Troubleshooting High Ct Values in Cancer Biomarker Detection: A Strategic Guide for Robust qPCR and dPCR Results
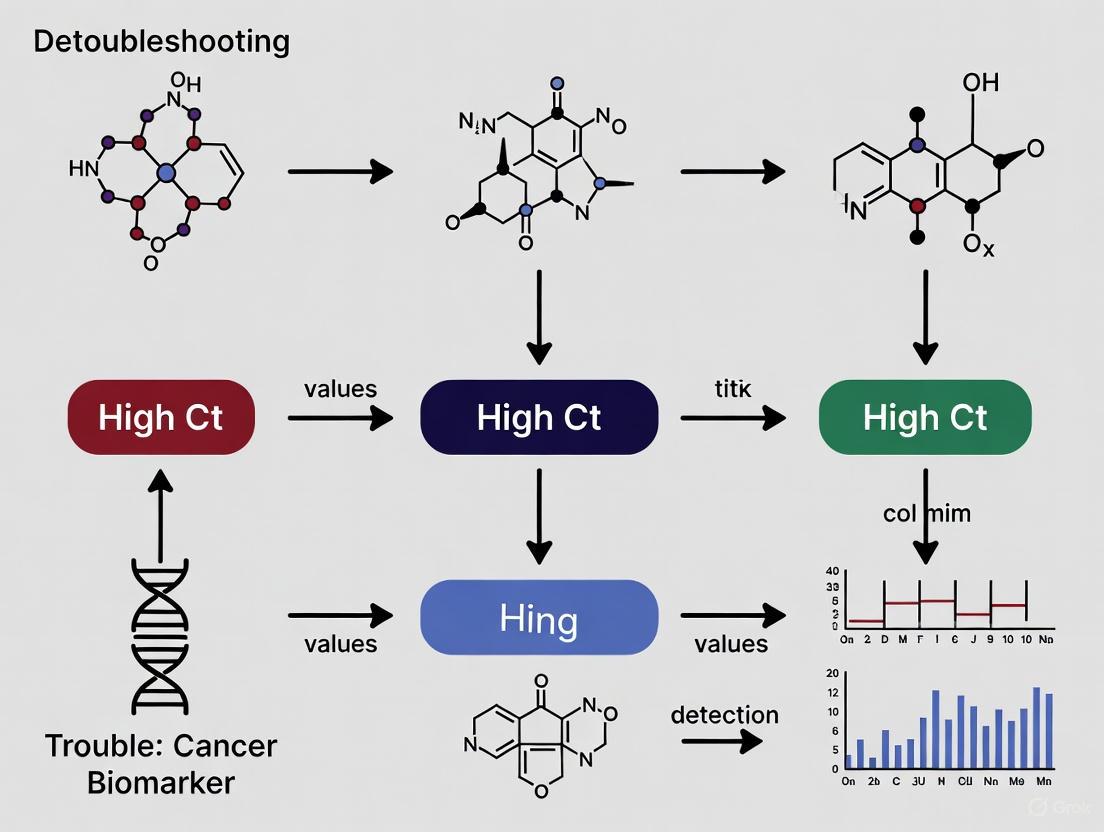
This article provides a comprehensive guide for researchers and drug development professionals facing the challenge of high cycle threshold (Ct) values in the detection of low-abundance cancer biomarkers.
Troubleshooting High Ct Values in Cancer Biomarker Detection: A Strategic Guide for Robust qPCR and dPCR Results
Abstract
This article provides a comprehensive guide for researchers and drug development professionals facing the challenge of high cycle threshold (Ct) values in the detection of low-abundance cancer biomarkers. Covering foundational principles to advanced validation, we explore the biological and technical origins of high Ct values, examine cutting-edge methodologies like digital PCR and next-generation sequencing that enhance sensitivity, detail systematic troubleshooting protocols for pre-analytical, analytical, and post-analytical phases, and establish rigorous frameworks for assay validation and performance benchmarking. By integrating insights from recent advancements in multi-omics and artificial intelligence, this resource aims to empower the development of reliable, clinically translatable biomarker assays for early cancer detection and personalized therapy.
Decoding High Ct Values: Biological and Technical Foundations in Cancer Biomarker Research
What is a Ct Value? The Threshold cycle (Ct) value is a critical metric in real-time PCR (qPCR) that indicates the PCR cycle number at which the fluorescence signal from amplification exceeds a predefined threshold, signifying the detection of the target sequence [1]. This value is central to both qualitative and quantitative analysis, as it is inversely correlated with the starting quantity of the target nucleic acid in the sample; a lower Ct value indicates a higher initial concentration of the target [1].
How is a Ct Value Determined? The determination of a Ct value follows a systematic process [1]:
- Amplification Plot: The real-time PCR instrument generates a plot of fluorescence (ΔRn) versus cycle number.
- Baseline Subtraction: The baseline fluorescence from early cycles is subtracted to normalize the data.
- Threshold Setting: A fluorescence threshold is set within the exponential phase of amplification. This threshold must be above the baseline but within the linear range of the plot to ensure precision and avoid high variability areas.
- Ct Calculation: The Ct value is the cycle at which the amplification curve intersects the threshold.
The following diagram illustrates the relationship between the amplification curve, the threshold, and the Ct value.
The Critical Link Between Ct Values and Low-Abundance Biomarker Detection
In cancer biomarker research, targets like circulating tumor DNA (ctDNA) and microRNA (miRNA) are often present in exceptionally low concentrations. ctDNA, for instance, can constitute less than 1% of the total cell-free DNA in early-stage cancer, making it a classic low-abundance target [2]. The detection of these biomarkers pushes qPCR technology to its sensitivity limits, directly resulting in high Ct values.
Why does this happen?
- Low Starting Concentration: The fundamental principle of qPCR is that the Ct value is a reflection of the initial target quantity. A scarce target, such as a specific ctDNA mutation or a miRNA molecule, requires more amplification cycles to generate a detectable fluorescent signal. This naturally leads to a high Ct value [1].
- Biomarker-Specific Challenges: ctDNA is not only low in concentration but also highly fragmented, which can further complicate primer and probe binding, potentially reducing assay efficiency and contributing to higher Ct values or false negatives [3] [4].
Consequently, a high Ct value in this context is a direct technical challenge. It operates at the limit of the assay's detection capability, where factors like background noise, inhibitors, and subtle efficiency losses have a magnified impact, threatening the reliability of the result.
Systematic Troubleshooting Guide for High Ct Values
When encountering high Ct values in the detection of ctDNA or miRNA, a systematic investigation is required. The following workflow outlines a step-by-step troubleshooting process, from sample preparation to data analysis.
Step 1: Assess Sample Quality and Nucleic Acid Integrity
- Problem: Degraded or poorly handled samples, especially with fragile targets like miRNA or fragmented ctDNA, are a primary cause of high Ct values.
- Solutions:
- Use Fresh or Properly Preserved Samples: For blood-based ctDNA, use specialized collection tubes that stabilize nucleated cells and prevent background DNA release. Process plasma within a few hours of collection [2].
- Verify Extraction Method: Ensure the nucleic acid extraction kit is validated for your specific biomarker type (e.g., small RNAs for miRNA, or short fragmented DNA for ctDNA). Manually check RNA Integrity Numbers (RIN) or DNA fragment size distribution if possible.
Step 2: Check Nucleic Acid Quantity and Purity
- Problem: Inaccurate quantification or the presence of inhibitors co-purified during extraction can severely hamper PCR efficiency.
- Solutions:
- Quantify with Fluorescence-based Methods: Avoid spectrophotometry (A260/A280) for low-concentration samples, as it is insensitive to degradation and can be skewed by contaminants. Use fluorescence dyes (e.g., Qubit, PicoGreen) that specifically bind to nucleic acids for accurate concentration measurement.
- Perform Dilution Test: Dilute the sample 1:5 and re-run the assay. If the Ct value decreases linearly with dilution, it suggests the presence of PCR inhibitors in the original sample. Re-purify the nucleic acid or use a cleaner extraction method.
Step 3: Verify Reaction Efficiency and Inhibition
- Problem: Suboptimal PCR efficiency, often caused by poor primer/probe design or reaction conditions, prevents robust amplification of low-abundance targets.
- Solutions:
- Run a Standard Curve: Prepare a 10-fold serial dilution of a known positive control or synthetic template. The ideal standard curve has a slope of -3.32, which corresponds to 100% PCR efficiency. A slope between -3.6 and -3.1 (90%-110% efficiency) is generally acceptable. A slope outside this range indicates poor efficiency that must be addressed [5].
- Use Unique Molecular Identifiers (UMIs): For ultra-rare targets like ctDNA, incorporate UMIs during reverse transcription or library preparation. UMIs tag individual molecules, allowing bioinformatic correction of PCR amplification biases and errors, leading to more accurate quantification at high Ct values [2].
Step 4: Optimize Assay Design and Thermocycling Conditions
- Problem: Even a well-designed assay may require fine-tuning for maximum sensitivity against challenging backgrounds.
- Solutions:
- Validate Primer/Probe Specificity: Use tools like BLAST to check for off-target binding. For miRNA, ensure the assay can discriminate between highly homologous family members.
- Consider Probe Chemistry: TaqMan probes are highly specific due to the 5' nuclease activity, reducing background and improving signal-to-noise ratio for low-level targets [5].
- Optimize Annealing Temperature: Perform a temperature gradient PCR to determine the optimal annealing temperature for your primer pair, which maximizes specific product yield.
Step 5: Validate with Appropriate Controls
- Problem: Without proper controls, it is impossible to distinguish between a true negative, a failed reaction, or a false negative due to a high Ct value.
- Solutions:
- Include a Positive Control: Use a synthetic oligonucleotide or a known positive sample at a concentration expected to yield a high Ct value (e.g., Ct 35-38). This verifies that the assay can detect low levels of the target under the current run conditions.
- Use a Internal Control: Spike-in a known amount of an exogenous control (e.g., synthetic non-human RNA or DNA) into each sample during lysis. A high Ct or failure for the spike-in control indicates a problem with the reaction itself (e.g., inhibition), invalidating a negative result for the target [1] [6].
Frequently Asked Questions (FAQs)
Q1: What is the maximum acceptable Ct value for a result to be considered reliable? There is no universal maximum Ct value. The cutoff is determined by assay validation. You must establish the Limit of Detection (LoD) for your specific assay by testing replicates of a known positive control at low concentrations. The LoD is typically the concentration at which 95% of the replicates are detected. Any result with a Ct value above the LoD's average Ct should be considered non-detectable or indeterminate. For clinically validated tests, this cutoff is strictly defined [6].
Q2: My negative control shows a Ct value. What does this mean? A Ct value in your no-template control (NTC) indicates contamination.
- If the NTC Ct is high (e.g., >38): This suggests low-level contamination, likely from amplicon carryover or contaminated reagents. You should discard the affected reagents, clean workspaces and equipment, and repeat the experiment.
- If the NTC Ct is low: This indicates significant contamination, and all results from the run are invalid. A systematic decontamination of your workflow is required.
Q3: How should I handle high Ct value data in my quantitative analysis? Exercise extreme caution. The widely used 2−ΔΔCT method assumes 100% PCR efficiency, an assumption that often breaks down in later cycles where efficiency can drop, making quantification at high Ct values inaccurate [7] [5]. For relative quantification, it is better to treat samples with very high Ct values as "non-detected" rather than assigning a numerical value. For absolute quantification, ensure your standard curve covers the high Ct range and that the linearity and efficiency are maintained in that region. Advanced statistical models like ANCOVA are recommended over the 2−ΔΔCT method for more robust analysis, especially when efficiency is not perfect [7].
Q4: Are there alternatives to qPCR for detecting targets that consistently yield high Ct values? Yes, more sensitive technologies are available:
- Digital PCR (dPCR): This method partitions a sample into thousands of individual reactions, allowing for absolute quantification without a standard curve. It is significantly more sensitive and robust for detecting rare targets like ctDNA mutations and can reliably detect sequences that yield Ct values >35 in qPCR [2] [5].
- Next-Generation Sequencing (NGS): Especially when using error-corrected sequencing methods (e.g., duplex sequencing), NGS can detect very low-frequency mutations with high specificity, overcoming the limitations of qPCR for complex, low-abundance biomarker detection [4] [2].
The Scientist's Toolkit: Essential Reagents and Materials
The following table lists key reagents and materials critical for optimizing assays designed to detect low-abundance biomarkers.
| Item | Function & Importance in Low-Abundance Detection |
|---|---|
| Nucleic Acid Stabilization Tubes | Preserves sample integrity from the moment of collection, preventing dilution of ctDNA or miRNA by background genomic DNA release from white blood cells [2]. |
| Nucleic Acid Extraction Kits (Size-Selective) | Designed to efficiently recover short, fragmented nucleic acids like ctDNA and miRNA, maximizing the yield of the target biomarker [3]. |
| Fluorometric Quantitation Kits | Provides accurate concentration measurements of precious, low-yield samples, which is critical for normalizing input material and avoiding false negatives [7]. |
| TaqMan Assays | The probe-based chemistry offers high specificity, reducing false positives from non-specific amplification, which is crucial when signal is near the background level [1] [5]. |
| Unique Molecular Identifiers (UMIs) | Tags individual molecules before amplification, enabling accurate counting and correction for PCR errors and biases, essential for quantifying rare variants [2]. |
| Digital PCR (dPCR) Reagents | Provides an absolute and highly sensitive quantification method, partitioning the sample to overcome PCR inhibition and detect rare targets with superior precision compared to qPCR [2] [5]. |
| Standard Curves & Positive Controls | Validates assay performance, defines the LoD, and is essential for accurate absolute quantification. A low-concentration positive control is vital for verifying high-Ct detection capability [6] [5]. |
FAQs on High Ct Values in Cancer Biomarker Detection
What biological factors can cause high Ct values in ctDNA detection assays?
High Ct values in circulating tumor DNA (ctDNA) detection can often be attributed to biological characteristics of the tumor itself rather than technical assay failure. The primary biological sources are low tumor DNA shedding and high molecular fragmentation.
Table 1: Biological Factors Contributing to High Ct Values
| Biological Factor | Impact on Ct Value | Underlying Mechanism |
|---|---|---|
| Low Tumor Shedding | Increases Ct (less template) | Some tumors release minimal DNA into circulation regardless of size [8] [2] |
| Apoptotic DNA Release | Variable impact | Produces short, fragmented DNA (~167 bp) which may be suboptimal for some assays [8] [9] |
| Necrotic DNA Release | Can improve signal | Releases longer DNA fragments; more prevalent in advanced/aggressive tumors [8] |
| Tumor Heterogeneity | Increases variability | Subclones with different shedding rates create fluctuating ctDNA levels [2] |
| Rapid ctDNA Clearance | Increases Ct | Short half-life (16 min to several hours) means levels can change rapidly [2] |
The amount of ctDNA in a patient's blood does not always correlate directly with tumor size. Some tumors are inherently "low-shedders," releasing minimal DNA into circulation, which directly reduces the template available for PCR amplification and results in higher Ct values [8] [2]. Furthermore, the mechanism of cell death affects the quality of the DNA; apoptosis produces short, nucleosome-bound fragments (~167 bp), while necrosis releases longer fragments. The fragmentation pattern of ctDNA can be more complex in cancer patients, and these shorter fragments may not be efficiently detected by all assay designs [8] [9].
How does tumor heterogeneity impact ctDNA levels and detection sensitivity?
Tumor heterogeneity profoundly affects ctDNA detection by creating a dynamic and variable pool of circulating DNA. Spatial heterogeneity means that different regions of a tumor, or different metastatic sites, may shed DNA at different rates [2]. Temporal heterogeneity refers to the evolution of the tumor over time, especially under treatment pressure, where subclones with different genetic profiles and shedding characteristics may emerge [2]. This can lead to inconsistent ctDNA levels and unexpected fluctuations in Ct values across longitudinal monitoring.
What methodologies can improve detection sensitivity for low-abundance ctDNA?
Overcoming the challenge of low-abundance ctDNA requires highly sensitive techniques and optimized workflows. Key methodological approaches include digital PCR (dPCR) and next-generation sequencing (NGS) with error correction.
Digital PCR (dPCR): This method partitions a single PCR reaction into thousands of nanoreactions, allowing for absolute quantification and detection of rare mutations present at very low frequencies (<0.1%) [2]. It is highly sensitive for tracking known mutations.
Next-Generation Sequencing (NGS): Targeted NGS panels allow for the simultaneous tracking of multiple patient-specific mutations, providing a more comprehensive view of the tumor burden. To overcome sequencing errors that obscure true low-frequency variants, methods incorporating Unique Molecular Identifiers (UMIs) are essential [2]. UMIs are molecular barcodes tagged onto DNA fragments before amplification, enabling bioinformatic filtering of PCR and sequencing errors. Advanced techniques like Duplex Sequencing provide the highest accuracy by sequencing both strands of the DNA duplex [2].
Fragmentation Pattern Analysis: Exploiting the unique size profile of ctDNA can enhance sensitivity. ctDNA fragments are often shorter than non-tumor cfDNA. Bioinformatic filtering for shorter fragments can effectively enrich the tumor-derived signal [8] [2].
Table 2: Experimental Protocols for Sensitive ctDNA Detection
| Method | Key Procedural Steps | Advantage for Low Abundance |
|---|---|---|
| Digital PCR (dPCR) | 1. Partition sample into thousands of droplets/nanowells.2. Perform endpoint PCR amplification.3. Count positive and negative partitions to calculate absolute concentration. | High sensitivity for known single mutations; ideal for monitoring MRD [2]. |
| NGS with UMIs | 1. Ligate UMIs to each DNA fragment during library prep.2. Perform deep sequencing (>10,000x coverage).3. Bioinformatically group reads by UMI to create consensus sequences and remove errors. | Broad panel allows multi-target tracking; error correction reduces false positives [2]. |
| Size Selection | 1. Extract plasma cfDNA.2. Perform gel electrophoresis or use automated size selection.3. Isolate DNA fragments in the 90-150 bp range for library construction. | Physically enriches for ctDNA by removing longer, non-tumor DNA fragments [8]. |
What are the technical versus biological root causes of high Ct values I should investigate?
A systematic investigation is crucial to diagnose the cause of high Ct values. The following workflow outlines a step-by-step troubleshooting guide to distinguish between technical and biological causes.
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials for ctDNA Analysis
| Item | Function in Experiment | Key Consideration |
|---|---|---|
| Cell-Free DNA BCT Tubes | Stabilizes blood samples to prevent white blood cell lysis and background cfDNA release. | Critical for pre-analytical phase; prevents false elevation of wild-type DNA [2]. |
| dPCR Master Mix | Provides reagents for highly sensitive partitioned PCR. | Select mixes designed for detecting rare variants in a high-background wild-type DNA. |
| UMI Adapter Kits | Adds unique molecular barcodes to each DNA fragment during NGS library preparation. | Essential for error correction in NGS-based ctDNA assays [2]. |
| Methylation-Specific Enzymes | Enzymes (e.g., for bisulfite-free conversion) to analyze ctDNA methylation patterns. | Provides an orthogonal method for detecting tumor DNA via epigenetic signatures [8]. |
| iRT Standard Peptides | For retention time calibration in LC-MS workflows, ensuring consistent peptide identification. | A key QC component in proteomic analyses of related biomarkers [10]. |
Frequently Asked Questions
1. What are pre-analytical variables and why do they matter for my qPCR results? Pre-analytical variables are all the steps that occur before the sample is analyzed, including collection, handling, transportation, stabilization, and storage. These steps are critical because studies show that 60-70% of all laboratory errors originate in the pre-analytical phase [11] [12]. Compromises during these stages can lead to nucleic acid degradation or the introduction of inhibitors, directly causing high Ct values, failed assays, and unreliable data in cancer biomarker detection.
2. I used a good extraction kit, but my RNA quality is still poor. What could have gone wrong? The quality of your starting material is the foundation for success. Even the best extraction kit cannot fully recover degraded nucleic acids. Key factors affecting quality include:
- Cold Ischemia Time: The time between tissue collection and preservation should be minimized (e.g., less than 1 hour for DNA PCR analysis) to prevent rapid RNA degradation by cellular nucleases [11].
- Fixation Type and Time: For formalin-fixed paraffin-embedded (FFPE) tissues, fixation in neutral buffered formalin for less than 72 hours is optimal. Prolonged fixation or use of unbuffered formalin causes nucleic acid fragmentation and cross-linking [11].
- Immediate Stabilization: For RNA work, samples should be immediately stabilized using reagents like RNAlater or through flash-freezing to halt nuclease activity [13].
3. My DNA concentrations measure fine, but my NGS results are poor. Why? Spectrophotometric methods (like Nanodrop) measure the concentration of all nucleic acids but do not assess integrity or the presence of inhibitors. Degraded or fragmented DNA, even in sufficient concentration, leads to inefficient library preparation during NGS. One study of FFPE tissues showed that samples with high DNA integrity had an NGS success rate of ~94%, which dropped to ~5.6% for low-integrity samples [14]. Always use fluorometric quantification (e.g., Qubit) and integrity assessment (e.g., TapeStation, Bioanalyzer) for sequencing applications [14].
4. How do freeze-thaw cycles affect my samples? Repeated freeze-thaw cycles progressively degrade nucleic acids and proteins. Each cycle causes physical shearing and can lead to inconsistent results between experiments. It is crucial to aliquot samples into single-use volumes to minimize freeze-thaw cycles [14] [12].
5. My Ct values are consistently high (>35) across multiple assays. What is the first thing I should check? The first and most critical step is to check the quality and integrity of your input nucleic acids [15]. High Ct values are often a direct result of degraded RNA/DNA or the presence of PCR inhibitors carried over from the sample or extraction process [16] [17]. Running your samples on a quality control instrument (e.g., Bioanalyzer) to determine the RNA Integrity Number (RIN) or DNA Integrity Number (DIN) is the most effective diagnostic step.
Sample-Specific Collection & Storage Guidelines
The table below summarizes evidence-based recommendations for handling common sample types to preserve nucleic acid integrity for downstream molecular assays, including cancer biomarker detection.
