Strategies to Minimize False Positives in qPCR Cancer Assays: From Foundational Principles to Clinical Validation
This article provides a comprehensive guide for researchers and drug development professionals on mitigating false positive results in quantitative PCR (qPCR) assays for cancer detection and monitoring.
Strategies to Minimize False Positives in qPCR Cancer Assays: From Foundational Principles to Clinical Validation
Abstract
This article provides a comprehensive guide for researchers and drug development professionals on mitigating false positive results in quantitative PCR (qPCR) assays for cancer detection and monitoring. It covers the foundational sources of error, methodological best practices in assay design and wet-lab procedures, systematic troubleshooting and optimization protocols, and rigorous validation frameworks. By synthesizing current research and proven techniques, this resource aims to enhance the specificity, reliability, and clinical applicability of qPCR-based cancer diagnostics, ultimately supporting the development of more accurate and trustworthy biomarker assays.
Understanding the Sources and Impact of False Positives in Cancer qPCR
In the realm of molecular oncology, quantitative polymerase chain reaction (qPCR) stands as a cornerstone technology for detecting cancer biomarkers, monitoring minimal residual disease, and guiding targeted therapy decisions. However, the clinical consequences of false positive results can be profound, leading to inappropriate treatment selections, unnecessary psychological distress for patients, and increased healthcare costs. A false positive result occurs when a qPCR assay incorrectly indicates the presence of a specific cancer-associated mutation or biomarker. In non-small cell lung cancer (NSCLC), for example, a recent study on EGFR S768I mutation detection revealed an 80% false positive rate when using a commercial qPCR system, with only one of five positive results confirmed by next-generation sequencing (NGS) [1]. Such inaccuracies in molecular diagnosis can directly impact therapeutic decisions, potentially steering patients toward ineffective or even harmful treatments.
The remarkably high sensitivity of qPCR, while advantageous for detecting low-abundance targets, also makes these assays particularly vulnerable to contamination and amplification artifacts [2]. In cancer diagnostics, where results directly influence treatment pathways, ensuring specificity is not merely an analytical concern but an ethical imperative. This technical support center provides researchers, scientists, and drug development professionals with evidence-based troubleshooting guides and FAQs to identify, prevent, and mitigate false positives in qPCR-based cancer assays, framed within the broader context of advancing precision oncology through more reliable molecular diagnostics.
FAQs: Understanding False Positives in Cancer qPCR
What are the primary sources of false positives in qPCR cancer assays?
False positives in qPCR cancer assays predominantly originate from three sources:
- Carryover contamination: Previously amplified PCR products (amplicons) from positive samples or controls can contaminate new reactions, generating false signals. This is particularly problematic in high-throughput laboratories processing numerous cancer samples daily [2] [3].
- Cross-contamination during sample processing: Aerosols created during pipetting, vortexing, or tube opening can transfer target nucleic acids between samples. In one documented case, false positives for Lyme disease led to inappropriate antibiotic therapy and subsequent patient complications [2].
- Assay design issues: Poorly designed primers and probes may bind nonspecifically to non-target sequences or form dimers that generate amplification signals. For instance, the use of primers targeting sequences only 25 bases long was postulated as a reason for false positives in SARS-CoV-2 rRT-PCR kits [2].
What are the clinical consequences of false positives in cancer diagnosis and treatment monitoring?
False positives in cancer qPCR assays can lead to several serious clinical outcomes:
- Inappropriate treatment selection: In NSCLC, false identification of EGFR mutations could lead to unnecessary tyrosine kinase inhibitor (TKI) therapy instead of more appropriate treatments, exposing patients to potential side effects without clinical benefit [1].
- Unnecessary additional testing and procedures: False positives may trigger additional invasive biopsies, imaging studies, or laboratory tests that increase patient risk and healthcare costs [2].
- Psychological distress: Patients and families experience unnecessary anxiety and stress when incorrectly informed about cancer diagnosis or disease progression [2].
- Delayed correct diagnosis: Time and resources spent pursuing false leads can delay identification of the actual molecular drivers of a patient's cancer, potentially compromising outcomes.
How can we validate the specificity of a new qPCR assay for cancer biomarker detection?
Assay validation should incorporate multiple strategies:
- In silico specificity checks: Regularly verify primer and probe sequences via BLAST search against databases like NCBI to ensure specificity and minimize cross-reactivity with non-target sequences [2].
- Experimental controls: Include no-template controls (NTCs) to detect contamination and non-specific template controls to identify primer-dimer formation or non-specific amplification [3].
- Comparison with orthogonal methods: Confirm positive results using alternative technologies such as next-generation sequencing (NGS), especially for rare mutations like EGFR S768I where qPCR systems have demonstrated high false positive rates [1].
- Dilution series analysis: Evaluate assay performance across a range of target concentrations to establish limits of detection and identify potential low-level contamination issues [4].
Troubleshooting Guide: Identifying and Resolving Common Causes of False Positives
Problem: Consistent False Positives Across Multiple Samples
Potential Cause: Environmental contamination of laboratory equipment, reagents, or workspace with amplicons or positive control material.
Solutions:
- Implement physical separation: Establish distinct pre-PCR and post-PCR areas with unidirectional workflow to prevent amplicon carryover [2].
- Enhance decontamination protocols: Clean workspaces and equipment with 10% sodium hypochlorite (minimum 10 minutes contact time) followed by 70% ethanol or 1M hydrogen chloride. Use UV irradiation for surface sterilization [2] [3].
- Utilize enzymatic prevention: Incorporate uracil-DNA-glycosylase (UNG) into PCR master mixes to degrade contaminating uracil-containing amplicons from previous reactions [2] [3].
- Service equipment: Regularly clean and service pipettes, especially their interiors, which can become contaminated through improper pipetting techniques [2].
Problem: False Positives for Specific Targets Despite Proper Controls
Potential Cause: Non-specific primer binding or probe degradation leading to aberrant amplification signals.
Solutions:
- Redesign suboptimal primers: Implement "hot start" PCR techniques that inhibit polymerase activity until high temperatures are reached, reducing nonspecific amplification during reaction setup [2].
- Apply touchdown PCR: Begin with an annealing temperature 5°C-10°C above the primer's estimated melting temperature, then gradually decrease to the optimal temperature over subsequent cycles to favor specific binding [2].
- Verify probe integrity: Use signal-to-noise assessment, mass spectrometry, or fluorometric scans to check for degraded probes that release signal molecules and cause high background noise [2].
- Optimize primer design: Create longer primers (targeting >100 base pairs when possible) with annealing-control primers containing polydeoxyinosine linkers that form bubble structures during annealing to prevent nonspecific binding [2].
Problem: Inconsistent False Positives with Low Signal Intensity
Potential Cause: Low-level contamination from synthetic control materials or plasmid DNA used as positive controls.
Solutions:
- Use chimeric plasmid DNA (cpDNA): Implement cpDNA with contamination indicator probes that emit distinct fluorescent signals, enabling differentiation between true target amplification and control contamination [4].
- Dilute positive controls: Prepare single-use aliquots of control materials at appropriate concentrations to minimize contamination risk [2].
- Implement dual-probe systems: Develop assays with separate probes for the target sequence and an exogenous control sequence to distinguish specific amplification from contamination [4].
Case Study: Troubleshooting EGFR S768I False Positives in NSCLC
A recent prospective study evaluating EGFR S768I mutation detection in NSCLC patients demonstrated the real-world impact of false positives and their resolution. When using the Idylla qPCR system, initial testing showed an 80% false positive rate, with only one of five positive results confirmed by NGS. The troubleshooting process revealed:
- Amplification curve analysis: False positives typically showed normalized fluorescence values below 12 points, distinguishing them from true positives [1].
- Repeat testing methodology: When initial tissue testing (Idylla1) produced false positives, repeat analysis using extracted DNA (Idylla2) showed significantly improved accuracy (0.833 vs. 0.333) and better agreement with NGS (Kappa = 0.571 vs. 0.077) [1].
- Algorithm refinement: The findings suggested a need to refine the system's interpretation algorithms, particularly for mutations with lower prevalence like S768I [1].
Experimental Protocols for False Positive Mitigation
Protocol: Establishing a Contamination-Free qPCR Workflow for Cancer Assays
This protocol implements stringent measures to prevent false positives in high-sensitivity cancer detection assays.
Materials Needed:
- Dedicated pre-PCR and post-PCR workspaces
- Aerosol-barrier pipette tips
- UNG-containing master mix
- Freshly prepared 10% sodium hypochlorite solution
- 70% ethanol solution
- UV irradiation cabinet
- Dedicated lab coats and gloves for each area
- Single-use reagent aliquots
Procedure:
- Spatial Separation: Perform reagent preparation, sample addition, amplification, and analysis in physically separated areas with unidirectional workflow [2].
- Pre-PCR Area Setup:
- Reagent Preparation:
- Control Implementation:
- Personal Protective Measures:
Protocol: Specificity Validation for Novel Cancer Biomarker Assays
This protocol ensures that newly developed qPCR assays for cancer biomarkers maintain high specificity against genomic backgrounds.
Materials Needed:
- Target-positive samples (cell lines or patient samples with known mutation status)
- Target-negative samples (cell lines or patient samples confirmed wild-type)
- Genomic DNA from various tissue sources
- NGS confirmation capability
- Standard qPCR equipment and reagents
Procedure:
- Analytical Specificity Testing:
- Test the assay against a panel of genomic DNA from different tissue types to check for tissue-specific non-specific amplification.
- Include samples with phylogenetically related sequences or highly homologous genes to assess cross-reactivity.
- Limit of Detection (LOD) Determination:
- Perform serial dilutions of positive control material in wild-type background.
- Identify the lowest concentration at which the target is detected in ≥95% of replicates [1].
- Comparison with Orthogonal Methods:
- Analyze a set of clinical samples (minimum 20-30) by both the new qPCR assay and an established reference method like NGS.
- Calculate sensitivity, specificity, and accuracy with 95% confidence intervals [1].
- Amplification Curve Analysis:
- Carefully examine amplification curves for atypical shapes that might indicate non-specific amplification.
- Establish normalized fluorescence thresholds to distinguish true positives from false signals, as demonstrated in the EGFR S768I study where false positives typically showed values below 12 points [1].
- Blinded Testing:
- Conduct blinded testing of known positive and negative samples by multiple operators to assess reproducibility and identify operator-dependent contamination issues.
Data Presentation: Quantitative Analysis of False Positive Rates in Cancer qPCR
Table 1: Performance Metrics of EGFR S768I Mutation Detection by qPCR Versus NGS [1]
| Test Method | Sample Type | Sensitivity (%) | Specificity (%) | Accuracy | False Positive Rate (%) |
|---|---|---|---|---|---|
| Idylla1 (initial tissue testing) | FFPE tissue | 100 | 20 | 0.333 | 80 |
| Idylla2 (extracted DNA testing) | Extracted DNA | 100 | 80 | 0.833 | 20 |
| NGS (reference standard) | FFPE tissue | 100 | 100 | 1.000 | 0 |
Table 2: Comparison of Contamination Prevention Methods in qPCR [2] [3]
| Method | Mode of Action | Advantages | Disadvantages |
|---|---|---|---|
| UNG/UDG Treatment | Enzymatic hydrolysis of uracil-containing DNA from previous amplifications | Easy to incorporate into existing protocols; effective against most common contamination | Added cost; may reduce amplification efficiency if not optimized |
| UV Irradiation | Forms thymidine dimers in contaminating DNA | Inexpensive; requires no change to PCR protocol | Ineffective against GC-rich and short (<300 bp) amplification products |
| Spatial Separation | Physical isolation of pre-and post-PCR activities | Highly effective when properly implemented; no chemical modifications needed | Requires significant laboratory space and workflow discipline |
| Psoralen Treatment | Forms cyclobutane adducts with DNA | Relatively inexpensive; requires minor protocol modification | Potential carcinogenicity; less effective for GC-rich amplicons |
| Hydroxylamine Treatment | Chemically modifies cytosine residues to prevent C-G pairing | Effective on short and GC-rich amplicons | Carcinogenic; may interfere with downstream analysis |
Table 3: Diagnostic Accuracy of Molecular Tests Compared to RT-PCR Reference Standard [5]
| Test Type | Sensitivity (95% CI) | Specificity (95% CI) | Positive Predictive Value (95% CI) | Negative Predictive Value (95% CI) |
|---|---|---|---|---|
| Rapid Antigen Tests (pooled) | 67.1% | Not reported | 97.7% | 95.2% |
| STANDARD Q COVID-19 Ag Test | 78.2% (58.7-90.0%) | 98.4% (94.9-99.5%) | Not reported | Not reported |
| PanBio COVID-19 Ag Test | 78.0% (61.0-88.9%) | 99.9% (99.3-100%) | Not reported | Not reported |
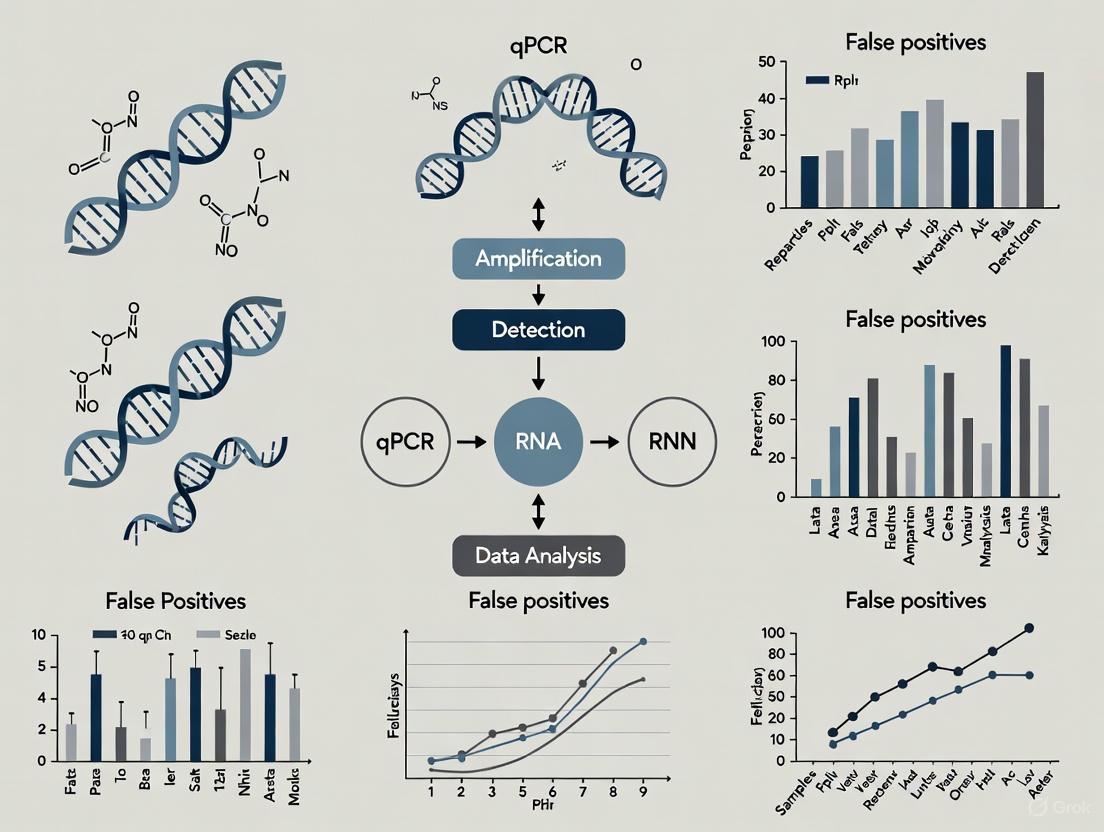
Visualization: Experimental Workflows and Diagnostic Pathways
Diagram 1: Comprehensive qPCR workflow and false positive investigation pathway illustrating the integrated approach required for reliable cancer diagnostics.
The Scientist's Toolkit: Essential Reagents and Controls for Reliable Cancer qPCR
Table 4: Research Reagent Solutions for False Positive Mitigation
| Reagent/Control | Function | Application Notes |
|---|---|---|
| UNG/UDG Enzyme | Degrades uracil-containing contaminating amplicons from previous reactions | Include in master mix with dUTP-containing nucleotides; incubate at 50°C for 2 minutes before amplification [2] [3] |
| No-Template Control (NTC) | Detects contamination in reagents or environment | Contains all reaction components except template nucleic acid; should always yield negative result [3] |
| Chimeric Plasmid DNA (cpDNA) | Positive control with contamination indicator | Contains target sequence plus exogenous sequence with separate probe; distinguishes true amplification from control contamination [4] |
| Annealing-Control Primers | Improve specificity through structural design | Incorporate polydeoxyinosine linkers that form bubble structures during annealing to prevent nonspecific binding [2] |
| Inhibition-Resistant Master Mixes | Reduce false positives from non-specific amplification | Formulations optimized with additives that increase specificity, especially for challenging templates [3] |
| SPUD Assay | Internal positive control for reaction inhibition | Amplification of specific non-target sequence confirms reaction efficiency; abnormal Cq indicates inhibition [3] |
In qPCR cancer assays, the reliability of your results is paramount. False positives can lead to incorrect data interpretation, wasted resources, and potentially affect downstream clinical decisions. The high sensitivity of qPCR makes it exceptionally vulnerable to contamination, which often manifests as amplification in No Template Controls (NTCs) [6] [3]. This guide details the major contamination sources and provides proven strategies to identify, prevent, and eliminate them, safeguarding the integrity of your research.
Frequently Asked Questions (FAQs)
1. What are the most common signs of contamination in my qPCR assay? The most direct indicator is amplification in your No Template Control (NTC) [6] [7]. Other red flags include an unexpected spike in positive results, particularly in a low-prevalence setting, or multiple samples with high Ct values clustering together on the plate [8].
2. How can I tell if my reagents are contaminated? If a contamination event affects a master mix or other shared reagent, you will typically see amplification in every NTC well containing that reagent, with similar Ct values across the wells [6]. Systematic testing of reagents and replacing suspected stocks is necessary in this case.
3. Why is amplicon carryover such a significant problem? Amplicons (the amplified PCR products) are present in extremely high concentrations following amplification. These products can aerosolize and contaminate laboratory environments, reagents, and equipment. Because they are perfect templates for the assay, even minute quantities can lead to robust false-positive signals [9] [10].
4. What is the single most effective practice to prevent contamination? Physical separation of pre- and post-amplification areas is the cornerstone of contamination prevention [6] [10]. Maintaining a unidirectional workflow—from reagent preparation to sample preparation to amplification and analysis—ensures that amplified products never re-enter clean areas where future reactions are set up [9].
Troubleshooting Guides
Guide 1: Identifying and Addressing Amplicon Carryover Contamination
Amplicon carryover, where PCR products from previous reactions contaminate new setups, is a primary source of false positives [9].
- Symptoms: Amplification in NTCs. A sudden, plate-wide increase in false positives.
- Primary Sources: Aerosols generated when opening tubes containing amplified products; contaminated pipettes or equipment used in both post- and pre-PCR areas.
Prevention and Control Strategies
- Laboratory Design: Implement a unidirectional workflow through physically separated rooms or dedicated areas for:
- Procedural Methods:
- Biochemical Methods:
- Uracil-N-Glycosylase (UNG): Use master mixes containing UNG and incorporate dUTP in your PCR reactions. UNG enzymatically degrades any uracil-containing carryover amplicons before thermal cycling begins, but it is inactivated at high temperatures and does not affect the new, natural-template DNA [6] [3] [2].
The following diagram illustrates the critical workflow designed to prevent amplicon carryover.
Guide 2: Managing Sample Cross-Contamination and Environmental Contaminants
This form of contamination involves the transfer of template between samples or the introduction of external DNA into reactions.
- Symptoms: Random positive results in NTCs with varying Ct values [6]; inconsistent results between sample replicates.
- Primary Sources: Contaminated gloves, lab coats, or surfaces; aerosol generation during pipetting, vortexing, or centrifugation; contaminated reagents or enzymes [3] [2].
Prevention and Control Strategies
- Personal Protective Equipment (PPE) and Technique:
- Surface and Equipment Decontamination:
- Regularly clean work surfaces, pipettes, and equipment with 10% bleach (sodium hypochlorite), allowing 10-15 minutes of contact time before wiping with de-ionized water or ethanol [6] [10]. Bleach chemically degrades DNA.
- Use UV irradiation in biosafety cabinets and on work surfaces to cross-link any contaminating DNA [10] [9].
- Reagent and Sample Management:
Guide 3: Systematic Decontamination and Validation Protocol
If contamination is suspected or confirmed, a rigorous decontamination process must be followed.
- Discard and Replace: Immediately discard all suspect reagents, including water, master mix, and primers [11].
- Deep Clean: Thoroughly decontaminate all work surfaces, equipment (especially pipettes), and racks with 10% bleach followed by 70% ethanol [10] [2].
- UV Irradiation: Expose pipettes, centrifuges, and biosafety cabinets to UV light for an extended period (e.g., overnight) [10].
- Validate: Before running patient or valuable samples, validate the clean environment by setting up multiple NTCs with fresh reagents. No amplification should be observed in the NTCs after a full qPCR run [6] [3].
Key Experimental Controls and Their Interpretation
Including the correct controls in every qPCR run is non-negotiable for detecting contamination and ensuring assay validity. The table below summarizes essential controls.
Table 1: Essential qPCR Controls for Contamination Monitoring
| Control Type | Composition | Expected Result | Interpretation of a Positive Result |
|---|---|---|---|
| No Template Control (NTC) [6] [3] | All reaction components except the nucleic acid template. | Negative (No amplification). | Indicates contamination in one of the reagents, primers, or the environment. |
| No Reverse Transcription Control (-RT) [3] [11] | RNA sample processed without the reverse transcriptase enzyme. | Negative. | Detects amplification from contaminating genomic DNA in RNA-based assays (RT-qPCR). |
| Positive Control | A known sample containing the target sequence. | Positive (Amplification at expected Ct). | Validates that the assay is functioning correctly. A negative result indicates assay failure. |
Research Reagent Solutions for Contamination Control
The following table lists key reagents and materials that are essential for implementing an effective contamination control strategy.
Table 2: Key Reagents and Materials for Contamination Control
| Item | Function | Considerations for Use |
|---|---|---|
| Aerosol-Resistant Filter Tips [9] | Prevents aerosols from contaminating the pipette shaft and subsequent samples. | Use for all liquid handling in pre-PCR areas. Do not autoclave. |
| Uracil-N-Glycosylase (UNG) [6] [9] | Enzymatically destroys carryover contamination from previous uracil-containing amplicons. | Requires the use of dUTP in the PCR reaction mix. Most effective for thymine-rich amplicons. |
| dUTP [6] | A nucleotide analog that incorporates into amplicons, making them susceptible to UNG degradation. | Used in place of dTTP in the PCR master mix. |
| Sodium Hypochlorite (Bleach) [6] [10] | Effective chemical decontaminant that degrades DNA on surfaces and equipment. | Use a freshly diluted 10% solution. Allow 10-15 minutes contact time. |
| DNase I [11] | Enzyme that degrades contaminating DNA in RNA samples. | Critical for RT-qPCR; use prior to the reverse transcription step. |
| Highly Purified Oligonucleotides | Primers and probes synthesized under controlled conditions. | Reduces risk of oligonucleotides being contaminated with template DNA during manufacturing [3]. |
Vigilance against contamination is a continuous requirement in any qPCR laboratory, especially in sensitive cancer research applications. By understanding the major sources—amplicon carryover, sample cross-contamination, and environmental contaminants—you can implement a robust defense-in-depth strategy. This combines rigorous laboratory practices, physical separation of workflows, systematic use of controls, and targeted biochemical methods. Adherence to these protocols will significantly reduce false positives, thereby enhancing the accuracy, reliability, and translational potential of your qPCR cancer assays.
