Tumor Mutational Burden Measurement by NGS: A Comprehensive Guide for Cancer Researchers and Drug Developers
This article provides a comprehensive examination of Tumor Mutational Burden (TMB) as a predictive biomarker for immunotherapy response, focusing on Next-Generation Sequencing (NGS) methodologies.
Tumor Mutational Burden Measurement by NGS: A Comprehensive Guide for Cancer Researchers and Drug Developers
Abstract
This article provides a comprehensive examination of Tumor Mutational Burden (TMB) as a predictive biomarker for immunotherapy response, focusing on Next-Generation Sequencing (NGS) methodologies. It covers the biological foundation of TMB, explores targeted panel sequencing as a practical alternative to whole exome sequencing, addresses critical technical challenges in measurement standardization, and discusses analytical validation approaches. Aimed at researchers, scientists, and drug development professionals, this review synthesizes current evidence and emerging best practices to guide robust TMB implementation in both research and clinical trial contexts, highlighting optimization strategies and future directions for this dynamic field.
The Biological and Clinical Foundation of Tumor Mutational Burden
Tumor Mutational Burden (TMB), defined as the total number of somatic mutations per megabase (mut/Mb) of interrogated genomic sequence, has emerged as a critical predictive biomarker for response to immune checkpoint inhibitors (ICIs) across multiple cancer types. The clinical significance of TMB stems from its role as a proxy for the generation of tumor-specific neoantigens—novel peptides arising from somatic mutations that are recognized by the immune system as foreign. This technical review examines the standardized definition of TMB, the biological pathway linking mutational burden to neoantigen genesis and antitumor immunity, current methodological approaches for TMB assessment, and the integration of this biomarker into clinical oncology practice. With the FDA's 2020 approval of pembrolizumab for TMB-high (≥10 mut/Mb) solid tumors based on the KEYNOTE-158 trial, standardized measurement and interpretation of TMB has become increasingly essential for translational researchers and drug development professionals.
The quantification of somatic mutations in tumor tissue has evolved from a research curiosity to a clinically validated biomarker that informs treatment selection. TMB measures the total number of non-inherited mutations detected per million bases (Mb) of sequenced genomic DNA [1]. This metric varies significantly across cancer types, with melanoma, non-small cell lung cancer (NSCLC), and squamous carcinomas typically demonstrating the highest TMB values, while leukemias and pediatric tumors show the lowest levels [1].
The biological rationale for TMB as a predictive biomarker lies in the immunogenic nature of mutation-derived neoantigens. As the mutational burden increases, so does the statistical probability that certain mutations will generate novel protein sequences that can be processed and presented as neoantigens on major histocompatibility complex (MHC) molecules [2]. These neoantigens are recognized as "non-self" by T cells, triggering an immune response that can be augmented by ICIs [3]. The FDA's landmark approval of pembrolizumab for TMB-high solid tumors in June 2020 established TMB as the first pan-cancer biomarker for immunotherapy response prediction [1] [4].
The Biological Pathway: From Somatic Mutations to Antitumor Immunity
The process by which somatic mutations lead to enhanced antitumor immunity involves multiple sequential steps, each with important implications for therapeutic response.
Neoantigen Genesis and Immunogenicity
Neoantigens arise primarily from non-synonymous somatic mutations—including single nucleotide variants (SNVs), insertions and deletions (INDELs), and gene fusions—that alter protein sequence and create novel peptide sequences absent in normal tissues [2]. These altered proteins are processed intracellularly into peptides, loaded onto MHC molecules, and transported to the cell surface for T-cell recognition. The immunogenic potential of neoantigens depends on multiple factors, including the binding affinity of mutant peptides to MHC molecules, the abundance of resulting peptide-MHC complexes on the tumor cell surface, and the presence of T-cell receptors capable of recognizing these complexes [3].
Not all mutations contribute equally to neoantigen generation. Frameshift INDELs often generate more immunogenic neoantigens compared to SNVs due to more substantial alterations in protein sequence [2]. Microsatellite instability-high (MSI-H) tumors, which result from deficient DNA mismatch repair (dMMR) mechanisms, accumulate numerous frameshift mutations that generate shared frameshift neoantigens across cancer types [2]. This explains the particularly high response rates to ICIs observed in MSI-H/dMMR tumors across multiple cancer types [5].
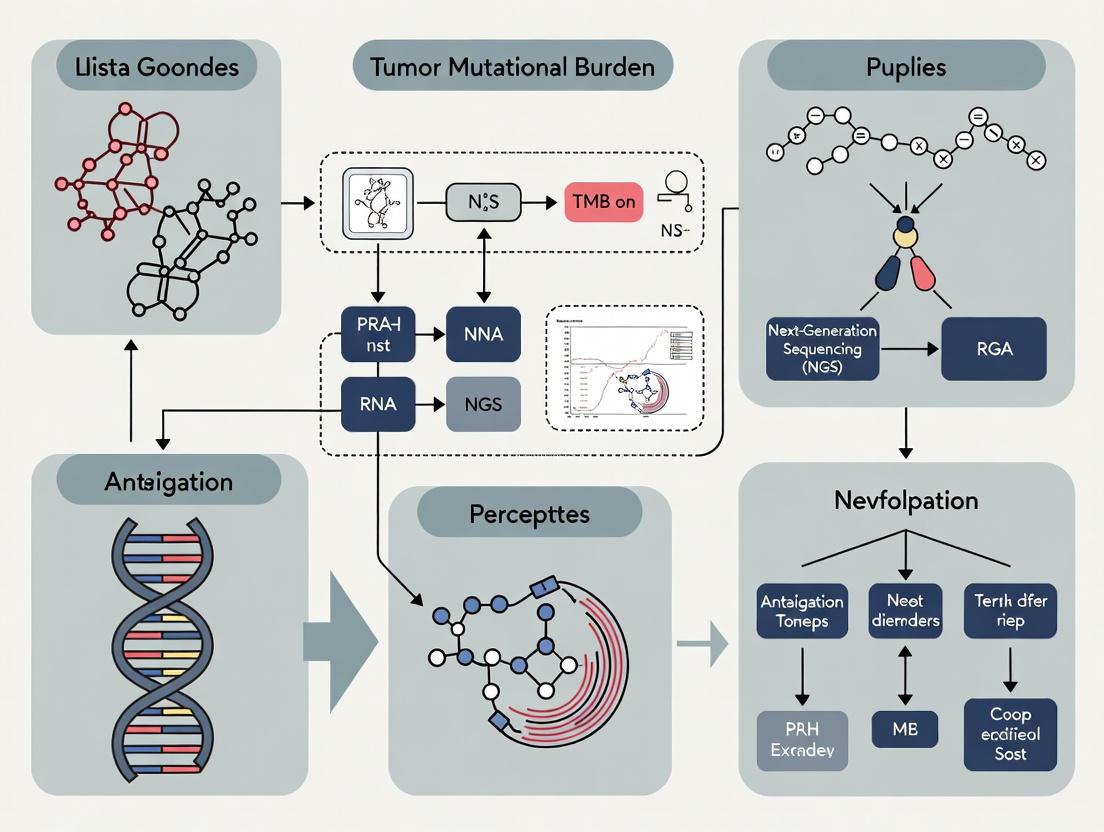
Figure 1: The pathway from somatic mutations to antitumor immunity through neoantigen genesis. Multiple mutation sources contribute to neoantigen formation, which enables immune recognition and is enhanced by checkpoint inhibition.
TMB as a Surrogate for Neoantigen Load
While neoantigen burden (the actual number of immunogenic mutations) would theoretically represent the ideal predictive biomarker, its assessment requires complex analyses incorporating HLA typing, peptide-MHC binding predictions, and T-cell recognition assays [6]. In contrast, TMB serves as a practical and robust surrogate that correlates with neoantigen load across diverse cancer types [3]. Research demonstrates that only a small fraction of somatic mutations (approximately 1-2%) ultimately generate immunogenic neoantigens, but this fraction remains relatively consistent across patients and cancer types [2]. This consistent ratio enables TMB to function as an effective clinical predictor of ICI response.
The relationship between TMB and neoantigen load explains the superior outcomes observed with ICIs in high-TMB cancers. Tumors with higher TMB present a broader repertoire of neoantigens to the immune system, increasing the probability of effective T-cell recognition and killing when immune checkpoints are blocked [4] [1]. This mechanism underpins the association between high TMB and improved response to ICIs across multiple cancer types, as demonstrated in pivotal trials such as KEYNOTE-158 [4].
Methodological Approaches for TMB Assessment
Accurate TMB measurement requires careful consideration of multiple technical factors, including sequencing methodology, bioinformatic processing, and variant filtering criteria.
Sequencing Platforms and Technical Considerations
TMB can be assessed using whole genome sequencing (WGS), whole exome sequencing (WES), or targeted next-generation sequencing (NGS) panels, each with distinct advantages and limitations for clinical application.
Table 1: Comparison of TMB Measurement Approaches
| Parameter | Whole Exome Sequencing (WES) | Large Targeted Panels (>1 Mb) | Small Targeted Panels (<1 Mb) |
|---|---|---|---|
| Genomic Coverage | ~30-40 Mb (entire exome) | 1.1-2.4 Mb (selected genes) | 0.8-1.0 Mb (limited genes) |
| TMB Correlation with WES | Gold standard | High (R² > 0.9) | Moderate to low |
| Clinical Feasibility | Low (cost, turnaround time) | High | High |
| Tumor Content Requirements | High (>30%) | Moderate (>20%) | High (>30%) |
| Variant Detection Sensitivity | High for coding regions | High for panel regions | Limited by panel size |
| Examples | Research standard | FoundationOneCDx, MSK-IMPACT, TSO500 | Various hotspot panels |
WES represents the historical gold standard for TMB assessment, interrogating approximately 30-40 megabases of coding sequence across ~20,000 genes [4]. While comprehensive, WES remains impractical for routine clinical use due to high cost, long turnaround time, and substantial tissue requirements [4] [1]. Targeted NGS panels covering 1.1-2.4 megabases have emerged as the preferred methodology for clinical TMB assessment, offering an optimal balance of comprehensiveness, cost-effectiveness, and clinical turnaround time [7].
The precision of TMB estimation depends significantly on panel size. The coefficient of variation of panel-based TMB decreases inversely with both the square root of the panel size and the square root of the TMB level [4]. Panels covering at least 1-1.5 Mb of coding sequence demonstrate improved correlation with WES-derived TMB and more reliable classification of TMB-high status [7].
Wet-Lab Protocols and Bioinformatics Analysis
Robust TMB assessment requires standardized wet-lab methodologies and bioinformatic pipelines to ensure reproducible results across laboratories.
Sample Processing and Sequencing
The typical workflow begins with DNA extraction from formalin-fixed paraffin-embedded (FFPE) tumor tissue or frozen specimens. FFPE specimens present particular challenges due to formalin-induced DNA damage, which can artifactually inflate TMB estimates if not properly addressed [5] [1]. After DNA extraction and quality control, libraries are prepared using targeted hybridization capture approaches, followed by next-generation sequencing on platforms such as Illumina's NextSeq 550Dx [7].
The Institut Curie protocol exemplifies a rigorous approach to TMB assessment, incorporating sample-specific quality thresholds and variant allele frequency (VAF) filters. Their methodology establishes optimal VAF cut-offs at 10% for FFPE samples and 5% for frozen samples to minimize false-positive mutations while retaining sensitivity [5]. This group also emphasizes the importance of pre-analytical DNA quality assessment, particularly for FFPE samples, where DNA degradation can significantly impact TMB accuracy [5].
Bioinformatic Processing and Variant Filtering
Bioinformatic pipelines for TMB calculation typically include sequence alignment, variant calling, and extensive filtering to exclude germline polymorphisms, sequencing artifacts, and driver mutations that may not contribute to neoantigen formation.
Table 2: Variant Filtering Criteria for TMB Calculation
| Filter Category | Inclusion Criteria | Exclusion Criteria |
|---|---|---|
| Variant Type | Non-synonymous SNVs, nonsense mutations, small indels | Synonymous mutations, intronic variants, large structural variants |
| Population Frequency | Absent from population databases (gnomAD, 1000 Genomes) | Variants with population frequency >0.1% |
| Variant Allele Frequency (VAF) | ≥10% for FFPE samples, ≥5% for frozen samples | Below threshold or >95% (potential germline) |
| Mutation Location | Protein-coding regions | Non-coding regions, promoter elements |
| Artifact Filtering | Passes strand bias, base quality, and mapping quality filters | FFPE-induced C>T transitions, sequencing errors |
| Driver Mutations | Included in some panels (MSK-IMPACT) | Excluded in some panels (FoundationOne CDx) |
The FoundationOne CDx algorithm exemplifies a tumor-only approach that includes synonymous mutations while excluding hotspot driver mutations, whereas MSK-IMPACT employs a tumor-normal paired approach with different filtering criteria [1]. These methodological differences highlight the importance of platform-specific validation and the current lack of complete harmonization across TMB assays [4].
The Researcher's Toolkit: Essential Reagents and Platforms
Table 3: Essential Research Reagents and Platforms for TMB Analysis
| Reagent/Platform | Function | Application in TMB Research |
|---|---|---|
| FFPE DNA Extraction Kits | Isolation of high-quality DNA from archived specimens | Ensures sufficient input material with minimal artifacts for reliable variant calling |
| Hybridization Capture Panels | Target enrichment for NGS | Focuses sequencing on clinically relevant genomic regions; panel size critical for TMB precision |
| UMI Adapters | Unique molecular identifiers | Reduces sequencing errors and improves variant calling accuracy by correcting PCR duplicates |
| Tumor-Normal Pair Analysis | Germline variant subtraction | Distinguishes somatic from inherited variants; requires matched normal tissue |
| Population Databases | Filtering of common polymorphisms | Identifies and excludes germline variants using databases like gnomAD and 1000 Genomes |
| Bioinformatic Tools | Variant calling and annotation | Platforms like Strelka for mutation detection; Kourami for HLA typing in neoantigen prediction |
TMB in Clinical Practice and Therapeutic Decision-Making
The translation of TMB from a research concept to a clinically actionable biomarker has progressed rapidly, culminating in regulatory approvals and inclusion in professional guidelines.
TMB Cutoffs and Predictive Value
The FDA-approved cutoff for TMB-high status is ≥10 mutations per megabase, based on data from the KEYNOTE-158 basket trial demonstrating significantly improved objective response rates to pembrolizumab in patients with TMB-high solid tumors [8] [4]. This pan-cancer threshold provides a standardized approach for patient selection, though evidence suggests optimal cutpoints may vary across cancer types [1].
Retrospective analyses demonstrate a clear relationship between TMB levels and response to ICIs. In one large cohort, patients with TMB ≥20 mut/Mb showed a 58% response rate to ICIs compared to 20% in patients with lower TMB [1]. The association between TMB and outcomes appears continuous rather than binary, with progressively higher TMB levels generally correlating with improved response, though exceptions exist in cancers such as renal cell carcinoma [4].
Integration with Other Biomarkers
TMB provides complementary information to other established biomarkers, including PD-L1 expression and microsatellite instability (MSI). While MSI-H/dMMR tumors typically exhibit high TMB, and MSI status predicts response to ICIs across cancer types, TMB can identify additional patients who may benefit from immunotherapy beyond those with MSI-H [4]. Similarly, the combination of TMB and PD-L1 expression may improve patient stratification compared to either biomarker alone [4] [7].
Emerging Approaches and Future Directions
Recent methodological advances aim to address current limitations in TMB assessment. Liquid biopsy approaches for blood-based TMB (bTMB) measurement offer a less invasive alternative to tissue biopsy, with promising data in non-small cell lung cancer suggesting bTMB ≥20 mut/Mb predicts improved outcomes with ICIs [7]. Additionally, novel methodologies for direct neoantigen identification from circulating tumor cells using apheresis and exome sequencing provide opportunities for minimally invasive neoantigen discovery [9].
The research community has initiated efforts to harmonize TMB measurement across platforms, including the Friends of Cancer Research TMB Harmonization Project, which aims to establish calibration standards and improve reproducibility across laboratory-developed tests [8]. Such initiatives are critical for ensuring consistent TMB assessment and clinical application across testing platforms.
Tumor Mutational Burden, defined as the number of somatic mutations per megabase of sequenced DNA, represents both a biological mediator of antitumor immunity and a clinically validated predictive biomarker for immunotherapy response. The connection between TMB and neoantigen genesis provides a mechanistic foundation for its predictive value, as increased mutational load enhances the probability of immunogenic neopeptide formation and T-cell recognition. Standardized measurement approaches using large targeted NGS panels have enabled TMB's translation into clinical practice, supported by level 1 evidence from prospective clinical trials. Ongoing efforts to harmonize assessment methodologies, refine predictive cutoffs across cancer types, and integrate TMB with complementary biomarkers will further optimize its utility for patient stratification and drug development in immuno-oncology.
Tumor Mutational Burden as a Predictive Biomarker for Immune Checkpoint Inhibitor Response
Tumor mutational burden (TMB) has emerged as a significant quantitative biomarker for predicting response to immune checkpoint inhibitors (ICIs) across multiple cancer types. Defined as the total number of somatic mutations per coding area of a tumor genome, TMB reflects the likelihood of neoantigen formation that can stimulate anti-tumor immune responses [10] [11]. This technical review examines the molecular basis of TMB, standardizes measurement methodologies, evaluates clinical validation evidence, and discusses integration with complementary biomarkers. While TMB shows considerable promise for personalizing immunotherapy, challenges remain in standardization, interpretation across cancer types, and accounting for tumor microenvironment influences that collectively impact clinical utility [10] [12].
TMB represents a quantifiable measure of genetic alterations accumulated within a tumor genome. The underlying hypothesis posits that tumors with higher mutation loads generate more neoantigens - novel peptides resulting from somatic mutations that are recognized as foreign by the immune system [10]. These neoantigens are presented on major histocompatibility complex (MHC) molecules, triggering T-cell activation and proliferation. In immunologically competent environments, this increased neoantigen burden enhances tumor immunogenicity and facilitates greater T-cell infiltration, ultimately rendering tumors more susceptible to immune checkpoint blockade [10] [11].
The relationship between TMB and ICI response extends beyond mere mutation quantity. Specific mutation classes, particularly nonsynonymous mutations that alter amino acid sequences, demonstrate stronger correlations with immunogenicity than silent mutations [13]. Additionally, mutational processes influencing TMB vary across cancer types, with ultraviolet light exposure in melanoma, tobacco smoking in lung cancer, and DNA repair deficiencies in various malignancies all contributing to distinct mutational signatures that differentially impact neoantigen quality and immune recognition [13].
Table 1: Key Molecular Processes Influencing TMB
| Biological Process | Impact on TMB | Representative Genes/Pathways |
|---|---|---|
| DNA Damage Repair | Defective repair dramatically increases mutation accumulation | MMR genes (MLH1, MSH2, MSH6, PMS2), POLE/POLD1 [11] |
| DNA Replication Fidelity | Polymerase errors increase mutation rate | POLE/POLD1 [11] |
| Carcinogen Exposure | Induces characteristic mutational signatures | Smoking (lung), UV light (melanoma) [13] |
| Homologous Recombination Repair | Deficiency increases genomic instability | BRCA1/2, ATM, RAD51 [10] |
Methodologies for TMB Assessment
Sequencing Approaches and Platforms
TMB measurement methodologies have evolved substantially, with next-generation sequencing (NGS) now representing the standard approach. Whole exome sequencing (WES) interrogates approximately 60 megabases (Mb) of protein-coding regions, providing the most comprehensive mutation assessment [14]. However, practical constraints including cost, turnaround time, and analytical complexity have driven development of targeted gene panels that estimate TMB from smaller genomic regions, typically ranging from 0.8 to 2.0 Mb [10] [14].
The FoundationOne CDx (324 genes) and MSK-IMPACT (468 genes) assays represent FDA-approved comprehensive genomic profiling platforms validated for TMB assessment [11] [13]. These targeted panels demonstrate strong correlation with WES when properly calibrated and provide a practical solution for clinical implementation [14]. Essential technical specifications for reliable TMB measurement include adequate tumor content (typically >20%), sufficient sequencing depth (>500x), and appropriate bioinformatic pipelines for germline mutation filtering [14].
Diagram 1: TMB Analysis Workflow
Blood-Based TMB (bTMB) Assessment
Liquid biopsy approaches for measuring TMB in circulating tumor DNA (ctDNA) address limitations of tissue sampling, including invasiveness, tumor heterogeneity, and serial monitoring challenges [15] [16]. The Foundation Medicine bTMB assay targets 1.1 Mb of genomic sequence and requires adequate ctDNA representation, typically defined as maximum somatic allele frequency (MSAF) ≥1% [16].
Recent validation studies demonstrate promising correlations between bTMB and tissue TMB, though technical challenges remain. The phase 2 B-F1RST trial evaluated bTMB as a predictive biomarker for first-line atezolizumab in non-small cell lung cancer (NSCLC), finding that bTMB ≥16 (approximately 14.5 mutations/Mb) was associated with improved overall survival (OS) despite not meeting the primary progression-free survival endpoint [16]. Similarly, the DART study in stage III NSCLC reported that high bTMB using both prespecified (8.5 mut/Mb) and median (6.6 mut/Mb) cutoffs correlated with longer progression-free survival following chemoradiotherapy and durvalumab [15].
Table 2: TMB Measurement Methodologies Comparison
| Parameter | Whole Exome Sequencing | Targeted NGS Panels | Blood-Based TMB |
|---|---|---|---|
| Genomic Coverage | ~60 Mb (entire exome) | 0.8-2.0 Mb (selected genes) | ~1.1 Mb (Foundation Medicine) [16] |
| Advantages | Comprehensive mutation detection; gold standard | Clinical feasibility; faster turnaround; lower cost | Minimally invasive; captures heterogeneity; enables monitoring [15] [16] |
| Limitations | Cost; analysis complexity; clinical turnaround | Requires validation against WES; panel size effects | Requires sufficient ctDNA (MSAF ≥1%); analytical sensitivity [16] |
| Clinical Implementation | Primarily research | FoundationOne CDx, MSK-IMPACT | Foundation Medicine bTMB assay [16] |
Clinical Validation of TMB as a Predictive Biomarker
Evidence Across Tumor Types
TMB demonstrates variable predictive value across cancer types, reflecting distinct immunobiological contexts. Consistent evidence supports TMB's predictive utility in NSCLC, melanoma, and urothelial carcinomas, while more limited associations appear in esophageal/gastric cancers and renal cell carcinoma [17] [12].
The phase 3 CheckMate 227 trial established TMB ≥10 mut/Mb as a predictive cutoff for first-line nivolumab plus ipilimumab in NSCLC, with significantly improved progression-free survival versus chemotherapy (7.2 vs. 5.5 months; HR 0.58) [13]. Similarly, a meta-analysis of 26 studies encompassing 5,712 patients demonstrated that high-TMB groups exhibited superior overall survival and progression-free survival with ICI treatment compared to low-TMB groups [10]. However, a VA population study found that while TMB ≥10 mut/Mb predicted improved survival in NSCLC, head and neck cancer, and urothelial cancer, no significant association was observed in melanoma or esophageal/gastric cancer, highlighting that fixed TMB thresholds may not apply universally across tumor types [17].
Tumor-Agnostic Approvals and Limitations
In 2020, the FDA granted accelerated approval to pembrolizumab for unresectable or metastatic solid tumors with TMB ≥10 mut/Mb that had progressed on prior treatments, based on the KEYNOTE-158 trial showing an overall response rate of 29% in the high-TMB cohort [12]. This tumor-agnostic approval represents a significant milestone but has generated controversy regarding optimal cutoffs, clinical utility across diverse malignancies, and absence of overall survival benefit in some analyses [12].
Research suggests that TMB thresholds may need tumor-specific optimization. A Northwestern University study found that in non-ICI-sensitive tumor types (those without FDA approval for ICI monotherapy), a higher TMB cutoff of ≥15 mut/Mb correlated with improved outcomes, whereas the standard ≥10 mut/Mb cutoff sufficed for ICI-sensitive tumors [12]. Additionally, specific mutational contexts influence TMB's predictive value; for instance, MYC pathway mutations and MLL2 alterations were associated with poorer ICI responses despite high TMB, while TERT mutations correlated with better responses [12].
Table 3: TMB Cutoffs and Associated Clinical Outcomes Across Selected Malignancies
| Cancer Type | Key Trial/Study | TMB Cutoff | Clinical Outcome |
|---|---|---|---|
| NSCLC | CheckMate 227 [13] | ≥10 mut/Mb | Improved PFS with nivolumab + ipilimumab vs chemo (7.2 vs 5.5 mo; HR 0.58) |
| Multiple Solid Tumors | KEYNOTE-158 [12] | ≥10 mut/Mb | ORR 29% with pembrolizumab; basis for FDA tumor-agnostic approval |
| SCLC | CheckMate 032 [18] | ≥248 mutations/tumor (WES) | Improved 1-year OS with nivolumab + ipilimumab (62.4% vs 23.4% in TMB-low) |
| NSCLC (Blood TMB) | B-F1RST [16] | ≥16 (≈14.5 mut/Mb) | Associated with longer OS with atezolizumab (36.5-month follow-up) |
| Non-ICI-sensitive Tumors | Northwestern Study [12] | ≥15 mut/Mb | Correlated with improved outcomes in tumors not typically ICI-sensitive |
Integration with Complementary Biomarkers
TMB alone provides incomplete predictive information, spurring investigation into multimodal biomarker strategies. PD-L1 expression represents the most established complementary biomarker, with evidence suggesting independent predictive value from TMB [15] [19]. The DART study in stage III NSCLC found that both PD-L1 ≥1% and high bTMB were independently associated with longer progression-free survival following chemoradiotherapy and durvalumab [15].
Specific mutational signatures and pathways further refine TMB's predictive capacity. Deficiencies in DNA damage response pathways, particularly mismatch repair (MMR) deficiencies leading to microsatellite instability (MSI-H), confer exceptionally high TMB and pronounced sensitivity to ICIs [11]. Additionally, mutations in STK11, KEAP1, and NFE2L2 have been associated with immunologically cold tumor microenvironments and resistance to ICIs despite high TMB [15]. These findings underscore the importance of evaluating both quantitative mutational burden and qualitative aspects of the tumor immune microenvironment.
Diagram 2: TMB and Modulating Factors in ICI Response
Emerging Approaches and Future Directions
Novel Predictive Models
Machine learning approaches integrating TMB with routinely available clinical and laboratory data show promise for improving prediction accuracy. The SCORPIO model, developed using data from 9,745 ICI-treated patients across 21 cancer types, utilizes complete blood counts, comprehensive metabolic profiles, and clinical characteristics to predict ICI outcomes [19]. In validation studies, SCORPIO significantly outperformed TMB alone for predicting overall survival (median time-dependent AUC 0.763 vs. 0.503) and clinical benefit (AUC 0.714 vs. 0.546), suggesting that composite models may surpass single-marker approaches [19].
Dynamic TMB assessment represents another emerging frontier. Longitudinal monitoring of TMB during treatment may provide early response indicators, with one melanoma study finding that early on-treatment changes in TMB (ΔTMB) strongly correlated with anti-PD-1 response and overall survival [11]. Liquid biopsy approaches facilitate such serial monitoring and may capture evolving clonal dynamics under therapeutic pressure.
Standardization Challenges and Research Needs
Substantial variability in TMB measurement methodologies, bioinformatic pipelines, and cutoff definitions currently hampers broader clinical implementation [10] [17]. The Friends of Cancer Research TMB Harmonization Project has demonstrated that while laboratory-specific differences exist, appropriate calibration can achieve consistent classification across platforms [10].
Key research priorities include establishing tumor-type-specific optimal cutoffs, validating blood-based TMB approaches, and refining integrated biomarker models that incorporate both tumor-intrinsic and host immune factors [12] [16]. Additionally, greater understanding of neoantigen quality rather than mere quantity may enhance prediction, as immunogenic potential varies substantially across mutation classes [10].
The Scientist's Toolkit: Essential Research Reagents and Platforms
Table 4: Key Experimental Resources for TMB Research
| Resource Category | Specific Examples | Application in TMB Research |
|---|---|---|
| Sequencing Platforms | Illumina NovaSeq, NextSeq | High-throughput sequencing for WES and targeted panels [14] |
| Targeted Panels | FoundationOne CDx, MSK-IMPACT | Clinical TMB measurement; validated against WES [11] [13] |
| Liquid Biopsy Assays | Foundation Medicine bTMB | Blood-based TMB assessment; requires MSAF ≥1% [16] |
| Bioinformatics Tools | Mutect2, VarScan, VEP | Somatic variant calling and annotation [14] |
| Reference Standards | Horizon Discovery, SeraCare | Method validation and cross-laboratory standardization |
| Data Resources | TCGA, cBioPortal | Reference TMB distributions across cancer types [14] |
Tumor mutational burden represents a fundamentally important biomarker with validated predictive capacity for immune checkpoint inhibitor responses across multiple cancer types. The biological rationale linking high mutation load to increased neoantigen formation and enhanced tumor immunogenicity provides a compelling mechanistic framework. However, clinical application requires careful consideration of measurement methodologies, tumor-type context, and integration with complementary biomarkers including PD-L1 expression and specific genomic alterations. Ongoing efforts to standardize assessment methodologies, validate blood-based approaches, and develop integrated predictive models will further solidify TMB's role in personalizing cancer immunotherapy and advancing precision oncology.
Tumor Mutational Burden (TMB) represents the total number of somatic mutations per megabase (mut/Mb) within a tumor genome's coding region [7]. As a quantifiable genomic biomarker, TMB functions as a surrogate for neoantigen load, with the underlying hypothesis that tumors possessing higher mutation counts are more likely to express neoantigens recognizable by the immune system, thereby enhancing susceptibility to immune checkpoint blockade therapy [7] [20]. The clinical validation of TMB represents a significant advancement in precision immuno-oncology, enabling better identification of patients who may derive exceptional benefit from immunotherapy across diverse cancer types.
This technical analysis examines the foundational evidence from two landmark clinical trials, KEYNOTE-158 and CheckMate 227, which prospectively validated TMB as a predictive biomarker for immunotherapy response. We explore their experimental methodologies, primary efficacy outcomes, and the subsequent impact on biomarker-driven drug development within the context of next-generation sequencing (NGS) research.
KEYNOTE-158: Prospective Validation of TMB in Advanced Solid Tumors
Study Design and Experimental Protocol
KEYNOTE-158 (NCT02628067) was a prospective, multi-cohort, open-label, phase 2 biomarker analysis that evaluated the efficacy of pembrolizumab monotherapy across multiple advanced solid tumors [21]. The trial was conducted across 81 academic and community institutions in 21 countries, enrolling patients aged ≥18 years with selected, previously treated advanced solid tumors (anal, biliary, cervical, endometrial, mesothelioma, neuroendocrine, salivary, small-cell lung, thyroid, and vulvar) who had progressed on or were intolerant to standard therapy [21].
Key Methodological Elements:
- Intervention: Pembrolizumab 200 mg intravenously every 3 weeks for up to 35 cycles
- TMB Assessment: Tissue TMB (tTMB) was evaluated in formalin-fixed paraffin-embedded (FFPE) tumor samples using the FoundationOne CDx assay
- Prespecified TMB-H Threshold: ≥10 mutations per megabase
- Primary Endpoint: Objective response rate (ORR) per RECIST 1.1 by independent central review
- Statistical Analysis: Efficacy was assessed in the treated population with evaluable tTMB data enrolled ≥26 weeks before data cutoff (June 27, 2019) [21]
Key Efficacy Findings and Clinical Outcomes
At data cutoff, 1073 patients were enrolled, with 1066 receiving treatment. Among these, 790 patients were evaluable for TMB and included in efficacy analyses. The TMB-high population (≥10 mut/Mb) comprised 102 patients (13%), while 688 patients (87%) had non-TMB-high status (<10 mut/Mb). After a median follow-up of 37.1 months, the study demonstrated a substantial differential response based on TMB status [21].