Table 1: Pre-analytical Guidelines for Common Sample Types in Cancer Research
| Specimen Type | Target | Short-Term Storage | Maximum Recommended Duration | Key Considerations |
|---|---|---|---|---|
| Whole Blood | DNA | Room Temperature (RT) or 2-8°C | 24h (RT), 72h (2-8°C) [11] | For RNA, use specialized RNA stabilization tubes (e.g., PAXgene, Tempus) [13]. |
| Plasma | Cell-free DNA (e.g., ctDNA) | 4°C or -20°C | 5 days (4°C), longer at -20°C [11] | Centrifuge soon after collection to separate plasma from cells. Critical for liquid biopsies [18]. |
| Tissue (Fresh) | DNA/RNA | Snap-freeze in liquid N₂ or place in RNAlater | Immediately | Minimize cold ischemia time. RNAlater allows for storage at 4°C for 24h before long-term storage [11] [13]. |
| FFPE Tissue | DNA/RNA | Room Temperature | Years (with degradation) | Limit formalin fixation to 6-72 hours in neutral buffered formalin [11]. |
| Stool | DNA | RT or 4°C | 4h (RT), 24-48h (4°C) [11] | For microbiome studies, use preservative kits to stabilize microbial community DNA. |
| Swabs (e.g., Cervical) | DNA | 2-8°C | Up to 10 days [11] | Store in appropriate viral transport medium (VTM). |
Troubleshooting Guide: High Ct Values in qPCR
High Ct values indicate delayed amplification, meaning it takes many cycles to detect the signal. This is a common problem in cancer biomarker research, often rooted in pre-analytical issues. The following workflow and table guide you through a systematic diagnosis.
Troubleshooting High Ct Values
Table 2: Diagnosing and Resolving Common Causes of High Ct Values
| Problem | Root Cause | Solution | Preventive Measure |
|---|---|---|---|
| Nucleic Acid Degradation | Extended cold ischemia; improper fixation; repeated freeze-thaw; nuclease contamination. | Re-extract from original sample if possible. For FFPE, use protocols designed for cross-linked nucleic acids. | Minimize time to preservation; use nuclease-free consumables; aliquot samples [11] [14]. |
| PCR Inhibition | Carryover of salts, phenol, ethanol, heparin, or humic acids from the sample or extraction. | Perform a nucleic acid clean-up (e.g., column-based purification, ethanol precipitation). Add a dilution series of your template to detect inhibition [16] [14]. | Ensure complete removal of wash buffers; use high-quality, inhibitor-free reagents; include a sample pre-wash step for complex matrices [14]. |
| Suboptimal Primer/Probe | Primer-dimer formation; non-specific binding; secondary structures. | Redesign primers using specialized software. Optimize annealing temperature via gradient PCR [16]. | Validate all primer sets with a positive control template before using on experimental samples. |
| Template Overload | Excess template DNA can scatter primers and probes, delaying specific binding. | Dilute the sample template (10x to 1000x) and re-run the assay [17]. | Perform accurate fluorometric quantification and establish a standard curve for optimal template input. |
| Low RNA Quality | RNA degradation during handling (very common). | Check RIN value; for degraded RNA, use a 3'-end sequencing method like BRB-seq, which is tolerant of lower RIN values [13]. | Immediately preserve samples in RNAlater or flash-freeze in liquid nitrogen [13]. |
The Scientist's Toolkit: Essential Research Reagents
The following table lists key reagents and tools that are fundamental for maintaining nucleic acid integrity throughout the pre-analytical phase.
Table 3: Key Reagent Solutions for Pre-Analytical Workflows
| Reagent / Tool | Function | Application Note |
|---|---|---|
| RNAlater Stabilization Solution | Rapidly permeates tissues to inactivate RNases, preserving RNA at room temp for short periods. | Ideal for field collection or when immediate freezing is impractical. Minimizes need for flash-freezing [13]. |
| PAXgene / Tempus Blood RNA Tubes | Specialized blood collection tubes containing reagents that stabilize RNA at the point of draw. | Critical for reliable gene expression studies from whole blood; prevents changes in transcript profiles [13]. |
| Neutral Buffered Formalin (NBF) | The recommended fixative for tissue histology and molecular pathology. Prevents acid-induced nucleic acid degradation. | Always prefer NBF over unbuffered formalin. Limit fixation time to under 72 hours for optimal DNA recovery [11]. |
| Magnetic Bead-Based Kits | For automated nucleic acid extraction. Provide high consistency and reduce hands-on time/cross-contamination. | Platforms like the Thermo Fisher KingFisher offer reproducible yields and are effective for high-throughput labs [14]. |
| Qubit Fluorometer & Assays | Provides highly accurate, dye-based quantification of DNA/RNA, specific for double-stranded DNA or RNA. | Essential for NGS. Prefer over spectrophotometry for library preparation to avoid concentration inaccuracies [14]. |
| Automated Liquid Handler (e.g., I.DOT) | Non-contact, tipless dispenser for nanoliter volumes. Reduces pipetting error and cross-contamination. | Improves accuracy and reproducibility of qPCR assays by ensuring consistent reagent volumes [16]. |
Limitations of Traditional Biomarkers and the Need for Advanced Detection Platforms
Cancer biomarkers are biological molecules, such as proteins, genes, or metabolites, that can be objectively measured to indicate the presence, progression, or behavior of cancer. They are indispensable in modern oncology for early detection, diagnosis, treatment selection, and monitoring of therapeutic responses [19]. However, traditional biomarkers often disappoint due to significant limitations in their sensitivity and specificity, resulting in overdiagnosis and/or overtreatment in patients [19].
For instance, Prostate-Specific Antigen (PSA) levels can rise due to benign conditions like prostatitis, leading to false positives and unnecessary invasive procedures. Similarly, CA-125 is not exclusive to ovarian cancer and can be elevated in other cancers or non-malignant conditions [19]. Furthermore, many established biomarkers do not emerge until the cancer is already advanced, reducing their value in early detection [19]. These shortcomings highlight the urgent need for more reliable screening tools and advanced detection platforms.
★ FAQs on Traditional Biomarker Limitations
1. What are the main limitations of traditional protein biomarkers like PSA and CA-125?
The primary limitations are poor sensitivity and specificity. These biomarkers are not exclusive to cancer, as their levels can be elevated in various benign conditions. This lack of specificity often leads to false positives, unnecessary invasive procedures, and patient anxiety [19]. Additionally, their sensitivity for early-stage disease is frequently low, meaning they often fail to detect cancer in its most treatable stages.
2. Why are single-biomarker tests increasingly being replaced?
There is a growing realization that biomarker panels or profiling is more valuable in cancer testing and personalized management than single-biomarker assessments [19]. Cancer is a complex and heterogeneous disease; a single molecule is often insufficient to capture its full biological reality. Multi-analyte panels that combine DNA mutations, methylation profiles, and protein biomarkers have demonstrated a superior ability to detect cancer simultaneously, with encouraging sensitivity and specificity [19].
3. What pre-analytical factors most commonly cause biomarker test failures?
Pre-analytical causes account for about 90% of all failed next-generation sequencing (NGS) cases. A study of 1,528 specimens found that 22.5% failed testing, with 65% of failures due to insufficient tissue and 28.9% due to insufficient DNA [20]. Factors strongly associated with failure include:
- Site and type of biopsy
- Clinical setting (initial diagnosis vs. recurrence)
- Age of the specimen and tumor viability [20]
Table 1: Factors Associated with Failed NGS Testing in a 1528-Specimen Cohort [20]
| Failure Category | Percentage of All Failures | Primary Associated Factors |
|---|---|---|
| Insufficient Tissue (INST) | 65% (223/343) | Site of biopsy, Type of biopsy, Clinical setting, Age of specimen, Tumor viability |
| Insufficient DNA (INS-DNA) | 28.9% (99/343) | Site of biopsy, Type of biopsy, Clinical setting, DNA purity, DNA degradation |
| Failed Library (FL) | 6.1% (21/343) | DNA purity, DNA degradation, Type of biopsy |
★ Troubleshooting Guide: Addressing High Ct Values in Biomarker Detection
A high Cycle Threshold (Ct) value in quantitative PCR (qPCR) indicates delayed amplification and low template quality or quantity. This is a common challenge when detecting scarce biomarkers, such as in liquid biopsies.
Problem: Ct values are higher than usual (>35) or undetectable in my qPCR-based biomarker assay.
Potential Causes and Solutions:
Cause 1: Poor Template Quality or Quantity
- Solution: Check RNA/DNA quality using recommended quality control checks. Use more input total RNA/DNA, or use the template at a lower dilution factor [15]. For DNA, ensure the input is within the functional range (e.g., 100 ng to 1 ng for gDNA); higher Ct values may indicate poor quality, degraded DNA, or inhibitors [21].
Cause 2: Excess Template or Inhibitors
Cause 3: Low or No Expression of Target
- Solution: The corresponding gene may not be expressed above the limit of detection. Use a template known to contain the gene of interest as a positive control to troubleshoot the PCR reagents and experimental procedure [15].
Table 2: Troubleshooting High Ct Values in qPCR Experiments
| Symptom | Potential Cause | Recommended Action |
|---|---|---|
| High Ct (>35) in all samples, including positive control | Inefficient reaction setup, degraded reagents | Prepare fresh reagents, run a new standard curve, optimize primer concentrations |
| High Ct only in patient samples | Poor sample quality, presence of PCR inhibitors | Check nucleic acid quality (degradation), dilute sample to reduce inhibitors, purify sample |
| High Ct for one biomarker, others are normal | Low expression of that specific target or suboptimal assay | Validate assay with a known positive sample; consider using a more abundant biomarker |
| Undetermined Ct (not detectable) | Target absent or below detection limit, major reaction failure | Increase input of template RNA/DNA; use a more sensitive technology (e.g., digital PCR) |
★ Advanced Detection Platforms: Moving Beyond Tradition
To overcome the limitations of traditional biomarkers and the technical challenges of qPCR, the field is rapidly evolving towards more sophisticated, multi-omics platforms.
1. Liquid Biopsies and Circulating Biomarkers Liquid biopsies, which analyze circulating tumor DNA (ctDNA), circulating tumor cells (CTCs), or exosomes from a blood sample, represent a non-invasive alternative to traditional tissue biopsies [19]. This method permits early detection and real-time monitoring. Key advancements include:
- Enhanced Sensitivity and Specificity: Advances in ctDNA analysis and exosome profiling are increasing the reliability of liquid biopsies for early disease detection and monitoring [22].
- Multi-Cancer Early Detection (MCED): Tests like the Galleri test, which analyzes ctDNA, are designed to detect over 50 cancer types simultaneously and are undergoing clinical trials [19].
2. Next-Generation Sequencing (NGS) and Multi-Omics NGS-based comprehensive genomic profiling allows for the simultaneous assessment of multiple biomarkers across many genes [19]. This is often coupled with multi-omics approaches that integrate genomics, proteomics, metabolomics, and transcriptomics to achieve a holistic understanding of disease mechanisms [23] [22]. This shift toward systems biology promotes a deeper understanding of how different biological pathways interact in health and disease [22].
3. Artificial Intelligence and Machine Learning AI and ML are revolutionizing biomarker analysis by identifying subtle patterns in large, complex datasets that human observers might miss [19] [23]. These tools enable the integration of various molecular data types with imaging to enhance diagnostic accuracy and therapy recommendations [19]. AI-driven algorithms are being developed for predictive analytics, automated data interpretation, and personalized treatment plans [22].
★ The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Reagents and Kits for Advanced Biomarker Detection
| Item | Function | Example Application |
|---|---|---|
| Nucleic Acid Extraction Kits (e.g., QIAamp DNeasy) | Isolation of high-quality DNA/RNA from complex samples (FFPE, blood, stool) | Pre-analytical step for NGS or qPCR; critical for obtaining sufficient, non-degraded material [20] |
| Multiplex PCR Primer Panels | Simultaneous amplification of multiple biomarker targets in a single reaction | Targeted NGS panels for comprehensive cancer gene profiling; increases efficiency and reduces sample input requirements [19] [24] |
| TaqMan Mutation Detection Assays | Allele-specific PCR for detecting known somatic mutations with high specificity | Validated assays for detecting key oncogenic drivers like EGFR, KRAS, and BRAF mutations [21] |
| Synthetic RNA/DNA Controls | Precisely quantified external controls for standard curve generation and assay validation | Determining the limit of detection and ensuring run-to-run reproducibility in qPCR and NGS [24] |
| Single-Cell RNA-Seq Kits | Profiling gene expression at the individual cell level | Uncovering tumor heterogeneity and identifying rare cell populations that drive disease [22] |
★ Experimental Protocol: Validating Novel mRNA Biomarkers from Stool for Colorectal Cancer Detection
The following workflow, derived from a 2025 study, details a robust method for identifying and validating novel mRNA biomarkers for detecting colorectal cancer (CRC) and advanced adenoma (AA) from stool samples [25]. This protocol exemplifies the multi-step process required to move from bioinformatic discovery to clinical validation.
Workflow for Stool mRNA Biomarker Validation
1. Bioinformatic Screening & Candidate Identification
- Data Acquisition: Download RNA-seq datasets from The Cancer Genome Atlas (TCGA) and Genotype-Tissue Expression (GTEx) databases. A combined dataset of 478 colon cancer and 692 normal colon/rectum tissue samples was used [25].
- Data Processing: Perform batch correction to merge datasets using a tool like ComBat-seq. Conduct a differential expression analysis comparing CRC tissue to healthy tissue using edgeR [25].
- Gene Ranking: Rank genes based on stringent criteria:
- Statistical Significance: False discovery rate (FDR) < 0.001.
- Discriminatory Power: Area under the curve (AUC) > 0.9 when comparing CRC to healthy tissue.
- Magnitude of Change: Log2 fold-change > 2.
- Expression Level: High median expression in CRC tissue.
- Output: A prioritized list of candidate genes (e.g., the top 20) for experimental validation [25].
2. Wet-Lab Validation on Clinical Samples
- Sample Cohort: Procure a well-characterized set of clinical stool samples (e.g., 33 CRC, 28 Advanced Adenoma, 53 Controls) [25].
- RNA Extraction & QC: Extract total RNA from stool samples. This is a critical step due to the complex and inhibitory nature of the stool matrix. Perform rigorous quality control.
- qRT-PCR Analysis: Test the expression of the top candidate genes via qRT-PCR across the sample cohort.
3. Analytical and Clinical Validation
- Statistical Correlation: Calculate the Pearson correlation coefficient between tissue and stool expression levels for the candidates (r=0.57, p=0.007 in the source study) [25].
- Performance Assessment: Evaluate the diagnostic performance by calculating the Area Under the Receiver Operator Curve (AUC). The combined 20-gene panel achieved an AUC of 0.94 for detecting CRC and 0.83 for detecting AA [25].
Advanced Methodologies for Enhancing Sensitivity in Low-Abundance Biomarker Detection
Frequently Asked Questions (FAQs) and Troubleshooting Guide
This technical support resource addresses common challenges in liquid biopsy research, providing targeted solutions for issues related to circulating tumor DNA (ctDNA), circulating tumor cells (CTCs), and exosomes, with a specific focus on troubleshooting high Ct values in cancer biomarker detection.
Circulating Tumor DNA (ctDNA)
FAQ: Why are my ctDNA assays yielding high Ct values or failing to detect known mutations?
High Ct values in ctDNA analysis typically indicate a low concentration of the target mutant DNA sequence relative to the wild-type background. This is a common challenge due to the inherent biological and technical complexities of working with ctDNA.
- Primary Cause: Low variant allele frequency (VAF), often below 0.1% in early-stage disease, is the most frequent cause [26] [27]. The amount of ctDNA can be vanishingly low, sometimes less than 1-100 copies per mL of plasma [27].
- Pre-analytical Factors: The use of improper blood collection tubes (e.g., regular EDTA tubes without rapid processing) can lead to genomic DNA contamination from lysed white blood cells, drastically diluting the ctDNA fraction [27]. Factors like recent physical exercise, surgical trauma, or underlying inflammatory conditions in the patient can also increase the background level of wild-type cell-free DNA [27].
Troubleshooting Guide for ctDNA Detection
| Challenge | Root Cause | Recommended Solution |
|---|---|---|
| Low Analytical Sensitivity | ctDNA concentration below assay detection limit [27]. | Use ultra-sensitive methods like droplet digital PCR (ddPCR) or ultra-deep next-generation sequencing (NGS) (>10,000x coverage) [28] [27]. |
| High Wild-Type Background | Contamination from lysed blood cells; patient's physiological condition [27]. | Use cell-stabilizing blood collection tubes (e.g., Streck cfDNA) and process plasma within 2-6 hours if using EDTA tubes [27]. |
| Pre-analytical DNA Degradation | Improple blood draw, handling, or storage [27]. | Use butterfly needles, avoid fine-gauge needles/prolonged tourniquet, and ensure immediate double-centrifugation for plasma separation [27]. |
| Rapid In Vivo Clearance | ctDNA is quickly eliminated by liver macrophages and nucleases [27]. | Research approaches to slow clearance (e.g., interfering with nucleases) are in development to increase yield [27]. |
Detailed Protocol: Optimized Plasma Collection for ctDNA Analysis
- Blood Draw: Use a 21-gauge butterfly needle and avoid prolonged tourniquet use to prevent hemolysis [27].
- Collection Tube: Draw a minimum of 10 mL of blood into cfDNA-specific BCTs (e.g., Streck, PAXgene). For EDTA tubes, process within 2-6 hours of collection [27].
- Plasma Separation: Perform a first centrifugation at 800-1600 RCF for 10 minutes at 4°C to separate plasma from cells.
- Plasma Clarification: Transfer the supernatant to a new tube and perform a second centrifugation at 16,000 RCF for 10 minutes to remove any remaining cellular debris.
- Storage: Aliquot the purified plasma and store at -80°C to prevent freeze-thaw cycles.
Circulating Tumor Cells (CTCs)
FAQ: Why is my CTC yield low, and how can I improve capture efficiency and purity?
The extreme rarity and heterogeneity of CTCs make their isolation and detection technically demanding. Low yields can stem from both biological factors and limitations of the chosen isolation technology.
- Primary Cause: CTCs are exceptionally rare, with as few as 1 CTC per billion blood cells, and fewer than 1 CTC per 10 mL of blood in early-stage cancer [29]. Furthermore, CTCs undergo epithelial-to-mesenchymal transition (EMT), leading to loss of epithelial markers like EpCAM, which are used in many capture technologies [29] [30].
- Technical Challenges: The complex blood environment causes non-specific binding, creating high background noise. High shear stress during isolation can also damage CTCs, reducing recovery and viability for downstream culture [29].
Troubleshooting Guide for CTC Isolation
| Challenge | Root Cause | Recommended Solution |
|---|---|---|
| Extreme Rarity | Low abundance of CTCs in blood [29]. | Process larger blood volumes (≥10 mL); use technologies that enable high-throughput processing [29] [30]. |
| Tumor Heterogeneity | Loss of epithelial markers (e.g., EpCAM) due to EMT [29] [30]. | Combine size-based (e.g., microfilters) and label-based (e.g., antibody) methods; use multiple biomarkers (e.g., EpCAM, vimentin) [29] [30]. |
| Low Purity & Viability | Non-specific binding of blood cells; harsh isolation conditions [29]. | Use negative enrichment (CD45+ depletion) or antifouling surfaces; employ low-shear microfluidic devices (e.g., Chip-based systems) [29] [30]. |
| Technical Complexity | Lack of standardized protocols across platforms [29]. | Automate capture and analysis where possible; use preservative tubes for sample integrity during transport [29]. |
Detailed Protocol: Combined EpCAM and Size-Based CTC Enrichment This protocol leverages the CellSearch system for immunomagnetic enrichment followed by microfluidic filtration for high-purity recovery.
- Reagents: Anti-EpCAM coated magnetic beads, anti-cytokeratin (CK) antibodies, anti-CD45 antibodies, 4′,6-diamidino-2-phenylindole (DAPI), fluorescence mounting medium.
- Equipment: CellSearch system or equivalent immunomagnetic separator, microfluidic filtration device (e.g., porous membrane filter with 8 µm diameter pores), fluorescent microscope.
Workflow:
- Immunomagnetic Enrichment: Incubate 7.5-10 mL of blood with anti-EpCAM magnetic beads for 15 minutes at room temperature. Place the tube in a magnetic separator and discard the supernatant.
- Washing: Resuspend the bead-bound cells in PBS and place in the magnet again. Repeat washing twice to remove unbound cells.
- Microfluidic Filtration: Resuspend the enriched cell fraction in PBS and load into a size-based microfluidic device. Apply a low pressure to pass the suspension through the filter, retaining larger CTCs.
- Immunofluorescence Staining: Fix the cells on the filter and stain with anti-CK (FITC), anti-CD45 (PE), and DAPI.
- Identification and Enumeration: Identify CTCs as CK+/DAPI+/CD45- under a fluorescent microscope [30].
Exosomes
FAQ: Why is my exosome detection signal weak, and how can I improve sensitivity?
Weak signals often result from low purity of isolated exosomes, inefficient capture on the sensor surface, or suboptimal detection probes.
- Primary Cause: The nanoscale size of exosomes (typically 30-150 nm) and their low concentration in complex biological fluids pose significant challenges for sensitive detection [31] [32]. Inefficient isolation methods or the use of a single, non-specific biomarker can further reduce the signal.
- Technical Challenges: Commonly used methods like ultracentrifugation can co-isolate contaminants like lipoproteins, while immunoaffinity methods can be limited by antibody cost and stability [32].
Troubleshooting Guide for Exosome Detection
| Challenge | Root Cause | Recommended Solution |
|---|---|---|
| Low Abundance & Small Size | Target exosomes are present at low concentrations and are difficult to label [32]. | Use high-affinity capture probes (e.g., aptamers against CD63); employ signal amplification strategies (e.g., enzymatic, nanomaterial-enhanced) [31] [32]. |
| Biomarker Heterogeneity | Reliance on a single marker (e.g., CD9) that is not universally expressed [32]. | Perform multiplexed profiling of several surface markers (e.g., CD9, CD63, CD81, EGFR) to capture heterogeneous populations [31]. |
| Low Purity & Reproducibility | Co-isolation of non-exosomal contaminants; tedious procedures [32]. | Combine isolation techniques (e.g., size-exclusion chromatography followed by affinity capture); use nanomaterial-based platforms (e.g., MXenes) for improved purity [32] [33]. |
| Matrix Effects | Signal interference from proteins/lipids in biofluids [33]. | Optimize blocking agents (e.g., BSA); validate assays in the specific biological matrix (e.g., plasma, urine) [31] [33]. |
Detailed Protocol: Paper-Based Vertical Flow Assay (VFA) for Exosome Profiling This protocol provides a rapid, cost-effective alternative to flow cytometry for exosome surface protein profiling [31].
