Transfer Learning for MRI Brain Tumor Detection: Advanced Models, Clinical Implementation, and Future Directions
This article comprehensively reviews the application of transfer learning (TL) for brain tumor detection in MRI scans, tailored for researchers and drug development professionals.
Transfer Learning for MRI Brain Tumor Detection: Advanced Models, Clinical Implementation, and Future Directions
Abstract
This article comprehensively reviews the application of transfer learning (TL) for brain tumor detection in MRI scans, tailored for researchers and drug development professionals. It explores the foundational principles of TL and its necessity in medical imaging, details state-of-the-art methodologies including hybrid CNN-Transformer architectures and attention mechanisms, and addresses key challenges like data scarcity and model interpretability. The scope also includes a rigorous comparative analysis of model performance and validation techniques, synthesizing findings to discuss future trajectories for integrating these AI tools into biomedical research and clinical diagnostics to enhance precision medicine.
The Foundation of Transfer Learning in Neuro-Oncology: From Basic Concepts to Clinical Imperatives
Defining Transfer Learning and its Core Mechanism in Medical Image Analysis
Transfer learning is a machine learning technique where knowledge gained from solving one problem is reused to improve performance on a different, but related, problem [1]. Instead of building a new model from scratch for each task, transfer learning uses pre-trained models as a starting point, leveraging patterns learned from large datasets to accelerate training and enhance performance on new tasks with limited data [2].
In medical image analysis, this approach is particularly valuable given the scarcity of large, annotated medical datasets and the substantial computational resources required to train deep learning models from scratch [1] [2]. For brain tumor detection in MRI scans, transfer learning enables researchers to adapt models initially trained on natural images to the specialized domain of medical imaging, significantly reducing development time while maintaining high diagnostic accuracy [3] [4].
Core Mechanisms of Transfer Learning
Fundamental Principles
The core mechanism of transfer learning operates on the principle that neural networks learn hierarchical feature representations. In computer vision applications, early layers typically detect low-level features like edges and textures, middle layers identify more complex shapes and patterns, while later layers specialize in task-specific features [2]. Transfer learning exploits this hierarchical structure by preserving and reusing the generic feature detectors from earlier layers while retraining only the specialized later layers for the new task.
This process involves two key types of layers:
- Frozen layers: Layers that retain knowledge from the original task and are not updated during retraining
- Modifiable layers: Layers that are retrained to adapt to the new task [2]
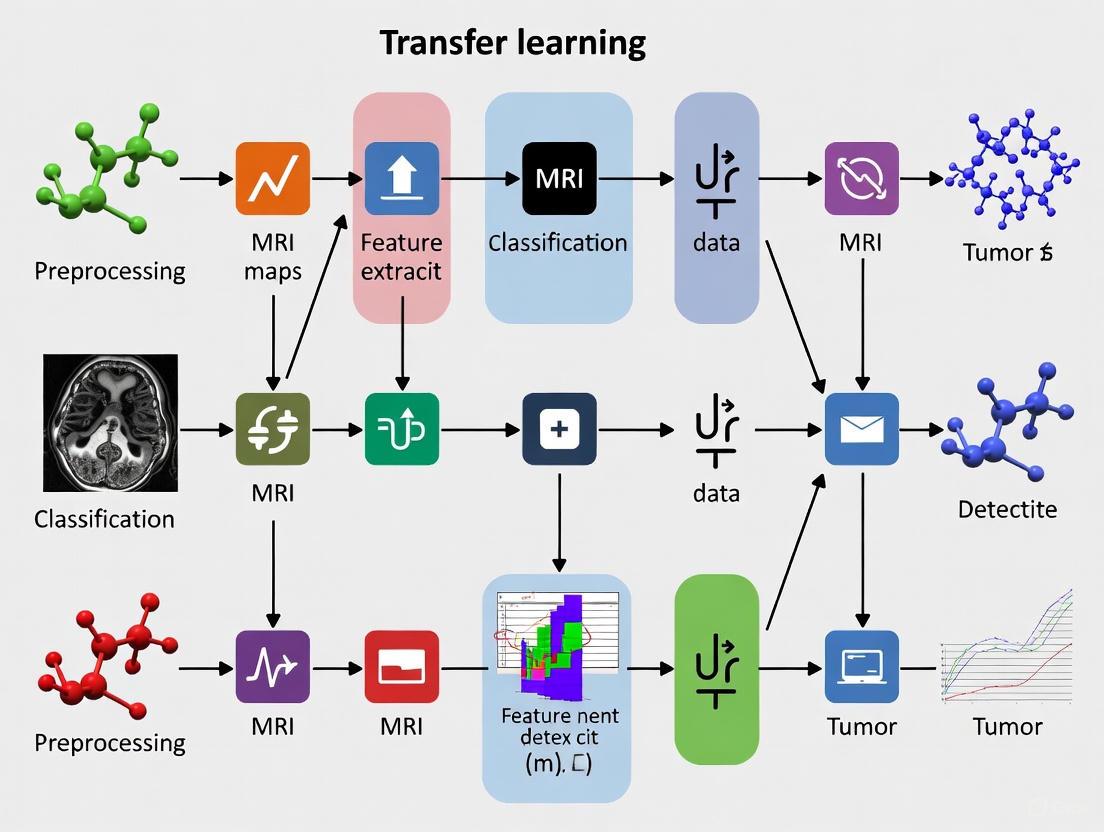
Transfer Learning Workflow for Medical Imaging
The following diagram illustrates the standard transfer learning pipeline for adapting a general image classification model to the specific task of brain tumor detection in MRI scans:
Types of Transfer Learning Approaches
Three primary approaches facilitate knowledge transfer across domains and tasks:
Inductive Transfer: Applied when source and target tasks differ, but domains may be similar or different. This commonly appears in computer vision where models pre-trained for feature extraction on large datasets are adapted for specific tasks like object detection [1].
Transductive Transfer: Used when source and target tasks are identical, but domains differ. Domain adaptation is a form of transductive learning that applies knowledge from one data distribution to the same task on another distribution [1].
Unsupervised Transfer: Employed when both source and target tasks are different, and data is unlabeled. This approach identifies common patterns across unlabeled datasets for tasks like anomaly detection [1].
Performance Comparison of Transfer Learning Models in Brain Tumor Detection
Quantitative Performance Metrics
Table 1: Comparative performance of transfer learning models for brain tumor classification
| Model Architecture | Dataset Size | Accuracy (%) | Preprocessing Techniques | Tumor Types Classified |
|---|---|---|---|---|
| GoogleNet [3] | 4,517 MRI scans | 99.2 | Data augmentation, class imbalance handling | Glioma, Meningioma, Pituitary, Normal |
| Enhanced YOLOv7 [4] | 10,288 images | 99.5 | Image enhancement filters, data augmentation | Glioma, Meningioma, Pituitary, Non-tumor |
| CNN with Feature Extraction [5] | 7,023 MRI images | 98.9 | Gaussian filtering, binary thresholding, contour detection | Glioma, Meningioma, Pituitary, Non-tumor |
| AlexNet [3] | 4,517 MRI scans | 98.1 | Data augmentation, class imbalance handling | Glioma, Meningioma, Pituitary, Normal |
| MobileNetV2 [3] | 4,517 MRI scans | 97.8 | Data augmentation, class imbalance handling | Glioma, Meningioma, Pituitary, Normal |
| YOLOv11 Pipeline [6] | Large diverse dataset + fine-tuning | 93.5 mAP | Two-stage transfer learning, geometric transformations | Glioma, Meningioma, Pituitary |
Advanced Implementation Frameworks
Table 2: Advanced transfer learning frameworks for brain tumor analysis
| Framework | Core Innovation | Transfer Learning Strategy | Key Advantages |
|---|---|---|---|
| YOLOv11 Pipeline [6] | Two-stage transfer learning with morphological post-processing | Base model trained on large dataset, then fine-tuned on smaller domain-specific dataset | High mAP (93.5%), generates segmentation masks, extracts clinical metrics |
| Enhanced YOLOv7 [4] | Integration of CBAM attention mechanism and BiFPN | Pre-trained model fine-tuned with domain-specific augmentation | 99.5% accuracy, improved small tumor detection, multi-scale feature fusion |
| Multi-Model Comparison [3] | Comprehensive analysis of AlexNet, MobileNetV2, GoogleNet | Individual model fine-tuning with data augmentation | Direct architecture comparison, GoogleNet achieved 99.2% accuracy |
Experimental Protocols and Methodologies
Standard Transfer Learning Protocol for Brain Tumor Classification
Phase 1: Data Preparation and Preprocessing
- Data Collection: Curate MRI dataset with balanced representation of tumor types (glioma, meningioma, pituitary) and normal scans [3] [5]
- Data Augmentation: Apply geometric transformations (rotation, flipping, scaling) to increase dataset diversity and prevent overfitting [4]
- Image Enhancement: Implement filters (Gaussian, binary thresholding) to improve contrast and highlight regions of interest [4] [5]
- Class Imbalance Handling: Employ sampling techniques or weighted loss functions to address unequal class distribution [3]
Phase 2: Model Selection and Adaptation
- Base Model Selection: Choose pre-trained model (GoogleNet, AlexNet, MobileNetV2, YOLO variants) based on task requirements [3] [4]
- Architecture Modification: Replace final classification layers with tumor-specific categories (glioma, meningioma, pituitary, non-tumor) [3]
- Layer Freezing: Preserve early and middle layers for generic feature extraction while enabling retraining of later layers [2]
Phase 3: Training and Optimization
- Two-Stage Training:
- Hyperparameter Tuning: Adjust learning rates, batch sizes, and optimization algorithms for medical imaging context
- Regularization: Apply techniques to prevent overfitting on limited medical data
Phase 4: Validation and Interpretation
- Performance Metrics: Evaluate using accuracy, precision, recall, F1-score, and mAP [3] [4]
- Clinical Validation: Assess model outputs against radiological expert annotations
- Interpretability: Implement visualization techniques (Grad-CAM, attention maps) to explain model decisions [4]
Advanced Two-Stage Transfer Learning Protocol
Stage 1: Base Model Development (Brain Tumor Detection Model - BTDM)
- Train model on large, diverse MRI dataset (10,000+ images) [6]
- Implement domain-specific augmentation: mosaic, cutmix, horizontal flipping [6]
- Continue training until mean Average Precision (mAP) exceeds 90% [6]
- Designate optimized model as Brain Tumor Detection Model (BTDM) [6]
Stage 2: Specialized Model Fine-tuning (Brain Tumor Detection and Segmentation - BTDS)
- Utilize structurally similar but smaller dataset for fine-tuning [6]
- Apply transfer learning from BTDM to maintain performance with limited data [6]
- Integrate morphological post-processing for segmentation mask generation [6]
- Extract clinically relevant metrics: tumor size, location, severity level [6]
Research Reagents and Computational Tools
Table 3: Essential research reagents and computational tools for transfer learning in medical imaging
| Resource Type | Specific Examples | Function/Application |
|---|---|---|
| Pre-trained Models | AlexNet, GoogleNet, MobileNetV2, ResNet, YOLO variants [3] [4] [2] | Provide foundation for transfer learning, feature extraction capabilities |
| Medical Imaging Datasets | Kaggle Brain Tumor MRI Dataset, Figshare dataset [3] [5] | Source of domain-specific data for fine-tuning and validation |
| Data Augmentation Tools | Geometric transformations, mosaic augmentation, cutmix [4] [6] | Increase dataset diversity, improve model generalization |
| Attention Mechanisms | Convolutional Block Attention Module (CBAM) [4] | Enhance feature extraction, focus on salient tumor regions |
| Feature Fusion Networks | Bi-directional Feature Pyramid Network (BiFPN) [4] | Enable multi-scale feature fusion, improve small tumor detection |
| Performance Metrics | Accuracy, mean Average Precision (mAP), F1-score [3] [6] | Quantify model performance, enable comparative analysis |
| Post-processing Modules | Morphological operations, segmentation mask generation [6] | Extract clinical metrics (tumor size, severity), enhance interpretability |
Technical Implementation Considerations
Optimization Strategies
Successful implementation of transfer learning for brain tumor detection requires addressing several technical challenges:
Data Scarcity Mitigation
- Leverage data augmentation techniques specifically tailored for medical images [4]
- Utilize two-stage transfer learning to maximize knowledge extraction from limited data [6]
- Implement class imbalance handling strategies to prevent model bias [3]
Architecture Optimization
- Integrate attention mechanisms (CBAM) to improve focus on tumor regions [4]
- Employ feature pyramid networks (BiFPN) for multi-scale feature detection [4]
- Balance computational efficiency with detection accuracy through model selection [3] [2]
Clinical Relevance Enhancement
- Develop post-processing modules for tumor segmentation and measurement [6]
- Generate clinically interpretable outputs (tumor size, location, severity) [6]
- Validate model performance against radiological expert assessments [4]
The strategic implementation of transfer learning mechanisms detailed in these protocols demonstrates significant potential for advancing automated brain tumor detection systems, ultimately contributing to improved diagnostic accuracy and patient outcomes in neuro-oncological care.
The accurate detection and diagnosis of brain tumors using Magnetic Resonance Imaging (MRI) are critical for determining appropriate treatment strategies and improving patient survival rates. However, the development of robust, automated diagnostic tools, particularly those powered by artificial intelligence (AI), faces two fundamental and interconnected challenges: the inherent scarcity of large, annotated medical datasets and the significant variability in clinical MRI data [7] [8]. Manual annotation of brain tumors by medical experts is time-consuming, expensive, and prone to inter-observer variability, leading to a natural limitation in dataset sizes [7]. Furthermore, MRI data acquired from different hospitals using various scanner manufacturers, models, and acquisition protocols exhibit substantial variations in image characteristics, such as intensity, contrast, and noise profiles, a phenomenon often termed "scanner effects" [7] [8]. This heterogeneity can severely degrade the performance and generalizability of AI models when deployed in real-world clinical settings. This Application Note details these challenges within the context of transfer learning research and provides structured protocols to effectively address them, enabling the development of more reliable and translatable diagnostic tools.
The following tables summarize the core data challenges and the performance of advanced methods designed to overcome them.
Table 1: Key Challenges in Brain Tumor MRI Data for AI Research
| Challenge Category | Specific Manifestation | Impact on AI Model Development |
|---|---|---|
| Data Scarcity | Limited number of annotated medical images [7] | Increased risk of model overfitting and poor generalization [7] |
| High cost and time required for expert labeling [7] | Limits the scale and diversity of datasets available for training | |
| Data Variability | Intensity inhomogeneity (bias field effects) [9] | Introduces non-biological variations, confusing feature extraction algorithms |
| "Scanner effects" from different protocols and equipment [7] [8] | Reduces model robustness and performance on external validation sets [7] | |
| Variations in tumor appearance (size, shape, morphology) [7] | Complicates the learning of consistent and generalizable tumor features | |
| Class Imbalance | Uneven distribution of tumor types (e.g., glioma, meningioma) and "no tumor" cases [10] | Introduces bias, causing models to perform poorly on underrepresented classes |
Table 2: Performance of Advanced Models Addressing Data Challenges
| Model Architecture | Core Strategy | Reported Performance | Reference |
|---|---|---|---|
| Fine-tuned VGG16 | Transfer Learning & Bounding Box Localization | Accuracy: 99.86% (Brain Tumor MRI Dataset) [10] | |
| GoogleNet (Transfer Learning) | Transfer Learning & Data Augmentation | Accuracy: 99.2% (4,517 image dataset) [3] | |
| DenseTransformer (DenseNet201 + Transformer) | Hybrid CNN-Attention & Transfer Learning | Accuracy: 99.41% (Br35H dataset) [11] | |
| CNN-SVM Hybrid | Hybrid Architecture (Feature Learning + Classification) | Accuracy: 98.5% [7] | |
| Swin Transformer | Advanced Transformer Architecture | Accuracy: Up to 99.9% [7] |
Experimental Protocols for Robust Model Development
This section outlines detailed methodologies for key experiments cited in this note, providing a reproducible framework for researchers.
Protocol: Transfer Learning for Brain Tumor Classification
This protocol is based on the methodology that achieved 99.86% accuracy using a fine-tuned VGG16 model [10].
1. Dataset Description and Preprocessing:
- Dataset: Use a curated brain tumor MRI dataset (e.g., the combined Figshare, SARTAJ, and Br35H dataset containing 7,023 images across four classes: glioma, meningioma, pituitary tumor, and no tumor) [10].
- Image Resizing: Load and resize all MRI images to a uniform 224 x 224 pixels to ensure consistency as input to the Convolutional Neural Network (CNN) model.
- Image Normalization: Scale pixel values to a range of 0 to 1 to enhance model convergence and reduce computational complexity [10].
- Data Splitting: Partition the dataset into training (80%), validation (10%), and test (10%) sets, ensuring a balanced distribution of classes across splits [10].
2. Data Augmentation (for addressing data scarcity and class imbalance): Apply the following augmentation techniques in real-time during training to increase the diversity of the training data and mitigate overfitting [10]:
- Shear (30%)
- Zoom (30%)
- Vertical and Horizontal Flip
- Fill Mode: 'nearest'
3. Model Selection and Fine-Tuning:
- Model Initialization: Select a pre-trained model (e.g., VGG16, ResNet50, Xception) initialized with weights from large-scale natural image datasets like ImageNet [10].
- Fine-Tuning Strategy:
- Unfreeze only the last 5 layers of the pre-trained model. This allows the model to adapt its high-level, task-specific features to the medical domain while retaining the general feature detectors learned from ImageNet.
- Replace the original classification head (top layers) with custom layers tailored for the specific brain tumor classification task (e.g., a new fully connected layer with 4 output nodes) [10].
- Training Hyperparameters:
- Epochs: 100 (with early stopping to prevent overfitting).
- Optimizer: Adam.
- Loss Function: Categorical Cross-Entropy.
Protocol: Multi-Scanner Harmonization and Preprocessing Pipeline
This protocol addresses data variability and is critical for ensuring model generalizability [8] [12].
1. Preprocessing Steps: Implement a sequential pipeline using tools like the FMRIB Software Library (FSL):
- Skull Stripping: Use FSL's Brain Extraction Tool (BET) to remove non-brain tissue [12].
- Bias Field Correction: Apply FSL's FMRIB's Automated Segmentation Tool (FAST) to correct for low-frequency intensity inhomogeneity (bias field) across the image [12].
- Denoising: Utilize an edge-preserving filter like FSL's SUSAN denoising to reduce high-frequency noise while preserving important structural details [12].
- Intensity Normalization: Perform Z-score normalization on the image to standardize intensities to a mean of zero and a standard deviation of one, reducing inter-scanner variability [12].
2. Harmonization Validation:
- Feature Reproducibility Analysis: Extract radiomic features from the processed images. Assess feature stability across different preprocessing pipelines and scanner types using the Intraclass Correlation Coefficient (ICC). Prefer features with high ICC (e.g., ≥ 0.90) for model development, as they are more robust to technical variations [12].
- Traveling Headers/Phantom Studies: Incorporate data from traveling human subjects or standardized phantoms scanned across multiple sites and scanners to quantitatively evaluate and correct for site-specific effects [8].
Workflow and Signaling Diagrams
The following diagram illustrates the integrated workflow for developing a robust brain tumor classification system that addresses data scarcity and variability.
Figure 1: Integrated workflow for robust brain tumor classification model development, illustrating how core solutions address key data challenges.