Table 1: KEYNOTE-158 Efficacy Outcomes by TMB Status
| Parameter | TMB-High (≥10 mut/Mb) | Non-TMB-High (<10 mut/Mb) |
|---|---|---|
| Patients, n | 102 | 688 |
| Objective Response Rate, % (95% CI) | 29% (21-39) | 6% (5-8) |
| Complete Response, n | 4 | 7 |
| Partial Response, n | 26 | 36 |
| Safety Population, n | 105 | - |
| Grade 3-5 Treatment-Related AEs, % | 15% | - |
| Treatment-Related Serious AEs, % | 10% | - |
The robust response rate in the TMB-high subgroup, which was nearly five-fold greater than in non-TMB-high patients, led the investigators to conclude that tTMB could serve as a novel and useful predictive biomarker for response to pembrolizumab monotherapy in patients with previously treated recurrent or metastatic advanced solid tumors [21].
CheckMate 227: TMB as a Biomarker for Dual Immunotherapy in NSCLC
Trial Methodology and Biomarker Assessment
CheckMate 227 was a pivotal phase 3 trial evaluating first-line immunotherapy in metastatic non-small cell lung cancer (NSCLC). Part 1 of this complex trial specifically examined the efficacy of nivolumab plus ipilimumab versus chemotherapy in patients with high TMB (≥10 mut/Mb), regardless of PD-L1 expression level [22].
Key Methodological Elements:
- Interventions: Nivolumab + ipilimumab versus chemotherapy
- TMB Assessment: Tissue TMB was evaluated using the FoundationOne CDx assay (324 genes)
- Prespecified TMB-H Threshold: ≥10 mutations per megabase
- Primary Endpoint: Progression-free survival (PFS) in the TMB-high population
- Statistical Design: The trial used a hierarchical testing strategy to evaluate multiple biomarker-defined populations [22]
Efficacy Outcomes and Long-Term Survival Data
CheckMate 227 Part 1 demonstrated that patients with high TMB (≥10 mut/Mb) experienced significantly improved progression-free survival with nivolumab plus ipilimumab compared to chemotherapy. Although initial reports indicated no significant overall survival difference in the TMB-high population, subsequent long-term follow-up analyses, particularly in patient subgroups, have confirmed durable clinical benefits [22] [23].
A recent pooled analysis of CheckMate 227 and CheckMate 9LA focusing on patients with tumor PD-L1 lower than 1% revealed substantial long-term benefits for nivolumab plus ipilimumab with or without chemotherapy. After a median follow-up of 73.7 months, the median overall survival was 17.4 months versus 11.3 months (hazard ratio [HR] = 0.64, 95% CI: 0.54-0.76), with 5-year survival rates of 20% versus 7% favoring the immunotherapy-based regimens [23].
Table 2: CheckMate 227/9LA Pooled Analysis in PD-L1 <1% Population
| Outcome Measure | Nivo+Ipi (±Chemo) | Chemotherapy | Hazard Ratio (95% CI) |
|---|---|---|---|
| Patients, n | 322 | 315 | - |
| Median OS, months | 17.4 | 11.3 | 0.64 (0.54-0.76) |
| 5-Year OS Rate, % | 20 | 7 | - |
| Median PFS, months | 5.4 | 4.9 | 0.72 (0.60-0.87) |
| 5-Year PFS Rate, % | 9 | 2 | - |
| Objective Response Rate, % | 29 | 22 | - |
| Median DoR, months | 18.0 | 4.6 | - |
The consistency of benefit across key subgroups, including patients with baseline brain metastases (HR = 0.44) and those with squamous histology (HR = 0.51), reinforces the clinical utility of this biomarker-driven approach [23].
Technical Methodologies for TMB Assessment
NGS-Based TMB Measurement Approaches
Accurate TMB quantification requires sophisticated genomic analysis methodologies. The two primary NGS-based approaches for somatic mutation identification in solid tumors are:
- Tumor-Only (TO) Sequencing: Analyzes tumor tissue alone, comparing sequencing data against population databases to distinguish somatic mutations [24]
- Tumor-Control (TC) Paired Sequencing: Simultaneously sequences tumor tissue and matched normal (white blood cells or normal tissue) to directly differentiate somatic from germline variants [24]
Recent comparative studies demonstrate that these different methodological approaches can impact TMB results, particularly near the critical 10 mut/Mb threshold. One analysis of 24 solid tumor samples revealed 92% consistency between TO and TC methods, but statistically significant differences in TMB classification (χ² = 16.667, p < 0.001), highlighting the importance of methodological standardization [24].
Emerging Approaches: Blood-Based TMB Assessment
The development of blood-based TMB (bTMB) represents an emerging approach that circumvents tissue availability limitations. bTMB is derived from circulating tumor DNA (ctDNA) using comprehensive genomic profiling. Early clinical data from studies such as MYSTIC and B-F1RST suggested potential utility, though subsequent trials like NEPTUNE and B-FAST (cohort C) failed to meet primary endpoints when using bTMB for patient selection [25].
The CheckMate 848 study evaluated concordance between tissue and blood TMB, demonstrating a statistically significant correlation across 1017 patients, particularly in samples with high maximum somatic allele frequency. However, discordant classification was observed in some cases, with patients exhibiting tTMB-high/bTMB-low status maintaining response rates of 35.0%, while those with bTMB-high/tTMB-low results showed reduced response rates of 9.7% [25].
Research Reagent Solutions for TMB Analysis
Table 3: Essential Research Tools for TMB Biomarker Development
| Research Tool | Primary Function | Key Features |
|---|---|---|
| FoundationOne CDx | Comprehensive genomic profiling for tTMB | 324-gene panel; FDA-approved companion diagnostic; validated for TMB assessment in KEYNOTE-158 and CheckMate 227 [21] [22] |
| FoundationOne Liquid CDx | Blood-based comprehensive genomic profiling | ctDNA analysis; provides bTMB score; approved in Japan for cancer genomic profiling [25] |
| TruSight Oncology 500 | Comprehensive genomic profiling for tumor-only TMB | 523-gene panel; utilizes hybrid capture-based NGS; detects multiple biomarker classes [24] |
| MSK-IMPACT | Targeted sequencing for cancer genomics | 468-gene panel; used for institutional genomic profiling and TMB calculation in research settings [20] |
| Shihe No.1 TMB Detection Kit | Tissue TMB detection with matched normal | 425-gene panel; designed for tumor-control paired analysis; includes white blood cell control [24] |
Conceptual Framework of TMB and Immunotherapy Response
Figure 1: Mechanism of TMB-Driven Response to Immunotherapy
Experimental Workflow for TMB Assessment in Clinical Trials
Figure 2: TMB Testing Workflow in Clinical Trials
The prospective evidence from KEYNOTE-158 and CheckMate 227 firmly established TMB as a clinically actionable biomarker for immunotherapy across multiple cancer types. KEYNOTE-158 validated the use of TMB ≥10 mut/Mb as a predictive biomarker for pembrolizumab monotherapy in previously treated advanced solid tumors, while CheckMate 227 demonstrated the utility of TMB for identifying NSCLC patients who benefit from first-line nivolumab-ipilimumab combination therapy.
Ongoing research continues to refine our understanding of TMB, including:
- Standardization of TMB measurement across different NGS platforms and methodologies [24]
- Integration of TMB with other biomarkers (MSI, PD-L1, gene signatures) for improved patient stratification [20] [26]
- Development of blood-based TMB assays to address tissue limitations [25]
- Exploration of TMB heterogeneity and its relationship with underlying mutational processes (APOBEC, DNA damage repair) [20]
These landmark trials represent a paradigm shift in biomarker-driven drug development, establishing comprehensive genomic profiling and TMB assessment as essential components of precision immuno-oncology research. The continued refinement of TMB quantification and interpretation will further optimize patient selection for immunotherapy across an expanding range of malignancies.
Tumor Mutational Burden (TMB) Variability Across Cancer Types and Etiologies (e.g., UV, Tobacco)
Tumor mutational burden (TMB), defined as the number of somatic mutations per megabase of interrogated genomic sequence, has emerged as a critical biomarker for predicting response to immune checkpoint inhibitors (ICIs) across multiple cancer types [4] [27]. Its value stems from the correlation between increased mutation load and enhanced neoantigen formation, which promotes T-cell-mediated anti-tumor immunity when checkpoint signals are inhibited [4] [27]. However, TMB demonstrates remarkable variability across different malignancies, influenced by distinct etiologies including carcinogen exposure (e.g., tobacco, UV radiation) and endogenous mutational processes [4] [28] [29]. This technical review examines the landscape of TMB distribution across cancers, explores the molecular mechanisms underlying etiology-specific mutational patterns, and discusses standardized methodologies for TMB assessment in clinical and research settings. Understanding these variables is paramount for optimizing TMB's predictive value in immunotherapy and advancing personalized cancer treatment strategies.
TMB quantifies the total number of somatic non-synonymous mutations within a tumor's genome, serving as a proxy for its potential neoantigen landscape [27] [30]. The fundamental premise is that tumors with higher mutation loads are more likely to express immunogenic neoantigens that can be recognized by the immune system, particularly when treated with ICIs [4] [27]. The clinical significance of TMB was solidified by the KEYNOTE-158 trial, which led to FDA approval of pembrolizumab for TMB-high (≥10 mut/Mb) solid tumors regardless of histology [4] [8].
The accurate measurement of TMB presents substantial challenges. While whole exome sequencing (WES) represents the gold standard, covering approximately 30-50 Mb of coding sequence, its clinical implementation is hampered by high cost, long turnaround time, and significant tissue requirements [4] [31]. Consequently, targeted sequencing panels have been developed as practical alternatives, though they introduce variability due to differences in panel size, genomic coverage, and bioinformatic pipelines [4] [28]. The coefficient of variation of TMB derived from panel sequencing decreases inversely with both the square root of the panel size and the square root of the TMB level, meaning halving the CV requires a four-fold increase in panel size [4].
Quantitative Landscape of TMB Across Cancers
The distribution of TMB varies dramatically across cancer types, spanning more than a 1,000-fold range from childhood malignancies with approximately 0.1 mutations/Mb to hypermutated tumors exceeding 400 mutations/Mb [31]. Analysis of 100,000 human cancer genomes revealed that nearly all cancer types contain a subset of patients with high TMB, including many rare tumors [28].
Table 1: TMB Distribution Across Selected Cancer Types
| Cancer Type | Typical TMB Range (mut/Mb) | Etiological Associations | Representative Alterations |
|---|---|---|---|
| Melanoma | Very High (often >100) [31] | UV radiation exposure [4] | BRAF, NRAS mutations [28] |
| Non-Small Cell Lung Cancer | Variable (0.6->10.5) [31] [29] | Tobacco smoke (dose-dependent) [29] | TP53, KRAS, EGFR mutations [29] |
| Cervical Cancer | 59% with TMB-high (≥10 mut/Mb) [32] | HPV infection (especially HPV52) [32] | PIK3CA, ARID1A mutations [32] |
| Breast Cancer | Mean: 4.6 mut/Mb; 6.7% with TMB≥10 [20] | Endogenous processes (APOBEC) [20] | PIK3CA, TP53, CDH1 mutations [20] |
| Colorectal Cancer (MSI-H) | Very High [4] | Mismatch repair deficiency [4] [28] | MLH1, MSH2, MSH6, PMS2 mutations [28] |
Table 2: Impact of Smoking on TMB in Lung Adenocarcinoma [29]
| Smoking Metric | Effect on TMB | Genetic Associations |
|---|---|---|
| Doubling pack-years | Significant increase | Increased KRASG12C; decreased EGFRdel19 and EGFRL858R |
| Doubling smoking-free months | Significant decrease | Increased EGFRL858R mutations |
| Current vs. former smokers | Higher median TMB (40 vs. 24 pack-years) | Distinct pathway alterations |
Large-scale genomic analyses demonstrate that TMB increases significantly with age, showing a 2.4-fold difference between ages 10 and 90 [28]. This relationship highlights the cumulative nature of mutagenesis and may partially explain the varying immunotherapy responses across age groups.
Etiological Factors and Mutational Mechanisms
Exogenous Carcinogens
Tobacco Smoke: Smoking history demonstrates a clear dose-response relationship with TMB in lung adenocarcinoma, with doubling pack-years associated with significant TMB increases after controlling for age, gender, and stage [29]. The mutagenic effects of tobacco carcinogens create a distinct mutational signature characterized by C>A transversions, with specific impacts on cancer-related pathways including increased KRASG12C mutations and decreased EGFR mutations [29].
Ultraviolet (UV) Radiation: Melanoma and other skin cancers exhibit some of the highest TMB values across malignancies, directly attributable to UV-induced DNA damage [4] [28]. This relationship is mechanistically explained by the formation of cyclobutane pyrimidine dimers and pyrimidine-pyrimidone photoproducts that introduce characteristic C>T and CC>TT transitions at dipyrimidine sites [28].
Endogenous Mutational Processes
APOBEC Mutagenesis: In breast cancer, APOBEC (apolipoprotein B mRNA-editing enzyme catalytic polypeptide) represents the dominant mutational signature in 64.7% of TMB-high cases [20]. TMB-high breast carcinomas with APOBEC signatures demonstrate significant enrichment in KMT2C, ARID1A, PTEN, NF1, and RB1 alterations, and show higher mean TMB (19.6 mut/Mb) compared to those with other signatures [20].
DNA Repair Deficiencies: Deficiencies in mismatch repair (MMR) pathways lead to microsatellite instability (MSI) and hypermutation across multiple cancer types [4] [28]. Similarly, mutations in polymerase epsilon (POLE) and polymerase delta (POLD1) proofreading domains result in ultra-hypermutated phenotypes [28]. A novel finding includes somatic mutations in the promoter of PMS2, occurring in 10% of skin cancers and associated with dramatically increased TMB [28].
Viral Associations: In cervical cancer, high TMB was identified in 59% of cases and was associated with nodal involvement, diabetes, and HPV52 infection, but not with the more common HPV16/18 subtypes or FIGO stage [32]. This suggests HPV type-specific interactions with host genomic stability mechanisms.
Diagram 1: Etiology to Immunotherapy Response Pathway
Methodologies for TMB Assessment
Sequencing Approaches
Whole Exome Sequencing (WES): WES remains the gold standard for TMB measurement, covering approximately 30-50 Mb of coding sequence representing all ~22,000 genes [4] [31]. The typical workflow requires 150-200 ng of genomic DNA from both tumor and matched normal samples to accurately identify tumor-specific variants [31]. At 50× coverage, 95% of single nucleotide variants and short indels with variant allele frequency ≥15% can be consistently detected, though deeper sequencing improves sensitivity in impure or heterogeneous samples [31].
Targeted Gene Panels: Multiple commercially available targeted sequencing panels have been developed for TMB assessment, offering practical advantages including lower cost, faster turnaround, and compatibility with limited tissue samples [4] [31]. The FoundationOne CDx (324 genes, ~0.8 Mb coding coverage) and MSK-IMPACT (468 genes, ~1.14 Mb coding coverage) are FDA-approved panels that demonstrate moderate concordance with WES [4]. The confidence intervals for TMB estimation vary significantly with panel size, with smaller panels (<0.5 Mb) showing substantially increased variance [28].
Standardization Challenges
Harmonizing TMB measurement across platforms represents a critical challenge for clinical implementation [4]. Key variables include:
- Panel size and genomic content: Larger panels (>1 Mb) generally provide more precise TMB estimates [4] [28]
- Mutation types included: Some panels count only non-synonymous mutations while others include synonymous variants to reduce sampling noise [4]
- Bioinformatic pipelines: Variant calling algorithms and germline mutation filtering approaches differ significantly between platforms [4] [31]
- Tumor content requirements: Most assays require minimum tumor cellularity (typically 20-30%) for accurate mutation detection [4] [31]
Diagram 2: TMB Assessment Workflow
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Research Reagents and Platforms for TMB Analysis
| Reagent/Platform | Type | Primary Function | Technical Notes |
|---|---|---|---|
| FoundationOne CDx | Targeted NGS Panel | Comprehensive genomic profiling and TMB assessment | 324 genes, ~0.8 Mb coding coverage; FDA-approved [4] |
| MSK-IMPACT | Targeted NGS Panel | Tumor mutational profiling and TMB calculation | 468 genes, ~1.14 Mb coding coverage; FDA-authorized [4] |
| Oncomine Tumor Mutation Load Assay | Targeted NGS Panel | TMB estimation from limited tissue samples | 409 genes, ~1.2 Mb coverage; optimized for FFPE samples [4] |
| TruSight Oncology 500 | Targeted NGS Panel | Comprehensive genomic profiling with TMB | 523 genes, ~1.33 Mb coverage; includes DNA and RNA sequencing [4] |
| NetMHCpan | Bioinformatics Algorithm | Neoantigen prediction from mutation data | Predicts peptide-MHC binding affinity; critical for neoantigen load estimation [27] |
| SigMA | Computational Tool | Mutational signature analysis from targeted sequencing | Infers dominant mutational patterns from panel data [20] |
Discussion and Future Directions
The variability of TMB across cancer types and etiologies presents both challenges and opportunities for personalized immunotherapy. While TMB serves as a robust predictive biomarker in lung cancer and melanoma, its utility in breast, prostate, and other malignancies with lower mutational burden remains limited [33]. The differential predictive power across cancers suggests that TMB thresholds may need cancer-type-specific optimization rather than a universal pan-cancer cutoff [4] [33].
Future research directions should focus on:
- Prospective validation of optimized TMB cutoffs specific to cancer types and etiological backgrounds
- Integration of TMB with complementary biomarkers including PD-L1 expression, MSI status, and tumor microenvironment characterization [27] [33]
- Standardization of TMB measurement across platforms through initiatives like the Friends of Cancer Research TMB Harmonization Project [8]
- Development of novel methodologies for neoantigen quality assessment beyond quantitative mutation load [4] [27]
Understanding the complex interplay between environmental exposures, endogenous mutational processes, and DNA repair mechanisms will enhance our ability to stratify patients for immunotherapy and develop novel combination strategies to overcome resistance mechanisms.
TMB represents a dynamic biomarker reflecting the cumulative impact of diverse mutational processes operating across different cancer types. The profound variability in TMB distributions, driven by distinct etiologies including UV exposure, tobacco carcinogens, viral infections, and endogenous mutagenesis, underscores the necessity for context-specific interpretation of TMB values. While technological challenges in measurement standardization remain substantial, ongoing efforts to harmonize methodologies and validate clinical thresholds promise to refine TMB's utility as a predictive biomarker. For researchers and drug development professionals, recognizing the intricate relationship between cancer etiology, mutational signatures, and TMB is fundamental to advancing precision immuno-oncology and developing more effective therapeutic strategies.
The Interrelationship Between TMB, MSI, and PD-L1 Expression
The advent of immune checkpoint inhibitors (ICIs) has revolutionized cancer treatment, yet a significant challenge remains: the majority of patients do not respond to these therapies. Predictive biomarkers are therefore critical for identifying patients most likely to benefit from treatment. Programmed death-ligand 1 (PD-L1) expression, tumor mutational burden (TMB), and microsatellite instability (MSI) have emerged as three pivotal biomarkers for guiding immunotherapy. These biomarkers reflect different aspects of tumor biology: PD-L1 represents adaptive immune resistance, TMB reflects tumor immunogenicity, and MSI indicates genomic instability due to deficient DNA mismatch repair.
Understanding the interrelationships between these biomarkers is essential for advancing precision oncology. This whitepaper, framed within the context of Next-Generation Sequencing (NGS) research, provides a technical examination of TMB, MSI, and PD-L1, detailing their clinical measurements, biological interactions, and combined utility in predicting response to immunotherapy.
Quantitative Landscape of TMB, MSI, and PD-L1 in Cancer
Clinical studies across various cancer types reveal distinct prevalence and interrelationships between these biomarkers. A study of 100 esophageal squamous cell carcinoma (ESCC) patients provides illustrative data on their distribution and overlap [34] [35].
Table 1: Biomarker Prevalence in ESCC (n=100) [34] [35]
| Biomarker | Prevalence | Classification Criteria |
|---|---|---|
| PD-L1 Positive | 54% (54/100) | Combined Positive Score (CPS) ≥ 1% |
| TMB-High (TMB-H) | 57% (57/100) | > 80% quantile of mutations/Mb |
| MSI-High (MSI-H) | 1% (1/100) | Instability in multiplex PCR loci |
Table 2: Biomarker Overlap in ESCC TMB-H Cases (n=57) [34] [35]
| Biomarker Profile | Number of Cases | Percentage of TMB-H Subset |
|---|---|---|
| TMB-H and PD-L1 Positive | 32 | 56.1% |
| TMB-H, PD-L1 Positive, and MSI-H | 1 | 1.8% |
| TMB-H, PD-L1 Low, and MSI Low | 21 | 36.8% |
The data demonstrates that PD-L1 and TMB-H are frequently expressed in ESCC, whereas MSI-H is rare. Critically, there was no statistically significant association between PD-L1 expression levels and TMB, suggesting they may provide independent predictive information [34]. Furthermore, clinicopathological correlations were observed: PD-L1 positivity was significantly associated with advanced TNM staging, and TMB-H was significantly linked to lymph node metastasis [35].
This pattern of variable association is consistent across other malignancies. In non-small cell lung cancer (NSCLC), for instance, high TMB is associated with improved outcomes on ICIs, independent of PD-L1 status [36]. Pan-cancer analyses confirm that elevated TMB, MSI-H, and PD-L1 positivity can identify distinct patient subgroups that benefit from immunotherapy, underscoring the limitation of relying on a single biomarker [37].
Technical Methodologies for Biomarker Assessment
Accurate measurement of these biomarkers is foundational to both clinical decision-making and research. NGS has become a transformative technology, enabling comprehensive genomic profiling from a single assay [38].
PD-L1 Expression Analysis
Experimental Protocol: Immunohistochemistry (IHC)
PD-L1 expression is typically quantified at the protein level using IHC on formalin-fixed, paraffin-embedded (FFPE) tumor specimens [35].
- Tissue Preparation: FFPE tumor tissue sections are cut at 4-5 µm thickness and mounted on slides.
- Antigen Retrieval: Heat-induced epitope retrieval is performed using Cell Conditioning Solution (CC1, Tris-EDTA buffer, pH 8.0) for 64 minutes at 95°C.
- Staining: Slides are incubated with a primary anti-PD-L1 antibody (e.g., Clone SP263). Detection is achieved using the OptiView DAB IHC Detection Kit, followed by counterstaining with hematoxylin.
- Scoring: PD-L1 expression is evaluated using the Combined Positive Score (CPS), calculated as: CPS = (Number of PD-L1-positive cells [tumor cells, lymphocytes, macrophages] / Total number of tumor cells) × 100 A CPS ≥ 1% is typically classified as PD-L1 positive [35].
An emerging, non-invasive alternative is the detection of exosomal PD-L1 (exo-PD-L1) from blood plasma. Exo-PD-L1 is derived from tumor cells and systemically suppresses T cell activity. Its levels dynamically reflect the tumor's immune status and show promise for predicting resistance to ICIs [39].
Tumor Mutational Burden (TMB) Analysis
Experimental Protocol: Next-Generation Sequencing
TMB is defined as the number of somatic mutations per megabase (mut/Mb) of the genome examined [34] [38] [37].
- DNA Extraction: Genomic DNA is extracted from FFPE tissue sections or liquid biopsy samples using specialized kits (e.g., Qiagen AllPrep DNA/RNA FFPE Kit). DNA quality and concentration are assessed (e.g., using Qubit dsDNA HS Assay Kit and Agilent TapeStation) [35].
- Library Preparation & Sequencing: A minimum of 120 ng of DNA is used for library preparation. Target capture is performed using comprehensive gene panels (e.g., a 733-gene panel). Sequencing is conducted on platforms like Illumina, which provides high throughput and low error rates (0.1–0.6%) [38] [40].
- Bioinformatic Analysis:
- Alignment: Sequencing reads are aligned to a reference human genome (e.g., hg19) using tools like BWA.
- Variant Calling: Somatic mutations (missense, nonsense mutations, and coding indels) are identified.
- TMB Calculation: TMB = (Total number of somatic mutations) / (Size of the targeted genomic region in Mb). TMB-H is often defined using percentile-based cut-offs (e.g., > 80% quantile) or a fixed threshold like 10 mut/Mb [34] [36] [37].
Microsatellite Instability (MSI) Analysis
Experimental Protocol: NGS-Based MSI Detection
While PCR-based methods have been the gold standard, NGS-based approaches offer expanded coverage and are highly concordant with traditional methods [40].
- Panel Design: An in-house NGS-based MSI detector (MSIDRL) can be developed by selecting hundreds of robust non-coding microsatellite (MS) loci. A training set of samples with predefined MSI status (e.g., by PCR) is used to establish a baseline [40].
- Sequencing & Analysis: For each MS locus in a sample, the number of reads supporting different repeat lengths is counted.
- Algorithm for MSI Calling: A novel algorithm involves:
- Defining a Diacritical Repeat Length (DRL): The repeat length that maximizes the read count difference between MSI-H and microsatellite stable (MSS) samples in the training set.
- Calculating Background Noise (B~i~): The baseline instability for each locus
iin MSS samples. - Statistical Testing: For each locus
iin a test samplej, the proportion of "unstable" reads (lengths ≤ DRL~i~) is calculated (b~ij~). A binomial test is used to compareb~ij~toB~i~. - Determining MSI Status: The Unstable Locus Count (ULC) is the number of loci significantly more unstable than the background. A ULC ≥ 11 (determined from a pan-cancer distribution) classifies a sample as MSI-H [40].
Diagram 1: NGS-based MSI calling workflow, based on a novel algorithm (MSIDRL) analyzed in 35,563 pan-cancer cases [40]. DRL: Diacritical Repeat Length.
Interrelationships and Biological Mechanisms
The interplay between TMB, MSI, and PD-L1 is complex and rooted in their shared role in anti-tumor immunity, yet they function through distinct mechanisms.
- TMB and Neoantigen Burden: High TMB leads to an increased generation of neoantigens—novel protein sequences that the immune system recognizes as foreign. This enhances tumor immunogenicity and T cell infiltration, creating a microenvironment more susceptible to immune checkpoint blockade [37].
- MSI as a Driver of TMB-H: MSI is a specific genomic signature caused by deficient mismatch repair (dMMR). This failure in DNA repair machinery results in a hypermutator phenotype, profoundly elevating TMB across numerous microsatellite regions [37] [40]. Thus, MSI-H is a direct genetic cause of exceptionally high TMB.
- PD-L1 as an Adaptive Immune Resistance Mechanism: The expression of PD-L1 on tumor cells or its secretion via exosomes is often an adaptive response to IFN-γ and other inflammatory signals released by tumor-infiltrating T cells. Therefore, a T cell-inflamed tumor microenvironment (often associated with high TMB) can drive the upregulation of PD-L1 as a primary mechanism of immune evasion [39].
- Independent and Complementary Biomarkers: Despite these connections, clinical data often show no direct statistical correlation between TMB and PD-L1 levels [34] [35]. This indicates that the processes governing mutational load and immune checkpoint expression are not perfectly coupled. They can be influenced by additional factors, such as tumor heterogeneity, the specific composition of the tumor microenvironment, and the dynamics of exosomal PD-L1 release, which can mediate systemic immunosuppression independent of tumor cell membrane PD-L1 [39].
Diagram 2: Logical relationships between dMMR/MSI, TMB, and PD-L1 expression. dMMR drives MSI-H, which causes high TMB. The resulting immune response triggers PD-L1 expression as an adaptive resistance mechanism [39] [37] [40].
The Scientist's Toolkit: Essential Research Reagents and Materials
Successful research in this field relies on a suite of specialized reagents, assays, and bioinformatic tools.
Table 3: Key Research Reagent Solutions for Biomarker Analysis
| Item / Reagent | Function / Application | Specific Examples / Notes |
|---|---|---|
| FFPE Tissue Sections | Preserves tumor morphology and biomolecules for IHC and DNA extraction. | Standard for clinical samples; requires quality control (e.g., Agilent TapeStation) [35]. |
| Anti-PD-L1 Antibodies | Detection of PD-L1 protein expression via IHC. | Clones SP263, 22C3, 28-8; scoring depends on tumor type (CPS or TPS) [35] [37]. |
| NGS Gene Panels | Targeted sequencing for TMB and MSI calculation. | Comprehensive panels (e.g., 733-gene); must cover sufficient genomic space for accurate TMB [38] [40]. |
| MSI Loci Panel | A set of microsatellite loci for NGS-based MSI detection. | Pan-cancer panels (e.g., 7-100 loci) can outperform traditional PCR panels for non-colorectal cancers [40]. |
| DNA Extraction Kits | Isolation of high-quality DNA from tissue or liquid biopsy. | Specialized kits for FFPE (e.g., Qiagen AllPrep DNA/RNA FFPE Kit) are essential [35]. |
| Bioinformatics Pipelines | Data analysis for variant calling, TMB, and MSI determination. | Tools like MSIsensor, BWA for alignment, GATK for variant calling [38] [40]. |
The interrelationship between TMB, MSI, and PD-L1 is multifaceted. While these biomarkers are functionally linked through the cancer immunity cycle, they provide non-redundant information. MSI can be a direct cause of high TMB, and the ensuing T-cell response can induce PD-L1 expression. However, the lack of a consistent statistical correlation between them underscores the complexity of tumor-immune interactions and the influence of other factors like exosomal PD-L1.
For researchers and drug development professionals, this has clear implications: a multi-modal biomarker approach is superior to reliance on any single marker for predicting response to immunotherapy. The integration of NGS, which allows for the simultaneous assessment of all three biomarkers from a single assay, is therefore paramount. Future research should focus on standardizing NGS-based biomarker assays, defining universal cut-off values, and further elucidating the dynamic crosstalk between the genome and the immune microenvironment to unlock the full potential of precision immuno-oncology.
From WES to Targeted Panels: NGS Methodologies for TMB Quantification
Whole exome sequencing (WES) has established itself as a fundamental tool in genomic research and clinical diagnostics, particularly in the context of cancer genomics and tumor mutational burden (TMB) assessment. By sequencing the protein-coding regions of the genome, WES provides comprehensive genetic information that enables researchers to identify mutations driving cancer development and progression. Its capacity to detect somatic mutations across all exonic regions has made WES the reference standard for TMB measurement, a critical biomarker predicting response to immune checkpoint inhibitors. However, significant technical and analytical limitations constrain its clinical application. This in-depth technical review examines WES methodologies, its established role in TMB quantification, and the inherent constraints researchers must navigate when implementing this technology in preclinical and clinical cancer research.
Whole exome sequencing is a next-generation sequencing (NGS) approach that targets the protein-coding regions of the human genome, comprising approximately 1% of the total genome but harboring an estimated 85% of disease-causing variants [41] [42]. The methodology involves selectively capturing and sequencing exonic regions from fragmented genomic DNA, generating data that encompasses single nucleotide variants (SNVs), small insertions/deletions (indels), and to a limited extent, copy number variations (CNVs) [42]. The fundamental premise of WES rests on its ability to provide comprehensive genetic information across all known genes without the excessive data burden and cost associated with whole genome sequencing (WGS), positioning it as a balanced solution for large-scale genomic studies [43].
In oncology research, WES has emerged as a particularly valuable tool for characterizing the mutational landscape of tumors. Unlike targeted gene panels that focus on predetermined genomic regions, WES allows for hypothesis-free exploration of all protein-coding sequences, enabling discovery of novel cancer-associated genes and pathways [4]. This agnostic approach is especially relevant for TMB assessment, which requires quantitative measurement of somatic mutations across a broad genomic territory to accurately estimate neoantigen load and predict immunotherapy responsiveness [4] [44].
WES as Gold Standard for Tumor Mutational Burden Assessment
TMB Definition and Clinical Significance
Tumor mutational burden refers to the number of somatic mutations per megabase of interrogated genomic sequence [4]. As a quantitative biomarker, TMB reflects the mutational accumulation within a tumor, which subsequently influences the generation of immunogenic neoantigens presented on major histocompatibility complex (MHC) molecules [4]. These neoantigens enable the immune system to recognize and target tumor cells, providing the mechanistic rationale for the observed correlation between high TMB and improved response to immune checkpoint inhibitors (ICIs) across multiple cancer types [4] [7].
The clinical validation of TMB as a predictive biomarker culminated in the 2020 FDA approval of pembrolizumab for solid tumors with TMB-high status (≥10 mutations/megabase), based on findings from the KEYNOTE-158 trial [4]. This regulatory milestone established TMB as a pan-cancer biomarker for immunotherapy selection, reinforcing the need for accurate and standardized TMB measurement in research and clinical contexts.