- Reagents: Nitrocellulose membrane, primary antibodies (e.g., anti-CD9, anti-CD63, anti-CD81, anti-EGFR), secondary antibody-ALP conjugate, NBT/BCIP substrate, blocking buffer (1% BSA in PBS).
- Equipment: VFA cartridge, vacuum manifold, smartphone or gel documentation system.
Workflow:
- Exosome Isolation: Isolate exosomes from cell culture supernatant or patient plasma using differential ultracentrifugation or a commercial kit [31].
- VFA Assembly: Place the nitrocellulose membrane into the VFA cartridge.
- Sample Application: Load the exosome sample onto the membrane and apply a gentle vacuum to facilitate perpendicular flow and capture.
- Immunodetection:
- Block the membrane with 1% BSA for 30 minutes.
- Incubate with primary antibody (e.g., anti-CD63) for 20 minutes.
- Wash and incubate with ALP-conjugated secondary antibody for 20 minutes.
- Add NBT/BCIP substrate to develop a colorimetric signal.
- Signal Quantification: Capture an image of the membrane with a smartphone and quantify the spot intensity using image analysis software like ImageJ [31].
The Scientist's Toolkit: Essential Research Reagents and Materials
| Item | Function/Benefit | Example Application |
|---|---|---|
| Cell-Stabilizing Blood Collection Tubes | Prevents white blood cell lysis for up to 7 days, preserving ctDNA VAF [27]. | ctDNA analysis from shipped blood samples. |
| Anti-EpCAM Coated Magnetic Beads | Immunoaffinity capture of epithelial CTCs from whole blood [30]. | Positive enrichment of CTCs using systems like CellSearch. |
| Microfluidic Chip Devices | Low-shear, high-purity CTC isolation based on size/deformability [29]. | Label-free capture of CTCs undergoing EMT. |
| Aptamers (e.g., CD63 aptamer) | Stable, synthetic alternatives to antibodies for exosome capture [32]. | Functionalization of electrochemical biosensors for exosome detection. |
| MXene (Ti3C2) Nanosheets | 2D material with high surface area and conductivity for biosensing [32]. | Signal amplification in electrochemical exosome sensors. |
| Stable Isotope-Labeled Internal Standards | Normalizes for variability in sample prep and analysis for LC-MS/MS [33]. | Absolute quantification of exosomal proteins. |
Experimental Workflows and Logical Diagrams
ctDNA Analysis Optimization Pathway
CTC Capture Strategy Selection
Exosome Detection and Characterization Workflow
Leveraging Next-Generation Sequencing (NGS) for Comprehensive Mutation Profiling
FAQs: NGS and qPCR in Cancer Biomarker Detection
Q1: How are qPCR Ct values and NGS quality control interconnected? The Cycle Threshold (Ct) value from qPCR is a critical quality control checkpoint in the NGS workflow. It represents the number of amplification cycles required for a target gene's signal to cross a fluorescence threshold, and it is inversely correlated with the starting template concentration [34]. In the context of NGS library preparation, qPCR is used to accurately quantify the concentration of "amplifiable" library fragments before sequencing, ensuring optimal loading on the sequencer for balanced run performance [35]. Anomalous Ct values can indicate issues that will compromise NGS results, such as low template quality or the presence of PCR inhibitors [34].
Q2: What are the primary sources of error in deep NGS for low-frequency variant detection? Sequencing errors are key confounding factors when detecting low-frequency variants, which are crucial for cancer diagnosis and monitoring. A comprehensive analysis identified that errors are introduced at various steps [36]:
- Sample Handling: Can lead to DNA damage, notably causing C>A/G>T substitution errors [36].
- Enrichment PCR: Target-enrichment PCR can lead to an approximately 6-fold increase in the overall error rate [36].
- Polymerase Errors: Incorrect nucleotide incorporation during amplification.
- Sequencing Chemistry: Platform-specific errors during the sequencing process itself.
The study found that different errors have characteristic rates, with A>G/T>C changes occurring at a rate of about 10⁻⁴, while A>C/T>G, C>A/G>T, and C>G/G>C changes occur at a lower rate of 10⁻⁵ [36].
Q3: What strategies can improve the detection of rare mutations in liquid biopsy? Detecting rare mutant alleles in circulating tumor DNA (ctDNA) is challenging due to the low abundance of ctDNA and the high error rates of conventional methods. Advanced methods involve using Unique Identifiers (UIDs). These are barcode sequences ligated to individual DNA molecules before amplification [37]. All copies derived from the same original molecule (sharing the same UID) are grouped to generate a consensus sequence, which helps distinguish true low-frequency mutations from random PCR or sequencing errors [37]. Newer PCR-based methods like SPIDER-seq are being developed to enable effective error correction with simpler, more cost-effective amplicon sequencing workflows [37].
Troubleshooting Guides
Guide 1: Addressing High Ct Values in Pre-NGS qPCR
High Ct values indicate low initial template concentration or reaction inhibition, which can lead to failed or low-quality NGS results. The table below summarizes common causes and solutions.
| Problem Cause | Specific Examples | Recommended Solutions |
|---|---|---|
| Low Template Concentration/Quality | Template degradation; insufficient input DNA/RNA [34]. | Increase template input; re-extract nucleic acids; check RNA integrity (RIN > 8) [34]. |
| PCR Inhibitors | Co-purified proteins, detergents from extraction; high concentration of reverse transcription reagents [34]. | Dilute the cDNA template; re-purify DNA/RNA; assess sample purity via A260/A280 and A260/A230 ratios [34]. |
| Low Reaction Efficiency | Suboptimal primer design (dimers, hairpins, mismatches); amplicon too long; unsuitable reaction conditions [34]. | Redesign primers; ensure amplicon length is 80-300 bp; optimize annealing temperature; use a two-step protocol [34]. |
| Reagent/Instrument Issues | Improper reagent mixing; pipetting errors; low polymerase activity or suboptimal buffer [34]. | Mix reagents thoroughly; calibrate pipettes; use a different, high-fidelity PCR kit [34]. |
Guide 2: Mitigating Sequencing Errors in NGS Data
Accurate detection of somatic mutations, especially at low frequencies, requires minimizing and correcting for errors. The following table outlines major error types and their mitigation strategies.
| Error Type / Source | Characteristic Error Profile | Recommended Mitigation Strategies |
|---|---|---|
| Sample Handling & DNA Damage | Elevated C>A/G>T substitutions [36]. | Optimize sample collection and storage; use gentle extraction methods. |
| PCR Amplification Errors | Overall increase in error rates (~6-fold); sequence context-dependent errors [36]. | Use high-fidelity polymerases; minimize PCR cycles; employ UID/barcoding consensus methods [36] [37]. |
| Sequencing Chemistry Errors | Platform-specific base substitution errors [36]. | Trim low-quality bases from read ends; filter low-quality reads; use bioinformatic error-suppression tools [36]. |
| Oxidative Damage | Not specified in results. | Include antioxidant additives in reaction buffers. |
Experimental Protocols for Key Methodologies
Protocol 1: qPCR-Based Quantification of NGS Libraries
Purpose: To accurately determine the concentration of amplifiable NGS library fragments prior to sequencing, ensuring equitable sample representation [35].
Materials:
- SYBR Green or EvaGreen qPCR master mix
- Adapter-specific primers
- DNA standards of known concentration
- Prepared NGS libraries
- Real-time PCR instrument
Method:
- Prepare Standards and Samples: Serially dilute the DNA standards to create a standard curve. Dilute the NGS library samples to within the dynamic range of the standard curve.
- Set Up qPCR Reactions: For each standard and unknown library sample, prepare a reaction mix containing the qPCR master mix, primers, and template.
- Run qPCR Program: Use the following cycling conditions:
- Initial Denaturation: 95°C for 2 minutes
- 40 Cycles of:
- Denaturation: 95°C for 7 seconds
- Annealing/Extension: 55°C for 15 seconds [38]
- Data Analysis: The instrument software will generate Ct values for all samples. Plot the standard curve (Ct vs. log concentration) and use it to calculate the concentration of amplifiable fragments in the library samples. Normalize the calculated molarity based on the average library size determined by a method like Fragment Analyzer or Bioanalyzer [35].
Protocol 2: Molecular Barcoding for Low-Frequency Variant Detection
Purpose: To sensitively detect rare mutations (e.g., in ctDNA) by reducing false positives from PCR and sequencing errors [37].
Materials:
- DNA samples (e.g., cfDNA from plasma)
- UID-containing adapters and primers
- High-fidelity DNA polymerase
- PCR purification kit
- NGS platform
Method:
- UID Ligation: Fragment genomic DNA and ligate UID-containing adapters to individual DNA molecules. Alternatively, for amplicon-based methods like SPIDER-seq, use primers with UIDs in the first PCR cycles [37].
- Library Amplification: Amplify the tagged library using a high-fidelity polymerase. The number of cycles should be optimized to avoid over-amplification, which can create artifacts and reduce library complexity [35].
- NGS Sequencing: Sequence the final library on an NGS platform to a sufficient depth.
- Bioinformatic Analysis:
- Demultiplexing: Assign reads to samples based on index sequences.
- Cluster Formation: Group reads that share a common UID, indicating they originated from the same original DNA molecule.
- Consensus Calling: Generate a single consensus sequence for each cluster of reads. A true mutation is one that appears in the consensus of a cluster, while random errors are eliminated through the consensus-building process [37].
Workflow Visualization
NGS Library Preparation and QC Workflow
Research Reagent Solutions
The following table lists key reagents and their critical functions in NGS and qPCR workflows for reliable mutation profiling.
| Reagent / Kit | Primary Function | Key Considerations for Quality Control |
|---|---|---|
| High-Fidelity DNA Polymerase | Amplifies DNA for library construction with minimal errors [36]. | Essential for reducing polymerase-induced errors during PCR enrichment; compare error rates of different polymerases [36]. |
| qPCR Quantification Kit | Precisely measures concentration of amplifiable NGS library fragments [35]. | Use adapter-specific primers for accurate quantification; normalize molarity based on library size from electrophoresis [35]. |
| DNA Extraction Kit | Ishes high-quality, intact nucleic acids from tumor samples. | Assess DNA quality via A260/A280 ratio (ideal: 1.7-2.2) [39]; ensure sufficient input mass (>20 ng) [39]. |
| UID/Barcoding Adapter Kit | Tags individual DNA molecules for error correction and rare variant detection [37]. | Critical for liquid biopsy and low-frequency variant applications; enables consensus sequencing to distinguish true mutations from noise [37]. |
| Microcapillary Electrophoresis Kit | Analyzes library size distribution and detects by-products like adapter dimers [35]. | Check for a sharp, dominant peak at expected size; by-products >3% of the total library should be removed by re-purification [35]. |
Digital PCR (dPCR) and its Superior Quantification of Rare Targets
In cancer biomarker detection research, the accurate quantification of rare targets, such as circulating tumor DNA (ctDNA), is paramount for early diagnosis, monitoring minimal residual disease, and guiding personalized therapy. However, researchers often face the challenge of high Ct (Cycle threshold) values in quantitative real-time PCR (qPCR), indicating low target abundance that borders on the limit of detection. These high Ct values introduce uncertainty, poor precision, and hinder reliable quantification. Digital PCR (dPCR) emerges as a powerful solution to this problem, fundamentally reimagining nucleic acid quantification. By providing absolute quantification without the need for standard curves and demonstrating superior tolerance to PCR inhibitors, dPCR is revolutionizing the detection of rare mutations in complex biological samples like plasma, thereby enabling more robust and reliable cancer diagnostics [40] [41] [42].
dPCR vs. qPCR: A Technical Comparison
Core Principles and Workflows
The fundamental difference between the two techniques lies in their approach to quantification.
- Quantitative Real-Time PCR (qPCR) relies on measuring the accumulation of fluorescent signal at each cycle during the exponential phase of amplification. The cycle at which the fluorescence crosses a predefined threshold (Ct value) is used, with reference to a standard curve, to determine the relative quantity of the starting nucleic acid material [40].
- Digital PCR (dPCR), in contrast, is an end-point measurement. The reaction mixture is partitioned into thousands of individual micro-reactions. After amplification, each partition is analyzed as either positive (containing the target) or negative (not containing the target). The absolute concentration of the target, in copies per microliter, is then calculated directly using Poisson statistics, without the need for a standard curve [40] [43] [42].
The following workflow diagram illustrates the core process of dPCR for ctDNA analysis:
Comparative Analysis: Key Quantitative Differences
The table below summarizes the critical differences that make dPCR particularly suited for quantifying rare targets.
Table 1: Key Operational Characteristics of qPCR versus dPCR
| Parameter | Quantitative Real-Time PCR (qPCR) | Digital PCR (dPCR) |
|---|---|---|
| Quantification Method | Relative (requires standard curve) | Absolute (no standard curve) [40] [43] |
| Detection of Rare Variants | >1% mutant allele frequency [43] | ≥0.1% mutant allele frequency [43] [44] |
| Precision & Sensitivity | Detects down to a 2-fold change [40] | High precision; capable of detecting small fold-change differences [40] |
| Tolerance to PCR Inhibitors | Impacted by inhibitors, affecting PCR efficiency [40] [43] | More tolerant due to sample partitioning [40] [43] |
| Ideal Application in ctDNA | Gene expression, high viral load quantification | Rare allele detection, copy number variation, low-level ctDNA quantification [40] [41] |
Troubleshooting High Ct Values: Transitioning from qPCR to dPCR
High Ct values in qPCR experiments for cancer biomarkers signal low template quality or quantity. The following guide addresses common issues and how dPCR overcomes them.
Troubleshooting Guide & FAQs
Table 2: Troubleshooting Common Issues in Rare Target Detection
| Problem | Possible Causes in qPCR | dPCR Solutions & Recommendations |
|---|---|---|
| High Ct/ Low Signal | Very low abundance of ctDNA in wild-type background [41] | Superior Sensitivity: dPCR reliably detects mutant alleles at fractional abundances as low as 0.01% [44]. |
| Poor Precision/ High Variability | Measurement at the plateau phase of PCR; reaction kinetics variability [40] | Absolute Quantification: End-point measurement and Poisson statistics provide a precise count, eliminating variability associated with reaction kinetics [40] [42]. |
| Inhibition & Poor Accuracy | Carry-over of PCR inhibitors (e.g., from plasma); affects reaction efficiency [45] | Enhanced Robustness: Partitioning dilutes inhibitors into many reactions, making the overall process more tolerant [40] [43]. |
| Need for Standard Curves | Relative quantification requires accurate and stable standard curves [40] | Standard-Free: Provides absolute quantification without reference materials, simplifying workflow and improving reliability [43] [42]. |
Frequently Asked Questions (FAQs)
Q1: My qPCR assays for TP53 mutations in patient plasma show Ct values >35, making quantification unreliable. Can dPCR help? Yes. dPCR is explicitly designed for this scenario. For instance, a study detecting TP53 mutations in head and neck cancer patients successfully quantified ctDNA with a mutant allele frequency down to 0.01%, far below the reliable detection limit of qPCR [44].
Q2: Are my existing qPCR assays (e.g., TaqMan) compatible with dPCR systems? In many cases, yes. Probe-based qPCR assays, especially TaqMan assays, can often be transferred directly to dPCR platforms with minimal optimization, allowing for a smooth transition of your validated assays [43].
Q3: We work with limited patient plasma samples. How much input DNA does dPCR require? dPCR is well-suited for limited samples. Protocols commonly use between 1-10 ng of cfDNA per reaction. The high sensitivity of dPCR allows for accurate data even from these low input amounts, which is typical in liquid biopsy workflows [41] [44].
Experimental Protocol: Detecting ctDNA in Breast Cancer Plasma via dPCR
The following protocol is adapted from clinical studies profiling mutations in genes like PIK3CA, ESR1, and TP53 in breast cancer patients [41].
Detailed Step-by-Step Methodology
- Sample Collection & Plasma Preparation: Collect blood in K2EDTA tubes. Centrifuge at 800-1600 g for 10 minutes to separate plasma. Transfer supernatant to a fresh tube and perform a second, high-speed centrifugation (16,000 g for 10 min) to remove any remaining cells. Aliquot and store plasma at -80°C until use.
- Cell-free DNA (cfDNA) Extraction: Use commercially available circulating nucleic acid extraction kits (e.g., QIAamp Circulating Nucleic Acid Kit). Elute DNA in a low-EDTA or EDTA-free buffer to prevent interference with the PCR reaction. A typical starting volume is 2-4 mL of plasma.
- dPCR Assay Setup:
- Design mutation-specific primers and TaqMan probes (FAM-labeled) and a reference assay (e.g., for a wild-type sequence, VIC-labeled).
- Prepare the dPCR reaction mix according to the manufacturer's instructions (e.g., Bio-Rad's ddPCR Supermix for Probes). A typical 20-22 µL reaction contains 1X supermix, primers and probes at optimized concentrations, and 2-8 µL of the extracted cfDNA.
- Partitioning and Emulsification: Load the reaction mixture into a droplet generator. This instrument partitions each sample into 20,000 nanoliter-sized water-in-oil droplets [44], effectively creating thousands of individual PCR reactions.
- PCR Amplification: Transfer the droplets to a 96-well PCR plate and run on a conventional thermal cycler. Use a standard thermal cycling profile: initial denaturation at 95°C for 10 min, followed by 40-55 cycles of denaturation at 94°C for 30 sec and annealing/extension at a primer-specific temperature (e.g., 55-60°C) for 60 sec, followed by a final enzyme deactivation step at 98°C for 10 min. A ramp rate of 2°C/sec is standard.
- Droplet Reading and Analysis: Place the plate in a droplet reader, which aspirates each sample sequentially. The reader measures the fluorescence in each droplet (FAM and VIC). Using the manufacturer's software (e.g., QuantaSoft), set thresholds to distinguish positive and negative droplets for each channel. The software automatically calculates the absolute concentration (copies/µL) of the mutant and wild-type DNA based on the fraction of positive droplets and Poisson statistics.
The logical flow of data analysis from droplet reading to final result is shown below:
The Scientist's Toolkit: Essential Research Reagents for dPCR
Successful dPCR experimentation relies on a set of key reagents and instruments.
Table 3: Essential Research Reagents and Materials for dPCR Experiments
| Item | Function | Example/Note |
|---|---|---|
| Circulating Nucleic Acid Kit | Isolation of high-quality, short-fragment cfDNA from plasma samples. | QIAamp Circulating Nucleic Acid Kit [44]. Critical for obtaining clean input material. |
| dPCR Supermix | Provides optimized buffer, dNTPs, and DNA polymerase for robust amplification in partitioned reactions. | ddPCR Supermix for Probes (no dUTP) [44]. Hot-start enzymes are recommended. |
| TaqMan Assay | Sequence-specific detection of wild-type and mutant alleles. Includes primers and fluorescent probes. | Can be adapted from existing qPCR assays or custom-designed [43]. Uses FAM/VIC dyes. |
| Droplet Generator & Reader | Instrumentation for creating nanodroplets and reading endpoint fluorescence. | QX200 Droplet Digital PCR System [44]. The core hardware of the workflow. |
| Negative Controls | To establish baseline and false-positive rates. | No-Template Control (NTC) and Wild-Type-Only DNA [44]. Essential for assay validation. |
Pre-Amplification Strategies and Probe Chemistry Optimization for qPCR
In cancer biomarker detection research, achieving low, reproducible Cycle threshold (Ct) values is paramount for sensitive and reliable results. A high Ct value indicates delayed amplification, often signaling issues with reaction efficiency or target availability. This technical support center provides targeted troubleshooting guides and FAQs to help researchers optimize their qPCR assays, focusing on robust pre-amplification strategies and refined probe chemistry to overcome the common challenge of high Ct values.
Troubleshooting Guides
Guide 1: Addressing High Ct Values and Poor Reproducibility
Problem: Your qPCR assay is producing high Ct values (typically above 30 in dye-based assays) with poor reproducibility between technical replicates.
Why this happens: High Ct values can stem from factors related to template quality, reaction efficiency, or the presence of inhibitors [15]. For low-expression genes, which are common in cancer biomarker studies, the inherent low abundance of the target transcript is a primary factor [46].
Solutions:
Optimize the Template:
- Input Amount: If the Ct value for the reference gene is normal but the target gene is high, increase the amount of cDNA template in the reaction. Avoid exceeding 1/10 of the total reaction volume [46].
- Purity and Integrity: Assess RNA integrity via agarose gel electrophoresis and check purity using a spectrophotometer (e.g., NanoDrop). Ensure the A260/A280 ratio is around 2.0 [46].
- Remove Inhibitors: Dilute the sample (10x to 1000x). This can reduce the impact of inhibitors and sometimes even lead to a lower Ct value by scattering oligos that may be bound to non-target DNA [47] [17].
Optimize the qPCR Program:
- Switch from a two-step to a three-step cycling protocol.
- Increase the extension time to improve amplification efficiency for longer or complex amplicons [46].
Refine Experimental Procedure:
- Increase the number of replicate wells (e.g., from duplicates to triplicates or more) to allow for statistical removal of outliers.
- Add inert carrier DNA or RNA to the reaction mix. This minimizes the loss of target molecules by preventing their adhesion to tube walls and pipette tips [46].
Table 1: Summary of Optimization Strategies for High Ct Values
| Factor | Problem | Solution | Expected Outcome |
|---|---|---|---|
| Template | Low input/ concentration | Increase cDNA input; use less diluted stock [46] | Lower Ct value |
| Presence of PCR inhibitors | Dilute sample (10-1000x) [17] | Improved efficiency, potentially lower Ct [47] | |
| qPCR Protocol | Inefficient cycling | Use a 3-step program; extend extension time [46] | Higher amplification efficiency |
| Reaction Setup | Stochastic variation in low-copy targets | Increase replicate wells; add carrier DNA/RNA [46] | Improved reproducibility |
Guide 2: Optimizing Primer and Probe Chemistry
Problem: Non-specific amplification, primer-dimers, or generally low amplification efficiency are leading to high Ct values and unreliable data.
