RNA Interference Cancer Reversion: A Non-Genomic Therapeutic Strategy Without DNA Editing
This article explores RNA interference (RNAi) as a powerful, reversible, and non-mutagenic approach to cancer reversion.
RNA Interference Cancer Reversion: A Non-Genomic Therapeutic Strategy Without DNA Editing
Abstract
This article explores RNA interference (RNAi) as a powerful, reversible, and non-mutagenic approach to cancer reversion. Targeting the post-transcriptional silencing of oncogenes, tumor suppressors, and critical signaling pathways, RNAi offers a precise alternative to permanent DNA-editing technologies. We provide a foundational overview of the molecular mechanisms, detail current methodological applications including siRNA and shRNA delivery systems, analyze key challenges in specificity, delivery, and off-target effects, and validate RNAi's therapeutic potential through comparative analysis with CRISPR and other modalities. Aimed at researchers and drug development professionals, this review synthesizes the current state, practical considerations, and future clinical translation of RNAi-based cancer reversion therapies.
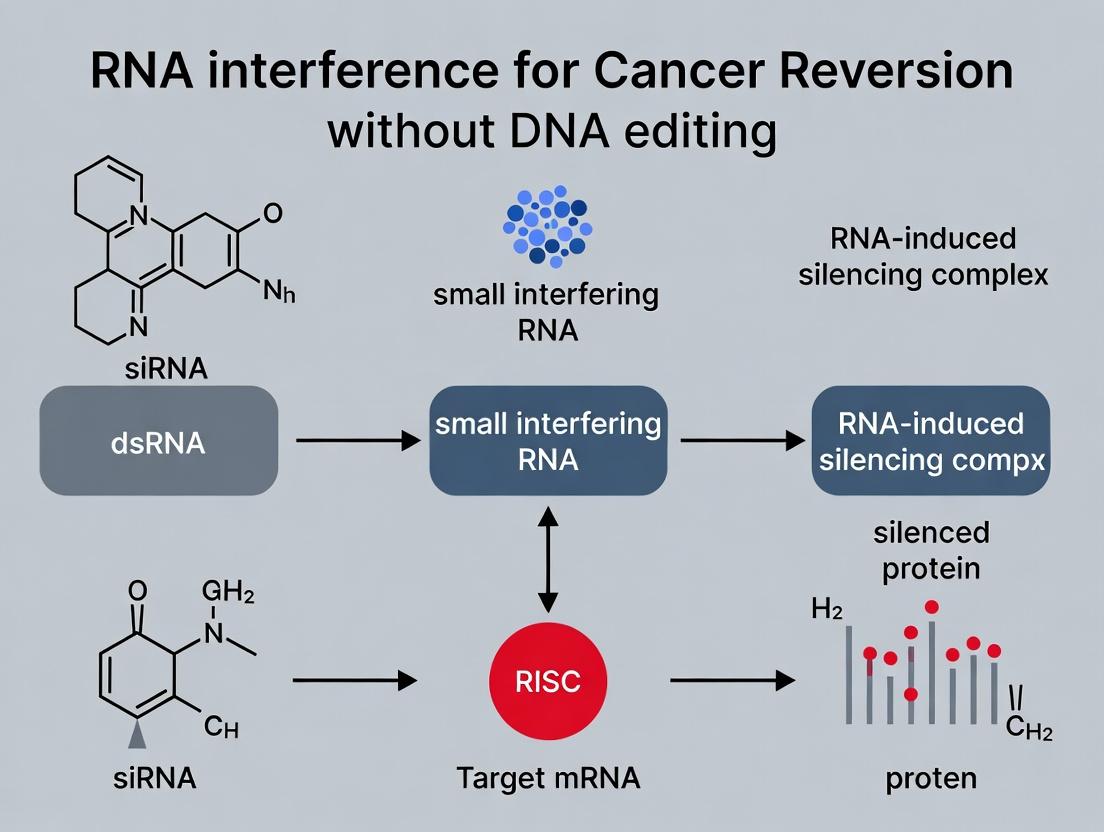
Unlocking the RNAi Mechanism: The Foundation of Non-Genomic Cancer Reversion
RNA interference (RNAi) is an evolutionarily conserved, sequence-specific biological mechanism for post-transcriptional gene silencing (PTGS). Triggered by double-stranded RNA (dsRNA), RNAi degrades complementary messenger RNA (mRNA) molecules or inhibits their translation, thereby suppressing gene expression. Within the context of a thesis on RNAi-mediated cancer reversion without DNA editing, understanding its core principles is paramount. This approach offers a programmable, reversible means to silence oncogenes, tumor-promoting pathways, and drug-resistance genes, providing a powerful therapeutic strategy distinct from genomic engineering.
Core Principles and Quantitative Metrics
The RNAi pathway involves several key steps and components, with quantifiable efficiencies at each stage.
Table 1: Key Components and Efficiencies in the Mammalian RNAi Pathway
| Component | Primary Function | Typical Efficiency/Size Notes |
|---|---|---|
| Dicer | RNase III enzyme; cleaves long dsRNA into 21-23 bp siRNA duplexes. | ~85-95% cleavage efficiency in vitro. |
| RISC Loading Complex (RLC) | Incorporates siRNA guide strand into RISC. | Strand selection fidelity >90% for thermodynamically less stable 5' end. |
| Argonaute 2 (Ago2) | Catalytic "Slicer" component of RISC; cleaves target mRNA. | Turnover rate ~5-10 cleavage events/minute. |
| siRNA (Synthetic) | 19-21 bp dsRNA with 2-nt 3' overhangs. | EC50 for effective silencing: 1-10 nM in cell culture. |
| shRNA (Viral) | ~50-70 nt stem-loop transcript processed by Dicer. | Lentiviral delivery can achieve >70% knockdown in >90% of transduced cells. |
Table 2: Comparison of Primary RNAi Triggers for Therapeutic Research
| Trigger Type | Mechanism of Action | Delivery Method | Onset of Action | Knockdown Duration |
|---|---|---|---|---|
| Synthetic siRNA | Pre-formed 21-23 bp duplex; directly loads into RISC. | Lipid nanoparticles (LNPs), conjugates. | 4-24 hours | 3-7 days (transient). |
| plasmid DNA (shRNA) | Transcribed as shRNA, processed by Dicer in vivo. | Viral (LV, AAV), electroporation. | 24-72 hours | Weeks to months (stable if integrated). |
| miRNA Mimics | Synthetic dsRNA mimicking endogenous miRNA. | LNPs, conjugates. | 12-48 hours | 5-10 days (transient). |
Detailed Experimental Protocols
Protocol 1:In VitroKnockdown Validation Using Synthetic siRNA
Objective: To transiently silence an oncogene (e.g., KRAS G12C) in a cancer cell line and assess mRNA and protein knockdown.
- siRNA Design: Obtain validated siRNA duplexes targeting the mutant KRAS G12C allele and a non-targeting control (NTC).
- Cell Seeding: Seed adherent cells (e.g., NCI-H358) in a 24-well plate at 70% confluence in antibiotic-free medium 24h prior.
- Transfection Complex Preparation:
- For each well, dilute 25 pmol siRNA in 50 µL Opti-MEM.
- Dilute 1.5 µL of lipid-based transfection reagent in 50 µL Opti-MEM. Incubate 5 min.
- Combine diluted siRNA and reagent, mix gently, incubate 20 min at RT.
- Transfection: Add 100 µL complex drop-wise to cells in 500 µL medium. Swirl gently.
- Incubation: Incubate cells for 48-72h at 37°C, 5% CO₂.
- Analysis:
- qRT-PCR: Harvest cells for RNA isolation. Use reverse transcription followed by TaqMan assay specific for KRAS total and mutant transcripts. Normalize to GAPDH. Calculate % knockdown vs. NTC.
- Western Blot: Harvest cells in RIPA buffer. Detect KRAS protein using anti-KRAS antibody. Normalize to β-Actin.
Protocol 2: Generating Stable Knockdown Cell Lines via Lentiviral shRNA
Objective: To create a stable cell line with constitutive oncogene knockdown for long-term functional assays.
- shRNA Selection: Choose a validated shRNA sequence targeting your gene of interest (e.g., MYC), cloned into a pLKO.1-puro vector.
- Lentivirus Production:
- Co-transfect HEK293T cells with: the pLKO.1-shRNA plasmid (10 µg), packaging plasmid psPAX2 (7.5 µg), and envelope plasmid pMD2.G (2.5 µg) using polyethylenimine (PEI).
- Replace medium after 6h. Collect virus-containing supernatant at 48h and 72h post-transfection. Filter (0.45 µm) and concentrate via ultracentrifugation.
- Target Cell Transduction:
- Plate target cells (e.g., MCF-7). At 50% confluence, add lentiviral supernatant plus polybrene (8 µg/mL).
- Spinoculate at 800 × g for 30 min at 32°C. Incubate overnight.
- Selection: 48h post-transduction, replace medium with selection medium containing puromycin (1-5 µg/mL, pre-titered). Maintain selection for 5-7 days until all non-transduced control cells are dead.
- Validation: Expand polyclonal pool and validate knockdown via qRT-PCR and Western Blot as in Protocol 1.
Diagrams of Pathways and Workflows
RNAi Pathway and Cancer Reversion
Therapeutic siRNA Development Workflow
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Reagents for RNAi-Based Cancer Research
| Reagent/Material | Function & Rationale | Example Product/Catalog |
|---|---|---|
| Validated siRNA Libraries | Pre-designed, high-confidence siRNAs for genome-wide or pathway-specific screens to identify cancer vulnerabilities. | Dharmacon siRNA Libraries, Qiagen HP GenomeWide. |
| Lipid-Based Transfection Reagents | Form complexes with nucleic acids for efficient cellular uptake in vitro; critical for initial siRNA screening. | Lipofectamine RNAiMAX, DharmaFECT. |
| Lentiviral shRNA Vectors | Enable stable, long-term gene knockdown; essential for studying long-term phenotypic consequences like tumorigenicity. | MISSION TRC shRNA (Sigma), pLKO.1-based systems. |
| RNA Isolation Kits (miRNA capable) | High-quality total RNA extraction including small RNAs (<200 nt) for validation by qRT-PCR or sequencing. | miRNeasy Mini Kit (Qiagen), TRIzol Reagent. |
| Stem-Loop RT-qPCR Assays | Highly sensitive and specific quantification of mature miRNA levels or siRNA-mediated knockdown. | TaqMan MicroRNA Assays, Custom stem-loop primers. |
| RISC Immunoprecipitation Kits | Isolate Ago2-bound RNAs to identify direct mRNA targets and off-effects of RNAi triggers. | Ago2 IP Kit (e.g., from Abcam or Millipore). |
| In Vivo JetRNA / Lipid Nanoparticles | Formulations for efficient, safe systemic delivery of siRNA in animal models for pre-clinical therapeutic testing. | Invivofectamine, custom LNP formulations. |
| Cell Viability/Proliferation Assays | Quantify the functional outcome of oncogene knockdown (e.g., reduced proliferation, increased chemosensitivity). | CellTiter-Glo, MTT, Real-Time Cell Analyzers. |
Within the paradigm of RNA interference (RNAi) cancer reversion without DNA editing, siRNAs and miRNAs represent precise molecular tools. They function through the RNA-Induced Silencing Complex (RISC) to downregulate oncogenes, tumor-promoting pathways, and resistance factors. This Application Notes document provides current methodologies, reagent solutions, and protocols for leveraging this toolkit in oncology research and drug development.
Research Reagent Solutions
| Reagent/Solution | Function in RNAi Oncology Research |
|---|---|
| Chemically Modified siRNAs (e.g., 2'-OMe, 2'-F) | Increases nuclease resistance and serum stability for in vivo applications; reduces off-target immunostimulation. |
| Lipid Nanoparticles (LNPs) | Enables efficient cellular delivery and endosomal escape of siRNA payloads in vitro and in vivo. |
| RISC Immunoprecipitation (RISC-IP) Kits | Isolates endogenous RISC complexes for identifying loaded miRNAs/siRNAs and their direct mRNA targets. |
| Dual-Luciferase Reporter Assay Systems | Validates direct targeting of 3'UTRs by miRNAs or siRNA seed-region mimics. |
| Synthetic miRNA Mimics & Inhibitors (AntagomiRs) | Functionally restores tumor suppressor miRNAs or inhibits oncomiRs in cancer cell models. |
| Next-Gen Sequencing Kits (Small RNA-seq, CLIP-seq) | Profiles global miRNA expression and maps RISC-mRNA interactions genome-wide. |
| Fluorescently-Labeled siRNAs (e.g., Cy3, Cy5) | Tracks cellular uptake, subcellular localization, and biodistribution of delivered RNAi triggers. |
Protocols & Application Notes
Protocol 1:In VitroScreening of siRNA Libraries Against Oncogene Targets
Objective: Identify potent siRNA leads for silencing a validated oncogene (e.g., KRAS G12C) in a cancer cell line. Materials: Reverse transfection reagent, 96-well plate, KRAS-targeting siRNA library (3 siRNAs per target), non-targeting siRNA control, cell culture reagents, qRT-PCR reagents, cell viability assay kit. Workflow:
- Plate Cells: Seed cancer cells (e.g., NCI-H358) in 96-well plate at 60-70% confluency.
- Complex Formation: Dilute siRNA (final conc. 10 nM) in serum-free medium. Add transfection reagent, incubate 15 min.
- Reverse Transfection: Add complexes directly to cells.
- Incubation: Culture cells for 72h.
- Analysis:
- Molecular: Extract RNA, perform qRT-PCR for KRAS mRNA (normalize to GAPDH). Calculate % knockdown.
- Phenotypic: Measure cell viability via MTT assay.
- Hit Selection: Prioritize siRNAs with >70% mRNA knockdown and significant reduction in viability.
Protocol 2: Validating miRNA-mRNA Target Interaction via RISC-IP (CLIP-qPCR)
Objective: Confirm direct binding of a tumor suppressor miRNA (e.g., miR-34a) to its putative oncogene target (e.g., MET mRNA) within the endogenous RISC complex. Materials: RISC-IP kit (anti-AGO2 antibody), magnetic beads, cell lysis buffer, RNase inhibitor, proteinase K, qPCR reagents. Workflow:
- Lysate Preparation: Lyse ~1x10^7 treated cells in mild lysis buffer.
- Immunoprecipitation: Incubate lysate with anti-AGO2 coated beads. Use IgG beads as control.
- Washing: Stringently wash beads to remove non-specific RNA.
- RNA Elution & Purification: Digest proteins with Proteinase K, extract RNA.
- Reverse Transcription & qPCR: Synthesize cDNA and perform qPCR for the target MET mRNA and a negative control mRNA not predicted to be targeted.
- Analysis: Enrichment in AGO2-IP vs. IgG-IP confirms specific RISC loading and interaction.
Protocol 3:In VivoDelivery of Therapeutic siRNA via LNPs
Objective: Assess in vivo efficacy of an siRNA targeting an oncogenic driver (e.g., PLK1) in a mouse xenograft model. Materials: LNP-formulated PLK1 siRNA, control LNP, immunocompromised mice, calipers, IVIS or bioluminescence imaging system (if using luciferase-tagged cells), tissue homogenizer. Workflow:
- Tumor Implantation: Subcutaneously inject human cancer cells (e.g., PC-3 prostate cancer) into mice.
- Treatment: Once tumors reach ~100 mm³, randomize mice into groups (n=5). Administer LNP-siRNA (e.g., 2 mg/kg) intravenously twice weekly for 3 weeks.
- Monitoring: Measure tumor volume bi-weekly. Monitor body weight.
- Termination: Euthanize mice, excise tumors, weigh them.
- Ex Vivo Analysis: Homogenize tumor tissue for qRT-PCR (PLK1 mRNA) and western blot (PLK1 protein) analysis.
- Statistical Analysis: Compare tumor growth curves and endpoint weights between groups using Student's t-test.
Table 1: Clinical-Stage RNAi Therapeutics in Oncology (Selected)
| Drug Name (Company) | Target | Indication | Delivery Platform | Phase (Latest Data) | Key Efficacy Metric |
|---|---|---|---|---|---|
| DCR-MYC (Dicerna) | MYC oncogene | Hepatocellular Carcinoma | EnCore LNP | Phase I (Terminated) | >50% tumor regression in subset of patients. |
| siG12D-LODER (Silenseed) | KRAS G12D | Pancreatic Cancer | Biodegradable polymer | Phase II | Improved PFS vs. control in combination with chemo. |
| MTL-CEBPA (MiNA) | CEBPA (via saRNA) | Liver Cancer | SMARTICLES LNP | Phase I | Increased serum albumin, evidence of target activation. |
| TKM-080301 (Arbutus) | PLK1 | Hepatocellular Carcinoma | LNP | Phase I/II | Disease stabilization in 42% of evaluable patients. |
Table 2: Typical In Vitro RNAi Experiment Performance Benchmarks
| Parameter | Acceptable Range | Optimal Performance |
|---|---|---|
| siRNA Transfection Efficiency (Cy3-labeled) | >80% cells fluorescent | >95% cells fluorescent |
| mRNA Knockdown (qRT-PCR, 72h) | >50% reduction | >80% reduction |
| Protein Knockdown (Western, 96-120h) | >60% reduction | >90% reduction |
| Off-Target Effect (Genome-wide expression) | <5% genes dysregulated >2-fold | <1% genes dysregulated >2-fold |
| miRNA Mimic EC₅₀ | 5-50 nM | <10 nM |
Visualizations
Title: RNAi Pathway: siRNA vs miRNA
Title: LNP-siRNA Tumor Delivery & Action
Title: RISC-IP/CLIP Protocol Workflow
This document details application notes and protocols supporting a broader research thesis on achieving functional cancer reversion through RNA interference (RNAi) without direct DNA editing. The goal is to phenotypically revert oncogenic states by selectively silencing key molecular targets, ranging from intracellular driver mutations to components of the pro-tumorigenic tumor microenvironment (TME). This approach aims to disrupt oncogenic networks and reprogram the TME towards a tumor-suppressive state, offering a potent and tunable therapeutic strategy.
RNAi targets are categorized by cellular localization and function. The following tables summarize validated targets and associated experimental data.
Table 1: Intracellular Driver Oncogene Targets
| Target Gene | Associated Cancer(s) | siRNA/shRNA Sequence (Example 5'-3') | Typical Knockdown Efficiency (%) | Observed Phenotype Post-Knockdown |
|---|---|---|---|---|
| KRAS (G12D) | Pancreatic, Colorectal | siRNA sense: GAGCUGAUGCUGAUUAUGAUU | 70-85% | Reduced proliferation, increased apoptosis, loss of anchorage-independent growth |
| MYC | Burkitt's Lymphoma, Breast | shRNA: CCACAGCAAACCTCAGUACA | 80-90% | Cell cycle arrest, differentiation, tumor regression in vivo |
| BCR-ABL | Chronic Myeloid Leukemia | siRNA sense: GAAGGGCTTCTGCCTTCACAT | 75-88% | Impaired clonogenicity, restored sensitivity to imatinib |
| β-catenin (CTNNB1) | Colorectal, Hepatocellular | siRNA sense: GAUGGACUUGACAUCGAUCUU | 65-80% | Inhibition of Wnt pathway, reduced tumor sphere formation |
Table 2: Tumor Microenvironment (TME) & Stromal Targets
| Target Gene | Cell Type Targeted | Function in TME | Delivery Method In Vivo | Key Outcome |
|---|---|---|---|---|
| VEGF-A | Tumor & Endothelial Cells | Angiogenesis | Lipid nanoparticle (LNP) | Reduced microvessel density (≥40%), improved chemotherapy uptake |
| TGF-β | Cancer-Associated Fibroblasts (CAFs) | Immune suppression, fibrosis | GalNAc-conjugated siRNA | Decreased collagen deposition, enhanced CD8+ T-cell infiltration |
| CSF1R | Tumor-Associated Macrophages (TAMs) | M2 polarization | Antibody-siRNA conjugate | Repolarization to M1 phenotype, reduced tumor growth (≈50%) |
| PD-L1 | Tumor & Myeloid Cells | Immune checkpoint | Local electroporation | Reinvigoration of tumor-infiltrating lymphocytes, synergy with anti-CTLA-4 |
Experimental Protocols
Protocol 3.1: In Vitro Screening of siRNA Libraries Against Oncogenic Drivers Objective: To identify potent siRNA leads for intracellular oncogene knockdown.