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials and Tools for Brain Tumor MRI Analysis
| Item/Tool Name | Function/Application | Explanation & Relevance |
|---|---|---|
| FSL (FMRIB Software Library) | Image Preprocessing & Analysis | A comprehensive library of analysis tools for fMRI, MRI, and DTI brain imaging data. Critical for implementing data harmonization pipelines (e.g., BET, FAST, SUSAN) [12]. |
| BraTS Dataset | Model Training & Benchmarking | A large-scale, multi-institutional benchmark dataset for brain tumor segmentation, providing multi-modal MRI scans with expert-annotated ground truth [7] [9]. |
| Pre-trained CNN Models (VGG16, ResNet50, DenseNet201) | Transfer Learning Base Models | Models pre-trained on ImageNet provide powerful, generic feature extractors. Fine-tuning them on medical images is a highly effective strategy when data is scarce [3] [10] [11]. |
| Grad-CAM / SHAP | Model Interpretability (XAI) | Techniques that produce visual explanations for decisions from CNN models, increasing clinical trust by highlighting regions of the MRI that influenced the classification [13] [11]. |
| Data Augmentation Tools (e.g., TensorFlow Keras ImageDataGenerator) | Mitigating Data Scarcity | Software tools that programmatically expand training datasets using transformations (rotation, flips, etc.), improving model robustness and combating overfitting [3] [10]. |
Pre-trained models have revolutionized the field of computer vision by providing powerful, ready-to-use solutions that save time and computational resources. These models, trained on large-scale datasets like ImageNet, capture intricate patterns and features, making them highly effective for image classification and other visual tasks [14]. Within medical imaging, and specifically for tumor detection in MRI scans, transfer learning with these models accelerates development and enhances the accuracy of diagnostic tools [3] [13]. This document provides a detailed overview of four common pre-trained models—VGG16, ResNet, DenseNet, and GoogleNet—framed within the context of brain tumor detection research. It includes architectural summaries, experimental protocols, and key reagents to equip researchers and scientists with the necessary knowledge for effective implementation.
Model Architectures and Principles
- VGG16: Developed by the Visual Geometry Group at the University of Oxford, VGG16 is characterized by its simplicity and depth, using only 3x3 convolutional filters stacked in a sequential manner. It consists of 13 convolutional layers and 3 fully connected layers, totaling 16 weight layers [15] [16]. Its uniform architecture makes it a strong baseline feature extractor.
- ResNet (Residual Networks): Introduced by Microsoft Research, ResNet revolutionized deep learning by solving the vanishing gradient problem through residual connections [14] [17]. These skip connections allow the network to learn residual functions by referencing the layer's inputs, expressed as
H(x) = F(x) + x, enabling the training of networks that are substantially deeper (e.g., ResNet-50, ResNet-101) than was previously feasible [17]. - DenseNet (Densely Connected Convolutional Network): DenseNet connects each layer to every other layer in a feed-forward fashion within a dense block [18] [19]. This architecture ensures maximum information flow between layers, encourages feature reuse, and significantly reduces the number of parameters, making it both efficient and powerful [18].
- GoogleNet (Inception v1): GoogleNet introduced the Inception module, which performs multiple convolution operations (1x1, 3x3, 5x5) in parallel, along with max pooling, and concatenates their outputs [20]. A key innovation is the use of 1x1 convolutions for dimensionality reduction, which decreases computational cost. It also uses auxiliary classifiers during training to combat the vanishing gradient problem and improve convergence in its 22-layer deep network [20].
Comparative Analysis for Tumor Detection
The table below summarizes the key architectural features and performance considerations of these models, particularly for medical image analysis.
Table 1: Comparative analysis of pre-trained models for tumor detection applications
| Aspect | VGG16 | ResNet | DenseNet | GoogleNet (Inception v1) |
|---|---|---|---|---|
| Core Innovation | Depth via small (3x3) filters [16] | Residual learning with skip connections [17] | Dense connectivity for feature reuse [18] | Inception module (multi-scale processing) [20] |
| Key Strength | Simple, robust feature extraction [14] | Trains very deep networks effectively [14] [17] | High parameter efficiency, strong gradient flow [18] | Computational efficiency, good accuracy [20] [21] |
| Depth (Layers) | 16 [16] | 50, 101, 152 (variants) [14] | 121, 169, 201 (variants) [14] [18] | 22 [20] |
| Parameter Count | High (~138 million) [16] | Moderate (e.g., ~25.6M for ResNet-50) | Low (e.g., ~8M for DenseNet-121) [18] | Low (~7M) [20] |
| Handling Vanishing Gradient | Prone | Mitigated via skip connections [17] | Mitigated via dense connections [18] | Mitigated via auxiliary classifiers [20] |
| Example Performance in Brain Tumor Classification | 94% accuracy (Hybrid CNN-VGG16) [13] | High accuracy in comparative studies [3] | Suitable for complex feature extraction [18] | 99.2% accuracy (highest in a 2025 study) [3] |
Experimental Protocol for Tumor Classification in MRI Scans
This protocol outlines a standardized methodology for leveraging pre-trained models to classify brain tumors from MRI scans, for instance, into categories like Glioma, Meningioma, Pituitary tumor, and Normal [3].
The following diagram illustrates the end-to-end experimental workflow for transfer learning-based tumor classification.
Detailed Methodology
Data Preprocessing and Augmentation
- Data Sourcing: Utilize publicly available datasets of brain MRI scans. A representative dataset includes 4,517 images across three tumor types (Glioma, Meningioma, Pituitary) and normal brains [3].
- Preprocessing Pipeline:
- Normalization: Scale pixel intensities to a range of [0, 1] by dividing by 255 [17].
- Resizing: Resize all images to the input size required by the pre-trained model (e.g., 224x224 for VGG16 and others) [15] [13].
- Data Augmentation: To address overfitting and class imbalance, apply real-time data augmentation during training. This includes random rotations, width and height shifts, shearing, zooming, and horizontal flipping [3] [15] [13]. This is efficiently implemented using tools like the
ImageDataGeneratorin Keras [15].
Model Setup and Fine-tuning
- Base Model Initialization: Load a pre-trained model (e.g., VGG16, ResNet, GoogleNet) without its top classification head. The convolutional base is used as a feature extractor [13].
- Custom Classifier Addition: Attach a new, randomly initialized classifier on top of the base model. This typically consists of a flattening layer, followed by one or more fully connected (Dense) layers with ReLU activation, and a final softmax output layer with a number of units equal to the tumor classes [15].
- Fine-tuning Strategy:
- Feature Extraction Phase: Initially, freeze the weights of the pre-trained base model and only train the newly added classifier layers. This allows the model to learn to interpret the pre-computed features for the new task.
- Fine-Tuning Phase: Unfreeze a portion of the deeper layers of the base model and train the entire network end-to-end with a very low learning rate (e.g., 1e-5). This carefully adapts the pre-trained features to the specifics of the medical imaging domain [13].
Training Configuration
- Optimizer: Use adaptive optimizers like Adam or SGD with Nesterov momentum. A learning rate scheduler (e.g., reducing the learning rate when validation accuracy plateaus) is highly recommended for stable fine-tuning [17].
- Loss Function: Use
Categorical Crossentropyfor multi-class classification. - Regularization: Employ techniques like Dropout in the fully connected layers and L2 regularization in convolutional layers to prevent overfitting [15] [17].
- Early Stopping: Halt training if the validation performance does not improve for a pre-defined number of epochs (e.g., 20) to avoid overfitting and save computational resources [15].
Model Validation and Explainability
- Performance Metrics: Evaluate the model on a held-out test set using metrics such as Accuracy, Precision, Recall, F1-Score, and Area Under the ROC Curve (AUC) [13].
- Explainable AI (XAI): Integrate XAI methods like SHapley Additive exPlanations (SHAP) or Gradient-weighted Class Activation Mapping (Grad-CAM) to generate visual explanations [13]. These heatmaps highlight the regions in the MRI scan that were most influential in the model's prediction, which is critical for building clinical trust and verifying that the model focuses on biologically relevant areas [13].
The Scientist's Toolkit: Research Reagent Solutions
The table below lists essential computational "reagents" and tools required to implement the described experimental protocol.
Table 2: Essential research reagents and computational tools for transfer learning in medical imaging
| Research Reagent / Tool | Specification / Function | Application Note |
|---|---|---|
| Pre-trained Model Weights | VGG16, ResNet, DenseNet, GoogleNet trained on ImageNet. | Serves as a robust feature extractor, providing a strong initialization for the medical task [14] [15]. |
| MRI Datasets | Curated public datasets (e.g., Figshare) with labeled tumor classes [3]. | The foundational data for training and evaluation. Requires careful partitioning into training, validation, and test sets. |
| Data Augmentation Generator | Keras ImageDataGenerator or PyTorch torchvision.transforms. |
Artificially expands the training dataset in real-time, improving model generalization and robustness [15]. |
| Optimizer | Adam or SGD with momentum and learning rate scheduling. | Controls the weight update process during training. Scheduling is crucial for effective fine-tuning [17]. |
| Explainability Framework | SHAP or Grad-CAM libraries. | Provides post-hoc interpretability of model predictions, a necessity for clinical validation and adoption [13]. |
| Computational Hardware | GPU with sufficient VRAM (e.g., NVIDIA Tesla V100, RTX 3090). | Accelerates the training of deep neural networks, which is computationally intensive, especially for 3D medical images. |
Within magnetic resonance imaging (MRI) research, the development of robust computer-aided diagnostic (CAD) systems, particularly those leveraging transfer learning, relies on access to high-quality, annotated datasets. These datasets serve as the foundational bedrock for training, validating, and benchmarking sophisticated deep learning models. For researchers and drug development professionals, selecting the appropriate dataset is a critical first step that directly influences the validity and generalizability of their findings. This application note provides a detailed overview of three pivotal resources in this domain—the BraTS, Figshare, and Kaggle datasets. It offers a structured comparison of their characteristics, outlines detailed experimental protocols for their use in transfer learning workflows, and visualizes the key methodologies to accelerate research in accurate brain tumor detection and classification.
Benchmark datasets provide the ground truth necessary for developing and evaluating automated brain tumor analysis systems. The BraTS, Figshare, and Kaggle collections are among the most widely used, each with distinct focuses and attributes.
BraTS (Brain Tumor Segmentation): The BraTS benchmark is a continuously evolving challenge focused primarily on the complex task of pixel-wise segmentation of glioma sub-regions. The BraTS 2025 dataset includes multi-parametric MRI (mpMRI) scans from both pre-treatment and post-treatment patients, featuring T1-weighted, post-contrast T1-weighted (T1ce), T2-weighted, and T2 FLAIR modalities [22]. Its annotations are exceptionally detailed, delineating the Enhancing Tumor (ET), Non-enhancing Tumor Core (NETC), Peritumoral Edema (also referred to as Surrounding Non-enhancing FLAIR Hyperintensity, SNFH), and Resection Cavity (RC). These are also combined to evaluate the Whole Tumor (WT) and Tumor Core (TC) [22]. With thousands of cases, it is a large-scale dataset designed for developing robust, clinically relevant segmentation models.
Figshare: The Figshare repository hosts several brain tumor datasets. A prominent, widely used dataset is the one contributed by Cheng et al., which contains 3,064 T1-weighted contrast-enhanced MRI images [23]. This dataset is curated for a three-class classification task (glioma, meningioma, pituitary tumor), making it a standard benchmark for image-level classification models rather than segmentation. A newer dataset, BRISC (Brain tumor Image Segmentation & Classification), addresses common limitations in existing collections. Announced in 2025, BRISC offers 6,000 T1-weighted MRI slices with physician-validated pixel-level masks and a balanced multi-class classification split, covering glioma, meningioma, pituitary tumor, and no tumor classes [24].
Kaggle: The Kaggle platform hosts community-driven datasets, often curated for specific learning and competition goals. One such public Brain Tumor MRI Dataset contains 7,023 T1-weighted images categorized for classification into four classes: glioma, meningioma, pituitary tumor, and no tumor [5] [25]. These datasets are typically structured for ease of use in deep learning pipelines, providing a straightforward path for applying transfer learning to classification problems.
Table 1: Quantitative Comparison of Key Brain Tumor MRI Datasets
| Dataset Name | Primary Task | Modality | Volume | Classes / Annotations | Key Features |
|---|---|---|---|---|---|
| BraTS 2025 [22] | Segmentation | Multi-parametric MRI (T1, T1ce, T2, FLAIR) | ~2,877 3D cases | • Enhancing Tumor (ET)• Non-Enhancing Tumor Core (NETC)• Edema (SNFH)• Resection Cavity (RC) | Focus on pre- & post-treatment glioma; standardized benchmark |
| Figshare (Cheng et al.) [23] | Classification | T1-weighted, contrast-enhanced | 3,064 2D images | • Glioma• Meningioma• Pituitary Tumor | Classic benchmark for three-class tumor classification |
| Figshare (BRISC 2025) [24] | Segmentation & Classification | T1-weighted | 6,000 2D slices | • Glioma, Meningioma, Pituitary, No Tumor• Pixel-wise binary masks | Balanced distribution; expert-validated masks; multi-plane slices |
| Kaggle (Brain Tumor MRI) [5] [25] | Classification | T1-weighted | 7,023 2D images | • Glioma, Meningioma, Pituitary, No Tumor | Large volume; readily usable for training classification models |
Table 2: Typical Performance Benchmarks of Transfer Learning Models on These Datasets
| Model | Dataset | Reported Accuracy | Key Strengths |
|---|---|---|---|
| GoogleNet [3] | Figshare (3-class) | 99.2% | High accuracy on balanced classification tasks |
| ResNet152 with SVM [25] | Kaggle (4-class) | 98.53% | Powerful feature extraction combined with robust classifier |
| CNN (Custom) [5] | Kaggle (4-class) | 98.9% | End-to-end learning; high precision in detection |
| Random Forest [26] | BraTS (for classification) | 87.0% | Can outperform complex DL models on certain classification tasks |
| MobileNetV2 [3] | Figshare (3-class) | High (Comparative) | Lightweight architecture suitable for resource-constrained deployment |
Experimental Protocols for Transfer Learning
This section outlines detailed methodologies for employing transfer learning on the aforementioned datasets, covering both classification and segmentation tasks.
Multi-class Tumor Classification Protocol
Objective: To fine-tune a pre-trained deep learning model for classifying brain MRI images into tumor types (e.g., Glioma, Meningioma, Pituitary) or "No Tumor" using datasets like Figshare or Kaggle.
Materials: Figshare (BRISC or Cheng et al.) or Kaggle Brain Tumor MRI Dataset [24] [23] [5].
Procedure:
- Data Preprocessing:
- Image Conversion: Convert all images to grayscale to reduce computational complexity, as essential features are based on intensity [5].
- Noise Reduction: Apply a Gaussian filter to blur images and suppress high-frequency noise [5] [25].
- Intensity Normalization: Rescale pixel values to a standard range (e.g., 0-1) to ensure stable model training.
- Size Standardization: Resize all images to match the input size required by the pre-trained model (e.g., 224x224 for models like ResNet or GoogleNet) [25].
- Data Augmentation (On-the-fly): To artificially expand the dataset and improve model generalization, apply random in-memory transformations to each training batch. These can include:
- Random rotations (±10°)
- Horizontal and vertical flipping
- Brightness and contrast variations
- Model Preparation & Transfer Learning:
- Select a Pre-trained Model: Choose a model pre-trained on a large natural image dataset (e.g., ImageNet). Common choices include ResNet152, GoogleNet, or MobileNetV2 [3] [25].
- Replace Classifier Head: Remove the final fully connected classification layer of the pre-trained model and replace it with a new one with output nodes equal to the number of tumor classes (e.g., 4).
- Fine-tuning: Train the model on the brain tumor dataset. It is common practice to use a lower learning rate for the pre-trained layers and a higher one for the newly added classifier head to avoid catastrophic forgetting.
- Evaluation: Evaluate the fine-tuned model on the held-out test set using metrics such as Accuracy, Precision, Recall, and F1-Score [25].
The workflow for this protocol is visualized below.
Tumor Segmentation Protocol with Advanced Augmentation
Objective: To train a model for pixel-wise segmentation of brain tumor sub-regions using the BraTS dataset, incorporating advanced on-the-fly data augmentation to improve robustness.
Materials: BraTS dataset (mpMRI scans) [22].
Procedure:
- Data Preprocessing:
- Co-registration and Normalization: The BraTS data is already pre-processed with co-registered MR sequences, interpolated to a uniform 1mm³ resolution, and skull-stripped [22].
- Intensity Normalization: Perform per-sequence (T1, T1ce, T2, FLAIR) Z-score normalization across each volume.
- Advanced On-the-Fly Augmentation:
- Synthetic Tumor Insertion: To address data scarcity and class imbalance, integrate a Generative Adversarial Network (GAN), such as GliGAN, into the training loop [22]. This approach dynamically inserts realistic synthetic tumors into healthy brain tissue or existing tumor scans during training, vastly increasing the model's exposure to diverse tumor appearances.
- Targeted Augmentation: Use the conditional nature of GliGAN to modify the input label masks, for instance, by scaling down lesions to create more small tumor examples or by swapping under-represented tumor class labels (e.g., converting Edema to Enhancing Tumor) to balance class distribution [22].
- Model Training:
- Architecture Selection: The nnU-Net framework is a robust, self-configuring baseline that has proven highly effective in BraTS challenges and is an excellent starting point [22].
- Training Loop: The model is trained on random 3D patches extracted from the mpMRI volumes. The on-the-fly augmentation (including synthetic tumor insertion) is applied to each batch before it is fed into the network.
- Evaluation: The model's performance is evaluated on the validation set using the BraTS-standard Dice similarity coefficient for the Enhancing Tumor (ET), Tumor Core (TC), and Whole Tumor (WT) regions [22].
The workflow for this advanced segmentation protocol is as follows.
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Tools and Models for Brain Tumor Analysis Research
| Tool / Reagent | Type | Function in Research | Exemplar Use Case |
|---|---|---|---|
| nnU-Net [22] | Deep Learning Framework | A self-configuring framework for medical image segmentation that automatically adapts to dataset properties. | Used as a robust baseline and core architecture for segmenting BraTS tumor sub-regions. |
| GliGAN [22] | Generative Adversarial Network | A pre-trained GAN for generating realistic synthetic brain tumors and inserting them into MRI scans. | Dynamic, on-the-fly data augmentation to increase model robustness and address class imbalance. |
| ResNet152 [25] | Pre-trained CNN Model | A very deep convolutional network for powerful hierarchical feature extraction from images. | Used as a feature extractor or fine-tuned for high-accuracy classification of tumor types. |
| GoogleNet [3] | Pre-trained CNN Model | A deep network with inception modules for efficient multi-scale feature computation. | Fine-tuned for brain tumor classification, achieving state-of-the-art accuracy. |
| Support Vector Machine (SVM) [25] | Machine Learning Classifier | A classical classifier that finds the optimal hyperplane to separate different classes in a high-dimensional space. | Used as the final classifier on deep features extracted by a pre-trained CNN (e.g., ResNet152). |
Implementing State-of-the-Art Transfer Learning Architectures and Techniques
Within the broader scope of thesis research on transfer learning for tumor detection in MRI scans, the fine-tuning of pre-trained Convolutional Neural Networks (CNNs) has emerged as a cornerstone technique. It effectively addresses the primary challenge in medical imaging: developing highly accurate models despite limited annotated datasets [27] [28]. This approach leverages feature hierarchies learned from large-scale natural image databases, such as ImageNet, and adapts them to the specific domain of neuroimaging, enabling robust classification of brain tumors like glioma, meningioma, and pituitary tumors [13].
The following sections provide a detailed examination of the state-of-the-art, presenting quantitative performance comparisons, structured experimental protocols, and essential toolkits to equip researchers and scientists with the practical knowledge for implementing these methods in diagnostic and drug development workflows.
Performance Analysis of Pre-trained Architectures
Recent studies have systematically evaluated various pre-trained architectures, demonstrating their efficacy in brain tumor classification. The table below summarizes the reported performance of several prominent models on standard datasets.
Table 1: Performance of Fine-Tuned Pre-trained Models in Brain Tumor Classification
| Model Architecture | Reported Accuracy | Dataset Used | Number of Classes | Key Findings / Context |
|---|---|---|---|---|
| InceptionV3 | 98.17% (Testing) [29] | Kaggle (7023 images) | 4 | Achieved impressive training accuracy of 99.28% [29]. |
| VGG19 | 98% (Classification Report) [29] | Kaggle (7023 images) | 4 | Demonstrated strong performance, beating other compared models [29]. |
| GoogleNet | 99.2% [3] | Dataset with 4,517 MRI scans | 4 | Outperformed previous studies using the same dataset [3]. |
| Fine-tuned ResNet-34 | 99.66% [27] | Brain Tumor MRI Dataset (7023 images) | 4 | Enhanced with Ranger optimizer and custom head; surpassed state-of-the-art [27]. |
| Proposed Automated DL Framework | 99.67% [30] | Figshare dataset | N/S | Used ensemble model after deep learning-based segmentation and attention modules [30]. |
| Xception | 98.57% [28] | Br35H dataset | 2 (Binary) | Part of a fine-tuned model for binary classification (abnormal vs. normal) [28]. |
| DenseTransformer (Hybrid) | 99.41% [11] | Br35H: Brain Tumor Detection 2020 | 2 (Binary) | Hybrid model combining DenseNet201 and Transformer with MHSA [11]. |
The performance of these models is heavily influenced by the specific fine-tuning strategies and data handling protocols employed. The following section details the core methodologies that underpin these results.