Why this happens: Suboptimal primer and probe design—including secondary structures, inappropriate melting temperatures (Tm), and non-specific binding—severely reduces PCR efficiency [48].
Solutions:
Primer Design Principles:
- Length and GC Content: Design primers 17-22 base pairs long with a GC content between 30-50% [48].
- Melting Temperature (Tm): Ensure the Tm values for the forward and reverse primers are within 2-3°C of each other [48].
- 3' End Stability: Avoid more than three G/C nucleotides within the last five bases at the 3' end to prevent non-specific extension [48].
- Specificity Check: Use tools like NCBI's Primer-BLAST to verify primer specificity and ensure a single amplicon product [48].
- Exon Boundaries: Where possible, design primers to span exon-exon junctions to prevent amplification of genomic DNA [48].
Probe Design and Validation:
- For TaqMan probes, ensure the probe's Tm is 5-10°C higher than the primers.
- Avoid guanine (G) residues at the 5' end of the probe, as this can quench the reporter dye fluorescence.
Concentration Optimization:
- Empirically test primer and probe concentrations. Using excessively high or low primer concentrations can lead to a significant drop in PCR efficiency and nonspecific amplification [48]. A typical starting concentration is 50-900nM for primers and 50-250nM for probes.
Table 2: Primer and Probe Design Criteria for Optimal qPCR [48]
| Parameter | Optimal Specification | Rationale |
|---|---|---|
| Primer Length | 17 - 22 bp | Balances specificity and efficient binding. |
| GC Content | 30 - 50% | Ensures stable binding without excessively high Tm. |
| Tm Difference | < 2 - 3 °C | Ensures both primers bind with similar efficiency. |
| 3' End Complementarity | Avoid >3 G/Cs | Minimizes mis-priming and non-specific amplification. |
| Amplicon Length | 50 - 150 bp | Shorter products amplify with higher efficiency. |
Frequently Asked Questions (FAQs)
Q1: Why are my Ct values too high (>35) or sometimes not detectable at all? [15]
A: Several factors can cause this:
- Biological: The target gene may not be expressed above the assay's detection limit.
- Technical:
- Poor RNA Quality: Check RNA integrity and purity.
- Insufficient Template: Use more input RNA or a less diluted cDNA sample.
- Experimental Error: Always include a positive control template to troubleshoot reagents and procedure.
- Primer-Template Mismatch: If using a vector system, ensure your primers are designed to match the transcribed regions (e.g., not just the UTRs present in the genomic DNA).
Q2: My amplification curves have an unusual shape or are jagged. What does this mean? [47]
A: Abnormal curve shapes often point to specific issues:
- Jagged Signal: Can be caused by poor amplification, a weak probe signal, or mechanical errors like bubbles in the well. Ensure sufficient probe concentration and mix reaction components thoroughly.
- Low Plateau Phase: Can result from limiting reagents, degraded dNTPs/master mix, or an inefficient reaction. Prepare fresh stock solutions and check reagent calculations.
- Unexpectedly Early Cq: Can indicate genomic DNA contamination in an RNA assay, poor primer specificity, or amplification of a multi-copy gene. Treat samples with DNase and redesign primers for specificity.
Q3: How can I validate my qPCR assay to ensure confidence in my results, especially for clinical cancer research? [49]
A: Proper validation is critical. Key parameters to check include:
- Amplification Efficiency: Calculate from a standard curve of serial dilutions. Efficiency should be between 90-110% (slope between -3.58 and -3.10) [48].
- Linearity (R²): The correlation coefficient for your standard curve should be ≥0.980 [49].
- Specificity: Ensure a single peak in the melt curve (for SYBR Green) or a single band of the expected size on a gel.
- Dynamic Range: The range of template concentrations over which the assay is linear and quantitative.
- Inclusivity/Exclusivity: Verify that your assay detects all intended target variants (inclusivity) and does not cross-react with genetically similar non-targets (exclusivity).
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Reagents for Optimized qPCR in Biomarker Research
| Reagent/Material | Function | Considerations for Optimization |
|---|---|---|
| Specialized qPCR Master Mix | Provides DNA polymerase, dNTPs, buffers, and fluorescent dye. | For low-expression targets, use kits specifically validated for high sensitivity and robust detection of low-copy templates [46]. |
| High-Quality Primers & Probes | Specifically amplifies and detects the target sequence. | HPLC or PAGE purification is recommended. Adhere to strict design principles to avoid secondary structures [48]. |
| Nuclease-Free Water | Solvent for preparing reagents and dilutions. | Ensures the reaction is free of RNases and DNases that could degrade components. |
| Positive Control Template | Plasmid or cDNA with a known copy number of the target. | Essential for assay validation, troubleshooting, and monitoring inter-run variation. |
Experimental Workflow and Pathway Diagrams
The following diagram outlines a logical workflow for diagnosing and troubleshooting high Ct values in a qPCR experiment.
This diagram illustrates the critical relationship between robust primer/probe design and successful qPCR amplification, which is fundamental to avoiding high Ct values.
The Role of Artificial Intelligence in Analyzing Complex Biomarker Patterns
Frequently Asked Questions (FAQs)
General AI Biomarker Concepts
Q1: What is the core advantage of using AI for biomarker discovery over traditional methods? AI-powered biomarker discovery transforms the process from a hypothesis-driven approach to a systematic, data-driven exploration. It uses machine learning and deep learning to analyze high-dimensional datasets (genomic, proteomic, imaging) to uncover complex, non-intuitive patterns that traditional methods often miss. This can reduce discovery timelines from years to months or even days [50].
Q2: In what ways can AI help with troubleshooting high Ct values or other assay inconsistencies? AI models can integrate multiple data types to provide context and alternative validation paths. For instance:
- Multi-modal Verification: If a qPCR assay shows high Ct values, AI can analyze concurrent digital pathology images of the biopsy sample to verify tumor cell content and quality, helping to distinguish a true negative from a failed assay [51] [52].
- Trend Analysis: AI can identify subtle patterns in sample metadata (e.g., storage time, extraction batch) that correlate with assay performance issues, pinpointing sources of technical variability [50].
Q3: What are the different types of biomarkers that AI can help identify? AI platforms are adept at finding several biomarker categories, each with a distinct clinical purpose [50]:
- Diagnostic Markers: Help identify the presence and type of cancer (e.g., AI-identified markers in liquid biopsies).
- Prognostic Markers: Predict the likely course of the disease, such as how aggressive a cancer is, independent of treatment.
- Predictive Markers: Determine which patients are most likely to benefit from a specific therapy (e.g., predicting response to immunotherapy).
Technical Implementation & Validation
Q4: What is a typical workflow for an AI-powered biomarker discovery project? A robust AI pipeline follows these key stages [50]:
- Data Ingestion: Collecting and harmonizing multi-modal data (genomics, imaging, clinical records).
- Preprocessing: Quality control, normalization, and feature engineering to clean and prepare data.
- Model Training: Using machine learning (e.g., random forests) or deep learning (e.g., neural networks) to train models, validated with holdout test sets.
- Validation: Rigorously testing the biomarker in independent patient cohorts and through biological experiments.
- Deployment: Integrating the validated biomarker into clinical workflows and diagnostic platforms.
Q5: How can we ensure that an AI-identified biomarker pattern is clinically actionable and not just a computational artifact? Validation is a multi-step process that goes beyond computational metrics [50] [53]:
- Analytical Validation: Does the test measure the biomarker accurately and reliably?
- Clinical Validation: Does the biomarker consistently predict the intended clinical outcome (e.g., treatment response) in a defined patient population?
- Clinical Utility Assessment: Does using the biomarker to guide decisions actually improve patient care and outcomes? This often requires prospective clinical trials.
Troubleshooting Guide: Addressing High Ct Values in AI-Integrated Biomarker Detection
Symptom: Inconsistent or high Ct values in qPCR/dPCR assays for candidate biomarkers, leading to unreliable data for AI model training or validation.
| Potential Cause | Investigation Steps | AI-Integrated Solution |
|---|---|---|
| Low Input Sample Quality/Quantity | - Check RNA/DNA integrity numbers (RIN/DIN).- Quantify nucleic acid concentration with fluorometry.- Review pathology reports on tumor cellularity. | Use AI-based digital pathology tools (e.g., from Paige or PathAI) on corresponding H&E slides to objectively quantify tumor cell percentage and necrosis in the source biopsy, confirming sample adequacy [52]. |
| Inhibition in Sample | - Perform spike-in controls with known template concentration.- Dilute sample and re-run assay. | Leverage AI models that are trained to recognize inhibition-specific patterns in amplification curves, which can distinguish inhibition from true low target concentration [50]. |
| Primer/Probe Design Issues | - Run BLAST for specificity.- Check for secondary structure using design software.- Test alternative assay designs. | Utilize AI-powered in silico platforms to simulate and optimize primer-probe binding kinetics and specificity across the genome, improving first-pass success rates [50]. |
| Suboptimal Data Normalization | - Evaluate stability of reference genes with geNorm or BestKeeper.- Test multiple normalization methods. | Employ AI-driven feature selection to identify the most stable reference genes from RNA-seq data or to discover novel, stable combination markers from high-dimensional data for robust normalization [50]. |
| True Biological Heterogeneity | - Perform single-cell RNA sequencing on a subset of samples.- Use immunohistochemistry to validate protein expression. | Integrate radiomic features from CT/MRI scans using AI models (e.g., ARTIMES). This provides an independent, non-invasive assessment of tumor heterogeneity that can explain variability in molecular biomarker levels [51]. |
Experimental Protocol: Correlating Digital Pathology with Molecular Data
This protocol is designed to troubleshoot discrepancies in molecular assays (like high Ct values) by using AI analysis of digitized tissue sections.
1. Objective: To objectively determine if high Ct values in a biomarker assay are due to low tumor cellularity in the source sample using an AI-based tumor detection algorithm.
2. Materials:
- Formalin-fixed, paraffin-embedded (FFPE) tissue block(s) corresponding to the analyzed sample.
- Microtome and slides.
- Hematoxylin and Eosin (H&E) staining reagents.
- Whole-slide scanner.
- Access to an AI-powered digital pathology platform (commercial or research-grade).
3. Methodology: * Sectioning and Staining: Cut a 4-5 micron section from the FFPE block and perform standard H&E staining. * Digitization: Scan the H&E slide using a whole-slide scanner at 20x magnification or higher to create a high-resolution digital image. * AI Analysis: Upload the digital image to the AI platform. Run a pre-trained tumor detection and segmentation model. * Data Extraction: The model will output quantitative data, including: * Percentage of the total tissue area classified as tumor. * Tumor cell density. * Spatial distribution of tumor regions. * Correlation: Correlate the AI-generated tumor percentage with the Ct value from the molecular assay. A high Ct value coupled with a low AI-measured tumor percentage strongly suggests the sample was not adequate for the molecular test.
4. Interpretation:
- Tumor Percentage > 30%: Suggests the sample was adequate. High Ct values are more likely due to technical issues in the molecular assay or true low expression of the biomarker.
- Tumor Percentage < 20%: Suggests the sample itself is the primary issue. The molecular result may be unreliable, and the assay should be repeated on a more cellular sample if available.
Key Research Reagent Solutions
The following table details essential reagents and tools used in AI-integrated biomarker research, particularly in studies like those cited from the ESMO Congress 2025 [51].
| Research Reagent / Tool | Function in AI Biomarker Research |
|---|---|
| Circulating Tumor DNA (ctDNA) Kits | Extraction and library preparation for liquid biopsies. Used to generate genomic data that AI models can fuse with imaging data to improve predictive power [51]. |
| Multiplex Immunofluorescence Panels | Allow simultaneous labeling of multiple protein biomarkers (e.g., immune cell markers) on a single tissue section. Provides rich, quantitative data on the tumor microenvironment for AI-based spatial analysis [51] [52]. |
| Whole-Slide Scanners | Digitize traditional glass pathology slides into high-resolution whole-slide images. This is the fundamental first step for any AI-driven digital pathology workflow [52]. |
| Next-Generation Sequencing (NGS) Panels | Targeted or whole-genome sequencing to identify mutations and genomic heterogeneity. The quantitative data on intratumoral heterogeneity is a key input for AI models predicting therapy response [51] [50]. |
| Cloud Computing & Federated Learning Platforms | Secure platforms that enable the analysis of sensitive patient data across multiple institutions without moving the data. This is critical for training robust AI models on large, diverse datasets while maintaining privacy [50]. |
Workflow and Relationship Diagrams
AI Biomarker Analysis Workflow
AI for High Ct Value Investigation
Systematic Troubleshooting and Protocol Optimization for High Ct Value Assays
This guide provides troubleshooting support for researchers and scientists troubleshooting high Ct (Cycle Threshold) values in PCR-based cancer biomarker detection. The pre-analytical phase—from sample collection to nucleic acid extraction—is a critical source of variability. Errors during this stage can degrade sample quality, reduce analyte concentration, and lead to elevated Ct values, compromising data reliability. The following FAQs and guides address specific, common pre-analytical challenges.
Troubleshooting Guides
Guide 1: Troubleshooting High Ct Values in Liquid Biopsies
Problem: Unexpectedly high Ct values during qPCR or RT-qPCR analysis of circulating tumor DNA (ctDNA) or other nucleic acid biomarkers from blood samples.
Background: High Ct values indicate low template quantity or quality in the PCR reaction. In the context of cancer biomarker research, this can be misinterpreted as low tumor DNA burden when it may actually stem from pre-analytical errors that degrade the sample or introduce inhibitors [18].
Investigation and Resolution:
| Phase | Investigation Step | Potential Cause | Corrective Action |
|---|---|---|---|
| Sample Collection & Handling | Check sample for hemolysis. | In-vitro hemolysis from traumatic draw or handling, releasing PCR inhibitors from red blood cells [54]. | Draw a new sample using proper phlebotomy technique. Avoid using hemolyzed samples. |
| Verify sample processing time. | Delay in processing, leading to degradation of target nucleic acids (e.g., ctDNA/RNA) by nucleases in the blood [55]. | Process plasma/serum within 1-2 hours of collection. Use stabilizing tubes if immediate processing is not possible. | |
| Confirm centrifugation protocol. | Incomplete separation of plasma from cells, leading to cellular contamination and degradation of nucleic acids. | Use a standardized, double-centrifugation protocol (e.g., 2,000 x g for 10 min, then 10,000 x g for 10 min). | |
| Nucleic Acid Extraction | Review extraction method and controls. | Inefficient extraction due to improper technique, wrong magnetic bead-to-sample ratio, or inhibitor carryover [55]. | Use a validated extraction kit. Include a positive control to monitor extraction efficiency. |
| Check extraction elution volume. | Over-dilution of the nucleic acid eluate in a large volume of buffer. | Elute in a smaller, consistent volume to increase final concentration. | |
| Assess for contamination. | PCR inhibitors (e.g., heparin, hemoglobin) co-purified with the nucleic acids, interfering with polymerase activity. | Use inhibitor removal steps during extraction. Perform a spike-in assay to check for inhibition. | |
| Storage | Confirm storage conditions. | Improper storage temperature or freeze-thaw cycles, causing fragmentation and degradation of target biomarkers like ctDNA [18]. | Store extracted nucleic acids at -80°C in single-use aliquots. Avoid repeated freeze-thaw cycles. |
Guide 2: Addressing Poor Sample Quality in Biobanked Tissues
Problem: Low yield or degraded nucleic acids extracted from archived tissue samples, leading to high Ct values or assay failure.
Background: The integrity of biomarkers in biobanked tissues is highly dependent on the initial stabilization and consistent storage conditions. Deviations can cause irreversible damage.
Investigation and Resolution:
| Investigation Step | Potential Cause | Corrective Action |
|---|---|---|
| Audit the cold chain. | Temperature fluctuations during storage or transport, accelerating nucleic acid degradation [55]. | Implement 24/7 temperature monitoring with alarms. Ensure backup freezers and documented transfer protocols. |
| Review fixation and processing records. | Prolonged formalin fixation can cause nucleic acid fragmentation and cross-linking [19]. | Standardize fixation time (e.g., 6-72 hours) and use neutral buffered formalin. |
| Check sample age and inventory system. | Long-term storage even at -80°C can lead to gradual degradation over many years. | Prioritize older samples for analysis. Use an inventory management system for first-in-first-out (FIFO) usage. |
Frequently Asked Questions (FAQs)
Q1: What are the most common pre-analytical errors that lead to unreliable biomarker data? Approximately 60-70% of all laboratory errors originate in the pre-analytical phase [54]. The most prevalent issues include:
- Sample Misidentification and Mislabeling: Account for a significant portion of phlebotomy errors [54] [56].
- Poor Sample Quality: Hemolysis, clotting, and improper volume constitute 80-90% of pre-analytical errors [54].
- Improper Handling and Transport: Delays in processing, exposure to incorrect temperatures, and improper centrifugation [55].
- Inconsistent Patient Preparation: Lack of fasting or recent medication use can interfere with tests [54].
Q2: How does hemolysis specifically affect PCR-based biomarker detection? Hemolysis releases intracellular components, including hemoglobin and ions, from red blood cells into the serum or plasma. Hemoglobin is a potent inhibitor of DNA polymerases used in PCR. Its presence can directly inhibit the amplification reaction, leading to decreased signal, elevated Ct values, or even false-negative results [54].
Q3: Our lab is considering moving to direct-to-PCR (D2P) methods to save time. What are the key trade-offs? While D2P (extraction-free) methods streamline workflow and reduce hands-on time, they come with risks:
- Increased Inhibitor Carryover: PCR inhibitors present in the original sample matrix are not removed, which can severely suppress amplification [57].
- Reduced Sensitivity: The absence of a nucleic acid concentration step may lower the effective amount of a low-abundance target (like ctDNA) in the reaction, potentially increasing Ct values or causing false negatives.
- Sample Compatibility: These methods may not be compatible with all sample types (e.g., tissues). Validation for your specific sample matrix and analyte is crucial.
Q4: Beyond traditional samples, what emerging biomarkers are sensitive to pre-analytical variation? Emerging biomarkers like circulating tumor DNA (ctDNA) and extracellular vesicles (exosomes) are highly sensitive to pre-analytical conditions [18].
- ctDNA: Is highly fragmented and present in low concentrations. Delays in plasma processing can lead to its degradation by nucleases or dilution by wild-type DNA released from lysing blood cells [18].
- Exosomes: Their yield, size distribution, and cargo (e.g., RNA, proteins) can be altered by centrifugation force, storage time, and temperature [18]. Standardizing these parameters is essential for reproducible data.
Q5: What strategies can reduce human error in sample processing?
- Automation: Implementing automated homogenizers and liquid handlers can drastically reduce cross-contamination and variability. One clinical genomics lab reported an 88% decrease in manual errors after automating their workflow [55].
- Barcoding Systems: Using barcodes for sample tracking reduces misidentification. One hospital histology department saw an 85% reduction in slide mislabeling after implementing a barcoding system [55].
- Robust Training & SOPs: Continuous education and strict adherence to detailed, clear Standard Operating Procedures (SOPs) are fundamental to minimizing operator-dependent variability [55] [56].
Quantitative Data for Pre-Analytical Quality Control
The following table summarizes quantitative findings on how pre-analytical factors can influence test interpretation, based on a study of SARS-CoV-2 RT-PCR, with principles applicable to biomarker detection [58].
Table: Stratification of False Positive Rates by Ct Value
| Ct Value Stratification | Interpretation & Risk of False Positives | Recommended Action for Biomarker Research |
|---|---|---|
| Ct < 30 | Low probability of false positives (≤ 1.72%). Strong signal [58]. | Results can be considered reliable. Focus on biological interpretation. |
| 30 ≤ Ct < 35 | Significant risk of false positives (0% - 9.14%), varying by reagents and lab protocols [58]. | Interpret with caution. Verify results with a repeat assay or orthogonal method. |
| Ct ≥ 35 | High probability of false positives (15.58% - 24.22%) [58]. | Retest the original sample before reporting. Investigate potential pre-analytical or analytical issues. |
Experimental Protocols for Audit
Protocol 1: Assessing the Impact of Plasma Processing Delay on ctDNA Ct Values
Objective: To quantitatively determine the maximum allowable time between blood draw and plasma freezing that maintains ctDNA integrity for your specific assay.
Methodology:
- Sample Collection: Draw blood from consented volunteers or patients into multiple dedicated ctDNA collection tubes (e.g., Streck, PAXgene).
- Processing Timepoints: Process the tubes in triplicate at different time points post-draw (e.g., 0.5h, 1h, 2h, 4h, 6h, 24h, 72h). Keep samples at room temperature until processing.
- Plasma Isolation: Follow a standardized double-centrifugation protocol to isolate plasma without cellular contamination.
- Storage: Immediately freeze all plasma aliquots at -80°C.
- Batch Analysis: Extract nucleic acids from all samples in a single batch to minimize inter-assay variation. Quantify a stable, specific ctDNA target (e.g., a known mutation via ddPCR) and report the Ct or concentration.
Expected Outcome: A time-course curve showing the degradation of ctDNA and a corresponding increase in Ct values over time, establishing your lab's optimal processing window.
Protocol 2: Evaluating Nucleic Acid Extraction Kit Performance
Objective: To compare the efficiency, purity, and consistency of different nucleic acid extraction kits for your sample type.
Methodology:
- Sample Pooling: Create a large, homogeneous pool of your target sample (e.g., plasma, tissue homogenate) to minimize source variability.
- Kit Comparison: Split the pooled sample into multiple aliquots and extract nucleic acids using different kits or methods (e.g., column-based, magnetic bead-based, direct-to-PCR) according to manufacturers' instructions. Perform extractions in triplicate.
- Quality Assessment: Measure the following for each eluate:
- Yield: Using a fluorometer (e.g., Qubit).
- Purity: A260/A280 and A260/A230 ratios via spectrophotometry.
- Inhibition: Perform a spike-in PCR with a known amount of external control.
- Functional Performance: Run your target qPCR assay and record the Ct values.