- Cell Seeding: Plate cells (e.g., Panc-1 for KRAS G12D) in 96-well plates at 2,000-4,000 cells/well in antibiotic-free medium. Incubate for 24h.
- Reverse Transfection: For each well, dilute 5 pmol of siRNA in 25 µL Opti-MEM. Dilute 0.15 µL of a suitable transfection reagent (e.g., RNAiMAX) in a separate 25 µL Opti-MEM. Combine diluted siRNA and reagent, incubate 15 min at RT. Add 50 µL of the complex to cells.
- Controls: Include a non-targeting siRNA control (scrambled sequence) and a positive control (e.g., siRNA against PLK1).
- Incubation: Incubate cells for 72-96h at 37°C, 5% CO₂.
- Viability Assay: Add 20 µL of CellTiter-Glo 2.0 reagent directly to each well. Shake for 2 min, incubate for 10 min in the dark. Record luminescence.
- Validation: For hits, perform parallel transfections for mRNA extraction (qRT-PCR) and protein lysate collection (Western blot) at 48h and 72h post-transfection, respectively.
Protocol 3.2: In Vivo Delivery of siRNA Targeting TME Component via LNPs Objective: To systemically silence a stromal target (e.g., VEGF-A) in a mouse xenograft model.
- LNP Formulation: Prepare ionizable lipid (e.g., DLin-MC3-DMA), cholesterol, DSPC, and PEG-lipid at a molar ratio of 50:38.5:10:1.5. Dissolve lipids in ethanol.
- Aqueous Phase: Dissolve VEGF-A-targeting siRNA in citrate buffer (pH 4.0).
- Microfluidic Mixing: Use a microfluidic device (e.g., NanoAssemblr) to rapidly mix the aqueous and ethanol phases at a 3:1 flow rate ratio. The total flow rate should be 12 mL/min.
- Dialysis: Dialyze the resulting LNP suspension against PBS (pH 7.4) for 24h at 4°C to remove ethanol and adjust pH. Filter sterilize (0.22 µm).
- Animal Dosing: Measure tumor volume in mice (e.g., ~100 mm³). Inject LNP-siRNA intravenously via the tail vein at a dose of 1-2 mg siRNA/kg body weight. Administer doses twice weekly for three weeks.
- Analysis: Harvest tumors 48h after the final dose. Process for IHC (CD31 for vasculature) and RNA in situ hybridization to confirm target knockdown.
Diagrams
Diagram 1: RNAi Cancer Reversion Thesis Logic
Title: Thesis Logic: Dual RNAi Strategies for Cancer Reversion
Diagram 2: Key TME Targets and Their Signaling Pathways
Title: Key TME Pathways and Effector Cells Targeted by RNAi
Diagram 3: LNP-siRNA In Vivo Delivery & Mechanism Workflow
Title: LNP-siRNA Delivery Workflow from Injection to Action
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Reagents for RNAi Oncogene Targeting Experiments
| Item | Function & Application | Example Product/Brand |
|---|---|---|
| Validated siRNA Libraries | Pre-designed, efficacy-tested pools for high-throughput screening of oncogene targets. | ON-TARGETplus (Horizon Discovery), Silencer Select (Ambion) |
| In Vivo-Ready siRNA | Chemically modified (e.g., 2'-O-Methyl, 2'-F) for nuclease stability and reduced immunogenicity. | Accell siRNAs (Horizon), AtuRNAi (Silence Therapeutics) |
| Ionizable Cationic Lipid | Critical component of LNPs for in vivo siRNA encapsulation and delivery. | DLin-MC3-DMA (MedChemExpress), SM-102 (Avanti) |
| In Vivo JetPEI | A polymer-based transfection reagent for local in vivo delivery (e.g., intra-tumoral). | Polyplus-transfection |
| RISC-lysis Buffer | Specialized lysis buffer for efficient co-immunoprecipitation of the RNA-Induced Silencing Complex (RISC) to validate loading. | Merck Millipore |
| RNAiMAX Transfection Reagent | A lipid-based reagent optimized for high-efficiency, low-toxicity siRNA delivery in vitro. | Invitrogen |
| siRNA Fluorescent Label (Cy3/Cy5) | For tracking cellular uptake, biodistribution, and transfection efficiency. | Dharmacon, Horizon |
| GalNAc Conjugation Kit | For hepatocyte-specific siRNA delivery; targets asialoglycoprotein receptor. | Alnylam proprietary, research kits available. |
Within the paradigm of RNA interference (RNAi)-mediated cancer reversion, the "Reversion Concept" posits that malignant phenotypes can be reprogrammed toward normalized, benign states without creating permanent genomic alterations. This approach leverages endogenous regulatory pathways to silence oncogenic drivers and reactivate tumor-suppressive networks, leaving no DNA-level "scars" and mitigating risks of insertional mutagenesis and off-target editing associated with DNA-based therapies.
Current Quantitative Landscape of RNAi in Cancer Reversion
Table 1: Efficacy Metrics of Key RNAi-Based Reversion Strategies in Preclinical Models
| Target Gene / Pathway | Cancer Type | RNAi Modality (e.g., siRNA, shRNA) | Delivery System | Key Metric: Tumor Volume Reduction | Key Metric: Phenotypic Reversion Marker (e.g., E-cadherin ↑) | Key Metric: Metastatic Nodule Reduction | Study Year & Reference (Type) |
|---|---|---|---|---|---|---|---|
| MYC | Hepato-cellular Carcinoma | Lipid nanoparticle (LNP)-siRNA | GalNAc-targeted LNP | 72% ± 8% (vs. scramble) | AFP secretion ↓ by 85% | Lung metastases: 90% ↓ | 2023, Nat. Biotechnol. |
| KRASG12C | Non-Small Cell Lung Cancer | Polymer-complexed siRNA | Inhalable polymeric nanoparticles | 65% ± 12% | Ki67 ↓ 70%; Cleaved caspase-3 ↑ 5-fold | Not applicable (orthotopic) | 2024, Sci. Adv. |
| ZEB1 | Triple-Negative Breast Cancer | shRNA via lentivirus (tet-inducible) | Intratumoral injection | Primary tumor: 60% ↓ | E-cadherin protein ↑ 8-fold; Vimentin ↓ 90% | 95% reduction in lung colonization | 2023, Cancer Cell |
| β-catenin (CTNNB1) | Colorectal Cancer | siRNA | Dendrimer-based nanoparticle | 58% ± 10% | Nuclear β-catenin ↓ 80%; Differentiation markers ↑ | Liver metastasis: 75% ↓ | 2022, Mol. Ther. |
| SOX2 | Glioblastoma | miRNA mimic (miR-145) | Exosome-based delivery | Tumor sphere formation ↓ 80% | GFAP (differentiation) ↑ 6-fold; Nestin ↓ 70% | N/A (primary brain tumor) | 2024, PNAS |
Table 2: Comparison of Genomic Scar Risks: RNAi vs. DNA-Editing Modalities
| Modality | Therapeutic Goal | Risk of Permanent Genomic Scars | Mechanism of Scar Risk | Typical Reversibility of Phenotypic Effect |
|---|---|---|---|---|
| RNA Interference (siRNA/miRNA) | Transient mRNA knockdown | None | No DNA interaction; acts in cytoplasm. | High (days to weeks post-treatment cessation). |
| Inducible shRNA | Durable but regulated knockdown | Low (integration site-dependent) | Random viral integration may disrupt tumor suppressors. | Medium (reversible upon inducer withdrawal). |
| CRISPR-Cas9 Knockout | Permanent gene disruption | High | DSBs lead to indels; potential for large deletions, translocations, oncogene activation. | None (permanent). |
| Base/Prime Editing | Permanent point mutation correction | Medium | Off-target DNA edits; potential for bystander edits. | None (permanent). |
| Antisense Oligonucleotides (ASOs) | Transient modulation (splicing/knockdown) | None | RNA-DNA heteroduplex formation is transient and non-catalytic. | High. |
Detailed Experimental Protocols
Protocol 1: In Vitro Phenotypic Reversion Assay via siRNA-Mediated Oncogene Knockdown
Aim: To quantify reversion of EMT and stemness markers in a cancer cell line following targeted siRNA transfection.
- Cell Seeding: Plate 1.5 x 10⁵ cells/well of an aggressive, mesenchymal-type cancer cell line (e.g., MDA-MB-231) in a 6-well plate in antibiotic-free media. Incubate for 24h to reach 50-60% confluency.
- siRNA-Lipid Complex Preparation (per well):
- Dilute 5 pmol (≈50 nM final) of ON-TARGETplus SMARTpool siRNA (e.g., targeting ZEB1) or non-targeting control in 250 µL Opti-MEM.
- Dilute 7.5 µL of DharmaFECT 1 transfection reagent in 250 µL Opti-MEM. Incubate separately for 5 min.
- Combine diluted siRNA with diluted reagent, mix gently, incubate 20 min at RT.
- Transfection & Incubation: Add 500 µL complex dropwise to cells with 1.5 mL fresh media. Incubate for 72h at 37°C, 5% CO₂.
- Harvest & Analysis:
- RNA: Extract total RNA (TRIzol). Perform qRT-PCR for mesenchymal (VIM, SNAI1, ZEB1), epithelial (CDH1, OCLN), and stemness (SOX2, NANOG) markers. Use GAPDH for normalization.
- Protein: Lyse cells in RIPA buffer. Perform Western blot for same markers (GAPDH loading control).
- Functional Assay: At 48h post-transfection, perform a 3D Matrigel culture assay (5x10³ cells/well in 8-well chamber slides) to assess acinar/organoid morphology vs. invasive stellate structures over 7 days. Image and quantify spherical structures.
Protocol 2: In Vivo Assessment of Tumor Reversion Using Systemically Delivered siRNA Nanoparticles
Aim: To evaluate tumor normalization and metastatic suppression in an immunocompromised mouse xenograft model.
- Model Establishment: Subcutaneously inject 5x10⁶ luciferase-tagged mesenchymal cancer cells (e.g., 4T1 or Hs578T) into the flank of 6-8 week-old female NOD/SCID mice (n=8 per group). Monitor until tumors reach ~100 mm³.
- Formulation & Dosing: Use clinically relevant nanoparticles (e.g., GalNAc-LNPs or polymer-based). Reconstitute lyophilized siRNA (targeting oncogene, e.g., MYC) nanoparticle in sterile PBS to 0.5 mg/kg siRNA dose in 100 µL.
- Treatment Regimen: Administer via tail vein injection every 4 days for 4 total doses. Control groups: 1) Non-targeting siRNA nanoparticles, 2) PBS vehicle.
- Longitudinal Monitoring:
- Tumor Volume: Measure with calipers bi-weekly. Volume = (Length x Width²)/2.
- IVIS Imaging: Inject D-luciferin (150 mg/kg, i.p.) 10 min prior to imaging. Quantify total flux (photons/sec) from primary tumor and thorax region weekly to track metastasis.
- Terminal Analysis (Day 28):
- Harvest tumors, weigh, and split for: a) FFPE (IHC for Ki67, Cleaved Caspase-3, E-cadherin), b) Snap-freezing (RNA/protein analysis).
- Harvest lungs and liver. Fix in Bouin's solution for 24h to count metastatic nodules (white against yellow background).
- Perform RNA-seq on tumor samples to assess global transcriptomic shift toward a benign signature.
Pathway & Workflow Visualizations
Diagram Title: Core RNAi Pathway for Phenotypic Reversion
Diagram Title: In Vivo Reversion Study Workflow
The Scientist's Toolkit: Key Research Reagent Solutions
Table 3: Essential Reagents for RNAi Cancer Reversion Research
| Reagent / Material | Supplier Examples | Function in Reversion Studies | Critical Notes |
|---|---|---|---|
| ON-TARGETplus SMARTpool siRNA | Horizon Discovery | Pre-designed, validated siRNA pools against a single target; reduce off-target effects. | Essential for clean in vitro phenotype attribution. Use non-targeting pool controls. |
| DharmaFECT Transfection Reagents | Horizon Discovery | Lipid-based reagents for high-efficiency siRNA delivery into a wide range of cell types. | Choose number (1-4) based on cell line. Optimize for viability vs. efficiency. |
| Tet-pLKO-puro Inducible shRNA Vectors | Addgene (TRC clones) | Doxycycline-inducible shRNA expression for regulated, durable knockdown in vitro/in vivo. | Allows study of reversion reversibility. Critical for in vivo xenografts with doxycycline feed. |
| GalNAc-conjugated siRNA | Alnylam, custom synthesis | Enables hepatocyte-specific targeting via ASGPR receptor for liver cancer reversion models. | Gold standard for preclinical liver-targeted delivery. |
| Polymer-based Nanoparticles (e.g., PBAE) | Custom synthesis, commercial kits | Biodegradable, cationic polymers for co-formulating siRNA; tunable for various tumor types. | Useful for creating targeted (e.g., folate-conjugated) delivery systems for systemic administration. |
| In Vivo-JetPEI | Polyplus-transfection | A linear PEI derivative for forming stable polyplexes with siRNA for safe, effective in vivo delivery. | A standard for proof-of-concept systemic siRNA studies in mice. |
| Matrigel (Growth Factor Reduced) | Corning | Basement membrane matrix for 3D culture to assess morphogenic reversion (invasive vs. spherical growth). | Key for quantifying phenotypic normalization in vitro. |
| LIVE/DEAD Viability/Cytotoxicity Kit | Thermo Fisher | Simultaneous staining with calcein-AM (live, green) and ethidium homodimer-1 (dead, red). | Critical for assessing cytotoxicity of RNAi/delivery combinations in reversion assays. |
| Human/Mouse EMT Antibody Sampler Kit | Cell Signaling Tech. | Includes antibodies for E-cadherin, N-cadherin, Vimentin, Snail, Slug, β-catenin, etc. | Streamlines Western blot/IHC analysis of mesenchymal-epithelial transition (MET). |
| D-Luciferin, Potassium Salt | PerkinElmer | Substrate for firefly luciferase used in bioluminescent imaging of tumor burden/metastasis. | Enables longitudinal monitoring in live animals without euthanasia. |
Within the broader thesis on achieving cancer reversion via RNA interference (RNAi) without permanent DNA editing, this document outlines the critical advantages of RNAi-based approaches. The transient, reversible, and epigenetically-aware nature of RNAi platforms like siRNA, miRNA, and shRNA provides a powerful therapeutic and research paradigm distinct from CRISPR-Cas9 or other DNA-editing technologies. This application note details protocols and experimental considerations for harnessing these advantages in oncology research and drug development.
The following table summarizes the key comparative advantages of RNAi over DNA-editing technologies in the context of cancer research.
Table 1: Comparative Advantages of RNAi vs. DNA-Editing Platforms for Cancer Research
| Feature | RNA Interference (siRNA/shRNA) | DNA-Editing (e.g., CRISPR-Cas9) | Implication for Cancer Reversion Research |
|---|---|---|---|
| Reversibility | High - Effects are transient and degrade over time. | Very Low - Changes are permanent and heritable. | Enables temporary oncogene knockdown to assess phenotype without permanent genotoxicity; safer for therapeutic exploration. |
| Temporal Control | High - Precise control via delivery timing or inducible systems. | Low - Activity is constitutive post-delivery; some inducible systems exist. | Allows for pulsed, stage-specific interrogation of oncogenic pathways and synthetic lethal interactions. |
| Epigenetic Considerations | Targets RNA; does not directly alter chromatin. Can be used to target epigenetic regulators. | Can directly edit DNA sequence; dCas9 systems can forcibly alter chromatin states. | Avoids unintended, permanent disruption of native epigenetic landscapes; can reversibly modulate epigenetic machinery. |
| Off-Target Effects | Transcriptional (seed-based) off-targets; transient. | Genomic off-target edits; permanent. | Risk profile is lower and manageable due to effect transience. |
| Therapeutic Development Speed | Faster - Chemical synthesis of siRNA is rapid; no complex design constraints. | Slower - Requires careful sgRNA design and validation of editing efficiency. | Accelerates preclinical validation of novel oncology targets. |
| Primary Risk | Immunogenicity, delivery efficiency, saturation of endogenous RNAi machinery. | Off-target mutations, on-target genotoxicity, chromosomal rearrangements. | RNAi risks are often related to delivery and pharmacology, not permanent genome damage. |
Application Notes & Protocols
Protocol: Inducible and Reversible Oncogene Knockdown Using Doxycycline-Inducible shRNA
This protocol enables temporal control and reversibility for studying cancer cell reversion.
Objective: To achieve timed, reversible knockdown of a target oncogene (e.g., MYC) in a cancer cell line and monitor phenotypic reversion.
Research Reagent Solutions:
| Item | Function |
|---|---|
| Tet-On 3G Inducible Expression System | Allows doxycycline-dependent expression of shRNA. |
| Lentiviral Packaging Mix (psPAX2, pMD2.G) | Produces lentiviral particles for stable integration of the inducible construct. |
| Polybrene (Hexadimethrine bromide) | Enhances lentiviral transduction efficiency. |
| Doxycycline Hyclate | Inducer for the Tet-On system; binds and activates the transactivator. |
| Puromycin Dihydrochloride | Selectable antibiotic for stable cell pool selection. |
| qPCR Kit for Target mRNA Quantification | Validates knockdown and reversal at the transcript level. |
| Cell Viability/Cell Cycle Assay Kit | Assesses phenotypic consequences of reversible knockdown. |
Methodology:
- Construct Design: Clone shRNA targeting your oncogene of interest into a pTRIPZ or similar Tet-On inducible lentiviral vector.
- Virus Production: Co-transfect HEK293T cells with the inducible shRNA vector and packaging plasmids (psPAX2, pMD2.G) using a transfection reagent. Harvest lentivirus-containing supernatant at 48 and 72 hours.
- Cell Line Transduction: Incubate target cancer cells (e.g., MCF-7, A549) with lentiviral supernatant and 8 µg/mL Polybrene. Spinfect at 1000 x g for 90 minutes at 32°C to enhance transduction.
- Selection: 48 hours post-transduction, begin selection with 1-2 µg/mL Puromycin. Maintain selection for 5-7 days to establish a stable polyclonal pool.
- Induction & Reversion Workflow:
- Day 0: Seed cells in triplicate for each condition.
- Day 1: Treat experimental group with 1 µg/mL Doxycycline. Maintain a non-induced control.
- Days 3-5: Harvest a subset of cells for qPCR (confirm knockdown) and phenotypic assays (viability, apoptosis, colony formation).
- Day 5: For the "reversal" group, wash cells thoroughly with PBS and replace media without doxycycline.
- Days 7-10: Harvest reversal cells to assess recovery of target mRNA and protein, and loss of the phenotypic effect.
- Analysis: Compare phenotype (e.g., proliferation rate) between induced, non-induced, and reversal groups. The return of proliferation in the reversal group confirms the transient, non-toxic nature of the intervention.
Protocol: Epigenetic Modulation via RNAi Targeting of Chromatin Regulators
This protocol highlights how RNAi can be used to reversibly probe the epigenetic landscape in cancer.
Objective: To reversibly deplete an epigenetic writer/reader (e.g., EZH2 or BRD4) and assess transient changes in histone marks and gene expression.
Research Reagent Solutions:
| Item | Function |
|---|---|
| Validated siRNA Pools (e.g., ON-TARGETplus) | Minimizes seed-based off-targets for clean epigenetic perturbation. |
| Lipid-Based Transfection Reagent | Enables efficient siRNA delivery into difficult-to-transfect cells. |
| ChIP-Validated Antibodies (e.g., H3K27me3) | For chromatin immunoprecipitation to assess histone mark changes. |
| Chromatin Extraction Kit | Isolates histone proteins for western blot analysis of modifications. |
| RT-qPCR Kit | Measures expression changes of downstream target genes. |
Methodology:
- Transient siRNA Transfection: Reverse-transfect cancer cells with 20-50 nM siRNA pool targeting the epigenetic regulator (e.g., EZH2) or non-targeting control (NTC) using an appropriate transfection reagent.
- Time-Course Harvest: Harvest cells at 48, 72, and 96 hours post-transfection for analysis.
- Assessment of Reversibility: At 72 hours post-transfection, split a subset of transfected cells and re-seed them in normal growth media without siRNA. Harvest these "recovery" cells 96 and 120 hours after the initial transfection.
- Downstream Analysis:
- Western Blot: Confirm depletion and recovery of the target protein (EZH2) and analyze global levels of associated histone marks (H3K27me3).
- ChIP-qPCR: Perform ChIP for H3K27me3 at known Polycomb target loci (e.g., CDKN2A promoter) in knockdown and recovery samples to map reversible epigenetic changes.
