Strategies to Minimize False Positives in Pharmacophore-Based Virtual Screening
This article provides a comprehensive guide for researchers and drug development professionals on addressing the pervasive challenge of false positives in pharmacophore-based virtual screening.
Strategies to Minimize False Positives in Pharmacophore-Based Virtual Screening
Abstract
This article provides a comprehensive guide for researchers and drug development professionals on addressing the pervasive challenge of false positives in pharmacophore-based virtual screening. It covers the fundamental causes of false positives, explores advanced methodological strategies like pharmacophore filtering and machine learning integration, details troubleshooting and optimization techniques using pre- and post-screening filters, and discusses rigorous validation protocols through ROC curves and enrichment factors. By synthesizing current best practices and emerging trends, this resource aims to enhance the efficiency and reliability of virtual screening campaigns in drug discovery.
Understanding False Positives: The Fundamental Challenge in Pharmacophore Screening
FAQs: Understanding False Positives in Virtual Screening
What is a false positive in computational drug discovery? A false positive occurs when a compound is computationally predicted to be biologically active but fails to show actual activity in experimental validation [1]. In virtual screening, only about 12% of top-scoring compounds typically show activity in biochemical assays, meaning the majority of predictions are false positives [2]. This represents a significant waste of resources as these compounds proceed to expensive experimental testing without providing real value.
How do false positives differ from false negatives? A false positive (Type I error) incorrectly identifies an inactive compound as active, while a false negative (Type II error) fails to identify a truly active compound [1]. The balance between these errors depends on research goals: reducing false negatives might be prioritized in early discovery to avoid missing potential hits, while later stages focus on reducing false positives to conserve resources [3].
What are the main causes of false positives in pharmacophore-based screening? False positives arise from multiple factors including:
- Simplistic scoring functions that cannot capture complex binding interactions [2]
- Insufficient training data with inadequate decoy compounds during model development [2]
- Assay interference mechanisms such as compound aggregation, chemical reactivity, or inhibition of reporter proteins [4]
- Inadequate treatment of receptor flexibility where each conformational model introduces its own false positives [5]
Troubleshooting Guides: Reducing False Positives
Problem: High False Positive Rate in Virtual Screening Hits
Issue: Too many computationally selected compounds show no activity in biochemical assays.
Solutions:
- Implement Multi-Conformation Docking
Use Advanced Machine Learning Classifiers
Apply Interference Prediction Tools
Problem: Compounds Showing Artificial Activity in Confirmatory Assays
Issue: Initial screening hits fail to show dose-dependent activity or demonstrate artifactual behavior.
Solutions:
- Employ Multiple Orthogonal Assays
- Implement Strategic Filtering
Experimental Protocols & Data
Quantitative Assessment of Screening Performance
Table 1: Virtual Screening Performance Metrics Across Methods
| Screening Method | Typical Hit Rate | Most Potent Hit (Median) | Key Limitations |
|---|---|---|---|
| Standard Structure-Based Virtual Screening | ~12% | ~3 μM Kd/Ki | High false positive rate from simplistic scoring functions [2] |
| Pharmacophore-Based Screening with Filters | Variable (15-25%) | Dependent on target and model quality | Requires careful model validation and interference filtering [6] |
| Machine Learning Classifiers (vScreenML) | Up to 43% (reported for AChE) | 280 nM IC50 (best hit) | Dependent on quality training data with compelling decoys [2] |
| Multi-Conformation Docking Strategy | Significantly improved enrichment | Better than single conformation | Computationally intensive; requires receptor dynamics data [5] |
Detailed Methodology: Structure-Based Pharmacophore Modeling
Protocol for Reduced False-Positive Pharmacophore Screening
Protein Structure Preparation
Pharmacophore Feature Generation
Virtual Screening Implementation
Hit Triage and Validation
Research Reagent Solutions
Table 2: Essential Tools for False Positive Reduction
| Tool/Resource | Function | Application in False Positive Reduction |
|---|---|---|
| Liability Predictor | Predicts assay interference compounds | Identifies thiol-reactive, redox-active, and luciferase-inhibiting compounds [4] |
| D-COID Dataset | Training set with compelling decoys | Machine learning model training for improved virtual screening [2] |
| vScreenML | Machine learning classifier | Distinguishes true actives from decoys in structure-based screening [2] |
| Multiple Receptor Conformations | Accounts for protein flexibility | Identifies compounds that bind favorably across different conformational states [5] |
| Pharmacophore Exclusion Volumes | Represents steric constraints | Filters compounds that would clash with binding site residues [7] |
| Orthogonal Assay Systems | Multiple detection methods | Confirms activity through different experimental readouts [3] |
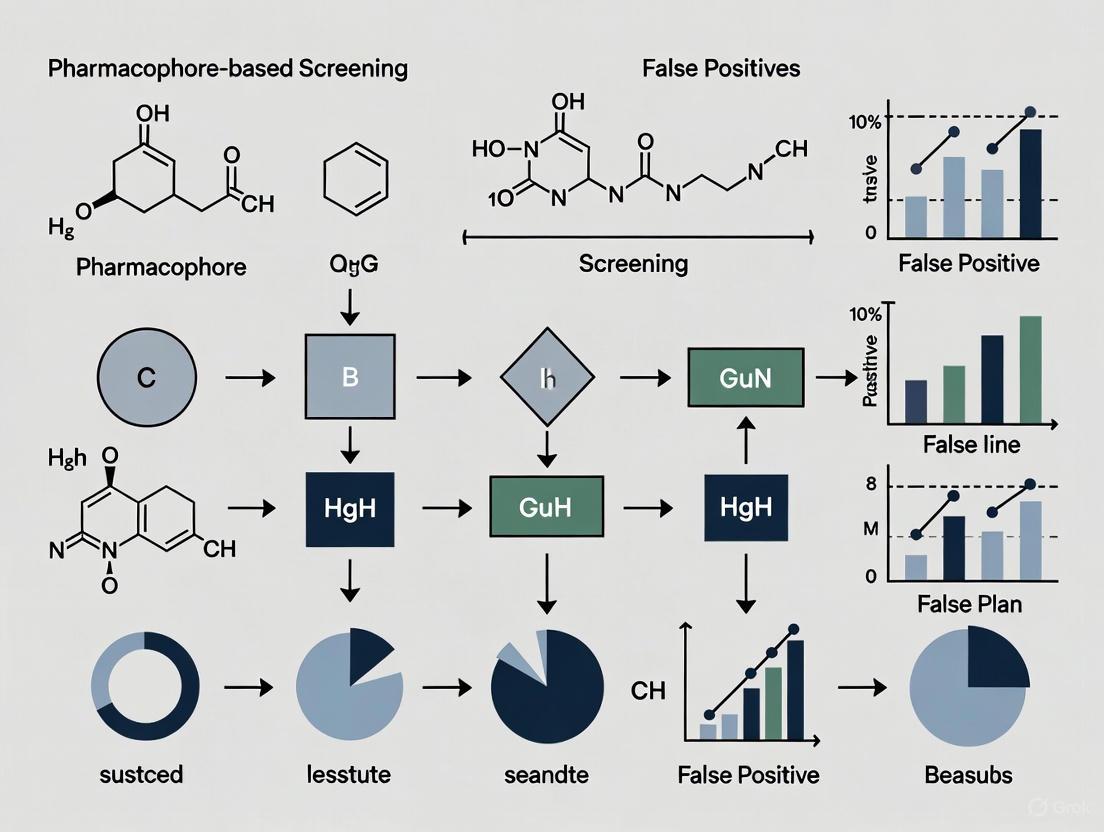
Workflow Visualization
Diagram: Integrated False Positive Reduction Strategy
Integrated Strategy for False Positive Reduction
Diagram: Assay Interference Mechanisms
Common Assay Interference Mechanisms
This technical support guide addresses two prevalent challenges in pharmacophore-based virtual screening that contribute to high false positive rates. The content is framed within a broader research thesis focused on improving the reliability of computational drug discovery.
Frequently Asked Questions
Q1: What are the consequences of setting my pharmacophore feature tolerances too loosely? Excessively permissive feature tolerances, or high "fuzziness," increase the risk of false positives by accepting compounds that match the spatial arrangement but lack the precise chemical complementarity required for strong binding. Overly loose tolerances can lead to poorer activity enrichment in virtual screening results, meaning fewer truly active compounds are retrieved among the top-ranked candidates [10].
Q2: How does conformer generation quality affect my screening results? Inadequate conformer sampling can cause bioactive conformations to be missed entirely during virtual screening. Since pharmacophore matching relies on pre-generated conformers, if the bioactive conformation isn't present in your ensemble, even perfect ligands will be rejected as false negatives. Research shows that for structure-based tasks, generating at least 250 conformers per compound using state-of-the-art methods like RDKit's ETKDG provides reasonable coverage of conformational space [11].
Q3: What strategies can help reduce false positives from pharmacophore screening? Combining docking with pharmacophore filtering has shown promise for reducing false positives. This approach uses docking for pose generation followed by pharmacophore filtering to eliminate poses lacking key interactions. Additionally, using multiple receptor conformations and selecting only compounds that rank highly across all conformations can help eliminate false positives that arise from fitting specific receptor states [12] [5].
Q4: Are there computational tools that help optimize these parameters? Yes, several specialized tools are available. ZINCPharmer provides an online interface for pharmacophore search of purchasable compounds and includes features for query refinement [13]. Pharmer uses efficient indexing algorithms for rapid exact pharmacophore search [14]. For conformer generation, RDKit with ETKDG parameters is widely used, while newer approaches like ABCR (Algorithm Based on Bond Contribution Ranking) aim to improve coverage of conformational space with fewer conformers [11] [15].
Troubleshooting Guides
Issue 1: High False Positive Rate in Virtual Screening
Symptoms:
- High computational hit rate but low experimental confirmation
- Retrieved compounds lack key interactions with binding site
- Poor correlation between computational ranking and experimental activity
Diagnosis and Resolution:
| Step | Action | Technical Details |
|---|---|---|
| 1 | Analyze feature tolerances | Reduce radii around pharmacophore features; start with 1.0Å tolerance and adjust based on target flexibility [11]. |
| 2 | Add exclusion volumes | Represent forbidden regions of binding site to eliminate sterically clashing compounds [7]. |
| 3 | Implement consensus filtering | Apply multiple receptor conformations and select only intersections from top-ranked lists [5]. |
| 4 | Validate with known actives/inactives | Test pharmacophore model against compounds with known activity to verify selectivity [12]. |
Issue 2: Poor Bioactive Conformation Recovery
Symptoms:
- Known active compounds missed in virtual screening
- Inability to reproduce crystallographic ligand poses
- High RMSD between generated and bioactive conformations
Diagnosis and Resolution:
| Step | Action | Technical Details |
|---|---|---|
| 1 | Increase conformer ensemble size | Generate 250+ conformers per compound for reasonable bioactive conformation recovery [11]. |
| 2 | Evaluate conformer generation methods | Compare RDKit's ETKDG vs. knowledge-based vs. machine learning approaches for your specific target class. |
| 3 | Apply energy minimization | Use force fields like UFF as post-processing to refine conformer geometries [11]. |
| 4 | Consider molecular flexibility | Allocate more conformers for compounds with high rotatable bond count (>10) [15]. |
Experimental Protocols
Protocol 1: Optimizing Pharmacophore Feature Tolerances
Purpose: To establish methodical approaches for setting pharmacophore feature tolerances that balance sensitivity and specificity.
Materials:
- Protein structure with binding site definition
- Set of known active compounds with diverse scaffolds
- Set of confirmed inactive compounds
- Pharmacophore modeling software (e.g., MOE, LigandScout, ZINCPharmer)
Methodology:
- Create initial pharmacophore model from protein-ligand complex or multiple active ligands
- Define key interaction features (H-bond donors/acceptors, hydrophobic areas, charged groups)
- Set initial tolerances based on:
- Test model performance using known actives and inactives
- Iteratively refine tolerances to maximize enrichment of actives while excluding inactives
- Validate optimized model with an independent test set not used in training
Protocol 2: Comprehensive Conformer Generation and Sampling
Purpose: To generate conformational ensembles that adequately represent bioactive conformations while maintaining computational efficiency.
Materials:
- Compound library in SMILES or 2D structure format
- Conformer generation software (RDKit, OMEGA, ABCR, or DMCG)
- High-performance computing resources for large libraries
- Reference set of protein-ligand complexes for validation
Methodology:
- Select appropriate conformer generator based on molecular flexibility:
- Set generation parameters:
- Validate ensemble quality using:
- RMSD to bioactive conformations from Platinum or PDBBind datasets
- Coverage of conformational space using diversity metrics
- Apply to virtual screening using tools like Pharmit or Pharmer for efficient searching [11] [14]
Workflow Diagrams
Figure 1: Iterative Optimization Workflow for addressing common pharmacophore screening pitfalls. The red nodes indicate critical points where false positives commonly originate and require particular attention.
Figure 2: Problem-Solution Mapping for two common pitfalls in pharmacophore-based screening, showing the direct relationship between specific issues and their targeted solutions.
Research Reagent Solutions
| Tool/Category | Examples | Function in Research | Key Considerations |
|---|---|---|---|
| Pharmacophore Modeling | MOE, LigandScout, ZINCPharmer | Create and refine pharmacophore hypotheses; screen compound libraries | Choose based on structure/ligand-based approach; check feature customization options [12] [13] [7] |
| Conformer Generation | RDKit/ETKDG, OMEGA, ABCR, DMCG | Generate 3D conformational ensembles for screening | Evaluate bioactive conformation recovery; consider computational efficiency [11] [15] |
| Virtual Screening Platforms | Pharmer, Pharmit, LIQUID | Efficient pharmacophore search of large compound libraries | Assess scalability to your library size; check alignment-based vs. fingerprint methods [13] [11] [14] |
| Validation Datasets | Platinum, PDBBind, DUDE | Benchmark performance using known actives/inactives | Ensure relevance to your target class; verify quality of experimental data [11] [2] |
| Post-Screening Analysis | GoldMine, Pose-Filter scripts, vScreenML | Filter results; apply machine learning to reduce false positives | Implement multiple filtering strategies; use consensus approaches [12] [2] [5] |
Frequently Asked Questions (FAQs)
1. What are promiscuous inhibitors and frequent hitters? Promiscuous inhibitors, or frequent hitters, are compounds that produce false-positive results across multiple high-throughput screening (HTS) assays, regardless of the biological target [16] [17]. They act through non-specific, spurious mechanisms rather than targeted, drug-like interactions. Their activity is often irreproducible in subsequent experiments, leading to wasted resources and effort [16] [18].
2. What are the common mechanisms by which these compounds interfere with assays? The primary mechanisms of interference include:
- Colloidal Aggregation: Compounds self-associate into particles (30-1000 nm in diameter) that non-specifically inhibit enzymes by adsorbing protein molecules onto their surface [16].
- Chemical Reactivity: Compounds contain reactive functional groups (e.g., aldehydes, epoxides) that form covalent bonds with protein targets, such as cysteine residues [17] [19].
- Assay Interference: Compounds interfere with the detection method itself, for example, by absorbing light in spectroscopic assays (autofluorescence) or inhibiting a reporter enzyme like firefly luciferase (FLuc) [17].
3. Are there specific chemical structures I should avoid? Yes, certain structural classes are notorious for promiscuous behavior. These include rhodanines, catechols, quinones, and 2-amino-3-carbonylthiophenes [18] [20]. These substructures are often identified by filters with names like PAINS (Pan-Assay Interference Compounds) [17] [20].
4. What computational tools can help identify these compounds early? Several computational tools have been developed to flag potential frequent hitters before experimental screening:
- ChemFH: An integrated online platform that uses machine learning to predict various types of interferents, including colloidal aggregators and reactive compounds [17].
- Hit Dexter: A set of machine learning models trained to predict frequent hitters in both target-based and cell-based assays [21].
- Aggregator Advisor: A tool specifically focused on identifying compounds likely to form colloidal aggregates [17].
5. My hit compound is inhibited by detergent. What does this mean? If your compound's inhibitory activity is significantly reduced or abolished by adding a small amount (e.g., 0.01%) of a non-ionic detergent like Triton X-100, it is a strong indicator that the compound acts through colloidal aggregation [16] [18] [20]. The detergent disrupts the aggregate particles, restoring enzyme activity.
Troubleshooting Guides
Guide 1: Diagnosing a Promiscuous Inhibitor in a Biochemical Assay
If you have a screening hit that you suspect is a false positive, this step-by-step guide helps you investigate.
- Objective: To experimentally determine if a hit compound is a promiscuous inhibitor acting via colloidal aggregation.
- Background: Colloidal aggregators form particles that non-specifically inhibit a wide range of enzymes. This behavior has a distinct experimental signature [16].
Experimental Protocol
Detergent Sensitivity Test
Enzyme Concentration Dependence
- Method: Repeat the inhibition assay at two or more different enzyme concentrations (e.g., 1 nM and 10 nM) [16].
- Interpretation: A decrease in apparent inhibition with increasing enzyme concentration suggests aggregator behavior. For a specific, well-behaved inhibitor, the percentage inhibition is largely independent of enzyme concentration within a reasonable range [16].
Steep Dose-Response Curves
Direct Observation of Particles
- Method: Use Dynamic Light Scattering (DLS) to analyze your compound solution in the assay buffer.
- Interpretation: The observation of particles in the 30-1000 nm size range supports the aggregation hypothesis [16].
The following workflow visualizes the key decision points in this diagnostic process:
Guide 2: Integrating Computational Filters into Virtual Screening
This guide outlines how to use computational tools to triage a virtual screening library before costly experimental work begins.
- Objective: To remove likely frequent hitters from a compound library prior to pharmacophore-based virtual screening.
- Background: Computational models can predict compounds with high propensity for assay interference based on their chemical structure, acting as a valuable first-pass filter [17] [21].
Workflow Protocol
Prepare Compound Library
- Standardize the structures in your virtual library (e.g., neutralize charges, remove duplicates) to ensure data quality [17].
Apply Substructure Filters
Utilize Machine Learning Models
Manual Inspection
- Review the remaining compounds, paying special attention to those with highly electrophilic character, which can be calculated using Density Functional Theory (DFT) and is associated with lack of biological selectivity [19].
Proceed with Pharmacophore Screening
- Use the cleaned, triaged library for your pharmacophore-based virtual screening, leading to a hit list with a potentially higher proportion of true positives.
The workflow for this computational triage process is as follows:
Table 1: Prevalence of Frequent Hitters in a Large-Scale HTS Analysis
This data, derived from a study of 93,212 compounds screened in six different assays, shows how a small fraction of compounds are responsible for a large number of hits [20].
| Number of Assays in Which Compound Was Active | Number of Compounds | Percentage of Total Library |
|---|---|---|
| 6 | 362 | 0.39% |
| 5 | 785 | 0.84% |
| 4 | 915 | 0.98% |
| 3 | 1,220 | 1.31% |
| 2 | 4,689 | 5.03% |
| 1 | 12,077 | 12.96% |
| 0 (Inactive) | 73,164 | 78.49% |
Table 2: Key Experimental Signatures of Colloidal Aggregators
This table summarizes the key experimental observations that can help distinguish colloidal aggregators from specific inhibitors [16] [18] [20].
| Experimental Observation | Expected Result for a Colloidal Aggregator | Expected Result for a Specific Inhibitor |
|---|---|---|
| Inhibition in presence of non-ionic detergent (Triton) | Significant attenuation or abolition of inhibition | Little to no effect on inhibition |
| Effect of increasing enzyme concentration | Decrease in apparent inhibition | No significant change in percentage inhibition |
| Shape of the dose-response curve | Unusually steep curve | Standard sigmoidal curve |
| Observation by Dynamic Light Scattering (DLS) | Particles present in the 30-1000 nm size range | No particles observed |
| Competitiveness of inhibition | Typically non-competitive | Can be competitive, non-competitive, or uncompetitive |
The Scientist's Toolkit: Essential Research Reagents & Materials
Table 3: Key Reagents for Identifying and Managing Promiscuous Inhibitors
| Reagent / Material | Function/Brief Explanation |
|---|---|
| Non-ionic Detergent (Triton X-100) | Disrupts colloidal aggregates; used to confirm aggregation as an inhibition mechanism [16] [18]. |
| Bovine Serum Albumin (BSA) | Can be used as an alternative to detergent in cell-based assays to sequester aggregators [16] [20]. |
| Dynamic Light Scattering (DLS) Instrument | Directly detects and measures the size of colloidal particles in compound solutions [16]. |
| Model Enzymes (e.g., β-lactamase, Chymotrypsin) | Well-characterized enzymes used in counter-screens to test for promiscuous inhibition across unrelated targets [16]. |
| Computational Tools (e.g., ChemFH, Hit Dexter) | Machine learning platforms for predicting frequent hitters from chemical structure prior to experimental screening [17] [21]. |
Quantitative Data on Virtual Screening Performance
The table below summarizes key quantitative findings from benchmark studies comparing virtual screening approaches and their strategies for handling false positives.