Expected Outcome: A comprehensive comparison allowing you to select the extraction kit that provides the best balance of high yield, low inhibitor carryover, and lowest Ct values for your application.
Workflow Visualization
Diagram 1: Pre-Analytical Workflow for Liquid Biopsies
Diagram 2: Troubleshooting High Ct Values
The Scientist's Toolkit: Research Reagent Solutions
Table: Essential Materials for Pre-Analytical Workflow Integrity
| Item | Function & Rationale |
|---|---|
| Cell-Free DNA Blood Collection Tubes (e.g., Streck, PAXgene) | Preserves blood cell integrity and stabilizes ctDNA for up to several days at room temperature, critical for mitigating delays in transport and processing [18]. |
| Magnetic Bead-Based Nucleic Acid Kits | Enable high-throughput, automated extraction with efficient binding and wash steps, reducing cross-contamination and improving yield consistency compared to manual column methods [55]. |
| PCR Inhibitor Removal Reagents | Specific additives or wash buffers designed to remove common inhibitors like hemoglobin, heparin, or humic acids, which are crucial for recovering amplifiable DNA from complex samples [55]. |
| Exogenous Internal Controls (e.g., Synthetic DNA/RNA Spikes) | Added to the sample at the beginning of extraction, these controls detect extraction efficiency and the presence of PCR inhibitors, helping to distinguish true target negativity from assay failure [57]. |
| Automated Homogenizer (e.g., Omni LH 96) | Provides consistent and reproducible disruption of tissue samples, reducing operator-dependent variability and the risk of cross-contamination through single-use tips, leading to more reliable biomarker data [55]. |
High Cycle threshold (Ct) values in quantitative PCR (qPCR) experiments present significant challenges in cancer biomarker detection research, potentially masking critical diagnostic information. Effective troubleshooting requires a systematic approach focusing on reaction component optimization and contaminant elimination. This guide provides researchers with targeted FAQs and methodologies to address these specific technical challenges, ensuring accurate and reproducible results in cancer biomarker studies.
FAQs on Master Mix and Inhibitor Troubleshooting
1. What are the primary causes of high Ct values in qPCR experiments for cancer biomarker detection?
High Ct values typically indicate delayed amplification, which can result from multiple factors related to reaction components. Low initial template concentration is a common cause, where each 10-fold dilution of cDNA can increase the Ct value by approximately 3.3 cycles [46]. The presence of PCR inhibitors in the reaction mixture can significantly reduce amplification efficiency, while suboptimal master mix formulations—including inadequate concentrations of DNA polymerase, magnesium ions, or fluorescent dyes—also contribute to poor performance [34] [46]. Additionally, low amplification efficiency due to problematic primer design or reaction conditions further exacerbates Ct value issues.
2. How can I determine if my master mix formulation requires optimization?
Several experimental indicators suggest suboptimal master mix performance. Consistently high Ct values (>30) across multiple assays despite adequate template quality signal potential formulation issues [34] [46]. Poor reproducibility between technical replicates indicates reaction inconsistency, while non-specific amplification (evidenced by multiple peaks in melt curves or high background signal) suggests inadequate reaction specificity. Additionally, reduced amplification efficiency (outside the ideal 90-110% range) calculated from standard curves clearly indicates the need for master mix optimization [34].
3. What strategies effectively remove inhibitors from qPCR reactions?
Comprehensive inhibitor removal begins with template purification. For RNA templates, evaluate integrity through agarose gel electrophoresis and assess purity using spectrophotometric ratios (A260/A280 and A260/A230) [46]. Increasing template dilution can reduce inhibitor concentration, though this must be balanced with maintaining sufficient template for detection [17]. Incorporating carrier nucleic acids that don't interfere with the target amplification can minimize adhesion to labware [46]. Additionally, using inhibitor-resistant DNA polymerases or specialized purification kits designed for challenging sample types can significantly improve results.
Troubleshooting Protocols and Methodologies
Protocol 1: Systematic Master Mix Optimization
This protocol provides a step-by-step approach to optimizing master mix components for sensitive detection of cancer biomarkers, particularly those with low expression levels.
Materials:
- Template DNA (serial dilutions of target plasmid or cDNA)
- Multiple master mix formulations for comparison
- Optimized primer pairs
- Nuclease-free water
- qPCR plates and sealing films
- Real-time PCR instrument
Procedure:
- Prepare Template Dilutions: Create a 10-fold serial dilution series of your target template, spanning at least 5 orders of magnitude (e.g., from 10^6 to 10^1 copies/μL).
Test Master Mix Formulations: Set up identical reaction series with different master mix formulations, ensuring consistent template inputs across all tests.
Amplification Conditions: For low-expression targets, consider using a three-step amplification program instead of a two-step protocol, or extend extension times to improve efficiency [46].
Data Analysis: Calculate amplification efficiencies from standard curves using the formula: Efficiency (%) = [10^(-1/slope) - 1] × 100. Ideal efficiency falls between 90-110% [34].
Sensitivity Assessment: Determine the limit of detection (LOD) for each formulation by identifying the lowest template concentration that reliably amplifies, following Poisson distribution principles for single-copy templates [46].
Protocol 2: Comprehensive Inhibitor Removal and Template Quality Control
This methodology focuses on identifying and eliminating PCR inhibitors that compromise qPCR efficiency in cancer biomarker detection.
Materials:
- TRIzol reagent or specialized nucleic acid purification kits
- NanoDrop spectrophotometer or equivalent
- Agarose gel electrophoresis system
- DNase/RNase-free tubes and tips
- Optional: inhibitor removal columns or reagents
Procedure:
- Nucleic Acid Extraction: Use optimized purification methods appropriate for your sample type (e.g., TRIzol for difficult tissues) [59].
Quality Assessment:
- Measure A260/A280 and A260/A230 ratios; ideal values are ~1.8-2.0 and >2.0 respectively [59].
- Evaluate RNA integrity via gel electrophoresis (clear 18S and 28S ribosomal bands indicate good quality).
- For cDNA, assess synthesis efficiency using control genes with known expression.
Inhibitor Removal:
- Increase dilution factors of template (10x-1000x) to reduce inhibitor concentration [17].
- Implement additional purification steps if ratios indicate contamination.
- For persistent issues, use specialized inhibitor removal kits.
Inhibition Testing: Include internal positive controls or spike-in templates to distinguish between true target absence and inhibition.
Data Presentation and Analysis
Table 1: Performance Comparison of Master Mix Formulations for Low-Abundance Cancer Biomarker Detection
| Formulation | Amplification Efficiency | Limit of Detection (copies) | Ct Value at LOD | Detection Rate at 1.75 Copies |
|---|---|---|---|---|
| Standard Master Mix | 95% | 10 | 32.5 | 45% |
| Optimized for Sensitivity | 102% | 1.75 | 29.8 | 75% |
| Inhibitor-Resistant | 98% | 5 | 31.2 | 65% |
Table 2: Troubleshooting Guide for High Ct Values Related to Reaction Components
| Problem | Possible Causes | Recommended Solutions | Expected Outcome |
|---|---|---|---|
| Consistently High Ct Values | Low template quality or concentration | Increase template input; improve purification methods [46] | Ct reduction of 3-5 cycles |
| Poor Reproducibility | PCR inhibitors present | Increase template dilution; use inhibitor-resistant enzymes [17] | Improved replicate consistency |
| Low Amplification Efficiency | Suboptimal master mix formulation | Test alternative buffers; adjust Mg2+ concentration [34] | Efficiency reaching 90-110% |
| Non-specific Amplification | Primer dimers or mispriming | Redesign primers; increase annealing temperature [16] | Clean melt curve with single peak |
Research Reagent Solutions
Table 3: Essential Reagents for Optimizing qPCR in Cancer Biomarker Research
| Reagent Category | Specific Examples | Function | Application Notes |
|---|---|---|---|
| Specialized Master Mixes | Taq Pro Universal SYBR qPCR Master Mix | Enhanced sensitivity for low-copy targets | Optimal for detecting low-expression biomarkers [46] |
| Nucleic Acid Purification Kits | TRIZOL reagent, Column-based kits | High-quality template isolation | Critical for challenging samples [59] |
| Reverse Transcription Kits | High-efficiency cDNA synthesis kits | Maximize cDNA yield from limited RNA | Important for low-abundance transcripts |
| Inhibitor Removal Reagents | Carrier nucleic acids, DNase/RNase | Reduce adsorption and degradation | Minimize template loss [46] |
| Quality Assessment Tools | Spectrophotometers, Electrophoresis systems | Verify template quality and quantity | Essential for troubleshooting [59] |
Experimental Workflow Visualization
Systematic Troubleshooting Workflow for High Ct Values
Advanced Optimization Strategies
For persistent issues with high Ct values in cancer biomarker detection, consider these advanced approaches:
Master Mix Component Titration: Systematically vary concentrations of critical components including magnesium ions (Mg2+), DNA polymerase, dNTPs, and buffer additives. Create matrix experiments to identify optimal combinations for your specific targets, as different master mix formulations can yield significantly different detection sensitivities for low-copy templates [46].
Inhibitor-Resistant Formulations: When working with challenging clinical samples prone to inhibition, incorporate specialized additives such as bovine serum albumin (BSA), betaine, or commercial inhibitor-resistant enzymes. These components can help overcome inhibitors commonly found in blood, tissue, and FFPE samples without requiring additional purification steps.
Temperature Gradient Optimization: Fine-tune annealing temperatures using gradient PCR to identify ideal conditions that maximize specificity and efficiency simultaneously. Small adjustments (1-2°C) can significantly impact Ct values, particularly for difficult targets with high secondary structure or GC-rich regions.
Effective troubleshooting of high Ct values in cancer biomarker research requires methodical optimization of master mix formulations and comprehensive inhibitor management. By implementing these standardized protocols and systematic approaches, researchers can significantly improve detection sensitivity for low-abundance targets, ultimately enhancing the reliability of cancer biomarker data. Regular validation and quality control measures ensure consistent performance across experiments, supporting robust and reproducible research outcomes.
Instrument Calibration and Prevention of Cross-Contamination
This technical support center provides targeted troubleshooting guides and FAQs to help researchers, scientists, and drug development professionals address challenges related to instrument calibration and cross-contamination, specifically within the context of troubleshooting high Ct values in cancer biomarker detection research.
Frequently Asked Questions (FAQs)
1. What are the immediate steps I should take if I observe inconsistent high Ct values across my qPCR replicates? Your first action should be to verify the calibration of your pipettes, as manual pipetting errors are a common cause of inconsistent template concentrations [16]. Subsequently, check the calibration status of other key instruments, including your real-time PCR machine and any equipment used to measure nucleic acid concentration [60] [61].
2. How can cross-contamination lead to false positives in cancer biomarker studies, and how is it identified? Cross-contamination can introduce trace amounts of target DNA into negative controls or low-concentration samples, leading to false-positive amplification and incorrect Ct values [62]. This is often identified by amplification in negative controls, unexpected clustering of samples in molecular epidemiology studies, or when a sample with a low bacterial yield is processed on the same day as a high-concentration sample [63] [62].
3. Why is regular calibration critical for the accuracy of quantitative measurements like Ct values? Regular calibration ensures the precision of instruments like pipettes, which directly affects reagent volumes, and qPCR machines, which affects fluorescence detection. Over time, instruments can drift from their calibrated state, introducing a constant offset or variability into all measurements [61]. This drift can directly impact Ct value consistency and the accuracy of quantitative results [64].
4. What are the common types of calibration errors I should be aware of? Several common calibration errors can affect instrument performance:
- Zero Error: The instrument does not read zero when the measured quantity is zero [61].
- Span Error: The instrument does not read correctly at the high-end of its measurement range [61].
- Linearity Error: The instrument's output deviates from a straight-line response across its operational range [61].
Troubleshooting Guide: High Ct Values
Problem: High and Inconsistent Ct Values in qPCR for Cancer Biomarker Detection
High Ct (Threshold Cycle) values indicate low initial quantities of your target nucleic acid, while inconsistent replicates suggest technical variability. In cancer research, this can obscure the detection of low-abundance biomarkers like circulating tumor DNA (ctDNA) [65] [1].
Step 1: Investigate Instrument Calibration
Begin by verifying the calibration of all equipment involved in your workflow.
Quantitative Data on Calibration Impact
| Instrument | Calibration Error Type | Potential Impact on Ct Values | Supporting Data |
|---|---|---|---|
| Pipettes | Volume inaccuracy (span error) | Inconsistent reagent volumes, high variability between replicates [16]. | Studies show uncalibrated pipettes are a primary cause of Ct value variation [16]. |
| PET/CT Scanner | Global scaling error | Incorrect standardized uptake value (SUV) measurements, affecting tumor quantification [64]. | One study found a 19.8% SUV deviation due to a calibration error [64]. Implementing QC reduced variability from 11% to 4% [64]. |
| qPCR Thermocycler | Optical detection error | Inaccurate fluorescence reading, leading to erroneous Ct value assignment [63]. | Erratic amplification curves can often be resolved by calibrating the optics of the system [63]. |
| Dose Calibrator | Activity measurement error | Incorrect activity concentration calculations, affecting all downstream quantitation [64]. | Dose calibrator variability was measured at <1%, though consistent bias was observed [64]. |
Experimental Protocol: Verifying Pipette Calibration
- Principle: Gravimetrically measure the mass of dispensed water to calculate the actual volume delivered.
- Materials: Analytical balance (0.01 mg precision), distilled water, temperature chamber, weighing vessel.
- Method:
- Pre-equilibrate water and pipettes to ambient temperature (e.g., 23°C) [61].
- Set the pipette to the desired volume (e.g., 10 µL for cDNA template addition).
- Dispense water into the weighing vessel and record the mass.
- Repeat 10 times for each pipette.
- Calculate the volume using the Z-factor (water density at the ambient temperature).
- Determine the accuracy (mean vs. target volume) and precision (coefficient of variation) [60].
- Expected Outcome: Properly calibrated pipettes should have an accuracy and precision of ≤2-3%. Pipettes outside this range require professional service.
Step 2: Address Cross-Contamination
If instrument calibration is verified, cross-contamination may be the culprit.
Common Scenarios and Control Strategies
| Contamination Scenario | Impact on Experiment | Prevention Strategy |
|---|---|---|
| Aerosols from high-concentration samples [62]. | False positives in subsequent low-concentration samples, lowering their Ct values and creating false clusters in data analysis [62]. | Use dedicated pipettes with aerosol barrier tips. Process high- and low-concentration samples in separate work areas or at different times [62]. |
| Carryover from shared equipment [66]. | Contamination of reagents or samples with foreign nucleic acids, leading to non-specific amplification or false positives [66]. | Use dedicated equipment for pre- and post-PCR steps. Decontaminate shared equipment thoroughly with validated agents like 10% bleach before and after use [66]. |
| Contaminated reagents [63]. | Amplification in negative controls, invalidating the entire experiment. | Use fresh, high-quality reagents. Aliquot reagents to minimize freeze-thaw cycles and exposure. Use commercial, certified contaminant-free polymerases [63]. |
| Personnel-mediated contamination on lab coats or gloves [66]. | Introduction of contaminants from one workstation to another. | Wear appropriate PPE, including lab coats and gloves. Change gloves between handling different samples and when moving between workstations [66]. |
Experimental Protocol: Decontaminating Work Surfaces and Equipment
- Principle: Use a chemical agent to degrade any contaminating nucleic acids on surfaces.
- Materials: Freshly prepared 10% sodium hypochlorite (bleach) solution, RNase Away or DNA Away solutions, clean wipes, 70% ethanol.
- Method:
- Before and after each use, thoroughly wipe down the work area inside the biosafety cabinet, pipettes, and tube racks with the 10% bleach solution.
- Allow a contact time of at least 5 minutes for the bleach to inactivate nucleic acids.
- Wipe down the same surfaces with 70% ethanol to remove residual bleach, which can corrode metal and affect some reactions.
- Allow the surfaces to air dry completely before use.
- Expected Outcome: Effective reduction of nucleic acid contaminants, as evidenced by clean negative controls in subsequent qPCR runs.
Step 3: Optimize Sample and Assay Quality
If calibration and contamination are ruled out, focus on sample and assay integrity.
- Check Template Quality: Assess DNA/RNA integrity and purity using spectrophotometry (e.g., Nanodrop) or capillary electrophoresis. Degraded or impure template can inhibit amplification, raising Ct values [63].
- Verify Primer Specificity: Redesign primers using specialized software to avoid self-complementarity and dimer formation, which cause non-specific amplification and reduce efficiency [16].
- Optimize Reaction Conditions: Perform a temperature gradient PCR to determine the optimal annealing temperature for your primers, which can maximize efficiency and yield [63].
Experimental Workflow for Troubleshooting High Ct Values
The following diagram outlines a logical pathway for diagnosing and resolving high Ct values.
The Scientist's Toolkit: Key Research Reagent Solutions
This table details essential materials and their functions for maintaining a reliable qPCR workflow in biomarker research.
| Item | Function/Benefit | Application Notes |
|---|---|---|
| Certified Reference Standards (NIST-traceable) | Provides a known, accurate reference point for calibrating equipment like dose calibrators, ensuring measurement traceability [60] [64]. | Essential for multi-site studies to ensure data consistency. |
| PCR Master Mix (Pre-mixed) | Contains optimized, consistent concentrations of Taq polymerase, dNTPs, and buffer, reducing pipetting steps and contamination risk [63]. | Use commercial master mixes to avoid contaminants from "homemade" preparations [63]. |
| Aerosol Barrier Pipette Tips | Prevents aerosols and liquids from entering the pipette shaft, protecting against cross-contamination between samples [62]. | Critical when pipetting high-concentration standards or templates. |
| Nuclease-Free Water | Free of RNases and DNases, ensuring reagents are not degraded by enzymatic contamination, which can raise Ct values. | Use for reconstituting primers, diluting samples, and preparing reaction mixes. |
| Contamination Control Mats (e.g., Dycem) | Antimicrobial mats placed at lab entry points and workstations capture and hold particulate contaminants from footwear [66]. | Reduces the introduction of external contaminants into sensitive pre-PCR areas. |
| ROX Dye (Passive Reference Dye) | Normalizes for non-PCR-related fluorescence fluctuations between wells, improving well-to-well reproducibility and Ct value accuracy [63] [1]. | Particularly useful for correcting for pipetting errors or plate abnormalities. |
Establishing Rigorous Controls and Standard Curves for Reliable Quantification
Why is my standard curve showing poor linearity (R² < 0.99) and what can I do to fix it?
Poor linearity in a standard curve often indicates issues with sample preparation, pipetting inaccuracy, or suboptimal assay conditions. To address this:
- Check Sample Integrity: Ensure your standard samples are not degraded. For RNA/cDNA in qPCR, use electrophoresis or a bioanalyzer to confirm integrity [16].
- Verify Pipetting Technique: Manual pipetting errors are a common cause. Use calibrated pipettes and proper technique, or consider automated liquid handling systems for better reproducibility [16].
- Prepare a Proper Dilution Series: Use a serial dilution spanning at least 5 to 7 orders of magnitude [49] [67]. Ensure dilutions are made accurately in the correct solvent and that all equipment, like volumetric flasks, is properly used [67].
- Review Primer Design: For qPCR, non-specific amplification or primer-dimer formation can affect linearity. Redesign primers using specialized software to ensure appropriate length, GC content, and melting temperature [16].
My qPCR assay has high Ct values. Does this point to a problem with my standard curve or my samples?
High Ct values indicate delayed amplification, which can be due to issues with either the standard curve/reaction efficiency or the sample itself.
| Potential Cause | Diagnostic Check | Troubleshooting Action |
|---|---|---|
| PCR Inhibitors in Sample [16] | Dilute the sample. If Ct decreases, inhibitor likely present. | Improve sample purification and cleanup procedures [16]. |
| Excess Template DNA [17] | Assess sample concentration via spectrophotometry. | Dilute samples (10x to 1000x) to reduce background signal and improve specificity [17]. |
| Suboptimal Reaction Efficiency [49] | Check primer efficiency from standard curve slope. Ideal efficiency is 90-110%. | Redesign primers or optimize annealing/extension temperature to make binding more specific [16] [17]. |
| Low Template Quality/Quantity [16] | Check RNA Integrity Number (RIN) or DNA purity (A260/A280). | Re-isolate nucleic acids to ensure high integrity and accurate quantification [16]. |
How do I validate the dynamic range and limit of detection for my quantification assay?
The linear dynamic range is the concentration range where the instrument's response is directly proportional to the analyte concentration. The Limit of Detection (LOD) is the lowest concentration that can be reliably detected [49] [68].
Experimental Protocol for Validation:
- Prepare Dilution Series: Create a minimum of a seven-point, 10-fold serial dilution of a known standard, performed in triplicate [49].
- Run the Assay: Process the entire dilution series alongside appropriate negative controls.
- Plot and Analyze Data: Plot the measured response (e.g., Ct for qPCR, Absorbance for UV-Vis) against the known concentration on a logarithmic scale [49] [67].
- Determine Linear Dynamic Range: Identify the range where the data fits a straight line with a coefficient of determination (R²) of ≥ 0.980 (or ≥0.990 for more stringent applications) [49].
- Calculate LOD: The LOD is typically defined as the concentration that produces a signal distinguishable from the blank, often determined as 3 standard deviations above the mean of the blank sample [68].
How do I ensure my assay is specific and does not cross-react with non-targets?
Assay specificity ensures your test detects the intended target and excludes genetically similar non-targets [49] [68].
- In Silico Analysis: Use available genetic databases to check your primer/probe sequences for homology with non-target sequences [49].
- Experimental Validation: Test your assay against a panel of well-defined strains or samples that include both target organisms (to check inclusivity) and non-target, closely related organisms (to check exclusivity or cross-reactivity) [49]. International standards recommend using up to 50 certified strains for a robust validation [49].
A Researcher's Guide to Creating a Reliable Standard Curve
A standard curve is a critical tool for quantifying the concentration of an unknown sample by relating a measurable signal to known concentrations of a standard [69] [67].
Step-by-Step Protocol:
- Prepare a Concentrated Stock Solution: Accurately weigh the solute and dissolve it in an appropriate solvent in a volumetric flask [67].