Experimental Protocols for TMB Measurement via WES
The established protocol for TMB assessment using WES involves a multi-step process that requires both tumor and matched normal DNA samples to distinguish somatic mutations from germline variants:
Sample Preparation and Sequencing
- DNA Extraction: Tumor DNA is typically isolated from formalin-fixed paraffin-embedded (FFPE) tissue sections, while normal DNA is obtained from peripheral blood, saliva, or adjacent normal tissue [44]. DNA quality and quantity are assessed using fluorometric methods (e.g., Qubit dsDNA HS Assay).
- Library Preparation: Fragmented DNA undergoes end-repair, adenylation, and adapter ligation. For WES, library preparation incorporates hybridization-based capture using biotinylated oligonucleotide probes that target the exonic regions (approximately 30-60 Mb) [4] [44].
- Sequencing: Captured libraries are sequenced on NGS platforms (e.g., Illumina HiSeq, NovaSeq) to achieve minimum coverage of 100-150x for tumor samples and 30-50x for normal samples [44].
Bioinformatic Analysis
- Alignment: Sequencing reads are aligned to the reference genome (e.g., GRCh38) using tools such as BWA-MEM [44].
- Variant Calling: Somatic variant calling identifies mutations present in tumor but not normal tissue using specialized algorithms (e.g., Mutect2, VarScan) [44]. The standard TMB calculation includes coding, non-synonymous mutations (missense, nonsense, indels) while typically excluding synonymous variants unless otherwise specified [4].
- TMB Calculation: The TMB value is derived using the formula:
TMB (mutations/Mb) = (Total number of somatic mutations) / (Size of the coding target region in Mb)
The coding target region for WES is approximately 30-38 Mb, though exact sizes vary by capture kit [4].
Table 1: Commercially Available Large Gene Panels for TMB Assessment
| Laboratory/Panel | Number of Genes | Total Region Covered (Mb) | TMB Region Covered (Mb) | Mutation Types Included |
|---|---|---|---|---|
| FoundationOne CDx | 324 | 2.20 | 0.80 | Non-synonymous, synonymous |
| MSK-IMPACT | 468 | 1.53 | 1.14 | Non-synonymous |
| TruSight Oncology 500 | 523 | 1.97 | 1.33 | Non-synonymous, synonymous |
| Oncomine TML Assay | 409 | 1.70 | 1.20 | Non-synonymous |
| TEMPUS Xt | 595 | 2.40 | 2.40 | Non-synonymous |
Source: Adapted from Merino et al. as cited in [4]
Comparative Performance of WES and Targeted Panels
While WES remains the gold standard for TMB measurement in research settings, targeted sequencing panels have gained traction in clinical practice due to practical advantages including lower cost, faster turnaround time, and reduced DNA input requirements [4]. Validation studies demonstrate that large panels (>1 Mb) show strong correlation with WES-derived TMB values, with reported Pearson correlation coefficients ranging from R=0.94 to R=0.98 [44]. However, this correlation strength is highly dependent on panel size and design, with smaller panels showing greater variability, particularly for intermediate TMB values [4].
The precision of TMB estimation improves with larger genomic regions, as the coefficient of variation decreases proportionally with the square root of both panel size and TMB level [4]. This relationship underscores the statistical advantage of WES for TMB quantification, as its larger target size (∼30 Mb versus 0.8-2.4 Mb for panels) provides more stable mutation counts, especially critical for tumors with intermediate TMB levels where clinical classification thresholds have significant therapeutic implications [4] [44].
Technical Limitations of Whole Exome Sequencing
Incomplete Exome Coverage and Capture Efficiency
Despite comprehensive target design, WES does not achieve complete coverage of all exonic regions due to technical limitations in capture efficiency and sequence context challenges:
- Regional Gaps: Current WES technologies typically capture approximately 97% of exons, with about 10% of exonic regions failing to achieve sufficient coverage depth (>20x) to reliably call heterozygous variants [43] [45]. These coverage gaps result from difficulties in capturing regions with extreme GC content, repetitive sequences, or homologous pseudogenes [43] [42].
- Capture Variability: Probe design limitations and hybridization efficiency variations create uneven coverage across the exome, with some clinically relevant genes exhibiting consistently poor capture [43]. This variability necessitates additional validation for genes of interest in specific research contexts.
- Comparative Performance: Interestingly, WGS has demonstrated more complete coverage of the exome than WES itself, highlighting a paradoxical limitation of exome-focused approaches [43].
Restricted Variant Detection Capability
WES is fundamentally limited in its ability to detect important classes of genomic alterations:
- Structural Variants: WES has low sensitivity for detecting structural variations including copy number variants (CNVs), inversions, and translocations [43] [42]. While some CNVs can be inferred from exome data, this requires specialized analytical approaches and remains inferior to detection by WGS or chromosomal microarrays [43] [46].
- Non-Coding Variants: By design, WES excludes the approximately 99% of the genome comprising non-coding regions, including regulatory elements, enhancers, and non-coding RNAs that increasingly demonstrate clinical significance in cancer [43] [46]. For example, non-coding regulatory variants have been shown to explain the majority of cases in TAR syndrome [43].
- Repeat Expansions: WES cannot reliably detect repeat expansion disorders (e.g., Huntington's disease) or other large repetitive elements that require specialized molecular techniques for accurate characterization [43] [46].
- Mitochondrial Genome: Standard WES protocols do not consistently cover the mitochondrial genome, necessitating separate assessment for mitochondrial DNA mutations [45].
Table 2: Variant Types and Their Detectability by Whole Exome Sequencing
| Variant Type | Detectable by WES | Detection Efficiency | Primary Limitations |
|---|---|---|---|
| Single Nucleotide Variants | Yes | High | Affected by regional coverage gaps |
| Small Insertions/Deletions | Yes | Moderate-High | Size limitations (<50bp) |
| Copy Number Variants | Limited | Low | Inference-based, high false-negative rate |
| Structural Variants | No | Not applicable | Requires long-read or specialized technologies |
| Non-Coding Variants | No | Not applicable | By design exclusion |
| Repeat Expansions | No | Not applicable | Requires repeat-primed PCR or long-read sequencing |
| Mitochondrial DNA Variants | Variable | Low | Inconsistent coverage in standard kits |
Analytical and Interpretation Challenges
The analytical pipeline for WES introduces additional layers of complexity that impact result reliability:
- Germline Contamination: In tumor-only sequencing designs, incomplete filtering of germline variants inflates TMB estimates by 3.9-5.8 mutations/Mb on average, potentially leading to false-positive TMB-high classifications [44]. This underscores the necessity for matched normal sequencing in research settings requiring accurate TMB quantification.
- Artifact Management: FFPE-derived DNA exhibits characteristic artifactual mutations resulting from cytosine deamination, oxidation, and other damage processes that must be distinguished from true somatic variants through specialized bioinformatic filters [44].
- Variant Interpretation: The extensive dataset generated by WES (approximately 50,000 variants per exome) creates challenges in prioritizing clinically relevant mutations, particularly for variants of uncertain significance (VUS) that require functional validation [41] [42].
The Scientist's Toolkit: Essential Research Reagents and Solutions
Table 3: Key Research Reagents and Platforms for WES-Based TMB Analysis
| Category | Product/Platform | Specifications | Research Application |
|---|---|---|---|
| Capture Kits | Agilent SureSelect Human All Exon V6 | ~60 Mb target size | Comprehensive exome capture for TMB reference standard |
| Illumina Nexome | ~40 Mb target size | Streamlined exome sequencing with integrated analysis | |
| Sequencing Platforms | Illumina NovaSeq 6000 | High-throughput, 20B reads/flow cell | Large cohort TMB studies |
| Illumina NextSeq 550 | Mid-throughput, 400M reads/flow cell | Moderate-scale TMB validation | |
| Bioinformatic Tools | GATK Mutect2 | Somatic variant caller | Standardized somatic mutation detection |
| BWA-MEM | Sequence aligner | Reference genome alignment | |
| Ion Reporter | Integrated analysis suite | Variant annotation and TMB calculation | |
| Reference Materials | Horizon TMB Reference Standard | Certified mutation load | Assay validation and QC |
| Coriell Institute DNA | Characterized biobank samples | Process control and reproducibility |
Whole exome sequencing maintains its position as the gold standard for tumor mutational burden assessment in research settings, providing comprehensive mutation profiling across protein-coding regions that enables robust correlation between mutational load and immunotherapy response. Its extensive target space offers statistical advantages over targeted panels for TMB quantification, particularly for tumors with intermediate mutation burdens where precise classification carries significant therapeutic implications.
However, researchers must acknowledge and address the technical limitations inherent to WES methodology, including incomplete exome coverage, inability to detect important variant classes such as structural variants and non-coding regulatory mutations, and analytical challenges in distinguishing true somatic events from germline polymorphisms and technical artifacts. These constraints necessitate complementary approaches—including WGS, transcriptomic analysis, and specialized structural variant detection—for comprehensive cancer genomic profiling.
As the field advances toward increasingly standardized and clinically applicable TMB measurement, WES continues to provide the foundational validation dataset against which emerging technologies are benchmarked. Its role in elucidating the complex relationship between tumor genetics and immune response ensures that WES will remain an essential component of the cancer research toolkit, even as its limitations guide the development of more comprehensive genomic characterization approaches.
Tumor Mutational Burden (TMB) has emerged as a critical biomarker for predicting patient response to immune checkpoint blockade (ICB) therapy. While whole-exome sequencing (WES) is the gold standard for TMB quantification, its high cost and complexity limit routine clinical use. This whitepaper details a data-driven framework for designing targeted gene panels that accurately estimate TMB and other exome-wide biomarkers, such as Tumor Indel Burden (TIB). We demonstrate that this approach facilitates a cost-effective and practical clinical alternative to WES, enabling broader access to biomarker-guided immunotherapy. Methodologies, experimental validation, and implementation protocols are provided to guide researchers and clinicians.
Immune checkpoint blockade (ICB) therapy has revolutionized cancer treatment, but determining which patients will benefit remains a significant challenge [47]. Exome-wide biomarkers, particularly Tumor Mutational Burden (TMB), defined as the total number of non-synonymous mutations in the tumor exome, are established predictors of response to ICB [47]. TMB serves as a proxy for how easily immune cells can recognize tumor cells as foreign [47].
However, the widespread clinical adoption of TMB is hindered by the cost and logistical challenges associated with Whole Exome Sequencing (WES) [47] [48]. This is especially problematic in scenarios requiring high-depth sequencing, such as with liquid biopsy samples using circulating tumor DNA (ctDNA) [47]. The same limitations apply to newer biomarkers like Tumor Indel Burden (TIB) [47].
Targeted gene panels, which sequence a small subset of genes, offer a potential solution. This technical guide outlines a robust, data-driven methodology for designing targeted panels and constructing accurate biomarker estimators, framing this approach within the broader thesis of advancing NGS research in clinical oncology.
Economic and Clinical Rationale for Targeted Panels
Comprehensive genomic profiling is essential for identifying patients eligible for targeted therapies. A 2025 economic model compared testing approaches for advanced/metastatic non-small cell lung cancer (NSCLC) [48].
Cost-Benefit Analysis of Testing Modalities
Table: Economic and Clinical Outcomes of Genomic Testing Strategies in NSCLC [48]
| Testing Strategy | Cost per Patient (USD) | Median Overall Survival Benefit | Key Limitations |
|---|---|---|---|
| No Genomic Testing | Reference | Reference | Patients excluded from targeted therapies |
| Sequential Single-Gene Tests | +$14,602 vs. WES/WTS | Minimal vs. WES/WTS | Cannot identify TMB, MSI; misses RNA fusions |
| WES/WTS (Whole Exome/Transcriptome) | Baseline | Baseline | High cost, tissue requirements, turnaround time |
| Targeted Gene Panel | Lower than WES/WTS | Comparable to WES/WTS when properly designed | Limited gene coverage; requires robust estimation models |
The analysis concluded that while WES/WTS improves outcomes versus no testing or single-gene tests, targeted panels offer a pathway to reduce costs while maintaining clinical utility [48]. Specifically, using WES/WTS reduced costs by $8,809 per patient compared to no testing and by $14,602 compared to sequential single-gene testing, while increasing median overall survival by an average of 3.9 months [48].
A Data-Driven Framework for Panel Design and Biomarker Estimation
Generative Model for Mutation Profiles
The core of the proposed methodology is a generative model that treats mutation counts as independent Poisson variables [47]. This model accounts for:
- Gene-dependent mutation rates: Different genes have varying predispositions to mutation.
- Variant type-dependent rates: Distinct mutation types (e.g., missense, indel) occur at different frequencies.
- Background Mutation Rate (BMR): The overall mutational landscape of the individual tumor.
Formally, let ( M{igs} ) represent the count of mutations in gene ( g ) of type ( s ) for sample ( i ). The model posits that ( M{igs} \sim \text{Poisson}(\lambda{gs} \mui) ), where ( \lambda{gs} ) is the expected mutation rate for gene ( g ) and type ( s ), and ( \mui ) is the BMR for sample ( i ) [47]. Due to the high-dimensional nature of the data, a regularization penalty is applied during parameter estimation to identify genes mutated above or below the background rate [47].
Constructing the Biomarker Estimator
The total biomarker value (e.g., TMB) for a sample is defined as: [ T = \sum{g \in G} \sum{s \in \bar{S}} M{0gs} ] where ( G ) is the set of all exonic genes, ( \bar{S} ) is the set of relevant variant types (e.g., all non-synonymous for TMB), and ( M{0gs} ) are the mutation counts for the test sample [47].
The model facilitates the construction of an estimator ( \hat{T} ) as a weighted linear combination of mutation counts in a selected gene panel ( P ): [ \hat{T} = \sum{g \in P} \sum{s \in S} w{gs} M{0gs} ] The vector of weights ( w ) is chosen to be sparse, meaning many entries are zero, so the estimation depends only on a subset of genes—the targeted panel [47]. This allows practitioners to select a panel of a pre-specified size or augment an existing panel.
Experimental Protocol and Validation
Data Preparation: The method requires an annotated mutation dataset from WES. For example, in the NSCLC validation study [47], data from 1144 tumors was used, considering seven non-synonymous variant types. Mutations are often grouped into two categories: indel mutations and all other non-synonymous mutations [47].
Model Fitting and Panel Selection:
- Split Data: Randomly split the dataset into training, validation, and test sets (e.g., 800, 171, and 173 samples, respectively) [47].
- Estimate Parameters: Fit the generative model on the training set using equation (4) from the source [47], determining the tuning parameter ( \kappa_1 ) via tenfold cross-validation. This yields estimates for ( \lambda ) and ( \eta ), identifying genes with mutation rates significantly different from the background [47].
- Construct Estimator: Derive the sparse weight vector ( w ) for estimating TMB based on the selected genes.
Validation: Assess the performance of the estimator on the held-out test set by comparing the predicted TMB (( \hat{T} )) to the true WES-derived TMB (( T )), using metrics like Pearson correlation or mean squared error [47].
Performance and Applications
Validation in Non-Small Cell Lung Cancer
The framework was validated on a NSCLC dataset from Campbell et al., comprising 1144 patient-derived tumors [47]. The training set had an average TMB of 252 and TIB of 9.25 [47]. The method demonstrated "excellent practical performance" in predicting TMB, outperforming existing state-of-the-art approaches [47]. This performance was further confirmed on two additional independent NSCLC studies [47].
Estimation of Tumor Indel Burden (TIB)
The model's flexibility allows for the estimation of biomarkers beyond TMB. By defining ( \bar{S} ) to include only frameshift insertion and deletion mutations, the same framework can be applied to predict TIB from a targeted panel, a task for which no other methods were known at the time of the study [47].
Utility Across Cancer Types
To investigate generalizability, the method was applied to six other cancer types beyond NSCLC. It proved effective in selecting targeted gene panels and estimating TMB across these diverse mutational profiles, underscoring its broad utility in oncology [47].
The Scientist's Toolkit: Essential Research Reagents and Platforms
Successful implementation relies on specific laboratory and computational tools.
Table: Key Research Reagent Solutions for Targeted Sequencing and Analysis
| Item / Platform | Function / Use Case | Key Characteristics |
|---|---|---|
| Illumina NGS Platforms [49] | Short-read sequencing for targeted panels. | High accuracy, uses sequencing-by-synthesis with reversible dye terminators. |
| Roche 454 Pyrosequencing [49] | Older NGS method for longer reads within short-read tech. | Detects pyrophosphate release; prone to indel errors in homopolymers. |
| Ion Torrent (Thermo Fisher) [49] | Semiconductor sequencing for targeted panels. | Detects H+ ion release during DNA synthesis; lower cost, homopolymer errors. |
| PacBio SMRT Sequencing [49] | Long-read sequencing for validation. | Real-time sequencing via zero-mode waveguides (ZMWs); average read length 10-25 kb. |
| Oxford Nanopore [49] | Long-read sequencing for complex variant detection. | Measures current changes as DNA strands pass through nanopores; very long reads. |
| ICBioMark R Package [47] | Implements the data-driven panel design and estimation framework. | Provides the methodology for generative modeling, panel selection, and biomarker estimation. |
Implementation Workflow: From Model to Clinical Assay
Translating the computational model into a validated clinical assay involves a multi-step process.
The data-driven design of targeted gene panels represents a sophisticated and economically viable strategy for bringing biomarker-guided immunotherapy to a broader patient population. By leveraging a generative model of tumor mutagenesis, this approach allows for the accurate estimation of exome-wide biomarkers like TMB and TIB from a limited gene set. As NGS technologies continue to evolve, becoming faster and more cost-effective [49], the integration of robust computational methods with targeted sequencing will be paramount for advancing personalized cancer therapy and solidifying the role of NGS in routine clinical practice.
Next-generation sequencing (NGS) panels have become the predominant method for assessing tumor mutational burden (TMB) in clinical settings, offering a practical alternative to whole exome sequencing (WES) by balancing cost, turnaround time, and analytical performance [50] [51] [4]. The accurate measurement of TMB is crucial for predicting response to immune checkpoint inhibitors (ICIs) across multiple cancer types [4] [52] [53]. However, the accuracy and consistency of panel-based TMB estimation can be compromised by variability in technical details across different laboratories [50]. This technical guide examines the three critical parameters—panel size, content, and genomic region selection—that laboratories must optimize to ensure reliable TMB assessment, framed within the broader context of standardizing TMB measurement for immunotherapy response prediction.
Panel Size: The Foundation for Reliable TMB Estimation
Panel size, specifically the size of the sequenced exonic regions, represents a fundamental determinant of TMB estimation accuracy. The coefficient of variation (CV) of panel sequencing-based TMB estimates decreases inversely proportional to the square root of both the panel size and the TMB level [4] [52].
Minimum Size Requirements and Optimal Ranges
Evidence from large-scale evaluations demonstrates that panels below a specific size threshold yield unacceptably high variability, while progressively larger panels deliver diminishing returns on improved precision.
Table 1: Panel Size Recommendations for TMB Assessment
| Size Category | Recommended Size | Impact on TMB Accuracy | Key Evidence |
|---|---|---|---|
| Minimum Threshold | >1.04 Mb [50] | Necessary for basic discrete accuracy | Multicenter study evaluating 38 unique methods |
| Optimal Range | 1.5 Mb to 3.0 Mb [52] | Ideal balance with small confidence intervals | Analysis of confidence variance relative to panel size |
| Clinical Standard | FoundationOne CDx: 0.8 Mb; MSK-IMPACT: 1.14 Mb; TSO500: 1.33-1.9 Mb [4] [53] | Moderate concordance with WES | FDA-approved panels with demonstrated clinical utility |
A comprehensive multicenter evaluation employing over 40,000 synthetic panels established that panel sizes beyond 1.04 Mb and 389 genes are necessary for basic discrete accuracy in TMB classification [50]. For optimal performance, panels between 1.5 Mb and 3.0 Mb demonstrate significantly smaller confidence intervals, providing the ideal cost-benefit ratio for reliable TMB estimation [52]. Most commercially available clinical panels range from 0.8 Mb to 2.4 Mb, with trends moving toward larger sizes to improve precision [4].
Panel Content: Mutation Types and Gene Selection
The specific mutation types included in TMB calculation and the selection of genes covered by the panel significantly influence TMB values and their correlation with WES-based measurement.
Mutation Types in TMB Calculation
The inclusion or exclusion of different mutation categories represents a substantial source of variability across TMB assays.
Table 2: Mutation Types in TMB Calculation and Their Impact
| Mutation Type | Inclusion in TMB | Biological Rationale | Prevalence in Panels |
|---|---|---|---|
| Missense | Universal [50] | Primary source of neoantigens | 100% of panels (38/38) [50] |
| Small Indels (frameshift and in-frame) | Universal [50] | Can generate novel peptide sequences | 100% of panels (38/38) [50] |
| Nonsense | Universal [50] | Truncated proteins may produce neoantigens | 100% of panels (38/38) [50] |
| Synonymous | Selective (34.2%) [50] [4] | Reduces sampling noise without contributing neoantigens | 13/38 panels [50] |
| Hotspot Mutations | Recommended with filtering [50] | Enhance accuracy but require careful implementation | Identified as important feature [50] |
While missense, nonsense, and small insertions and deletions (indels) are included in all panel-based TMB assays, the handling of synonymous mutations varies significantly [50]. Approximately 34.2% (13/38) of panels include synonymous mutations in TMB calculation, which do not contribute to neoantigen generation but may reduce sampling noise and improve the approximation of genome-wide TMB when tumor-normal pairs are sequenced [50] [4] [52]. The Friends of Cancer Research (FOCR) has recommended including synonymous mutations to improve the correlation between panel-based TMB and WES-TMB [50].
Gene Content and Driver Mutations
Panel design must balance the inclusion of established cancer driver genes with the need for a representative genomic sample for TMB estimation. Commercially available pan-cancer panels typically cover 300-600 genes, encompassing the 375 known cancer driver genes [52]. The presence of driver gene mutations frequently correlates with higher TMB across multiple cancer types [52]. The SHapley Additive exPlanations (SHAP) value analysis has identified that including hotspot mutations with appropriate filtering enhances the accuracy of panel-based TMB assessment [50].
Genomic Region Selection and Technical Considerations
The specific genomic regions targeted by sequencing panels, along with pre-analytical and bioinformatic factors, substantially influence TMB measurement accuracy.
Coding vs. Non-Coding Regions
While TMB specifically quantifies mutations in coding regions, panel designs often include non-coding sequences to enable simultaneous assessment of other biomarkers.
- Coding Regions: Essential for TMB calculation as they encompass protein-altering mutations that may generate neoantigens [52]
- Intronic Regions: Frequently included in panels (e.g., for fusion detection) but should be excluded from TMB calculation [54] [52]
- Panel Design Implications: Laboratories must clearly define which regions contribute to TMB calculation, as panels often include both exonic and intronic regions for comprehensive genomic profiling [54]
The TruSight Oncology 500 kit, for example, targets 523 cancer-related genes but requires careful bioinformatic separation of coding mutations for TMB calculation from intronic sequences included for structural variant detection [54] [53].
Tumor Purity and Variant Allele Frequency Threshold
The accuracy of TMB estimation depends on adequate tumor content and appropriate variant calling parameters. A 5% variant allele frequency (VAF) cut-off is suitable for TMB assays using tumor samples with at least 20% tumor purity [50]. Below this purity threshold, performance degrades significantly, leading to TMB overestimation [50]. Both tumor-only (TO) and tumor-control (TC) approaches demonstrate high consistency (kappa = 0.833) in TMB classification, though they may identify different mutation sets due to varying germline filtration strategies [54].
Experimental Protocols for Panel Validation
Robust validation of NGS panels for TMB assessment requires systematic evaluation using reference materials and real-world samples.
Multicenter Validation Framework
A comprehensive protocol for validating panel-based TMB assays should incorporate the following steps derived from recent multicenter studies:
Reference Sample Preparation: Utilize CRISPR-edited cell line subclones with known mutation loads to establish truth sets [50]. Include samples with varying tumor purities (e.g., 20%-40%) to assess performance across clinically relevant conditions [50].
In Silico Validation: Employ large cancer genomics datasets (e.g., TCGA MC3) to assemble over 40,000 synthetic panels evaluating different size, content, and region parameters [50].
Wet-Lab Validation: Process reference samples through the entire NGS workflow, including:
Bioinformatic Analysis:
Performance Metrics Assessment:
Reagent Solutions for TMB Panel Development
The following research reagents represent essential components for developing and validating NGS panels for TMB assessment.
Table 3: Essential Research Reagents for TMB Panel Development
| Reagent/Category | Specific Examples | Function in TMB Workflow |
|---|---|---|
| DNA Extraction Kits | MagCore Genomic DNA FFPE One-Step Kit [53], Kaijie FFPE magnetic bead extraction [54] | Isolation of high-quality DNA from challenging FFPE samples |
| Target Enrichment Panels | TruSight Oncology 500 (523 genes) [54] [53], MSK-IMPACT (468 genes) [4], FoundationOne CDx (324 genes) [4] | Hybrid capture-based enrichment of genomic regions for TMB calculation |
| Library Prep Kits | Illumina TruSight Oncology 500 kit [53], Nonacus GALEAS Tumor panel [52] | Preparation of sequencing libraries with unique molecular identifiers (UMIs) |
| QC Assays | Qubit dsDNA HS Assay Kit [54], FFPE QC Kit (Illumina) [53] | Quantification and quality assessment of input DNA and final libraries |
| Bioinformatic Tools | Burrows-Wheeler Aligner (BWA) [53], Population frequency databases (dbSNP, ExAC, gnomAD) [54] | Sequence alignment, variant calling, and germline mutation filtering |
Optimal design of NGS panels for TMB assessment requires careful consideration of size (>1.5 Mb for optimal precision), content (inclusion of synonymous and hotspot mutations with appropriate filtering), and genomic region selection (focus on coding sequences). Evidence from multicenter studies indicates that mutation detection must maintain a reciprocal gap of recall and precision less than 0.179 for reliable TMB calculation [50]. As TMB continues to evolve as a predictive biomarker for immunotherapy response across multiple cancer types [4] [53] [56], standardization of these critical panel design parameters will be essential for ensuring consistent and clinically actionable results across laboratories and platforms. Future efforts should focus on harmonizing TMB measurement through consensus guidelines that address these fundamental design considerations while maintaining flexibility for technological innovation.
Comparison of Commercially Available Platforms (e.g., MSK-IMPACT, FoundationOne CDx)
The advent of Next-Generation Sequencing (NGS) has fundamentally transformed cancer research and therapeutic development, enabling comprehensive molecular profiling of tumors at unprecedented scale and resolution. Within this landscape, tumor mutational burden (TMB) has emerged as a critical biomarker for predicting response to immune checkpoint inhibitors (ICIs) across multiple cancer types [57] [24]. TMB quantifies the number of somatic mutations per megabase of DNA, with higher levels theoretically generating more neoantigens that can be recognized by the immune system when unleashed from checkpoint inhibition [57]. The clinical validation of TMB has created an urgent need for standardized, reliable NGS platforms that can accurately quantify this biomarker while simultaneously identifying other actionable genomic alterations. This technical guide provides an in-depth comparison of two pioneering NGS platforms—MSK-IMPACT and FoundationOne CDx—with particular emphasis on their methodological approaches, technical performance, and application in TMB research and drug development.
MSK-IMPACT (Memorial Sloan Kettering-Integrated Mutation Profiling of Actionable Cancer Targets)
MSK-IMPACT is a targeted tumor-sequencing test developed by Memorial Sloan Kettering Cancer Center that utilizes hybridization capture and NGS technology to detect mutations and other critical genomic alterations in both rare and common cancers [58]. A distinctive feature of MSK-IMPACT is its use of matched tumor-normal sequencing, where DNA from tumor tissue is directly compared to DNA from normal tissue (typically white blood cells) to ensure that detected mutations are specific to cancer cells [58]. This approach allows for unambiguous discrimination between somatic and germline variants, a critical consideration for accurate TMB calculation [24] [59].
The platform initially targeted 341 cancer-related genes but has been regularly updated; the current panel comprises 505 genes selected by MSK researchers for their role in cancer development and behavior [58]. The test detects multiple classes of genomic alterations including single-nucleotide variants, small insertions and deletions, copy number alterations, chromosomal rearrangements, microsatellite instability (MSI), and TMB [58]. MSK-IMPACT was the first NGS-based tumor profiling test to receive FDA authorization through the FDA-CMS parallel review program in 2017 [60] [61].
FoundationOne CDx
FoundationOne CDx is a comprehensive genomic profiling test developed by Foundation Medicine, Inc. that was approved by the FDA in December 2017 as the first broad companion diagnostic for solid tumors [62] [61]. This tissue-based test analyzes 324 genes known to drive cancer growth and is clinically and analytically validated to provide clinically actionable information for therapy selection [62] [63].
The test identifies all four major types of genomic alterations—base substitutions, insertions and deletions, copy number alterations, and rearrangements—while also assessing genomic signatures including TMB, MSI, and homologous recombination deficiency (HRD) [62]. FoundationOne CDx utilizes a tumor-only approach for mutation detection, relying on population frequency databases (such as dbSNP, ExAC, and gnomAD) to filter out potential germline mutations [24] [63]. The test has obtained national coverage for qualifying Medicare patients across all solid tumors and is covered by numerous commercial health plans [62].
Table 1: Core Technical Specifications of MSK-IMPACT and FoundationOne CDx
| Specification | MSK-IMPACT | FoundationOne CDx |
|---|---|---|
| Developer | Memorial Sloan Kettering Cancer Center | Foundation Medicine, Inc. |
| FDA Approval Date | November 2017 [61] | December 2017 [61] |
| Genes Analyzed | 505 genes (current version) [58] | 324 genes [62] |
| Variant Types Detected | SNVs, indels, CNAs, rearrangements, MSI, TMB [58] | SNVs, indels, CNAs, rearrangements, MSI, TMB [62] |
| Methodology | Hybridization capture NGS [58] | Hybridization capture NGS [63] |
| Sample Input | FFPE tumor tissue + matched normal [58] | FFPE tumor tissue [63] |
| TMB Calculation | Based on somatic coding mutations from matched normal [58] | Based on mutations filtered against population databases [63] |
| Regulatory Status | FDA-approved; NY State-approved [58] | FDA-approved companion diagnostic [62] |
Methodological Approaches to TMB Assessment
TMB Definition and Clinical Significance
Tumor mutational burden (TMB) is formally defined as the total number of somatic mutations per megabase (mut/Mb) of the tumor genome coding region [24]. This biomarker indicates genomic instability of tumor cells, with higher TMB values associated with increased neoantigen load and enhanced response to immune checkpoint blockade across multiple tumor types [57] [24]. Based on the KEYNOTE-158 study, the FDA approved pembrolizumab for adult and pediatric patients with unresectable or metastatic TMB-high (TMB-H ≥10 muts/Mb) solid tumors, establishing this threshold as a clinically relevant cutoff [24].
The accurate calculation of TMB presents significant technical challenges due to methodological variations in mutation detection, germline variant filtering, and panel size considerations. While whole exome sequencing (WES) is considered the gold standard for TMB analysis, its high cost and large sample requirements limit widespread clinical application [24]. Targeted NGS panels provide a practical alternative for TMB assessment, offering deeper sequencing depth at lower cost while maintaining accuracy for biomarker calculation [24].
MSK-IMPACT: Matched Tumor-Normal Approach
MSK-IMPACT employs a tumor-control (TC) method for somatic mutation identification, which involves simultaneous sequencing of a patient's tumor tissue and matched normal tissue (white blood cells) [58] [24]. This methodological approach provides several advantages for TMB calculation:
Precise Germline Filtering: Direct comparison of tumor and normal sequences enables unambiguous discrimination between true somatic mutations and germline variants, eliminating false positives that could inflate TMB values [24] [59].
Reduced Ancestral Bias: The matched normal control avoids potential errors from population frequency databases that may underrepresent certain ancestral groups [24].
Comprehensive Variant Detection: The MSK-IMPACT pipeline detects single nucleotide variants, small insertions and deletions using a combination of MuTect and GATK HaplotypeCaller, with thresholds of coverage depth ≥50X and variant frequency ≥20% for exonic variants [59].