Table 1: Performance Metrics of Virtual Screening and Refinement Methods
| Method Category | Specific Method/Strategy | Performance Metric | Result | Reference |
|---|---|---|---|---|
| Virtual Screening Approach | Pharmacophore-Based Virtual Screening (PBVS) | Average Enrichment Factor | Outperformed DBVS in 14 out of 16 test cases | [22] |
| Docking-Based Virtual Screening (DBVS) | Average Enrichment Factor | Lower performance compared to PBVS | [22] | |
| False Positive Reduction | Multiple Receptor Conformations (MRC) with Intersection Selection | Success in Identifying High-Affinity Controls | Correctly identified all added high-affinity control molecules | [5] |
| Model Refinement | AF2 Recycling (Monomeric, non-AF2 models) | Model Improvement Rate (lDDT) | 81.25% (single sequence) to 100% (MSA) | [23] |
| AF2 Recycling (Multimeric, non-AF2 models) | Model Improvement Rate (lDDT) | 94% (single sequence) to 100% (MSA) | [23] | |
| Protein-Peptide Prediction | AF2-Multimer with Full-Length Input | Success Rate (Unbiased Benchmark) | 40% | [24] |
| AF2-Multimer with Fragment Scanning & MSA Mix | Success Rate (Unbiased Benchmark) | >90% | [24] |
Troubleshooting Guides and FAQs
FAQ 1: Why does considering receptor flexibility in virtual screening often increase false positives, and how can I mitigate this?
- Problem: Each distinct conformational state of a protein receptor can bind compounds that are not true binders, generating unique lists of top-ranked hits. When multiple receptor conformations (MRCs) are used, the union of these lists can lead to an unmanageable number of false positives [5].
- Solution: Implement a consensus or intersection strategy. The hypothesis is that a true bioactive ligand will bind favorably to multiple conformations of the binding site.
- Experimental Protocol:
- Generate Multiple Receptor Conformations (MRCs): Use molecular dynamics (MD) simulations [5] or other sampling methods to generate a set of distinct, biologically relevant protein conformations.
- Perform Docking: Dock your virtual compound library against each conformation separately.
- Rank and Intersect: For each receptor conformation, generate a list of top-ranked compounds (e.g., top 100). The final list of high-confidence hits consists only of the compounds that appear in the top-ranked lists of all (or a majority) of the receptor conformations [5].
- Validation: This method has been shown to successfully distinguish high-affinity controls from low-affinity controls and decoys [5].
- Experimental Protocol:
FAQ 2: How can I refine initial protein models to correct for steric clashes and improve model quality?
- Problem: Initial protein structural models, even from high-accuracy predictors like AlphaFold2, may contain local steric clashes or backbone inaccuracies that limit their use in drug design.
- Solution: Use a quality-aware molecular dynamics (MD) refinement protocol.
- Experimental Protocol (Based on ReFOLD4):
- Obtain Local Quality Estimates: Use the per-residue predicted lDDT (pLDDT) score from AlphaFold2, which is often stored in the B-factor column of the PDB file [23].
- Apply Fine-Grained Restraints: In your MD simulation, apply harmonic positional restraints to all atoms of each residue. The key is to set the force constant of these restraints proportional to the residue's pLDDT score.
- Run MD Simulation: Perform the simulation using standard parameters (e.g., CHARMM force field, TIP3 water model, neutralization with ions, 298 K) [23]. This protocol is optimized for modest computational resources.
- Experimental Protocol (Based on ReFOLD4):
FAQ 3: How can I accurately identify the binding interface for a protein-protein interaction involving a disordered region?
- Problem: When using full-length protein sequences as input for AlphaFold2-Multimer, the success rate for predicting the correct structure of a complex with an intrinsically disordered ligand can be low (~40%) [24].
- Solution: Employ a fragment-scanning approach to pinpoint the interaction site before full complex prediction.
- Experimental Protocol:
- Define the Search Space: Identify the protein partner that contains the suspected disordered region.
- Generate Fragments: Divide the sequence of this partner into consecutive fragments of a fixed size (e.g., 100 amino acids) [24].
- Screen Fragments: Run AlphaFold2-Multimer predictions for the receptor paired with each individual fragment.
- Identify the Binding Fragment: The fragment that yields the model with the highest interface prediction score (ipTM) is highly likely to contain the true binding site. This strategy can successfully identify the correct region in up to 89% of cases [24].
- Refine the Model: Once the binding region is identified, a final, high-confidence model can be generated by using the defined fragment and combining multiple sequence alignment (MSA) strategies.
- Experimental Protocol:
Research Reagent Solutions
The table below lists key software and computational tools essential for experiments dealing with steric clashes and model refinement.
Table 2: Essential Research Reagents and Software Tools
| Item Name | Function/Brief Explanation | Example Use Case |
|---|---|---|
| GOLD | Docking software used for structure-based virtual screening, capable of handling protein flexibility [5]. | Identifying potential ligand candidates by docking compound libraries into flexible binding pockets [5]. |
| LigandScout/Catalyst | Software for creating pharmacophore models and performing pharmacophore-based virtual screening [22]. | Filtering large compound libraries to find molecules that match essential 3D chemical features for binding, often as a pre- or post-processing step for docking [22]. |
| AlphaFold2/AlphaFold-Multimer | Deep learning system for predicting protein tertiary and quaternary structures from amino acid sequences [23] [24]. | Generating initial structural models for targets with unknown structures, or refining existing models via its recycling function [23] [24]. |
| NAMD | Molecular dynamics simulation program used for refining protein structures and simulating biomolecular systems [23]. | Running refinement protocols (e.g., ReFOLD) to resolve steric clashes and improve local backbone geometry in protein models [23]. |
| ColabFold | A fast and user-friendly implementation of AlphaFold2 that includes a custom template function [23]. | Recycling and refining existing 3D models by feeding them back as custom templates into the AlphaFold2 inference loop [23]. |
Experimental Workflow Visualizations
Detailed View of the Model Refinement Process
Advanced Strategies to Reduce False Positives: Methodological Solutions
Frequently Asked Questions (FAQs)
Q1: What is the primary advantage of combining docking with pharmacophore filtering?
The primary advantage is a significant reduction in false positive rates. Traditional docking, which relies on scoring functions, often prioritizes compounds that score well in silico but do not bind in reality. By adding a pharmacophore filtering step, you enforce essential chemical complementarity with the target, ensuring that only poses which form key interactions (like specific hydrogen bonds or hydrophobic contacts) are advanced. This hybrid approach leverages docking's ability to generate plausible poses and pharmacophore's ability to define critical interaction patterns, leading to a more enriched and reliable list of candidate molecules [25].
Q2: My virtual screening results contain many compounds that fit the pharmacophore but have poor drug-like properties. How can I address this?
This is a common challenge. The solution is to integrate Absorption, Distribution, Metabolism, Excretion, and Toxicity (ADMET) profiling early in your screening pipeline. After the pharmacophore filtering step, subject the resulting hit compounds to in silico ADMET prediction. This allows you to filter out molecules with unfavorable properties, such as poor solubility or predicted toxicity, before they are selected for costly synthesis or experimental testing. Modern computational pipelines routinely combine pharmacophore screening, molecular docking, and ADMET analysis to prioritize leads with not only high binding potential but also a high probability of success in later development stages [26] [27].
Q3: After applying pharmacophore constraints, I get very few or no hits. What could be the reason?
This issue can stem from several sources:
- Overly Restrictive Pharmacophore Model: Your model may have too many features or the tolerance radii for each feature might be set too tightly. Solution: Re-evaluate your pharmacophore hypothesis. Consider if all features are absolutely essential. Start with a core set of critical interactions and slightly increase the tolerance radii to allow for more flexibility in ligand matching [25].
- Inadequate Conformational Sampling: The docking program may not have generated a pose where the ligand conformation aligns perfectly with your pharmacophore. Solution: Increase the conformational sampling parameters in your docking software or use a stochastic docking algorithm that generates more diverse poses [25].
- Incorrect Binding Site Preparation: The protein structure's protonation states or side-chain orientations might not be optimal for forming the expected interactions. Solution: Carefully prepare the protein structure, ensuring correct protonation states of key residues at physiological pH [28].
Q4: How do I validate the performance of my pharmacophore model before using it for screening?
The standard method is to calculate the Enrichment Factor (EF), which measures how well your model can identify true active compounds from a database that also contains decoys (inactive molecules). A high EF indicates good model performance [29]. Additionally, you can use ROC curve analysis (Receiver Operating Characteristic) to quantify the model's ability to distinguish between active and inactive compounds. The Area Under the Curve (AUC) provides a threshold-independent metric of model quality, with values closer to 1.0 indicating superior discriminatory power [27].
Troubleshooting Guides for Common Experimental Issues
Problem: High False Positive Rate in Initial Docking Hits
Symptoms: A large number of top-ranked compounds from docking fail to show activity in subsequent experimental assays.
| Potential Cause | Diagnostic Steps | Corrective Actions |
|---|---|---|
| Limitations of scoring functions scoring functions often prioritize steric fit over chemical logic. | Check if highly scored poses lack key interactions with functional groups in the binding site (e.g., an unpaired hydrogen bond donor/acceptor). | Implement pharmacophore filtering as a post-docking step to remove poses that do not fulfill essential interaction constraints [25]. |
| Nonspecific compound binding | Analyze ligand structures for promiscuous motifs (e.g., pan-assay interference compounds, or PAINS). | Apply structural filtration rules to remove compounds with undesirable functional groups or properties [30]. |
| Insufficient structural constraints in docking | Review if the binding site is too open or solvent-exposed, allowing many different molecules to score well. | Use a multi-tiered docking approach (e.g., HTVS -> SP -> XP in Glide) with increasing rigor, and combine results with pharmacophore constraints [27]. |
Problem: Inconsistent Results During Pharmacophore-Based Screening
Symptoms: The same pharmacophore query yields different hit lists on different runs or with slightly modified parameters.
| Potential Cause | Diagnostic Steps | Corrective Actions |
|---|---|---|
| Inconsistent preparation of the compound library | Ensure all ligands are prepared with the same protocol (e.g., ionization states, tautomers, stereochemistry). | Standardize ligand preparation using a consistent workflow (e.g., using Schrödinger's LigPrep or MOE) before screening [27]. |
| Poorly defined pharmacophore feature tolerances | Test the sensitivity of your results by slightly varying the tolerance radii of key pharmacophore features. | Optimize feature radii based on a known set of active and inactive compounds. Avoid overly strict tolerances that eliminate true actives [25]. |
| Software-specific interpretation of features | If possible, test the same pharmacophore model in different software platforms (e.g., LigandScout, MOE, Phase) to compare results. | Validate the model across platforms and understand the specific definitions and algorithms used by your chosen software [31]. |
Problem: Poor Correlation Between Computational Predictions and Experimental Binding Affinity
Symptoms: Compounds predicted to bind strongly show weak or no activity in biochemical assays.
| Potential Cause | Diagnostic Steps | Corrective Actions |
|---|---|---|
| Inadequate treatment of solvation and entropy | Docking scores are simplified and may not accurately reflect true binding free energy. | Employ more advanced post-docking scoring methods such as Molecular Mechanics with Generalized Born and Surface Area Solvation (MM-GBSA) to refine your predictions [26] [27]. |
| Rigid receptor approximation | The protein's flexibility and induced-fit effects upon ligand binding are not accounted for. | Perform Molecular Dynamics (MD) simulations (e.g., 100-200 ns) on top hits to assess binding stability and account for protein flexibility [26] [31]. |
| Incorrect binding pose | The docked and pharmacophore-matched pose may not be the true binding mode. | Use composite scoring: rank compounds by a combination of docking score, pharmacophore fit score, and interaction energy from MD/MM-GBSA [25] [27]. |
Experimental Protocols for Key Methodologies
Protocol: Implementing a Basic Pharmacophore Filtering Workflow
This protocol outlines the steps for using a pharmacophore model to filter docking results, as conceptualized in the research [25].
Principle: Docking generates aligned poses, and a structure-based pharmacophore model defines the essential interactions a ligand must make within the binding site. Filtering removes poses that are chemically complementary.
Procedure:
- Pose Generation: Run a molecular docking program (e.g., GOLD, Glide) on your compound library. Configure the software to output a large number of poses per ligand (e.g., 10-50) without heavy reliance on the native scoring function for ranking.
- Pharmacophore Model Definition: Using the target's 3D structure (with or without a co-crystallized ligand), define a set of essential pharmacophore features. These typically include:
- Hydrogen Bond Donor (HBD)
- Hydrogen Bond Acceptor (HBA)
- Hydrophobic (HY)
- Aromatic Ring (AR)
- Positively/Negatively Charged groups (PI/NI)
- Feature Placement: Place these features in 3D space based on complementary functional groups in the protein's binding site. For example, place an HBA feature near a key histidine residue that can act as a hydrogen bond donor.
- Filtering: Process the file containing all saved docking poses. For each pose, check if its atoms satisfy the spatial and chemical constraints of all mandatory pharmacophore features. Poses that fail to match one or more critical features are discarded.
- Ranking: Rank the filtered hits based on a combination of their docking score and their pharmacophore fit score.
Protocol: Structure-Based Pharmacophore Model Generation
This protocol describes the generation of a Shared Feature Pharmacophore (SFP) model from multiple protein-ligand complexes, a method employed in recent studies [31].
Principle: By analyzing several ligand-bound structures of the same target, a consensus pharmacophore model can be built that captures the common, essential interactions shared across different chemotypes, making it more robust.
Procedure:
- Structure Retrieval and Preparation: Obtain high-resolution crystal structures of your target protein in complex with different active ligands from the Protein Data Bank (PDB). Prepare each structure by adding hydrogens, correcting protonation states, and optimizing hydrogen bonds.
- Individual Pharmacophore Generation: For each protein-ligand complex, use structure-based pharmacophore software (e.g., LigandScout) to automatically generate a pharmacophore model. This model will identify features like HBD, HBA, and HY regions based on the observed ligand-protein interactions.
- Model Alignment and Comparison: Align the individual pharmacophore models based on the 3D structure of the protein. The software will identify features that are common across all or most of the models.
- Consensus (SFP) Model Generation: Create a final Shared Feature Pharmacophore model that includes only the overlapping features from the individual models. This model represents the minimal set of interactions necessary for binding.
- Model Validation: Validate the model's ability to distinguish known active compounds from decoys using enrichment calculations or ROC curve analysis [27].
Workflow Visualization
The Scientist's Toolkit: Essential Research Reagents & Software
The following table details key computational tools and resources used in the featured experiments and this field of research.
| Item Name | Type/Supplier | Function in the Workflow |
|---|---|---|
| MOE (Molecular Operating Environment) | Software Suite (Chemical Computing Group) | Used for ligand-based pharmacophore modeling, molecular docking, and molecular dynamics simulations [26]. |
| LigandScout | Software (Inte:Ligand) | Enables advanced structure-based and ligand-based pharmacophore model generation, and performs virtual screening [31]. |
| Schrödinger Suite | Software Suite (Schrödinger) | Provides an integrated platform for protein preparation (Protein Prep Wizard), pharmacophore modeling (Phase), molecular docking (Glide), and energy calculations (MM-GBSA) [27]. |
| ZINC Database | Online Compound Library | A curated collection of commercially available chemical compounds, often used as a source for virtual screening libraries [25]. |
| DOCK3.7 | Docking Software (Academic) | A widely used academic docking program for large-scale virtual screening of ultra-large chemical libraries [28]. |
| ELIXIR-A | Software Tool (Open Source) | A Python-based tool for refining and comparing pharmacophore models from multiple ligands or receptors, aiding in the identification of the best set of pharmacophores [29]. |
| Enamine MAKE-ON-DEMAND | Virtual Compound Library | A pragmatically accessible virtual library of billions of molecules that can be synthesized on demand, used for ultra-large virtual screening [28]. |
Integration of Machine Learning to Predict Docking Scores and Accelerate Screening
FAQs and Troubleshooting Guides
This technical support resource addresses common challenges researchers face when integrating machine learning (ML) with pharmacophore-based virtual screening, with a specific focus on mitigating false positives.
FAQ 1: How can I reduce false positives when my ML model performs well on training data but poorly in prospective screening?
Problem: Your model has high training accuracy but selects an excessive number of false positives during virtual screening of new chemical libraries.
Solutions:
- Apply a Consensus Scoring Strategy: Screen your library against multiple, distinct conformations of the target receptor. Select only the compounds that are top-ranked across all the receptor models. This strategy leverages the concept that a true binder typically fits favorably to different conformations of the binding site, while false positives are often only highly ranked in a single conformation [5].
- Implement Conformal Prediction: Use the conformal prediction (CP) framework with your ML classifier. The CP framework allows you to control the error rate of predictions. By setting a significance level (e.g., ε=0.1), you can define a "virtual active" set with a guaranteed maximum percentage of incorrectly classified compounds, thus filtering out many false positives before they reach the docking stage [32].
- Re-evaluate Your Training Data Splitting: Avoid random splits of your data for training and testing. Instead, split the data based on compound Bemis-Murcko scaffolds. This ensures that the model is tested on chemotypes that differ from those used in training, providing a more realistic assessment of its screening capability and generalizability to novel compounds [33].
FAQ 2: What is the most efficient way to apply ML to screen ultra-large, multi-billion compound libraries?
Problem: Classical molecular docking is computationally infeasible for libraries containing billions of molecules.
Solutions:
- Adopt a Two-Stage ML-Docking Workflow: Use a fast ML classifier as a pre-filter to drastically reduce the library size before any docking occurs.
- Stage 1 - ML Pre-screening: Train a classification algorithm (e.g., CatBoost) on molecular fingerprints (e.g., Morgan fingerprints) using docking scores from a smaller, representative subset (e.g., 1 million compounds) of the large library. Apply this model to predict and select a "virtual active" set from the multi-billion compound library [32].
- Stage 2 - Docking Validation: Perform molecular docking only on the significantly reduced "virtual active" set identified by the ML model. This protocol can reduce the computational cost of structure-based virtual screening by more than 1,000-fold [33] [32].
- Algorithm and Descriptor Selection: For optimal balance between speed and accuracy, use the CatBoost classifier with Morgan2 fingerprints. This combination has been shown to achieve high precision while requiring the least computational resources for training and prediction [32].
FAQ 3: How can I integrate pharmacophore constraints with an ML-based docking prediction model?
Problem: You want to ensure that ML-predicted hits not only have a favorable docking score but also satisfy key pharmacophoric features essential for binding.
Solutions:
- Sequential Filtering Protocol:
- Pharmacophore Filter: First, screen your initial compound database using a well-validated pharmacophore model. This model, which encapsulates steric and electronic features essential for binding, will filter out compounds lacking these critical features [34] [35].
- ML Scoring Filter: Next, apply your ML model trained to predict docking scores to the pharmacophore-filtered subset. This prioritizes compounds that both match the pharmacophore and are predicted to have high affinity [33].
- Use Pharmacophore-Based Fingerprints: Employ a pharmacophore-based fingerprint, such as the Extended Reduced Graph (ErG), as the molecular representation for your ML model. This directly encodes the pharmacophoric features of a molecule (e.g., hydrogen bond donors/acceptors, hydrophobic regions) and has proven effective in creating models that can assign compounds to specific target classes based on these features [36] [37].
Experimental Protocols
Protocol 1: Implementing Consensus Docking to Reduce False Positives
This methodology is designed to select true ligands and minimize false positives when receptor flexibility is considered [5].
- Generate Multiple Receptor Conformations (MRCs): Use molecular dynamics (MD) simulations or available crystal structures to generate an ensemble of distinct conformations of your target protein.
- Docking Screen: Dock your entire compound library (including known high-affinity and low-affinity controls) separately into each receptor conformation in the MRCs.
- Rank and Compare: Generate a ranked list of top-scoring compounds (e.g., top 100) for each individual receptor conformation.
- Identify Intersection Compounds: Select only the compounds that appear in the top-ranked lists across all (or a defined majority) of the receptor conformations. These intersection compounds are your high-confidence hits.
Protocol 2: Machine Learning-Guided Docking Screen of Ultra-Large Libraries
This workflow enables virtual screening of billion-compound libraries at a modest computational cost [32].
- Data Preparation & Docking: Select a random subset (e.g., 1 million compounds) from your ultra-large library. Dock these compounds against your target to generate docking scores.
- Model Training: Define an activity threshold (e.g., top 1% of docking scores) to create a binary classification. Train an ensemble of machine learning classifiers (e.g., five CatBoost models) using molecular fingerprints (e.g., Morgan2) of the 1-million compound set and their class labels.
- Conformal Prediction & Calibration: Use a separate calibration set to calculate nonconformity scores and apply the Mondrian conformal prediction framework.
- Virtual Screening & Selection: Apply the trained conformal predictor to the entire ultra-large library. Using a predefined significance level (ε), the framework will output a "virtual active" set. This set is guaranteed to have an error rate below ε and will be orders of magnitude smaller than the original library.
- Experimental Validation: Perform molecular docking on the reduced "virtual active" set and select top-ranking compounds for synthesis and biological testing.
The table below summarizes key quantitative findings from recent studies on ML-accelerated screening.
