Optimizing qPCR for Minimal Residual Disease Detection: Protocols, Pitfalls, and Future Directions
This article provides a comprehensive guide for researchers and drug development professionals on implementing quantitative PCR (qPCR) for minimal residual disease (MRD) detection.
Optimizing qPCR for Minimal Residual Disease Detection: Protocols, Pitfalls, and Future Directions
Abstract
This article provides a comprehensive guide for researchers and drug development professionals on implementing quantitative PCR (qPCR) for minimal residual disease (MRD) detection. It covers the foundational principles of MRD as a critical prognostic marker in hematologic malignancies, details robust methodological workflows including sample handling and the comparative ΔΔCt method, and addresses key challenges such as inhibitor management and reference gene validation. Furthermore, it evaluates the performance of qPCR against emerging next-generation sequencing (NGS) technologies, emphasizing the importance of adhering to MIQE guidelines for rigor and reproducibility in clinical and research settings.
Understanding Minimal Residual Disease (MRD) and the Role of qPCR
Measurable residual disease (MRD), also referred to as minimal residual disease, represents the small population of cancer cells that persist in patients after treatment, typically at levels below the detection limit of conventional morphological microscopy (which has a sensitivity of only 1-5%) [1] [2]. In patients who have achieved complete remission (CR), MRD originates from resistant tumor cells that may eventually lead to disease relapse [1] [2]. The clinical significance of MRD monitoring has been firmly established in hematological malignancies and is increasingly being explored in solid tumors [3].
MRD testing provides a powerful tool for risk stratification, prognosis prediction, and therapeutic decision-making. Patients with undetectable MRD or favorable MRD responses consistently demonstrate lower relapse risk and better survival outcomes compared to those with MRD positivity [1]. This application note details the clinical significance of MRD across cancer types and provides detailed methodological protocols for its detection, with particular emphasis on qPCR-based approaches within the broader context of MRD research.
MRD Detection Methods and Performance Characteristics
Multiple technologies with varying sensitivities and applications have been developed for MRD detection. The choice of method depends on cancer type, available biomarkers, required sensitivity, and laboratory capabilities.
Table 1: Comparison of Major MRD Detection Technologies
| Method | Applicability | Sensitivity | Key Advantages | Major Limitations |
|---|---|---|---|---|
| Multiparameter Flow Cytometry (MFC) | Nearly 100% for acute leukemia [2] | 10-3 to 10-5 [1] | Fast (hours); wide applicability; relatively inexpensive [1] [2] | Lack of standardization; fresh cells required; phenotypic changes [1] [2] |
| Quantitative PCR (qPCR) | 40-50% [2] | 10-4 to 10-6 [2] | High sensitivity; standardized; lower costs [2] | Only one gene assessed per assay [2] |
| Next-Generation Sequencing (NGS) | >95% [2] | 10-2 to 10-6 [2] | Multiple genes analyzed simultaneously; broad applicability [2] | High cost; complex data analysis; not yet standardized [2] |
| Digital PCR (dPCR) | Information missing | Information missing | Absolute quantification without standard curves; high sensitivity | Limited multiplexing capability; not covered in sources |
| Karyotyping | ~50% [2] | 5×10-2 [2] | Widely used; standardized [2] | Slow; labor-intensive; low sensitivity [2] |
Method Selection Considerations
The optimal MRD detection method varies by clinical context. For acute leukemias, flow cytometry approaches include Leukemia-Associated ImmunoPhenotype (LAIP) and "Different from Normal" (DFN) strategies [1]. Molecular methods like qPCR and NGS are preferred when specific genetic biomarkers are available, such as fusion transcripts (e.g., BCR::ABL1 in CML) or clonal immunoglobulin/T-cell receptor rearrangements [1] [3]. The European LeukemiaNet recommends using highly sensitive methods with detection limits of at least 10-4 for MRD assessment in AML [4].
Clinical Significance of MRD Testing
Prognostic Value Across Malignancies
MRD status represents the strongest independent prognostic factor in acute leukemia, outperforming conventional risk stratification based on disease biology alone [1] [4]. The predictive power of MRD testing has been quantified in recent large-scale analyses.
Table 2: Predictive Value of MRD Testing for Relapse Across Cancer Types
| Cancer Category | Odds Ratio for Relapse (MRD+ vs MRD-) | 95% Confidence Interval | Common Assays | Typical Time Points |
|---|---|---|---|---|
| All Hematological Cancers | 3.5 | [2.3, 5.4] [3] | MPFC, PCR [3] | Post-induction, pre-transplant [3] |
| Acute Myeloid Leukemia (AML) | 4.7 | [2.6, 8.6] [3] | MPFC, NGS [3] | After consolidation [3] |
| Acute Lymphoblastic Leukemia (ALL) | 2.5 | [1.3, 4.5] [3] | MPFC, IG/TCR PCR [3] | Early treatment (e.g., day 8) [1] |
| Solid Cancers | 9.1 | [3.3, 24.9] [3] | ctDNA NGS [3] | Post-resection [3] |
The higher odds ratio in solid cancers may reflect that MRD detection in blood implies established metastatic capability [3]. In hematologic malignancies, MRD assessment times vary by disease: in B-cell ALL, early assessment during induction (e.g., day 8) can evaluate leukemia clearance kinetics, while post-consolidation and pre-transplant timepoints provide strong prognostic information [1] [3].
Clinical Applications
Risk Stratification and Treatment Guidance
MRD monitoring enables dynamic risk assessment that can overcome limitations of initial risk stratification. In AML, MRD status can supersede pre-treatment prognostic stratification based on disease biology [4]. This allows for risk-adapted therapy approaches, where MRD-positive patients may receive intensified treatment (e.g., allogeneic stem cell transplantation) while MRD-negative patients may be spared excessive toxicity [1] [2].
Surrogate Endpoint and Drug Development
MRD has emerged as a surrogate endpoint in clinical trials, accelerating the testing and approval process for novel therapeutics [1]. MRD response can provide early evidence of drug efficacy before overall survival data mature, particularly valuable in slow-progressing diseases.
Early Relapse Detection and Monitoring
Serial MRD monitoring can detect molecular relapse weeks to months before clinical manifestation, creating a therapeutic window for early intervention [1]. In CML, rising BCR::ABL1 levels trigger intervention before hematologic relapse occurs [3].
MRD in Solid Tumors: Emerging Applications
While MRD testing is most established in hematologic malignancies, the concept is rapidly expanding to solid tumors using circulating tumor DNA (ctDNA) analysis. In solid cancers, MRD assessment typically occurs after surgical resection of localized disease, unlike the remission monitoring approach used in hematologic cancers [3].
Recent studies demonstrate that ctDNA-based MRD detection post-resection predicts recurrence with high accuracy in colorectal, breast, and other solid tumors [3]. The technical approach differs, focusing primarily on identifying cancer-related mutations in blood rather than cellular immunophenotypes or fusion transcripts [3].
In neuroblastoma, a pediatric solid tumor, multimodal approaches combining automatic immunofluorescence plus interphase FISH (AIPF) with RT-qPCR panels have significantly improved MRD detection compared to standard morphological assessment [5]. These techniques also enable monitoring of therapeutic targets like GD2 expression and tumor cell plasticity between adrenergic and mesenchymal states [5].
Experimental Protocols for MRD Detection
qPCR-Based MRD Detection Protocol
Sample Preparation and Nucleic Acid Extraction
Bone Marrow Aspirate Collection:
- Collect bone marrow aspirate (first pull, <5 mL) into EDTA or sodium heparin tubes [1]
- Process within 48 hours of collection; transport at room temperature [1]
- For RNA extraction, preserve samples in Trizol or PAXgene blood RNA tubes within 24 hours [5]
Cell-Free DNA Extraction:
- Use cell-free DNA blood collection tubes (e.g., Streck) [6]
- Extract cfDNA using specialized kits (e.g., QIAamp Circulating Nucleic Acid Kit) [6]
- Quantify yield with fluorometric methods (e.g., Qubit Fluorometer) [6]
- Assess quality with PreSeq DNA QC Assay or similar quality control measures [6]
Reverse Transcription and qPCR Setup
Reverse Transcription:
- Use high-temperature reverse transcriptase for structured RNA regions [7]
- Employ random hexamers and/or gene-specific primers
- Use ReadyScript cDNA Synthesis Mix or equivalent systems [7]
qPCR Reaction Components:
- Template: 100 pg gDNA or cDNA equivalent [7]
- Primers: Optimized concentration to minimize dimer formation [7]
- dNTPs: Standard mix or dUTP/UNG system for contamination control [7]
- MgCl2: 3-6 mM final concentration (optimize for each assay) [7]
- Taq DNA Polymerase: Use "hot-start" versions to reduce non-specific amplification [7]
- Reference dye: ROX or similar for signal normalization where required [7]
Thermal Cycling Conditions:
- UNG incubation (if using dUTP): 50°C for 2 minutes
- Initial denaturation: 95°C for 2-10 minutes
- Amplification (40-45 cycles):
- Denaturation: 95°C for 15-30 seconds
- Annealing: Primer-specific temperature (55-65°C) for 30-60 seconds
- Extension: 72°C for 30-60 seconds
- Melting curve analysis (for SYBR Green): 65°C to 95°C with continuous fluorescence monitoring [7]
Data Analysis and Interpretation
Quantification Methods:
- Absolute Quantification: Use external standards with identical primer binding sites to target sequence [7]
- Relative Quantification: Calculate target template ratio to reference gene (e.g., GAPDH, ABL1) [7]
Quality Control:
- Include no-template controls in each run
- Ensure PCR efficiency of 90-110%
- Maintain correlation coefficient (R2) >0.98 for standard curves
- A260/A280 ratio of 1.8-2.0 for DNA purity assessment [7]
Next-Generation Sequencing Protocol for MRD
Library Preparation and Sequencing
Library Preparation:
- Use targeted gene panels (e.g., VariantPlex Core AML, ArcherDx) [6]
- Incorporate molecular barcodes for error correction
- Amplify libraries with appropriate cycle number
Sequencing:
- Platform: Illumina MiSeq or NextSeq systems [6]
- Read length: 150 bp paired-end [6]
- Minimum reads: 0.75-3×106 depending on panel size [6]
Bioinformatic Analysis
Variant Calling:
- Use dedicated pipelines (e.g., Archer Analysis) with error correction enabled [6]
- Set minimum depth threshold (e.g., 500-1000× for sensitivity to 0.1% VAF)
- Manually review mutations previously identified by routine diagnostics [6]
Variant Annotation:
- Cross-reference with clinical databases (COSMIC, ClinVar) [6]
- Apply computational prediction algorithms (FATHMM, PolyPhen2, PROVEAN, SIFT) [6]
- Filter for pathogenic/likely pathogenic variants only [6]
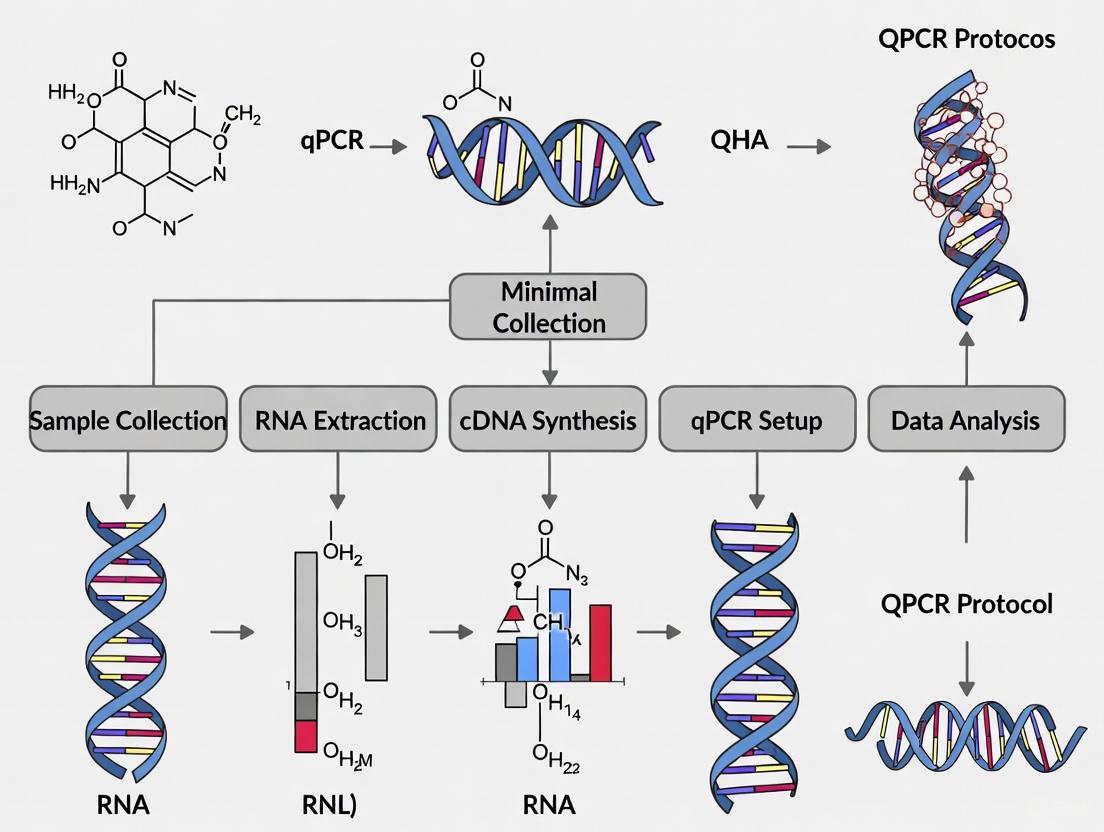
Visualization of MRD Testing Workflow
MRD Testing Workflow: From Sample to Clinical Application
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Research Reagent Solutions for MRD Detection
| Reagent/Category | Specific Examples | Function/Application | Technical Notes |
|---|---|---|---|
| Nucleic Acid Stabilization | PAXgene Blood RNA Tubes, Streck cfDNA BCT | Preserves sample integrity during transport | PAXgene for RNA/DNA; Streck for cell-free DNA [6] [5] |
| Nucleic Acid Extraction | QIAamp Circulating Nucleic Acid Kit, Trizol-based methods | Isolation of high-quality nucleic acids | QIAamp optimized for cfDNA; Trizol for RNA [6] [5] |
| Reverse Transcription | ReadyScript cDNA Synthesis Mix, High-temperature RT enzymes | cDNA synthesis from RNA templates | High-temperature enzymes for structured RNAs [7] |
| qPCR Master Mixes | SYBR Green, TaqMan probes, UNG-containing systems | Amplification and detection of targets | SYBR Green for melting curve; TaqMan for specificity [7] |
| Targeted Gene Panels | VariantPlex Core AML, Core Myeloid panels | NGS-based mutation detection | 10-37 gene panels cover common mutations [6] |
| Reference Genes | ABL1, GAPDH, β-actin | Normalization of qPCR data | ABL1 preferred in hematologic malignancies [7] |
| Quality Control Assays | PreSeq DNA QC Assay, Qubit assays, Bioanalyzer | Assess nucleic acid quantity/quality | Essential for reliable MRD detection [6] |
MRD testing represents a transformative approach in oncology, enabling前所未有的 sensitive monitoring of treatment response and disease recurrence across hematological malignancies and solid tumors. The clinical utility of MRD assessment is well-established for risk stratification, treatment guidance, and as a surrogate endpoint in drug development.
qPCR-based methods provide a robust, sensitive, and relatively accessible platform for MRD detection, particularly when specific genetic biomarkers are available. However, method selection should be guided by disease context, available biomarkers, and required sensitivity. As MRD technologies continue to evolve with innovations in digital PCR, next-generation sequencing, and liquid biopsy applications, the implementation of standardized protocols and analytical frameworks will be essential for maximizing clinical utility across diverse cancer types.
Why qPCR? Principles of Quantitative Real-Time PCR for Sensitive Detection
Quantitative real-time polymerase chain reaction (qPCR), also known as real-time PCR, is a powerful molecular biology technique that allows for the amplification and simultaneous quantification of targeted DNA molecules. Unlike conventional PCR, which provides only endpoint detection, qPCR enables researchers to monitor the accumulation of PCR products in real time as the reaction progresses. This capability for precise quantification, combined with high sensitivity and specificity, has established qPCR as the gold standard for nucleic acid quantification in various applications, including gene expression analysis, pathogen detection, and biomedical diagnostics [8] [9].
In the context of minimal residual disease (MRD) research, qPCR plays a particularly crucial role. MRD refers to the small number of cancer cells that remain in a patient during or after treatment, often at levels undetectable by conventional microscopy. Sensitive MRD monitoring in acute lymphoblastic leukemia (ALL), for instance, requires technologies capable of detecting one leukemic cell among 100,000 normal cells or more. qPCR-based methods using patient-specific immunoglobulin (IG) and T-cell receptor (TCR) gene rearrangements as molecular markers have proven essential for this purpose, providing critical prognostic information that guides therapeutic decisions [10].
Basic Principles and Chemistries
Core Principle of Quantification
The fundamental principle of qPCR quantification relies on monitoring the fluorescence signal generated during each PCR cycle. The more copies of a DNA template present at the beginning of the experiment, the fewer PCR cycles are needed to generate enough product for detection. The key measurement is the quantification cycle (Cq), previously known as threshold cycle (Ct), which represents the number of cycles required for the fluorescence signal to cross a predetermined threshold above the background level. Lower Cq values indicate higher initial target concentrations [9].
Detection Chemistries
qPCR utilizes two primary types of detection chemistries, each with distinct advantages:
DNA-Binding Dyes (e.g., SYBR Green): These dyes bind non-specifically to double-stranded DNA and emit fluorescence upon excitation. SYBR Green is widely used due to its cost efficiency and ease of use. A significant advantage is that it does not require probe design, making it suitable for initial screening and expression profiling. However, a potential disadvantage is that it binds to any double-stranded DNA, including non-specific reaction products and primer dimers, which may lead to overestimation of the target concentration. Melt curve analysis is therefore essential post-amplification to verify reaction specificity [9].
Sequence-Specific Probes (e.g., TaqMan Probes): These oligonucleotide probes are labeled with a 5' fluorophore and a 3' quencher. When intact, the proximity of the quencher suppresses fluorescence. During PCR amplification, the 5' nuclease activity of the DNA polymerase cleaves the probe, separating the fluorophore from the quencher and generating a fluorescent signal. This method provides increased specificity and sensitivity over DNA-binding dyes, as fluorescence is generated only when the specific target sequence is amplified. This makes probe-based assays particularly valuable for applications requiring high specificity, such as MRD detection and multiplex PCR, where multiple targets are amplified in a single reaction [11] [9].
Table 1: Comparison of qPCR Detection Chemistries
| Feature | DNA-Binding Dyes (SYBR Green) | Sequence-Specific Probes (TaqMan) |
|---|---|---|
| Specificity | Lower - binds to any dsDNA | Higher - specific hybridization required |
| Cost | Lower | Higher |
| Probe Design | Not required | Required |
| Multiplexing Capability | No | Yes |
| Best For | Gene scanning, initial screening | High-specificity applications (e.g., MRD) |
| Verification Step | Melt curve analysis required | Not required |
Quantitative Approaches in qPCR
Absolute Quantification
Absolute quantification determines the exact number of target DNA molecules in a sample. This is typically achieved using a standard curve generated from serially diluted standards of known concentrations. The curve establishes a linear relationship between the Cq values and the logarithm of the initial template amount. The reliability of this method depends heavily on the accuracy of the standards and the amplification efficiencies. More recently, digital PCR (dPCR) has emerged as an alternative method for absolute quantification without standard curves. dPCR partitions a sample into thousands of individual reactions, applying a Poisson statistical analysis to provide absolute quantification with potentially higher precision and robustness to amplification efficiency variations compared to qPCR [12] [9].
