qPCR in Modern Medicine: Powering Precision Diagnostics and Personalized Therapies
This article explores the pivotal role of quantitative Polymerase Chain Reaction (qPCR) in advancing molecular diagnostics and personalized medicine.
qPCR in Modern Medicine: Powering Precision Diagnostics and Personalized Therapies
Abstract
This article explores the pivotal role of quantitative Polymerase Chain Reaction (qPCR) in advancing molecular diagnostics and personalized medicine. Tailored for researchers, scientists, and drug development professionals, it provides a comprehensive analysis spanning from the foundational principles and booming market landscape of qPCR to its cutting-edge methodological applications in oncology and infectious diseases. The content delves into critical troubleshooting and optimization strategies for data accuracy, examines qPCR's position against emerging technologies like digital PCR and NGS, and forecasts future trends driven by AI integration and point-of-care testing. This resource synthesizes the current state and future trajectory of qPCR, offering valuable insights for professionals leveraging this technology in clinical and research settings.
The qPCR Revolution: From Basic Principles to a Multi-Billion Dollar Market
Quantitative PCR (qPCR), also known as real-time PCR, has revolutionized molecular biology by enabling the accurate and quantitative measurement of nucleic acids during the amplification process itself [1]. This powerful technique represents a significant advancement over traditional PCR, which could only provide end-point detection. The core innovation of qPCR lies in its ability to monitor PCR product accumulation in real-time through fluorescence detection, transforming PCR from a qualitative tool into a precise quantitative one [1]. In the context of molecular diagnostics and personalized medicine, this quantification capability is paramount—it allows researchers and clinicians not just to detect the presence of specific genetic markers, but to measure their abundance, enabling applications from viral load monitoring to gene expression profiling for therapeutic decision-making [2].
The fundamental difference between traditional PCR and qPCR lies in their measurement approaches. Traditional PCR relies on end-point detection, where results are collected after the reaction is complete, making it impossible to determine the precise starting concentration of nucleic acid [1]. In contrast, qPCR focuses on the exponential phase of amplification, where reaction efficiency is highest and most consistent, providing the most precise and accurate data for quantitation [1]. This real-time monitoring capability, combined with the technique's exceptional sensitivity (detection down to a single copy) and broad dynamic range, has established qPCR as a cornerstone technology in modern molecular diagnostics [1].
Core Principles of Real-Time Detection
The qPCR Workflow and Kinetic Phases
The qPCR process follows three distinct kinetic phases that are crucial for understanding its quantification capabilities. The exponential phase represents the ideal period for quantification, where exact doubling of product occurs at every cycle (assuming 100% reaction efficiency) [1]. During this phase, all reagents are fresh and available, and the reaction kinetics favor amplicon doubling. The linear phase follows as some reagents become consumed, causing the reaction to slow down so the PCR product is no longer doubled at each cycle [1]. Finally, the plateau phase occurs when the reaction stops entirely, and if left long enough, PCR products begin to degrade [1].
Traditional PCR methods take measurements at this plateau phase, which provides poor quantification because each reaction reaches plateau at different points due to varying reaction kinetics [1]. qPCR fundamentally improves upon this by focusing measurement during the exponential phase, where the relationship between the number of amplification cycles and the amount of product is most predictable and reproducible.
Fluorescence Detection and Cq Values
The real-time monitoring capability of qPCR is enabled by fluorescent reporter molecules that track PCR product accumulation. As the quantity of target amplicon increases, so does the amount of fluorescence emitted from the fluorophore [1]. The key quantitative measurement in qPCR is the Cq (quantification cycle) value, defined as the PCR cycle at which the sample's fluorescence intensity crosses a predetermined threshold above background levels [1].
The relationship between Cq and starting quantity is inverse and logarithmic: samples with higher starting concentrations of the target sequence will display lower Cq values, as they require fewer cycles to reach the detection threshold. This fundamental relationship enables precise quantification through the comparison of Cq values between samples and standards [3].
Critical Parameters for Accurate Quantification
Baseline Correction and Threshold Setting
Accurate Cq determination relies on proper baseline correction and threshold setting. The baseline represents background fluorescence during initial cycles before detectable amplification occurs, typically calculated from cycles 5-15 [3]. Proper baseline correction is essential because background fluorescence variations can significantly impact Cq values—incorrect baseline settings can cause Cq value variations of multiple cycles [3].
The threshold should be set high enough to be above background fluorescence but within the exponential phase of all amplification plots [3]. When amplification plots display parallel logarithmic phases, the specific threshold position doesn't affect relative quantification between samples (ΔCq), but when plots aren't parallel due to efficiency differences at higher Cq values, threshold positioning becomes critical for accurate quantification [3].
Table 1: Critical Parameters for qPCR Data Analysis
| Parameter | Optimal Setting | Impact on Quantification | Common Issues |
|---|---|---|---|
| Baseline Correction | Cycles 5-15 or the last pre-amplification cycle | Corrects for background fluorescence variations | Incorrect cycles can shift Cq values by multiple cycles [3] |
| Threshold Setting | Above background, within parallel exponential phases | Determines Cq value for quantification | Non-parallel amplification curves make ΔCq threshold-dependent [3] |
| Cq Value | Cycle where fluorescence crosses threshold | Inverse log relationship to starting quantity | High Cq values (>35) show increased variability and reduced precision [3] |
| Amplification Efficiency | 90-110% (ideal: 100%) | Affects accuracy of quantification calculations | Efficiency outside range reduces sensitivity and linear dynamic range [1] |
Detection Chemistries and Mechanisms
DNA-Binding Dyes: SYBR Green Chemistry
SYBR Green-based qPCR represents the simpler of the two main detection approaches. The SYBR Green I dye binds to the minor groove of all newly synthesized double-stranded DNA complexes and fluoresces when bound [4]. As PCR cycling continues, fluorescence accumulates and is measured at the end of each PCR cycle [4]. The primary advantage of this method is that it monitors amplification of any double-stranded DNA sequence without requiring target-specific probes, reducing assay setup and running costs [4]. Additionally, multiple dye molecules can bind to a single amplified molecule, increasing sensitivity for detecting amplification products [4].
The main limitation of SYBR Green chemistry is its lack of inherent specificity—it detects all double-stranded DNA, including non-specific products and primer-dimers. This necessitates careful assay optimization and melt curve analysis to verify reaction specificity.
Target-Specific Probes: TaqMan Chemistry
Probe-based qPCR, commonly implemented as TaqMan chemistry (also known as "fluorogenic 5´ nuclease chemistry"), provides higher specificity through the use of target-specific probes [1]. These probes are oligonucleotides complementary to the target sequence, labeled with both a reporter fluorophore and a quencher molecule [4]. When intact, the proximity of the quencher suppresses reporter fluorescence through Fluorescence Resonance Energy Transfer (FRET). During the extension phase of PCR, the DNA polymerase displaces and cleaves the probe, separating the reporter from the quencher and resulting in measurable fluorescence [4].
The targeted nature of probe-based qPCR leads to low background and eliminates false positives from non-specific amplification [4]. Additionally, probes can be labeled with different, distinguishable reporter dyes to allow for amplification of two distinct sequences in one reaction tube (duplex PCR) or even more targets in multiplex configurations [4] [1].
Table 2: Comparison of qPCR Detection Chemistries
| Characteristic | SYBR Green Chemistry | TaqMan Probe Chemistry |
|---|---|---|
| Specificity | Lower - binds any dsDNA | Higher - requires specific hybridization |
| Cost | Lower - no probe required | Higher - requires labeled probe |
| Setup Complexity | Simple | More complex - requires probe design |
| Multiplexing Capability | None - single target per reaction | Yes - multiple targets with different dyes |
| Background Signal | Higher - binds non-specific products | Lower - specific cleavage required |
| False Positives | Possible from primer-dimers | Minimal with proper design |
| Optimal Use Cases | Single target studies, cost-sensitive applications | Multiplexing, high-specificity requirements |
Advanced Multiplexing Strategies
Multicolor Combinatorial Probe Coding (MCPC)
The MCPC strategy represents a significant innovation in qPCR multiplexing capability. This approach uses a limited number (n) of differently colored fluorophores in various combinations to label each probe, enabling detection of up to 2^n-1 genetic targets in one reaction [5]. For example, with four different fluorophores, the maximum number of uniquely labeled probes is 15 (four with single colors, six with two-color combinations, four with three-color combinations, and one with all four colors) [5].
The MCPC strategy is particularly valuable for applications where only one out of many potential targets needs to be identified, such as in pathogen identification from normally sterile sites (e.g., blood) or genetic disease diagnosis where coexistence of multiple genotypes in the same sample is rare [5]. The proof-of-principle of MCPC was validated by identification of one of 15 possible human papillomavirus types in one reaction using a 4-color channel instrument [5].
Technical Implementation of MCPC
Implementing MCPC requires careful experimental design. To make one probe labeled with a combination of different colors, the most practical approach is to mix equal molar quantities of probes each labeled with a single but different color to function as a single probe set [5]. Each combinatorially labeled probe receives a unique digital code (MCPC signature) for identification [5].
A key challenge in highly multiplexed PCR is maintaining analytical sensitivity, as heavily multiplexed settings often experience significant decreases in sensitivity compared to uniplex PCRs [5]. This can be addressed through strategies like the Homo-Tag Assisted Non-Dimer (HAND) system, which alleviates primer dimer formation by designing primers so that if dimerization occurs, it forms separate hairpin structures that hinder further amplification rather than double-stranded structures that amplify efficiently [5]. This approach has demonstrated the ability to improve analytical sensitivity of a 10-plex MCPC assay to the same level as uniplex real-time PCR [5].
Quantitative Analysis Methods
Absolute vs. Relative Quantification
qPCR supports two primary quantification approaches: absolute and relative quantification. Absolute quantification determines the exact copy number or concentration of a target sequence in a sample using a standard curve with known concentrations [3] [1]. This method requires running additional external standards alongside test samples and careful selection of standard curve material that matches the amplification efficiency of the target [3].
Relative quantification compares the expression level of a target gene between different samples without determining absolute copy numbers [1]. The data output is typically expressed as fold-change or fold-difference, such as when comparing gene expression in treated versus untreated samples [1]. Relative quantification is generally more practical for gene expression studies where the exact copy number is less important than the change in expression levels between conditions.
The ΔΔCq Method for Relative Quantification
The comparative CT (ΔΔCT) method is widely used for relative quantitation of gene expression [1]. This approach uses the formula 2^(-ΔΔCT) to calculate fold changes in gene expression relative to a reference sample [6]. The calculation involves two key normalization steps: first, normalization to an endogenous control (reference gene) to account for variations in RNA input and reverse transcription efficiency (ΔCT = CT,target - CT,reference); and second, normalization to a calibrator sample (such as untreated control) to calculate the ΔΔCT value (ΔΔCT = ΔCT,test - ΔCT,calibrator) [6].
This method originally assumed 100% PCR efficiency for all reactions, meaning a ΔC_T of 1 represented a 2-fold difference in target quantity [3]. However, the efficiency-adjusted (Pfaffl) model improves accuracy by incorporating actual PCR efficiencies determined from standard curves, replacing the factor of 2 with the actual efficiency values for both target and reference genes [3].
Standard Curve Quantification
The standard curve method involves generating a dilution series of standards with known concentrations and plotting their Cq values against the logarithm of concentration [3]. This creates a linear relationship from which unknown sample concentrations can be interpolated [3]. When using plasmid DNA as standards, consistency in DNA conformation is critical—supercoiled versus linearized plasmids can yield different Cq values, and plasmid preparations should be handled consistently to avoid variations caused by freeze/thaw cycles and pipetting shearing forces [6].
Table 3: Quantitative Analysis Methods in qPCR
| Method | Principle | Applications | Requirements | Limitations |
|---|---|---|---|---|
| Standard Curve (Absolute) | Interpolates unknowns from standards of known concentration | Viral load quantification, pathogen counting | Standard curve with known concentrations | Requires accurate standard quantification [6] |
| Comparative C_T (Relative) | 2^(-ΔΔC_T) calculation normalized to reference genes | Gene expression studies, fold-change analysis | Validated reference genes, similar amplification efficiencies | Assumes optimal and similar reaction efficiencies [6] |
| Efficiency-Adjusted (Pfaffl) | Incorporates actual PCR efficiency values | High-accuracy gene expression studies | Standard curves for efficiency determination | More complex calculations [3] |
| Multiplex Relative | Simultaneous target/reference amplification in same well | High-precision clinical diagnostics | Optimized multiplex conditions, different fluorescent dyes | Complex optimization, potential interference [1] |
The Scientist's Toolkit: Essential Reagents and Materials
Table 4: Essential Research Reagent Solutions for qPCR
| Reagent/Material | Function | Key Considerations | Application Context |
|---|---|---|---|
| SYBR Green Dye | Binds double-stranded DNA nonspecifically | Cost-effective but requires specificity verification | General gene expression, genotyping [4] |
| TaqMan Probes | Target-specific hybridization and cleavage | Higher specificity but more expensive | High-specificity applications, multiplexing [1] |
| HEX (Hexachlorofluorescein) | Fluorescent dye for probe labeling | Excitation: 533 nm, Emission: 549 nm | Multiplexing, internal controls [7] |
| Reverse Transcriptase | Converts RNA to cDNA for gene expression | Choice affects efficiency and representation | Gene expression analysis (RT-qPCR) [1] |
| Hot-Start DNA Polymerase | Reduces non-specific amplification | Activated at high temperatures | Improves specificity, especially in multiplex [5] |
| dNTPs | Building blocks for DNA synthesis | Quality affects amplification efficiency | All qPCR applications |
| Primers | Target sequence recognition | Specificity, efficiency, dimer formation potential | All qPCR applications [6] |
| Reference Genes | Normalization controls | Must be stable across experimental conditions | Gene expression normalization [6] |
Best Practices and Quality Control
MIQE Guidelines and Experimental Rigor
The Minimum Information for Publication of Quantitative Real-Time PCR Experiments (MIQE) guidelines, established by Stephen Bustin and colleagues, have become the essential framework for standardizing qPCR experiments to ensure reproducibility and reliability [6]. These guidelines serve as a comprehensive checklist for assay development and reporting, covering essential information such as primer and probe sequences, reaction conditions, and any modifications to commercial kits [6]. Adherence to MIQE guidelines is particularly crucial in molecular diagnostics and personalized medicine research, where results may inform clinical decisions.
Key considerations highlighted in best practices include subsampling error due to pipetting aliquots of nucleic acid extract, quality control of experiments using internal controls to monitor PCR inhibition, and evaluation of the end-to-end procedure including consistent storage and handling of biological samples [6]. For multiplexing applications, additional considerations include dye compatibility in a single tube and off-target amplification of primers [6].
Reference Gene Validation
Proper normalization using validated reference genes (often called housekeeping genes) is critical for accurate gene expression analysis. The common assumption that reference genes maintain constant expression across all experimental conditions is often incorrect—so-called housekeeping genes can vary in their expression levels and can be affected by different experimental conditions or treatments [6]. Using an inappropriate reference gene can significantly distort results, as demonstrated in case studies comparing TLR2 gene expression normalized against different housekeeping genes [6].
The geometric averaging of multiple internal control genes, as proposed by Vandesompele et al., provides a more robust normalization approach [6]. This method recommends using at least three validated reference genes to normalize RT-qPCR results, substantially improving quantification accuracy [6]. The specific reference genes selected should be appropriate for the source tissue or cell line and should be empirically validated for stability under the specific experimental conditions.
Efficiency Optimization and Validation
PCR amplification efficiency directly impacts quantification accuracy. The recommended amplification efficiency for reliable assays is between 90-110%, with ideal efficiency at 100% [1]. Less efficient assays result in reduced sensitivity and linear dynamic range, limiting the ability to detect low-abundance transcripts [1]. Efficiency should be determined using standard curve analysis with the formula: Efficiency = [10^(-1/slope) - 1] × 100% [6].
Factors affecting efficiency include primer design, template quality, reaction conditions, and inhibitor presence. Efficiency validation should be performed for each new assay and periodically verified, especially when using the assay in different sample matrices or after reagent lot changes. For gene expression studies, both target and reference gene assays should have similar efficiencies to ensure accurate ΔΔC_T calculations [6].
The core technology of real-time amplification and quantification represents a sophisticated integration of biochemical principles, optical detection systems, and computational analysis. From the fundamental fluorescence detection mechanisms to advanced multiplexing strategies like MCPC, qPCR technology continues to evolve, pushing the boundaries of what's possible in molecular quantification. The precision of Cq determination through proper baseline correction and threshold setting, combined with robust quantification methods like the efficiency-adjusted ΔΔC_T calculation, enables researchers to obtain reliable, reproducible data essential for both basic research and clinical applications.
In the context of molecular diagnostics and personalized medicine, these technological foundations support increasingly sophisticated applications—from cancer companion diagnostics that blur the lines between diagnosis and treatment, to liquid biopsy approaches for minimal residual disease testing [2]. As the field advances with innovations in artificial intelligence, digital PCR, and single-cell analysis, the core principles of real-time amplification and quantification remain fundamental to extracting meaningful biological insights from minute quantities of genetic material, ultimately supporting more precise and personalized healthcare interventions.
The global diagnostic landscape is undergoing a profound transformation, driven by technological advancements and a paradigm shift toward personalized medicine. At the heart of this transformation lies quantitative polymerase chain reaction (qPCR) technology, a cornerstone of molecular diagnostics that enables precise amplification and quantification of nucleic acids in real-time. The integration of qPCR into clinical and research workflows has catalyzed advancements across infectious disease detection, oncology, genetic disorder testing, and pharmacogenomics, establishing it as an indispensable tool in modern biomedical science. This whitepaper provides a comprehensive analysis of the multi-billion dollar qPCR instruments market, examining its growth trajectory, key technological trends, regional dynamics, and future opportunities. Framed within the broader context of molecular diagnostics and personalized medicine research, this analysis offers drug development professionals and researchers a detailed assessment of how qPCR continues to evolve and integrate with emerging technologies to address complex diagnostic challenges.
The qPCR instruments market represents a substantial and rapidly expanding segment of the broader molecular diagnostics landscape. Current market evaluations indicate robust growth driven by increasing adoption across clinical diagnostics, pharmaceutical research, and academic institutions. The global qPCR instruments market was valued at approximately USD 1.76 billion in 2024 and is projected to reach USD 5.5 billion by 2033, growing at a compound annual growth rate (CAGR) of 13.5% during the forecast period (2025-2033) [8]. Alternative market assessments that include related technologies provide additional context for this growth trajectory, with the combined digital PCR (dPCR) and real-time PCR (qPCR) market size calculated at USD 10.15 billion in 2024 and projected to reach USD 21.87 billion by 2034, reflecting a CAGR of 7.97% [9]. When considering the even broader PCR technologies market (encompassing instruments, reagents, and services), market size was approximately USD 15.78 billion in 2024 and is predicted to increase to USD 31.39 billion by 2034, expanding at a CAGR of 7.12% from 2025 to 2034 [10].
Table 1: qPCR Instruments Market Size Projections
| Market Segment | 2024 Base Value | Projected Value | Time Period | CAGR | Source |
|---|---|---|---|---|---|
| qPCR Instruments Market | USD 1.76 billion | USD 5.5 billion | 2025-2033 | 13.5% | [8] |
| dPCR & qPCR Combined Market | USD 10.15 billion | USD 21.87 billion | 2024-2034 | 7.97% | [9] |
| Overall PCR Technologies Market | USD 15.78 billion | USD 31.39 billion | 2024-2034 | 7.12% | [10] |
This growth is fueled by several key factors, including the rising prevalence of infectious diseases, increasing application of qPCR in oncology and genetic testing, expanding research in genomics and biomarker discovery, and the ongoing shift toward personalized medicine [8] [10]. The COVID-19 pandemic served as a significant catalyst, accelerating the adoption of qPCR technology and driving massive infrastructure investments in clinical laboratories worldwide [11]. This established foundation continues to support market expansion as laboratories apply existing qPCR capabilities to new diagnostic applications beyond pandemic response.
Key Market Dynamics
Growth Drivers
The expansion of the qPCR market is underpinned by several powerful drivers that create sustained demand for molecular diagnostic solutions:
Rising Infectious Disease Burden: The increasing global prevalence of infectious diseases such as HIV, tuberculosis, hepatitis, and respiratory infections continues to drive demand for rapid, accurate diagnostic tools. The World Health Organization reports approximately 40.8 million people were living with HIV globally in 2024, with 630,000 deaths from HIV-related illnesses, creating substantial need for sensitive detection methods [10]. qPCR's ability to identify pathogens from minimal genetic material with high sensitivity has established it as the gold standard for infectious disease detection.
Expansion in Oncology and Genetic Testing: qPCR is increasingly utilized in cancer diagnostics for mutation detection, gene expression profiling, and liquid biopsy applications. The technology enables identification of cancer biomarkers, gene mutations, and hereditary conditions, facilitating early detection and informed treatment decisions [10]. The growing incidence of cancer worldwide and advancements in liquid biopsy methods are further solidifying qPCR's role in oncology workflows [9].
Advancements in PCR Platforms: Continuous innovation in qPCR technology, including improvements in sensitivity, speed, automation, and multiplexing capabilities, continues to drive market growth. The development of high-throughput systems, advanced optics, microfluidics, and automation technologies has enhanced performance while expanding the range of applications [8]. These innovations make qPCR increasingly adaptable to various settings, from research laboratories to point-of-care diagnostics.
Growing Emphasis on Personalized Medicine: The shift toward personalized healthcare approaches, which accounted for a market projected to reach nearly $590 billion by 2028, drives demand for molecular diagnostic tools that can guide tailored therapeutic interventions [12]. qPCR plays a critical role in genetic testing and drug development, supporting the trend toward treatments customized to individual genetic profiles.
Market Challenges and Restraints
Despite strong growth prospects, the qPCR market faces several significant challenges that may impact broader adoption:
High Instrumentation Costs: The substantial upfront investment required for qPCR systems presents a barrier to adoption, particularly for smaller research institutions and laboratories in resource-limited settings. High-end qPCR instruments were priced between $30,000 and $50,000 in 2022, with additional annual expenses of $15,000 to $25,000 for maintenance, consumables, and reagents [8]. These costs can be prohibitive for organizations with constrained budgets.
Technical Complexity and Operational Challenges: qPCR workflows require specialized technical expertise for assay design, validation, and data interpretation. The technology remains susceptible to issues such as PCR inhibition, sample contamination, and reagent compatibility problems [13]. The requirement for precise normalization against reference genes and the use of standard curves can introduce variability in quantification, potentially affecting result reproducibility [14].
Risk of False Positive Results: Concerns about potential false positives, particularly at high cycle threshold (Ct) values or due to sample contamination, present challenges for large-scale screening applications. Analyses indicate that PCR performed at Ct values exceeding 35-40 cycles may detect residual viral fragments rather than live virus, potentially leading to misleading diagnostic conclusions [10]. These concerns have prompted regulatory bodies to impose stricter protocols that may increase operational complexity and costs.
Competition from Alternative Technologies: While qPCR remains a cornerstone technology, it faces increasing competition from emerging methods such as next-generation sequencing (NGS), which offers broader genomic coverage and the ability to detect novel variants without prior sequence knowledge [12]. Digital PCR (dPCR) also presents competition for applications requiring absolute quantification or detection of rare mutations, as it provides enhanced precision for low-abundance targets [9] [14].
Technological Trends and Innovations
The qPCR landscape is evolving rapidly through multiple technological advancements that enhance performance, expand applications, and improve accessibility:
Automation and High-Throughput Systems: The integration of automation technologies is transforming qPCR workflows by increasing processing capacity, reducing manual intervention, and improving reproducibility. High-throughput systems can increase sample processing capacity by up to 80% compared to traditional methods, significantly reducing both time and costs [8]. Automated solutions are particularly valuable for clinical laboratories with high testing volumes and for applications in drug development and biomarker validation.
Multiplexing Capabilities: Advanced multiplex qPCR systems enable simultaneous detection and quantification of multiple targets in a single reaction, conserving precious samples while providing comprehensive pathogen profiling. This capability is especially valuable for infectious disease panels that differentiate between pathogens with similar symptoms, such as influenza and SARS-CoV-2 [11], and for oncology applications requiring parallel assessment of multiple biomarkers [13].
Point-of-Care and Portable Systems: The development of compact, portable qPCR systems is extending molecular diagnostics beyond central laboratories to decentralized settings such as clinics, field locations, and resource-limited areas. This trend addresses the growing demand for rapid, on-site testing and supports global health initiatives aimed at making molecular testing accessible in underserved regions [10]. Companies including Bio-Rad Laboratories have announced developments in portable Droplet Digital PCR (ddPCR) platforms suitable for point-of-care use [10].
Integration of Artificial Intelligence: AI and machine learning algorithms are increasingly being applied to optimize qPCR assay design, enhance data analysis, and improve diagnostic accuracy. These technologies enable real-time analysis of complex gene expression patterns, reduce turnaround times, and minimize the risk of human error [13] [9]. AI-powered systems also show promise in identifying subtle patterns in amplification curves that may not be detectable through conventional analysis methods.
Digital PCR Convergence: The boundaries between qPCR and digital PCR (dPCR) are blurring as technologies evolve and converge. dPCR provides absolute quantification of nucleic acids without requiring standard curves, offering advantages for detecting rare mutations, copy number variations, and minimal residual disease [14]. The emerging hybrid platforms combine the quantitative capabilities of qPCR with the precision of dPCR, particularly benefiting applications in oncology and liquid biopsy [13].
Table 2: Comparison of PCR-Based Technologies
| Parameter | qPCR | Digital PCR (dPCR) | Next-Generation Sequencing (NGS) |
|---|---|---|---|
| Quantification Approach | Relative quantification using standard curves | Absolute quantification by Poisson statistics | Relative or absolute with standards |
| Sensitivity | High (detects down to few copies) | Very high (detects single molecules) | Variable (depends on coverage depth) |
| Multiplexing Capability | Moderate (typically 4-6 targets) | Moderate | High (hundreds to thousands of targets) |
| Throughput | High | Moderate to High | Very High |
| Primary Applications | Gene expression, pathogen detection, routine diagnostics | Rare mutation detection, copy number variation, liquid biopsy | Variant discovery, comprehensive genomic profiling, transcriptomics |
| Cost per Sample | Low to Moderate | Moderate | Moderate to High |
| Infrastructure Requirements | Standard molecular biology lab | Specialized instrumentation | Specialized instrumentation and bioinformatics |
Regional Market Analysis
The qPCR instruments market demonstrates distinct regional patterns influenced by varying levels of healthcare infrastructure, research funding, regulatory frameworks, and adoption of molecular diagnostics:
North America: North America dominates the global qPCR instruments market, accounting for approximately 44% of the broader PCR technologies market share in 2024 [10]. This leadership position is attributed to well-established biotechnology and pharmaceutical industries, extensive research and development activities, strong focus on genomic and molecular diagnostics, and significant investments in personalized medicine [8]. The region benefits from numerous collaborations between industry and academic research institutes, advanced healthcare IT infrastructure, and high rates of automation in PCR technologies. The United States represents the largest market within North America, driven by continuing investments in molecular diagnostics, life sciences research, and infectious disease surveillance [13].
Europe: Europe represents a significant and rapidly growing market for qPCR instruments, characterized by robust emphasis on life sciences research and advanced diagnostic technologies. Germany, the United Kingdom, and France are pivotal contributors, supported by strong research infrastructure and substantial investments in molecular biology [8]. Europe's stringent regulatory frameworks, particularly the In Vitro Diagnostic Regulation (IVDR), impose rigorous requirements on diagnostic devices, driving demand for sophisticated qPCR instruments that comply with these standards [13]. The European Molecular Biology Organization (EMBO) underscores the region's significant market presence, attributing this to leadership in genetic and genomic research.
Asia-Pacific: The Asia-Pacific region represents the fastest-growing market for qPCR technologies, with expanding production capabilities, government-driven innovation programs, and increasing healthcare expenditures [10]. Growth is particularly strong in China, India, Japan, and South Korea, supported by government spending on public health laboratories, infectious disease control, and biotech innovation ecosystems [13]. China is expanding its domestic qPCR manufacturing capacity and scaling lab automation in hospitals, while countries like India are implementing qPCR for tuberculosis, dengue, and cancer screening programs [13]. Japan's market is supported by innovations in precision medicine and demands of an aging population, while South Korea benefits from government-funded genomics initiatives and growing biotech clusters [13].
Latin America and Middle East & Africa: These regions are witnessing gradual market progression, supported by improving economic conditions, rising urbanization, and growing awareness of advanced diagnostic solutions [15]. The COVID-19 pandemic significantly accelerated qPCR infrastructure development in many of these regions; for example, Nigeria expanded from four to seventy-two qPCR-capable laboratories between January 2020 and January 2021 [11]. This expanded capacity creates opportunities for applying qPCR to other public health challenges, though resource constraints and infrastructure limitations continue to present challenges for widespread adoption.