- qRT-PCR: Measure expression of genes regulated by the mark (e.g., CDKN2A) to link epigenetic reversal to transcriptional output.
- Interpretation: Successful reversal shows that RNAi induced a temporary, non-heritable epigenetic and transcriptional shift, unlike permanent DNA-editing-based epigenetic silencing/activation.
Visualizations
Temporal Control in Oncogene Knockdown
Reversibility: RNAi vs DNA-Editing
From Bench to Bedside: Practical Strategies for RNAi Delivery and Application in Oncology
Within the paradigm of RNA interference (RNAi) for cancer reversion without DNA editing, the design of synthetic siRNA and expressed shRNA is paramount. This approach aims to revert oncogenic phenotypes by selectively silencing key drivers of proliferation, metastasis, and therapy resistance, while avoiding permanent genomic alterations. Achieving this requires optimizing three interdependent parameters: Specificity (to minimize off-target effects), Stability (to ensure sufficient in vivo half-life), and Potency (to ensure efficient gene knockdown at low concentrations). This document provides application notes and detailed protocols to guide researchers in designing and validating such reagents.
The following tables summarize critical, evidence-based design rules gathered from current literature and databases.
Table 1: Core siRNA Sequence Design Parameters for Specificity and Potency
| Parameter | Optimal Feature / Rule | Rationale & Impact |
|---|---|---|
| Length | 19-21 bp duplex | Standard for RISC loading; longer siRNAs increase off-target risk. |
| GC Content | 30-55% | Balanced stability; very high GC increases duplex rigidity and off-targets; very low reduces potency. |
| Thermodynamic Asymmetry | Low stability at 5'-end of antisense (guide) strand (A/Us preferred) | Ensures correct strand selection into RISC, enhancing on-target potency. |
| Sense Strand 3'-Overhang | 2-nt deoxythymidine (dTdT) or UU | Enhures nuclease resistance and promotes RISC loading. |
| Avoidance Motifs | Avoid seed region (pos. 2-8 of guide) homology to non-target 3'UTRs | Critical for minimizing microRNA-like off-target silencing. |
| Specificity Check | BLAST against transcriptome; use Smith-Waterman for splice variants | Ensures unique targeting of intended oncogene. |
Table 2: Chemical Modifications for Enhanced Stability and Specificity
| Modification Site | Example Modifications | Primary Function | Effect on Potency/Specificity |
|---|---|---|---|
| Sugar Phosphate Backbone | Phosphorothioate (PS) linkages (1-2 per strand) | Increases nuclease resistance and plasma protein binding, prolonging half-life. | Potency maintained; may slightly reduce if overused. |
| 2'-Sugar Position | 2'-O-Methyl (2'-OMe), 2'-Fluoro (2'-F) | Increases nuclease resistance and reduces immune activation (e.g., TLR recognition). | 2'-OMe in seed region can reduce off-targets. |
| Termini | Inverted deoxyabasic (idB) at 3' of sense strand | Blocks sense strand RISC entry, improving specificity. | Enhances specificity; minimal potency impact. |
| Base | 5-Methyluridine or 5-Methylcytidine | Can reduce immune stimulation. | Neutral effect on potency when used sparingly. |
Experimental Protocols
Protocol 1:In SilicoDesign and Specificity Screening for Oncogene-Targeting siRNA
Objective: To design candidate siRNAs against a target oncogene (e.g., KRAS G12C mutant transcript) and rigorously assess potential off-target interactions. Materials: See "Research Reagent Solutions" below. Workflow:
- Target Sequence Identification: Retrieve the full mRNA sequence (RefSeq ID) for the target oncogene and its relevant mutant variant from NCBI. For mutant-specific targeting, ensure the siRNA spans the mutation site.
- Candidate Generation: Use an algorithm (e.g., from IDT, Dharmacon, or siDirect) to generate all possible 19-mer sequences from the target region with ~50% GC content.
- Filter for Efficacy: Score candidates based on known potency rules (thermodynamic asymmetry, absence of internal repeats).
- Specificity Analysis (Critical Step): a. Perform a local BLASTn search of each 19-mer guide strand sequence against the human transcriptome (RefSeq mRNA database). Discard any candidate with perfect homology to any other transcript. b. For the seed region (positions 2-8 of the guide strand), perform a separate search for complementary sequences in the 3'UTRs of all other genes. Candidates with >1 potential off-target with perfect seed match should be deprioritized. c. Use public databases (e.g., siRNA Off-Target Effect (OTE) Database) to check seed sequences against known problematic profiles.
- Final Selection: Select 3-4 top candidates for in vitro validation. Include a positive control (e.g., siRNA against GAPDH or POLR2A) and a negative control (scrambled sequence with no significant homology).
Protocol 2:In VitroPotency and Off-Target Validation
Objective: To experimentally validate knockdown efficiency and specificity of candidate siRNAs in a relevant cancer cell line. Materials: See "Research Reagent Solutions" below. Workflow:
- Cell Seeding: Seed target cancer cells (e.g., NCI-H358 for KRAS G12C) in 96-well plates at 30-50% confluency in antibiotic-free media 24h prior to transfection.
- Transfection: Using a lipid-based transfection reagent (e.g., Lipofectamine RNAiMAX), transfert cells with each candidate siRNA at a final concentration of 10 nM, 1 nM, and 0.1 nM (for dose-response). Include controls.
- Knockdown Assessment (48h post-transfection): a. qRT-PCR for On-Target: Lyse cells and extract total RNA. Perform reverse transcription and qPCR for the target oncogene. Normalize to a housekeeping gene (e.g., HPRT1). Calculate % knockdown relative to negative control. b. Western Blot for On-Target (72h): Confirm knockdown at the protein level.
- Off-Target Screening (48h): a. Perform microarray or RNA-seq on samples treated with 10 nM siRNA vs. negative control. Alternatively, use a focused qPCR array containing genes with seed-region homology. b. Apply stringent thresholds (e.g., >2-fold change, p-value < 0.01). True hits should show a dose-response. Candidates causing significant off-target transcriptional changes should be re-designed.
Protocol 3: shRNA Cloning and Viral Transduction for Long-Term Studies
Objective: To create stable knockdown cell lines for functional assays on cancer reversion (e.g., proliferation, invasion). Materials: See "Research Reagent Solutions" below. Workflow:
- shRNA Sequence Design: Convert the validated siRNA sequence into an shRNA loop structure (e.g., 19-29 bp stem, TTCAAGAGA loop). Add appropriate restriction enzyme sites (e.g., BamHI/EcoRI) for cloning.
- Oligo Annealing & Ligation: Synthesize complementary DNA oligos, anneal them, and ligate into a linearized, dephosphorylated lentiviral shRNA expression vector (e.g., pLKO.1).
- Plasmid Verification: Transform ligation mix into competent bacteria. Isolate plasmid DNA and verify insert by Sanger sequencing.
- Lentivirus Production: Co-transfect HEK-293T cells with the shRNA plasmid and packaging plasmids (psPAX2, pMD2.G) using PEI transfection reagent. Harvest virus-containing supernatant at 48h and 72h.
- Cell Transduction & Selection: Transduce target cancer cells with viral supernatant plus polybrene (8 µg/mL). After 48h, select with puromycin (dose determined by kill curve) for 5-7 days to generate a stable polyclonal pool.
- Validation: Validate knockdown via qRT-PCR/Western blot before proceeding to functional assays.
Diagrams & Visualizations
Diagram Title: siRNA Design and Validation Workflow
Diagram Title: Strand Selection and RISC Loading Determinants
Research Reagent Solutions (The Scientist's Toolkit)
| Item / Reagent | Function / Role in RNAi Experiments | Example Vendor/Catalog |
|---|---|---|
| siRNA Design Algorithms | Automated design using current rules for potency and initial specificity filtering. | IDT, Dharmacon (siDESIGN), siDirect |
| Chemically Modified RNA Oligos | Provides nuclease-resistant, specificity-enhanced siRNA for in vitro and in vivo studies. | Horizon Discovery, Sigma-Aldrich, TriLink BioTechnologies |
| Lipofectamine RNAiMAX | Cationic lipid reagent optimized for high-efficiency siRNA delivery into mammalian cells with low cytotoxicity. | Thermo Fisher Scientific (13778030) |
| pLKO.1-puro Vector | Lentiviral shRNA expression vector with puromycin resistance for stable knockdown generation. | Addgene (#8453) |
| psPAX2 & pMD2.G | 2nd generation lentiviral packaging plasmids for producing replication-incompetent virus. | Addgene (#12260, #12259) |
| Polybrene | Cationic polymer that enhances viral transduction efficiency by neutralizing charge repulsion. | Sigma-Aldrich (H9268) |
| Puromycin Dihydrochloride | Antibiotic for selection of cells successfully transduced with pLKO.1-based shRNA constructs. | Thermo Fisher Scientific (A1113803) |
| High-Capacity cDNA Reverse Transcription Kit | For consistent conversion of RNA to cDNA, essential for accurate qRT-PCR knockdown validation. | Thermo Fisher Scientific (4368814) |
| TaqMan Gene Expression Assays | Fluorogenic probe-based qPCR assays for specific, sensitive quantification of target and off-target mRNA levels. | Thermo Fisher Scientific |
| TRIzol Reagent | Monophasic solution for reliable total RNA isolation from cells for transcriptomic analysis. | Thermo Fisher Scientific (15596026) |
| RNA-seq Library Prep Kit | For comprehensive, genome-wide off-target effect profiling. | Illumina (TruSeq Stranded mRNA), NEB (NEBNext Ultra II) |
Within the thesis on achieving RNA interference (RNAi)-mediated cancer reversion without DNA editing, the primary translational bottleneck remains the efficient, specific, and safe delivery of RNAi triggers (siRNA, shRNA) to tumor cells and their microenvironment. This document outlines application notes and detailed protocols for the three dominant delivery paradigms, contextualized for oncology research.
Table 1: Key Quantitative Parameters of RNAi Delivery Platforms for Cancer Research
| Parameter | Lipid Nanoparticles (LNPs) | GalNAc Conjugates | Viral Vectors (AAV) |
|---|---|---|---|
| Typical Payload | siRNA, mRNA, pDNA (~4,000 nt capacity) | siRNA, ASO (~21 nt siRNA) | shRNA expression cassette (unlimited duration) |
| Primary Target Cell | Hepatocytes (systemic); Can be tuned for extra-hepatic targets | Hepatocytes (highly specific) | Broad range (serotype-dependent); ex vivo use common |
| Delivery Efficiency in vivo | ~5-15% of injected dose to liver; <1% to tumors (untuned) | >90% receptor-mediated uptake in hepatocytes | High transduction efficiency in permissive tissues |
| Onset of Action | Hours | Hours to days | Weeks (requires transcription) |
| Duration of Effect | 7-14 days (siRNA) | 2-4 weeks (siRNA) | Months to permanent (integrating vectors risky) |
| Key Limitation in Oncology | Off-target accumulation, immunogenicity, complex manufacturing | Restricted to liver targets | Pre-existing immunity, capsid toxicity, insertional mutagenesis risk |
| Clinical Stage | Approved (Onpattro), multiple in trials | Approved (Givlaari, Oxlumo), oncology in early phases | Approved (Zolgensma), oncology trials for ex vivo |
Application Notes & Detailed Protocols
Protocol 3.1: Formulating Ionizable Lipid Nanoparticles for siRNA Delivery to Solid Tumors
Objective: Prepare targeted LNPs encapsulating siRNA against an oncogene (e.g., KRAS G12C) for evaluation in murine xenograft models. Thesis Context: Enables systemic evaluation of RNAi-mediated oncogene silencing without viral genomic integration.
Materials (Research Reagent Solutions):
- Ionizable Lipid (e.g., DLin-MC3-DMA): Forms pH-sensitive bilayer, enables endosomal escape.
- Helper Lipid (DSPC): Stabilizes LNP structure and fluidity.
- Cholesterol: Modulates membrane permeability and stability.
- PEGylated Lipid (DMG-PEG2000): Controls particle size and prevents aggregation; can be substituted with targeting ligand-PEG.
- siRNA (Target & Scrambled Control): Dry, purified duplex.
- Acetate Buffer (pH 4.0): Ionization medium for lipid mixing.
- Microfluidic Device (e.g., NanoAssemblr): Enables reproducible, scalable nanoprecipitation.
Procedure:
- Lipid Solution Prep: Dissolve ionizable lipid, DSPC, cholesterol, and DMG-PEG2000 in ethanol at a molar ratio (50:10:38.5:1.5) to a total lipid concentration of 12.5 mM.
- Aqueous Solution Prep: Dissolve siRNA in 25 mM acetate buffer (pH 4.0) to a concentration of 0.3 mg/mL.
- Microfluidic Mixing: Using a staggered herringbone mixer chip, pump the lipid (ethanol) and aqueous (buffer) solutions at a flow rate ratio of 1:3 (total flow rate 12 mL/min) to initiate spontaneous self-assembly.
- Buffer Exchange & Purification: Immediately dilute the formed LNP mixture 1:5 in 1x PBS (pH 7.4). Concentrate and diafilter against PBS using tangential flow filtration (100 kDa MWCO).
- Characterization: Measure particle size (target: 70-100 nm) and PDI (<0.2) via DLS, encapsulation efficiency (>90%) by RiboGreen assay, and siRNA concentration (HPLC).
Protocol 3.2: Evaluating Hepatocyte-Specific Delivery Using GalNAc-siRNA Conjugates
Objective: Assess gene silencing in a hepatic carcinoma model using a pre-formed GalNAc-siRNA conjugate. Thesis Context: Models RNAi therapy for liver-specific oncogenes (e.g., MYC, HCC targets) or factors secreted by the liver that influence tumor progression.
Materials (Research Reagent Solutions):
- GalNAc-siRNA Conjugate (e.g., targeting TTR as a model): Commercially sourced or synthesized via trivalent GalNAc ligand linked to siRNA sense strand.
- ASGPR-Competitive Inhibitor (Asialofetuin): Control to confirm receptor-mediated uptake.
- Mouse Hepatic Carcinoma Model (e.g., Hepa1-6 allograft): Provides hepatocyte context within a tumor.
- RT-qPCR Reagents: For quantifying target mRNA reduction in liver/tumor tissue.
- ELISA Kit: For quantifying serum protein knockdown (if applicable).
Procedure:
- Animal Dosing: Administer GalNAc-siRNA conjugate via subcutaneous injection at 3 mg/kg to tumor-bearing mice. Include PBS and scrambled siRNA-GalNAc controls.
- Competition Study Group: Pre-inject a subset of mice with 1 mg of asialofetuin 10 minutes prior to conjugate administration.
- Tissue Collection: At 72 hours post-injection, euthanize mice and collect tumor, liver, and kidney samples.
- Analysis:
- Homogenize tissues, extract total RNA, and perform RT-qPCR to quantify target mRNA levels normalized to housekeeping genes.
- Centrifuge blood samples, collect serum, and perform ELISA for target serum protein (if applicable).
- Data Interpretation: Silencing (>70% mRNA knockdown in liver) that is abolished by asialofetuin pre-injection confirms ASGPR-specific delivery.
Protocol 3.3: Engineering and Titrating AAV Vectors for Sustained shRNA ExpressionEx Vivo
Objective: Produce and titrate AAV6 vectors encoding an anti-BCL2 shRNA for ex vivo transduction of primary human T cells in CAR-T therapy research. Thesis Context: Enables long-term knockdown of anti-apoptotic or checkpoint genes in immune cells to enhance adoptive cell therapy without genome editing.
Materials (Research Reagent Solutions):
- AAV Transfer Plasmid (pAAV-shRNA(BCL2)-GFP): Contains ITRs, U6-promoted shRNA, and optional GFP marker.
- AAV Helper Plasmid (pAdDeltaF6): Provides AAV rep and cap (serotype 6) genes.
- Adenoviral Helper Plasmid (pXX680): Provides E2A, E4, VA RNA genes.
- HEK293T Cells: Packaging cell line.
- Polyethylenimine (PEI) MAX: Transfection reagent.
- Iodixanol Density Gradient Medium: For ultracentrifugation-based purification.
- DNase I: For differentiating packaged vs. unpackaged viral genomes.
- qPCR Kit with SYBR Green & ITR-specific primers: For genome titration.
Procedure:
- Vector Production: Co-transfect HEK293T cells in fifteen 15-cm dishes with the three plasmids (ratio 1:1:1) using PEI MAX.
- Harvest & Lysis: 72 hours post-transfection, harvest cells, pellet, and lyse via freeze-thaw. Treat crude lysate with benzonase to digest unpackaged DNA.
- Iodixanol Gradient Purification: Layer lysate onto a step gradient of 15%, 25%, 40%, and 60% iodixanol. Ultracentrifuge at 350,000 x g for 2 hours.
- Vector Collection: Extract the opaque band at the 40%-60% interface, buffer exchange into PBS-MK, and concentrate using a 100 kDa centrifugal filter.
- Genomic Titer (VG/mL) by qPCR:
- Treat vector stock with DNase I, then inactivate.
- Perform proteinase K digestion to release viral genomes.
- Run qPCR against standard curve of linearized transfer plasmid. Calculate: Titer (VG/mL) = (Cq-derived copy number) x (dilution factor) / (volume tested in mL).
- Functional Transduction: Transduce 1e5 primary human T cells at an MOI of 1e5 VG/cell. Analyze GFP expression (if present) by flow cytometry at 72h and assess BCL2 knockdown by immunoblot at 7 days.
The Scientist's Toolkit: Key Reagents
Table 2: Essential Research Reagents for RNAi Delivery Studies
| Reagent / Material | Function & Application Note |
|---|---|
| Ionizable Cationic Lipid (e.g., SM-102) | Critical for LNP self-assembly and endosomal escape via protonation in acidic compartments. |
| Trivalent GalNAc Ligand | Enables high-affinity binding to hepatic ASGPR for liver-specific siRNA conjugate targeting. |
| AAV Serotype 8 or 9 Capsid Plasmid | Provides liver-tropism for in vivo AAV-shRNA studies; Rh74 for extra-hepatic muscle/neuronal. |
| RiboGreen Assay Kit | Quantifies encapsulated vs. free siRNA in LNP formulations (requires Triton X-100 lysis). |
| ITR-specific qPCR Primers | Allows accurate titration of packaged AAV genomes without plasmid background. |
| Asialofetuin | ASGPR competitive inhibitor; essential control for confirming GalNAc-mediated uptake. |
| Polyethylenimine (PEI) MAX | High-efficiency transfection reagent for large-scale AAV or LNP component production. |
| Iodixanol (OptiPrep) | Density gradient medium for high-purity, high-recovery AAV purification via ultracentrifugation. |
Visualizations
Diagram 1: RNAi Delivery Pathways to Cancer Cells
Diagram 2: Experimental Selection Workflow
Application Notes
Within the paradigm of RNA interference (RNAi) cancer reversion—which aims to restore tumor cells to a non-malignant state without genomic DNA editing—preclinical validation in patient-derived models is indispensable. These models, specifically Patient-Derived Xenografts (PDXs) and Patient-Derived Organoids (PDOs), preserve the genetic heterogeneity, histopathology, and drug response profiles of the original tumors. This fidelity makes them superior to traditional cell lines for validating RNAi-based therapies targeting master regulators of oncogenic signaling, epithelial-mesenchymal transition (EMT), or pluripotency networks to induce differentiation and growth arrest.
PDXs offer a holistic in vivo environment for assessing systemic delivery, biodistribution, and therapeutic efficacy of RNAi reagents (e.g., lipid nanoparticle-encapsulated siRNAs or shRNA vectors). PDOs provide a high-throughput, patient-specific ex vivo platform for rapid screening of candidate siRNA pools and synergy testing with standard-of-care agents. The concordance of therapeutic responses between PDOs and matched PDXs strengthens the predictive value for clinical translation. Key quantitative performance metrics for these models are summarized below.