Relative Quantification
Relative quantification compares the expression level of a target gene between different experimental conditions relative to one or more reference genes. This method avoids the need for standard curves and is widely used in gene expression studies. The two most common mathematical models are:
The Livak Method (2^(-ΔΔCq) Method): This method assumes that the target and reference genes amplify with near-perfect efficiency (close to 100%). It calculates the fold change in gene expression by normalizing the target gene's Cq to a reference gene and then to a calibrator sample (e.g., untreated control) [13].
The Pfaffl Method: This approach offers greater flexibility by incorporating the actual amplification efficiencies of both target and reference genes into the calculation. This provides a more accurate representation of relative gene expression levels when amplification efficiencies differ from 100% [13].
Table 2: Comparison of Quantitative Approaches in qPCR
| Quantification Method | Principle | Requirements | Applications |
|---|---|---|---|
| Absolute (Standard Curve) | Relates Cq to known standard concentrations | Accurate standard dilutions | Viral load, copy number variation |
| Absolute (Digital PCR) | Partitioning and Poisson statistics | Digital PCR system | Absolute quantification without standards |
| Relative (Livak Method) | 2^(-ΔΔCq) calculation with efficiency assumption | Stable reference genes, ~100% efficiency | Gene expression (efficiency ~100%) |
| Relative (Pfaffl Method) | Efficiency-corrected calculation | Precisely determined PCR efficiencies | Gene expression (variable efficiencies) |
Application to Minimal Residual Disease Detection
MRD Detection Using IG/TCR Rearrangements
In acute lymphoblastic leukemia, qPCR-based MRD monitoring frequently targets patient-specific immunoglobulin (IG) and T-cell receptor (TCR) gene rearrangements. During lymphoid development, each cell undergoes V(D)J recombination, creating unique DNA sequences that serve as clonal markers for the leukemic population. At diagnosis, these specific rearrangements are identified in the patient's leukemic cells. Subsequently, complementary allele-specific oligonucleotide (ASO) primers are designed for highly sensitive MRD monitoring during treatment, allowing detection of up to 1 leukemic cell in 100,000 normal cells (sensitivity of 10^-5) [10].
Workflow for MRD Detection
The standard workflow for MRD detection using qPCR involves several critical steps from sample collection to data interpretation, as illustrated below:
Emerging Technologies in MRD Detection
While qPCR remains a cornerstone for MRD assessment, new technologies are emerging. Next-generation sequencing (NGS)-based methods enable deeper analysis of IG/TCR gene rearrangements and can overcome certain limitations of qPCR, such as clonal evolution that may lead to false-negative results. Additionally, droplet digital PCR (ddPCR) has shown promise in recent studies, demonstrating significantly better quantitative limit of detection and sensitivity compared to traditional qPCR, particularly for critical low-positive samples [10] [12].
Detailed Experimental Protocol for qPCR-Based MRD Detection
Sample Preparation and DNA Extraction
- Sample Source: Bone marrow aspirates are the preferred material for MRD assessment in ALL. Peripheral blood is not recommended as MRD levels are typically 1-3 logs lower than in bone marrow [10].
- DNA Extraction: Use standardized commercial kits for genomic DNA extraction. Ensure high DNA quality and quantity, measuring concentration using spectrophotometry.
- DNA Storage: Extract DNA in sufficient quantities from the diagnostic sample to serve as a positive control and for all future MRD assessments.
Identification of Clonal Markers at Diagnosis
- PCR Amplification: Perform multiplex PCR assays to identify clonal IG and/or TCR gene rearrangements.
- Clonality Confirmation: Analyze PCR products by capillary electrophoresis or heteroduplex analysis to confirm clonality.
- Sequencing: Sequence clonal PCR products to identify the specific V(D)J junctional regions that will serve as patient-specific markers.
ASO Primer and Probe Design
- Primer Design: Design allele-specific oligonucleotide (ASO) primers complementary to the unique junctional regions identified during sequencing.
- Probe Design: For probe-based qPCR, design dual-labeled hydrolysis probes (e.g., TaqMan) according to these criteria:
- Tm: 5-10°C higher than primers (typically 65-70°C)
- Length: 20-30 nucleotides
- GC Content: 30-80%
- 5' Base: Avoid G at the 5' end as it can quench common dyes like FAM [11]
- Specificity Check: Validate primer and probe specificity using BLAST analysis against the human genome.
qPCR Assay Validation
- Sensitivity Testing: Prepare serial dilutions of diagnostic DNA in polyclonal normal DNA (e.g., 10^-2 to 10^-5) to establish the quantitative range and limit of detection.
- Efficiency Calculation: Perform a standard curve with at least 3 replicates per dilution point. Calculate PCR efficiency using the formula: Efficiency (%) = (10^(-1/slope) - 1) × 100. Acceptable efficiency ranges from 90-110% [14].
- Reproducibility Assessment: Determine intra- and inter-assay coefficients of variation.
MRD Quantification in Follow-up Samples
- Experimental Setup: Include appropriate controls in each run:
- No template control (NTC): Identifies contamination
- Positive control: Diagnostic DNA diluted in normal DNA
- Negative control: Polyclonal normal DNA
- PCR Conditions:
- Reaction Volume: 20-50 μL
- Thermal Cycling: Initial denaturation (95°C for 10 min); 45-50 cycles of denaturation (95°C for 15 sec), annealing (60°C for 30-60 sec), and extension (72°C for 30 sec)
- Data Analysis: Use the ΔΔCq method or efficiency-corrected model (Pfaffl method) for quantification relative to the diagnostic sample.
Critical Controls and Data Interpretation
Essential Controls for Reliable Results
- No Reverse Transcriptase Control (-RT): For RT-qPCR applications, this control checks for genomic DNA contamination by omitting the reverse transcriptase enzyme [15] [11].
- No Template Control (NTC): Contains all reaction components except the DNA template to identify reagent contamination.
- Positive Controls: Include dilution series of known targets to validate assay sensitivity and efficiency.
- Reference Genes: Use at least two validated reference genes with stable expression across all experimental conditions for normalization in relative quantification [11].
Data Analysis and Quality Assessment
- Baseline and Threshold Setting: The baseline represents the background fluorescence during early cycles (typically cycles 3-15). The threshold should be set in the exponential phase of amplification, sufficiently above the baseline but within the linear range of amplification [14].
- Amplification Efficiency Calculation: Prepare a standard curve with serial dilutions. Plot the log of the initial template amount against the Cq values. The slope of the line is used to calculate efficiency: Efficiency = 10^(-1/slope) - 1. Ideal efficiency is 100% (slope = -3.32) [14].
- Quantification Methods: Based on the experimental design and validation data, choose between absolute quantification (standard curve) or relative quantification (ΔΔCq or Pfaffl method).
The Scientist's Toolkit: Essential Reagents and Materials
Table 3: Research Reagent Solutions for qPCR-Based MRD Detection
| Reagent/Material | Function | Specifications/Considerations |
|---|---|---|
| DNA Extraction Kits | Isolation of high-quality genomic DNA from patient samples | Ensure high molecular weight and purity (A260/A280 ~1.8) |
| qPCR Master Mix | Provides optimized buffer, enzymes, dNTPs for amplification | Choose probe-based or SYBR Green format; hot-start recommended |
| Sequence-Specific Probes | Target-specific detection (e.g., TaqMan) | Dual-labeled with 5' fluorophore (FAM, HEX) and 3' quencher |
| Allele-Specific Primers | Amplification of patient-specific IG/TCR rearrangements | Designed to complement unique V(D)J junctional regions |
| Reference Gene Assays | Normalization of sample input variation | Use validated, stably expressed genes (e.g., ABL, GUSB) |
| DNase/RNasin | Prevention of nucleic acid degradation | Essential for RNA workflows in RT-qPCR |
| Standard Curve Templates | Quantification and efficiency calculation | Serial dilutions of known target concentration |
Comparison of MRD Detection Technologies
The landscape of MRD detection methodologies continues to evolve, with each technology offering distinct advantages and limitations as summarized below:
Quantitative real-time PCR remains an indispensable technology for sensitive detection of minimal residual disease in leukemia and other malignancies. Its robust quantification capabilities, combined with well-established standardization through consortia like EuroMRD, make it a cornerstone of modern clinical diagnostics and research. While emerging technologies like digital PCR and next-generation sequencing offer promising enhancements for specific applications, qPCR continues to provide the sensitivity, specificity, and reproducibility required for reliable MRD assessment. The continued refinement of qPCR protocols, primer design strategies, and data analysis methods will further solidify its role in personalized medicine and treatment response monitoring.
Minimal residual disease (MRD) refers to the small population of leukemic cells that persists in patients after treatment at levels undetectable by conventional microscopy [2]. The accurate detection of MRD is a powerful independent prognostic factor in acute lymphoblastic leukemia (ALL), guiding risk stratification and therapeutic decisions [16] [17]. Real-time quantitative PCR (qPCR) has established itself as a cornerstone technology for MRD monitoring due to its exceptional sensitivity, capable of detecting one leukemic cell among 100,000 normal cells (sensitivity of 10⁻⁵) [2] [17].
The clinical significance of MRD detection is profound. Patients who achieve MRD negativity demonstrate significantly superior outcomes, with 5-year overall survival rates of approximately 68% compared to only 34% for MRD-positive patients [17]. Within the framework of a comprehensive thesis on qPCR-MRD protocols, this application note details the three principal categories of molecular biomarkers—fusion gene transcripts, immunoglobulin and T-cell receptor gene rearrangements, and specific mutations—alongside their associated experimental methodologies.
Key Biomarker Categories for qPCR-MRD
The selection of an appropriate biomarker is critical for successful MRD tracking. The applicability and performance of each biomarker category vary, influencing their suitability for different clinical contexts.
Table 1: Key Biomarker Categories for qPCR-MRD in ALL
| Biomarker Category | Examples | Applicability | Advantages | Limitations |
|---|---|---|---|---|
| Fusion Gene Transcripts | BCR::ABL1, ETV6::RUNX1, KMT2A rearrangements | ~40-50% of ALL cases [2] | Very high sensitivity (10⁻⁶); stable target; no patient-specific reagents needed [16] [2] | Limited applicability; cannot track clonal evolution [16] |
| Immunoglobulin (IG)/T-Cell Receptor (TCR) Gene Rearrangements | IGH, IGK, TRG, TRD rearrangements | >90% of ALL cases [18] | High sensitivity (10⁻⁵); highly patient-specific; broad applicability [2] [18] | Requires diagnostic sample; time-consuming setup; clonal evolution may cause false negatives [16] |
| Recurrent Somatic Mutations | NPM1 mutations | Subset of AML and ALL cases | Stable marker; direct targeting of driver mutation | Lower applicability in ALL; requires knowledge of specific mutation [17] |
The workflow for implementing these biomarkers in a qPCR-MRD protocol involves sequential steps from sample collection to final data interpretation, guided by international consortia like EuroMRD to ensure standardization and quality [18].
Fusion Gene Transcripts as Biomarkers
Principle and Clinical Relevance
Fusion genes result from chromosomal rearrangements that create novel chimeric transcripts, serving as highly specific leukemia markers. These aberrations are not only drivers of leukemogenesis but also ideal MRD targets due to their stability throughout the disease course [16]. In Philadelphia chromosome-positive ALL, the BCR::ABL1 fusion is a critical target, while in pediatric B-ALL, ETV6::RUNX1 is a common favorable prognostic marker [16] [17].
Detailed Protocol: RT-qPCR for Fusion Transcript Detection
Sample Preparation and RNA Extraction:
- Sample Collection: Collect bone marrow aspirate or peripheral blood in appropriate anticoagulant tubes (e.g., EDTA). Process samples within 24-48 hours.
- RNA Extraction: Use commercial kits (e.g., Qiagen AllPrep DNA/RNA kits) for simultaneous DNA/RNA extraction or dedicated RNA isolation kits. For FFPE samples, use specialized kits like the AllPrep DNA/RNA FFPE Kit [19].
- Quality Control: Assess RNA concentration using a fluorometer (e.g., Qubit 2.0) and purity/integrity with a spectrophotometer (e.g., NanoDrop) and automated electrophoresis system (e.g., TapeStation). RNA Integrity Number (RIN) >7.0 is recommended for reliable RT-qPCR [19].
Reverse Transcription and qPCR Setup:
- cDNA Synthesis: Convert 100 ng - 1 µg of total RNA to cDNA using a High-Capacity cDNA Reverse Transcription Kit with random hexamers. Include a no-reverse transcriptase control (-RT) for each sample to detect genomic DNA contamination.
- Assay Design: Use publicly available primer/probe sequences or design assays spanning the fusion junction to ensure specificity. The EuroMRD consortium provides standardized assays for common fusions like BCR::ABL1 [18].
- Reaction Setup: Prepare reactions in a 96- or 384-well plate format. A typical 20 µL reaction contains: 1x TaqMan Master Mix, 900 nM forward and reverse primers, 250 nM TaqMan probe (FAM-labeled), and 5 µL of cDNA template.
- Standard Curve: Include a 5-6 point standard curve in each run using serial dilutions (e.g., 1:10 from 10⁻¹ to 10⁻⁵) of plasmid DNA containing the target fusion sequence or cDNA from a positive control cell line with known copy number.
Thermocycling Conditions:
- Step 1: 50°C for 2 minutes (UNG incubation, if applicable)
- Step 2: 95°C for 10 minutes (polymerase activation)
- Step 3: 45 cycles of:
- 95°C for 15 seconds (denaturation)
- 60°C for 1 minute (annealing/extension)
- Data collection occurs at the annealing/extension step of each cycle.
Data Interpretation and Quality Control
Data analysis requires precise calculation based on the standard curve. The quality of the entire process must be assured through stringent controls.
Table 2: Essential Controls for Fusion Gene qPCR-MRD
| Control Type | Purpose | Acceptance Criteria |
|---|---|---|
| No Template Control (NTC) | Detects reagent contamination | Cq value >40 or undetermined |
| Positive Control | Verifies assay functionality | Cq value within expected range |
| Negative Control (Normal PBMMC) | Confirms assay specificity | Cq value >40 or undetermined |
| Standard Curve | Enables quantification | PCR efficiency: 90-110%; R² > 0.98 |
| Housekeeping Gene (e.g., ABL1, GUSB) | Assesses RNA quality and input | Cq value within normal range for sample type |
Results are typically reported as normalized copy numbers, for instance, as BCR::ABL1⁰¹⁰/ABL1 ratio, with a sensitivity of 10⁻⁴ to 10⁻⁶ achievable under optimal conditions [2]. The MIQE 2.0 guidelines provide a comprehensive framework for ensuring experimental rigor and transparent reporting of all qPCR parameters [20].
Immunoglobulin and T-Cell Receptor Gene Rearrangements
Principle and Clonality Assessment
During lymphocyte development, the genes encoding immunoglobulin (IG) and T-cell receptors (TCR) undergo V-(D)-J recombination, creating unique nucleotide sequences in the complementarity-determining regions (CDR3) that serve as a "clonal fingerprint" for each lymphocyte and its malignant progeny [16] [18]. This principle allows for the design of patient-specific qPCR assays to track the leukemic clone with high sensitivity. Notably, cross-lineage rearrangement is common; for example, TCR rearrangements can be found in up to 90% of B-ALL cases, expanding the applicability of this approach [17].
Detailed Protocol: IG/TR Rearrangement Analysis
Diagnostic Marker Identification and Assay Design:
- DNA Extraction from Diagnostic Sample: Extract high-quality DNA from a bone marrow sample with known leukemic infiltration. Use kits designed for genomic DNA extraction (e.g., QIAamp DNA Blood Mini Kit). Assess DNA purity (A260/A280 ~1.8) and integrity via agarose gel electrophoresis or Fragment Analyzer.
- Clonality Assessment: Perform multiplex PCR followed by fragment analysis or Sanger sequencing to identify the specific clonal IG/TR rearrangements (e.g., IGH, IGK, TRG, TRD) present in the leukemic cells. The EuroMRD Consortium provides standardized multiplex PCR protocols [18].
- Patient-Specific Primer/Probe Design: Design a TaqMan probe that binds to the unique CDR3 sequence of the identified clone. The allele-specific oligonucleotide (ASO) primer is designed to span the V-N-J junction, with its 3' end being patient-specific.
RQ-PCR for MRD Quantification in Follow-Up Samples:
- Reaction Setup: For each follow-up sample, set up a 20 µL reaction containing: 1x TaqMan Master Mix, 200-600 nM ASO primer, 200-600 nM reverse primer, 100-300 nM TaqMan probe (FAM-labeled), and 500 ng of patient DNA.
- Control Reactions: Include a polyclonal control (DNA from healthy donors) to confirm the absence of background amplification and a positive control (diluted diagnostic DNA) to assess assay performance.
- Standard Curve and Sensitivity Dilution Series: Prepare a standard curve using serial dilutions of the diagnostic DNA into polyclonal normal DNA (e.g., 10⁻², 10⁻³, 10⁻⁴, 10⁻⁵). A separate dilution series (e.g., 10⁻⁴, 10⁻⁵) should be included to empirically determine the sensitivity of the assay for that specific sample.
- Thermocycling Conditions: Use the same profile as described for fusion genes (Section 3.2).
Data Interpretation and EuroMRD Guidelines
Data interpretation must follow international guidelines, such as those established by the EuroMRD Consortium, which define specific categories for result reporting [18]. Adherence to these guidelines is critical for inter-laboratory comparability and consistent clinical decision-making.
- Quantitative Range (QR): The MRD level is considered quantitative if the result lies within the linear range of the standard curve and the corresponding sensitivity dilution is positive.
- Positive, Below Quantitative Range (pos_bqL): A recently refined category. A sample is positive with a non-quantifiable result if the target is detected below the QR, but the sensitivity of the assay is sufficient to detect MRD at that level.
- Negative: The target is not detected, and the sensitivity of the assay is sufficient (e.g., at least 10⁻⁴) to rule out the presence of the leukemic clone at that threshold.
- MRD of Uncertain Significance: A new category introduced in updated guidelines for low-level signals that cannot be definitively classified due to technical or biological factors [18].
Laboratories performing this analysis are strongly encouraged to participate in the EuroMRD external quality assessment (QA) scheme to ensure proficiency and standardization [18].
Successful implementation of qPCR-MRD assays requires a suite of validated reagents, specialized equipment, and bioinformatics resources.
Table 3: Research Reagent Solutions for qPCR-MRD
| Category | Item | Function/Application | Examples/Notes |
|---|---|---|---|
| Nucleic Acid Extraction | DNA/RNA Co-extraction Kit | Simultaneous purification of DNA (for IG/TR) and RNA (for fusions) from a single sample | Qiagen AllPrep DNA/RNA Mini Kit (for fresh tissue) [19] |
| FFPE-specific Extraction Kit | Optimized isolation of fragmented nucleic acids from archival tissue | Qiagen AllPrep DNA/RNA FFPE Kit [19] | |
| Reverse Transcription | cDNA Synthesis Kit | Converts RNA to cDNA for fusion transcript analysis | Kits including random hexamers and reverse transcriptase |
| qPCR Core Reagents | TaqMan Universal PCR Master Mix | Provides enzymes, dNTPs, and buffer for probe-based qPCR | Must include dUTP and Uracil-N-Glycosylase (UNG) for carryover contamination prevention |
| Assay Design | EuroMRD Primer/Probe Sequences | Standardized, validated assays for common fusion genes and IG/TR frameworks | Available through the EuroMRD Consortium [18] |
| Critical Controls | Standard Curve Template | Quantification benchmark for both fusion and IG/TR assays | Plasmid DNA or cell line cDNA/DNA with known target copy number |
| Polyclonal Control DNA | Background signal control for IG/TR assays | Pooled DNA from healthy donor peripheral blood mononuclear cells (PBMCs) | |
| Quality Control | RNA Integrity Number (RIN) Assessment | Evaluates RNA quality pre-reverse transcription | Agilent TapeStation system [19] |
| Software & Guidelines | MIQE 2.0 Guidelines | International standard for reporting qPCR experiments; ensures rigor and reproducibility [20] | |
| EuroMRD QA Scheme | External proficiency testing and standardized data interpretation for MRD in ALL [18] |
The robust detection of MRD using qPCR relies on the precise targeting of fusion gene transcripts, immunoglobulin and T-cell receptor gene rearrangements, and specific mutations. The protocols and guidelines detailed in this application note, grounded in international standards like those from the EuroMRD Consortium and MIQE 2.0, provide a framework for generating reliable, clinically actionable data. As the field advances, the integration of these well-established qPCR methods with emerging technologies like droplet digital PCR (ddPCR) and next-generation sequencing (NGS) will further enhance the sensitivity and comprehensive nature of MRD assessment, ultimately refining risk stratification and personalizing treatment strategies for patients with acute leukemias [16] [12].