Applications in Personalized Medicine and Clinical Trials
qPCR technology plays an increasingly vital role in advancing personalized medicine and optimizing clinical trial designs across multiple therapeutic areas:
Biomarker-Guided Therapeutic Strategies
The development of biomarker-guided personalized therapies represents a paradigm shift in oncology and other therapeutic areas, with qPCR serving as an essential tool for patient stratification and treatment selection. Clinical trial designs have evolved to incorporate biomarker-based enrichment strategies that selectively enroll patients most likely to respond to targeted therapies [16]. These approaches use qPCR and related molecular techniques to identify relevant biomarkers, including individual genes, proteins, or gene expression signatures that predict therapeutic response [16]. The successful implementation of these strategies requires careful consideration of biomarker measurement technologies (e.g., quantitative RT-PCR, immunohistochemistry, phospho-flow) and appropriate clinical trial designs (e.g., biomarker-stratified, enrichment, or adaptive designs) to validate biomarker-therapy relationships [16].
Pharmacogenomics and Treatment Optimization
qPCR enables pharmacogenomic profiling that guides drug selection and dosing based on individual genetic variations affecting drug metabolism and response. Applications include determining cytochrome P450 enzyme polymorphisms that influence drug metabolism, identifying genetic variants associated with drug efficacy or adverse effects, and monitoring expression of drug target genes [14]. These approaches help optimize medication regimens, reduce adverse drug reactions, and improve therapeutic outcomes—core objectives of personalized medicine implementation.
Clinical Trial Monitoring and Endpoint Assessment
qPCR supports multiple aspects of clinical trial execution, from patient screening to endpoint assessment across various therapeutic modalities:
Oncology Trials: qPCR facilitates detection of circulating tumor DNA (ctDNA) for minimal residual disease monitoring, quantification of gene expression changes in response to targeted therapies, and validation of biomarker status for patient stratification [14]. The technology's sensitivity and quantitative capabilities make it particularly valuable for assessing pharmacodynamic biomarkers and early response indicators.
Gene and Cell Therapy Trials: qPCR applications in advanced therapy medicinal products include vector copy number determination, biodistribution studies, detection of replication-competent viruses, and transgene expression analysis [17]. These applications support dose-finding, safety assessment, and efficacy evaluation throughout clinical development.
Exon-Skipping Therapies: For neuromuscular disorders such as Duchenne muscular dystrophy (DMD), qPCR and digital PCR enable precise quantification of exon-skipping efficiency in response to antisense oligonucleotide therapies [14]. These methods provide absolute counts of skipped and non-skipped transcript isoforms, supporting therapeutic response monitoring and dose optimization in clinical trials.
Companion Diagnostic Development
qPCR serves as a platform for developing and implementing companion diagnostics that identify patients likely to benefit from specific targeted therapies. These assays detect genetic mutations, gene amplifications, or expression signatures that predict response to targeted agents, enabling more precise therapeutic targeting and improving drug development efficiency [16]. The speed, reproducibility, and regulatory familiarity with qPCR platforms facilitate the translation of biomarker assays into validated companion diagnostics suitable for clinical deployment.
Experimental Protocols and Methodologies
qPCR Assay Design and Validation
Robust qPCR assay design requires careful attention to multiple parameters to ensure specificity, sensitivity, and reproducibility:
Primer and Probe Design: Primers should be 18-22 nucleotides long with GC content between 40-60%, melting temperatures (Tm) of 58-60°C, and amplicon lengths of 75-150 base pairs for optimal efficiency [14]. Probe-based systems (e.g., TaqMan) require fluorescence-quencher combinations with minimal spectral overlap and should be positioned to avoid polymorphic regions or secondary structures.
Validation Parameters: Each qPCR assay requires comprehensive validation including:
- Amplification Efficiency: Determined from standard curve slope (ideal range: 90-110%)
- Dynamic Range: Typically 5-7 orders of magnitude for quantitative applications
- Limit of Detection (LOD) and Limit of Quantification (LOQ): Established through dilution series
- Specificity: Verified by melt curve analysis (for SYBR Green) or sequence verification
- Reproducibility: Assessed through intra- and inter-assay coefficient of variation [14]
Reference Gene Selection: Appropriate reference genes (e.g., GAPDH, β-actin, ribosomal genes) should demonstrate stable expression across experimental conditions and be validated using algorithms such as geNorm or NormFinder [14]. The use of multiple reference genes is recommended for improved normalization accuracy.
Liquid Biopsy Analysis Using dPCR
Droplet Digital PCR (ddPCR) provides enhanced sensitivity for liquid biopsy applications requiring detection of rare mutations in circulating tumor DNA:
Sample Preparation: Cell-free DNA is extracted from 4-10 mL of plasma using specialized kits designed for low-abundance targets. Input DNA is quantified by fluorometry to determine appropriate partitioning density [14].
Droplet Generation and Amplification: The reaction mixture is partitioned into 10,000-20,000 nanoliter-sized droplets using a droplet generator. PCR amplification is performed with mutation-specific probes and reference assays with cycling conditions optimized for target sequence and background wild-type DNA [14].
Droplet Reading and Analysis: Following amplification, droplets are streamed through a fluorescence reader that categorizes each droplet as positive (mutant), positive (reference), double-positive, or negative. Absolute quantification is calculated using Poisson statistics to account for multiple targets per droplet [14].
Validation and Quality Control: Assay validation includes determination of false-positive rate in control samples, analytical sensitivity using dilution series in wild-type background, and establishment of threshold for positive calls (typically ≥3 positive droplets for rare variant detection) [14].
Liquid Biopsy dPCR Workflow
Biomarker Stratification in Clinical Trials
Implementation of biomarker-guided strategies in clinical trials requires specific methodological considerations:
Biomarker Assay Development: Biomarker measurements should demonstrate analytical validity with established performance characteristics including sensitivity, specificity, reproducibility, and pre-defined cutoffs for patient stratification [16]. The choice of technology (qPCR, dPCR, NGS) depends on the nature of the biomarker, required sensitivity, and sample type.
Adaptive Randomization Designs: Bayesian adaptive randomization approaches use accumulating response data to preferentially assign patients to more effective treatments based on their biomarker profile [16]. These designs require real-time biomarker assessment and statistical models that update treatment allocation probabilities as trial data accumulates.
Enrichment Design Considerations: Enrichment designs that restrict enrollment to biomarker-positive patients require careful consideration of biomarker prevalence, assay performance characteristics, and potential for biomarker false negatives that could exclude potentially responsive patients [16].
The Scientist's Toolkit: Essential Research Reagent Solutions
Successful implementation of qPCR-based assays requires careful selection of reagents and consumables optimized for specific applications:
Table 3: Essential Research Reagent Solutions for qPCR Applications
| Reagent Category | Key Functions | Application Notes | Representative Products |
|---|---|---|---|
| Master Mixes | Provides buffer, enzymes, dNTPs for amplification | Formulations with dUTP prevent carryover contamination; lyo-ready versions enable ambient-temperature stability | dUTP master mixes, Lyo-Ready master mixes [12] |
| Polymerase Systems | Catalyzes DNA amplification during thermal cycling | Hot-start versions reduce non-specific amplification; high-concentration, glycerol-free formulations compatible with lyophilization | High-concentration, glycerol-free enzymes [12] |
| Fluorescent Probes & Dyes | Enables real-time detection of amplification | Intercalating dyes (SYBR Green) for general use; sequence-specific probes (TaqMan) for multiplexing; minimal spectral overlap in multiplex panels | Hydrolysis probes, intercalating dyes [14] |
| Sample Preparation Kits | Nucleic acid extraction and purification | Specialized formulations for different sample types (blood, tissue, cells); optimized for low-abundance targets in liquid biopsy | cfDNA extraction kits, RNA extraction kits [14] |
| Reference Assays | Normalization and quality control | Pre-validated reference genes; DNA quality assessment assays; RNA integrity number (RIN) measurement | Reference gene panels, DNA/RNA quality control assays [14] |
| NGS Library Prep | Complementary technology integration | Enables sequential qPCR-NGS workflows; glycerol-free formulations reduce cost and improve portability | Glycerol-free NGS library preparation kits [12] |
Future Outlook and Strategic Directions
The qPCR instruments market continues to evolve through technological convergence, expanding applications, and shifting market dynamics:
Technology Integration and Hybrid Approaches: The future qPCR landscape will be characterized by increased integration with complementary technologies, particularly NGS and dPCR. Hybrid approaches that leverage the speed and cost-effectiveness of qPCR for initial screening followed by the comprehensive profiling capabilities of NGS for complex cases are emerging as efficient diagnostic pathways [12]. Similarly, qPCR-dPCR combinations enable initial quantification followed by highly sensitive detection of rare variants, particularly in oncology and infectious disease monitoring [13].
Digital Transformation and Connectivity: Next-generation qPCR platforms will increasingly incorporate digital features including cloud connectivity, remote device management, blockchain-based result verification, and integration with patient-linked genomic databases [13]. These capabilities support decentralized testing models, real-time epidemiological mapping, and enhanced data security while facilitating collaboration across distributed research networks.
Sustainability Initiatives: Growing emphasis on environmental impact is driving development of reusable consumables, low-energy thermocyclers, and eco-friendly reagent packaging [13]. These initiatives address concerns about single-use plastics and energy consumption while potentially reducing long-term operational costs through reusable components and reduced waste streams.
Expansion in Non-Traditional Applications: qPCR technology is expanding beyond traditional clinical and research settings into veterinary diagnostics, environmental biosensing, food safety testing, and synthetic biology workflows [13]. These emerging applications represent new growth avenues while contributing to one health approaches that integrate human, animal, and environmental health monitoring.
Personalized Medicine Integration: As personalized medicine continues to evolve, qPCR will play an increasingly critical role in routine clinical practice through companion diagnostics, therapy monitoring, and population health screening programs. The technology's versatility, established regulatory pathways, and relatively low cost position it as an enabling platform for the broad implementation of genetically-guided healthcare [12].
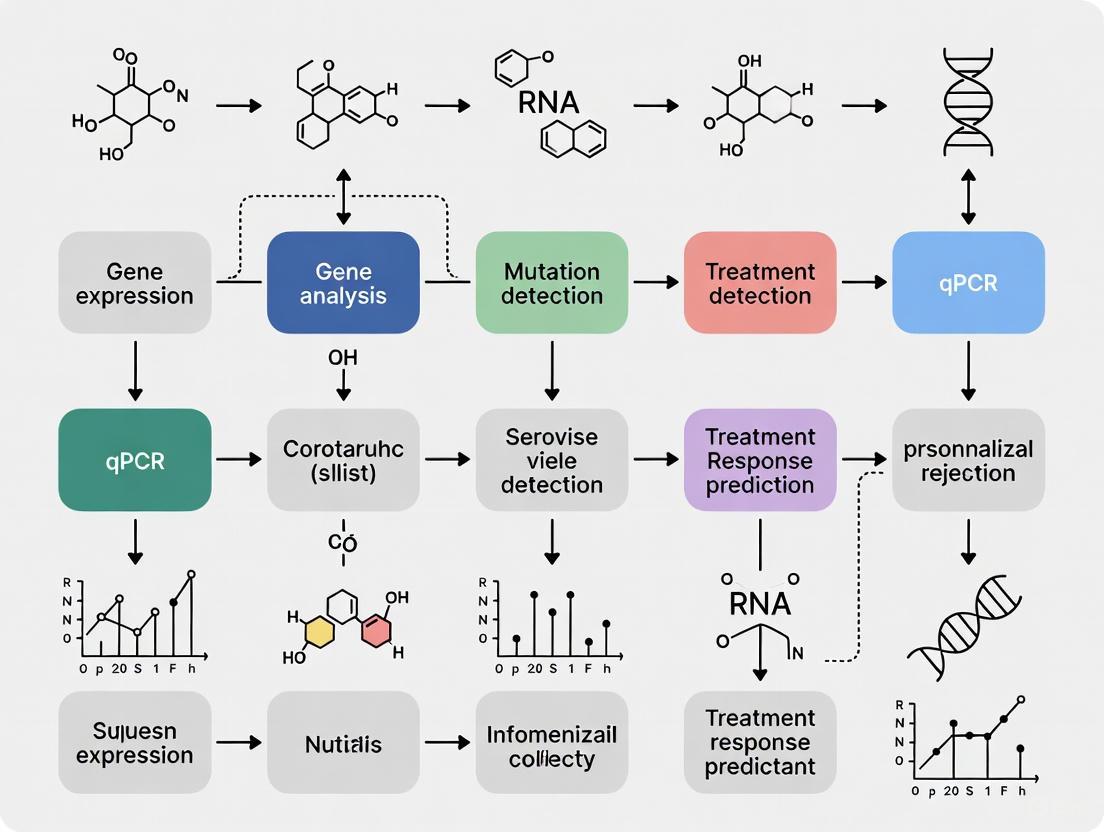
Future qPCR Technology Directions
The qPCR instruments market represents a dynamic and expanding segment of the global diagnostic landscape, characterized by continuous technological innovation and broadening applications across healthcare and research. With projected growth to USD 5.5 billion by 2033 and a robust CAGR of 13.5%, the market demonstrates strong momentum driven by infectious disease testing, oncology applications, personalized medicine initiatives, and expanding research capabilities. The convergence of qPCR with emerging technologies including artificial intelligence, digital PCR, and next-generation sequencing creates new opportunities for enhanced diagnostic precision and comprehensive genomic analysis. Despite challenges related to cost, complexity, and competition from alternative technologies, qPCR maintains its position as a cornerstone of molecular diagnostics through continuous innovation, established regulatory pathways, and proven utility across diverse applications. For researchers, scientists, and drug development professionals, understanding the evolving qPCR landscape is essential for leveraging this technology to advance personalized medicine, optimize therapeutic development, and address emerging diagnostic challenges in an increasingly precision-focused healthcare environment.
The fields of molecular diagnostics and personalized medicine are undergoing a rapid transformation, driven by converging technological advancements and pressing clinical needs. This whitepaper examines the two key drivers—the rise of personalized medicine and the growing demand for rapid infectious disease testing—that are shaping the current and future landscape of molecular diagnostics, with a specific focus on the role of qPCR (quantitative Polymerase Chain Reaction) technology. For researchers and drug development professionals, understanding this synergistic relationship is critical for developing next-generation diagnostic and therapeutic strategies. The integration of genetic, environmental, and lifestyle data enables a shift from a one-size-fits-all model to tailored approaches that improve patient outcomes, particularly in complex areas like oncology and infectious diseases [12]. This document provides a detailed analysis of the market context, technological comparisons, experimental frameworks, and essential reagent solutions underpinning this evolution.
Market Context and Growth Dynamics
The molecular diagnostics market is experiencing significant growth, fueled by its central role in personalized medicine and infectious disease testing. In the United States, the molecular diagnostics market was valued at USD 4.91 billion in 2024 and is projected to reach USD 8.40 billion by 2033, growing at a CAGR of 6.15% [18]. The global infectious disease diagnostics market, a critical segment, reflects an even steeper growth trajectory, projected to expand from USD 25.01 billion in 2024 to USD 62.95 billion by 2034, at a CAGR of 9.67% [19]. Another analysis estimates this market will grow from USD 26.58 billion in 2025 to USD 42.20 billion by 2030 at a CAGR of 9.7% [20].
Table 1: Global Market Outlook for Key Diagnostic Segments
| Market Segment | Base Year Value (USD) | Projected Year Value (USD) | CAGR | Key Drivers |
|---|---|---|---|---|
| U.S. Molecular Diagnostics Market [18] | $4.91 Billion (2024) | $8.40 Billion (2033) | 6.15% | Rising demand for personalized medicine; incidence of infectious diseases and cancer. |
| Global Infectious Disease Diagnostics Market [19] | $25.01 Billion (2024) | $62.95 Billion (2034) | 9.67% | Rising prevalence of infectious diseases; demand for rapid, accurate testing; technological advancements. |
| Global Infectious Disease Diagnostics Market [20] | $26.58 Billion (2025) | $42.20 Billion (2030) | 9.7% | Global burden of infectious diseases; innovation in diagnostic technologies; government initiatives. |
| Global PCR, dPCR, and qPCR Market [15] | $7.18 Billion (2025) | $16.98 Billion (2033) | 15.43% | Expanding applications in healthcare and research; demand for precise molecular diagnostics. |
This growth is geographically diverse. North America currently holds the dominant market share, attributed to its advanced healthcare infrastructure and high adoption of innovative technologies [19] [21]. However, the Asia-Pacific region is poised to be the fastest-growing market, driven by rapid industrialization, improving healthcare infrastructure, and government-led innovation programs [19] [15].
Technological Foundations: qPCR and NGS
The execution of personalized medicine and advanced infectious disease testing is enabled by a suite of molecular technologies, primarily qPCR and Next-Generation Sequencing (NGS). Each technology has distinct strengths, making them suitable for different applications within the diagnostic and research workflow.
Comparative Analysis of qPCR and NGS
qPCR has been the cornerstone of molecular diagnostics for decades, prized for its speed, sensitivity, cost-effectiveness, and ease of use in detecting specific, known nucleic acid sequences [12]. It is the gold standard for applications like pathogen detection (e.g., SARS-CoV-2, HIV, influenza) and quantifying known genetic biomarkers [12] [18].
In contrast, NGS provides a comprehensive, hypothesis-free approach by sequencing entire genomes, exomes, or targeted gene panels in a single assay. This allows for the discovery of novel variants and a holistic view of the genetic landscape, which is indispensable in oncology for identifying rare mutations and guiding targeted therapies [12].
Table 2: Key Technical Characteristics of qPCR vs. NGS
| Characteristic | qPCR | NGS |
|---|---|---|
| Primary Strength | Rapid, sensitive detection of known targets | Discovery of known and novel variants; comprehensive profiling |
| Throughput | Low to medium (single to multiplexed targets) | Very high (entire genomes to large gene panels) |
| Turnaround Time | Short (minutes to a few hours) | Longer (days to weeks) |
| Cost per Test | Low | High, though decreasing |
| Ideal Application | Routine diagnostics, rapid screening, high-volume targeted testing | Oncology genomics, rare disease diagnosis, pathogen discovery, outbreak surveillance |
| Data Complexity | Low (quantification of specific targets) | High (requires sophisticated bioinformatics analysis) |
A Complementary Workflow
The most powerful diagnostic strategies often leverage both technologies in a complementary manner [12]. A common workflow involves using qPCR as a rapid, first-pass screening tool for known mutations or pathogens. If results are inconclusive or a deeper understanding is needed, the sample can be subjected to NGS analysis. This hybrid approach was successfully deployed during the COVID-19 pandemic, where qPCR was used for widespread testing while NGS was employed to sequence viral genomes and track the emergence of new variants [12].
A Framework for Personalized Medicine Integration
Implementing personalized medicine requires more than just advanced technology; it demands a structured approach to integrating testing, data, and leadership within a healthcare or research organization. A quantitative framework for assessing PM integration maturity is based on eight key criteria across multiple clinical areas (e.g., oncology, rare diseases) [22].
Key Evaluation Criteria for PM Maturity [22]:
- Testing Guidance & Data Accessibility: Moving from physician-driven, manual test processes to reflexive testing pathways with automated EHR integration.
- Leadership: Evolving from individual physician champions to C-Suite supported, organization-wide initiatives.
- Internal Funding: The percentage of PM initiatives funded internally, indicating institutional commitment.
- Utilization of Data: Using data to inform standard of care, enable off-label treatments/clinical trial matching, and support research.
- Data Sharing: Progressing from data used by individual physicians to sharing across multidisciplinary teams, departments, and external organizations.
- Collection of Genomic Data: Advancing from disparate biomarkers to multigene panels and ultimately whole-genome or whole-exome sequencing.
- Collection of Other Omics Data: Incorporating proteomic, epigenetic, and metabolomic data.
- Collection of Non-Laboratory Data: Integrating social determinants of health, clinical outcomes, and economic outcomes.
This framework uses a points-based system to assign organizations a maturity level from 1 (lowest) to 5 (highest). A 2021 survey of 153 US healthcare organizations using this model revealed significant heterogeneity in PM adoption, with high-performing organizations typically excelling in data sophistication, sharing practices, and internal funding [22].
Experimental Protocols for qPCR-based Research
For scientists developing qPCR-based diagnostic assays, following a rigorous experimental protocol is paramount. The following section outlines a generalized workflow for a multiplex qPCR assay, which is highly relevant for detecting multiple pathogens or genetic biomarkers simultaneously.
Detailed Protocol: Multiplex qPCR Assay
Objective: To simultaneously detect and quantify multiple specific nucleic acid targets in a single reaction.
Materials:
- Extracted DNA/RNA samples
- Multiplex qPCR Master Mix: Contains Hot Start DNA Polymerase, dNTPs, and optimized buffer salts. Must be formulated for multiplexing to maintain sensitivity and specificity [12].
- Sequence-Specific Primers and Probes: Each pair of primers and a corresponding hydrolysis probe (e.g., TaqMan) labeled with a distinct fluorophore (e.g., FAM, VIC, Cy5).
- Nuclease-Free Water
- qPCR Instrument (e.g., from Roche, Thermo Fisher, Bio-Rad)
Methodology:
Assay Design:
- Design primers and probes to have similar melting temperatures (Tm ~60°C).
- Verify specificity using tools like BLAST to avoid cross-homology.
- Ensure fluorophore and quencher combinations are compatible with your qPCR instrument's optical channels.
Template Preparation:
- Extract high-quality DNA/RNA from samples using a commercial kit.
- If using RNA, perform reverse transcription to generate cDNA.
- Quantify nucleic acid concentration and purity using a spectrophotometer.
Reaction Setup:
- Prepare reactions on ice in a low-binding microcentrifuge tube. A typical 20 µL reaction may contain:
- 10 µL of 2x Multiplex Master Mix
- Primer and probe mix (optimized concentrations, typically 100-900 nM for primers and 50-250 nM for probes)
- 2 µL of template DNA/cDNA
- Nuclease-free water to 20 µL
- Critical: Include negative controls (no-template control) and positive controls (samples with known target) in each run.
- Prepare reactions on ice in a low-binding microcentrifuge tube. A typical 20 µL reaction may contain:
qPCR Run:
- Program the thermocycler with the following standard cycling conditions:
- Initial Denaturation: 95°C for 2-5 minutes (activates the Hot Start enzyme).
- 40-50 Cycles of:
- Denaturation: 95°C for 15 seconds
- Annealing/Extension: 60°C for 60 seconds (data acquisition occurs at this step)
- Set the instrument to monitor fluorescence for each fluorophore at the end of each annealing/extension step.
- Program the thermocycler with the following standard cycling conditions:
Data Analysis:
- Set the fluorescence threshold in the cycle where the amplification signal is in the exponential phase. The cycle threshold (Ct) is determined for each reaction.
- For absolute quantification, generate a standard curve using serially diluted samples of known concentration for each target.
- For relative quantification, use the ΔΔCt method with a validated reference gene.
Troubleshooting:
- High Background/Nonspecific Amplification: Optimize primer/probe concentrations; increase annealing temperature; use a Hot Start enzyme formulation [12].
- Poor Multiplexing Efficiency: Ensure master mix is optimized for multiplexing; check for spectral overlap between fluorophores.
- Inconsistent Replicates: Mix all reaction components thoroughly before aliquoting; ensure template is homogenous.
The Scientist's Toolkit: Key Research Reagent Solutions
The performance and reliability of qPCR-based research and diagnostics are heavily dependent on the quality and suitability of the reagents used. The following table details essential solutions for developing robust assays.
Table 3: Key Research Reagent Solutions for qPCR Assays
| Reagent Solution | Core Function | Key Considerations for Selection |
|---|---|---|
| dUTP Master Mixes [12] | Contains dUTP instead of dTTP. Used with Uracil-DNA Glycosylase (UDG) to prevent amplicon carryover contamination in high-throughput or reusable equipment settings. | Essential for high-sensitivity applications and when reusing reaction plates/tubes to eliminate false positives from previous amplifications. |
| Lyo-Ready / Air-Dryable Master Mixes [12] | Specially formulated reagents for creating ambient-temperature stable assays via lyophilization or air-drying. | Critical for developing point-of-care tests, shelf-stable kits, and assays for use in resource-limited settings without reliable cold chain. |
| High-Concentration, Glycerol-Free Enzymes [12] | Purified enzymes supplied in glycerol-free buffers at high concentrations. | Enables compatibility with lyophilization and improves performance in high-throughput automated workflows. Allows for custom formulation of master mixes. |
| Optimized Multiplex Master Mix [12] | A proprietary buffer formulation that allows for simultaneous amplification of multiple targets in a single reaction without loss of sensitivity or specificity. | Required for developing assays that detect several pathogens (e.g., COVID-19/Flu/RSV) or genetic biomarkers concurrently, saving time, sample, and reagents. |
The convergence of personalized medicine and rapid infectious disease testing represents a paradigm shift in molecular diagnostics, with qPCR technology playing an indispensable role. The powerful, complementary relationship between high-throughput, discovery-oriented NGS and rapid, targeted qPCR is creating robust, hybrid diagnostic workflows. For researchers and drug development professionals, success in this evolving landscape hinges on a deep understanding of the technological strengths of each platform, the application of rigorous experimental protocols, and the strategic selection of advanced reagent solutions. As the field advances, driven by data science and automation, the integration of these tools will continue to accelerate the delivery of precise, personalized healthcare on a global scale.
The COVID-19 pandemic served as an unprecedented catalyst for molecular diagnostics, propelling quantitative polymerase chain reaction (qPCR) from a specialized research tool to a cornerstone of global public health response. This whitepaper examines the evolving role of qPCR within the molecular diagnostics landscape, with particular emphasis on its integration into personalized medicine research. We explore how pandemic-driven advancements in throughput, automation, and point-of-care applications are being channeled toward precision oncology, infectious disease surveillance, and biomarker validation. Technical protocols for rigorous data analysis, reagent solutions, and emerging technological synergies with digital PCR (dPCR) and next-generation sequencing (NGS) are detailed to provide researchers and drug development professionals with a comprehensive framework for leveraging qPCR in post-pandemic diagnostic development.
The COVID-19 crisis transformed laboratory operations on an unprecedented scale, driving a global surge in PCR testing evolution that placed speed, precision, and scalability at the forefront of diagnostic priorities [23]. Instruments once used primarily for specialized testing became essential tools for infectious disease diagnostics, detecting SARS-CoV-2 alongside influenza, tuberculosis, and other pathogens in record time [23]. This transformation established a new paradigm for molecular diagnostics, demonstrating the critical importance of rapid, accurate nucleic acid detection in managing public health crises.
As the world enters a post-pandemic diagnostics era, qPCR maintains its position as the gold standard for nucleic acid quantification due to its well-established protocols, sensitivity, and cost-effectiveness [24] [25]. The pandemic-induced acceleration in diagnostic innovation has created lasting momentum, with qPCR now positioned as an integral component in the personalized medicine pipeline, particularly for applications requiring rapid turnaround of targeted molecular data [23] [25]. The convergence of pandemic-proven qPCR methodologies with growing demand for personalized healthcare solutions represents a significant opportunity for researchers and drug developers working to translate molecular insights into clinical applications.
The Evolving Diagnostic Landscape: qPCR in the Post-Pandemic Era
From Crisis Response to Strategic Implementation
The legacy of COVID-19 on molecular diagnostics is characterized by widespread adoption of high-throughput platforms and automated workflows that permanently elevated laboratory testing capabilities [23]. Real-time RT-PCR (or qRT-PCR), the standard for viral detection, was implemented on a global scale due to its precision, automation, and high-throughput capabilities [23]. This infrastructure now provides a foundation for expanding diagnostic applications beyond infectious diseases into areas such as oncology profiling, pharmacogenomics, and comprehensive pathogen detection [23].
The post-pandemic era is witnessing a strategic shift from reactive crisis response to proactive integration of qPCR within broader diagnostic ecosystems. Laboratories are now leveraging investments made during the pandemic to create more resilient, flexible testing infrastructures capable of addressing diverse clinical needs [23]. This transition is supported by a growing emphasis on cost-efficient refurbished platforms that maintain high performance standards while conserving resources, enabling laboratories to sustain expanded testing capabilities despite budgetary constraints [23].
qPCR in the Personalized Medicine Paradigm
Personalized medicine, which tailors treatment according to individual genomic profiles, increasingly depends on tools that provide high sensitivity, reproducibility, and throughput [25]. The personalized healthcare market is projected to grow at a CAGR of 10.8%, reaching nearly $590 billion by 2028, driven by rising demand for personalized therapeutics and diagnostics [12]. qPCR occupies a pivotal role in this ecosystem through its capacity to quantify nucleic acids in real time, supporting precision in interpreting gene expression, pathogen load, and molecular biomarkers [25].
qPCR applications in precision medicine include:
- Pharmacogenomic profiling for optimized drug choice and dosing through detection of single-nucleotide polymorphisms or allele-specific expression [25]
- Minimal residual disease monitoring in cancer through detection of specific transcripts or fusion genes in hematologic malignancies and solid tumors [25]
- Vector copy number quantification in cell and gene therapy monitoring [25]
- Validation of biomarker signatures discovered through high-throughput methodologies such as NGS [26]
Table 1: RNA Biomarkers Detectable by qPCR in Liquid Biopsies
| RNA Type | Example Biomarker | Disease Context | Potential Application |
|---|---|---|---|
| mRNA | PON2 (Paraoxonase-2) | Bladder cancer | Diagnostic [26] |
| lncRNA (>200 nt) | XLOC_009167 | Lung cancer | Diagnostic [26] |
| miRNA (~22 nt) | miR-141 | Prostate cancer | Diagnostic [26] |
| isomiR (~22 nt) | miR-574-3p (3´ deletion A) | Esophageal squamous cell carcinoma | Diagnostic [26] |
| piRNA (26-31 nt) | piR-1245 | Colorectal cancer | Prognostic [26] |
Technical Foundations: qPCR Methodologies and Analysis
Core qPCR Technologies and Applications
qPCR technologies have evolved to address diverse diagnostic needs across clinical specialities. The primary variations include:
Quantitative PCR (qPCR) monitors amplification in real-time using fluorescence signals to quantify DNA, enabling both dye-based (e.g., SYBR Green) and probe-based (e.g., TaqMan) approaches [24]. Multiplex detection for diagnosing various infectious diseases is achievable using different fluorophores attached to probes [24]. qPCR remains faster and less complex than next-generation sequencing (NGS) in many diagnostic settings, particularly when targeting defined genes or panels [25].
