification of ... [https://pubmed.ncbi.nlm.nih.gov/41167182/]
- 93. EuroMRD: Home [https://euromrd.org/]
- 94. Analysis of measurable residual disease by IG/TR gene ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11147754/]
- 95. Guidelines for RQ-PCR MRD [https://euromrd.org/guidelines/]
- 96. Introduction to Quantitative PCR (qPCR) Gene Expression ... [https://www.thermofisher.com/us/en/home/life-science/pcr/real-time-pcr/real-time-pcr-learning-center/gene-expression-analysis-real-time-pcr-information/introduction-gene-expression.html]
- 97. How Digital PCR Enables Early Molecular Relapse Detection [https://www.thermofisher.com/blog/behindthebench/early-molecular-relapse-detection-dpcr/]
- 98. dPCR vs end-point qPCR vs PCR [https://www.qiagen.com/us/knowledge-and-support/knowledge-hub/bench-guide/pcr/digital-pcr/digital-pcr-vs-quantitative-pcr-vs-end-point-pcr]
- 99. Real-Time vs Traditional Digital | Thermo Fisher Scientific - SG vs PCR [https://www.thermofisher.com/sg/en/home/life-science/pcr/real-time-pcr/real-time-pcr-learning-center/real-time-pcr-basics/real-time-vs-digital-vs-traditional-pcr.html]
- 100. Digital PCR or Quantitative Real-Time PCR: Which Method ... [https://bitesizebio.com/19734/digital-pcr-or-quantitative-real-time-pcr-which-method-is-best-for-your-quantitative-pcr-application/]
- 101. Digital droplet PCR is an accurate and precise method to ... [https://www.nature.com/articles/s41598-025-20944-4]
- 102. Simultaneous detection of eight cancer types using a ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11705734/]
- 103. Supporting Biomarker-Driven Therapies in Oncology [https://pmc.ncbi.nlm.nih.gov/articles/PMC10166172/]
- 104. NGS, qPCR, or Sanger Sequencing: An Assay Selection ... [https://blog.genewiz.com/ngs-qpcr-or-sanger-sequencing-an-assay-selection-guide]
- 105. The Growing Demand for Personalized Diagnostics [https://www.meridianbioscience.com/lifescience-blog/the-growing-demand-for-personalized-diagnostics-navigating-the-benefits-and-limits-of-qpcr-vs-ngs/]
- 106. NGS vs qPCR [https://www.illumina.com/science/technology/next-generation-sequencing/beginners/advantages/ngs-vs-qpcr.html]
- 107. The Advantage of Targeted Next-Generation Sequencing ... [https://www.mdpi.com/1422-0067/25/14/7908]
- 108. Comparison of Next-Generation Sequencing, Quantitative ... [https://pubmed.ncbi.nlm.nih.gov/27215089/]
- 109. Real-Time PCR (qPCR) and Whole-Transcriptome NGS [https://www.thermofisher.com/us/en/home/life-science/pcr/real-time-pcr/ngs-comparison.html]
- 110. Next-Generation Sequencing versus qPCR and Microarrays [https://www.rna-seqblog.com/next-generation-sequencing-versus-qpcr-and-microarrays/]
- 111. Cost of genetic testing, delayed care, and suboptimal ... [https://pubmed.ncbi.nlm.nih.gov/38391239/]
- 112. Essential Assays in Clinical Trials: Reporting Requirements ... [https://dctd.cancer.gov/drug-discovery-development/assays/essential-assays]
- 113. FDA's New Plausible Mechanism Pathway [https://www.avancebio.com/fdas-new-plausible-mechanism-pathway-how-it-compares-to-existing-approval-routes/]
- 114. qPCR assays and IVDR regulation in clinical trials [https://medicover-mics.com/qpcr-assays-and-ivdr-regulation/]
- 115. Multicolor Combinatorial Probe Coding for Real-Time PCR [https://pmc.ncbi.nlm.nih.gov/articles/PMC3021529/]