Minimal Residual Disease (MRD), also referred to as Measurable Residual Disease, describes the small population of cancer cells that persist in patients after treatment who have achieved clinical and hematological remission [2]. These residual cells, often present at levels undetectable by conventional morphological microscopy, represent a latent reservoir of disease that can ultimately lead to clinical relapse [2]. In hematological malignancies, the detection and monitoring of MRD have become integral to modern clinical management, providing a significantly more sensitive assessment of treatment response than traditional methods such as morphological examination of bone marrow, which has a sensitivity of only 5% (1 in 20 cells) [2] [21]. The evolving role of MRD extends beyond prognosis into therapeutic decision-making, enabling risk-adapted treatment strategies and serving as a powerful surrogate endpoint in clinical trials [21].
The Prognostic Power of MRD in Risk Stratification
MRD status has emerged as a universally significant prognostic biomarker across hematologic malignancies. The presence of MRD (MRD-positivity) signifies residual treatment-resistant disease and is consistently associated with worse clinical outcomes, while MRD negativity correlates with superior survival rates [21].
Table 1: Prognostic Impact of MRD Status Across Hematologic Malignancies
| Malignancy | Impact on Progression-Free Survival (PFS) | Impact on Overall Survival (OS) |
|---|---|---|
| Acute Myeloid Leukemia (AML) | Not Specified | 5-year OS: 68% if MRD-negative vs. 34% if MRD-positive [21] |
| Acute Lymphoblastic Leukemia (ALL) | HR 0.23 for EFS in pediatric patients; HR 0.28 for EFS in adult patients [21] | HR 0.28 for both pediatric and adult patients [21] |
| Chronic Lymphocytic Leukemia (CLL) | HR 0.28 (72% reduction in risk of progression/death); HR 0.24 in first-line setting [21] | Not Specified |
| Multiple Myeloma | HR 0.33 [21] | HR 0.45 [21] |
The correlation between MRD status and patient outcomes provides the foundation for its use in risk stratification. Patients who achieve MRD negativity, particularly when sustained, belong to a favorable risk group with significantly better long-term prospects. Conversely, MRD-positive patients are identified as having higher-risk disease, warranting more aggressive monitoring and intervention strategies [2] [21]. The depth of MRD clearance also holds prognostic importance, with earlier clearance during treatment often portending improved outcomes [21].
MRD-Guided Treatment Decisions
The ability of MRD testing to identify patients at varying levels of relapse risk enables more personalized and dynamic treatment approaches. The clinical application of MRD results can be visualized in the following decision pathway.
Treatment Intensification and Escalation
For patients with persistent MRD positivity, clinical evidence supports the consideration of treatment intensification to eradicate resistant disease clones. This may involve switching to alternative drug classes, pursuing allogeneic stem cell transplantation where appropriate, or enrolling in clinical trials of novel agents [21]. In diseases like Acute Promyelocytic Leukemia (APL) and Chronic Myeloid Leukemia (CML), MRD assessment by RT-PCR is successfully integrated into treatment algorithms to guide therapy duration and identify when treatment changes are needed [21].
Treatment De-Escalation
A promising application of MRD testing is identifying patients who may benefit from treatment de-escalation to reduce therapy-related toxicity. Patients who achieve sustained MRD negativity may be candidates for reduced treatment duration or intensity, including avoidance of more toxic interventions like stem cell transplantation [21]. In solid tumors, studies are investigating whether MRD-negative patients can delay or avoid systemic therapies, thereby sparing them from serious side effects [22].
Dynamic Monitoring and Early Intervention
Serial MRD monitoring enables earlier detection of molecular relapse before clinical or radiographic recurrence becomes apparent [21] [23]. This "lead time" allows clinicians to intervene at a lower disease burden, potentially improving treatment efficacy. In the post-transplant setting, MRD detection can signal impending relapse well before it becomes morphologically evident, enabling preemptive interventions such as rapid immunosuppression withdrawal or donor lymphocyte infusion [21] [6].
MRD Detection Methodologies
Multiple laboratory techniques are available for MRD detection, each with distinct sensitivities, advantages, and limitations. The choice of methodology depends on disease type, available genetic markers, and required sensitivity.
Table 2: Comparison of Major MRD Detection Techniques
| Method | Applicability | Sensitivity | Key Advantages | Key Limitations |
|---|---|---|---|---|
| Multiparametric Flow Cytometry (MFC) | ~100% [2] | 10⁻³ to 10⁻⁶ [2] | Fast turnaround; Wide applicability [2] | Lack of standardization; Phenotype changes [2] |
| Quantitative PCR (qPCR) | ~40-50% [2] | 10⁻⁴ to 10⁻⁶ [2] | Highly standardized; Lower cost [2] | Only one gene/assay; Primer-specific [2] |
| Next-Generation Sequencing (NGS) | >95% [2] | 10⁻² to 10⁻⁶ [2] | Multiple genes simultaneously; Broad applicability [2] | High cost; Complex analysis [2] |
| Digital PCR (ddPCR) | Not Specified | Not Specified | Absolute quantification; High sensitivity | Not widely standardized [24] |
| Liquid Biopsy (ctDNA) | Emerging for solid tumors & AML [22] [6] | Varies by platform | Minimally invasive; Whole genome coverage [22] | Lower tumor fraction in some cancers [22] |
qPCR Workflow for MRD Detection
Quantitative polymerase chain reaction (qPCR) remains a cornerstone technique for MRD detection, particularly in malignancies with well-defined genetic markers. The following protocol outlines a standardized qPCR workflow for MRD assessment.
Detailed qPCR Experimental Protocol
Sample Collection and Processing
- Sample Types: Bone marrow (preferred for highest sensitivity) or peripheral blood collected in appropriate anticoagulant tubes (e.g., EDTA or cell-free DNA collection tubes) [6].
- Cell Processing: For cellular DNA/RNA analysis, isolate mononuclear cells using density gradient centrifugation. For plasma cfDNA analysis, centrifuge blood samples within specified timeframes to prevent cellular degradation [6].
- Nucleic Acid Extraction: Use commercial kits (e.g., QIAamp Circulating Nucleic Acid Kit) optimized for the sample type. Quantify extracted DNA/RNA using fluorometric methods (e.g., Qubit Fluorometer) for accurate concentration measurement [6].
Reverse Transcription (for RNA Targets)
- For fusion transcript detection (e.g., BCR-ABL1, PML-RARA), convert RNA to cDNA using reverse transcriptase.
- Use gene-specific primers or random hexamers with temperature conditions according to enzyme manufacturer specifications.
- Include negative controls (no template and no enzyme) to monitor contamination.
Primer and Probe Design
- Design primers and probes to span rearrangement-specific junctional regions for maximal specificity.
- Validate primer specificity using in silico analysis and experimental testing against positive and negative controls.
- For DNA targets, design amplicons of 50-150 bp for optimal qPCR efficiency [25].
qPCR Reaction Setup
- Reaction Components: TaqMan or SYBR Green master mix, forward and reverse primers, probe (if using TaqMan), template DNA/cDNA, and nuclease-free water.
- Automated Liquid Handling: Utilize systems like the I.DOT Liquid Handler to improve pipetting precision, reduce cross-contamination risk, and increase throughput [25].
- Controls: Include positive controls (diagnostic sample with known mutation), negative controls (healthy donor), no template controls, and standard curve dilutions for quantification.
Thermal Cycling Conditions
- Initial Denaturation: 95°C for 2-10 minutes
- Amplification Cycles (40-50 cycles): Denaturation at 95°C for 15-30 seconds, Annealing/Extension at 60°C for 30-60 seconds (temperature optimized for primer Tm)
- Data Acquisition: Collect fluorescence data during the annealing/extension phase of each cycle.
Data Analysis and Interpretation
- Determine Cycle threshold (Ct) values for samples and standards.
- Generate a standard curve from serial dilutions of positive control material to quantify target levels.
- Calculate MRD levels relative to reference genes (e.g., ABL1, GUSB) to normalize for sample quality and quantity.
- Report results as target:control gene ratio with assay sensitivity limit.
Critical Reagents and Materials
Table 3: Essential Research Reagent Solutions for qPCR-based MRD Detection
| Reagent/Material | Function | Examples/Specifications |
|---|---|---|
| Nucleic Acid Extraction Kits | Isolation of high-quality DNA/RNA from patient samples | QIAamp Circulating Nucleic Acid Kit [6] |
| Cell-Free DNA Collection Tubes | Stabilization of blood samples for plasma separation | Streck cell-free DNA Blood Collection Tubes [6] |
| Reverse Transcriptase Enzyme | cDNA synthesis from RNA targets | Moloney Murine Leukemia Virus (M-MLV) RT |
| Hot-Start DNA Polymerase | Specific amplification with reduced primer-dimer formation | Taq DNA Polymerase |
| Fluorescent Probes/Dyes | Real-time detection of amplification products | TaqMan probes, SYBR Green dye [25] |
| qPCR Master Mix | Optimized buffer system for efficient amplification | Contains dNTPs, MgCl₂, reaction buffer |
| Primers and Probes | Target-specific amplification | Designed to detect fusion genes or rearrangements [2] |
| Quantification Standards | Standard curve generation for absolute quantification | Plasmid standards, cell line DNA with known targets |
| Reference Gene Primers | Amplification control and normalization | ABL1, GUSB, BCR [2] |
Troubleshooting Common qPCR Challenges in MRD Detection
Successful MRD detection by qPCR requires optimization to address several technical challenges that can impact assay sensitivity and reliability.
- Low Yield/Amplification Efficiency: Poor RNA quality or inefficient cDNA synthesis can reduce sensitivity. Remedy by optimizing RNA purification steps, performing appropriate clean-up procedures, and adjusting cDNA synthesis conditions. Verify RNA integrity prior to reverse transcription [25].
- Non-Specific Amplification: Primer-dimer formation or mispriming can lead to false positives. Address by redesigning primers using specialized software, optimizing annealing temperature, and implementing touchdown PCR protocols. Use hot-start polymerase to minimize non-specific amplification at lower temperatures [25].
- Ct Value Variations: Inconsistent pipetting techniques cause template concentration differences across replicates. Improve by implementing proper pipetting techniques, using automated liquid handling systems, and ensuring thorough mixing of reaction components [25].
- Inhibition: Substances co-purified with nucleic acids can inhibit PCR. Detect through dilution series or internal controls. Remedies include additional purification steps, dilution of template, or use of inhibitor-resistant polymerase formulations [25].
Emerging Technologies and Future Directions
The field of MRD detection is rapidly evolving with several promising technological advances. Next-generation sequencing (NGS) approaches, particularly error-corrected sequencing, are achieving sensitivities of 10⁻⁶ and enabling comprehensive assessment of the clonal landscape [2]. Liquid biopsy using circulating tumor DNA (ctDNA) analysis represents a minimally invasive alternative for MRD monitoring, with applications expanding from solid tumors to hematologic malignancies like AML [22] [6]. Tumor-informed, whole genome sequencing-based tests (e.g., Precise MRD) can monitor hundreds to thousands of tumor-specific variants, enabling exceptional sensitivity and quantification of ctDNA even in cancers with low tumor fraction [22]. Standardization efforts led by consortia such as EuroFlow and EuroMRD continue to harmonize MRD assessment protocols across laboratories, though comparable standardization in AML remains an unmet need [21].
MRD assessment has transformed the clinical management of hematologic malignancies, providing an powerful tool for risk stratification and treatment personalization. The integration of sensitive molecular techniques like qPCR into standardized clinical protocols enables dynamic monitoring of disease burden, guiding critical therapeutic decisions. As detection technologies continue to advance and standardization improves, MRD-directed therapy promises to further optimize outcomes through truly personalized treatment approaches.
A Step-by-Step qPCR Protocol for Robust MRD Detection
The accurate detection of Minimal Residual Disease (MRD) via quantitative PCR (qPCR) is a powerful independent predictor of clinical outcomes for patients with hematologic malignancies such as Acute Lymphoblastic Leukemia (ALL) [26]. The sensitivity of these molecular assays, which can detect as low as one cancer cell among 100,000 normal cells, means that the pre-analytical phase—specifically, sample collection and nucleic acid stabilization—is a critical determinant of assay success [26] [12]. Variations in collection techniques, sample handling, and storage can profoundly impact nucleic acid integrity, leading to false-negative results or inaccurate MRD quantification, which in turn can misguide therapeutic decisions. This application note details standardized, evidence-based protocols for the collection and processing of blood and bone marrow to preserve nucleic acid integrity, ensuring reliable and reproducible results in MRD research.
Sample Collection Protocols
Bone Marrow Aspiration for MRD Analysis
The following protocol, adapted from a comprehensive methodological guide, is designed to obtain high-quality bone marrow aspirates while minimizing hemodilution, which can confound MRD results [27].
- Patient Preparation and Positioning: Place the patient in a lateral decubitus position. Locate the posterior superior iliac spine (typically one hand width distal to the iliac crest and one hand width lateral to the midline) and mark the site. Disinfect the skin thoroughly with a chlorhexidine-ethanol solution [27].
- Anesthesia: Infiltrate the skin, subcutaneous tissue, and periosteum with 1% lidocaine. Adequate anesthesia of the periosteum is crucial for patient comfort. Test the anesthetized area by tapping with the needle; the patient should feel pressure but no pain [27].
- Aspiration Technique:
- Introduce a sterile bone marrow aspiration needle (e.g., 15 or 16 gauge) with a rotating motion until a loss of resistance indicates entry into the marrow cavity [27].
- Remove the stylet and attach a 10-20 mL syringe. Apply negative pressure with a gentle pull. Aspirate only 1-2 mL of marrow to avoid hemodilution, which is a critical source of pre-analytical error. The first 1-2 mL contains the highest concentration of bone marrow spicules [27].
- Warn the patient they may feel a momentary cramping sensation.
- Sample Handling:
- Immediately transfer the aspirate into a tube containing an anticoagulant, such as EDTA or heparin, and invert the tube several times to ensure adequate mixing and prevent coagulation [27] [28].
- For MRD analysis, a successful aspirate should yield at least 10 million viable cells to perform advanced analyses like Leukemia-Associated Immunophenotype (LAIP) and leukemia stem cell (LSC) detection [27].
Peripheral Blood Collection for Molecular Analysis
While bone marrow is the preferred matrix for MRD, peripheral blood is increasingly used, and its proper collection is equally important.
- Collection: Collect venous blood into EDTA Vacutainer tubes [29].
- Storage: Store samples at -70 °C or lower until analysis to preserve nucleic acid integrity. Repeated thawing and freezing cycles should be strictly avoided [29].
Sample Processing & Nucleic Acid Stabilization
Processing of Bone Marrow Aspirates
- Timing: All specimens for immunophenotyping and molecular analysis should be processed preferentially within 24 hours of collection [27]. While samples can sometimes be analyzed after up to 72 hours at ambient temperature, this is not recommendable for optimal results [27].
- Conditions: Perform all handling under sterile conditions to enable potential cryopreservation of cells for future research or quality assessment [27].
A Rapid Whole Blood Processing Protocol
For certain qPCR applications, standard DNA extraction can be bypassed with a rapid whole-blood processing method, saving significant time and cost without compromising genotyping accuracy [29]. The workflow below outlines this protocol and its application context.
Detailed Protocol:
- Dilution: Dilute 20 µL of EDTA-anticoagulated whole blood with 20 µL of deionized water [29].
- Incubation: Incubate the diluted blood at 90 °C for 3 minutes. This heat treatment helps to lyse cells and inactivate nucleases [29].
- Centrifugation: Centrifuge the sample at 10,000 × g for 2 minutes to pellet cell debris [29].
- Supernatant Collection: The resulting supernatant contains amplifiable DNA and can be used directly as a template in subsequent real-time PCR reactions (use 4 µL per 16 µL PCR mixture) [29].
Impact of Sample Stabilization on RNA Integrity
For gene expression assays, the stabilization method is a critical pre-analytical factor affecting RNA integrity. Research comparing different methods for human lung tissue demonstrates clear differences in RNA quality [30]. The table below summarizes key performance data for DNA and RNA samples processed for qPCR analysis.
Table 1: Quantitative Data from Nucleic Acid Analysis in Blood and Bone Marrow
| Sample Type / Method | Analyte | Key Performance Metric | Result / Value | Citation |
|---|---|---|---|---|
| Modified Whole Blood (Rapid protocol) | DNA | Median Ct value (FV Leiden, wt/wt) | 25.3 | [29] |
| Standard DNA Extract (from blood) | DNA | Median Ct value (FV Leiden, wt/wt) | 18.5 | [29] |
| Bone Marrow (for Leishmania detection) | DNA | Correlation: Amastigote count vs. Ct value | Spearman's ρ = -0.89 | [28] |
| RNA from RNAlater | RNA | Average RIN (RNA Integrity Number) | 7.6 | [30] |
| RNA from Snap-Freezing with OCT | RNA | Average RIN (RNA Integrity Number) | 8.1 | [30] |
| RNA from Formalin-Fixed, Paraffin-Embedded (FFPE) | RNA | Average RIN (RNA Integrity Number) | 1.4 | [30] |
Molecular Analysis & Quality Control
DNA Extraction and qPCR Setup
- DNA Extraction: For conventional protocols, genomic DNA can be isolated from 200 µL of blood or bone marrow aspirate using commercial kits (e.g., MagCore Genomic DNA Whole Blood Kit) according to manufacturer's instructions [29] [28]. Automated systems like the KingFisher Flex can improve reproducibility for high-throughput labs [28].
- qPCR Reaction Setup:
Quality Control and Assay Validation
Ensuring the integrity of nucleic acids and validating the qPCR assay are non-negotiable for reliable MRD quantification. The following diagram and table outline the core components and reagents for this critical phase.
Table 2: The Scientist's Toolkit: Key Reagents and Materials
| Item | Function / Application | Examples / Notes |
|---|---|---|
| EDTA or Heparin Tubes | Anticoagulant for blood and bone marrow collection | Prevents coagulation; EDTA is preferred for molecular studies. |
| RNAlater / RNA Stabilization Reagents | Preserves RNA integrity in fresh tissues/cells by stabilizing and protecting RNA. | Critical for gene expression studies from tissue samples [30]. |
| DNA Extraction Kit | Isolation of high-purity genomic DNA from whole blood or bone marrow. | MagCore Genomic DNA Whole Blood Kit; automated systems available [29] [28]. |
| qPCR Master Mix | Contains enzymes, dNTPs, buffer, and passive reference dye for real-time PCR. | Should include a passive reference dye (e.g., ROX) to normalize fluorescence [31]. |
| Hydrolytic (TaqMan) Probes | Sequence-specific detection providing high specificity for target amplification. | Used with CE-IVD certified kits for allelic discrimination (e.g., thrombophilic mutations) [29]. |
| Validated Primer/Probe Sets | For specific detection of MRD targets (e.g., IG/TR rearrangements, fusion transcripts). | Must be validated for inclusivity, exclusivity, and dynamic range [32] [33]. |
| Internal Extraction Control (IEC) | Non-target DNA added to samples to monitor extraction efficiency. | Helps identify PCR inhibition or extraction failures [28]. |
Key QC Steps:
- Nucleic Acid Purity and Integrity: Assess DNA/RNA concentration and purity via spectrophotometry (A260/A280 ratio >1.8). For RNA, the RNA Integrity Number (RIN) is a key metric; values above 8.0 indicate intact RNA, while values below 5.0 suggest significant degradation [34] [30].