Table 1: Performance Metrics of ML-Accelerated Virtual Screening
| Metric | Reported Performance | Context and Methodology |
|---|---|---|
| Speed Acceleration | >1,000-fold [33] [32] | ML-based prediction of docking scores versus classical docking-based screening. |
| Library Size Reduction | ~90% (234M to 25M compounds) [32] | Using CP to pre-filter an ultralarge library before docking. |
| Sensitivity (Recall) | 0.87 - 0.88 [32] | CP workflow identified 87-88% of true virtual actives while docking only ~10% of the library. |
| Model Accuracy | 93.8% [36] | Accuracy of a pharmacophore-fingerprint (ErG) based multi-class model for classifying E3 ligase binders. |
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Resources for ML-Guided Virtual Screening
| Research Reagent / Tool | Function in Experiment | Specific Examples / Notes |
|---|---|---|
| Docking Software | Predicts binding pose and affinity of a ligand to a protein target. | Smina [33], GOLD [5]. Crucial for generating training data for the ML model. |
| Chemical Databases | Source of compounds for virtual screening. | ZINC [33], Enamine REAL Space [32]. Provide ultra-large libraries of purchasable compounds. |
| Molecular Fingerprints | Numerical representation of chemical structure used as input for ML models. | Morgan fingerprints (ECFP4) [33] [32], Extended Reduced Graph (ErG) [36] [37]. ErG is a pharmacophore-based fingerprint. |
| Machine Learning Classifiers | Algorithm that learns to predict docking scores or activity classes from fingerprints. | CatBoost [32], XGBoost [36], Deep Neural Networks [32]. CatBoost offers a good speed/accuracy balance. |
| Conformal Prediction Framework | Provides a mathematically rigorous measure of confidence for ML predictions, controlling error rates. | Mondrian Conformal Predictors [32]. Key for managing false positives and defining the size of the "virtual active" set. |
| Pharmacophore Modeling Software | Creates abstract models of steric and electronic features essential for binding. | Used as a primary filter or to generate pharmacophore-based fingerprints [34] [36] [35]. |
Workflow Visualization
Integrated Screening Workflow for False Positive Reduction
Logic of Consensus Docking Strategy
Frequently Asked Questions (FAQs)
Q1: What is the fundamental definition of a structure-based pharmacophore model? A structure-based pharmacophore model is an abstract representation of the steric and electronic features that are necessary for a molecule to achieve optimal supramolecular interactions with a specific biological target. It is generated directly from the three-dimensional structure of a macromolecule, typically a protein, often in complex with a ligand. These models represent key chemical functionalities—such as hydrogen bond acceptors (HBA), hydrogen bond donors (HBD), hydrophobic areas (H), and ionizable groups—as geometric entities like spheres, planes, and vectors to define the essential interaction points for biological activity [7].
Q2: What are the most common features in a structure-based pharmacophore, and how are they represented? The most common features include [7]:
- Hydrogen Bond Acceptor (HBA): Represented as a vector projecting from an electronegative atom (e.g., oxygen).
- Hydrogen Bond Donor (HBD): Represented as a vector projecting from a hydrogen atom attached to an electronegative atom.
- Hydrophobic (H): Represented as a sphere centered on a carbon atom in a non-polar region.
- Positive/Negative Ionizable (PI/NI): Represented as a sphere centered on an atom capable of holding a formal charge.
- Aromatic (AR): Represented as a ring or plane.
- Exclusion Volumes (XVOL): Represented as spheres that define regions in space occupied by the protein, which the ligand must avoid.
Q3: What is the primary cause of false positives in pharmacophore-based virtual screening? The primary cause is insufficient selectivity in the initial pharmacophore hypothesis. A model that is too generic or lacks critical spatial constraints may match compounds that fit the pharmacophore's geometric and chemical criteria but cannot actually bind to the target protein due to unaccounted-for steric clashes or subtle electronic mismatches [7] [38]. This often occurs when the model does not adequately represent the shape and steric restrictions of the entire binding pocket.
Q4: How can exclusion volumes be used to reduce false positive rates? Exclusion volumes are a direct method to incorporate the shape of the binding pocket into the model. They define "forbidden" regions in space that are occupied by the protein's atoms. During virtual screening, any compound whose atoms intrude into these exclusion volume spheres is penalized or filtered out. This directly addresses steric incompatibility and is a crucial tool for improving the selectivity of a pharmacophore model and reducing false positives [7].
Q5: What validation metrics are used to assess a model's ability to distinguish active from inactive compounds before screening? The standard method involves using a decoy set containing known active compounds and property-matched inactive molecules (e.g., from the DUD-E database). The model is used to screen this set, and its performance is evaluated using [39]:
- Receiver Operating Characteristic (ROC) Curve: A plot of the true positive rate against the false positive rate.
- Area Under the Curve (AUC): A value of 1.0 indicates perfect discrimination, while 0.5 indicates a random classifier. An excellent model typically has an AUC value above 0.9 [39].
- Enrichment Factor (EF): Measures the concentration of active compounds at the top of the screening list. For example, an EF of 10.0 at a 1% threshold means that actives are 10 times more concentrated in the top 1% of results than in the entire database [39].
Q6: Beyond exclusion volumes, what advanced strategies can improve model selectivity? Advanced strategies include:
- Enrichment-Driven Optimization: Tools like BR-NiB (Brute Force Negative Image-Based Optimization) or the O-LAP algorithm can iteratively refine a model's features and their positions based on its performance on a training set of known actives and inactives. This process optimizes the model specifically for high enrichment [38].
- Shape-Focused Models: Algorithms like O-LAP generate cavity-filling models by clustering overlapping atoms from docked active ligands. These models prioritize the overall shape and electrostatic potential complementarity to the binding site, which can be more selective than feature-based models alone [38].
- Integration with Machine Learning: ML classifiers can be trained on chemical descriptors of known active and inactive compounds to further filter virtual screening hits, adding another layer of selectivity [40].
Troubleshooting Guides
Problem: High False Positive Rate in Virtual Screening
Issue: Your pharmacophore model retrieves a large number of hits during virtual screening, but subsequent molecular docking or experimental testing shows a very low confirmation rate.
Solutions:
- Incorporate Exclusion Volumes: Add exclusion volumes to your model based on the protein's binding site structure. This is the most direct way to filter out compounds that sterically clash with the protein [7].
- Refine Feature Selection: Re-evaluate the generated features. Remove redundant or non-essential features that may not critically contribute to binding affinity. Prioritize features that interact with key conserved residues in the binding site [7].
- Optimize with a Training Set: If a set of known active and inactive compounds is available, use enrichment-driven optimization (e.g., with O-LAP) to adjust feature positions, types, and weights to maximize the model's ability to separate actives from inactives [38].
- Apply a Shape Constraint: Use the entire binding cavity to generate a shape-focused pharmacophore model (e.g., a negative image-based model) and use it to rescore or pre-filter the results from your initial feature-based screening. This ensures hits not only match the chemical features but also the overall shape of the pocket [38].
Table 1: Strategies for Mitigating False Positives in Pharmacophore Screening
| Strategy | Mechanism | Tools/Methods |
|---|---|---|
| Exclusion Volumes | Defines steric constraints from the protein, filtering compounds that cause clashes. | LigandScout, structure-based modelers [7]. |
| Enrichment Optimization | Iteratively refines the model to improve its discrimination of active vs. inactive compounds. | O-LAP, BR-NiB [38]. |
| Shape-Focused Rescoring | Evaluates the overall shape and electrostatic complementarity of hits to the binding cavity. | ShaEP, R-NiB (Negative Image-Based Rescoring) [38]. |
| Machine Learning Filtering | Uses trained classifiers to predict activity based on chemical descriptors, post-screening. | PaDEL-Descriptors, ML classifiers (e.g., from Scikit-learn) [40]. |
Problem: Poor Validation Metrics in Model Assessment
Issue: During validation with a decoy set, your model shows a low AUC value or a low enrichment factor, indicating it cannot reliably distinguish active compounds.
Solutions:
- Verify Input Data Quality: Ensure the source protein-ligand complex structure is of high resolution and the ligand's binding pose is biologically relevant. The quality of the input structure directly dictates the quality of the pharmacophore model [7].
- Check Feature Conservation: Analyze if the selected pharmacophore features are conserved across multiple known active ligands or different protein-ligand complex structures. A feature that is not conserved may not be critical for binding [7].
- Adjust Feature Tolerance: Increase the tolerance radii (the size of the feature spheres) slightly to account for minor conformational flexibility, but avoid making them too large, which reduces selectivity.
- Review Decoy Set: Confirm that the decoy set (e.g., from DUD-E) is appropriately matched to the active compounds in terms of molecular weight and other physicochemical properties but is topologically distinct to ensure a fair validation [39] [38].
Problem: Low Hit Rate or Overly Stringent Screening
Issue: Your pharmacophore model retrieves very few or no hits from a large database, potentially missing valid active compounds.
Solutions:
- Relax Feature Constraints: Remove the least critical feature from your hypothesis and re-run the screening. Alternatively, increase the tolerance radii of the features.
- Review Exclusion Volumes: Excessively large or misplaced exclusion volumes can over-constrain the model. Visually inspect the model within the binding pocket to ensure exclusion volumes accurately represent protein atoms.
- Implement Multiple Hypotheses: If the binding site can accommodate ligands in different ways, generate several alternative pharmacophore models (multiple hypotheses) and screen the database against each one independently [7].
Experimental Protocols & Data Presentation
Standard Workflow for Structure-Based Pharmacophore Modeling
The following diagram illustrates the general workflow for creating and applying a structure-based pharmacophore model, integrated with key steps for managing false positives.
Graph 1: Structure-Based Pharmacophore Modeling and Optimization Workflow
Core Protocol: Generating and Validating a Model
This protocol is based on methodologies detailed in multiple studies [39] [7].
1. Protein Structure Preparation:
- Source: Obtain a high-resolution 3D structure of the target protein, preferably in complex with a bioactive ligand, from the Protein Data Bank (PDB).
- Preparation Steps:
- Add hydrogen atoms and correct protonation states of residues (especially in the binding site) at physiological pH.
- Remove crystallographic water molecules unless they are known to mediate key interactions.
- Perform energy minimization to relieve steric clashes and ensure correct stereochemistry.
2. Binding Site Definition and Pharmacophore Feature Generation:
- Define Site: The binding site can be defined as the region surrounding a co-crystallized ligand.
- Generate Features: Use software like LigandScout to automatically interpret the protein-ligand interactions and convert them into pharmacophore features. The software identifies features like HBA, HBD, H, and PI/NI based on the spatial arrangement and chemical nature of the interacting atoms [39].
- Feature Selection: Manually review and curate the automatically generated features. Retain those that represent strong, conserved interactions (e.g., hydrogen bonds with key catalytic residues, crucial hydrophobic contacts) and remove redundant or weak features.
3. Model Validation (Critical Step):
- Prepare Test Set: Compile a set of 10-30 known active compounds and a large set (e.g., 1000-5000) of property-matched decoy molecules. The DUD-E database is a standard source for such decoys [39] [38].
- Run Validation Screening: Use the pharmacophore model as a query to screen the combined set of actives and decoys.
- Calculate Performance Metrics:
- AUC-ROC: Calculate the Area Under the Receiver Operating Characteristic curve. An AUC > 0.7 is acceptable, >0.8 is good, and >0.9 is excellent [39].
- Enrichment Factor (EF): Calculate the EF at 1% of the screened database. For example, a study on XIAP inhibitors achieved an EF1% of 10.0, indicating high early enrichment [39].
Table 2: Key Performance Metrics from a Validated XIAP Inhibitor Pharmacophore Model [39]
| Metric | Value | Interpretation |
|---|---|---|
| AUC (Area Under the ROC Curve) | 0.98 | Excellent model; 98% chance of ranking a random active compound higher than a random decoy. |
| Enrichment Factor (EF) at 1% | 10.0 | In the top 1% of screening results, active compounds are 10 times more concentrated than in the entire database. |
| Number of Actives in Test Set | 10 | The model was validated against 10 known active XIAP antagonists. |
| Number of Decoys in Test Set | 5199 | A large set of decoys was used to ensure statistical robustness. |
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Software and Databases for Structure-Based Pharmacophore Modeling
| Tool/Resource | Type | Primary Function | Key Application in the Workflow |
|---|---|---|---|
| RCSB PDB | Database | Repository of experimentally determined 3D protein structures. | Source of the initial target protein structure (e.g., PDB ID: 5OQW for XIAP) [39]. |
| LigandScout | Software | Advanced molecular design software for structure- and ligand-based pharmacophore modeling. | Generation and visualization of pharmacophore features from protein-ligand complexes [39]. |
| ZINC Database | Database | Curated collection of commercially available compounds for virtual screening. | Source of natural compounds or drug-like molecules for pharmacophore-based screening [39] [40]. |
| DUD-E | Database | Database of Useful Decoys: Enhanced. Contains decoy molecules for validation. | Provides property-matched decoys to validate the model's ability to distinguish actives from inactives [39] [38]. |
| O-LAP | Software | Algorithm for generating shape-focused pharmacophore models via graph clustering. | Creates cavity-filling models to improve screening selectivity and reduce false positives [38]. |
| PaDEL-Descriptor | Software | Calculates molecular descriptors and fingerprints from chemical structures. | Generates features for machine learning-based filtering of screening hits [40]. |
| AutoDock Vina/PLANTS | Software | Molecular docking programs. | Used for flexible docking of hits for post-screening validation and pose analysis [40] [38]. |
For researchers developing ligand-based models, public databases are indispensable sources of experimentally validated protein-ligand interaction data. These resources provide the foundational information for building predictive models in virtual screening campaigns.
Table 1: Primary Databases for Ligand-Based Model Development
| Database Name | Primary Content & Specialization | Key Statistics | Data Sources & Licensing |
|---|---|---|---|
| BindingDB [41] | Measured binding affinities of drug-like small molecules against protein targets. | - 3.2M binding data points- 1.4M Compounds- 11.4K Protein Targets [41] | Data extracted from scientific literature and patents; provided under Creative Commons Attribution 3.0 License [41]. |
| ChEMBL [2] | Bioactive molecules with drug-like properties, containing binding, functional, and ADMET information. | (Imported into BindingDB, a major source of curated data) [41] | Data provided under Creative Commons Attribution-Share Alike 3.0 Unported License [41]. |
| Pocketome [42] | An encyclopedia of crystallographically observed conformations of binding pockets in complex with diverse chemicals. | - ~2,050 binding site ensembles- Covers major target families (GPCRs, Kinases, Nuclear Receptors) [42] | Derived from Protein Data Bank (PDB) and UniProt Knowledgebase [42]. |
| PDBbind [43] | Experimentally measured binding affinity data for biomolecular complexes housed in the PDB. | Used to train and test computational models (e.g., 3,875 complexes in one curated set) [43] | Linked to the primary PDB structure repository. |
FAQs: Data Curation and Preparation
1. How can I assess and improve the quality of data sourced from public databases for my model? The quality of your model is directly dependent on the quality of the input data. Begin by applying stringent filtering based on experimental conditions. For binding affinity data (e.g., Ki, IC50), prioritize measurements obtained under consistent and physiologically relevant conditions (e.g., pH, temperature) [41]. Furthermore, check for chemical structure integrity. Ensure structures are standardized, with correct valence, defined stereochemistry, and removal of counterions and salts. Utilize the curated subsets provided by databases like BindingDB, which contain over 1.5 million data points meticulously curated by experts, to start with a higher-quality foundation [41].
2. What are the best practices for selecting an appropriate benchmark decoy set to test my model's performance? The choice of decoy set is critical for a realistic assessment of your model's ability to distinguish true actives from inactives. Avoid using decoys that are trivially different from actives. Instead, employ a strategy that generates "compelling decoys" – molecules that are individually matched to active complexes and are challenging to distinguish, forcing the model to learn the nuanced features of true binding [2]. This approach prevents model overfitting and more accurately reflects the challenge of a real virtual screen, where the vast majority of compounds are plausible but inactive [2].
3. My model performs well on training data but poorly in prospective virtual screening. What might be the cause? This is a classic sign of overfitting or dataset bias. This often occurs when a model is trained on a limited set of examples and cannot generalize to new chemical scaffolds. To address this:
- Expand Structural Diversity: Incorporate data from ensembles of protein-ligand structures, such as those provided by the Pocketome, to expose your model to the natural conformational variability of binding sites [42].
- Analyze Applicability Domain: Ensure your screening library falls within the chemical space covered by your training data. Models fail when applied to "out-of-distribution" compounds [2].
- Integrate Structure-Based Insights: If possible, use 3D ligand-based methods that project ligand properties into specific spatial locations, which are less biased toward known chemical scaffolds and better for "scaffold-hopping" than 2D similarity measures [42].
FAQs: Model Development and Validation
4. What are the main computational approaches for building ligand activity models? There are two primary types of 3D models you can build, each with its own strengths.
- Pocket-Based Models (Structure-Based): These models rely on the 3D structures of binding pockets from sources like the Pocketome. They evaluate new ligands by computationally docking them and scoring their complementarity to the pharmacophore features of the pocket. They do not require known ligands to start, making them suitable for novel targets [42].
- Ligand Property-Based Models (Ligand-Based): These models use the 3D structures of known active ligands in their bound conformations. They define the optimal spatial distribution of pharmacophore features required for binding and evaluate new compounds by their 3D similarity to this template. These methods are excellent for scaffold-hopping as they focus on interaction patterns rather than chemical graphs [42].
5. How do I rigorously validate my ligand-based model before prospective use? Robust validation is non-negotiable. Move beyond simple random splits of your data.
- Use Temporal Splits: A more realistic validation involves training your model on data published before a certain date and testing it on data published after. BindingDB facilitates this by providing publication and curation dates for measurements [41].
- Benchmark on Challenging Sets: Test your model's performance on external benchmark datasets designed to be difficult, such as those containing the "compelling decoys" mentioned earlier [2].
- Employ Multiple Metrics: Don't rely on a single metric. Use a composite of metrics including Area Under the ROC Curve (AUC) to measure overall enrichment, and also examine the hit rate in the top-ranked compounds. A good model should achieve a high AUC and a high proportion of true actives in its top ranks [42].
Troubleshooting Guides
Problem 1: High False Positive Rate in Virtual Screening
Symptoms
- A high number of top-ranked compounds from a virtual screen show no activity in subsequent experimental assays.
- The observed hit rate is significantly lower than the expected hit rate based on model confidence scores.
Investigation and Resolution Steps
1. Interrogate Decoy Set Quality: A major cause of high false positives is an inadequate decoy set used during model training or validation. If the decoys are trivially different from actives (e.g., lacking key functional groups), the model will not learn the true, complex features of binding and will fail in real screens [2].
- Solution: Adopt a rigorous decoy selection strategy like the D-COID method, which aims to generate highly compelling decoy complexes that are individually matched to available active complexes, ensuring the model is trained on a challenging and realistic task [2].
2. Check for Model Overfitting: The model may have memorized the training data without learning generalizable rules.
- Solution: Validate your model using a temporal split (training on older data, testing on newer data) rather than a random split. This better simulates a prospective screening scenario. Furthermore, ensure your training set encompasses a diverse range of chemical scaffolds and target conformations to improve generalizability [41] [42].
3. Inspect Binding Pocket Conformation: For structure-aware models, using a single, rigid protein structure can lead to false positives for compounds that would be sterically or electrostatically incompatible with other relevant pocket conformations.
- Solution: Utilize an ensemble of pocket conformations from resources like the Pocketome. Docking against multiple representative structures can help identify compounds whose binding is sensitive to minor structural changes, which are less promising leads [42].
4. Integrate Machine Learning-Based Re-scoring: Traditional scoring functions can be misled by specific, favorable interactions that are not sufficient for overall high-affinity binding.
- Solution: Implement a machine learning classifier like vScreenML as a post-docking filter. Such classifiers, trained on challenging decoys, can more effectively distinguish true actives from false positives by considering nonlinear interactions and complex patterns that traditional functions miss [2] [43].
Problem 2: Low Hit Rate and Inability to Find Novel Scaffolds
Symptoms
- The model successfully identifies known chemotypes but fails to find new chemical scaffolds (i.e., poor at "scaffold-hopping").
- All top-ranked compounds are structurally very similar to the training set actives.
Investigation and Resolution Steps
1. Evaluate the 3D Nature of the Pharmacophore Model: If your model is primarily based on 2D chemical similarity, it is inherently biased toward recovering compounds that are structurally similar to the training set.
- Solution: Shift to a 3D ligand property-based model. These methods represent ligands as 3D fields of pharmacophore features, free from the constraints of the underlying chemical graph. This makes them more realistic and suitable for scaffold-hopping, as they focus on the spatial arrangement of interactions rather than the specific atoms creating them [42].
2. Analyze the Diversity of the Training Set: The model cannot learn what it has never seen. If the training data is composed of a few, highly similar chemical series, the model's applicability domain will be narrow.
- Solution: Actively curate a more diverse training set. Augment your data by incorporating ligands from different sources like ChEMBL and BindingDB that bind to the same target but belong to distinct structural classes. The use of diverse data is critical for expanding the model's recognition capabilities [41] [42].
3. Leverage Multiple Pocket Conformations: Different chemical scaffolds often bind by stabilizing distinct conformations of the target protein. A model based on a single protein structure may be optimized for only one specific scaffold.
- Solution: As with reducing false positives, using a pocket ensemble from the Pocketome can help. Different scaffolds may be best identified using different representative structures from the ensemble, increasing the chances of finding novel chemotypes [42].