In quantitative PCR (qPCR) research, particularly in the high-stakes field of cancer diagnostics, the fidelity of your signal is paramount. False positives can lead to incorrect data interpretation, misdiagnosis, and flawed scientific conclusions. A significant source of this error stems from fundamental assay design flaws, primarily concerning primer specificity and amplicon characteristics. This guide addresses these critical issues through targeted troubleshooting and frequently asked questions, providing a framework for developing robust, reliable qPCR cancer assays.
Primer Design and Specificity
What are the fundamental principles of robust qPCR primer design?
Adherence to established design parameters is the first defense against false positives. The table below summarizes the core criteria for robust primers.
Table 1: Key Criteria for qPCR Primer Design
| Parameter | Optimal Value/Range | Rationale |
|---|---|---|
| Primer Length | 18–30 bases [12] | Balances specificity and binding efficiency. |
| Melting Temperature (Tm) | 60–64°C [12] | Ideal for standard enzyme function; forward and reverse primer Tms should not differ by more than 2°C. |
| GC Content | 35–65% (ideal: 50%) [12] | Provides sufficient sequence complexity while avoiding stable secondary structures. |
| 3'-End Complementarity | Avoid >2 complementary bases, especially GC [13] [14] | Greatly reduces the potential for primer-dimer formation. |
| Secondary Structures | ΔG of hairpins/self-dimers > -9.0 kcal/mol [12] | Ensures primers remain available for binding to the template rather than themselves. |
Beyond these rules, always verify primer specificity using tools like NCBI BLAST to ensure they are unique to your intended target [12]. Remember that the optimal annealing temperature (Ta) must be determined empirically, as it is influenced by your specific reaction buffer and master mix [13].
How do primer dimers lead to false positives, and how can I prevent them?
Primer dimers are small, unintended DNA fragments formed when primers anneal to each other instead of the target DNA. During qPCR, fluorescent dyes like SYBR Green bind to this double-stranded DNA, producing a false signal that can be mistaken for true target amplification, especially at low template concentrations or high cycle thresholds [14] [15].
Prevention Strategies:
- Design with Low 3' Complementarity: Use primer design tools to avoid primers that can base-pair with each other at their 3' ends [14].
- Optimize Reaction Conditions: Lower primer concentrations or increase template concentration to improve the primer-to-template ratio [14].
- Apply Hot-Start DNA Polymerase: These enzymes are inactive until a high-temperature activation step, minimizing nonspecific amplification during reaction setup [14].
- Increase Annealing Temperature: A higher Ta reduces the likelihood of primers binding nonspecifically to each other or to off-target sites [14].
Amplicon Characteristics and Validation
What amplicon features are critical for signal fidelity?
The amplicon—the DNA fragment amplified by PCR—is at the heart of your assay. Its characteristics directly influence specificity and efficiency.
Table 2: Optimal Amplicon Characteristics for qPCR Assays
| Characteristic | Recommendation | Impact on Assay |
|---|---|---|
| Length | 70–150 bp [12] | Shorter fragments amplify with higher efficiency and are ideal for standard cycling conditions. |
| Location | Span an exon-exon junction [12] | Prevents amplification of genomic DNA contamination, a major source of false positives. |
| Uniqueness | Unique in the genome; check for pseudogenes [13] | Ensures amplification is specific to the intended transcript or genetic locus. |
| Secondary Structure | Avoid regions with high stability at primer binding sites [13] | Allows primers to bind efficiently to the template, preventing delayed amplification or failure. |
Why is a melt curve analysis non-negotiable for SYBR Green assays, and how do I troubleshoot it?
SYBR Green dye binds to any double-stranded DNA, including non-specific products and primer dimers. Melt curve analysis is the primary quality control step to verify that the fluorescence signal originates from a single, specific amplicon [15]. After amplification, the temperature is gradually increased while fluorescence is measured. A single, sharp peak typically indicates a single, specific product. Multiple peaks, broad peaks, or peaks at unexpected temperatures indicate problems [16] [15].
Table 3: Troubleshooting Common Melt Curve Anomalies
| Melt Curve Appearance | Likely Cause | Corrective Actions |
|---|---|---|
| Single peak, but Tm < 80°C | Primer dimer formation with no true product [16]. | Redesign primers; check primer specificity. |
| Double peaks; minor peak < 80°C | Primer dimers or short nonspecific products [16]. | Increase annealing temperature; lower primer concentration; increase template amount. |
| Double peaks; minor peak > 80°C | Non-specific amplification [16]. | Increase annealing temperature; check and remove genomic DNA contamination. |
| Irregular or noisy peaks | Template contamination or instrument issues [16]. | Prepare fresh, high-quality template; perform instrument maintenance. |
| Single peak, but not sharp | Broad peaks can be related to reagent composition or instrument sensitivity. If the temperature range is ≤ 7°C, the result is often still usable [16]. | If problematic, try different master mixes or optimize conditions. |
Experimental Protocols for Validation
How do I empirically validate and optimize a new qPCR assay?
Theoretical design is only the beginning. The following workflow, derived from established best practices, is essential for validating a robust assay [13].
Detailed Methodology:
- No-Template Control (NTC): Always include a reaction containing all components except the template DNA. Amplification in the NTC indicates contamination or severe primer-dimer formation [14].
- Standard Curve and Efficiency Calculation: Prepare a dilution series (e.g., 1:10, 1:100, 1:1000) of your cDNA sample. Run qPCR with this series to generate a standard curve.
- Annealing Temperature Optimization: Use a thermal gradient on your qPCR instrument to test a range of annealing temperatures (e.g., 55°C to 65°C). The optimal temperature produces the lowest Cq value with a single, specific peak in the melt curve [13]. An assay that works well over a broad temperature range is considered robust.
How do I select and validate reference genes for reliable normalization in cancer studies?
Using unstable reference genes is a major source of inaccurate results. This is particularly critical in cancer research, where treatments can alter the expression of commonly used "housekeeping" genes.
Validation Protocol [18]:
- Select Candidate Genes: Choose 3–5 potential reference genes from different functional classes (e.g., GAPDH, ACTB, B2M, YWHAZ, TBP).
- Test Expression Stability: Run qPCR for all candidate genes across all your experimental conditions (e.g., different cancer cell lines, treated vs. untreated samples).
- Analyze with Stability Algorithms: Use software like NormFinder or geNorm to statistically determine the most stably expressed genes.
- Report Findings: Always report the genes selected and the validation data. For example, a 2025 study found that ACTB and ribosomal protein genes were unstable in mTOR-inhibited cancer cells, while B2M and YWHAZ were more reliable [18].
Table 4: Research Reagent Solutions for qPCR Assay Development
| Item | Function | Key Considerations |
|---|---|---|
| Hot-Start DNA Polymerase | Enzyme activated only at high temperatures, drastically reducing primer-dimer and non-specific amplification at setup [14]. | Essential for complex targets and multiplex PCR. |
| SYBR Green Master Mix | A ready-to-use mixture containing SYBR Green dye, buffer, dNTPs, and polymerase for simple, cost-effective qPCR [15]. | Always requires melt curve analysis for specificity confirmation. |
| TaqMan Probes & Master Mix | Hydrolysis probes that provide target-specific fluorescence, eliminating the need for post-run melt curve analysis and enabling multiplexing [12] [19]. | More expensive than SYBR Green, but superior for specificity. |
| DNase I, RNase-free | Enzyme used to degrade residual genomic DNA in RNA samples before cDNA synthesis, preventing false positives [12]. | Critical when amplicons do not span exon-exon junctions. |
| Reverse Transcriptase | Enzyme for synthesizing cDNA from an RNA template. The choice of enzyme and protocol can introduce bias [15]. | Investigate potential reverse transcription bias using standard curves. |
Adherence to MIQE Guidelines
To ensure the rigor, reproducibility, and transparency of your qPCR data, adherence to the MIQE (Minimum Information for Publication of Quantitative Real-Time PCR Experiments) guidelines is critical [20] [19]. This includes comprehensive reporting of:
- Sample details: Origin, processing, and nucleic acid quality metrics (e.g., RIN for RNA) [20].
- Assay information: Primer and probe sequences, or amplicon context sequence and unique assay ID for commercial assays [19].
- Validation data: PCR efficiency, R², LOD, and evidence of specificity for each assay [13] [19].
- qPCR protocol: Complete reaction conditions and data analysis method [17] [19].
Failure to provide this information undermines the credibility of reported findings. As stated in a 2025 commentary, "if the data cannot be reproduced, they are not worth publishing" [20].
The Role of Non-Specific Amplification and Primer-Dimer Formation in Generating Background Noise
Frequently Asked Questions (FAQs)
1. What are the primary causes of non-specific amplification and primer-dimer formation? Non-specific amplification and primer-dimers result from a combination of factors, including inadequate primer design (e.g., self-complementarity or complementarity between primers), low annealing temperatures, excessive primer concentration, and the use of low-quality reagents. These conditions promote unintended primer interactions and amplification of off-target sequences [21] [2].
2. How can I confirm that background noise in my qPCR results is due to primer-dimers? The presence of primer-dimers can be confirmed by performing a dissociation curve (melt curve) analysis after the qPCR run. Primer-dimers typically appear as an additional peak at a lower melting temperature than your specific amplicon. Alternatively, running the qPCR products on an agarose gel will show a fuzzy smear or band below 100 bp [22] [7].
3. Why is controlling for non-specific amplification particularly critical in cancer research assays? In cancer research, assays often detect rare events, such as somatic mutations or low-abundance fusion transcripts, against a high background of wild-type DNA. Non-specific amplification can generate false positives, leading to incorrect mutation calls, or mask true low-abundance signals, compromising the accuracy of diagnosis and treatment decisions [23] [24].
4. What are the best practices for preventing contamination, a major source of false positives? To prevent contamination, use separate, dedicated work areas for pre- and post-PCR steps. Employ good laboratory practices, including using filter pipette tips, preparing single-use reagent aliquots, and routinely decontaminating surfaces with 10% bleach or UV irradiation. Always include a No-Template Control (NTC) to monitor for contamination [22] [2].
5. Are there advanced molecular techniques to suppress non-specific background? Yes, several advanced techniques exist. Xeno Nucleic Acid (XNA) molecular clamping uses synthetic DNA analogs to block the amplification of non-target sequences (e.g., wild-type DNA), allowing for the selective detection of mutations or fusions [23]. Competitive Allele-Specific TaqMan PCR (castPCR) uses an MGB blocker oligonucleotide to suppress the wild-type background, enabling highly specific detection of mutant alleles [24].
Troubleshooting Guides
Issue 1: Amplification in the No-Template Control (NTC)
A positive signal in the NTC indicates contamination or significant primer-dimer formation.
Step 1: Identify the Source
- Perform a Melt Curve Analysis: If the melt curve shows a peak at a lower temperature than your target amplicon, it is likely primer-dimer [22] [7].
- Check the Cq Value: Late amplification (Cq >34 for SYBR Green assays) in the NTC can be a result of dimer amplification rather than true contamination [22].
Step 2: Apply Corrective Measures
- If due to contamination: Replace all reagents. Decontaminate workspaces and equipment thoroughly. Use uracil-DNA-glycosylase (UNG) in the reaction mix to degrade carryover contamination from previous PCR products [2].
- If due to primer-dimer: Optimize your reaction conditions as outlined in Issue 2.
Issue 2: Non-Specific Bands or High Background with SYBR Green Chemistry
This is a classic sign of non-specific amplification or primer-dimer formation.
Step 1: Optimize Thermal Cycling Conditions
- Increase Annealing Temperature: Use a temperature gradient to find the highest possible annealing temperature that still yields your specific product [14] [21].
- Use a Hot-Start DNA Polymerase: This enzyme is inactive at room temperature, preventing primer-dimer formation during reaction setup. It is activated only at high temperatures, improving specificity [14] [2].
- Employ Touchdown PCR: Start with an annealing temperature 5–10°C above the primer's Tm and gradually decrease it over subsequent cycles. This early stringent annealing favors specific binding [2].
Step 2: Optimize Reaction Components
- Lower Primer Concentration: High primer concentration is a common cause. Reduce the concentration, typically testing a range of 50–900 nM, to find the lowest concentration that provides efficient amplification [14] [21].
- Improve Primer Design: Re-design primers using trusted software to avoid self-complementarity (especially at the 3' ends) and complementarity between forward and reverse primers. The annealing temperatures for the primer pair should not differ by more than 3°C [21].
Step 3: Verify Primer Specificity
- Run a BLAST Search: Ensure your primer sequences are specific to the intended target and will not cross-react with other sequences in the sample [2].
The following workflow summarizes the systematic approach to troubleshooting background noise:
Quantitative Data and Experimental Protocols
Table 1: Impact of Common Factors on Non-Specific Amplification
| Factor | Typical Optimal Range / Condition | Effect of Deviation | Reference |
|---|---|---|---|
| Primer Concentration | 50–900 nM (often ~200 nM) | High concentration increases primer-dimer risk. | [14] [21] |
| Annealing Temperature | Primer Tm ± 3°C | Low temperature promotes non-specific binding. | [14] [21] |
| Cycle Number | 30–40 cycles | Excessive cycles increase primer-dimer formation after target exhaustion. | [21] |
| Primer Dimer Cq in NTC | >34 cycles (SYBR Green) | Cq <34 suggests contamination or severe dimerization. | [22] |
| Enzyme Type | Hot-Start Polymerase | Standard polymerase can extend dimers during reaction setup. | [14] [2] |
Table 2: Advanced Techniques for Noise Suppression in Cancer Assays
| Technique | Core Principle | Key Performance Metrics | Application Context |
|---|---|---|---|
| XNA Molecular Clamping | Synthetic XNA binds to and blocks amplification of non-target sequences (e.g., wild-type DNA). | LOD: 50 copies for fusion genes. Effectively blocks wild-type. | Detection of gene fusions (ALK, RET, ROS1) in NSCLC [23]. |
| castPCR Technology | Uses an MGB blocker oligonucleotide to suppress wild-type DNA amplification. | Detects 1 mutant in 1,000 wild-type cells. | Somatic mutation detection (e.g., KRAS, BRAF) [24]. |
| Nicking Endonuclease-based RCA (NER/Cas12a) | Exponential amplification with two circular templates to minimize nonspecific initiation. | LOD: 0.77 fM. Recognizes single-base mismatches. | Ultrasensitive detection of tumor suppressor genes (e.g., p53) [25]. |
Experimental Protocol: XNA-Based Clamping for Fusion Gene Detection
This protocol is adapted from an assay developed to detect ALK, RET, and ROS1 fusions in lung cancer FFPE samples [23].
- RNA Extraction: Extract total RNA from FFPE samples using a silica spin-column-based kit (e.g., RNeasy FFPE kit). Quantify RNA and assess quality.
- Reverse Transcription: Convert 50 ng of total RNA into cDNA using a reverse transcriptase kit with random hexamers or oligo-dT primers.
- qPCR with XNA Clamp:
- Reaction Mix: Prepare a multiplex qPCR master mix containing:
- Primers specific for the target fusion variants.
- XNA oligonucleotides designed to be complementary to the wild-type sequence.
- Hot-Start DNA Polymerase, dNTPs, and buffer.
- A fluorescent probe (e.g., TaqMan) for detection.
- Thermal Cycling:
- Initial Denaturation: 95°C for 5 min.
- 45 cycles of:
- Denaturation: 95°C for 15 sec.
- Annealing/Extension: 60°C for 60 sec (acquire fluorescence).
- Controls: Include positive controls (synthetic templates or cell lines with known fusions), negative controls (fusion-negative cell lines like A549), and a No-Template Control (NTC).
- Reaction Mix: Prepare a multiplex qPCR master mix containing:
- Data Analysis: The XNA clamp binds stably to the wild-type sequence, preventing its amplification. Only samples containing the fusion gene, which has a mismatched sequence at the XNA binding site, will produce a fluorescent signal.
The logic of this clamping mechanism is illustrated below:
The Scientist's Toolkit: Essential Reagents and Materials
Table 3: Research Reagent Solutions for Reducing Background Noise
| Item | Function in Noise Reduction | Example / Specification |
|---|---|---|
| Hot-Start DNA Polymerase | Prevents enzymatic activity during reaction setup, reducing primer-dimer formation. | Various commercial master mixes. |
| XNA Molecular Clamps | Synthetic nucleotides that block polymerase extension on non-target sequences, suppressing wild-type amplification. | Custom-designed for wild-type sequence [23]. |
| Uracil-DNA-Glycosylase (UNG) | Enzyme that degrades uracil-containing DNA, preventing carryover contamination from previous PCR products. | Often included in commercial master mixes [2]. |
| Competitive Allele-Specific Blocker | Oligonucleotide blocker that suppresses amplification of the wild-type allele in mutation detection assays. | TaqMan Mutation Detection Assays [24]. |
| High-Purity Primers | Minimizes synthesis errors and truncated sequences that can contribute to non-specific amplification. | HPLC-purified primers [21]. |
| Nuclease-Free Water & Tubes | Ensures the reaction is not compromised by external nucleases or contaminants. | Certified nuclease-free, DNase-free, RNase-free. |
For patients with advanced (stage IV) cancer, conventional imaging can take 6 to 8 weeks to determine whether a new treatment is working, leading to stressful delays that keep patients on ineffective therapies and exposed to unnecessary toxicity [26]. A novel blood test has been developed to detect treatment failure in just 2–3 weeks, addressing this critical unmet need in oncologic care [26].
This innovative assay is a quantitative PCR (qPCR)-based test that measures specific tumor-derived cell-free DNA (cfDNA) fragments in the blood. It reports a "Progression Score" (PS) ranging from 0 to 100, where high scores indicate likely rapid cancer growth and low scores suggest the therapy is effective [26]. Because the test is quick, noninvasive, and does not rely on specific genetic mutations, it can be used across many cancer types and treatments, helping oncologists decide sooner whether to continue, modify, or discontinue a patient's therapy [26] [27].
The Progression Score (PS) assay is based on the principle of cfDNA fragmentomics, which exploits the observation that cfDNA fragments from tumor cells exhibit distinct size distributions compared to healthy cfDNA [26] [28]. The assay specifically targets multi-copy retrotransposon elements (ALU elements) via qPCR, quantifying fragments of different size thresholds: >80 bp, >105 bp, and >265 bp, along with an internal control [26] [27]. A logistic regression model then integrates these quantitative measurements into the single Progression Score [26].
In a prospective study of 128 patients with metastatic lung, breast, or colorectal cancer, the PS model yielded an area under the receiver-operating-characteristic (ROC) curve of 0.93 for predicting radiographic progression at the first imaging timepoint [26] [27]. The scores were strongly bimodal: 92% of patients with PS > 90 experienced disease progression, while 95% with PS < 10 did not [26]. This performance demonstrates the potential of fragmentomics to provide an earlier, tumor-agnostic signal of treatment response.
Troubleshooting Guide: Addressing False Positives in qPCR-Based Assays
The extreme sensitivity of qPCR methodology, while a great advantage, also makes it vulnerable to contamination and false-positive results. The following section provides a targeted troubleshooting guide for issues specifically relevant to cfDNA fragmentomic assays.
Frequently Asked Questions (FAQs)
Q1: My No Template Control (NTC) shows amplification. What are the most likely causes?
- Reagent Contamination: Trace amounts of bacterial DNA in enzyme preparations or contaminants in oligonucleotides, buffers, or water can be amplified [3] [22].
- Amplicon Carryover: Aerosolized amplification products from previous PCR runs are a very common source of contamination [3] [2].
- Cross-Contamination: This can occur during sample handling when a positive sample contaminates a negative one or from contaminated laboratory equipment like pipettes [3].
- Primer-Dimer Formation: Primers can anneal to each other and amplify, especially in late cycles (>34 cycles for SYBR Green assays), producing a false signal [22] [2].
Q2: How can I distinguish primer-dimer formation from specific amplification in my NTC?
Perform a melting curve analysis after the PCR run. Specific amplification products will have a distinct, sharp melt peak at a higher temperature, while primer-dimers will generate a broader peak at a lower melting temperature [22] [2].
Q3: Our lab runs this assay frequently. What specific procedures can prevent amplicon carryover?
- Uracil-DNA-Glycosylase (UNG) Treatment: Incorporate a master mix containing dUTP and UNG. UNG enzymatically degrades any uracil-containing carryover amplicons from previous reactions before the new PCR begins, preventing their re-amplification [3] [2].
- Physical Separation: Maintain separate, dedicated rooms or hoods for reagent preparation, sample setup, and post-PCR analysis. A unidirectional workflow is critical [2].
Q4: What should I do if I confirm a contamination event in my lab?
- Replace all reagents: Discard all open tubes of buffers, enzymes, primers, and probes, and prepare fresh aliquots [22] [2].
- Decontaminate surfaces and equipment: Thoroughly clean work areas, pipettes, and equipment with a 10% bleach solution, followed by 70% ethanol or RNase/DNase-free water [3] [2].
- Use UV irradiation: If available, expose the PCR setup hood to UV light to cross-link any residual contaminating DNA [2].
Troubleshooting Table: Common qPCR False-Positive Issues
| Problem | Potential Cause | Detection Method | Corrective & Preventive Actions |
|---|---|---|---|
| Amplification in NTC | Contaminated reagents (enzymes, water) | Systematic testing of individual reagent components | Prepare fresh aliquots; use certified nuclease-free reagents and water [3] [2] |
| Amplification in NTC | Amplicon carryover from previous runs | Review of workflow and lab layout | Implement UNG treatment; enforce physical separation of pre- and post-PCR areas [3] [2] |
| Amplification in NTC | Primer-dimer artifacts | Melt curve analysis (shows low-Tm peak) | Re-optimize primer concentrations; use hot-start PCR [22] [2] |
| Amplification in NTC | Cross-contamination from samples | Tracking sample placement on plate | Use filter pipette tips; place NTC wells away from positive samples [2] |
| High Background Noise | Degraded fluorescent probe | Fluorometric scan or mass spectrometry | Aliquot probes to minimize freeze-thaw cycles; protect from light [22] |
| Non-specific Amplification | Poor primer specificity | In silico BLAST analysis for cross-reactivity | Redesign primers to target unique hypervariable regions [22] |
Experimental Protocol: Core Methodology of the cfDNA Fragmentomic Assay
The following protocol details the key steps for the novel cfDNA fragmentomic assay as described in the foundational study, providing a framework for researchers to implement and validate similar approaches [26].
Sample Collection and Processing
- Blood Collection: Collect 8–10 mL of peripheral blood into Streck Cell-Free DNA BCT tubes.
- Transport: Transport tubes at ambient temperature via overnight courier. Critical Step: Process samples within 120 hours (5 days) of collection, as delays can affect cfDNA concentrations [26].
- Plasma Separation: Use a two-step centrifugation protocol.
- Centrifuge Streck tubes at 1,600× g for 10 minutes at 15°C to separate plasma.
- Transfer the plasma to a new tube and centrifuge at 16,000× g for 10 minutes at room temperature to remove any remaining cellular debris.
- Storage: Aliquot the clarified plasma into cryogenic tubes and store at -80°C until cfDNA extraction [26].
Cell-Free DNA Extraction
- Extraction Kit: Use the QIAamp Circulating Nucleic Acid Kit.
- Starting Volume: Use 500 µL of plasma.
- Protocol Modification: Omit the carrier RNA from the ACL buffer during the extraction procedure [26].
Quantitative PCR (qPCR) Setup and Analysis
- Targets: Design qPCR assays to target multi-copy retrotransposon elements (e.g., ALU) for three fragment size ranges: >80 bp, >105 bp, and >265 bp. Include an internal control [26] [27].