- Perform a Serial Dilution: Label a series of volumetric flasks or microtubes. Create a dilution series (e.g., 1:10, 1:100) by sequentially transferring a precise volume from the previous concentration to the next and adding the required volume of solvent. Mix thoroughly at each step. A minimum of five standards is recommended [67].
- Prepare the Assay Plate/Cuvettes: Transfer the diluted standards and your unknown samples to the assay platform (e.g., a qPCR plate or spectrophotometer cuvette). Ensure the unknown samples are in the same buffer and at the same pH as the standards [69] [67].
- Measure the Response: Run the standards and unknowns in your instrument (qPCR machine, UV-Vis spectrophotometer). Obtain between three and five technical readings for each standard to account for variability [67].
- Plot the Data and Fit the Curve: Create a plot with the measured response (Y-axis) against the known concentration (X-axis). Use statistical software to fit the data to an appropriate model:
- Calculate Unknown Concentrations: Use the equation from your fitted curve to calculate the concentration of your unknown samples based on their measured response [69] [67].
Experimental Workflow for qPCR Assay Validation
The following diagram outlines the critical stages of establishing a validated qPCR assay, from pre-analytical steps to final data analysis, ensuring reliable quantification for clinical research.
The Scientist's Toolkit: Essential Materials for Reliable Quantification
This table lists key reagents and equipment necessary for establishing robust standard curves and controls in quantitative experiments, particularly in qPCR workflows.
| Item | Function | Key Considerations |
|---|---|---|
| Standard Solution [67] | A solution of known analyte concentration used to create the calibration curve. | Should be pure and traceable to a reference material. Prepare a series of dilutions covering the expected sample concentration range [69] [67]. |
| High-Quality Solvent [67] | Used to prepare standard dilutions and dissolve samples. | Must be compatible with the analyte and instrument (e.g., nuclease-free water for qPCR, specific buffers for proteins) [67]. |
| Precision Pipettes & Tips [67] | For accurate measurement and transfer of liquid volumes. | Must be properly calibrated. Using low-retention tips is recommended for small volumes and viscous liquids [16] [67]. |
| Volumetric Flasks / Microtubes [67] | For preparing standard solutions with precise final volumes. | Ensure they are clean and appropriate for the volume being handled [67]. |
| qPCR Plates & Seals | Hold samples during qPCR runs. | Opt for thin-wall plates for optimal thermal conductivity. Use optical-grade seals to prevent well-to-well contamination and evaporation [16]. |
| UV-Vis Spectrophotometer & Cuvettes [67] | Measures the absorbance of light by a solution to determine analyte concentration. | Cuvettes must be compatible with the wavelength range (e.g., quartz for UV) [67]. |
| Automated Liquid Handler [16] | Automates pipetting steps. | Significantly improves accuracy, reproducibility, and throughput while reducing contamination risk and human error [16]. |
Implementing Reflex Testing and Multi-Analyte Panels to Overcome Specificity Issues
FAQ: Addressing Specificity in Cancer Biomarker Detection
Q1: What are multi-analyte panels and how do they improve test specificity? Multi-analyte panels combine the measurement of several biomarkers (such as proteins and circulating tumor DNA) into a single test. By using an algorithm to interpret the combined results, these panels can achieve higher specificity than any single biomarker. For example, the EarlySEEK test for ovarian cancer combines ctDNA with protein biomarkers (including CA125 and HE4), achieving a 94.2% sensitivity while maintaining 95% specificity [70]. This approach helps mitigate the risk of false positives that can occur when relying on a single, less-specific analyte.
Q2: My qPCR assays for cancer biomarkers show high Ct values (>35). Is this a specificity issue? High Ct values can stem from several issues, not all related to specificity. To troubleshoot, please refer to the table below. However, non-specific amplification, where primers bind to non-target sequences, can consume reaction resources and reduce efficient amplification of your true target, leading to higher Ct values. Ensuring optimal primer design and efficiency (90-110%) is crucial for specificity [46] [71].
Q3: What is reflex testing and how can it be used in a research setting? Reflex testing is a protocol where the laboratory automatically performs a second, more specific test based on the results of an initial test. This is governed by predefined rules [72]. In cancer research, a common application is in genetic testing. For instance, after a targeted gene panel returns negative or inconclusive results, the protocol can automatically "reflex" to a more comprehensive whole exome sequencing (WES) analysis on the same stored sample, potentially increasing diagnostic yield without requiring a new sample [73].
Q4: How can machine learning enhance traditional rule-based reflex testing? Traditional reflex testing uses simple "if-then" rules, which can't handle complex, multi-factor decision-making. Machine learning (ML) models can analyze a broader set of patient data (e.g., multiple CBC parameters and historic results) to predict the need for a second-line test with greater nuance. A proof-of-concept study for ferritin testing showed that an ML-based "smart" reflex protocol outperformed all possible rule-based approaches, offering a promising path to more accurate and automated test utilization [74].
Troubleshooting Guide: High Ct Values in Biomarker Detection
High Ct values in qPCR can significantly hinder the detection of low-abundance cancer biomarkers. The following table summarizes common causes and their solutions [15] [46].
| Issue Category | Specific Problem | Recommended Solution |
|---|---|---|
| Template Quality & Quantity | Poor RNA purity, degradation, or low input amount. | - Check RNA integrity via gel electrophoresis and purity with a spectrophotometer (e.g., NanoDrop).- Increase RNA input in the reverse transcription reaction.- Use a more concentrated cDNA dilution (each 10-fold dilution increases Ct by ~3.3) [46]. |
| Primer Design & Performance | Non-specific amplification or suboptimal primer efficiency. | - Redesign primers following best-practice principles to avoid non-target binding.- Validate primer efficiency using a standard curve; it should be between 90% and 110% [46] [71]. |
| qPCR Reagents & Protocol | Kit formulation is not optimal for low-copy targets, or the thermal cycling program is inefficient. | - Use qPCR kits specially validated for sensitive detection of low-expression genes [46].- Switch from a two-step to a three-step qPCR program or increase extension time [46]. |
| Experimental Procedure | Low-copy target loss or poor reproducibility. | - Increase the number of replicate wells and statistically remove outliers.- Add inert carrier DNA/RNA to tubes to minimize sample adhesion during liquid handling [46]. |
Experimental Protocol: Optimizing qPCR for Low-Abundance Biomarkers
For researchers consistently encountering high Ct values while detecting low-expression cancer biomarkers, the following detailed protocol can enhance sensitivity and reproducibility [46].
Sample Quality Control:
- RNA Assessment: Evaluate 1 µL of RNA sample on a 1% agarose gel. Sharp 28S and 18S ribosomal RNA bands are indicative of high-quality, non-degraded RNA. The 28S band should be approximately twice the intensity of the 18S band.
- Purity Check: Use a spectrophotometer to measure absorbance ratios. Acceptable ratios are A260/A280 ≥ 1.8 and A260/A230 ≥ 2.0. Deviations suggest protein or chemical contamination.
Reverse Transcription and Template Input:
- Use 500 ng to 1 µg of total RNA as input for the reverse transcription reaction to ensure sufficient cDNA yield.
- For the subsequent qPCR reaction, do not use a cDNA dilution that exceeds 1/10 of the total reaction volume. Using a more concentrated template directly addresses the issue of low target abundance.
qPCR Master Mix and Program Optimization:
- Select a qPCR master mix specifically formulated for robust amplification of low-copy templates, which often contains optimized polymerases, buffer components, and Mg2+ concentrations.
- Modify the thermal cycling protocol:
- Use a three-step protocol (denaturation, annealing, extension) instead of a two-step protocol to improve stringency and efficiency.
- Increase the extension time by 50-100% to ensure complete amplification of the target sequence in each cycle.
Research Reagent Solutions
The table below lists essential reagents and their functions for developing and running sensitive multi-analyte and reflex-testing workflows.
| Reagent / Material | Function in the Experiment |
|---|---|
| Taq Pro Universal SYBR qPCR Master Mix | A pre-mixed solution containing a specialized blend of Taq DNA polymerase, buffers, Mg2+, dNTPs, and a fluorescent dye for highly sensitive detection of low-copy number targets in qPCR [46]. |
| Simoa HD-X Analyzer | A fully automated digital immunoassay analyzer that uses single-molecule detection technology to achieve attomolar sensitivity for measuring protein biomarkers in plasma (e.g., GFAP, NfL in neurological tests) [75]. |
| TaqMan Probes | Fluorescently labeled hydrolysis probes used in real-time PCR assays that provide high specificity by only emitting a signal when they bind to the exact target sequence during amplification [1]. |
| Family Member Comparator Specimens | Biological samples from a patient's parents or other relatives used as comparators in whole exome sequencing reflex tests to help filter out inherited benign variants and identify disease-causing mutations [73]. |
Workflow Diagrams for Reflex Testing and Multi-Analyte Analysis
Rule-Based Reflex Testing Workflow
This diagram illustrates the traditional, rule-based reflex testing process as used in clinical laboratories, such as for urinalysis or genetic testing [72] [73].
Multi-Analyte Algorithmic Analysis
This diagram shows the process of combining multiple analytes (e.g., ctDNA and proteins) using an algorithm to generate a single, more specific diagnostic result, as seen in tests like EarlySEEK and CancerSEEK [76] [70] [75].
Machine Learning Smart Reflex Workflow
This diagram outlines the advanced "smart reflex" process that uses a machine learning model to decide on second-line testing, moving beyond simple rules [74].
Validation Frameworks and Comparative Analysis for Clinical-Grade Biomarker Assays
This technical support guide provides troubleshooting and FAQs for researchers establishing analytical methods, specifically framed within the context of troubleshooting high Ct values in cancer biomarker detection research.
FAQs: Core Concepts and Definitions
Q1: What are LOD and LOQ, and why are they critical in cancer biomarker research?
A: The Limit of Detection (LOD) and Limit of Quantitation (LOQ) are fundamental figures of merit that define the capabilities of an analytical method at low analyte concentrations [77] [78].
- LOD is the lowest concentration of an analyte that can be reliably detected by the method, but not necessarily quantified as an exact value. It signifies the point where an analyte's signal can be distinguished from background noise [77] [79].
- LOQ is the lowest concentration that can be quantitatively measured with stated accuracy and precision [77] [80]. For bioanalytical methods, a common acceptance criterion is that the LOQ has precision (CV%) and accuracy within ±20% [80].
In cancer biomarker research—such as detecting low levels of circulating tumor DNA (ctDNA)—a method with a low LOD and LOQ is essential. It allows for the early detection of minimal residual disease or rare molecular events that occur at extremely low concentrations, which might otherwise be missed by less sensitive assays [65].
Q2: How do high Ct values in qPCR relate to LOD and LOQ?
A: In real-time PCR (qPCR), the Ct (threshold cycle) value indicates the cycle number at which the amplification curve crosses the threshold. A high Ct value signifies a low starting quantity of the target nucleic acid [1].
- The precision and accuracy of measurements near the LOQ directly impact the reliability of high Ct value data. High variation (poor precision) at these low concentrations makes it difficult to trust the results.
- If your target biomarker concentration is near the assay's LOD, you can only reliably report its presence or absence. For accurate quantification, the concentration must be at or above the LOQ [77] [78]. Therefore, an assay with an improperly characterized LOQ may produce high Ct values that are not quantitatively meaningful.
Q3: What are the primary methods for determining LOD and LOQ?
A: The ICH Q2(R1) guideline outlines several approaches, with the following being most common [78] [81] [79]:
Table 1: Methods for Determining LOD and LOQ
| Method | Description | Typical Use Case | Key Formulas |
|---|---|---|---|
| Standard Deviation of Response & Slope | Uses the variability of the calibration curve and its slope. Considered robust and scientifically satisfying [81]. | Quantitative methods, especially with calibration curves (e.g., HPLC, qPCR standard curves). | LOD = 3.3 × σ / SLOQ = 10 × σ / SWhere σ = standard deviation of the response, S = slope of the calibration curve [78] [81] [82]. |
| Signal-to-Noise (S/N) | Compares the analyte signal to the background noise. | Instrumental methods with a observable baseline noise (e.g., chromatography) [78]. | LOD: S/N of 2:1 or 3:1LOQ: S/N of 10:1 [78] [80] [79]. |
| Visual Evaluation | Determination based on analyst observation of a known concentration. | Non-instrumental or qualitative methods (e.g., inhibition assays) [78] [79]. | The lowest concentration at which the analyte can be consistently observed [79]. |
The following workflow can guide the selection and execution of the appropriate method:
Troubleshooting Guide: Addressing High Ct Values and Poor Sensitivity
High Ct values in qPCR for cancer biomarkers can stem from issues that also affect LOD, LOQ, precision, and accuracy. This guide helps diagnose and resolve these problems.
Problem: High Ct values, indicating low sensitivity and potential precision issues near the LOQ.
Table 2: Troubleshooting High Ct Values and Poor Sensitivity
| Symptoms | Potential Root Cause | Troubleshooting Experiments & Solutions |
|---|---|---|
| High Ct values, low signal, or non-detect in samples with known low concentrations. | Poor RNA/DNA Quality or Presence of Inhibitors: Degraded nucleic acids or contaminants can reduce amplification efficiency [16]. | Experiment: Run samples on a bioanalyzer or gel to check integrity. Perform a spike-in experiment with a control analyte to check for inhibition.Solution: Optimize RNA purification steps, include clean-up procedures, and use high-quality reagents [16]. |
| High variation in replicate Ct values (poor precision), especially at low concentrations. | Pipetting Inconsistencies: Manual errors can lead to significant variations in template and reagent volumes, critically impacting precision at the LOQ [16]. | Experiment: Compare the CV of results from manually prepared replicates versus those prepared using an automated liquid handler.Solution: Implement proper pipetting techniques, use calibrated equipment, and consider automation to improve accuracy and reproducibility [16]. |
| High Ct values and non-specific amplification (e.g., primer-dimer). | Suboptimal Primer Design or Annealing Conditions: Primers binding non-specifically reduce the efficiency of the target amplification [16]. | Experiment: Run a melt curve analysis to check for multiple products. Test a gradient of annealing temperatures.Solution: Redesign primers using specialized software to ensure appropriate length, GC content, and absence of secondary structures. Optimize the annealing temperature [16]. |
| High Ct values even with a well-characterized assay. | Incorrect Threshold Setting in qPCR Analysis: The threshold is set outside the exponential phase of amplification, leading to artificially high Ct values [1]. | Experiment: Re-analyze the amplification plot on a log scale. The threshold should be set in the linear, exponential phase of the plot, above the background variability but well before the plateau [1].Solution: Visually assess and adjust the threshold within the exponential phase for consistent Ct value calculation across all runs [1]. |
Experimental Protocol: Determining LOQ via the Calibration Curve Method
This is a detailed protocol for establishing the LOQ using the standard deviation and slope method, which is highly applicable to qPCR data.
Objective: To determine the lowest concentration of a cancer biomarker (e.g., a specific gene mutation in ctDNA) that can be quantified with acceptable precision and accuracy using a qPCR-based assay.
Methodology:
Preparation of Calibration Standards:
- Prepare a series of at least five standard solutions in the relevant matrix (e.g., human plasma, buffer) with concentrations expected to be in the low, sub-LOQ range. A recommended practical number of replicates for establishing these parameters is 60 for a manufacturer, while a verifying laboratory might use 20 [77].
Sample Analysis:
- Analyze each calibration standard using the validated qPCR method. The data (concentration and corresponding response, e.g., Ct value or calculated concentration from standard curve) should be collected.
Data Analysis and LOQ Calculation:
- Plot a Standard Curve: Plot the known concentration (X-axis) against the instrument response (Y-axis). Perform a linear regression analysis [81] [82].
- Extract Key Parameters: From the regression analysis, obtain the slope (S) of the calibration curve and the standard error of the regression (σ) or the standard deviation of the y-intercepts [78] [81].
- Calculate LOQ: Use the formula: LOQ = 10 × σ / S [78] [81] [82]. This provides a theoretical concentration for the LOQ.
Experimental Validation (Mandatory):
- The calculated LOQ is an estimate and must be experimentally confirmed [81] [79].
- Prepare a minimum of five (recommended) replicate samples at the calculated LOQ concentration [80].
- Analyze these samples and determine their measured concentrations.
- Acceptance Criteria: The measured concentrations at the LOQ must demonstrate a precision (CV%) and an accuracy (relative error to the nominal concentration) of ≤20% [80]. If these criteria are not met, the LOQ must be re-estimated at a slightly higher concentration and re-validated.
The Scientist's Toolkit: Essential Reagents and Materials
Table 3: Key Research Reagent Solutions for Sensitive qPCR Assays
| Item | Function/Benefit | Considerations for High-Sensitivity Assays |
|---|---|---|
| High-Fidelity DNA Polymerase | Catalyzes DNA amplification; high fidelity reduces errors during replication. | Essential for accurately detecting low-frequency mutations in ctDNA, preventing false positives from polymerase errors. |
| TaqMan Probes or SYBR Green Dye | Fluorescent reporters for real-time detection of amplification. | TaqMan probes offer greater specificity for mutation detection. SYBR Green is more cost-effective but requires careful optimization to avoid non-specific signal. |
| Ultra-Pure dNTPs and MgCl₂ | Building blocks and co-factor for PCR. | Consistent quality and concentration are vital for maintaining robust amplification efficiency, which directly impacts Ct values and precision. |
| Nucleic Acid Purification Kits | Isolate and clean DNA/RNA from complex samples like blood or tissue. | Select kits designed for high recovery of low-concentration cfDNA/ctDNA. Effective removal of inhibitors (e.g., heparin, hemoglobin) is critical [16]. |
| Automated Liquid Handler | Performs precise, nanoliter-scale liquid transfers (e.g., I.DOT Liquid Handler) [16]. | Dramatically reduces pipetting errors, improving accuracy and precision of replicates—especially crucial for measurements near the LOD/LOQ. Minimizes cross-contamination risk [16]. |
| qPCR Plates and Seals | Reaction vessels for amplification. | Use optically clear plates and seals compatible with your qPCR instrument to ensure accurate fluorescence detection without signal loss. |
In cancer biomarker detection research, accurate and sensitive molecular diagnostics are paramount. Quantitative PCR (qPCR), digital PCR (dPCR), and Next-Generation Sequencing (NGS) each offer distinct advantages and limitations. This technical support center focuses on troubleshooting a common challenge across these platforms: high cycle threshold (Ct) values, which can indicate low abundance of target molecules and impact assay reliability. The following guides and FAQs provide targeted solutions for researchers, scientists, and drug development professionals.
FAQs: Platform Selection and Core Concepts
FAQ 1: What is a Ct value in qPCR and what is considered an acceptable range?
The Ct (Cycle Threshold) value is the number of amplification cycles required for the fluorescence signal of a qPCR reaction to cross a predetermined threshold, indicating detection of the target sequence [34] [1]. It is inversely related to the starting quantity of the target nucleic acid; a lower Ct value indicates a higher initial concentration [34] [1]. The generally accepted reasonable range for Ct values is between 15 and 35 [34]. Values below 15 are often in the baseline phase, while values above 35 may indicate that the initial template copy number is less than 1, making the result statistically insignificant [34].
FAQ 2: When should I choose dPCR over qPCR for my cancer biomarker study?
Digital PCR (dPCR) is particularly advantageous when you require absolute quantification without a standard curve, need to detect rare genetic mutations amidst a background of wild-type genes, or are working with very low-abundance targets where superior sensitivity and precision are critical [83] [84]. It is also more resistant to PCR inhibitors, making it suitable for complex clinical samples like liquid biopsies (e.g., analyzing circulating tumor DNA, ctDNA) [83] [85] [84]. A 2025 study on respiratory viruses demonstrated that dPCR provided greater consistency and precision than Real-Time RT-PCR, especially for medium and low viral loads [83].
FAQ 3: What is the primary role of NGS in cancer biomarker discovery?
NGS enables comprehensive genomic profiling by simultaneously evaluating a wide panel of genes for mutations, fusions, and other alterations [86]. It is the recommended technique for identifying multiple actionable mutations concurrently from both tissue and liquid biopsy samples, facilitating the initiation of personalized therapy [86]. A 2025 meta-analysis confirmed that NGS demonstrates high diagnostic accuracy in tissue for mutations like EGFR (sensitivity: 93%, specificity: 97%) and is effective for detecting several key mutations in liquid biopsy [86].
Troubleshooting Guide: Resolving High Ct Values
High Ct values are a common issue in qPCR and can also impact data interpretation in dPCR and NGS library preparation. The causes and solutions are multifaceted.
Q: My qPCR assays are consistently showing high Ct values for my target cancer biomarkers. What are the potential causes and solutions?
High Ct values can stem from issues related to template quality, reaction efficiency, or instrumentation. The table below summarizes the primary causes and their solutions.
Table: Troubleshooting High Ct Values in qPCR
| Problem Category | Specific Cause | Recommended Solution |
|---|---|---|
| Template Quality | Low template concentration or purity; degradation [71] [34]. | Increase template input; re-purify nucleic acids; check absorbance ratios (A260/280 ~1.8-2.0) [71] [34] [87]. |
| Template Quality | Presence of PCR inhibitors (e.g., heparin, phenol, proteins) [34] [87]. | Dilute the template; use a master mix resistant to inhibitors; add a carrier nucleic acid [71] [87]. |
| Reaction Efficiency | Non-optimal primer design leading to dimers, hairpins, or non-specific binding [71] [34]. | Redesign primers following best practices; check for specificity; optimize annealing temperature [71] [34]. |
| Reaction Efficiency | Suboptimal reagent concentrations or reaction conditions [71] [34]. | Use a three-step qPCR program instead of two-step; increase extension time; use kits designed for low-expression targets [71]. |
| Experimental Procedure | Low abundance of the target gene (e.g., low-copy ctDNA) [71]. | Increase the number of technical replicate wells; use a more sensitive platform like dPCR [71] [83]. |
The following workflow diagram outlines a logical, step-by-step process for diagnosing and resolving high Ct value issues in the lab.
Experimental Protocols for Performance Validation
Protocol 1: Determining qPCR Primer Efficiency
Accurate quantification in qPCR relies on primers with high amplification efficiency (ideally 90-110%) [87].
- Prepare Dilutions: Create a minimum of three (preferably five) serial dilutions (e.g., 1:10, 1:100) of your template cDNA or DNA [71] [87].