Table 2: Key Computational Tools and Resources for Ligand-Based Modeling
| Tool/Resource Name | Type | Primary Function in Model Development |
|---|---|---|
| BindingDB [41] | Database | Source for curated binding affinity and small molecule bioactivity data to train and validate models. |
| ChEMBL [41] | Database | Large-scale repository of bioactive molecules with drug-like properties, used as a data source. |
| The Pocketome [42] | Database | Provides ensembles of binding pocket conformations for incorporating target flexibility into models. |
| PDBbind [43] | Database | Provides a refined set of protein-ligand complexes with binding affinity data for benchmarking. |
| LigPlot+ [44] | Visualization Tool | Generates schematic 2D diagrams of protein-ligand interactions to visualize and analyze binding modes. |
| vScreenML [2] | Software/Classifier | A machine learning classifier trained to reduce false positives in structure-based virtual screening. |
| D-COID Dataset [2] | Training Dataset | A strategy for building a dataset of "compelling decoys" to train robust ML classifiers for virtual screening. |
| MedusaNet [43] | Software/Scoring | A 3D Convolutional Neural Network (CNN) model used to predict the stability of protein-ligand complexes. |
Advanced Experimental Protocol: Building a vScreenML-like Classifier
This protocol outlines the methodology for creating a machine learning classifier to reduce false positives in virtual screening, based on the approach described in [2].
1. Objective: To train a general-purpose binary classifier (vScreenML) that can effectively distinguish between active and "compelling decoy" protein-ligand complexes.
2. Materials and Data Sources:
- Active Complexes: Source experimentally determined protein-ligand structures from the Protein Data Bank (PDB). Filter these to include only ligands that adhere to the desired physicochemical properties for your drug discovery campaign (e.g., molecular weight, logP) [2].
- Decoy Complexes: Generate a set of "compelling decoys" using the D-COID strategy. This involves creating decoy complexes that are individually matched to the active complexes and are difficult to distinguish based on simple criteria, ensuring the model learns non-trivial aspects of molecular recognition [2].
3. Methodology:
- Step 1: Data Compilation and Preparation.
- Compile a set of active complexes from the PDB, ensuring they meet your ligand property criteria.
- For each active complex, generate a set of matched decoy complexes using a docking program to pose the decoys in the binding site.
- Step 2: Feature Extraction.
- For each complex (both active and decoy), calculate a set of features that describe the protein-ligand interaction. These may include:
- Interaction fingerprints: Hydrogen bonds, hydrophobic contacts, ionic interactions.
- Geometric descriptors: Buried surface area, shape complementarity.
- Energetic terms: Components from traditional scoring functions (e.g., vdW, electrostatics).
- For each complex (both active and decoy), calculate a set of features that describe the protein-ligand interaction. These may include:
- Step 3: Model Training.
- Use the XGBoost framework, a powerful and efficient implementation of gradient-boosted trees, to train the classifier.
- The model is trained on the labeled dataset where active complexes are the positive class and compelling decoy complexes are the negative class.
- Step 4: Validation.
- Perform rigorous retrospective benchmarks to evaluate the classifier's performance against other scoring functions.
- The key metric is the enrichment of true actives in the top-ranked compounds compared to traditional methods.
4. Prospective Application:
- In a new virtual screening campaign, the trained
vScreenMLclassifier is used to re-score the output poses from a molecular docking run. The top-ranked compounds by the classifier are selected for experimental testing [2].
Frequently Asked Questions
1. What are the most common causes of false positives after the initial pre-screening filters? False positives often persist due to an overestimation of conformational flexibility during the 3D alignment step or an inability of the 2D pre-filters to account for specific stereochemical constraints [8]. Furthermore, if the pre-filtering steps are not "lossless," they may mathematically discard molecules that could actually fit the query, but this is often accepted for the benefit of higher screening efficiency [8].
2. How can I validate that my pre-filtering steps are not discarding potential true positives? You can validate your workflow by using a set of known active compounds. A best practice is to apply "lossless" filters that guarantee all discarded molecules are geometrically incapable of matching the query, thus preserving all potential true positives [8]. Additionally, comparing your results against a strategy that docks molecules to multiple receptor conformations can serve as a cross-validation; true binders are often identified as the common top-ranked hits across different receptor models [5].
3. My pharmacophore key search is returning no hits. What should I check? First, verify the complexity of your query. A pharmacophore key is a binary fingerprint representing possible 2-point, 3-point, or 4-point pharmacophores from a molecule's conformations [8]. If your query contains too many features or overly restrictive distance tolerances, it may not match any database entries. Widen the distance tolerance bins in your fingerprint generation algorithm and ensure it is at least twice the binning size of the partitioning tree to enable self-matches [8]. Second, check that the feature definitions (e.g., hydrogen-bond acceptor, hydrophobic) in your query are consistent with those used to generate the database's pharmacophore keys [8].
4. Can these filtering techniques be applied to fragment-based screening? Yes, and they are particularly powerful in this context. Novel workflows like FragmentScout have been developed to aggregate pharmacophore feature information from multiple experimental fragment poses—such as those from XChem crystallographic screening—into a single joint pharmacophore query [45]. This query, which can contain many features, is then used to screen large 3D databases. The efficiency of modern alignment algorithms, like the Greedy 3-Point Search in LigandScout XT, makes it feasible to handle these complex queries and identify micromolar hits from millimolar fragments [45].
Troubleshooting Guides
Problem: High Number of False Positives After Feature-Count Pre-screening
- Symptoms: The virtual screening hit-list is large and contains many chemically diverse compounds that do not show activity in subsequent experimental assays.
- Investigation & Diagnosis:
- Verify Filter Specificity: A feature-count filter is a simple 0D descriptor that checks if a database molecule possesses at least the same number of each pharmacophoric feature type as the query [8]. While it can quickly eliminate a large fraction of a database, it is not geometrically specific. Investigate if the chemical features in your false positives are sterically incapable of aligning with the query's 3D arrangement.
- Check Conformational Sampling: The pre-computed conformer database used for screening may not contain the specific bioactive conformation. Ensure your conformer generation protocol is sufficiently exhaustive to cover the relevant conformational space [8].
- Resolution:
- Implement a More Restructive Pre-filter: Introduce a pharmacophore key filter immediately after the feature-count check. This provides an intermediate level of complexity by checking for the presence of key 2, 3, and 4-point distance combinations between features, offering some geometric filtering before the computationally expensive 3D alignment [8].
- Apply a Consensus Strategy: To specifically tackle false positives arising from receptor flexibility, use multiple receptor conformations for screening. Select only those hits that appear in the top-ranked lists across all or most of the different conformations. This strategy is proven to effectively distinguish high-affinity binders from false positives [5].
Problem: Inconsistent Screening Results with a Valid Pharmacophore Query
- Symptoms: Different screening runs with the same query and database yield varying hit-lists, or known active compounds are not retrieved.
- Investigation & Diagnosis:
- Review Feature Definitions: Inconsistent results can stem from differences in how pharmacophore features are defined and placed by various software platforms (e.g., Catalyst, MOE, Phase, LigandScout) [8]. Confirm the exact definition and spatial placement of features like hydrogen-bond donors/acceptors in your query model.
- Analyze Tolerance Radii: The radius of a pharmacophore feature sphere determines how closely a database molecule must match. Excessively small radii may miss valid hits, while overly large radii can permit geometrically implausible matches and increase false positives [46].
- Resolution:
- Standardize the Workflow: Use the same software platform for both query generation and database screening to ensure internal consistency in feature handling.
- Calibrate Tolerances: Adjust feature radii based on the flexibility of the binding site and the known variability in your active ligand set. Using a test set of known actives and inactives can help optimize these parameters.
Problem: Slow Screening Performance with Large Compound Libraries
- Symptoms: The virtual screening process takes an impractically long time to complete, hindering research progress.
- Investigation & Diagnosis:
- Evaluate Filter Order: The screening workflow should follow a cascade of increasing computational complexity [8]. Confirm that the fastest, least restrictive filters (like feature-count) are applied first, followed by medium-complexity filters (like pharmacophore keys), with the slow, accurate 3D alignment performed last on a greatly reduced subset.
- Check Database Indexing: If using pharmacophore keys or other fingerprint methods, ensure the screening database is properly pre-processed and indexed for rapid similarity searches [8].
- Resolution:
- Optimize the Filtering Cascade: Implement a multi-step workflow as described in the diagnosis. The goal of pre-filtering is to quickly identify and eliminate molecules that cannot possibly fit the query before they reach the time-limiting 3D alignment step [8].
- Utilize Pre-computed Conformations: As noted in current strategies, pre-generating a conformational database once and reusing it for multiple screening campaigns is strongly preferred over on-the-fly conformation generation, as it provides a significant speed-up [8].
Research Reagent Solutions
The following tools and materials are essential for implementing robust multi-step filtering workflows.
| Tool/Reagent | Function in the Workflow |
|---|---|
| Conformational Database | A pre-computed database of multiple 3D conformations for each compound in a screening library. It is essential for efficiently handling molecular flexibility during screening [8]. |
| Pharmacophore Modeling Software (e.g., LigandScout, Catalyst, Phase, MOE) | Platforms used to create and validate the 3D pharmacophore query, and often to conduct the virtual screening itself. They provide the algorithms for feature placement and 3D alignment [8]. |
| Pharmacophore Keys / Fingerprints | A binary representation of a molecule that encodes the presence or absence of specific 2, 3, and 4-point pharmacophoric patterns, considering conformational flexibility. Used as a medium-complexity pre-filter [8]. |
| Multiple Receptor Conformations (MRCs) | A set of distinct 3D structures of the target protein (from MD simulations, NMR, or crystal structures). Docking or screening against MRCs and selecting intersection hits is a proven strategy to reduce false positives stemming from receptor plasticity [5]. |
| Fragment Libraries (e.g., XChem) | Collections of small, simple molecules used in fragment-based screening. They are the starting point for workflows like FragmentScout, which builds a joint pharmacophore query from multiple bound fragment poses to discover novel leads [45]. |
Experimental Protocols
Protocol 1: Implementing a Standard Multi-Step Filtering Workflow
This protocol outlines the general workflow for pharmacophore-based virtual screening using sequential filters to maximize efficiency and minimize false positives [8].
Query Pharmacophore Generation:
- Structure-Based Method: If a protein-ligand complex structure is available, use software like LigandScout to automatically extract interaction features (H-bond donors/acceptors, hydrophobic contacts, charged groups) from the binding site. Add exclusion volumes to define the steric boundaries [8] [45].
- Ligand-Based Method: If structural data is unavailable, align a set of known active ligands and use software (e.g., Catalyst/HipHop, Phase) to identify the 3D arrangement of chemical features common to all actives.
Database Pre-processing:
Multi-Step Filtering:
- Step 1 - Feature-Count Filtering: Calculate the number of each type of pharmacophoric feature (e.g., 2 HBA, 1 Hy-Ali, 1 Hy-Ar [6]) for both the query and all database molecules. Quickly discard any molecule that does not possess the minimum required count of each feature [8].
- Step 2 - Pharmacophore Key Filtering: Generate a pharmacophore key (a fixed-length binary fingerprint) for the query and the remaining database molecules. The fingerprint should encode 2-, 3-, and 4-point distance patterns between features. Perform a fast fingerprint intersection to eliminate molecules that lack the essential geometric pharmacophores of the query [8].
- Step 3 - 3D Geometric Alignment: For the molecules that pass the first two filters, perform an accurate 3D alignment. This involves finding a subset of the molecule's features that matches the query's spatial arrangement within defined tolerances, typically by minimizing the RMSD between associated feature pairs. This step finally produces the virtual screening hit-list [8].
Protocol 2: A False Positive Reduction Strategy Using Multiple Receptor Conformations
This protocol leverages receptor flexibility to discriminate true binders from false positives, based on the hypothesis that a true inhibitor can bind favorably to different conformations of the binding site [5].
Generate Multiple Receptor Conformations (MRCs):
- Use molecular dynamics (MD) simulations of the apo (unliganded) or holo (liganded) receptor to sample its flexible states. Extract several (e.g., 5-6) structurally distinct snapshots from the trajectory [5].
Perform Parallel Docking/Screening:
- Using each distinct receptor conformation as a separate model, dock the entire compound library (including known high-affinity and low-affinity controls). Perform this docking separately for each conformation [5].
Identify Intersection Hits:
- For each receptor model, generate a list of top-ranked molecules (e.g., top 50, top 100). The final hit-list is composed of the intersection—the molecules that appear in the top-ranked lists from all or a defined majority of the receptor models. This selectively identifies compounds that bind robustly across different conformations while filtering out the unique false positives introduced by each individual model [5].
Workflow Diagrams
Multi-Step Pharmacophore Screening
Pharmacophore Key Generation
Troubleshooting and Workflow Optimization: A Practical Guide
Troubleshooting Guides
FAQ: Managing Tautomeric and Protonation States
Q1: Why do my pharmacophore models generate false positives in virtual screening?
False positives often occur due to inadequate handling of molecular tautomerism and protonation states during library preparation. Tautomeric rearrangements create distinct equilibrated structural states of the same compound, significantly impacting ligand-protein interaction patterns. When these states are not properly considered, derived pharmacophore models may misrepresent binding modes, leading to inaccurate virtual screening results [47].
Q2: How can I systematically account for tautomerism in structure-based pharmacophore modeling?
Implement a multiple species, multiple mode approach. This involves:
- Enumeration: Generate all possible tautomers and relevant protonation states for each ligand at biological pH.
- Representation: Create multiple representations for each compound, concatenating them into a unique fingerprint that accounts for most of its chemical and conformational diversity [48].
- Validation: Use an exhaustive cross-validation scheme to ensure model robustness and predictive power. An algorithm that enumerates all possible tautomers under the constraints of a fixed active ligand conformation can be employed for this purpose [47].
Q3: What is the critical first step in preparing a compound library for pharmacophore-based screening?
The most critical step is the comprehensive generation and consideration of all plausible tautomeric and protonation states for each molecule in the library. Overlooking this step creates an inherent bias in the chemical representation, which propagates through model creation and ultimately leads to misinterpretation of ligand-binding interactions and false positives in screening [47].
Q4: My virtual screening results are inconsistent. Could this be related to conformer generation?
Yes, inconsistencies are frequently traced to incomplete conformational sampling. Relying on a single, low-energy conformer is insufficient. A robust protocol must generate multiple 3D conformations for each tautomeric/protonated state to adequately represent the molecule's flexibility and identify the bioactive conformation relevant to the protein target.
Experimental Protocols
Protocol 1: Generating a Tautomer-Aware Compound Library
Purpose: To create a comprehensive screening library that accurately represents the tautomeric and protonation diversity of each compound.
Methodology:
- Input Preparation: Start with a curated set of compounds in a standard format (e.g., SMILES or SDF).
- Tautomer Enumeration: Use software (e.g., MOE, ChemAxon, or RDKit) to generate all possible tautomers for each compound. The algorithm should consider constraints like the molecular environment of the protein active site [47].
- Protonation State Assignment: At a physiological pH (e.g., 7.4), calculate and generate the major microspecies for each tautomer.
- 3D Conformer Generation: For each resulting unique molecular representation, generate multiple low-energy 3D conformers. The number of conformers should be sufficient for coverage (e.g., a maximum of 250 conformers per molecule with an energy cutoff of 10 kcal/mol).
- Fingerprint Creation: Encode all representations and conformations of a compound into a unified pharmacophore fingerprint to capture its full chemical diversity [48].
Troubleshooting Table: Tautomer and Conformer Generation Issues
| Problem | Potential Cause | Solution |
|---|---|---|
| Excessive library size | Too many tautomers/protonation states generated | Apply stricter energy filters (e.g., < 5-7 kcal/mol from global minimum); focus on states relevant at physiological pH. |
| Missed bioactive state | Enumeration algorithm limitations | Use multiple software tools for enumeration and compare results; manually inspect key compounds. |
| Long computation time | Large number of conformers per molecule | Reduce the maximum number of conformers; use a faster, less precise conformer generation method initially. |
| Poor model performance | Inadequate representation of molecular diversity | Ensure the concatenated fingerprint includes all tautomers and conformers; validate with known active compounds [48]. |
Protocol 2: Building a Robust 3D Pharmacophore Model
Purpose: To develop a predictive pharmacophore model that is invariant to tautomeric and protonation state changes.
Methodology:
- Input Structures: Use a set of known active ligands, prepared according to Protocol 1 to include their multiple states and conformations.
- Pharmacophore Feature Mapping: For each ligand representation, identify key pharmacophore features (e.g., hydrogen bond donors/acceptors, hydrophobic regions, aromatic rings, charged groups).
- Common Feature Identification: Align the multiple conformations of the active ligands to identify common 3D spatial arrangements of pharmacophore features that are critical for biological activity.
- Model Validation: Employ a rigorous cross-validation scheme. The model's ability to correctly identify active compounds (sensitivity) and reject inactives (specificity) should be tested against an external validation set [48].
- Virtual Screening: Apply the validated model to screen large compound libraries that have been prepared with the same rigorous tautomer and conformer protocols.
Workflow for Tautomer-Aware Library Preparation
The Scientist's Toolkit: Research Reagent Solutions
Table: Essential Computational Tools for Managing Molecular Diversity
| Item | Function | Application Note |
|---|---|---|
| Tautomer Enumeration Software (e.g., from MOE, ChemAxon) | Automatically generates all possible tautomeric forms of a molecule. | Critical for ensuring the chemical structure considered is the correct one for ligand-protein interaction analysis [47]. |
| Protonation State Calculator (e.g., Epik, MOE) | Predicts the major microspecies of a molecule at a specified pH. | Essential for accurately modeling the ionic states of compounds under physiological conditions. |
| Conformer Generation Algorithm (e.g., ConfGen, OMEGA) | Produces multiple, low-energy 3D shapes of a molecule. | A "multiple species, multiple mode" approach that accounts for conformational diversity is key to building predictive models [48]. |
| Pharmacophore Modeling Platform (e.g., MOE, Phase) | Identifies and models 3D arrangements of features essential for biological activity. | Must be used with tautomer- and protonation-aware libraries to derive accurate, tautomer-invariant pharmacophore patterns [47]. |
| 3D-Pharma Fingerprinting | Creates a unified fingerprint from all species and conformations of a compound. | This concatenated fingerprint improves virtual screening performance by capturing a molecule's full diversity [48]. |
Troubleshooting Path for Model Improvement
Troubleshooting Guides
Guide 1: Troubleshooting High False Positive Rates in Pharmacophore-Based Screening
Problem: Your virtual screening results in an unmanageably high number of hits, many of which are likely false positives or promiscuous compounds.
Solution: Implement a structured cascade of filters to remove non-lead-like and problematic compounds early in the workflow.
- Step 1: Apply Lead-Likeness Filters. Begin by filtering your initial compound library using strict lead-like criteria. This removes molecules that are too complex to be viable starting points for optimization. The "Rule of Three" is appropriate here: Molecular Mass < 300 Da, log P ≤ 3, Hydrogen Bond Donors ≤ 3, Hydrogen Bond Acceptors ≤ 3, Rotatable Bonds ≤ 3 [49].
- Step 2: Eliminate Functional Group Alerts. Screen the remaining compounds against functional group filters to remove pan-assay interference compounds (PAINS), rapid elimination of swill (REOS), and other promiscuous or reactive molecules. These filters use SMARTS strings to identify undesirable moieties such as rhodanines, quinones, and curcumin-based structures that are known to cause false positives [50] [51].
- Step 3: Enforce Drug-Likeness Rules. Further refine the library by applying drug-likeness rules like Lipinski's Rule of Five. This focuses the chemical space on compounds with a higher probability of oral bioavailability [49] [51].
- Step 4: Conduct Specificity Checks. Before final selection, perform a final check against aggregator databases and use predictive models for specific toxicity endpoints (e.g., cardiotoxicity via hERG blockade) to flag compounds with potential off-target effects or mechanism-based toxicity [52] [51].
The following workflow diagram illustrates this multi-step troubleshooting process:
Guide 2: Addressing Poor Synthesizability of Screening Hits
Problem: Identified hit compounds are theoretically promising but are predicted to be difficult or impractical to synthesize, halting project progression.
Solution: Integrate synthesizability assessment tools directly into the hit identification and prioritization workflow.
- Step 1: Early-Stage Feasibility Estimation. For all compounds passing initial drug-likeness filters, use a tool like RDKit's synthetic accessibility (SA) score to get a rapid, preliminary estimate of synthesis difficulty. This helps in prioritization [52].
- Step 2: AI-Powered Retrosynthetic Analysis. For top-ranked hits, perform a detailed retrosynthetic analysis using AI-based tools. The
druglikeFiltertool, for example, integrates the Retro* algorithm, which deconstructs complex molecules into simpler building blocks to identify viable synthetic pathways [52]. - Step 3: Prioritize by Synthetic Tractability. When choosing between several hits with similar predicted activity and drug-likeness, prioritize the compounds with clearer and shorter predicted synthetic routes. This saves significant time and resources downstream [52].
- Step 4: Consult a Medicinal Chemist. No computational tool is infallible. Always have a medicinal chemist review the proposed structures and synthetic routes suggested by the software to assess real-world feasibility [50].
Frequently Asked Questions (FAQs)
FAQ 1: What is the fundamental difference between "drug-likeness" and "lead-likeness," and why is the distinction important in early screening?
Drug-likeness describes properties of a molecule that make it a likely oral drug, typically assessed by rules like Lipinski's Rule of Five (Ro5). In contrast, lead-likeness describes a more restrictive set of properties designed for a viable starting point for optimization. A good lead compound is typically smaller and less complex than a final drug, providing "chemical space" for medicinal chemists to optimize its potency and selectivity without breaking drug-likeness rules later. Applying lead-like filters first increases the chance that optimized candidates will remain drug-like [49] [51].
FAQ 2: My promising compound violates Lipinski's Rule of Five. Should I automatically discard it?