Digital PCR (dPCR) enhances the limit of detection and provides more reliable sensitivity for low-abundance targets by partitioning samples into numerous individual PCR reactions, allowing absolute quantification of nucleic acids without calibration curves [23] [25]. This partitioning effectively increases the local concentration of the target within each reaction volume and reduces inhibition and contamination [24]. dPCR is particularly valuable for detecting rare variants or very low levels of viruses [23].
Table 2: Comparative Analysis of PCR Technologies in Clinical Diagnostics
| Parameter | qPCR | Digital PCR | Next-Generation Sequencing |
|---|---|---|---|
| Quantification Approach | Relative to standard curve | Absolute counting of molecules | Relative to reference genome |
| Sensitivity | High | Very high (detection of rare variants) | Variable (depends on coverage depth) |
| Multiplexing Capacity | Moderate (limited by fluorescence channels) | Moderate | Very high (entire genomes) |
| Throughput | High | Moderate | High (parallel processing) |
| Cost per Sample | Low | Moderate | High |
| Best Applications | Routine pathogen detection, gene expression quantification | Rare variant detection, liquid biopsy, absolute quantification | Discovery, unknown pathogen identification, comprehensive genomic profiling |
Experimental Protocol: The Double Delta Ct Analysis Method
The double delta Ct (2^(-ΔΔCt)) method remains a widely used approach for analyzing relative gene expression data in qPCR experiments [27]. Below is a detailed protocol for implementing this methodology:
Assumptions and Prerequisites:
- Primer efficiency between primer sets should be approximately equal (within 5%)
- Near 100% amplification efficiency for both reference and target genes
- Internal control genes must be constantly expressed and unaffected by experimental treatment [27]
Step-by-Step Procedure:
Calculate Average Ct Values
- Take the average of the Ct values for the housekeeping gene and the gene of interest in both experimental and control conditions
- This yields four values: Gene Being Tested Experimental (TE), Gene Being Tested Control (TC), Housekeeping Gene Experimental (HE), and Housekeeping Gene Control (HC)
Determine ΔCt Values
- Calculate ΔCt experimental (ΔCTE) = TE - HE
- Calculate ΔCt control (ΔCTC) = TC - HC
- These calculations normalize the gene of interest to the reference/housekeeping gene within each condition [27]
Calculate ΔΔCt Value
- ΔΔCt = ΔCTE - ΔCTC
- This represents the normalized difference in expression between experimental and control conditions [27]
Compute Fold Change
- Fold Change = 2^(-ΔΔCt)
- Since all calculations are in logarithm base 2, this conversion translates the logarithmic data into a linear fold change value [27]
Interpretation of Results:
- Fold change of 1 = No change in expression (100% of control)
- Fold change > 1 = Upregulation (e.g., 1.5 = 150% expression relative to control)
- Fold change < 1 = Downregulation (e.g., 0.5 = 50% expression relative to control) [27]
Advanced Data Analysis: Ensuring Rigor and Reproducibility
Despite the widespread use of the 2^(-ΔΔCt) method, advanced analysis approaches are emerging to address its limitations. Analysis of Covariance (ANCOVA) enhances statistical power compared to the 2^(-ΔΔCt) method and provides P-values that are not affected by variability in qPCR amplification efficiency [28]. This flexible multivariable linear modeling approach generally offers greater statistical power and robustness [28].
Key considerations for rigorous qPCR data analysis include:
Baseline Correction: Proper baseline setting is crucial for accurate Cq determination. The baseline should be set using early cycles (e.g., cycles 5-15) where fluorescence intensity represents background fluorescence rather than amplification signal [29]. Incorrect baseline adjustment can significantly alter Cq values and lead to erroneous conclusions [29].
Threshold Setting: The quantification threshold should be set:
- Sufficiently above background fluorescence to avoid premature threshold crossing
- Within the exponential phase of amplification,不受高原阶段的影响
- Where all amplification plots are parallel [29]
Efficiency Correction: The assumption of 100% amplification efficiency in basic ΔΔCt calculations introduces significant bias [30]. Efficiency-adjusted models incorporate actual reaction efficiencies determined from standard curves, substantially improving quantification accuracy [29].
MIQE Compliance: The Minimum Information for Publication of Quantitative Real-Time PCR Experiments (MIQE) guidelines establish best practices for reporting, including transparency in assay design and controls [25]. Recent analyses reveal ongoing deficiencies in reporting transparency and experimental validation in qPCR studies [25]. Adherence to MIQE principles and FAIR (Findable, Accessible, Interoperable, Reproducible) data principles enhances reproducibility and scientific rigor [28].
Essential Research Reagents and Solutions
Successful qPCR implementation requires careful selection and optimization of research reagents. The following table details essential components for robust qPCR assays:
Table 3: Essential Research Reagent Solutions for qPCR Assays
| Reagent Category | Specific Examples | Function and Application | Technical Considerations |
|---|---|---|---|
| Polymerase Master Mixes | dUTP master mixes | Prevents carryover contamination in high-throughput settings | Essential when reusing equipment between reactions [12] |
| Lyo-Ready and Air-Dryable master mixes | Enables creation of ambient-temperature stable assays | Critical for point-of-care and resource-limited settings [12] | |
| Inhibitor-tolerant qPCR mixes | Optimized for challenging sample types (saliva, whole blood) | Increases resilience to inhibitors, reduces preprocessing [25] | |
| Reverse Transcriptase | High-concentration, glycerol-free enzymes | cDNA synthesis for RT-qPCR applications | Compatible with lyophilization [12] |
| Probes and Dyes | Hydrolysis probes (TaqMan) | Sequence-specific detection with high specificity | Enables multiplexing with different fluorophores [24] |
| DNA binding dyes (SYBR Green) | Cost-effective detection for single-plex applications | Requires verification of reaction specificity [24] | |
| Reference Assays | Validated reference genes | Normalization of sample input and RNA quality | Must demonstrate stable expression across experimental conditions [26] |
| Sample Preparation Kits | Silica-based columns, magnetic beads | Nucleic acid extraction and purification from clinical samples | Critical for removing PCR inhibitors from complex matrices [24] |
Integrated Diagnostic Approaches: qPCR in Multi-Technology Workflows
Complementary Technology Integration
qPCR increasingly functions within integrated diagnostic workflows that leverage the complementary strengths of multiple technologies:
qPCR-NGS Synergy: NGS offers comprehensive genomic coverage and discovery potential, while qPCR provides rapid, cost-effective validation and quantification of specific biomarkers [12]. A hybrid approach uses qPCR for initial screening of known mutations or pathogens, followed by NGS to explore novel variants or broader genomic regions when needed [12]. This strategy was successfully deployed during the COVID-19 pandemic to track and monitor emerging variants [12].
qPCR-dPCR Integration: Digital PCR provides absolute quantification and higher precision for detecting rare variants or small expression changes [25]. Clinical workflows may employ qPCR for preliminary screening with confirmation of ambiguous findings via dPCR [25]. Emerging real-time digital PCR (rdPCR) represents a hybrid approach combining real-time detection with partitioned absolute quantification [25].
CRISPR-qPCR Combinations: CRISPR-based diagnostics enable rapid, point-of-care nucleic acid detection, while qPCR remains established, validated, and scalable for centralized laboratory settings [25]. Integration of these technologies creates complementary diagnostic pathways appropriate for different healthcare scenarios.
Point-of-Care Innovations: The QUICK-PCR Paradigm
The pandemic accelerated development of point-of-care molecular diagnostics, creating momentum for QUICK-PCR (Quick, Ubiquitous, Integrated, Cost-efficient Molecular Diagnostic Kit) systems [24]. These platforms aim to deliver 6S performance: simplicity, speed, small size, sustainability, sensitivity, and specificity [24].
Innovations driving QUICK-PCR development include:
- Rapid thermal cycling using Joule heating, thermoelectric heating, and plasmonic heating technologies
- Integrated sample preparation reducing processing time and complexity
- Compact readout systems utilizing fluorescence, colorimetry, and electrochemical detection techniques [24]
- Microfluidic implementations enabling automated fluid handling and reaction partitioning
Despite these advances, practical QUICK-PCR implementation faces challenges including complex operation processes, lengthy sample-to-answer turnaround times, and limitations of bulky equipment for result analysis [24]. Typical sample preparation alone requires approximately 30 minutes through a complex multi-step process needing skilled personnel [24].
Future Perspectives and Research Directions
The future evolution of qPCR in clinical diagnostics will be shaped by several converging technological trends:
Artificial Intelligence Integration: AI and machine learning are increasingly employed for curve fitting, baseline correction, outlier detection, and assay quality checking [25]. These tools reduce human error and increase throughput while improving analytical accuracy. Interpretable digital PCR methods incorporating machine learning, such as I²ddPCR which synergizes front-end predictive models and language model components to automate droplet classification, may influence future qPCR/dPCR hybrid pipelines [25].
Portable qPCR Systems: The advent of point-of-care qPCR systems may shift some diagnostics to decentralized settings [25]. Portable qPCR instruments that maintain high precision could support near-patient testing in oncology, infectious disease, or pharmacogenomic contexts, potentially improving healthcare access in resource-limited environments [24] [25].
Enhanced Multiplexing Capabilities: Reagent and chemistry innovations continue to enhance qPCR robustness for complex applications [25]. Multiplex qPCR panels are expanding to cover broader pathogen detection and complex genetic signatures, enabled by improved probe chemistries and signal deconvolution algorithms [31].
Sustainability Considerations: Environmental impact concerns are driving development of sustainable manufacturing systems for disposable parts and attention to landfill implications of single-use diagnostic components [24]. This focus on sustainability will likely influence both product design and end-of-life management for diagnostic platforms.
The global market for real-time polymerase chain reaction systems is projected to grow from USD 4.93 billion in 2022 to USD 7.01 billion by 2030, representing a CAGR of 4.57% [25]. This growth reflects the enduring value of qPCR technology alongside complementary molecular diagnostic approaches.
qPCR maintains an essential role in the post-pandemic clinical diagnostics landscape, bridging the gap between high-throughput discovery platforms and routine clinical implementation. The technology's balance of speed, sensitivity, specificity, and cost-effectiveness ensures its continued relevance in personalized medicine, particularly for applications requiring rapid, quantitative assessment of defined molecular targets. Pandemic-driven innovations in automation, throughput, and point-of-care applications have expanded qPCR's utility beyond traditional laboratory settings, creating new opportunities for decentralized testing and rapid response capabilities.
Future diagnostic ecosystems will increasingly leverage qPCR within integrated workflows that capitalize on the complementary strengths of multiple technologies. The convergence of AI-enhanced analysis, portable platforms, and sustainable design principles will further enhance qPCR's value in advancing precision medicine. For researchers and drug development professionals, understanding both the capabilities and limitations of modern qPCR methodologies remains crucial for designing robust diagnostic approaches that can successfully translate molecular insights into improved patient care.
qPCR in Action: Advanced Applications in Oncology, Infectious Diseases, and Pharmacogenomics
Multiplex Panels for Comprehensive Pathogen Detection and Strain Differentiation
Multiplex polymerase chain reaction (PCR) panels represent a significant advancement in molecular diagnostics, enabling the simultaneous detection and differentiation of multiple pathogens or genetic variants in a single reaction. Within the expanding field of personalized medicine, these panels provide the rapid, precise pathogen identification necessary for tailoring therapeutic strategies to individual patients, thereby improving clinical outcomes and supporting antimicrobial stewardship [12]. The technology is particularly valuable in infectious disease management, where differentiating between pathogens with overlapping symptomatology—such as SARS-CoV-2, influenza, and respiratory syncytial virus (RSV)—is critical for initiating targeted treatment and implementing appropriate infection control measures [32].
The transition from single-plex to highly multiplexed assays addresses a pressing clinical need for comprehensive diagnostic data without increasing turnaround times. This is especially true in resource-limited settings, where access to broad genomic testing may be constrained [33]. The growing market for PCR, dPCR, and qPCR technologies, projected to reach $16.98 billion by 2033, underscores the pivotal role these tools play in contemporary healthcare and biomedical research [15]. This technical guide explores the core principles, design strategies, implementation protocols, and data analysis frameworks for developing and utilizing multiplex PCR panels for sophisticated pathogen detection and strain differentiation.
Technical Design of Multiplex PCR Panels
Primer and Probe Design Strategies
The design of a highly multiplexed PCR primer set is a computationally complex challenge. The primary obstacle is the quadratic increase in potential primer-dimer interactions relative to the number of primers. For an N-plex assay with 2N primers, the number of potential pairwise interactions is (2N choose 2), which amounts to 4950 potential interactions for a 50-plex assay [34]. To address this, advanced algorithms like the Simulated Annealing Design using Dimer Likelihood Estimation (SADDLE) have been developed. SADDLE is a stochastic optimization algorithm that navigates the non-convex fitness landscape of primer selection to minimize primer dimer formation [34].
The SADDLE workflow involves:
- Primer Candidate Generation: For each genetic target, multiple "proto-primers" are generated. These are subsequently trimmed to achieve an optimal hybridization free energy (ΔG°) of approximately -11.5 kcal/mol, balancing amplification efficiency and specificity [34].
- Initial Primer Set Selection: A primer pair candidate is randomly selected for each target to form an initial set, S₀.
- Loss Function Evaluation: A computationally efficient Loss function, L(S), sums the "Badness" of all potential primer-primer interactions within the set, estimating the overall severity of dimer formation.
- Iterative Optimization: The algorithm generates new primer sets (T) by randomly swapping primers from the candidate pool. A new set is accepted probabilistically based on its improved Loss value, following the simulated annealing optimization technique [34].
This approach has demonstrated remarkable efficacy, reducing primer dimer fractions from 90.7% in a naively designed 96-plex set (192 primers) to just 4.9% in the optimized set [34].
Assay Configuration and Target Selection
Effective multiplex panels are configured to address specific clinical or research questions, such as differentiating hypervirulent and carbapenem-resistant Klebsiella pneumoniae pathotypes or identifying the causative agent of a lower respiratory tract infection (LRTI).
Defining Pathotypes with Biomarkers: For bacterial strain differentiation, assays target a combination of virulence and resistance genes. For example, a multiplex PCR for Klebsiella pneumoniae can be designed to detect:
- Hypervirulence Markers:
rmpA,rmpA2,iucA,peg344,iroB[33]. - Carbapenem-Resistance Markers:
blaNDM,blaOXA-48-like,blaKPC[33]. Strains are then classified based on their gene profiles; for instance, a hypervirulent (hvKp) strain may be strictly defined as one possessing all five canonical virulence genes [33].
Comprehensive Pathogen Panels: Respiratory panels exemplify syndromic testing, simultaneously screening for multiple bacterial and viral pathogens. A typical panel might target:
- Bacterial Targets: Pseudomonas aeruginosa, Klebsiella pneumoniae, Staphylococcus aureus, Streptococcus pneumoniae, Haemophilus influenzae, Legionella pneumophila [35].
- Viral Targets: Influenza A/B, Respiratory syncytial virus, Adenoviruses, Human rhinovirus, Mycoplasma pneumoniae [35].
The design must also consider the required clinical sensitivity. Analytical validation of a novel FMCA-based multiplex PCR for six respiratory pathogens reported limits of detection (LOD) between 4.94 and 14.03 copies/µL, ensuring high sensitivity for clinical application [32].
Workflow Diagram: Multiplex PCR Assay Design and Validation
The following diagram illustrates the comprehensive workflow for designing, optimizing, and validating a multiplex PCR panel, from initial genomic analysis to clinical application.
Implementation and Experimental Protocols
Detailed Methodology for a HypervirulentK. pneumoniaeAssay
The following protocol is adapted from a study that developed a multiplex PCR for detecting hypervirulent and carbapenem-resistant K. pneumoniae [33].
1. Nucleic Acid Extraction:
- Use a commercial kit for genomic DNA extraction from bacterial isolates or clinical samples.
- Elute DNA in nuclease-free water or TE buffer. The assay is sensitive enough to work with DNA inputs as low as 1 ng/µL [33].
- Quantify DNA concentration using a spectrophotometer and store at -20°C until use.
2. Multiplex PCR Reaction Setup:
- Prepare a master mix on ice. A sample 25 µL reaction volume may contain:
- 1X PCR Buffer (with MgCl₂)
- 200 µM of each dNTP
- 0.2-0.5 µM of each primer (see table below)
- 1.25 U of DNA Polymerase
- 1-100 ng of template DNA
- Nuclease-free water to volume.
- Gently mix and briefly centrifuge the reactions.
3. Thermal Cycling Conditions:
- Initial Denaturation: 95°C for 5 minutes.
- Amplification (35 cycles):
- Denaturation: 95°C for 30 seconds.
- Annealing: 60°C for 30 seconds (optimize temperature based on primer Tm).
- Extension: 72°C for 1 minute (adjust based on amplicon size).
- Final Extension: 72°C for 7 minutes.
- Hold: 4°C.
4. Amplicon Analysis:
- Separate PCR products by gel electrophoresis (e.g., 2% agarose gel).
- Visualize bands under UV light and document.
- Confirm the identity of amplicons by Sanger sequencing for validation [33].
Research Reagent Solutions Toolkit
The table below lists essential reagents and their functions for establishing a multiplex PCR assay, based on the protocols cited.
| Research Reagent | Function in the Assay | Technical Specification / Example |
|---|---|---|
| Primers & Probes | Specific binding to target DNA sequences. | Designed for virulence (iucA, rmpA) and resistance (blaKPC, blaNDM) genes [33]. |
| DNA Polymerase | Enzymatic amplification of target DNA. | Thermostable enzyme with high processivity and fidelity. |
| dNTP Mix | Building blocks for new DNA strands. | 200 µM of each dNTP in the final reaction [33]. |
| PCR Buffer | Provides optimal chemical environment. | Includes MgCl₂ (1.5-2.5 mM final concentration) as a co-factor [33]. |
| Template DNA | Sample containing the target genetic material. | 1-100 ng of genomic DNA from bacterial isolates or clinical samples [33]. |
| Fluorescent Probes | Target-specific detection in real-time assays. | Probes labeled with dyes (FAM, HEX, CY5) for FMCA or qPCR [32]. |
Data Analysis and Interpretation
qPCR Data Analysis: For quantitative real-time PCR (qPCR) data, robust mathematical models are essential. The rtpcr R package provides a comprehensive framework, supporting analyses with up to two reference genes [36].
- Pfaffl Method: This is a preferred method as it accounts for potential differences in amplification efficiencies between target and reference genes. The fold change (FC) is calculated as:
- FC = (Etarget)^(-ΔCTTarget) / (Eref)^(-ΔCTRef) [36] where E is the amplification efficiency and ΔCT is the difference in threshold cycles between treatment and control conditions.
- Statistical Analysis: The package can perform t-tests, analysis of variance (ANOVA), or analysis of covariance (ANCOVA) on efficiency-weighted ΔCT values, which are expected to be normally distributed, to calculate significance and confidence intervals [36].
Pathogen Detection and Co-infection Analysis: In clinical samples, multiplex panels frequently reveal co-infections. A large multicenter study of a respiratory panel found that 19.8% (144/728) of bronchoalveolar lavage samples contained multiple pathogens [35]. The interpretation of results, particularly for bacteria that can be colonizers, requires correlating the pathogen detection with clinical symptoms. For example, a high semi-quantitative signal (low Ct value, e.g., ≤30) is more strongly associated with clinical infection than a low-level detection [35] [37].
Performance Validation and Clinical Applications
Analytical and Clinical Performance Metrics
Rigorous validation is mandatory before a multiplex panel can be deployed in clinical or research settings. The following table summarizes key performance metrics from recent studies.
| Performance Metric | Result from Validation Studies | Context & Implications |
|---|---|---|
| Specificity | 100% (vs. WGS) [33] | No cross-reactivity observed in the K. pneumoniae pathotype assay, ensuring reliable strain differentiation. |
| Sensitivity (LOD) | 4.94 - 14.03 copies/µL [32] | High analytical sensitivity of an FMCA-based respiratory panel enables detection of low viral loads. |
| Positive Percent Agreement (PPA) | 96.3% (Bacterial Targets) [37] | The BioFire FilmArray Pneumonia panel showed high agreement with culture for detecting bacteria in sputum. |
| Negative Percent Agreement (NPA) | 54.9% (Bacterial Targets) [37] | Lower NPA in sputum highlights the assay's higher sensitivity compared to culture, detecting unculturable targets. |
| Precision (CV) | Intra-assay: ≤0.70%; Inter-assay: ≤0.50% [32] | High repeatability and reproducibility of the FMCA-based assay's melting temperature (Tm) measurements. |
| Clinical Concordance | 98.81% (vs. RT-qPCR) [32] | High overall agreement between the novel FMCA panel and approved commercial RT-qPCR tests. |
Application in Personalized Medicine and Drug Development
The integration of multiplex PCR panels into the paradigm of personalized medicine is transformative. In oncology, these panels are used for companion diagnostics, identifying specific mutations (e.g., EGFR, BRAF) to guide the use of targeted therapies [38]. The ability to rapidly distinguish between viral and bacterial infections, or to identify a multidrug-resistant pathogen, directly informs antimicrobial stewardship, ensuring patients receive the most effective treatment while minimizing unnecessary antibiotic exposure [33] [12].
For drug development professionals, multiplex panels offer a powerful tool for patient stratification in clinical trials. By categorizing patients based on their infectious agent or specific pathogen strain, trials can achieve more homogeneous study arms, potentially leading to clearer efficacy signals. Furthermore, the trend towards liquid biopsy in cancer diagnostics leverages highly multiplexed PCR and NGS to monitor tumor DNA in blood, enabling non-invasive assessment of treatment response and emergence of resistance [38].
Multiplex PCR panels are a cornerstone of modern molecular diagnostics, providing a rapid, sensitive, and specific means for comprehensive pathogen detection and strain differentiation. The sophisticated computational design of these panels, exemplified by the SADDLE algorithm, allows for high-level multiplexing that was previously unattainable. When combined with advanced detection methods like FMCA and robust data analysis pipelines, these panels deliver actionable insights that are critical for both clinical decision-making and biomedical research.
As the field of personalized medicine continues to evolve, the demand for precise, multiplexed diagnostic tools will only intensify. The ongoing innovation in PCR technologies, coupled with a deeper understanding of pathogen genomics, ensures that multiplex panels will remain at the forefront of efforts to tailor healthcare to the individual patient, ultimately improving outcomes in infectious disease management, oncology, and beyond.
Quantitative PCR (qPCR) stands as a foundational technology in molecular diagnostics and personalized medicine research, enabling precise detection and quantification of nucleic acids in oncology. This guide explores core oncology applications—gene expression profiling, mutation detection, and liquid biopsy analysis—framed within the context of qPCR's evolving role in clinical research. The emergence of liquid biopsy has revolutionized cancer management by providing a minimally invasive alternative to traditional tissue biopsies, allowing for real-time monitoring of tumor dynamics through analysis of circulating tumor biomarkers [39] [40]. These advances align with the growing emphasis on precision medicine, where molecular profiling guides therapeutic decisions tailored to individual patients' tumor characteristics.
qPCR technologies serve as critical tools for validating biomarkers discovered through high-throughput methodologies, bridging the gap between research discovery and clinical application. The technical standardization of qPCR remains essential for translating promising molecular findings into reliable clinical tests, particularly in the context of liquid biopsy where analyte concentrations can be extremely low [41]. This guide provides researchers, scientists, and drug development professionals with comprehensive technical resources for implementing these technologies in oncology research, with a focus on practical experimental protocols and analytical frameworks.
Liquid Biopsies in Oncology: Components and Applications
Circulating Biomarkers for Cancer Detection and Monitoring
Liquid biopsy involves the isolation and analysis of tumor-derived components from bodily fluids, primarily blood, but also including urine, cerebrospinal fluid, and pleural effusions [39] [40]. The primary analytes include:
Circulating Tumor Cells (CTCs): Intact cancer cells shed from primary and metastatic tumors into circulation. Despite their low abundance (approximately 1 CTC per 1 million leukocytes), CTCs provide valuable information about cancer biology and metastatic potential [40]. The CellSearch system remains the only FDA-cleared method for CTC enumeration in metastatic breast, colorectal, and prostate cancers [40].
Circulating Tumor DNA (ctDNA): Short DNA fragments (20-50 base pairs) released into the bloodstream through tumor cell apoptosis and necrosis. ctDNA typically represents 0.1-1.0% of total cell-free DNA (cfDNA) in cancer patients [40]. The short half-life of ctDNA (approximately 2 hours) enables real-time monitoring of tumor dynamics [40].
Extracellular Vesicles (EVs): Membrane-bound particles, including exosomes, released by tumor cells that contain proteins, nucleic acids, and metabolites. EVs protect their molecular cargo from degradation, making them stable biomarkers [39] [42].
Cell-free RNA (cfRNA): Various RNA species, including microRNA (miRNA) and messenger RNA (mRNA), released from tumor cells. miRNAs are particularly stable in circulation and can serve as biomarkers for cancer detection [42].
Table 1: Comparison of Liquid Biopsy Analytes and Their Characteristics
| Analyte | Typical Concentration | Half-Life | Primary Origins | Key Applications |
|---|---|---|---|---|
| CTC | 1-10 cells/mL blood | 1-2.5 hours | Primary & metastatic tumors | Prognostic assessment, metastasis research, drug resistance studies |
| ctDNA | 0.1-1.0% of cfDNA | ~2 hours | Tumor cell apoptosis/necrosis | Mutation detection, treatment response monitoring, MRD assessment |
| EVs | 10^9-10^11 particles/mL | Hours to days | Active secretion from cells | Biomarker discovery, intercellular communication studies |
| cfRNA | Variable | Minutes to hours | Cell death, active secretion | Gene expression profiling, miRNA signatures |
Clinical Applications and Advantages
Liquid biopsy addresses several limitations of traditional tissue biopsies, particularly regarding tumor heterogeneity and the practical challenges of serial sampling [39] [40]. Key applications include:
Early Detection and Screening: Identifying cancer-associated molecular alterations in blood samples before clinical symptoms manifest. Studies have demonstrated the potential of ctDNA and CTC analysis for early detection in high-risk populations [42].
Treatment Selection and Personalized Therapy: Detecting actionable mutations to guide targeted therapy. For example, ctDNA testing for EGFR mutations in non-small cell lung cancer can identify patients likely to respond to EGFR tyrosine kinase inhibitors [40] [43].
Monitoring Treatment Response and Resistance: Serial liquid biopsies can track molecular changes associated with treatment efficacy and emerging resistance mechanisms. The dynamic monitoring of ctDNA mutation levels correlates with tumor burden and treatment response [40] [42].
Minimal Residual Disease (MRD) Detection: Identifying molecular evidence of residual disease after curative-intent treatment, often at levels undetectable by conventional imaging [39].
Assessment of Tumor Heterogeneity: Liquid biopsies capture material from multiple tumor sites, providing a more comprehensive molecular profile than single-site tissue biopsies [39] [42].
The advantages of liquid biopsy over tissue biopsy include minimal invasiveness, enabling repeated sampling; real-time monitoring of tumor evolution; accessibility when tissue is difficult to obtain; and potentially lower cost [39]. However, challenges remain regarding sensitivity and specificity, particularly in early-stage disease where analyte concentrations are lowest [39].
Technical Approaches and Detection Platforms
Comparison of Detection Methodologies
Multiple technological platforms are available for analyzing liquid biopsy samples, each with distinct performance characteristics, sensitivity thresholds, and appropriate applications.
Table 2: Performance Comparison of Liquid Biopsy Detection Platforms
| Platform | Sensitivity | Specificity | Key Advantages | Limitations | Representative Applications |
|---|---|---|---|---|---|
| qPCR | Moderate (0.1-1% VAF) | High | Rapid, cost-effective, easily implemented | Limited multiplexing capability, lower sensitivity than newer methods | Targeted mutation detection (e.g., EGFR, KRAS) |
| Digital Droplet PCR (ddPCR) | High (0.01-0.1% VAF) | High | Absolute quantification, high sensitivity, no standard curve required | Limited multiplexing capability, targeted approach only | Low-frequency mutation detection, MRD monitoring |
| Next-Generation Sequencing (NGS) | Variable (0.1-1% VAF for standard; <0.1% for error-corrected) | Variable | Comprehensive profiling, multiplexing capability, discovery potential | Higher cost, complex data analysis, longer turnaround time | Comprehensive mutation profiling, novel biomarker discovery |
A 2024 meta-analysis comparing detection platforms for human papillomavirus (HPV)-associated cancers demonstrated that sensitivity was greatest with NGS, followed by ddPCR and then qPCR, while specificity was similar across platforms [44]. The analytical sensitivity of NGS-based approaches can be enhanced through error-reduction methods such as unique molecular identifiers (UMIs) and molecular amplification pools (MAPs), which help distinguish true low-frequency variants from technical artifacts [43].