Experimental Protocols for Fine-Tuning
A successful fine-tuning experiment for brain tumor classification involves a structured pipeline from data preparation to model training. The protocol below synthesizes best practices from recent high-performing studies [27] [28].
Data Preprocessing and Augmentation Protocol
Objective: To prepare a robust and generalized dataset for model training. Materials: Raw MRI dataset (e.g., Figshare, Br35H), Python with OpenCV/TensorFlow/PyTorch libraries.
- Data Cleansing: Identify and remove duplicate images using algorithms like MD5 hashing to prevent overfitting [27].
- Normalization: Normalize pixel intensities using the mean and standard deviation from the ImageNet dataset (
mean = [0.485, 0.456, 0.406],std = [0.229, 0.224, 0.225]) to align with the pre-trained model's expected input distribution [27]. - Resizing and Cropping: Resize all images to a larger dimension (e.g., 256x256 pixels) followed by a random center crop to the target input size of the network (e.g., 224x224 for ResNet). This preserves important anatomical details while introducing variability [27].
- Data Augmentation: Apply real-time augmentation during training to increase dataset diversity and improve model generalization. Common techniques include:
- Vertical/Horizontal Flipping: Addresses orientation variability in MRI scans [27].
- Random Rotation (±20 degrees): Improves model invariance to slight angular differences [27].
- Random Zoom (e.g., 0.2): Helps the model learn features at different scales [27].
- Brightness Adjustment (e.g., max_delta=0.4): Accounts for differences in MRI scanner settings and imaging protocols [27].
Table 2: Standard Data Augmentation Parameters
| Augmentation Technique | Typical Parameter Value | Purpose |
|---|---|---|
| Rotation | ±20 degrees | Invariance to patient head tilt |
| Zoom | 0.2 (20%) | Robustness to tumor size variance |
| Width/Height Shift | 0.2 (20%) | Invariance to tumor location |
| Horizontal Flip | True | Positional invariance |
| Brightness Adjustment | Max Delta = 0.4 | Robustness to scanner intensity variation |
Model Fine-Tuning and Training Protocol
Objective: To adapt a pre-trained CNN for the specific task of brain tumor classification. Materials: Pre-trained model (e.g., ResNet, VGG, Inception), deep learning framework (TensorFlow/PyTorch).
Base Model Selection and Initial Setup:
Custom Classification Head:
- Remove the original fully connected (FC) head of the pre-trained model.
- Replace it with a new, randomly initialized head. A typical structure includes:
- A Global Average Pooling 2D (GAP2D) layer to convert feature maps into a vector, reducing parameters and overfitting compared to a flattening layer [28].
- One or more Dense layers (e.g., 512, 256 units) with ReLU activation and Dropout regularization (e.g., rate=0.5) to combat overfitting [28].
- A final Dense layer with Softmax activation, with units equal to the number of tumor classes (e.g., 4 for glioma, meningioma, pituitary, no tumor) [27].
Two-Phase Training:
- Phase 1: Train only the newly added classification head for a few epochs using a frozen convolutional base. This allows the head to learn to interpret the existing features.
- Phase 2: Unfreeze a portion (or all) of the convolutional base for fine-tuning. Use a significantly lower learning rate (e.g., 10 times smaller) than used in Phase 1 to make small, precise adjustments to the pre-trained features [13].
Optimization and Compilation:
- Use optimizers that contribute to stable convergence, such as Ranger (a combination of RAdam and Lookahead) [27] or Adam.
- Compile the model with a loss function like
categorical_crossentropyfor multi-class classification. - Implement learning rate scheduling or early stopping to prevent overfitting and optimize training time.
The Scientist's Toolkit: Research Reagent Solutions
This section catalogs the essential "research reagents"—key datasets, software, and hardware—required to conduct experiments in fine-tuning CNNs for brain tumor classification.
Table 3: Essential Research Reagents for Fine-Tuning Experiments
| Reagent / Resource | Type | Specification / Example | Primary Function in Experiment |
|---|---|---|---|
| Benchmark MRI Datasets | Data | Figshare (3064+ images), Br35H (3000 images), Kaggle Brain Tumor MRI Dataset (7023 images) [29] [27] [28] | Provides standardized, annotated data for model training, validation, and comparative performance benchmarking. |
| Pre-trained Model Weights | Software | ImageNet-pretrained models (ResNet34, VGG19, InceptionV3, Xception, DenseNet201) [29] [11] [28] | Serves as the foundational feature extractor, providing a robust starting point for transfer learning. |
| Deep Learning Framework | Software | TensorFlow 2.x / Keras, PyTorch | Offers the programming environment and high-level APIs for building, fine-tuning, and evaluating deep learning models. |
| Data Augmentation Library | Software | TensorFlow ImageDataGenerator, Torchvision transforms |
Systematically generates variations of training data to improve model generalization and combat overfitting. |
| Optimizer | Algorithm | Ranger (RAdam + Lookahead), Adam, SGD | Controls the model's weight update process during training, impacting convergence speed and final performance [27]. |
| Explainable AI (XAI) Tool | Software | Grad-CAM, LIME, SHAP [11] [13] | Provides visual and quantitative explanations for model predictions, building trust and enabling clinical validation. |
| Computing Hardware | Hardware | GPU with ≥ 8GB VRAM (NVIDIA RTX 3080, A100) | Accelerates the computationally intensive process of model training and inference. |
Advanced Architectural Strategies
Beyond basic fine-tuning, recent research has focused on hybrid and advanced architectural strategies to push performance boundaries.
Integration of Attention Mechanisms
Attention modules, such as Multi-Head Self-Attention (MHSA) and Squeeze-and-Excitation Attention (SEA), can be integrated after the CNN backbone. These mechanisms allow the model to focus on diagnostically salient regions in the MRI scan by capturing global contextual relationships and channel-wise dependencies, which is crucial for identifying irregular or small tumors [11].
Hybrid CNN-Transformer Frameworks
Models like the DenseTransformer combine the strengths of CNNs in local feature extraction with the ability of Transformers to model long-range dependencies. These hybrid frameworks leverage a pre-trained CNN (e.g., DenseNet201) for initial feature extraction and then process the reshaped features through a Transformer encoder to capture global context, achieving state-of-the-art accuracy [11].
Explainable AI (XAI) for Model Interpretation
For clinical deployment, model interpretability is paramount. Techniques like Gradient-weighted Class Activation Mapping (Grad-CAM) and SHapley Additive exPlanations (SHAP) are used to generate heatmaps that highlight the regions of the MRI scan that most influenced the model's decision. This aligns the AI's reasoning with clinical expertise, fostering trust and facilitating validation by radiologists [11] [13].
The application of deep learning to medical image analysis, particularly for brain tumor detection in Magnetic Resonance Imaging (MRI) scans, represents a critical frontier in modern computational oncology. Within the broader context of transfer learning research for tumor detection, hybrid models that integrate Convolutional Neural Networks (CNNs) with attention mechanisms and Transformer architectures have emerged as a particularly powerful paradigm. These models synergistically combine the proven feature extraction capabilities of CNNs, honed on large-scale natural image datasets, with the powerful global contextual reasoning of Transformers, which excel at capturing long-range dependencies in images [31] [32]. This fusion addresses fundamental limitations of pure architectures: CNNs are limited by their local receptive fields, while Transformers are often computationally intensive and data-hungry for high-resolution medical images [32]. The resulting hybrid frameworks achieve state-of-the-art performance in classification, detection, and segmentation tasks, enabling more precise, interpretable, and clinically actionable tools for researchers, scientists, and drug development professionals working in neuro-oncology.
Quantitative Performance of Hybrid Architectures
Recent research demonstrates that hybrid models consistently outperform traditional CNN and pure Transformer approaches across multiple benchmark datasets. The table below summarizes the performance of key hybrid architectures in brain tumor classification.
Table 1: Performance of Hybrid Models for Brain Tumor Classification on MRI Scans
| Model Name | Architecture Type | Reported Accuracy | Key Metrics | Dataset Used |
|---|---|---|---|---|
| HybLwDL [33] | Lightweight Hybrid Twin-Attentive Pyramid CNN | 99.5% | High computational efficiency | Brain Tumor Detection 2020 |
| VGG16 + Custom Attention [34] | CNN (VGG16) + SoftMax-weighted Attention | 99% | Precision and Recall ~99% | Kaggle (7023 images) |
| Hierarchical Multi-Scale ViT [32] | Vision Transformer with Multi-Scale Attention | 98.7% | Precision: 0.986, F1-Score: 0.987 | Brain Tumor MRI Dataset |
| ShallowMRI Attention [35] | Lightweight CNN with Novel Attention | 98.24% (Multiclass) | Computational cost: 25.4 G FLOPs | Kaggle Multiclass, BR35H |
| ANSA_Ensemble [36] | Shallow Attention-guided CNN | 98.04% (Best) | Cross-dataset validation | Cheng, Bhuvaji, Sherif |
| Ensemble CNN (VGG16) [37] | Transfer Learning (VGG16) | 98.78% (Test) | Specificity >0.98 | Kaggle (4 classes) |
These quantitative results underscore a clear trend: the integration of attention and Transformer components into established CNN pipelines reliably pushes classification accuracy into the high 98th and 99th percentiles. Furthermore, the development of lightweight hybrid models like ShallowMRI and HybLwDL proves that this performance gain does not necessarily come at the cost of computational intractability, making such models suitable for deployment in resource-constrained environments, including potential edge computing applications in clinical settings [33] [35] [36].
Core Architectural Components and Signaling Pathways
The superior performance of hybrid models stems from the seamless integration of distinct, complementary components into a cohesive analytical pipeline.
The Convolutional Backbone: Local Feature Extraction
The foundation of most hybrid models is a pre-trained CNN (e.g., VGG16, ResNet, EfficientNet) used as a feature extraction backbone [34] [38] [37]. This leverages the principle of transfer learning, where knowledge from a source domain (e.g., ImageNet) is transferred to the target medical domain. CNNs provide an inductive bias for images—namely, translation invariance and locality—making them exceptionally efficient at extracting hierarchical features like edges, textures, and complex patterns from local pixel neighborhoods [32]. This process converts a raw input MRI image into a rich, multi-dimensional feature map that serves as a structured input for subsequent stages.
The Attention Mechanism: Dynamic Feature Re-calibration
Attention mechanisms act as an intermediary, intelligent filter between the CNN and the Transformer. They can be integrated directly into the CNN backbone or as separate modules. The core function of attention is to dynamically weight the importance of different features or spatial regions. For instance:
- Channel Attention (e.g., as in Squeeze-and-Excitation networks) re-calibrates feature maps across channels, allowing the model to emphasize more informative diagnostic features [35].
- Spatial Attention generates a mask that highlights the most semantically relevant regions of the image, such as the probable tumor location, while suppressing irrelevant background information [34].
This "focusing" mechanism mimics a radiologist's ability to concentrate on salient areas, thereby improving feature quality and model interpretability before data is passed to the Transformer encoder.
The Transformer Encoder: Global Context Modeling
The processed feature maps from the CNN and attention modules are then transformed into a sequence of tokens and fed into a Transformer encoder. The encoder's multi-head self-attention mechanism is the core of its power. It allows every element in the sequence to interact with every other element, regardless of distance. This enables the model to capture long-range dependencies and global contextual relationships—for example, understanding the spatial relationship between a tumor's core and its diffuse boundaries across the entire brain slice, something CNNs struggle with due to their progressively limited receptive fields [31] [32]. The output is a set of features enriched with both local detail and global context, ready for the final classification or segmentation head.
Diagram 1: High-level workflow of a generic hybrid CNN-Transformer model for tumor classification.
Experimental Protocols for Model Implementation
This section provides a detailed, actionable protocol for developing and validating a hybrid CNN-Transformer model, framed within a transfer learning paradigm.
Data Preprocessing and Augmentation Protocol
Objective: To prepare a raw MRI dataset for model training, enhancing robustness and generalizability.
- Data Sourcing: Utilize a public benchmark dataset such as the Kaggle Brain Tumor MRI Dataset (7023 images) or the Figshare dataset [34] [31]. Ensure the data is partitioned into training, validation, and test sets (e.g., 70-15-15 split).
- Noise Reduction: Apply a filtering technique to raw images to improve signal-to-noise ratio. Median Filtering or a Gaussian Bilateral Network Filter (GANF) are common choices that effectively reduce noise while preserving edges [33] [38].
- Intensity Normalization: Standardize the intensity values of all images to a common scale (e.g., 0 to 1) to ensure consistent model convergence.
- Data Augmentation: Artificially expand the training dataset to prevent overfitting. Apply real-time transformations including:
- Random rotation (±10 degrees)
- Horizontal and vertical flipping
- Brightness and contrast adjustments
- Zoom and shear operations [34]
Model Construction and Training Protocol
Objective: To build a hybrid architecture leveraging transfer learning and optimize its parameters.
- Backbone Initialization: Select a pre-trained CNN (e.g., VGG16, EfficientNet-B0) and remove its classification head. This network serves as a feature extractor [34] [37].
- Attention Integration: Introduce an attention module to process the CNN's feature maps. A standard approach is to use a Custom Attention (CA) layer that employs SoftMax-weighted attention to dynamically weigh tumor-specific features [34].
- Transformer Integration:
- Classification Head: Attach a fully connected Multi-Layer Perceptron (MLP) to the output of the Transformer's [CLS] token or averaged tokens for the final classification into categories (e.g., Glioma, Meningioma, Pituitary, No Tumor).
- Hyperparameter Tuning: Utilize an optimization algorithm like the Stellar Oscillation Optimizer (SOO) or other nature-inspired metaheuristics to fine-tune hyperparameters such as learning rate, batch size, and the number of attention heads [33].
Model Evaluation and Explainability Protocol
Objective: To validate model performance and ensure its predictions are interpretable for clinical stakeholders.
- Performance Metrics: Calculate standard classification metrics on the held-out test set: Accuracy, Precision, Recall/Sensitivity, Specificity, and F1-Score (see Table 1 for benchmarks).
- Explainability Analysis: Implement Grad-CAM (Gradient-weighted Class Activation Mapping) to generate heatmaps that visually highlight the regions of the input MRI that were most influential in the model's prediction. This step is critical for building clinical trust and verifying that the model focuses on biologically plausible areas [33] [34].
- Cross-Dataset Validation: Test the final model on a different, external dataset (e.g., BraTS) to evaluate its generalization capability and robustness to domain shift [36].
Diagram 2: Detailed protocol for developing and validating a hybrid model.
The Scientist's Toolkit: Research Reagent Solutions
For researchers embarking on replicating or building upon these hybrid models, the following table catalogs the essential "research reagents" and computational tools required.
Table 2: Essential Research Reagents and Computational Tools for Hybrid Model Development
| Category | Item / Technique | Specific Function | Exemplars / Alternatives |
|---|---|---|---|
| Data | Public MRI Datasets | Provides standardized, annotated data for training and benchmarking. | Kaggle Brain Tumor, Figshare, BraTS [34] [31] |
| Computational Backbone | Pre-trained CNN Models | Serves as a feature extractor; foundation of transfer learning. | VGG16, ResNet, EfficientNet [34] [38] [37] |
| Architectural Components | Attention Modules | Dynamically highlights salient features and spatial regions. | Custom SoftMax-weighted Attention, Channel Attention [34] [35] |
| Transformer Encoders | Captures global contextual relationships between all image features. | Standard ViT Encoder, Swin Transformer [31] [32] | |
| Optimization & Training | Hyperparameter Optimizers | Automates the tuning of model parameters for peak performance. | Stellar Oscillation Optimizer (SOO), Manta Ray Foraging Optimizer [33] |
| Validation & Analysis | Explainability Tools | Generates visual explanations to build trust and verify model focus. | Grad-CAM, SHAP [33] [34] [31] |
| Performance Metrics | Statistical Measures | Quantifies model performance across multiple dimensions. | Accuracy, Precision, Recall, F1-Score, Specificity [33] [36] |
The application of deep learning, particularly through transfer learning, has revolutionized the analysis of Magnetic Resonance Imaging (MRI) for brain tumor detection. Pre-trained models such as DenseNet169, ResNet50, VGG16, and GoogleNet, when fine-tuned on medical datasets, have demonstrated exceptional classification accuracy, often exceeding 98% [39] [3] [40]. However, the "black-box" nature of these high-performing models poses a significant barrier to their clinical adoption, as medical professionals require understanding the reasoning behind a diagnostic decision to trust and validate it [41] [42].
Explainable AI (XAI) has emerged as a critical subfield of artificial intelligence aimed at making the decision-making processes of complex models transparent, interpretable, and trustworthy [41]. Techniques such as Grad-CAM, LIME, and SHAP provide visual and quantitative explanations for model predictions, highlighting the specific image regions or features that influence the classification outcome [39] [40] [43]. Within the context of transfer learning for tumor detection, integrating XAI is not merely an add-on but a fundamental component for bridging the gap between algorithmic performance and clinical utility. It enables researchers and clinicians to verify that a model focuses on biologically relevant tumor hallmarks rather than spurious artifacts, thereby enhancing diagnostic confidence, facilitating earlier and more accurate treatment planning, and ultimately improving patient outcomes [44] [45] [13].
The integration of Explainable AI (XAI) with transfer learning models has yielded remarkable performance in brain tumor classification using MRI data. The following table summarizes the quantitative results from recent key studies, demonstrating the synergy between model accuracy and interpretability.
Table 1: Performance of Various XAI-Integrated Models in Brain Tumor Classification
| Model Architecture | XAI Method | Dataset Size | Key Performance Metrics | Reference |
|---|---|---|---|---|
| DenseNet169-LIME-TumorNet | LIME | 2,870 images | Accuracy: 98.78% [39] | |
| Parallel Model (ResNet101 + Xception) | LIME | Information Missing | Accuracy: 99.67% [44] | |
| Improved CNN (from DenseNet121) | Grad-CAM++ | 2 datasets | Accuracy: 98.4% and 99.3% [45] | |
| ResNet50 + SSPANet | Grad-CAM++ | Information Missing | Accuracy: 97%, Kappa: 95% [40] | |
| GoogleNet | Not Specified | 4,517 scans | Accuracy: 99.2% [3] | |
| Custom CNN & SVC | SHAP | 7,023 images | CNN Accuracy: 98.9%, SVC Accuracy: 96.7% [5] [43] | |
| Hybrid CNN-VGG16 | SHAP | 3 datasets | Accuracy: 94%, 81%, 93% [13] |
These results underscore a critical trend: the pursuit of transparency through XAI does not compromise diagnostic accuracy. On the contrary, the most interpretable models are often among the most accurate. For instance, the DenseNet169-LIME-TumorNet model not only achieved a state-of-the-art accuracy of 98.78% but also provided visual explanations that build trust and facilitate clinical validation [39]. Similarly, an improved CNN model based on DenseNet121, when coupled with Grad-CAM++, achieved up to 99.3% accuracy, demonstrating exceptional performance in localizing complex tumor instances [45].
Detailed Experimental Protocols for XAI in Tumor Detection
To ensure reproducibility and robust implementation of XAI techniques, the following section outlines standardized experimental protocols. These protocols cover the essential workflow from data preparation to model explanation.
Protocol 1: Model Training with Integrated Grad-CAM Explanations
This protocol details the procedure for training a brain tumor classifier and generating explanations using Grad-CAM or its advanced variant, Grad-CAM++.