No. Lipinski's Rule of Five is a guideline, not an absolute rule. It was developed based on an analysis of orally administered drugs and has notable exceptions. For instance, several natural products, antibiotics, and drugs that utilize active transporters are successful despite violating the rule. A violation should be a flag for further investigation, not immediate discard. Evaluate the reason for the violation, consider the intended route of administration, and use additional tools to assess its ADMET properties more comprehensively [49].
FAQ 3: What are PAINS, and why are they so problematic in virtual screening?
PAINS (Pan-Assay Interference Compounds) are chemical compounds that appear as hits in many different biological screening assays but do not work through a specific, drug-like mechanism. Instead, they interfere with the assay technology itself through various means, such as covalent modification of the protein target, chelation of metal ions, or aggregation. Because they are promiscuous, they are a major source of false positives. Filtering them out early using dedicated PAINS filters is critical to avoid wasting resources on optimizing compounds that will inevitably fail [50] [51].
FAQ 4: Are there comprehensive tools that integrate multiple types of filters into a single workflow?
Yes, integrated platforms are being developed to streamline this process. For example, the AI-powered druglikeFilter tool allows for the collective evaluation of drug-likeness across four critical dimensions: physicochemical properties, toxicity alerts, binding affinity, and compound synthesizability. This provides a more holistic assessment than applying individual rules in sequence [52]. Similarly, KNIME analytics platforms can be configured with nodes that apply various medicinal chemistry filters to tailor chemical libraries effectively [51].
Data Presentation
Table 1: Key Property-Based Filters for Drug and Lead Discovery
This table summarizes the most widely used rules for defining drug-like and lead-like chemical space.
| Filter Name | Core Criteria | Primary Objective | Common Applications |
|---|---|---|---|
| Lipinski's Rule of Five (Ro5) [49] [51] | MW ≤ 500, log P ≤ 5, HBD ≤ 5, HBA ≤ 10 | Identify compounds with a high probability of oral bioavailability. | Primary filter for drug-likeness in late-stage screening and candidate triage. |
| Veber's Rules [49] [51] | Rotatable Bonds ≤ 10, TPSA ≤ 140 Ų | Predict good oral bioavailability based on molecular flexibility and polarity. | Often used alongside or as an extension to Ro5. |
| Lead-like (Rule of Three) [49] | MW < 300, log P ≤ 3, HBD ≤ 3, HBA ≤ 3, Rotatable Bonds ≤ 3 | Identify simple compounds with room for medicinal chemistry optimization. | Early-stage screening to define a high-quality, optimizable starting library. |
| Ghose Filter [49] | MW 180-480, log P -0.4 to 5.6, Molar Refractivity 40-130, Total Atoms 20-70 | A more quantitative and constrained definition of drug-likeness. | Refining large commercial or virtual compound libraries. |
Table 2: Key Functional Group Filters to Minimize False Positives
This table lists critical functional group filters used to identify and remove problematic compounds.
| Filter Type | Key Examples of Flagged Motifs | Reason for Filtering | How to Apply |
|---|---|---|---|
| PAINS [50] [51] | Rhodanines, Quinones, Curcumin, 2-Aminothiophenes | Compounds are promiscuous assay interferers and likely false positives. | Screen compound libraries against defined SMARTS patterns before virtual screening. |
| REOS [51] | 117+ SMARTS strings for reactive moieties and toxicophores | Remove compounds with reactive functional groups or known toxicity issues. | Apply as a functional group filter to eliminate "swill" and unworthy leads. |
| Aggregators [51] | Known aggregators with high lipophilicity (SlogP >3) | Eliminate compounds that form colloidal aggregates, a common source of false positives. | Use a combination of structural similarity checks and property-based cut-offs. |
Experimental Protocols
Protocol 1: Implementing a Standard Pre-Virtual Screening Filtering Cascade
This protocol details a standard methodology for preparing a compound library for structure-based virtual screening (e.g., molecular docking) to minimize false positives.
1. Library Acquisition and Preparation:
- Obtain your compound library in SMILES or SDF format from a commercial, public (e.g., PubChem), or proprietary source [50].
- Standardize the structures: neutralize charges, remove duplicates, and generate canonical tautomers and stereochemistry. This ensures consistency in subsequent calculations [50].
2. Sequential Filtering Steps:
- Step 2.1: Lead-likeness Filter. Apply the "Rule of Three" (see Table 1) to focus on optimizable starting points [49].
- Step 2.2: Functional Group Filter. Screen the lead-like subset against PAINS and REOS filters (see Table 2) using SMARTS pattern matching to remove promiscuous and reactive compounds [51].
- Step 2.3: Drug-likeness Filter. Apply Lipinski's Rule of Five and Veber's rules to prioritize compounds with favorable ADMET properties [49] [51].
3. Output:
- The output is a refined, focused library ready for more computationally intensive virtual screening methods like molecular docking. This protocol significantly enriches the library with high-quality, tractable candidates [50].
The workflow for this protocol is visualized below:
Protocol 2: A Multi-Dimensional Drug-Likeness Evaluation UsingdruglikeFilter
This protocol uses the AI-powered druglikeFilter framework for a comprehensive assessment that goes beyond traditional rules [52].
1. Input and Setup:
- Access the web server at
https://idrblab.org/drugfilter/. The platform is browser-based and does not require login. - Prepare your compound library (up to 10,000 molecules) in SMILES or SDF format. If evaluating binding affinity, prepare the target protein structure (PDB format) or sequence (FASTA format).
2. Configure the Evaluation Dimensions:
- Physicochemical Properties: The tool automatically calculates 15 common descriptors (e.g., MW, LogP, TPSA, HBD/HBA) and evaluates them against 12 integrated medicinal chemistry rules [52].
- Toxicity Alert Screening: The tool screens compounds against ~600 structural alerts for various toxicity endpoints (acute toxicity, genotoxicity, etc.) and uses a deep learning model (CardioTox net) to predict cardiotoxicity risk via hERG blockade [52].
- Binding Affinity Measurement: Choose the appropriate path based on your target data.
- Structure-based: The tool uses AutoDock Vina for molecular docking into a defined binding pocket.
- Sequence-based: If no structure is available, the tool uses the transformerCPI2.0 AI model to predict binding from the protein sequence alone [52].
- Synthesizability Assessment: The tool provides a synthetic accessibility score and can perform retrosynthetic analysis using the Retro* algorithm to propose viable synthetic routes [52].
3. Analysis and Output:
druglikeFilterprovides a comprehensive report and allows for automated filtering and ranking of compounds based on the integrated results across all four dimensions. This facilitates the selection of the most promising and viable drug candidates [52].
The Scientist's Toolkit: Essential Research Reagents & Solutions
This table details key computational tools and resources used in the application of drug-likeness filters.
| Tool/Resource Name | Function/Brief Explanation | Typical Use Case |
|---|---|---|
| RDKit [52] [51] | An open-source cheminformatics toolkit used for calculating molecular descriptors, handling SMILES/SDF, and generating fingerprints. | The computational engine behind many property calculations and structural manipulations in custom scripts and workflows. |
| PAINS/REOS Filters [51] | Libraries of SMARTS strings (text-based representations of molecular patterns) that define problematic functional groups. | Integrated into screening pipelines (e.g., in KNIME) to automatically flag and remove promiscuous or reactive compounds. |
| druglikeFilter [52] | A comprehensive, AI-powered web tool that collectively evaluates drug-likeness across physicochemical, toxicity, binding, and synthesizability dimensions. | A one-stop shop for a multi-parameter assessment of compound libraries, minimizing the need to use multiple disjointed tools. |
| ADMETlab / SwissADME [52] | Specialized web servers that provide systematic predictions of Absorption, Distribution, Metabolism, Excretion, and Toxicity (ADMET) parameters. | Used for a deeper dive into the ADMET profile of a shortlisted set of compounds after initial filtering. |
| KNIME [51] | A visual programming platform for data analytics. Pre-configured nodes are available for applying various medicinal chemistry filters. | Building, customizing, and executing automated, reproducible virtual screening and filtering workflows. |
Frequently Asked Questions
FAQ 1: What are the most common types of problematic compounds we encounter in screening? Problematic compounds, often called frequent hitters or pan-assay interference compounds (PAINS), exhibit several common mechanisms that lead to false-positive results. The primary types are summarized in the table below [53]:
| Interference Type | Principle of Interference | Common Chemotypes |
|---|---|---|
| Covalent Interaction | Covalently bind to various macromolecules, often irreversibly. | Quinones, rhodanines, enones, Michael acceptors [53]. |
| Colloidal Aggregation | Form aggregates that non-specifically bind to proteins, confounding enzymatic assays. | Miconazole, staurosporine aglycone, trifluralin [53]. |
| Redox Cycling | Generate reactive oxygen species (ROS) that indirectly inhibit protein activity. | Quinones, catechols, arylsulfonamides [53]. |
| Ion Chelation | Chelate metal ions, disrupting the function of metalloproteins or assay components. | Hydroxyphenyl hydrazones, catechols, rhodanines [53]. |
| Assay Signal Interference | Interfere with assay detection methods, e.g., through autofluorescence or luciferase inhibition. | Curcuminoids, quinoxalin-imidazolium substructures [53]. |
FAQ 2: Are all compounds flagged by PAINS filters truly "bad"? Not necessarily. There is a significant debate in the field. While these filters are crucial for identifying potential false positives, they can sometimes incorrectly label a compound as problematic [54]. Many approved drugs would have been flagged by these filters but are effective because their promiscuity or multi-target action is integral to their therapeutic effect [54]. It is essential to use these filters as a triage tool, not an absolute verdict, and to follow up with experimental validation [53].
FAQ 3: What is a robust step-by-step workflow for filtering a new compound library? A comprehensive strategy involves both computational pre-filtering and subsequent experimental confirmation. The following workflow provides a general guide [50] [17]:
FAQ 4: What experimental methods can confirm if a hit is a false positive? After computational filtering, several orthogonal experimental assays can help confirm the authenticity of a hit [53] [54]:
| Experimental Method | Function | Key Detail |
|---|---|---|
| Detergent Addition | Disrupts colloidal aggregates; a true hit's activity remains, while an aggregator's is lost. | Use non-ionic detergents like Triton X-100 [17]. |
| Counter-Screen Assays | Identifies compounds that interfere with the assay technology itself. | Use a luciferase inhibitor counter-screen for assays using this reporter [17]. |
| Orthogonal Assays | Confirms activity using a different assay format or readout. | Switch from a fluorescence-based to a radioactivity-based assay [53]. |
| Covalent Trapping | Identifies chemically reactive compounds. | Use scavenger reagents like glutathione (GSH) or dithiothreitol (DTT) [53]. |
Troubleshooting Guides
Problem 1: A high number of hits from a virtual screen are flagged as PAINS.
- Potential Cause: The initial compound library may be enriched with promiscuous scaffolds or lack diversity, leading to a high rate of false positives.
- Solution:
- Re-evaluate Library Source: Consider sourcing compounds from diverse commercial or natural product databases to improve chemical space coverage [50].
- Apply Lead-like Filters: Before PAINS filters, apply lead-like property filters (e.g., molecular weight < 350, clogP < 3) to focus on more optimizable starting points [50].
- Use Multiple Filtering Tools: Do not rely on a single PAINS list. Use integrated platforms like ChemFH, which combines multiple prediction models and substructure rules for a more comprehensive assessment [17].
Problem 2: A promising hit compound is flagged by a PAINS filter, but you suspect it might be a true active.
- Potential Cause: The computational filter may be generating a false alarm for a potentially valuable "privileged structure" or multi-target-directed ligand (MTDL).
- Solution: Implement a "Fair Trial Strategy" [53]:
- Dose-Response Analysis: Confirm a clean, saturable dose-response curve. Promiscuous inhibitors often have shallow curves.
- Specificity Testing: Test the compound against unrelated targets. A true specific hit will be inactive against these.
- Analogue Analysis: Synthesize or acquire close structural analogues. A true structure-activity relationship (SAR) will show predictable changes in potency, whereas PAINS often have a "cliff" or no clear SAR.
- Engage a Medicinal Chemist: Have a chemist evaluate the structure to assess its potential for optimization and the likelihood of intrinsic reactivity.
Problem 3: Hits show activity in an initial biochemical assay but fail in a cellular or phenotypic assay.
- Potential Cause: The compounds may be acting through mechanisms that are irrelevant in a cellular context, such as colloidal aggregation, or they may have poor cell permeability.
- Solution:
- Test for Aggregation: Perform the initial biochemical assay in the presence and absence of a non-ionic detergent (e.g., 0.01% Triton X-100). A significant drop in activity with detergent suggests aggregation [17].
- Check Cellular Cytotoxicity: Use a simple cell viability assay (e.g., MTT, ATP-based) to rule out that the observed effect is due to general cell death.
- Assess Membrane Permeability: Utilize computational models to predict logP and other permeability-related properties, or run experimental assays like Caco-2 to confirm the compound can enter cells [50].
The Scientist's Toolkit
This table details key computational and experimental resources for identifying and managing problematic compounds [50] [17] [53].
| Tool / Reagent Name | Type | Primary Function |
|---|---|---|
| ChemFH | Integrated Online Platform | A comprehensive tool for predicting various false positives, including aggregators, fluorescent compounds, and reactive molecules using advanced machine learning models [17]. |
| PAINS Filters | Structural Alert Filter | A set of substructure rules designed to identify compounds known to frequently produce false-positive results in bioassays [50] [53]. |
| Triton X-100 | Laboratory Reagent | A non-ionic detergent used in secondary assays to disrupt colloidal aggregates and confirm a specific mechanism of action [17]. |
| Glutathione (GSH) | Laboratory Reagent | A scavenger molecule used to trap chemically reactive compounds and confirm whether a hit's activity is due to covalent modification [53]. |
| Lead-like Filters | Computational Filter | Property-based filters (e.g., MW, clogP) more stringent than drug-like rules, applied to identify compounds with better optimization potential [50]. |
Frequently Asked Questions
1. How does adjusting the radius of a pharmacophore feature affect my virtual screening results? Adjusting the feature radius directly controls the stringency of the search. A larger radius will retrieve more compounds (increasing recall but also the risk of false positives), as a molecule's feature only needs to fall within this spherical tolerance to match the query. Conversely, a smaller radius demands a more geometrically precise match, which can reduce false positives but may also exclude some true active compounds [46]. Fine-tuning this parameter is essential for balancing sensitivity and specificity in your screening campaign.
2. What is the purpose of vector directions on features like hydrogen bond donors and acceptors? Vector directions encode the geometry of directional interactions, such as hydrogen bonds. A hydrogen bond donor feature, for example, includes a vector representing the trajectory from the donor atom (e.g., Nitrogen) to the hydrogen atom. For a molecule to match this feature, it must not only have an atom in the spherical tolerance zone but also have a complementary vector (from an acceptor atom to its lone pair) that is aligned with the query's direction. Ignoring this can lead to geometrically implausible binding modes and false positives [55] [14].
3. My model is retrieving too many false positives. What are the first parameters I should adjust? Your first step should be a two-pronged approach:
- Reduce Feature Radii: Systematically decrease the radius of your key pharmacophore features, especially those critical for binding, to enforce stricter geometric matching [46].
- Utilize Exclusion Volumes: Introduce exclusion spheres (or shape constraints) in regions of the binding site that are occupied by protein atoms. This prevents molecules from being flagged as hits if their atoms sterically clash with the receptor [46] [55].
4. Can I automate the process of pharmacophore refinement and screening? Yes, recent advances have introduced AI-driven tools that automate and enhance this process. For instance, DiffPhore is a knowledge-guided diffusion framework that generates ligand conformations which maximally map to a given pharmacophore model, inherently handling feature types and directional constraints during its "on-the-fly" 3D mapping process [55]. Other tools like ELIXIR-A use point cloud registration algorithms to automatically refine and consensus pharmacophore models from multiple ligand-receptor complexes [29].
Troubleshooting Guides
Problem: High Rate of False Positive Hits
Potential Causes and Solutions:
Cause: Overly Permissive Feature Tolerances.
- Solution: Implement a stepwise reduction of feature radii. Start with your original model and create versions with progressively smaller radii (e.g., reduce by 0.5 Å increments). Screen a small, well-characterized validation set (containing known actives and inactives) to identify the radius that maximizes enrichment [29] [56].
Cause: Lack of Steric or Shape Constraints.
- Solution: Incorporate exclusion volumes. Derive these volumes from the binding site structure by placing spheres in areas where ligand atoms should not be present. Many platforms, such as Pharmit, allow you to define an exclusive shape constraint based on the receptor's surface [46].
Cause: Ignoring Protein Flexibility and Multiple Receptor Conformations.
- Solution: A pharmacophore model derived from a single, static protein structure may be overfitted. To create a more robust model, generate pharmacophores from multiple snapshots of a Molecular Dynamics (MD) simulation or from several crystal structures. Tools like HGPM (Hierarchical Graph Representation of Pharmacophore Models) can help visualize and select consensus models from an MD trajectory [57]. The strategy of selecting compounds that are top-ranked across multiple conformations has been proven to effectively reduce false positives [5].
Problem: High Rate of False Negative Hits (Missing Known Actives)
Potential Causes and Solutions:
Cause: Excessively Stringent Feature Tolerances or Directions.
Cause: Inadequate Sampling of Ligand Conformational Flexibility.
- Solution: Ensure your virtual screening protocol generates a sufficient number of diverse, low-energy conformers for each database molecule. A molecule might possess the correct pharmacophore, but not in the specific conformer you are testing [56].
Cause: Missing a Critical but Subtle Pharmacophore Feature.
- Solution: Re-evaluate the ligand-receptor interaction pattern. You may have missed a weak but important hydrophobic contact or a water-mediated hydrogen bond. Consider using a tool like SILCS-Pharm or Pharmmaker that can identify pharmacophore features from MD simulations in the presence of organic probes, revealing cryptic binding hotspots [29].
Quantitative Data for Parameter Tuning
The following table summarizes general guidelines for adjusting key pharmacophore parameters based on desired screening outcomes.
Table 1: Pharmacophore Parameter Adjustment Guide
| Parameter | Typical Range | Effect of Increasing Value | Effect of Decreasing Value | Recommended Use Case |
|---|---|---|---|---|
| Feature Radius | 1.0 - 2.5 Å [46] | Increases hits, higher recall, more false positives | Reduces hits, higher precision, risk of false negatives | Start at ~1.5 Å, increase if missing actives, decrease for too many false positives. |
| Directional Angle Tolerance | 15° - 45° [55] | Allows more deviation from ideal geometry | Enforces stricter directional alignment | Use narrower tolerance (e.g., 30°) for critical, rigid H-bonds. |
| Exclusion Volume Radius | 1.2 - 2.0 Å [46] [55] | Increases steric penalty, more excluded compounds | Reduces steric penalty, fewer excluded compounds | Place with radius ~1.5 Å in protein-occupied regions to eliminate clashing poses. |
Experimental Protocols for Systematic Optimization
Protocol 1: Optimization of Feature Tolerances Using a Validation Set
This protocol uses a dataset of known active and inactive compounds to empirically determine the optimal feature radii.
- Preparation: Curate a validation set containing known active compounds and decoys (inactive compounds with similar physicochemical properties) [29] [5].
- Model Generation: Create your initial structure-based or ligand-based pharmacophore model.
- Parameter Variation: Generate several versions of the model where the radii of all features are uniformly set to different values (e.g., 1.0, 1.5, 2.0, 2.5 Å).
- Virtual Screening: Perform virtual screening on the validation set with each model variant.
- Evaluation: For each variant, calculate the Enrichment Factor (EF) and plot the ROC curve.
- Enrichment Factor (EF) is calculated as: EF = (Hitssampled / Nsampled) / (Hitstotal / Ntotal), where "Hitssampled" is the number of known actives found in the top-ranked subset of the database, and "Hitstotal" is the total number of known actives in the entire database [29].
- Selection: Choose the radius parameter set that yields the highest early enrichment (e.g., EF1%).
Protocol 2: Consensus Pharmacophore Selection from Molecular Dynamics
This protocol uses MD simulations to account for protein flexibility and generate a more robust pharmacophore model [5] [57].
- Simulation: Run an MD simulation of the protein-ligand complex (or the apo protein) to sample multiple receptor conformations.
- Snapshot Extraction: Extract a representative set of snapshots from the MD trajectory (e.g., every 10 ns).
- Pharmacophore Generation: Generate a structure-based pharmacophore model from each snapshot using software like LigandScout.
- Analysis and Clustering: Use a tool like HGPM to analyze and cluster the generated models based on their feature composition and spatial arrangement. This visualizes the hierarchy and frequency of observed pharmacophore features [57].
- Consensus Model Building: Select the most persistent features (those that appear in a high percentage of snapshots) to build a consensus pharmacophore model. This model captures the essential, stable interactions while filtering out transient ones.
Workflow Visualization
Diagram 1: A logical workflow for troubleshooting a high false positive rate in pharmacophore-based screening.