Analytical Validation Considerations
For liquid biopsy tests to transition from research to clinical applications, rigorous analytical validation is essential. Key performance characteristics include [41]:
- Analytical Sensitivity: The ability to detect the analyte of interest at low concentrations. For ctDNA assays, this is typically expressed as the limit of detection (LOD) in variant allele frequency (VAF) or copy number.
- Analytical Specificity: The ability to distinguish the target analyte from similar molecules and avoid false positives.
- Precision: The closeness of agreement between repeated measurements of the same sample, including both repeatability (within-run) and reproducibility (between-run, between-laboratory).
- Trueness: The closeness of agreement between the measured value and the true value.
The validation approach should follow a "fit-for-purpose" principle, where the level of validation matches the intended context of use [41]. For example, assays intended for clinical decision-making require more stringent validation than those for research use only.
Experimental Protocols for Liquid Biopsy Analysis
Sample Collection and Processing
Proper sample collection and processing are critical for reliable liquid biopsy results. Variations in preanalytical conditions can significantly impact assay performance [41].
Blood Collection and Plasma Separation Protocol:
- Collect blood into EDTA or specialized cell-free DNA blood collection tubes (e.g., Streck, PAXgene).
- Invert tubes gently 8-10 times immediately after collection to ensure proper mixing with anticoagulant.
- Process samples within 2-4 hours of collection for EDTA tubes, or within up to 7 days for stabilized collection tubes.
- Centrifuge at 1,600-2,000 × g for 10 minutes at 4°C to separate plasma from cellular components.
- Transfer the supernatant to a fresh tube and perform a second centrifugation at 16,000 × g for 10 minutes to remove residual cells.
- Aliquot plasma and store at -80°C until DNA extraction.
Cell-Free DNA Extraction Protocol:
- Use commercial cfDNA extraction kits (e.g., QIAamp Circulating Nucleic Acid Kit, MagMAX Cell-Free DNA Isolation Kit) following manufacturer's instructions.
- Include appropriate quality control measures, such as spiked-in synthetic DNA standards to assess extraction efficiency.
- Elute cfDNA in low-EDTA TE buffer or nuclease-free water.
- Quantify cfDNA using fluorometric methods (e.g., Qubit dsDNA HS Assay) rather than spectrophotometry, as the latter is less accurate for low-concentration samples.
- Assess fragment size distribution using bioanalyzer or tape station systems if available.
qRT-PCR Protocol for Gene Expression Analysis in Liquid Biopsies
This protocol outlines the steps for analyzing gene expression patterns from circulating tumor cells or cell-free RNA, with applications in cancer subtype classification and monitoring of treatment response [41].
RNA Extraction and Reverse Transcription:
- Extract total RNA from CTCs or plasma using appropriate RNA isolation kits with carrier RNA to improve yields.
- Treat samples with DNase I to remove genomic DNA contamination.
- Assess RNA quality and quantity using sensitive methods appropriate for low-input samples (e.g., Bioanalyzer RNA Pico chip).
- Perform reverse transcription using random hexamers and/or gene-specific primers with a high-fidelity reverse transcriptase.
qPCR Setup and Analysis:
- Design primers and probes according to MIQE guidelines, with amplicon lengths of 60-150 bp for optimal efficiency [41].
- Include no-template controls (NTCs) and positive controls in each run.
- Prepare reaction mix containing:
- 10 μL 2× qPCR master mix
- 1 μL each of forward and reverse primer (final concentration 200-500 nM)
- 0.5-1 μL probe (final concentration 100-250 nM) if using probe-based chemistry
- 5-8 μL template cDNA
- Nuclease-free water to 20 μL total volume
- Run qPCR using the following cycling conditions:
- Initial denaturation: 95°C for 2-5 minutes
- 40-50 cycles of:
- Denaturation: 95°C for 15-30 seconds
- Annealing/extension: 60°C for 30-60 seconds
- Analyze data using the comparative Ct (ΔΔCt) method or efficiency-calibrated models for relative quantification [45].
- Include multiple reference genes for normalization (e.g., GAPDH, ACTB, B2M) and validate their stability in the sample type of interest.
ddPCR Protocol for Low-Abundance Mutation Detection
Droplet digital PCR provides absolute quantification of mutant alleles without the need for standard curves and offers enhanced sensitivity for detecting rare mutations in ctDNA [43].
Reaction Setup and Droplet Generation:
- Design mutant-specific primers and probes following manufacturer guidelines for ddPCR assays.
- Prepare reaction mix containing:
- 11 μL 2× ddPCR Supermix
- 1.1 μL 20× primer-probe assay
- 5-10 μL template DNA (up to 20 ng cfDNA)
- Nuclease-free water to 22 μL total volume
- Generate droplets using the droplet generator according to manufacturer's instructions.
- Transfer the droplet emulsion to a 96-well PCR plate and seal firmly with a pierceable foil heat seal.
PCR Amplification and Analysis:
- Perform PCR amplification using the following cycling conditions:
- Enzyme activation: 95°C for 10 minutes
- 40 cycles of:
- Denaturation: 94°C for 30 seconds
- Annealing/extension: 55-60°C (assay-specific) for 60 seconds
- Enzyme deactivation: 98°C for 10 minutes
- Hold at 4°C
- Read the plate on a droplet reader to count positive and negative droplets for each target.
- Calculate the mutant allele concentration using the manufacturer's software and Poisson statistics for absolute quantification.
- Report results as copies/μL or variant allele frequency (VAF).
Visualization of Experimental Workflows and Signaling Pathways
Liquid Biopsy Experimental Workflow
Liquid Biopsy Analysis Workflow
Molecular Pathways in Cancer Biomarker Detection
Biomarker Pathways to Clinical Application
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Essential Reagents and Materials for Liquid Biopsy Research
| Category | Specific Reagents/Materials | Function/Purpose | Examples/Notes |
|---|---|---|---|
| Sample Collection | Cell-free DNA blood collection tubes | Preserve blood samples and prevent cell lysis during storage/transport | Streck Cell-Free DNA BCT, PAXgene Blood cDNA Tube |
| Nucleic Acid Extraction | Circulating nucleic acid isolation kits | Isolve and purify cfDNA/RNA from plasma/serum | QIAamp Circulating Nucleic Acid Kit, MagMAX Cell-Free DNA Isolation Kit |
| Quality Assessment | Fluorometric DNA/RNA quantification kits | Accurately measure low concentrations of nucleic acids | Qubit dsDNA HS Assay, RNA HS Assay |
| qPCR Reagents | Master mixes with UDG treatment | Prevent carryover contamination and ensure robust amplification | TaqMan Fast Advanced Master Mix, SYBR Green with UDG |
| ddPCR Reagents | ddPCR supermix and droplet generation oil | Enable droplet formation and PCR amplification in water-oil emulsion | Bio-Rad ddPCR Supermix for Probes, Droplet Generation Oil |
| Reference Materials | Synthetic DNA/RNA controls | Monitor assay performance and extraction efficiency | gBlocks, Spike-in synthetic mutation controls |
| Primers & Probes | Sequence-specific oligonucleotides | Target amplification and detection of mutations or expression markers | TaqMan assays, Custom-designed primers with dual-labeled probes |
The integration of qPCR and related molecular technologies into liquid biopsy applications represents a significant advancement in oncology research and personalized medicine. These approaches enable non-invasive monitoring of tumor dynamics, providing insights into tumor heterogeneity and evolution that are difficult to obtain through traditional tissue biopsies [39] [40]. As detection technologies continue to improve in sensitivity and multiplexing capability, liquid biopsies are poised to expand their role in early cancer detection, minimal residual disease monitoring, and comprehensive profiling of therapeutic resistance.
The future of liquid biopsy research will likely focus on standardizing preanalytical and analytical processes to improve reproducibility across laboratories [41], developing multimodal approaches that integrate information from multiple analyte types (CTCs, ctDNA, EVs), and validating clinical utility in prospective interventional trials. The ongoing development of error-corrected sequencing methods and advanced bioinformatics approaches will further enhance the sensitivity and specificity of liquid biopsy assays, particularly for early-stage disease where analyte concentrations are lowest [43]. As these technologies mature, they will increasingly inform clinical decision-making and contribute to the realization of personalized cancer medicine.
The foundational goal of personalized medicine is to tailor medical treatment to the individual characteristics of each patient. At the heart of this paradigm shift are pharmacogenomics (PGx) and biomarker discovery, which aim to understand how genetic makeup influences an individual's response to drugs. Quantitative Polymerase Chain Reaction (qPCR) has emerged as a cornerstone technology in this field, providing a rapid, sensitive, and reliable method for genotyping genetic variants that predict drug efficacy and toxicity. In the broader thesis of molecular diagnostics, qPCR represents a critical translational bridge between foundational genetic research and routine clinical application, enabling the move from a one-size-fits-all treatment model to a more precise, predictive, and personalized approach [46] [11] [47].
The clinical need is clear: interindividual variability in drug response is a major challenge, often leading to adverse drug reactions or therapeutic failure. Variations in drug pharmacokinetics (how the body processes a drug) and pharmacodynamics (how the drug affects the body) can be significantly explained by polymorphic variants in genes encoding drug-metabolizing enzymes, transporters, and drug targets [48]. qPCR technology is uniquely positioned to detect these variants efficiently in clinical settings, facilitating timely decision-making to optimize tailored drug therapy, maximize efficacy, and minimize harmful side effects [47].
The Biomarker Discovery and Validation Pipeline
The journey of a biomarker from discovery to clinical application is a rigorous, multi-stage process. The following workflow outlines the key stages from initial discovery to clinical translation, highlighting how qPCR is integrated at critical validation points.
Discovery and Candidate Identification
The process often begins with high-throughput approaches like genome-wide association studies (GWAS) that scan the entire genome to identify genetic markers associated with specific drug responses [48]. These studies generate vast lists of candidate biomarkers. More recently, traditional machine learning methods applied to large, public transcriptomic datasets have proven powerful for identifying robust, multi-gene signatures. For instance, one study analyzed 14 independent pancreatic cancer datasets using random-effects meta-analysis and forward-search optimization to identify a diagnostic and therapeutic five-gene signature (LAMC2, TSPAN1, MYO1E, MYOF, and SULF1) [49]. This computational prioritization is crucial for selecting the most promising candidates for downstream validation.
Analytical and Clinical Validation with qPCR
Computational predictions require robust experimental confirmation. qPCR is a gold-standard technology for this validation phase due to its quantitative capabilities, high sensitivity, and specificity [50] [47]. Analytical validation involves confirming that the assay itself accurately and reliably measures the biomarker. This includes determining key performance parameters like the lower limit of detection (LOD) and the lower limit of quantitation (LOQ), which define the assay's dynamic range and reliability [51].
Clinical validation tests whether the biomarker accurately predicts the clinical outcome (e.g., drug response or toxicity) in relevant patient populations. This often requires the analysis of well-characterized clinical samples. The case study in Section 4.1 demonstrates this process, where a computationally derived gene signature was successfully validated using qPCR on peripheral blood samples from 55 patients, confirming its utility as a non-invasive diagnostic tool [49].
qPCR Methodologies and Data Analysis for PGx
Core qPCR Principles in Genotyping
qPCR, also known as real-time PCR, enables both the amplification and simultaneous quantification of target DNA sequences. Unlike traditional PCR, which provides end-point analysis, qPCR monitors the accumulation of amplified product in real-time during the exponential phase of amplification, which is critical for accurate quantification [46] [51]. The key quantitative output is the Cycle threshold (Ct), which is the cycle number at which the fluorescence signal crosses a predetermined threshold. The Ct value is inversely proportional to the starting quantity of the target nucleic acid in the sample [50] [51].
For PGx applications, two primary chemistries are used:
- TaqMan Probe-Based Assays: These use sequence-specific fluorescently labeled probes, offering high specificity and are ideal for multiplexing (detecting multiple targets in a single reaction), a common requirement in PGx where multiple variants may need to be assessed simultaneously [51].
- SYBR Green Dye-Based Assays: This DNA-binding dye fluoresces when bound to double-stranded DNA. It is more cost-effective but requires careful optimization to ensure specificity, as it binds to any double-stranded DNA product, including non-specific amplicons [50].
Statistical Analysis and Quantification Models
Robust statistical analysis is paramount for reliable qPCR data interpretation. A common method for relative quantification (sufficient for most PGx applications where the ratio of expression or the presence of an allele is determined) is the ΔΔCt method [50]. This model assumes that the PCR amplification efficiency is close to 100% (i.e., the amount of product doubles with each cycle during the exponential phase). The formula for calculating the relative expression or allele frequency ratio is:
Ratio = 2^(-ΔΔCt) [50]
Where:
- ΔΔCt = (Cttarget - Ctreference)treatment - (Cttarget - Ctreference)control
For results to be statistically valid, confidence intervals and significance testing should be applied. Several statistical models can be used, including multiple regression analysis and Analysis of Covariance (ANCOVA), which can derive ΔΔCt from the estimation of the interaction between gene and treatment effects [50].
Essential Research Reagent Solutions
A successful qPCR-based PGx assay relies on a suite of specialized reagents and instruments. The table below details the key components of the qPCR workflow.
Table 1: Key Research Reagent Solutions for qPCR-based Pharmacogenomics
| Reagent/Instrument | Function | Example Application in PGx |
|---|---|---|
| Nucleic Acid Extraction Kits | Isolate high-quality DNA/RNA from patient samples (blood, tissue). | Preparing template for genotyping or gene expression analysis from patient whole blood [49]. |
| Reverse Transcription Kits | Convert RNA into complementary DNA (cDNA). | Essential for analyzing gene expression biomarkers from RNA samples. |
| TaqMan Genotyping Assays | Sequence-specific probes and primers for allele discrimination. | Gold-standard for detecting single nucleotide polymorphisms (SNPs) in drug metabolism enzymes (e.g., CYP450 genes) [47]. |
| SYBR Green Master Mix | Fluorescent dye for detecting double-stranded DNA. | Cost-effective option for validating gene expression signatures discovered via transcriptomics [49]. |
| Real-Time PCR Instruments | Thermal cyclers with optical systems for fluorescence detection. | Platforms like the QuantStudio series enable high-throughput, automated genotyping for clinical research [46]. |
| Quality Control Standards | External or internal standards for quantification. | Critical for ensuring analytical validity and inter-laboratory consistency, especially in viral load monitoring [51]. |
Applications and Case Studies in Personalized Medicine
Case Study: Validation of a Pancreatic Cancer Gene Signature
A 2025 study exemplifies the integration of computational discovery and qPCR validation. Researchers first used traditional machine learning on 14 public datasets to identify a five-gene signature (LAMC2, TSPAN1, MYO1E, MYOF, SULF1) for pancreatic cancer diagnosis [49]. To translate this finding towards clinical utility, they performed independent validation using qPCR.
Experimental Protocol Overview [49]:
- Sample Collection: 55 participants (30 pancreatic cancer patients, 25 healthy controls) were recruited, with peripheral blood samples collected in EDTA tubes.
- RNA Extraction: Total RNA was isolated from blood using TRIzol LS reagent. RNA quality was assessed, and only samples with an RNA Integrity Number (RIN) >7 were used.
- cDNA Synthesis: First-strand cDNA was synthesized from 1 μg of total RNA using the SuperScript III First-Strand Synthesis System.
- Quantitative PCR: qPCR was performed using SYBR Green Master Mix on an ABI 7900HT Real-Time PCR System. Each reaction was run in triplicate with GAPDH as the internal reference control.
- Data Analysis: Relative gene expression was calculated using the 2^(-ΔΔCt) method. The differential expression of all five genes was confirmed, and the signature achieved an Area Under the Curve (AUC) of 0.83 for distinguishing cancer from normal conditions, demonstrating strong diagnostic potential in a minimally invasive liquid biopsy format.
Infectious Disease and Virology Management
qPCR is the gold standard for quantifying viral loads, which is essential for managing infections like Human Immunodeficiency Virus (HIV) and Cytomegalovirus (CMV). In HIV, viral load monitoring via qPCR is critical for assessing the effectiveness of antiretroviral therapy (ART) and detecting the emergence of drug resistance [51]. The high sensitivity and quantitative nature of qPCR allow clinicians to make precise therapeutic decisions, such as switching drug regimens when viral suppression is not achieved. Standardization of these assays to international units (IU/mL) is crucial for inter-laboratory consistency and applying universal clinical guidelines [51].
Market Outlook and Future Perspectives
The PCR technologies market is experiencing robust growth, driven significantly by the demand for personalized medicine. The global market is projected to grow at a CAGR of 7.12% from 2025 to 2034, reaching approximately USD 31.39 billion [10]. Key trends fueling this growth in the PGx and biomarker space include:
- Rising Demand for Precision Medicine: The need for companion diagnostics to guide targeted therapies, especially in oncology, is a major driver [52].
- Technological Innovations: Digital PCR (dPCR) is emerging as a highly sensitive technology for detecting rare genetic variants and low-abundance targets, further pushing the boundaries of detection [10] [52].
- Automation and AI Integration: Automation of qPCR workflows increases throughput and reduces human error. Furthermore, artificial intelligence (AI) is beginning to transform the field by analyzing complex qPCR data patterns, improving quality control, and accelerating primer/probe design [10] [52].
Despite the promise, challenges remain, including the high cost of advanced instrumentation, regulatory complexity for assay approval, and the risk of false positives/negatives if assays are not meticulously optimized and validated [10] [52]. The recent FDA ruling on laboratory-developed tests (LDTs) adds another layer of regulatory consideration for labs developing in-house PGx tests [52].
Table 2: Key Market Drivers and Restraints for PCR in Personalized Medicine
| Driver | Impact | Restraint | Impact |
|---|---|---|---|
| Rising prevalence of infectious diseases & cancer | +1.8% impact on CAGR forecast [52] | High capital & consumable costs | -1.0% impact on CAGR forecast [52] |
| Rising demand for precision medicine | +1.1% impact on CAGR forecast [52] | Regulatory complexity & reimbursement uncertainty | -0.9% impact on CAGR forecast [52] |
| Technological innovation (e.g., dPCR, automation) | +1.2% impact on CAGR forecast [52] | Limited availability of a skilled workforce | -0.7% impact on CAGR forecast [52] |
| Adoption of syndromic & multiplex panels | +0.8% impact on CAGR forecast [52] | Competition from alternative diagnostics (e.g., CRISPR) | -0.6% impact on CAGR forecast [52] |
qPCR stands as a pivotal, robust, and accessible technology firmly embedded in the molecular diagnostics ecosystem for biomarker discovery and pharmacogenomics. Its ability to provide sensitive, specific, and quantitative genetic data in a timely manner makes it an indispensable tool for validating genomic biomarkers and translating them into clinically actionable tests. As the field of personalized medicine continues to evolve, driven by larger genomic datasets and more sophisticated bioinformatics, qPCR will remain the workhorse for robust, translational validation, ensuring that promising discoveries in the research lab can be reliably implemented to enable truly personalized treatment strategies, ultimately improving patient outcomes and advancing public health.
Quantitative Polymerase Chain Reaction (qPCR) maintains a pivotal role in molecular diagnostics, supporting precision medicine through its capacity to quantify nucleic acids with high sensitivity, specificity, and reproducibility [25]. The global real-time PCR systems market, valued at approximately USD 4.93 billion in 2022, reflects this critical role and is projected to grow steadily, underscoring the technology's entrenched position in laboratories worldwide [25]. In the era of personalized healthcare, which aims to tailor treatments to individual genetic profiles, the demand for reliable molecular diagnostic tools has intensified. The personalized medicine market itself is projected to grow at a CAGR of 10.8%, reaching nearly $590 billion by 2028 [12]. qPCR excels in scenarios requiring rapid, sensitive detection of specific, known genetic markers, making it the preferred choice for routine testing, such as identifying pathogens or confirming well-characterized mutations [12]. Roche's LightCycler PRO system emerges as a next-generation platform designed to bridge the gap between translational research and in-vitro diagnostics, offering the flexibility and accuracy required to advance both clinical diagnostics and personalized medicine research [53] [54].
The LightCycler PRO system is engineered as a comprehensive qPCR solution, combining instrumentation, consumables, reagents, and data management to support semi-automated workflows for nucleic acid testing [53]. It leverages the proven robustness of the LightCycler 480 platform while integrating innovative technologies to enhance performance and user experience [53] [55].
Core Technical Specifications
The system's architecture is designed for precision, flexibility, and operational efficiency. Key specifications are detailed in the table below.
Table 1: Technical Specifications of the LightCycler PRO System
| Feature Category | Specification | Performance Detail |
|---|---|---|
| Temperature Control | Heating/Cooling Method | Peltier-based (20°C-99°C) [53] |
| Temperature Uniformity | Integrated vapor chamber for optimal distribution [53] [55] | |
| Heating Rate | 4.4 °C/s (96-well); 4.8 °C/s (384-well) [53] | |
| Optical System | Light Source | White LED lamp [53] |
| Detector | CMOS Camera [53] | |
| Channels | 7 Excitation and 7 Emission filters for multiplexing [53] [55] | |
| Data Management & Connectivity | Interfaces | 6x USB 2.0 (back), 2x USB 2.0 (front), 1x HDMI, 1x Ethernet [53] |
| Software Compliance | Compatibility with 21 CFR Part 11 [53] | |
| Integration | HL7-based LIS interface; barcode-assisted plate scanning [53] | |
| Physical Dimensions | Instrument Size | 45.3 x 54.3 x 50.4 cm (W x H x D) [53] |
| Weight | 54.5 kg [53] | |
| Power Supply | 100-240 VAC, 50/60 Hz [53] |
Key Technological Innovations
The system incorporates several advanced features that underpin its performance:
- Patented Vapor Chamber Mount: This design ensures precise temperature regulation and uniform heat distribution across the block, which is critical for reaction fidelity and enhanced sensitivity [55].
- Seven-Channel Optical System: The optical module allows for uniform excitation and simultaneous data capture across seven channels. This design minimizes edge effects and enables high-level multiplexing, increasing hourly throughput and allowing for a greater diversity of tests per run [55].
- Interchangeable Blocks: The thermal cycler supports both 96- and 384-well plates, providing laboratories with variable throughput options to match specific workload needs [55].
- Enhanced Software Algorithms: The system features new adaptive algorithms for improved color compensation across all seven channels, preventing signal crosstalk and ensuring result purity. An updated derivative algorithm automatically determines the Cq (Quantification Cycle) value from PCR run data, instilling confidence in results calling [53] [55].
Figure 1: System Architecture and Workflow of the LightCycler PRO. The diagram illustrates the integration of hardware components and software algorithms that enable the automated qPCR workflow, from sample loading to result reporting.
Workflow Integration for Research and Diagnostic Laboratories
A defining feature of the LightCycler PRO system is its ability to seamlessly support both research and clinical diagnostic workflows within a single platform. This dual capability allows laboratories to compliantly transition from discovery research to patient sample testing, maximizing the utility of the instrument [54].
Data Management and Connectivity
The system is designed for modern, connected laboratory environments. Key features that facilitate workflow integration include:
- Remote Monitoring and Access: Users can remotely monitor processes and review data, enhancing operational flexibility [53].
- Laboratory Information System (LIS) Connectivity: An HL7-based host interface enables direct communication with a customer's LIS, streamlining data transfer and sample tracking [53].
- Barcode-Assisted Scanning: Integrated barcode scanning of multi-well plates minimizes manual entry errors and improves sample traceability [53].
- User-Friendly Interface: A large 15.7-inch touchscreen provides an improved user interface for easy access to workflow and data management options [55].
Reagent and Assay Menu
The system's workflow is supported by an extensive portfolio of assays and reagents. Roche's subsidiary, TIB Molbiol, provides a comprehensive menu, including over 200 LightMix Modular research assays and over 60 CE-IVD assays [53] [54]. These assays are meticulously tailored for optimal performance on the LightCycler PRO system, ensuring reliability and reproducibility without compromising on user convenience [53]. The platform also offers open flexibility for users to develop and optimize their own tests, making it adaptable to specific research or diagnostic needs [56].
Experimental Protocols and Performance Validation
Robust experimental protocols are fundamental to obtaining reliable qPCR results. The following section outlines a generalized methodology for a multiplex qPCR experiment on the LightCycler PRO system, utilizing its advanced capabilities.
Detailed Protocol: 7-Target Multiplex Detection
This protocol is adapted from the Gastro Bacteria 7-target multiplexed assay optimized for the LightCycler PRO [53] [55].
Table 2: Key Research Reagent Solutions for Multiplex qPCR
| Reagent/Material | Function | Example/Note |
|---|---|---|
| Master Mix | Contains DNA polymerase, dNTPs, buffer, and salts for amplification. | Optimized for multiplexing; may include inhibitor-resistant formulations [25]. |
| Multiplex Assay Probes | Fluorescently-labeled probes for simultaneous detection of multiple targets. | LightMix Modular Assays; requires distinct, non-overlapping dyes for each channel [53]. |
| Template DNA | The target nucleic acid to be amplified and quantified. | Extracted from sample (e.g., stool, tissue, liquid biopsy). |
| Optical Plate & Seals | Reaction vessel for thermal cycling and fluorescence detection. | Roche-compatible multi-well plates; ensure optical clarity. |
Step-by-Step Procedure:
Assay Design and Validation: For in-house assays, design primers and probes according to MIQE (Minimum Information for Publication of Quantitative Real-Time PCR Experiments) guidelines to ensure specificity, efficiency, and transparent reporting [26] [25]. For pre-validated assays like the LightMix kits, reconstitute reagents as per the manufacturer's instructions.
Reaction Plate Setup:
- Thaw and gently mix all reagents. Centrifuge briefly to collect contents at the bottom of the tube.
- Prepare a master mix in a sterile tube, calculating volumes for the total number of reactions plus excess to account for pipetting error. A single reaction might contain:
- 10.0 µL of 2x Master Mix
- 2.0 µL of Primer-Probe Mix (for all 7 targets)
- 3.0 µL of Nuclease-Free Water
- 5.0 µL of Template DNA
- Gently mix the master mix and aliquot 20 µL into each well of a 96-well or 384-well optical plate.
- Seal the plate with an optical adhesive film, ensuring a tight seal to prevent evaporation and cross-contamination.
Instrument Setup and Run:
- Load the sealed plate into the LightCycler PRO instrument. The system will automatically detect the barcode if present.
- Select the appropriate pre-configured or custom run protocol on the touchscreen interface. A typical thermal cycling protocol is:
- Initial Denaturation: 95°C for 2 minutes (1 cycle)
- Amplification: 95°C for 15 seconds (denaturation) → 60°C for 60 seconds (annealing/extension with fluorescence acquisition) (45 cycles)
- Initiate the run. The system will automatically execute the protocol, with the vapor chamber ensuring temperature homogeneity and the optical system acquiring fluorescence data from all seven channels at the end of each annealing/extension step.
Data Analysis:
- Upon run completion, the software's adaptive color compensation algorithm will process the raw fluorescence data to prevent spectral crosstalk between channels.
- The updated derivative algorithm will then automatically analyze the amplification curves and assign Cq values for each target in each well.
- Results can be reviewed on the instrument's touchscreen, exported for further analysis, or directly transmitted to a LIS via the HL7 interface.
Performance Metrics and Validation
The LightCycler PRO system demonstrates high precision and accuracy across a wide dynamic range. Validation data shows a dilution series from 10^1 to 10^8 copies can be reliably detected, with the system maintaining linearity and sensitivity even at low concentrations [53] [55]. The precision of the system is underpinned by the temperature uniformity provided by the vapor chamber and the accuracy of the optical detection system. These performance characteristics are critical for applications in both research and clinical diagnostics, where reliable and reproducible data is paramount.
The Broader Diagnostic Ecosystem: qPCR, NGS, and dPCR
The LightCycler PRO system does not operate in isolation but is part of a broader, evolving molecular diagnostics landscape where qPCR, digital PCR (dPCR), and Next-Generation Sequencing (NGS) play complementary roles.
Comparative Analysis of Nucleic Acid Detection Technologies
Table 3: Comparison of Key Molecular Diagnostic Technologies
| Technology | Primary Strengths | Inherent Limitations | Ideal Application Context |
|---|---|---|---|
| qPCR (LightCycler PRO) | High speed, cost-effectiveness, excellent sensitivity and specificity for known targets, well-established workflows, high throughput [12] [25]. | Relies on pre-designed primers/probes; limited to detecting known sequences; relative quantification requires standard curves; lower precision for rare alleles vs. dPCR [12] [25]. | Routine infectious disease testing, rapid screening of known mutations, gene expression analysis, validation of NGS findings. |
| Next-Generation Sequencing (NGS) | Comprehensive, hypothesis-free discovery; detects known and novel variants; analyzes entire genomes/transcriptomes [12]. | Higher cost per sample; longer turnaround time; complex data analysis and storage requirements [12]. | Discovery of novel biomarkers, comprehensive genomic profiling in oncology, analysis of complex genetic disorders. |
| Digital PCR (dPCR) | Absolute quantification without standard curves; high sensitivity and precision for detecting rare mutations; resistant to inhibitors [57] [25]. | Lower throughput; higher cost per sample than qPCR; more limited multiplexing capabilities [57]. | Liquid biopsy for rare allele detection (e.g., in oncology), copy number variation analysis, validation of qPCR results, and gene therapy monitoring. |
Figure 2: Technology Selection Workflow in Molecular Diagnostics. This decision tree outlines how qPCR (e.g., LightCycler PRO), NGS, and dPCR can be integrated into a complementary diagnostic workflow based on the clinical or research question.