Table 2: Protocol for Model Training with Grad-CAM/Grad-CAM++
| Step | Component | Description | Purpose & Rationale |
|---|---|---|---|
| 1. Data Preparation | Dataset | Utilize a public Brain Tumor MRI Dataset (e.g., Kaggle). A typical dataset may contain 2,870 - 7,023 T1-weighted, T2-weighted, and FLAIR MRI sequences [39] [5]. | Provides a standardized benchmark for training and evaluation. |
| Preprocessing | Convert images to grayscale. Apply Gaussian filtering for noise reduction. Use binary thresholding and contour detection to crop the Region of Interest (ROI). Normalize pixel intensities [5] [13]. | Reduces computational complexity, minimizes irrelevant background data, and standardizes input. | |
| Augmentation | Apply affine transformations, intensity scaling, and noise injection to augment the training dataset [13]. | Improves model robustness and mitigates overfitting, especially with limited data. | |
| 2. Model & Training | Base Model | Employ a pre-trained model like ResNet50 or DenseNet121 as the feature extractor [40] [45]. | Leverages transfer learning to utilize features learned from large datasets (e.g., ImageNet). |
| Fine-Tuning | Replace and train the final fully connected layer for tumor classification. Optionally unfreeze and fine-tune deeper layers of the network [3] [13]. | Adapts the pre-trained model to the specific task of brain tumor classification. | |
| Training Loop | Train using a standard optimizer (e.g., Adam) and a cross-entropy loss function. | Standard procedure for supervised learning in classification tasks. | |
| 3. XAI Explanation | Explanation Generation | For a given input image, compute the gradients of the target class score flowing into the final convolutional layer. Generate a heatmap by weighing the feature maps by these gradients and applying a ReLU activation [40] [45]. | Produces a coarse localization map highlighting important regions for the prediction. |
| Visualization | Overlay the generated heatmap onto the original MRI scan. Use a color map (e.g., jet) to visualize regions of high and low importance. | Provides an intuitive visual explanation that clinicians can interpret. |
Protocol 2: Generating Model-Agnostic Explanations with LIME
LIME (Local Interpretable Model-agnostic Explanations) explains individual predictions by approximating the complex model locally with an interpretable one.
Table 3: Protocol for Generating Explanations with LIME
| Step | Component | Description | Purpose & Rationale |
|---|---|---|---|
| 1. Model & Data | Pre-trained Model | Use a fully trained and fine-tuned model (e.g., DenseNet169) for brain tumor classification [39] [44]. | Provides the "black-box" model whose predictions need to be explained. |
| Instance Selection | Select a specific MRI image (a single instance) for which an explanation is required. | LIME is designed to explain individual predictions. | |
| 2. LIME Process | Perturbation | Generate a set of perturbed versions of the original image by randomly turning parts of the image (superpixels) on or off [39]. | Creates a local neighborhood of data points around the instance to be explained. |
| Prediction | Obtain predictions from the black-box model for each of these perturbed samples. | Maps the perturbed inputs to the model's output. | |
| Interpretable Model | Train a simple, interpretable model (e.g., a linear model with Lasso regression) on the dataset of perturbed samples and their corresponding predictions. The features are the binary vectors indicating the presence of superpixels. | Learns a locally faithful approximation of the complex model's behavior. | |
| 3. Explanation | Feature Importance | The trained linear model yields weights (coefficients) for each superpixel, indicating its importance for the specific prediction. | Identifies which image segments (superpixels) most strongly contributed to the classification. |
| Visualization | Highlight the top-K most important superpixels on the original image. | Provides an intuitive, visual explanation for the specific prediction. |
The Scientist's Toolkit: Essential Research Reagents & Materials
Successful implementation of XAI for tumor detection relies on a suite of computational tools, datasets, and software libraries. The following table catalogs the key "research reagents" essential for experiments in this field.
Table 4: Essential Research Reagents and Tools for XAI in Tumor Detection
| Category | Item / Solution | Specifications / Function | Example Use Case |
|---|---|---|---|
| Datasets | Brain Tumor MRI Dataset (Kaggle) | A public dataset often containing 2,000+ T1-weighted, T2-weighted, and FLAIR MRI sequences, classified into tumor subtypes (Glioma, Meningioma, Pituitary) and non-tumor cases [5]. | Serves as the primary benchmark for training and evaluating models [39] [5]. |
| Figshare Dataset | A large-scale, publicly available dataset of brain MRIs, often used for multi-class classification and segmentation tasks [3]. | Used for validating model generalization power on larger, diverse data [3] [44]. | |
| Software & Libraries | Python | The primary programming language for deep learning and XAI research, preferred for its extensive ecosystem of scientific libraries (used in ~32% of studies) [42]. | Core programming environment for implementing all workflows. |
| TensorFlow / PyTorch / Keras | Open-source deep learning frameworks that provide the backbone for building, training, and fine-tuning convolutional neural networks [44]. | Used to implement transfer learning with architectures like ResNet, DenseNet, and VGG. | |
| XAI Libraries (SHAP, LIME, TorchCam) | Specialized libraries for generating explanations. SHAP explains output using game theory, LIME creates local surrogate models, and TorchCam provides Grad-CAM variants for PyTorch. | Generating visual and quantitative explanations for model predictions [39] [43] [13]. | |
| Computational Hardware | GPUs (NVIDIA) | Graphics Processing Units are critical for accelerating the training of deep learning models, reducing computation time from weeks to hours. | Essential for all model training and extensive hyperparameter tuning. |
| Pre-trained Models | DenseNet169 / ResNet50 / VGG16 | Established Convolutional Neural Network architectures pre-trained on the ImageNet dataset. They serve as powerful and efficient feature extractors. | Used as the backbone for transfer learning, where they are fine-tuned on medical image data [39] [40] [13]. |
The application of deep learning, particularly transfer learning, for brain tumor detection in MRI scans represents a significant advancement in medical imaging. This approach leverages pre-trained convolutional neural networks (CNNs), fine-tuned on medical datasets, to achieve high diagnostic accuracy even with limited data. By transferring knowledge from large-scale natural image datasets, these models can learn robust feature representations, overcoming the common challenge of small, annotated medical imaging datasets. The integration of data augmentation and explainable AI (XAI) further enhances model robustness and clinical trust, providing a comprehensive framework for assisting researchers and clinicians in accurate, efficient diagnosis.
Data Acquisition and Preprocessing
Publicly available datasets are crucial for benchmarking and developing brain tumor classification models. The following table summarizes commonly used datasets in recent studies.
Table 1: Summary of Brain Tumor MRI Datasets Used in Research
| Dataset | Sample Size | Classes | Key Characteristics | Citation |
|---|---|---|---|---|
| Figshare (Cheng, 2017) | 4,517 images | Glioma (1,129), Meningioma (1,134), Pituitary (1,138), Normal (1,116) | Large, multi-class; used for comprehensive model comparison | [3] |
| Br35H | 3,000 images | Normal, Tumor | Designed for binary classification (normal vs. tumor) | [11] |
| Kaggle Brain Tumor MRI | 2,000 - 7,023 images | Glioma, Meningioma, Pituitary, Normal | Often used in two variants (small and large) for testing generalization | [5] |
Preprocessing Pipeline
A standardized preprocessing pipeline is essential to ensure data quality and model performance.
- Grayscale Conversion: Images are often converted to grayscale to reduce computational complexity, as key diagnostic features are captured in intensity variations [5].
- Noise Reduction: A Gaussian filter is applied to blur images, reducing high-frequency noise and allowing the model to focus on relevant features [5].
- Intensity Normalization: Pixel intensities are normalized (e.g., min-max scaling) to a standard range (e.g., [0, 1]) to stabilize and accelerate the training process [13].
- Contrast Enhancement: Techniques like min-max normalization or histogram equalization can be used to improve the contrast between tumor regions and healthy tissue [13].
- Region of Interest (ROI) Extraction: Contour detection methods identify the largest contour, presumed to be the tumor region, and images are cropped to this ROI to eliminate irrelevant background information [5].
- Resizing: All images are resized to a uniform dimension compatible with the input layer of the chosen pre-trained model (e.g., 224x224 for models like VGG16 and DenseNet201) [13] [11].
Figure 1: Data Preprocessing Workflow for MRI Brain Scans
Data Augmentation Strategies
Data augmentation artificially expands the training dataset, improving model generalization and combating overfitting. This is especially critical in medical imaging where data scarcity is common [7] [46].
Conventional and Deep Learning-Based Augmentation
Table 2: Data Augmentation Techniques for Brain Tumor MRI
| Category | Technique | Description | Purpose |
|---|---|---|---|
| Geometric Transformations | Rotation, Flipping, Translation, Scaling | Affine transformations that alter image geometry while preserving tumor labels. | Increases invariance to object orientation and position. |
| Photometric Transformations | Brightness, Contrast, Gamma Adjustments | Modifies pixel intensity values across the image. | Improves robustness to variations in scanning protocols and lighting. |
| Noise Injection | Adding Gaussian or Salt-and-Pepper Noise | Introduces random noise to simulate image acquisition artifacts. | Enhances model robustness to noisy clinical data. |
| Advanced Generative Models | Generative Adversarial Networks (GANs), Denoising Diffusion Probabilistic Models (DDPMs) | Generates entirely new, realistic tumor images. The Multi-Channel Fusion Diffusion Model (MCFDiffusion) converts healthy images to tumor images. [47] | Addresses severe class imbalance; creates diverse and complex tumor morphologies. |
Transfer Learning Model Architectures and Training
Transfer learning involves using a pre-trained CNN model (typically on ImageNet) and fine-tuning it on the medical imaging task.
Model Selection and Performance
Researchers have evaluated numerous pre-trained architectures. The table below summarizes reported performance metrics from recent studies.
Table 3: Performance Comparison of Transfer Learning Models for Brain Tumor Classification
| Model Architecture | Reported Accuracy | Key Strengths | Citation |
|---|---|---|---|
| GoogleNet | 99.2% | High accuracy on multi-class classification (Figshare dataset). | [3] |
| Proposed DenseTransformer (DenseNet201 + Transformer) | 99.41% | Captures both local features and long-range dependencies via self-attention. | [11] |
| Lightweight CNN (5-layer custom) | 99% | Effective with limited data (189 images); suitable for resource-constrained environments. | [48] |
| Hybrid CNN-VGG16 | 94% | Demonstrates effective knowledge transfer across multiple neurological datasets. | [13] |
| MobileNetV2 | >95% (Comparative) | Lightweight architecture, efficient for potential clinical deployment. | [3] |
End-to-End Model Training Workflow
The following diagram and protocol describe the standard workflow for adapting a pre-trained model for brain tumor classification.
Figure 2: Transfer Learning and Fine-tuning Workflow
Experimental Protocol: Model Fine-tuning
Base Model and Classifier Replacement:
- Select a pre-trained model (e.g., DenseNet201, VGG16) [13] [11].
- Remove the original final fully-connected classification head.
- Append a new, randomly initialized classifier tailored to the brain tumor task. This typically consists of a global average pooling layer, followed by one or more dense layers with ReLU activation and dropout for regularization, and a final softmax/output layer with units equal to the number of classes (e.g., 4 for Figshare dataset).
Layer Freezing and Initial Training:
- Freeze the weights of the pre-trained convolutional base. This prevents the pre-learned, general-purpose features from being destroyed in the initial training phase.
- Compile the model with an optimizer (e.g., Adam) and a loss function (e.g., categorical cross-entropy).
- Train only the new, custom classifier head on the preprocessed and augmented brain MRI dataset for a limited number of epochs.
Fine-tuning:
- Unfreeze a portion of the higher-level layers in the convolutional base. These layers are more task-specific and benefit from fine-tuning on the medical domain.
- Use a significantly lower learning rate (e.g., 10 times smaller) than that used for the initial classifier training to avoid catastrophic forgetting and allow for gentle weight adjustments.
- Continue training the model, now updating the weights of both the unfrozen base layers and the classifier head.
Advanced Architectures: Integrating Attention and Explainability
Hybrid models combining CNNs with attention mechanisms have shown state-of-the-art performance.
Figure 3: Hybrid CNN-Transformer Model Architecture
Experimental Protocol: Hybrid CNN-Transformer Model
- Feature Extraction: The input MRI is passed through a pre-trained CNN backbone (e.g., DenseNet201) to extract rich spatial feature maps [11].
- Tokenization: The resulting feature maps are reshaped into a sequence of feature vectors (tokens) to be processed by the Transformer component.
- Self-Attention Processing: The token sequence is fed into a Multi-Head Self-Attention (MHSA) block. This mechanism allows the model to weigh the importance of different features across all spatial locations, capturing long-range dependencies and global context crucial for identifying irregular tumor boundaries [11].
- Classification: The output from the attention block is aggregated and passed through a standard Multi-Layer Perceptron (MLP) classifier for final prediction.
To address the "black box" nature of deep learning models, Explainable AI (XAI) techniques like Gradient-weighted Class Activation Mapping (Grad-CAM) and SHapley Additive exPlanations (SHAP) are integrated. These methods generate heatmaps that highlight the regions of the input MRI that were most influential in the model's decision, providing visual explanations that can be validated by clinicians [13] [5] [11].
The Scientist's Toolkit: Research Reagent Solutions
Table 4: Essential Tools and Frameworks for Implementation
| Category / Item | Specific Examples | Function / Application |
|---|---|---|
| Programming Languages & Core Libraries | Python 3.x | Core programming environment for model development and data handling. |
| Deep Learning Frameworks | TensorFlow, Keras, PyTorch | Provides high-level APIs for building, training, and evaluating deep learning models. |
| Medical Image I/O | PyDICOM, ITK, SimpleITK | Reading and processing DICOM files and other medical image formats. |
| Image Augmentation Libraries | TensorFlow ImageDataGenerator, Albumentations, Torchvision Transforms |
Implementing geometric and photometric transformations for data augmentation. |
| Generative Models for Augmentation | Custom DDPM/DDIM implementations (e.g., for MCFDiffusion [47]), GANs (e.g., StyleGAN2) | Generating synthetic medical images to address data scarcity and class imbalance. |
| Pre-trained Models | Keras Applications, Torchvision Models | Providing access to pre-trained architectures like VGG16, DenseNet201, and ResNet for transfer learning. |
| Explainable AI (XAI) Tools | SHAP, Grad-CAM implementation, LIME | Interpreting model predictions and generating heatmaps for clinical validation. |
| Hardware Acceleration | NVIDIA GPUs (CUDA cores) | Drastically reducing training and inference time for complex deep learning models. |
Overcoming Practical Challenges: Data, Performance, and Computational Efficiency
Addressing Data Imbalance and Limited Annotations with Augmentation Strategies
The development of robust deep learning models for brain tumor detection in MRI scans is critically hampered by two interconnected data challenges: class imbalance and limited annotations. Medical imaging datasets often exhibit a significant imbalance, where certain tumor types or healthy cases are over-represented, leading to models that perform poorly on minority classes [5]. Simultaneously, obtaining pixel-level annotations for segmentation tasks is costly, time-consuming, and requires specialized expertise, resulting in limited labeled data [49] [50]. These constraints are particularly pronounced in brain tumor MRI analysis, where tumor heterogeneity, varying imaging protocols, and the complexity of manual segmentation further exacerbate the problem [22].
Data augmentation strategies present a powerful solution to these challenges by artificially expanding the diversity and size of training datasets. Within a broader thesis on transfer learning for tumor detection, augmentation serves as a force multiplier, enhancing the generalization capability of pre-trained models when fine-tuned on limited medical data. This document provides detailed application notes and experimental protocols for implementing cutting-edge augmentation strategies specifically for brain tumor MRI analysis.
A diverse set of data augmentation strategies has been developed to address data scarcity and imbalance, each with distinct mechanisms and applications. The table below summarizes the primary categories, their representative techniques, and primary functions.
Table 1: Taxonomy of Data Augmentation Strategies for Brain Tumor MRI Analysis
| Category | Representative Techniques | Primary Function | Key Advantages |
|---|---|---|---|
| Traditional Image Transformations | Rotation, Flipping, Scaling, Elastic Deformations [13] | Increases basic spatial variance | Simple to implement; computationally cheap |
| Generative AI-Based | GliGAN (GAN-based) [22], MCFDiffusion (Diffusion Model) [51] | Synthesizes entirely new, realistic tumor images | Directly tackles class imbalance; generates highly diverse data |
| Advanced Mixing-Based | HSMix (Hard & Soft Mixing) [50] | Creates novel samples by blending regions from multiple images | Preserves contour information; enriches semantic diversity |
| On-the-Fly / Dynamic | On-the-fly tumor insertion with GliGAN [22] | Dynamically augments data during the training loop | Avoids massive storage overhead; allows for targeted augmentation |
| MRI-Specific Artifact Simulation | Motion artifact simulation [52] | Introduces common MRI-specific corruptions | Improves model robustness to real-world clinical imperfections |
Quantitative Performance of Augmentation Strategies
Empirical results from recent literature demonstrate the significant impact of advanced augmentation on model performance for classification and segmentation tasks.
Table 2: Quantitative Performance Gains from Data Augmentation
| Study & Model | Augmentation Strategy | Task | Performance Gain |
|---|---|---|---|
| MCFDiffusion [51] | Multi-channel fusion diffusion model | Image Classification | ~3% increase in accuracy |
| MCFDiffusion [51] | Multi-channel fusion diffusion model | Tumor Segmentation | 1.5% - 2.5% improvement in Dice score |
| HSMix [50] | Hard and Soft Mixing with superpixels | Medical Image Segmentation | Superior performance vs. CutOut, CutMix, and Mixup |
| MRI-Specific Augmentation [52] | Simulated motion artifacts | Segmentation under artifacts | Mitigated performance drop; maintained precise angle measurements (ICC: 0.86 vs. -0.10 baseline) |
Detailed Experimental Protocols
Protocol 1: On-the-Fly Synthetic Tumor Insertion for Glioma Segmentation
This protocol is based on the winning solution of the BraTS 2025 challenge and is designed to address data scarcity and class imbalance in segmenting glioma sub-regions [22].
Research Reagent Solutions:
- Software Framework: nnU-Net (self-configuring framework for medical image segmentation).
- Generative Model: Pre-trained GliGAN weights (Swin UNETR-based generator).
- Data: BraTS multi-parametric MRI (mpMRI) datasets in NIfTI format (T1, T1ce, T2, FLAIR).
Methodology:
- Data Preparation: Utilize the default nnU-Net pipeline for preprocessing, which includes resampling to an isotropic resolution of 1mm³ and normalizing intensity values.
- Integration of GliGAN: Incorporate the pre-trained GliGAN generator into the nnU-Net training loop. Instead of a separate preprocessing step, the augmentation occurs dynamically for each training batch.
- On-the-Fly Augmentation Process:
- For a batch of training images, with a predefined probability
p, select an image for augmentation. - Label Modification (To Handle Imbalance): To address the under-representation of certain tumor classes like Enhancing Tumor (ET) and Non-Enhancing Tumor Core (NETC), modify a randomly selected label mask from another patient. With a probability of 0.7, replace Surrounding Non-enhancing FLAIR Hyperintensity (SNFH) labels with ET, and subsequently replace ET with NETC.
- Scale Adjustment (For Small Lesions): Apply a scale factor to the label mask to generate smaller synthetic lesions, forcing the model to learn features of under-represented small tumors.
- Tumor Insertion: The GliGAN generator takes the original image (with added noise in the target region) and the modified label mask as input, outputting a realistic synthetic tumor seamlessly blended into the healthy tissue.
- For a batch of training images, with a predefined probability
- Training: Train the nnU-Net model using the standard combination of Dice and Cross-Entropy loss. The augmented and non-augmented batches are used interchangeably throughout the training process.
Protocol 2: MCFDiffusion for Data Imbalance in Tumor Classification
This protocol uses a multi-channel fusion diffusion model (MCFDiffusion) to convert healthy brain MRIs into images containing tumors, effectively balancing the dataset [51].
Research Reagent Solutions:
- Model Architecture: Denoising Diffusion Implicit Model (DDIM) adapted for multi-channel medical images.
- Data: Public brain tumor datasets (e.g., Figshare). Requires paired healthy and tumorous images or a pre-trained healthy-tumor translation model.
Methodology:
- Model Training:
- Train the MCFDiffusion model on a dataset containing healthy brain MRIs and MRIs with tumors. The model learns the complex data distribution of pathological changes.
- The "multi-channel fusion" mechanism ensures that the synthetic tumors are generated in anatomically plausible locations and with realistic appearance across all MRI sequences (T1, T1ce, T2, FLAIR).