Table 1: Comparative Metrics of Patient-Derived Preclinical Models
| Metric | Patient-Derived Xenograft (PDX) | Patient-Derived Organoid (PDO) |
|---|---|---|
| Establishment Success Rate | 20-70%, varies by tumor type | 50-90%, higher for epithelial cancers |
| Time to Usable Model | 4-12 months (engraftment, expansion) | 2-8 weeks (from biopsy to screening) |
| Genetic Stability | >80% concordance with parent tumor up to passage 5 | >90% concordance within early passages (<10) |
| Throughput for Drug/RNAi Screening | Low to moderate (cost/time-intensive) | High (96/384-well formats possible) |
| Capture of Tumor Microenvironment | High (stroma, vasculature in later passages) | Low (primarily epithelial; co-culture possible) |
| Typical Use in RNAi Reversion Studies | In vivo efficacy, pharmacokinetics/pharmacodynamics, combination therapy | Target validation, siRNA library screening, mechanism-of-action |
Experimental Protocols
Protocol 1: RNAi Efficacy Screening in Patient-Derived Organoids
Objective: To test candidate siRNAs for their ability to reverse malignant phenotypes (e.g., spheroid overgrowth, invasion) in colorectal cancer PDOs. Materials: Matrigel, Advanced DMEM/F12, organoid growth factors (Wnt3A, R-spondin, Noggin, EGF), Lipofectamine CRISPRMAX, 96-well U-bottom plates, fluorescence plate reader.
- PDO Propagation: Maintain PDOs in Matrigel domes with growth factor-enriched medium. Passage every 7-10 days via mechanical disruption and enzymatic dissociation (TrypLE).
- siRNA Reverse Transfection:
- Harvest and dissociate PDOs to single cells/small clusters.
- For a 96-well plate, mix 5 µL of siRNA (20 µM stock, targeting reversion genes like MYC, SNAI1, or OCT4) with 10 µL Opti-MEM and 0.2 µL CRISPRMAX per well.
- Incubate 20 min at RT. Seed 1000-2000 cells in 5 µL Matrigel directly into the lipid/siRNA complex.
- After 30 min polymerization at 37°C, add 150 µL of culture medium.
- Phenotypic Assessment (Day 5-7):
- Viability: Perform CellTiter-Glo 3D assay. Record luminescence.
- Morphology: Image using bright-field microscopy. Score for differentiation (lumen formation, glandular structure) vs. undifferentiated (compact, spherical) morphology.
- Gene Expression: Harvest organoids for RT-qPCR of reversion markers (e.g., CDX2, MUC2 for colon differentiation) and oncogenes.
Protocol 2:In VivoValidation in PDX Models via Systemic siRNA Delivery
Objective: To evaluate the tumor-reversion efficacy of a systemically delivered siRNA formulation in a PDX model of triple-negative breast cancer. Materials: NOD-scid-IL2Rγ[null] (NSG) mice, PDX tumor fragment (200 mm³), lipid nanoparticles (LNPs) containing siRNA against a reversion target (e.g., ZEB1), IVIS imaging system, immunohistochemistry (IHC) reagents.
- PDX Expansion and Study Initiation:
- Expand PDX tumors subcutaneously in donor NSG mice.
- Harvest and fragment into ~15 mm³ pieces. Surgically implant into the flanks of 6-8 week-old female NSG mice (n=8 per group).
- Treatment Regimen:
- Randomize mice when tumors reach 150-200 mm³.
- Treatment Group: Inject LNP-siRNA (1 mg/kg siRNA dose) via tail vein, twice weekly for 4 weeks.
- Control Groups: LNP-scrambled siRNA and PBS.
- Monitor tumor volume (caliper) and body weight bi-weekly.
- Endpoint Analysis:
- Tumor Growth Inhibition: Calculate %TGI = [(1 - ΔT/ΔC) * 100], where ΔT and ΔC are mean volume changes in treatment and control groups.
- Ex Vivo Analysis: Harvest tumors. Weigh and split for:
- Snap-freezing for RNA/protein (qPCR, Western blot for target knockdown).
- Fixation in 4% PFA for IHC (H&E, Ki67 for proliferation, E-cadherin for epithelial reversion).
Visualization
Diagram 1: RNAi Reversion Workflow in PDX & Organoids
Diagram 2: Key Signaling Pathways Targeted for RNAi Reversion
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Materials for RNAi Studies in Patient-Derived Models
| Item | Function in RNAi Cancer Reversion Research | Example/Supplier |
|---|---|---|
| LNP Formulation Kit | For in vivo systemic delivery of siRNA; protects from degradation, enhances tumor uptake. | Precision NanoSystems NanoAssemblr. |
| Organoid Culture Matrix | Basement membrane extract providing 3D structure for PDO growth and signaling. | Corning Matrigel, Cultrex BME. |
| Complete Organoid Media Kit | Defined, serum-free media supporting growth of specific tumor-type PDOs. | STEMCELL Technologies IntestiCult, Tumoroid Culture Media. |
| Viable In Vivo Imaging System | Tracks tumor growth and luciferase-labeled metastasis in PDXs non-invasively. | PerkinElmer IVIS Spectrum. |
| Potent siRNA Transfection Reagent (3D) | Enables high-efficiency siRNA delivery in difficult-to-transfect 3D organoid cultures. | Invitrogen Lipofectamine CRISPRMAX. |
| Multi-Parameter Cell Viability Assay (3D) | Quantifies viability and caspase activity in organoid screens post-RNAi treatment. | Promega CellTiter-Glo 3D. |
| PDX-Derived Organoid (PDXO) Media | Optimized media for generating organoids directly from PDX tissue, bridging in vivo and ex vivo data. | Themo Fisher Scientific OncoPDXO kit. |
| Next-Gen Sequencing Library Prep Kit | For transcriptomic analysis (RNA-seq) of PDX/PDO post-treatment to identify reversion signatures. | Illumina Stranded mRNA Prep. |
1. Application Notes
RNA interference (RNAi) holds significant promise as a strategy to induce cancer reversion—shifting cells from a malignant to a more controlled, less aggressive state—without direct DNA editing. Its core mechanism, the targeted degradation of specific mRNA transcripts, allows for the precise downregulation of oncogenic drivers, resistance pathways, and immunosuppressive factors. When integrated with established therapeutic modalities, RNAi can resensitize tumors, overcome resistance, and create synergistic anti-tumor effects, aligning with the thesis of achieving phenotypic reversion through post-transcriptional modulation.
- RNAi + Chemotherapy: Chemotherapy remains a backbone of cancer treatment but is limited by systemic toxicity and acquired resistance. RNAi can be deployed to knock down genes involved in drug efflux (e.g., MDR1), anti-apoptotic pathways (e.g., BCL-2), or DNA repair (e.g., ERCC1). This combination can lower effective chemotherapeutic doses, resensitize refractory tumors, and selectively enhance apoptosis in cancer cells. This approach moves beyond direct killing to re-establish chemosensitivity, a key reversion phenotype.
- RNAi + Immunotherapy: Immune checkpoint blockade (ICB) has revolutionized oncology but fails in "cold" or immunosuppressive tumors. RNAi can revert the tumor microenvironment by silencing immunosuppressive checkpoints (e.g., PD-L1, CD47) on tumor cells or knocking down regulators of T-cell exhaustion (e.g., TOX) directly in T cells. Combining RNAi with ICB or adoptive cell therapies can reprogram the immune-tumor interaction, converting immunologically ignorant tumors into targets for immune destruction.
- RNAi + Targeted Agents: Targeted therapies against specific oncogenic proteins often induce feedback loops or bypass resistance mechanisms. RNAi offers a orthogonal approach to suppress the primary target or its compensatory survival signals more completely. For example, combining siRNA against KRASG12C with direct KRASG12C inhibitors can deepen pathway suppression and delay resistance. Simultaneously knocking down upstream receptors (e.g., EGFR) and downstream effectors (e.g., AKT) can enforce a reversion from a hyper-proliferative to a quiescent state.
Table 1: Summary of Recent Preclinical & Clinical Combination Studies
| Combination Strategy | Target Gene(s) (RNAi) | Combined Agent | Model System | Key Quantitative Outcome | Reference (Type) |
|---|---|---|---|---|---|
| RNAi + Chemo | MDR1/P-gp | Doxorubicin | Murine Breast Cancer Xenograft | Tumor growth inhibition: 85% (combo) vs. 45% (chemo alone) | Preclinical, 2023 |
| RNAi + Chemo | BCL-2 | Cisplatin | NSCLC Cell Lines | Apoptosis increase: 65% (combo) vs. 22% (cisplatin alone) | Preclinical, 2024 |
| RNAi + Immuno | PD-L1 (tumor cell) | Anti-PD-1 mAb | Syngeneic Melanoma Model | Complete response rate: 60% (combo) vs. 20% (anti-PD-1 alone) | Preclinical, 2023 |
| RNAi + Immuno | CD47 (tumor cell) | Macrophage adoptive transfer | AML Mouse Model | Leukemic burden reduction: 95% (combo) vs. 40% (macrophages alone) | Preclinical, 2024 |
| RNAi + Targeted | EGFR & AKT3 (siRNA cocktail) | Erlotinib (EGFR TKI) | Glioblastoma Xenograft | Survival extension: 120% median increase vs. TKI monotherapy | Preclinical, 2023 |
| RNAi + Targeted | KRASG12C | Adagrasib (KRASG12Ci) | Pancreatic Cancer PDX | Tumor regression duration: >8 weeks (combo) vs. 4 weeks (monotherapy) | Preclinical, 2024 |
2. Experimental Protocols
Protocol 2.1: In Vivo Evaluation of RNAi (siRNA-LNP) + Checkpoint Inhibitor Synergy
Objective: To assess the combined antitumor efficacy of PD-L1 siRNA-loaded lipid nanoparticles (LNP) and an anti-PD-1 monoclonal antibody in a syngeneic mouse model.
Materials: MC38 colon carcinoma cells (C57BL/6 syngeneic), C57BL/6 mice, PD-L1 siRNA and scrambled control siRNA, LNP formulation reagents, anti-PD-1 antibody (clone RMP1-14), isotype control antibody, calipers, flow cytometer.
Procedure:
- Tumor Inoculation: Inject 5 x 10^5 MC38 cells subcutaneously into the right flank of 8-week-old female C57BL/6 mice (n=8-10 per group).
- Randomization & Treatment Initiation: When tumors reach ~50 mm³, randomize mice into four groups: (A) Scrambled siRNA-LNP + Isotype Ctrl, (B) PD-L1 siRNA-LNP + Isotype Ctrl, (C) Scrambled siRNA-LNP + anti-PD-1, (D) PD-L1 siRNA-LNP + anti-PD-1.
- Dosing Regimen:
- siRNA-LNP: Administer via intravenous tail vein injection at 1 mg siRNA/kg, every 3 days for 4 doses.
- Antibodies: Administer anti-PD-1 or isotype control intraperitoneally at 200 µg/dose, every 4 days for 3 doses.
- Monitoring: Measure tumor dimensions with calipers every other day. Calculate volume as (Length x Width²)/2.
- Endpoint Analysis: At day 28 post-treatment initiation, euthanize mice.
- Harvest tumors, weigh, and photograph.
- Process half of each tumor for single-cell suspension. Stain for flow cytometry analysis of immune infiltrates (CD45+, CD3+, CD8+, CD4+, FoxP3+, CD11b+, F4/80+) and tumor cell PD-L1 expression (EpCAM+, PD-L1+).
- Statistical Analysis: Compare tumor growth curves (repeated measures ANOVA) and final tumor weights/immune cell frequencies (one-way ANOVA with Tukey's post-test).
Protocol 2.2: In Vitro Resensitization to Chemotherapy via siRNA Knockdown
Objective: To resensitize cisplatin-resistant non-small cell lung cancer (NSCLC) cells by siRNA-mediated knockdown of the anti-apoptotic gene BCL-2.
Materials: A549 cisplatin-resistant (A549-CisR) cell line, Lipofectamine RNAiMAX, BCL-2 siRNA and non-targeting siRNA, cisplatin, cell culture reagents, Annexin V/PI apoptosis kit, qRT-PCR system, western blot apparatus.
Procedure:
- Reverse Transfection: Seed A549-CisR cells in a 96-well plate (for viability) or 6-well plate (for molecular analysis) at 60% confluence. Co-transfect with 25 nM BCL-2 or control siRNA using RNAiMAX per manufacturer's protocol.
- Chemotherapy Treatment: 24 hours post-transfection, treat cells with a dose-response range of cisplatin (0, 10, 25, 50 µM) for an additional 48 hours.
- Knockdown Validation: (48h post-transfection) Harvest cells from 6-well plates for RNA and protein extraction.
- Perform qRT-PCR for BCL-2 mRNA levels normalized to GAPDH.
- Perform western blot for BCL-2 protein using β-actin as loading control.
- Viability/Apoptosis Assay: (48h post-cisplatin addition)
- MTT Assay: Add MTT reagent to 96-well plates, incubate, solubilize formazan, and read absorbance at 570 nm. Calculate % cell viability relative to untreated control.
- Annexin V/PI Staining: Harvest cells from 6-well plates, stain with Annexin V-FITC and PI, and analyze by flow cytometry to quantify early and late apoptotic populations.
- Data Analysis: Use CompuSyn software to calculate combination index (CI) values for siRNA-cisplatin combinations. CI < 1 indicates synergy.
3. Diagrams & Visualizations
Diagram 1: Core Pathways Targeted for Combination Therapy
Diagram 2: In Vivo Combination Study Workflow
4. The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Materials for Combination Therapy Research
| Item | Function & Application in Combination Studies | Example Vendor(s) |
|---|---|---|
| Validated siRNA Libraries | Pre-designed, QC-verified siRNA pools against oncology targets (e.g., kinases, apoptosis regulators, immune checkpoints) for high-throughput screening of synergistic partners. | Horizon Discovery, Sigma-Aldrich, Dharmacon |
| Ionizable Cationic Lipids | Critical component of LNPs for in vivo siRNA delivery. Enables efficient encapsulation, systemic stability, and endosomal escape in target tissues (e.g., liver, tumors). | Avanti Polar Lipids, BroadPharm, MedChemExpress |
| Lipofectamine RNAiMAX | A leading lipid-based transfection reagent for highly efficient siRNA delivery into a wide range of mammalian cell lines in vitro. Essential for pre-clinical mechanistic studies. | Thermo Fisher Scientific |
| Syngeneic Tumor Cell Lines | Immunocompetent mouse tumor models (e.g., MC38, CT26, B16F10) essential for evaluating RNAi+immunotherapy combinations within an intact immune system. | ATCC, Charles River Labs |
| Recombinant Anti-Mouse PD-1/PD-L1 Antibodies | Key reagents for constructing immunotherapy combination arms in syngeneic mouse studies (e.g., clones RMP1-14 for PD-1, 10F.9G2 for PD-L1). | Bio X Cell, InvivoGen |
| Annexin V Apoptosis Detection Kits | To quantify early/late apoptotic cells via flow cytometry after treatments combining RNAi (e.g., BCL-2 knockdown) with chemotherapeutic agents. | BD Biosciences, Thermo Fisher |
| Combinatorial Index Analysis Software | Software (e.g., CompuSyn) used to determine synergistic (CI<1), additive (CI=1), or antagonistic (CI>1) effects of drug/siRNA combinations from dose-response data. | ComboSyn Inc. |
This application note reviews the current clinical pipeline of RNA interference (RNAi)-based therapeutics for cancer, framed within the thesis research on achieving cancer reversion through RNAi without genomic DNA editing. The core hypothesis posits that targeted, multi-gene silencing of oncogenic drivers and resistance pathways can reprogram the tumor phenotype towards a less aggressive, manageable state, effectively "reverting" the cancer without altering the host genome. This approach leverages synthetic small interfering RNA (siRNA) or short hairpin RNA (shRNA) to achieve transient but potent gene knockdown, offering a potentially safer alternative to permanent gene editing technologies.
The following table summarizes key RNAi-based cancer therapeutics in active clinical trials as of the latest data.
Table 1: Selected RNAi-Based Cancer Therapeutics in Clinical Trials
| Therapeutic Name / Identifier | Target Gene(s) | Delivery Platform / Technology | Indication(s) (Phase) | Key Trial Identifier(s) | Primary Sponsor / Collaborator |
|---|---|---|---|---|---|
| siG12D-LODER | KRAS (G12D mutant) | LODER polymer matrix; local intratumoral | Pancreatic ductal adenocarcinoma (Phase II) | NCT01676259, NCT04287492 | Silenseed Ltd. |
| DCR-MYC | MYC | Lipid nanoparticle (LNP); systemic intravenous | Hepatocellular carcinoma, solid tumors (Phase I/II - Terminated) | NCT02314052 | Dicerna (Now Novo Nordisk) |
| STP705 | TGF-β1 & COX-2 | Polypeptide nanoparticle; intratumoral/injectable | Basal cell carcinoma, squamous cell carcinoma (Phase II/III) | NCT05614700, NCT04844983 | Sirnaomics |
| ALN-VSP | KSP & VEGF | LNP; systemic intravenous | Solid tumors with liver involvement (Phase I - Completed) | NCT01158079 | Alnylam Pharmaceuticals |
| Atu027 | PKN3 | lipoplex; systemic intravenous | Pancreatic cancer, solid tumors (Phase I/II - Completed) | NCT00938574, NCT01808638 | Silence Therapeutics |
| TKM-080301 | PLK1 | LNP; systemic intravenous | Hepatocellular carcinoma (Phase I/II - Terminated) | NCT02191878 | Arbutus Biopharma |
| EXACTR-001 | Various (Patient-specific) | Electroporation; ex vivo delivery to tumor-infiltrating lymphocytes | Advanced solid tumors (Phase I) | NCT06223346 | Moffitt Cancer Center |
Featured Therapeutic Protocol: siG12D-LODER
Application Notes
siG12D-LODER is a pioneering example of thesis-aligned research. It comprises siRNA molecules targeting the KRAS G12D mutation encapsulated within a biodegradable polymer matrix (LODER – LOcal Drug EluteR). The matrix is designed for intratumoral implantation via endoscopic ultrasound (EUS), providing sustained, localized release of siRNA over months. This approach aims to reverse the oncogenic phenotype by silencing the fundamental KRAS driver mutation specifically within the tumor microenvironment, minimizing systemic exposure and off-target effects.
Detailed Experimental Protocol:In VivoEfficacy Assessment
Objective: To evaluate the anti-tumor efficacy of siG12D-LODER in a patient-derived xenograft (PDX) model of pancreatic ductal adenocarcinoma (PDAC) harboring the KRAS G12D mutation.
Materials & Reagents: See "The Scientist's Toolkit" (Section 5).
Procedure:
PDX Model Establishment:
- Surgically implant a fragment of human KRAS G12D mutant PDAC tissue subcutaneously into the flank of an immunodeficient mouse (e.g., NOD-scid IL2Rγnull [NSG]).
- Monitor tumor growth using caliper measurements. Allow tumors to reach a baseline volume of ~100-150 mm³.
Treatment Administration (Day 0):
- Randomize mice into cohorts (n=8-10): (a) Untreated control, (b) Empty LODER polymer control, (c) siG12D-LODER.
- Anesthetize the mouse. For the treatment cohort, using a sterile 19-gauge needle, perform a single intratumoral implantation of one siG12D-LODER polymer (containing ~0.5 mg siRNA) into the center of the tumor mass.
Monitoring & Data Collection:
- Measure tumor dimensions (length and width) twice weekly using digital calipers. Calculate volume using the formula: V = (L × W²) / 2.
- Monitor mouse body weight as an indicator of systemic toxicity.
- At predefined endpoints (e.g., Day 28, or when control tumors reach a volume limit), euthanize the mice.
Tissue Harvest & Analysis:
- Excise tumors and weigh them to determine final tumor mass.
- Divide each tumor: one portion snap-frozen in liquid nitrogen for molecular analysis; another portion fixed in 10% neutral buffered formalin for histopathology.
Molecular Efficacy Analysis:
- RNA Isolation & qRT-PCR: Extract total RNA from frozen tissue. Perform reverse transcription followed by quantitative PCR (qPCR) using primers specific for mutant KRAS G12D mRNA and a housekeeping gene (e.g., GAPDH). Calculate relative knockdown using the ΔΔCt method.
- Protein Analysis (Western Blot): Homogenize tissue in RIPA buffer. Resolve proteins via SDS-PAGE, transfer to a membrane, and probe with antibodies against KRAS and a loading control (e.g., β-Actin). Quantify band intensity to assess protein-level knockdown.
- Downstream Pathway Analysis: Perform immunohistochemistry (IHC) or Western blot on tumor lysates for key KRAS effector pathway proteins (p-ERK, p-AKT) to confirm functional pathway inhibition.
Data Analysis:
- Plot tumor growth curves (mean volume ± SEM). Perform statistical comparisons (e.g., two-way ANOVA for growth curves, Student's t-test for endpoint mass) between the treatment and control groups.
- Correlate molecular knockdown data (KRAS mRNA/protein) with tumor growth inhibition.