The Hybrid Approach in Personalized Medicine
A growing trend in molecular diagnostics is the adoption of hybrid workflows that leverage the strengths of multiple technologies [12]. For instance:
- Stepwise Testing: A laboratory might use the LightCycler PRO for rapid, cost-effective screening of a patient sample for a panel of known cancer mutations. If the result is ambiguous or negative despite a strong clinical suspicion, the sample could be reflexed to an NGS panel to search for novel or rare variants not covered by the qPCR assay [12].
- Layered Surveillance: In infectious disease monitoring, the LightCycler PRO can be used for high-throughput testing to track specific variants of concern in real-time, while NGS is used periodically to sequence the full pathogen genome for comprehensive surveillance and to identify emerging variants, as demonstrated during the COVID-19 pandemic [12].
- Validation and Monitoring: Discovered biomarkers from NGS studies can be transitioned into validated, routine clinical tests using robust qPCR platforms like the LightCycler PRO. For applications requiring extreme precision, such as monitoring minimal residual disease in cancer patients, dPCR may be used to confirm qPCR results due to its superior sensitivity for rare events [57] [25].
Roche's LightCycler PRO system represents a significant evolution in qPCR technology, designed to meet the dual demands of modern research and clinical diagnostics. Its technical innovations—including the vapor chamber for temperature uniformity, 7-channel multiplexing capability, and advanced software algorithms—ensure the delivery of precise, reliable, and actionable data. The platform's flexibility for workflow integration, supported by a broad assay menu and open architecture, makes it a powerful tool for laboratories navigating the transition from biomarker discovery to validated clinical testing. As the field of personalized medicine continues to expand, driving a projected market growth to nearly $590 billion by 2028 [12], the role of reliable, quantitative nucleic acid detection will only become more critical. Within the evolving molecular diagnostic ecosystem, the LightCycler PRO is positioned not as a replacement for technologies like NGS or dPCR, but as a complementary cornerstone. Its speed, accuracy, and workflow efficiency make it an indispensable component of a holistic, integrated approach to precision medicine, ultimately supporting the advancement of personalized healthcare and improved patient outcomes.
Mastering qPCR: Strategies for Overcoming Contamination, Normalization, and Technical Challenges
In the advancing field of molecular diagnostics and personalized medicine, quantitative PCR (qPCR) remains a cornerstone technology for its sensitivity and speed. However, the reliability of its results is perpetually challenged by two critical pitfalls: contamination from extraneous nucleic acids and inhibition from substances within biological samples. Effectively managing these issues is paramount for accurate patient stratification, therapy monitoring, and biomarker validation in precision medicine. This guide details modern strategies and protocols to overcome these obstacles, ensuring data integrity.
Understanding and Mitigating Contamination Risks
Contamination in qPCR, particularly from amplicon carryover or sample-to-sample cross-contamination, can lead to false-positive results, compromising diagnostic conclusions and research outcomes. In the context of cell and gene therapy manufacturing, a field projected to see 10-20 new product approvals per year by 2025, residual host cell DNA from production systems like HEK293 cells poses a significant safety and regulatory risk [58].
Strategies for Contamination Control
A robust contamination control strategy is multi-layered, focusing on prevention, detection, and the use of advanced technologies.
- Physical Segregation and Pre-PCR Processing: The most effective single measure is physically separating the pre- and post-PCR areas. Reagent preparation, sample handling, and PCR setup should occur in a dedicated, isolated clean room with dedicated equipment and unidirectional workflow to prevent amplicon carryback [58].
- Enzymatic and Chemical Decontamination: Incorporate uracil-DNA glycosylase (UDG) or dUTP systems into the qPCR master mix. This method selectively degrades uracil-containing contaminating amplicons from previous reactions without affecting the native thymine-containing DNA template. Regular decontamination of workspaces and equipment with sodium hypochlorite (bleach) or DNA-degrading solutions is also critical.
- Adoption of Digital PCR (dPCR) for Sensitive Detection: For highly sensitive applications like testing residual DNA in biotherapeutics, droplet digital PCR (ddPCR) is becoming the gold standard. It does not require a standard curve and provides absolute quantification. Its high tolerance to inhibitors often eliminates the need for extensive sample purification, thereby reducing manipulation and the associated contamination risk [58].
Table: Key Reagent Solutions for Contamination and Inhibition Management
| Reagent/Material | Primary Function | Application Context |
|---|---|---|
| UDG/dUTP System | Enzymatically degrades carryover contaminant amplicons from previous PCR runs. | Essential for high-throughput labs and diagnostic assays to prevent false positives [58]. |
| Inhibitor-Resistant Polymerase Mixes | Engineered polymerases maintain activity in the presence of common PCR inhibitors. | Critical for analyzing complex samples (blood, soil, plant, food) without extensive cleanup [59] [60]. |
| Droplet Digital PCR (ddPCR) Assays | Enables absolute quantification of targets without a standard curve; highly inhibitor-tolerant. | Gold standard for detecting trace contaminants (e.g., host cell DNA) in cell and gene therapies [58]. |
| SPUD Assay | A qPCR-based assay that detects the presence of inhibitors in nucleic acid preparations. | Used for quality control of extracted DNA/RNA to pre-emptively identify failed reactions [60]. |
| Nucleic Acid Extraction Kits with Clean-up | Selectively binds nucleic acids, removing a wide array of inhibitors and contaminants. | First-line defense for obtaining high-quality template from complex biological matrices [60]. |
The following workflow integrates these strategies into a comprehensive contamination control plan.
Overcoming qPCR Inhibition Issues
Inhibition occurs when substances co-purified with nucleic acids interfere with the polymerase, primer binding, or fluorescence detection, leading to reduced sensitivity, efficiency, or reaction failure. This is a major concern in personalized medicine, where samples like blood, biopsies, and wastewater are inherently complex [60].
Detection and Identification of Inhibition
Before attempting to overcome inhibition, it must be correctly identified. Key indicators in qPCR data include [60]:
- Delayed Cq Values: A systematic increase in Cq values across samples and controls suggests general inhibition.
- Poor Amplification Efficiency: Calculated efficiency outside the ideal 90–110% range (slope -3.6 to -3.1).
- Abnormal Amplification Curves: Flattened curves, inconsistent exponential phases, or a failure to reach the detection threshold.
- Use of Internal Controls: Adding an internal positive control (IPC) is the most reliable method. A delayed IPC Cq confirms the presence of inhibitors, distinguishing it from low target concentration.
Strategies to Overcome Inhibition
A combination of sample preparation, reaction optimization, and reagent selection is most effective.
- Enhanced Sample Purification and Dilution: Using silica-membrane column kits designed for specific sample types (e.g., stool, blood) is fundamental. For heavily inhibited samples, an additional clean-up step or template dilution can reduce inhibitor concentration to a non-critical level, though this may also dilute the target [60].
- Reaction Optimization with Additives: The addition of enhancers like bovine serum albumin (BSA) or trehalose can bind to inhibitors and stabilize the polymerase. Adjusting MgCl₂ concentration can counteract chelators like heparin [60].
- Selection of Inhibitor-Resistant Enzymes: Utilizing engineered DNA polymerases with innate inhibitor tolerance is a powerful solution. A recent 2025 study used a live culture-based screening method to identify novel Taq polymerase variants (e.g., Taq C-66 and Klentaq1 H101) with superior resistance to a wide range of inhibitors, including those from blood, humic acid, chocolate, and black pepper [59]. These variants offer intrinsic tolerance that persists after enzyme purification.
The experimental workflow below outlines a protocol for screening and validating such inhibitor-resistant polymerases.
Table: Common qPCR Inhibitors and Their Effects
| Inhibitor Source | Example Compounds | Primary Effect on qPCR |
|---|---|---|
| Biological Samples | Hemoglobin (blood), Heparin (plasma), Immunoglobulin G (serum), Lactoferrin (milk) | Polymerase inhibition, co-factor chelation [60]. |
| Environmental Samples | Humic and Fulvic Acids (soil/water), Tannins (plants), Polysaccharides (plants) | DNA degradation, fluorescence interference [59] [60]. |
| Food & Consumer Products | Polyphenols (food), Collagen (tissues), Calcium ions (feces) | Template precipitation, primer binding disruption [59]. |
| Laboratory Reagents | SDS, Ethanol, Phenol | Denaturation of enzyme, disruption of reaction kinetics [60]. |
Experimental Protocol: Validating an Inhibitor-Resistant qPCR Assay
This protocol is adapted from recent research on evolving resistant polymerases and MIQE 2.0 guidelines [59] [61].
Sample Preparation and Nucleic Acid Extraction:
- Spike a constant amount of target DNA (e.g., a synthetic construct) into a series of inhibitor-containing matrices (e.g., blood extract, humic acid solution). Use a negative control (nuclease-free water).
- Extract nucleic acids using a standard kit protocol. For a comparison arm, include an additional purification clean-up step for a subset of samples.
- Quantify and assess purity via spectrophotometry (A260/280 and A260/230 ratios).
qPCR Reaction Setup and Experimental Design:
- Prepare two master mixes: one with a standard polymerase and one with an inhibitor-resistant polymerase.
- The reaction mix should contain: 1X master mix (including buffer, dNTPs, MgCl₂), forward and reverse primers (e.g., 400 nM each), fluorescent probe (e.g., 200 nM), and template DNA (e.g., 5 µL of extracted sample).
- Critical Step: Include a standard curve using the target DNA serially diluted in nuclease-free water. This is essential for calculating amplification efficiency as per MIQE 2.0 [61].
- Run all reactions in triplicate on a real-time PCR instrument.
Data Analysis and Validation:
- Calculate amplification efficiency (E) from the standard curve slope: E = 10^(-1/slope) - 1. Efficiency should be 90-110% for an optimal, uninhibited reaction [60].
- Compare the Cq values and efficiency between the two polymerases for each inhibitor matrix. A significantly lower Cq and efficiency closer to 100% for the resistant variant indicates successful tolerance.
- Report the results with thorough documentation as per MIQE 2.0, including primer sequences, exact reaction conditions, and Cq values [61].
The Scientist's Toolkit: Essential Reagents and Materials
Success in managing contamination and inhibition relies on a toolkit of specialized reagents and materials. The table below details key solutions referenced in this guide.
Table: Essential Research Reagent Solutions
| Reagent/Material | Primary Function | Application Context |
|---|---|---|
| UDG/dUTP System | Enzymatically degrades carryover contaminant amplicons from previous PCR runs. | Essential for high-throughput labs and diagnostic assays to prevent false positives [58]. |
| Inhibitor-Resistant Polymerase Mixes | Engineered polymerases maintain activity in the presence of common PCR inhibitors. | Critical for analyzing complex samples (blood, soil, plant, food) without extensive cleanup [59] [60]. |
| Droplet Digital PCR (ddPCR) Assays | Enables absolute quantification of targets without a standard curve; highly inhibitor-tolerant. | Gold standard for detecting trace contaminants (e.g., host cell DNA) in cell and gene therapies [58]. |
| SPUD Assay | A qPCR-based assay that detects the presence of inhibitors in nucleic acid preparations. | Used for quality control of extracted DNA/RNA to pre-emptively identify failed reactions [60]. |
| Nucleic Acid Extraction Kits with Clean-up | Selectively binds nucleic acids, removing a wide array of inhibitors and contaminants. | First-line defense for obtaining high-quality template from complex biological matrices [60]. |
Navigating the pitfalls of contamination and inhibition is non-negotiable for leveraging qPCR in sensitive molecular diagnostics and personalized medicine research. A proactive, layered strategy is most effective. This includes adhering to strict physical segregation and enzymatic clean-up to prevent contamination, while combining robust nucleic acid extraction, the use of additive enhancers, and—most powerfully—the adoption of novel, inhibitor-resistant polymerase enzymes to overcome inhibition. By integrating these protocols and tools into their workflow, researchers and drug developers can ensure the generation of precise, reproducible, and clinically actionable data.
In the evolving fields of molecular diagnostics and personalized medicine, quantitative PCR (qPCR) remains a cornerstone technology for precise gene expression measurement. The accuracy of this data critically depends on robust normalization strategies to control for technical variability. This technical guide provides researchers and drug development professionals with a comprehensive framework for implementing the MIQE (Minimum Information for Publication of Quantitative Real-Time PCR Experiments) guidelines, with particular emphasis on reference gene validation. Through evidence-based protocols, comparative analysis of normalization methods, and practical visualization tools, we establish a pathway to achieving reproducible, reliable gene expression data that meets the rigorous standards required for diagnostic and therapeutic applications.
Quantitative PCR has established itself as one of the most sensitive and reproducible methods for gene expression analysis in research settings that inform molecular diagnostics. The accuracy and reliability of qPCR experiments are of paramount importance when results contribute to diagnostic decisions or therapeutic development [62]. Normalization serves as the foundational process to eliminate technical variability introduced during sample processing, RNA extraction, cDNA synthesis, and PCR amplification, thereby ensuring that measured expression differences reflect true biological variation rather than experimental artifacts [63].
The MIQE guidelines provide a standardized framework for the execution and reporting of qPCR experiments, aimed at achieving reproducibility and credibility of experimental results [62]. Compliance with MIQE guidelines gives researchers the tools to comprehensively document all aspects of their qPCR experiments, from sample preparation to data analysis. Within this framework, the selection and validation of appropriate reference genes represents one of the most critical steps, as improper normalization can lead to significant errors in data interpretation with potentially serious consequences in diagnostic and therapeutic contexts.
The MIQE Framework: Ensuring Reproducibility and Reliability
Core Principles and Requirements
The MIQE guidelines establish minimum information requirements for publishing qPCR experiments, creating a standardized framework that enhances experimental transparency and reproducibility. These guidelines cover all aspects of qPCR, including experimental design, sample quality, assay validation, and data analysis [62]. By following MIQE, researchers ensure their experiments are well-documented and that results can be independently verified by other scientists, a crucial consideration for diagnostic applications.
A key MIQE requirement is comprehensive disclosure of assay sequences. As outlined in the guidelines, "to fully comply with MIQE guidelines on assay sequence disclosure, the probe or amplicon context sequence in addition to the Assay ID will need to be provided" [62]. For TaqMan assays, this information is typically available through the Assay Information File (AIF) provided by manufacturers, which contains the required context sequences.
Documentation and Reporting Standards
MIQE-compliant reporting requires detailed documentation of several critical parameters:
- Sample metadata: Includes information on sample origin, handling, and storage conditions
- Nucleic acid quality: Assessment of RNA integrity and purity metrics
- Reverse transcription: Detailed protocol including priming method and enzyme used
- qPCR efficiency: For each assay, with acceptable ranges typically between 90-110%
- Normalization strategy: Clear description of reference gene selection and validation process
This comprehensive documentation ensures that experiments can be properly evaluated and replicated, establishing the foundation for reliable data interpretation in diagnostic development.
Reference Gene Validation: Methodologies and Best Practices
Experimental Design for Validation Studies
Proper validation of reference genes requires careful experimental design that encompasses the full range of conditions expected in the main study. The design should include:
- Biological replicates: A sufficient number to account for biological variability (typically n≥5-8 per group)
- Technical replication: Duplicate or triplicate measurements to assess technical variability
- Coverage of experimental conditions: Including all tissue types, disease states, treatments, or time points under investigation
As demonstrated in a study on canine gastrointestinal tissues, experimental designs should include samples representing all biological conditions to be compared—in this case, tissues from healthy dogs and those with gastrointestinal cancer or chronic inflammatory enteropathy [63].
Computational Tools for Stability Analysis
Multiple algorithms have been developed to evaluate reference gene stability, each employing distinct statistical approaches:
Table 1: Computational Tools for Reference Gene Validation
| Tool | Statistical Approach | Output Metrics | Key Strengths |
|---|---|---|---|
| geNorm | Pairwise variation | M-value (lower = more stable) | Identifies best-performing gene pairs; suggests optimal number of reference genes |
| NormFinder | Model-based approach | Stability value (lower = more stable) | Considers both intra- and inter-group variation; less sensitive to co-regulation |
| BestKeeper | Correlation analysis | Standard deviation, coefficient of variation | Uses raw Cq values; provides direct measure of expression variability |
| RefFinder | Comprehensive ranking | Geometric mean of rankings | Integrates results from all three algorithms for consolidated stability assessment |
These tools should be used in combination, as they provide complementary insights into gene stability. For instance, a study on 3T3-L1 adipocytes treated with postbiotic supernatants employed all four algorithms, revealing HPRT as the most stable internal control, followed by HMBS and 36B4 [64]. This comprehensive approach mitigates the limitations inherent in any single algorithm.
Step-by-Step Validation Protocol
Based on recent studies, the following protocol provides a robust framework for reference gene validation:
Select candidate reference genes: Choose 3-10 genes representing different functional pathways to minimize chance of co-regulation. Traditional housekeeping genes (GAPDH, ACTB, 18S rRNA) may be included but should not be assumed stable without validation.
Design and validate primers:
- Design primers to span exon-exon junctions where possible to exclude genomic DNA amplification
- Verify primer specificity through melt curve analysis and gel electrophoresis
- Confirm amplification efficiency between 90-110% with R² > 0.98
- Test for absence of primer-dimer formation
Perform qPCR on experimental samples:
- Include all biological conditions under investigation
- Run technical replicates to assess assay precision
- Include no-template controls to detect contamination
Analyze stability using multiple algorithms:
- Input Cq values into geNorm, NormFinder, BestKeeper, and RefFinder
- Compare rankings across different algorithms
- Identify the most stable genes and optimal number required
Validate selected reference genes:
- Test impact of normalization on known positive and negative controls
- Compare normalization performance against alternative methods if possible
This protocol was successfully applied in a wheat gene expression study, where researchers evaluated ten candidate genes across different tissues and identified Ref 2 and Ta3006 as the most stable for normalization in developing wheat organs [65].
Figure 1: Reference Gene Validation Workflow - This diagram illustrates the step-by-step process for validating reference genes, from initial selection through final implementation in main study.
Comparative Analysis of Normalization Strategies
Reference Gene Method
The use of internal reference genes remains the most common normalization approach for qPCR. The MIQE guidelines recommend using at least two validated reference genes to improve normalization accuracy [64]. However, the expression stability of these genes must be rigorously validated for each specific experimental condition, as commonly used reference genes can show significant variability under different physiological or pathological conditions.
For example, a study on canine intestinal tissues demonstrated that while three reference genes (RPS5, RPL8, and HMBS) showed suitable stability for normalizing qPCR data in gastrointestinal tissue with different pathologies, the performance varied across tissue types and disease states [63]. Similarly, research on Escherichia coli subjected to antimicrobial blue light treatment identified ihfB as the most stable reference gene, followed by cysG and gyrA [66].
Global Mean Normalization
The global mean (GM) method represents an alternative normalization approach that uses the geometric mean of all expressed genes in the dataset as a normalization factor. This method is particularly valuable when profiling large sets of genes, as it avoids the potential bias introduced by selecting a small number of reference genes.
In the canine gastrointestinal tissue study, researchers compared normalisation strategies including one to five of the most stable reference genes and the global mean of the expression of all tested genes. They found that "the global mean expression was the best-performing normalisation method" when profiling larger sets of genes, specifically recommending its implementation when a set greater than 55 genes is profiled [63].
Algorithm-Only Approaches
Algorithm-based normalization methods such as NORMA-Gene provide an alternative that doesn't require reference genes. NORMA-Gene uses a least squares regression to calculate a normalization factor that reduces variation in gene expression across experimental samples [67].
A comparative study on sheep liver samples found that "NORMA-Gene was better at reducing the variance in the expression of the target genes than was any of the other normalization methods" and offered the practical advantage of requiring fewer resources than the reference gene method [67].
Table 2: Comparison of Normalization Methods
| Method | Principle | Optimal Use Case | Advantages | Limitations |
|---|---|---|---|---|
| Single Reference Gene | Normalization to one internal control | Preliminary studies; when a universally stable gene is known | Simple, cost-effective | High risk of inaccurate normalization; not MIQE compliant |
| Multiple Reference Genes | Geometric mean of 2+ validated genes | Most qPCR studies; MIQE-compliant reporting | Improved accuracy; accounts for co-regulation | Requires validation; increased cost and effort |
| Global Mean | Mean of all expressed genes | High-throughput studies (>55 genes) [63] | No selection bias; data-driven | Requires large gene sets; computationally intensive |
| NORMA-Gene | Algorithm-based normalization | Studies with limited pre-validated references | No reference genes needed; reduces variance | Requires expression data of multiple genes |
Advanced Applications in Molecular Diagnostics and Personalized Medicine
Implementation in Disease-Specific Contexts
The validation of appropriate reference genes becomes particularly critical in molecular diagnostics, where expression patterns may be altered by disease states. For instance, in cancer diagnostics, commonly used reference genes like GAPDH and ACTB often show significant variability in tumor tissues [63]. Similarly, in inflammatory conditions, the expression stability of reference genes must be verified across disease states and tissue types.
A study on canine gastrointestinal tissues with different pathologies highlighted this challenge, demonstrating that reference gene stability varied between healthy tissues and those affected by cancer or inflammatory disease [63]. This underscores the necessity of validating reference genes specifically within the pathological context under investigation.
Quality Control in Diagnostic Applications
For qPCR-based diagnostics, implementing a rigorous normalization strategy is essential for quality control. This includes:
- Process control genes: To monitor RNA quality and reverse transcription efficiency
- Reference genes: Validated for the specific tissue and disease context
- Positive controls: To confirm assay performance across runs
- Inter-laboratory standardization: Essential for multi-center trials or diagnostic networks
The MIQE guidelines provide a framework for establishing these quality control measures, ensuring that results are comparable across different laboratories and over time [62].
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Reagents and Tools for MIQE-Compliant qPCR
| Item | Function | Application Notes |
|---|---|---|
| RNA Integrity Number (RIN) | Assesses RNA quality | Critical for sample inclusion; RIN >7 typically recommended |
| Reverse Transcriptase | cDNA synthesis | Choice of enzyme affects efficiency; document lot number |
| Pre-amplification Mix | Target enrichment | For limited samples; requires validation of linearity |
| qPCR Master Mix | Amplification reaction | SYBR Green or probe-based; requires efficiency validation |
| Stability Analysis Software | Reference gene validation | geNorm, NormFinder, BestKeeper, RefFinder |
| MIQE Checklist | Documentation aid | Ensures comprehensive reporting of all essential parameters |
Robust data normalization is not merely a technical requirement for publication but a fundamental component of reliable gene expression analysis in molecular diagnostics and personalized medicine research. Implementation of the MIQE guidelines, coupled with rigorous validation of reference genes appropriate for the specific biological context, establishes a foundation for generating clinically relevant, reproducible data. As qPCR applications continue to evolve in diagnostic and therapeutic development, adherence to these standardized approaches ensures that expression data contributes meaningfully to advancing personalized medicine while maintaining the rigorous standards required for clinical application.
The choice of normalization strategy should be guided by experimental context—while validated reference genes remain the standard for targeted gene expression studies, global mean normalization and algorithm-based approaches offer powerful alternatives for high-throughput applications. By systematically applying these principles, researchers can master data normalization to produce the reliable, reproducible results that drive advances in molecular diagnostics.
Accurate normalization is a foundational requirement for reliable gene expression data in reverse transcription quantitative polymerase chain reaction (RT-qPCR), a gold-standard technique in molecular diagnostics and personalized medicine research. Normalization controls for technical variations arising from differences in sample quantity, RNA integrity, reverse transcription efficiency, and pipetting inaccuracies [68] [69]. Without proper normalization, observed changes in gene expression may reflect experimental artifacts rather than true biological signals, potentially leading to incorrect conclusions in clinical diagnostics or drug development studies.
The two dominant normalization paradigms are the traditional reference gene method and emerging algorithm-only approaches such as NORMA-Gene. The traditional method relies on measuring one or more constitutively expressed reference genes as internal controls [70]. In contrast, algorithm-only methods perform data-driven normalization using the entire dataset of target genes without requiring separate reference gene assays [71] [72]. This technical guide provides an in-depth comparison of these methodologies, offering researchers a evidence-based framework for selecting appropriate normalization strategies in molecular diagnostics and personalized medicine research.
Traditional Reference Gene Normalization: Principles and Workflow
Theoretical Foundation and Assumptions
The reference gene method operates on the principle that carefully selected endogenous controls maintain stable expression across all experimental conditions, cell types, and treatments. These genes, often involved in basic cellular maintenance functions, serve as internal calibrators to distinguish technical variation from biological changes in target gene expression [70]. The method assumes that any variation affecting the target gene measurement affects the reference gene proportionally, enabling correction through relative quantification using the ∆∆Cq method [68].
Experimental Protocol and Validation Workflow
Implementing reference gene normalization requires a rigorous, multi-step process to identify and validate suitable controls for specific experimental conditions.
Step 1: Candidate Gene Selection
Researchers typically select candidate reference genes from classical housekeeping genes (e.g., GAPDH, ACTB, 18S rRNA) or genes previously reported as stable in similar experimental systems. For human studies, pre-designed panels such as the TaqMan Endogenous Control Plate provide 32 candidate genes for systematic screening [70].
Step 2: Experimental Validation
Candidate genes must be experimentally validated across representative conditions. The protocol involves:
- RNA Extraction: Purify RNA from all samples across different test conditions using the same method.
- cDNA Synthesis: Quantify RNA and use identical amounts and methods for cDNA synthesis.
- qPCR Amplification: Test each candidate gene across all experimental conditions in at least triplicate qPCR reactions.
- Stability Assessment: Calculate the variation in Cq values for each gene under different conditions [70].
Step 3: Stability Analysis Using Specialized Algorithms
Several algorithms have been developed to rank candidate genes by expression stability:
- geNorm: Determines the most stable genes by pairwise variation and calculates a normalization factor based on the geometric mean of the best performers [73] [69].
- NormFinder: Identifies the most stable gene(s) using model-based approaches that consider intra- and inter-group variation [73] [74].
- BestKeeper: Assesses gene stability based on the coefficient of variance and standard deviation of Cq values [73] [75].
- RefFinder: Aggregates results from multiple algorithms to provide a comprehensive stability ranking [73].
Limitations and Challenges
Despite widespread use, the reference gene approach faces significant limitations. A fundamental issue is the circular logic inherent in the method: target gene data is normalized using reference gene data obtained with the same technique [71]. Furthermore, no universally stable reference genes exist; their expression varies by species, tissue type, and experimental conditions [76]. Research shows that commonly used reference genes like GAPDH and ACTB can exhibit significant variability in certain contexts [76] [70]. Finding and validating suitable references is resource-intensive, requiring additional laboratory work, reagents, and sample material [71] [73]. This challenge is particularly acute in heterogeneous clinical samples or when studying conditions that broadly affect gene expression [71].
NORMA-Gene: An Algorithm-Only Normalization Approach
Theoretical Foundation and Mathematical Principles
NORMA-Gene (Normalization Of Real-time PCR Data by Model Averages) represents a paradigm shift in qPCR normalization by eliminating the need for separate reference genes. This data-driven algorithm utilizes the entire set of target genes being studied to calculate a normalization factor that reduces systematic, between-replicate bias [71] [72].
The method operates on two distinct levels of variance:
- Among-replicate variation (bias): Encompasses biological variation and technical variations in RNA extraction and reverse transcription efficiency.
- Among-gene variation within a single replicate: Reflects technical and random variation specific to the qPCR process [71].
NORMA-Gene specifically addresses the first level by calculating mean expression values for each replicate across all studied target genes and applying a Least Squares method to estimate and minimize systematic bias. The normalization factor for each replicate within a treatment is calculated as:
[aj = \frac{\sum{i=1}^{Nj} \left( \log X{i,j} - \frac{1}{Nj} \sum{i=1}^{Nj} \log X{i,j} \right)}{N_j}]
Where (aj) is the bias coefficient for replicate (j), (X{i,j}) is the measured gene expression value for sample (j) and gene (i), and (N_j) is the number of genes recorded for replicate (j) [71].
Implementation Workflow
Implementing NORMA-Gene requires a specific data structure and analytical process:
Step 1: Experimental Design and Data Collection
- Measure at least five target genes across all experimental replicates [71].
- Ensure consistent data quality through standard qPCR quality controls (verifying PCR efficiencies, inspecting melting curves, etc.) [71].
- Export raw Cq or fluorescence values for analysis.
Step 2: Data Preprocessing and Log Transformation
- Perform log transformation of the raw expression data, as the algorithm operates on log-transformed values [71].
- The NORMA-Gene workbook (a macro-enabled Excel tool available from the original authors) can automate this process [71].
Step 3: Normalization Factor Calculation
- The algorithm calculates normalization factors for each replicate within a treatment group using the Least Squares method.
- It estimates the remaining variance not explained by experimental bias and calculates the precision of the identified bias [71].