- Data Synthesis:
- To address a lack of images for a specific tumor class (e.g., glioma), use healthy brain images as the input to the trained diffusion model.
- Condition the model to generate the specific, under-represented tumor type.
- Generate a sufficient number of synthetic tumor images to balance the class distribution in the original training set.
- Model Evaluation:
- Combine the original imbalanced dataset with the synthetically generated images to create a balanced training set.
- Train a downstream brain tumor classification model (e.g., CNN, VGG16, ResNet) on this augmented dataset.
- Evaluate the model's performance on a held-out test set, comparing metrics like accuracy, precision, and recall for the previously under-represented classes against a model trained only on the original data.
Protocol 3: HSMix Augmentation for Semantic Segmentation
HSMix is a plug-and-play augmentation method that combines hard and soft mixing of superpixels to preserve contour information and enhance diversity [50].
Research Reagent Solutions:
- Core Technique: Superpixel generation algorithm (e.g., SLIC).
- Software: Compatible with any deep learning framework (PyTorch, TensorFlow). Designed for segmentation architectures like U-Net.
Methodology:
- Superpixel Generation: For two randomly selected source medical images (Ia and Ib) and their corresponding segmentation masks (Ma and Mb), decompose each image into superpixels (homogeneous regions).
- Hard Mixing:
- Randomly select a set of superpixels from Ib.
- Cut these superpixels from Ib and paste them into the same spatial location in Ia to create a "hard-mixed" image Ihard.
- Perform the identical operation on the segmentation masks to create the corresponding hard-mixed mask Mhard.
- Soft Mixing:
- For the same set of selected superpixels, instead of a direct paste, perform a pixel-wise brightness blending between Ia and Ib.
- The blending coefficient for each pixel is determined by a locally aggregated saliency coefficient, which emphasizes semantically important regions.
- This creates a "soft-mixed" image Isoft and its mask Msoft, where the transition between pasted and original regions is more gradual and natural.
- Training: Use both Ihard/Mhard and Isoft/Msoft pairs as additional training samples during the segmentation model's training. This forces the model to learn robust features from contoured, blended, and saliency-weighted examples.
Workflow Visualization
The following diagram illustrates the logical integration of these augmentation strategies within a comprehensive transfer learning pipeline for brain tumor research.
Diagram 1: Augmentation-Enhanced Transfer Learning Pipeline. This workflow integrates specialized data augmentation strategies to bridge the gap between a generic pre-trained model and a robust clinical application, directly addressing data limitations in medical imaging.
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Research Reagents and Tools for Implementation
| Item | Function / Application | Exemplar / Source |
|---|---|---|
| nnU-Net Framework | Self-configuring baseline framework for medical image segmentation; serves as a robust foundation for implementing custom augmentations [22]. | https://github.com/MIC-DKFZ/nnU-Net |
| Pre-trained GliGAN Weights | Enables realistic synthetic tumor generation and insertion into healthy MRI scans for on-the-fly augmentation [22]. | Publicly released weights from BraTS 2023-24 winners |
| BraTS Datasets | Benchmark multi-parametric MRI datasets with expert-annotated tumor sub-regions for training and evaluation [22]. | https://www.synapse.org/ BraTS challenges |
| DICOM Annotation Tools | Specialized software for creating pixel-level annotations on medical images, crucial for generating ground truth data [49]. | Commercial and open-source platforms (e.g., ITK-SNAP, 3D Slicer) |
| MCFDiffusion Code | Implementation of the multi-channel fusion diffusion model for generating synthetic tumor images to correct class imbalance [51]. | https://github.com/feiyueaaa/MCFDiffusion |
| HSMix Code | Implementation of the hard and soft mixing augmentation technique for semantic segmentation tasks [50]. | https://github.com/DanielaPlusPlus/HSMix |
Hyperparameter Optimization and Avoiding Overfitting in Small Datasets
In the field of medical image analysis, particularly for tumor detection in MRI scans, the confluence of limited data availability and complex deep learning models presents a significant challenge. The performance of these models is critically dependent on the proper configuration of hyperparameters, which govern the training dynamics and architectural complexity [53]. However, when working with small datasets—a common scenario in medical research due to privacy concerns and costly annotations—improper hyperparameter settings dramatically increase the risk of overfitting, where models memorize dataset-specific noise rather than learning generalizable features [54]. This application note provides structured protocols and analytical frameworks for optimizing hyperparameters while mitigating overfitting within the specific context of transfer learning for tumor detection in MRI, enabling researchers to develop more robust and reliable diagnostic tools.
Theoretical Foundations and Challenges
Hyperparameter Optimization in Medical Imaging
Hyperparameter optimization is the process of identifying the optimal set of parameters that control the learning process itself before training begins [55]. In deep learning-based tumor detection, these parameters may include learning rate, batch size, optimization algorithm settings, and architectural elements like the number of layers or filters. Traditional methods like grid search perform exhaustive searches through manually specified subsets of hyperparameter space but suffer from the curse of dimensionality and computational inefficiency, especially when dealing with complex models and limited data [55].
More advanced approaches include:
- Bayesian Optimization: Builds a probabilistic model of the function mapping from hyperparameter values to the objective measured on a validation set, balancing exploration and exploitation to find optimum configurations in fewer evaluations [55] [56].
- Population-Based Training (PBT): Simultaneously learns both hyperparameter values and network weights, with poorly performing models iteratively replaced by models that adopt modified hyperparameters and weights from better performers [55].
- Evolutionary Optimization: Uses evolutionary algorithms to search hyperparameter space through processes inspired by biological evolution, including mutation, crossover, and selection [55].
The Overfitting Dilemma in Small Medical Datasets
Overfitting occurs when a model learns the specific patterns, noise, and random fluctuations in the training data to such an extent that it negatively impacts performance on new, unseen data [54] [57]. In healthcare AI, this can lead to inaccurate diagnoses, ineffective treatments, and compromised patient safety when models that performed well during development fail in clinical deployment [54].
The challenge is particularly acute in medical imaging domains like brain tumor detection using MRI, where datasets may be limited due to:
- Privacy concerns and data sharing restrictions
- Costly expert annotation requirements
- Rare conditions or specific tumor subtypes
- Institutional data silos [3] [54]
Methodological Framework
Hyperparameter Optimization Techniques for Small Datasets
Table 1: Hyperparameter Optimization Methods for Small Datasets in Medical Imaging
| Method | Key Principle | Advantages for Small Datasets | Implementation Considerations |
|---|---|---|---|
| Bayesian Optimization | Builds probabilistic model of objective function; balances exploration/exploitation [55] | Efficient evaluation; good for expensive-to-evaluate functions [56] | Requires careful definition of search space; parallelization challenges |
| Multi-Strategy Parrot Optimizer (MSPO) | Enhances original Parrot Optimizer with Sobol sequence, nonlinear decreasing inertia weight, chaotic parameter [53] | Improved global exploration and convergence steadiness; reduced premature convergence [53] | Complex implementation; requires parameter tuning itself |
| Random Search | Randomly samples hyperparameter space according to specified distributions [55] | Simpler than grid search; easily parallelized; good baseline [55] | May miss optimal regions; inefficient for high-dimensional spaces |
| Successive Halving/ Hyperband | Early stopping-based; allocates more resources to promising configurations [55] | Computational efficiency; rapidly discards poor performers [55] | Aggressive pruning may eliminate configurations needing longer training |
Overfitting Prevention Strategies
Table 2: Comprehensive Overfitting Prevention Techniques for Medical Imaging
| Technique Category | Specific Methods | Application Context | Expected Impact |
|---|---|---|---|
| Data-Centric Approaches | Data augmentation (rotation, flipping, scaling) [58] [56], Synthetic data generation (GANs, diffusion models) [58], Transfer learning from pre-trained models [58] [3] | Limited dataset sizes; class imbalance; domain shift | Increases effective dataset size; improves model generalization [58] |
| Model-Centric Approaches | L1/L2 regularization [54] [57], Dropout (0.2-0.5 rate) [58] [57], Early stopping [58] [57], Simplified architectures (fewer layers) [58] | Complex models prone to memorization; limited training data | Reduces model complexity; prevents overtraining; encourages simpler solutions [54] |
| Training Strategies | Cross-validation [58] [55], Learning rate scheduling [58], Ensembling multiple models [58] | Hyperparameter tuning; model selection; performance estimation | Provides more reliable performance estimates; stabilizes training [58] |
Experimental Protocols
Protocol 1: Bayesian Hyperparameter Optimization for MRI Tumor Classification
Objective: Optimize hyperparameters for a transfer learning-based brain tumor classification model using a small MRI dataset.
Materials:
- Dataset: Brain Tumor MRI Dataset (e.g., 2,000-7,000 images) [5]
- Base Architecture: Pre-trained ResNet18 or GoogleNet [53] [3]
- Framework: PyTorch or TensorFlow with Bayesian optimization library (e.g., Ax, Optuna)
Procedure:
- Data Preparation:
- Split data into training (70%), validation (15%), and test (15%) sets
- Apply minimal preprocessing: resizing to match pre-trained model input dimensions, normalization using ImageNet statistics
- Implement basic augmentation: random horizontal flipping (±10° rotation) [56]
Search Space Definition:
- Learning rate: Log-uniform distribution between 1e-5 and 1e-2
- Batch size: Categorical choice from {16, 32, 64} based on GPU memory
- Dropout rate: Uniform distribution between 0.1 and 0.5
- Optimizer: Choice between Adam, SGD with momentum
- Fine-tuning strategy: Choice of freezing early layers vs. full fine-tuning
Optimization Loop:
- Initialize Bayesian optimization with 10 random configurations
- For each iteration (total 50 iterations):
- Sample hyperparameter configuration from acquisition function
- Train model for 50 epochs with early stopping patience of 10 epochs
- Evaluate on validation set using accuracy as primary metric
- Update surrogate model with (configuration, validation accuracy) pair
- Select best-performing configuration on validation set
- Final evaluation on held-out test set
Validation Metrics:
- Primary: Accuracy, F1-score
- Secondary: Precision, Recall, AUC-ROC [53]
Protocol 2: Comprehensive Overfitting Assessment and Mitigation
Objective: Systematically evaluate and mitigate overfitting in a liver and liver tumor segmentation model using a small CE-MRI dataset.
Materials:
- Dataset: ATLAS dataset (60 3D CE-MRI scans) [56]
- Architecture: Hybrid CNN-transformer models (e.g., UNet with transformer bottlenecks)
- Framework: nnUNet framework or custom implementation in PyTorch [56]
Procedure:
- Baseline Model Training:
- Train model with default hyperparameters for 1000 epochs
- Track training vs. validation Dice coefficient every epoch
- Calculate overfitting gap: (Training Dice - Validation Dice) at convergence
Overfitting Detection Battery:
- Performance Discrepancy Analysis: Compare training vs. validation performance across epochs [54]
- Feature Visualization: Use Grad-CAM or SHAP to identify if model relies on clinically irrelevant features [59]
- Simplified Data Test: Evaluate on artificially simplified data to detect reliance on spurious correlations [59]
- Cross-Validation: Perform 5-fold cross-validation to assess performance variance [58]
Mitigation Implementation:
- Data Augmentation Pipeline:
- Spatial transformations: random rotation (±15°), scaling (0.85-1.15), elastic deformations
- Intensity transformations: Gaussian noise, brightness/contrast adjustments
- MixUp/CutMix: Implement with α=0.2 for regularizing effect [58]
- Regularization Stack:
- Weight decay: 1e-4 for all parameters
- Dropout: 0.3 after convolutional blocks
- Early stopping: Patience of 100 epochs based on validation Dice
- Architecture Selection:
- Compare CNN vs. transformer vs. hybrid architectures
- Select model with smallest overfitting gap while maintaining performance
- Data Augmentation Pipeline:
Evaluation:
- Report Dice coefficients for liver and tumor segmentation pre- and post-mitigation
- Quantify reduction in overfitting gap
- Perform statistical significance testing using paired t-test across folds
The Scientist's Toolkit
Table 3: Essential Research Reagent Solutions for Hyperparameter Optimization in Medical Imaging
| Reagent/Tool | Function | Application Notes |
|---|---|---|
| Pre-trained Models (ImageNet) | Transfer learning initialization; feature extraction [3] | Models like ResNet18, GoogleNet, MobileNetV2 provide strong baselines; adjust input channels for MRI [53] [3] |
| Bayesian Optimization Frameworks (Ax, Optuna) | Efficient hyperparameter search; parallel experimentation [55] [56] | Define appropriate search spaces; use ASHA for early stopping; budget ~50-100 trials for convergence |
| Data Augmentation Pipelines (TorchIO, Albumentations) | Dataset expansion; domain randomization [58] [56] | Medical-specific transformations; careful with anatomical plausibility; monitor validation performance |
| Regularization Modules (Dropout, L2, Early Stopping) | Overfitting prevention; model simplification [58] [57] | Dropout rate 0.2-0.5; L2 weight decay 1e-4; early stopping patience 10-100 epochs depending on task |
| Model Interpretation Tools (Grad-CAM, SHAP) | Overfitting detection; feature importance analysis [59] | Identify Clever Hans effects; ensure model uses clinically relevant features; qualitative validation |
| Cross-Validation Frameworks | Performance estimation; hyperparameter selection [58] [55] | 5-fold common for medical tasks; stratified sampling for class imbalance; compute mean and variance |
Workflow Visualization
Workflow for MRI Analysis with Small Datasets
Overfitting Mitigation Strategies
Effective hyperparameter optimization and overfitting prevention are critical components for successful implementation of deep learning models in tumor detection from MRI scans, particularly when working with limited datasets. The integration of systematic HPO methods like Bayesian optimization with comprehensive overfitting mitigation strategies—including data augmentation, regularization, and careful model selection—enables researchers to develop more robust and generalizable models. Future research directions should focus on automated detection of shortcut learning [59], federated learning approaches for leveraging multi-institutional data without sharing, and the development of more sample-efficient architectures that inherently resist overfitting. By adopting the protocols and frameworks outlined in this document, researchers can enhance the reliability and clinical applicability of their tumor detection systems, ultimately contributing to improved patient outcomes through more accurate and early diagnosis.
Balancing Accuracy and Computational Cost for Clinical Deployment
The integration of artificial intelligence (AI) in medical imaging represents a paradigm shift in neuro-oncology, offering unprecedented opportunities for enhancing diagnostic precision while imposing significant computational burdens. For brain tumor detection using Magnetic Resonance Imaging (MRI), deep learning models, particularly those leveraging transfer learning, have demonstrated remarkable accuracy, with some studies reporting performance exceeding 99% [34] [60]. However, this diagnostic precision often comes with substantial computational requirements that challenge practical clinical deployment. This document establishes a framework for achieving an optimal balance between these competing priorities—maximizing diagnostic accuracy while minimizing computational costs—to facilitate the transition of research models into viable clinical tools. By providing structured protocols and comparative analyses, we aim to equip researchers and clinicians with practical strategies for implementing robust, efficient, and clinically viable AI solutions for brain tumor detection.
Quantitative Performance Analysis of Model Architectures
Comprehensive evaluation of current deep learning architectures reveals distinct trade-offs between classification accuracy and computational efficiency. The table below synthesizes performance metrics from recent studies to guide model selection decisions.
Table 1: Comparative performance of deep learning models for brain tumor classification
| Model Architecture | Reported Accuracy | Computational Efficiency | Key Advantages | Clinical Implementation Considerations |
|---|---|---|---|---|
| Xception | 98.73% [61] | Moderate | Exceptional generalization capabilities, effective for class imbalance | Suitable for well-resourced clinical settings with dedicated computing infrastructure |
| ResNet18 | 99.77% [60] | High | Strong baseline performance, residual connections prevent vanishing gradient | Ideal for deployment in resource-constrained environments |
| YOLOv7 with CBAM | 99.5% [4] | Moderate to High | Simultaneous localization and classification, enhanced feature extraction | Appropriate for clinical workflows requiring both detection and segmentation |
| VGG16 + Attention | 99% [34] | Low | Interpretable predictions via Grad-CAM, enhanced feature selection | Valuable when model explainability is prioritized over speed |
| DenseNet201 + Transformer | 99.41% [11] | Low | Captures both local and global features, strong contextual understanding | Suitable for research settings with ample computational resources |
| MobileNetV3 | 99.75% [34] | Very High | Optimized for mobile deployment, minimal parameters | Optimal for point-of-care applications or edge computing devices |
| SVM + HOG | 97% [60] | Very High | Low computational requirements, transparent decision process | Useful as baseline model or when training data is extremely limited |
Beyond these standardized architectures, hybrid approaches combining convolutional neural networks with attention mechanisms have demonstrated particular promise for balancing performance and efficiency. For instance, models incorporating Convolutional Block Attention Module (CBAM) within the YOLOv7 framework achieve high accuracy while maintaining reasonable computational demands through selective feature refinement [4]. Similarly, squeeze-and-excitation attention blocks integrated with DenseNet architectures have shown enhanced focus on tumor-relevant regions without dramatically increasing inference time [11].
Experimental Protocols for Model Development and Evaluation
Data Preparation and Preprocessing Protocol
Objective: To ensure consistent, high-quality input data for model training while enhancing generalizability through controlled augmentation.
Figure 1: MRI Data Preprocessing and Augmentation Workflow
Step-by-Step Procedure:
- Data Sourcing: Utilize publicly available brain MRI datasets (e.g., Brain Tumor MRI Dataset on Kaggle with 7,023 images or Figshare dataset with 2,870 images) [61] [60].
- Grayscale Conversion: Convert all images to single-channel grayscale to reduce computational complexity while preserving structural information [61].
- Standardized Resizing: Resize images to 224×224 pixels using bilinear interpolation to ensure consistent input dimensions across models [60].
- Intensity Normalization: Apply z-score normalization with mean=0.5 and standard deviation=0.5 to standardize pixel value distributions [60].
- Data Augmentation: Implement a comprehensive augmentation pipeline including:
- Random affine transformations with shear up to ±5 degrees
- Random scaling between 95% and 105%
- Small random rotations up to ±3 degrees
- Horizontal flipping (applied to 50% of images)
- Vertical flipping (applied to 30% of images)
- Gaussian blur with kernel size of 3 and sigma randomly selected between 0.1-1.0 [60]
- Data Partitioning: Split data into training (70%), validation (15%), and test (15%) sets, ensuring balanced class distribution across splits [60].
Transfer Learning Implementation Protocol
Objective: To leverage pre-trained models for reduced training time and computational requirements while maintaining high accuracy.
Step-by-Step Procedure:
- Base Model Selection: Choose appropriate pre-trained models (Xception, ResNet18, MobileNetV3, DenseNet201) based on accuracy-efficiency trade-offs [61] [34] [11].
- Feature Extraction Layer Freezing: Freeze all pre-trained layers except the final 3 residual blocks and the classification head to preserve learned feature representations while allowing domain adaptation [60].
- Progressive Unfreezing: After initial training, progressively unfreeze deeper layers with a reduced learning rate (one-tenth of initial rate) to fine-tune domain-specific features [61].
- Custom Classification Head: Replace original fully connected layers with task-specific heads:
- Global average pooling layer
- Dense layer with 512 units and ReLU activation
- Dropout layer with 40% rate
- Final softmax layer with 4 units (glioma, meningioma, pituitary, no tumor) [60]
- Differential Learning Rates: Apply higher learning rates to newly added layers (1e-3) and lower rates to pre-trained layers (1e-4) to balance stability and adaptability [61].
Attention Mechanism Integration Protocol
Objective: To enhance model focus on diagnostically relevant regions while minimizing computational overhead.
Figure 2: Attention Mechanism Integration Architecture
Step-by-Step Procedure:
- Attention Module Selection: Implement Convolutional Block Attention Module (CBAM) which sequentially applies channel and spatial attention [4].
- Channel Attention: Generate channel attention maps using global average and max pooling followed by a shared multi-layer perceptron with sigmoid activation [4].
- Spatial Attention: Create spatial attention maps by applying mean and max pooling along the channel dimension followed by a convolutional layer with sigmoid activation [4].
- Feature Refinement: Multiply input feature maps with the computed attention maps to emphasize relevant features and suppress less informative ones [4].
- Integration Points: Insert attention modules after the final convolutional layer of the base architecture or between residual blocks in deeper networks [11] [4].