- Assay Validation Parameters: Following MIQE guidelines and related consensus statements is essential [32] [33].
- Dynamic Range and Efficiency: Test a 7-log 10-fold dilution series of the target. The assay should have a linear range of 6-8 orders of magnitude with an amplification efficiency between 90-110% and an R² value of ≥0.980 [32].
- Inclusivity and Exclusivity: Ensure the assay detects all intended target variants (inclusivity) and does not cross-react with genetically similar non-targets (exclusivity), both in silico and experimentally [32] [33].
- Precision: Measure the Coefficient of Variation (CV) across technical and biological replicates. Low CV indicates high precision and reliable ability to detect fold changes [31].
Data Analysis and Interpretation
- Absolute vs. Relative Quantification: MRD analysis often uses absolute quantification to determine the exact number of leukemic cells per total number of normal cells (e.g., 10⁻⁴) [26] [31]. This requires a standard curve from diagnostic DNA diluted in normal DNA [26].
- Digital PCR (dPCR) as an Emerging Tool: dPCR technologies, such as droplet digital PCR (ddPCR), offer absolute quantification without a standard curve. Recent studies show ddPCR can outperform qPCR in MRD monitoring, providing better sensitivity and reducing the number of non-quantifiable low-positive results [26] [12].
- Replicates and Statistics:
- Use at least technical triplicates to account for system variation and allow for outlier detection [31].
- Employ sufficient biological replicates to account for true variation within a sample group [31].
- Use appropriate statistical tests (e.g., t-test) to determine if observed fold changes are significant, considering both statistical and physiological relevance [31].
Robust MRD research begins long before the qPCR machine starts running. Meticulous attention to sample collection, processing, and nucleic acid stabilization is fundamental to preserving the integrity of the genetic template. By adhering to the standardized protocols outlined here—from the technique of bone marrow aspiration to the implementation of rigorous quality control measures—researchers can significantly enhance the accuracy, sensitivity, and reproducibility of their qPCR data. This, in turn, provides a more reliable foundation for understanding disease progression and guiding therapeutic development in oncology.
Quantitative PCR (qPCR) is a foundational technique in molecular biology, enabling the accurate quantification of nucleic acids. In the context of Minimal Residual Disease (MRD) detection in hematological malignancies, qPCR serves as a critical tool for monitoring residual cancer cells after treatment, with sensitivities reaching 10⁻⁴ to 10⁻⁶ [2]. This high sensitivity allows clinicians to identify patients at risk of relapse and guide treatment decisions. The accuracy of MRD detection hinges on a robustly designed qPCR assay, where careful selection of primers and probes, along with meticulous optimization of amplification efficiency, is paramount for generating reliable, reproducible data that can inform clinical decision-making [2] [18].
Primer and Probe Design Fundamentals
Core Principles for Primer Design
Designing effective primers requires adherence to several key parameters to ensure specificity, sensitivity, and high efficiency.
- Length and Melting Temperature (Tm): Primers should be 18-30 bases long, with an optimal Tm between 58°C and 65°C [35] [36]. For two-step qPCR protocols, a Tm of 58-60°C is recommended [35]. The Tms of the forward and reverse primers should not differ by more than 2°C to ensure simultaneous binding [36].
- GC Content and Sequence: The optimal GC content is between 40% and 60% [35]. Sequences should avoid runs of identical nucleotides, particularly more than three consecutive G or C bases, and the 3' end should not contain more than two Gs or Cs in the last five nucleotides to prevent mispriming [35] [36].
- Specificity and Secondary Structures: Primers must be specific to the target sequence. Tools like NCBI BLAST should be used to verify uniqueness [35] [36]. Self-complementarity should be avoided, and the ΔG value for any potential hairpins or dimers should be weaker (more positive) than -9.0 kcal/mol [36].
Core Principles for Probe Design
Hydrolysis probes (e.g., TaqMan) must be designed with distinct criteria to ensure specific signal generation.
- Location and Melting Temperature: The probe should be located in close proximity to a primer-binding site but must not overlap with it [36]. The Tm of the probe should be 5-10°C higher than the Tm of the primers to ensure it binds before the primers [35] [36].
- Sequence and Quenching: GC content should be 30-70%, and a guanine (G) base at the 5' end should be avoided as it can quench the fluorophore reporter [35] [36]. Double-quenched probes are recommended over single-quenched probes to achieve lower background and higher signal-to-noise ratios [36].
Assay Design Considerations
- Amplicon Characteristics: The ideal amplicon length for qPCR is 70-150 base pairs, balancing efficient amplification and the need for sufficient sequence for primer/probe design [36]. For MRD detection using DNA targets, shorter fragments (50-200 bp) are more tolerant of PCR conditions and amplify quickly [35].
- Specificity for Gene Expression: When designing assays for gene expression analysis (RT-qPCR), amplicons should span an exon-exon junction where possible. This design prevents the amplification of genomic DNA, thereby ensuring that the signal originates specifically from cDNA [36].
Table 1: Summary of Primer and Probe Design Guidelines
| Parameter | Primer Guidelines | Probe Guidelines |
|---|---|---|
| Length | 18-30 bases [36] | 9-40 bases; 20-30 bp for single-quenched [35] [36] |
| Melting Temperature (Tm) | 58-65°C; within 2°C for primer pair [35] [36] | 5-10°C higher than primers [35] [36] |
| GC Content | 40-60% [35] | 30-70% [35] |
| Sequence to Avoid | ≤3 consecutive G/C; avoid 3' end GC-rich [35] | G at the 5' end [36] |
| Specificity Check | BLAST analysis; avoid secondary structures (ΔG > -9 kcal/mol) [36] | BLAST analysis; ensure binding to correct strand [36] |
Optimization of Amplification Efficiency
Defining and Calculating qPCR Efficiency
Amplification efficiency (E) is a critical metric in qPCR, defining the fold-increase of amplicon per cycle. An ideal reaction has 100% efficiency (E=2), meaning the product doubles every cycle [37] [38]. Efficiency is typically calculated from a standard curve of serial dilutions. The Cq values are plotted against the logarithm of the starting concentration, and the slope of the trend line is used in the equation: E = -1 + 10(-1/slope) [38]. The desired efficiency range for a well-optimized assay is 90-110% [39] [38].
Thermocycling Protocol Optimization
The thermocycling protocol can be systematically optimized to achieve high efficiency.
- Initial Denaturation/Activation: A step of 95°C for 30 seconds is often sufficient for genomic DNA. For cDNA, this can be lower. Note that hot-start polymerases may require a longer initial activation step as per the manufacturer's protocol [35].
- Denaturation: During cycling, a short denaturation step of 95°C for 5-15 seconds is adequate for most templates [35].
- Annealing and Extension: For many assays, a two-step PCR (combining annealing and extension) at 60°C for 1 minute is a good starting point [35]. The annealing temperature (Ta) should be set no more than 5°C below the primer Tm and can be optimized using a thermal gradient cycler [35] [36]. If annealing and extension are separate, the Ta should be approximately equal to the primer Tm, and the extension time is based on polymerase speed (e.g., 15-30 seconds per 100 bp) [35].
- Cycle Number: While 40 cycles is standard, this can be reduced to 30 if the amplification reaches the plateau phase early [35].
Troubleshooting Amplification Efficiency
Deviations from the ideal efficiency range indicate problems with the assay.
- Efficiency >110%: This is often caused by the presence of polymerase inhibitors in concentrated samples, which flatten the standard curve slope. Other causes include pipetting errors, inaccurate dilution series, or primer-dimer formation with intercalating dyes [38]. Remedies include diluting the sample, re-purifying the nucleic acid, and checking for A260/280 purity ratios (≥1.8 for DNA, ≥2.0 for RNA) [38].
- Efficiency <90%: This is typically due to suboptimal primer design (e.g., secondary structures, low Tm), poor probe binding, or non-optimal reagent concentrations or reaction conditions [35] [38]. Re-designing primers and probes or re-optimizing the Ta is necessary.
Table 2: Troubleshooting qPCR Amplification Efficiency
| Symptom | Potential Causes | Solutions |
|---|---|---|
| Low Efficiency (<90%) | Poor primer/probe design, secondary structures, low Ta, reagent limitations [35] [38] | Re-design oligonucleotides; optimize Ta; check reagent quality and concentrations [35] |
| High Efficiency (>110%) | Polymerase inhibitors in sample, pipetting errors, primer dimers (SYBR Green) [38] | Dilute or re-purify sample; improve pipetting technique; use inhibitor-tolerant master mix [38] |
| Poor Reproducibility | Primer-dimer formation, assay design, pipetting inaccuracies [39] | Use double-quenched probes; ensure precise pipetting; use white wells with clear seals [35] [36] |
| Non-Homogeneous Amplification (Multiplex) | Sequence-specific efficiency differences, adapter-mediated self-priming [40] | Use deep learning tools for homogeneous library design; check for inhibitory motifs near primers [40] |
Advanced Optimization Strategies and MRD-Specific Workflow
Statistical and Computational Optimization Methods
Advanced methods can streamline the optimization process and address complex issues.
- Design of Experiments (DOE): A statistical DOE approach can efficiently optimize multiple factors simultaneously. For probe optimization, this method has been shown to increase PCR efficiency by up to 10% while significantly reducing the number of required experiments compared to a one-factor-at-a-time approach [41].
- Deep Learning for Efficiency Prediction: For multi-template PCR, such as in NGS library preparation, non-homogeneous amplification can skew results. Recent studies use one-dimensional convolutional neural networks (1D-CNNs) to predict sequence-specific amplification efficiencies, identifying specific motifs (e.g., near adapter priming sites) that cause poor amplification [40]. This allows for the design of inherently homogeneous amplicon libraries.
Application in MRD Detection: A Workflow
In MRD detection for acute lymphoblastic leukemia (ALL), qPCR of immunoglobulin (IG) and T-cell receptor (TR) gene rearrangements is a gold standard [18]. The workflow involves identifying a patient-specific clonal rearrangement at diagnosis and designing allele-specific primers for highly sensitive monitoring during remission. Adherence to international guidelines, like those from the EuroMRD Consortium, is crucial for data interpretation and quality assurance [18]. These guidelines define categories such as "quantifiable MRD," "positive below quantitative range," and "negative" to ensure consistent and accurate reporting across laboratories [18].
Table 3: Research Reagent Solutions for qPCR Assay Development
| Item | Function/Description | Example/Benefit |
|---|---|---|
| High-Quality qPCR Master Mix | A pre-mixed solution containing DNA polymerase, dNTPs, buffer, and Mg²⁺. | Ensures consistent performance; some mixes are more tolerant of inhibitors [35] [38]. |
| Validated Primer/Probe Assays | Pre-designed and tested oligonucleotide sets for specific targets. | Saves time and optimization; available from vendors like Qiagen and Thermo Fisher [39] [42]. |
| White qPCR Plates with Ultra-Clear Seals | Plates and seals designed for optimal optical clarity and signal reflection. | Reduces light distortion and increases fluorescent signal detection [35]. |
| Nucleic Acid Isolation Kits | Kits for purifying high-quality, inhibitor-free DNA/RNA. | Critical for sample prep; ensures high purity (A260/280 ratio) [35] [38]. |
| qPCR Instrument with Gradient Function | A thermal cycler with real-time detection and temperature gradient capability. | Allows parallel optimization of annealing temperatures in a single run [35]. |
| Online Design & Analysis Tools | Free software for oligonucleotide design and analysis. | IDT's OligoAnalyzer, PrimerQuest; used for Tm calculation, secondary structure check [36]. |
| Public Primer Databases | Online repositories of published primer sequences. | PrimerBank, RT PrimerDB; provide starting points for assay design [42]. |
Within minimal residual disease (MRD) detection research, the accurate quantification of rare disease-specific nucleic acid targets is paramount. Reverse transcription quantitative polymerase chain reaction (RT-qPCR) serves as a cornerstone technology for this application, enabling researchers to monitor treatment efficacy and predict disease recurrence with high sensitivity. This application note provides a detailed protocol for the entire RT-qPCR workflow, framed within the context of MRD detection, to ensure precise and reliable gene expression quantification for researchers, scientists, and drug development professionals. The methodology outlined emphasizes robust assay design, optimized reaction conditions, and rigorous data analysis tailored to the challenges of detecting low-abundance targets.
The RT-qPCR process for MRD detection involves a series of critical steps, from sample preparation to data interpretation. The following diagram illustrates the complete workflow, highlighting the two main procedural pathways and key decision points.
RNA Isolation and Reverse Transcription
RNA Extraction and Quality Control
The accuracy of MRD detection begins with high-quality RNA. Extract RNA from patient blood or bone marrow samples using column-based purification methods or reagents like TRIzol, ensuring efficient cell lysis and RNase inactivation [43]. Critical steps include:
- DNase Treatment: Treat extracted RNA with DNase I to eliminate genomic DNA contamination, which is a significant source of false positives in MRD detection [43].
- Quality Assessment: Evaluate RNA integrity and purity using spectrophotometry (A260/A280 ratio of 1.8-2.0) and agarose gel electrophoresis [44]. High-quality RNA is essential for reliable cDNA synthesis.
Reverse Transcription to cDNA
Convert purified RNA into complementary DNA (cDNA) using reverse transcriptase enzymes (e.g., M-MLV or AMV) [43]. The choice of priming strategy affects cDNA representation and assay sensitivity:
- Oligo(dT) Primers: Prime reverse transcription from the poly-A tails of mRNA, suitable for amplifying protein-coding genes [45].
- Random Hexamers: Prime throughout the RNA transcriptome, enabling detection of non-polyadenylated transcripts and providing more comprehensive coverage [45].
- Gene-Specific Primers: Offer the highest sensitivity for specific MRD targets but limit analysis to predefined genes [43].
Table 1: Comparison of One-Step vs. Two-Step RT-qPCR Approaches
| Parameter | One-Step RT-qPCR | Two-Step RT-qPCR |
|---|---|---|
| Procedure | Reverse transcription and PCR amplification occur in a single tube [43] | Reverse transcription and PCR amplification are performed in separate tubes [43] |
| Advantages | Reduced hands-on time, lower contamination risk, easier automation [43] | cDNA can be stored and used for multiple assays, greater flexibility in optimization [43] |
| Disadvantages | Limited to specific targets, no cDNA archive for future use [43] | Increased pipetting steps, higher contamination risk [43] |
| Ideal for MRD | High-throughput screening of defined targets | Research requiring analysis of multiple targets from precious samples |
qPCR Amplification and Detection
Reaction Setup and Optimization
Establish robust qPCR conditions to ensure specific and efficient amplification of MRD targets:
- Master Mix Components: Prepare reactions containing DNA polymerase, dNTPs, primers, fluorescent detection system (dye or probe), and cDNA template [46]. Use "hot-start" polymerases to minimize non-specific amplification at lower temperatures [44].
- Primer Design: Design primers with melting temperatures (Tm) of 60-65°C, length of 15-30 base pairs, and GC content of 40-60% to ensure specificity and efficiency [46]. For MRD applications, design amplicons of 70-200 base pairs for optimal amplification efficiency.
- Thermal Cycling Conditions: Program thermal cyclers with an initial denaturation step (94-98°C), followed by 35-40 cycles of denaturation, annealing (50-70°C), and extension (68-72°C) [46].
Detection Chemistries
Select appropriate detection methods based on the specificity requirements of your MRD assay. The following diagram illustrates the mechanisms of the two primary detection chemistries.
Table 2: Comparison of qPCR Detection Methods for MRD Applications
| Detection Method | Mechanism | Advantages | Limitations | MRD Applicability |
|---|---|---|---|---|
| Hydrolysis Probes (TaqMan) | Fluorogenic probes cleaved by 5'→3' exonuclease activity of DNA polymerase [47] | High specificity, multiplexing capability, low background [47] | Requires custom probe design, higher cost [47] | Ideal for specific mutation detection and multiplex assays |
| SYBR Green Dye | Fluorescent dye intercalating into double-stranded DNA [43] | Cost-effective, flexible (no probe needed), easy optimization [43] | Less specific, requires melt curve analysis [43] | Suitable for abundant targets with optimized primer specificity |
| Molecular Beacons | Hairpin-shaped probes with reporter and quencher; fluorescence upon hybridization [43] | High specificity for SNP detection, stable signal [43] | Complex design, optimization required [43] | Useful for distinguishing closely related genetic sequences |
Essential Controls for MRD Detection
Implement rigorous controls to ensure assay validity and prevent false results:
- No Template Control (NTC): Contains all reaction components except template cDNA to detect contamination [46].
- Positive Control: Includes a known amount of target sequence to verify reaction efficiency [46].
- Negative Biological Control: Sample lacking the MRD target to establish background signal [46].
- Reference Gene Control: Endogenous housekeeping gene with stable expression for normalization [46].
Data Analysis and Normalization
Quantification Methods and Threshold Cycle (Ct)
qPCR data analysis centers on the threshold cycle (Ct), the cycle number at which the fluorescent signal exceeds the background threshold [46]. For MRD detection, lower Ct values indicate higher target abundance, while higher Ct values reflect lower target levels.
- Absolute Quantification: Determines the exact copy number of MRD targets using a standard curve with known concentrations [48]. Essential for establishing clinically relevant MRD thresholds.
- Relative Quantification: Measures changes in MRD target expression relative to a reference sample (e.g., diagnosis sample) and normalized to reference genes [48]. The comparative ΔΔCt method is commonly used [46].
Reference Gene Selection and Validation
Proper normalization is critical for accurate MRD quantification. While traditional housekeeping genes (e.g., GAPDH, β-actin) are commonly used, their expression may vary under different experimental conditions [49]. For MRD studies:
- Validate Reference Genes: Confirm stable expression of reference genes across all sample types and treatment conditions [49].
- Use Multiple Reference Genes: Improve normalization accuracy by using the geometric mean of multiple validated reference genes [49].
- Leverage RNA-Seq Data: Mine RNA-Seq databases to identify stably expressed gene combinations specifically for your experimental system [49].
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Reagents and Materials for RT-qPCR in MRD Research
| Reagent/Material | Function | Application Notes |
|---|---|---|
| Column-Based RNA Purification Kits | Isolation of high-quality RNA from clinical samples | Ensure high RNA integrity numbers (RIN >8) for MRD detection [43] |
| Reverse Transcriptase (e.g., M-MLV) | Synthesis of cDNA from RNA templates | Select enzymes with high thermal stability for GC-rich targets [44] |
| Hot-Start DNA Polymerase | DNA amplification during PCR | Reduces non-specific amplification in early cycles [44] |
| dNTP Mix | Building blocks for DNA synthesis | Consider dUTP-containing mixes for UNG-mediated contamination control [44] |
| Sequence-Specific Probes (TaqMan) | Target-specific detection | Fluorophore selection depends on instrument capabilities and multiplexing needs [47] |
| SYBR Green I Dye | Non-specific DNA detection | Cost-effective for single-plex assays; requires melt curve analysis [43] |
| qPCR Plates and Seals | Reaction vessels | Ensure optical clarity and secure sealing to prevent evaporation |
| DNase I Enzyme | Degradation of contaminating genomic DNA | Critical for preventing false positives in MRD detection [43] |
| Reference Gene Assays | Normalization controls | Validate stability across patient samples and disease stages [49] |
The RT-qPCR workflow for minimal residual disease detection demands meticulous attention to each procedural step, from RNA extraction through data analysis. By implementing the detailed protocols and considerations outlined in this application note, researchers can establish robust, sensitive, and reproducible MRD detection assays. The selection of appropriate detection chemistries, rigorous validation of reference genes, and implementation of comprehensive controls are particularly critical for the reliable quantification of low-abundance targets in clinical research settings. This optimized workflow provides a foundation for generating high-quality data that can inform therapeutic decisions and advance drug development in oncology.
In the context of minimal residual disease (MRD) detection research, precise and reproducible quantitative PCR (qPCR) data is paramount. Relative quantification determines the change in expression of a target gene in a test sample relative to a control sample, normalized to one or more reference genes. This approach is fundamental in MRD research to compare gene expression signatures between minimal disease states and healthy controls. The two predominant methods for relative quantification are the ΔΔCt method and the standard curve-based method, each with specific applications and assumptions critical to reliable MRD assessment.