The TMB calculation includes synonymous and non-synonymous non-hot spot somatic coding variants with ≥5% variant allele frequency, divided by the size of the coding region covered by the panel [24].
FoundationOne CDx: Tumor-Only with Bioinformatic Filtering
FoundationOne CDx utilizes a tumor-only (TO) method for mutation detection, relying on computational approaches to distinguish somatic from germline variants:
Database Filtering: Potential germline mutations are identified and filtered using population frequency databases (dbSNP, ExAC, gnomAD), with mutations having ≥50 population allele count typically classified as germline [24] [63].
Algorithmic Classification: A proprietary bioinformatics pipeline analyzes sequencing data to identify somatic mutations while excluding likely germline variants and sequencing artifacts [63].
TMB Calculation: The FoundationOne TMB algorithm counts somatic mutations (including synonymous and non-synonymous) across the coding region of the panel, excluding known driver mutations to avoid bias, and normalizes to the total megabases of covered genome [63].
This tumor-only approach enables broader application when matched normal tissue is unavailable but may be susceptible to germline contamination in populations underrepresented in genomic databases [24].
Diagram: Methodological Differences in TMB Calculation Between Platforms
Comparative Performance and Analytical Validation
TMB Concordance and Methodological Variability
Recent studies have directly compared the impact of different NGS methodologies on TMB assessment, revealing both concordance and significant variability. A 2025 study examining different NGS identification methods for somatic mutations in solid tumors found that while TO and TC methods showed 92% consistency in TMB classification, there was a statistically significant difference in TMB results (χ² = 16.667, p < 0.001) [24]. The Cohen's kappa analysis demonstrated good consistency between methods (kappa = 0.833, p < 0.001), indicating generally reproducible TMB classification despite methodological differences [24].
The study further revealed that TO and TC methods identify and incorporate different mutation sites for TMB calculation, directly impacting the final TMB values [24]. This variability is particularly consequential when TMB values fall near the clinically relevant 10 mut/Mb threshold, where different methods may yield different classifications that directly impact treatment decisions [24].
Platform-Specific Validation and Performance
MSK-IMPACT has demonstrated robust performance in analytical validations, with one study reporting detection of all germline variants in 233 unique patient DNA samples previously confirmed by single-gene testing [59]. The assay achieved high sequencing coverage across targeted regions, with mean coverage of 844X across exons of cancer predisposition genes and 99.3% of exons covered to a minimum of 50X [59]. Power analysis demonstrated that with 17X coverage, MSK-IMPACT can detect heterozygous variants (50% allele frequency) with 99% sensitivity [59].
FoundationOne CDx has shown similarly strong performance characteristics, with a prospective study reporting a 96.7% success rate (175/181 samples) in generating genomic data from FFPE tumor specimens [63]. The test demonstrated a median turnaround time of 41 days (range: 21-126 days) and detected known or likely pathogenic variants in TP53 (n=113), PIK3CA (n=33), APC (n=32), and KRAS (n=29) among 175 successfully sequenced samples [63]. In TMB assessment, the median TMB was 4 mutations/Mb across 153 patients, with TMB-high tumors significantly more prevalent in lung cancer (11/32) than in other solid tumor types (9/121, p < 0.01) [63].
Table 2: Performance Characteristics in Clinical and Research Settings
| Performance Metric | MSK-IMPACT | FoundationOne CDx |
|---|---|---|
| Success Rate | Not explicitly stated (high, based on coverage) | 96.7% (175/181 samples) [63] |
| Median Coverage | ~787X (blood normal samples) [59] | >500X (typical median depth) [63] |
| Turnaround Time | Not explicitly stated | 41 days (median, range: 21-126) [63] |
| TMB Median | Not explicitly stated | 4 mut/Mb (across 153 patients) [63] |
| Common Mutations Detected | Not explicitly stated for validation | TP53 (113), PIK3CA (33), APC (32), KRAS (29) [63] |
| Clinical Actionability | 37% of patients with advanced cancers had actionable mutations [61] | 14% (24/174) received matched targeted therapy [63] |
Research Applications and Integration in Drug Development
Clinical Trial Design and Patient Stratification
Both platforms have significantly advanced precision oncology research through their integration into clinical trial design and patient stratification strategies. MSK-IMPACT has facilitated basket trial designs that enroll patients based on specific genetic alterations rather than tumor histology, dramatically increasing clinical trial enrollment at MSKCC [58] [61]. Research using MSK-IMPACT has identified actionable genetic changes in 37% of patients with advanced solid cancers, enabling matching to appropriate targeted therapies or clinical trials [61].
FoundationOne CDx has supported over 850 clinical trials and holds nearly 60% of all approved companion diagnostic indications for NGS testing across the United States and Japan—the most of any diagnostic company [64]. The platform's comprehensive genomic profiling enables identification of patients for trials based on complex biomarkers including TMB, MSI, and specific gene alterations, with capabilities to detect challenging variant types like fusions and multi-gene signatures [64].
Data Sharing and Collaborative Research
A distinctive feature of MSK-IMPACT is its integration with publicly accessible knowledge bases and data sharing initiatives. Results from clinical testing are available to MSK researchers through the cBioPortal for Cancer Genomics and are shared more broadly with the scientific community through AACR Project GENIE, enabling aggregation of tumor-sequencing data from multiple institutions [58]. This approach is particularly valuable for studying rare cancer types and infrequently mutated genes, accelerating collaborative research discoveries [58].
Foundation Medicine has developed a Clinico-Genomic Database (CGDB) that combines comprehensive genomic profiling data with longitudinal clinical data, providing real-world evidence to support companion diagnostic submissions and drug development programs [64]. This real-world data resource enhances the efficiency of clinical trial design and provides insights into therapeutic performance in diverse patient populations.
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Key Research Reagents and Materials for NGS-Based TMB Analysis
| Reagent/Material | Function | Platform Application |
|---|---|---|
| FFPE Tissue Samples | Preservation of tumor tissue for DNA extraction | Both platforms; requires tumor content >20% for optimal results [63] |
| Blood Collection Tubes | Procurement of matched normal DNA (germline control) | Essential for MSK-IMPACT TC method [58] |
| DNA Extraction Kits | Isolation of high-quality DNA from FFPE and blood samples | Both platforms; minimum 300ng DNA required [24] |
| Hybridization Capture Probes | Target enrichment of specific gene panels | Platform-specific probe sets (505 genes for MSK-IMPACT, 324 for F1CDx) [58] [62] |
| Library Preparation Kits | Preparation of sequencing-ready libraries | Both platforms; includes fragmentation, end repair, adapter ligation [24] |
| Population Databases | Bioinformatic filtering of germline variants | Critical for FoundationOne CDx TO method (dbSNP, ExAC, gnomAD) [24] |
| UMI (Unique Molecular Identifiers) | Error correction and artifact removal | Used in some TMB detection kits to improve accuracy [24] |
The methodological comparison between MSK-IMPACT and FoundationOne CDx reveals a fundamental trade-off in NGS-based TMB assessment between technical rigor and practical applicability. The matched tumor-normal approach of MSK-IMPACT provides superior accuracy in somatic variant detection and eliminates germline contamination, making it particularly valuable for research settings where precision is paramount. Conversely, the tumor-only methodology of FoundationOne CDx offers broader accessibility and has demonstrated robust performance in real-world clinical applications, supported by extensive regulatory approvals and companion diagnostic indications.
For researchers and drug development professionals, platform selection should be guided by specific research objectives, sample availability, and regulatory requirements. MSK-IMPACT offers advantages for comprehensive genomic studies requiring high-confidence somatic mutation calls, while FoundationOne CDx provides a streamlined pathway for clinical trial enrollment and companion diagnostic development. As TMB continues to evolve as a predictive biomarker, both platforms are likely to incorporate emerging biomarkers and methodological refinements to enhance the accuracy and clinical utility of genomic profiling in oncology research.
Blood-Based TMB (bTMB) and Circulating Tumor DNA
Blood-based tumor mutational burden (bTMB) represents a transformative approach in immuno-oncology, serving as a minimally invasive surrogate for tissue TMB that predicts response to immune checkpoint inhibitors (ICIs). This whitepaper delineates the technical foundations, measurement methodologies, and clinical validation of bTMB assessment through circulating tumor DNA (ctDNA) analysis. Framed within next-generation sequencing (NGS) research, we examine the pre-analytical requirements, computational pipelines, and analytical validation necessary for robust bTMB quantification. Emerging evidence demonstrates that bTMB reliably stratifies patient survival outcomes in multiple malignancies, particularly non-small cell lung cancer (NSCLC), while overcoming limitations of tissue sampling. This comprehensive technical guide provides researchers and drug development professionals with experimental protocols, reagent specifications, and standardized workflows to advance bTMB implementation in precision oncology.
Circulating tumor DNA (ctDNA) comprises fragmented tumor-derived DNA molecules shed into the bloodstream through apoptosis, necrosis, and active secretion from cancer cells. These fragments typically range between 150-200 base pairs and carry the full complement of somatic mutations present in the parent tumor tissue. Blood-based tumor mutational burden (bTMB) quantifies the number of somatic mutations per megabase (mut/Mb) detected in ctDNA, serving as a proxy for neoantigen load and potential immunogenicity. The half-life of ctDNA is remarkably short (approximately 16 minutes to several hours), enabling real-time monitoring of tumor dynamics and treatment response.
The fundamental biological rationale linking elevated TMB to improved ICI response centers on neoantigen generation. Somatic mutations create altered protein sequences that can be recognized as foreign by the immune system when presented as neoantigens on major histocompatibility complex molecules. Higher mutation loads increase the probability of generating immunogenic neoantigens, thereby enhancing T-cell recognition and tumor cell killing when immune checkpoints are blocked. bTMB effectively captures this mutational landscape through a minimally invasive liquid biopsy, circumventing the invasiveness and sampling bias associated with traditional tissue biopsies while providing a comprehensive representation of tumor heterogeneity.
Technical Foundations of bTMB Measurement
Pre-analytical Considerations
Standardized blood collection and processing protocols are critical for reliable bTMB assessment due to the low abundance of ctDNA relative to total cell-free DNA (typically 0.025%-2.5% in plasma). The following technical requirements must be rigorously implemented:
Blood Collection: A minimum of 2×10 mL blood drawn into specialized blood collection tubes (BCTs) containing cell-stabilizing preservatives (e.g., cfDNA BCT tubes from Streck, PAXgene Blood ccfDNA tubes from Qiagen). These tubes prevent leukocyte lysis and genomic DNA contamination, maintaining sample integrity for up to 7 days at room temperature during transport. Conventional EDTA tubes require processing within 2-6 hours at 4°C.
Plasma Separation: Two-step centrifugation protocol: initial low-speed centrifugation (800-1,600×g for 10-20 minutes at 4°C) to separate plasma from blood cells, followed by high-speed centrifugation (16,000×g for 10-20 minutes at 4°C) to remove remaining cellular debris.
cfDNA Extraction: Automated or manual extraction from 4-8 mL plasma using specialized kits (e.g., Mag-Bind cfDNA Kit from Omega Bio-Tek) with final elution in 20-100 μL buffer. DNA concentration and quality assessment via fluorometry (Qubit) and fragment analysis (TapeStation).
Sequencing Methodologies
bTMB quantification requires targeted next-generation sequencing panels covering sufficient genomic territory to accurately estimate whole-exome mutational load:
Panel Size Requirements: Minimum coverage of 0.5-1.25 Mb of coding sequence, with panels ≥1.1 Mb demonstrating optimal concordance with whole-exome sequencing. The FoundationOne CDx assay (1.1 Mb), MSK-IMPACT, and NeoThetis Pan Cancer Plus assay (1.25 Mb) represent validated platforms.
Sequencing Parameters: Minimum median exon coverage of 250-300× with ≥95% of exons covered at ≥100×. Unique molecular identifiers (UMIs) are essential for error correction and accurate variant calling, with duplex sequencing methods providing the highest accuracy.
Variant Calling: Bioinformatic pipelines must filter germline variants using matched white blood cell DNA or population databases. Somatic variants are called with minimum variant allele frequency thresholds typically set at 0.5%-1.0%, though lower thresholds may be applied for ultra-sensitive detection.
Table 1: Comparison of bTMB Assay Characteristics
| Assay Parameter | Minimum Requirement | Optimal Specification | Technical Justification |
|---|---|---|---|
| Panel Size | 0.5 Mb | ≥1.1 Mb | Improves correlation with WES-derived TMB; reduces variability |
| Sequencing Depth | 150× | 250-300× | Enables detection of low VAF variants; improves sensitivity |
| VAF Sensitivity | 1% | 0.5% | Captures subclonal mutations in heterogeneous tumors |
| Input Plasma | 4 mL | 8-10 mL | Increases ctDNA yield for low-shedding tumors |
| UMI Incorporation | Recommended | Essential | Reduces sequencing artifacts; improves variant calling accuracy |
bTMB Analysis Workflow
The following diagram illustrates the complete bTMB analysis workflow from blood collection to final reporting:
Computational Analysis Pipeline
The bioinformatic workflow for bTMB calculation involves multiple quality control checkpoints and analytical steps:
Key computational steps include:
- Sequence Alignment: Mapping reads to reference genome (GRCh38) using optimized aligners (BWA-MEM2)
- Variant Calling: Simultaneous application of multiple callers (GATK Mutect2, Strelka2) with integration of results
- Germline Filtering: Removal of germline polymorphisms using matched normal DNA or population databases (gnomAD)
- bTMB Calculation: Summation of synonymous and non-synonymous mutations in targeted regions, divided by the total coding megabases sequenced, with exclusion of known driver mutations
Clinical Validation and Cut-off Determination
bTMB has demonstrated predictive value across multiple cancer types, with varying optimal cut-offs observed in clinical studies:
Table 2: bTMB Clinical Validation Studies and Cut-off Values
| Study/Cancer Type | bTMB Cut-off | Clinical Outcome | Statistical Significance |
|---|---|---|---|
| B-F1RST Trial (NSCLC) [65] | ≥16 (≈14.5 mut/Mb) | Improved OS with atezolizumab | HR=0.75 for OS |
| DART Study (Stage III NSCLC) [66] | ≥8.5 mut/Mb | Longer PFS with durvalumab | HR=0.65, p=0.088 |
| DART Study (Stage III NSCLC) [66] | ≥6.6 mut/Mb (median) | Longer PFS with durvalumab | HR=0.52, p=0.016 |
| Breast/Prostate Cancers [67] | ≥10 mut/Mb | Limited predictive value | No significant PFS benefit |
| Illumina Recommendations [7] | ≥20 mut/Mb | Improved outcomes in mNSCLC | Associated with ICI benefit |
The DART study (2025) prospectively validated bTMB in 86 patients with unresectable stage III NSCLC treated with chemoradiotherapy followed by durvalumab, employing a targeted NGS panel covering 1.25 Mb. This study demonstrated that bTMB acts as an independent biomarker, with high bTMB (using both 8.5 mut/Mb and median 6.6 mut/Mb cut-offs) significantly associated with longer progression-free survival in multivariable analysis. Additional findings revealed that PD-L1 expression ≥1% and absence of STK11/KEAP1/NFE2L2 mutations in ctDNA provided complementary predictive information, supporting a multi-biomarker approach for optimal patient stratification.
Research Reagent Solutions
Table 3: Essential Research Reagents for bTMB Analysis
| Reagent/Category | Specific Examples | Function/Application |
|---|---|---|
| Blood Collection Tubes | cfDNA BCT tubes (Streck), PAXgene Blood ccfDNA tubes (Qiagen) | Preserves blood sample integrity during transport/storage |
| DNA Extraction Kits | Mag-Bind cfDNA Kit (Omega Bio-Tek), AllPrep DNA/RNA FFPE Kit (Qiagen) | Isolation of high-quality cfDNA from plasma/tissue |
| Library Preparation | Twist Biosciences Library Preparation Kit, Illumina TruSight Oncology | NGS library construction with UMI incorporation |
| Target Capture Panels | NeoThetis Pan Cancer Plus (1.25 Mb), FoundationOne CDx (1.1 Mb) | Hybridization capture of genomic regions for TMB calculation |
| Sequencing Platforms | Illumina NovaSeq 6000, NextSeq 550Dx | High-throughput sequencing with required coverage |
| Bioinformatic Tools | GATK Mutect2, Strelka2, BWA-MEM2 | Variant calling, alignment, and bTMB calculation |
Experimental Protocol for bTMB Assessment
Sample Collection and Processing
- Blood Collection: Draw 20 mL peripheral blood (2×10 mL) into cell-stabilizing BCTs using 21-gauge or larger butterfly needles with minimal tourniquet time.
- Plasma Separation: Process within 30 minutes-6 hours (EDTA tubes) or up to 7 days (stabilizing BCTs). First centrifugation: 800×g for 10 minutes at 4°C. Transfer supernatant to fresh tube. Second centrifugation: 16,000×g for 10 minutes at 4°C. Aliquot plasma and store at -80°C.
- cfDNA Extraction: Extract from 4-8 mL plasma using silica-membrane or magnetic bead-based kits. Elute in 20-50 μL elution buffer. Quantify using fluorometric methods (≥1 ng/μL required).
Library Preparation and Sequencing
- DNA Quality Control: Assess fragment size distribution (Agilent TapeStation), confirming predominant 150-200 bp fragments.
- Library Construction: Convert 10-100 ng cfDNA to sequencing library with UMI tagging (Twist Library Preparation Kit). Include dA-tailing, adapter ligation, and limited-cycle PCR.
- Target Enrichment: Hybridize with biotinylated probes targeting ≥1.1 Mb cancer-related genes (NeoThetis Pan Cancer Plus). Capture with streptavidin beads, wash, and amplify.
- Sequencing: Pool libraries and sequence on Illumina platform (NovaSeq 6000) targeting 250-300× median coverage with ≥95% uniformity.
Bioinformatic Analysis
- Data Processing: Demultiplex raw sequencing data (bcl2fastq), assess quality (FastQC).
- Alignment: Map reads to GRCh38 reference genome (BWA-MEM2), generate UMI consensus sequences.
- Variant Calling: Identify somatic mutations using dual caller approach (GATK Mutect2, Strelka2) with minimum VAF 0.5%.
- bTMB Calculation: Filter out germline variants (using matched normal or population databases) and known driver mutations. Calculate bTMB = (total synonymous + non-synonymous mutations) / (panel size in Mb).
Blood-based TMB represents a significant advancement in immuno-oncology biomarker research, offering a minimally invasive approach for quantifying tumor mutational burden and predicting response to immune checkpoint inhibitors. The technical framework outlined in this whitepaper provides researchers with standardized methodologies for bTMB assessment, from pre-analytical sample handling through computational analysis. While clinical validation across diverse cancer types continues to evolve, current evidence strongly supports bTMB as a robust predictive biomarker in NSCLC, particularly when integrated with complementary biomarkers such as PD-L1 expression and specific resistance mutations. Future directions include harmonization of bTMB thresholds across platforms, validation in prospective clinical trials, and development of integrated biomarker models that leverage the dynamic capabilities of ctDNA analysis throughout treatment.
Overcoming Technical Challenges in TMB Measurement and Standardization
In the era of precision oncology, tumor mutational burden (TMB) has emerged as a significant predictive biomarker for response to immune checkpoint inhibitors (ICIs). Defined as the number of somatic mutations per megabase of interrogated genomic sequence, TMB measurement relies heavily on next-generation sequencing (NGS) technologies [4]. However, the accuracy and reliability of TMB assessment are profoundly influenced by pre-analytical variables—factors affecting samples before they reach sequencing [68]. These variables, including tissue quality, tumor purity, and input DNA characteristics, introduce substantial variability that can compromise TMB measurement accuracy and consequently affect clinical decision-making [69] [5].
The standardization of pre-analytical variables remains challenging due to the plethora of specimen acquisition and processing methods used across institutions [68]. Specimen acquisition, fixation, sectioning, and post-fixation processing all contribute to the reliability of NGS analysis [68]. This technical guide examines these critical pre-analytical factors within the context of TMB research, providing researchers and drug development professionals with evidence-based methodologies to optimize workflow consistency and data quality.
Tissue Quality: Foundation for Reliable NGS
Effects of Specimen Handling and Fixation
Formalin-fixed, paraffin-embedded (FFPE) tissue represents the most common specimen source for clinical cancer sequencing, but its processing introduces specific challenges for molecular analysis. Formalin fixation causes various types of crosslinks between amino acids and nucleic acids, leading to DNA fragmentation and nucleotide alterations that can confound molecular testing [69]. The most significant artifacts include:
- DNA fragmentation: Methylene crosslinks result in DNA strand breaks, limiting template length for sequencing [69].
- Deamination artifacts: Formalin fixation can cause nucleotide deaminations, particularly C>T transitions at CpG dinucleotides, which manifest as false positive variant calls [69].
- Oxidative damage: Formalin can cause nucleotide oxidation, further compromising DNA integrity [69].
A systematic review of breast cancer samples demonstrated that while FFPE and fresh-frozen (FF) tissues show high concordance in various downstream applications, proper handling and fixation protocols are essential to minimize artifacts [70]. Exclusion of variants below 5% variant allele frequency (VAF) was particularly important to overcome FFPE-induced artifacts [70].
DNA Quality Assessment and Quality Control
Robust quality control (QC) measures are essential before proceeding with NGS library preparation. A PCR-based QC assay utilizing multiple amplicon sizes (e.g., 105bp and 236bp) effectively determines DNA fragmentation levels and suitability for sequencing [69]. This approach calculates a QC ratio by comparing sample amplification to non-degraded control DNA, with ratios above 0.20 indicating favorable quality [69].
Additional QC parameters include:
- Spectrophotometric purity assessment (A260/A280 ratios) to detect protein contamination [70].
- Fragment size distribution analysis using automated electrophoresis systems [69].
- DNA quantification using fluorescence-based methods superior to spectrophotometry for FFPE-derived DNA [69].
Table 1: Impact of FFPE Storage Time on Sequencing Metrics [69]
| Storage Time (years) | Target Base Coverage | Alignment Rate (%) | Duplicate Read Rate (%) | Insert Size (bp) |
|---|---|---|---|---|
| <5 | 98.5% | 99.2% | 12.5% | 135 |
| 5-10 | 97.8% | 98.7% | 15.3% | 128 |
| >10 | 95.2% | 96.1% | 22.8% | 117 |
Tumor Purity: Critical Determinant of Variant Calling
Definition and Estimation Methods
Tumor purity refers to the proportion of malignant cells within a analyzed tissue sample [71]. Accurate determination is crucial for TMB assessment as low purity can lead to false negative calls and inaccurate mutation burden calculations [72]. Tumor purity estimation methods include:
- Pathological assessment: Conventional microscopic evaluation of H&E-stained slides by pathologists, though this method shows notable inter-observer variability [71] [72].
- Digital pathology: Semi-automated image analysis of scanned H&E slides using platforms like QuPath, providing more objective and reproducible purity measurements [72].
- Bioinformatic estimation: Computational tools like Sequenza and Sclust infer purity from sequencing data by analyzing allele-specific copy number alterations [72].
- Transcriptome-based estimation: Methods like PUREE (Pan-cancer Tumor Purity Estimation) use machine learning models trained on gene expression data to infer purity, demonstrating high accuracy across solid tumor types [71].
A comparative study in ovarian carcinomas found that conventional pathology systematically overestimated tumor purity by approximately 8% compared to digital pathology [72]. This overestimation can significantly impact homologous recombination deficiency (HRD) scores, which share similar purity dependencies with TMB calculation [72].
Impact on TMB Assessment and Variant Calling
Tumor purity directly affects variant allele frequency (VAF) measurements, with low purity samples exhibiting depressed VAFs that may fall below detection thresholds [72] [5]. The relationship between tumor purity and minimal detectable VAF follows:
Detectable VAF ≈ (Mutation Copies) / (Total DNA × Purity)
For TMB assessment, establishing appropriate VAF thresholds is essential to balance sensitivity and specificity. Research indicates that optimal VAF cutoffs differ between sample types: 5% for frozen samples and 10% for FFPE specimens [5]. This higher threshold for FFPE samples helps mitigate false positives from formalin-induced artifacts while maintaining sensitivity for true somatic variants.
Table 2: Tumor Purity Estimation Methods Comparison [71] [72]
| Method | Principle | Advantages | Limitations | Concordance with Digital Pathology |
|---|---|---|---|---|
| Conventional Pathology | Visual estimation of tumor cell percentage on H&E slides | Rapid, cost-effective, widely available | Subjective, inter-observer variability, ~8% overestimation | 0.72 (Pearson correlation) |
| Digital Pathology | Semiautomated image analysis of scanned H&E slides | Objective, reproducible, precise | Requires specialized equipment and training | 1.00 (reference method) |
| Genomics-based (Sequenza) | Bayesian modeling of allele-specific copy numbers from sequencing data | Purity and ploidy simultaneously, no additional cost | Requires matched normal, affected by aneuploidy | 0.85 (Pearson correlation) |
| Transcriptomics-based (PUREE) | Machine learning model using gene expression patterns | High accuracy, works with RNA-seq data only | Pan-cancer model may miss type-specific features | 0.78 (Pearson correlation) |
Figure 1: Tumor Purity Estimation Workflow and Impact on TMB Calculation
Input DNA: Quantity, Quality, and Library Preparation
DNA Input Requirements and Optimization
The quantity and quality of input DNA significantly impact NGS library complexity and sequencing uniformity. Different NGS approaches have varying requirements:
- Hybridization-capture panels: Typically require 50-200ng of input DNA, with higher inputs recommended for degraded FFPE samples [69].
- Whole exome sequencing (WES): Generally requires 100-500ng of high-quality DNA for optimal coverage.
- Liquid biopsy assays: Can work with much lower inputs (5-30ng) due to the fragmented nature of cell-free DNA [73] [74].
For FFPE-derived DNA, a study on lung tumor specimens demonstrated that DNA input amount significantly correlated with sequencing efficiency metrics including depth of coverage, alignment rate, and read quality [69]. The relationship between input amount and coverage uniformity was particularly important in genomic regions with extreme GC content, where suboptimal samples showed markedly worse performance [69].
Library Preparation Considerations
Library preparation methods must be optimized for FFPE-derived DNA, which is typically more fragmented than DNA from fresh tissues. Key considerations include:
- Fragmentation method: Sonication versus enzyme-based fragmentation approaches show different performance characteristics with degraded samples [69].
- Capture efficiency: Varies based on DNA integrity, with lower efficiency observed in highly degraded samples [69].
- Unique molecular identifiers (UMIs): Essential for distinguishing true low-frequency variants from sequencing artifacts, particularly important for low-purity samples [74].
- PCR cycle optimization: Excessive amplification can reduce library complexity and increase duplicate rates, particularly critical for low-input samples [69].
Table 3: DNA Input Recommendations for Different NGS Applications [69] [74] [70]
| NGS Application | Recommended Input DNA | Minimum Input DNA | Optimal DNA Integrity | QC Method |
|---|---|---|---|---|
| Large Panels (>1Mb) | 200ng | 50ng | DV200 > 30% | PCR-based QC assay |
| Small Panels (<0.5Mb) | 100ng | 20ng | DV200 > 20% | Fragment analyzer |
| Whole Exome Sequencing | 500ng | 100ng | DV200 > 50% | Qubit + TapeStation |
| Liquid Biopsy (ctDNA) | 30ng | 5ng | N/A (naturally fragmented) | ddPCR for input |
TMB Calculation: Standardization Across Platforms
Panel Design and Bioinformatics Considerations
TMB estimation using targeted NGS panels requires careful consideration of multiple factors:
- Panel size: Larger panels (typically >1Mb) provide more reliable TMB estimates, with the coefficient of variation inversely proportional to both the square root of panel size and TMB level [4].
- Genomic content: Panels must be carefully designed to avoid regions with inherent instability or germline polymorphisms [4] [5].
- Variant types included: Most TMB algorithms focus on coding, non-synonymous mutations, though some panels include synonymous mutations to reduce sampling noise [4].
- Bioinformatic filtering: Proper filtering for germline variants, sequencing artifacts, and driver mutations is essential for accurate TMB calculation [5].
Different commercial panels show variability in TMB estimation due to differences in panel size, genomic content, and bioinformatic pipelines. The FoundationOne CDx assay covers 0.8Mb across 324 genes, while MSK-IMPACT covers 1.14Mb across 468 genes [4]. This variability necessitates careful cross-platform validation when comparing TMB results.
VAF Thresholds and Filtering Strategies
Establishing appropriate VAF thresholds is critical for accurate TMB estimation. Studies comparing FFPE and frozen sample pairs have demonstrated that:
- Frozen samples reach a TMB plateau at VAF thresholds around 5%, representing the "true" mutational burden [5].
- FFPE samples require higher VAF thresholds (10% for high-quality FFPE DNA, potentially higher for low-quality specimens) to eliminate formalin-induced artifacts [5].
- Low-quality FFPE samples may never reach a clear TMB plateau, making them suboptimal for reliable TMB assessment [5].
Additionally, biological curation of high-TMB cases is recommended, as a significant proportion (21% in one study) may harbor undetected MSI or POLE deficiencies that explain the elevated mutation burden [5].
Figure 2: TMB Calculation Bioinformatics Workflow
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 4: Essential Research Reagents and Platforms for Pre-analytical Workflow [69] [72] [70]
| Reagent/Platform | Specific Examples | Function in Workflow | Key Considerations |
|---|---|---|---|
| Nucleic Acid Extraction Kits | QIAamp DNA FFPE Tissue Kit, AllPrep DNA/RNA FFPE Kit | Simultaneous DNA/RNA extraction from FFPE tissue | Yield and quality preservation from degraded samples |
| DNA Quality Assessment | Agilent 2200 TapeStation, Bioanalyzer | Fragment size distribution analysis | DV200 metric calculation for FFPE samples |
| Digital Pathology Platforms | QuPath software | Objective tumor purity estimation | Requires pathologist training and validation |
| Targeted NGS Panels | MSK-IMPACT, FoundationOne CDx, TruSight Oncology 500 | TMB estimation and comprehensive genomic profiling | Panel size >1Mb recommended for reliable TMB |
| Bioinformatic Tools for Purity | Sequenza, Sclust, PUREE | Computational tumor purity estimation | Different underlying algorithms and input requirements |
| Unique Molecular Identifiers (UMIs) | Duplex Sequencing, Safe-SeqS | Error correction and artifact removal | Essential for low-frequency variant detection |
| QC Assays | PCR-based QC assay with multiple amplicon sizes | DNA quality assessment prior to library preparation | QC ratio >0.20 indicates adequate quality |
The reliable determination of tumor mutational burden depends critically on careful attention to pre-analytical variables. Tissue quality, tumor purity, and input DNA characteristics collectively influence the accuracy and reproducibility of TMB measurements, with implications for both clinical decision-making and research applications. Standardization of specimen processing, implementation of robust quality control measures, and application of appropriate bioinformatic corrections are essential steps toward harmonizing TMB assessment across platforms and institutions.
As TMB continues to evolve as a predictive biomarker for immunotherapy response, the research community must prioritize pre-analytical standardization to ensure the reliability and clinical utility of this important molecular marker. Future directions include the development of integrated quality metrics, reference standards, and automated systems that minimize pre-analytical variability while maximizing data quality for precision oncology applications.
Bioinformatic Pipeline Optimization for Somatic Variant Calling
The accurate identification of somatic mutations is a cornerstone of precision oncology, essential for understanding tumorigenesis, developing targeted therapies, and advancing cancer research [75]. Within this context, Tumor Mutational Burden (TMB), defined as the quantifiable number of acquired somatic mutations per megabase of sequenced genome, has emerged as a significant biomarker [20]. TMB serves as a potential surrogate for neoantigen load and an indicator of likely response to immune checkpoint blockade therapy [20]. However, the biological and clinical significance of TMB, particularly in specific cancer types like breast cancer, is not yet fully understood, necessitating robust bioinformatic pipelines for its accurate measurement [20].