Model Optimization and Compression Protocol
Objective: To reduce model size and computational requirements while preserving diagnostic accuracy.
Step-by-Step Procedure:
- Pruning: Implement iterative magnitude-based pruning to remove redundant weights with values below a specified threshold, gradually increasing sparsity from 0% to 80% over training epochs [60].
- Quantization: Apply post-training quantization to reduce precision from 32-bit floating point to 16-bit or 8-bit integers, decreasing model size and accelerating inference [60].
- Knowledge Distillation: Train a compact student model (e.g., MobileNetV3) to mimic predictions of a larger teacher model (e.g., Xception or DenseNet201), transferring knowledge while reducing parameters [34].
- Architecture Optimization: Utilize neural architecture search (NAS) to identify optimal layer configurations specifically optimized for brain tumor detection tasks [34].
Evaluation and Interpretability Protocol
Objective: To ensure model reliability and provide clinical interpretability through comprehensive validation and explanation techniques.
Step-by-Step Procedure:
- Performance Metrics: Evaluate models using comprehensive metrics including:
- Cross-Domain Validation: Assess generalization on external datasets with different demographic characteristics and acquisition parameters to evaluate real-world robustness [60].
- Explainability Techniques: Implement interpretability methods:
- Statistical Validation: Perform statistical tests including:
- McNemar's test based on F1-score
- DeLong's test based on AUC
- Z-test based on Cohen's Kappa Score [11]
- Clinical Correlation: Validate model focus regions against radiological annotations to ensure alignment with clinical expertise [34].
Table 2: Key research reagents and computational resources for brain tumor detection research
| Resource Category | Specific Examples | Function/Purpose | Implementation Notes |
|---|---|---|---|
| Public Datasets | Brain Tumor MRI Dataset (Kaggle, 7,023 images) [61]; Figshare Brain Tumor Dataset (2,870 images) [60]; BraTS Challenge Datasets [62] [63] | Model training and benchmarking | Ensure proper data partitioning; implement duplicate detection using phash algorithm [60] |
| Pre-trained Models | Xception, ResNet18, DenseNet201, MobileNetV3, VGG16 [61] [34] [11] | Transfer learning backbone | Select based on accuracy-efficiency trade-offs; freeze initial layers during fine-tuning |
| Attention Modules | Convolutional Block Attention Module (CBAM) [4]; Squeeze-and-Excitation Attention [11]; Multi-Head Self-Attention [11] | Feature refinement and focus | Insert before classification heads; helps model focus on tumor regions |
| Evaluation Frameworks | Grad-CAM [34] [11]; LIME [11]; Statistical testing suites [11] | Model interpretability and validation | Essential for clinical translation; builds trust with radiologists |
| Optimization Tools | Magnitude-based pruning; quantization; knowledge distillation [34] [60] | Model compression for deployment | Enables deployment on resource-constrained hardware |
The strategic balance between diagnostic accuracy and computational efficiency represents a critical frontier in the clinical translation of AI systems for brain tumor detection. Our analysis demonstrates that through careful architecture selection, targeted optimization, and comprehensive validation, it is feasible to achieve diagnostic accuracy exceeding 99% while maintaining computationally efficient profiles suitable for diverse clinical environments [61] [34] [60]. The protocols and frameworks presented herein provide a structured pathway for researchers to navigate the complex trade-offs inherent in medical AI deployment.
Future advancements in this domain will likely focus on several key areas: (1) development of more sophisticated neural architecture search techniques to automatically discover optimal architectures balancing accuracy and efficiency; (2) integration of federated learning approaches to enhance model generalizability while addressing data privacy concerns [64]; and (3) creation of standardized benchmarking frameworks specifically designed to evaluate the real-world clinical viability of AI systems beyond traditional performance metrics. As the field progresses, the harmonization of diagnostic excellence and computational practicality will remain paramount for fulfilling the promise of AI-enhanced neuro-oncology in routine clinical practice.
In the domain of magnetic resonance imaging (MRI)-based tumor detection, the development of robust and generalizable deep learning models is fundamentally challenged by intensity heterogeneity and scanner variability. These technical inconsistencies, stemming from differences in acquisition protocols, magnetic field strengths, and scanner manufacturers, introduce non-biological noise that can significantly degrade model performance and limit clinical applicability [12]. Within the broader research context of transfer learning for tumor detection, addressing these sources of variation is not merely a preprocessing step but a critical prerequisite for enabling knowledge transfer across imaging domains. This document outlines standardized protocols and analytical frameworks designed to mitigate these challenges, thereby enhancing the reliability and reproducibility of predictive models in neuro-oncological research and drug development.
Background and Significance
Intensity heterogeneity in MRI, often manifested as bias fields or intensity non-uniformity, refers to slow, spatially varying artifacts that cause the same tissue type to have different signal intensities across the image [12]. Concurrently, scanner variability—encompassing differences in hardware, software, and imaging parameters—leads to domain shifts between datasets, causing models trained on one source to underperform on others. For transfer learning approaches, which aim to leverage knowledge from a source domain (e.g., a large, labeled glioma dataset) to a target domain (e.g., a smaller meningioma dataset from a different institution), these variabilities pose a substantial risk. If not corrected, the model may learn to recognize scanner-specific artifacts rather than true pathological features, thereby compromising its utility in multi-center clinical trials and real-world deployment [65] [66].
Quantitative Analysis of Preprocessing Impact
The choice of preprocessing pipeline directly influences data homogeneity and subsequent model performance. The following table summarizes the impact of different methods on feature reproducibility and classification accuracy, as demonstrated in radiomics studies.
Table 1: Impact of MRI Preprocessing Methods on Feature Reproducibility and Classification Performance
| Preprocessing Method | Key Processing Steps | Effect on Feature Reproducibility | Reported AUC / Performance Change |
|---|---|---|---|
| S+B+ZN [12] | SUSAN Denoising → Bias Field Correction → Z-score Normalization | – | Achieved the highest AUC (0.88) before reproducible feature selection |
| B+ZN [12] | Bias Field Correction → Z-score Normalization | – | AUC improved from 0.49 to 0.64 after excluding non-reproducible features |
| Z-score Normalization (ZN) [12] | Standardization of image intensities to zero mean and unit variance | Reduces inter-scanner and inter-subject variability [12] | – |
| Wavelet-based Features [12] | Transformation of images to wavelet domain for feature extraction | 37% demonstrated excellent reproducibility (ICC ≥ 0.90) | – |
| Texture-based Features (GLCM, GLSZM) [12] | Calculation of texture matrices from original images | Among the most reproducible across preprocessing methods | – |
Experimental Protocols for Robustness Evaluation
Protocol: Evaluation of Preprocessing Pipelines for Feature Stability
This protocol provides a framework for assessing the robustness of radiomic features across different image preprocessing methods.
- Data Preparation: Collect a multi-scanner MRI dataset, ideally from public archives like the Parkinson’s Progression Markers Initiative (PPMI) or Brain Tumor Segmentation (BraTS) challenges [12] [65]. The dataset should include T1-weighted scans and be representative of the expected variability.
- Preprocessing: Apply multiple preprocessing pipelines to the raw images. Example pipelines include:
- ZN: Z-score normalization alone.
- B+ZN: Bias field correction followed by Z-score normalization.
- S+ZN: SUSAN denoising followed by Z-score normalization.
- S+B+ZN: SUSAN denoising followed by bias field correction and Z-score normalization [12].
- Tools: FSL (FMRIB Software Library) can be used for steps like bias field correction (FAST) and denoising (SUSAN) [12].
- Feature Extraction: From each preprocessed image, extract a large set of radiomic features (e.g., 22,560 features) from defined volumes of interest (VOIs). These should include first-order, shape, and texture features (e.g., from GLCM and GLSZM) [12].
- Stability Assessment: Calculate the Intraclass Correlation Coefficient (ICC) for each feature across the different preprocessing pipelines. Features with an ICC ≥ 0.90 are typically considered excellently reproducible [12].
- Downstream Analysis: Train machine learning models (e.g., Support Vector Machines) using two sets of features: (a) all extracted features, and (b) only reproducible features (ICC ≥ 0.90). Compare the classification performance (e.g., AUC) between the two sets to quantify the value of feature stability.
Protocol: Meta-Transfer Learning for Cross-Tumor Generalization
This protocol uses a meta-learning strategy to adapt a segmentation model trained on one tumor type to others, improving performance despite dataset shifts and limited data.
- Base Model Pretraining: Start with a state-of-the-art segmentation model like nnUNet, pretrained on a large, well-annotated dataset of a common tumor type (e.g., gliomas from BraTS) [65].
- Meta-Fine-Tuning:
- Objective: Reformulate the problem as a few-shot learning task. The goal is to find model parameters that can be rapidly adapted to new tumor types (e.g., meningioma, metastasis) with only a few gradient steps.
- Process: Use an algorithm like Model-Agnostic Meta-Learning (MAML). In the inner loop, the model is temporarily fine-tuned on small "tasks" (episodes) of meningioma or metastasis data. In the outer loop, the model's initial parameters are updated based on its performance on held-out data from these tasks, encouraging generalizable features [65].
- Loss Function: Employ a loss function like the Focal Tversky Loss to handle class imbalance between tumor sub-regions and background [65].
- Evaluation: Benchmark the performance of the resulting Meta-nnUNet model on independent test sets of the target tumor types, using metrics like the Dice coefficient for Whole Tumor (WT), Tumor Core (TC), and Enhancing Tumor (ET) [65].
Table 2: Key Research Reagent Solutions for Robust MRI Analysis
| Reagent / Tool | Type | Primary Function | Application Note |
|---|---|---|---|
| FSL [12] | Software Library | Provides tools for MRI brain analysis (BET, FAST, SUSAN) | Used for bias field correction, denoising, and skull-stripping in preprocessing pipelines. |
| nnUNet [65] | Deep Learning Framework | A self-configuring framework for medical image segmentation. | Serves as a powerful baseline and backbone for meta-transfer learning approaches. |
| BraTS Datasets [65] | Data | Multi-institutional MRI datasets with tumor segmentations. | Essential for pretraining (BraTS 2020) and evaluating generalization (BraTS 2023) across tumor types. |
| Focal Tversky Loss [65] | Algorithm | A loss function that handles class imbalance in segmentation. | Critical for training models on datasets with unequal class distributions (e.g., small lesions). |
| Model-Agnostic Meta-Learning (MAML) [65] | Algorithm | A meta-learning algorithm for fast adaptation to new tasks. | The core optimizer in meta-transfer learning to prepare models for adaptation with few labels. |
Visualizing Workflows for Robust Model Development
The following diagrams illustrate key experimental and computational workflows described in these protocols.
Radiomics Robustness Evaluation Workflow
Meta-Transfer Learning for Tumor Segmentation
Benchmarking Performance: A Comparative Analysis of Models and Metrics
In the field of tumor detection using MRI scans, the transition from experimental deep learning models to clinically viable tools demands rigorous quantitative assessment. Performance metrics—accuracy, precision, recall, and F1-score—serve as the critical bridge between algorithmic outputs and clinical decision-making, providing standardized measures to evaluate model effectiveness and safety. Within translational research frameworks, particularly those utilizing transfer learning, these metrics enable researchers to quantify a model's diagnostic capability, assess its potential impact on patient care, and identify areas requiring improvement before clinical deployment.
The fundamental challenge in medical AI lies in balancing detection sensitivity with diagnostic specificity. In brain tumor detection, for instance, a model must identify subtle pathological features while minimizing false alarms that could lead to unnecessary interventions. Research demonstrates that these metrics provide complementary insights: a model might achieve high overall accuracy yet miss critical cases (low recall), or identify tumors with high precision but miss too many actual cases. By comprehensively evaluating these metrics, researchers can optimize models to align with clinical priorities, whether prioritizing recall to minimize missed diagnoses in screening contexts or emphasizing precision to reduce false positives in confirmatory testing [67] [68].
Theoretical Foundations of Core Performance Metrics
Metric Definitions and Clinical Interpretations
The four core metrics are derived from a 2x2 confusion matrix that cross-tabulates predicted classifications against actual conditions. In the context of tumor detection:
- True Positive (TP): The model correctly identifies a tumor present in the MRI.
- False Positive (FP): The model incorrectly flags a healthy region as tumorous.
- True Negative (TN): The model correctly identifies a healthy region.
- False Negative (FN): The model misses an actual tumor.
Table 1: Fundamental Performance Metrics and Their Clinical Significance
| Metric | Formula | Clinical Interpretation |
|---|---|---|
| Accuracy | (TP+TN)/(TP+FP+TN+FN) | Overall correctness in classifying scans |
| Precision | TP/(TP+FP) | Reliability when a tumor is predicted |
| Recall (Sensitivity) | TP/(TP+FN) | Ability to detect all actual tumors |
| F1-Score | 2×(Precision×Recall)/(Precision+Recall) | Balanced measure when class distribution is uneven |
Clinical Consequences of Metric Trade-offs
Each metric illuminates different aspects of model performance with direct clinical implications:
High Recall as a "Lifeline" in Screening: In cancer screening, high recall is paramount as it minimizes false negatives where actual tumors go undetected. A recall rate of 80% means 20% of cancerous cases are missed, potentially delaying critical treatment. For diseases like brain tumors where early detection significantly impacts survival, maximizing recall is often prioritized, even at the expense of increased false positives [68].
Precision for Efficient Resource Utilization: High precision reduces false alarms, preventing unnecessary patient anxiety, follow-up tests, and invasive procedures like biopsies. In a case study of cancer screening, a precision of 53.3% meant nearly half of those flagged for cancer were actually healthy, leading to potential overtreatment and resource waste [68].
Accuracy's Limitations in Imbalanced Datasets: While accuracy provides an intuitive overall measure, it can be misleading when tumors are rare. A model might achieve 91% accuracy simply by correctly identifying mostly healthy scans while missing actual tumors. This phenomenon underscores why accuracy should not be evaluated in isolation, particularly for rare conditions [68].
F1-Score for Holistic Assessment: The F1-score, as the harmonic mean of precision and recall, provides a single metric that balances both concerns, particularly valuable when class distribution is uneven—a common scenario in medical imaging where pathological cases are often outnumbered by normal scans [69].
Quantitative Benchmarking in Tumor Detection Research
Performance Comparisons Across Model Architectures
Research directly comparing multiple deep learning architectures with standardized metrics provides crucial insights for model selection in transfer learning pipelines. One comprehensive study evaluated five pre-trained models—VGG16, MobileNetV2, DenseNet121, InceptionV3, and ResNet50—for brain tumor detection using identical optimization conditions, with results demonstrating significant performance variations.
Table 2: Comparative Performance of Pre-trained Models in Brain Tumor Detection
| Model Architecture | Accuracy | Precision | Recall | F1-Score |
|---|---|---|---|---|
| MobileNetV2 | 96% | 96% | 94% | 95% |
| DenseNet121 | 95% | - | - | - |
| VGG16 | 94% | - | - | - |
| InceptionV3 | 93% | 93% | 91% | 92% |
| ResNet50 | 77% | 78% | 76% | 76% |
This benchmark analysis revealed MobileNetV2 as the top performer when paired with the Adam optimizer, achieving an optimal balance across all metrics. The substantial performance gap with ResNet50 (96% vs. 77% accuracy) highlights how architectural differences significantly impact detection capability, guiding researchers toward more effective base models for transfer learning applications [67].
Advanced Architectures and Their Metric Profiles
Beyond standard architectures, specialized models customized for medical imaging demonstrate how architectural innovations impact metric performance. The YOLOv7 model, enhanced with attention mechanisms and specialized pooling, achieved remarkable 99.5% accuracy in brain tumor detection, though researchers acknowledged limitations in detecting small tumors—a challenge reflected in potentially lower recall for subtle lesions [4].
Similarly, a 3D CNN approach for early lung adenocarcinoma classification achieved an AUC of 0.871 for binary classification (non-invasive vs. invasive) and 0.879 for three-class classification, with corresponding F1-scores of 76.46%, demonstrating robust performance in complex diagnostic tasks with multiple outcome categories [69].
Experimental Protocols for Metric Evaluation
Standardized Model Training and Assessment Framework
To ensure reproducible metric evaluation in transfer learning research, the following protocol provides a standardized approach:
Protocol 1: Comprehensive Model Assessment for Tumor Detection
Data Preparation and Augmentation
- Curate a balanced dataset representing tumor and non-tumor cases (e.g., 2000 MRI images with 1000 tumor and 1000 non-tumor cases) [5].
- Apply standardized preprocessing: convert to grayscale, apply Gaussian filtering for noise reduction, and implement binary thresholding for tumor region highlighting [5].
- Employ data augmentation techniques including rotation, scaling, and elastic deformation to increase dataset diversity and enhance model generalization [67] [4].
- Implement brightness and contrast adjustments specifically to improve model robustness to imaging variations [67].
Model Selection and Transfer Learning Implementation
- Select pre-trained models with proven efficacy in medical imaging (VGG16, MobileNetV2, DenseNet121, InceptionV3, ResNet50) [67].
- Replace final classification layers to align with tumor detection objectives (binary or multi-class).
- Apply fine-tuning with differential learning rates, prioritizing higher rates for newly added layers.
Optimization Strategy
- Compare multiple optimizers (Adam, Stochastic Gradient Descent, Adamax) to identify optimal pairing with each architecture [67].
- Conduct systematic hyperparameter tuning using grid search for learning rate, batch size, and dropout rate [67].
- Implement cross-validation with consistent data splits to ensure comparable results across experiments.
Performance Quantification
- Calculate all four core metrics (accuracy, precision, recall, F1-score) against a hold-out test set.
- Generate confusion matrices for detailed error analysis [67] [69].
- Compute AUC values for different classification thresholds and generate ROC curves [69].
- Perform statistical significance testing on metric differences between model configurations.
Specialized Protocol for Challenging Segmentation Tasks
Medical images with uncertain, small, or empty reference annotations present unique challenges that conventional metrics may not adequately capture. The USE-Evaluator protocol addresses these scenarios:
Protocol 2: Evaluation Under Domain Shift and Annotation Uncertainty
Data Characterization
- Quantify reference annotation uncertainty using the Uncertainty score (U-score) [70].
- Analyze the distribution of reference annotation volumes, identifying cases where target pathology represents <1% of total volume [70].
- Document the prevalence of empty reference annotations where the pathology was not visible to annotators [70].
Metric Adaptation
- For small annotations (<1% of organ volume), implement volumetric thresholds where voxel-wise agreement extends beyond clinical relevance [70].
- For empty reference annotations, supplement segmentation metrics with image-level classification assessment (e.g., lesion present/absent) [70].
- Report metric distributions across different annotation size quartiles rather than relying solely on aggregate values [70].
Domain Shift Mitigation
- Train models on multi-institutional datasets with diverse scanner types, magnetic field strengths, and imaging protocols [71].
- Evaluate performance separately on internal vs. external datasets to quantify generalization gap [71].
- Implement domain adaptation techniques when performance disparities exceed clinically acceptable thresholds.
Diagram: Tumor Detection Model Development Workflow
Table 3: Essential Research Reagents and Computational Tools
| Resource Category | Specific Tools/Models | Application in Research |
|---|---|---|
| Pre-trained Models | VGG16, MobileNetV2, DenseNet121, InceptionV3, ResNet50, YOLOv7/YOLOv8 | Base architectures for transfer learning in tumor detection [67] [4] [72] |
| Optimization Algorithms | Adam, Stochastic Gradient Descent (SGD), Adamax | Fine-tuning model parameters during training [67] |
| Attention Mechanisms | Convolutional Block Attention Module (CBAM) | Enhanced feature extraction focusing on salient tumor regions [4] |
| Data Augmentation Tools | Brightness/contrast adjustment, rotation, scaling, elastic deformation | Increased dataset diversity and model generalization [67] [4] |
| Performance Evaluation Frameworks | USE-Evaluator, nnU-Net evaluation protocols | Specialized assessment under annotation uncertainty [70] |
| Domain Adaptation Resources | Multi-site datasets, harmonization algorithms | Improved model generalizability across imaging protocols [71] |
Metric Interpretation in Clinical Translation
The ultimate value of performance metrics emerges through their interpretation within specific clinical contexts. Different diagnostic scenarios demand distinct metric prioritization:
Screening vs. Confirmatory Testing: In population-level screening (e.g., early brain tumor detection), high recall is prioritized to minimize missed cases, accepting lower precision to ensure comprehensive detection. Conversely, in confirmatory testing or treatment planning, high precision becomes critical to avoid unnecessary interventions, with recall being relatively less crucial [68].