The ΔΔCt Method: Principles and Protocol
Core Principles and Assumptions
The 2–ΔΔCt method is a widely used approach for calculating the relative fold change in gene expression [50]. Its validity, however, rests on several key assumptions that must be verified for robust MRD data:
- Primer Efficiency: The amplification efficiencies of the target gene and the reference gene must be approximately equal and near 100% [50] [51]. Efficiency between 90-110% is generally considered acceptable, but efficiencies between 95-105% are ideal for the ΔΔCt method [52].
- Reference Gene Stability: The expression of the endogenous control (reference) genes must remain constant across all experimental conditions, including in patient-derived MRD samples and control samples [50].
Step-by-Step Experimental Protocol
Step 1: Calculate Average Ct Values
- Run qPCR reactions for your target gene(s) and reference gene(s) in all experimental and control samples. Include at least three technical replicates for each sample-gene combination [53].
- Calculate the average Ct value for the target gene and the reference gene in both the experimental (e.g., MRD-positive) and control (e.g., healthy) groups [50].
Step 2: Calculate ΔCt Values
- For each condition (experimental and control), subtract the average reference gene Ct from the average target gene Ct.
Step 3: Calculate ΔΔCt Value
- Subtract the control ΔCt from the experimental ΔCt.
Step 4: Calculate Fold Change
- The fold change in gene expression is calculated using the formula:
- A fold change greater than 1 indicates upregulation in the experimental group, while a value less than 1 indicates downregulation [50].
Table 1: Example ΔΔCt Calculation for an MRD Marker Gene
| Sample Group | Avg. Target Gene Ct | Avg. Reference Gene Ct | ΔCt | ΔΔCt | Fold Change (2–ΔΔCt) |
|---|---|---|---|---|---|
| MRD (Experimental) | 22.5 | 20.1 | 2.4 | 1.3 | 0.41 (Downregulation) |
| Healthy (Control) | 23.8 | 21.5 | 2.3 | 0.0 | 1.00 |
Data Analysis Workflow
The following diagram illustrates the logical workflow and calculations involved in the ΔΔCt method:
Standard Curves: Principles and Protocol for Efficiency Analysis
The Role of Standard Curves
A standard curve is an essential control used to determine the amplification efficiency (E) of a qPCR assay [53]. This is a critical pre-qualification step before employing the ΔΔCt method, especially when developing novel assays for MRD detection. The efficiency indicates the rate at of amplicon accumulation during the exponential phase of PCR, with an ideal E of 100% representing a perfect doubling of product each cycle [53].
Step-by-Step Protocol for Standard Curve Generation
Step 1: Prepare Serial Dilutions
- Start with a known concentration of the DNA template (e.g., a plasmid, PCR product, or synthetic gBlock fragment containing the target sequence) [55] [53].
- Create a serial dilution series (e.g., 1:10, 1:100, 1:1000, 1:10000) covering at least five orders of magnitude [55] [53]. This range ensures an accurate assessment of the assay's dynamic range.
Step 2: Run qPCR and Analyze Ct Values
- Perform qPCR on each dilution in triplicate [53].
- Record the average Ct value for each dilution point.
Step 3: Plot the Standard Curve and Calculate Efficiency
- Plot the log10 of the starting quantity or dilution factor (X-axis) against the average Ct value (Y-axis) [52] [53].
- Perform linear regression analysis. The slope and R² value of the trend line are used for quality assessment and efficiency calculation [52].
- Calculate PCR Efficiency using the formula: Efficiency (%) = [10(–1/slope) – 1] × 100 [52] [53].
- An acceptable efficiency typically falls between 90% and 110%, with an R² value > 0.99 [52] [53].
Table 2: Example Standard Curve Data and Efficiency Calculation
| Dilution Factor | Log10(Dilution) | Average Ct | Standard Deviation |
|---|---|---|---|
| 1:10 (0.1) | -1 | 20.5 | 0.08 |
| 1:100 (0.01) | -2 | 24.1 | 0.12 |
| 1:1000 (0.001) | -3 | 27.6 | 0.15 |
| 1:10000 (0.0001) | -4 | 31.0 | 0.09 |
| Result | Slope = -3.33 | R² = 0.998 | Efficiency = 99.6% |
Experimental Workflow
The workflow for generating and using a standard curve in assay validation is as follows:
Advanced Topics and Methodological Considerations
Alternative Quantification Methods and Templates
When the assumptions of the ΔΔCt method are not met, several robust alternatives exist:
- Pfaffl Method: This method is recommended when the amplification efficiencies of the target and reference genes are significantly different and known. It incorporates the actual efficiency values into the fold change calculation, providing a more accurate result [52].
- Multivariable Linear Models (MLM)/ANCOVA: Emerging research suggests that using MLMs directly on Ct data can be superior to the 2–ΔΔCt method. MLMs do not assume that amplification efficiency is exactly 2 (100%) for all genes and can provide correct significance estimates even when efficiencies differ [56].
- Artificial DNA Templates (gBlocks): For absolute quantification or robust standard curves, synthetic double-stranded DNA fragments (gBlocks Gene Fragments) can be used. They are ideal for creating multi-target constructs, reducing pipetting steps and experimental variability in multiplex MRD assays [55]. A key benefit is the ability to design artificial sequences distinguishable from wild-type sequences via melt curve analysis, a crucial feature for contamination control in a clinical MRD setting [55].
The Scientist's Toolkit: Essential Reagents and Software
Table 3: Key Research Reagent Solutions and Computational Tools
| Item | Function/Benefit | Application in MRD Research |
|---|---|---|
| gBlocks Gene Fragments | Synthetic double-stranded DNA fragments (up to 3000 bp); used as a quantifiable standard or multi-assay control template [55]. | Generating standard curves for multiple MRD targets from a single construct, reducing cost and variability [55]. |
| SYBR Green dye | Fluorescent intercalating dye that binds double-stranded DNA; used for monitoring amplification in real-time. | Detecting amplicon accumulation in assays without a specific probe; requires subsequent melt curve analysis for specificity [55]. |
| BHQ (Black Hole Quencher) Probes | Dual-labeled hydrolysis probes (e.g., TaqMan) with a non-fluorescent quencher; offer low background and high signal-to-noise ratio [57]. | Multiplex detection of several MRD markers in a single reaction due to their high specificity and compatibility with multiple fluorophores [57]. |
| R Package: RQdeltaCT | An open-source R package for relative quantification using 2–dCt and 2–ddCt methods; includes quality control and publication-ready visuals [54]. | Streamlining and standardizing the data analysis pipeline for high-throughput MRD qPCR data, ensuring reproducibility [54]. |
| R Package: qPCRtools | An R package for processing qPCR data, including calculating amplification efficiency and gene expression via multiple methods [51]. | Efficiently calculating primer efficiencies during assay validation and processing large Ct data tables from MRD experiments [51]. |
| RealTimeDesign Software | Free, web-based software for optimal design of qPCR assays, primers, and probes (Note: To be retired in 2026, migrating to PCR Forge) [57]. | Designing highly specific primer and probe sets for novel MRD markers to ensure high amplification efficiency and specificity from the start [57]. |
Adherence to MIQE Guidelines
For publication-quality MRD research, adherence to the MIQE (Minimum Information for Publication of Quantitative Real-Time PCR Experiments) guidelines is crucial. The recently updated MIQE 2.0 guidelines emphasize transparent reporting of all experimental details, including [58]:
- Sample handling and nucleic acid quantification methods.
- Assay validation data, including amplification efficiencies and dynamic ranges for each target.
- Normalization strategies based on stable reference genes.
- Raw data export to allow independent re-evaluation of results. Following these guidelines ensures the repeatability, reproducibility, and reliability of your qPCR data in the sensitive context of minimal residual disease detection.
In minimal residual disease (MRD) detection, quantitative polymerase chain reaction (qPCR) serves as a cornerstone technology due to its exceptional sensitivity, capable of detecting residual leukemic cells at frequencies as low as 10⁻⁶ [2]. Accurate MRD assessment is clinically critical, as the presence of residual disease is a powerful predictor of relapse risk and overall survival in hematological malignancies [2] [6]. However, achieving this level of analytical precision and clinical reliability is entirely dependent on the rigorous implementation of experimental controls. These controls are indispensable for verifying assay specificity, monitoring reaction efficiency, and normalizing sample input, thereby ensuring that the final quantitative data truly reflects the patient's disease burden [59] [60]. This application note details the essential roles and implementation protocols for three fundamental control types—No-Template Controls, Positive Controls, and Endogenous Reference Genes—within the context of an MRD-optimized qPCR workflow.
The Role of Controls in MRD qPCR
The following diagram illustrates the integrated workflow for incorporating these essential controls into an MRD qPCR experiment, highlighting the specific objective and data interpretation for each control type.
No-Template Controls (NTC)
Purpose and Application
No-Template Controls (NTCs), also referred to as negative controls, are critical for diagnosing contamination within the qPCR assay. An NTC consists of all reaction components—primers, probe, master mix, and water—except for the template nucleic acid [60]. The primary function of the NTC is to confirm that the amplification signal generated in experimental wells originates solely from the specific target sequence present in the patient sample, and not from environmental contaminants, amplicon carryover, or contaminated reagents. In the context of MRD detection, where sensitivity is paramount and false positives can have significant clinical consequences, the NTC is a non-negotiable element of quality assurance.
Protocol for Implementation and Interpretation
- Preparation: For each primer-probe set used in the MRD assay, prepare at least one NTC well. The NTC should be set up in the same reaction plate and under the same conditions as the test samples.
- Formulation: Use nuclease-free water or the buffer used to suspend the sample cDNA/cfDNA as the substitute for the template. All other reagents must be identical and sourced from the same batches used for the test reactions.
- Amplification: Run the NTC through the entire qPCR cycling protocol alongside the patient samples and other controls.
- Interpretation:
- Acceptable Result: The NTC must show no amplification throughout the entire 40-45 cycle run, manifested as a flat amplification curve that does not cross the fluorescence threshold [60].
- Unacceptable Result: Any amplification curve in the NTC that crosses the threshold, resulting in a reported Cq value, indicates contamination. The experiment must be rejected, and the source of contamination investigated before proceeding. Common sources include aerosolized amplicons, contaminated reagents, or template cross-contamination during sample setup.
Positive Controls
Purpose and Application
Positive controls serve to verify the functionality and efficiency of the entire qPCR process. A positive result confirms that the enzymes, nucleotides, buffers, primers, and probes are all active and combined in a manner that permits specific amplification of the intended target. For MRD assays, which often rely on patient-specific mutations or rearrangements, the positive control validates the entire analytical process from nucleic acid extraction to final detection.
Protocol for Implementation and Interpretation
- Types of Positive Controls:
- Assay Positivity Control: A synthetic oligonucleotide or plasmid containing the target sequence (e.g., the specific mutation or fusion gene like BCR-ABL1). This controls for the qPCR reaction itself.
- Extraction Control: A pre-quantified positive sample (e.g., cell line DNA with a known mutation) taken through the nucleic acid extraction process alongside patient samples. This controls for the efficiency of the extraction and cDNA synthesis steps.
- Formulation and Use: The positive control should be included in every run. For quantitative accuracy, it is advisable to run a dilution series of the positive control to generate a standard curve, allowing for the calculation of PCR efficiency [60].
- Interpretation:
- Acceptable Result: The positive control must produce an amplification curve with a Cq value within an expected, pre-defined range. The standard curve should demonstrate a linear dynamic range with a PCR efficiency (E) between 90% and 110% (slope of -3.1 to -3.6), and a correlation coefficient (R²) > 0.98 [60].
- Unacceptable Result: A significantly delayed Cq, complete lack of amplification, or poor standard curve parameters indicate a failure in the assay system. Potential causes include degraded reagents, incorrect reaction setup, or instrument malfunction.
Endogenous Reference Genes
Purpose and Application
Endogenous reference genes (RGs), or housekeeping genes, are essential for normalizing target gene expression levels in RT-qPCR experiments [59]. They account for technical variations inherent in the process, including differences in sample collection, RNA quality and quantity, cDNA synthesis efficiency, and pipetting inaccuracies [59] [61]. In MRD analysis using cell-free DNA (cfDNA), stable genomic reference genes can be used to quantify total cfDNA input. Normalization against a stable RG ensures that changes in the measured level of the disease-specific target (e.g., a mutant allele) are biologically real and not merely reflective of variations in sample input or quality [59]. The use of an invalidated, unstable RG can lead to severe misinterpretation of data [62] [61].
Selection and Validation of Reference Genes
A critical finding in recent years is that there is no universal "perfect" reference gene. The expression stability of commonly used genes like GAPDH and ACTB can vary significantly across different tissue types, cell lines, and experimental conditions [59] [61] [63]. Therefore, RGs must be empirically validated for each specific experimental setting.
Candidate Gene Selection: Begin by selecting 3-8 candidate RGs from the literature relevant to your sample type (e.g., hematopoietic cells) [59]. The table below lists commonly used candidate genes.
Stability Analysis: The expression stability of the candidate RGs is evaluated using specialized algorithms that analyze the Cq values obtained from all test samples (e.g., different patient samples, time points). Key statistical tools include:
- geNorm: Ranks genes by stability measure (M) and determines the optimal number of RGs required for accurate normalization [62] [63].
- NormFinder: Employs a model-based approach to estimate intra- and inter-group variation, providing a stability value [62] [63].
- BestKeeper: Relies on pairwise correlations of the Cq values of all candidate genes [62] [63].
- RefFinder: A comprehensive tool that integrates the results from geNorm, NormFinder, BestKeeper, and the comparative ΔCq method to provide a overall consensus ranking [62].
Validation: The selected RG(s) should be used to normalize the expression of a well-characterized target gene in a pilot experiment to confirm that the normalization scheme produces biologically plausible results.
Table 1: Statistical Algorithms for Reference Gene Validation
| Algorithm | Core Principle | Primary Output | Key Advantage |
|---|---|---|---|
| geNorm [62] [63] | Pairwise comparison of expression stability between all candidate genes. | Stability measure (M); determines optimal number of reference genes. | Intuitively determines if multiple genes are needed. |
| NormFinder [62] [63] | Model-based estimation of intra- and inter-group variation. | Stability value; less sensitive to co-regulated genes. | Identifies the single most stable gene. |
| BestKeeper [62] [63] | Pairwise correlation analysis using raw Cq values. | Standard deviation (SD) and coefficient of variance (CV). | Provides a simple index based on Cq variability. |
| RefFinder [62] | Comprehensive ranking by integrating geNorm, NormFinder, BestKeeper, and ΔCt. | Overall final ranking of candidate genes. | Provides a robust consensus from multiple methods. |
Protocol for Implementation
- Select Candidate RGs: Choose a panel of candidate genes (e.g., ABL1, GUSB, B2M, PGK1, TBP, RPL30) based on published studies in hematological malignancies or AML [2] [6].
- RNA Extraction & cDNA Synthesis: Extract total RNA from patient samples (e.g., peripheral blood or bone marrow mononuclear cells) using a standardized kit. Treat samples with DNase I to remove genomic DNA contamination. Synthesize cDNA using a high-capacity reverse transcription kit with random hexamers, ensuring all reactions are performed with the same amount of input RNA (e.g., 200-1000 ng) [62] [63].
- qPCR Amplification: Perform qPCR for all candidate RGs and the MRD target gene across all cDNA samples. Run all reactions in triplicate. Include no-template and positive controls.
- Data Analysis: Calculate the average Cq for each gene in each sample. Input the Cq values into the stability analysis software (geNorm, NormFinder, etc.) to rank the candidate genes and select the most stable one(s).
- Normalization Calculation: Use the Cq values of the validated RG(s) to normalize the target gene expression. The most common method is the ΔΔCq method [13], but the Pfaffl method is more accurate when the amplification efficiencies of the target and reference gene are not equal and precisely 100% [13] [60].
The Pfaffl formula is:
[ FC = \frac{(E{target})^{-\Delta Cq{target}}}{(E{ref})^{-\Delta Cq{ref}}} ]
...where E is the amplification efficiency (between 1.9 and 2.1) and ΔCq is the difference in Cq values between test and control conditions [13].
The Scientist's Toolkit: Research Reagent Solutions
The following table lists essential reagents and tools required for implementing the controls described in this protocol.
Table 2: Essential Reagents and Tools for qPCR Controls in MRD Research
| Item | Function/Description | Example Application in MRD Protocol |
|---|---|---|
| Nuclease-Free Water | Solvent for preparing NTCs and diluting reagents; certified free of RNases and DNases. | Used as the template substitute in the No-Template Control (NTC) reaction. |
| TaqMan Endogenous Control Assays [59] | Pre-optimized, gene-specific primer-probe sets for stable human genes (e.g., GUSB, ABL1, B2M). | Provides reliable reagents for quantifying candidate reference genes during the validation process. |
| Commercial Reference Gene Panels [59] | Multi-well plates pre-configured with assays for dozens of candidate reference genes. | Enables high-throughput screening of many candidate genes to identify the most stable ones for a specific study. |
| Synthetic Oligonucleotides or G-Blocks | Custom-designed double-stranded DNA fragments containing the exact target sequence. | Serves as a well-defined positive control for patient-specific mutations or fusion genes (e.g., NPM1, BCR-ABL1). |
| Universal cDNA Reverse Transcription Kit | Kits for converting RNA to cDNA, often including components to remove genomic DNA. | Essential for standardizing the first step of RT-qPCR, ensuring high-quality cDNA from patient RNA samples. |
| Stability Analysis Software | Algorithms (geNorm, NormFinder, BestKeeper) packaged in software or web tools. | Used to analyze Cq values from candidate RGs and objectively select the most stable genes for normalization. |
The path to reliable and clinically actionable MRD data is paved with rigorous quality control. The systematic implementation of No-Template, Positive, and Endogenous Reference Gene controls is not optional but fundamental to the qPCR workflow. These controls work in concert to safeguard the assay from false positives, monitor its analytical performance, and correct for sample-to-sample variations. By adhering to the detailed protocols outlined in this application note—particularly the critical step of empirically validating reference genes for each specific experimental context—researchers and clinicians can ensure the highest standards of data integrity, ultimately supporting accurate risk stratification and treatment decisions for patients with hematological malignancies.
Overcoming Common qPCR Challenges in MRD Assays
Identifying and Mitigating PCR Inhibitors from Biological Samples
Accurate minimal residual disease (MRD) detection via quantitative polymerase chain reaction (qPCR) is paramount for assessing treatment efficacy, predicting relapse, and guiding therapeutic decisions in hematological malignancies [2]. The sensitivity of this powerful biomarker technology, capable of detecting up to one leukemic cell in a million, can be severely compromised by the presence of PCR inhibitors in biological samples [2]. These substances, which can originate from the sample matrix, sample collection materials, or laboratory reagents, interfere with the enzymatic amplification process, potentially leading to false-negative results or inaccurate quantification [64] [65]. Such errors can directly impact clinical outcomes by misinforming risk stratification and treatment strategies. This application note details the common sources and mechanisms of PCR inhibition, provides methodologies for its identification, and outlines robust, practical protocols for mitigation, all framed within the critical context of MRD research.
Understanding PCR Inhibitors in MRD Sample Contexts
PCR inhibitors are a heterogeneous class of substances that can derail the biochemical and biophysical processes essential for in vitro DNA polymerization [64] [65]. Their impact in MRD analysis ranges from a partial reduction in amplification efficiency—causing an underestimation of the target nucleic acid amount—to complete amplification failure [65]. The mechanisms of inhibition are diverse. Inhibitors can bind directly to single- or double-stranded nucleic acids, making the template unavailable for amplification [65]. They may also degrade, denature, or alter the DNA polymerase enzyme itself, or chelate co-factors like magnesium ions that are essential for polymerase activity [65] [66]. Furthermore, in qPCR, certain compounds can quench the fluorescent signal or increase background fluorescence, thereby interfering with detection [64] [65].