The primary challenge in somatic variant calling lies in the reliable discrimination of true somatic variants from an overwhelming background of germline variants and technical artifacts introduced during sequencing [75]. This challenge is compounded in tumor-only sequencing scenarios, where the absence of a matched normal sample makes it difficult to distinguish somatic variants with a variant allelic fraction (VAF) close to germline heterozygotes from those with low VAF that may be mistaken for background noise [75]. The entire process, from nucleic acid isolation to final data interpretation, must be meticulously optimized to ensure the validity of the resulting TMB calculations and variant profiles. This guide details the key stages of pipeline optimization, provides benchmarking for modern variant callers, and outlines essential reagents, providing a comprehensive framework for researchers and drug development professionals.
Foundational NGS Workflow and Technical Considerations
A optimized bioinformatic pipeline for somatic variant discovery is built upon a foundation of a rigorous and well-controlled laboratory workflow. The principal stages of the next-generation sequencing (NGS) process must be carefully executed to generate high-quality data suitable for sensitive variant detection [76].
Key Steps in the NGS Wet-Lab Workflow
- Nucleic Acid Isolation: The initial step is critical for success. Isolated DNA must possess sufficient yield, purity, and quality for library preparation [76] [77]. For formalin-fixed, paraffin-embedded (FFPE) samples, which contain fragmented nucleic acids, the isolation method must be optimized to obtain a sufficient quantity of material [76]. Purity is vital to avoid contaminants that can inhibit enzymatic reactions in later steps [76]. Quality assessment often involves UV spectrophotometry, fluorometric assays, and gel electrophoresis [76].
- Library Preparation: This process prepares nucleic acids for sequencing and involves fragmentation, adapter ligation, and library quantification [76]. For Illumina systems, fragmentation size should be optimized for the specific sequencer and application [76]. Platform-specific adapters (e.g., P5 and P7 for Illumina) are ligated to fragment ends [76]. Accurate library quantification via fluorometry or qPCR is necessary to ensure optimal loading concentration on the sequencer, which maximizes data output and quality [76].
- Clonal Amplification and Sequencing: Prior to sequencing, DNA libraries undergo clonal amplification on a flow cell to generate clusters of identical molecules, ensuring fluorescent signals from sequencing-by-synthesis are detectable [76]. The Illumina platform then uses sequencing-by-synthesis (SBS) with fluorescently-labeled, reversibly-terminated nucleotides. Fluorescent signals are captured cycle-by-cycle to determine the base sequence of each cluster [76].
Workflow Automation and Optimization
Integrating automation into the NGS workflow significantly enhances efficiency, consistency, and reproducibility [77]. An automation plan developed at the project's outset helps optimize tools, protocols, and reagents. Strategies include [77]:
- Tailoring Hardware: Selecting appropriate hardware and protocols for specific sample types (e.g., RNA vs. DNA, cfDNA vs. high molecular weight DNA).
- Choosing Optimal Consumables: Ensuring compatibility between consumables and liquid reagents is crucial; contaminants from labware can inhibit sensitive enzymatic reactions [77].
- Planning for Flexibility: Selecting vendor-agnostic systems and modular platforms allows workflows to adapt to changing project needs, such as scaling throughput or switching chemistries [77].
The following diagram illustrates the core stages of the NGS workflow that forms the basis for somatic variant analysis.
Core NGS Wet-Lab Workflow
Computational Pipeline for Somatic Variant Calling
Once raw sequencing data (FASTQ files) are generated, the computational phase begins. This phase involves processing the data to identify somatic variants with high confidence, a process that is particularly challenging in tumor-only contexts.
Bioinformatic Data Processing Stages
The bioinformatic analysis can be categorized into three main stages [76]:
- Stage 1: Data Processing and Cleanup. This involves base calling, determining read numbers and lengths, applying quality filters (e.g., clusters passing filters), trimming adapter sequences, and demultiplexing samples if multiple libraries were sequenced together [76].
- Stage 2: Sequence Analysis. The processed reads are mapped or aligned to a reference genome (e.g., GRCh37/hg19, GRCh38/hg38). Following alignment, duplicate reads (often PCR artifacts) are removed. For tumor-only analysis, this stage heavily relies on sophisticated algorithms to differentiate potential somatic variants from germline polymorphisms and technical artifacts [75].
- Stage 3: Biological Interpretation. The final stage focuses on extracting biological meaning from the variant calls. This includes genome annotation, detecting sequence variants, determining gene counts, analyzing biological pathways, and identifying biomarkers or drug targets [76].
The Challenge of Tumor-Only Variant Calling
In many real-world clinical scenarios, a matched normal sample from the same patient is unavailable [75]. Tumor-only somatic variant calling is exceptionally challenging because the algorithm must distinguish true somatic variants from a much larger number of germline variants and technical artifacts without a direct reference [75]. This requires "more proficient algorithms" that can learn the characteristics of true somatic signals [75].
Advanced methods like ClairS-TO have been developed to address this. ClairS-TO is a deep-learning-based method designed for long-read tumor-only somatic variant calling. It uses an ensemble of two disparate neural networks: an affirmative network (AFF) that determines how likely a candidate is a somatic variant, and a negational network (NEG) that determines how likely it is not [75]. A posterior probability is calculated from the outputs of these networks. The method is further refined using hard-filters, panels of normals (PoNs), and a statistical "Verdict" module to classify variants as germline, somatic, or subclonal somatic [75]. The diagram below illustrates this sophisticated computational workflow.
ClairS-TO Tumor-Only Variant Calling Workflow
Performance Benchmarking and Mutational Signature Analysis
Selecting and optimizing a somatic variant calling pipeline requires an understanding of the performance characteristics of available tools under various experimental conditions. Furthermore, the biological interpretation of the results, particularly regarding TMB, is enriched by analyzing the underlying mutational signatures.
Benchmarking Somatic Variant Callers
Comprehensive benchmarking using well-characterized cancer cell lines like COLO829 (melanoma) and HCC1395 (breast cancer) provides critical performance data. The table below summarizes the Area Under the Precision-Recall Curve (AUPRC) for Single Nucleotide Variant (SNV) detection using Oxford Nanopore Technologies (ONT) long-read data, comparing ClairS-TO against other callers [75].
Table 1: Benchmarking Performance of Somatic Variant Callers on ONT Data (AUPRC for SNVs)
| Variant Caller | Description | 25x Coverage | 50x Coverage | 75x Coverage |
|---|---|---|---|---|
| ClairS-TO (SSRS) | Deep learning model (synthetic & real sample training) | 0.6489 | 0.6634 | 0.6685 |
| ClairS-TO (SS) | Deep learning model (synthetic sample training only) | 0.5820 | 0.5980 | 0.6042 |
| DeepSomatic | Deep-learning-based, multi-cancer model | 0.5507 | 0.5625 | 0.5661 |
| smrest | Haplotype-resolved statistical method | 0.5104 | 0.5226 | 0.5258 |
Key insights from this benchmark include [75]:
- ClairS-TO SSRS consistently outperforms other methods across all coverages, demonstrating the value of training with real tumor samples.
- Performance gains are more pronounced when increasing coverage from 25x to 50x than from 50x to 75x, informing cost-effective experimental design.
- ClairS-TO is also applicable to short-read (Illumina) data, where it has been shown to outperform Mutect2, Octopus, and Pisces at 50-fold coverage [75].
TMB and Mutational Signature Integration
Beyond counting mutations, understanding their origin is crucial. Mutational signature analysis reveals the underlying biological processes active in a tumor. In TMB-high breast carcinomas, the predominant mutational signature is often attributed to the APOBEC (apolipoprotein B mRNA editing enzyme catalytic polypeptide) family of cytidine deaminases [20].
Table 2: Characteristics of TMB-High Breast Carcinomas
| Feature | Characteristic in TMB-High Breast Cancer | Implication |
|---|---|---|
| Predominant Signature | APOBEC (64.7% of tumors) [20] | Suggests a specific mutagenic process; potential therapeutic target. |
| Commonly Altered Genes | Enrichment in KMT2C, ARID1A, PTEN, NF1, RB1 [20] | These alterations are associated with APOBEC mutagenesis. |
| Immune Context | Loss-of-function in ARID1A and PTEN linked to immune cell exclusion [20] | May explain resistance to immunotherapy despite high TMB. |
| Metastatic Site Genetics | ESR1 mutations in 27% of liver mets; CDH1 mutations & ERBB2 amps in bone/brain [20] | Informs on patterns of progression and site-specific therapy. |
Studies show that TMB-high breast cancers are enriched in specific somatic alterations beyond common drivers like PIK3CA and TP53. These include KMT2C, ARID1A, PTEN, NF1, and RB1, which have been linked to APOBEC mutagenesis [20]. Furthermore, loss-of-function alterations in ARID1A and PTEN are associated with immune cell exclusion from the tumor microenvironment, which may impact response to immune checkpoint blockade even in the context of high TMB [20]. The relationship between these genomic features is illustrated below.
Genomic Interplay in TMB-High Tumors
Essential Research Reagent Solutions and Materials
The successful implementation of an optimized somatic variant calling pipeline relies on a foundation of high-quality laboratory reagents and materials. The following table details key solutions used in the featured experiments and the broader field.
Table 3: Essential Research Reagent Solutions for Somatic Variant Calling and TMB Analysis
| Item | Function / Application | Specific Examples / Considerations |
|---|---|---|
| Targeted NGS Panels | Hybrid-capture panels for focused sequencing of cancer-related genes and TMB calculation. | ONCOaccuPanel (344 genes); MSK-IMPACT [32] [20]. |
| DNA Isolation Kits | Extraction of high-yield, pure, high-quality DNA from tumor samples, including challenging FFPE tissue. | Kits optimized for FFPE, fresh frozen tissue, or blood (for cfDNA); should minimize inhibitors [76] [77]. |
| Library Prep Kits | Preparation of sequencing libraries via fragmentation, adapter ligation, and amplification. | Illumina DNA Prep kits; should be selected based on input DNA type and quantity [76]. |
| Whole Genome Amplification (WGA) Kits | Amplification of genomic DNA from low-input or single-cell samples to increase template for library prep. | Kits utilizing phi29 DNA polymerase for high processivity and reduced bias [76]. |
| Bioinformatic Software Suites | Platforms for secondary data analysis, including alignment, variant calling, and annotation. | NGeneAnalySys; custom pipelines using BWA, GATK; specialized tools like ClairS-TO [32] [75]. |
| Automation-Compatible Consumables | DNase/RNase-free, endotoxin-free plates and tubes that prevent enzymatic inhibition in automated workflows. | Certified "PCR-clean" or "non-binding" labware to ensure reagent compatibility and reaction efficiency [77]. |
Optimizing a bioinformatic pipeline for somatic variant calling is a multi-faceted endeavor, integral to the accurate determination of Tumor Mutational Burden and other genomic biomarkers in cancer research. It requires tight integration of wet-lab procedures—from nucleic acid isolation using specialized reagents to streamlined library preparation—with advanced computational methods. The adoption of sophisticated, deep-learning-based tools like ClairS-TO for tumor-only analysis significantly improves the accuracy of somatic variant discovery, especially when paired with long-read sequencing technologies. Furthermore, moving beyond a simple TMB score to incorporate mutational signature analysis provides deeper biological insights into tumor etiology and potential therapeutic vulnerabilities. By adhering to the rigorous experimental protocols, benchmarking standards, and utilizing the essential research tools outlined in this guide, researchers and drug developers can enhance the precision and reliability of their genomic analyses, ultimately accelerating progress in personalized cancer medicine.
Next-generation sequencing (NGS) has revolutionized oncology research and precision medicine by enabling comprehensive genomic profiling of tumors. Within this framework, tumor mutational burden (TMB) has emerged as a critical biomarker for predicting response to immunotherapy. However, accurate TMB calculation and therapeutic interpretation depend heavily on the precise discrimination between somatic mutations and germline variants. This technical review examines the core methodologies for germline variant filtering, comparing the efficiency, limitations, and clinical implications of tumor-only versus tumor-normal paired sequencing approaches. We provide detailed experimental protocols, quantitative comparisons, and pathway analyses to guide researchers and drug development professionals in optimizing NGS strategies for accurate mutational burden assessment.
Tumor mutational burden (TMB), defined as the number of somatic mutations per megabase of interrogated genomic sequence, has gained significant traction as a predictive biomarker for immune checkpoint blockade response. The underlying principle suggests that higher TMB increases neoantigen load, enhancing T-cell-mediated tumor recognition and destruction. However, accurate TMB quantification requires precise exclusion of germline polymorphisms, as their inadvertent inclusion artificially inflates TMB values, potentially leading to false-positive predictions of immunotherapy responsiveness.
The prevailing clinical practice utilizes two primary NGS approaches for tumor genotyping: tumor-only sequencing (analyzing DNA from tumor tissue alone) and tumor-normal paired sequencing (analyzing matched tumor and normal DNA from the same patient). While 90% of clinical NGS laboratories perform tumor-only testing due to cost and efficiency considerations, this approach presents significant challenges for definitive germline variant identification [78]. Research demonstrates that integrated germline sequencing improves the accuracy of somatic mutation calls and enhances the identification of hereditary cancer risk variants, with substantial implications for both TMB calculation and therapeutic interpretation [78] [79].
Technical Foundations of NGS for Cancer Genomics
Next-generation sequencing technologies enable massive parallel sequencing of DNA fragments, providing a comprehensive view of cancer genomes. The basic NGS workflow involves: (1) nucleic acid extraction from tumor samples (e.g., FFPE tissue, blood), (2) library preparation through fragmentation and adapter ligation, (3) target enrichment (for panel sequencing), (4) massive parallel sequencing, and (5) bioinformatic data analysis including alignment, variant calling, and annotation [80] [81].
Key NGS methods employed in oncology research include:
- Whole Genome Sequencing (WGS): Provides the most comprehensive analysis but requires high DNA input and is less practical for FFPE samples.
- Whole Exome Sequencing (WES): Focuses on protein-coding regions with higher coverage depth than WGS.
- Targeted Sequencing Panels: Most widely used in clinical research; focuses on predefined cancer-associated genes with lower input requirements and better compatibility with degraded samples like FFPE [80].
- RNA Sequencing: Assesses transcriptome changes and fusion events.
For TMB calculation, targeted panels of several hundred genes have been developed and validated against whole exome sequencing, providing a practical approach for clinical research applications [20] [32].
Germline Filtering in Tumor-Only Sequencing
Computational Filtering Strategies
Tumor-only sequencing relies heavily on bioinformatic filters to remove potential germline variants from the final somatic variant calls. The primary strategies include:
- Population Frequency Filtering: Variants present in population databases (e.g., gnomAD, NHLBI ESP) at frequencies exceeding a set threshold (typically >0.1-1%) are filtered out as likely polymorphisms [78].
- Panel of Normals (PON): A database of non-tumor samples sequenced using the same platform and pipeline is used to identify and remove recurrent sequencing artifacts and germline variants present in the reference population.
- Variant Allele Fraction (VAF) Considerations: While sometimes used heuristically, VAF has proven insufficient for reliable germline-somatic discrimination, as heterozygotic germline variants typically present at ~50% VAF but can be altered by tumor ploidy, stromal contamination, and copy-number changes [78].
Limitations and Clinical Implications
Studies examining tumor-only sequencing followed by confirmatory germline testing reveal significant limitations in computational filtering alone:
- Incomplete Germline Variant Removal: In a study of 160 pediatric solid tumors, 71% (308/434) of single-nucleotide variants reported in tumor-only sequencing were subsequently confirmed as germline in origin [78]. This substantial contamination directly impacts TMB calculation accuracy.
- Failure to Identify Pathogenic Variants: The same study found that only 66% (25/38) of pathogenic/likely pathogenic germline variants were included in the original tumor-only reports. The remaining variants were filtered out due to population frequency thresholds or masked by tumor copy-number alterations [78].
- Expert Review Inconsistency: While molecular pathologists may comment on potential germline origin in tumor-only reports, this process is subjective and inconsistently applied across institutions.
The following table summarizes quantitative findings from comparative studies:
Table 1: Quantitative Comparison of Germline Variant Detection in Tumor-Only vs. Integrated Analysis
| Metric | Tumor-Only Sequencing | Integrated Tumor-Normal | Study Details |
|---|---|---|---|
| Reported variants later confirmed germline | 71% (308/434 SNVs) | Not applicable | 160 pediatric solid tumors [78] |
| Pathogenic/likely pathogenic germline variants detected | 66% (25/38) | 100% (38/38) | Same cohort with confirmatory testing [78] |
| Patients with pathogenic germline variants | Not fully detected | 22% (35/160) | High-risk pediatric solid tumors [78] |
Diagram 1: Tumor-Only Germline Filtering Workflow
Integrated Tumor-Normal Paired Sequencing
Methodological Approach
Tumor-normal paired sequencing provides the definitive method for distinguishing somatic from germline variants by analyzing matched tumor and normal (typically blood, buccal swab, or skin) DNA samples from the same patient in parallel. The methodological framework involves:
- Sample Collection: Concurrent collection of tumor tissue (FFPE, fresh frozen, or biopsy) and matched normal tissue (peripheral blood mononuclear cells or saliva) during the initial diagnostic process.
- Parallel Library Preparation: DNA extraction and library preparation for both tumor and normal samples using identical protocols and sequencing platforms to minimize technical variability.
- Sequencing and Analysis: Simultaneous sequencing of tumor-normal pairs with subsequent bioinformatic analysis that directly compares variant calls between the two samples. True somatic mutations are identified as variants present in the tumor but absent in the matched normal, while germline variants appear in both samples.
Advantages for TMB Research
The integrated approach offers several critical advantages for accurate TMB determination and beyond:
- Definitive Somatic-Germline Discrimination: Direct comparison eliminates guesswork from germline filtering, providing definitive classification of somatic mutations for precise TMB calculation [78] [79].
- Comprehensive Germline Variant Detection: Enables simultaneous identification of pathogenic germline variants (PGVs) with cancer predisposition implications, which is crucial for both the patient and family members [78] [82].
- Detection of Loss of Heterozygosity (LOH): Facilitates identification of somatic LOH events, where the wild-type allele of a germline variant is lost in the tumor, a common oncogenic mechanism in hereditary cancer syndromes [78] [83].
- Reduced Curation Burden: Automates the variant classification process, reducing the need for labor-intensive expert curation and computational filtering approximations.
Table 2: Tumor-Normal Sequencing Impact on Clinical Interpretation
| Analysis Aspect | Tumor-Only Approach | Tumor-Normal Paired Approach |
|---|---|---|
| Germline-Somatic Discrimination | Indirect, probabilistic | Direct, definitive |
| TMB Calculation Accuracy | Potentially inflated | Highly accurate |
| Cancer Predisposition Detection | Limited, incomplete | Comprehensive |
| LOH Identification | Challenging, indirect | Straightforward, direct |
| Expert Curation Time | Significant | Reduced |
| Therapeutic Interpretation | Potentially confounded | Precise |
Experimental Protocols for Germline Filtering
Tumor-Only Bioinformatic Filtering Protocol
For laboratories utilizing tumor-only sequencing, the following detailed protocol implements a multi-layered filtering approach:
Variant Calling: Perform initial variant calling using established somatic callers (MuTect2, VarDict, or similar) with standard parameters.
Population Frequency Filtering:
- Annotate variants against population databases (gnomAD, ESP, 1000 Genomes)
- Filter out variants with population allele frequency >0.1% in any subpopulation
- Retain variants with frequency <0.1% or absent from databases
Panel of Normals (PON) Application:
- Create institution-specific PON from blood samples or non-tumor tissues
- Sequence PON samples using identical library prep and sequencing protocols
- Filter variants recurrently appearing in PON (>2% of samples)
Artifact Removal:
- Implement orientation bias filters for FFPE-derived artifacts
- Apply sequencing context-specific filters (e.g., homopolymer regions)
- Remove low-quality calls with strand bias or poor mapping quality
Expert Review:
- Manually review variants with VAF 30-70% for potential germline origin
- Assess variants in known cancer predisposition genes (ACMG list) for possible germline etiology
- Rescue variants with strong clinical or functional evidence despite filtering
Tumor-Normal Paired Analysis Protocol
For laboratories implementing matched sequencing, this protocol ensures optimal germline-somatic discrimination:
Sample Preparation:
- Extract DNA from tumor and matched normal using identical methods
- Assess DNA quality: tumor content >20%, normal sample purity
- Utilize targeted panels covering 300-500 genes for optimal TMB assessment
Library Preparation and Sequencing:
- Process tumor-normal pairs in the same sequencing batch
- Use unique dual indices to prevent cross-contamination
- Sequence to adequate depth: ≥500× for tumor, ≥200× for normal
Somatic Variant Calling:
- Use paired callers (MuTect2 in tumor-normal mode)
- Call SNVs, indels, and copy-number alterations
- Apply strict contamination checks between tumor-normal pairs
Germline Variant Calling:
- Process normal sample through germline variant caller (GATK HaplotypeCaller)
- Annotate against population databases and clinical databases (ClinVar)
- Classify according to ACMG/AMP guidelines
Integrated Reporting:
- Generate separate somatic and germline reports
- Calculate TMB using confirmed somatic variants only
- Flag potential germline findings in somatic report when appropriate
Diagram 2: Tumor-Normal Paired Analysis Workflow
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Essential Research Reagents for Germline Filtering Studies
| Reagent/Resource | Specifications | Research Application |
|---|---|---|
| Targeted NGS Panels | 300-500 gene content (e.g., OncoPanel, MSK-IMPACT) | Balanced TMB assessment and therapeutic target identification [78] [20] |
| Matched Normal Collection Kits | Blood collection tubes (EDTA, Streck), buccal swab kits | Source of germline DNA for tumor-normal paired analysis |
| FFPE DNA Extraction Kits | Optimized for cross-linked, fragmented DNA | Extraction of quality DNA from archival clinical samples [80] |
| Hybrid Capture Reagents | Biotinylated probes, streptavidin beads | Target enrichment for targeted sequencing approaches |
| Population Databases | gnomAD, NHLBI ESP, 1000 Genomes | Reference for germline variant filtering in tumor-only analysis [78] |
| Somatic-Germline Classifiers | Bioinformatics pipelines (MuTect2, VarDict) | Distinguishing somatic mutations from germline variants [83] |
| ACMG Classification Guidelines | Standardized variant interpretation framework | Pathogenicity assessment of germline findings [79] [32] |
The accurate discrimination between germline and somatic variants is fundamental to precise TMB calculation and meaningful interpretation in cancer research. While tumor-only sequencing offers practical advantages in cost and turnaround time, its limitations in germline variant filtering pose significant challenges for TMB reliability and comprehensive genomic assessment. Integrated tumor-normal paired sequencing represents the methodological gold standard, providing definitive somatic-germline discrimination while simultaneously identifying cancer predisposition variants with clinical utility.
Future methodological developments will likely focus on refined computational approaches that improve germline variant prediction in tumor-only data, potentially through machine learning algorithms trained on large paired sequencing datasets. Additionally, the growing recognition of germline-somatic interactions in shaping tumor evolution and therapeutic response underscores the importance of comprehensive germline assessment in oncology research beyond traditional risk prediction [82] [83]. As TMB continues to evolve as a biomarker for immunotherapy response, standardized approaches to germline filtering will be essential for generating comparable results across studies and institutions, ultimately advancing drug development and personalized cancer care.
Algorithm Development for Population-Specific TMB Calculation
Tumor Mutational Burden (TMB) is defined as the total number of somatic mutations per megabase (mut/Mb) of interrogated genomic sequence in a tumor genome [4]. It has emerged as a crucial predictive biomarker for assessing response to immune checkpoint inhibitors (ICIs) across various cancer types [54] [4]. The biological rationale stems from the principle that tumors with higher TMB generate more neoantigens, which can be recognized by the immune system, leading to enhanced anti-tumor immune responses when checkpoint inhibition is applied [10]. Based on the KEYNOTE-158 trial, the U.S. Food and Drug Administration (FDA) approved pembrolizumab for adult and pediatric patients with unresectable or metastatic TMB-high (TMB-H ≥ 10 muts/Mb) solid tumors, establishing TMB as a pan-cancer biomarker [54] [4].
While whole exome sequencing (WES) represents the gold standard for TMB assessment, its clinical implementation faces practical challenges including high cost, long turnaround time, and substantial tissue requirements [4] [5]. Targeted next-generation sequencing (NGS) panels have consequently emerged as a practical alternative for TMB estimation in clinical settings [54] [4]. However, the development of robust algorithms for TMB calculation, particularly those accounting for population-specific genetic variations, remains technically challenging due to factors such as panel size, genomic content, bioinformatic pipelines, and germline mutation filtering strategies [4] [5]. This technical guide outlines a comprehensive framework for developing population-specific TMB calculation algorithms within the context of NGS research.
Foundational Concepts in TMB Measurement
Key Definitions and Methodological Approaches
TMB quantification relies on accurate identification of somatic mutations from tumor tissue sequencing data. Two primary methodological approaches exist for this purpose:
- Tumor-Only (TO) Method: Analyzes patient tumor tissue alone and identifies somatic mutations by comparing tumor sequencing data with population frequency databases (e.g., dbSNP, ExAC, gnomAD) to filter out germline polymorphisms [54]. While less costly and requiring only tumor tissue, this method faces challenges in distinguishing rare germline variants from true somatic mutations.
- Tumor-Control (TC) Method: Simultaneously sequences patient tumor tissue and matched normal tissue (typically white blood cells or adjacent normal tissue) to directly identify somatic mutations by comparative analysis [54]. This approach provides more accurate somatic mutation calling but increases sequencing costs and sample requirements.
Critical Technical Considerations in TMB Algorithm Development
Multiple technical factors significantly influence TMB calculation accuracy and reproducibility:
- Panel Size and Genomic Content: The size of the targeted sequencing panel directly impacts TMB estimation precision. Studies indicate that the coefficient of variation (CV) of TMB decreases inversely with both the square root of panel size and TMB level [4]. Commercially available panels cover between 0.80 and 2.40 Mb, representing less than 5% of the total coding sequence [4].
- Variant Allele Frequency (VAF) Thresholds: Optimal VAF thresholds differ by sample type. Research suggests 5% VAF for frozen samples and 10% VAF for FFPE samples due to increased background noise in preserved specimens [5].
- Variant Classification and Filtering: Accurate TMB calculation requires careful inclusion of specific mutation types. Most algorithms incorporate non-synonymous mutations (single nucleotide variants, splice-site variants, and short insertions/deletions), while the inclusion of synonymous mutations varies by platform [4].
Table 1: Commercially Available NGS Panels for TMB Assessment
| Laboratory | Panel Name | Number of Genes | Total Region Covered (Mb) | TMB Region Covered* (Mb) | Type of Exonic Mutations Included |
|---|---|---|---|---|---|
| Foundation Medicine | FoundationOne CDx | 324 | 2.20 | 0.80 | Non-synonymous, synonymous |
| Illumina | TSO500 (TruSight Oncology 500) | 523 | 1.97 | 1.33 | Non-synonymous, synonymous |
| Memorial Sloan Kettering Cancer Center | MSK-IMPACT | 468 | 1.53 | 1.14 | Non-synonymous |
| Tempus | TEMPUS Xt | 595 | 2.40 | 2.40 | Non-synonymous |
Coding region used to estimate TMB regardless of the size of the region assessed by the panel. Adapted from Merino et al [4].
Core Components of TMB Calculation Algorithms
Bioinformatic Processing Pipeline
A robust bioinformatics pipeline for TMB calculation requires multiple processing steps to ensure accurate variant identification and classification:
Figure 1: Bioinformatic Workflow for TMB Calculation
Variant Filtering Strategies for Population-Specific Applications
Population-specific TMB algorithm development requires specialized filtering approaches to address genetic diversity across ethnic groups:
- Germline Mutation Filtering: In Tumor-Only protocols, population frequency databases are critical for filtering germline polymorphisms. Population-specific algorithm development must incorporate ethnically diverse reference databases to avoid misclassifying population-specific germline variants as somatic mutations [54]. Databases such as gnomAD, which include multi-ethnic population data, should be prioritized.
- Variant Type Selection: TMB algorithms typically focus on coding sequence variants with demonstrated immunogenic potential. The Institut Curie algorithm includes "high-quality, coding, non-synonymous, nonsense, driver variants, and small insertion/deletions (indels), absent from known polymorphisms/germline database" [5].
- Quality Control Parameters: Implementation of sample-specific quality thresholds is essential. Parameters include minimum sequencing depth (typically >100× for reliable mutation detection), minimum VAF thresholds (5-10% depending on sample type), and tumor purity requirements (>20% tumor cell content) [54] [5].
Table 2: Key Variant Filtering Criteria for TMB Calculation
| Filtering Category | Specific Criteria | Impact on TMB Calculation |
|---|---|---|
| Variant Type | Inclusion of non-synonymous SNVs, indels; optional inclusion of synonymous variants | Affects the absolute TMB value and correlation with neoantigen load |
| Population Frequency | Exclusion of variants with frequency >0.1% in population databases | Critical for minimizing false positives in tumor-only approaches |
| Quality Metrics | Minimum read depth (typically >100×), mapping quality, VAF thresholds | Ensures reliable variant detection and reduces technical noise |
| Functional Impact | Focus on coding sequences; exclusion of non-coding regions | Improves correlation with immunogenic neoantigen production |
TMB Calculation Formula and Normalization
The fundamental formula for TMB calculation is:
TMB (mut/Mb) = (Total Number of Eligible Somatic Mutations) / (Size of Coding Region Interrogated in Mb)
The Institut Curie algorithm exemplifies a rigorous approach: "TMB variants (including synonymous and non-synonymous non-hot spot somatic coding variants, i.e., single nucleotide variants or small insertions/deletions, with a ≥ 5% variant allele frequency) divided by the size of the coding region defined by the quality control criteria of the reagent" [54]. These calculations typically exclude mutations below established thresholds and mutations in mitochondria and non-eligible regions [54].
Experimental Design and Validation Framework
Sample Selection and Preparation Protocols
Robust TMB algorithm validation requires carefully characterized sample sets:
- Sample Type Considerations: Both Fresh Frozen and Formalin-Fixed Paraffin-Embedded (FFPE) samples can be utilized, with appropriate adjustments for each sample type. Studies indicate that FFPE samples require higher VAF thresholds (10% vs 5%) due to increased background noise [5].
- Tumor Content Requirements: Pathological review with H&E staining should confirm tumor cell content >20% to ensure reliable mutation detection [54].
- Nucleic Acid Quality Control: DNA extraction should yield sufficient quantity (>300ng for tumor tissue, >50ng for control samples) with quality parameters including A260/280 ratio ≥1.8 for purity assessment [54].
Reference Materials and Analytical Validation
Analytical validation requires well-characterized reference materials:
- Standard References: Commercially available standard references containing hotspot mutation sites of solid tumors should be used to evaluate detection accuracy and specificity [54].
- Performance Metrics: Validation should demonstrate high accuracy and specificity with coefficient of variation (CV%) between detected variant frequencies and true mutation frequencies <10% [54].
- Cross-Platform Comparison: Comparing TMB values with orthogonal methods, such as WES or established commercial tests (e.g., FoundationOneCDx), provides important validation [5].
Algorithm Validation and Statistical Assessment
Comprehensive validation requires multiple statistical approaches:
- Concordance Analysis: Statistical tests including Chi-square tests and Cohen's kappa analysis should demonstrate significant consistency between different TMB methods. One study reported high consistency (kappa = 0.833, p < 0.001) between Tumor-Only and Tumor-Control methods [54].
- Threshold Validation: For binary TMB classification (TMB-H vs TMB-L), receiver operating characteristic (ROC) analysis against clinical response data should validate chosen cutoffs, particularly around critical thresholds like 10 mut/Mb [54] [5].
- Precision Assessment: Inter- and intra-assay precision should be evaluated through replicate testing, with demonstration of low coefficient of variation across replicates.
Population-Specific Implementation Considerations
Database Development for Population-Specific Filtering
Developing population-appropriate TMB algorithms requires customized bioinformatic resources:
- Population-Specific Germline Databases: Create or integrate region-specific germline variant databases containing genetic information from the target population to improve germline mutation filtering accuracy.
- Ethnically-Balanced Reference Sets: Utilize reference materials that include genetic variants representative of the target population's ethnic composition to minimize reference bias.
- Local Pathogenic Variant Curations: Incorporate population-specific pathogenic variant annotations from local clinical genetics databases to improve variant classification accuracy.