- Controls: Each run must include:
- qPCR Method: The published study used a standard qPCR methodology. To enhance specificity, consider Hot-Start PCR to suppress polymerase activity until the high temperatures of the first denaturation step are reached, thereby reducing non-specific amplification and primer-dimer formation at room temperature [2].
- Data Analysis: Input the qPCR quantification cycle (Cq) values for the different fragment sizes into the proprietary logistic regression model to calculate the Progression Score (PS) on a scale of 0–100 [26].
Diagram 1: Experimental workflow of the cfDNA fragmentomic assay, highlighting key steps and critical quality control points.
The Scientist's Toolkit: Essential Reagents and Materials
The following table details key reagents and materials essential for implementing the cfDNA fragmentomic assay, with a focus on components that impact assay reliability and contamination control.
Table: Key Research Reagent Solutions
| Item | Function / Role | Key Considerations for False-Positive Reduction |
|---|---|---|
| Streck Cell-Free DNA BCT Tubes | Stabilizes blood samples for cfDNA analysis during transport. | Prevents release of genomic DNA from white blood cells, which can contaminate the cfDNA sample and alter fragmentomic profiles [26]. |
| QIAamp Circulating Nucleic Acid Kit | Extraction of high-quality cfDNA from plasma. | The protocol's omission of carrier RNA is a specific modification that prevents potential interference in downstream qPCR [26]. |
| Hot-Start DNA Polymerase | Enzyme for qPCR amplification. | Reduces non-specific amplification and primer-dimer formation by remaining inactive until the initial high-temperature denaturation step [2]. |
| UNG (Uracil-N-Glycosylase) | Enzyme for contamination control. | Degrades carryover amplicons from previous PCR runs when dUTP is incorporated, critically preventing false positives [3] [2]. |
| Nuclease-Free Water | Solvent for preparing PCR master mixes. | Must be certified sterile and nuclease-free to avoid introduction of contaminating DNA or PCR inhibitors [2]. |
| Filter Pipette Tips | For accurate and sterile liquid handling. | Prevents aerosol-based cross-contamination between samples; essential for both sample and reagent handling [2]. |
Strategic Contamination Control Framework
Beyond immediate troubleshooting, a proactive, systematic strategy is required to safeguard the integrity of sensitive qPCR assays in a clinical research setting. The following diagram and table outline a comprehensive defense strategy.
Diagram 2: A multi-phase strategic framework for preventing contamination in qPCR workflows.
Table: Proactive Contamination Control Measures
| Phase | Measure | Implementation Example |
|---|---|---|
| Pre-PCR | Spatial Segregation | Maintain physically separate rooms for reagent preparation, sample setup, and post-PCR analysis. Enforce a unidirectional workflow for personnel [2]. |
| Pre-PCR | Reagent Management | Prepare single-use aliquots of all reagents, primers, and probes. Use certified nuclease-free water and buffers [22] [2]. |
| Pre-PCR | Environmental Decontamination | Regularly clean surfaces and equipment with 10% bleach (sodium hypochlorite), followed by ethanol or water to remove residue. Use UV irradiation in hoods when unoccupied [3] [2]. |
| PCR | In-Reaction Safeguards | Use a master mix containing UNG and dUTP for carryover prevention. Employ Hot-Start polymerase chemistry to improve specificity [2]. |
| PCR | Control Strategy | Include NTCs and positive controls on every plate. Place NTCs away from high-concentration samples to monitor for well-to-well contamination [3] [2]. |
| Post-PCR | Amplicon Containment | Perform all analysis of amplified products in the dedicated post-PCR area. Prefer closed-tube detection systems to avoid opening plates containing amplicons [2]. |
Best Practices in Assay Design and Laboratory Workflow to Enhance Specificity
FAQs: Core Design Principles
1. What are the optimal physicochemical properties for qPCR primers and probes?
The table below summarizes the critical parameters for designing effective primers and probes to ensure high specificity and yield in qPCR assays, crucial for sensitive applications like cancer research [29] [30].
Table 1: Optimal Design Parameters for qPCR Primers and Probes
| Parameter | Primers | Probes | Rationale |
|---|---|---|---|
| Length | 18–24 nucleotides [29] | 15–30 nucleotides [29] | Balances specificity and efficient binding. |
| GC Content | 40–60% [30] | 35–60% [29] | Prevents overly stable (high GC) or unstable (low GC) duplexes. |
| Melting Temperature (Tm) | 54°C–65°C; ideally ≥60°C [29] [31] | 5-10°C higher than primer Tm [30] | Ensures specific hybridization; higher probe Tm guarantees probe binding before primers. |
| 3'-End Stability (GC Clamp) | Max. 3 G/C bases in last 5 bases [30] | Avoid G at the 5' end [29] | Promotes specific initiation of amplification; avoids fluorescence quenching. |
2. Why is it critical to avoid secondary structures, and how can I check for them?
Secondary structures such as hairpins (intramolecular folding) and primers-dimers (intermolecular binding) compete with template binding, drastically reducing amplification efficiency and increasing false negatives [29] [30]. Their formation is governed by Gibbs Free Energy (ΔG), where larger negative values indicate more stable, problematic structures [30].
Table 2: Guidelines for Tolerable Secondary Structure Stability (ΔG)
| Structure Type | Acceptable ΔG Threshold |
|---|---|
| 3' End Hairpin | > -2 kcal/mol [30] |
| Internal Hairpin | > -3 kcal/mol [30] |
| 3' End Self-Dimer | > -5 kcal/mol [30] |
| Internal Self-Dimer | > -6 kcal/mol [30] |
Use in-silico tools like OligoAnalyzer [32] or Primer Premier [30] to simulate and calculate the ΔG values for your sequences. These tools help identify self-complementarity and self 3'-complementarity, which should be kept as low as possible [29].
3. How do I calculate the annealing temperature (Ta) from the Tm?
The annealing temperature (Ta) is distinct from the Tm and is critical for specificity. While a common rule of thumb is to set the Ta 2–5°C below the primer Tm [29], a more precise method uses the Rychlik formula [30]:
Ta Opt = 0.3 x Tm(primer) + 0.7 x Tm(product) – 14.9
Where:
Tm(primer)is the melting temperature of the less stable primer-template pair.Tm(product)is the melting temperature of the PCR product.
For the highest specificity, always empirically determine the optimal Ta using a temperature gradient PCR [33]. A robust assay will perform well over a broad temperature range, whereas an assay that only works in a narrow window is prone to failure with minor condition changes [13].
Troubleshooting Guides
Problem: Amplification in No-Template Control (NTC) indicates contamination or primer-dimer formation.
Amplification in the NTC is a classic sign of false positives, which can severely compromise data integrity in cancer biomarker detection [3] [22].
Table 3: Troubleshooting False Positives in the NTC
| Observation | Probable Cause | Corrective Actions |
|---|---|---|
| Melt curve of NTC matches specific product. | Contamination from amplicon carryover or contaminated reagents [3] [31]. | 1. Replace all reagents and thoroughly clean workspace with 10% bleach [22] [31]. 2. Use UNG/UDG treatment in the master mix to degrade carryover contaminants [3] [31]. 3. Implement physical separation of pre- and post-PCR areas [22]. |
| Melt curve of NTC shows a lower Tm (e.g., primer-dimer). | Non-specific amplification due to primer secondary structures [31]. | 1. Redesign primers with stricter adherence to design rules (see Table 1) [31]. 2. Re-optimize primer concentrations [31]. 3. Use a primer design tool to minimize self- and cross-dimerization potential [32]. |
| Using universal primers (e.g., for 16S rRNA). | Amplification of bacterial DNA present in enzymes or consumables [22]. | 1. Design primers for a hypervariable region [22]. 2. Use blocking oligonucleotides to suppress background amplification [22]. 3. Perform a BLAST search to check for cross-reactivity with common contaminants [22]. |
The following workflow outlines a systematic approach to diagnosing and resolving false positives:
Diagnosing NTC Amplification
Problem: My primers are well-designed, but I still get low yield or no amplification.
- Cause: Template Secondary Structure. Stable secondary structures in the RNA/DNA template at the primer binding site can prevent primer annealing [30]. This is a common issue when working with complex biological samples.
- Solution:
- Use software that predicts template secondary structure and designs primers in accessible regions [30].
- Consider using touch-down PCR protocols, which start with a higher annealing temperature and gradually lower it, thereby favoring specific amplification before secondary structures can interfere once the reaction is established [34].
- Ensure you are using a master mix formulated for high GC-rich or structured templates.
Experimental Protocols for Validation
Protocol: Empirical Determination of Optimal Annealing Temperature (Ta)
- Design Primers: Design your primer pair according to the parameters in Table 1.
- Calculate Theoretical Tm: Use a reliable Tm calculator, such as the one from Thermo Fisher Scientific [33] or IDT's OligoAnalyzer [32], which uses the nearest-neighbor thermodynamic method.
- Set Up Gradient PCR:
- Prepare a master mix containing all reaction components (polymerase, buffer, dNTPs, primers, and a validated positive control template).
- Aliquot the master mix into your qPCR plate.
- On your thermal cycler, set an annealing temperature gradient. The range should start at approximately 5°C below the calculated Tm and extend up to the extension temperature (e.g., 60°C for two-step PCR) [33].
- Analyze Results:
- After the run, analyze the amplification curves and efficiency.
- The optimal Ta is the highest temperature that yields a single, specific product with the lowest Cq (quantification cycle) and highest fluorescence [13].
- Confirm product specificity with melt curve analysis.
Protocol: Validating Assay Specificity and Efficiency
- Run Controls: Include a No-Template Control (NTC) and a no-reverse-transcription control (for RNA targets) to check for genomic DNA contamination or primer-dimer artifacts [3].
- Generate a Standard Curve: Prepare a serial dilution (at least 5 points) of a known quantity of your target template.
- Calculate Efficiency: Perform qPCR on the dilution series. The amplification efficiency (E) is calculated from the slope of the standard curve using the formula: E = -1 + 10^(-1/slope) [34].
- Interpret Results: An ideal, highly specific assay will have an efficiency between 90% and 105%, with a correlation coefficient (R²) of >0.99 [31]. Efficiency outside this range suggests issues with primer design or reaction conditions that require optimization.
The Scientist's Toolkit
Table 4: Essential Research Reagent Solutions for Robust qPCR Assays
| Item | Function & Importance |
|---|---|
| High-Fidelity DNA Polymerase | Enzymes like Phusion or Platinum SuperFi offer high specificity, crucial for distinguishing true targets in complex cancer samples [33]. |
| Master Mix with UNG/UDG | Contains Uracil-N-Glycosylase, which degrades PCR products from previous reactions, effectively controlling carryover contamination [3] [31]. |
| Nuclease-Free Water | A critical, often overlooked reagent. Must be certified free of nucleases and contaminants to prevent degradation of oligonucleotides and false results [22]. |
| Validated Positive Control Template | Synthetic or cloned DNA/RNA used to validate assay performance, calculate efficiency, and serve as a run control [3]. |
| qPCR Probes (Dual-Labeled) | Hydrolysis probes (e.g., TaqMan) provide superior specificity over intercalating dyes by requiring hybridization to the target for signal generation [29]. |
| RT-qPCR Kit for FFPE Samples | Specialized kits are optimized to overcome the challenges of fragmented and cross-linked RNA from formalin-fixed paraffin-embedded (FFPE) tissue, a common source in cancer research [34] [23]. |
In quantitative PCR (qPCR) research, particularly in sensitive applications like cancer biomarker detection, false positives can severely compromise data integrity and lead to incorrect conclusions. The extreme sensitivity of qPCR, which allows for the detection of minute amounts of DNA, also makes it vulnerable to contamination from amplified DNA products (amplicons) generated in previous experiments [6] [3]. Implementing robust physical separation of pre- and post-PCR areas and a strict unidirectional workflow is not merely a recommendation but a fundamental necessity for generating reliable, reproducible results in cancer research and drug development. This guide provides detailed protocols and troubleshooting advice to help researchers establish and maintain a contamination-free laboratory environment.
Core Concepts: Physical Separation and Unidirectional Workflow
What are a unidirectional workflow and why are they critical for qPCR?
A unidirectional workflow is a system where materials and personnel move in one direction only: from "clean" areas (where pre-PCR steps are performed) to "dirty" areas (where post-PCR steps are handled) [35] [36]. The primary goal is to prevent the backflow of amplified DNA (amplicons) from post-PCR areas into pre-PCR areas. Since qPCR can produce millions of copies of a DNA target, even microscopic aerosols containing these amplicons can contaminate reagents, equipment, or new reaction setups, leading to false-positive results [6]. This is especially crucial in cancer research, where detecting low-abundance circulating tumour DNA (ctDNA) requires pristine conditions to avoid reporting false biomarkers [37].
The following diagram illustrates the ideal unidirectional workflow and the specific activities permitted in each designated zone.
FAQ: How can PCR amplicons cause contamination?
During the post-PCR phase, when tubes or plates are opened, significant quantities of amplified DNA product can become aerosolized and disperse into the lab environment [6]. These aerosolized amplicons are stable and can settle on surfaces, equipment, gloves, and lab coats. If introduced into a new qPCR reaction mix—either through contaminated reagents, pipettes, or personnel—they act as a ready-made template for amplification. This leads to amplification signals in "No Template Control" (NTC) wells and can cause false positives in experimental samples, critically misleading cancer diagnostics and research outcomes [6] [3].
Implementation Guide: Setting Up Your Laboratory
Physical Laboratory Layout
The gold standard is to have four separate rooms. However, if space is limited, physically separated, dedicated areas with dedicated equipment are the minimum requirement [35].
Table 1: Laboratory Area Specifications and Functions
| Laboratory Area | Primary Function | Key Equipment & Materials | What is FORBIDDEN |
|---|---|---|---|
| Reagent Preparation [35] | Preparation of master mixes; aliquoting of pristine reagents. | Dedicated pipettes, filter tips, microcentrifuge, vortex, master mix reagents, nuclease-free water. | Any DNA template, samples, or PCR products. |
| Sample Preparation / Template Addition [35] | Nucleic acid extraction from samples; addition of DNA template to master mix. | Dedicated pipettes, filter tips, centrifuge, vortex, extracted DNA/RNA samples. | PCR amplifiers or amplified products. |
| Amplification [35] | Housing of qPCR thermocyclers; running the amplification reaction. | qPCR thermocyclers, sealed reaction plates/tubes. | Unsealing reaction plates/tubes after the run. |
| Post-PCR Analysis [35] [36] | Analysis of amplified products (e.g., gel electrophoresis). | Gel documentation systems, tube openers. | Bringing anything from this area back to a pre-PCR area. |
Standard Operating Procedures for a Unidirectional Workflow
- Movement of Personnel: Lab members must not move from a post-PCR area back to a pre-PCR area on the same day. If unavoidable, they must thoroughly wash hands, change lab coats, and use dedicated PPE for the clean area [35].
- Movement of Equipment and Consumables: Supplies (e.g., pipettes, tip boxes, lab coats) must be dedicated to each area. Never move equipment or consumables from a "dirty" (post-PCR) area to a "clean" (pre-PCR) area. If an essential item must be moved backward, it must be decontaminated first [35].
- Data Handling: Lab books, paperwork, and electronic devices that have been in a post-PCR area should not be taken into pre-PCR areas. Use duplicate print-outs of protocols or digital copies on dedicated computers if necessary [35].
The Scientist's Toolkit: Essential Reagent Solutions
Table 2: Key Reagents and Materials for Contamination Control
| Item | Function in Contamination Control |
|---|---|
| Aerosol-Resistant Filtered Pipette Tips [6] [35] | Prevent aerosols and liquids from entering the pipette shaft, protecting the instrument from becoming a source of contamination. |
| Uracil-N-Glycosylase (UNG) [6] [3] | An enzymatic system to destroy carryover contamination from previous PCRs. It requires using dUTP in the PCR mix instead of dTTP. UNG selectively degrades any uracil-containing DNA from prior amplifications before the new PCR begins. |
| Fresh 10% Bleach Solution [6] [35] | A potent DNA-destroying decontaminant for surfaces. It must be made fresh frequently and allowed 10-15 minutes of contact time for effectiveness. |
| 70% Ethanol [6] [35] | Effective for general cleaning and degreasing. For DNA decontamination, it should be used after bleach or in conjunction with UV irradiation. |
| Aliquoted Reagents [6] [35] | Dividing bulk reagents into single-use aliquots prevents repeated freeze-thaw cycles and avoids contaminating the entire stock. |
| No-Template Controls (NTCs) [6] [3] | The essential quality control. Contains all reaction components except the DNA template. Amplification in the NTC indicates contamination. |
Troubleshooting Common Contamination Scenarios
FAQ: Amplification is observed in my No-Template Control (NTC). What should I do?
- Interpret the NTC Result:
- Consistent Ct across all NTCs: Suggests a reagent is contaminated. The source could be the water, master mix, or primers/probes [6] [3].
- Random Ct values in NTCs: Suggests random environmental contamination or aerosol contamination during plate setup, potentially from a nearby open tube of positive control or sample [6].
- Systematic Response:
- Replace Reagents: Systematically replace reagents, starting with water and master mix, to identify the contaminated component [6].
- Decontaminate Workspace: Thoroughly clean all work surfaces, equipment, and pipettes in the pre-PCR areas with 10% bleach followed by 70% ethanol or a commercial DNA decontaminant [6] [35].
- Review Practices: Ensure you are using filter tips, centrifuging tubes before opening, and that your physical separation is being strictly followed [6].
FAQ: My laboratory space is limited. How can I implement physical separation?
- Use Designated Benches or Cabinets: Designate specific bench areas at opposite ends of the lab for pre- and post-PCR work. A laminar flow cabinet or dead air box can serve as an excellent clean "room" for reagent preparation and reaction assembly [35] [36].
- Temporal Separation: Perform all pre-PCR work first in the morning, before any post-PCR analysis is conducted. Clean the area thoroughly afterward.
- Dedicated Equipment is Non-Negotiable: Even in a shared space, you must use separate, clearly labelled pipettes, tip boxes, and lab coats for pre- and post-PCR work [35].
Decontamination Protocols and Best Practices
Surface and Equipment Decontamination
- For surfaces (bench tops): Clean with a 10% (v/v) bleach solution (sodium hypochlorite). Allow it to wet the surface and remain for 10-15 minutes, then wipe down with de-ionized water or 70% ethanol to remove residue [6] [35].
- For sensitive equipment (pipettes, centrifuges): Do not use bleach as it can damage metals and plastics. Wipe down thoroughly with 70% ethanol. If possible, expose to UV light inside a closed cabinet for 30 minutes for more effective DNA destruction [35].
- Pipette Sterilization: Autoclave pipettes regularly if the manufacturer permits. For non-autoclavable pipettes, disassemble and clean components with 70% ethanol or a commercial DNA decontaminant [35].
Procedural Best Practices
- Pipetting Technique: Use slow, smooth pipetting actions to minimize aerosol creation. Always centrifuge tubes briefly before opening to collect contents at the bottom [6] [35].
- Glove Management: Change gloves frequently, especially after touching potentially contaminated surfaces, your face, or phone. Always change gloves when moving between different designated areas [6] [35].
- Aliquot Everything: Never use a stock reagent bottle directly in an experiment. Always prepare aliquots to limit exposure and potential contamination of the entire stock [6] [35].
By meticulously implementing these guidelines for physical separation, unidirectional workflow, and rigorous decontamination, research laboratories can significantly reduce the risk of false positives, thereby ensuring the integrity and reliability of their qPCR data in critical cancer research and drug development.
Utilizing Hot-Start PCR and Touchdown Protocols to Suppress Early Mis-Priming
Frequently Asked Questions (FAQs)
Q1: What is the primary cause of false positives in qPCR cancer assays, and how do these techniques help? False positives in qPCR often arise from non-specific amplification and primer-dimer formations, especially during reaction setup and the initial cycles before thermal cycling begins. Hot-Start PCR and Touchdown PCR are designed to suppress this early mis-priming. Hot-Start PCR inhibits the DNA polymerase's activity at room temperature, preventing non-specific synthesis from occurring before the first denaturation step [38] [39]. Touchdown PCR enhances specificity by starting with an annealing temperature too high for imperfect primer binding, then gradually lowering it, which gives a "head start" to the correct target amplicon and allows it to outcompete non-specific products [40] [41].
Q2: Can Hot-Start PCR and Touchdown PCR be used together? Yes, these techniques are highly complementary. Using a Hot-Start polymerase ensures the reaction remains pristine during setup, while the Touchdown cycling protocol further enriches specificity during the early amplification cycles. This powerful combination is highly recommended for challenging applications like detecting low-abundance cancer biomarkers to maximize specificity and sensitivity [40].
Q3: My qPCR assay has low yield despite high template quality. What optimization should I try? Low yield can result from an annealing temperature that is too high or insufficient enzyme activity. Consider these steps:
- Verify Annealing Temperature: Use a Tm calculator and run a temperature gradient. With Touchdown PCR, ensure your starting temperature is not excessively high [42] [43].
- Incorporate Additives: For difficult templates (e.g., GC-rich regions), use enhancers like DMSO (1-10%), formamide (1.25-10%), or Betaine (0.5 M to 2.5 M) [42].
- Check Mg²⁺ Concentration: Optimize the Mg²⁺ concentration in 0.2-1 mM increments, as it is crucial for polymerase activity [43].
Q4: How do I choose between different types of Hot-Start polymerases? The choice depends on your priorities for activation speed, specificity, and potential for contamination. The table below compares the common inhibition methods.
| Inhibition Method | Mechanism | Activation | Key Advantages | Potential Drawbacks |
|---|---|---|---|---|
| Antibody-based | A monoclonal antibody binds the enzyme's active site [38]. | Initial denaturation (1-3 minutes) [38]. | Fast, full activation; high specificity [38]. | Animal-derived antibodies risk mammalian DNA contamination [38]. |
| Aptamer-based | Specific oligonucleotides bind the active center [38]. | Very fast activation (~30 seconds) [38]. | Fully synthetic; no animal contaminants; fast [38]. | Potentially less stringent binding, may allow minor non-specificity [38]. |
| Chemical Modification | Enzyme is covalently modified to block activity [38]. | Longer heat activation (>10 minutes) [38]. | Highly stable; allows gradual activation for higher efficiency [38]. | Long activation can damage DNA; not suitable for long fragments (>3kb); inhibitor may not fully detach [38]. |
Q5: What are the critical steps to prevent contamination in sensitive qPCR assays for cancer research? Preventing contamination requires strict laboratory practice:
- Physical Separation: Use separate, dedicated rooms or areas for pre-PCR (reagent prep, sample handling), PCR amplification, and post-PCR analysis [2].
- Unidirectional Workflow: Maintain a one-way flow of materials and personnel from clean to post-amplification areas. Never bring post-PCR products into pre-PCR areas [2].
- Meticulous Technique: Use aerosol-resistant pipette tips, fresh gloves, and dedicated lab coats. Regularly decontaminate surfaces with 10% sodium hypochlorite or UV light [2].
- Essential Controls: Always include a no-template control (NTC) to detect reagent or environmental contamination [2].