Accounting for Prevalence: The clinical implications of metric values depend heavily on disease prevalence. A precision of 50% in a screening context with 5% prevalence has dramatically different consequences than the same precision in a high-risk population with 50% prevalence. Similarly, the acceptable false negative rate varies with tumor aggressiveness—lower for fast-growing malignancies like glioblastoma compared to slower-progressing tumors [68] [4].
Domain Shift Considerations: Models achieving excellent metrics on curated research datasets may experience significant performance degradation in clinical practice due to domain shift—discrepancies in scanner manufacturers, imaging protocols, or patient populations. One study found scanner differences caused the most significant performance drop (ΔDSC=0.33), underscoring the necessity of external validation [71]. Models trained on multi-institutional datasets consistently demonstrate superior generalizability compared to single-institution models, though the latter may achieve higher performance on internal validations [71].
Diagram: Clinical Context Determines Metric Priority
Accuracy, precision, recall, and F1-score collectively provide the essential quantitative framework for evaluating tumor detection models in MRI research. Rather than pursuing universal optimization across all metrics, successful clinical translation requires deliberate metric prioritization aligned with specific clinical needs—whether emphasizing recall for screening applications or precision for treatment planning. The integration of these metrics throughout the model development pipeline, from initial transfer learning experiments to final clinical validation, ensures that computational advances translate into genuine improvements in patient care. As deep learning approaches increasingly mature toward clinical deployment, rigorous metric evaluation remains foundational to building systems that clinicians can trust and patients can rely on for accurate diagnosis.
Within the framework of a broader thesis on transfer learning for tumor detection in MRI scans, this application note provides a comparative analysis of four prominent deep learning architectures: GoogleNet, MobileNetV2, VGG16, and ResNet152. The accurate classification of brain tumors from Magnetic Resonance Imaging (MRI) is a critical step in diagnosis and treatment planning, directly impacting patient survival rates [73]. Transfer learning, which leverages pre-trained models on large-scale datasets like ImageNet, has emerged as a pivotal technique to address the challenge of limited annotated medical data, enabling researchers to achieve high performance with reduced computational overhead and training time [74] [75]. This document details the experimental protocols and performance metrics for these architectures, serving as a practical guide for researchers, scientists, and drug development professionals working in the field of neuro-oncology and medical image analysis.
A synthesis of recent research reveals the distinct performance characteristics of each architecture when applied to brain tumor classification tasks. The following table summarizes key quantitative findings from the literature.
Table 1: Performance Metrics of Deep Learning Architectures in Brain Tumor Classification
| Architecture | Reported Accuracy | Key Strengths | Notable Applications/Findings |
|---|---|---|---|
| GoogleNet | 89% [73] | Effective feature extraction with inception modules [9]. | Utilized for feature encoding and retrieval using Siamese Neural Networks [9]. |
| MobileNetV2 | 97.32% [76], 99.16% [77] | Computational efficiency, lightweight, suitable for mobile/edge deployment [78] [77]. | Hybrid MobileNetV2-SVM model achieved high AUC scores (e.g., 1.0 for pituitary tumors) [78]. |
| VGG16 | 90.97% (Testing) [79], 97.72% [75] | Simple, uniform architecture with strong feature representation [79]. | Enhanced versions have been reported to achieve detection accuracy up to 98.69% [74]. |
| ResNet152 | 98.85% [80] | Superior ability to capture complex features, mitigates vanishing gradient [73] [80]. | Used as a pre-trained model in DCNN for classifying meningioma, glioma, and pituitary tumors [80]. |
| ResNet50 (Benchmark) | 99.88% [73] | High accuracy with residual learning blocks. | Surpassed a classic CNN architecture (94.55%) in a three-class tumor classification task [73]. |
Detailed Experimental Protocols
Dataset Preparation and Preprocessing
A consistent dataset and preprocessing pipeline is fundamental for a fair comparative analysis.
- Data Source: The Kaggle brain tumor dataset (MRI images) is commonly used, which includes images categorized into glioma, meningioma, pituitary tumor, and occasionally "no tumor" [73] [78] [74]. The Figshare dataset is another validated source [80] [76].
- Data Split: A standard 80:20 split for training and testing is widely adopted, though cross-validation is also employed for robust evaluation [73] [77] [75].
- Image Preprocessing: A standardized preprocessing workflow is critical:
- Resizing: Images are typically resized to match the input requirements of the pre-trained models (e.g., 224×224 pixels for VGG16, MobileNetV2) [73] [77].
- Grayscale Conversion & Enhancement: Conversion to grayscale and application of Contrast-Limited Adaptive Histogram Equalization (CLAHE) to improve contrast [77].
- Noise Reduction: Use of median and Gaussian filters for noise removal [77].
- Data Augmentation: To address class imbalance and increase dataset diversity, techniques such as rotation, flipping, and scaling are applied [74] [80].
- Normalization: Pixel values are normalized to a standard range (e.g., 0-1) to ensure stable and efficient model training.
Architecture-Specific Configuration and Fine-Tuning
The following protocols outline the setup for each model, emphasizing transfer learning and fine-tuning.
GoogleNet (InceptionV1) Protocol:
- Feature Extraction: GoogleNet's inception modules are effective for multi-scale feature extraction. A common protocol involves using pre-trained GoogleNet encodings and representing them in a lower-dimensional feature space using a Siamese Neural Network (SNN) for retrieval and comparison tasks [9].
- Fine-Tuning: Replace the final fully connected layer with a new one matching the number of tumor classes. The base learning rate for the new layers should be set higher than that of the pre-trained layers to allow for adaptive learning.
MobileNetV2 Protocol:
- Base Model: Utilize MobileNetV2 pre-trained on ImageNet, leveraging its depth-wise separable convolutions for efficiency [78] [77].
- Hybrid Classification: A proven approach is to use MobileNetV2 as a feature extractor and pair it with a Support Vector Machine (SVM) classifier. This hybrid model (MobileNetV2-SVM) reduces computational overhead while maintaining high accuracy [78].
- Hyperparameter Optimization: Employ optimization algorithms like the Contracted Fox Optimization Algorithm (CFO) to select optimal hyperparameters for MobileNetV2, further enhancing accuracy [76].
VGG16 Protocol:
- Base Model: Utilize the VGG16 architecture pre-trained on ImageNet, known for its simplicity and depth using small convolutional filters [79].
- Transfer Learning: Remove the top layers and add custom fully connected layers for classification. Due to VGG16's high parameter count, focus on fine-tuning the later blocks while keeping earlier layers frozen to prevent overfitting.
- Ensemble Methods: To boost performance, VGG16 can be integrated into an ensemble model, such as combining a Shallow CNN with VGG16, which has been shown to achieve high accuracy (97.77%) and robustness against overfitting on imbalanced datasets [77].
ResNet152 Protocol:
- Base Model: Employ ResNet152 pre-trained on ImageNet. Its deep architecture with residual connections is highly effective for complex feature learning [80].
- Feature Extraction and Selection: Use ResNet152 as a deep convolutional feature extractor. Following feature extraction, apply feature selection algorithms like the Enhanced Chimpanzee Optimization Algorithm (EChOA) to reduce feature dimensionality and remove redundancies, which can lead to higher classification accuracy [80].
- Classification: The selected features are then classified using a softmax classifier [80].
Diagram 1: Experimental workflow for comparative analysis
The Scientist's Toolkit: Key Research Reagents and Materials
Table 2: Essential Research Reagents and Computational Tools for MRI-Based Tumor Classification
| Reagent / Tool | Function / Description | Example in Use |
|---|---|---|
| Kaggle / Figshare MRI Datasets | Publicly available benchmark datasets containing labeled MRI scans of brain tumors (e.g., glioma, meningioma, pituitary) for model training and validation. | Primary data source for most comparative studies [73] [78] [80]. |
| Pre-trained Models (ImageNet) | Models pre-trained on large-scale vision datasets provide powerful initial feature extractors, enabling effective transfer learning and reducing data requirements. | Base for all four architectures (GoogleNet, MobileNetV2, VGG16, ResNet152) [74] [75]. |
| Data Augmentation Tools | Software modules (e.g., in TensorFlow/PyTorch) to artificially expand training datasets using transformations, improving model generalization and robustness. | Applied to address class imbalance and prevent overfitting [74] [77]. |
| Support Vector Machine (SVM) | A robust machine learning classifier that can be paired with deep feature extractors to create hybrid models, potentially enhancing performance. | Used with MobileNetV2 features to form a high-accuracy hybrid classifier [78]. |
| Optimization Algorithms (e.g., EChOA, CFO) | Metaheuristic algorithms used for hyperparameter tuning and feature selection to optimize model performance and efficiency. | EChOA for feature selection with ResNet152 [80]; CFO for tuning MobileNetV2 [76]. |
This comparative analysis demonstrates that while all four architectures are viable for brain tumor classification, they offer different trade-offs. ResNet152 and highly optimized MobileNetV2 models currently achieve the highest reported accuracy, surpassing 98% [80] [77]. GoogleNet provides a solid baseline, while VGG16 offers a straightforward and effective architecture. The choice of model should be guided by the specific constraints of the clinical or research application, balancing the need for high precision against computational resources and latency requirements. The continued advancement and fine-tuning of these architectures, particularly through hybrid models and sophisticated optimization techniques, hold significant promise for enhancing diagnostic accuracy and ultimately improving patient outcomes in clinical oncology.
Statistical Validation of Model Reliability and Significance
Within the broader scope of thesis research on transfer learning for tumor detection in MRI scans, establishing the statistical reliability and significance of model performance is paramount. Moving beyond simple accuracy metrics is essential for developing models that are not only high-performing but also clinically trustworthy. This document provides detailed application notes and protocols for researchers and scientists, focusing on rigorous statistical validation practices specifically tailored for neuroimaging-based classification models. The content covers prevalent pitfalls in model comparison, standardized experimental protocols from recent literature, and practical tools to ensure that reported improvements in brain tumor detection are statistically sound and reproducible.
Statistical Testing and Cross-Validation Frameworks
A critical challenge in model development is the statistically sound comparison of different algorithms. A common but flawed practice is using a paired t-test on accuracy scores obtained from a repeated K-fold cross-validation (CV). Research has demonstrated that this approach is highly sensitive to the specific CV setup, such as the number of folds (K) and repetitions (M). Despite applying two classifiers with the same intrinsic predictive power, the outcome of the model comparison can be misleadingly deemed significant simply by varying K and M [81].
Key Pitfalls of Common Practices:
- Violation of Independence: The overlapping training folds between different CV runs create implicit dependencies in the accuracy scores, violating the core assumption of independence in standard statistical tests like the paired t-test [81].
- Sensitivity to CV Configuration: The likelihood of detecting a statistically significant difference (i.e., the "Positive Rate") artificially increases with higher numbers of folds (K) and repetitions (M). This variability can lead to p-hacking and inconsistent conclusions about model superiority [81].
Table 1: Impact of Cross-Validation Setup on Statistical Significance
| Dataset | CV Folds (K) | CV Repetitions (M) | Observed Positive Rate* | Recommended Practice |
|---|---|---|---|---|
| ABCD | 2 | 1 | Low (e.g., ~0.1) | Use corrected statistical tests (e.g., Nadeau and Bengio's correction). |
| ABCD | 50 | 10 | High (e.g., ~0.6) | Report all CV parameters (K, M) transparently. |
| ABIDE | 2 | 1 | Low | Avoid using paired t-tests on raw CV scores. |
| ABIDE | 50 | 10 | High | Focus on effect sizes and confidence intervals alongside p-values. |
| ADNI | 2 | 1 | Low | Utilize nested cross-validation for unbiased performance estimation. |
| ADNI | 50 | 10 | High | Source: Adapted from [81] |
*Positive Rate: The probability of a test incorrectly declaring a significant difference between models of equivalent power.
Figure 1: Flawed Model Comparison Workflow. This diagram illustrates a common but statistically problematic method for comparing models, where the outcome is overly sensitive to cross-validation configuration.
Experimental Protocols for Brain Tumor Classification
The following protocols summarize detailed methodologies from recent studies on brain tumor classification using MRI scans. These protocols highlight the use of transfer learning, data augmentation, and architectural modifications to achieve high performance.
Protocol 1: Refined YOLOv7 with Attention and Multi-Scale Fusion
This protocol is designed for accurate localization and classification of gliomas, meningiomas, and pituitary tumors [4].
1. Dataset Curation:
- Source: Open-source brain tumor datasets.
- Composition: The curated dataset includes:
- Glioma: 2548 images
- Pituitary: 2658 images
- Meningioma: 2582 images
- Non-tumor: 2500 images
2. Image Preprocessing:
- Apply image enhancement filters to improve the visual quality of low-resolution MRI scans.
- Implement aspect ratio normalization and resizing to standardize input dimensions.
3. Data Augmentation:
- Apply techniques to mitigate overfitting and improve model generalization on limited datasets.
4. Model Architecture & Training:
- Base Model: Adopt a pre-trained YOLOv7 model.
- Key Modifications:
- Integrate a Convolutional Block Attention Module (CBAM) to enhance feature extraction from salient tumor regions.
- Add a Spatial Pyramid Pooling Fast+ (SPPF+) layer to the network core.
- Incorporate a Bi-directional Feature Pyramid Network (BiFPN) to accelerate multi-scale feature fusion and improve detection of small tumors.
- Use decoupled heads to efficiently learn from diverse data.
- Training Paradigm: Utilize transfer learning by fine-tuning the pre-trained model on the brain tumor dataset.
5. Performance Outcomes:
- Achieved an overall accuracy of 99.5% on the test dataset [4].
Protocol 2: Certainty-Aware VGG19 for Reliable Classification
This protocol emphasizes not only accuracy but also the certainty of model predictions, which is critical for clinical application [82].
1. Dataset:
- An MRI dataset comprising glioma, meningioma, pituitary tumors, and non-tumor cases.
2. Model Architecture & Training:
- Base Model: A VGG19 architecture pre-trained on large-scale image datasets.
- Customization: Replace and customize the classification layers of VGG19 for the specific task of brain tumor classification.
- Training Focus: Explicitly minimize the loss function during training, as lower loss is correlated with higher prediction certainty.
3. Evaluation Metrics:
- Assess models using accuracy, precision, recall, and loss.
- The "Proposed Model" (customized VGG19) achieved 96.95% accuracy with a loss of 0.087, outperforming baseline CNN, ResNet50, and XceptionNet models in terms of both accuracy and certainty [82].
Protocol 3: Hybrid VGG16 with Attention and Explainability
This protocol combines transfer learning, attention mechanisms, and explainable AI to create a high-performance, interpretable model [34].
1. Dataset:
- Source: Publicly available Kaggle brain MRI dataset.
- Size: 7023 MRI images.
- Classes: Glioma, meningioma, pituitary tumor, and no tumor.
2. Preprocessing:
- Apply state-of-the-art preprocessing techniques to normalize the data.
3. Model Architecture:
- Backbone: A pre-trained VGG16 model for feature extraction.
- Attention Mechanism: Integrate a custom SoftMax-weighted attention layer to dynamically weigh tumor-specific features and suppress irrelevant image regions.
- Classification Head: A fully connected layer for final classification.
4. Explainability:
- Employ Gradient-weighted Class Activation Mapping (Grad-CAM) to produce heatmaps that visually identify the regions of the MRI scan that most influenced the classification decision.
5. Performance Outcomes:
- The hybrid model achieved 99% test accuracy and impressive precision and recall figures, significantly outperforming traditional machine learning approaches [34].
Table 2: Summary of Experimental Protocols and Key Outcomes
| Protocol | Base Model | Key Technical Innovations | Reported Accuracy | Primary Advantage |
|---|---|---|---|---|
| Protocol 1 [4] | YOLOv7 | CBAM, BiFPN, SPPF+, Decoupled Head | 99.5% | High precision in localization and small tumor detection. |
| Protocol 2 [82] | VGG19 | Custom Classifier Layers, Loss Minimization for Certainty | 96.95% | High prediction certainty and reliability. |
| Protocol 3 [34] | VGG16 | SoftMax-Weighted Attention, Grad-CAM Visualization | 99% | High accuracy with model interpretability/explainability. |
| GoogleNet TL [3] | GoogleNet | Transfer Learning, Data Augmentation for Class Imbalance | 99.2% | Effective handling of class imbalance in multi-class classification. |
Figure 2: Generalized Experimental Workflow. A high-level overview of the key stages in developing and validating a deep learning model for brain tumor classification.
The Scientist's Toolkit: Research Reagent Solutions
This section details essential materials, datasets, and software tools used in the featured experiments.
Table 3: Essential Research Reagents and Tools for Brain Tumor Detection Research
| Item Name | Type | Function / Application | Example / Source |
|---|---|---|---|
| Brain Tumor MRI Datasets | Data | Provides labeled images for model training, validation, and testing. | Kaggle Brain MRI, Figshare, BraTS [4] [34] |
| Pre-trained Models | Software | Serves as a foundation for transfer learning, reducing training time and data requirements. | YOLOv7, VGG16, VGG19, GoogleNet, ResNet50 [4] [3] [82] |
| Attention Modules | Algorithm | Enhances feature extraction by focusing model attention on salient tumor regions. | Convolutional Block Attention Module (CBAM) [4] |
| Data Augmentation Tools | Software | Artificially expands training datasets to prevent overfitting and improve model robustness. | Image transformations (rotation, flip) in PyTor/TensorFlow [4] |
| Explainability Tools | Software | Generates visual explanations for model predictions, building trust and aiding clinical validation. | Grad-CAM (Gradient-weighted Class Activation Mapping) [34] |
| Statistical Testing Libraries | Software | Provides functions for rigorous statistical comparison of model performance. | SciPy, scikit-posthocs (for corrected tests) [81] |
Statistical validation is the cornerstone of reliable and significant research in transfer learning for brain tumor detection. This document has outlined critical pitfalls in model comparison, underscored the importance of proper cross-validation practices, and provided detailed protocols from cutting-edge research. By adhering to these application notes and leveraging the provided toolkit, researchers can ensure their findings are not only high-performing but also statistically sound and clinically relevant, thereby advancing the field toward more robust and deployable diagnostic solutions.
In the field of medical artificial intelligence (AI), particularly for tumor detection in MRI scans, a model's performance on a single, curated test set is often an insufficient indicator of its real-world clinical utility. The ultimate challenge lies in generalizability—the ability of a model to maintain high performance across diverse, unseen datasets that vary in patient demographics, imaging protocols, scanner manufacturers, and clinical practices. This application note examines the critical factors affecting model generalizability, provides protocols for its rigorous evaluation, and synthesizes quantitative findings from recent research to guide the development of robust, clinically applicable tools for researchers and drug development professionals.
The Generalizability Challenge in Neuro-Oncology
Deep learning models for brain tumor analysis have achieved performance metrics surpassing 95% accuracy on benchmark datasets [3] [34]. However, these models often experience significant performance degradation when applied to data from new institutions. This "generalizability gap" stems from several sources:
- Dataset Shift: Public datasets like the Brain Tumor Segmentation (BraTS) challenges are invaluable but can introduce bias. Models may learn to recognize dataset-specific artifacts or annotation styles rather than the underlying pathology [62].
- Technical Heterogeneity: Variations in MRI scanners, imaging sequences (e.g., T1-weighted, T2-weighted, FLAIR), acquisition parameters, and pre-processing pipelines create a high-dimensional variability that models must overcome [83].
- Pathological and Anatomical Diversity: Brain tumors, including gliomas, meningiomas, and metastases, exhibit vast heterogeneity in size, shape, location, and appearance. A model trained predominantly on one tumor type may not generalize well to others [84] [62].
Addressing these challenges is not merely an academic exercise; it is a prerequisite for the integration of AI into clinical workflows and multi-center drug development trials, where reliable performance across diverse patient populations is paramount.
Quantitative Synthesis of Model Performance
The following tables synthesize key quantitative findings from recent studies, highlighting the relationship between model architectures, data strategies, and generalizability outcomes.