Validation in Diverse Cohorts
Population-specific validation requires representative sample sets:
- Diverse Cancer Type Inclusion: Ensure validation across cancer types prevalent in the target population, as TMB distributions vary significantly across cancer types [4] [5].
- Demographically Representative Sampling: Include samples that reflect the ethnic, geographic, and demographic diversity of the target population to identify potential biases.
- Clinical Outcome Correlation: When possible, correlate TMB measurements with clinical outcomes from patients within the target population to validate predictive performance.
Figure 2: Population-Specific TMB Algorithm Development Workflow
Research Reagent Solutions for TMB Algorithm Development
Table 3: Essential Research Tools for TMB Algorithm Development
| Category | Specific Product/Technology | Application in TMB Research |
|---|---|---|
| Nucleic Acid Extraction | Kaijie FFPE magnetic bead extraction reagent [54] | Isolation of high-quality DNA from challenging FFPE samples |
| Targeted Sequencing Panels | Illumina TruSight Oncology 500 kit (523 genes) [54] | Comprehensive profiling of cancer-associated genes for TMB estimation |
| Hybrid Capture Reagents | Shihe No.1 Non-Small Cell Lung Cancer TMB Detection Kit [54] | Target enrichment for specific cancer types |
| Library Preparation | Fragmentation using Covaris M220 [54] | Generation of appropriately sized DNA fragments for library construction |
| Sequencing Platforms | Illumina NextSeq 550 system [54] | High-throughput sequencing with appropriate depth for variant detection |
| Quality Control Instruments | Agilent 2100 fragment analyzer [54] | Assessment of library quality and size distribution before sequencing |
The development of robust, population-specific TMB calculation algorithms requires meticulous attention to multiple technical parameters, including panel design, bioinformatic filtering strategies, variant classification, and validation frameworks. As research continues, several emerging areas warrant attention:
- Standardization Efforts: Harmonization of TMB measurement across test platforms remains crucial for clinical implementation [4].
- Liquid Biopsy Applications: Blood-based TMB (bTMB) assessment presents unique analytical validation challenges, including differentiation of tumor-specific alterations from clonal hematopoiesis [84].
- Artificial Intelligence Integration: AI approaches show promise in extracting imaging features that predict mutational status, potentially complementing molecular TMB assessment [85].
- Combination Biomarkers: Integrating TMB with other biomarkers, such as PD-L1 expression and MSI status, may improve predictive accuracy for immunotherapy response [10] [86].
By addressing these technical considerations and validation requirements, researchers can develop population-optimized TMB algorithms that enhance precision oncology initiatives across diverse patient populations.
Tumor Mutational Burden (TMB), defined as the total number of somatic mutations per megabase (mut/Mb) of DNA in a tumor genome, has emerged as a critical predictive biomarker for response to immune checkpoint inhibitors (ICIs) [3]. The biological rationale stems from the principle that a higher mutational load increases the likelihood of generating immunogenic neoantigens, which enables the immune system to recognize and attack tumor cells [3] [87]. Following the KEYNOTE-158 trial, the U.S. Food and Drug Administration (FDA) approved pembrolizumab for treating unresectable or metastatic TMB-high (TMB-H) solid tumors, defined by a threshold of ≥10 mut/Mb as determined by the FoundationOneCDx assay [20] [5]. This regulatory action established TMB as a pan-cancer biomarker of paramount importance for clinical decision-making.
However, the application of a universal TMB-H threshold across all populations and cancer types presents significant challenges. Growing evidence indicates that TMB distribution is influenced by a complex interplay of technical, biological, and population-specific factors [87] [88]. A one-size-fits-all threshold risks misclassifying patients who could benefit from immunotherapy, particularly in populations with generally lower TMB backgrounds, such as East Asians [88]. This whitepaper examines the sources of TMB threshold discordance, summarizes the evidence for population-specific optimization, and provides a technical framework for developing and validating robust, context-aware TMB cut-offs.
Factors Contributing to TMB Threshold Discordance
Technical and Methodological Variability
The accurate measurement of TMB is technically complex, and variations in laboratory methods and bioinformatics pipelines introduce substantial variability, complicating the comparison of results across different testing platforms.
- Sequencing and Analysis Methods: The choice between Tumor-Only (TO) and Tumor-Control (TC) sequencing methods significantly impacts TMB results. TO methods, which compare tumor tissue sequencing data against population databases, and TC methods, which use a patient-matched normal sample (e.g., white blood cells) to distinguish somatic from germline mutations, can identify different mutation sets, thereby affecting the final TMB calculation [24]. One study found a 92% consistency rate in TMB classification between TO and TC methods, but a significant statistical difference in the results, particularly near the 10 mut/Mb threshold [24].
- Bioinformatics Pipelines and Parameters: The specific bioinformatics algorithm used for TMB calculation is a major source of discrepancy. Factors such as the Variant Allele Frequency (VAF) cut-off profoundly influence the result. For example, one study established an optimal VAF cut-off of 10% for Formalin-Fixed Paraffin-Embedded (FFPE) samples and 5% for frozen samples to minimize false positives [5]. Furthermore, the inclusion or exclusion of specific mutation types (e.g., synonymous, nonsense, and hotspot mutations) in the TMB count alters the final value [50].
- Panel Design and Size: Targeted panel sequencing, the most common clinical method for TMB assessment, is highly sensitive to panel design. Research shows that panel sizes beyond 1.04 Mb and 389 genes are necessary for basic discrete accuracy [50]. Smaller panels lead to higher variance and less reliable TMB estimates [28].
Biological and Population-Specific Factors
- Ethnic and Racial Differences: Genomic studies have consistently revealed differences in TMB distributions across ethnicities. Data indicates that East Asian populations generally exhibit lower TMB across multiple cancer types compared to European and American populations [88]. Applying a uniform 10 mut/Mb threshold to these populations risks excluding a substantial subset of patients who may still derive clinical benefit from ICIs.
- Cancer Type and Mutational Signatures: The underlying biological processes driving mutagenesis vary by cancer type and influence TMB. For instance, in breast cancer, a dominant APOBEC mutational signature is frequently observed in TMB-high cases and is associated with a higher TMB compared to signatures like homologous recombination deficiency (HRD) [20]. This suggests that optimal thresholds may need to be calibrated for specific cancer types and etiologies.
Table 1: Key Factors Contributing to TMB Threshold Discordance
| Category | Factor | Impact on TMB Assessment |
|---|---|---|
| Technical | Sequencing Method (TO vs. TC) | Affects accuracy of somatic mutation calling; can lead to different TMB values near clinical thresholds [24]. |
| Technical | Bioinformatics Algorithm & VAF Cut-off | Influences sensitivity/specificity; optimal VAF differs by sample type (FFPE vs. frozen) [5]. |
| Technical | Panel Size & Design | Smaller panels (<~1 Mb) increase variance and reduce accuracy; gene content also affects performance [50] [28]. |
| Biological | Ethnic/Racial Background | Underlying germline genetics and mutagen exposures lead to different TMB distributions (e.g., lower in East Asians) [88]. |
| Biological | Cancer Type & Mutational Signature | TMB distribution and underlying biology (e.g., APOBEC, MSI, POLE) vary widely across cancer types [20]. |
Evidence for Population-Specific TMB Cut-offs
The Case for East Asian Populations
Compelling evidence calls for re-evaluating the 10 mut/Mb cut-off in East Asian populations. A pivotal study systematically analyzed East Asian lung cancer patients treated with ICIs to determine an optimal threshold [88]. Using a training cohort of 66 patients and a validation cohort of 69 patients, researchers performed receiver operating characteristic (ROC) curve and log-rank analysis to correlate TMB with durable clinical benefit (DCB) and survival.
The results demonstrated that a cut-off of 7 mut/Mb, rather than 10 mut/Mb, was optimal for this population. Patients with a TMB ≥7 mut/Mb had significantly better outcomes following ICI treatment than those with a TMB below this threshold [88]. This finding underscores that the FDA-approved threshold, while validated in predominantly Western cohorts, is not universally applicable and that population-specific optimization is both feasible and necessary to guide clinical practice and ensure equitable access to effective therapies.
Statistical Optimization for Threshold Determination
The process of defining a TMB threshold is further complicated by measurement errors in both TMB assessment and clinical endpoint evaluation. To address this, advanced statistical models like TMBocelot have been developed [89]. TMBocelot is a Bayesian framework that accounts for pairwise measurement errors in TMB values and clinical outcomes (e.g., tumor response and survival time). By modeling these errors and utilizing Markov Chain Monte Carlo (MCMC) sampling, it stabilizes the determination of hierarchical thresholds, leading to more accurate and reliable TMB-positive cut-offs tailored to specific datasets and patient populations [89].
Technical Framework for TMB Assessment and Optimization
Standardized TMB Wet-Lab Protocol
A robust TMB workflow begins with stringent pre-analytical and analytical steps.
- Sample Collection and QC: Use pathologically confirmed FFPE tumor samples or frozen tissue. The tumor cell content should be >20% for FFPE samples, and the extracted DNA should have a total amount >300 ng with high purity (A260/280 ≥ 1.8) [24] [28].
- Library Construction and Sequencing:
- DNA Shearing: Fragment DNA to 90-250 bp using a focused-ultrasonicator (e.g., Covaris M220).
- Library Prep: Perform end repair, A-tailing, and ligation of indexed adapters.
- Hybridization Capture: Use a panel that covers >1.04 Mb of the exonic genome [50]. Two rounds of hybridization capture can enhance specificity.
- Sequencing: Sequence on an NGS platform (e.g., Illumina NextSeq 550) to a high, uniform depth of >500x to ensure accurate variant calling [28].
Bioinformatics Analysis for TMB Calculation
The bioinformatics pipeline must be meticulously designed to ensure accurate somatic mutation calling and TMB calculation.
- Sequence Data Processing:
- Raw Data QC: Filter reads with >10% N rate or >10% bases with quality score <20.
- Alignment: Map cleaned reads to the reference genome (e.g., hg19/GRCh37) using an aligner like BWA.
- Variant Calling and Filtration:
- Somatic Calling: Use tools like VarScan or MuTect to call somatic single nucleotide variants (SNVs) and small insertions/deletions (indels) [88]. For TO assays, optimized algorithms like the Somatic-Germline-Zygosity (SGZ) algorithm, calibrated for the target population (e.g., East Asian), are essential [88].
- Variant Filtration: Apply a VAF cut-off of 5-10%, with the specific value optimized for sample type (5% for frozen, 10% for FFPE) [5]. Filter against population frequency databases (e.g., gnomAD, dbSNP) to remove potential germline polymorphisms.
- TMB Calculation:
Diagram 1: Bioinformatics Workflow for TMB Calculation. This diagram outlines the key computational steps for processing NGS data to derive a TMB score, from raw data to final value.
Experimental Protocol for Validating Population-Specific Cut-offs
To establish a validated TMB cut-off for a specific population (e.g., East Asian lung cancer), the following study design is recommended, based on published methodologies [88].
- Patient Cohorts:
- Training Cohort: Retrospectively collect tumor samples from a minimum of 60 patients from the target population who were treated with ICIs. Clinical outcomes, including objective response and survival, must be well-annotated.
- Validation Cohort: An independent cohort of a similar size and matching clinical characteristics.
- Sequencing and TMB Calculation: Perform NGS on all samples using a validated targeted panel. Calculate TMB for each patient using the standardized bioinformatics pipeline outlined above.
- Statistical Analysis:
- Correlation with Clinical Benefit: Define a clinical endpoint such as Durable Clinical Benefit (DCB: complete/partial response or stable disease ≥24 weeks) vs. Non-Durable Benefit (NDB).
- ROC Analysis: In the training cohort, perform ROC analysis to assess the predictive power of TMB for DCB and identify the cut-off value that maximizes the sum of sensitivity and specificity.
- Survival Analysis: Conduct log-rank analysis to compare progression-free or overall survival between patients above and below the candidate cut-offs.
- Validation: Apply the final chosen cut-off to the independent validation cohort to confirm its predictive value for clinical outcomes.
Diagram 2: Threshold Validation Workflow. This diagram illustrates the key steps for empirically deriving and validating a TMB cut-off specific to a patient population.
Table 2: Key Research Reagents and Solutions for TMB Analysis
| Item | Function/Description | Example/Specification |
|---|---|---|
| FFPE DNA Extraction Kit | Isolation of high-quality DNA from archived clinical tumor samples. | Qiagen GeneRead DNA FFPE kit [88]. |
| Blood DNA Extraction Kit | Isolation of germline DNA from patient-matched blood for TC sequencing. | Qiagen DNA Blood Mini Kit [88]. |
| DNA Quantitation Assay | Accurate quantification of DNA concentration and quality prior to library prep. | Qubit dsDNA HS Assay Kit [24]. |
| Hybridization Capture Panel | Enrichment of target genomic regions prior to sequencing. | Custom panels covering >1.04 Mb (e.g., OncoScreen Plus, Onco1021plus) [88] [50]. |
| NGS Platform | High-throughput sequencing of prepared libraries. | Illumina NextSeq 550 or MGISEQ-T7 [88]. |
| Reference Standards | Cell line-derived genomic DNA with known mutations for assay validation and QC. | CRISPR-edited 293T subclones [50]. |
The pursuit of precision immuno-oncology demands a nuanced approach to biomarker application. The establishment of TMB as a predictive biomarker for immunotherapy response represents a significant advance, but the initial universal threshold of 10 mut/Mb is an oversimplification. As detailed in this whitepaper, evidence from technical performance studies and clinical cohorts strongly supports the need for optimized, context-aware TMB cut-offs. Key to this effort is the recognition of population-specific TMB distributions, as exemplified by the 7 mut/Mb threshold validated in East Asian lung cancer patients [88].
Moving forward, the field must adopt standardized, transparent methodologies for TMB measurement and threshold determination. This involves using adequately sized NGS panels, robust bioinformatics pipelines with appropriate filters, and statistical models that account for real-world measurement errors [89] [50]. The integration of TMB with other biomarkers, such as PD-L1 expression, microsatellite instability, and mutational signatures, will further refine patient stratification [3] [20] [5]. By embracing this comprehensive and tailored framework, researchers and drug developers can optimize TMB's predictive power, ensure equitable patient benefit across diverse populations, and fully realize the promise of precision cancer immunotherapy.
Analytical Validation, Harmonization, and Comparative Performance
Frameworks for Analytical Validation of Complex TMB Assays
Tumor Mutational Burden (TMB) has emerged as a pivotal biomarker in immuno-oncology, quantifying the total number of somatic mutations per megabase of tumor DNA. It serves as a proxy for neoantigen load and a predictor of response to immune checkpoint inhibitors (ICI) across multiple cancer types [27] [32]. The clinical adoption of TMB, however, is complicated by its inherent nature as a complex, derived biomarker rather than a single, directly measured analyte. This complexity introduces significant challenges in analytical validation, as TMB measurement is influenced by pre-analytical variables, bioinformatics pipelines, panel design, and the nearly infinite combinatorial possibility of single-nucleotide variants (SNVs) and insertions/deletions (indels) that constitute a specific TMB score [25]. Consequently, robust analytical validation frameworks are essential to ensure that technical and biological limitations do not confound clinical interpretation and that results are reliable, reproducible, and comparable across different testing platforms [25] [90]. This guide synthesizes current consensus recommendations and methodologies for the analytical validation of TMB assays, providing a structured approach for researchers and developers in the field of next-generation sequencing (NGS) based cancer genomics.
Foundational Validation Frameworks and Consensus Recommendations
Core Principles from Professional Organizations
The validation of NGS-based oncology tests, including TMB assays, is guided by best practice recommendations established by professional organizations. The Association for Molecular Pathology (AMP) and the College of American Pathologists (CAP) have provided foundational guidelines emphasizing an "error-based approach" that identifies potential sources of errors throughout the analytical process and addresses them through test design, method validation, or quality controls [55]. These guidelines cover critical aspects such as panel content selection, utilization of reference materials, determination of positive percentage agreement and positive predictive value for each variant type, and requirements for minimal depth of coverage [55]. More recently, recognizing the specific challenges of TMB measurement, a joint consensus from AMP, CAP, and the Society for Immunotherapy of Cancer (SITC) has provided targeted recommendations for TMB assay validation and reporting, encompassing pre-analytical, analytical, and post-analytical factors to ensure comparability between assays [90].
Specialized Framework for Blood-Based TMB (bTMB)
The BLOODPAC consortium has further advanced the field by developing a specialized conceptual framework for the analytical validation of blood-derived TMB (bTMB) assays. This perspective addresses the unique technical and biological challenges associated with measuring TMB from circulating tumor DNA (ctDNA), where the low fractional abundance of tumor-derived DNA in a background of normal cell-free DNA necessitates exceptional assay sensitivity and specificity [25] [91] [92]. The BLOODPAC working group emphasizes that while bTMB is a promising biomarker for predicting immunotherapy response in patients with advanced solid tumors, its complexity demands careful validation to avoid confounding clinical results [91]. Key considerations include managing pre-analytical variables and incorporating methods to differentiate tumor-specific alterations from those associated with germline polymorphisms or clonal hematopoiesis [25] [93].
Table 1: Key Analytical Validation Guidelines and Their Scope
| Organization / Consortium | Primary Focus | Key Contributions |
|---|---|---|
| Association for Molecular Pathology (AMP) / College of American Pathologists (CAP) [55] | NGS-based somatic variant detection | Foundational guidelines for NGS test validation; error-based approach; requirements for accuracy, precision, and coverage. |
| AMP, CAP, & Society for Immunotherapy of Cancer (SITC) [90] | TMB-specific assay validation | Joint consensus on TMB pre-analytical, analytical, and post-analytical factors; emphasizes reporting transparency. |
| BLOODPAC [25] [91] | Blood-derived TMB (bTMB) | Conceptual framework for complex ctDNA biomarker validation; addresses low ctDNA fraction and clonal hematopoiesis. |
Methodological Considerations for TMB Assay Validation
Experimental Design for Key Analytical Performance Metrics
The analytical validation of a TMB assay requires a study design that adequately characterizes its performance across critical metrics. The BLOODPAC group has adapted traditional clinical laboratory validation protocols to address the specific challenges of a complex biomarker like TMB and the limited availability of clinical plasma samples [25].
- Analytical Accuracy: Due to the combinatorial nature of TMB, a test's accuracy should be established by evaluating the performance of its constituent variant classes (SNVs and indels). The study design must account for limited sample availability, often requiring the use of surrogate samples. However, it is crucial to recognize the limitations of these surrogates, as they may not fully replicate the variant clonality and fragmentation profiles of real clinical samples [25].
- Precision, Reproducibility, and Repeatability: Evaluation of precision is modified to account for the lack of suitable contrived sample models and the scarcity of clinical samples with a stable TMB value. The nearly infinite mutation combinations leading to a given TMB score can cause sample-specific variability in performance estimates [25].
- Limit of Detection (LOD): A singular LOD for the TMB test cannot be determined because the LOD for individual variants contributing to the score varies based on genomic context, allele frequency, and variant type. Instead, the LOD should be characterized for the individual SNVs and indels that are inputs to the TMB algorithm [25].
- Limit of Blank (LOB): This can be assessed using plasma from cancer-free donors that are representative of the intended use population. This helps establish the background signal and define the threshold for distinguishing true TMB signal from noise [25].
Table 2: Summary of Analytical Validation Protocols for TMB Assays
| Performance Metric | Traditional Approach | TMB-Specific Considerations |
|---|---|---|
| Accuracy | Comparison to a reference method or known truth set. | Accuracy is inferred from the performance of SNV and indel detection. Limited clinical sample availability necessitates surrogate samples. |
| Precision | Repeated testing of the same sample over time, across operators, etc. | Study design is modified due to lack of stable contrived samples and limited clinical sample availability. |
| Limit of Detection (LOD) | The lowest concentration that can be reliably detected. | A single test-specific LOD is not feasible. LOD is characterized for the underlying SNVs and indels. |
| Limit of Blank (LOB) | Testing of samples without the analyte (e.g., cancer-free donors). | Can be applied as for other ctDNA assays using representative cancer-free donor plasma. |
Integrated DNA and RNA Sequencing Approaches
Emerging evidence supports the clinical value of integrating whole exome sequencing (WES) with RNA sequencing (RNA-seq). One recent study demonstrated a comprehensive validation approach for a combined assay in a large tumor cohort [94]. Their three-step process provides a model for robust validation of more complex genomic assays:
- Analytical Validation: Using custom reference samples containing thousands of SNVs and copy number variations (CNVs) across multiple sequencing runs at varying tumor purities.
- Orthogonal Testing: Validation of results in patient samples using alternative methods or platforms.
- Clinical Utility Assessment: Evaluation of the assay's performance and impact in real-world clinical cases [94].
This integrated approach not only improves the detection of actionable alterations, such as gene fusions but also allows for direct correlation of somatic alterations with gene expression, providing a more comprehensive genomic profile [94].
Diagram 1: TMB Assay Workflow. This diagram outlines the key steps in a TMB testing workflow, from sample preparation to final validation.
The Scientist's Toolkit: Essential Reagents and Materials
The successful development and validation of a TMB assay rely on a suite of critical research reagents and materials. The table below details key components and their functions in the validation process.
Table 3: Research Reagent Solutions for TMB Assay Validation
| Reagent / Material | Function in Validation | Key Considerations |
|---|---|---|
| Reference Cell Lines & contrived samples [25] [55] | Assess assay accuracy, precision, and LOD for SNVs/indels. | Used to spike-in known mutations at varying allele frequencies. May have limitations in representing clinical sample fragmentation and clonality. |
| Formalin-Fixed, Paraffin-Embedded (FFPE) Tumor Samples [94] [32] | Mirror real-world clinical specimens for validation studies. | Tumor cell content must be assessed by a pathologist; DNA may be fragmented, impacting quality. |
| Cancer-Free Donor Plasma [25] | Determine the Limit of Blank (LOB) and specificity. | Establishes background mutation rate; donors should represent the intended use population. |
| Targeted NGS Panels / Whole Exome Kits [94] [27] [32] | Interrogate genomic regions for mutation detection. | Panel size and gene content significantly impact TMB calculation; WES is the gold standard but targeted panels are more clinically practical. |
| Bioinformatic Pipelines [25] [94] | Align sequences, call variants, filter artifacts, and calculate TMB. | Critical for distinguishing somatic mutations from germline variants and clonal hematopoiesis; requires their own validation. |
Navigating Technical and Biological Complexities
Distinguishing Tumor-Specific Mutations
A paramount challenge in TMB calculation, especially for bTMB, is the accurate discrimination of true somatic tumor mutations from background biological noise. Two major sources of confounding alterations are:
- Germline Polymorphisms: These are inherited variants present in all cells of an individual. Their misinterpretation as somatic events would artificially inflate TMB. This is typically addressed by sequencing a matched normal sample (e.g., from peripheral blood) and subtracting germline variants from the tumor profile [25] [55].
- Clonal Hematopoiesis (CH): Mutations that arise in blood-forming stem cells can be shed into the plasma and are not of tumor origin. Failing to identify and remove CH-associated mutations is a significant source of inaccuracy in bTMB assays. Bioinformatic filters and databases of common CH genes are used to mitigate this effect [25] [93].
Impact of Panel Design and Bioinformatics
The design of the targeted sequencing panel and the bioinformatics pipeline are not mere technical details but are fundamental determinants of the TMB result.
- Panel Size and Content: Larger panels that cover more genomic territory generally provide more stable and accurate TMB estimates [27]. The specific genes selected can also influence the result, particularly if they are enriched for mutations in certain cancer types.
- Bioinformatic Algorithms: The stringency of variant-calling filters, the handling of low-frequency alleles, and the methods for excluding sequencing artifacts and false positives directly impact the final TMB score. The algorithms used to calculate TMB from the list of filtered mutations are also a source of inter-assay variability [25] [94].
Diagram 2: TMB Calculation Refinement. This diagram illustrates the essential bioinformatic filtering steps required to derive an accurate TMB score from raw variant calls.
The analytical validation of complex TMB assays requires a thoughtful and multifaceted approach that moves beyond traditional single-analyte validation frameworks. As summarized in this guide, success depends on adhering to consensus recommendations from professional organizations, designing rigorous experiments that account for the combinatorial nature of TMB, and proactively addressing technical and biological confounders such as panel design, bioinformatics, and clonal hematopoiesis. The ongoing work of consortia like BLOODPAC to refine these frameworks and promote data sharing is critical for achieving harmonization across the field. For researchers and drug developers, a robust and transparent analytical validation is the indispensable foundation upon which reliable clinical utility and patient stratification for immunotherapy can be built.
Tumor Mutational Burden (TMB) has emerged as a critical predictive biomarker for response to immune checkpoint inhibitors in cancer immunotherapy. While whole exome sequencing (WES) is considered the gold standard for TMB quantification, targeted gene panels are widely adopted in clinical settings due to their cost-effectiveness and faster turnaround times. This whitepaper provides a technical guide to assessing the concordance between panel-based TMB estimates and WES-derived values. We synthesize current evidence on key methodological variables affecting concordance, including panel size, bioinformatics pipelines, and mutation filtering criteria. Furthermore, we present standardized experimental protocols for validation studies and visualize critical workflows. For researchers and drug development professionals, this review offers a comprehensive framework for evaluating and improving the accuracy of panel-based TMB measurement, thereby supporting robust biomarker development in precision oncology.
Tumor Mutational Burden (TMB) is defined as the total number of somatic mutations per megabase (mut/Mb) of the genome sequenced and reflects the level of genomic instability within a tumor [33] [31]. Tumors with high TMB (TMB-H) are more likely to express neoantigens, which can be recognized by the immune system, leading to improved responses to immune checkpoint inhibitors (ICIs) across various cancer types, including non-small cell lung cancer (NSCLC) and melanoma [95] [33]. The clinical utility of TMB was solidified by the KEYNOTE-158 trial, leading to the FDA approval of pembrolizumab for any solid tumor with TMB-H (≥10 mut/Mb) [54].
The gold standard for TMB measurement is whole exome sequencing (WES), which comprehensively sequences all protein-coding regions (~30-50 Mb) [95] [31]. However, WES is expensive, requires large amounts of DNA, and involves complex data analysis, making it unsuitable for routine clinical practice [95] [96]. Consequently, targeted gene panels have become the predominant method for TMB estimation in clinical and research settings [96]. These panels focus on a subset of genes (e.g., 300-500 genes) covering a smaller genomic region (e.g., 0.3-1.5 Mb), offering a more cost-effective and rapid alternative [54] [95].
The central challenge lies in the concordance between panel-based TMB (psTMB) and WES-based TMB (wesTMB). The accuracy of extrapolating the mutational burden from a small genomic subset to the entire exome is influenced by multiple technical factors. Understanding and quantifying this concordance is paramount for ensuring that panel-based results are reliable and clinically actionable [95] [96]. This guide details the critical factors affecting concordance, provides experimental protocols for its assessment, and visualizes the key processes involved.
Quantitative Comparison of TMB Methodologies
The following tables summarize the key performance metrics and technical specifications that influence concordance between panel-based TMB and WES.
Table 1: Performance Metrics of Panel-based TMB vs. Whole Exome Sequencing
| Metric | WES (Gold Standard) | Targeted Gene Panels | Impact on Concordance |
|---|---|---|---|
| Genomic Space | 30-50 Mb [31] | 0.3 - 2.0 Mb (typically 1.0+ Mb recommended) [96] | Larger panel size (>1.0 Mb) improves correlation and reduces sampling error [95] [96]. |
| Correlation with WES | N/A | R² > 0.9 reported for large, well-designed panels (e.g., F1CDx, TSO 500) [95] | High correlation is necessary but insufficient; Bland-Altman analysis is needed to assess bias [96]. |
| Overall Percent Agreement (OPA) | N/A | 73.3% - 96.7% (varies by panel design and calculation method) [97] | OPA with WES-TMB status improves when non-coding regions are leveraged to supplement panel size [97]. |
| TMB-H Threshold | Variable (e.g., ≥10 mut/Mb) [98] | Calibrated to WES (e.g., ≥10 mut/Mb) | Consistency in threshold application is critical; discordance is highest near the cut-off [54] [96]. |
| Cost & Turnaround Time | High cost and longer time [95] | Lower cost and shorter turnaround [95] | Makes panels clinically practical but requires rigorous validation against WES. |
Table 2: Technical Specifications Influencing TMB Concordance
| Specification | WES | Targeted Panels | Recommendation for Concordance |
|---|---|---|---|
| DNA Input | 150-200 ng [31] | 40-80 ng (for assays like TSO 500) [99] [100] | Adhere to panel-specific input requirements; low input can affect sensitivity. |
| VAF Cut-off | Not standardized; often low (e.g., 2-5%) | Typically 5% for TMB calculation [96] [98] | A 5% VAF is suitable for samples with ≥20% tumor purity [96]. |
| Mutation Types Included | All somatic coding, nonsynonymous, and synonymous. | Varies by lab; often excludes synonymous [96] | Inclusion of synonymous mutations improves accuracy and is a key feature of reliable assays [96]. |
| Bioinformatics Pipeline | Complex, custom pipelines (e.g., GATK) [97] | Vendor-specific or lab-developed (e.g., MSIsensor, VarSome) [40] [98] | Pipeline choice significantly impacts somatic mutation detection and germline filtering [54] [96]. |
| Matched Normal | Highly recommended for germline subtraction [31] | Used in Tumor-Control (TC); not in Tumor-Only (TO) [54] | Tumor-Control (TC) method is more accurate than Tumor-Only (TO) for somatic mutation identification [54]. |
Critical Factors Determining Concordance Between Methods
Panel Size and Design
Panel size is one of the most critical determinants of concordance. In silico studies demonstrate that the accuracy of psTMB drops significantly when the panel covers less than 0.5 Mb of coding regions [95] [96]. A multicenter study established that a panel size beyond 1.04 Mb and 389 genes is necessary for basic discrete accuracy [96]. This is due to statistical sampling effects; smaller panels are less precise, especially for tumors with low to moderate TMB, and can lead to overestimation [95] [96]. Furthermore, innovative panel designs that leverage non-coding regions (e.g., introns) to supplement the effective genomic size have shown improved concordance. One study reported that adding non-coding regions increased the Overall Percent Agreement (OPA) with WES from 73.3% to 96.7% [97].
Wet-Lab and Bioinformatics Protocols
The entire workflow, from sample processing to data analysis, introduces variability.
- Sample Type and Quality: DNA derived from Formalin-Fixed Paraffin-Embedded (FFPE) tissues, the most common clinical sample, is often degraded, which can impact library complexity and variant calling. Fresh-Frozen (FF) tissues provide higher-quality nucleic acids and demonstrate better performance for detecting biomarkers like TMB and MSI [99] [100].
- Somatic Mutation Detection: The method used to distinguish somatic from germline mutations is crucial. The Tumor-Control (TC) method, which sequences a matched normal sample (e.g., blood), allows for direct identification of somatic mutations. In contrast, the Tumor-Only (TO) method relies on population frequency databases (e.g., gnomAD) to filter germline variants, which can lead to misclassification and affect TMB calculation. Studies show a significant difference in TMB results between TO and TC methods, although their consistency can be good (kappa = 0.833) [54].
- Variant Filtering and TMB Calculation Rules: The bioinformatics pipeline for variant calling, filtering, and TMB calculation must be standardized. Key decisions include:
- Inclusion of Synonymous Mutations: While some panels count only non-synonymous mutations, evidence indicates that including synonymous mutations enhances the accuracy of psTMB estimation [96].
- Variant Allele Frequency (VAF) Cut-off: A consistent VAF cut-off (e.g., 5%) is recommended for samples with tumor purity ≥20% to avoid noise from sequencing errors or subclonal mutations [96] [98].
- Calibration: psTMB values often require calibration against WES-derived TMB from reference datasets (e.g., TCGA) to ensure the slope of the linear model is close to 1 and to correct for over- or underestimation tendencies [96] [98].
Experimental Protocols for Concordance Assessment
For researchers seeking to validate a panel-based TMB assay against WES, the following detailed protocol provides a robust methodological framework.
Sample Selection and Preparation
- Cohort Definition: Select a minimum of 30 paired tumor-normal samples, ideally representing multiple cancer types with a wide range of expected TMB values (e.g., lung cancer, melanoma, colorectal cancer, and cancers with low TMB). This ensures validation across the clinical dynamic range [97] [33].