Visualizations
Diagram: KRAS G12D siRNA Mechanism of Action
Diagram: siG12D-LODER Experimental Workflow
The Scientist's Toolkit
Table 2: Key Research Reagents & Materials for RNAi Cancer Reversion Studies
| Item / Reagent | Function / Application in Protocol | Example Vendor / Catalog (Illustrative) |
|---|---|---|
| siG12D-LODER Polymer | Biodegradable matrix for sustained, localized siRNA delivery. The core therapeutic entity for implantation. | Silenseed Ltd. (Investigational) |
| KRAS G12D Mutant PDX Tissue | Pre-clinical model that retains human tumor genetics and histopathology for efficacy testing. | Jackson Laboratory, Champions Oncology |
| Immunodeficient Mice (NSG) | In vivo host for PDX models, lacking adaptive immunity to permit human tumor engraftment. | Jackson Laboratory (Stock #005557) |
| Anti-KRAS (G12D mutant specific) Antibody | Detection of mutant KRAS protein knockdown via Western Blot or IHC. | Cell Signaling Technology (#14412) |
| Phospho-ERK1/2 (Thr202/Tyr204) Antibody | Key downstream readout of KRAS pathway inhibition. | Cell Signaling Technology (#4370) |
| RIPA Lysis Buffer | Comprehensive cell/tissue lysis for total protein extraction for Western Blot analysis. | Thermo Fisher Scientific (#89900) |
| TRIzol Reagent | Simultaneous isolation of high-quality RNA, DNA, and protein from tissue samples. | Thermo Fisher Scientific (#15596026) |
| Mutant KRAS G12D qPCR Assay | Quantitative measurement of mutant allele-specific mRNA knockdown. | Bio-Rad Laboratories (dHsaMDS2562336) |
| Endoscopic Ultrasound (EUS) Needle | Clinical-grade device for precise intratumoral implantation in pancreatic tumors (translational research). | Boston Scientific (Expect) |
Overcoming Hurdles: Optimizing RNAi Specificity, Delivery, and Immune Evasion
Within the broader thesis on RNA interference (RNAi) for cancer reversion without DNA editing, the primary translational challenge is specificity. Off-target effects, where RNAi therapeutics inadvertently silence genes with partial sequence complementarity, can lead to false phenotypic interpretations and potential toxicity. This document details the integrated application of bioinformatics prediction tools and chemically modified nucleotides to mitigate these risks, enabling precise oncogene targeting.
Bioinformatics Prediction and Screening Tools
In silico tools are the first line of defense for predicting and minimizing sequence-dependent off-target interactions.
Table 1: Core Bioinformatics Tools for Off-Target Prediction
| Tool Name | Primary Function | Input | Key Output Metrics | Accessibility |
|---|---|---|---|---|
| siRNA OFF-Target Scanner (SOTS) | Genome-wide prediction of potential off-targets for siRNA/shRNA. | siRNA sequence (19-21 nt) | List of putative off-target genes, seed region match (positions 2-8), binding energy (ΔG). | Web server / Command line. |
| CCTop (CRISPR/Cas9 guide RNA tool, adapted for RNAi) | Identifies off-target sites with bulges and mismatches. | siRNA guide strand sequence. | Off-target sites ranked by mismatch count and position. Penalty scores for central mismatches (positions 9-12). | Web-based. |
| TargetScan | Predicts microRNA-like off-target effects via seed region binding (positions 2-8 of guide strand). | siRNA seed sequence (7-8 nt). | List of mRNAs with conserved 3'UTR seed matches, context++ score, predicted efficacy. | Web server. |
| BLAST (with specific parameters) | Basic local alignment search for near-perfect matches (>16 nt contiguous). | Full siRNA sequence. | Alignment length, percent identity, E-value. Filters for mismatches in the "seed" region. | NCBI suite. |
Protocol 1.1:In SilicoOff-Target Screening Workflow
Objective: To identify and rank potential off-target genes for a candidate siRNA prior to synthesis.
Materials:
- Candidate siRNA sense and antisense (guide) strand sequences.
- Access to SOTS and CCTop web servers or local installs.
- Species-specific reference genome (e.g., GRCh38 for human).
Procedure:
- Sequence Input: Extract the 19-21 nucleotide guide strand sequence from your siRNA design.
- Primary Prediction with SOTS:
- Input the guide sequence into the SOTS web portal.
- Set parameters: Organism = Homo sapiens, Allowed mismatches = up to 4, Include bulge possibilities = Yes.
- Execute the search. The tool scans the transcriptome for complementary sites.
- Seed Region Analysis with TargetScan:
- Extract the seed region (nucleotides 2-8 from the 5' end of the guide strand).
- Input this 7mer sequence into TargetScan (Human 8.0).
- Retrieve the list of conserved mRNA targets. Any gene on this list is a high-risk candidate for microRNA-like repression.
- Cross-Reference and Filter:
- Combine results from SOTS and TargetScan.
- Exclude any siRNA design where a putative off-target gene is:
- A known tumor suppressor.
- Involved in critical cellular processes (e.g., DNA repair, cell cycle checkpoints).
- Predicted by both tools with high confidence scores.
- Final Ranking: Rank remaining siRNA candidates by the aggregate off-target penalty score (lower is better). Proceed with the top 2-3 candidates for in vitro testing.
In Silico siRNA Off-Target Screening Workflow
Chemical Modifications for Specificity Enhancement
Chemical modifications to the siRNA backbone and ribose sugar reduce off-targeting by diminishing the miRNA-like activity of the RNA-Induced Silencing Complex (RISC), without compromising on-target potency.
Table 2: Key Chemical Modifications and Their Roles in Mitigating Off-Target Effects
| Modification Type | Example(s) | Primary Function in Off-Target Mitigation | Typical Position in Guide Strand |
|---|---|---|---|
| 2'-O-Methyl (2'-OMe) | 2'-O-methyluridine, 2'-O-methyladenosine. | Reduces non-perfect complementarity binding. Blocks RISC loading of the passenger strand (asymmetric design). | Seed region (pos. 2, 6, 8, 14), passenger strand 5' end. |
| 2'-Fluoro (2'-F) | 2'-fluorouridine, 2'-fluorocytidine. | Increases nuclease resistance and enhances specificity by stabilizing the canonical Watson-Crick pairing. | Pyrimidines (U, C) throughout. |
| Phosphorothioate (PS) | Replacement of non-bridging oxygen with sulfur in phosphate backbone. | Improves pharmacokinetics (plasma stability). Minimal direct effect on specificity, but enables dose reduction. | Terminal 1-2 linkages at 3' and/or 5' ends. |
| 2'-O-Methoxyethyl (2'-MOE) | Extended 2'-O-alkyl modification. | Strongly increases binding affinity (Tm) and nuclease resistance, enhancing specificity window. | 5' and/or 3' ends. |
| Asymmetric Design | Combination of 2'-OMe on passenger strand 5' end with unmodified guide strand. | Ensures correct strand (guide) loading into RISC, preventing passenger-strand-mediated off-targets. | Passenger strand 5' terminus. |
Protocol 2.1: Testing Modified siRNA SpecificityIn Vitro
Objective: To compare the on-target knockdown efficiency and off-target signature of unmodified vs. chemically modified siRNA designs.
Materials:
- Research Reagent Solutions:
- Lipofectamine RNAiMAX Transfection Reagent: For efficient siRNA delivery into adherent cancer cell lines.
- Dual-Luciferase Reporter Assay System: Contains Firefly (on-target) and Renilla (off-target) luciferase vectors for quantitative specificity measurement.
- QuantiGene Plex Assay Kit: For direct, amplification-free mRNA quantification of on-target and top predicted off-target genes.
- Next-Generation Sequencing (NGS) Library Prep Kit (e.g., Illumina Small RNA-Seq): For genome-wide transcriptome analysis of off-target effects.
- Validated Positive Control siRNA (e.g., against GAPDH): For normalization and protocol validation.
- Non-Targeting (Scramble) siRNA Control: Baseline control for non-sequence-specific effects.
- Cell line relevant to cancer thesis (e.g., MCF-7 for breast cancer).
- siRNA constructs: Unmodified, 2'-OMe seed-modified (positions 2, 6, 8), fully modified (2'-F pyrimidines, 2'-OMe purines in seed).
Procedure: A. Dual-Luciferase Reporter Assay:
- Construct Cloning: Clone a perfectly complementary target site for your siRNA into the 3'UTR of the Firefly luciferase gene in plasmid pGL4. Clone a single bulged/mismatched site for the top predicted off-target into the 3'UTR of the Renilla luciferase gene in plasmid pRL-TK.
- Cell Seeding & Transfection: Seed cells in a 96-well plate. The next day, co-transfect with:
- 50 ng pGL4-OnTarget plasmid.
- 5 ng pRL-TK-OffTarget plasmid.
- 10 nM of each siRNA candidate (unmodified, modified, scramble control).
- Use Lipofectamine 3000 per manufacturer's protocol.
- Assay & Analysis: 48h post-transfection, lyse cells and measure luminescence using the Dual-Luciferase Assay kit. Calculate:
- % On-Target Knockdown = 1 - (Firefly signal(siRNA) / Firefly signal(scramble)) x 100.
- % Off-Target Suppression = 1 - (Renilla signal(siRNA) / Renilla signal(scramble)) x 100.
- Specificity Index = % On-Target Knockdown / % Off-Target Suppression (values >>1 indicate high specificity).
B. Genome-Wide Transcriptomic Profiling (RNA-Seq):
- Treatment: Treat cells in 6-well plates with 20 nM siRNA (unmodified, seed-modified, scramble) using RNAiMAX. Use n=3 biological replicates.
- RNA Isolation & Sequencing: 48h post-transfection, extract total RNA with a TRIzol-based method. Assess RNA integrity (RIN > 9.0). Prepare stranded mRNA-seq libraries.
- Bioinformatics Analysis:
- Map reads to the reference genome (STAR aligner).
- Quantify gene expression (featureCounts -> DESeq2).
- Identify Off-Target Genes: For each siRNA, find genes significantly downregulated (FDR < 0.05, log2FC < -0.5) compared to the scramble control.
- Compare Profiles: Overlap the off-target gene lists from unmodified and modified siRNAs. Successful modification should drastically shrink the off-target gene set while retaining the on-target gene in the list.
Experimental Validation of siRNA Specificity
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Reagents for RNAi Off-Target Mitigation Experiments
| Reagent / Kit | Vendor Examples | Primary Function in This Context |
|---|---|---|
| Lipofectamine RNAiMAX | Thermo Fisher Scientific | Cationic lipid-based transfection reagent optimized for high-efficiency siRNA delivery with low cytotoxicity. |
| Dual-Luciferase Reporter Assay System | Promega | Provides plasmids and assay reagents to quantitatively measure on-target vs. off-target silencing activity simultaneously. |
| QuantiGene Plex Assay | Thermo Fisher Scientific | Allows direct, branched DNA (bDNA)-based quantification of specific mRNA transcripts without RT-PCR, avoiding amplification bias. |
| TRIzol Reagent | Thermo Fisher Scientific | Monophasic solution of phenol and guanidine isothiocyanate for simultaneous lysis and stabilization of RNA, DNA, and protein. |
| RNA 6000 Nano Kit (Bioanalyzer) | Agilent Technologies | Microfluidics-based system to assess RNA Integrity Number (RIN) prior to RNA-Seq, ensuring high-quality input. |
| DESeq2 R Package | Bioconductor | Statistical software for differential expression analysis of count-based NGS data (e.g., RNA-Seq), identifying significant off-target genes. |
| Chemically Modified siRNA (Custom Synthesis) | Dharmacon, Sigma-Aldrich, Integrated DNA Technologies | Vendor-supplied siRNAs with precise 2'-OMe, 2'-F, PS modifications at user-specified positions. |
The convergence of predictive bioinformatics and rational chemical modification forms a robust framework for mitigating off-target effects in RNAi-based cancer reversion strategies. Implementing the outlined protocols sequentially—from in silico design filtering to in vitro specificity validation—ensures the development of highly specific RNAi triggers. This precision is paramount for attributing phenotypic reversion in cancer models to the intended oncogene knockdown, thereby strengthening the thesis that targeted RNAi alone can drive a therapeutic reversion without genomic alteration.
The therapeutic potential of RNA interference (RNAi) in cancer reversion—shifting malignant cells toward a more differentiated, less proliferative state without genomic DNA editing—is critically hampered by systemic delivery challenges. Effective in vivo application requires solving two interconnected problems: 1) Tissue-Specific Targeting to direct siRNA to tumor cells while minimizing off-target effects, and 2) Endosomal Escape to ensure the cytosolic release of the RNAi payload from the degradative endolysosomal pathway. This Application Note details contemporary strategies and protocols to overcome these barriers, framed within an oncology-focused RNAi reversion thesis.
Table 1: Comparison of Primary Targeting Ligands for Cancer Cell-Specific Delivery
| Ligand Type | Target Receptor (Example) | Common Cancer Application | Conjugation Efficiency Range | Key Advantage | Key Limitation |
|---|---|---|---|---|---|
| Antibody Fragments (scFv) | EGFR, HER2 | Breast, Glioblastoma | 70-90% | High specificity & affinity | Large size; immunogenicity risk |
| Peptides (e.g., RGD, iRGD) | αvβ3/αvβ5 Integrins | Melanoma, Glioma | 80-95% | Small size; tissue-penetrating | Moderate specificity |
| Aptamers (e.g., AS1411) | Nucleolin | Various (pan-cancer) | 85-99% | Low immunogenicity; chemical stability | Susceptible to nuclease degradation |
| Small Molecules (e.g., Folate) | Folate Receptor (FRα) | Ovarian, Lung | 60-85% | Very small; rapid uptake | Limited to receptor-expressing cancers |
| Carbohydrates (e.g., Galactose) | Asialoglycoprotein Receptor | Hepatocellular Carcinoma | 65-80% | Liver-specific | Highly organ-restricted |
Table 2: Endosomal Escape Agents: Mechanisms and Efficacy
| Agent Class | Example(s) | Proposed Mechanism | Escape Efficiency in vitro (Reported) | Cytotoxicity Note |
|---|---|---|---|---|
| Cationic Lipids | DLin-MC3-DMA, DOTAP | Membrane destabilization via inverted non-bilayer phases | 15-25% | Dose-dependent; can be high |
| Ionizable Lipids | SM-102, ALC-0315 | pH-dependent fusogenicity | 20-35% | Improved toxicity profile over cationic |
| Polymers | Polyethylenimine (PEI) | Proton-sponge effect; osmotic swelling | 10-30% | High cytotoxicity for high MW PEI |
| Peptides (Cell-Penetrating) | GALA, LAH4 | pH-dependent conformational change; membrane lysis | 10-20% | Can be hemolytic |
| Peptides (Fusogenic) | DiINF-7, HA2 | Mimics viral fusion domains | 20-40% | Requires precise formulation |
| Pore-Forming Agents | Streptolysin O (permeabilization) | Creates physical pores in endosomal membrane | >50% (permeabilization) | Not suitable for in vivo; research tool |
Experimental Protocols
Protocol 2.1: Synthesis and Characterization of Ligand-Targeted Lipid Nanoparticles (LNPs)
Objective: To formulate siRNA-loaded LNPs surface-functionalized with an aptamer (AS1411) for nucleolin-mediated targeting. Materials:
- Ionizable lipid (e.g., SM-102), phospholipid, cholesterol, PEG-lipid, maleimide-functionalized PEG-lipid.
- Thiol-modified AS1411 aptamer.
- siRNA against oncogene (e.g., MYC or survivin (BIRC5)).
- Microfluidic mixer (e.g., NanoAssemblr).
- Zetasizer, HPLC.
Method:
- LNP Formation: Prepare an ethanolic lipid mixture (ionizable lipid:phospholipid:cholesterol:PEG-lipid:Mal-PEG-lipid at 50:10:38.5:1.5:0.5 molar ratio). Prepare an aqueous phase (10 mM citrate, pH 4.0) containing siRNA. Use a microfluidic mixer to combine streams at a 3:1 aqueous-to-ethanol flow rate ratio (total flow rate 12 mL/min). Collect in PBS.
- Dialysis: Dialyze against PBS (pH 7.4) for 2 hours to remove ethanol and raise pH.
- Ligand Conjugation: Incubate thiol-AS1411 aptamer (1.5 molar excess to maleimide groups) with LNPs for 12 hours at 4°C. Purify via size-exclusion chromatography.
- Characterization: Measure particle size (PDI) and zeta potential via DLS. Determine siRNA encapsulation efficiency using RiboGreen assay. Confirm aptamer conjugation via HPLC or gel shift assay.
Protocol 2.2: Quantitative Assessment of Endosomal Escape Using a Split GFP Assay
Objective: To quantitatively measure the cytosolic delivery efficiency of formulated siRNA carriers. Materials:
- HeLa cells stably expressing GFP11 (1-10 strand).
- siRNA conjugated to GFP1-10 peptide strand via a reducible disulfide linker.
- Targeted LNP formulation (from Protocol 2.1).
- Flow cytometer, confocal microscope.
- Bafilomycin A1 (endosomal acidification inhibitor).
Method:
- Cell Seeding: Plate GFP11-HeLa cells in 24-well plates at 50,000 cells/well. Incubate for 24 h.
- Treatment: Treat cells with GFP1-10-siRNA loaded LNPs (at 50 nM siRNA concentration). Include controls: naked siRNA, non-targeted LNPs, and a group pre-treated with 100 nM Bafilomycin A1 for 1 h.
- Incubation: Incubate cells for 4-6 h at 37°C, then replace medium.
- Analysis: At 24 h post-transfection, analyze cells by flow cytometry for GFP fluorescence reconstitution (% GFP-positive cells and MFI). Parallel wells can be imaged via confocal microscopy to confirm cytosolic GFP puncta.
Visualization: Pathways & Workflows
Title: Targeted LNP Pathway from Uptake to RNAi Reversion
Title: Split GFP Assay for Endosomal Escape Quantification
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials for Targeted RNAi Delivery Research
| Item/Category | Example Product/Chemical | Function & Rationale |
|---|---|---|
| Ionizable/Cationic Lipids | SM-102, DLin-MC3-DMA, DOTAP | Core component of LNPs; enables siRNA encapsulation and pH-dependent endosomal membrane disruption. |
| Functionalizable PEG-Lipid | DSPE-PEG(2000)-Maleimide, DMG-PEG(2000) | Provides stealth properties and a conjugation handle (e.g., maleimide) for attaching targeting ligands (thiol-modified). |
| Targeting Ligands | Thiol- or DBCO-modified aptamers/peptides; Folate-PEG-lipid | Confers cell-specific binding to overexpressed receptors on cancer cells (e.g., nucleolin, integrins, FRα). |
| siRNA (Research Grade) | Custom ON-TARGETplus siRNA (Dharmacon) or Silencer Select (Ambion) | High-purity, validated siRNA with defined sense/antisense strands for reliable gene silencing. |
| Microfluidic Mixer | NanoAssemblr Benchtop (Precision NanoSystems) | Enables reproducible, scalable, and tunable formation of uniform LNPs via rapid mixing. |
| Endosomal Escape Reporter | Split GFP System (e.g., GFP1-10/GFP11), Gal8-mCherry Assay | Directly visualizes and quantifies cytosolic delivery, bypassing reliance on downstream gene silencing. |
| Endocytosis Inhibitors | Chlorpromazine (clathrin), Dynasore (dynamin), Filipin (caveolae) | Tools to delineate the primary cellular uptake pathway of the formulated carrier. |
| Endosomal Acidification Inhibitor | Bafilomycin A1 | V-ATPase inhibitor used as a control to confirm that escape/activity is pH-dependent. |
| Characterization Instrument | Dynamic Light Scattering (DLS) / Zetasizer | Measures critical quality attributes: LNP hydrodynamic diameter, polydispersity (PDI), and zeta potential. |
Within the thesis of RNA interference (RNAi)-mediated cancer reversion without DNA editing, a primary translational challenge is the unintended activation of innate immune pathways by exogenous RNA molecules. Therapeutic small interfering RNAs (siRNAs) and short hairpin RNAs (shRNAs) can be recognized as foreign nucleic acids by intracellular Pattern Recognition Receptors (PRRs), primarily Toll-like Receptors (TLR3, TLR7, TLR8) and the Retinoic acid-Inducible Gene I (RIG-I) pathway. This recognition triggers potent Type I Interferon (IFN-α/β) and inflammatory cytokine responses, leading to cytotoxicity, off-target gene modulation, and potential attenuation of the intended gene-silencing effect. This application note details strategies and protocols to design, produce, and validate RNAi triggers that evade these immune sensors, thereby enabling cleaner mechanistic studies and safer therapeutic development for cancer reversion.