Troubleshooting Guides
Guide 1: Addressing Non-Specific Amplification and False Positives
| Observation | Possible Cause | Recommended Solution |
|---|---|---|
| Multiple bands or smears on gel/post-run analysis | Primer annealing temperature is too low [43]. | Increase annealing temperature. Implement Touchdown PCR: start 5-10°C above Tm and decrease by 1°C every cycle/2nd cycle [40] [41]. |
| False positive in No-Template Control (NTC) | Contamination from amplicons, reagents, or environment [2]. | Use Uracil-DNA-glycosylase (UNG): incorporate dUTP in place of dTTP; UNG degrades contaminating amplicons from previous runs before PCR starts [2]. |
| Non-specific products form during reaction setup | Polymerase activity at room temperature [38]. | Switch to a Hot-Start polymerase (antibody or aptamer-based for fast activation). Keep all reagents on ice until cycler start [38] [40]. |
| Primer-dimer formation | Primers annealing to themselves or each other at 3' ends [42]. | Redesign primers to avoid 3' end complementarity. Use a Hot-Start polymerase. Increase annealing temperature. |
Guide 2: Resolving Low or No Amplification
| Observation | Possible Cause | Recommended Solution |
|---|---|---|
| No product | Excessive annealing temperature [43]. | Recalculate primer Tm. For Touchdown PCR, verify the final annealing temperature is not set too high. Use a temperature gradient. |
| Low yield | Poor primer design or inefficient amplification [43]. | Redesign primers per guidelines (length 18-30 bp, GC% 40-60%, avoid repeats). Use Touchdown qPCR (TqPCR): proven to reduce Cq values and improve detection sensitivity for low-abundance targets [44]. |
| Inconsistent results | Complex or GC-rich template [43]. | Use a high-fidelity polymerase. Include PCR enhancers like DMSO, BSA, or commercial GC buffers [42] [43]. |
| Inhibition of reaction | Carryover of inhibitors from sample (e.g., heparin, phenol) [43]. | Further purify the template DNA. Add BSA (10-100 μg/ml) to the reaction to bind certain inhibitors [42] [2]. |
Experimental Protocols
Protocol 1: Setting Up a Hot-Start qPCR Reaction
This protocol is ideal for detecting cancer biomarkers like circulating tumor DNA (ctDNA), where specificity is critical.
Design Primers: Follow stringent rules for specificity [42].
- Length: 18-30 nucleotides.
- GC content: 40-60%.
- Avoid 3' end complementarity to prevent primer-dimers.
- Verify specificity with a BLAST search against the NCBI database [2].
Prepare Reaction Mix on Ice: Thaw all reagents and keep them on ice. Assemble the following in a sterile, nuclease-free tube [42]:
- Sterile Water: Q.S. to 50 μl
- 10X PCR Buffer: 5 μl
- dNTPs (10 mM): 1 μl
- MgCl₂ (25 mM): Optional, if not in buffer; typically 1.5-4.0 mM final [42]
- Forward Primer (20 μM): 1 μl
- Reverse Primer (20 μM): 1 μl
- DNA Template (1-1000 ng): variable
- Hot-Start DNA Polymerase (e.g., 0.5 U/μl): 0.5 μl
Run qPCR Program:
Protocol 2: Incorporating a Touchdown qPCR (TqPCR) Program
This protocol, adapted from published research, enhances sensitivity for lowly-expressed transcripts [44].
- Initial Denaturation: 95°C for 3 minutes (also activates Hot-Start polymerase).
- Touchdown Phase (4 cycles):
- Denature: 95°C for 20 seconds.
- Anneal: Start at 66°C for 10 seconds.
- Decrease the annealing temperature by 3°C per cycle over these 4 cycles.
- Quantification Phase (40 cycles):
- Denature: 95°C for 20 seconds.
- Anneal/Extend: 55°C for 10 seconds, 70°C for 1 second with a plate read [44].
The Scientist's Toolkit: Key Research Reagent Solutions
| Item | Function | Application Note |
|---|---|---|
| Hot-Start Polymerase (Aptamer-based) | Inhibits polymerase at room temperature via oligonucleotide binding; activated by heat. | Ideal for fast setups and avoiding mammalian DNA contamination from antibody-based systems [38]. |
| Hot-Start Polymerase (Antibody-based) | Inhibits polymerase via antibody; activated during initial denaturation. | Provides strong inhibition for maximum specificity in standard assays [38] [39]. |
| dNTP Mix | Provides nucleotides (dATP, dCTP, dGTP, dTTP) for DNA synthesis. | Use a balanced, high-quality mix. For contamination control, use dUTP instead of dTTP [2]. |
| PCR Additives (DMSO, BSA, Betaine) | Enhancers that reduce secondary structure, neutralize inhibitors, or improve efficiency on complex templates [42]. | Critical for amplifying GC-rich sequences or when sample purity is suboptimal. |
| Uracil-DNA-Glycosylase (UNG) | Enzyme that degrades uracil-containing DNA, preventing carryover contamination from previous PCR products [2]. | Essential in high-throughput labs to eliminate one of the most common contamination sources. |
Technical Diagrams
Touchdown PCR Specificity Mechanism
Hot-Start PCR Inhibition Methods
Incorporating Uracil-DNA Glycosylase (UNG) to Combat Carryover Contamination from Amplicons
Carryover contamination, where amplification products (amplicons) from previous polymerase chain reaction (PCR) reactions contaminate new setups, is a major source of false positives in quantitative PCR (qPCR)-based cancer research. This contamination can lead to inaccurate gene expression quantification in circulating tumor cell (CTC) analysis or misinterpretation of oncogene mutation status. Uracil-DNA Glycosylase (UNG), also referred to as UDG, provides an effective enzymatic barrier against this specific type of contamination, thereby safeguarding the integrity of sensitive assays in oncology research and drug development [45] [46].
The core principle of the UNG system is the substitution of dTTP with dUTP in the PCR master mix. This results in all newly synthesized amplicons incorporating uracil instead of thymine. In subsequent PCR setups, a pre-PCR incubation with the UNG enzyme selectively degrades any uracil-containing contaminating DNA from earlier runs. The native, thymine-containing DNA template of interest remains unaffected, ensuring that only the intended target is amplified [45] [46] [47].
Implementing the UNG Carryover Prevention System
Core Mechanism and Workflow
The UNG-mediated carryover prevention system operates through a precise biochemical pathway prior to the start of the thermal cycling process. The following diagram illustrates the sequence of events that ensures the degradation of contaminating amplicons while preserving the original DNA template.
Experimental Protocol for qPCR Cancer Assays
Integrating UNG into your qPCR workflow requires modifications to the master mix and thermal cycler protocol. The table below summarizes the key modifications, and the detailed methodology follows.
| Parameter | Standard qPCR Protocol | UNG-Protected qPCR Protocol |
|---|---|---|
| dNTP Mix | Standard dNTPs (dATP, dCTP, dGTP, dTTP) | dUTP replaces dTTP (dATP, dCTP, dGTP, dUTP) |
| Additional Reagent | None | UNG Enzyme (e.g., E. coli UNG or Cod UNG) |
| Thermal Cycler Program | Direct start at denaturation temperature (e.g., 95°C) | Pre-PCR incubation at 50°C for 2 minutes, then denaturation |
Detailed Step-by-Step Methodology:
- Master Mix Preparation: For each qPCR reaction, prepare a master mix containing all standard components: buffer, primers, probe (if used), DNA polymerase, and a modified dNTP mix where dUTP fully substitutes dTTP. Finally, add UNG enzyme at the manufacturer's recommended concentration (e.g., 0.01 - 0.1 U/µL) [45] [47].
- Reaction Setup: Aliquot the master mix into reaction tubes or plates and add the template nucleic acid (DNA or RNA). Include a No-Template Control (NTC) containing nuclease-free water to monitor for carryover contamination.
- Pre-PCR Incubation: Program your thermal cycler to begin with a hold at 50°C for 2 minutes. During this step, UNG is active and cleaves the glycosidic bond of uracil bases in any contaminating dUTP-containing amplicons, creating abasic sites that fragment during the subsequent denaturation step [45] [46].
- UNG Inactivation and PCR Amplification: Following the incubation, increase the temperature to 95°C for 2-10 minutes. This step serves a dual purpose: it inactivates the UNG enzyme (preventing it from degrading newly synthesized dUTP-containing products later in the run) and initiates the standard denaturation of the native template.
- Proceed with Standard qPCR Cycling: Continue with the optimized cycling conditions for your specific cancer assay (e.g., 40-45 cycles of 95°C denaturation, 60°C annealing/extension).
Research Reagent Solutions
The successful implementation of a UNG-based carryover prevention system relies on key reagents. The table below lists essential materials and their functions.
| Reagent/Material | Function & Importance |
|---|---|
| dUTP | A direct substitute for dTTP in the PCR mix; allows for the incorporation of uracil into all newly synthesized amplicons, marking them for future degradation by UNG [46] [47]. |
| UNG Enzyme | The core enzyme that recognizes and excises uracil bases from DNA strands, fragmenting contaminating amplicons and preventing their amplification [45]. |
| dUTP-Compatible Polymerase | A DNA polymerase that efficiently incorporates dUTP into nascent DNA strands without a reduction in amplification efficiency or specificity. |
| UNG-Compatible Buffer | An optimized reaction buffer that supports both maximum PCR efficiency and robust UNG enzymatic activity during the pre-incubation step. |
Troubleshooting and FAQs
Q1: Our No-Template Control (NTC) still shows amplification after implementing UNG. What could be wrong? Amplification in an NTC after UNG implementation suggests the contamination source is not dUTP-containing amplicons. UNG only degrades uracil-containing DNA. Potential alternative sources include:
- Contamination of reagents, primers, or probes with the native target sequence [22] [46].
- Carryover of standard dTTP-containing amplicons from before UNG was implemented, which UNG cannot recognize [46].
- Aerosol contamination during pipetting. Solution: Decontaminate workspaces and equipment with 10% bleach and UV irradiation. Use fresh reagent aliquots and filter tips. Ensure all previous amplicons in the lab were generated with dUTP [22].
Q2: We observed a loss of PCR efficiency or sensitivity after switching to a dUTP/UNG system. How can we resolve this? Some DNA polymerases incorporate dUTP less efficiently than dTTP, which can slightly reduce yield or sensitivity. Solution:
- Optimize dUTP concentration: Test a dUTP/dTTP mixture (e.g., a 3:1 ratio of dUTP:dTTP) rather than a complete substitution, as this can sometimes restore efficiency while still providing sufficient uracil incorporation for UNG to function [46].
- Use high-performance enzymes: Select polymerases specifically engineered for high processivity with dUTP.
- Verify UNG concentration: Excessive UNG can lead to partial degradation of your new dUTP-containing products if any residual activity remains during cycling.
Q3: Is the UNG system compatible with one-step RT-qPCR for gene expression analysis in tumor samples? Yes, but it requires a specific type of UNG. Standard E. coli UNG retains activity up to ~55°C and would degrade the dUTP-containing cDNA synthesized during the reverse transcription step, which typically occurs between 42°C and 55°C [47]. Solution: Use a heat-labile UNG, such as Cod UNG, which is irreversibly inactivated at 55°C. This allows for a pre-PCR incubation at 25-40°C to destroy contaminants, after which the enzyme is inactivated during the reverse transcription step, protecting your newly synthesized cDNA [47].
Q4: In our multiplex qPCR assay for mutation detection, we see primer-dimer formation. Will UNG help with this? UNG has limited effectiveness against primer-dimers. While it can degrade dimer products that contain dA-nucleotides near the 3' end, it is not a reliable solution for primer-dimer issues [45]. Solution: Redesign primers to avoid 3' complementarity. Optimize annealing temperature and MgCl2 concentration. Use a hot-start polymerase to prevent non-specific amplification during reaction setup.
The UNG system is particularly valuable in sensitive cancer research applications where false positives can have significant consequences. For instance, in studies detecting minimal residual disease (MRD) or analyzing circulating tumor DNA (ctDNA), where the target is rare against a high background of wild-type DNA, preventing false signals is paramount [48]. Digital PCR (dPCR), a technology increasingly used in oncology for its absolute quantification and sensitivity, also benefits from integrating UNG to ensure the integrity of its partitions is not compromised by contaminating amplicons [48].
In conclusion, incorporating a dUTP/UNG system is a highly effective and relatively low-cost strategy to combat one of the most pervasive problems in a high-throughput molecular biology lab: carryover contamination. By meticulously degrading uracil-labeled amplicons from previous runs, it adds a critical layer of quality control to qPCR workflows, ensuring the reliability and accuracy of data in critical cancer research and diagnostic development.
Selection and Validation of Stable Reference Genes for Accurate Normalization in Complex Matrices
Core Concepts: The Critical Role of Reference Genes in Reducing False Positives
Accurate normalization is a critical step in qPCR analysis, especially in cancer research where false positives can lead to incorrect conclusions about therapeutic efficacy or disease mechanisms. Using inappropriate reference genes for normalization is a significant source of inaccurate gene expression data. Proper validation is essential to ensure that observed expression changes in target genes are biologically real and not artifacts of unstable controls [49] [17].
The stability of traditionally used "housekeeping" genes can be dramatically altered under various experimental conditions, including cancer cell dormancy models, nutrient stress, and across different cell line passages [49] [50]. For instance, in dormant cancer cells induced by mTOR inhibition, genes like ACTB (cytoskeleton) and ribosomal genes (RPS23, RPS18, RPL13A) undergo such dramatic expression changes that they are categorically inappropriate for normalization [49]. Similarly, in studies using MCF-7 breast cancer cell sub-clones, common reference genes like GAPDH and ACTB showed significant variability, making them unreliable as single internal controls [50].
The following workflow outlines the essential process for selecting and validating reference genes to minimize false positives:
Troubleshooting Guide & FAQs
Frequently Asked Questions
Q1: Why can't I use a single, well-known reference gene like GAPDH or ACTB for all my experiments in cancer cell lines? A1: Extensive research has demonstrated that the expression of common reference genes is not universal. Their stability can be affected by the specific cancer cell line, experimental treatment, and even sub-clones of the same cell line [50]. For example:
- In MCF-7 breast cancer cells, GAPDH and ACTB showed variable expression across different passages and sub-clones [50].
- In A549, T98G, and PA-1 cancer cells treated with an mTOR inhibitor, ACTB and ribosomal protein genes were among the least stable [49]. Relying on a single, unvalidated gene can introduce significant bias and lead to false positives or false negatives in your data.
Q2: My Ct values for biological replicates are highly inconsistent. What could be the cause? A2: Inconsistency among biological replicates often indicates issues with sample quality or handling. Key culprits include:
- RNA Degradation: Always check RNA integrity prior to reverse transcription using a spectrophotometer (aim for 260/280 ratio of 1.9–2.0) and/or an agarose gel [7].
- Minimal Starting Material: This is especially critical when working with rare cells like disseminated cancer cells [51].
- Inefficient cDNA Synthesis: Optimize reaction conditions and ensure consistent reagent volumes [52].
- Pipetting Errors: Inconsistent pipetting can cause significant Ct value variations; consider using automated liquid handlers for improved reproducibility [52].
Q3: What does it mean if my No Template Control (NTC) shows amplification? A3: Amplification in the NTC indicates contamination or primer-dimer formation.
- Contamination: Clean your work area and pipettes with 70% ethanol or 10% bleach if reagents have spilled. Prepare fresh primer dilutions and use new reagents if necessary [7].
- Primer-Dimer: Add a dissociation (melt) curve at the end of qPCR cycling. An additional peak at a lower temperature indicates primer-dimer formation. Redesigning primers using specialized software may be required [52] [7].
- Splash Contamination: Be extremely cautious when pipetting template to prevent splashing into adjacent NTC wells. Physically separate NTC wells from sample wells on the plate [7].
Q4: How many reference genes should I use for reliable normalization? A4: Normalization against a single reference gene is strongly discouraged by the MIQE guidelines [17] [53]. It is recommended to use the top two or three most stable genes identified from a validation experiment for your specific experimental conditions [54] [50]. This approach minimizes the normalization error and provides a more robust foundation for your gene expression data.
Reference Gene Stability in Different Experimental Models
The table below summarizes findings on reference gene stability from recent studies, highlighting that optimal choices are highly context-dependent.
Table 1: Reference Gene Performance Across Different Experimental Models
| Experimental Model/Condition | Recommended Stable Genes | Genes to Avoid (Unstable) | Primary Citation |
|---|---|---|---|
| Dormant Cancer Cells (A549, T98G, PA-1; mTOR-inhibited) | A549: B2M, YWHAZT98G: TUBA1A, GAPDH | ACTB, RPS23, RPS18, RPL13A | [49] |
| MCF-7 Breast Cancer Cell Line (across passages & nutrient stress) | GAPDH, CCSER2, PCBP1 (as a triplet) | ACTB, PGK1 as single controls | [50] |
| Dystrophic Mouse Muscle (BL10-mdx & D2-mdx models) | Htatsf1, Pak1ip1, Zfp91 | Actb, Gapdh, Rpl13a | [54] |
| Turbot Gonad Development (across temperatures) | UBQ, RPS4 | B2M | [53] |
Experimental Protocols
Protocol: Validation of Reference Genes for a New Experimental Condition
This protocol provides a framework for identifying the most stable reference genes in your specific experimental system, such as a new cancer drug treatment or a novel cell culture condition.
1. Candidate Gene Selection:
- Select 8-12 candidate genes from the literature relevant to your field (e.g., cancer research) [49] [50].
- Include both traditional genes (e.g., GAPDH, ACTB) and newer, potentially more stable candidates (e.g., YWHAZ, B2M, TBP) [49] [54].
2. Primer Design and Validation:
- Design primers using specialized software to ensure appropriate length, GC content, and melting temperature (Tm). Check for potential secondary structures or dimer formation [52].
- Validate primer specificity using:
3. qPCR Run and Data Collection:
- Run qPCR on all candidate genes across all test samples (including all experimental conditions and replicates).
- Include No Template Controls (NTCs) for each primer pair.
- Ensure replicate consistency (Cq differences should be <1 cycle) [53].
4. Stability Analysis:
- Analyze the resulting Cq data using multiple algorithms to ensure a robust conclusion. The most common are:
- NormFinder: Considers both intra- and inter-group variation; often recommended for its reliability [53].
- geNorm: Determines the pairwise variation and recommends the optimal number of reference genes [54] [53].
- BestKeeper: Ranks genes based on the standard deviation of their Cq values [54] [53].
- Comparative ΔCq method: A straightforward method based on pairwise comparisons [54].
- Consensus: Select the top 2-3 genes that are consistently ranked as the most stable across the different algorithms [54] [50].
5. Final Validation:
- Use the selected gene panel to normalize the expression of a well-characterized target gene in your system. If the normalized results align with expected outcomes or other validation data, the panel is confirmed as suitable [50].
The following diagram illustrates the four major algorithms used to determine the most stable reference genes from your qPCR data:
The Scientist's Toolkit: Essential Research Reagents & Materials
Table 2: Key Reagents and Materials for Reference Gene Validation
| Item | Function/Benefit | Considerations for Reducing False Positives |
|---|---|---|
| Validated Primer Panels | Pre-designed sets of primers for common candidate reference genes. | Reduces risk of non-specific amplification and primer-dimers, a common source of false positives [52]. |
| RNA Integrity Number (RIN) | Quantitative measure of RNA quality (e.g., via Bioanalyzer). | High-quality RNA (RIN >8) is crucial for accurate cDNA synthesis and prevents false negatives from degraded targets [7]. |
| DNase I Treatment | Removes genomic DNA contamination from RNA samples. | Prevents amplification of genomic DNA, a major contributor to false positive signals [7]. |
| SYBR Green Master Mix | Fluorescent dye for detecting PCR products in real-time. | Use mixes that include additives to inhibit primer-dimer formation. Always run with a melt curve analysis to confirm specificity [53]. |
| Automated Liquid Handler | Precision robot for pipetting (e.g., I.DOT Liquid Handler). | Minimizes pipetting errors and Ct value variations between replicates, enhancing reproducibility and data reliability [52]. |
| Stability Analysis Software | Tools for running geNorm, NormFinder, BestKeeper. | Using multiple algorithms cross-validates results, leading to a more robust and reliable selection of reference genes [54] [53]. |
Systematic Optimization and Troubleshooting of qPCR Protocols
In quantitative PCR (qPCR) assays for cancer research, the high sensitivity required to detect low-abundance biomarkers also makes the technique vulnerable to false positives. These inaccuracies can compromise research integrity, leading to incorrect conclusions about gene expression or mutational status. Proper implementation and interpretation of No-Template Controls (NTC) and No Reverse Transcription Controls (NoRT) are foundational to data validity. This guide details the design, interpretation, and troubleshooting of these essential controls to enhance the reliability of your qPCR cancer assays.
Frequently Asked Questions (FAQs)
1. What is the fundamental purpose of an NTC and a NoRT control?
- No-Template Control (NTC): This reaction contains all qPCR components—master mix, primers, probe, and water—except for the template nucleic acid [55]. Its primary purpose is to detect contamination in the reagents or the assay setup process. Amplification in the NTC indicates that one of the reagents is contaminated with the target sequence, such as amplicon carryover from previous PCRs or environmental contamination [56] [2].
- No Reverse Transcription Control (NoRT): This control is specific to reverse transcription qPCR (RT-qPCR). It contains all components for the RT step, including the RNA sample, but lacks the reverse transcriptase enzyme [55]. A positive signal in the NoRT control reveals the presence of contaminating genomic DNA (gDNA) in the RNA sample, which is being amplified directly and could be mistaken for cDNA [55] [57].
2. How do I interpret amplification in my NTC?
Amplification in the NTC signifies a false positive. The Cycle of Quantification (Cq) value and melting curve analysis are critical for diagnosing the source. The table below outlines the common causes and characteristics.
Table 1: Diagnosing Amplification in the No-Template Control (NTC)
| Observation | Probable Cause | Characteristics | Confirmation Method |
|---|---|---|---|
| Late amplification (Cq >34-38) [22] [2] | Primer-dimer formation [56] | Dissociation curve shows a low-temperature peak distinct from the specific amplicon's peak [56] [7]. | Melt curve analysis [56] [22]. |
| Early amplification (Cq <34-38), consistent across replicates [56] | Reagent contamination | All NTC replicates show similar, early Cq values. The melt curve peak matches your specific amplicon [56] [3]. | Compare melt curve of NTC to positive samples [57]. |
| Early amplification, random across replicates [56] | Cross-contamination during plate setup | NTCs show amplification at varying Cq values; not all NTCs may be affected [56]. | Review pipetting technique and plate layout. |
3. What does amplification in my NoRT control mean, and why is it a problem in cancer research?
Amplification in the NoRT control indicates that your RNA sample is contaminated with genomic DNA (gDNA) [55] [57]. In cancer research, this is particularly problematic because:
- Inaccurate Quantification: The signal from gDNA inflates the apparent expression level of your target gene, leading to false conclusions about gene overexpression, a common event in cancer.
- Masking True Regulation: It can obscure the true up- or down-regulation of oncogenes or tumor suppressor genes.
- False Positives: For assays designed to detect fusion transcripts or viral oncogenes (e.g., HPV in cervical cancer), gDNA amplification can produce a false positive result.
4. What are the best practices for preventing contamination and false positives?
- Physical Separation: Use separate, dedicated rooms or workstations for reagent preparation, sample/template addition, and post-PCR analysis [56] [22] [2].
- Meticulous Lab Practice: Use filter pipette tips, clean surfaces and pipettes regularly with 10% bleach or ethanol, and wear gloves [22] [2].
- Enzymatic Prevention: Use a master mix containing Uracil-N-Glycosylase (UNG). This enzyme degrades PCR products from previous reactions that incorporate dUTP (substituted for dTTP), preventing "carryover" contamination [56] [2] [3].
- Robust Assay Design: For RT-qPCR, design primers to span an exon-exon junction so they will not efficiently bind to gDNA [58] [7]. As an additional measure, treat RNA samples with DNase I prior to reverse transcription [57] [2].
- Reagent Management: Prepare small, single-use aliquots of all reagents, primers, and probes to minimize freeze-thaw cycles and prevent widespread contamination [22].
5. Where should I place the NTC on my qPCR plate?
Place the NTC wells as far away from positive samples and positive controls as possible on the plate [22]. This minimizes the risk of cross-contamination via aerosols or splashing during pipetting.