The Scientist's Toolkit: Essential Research Reagents & Software
Table 2: Key Software Tools for Pharmacophore Modeling and Refinement
| Tool Name | Primary Function | Relevance to Fine-Tuning |
|---|---|---|
| Pharmit [46] | Interactive pharmacophore-based virtual screening web server. | Allows real-time adjustment of feature radii, types, and vector directions. Supports inclusive/exclusive shape constraints. |
| ELIXIR-A [29] | Python-based pharmacophore refinement tool. | Uses point cloud algorithms (RANSAC, colored ICP) to align and refine pharmacophores from multiple complexes, aiding consensus model building. |
| LigandScout [29] [57] [56] | Create structure-based and ligand-based pharmacophore models. | Provides advanced options for defining feature tolerances and directional constraints. Used to generate models from MD snapshots. |
| DiffPhore [55] | AI-based 3D ligand-pharmacophore mapping. | Employs a diffusion model to generate conformations that match a pharmacophore's features and directions, automating the mapping process. |
| HGPM [57] | Hierarchical Graph Representation of Pharmacophore Models. | Visualizes multiple pharmacophore models from MD simulations as an interactive graph, aiding in the selection of optimal feature sets. |
Frequently Asked Questions (FAQs)
Q1: What are the most common causes of false positives in pharmacophore-based virtual screening?
False positives in virtual screening can arise from several sources. Assay interference is a primary cause, where compounds exhibit signals not related to the intended biological activity, for instance, through colloidal aggregation, autofluorescence, or chemical reactivity with assay components [58]. Furthermore, oversimplified computational models can contribute to the problem. Many virtual screening workflows use a single, rigid protein structure, which fails to account for natural receptor plasticity. This can cause the model to favor compounds that fit that one conformation but are poor binders to the actual, dynamic protein in a biological system, generating false positives [5]. The chemical features in a pharmacophore model itself can sometimes be too general, inadvertently matching compounds that lack true biological activity against the target [7].
Q2: How can ADMET predictions help prioritize hits after a pharmacophore-based screen?
Integrating ADMET (Absorption, Distribution, Metabolism, Excretion, and Toxicity) predictions early in the screening process helps identify and deprioritize compounds with undesirable properties before investing in costly experimental validation. This approach addresses the leading causes of clinical trial failures [59] [60]. You can use these predictions to filter out compounds with:
- Poor pharmacokinetics: Low intestinal absorption, high metabolic lability, or unfavorable distribution profiles.
- Toxicity liabilities: Potential for cardiotoxicity (e.g., hERG channel inhibition), mutagenicity (e.g., Ames test positivity), or drug-induced liver injury (DILI) [61].
- Unfavorable physicochemical properties: Properties that violate established drug-likeness rules, such as excessive molecular weight or lipophilicity [61].
By scoring or ranking hits based on a combination of their predicted pharmacological activity and ADMET profile, you can prioritize compounds that have a higher probability of success in later-stage development [61] [59].
Q3: What is the difference between rule-based and data-driven ADMET risk assessment?
Rule-based and data-driven approaches offer complementary ways to assess ADMET risk.
- Rule-Based (e.g., Extended "Rule of 5"): These methods use predefined, often binary, thresholds for specific molecular properties. For example, a rule might flag any compound with a calculated logP (MLogP) > 4.15 as having a risk of poor absorption [61]. They are transparent and easy to interpret.
- Data-Driven / AI-Based (e.g., ADMET Predictor, ADMETlab): These methods use machine learning models trained on large, experimental datasets to predict properties and overall risk [61] [60]. They can capture complex, non-linear relationships between chemical structure and biological outcomes. Some platforms provide a comprehensive ADMET Risk Score, which is a weighted sum of individual risks (e.g., absorption risk, CYP metabolism risk, toxicity risk), offering a more nuanced assessment than simple rules [61].
Q4: My hit list contains compounds that are flagged as frequent hitters or pan-assay interferents (PAINS). What should I do?
The presence of PAINS or other structural alerts should be a major consideration in triage, but not the sole reason for automatic exclusion. Use these alerts as a filtering and prioritization guide rather than a hard elimination rule [58] [62]. It is recommended to:
- Investigate the chemical context: Some structural motifs can be problematic in certain assay technologies but not others.
- Corroborate with other data: Cross-reference the alert with other predictive data. A compound flagged as a PAINS but that also has a favorable predicted ADMET profile and strong, clean activity in orthogonal assays may still be worth investigating [62].
- Apply modern machine learning tools: Use advanced, assay-adapted tools like Minimum Variance Sampling Analysis (MVS-A) that can help distinguish true bioactivity from assay-specific interference without relying solely on predefined structural rules [58].
Q5: How can I visualize the key properties of my screened compounds to quickly identify promising leads?
Creating a property dashboard is an effective way to visualize multiple parameters simultaneously. The table below outlines key properties and their ideal ranges for a typical oral drug candidate.
Table 1: Key Properties for Hit Prioritization and Their Ideal Ranges
| Property Category | Specific Property | Ideal Range or Target | Interpretation & Rationale |
|---|---|---|---|
| Pharmacophore Fit | Fit Value | > (Model-Defined Threshold) | Higher values indicate a better match to the hypothesized active conformation [7]. |
| Physicochemical | Molecular Weight (MW) | ≤ 500 g/mol | Lower molecular weight is generally associated with better oral absorption [61]. |
| Calculated LogP (MLogP) | ≤ 4.15 | Controls lipophilicity; high values can lead to poor solubility and metabolic clearance [61]. | |
| ADMET Profile | ADMET Risk Score | Lower is better | A composite score predicting overall developability; a high score indicates multiple potential liabilities [61]. |
| hERG Inhibition | Low probability | Critical for avoiding cardiotoxicity; a high predicted risk is a significant liability [59]. | |
| Human Liver Microsomal Stability | Stable | Predicts low metabolic clearance, suggesting a desirable longer half-life [61]. |
Troubleshooting Guides
Problem 1: High Number of False Positives from Virtual Screening
Issue: Your pharmacophore-based virtual screening returns a large number of hits, but subsequent experimental validation shows a very low confirmation rate.
Solution:
- Apply a Robust Multi-Conformation Docking Strategy: To account for receptor flexibility, which is a major source of false positives, dock your hit list against multiple receptor conformations (MRCs). These MRCs can be obtained from molecular dynamics simulations or multiple crystal structures. A true positive is more likely to bind favorably to different conformations of the binding site. Select only the compounds that are top-ranked across most or all the different receptor models for further study [5].
- Integrate Machine Learning-Based Hit Prioritization: Employ tools like Minimum Variance Sampling Analysis (MVS-A). This method trains a gradient boosting machine (GBM) on your primary HTS data and computes an influence score for each hit. Compounds with high scores are likely false positives, while those with low scores are likely true positives. This method is fast and does not rely on pre-defined interference mechanisms, making it broadly applicable [58] [62].
- Implement a Tiered Filtering Workflow: Subject your virtual hit list to a sequential filtering process:
- Pharmacophore Fit: Initial selection based on the pharmacophore model.
- Structural Alert Filtering: Filter or flag compounds containing PAINS and other undesirable substructures.
- ADMET Prediction: Use a platform like ADMETlab or ADMET Predictor to filter out compounds with poor predicted absorption, high toxicity risk, or unfavorable metabolic profiles [60] [61].
- Consensus Scoring: Combine scores from pharmacophore mapping, molecular docking, and ADMET predictions to create a consensus rank for final hit prioritization.
The following workflow diagram illustrates this multi-step troubleshooting process:
Problem 2: Promising Hits Exhibit Poor ADMET Properties
Issue: Hits with excellent activity in the primary pharmacological assay show poor solubility, high metabolic instability, or toxicity in early testing.
Solution:
- Front-Load ADMET Prediction in the Workflow: The most effective strategy is to integrate ADMET predictions before experimental testing. Use computational tools to evaluate your virtual hit list and deprioritize or eliminate compounds with predicted liabilities. This shifts the focus to chemotypes with a higher probability of success [59] [60].
- Conduct a Mechanistic Toxicity Analysis: Move beyond simple "yes/no" toxicity predictions. Use advanced tools that provide mechanistic insights, such as predicting specific CYP enzyme inhibition or the mechanism of drug-induced liver injury (DILI). This information can help medicinal chemists understand the root cause of the toxicity and guide structural modifications [61].
- Perform a Matched Molecular Pair Analysis: If you have a series of analogs, use this technique to systematically identify structural changes that improve ADMET properties while maintaining potency. For example, you can identify a specific R-group substitution that reduces hERG inhibition or improves metabolic stability [61].
Problem 3: In Vitro Activity Does Not Translate to Cellular or In Vivo Efficacy
Issue: Compounds that are potent in biochemical assays show no activity in cell-based assays or in animal models.
Solution:
- Verify Cellular Permeability and Efflux: Use predictive models for properties like Caco-2 permeability and P-glycoprotein (P-gp) efflux. A compound might be a potent enzyme inhibitor but fail to reach its intracellular target due to poor membrane permeability or active efflux. Prioritize compounds with high predicted permeability and low efflux risk [60].
- Simulate Preliminary Pharmacokinetics: Employ high-throughput PBPK (Physiologically Based Pharmacokinetic) modeling, available in some advanced platforms, to predict a compound's concentration-time profile in plasma. This can help you determine if the compound is likely to achieve sufficient exposure at the target site to elicit an effect [61].
- Check for Plasma Protein Binding (PPB): Highly lipophilic compounds often bind strongly to plasma proteins, which reduces the free fraction of drug available to interact with the target. Predict PPB and prioritize compounds with a moderate to low binding percentage to ensure adequate free drug concentration [61].
The Scientist's Toolkit: Essential Research Reagents & Computational Solutions
Table 2: Key Resources for Post-Screening Analysis
| Tool / Resource Name | Type | Primary Function in Hit Prioritization |
|---|---|---|
| ADMET Predictor [61] | Commercial Software Platform | Predicts over 175 ADMET properties and provides an integrated ADMET Risk score for early developability assessment. |
| ADMETlab [60] | Free Web Platform | Provides systematic evaluation of 31 ADMET endpoints, useful for virtual screening and filtering large compound libraries. |
| MVS-A (Minimum Variance Sampling Analysis) [58] | Open-Source Machine Learning Tool | Distinguishes true bioactive compounds from assay interferents directly from HTS data, reducing false positive rates. |
| GOLD [5] | Molecular Docking Software | Used for structure-based virtual screening and studying ligand binding modes; can be applied in multi-conformation strategies. |
| PAINS Filters [58] | Structural Alert Filters | Identifies compounds with substructures known to frequently cause assay interference, serving as an initial triage tool. |
| Rule of 5 and Extensions [61] | Drug-Likeness Rules | Provides a quick assessment of a compound's potential for oral absorption based on fundamental physicochemical properties. |
Experimental Protocols
Protocol 1: Minimum Variance Sampling Analysis (MVS-A) for Hit Triage
Purpose: To prioritize true bioactive compounds and identify false positives directly from high-throughput screening (HTS) data using machine learning [58].
Methodology:
- Data Preparation: Format your primary HTS data, ensuring each compound is labeled as either a "Hit" or "Inactive" based on the primary assay readout.
- Model Training: Train a Gradient Boosting Machine (GBM) classifier (e.g., using libraries like XGBoost or Scikit-learn) on the HTS data to distinguish hits from inactives based on chemical descriptors or fingerprints.
- Influence Score Calculation: For every compound labeled as a hit in the training set, compute its MVS-A score. This score quantifies how "unusual" the hit is according to the learned GBM model. A high score suggests the model finds it difficult to classify the compound as active based on the patterns it learned, indicating a potential false positive.
- Hit Prioritization: Rank all hits by their MVS-A score in ascending order. Compounds with the lowest scores are the most trustworthy and should be prioritized for confirmation. Compounds with the highest scores are likely false positives and can be deprioritized.
The following diagram illustrates the MVS-A workflow:
Protocol 2: Structure-Based Virtual Screening with Multiple Receptor Conformations
Purpose: To reduce false positives in structure-based virtual screening by accounting for inherent protein flexibility [5].
Methodology:
- Generate Receptor Conformations: Obtain multiple 3D structures of the target protein. These can be from:
- Experimental sources (e.g., different crystal structures from the PDB).
- Computational methods (e.g., molecular dynamics simulations, normal mode analysis).
- Parallel Docking: Dock the entire compound library against each individual protein conformation separately, using molecular docking software like GOLD.
- Generate Ranked Lists: For each receptor conformation, generate a list of top-ranked compounds based on docking scores.
- Intersection Analysis: Identify the intersection set of compounds that appear in the top-ranked lists (e.g., top 100) across all or most of the different receptor conformations.
- Selection: Select this intersection set as the final hit list. The underlying hypothesis is that a true positive will bind favorably to various representations of the binding site, while false positives will only rank highly in one or a few specific conformations.
Validation, Benchmarking, and Comparative Analysis
This technical support resource addresses the critical challenge of false positives in pharmacophore-based virtual screening. A robust validation protocol is your most effective defense, ensuring that your computational models are reliable and predictive. This guide provides clear, actionable methods to assess and confirm the quality of your pharmacophore models before proceeding to costly experimental stages.
FAQs: Core Concepts for Researchers
Q1: What is the specific role of an ROC curve in validating a pharmacophore model?
A Receiver Operating Characteristic (ROC) curve is a graphical plot that illustrates the diagnostic ability of a binary classifier system, like a pharmacophore model used to distinguish "active" from "inactive" molecules [63]. Its role in validation is to provide a visual and quantitative measure of how well your model can discriminate between these two classes.
In practice, you test your model on a dedicated decoy set—a collection of known active molecules and presumed inactive molecules (decoys) that are physically similar but chemically distinct to avoid bias [64]. The ROC curve is created by plotting the True Positive Rate (TPR or Sensitivity) against the False Positive Rate (FPR) at various classification thresholds [63]. A model that performs perfectly would produce a curve that goes straight up the left side and across the top, while a random guess would follow the diagonal line from the bottom-left to the top-right [63].
Q2: How do I interpret the AUC value to determine if my model is good enough?
The Area Under the ROC Curve (AUC) is a single numerical value that summarizes the overall performance of your model.
- AUC = 1.0: Represents a perfect classifier.
- AUC = 0.5: Represents a classifier with no discriminative power, equivalent to random guessing [63].
- AUC > 0.5: Indicates a model that is better than random chance. The closer the value is to 1.0, the better the model's predictive power.
For a pharmacophore model, an AUC value of 0.819 at a 1% threshold has been demonstrated to prove the model's ability to distinguish between truly active substances and decoy compounds, indicating a good predictive capability [65]. The table below provides a general guide for interpreting AUC values.
Table: Interpretation Guide for AUC Values
| AUC Value Range | Classification Performance |
|---|---|
| 0.90 - 1.00 | Excellent discrimination |
| 0.80 - 0.90 | Good discrimination |
| 0.70 - 0.80 | Fair discrimination |
| 0.60 - 0.70 | Poor discrimination |
| 0.50 - 0.60 | Failure (no discrimination) |
Q3: Beyond ROC/AUC, what other validation methods should I use?
While ROC/AUC analysis is crucial, a comprehensive validation protocol should include multiple methods to test different aspects of model robustness [64]:
- Fisher's Randomization Test: This test assesses the statistical significance of your model. The biological activities of your training set compounds are randomly shuffled, and new models are generated from this scrambled data. If these randomized models consistently show lower correlation than your original model, it confirms that your original model's performance is not due to a chance correlation [64].
- Test Set Prediction: A dedicated test set of compounds, not used in model generation, is used to evaluate the model's predictive power. An R²pred value greater than 0.50 is generally considered acceptable [64].
- Cost Function Analysis: During model generation, a low configuration cost (typically below 17) and a high total cost difference (null cost, Δ) of more than 60 bits compared to a null hypothesis model signify a robust model that is not a product of chance [64].
Troubleshooting Guide: Addressing Common Experimental Issues
Problem: My model has a high AUC but still selects many false positives in virtual screening.
Solution: This is a common challenge when receptor plasticity is considered, as each distinct protein conformation can introduce its own set of false positives [5]. A proven strategy to defeat this is ensemble docking and consensus scoring.
- Hypothesis: A true inhibitor will bind favorably to different conformations of the binding site, while false positives will only rank highly in a few [5].
- Protocol:
- Generate Multiple Receptor Conformations (MRCs): Use molecular dynamics (MD) simulations or select multiple crystal structures to create an ensemble of receptor models that represent the flexibility of the binding site [5].
- Dock Your Compound Library: Perform virtual screening by docking your compound library against each distinct receptor conformation separately [5].
- Apply Consensus Scoring: For each receptor model, generate a list of top-ranked molecules. The true ligands will be the intersection molecules—those that appear in the top-ranked lists across all or most of the different receptor conformations [5]. This strategy has been shown to successfully identify high-affinity controls while filtering out false positives.
Problem: The predictive power of my model drops significantly when tested on new chemical scaffolds.
Solution: This indicates that your model may be over-fitted to the specific chemotypes in your training set and lacks generalizability.
- Preventive Measure during Data Splitting: When preparing your data for model development, avoid simple random splitting. Instead, use a scaffold-based splitting method. This ensures that the training and test sets contain different molecular frameworks (Bemis-Murcko scaffolds), which rigorously tests the model's ability to generalize to truly novel chemotypes [66].
- Validation Step: Always perform the test set prediction validation on a structurally diverse test set as described in the FAQs. A low R²pred value for such a set is a clear indicator of this problem [64].
Essential Research Reagents and Computational Tools
The following table lists key resources used in establishing the validation protocols discussed above.
Table: Key Research Reagent Solutions for Validation Protocols
| Item Name | Function in Validation |
|---|---|
| Decoy Set (e.g., from DUD-E) | A collection of pharmaceutically relevant "inactive" molecules used with known actives to test a model's ability to discriminate in ROC/AUC analysis [64]. |
| Test Set Compounds | A dedicated set of compounds with known activity, withheld from model training, used to independently evaluate the model's predictive power (R²pred) [64]. |
| Molecular Dynamics (MD) Software | Used to generate an ensemble of protein conformations, helping to account for receptor flexibility and reduce false positives during virtual screening [5]. |
| Docking Software (e.g., AutoDock, GOLD, Smina) | Used to perform the virtual screening and generate scores for the top-ranked molecules against different receptor conformations for consensus analysis [5] [66]. |
Workflow Diagram: Comprehensive Pharmacophore Model Validation
The following diagram illustrates the integrated workflow for establishing a robust validation protocol, incorporating the key troubleshooting and validation strategies.
Within pharmacophore-based virtual screening, a significant challenge is the high rate of false positives—compounds predicted to be active that are, in fact, inactive during experimental testing [5] [7]. Effectively quantifying your workflow's ability to distinguish these false positives from true active compounds is paramount. The Enrichment Factor (EF) is a key, widely used metric that provides a clear and direct measure of this performance [67] [68]. This guide will detail how to calculate and interpret the EF, integrate it into your screening protocol, and troubleshoot common issues to optimize your research.
Frequently Asked Questions (FAQs)
What is the Enrichment Factor (EF) and why is it critical for my screening?
The Enrichment Factor (EF) is a metric used in virtual screening to measure the added value of your computational method over a random selection of compounds [68]. In practical terms, it tells you how much more likely you are to find a true active compound within a selected top-ranked subset of your screening library compared to picking compounds at random from the entire library.
It is critical because:
- It measures early recognition: EF is particularly valuable for assessing performance where it matters most—in the early, resource-limited stage of selecting a small number of compounds for experimental testing [67].
- It directly evaluates false positive filtration: A high EF indicates that your workflow (e.g., your pharmacophore model and its parameters) is successfully enriching true actives and deprioritizing false positives and decoys.
How do I calculate the Enrichment Factor?
The EF is calculated using the following formula [68]:
EF = (Hitssampled / Nsampled) / (Hitstotal / Ntotal)
Where:
- Hitssampled is the number of known active compounds found in the top-ranked subset of your screening library.
- Nsampled is the total number of compounds in that top-ranked subset (e.g., the top 1% or top 100 compounds).
- Hitstotal is the total number of known active compounds in the entire screening library.
- Ntotal is the total number of compounds in the entire screening library.
Example Calculation: Imagine you have a virtual screening library of 10,000 compounds (Ntotal), which contains 50 known active compounds (Hitstotal). You run your pharmacophore screen and examine the top 500 ranked compounds (Nsampled). Within this top 500, you find 25 of the known actives (Hitssampled).
- Random selection rate: (50 / 10,000) = 0.005 (or 0.5%)
- Your method's hit rate in the top 5%: (25 / 500) = 0.05 (or 5%)
- EF = 0.05 / 0.005 = 10
This result means your pharmacophore screening method was 10 times better than random selection at finding active compounds in the top 5% of the list.
What is EFmax and what does the EF/EFmax ratio tell me?
There is a ceiling to the best possible enrichment you can achieve, which is limited by the total number of actives in your library. The maximum achievable EF, or EFmax, is the enrichment you would get if you perfectly selected only active compounds in your top subset [68].
EFmax = (Nsampled / Nsampled) / (Hitstotal / Ntotal) = 1 / (Hitstotal / Ntotal)
The EF/EFmax ratio is a normalized metric that provides a more consistent way to compare enrichment across different datasets or against other published methods [68]. A ratio closer to 1.0 indicates your method is performing near the theoretical maximum.
My Enrichment Factor is low. What are the common causes and solutions?