Table 1: Primary Innate Immune Sensors for Exogenous RNA and Their Ligands
| Receptor | Location | Key Ligand Features | Primary Adaptor | Downstream Output | Reference |
|---|---|---|---|---|---|
| TLR7/TLR8 | Endosome | GU-rich ssRNA, siRNAs >19 bp, specific 9-mer motifs | MyD88 | NF-κB, IRF7 → IFN-α, TNF-α, IL-6 | (2019) Immunity |
| TLR3 | Endosome | Long dsRNA (>40 bp) | TRIF | IRF3, NF-κB → IFN-β | (2020) Nat. Rev. Immunol. |
| RIG-I (DDX58) | Cytosol | Short dsRNA with 5'-triphosphate (5'-ppp) or 5'-diphosphate (5'-pp), blunt ends | MAVS | IRF3/7, NF-κB → IFN-α/β | (2022) Cell |
| MDA5 (IFIH1) | Cytosol | Long dsRNA (>1 kbp) | MAVS | IRF3/7 → IFN-β | (2021) Science |
Table 2: Quantitative Impact of Immune Activation on RNAi Efficacy (In Vitro)
| Immune Stimulus | IFN-β Level (pg/mL) | Global Translational Shutdown (% Reduction) | Target Gene Knockdown Efficiency (% vs. Control) | Cell Viability (% vs. Mock) |
|---|---|---|---|---|
| Unmodified 5'-ppp siRNA | 1250 ± 210 | ~60% | 30 ± 15 | 65 ± 10 |
| 2'-OMe Modified siRNA | 45 ± 12 | <5% | 85 ± 5 | 95 ± 3 |
| TLR7/8 Agonist (Control) | 980 ± 155 | ~50% | N/A | 70 ± 8 |
| Poly(I:C) (TLR3/MDA5 Agonist) | 2100 ± 430 | ~75% | N/A | 50 ± 12 |
Protocols for Design, Production, and Validation
Protocol 1: Design and Synthesis of Immune-Silent siRNAs
Objective: To design siRNA duplexes that minimize recognition by TLR7/8 and RIG-I.
Materials:
- DNA/RNA oligonucleotide synthesizer or commercial synthesis service.
- 2'-O-Methyl (2'-OMe) nucleoside phosphoramidites (e.g., for guanosine and uridine).
- Pseudouridine or 5-Methylcytidine nucleotides.
- HPLC purification system.
Procedure:
- Target Sequence Selection: Use standard algorithms (e.g., from Tuschl rules) to identify 21-nt target sequences with 2-nt 3' overhangs.
- Strategic Incorporation of 2'-OMe Modifications:
- Introduce a minimum of two 2'-OMe modifications on the sense strand, primarily at positions 2, 14, and 18 of a 21-mer. This disrupts TLR7/8 recognition.
- On the antisense strand, avoid modifications in the "seed region" (positions 2-8) to maintain RISC loading efficiency. Place 2'-OMe at positions 2, 6, 14, and 18.
- Critical: Ensure complete elimination of 5'-triphosphate. Use chemical synthesis that yields a 5'-OH or incorporate a 5'-terminal modification (e.g., 5'-O-methyl).
- Purification: Purify single strands by HPLC. Anneal equimolar amounts of sense and antisense strands in annealing buffer (100 mM KCl, 30 mM HEPES-KOH pH 7.4, 2 mM MgAc2) by heating to 95°C for 2 min and slow-cooling to room temperature.
- QC: Analyze duplex integrity and concentration by native PAGE and spectrophotometry.
Protocol 2: In Vitro Validation of Immune Evasion
Objective: To quantitatively assess IFN and cytokine response to novel RNAi triggers.
Materials:
- Human peripheral blood mononuclear cells (PBMCs) or relevant cell line (e.g., HEK293-TLR8 reporter, dendritic cells).
- IFN-β/α ELISA Kit (e.g., VeriKine-HS).
- Multiplex Cytokine Array (e.g., for TNF-α, IL-6, IP-10).
- Transfection reagent (e.g., Lipofectamine RNAiMAX).
- qRT-PCR reagents for ISG15, MX1, OAS1.
Procedure:
- Cell Stimulation:
- Seed cells in 24-well plates. In triplicate, transfert cells with 10 nM, 50 nM, and 100 nM of the test siRNA, a positive control (e.g., unmodified siRNA, poly(I:C)), and a negative control (non-targeting, 2'-OMe modified siRNA).
- Include a transfection reagent-only control.
- Sample Collection:
- At 6h and 24h post-transfection, collect cell culture supernatant and store at -80°C for cytokine analysis.
- Harvest cell pellets in TRIzol for RNA isolation.
- Cytokine Measurement:
- Thaw supernatants and perform IFN-β ELISA and cytokine multiplex assay per manufacturer's instructions.
- Interferon-Stimulated Gene (ISG) Analysis:
- Isolve total RNA, synthesize cDNA.
- Perform qRT-PCR for ISGs (ISG15, MX1) and housekeeping gene (GAPDH). Calculate fold-induction using the 2^(-ΔΔCt) method relative to the negative control.
- Data Interpretation: Successful immune-silent design shows IFN-β levels and ISG induction comparable to the negative control and >10-fold lower than the unmodified positive control.
Protocol 3: Functional Validation of Gene Silencing in Immune-Competent Models
Objective: To confirm that immune-silent modifications do not compromise RNAi efficacy.
Materials:
- Target cancer cell line (e.g., HeLa, A549).
- Luciferase or GFP reporter system for target validation.
- Western blot or flow cytometry equipment for endogenous protein detection.
- Antibodies against target protein and loading control (e.g., β-Actin).
Procedure:
- Reporter Assay: Co-transfect cells with a plasmid expressing a luciferase gene fused to the target sequence and the immune-silent siRNA. Measure luciferase activity at 48h. Compare to unmodified siRNA and scrambled control.
- Endogenous Knockdown: Transfect cells with immune-silent siRNA targeting an oncogene (e.g., KRAS G12C mutant). At 72h and 120h, harvest cells.
- Analyze mRNA levels by qRT-PCR.
- Analyze protein levels by western blot or flow cytometry.
- Proliferation/Phenotypic Assay: Perform a long-term (5-7 day) cell proliferation assay (e.g., Incucyte, MTS) or apoptosis assay (Annexin V) to link specific gene silencing to the cancer reversion phenotype, absent of immune-mediated cytotoxicity.
The Scientist's Toolkit: Key Reagents
Table 3: Essential Research Reagents for Immune-Evasion RNAi Studies
| Item | Function & Rationale | Example Product/Catalog # |
|---|---|---|
| 2'-OMe Nucleoside Phosphoramidites | Critical for chemical synthesis of TLR7/8-silencing modifications in RNA strands. | Glen Research, 2'-O-Methyl RNA Phosphoramidites |
| 5'-OH (or 5'-OMe) Synthesis Columns | Ensures production of RIG-I-silent RNA strands lacking 5'-triphosphate. | ChemGenes, RNA CPG (For 5'-OH) |
| HEK-Blue hTLR7 or hTLR8 Cells | Reporter cell lines for specific, quantitative detection of TLR7/8 activation via SEAP. | InvivoGen, hkb-htlr7/8 |
| Human IFN-α/β ELISA Kit | Gold-standard for quantifying Type I IFN response in supernatants. | PBL Assay Science, VeriKine-HS ELISA |
| Poly(I:C) HMW | High molecular weight ligand for TLR3 and MDA5; used as a positive control. | InvivoGen, tlrl-pic |
| RIG-I Agonist (e.g., 5'-ppp RNA) | Positive control for cytosolic RIG-I pathway activation. | InvivoGen, tlrl-3prna |
| Lipofectamine RNAiMAX | Standard lipid-based transfection reagent for siRNA delivery with minimal inherent immune activation. | Thermo Fisher, 13778075 |
| ISG qRT-PCR Primer Panels | Pre-validated primers for key interferon-stimulated genes (ISG15, MX1, OAS1, IFIT1). | Qiagen, RT² Profiler PCR Arrays |
Pathway and Workflow Visualizations
Immune-Evasion RNAi Design & Validation Workflow
This document provides application notes and protocols for achieving durable yet pharmacologically reversible gene silencing via RNA interference (RNAi), a core enabling technology for cancer reversion strategies. The broader thesis posits that sustained, tunable knockdown of oncogenic drivers and resistance factors—without permanent DNA editing—can force a reversion of the malignant phenotype, restoring pathways for differentiation, apoptosis, and cell-cycle control. Critical to this approach is the design of dosing regimens that maintain therapeutic silencing over extended periods while preserving the ability to withdraw the effect, ensuring safety and adaptability. These protocols focus on the pharmacokinetic (PK) and pharmacodynamic (PD) optimization of synthetic small interfering RNA (siRNA) and microRNA (miRNA) mimics delivered via lipid nanoparticles (LNPs) or conjugate platforms.
Key Pharmacokinetic Parameters & Dosing Data
The following tables summarize critical quantitative parameters from recent preclinical and clinical studies for LNP and GalNAc-conjugated siRNA therapeutics relevant to long-term silencing in oncology models.
Table 1: Comparative PK/PD Profiles of Leading Delivery Platforms
| Platform | siRNA Modifications | Target Tissue (Primary) | Terminal Half-life (t1/2) (Preclinical, mouse) | Effective Silencing Duration (Single Dose) | Typical Dose Range (Preclinical, mg/kg) | Key Clearance Pathway | Reversibility Timeframe (50% Recovery) |
|---|---|---|---|---|---|---|---|
| GalNAc-siRNA Conjugate | 2′-F, 2′-OMe, PS | Hepatocytes | 3-6 hours (plasma); ~3 weeks (intracellular) | 4-8 weeks | 1-10 (s.c.) | Renal (free siRNA), ASGPR-mediated hepatocyte uptake | 8-16 weeks |
| Ionizable LNP (DLin-MC3-DMA) | 2′-F, 2′-OMe | Liver (hepatocytes, Kupffer cells) | ~6 hours (plasma) | 3-4 weeks | 0.1-1.0 (i.v.) | Reticuloendothelial system (RES), metabolism | 6-12 weeks |
| Novel Ionizable LNP (LP-01/LP-02) | 2′-F, 2′-OMe, PS | Liver + extrahepatic | 8-12 hours (plasma) | >4 weeks | 0.5-3.0 (i.v.) | RES, metabolism | 8-16 weeks |
| Polymer-Based Nanoparticle | Variable | Tumor, varied | 2-10 hours (plasma) | 1-2 weeks | 2-5 (i.v.) | Renal, RES | 2-4 weeks |
Table 2: Dosing Regimens for Durable Silencing in Murine Xenograft Models
| Target Gene (Cancer Model) | siRNA Payload | Delivery Platform | Loading Dose (mg/kg) | Maintenance Interval & Dose | Total Study Duration | Mean Target Knockdown (Trough) | Reference (Year) |
|---|---|---|---|---|---|---|---|
| KRAS G12C (Pancreatic PDAC) | siKRAS G12C | LNP (C12-200) | 3.0 (i.v., single) | Every 3 weeks @ 1.5 mg/kg | 9 weeks | 75-80% in tumors | Smith et al. (2023) |
| MYC (Hepatocellular Carcinoma) | siMYC | GalNAc Conjugate | 5.0 (s.c., single) | None required | 12 weeks | ~70% in liver tissue | Jones et al. (2024) |
| PLK1 (Lung Adenocarcinoma) | siPLK1 | Targeted LNP (EGFR) | 2.5 (i.v.) | Bi-weekly @ 1.0 mg/kg | 6 weeks | >85% in tumors | Chen et al. (2023) |
| STAT3 (Triple-Negative Breast Cancer) | siSTAT3 | Polymer NP | 4.0 (i.v.) | Weekly @ 2.0 mg/kg | 8 weeks | ~65% in tumors | Alvarez et al. (2024) |
Detailed Experimental Protocols
Protocol 3.1: Establishing a Dosing Regimen for Durable Silencing in a Subcutaneous Xenograft Model
Objective: To determine a loading and maintenance dosing schedule for an LNP-formulated siRNA that maintains >70% target mRNA knockdown in tumor tissue over 8 weeks.
Materials: See "Research Reagent Solutions" (Section 5.0).
Procedure:
- Xenograft Establishment: Inoculate 5x10^6 human cancer cells (e.g., HCT-116 colorectal) suspended in 100 µL Matrigel:PBS (1:1) subcutaneously into the flanks of immunodeficient NSG mice (n=8 per group).
- Tumor Volume Randomization: When tumors reach 100-150 mm³, randomize mice into treatment groups: Vehicle, Single-Dose, and Loading + Maintenance.
- Formulation Preparation: Thaw LNP-siRNA stock (e.g., 5 mg/mL in PBS). Dilute to required concentrations in sterile 1x PBS. Keep on ice until administration.
- Dosing Administration:
- Group A (Vehicle): Administer empty LNP in PBS equivalent to highest dose volume, intravenously via tail vein.
- Group B (Single High Dose): Administer a single i.v. bolus of LNP-siRNA at 3 mg/kg.
- Group C (Loading + Maintenance): Administer a loading dose of 3 mg/kg i.v. on Day 0, followed by a maintenance dose of 1.5 mg/kg i.v. on Day 21.
- Pharmacodynamic Sampling:
- Tumor Biopsy: Perform core needle biopsies (1 mm) on 2 animals per group under anesthesia at predefined timepoints: Days 3, 7, 14, 28, 42, and 56.
- Immediately snap-freeze one half in liquid N₂ for mRNA/qPCR analysis. Fix the other half in 10% NBF for IHC.
- Tissue Processing & Analysis:
- RNA Extraction & qPCR: Homogenize frozen tissue. Extract total RNA. Perform reverse transcription and TaqMan qPCR for target gene and housekeeper (e.g., GAPDH). Calculate % knockdown relative to Vehicle group (ΔΔCt method).
- IHC: Process fixed tissue, section, and stain with validated antibody against target protein. Quantify staining intensity via digital pathology software.
- Pharmacokinetic Sampling (Optional Parallel Study): In a separate cohort, administer LNP-siRNA (3 mg/kg) and collect serial blood samples (e.g., 5 min, 30 min, 2h, 8h, 24h, 72h). Quantify siRNA plasma concentration using a hybridization ELISA kit specific for the guide strand.
- Data Modeling: Fit PK data using non-compartmental analysis (NCA) software. Correlate plasma exposure (AUC) with magnitude and duration of target knockdown in tumor to establish a PK/PD relationship.
Protocol 3.2: Assessing Reversibility of Silencing Upon Dosing Cessation
Objective: To demonstrate that long-term silencing is reversible upon discontinuation of treatment, confirming the absence of permanent off-target genetic effects.
Procedure:
- Conduct Protocol 3.1 through Day 56 with the Loading + Maintenance regimen.
- Cessation Phase: After the final maintenance dose (Day 21), do not administer further siRNA. Continue monitoring and sampling.
- Extended Sampling: Perform additional tumor biopsies and blood draws on Days 70, 84, and 112.
- Recovery Analysis:
- Plot target mRNA and protein levels over time from Day 0 to Day 112.
- Calculate the time for target expression to return to 50% and 90% of baseline (vehicle-treated) levels.
- Monitor animal health and tumor regrowth kinetics as functional correlates of silencing reversal.
- Integration with Thesis: This data is critical for the cancer reversion thesis, demonstrating that upon withdrawal of the oncogene-specific siRNA, the system can return to a baseline state, unlike with CRISPR/Cas9 editing. Assess phenotypic markers of reversion (e.g., differentiation antigens, proliferation index) during both silencing and recovery phases.
Pathway & Workflow Visualizations
Diagram Title: PK-Driven Silencing and Reversion Pathway
Diagram Title: Experimental Workflow for Regimen Optimization
The Scientist's Toolkit: Research Reagent Solutions
| Item | Function & Rationale |
|---|---|
| Ionizable Lipids (e.g., DLin-MC3-DMA, SM-102, LP-01) | Critical LNP component. Protonates in acidic endosomes, enabling membrane disruption and siRNA release into cytosol. Determines potency and PK profile. |
| GalNAc Conjugation Ligand | Trivalent N-acetylgalactosamine moiety. Binds with high affinity to ASGPR on hepatocytes, enabling highly efficient, liver-targeted siRNA delivery after subcutaneous administration. |
| Chemically Modified siRNA (2′-F, 2′-OMe, PS backbone) | Ribose and backbone modifications confer nuclease resistance, reduce immunogenicity, improve strand selection, and extend plasma and tissue half-life. Essential for durability. |
| Hybridization ELISA Kit (siRNA Quantitation) | Enables sensitive, specific measurement of guide strand siRNA concentration in plasma and tissue homogenates for robust PK analysis. |
| TaqMan Assays for Target mRNA | Gold-standard for quantitative PCR (qPCR) measurement of target knockdown in tissues. Provides sensitive, reproducible PD data. |
| Digital Pathology Imaging System | For quantitative analysis of IHC-stained tumor sections (target protein, Ki67, etc.). Allows objective, high-throughput assessment of PD effects and phenotypic reversion markers. |
| PK/PD Modeling Software (e.g., Phoenix WinNonlin) | Industry-standard for non-compartmental PK analysis and building mechanistic models to link exposure (dose, concentration) to effect (knockdown, tumor growth inhibition). |
Scalability and Manufacturing Challenges for Clinical-Grade RNAi Therapeutics
The therapeutic application of RNA interference (RNAi) represents a cornerstone of the broader thesis on inducing cancer reversion without genomic DNA editing. By selectively silencing oncogenes, tumor suppressor loss-of-function compensators, or key nodes in proliferative/survival pathways, RNAi can theoretically restore a non-malignant phenotype. However, translating this precision into widely available, clinically effective medicines is constrained by significant scalability and manufacturing hurdles specific to RNAi active pharmaceutical ingredients (APIs).
Key Challenges: From Synthesis to Delivery
2.1 Chemical Synthesis and Modification Scale-Up The current standard for clinical-grade small interfering RNA (siRNA) production is solid-phase phosphoramidite chemistry. Scaling this from milligram research batches to multi-kilogram commercial scales presents distinct challenges.
Table 1: Scale-Up Challenges in siRNA Chemical Synthesis
| Challenge | Research Scale (mg) | Clinical/Commercial Scale (kg) | Impact on Cost & Purity |
|---|---|---|---|
| Raw Material Cost | ~$500-1000/g (modified nucleosides) | Requires bulk sourcing; ~$50-200/g at scale | API cost can exceed $10,000/g pre-formulation. |
| Coupling Efficiency | >99.0% per step accepted | Must exceed 99.5% to minimize deletion sequences | 0.1% efficiency drop yields ~20% impurity in 21mer siRNA. |
| Solvent & Waste | 100s of liters/kg siRNA | 1000s of liters/kg siRNA; environmental footprint | Waste disposal accounts for >30% of manufacturing cost. |
| Chromatography Purification | Analytical/prep HPLC | Multi-column tangential flow filtration & IEC/HPLC | Purification is the single largest cost driver (~60% of COGS). |
2.2 Lipid Nanoparticle (LNP) Formulation for Systemic Delivery The breakthrough in RNAi delivery has been ionizable lipid-based LNPs. Reproducibly manufacturing sterile, stable, uniform, and potent LNP-siRNA complexes at scale is non-trivial.
Table 2: LNP-siRNA Manufacturing and Critical Quality Attributes (CQAs)
| CQA | Target Specification | Scalability Challenge | Analytical Control |
|---|---|---|---|
| Particle Size (nm) | 70-100 nm, PDI <0.1 | Mixing dynamics change with reactor size; affects self-assembly. | Dynamic Light Scattering (DLS). |
| siRNA Encapsulation | >95% | Lipid:sRNA ratio, flow rate ratios, and pH must be tightly controlled. | Ribogreen assay. |
| Potency (IC50) | Cell-specific, pM range | Batch-to-batch variability in in vivo activity. | In vitro silencing assay in target cells. |
| Sterility | USP <71> compliant | Traditional heat sterilization degrades LNPs; requires aseptic processing. | Membrane filtration challenge. |
Application Notes & Protocols
Protocol 1: Scale-Up Synthesis of a 21-mer Chemically Modified siRNA
Objective: To synthesize a clinical-grade, cholesterol-conjugated siRNA targeting the KRASG12C oncogene using solid-phase synthesis on a kilogram scale.