Table 1: Performance of Segmentation Models Across MRI Sequence Combinations. This table compares deep learning model performance in segmenting tumor subregions using different input MRI sequences, demonstrating that minimized input data can achieve high accuracy. Data sourced from [63] [85].
| MRI Sequences Used | Dice Score (Enhancing Tumor) | Dice Score (Tumor Core) | Sensitivity | Hausdorff Distance (mm) |
|---|---|---|---|---|
| T1 + T2 + T1C + FLAIR | 0.785 | 0.841 | 0.754 | 17.622 - 33.812 |
| T1C + FLAIR | 0.814 | 0.856 | 0.829 | 5.964 |
| T1C-only | 0.781 | 0.852 | 0.737 | - |
| FLAIR-only | 0.008 | 0.619 | - | - |
Table 2: Generalizability of a Raman Spectroscopy Model Across Tumor Types. This table illustrates how a single diagnostic model can exhibit variable performance when applied to different brain tumor pathologies, underscoring the need for targeted validation. Data sourced from [84].
| Tumor Type | Positive Predictive Value (PPV) | Key Challenge / Note |
|---|---|---|
| Glioblastoma | 91% | Model trained primarily on this type |
| Brain Metastases | 97% | Model trained primarily on this type |
| Meningioma | 96% | Model trained primarily on this type |
| Astrocytoma | 70% | Performance drop on unseen tumor type |
| Oligodendroglioma | 74% | Performance drop on unseen tumor type |
| Ependymoma | 100% | High performance on small sample |
| Pediatric Glioblastoma | 100% | High performance on small sample |
Table 3: Classification Performance of Deep Learning Models on Public Datasets. This table summarizes the high accuracy achieved by various deep learning models on common public benchmarks, which serve as a baseline for initial performance assessment. Data sourced from [3] [5] [34].
| Model Architecture | Reported Accuracy | Dataset | Key Feature |
|---|---|---|---|
| GoogleNet | 99.2% | Kaggle (4,517 images) | Transfer Learning |
| Custom CNN | 98.9% | Kaggle (7,023 images) | Local Binary Patterns |
| Hybrid VGG16 + Attention | 99.0% | Kaggle (7,023 images) | Explainable AI (Grad-CAM) |
| MobileNetV3 | 99.75% | Kaggle Brain MRI | Transfer Learning |
Experimental Protocols for Generalizability Evaluation
A robust evaluation framework is essential to properly assess a model's readiness for real-world application. The following protocols provide a structured approach.
Protocol: Multi-Center External Validation
This protocol outlines the gold-standard method for evaluating model generalizability using completely independent datasets [86].
1. Objective: To assess the performance and calibration of a pre-trained model on external data from institutions not involved in the training process.
2. Materials:
- Trained Model: A frozen model weights file.
- External Test Set: MRI data from at least two independent clinical centers, with corresponding ground-truth annotations. The dataset should be cohort- and distribution-shifted relative to the training data (e.g., the ISMF-Net external test set with 281 patients [86]).
- Computing Environment: Hardware and software capable of running the model inference.
3. Procedure:
- Step 1: Data Curation. Collect and anonymize DICOM files and ground-truth labels from the external centers. Ensure ethical approval for data usage.
- Step 2: Harmonization. Apply identical pre-processing steps used during model training (e.g., intensity normalization, skull-stripping, resampling) to the external data. Do not re-train or fine-tune the model.
- Step 3: Inference. Run the model on the pre-processed external test set to generate predictions (segmentations or classifications).
- Step 4: Quantitative Analysis. Calculate performance metrics (Dice Score, Accuracy, Sensitivity, Specificity) by comparing predictions to the ground truth.
- Step 5: Statistical Comparison. Use statistical tests (e.g., paired t-tests, Wilcoxon signed-rank test) to compare the model's performance on the internal versus external test sets. A significant performance drop indicates poor generalizability.
4. Interpretation: A generalizable model will maintain high performance metrics across all test sets without significant degradation. The external validation performance, not the internal test performance, is the best indicator of real-world utility.
Protocol: Cross-Validation on Heterogeneous Data Splits
This protocol is used during model development to estimate generalizability and mitigate overfitting to site-specific biases.
1. Objective: To evaluate model robustness by training and validating on data splits that maximize heterogeneity between folds.
2. Materials:
- Multi-Institutional Dataset: A combined dataset from multiple sources (e.g., BraTS 2018 and 2021 [63]).
- Training Infrastructure: Sufficient computational resources for multiple training runs.
3. Procedure:
- Step 1: Data Stratification. Instead of a simple random split, partition the data such that all studies from a single institution or scanner are contained entirely within one fold. This is known as "leave-site-out" cross-validation.
- Step 2: Iterative Training and Validation. For each fold, train the model on data from all but one institution and validate on the held-out institution's data.
- Step 3: Performance Aggregation. Calculate the final model performance by averaging the metrics across all held-out validation folds.
The following workflow diagram illustrates this process for a hypothetical dataset comprising three institutions.
Protocol: Ablation Study for Data Efficiency
This protocol evaluates the minimum data requirements for effective model performance, which is critical for applications in resource-constrained settings [63] [85].
1. Objective: To determine the impact of different input MRI sequences on segmentation accuracy, identifying a minimal yet sufficient subset for clinical use.
2. Materials:
- Dataset: A public dataset with multiple MRI sequences per patient (e.g., BraTS with T1, T1C, T2, FLAIR).
- DL Framework: A standard segmentation architecture like 3D U-Net.
3. Procedure:
- Step 1: Model Variant Training. Train multiple instances of the same model architecture, but vary the input MRI sequences provided to each (e.g., T1C-only, FLAIR-only, T1C+FLAIR, All sequences).
- Step 2: Consistent Evaluation. Evaluate all model variants on the same, held-out test dataset.
- Step 3: Comparative Analysis. Compare performance metrics (Dice Score, Hausdorff Distance) across the different model variants.
4. Interpretation: As shown in Table 1, a model trained on only T1C and FLAIR can match or even exceed the performance of a model trained on all four conventional sequences. This finding suggests that a reduced sequence dependency can enhance model generalizability by lowering the barrier for clinical deployment.
The Scientist's Toolkit: Research Reagent Solutions
The following table details key resources and their functions for developing and evaluating generalizable models in neuro-oncology AI.
Table 4: Essential Research Reagents and Resources for Model Development.
| Resource / Solution | Function in Research | Example & Notes |
|---|---|---|
| Public Datasets (BraTS) | Benchmarking, pre-training, and initial validation of segmentation models. | MICCAI BraTS: Contains multi-institutional gliomas with T1, T1C, T2, FLAIR sequences and expert annotations [62]. |
| Longitudinal Metastasis Datasets | Studying treatment response and temporal generalizability. | Brain Metastases dataset [83]: Includes 744 MRI scans with segmentations of enhancing tumor, edema, and necrotic core across multiple time points. |
| Pre-trained CNN Models | Leveraging transfer learning for classification tasks, improving data efficiency. | VGG16, GoogleNet, MobileNet [3] [34]: Models pre-trained on natural images (e.g., ImageNet) can be fine-tuned for medical image analysis. |
| 3D U-Net Architecture | Standard baseline model for volumetric medical image segmentation. | As used in [63] [85]: Effectively handles 3D context with encoder-decoder structure and skip connections. |
| Explainability Tools (Grad-CAM) | Providing visual explanations for model predictions, building clinical trust. | Gradient-weighted Class Activation Mapping [34]: Generates heatmaps highlighting image regions most important for the classification decision. |
| Raman Spectroscopy Systems | Intraoperative real-time decision support and tissue characterization. | As described in [84]: Provides biochemical contrast based on inelastic light scattering, complementing MRI findings. |
Evaluating model generalizability is a critical step that transcends the pursuit of high accuracy on benchmark leaderboards. For AI tools to be integrated into clinical practice and drug development pipelines, they must demonstrate consistent performance across diverse and unpredictable real-world data. This requires a shift in methodology, prioritizing rigorous external validation, heterogeneous data splitting, and data-efficient model design. By adopting the protocols and frameworks outlined in this document, researchers can develop more robust and reliable AI solutions, ultimately accelerating their translation into tools that improve patient care and advance neuro-oncological research.
Conclusion
Transfer learning has unequivocally established itself as a powerful paradigm for brain tumor detection in MRI, demonstrating remarkable accuracy often exceeding 98% in research settings. The synthesis of this review confirms that hybrid models, which combine the feature extraction prowess of pre-trained CNNs with the contextual understanding of attention mechanisms and transformers, represent the current state-of-the-art. The critical integration of Explainable AI (XAI) is paving the way for clinical trust and adoption by making model decisions transparent. Future directions should focus on the development of large, multi-institutional foundation models, robust validation in real-world clinical workflows, and exploration of sequential transfer learning across related neurological conditions. For biomedical research, these advancements promise not only enhanced diagnostic tools but also new avenues for discovering imaging biomarkers and assessing treatment response, ultimately accelerating the path toward personalized medicine in neuro-oncology.
References
- 1. What is transfer learning? [https://www.ibm.com/think/topics/transfer-learning]
- 2. What Is Transfer Learning? A Guide for Deep Learning [https://builtin.com/data-science/transfer-learning]
- 3. Transfer learning for accurate brain tumor classification in MRI [https://pmc.ncbi.nlm.nih.gov/articles/PMC12149374/]
- 4. Brain Tumor Detection Based on Deep Learning Approaches ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10453020/]
- 5. Enhanced MRI brain tumor detection using deep learning ... [https://www.nature.com/articles/s41598-025-14901-4]
- 6. An Advanced Transfer Learning Pipeline Using YOLO11 ... [https://www.mdpi.com/2313-433X/11/8/282]
- 7. Machine Learning in MRI Brain Imaging: A Review ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12609805/]
- 8. ESMRMB 2025 focus topic: cycle of quality—from concept to ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12255560/]
- 9. Deep learning-integrated MRI brain tumor analysis [https://www.nature.com/articles/s41598-024-84386-0]
- 10. A Comprehensive MRI Tumor Framework [https://arxiv.org/html/2509.24149v1]
- 11. Hybrid transfer learning and self-attention framework for ... [https://www.nature.com/articles/s41598-025-09311-5]
- 12. Impact of image preprocessing methods on MRI radiomics ... [https://www.nature.com/articles/s41598-025-23702-8]
- 13. Transfer deep learning and explainable AI framework for ... [https://www.frontiersin.org/journals/medicine/articles/10.3389/fmed.2025.1618550/full]
- 14. Top Pre-Trained Models for Image Classification [https://www.geeksforgeeks.org/computer-vision/top-pre-trained-models-for-image-classification/]
- 15. Everything you need to know about VGG16 [https://medium.com/@mygreatlearning/everything-you-need-to-know-about-vgg16-7315defb5918]
- 16. VGG-16 | CNN model [https://www.geeksforgeeks.org/computer-vision/vgg-16-cnn-model/]
- 17. Residual Networks (ResNet) - Deep Learning [https://www.geeksforgeeks.org/deep-learning/residual-networks-resnet-deep-learning/]
- 18. DenseNet Explained [https://www.geeksforgeeks.org/computer-vision/densenet-explained/]
- 19. Deep Learning Architecture 7 : DenseNet | by Abhishek Jain [https://medium.com/@abhishekjainindore24/deep-learning-architecture-7-densenet-feee44d57f89]
- 20. Understanding GoogLeNet Model - CNN Architecture [https://www.geeksforgeeks.org/machine-learning/understanding-googlenet-model-cnn-architecture/]
- 21. Comparison and Architecture of Pre-Trained Models ... [https://medium.com/@muradatcorvit23/comparison-and-architecture-of-pre-trained-models-alexnet-vgg-16-vgg-19-resnet-googlenet-05f83214fc47]
- 22. On-the-Fly Data Augmentation for Brain Tumor Segmentation [https://arxiv.org/html/2509.24973v1]
- 23. brain tumor dataset [https://figshare.com/articles/dataset/brain_tumor_dataset/1512427]
- 24. BRISC: Annotated Dataset for Brain Tumor Segmentation ... [https://figshare.com/articles/dataset/_b_BRISC_Annotated_Dataset_for_Brain_Tumor_Segmentation_and_Classification_b_/30533120]
- 25. Detection of brain tumors using a transfer learning-based ... [https://www.sciencedirect.com/science/article/abs/pii/S0010482525001404]
- 26. Comparative analysis of machine learning techniques on ... [https://pubmed.ncbi.nlm.nih.gov/41030946/]
- 27. Fine-tuned ResNet34 for efficient brain tumor classification [https://www.nature.com/articles/s41598-025-20872-3]
- 28. Enhancing brain tumor classification in MRI images [https://www.sciencedirect.com/science/article/pii/S026288562500143X]
- 29. Fine-Tuning Pre-trained Convolutional Neural Network ... [https://link.springer.com/10.1007/978-3-031-92625-9_1]
- 30. An automated deep learning framework for brain tumor ... [https://www.nature.com/articles/s41598-025-02209-2]
- 31. A comprehensive review of transformer models in brain ... [https://www.sciencedirect.com/science/article/abs/pii/S0957417425041247]
- 32. Hierarchical multi-scale vision transformer model for ... [https://www.nature.com/articles/s41598-025-23100-0]
- 33. An intelligent brain tumor detection model using lightweight ... [https://www.nature.com/articles/s41598-025-23813-2]
- 34. Optimized deep learning for brain tumor detection: a hybrid ... [https://www.nature.com/articles/s41598-025-04591-3]
- 35. ShallowMRI: A novel lightweight CNN with novel attention ... [https://www.sciencedirect.com/science/article/abs/pii/S174680942500936X]
- 36. Brain Tumor Classification in MRI Scans Using Edge ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12561617/]
- 37. A Deep Learning Framework for Brain Tumor Detection ... [https://www.sciencedirect.com/science/article/pii/S277294192500208X]
- 38. Leveraging transfer learning-driven convolutional neural ... [https://www.nature.com/articles/s41598-024-81966-y]
- 39. Transparent brain tumor detection using DenseNet169 and ... [https://www.nature.com/articles/s41598-025-13233-7]
- 40. Enhancing brain tumor classification with a novel attention ... [https://www.sciencedirect.com/science/article/pii/S1746809425011474]
- 41. Exploring the potential of explainable AI in brain tumor ... [https://link.springer.com/article/10.1007/s10462-025-11410-8]
- 42. Leveraging explainable artificial intelligence for ... [https://pubmed.ncbi.nlm.nih.gov/40839960/]
- 43. Enhanced MRI brain tumor detection using deep learning ... [https://pubmed.ncbi.nlm.nih.gov/40790336/]
- 44. Hybrid model integration with explainable AI for brain ... [https://www.nature.com/articles/s41598-025-06455-2]
- 45. Revolutionizing Brain Tumor Detection Using Explainable ... [https://pubmed.ncbi.nlm.nih.gov/39948696/]
- 46. A systematic review of deep learning data augmentation in ... [https://www.sciencedirect.com/science/article/pii/S277244252400042X]
- 47. Multi channel fusion diffusion models for brain tumor MRI ... [https://www.nature.com/articles/s41598-025-06529-1]
- 48. Lightweight CNN for accurate brain tumor detection from ... [https://www.frontiersin.org/journals/medicine/articles/10.3389/fmed.2025.1636059/full]
- 49. Medical Image Annotation and Labeling Services Guide ... [https://www.cogitotech.com/blog/medical-image-annotation-labeling-guide-2025/]
- 50. Hard and Soft Mixing Data Augmentation for Medical ... [https://arxiv.org/html/2511.17614v1]
- 51. Multi channel fusion diffusion models for brain tumor MRI ... [https://pubmed.ncbi.nlm.nih.gov/40594886/]
- 52. AI in motion: the impact of data augmentation strategies on ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12559149/]
- 53. MSPO: A machine learning hyperparameter optimization ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12277558/]
- 54. Overfitting In Healthcare AI [https://www.meegle.com/en_us/topics/overfitting/overfitting-in-healthcare-ai]
- 55. Hyperparameter optimization [https://en.wikipedia.org/wiki/Hyperparameter_optimization]
- 56. comparative analysis and hyperparameter optimisation of ... [https://www.nature.com/articles/s41598-024-53528-9]
- 57. Overfitting Prevention Techniques [https://www.meegle.com/en_us/topics/overfitting/overfitting-prevention-techniques]
- 58. How do you prevent in deep learning with small datasets? [https://medium.com/@sharetonschool/how-do-you-prevent-in-deep-learning-with-small-datasets-745acb036f71]
- 59. Detecting and Mitigating the Clever Hans Effect in Medical ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12344020/]
- 60. Trade-Off Analysis of Classical Machine Learning and Deep ... [https://ai.jmir.org/2025/1/e76344]
- 61. Advanced Brain Tumor Classification in MR Images Using ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11719945/]
- 62. A review of deep learning for brain tumor analysis in MRI [https://www.nature.com/articles/s41698-024-00789-2]
- 63. Brain tumor segmentation using deep learning [https://www.frontiersin.org/journals/radiology/articles/10.3389/fradi.2025.1616293/full]
- 64. A review on brain tumor segmentation based on deep ... [https://www.sciencedirect.com/science/article/pii/S0895611123001313]
- 65. Meta transfer learning for brain tumor segmentation using ... [https://www.nature.com/articles/s41598-025-20957-z]
- 66. A novel federated learning framework for medical imaging [https://pmc.ncbi.nlm.nih.gov/articles/PMC12409104/]
- 67. 用于优化脑肿瘤检测的增强多模态融合:评估和比较分析 [https://www.jove.com/cn/t/67822/augmented-multimodal-fusion-for-optimized-brain-tumor-detection]
- 68. 癌症筛查中精确率、准确率和召回率的协同分析与医疗决策原创 [https://blog.csdn.net/Kent_Li/article/details/148973843]
- 69. Clinical Study of Artificial Intelligence-assisted Diagnosis ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9051300/]
- 70. USE-Evaluator: Performance metrics for medical image ... [https://www.sciencedirect.com/science/article/abs/pii/S1361841523001871]
- 71. 基于人工智能的前列腺MRI自动轮廓分割在放疗中的领域偏 ... [https://www.ebiotrade.com/newsf/2025-11/20251116004303297.htm]
- 72. 基于YOLOv8的原发性中枢神经系统淋巴瘤检测分类方法及 ... [https://patents.google.com/patent/CN118485864A/zh]
- 73. Learning Architecture for Brain Tumor Classification Based ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11898819/]
- 74. Brain Tumor Detection and Prediction in MRI Images ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11944010/]
- 75. T1-weighted MRI-based brain tumor classification using ... [https://www.nature.com/articles/s41598-025-92020-w]
- 76. Brain tumor diagnosis from MRI based on Mobilenetv2 ... [https://www.sciencedirect.com/science/article/pii/S2405844023110747]
- 77. Enhanced Brain Tumor Classification Using MobileNetV2 [https://www.mdpi.com/2673-7426/5/2/30]
- 78. Efficient and Accurate Brain Tumor Classification Using Hybrid ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11674380/]
- 79. The VGG16 Method Is a Powerful Tool for Detecting Brain ... [https://www.mdpi.com/2673-4591/59/1/46]
- 80. Feature Extraction Using a Residual Deep Convolutional ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9955169/]
- 81. Statistical variability in comparing accuracy of ... [https://www.nature.com/articles/s41598-025-12026-2]
- 82. Evaluating certainty of AI models for brain tumour detection [https://www.sciencedirect.com/science/article/abs/pii/S0010482525007267]
- 83. A longitudinal MRI dataset of brain metastases with tumor ... [https://www.nature.com/articles/s41597-025-06131-0]
- 84. Quantitative assessment of the generalizability of a brain ... [https://pubmed.ncbi.nlm.nih.gov/39866856/?utm_source=FeedFetcher&utm_medium=rss&utm_campaign=None&utm_content=1fILiDRVSw3cwZwfjHzy68f--yYPFWex_KPhHaWrY8u8d8LYTj&fc=None&ff=20250128123549&v=2.18.0.post9+e462414]
- 85. Brain tumor segmentation using deep learning [https://pubmed.ncbi.nlm.nih.gov/40697313/]
- 86. Development and validation of a multi-modal MRI-based ... [https://www.sciencedirect.com/science/article/pii/S258953702500570X]