- Sample Type: Use paired FFPE and Fresh-Frozen (FF) tissue samples from the same tumor resection when possible. This allows for direct comparison of sample type impact on concordance [99] [100].
Tumor Purity Assessment: Ensure all samples have a tumor cell content of >20%,
as determined by a pathologist's review of haematoxylin and eosin-stained sections. This is a standard requirement for reliable TMB assessment [99] [54].
- Nucleic Acid Extraction:
- For FFPE samples, use dedicated kits (e.g., AllPrep DNA/RNA FFPE Kit) with a gentle deparaffinization step. Quantify DNA using a fluorometer (e.g., Qubit) and assess quality with an FFPE-specific QC assay (e.g., Illumina FFPE QC kit, requiring ∆Cq ≤5) [99] [100].
- For FF samples, use simultaneous DNA/RNA extraction kits (e.g., AllPrep DNA/RNA Micro Kit). Assess DNA quality via bioanalyzer (e.g., Agilent 2100), looking for an average fragment size ≥4,500 bp [99] [100].
- For the matched normal control, extract genomic DNA from peripheral blood or adjacent normal tissue.
Library Preparation and Sequencing
- Parallel Processing: Subject all samples to both WES and the targeted panel sequencing in parallel to minimize batch effects.
- WES Library Preparation:
- Fragment 150-200 ng of genomic DNA using a sonicator (e.g., Covaris).
- Prepare libraries using a kit such as the SureSelect XT HS reagent and hybridize with a whole exome capture library (e.g., SureSelect XT Human All Exon V6).
- Sequence on a platform like Illumina NovaSeq 6000 to a median coverage of >150x for tumor and >100x for normal samples [97].
- Targeted Panel Library Preparation:
- Use the commercial or lab-developed panel of choice (e.g., Illumina TSO 500, FoundationOne CDx, MSK-IMPACT).
- Follow manufacturer instructions precisely. For example, the TSO 500 assay uses 80 ng DNA for library prep, followed by hybridization capture, and sequencing on platforms like Illumina NextSeq 550 [99] [54].
- Sequencing Depth: Ensure a high and uniform sequencing depth for the panel (e.g., >500x) to enable sensitive variant detection.
Bioinformatics Analysis
- Primary Analysis: Process raw sequencing data (FASTQ files) through standard steps: adapter trimming, alignment to a reference genome (e.g., GRCh38), and duplicate marking using tools like BWA and GATK.
- Somatic Variant Calling:
- For WES data, analyze tumor-normal pairs using a validated pipeline like the "GATK best practices" for somatic variant calling [97].
- For targeted panel data, use the vendor-recommended bioinformatics pipeline (e.g., PierianDx CGW for TSO 500, VarSome Clinical) for both TO and TC analyses if possible [99] [98].
- TMB Calculation:
- WES-TMB: Calculate as the total number of somatic (non-synonymous and synonymous) coding mutations, divided by the size of the covered exonic space in megabases (e.g., ~38 Mb). Follow the "Parameters for the Uniform TMB Calculation Method" from the TMB Harmonization Project where applicable [97] [98].
- Panel-TMB (psTMB): Calculate as the number of qualifying somatic mutations (following the panel's specific rules for mutation types and VAF filter, e.g., ≥5%) divided by the panel's exonic footprint in Mb [96] [98].
- Calibration (Optional): For the panel-based TMB, apply a calibration model (e.g., simple linear regression) derived from a reference dataset to convert psTMB to an estimated WES-TMB value [96] [98].
Concordance and Statistical Analysis
- Correlation Analysis: Perform Pearson or Spearman correlation analysis between WES-TMB and psTMB (both raw and calibrated) across all samples.
- Categorical Agreement: Classify samples as TMB-High (e.g., ≥10 mut/Mb) or TMB-Low based on both WES and panel TMB. Calculate the Overall Percent Agreement (OPA), Positive Percent Agreement (PPA), and Negative Percent Agreement (NPA) [97].
- Statistical Tests: Use Cohen’s kappa statistic to evaluate the agreement in TMB status categorization beyond chance [54]. A kappa value > 0.8 indicates excellent agreement.
- Bland-Altman Plot: Generate a Bland-Altman plot to visualize the mean difference between the two methods (bias) and the limits of agreement, identifying any TMB-dependent bias [96].
Visualizing Key Workflows and Relationships
The following diagrams illustrate the core experimental workflows and logical relationships involved in TMB concordance assessment.
Sample Processing and Nucleic Acid Extraction Workflow
Wet-Lab and Bioinformatics Analysis Pipeline
Factors Influencing Panel-Based TMB Concordance
The Scientist's Toolkit: Essential Research Reagents and Platforms
Table 3: Key Research Reagent Solutions for TMB Concordance Studies
| Item | Function | Example Products & Kits |
|---|---|---|
| Nucleic Acid Extraction Kits | Isolate high-quality DNA and RNA from challenging clinical samples. | - AllPrep DNA/RNA FFPE Kit (Qiagen): For simultaneous DNA/RNA extraction from FFPE tissue.- AllPrep DNA/RNA Micro Kit (Qiagen): For co-extraction from small FF tissue samples.- QIAamp DNA FFPE Tissue Kit (Qiagen) [99] [97] [100]. |
| Nucleic Acid QC Instruments | Accurately quantify and qualify DNA/RNA to ensure input material meets NGS standards. | - Qubit Fluorometer (Thermo Fisher): For precise dsDNA/RNA concentration.- Agilent 2100 Bioanalyzer/TapeStation: For assessing DNA integrity (DIN) and RNA quality (DV200) [99] [97] [100]. |
| Targeted NGS Panels | Comprehensive genomic profiling to detect variants and calculate TMB from a targeted gene set. | - Illumina TruSight Oncology 500 (TSO 500): Analyzes 523 genes for SNVs, indels, fusions, TMB, MSI.- FoundationOne CDx: FDA-approved panel for TMB and other biomarkers.- MSK-IMPACT: A large panel used in clinical research [99] [54] [95]. |
| Library Prep & Sequencing | Prepare sequencing libraries from extracted DNA and perform high-throughput sequencing. | - Covaris Sonicator: For DNA shearing.- Illumina NextSeq 550/550Dx, NovaSeq 6000: Sequencing platforms [99] [54] [97]. |
| Bioinformatics Platforms | Analyze NGS data, call somatic variants, and calculate TMB following standardized methods. | - PierianDx Clinical Genomics Workspace: For annotating variants from TSO 500.- VarSome Clinical: Supports TMB estimation for WES and targeted panels, following the Uniform TMB Calculation Method.- MSIsensor: A tool for MSI detection from NGS data [99] [40] [98]. |
| Reference Materials | Act as a gold standard for validating and benchmarking TMB assay performance. | - Seraseq gDNA TMB Mix (Seracare): Commercially available reference materials with predefined TMB scores [97]. |
Achieving high concordance between panel-based TMB and WES is technically demanding but essential for translating this biomarker into reliable clinical and research applications. The key to success lies in the rigorous optimization and standardization of the entire process. Researchers must prioritize the use of large panels (>1.04 Mb), employ Tumor-Control (TC) methods for accurate somatic calling, adopt standardized bioinformatics pipelines that include synonymous mutations, and calibrate results against WES where necessary. Furthermore, understanding the limitations imposed by sample quality, particularly from FFPE tissue, is critical. As the field moves forward, ongoing harmonization efforts and the development of best practice guidelines will be crucial to ensure that panel-based TMB remains a robust and predictive biomarker, ultimately enabling more effective and personalized cancer immunotherapy.
The accurate estimation of tumor mutational burden (TMB) using targeted next-generation sequencing (NGS) panels is critical for predicting response to immune checkpoint inhibitors in oncology. While the coefficient of determination (R-squared) has been the mainstream statistical metric for evaluating the correlation between panel-based TMB and whole-exome sequencing (WES) gold standard, significant limitations in its application to long-tailed TMB distributions have emerged. This technical review examines angular distance as a more robust alternative for assessing TMB estimation performance, alongside other emerging metrics. We provide comprehensive experimental protocols, comparative data analyses, and visualization tools to guide researchers and drug development professionals in implementing these advanced statistical approaches for NGS panel validation and optimization.
Tumor mutational burden has emerged as a crucial genomic biomarker predicting response to immune checkpoint inhibitor therapy across multiple cancer types [101] [4]. Defined as the total number of somatic mutations per megabase of interrogated genomic sequence, TMB quantifies mutational load that may generate immunogenic neoantigens recognizable by the immune system upon checkpoint blockade [4]. The clinical significance of TMB was solidified when the KEYNOTE-158 trial demonstrated that TMB-high status (≥10 mut/Mb) was associated with significantly improved response to pembrolizumab, leading to FDA approval for this tissue-agnostic indication [4].
While whole-exome sequencing represents the gold standard for TMB assessment, its clinical implementation is hampered by high costs, extended turnaround times, and substantial tissue requirements [4] [24]. Consequently, targeted NGS panels have been developed as practical alternatives for TMB estimation in clinical settings [102] [7]. The growing proliferation of these panels necessitates robust statistical methods to evaluate and compare their performance against WES-derived TMB values [102]. Traditional evaluation relying primarily on R-squared values has proven inadequate due to the characteristic long-tailed distribution of TMB values across cancer populations [102]. This review examines the limitations of R-squared in this context and explores angular distance as a more veritable, objective, and logical measurement for evaluating TMB estimation accuracy in gene-targeted panels.
The R-squared Problem in TMB Distribution Context
Mathematical Limitations of R-squared
The coefficient of determination (R-squared) represents the proportion of variance in the dependent variable (WES-based TMB) that is predictable from the independent variable (panel-based TMB) in a linear regression model. The mathematical formulation follows:
y = ax + b [102]
Where y represents WES-based TMB, x represents panel-based TMB, a is the slope, and b is the Y-intercept. The R-squared value is calculated as:
R² = 1 - (∑(yᵢ - axᵢ - b)² / ∑(yᵢ - ȳ)²) [102]
This mathematical formulation reveals two critical limitations when applied to TMB distribution:
- Denominator Dominance: The denominator represents the total sum of squares, heavily influenced by TMB distribution across the entire dataset. In real-world cancer populations, TMB distribution follows a pronounced long-tailed pattern where most patients exhibit low to moderate TMB values, while a small subset displays hypermutated phenotypes [102].
- Squared Residual Bias: The numerator sums squared residuals, giving exponentially more weight to higher-TMB patients. For a patient with WES-based TMB
kym(where k >> 1) versus a patient with TMBym, the squared residual of the higher-TMB patient is approximatelyk²-fold greater, causing R-squared to be predominantly determined by extreme outliers [102].
Impact of TMB Distribution on Statistical Evaluation
Analysis of The Cancer Genome Atlas dataset reveals that TMB distribution follows a pronounced long-tailed pattern across cancer types (Figure 1A) [102]. The average TMB value is approximately 9.64 mutations/Mb, yet about 83% of patients fall below this average value. Conversely, hypermutated patients (TMB > 50 mutations/Mb) exhibit an average TMB of 151.51 mutations/Mb, creating a variance of 1559.63 for the entire dataset [102]. This distribution characteristic profoundly impacts R-squared calculation:
Table 1: Impact of TMB Distribution on R-squared Calculation
| Aspect | Effect on R-squared | Clinical Interpretation |
|---|---|---|
| Hypermutated cases (TMB > 50 mut/Mb) | Disproportionately influence denominator and numerator | Small number of patients disproportionately determines perceived panel performance |
| Low-TMB cases (0-2 mut/Mb) ~40% of population | Minimal contribution to R-squared value | Poor performance in majority of cases may be masked |
| Y-intercept (b) not接近 0 | Large relative bias for low-TMB patients: ym/xm ≈ a + b/xm |
Clinically critical low-TMB range shows highest estimation error |
These mathematical properties explain why R-squared values reach a plateau once panel size exceeds approximately 0.5 Mb, failing to adequately characterize panel performance as panel size increases further [102]. This plateau effect creates a false sense of optimization and obscures meaningful differences between panel designs and analytical approaches.
Angular Distance: A Robust Alternative Metric
Conceptual Foundation and Mathematical Formulation
Angular distance provides a geometrically intuitive alternative to R-squared that directly measures estimation bias for each individual patient. The conceptual framework transforms the Cartesian coordinates of panel-based TMB (x) and WES-based TMB (y) into polar coordinates, where the angle relative to the ideal prediction line (y = x) quantifies estimation accuracy [102].
For a patient i with panel-based TMB xi and WES-based TMB yi, the polar coordinate conversion follows:
ri = √(xi² + yi²)
φi = arctan(yi/xi) [102]
The angular distance (θi) representing the estimation bias is calculated as:
θi = |π/4 - φi| = |π/4 - arctan(yi/xi)| [102]
Theoretical range of angular distance extends from 0 (perfect estimation where panel-based TMB equals WES-based TMB) to π/4 (maximum estimation error) [102]. This direct measurement of individual patient bias addresses the fundamental limitation of R-squared, which only assesses aggregate variance explanation without quantifying directional estimation error.
Comparative Performance Evidence
Empirical evidence demonstrates the superior sensitivity of angular distance for evaluating TMB estimation performance compared to R-squared. In silico analysis reveals that while R-squared values plateau after panel size reaches approximately 0.5 Mb, angular distance remains sensitive to changes in panel sizes up to 6 Mb [102]. This continued sensitivity enables more discriminating evaluation of panel optimization and design improvements.
Furthermore, when applied to datasets with and without hypermutated patients, R-squared values differ substantially across cancer types, whereas angular distances remain highly consistent [102]. This consistency across diverse TMB distributions makes angular distance particularly valuable for pan-cancer applications where TMB ranges vary dramatically between cancer types.
Table 2: Comparative Performance of Angular Distance vs. R-squared
| Evaluation Criterion | R-squared | Angular Distance |
|---|---|---|
| Sensitivity to panel size increases | Plateaus at ~0.5 Mb | Remains sensitive up to ~6 Mb |
| Effect of hypermutation inclusion | Varies widely across cancer types | Highly consistent across cancer types |
| Mathematical basis | Proportion of variance explained | Direct measurement of individual bias |
| Weighting of patients | Exponentially favors high-TMB patients | Equitably weights all patients |
| Clinical interpretation | Abstract statistical concept | Geometrically intuitive bias measure |
Experimental Protocols for Metric Evaluation
Sample Preparation and Sequencing
Robust evaluation of TMB estimation metrics requires carefully controlled experimental designs. The following protocol outlines key considerations:
Sample Selection and Preparation:
- Select tumor samples representing diverse cancer types with expected TMB range variation [5]
- Ensure tumor cellularity >20% through pathologist review of hematoxylin and eosin-stained sections [24]
- Extract DNA from both formalin-fixed paraffin-embedded (FFPE) tissue and frozen tissue when possible for comparison [5]
- Assess DNA quality and quantity using appropriate methods (e.g., Nanodrop for purity with A260/280 ≥ 1.8) [24]
Sequencing Approach:
- Perform whole-exome sequencing as gold standard reference (targeting ~30 Mb coding region) [4]
- Conduct targeted panel sequencing using investigated panels (typically 0.8-2.4 Mb target regions) [4] [7]
- Utilize hybrid capture-based NGS methods for targeted sequencing [24]
- Sequence at appropriate depths: ≥100× for WES, ≥500× for targeted panels [4]
Bioinformatics Processing
Variant Calling and Filtering:
- Implement tumor-only or tumor-normal paired analysis approaches based on available samples [24]
- Apply minimum variant allele frequency thresholds: 10% for FFPE samples, 5% for frozen samples [5]
- Filter out known polymorphisms using population databases (dbSNP, ExAC, gnomAD) [5] [24]
- Include specific mutation types: non-synonymous, nonsense, small insertions/deletions [5]
TMB Calculation:
- Calculate WES-based TMB: (total somatic mutations / 30 Mb) [4]
- Calculate panel-based TMB: (total somatic mutations / panel size in Mb) [4]
- For targeted panels, normalize to mutations per megabase regardless of panel size [4]
Statistical Evaluation Protocol
Data Collection:
- Compile paired TMB values (panel-based
xi, WES-basedyi) for all samples - Document cancer types, sequencing quality metrics, and sample characteristics
Metric Calculation:
- Calculate R-squared value via linear regression [102]
- Compute angular distance for each patient:
θi = |π/4 - arctan(yi/xi)|[102] - Determine mean angular distance across dataset
- Perform subgroup analyses by cancer type, TMB range, and sample quality
Essential Research Reagents and Computational Tools
Table 3: Research Reagent Solutions for TMB Metric Evaluation
| Reagent/Tool Category | Specific Examples | Function in TMB Assessment |
|---|---|---|
| NGS Panels | FoundationOne CDx (324 genes, 0.8 Mb TMB region) [4] | Targeted TMB estimation with FDA approval |
| MSK-IMPACT (468 genes, 1.14 Mb TMB region) [4] | Targeted TMB estimation with FDA authorization | |
| TruSight Oncology 500 (523 genes, 1.33 Mb TMB region) [4] | Comprehensive genomic profiling for TMB | |
| Bioinformatics Tools | MSIsensor [5] | Microsatellite instability assessment |
| Population frequency databases (dbSNP, ExAC, gnomAD) [5] [24] | Germline variant filtering | |
| Custom TMB algorithms [5] | Laboratory-specific TMB calculation | |
| Reference Materials | Standard reference samples with known mutations [24] | Assay validation and quality control |
| FFPE and frozen sample pairs [5] | Evaluation of pre-analytical effects |
Visualization of Analytical Workflows
Angular Distance Calculation Diagram
Comprehensive TMB Metric Evaluation Workflow
The evaluation of TMB estimation performance for targeted NGS panels requires statistical approaches that address the unique challenges posed by long-tailed TMB distributions in cancer populations. While R-squared has been widely used for this purpose, its mathematical properties render it suboptimal due to disproportionate influence from hypermutated cases and insensitivity to panel size improvements beyond minimal thresholds. Angular distance provides a geometrically intuitive, robust alternative that directly measures estimation bias for individual patients and maintains sensitivity across diverse TMB ranges and panel sizes.
Implementation of angular distance alongside traditional metrics offers researchers, scientists, and drug development professionals a more comprehensive framework for evaluating TMB estimation accuracy. The experimental protocols and analytical workflows presented in this review provide practical guidance for incorporating these advanced statistical approaches into NGS panel validation and optimization processes. As TMB continues to evolve as a critical biomarker for immunotherapy response, refined statistical evaluation methods will play an increasingly important role in ensuring accurate and reliable measurement across testing platforms.
Inter-laboratory Reproducibility and Cross-Platform Harmonization Efforts
Tumor Mutational Burden (TMB) has emerged as a significant predictive biomarker for response to immune checkpoint inhibitors across various cancer types, quantified as the total number of somatic mutations per megabase of the interrogated tumor genome [103]. Despite its clinical utility, significant variability in TMB measurement has been observed across different laboratories and sequencing platforms, creating substantial challenges for consistent clinical application and data interpretation [103]. This variability stems from differences in pre-analytical and laboratory methods, panel size and design, bioinformatics pipelines, and analytical thresholds, leading to confusion and disparity in the field [103]. The fundamental challenge lies in enabling consistent estimation and reporting of TMB scores from samples analyzed across different assays, platforms, and centers, thus necessitating comprehensive standardization efforts [103].
The reproducibility crisis in TMB measurement affects both tissue-based TMB (tTMB) and blood-based TMB (bTMB) approaches, though each presents unique challenges. While tissue TMB faces issues with tumor heterogeneity and sample availability, blood TMB must contend with low levels of tumor DNA shedding and the potential interference from clonal hematopoiesis, which could elevate the number of apparent somatic mutations and result in higher predicted bTMB scores [103]. With clinical evidence growing for the use of TMB as a predictive biomarker for immunotherapy, standardization efforts have become increasingly critical for both research and clinical applications [90].
Pre-analytical and Analytical Factors
The journey toward reliable TMB measurement begins with pre-analytical considerations that introduce significant variability. Formalin-fixed paraffin-embedded (FFPE) sample quality, tumor content, nucleic acid integrity, and extraction methods all substantially impact downstream results [54] [104]. Studies have demonstrated that the optimized proportion of tumor cells in FFPE samples should exceed 20% by HE staining, with minimum DNA input thresholds varying by platform (typically 40-300ng) to ensure reliable results [54]. Library preparation methods further contribute to variability, with differences emerging between hybridization capture-based approaches and amplification-based techniques, each with distinct strengths and limitations in genomic coverage and technical performance [104].
The sequencing platform itself introduces another layer of complexity, with different vendors applying different detection methods, and each platform requiring specific assay designs to optimize detection of different genomic variant types [104]. Depth of coverage represents a critical parameter, with higher sequencing depths enabling more reliable detection of low-frequency variants but increasing costs and computational requirements [54]. The dynamic range of quantification differs substantially across platforms, with digital PCR providing higher precision of quantification than qPCR, even when used on identical nucleic acid targets and molecular assays [105].
Bioinformatics and Computational Variability
The bioinformatics pipeline constitutes a major source of inter-laboratory variability in TMB assessment. Data processing beginning from the detector signal all the way to variant identification involves multiple steps where decisions dramatically impact final TMB scores [104]. Variant calling algorithms differ in their approaches to distinguishing true somatic mutations from sequencing artifacts and germline variants, with significant consequences for TMB calculation [54]. The choice of population frequency databases (such as dbSNP, ExAC, and gnomAD) for filtering germline mutations influences which variants are considered somatic, directly impacting the final TMB value [54].
The bioinformatic filtration steps required to account for low variant allele frequency (VAF) artifact variants present another challenge, as different thresholds and approaches can yield substantially different results [103]. Studies have demonstrated that a bioinformatic filtration step is necessary to account for low-VAF artifact variants, typically achieved by filtering for known somatic tumor variants with minor allele frequency >1-2% in well-characterized cell-line gDNA [103]. Additionally, the handling of specific mutation types—including synonymous single nucleotide variants (SNVs), insertions/deletions (indels), and structural variants—varies considerably across pipelines, further complicating cross-platform comparisons [103] [54].
Table 1: Key Sources of Variability in TMB Measurement
| Category | Specific Source of Variability | Impact on TMB Results |
|---|---|---|
| Pre-analytical | FFPE sample quality & tumor content | Affects input DNA quality and variant detection sensitivity |
| DNA/RNA integrity & extraction methods | Influences library complexity and sequencing quality | |
| Analytical | Sequencing platform & chemistry | Impacts error rates, coverage uniformity, and sensitivity |
| Panel size & genomic coverage | Affects the statistical robustness of TMB estimation | |
| Depth of coverage & sequencing parameters | Influences detection of low-frequency variants | |
| Bioinformatic | Variant calling algorithms & thresholds | Affects sensitivity/specificity of mutation detection |
| Germline filtration databases & methods | Influences which variants are counted as somatic | |
| VAF thresholds & artifact filtering | Impacts final mutation count and TMB calculation |
Reference Materials and Standards Development
Contrived Reference Materials for bTMB
The development of standardized reference materials represents a crucial advancement in TMB harmonization. Research has demonstrated the feasibility of producing contrived bTMB reference materials using DNA from tumor cell lines and donor-matched lymphoblastoid cell lines to support calibration and alignment across different laboratories and bTMB platforms [103]. These materials are developed using genomic DNA from WES TMB-characterized, human-derived lung tumor cell lines that are individually blended by mass into gDNA from donor-matched lymphoblastoid cell lines at specific tumor content percentages (typically 0.5% and 2%) [103].
The manufacturing process involves fragmenting DNA using proprietary shearing techniques and size-selecting to mirror the size profile of circulating cell-free tumor DNA (ctDNA), with the target size range for DNA fragments being 135-205 bp, which comprises approximately half of the total DNA in each sample [103]. Quality control of these contrived reference materials involves analysis using the Bioanalyzer High Sensitivity DNA assay to determine fragment sizes, with comparisons to amplified cfDNA samples from cancer patients to verify biological relevance [103]. These reference materials are further validated using NGS assays such as the Archer Reveal ctDNA 28 assay to quantify cell line-specific mutations in genes including KRAS, MAP2K1, and TP53 to verify blending accuracy [103].
Table 2: Contrived bTMB Reference Material Characteristics
| TMB Score (mut/Mb) | Tumor Content | Development Method | Validation Platform | Key Applications |
|---|---|---|---|---|
| 7, 9, 20, 26 | 0.5% & 2.0% | Method A (shearing & size selection) | PredicineATLAS, GuardantOMNI | Platform calibration & alignment |
| 7, 9, 26 | 2.0% | Method B (amplification-based) | GuardantOMNI | High-volume reference material production |
| 20 | 0.5% & 2.0% | Method A & B | PredicineATLAS | Sensitivity assessment at low tumor content |
Standardization Initiatives and Guidelines
Numerous organizations have developed standards, guidelines, and quality control metrics for NGS workflows to address harmonization challenges [104]. The Centers for Disease Control and Prevention (CDC), in collaboration with the Association of Public Health Laboratories (APHL), launched the Next Generation Sequencing Quality Initiative in 2019, providing laboratories with over 100 free guidance documents and standard operating procedures (SOPs) to support high-quality sequencing data and adherence to standards [104]. The Global Alliance for Genomics and Health (GA4GH), an international consortium founded in 2013, develops standards for responsibly collecting, storing, analyzing, and sharing genomic data, aiming to enable an "internet of genomics" that integrates genomic data, computational tools, and stakeholders globally [104].
Professional guidelines have also emerged from organizations including the American College of Medical Genetics and Genomics (ACMG), which has developed comprehensive guidelines for clinical laboratories utilizing NGS, covering the interpretation and reporting of variants, with technical standards revised in 2021 to reflect technological advancements and current best practices [104]. More specifically for TMB, the Association for Molecular Pathology convened a multidisciplinary collaborative working group with representation from the American Society of Clinical Oncology, the College of American Pathologists, and the Society for the Immunotherapy of Cancer to review laboratory practices surrounding TMB and develop recommendations for the analytical validation and reporting of TMB testing based on survey data, literature review, and expert consensus [90].
Methodological Comparisons and Their Impact on TMB
Tumor-Only versus Tumor-Control Approaches
Significant methodological differences exist in NGS approaches for TMB detection, primarily between tumor-only (TO) and tumor-control (TC) methods. The TO method analyzes the patient's tumor tissue to identify somatic mutations by comparing the tumor tissue sequencing data with population databases, while the TC method simultaneously detects the patient's tumor tissue and white blood cells or normal tissue, allowing direct comparison [54]. Studies comparing these approaches have revealed that while they share substantial overlap in detected genes (298 common genes in one comparison), they identify and incorporate different TMB sites, which in turn affects the TMB calculation results [54].
The consistency rate of TMB classification (high vs. low) between TO and TC methods has been observed to be 92% (22/24 samples), with chi-square tests indicating a significant difference in TMB results between TO and TC (χ² = 16.667, p = 0.000, p < 0.001) [54]. Despite this difference, Cohen's kappa analysis shows consistency in the TMB values detected by TO and TC methods, which were good and had high repeatability (kappa = 0.833, p = 0.000, p < 0.001) [54]. This suggests that while absolute TMB values may differ between approaches, categorical classification (high vs. low) shows reasonable concordance. The critical implication is that when the TMB result is near the 10 mut/Mb threshold, different methods may yield different clinical classifications, potentially affecting treatment decisions [54].
Panel Size and Design Considerations
The size and design of targeted sequencing panels significantly impact TMB estimation accuracy and reliability. While whole exome sequencing (WES) is considered the gold standard for TMB analysis, it has high cost and requires large sample sizes, limiting its wide application in clinical practice [54]. Large panels provide deeper sequencing depth (typically 1000×) within a reasonable cost range, allowing more accurate calculation of molecular indicators such as TMB [54]. However, significant variability exists in panel sizes and genomic coverage, with different panels covering anywhere from 425 to 523 genes in comparative studies, with detection ranges primarily comprising exons and some introns [54].
The specific algorithm used for TMB calculation varies across platforms, with some including complete detection of synonymous single nucleotide variants (SNVs) and insertions/deletions (indels) at all VAFs within the sensitivity range for the assay (≥0.25%), while others incorporate somatic SNVs, including synonymous SNVs, and indels at all VAFs and are optimized to calculate TMB on plasma samples with low ctDNA content [103]. The TMB calculation method typically involves dividing the number of TMB variants (including synonymous and non-synonymous non-hot spot somatic coding variants with a ≥5% variant allele frequency) by the size of the coding region defined by the quality control criteria of the reagent, while excluding mutations below the threshold and mutations in mitochondria and non-eligible regions [54].
Table 3: Comparison of TMB Detection Methodologies
| Parameter | Tumor-Only (TO) Method | Tumor-Control (TC) Method |
|---|---|---|
| Sample Requirements | Tumor tissue only | Tumor tissue + white blood cells/normal tissue |
| Germline Variant Filtering | Population databases (dbSNP, ExAC, gnomAD) | Direct comparison with matched normal |
| Key Advantages | Less sample required, lower cost | More accurate germline mutation discrimination |
| Key Limitations | Potential false positives from germline variants | Higher sample requirements, increased cost |
| Consistency with Other Method | 92% categorical consistency (TMB-H/TMB-L) | 92% categorical consistency (TMB-H/TMB-L) |
| Statistical Significance | χ² = 16.667, p < 0.001 | χ² = 16.667, p < 0.001 |
| Cohen's Kappa | kappa = 0.833, p < 0.001 | kappa = 0.833, p < 0.001 |
Experimental Protocols for TMB Validation
Reference Material Development and Validation
The development of contrived bTMB reference materials follows a rigorous experimental protocol to ensure reproducibility and accuracy. The process begins with genomic DNA from each of four WES TMB-characterized, human-derived lung tumor cell lines that are previously analyzed by the Friends of Cancer Research TMB Harmonization Consortium [103]. These are individually blended by mass into gDNA from donor-matched lymphoblastoid cell lines at 2% and 0.5% tumor content, with careful consideration that tumor lines are aneuploid, meaning a given tumor cell does not necessarily contain the same mass of DNA per genome as a normal euploid cell [103].
DNA fragmentation employs a proprietary shearing technique followed by size-selection to mirror the size profile of circulating cell-free tumor DNA with TMB scores of 7, 9, 20, and 26 mut/Mb, matching those of the parent lung tumor cell lines [103]. Approximately 100 ng of each mixture is amplified to generate a large batch of the same material using a method designed to take cfDNA or cfDNA-like material and amplify it in a way that generally preserves the fragment length distributions and genetic content, enabling simpler generation of high volumes of reference materials [103]. Validation of these materials involves assessing VAF and bTMB scores using established NGS platforms such as PredicineATLAS (comprising 600 genes with 2.4 Mb genome coverage) and GuardantOMNI (comprising 500 genes with 2.145 Mb genome coverage) [103].
Cross-Platform Validation Framework
A comprehensive computational framework has been proposed to improve cross-platform implementation of transcriptomic signatures, with principles applicable to TMB harmonization [105]. This framework emphasizes embedding constraints related to cross-platform implementation in the process of signature discovery, including technical limitations of amplification platform and chemistry, the maximal number of targets imposed by the chosen multiplexing strategy, and the genomic context of identified RNA biomarkers [105]. The framework integrates these constraints with existing statistical and machine learning models used for signature identification, accelerating the integration of discoveries made by high-throughput technologies into approaches suitable for clinical applications [105].
The validation process must account for the biochemical and thermodynamic criteria that impact molecular assay design, such as primer melting temperature, amplicon length, GC content, specificity of primer binding on the region of interest, and avoidance of primer-dimers, especially in single-tube multiplex PCR assays [105]. These constraints may differ across implementation chemistries—for instance, the minimal amplicon length necessary for successful implementation on a LAMP-based platform might be longer than on a PCR-based platform, since a typical LAMP assay usually relies on a total of six primers targeting eight genomic regions per amplicon and spanning across 200–250 base pairs [105].
Quality Control and Proficiency Testing
Quality Management Systems and Metrics
Quality management systems for NGS encompass comprehensive frameworks based on the Clinical & Laboratory Standards Institute's 12 Quality Systems Essentials (QSEs), addressing challenges in developing and implementing NGS-based tests [104]. These systems provide laboratories with extensive guidance documents and standard operating procedures to support high-quality sequencing data and adherence to standards [104]. The establishment of condition-specific, data-driven guidelines offers a robust framework to ensure the consistency and accuracy of results while promoting the harmonization of quality management in NGS workflows [104].