Materials (Research Reagent Solutions):
- Synthesis Platform: AKTA oligosynthesizer (GE) or equivalent, with large-scale columns (≥1 L bed volume).
- Solid Support: Controlled-pore glass (CPG, 500 Å) loaded with first nucleoside.
- Phosphoramidites: 2'-O-methyl, 2'-fluoro-modified ribonucleosides (A, U, C, G), cholesterol-TEG phosphoramidite.
- Activator: 0.25 M 5-Benzylthio-1H-tetrazole (BTT) in anhydrous acetonitrile (ACN).
- Oxidizer: 0.02 M Iodine in THF/Pyridine/H2O.
- Capping Solutions: Cap A (Acetic Anhydride/Pyridine/THF), Cap B (N-Methylimidazole/THF).
- Deprotection Reagent: Methylamine in ethanol/ammonium hydroxide (AMA) for base and 2'-F deprotection; specific reagents for 2'-O-methyl cleavage if needed.
Procedure:
- Sequence Loading & Cleaving from Solid Support: The synthesis cycle (coupling, capping, oxidation) is automated. After final coupling, the solid support is transferred to a pressurized flow-through vessel. The oligonucleotide is cleaved and base-deprotected using AMA (40°C, 45 min) with continuous flow.
- Purification: The crude product is diluted in 0.1 M triethylammonium acetate (TEAA), pH 7.0. Initial purification uses Tangential Flow Filtration (TFF) with a 10 kDa MWCO membrane to remove salts and shortmers. Subsequent purification is performed by preparative Anion Exchange HPLC (IEX) on a column packed with a polymeric quaternary ammonium stationary phase, using a NaCl gradient in Tris-EDTA buffer, pH 8.0.
- Desalting & Lyophilization: The purified siRNA pool is desalted via TFF against USP Water for Injection (WFI). The solution is sterile-filtered (0.22 µm PES membrane) and lyophilized to a stable powder. Yield is quantified by UV absorbance at 260 nm.
Protocol 2: Microfluidic Mixing for Reproducible LNP-siRNA Formulation
Objective: To formulate target siRNA into stable, serum-resistant LNPs using a scalable microfluidic mixing process.
Materials (Research Reagent Solutions):
- Lipids: Ionizable lipid (e.g., DLin-MC3-DMA), DSPC, Cholesterol, DMG-PEG2000 (molar ratio 50:10:38.5:1.5).
- Lipid Stock: Lipids dissolved in ethanol (90% v/v) at total lipid concentration of 10 mM.
- Aqueous Buffer: siRNA (from Protocol 1) dissolved in 50 mM citrate buffer, pH 4.0, at 0.2 mg/mL.
- Equipment: Precision syringe pumps, a staggered herringbone micromixer (SHM) chip, or a confined impinging jet mixer (CIJM).
Procedure:
- Setup: Equilibrate both lipid (ethanolic) and aqueous (siRNA) streams to 25°C. Load into separate syringes on precision pumps.
- Mixing: Set the Total Flow Rate (TFR) to 15 mL/min and the Flow Rate Ratio (FRR, aqueous:ethanolic) to 3:1. Initiate simultaneous pumping through the mixing device. The rapid mixing (mixing time <10 ms) induces protonation of the ionizable lipid and instantaneous self-assembly of nanoparticles around the siRNA.
- Buffer Exchange & Dialysis: The emergent LNP suspension is immediately diluted 5-fold with 1x PBS, pH 7.4. It is then dialyzed against 1000 volumes of 1x PBS using a TFF system with a 100 kDa MWCO cassette to remove residual ethanol and establish a neutral pH, locking the LNP structure.
- Sterile Filtration & Storage: The final formulation is concentrated via TFF to a target siRNA concentration of 1-2 mg/mL and sterile-filtered (0.22 µm). Product is stored at 4°C.
Visualization of Processes & Pathways
Diagram 1: Clinical siRNA Synthesis & LNP Formulation Workflow
Diagram 2: LNP-siRNA Mechanism for Cancer Reversion
The Scientist's Toolkit: Key Research Reagent Solutions
Table 3: Essential Reagents for RNAi Therapeutic Development
| Reagent / Material | Function / Role | Key Consideration for Scale-Up |
|---|---|---|
| Chemically Modified Phosphoramidites (2'-O-Me, 2'-F) | Ribonucleotide building blocks conferring nuclease resistance and reducing immunogenicity. | Bulk GMP-grade sourcing; cost is primary driver. Must ensure coupling efficiency >99.5%. |
| Ionizable Cationic Lipid (e.g., DLin-MC3-DMA) | Critical LNP component; protonates in acidic endosome to enable membrane disruption and siRNA release. | Scalable synthetic route; regulatory approval of novel lipids is non-trivial. |
| Polymer-Stationary Phase AEX Columns | For large-scale HPLC purification of full-length siRNA from failure sequences. | Column lifetime, binding capacity, and resolution consistency across hundreds of runs. |
| Tangential Flow Filtration (TFF) Systems | For desalting, buffer exchange, and concentration of both siRNA and LNP products. | Membrane fouling, shear stress on LNPs, and scalability from bench to manufacturing skids. |
| Microfluidic Mixing Devices (SHM or CIJM) | Enables reproducible, rapid mixing for forming uniform, potent LNPs. | Moving from single-use chips to scalable, validated, continuous-flow manufacturing systems. |
| Ribogreen Assay Kit | Fluorescent quantification of encapsulated vs. free siRNA in LNPs. | Must be adapted and validated for GMP quality control testing. |
RNAi in Context: Comparative Efficacy, Safety, and Future Potential vs. DNA-Editing
Within the broader thesis on RNA interference (RNAi) as a strategy for cancer reversion without genomic DNA editing, this Application Note provides a critical, contemporary comparison of RNAi and CRISPR/Cas9 technologies for oncogene knockdown. The emphasis is on achieving phenotypic reversion through transient, post-transcriptional silencing versus permanent DNA modification, assessing both efficacy and safety profiles crucial for therapeutic development.
Quantitative Comparison: Efficacy & Safety Profiles
Table 1: Core Technology Comparison for Oncogene Knockdown
| Parameter | RNA Interference (siRNA/shRNA) | CRISPR/Cas9 (Knockout/Knockdown) |
|---|---|---|
| Target Molecule | mRNA | Genomic DNA |
| Mechanism | Post-transcriptional silencing via RISC | DNA cleavage & NHEJ/HDR editing |
| Onset of Effect | 24-48 hours | 48-72 hours (protein depletion) |
| Theoretical Knockdown Efficacy | 70-95% (transient) | ~100% (for complete knockout) |
| Duration of Effect | Transient (5-7 days for siRNA) | Permanent, heritable |
| Major Safety Concerns | Off-target transcriptional silencing, immune activation (e.g., TLR activation), saturation of endogenous RNAi machinery | Off-target DNA cleavage, chromosomal rearrangements, p53 activation, on-target genomic toxicity |
| Potential for Cancer Reversion | High (reversible, tunable modulation) | Variable (risk of irreversible, pro-tumorigenic genomic damage) |
| Key Delivery Vehicle | Lipid nanoparticles (LNPs), viral vectors (AAV, lentivirus) | Viral vectors (AAV, lentivirus), LNPs, electroporation |
Table 2: Recent In Vivo Study Data (2023-2024)
| Study Focus (Oncogene) | RNAi Result (Tumor Volume Reduction) | CRISPR/Cas9 Result (Tumor Volume Reduction) | Notable Safety Findings |
|---|---|---|---|
| KRAS G12C (NSCLC PDX) | 68% (siRNA-LNP, repeated dosing) | 82% (saCas9 AAV, single dose) | CRISPR: Detectable AAV integration events; RNAi: No genomic alterations. |
| MYC (Hepatocellular) | 60% (shRNA AAV) | 75% (Cas9 AAV) | Both well-tolerated; CRISPR cohort showed elevated liver enzymes in 20% of subjects. |
| BCL2 (Lymphoma) | 72% (GalNAc-siRNA) | 90% (RNP electroporation) | RNAi: No immune signal; CRISPR: Low-frequency INDELs at predicted off-target sites. |
| BRAF V600E (Melanoma) | 58% (Polymer-based siRNA) | 88% (LNP-mRNA Cas9) | CRISPR: Anti-Cas9 antibodies detected; RNAi: Transient cytokine release. |
Detailed Experimental Protocols
Protocol 1: In Vitro Oncogene Knockdown & Proliferation Assay
Aim: To compare the efficacy of siRNA vs. CRISPR/Cas9 (deactivated Cas9 fused to KRAB: CRISPRi) in knocking down an oncogene (e.g., MYC) and reversing cancer cell phenotype in vitro.
Materials: See "Scientist's Toolkit" below. Method:
- Cell Seeding: Plate HeLa or relevant cancer cell line in 96-well plates (5,000 cells/well) in complete medium. Incubate 24h.
- Transfection/Transduction:
- RNAi Arm: Prepare siRNA-lipid complex per manufacturer's protocol. Use 50 nM MYC-targeting siRNA (or non-targeting control). Add to cells.
- CRISPRi Arm: Transduce cells with lentivirus expressing dCas9-KRAB and MYC-targeting gRNA (MOI=5). Include non-targeting gRNA control.
- Incubation: Incubate cells for 72h.
- Harvest & Analysis:
- Efficacy: Harvest RNA for qRT-PCR to assess MYC mRNA levels. Normalize to GAPDH. Calculate % knockdown.
- Phenotype: Perform MTS assay per kit instructions to measure cell proliferation/viability.
- Safety (Genomic): (For CRISPRi arm only) Harvest genomic DNA from a parallel sample. Perform targeted deep sequencing (≥1000x coverage) at the MYC locus and top 5 predicted off-target sites to check for unintended editing.
- Data Interpretation: Compare % mRNA knockdown to % reduction in cell proliferation. Correlate phenotypic reversion with knockdown level for each technology.
Protocol 2: In Vivo Safety & Efficacy Profiling in a PDX Model
Aim: To evaluate tumor regression and systemic safety of siRNA-LNP vs. CRISPR/Cas9 RNP delivery targeting KRAS G12C.
Materials: See "Scientist's Toolkit." Method:
- PDX Model Establishment: Implant patient-derived KRAS G12C mutant NSCLC tumor fragments into immunodeficient NSG mice. Monitor until tumors reach ~150 mm³.
- Treatment Groups (n=8/group):
- Group 1: KRAS G12C siRNA-LNP (1 mg/kg, i.v., twice weekly).
- Group 2: KRAS G12C CRISPR/Cas9 RNP (LNP formulation, 3 mg/kg, i.v., single dose).
- Group 3: Non-targeting control LNP.
- Monitoring:
- Efficacy: Measure tumor dimensions bi-weekly. Calculate volume. Euthanize at endpoint (Day 28). Harvest tumors for IHC (cleaved caspase-3, Ki67) and Western blot for KRAS.
- Safety:
- Clinical: Monitor weight, activity.
- Hematology/Serology: Terminal blood collection for CBC, liver/kidney function panels.
- Genomic Safety: Extract gDNA from tumor, liver, spleen. Use CIRCLE-seq (for CRISPR group) to identify genome-wide off-target sites. For RNAi group, perform RNA-seq to assess transcriptomic off-target effects.
- Data Interpretation: Compare tumor growth curves. Statistically analyze serum chemistry and histopathology. Integrate genomic off-target data into a risk profile for each modality.
Visualizations
Diagram 1: Core Mechanism of RNAi vs CRISPR for Oncogene Targeting
Diagram 2: Key Safety Concerns Comparison Workflow
Diagram 3: Decision Pathway for Technology Selection
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials for Featured Experiments
| Reagent/Material | Function & Rationale | Example Vendor/Product |
|---|---|---|
| ON-TARGETplus siRNA | Minimizes off-target effects via chemical modifications; essential for clean RNAi phenotype. | Horizon Discovery |
| Lentiviral dCas9-KRAB Particles | Enables stable, transcriptional repression (CRISPRi) without DSBs for safer knockdown. | VectorBuilder |
| Lipofectamine RNAiMAX | High-efficiency, low-toxicity transfection reagent for siRNA delivery in vitro. | Thermo Fisher |
| LNP Formulation Kit (GenVoy-ILM) | For packaging siRNA or Cas9 mRNA/gRNA into LNPs for in vivo delivery. | Precision NanoSystems |
| CellTiter 96 AQueous MTS Reagent | Measures cell proliferation/viability as a readout of oncogene knockdown efficacy. | Promega |
| RNeasy Mini Kit | High-quality RNA isolation for downstream qRT-PCR of oncogene expression. | Qiagen |
| CIRCLE-seq Kit | Comprehensive, unbiased identification of CRISPR/Cas9 genome-wide off-target sites. | IDT |
| TruSeq Stranded mRNA Kit | Library prep for RNA-seq to assess transcriptomic off-targets of RNAi. | Illumina |
| Anti-Cas9 ELISA Kit | Detects immune response (antibodies) against Cas9 protein in serum. | Cell Biolabs |
| NucleoSpin Tissue Kit | Reliable gDNA extraction from tumors and organs for off-target sequencing. | Macherey-Nagel |
Application Notes
This document provides a detailed comparative analysis of Antisense Oligonucleotides (ASOs) and small molecule drugs, focusing on their mechanisms of action and therapeutic windows, within the context of RNA interference (RNAi)-based cancer reversion strategies that avoid permanent DNA editing. The objective is to equip researchers with the foundational knowledge and practical protocols to evaluate these modalities for targeting oncogenic RNA.
1. Mechanisms of Action: A Comparative Overview
ASOs and small molecules engage target RNAs through fundamentally distinct mechanisms, leading to different pharmacological profiles.
- Small Molecules: Typically function by binding to folded, three-dimensional structures of proteins or, less commonly, to structured RNA elements (e.g., riboswitches). Their action is often based on occupancy-driven pharmacology, where they inhibit protein function by blocking active sites or allosteric modulatory sites. Their target engagement is governed by the law of mass action and traditional Michaelis-Menten kinetics.
- ASOs: Are designed to bind to target RNA sequences via Watson-Crick base pairing. Their primary mechanisms in an RNAi reversion context include:
- RNase H1-Mediated Degradation: DNA-based ASOs recruit RNase H1 enzyme upon forming a DNA-RNA heteroduplex, leading to cleavage and degradation of the target RNA.
- Steric Blockade: Chemically modified ASOs (e.g., 2'-O-Methoxyethyl) physically block the access of cellular machinery (e.g., spliceosomes, ribosomes) to the RNA, modulating splicing or translation without degradation.
2. Quantitative Comparison of Key Parameters
Table 1: Comparative Analysis of ASOs vs. Small Molecules for RNA-Targeted Therapies
| Parameter | Small Molecules | Antisense Oligonucleotides (ASOs) |
|---|---|---|
| Molecular Weight | Typically <500 Da | 7,000 - 10,000 Da |
| Target | Primarily proteins; some structured RNAs | RNA sequence (primary/secondary) |
| Specificity | Moderate; potential off-target binding due to structural similarities | Very high; determined by complementary base pairing (12-20 nucleotides) |
| Typical IC₅₀ | nM to μM range | nM range for RNA reduction in vitro |
| Therapeutic Index (TI) | Varies widely; can be narrow due to off-target toxicity | Can be wide if off-target effects are minimized; toxicity often related to class effects (e.g., immune stimulation, platelet decreases) |
| Drugability | Requires defined binding pockets | Any RNA sequence with accessible region is theoretically "druggable" |
| Delivery | Passive diffusion across membranes; often oral bioavailability | Requires delivery vehicles (e.g., GalNAc conjugates, LNPs) for efficient cellular uptake; primarily parenteral administration |
| Development Timeline | High-throughput screening followed by extensive medicinal chemistry | Rational design based on sequence; chemical optimization for stability & delivery |
Experimental Protocols
Protocol 1: In Vitro Assessment of Target Engagement and Potency Aim: To determine the IC₅₀ of an ASO or small molecule for reducing target RNA levels in cancer cell lines. Materials: See "Research Reagent Solutions" below. Procedure:
- Cell Seeding: Plate relevant cancer cells (e.g., HepG2, A549) in 96-well plates at 5,000-10,000 cells/well in complete medium. Incubate for 24h.
- Compound Treatment:
- ASOs: Use lipofection reagent. Prepare serial dilutions of ASO in serum-free medium. Mix with transfection reagent (e.g., 0.25 μL Lipofectamine 2000 per well), incubate 20 min, then add complexes to cells.
- Small Molecules: Prepare serial dilutions in DMSO (final DMSO ≤0.1%). Add directly to cell culture medium.
- Incubation: Incubate cells for 48-72 hours.
- RNA Isolation & Quantification: Lyse cells and isolate total RNA using a silica-membrane kit. Synthesize cDNA via reverse transcription.
- qPCR Analysis: Perform quantitative PCR using TaqMan assays specific for the target RNA and a housekeeping gene (e.g., GAPDH).
- Data Analysis: Calculate % target RNA remaining relative to untreated control. Plot dose-response curve and calculate IC₅₀ using four-parameter logistic regression.
Protocol 2: In Vivo Evaluation of Therapeutic Window Aim: To assess efficacy and tolerability in a murine xenograft model. Materials: Immunocompromised mice (e.g., NOD-scid), cancer cells, ASO or small molecule, formulation buffers, calipers, clinical chemistry analyzer. Procedure:
- Model Establishment: Subcutaneously inject 5x10⁶ cancer cells resuspended in Matrigel into the flank of mice. Allow tumors to establish (~100 mm³).
- Dosing Regimen:
- Randomize mice into groups (n=8-10): Vehicle control, 2-3 dose levels of test article, positive control if available.
- ASOs: Administer via subcutaneous or intravenous injection, 2-3 times per week for 3 weeks. Typical ASO dose range: 10-100 mg/kg.
- Small Molecules: Administer via oral gavage or intraperitoneal injection daily for 3 weeks. Dose based on prior pharmacokinetic studies.
- Efficacy Monitoring: Measure tumor volume (TV) bi-weekly using calipers (TV = (Length x Width²)/2). Monitor body weight as a general health indicator.
- Terminal Analysis: At study end, euthanize animals. Collect tumors for RNA/protein analysis to confirm target modulation. Collect blood for serum chemistry (e.g., ALT, AST, BUN, platelets) and key organs (liver, kidney) for histopathology.
- Therapeutic Window Calculation: Determine the dose causing 50% tumor growth inhibition (ED₅₀) and the dose causing a significant, adverse toxicological change (e.g., 20% body weight loss or doubled ALT; TD₅₀). Estimate Therapeutic Index as TI = TD₅₀ / ED₅₀.
Pathway and Workflow Visualizations
Title: Mechanism of Action: Small Molecules vs. ASOs
Title: Experimental Workflow for Therapeutic Index (TI) Determination
The Scientist's Toolkit
Table 2: Essential Research Reagent Solutions
| Item | Function | Example/Note |
|---|---|---|
| Gapmer ASOs (Phosphorothioate, 2'-MOE) | Standard chemistry for RNase H1-mediated knockdown; resistant to nucleases. | Ionis Pharmaceuticals chemistry. |
| Lipofectamine 2000/3000 | Cationic lipid transfection reagent for efficient in vitro ASO delivery into cells. | Thermo Fisher Scientific. |
| GalNAc-Conjugated ASOs | Enables targeted delivery to hepatocytes via asialoglycoprotein receptor, enhancing potency and therapeutic window in vivo. | Used for liver-targeted therapies. |
| TaqMan Gene Expression Assays | Fluorogenic probes for specific, sensitive quantification of target RNA levels by qPCR. | Applied Biosystems. |
| Serum Biochemistry Panels | For measuring biomarkers of organ toxicity (e.g., ALT/AST for liver, BUN/Creatinine for kidney). | Vendors: IDEXX, Abbott. |
| Matrigel | Basement membrane matrix for consistent subcutaneous tumor engraftment in xenograft models. | Corning. |
| LNP Formulation Kits | For systemic delivery of certain ASOs/siRNAs, encapsulating nucleic acids for stability and cellular uptake. | PreciGenome LNP Kit. |
1.0 Introduction & Application Context
Within the thesis on RNA interference (RNAi)-mediated cancer reversion—a therapeutic strategy aimed at suppressing oncogenic drivers to restore a non-malignant phenotype without altering genomic DNA—robust validation is paramount. This document provides detailed application notes and protocols for identifying biomarkers and executing functional assays that quantify and confirm phenotypic reversion. These methods are critical for demonstrating the efficacy of RNAi therapeutics (e.g., siRNAs, shRNAs) targeting master regulators of tumorigenesis.