The table below catalogs common inhibitors relevant to MRD and clinical research, detailing their sources and primary mechanisms of action.
Table 1: Common PCR Inhibitors in Biological and Clinical Samples
| Inhibitor Source | Specific Examples | Mechanism of Inhibition |
|---|---|---|
| Blood-Derived Samples | Hemoglobin, Immunoglobulin G (IgG), Lactoferrin, Heparin (anticoagulant) | IgG binds single-stranded DNA; Hemoglobin and heparin inhibit polymerase activity; Heparin chelates Mg²⁺ [64] [65] [67]. |
| Sample Collection & Prep | EDTA, Phenol, Ethanol, Isopropanol, Ionic Detergents (SDS) | EDTA chelates Mg²⁺; Phenol/ethanol denature enzymes; SDS inhibits polymerase [65] [67]. |
| Bone Marrow Aspirates | Complex biological matrix, Hematin, Lipids, Proteins | Degrade or sequester nucleic acids; inhibit polymerase activity; fluorescence interference [64] [66]. |
Detecting Inhibition in MRD qPCR Assays
Recognizing inhibition is the first critical step in ensuring data fidelity. In qPCR, inhibition can be detected through several tell-tale signs in the amplification data and by employing specific controls.
3.1 Indicators from Amplification Kinetics
- Delayed Quantification Cycle (Cq): A uniform increase in Cq values across samples and controls suggests the presence of inhibitors affecting the reaction kinetics [66].
- Poor Amplification Efficiency: The generation of a standard curve with a slope steeper than -3.6 indicates reduced amplification efficiency, often a consequence of inhibition [66] [68].
- Abnormal Amplification Curves: Flattened curves, a lack of a distinct exponential phase, or a failure to cross the detection threshold are visual indicators of interference with the polymerase, template, or fluorescence detection [66].
3.2 Internal Amplification Controls (IAC) The use of an IAC is a robust and highly recommended method for diagnosing inhibition in diagnostic and MRD assays [68]. An IAC is a non-target DNA sequence added at a known concentration to the qPCR reaction. A significant delay in the Cq value of the IAC in a test sample compared to its Cq in a clean reaction (e.g., nuclease-free water) confirms the presence of PCR inhibitors [68]. This approach effectively differentiates between true target absence (low input) and amplification failure due to inhibition.
The following diagram illustrates the decision workflow for identifying and responding to signs of PCR inhibition in an MRD qPCR experiment.
Protocols for Mitigating PCR Inhibition
Once inhibition is identified, researchers can employ a multi-faceted approach to overcome it. The strategies below are listed from least to most disruptive to the standard workflow.
4.1 Protocol: Dilution of Nucleic Acid Eluates Simple dilution of the DNA extract reduces the concentration of inhibitors to a sub-critical level while ideally retaining a detectable quantity of the target MRD sequence [65] [69].
- Procedure: Prepare a series of log dilutions (e.g., 1:5, 1:10) of the extracted DNA sample using nuclease-free water or TE buffer.
- qPCR Analysis: Amplify each dilution using your standard MRD qPCR assay.
- Interpretation: Identify the dilution at which the Cq value shifts to that expected from a clean, uninhibited reaction. The target concentration is then calculated by correcting for the dilution factor. Note that excessive dilution may render low-abundance MRD targets undetectable [69].
4.2 Protocol: Optimizing Reaction Chemistry with Additives The addition of facilitator compounds to the qPCR master mix can neutralize specific inhibitors.
- Preparation: Prepare separate master mix aliquots containing different facilitators.
- Bovine Serum Albumin (BSA): Final concentration of 0.1 - 0.5 μg/μL [65] [69]. Effective against humic acids, phenolics, and inhibitors in blood [65].
- T4 Gene 32 Protein (gp32): Final concentration of 0.1 - 1 nM [69] [70]. Binds single-stranded DNA, stabilizing the template and counteracting inhibitors like humic acid.
- Non-Ionic Detergents (e.g., Tween-20): Final concentration of 0.1 - 1% (v/v) [65] [69]. Can stimulate polymerase activity and reduce false terminations.
- Optimization: Run the qPCR assay with both inhibited and control samples to determine the optimal type and concentration of additive for your specific sample matrix.
4.3 Protocol: Enhanced Sample Purification If dilution and additives are insufficient, revisiting the nucleic acid extraction step is necessary.
- Column-Based Clean-up: Apply the extracted DNA to a new silica-membrane column. Perform the wash steps as recommended, ensuring complete removal of ethanol by letting the column air dry for 5 minutes before elution [65] [66].
- Organic Extraction (for severe inhibition): For heavily inhibited samples, re-purify the DNA using a phenol-chloroform extraction followed by ethanol precipitation [71]. This method effectively removes proteins and other organic contaminants.
4.4 Strategic Selection of Polymerase Enzymes The choice of DNA polymerase is a critical factor. Several engineered DNA polymerases demonstrate superior resistance to inhibitors found in blood and other complex matrices compared to wild-type Taq [64] [65]. When establishing an MRD protocol, select a master mix specifically formulated for high inhibitor tolerance, as this provides a robust foundation for reliable quantification [66].
Table 2: Summary of PCR Inhibition Mitigation Strategies
| Strategy | Key Reagents | Mechanism of Action | Advantages | Limitations |
|---|---|---|---|---|
| Sample Dilution | Nuclease-free water, TE Buffer | Reduces inhibitor concentration below inhibitory threshold. | Simple, fast, low-cost. | Risk of losing detection of low-copy targets [69]. |
| Chemical Additives | BSA, gp32, Tween-20, DMSO | Binds inhibitors, stabilizes enzymes/templates, lowers DNA Tm. | Easy to implement, cost-effective. | Requires optimization; effect is inhibitor-dependent [65] [69]. |
| Enhanced Purification | Silica columns, Phenol-chloroform | Physically separates inhibitors from nucleic acids. | Highly effective for a broad inhibitor range. | Time-consuming; can lead to significant DNA loss [64] [71]. |
| Robust Polymerase | Inhibitor-resistant enzyme blends | Polymerase structure is less susceptible to inhibition. | Built-in resilience; minimal protocol change. | Can be more expensive than standard polymerases [64] [66]. |
The Scientist's Toolkit: Research Reagent Solutions
The following table lists key reagents and their functions for implementing the protocols described in this note.
Table 3: Essential Reagents for Inhibition Management in MRD qPCR
| Reagent / Kit | Function / Application |
|---|---|
| Inhibitor-Resistant qPCR Master Mix (e.g., GoTaq Endure) | Provides a robust enzyme and buffer system designed for reliable amplification from challenging samples like blood [66]. |
| Internal Amplification Control (IAC) | Non-target sequence used as a spike-in control to diagnostically confirm the presence of PCR inhibitors in a reaction [68]. |
| Bovine Serum Albumin (BSA), Molecular Biology Grade | Acts as a chemical facilitator by binding to a wide range of PCR-inhibitory substances, neutralizing their effect [65] [69]. |
| T4 Gene 32 Protein (gp32) | A single-stranded DNA binding protein used as a facilitator to stabilize DNA templates and counteract inhibition [69] [70]. |
| High-Quality Nucleic Acid Purification Kits | Silica-membrane or magnetic bead-based kits designed for maximal inhibitor removal during DNA extraction from blood and tissues [66]. |
| PCR-Grade Water | Used for preparing sample dilutions to mitigate inhibition and for reconstituting master mixes and controls [65]. |
The integrity of MRD data generated by qPCR is fundamentally dependent on the successful management of PCR inhibitors. By integrating systematic detection methods—such as the use of internal amplification controls and kinetic analysis—with practical mitigation protocols—including dilution, chemical facilitation, and enhanced purification—researchers can significantly improve the reliability and accuracy of their results. A proactive approach, beginning with the selection of an inhibitor-resistant polymerase and validated nucleic acid extraction methods, provides the strongest foundation for generating clinically actionable MRD data that can confidently guide patient management in hematological malignancies.
In the context of minimal residual disease (MRD) detection, the accuracy of real-time quantitative PCR (qPCR) can directly influence patient management decisions. This technique is considered the most reliable and accurate method for molecular diagnosis and MRD monitoring due to its high sensitivity and specificity [72]. However, the process is susceptible to variations from multiple sources, including sample quality, RNA extraction efficiency, and reverse transcription yield. Normalization, the process of correcting for these technical variations, is therefore an "absolute necessity" to achieve reliable and interpretable results [72]. The use of stable reference genes, also known as housekeeping genes or endogenous controls, is widely regarded as one of the most effective normalization methods [72].
A valid reference gene must be expressed at a constant level across different tissue types, physiological states, and experimental conditions. This is especially critical in oncology, where the complex physiology of cancer can greatly alter gene expression patterns [72]. Contrary to past assumptions, commonly used housekeeping genes do not always show constant expression. Their expression levels can be affected by the type of tissue, developmental stage, diseases such as cancer, and even medical treatment [72] [73]. Therefore, the validation of reference gene stability is not an optional step but a critical prerequisite for any accurate relative qRT-PCR study, particularly in MRD research where detecting minute changes in gene expression is paramount.
The Consequences of Improper Normalization
Using an inappropriate or unstable reference gene can lead to misleading data, resulting in incorrect biological conclusions. This risk is profoundly significant in clinical research, such as MRD detection, where qPCR data may inform therapeutic choices. For instance, a study on neuroblastoma MRD monitoring highlighted that PCR target expression (e.g., PHOX2B and TH) can vary during treatment or at relapse. If the marker genes used for monitoring are not stably expressed, the estimation of MRD levels in bone marrow or peripheral blood will be hampered [74].
Gene expression patterns of housekeeping genes can vary in different malignant tissues, different malignant cell subtypes, or even in the same type of carcinoma. This illustrates the difference in the personalized metabolism drivers of cancer cells [73]. For example, in acute leukemia research, the genes GAPDH and HPRT were found to have high standard deviations and great variability between groups, indicating low stability and rendering them poor choices as single reference genes [72]. Without proper validation, the results of gene expression studies are less reliable due to such unexpected behavior of housekeeping genes [73]. The consequences can include both false positives and false negatives in MRD detection, potentially impacting patient care.
Selecting Candidate Reference Genes and Experimental Design
Choosing a Panel of Candidates
The first step in the validation process is to select a panel of candidate reference genes for evaluation. A typical panel consists of 6 to 12 genes [75]. Selection should be based on a systematic literature search for the specific tissue and disease model under investigation. It is crucial to choose genes with diverse cellular functions to avoid selecting co-regulated genes that might share expression patterns. Genes belonging to the same biological pathway may be co-regulated, which would undermine the normalization process [75].
Commonly investigated candidate genes include:
- GAPDH: Glyceraldehyde-3-phosphate dehydrogenase (glycolysis)
- ACTB: β-actin (cytoskeletal structure)
- HPRT1: Hypoxanthine phosphoribosyl-transferase 1 (purine synthesis)
- B2M: Beta-2-microglobulin (component of MHC class I molecules)
- RPLP0: Ribosomal protein lateral stalk subunit P0 (protein translation)
- TBP: TATA box binding protein (transcription initiation)
- UBC: Polyubiquitin-C (protein degradation)
- 18S rRNA: 18S ribosomal RNA (component of the ribosome)
Experimental Design for Validation
A robust validation experiment requires analyzing the candidate genes in a representative set of samples that reflect the full scope of the planned study. For MRD research, this should include samples from both disease (e.g., primary tumor) and normal tissues, and if possible, paired samples from the same patient at different time points (e.g., diagnosis, during treatment, and at relapse) [74].
Table 1: Example Sample Cohort for Reference Gene Validation in Leukemia MRD Research
| Sample Group | Source | Number of Samples | Purpose |
|---|---|---|---|
| Acute Myeloid Leukemia (AML) | Bone Marrow / Peripheral Blood | 24 | Represent the target disease state [72] |
| Acute Lymphoblastic Leukemia (ALL) | Bone Marrow / Peripheral Blood | 25 | Represent another target disease state [72] |
| Paired Normal Tissue | Bone Marrow / Peripheral Blood | 15 | Provide a normal baseline expression level [72] |
| Control Group | Peripheral Blood | 15 | From healthy individuals [72] |
Step-by-Step Validation Protocol
RNA Extraction and cDNA Synthesis
- RNA Extraction: Extract total RNA from samples using a standardized method, such as TRIzol Reagent, according to the manufacturer's instructions [72]. Assess the concentration and purity of the RNA using a spectrophotometer (e.g., Nanodrop). An A260/A280 ratio of approximately 1.8-2.0 is generally accepted as pure. RNA integrity should be checked using an instrument like the Agilent 2100 Bioanalyzer [75].
- DNAse Treatment: Treat RNA samples with a DNAse kit (e.g., Ambion TURBO DNA-free Kit) to remove any contaminating genomic DNA [75].
- cDNA Synthesis: Convert a fixed amount of total RNA (e.g., 1 µg) to cDNA using a High-Capacity cDNA Reverse Transcriptase Kit with random primers [72]. Use a thermal cycler with a standardized protocol (e.g., 10 minutes at 25°C, 120 minutes at 37°C, 5 minutes at 85°C). The resulting cDNA library can be stored at -20°C until use.
Quantitative Real-Time PCR (qPCR)
- Reaction Setup: Perform qPCR reactions in triplicate for each candidate gene and each sample. A typical 20 µL reaction may contain [72]:
- 1 µL of cDNA
- 0.5 µL of each primer/probe
- 5 µL of TaqMan Gene Expression Master Mix
- 3.5 µL of ultra-pure water
- PCR Cycling Conditions: Use standard cycling conditions on a real-time PCR system (e.g., Quantstudio 7 FLEX) [75]:
- Hold Stage: 95°C for 2 minutes
- PCR Cycle (40 repeats): 95°C for 10 seconds (denaturation) followed by 60°C for 1 minute (annealing/extension)
- Quality Control: Include a no-template control (NTC) for each gene to check for contamination. Perform melt-curve analysis at the end of the run to confirm the specificity of amplification and the presence of a single product [73].
Data Analysis and Stability Evaluation
The analysis of the resulting Ct (Cycle threshold) values is performed using specialized algorithms to rank the genes by their expression stability. The use of multiple algorithms is recommended for a robust conclusion.
Figure 1: Workflow for analyzing Ct values to select the most stable reference genes.
- GeNorm Algorithm: This algorithm calculates a gene stability measure (M) based on the average pairwise variation between a particular gene and all other tested reference genes. The gene with the highest M-value (least stable) is stepwise eliminated. A lower M-value indicates higher stability. GeNorm also calculates a pairwise variation (V) value to determine the optimal number of reference genes required for reliable normalization. A common threshold is V<0.15, indicating that adding more genes does not significantly improve normalization [75] [73].
- NormFinder Algorithm: This method uses a model-based approach to estimate not only the overall expression variation but also the variation between sample subgroups. It provides a stability value for each gene, where a lower value indicates greater stability. NormFinder is particularly useful for identifying the best combination of two genes [73].
- BestKeeper Algorithm: This Excel-based tool uses pairwise correlation analysis to determine the stable genes. It calculates the geometric mean of the Ct values of all candidate genes and then correlates the Ct values of each individual gene to this index. It also provides standard deviation (SD) and coefficient of variation (CV) values; genes with a SD greater than 1 are considered unstable [73].
Case Studies and Application to MRD Research
Validation studies across different cancers consistently demonstrate that the most stable reference genes are tissue and disease-specific.
Table 2: Stable Reference Genes Identified in Various Cancer Studies
| Cancer Type | Most Stable Reference Genes | Key Findings | Source |
|---|---|---|---|
| Acute Leukemias | ACTB, ABL, TBP, RPLP0 | GAPDH and HPRT1 showed high variability and low stability in peripheral blood and bone marrow. | [72] |
| Papillary Thyroid Carcinoma | GUSB, HPRT1 | The combination of GUSB with HPRT1, HMBS, or PGM1 was recommended. Three genes were optimal for normalization. | [73] |
| Neuroblastoma (MRD) | Panel of markers (e.g., PHOX2B, TH) | Using the median value of a panel of PCR targets levels out variations due to treatment and subclone outgrowth. | [74] |
| HEK293 Cell Line | UBC, TOP1, ATP5B, CYC1, GAPDH | UBC and TOP1 showed the least variation. The optimal number of reference genes was two. | [75] |
In the context of MRD, a study on neuroblastoma highlighted that while PCR target expression at diagnosis is quite stable, it can alter upon treatment and at relapse [74]. This underscores the necessity of validating the stability of MRD markers themselves, not just classical housekeeping genes. The study found that using the median value of the relative expression of a panel of PCR targets helped to "level out" most variations caused by treatment and the outgrowth of subclones [74]. This suggests that for MRD detection, employing a panel of several validated markers and reference genes provides the most reliable quantification.
The Scientist's Toolkit: Essential Reagents and Materials
Table 3: Key Research Reagent Solutions for Reference Gene Validation
| Reagent / Material | Function / Purpose | Example Product / Note |
|---|---|---|
| RNA Extraction Kit | Isolate high-purity, intact total RNA from samples. | TRIzol Reagent; assess RNA integrity with Bioanalyzer. |
| DNAse Treatment Kit | Remove contaminating genomic DNA to prevent false positives. | Ambion TURBO DNA-free Kit. |
| Reverse Transcriptase Kit | Synthesize cDNA from RNA templates. | High-Capacity cDNA Reverse Transcriptase Kit. |
| qPCR Master Mix | Provides enzymes, dNTPs, and buffer for efficient amplification. | TaqMan Gene Expression Master Mix (for probe-based assays). |
| Primers/Probes | Gene-specific oligonucleotides for amplification and detection. | Validated primer sets or TaqMan assays for candidate genes. |
| Reference Gene Panels | Pre-designed assays for common candidate reference genes. | Commercial panels available from various suppliers (e.g., PrimerDesign). |
| Real-Time PCR System | Instrument to run qPCR and detect fluorescence in real-time. | Quantstudio 7 FLEX, Applied Biosystems instruments. |
Validating reference genes is a non-negotiable step in designing a robust qPCR assay for minimal residual disease detection. The process involves selecting a panel of candidate genes, running a well-designed validation experiment, and analyzing the data with multiple statistical algorithms. The following best practices are recommended:
- Never Assume Stability: Do not rely on a single, unvalidated housekeeping gene like GAPDH or ACTB.
- Use Multiple Genes: Always use the geometric mean of at least two or three validated reference genes for normalization. This greatly improves reliability [73].
- Context is Key: The stability of a reference gene must be confirmed for your specific sample type, disease model, and experimental conditions.
- Verify in MRD Context: For MRD studies, confirm that the chosen reference genes remain stable not only at diagnosis but also in treated samples and at potential relapse, as expression profiles can shift during therapy [74].
By following this detailed protocol, researchers in MRD and drug development can ensure that their qPCR data is accurate, reproducible, and clinically meaningful.
Quantitative PCR (qPCR) is a cornerstone technology in minimal residual disease (MRD) detection, where analytical sensitivity and reproducibility are paramount for accurate risk stratification. This application note details a systematic framework for troubleshooting common qPCR amplification curve anomalies—including poor efficiency, high quantification cycle (Cq), and abnormal baselines—that compromise data integrity in sensitive MRD workflows. By integrating precise diagnostic protocols with targeted corrective methodologies, we provide a standardized approach to ensure robust, reliable, and clinically actionable qPCR results in oncology research and drug development.
In the context of minimal residual disease (MRD) detection, qPCR assays are pushed to their technical limits to identify rare leukemic cells persisting after treatment at sensitivities reaching 10⁻⁴ to 10⁻⁶ [2] [6]. The accurate interpretation of amplification curves is not merely a technical exercise but a critical determinant of clinical prognosis. The fundamental relationship between the initial target quantity (N₀), amplification efficiency (E), and the quantification cycle (Cq) is described by the equation: N₀ = Fq / E^Cq, where Fq is the fluorescence at the quantification threshold [37]. In MRD monitoring, subtle biases introduced by non-optimal amplification efficiency or incorrect baseline setting can significantly alter the calculated MRD burden, leading to erroneous clinical conclusions regarding relapse risk and therapeutic efficacy [37] [2]. This note establishes a rigorous protocol for identifying and rectifying common amplification curve artifacts to safeguard the validity of MRD data.