A low EF indicates that your virtual screening workflow is not effectively distinguishing active compounds from inactives. Here are common causes and troubleshooting actions:
| Cause | Description | Troubleshooting Actions |
|---|---|---|
| Poor Pharmacophore Model Quality | The hypothesis (features, geometry) does not accurately represent the essential interactions for binding. | For ligand-based models: Verify the training set ligands are diverse and the model is validated. For structure-based models: Check the protein structure preparation and ensure features map to key binding site residues [7]. |
| Inadequate Handling of Receptor Flexibility | A single, rigid receptor conformation may not accommodate all true binders, incorrectly flagging them as false positives. | Consider using multiple receptor conformations (e.g., from molecular dynamics simulations) and select consensus hits [5]. |
| Limitations of the Screening Algorithm | The shape-matching or scoring function may be inadequate, leading to poor pose ranking [67]. | Experiment with different scoring functions or post-processing with more rigorous methods like absolute binding free energy calculations [69]. |
| Library Bias | The decoy or compound library may not be challenging enough, or actives may be too similar to each other. | Use a standardized, validated benchmark like the Directory of Useful Decoys (DUD) to ensure a fair assessment [67]. |
Standard Protocol: Calculating EF for a Pharmacophore Screen
This protocol outlines the steps to validate a new pharmacophore model using a library containing known actives and decoys.
Objective: To quantify the enrichment performance of a pharmacophore model by screening a library with known actives and decoys.
Materials and Reagents:
- Pharmacophore Modeling Software: (e.g., Catalyst, Phase, MOE).
- Screening Library: A database of compounds, such as the DUD-E, which includes known actives and property-matched decoys [67] [69].
- Known Actives: A set of confirmed active compounds for the target.
- Decoys: Inactive molecules with similar physicochemical properties to the actives, used to mimic a real screening scenario and test selectivity [69].
Methodology:
- Library Preparation: Prepare your screening library, ensuring known actives and decoys are clearly labeled. Standardize the structures and generate relevant 3D conformations.
- Virtual Screening: Execute the virtual screen using your pharmacophore model as the query. Export the results, ranked by the software's scoring function (e.g., fit value).
- Data Analysis at Various Cutoffs: Analyze the ranked list at different early recognition thresholds (e.g., top 1%, 2%, 5%, 10%).
- For each threshold, count how many of the known actives (
Hitssampled) are present.
- For each threshold, count how many of the known actives (
- EF Calculation: For each threshold, calculate the EF using the formula provided in FAQ #2.
- Visualization: Plot the EF or the EF/EFmax ratio against the fraction of the screened library to visualize the enrichment profile.
The workflow below summarizes this protocol:
Advanced Protocol: Multi-Conformation Screening to Reduce False Positives
This advanced protocol leverages receptor flexibility to improve selectivity and reduce false positives, directly addressing the thesis context.
Objective: To improve EF by using multiple receptor conformations and selecting consensus hits, thereby minimizing false positives associated with a single rigid receptor structure [5].
Materials and Reagents:
- Receptor Structures: A set of distinct protein conformations. These can be obtained from:
- Multiple crystal/NMR structures.
- Molecular Dynamics (MD) simulation snapshots [5].
- Docking/Virtual Screening Software: Software capable of docking against multiple receptor conformations (e.g., GOLD) [5].
Methodology:
- Generate Receptor Conformations: Perform MD simulations of the apo or holo receptor and cluster the trajectory to obtain a set of distinct, representative conformations [5].
- Parallel Docking/Screening: Dock the entire screening library (actives and decoys) against each receptor conformation separately.
- Generate Ranked Lists: For each receptor conformation, generate a separate ranked list of top-scoring compounds.
- Select Consensus Hits: Identify the "intersection ligands"—compounds that appear in the top-ranked lists (e.g., top 100) across all or most of the receptor models [5].
- Calculate Cross-Model EF: Treat the set of consensus hits as your final selection. Calculate the EF for this set using the standard formula. This "Cross-Model EF" reflects the power of your multi-conformation strategy to select for true binders.
The following diagram visualizes this multi-conformation screening and validation workflow:
The Scientist's Toolkit: Key Research Reagent Solutions
| Item | Function in EF Analysis |
|---|---|
| DUD/E Database | A public database containing known actives and property-matched decoys for many targets, providing a standardized benchmark for virtual screening methods and EF calculation [67] [69]. |
| Molecular Dynamics (MD) Software | Used to simulate the dynamic motion of a protein, generating an ensemble of conformations for multi-conformation screening to account for receptor flexibility and reduce false positives [5]. |
| Absolute Binding Free Energy (ABFE) Calculations | A more computationally intensive method that can be applied to top-ranked docking hits to provide a more accurate ranking and improve the final enrichment of actives, serving as a powerful post-docking filter [69]. |
| ROC Curves | A graphical plot (Receiver Operating Characteristic) that shows the diagnostic ability of a binary classifier system. The Area Under the Curve (AUC) is often reported alongside EF to provide a more complete picture of screening performance across all thresholds [67]. |
In pharmacophore-based virtual screening, a false positive is a compound predicted by the computational model to be active against the target protein but which fails to demonstrate meaningful biological activity in experimental validation. These false hits consume significant resources and can derail research progress. This technical support guide analyzes successful case studies targeting Bromodomain-containing protein 4 (BRD4) and Monoamine Oxidases (MAOs) to provide proven strategies for mitigating false positives throughout the screening workflow.
FAQ: Understanding and Addressing False Positives
Q1: What are the primary sources of false positives in pharmacophore-based screening?
A1: False positives typically originate from several key areas:
- Oversimplified Pharmacophore Models: Models lacking essential exclusion volumes may select compounds that fit the positive features but clash with the protein structure [70].
- Inadequate Conformational Sampling: If the bioactive conformation of a ligand is not generated during screening, the process may select compounds for the wrong reasons [71].
- Ignoring Chemical Reactivity/Promiscuity: Compounds with pan-assay interference (PAINS) properties can show apparent activity through undesirable mechanisms like covalent modification or aggregation [71].
- Insufficient ADMET Filtering: Compounds that appear potent may have poor pharmacokinetic properties (e.g., low solubility, high metabolic instability) that prevent cellular activity [72].
Q2: How can researchers validate their pharmacophore model before full-scale screening?
A2: Proper model validation is crucial and should include:
- Decoy Set Screening: Use tools like the DUD-E database or DecoyFinder to challenge your model with inactive compounds that are physically similar to actives. A good model should successfully enrich active compounds over inactives [71] [70].
- Test with Known Actives and Inactives: Screen a small set of compounds with established experimental activity to ensure your model correctly identifies true actives and rejects inactives [70].
- Retrospective Screening: Apply your model to a library where active compounds are known but hidden, measuring its ability to retrieve these known actives early in the screening process.
Q3: What orthogonal screening methods can help eliminate false positives after the initial pharmacophore hit?
A3: Implementing a multi-stage screening workflow significantly reduces false positives:
- Structure-Based Molecular Docking: Follow pharmacophore screening with molecular docking to assess binding pose realism and complementarity with the protein binding site [72] [73].
- Machine Learning Scoring: Train ML models on docking results or experimental data to prioritize compounds with higher confidence [66] [74].
- Experimental Cross-Validation: Use multiple biochemical assay formats (e.g., AlphaScreen followed by HTRF or SPR) to confirm activity through different detection mechanisms [75] [73].
Troubleshooting Guide: Common Experimental Issues and Solutions
Problem: Hits from screening show good binding affinity in biochemical assays but no cellular activity
Potential Causes and Solutions:
Cause 1: Poor Cellular Permeability
- Solution: Implement early ADMET prediction in your workflow. Use tools like SwissADME or QikProp to calculate properties like logP, polar surface area, and P-glycoprotein substrate probability [72] [71]. For BRD4 inhibitors targeting neuroblastoma, ensure compounds can cross cell membranes by adhering to Lipinski's Rule of Five parameters during selection [72].
Cause 2: High Protein Binding in Serum
Cause 3: Metabolic Instability
- Solution: Incorporate metabolic stability predictions early in the screening process. Use tools that predict cytochrome P450 metabolism and phase II conjugation reactions [71].
Problem: Inconsistent results between different assay formats for the same compounds
Potential Causes and Solutions:
Cause 1: Assay Interference Compounds
- Solution: Test compounds in multiple assay formats (e.g., AlphaScreen and HTRF) to identify format-specific interferers. The successful BRD4 case study used both assays to confirm activity, with HTRF particularly valuable for eliminating fluorescent compound interference [75].
Cause 2: Compound Aggregation
- Solution: Include detergent (e.g., 0.01% Triton X-100) in assays to disrupt aggregates. Check for concentration-dependent activity that deviates from typical hyperbolic binding curves [71].
Cause 3: Solubility Issues
- Solution: Physically measure compound solubility in assay buffers rather than relying solely on predictions. Use DMSO stocks at appropriate concentrations (<0.1% final concentration) to prevent precipitation [75].
Case Study 1: BRD4 Inhibitor Discovery with Validated Workflow
Experimental Protocol: Integrated Pharmacophore and Structure-Based Screening
This protocol follows the successful approach documented in recent BRD4 inhibitor discovery campaigns [72] [73] [70].
Step 1: Pharmacophore Model Development
- Template Selection: Use a high-resolution crystal structure of BRD4 in complex with a known inhibitor (e.g., PDB ID: 4BJX or 3MXF) [72] [73].
- Feature Identification: Using Pharmit or Ligand Scout, define key pharmacophore features from the co-crystal ligand: hydrogen bond acceptors (to Asn140), hydrophobic features, and aromatic rings [72] [70].
- Exclusion Volumes: Add exclusion volumes based on the protein structure to prevent selection of compounds that would sterically clash with the binding site [70].
Step 2: Virtual Screening Implementation
- Database Preparation: Screen databases like ZINC, ChEMBL, or in-house libraries pre-filtered by drug-like properties (MW <500, LogP <5, HBD <5, HBA <10) [72].
- Conformational Sampling: Use OMEGA or RDKit's ETKDG method to generate representative conformational ensembles for each compound [71].
- Screening Parameters: Require matches to 5 out of 7 key pharmacophore features to balance selectivity and chemical diversity [73].
Step 3: Orthogonal Validation with Molecular Docking
- Protein Preparation: Using Maestro's Protein Preparation Wizard or similar tools, add hydrogens, optimize hydrogen bonding, and minimize the protein structure using OPLS_2005 force field [72].
- Grid Generation: Define the binding site using coordinates from the native ligand (e.g., X=14.09, Y=0.72, Z=9.68 for BRD4) [72].
- Docking Execution: Dock screened hits using Glide (SP mode) or Smina, generating multiple poses per compound to explore binding orientations [72] [66].
Step 4: Experimental Validation
- Primary Screening: Use AlphaScreen assay with BRD4 BD1 domain and biotinylated acetylated histone H4 peptide to test inhibition [75] [73].
- Secondary Confirmation: Validate hits using HTRF assay format to eliminate false positives from AlphaScreen interference [75].
- Cellular Assay: Test cytotoxicity in BRD4-dependent cell lines (e.g., Ty82 NUT midline carcinoma) with WST-1 viability assay after 72-hour treatment [75].
Quantitative Results from Successful BRD4 Screening Campaigns
Table 1: Performance Metrics from Published BRD4 Inhibitor Discoverys
| Study Reference | Initial Library Size | Pharmacophore Hits | Confirmed Active | Success Rate | Best Compound IC50/Ki |
|---|---|---|---|---|---|
| Natural Compound Screening [70] | ~200,000 natural compounds | 136 | 4 | 2.9% | ~nM range (docking score ≤-9.0 kcal/mol) |
| Drug Repositioning Campaign [73] | 273 repurposed compounds | 6 | 3 | 50.0% | 0.60 ± 0.25 µM |
| Naphthalene-1,4-dione Scaffold [75] | Not specified | 1 novel scaffold | 1 | N/A | Cytotoxic in Ty82 cells |
Research Reagent Solutions for BRD4 Screening
Table 2: Essential Research Reagents for BRD4 Pharmacophore Screening and Validation
| Reagent/Resource | Function in Workflow | Example Sources/Parameters |
|---|---|---|
| BRD4 Protein (BD1 domain) | Biochemical assay target | Recombinant expression (amino acids 47-170) with GST/His6 tags [75] |
| Acetylated Histone Peptide | Binding partner for competition assays | Biotinylated SGRGK(Ac)GGK(Ac)GLGK(Ac)GGAK(Ac)RHRK peptide [75] |
| AlphaScreen Beads | Detection system for biochemical assay | Streptavidin-coated donor beads, anti-GST acceptor beads [75] [73] |
| Pharmacophore Software | Model development and screening | Pharmit, Ligand Scout, Schrödinger Phase [72] [73] [70] |
| Molecular Docking Tools | Structure-based validation | Glide (Schrödinger), Smina, AutoDock Vina [72] [66] |
Case Study 2: MAO Inhibitor Discovery with Machine Learning Enhancement
Experimental Protocol: Machine Learning-Accelerated MAO Inhibitor Screening
This protocol follows the innovative approach that achieved 1000x acceleration in MAO inhibitor discovery [66] [74].
Step 1: Data Curation for Machine Learning
- Activity Data Collection: Download MAO-A and MAO-B inhibitors with IC50/Ki values from ChEMBL database (2,850 MAO-A and 3,496 MAO-B records in the referenced study) [66].
- Descriptor Calculation: Generate multiple molecular representations including ECFP fingerprints, molecular descriptors, and 3D pharmacophore features.
- Data Splitting: Implement scaffold-based splitting to ensure models can generalize to new chemical classes, not just similar analogs [66].
Step 2: Machine Learning Model Training
- Docking Score Prediction: Train ensemble models to predict docking scores from 2D structures, bypassing expensive docking calculations [66].
- Model Validation: Use five-fold cross-validation with multiple random splits, reporting mean scores and standard deviations.
- Performance Benchmarking: Compare ML-predicted docking scores with actual docking results to ensure correlation (r² > 0.7 in successful implementations) [66].
Step 3: Pharmacophore-Constrained Screening
- Feature Definition: For MAO-A, define features complementary to the bipartite cavity (F208, I335 in MAO-A vs I199, Y326 in MAO-B for selectivity) [66] [77].
- Selectivity Filtering: Incorporate features that exploit differences between MAO-A and MAO-B substrate cavities to enhance selectivity [77].
Step 4: Experimental Validation with Selectivity Profiling
- Enzyme Inhibition Assays: Test compounds against both MAO-A and MAO-B isoforms to determine selectivity index [66] [77].
- Cellular Activity: Assess inhibition in relevant cell models, noting that MAO-B expression increases with age and in neurodegenerative conditions [77].
- Toxicity Screening: Evaluate tyramine-induced pressor response potential (cheese effect) for MAO inhibitors early in development [76].
Workflow Visualization: Integrated Screening with False Positive Mitigation
Quantitative Results from MAO Inhibitor Screening
Table 3: Performance Metrics from MAO Inhibitor Discovery Campaigns
| Study Reference | Screening Approach | Compounds Screened | Synthesized/Tested | Active Compounds | Best Inhibitor IC50 |
|---|---|---|---|---|---|
| Machine Learning MAO Screening [66] | ML-accelerated docking prediction | 1.3 million in ZINC (pharmacophore-constrained) | 24 | 8 (33% MAO-A inhibition) | Weak inhibitors identified |
| Traditional MAO Inhibitor Design [77] | Structure-based design | Not specified | Focused library | Multiple selective inhibitors | Varies by compound |
Essential Research Reagents for Protein-Targeted Screening
Table 4: Core Research Toolkit for Pharmacophore-Based Screening Campaigns
| Tool Category | Specific Tools | Application in Workflow |
|---|---|---|
| Pharmacophore Modeling | Pharmit, Ligand Scout, Schrödinger Phase | Model development, virtual screening, hit identification [72] [73] [70] |
| Molecular Docking | Glide, Smina, AutoDock Vina | Binding pose prediction, affinity estimation, structure-based validation [72] [66] |
| Machine Learning | Qsarna, RDKit, Scikit-learn | Docking score prediction, activity classification, false positive reduction [66] [74] |
| Compound Libraries | ZINC, ChEMBL, Enamine, ChemDiv | Sources of screening compounds with diverse chemical space [72] [66] |
| Biochemical Assays | AlphaScreen, HTRF, Fluorescence-based | Experimental validation, dose-response testing, selectivity profiling [75] [73] |
| ADMET Prediction | QikProp, SwissADME, FAF-Drugs4 | Property optimization, toxicity screening, drug-likeness assessment [72] [71] |
Successful targeting of proteins like BRD4 and MAOs demonstrates that false positives in pharmacophore screening can be effectively managed through integrated workflows that combine computational and experimental approaches. The key strategies emerging from these case studies include: (1) implementing multi-stage filtering with orthogonal methods; (2) incorporating machine learning to prioritize compounds with higher confidence; (3) using multiple biochemical assay formats to eliminate technological artifacts; and (4) applying ADMET prediction early in the screening process. By adopting these practices, researchers can significantly improve the efficiency of their pharmacophore-based screening campaigns and accelerate the discovery of genuine bioactive compounds.
Frequently Asked Questions
1. How can I improve the accuracy of my pharmacophore model and reduce false positives? A combination of structure-based modeling and rigorous validation is key. Start by creating a structure-based pharmacophore from a high-resolution protein-ligand complex (e.g., in LigandScout) to capture essential binding features. Then, validate its predictive power using a set of known active and decoy compounds. A good model should have a high Area Under the Curve (AUC) value (≥0.7) and a high enrichment factor, which indicates its ability to distinguish true actives from inactives [78].
2. What is the benefit of using multiple receptor conformations (MRCs) in docking? Using a single, rigid receptor structure often leads to inaccurate binding energy estimates and poor binding mode predictions, which generates false positives. The MRC approach, such as ensemble docking, accounts for natural protein flexibility. By docking against multiple distinct conformations, you can identify ligands that bind favorably across different protein shapes, which is a hallmark of a true binder [5].
3. My virtual screening retrieved many hits that are likely false positives. How can I narrow down the list? A robust strategy is to use the intersection of top-ranked hits from multiple independent screenings. For example, dock your library against several distinct conformations of your target receptor. Then, only select the ligands that appear in the top-ranked lists (e.g., top 50 or 100) across all or most of the conformations. This method effectively filters out compounds that scored highly by chance in a single rigid receptor setup [5].
4. What are the advantages of parallel screening or activity profiling? Screening a single compound against a collection of pharmacophore models (a Pharmacophore Model Collection or PMC) representing various pharmacological targets allows you to predict its activity profile. This helps identify not only the desired therapeutic effect but also potential off-target interactions that could lead to adverse effects, thereby flagging compounds with a high risk of failure early in the process [79].
5. Can I use a pharmacophore model created in LigandScout with other software like MOE?
Yes, but interoperability requires careful steps. LigandScout recommends using its "Create Simplified Pharmacophore" function to achieve the best compatibility with external software like MOE. After simplification, you can export the pharmacophore in the MOE format (.ph4) for subsequent virtual screening tasks [80].
Troubleshooting Guides
Problem: High False Positive Rate in Structure-Based Virtual Screening
Issue: Your virtual screening returns a large number of hits, but subsequent experimental validation shows most have no inhibitory effect.
Solution: Implement a multiple receptor conformation (MRC) strategy with consensus scoring.
Required Materials & Tools:
- Receptor Structures: A crystal structure (from PDB) and multiple conformations from Molecular Dynamics (MD) simulations [5].
- Screening Library: A diverse molecule library (e.g., Otava PrimScreen1 library used in the cited study) [5].
- Docking Software: Software with docking capabilities, such as GOLD [5].
- Analysis Tools: Scripts or software to compare and intersect hit lists from different docking runs.
Step-by-Step Protocol:
- Generate Multiple Receptor Conformations: Perform molecular dynamics (MD) simulations of the apo (unliganded) form of your receptor to explore its structural flexibility. Extract several (e.g., 5-6) distinct snapshots from the trajectory [5].
- Prepare Structures: Prepare the original crystal structure and the MD-derived structures using your software's standard preparation protocol (e.g., protonation, energy minimization).
- Dock the Library: Separately dock the entire molecule library, including known high-affinity and low-affinity control molecules, into each of the prepared receptor models [5].
- Generate Ranked Lists: For each receptor model, generate a list of top-ranked ligands (e.g., top 100 or 200) based on docking scores.
- Apply Consensus Selection: Identify the "intersection ligands"—the compounds that appear in the top-ranked lists across all or a majority of the receptor models. These consensus hits are your refined, high-confidence candidates [5].
Expected Outcome: This protocol significantly reduces false positives. In a study on influenza A nucleoprotein, this method successfully identified all added high-affinity control molecules while filtering out low-affinity ones. The number of final candidates decreases sharply as more receptor conformations are considered, leading to a more focused and reliable hit list [5].
Problem: Validating a Pharmacophore Model Before Screening
Issue: You have built a pharmacophore model but are unsure of its quality and predictive power before applying it to a large database.
Solution: Validate the model using a set of known active and decoy compounds to calculate statistical metrics.
Required Materials & Tools:
- Validated Software: Pharmacophore modeling software (e.g., LigandScout, MOE, Catalyst/Discovery Studio) [78] [79].
- Active Compounds: A set of known active compounds (e.g., from ChEMBL database) for the target [78].
- Decoy Molecules: A set of presumed inactive molecules with similar physicochemical properties but different 2D structures. These can be generated from databases like DUD-E [78].
Step-by-Step Protocol:
- Create the Model: Develop your initial pharmacophore model, either from a protein-ligand complex (structure-based) or a set of active ligands (ligand-based).
- Prepare Test Sets: Compile your set of known active compounds and a much larger set of decoy molecules.
- Run the Validation Screening: Use your pharmacophore model to screen the combined set of actives and decoys.
- Analyze the Results: Based on the screening hits, classify compounds as True Positives (TP), False Positives (FP), True Negatives (TN), and False Negatives (FN).