Quality control parameters for NGS-based TMB testing must be systematically monitored and standardized to enable comparability across laboratories. Key metrics include sample quality, DNA/RNA integrity, library QC (insert size, etc.), depth of coverage, and base quality (e.g., Q30) [104]. Different organizations emphasize different QC parameters—for instance, reads mapped is recommended in EuroGentest guidelines but not by CAP or RCPA, while CAP does not require monitoring of GC Bias, whereas it is considered important by EuroGentest [104]. This variability in quality monitoring approaches underscores the need for harmonized quality metrics specifically for TMB testing.
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 4: Essential Research Reagents and Materials for TMB Harmonization
| Reagent/Material | Specification/Example | Primary Function | Key Considerations |
|---|---|---|---|
| Reference Materials | Contrived bTMB standards (7, 9, 20, 26 mut/Mb) | Platform calibration & alignment | Tumor content (0.5%, 2.0%), fragment size (135-205 bp) |
| Cell Lines | WES TMB-characterized lung tumor cell lines | Reference material development | Donor-matched lymphoblastoid lines for blending |
| Extraction Kits | FFPE magnetic bead extraction reagents | Nucleic acid isolation | Minimum input (40-300ng), A260/280 ≥ 1.8 |
| NGS Library Prep | Hybridization capture-based kits (e.g., Archer, TSO 500) | Library construction | Panel size (425-600 genes), coverage uniformity |
| Sequencing Platforms | Illumina NovaSeq 6000, Ion PGM Dx System | DNA sequencing | DRAGEN onboard analysis, depth of coverage |
| Bioinformatics Tools | Variant callers, population frequency databases | Data analysis | Germline filtration, artifact removal algorithms |
Future Directions and Implementation Strategies
Computational and Analytical Advancements
The future of TMB harmonization lies in advanced computational frameworks that embed cross-platform implementation constraints directly into the discovery process [105]. This approach involves integrating biochemical and thermodynamic criteria that impact molecular assay design with statistical and machine learning models used for feature selection [105]. By considering the technical limitations of the eventual implementation platform during the discovery phase, researchers can ensure that classification performance is maintained when transitioning from high-throughput discovery platforms to clinically applicable diagnostic tools [105].
Another promising direction involves the development of novel partnership models between technology companies and research institutions to advance NGS capabilities. For instance, the collaboration between Integrated DNA Technologies and Molecular Health pairs IDT's Archer NGS research assay platform with Molecular Health's variant annotation and reporting software to equip molecular researchers with tertiary analysis for their NGS data, maximizing lab efficiency and streamlining genomics data workflows to accelerate cancer discoveries [106]. Such partnerships reflect the ongoing efforts to address the cancer research community's need for more complete tools inclusive of high-performance chemistries along with the ability to manage and annotate an ever-expanding biomarker knowledgebase [106].
Implementation Roadmap for Laboratories
Implementing harmonized TMB testing requires a systematic approach encompassing pre-analytical, analytical, and post-analytical phases. Laboratories should establish standardized protocols for sample processing, including FFPE sample quality control with tumor content >20% by HE staining, DNA extraction with minimum thresholds (typically >300ng for FFPE samples), and purity requirements (A260/280 ≥1.8) [54]. Analytical validation must include cross-platform comparison using standardized reference materials and established bioinformatics pipelines with clearly defined VAF thresholds and germline filtration approaches [103] [54].
The adoption of FAIR (Findable, Accessible, Interoperable, Reusable) data principles facilitates the development of harmonized datasets that can be integrated to enable the broader scientific community to address complex scientific questions [107]. This requires harmonizing as many elements of the data collection and processing pipeline as possible, including the types, levels, and sources of data in formats that are compatible and comparable so that they can be integrated [107]. Establishing a common framework for collecting data across sites ensures that points of commonality between datasets are clear to both humans and machines, enabling different types of data to be meaningfully combined [107].
Successful implementation also requires a cultural shift in current scientific practices, with comprehensive support and training in data management and sharing practices [107]. For academic scientists to pursue and contribute to team science initiatives, the entire academic enterprise must shift so that effective data sharing strategies are valued on par with publications and other standards that are commonly used for tenure and promotion decisions [107]. This culture shift toward open data sharing in academic biomedical research is particularly urgent given the artificial intelligence revolution already underway, which requires open, high-quality, well-annotated and structured data on which to operate [107].
Tumor Mutational Burden (TMB) has emerged as a significant biomarker for predicting response to immune checkpoint inhibitors (ICIs) across various solid tumors. The clinical interpretation of TMB, typically dichotomized as "high" or "low" using a specific mutations per megabase (mut/Mb) threshold, depends entirely on the rigorous validation of these cut-off values. The journey from initial retrospective analysis to definitive prospective confirmation represents a critical pathway in biomarker development that ensures clinical utility and reliability. This process is particularly complex for TMB due to methodological variations in next-generation sequencing (NGS) approaches, biological heterogeneity across cancer types, and the intricate relationship between mutational load and immune response.
The validation of TMB cut-offs extends beyond mere technical performance, encompassing both analytical validation (ensuring the test itself reliably measures TMB) and clinical validation (demonstrating that the TMB result accurately predicts treatment outcome). As the BLOODPAC Analytical Validation Working Group emphasizes, "bTMB tests require additional standardization and harmonization before broad clinical use with a threshold to dichotomize the quantitative result" [25]. This guide examines the comprehensive framework for establishing and validating these critical clinical decision points within the context of modern NGS research.
Analytical Validation Foundations
Addressing the Complexities of TMB as a Biomarker
TMB represents a uniquely complex biomarker that differs fundamentally from single-analyte biomarkers. The nearly infinite combination of single-nucleotide variants (SNVs) and insertions/deletions (indels) that can yield an identical TMB score introduces significant challenges for traditional analytical validation approaches. According to the BLOODPAC consortium, this complexity leads to "sample-specific variability in estimates of analytical performance of bTMB due to the underlying variant heterogeneity, including composition of SNVs and indels, genomic context, variant clonality, variant allele frequency, and shedding rates of primary and metastatic lesions" [25].
Additional confounding factors include differences in targeted panel content, variant detection algorithms, and TMB classification models across testing platforms. These variables collectively impact the assessment of analytical performance and necessitate specialized validation approaches beyond those used for conventional biomarkers.
Key Analytical Performance Metrics
When designing analytical validation studies for TMB assays, researchers must adapt traditional clinical laboratory standards to address the biomarker's unique characteristics. The BLOODPAC Working Group has provided specific guidance on which analytical metrics can be directly applied from established circulating tumor DNA (ctDNA) assays and which require substantial modification for TMB assessment [25].
Table 1: Analytical Validation Considerations for TMB Assays
| Protocol Name | TMB-Specific Considerations | Recommended Approach |
|---|---|---|
| Limit of Blank | Can be applied as outlined for ctDNA assays | Use cancer-free reference donors representative of intended use population |
| Interfering Substances | Can be applied for SNVs and Indels | Evaluation of contributing variant classes is sufficient |
| Analytical Accuracy | Requires modified study design | Account for complex biomarker nature and limited sample availability |
| Limit of Detection | Test-specific measurement cannot be determined | bTMB is a complex biomarker without a single limit of detection |
| Precision/Reproducibility | Modified design needed | Address lack of contrived sample models and limited clinical sample availability |
| Contrived Sample Characterization | Standardized models don't represent intended use population | Use clinical samples where possible; recognize limitations of surrogate samples |
Experimental Protocol: Contrived Sample Functional Characterization
- Identify potential surrogate samples (biosynthetic constructs, cell line-derived DNA)
- Account for pre-analytical processing limitations (fragmentation artifacts)
- Use matched nontumor sample as proper diluent to modify tumor content
- Validate against a subset of clinical samples to establish correlation
- Document all limitations of surrogate models in final validation report
The limited availability of plasma from the intended use population presents particular challenges for executing traditional analytical validation studies. While surrogate samples have been proposed, they often suffer from limitations including "pre-analytical processing (e.g., biosynthetic constructs and immortalized cell line fragmentation-related artifacts), variant clonality, and presence of a matched nontumor sample as a proper diluent to modify tumor content" [25].
Retrospective Analysis for Cut-off Identification
Distribution-Based Approaches for Initial Cut-off Determination
Retrospective analysis of existing datasets represents the initial stage in TMB cut-off development. The study by Jun et al. demonstrates how real-world data can be leveraged to establish tumor-type-specific TMB thresholds using an interquartile range (IQR)-based method [108]. This approach identified TMB cut-offs that showed significant association with longer progression-free survival (PFS) in ICI-treated patients (HR=0.85, 95% CI: 0.73-0.98, p=0.02), outperforming the universal 10 mut/Mb cutoff which showed no statistical significance [108].
Experimental Protocol: IQR-Based Cut-off Determination
- Collect targeted NGS data from a large cohort of patients (n=9,459 in the Jun et al. study)
- Calculate TMB values for all samples using established bioinformatics pipelines
- Determine the IQR for TMB values within specific tumor types
- Set preliminary cut-offs based on upper quartile values or statistical outliers
- Validate preliminary cut-offs against clinical outcomes in ICI-treated subsets
The significant finding that "IQR-based TMB-H was significantly associated with longer PFS in the ICI-treated cohort" while "the universal 10 mut/Mb cutoff showed no statistical significance" highlights the importance of distribution-based approaches tailored to specific cancer types and populations [108].
Assessing Methodological Impact on TMB Calculation
Different NGS methodologies significantly impact TMB measurement, particularly near critical decision thresholds. A recent comparative study evaluating Tumor-Only (TO) versus Tumor-Control (TC) approaches found that while both methods showed 92% consistency in TMB classification, a significant difference existed in their results (χ2 = 16.667, p = 0.000) [24]. This demonstrates how methodological choices affect TMB quantification, particularly near the 10 mut/Mb threshold commonly used for clinical decision-making.
The study further revealed that "different algorithms and design panels for mutation filtering affect the TMB test results" and noted that "when the TMB result is near the 10 mut/Mb threshold, different methods may yield different results" [24]. This has direct implications for clinical management, as a single test result can determine treatment eligibility.
Prospective Confirmation of Clinical Utility
Designing Prospective Validation Studies
Prospective confirmation represents the gold standard for establishing clinical utility of TMB cut-offs. The DART study exemplifies this approach in unresectable stage III non-small cell lung cancer (NSCLC) treated with chemoradiotherapy followed by durvalumab [15]. This multicenter, prospective cohort study evaluated blood-based TMB (bTMB) alongside other biomarkers, with pre-specified statistical plans and endpoints.
Experimental Protocol: Prospective Validation Study Design
- Define primary endpoint (e.g., progression-free survival, overall survival)
- Establish inclusion/exclusion criteria matching intended use population
- Pre-specify TMB cut-off values based on retrospective data
- Implement standardized sample collection and processing protocols
- Plan for multivariable analysis including potential confounders (PD-L1, specific mutations)
- Include statistical power calculation to determine sample size
In the DART study, researchers found that "high bTMB was associated with longer PFS using both the prespecified 8.5 mut/Mb cut-off (HR: 0.65; p = 0.088) and the median 6.6 mut/Mb cut-off (HR: 0.52; p = 0.016)" [15]. This demonstrates how different cut-offs may show varying levels of predictive power, even within the same study population.
Integrating TMB with Complementary Biomarkers
Prospective studies increasingly recognize that TMB does not function in isolation. The DART study simultaneously evaluated PD-L1 expression and specific mutations in genes such as STK11, KEAP1, and NFE2L2, finding that "PD-L1 ≥ 1% was associated with longer PFS (HR: 0.38; p = 0.0003), while STK11, KEAP1, or NFE2L2 mutations in ctDNA were linked to shorter PFS (HR: 1.84; p = 0.040)" [15]. This multi-biomarker approach provides a more nuanced understanding of treatment response.
The study further demonstrated that in multivariable analysis, "PD-L1 remained significantly associated with PFS in both models, while bTMB and STK11/KEAP1/NFE2L2 mutations were significant using the 6.6 mut/Mb cut-off" [15]. This highlights the importance of evaluating TMB in the context of other relevant biomarkers during prospective validation.
Technical Considerations in TMB Measurement
NGS Methodologies and Their Impact on TMB Quantification
The specific NGS methodology employed significantly influences TMB measurement, particularly through its effect on germline mutation filtering. The fundamental difference between Tumor-Only (TO) and Tumor-Control (TC) approaches lies in their ability to distinguish somatic from germline variants [24].
Table 2: Comparison of NGS Methodologies for TMB Assessment
| Parameter | Tumor-Only (TO) Approach | Tumor-Control (TC) Approach |
|---|---|---|
| Sample Requirements | Tumor tissue only | Tumor tissue + matched normal (blood or tissue) |
| Germline Filtering | Computational using population databases (dbSNP, ExAC, gnomAD) | Direct comparison with patient's normal DNA |
| Key Advantages | Lower cost, simpler workflow | More accurate somatic mutation identification |
| Key Limitations | Potential for false positives (germline variants misclassified as somatic) | Higher cost, more complex workflow |
| TMB Consistency | 92% with TC method, but significant differences near cut-offs | Gold standard for somatic variant identification |
Experimental Protocol: Tumor-Only Versus Tumor-Control Comparison
- Collect paired tumor and normal samples from the same patients (n=24 in validation study)
- Process samples using both TO and TC approaches in parallel
- Apply respective bioinformatics pipelines for each method
- Calculate TMB values using identical coding region definitions
- Compare results using statistical methods (chi-square, Cohen's kappa)
- Resolve discordant cases through orthogonal validation methods
The comparative study found that "different algorithms and design panels for mutation filtering affect the TMB test results" and specifically noted that "when the TMB result is near the 10 mut/Mb threshold, different methods may yield different results" [24]. This technical variability has direct clinical implications, potentially altering treatment decisions for borderline cases.
The Scientist's Toolkit: Essential Research Reagents and Materials
Robust TMB cut-off validation requires carefully selected reagents and materials throughout the analytical workflow. The following table details essential components based on current validation studies.
Table 3: Research Reagent Solutions for TMB Validation Studies
| Reagent/Material | Function | Example Products | Key Quality Controls |
|---|---|---|---|
| FFPE DNA Extraction Kits | Nucleic acid isolation from archival tissue | AllPrep DNA/RNA FFPE Kit (Qiagen), Kaijie FFPE magnetic bead extraction reagent | Tumor cell content >20%, DNA amount >300 ng, A260/280 ≥1.8 |
| Targeted NGS Panels | Hybridization capture of genomic regions | Illumina TruSight Oncology 500, Shihe No.1NSCLC TMB Detection Kit | Panel size ≥1 Mb, coverage of key cancer genes |
| Library Preparation | NGS library construction for sequencing | Manufacturer-specific kits with hybridization capture | Fragment size 90-250 bp, unique molecular identifiers (UMIs) |
| Sequence Platforms | High-throughput DNA sequencing | Illumina NextSeq 550, similar platforms | Minimum depth 1000×, >80% bases at 100× |
| Bioinformatics Tools | Variant calling and TMB calculation | NGeneAnalySys, custom pipelines | dbSNP/ExAC/gnomAD for germline filtering, ≥5% VAF threshold |
Clinical Implementation and Ongoing Challenges
Tissue-Specific versus Universal Cut-offs
The debate between universal versus tissue-specific TMB cut-offs continues to evolve as more evidence accumulates. The Jun et al. study demonstrated that "IQR-based TMB-H was significantly associated with longer PFS" in specific cancer types including "bladder (p=0.014), bowel (p=0.013), and uterine cancers (p=0.006)" [108], supporting tissue-specific approaches. Furthermore, their research showed that "in lung cancer, patients with both TMB-H and very high PD-L1 expression (≥90%) had the longest PFS (HR=0.64, 95% CI: 0.44-0.93, p=0.021)" [108], highlighting the potential for combination biomarker strategies.
However, practical implementation of tissue-specific cut-offs faces challenges including sufficient sample sizes for rare cancers, standardization across platforms, and regulatory considerations. The pursuit of both universal and tissue-specific thresholds continues in parallel, with each approach offering distinct advantages for different clinical contexts.
Biological Context and Mutational Signatures
Understanding the biological context of high TMB provides additional refinement beyond simple cut-off values. Research in breast cancer has revealed that "the predominant mutational signature was apolipoprotein B mRNA-editing enzyme catalytic polypeptide (APOBEC) in 64.7% of tumors" and that "TMB-high BCs were enriched in KMT2C, ARID1A, PTEN, NF1, and RB1 alterations, which are associated with APOBEC mutagenesis" [20]. This biological insight helps explain why not all high-TMB tumors respond equally to immunotherapy.
Additionally, the study found that "TMB-high BCs exhibited a dominant APOBEC signature" and that "TMB values were significantly higher in tumors with a dominant APOBEC signature when compared to HRD (p = 1.6 × 10−12), clock (p = 0.002), and ROS/5FU (p = 0.005)" [20]. This suggests that mutational signatures may provide important contextual information alongside TMB values in future clinical implementation.
The validation of TMB cut-offs represents an ongoing journey from retrospective discovery to prospective confirmation, requiring rigorous analytical validation, thoughtful clinical study design, and careful consideration of technical and biological variables. The evolving landscape continues to refine our understanding of how to best implement TMB as a biomarker for immunotherapy response across different cancer types and clinical contexts.
As research advances, the integration of TMB with complementary biomarkers such as PD-L1 expression, specific mutational signatures, and genomic alterations will likely provide more nuanced predictive models. Furthermore, standardization of testing methodologies and analytical approaches will be essential for consistent clinical implementation. The pathway from retrospective analysis to prospective confirmation remains fundamental to establishing TMB as a reliable biomarker that genuinely improves patient outcomes through better treatment selection.
Conclusion
The integration of TMB as a biomarker in oncology represents a significant advancement in personalized cancer therapy, yet its full potential is contingent on resolving key methodological challenges. Successful implementation requires robust NGS panel design, standardized bioinformatic pipelines, and rigorous analytical validation. Future efforts must focus on prospective validation of context-specific TMB thresholds, refinement of blood-based TMB assays, and integration of TMB with other biomarkers like neoantigen quality and tumor microenvironment features. For researchers and drug developers, addressing these areas is crucial for enhancing the predictive power of TMB and expanding the benefits of immunotherapy to broader patient populations, ultimately guiding more precise and effective therapeutic strategies.
References
- 1. Tumor mutational burden [https://en.wikipedia.org/wiki/Tumor_mutational_burden]
- 2. Neoantigens: promising targets for cancer therapy [https://www.nature.com/articles/s41392-022-01270-x]
- 3. The role of neoantigens and tumor mutational burden in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12406617/]
- 4. Tumor Mutational Burden (TMB) as a Predictive Biomarker ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7710563/]
- 5. Tumor mutational burden assessment and standardized bioinformatics approach using custom NGS panels in clinical routine | BMC Biology | Full Text [https://bmcbiol.biomedcentral.com/articles/10.1186/s12915-024-01839-8]
- 6. The Neoantigen Landscape of the Coding and Noncoding ... [https://www.sciencedirect.com/science/article/pii/S1525157822000721]
- 7. Tumor Mutational Burden | TMB NGS testing [https://www.illumina.com/areas-of-interest/cancer/ngs-in-oncology/biomarkers/tumor-mutational-burden.html]
- 8. Tumor Mutational Burden (TMB) [https://www.carislifesciences.com/physicians/physician-tests/whole-exome-sequencing/tumor-mutational-burden-tmb/]
- 9. A method for identifying neoantigens through isolation of ... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2025.1609116/full]
- 10. TMB as a predictive biomarker for ICI response in TNBC [https://pmc.ncbi.nlm.nih.gov/articles/PMC12628467/]
- 11. Predictive biomarkers for cancer immunotherapy with immune... [https://biomarkerres.biomedcentral.com/articles/10.1186/s40364-020-00209-0]
- 12. Clinical and Molecular Differences Suggest ... [https://www.mdpi.com/2072-6694/17/16/2673]
- 13. Tumor mutation burden in lung cancer: a new predictive ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6297473/]
- 14. Analysis Tumor Mutational Burden [https://labs.iqvia.com/genomics/tumor-mutational-burden-analysis]
- 15. Frontiers | Blood-based tumor as a mutational in... burden biomarker [https://www.frontiersin.org/journals/oncology/articles/10.3389/fonc.2025.1681420/full]
- 16. Blood-based tumor as a mutational for... burden biomarker [https://www.nature.com/articles/s41591-022-01754-x?error=cookies_not_supported&code=c02bd047-035b-458e-a9bc-a1a22c01b70a]
- 17. Utility of Tumor as a Mutational for Burden to... Biomarker Response [https://pubmed.ncbi.nlm.nih.gov/38039430/]
- 18. (TMB) as a Tumor of mutational to... burden biomarker response [https://jtd.amegroups.org/article/view/23082/html]
- 19. Prediction of checkpoint inhibitor immunotherapy efficacy ... [https://www.nature.com/articles/s41591-024-03398-5]
- 20. Genomic characterization of tumor mutational burden-high ... [https://www.nature.com/articles/s41698-025-01045-x]
- 21. Association of tumour with outcomes in patients... mutational burden [https://pubmed.ncbi.nlm.nih.gov/32919526/]
- 22. as Biomarker in Stage IV NSCLC Tumor Mutation Burden [https://decisionpoint.medscape.com/oncology/viewarticle/925933]
- 23. Long-Term Survival Outcomes With First-Line Nivolumab ... [https://www.sciencedirect.com/science/article/pii/S1556086424023554]
- 24. Different NGS identification methods of somatic mutation sites in solid... [https://bmccancer.biomedcentral.com/articles/10.1186/s12885-025-13719-7]
- 25. Analytical Validation of Blood-Derived Tumor Mutation ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12597528/]
- 26. A phase 2 trial of pembrolizumab for recurrent Lynch-like ... [https://www.sciencedirect.com/science/article/abs/pii/S0090825825008170]
- 27. The role of neoantigens and tumor mutational burden in ... [https://jhoonline.biomedcentral.com/articles/10.1186/s13045-025-01732-z]
- 28. Analysis of 100000 human cancer genomes reveals the ... [https://genomemedicine.biomedcentral.com/articles/10.1186/s13073-017-0424-2]
- 29. Association between smoking history and tumor mutation ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8137661/]
- 30. Tumour mutational burden: an overview for pathologists [https://www.sciencedirect.com/science/article/pii/S0031302522000307]
- 31. Methods of measurement for tumor mutational burden in tumor ... [https://tlcr.amegroups.org/article/view/23823/html]
- 32. Tumor Mutational Burden in Cervical Cancer as Potential ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12468667/]
- 33. Evaluating Tumour Mutational Burden as a Key Biomarker ... [https://www.mdpi.com/2072-6694/17/3/480]
- 34. Clinicopathological characteristics and the relationship of ... [https://pubmed.ncbi.nlm.nih.gov/40165109/]
- 35. Clinicopathological characteristics and the relationship of PD - L status... 1 [https://bmccancer.biomedcentral.com/articles/10.1186/s12885-025-13938-y]
- 36. as a Potential Tumor for... Mutation Burden Biomarker [https://pubmed.ncbi.nlm.nih.gov/32052340/]
- 37. Immunotherapy Biomarkers | Foundation Medicine [https://www.foundationmedicine.com/resource/immunotherapy-biomarkers]
- 38. Next-Generation Sequencing: A Review of Its Transformative ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12523276/]
- 39. Frontiers | Exosomal PD - L detection in cancer predictive 1 ... biomarker [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2025.1603855/full]
- 40. Applying next-generation sequencing to detect ... [https://www.nature.com/articles/s41698-025-01096-0]
- 41. Limitations of Whole Genome Sequencing in Genetic Testing [https://3billion.io/blog/limitation-of-whole-genome-sequencing]
- 42. Whole exome sequencing — Knowledge Hub [https://www.genomicseducation.hee.nhs.uk/genotes/knowledge-hub/whole-exome-sequencing/]
- 43. Limitations of Whole Exome Sequencing [https://3billion.io/blog/limitations-of-whole-exome-sequencing]
- 44. Analysis of tumor mutational burden: correlation of five ... [https://www.nature.com/articles/s41598-020-68394-4]
- 45. Limitations of the exome sequencing [https://www.asperbio.com/ngs-service/limitations-of-the-exome-sequencing/]
- 46. Limitations of exome sequencing in detecting rare and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8057342/]
- 47. Data-driven design of targeted gene panels for estimating ... [https://www.nature.com/articles/s42003-022-03098-1]
- 48. Costs and Benefits of Whole-Exome, Whole-Transcriptome ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12184969/]
- 49. Next-Generation Sequencing Technology: Current Trends ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10376292/]
- 50. Enhancing the quality of panel-based tumor mutation ... [https://www.nature.com/articles/s41698-024-00504-1]
- 51. Demystifying the Discussion of Sequencing Panel Size in ... [https://www.emjreviews.com/flagship-journal/article/demystifying-the-discussion-of-sequencing-panel-size-in-oncology-genetic-testing-j190222/]
- 52. Can you use NGS panels to test for Tumor Mutational ... [https://nonacus.com/blog-can-you-use-ngs-panels-to-test-for-tumor-mutational-burden/]
- 53. High tumor mutational burden assessed through next ... [https://translational-medicine.biomedcentral.com/articles/10.1186/s12967-024-05927-9]
- 54. Different NGS identification methods of somatic mutation ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11892244/]
- 55. Guidelines for Validation of Next-Generation Sequencing– ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6941185/]
- 56. To be or low TMB (tumor mutational burden) - Falk [https://tcr.amegroups.org/article/view/97043/html]
- 57. To be or low TMB ( tumor ) - PMC mutational burden [https://pmc.ncbi.nlm.nih.gov/articles/PMC11912084/]
- 58. MSK-IMPACT: A Comprehensive Tumor Sequencing Test ... [https://www.mskcc.org/msk-impact]
- 59. Comprehensive detection of germline variants by MSK ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5437632/]
- 60. Regulations, Open Data and Healthcare Innovation [https://pmc.ncbi.nlm.nih.gov/articles/PMC8304506/]
- 61. FDA Approves Two Genomic Profiling Tests for Cancer - NCI [https://www.cancer.gov/news-events/cancer-currents-blog/2017/genomic-profiling-tests-cancer]
- 62. FoundationOne CDx | Foundation ... [https://www.foundationmedicine.com/test/foundationone-cdx]
- 63. Clinical Application of the FoundationOne CDx Assay to ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8018334/]
- 64. Clinical Trial & CDx Development [https://www.foundationmedicine.com/service/clinical-development-and-cdx]
- 65. Blood-based tumor mutational burden as a biomarker for ... [https://www.nature.com/articles/s41591-022-01754-x]
- 66. Blood-based tumor mutational burden as a biomarker in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12586078/]
- 67. Blood-based tumor mutational burden impacts clinical ... [https://www.nature.com/articles/s43856-024-00687-5]
- 68. Preanalytic Variables and Tissue Stewardship for Reliable ... [https://www.sciencedirect.com/science/article/pii/S1525157819300030]
- 69. Impact of Pre-Analytical Variables on Cancer Targeted ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4659597/]
- 70. Systematic review and feasibility study on pre-analytical ... [https://www.nature.com/articles/s41598-024-69285-8]
- 71. PUREE: accurate pan-cancer tumor purity estimation from ... [https://www.nature.com/articles/s42003-023-04764-8]
- 72. Accurate tumor purity determination is critical for the ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10285282/]
- 73. Techniques of using circulating tumor DNA as a liquid ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6197739/]
- 74. Circulating tumor DNA to monitor treatment response in ... [https://www.nature.com/articles/s41698-025-00876-y]
- 75. ClairS-TO: a deep-learning method for long-read tumor ... [https://www.nature.com/articles/s41467-025-64547-z]
- 76. Next-Generation Sequencing Illumina Workflow–4 Key Steps [https://www.thermofisher.com/us/en/home/life-science/cloning/cloning-learning-center/invitrogen-school-of-molecular-biology/next-generation-sequencing/illumina-workflow.html]
- 77. Key Strategies for Optimizing NGS Workflows [https://www.technologynetworks.com/genomics/articles/key-strategies-for-optimizing-ngs-workflows-395232]
- 78. Germline Sequencing Improves Tumor-Only ... - PubMed Central [https://pmc.ncbi.nlm.nih.gov/articles/PMC8710335/]
- 79. Detecting likely germline variants during tumor-based ... [https://www.jci.org/articles/view/190264]
- 80. NGS Basics for Cancer Research [https://www.thermofisher.com/us/en/home/life-science/sequencing/sequencing-learning-center/next-generation-sequencing-information/cancer-research/basics.html]
- 81. Next-generation sequencing in cancer diagnosis and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12009796/]
- 82. Germline Variants that Affect Tumor Progression - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC8043969/]
- 83. Germline genetic variation impacts clonal hematopoiesis ... [https://www.nature.com/articles/s41588-025-02250-x]
- 84. Analytical Validation of Blood-Derived Tumor Mutation ... [https://www.sciencedirect.com/science/article/pii/S1525157825001850]
- 85. The Future of Precision Oncology: Biomarkers and Drug ... [https://binaytara.org/cancernews/article/the-future-of-precision-oncology-biomarkers-and-drug-development]
- 86. Cancer Biomarkers and Precision Oncology: A Review of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11571259/]
- 87. Tumor mutational burden for the prediction of PD-(L)1 ... [https://www.sciencedirect.com/science/article/pii/S092375342400084X]
- 88. Systematic assessment and optimizing algorithm of tumor ... [https://www.frontiersin.org/journals/oncology/articles/10.3389/fonc.2022.972972/full]
- 89. TMBocelot: an omnibus statistical control model optimizing the ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11788372/]
- 90. Recommendations for Tumor Mutational Burden Assay ... [https://www.sciencedirect.com/science/article/pii/S1525157824001156]
- 91. Analytical Validation of Blood-Derived Tumor Mutation ... [https://www.bloodpac.org/publications/analytical-validation-of-blood-derived-tumor-mutation-burden-btmb-assays-a-joint-consensus-recommendation-of-the-bloodpac-btmb-analytical-validation-working-group]
- 92. Understanding BLOODPAC's Analytical Validation Protocols [https://www.bloodpac.org/bloodpac-blog/understanding-bloodpacs-analytical-validation-protocols-for-ctdna-assays]
- 93. Analytical Validation of Blood-Derived Tumor Mutation ... [https://pubmed.ncbi.nlm.nih.gov/40998494/]
- 94. Clinical and analytical validation of a combined RNA ... [https://www.nature.com/articles/s43856-025-00934-3]
- 95. Tumor mutational burden quantification from targeted gene panels ... [https://link.springer.com/article/10.1186/s40425-019-0647-4]
- 96. Enhancing the quality of panel - based tumor mutation burden... [https://www.nature.com/articles/s41698-024-00504-1?error=cookies_not_supported]
- 97. Leveraging non‐coding regions to guarantee the accuracy of... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11611766/]
- 98. Tumor Mutational Burden Estimation with VarSome Clinical [https://docs.varsome.com/en/tmb]
- 99. Comparison of next‑generation sequencing quality metrics ... [https://www.spandidos-publications.com/10.3892/etm.2025.12814]
- 100. Comparison of next‑generation sequencing quality metrics ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11843196/]
- 101. Challenges and Future Directions in the Management of ... [https://www.mdpi.com/2072-6694/15/24/5841]
- 102. Optimizing the evaluation of gene-targeted panels ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8548549/]
- 103. Development and validation of blood tumor mutational burden ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10107199/]
- 104. Evolving Standards in Clinical NGS (updated) [https://www.euformatics.com/blog-post/evolving-standards-in-clinical-ngs]
- 105. A computational framework to improve cross-platform ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11245942/]
- 106. New Global Partnership Enhances NGS for Advanced ... [https://clpmag.com/diagnostic-technologies/molecular-diagnostics/new-global-partnership-enhances-ngs-for-advanced-cancer-research/]
- 107. A Guide to Developing Harmonized Research Workflows in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12233188/]
- 108. Tumor-Type-Specific TMB Cutoffs for Improved ICI ... [https://pubmed.ncbi.nlm.nih.gov/40968606/]