Troubleshooting Common Amplification Curve Anomalies
A systematic approach to diagnosing and correcting amplification curve aberrations is essential for reliable MRD quantification. Key anomalies, their common causes, and validated solutions are summarized below.
Poor Amplification Efficiency
PCR efficiency (E), defined as the fold-increase in amplicons per cycle, should ideally be 100% (E=2), meaning the target doubles every cycle. Efficiencies significantly below 90% or above 110% indicate assay problems [38] [76].
- Primary Causes: Inefficient primer design (secondary structures, dimers, suboptimal Tm), non-optimal reagent concentrations, or the presence of polymerase inhibitors (e.g., heparin, hemoglobin, ethanol, phenol carryover) are common culprits [38].
- Impact on MRD: Poor efficiency directly distorts the calculated initial target quantity, leading to an inaccurate estimation of the MRD level [37].
- Corrective Protocols:
- Redesign Primers: Ensure primers are specific, have appropriate Tm, and are devoid of self-complementarity or dimerization potential. Use validated primer design software.
- Purify Nucleic Acid Template: Assess sample purity via spectrophotometry (A260/A280 ratios ~1.8 for DNA, ~2.0 for RNA). Re-purify samples with suboptimal ratios to remove inhibitors [38].
- Optimize Reaction Conditions: Titrate Mg²⁺ concentration, adjust annealing temperature using a gradient PCR block, and use a high-quality, inhibitor-tolerant master mix.
- Validate Efficiency: Perform a standard curve with a minimum 5-point, 10-fold serial dilution of the target. Plot Cq vs. log(quantity) and calculate efficiency from the slope: E = 10^(-1/slope). The R² value should be >0.99. A slope of -3.32 corresponds to 100% efficiency [77] [76].
High Cq Values
In MRD detection, high Cq values (typically >35-38 cycles) can indicate either a genuinely low target copy number or a technical failure [77].
- Primary Causes:
- Low Template Concentration: A common and expected cause in MRD samples.
- Low Amplification Efficiency: As above.
- Suboptimal Nucleic Acid Isolation: Inadequate yield or quality.
- PCR Inhibition: As described for poor efficiency.
- Degraded RNA/cDNA: Improper handling or multiple freeze-thaw cycles [77].
- Corrective Protocols:
- Increase Template Input: If possible, use more template cDNA/DNA per reaction, ensuring it does not introduce additional inhibitors.
- Verify Isolation Protocol: Quantify nucleic acids and run an agarose gel to check for integrity. Consider alternative isolation methods designed for low-abundance targets.
- Check Reverse Transcriptase Activity: Use a fresh, high-quality reverse transcriptase for cDNA synthesis [77].
- Confirm Specificity: Ensure high Cq is not due to non-specific amplification or primer-dimer by analyzing the melt curve.
Abnormal Baselines and Curve Shapes
The baseline phase consists of initial cycles where fluorescence is amplification-independent. Its improper correction propagates error throughout the analysis [37] [78].
- Abnormalities and Solutions:
- Increasing or Decreasing Baseline Trend: Caused by improper baseline cycle setting that includes early exponential phase cycles or high variation in ground phase fluorescence.
- Solution: Manually adjust the baseline endpoints to cycles where all reactions are in the true ground phase. Disable the instrument's "dynamic" photomultiplier sensitivity setting [37].
- "Sagging" Plateau or Plateau Not Reached: Can be caused by cDNA concentration being too high, reagent degradation, or template concentration being too low, respectively [78].
- Solution: For sagging, dilute the template. For failure to plateau, increase the number of PCR cycles or template concentration.
- Non-Smooth or "Zigzag" Curves: Often result from instrument calibration issues, bubbles in the reaction mix, or poor RNA purity [78].
- Solution: Calibrate the qPCR instrument, centrifuge plates thoroughly to remove bubbles, and re-purify the RNA template.
- Increasing or Decreasing Baseline Trend: Caused by improper baseline cycle setting that includes early exponential phase cycles or high variation in ground phase fluorescence.
The following workflow provides a logical, step-by-step guide for diagnosing and addressing these common issues.
Quantitative Data and Method Comparisons in MRD Context
Sensitivity is a critical performance metric in MRD detection. The table below compares common MRD detection methods, highlighting the role of qPCR.
Table 1: Comparison of MRD Detection Method Sensitivities
| Platform | Typical Sensitivity | Key Advantages for MRD | Key Limitations for MRD |
|---|---|---|---|
| qPCR (Fusion gene, IgH/TCR) | 10⁻⁴ – 10⁻⁶ [2] | Widely used, standardized, lower cost, high sensitivity for specific targets [2] | Only one gene assessed per assay; requires a pre-identified genetic target [2] |
| Flow Cytometry (FCM) | 10⁻³ – 10⁻⁶ (depends on colors) [2] | Wide applicability, fast, can analyze many cells without a pre-defined target [2] | Lack of standardization; changes in immunophenotype can lead to false negatives [2] |
| Next-Generation Sequencing (NGS) | 10⁻² – 10⁻⁶ [2] | Comprehensive detection of clonal rearrangements and mutations; high sensitivity [2] [6] | High cost, complex data analysis, not yet fully standardized [2] |
| Morphology (Cytology) | 5 x 10⁻² (5% blasts) [2] | Traditional gold standard for remission assessment | Far too insensitive for meaningful MRD detection [2] |
For qPCR itself, understanding the expected values for key parameters is crucial for quality control.
Table 2: Key qPCR Amplification Characteristics and Acceptable Ranges
| Parameter | Ideal Value / Range | Interpretation and Clinical Relevance |
|---|---|---|
| Amplification Efficiency (E) | 90% - 110% [38] [76] | E=100% (slope of -3.32) is ideal. Values outside this range quantifiably bias MRD load calculations. |
| Cq Value for MRD | Variable; can be >35 [77] | High Cq can indicate low disease burden. Requires validation of specificity and efficiency to be trusted. |
| ΔCq between dilutions | ~3.3 [77] | For a 10-fold dilution with 100% efficiency, the Cq difference should be approximately 3.3 cycles. |
| Standard Curve R² | >0.99 [77] [76] | Indicates a highly precise and linear relationship between Cq and log concentration. |
| Baseline | Flat, stable fluorescence in early cycles [37] [79] | An unstable baseline necessitates manual correction to prevent erroneous Cq calling. |
Detailed Experimental Protocols
Protocol: Determining qPCR Amplification Efficiency
This protocol is essential for validating any qPCR assay before its use in MRD detection.
- Standard Curve Preparation: Create a minimum 5-point, 10-fold serial dilution series of a template with known high concentration (e.g., plasmid DNA, synthetic gBlock, or patient sample with high mutant allele frequency).
- qPCR Run: Run all dilution points in triplicate on the same qPCR plate alongside a no-template control (NTC).
- Data Analysis:
- The qPCR software will generate a standard curve by plotting the Log10(Starting Quantity) of each dilution against its mean Cq value.
- Obtain the slope of the linear regression trendline from the standard curve.
- Calculate the efficiency using the formula: Efficiency (%) = [10^(-1/slope) - 1] * 100.
- Interpretation: An efficiency of 100% corresponds to a slope of -3.32. Assays with efficiencies between 90% and 110% are generally acceptable for relative quantification, but efforts should be made to achieve near 100% efficiency for MRD work [76].
Protocol: Systematic Analysis of Amplification Curves
Implement this checklist for every qPCR run to ensure data quality.
- Visual Inspection (Log Scale): Plot amplification curves with fluorescence on a logarithmic (log10) axis. The exponential phase should appear as a straight line. Check that all curves for the same target have parallel exponential phases, indicating consistent efficiency [76].
- Baseline Setting: Verify that the automatically set baseline cycles occur before any signal emergence. If the baseline shows a trend or includes the start of amplification, manually redefine the start and end cycles to an earlier, flat section of the curve [37].
- Threshold Setting: Set the quantification threshold within the exponential phase of all samples (visible as the linear portion on the log plot). Avoid setting it in the noisy baseline or the curving plateau phase [37] [79].
- Melt Curve Analysis: For dye-based qPCR, analyze the dissociation curve immediately after amplification. A single sharp peak indicates specific amplification. Multiple peaks or a broad peak suggest primer-dimer or non-specific amplification, invalidating the Cq value [78].
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Reagents and Materials for Robust qPCR in MRD Research
| Item | Function | Application Note |
|---|---|---|
| Inhibitor-Tolerant Master Mix | A specialized buffer/enzyme mix resistant to common PCR inhibitors found in clinical samples (e.g., heparin, hemoglobin). | Critical for analyzing unpurified or difficult clinical samples; improves amplification efficiency and reliability [38]. |
| qPCR Plates with Optical Seals | Microplates and seals designed for optimal thermal conductivity and fluorescence reading with minimal background. | Using instrument-compatible consumables prevents signal aberrations and well-to-well contamination [78]. |
| Nucleic Acid Purification Kits (cfDNA/RNA) | Kits optimized for high-yield isolation of circulating cell-free DNA (cfDNA) or intact RNA from blood or bone marrow. | Essential for obtaining high-quality template from MRD sample sources. Purity (A260/280) should be verified [6]. |
| Pre-designed, Validated Assays | Assays (e.g., TaqMan) for known fusion genes or mutations (e.g., NPM1, BCR-ABL1). | Off-the-shelf assays are often guaranteed to have ~100% efficiency, reducing validation time and improving inter-lab reproducibility [76]. |
| Passive Reference Dye (e.g., ROX) | A fluorescent dye included in the master mix that does not participate in amplification. | Used by the instrument to normalize for well-to-well volume variations and pipetting inaccuracies, reducing noise [78] [77]. |
The accurate interpretation of qPCR amplification curves is a non-negotiable requirement for generating meaningful MRD data. By adhering to the systematic troubleshooting and validation protocols outlined in this document—specifically addressing efficiency loss, high Cq values, and baseline anomalies—researchers can significantly enhance the rigor and reproducibility of their findings. Implementing these standardized procedures ensures that qPCR remains a powerful, reliable tool for guiding treatment decisions and improving patient outcomes in oncology research.
Quantitative PCR (qPCR) remains a cornerstone technique in molecular diagnostics and research, particularly in sensitive applications like minimal residual disease (MRD) detection. The accurate quantification of low-abundance targets in MRD research is paramount for clinical decision-making. The Minimum Information for Publication of Quantitative Real-Time PCR Experiments (MIQE) guidelines, established in 2009 and recently updated to version 2.0, provide a foundational framework to ensure the rigor, reproducibility, and transparency of qPCR experiments [58]. Widespread adherence to these principles is critical, as studies suggest that a significant majority of researchers have encountered irreproducible findings, underscoring a pressing need for standardized practices [80] [81]. This application note details a comprehensive protocol for implementing MIQE 2.0 guidelines specifically within the context of developing a robust qPCR assay for MRD detection.
Core Principles of the MIQE 2.0 Guidelines
The revised MIQE 2.0 guidelines emphasize transparent and comprehensive reporting of all experimental details to ensure the repeatability and reproducibility of qPCR results [58]. For MRD research, where detecting minute quantities of disease-specific markers is critical, these principles are non-negotiable.
Key advancements in MIQE 2.0 include:
- Emphasis on Raw Data: Encouraging instrument manufacturers to enable the export of raw fluorescence data to permit independent re-analysis [58].
- Robust Quantification: Stating that quantification cycle (Cq) values must be converted into efficiency-corrected target quantities and reported with prediction intervals [58].
- Assay Characterization: Requiring the determination and reporting of the dynamic range and limit of detection for each assay, a vital consideration for MRD where target concentration is extremely low [58].
- Streamlined Reporting: Clarifying and simplifying reporting requirements to facilitate compliance without undue burden on researchers [58].
Experimental Workflow for MRD qPCR Assay Development
The following diagram illustrates the core workflow for developing and validating a MIQE-compliant qPCR assay for minimal residual disease detection.
Detailed Experimental Protocols
Sample Processing and Nucleic Acid Extraction
Principle: The accuracy of MRD quantification is fundamentally dependent on sample quality. Proper handling and extraction are critical to prevent degradation and ensure high yields of intact nucleic acids.
Protocol:
- Sample Collection: Collect patient samples (e.g., bone marrow, blood) in appropriate anticoagulant tubes. Process within 2 hours of collection to preserve RNA/DNA integrity.
- Cell Lysis: Use a validated lysis protocol or kit that efficiently lyses cells while inhibiting nucleases.
- Nucleic Acid Extraction: Employ a column-based or magnetic bead-based extraction method. For MRD, methods that recover small fragments and provide high purity are preferred.
- Quality Control:
- Purity: Measure the absorbance at 260nm, 280nm, and 230nm using a spectrophotometer. Acceptable ratios are A260/280 ≥ 1.8 and A260/230 ≥ 2.0.
- Integrity: Assess RNA integrity using a microfluidic capillary electrophoresis system (e.g., Bioanalyzer). An RNA Integrity Number (RIN) > 7.0 is recommended for gene expression studies in MRD.
Assay Design and Validation
Principle: The specificity and efficiency of the qPCR assay are determined during the design and validation phase. For MRD, assays must be highly specific to the disease-associated genetic marker (e.g., fusion gene, mutation) with minimal background.
Protocol:
- In Silico Design:
- Design primers and probes (if using hydrolysis probes) to span exon-exon junctions to avoid amplification of genomic DNA.
- Verify specificity using BLAST or similar tools against the appropriate genome database.
- Ensure amplicon length is between 70-150 bp for optimal amplification efficiency.
- Experimental Validation:
- Perform a standard curve analysis using a serial dilution (at least 5 points) of a synthetic oligonucleotide or a well-characterized positive control sample with known copy number.
- Run each dilution in triplicate.
- Calculate PCR efficiency using the slope of the standard curve: Efficiency (%) = (10^(-1/slope) - 1) * 100 [82]. Acceptable efficiency ranges from 90% to 110% [83] [82].
- Determine the linear dynamic range and the limit of detection (LoD) and limit of quantification (LoQ) from the standard curve data.
qPCR Setup, Data Acquisition, and Analysis
Principle: Accurate data acquisition and rigorous analysis are required to convert Cq values into biologically meaningful quantitative data. This involves proper baseline and threshold settings and efficiency-corrected calculations.
Protocol:
- Reaction Setup:
- Use a master mix with proven high reproducibility, such as those based on QuantiNova chemistry [80].
- Include no-template controls (NTCs) to check for contamination.
- Include an inter-run calibrator on each plate to control for run-to-run variation.
- Baseline and Threshold Setting:
- Baseline: Set the baseline to the fluorescence intensity during early cycles (e.g., cycles 3-15) where there is little change, establishing the background signal [83]. Avoid the first few cycles which may have stabilization artifacts.
- Threshold: Set the threshold within the exponential phase of all amplification curves, where the curves are parallel. This ensures that ΔCq values between samples are consistent and not affected by the chosen threshold level [83].
- Data Analysis with ANCOVA:
- Export raw fluorescence data for independent analysis [58] [81].
- Instead of relying solely on the 2^−ΔΔCq method, which assumes perfect and equal amplification efficiencies, use a more robust statistical approach like Analysis of Covariance (ANCOVA). This method uses the entire amplification curve and offers greater statistical power and robustness, especially when efficiencies deviate from 100% [81].
- For relative quantification (e.g., target gene vs. reference gene), use the efficiency-adjusted Pfaffl method if the efficiencies of the target and reference genes are not equal [83] [82].
Table 1: Key Quantitative Parameters for MIQE-Compliant MRD Assay Reporting
| Parameter | Definition | Acceptable Range for MRD | Reporting Requirement |
|---|---|---|---|
| Amplification Efficiency | The efficiency of target amplification per cycle. | 90% - 110% [82] | Calculated from standard curve slope. |
| Standard Curve R² | The goodness-of-fit of the standard curve. | > 0.985 | Reported for each run. |
| Dynamic Range | The range of concentrations over which the assay is linear. | At least 5 orders of magnitude for MRD. | Log10 starting quantity vs. Cq. |
| Limit of Detection (LoD) | The lowest concentration detectable but not necessarily quantifiable. | Defined per assay; must be clinically relevant. | Determined from dilution series. |
| Limit of Quantification (LoQ) | The lowest concentration that can be quantified with acceptable precision and accuracy. | Defined per assay; must be clinically relevant. | Determined from dilution series. |
| Cq Variation (SD) | The standard deviation of replicate Cq values. | < 0.167 for technical replicates [83] | Reported for all sample replicates. |
The Scientist's Toolkit: Essential Research Reagent Solutions
Table 2: Key Reagents and Materials for a MIQE-Compliant MRD qPCR Workflow
| Item | Function / Description | Example / Consideration |
|---|---|---|
| Nucleic Acid Extraction Kit | Isolates high-purity RNA/DNA from complex patient samples. | Kits with high recovery efficiency for low-abundance targets are critical for MRD. |
| Reverse Transcriptase | Synthesizes complementary DNA (cDNA) from RNA templates. | Use enzymes with high fidelity and efficiency, especially for long transcripts. |
| qPCR Master Mix | Contains DNA polymerase, dNTPs, buffers, and salts for the reaction. | Use kits with high lot-to-lot reproducibility (e.g., QuantiNova) [80]. |
| Sequence-Specific Probes | Provides high specificity for detection (e.g., TaqMan, Molecular Beacons). | Essential for discriminating single-nucleotide variants in some MRD targets. |
| Validated Primers/Probes | Assays designed against the specific MRD target (e.g., BCR-ABL1). | Must be validated for specificity and efficiency as per MIQE. |
| Reference Gene Assay | A stably expressed gene used for normalization of target gene expression. | Must be validated for stable expression in the specific sample matrix under study. |
| Nuclease-Free Water | A reagent-grade water used to make up reaction mixes. | Ensures no enzymatic degradation of reaction components. |
| Positive Control Template | A synthetic or cloned DNA/RNA with the target sequence. | Used for standard curve generation and as an inter-run calibrator. |
Data Analysis and Reporting Workflow
The process of analyzing raw qPCR data to generate a final report involves several critical steps to ensure accuracy. The following diagram outlines this workflow, emphasizing steps that prevent the introduction of bias.
Adherence to the MIQE 2.0 guidelines is not merely an academic exercise but a fundamental requirement for generating reliable and actionable data in minimal residual disease research. The framework presented here—encompassing meticulous sample handling, rigorous assay validation, transparent data analysis, and comprehensive reporting—provides a clear path to achieving the rigor and reproducibility demanded by both the scientific community and clinical applications. By integrating these practices and leveraging available tools and reagents designed for reproducibility, researchers can significantly enhance the credibility of their findings and contribute to meaningful advances in the management and treatment of cancer.
Troubleshooting False Positives and Negatives in Low-Abundance Targets
In the context of minimal residual disease (MRD) detection, the precision of quantitative PCR (qPCR) is paramount. MRD refers to the small number of cancer cells that persist in patients after treatment, often at concentrations as low as 1 malignant cell in 10^4 to 10^6 normal cells [2]. Accurate detection at this level is crucial for risk stratification, treatment adjustment, and predicting clinical relapse [2] [6]. However, the exquisite sensitivity required for low-abundance targets makes MRD testing particularly susceptible to both false-positive and false-negative results. False positives can lead to unnecessary further treatment and patient distress, while false negatives risk missing a relapsing disease [84]. This application note details the primary sources of these errors and provides validated protocols to mitigate them, ensuring data integrity in critical MRD research.
Understanding and Controlling for False Positives
False positive results in MRD qPCR typically arise from contamination or nonspecific amplification. Identifying and controlling these sources is the first step toward robust assay performance.
The table below summarizes the major culprits and corresponding corrective actions.