Troubleshooting Guides
Issue 1: Amplification in No-Template Control (NTC)
The following workflow diagram outlines a systematic approach to diagnosing and resolving NTC amplification.
Recommended Actions:
- If Primer-Dimer is Diagnosed:
- Optimize Primer Concentrations: Test a matrix of forward and primer concentrations (e.g., from 100-400 nM each) to find a combination that minimizes dimerization while maintaining efficient amplification [56].
- Redesign Primers: Use primer design software to create primers with minimal self-complementarity and a Tm of ~60°C [57].
- If Contamination is Diagnosed:
- Replace Reagents: Discard all suspect reagents, including water, master mix, and primer/probe stocks. Use fresh aliquots [22] [57].
- Decontaminate: Thoroughly clean work areas, pipettes, and equipment with 10% bleach, followed by ethanol or RNAase-free water [22] [2] [3].
- Implement UNG: Switch to a master mix containing Uracil-N-Glycosylase (UNG) to prevent future carryover contamination [56] [3].
Issue 2: Amplification in No Reverse Transcription (NoRT) Control
The workflow below guides you through addressing genomic DNA contamination.
Recommended Actions:
- DNase I Treatment: The most direct solution is to treat your RNA samples with DNase I during the RNA purification process or immediately before the RT reaction to digest any contaminating gDNA [57] [2].
- Primer Redesign: Design new primers so that the binding sites are on two different exons, with the probe spanning the exon-exon junction. This ensures the primer pair cannot amplify gDNA efficiently because of the presence of large introns [58] [7].
The Scientist's Toolkit: Key Reagent Solutions
Table 2: Essential Reagents for Controlling False Positives in qPCR
| Reagent / Solution | Function in Control | Key Considerations |
|---|---|---|
| Nuclease-Free Water [22] | The liquid component for NTCs; must be sterile to avoid introducing template. | Always aliquot to prevent contamination of the main stock. |
| UNG/Uracil DNA Glycosylase (UDG) [56] [3] | Enzymatically degrades carryover PCR products from previous reactions, preventing false positives in NTCs. | Requires incorporation of dUTP in the PCR master mix. A pre-PCR incubation step is needed. |
| DNase I, RNase-free [57] | Digests contaminating genomic DNA in RNA samples to prevent amplification in NoRT controls. | Requires an inactivation step (e.g., with EDTA or heat) post-treatment to avoid degrading cDNA. |
| qPCR Probes & Primers [22] [58] | Sequence-specific reagents for detection. Can be a source of contamination. | Aliquot upon arrival. Verify specificity with BLAST. Design primers to span exon-exon junctions. |
| Positive Control Template [55] [59] | A synthetic or purified template of known concentration used to validate assay performance. | Use at a defined, low copy number. Keep separate from pre-PCR areas to avoid contamination. |
In quantitative PCR (qPCR) for cancer research, the precision of thermal cycler parameters is a critical determinant in the fight against false positives. Non-specific amplification, often manifesting as false positive signals, can directly lead to inaccurate data, potentially compromising experimental conclusions and subsequent research directions [2]. The annealing temperature and the number of amplification cycles are two of the most pivotal factors under your direct control. Optimizing these parameters enhances the stringency of the reaction, ensuring that primers bind only to their perfectly matched target sequences, thereby safeguarding the integrity of your results, especially in sensitive applications like detecting low-frequency cancer mutations [60] [61]. This guide provides detailed troubleshooting and protocols to methodically optimize these settings, reducing the risk of false positives in your qPCR cancer assays.
Key Concepts and Definitions
To effectively troubleshoot and optimize your qPCR assays, a firm grasp of the underlying concepts and components is essential. The following table defines key terms and reagents central to this process.
- Table: Key qPCR Concepts and Research Reagent Solutions
| Term/Reagent | Definition / Function |
|---|---|
| Annealing Temperature (Ta) | The temperature during the thermal cycling protocol at which primers bind to their complementary template sequence. Optimal Ta is crucial for specificity [61]. |
| Cycle Threshold (Ct) | The thermal cycle number at which the fluorescence of a reaction crosses a threshold level, indicating amplification detection. High Ct values (>34-38) can indicate low-level noise or false amplification [22] [60]. |
| Primer-Dimer | A non-specific amplification artifact formed by the interaction of two primers, which can be misinterpreted as a positive signal, particularly in intercalating dye assays [62] [61]. |
| No-Template Control (NTC) | A critical control reaction containing all reagents (master mix, primers, water) except the template nucleic acid. Amplification in the NTC indicates contamination or primer-dimer formation [22] [3]. |
| Hot-Start Polymerase | A modified polymerase that is inactive at room temperature, preventing non-specific amplification and primer-dimer formation during reaction setup. It is activated by the initial high-temperature denaturation step [2]. |
| dUTP/UNG System | A contamination control system where dUTP is incorporated into PCR amplicons. Uracil-N-Glycosylase (UNG) then degrades any contaminating carryover PCR products from previous reactions before amplification begins [3] [2]. |
| Passive Reference Dye (e.g., ROX) | A dye included in some master mixes to normalize for non-PCR-related fluorescence fluctuations between wells, improving well-to-well and run-to-run reproducibility [61]. |
| Hydrolysis Probes (e.g., TaqMan) | Target-specific probes that increase assay specificity by generating a fluorescent signal only upon hybridization and cleavage during amplification. They are less susceptible to primer-dimer artifacts than intercalating dyes [62] [61]. |
Thermal Cycler Parameter Optimization Guide
Systematic optimization of thermal cycler parameters is the most effective strategy to enhance assay specificity. The following workflow and table provide a structured approach to this process.
Detailed Optimization Parameters
After following the workflow, use the table below to fine-tune specific parameters. The quantitative data are synthesized from multiple studies to guide your experiments.
- Table: Quantitative Optimization Parameters for Thermal Cycling
| Parameter | Sub-Parameter | Recommended Range / Optimal Value | Effect on Specificity & False Positives | Experimental Evidence |
|---|---|---|---|---|
| Annealing Temperature | Gradient Range | 55°C - 65°C (start) [61] | Higher temperatures increase stringency, reducing non-specific binding. | A study on SARS-CoV-2 N2 assay found increasing Ta from 60°C to 63°C was critical in reducing false positives from 56.4% to 11.5% [62]. |
| Optimal Selection | 5-10°C above primer Tm for Touchdown PCR [2] | Favors specific primer-template binding from the first cycles. | - | |
| Probe Consideration | Tm of probe should be ~10°C higher than primers [63] | Ensures probe binds before primers, maximizing signal specificity. | - | |
| Cycle Number | General Guideline | 40 cycles (standard) [61] | - | - |
| Cut-off for Positives | ≤34 cycles for SYBR Green [22]≤38 cycles for probe-based assays [22] [60] | Amplification beyond these cycles is often non-specific (primer-dimers) or from very low-level contamination. | Research on EGFR S768I mutation showed false positives were associated with late Cq values; confirming positives with an orthogonal method (NGS) is advised for high Cq results [60]. | |
| Reduction Strategy | Reduce to 30 cycles if plateau is reached early [63] | Saves time and reduces opportunity for late-cycle noise. | - | |
| Other Critical Parameters | Denaturation Time | 5-15 sec for templates <300 bp [63] | Sufficient for complete denaturation without excessive enzyme stress. | - |
| MgSO4 Concentration | Adjust between 3-6 mM [62] | Higher concentrations can increase non-specific binding; optimization is key. | In the same SARS-CoV-2 study, optimizing MgSO4 to 6 mM helped reduce false positives [62]. | |
| Primer/Probe Concentration | Test 50-400 nM primers; 33-100 nM probe [62] [64] | Lower concentrations can minimize primer-dimer potential. | A study demonstrated that suboptimal primer concentrations (too high or too low) can cause a significant drop in PCR efficiency (e.g., -13%) [64]. |
Troubleshooting FAQs: Addressing Common qPCR Problems
Q1: My no-template control (NTC) shows amplification late in the run (e.g., after cycle 34). Is this a false positive and how should I address it?
A: Yes, late amplification in the NTC is a classic sign of a false positive, most commonly caused by primer-dimer formation or low-level contamination [22]. To address this:
- Confirm the Artifact: Perform melt curve analysis. A single, sharp peak at the same temperature as your positive sample indicates specific product contamination. A lower-temperature, broader peak suggests primer-dimers [22] [61].
- Optimize Annealing Temperature: Increase the annealing temperature in 1-2°C increments. A higher temperature increases stringency, reducing the chance for primers to bind non-specifically to each other or non-target sequences [62] [61].
- Adjust Reagent Concentrations: Lower the concentration of primers and/or magnesium in the reaction mix, as both can promote dimer formation at high concentrations [62] [64].
- Decontaminate: If contamination is confirmed, replace all aliquots of reagents (water, master mix, primers) and thoroughly decontaminate workspaces and equipment with 10% bleach followed by UV irradiation [22] [2].
Q2: After optimizing my annealing temperature with a gradient, I still get inconsistent results and high variation between replicates. What could be wrong?
A: Inconsistency between replicates often points to issues with pipetting accuracy or reaction mix homogeneity, which become critically important when using reduced volumes or highly specific conditions [52].
- Check Pipetting Technique and Calibration: Ensure pipettes are regularly calibrated. Use proper pipetting techniques and consider using automated liquid handlers for improved precision and reproducibility [52] [2].
- Review Master Mix Preparation: Always prepare a master mix for all samples and controls (except template) to minimize tube-to-tube variation. Vortex and centrifuge the master mix thoroughly before aliquoting [61].
- Verify Primer Quality and Design: Use in silico tools (e.g., OligoAnalyzer) to check for primer self-complementarity and dimer formation. Poorly designed primers with stable secondary structures will yield inconsistent results regardless of thermal profile [62] [64]. Redesign primers if necessary, ensuring they are 28bp or larger and have a Tm between 58-65°C [63].
Q3: My assay detected a rare cancer mutation, but orthogonal confirmation (e.g., NGS) was negative. What thermal cycler-related issues could have caused this false positive?
A: This scenario highlights the risk of method-specific false positives, as documented in studies of the EGFR S768I mutation, where one platform showed an 80% false positive rate [60].
- Establish a Cycle Threshold (Ct) Cut-off: For rare mutations, define a maximum Ct value for reporting positives. The Idylla system false positives for EGFR S768I were often near the detection limit. Setting a conservative Ct cut-off (e.g., <36-38) can help filter these out [60] [65].
- Increase Annealing Stringency: Re-optimize using a higher annealing temperature gradient. The increased stringency can discriminate perfectly between the true mutation and a sequence with a single nucleotide mismatch that might be amplified less efficiently [61].
- Mandatory Orthogonal Confirmation: For results with significant clinical or research implications—especially those with high Ct values or low allele frequency—always plan for confirmation using a different technological principle, such as NGS or digital PCR [60]. Digital PCR can be particularly useful for absolutely quantifying template and setting a logical Ct cut-off [65].
Using Melting Curve Analysis to Identify and Eliminate Non-Specific Products and Primer Dimers
Core Concepts: Understanding Melt Curve Analysis
What is melt curve analysis and why is it critical for qPCR specificity?
Melt curve analysis is a quality control step performed after a SYBR Green qPCR run to verify that the fluorescence detected during the reaction comes from a single, specific amplicon [15]. The SYBR Green dye binds to any double-stranded DNA (dsDNA), including non-specific products and primer dimers. The melt curve helps distinguish desired products from these artifacts, which is crucial for the accuracy of quantification, especially in sensitive applications like cancer assay research where false positives must be minimized [15].
How does a melt curve analysis work?
After amplification, the thermal cycler gradually increases the temperature while monitoring fluorescence. As the temperature rises, the dsDNA denatures, the SYBR Green dye is released, and the fluorescence decreases [66] [15]. This raw data is often presented as the negative derivative of the fluorescence over temperature (-dF/dT). This conversion turns the point of most rapid fluorescence drop into a distinct, easy-to-interpret peak, with the peak's location indicating the melting temperature (Tm) of the PCR product [15].
FAQs: Interpreting Your Results
1. A single, sharp peak on my melt curve derivative plot—does this guarantee a single, specific product?
A single, sharp peak strongly suggests a single, dominant PCR product, but it is not absolute proof [66] [15]. It is possible for a single amplicon to exhibit multiple peaks if it has distinct domains with different stability, such as very G/C-rich regions that melt at a higher temperature than A/T-rich regions [66]. For definitive confirmation, you should analyze the PCR product by agarose gel electrophoresis. A single, clean band of the expected size on the gel corroborates the melt curve result [66] [15].
2. What does a single peak at a very low temperature (e.g., below 75°C) typically indicate?
A single peak with a low Tm is a classic signature of primer-dimer formation [15]. Primer dimers are very short, double-stranded artifacts formed by the primers amplifying themselves. Due to their small size and low stability, they melt at significantly lower temperatures than a specific, longer amplicon.
3. My melt curve shows multiple peaks. What does this mean and how should I proceed?
Multiple peaks indicate a mixture of DNA species with different melting temperatures. This means your reaction has produced:
- Non-specific amplification: Your primers have bound to and amplified unintended regions of the genome [15].
- A mixture of primer dimers and your specific product: This often appears as a large, correct peak and a smaller, low-temperature peak [15].
- A single, complex amplicon: In rarer cases, a single product with internal sequence variations can melt in multiple phases [66].
Your first step should be to use prediction software like uMelt to model the expected melt curve for your specific target sequence. If the predicted curve matches your single-peak result, you can be more confident. If not, you need to optimize your assay to eliminate the extra products [66].
4. My peak is very broad or asymmetrical. What could be the cause?
Unusual peak shapes like broad or asymmetrical peaks suggest an anomaly that is more difficult to diagnose and may merit re-running the experiment or redesigning the primers [15]. This can sometimes occur with a highly heterogeneous PCR product population or other complex issues.
Troubleshooting Guide: From Problem to Solution
This guide provides a structured approach to resolving common melt curve issues.
| Observation | Possible Cause | Recommended Solution |
|---|---|---|
| Multiple Peaks | Non-specific binding of primers to off-target sequences [15]. | 1. Increase annealing temperature by 2-5°C [67] [15]. 2. Redesign primers using BLAST analysis to ensure specificity [12]. 3. Use a hot-start polymerase to prevent activity at low temperatures [67]. |
| Single Low-Tm Peak (~70-75°C) | Primer-dimer formation [15]. | 1. Increase annealing temperature [15]. 2. Lower primer concentration (e.g., from 0.5µM to 0.1-0.3µM) [67] [15]. 3. Redesign primers to avoid 3'-end complementarity [12] [42]. 4. Use a primer design tool to check for self-dimers and hairpins [12]. |
| No Product / Broad Peaks | Suboptimal reaction conditions, inhibitors, or poor primer design. | 1. Check primer design: Ensure Tm of 60-64°C, 40-60% GC content, and no long repeats [12] [42]. 2. Optimize Mg2+ concentration in 0.5-1 mM increments [67]. 3. Purify template DNA to remove inhibitors like salts or phenols [67]. |
| High Variation Between Replicates | Pipetting errors or inconsistent reaction mixtures [52]. | 1. Use a master mix for all common reagents. 2. Employ proper pipetting technique or an automated liquid handler to improve precision [52]. |
Experimental Protocol: A Step-by-Step Optimization Workflow
The following diagram outlines a systematic workflow for using melt curve analysis to troubleshoot and optimize a qPCR assay.
Step 1: Initial Run and Analysis
- Set up your SYBR Green qPCR reaction as planned.
- Program the thermal cycler to run a melt curve analysis after the amplification cycles. A standard protocol is to heat from 60°C to 95°C, with continuous fluorescence measurement [15].
- After the run, view the derivative melt curve plot (-dF/dT) in your qPCR software.
Step 2: Result Interpretation and Action
- If you observe a single, sharp peak at the expected Tm:
- If you observe multiple peaks, a single low-Tm peak, or a broad peak:
- Consult the troubleshooting table above. Begin with the simplest solutions, such as increasing the annealing temperature and lowering primer concentration.
- If optimization fails, redesign your primers. Use design tools to ensure they meet optimal criteria: length of 18-30 bases, Tm of 60-64°C, and GC content of 40-60% [12] [42]. Crucially, screen for self-dimers and hairpins [12].
- Validate the new primer set by repeating Step 1.
Research Reagent Solutions for Robust qPCR
This table lists essential reagents and their roles in achieving specific amplification and reliable melt curve analysis.
| Reagent / Material | Function in Assay | Key Considerations for Specificity |
|---|---|---|
| SYBR Green Dye | Fluorescent dye that binds dsDNA; enables real-time quantification and melt curve analysis [15]. | Binds to all dsDNA (specific and non-specific); makes post-run melt curve analysis essential [15]. |
| Hot-Start DNA Polymerase | Enzyme engineered to be inactive at room temperature; prevents pre-amplification activity. | Reduces primer-dimer formation and non-specific amplification during reaction setup [67]. |
| Primer Pairs | Oligonucleotides that define the start and end of the target amplicon. | Design is critical: use tools to ensure specificity, optimal Tm (~62°C), and avoid self-complementarity [12] [42]. |
| dNTPs | Nucleotide building blocks for DNA synthesis. | Use balanced concentrations to prevent incorporation errors that can lead to spurious results [67]. |
| MgCl2 | Cofactor for DNA polymerase activity; concentration affects primer binding and fidelity. | Optimize concentration (e.g., 1.5-4.0 mM); too much can promote non-specific binding [67]. |
| qPCR Plates & Seals | Reaction vessels for thermal cycling. | Ensure a tight seal to prevent evaporation, which can cause well-to-well variation and affect melt curve shape. |
| Automated Liquid Handler | Instrument for precise dispensing of reaction components. | Improves accuracy and reproducibility of replicates, reducing Ct value variations caused by pipetting errors [52]. |
Frequently Asked Questions
What is the primary cause of false positives in my qPCR assay? The most common source of false positives is contamination, which can originate from amplicon carryover from previous reactions, contaminated reagents, or cross-contamination from positive samples or controls during sample handling [2] [3]. Even microscopic aerosols created during pipetting can introduce enough template to generate a signal.
Why should I not use DEPC-treated water for PCR? While effective for inactivating RNases in RNA work, DEPC-treated water is not recommended for PCR. Residual DEPC or its by-products (ethanol and CO₂) can inhibit DNA polymerase activity, compromising the efficiency and reliability of the PCR reaction [68].
My No Template Control (NTC) shows amplification. What does this mean? Amplification in your NTC indicates contamination in one of your reagent components or from the environment [22] [3]. It means that your primers, master mix, or water contain a template that is being amplified. This is a critical red flag that must be addressed before trusting any experimental results.
What is the function of ROX dye in my master mix? ROX is a passive reference dye. Its fluorescence is not affected by PCR amplification. It serves to normalize the reporter dye signal (like FAM or SYBR Green) against non-amplification-related fluctuations caused by bubbles, evaporation, condensation, or instrument variability, leading to more precise data from technical replicates [69].
How can master mix composition help reduce false positives? Many modern master mixes incorporate features to enhance specificity and prevent contamination. Hot-start polymerases prevent non-specific amplification during reaction setup by remaining inactive until a high temperature is reached [2]. Furthermore, master mixes containing uracil-N-glycosylase (UNG) can degrade carryover contamination from previous PCR reactions that contain dUTP (which is incorporated instead of dTTP), thereby preventing its amplification [2] [3].
Troubleshooting Guides
Problem: Contamination and False Positives
Symptoms:
- Consistent amplification signal in the No Template Control (NTC) wells.
- Unexpected positive results in known negative samples.
- High background noise or early amplification in negative controls.
Solutions and Preventive Measures:
Implement Rigorous Laboratory Practices:
- Physical Separation: Use separate, dedicated rooms or work areas for reagent preparation, sample preparation, and post-PCR analysis [2].
- Unidirectional Workflow: Maintain a one-way flow of personnel and materials from "clean" (reagent prep) to "dirty" (post-PCR) areas [2].
- Decontaminate Surfaces: Regularly clean benches, pipettes, and equipment with 10% bleach (sodium hypochlorite), followed by 70% ethanol to remove the bleach residue [22] [2]. UV irradiation of workstations and consumables can also be effective [22].
Use Molecular Biology Grade Reagents:
- Nuclease-Free Water: Use certified nuclease-free, PCR-grade water to prevent the degradation of nucleic acids and avoid introducing contaminants [68] [2].
- Sterile, Filter Tips: Always use aerosol-barrier pipette tips to prevent cross-contamination and pipette contamination [22].
- Aliquot Reagents: Prepare single-use aliquots of all primers, probes, and master mixes to minimize freeze-thaw cycles and reduce the chance of contaminating a bulk stock [22].
Employ Biochemical Deterrents:
- UNG Treatment: Use a master mix that contains uracil-N-glycosylase (UNG) and substitute dUTP for dTTP in your reactions. UNG will enzymatically degrade any uracil-containing contaminants from previous amplifications before the PCR cycle begins, preventing re-amplification [2] [3].
- Hot-Start Polymerases: Always use a hot-start polymerase to inhibit enzyme activity until the initial denaturation step, preventing primer-dimer formation and non-specific amplification at room temperature [2].
Summary of Contamination Sources and Actions
| Contamination Source | Result | Recommended Action |
|---|---|---|
| PCR Product Carryover | False Positive | Implement UNG/dUTP system; decontaminate workspaces with bleach [2] [3]. |
| Contaminated Reagents | False Positive | Replace all reagents; use new aliquots; test components with NTCs [3]. |
| Cross-contamination during pipetting | False Positive | Use filter tips; maintain separate pipettes for pre- and post-PCR; improve technique [2]. |
| Contaminated Master Mix (e.g., bacterial DNA) | False Positive (in bacterial assays) | Source enzymes from suppliers that test for bacterial genomic DNA contamination [3]. |
| Primer-Dimers | Late amplification in NTC | Redesign primers; check with melt curve analysis; optimize primer concentrations [22] [7]. |
Problem: Inconsistent Results and Poor Precision
Symptoms:
- High variation between technical replicates.
- Standard curves with poor R² values or irregular amplification plots.
Solutions:
Normalize with a Passive Reference Dye:
- Ensure your master mix contains a passive reference dye like ROX and that your instrument's software is configured to use it for normalization. This corrects for well-to-well variations caused by bubbles, evaporation, or minor pipetting errors, significantly improving replicate precision [69].
Verify Pipetting Accuracy and Reagent Homogeneity:
- Calibrate Pipettes: Ensure pipettes are regularly serviced and calibrated [2].
- Mix Thoroughly: Gently but thoroughly vortex all reagents before use and briefly centrifuge to collect contents at the bottom of the tube.
- Prepare Fresh Dilutions: Use freshly diluted standards and templates to avoid concentration changes due to evaporation [7].
Experimental Protocols for Quality Control
Protocol 1: Testing Water and Reagents for Nuclease Contamination
Purpose: To verify that your nuclease-free water and other liquid reagents are free of contaminating nucleases and DNA.
Methodology:
- Prepare a test reaction using the reagent water as the template instead of a sample.
- Use a highly sensitive and robust assay, such as one targeting a bacterial 16S rRNA gene or a human housekeeping gene.
- Run the test on a qPCR instrument for at least 40-45 cycles.
- Interpretation: A late amplification signal (Cq > 34-38, depending on assay sensitivity) may indicate low-level contamination or primer-dimer formation. A strong, early Cq in the NTC indicates significant contamination of the tested reagent [22].
Protocol 2: Using Controls to Monitor Assay Integrity
Including the correct controls in every run is non-negotiable for diagnostic-quality qPCR.