- Run qPCR: Perform qPCR on all dilution samples in replicate.
- Generate Standard Curve: Plot the Ct values obtained against the logarithm of the initial template concentration for each dilution. The qPCR software can often do this automatically [71] [87].
- Calculate Efficiency: Obtain the slope of the standard curve. Calculate primer efficiency (E) using the formula: E = -1 + 10(-1/slope). Efficiency of 100% corresponds to a slope of -3.32 [87].
Protocol 2: Performing a Digital PCR Assay for Absolute Quantification
dPCR partitions a sample into thousands of individual reactions, allowing for absolute quantification of nucleic acids without a standard curve [84].
- Sample and Master Mix Preparation: Prepare the PCR mixture containing the sample, primers, probes, and dPCR supermix.
- Partitioning: Load the mixture into a dPCR instrument (e.g., droplet-based or nanowell-based like QIAcuity). The instrument automatically partitions the sample into thousands of nanoliter-scale reactions [83] [84].
- Endpoint PCR Amplification: Run a standard PCR protocol on the partitioned sample to amplify the target.
- Fluorescence Reading and Analysis: After amplification, each partition is analyzed for fluorescence. Partitions are scored as positive (containing the target) or negative (not containing the target) [84].
- Absolute Quantification Calculation: The instrument software uses Poisson statistics to calculate the absolute concentration of the target in the original sample (e.g., copies per microliter), based on the ratio of positive to negative partitions [84].
The workflow for a standard dPCR experiment, from sample preparation to result, is visualized below.
The Scientist's Toolkit: Research Reagent Solutions
Table: Essential Reagents for Sensitive Nucleic Acid Detection
| Item | Function | Application Notes |
|---|---|---|
| SYBR Green qPCR Master Mix | Fluorescent dye that binds double-stranded DNA, enabling real-time detection [71]. | Cost-effective; requires optimization to prevent non-specific signal. Use kits formulated for low-expression genes [71]. |
| TaqMan Probe qPCR Master Mix | Sequence-specific fluorescent probes provide higher specificity than intercalating dyes [1]. | Ideal for multiplexing; reduces false positives from primer dimers. |
| dPCR Supermix | Specialized buffer formulation for stable and efficient amplification within partitions (droplets or nanowells) [83] [84]. | Essential for robust digital PCR; often contains stabilizers for partition integrity. |
| NGS Library Prep Kit | Reagents for fragmenting, adapter ligating, and amplifying DNA/cDNA for sequencing [86]. | Select panels based on the number of genes and types of variants (SNVs, fusions, CNVs) to be analyzed [86]. |
| Nucleic Acid Purification Kit | Isolates high-purity DNA/RNA from complex samples (tissue, blood, cells) [83]. | Critical for removing contaminants that inhibit polymerase activity and cause high Ct values [34] [87]. |
Table: Comparative Analysis of qPCR, dPCR, and NGS
| Feature | qPCR | dPCR | NGS |
|---|---|---|---|
| Quantification Method | Relative (requires standard curve) | Absolute (Poisson statistics) | Relative (requires calibration) |
| Sensitivity | High | Very High (can detect single molecules) | High (depends on sequencing depth) |
| Precision | Good | Superior, especially at low target concentrations [83] | Good |
| Multiplexing Capability | Moderate (limited by fluorescence channels) | Moderate | Very High (can assay hundreds of genes simultaneously) [86] |
| Throughput | High | Medium to High | Very High |
| Cost | Low | Medium | High |
| Primary Clinical/Research Use | Gene expression, pathogen detection (qualitative/quantitative) | Rare mutation detection, liquid biopsy, copy number variation [84] | Comprehensive genomic profiling, discovery of novel biomarkers [86] |
| Best Suited For | Rapid, high-throughput quantification of known targets | Absolute quantification of rare targets or in inhibitor-rich samples [85] | Unbiased discovery and parallel analysis of many targets |
In cancer biomarker research, establishing a test's diagnostic accuracy is as crucial as discovering a statistically significant association. A low p-value might indicate that a biomarker's level differs between diseased and healthy populations, but it reveals nothing about how well the test can actually classify individuals. This technical support guide focuses on the essential statistical practices—specifically Classification Error metrics and Receiver Operating Characteristic (ROC) Analysis—that researchers must employ to robustly validate the performance of diagnostic biomarkers, particularly when troubleshooting challenges like high Ct values in qPCR experiments.
Core Concepts: From p-Values to Performance Metrics
What is the fundamental limitation of the p-value in diagnostic test development?
A p-value helps determine if a difference in biomarker levels between groups is likely due to chance. However, it does not quantify the test's ability to correctly identify individuals with and without the condition. A biomarker can show a statistically significant difference (low p-value) yet still have substantial overlap in values between groups, leading to poor classification performance [88] [89].
Which metrics should I use to evaluate the real-world performance of a diagnostic biomarker?
To fully understand your biomarker's diagnostic capability, you need a suite of metrics derived from its classification performance. The foundation for these metrics is the Confusion Matrix, a table that compares the biomarker's predictions against the true disease status (the gold standard) [90] [91].
Confusion Matrix Structure:
- True Positive (TP): The test correctly identifies a person with the disease.
- False Positive (FP): The test incorrectly labels a healthy person as diseased (Type I error).
- True Negative (TN): The test correctly identifies a healthy person.
- False Negative (FN): The test incorrectly labels a person with the disease as healthy (Type II error) [91].
From the confusion matrix, key performance metrics can be calculated. The table below summarizes the most critical ones for biomarker research.
Table 1: Key Performance Metrics for Diagnostic Biomarkers
| Metric | Formula | Interpretation | Clinical Context |
|---|---|---|---|
| Sensitivity (Recall) | TP / (TP + FN) | Ability to correctly identify those with the disease. | Crucial for "rule-out" tests where missing a case is dangerous. |
| Specificity | TN / (TN + FP) | Ability to correctly identify those without the disease. | Crucial for "rule-in" tests where a false alarm is costly. |
| Precision (PPV) | TP / (TP + FP) | Proportion of positive test results that are true positives. | Important when the cost of a false positive is high. |
| F1-Score | 2 × (Precision × Recall) / (Precision + Recall) | Harmonic mean of precision and recall. | Useful when seeking a balance between precision and recall on imbalanced data [90]. |
| Accuracy | (TP + TN) / (TP+TN+FP+FN) | Overall proportion of correct classifications. | Can be misleading with imbalanced datasets [91]. |
| Matthews Correlation Coefficient (MCC) | (TP×TN - FP×FN) / √((TP+FP)(TP+FN)(TN+FP)(TN+FN)) | A balanced measure even on imbalanced classes. Ranges from -1 to +1 [90]. |
Troubleshooting High Ct Values: An ROC Analysis Framework
High Cycle Threshold (Ct) values in quantitative PCR indicate low concentrations of the target biomarker. This can lead to misclassification and requires a rigorous analytical approach to determine the optimal cut-off point.
How can ROC analysis help me determine the best cut-point for a biomarker with high Ct values?
ROC analysis is a powerful method that visualizes the trade-off between sensitivity and specificity across all possible cut-points of a continuous biomarker [88] [89]. This is essential for finding the most effective threshold, even when signal is low (high Ct).
Workflow for Implementing ROC Analysis:
How do I interpret the Area Under the Curve (AUC) value?
The Area Under the ROC Curve (AUC) is a single metric that summarizes the overall diagnostic ability of the biomarker across all possible thresholds [88] [89].
Table 2: Interpretation of AUC Values for Diagnostic Tests
| AUC Value | Interpretation | Clinical Usability |
|---|---|---|
| 0.9 - 1.0 | Excellent discrimination | High clinical utility |
| 0.8 - 0.9 | Considerable/good discrimination | Clinically useful |
| 0.7 - 0.8 | Fair discrimination | Limited clinical utility |
| 0.6 - 0.7 | Poor discrimination | Not very useful |
| 0.5 - 0.6 | Fail (no discrimination) | Test is uninformative [88] |
It is critical to always report the 95% confidence interval for the AUC, as a wide interval indicates uncertainty about the true performance of the test [88].
What methods can I use to select the optimal cut-point from an ROC curve?
Several statistical methods exist to identify the optimal cut-point. The choice can depend on the clinical context and the relative importance of sensitivity versus specificity.
Table 3: Methods for Determining the Optimal Cut-Point in ROC Analysis
| Method | Calculation | Rationale | Best Used When... |
|---|---|---|---|
| Youden Index | J = Sensitivity + Specificity - 1 | Maximizes the overall correct classification rate (sensitivity + specificity) [88] [89]. | The clinical costs of false positives and false negatives are approximately equal. |
| Euclidean Index | Minimizes the Euclidean distance to the point (0,1) on the ROC curve. | Identifies the point on the ROC curve closest to perfect discrimination (100% sensitivity and 100% specificity) [89]. | Seeking a point that balances Se and Sp geometrically. |
| Product of Sensitivity and Specificity | P = Sensitivity × Specificity | Maximizes the product of Se and Sp, another way to balance the two metrics [89]. | Similar to the Youden Index; often produces similar results. |
| Clinical Utility | Based on pre-defined clinical requirements (e.g., Sensitivity > 90%). | Chooses a point that meets the minimal acceptable performance for a specific clinical application. | The test has a defined "rule-out" (high sensitivity) or "rule-in" (high specificity) purpose. |
Advanced Protocols & Statistical Validation
Protocol: Conducting a Robust ROC Analysis
Objective: To determine the diagnostic accuracy of a continuous cancer biomarker and identify its optimal classification cut-point. Materials: NCSS, R (pROC package), SPSS, SAS, Python (scikit-learn).
- Data Preparation: Assemble a dataset with two columns: the continuous biomarker measurements (e.g., Ct values, concentration) and the confirmed disease status (True=Disease, False=Control) based on the gold standard.
- Software Execution: Use the ROC analysis procedure in your chosen software. Input the biomarker as the "test variable" and the disease status as the "state variable."
- Output Generation:
- Generate the ROC curve plot.
- Calculate the AUC with its 95% confidence interval.
- Request a coordinate table listing sensitivity and specificity for every possible cut-point.
- Cut-Point Selection: Apply the Youden Index (or your preferred method) to the coordinate table to identify the optimal cut-point. The cut-point is the value that yields the maximum Youden Index.
- Validation: Report the sensitivity, specificity, positive predictive value (PPV), and negative predictive value (NPV) at the chosen cut-point [89].
How do I statistically compare two biomarkers or two models?
To determine if one biomarker has a significantly higher AUC than another, use the De-Long test [88]. This is a specialized statistical test for comparing correlated AUCs derived from the same set of patients. Most statistical software with ROC analysis capabilities (e.g., R's pROC package) include an implementation of this test. A significant p-value from the De-Long test indicates a real difference in the discriminatory power of the two biomarkers.
Frequently Asked Questions (FAQs)
Q1: My biomarker's AUC is 0.75 and statistically significant (p < 0.01), but my colleagues say it's not clinically useful. Are they correct? Yes, they are likely correct. Statistical significance (p < 0.01) means we can be confident the AUC is not 0.5 (random chance). However, an AUC of 0.75 falls into the "fair" or "limited clinical utility" category [88]. The clinical value depends on the context, but for many applications, an AUC above 0.80 or even 0.90 is required for a test to be considered clinically impactful.
Q2: Why does the optimal cut-point I calculated differ from the one used in a published paper on the same biomarker? Optimal cut-points are not universal constants. They can vary significantly due to:
- Population Differences: The prevalence and severity of the disease in your study population.
- Technical Variation: Differences in assay protocols, reagents, or laboratory equipment, which can be a source of measurement error [92].
- Choice of Method: The use of a different statistical method (Youden vs. Euclidean, etc.) for cut-point selection [89]. It is often necessary to establish a laboratory-specific reference range or cut-point.
Q3: My dataset is highly imbalanced (95% controls, 5% cases). Which metrics should I avoid, and which should I trust? With imbalanced data, accuracy is a highly misleading metric and should not be relied upon. A naive classifier that always predicts "control" would achieve 95% accuracy, falsely indicating excellent performance. Instead, focus on:
- Sensitivity and Specificity: These are independent of prevalence and provide a clearer picture.
- AUC-ROC: Provides a good summary of performance across thresholds.
- Matthews Correlation Coefficient (MCC): Specifically designed to be reliable on imbalanced datasets [93] [90].
Q4: How can measurement error in my biomarker assay impact these classification metrics? Measurement error, a common issue in biomarker research, typically attenuates (reduces) the observed diagnostic performance [92]. This means:
- The observed AUC will be lower than the true AUC.
- The estimates of sensitivity and specificity will be biased towards the performance of a random classifier.
- The ability to find a reliable optimal cut-point is diminished. It is critical to optimize your assay to minimize technical variability and account for measurement error in your statistical models where possible.
The Scientist's Toolkit: Research Reagent Solutions
Table 4: Essential Materials for Cancer Biomarker Validation Studies
| Item | Function in Biomarker Research |
|---|---|
| Reference Standard (Gold Standard) | The definitive method for diagnosing the disease (e.g., histopathology, clinical follow-up). Serves as the benchmark against which the new biomarker is evaluated [93]. |
| Automated Homogenizer (e.g., Omni LH 96) | Standardizes sample preparation (e.g., tissue, biofluids), reducing contamination and pre-analytical variability that can introduce measurement error [55]. |
| Next-Generation Sequencing (NGS) | Enables comprehensive genomic profiling for the discovery of novel biomarkers, such as specific mutations or fusion genes [19] [18]. |
| Liquid Biopsy Kits | Facilitate the non-invasive collection and analysis of circulating tumor DNA (ctDNA), circulating tumor cells (CTCs), and exosomes from blood [19] [18]. |
| Multiplex Immunoassay Panels | Allow simultaneous measurement of multiple protein biomarkers from a single small-volume sample, enabling the creation of diagnostic panels. |
| Artificial Intelligence (AI) / Machine Learning Platforms | Used to identify complex, hidden patterns in multi-omics data to discover novel biomarker signatures and improve image-based diagnostics [19] [90]. |
Assessing Clinical Validity and Utility for Early Detection and Treatment Monitoring
FAQs: Troubleshooting High Ct Values in qPCR for Cancer Biomarkers
FAQ: Why are my qPCR Ct values too high (>35) or undetectable in my cancer biomarker assays?
High Ct values in qPCR experiments can stem from various issues across your experimental workflow. The most common causes and solutions are outlined below [94]:
- Low Gene Expression or Transcript Abundance: The target biomarker may not be expressed above the detection limit in your sample type.
- Poor RNA Sample Quality: Degraded or impure RNA is a frequent culprit. Always perform rigorous quality control checks on your RNA samples.
- Insufficient Template Amount: The amount of input RNA may be too low. Consider using more total RNA, a higher concentration of template, or a larger reaction volume.
- Experimental Error: Include a known positive control template containing your gene of interest to troubleshoot your PCR reagents and procedure.
- Primer/Transcript Mismatch: If detecting expression from an exogenous vector containing only the open reading frame (ORF), ensure your primers are not designed to target untranslated regions (UTRs) that are not present [94].
FAQ: My biomarker data is inconsistent across replicates. What are common lab issues I should check?
Inconsistent data often originates from pre-analytical and analytical stages. Key areas to investigate include [55]:
- Sample Contamination: Contaminants can skew biomarker profiles. Implement strict contamination controls, such as using dedicated clean areas, routine equipment decontamination, and automated homogenization systems to minimize cross-contamination.
- Inconsistent Sample Preparation: Variability in processing, such as during homogenization or extraction, introduces bias and background noise. Standardize your protocols and use validated reagents.
- Improper Temperature Regulation: Biomarkers like nucleic acids are sensitive to temperature fluctuations. Ensure consistent cold-chain logistics and correct storage conditions to prevent degradation.
- Human Factors and Procedure Complexity: Complex, multi-step procedures are prone to human error. Comprehensive training, strict adherence to Standard Operating Procedures (SOPs), and lab automation can significantly reduce these errors [55].
Troubleshooting Guide: Resolving High Ct Values
A systematic approach to troubleshooting is essential for resolving high Ct values. Follow this guide to diagnose and correct common issues.
Step-by-Step Diagnostic Guide
| Step | Action | Expected Outcome |
|---|---|---|
| 1. Check Positive Controls | Run a template known to contain your gene of interest. | A low, expected Ct value confirms your reagents and procedure are working correctly [94]. |
| 2. Assess RNA Quality | Use spectrophotometry (A260/A280 ratio) and/or electrophoresis (e.g., Bioanalyzer) to check for purity and degradation. | High-quality RNA (A260/A280 ~2.0, clear ribosomal bands) is essential for efficient reverse transcription and PCR [94]. |
| 3. Quantify Template Input | Precisely measure RNA concentration and ensure sufficient amount is used per reaction. | Increasing input RNA or using a less diluted template should lower the Ct value, provided inhibition is not an issue [94]. |
| 4. Verify Primer Specificity | Ensure primers are designed to match the specific transcript isoforms in your sample (e.g., for transfected constructs, target the ORF). | Correct primer binding ensures amplification of the intended target and prevents false negatives [94]. |
| 5. Review Experimental Logs | Check for deviations in protocol, reagent lot numbers, or equipment calibration. | Identifying a change in the process can pinpoint the source of the problem [55]. |
Advanced Issues and Solutions
For persistent problems, consider these less common but critical issues:
| Issue | Description | Solution |
|---|---|---|
| PCR Inhibition | Substances co-purified with nucleic acids can inhibit the polymerase. | Dilute the template, use a cleanup column, or add bovine serum albumin (BSA) to the reaction. |
| Poor Reverse Transcription Efficiency | The initial cDNA synthesis step is inefficient. | Use a high-quality reverse transcriptase and ensure primers (oligo-dT and/or random hexamers) are included. |
| Equipment Malfunction | Thermocycler block temperature uniformity or calibration is off. | Validate cycler performance using a calibration kit. |
| Probe Degradation | Fluorescent probes, especially those with fluorophores sensitive to light, have degraded. | Use fresh aliquots of probes and minimize exposure to light. |
Experimental Protocols for Validation
Protocol 1: RNA Integrity and QC Check for Biomarker Research
Purpose: To ensure RNA quality is sufficient for sensitive qPCR detection of biomarkers. Reagents: High-quality RNA sample, RNase-free water, agarose, formaldehyde (or commercial RNA analysis kit). Procedure:
- Use a nanodrop spectrophotometer to measure RNA concentration and purity. Acceptable A260/A280 ratios are typically 1.8-2.1.
- To assess integrity, run an RNA sample on a denaturing agarose gel or a microfluidic system (e.g., Bioanalyzer).
- On a gel, intact total RNA should show sharp ribosomal RNA bands (28S and 18S for eukaryotic RNA), with the 28S band approximately twice the intensity of the 18S band.
- RNA with a RNA Integrity Number (RIN) greater than 8.0 (on a scale of 1-10) is generally considered high-quality for qPCR applications.
Protocol 2: Establishing a Standard Curve for Assay Validation
Purpose: To evaluate the efficiency, dynamic range, and limit of detection of your qPCR assay. Reagents: Serially diluted standard template (e.g., cDNA of known concentration, synthetic gBlock), qPCR master mix, primers, probe. Procedure:
- Prepare a 10-fold serial dilution of your standard template over at least 5 orders of magnitude.
- Run all dilutions in duplicate or triplicate on the same qPCR plate as your test samples.
- Plot the Ct values against the logarithm of the template concentration. The slope of the resulting standard curve is used to calculate amplification efficiency: Efficiency % = (10^(-1/slope) - 1) * 100.
- An ideal assay has an efficiency between 90% and 105%, a correlation coefficient (R²) >0.99, and a defined limit of detection.
Workflow and Process Diagrams
Sample Prep to Data Analysis Workflow
The Scientist's Toolkit: Research Reagent Solutions
Essential materials and reagents for robust qPCR-based biomarker detection.
| Item | Function | Key Considerations |
|---|---|---|
| RNA Stabilization Reagents | Preserve RNA integrity immediately upon sample collection (e.g., RNAlater). | Prevents degradation by RNases; critical for clinical samples. |
| High-Quality Nucleic Acid Extraction Kits | Isolate pure DNA/RNA from complex biological samples (tissue, blood, FFPE). | Look for high yield, consistency, and effective removal of inhibitors. |
| Automated Homogenization Systems | Standardize and streamline sample lysis (e.g., Omni LH 96). | Reduces cross-contamination and operator-dependent variability [55]. |
| Reverse Transcriptase Enzymes | Synthesize complementary DNA (cDNA) from an RNA template. | High efficiency and processivity are vital for representing low-abundance transcripts. |
| Hot-Start DNA Polymerases | Amplify target cDNA sequences during qPCR. | Reduces non-specific amplification and primer-dimer formation, improving sensitivity. |
| Target-Specific Primers & Probes | Enable specific amplification and detection of the biomarker of interest. | Meticulous in silico design and empirical validation are required. |
| Standardized Reference Materials | Serve as positive controls and for generating standard curves. | Essential for assay calibration and inter-laboratory reproducibility [95]. |
Navigating Regulatory Pathways and Biomarker Qualification for Clinical Implementation
Understanding Ct Values in Cancer Biomarker Detection
In real-time PCR (qPCR) experiments, the Ct (Threshold Cycle) value is the number of amplification cycles required for the fluorescent signal of a PCR product to cross a predetermined threshold, indicating detectable amplification [1]. This value is crucial for cancer biomarker research as it provides quantitative information about the initial amount of the target genetic sequence in a sample.
The Ct value is fundamentally linked to template concentration: a lower Ct value indicates a higher starting concentration of the target sequence, while a higher Ct value indicates a lower starting concentration [1] [34]. In ideal conditions with 100% amplification efficiency, the Ct value for quantifying a single gene copy is theoretically around 35 [34]. Ct values exceeding 35 may suggest the initial template copy number is less than 1, making the result statistically questionable [34].
Frequently Asked Questions (FAQs) on High Ct Values
FAQ 1: What range of Ct values is considered reasonable, and when are values considered too high?