Step 4: Handling Missing Data
- NORMA-Gene is robust to missing data points, requiring only a minimum of five data points within a replicate across genes.
- Unlike reference gene methods where missing a reference gene replicate can lead to loss of an entire biological replicate, NORMA-Gene can proceed with extensive missing data provided minimum requirements are met [71].
Comparative Analysis: Performance and Practical Implementation
Performance Comparison in Experimental Studies
Direct comparisons between normalization methods reveal significant differences in performance and outcomes.
Table 1: Comparative Performance of Normalization Methods in Experimental Studies
| Study Context | Reference Gene Method Performance | NORMA-Gene Performance | Key Findings |
|---|---|---|---|
| Oxidative Stress in Sheep Liver (2025) [73] | Interpretation of GPX3 expression effect differed significantly depending on reference genes used | Better reduction of variance in target gene expression; More reliable normalization requiring fewer resources | NORMA-Gene provided more consistent interpretation and superior variance reduction |
| Artificial Dataset Benchmarking [71] | Precision affected by ratio of reference gene variation to target gene variation | Yielded more precise results across a large range of tested parameters | NORMA-Gene demonstrated superior precision under most experimental conditions |
| Tomato Model Plant Study [77] | Standard reference genes showed variable stability across conditions | Not directly tested, but gene combination method outperformed standard references | Highlights limitation of assuming universal reference gene stability |
Practical Implementation Considerations
Table 2: Practical Implementation Requirements Comparison
| Parameter | Reference Gene Method | NORMA-Gene |
|---|---|---|
| Minimum Gene Requirements | 1-3 reference genes typically recommended [73] | Minimum 5 target genes total [71] |
| Experimental Workload | High (requires additional assays for reference genes) | Reduced (uses target gene data only) |
| Resource Requirements | Additional reagents, samples, and processing time for reference genes | No additional resources beyond target gene measurement |
| Handling of Missing Data | Problematic (may lose entire replicates) | Robust (can proceed with missing data points) |
| Suitability for Limited Samples | Challenging (requires sufficient material for reference assays) | Ideal (maximizes information from limited target genes) |
| Adaptability to New Conditions | Requires re-validation for new conditions [76] | Automatically adapts to new experimental conditions |
Conceptual Workflow Comparison
The following diagram illustrates the fundamental differences in workflow between the two normalization approaches:
Advanced Applications and Emerging Approaches
NORMA-Gene in Research Contexts
NORMA-Gene has been successfully applied across diverse biological systems, demonstrating its broad applicability. Research applications include studies in various insect species, fish, hamsters, and humans [73]. A 2025 study on oxidative stress genes in sheep liver demonstrated NORMA-Gene's practical utility in livestock research, where it provided a more reliable normalization method that required fewer resources than reference genes [73].
RNA-Seq Informed Normalization
Emerging approaches leverage comprehensive RNA-Seq databases to identify optimal normalization genes or combinations. One innovative method identifies a stable combination of non-stable genes whose expressions balance each other across experimental conditions [77]. This approach uses RNA-Seq data to find optimal gene combinations through mathematical variance calculations, demonstrating superiority over commonly used housekeeping genes in tomato model systems [77].
The methodology involves:
- Accessing a comprehensive RNA-Seq database relevant to the research context
- Calculating mean expressions and variances for all genes across conditions of interest
- Identifying the optimal combination of genes whose geometric mean has similar expression to the target gene and whose arithmetic mean has minimal variance
- Experimental validation of the identified gene combinations [77]
Hybrid Approaches and Future Directions
The integration of algorithm-based methods with RNA-Seq data represents a promising direction for qPCR normalization. As transcriptomic databases expand, researchers can increasingly identify condition-specific normalizers that outperform classical reference genes [77] [76]. Future developments will likely focus on:
- Developing organism-specific and tissue-specific normalization databases
- Creating user-friendly tools that integrate multiple normalization strategies
- Establishing guidelines for method selection based on experimental design constraints
Table 3: Key Research Reagents and Resources for qPCR Normalization Studies
| Resource Category | Specific Examples | Function/Application |
|---|---|---|
| Reference Gene Assays | TaqMan Endogenous Control Panel (Human) [70] | Pre-validated assays for systematic screening of candidate reference genes |
| Stability Analysis Software | geNorm, NormFinder, BestKeeper [73] [69] [74] | Algorithms for ranking candidate reference genes by expression stability |
| NORMA-Gene Implementation | NORMA-Gene Excel Workbook [71] | Macro-based tool for automated implementation of NORMA-Gene normalization |
| RNA-Seq Databases | TomExpress (Tomato) [77], Genevestigator [76] | Comprehensive gene expression databases for identifying condition-specific normalizers |
| Quality Control Tools | DART-PCR algorithm [71] | Tool for computing fluorescence data and ensuring data quality pre-normalization |
The choice between traditional reference genes and algorithm-only normalization methods depends on specific research contexts, experimental constraints, and application requirements.
Context-Specific Recommendations
- For studies with limited sample material or resources: NORMA-Gene provides a significant advantage by eliminating the need for additional reference gene assays, maximizing information from minimal target genes [71] [73].
- For heterogeneous samples or conditions with broadly affected gene expression: NORMA-Gene or RNA-Seq informed approaches may outperform traditional reference genes, which can be challenging to validate in these contexts [71] [77].
- For diagnostic applications requiring strict standardization: Well-validated reference gene panels may be preferable when established for specific tissue types or conditions [70].
- For exploratory studies in non-model systems: NORMA-Gene offers adaptability to new biological contexts without prior knowledge of stable reference genes [71].
Future Perspectives in Molecular Diagnostics
As molecular diagnostics and personalized medicine increasingly rely on precise gene expression quantification, robust normalization methods become critical for accurate clinical interpretation. Algorithm-only approaches like NORMA-Gene offer promising alternatives to traditional methods, particularly when sample material is limited or reference gene validation is impractical. The integration of comprehensive transcriptomic databases with algorithm-based normalization represents the future of precise, context-specific qPCR normalization in both basic research and clinical applications.
Researchers should select normalization methods based on careful consideration of their specific experimental design, resource constraints, and the biological system under investigation. Whichever method is chosen, proper validation and transparent reporting of normalization approaches remain essential for generating reliable, reproducible gene expression data in molecular diagnostics and personalized medicine research.
Quantitative PCR (qPCR) and reverse transcription qPCR (RT-qPCR) are cornerstone techniques in molecular diagnostics and personalized medicine research, enabling the precise quantification of genetic material [1]. The optimization of qPCR workflows through the integration of automation, high-throughput systems, and reagent standardization is critical for enhancing data reproducibility, increasing laboratory throughput, and reducing manual errors [78]. In fields such as oncology and infectious disease diagnostics, where results directly influence therapeutic decisions, robust and efficient qPCR processes are non-negotiable. This guide details the methodologies and technologies that researchers and drug development professionals can deploy to refine their qPCR workflows, ensuring that they meet the stringent demands of modern clinical research and diagnostic applications.
The drive toward personalized medicine, particularly in oncology, is accelerating the adoption of advanced molecular diagnostics [2]. Technologies such as PCR are dominating the market, accounting for over 50% of its share, a testament to their fundamental role [79]. The global molecular diagnostics market, valued at US$21.01 billion in 2024, is projected to grow, further underlining the importance of efficient and scalable diagnostic workflows [79]. Automation stands out as a key solution, revolutionizing laboratories by enhancing efficiency, ensuring compliance with regulatory standards, and allowing for scalable operations without compromising data quality [78].
The Case for Automation and Standardization
The Impact of Automation on Data Quality and Throughput
Automation in qPCR workflows transcends mere convenience; it significantly enhances data integrity and operational efficiency. A primary benefit is the substantial reduction in manual errors associated with pipetting and sample handling [78]. In high-throughput settings, where hundreds or thousands of reactions are processed simultaneously, manual processing becomes a significant source of variability. Automated liquid handling systems ensure consistent reagent dispensing across all wells, directly improving the reproducibility of results [78].
Furthermore, automation seamlessly integrates with laboratory information management systems (LIMS) or cloud-based platforms, enabling the automated transfer of run data [78]. This minimizes manual data handling, reduces transcription errors, and ensures data integrity, which is particularly crucial in regulated environments like clinical diagnostics and biopharma that must comply with standards such as U.S. FDA 21 CFR Part 11 [78]. The capability for remote monitoring and control of instruments via cloud platforms also facilitates centralized management and flexibility [78].
The Role of Reagent Standardization
Reagent standardization is the complement to automation. Using consistent, high-quality reagents that are specifically designed for automated workflows is fundamental to achieving reliable and reproducible qPCR data [80]. Key considerations include:
- Reagent Stability: Reagents that are room-temperature stable for extended periods (e.g., 24 hours) are ideal for automated dispensing, as they do not require cooling blocks that can complicate robotic workflows [78].
- Optimized Formulations: Master mixes should be optimized for robust amplification and consistent performance with both specific dyes (like TaqMan probes) and non-specific dyes (like SYBR Green) [80] [78].
- Automation-Compatible Packaging: Reagents offered in bulk formats or custom packaging are tailored for the demands of high-throughput automated systems, facilitating uninterrupted runs [78].
High-Throughput Systems and Miniaturization Strategies
Automated qPCR Instrumentation
Modern real-time PCR systems are engineered with automation and high-throughput as core design principles. Instruments like the CFX Opus Real-Time PCR System can be integrated directly with automated liquid handlers for hands-off reaction setup and plate loading [78]. These systems often feature application programming interfaces (APIs) that allow them to communicate with and be controlled by robotic workstations, creating a fully automated pipeline from sample preparation to data analysis [78]. The high-density 384-well format of some thermal cyclers is specifically optimized for laboratories requiring higher sample throughput, which is common in genotyping studies and large-scale screening applications [78].
Miniaturization of Reaction Volumes
Miniaturization is a powerful strategy for reducing reagent costs and enabling high-throughput analysis, particularly when working with precious or limited sample types, such as patient biopsies. Research has demonstrated that careful miniaturization of qPCR reactions is feasible without sacrificing data quality.
Table 1: Performance of Miniaturized qPCR Reaction Conditions
| Reaction Condition | Success Rate / Amplification Performance | Correlation with Manual Full Reaction |
|---|---|---|
| Full Reaction (FR) | Successful amplification [81] | Baseline for manual processing [81] |
| 1.5x Miniaturization | Successful amplification; >70% success rate with biological samples [81] | Strong significant positive correlation [81] |
| 2.5x Miniaturization | Suboptimal amplification; lower success rate [81] | Excluded from further analysis [81] |
| 5x Miniaturization | No amplification [81] | Excluded from further analysis [81] |
A study automating a gene expression workflow found that a 1.5x miniaturization condition yielded a success rate greater than 70% when testing biological RNA samples on immunology and pregnancy gene expression panels [81]. Critically, the data from these miniaturized, automated runs showed a "strong significant positive correlation" with data from manual full-reaction workflows, underscoring the robustness of this approach [81]. However, the study also highlights that excessive miniaturization (e.g., 2.5x and 5x) leads to suboptimal or failed amplification, indicating that optimization is essential [81].
Experimental Protocols for Workflow Integration and Validation
Protocol: Automating a Gene Expression Workflow
This protocol is adapted from a published study on the automation and miniaturization of high-throughput qPCR for gene expression profiling [81].
- Workflow Scripting: Script the entire gene expression workflow, including all liquid handling steps, on the software of an automated liquid handler (e.g., Mosquito HV genomics software) [81].
- Sample Preparation: Isolate RNA from biological samples (e.g., from patient cohorts). Use qualified collection tools and isolation kits to ensure high-quality, consistent input material [81] [80].
- Quality Control: Never skip the integrity check. Test the purity and integrity of the purified RNA using a method such as gel electrophoresis or a bioanalyzer. High-quality RNA is critical for reliable results [80].
- Reverse Transcription (Two-Step RT-qPCR): Convert RNA to cDNA using a high-quality reverse transcription kit. This two-step approach offers flexibility for storing cDNA and analyzing multiple targets from a single sample [1].
- Automated qPCR Setup: a. Use an automation-compatible qPCR master mix, selected for its stability and performance with automated dispensers [78]. b. Prime the liquid handler to dispense the master mix, primers/probes, and cDNA samples into a robust, automation-designed PCR plate (e.g., a rigid Hard-Shell PCR plate) [78]. c. Seal the plate using an automated plate sealer to ensure sample integrity [78]. d. Automatically transfer the sealed plate to the real-time PCR instrument via an integrated robotic arm [81].
- qPCR Amplification: Run the plate using a standardized thermal cycling protocol. The CFX Opus system, for example, can be triggered automatically to start the run [78].
- Data Analysis: Use integrated software (e.g., CFX Maestro) to automatically process the qPCR data. The expression of each gene can be calculated using the 2^(-ΔΔCt) method for relative quantification, which is ideal for comparing gene expression across different treatment groups [81] [1] [82].
Protocol: qPCR Assay Optimization in 9 Steps
Before implementing any assay in an automated workflow, it must be rigorously optimized. The following steps are crucial [80]:
- Primer Design: Design primers to be 28bp or larger with an optimal GC content between 40%-60%. The melting temperature (Tm) should be between 58°C-65°C, with a difference of no more than 4°C between forward and reverse primers. The 3' end should have no more than two Gs or Cs in the last five nucleotides to minimize primer-dimer formation [80].
- Probe Design (if applicable): The probe Tm should be ~10°C higher than the primer Tm to ensure it binds first. Avoid G repeats, especially at the 5' end, as this can quench the reporter dye [80].
- Thermocycler Optimization: a. Initial Denaturation: 95°C for 30 seconds is sufficient for short genomic DNA templates [80]. b. Cycling Denaturation: For short templates (<300 bp), 95°C for 5-15 seconds is adequate [80]. c. Annealing/Extension: A two-step (shuttle) PCR is often used. Start at 60°C for 1 minute and optimize in 0.1°C steps. The time depends on the detection speed of your system [80].
- Efficiency Calculation: Perform a serial dilution of a known template amount (e.g., 1/10, 1/100, 1/1000). Plot the Log(10) dilution factor against the resulting Ct values. Use the slope of the standard curve in the formula: Efficiency (%) = (10^(-1/slope) - 1) x 100. An efficiency between 90% and 110% is acceptable [82].
- Validation: Consistently use automation-compatible plastics, such as white wells with ultra-clear caps, to reduce light distortion and improve signal detection [80] [78].
The Scientist's Toolkit: Essential Reagents and Materials
Selecting the right tools is the foundation of any optimized and automated qPCR workflow. The following table details key reagent solutions and their specific functions.
Table 2: Research Reagent Solutions for Automated qPCR Workflows
| Item Category | Specific Product Examples | Function in Automated Workflow |
|---|---|---|
| qPCR Master Mix | Reliance One-Step Multiplex Supermix; SsoAdvanced Universal Probes Supermix [78] | Room-temperature stable enzymes optimized for automated dispensing; provide consistent, robust amplification for probe-based or dye-based detection [78]. |
| Automation-Compatible Plates | Hard-Shell PCR Plates (96-/384-well) [78] | Rigid construction minimizes warping for easy robotic handling; ensures flatness for optimal thermal conductivity and seal integrity [78]. |
| Plate Seals | Adhesive or Heat Seals [78] | Compatible with automated sealers to prevent cross-contamination and evaporation, maintaining sample integrity during runs [78]. |
| dNTPs & Buffers | dNTP Mixes in bulk formats [78] | Supplied in bulk packaging suitable for automated dispensing systems, ensuring a continuous supply for high-throughput applications [78]. |
| Liquid Handler | Mosquito HV [81] | Automated liquid handling system capable of accurately pipetting and dispensing nanoliter volumes for reaction setup and miniaturization [81]. |
| Real-Time PCR System | CFX Opus System; BioMark HD [81] [78] | High-throughput real-time PCR instruments with API for integration into automated workstations; enable remote monitoring and automated data export [81] [78]. |
Data Analysis and Interpretation in Automated Systems
Fundamentals of the qPCR Amplification Curve
Understanding the components of a qPCR amplification curve is vital for troubleshooting automated runs. Key elements include [82]:
- Baseline: The initial cycles (5-15) where fluorescent signal is background noise. The instrument uses this to establish a baseline fluorescence level [82].
- Threshold: A fluorescence level set sufficiently above the baseline to indicate a significant, exponential increase in signal. It is used to determine the Ct value [82].
- Ct (Cycle Threshold): The PCR cycle number at which the sample's amplification curve crosses the threshold. It is a relative measure of the target's starting concentration [1] [82].
- Amplification Curve: The S-shaped plot representing DNA accumulation. The exponential phase is where the most accurate quantitative data is derived [1] [82].
- Plateau Phase: The final phase where reaction kinetics slow and signal accumulation stops, due to reagent consumption or enzyme inactivation [1] [82].
Quantitative Analysis Methods
For gene expression studies in personalized medicine, relative quantification is the most common approach, as it allows for the comparison of gene expression levels between different sample groups (e.g., treated vs. control, diseased vs. healthy) [1] [82].
The Comparative C_T (ΔΔCT) Method is widely used and can be easily automated with software like CFX Maestro [1] [78]. The steps are as follows [82]:
- Normalize to Endogenous Control: Calculate ΔCT for each sample.
- ΔCT = CT (Target Gene) - C_T (Reference Gene)
- A stable reference gene (e.g., ACTB, GAPDH) is critical for accurate normalization [1].
- Normalize to Reference Sample: Calculate ΔΔCT.
- ΔΔCT = ΔCT (Test Sample) - ΔCT (Calibrator Sample)
- The calibrator is often an untreated control or a baseline sample.
- Calculate Fold Change:
- Fold Change = 2^(-ΔΔC_T)
This method assumes that the amplification efficiencies of the target and reference genes are approximately equal and close to 100% [82]. If efficiencies are not optimal, alternative methods like the one described by Pfaffl should be employed [82].
The integration of automation, high-throughput systems, and reagent standardization represents the definitive path forward for qPCR in molecular diagnostics and personalized medicine research. The technical protocols and solutions outlined in this guide provide a framework for laboratories to achieve higher levels of efficiency, reproducibility, and throughput. As the molecular diagnostics market continues its rapid growth and the demand for companion diagnostics in oncology and other fields intensifies, the reliance on these optimized workflows will only deepen [2] [79]. The future will likely see a greater emphasis on fully integrated robotic workstations that automate the entire process from sample to answer, alongside continued innovation in miniaturization and multiplexing capabilities. By adopting and refining these integrated workflows, researchers and clinical professionals can ensure they are at the forefront of delivering precise, reliable, and actionable genetic data that is essential for advancing personalized patient care.
qPCR in the Evolving Diagnostic Arena: Benchmarking Against dPCR, NGS, and CRISPR
In the evolving landscape of molecular diagnostics, quantitative PCR (qPCR), digital PCR (dPCR), and Next-Generation Sequencing (NGS) have emerged as cornerstone technologies, each with distinct strengths and applications. While qPCR remains the established workhorse for high-throughput, cost-effective routine testing, dPCR offers superior precision and sensitivity for absolute quantification of rare targets. NGS provides an unparalleled breadth of discovery, enabling comprehensive genomic analysis. The selection of an appropriate technology is not a question of superiority but of strategic alignment with specific research objectives, sample types, and logistical constraints. Within the broader thesis of personalized medicine, these technologies form a complementary toolkit: qPCR for rapid screening, dPCR for precise validation, and NGS for exploratory discovery, collectively driving the transition from reactive diagnostics to proactive, patient-centered care.
The polymerase chain reaction (PCR), invented in 1986, revolutionized molecular biology by allowing for the exponential amplification of specific DNA sequences [83]. This foundational technology has since evolved through several generations. The initial end-point PCR provided qualitative or semi-quantitative analysis but lacked robust quantification capabilities [84]. The advent of quantitative PCR (qPCR), also known as real-time PCR, in the early 1990s introduced the ability to monitor DNA amplification in real-time using fluorescent probes, enabling relative quantification of the target nucleic acid [83] [84]. The third generation, digital PCR (dPCR), developed in the late 1990s and commercialized in the 2000s, transformed quantification by using limiting dilution and Poisson statistics to provide absolute quantification of DNA molecules without the need for a standard curve [83] [85].
Parallel to these developments, Next-Generation Sequencing (NGS) emerged in the late 2000s as a transformative technology capable of sequencing millions of DNA fragments simultaneously [12] [86]. Unlike PCR-based methods that target specific, known sequences, NGS offers a hypothesis-free approach, allowing for the discovery of novel variants and comprehensive analysis of entire genomes, exomes, or transcriptomes [12] [87]. The convergence of these technologies is accelerating the advancement of personalized medicine, which aims to tailor therapeutic and diagnostic approaches to an individual's unique genetic profile [12] [88].
Quantitative PCR (qPCR)
qPCR functions by amplifying a target DNA sequence and monitoring the accumulation of fluorescent signal at the end of each PCR cycle. The core quantitative metric is the quantification cycle (Cq), the cycle number at which the fluorescence crosses a predetermined threshold. The Cq value is inversely proportional to the initial amount of target nucleic acid. To determine concentration, the Cq values of unknown samples are compared to a standard curve generated from samples with known concentrations [84] [11]. This reliance on a standard curve and the fact that the reaction occurs in a bulk mixture are defining characteristics of qPCR. Its high throughput, established workflows, and cost-effectiveness have made it the gold standard for a vast range of applications, from infectious disease testing to gene expression analysis [12] [11].
Digital PCR (dPCR)
dPCR operates on a fundamentally different principle by partitioning a single PCR reaction into thousands to millions of individual compartments (nanowell arrays or droplets) such that each contains either zero, one, or a few target molecules [83] [84]. Following end-point PCR amplification, each partition is analyzed for fluorescence. Partitions containing the target sequence (positive) are counted against those without (negative). Using Poisson statistics, the absolute concentration of the target in the original sample is calculated without the need for a standard curve [83] [85]. This partitioning confers key advantages, including exceptional sensitivity, high tolerance to PCR inhibitors, and the ability to detect minute (e.g., 0.1% variant allele frequency) differences, making it ideal for detecting rare mutations and copy number variations [84] [85].
Next-Generation Sequencing (NGS)
NGS is a high-throughput technology that enables the massively parallel sequencing of millions of DNA fragments. While platforms like Illumina (short-read), Pacific Biosciences, and Oxford Nanopore (long-read) differ in their underlying chemistry, they all share the ability to generate enormous amounts of sequence data in a single run [87] [86]. Unlike qPCR and dPCR, which are targeted methods, NGS can be applied in a targeted (specific gene panels), whole-exome, or whole-genome manner. This allows for the comprehensive detection of a wide spectrum of genetic variations—single nucleotide variants (SNVs), insertions/deletions (indels), copy number variations (CNVs), and gene fusions—in a single assay, making it a powerful discovery tool [12] [86].
Table 1: Core Technological Principles and Key Characteristics
| Feature | qPCR | Digital PCR (dPCR) | Next-Generation Sequencing (NGS) |
|---|---|---|---|
| Fundamental Principle | Real-time fluorescence monitoring in a bulk reaction | End-point fluorescence detection in partitioned reactions | Massively parallel sequencing of DNA fragments |
| Quantification Method | Relative (based on Cq & standard curve) | Absolute (based on Poisson statistics of positive partitions) | Relative (based on read counts and alignment) |
| Throughput | High (number of samples) | Medium | Very High (amount of data per sample) |
| Typical Applications | Pathogen detection, gene expression, genotyping | Rare mutation detection, copy number variation, liquid biopsy | Whole genome/exome sequencing, variant discovery, transcriptomics, metagenomics |
| Key Strength | Speed, cost-effectiveness, high-throughput screening | Absolute quantification, high precision, sensitivity for rare targets | Comprehensive, untargeted discovery of known and novel variants |
| Primary Limitation | Requires standard curve, lower precision & sensitivity vs. dPCR | Limited dynamic range, higher cost per sample than qPCR | High computational demand, complex data analysis, higher cost for targeted applications |
Comparative Technical Performance and Application Fit
Quantitative Data Comparison
A direct comparison of key performance metrics reveals the specific niches for each technology.
Table 2: Head-to-Head Performance Metric Comparison
| Performance Metric | qPCR | Digital PCR (dPCR) | Next-Generation Sequencing (NGS) |
|---|---|---|---|
| Sensitivity (Limit of Detection) | Moderate (e.g., 1% VAF for mutations) [85] | High (e.g., 0.1% VAF for mutations; can reach 0.01% with BEAMing) [85] | Variable (Moderate to High; depends on coverage depth) |
| Precision | ++ (Good) [84] | +++ (Excellent) [84] | + to ++ (Varies with platform and bioinformatics) |
| Dynamic Range | >10^5 (Wide) [84] | ~10^4 (Constrained by partition count) [84] [89] | Extremely Wide |
| Multiplexing Capability | + (Limited, typically 2-6 plex) [84] | +++ (High potential in each partition) [84] | ++++ (Virtually unlimited) |
| Absolute Quantification | No (Requires standard curve) | Yes (Calibration-free) [84] [85] | No (Relative to total reads) |
| Cost per Sample | $ (Low) | $$ (Medium) | $$$ (High for WGS, lower for panels) |
| Ease of Use / Workflow | Established, familiar workflow | Simplified analysis, less prone to inhibitor effects [84] | Complex, requires specialized bioinformatics expertise [87] |
Application Scenarios in Personalized Medicine
Infectious Disease Diagnostics: qPCR is the undisputed leader for high-volume, routine pathogen detection due to its speed and low cost, a role solidified during the COVID-19 pandemic [12] [11]. NGS is invaluable for public health surveillance, as it can sequence entire viral genomes to track emerging variants and understand transmission dynamics [12]. dPCR finds utility in precisely quantifying viral load, especially for pathogens that are difficult to culture or when monitoring minimal residual disease [83].
Oncology and Liquid Biopsy: This area highlights the complementary nature of these technologies. qPCR can serve as a first-pass, cost-effective screen for common, known cancer mutations [12]. dPCR excels in the precise monitoring of circulating tumor DNA (ctDNA), where it can detect and quantify rare mutant alleles in a high background of wild-type DNA with a sensitivity crucial for assessing treatment response and early recurrence [83] [85]. NGS is the technology of choice for comprehensive genomic profiling of tumors, identifying a wide array of actionable mutations, fusions, and biomarkers to guide targeted therapy selection [12] [87].
Genetic Disorder Diagnosis: For screening known, high-frequency mutations, qPCR is highly efficient. dPCR offers robust and precise quantification of gene copy number variations (CNVs), such as in the diagnosis of certain hereditary conditions [83] [84]. NGS, particularly through whole-exome or whole-genome sequencing, is transformative for diagnosing rare and undiagnosed genetic diseases, as it can interrogate the entire coding genome without prior knowledge of the causative variant [87].
Experimental Workflows and Protocols
The experimental pathways for these technologies differ significantly, from sample preparation to data analysis. The following diagrams and protocols outline the core workflows.
qPCR and dPCR Workflow
Detailed qPCR Protocol for Gene Expression Analysis
- RNA Extraction: Purify total RNA from cells or tissue using a silica-column or magnetic bead-based kit. Assess RNA integrity and concentration using a spectrophotometer.
- Reverse Transcription: Convert 0.1–1 µg of total RNA into complementary DNA (cDNA) using a reverse transcriptase enzyme and oligo(dT) or random hexamer primers.
- Reaction Setup: Prepare a 20 µL qPCR reaction mix containing:
- 1X TaqMan Gene Expression Master Mix (includes DNA polymerase, dNTPs, and optimized buffer).
- 1X TaqMan Gene Expression Assay (contains sequence-specific forward and reverse primers and a FAM-labeled probe).
- 10–50 ng of cDNA template.
- Nuclease-free water to volume.
- Amplification and Detection: Load the plate into a real-time PCR instrument. Run the following thermal cycling protocol:
- UNG Incubation (Optional): 50°C for 2 minutes to prevent amplicon carryover.
- Polymerase Activation: 95°C for 10–20 minutes.
- 40–50 Cycles of:
- Denaturation: 95°C for 15 seconds.
- Annealing/Extension: 60°C for 1 minute (with fluorescence data collection).
- Data Analysis: Use the instrument's software to determine the Cq value for each reaction. Normalize the Cq of the target gene to the Cq of one or more reference genes (e.g., GAPDH, ACTB) using the ∆∆Cq method to calculate relative fold-change in expression [84] [11].
Detailed dPCR Protocol for Rare Mutation Detection
- DNA Extraction: Purify genomic DNA or cell-free DNA (cfDNA) from plasma. Precisely quantify the DNA using a fluorometer.
- Reaction Setup: Prepare a 20–40 µL dPCR reaction mix containing:
- 1X ddPCR Supermix for Probes (or equivalent).
- 1X primer-probe assay for the mutant allele (FAM-labeled) and wild-type allele (HEX/VIC-labeled) if performing duplex detection.
- 1–100 ng of DNA template.
- Partitioning:
- PCR Amplification: Place the partitions in a thermal cycler and run a standard endpoint PCR protocol with optimized cycle numbers (e.g., 40 cycles) to amplify the target within each partition.
- Signal Readout:
- For Droplets: Transfer the droplet emulsion to a droplet reader that flows them single-file past a fluorescence detector to classify each as FAM-positive (mutant), HEX-positive (wild-type), double-positive, or negative [83].