Essential Controls and Their Expected Results [3]:
| Control | Composition | Expected Result | Interpretation of a False Positive |
|---|---|---|---|
| No Template Control (NTC) | Master mix, primers/probe, nuclease-free water | No amplification | Indicates contamination in the master mix, primers, probe, or water. |
| No Reverse Transcription Control (NRT) | RNA sample, master mix, but no reverse transcriptase | No amplification | Indicates contamination of the RNA sample with genomic DNA. |
| Positive Control | Master mix with a known, low-copy number of the target sequence | Amplification at expected Cq | — |
Protocol 3: Distinguishing Specific Amplification from Primer-Dimers
Purpose: To confirm that the signal in your reaction, especially a late-amplifying one, is from your specific target and not from non-specific primer-dimer artifacts.
Methodology (for intercalating dye assays like SYBR Green):
- After the final PCR cycle, add a dissociation (melt) curve step.
- The instrument will slowly heat the amplicons and measure fluorescence as the DNA melts.
- Interpretation: A single, sharp peak in the melt curve indicates a single, specific amplification product. Multiple peaks or a broad peak at a lower temperature indicates the presence of non-specific products like primer-dimers [22] [7].
The Scientist's Toolkit: Essential Reagents for Robust qPCR
| Reagent / Material | Function & Importance in Reducing False Positives |
|---|---|
| PCR-Grade Nuclease-Free Water | Certified free of DNases, RNases, and contaminating nucleic acids. Prevents degradation of templates and primers, and avoids introduction of background DNA that can lead to false signals [68] [70]. |
| Hot-Start Master Mix | Contains a modified polymerase that is inactive at room temperature. Prevents non-specific amplification and primer-dimer formation during reaction setup, improving assay specificity and sensitivity [2]. |
| UNG-Enabled Master Mix | Includes the enzyme Uracil-N-Glycosylase (UNG) for the prevention of carryover contamination. Degrades PCR products from previous runs that contain dUTP, making them unamplifiable [2] [3]. |
| Passive Reference Dye (e.g., ROX) | An inert dye used to normalize fluorescent data. Corrects for well-to-well volume variations and other non-biological fluctuations, increasing the precision and reliability of replicate measurements [69]. |
| Aerosol-Barrier Pipette Tips | Prevent aerosols and liquids from entering the pipette shaft, thereby eliminating a major source of cross-contamination between samples [22] [2]. |
| Molecular Biology Grade Primers & Probes | Oligonucleotides synthesized and purified in a controlled environment to minimize cross-contamination with other synthetic templates, which can be a catastrophic source of false positives [3]. |
Experimental Workflow: From Reagent to Result
The diagram below illustrates the logical workflow for evaluating reagent quality and its direct impact on qPCR results, highlighting critical control points.
Step-by-Step Guide to Diagnosing and Resolving Persistent Fluorescence in Negative Controls
A critical protocol for ensuring the integrity of your qPCR cancer assay data
In the sensitive context of qPCR cancer assays, amplification in your negative controls—often flagged as AMPNC [71]—is a significant red flag. This persistent fluorescence indicates contamination or systematic error that can severely compromise data integrity, leading to false conclusions about oncogene expression, cancer subtyping, and therapeutic targets [34]. This guide provides a systematic, step-by-step approach to diagnose and resolve this critical issue, safeguarding your research on biomarkers like HER2, ESR, and PGR [34].
Phase 1: Problem Identification & Initial Assessment
The first step is to correctly identify the nature of the amplification in your No Template Control (NTC).
Step 1: Interpret the Amplification Curve
Examine the amplification plot of your NTC. A true problem is indicated by exponential amplification that crosses the threshold before cycle 34-38 [22] [72]. Late amplification (beyond cycle 34-38) may instead be due to non-specific byproducts like primer-dimers, which can be confirmed with a melt curve analysis [22].
Step 2: Document the Observation
Record the Cq value, the shape of the curve, and the fluorescence intensity. This baseline information is crucial for diagnosing the cause and tracking the effectiveness of your decontamination efforts.
Phase 2: Systematic Diagnosis of the Root Cause
Follow the diagnostic workflow below to pinpoint the most likely source of your contamination. The causes can be broadly categorized, and the flowchart guides you to the most probable culprit.
Table 1: Common Causes of Amplification in Negative Controls
| Category | Specific Cause | Typical Cq Indication |
|---|---|---|
| Laboratory Contamination [73] [72] | Aerosols from high-concentration samples or previous runs contaminating reagents, pipettes, or work surfaces. | Can vary; often low Cq if contamination is significant. |
| Reagent Contamination [22] [72] | Master mixes, polymerases, or water contaminated with target DNA or bacterial genomic DNA (e.g., 16S rRNA). | Consistent Cq across multiple experiments. |
| Amplicon Carryover [73] | Improper handling of post-PCR products near pre-PCR setup areas. | Typically low Cq (high concentration). |
| Assay Design Issues [72] | Primer-dimers or non-specific amplification, especially with poorly optimized assays. | High Cq (late amplification, often >34 cycles). |
Phase 3: Resolution Protocols & Corrective Actions
Once you have a hypothesis for the source, implement these targeted corrective actions.
Protocol A: Eradicating Laboratory Contamination
If you suspect general laboratory contamination (amplicon carryover or aerosols), execute this comprehensive decontamination protocol.
Physical Workspace Decontamination:
- Clean Thoroughly: Wipe down all work surfaces, pipettes, and equipment with a DNA degradative agent, such as 10% bleach solution [22] [72].
- Neutralize and Rinse: Follow the cleaning by wiping with nuclease-free water or 70% ethanol to remove residual bleach that could degrade your oligonucleotides [73].
- UV Irradiation: If available, irradiate the PCR setup hood with UV light for at least 30 minutes to cross-link any residual DNA [22].
Implement Strict Workflow Segregation:
Use Aerosol-Free Consumables:
Protocol B: Replacing Contaminated Reagents
If you suspect your reagents are the source, follow this reagent management protocol.
Discard and Replace:
Implement Proper Reagent Handling:
- Create Aliquots: Aliquot probes and primers into small, single-use volumes. This minimizes freeze-thaw cycles (which degrade quality) and prevents repeated exposure of your main stock to potential contamination [73] [22].
- Use Positive Controls: Always include a well-characterized positive control and a no-template control (NTC) in every run to validate your reagents.
Protocol C: Optimizing Assay Design and Reaction Chemistry
If the problem is due to assay design, take these optimization steps.
Incorporate UNG Treatment:
- Use Uracil-N-Glycosylase (UNG) in your master mix. This enzyme degrades any PCR products from previous reactions that contain dUTP (which you can incorporate in place of dTTP), effectively preventing their re-amplification and eliminating carryover contamination [73].
Redesign Suboptimal Assays:
- Check Specificity: Perform a BLAST search to ensure your primers and probe are specific to your intended target and do not cross-react with common contaminants or other sequences in your sample [22].
- Optimize Primers: If primer-dimers are the issue, redesign primers to avoid self-complementarity. Aim for primers with similar melting temperatures (within 2-5°C) and a GC content between 30-50% [72].
- Target Unique Sequences: If using universal targets (e.g., 16S rRNA for bacterial identification), design your assay to target a hypervariable region or a novel, species-specific gene to avoid amplifying background contamination [22].
The Scientist's Toolkit: Essential Reagents for Resolving NTC Amplification
Table 2: Key Research Reagent Solutions for Troubleshooting False Positives
| Reagent / Tool | Function in Troubleshooting |
|---|---|
| UNG (Uracil-N-Glycosylase) [73] | Enzyme that digests carryover contaminant DNA from previous PCR reactions, preventing its amplification. |
| DNA Degradative Agent (e.g., 10% Bleach) [22] [72] | Used for decontaminating work surfaces and equipment by degrading DNA. |
| Sterile, Filtered Pipette Tips [73] [22] | Prevents aerosol contamination from pipettes, a common source of false positives. |
| Fresh Reagent Aliquots [73] [22] | Minimizes contamination risk and freeze-thaw cycles that degrade oligonucleotide quality. |
| Blocking Oligos / Clamps [22] | Can be used to block the amplification of common contaminant sequences (e.g., 16S rRNA), allowing your specific target to be amplified. |
| Nuclease-Free Water [22] | Certified to be free of nucleases and contaminants, used as a solvent and for dilutions. |
Frequently Asked Questions (FAQs)
Q1: My NTC shows late amplification (Cq > 38). Is this a major concern? While exponential amplification in the NTC is always a concern, late amplification is often due to primer-dimer formation rather than target contamination. Perform a melt curve analysis to confirm. If it's primer-dimer, you should still optimize your primer design or concentration to improve assay efficiency and specificity [22] [72].
Q2: I've cleaned everything and used new reagents, but my NTC is still amplifying. What now? The contaminant might be a pervasive sequence. If you are using primers for a common gene (like bacterial 16S rRNA), the contaminant could be present in the enzyme or another reagent itself. In this case, redesign your assay to target a unique, hypervariable region or use blocking oligos to suppress the contaminant's amplification [22].
Q3: How can I prevent this issue from recurring in my lab? Prevention is rooted in consistent, good laboratory practices:
- Maintain physical separation of pre-and post-PCR areas.
- Always use filtered tips and dedicated pipettes.
- Regularly decontaminate work surfaces with bleach.
- Aliquot all reagents upon receipt.
- Incorporate UNG into your standard qPCR protocol [73] [22].
In cancer research, where qPCR results directly influence the understanding of gene expression profiles like HER2 and ESR1 [34], the integrity of your negative controls is non-negotiable. By adopting this systematic, phased approach—identifying the problem, diagnosing the root cause with a logical workflow, and implementing targeted resolution protocols—you can eliminate false positives at their source. This rigorous framework not only rescues compromised experiments but also establishes a robust, contamination-aware laboratory culture, ensuring that your findings on cancer biomarkers and subtypes are both accurate and reliable.
Establishing Assay Robustness through Rigorous Validation and Comparative Analysis
Frequently Asked Questions
1. What are LOD and LoQ, and how do they differ in qPCR? The Limit of Detection (LOD) is the lowest amount of analyte in a sample that can be detected with a stated probability (e.g., 95% confidence), but not necessarily quantified as an exact value. The Limit of Quantification (LoQ), is the lowest amount of analyte that can be quantitatively determined with stated acceptable precision and accuracy [74]. In practice for qPCR, the LOD defines the minimal copy number that can be reliably detected, while the LoQ defines the level at which you can also trust the quantitative value [74] [75].
2. How can I determine the LOD for my qPCR assay? The LOD is determined through a statistical approach using a dilution series of the target. It is based on the concentration at which 95% of the positive samples are detected. This involves running multiple replicates (e.g., n=64) at very low template concentrations and applying a logistic regression model to the results to find the concentration at which the detection probability is 95% [74].
3. My no-template control (NTC) shows amplification. What should I do? Amplification in the NTC indicates contamination or primer-dimer formation [22] [3]. You should:
- Replace all reagents and thoroughly clean the PCR preparation area with 10% bleach followed by ethanol [22] [2].
- Check for primer-dimers by performing melt curve analysis [22].
- Verify probe integrity, as degraded probes can cause high background signal [22].
- Use a master mix containing Uracil-N-Glycosylase (UNG) to degrade carryover contamination from previous PCR amplifications [2] [3].
4. What are the key metrics for ensuring qPCR assay precision? Precision should be evaluated by running multiple replicates of the same sample. The variation between these replicates, especially at low copy numbers, is a key metric. Data should be highly reproducible, with replicate Cq values typically not varying by more than 1 cycle [75]. The coefficient of variation (CV) for calculated concentrations should also be determined [74].
5. How is analytical specificity validated for a cancer mutation assay? Specificity ensures the assay only detects the intended target. For cancer assays, this is critical for distinguishing mutant from wild-type sequences. Techniques include:
- In silico specificity checks using BLAST to ensure primers/probes are unique [22] [2].
- Experimental validation using samples with known mutations and wild-type-only controls to establish the false-positive rate [76].
- Using specialized chemistries like hydrolysis probes, LNA (Locked Nucleic Acid) probes, or ARMS (Amplification Refractory Mutation System) primers to enhance allele discrimination [76] [37].
Troubleshooting Guides
Guide 1: Addressing High False Positive Rates and Poor Specificity
| Symptom | Possible Cause | Corrective Action |
|---|---|---|
| Amplification in No-Template Control (NTC) | Contaminated reagents or labware [2] | Aliquot reagents; use sterile, nuclease-free tubes and filter tips; decontaminate surfaces with 10% bleach/UV [22] [2]. |
| Amplicon carryover contamination [2] [3] | Use separate physical areas for pre- and post-PCR; incorporate UNG enzyme into the master mix [2] [3]. | |
| Primer-dimer formation or non-specific amplification [22] [75] | Perform melt curve analysis; optimize primer design and annealing temperature; use "Hot-Start" PCR [2]. | |
| False positive calls in wild-type samples | Poor allele discrimination by the assay [76] | Redesign assay using specialized probes (e.g., LNA) or primers (e.g., ARMS); optimize primer/probe concentrations [76] [37]. |
Guide 2: Addressing Poor Precision and Inaccurate LoD
| Symptom | Possible Cause | Corrective Action |
|---|---|---|
| High variability between replicate Cq values | Pipetting errors or inaccurate equipment [2] | Service and calibrate pipettes regularly; use good pipetting technique; increase replicate number for low-copy targets [2] [75]. |
| PCR inhibitors in the sample [77] [3] | Purify sample DNA/RNA more thoroughly; use an internal positive control (IPC) like SPUD to detect inhibition; add BSA to the reaction mix to counteract some inhibitors [2] [3]. | |
| Inconsistent LoD determination | Insufficient number of replicates at low concentrations [74] | Perform a minimum of 16-24 replicates per dilution near the expected LoD to get a statistically robust result [74]. |
| Low PCR efficiency [75] | Re-optimize the assay; check the standard curve. Efficiency should be 90-110% [75]. |
Experimental Protocols & Data
This table shows the high sensitivity and specificity achievable with dPCR for detecting cancer mutations, which is a benchmark for qPCR validation.
| Assay Target | False Positive Rate | LoD (95% Confidence) | Amount of DNA Analyzed |
|---|---|---|---|
| EGFR L858R | 1 in 14 million | 1 mutant in 180,000 wild-type | 3.3 μg genomic DNA |
| EGFR L858R (theoretical) | (As above) | 1 mutant in >4 million wild-type | 70 million DNA copies |
| EGFR T790M | Not specified | 1 mutant in 13,000 wild-type | 3.3 μg genomic DNA |
Use this table to score the overall quality of your qPCR runs. A high-quality assay should meet these criteria.
| Metric | Ideal Result for Intercalating Dye | Ideal Result for Hydrolysis Probe |
|---|---|---|
| Linearity (R²) | ≥ 0.98 | ≥ 0.98 |
| Reproducibility | Replicate Cq variation ≤ 1 cycle | Replicate Cq variation ≤ 1 cycle |
| RFU Consistency | Max plateau fluorescence within 20% of mean | Fluorescence increase is consistent and parallel |
| Curve Steepness | Rises from baseline to plateau in ≤10 Cq | Rises to 50% max RFU in ≤10 Cq |
| Curve Shape | Sigmoidal | Reaches a horizontal asymptote |
Protocol: Determining Limit of Detection (LOD) for a qPCR Assay
- Prepare a Dilution Series: Create a serial dilution of the target nucleic acid, extending to concentrations expected to be near the detection limit (e.g., from 1000 copies/reaction down to 1 copy/reaction) [74] [75].
- Run Multiple Replicates: For each dilution, run a high number of replicates. To achieve statistical confidence at the LoD, a minimum of 16-24 replicates per dilution is recommended, with some studies using 64 or more [74].
- Include Controls: Include no-template controls (NTCs) in the run to monitor for contamination [3].
- Perform Data Analysis:
- Record the number of positive detections (e.g., Cq < cut-off) for each dilution [74].
- Use a statistical model, such as logistic regression, to analyze the proportion of positive replicates versus the log concentration.
- The LOD is defined as the concentration at which the probability of detection is 95% [74].
Protocol: Establishing Assay Specificity and False Positive Rate
- Test Wild-Type-Only Samples: Analyze a large number of replicates (e.g., N=58-71) that contain only wild-type DNA [76].
- Quantify False Positives: Count the number of wells that incorrectly show a positive signal for the mutant target.
- Calculate the False Positive Rate: The rate is calculated as the average number of false-positive events divided by the number of wild-type molecules tested (RFP = ΛFP / #WT) [76]. A robust assay will have an exceptionally low false-positive rate, such as 1 in 14 million [76].
Research Reagent Solutions
| Reagent / Material | Function in Validation | Example / Consideration |
|---|---|---|
| Synthetic Template (e.g., gBlocks, Plasmids) | Positive control for assay optimization; creating standard curves for LoD/LoQ [76] | Use linearized plasmid or fragmented synthetic DNA to mimic real sample templates [76]. |
| Wild-Type Genomic DNA | Determining the false-positive rate and analytical specificity [76] | Use commercially available high-quality genomic DNA from healthy donors. |
| LNA/DNA Probes | Increases hybridization affinity and specificity, improving allele discrimination in mutation detection [76] [37] | Ideal for distinguishing single-nucleotide variants (e.g., EGFR T790M) [76]. |
| UNG/Uracil-DNA-glycosylase | Prevents false positives by degrading carryover contamination from previous PCR amplicons [2] [3] | Often included in commercial master mixes. |
| Blocking Oligos / Clamps | Suppresses amplification of wild-type sequences, enriching for mutant targets and improving sensitivity [37] | Used in techniques like PNA-clamping or the PNB-qPCR method [37]. |
| ARMS Primers | Selectively amplifies mutant alleles by exploiting the low efficiency of primers with a 3'-mismatch, enhancing specificity [37] | A core component in many allele-specific PCR assays. |
Workflow Diagrams
Workflow for Determining the Limit of Detection (LOD)
Troubleshooting Guide for Contamination and Specificity
Core Chemistry and Mechanism
Frequently Asked Questions
What are the fundamental mechanism differences between SYBR Green and hydrolysis probes? SYBR Green is a fluorescent dye that binds non-specifically to the minor groove of all double-stranded DNA (dsDNA) present in the reaction. The fluorescence increases 1,000-fold upon binding to dsDNA, providing a direct measure of total amplified DNA accumulation [78]. In contrast, hydrolysis probes (like TaqMan) are sequence-specific, dual-labeled oligonucleotides that rely on the 5' nuclease activity of Taq DNA polymerase. The probe contains a fluorescent reporter dye on the 5' end and a quencher dye on the 3' end. When intact, the quencher suppresses the reporter's fluorescence through fluorescence resonance energy transfer (FRET). During amplification, the polymerase cleaves the probe, separating the reporter from the quencher and generating a fluorescent signal proportional to target amplification [78] [79].
Which chemistry provides better specificity for detecting cancer targets, and why? Hydrolysis probes provide inherently higher specificity for cancer targets because fluorescence generation requires specific hybridization between the probe and its complementary target sequence [79]. This is particularly crucial in cancer research where distinguishing between homologous sequences or single nucleotide polymorphisms (SNPs) can be vital. SYBR Green detects all dsDNA, including non-specific products and primer-dimers, which can lead to false positives. However, its specificity can be significantly improved through rigorous primer optimization and melt curve analysis [78] [79].
Experimental Workflow
The diagram below illustrates the key procedural differences when using these two chemistries in a typical experiment for cancer target detection.
Performance Comparison for Cancer Research
The table below summarizes the comparative performance of SYBR Green and Hydrolysis Probes, drawing from general qPCR principles and specific cancer study data [78].
Table 1: Performance Comparison of SYBR Green vs. Hydrolysis Probes
| Parameter | SYBR Green | Hydrolysis Probes (TaqMan) |
|---|---|---|
| Specificity | Lower* | Higher |
| Sensitivity (Low Copy Detection) | Variable* | 1-10 copies |
| Reproducibility | Medium* | High |
| Multiplexing Capability | No | Yes |
| Assay Design Complexity | User-designed primers required | Predesigned assays available |
| Cost | Lower | Higher |
| Efficiency | >95% (when optimized) [78] | >97% [78] |
| Key Applications in Cancer Research | Mycoplasma testing, NGS library quantification, Telomere length, ChIP [79] | Gene expression, miRNA analysis, Copy number variation, SNP genotyping, MRD detection [80] [79] |
*Depends heavily on template quality and primer design/optimization [79].
Key Experimental Protocol: Comparative Gene Expression Analysis
A study comparing SYBR Green and TaqMan methods for analyzing adenosine receptor gene expression in breast cancer tissues provides a robust methodological framework [78].
Sample Preparation:
- Breast cancer tissue samples were obtained and immediately stored in liquid nitrogen at -80°C.
- Total RNA was extracted using a commercial kit (e.g., RNeasy plus mini kit, Qiagen).
- RNA quality and concentration were verified using UV absorption (260/280 nm) and denaturing agarose gel electrophoresis.
cDNA Synthesis:
- 1 μg of total RNA was reverse transcribed using a commercial reverse transcription kit (e.g., Quantitect Rev. transcription kit, Qiagen).
qPCR Setup:
- TaqMan Assay: Reaction mixtures contained cDNA template, Assays-on-Demand primer and probe mix, and TaqMan Universal PCR master mix. Cycling conditions: 95°C for 10 min, followed by 40 cycles of 95°C for 10 s and 60°C for 20 s.
- SYBR Green Assay: Reaction mixtures contained cDNA template, custom-designed primers (designed with Beacon Designer software), and Quantitect SYBR Green master mix. Cycling conditions were comparable to the TaqMan protocol.
Data Analysis:
- All samples were run in triplicate.
- Threshold cycle (Ct) values were determined.
- Gene expression data were normalized to the Beta-actin (ACTB) reference gene using the ΔCt method: ΔCt = Ct (Gene of Interest) - Ct (ACTB).
Troubleshooting False Positives
Troubleshooting Guide
Problem: Amplification in No-Template Control (NTC) wells.
- Potential Causes & Solutions:
- Contaminated Reagents: Replace all reagents, enzymes, and buffers with fresh aliquots. Use sterile, nuclease-free water and tubes [22] [2].
- Environmental Contamination: Decontaminate PCR work areas, pipettes, and equipment with 10% bleach, followed by 70% ethanol or UV irradiation. Use separate work areas for pre- and post-PCR steps [22] [2].
- Carry-over Contamination: Use a master mix containing Uracil-DNA-glycosylase (UNG) to degrade PCR products from previous reactions [2] [3].
- Primer-Dimers (SYBR Green): If amplification occurs late (e.g., beyond cycle 34), perform melt curve analysis. Redesign primers if a lower-temperature peak indicates primer-dimer formation [22] [81].
- Probe Degradation (TaqMan): Check probe integrity via signal-to-noise assessment, mass spectrometry, or a fluorometric scan. Use fresh probe aliquots [22].
Problem: Non-specific peaks in melt curve (SYBR Green only).
- Potential Causes & Solutions:
- Non-specific Amplification: Optimize primer annealing temperature. Use touchdown PCR, starting 5°C–10°C above the primer Tm and decreasing incrementally [2].
- Primer-Dimers: Redesign primers to avoid self-complementarity. Utilize hot-start PCR to prevent spurious amplification during reaction setup [2].
- gDNA Contamination: Treat samples with DNase I during RNA isolation. Include a no-reverse transcription control (no-RT) to detect genomic DNA contamination [81] [3].
Problem: High background noise (TaqMan only).
- Potential Causes & Solutions:
Advanced Specificity Techniques for Cancer Targets
How can I enhance specificity for detecting single-nucleotide variants or low-abundance transcripts in cancer?
- Use TaqMan MGB Probes: These probes incorporate a Minor Groove Binder moiety at the 3' end, which increases the probe's melting temperature (Tm) and allows for the use of shorter probes. This results in greater discrimination between matched and mismatched targets, making them ideal for SNP genotyping and allelic discrimination in cancer genes [79].