In qPCR experiments, the generally accepted reasonable range for Ct values is between 15 and 35 [34]. Values below 15 may fall within the baseline phase and not reliably exceed the fluorescence threshold, while values above 35 often indicate a very low initial template concentration that may be statistically insignificant [34]. Ct values greater than 35 or undetectable values are typically considered too high and can compromise reliable quantification [15].
FAQ 2: What are the primary causes of unusually high Ct values across all wells in an experiment?
High Ct values, indicating delayed amplification, can stem from several technical issues [17]:
- Low Template Quantity or Quality: Too little DNA template [96], poor RNA/DNA quality (degradation or insufficient purity) [96] [15], or the presence of PCR inhibitors [34] can all lead to high Ct values.
- Suboptimal Reaction Efficiency: Factors that reduce the efficiency of the PCR reaction itself will delay amplification. These include incorrect cycling conditions (e.g., temperature profile) [96], low primer annealing efficiency due to poor design [34], and suboptimal reagent composition (e.g., low polymerase concentration or incorrect buffer) [34].
- Experimental Error: Inconsistent pipetting can cause variations in template concentration, leading to high and variable Ct values [16].
FAQ 3: What troubleshooting steps can I take to resolve high Ct values?
- Assess and Improve Template: Ensure proper quantification of DNA/RNA and verify its quality, checking for degradation or contamination [96] [34]. Re-purify the template if necessary to remove inhibitors [34]. Consider increasing the amount of input RNA or using a template at a higher concentration [15].
- Optimize Reaction Components and Conditions: Dilute the sample (10x-1000x) to mitigate the effects of potential inhibitors or excess background DNA that can scatter oligonucleotides [17]. Increase the annealing/extension temperature to enhance the specificity of primer binding [17]. Redesign primers if they form dimers, hairpins, or have mis-matches [34].
- Verify Protocols and Equipment: Double-check the cycler's temperature profile against the recommended protocol [96]. Use a positive control template known to contain the gene of interest to troubleshoot reagents and procedures [15]. Ensure proper pipetting technique and consider using automated liquid handling systems for improved accuracy [16].
FAQ 4: How do high Ct values impact the validation of cancer biomarkers for regulatory submission?
The reliability of qPCR data is critical when generating evidence for biomarker validation and subsequent regulatory qualification. High Ct values, indicative of low target abundance or poor assay efficiency, can negatively impact key validation parameters [97]:
- Sensitivity: High Ct values can reduce the assay's ability to detect a meaningful change in the biomarker, potentially failing to reflect a true change in the clinical endpoint [97].
- Specificity: Assays with non-optimal efficiency (leading to high Ct values) may struggle to distinguish between responders and non-responders to a therapeutic intervention [97].
- Reproducibility: High Ct values are often associated with greater data variability, which undermines the precision required for a robust and reliable biomarker assay [97].
Table 1: Troubleshooting Guide for High Ct Values
| Problem Category | Specific Cause | Recommended Solution |
|---|---|---|
| Template Issues | Low concentration [15] | Increase template amount; use less diluted cDNA [34] |
| Poor quality/Degradation [96] | Repurify template; check A260/A280 ratios; run agarose gel [34] | |
| Presence of PCR inhibitors [34] | Increase dilution factor of RNA/cDNA; prepare template again [34] | |
| Reaction Efficiency | Low primer annealing efficiency [34] | Lower annealing temperature; use two-step amplification; redesign primers [34] |
| Suboptimal reagent composition [34] | Try different qPCR reagent kits; ensure components are mixed thoroughly [34] | |
| Non-specific amplification [17] | Increase annealing temperature; optimize primer design [16] [17] | |
| Experimental Procedure | Incorrect cycler program [96] | Verify and correct the thermal cycler temperature profile [96] |
| Pipetting errors [16] | Use proper pipetting technique; employ automated liquid handlers [16] |
The Scientist's Toolkit: Essential Reagents and Materials
Table 2: Key Research Reagent Solutions for qPCR Experiments
| Item | Function | Key Considerations |
|---|---|---|
| High-Quality Nucleic Acid Isolation Kits | To purify RNA/DNA from complex biological samples (e.g., tumor tissue, blood) with high integrity and minimal inhibitors [96]. | Select kits suitable for your sample type (e.g., FFPE); include RNase digestion for DNA isolation to prevent RNA contamination [96]. |
| Reverse Transcription Kits | To convert RNA into complementary DNA (cDNA) for gene expression analysis. | Ensure high efficiency and fidelity; the resulting cDNA may need dilution to reduce inhibitors from the RT reaction [34]. |
| qPCR Master Mix | A pre-mixed solution containing DNA polymerase, dNTPs, salts, and optimized buffer. | Choose mixes with high polymerase concentration and buffer formulations that maximize enzyme activity and specificity [34]. |
| Validated Primers and Probes | Oligonucleotides designed to specifically amplify and detect the target biomarker sequence. | Use specialized software for design; check for dimers/hairpins; aim for amplicon length of 80-300 bp [34]. |
| Automated Liquid Handler (e.g., I.DOT) | To perform precise, low-volume liquid transfers. | Improves accuracy, reduces human error and cross-contamination, and ensures consistent Ct values [16]. |
Regulatory Pathways for Biomarker Integration
For a cancer biomarker to be used in regulatory decision-making, it must undergo a rigorous process of analytical validation and clinical qualification. The U.S. FDA's Center for Drug Evaluation and Research (CDER) provides two primary pathways for this integration [98]:
- The Drug Approval Process: This is the most common pathway. A drug developer uses a biomarker, established or novel, within the context of a specific drug's clinical trials. The developer is responsible for all aspects of the biomarker's validation. If the biomarker proves useful, its application may be included in the drug's labeling or in guidance documents [98].
- The Biomarker Qualification Program (BQP): This is a formal, drug-independent pathway for biomarkers intended for use across multiple drug development programs. Once a biomarker is "qualified" for a specific Context of Use (COU), it becomes publicly available and can be used by any sponsor for that qualified purpose in their Investigational New Drug (IND), New Drug Application (NDA), or Biologics License Application (BLA) submissions [98] [99].
A qualified biomarker is independent of any specific test kit. While a reliable measurement method is required for qualification, drug sponsors are free to use any analytically validated assay to measure the biomarker in their submissions, provided it demonstrates performance characteristics comparable to the method used during qualification [99].
Regulatory Pathways for Biomarkers
Biomarker Validation and Qualification Framework
The journey of a biomarker from discovery to regulatory acceptance involves distinct stages of evidence generation. The terminology is critical: validation refers to assessing the biomarker's measurement performance characteristics (the assay itself), while qualification is the evidentiary process of linking the biomarker with biological processes and clinical endpoints [97].
The validation process evaluates several key properties of a biomarker [97]:
- Sensitivity: The ability of the biomarker (and its assay) to be measured with adequate precision and to reflect a meaningful change in a clinical endpoint.
- Specificity: The ability of the biomarker to distinguish between patients who respond to a therapy and those who do not.
A biomarker progresses through stages of evidence towards acceptance: from exploratory, to probable valid, to known valid or "fit-for-purpose." [97]. The further a biomarker advances toward being considered a surrogate endpoint, the more thorough its validation must be [97]. This requires a scientific program planned early in drug discovery, with data progressively accumulated from preclinical studies through all phases of clinical trials [97].
Biomarker Validation & Qualification Stages
Successfully navigating the regulatory landscape for cancer biomarkers requires a dual focus. Researchers must first master the technical aspects of qPCR, ensuring robust and reproducible data by systematically troubleshooting issues like high Ct values. Simultaneously, a clear strategic understanding of the FDA's pathways—leveraging the drug approval process for specific applications or pursuing broader qualification through the BQP—is essential. By integrating precise laboratory practice with a forward-looking regulatory strategy, scientists can effectively translate promising biomarkers from the bench to the clinic, accelerating the development of targeted cancer therapies.
Conclusion
Effectively troubleshooting high Ct values is paramount for unlocking the full potential of cancer biomarkers in precision medicine. A systematic approach that integrates a deep understanding of biomarker biology, adopts advanced sensitive methodologies like dPCR and NGS, implements rigorous troubleshooting protocols, and adheres to robust statistical validation frameworks is essential. Future directions will be shaped by the integration of multi-omics data, the application of AI for pattern recognition in complex datasets, and the development of standardized, scalable workflows. By addressing these challenges, researchers can enhance the reliability of biomarker detection, accelerating the development of non-invasive tools for early cancer diagnosis, personalized treatment selection, and improved patient outcomes.
References
- 1. Understanding Ct Values in Real-Time PCR [https://www.thermofisher.com/blog/behindthebench/understanding-ct-values/]
- 2. Circulating tumor DNA to monitor treatment response in ... [https://www.nature.com/articles/s41698-025-00876-y]
- 3. Emerging biomarkers for early cancer detection and diagnosis [https://pmc.ncbi.nlm.nih.gov/articles/PMC12359849/]
- 4. Circulating tumor DNA methylation detection as biomarker ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11550092/]
- 5. Principles of Real-time Quantitative PCR [https://www.cd-genomics.com/diseasepanel/resource/principles-real-time-quantitative-pcr.html]
- 6. Comprehensive performance evaluation of a high-throughput ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12206697/]
- 7. Analyzing qPCR data: Better practices to facilitate rigor and ... [https://www.sciencedirect.com/science/article/pii/S2405580825004431]
- 8. Circulating Tumor DNA as a Cancer Biomarker [https://pmc.ncbi.nlm.nih.gov/articles/PMC9350013/]
- 9. Circulating tumor nucleic acids: biology, release mechanisms ... [https://molecular-cancer.biomedcentral.com/articles/10.1186/s12943-022-01710-w]
- 10. Avoiding Failure in DIA Proteomics: Common Pitfalls and ... [https://www.creative-proteomics.com/ngpro/resource-dia-proteomics-failure-pitfalls-fixes.html]
- 11. - Pre Practices in the Molecular Diagnostic Tests, A Concise... analytical [https://pmc.ncbi.nlm.nih.gov/articles/PMC7691716/]
- 12. Top 5 quality factors that make or break biospecimen research [https://blog.crownbio.com/top-5-quality-factors-that-make-or-break-biospecimen-research]
- 13. RNA Preservation Methods to Improve RNA Quality and ... [https://alitheagenomics.com/blog/rna-preservation-methods-to-improve-rna-quality-and-quantity]
- 14. Sample Preparation for High-Quality Sequencing Results [https://www.cd-genomics.com/resource-sample-preparation-for-sequencing.html]
- 15. Why are my qPCR Ct values too high (> 35 or not ... [https://www.qiagen.com/us/resources/faq/2685]
- 16. qPCR Troubleshooting: How to Ensure Successful ... [https://dispendix.com/blog/qpcr-troubleshooting]
- 17. What troubleshooting is recommended when Ct values are ... [https://pcrbio.com/resources/faqs/qpcrbio-probe-mix/what-troubleshooting-is-recommended-when-ct-values-are-higher-than-usual/]
- 18. Emerging biomarkers for early cancer detection and diagnosis [https://eurjmedres.biomedcentral.com/articles/10.1186/s40001-025-03003-6]
- 19. Cancer Biomarkers: Reflection on Recent Progress, Emerging ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12468363/]
- 20. Identification of major factors associated with failed clinical ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5528718/]
- 21. Mutation Detection Support—Troubleshooting [https://www.thermofisher.com/us/en/home/technical-resources/technical-reference-library/real-time-digital-PCR-applications-support-center/mutation-detection-support/mutation-detection-support-troubleshooting.html]
- 22. Challenges and Future Trends in Biomarker Analysis for ... [https://blog.crownbio.com/challenges-and-future-trends-in-biomarker-analysis-for-clinical-research-whats-ahead-in-2025]
- 23. Applications and challenges of biomarker-based predictive ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12399543/]
- 24. A multiplexed, next generation sequencing platform for ... [https://www.nature.com/articles/s41467-021-21653-y]
- 25. Bioinformatic screen with clinical validation for the ... [https://www.nature.com/articles/s41598-025-13074-4]
- 26. Liquid biopsy in cancer: current status, challenges and ... [https://www.nature.com/articles/s41392-024-02021-w]
- 27. Improvement of the sensitivity of circulating tumor DNA- ... [https://www.explorationpub.com/Journals/etat/Article/1002333]
- 28. Liquid biopsy in cancer management: Integrating diagnostics ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11743551/]
- 29. Circulating tumor cells: overcoming challenges of detecting ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12123222/]
- 30. Isolation of circulating tumor cells: recent progress and ... [https://link.springer.com/article/10.1007/s44258-024-00044-0]
- 31. Exosome Biomarker Profiling Using a Paper-Based ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12563862/]
- 32. MXenes for exosome detection: a new frontier in biomolecular ... [https://pubs.rsc.org/en/content/articlehtml/2025/ma/d5ma00394f]
- 33. Analytical Validation of Exosome Diagnostics for Clinical ... [https://www.sepscience.com/analytical-validation-of-exosome-diagnostics-for-clinical-applications-12159]
- 34. The Reasonable Range of Ct Values in qPCR Experiments [https://www.yeasenbio.com/blogs/molecular-biology/the-reasonable-range-of-ct-values-in-qpcr-experiments]
- 35. Library Preparation Quality Control and Quantification [https://www.lexogen.com/blog/rna-lexicon-library-preparation-quality-control-and-quantification/]
- 36. Analysis of error profiles in deep next-generation ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6417284/]
- 37. Correcting errors in PCR-derived libraries for rare allele ... [https://www.nature.com/articles/s42003-025-08537-3]
- 38. Comparison and evaluation of metagenomic next- ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12634516/]
- 39. Clinical implementation of next-generation sequencing ... [https://www.nature.com/articles/s41598-024-84909-9]
- 40. Real-Time vs Digital vs Traditional PCR [https://www.thermofisher.com/lc/en/home/life-science/pcr/real-time-pcr/qpcr-education/qpcr-vs-digital-pcr-vs-traditional-pcr.html]
- 41. The Clinical Utility of Droplet Digital PCR for Profiling Circulating Tumor DNA in Breast Cancer Patients - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC9776872/]
- 42. Medical diagnostic value of digital PCR (dPCR): A systematic review - ScienceDirect [https://www.sciencedirect.com/science/article/pii/S2667099223000221]
- 43. dPCR vs qPCR [https://www.qiagen.com/us/applications/digital-pcr/beginners/dpcr-vs-qpcr]
- 44. Droplet digital PCR for detection and quantification of circulating tumor DNA in plasma of head and neck cancer patients | BMC Cancer | Full Text [https://bmccancer.biomedcentral.com/articles/10.1186/s12885-017-3424-0]
- 45. PCR Troubleshooting Guide | Thermo Fisher Scientific - US [https://www.thermofisher.com/us/en/home/life-science/cloning/cloning-learning-center/invitrogen-school-of-molecular-biology/pcr-education/pcr-reagents-enzymes/pcr-troubleshooting.html]
- 46. Troubleshoot High Ct Values: qPCR Optimization [https://www.vazymeglobal.com/News/MediaReleases/1707309414879432705.html]
- 47. Troubleshooting qPCR: Interpreting Amplification Curves [https://blog.biosearchtech.com/thebiosearchtechblog/bid/63622/qpcr-troubleshooting]
- 48. Troubleshooting fine‐tuning procedures for qPCR system ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6647679/]
- 49. Quantitative PCR validation for research scientists: Part 1 of 2 [https://virologyresearchservices.com/2023/01/13/quantitative-pcr-validation-part-1-of-2/]
- 50. AI-Powered Biomarker Discovery: 7 ... [https://lifebit.ai/blog/ai-powered-biomarker-discovery/]
- 51. New AI-based biomarkers offer insight into treatment ... [https://dailyreporter.esmo.org/esmo-congress-2025/ai-digital-oncology/new-artificial-intelligence-based-biomarkers-offer-early-insight-into-treatment-response]
- 52. How Artificial Intelligence Is Transforming Cancer Care in ... [https://oncodaily.com/oncolibrary/artificial-intelligence-ai]
- 53. Tumor markers in clinical practice: General principles and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC2902207/]
- 54. Preanalytical Errors in Clinical Laboratory Testing at a ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10981510/]
- 55. Common Lab Issues That Impact Biomarker Data [https://blog.omni-inc.com/blog/common-lab-issues-that-impact-biomarker-data]
- 56. Reducing Pre-Analytical Errors in Clinical Diagnostics [https://clpmag.com/lab-essentials/quality-systems/quality-control-programs/reducing-pre-analytical-errors-clinical-diagnostics/]
- 57. Evaluation of direct-to-PCR (D2P) method for molecular ... [https://www.sciencedirect.com/science/article/pii/S001448002500022X]
- 58. Learn from the SARS-CoV-2 nucleic acid test to increase ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12020272/]
- 59. Optimization of internal reference genes for qPCR in human ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8797320/]
- 60. Instrumentation Calibration Do's & Don'ts [https://www.linkedin.com/pulse/instrumentation-calibration-dos-donts-nagaraj-kumbar-3zxwc]
- 61. How to Avoid Common Lab Equipment Calibration Errors [https://ifm.flagshipinc.com/common-calibration-errors]
- 62. Impact of Laboratory Cross-Contamination on Molecular ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC1594630/]
- 63. PCR Troubleshooting Guide & Solutions [https://www.bosterbio.com/protocol-and-troubleshooting/pcr-troubleshooting?srsltid=AfmBOoqPvT0sY2Zc3Ks2u-GiCdhm0o-EdLx6fj3mI7ZmafKrTA3yKpDW]
- 64. Quantifying and Reducing the Effect of Calibration Error on ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4491194/]
- 65. Exploring Circulating Tumor DNA (CtDNA) and Its Role in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10516512/]
- 66. Controlling Cross-Contamination in Research Facilities [https://dycem.com/blog/controlling-cross-contamination-in-research-facilities/]
- 67. How to Make a Calibration Curve: A Step-by-Step Guide [https://www.labmanager.com/how-to-make-a-calibration-curve-28411]
- 68. Consensus guidelines for the validation of qRT-PCR ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8792405/]
- 69. How Do I Calculate Values from a Standard Curve [https://www.creative-diagnostics.com/how-do-i-calculate-values-from-a-standard-curve.htm]
- 70. Multi-analyte approach combining cfDNA sequencing and ... [https://www.sciencedirect.com/science/article/pii/S2589004225008788]
- 71. Troubleshoot High Ct Values: qPCR Optimization in Three ... [https://www.linkedin.com/pulse/science-lab-troubleshoot-high-ct-values-qpcr-optimization-three]
- 72. Don't Forget Your Rules When Harmonizing Laboratory ... [https://www.cap.org/member-resources/clinical-informatics-resources/dont-forget-your-rules-when-harmonizing-laboratory-testing-across-multiple-sites]
- 73. Panel to Whole Exome Sequencing Reflex Test, Varies [https://www.mayocliniclabs.com/test-catalog/overview/621326]
- 74. Using machine learning to develop smart reflex testing ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10797267/]
- 75. Clinical performance of scalable automated p‐tau 217 multi ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12635865/]
- 76. Multi-analyte assays and early detection of common cancers [https://pmc.ncbi.nlm.nih.gov/articles/PMC6072951/]
- 77. Limit of Blank, Limit of Detection and Limit of Quantitation [https://pmc.ncbi.nlm.nih.gov/articles/PMC2556583/]
- 78. What is meant by the limit of detection and quantification (LOD ... [https://mpl.loesungsfabrik.de/en/english-blog/method-validation/limit-of-detection-quantifcation]
- 79. Method Validation Essentials, Limit of Blank ... [https://www.biopharminternational.com/view/method-validation-essentials-limit-blank-limit-detection-and-limit-quantitation]
- 80. Limit of Quantitation - an overview [https://www.sciencedirect.com/topics/nursing-and-health-professions/limit-of-quantitation]
- 81. Determining LOD and LOQ Based on the Calibration Curve [https://www.sepscience.com/hplc-solutions-126-chromatographic-measurements-part-5-determining-lod-and-loq-based-on-the-calibration-curve-6959]
- 82. Calculate LOD and LOQ with Microsoft Excel [https://bitesizebio.com/48459/excel-lod-loq/]
- 83. Comparative Performance of Digital PCR and Real-Time RT ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12474457/]
- 84. Digital PCR: from early developments to its future application ... [https://pubs.rsc.org/en/content/articlehtml/2025/lc/d5lc00055f]
- 85. Detection of bacterial pathogens directly from synovial ... [https://www.sciencedirect.com/science/article/pii/S0732889325000720]
- 86. Diagnostic accuracy of next-generation sequencing (NGS) ... [https://link.springer.com/article/10.1007/s12094-025-04040-7]
- 87. Understanding qPCR Efficiency and Why It Exceeds 100% [https://biosistemika.com/blog/qpcr-efficiency-over-100/]
- 88. A guide to interpreting the area under the curve value - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC10664195/]
- 89. Methods of determining optimal cut-point of diagnostic ... [https://bmcmedresmethodol.biomedcentral.com/articles/10.1186/s12874-024-02198-2]
- 90. Evaluation metrics and statistical tests for machine learning [https://www.nature.com/articles/s41598-024-56706-x]
- 91. Evaluation Metrics For Classification Model [https://www.analyticsvidhya.com/blog/2021/07/metrics-to-evaluate-your-classification-model-to-take-the-right-decisions/]
- 92. Biomarker data with measurement error in medical research [https://pmc.ncbi.nlm.nih.gov/articles/PMC11305697/]
- 93. Challenges in the real world use of classification accuracy ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10550141/]
- 94. Why are my qPCR Ct values too high (> 35 or not detectable) in ... [https://www.qiagen.com/us/resources/faq?id=25fdb628-8670-41c2-9e50-b2fc5e88b9e9&lang=en]
- 95. Causes behind error rates for predictive biomarker testing [https://pmc.ncbi.nlm.nih.gov/articles/PMC8099794/]
- 96. What could have gone wrong if the CT values are ... [https://www.qiagen.com/us/resources/faq/3412]
- 97. A Pathway and Approach to Biomarker Validation ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3261486/]
- 98. Pathways for Biomarker Integration in Drug Development [https://www.fda.gov/drugs/biomarker-qualification-program/pathways-biomarker-integration-drug-development]
- 99. Qualifying a Biomarker through the Biomarker Qualification ... [https://www.fda.gov/drugs/biomarker-qualification-program/qualifying-biomarker-through-biomarker-qualification-program]