- For Nanowells: Image the entire chip using a fluorescence microscope or scanner to determine the fluorescence signature of each well [85].
- Data Analysis: The instrument software applies Poisson statistics to the count of positive and negative partitions to calculate the absolute concentration of the mutant and wild-type targets (in copies/µL) and the variant allele frequency (VAF) [84] [85].
NGS Workflow
Detailed NGS Protocol for Targeted Gene Panel Sequencing
- DNA Extraction & QC: Extract high-quality genomic DNA. Precisely quantify using a fluorometric method (e.g., Qubit) and assess integrity using a fragment analyzer or agarose gel.
- Library Preparation:
- Fragmentation: Use enzymatic or acoustic shearing to fragment 50–200 ng of DNA to a target size of 200–500 bp.
- End-Repair & A-Tailing: Perform enzymatic reactions to create blunt-ended, 5'-phosphorylated fragments with a single 3'-A overhang.
- Adapter Ligation: Ligate platform-specific sequencing adapters (containing index sequences for sample multiplexing) to the fragments.
- PCR Amplification: Perform a limited-cycle PCR (e.g., 8–10 cycles) to enrich for adapter-ligated fragments and add full-length adapters and indices.
- Target Enrichment (for Panel Sequencing): Hybridize the library to biotinylated probes complementary to the target genomic regions. Capture the probe-bound library fragments using streptavidin-coated magnetic beads. Wash away non-target fragments and perform a post-capture PCR to amplify the enriched library.
- Library QC and Pooling: Quantify the final library using qPCR to measure the concentration of amplifiable fragments. Pool (multiplex) equimolar amounts of up to hundreds of individually indexed libraries into a single sequencing run.
- Sequencing: Denature the pooled library and load it onto the NGS platform (e.g., Illumina MiSeq/HiSeq/NovaSeq) for cluster generation and sequencing-by-synthesis, typically generating paired-end reads [87] [86].
- Bioinformatic Analysis:
- Primary Analysis: The sequencer's software performs base calling and demultiplexing, generating FASTQ files for each sample.
- Secondary Analysis: Sequence reads (FASTQ) are aligned to a reference genome (e.g., GRCh38) using aligners like BWA or Bowtie2, producing BAM files. PCR duplicates are marked, and base quality scores are recalibrated.
- Tertiary Analysis: Variant callers (e.g., GATK) are used to identify SNVs and indels from the BAM files, generating VCF files. Variants are filtered, annotated for functional impact (using databases like ClinVar, gnomAD), and interpreted in the context of the clinical or research question [87].
The Scientist's Toolkit: Essential Research Reagents & Materials
Successful implementation of these technologies relies on a suite of specialized reagents and instruments.
Table 3: Key Research Reagent Solutions and Their Functions
| Category | Specific Product Examples | Critical Function in Workflow |
|---|---|---|
| Nucleic Acid Polymerases | Hot-start Taq DNA Polymerase, Bst 2.0 Polymerase (for isothermal), Reverse Transcriptase | Enzymatic engine of amplification; critical for specificity, efficiency, and yield. |
| Master Mixes | qPCR Master Mix (e.g., with UNG), ddPCR Supermix for Probes, Lyo-Ready formulations | Pre-mixed, optimized solutions of buffers, dNTPs, polymerase, and salts for robust and reproducible reactions [12]. |
| Primers & Probes | TaqMan Assays, Double-Quenched Probes, Target-Specific Primers | Confer assay specificity; fluorescent probes enable real-time detection or endpoint classification. |
| Library Prep Kits | Illumina DNA Prep, Nextera Flex, Amplicon-based Panels | Streamlined reagent kits for converting sample DNA into sequencing-ready NGS libraries [86]. |
| Target Enrichment | IDT xGen Lockdown Probes, Twist Human Core Exome | Biotinylated oligonucleotide probes for capturing genomic regions of interest in hybrid capture-based NGS [87]. |
| Quality Control Kits | Qubit dsDNA HS Assay, Agilent Bioanalyzer Kits, qPCR-based Library Quant Kits | Essential for accurately quantifying input nucleic acids and final libraries to ensure sequencing success [86]. |
The choice between qPCR, dPCR, and NGS is not a matter of selecting a single superior technology but of strategically deploying the right tool for the specific research question. qPCR remains the most efficient and cost-effective solution for high-throughput targeted screening. dPCR has carved out a critical niche where absolute quantification, high precision, and superior sensitivity for rare targets are paramount. NGS stands alone in its ability to conduct comprehensive, hypothesis-free genomic exploration.
The future of molecular diagnostics lies not in the isolation of these technologies but in their integration. A powerful emerging paradigm is the use of qPCR for initial rapid screening, followed by dPCR for sensitive validation and longitudinal monitoring, and NGS for comprehensive discovery and panel development [12]. Furthermore, the convergence of these technologies with artificial intelligence (AI) for data analysis, multi-omics integration, and the development of point-of-care (POC) applications is set to redefine the boundaries of personalized medicine [87] [88]. As these tools continue to evolve, becoming faster, more affordable, and more accessible, they will collectively empower researchers and clinicians to deliver on the promise of truly personalized healthcare.
Quantitative Polymerase Chain Reaction (qPCR) occupies a pivotal role in molecular diagnostics and personalized medicine research due to its capacity to precisely quantify nucleic acids in real time [25]. This technique supports precision in interpreting gene expression, pathogen load, and molecular biomarkers, forming the foundation for patient stratification and tailored therapeutic interventions [25]. The evolving landscape of personalized medicine, which tailors treatment according to individual genomic profiles, increasingly depends on qPCR and related technologies that provide high sensitivity, reproducibility, and throughput [25] [90]. This technical guide provides a comprehensive analysis of qPCR performance characteristics, establishes its optimal use cases against competing technologies, and outlines validated experimental protocols to ensure research and diagnostic reliability.
Table 1: Key Performance Characteristics of qPCR
| Performance Metric | Typical qPCR Performance | Impact on Diagnostic Utility |
|---|---|---|
| Analytical Sensitivity | Can detect down to single copies of nucleic acids; single-cell sensitivity demonstrated in optimized protocols [91] | Enables early disease detection and monitoring of minimal residual disease |
| Assay Specificity | High, dependent on primer design and reaction optimization; can distinguish single-nucleotide polymorphisms [25] | Critical for accurate mutation detection and pathogen identification |
| Dynamic Range | 7-8 logarithms of magnitude [25] | Allows quantification of targets across wide concentration ranges without sample dilution |
| Throughput | Medium to High (96- and 384-well formats); automation can process thousands of reactions daily [92] | Supports large-scale screening and epidemiological studies |
| Turnaround Time | 2-4 hours for results [93] | Facilitates rapid clinical decision-making |
| Multiplexing Capacity | Limited by spectral overlap of fluorescent probes; typically 4-6 targets per reaction [25] | Enables parallel detection of multiple pathogens or genetic markers |
qPCR Workflows and Technical Considerations
Core qPCR Methodology and Optimization
The qPCR technique amplifies target DNA sequences while monitoring fluorescence signals in each cycle, allowing determination of nucleic acid quantity during the exponential phase rather than at reaction end [25]. The method uses fluorescent dyes or sequence-specific probes to measure amplified products through a three-step process: (1) Denaturation, where template DNA double-strand dissociates to single strand at high temperature (94°C); (2) Annealing, where specific primers and target DNA complementary combine according to base pairing principle (50-60°C); and (3) Extension, where single-stranded DNA serves as a template for complementary DNA replication with primer extension at 72°C [93].
A critical advancement in qPCR application is the development of high-throughput screening (HTS) protocols that maintain sensitivity while dramatically reducing costs. One systematically optimized RT-qPCR protocol reduced reagent volumes to 25% of manufacturer recommendations, achieving a nearly 90% cost reduction while maintaining excellent HTS performance metrics (Z' factor >0.5) [91]. This protocol demonstrated single-cell analytical sensitivity and diagnostic sensitivity equivalent to detecting 1:10,000 responding cells with over 90% accuracy, making it particularly valuable for limited samples such as PBMCs [91].
Experimental Protocol: High-Throughput, Cost-Optimized RT-qPCR
Application: Quantification of surrogate markers of immunity (e.g., IFN-γ mRNA) from peripheral blood mononuclear cells (PBMCs) for immunology research and vaccine development [91].
Table 2: Research Reagent Solutions for HTS qPCR
| Reagent/Consumable | Function | Specific Example |
|---|---|---|
| MagMAX mirVana Total RNA Isolation Kit | RNA extraction from PBMCs | Provides high-quality RNA with minimal inhibitors |
| SuperScript IV First-Strand Synthesis System | Reverse transcription of RNA to cDNA | Creates stable cDNA template for qPCR |
| ssoAdvanced Universal SYBR Green Master-Mix | Fluorescent detection of amplified DNA | Intercalating dye for real-time quantification |
| QuantStudio 5 Real-Time PCR System | Thermal cycling with fluorescence detection | Instrument platform for reaction execution and data collection |
| PrimerBank Primers | Sequence-specific amplification | Ensures targeted amplification of genes of interest |
| 96- or 384-Well Reaction Plates | Reaction vessels | Compatible with automated liquid handling systems |
Step-by-Step Methodology:
- Cell Stimulation & Lysis: Incubate PBMCs (50,000-100,000 cells) with antigenic stimulants (e.g., peptide epitopes, PMA/Ionomycin) in 96-well U-bottom plates for 3-9 hours at 37°C, 5% CO₂. Pellet cells and lyse for RNA extraction [91].
- RNA Extraction: Use magnetic bead-based RNA extraction kits (e.g., MagMAX mirVana) following manufacturer's instructions. For HTS, consider semi-automated purification systems [91].
- Reverse Transcription (Cost-Optimized): Convert extracted RNA to cDNA using a quarter-volume protocol: Use 25% of recommended reagent volumes (reverse transcriptase, buffers, dNTPs) while maintaining total reaction volume with DEPC-treated H₂O. Incubate at 50°C for 10 minutes, then 80°C for 10 minutes [91].
- qPCR Reaction Setup: Prepare 5µL reactions containing:
- 2.5µL SYBR Green master mix
- 0.5µL primer mix (500nM final concentration)
- 1µL diluted cDNA (1:4 dilution in Ultra-Pure H₂O)
- 1µL DEPC-treated H₂O
- Thermal Cycling: Program thermocycler with:
- Initial denaturation: 95°C for 2 minutes
- 40 cycles of: 95°C for 5 seconds (denaturation), 60°C for 30 seconds (annealing/extension)
- Melt curve analysis: 95°C for 15 seconds, 60°C for 1 minute, then gradual increase to 95°C [91].
- Data Analysis: Calculate mRNA copies/reaction using absolute quantification based on a standard curve. Normalize data to reference genes and analyze using appropriate statistical methods.
Validation Parameters: For HTS applications, validate assay uniformity through coefficient of variation (CV) calculations and Z-Prime factor determination from the mean and standard deviation of qPCR cycle threshold values for minimal, medium, and maximal signals [91].
Comparative Technology Analysis in Clinical Applications
qPCR Versus Alternative Platforms
The positioning of qPCR within the molecular diagnostics landscape requires clear understanding of its performance relative to emerging technologies, particularly next-generation sequencing (NGS) and digital PCR (dPCR).
Table 3: Technology Comparison for Molecular Diagnostics
| Parameter | qPCR | Digital PCR (dPCR) | Next-Generation Sequencing (NGS) |
|---|---|---|---|
| Absolute Quantification | Relative quantification (requires standard curve) [25] | Yes (absolute without standard curve) [25] | Relative (requires normalization) |
| Sensitivity | High (detects 1:10,000 responding cells) [91] | Very High (superior for rare variants) [25] | Variable (depends on coverage depth) |
| Multiplexing Capacity | Limited (typically 4-6 targets) [25] | Limited | Excellent (thousands of targets simultaneously) [90] |
| Throughput | High (especially with automation) [92] [94] | Medium | Very High (massively parallel) |
| Cost Per Sample | Low [91] [90] | Medium | High (though decreasing) [90] |
| Turnaround Time | 2-4 hours [93] | 3-5 hours | Days to weeks |
| Variant Discovery | Limited to known targets | Limited to known targets | Excellent for novel variant discovery [90] |
| Best Applications | Routine diagnostics, high-throughput screening, rapid pathogen detection [90] | Rare variant detection, absolute quantification needed [25] | Comprehensive genomic analysis, discovery research [90] |
Clinical Utility in Personalized Medicine
qPCR delivers particular clinical value in scenarios requiring rapid, sensitive detection of predefined targets. In oncology, qPCR methods remain widely used to assess transcripts or fusion genes in hematologic malignancies and solid tumors, with applications in minimal residual disease monitoring [25]. For pharmacogenomic profiling, qPCR effectively detects single-nucleotide polymorphisms or allele-specific expression that guide optimized drug choice and dosing [25]. In infectious disease management, qPCR provides rapid pathogen identification and quantification, enabling targeted therapeutic interventions and infection control [93].
The integration of qPCR with complementary technologies creates powerful diagnostic workflows. A hybrid approach uses qPCR for rapid screening of known mutations or pathogens, followed by NGS to explore novel variants or broader genomic regions when results are inconclusive [90]. Similarly, qPCR can serve as a first-pass tool in oncology workflows, with dPCR confirmation for ambiguous cases requiring absolute quantification [25].
Figure 1: Technology Selection Workflow for Molecular Diagnostics. This decision tree guides selection of qPCR, dPCR, or NGS based on application requirements.
Implementation Considerations for Research and Clinical Settings
Quality Assurance and Regulatory Compliance
Reliable qPCR implementation requires strict adherence to quality standards. The MIQE guidelines (Minimum Information for Publication of Quantitative Real-Time PCR Experiments) establish best practices for reporting, including transparency in assay design and controls [25] [26]. For clinical applications, laboratories must follow regulatory frameworks like CLIA, ISO 15189, or equivalent national standards [25] [41].
Key validation parameters for clinical research assays include [41]:
- Analytical Sensitivity: Determine the limit of detection (LoD) through serial dilution of target nucleic acid.
- Analytical Specificity: Evaluate cross-reactivity with closely related organisms or genetic variants.
- Precision: Assess repeatability (within-run) and reproducibility (between-run, between-operator, between-instrument).
- Accuracy: Compare results to a reference method or certified reference materials.
The fit-for-purpose validation approach recognizes that the required rigor of validation depends on the intended context of use [41]. For example, a qPCR assay for research screening requires different validation than a companion diagnostic determining therapeutic selection.
Automation and Workflow Efficiency
Investment in qPCR automation addresses significant limitations in manual workflows, particularly regarding time, labor, and error rates [92]. Automated liquid handling systems provide:
- Increased Throughput: Simultaneous processing of numerous samples, accelerating research timelines [92] [94].
- Reduced Labor Costs: Freeing highly-trained personnel from repetitive pipetting tasks for higher-value activities [92].
- Minimized Errors: Precise and consistent reagent dispensing reduces pipetting inaccuracies and cross-contamination [92].
- Enhanced Reproducibility: Standardized protocols ensure consistent results regardless of operator [92].
The economic analysis reveals that while initial automation investment is required, the long-term return on investment is substantial due to reagent savings, reduced repeat experiments, and more efficient personnel utilization [92].
qPCR remains an indispensable technology in molecular diagnostics and personalized medicine research, offering an optimal balance of sensitivity, speed, and cost-effectiveness for defined applications. Its utility is maximized in scenarios requiring detection of known biomarkers, high-throughput screening, and rapid diagnostic results. The evolving landscape features increased automation, integration with complementary technologies like NGS and dPCR, and development of more sustainable practices. By understanding its performance characteristics relative to alternative platforms and implementing validated experimental protocols, researchers and clinicians can leverage qPCR to advance personalized medicine and improve patient outcomes. Future directions point toward more streamlined workflows, point-of-care applications, and enhanced computational integration for data analysis and interpretation.
Quantitative PCR (qPCR) remains a foundational technology in modern molecular diagnostics, not as a standalone method but as a powerfully synergistic component that enhances and validates next-generation diagnostic platforms. This technical guide examines how qPCR's unique attributes—quantitative precision, rapid turnaround, and methodological robustness—create complementary relationships with emerging technologies across the diagnostic workflow. As the molecular diagnostics market accelerates toward a projected $37.19 billion by 2033 with PCR technology maintaining over 50% market share [79], understanding these integrative workflows becomes essential for researchers, clinical laboratories, and drug development professionals implementing personalized medicine approaches. The continued innovation in qPCR platforms, including automated systems supporting end-to-end IVD and LDT workflows [95], ensures its persistent relevance in an evolving diagnostic ecosystem where multi-platform strategies are becoming standard practice.
The landscape of molecular diagnostics has expanded dramatically with the advent of technologies ranging from next-generation sequencing (NGS) to digital PCR (dPCR) and various isothermal amplification methods. Yet qPCR maintains a central position in clinical and research settings due to its well-established standardization, regulatory acceptance, and continuous technical evolution. The "gold standard" status of PCR in molecular diagnosis is supported by decades of clinical validation and well-established international standards and regulatory systems [24]. What has evolved is qPCR's role from a primary standalone technology to an integral component in multi-technology workflows that leverage the respective strengths of complementary platforms.
This integration is particularly valuable in personalized medicine, where qPCR plays a crucial role in companion diagnostics that identify biomarkers predicting patient response to specific therapies, especially in oncology, infectious diseases, and autoimmune disorders [79]. The rising adoption of these companion diagnostics exemplifies how qPCR's reliability and quantitative capabilities complement the discovery power of other technologies in targeted therapeutic applications.
Market Context and Technological Positioning
Molecular Diagnostics Market Landscape
The molecular diagnostics market is experiencing substantial growth, driven by technological advancements and expanding applications across healthcare and research sectors. This expansion creates opportunities for integrated platform approaches that combine qPCR with complementary technologies.
Table 1: Molecular Diagnostics Market Outlook
| Metric | 2024 Value | 2033 Projection | CAGR (2025-2033) |
|---|---|---|---|
| Global Market Size | US$21.01 billion | US$37.19 billion | 5.8% |
| PCR Technology Market Share | >50% | Maintains dominance | - |
| North America Market (2022) | US$13.27 billion | Continued leadership | - |
Data compiled from market analysis reports [79] [2].
The instrument segment of the molecular diagnostics market is experiencing particularly rapid growth, advancing from US$8.55 billion in 2022 to US$8.97 billion in 2023 [79], reflecting continued investment in platform technologies including qPCR systems. This growth is fueled by the rising emphasis on personalized medicine and early disease detection, which demand the sophisticated capabilities of modern qPCR systems alongside complementary technologies.
qPCR Technological Fundamentals
qPCR's value in integrated workflows stems from its core technical attributes:
- Quantitative Precision: qPCR provides accurate quantification of nucleic acids across a wide dynamic range, typically 7-8 orders of magnitude [1], enabling reliable measurement of gene expression, pathogen load, and genetic variations.
- Probe-Based Specificity: Technologies such as TaqMan probes offer sequence-specific detection through fluorescent reporter-quencher systems, allowing multiplexed detection of multiple targets in a single reaction [96].
- Rapid Turnaround: Modern qPCR systems can provide results in as few as 30 minutes using fast cycling protocols [95], making them invaluable for time-sensitive diagnostic applications.
- Automation Compatibility: Contemporary systems like the QuantStudio 7 Pro Dx support end-to-end IVD and LDT workflows with interchangeable 96-well and 384-well blocks that integrate with liquid handling systems [95].
Complementary Workflows: qPCR in Multi-Platform Diagnostics
qPCR-NGS Integration
The relationship between qPCR and NGS represents one of the most powerful synergies in modern molecular diagnostics, with each technology compensating for the other's limitations:
Target Discovery Clinical Validation: NGS enables hypothesis-free discovery of novel biomarkers, mutations, and expression profiles across the entire genome or transcriptome, while qPCR provides the high-throughput validation required to confirm findings in larger patient cohorts [2]. This complementary relationship efficiently bridges the discovery-to-validation gap in biomarker development.
Comprehensive Profiling Targeted Quantification: While NGS offers unparalleled comprehensive profiling capabilities, its relatively higher cost and computational demands make it impractical for routine monitoring of established biomarkers. qPCR excels at cost-effective, repetitive quantification of predefined targets, creating a natural workflow where NGS identifies candidates and qPCR handles ongoing assessment [97].
Sensitivity Challenges Amplification Power: For targets with low abundance, qPCR can detect down to single-digit copy numbers [98], providing superior sensitivity for rare transcripts or low-level infections that might be missed by NGS, especially when material is limited.
Figure 1: qPCR-NGS Complementary Workflow. This synergy bridges discovery and clinical application.
qPCR-dPCR Relationship
Digital PCR (dPCR) has emerged as a complementary technology to qPCR rather than a replacement, with each method serving distinct purposes in the diagnostic workflow:
Absolute vs. Relative Quantification: dPCR provides absolute quantification without standard curves by partitioning samples into thousands of individual reactions [97], making it ideal for applications requiring precise copy number determination. qPCR remains superior for high-throughput relative quantification where comparison across many samples is required.
Low Abundance Target Detection: dPCR demonstrates greater precision and reproducibility for detecting rare mutations and low-abundance targets [97], particularly in liquid biopsy applications where tumor DNA represents a minute fraction of total cell-free DNA.
Practical Implementation Considerations: While dPCR offers advantages for specific applications, qPCR maintains practical benefits in throughput, cost-effectiveness, and established regulatory pathways that ensure its continued dominance in routine clinical diagnostics.
qPCR-Isothermal Amplification Synergy
Isothermal amplification methods like LAMP and RPA have gained attention for point-of-care applications, but they complement rather than replace qPCR:
Point-of-Care vs. Central Laboratory: Isothermal methods excel in decentralized settings due to minimal equipment requirements, while qPCR remains the gold standard in central laboratories where its superior specificity and quantification capabilities are essential [24].
Specificity Considerations: Isothermal methods like LAMP can suffer from higher non-specific amplification compared to qPCR [24], making qPCR the preferred method for applications demanding high specificity.
Multiplexing Capabilities: qPCR supports robust multiplex detection (currently up to 5-plex in standard systems) [98], whereas isothermal methods face significant challenges in multiplexed detection due to primer complexity.
Experimental Protocols for Integrated Workflows
qPCR-NGS Validation Protocol
This protocol describes a standardized approach for validating NGS-derived biomarkers using qPCR, suitable for gene expression studies or variant confirmation:
Sample Preparation:
- Extract high-quality RNA/DNA using silica-column or magnetic bead-based methods. For blood samples, consider PAXgene RNA systems for stabilized RNA.
- Quantify nucleic acids using fluorescence-based methods (e.g., Qubit) rather than spectrophotometry for accurate concentration measurement.
- For RNA targets, perform reverse transcription using random hexamers and oligo(dT) primers (ratio 1:1) in a 20 µL reaction with 1 µg total RNA input.
qPCR Assay Configuration:
- Use TaqMan probe chemistry for maximum specificity, particularly for single-nucleotide variant detection.
- Design assays with amplicon sizes between 60-150 bp to match typical NGS library insert sizes.
- Implement multiplex reactions incorporating both target assays and reference genes (e.g., GAPDH, β-actin) for normalization.
- Perform efficiency validation using 5-point 1:4 serial dilution curves, accepting assays with 90-110% efficiency and R² > 0.985 [1].
Data Analysis:
- Apply baseline correction using early cycles (typically 3-15) to eliminate background fluorescence [99].
- Set threshold in the logarithmic phase of amplification where all curves display parallel trajectories.
- Use the ΔΔCq method for relative quantification or standard curve approach for absolute quantification [99].
qPCR-dPCR Concordance Testing
For applications requiring the utmost precision, this protocol establishes analytical validity between qPCR and dPCR measurements:
Sample Processing:
- Prepare sample aliquots from the same source material for parallel qPCR/dPCR analysis.
- For dPCR, partition samples according to platform specifications (20,000 partitions for droplet-based systems).
- For qPCR, run triplicate technical replicates on a calibrated instrument.
Data Normalization:
- Apply Poisson correction to dPCR data to account for partitions containing multiple copies.
- For qPCR, use standard curves derived from reference materials with known concentrations.
- Compare absolute quantification values between platforms, accepting <25% coefficient of variation as acceptable concordance.
Table 2: Research Reagent Solutions for Integrated qPCR Workflows
| Reagent Category | Specific Examples | Function in Workflow | Technical Considerations |
|---|---|---|---|
| Reverse Transcriptase | LunaScript RT SuperMix | cDNA synthesis from RNA templates | Includes aptamer-based enzyme control for room temperature setup [98] |
| qPCR Master Mix | Luna Universal qPCR Master Mix | Amplification and detection | Compatible with multiplexing (up to 5-plex) and carryover prevention [98] |
| Probe Chemistry | TaqMan Hydrolysis Probes | Sequence-specific detection | Fluorophore choices (FAM, VIC, ROX) enable multiplexing [96] |
| Reference Genes | GAPDH, β-actin, 18S rRNA | Normalization controls | Require validation for specific sample types [1] |
| Inhibition Resistance | Tween-20, BSA | Enhanced robustness | Critical for direct amplification without extraction [98] |
Diagnostic Applications in Personalized Medicine
Oncology Companion Diagnostics
qPCR plays an essential role in oncology companion diagnostics, where it complements broader genomic profiling approaches:
Therapy Selection: qPCR efficiently detects specific mutations (e.g., EGFR, BRAF, KRAS) that determine eligibility for targeted therapies, providing rapid turnaround compared to NGS while offering higher specificity than traditional methods [2].
Minimal Residual Disease (MRD) Monitoring: qPCR assays targeting patient-specific rearrangements enable highly sensitive MRD detection with a sensitivity of 1 in 10⁵ - 10⁶ cells, complementing dPCR for absolute quantification in cases requiring extreme sensitivity [2].
Liquid Biopsy Applications: While NGS identifies novel circulating tumor DNA markers, qPCR provides the practical solution for routine monitoring of established markers, with emerging technologies like AnchorDx and AccuStem developing specialized liquid biopsy panels [2].
Infectious Disease Management
In infectious disease diagnostics, qPCR serves as the frontline detection method while complementing other technologies:
Multiplex Pathogen Panels: qPCR multiplex panels (e.g., BioFire FilmArray) simultaneously detect 20+ pathogens, with positive results potentially triggering reflex testing by sequencing for strain typing or resistance marker identification [98].
Antiviral Resistance Monitoring: qPCR assays specifically detect known resistance mutations (e.g., influenza neuraminidase, HIV reverse transcriptase), while NGS identifies emerging novel resistance patterns [79].
Point-of-Care Adaptation: Simplified qPCR workflows like saliva-based direct amplification eliminate RNA extraction steps, making molecular testing more accessible while maintaining the gold standard accuracy [98].
Emerging Trends and Future Directions
QUICK-PCR for Point-of-Care Testing
The future of qPCR integration lies in the development of QUICK-PCR (Quick, Ubiquitous, Integrated, Cost-efficient) systems that maintain the technology's gold standard accuracy while expanding its accessibility [24]. These systems aim to deliver:
- Simplified Workflows: Integration of sample preparation, amplification, and detection in single disposable cartridges.
- Rapid Thermal Cycling: Advanced heating technologies including Joule heating, thermoelectric heating, and plasmonic heating to reduce amplification time [24].
- Integrated Readout Systems: Compact detection systems utilizing smartphone cameras and LEDs to replace bulky conventional optics [24].
Artificial Intelligence Integration
AI and machine learning are enhancing qPCR integration in several key areas:
- Automated Data Analysis: AI algorithms assist in baseline correction, threshold setting, and amplification efficiency calculation, reducing inter-operator variability [2].
- Quality Control: Machine learning models identify anomalous amplification curves, contamination patterns, and sample quality issues that might compromise results [95].
- Predictive Analytics: Integration of qPCR data with clinical parameters through AI models improves diagnostic and prognostic accuracy in personalized treatment planning [2].
Standardization and Data Exchange
Future integration will rely heavily on improved standardization:
- RDML Data Format: Widespread adoption of the Real-time PCR Data Markup Language (RDML) standard will facilitate data exchange between qPCR instruments, analysis tools, and researchers [97].
- MIQE Compliance: Adherence to Minimum Information for Publication of Quantitative Real-Time PCR Experiments (MIQE) guidelines ensures data quality and reproducibility across platforms [97].
- Regulatory Harmonization: Efforts to harmonize regulatory requirements across regions will accelerate the implementation of integrated diagnostic systems combining qPCR with complementary technologies [79].
qPCR maintains an indispensable position in the molecular diagnostics ecosystem through strategic complementarity with next-generation technologies rather than competition. Its quantitative precision, methodological robustness, and continuous innovation create natural synergies with NGS, dPCR, and isothermal amplification methods across diverse diagnostic applications. As personalized medicine advances, integrated workflows leveraging qPCR's strengths alongside complementary technologies will deliver the comprehensive yet practical diagnostic solutions required for modern healthcare. The ongoing development of QUICK-PCR systems, AI-enhanced analytics, and standardized data exchange will further strengthen these synergistic relationships, ensuring qPCR's central role in the future of integrated diagnostics.