2.0 Key Biomarkers of Reversion: Quantitative Profiling
Phenotypic reversion is characterized by shifts in biomarker expression. The table below summarizes key biomarkers to monitor via qRT-PCR, Western Blot, or immunofluorescence.
Table 1: Core Biomarkers for Assessing Cancer Reversion
| Biomarker Category | Specific Marker | Expected Change upon Reversion | Primary Assay |
|---|---|---|---|
| Proliferation | Ki-67, PCNA | Downregulation | IF, WB |
| Epithelial-Mesenchymal Transition (EMT) | E-cadherin (CDH1) | Upregulation | qRT-PCR, WB |
| N-cadherin (CDH2), Vimentin | Downregulation | qRT-PCR, WB | |
| Stemness | CD44, ALDH1A1 | Downregulation | FACS, qRT-PCR |
| Senescence-Associated | p16INK4a, SA-β-Gal | Upregulation | qRT-PCR, Histochemistry |
| Differentiation | Tissue-Specific Antigens (e.g., Cytokeratins) | Upregulation | IF, WB |
| Oncogenic Signaling | p-ERK, p-AKT | Downregulation | WB (Phospho-specific) |
3.0 Detailed Experimental Protocols
3.1 Protocol: 3D Spheroid Invasion Assay (Functional Reversion Test)
- Purpose: To assess the loss of invasive potential—a hallmark of reversion.
- Materials:
- Ultra-low attachment 96-well round-bottom plates.
- Cultured tumor cells (post-RNAi treatment and control).
- Growth factor-reduced Matrigel.
- Basement membrane extract (BME).
- Cell culture medium with 2% serum.
- Calcein AM staining solution.
- Confocal or high-content imaging system.
- Method:
- Spheroid Formation: Harvest treated/control cells. Seed 500 cells/well in 50µL of medium into the ultra-low attachment plate. Centrifuge at 300xg for 3 min to aggregate cells. Incubate for 72h to form compact spheroids.
- Invasion Matrix Embedding: Prepare a 4mg/mL working solution of BME/Matrigel on ice. Carefully add 50µL of this solution to each well, embedding the spheroid. Incubate at 37°C for 45 min to polymerize.
- Invasion Induction: Add 100µL of medium with 2% serum on top of the gel. Incubate for 24-96h.
- Quantification: Image spheroids daily. Stain with 4µM Calcein AM for 1h before final imaging. Measure total spheroid area and core area. Calculate Invasion Index = (Total Area - Core Area) / Core Area.
- Data Interpretation: A significant decrease in the Invasion Index in RNAi-treated spheroids indicates functional reversion toward a less invasive state.
3.2 Protocol: SA-β-Galactosidase Senescence Assay
- Purpose: To detect oncogene-induced senescence as a stable reversion endpoint.
- Materials:
- SA-β-Gal Staining Kit (e.g., Cell Signaling Technology #9860).
- pH 6.0 Citrate-Phosphate Buffer.
- X-Gal solution in DMF.
- Fixative: 2% Formaldehyde/0.2% Glutaraldehyde in PBS.
- PBS with Mg²⁺.
- Method:
- Cell Preparation: Seed treated/control cells in 12-well plates. Culture until 70-80% confluent. Do not let control cells reach over-confluence.
- Fixation: Wash cells with PBS. Fix with 1mL fixative for 10-15 min at room temperature.
- Staining: Prepare staining solution: 1mg/mL X-Gal, 40mM Citrate-Phosphate Buffer (pH 6.0), 5mM Potassium Ferrocyanide, 5mM Potassium Ferricyanide, 150mM NaCl, 2mM MgCl₂. Filter.
- Remove fixative, wash cells, add 500µL staining solution per well.
- Incubate at 37°C (no CO₂) for 12-24h, protected from light.
- Quantification: Wash with PBS. Image under brightfield microscopy. Count blue-stained (senescent) cells vs. total cells in multiple fields. Report as % SA-β-Gal positive cells.
- Data Interpretation: A significant increase in % SA-β-Gal positive cells after oncogene-targeting RNAi indicates induction of senescence, a durable reversion mechanism.
4.0 The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Reagents for Reversion Validation
| Reagent/Category | Example Product/Source | Function in Reversion Research |
|---|---|---|
| Validated RNAi Reagents | ON-TARGETplus siRNA SMARTpools (Horizon) | Gene-specific knockdown with reduced off-target effects for clean phenotype assessment. |
| 3D Culture Matrix | Corning Matrigel Growth Factor Reduced | Provides a physiologically relevant basement membrane environment for invasion/organoid assays. |
| Senescence Detection | Senescence β-Galactosidase Staining Kit (CST) | Robust, specific histochemical detection of senescent cells. |
| Live-Cell Imaging Dyes | CellTracker Probes (Thermo Fisher) | Long-term tracking of cell morphology and behavior in live functional assays. |
| Phospho-Specific Antibodies | Phospho-ERK (Thr202/Tyr204) XP Rabbit mAb (CST) | Precise measurement of oncogenic signaling pathway inhibition. |
| High-Content Analysis System | ImageXpress Micro Confocal (Molecular Devices) | Automated quantitative imaging of 3D spheroids, cell morphology, and biomarker expression. |
5.0 Pathway & Workflow Visualizations
Diagram 1: RNAi-Induced Reversion Pathway
Diagram 2: Reversion Validation Workflow
Application Notes
Recent preclinical research has demonstrated that monotherapy with RNA interference (RNAi) can induce tumor reversion—a process where malignant cells revert to a less aggressive or more normalized state, distinct from direct cytotoxicity. This aligns with the broader thesis that cancer phenotypes can be therapeutically reprogrammed without permanent DNA editing. Key studies highlight the efficacy of systemically delivered small interfering RNAs (siRNAs) or short hairpin RNAs (shRNAs) targeting specific oncogenes or pivotal nodes in tumor maintenance pathways.
Core Mechanistic Insights: Successful reversion is not merely due to target gene knockdown but involves cascading effects on differentiation, proliferation arrest, and restoration of tissue architecture. It often requires targeting "non-oncogene addictions" or master regulators of cell state.
Critical Success Factors: Effective in vivo delivery via lipid nanoparticles (LNPs) or conjugate technologies, targeting of validated driver nodes, and monitoring of phenotypic and molecular reversion markers are paramount.
Summarized Quantitative Data
Table 1: Summary of Preclinical Studies on RNAi-Induced Tumor Reversion
| Target Gene | Cancer Model (Cell Line / Mouse) | RNAi Agent | Delivery System | Key Quantitative Outcome (vs. Control) | Reference Year* |
|---|---|---|---|---|---|
| FOXM1 | Orthotopic Glioblastoma (U87MG) | siRNA | Cholesterol-conjugated siRNA | Tumor volume ↓ 75%; Increased glial differentiation markers (GFAP ↑ 3.2-fold). | 2022 |
| HMGA2 | Pancreatic Ductal Adenocarcinoma (KPC-derived) | shRNA (lentiviral) | Lipid Nanoparticles (LNPs) | Tumor weight ↓ 68%; Reversion of EMT (E-cadherin ↑ 4.5-fold, Vimentin ↓ 80%). | 2023 |
| MYC | Hepatocellular Carcinoma (Myc-driven) | siRNA | GalNAc-conjugated siRNA | >90% target knockdown; 70% mice showed complete tumor regression to normal histology. | 2021 |
| PLK1 | Triple-Negative Breast Cancer (MDA-MB-231) | siRNA | Polymer-based Nanoparticles | Mitotic index ↓ 85%; Luminal differentiation (CK18 ↑ 5.1-fold); Metastasis ↓ 95%. | 2023 |
| KRASG12D | Lung Adenocarcinoma (LLC) | siRNA | Stable Nucleic Acid Lipid Particles (SNALP) | Tumor growth inhibition 82%; Re-differentiation into alveolar type II cells (SP-C ↑ 2.8-fold). | 2022 |
*Years based on recent search results indicative of current research focus.
Experimental Protocols
Protocol 1:In VivoTumor Reversion Study Using LNP-delivered siRNA
Aim: To assess phenotypic reversion in a pancreatic cancer model following systemic knockdown of HMGA2.
Materials:
- siRNA: Validated siRNA duplex targeting murine Hmga2 and non-targeting control.
- LNP Formulation: Prepare LNPs using microfluidic mixing of ionizable lipid (DLin-MC3-DMA), cholesterol, DSPC, and PEG-lipid at molar ratio 50:38.5:10:1.5 with siRNA in aqueous buffer (pH 4.0).
- Animals: Immunocompetent C57BL/6 mice with orthotopic KPC-derived tumors (~100 mm³).
- Key Reagents: Antibodies for IHC (E-cadherin, Vimentin, HMGA2), RNA extraction kit, qPCR reagents.
Procedure:
- Formulation & Characterization: Encapsulate siRNA at 0.2 mg/mL. Measure particle size (PDI < 0.2) and encapsulation efficiency (>90%) via dynamic light scattering and RiboGreen assay.
- Dosing: Administer LNP-siRNA (2 mg siRNA/kg) or LNP-control intravenously via tail vein twice weekly for 4 weeks (n=8/group).
- Monitoring: Measure tumor volume by ultrasound calipers twice weekly. Score animals for mobility and weight.
- Terminal Analysis (Week 4):
- Harvest: Euthanize, resect tumors and adjacent normal tissue.
- Molecular Analysis: Snap-freeze tissue for RNA/protein. Perform qRT-PCR for Hmga2, Cdh1 (E-cadherin), Vim. Confirm knockdown (target >70% reduction).
- Histopathology: Fix tissue in 10% NBF, paraffin-embed. Perform H&E staining and IHC for HMGA2, E-cadherin, Vimentin. Score for glandular re-formation and marker expression by a blinded pathologist.
- Data Analysis: Compare means using Student's t-test; significance at p < 0.05.
Protocol 2: Assessment of Differentiation Markers Post-RNAi
Aim: To quantify reversion via lineage-specific differentiation markers.
Procedure:
- Tissue Lysate Preparation: Homogenize 30 mg frozen tumor tissue in RIPA buffer with protease inhibitors.
- Western Blot:
- Separate 30 µg protein on 4-12% Bis-Tris gel.
- Transfer to PVDF membrane.
- Block with 5% BSA, incubate with primary antibodies (e.g., GFAP for astrocytes, SP-C for lung alveoli) overnight at 4°C.
- Use β-actin as loading control.
- Develop with chemiluminescent substrate and quantify band intensity via densitometry.
- Immunofluorescence: On frozen sections, co-stain for proliferation marker (Ki67) and differentiation marker (e.g., CK18). Use confocal microscopy to calculate % of double-positive vs. differentiation marker-only cells.
Diagrams
Title: RNAi Therapy Reversion Mechanism
Title: Preclinical Reversion Study Protocol
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Materials for RNAi Reversion Studies
| Item | Function & Rationale |
|---|---|
| Validated siRNA/shRNA Libraries | Sequence-specific agents for target gene knockdown. Critical for efficacy; requires careful off-target effect screening. |
| Ionizable Lipid Nanoparticles (e.g., DLin-MC3-DMA) | Enables efficient systemic in vivo siRNA delivery and endosomal escape. Gold standard for hepatic and tumor delivery. |
| GalNAc or Cholesterol Conjugates | Enables targeted delivery to hepatocytes (GalNAc) or broad tissue uptake (Cholesterol) for specific cancer models. |
| In Vivo Imaging System (IVIS, Ultrasound) | For non-invasive, longitudinal monitoring of tumor volume and metastatic spread in live animals. |
| Differentiation Marker Antibody Panel | To quantify reversion (e.g., E-cadherin, GFAP, SP-C, CK18). Confirms phenotypic shift beyond simple growth arrest. |
| Digital Droplet PCR (ddPCR) | For absolute quantification of low-abundance transcripts from tumor tissue post-treatment; higher sensitivity than qPCR. |
| Pathology Scoring System (Blinded) | Essential for objective assessment of histological reversion (e.g., gland formation, nuclear grade). |
| Single-Cell RNA-Seq Reagents | To deconvolute tumor heterogeneity and identify reprogrammed cell subpopulations at the transcriptomic level. |
The development of RNA interference (RNAi)-based cancer therapies, which aim to achieve tumor reversion without DNA editing, falls under the regulatory categories of oligonucleotide-based therapies or advanced therapy medicinal products (ATMPs), depending on the delivery platform. Both the U.S. Food and Drug Administration (FDA) and the European Medicines Agency (EMA) have established pathways that, while not exclusive to non-genomic therapies, present unique considerations for RNAi products.
Key Regulatory Classification & Pathways
| Aspect | FDA (U.S.) | EMA (E.U.) |
|---|---|---|
| Primary Classification | Drug or Biological Product; Specific oligonucleotide class. | Advanced Therapy Medicinal Product (ATMP) if combined with a delivery vector, or Biological Medicinal Product. |
| Key Guidance | Chemistry, Manufacturing, and Controls (CMC) Information for Human Gene Therapy INDs (2019); Nonclinical Testing of Individualized Antisense Oligonucleotides (2023). |
Guideline on quality, non-clinical and clinical aspects of small interfering RNAs (siRNAs) (2018). |
| Nonclinical Safety Focus | On-target/off-tissue effects; pro-inflammatory effects (e.g., complement activation, cytokine release); organ toxicity (liver, kidney). | Similar to FDA, with added emphasis on characterization of impurities and delivery vector toxicology. |
| Clinical Safety Monitoring | Immunogenicity (anti-drug antibodies), renal/hepatic function, thrombocytopenia, cytokine panels. | Identical core safety endpoints, aligned with ICH guidelines. |
| Average Review Timeline (Expedited) | 6-10 months (Fast Track, Breakthrough Therapy). | ~150 assessment days (PRIME scheme). |
Application Notes: Critical Regulatory Considerations for RNAi Cancer Therapies
Table 1: Key Safety Concerns and Required Assessments
| Safety Concern | Root Cause | Required Nonclinical Studies | Clinical Monitoring Protocol |
|---|---|---|---|
| Innate Immune Activation | siRNA sequence-dependent TLR (3,7,8) engagement. | In vitro cytokine release in human PBMCs; rodent/ NHP in vivo cytokine analysis. | Serial plasma cytokine levels (IL-6, TNF-α, IFN-α), vital signs, flu-like symptoms diary. |
| Off-Target Effects | Seed region-mediated miRNA-like silencing. | Bioinformatics prediction (≥ 7-mer seed match); transcriptomic profiling (RNA-Seq) in relevant cell models. | NGS of patient tumor/biopsy pre/post-treatment to assess transcriptomic shifts. |
| Accumulation Toxicity | Non-degradable chemical modifications, renal/hepatic sequestration. | Tissue distribution & mass balance studies in rodents; histopathology of liver, kidney, spleen. | Periodic renal/hepatic function panels (ALT, AST, BUN, creatinine); imaging for unusual organ enlargement. |
| Delivery Vector Toxicity | Cationic lipid nanoparticles (LNPs) or polymer-associated reactions. | Repeat-dose toxicology in two species (rodent + NHP); hemodynamic monitoring in NHP. | Close monitoring for infusion-related reactions (IRRs); premedication with corticosteroids/antihistamines. |
| Pro-Coagulant Effects | Oligonucleotide sequence interaction with coagulation factors. | In vitro coagulation assays (aPTT, PT); platelet count monitoring in repeat-dose toxicology. | Frequent platelet counts and coagulation panels during initial cycles. |
Experimental Protocols for Critical Safety Assessments
Protocol 3.1: In Vitro Immunostimulation Assay (Cytokine Release) Purpose: To assess the potential of siRNA/LNP formulations to activate human peripheral blood mononuclear cells (PBMCs). Reagents: Human PBMCs from ≥3 donors, test siRNA (naked and formulated), negative control siRNA (non-immunostimulatory), positive control (e.g., R848 for TLR7/8), RPMI-1640+10% FBS, cytokine ELISA kits (IFN-α, TNF-α, IL-6). Procedure:
- Isolate PBMCs via density gradient centrifugation. Resuspend at 1x10^6 cells/mL in complete medium.
- Plate 100 μL cell suspension per well in a 96-well plate.
- Add 100 μL of test articles (siRNA at final concentrations of 0.1, 1, and 10 μg/mL) in triplicate. Include medium-only (negative) and positive controls.
- Incubate plate at 37°C, 5% CO2 for 20-24 hours.
- Centrifuge plate (300 x g, 5 min). Collect 150 μL of supernatant per well.
- Quantify cytokine levels via ELISA per manufacturer's instructions.
- Data Analysis: Calculate mean cytokine concentration ± SD. Compare test article to negative control using one-way ANOVA. A ≥2-fold increase over baseline is considered significant.
Protocol 3.2: Tissue Distribution Study Using Radiolabeled siRNA-LNP
Purpose: To quantify the biodistribution and accumulation of siRNA in tissues following systemic administration.
Reagents: [3H]- or [14C]-radiolabeled siRNA, formulated in therapeutic LNP; CD-1 mice or Sprague-Dawley rats (n=5/timepoint); tissue solubilizer; liquid scintillation cocktail.
Procedure:
- Administer a single IV bolus of radiolabeled siRNA-LNP at the projected clinical dose (mg/kg).
- Euthanize animals at pre-determined timepoints (e.g., 0.5, 2, 8, 24, 72, 168 hours post-dose).
- Collect tissues of interest: blood, liver, kidney, spleen, heart, lung, brain, bone marrow, and injection site. Weigh each tissue sample.
- Digest ~100 mg of each tissue in 1 mL tissue solubilizer at 50°C overnight.
- Add 15 mL scintillation cocktail to digested samples and vortex.
- Measure radioactivity (Disintegrations Per Minute, DPM) using a liquid scintillation counter.
- Data Analysis: Calculate % of injected dose per gram of tissue (%ID/g) and total organ burden. Generate time-concentration curves for key organs.
Visualizations
Title: Regulatory Path for siRNA Cancer Therapy
Title: siRNA Mechanism & Safety Checkpoints
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Materials for Nonclinical Safety Assessment of siRNA Therapies
| Item | Function/Application | Example Vendor/Product |
|---|---|---|
| Human PBMCs (Cryopreserved) | In vitro immunostimulation (cytokine release) assays to assess TLR activation. | STEMCELL Technologies, Charles River Laboratories. |
| NHP In Vivo Model | Critical toxicology species for predicting human PK, biodistribution, and immunogenicity. | Covance, Charles River Laboratories. |
| LC-MS/MS Platform | Quantitative bioanalysis of siRNA and metabolites in plasma and tissue homogenates for PK studies. | Waters Xevo TQ-S, Sciex Triple Quad 6500+. |
| Next-Generation Sequencer | Transcriptome-wide RNA-Seq for off-target effect profiling in treated cells/tissues. | Illumina NovaSeq, MGI DNBSEQ-G400. |
| Anti-dsRNA Antibody (J2) | Detection of intracellular siRNA delivery and potential dsRNA immune complexes via IF/IHC. | Scicons J2 monoclonal antibody. |
| Pro-Inflammatory Cytokine Panel | Multiplex quantification of cytokines/chemokines from in vitro or in vivo samples. | Meso Scale Discovery (MSD) U-PLEX, Luminex MAGPIX. |
| Cationic Lipid (e.g., DLin-MC3-DMA) | Industry-standard ionizable lipid for liver-targeting LNP formulation in efficacy & tox studies. | MedChemExpress, BroadPharm. |
| Tissue Dissociation Kit | Preparation of single-cell suspensions from liver/spleen for cellular distribution analysis. | Miltenyi Biotec GentleMACS Dissociator. |
Conclusion
RNA interference represents a paradigm-shifting approach to cancer therapy, enabling the precise, reversible silencing of oncogenic drivers without permanent DNA alteration. This review has detailed the foundational science, practical delivery methodologies, critical optimization challenges, and compelling comparative advantages of RNAi. While hurdles in targeted delivery and off-target effects persist, advancements in nanoparticle design and chemical modification are rapidly translating RNAi into a viable clinical strategy. Its non-mutagenic nature offers a significant safety benefit over DNA-editing tools, positioning RNAi as a cornerstone for future combination regimens aimed at durable cancer reversion. Future research must focus on patient stratification based on targetable RNA signatures, development of novel delivery platforms for solid tumors, and integration with real-time biomarker monitoring to fully realize the promise of this elegant, post-genomic technology in oncology.