- Locked Nucleic Acid (LNA) Probes: LNA nucleotides can be incorporated into probes or primers to dramatically increase binding affinity and specificity. This technology has been successfully applied in sensitive quantitative PCR assays for minimal residual disease (MRD) detection in lymphomas, such as those with t(11;14) and t(14;18) translocations [80].
- Blocking Oligos: For assays where universal primers (e.g., targeting conserved regions) might bind to non-target sequences, use blocking oligonucleotides to suppress amplification of common background sequences and enhance the amplification of your rare cancer target [22].
Research Reagent Solutions
The table below lists essential materials and reagents for implementing these qPCR chemistries in a cancer research setting, based on the protocols and troubleshooting advice cited.
Table 2: Essential Research Reagent Solutions for qPCR Cancer Assays
| Item | Function | Example Products/Brands |
|---|---|---|
| Hot-Start DNA Polymerase | Reduces non-specific amplification and primer-dimer formation by inhibiting polymerase activity at low temperatures. | Various commercial Hot-Start Master Mixes |
| UNG/UDG Enzyme | Prevents carry-over contamination by degrading uracil-containing PCR products from previous runs. | Included in many commercial master mixes [3] |
| TaqMan MGB Probes | Provides superior mismatch discrimination for SNP detection and allelic discrimination in cancer genes. | Applied Biosystems TaqMan MGB Probes [79] |
| LNA-containing Oligos | Enhances hybridization affinity and specificity for challenging targets like low-abundance transcripts. | LNA probes and primers [80] |
| Nuclease-free Water & Tubes | Prevents sample degradation and external nucleic acid contamination. | Various suppliers (e.g., IDT buffers [22]) |
| RNA Isolation Kit | Ensures high-quality, intact RNA from tissue samples (e.g., tumor biopsies). | RNeasy plus mini kit (Qiagen) [78] |
| Reverse Transcription Kit | Produces high-yield cDNA for sensitive detection of low-expression genes. | Quantitect Rev. transcription kit (Qiagen) [78] |
Chemistry Selection Workflow
To aid in selecting the appropriate chemistry for a given project, use the following decision workflow.
In cancer research, quantitative PCR (qPCR) serves as a powerful technique for detecting and quantifying biomarkers with high sensitivity. However, this same sensitivity makes it vulnerable to false positives, which can compromise research validity and clinical translation. Benchmarking against gold standards—highly accurate experimental procedures like imaging and histopathology—provides an essential framework for verifying qPCR assay performance. This process uses robust, comprehensive evaluations to establish ground truth, enabling researchers to distinguish true biological signals from artifacts. For molecular diagnostics in oncology, where treatment decisions may hinge on detecting minute quantities of cancer DNA or RNA, rigorous correlation with established gold standard methods is not merely beneficial but essential for ensuring reliable, clinically actionable results [82] [83].
This technical support guide provides a structured approach to validating qPCR results against gold standard methodologies, offering troubleshooting advice and detailed protocols to enhance the reliability of your cancer assays.
Core Principles of Benchmarking qPCR Assays
What Constitutes a Gold Standard in Cancer Research?
In the context of qPCR for cancer research, a "gold standard" refers to a method or combination of methods with proven, high diagnostic accuracy for confirming the presence or absence of a specific cancer biomarker or pathological state. These often include:
- Histopathological analysis: Microscopic examination of tissue sections by a qualified pathologist remains the definitive standard for diagnosing cancer type, grade, and stage [82].
- Immunohistochemistry (IHC): Detection of specific protein biomarkers in tissue sections provides spatial context and protein-level validation.
- High-accuracy sequencing methods: Techniques like Sanger sequencing, though slower and more costly, are often used to validate DNA-level variations such as single-nucleotide variants (SNVs) and insertions/deletions (indels) identified in screening assays [84].
- Imaging techniques: Modalities like MRI, CT, and PET scans serve as in vivo standards for tumor localization, size, and metastatic burden.
The fundamental principle of benchmarking is to run your qPCR assay on samples with well-characterized status as determined by these gold standards, then compare the results to calculate performance metrics such as sensitivity, specificity, and predictive values [82] [85].
The Consequences of Inadequate Validation
Failure to properly validate qPCR assays against appropriate standards can have profound consequences. In research, it can lead to the publication of incorrect conclusions and wasted resources pursuing false leads. In the clinical realm, the implications are even more serious, potentially resulting in misdiagnosis, inappropriate treatment choices, and undue patient stress [3] [83]. A survey of qPCR studies in colorectal cancer research revealed that 97% of publications could not be reliably assessed for validity, primarily due to inadequate normalization procedures and lack of proper validation [86]. This highlights a pervasive problem in the field and underscores the necessity of the rigorous benchmarking approach outlined in this guide.
Experimental Protocols for Benchmarking
Protocol 1: Correlating qPCR with Histopathology for Tumor Detection
Objective: To validate a qPCR assay designed to detect a specific cancer biomarker by comparing its results with histopathological findings.
Materials:
- Matatched tissue samples: Fresh-frozen for qPCR and FFPE for histopathology from the same biopsy
- RNA/DNA extraction kits
- qPCR reagents: primers, probes, master mix
- Histopathology supplies: staining reagents, antibodies for IHC if applicable
Methodology:
- Sample Processing: Divide each patient biopsy, processing one portion for standard histopathology (FFPE embedding) and another for nucleic acid extraction (snap-freezing).
- Pathology Assessment: A pathologist, blinded to the qPCR results, examines the H&E-stained sections and performs IHC for relevant markers, documenting tumor content, grade, and marker status.
- Nucleic Acid Extraction: Isolve DNA/RNA from the frozen portion, quantifying yield and quality.
- qPCR Analysis: Perform qPCR for the target biomarker using validated assays with appropriate controls.
- Data Correlation: Create a contingency table comparing qPCR results (positive/negative) against the pathological diagnosis.
Table 1: Example Data Structure for Correlation with Histopathology
| Sample ID | Pathology Result | qPCR Ct Value | qPCR Interpretation | Concordance |
|---|---|---|---|---|
| PT_01 | Positive | 22.5 | Positive | Yes |
| PT_02 | Positive | 35.2 | Negative | No |
| PT_03 | Negative | Undetermined | Negative | Yes |
| PT_04 | Negative | 28.1 | Positive | No |
Protocol 2: Orthogonal Validation Using Sequencing Methods
Objective: To confirm the specificity of qPCR-detected genetic alterations using an orthogonal sequencing method.
Materials:
- DNA/cDNA samples
- qPCR reagents
- Sequencing reagents and platform (e.g., Sanger, NGS)
- Bioinformatics tools for sequence analysis
Methodology:
- Sample Selection: Choose samples spanning a range of qPCR results (positive, negative, equivocal).
- qPCR Analysis: Run the qPCR assay under standard conditions.
- Amplicon Sequencing: Design primers to amplify the region of interest for sequencing. Purify PCR products and perform Sanger sequencing or prepare libraries for NGS.
- Sequence Alignment: Align resulting sequences to the reference genome to identify mutations or expression variants.
- Discrepancy Resolution: Investigate samples with discordant results between qPCR and sequencing. This may involve repeating assays, trying different techniques, or using a third method for arbitration [82] [84].
Table 2: Performance Metrics for qPCR vs. Sequencing Gold Standard
| Metric | Calculation | Target Value | Experimental Result |
|---|---|---|---|
| Sensitivity | TP/(TP+FN) | >95% | |
| Specificity | TN/(TN+FP) | >95% | |
| PPV | TP/(TP+FP) | >95% | |
| NPV | TN/(TN+FN) | >95% | |
| Overall Accuracy | (TP+TN)/Total | >98% |
Troubleshooting Common Benchmarking Challenges
FAQ 1: My qPCR results show poor concordance with histopathology. What could be causing this?
Potential Causes and Solutions:
- Sample heterogeneity: Tumor tissue is often heterogeneous, and the portions used for histology and molecular analysis may contain different proportions of tumor cells.
- Solution: Macrodissect or laser-capture microdissect the histology slide to enrich for tumor cells from the exact same area before nucleic acid extraction.
- Assay limit of detection (LOD): Your qPCR assay may not be sensitive enough to detect low-level biomarkers in samples with low tumor content.
- Solution: Determine the LOD of your qPCR assay using a dilution series of positive control material. Consider using digital PCR for absolute quantification and improved sensitivity at low target concentrations [76].
- Pre-analytical variables: Differences in sample handling, fixation times, or nucleic acid extraction methods can significantly impact results.
- Solution: Standardize pre-analytical conditions across all samples and document any deviations meticulously.
FAQ 2: How do I handle discrepant results between qPCR and the gold standard method?
Systematic Approach:
- Repeat the assays: Technical errors can occur in both qPCR and gold standard methods.
- Employ a third arbitration method: Use an alternative technology to break the tie. For example, if qPCR and IHC disagree, use RNA in situ hybridization to visualize RNA expression directly in tissue sections.
- Review assay design: For qPCR, check primer/probe specificity using BLAST and ensure optimal reaction efficiency (90-110%). Update assays if in silico analysis reveals potential cross-reactivity [83] [22].
- Consider biological context: Some discrepancies may reflect genuine biological differences, such as post-transcriptional regulation causing mRNA-protein discordance.
Essential Controls and Reagents for Robust Benchmarking
Critical Experimental Controls
Implementing appropriate controls is fundamental for distinguishing true results from false positives:
- No template controls (NTCs): Contain all reaction components except the nucleic acid template. Amplification in NTCs indicates contamination [3] [22].
- No reverse transcription controls (for RNA assays): Detect amplification of contaminating genomic DNA.
- Positive controls: Samples with known status verify assay functionality.
- Reference genes: For gene expression studies, use multiple validated reference genes with stable expression in your specific sample type. Common reference genes like GAPDH and β-actin can vary significantly in cancer tissues [86] [84].
Research Reagent Solutions
Table 3: Essential Reagents for qPCR Benchmarking Studies
| Reagent/Category | Function | Key Considerations |
|---|---|---|
| Nucleic Acid Isolation Kits | Extract high-quality DNA/RNA from tissue | Choose kits validated for your sample type (e.g., FFPE); assess integrity (RNA Integrity Number) |
| qPCR Master Mixes | Provide enzymes, buffers, dNTPs for amplification | Select with UNG/Uracil DNA Glycosylase to prevent amplicon contamination; verify efficiency |
| Validated Primers/Probes | Specifically amplify and detect target sequence | Design to span exon-exon junctions (RNA); perform BLAST for specificity; test efficiency |
| Reference Gene Assays | Normalize sample-to-sample variation | Use multiple validated genes; avoid commonly variable genes like GAPDH without validation |
| Quantified Control Materials | Generate standard curves; assess assay performance | Use synthetic oligonucleotides or cell line DNA with known copy numbers |
Quality Assurance and Data Interpretation
Establishing Analytical Performance Metrics
Before comparing qPCR to gold standards, fully characterize your assay's analytical performance:
- Linear dynamic range: The range of template concentrations over which the fluorescent signal is directly proportional to DNA concentration. Test using a 7-point, 10-fold dilution series of control material with at least three replicates per dilution. Acceptable linearity requires R² ≥ 0.980 [83].
- Limit of detection (LOD): The lowest concentration of analyte that can be reliably detected. Determine using a dilution series approaching the expected lower limit, with LOD typically defined as the concentration detected in 95% of replicates [76] [85].
- Precision: The closeness of agreement between independent measurements. Assess through repeatability (same operator, same day) and reproducibility (different operators, different days) experiments [85].
Implementing a Standardized Benchmarking Workflow
The following workflow diagram illustrates a systematic approach to benchmarking qPCR assays against gold standards:
Correlating qPCR results with imaging and histopathology gold standards is not a single experiment but an ongoing quality assurance process. By implementing the protocols, controls, and troubleshooting approaches outlined in this guide, researchers can significantly enhance the reliability of their qPCR data. This rigorous approach to validation is especially critical in cancer research, where the stakes for accurate detection and quantification are high, and the consequences of false positives can ripple from benchtop to bedside. As technologies evolve and new biomarkers emerge, the principles of systematic benchmarking remain constant—providing the foundation for trustworthy molecular analyses that can confidently inform both scientific understanding and clinical practice.
Utilizing Computational Algorithms (geNorm, NormFinder, BestKeeper) for Reference Gene Stability Assessment
Accurate gene expression analysis using quantitative real-time PCR (qRT-PCR) is fundamental in cancer research, particularly in the quest to identify reliable biomarkers and therapeutic targets. A crucial, yet often overlooked, step in ensuring data accuracy is the normalization of qPCR results using stably expressed reference genes, also known as housekeeping genes (HKGs). The use of inappropriate reference genes is a significant source of technical variability that can lead to false positives or false negatives, ultimately compromising research validity and the development of clinical assays [18] [87].
The Minimum Information for Publication of Quantitative Real-Time PCR Experiments (MIQE) guidelines strongly recommend the validation of reference gene stability for each specific experimental condition [87] [88]. This is because the expression of commonly used HKGs, such as GAPDH and ACTB, can vary considerably under different pathological or treatment conditions, including cancer [18] [87] [89]. For instance, in dormant cancer cells induced by mTOR inhibition, genes like ACTB, RPS23, RPS18, and RPL13A undergo dramatic expression changes and are categorically unsuitable for normalization [18].
To address this challenge, computational algorithms such as geNorm, NormFinder, and BestKeeper have been developed to objectively rank candidate reference genes based on their expression stability. This technical support guide provides detailed troubleshooting and best practices for employing these algorithms to enhance the reliability of your qPCR data in cancer research.
Three primary algorithms are widely used for reference gene stability assessment. The table below summarizes their core methodologies, outputs, and key considerations.
Table 1: Key Computational Algorithms for Reference Gene Stability Assessment
| Algorithm | Core Principle | Stability Measure | Key Output | Special Consideration |
|---|---|---|---|---|
| geNorm [90] [87] | Pairwise comparison of expression ratios between candidate genes. | M-value: Lower M-value indicates higher stability. A value ≤ 1.5 is generally acceptable [91]. | Ranks genes by stability; Determines the optimal number of genes via pairwise variation (Vn/Vn+1). A V-value < 0.15 suggests that 'n' genes are sufficient [92] [87]. | Does not directly evaluate co-regulation; prone to selecting genes with co-regulated expression. |
| NormFinder [87] [89] | Model-based approach to estimate intra- and inter-group variation. | Stability Value: Lower value indicates higher stability. Considers sample subgroups (e.g., healthy vs. diseased). | Ranks genes by stability; Favors genes that are stable across defined groups, reducing group-specific bias. | Superior to geNorm when sample sets contain distinct subgroups. |
| BestKeeper [87] [91] | Analyses the raw Cq (quantification cycle) values of each candidate gene. | Standard Deviation (SD) & Coefficient of Variation (CV): Lower SD/CV indicates higher stability. Genes with SD > 1 are considered unstable [91]. | Provides an index based on the geometric mean of the best genes. | Works best with a small number of pre-defined candidate genes. Uses raw Cq values, not transformed data. |
| RefFinder [92] [93] | A comprehensive web-based tool that integrates the other algorithms. | Geomean of Ranking Values: Provides an overall final ranking. | Combines results from geNorm, NormFinder, BestKeeper, and the comparative ΔCt method into a single consensus ranking. | Offers a robust, consolidated recommendation, minimizing the limitations of any single algorithm. |
The following workflow diagram illustrates a recommended strategy for integrating these tools:
Diagram 1: Workflow for reference gene validation.
Frequently Asked Questions (FAQs) and Troubleshooting Guides
FAQ 1: Why is it necessary to use multiple algorithms instead of just one?
Each algorithm has unique strengths and potential biases. Using multiple tools provides a consensus view, increasing confidence in the final gene selection.
- geNorm is highly effective at finding the most stable pair of genes but may select co-regulated genes, which is not ideal [90].
- NormFinder is better at handling experimental subgroups (e.g., tumor vs. normal tissue) and is less likely to be misled by co-regulation [89].
- BestKeeper uses raw Cq values and provides a straightforward measure of variability [91].
- Solution: Always use at least two algorithms, such as geNorm and NormFinder. For the most robust validation, use all three and compile the results with RefFinder to get a comprehensive ranking [92] [93]. This integrated approach is considered best practice.
FAQ 2: I have my candidate gene rankings, but how do I decide on the final number of reference genes to use?
The optimal number is determined using geNorm's pairwise variation (V), calculated as Vn/Vn+1.
- Interpretation: A pairwise variation value below 0.15 indicates that the inclusion of an additional reference gene is not necessary, and 'n' genes are sufficient for reliable normalization [92] [87].
- Example: If V2/3 (the pairwise variation between the 2-gene and 3-gene normalization factors) is 0.12, then using the top two most stable genes is acceptable. If it is above 0.15, you should include the third gene and check V3/4.
- Best Practice: The MIQE guidelines recommend using a minimum of two validated reference genes [87] [88]. In cancer research, where heterogeneity is high, using a combination of three genes is often advisable.
FAQ 3: My most stable genes are all from the same functional pathway (e.g., ribosomal proteins). Is this a problem?
Yes, this can be problematic. Genes from the same functional pathway are often co-regulated, meaning their expression may change in a correlated manner under certain conditions. This violates the principle that reference genes should be independent.
- The Risk: Using co-regulated genes for normalization can mask true biological variation or introduce bias, leading to inaccurate results [94].
- Solution: If your top-ranked genes are functionally related (e.g., multiple ribosomal proteins), consult the NormFinder ranking. NormFinder is less susceptible to this issue. Consider selecting the highest-ranked gene from a different functional class to create a combination of non-co-regulated genes [90] [94]. For example, pair a ribosomal protein gene with a gene involved in a different cellular process, like HPRT or B2M.
FAQ 4: What are some common pitfalls when preparing data for these algorithms?
- Pitfall 1: Incorrect Data Input. A common error is using transformed expression data (like 2^-ΔΔCq) instead of the raw Cq values for geNorm and NormFinder.
- Solution: geNorm and NormFinder require Cq values as input. BestKeeper also uses raw Cq values. Do not transform your data before analysis [91].
- Pitfall 2: Ignoring PCR Efficiency.
- Solution: The algorithms assume that the PCR amplification efficiencies of your candidate genes are similar and close to 100%. Always calculate primer efficiency from a standard curve (slope of -3.32 indicates 100% efficiency). Efficiencies between 90% and 110% are generally acceptable. Genes with widely different efficiencies should not be compared directly [95].
- Pitfall 3: Overlooking Sample Subgroups.
Case Study in Cancer Research: Reference Gene Validation in Dormant Cancer Cells
Context: A 2025 study investigated gene expression in dormant cancer cells generated by pharmacological inhibition of the mTOR kinase, a common mechanism in cancer cell survival [18].
Challenge: mTOR inhibition causes a global rewiring of cellular functions, profoundly affecting the expression of many standard housekeeping genes. Using an unstable reference gene would severely distort the expression profile of target genes.
Methodology: Researchers analyzed 12 candidate reference genes (GAPDH, ACTB, TUBA1A, RPS23, RPS18, RPL13A, PGK1, EIF2B1, TBP, CYC1, B2M, and YWHAZ) in three cancer cell lines (A549, T98G, PA-1) treated with the mTOR inhibitor AZD8055. Expression stability was assessed using geNorm, NormFinder, and BestKeeper.
Key Findings:
- Unstable Genes: ACTB (cytoskeleton) and ribosomal genes RPS23, RPS18, and RPL13A underwent "dramatic changes" and were deemed "categorically inappropriate" for normalization in this model.
- Stable Genes: The optimal reference genes were cell line-specific:
- A549 cells: B2M and YWHAZ
- T98G cells: TUBA1A and GAPDH
- PA-1 cells: No single optimal gene was found, highlighting the need for rigorous validation in each model system.
Conclusion: The study demonstrated that an incorrect selection of a reference gene resulted in a "significant distortion of the gene expression profile in dormant cancer cells," underscoring the critical importance of algorithm-based validation in specific cancer models to avoid false conclusions [18].
Essential Research Reagent Solutions
The following table lists key reagents and resources commonly used in reference gene validation studies, as cited in recent literature.
Table 2: Key Research Reagents and Resources for Reference Gene Validation
| Reagent / Resource | Function / Description | Example from Literature |
|---|---|---|
| RNA Isolation Kit | To extract high-quality, intact total RNA from samples. | RNeasy Plant Mini Kit (Qiagen) [92]; RNeasy Mini Lipid Tissue Kit (Qiagen) [87] |
| cDNA Synthesis Kit | To reverse transcribe RNA into stable cDNA for qPCR amplification. | Maxima H Minus Double-Stranded cDNA Synthesis Kit (Thermo Scientific) [92]; RevertAid First Strand cDNA Synthesis Kit (Thermo Scientific) [87] |
| qPCR Master Mix | A optimized cocktail containing polymerase, dNTPs, buffers, and fluorescent dye for real-time detection. | SYBR Green-based kits are widely used for gene expression studies [95]. |
| Statistical Algorithm Software | Tools to calculate gene expression stability from raw Cq values. | geNorm, NormFinder, BestKeeper: Often integrated into qPCR platform software or available as standalone tools. RefFinder: A free, web-based tool that integrates all three [92] [93]. |
| Validated Primer Sets | Gene-specific primers with high amplification efficiency (~90-110%) and a single, specific amplification product. | Primers must be designed and validated for each candidate gene and species. Efficiency is confirmed via standard curve; specificity by melt curve analysis [18] [95]. |
Standard Operating Protocol: Establishing Inter-laboratory Reproducibility
This guide provides a detailed methodology for validating the inter-laboratory reproducibility of qPCR assays, which is essential for reducing false positives in cancer research and ensuring reliable clinical translation.
Experimental Design and Sample Preparation
A properly designed inter-laboratory study requires careful planning and sample characterization. Follow this validated protocol to establish reproducibility for your qPCR assay.
Sample Selection and Characterization:
- Sample Size and Composition: Select a minimum of 510 samples to achieve statistical power, following international validation guidelines. The sample set should contain approximately 30% positive specimens as determined by a clinically validated reference assay [96].
- Sample Processing: Collect cervical samples in PreservCyt liquid-based cytology media (ThinPrep) according to manufacturer recommendations and European guidelines. Prepare three 1mL aliquots from the original solution within 3 days of collection and store at room temperature [96].
- Blinded Testing: Code all samples to ensure blinding and minimize bias during testing and analysis [97] [96].
Reference Method Validation:
- Validate all samples using a clinically validated reference method prior to inter-laboratory testing. The RIATOL qPCR assay targeting E6/E7 genes of 18 HPV genotypes represents one such validated approach [96].
- Ensure the reference method demonstrates high sensitivity and specificity for the targets of interest through prior clinical validation [96].
Laboratory Testing Protocol
Intra-laboratory Testing:
- Conduct two independent testing runs in the primary laboratory with a minimum 4-week interval between runs using the same equipment and reagents [96].
- Follow manufacturer instructions precisely for cartridge-based systems. For tissue samples, use sections totaling 5-10μm thickness with minimum 20% tumor cell content [60].
Inter-laboratory Testing:
- Select participating laboratories with demonstrated competency in molecular diagnostics and qPCR techniques.
- Distribute identical aliquots to all participating laboratories with standardized operating procedures.
- For the third aliquot, ship to the validation laboratory under appropriate conditions while maintaining sample stability [96].
Quality Control Measures:
- Include internal controls for sample processing and amplification in each run [60].
- Monitor amplification curves and Cq values for consistency. For the IdyllaTM system, review results through the manufacturer's web application [60].
- Re-test any samples yielding "INVALID" results, as initial failures may indicate assay rather than sample issues [96].
Data Analysis and Interpretation
Statistical Analysis:
- Calculate overall percentage agreement as the proportion of concordant results (positive + negative) over all test results.
- Compute binomial exact 95% confidence intervals for agreement percentages.