- Calculate Key Metrics:
- ROC Curve & AUC: Plot the Receiver Operating Characteristic (ROC) curve and calculate the Area Under the Curve (AUC). An AUC of 0.7-0.8 is "good," and 0.8-0.9 is "excellent" [78].
- Enrichment Factor (EF): This measures how much the model enriches active compounds in the hit list compared to a random selection. A higher EF indicates better performance [78] [79].
Expected Outcome: A reliable model will show a high AUC (e.g., >0.7) and a high enrichment factor in early enrichment (e.g., EF1% > 10). This gives you confidence that the model can effectively prioritize active compounds during virtual screening [78].
Experimental Protocols & Data
Detailed Methodology: Reducing False Positives via MRC Docking
This protocol is adapted from a study on influenza A nucleoprotein [5].
- System Setup: Obtain the crystal structure of the target (e.g., PDB ID for influenza NP). Place it in a solvated simulation box.
- Molecular Dynamics (MD): Run MD simulations (e.g., using GROMACS, AMBER, or NAMD) for the apo receptor to sample flexible states.
- Conformation Sampling: Extract multiple (e.g., 5-6) snapshots from the stable phase of the MD trajectory that represent distinct conformations of the binding site.
- Virtual Screening: Using docking software (e.g., GOLD):
- Prepare each receptor conformation.
- Dock the entire compound library against each conformation separately.
- For each run, generate a ranked list of the top N molecules (e.g., top 200).
- Data Analysis: Compare all ranked lists. Select only the ligands that are present in the top N of every list. These intersection molecules are your high-confidence hits.
Quantitative Data from Case Study [5]: The table below shows how applying this consensus strategy narrowed down candidates for two binding sites on influenza A nucleoprotein.
| Binding Site | Level of Comparison | Molecules Selected | Key Result |
|---|---|---|---|
| T-Loop Binding Pocket | Top-ranked 50 | 1 (Molecule A) | Successfully identified the most potent molecule. |
| T-Loop Binding Pocket | Top-ranked 100 | 2 (HAC and B) | Identified the added High-Affinity Control (HAC). |
| T-Loop Binding Pocket | Top-ranked 200 | 14 total | Final list of 14 selected candidates from the initial library. |
| RNA Binding Site | Top-ranked 50 | 7 total | Final list included three known HACs (HAC1, HAC2, HAC3). |
Key Research Reagent Solutions
| Reagent / Resource | Function in the Experiment | Example / Source |
|---|---|---|
| Protein Data Bank (PDB) | Source of high-resolution 3D structures of target proteins to initiate structure-based design. | PDB ID: 4BJX (Brd4 protein used for pharmacophore generation) [78]. |
| ZINC Database | A freely available database of commercially available compounds for virtual screening. | Used for screening natural active compounds [78]. |
| ChEMBL Database | A manually curated database of bioactive molecules with drug-like properties, used for model validation. | Source for known active antagonists of a target [78]. |
| DUD-E Server | Database of useful decoys for virtual screening benchmark studies; provides decoy molecules for validation. | Used to retrieve decoy sets to test a model's false positive rate [78]. |
| Control Molecules | Known high-affinity and low-affinity ligands for the target, used to benchmark and validate the screening process. | Added to the screening library to test the selection strategy [5]. |
Workflow Diagrams
Workflow for False Positive Reduction
Pharmacophore Model Validation
Frequently Asked Questions (FAQs)
1. What are DUD-E and MUV, and why are they important for virtual screening?
DUD-E (Directory of Useful Decoys, Enhanced) and MUV (Maximum Unbiased Validation) are benchmarking data sets used to evaluate the performance of virtual screening (VS) approaches, a key technique in early-stage drug discovery [81]. They are crucial because they provide researchers with a set of known active ligands and presumed inactive decoy molecules. This allows for the retrospective assessment of VS methods by measuring their ability to "enrich" the active ligands at the top of a screening list, thereby estimating the method's potential for real-world, prospective drug discovery campaigns [82] [81].
2. My pharmacophore model performs well on DUD-E but poorly on MUV. What could be the cause?
This is a common scenario often pointing to "analogue bias" in your screening strategy [81]. The DUD-E set is designed to cluster ligands by their Bemis-Murcko atomic frameworks to reduce this bias, but it can still be present [82]. MUV, however, is specifically designed to be maximum-unbiased and correct for this by ensuring decoys are topologically dissimilar and by avoiding artificial enrichment [81]. If your model is highly tuned to recognize a specific chemical scaffold, it may struggle with the structurally diverse actives in MUV. You should refine your pharmacophore model to capture the essential, abstract interaction features (e.g., hydrogen bonds, hydrophobic regions) shared by diverse chemotypes, rather than overfitting to a single scaffold [83].
3. What is the recommended ratio of decoys to active ligands for a reliable benchmark?
A ratio of approximately 1:50 (active molecules to decoys) is recommended [83]. This ratio reflects the reality of prospective screening, where only a few active molecules are distributed among a vast library of inactive compounds. Using this proportion helps to generate statistically significant enrichment metrics and provides a challenging test for the virtual screening method.
4. How can I minimize false positives when using these decoy sets?
False positives in benchmarking can arise from "false decoys"—molecules in the decoy set that may actually bind to the target [82]. To address this:
- Use Tightly Matched Decoys: DUD-E generates decoys that are matched to the ligands' physical properties (e.g., molecular weight, logP, number of rotatable bonds, hydrogen bond donors/acceptors) but are topologically dissimilar to minimize the likelihood of binding [82].
- Incorporate Experimental Decoys: Where possible, use decoys with experimentally confirmed inactivity. DUD-E includes such molecules for some targets [82].
- Validate with Multiple Sets: Cross-validate your pharmacophore model against both DUD-E and MUV. Consistent performance across different sets increases confidence in your model's robustness and reduces the risk of false positives stemming from set-specific biases [81].
5. How do I choose between a structure-based and ligand-based pharmacophore approach for benchmarking?
The choice depends on the data available for your target:
- Structure-Based Approach: Use this when an experimentally determined (e.g., X-ray crystallography) structure of the target protein with a bound ligand is available. You can directly extract the interaction pattern from the complex to create the model [83]. This approach is less susceptible to analogue bias.
- Ligand-Based Approach: Use this when no 3D protein structure is available, but you have a set of known active molecules. This method aligns the 3D structures of multiple active ligands to identify their common pharmacophore features [83]. Be cautious of analogue bias with this method, and ensure your training set is as diverse as possible.
Troubleshooting Guide: Common Issues and Solutions
| Problem | Possible Cause | Solution |
|---|---|---|
| Poor enrichment on both DUD-E and MUV | Pharmacophore model features are too generic or do not reflect key ligand-target interactions. | Re-evaluate the binding mode. For structure-based models, check key protein-ligand interactions. For ligand-based models, ensure the training set is diverse and the common features are essential [83]. |
| High rate of false positives | Decoys are too chemically similar to active ligands; model is not specific enough. | Use the "dissimilarity" filter in DUD-E generation. Add exclusion volumes to your pharmacophore model to sterically prevent decoy binding [82] [83]. |
| Model fails to identify active ligands with novel scaffolds | Analogue bias; model is over-fitted to a specific chemical scaffold present in the training set. | Use the clustered ligands in DUD-E. For ligand-based modeling, incorporate active ligands with diverse Bemis-Murcko frameworks into your training set [82] [81]. |
| Inconsistent results between different decoy sets | Fundamental differences in the design philosophy and correction for biases in the benchmarking sets [81]. | Understand the strengths of each set: Use DUD-E for its size and target diversity. Use MUV to rigorously test for scaffold hopping ability and avoid artificial enrichment. |
Benchmarking Database Characteristics and Applications
The table below summarizes the key features of the DUD-E and MUV databases to guide your selection.
| Feature | DUD-E (Directory of Useful Decoys, Enhanced) | MUV (Maximum Unbiased Validation) |
|---|---|---|
| Primary Design | Structure-based VS (SBVS) specific [81]. | Ligand-based VS (LBVS) specific [81]. |
| Target Coverage | 102 targets, including kinases, proteases, GPCRs, ion channels [82]. | 17 targets, derived from PubChem HTS data [81]. |
| Ligand Source | ChEMBL, with measured affinities [82]. | PubChem Bioassay HTS data [81]. |
| Decoy Selection | Property-matched (MW, logP, HBD/HBA) but topologically dissimilar [82]. | Corrects for "analogue bias" and "artificial enrichment"; uses nearest-neighbor analysis [81]. |
| Key Strength | Large size, diverse target classes, includes experimental decoys for some targets [82]. | Maximum-unbiased sets, ideal for testing scaffold hopping and avoiding over-optimistic results [81]. |
| Common Application | Evaluating docking programs and structure-based pharmacophore models [82]. | Validating ligand-based similarity searches and pharmacophore models [81]. |
Experimental Protocol: Conducting a Retrospective Benchmarking Study
1. Define Your Objective Determine the goal: for example, to benchmark a new pharmacophore model, compare multiple VS tools, or optimize a scoring function.
2. Select and Prepare the Benchmarking Set
- Download: Obtain the ligand and decoy sets for your target from http://dude.docking.org (DUD-E) or the MUV repository.
- Curation: Ensure the ligands are in the appropriate protonation state for your target. Filter decoys based on your desired molecular properties if necessary.
- Combine: Merge the active ligands and decoys into a single screening library, maintaining the recommended ~1:50 ratio [83].
3. Execute the Virtual Screening
- Pharmacophore Screening: Screen the combined library against your pharmacophore model using software like Catalyst, LigandScout, or PHASE [81].
- Pose Generation: For structure-based models, ensure the screening algorithm generates multiple conformations for each molecule to find one that matches the pharmacophore.
4. Analyze and Validate Results
- Calculate Enrichment: Rank the screened compounds based on the pharmacophore fit value or scoring function. Calculate enrichment factors (EF) and plot Receiver Operating Characteristic (ROC) curves to evaluate performance [83].
- Inspect Hits: Visually inspect the top-ranking compounds, both actives and decoys, to understand why they were selected. This can reveal model strengths or flaws.
The workflow for this protocol is summarized in the diagram below:
| Item | Function in Research |
|---|---|
| DUD-E Database | Provides a large, diverse set of targets with property-matched decoys for benchmarking structure-based virtual screening methods [82]. |
| MUV Database | Offers bias-corrected datasets designed for validating ligand-based virtual screening and assessing scaffold-hopping capability [81]. |
| Pharmacophore Modeling Software (e.g., LigandScout, Catalyst) | Tools used to create, visualize, and run virtual screens using structure-based or ligand-based pharmacophore models [83] [81]. |
| CHEMBL Database | A public repository of bioactive molecules with drug-like properties and binding affinities; a primary source for DUD-E ligands [83]. |
| PubChem Bioassay | A public database containing biological test results for small molecules, used as a source for active and inactive compounds in MUV [83] [81]. |
| Bemis-Murcko Frameworks | A method for clustering molecules by their central scaffold; used in DUD-E to reduce "analogue bias" in the ligand set [82]. |
Conclusion
Effectively managing false positives is not a single-step solution but requires a holistic, multi-layered strategy integrating careful model construction, robust filtering protocols, and rigorous validation. The integration of pharmacophore filtering with docking, the application of machine learning for rapid score prediction, and the diligent use of pre- and post-screening filters collectively create a powerful defense against spurious hits. As virtual screening libraries expand into the billions of compounds, these strategies become increasingly critical for maintaining efficiency in drug discovery. Future directions will likely involve greater automation of these workflows, the development of more sophisticated machine learning models trained on diverse target classes, and the wider adoption of high-fidelity activity profiling to de-risk candidates early. Embracing these comprehensive approaches will significantly improve the success rate of translating computational hits into validated lead compounds for biomedical and clinical research.
References
- 1. Practices of Science: False Positives and False Negatives [https://manoa.hawaii.edu/exploringourfluidearth/chemical/matter/properties-matter/practices-science-false-positives-and-false-negatives]
- 2. Machine learning classification can reduce false positives ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7414157/]
- 3. How to Avoid False Positives and False Negatives in ... [https://www.acdlabs.com/blog/how-to-avoid-false-positives-and-false-negatives-in-analytical-chemistry/]
- 4. Lies and Liabilities: Computational Assessment of High- ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11724736/]
- 5. Reduction of False Positives in Structure-Based Virtual ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6272817/]
- 6. Pharmacophore-based virtual screening and density ... [https://www.nature.com/articles/aps201221]
- 7. Drug Design by Pharmacophore and Virtual Screening ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9145410/]
- 8. Strategies for 3D pharmacophore-based virtual screening [https://www.sciencedirect.com/science/article/abs/pii/S1740674910000375]
- 9. Machine learning reveals that structural features ... [https://www.nature.com/articles/s41598-021-87042-z]
- 10. 'Fuzziness' in pharmacophore-based virtual screening and ... [https://www.sciencedirect.com/science/article/abs/pii/S1740674910000338]
- 11. Conformer Generation for Structure-Based Drug Design [https://pmc.ncbi.nlm.nih.gov/articles/PMC10647020/]
- 12. Combining docking with pharmacophore filtering for improved virtual screening - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC3152774/]
- 13. ZINCPharmer: pharmacophore search of the ZINC database [https://pmc.ncbi.nlm.nih.gov/articles/PMC3394271/]
- 14. Pharmer: Efficient and Exact Pharmacophore Search - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC3124593/]
- 15. An optimization algorithm for conformer generation based ... [https://www.sciencedirect.com/science/article/abs/pii/S1476927122001311]
- 16. Promiscuous Ligands - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC7151901/]
- 17. ChemFH: an integrated tool for screening frequent false ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11223804/]
- 18. Frequent Hitters, False Positives, Promiscuous Compounds [https://www.cambridgemedchemconsulting.com/DDResources/Hit_iden/promiscous.html]
- 19. Exploring the biological promiscuity of high-throughput ... [https://www.sciencedirect.com/science/article/abs/pii/S0968089614001709]
- 20. Frequent Hitters [https://www.cambridgemedchemconsulting.com/resources/hit_identification/promiscous.html]
- 21. Computational prediction of frequent hitters in target-based ... [https://www.sciencedirect.com/science/article/pii/S2667318521000076]
- 22. -based virtual Pharmacophore versus docking-based virtual... screening [https://pmc.ncbi.nlm.nih.gov/articles/PMC4007494/]
- 23. Improvement of protein tertiary and quaternary structure ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10290552/]
- 24. From interaction networks to interfaces, scanning ... [https://www.nature.com/articles/s41467-023-44288-7]
- 25. Combining docking with pharmacophore filtering for improved ... [https://jcheminf.biomedcentral.com/articles/10.1186/1758-2946-1-6]
- 26. Pharmacophore-based approach for the identification of ... [https://www.sciencedirect.com/science/article/pii/S266702242500012X]
- 27. Discovery of Novel FGFR1 Inhibitors via Pharmacophore ... [https://www.mdpi.com/2813-3137/3/4/35]
- 28. A practical guide to large-scale docking - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC8522653/]
- 29. ELIXIR-A: An Interactive Visualization Tool for Multi-Target ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9025992/]
- 30. Editorial: Approaches to improve the performance of virtual ... [https://www.frontiersin.org/journals/pharmacology/articles/10.3389/fphar.2025.1658699/abstract]
- 31. Structure‐based pharmacophore modeling for precision ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11299079/]
- 32. Rapid traversal of vast chemical space using machine ... [https://www.nature.com/articles/s43588-025-00777-x]
- 33. Machine learning accelerates pharmacophore-based virtual ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11369158/]
- 34. Virtual screening based on pharmacophore model ... [https://pubmed.ncbi.nlm.nih.gov/27133076/]
- 35. Docking compared to 3D-pharmacophores: the scoring ... [https://www.sciencedirect.com/science/article/abs/pii/S1740674910000557]
- 36. Pharmacophore-Based Machine Learning Model To ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10448689/]
- 37. Pharmacophore-based ML model to filter candidate E3 ... [https://www.sciencedirect.com/science/article/pii/S2352914823002708]
- 38. Building shape-focused pharmacophore models for effective ... [https://jcheminf.biomedcentral.com/articles/10.1186/s13321-024-00857-6]
- 39. Structure based pharmacophore modeling, virtual ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7892887/]
- 40. Structure based drug design and machine learning ... [https://www.nature.com/articles/s41598-025-17708-5]
- 41. Info [https://www.bindingdb.org/rwd/bind/info.jsp]
- 42. Compound activity prediction using models of binding pockets or ligand properties in 3D - PMC [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4085113/]
- 43. Guiding Conventional Protein–Ligand Docking Software ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10706896/]
- 44. LigPlot+ Operating Manual [https://www.ebi.ac.uk/thornton-srv/software/LigPlus/manual/manual.html]
- 45. A New Fragment‐Based Pharmacophore Virtual Screening ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12412281/]
- 46. interactive exploration of chemical space [https://pharmit.csb.pitt.edu/help.html]
- 47. Tautomerism in structure-based 3 modeling - PMC D pharmacophore [https://pmc.ncbi.nlm.nih.gov/articles/PMC4236210/]
- 48. (PDF) 3 -Pharma, A Ligand-based Virtual D tool using... Screening [https://www.academia.edu/123519625/3D_Pharma_A_Ligand_based_Virtual_Screening_tool_using_3D_Pharmacophore_Fingerprints]
- 49. Lipinski's rule of five [https://en.wikipedia.org/wiki/Lipinski%27s_rule_of_five]
- 50. Using filters in virtual screening: A comprehensive guide to ... [https://www.sciencedirect.com/science/article/abs/pii/S0065774322000100]
- 51. Molecular Filters in Medicinal Chemistry [https://www.mdpi.com/2673-8392/3/2/35]
- 52. druglikeFilter 1.0: An AI powered filter for collectively ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12268052/]
- 53. Gains from no real PAINS: Where 'Fair Trial Strategy' stands in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8642439/]
- 54. Filtering promiscuous compounds in early drug discovery [https://www.sciencedirect.com/science/article/abs/pii/S1359644616300307]
- 55. Knowledge-guided diffusion model for 3D ligand ... [https://www.nature.com/articles/s41467-025-57485-3]
- 56. Pharmacophore - an overview | ScienceDirect Topics [https://www.sciencedirect.com/topics/immunology-and-microbiology/pharmacophore]
- 57. Hierarchical Graph Representation of Pharmacophore ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7793842/]
- 58. Machine Learning Assisted Hit Prioritization for High ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11046457/]
- 59. ADMET Prediction - Rowan Scientific [https://www.rowansci.com/tools/admet]
- 60. ADMETlab: a platform for systematic ADMET evaluation based on a comprehensively collected ADMET database | Journal of Cheminformatics | Full Text [https://jcheminf.biomedcentral.com/articles/10.1186/s13321-018-0283-x]
- 61. ADMET Predictor® Modules [https://www.simulations-plus.com/software/admetpredictor/]
- 62. Hit Prioritization for High Throughput Screening with MVS-A [https://medium.com/@kapeluha.ann00/hit-prioritization-for-high-throughput-screening-with-mvs-a-d6750540b89f]
- 63. Receiver operating characteristic [https://en.wikipedia.org/wiki/Receiver_operating_characteristic]
- 64. Validation of pharmacophore model [https://bio-protocol.org/exchange/minidetail?id=19108364&type=30]
- 65. Structure-Based Pharmacophore Modeling, Virtual ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8777599/]
- 66. Machine learning accelerates pharmacophore-based ... [https://www.nature.com/articles/s41598-024-58122-7]
- 67. Ligand-Based Virtual Screening Approach Using a New ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3405195/]
- 68. What is the significance of enrichment factor regarding ... [https://bioinformatics.stackexchange.com/questions/11020/what-is-the-significance-of-enrichment-factor-regarding-machine-learning-methods]
- 69. Absolute binding free energy calculations improve ... [https://www.nature.com/articles/s41598-022-17480-w]
- 70. Pharmacophore-Model-Based Virtual-Screening ... [https://www.mdpi.com/1467-3045/44/10/329]
- 71. The Light and Dark Sides of Virtual Screening [https://pmc.ncbi.nlm.nih.gov/articles/PMC6470506/]
- 72. Computational discovery of BRD4 inhibitors for ... [https://www.nature.com/articles/s41598-025-20714-2]
- 73. Identification of Novel Bromodomain-Containing Protein 4 ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11397543/]
- 74. Qsarna: An Online Tool for Smart Chemical Space ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12344758/]
- 75. Novel brd with a unique scaffold exhibit antitumor effects 4 inhibitors [https://www.spandidos-publications.com/10.3892/ol.2021.12734?text=fulltext]
- 76. Monoamine Oxidase Inhibitors (MAOI) - StatPearls - NCBI - NIH [https://www.ncbi.nlm.nih.gov/books/NBK539848/]
- 77. Discovery of monoamine oxidase inhibitors by medicinal ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6350766/]
- 78. Pharmacophore-Model-Based Virtual-Screening Approaches ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9600652/]
- 79. 3D pharmacophores as tools for activity profiling [https://www.sciencedirect.com/science/article/abs/pii/S1740674910000430]
- 80. A Review of LigandScout [https://macinchem.org/2023/03/13/a-review-of-ligandscout/]
- 81. Benchmarking methods and data sets for ligand ... [https://www.sciencedirect.com/science/article/abs/pii/S1046202314003788]
- 82. Directory of Useful Decoys, Enhanced (DUD-E) [https://pmc.ncbi.nlm.nih.gov/articles/PMC3405771/]
- 83. Concepts and Applications Exemplified on Hydroxysteroid ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6332202/]