Navigating the Regulatory and Reimbursement Landscape for Clinical Assay Validation
The integration of quantitative Polymerase Chain Reaction (qPCR) into molecular diagnostics and personalized medicine represents a cornerstone of modern clinical research and therapeutic development. This powerful technology enables precise quantification of nucleic acids, facilitating applications ranging from gene expression analysis and pathogen detection to genotyping and mutation analysis in precision oncology [100]. The global market for qPCR assay design and validation services, valued at $408.2 million in 2024 and projected to reach $866.3 million by 2033, reflects the critical importance of robust, reliable assay validation in the clinical ecosystem [100].
For researchers, scientists, and drug development professionals, navigating the complex regulatory and reimbursement landscape is paramount for successfully translating qPCR assays from research tools to clinically validated diagnostics. The process requires meticulous attention to analytical validation, regulatory compliance, and reimbursement strategy—each representing a critical milestone on the path to clinical adoption. This technical guide provides a comprehensive framework for this journey, addressing both the scientific rigor required for validation and the practical considerations for regulatory approval and reimbursement success.
Global Regulatory Frameworks for qPCR Assays
United States Food and Drug Administration (FDA) Pathways
The FDA regulates clinical assays through several distinct pathways, each with specific requirements and considerations for qPCR-based tests:
Emergency Use Authorization (EUA): Under Section 564 of the FD&C Act, the EUA pathway allows for accelerated authorization of unapproved medical products during public health emergencies when no adequate alternatives exist [101]. This mechanism was extensively utilized during the COVID-19 pandemic for molecular diagnostics and continues to be relevant for emerging threats, as demonstrated by its application during the 2022 mpox outbreak [101].
Premarket Approval (PMA) and 510(k): For routine clinical use, qPCR assays typically require traditional marketing authorization through either the PMA pathway (for higher-risk Class III devices) or the 510(k) pathway (for moderate-risk Class II devices demonstrating substantial equivalence to a predicate device).
Breakthrough Device Designation: This voluntary program provides prioritized review and interactive communication for devices that demonstrate potential for more effective treatment or diagnosis of life-threatening diseases [102].
The FDA emphasizes rigorous analytical and clinical validation, requiring comprehensive documentation of assay performance characteristics, manufacturing quality controls, and clinical utility evidence.
European Union In Vitro Diagnostic Regulation (IVDR)
The implementation of the EU's In Vitro Diagnostic Regulation (IVDR) in 2022 significantly heightened regulatory requirements for qPCR assays in European markets [103]. Key aspects include:
Stratified Risk Classification: IVDR implements a risk-based classification system (Class A-D) that determines the level of regulatory scrutiny, with most qPCR assays falling into Class C (high individual risk) or Class D (high public health risk) categories.
Enhanced Technical Documentation: The regulation mandates exhaustive technical documentation including performance evaluation reports, scientific validity evidence, analytical performance data, and clinical performance data [103].
Strict Quality Management System Requirements: Manufacturers must implement comprehensive quality management systems conforming to IVDR standards, encompassing the entire device lifecycle from design to post-market surveillance.
For clinical trials utilizing qPCR assays within the EU, IVDR compliance requires stringent validation studies covering accuracy, precision, specificity, sensitivity, and reproducibility, accompanied by detailed validation reports and risk management documentation [103].
International Harmonization Initiatives
Global regulatory harmonization continues to evolve through initiatives such as:
International Council for Harmonisation (ICH) Guidelines: Many regulatory authorities, including China's NMPA, have adopted ICH guidelines to align technical requirements for pharmaceutical products, creating consistency in companion diagnostic development [102].
Project Orbis: This FDA-led initiative facilitates simultaneous submission and review of oncology products among multiple international regulatory agencies, potentially streamlining approval for companion diagnostics [102].
Table 1: Comparative Analysis of Major Regulatory Pathways for qPCR Assays
| Regulatory Aspect | U.S. FDA | EU IVDR | China NMPA |
|---|---|---|---|
| Review Timeline | 180 days (PMA) | 90-120 days (Class C) | 60-120 days (Category 1 innovative) |
| Clinical Evidence Requirements | Analytical & clinical performance with intended use population | Analytical & clinical performance with scientific validity | Analytical & clinical performance with Chinese population data |
| Quality System Requirements | QSR (21 CFR Part 820) | QMS per Annexes IX & XI | GMP per NMPA guidelines |
| Post-Market Surveillance | Mandatory reporting (MDR) | Post-market performance follow-up (PMPF) | Annual reporting and re-evaluation |
Reimbursement Strategies for Validated qPCR Assays
United States Reimbursement Framework
The U.S. reimbursement landscape for molecular diagnostics centers on several key mechanisms:
Medicare's MolDX Program: This program provides a structured framework for coverage of molecular diagnostics, requiring technical assessment and demonstrated clinical utility for payment determination [104]. The program has established specific coverage for qPCR-based tests in areas such as oncology, infectious diseases, and transplantation medicine.
Current Procedural Terminology (CPT) Codes: Obtaining appropriate CPT codes is essential for reimbursement, with options including:
- Category I CPT Codes: Established codes for widely adopted tests with demonstrated clinical utility
- Proprietary Laboratory Analyses (PLA) Codes: Specific identifiers for unique laboratory-developed tests
- Category III CPT Codes: Temporary codes for emerging technologies, services, and procedures
Local Coverage Determinations (LCDs): Regional Medicare Administrative Contractors (MACs) issue LCDs that outline coverage policies for specific tests, creating geographic variability in reimbursement [104].
Recent trends show increasing coverage for qPCR-based liquid biopsy assays in oncology, particularly for monitoring minimal residual disease and treatment response [104].
International Reimbursement Considerations
European Health Technology Assessment: EU member states utilize varying health technology assessment frameworks to evaluate clinical and economic value, with growing emphasis on cost-effectiveness analyses for diagnostic reimbursement decisions.
Emerging Market Dynamics: Markets such as China are rapidly evolving their reimbursement frameworks for innovative diagnostics, with the NMPA streamlining approval pathways for novel assays [102]. Between 2019-2023, China demonstrated significant progress in innovative drug development, creating parallel opportunities for companion diagnostics [102].
Table 2: Key Reimbursement Considerations for qPCR Clinical Assays
| Reimbursement Factor | Technical Requirements | Evidence Expectations | Documentation Needs |
|---|---|---|---|
| Analytical Validity | Sensitivity, specificity, accuracy, precision, reportable range, reference range | CLSI guideline compliance (EP05, EP06, EP07, EP09, EP12, EP17, EP25) | Complete validation reports with statistical analysis |
| Clinical Validity | Positive/negative predictive value, clinical sensitivity/specificity, prevalence | Well-designed clinical studies establishing clinical performance | Published peer-reviewed literature, clinical study reports |
| Clinical Utility | Impact on clinical decision-making, patient outcomes, economic value | Comparative effectiveness research, health economic analyses | Real-world evidence, clinical guidelines endorsements |
| Economic Evidence | Cost-effectiveness, budget impact, cost-benefit analysis | Health economic models comparing to standard of care | Detailed economic analyses using accepted methodologies |
Experimental Design for qPCR Assay Validation
Analytical Validation Protocols
Comprehensive analytical validation establishes that an assay consistently and accurately measures the analyte of interest. For clinical qPCR assays, the following performance characteristics must be rigorously evaluated:
Accuracy and Precision Studies:
- Protocol: Test at least three levels of controls (low, medium, high) across a minimum of 20 replicates over five separate runs [103].
- Acceptance Criteria: Total precision (CV) ≤15% for RNA assays, ≤10% for DNA assays; mean observed concentration within 15% of true value for accuracy.
Limit of Detection (LoD) Determination:
- Protocol: Serially dilute target nucleic acid in appropriate matrix, testing a minimum of 60 replicates across the expected detection limit [103].
- Statistical Analysis: Probit analysis recommended with 95% detection rate establishing LoD.
Linearity and Reportable Range:
- Protocol: Test at least five concentrations spanning the assay's measuring range with multiple replicates at each level.
- Analysis: Linear regression with R² ≥0.98, back-calculated concentrations within 15% of expected values.
Specificity Testing:
- Cross-Reactivity: Evaluate against genetically related organisms, commensal flora, and human genomic DNA.
- Interfering Substances: Assess effects of common interferents (hemoglobin, lipids, heparin, etc.) at clinically relevant concentrations.
Clinical Validation Methodologies
Clinical validation establishes the assay's performance characteristics in the intended use population:
Comparator Method Studies:
- Protocol: Prospective testing of clinical specimens using both the new qPCR assay and an established comparator method (gold standard).
- Sample Size: Minimum of 100 positive and 100 negative samples recommended for statistical power.
Precision Medicine Applications:
- For companion diagnostics, demonstrate capability to accurately stratify patients for targeted therapies through well-controlled clinical trials [100] [102].
Essential Research Reagent Solutions for qPCR Validation
Successful validation of clinical qPCR assays requires carefully selected, quality-controlled reagents and materials. The following table outlines essential components and their functions in the validation workflow:
Table 3: Research Reagent Solutions for qPCR Assay Validation
| Reagent/Material | Function in Validation | Quality Considerations |
|---|---|---|
| Reference Standards | Quantification calibrators, positive controls for accuracy determination | Traceability to international standards, certified concentrations, stability data |
| Extraction Kits | Nucleic acid purification from clinical matrices | Consistent yield, purity (A260/A280), inhibitor removal, minimal cross-contamination |
| PCR Master Mixes | Amplification reaction foundation | Lot-to-lot consistency, inhibitor tolerance, efficiency documentation |
| Primers/Probes | Target-specific detection | HPLC purification, sequence verification, specificity confirmation, minimal self-complementarity |
| Internal Controls | Extraction and amplification monitoring | Non-competitive design, non-interference with target amplification, clinically relevant concentration |
| Negative Controls | Contamination monitoring | Nuclease-free water, human genomic DNA, matrix-matched negative samples |
Quality Control and Assurance Systems
Implementing External Quality Control
External Quality Control (EQC) provides independent verification of assay performance through inter-laboratory comparison programs [105]. Key components include:
- Proficiency Testing: Regular participation in recognized proficiency testing programs using blinded samples with undisclosed target concentrations [105].
- External Quality Assessment Schemes: Systematic programs that provide external validation of laboratory testing quality, often mandated by regulatory bodies like the FDA and WHO [105].
- Standardized Operating Procedures: Implementation of comprehensive SOPs for all aspects of the testing process, regularly reviewed and updated to reflect current best practices [105].
Continuous Monitoring and Improvement
Robust quality systems incorporate ongoing monitoring mechanisms:
- Statistical Process Control: Implement control charts tracking quality control results to identify trends and shifts in assay performance.
- Root Cause Analysis: Structured investigation protocols for identifying underlying causes of assay failures or performance degradation.
- Preventive Action Programs: Proactive systems for addressing potential issues before they impact clinical results.
Workflow Visualization for Regulatory Strategy
The following diagram illustrates the comprehensive workflow for navigating the regulatory and reimbursement pathway for clinical qPCR assays:
Regulatory Strategy Workflow for Clinical qPCR Assays
Successfully navigating the regulatory and reimbursement landscape for clinical qPCR assays demands a systematic, evidence-based approach integrating rigorous scientific validation with comprehensive regulatory strategy. The evolving nature of both molecular technologies and regulatory frameworks requires ongoing vigilance and adaptation from research and development professionals.
Key success factors include early engagement with regulatory authorities, robust analytical and clinical validation study designs, strategic reimbursement planning, and implementation of sustainable quality systems. By adopting the structured approaches outlined in this guide, researchers and drug development professionals can effectively advance qPCR assays through the complex pathway from research tool to clinically adopted diagnostic, ultimately supporting the continued advancement of personalized medicine and improved patient care.
The future of clinical qPCR validation will likely see increased harmonization of international standards, expanded applications in liquid biopsy and minimal residual disease monitoring, and greater integration of artificial intelligence in quality control and data analysis—all areas requiring continued attention from the scientific community.
Conclusion
qPCR remains an indispensable and dynamically evolving technology in molecular diagnostics, firmly establishing itself as a gold standard for nucleic acid quantification. Its robustness, quantitative capability, and adaptability continue to make it fundamental for applications ranging from infectious disease diagnostics to oncology and pharmacogenomics. The future of qPCR is being shaped by powerful trends, including the integration of artificial intelligence for data analysis, the development of portable point-of-care devices for decentralized testing, and the creation of sophisticated multiplex assays. Furthermore, its role is increasingly defined by synergy rather than competition, as it integrates into larger diagnostic workflows alongside dPCR and NGS. For researchers and drug developers, mastering both the technical execution—including rigorous normalization and troubleshooting—and the strategic application of qPCR within this expanding technological ecosystem is paramount. This expertise will be crucial for driving the next wave of innovation in precision medicine, ultimately enabling faster, more accurate diagnoses and more effective, personalized patient therapies.
References
- 1. Introduction to Quantitative PCR (qPCR) Gene Expression ... [https://www.thermofisher.com/us/en/home/life-science/pcr/real-time-pcr/real-time-pcr-learning-center/gene-expression-analysis-real-time-pcr-information/introduction-gene-expression.html]
- 2. Molecular Diagnostics for Cancer Markets Forecasts 2025 ... [https://www.businesswire.com/news/home/20251104680914/en/Molecular-Diagnostics-for-Cancer-Markets-Forecasts-2025-2030-by-Cancer-Type-Product-and-Place-with-Executive-and-Consultant-Guides-and-Impact-of-Artificial-Intelligence---ResearchAndMarkets.com]
- 3. PCR/qPCR Data Analysis [https://www.sigmaaldrich.com/US/en/technical-documents/technical-article/genomics/qpcr/data-analysis?srsltid=AfmBOoqhavXKxAM4ymLnbURIZQLwMUvo0EQ_oR1ROZUFClVlgnjnhKas]
- 4. How qPCR Works [https://www.sigmaaldrich.com/US/en/technical-documents/technical-article/genomics/qpcr/how-qpcr-works?srsltid=AfmBOoqJA1i4rbBeG5J4j-d6isasK7phWCoD2xAZH2qtvw0RwFr6sVyR]
- 5. Multicolor Combinatorial Probe Coding for Real-Time PCR [https://pmc.ncbi.nlm.nih.gov/articles/PMC3021529/]
- 6. Top 11 qPCR Papers Every Researcher Should Know [https://bitesizebio.com/62143/qpcr-papers/]
- 7. HEX (Hexachlorofluorescein) in Fluorophores [https://www.lumiprobe.com/t/fluorophores/hex]
- 8. qPCR Instruments Market Size & Demand Analysis | 2033 [https://straitsresearch.com/report/qpcr-instruments-market]
- 9. Digital PCR (dPCR) and Real-time PCR (qPCR) Market to ... [https://www.towardshealthcare.com/insights/digital-pcr-dcpr-and-real-time-pcr-qpcr-market-sizing]
- 10. PCR Technologies Market Size to Hit USD 31.39 Billion ... [https://www.precedenceresearch.com/pcr-technologies-market]
- 11. The rise of qPCR testing in clinical diagnostics [https://www.nature.com/articles/d42473-022-00012-5]
- 12. The Growing Demand for Personalized Diagnostics [https://www.meridianbioscience.com/lifescience-blog/the-growing-demand-for-personalized-diagnostics-navigating-the-benefits-and-limits-of-qpcr-vs-ngs/]
- 13. qPCR Instruments Market Size, Trends & Forecast 2025- ... [https://www.futuremarketinsights.com/reports/qpcr-instruments-market]
- 14. Introductory Chapter: Molecular Diagnostics in the Era of ... [https://www.intechopen.com/chapters/1236960]
- 15. Pcr (Dpcr) And Qpcr Market Size 2025 Report [https://www.linkedin.com/pulse/pcr-dpcr-qpcr-market-size-2025-report-cagr-industry-3oz8e]
- 16. Clinical trial designs for testing biomarker-based ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4296980/]
- 17. Breaking Barriers with PCR: Strategies for clinical trial ... [https://www.precisionformedicine.com/breaking-barriers-with-pcr-in-clinical-trials]
- 18. United States Molecular Diagnostics Market Forecast ... [https://crisprmedicinenews.com/press-release-service/card/united-states-molecular-diagnostics-market-forecast-report-and-company-analysis-2025-2033-featuring/]
- 19. Infectious Disease Diagnostics Market to Surge USD 62.95 ... [https://www.towardshealthcare.com/insights/infectious-disease-diagnostics-market-sizing]
- 20. Infectious Disease Diagnostics Market Size & Growth ... [https://www.marketsandmarkets.com/Market-Reports/infectious-disease-diagnostics-market-116764589.html]
- 21. Infectious Disease In Vitro Diagnostics Market Set to Reach ... [https://www.biospace.com/press-releases/infectious-20disease-20in-20vitro-20diagnostics-20market]
- 22. A Quantitative Framework for Measuring Personalized ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8000405/]
- 23. Molecular Diagnostics Trends: What's Next After COVID-19? [https://www.diamonddiagnostics.com/blog/molecular-diagnostics-trends-whats-next-after-covid-19]
- 24. Towards practical point-of-care quick, ubiquitous ... [https://www.nature.com/articles/s41378-025-01057-4]
- 25. qPCR in Personalized Medicine: Advancing Precision ... [https://www.kingsresearch.com/blog/exploring-real-time-polymerase-chain-reaction-systems]
- 26. Obtaining Reliable RT-qPCR Results in Molecular ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8953338/]
- 27. qPCR Double Delta Ct Analysis in 4 Easy Steps [https://bitesizebio.com/24894/4-easy-steps-to-analyze-your-qpcr-data-using-double-delta-ct-analysis/]
- 28. Analyzing qPCR data: Better practices to facilitate rigor and ... [https://www.sciencedirect.com/science/article/pii/S2405580825004431]
- 29. PCR/qPCR Data Analysis [https://www.sigmaaldrich.com/US/en/technical-documents/technical-article/genomics/qpcr/data-analysis?srsltid=AfmBOopy47TJWZ6opBOrVAp1uY9fDFsRWedjypRMHtlam6RmEJLPlpk8]
- 30. Analysis of qPCR Data: From PCR Efficiency to Absolute ... [https://www.preprints.org/manuscript/202510.2485]
- 31. PCR (qPCR, dPCR, Singleplex, Multiplex) Markets ... [https://www.businesswire.com/news/home/20250616322572/en/PCR-qPCR-dPCR-Singleplex-Multiplex-Markets-Forecasts-2025-2030---Revolutionizing-Diagnostics-with-Cutting-Edge-Precision-Fueling-Opportunities---ResearchAndMarkets.com]
- 32. Development and clinical validation of a novel multiplex ... [https://www.nature.com/articles/s41598-025-16434-2]
- 33. Multiplex PCR assay for the rapid detection of Klebsiella ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12578128/]
- 34. Designing highly multiplex PCR primer sets with Simulated ... [https://www.nature.com/articles/s41467-022-29500-4]
- 35. Multicenter evaluation of fast multiplex PCR for detection ... [https://www.frontiersin.org/journals/cellular-and-infection-microbiology/articles/10.3389/fcimb.2025.1643991/full]
- 36. rtpcr: a package for statistical analysis and graphical ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12530193/]
- 37. Performance evaluation of a commercial multiplex ... [https://pubmed.ncbi.nlm.nih.gov/40952331/]
- 38. Molecular Diagnostics for Cancer Markets Forecasts 2025 ... [https://finance.yahoo.com/news/molecular-diagnostics-cancer-markets-forecasts-113700384.html]
- 39. Liquid biopsy – a narrative review with an update on current ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12333414/]
- 40. Liquid biopsy in cancer: current status, challenges and ... [https://www.nature.com/articles/s41392-024-02021-w]
- 41. Consensus guidelines for the validation of qRT-PCR ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8792405/]
- 42. Current Trends in Liquid Biopsy Tracking Resistance ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12027453/]
- 43. Sensitivity, specificity, and accuracy of a liquid biopsy ... [https://www.nature.com/articles/s41598-021-89592-8]
- 44. Comparing the Diagnostic Performance of Quantitative PCR ... [https://pubmed.ncbi.nlm.nih.gov/38103593/]
- 45. Statistical analysis of real-time PCR data - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC1395339/]
- 46. The qPCR Ecosystem and State of qPCR in Molecular ... [https://www.thermofisher.com/blog/clinical-conversations/the-qpcr-ecosystem-and-state-of-qpcr-in-molecular-diagnostics/]
- 47. Pharmacogenomics (PGx) using Real-Time PCR [https://www.thermofisher.com/us/en/home/clinical/clinical-translational-research/pharmacogenomics/real-time-pcr-solutions.html]
- 48. Pharmacogenomics Biomarker Discovery and Validation ... [https://pubmed.ncbi.nlm.nih.gov/33089968/]
- 49. Integrating traditional machine learning with qPCR ... [https://www.frontiersin.org/journals/pharmacology/articles/10.3389/fphar.2024.1539120/full]
- 50. Statistical analysis of real-time PCR data - BMC Bioinformatics [https://bmcbioinformatics.biomedcentral.com/articles/10.1186/1471-2105-7-85]
- 51. Clinical Applications of Quantitative Real-Time PCR in Virology [https://pmc.ncbi.nlm.nih.gov/articles/PMC7148891/]
- 52. PCR Molecular Diagnostics Market Size & Share Analysis [https://www.mordorintelligence.com/industry-reports/pcr-molecular-diagnostics]
- 53. LightCycler® PRO system [https://diagnostics.roche.com/us/en/products/instruments/lightcycler-pro-ins-6284.html]
- 54. Roche launches next-generation qPCR system to advance ... [https://diagnostics.roche.com/global/en/news-listing/2023/roche-launches-next-generation-qpcr-system-to-advance-clinical-needs.html]
- 55. LightCycler® PRO System [https://sequencing.roche.com/us/en/products/group/lightcycler-pro-system.html]
- 56. High-performance real-time quantitative PCR for your ... [https://diagnostics.roche.com/us/en/products/product-category/brand/lightcycler.html]
- 57. Digital PCR: from early developments to its future application ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12278255/]
- 58. Leaving DNA contamination at the lab bench | Drug Discovery [https://www.drugdiscoverytrends.com/leaving-dna-contamination-at-the-lab-bench/]
- 59. Live culture-based qPCR screening of Taq DNA ... [https://pubmed.ncbi.nlm.nih.gov/40948961/]
- 60. Overcoming qPCR Inhibitors: Strategies for Reliable ... [https://www.promegaconnections.com/overcoming-qpcr-inhibitors-strategies-for-reliable-quantification/]
- 61. MIQE 2.0: Revision of the Minimum Information for ... [https://pubmed.ncbi.nlm.nih.gov/40272429/]
- 62. MIQE Guidelines | Thermo Fisher Scientific - US [https://www.thermofisher.com/us/en/home/life-science/pcr/real-time-pcr/real-time-pcr-assays/why-choose-taqman-assays/publish-real-time-pcr-results.html]
- 63. Evaluation of normalisation strategies for qPCR data ... [https://www.nature.com/articles/s41598-025-06657-8]
- 64. Comparative Evaluation of Computational Methods for ... [https://www.mdpi.com/2227-9059/13/8/2036]
- 65. Validated reference genes for normalization of RT-qPCR in ... [https://www.nature.com/articles/s41598-025-08295-6]
- 66. Identification and validation of reference genes for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11743365/]
- 67. A comparison of normalization methods for the expression of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12312509/]
- 68. PCR/qPCR 数据分析 [https://www.sigmaaldrich.com/HK/zh/technical-documents/technical-article/genomics/qpcr/data-analysis?srsltid=AfmBOor5T1OtwW3hhFeT6Ta8l5XMk45wuZMfQRXc_L2DPR6uFFxpa4HO]
- 69. Reference genes for quantitative real-time PCR normalization ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8167929/]
- 70. How to Select Endogenous Controls for Real-Time PCR [https://www.thermofisher.com/us/en/home/life-science/pcr/real-time-pcr/real-time-pcr-learning-center/gene-expression-analysis-real-time-pcr-information/choosing-endogenous-control-gene-expression-analysis-real-time-pcr.html]
- 71. NORMA-Gene: A simple and robust method for qPCR ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3223928/]
- 72. NORMA-Gene: a simple and robust method for qPCR ... [https://pubmed.ncbi.nlm.nih.gov/21693017/]
- 73. A comparison of normalization methods for the expression of ... [https://bmcgenomdata.biomedcentral.com/articles/10.1186/s12863-025-01345-y]
- 74. Identification of reference genes for RT-qPCR data ... [https://www.nature.com/articles/s41598-019-50035-0]
- 75. Selection and validation of reference genes for ... [https://www.sciencedirect.com/science/article/pii/S1878614623001368]
- 76. RefGenes:用于RT-qPCR 数据归一化的可靠和条件特异性 ... [https://suppr.wilddata.cn/browses/detail/pubmed/21418615]
- 77. A stable combination of non-stable genes outperforms ... [https://www.nature.com/articles/s41598-024-82651-w]
- 78. Automated PCR and qPCR Solutions [https://www.bioradiations.com/automated-pcr-and-qpcr-solutions-225/]
- 79. Molecular Diagnostics Market Outlook 2025–2033 [https://www.datamintelligence.com/research-report/molecular-diagnostics-market]
- 80. How to optimize qPCR in 9 steps? [https://westburg.eu/knowledge/pcr_qpcr/hate_optimizing_qpcr]
- 81. Automation and miniaturization of high-throughput qPCR ... [https://www.sciencedirect.com/science/article/pii/S2472630324001237]
- 82. How To Interpret RT-qPCR Results [https://www.goldbio.com/blogs/articles/how-to-interpret-rt-qpcr-results?srsltid=AfmBOoprgLQRGEE41Ps-Yzu69XlFK7CW86P1rgy_-FM1EGqxU33q6dIe]
- 83. Digital PCR: from early developments to its future application ... [https://pubs.rsc.org/en/content/articlehtml/2025/lc/d5lc00055f]
- 84. dPCR vs qPCR vs end-point PCR [https://www.qiagen.com/us/knowledge-and-support/knowledge-hub/bench-guide/pcr/digital-pcr/digital-pcr-vs-quantitative-pcr-vs-end-point-pcr]
- 85. Analytical techniques for nucleic acid and protein detection ... [https://www.nature.com/articles/s12276-025-01453-w]
- 86. Next-Generation Sequencing Technology: Current Trends ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10376292/]
- 87. 2025 and Beyond: The Future of Genomic Data Analysis ... [https://blog.crownbio.com/2025-and-beyond-the-future-of-genomic-data-analysis-and-innovations-in-genomics-services]
- 88. Applications and challenges of biomarker-based predictive ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12399543/]
- 89. The hidden limits of digital PCR and what comes next [https://countablelabs.com/blog/the-hidden-limits-of-digital-pcr-and-what-comes-next]
- 90. The Growing Demand for Personalized : Navigating the... Diagnostics [https://www.meridianbioscience.com/lifescience-blog/the-growing-demand-for-personalized-diagnostics-navigating-the-benefits-and-limits-of-qpcr-vs-ngs/?country=RU]
- 91. A high-throughput screening RT-qPCR assay for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9469018/]
- 92. Investing in qPCR Automation: Time & Money Saved is ... [https://dispendix.com/blog/investing-in-qpcr-automation-time-money-saved-is-research-gained]
- 93. PCR Techniques and Their Clinical Applications [https://www.intechopen.com/chapters/86086]
- 94. Innovations in qPCR Technology: What Researchers Need ... [https://www.thermofisher.com/blog/behindthebench/innovations-in-qpcr-technology/]
- 95. A qPCR System for the Future of Molecular Diagnostics [https://www.thermofisher.com/blog/clinical-conversations/qpcr-system-future-molecular-diagnostics/]
- 96. How qPCR Works [https://www.sigmaaldrich.com/US/en/technical-documents/technical-article/genomics/qpcr/how-qpcr-works?srsltid=AfmBOoo3Faq24DrSTUB7gs4dX4tvecmuaoyMxFPstZc8P1voaqEj2p2q]
- 97. A survey of tools for the analysis of quantitative PCR ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5129434/]
- 98. RT-qPCR strategies for molecular diagnostics, OEM and ... [https://www.neb.com/en/nebinspired-blog/rt-qpcr-strategies-for-molecular-diagnostics-and-oem?srsltid=AfmBOopP3HYVjGkwsySm-wj-036ECHuyRF1YrtLwrGWScLJSwzWKDf7L]
- 99. PCR/qPCR Data Analysis [https://www.sigmaaldrich.com/US/en/technical-documents/technical-article/genomics/qpcr/data-analysis?srsltid=AfmBOordVrKETn1z3LSYZr4tlvsm20cGdbABbK0leXo6BPx7lFej2CK5]
- 100. qPCR Assay Design and Validation Services Market [https://dataintelo.com/report/qpcr-assay-design-and-validation-services-market]
- 101. Emergency Use Authorization [https://www.fda.gov/emergency-preparedness-and-response/mcm-legal-regulatory-and-policy-framework/emergency-use-authorization]
- 102. Current landscape of innovative drug development and ... [https://www.nature.com/articles/s41392-025-02267-y]
- 103. qPCR assays and IVDR regulation in clinical trials [https://medicover-mics.com/qpcr-assays-and-ivdr-regulation/]
- 104. Digital PCR Market Size, Forecast Report [https://www.mordorintelligence.com/industry-reports/digital-pcr-market]
- 105. Ensuring Precision and Reliability in Molecular Diagnostics [https://ahfad.org/pcr-external-quality-control-ensuring-precision-and-reliability-in-molecular-diagnostics/]