- Determine Cohen's Kappa values with 95% confidence intervals as proposed by Fleiss to measure agreement beyond chance [96].
Interpretation Against Validation Criteria: The international validation criteria for HPV assays require:
- Lower bound of the 95% confidence interval for intra- and inter-laboratory agreement must exceed 87%
- Kappa value must be ≥0.5 [97] [96]
Exemplary performance was demonstrated by the RIATOL qPCR assay with intra-laboratory agreement of 98.2% (95% CI: 96.6-99.1%) and kappa of 0.96, and inter-laboratory agreement of 98.5% (95% CI: 97.1-99.4%) with kappa of 0.97 [97].
Table 1: Exemplary Reproducibility Results from Validation Studies
| Assay Name | Type of Reproducibility | Overall Agreement % (95% CI) | Kappa Value (95% CI) | Meeting Validation Criteria? |
|---|---|---|---|---|
| RIATOL qPCR HPV assay | Intra-laboratory | 98.2% (96.6-99.1%) | 0.96 (0.888-0.961) | Yes |
| RIATOL qPCR HPV assay | Inter-laboratory | 98.5% (97.1-99.4%) | 0.97 (0.917-0.978) | Yes |
| Xpert HPV assay | Intra-laboratory | 96.9% (95.0-98.2%) | 0.925 (0.888-0.961) | Yes |
| Xpert HPV assay | Inter-laboratory | 97.8% (96.2-98.9%) | 0.948 (0.917-0.978) | Yes |
Troubleshooting Guide: Addressing Common Inter-laboratory Validation Challenges
Problem 1: False Positive Results in Mutation Detection
Background: A 2025 study investigating EGFR S768I mutation detection in NSCLC found an 80% false positive rate with the IdyllaTM qPCR system, where only 1 of 5 positive results was confirmed by NGS [60].
Symptoms:
- Positive results with normalized fluorescence values below 12 points
- Discordant results between different testing methods
- No clear correlation with sample quantity or tumor content [60]
Solutions:
- Confirmatory Testing: Implement orthogonal verification using Next-Generation Sequencing (NGS) for all positive results, particularly when making therapeutic decisions [60].
- Protocol Modification: Use extracted DNA instead of direct tissue analysis, which demonstrated improved accuracy (0.833 vs. 0.333) and better agreement with NGS (Kappa = 0.571 vs. 0.077) [60].
- Threshold Adjustment: Review and adjust interpretation algorithms, as false positives typically show low fluorescence values [60].
Problem 2: Inconsistent Ct Values Across Laboratories
Background: The Xpert HPV assay validation showed inconsistencies in Ct values, particularly in fluorescent channel 3 (HPV types 31, 33, 35, 52, 58), with differences up to 8.6 cycles [96].
Symptoms:
- Large variations in Ct values for the same samples across laboratories
- Highest discrepancies in multi-target detection channels
- Borderline results near the detection limit [96]
Solutions:
- Standardized Analysis: Implement uniform thresholding algorithms across laboratories
- Data Review: Regularly review amplification curves and Ct values through manufacturer web applications
- Threshold Optimization: Apply no-template control-informed thresholding (ddpcRquant) to mitigate false-positive/false-negative findings, particularly for low-level targets [98]
Problem 3: Invalid Results and Assay Failures
Background: During Xpert HPV validation, 16 of 1530 runs (approximately 1%) produced invalid results initially, though re-testing yielded valid results [96].
Symptoms:
- Invalid result flags despite proper sample collection
- Internal control failures indicating assay rather than sample issues
- Inconsistent failure patterns across laboratories [96]
Solutions:
- Re-testing Protocol: Automatically re-test samples yielding invalid results, as initial failures often resolve on repeat testing [96].
- Equipment Maintenance: Ensure regular calibration and maintenance of instrumentation
- Process Control: Implement automated liquid handling systems to reduce human error and improve reproducibility [52]
Problem 4: Poor RNA Quality Affecting Gene Expression Analysis
Background: In cancer research, particularly studies involving dormant cancer cells, RNA quality significantly impacts reference gene stability and overall results [18].
Symptoms:
- Unstable reference gene expression across experimental conditions
- Inconsistent results between replicates
- Poor amplification efficiency [18]
Solutions:
- Reference Gene Validation: Systematically evaluate reference gene stability under specific experimental conditions. For example, in dormant cancer cells generated by mTOR inhibition, avoid ACTB, RPS23, RPS18, and RPL13A, which show dramatic expression changes [18].
- RNA Quality Control: Implement rigorous RNA purification and clean-up procedures to ensure high integrity and absence of inhibitors [52].
- Primer Validation: Assess primer specificity using determination coefficients (R²) and efficiency coefficients (E) from serial cDNA dilutions, supplemented by melt curve analyses [18].
Frequently Asked Questions (FAQs)
What are the international validation criteria for inter-laboratory reproducibility of qPCR assays?
The international criteria for HPV assays, which can be generalized to cancer qPCR assays, require that the lower bound of the 95% confidence interval for both intra- and inter-laboratory agreement exceeds 87%, with a kappa value ≥0.5. These criteria ensure sufficient reproducibility for clinical application [97] [96].
How many samples are needed for a proper inter-laboratory validation study?
Validation studies should include at least 510 samples with approximately 30% positive specimens as determined by a clinically validated reference method. This provides sufficient statistical power to demonstrate reproducibility [96].
What is the difference between analytical and clinical performance validation?
Analytical performance includes trueness, precision, analytical sensitivity, and specificity, while clinical performance includes diagnostic sensitivity, specificity, and predictive values. Both must be validated for clinical translation [85].
How can we handle discordant results between laboratories?
First, review amplification curves and Cq values. Discordant results often occur near the detection limit. Establish a predefined protocol for arbitration testing using a reference method or alternative technology [60] [96].
What reference genes are most stable for cancer cell qPCR studies?
Reference gene stability varies by cell type and treatment. In mTOR-inhibited cancer cells, ACTB, RPS23, RPS18, and RPL13A are unstable. Instead, use B2M and YWHAZ for A549 cells, TUBA1A and GAPDH for T98G cells [18].
How can automation improve inter-laboratory reproducibility?
Automated systems enhance precision in liquid handling, reduce human error, minimize contamination risk, and increase throughput. Systems like the I.DOT Liquid Handler accurately handle volumes as low as 4nL, ensuring consistent Ct values [52].
The Scientist's Toolkit: Essential Materials for Validation Studies
Table 2: Key Research Reagent Solutions for Inter-laboratory Validation
| Reagent/Kit | Manufacturer | Function in Validation | Key Considerations |
|---|---|---|---|
| IdyllaTM EGFR Mutation Test | Biocartis | Fully automated EGFR mutation detection | Integrated sample processing; detects 51 mutations in exons 18-21; 2.5h processing time [60] |
| PreservCyt Medium | Hologic | Sample collection and preservation | Liquid-based cytology medium; maintains sample stability for inter-laboratory studies [96] |
| RecoverAll Total Nucleic Acid Isolation Kit | Invitrogen | Nucleic acid extraction from FFPE samples | Purifies RNA/DNA from challenging samples; essential for archival tissue analysis [60] |
| Oncomine Focus Assay | ThermoFisher | NGS validation of qPCR results | 52-gene panel; orthogonal verification for false-positive reduction [60] |
| I.DOT Liquid Handler | Dispendix | Automated liquid handling | Non-contact dispensing; reduces Ct value variation; minimizes cross-contamination [52] |
Experimental Workflow Visualization
Inter-laboratory Validation Workflow
Decision Framework for Discordant Results
Discordant Results Resolution Protocol
Conclusion
Minimizing false positives in qPCR cancer assays is not a single-step fix but requires a holistic, multi-faceted strategy that integrates foundational knowledge, meticulous methodology, systematic optimization, and rigorous validation. The convergence of careful assay design, uncompromising laboratory practice, and robust analytical frameworks is essential to achieve the high specificity demanded in clinical and research settings. Future directions will likely involve the deeper integration of computational tools for assay design and data analysis, the adoption of novel chemistries that further enhance specificity, and the establishment of universal standards for validating liquid biopsy and other qPCR-based oncological applications. By adhering to these principles, researchers can significantly improve the reliability of their data, accelerating the development of precise molecular diagnostics and contributing to more effective cancer management strategies.
References
- 1. High Incidence of False Positives in EGFR S768I Mutation ... [https://www.mdpi.com/2075-4418/15/3/321]
- 2. Preventing False Positive and False Negative PCR Results [https://www.clinicallab.com/preventing-false-positive-and-false-negative-pcr-results-26261]
- 3. Controlling for contamination in qPCR testing - LGC [https://blog.biosearchtech.com/how-to-control-for-contamination-in-qpcr-testing]
- 4. Development of a novel strategy to reduce diagnostic ... [https://www.nature.com/articles/s41598-024-78654-2]
- 5. Comparison of diagnostic accuracy of rapid antigen tests for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11462910/]
- 6. Avoiding Contamination | Thermo Fisher Scientific - ES [https://www.thermofisher.com/us/en/home/life-science/pcr/real-time-pcr/real-time-pcr-learning-center/real-time-pcr-basics/good-laboratory-practice-avoid-contamination-qpcr-experiments.html]
- 7. qPCR Troubleshooting Guide [https://azurebiosystems.com/qpcr-resources/troubleshooting/]
- 8. False Positive Results With SARS-CoV-2 RT-PCR Tests ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7934325/]
- 9. Amplicon - an overview [https://www.sciencedirect.com/topics/biochemistry-genetics-and-molecular-biology/amplicon]
- 10. The Devil in the Details: Contamination in a PCR Lab [https://www.rapidmicrobiology.com/news/the-devil-in-the-details-contamination-in-a-pcr-lab]
- 11. Could your PCR be affected by contamination? | IDT [https://www.idtdna.com/page/support-and-education/decoded-plus/could-your-pcr-be-affected-by-contamination/]
- 12. Rules and Tips for PCR & qPCR Primer Design | IDT [https://www.idtdna.com/page/support-and-education/decoded-plus/how-to-design-primers-and-probes-for-pcr-and-qpcr/]
- 13. qPCR primer design revisited - PMC - PubMed Central - NIH [https://pmc.ncbi.nlm.nih.gov/articles/PMC5702850/]
- 14. Troubleshooting primer dimer in PCR [https://www.minipcr.com/primer-dimer-pcr/]
- 15. Trust your SYBR Green qPCR Data [https://www.thermofisher.com/blog/behindthebench/trust-your-sybr-green-qpcr-data/]
- 16. Why Does Your Melt Curve Look So Strange? - Yeasen [https://www.yeasenbio.com/blogs/molecular-biology/why-does-your-melt-curve-look-so-strange]
- 17. Analyzing qPCR data: Better practices to facilitate rigor and ... [https://www.sciencedirect.com/science/article/pii/S2405580825004431]
- 18. Selection and validation of reference genes for RT-qPCR ... [https://www.nature.com/articles/s41598-025-02951-7]
- 19. MIQE Guidelines | Thermo Fisher Scientific - US [https://www.thermofisher.com/us/en/home/life-science/pcr/real-time-pcr/real-time-pcr-assays/why-choose-taqman-assays/publish-real-time-pcr-results.html]
- 20. MIQE 2.0 and the Urgent Need to Rethink qPCR Standards [https://www.mdpi.com/1422-0067/26/11/4975]
- 21. PCR Troubleshooting 103: How to Address Primer-Dimers [https://geneticeducation.co.in/pcr-troubleshooting-103-how-to-address-primer-dimers/]
- 22. Avoiding false positives with PCR | IDT [https://www.idtdna.com/page/support-and-education/decoded-plus/how-to-avoid-false-positives-in-pcr-and-what-to-do-if-you-get-them/]
- 23. A Highly Sensitive XNA-Based RT-qPCR Assay for the ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10930897/]
- 24. Mutation Detection Analysis Using TaqMan Assays [https://www.thermofisher.com/us/en/home/life-science/pcr/real-time-pcr/real-time-pcr-assays/taqman-mutation-detection-assays.html]
- 25. Programmable no-nonspecific genetic analytical system ... [https://www.nature.com/articles/s41598-025-24565-9]
- 26. A Novel Cell-Free DNA Fragmentomic Assay and Its ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12606779/]
- 27. A Novel Cell-Free DNA Fragmentomic Assay and Its ... [https://pubmed.ncbi.nlm.nih.gov/41228374/]
- 28. Circulating tumor DNA to monitor treatment response in ... [https://www.nature.com/articles/s41698-025-00876-y]
- 29. Primer design guide - 5 tips for best PCR results [https://the-dna-universe.com/2022/09/05/primer-design-guide-the-top-5-factors-to-consider-for-optimum-performance/]
- 30. Primer Design Guide for PCR :: Learn Designing Primers for PCR [http://www.premierbiosoft.com/tech_notes/PCR_Primer_Design.html]
- 31. Luna® One-Step RT-qPCR Troubleshooting Guide [https://www.neb.com/en-us/tools-and-resources/troubleshooting-guides/luna-one-step-rt-qpcr-troubleshooting-guide?srsltid=AfmBOoplclqWwAk9Q05ofc0EPiXkPpNDVyGJIpQlm3U_lsPPuI3baa0R]
- 32. Primer Analysis Tool and Tm Calculator | IDT [https://www.idtdna.com/pages/tools/oligoanalyzer]
- 33. Tm Calculator for Primers | Thermo Fisher Scientific - US [https://www.thermofisher.com/us/en/home/brands/thermo-scientific/molecular-biology/molecular-biology-learning-center/molecular-biology-resource-library/thermo-scientific-web-tools/tm-calculator.html]
- 34. Advanced breast cancer diagnosis: Multiplex RT-qPCR for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10776909/]
- 35. Dos and don'ts for molecular testing [https://www.who.int/teams/global-malaria-programme/case-management/diagnosis/nucleic-acid-amplification-based-diagnostics/dos-and-don-ts-for-molecular-testing]
- 36. Organizing and Optimizing Laboratory Space for Molecular ... [https://www.aphl.org/programs/newborn_screening/Pages/Molecular-Workflow.aspx]
- 37. Establishing PNB-qPCR for quantifying minimal ctDNA ... [https://www.nature.com/articles/s41598-017-09137-w]
- 38. Hot-Start PCR: Higher specificity, higher yield, ... [https://www.genaxxon.com/shop/en/blog/hot-start-pcr-higher-specificity-higher-yield-higher-sensitivity]
- 39. Reduce false positives with hot start PCR - News Blog [https://www.jenabioscience.com/about-us/news-blog/3455-reduce-false-positives-with-hot-start-pcr]
- 40. Touchdown PCR: Easy Intro Plus 5 Expert Tips [https://bitesizebio.com/2203/touchdown-pcr-a-primer-and-some-tips/]
- 41. Touchdown polymerase chain reaction [https://grokipedia.com/page/Touchdown_polymerase_chain_reaction]
- 42. Polymerase Chain Reaction: Basic Protocol Plus ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4846334/]
- 43. PCR Troubleshooting Guide [https://www.neb.com/en-us/tools-and-resources/troubleshooting-guides/pcr-troubleshooting-guide?srsltid=AfmBOop4ZwbA0czoush50P7bJJjCl2TncjP73-50NsxZjfZmlRsC8ARo]
- 44. TqPCR: A Touchdown qPCR Assay with Significantly ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4501803/]
- 45. What is UNG/UDG? [https://www.thermofisher.com/us/en/home/life-science/pcr/real-time-pcr/real-time-pcr-learning-center/real-time-pcr-basics/what-is-ung-udg.html]
- 46. Eliminate PCR Amplicon (but not real-time PCR?) Carry- ... [https://bitesizebio.com/4813/eliminate-pcr-amplicon-but-not-rtpcr-carry-over-with-ung/]
- 47. PCR Carry-Over Prevention Solutions [https://www.arcticzymes.com/application/pcr-carry-over-prevention]
- 48. - Digital Cancer | GeneGlobe Research PCR Assays [https://geneglobe.qiagen.com/us/applications/digital-pcr/cancer-research]
- 49. Selection and validation of reference for RT- genes ... qPCR [https://pmc.ncbi.nlm.nih.gov/articles/PMC12126485/]
- 50. a comprehensive analysis in MCF-7 breast cancer cell line [https://bmcmolcellbiol.biomedcentral.com/articles/10.1186/s12860-020-00313-x]
- 51. Targeted transcript quantification in single disseminated cancer cells... [https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0216442]
- 52. qPCR Troubleshooting: How to Ensure Successful ... [https://dispendix.com/blog/qpcr-troubleshooting]
- 53. Analysis of qPCR determination methods and... reference gene stability [https://bmcgenomics.biomedcentral.com/articles/10.1186/1471-2164-15-648]
- 54. Identification of suitable qPCR reference genes for the ... [https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0318944]
- 55. PCR controls [https://www.qiagen.com/us/knowledge-and-support/knowledge-hub/bench-guide/pcr/reference-genes-and-controls/pcr-controls]
- 56. Amplification of the No Template Control (NTC) [https://www.thermofisher.com/us/en/home/life-science/pcr/real-time-pcr/real-time-pcr-learning-center/real-time-pcr-basics/real-time-pcr-troubleshooting-tool/gene-expression-quantitation-troubleshooting/amplification-no-template-control.html]
- 57. Luna® One-Step RT-qPCR Troubleshooting Guide [https://www.neb.com/en-us/tools-and-resources/troubleshooting-guides/luna-one-step-rt-qpcr-troubleshooting-guide?srsltid=AfmBOopu5mFW5iWPRijbRji_f8lNTXJKctDihLZQJEqLm3TzX7uLBBco]
- 58. qPCR Steps: Creating a Successful Experiment | IDT [https://www.idtdna.com/page/support-and-education/decoded-plus/successful-qpcr/]
- 59. PCR Quantification Standards [https://minervabiolabs.us/dna-standards-en/1216-pcr-quantification-standards.html]
- 60. High Incidence of False Positives in EGFR S768I Mutation ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11816987/]
- 61. qPCR optimization in focus: tips and tricks for excellent ... [https://www.genaxxon.com/shop/en/blog/qpcr-optimization-in-focus-tips-and-tricks-for-excellent-analyses]
- 62. Adjusting RT-qPCR conditions to avoid unspecific ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7598553/]
- 63. How to optimize qPCR in 9 steps? [https://westburg.eu/knowledge/pcr_qpcr/hate_optimizing_qpcr]
- 64. Troubleshooting fine‐tuning procedures for qPCR system ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6647679/]
- 65. Optimization of TaqMan-based quantitative PCR diagnosis ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12165414/]
- 66. Explaining multiple peaks in qPCR melt curve analysis | IDT [https://www.idtdna.com/page/support-and-education/decoded-plus/interpreting-melt-curves-an-indicator-not-a-diagnosis/]
- 67. PCR Troubleshooting Guide [https://www.neb.com/en-us/tools-and-resources/troubleshooting-guides/pcr-troubleshooting-guide?srsltid=AfmBOootOXeAwEDh4xY_ZnRkVxJ3kGLlaa60Zf32a2Lf5Uzk06QB56Dr]
- 68. Nuclease-Free Water | Thermo Fisher Scientific - US [https://www.thermofisher.com/us/en/home/life-science/dna-rna-purification-analysis/rna-extraction/rna-extraction-products/nuclease-free-tubes-tips-and-buffers/nuclease-free-water.html]
- 69. The Purpose of ROX Reference Dye in Real-Time PCR ... [https://www.thermofisher.com/blog/behindthebench/the-purpose-of-rox-reference-dye-in-real-time-pcr-qpcr/]
- 70. Nuclease Free Water - Its Importance in Biological Research [https://norgenbiotek.com/blog/importance-water-quality-biological-research?srsltid=AfmBOopfBDrkyIGQabidzS4LLA6yIq1kFIAcQe_ZlmM2RiiARG1GrDcC]
- 71. AMPNC flag (amplification in negative control) [https://apps.thermofisher.com/apps/help/MAN0010504/GUID-C8E5C9E4-A763-4E49-B73A-67BF018D0BD0.html]
- 72. Troubleshooting qPCR: Interpreting Amplification Curves [https://blog.biosearchtech.com/thebiosearchtechblog/bid/63622/qpcr-troubleshooting]
- 73. I am performing real time qPCR and my negative controls ... [https://oligos.biosearchtech.com/support/faqs/qpcr-applications-calibration-troubleshooting/i-am-performing-real-time-qpcr-and-my-negative-controls-are-amplifying-why-would-this-happen]
- 74. Methods to determine limit of detection and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5496743/]
- 75. High-Throughput Data Analysis for qPCR [https://www.neb.com/en-us/tools-and-resources/feature-articles/development-of-a-high-throughput-data-analysis-method-for-quantitative-real-time-pcr?srsltid=AfmBOoo1RauIjN1rvJTuTL_BNSuiWmUCNEh_NnkQewK8UEN2X1_eSF6p]
- 76. Determining lower limits of detection of digital PCR assays ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5129438/]
- 77. Minimizing errors in RT-PCR detection and quantification of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8386095/]
- 78. Comparison of SYBR Green and TaqMan methods in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3988599/]
- 79. TaqMan vs. SYBR Chemistry for Real-Time PCR [https://www.thermofisher.com/us/en/home/life-science/pcr/real-time-pcr/real-time-pcr-learning-center/real-time-pcr-basics/taqman-vs-sybr-chemistry-real-time-pcr.html]
- 80. vehicles for minimal residual disease detection in t(11;14) ... [https://pubmed.ncbi.nlm.nih.gov/24631717/]
- 81. Real-Time PCR Basics Support—Troubleshooting [https://www.thermofisher.com/us/en/home/technical-resources/technical-reference-library/real-time-digital-PCR-applications-support-center/real-time-pcr-basics-support/real-time-pcr-basics-support-troubleshooting.html]
- 82. Systematic benchmarking of omics computational tools - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC6437167/]
- 83. Quantitative PCR validation for research scientists: Part 1 of 2 [https://virologyresearchservices.com/2023/01/13/quantitative-pcr-validation-part-1-of-2/]
- 84. Cancer Research to Microbes: Harnessing the Power of ... [https://www.thermofisher.com/blog/behindthebench/harnessing-the-power-of-qpcr/]
- 85. Consensus guidelines for the validation of qRT-PCR ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8792405/]
- 86. Critical appraisal of quantitative PCR results in colorectal ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5528534/]
- 87. Comparative Evaluation of Computational Methods for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12383485/]
- 88. Comparative Evaluation of Computational Methods for ... [https://www.mdpi.com/2227-9059/13/8/2036]
- 89. Identification and validation of stable reference genes for ... [https://www.sciencedirect.com/science/article/abs/pii/S092144882500224X]
- 90. A stable combination of non-stable genes outperforms ... [https://www.nature.com/articles/s41598-024-82651-w]
- 91. Identification of Reliable Housekeeping Genes for qRT- ... [https://brieflands.com/journals/gct/articles/161203]
- 92. Identification of best housekeeping gene for normalization in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12475163/]
- 93. Validation and Selection of New Reference Genes for RT ... [https://www.mdpi.com/2073-4425/12/9/1335]
- 94. Evaluation of normalisation strategies for qPCR data ... [https://www.nature.com/articles/s41598-025-06657-8]
- 95. Selection of Stable Reference Genes for Gene Expression ... [https://www.mdpi.com/1422-0067/26/14/6790]
- 96. and inter-laboratory reproducibility of the Xpert HPV assay ... [https://virologyj.biomedcentral.com/articles/10.1186/s12985-018-1076-6]
- 97. and interlaboratory reproducibility of the RIATOL qPCR ... [https://pubmed.ncbi.nlm.nih.gov/37702556/]
- 98. Regular article Comparison of Real-Time PCR and Digital ... [https://www.sciencedirect.com/science/article/pii/S1525157823000740]