Table 1: Common Sources of False Positives and Prevention Strategies
| Source | Impact | Prevention Strategy |
|---|---|---|
| Contamination (Amplicons, Templates) [85] [84] | Carry-over of amplification products from previous runs, leading to erroneous signal. | Use separate pre- and post-PCR workstations; decontaminate with 10% bleach and UV irradiation [85] [84]. |
| Reagent/Labware Contamination [85] [86] | Bacterial DNA in reagents or human DNA on consumables can be amplified. | Use sterile, aliquoted reagents; request nuclease/human DNA-free certification from manufacturers [85] [86]. |
| Nonspecific Amplification [84] [87] | Primer-dimers or mis-priming on non-target sequences, especially with low template. | Optimize primer design and use hot-start polymerase; perform melt curve analysis [84] [87]. |
| Probe Degradation [85] | Free fluorescent dye released from degraded probes causes high background noise. | Aliquot probes; assess health via fluorometric scan or mass spectrometry [85]. |
Protocol: Establishing a Contamination-Free Workflow
A rigorous spatial separation is the most effective defense against contamination.
Procedure:
- Dedicated Work Areas: Maintain physically separate rooms or dedicated biosafety cabinets for:
- Reaction Setup (Clean Area): This area should contain dedicated pipettes, tips, lab coats, and reagents. It must never come into contact with amplified PCR products or high-concentration template DNA [84].
- Post-PCR Analysis (Contaminated Area): All work involving opened post-amplification tubes, including gel electrophoresis, must be confined to this area [85].
- Unidirectional Workflow: Personnel must move from the clean area to the contaminated area, but never in reverse, without a complete change of lab coat and gloves [84].
- Decontamination: Routinely clean the pre-PCR workstation with 10% sodium hypochlorite (bleach), allowing a minimum of 10 minutes of contact time, followed by rinsing with nuclease-free water and UV irradiation [85] [84].
- Technical Replicates: Include a No-Template Control (NTC) in every run. Place the NTC wells as far as possible from positive samples during plate setup [85]. A positive signal in the NTC indicates contamination.
Understanding and Controlling for False Negatives
False negatives in MRD testing are often more dangerous than false positives, as they can provide a false sense of security. These errors typically stem from factors that inhibit or prevent amplification.
Table 2: Common Sources of False Negatives and Prevention Strategies
| Source | Impact | Prevention Strategy |
|---|---|---|
| PCR Inhibition [84] [88] | Substances co-extracted from samples (e.g., heparin, hemoglobin) inhibit the polymerase enzyme. | Include an Internal Positive Control (IPC); use inhibitors like BSA to bind phenolic compounds [84]. |
| Nucleic Acid Degradation [84] | RNA/DNA is degraded during collection, storage, or extraction, reducing amplifiable template. | Use nuclease-free reagents and tubes; store samples at low temperatures in small aliquots [84]. |
| Suboptimal PCR Efficiency [87] [89] | Poor primer design or reaction conditions lead to inefficient amplification of the target. | Validate primer efficiency with a standard curve; consider hot-start or touchdown PCR [84] [87]. |
| Instrument/Pipette Calibration [84] [86] | Inaccurate liquid handling or thermal cycling leads to failed reactions. | Service and calibrate pipettes and instruments regularly [84]. |
| Reagent Batch Failure [89] | A specific batch of a critical reagent (e.g., polymerase) fails for a particular assay. | Quality-check new reagent batches with multiple assays; maintain a backup supplier [89]. |
Protocol: Implementing a System of Controls
A robust system of controls is non-negotiable for identifying and troubleshooting false negatives. The following workflow provides a logical pathway for interpretation and corrective action.
Procedure:
- Internal Positive Control (IPC):
- Purpose: Distinguishes between a true negative result and a failed reaction due to inhibition or degradation.
- Implementation: Spike a known, non-interfering control sequence (e.g., a synthetic RNA/DNA or a housekeeping gene like GAPDH) into each patient sample reaction [84]. Amplification of the IPC confirms the reaction was viable.
- Interpretation: If the target is negative but the IPC is also negative or has a significantly delayed Cq, the sample is likely inhibited.
External Positive Control:
- Purpose: Verifies that the entire assay process, from extraction to amplification, is functioning correctly.
- Implementation: Include a positive control containing a known low copy number of the target sequence. This can be a synthetic construct or a reference material spiked into a negative matrix [84].
- Interpretation: Failure of the positive control indicates a global assay failure, such as a bad reagent batch or incorrect thermal cycling parameters [89].
Inhibition Mitigation:
- If inhibition is suspected, dilute the sample template and re-run the PCR. Alternatively, re-purify the nucleic acid or add bovine serum albumin (BSA) to the reaction mix (200–400 ng/µL) to bind common inhibitors [84].
The Scientist's Toolkit: Essential Reagents and Materials
Table 3: Key Research Reagent Solutions for MRD qPCR
| Item | Function & Importance | Specifications & Quality Control |
|---|---|---|
| Hot-Start DNA Polymerase [84] | Prevents non-specific amplification and primer-dimer formation by remaining inactive until high temperatures are reached. Essential for specificity. | Use master mixes validated for high sensitivity. Verify performance with a new batch using multiple assays, not just one [89]. |
| Nuclease-Free Water & Tubes [84] [86] | Serves as the reaction solvent. Contamination with nucleases can degrade primers/probes/template, leading to false negatives. | Use certified nuclease-free, sterile water. Request a Certificate of Analysis for human DNA contamination from the manufacturer [86]. |
| Ultra-Pure dNTPs & Buffer | The building blocks and optimal chemical environment for PCR. Impurities can inhibit the reaction. | Purchase as ready-to-use master mixes or aliquot high-quality stocks to minimize freeze-thaw cycles. |
| Validated Primers/Probes [85] [87] | Ensure specific and efficient amplification of the intended low-abundance target. | Design primers with amplicons 75-150 bp; perform BLAST search for specificity; validate efficiency (90-110%); aliquot to prevent degradation [85] [87]. |
| qPCR Plates/Tubes [86] | The reaction vessel. Suboptimal optical clarity or fit can cause signal variation and evaporation. | Use thin-walled, white-well plates for reduced crosstalk and enhanced fluorescence. Ensure seals are optically clear and provide a tight fit [86]. |
Reliable detection of low-abundance targets in MRD research hinges on a vigilant and proactive approach to troubleshooting. By understanding the root causes of false positives and negatives, and by systematically implementing the detailed protocols for contamination control, inhibition monitoring, and reagent validation outlined herein, researchers can significantly enhance the fidelity of their qPCR data. This rigorous practice is fundamental to generating results that can confidently inform clinical decision-making in the management of hematological malignancies.
Benchmarking qPCR: Validation, Standards, and Comparison with NGS
Quantitative Real-Time Polymerase Chain Reaction (qPCR) stands as the most sensitive and specific technique for nucleic acid detection, playing a pivotal role in minimal residual disease (MRD) monitoring in hematological malignancies such as acute lymphoblastic leukemia [90] [2]. The accurate determination of the Limit of Detection (LoD) and Limit of Quantification (LoQ) is fundamental for assessing qPCR assay performance, guiding clinical treatment decisions, risk stratification, and evaluating patient outcomes [90] [2]. This application note provides detailed protocols for establishing LoD and LoQ within the context of MRD detection, presenting standardized methodologies and analytical frameworks essential for research and diagnostic implementation.
In clinical diagnostics and biomedical research, particularly in MRD detection, understanding the lower limits of an assay's capability is crucial [2]. MRD refers to the small number of cancer cells that persist in patients after treatment who have achieved clinical and hematological remission [2]. Accurate and early detection of MRD allows clinicians to identify residual cancer cells before they lead to relapse, enabling timely intervention and personalized treatment adjustments [2].
The parameters describing these lower detection capabilities are the LoD and LoQ. The Clinical Laboratory Standards Institute (CLSI) defines LoD as "the lowest amount of analyte in a sample that can be detected with (stated) probability, although perhaps not quantified as an exact value," and LoQ as "the lowest amount of measurand in a sample that can be quantitatively determined with stated acceptable precision and stated, acceptable accuracy, under stated experimental conditions" [90]. For MRD detection in conditions like neuroblastoma and leukemia, techniques such as reverse transcriptase qPCR (RT-qPCR) can reliably detect tumor cells with a sensitivity of up to 1 in 1 million normal nucleated bone marrow cells [5].
Theoretical Foundations: LoD and LoQ in qPCR
qPCR presents unique analytical challenges because the measured quantification cycle (Cq) values are proportional to the logarithm of the target concentration, creating a logarithmic response rather than a linear one [90]. This fundamental characteristic means that conventional linear approaches for determining LoD and LoB (Limit of Blank) are not directly applicable [90].
The standard CLSI EP17 approach for linear assays defines:
- LoB = meanblank + 1.645 × SDblank (at 95% confidence)
- LoD = LoB + 1.645 × SD_low concentration sample [90]
However, in qPCR, negative samples do not yield a Cq value, making it impossible to calculate a standard deviation for blank measurements in the linear domain [90]. Consequently, estimating LoD in qPCR requires a probability-based approach using sample replicates across different dilutions to determine the concentration at which a specified percentage of samples test positive [90].
Experimental Protocol for Determining LoD and LoQ in qPCR-based MRD Detection
Reagent and Material Requirements
Table 1: Essential Research Reagent Solutions for LoD/LoQ Establishment in qPCR MRD Assays
| Reagent/Material | Function/Description | Example Specifications |
|---|---|---|
| Calibrated DNA Standard | Provides accurate reference material for dilution series | Human genomic DNA calibrated against NIST SRM 2372 [90] |
| qPCR Master Mix | Contains enzymes, dNTPs, and buffers for amplification | TATAA Probe GrandMaster Mix [90] |
| Sequence-Specific Assay | Enables specific target amplification | ValidPrime assay: 200 nM FAM-labeled probe, 400 nM of each primer [90] |
| MRD Target Assays | Detect disease-specific markers | IgH/TCR rearrangement primers; ADRN/MES phenotype mRNA panels [2] [5] |
Step-by-Step LoD/LoQ Establishment Protocol
Step 1: Preparation of Dilution Series
- Prepare a dilution series of the target nucleic acid covering the range from below the expected detection limit to well above it [90].
- For MRD detection, a 2-fold dilution series is recommended, covering a range of 1 to 2048 molecules per reaction volume [90].
- Use a calibrated reference material to ensure accuracy throughout the dilution series [90].
Step 2: qPCR Amplification
- Perform amplification with sufficient replicates at each concentration level to enable robust statistical analysis [90].
- Recommended replicate numbers: 64 replicates per concentration, with 128 replicates for the most diluted sample to better characterize detection probability at the lowest concentrations [90].
- Use a two-step qPCR protocol: 1 min enzyme activation at 95°C, followed by 50 cycles of 10 s at 95°C and 30 s at 60°C [90].
Step 3: Data Preprocessing
- Identify and remove outliers using appropriate statistical methods such as Grubb's test [90].
- Set a consistent threshold line in the region of exponential amplification across all amplification plots for Cq value determination [90].
Step 4: Logistic Regression Analysis
- For each concentration, calculate the proportion of positive replicates (detection rate) [90].
- Use a binary indicator function (1 for Cq < cut-off value, 0 for Cq > cut-off value) [90].
- Fit a logistic regression model to the binary outcomes versus the logarithm of the concentration [90].
- The logistic regression curve is defined as: fi = 1 / (1 + e^(-(β0 + β1 × xi))), where xi = log2(ci) [90].
Step 5: LoD and LoQ Determination
- The LoD is typically defined as the concentration at which 95% of the replicates test positive, derived from the logistic regression curve [90].
- The LoQ is the lowest concentration at which acceptable precision (as measured by coefficient of variation) and accuracy are maintained, based on clinical or analytical requirements [90].
Figure 1: Experimental workflow for establishing LoD and LoQ in qPCR assays.
Data Analysis and Interpretation
Statistical Analysis of Detection Limits
For the logistic regression model, the likelihood function is: L = Π (n choose zi) × fi^zi × (1 - fi)^(n - zi) = Π (n choose zi) × e^(β0y1 + β1y2 - φ) where y1 = Σzi, y2 = Σzixi, and φ = Σ n × ln(1 + e^(β0 + β1xi)) [90]
The maximum likelihood estimates of β0 and β1 are obtained by solving the system of equations: y1 - Σ [n / (1 + e^(-β0 - β1xi))] = 0 y2 - Σ [n × xi / (1 + e^(-β0 - β1xi))] = 0 [90]
The standard error for the estimated detection probability is given by: σ̂ = [Σ (∂t/∂yi) × (∂²φ/∂βi∂βj) × (∂t/∂yj)]^(1/2) [90]
MRD Detection Method Comparison
Table 2: Comparison of MRD Detection Methods: Sensitivity and Applications
| Method | Sensitivity | Advantages | Limitations | Applicability in MRD |
|---|---|---|---|---|
| qPCR | 10⁻⁴ to 10⁻⁶ [2] | Widely used, standardized, lower costs [2] | Only one gene assessed per assay [2] | ~40-50% of patients [2] |
| Flow Cytometry | 10⁻³ to 10⁻⁶ [2] | Wide applicability, fast, relatively inexpensive [2] | Lack of standardization, fresh cells often required [2] | Almost 100% [2] |
| Next-Generation Sequencing (NGS) | 10⁻² to 10⁻⁶ [2] | Multiple genes analyzed, broad applicability [2] | High cost, complex analysis, not standardized [2] | >95% [2] |
| Digital PCR (ddPCR) | Comparable or better than qPCR [12] | Absolute quantification, better precision and sensitivity [12] | Emerging technology, limited standardization [12] | Similar to qPCR [12] |
Recent advances in MRD detection have introduced methods such as droplet digital PCR (ddPCR), which shows significantly better quantitative limits of detection and sensitivity compared to qPCR, reducing the number of critical MRD estimates below the quantitative limit by threefold to sixfold [12]. Furthermore, multimodal approaches that combine techniques like automatic immunofluorescence plus interphase fluorescence in situ hybridization (AIPF) with RT-qPCR can improve MRD detection and allow monitoring of phenotypic switches and immunotherapy targets [5].
Implementation in MRD Research
Clinical Implications and Applications
In high-risk neuroblastoma, studies have demonstrated the feasibility of integrating high-sensitivity techniques like AIPF and RT-qPCR with standard-of-care assessments in an international multicenter setting [5]. This multi-modal MRD detection approach is crucial for:
- Early detection of disease progression and relapse
- Monitoring plasticity of tumor cell states (ADRN and MES phenotypes)
- Assessing expression of immunotherapy targets (e.g., GD2) on rare, therapy-resistant cells [5]
For hematological malignancies, continuous monitoring of MRD status during and after treatment serves as a key prognostic factor, predicting disease recurrence and assessing therapeutic efficacy [2]. This monitoring helps identify patients at high and low recurrence risk, guiding treatment adjustments and offering insights for risk stratification [2].
Figure 2: Multi-modal approach to MRD detection enhances sensitivity and characterization.
Quality Assurance Considerations
To ensure reliable LoD and LoQ determinations:
- Implement rigorous outlier detection methods such as Grubb's test to identify and remove anomalous data points [90].
- Calculate the coefficient of variation using the formula for log-normal distribution: CV = √[exp(SD_ln(conc)²) - 1] [90].
- Account for the log-normal distribution of qPCR data by performing statistical analyses on logarithmic transformed concentrations [90].
- Validate LoD estimates with confidence intervals derived from the logistic regression model to communicate uncertainty appropriately [90].
Establishing accurate LoD and LoQ parameters is essential for developing robust qPCR assays for MRD detection. The probability-based approach using logistic regression on replicated dilution series addresses the unique challenges posed by the logarithmic nature of qPCR data [90]. As MRD detection technologies evolve, with emerging methods like ddPCR showing enhanced sensitivity and precision, the fundamental principles of properly characterizing detection and quantification limits remain paramount [12]. Implementing these protocols with appropriate statistical rigor ensures reliable assay performance, ultimately supporting improved patient management through sensitive MRD monitoring and personalized treatment strategies [2] [5].
The detection and quantification of minimal residual disease (MRD) are critical for prognostic assessment, therapeutic stratification, and relapse monitoring in hematological malignancies. This application note provides a detailed comparative analysis of two cornerstone MRD detection technologies: quantitative polymerase chain reaction (qPCR) and multiparametric flow cytometry (MFC). We evaluate their analytical performance, operational characteristics, and clinical applicability, supported by experimental data and standardized protocols. Within the broader context of MRD research, understanding the complementary strengths and limitations of these methods is essential for optimizing clinical diagnostics and drug development workflows.
Minimal residual disease (MRD) refers to the presence of residual leukemic cells below the detection limit of conventional microscopy in patients who have achieved morphological remission. In acute lymphoblastic leukemia (ALL), MRD monitoring has emerged as one of the most substantial independent prognostic factors [10]. The accurate quantification of MRD requires highly sensitive and specific methods, primarily qPCR and MFC, each with distinct technological foundations and application landscapes. This document frames the comparison within the ongoing research into refining qPCR protocols for MRD detection, highlighting how these methods relate and contribute to the field.
Comparative Performance Data
The following tables summarize key performance characteristics of qPCR and MFC as evidenced by recent clinical and research studies.
Table 1: Overall Method Comparison for MRD Detection
| Feature | Quantitative PCR (qPCR) | Multiparametric Flow Cytometry (MFC) |
|---|---|---|
| Measured Target | CAR transgene copy number or specific gene rearrangements/fusions [91] [10] | CAR protein expression or leukemia-associated immunophenotypes (LAIPs) on cell surfaces [91] [92] |
| Sensitivity | Up to 10-5 (1 in 100,000 cells) for IG/TCR rearrangements [10] | Typically 10-4 to 10-5 (1 in 10,000 to 100,000 cells) [10] [93] |
| Applicability | ~90-95% of ALL patients (requires a defined marker at diagnosis) [10] | ~90% of Acute Myeloid Leukemia (AML) patients [92] |
| Turnaround Time | Longer (several hours to days, including analysis); can be time-consuming and laborious [94] [10] | Rapid (a few hours for analysis); quick results possible [10] |
| Key Advantage | High sensitivity and specificity for defined molecular targets; well-standardized for ALL [10] | Broad applicability, high throughput, and ability to analyze millions of cells rapidly [92] [10] |
| Key Limitation | Cannot distinguish between living and dead cells carrying the transgene; prone to PCR inhibition [91] [94] | Requires immediate sample processing; subjective analysis potential and need for expert operators [92] [10] |
Table 2: Quantitative Correlation and Sensitivity Data from Recent Studies
| Study Context | qPCR Performance | MFC Performance | Comparative Findings |
|---|---|---|---|
| CAR-T Cell Kinetics (4 Phase 1 studies) | - | - | CAR transgene copy number correlated more strongly with the ratio of CAR-T cells to WBCs (r=0.95) than with the absolute CAR-T cell count (r=0.43) [91]. |
| CAR-T Cell Monitoring | Sensitivity: 1% [95] | Sensitivity: 0.1% [95] | Digital PCR (dPCR) showed high correlation with both MFC (r=0.97) and qPCR (r=0.87), offering a superior sensitivity of 0.01% [95]. |
| ALL MRD Monitoring (Blinded Study) | Higher number of "positive-not-quantifiable" (PNQ) results [12] | - | Droplet Digital PCR (ddPCR) outperformed qPCR, reducing PNQ results and showing higher concordance with MFC quantitative values [12]. |
| Correlation with Cytokines (CAR-T studies) | Correlated with cytokine levels [91] | Correlated with cytokine levels; had higher correlation coefficients (r) and lower p-values than qPCR [91] | Flow cytometry data showed a stronger statistical association with pharmacodynamic responses [91]. |
Experimental Protocols
Protocol: qPCR for MRD Detection via IG/TCR Gene Rearrangements
This protocol is adapted from standardized guidelines for MRD detection in ALL [10].
1. Sample Preparation and DNA Isolation
- Source: Obtain genomic DNA from patient bone marrow samples collected at diagnosis and during follow-up. Bone marrow is preferred over peripheral blood as MRD levels are typically 1-3 logs higher [10].
- Extraction: Use a commercial DNA extraction kit (e.g., DNeasy Blood & Tissue Kit) to isolate high-quality genomic DNA. Quantify DNA using spectrophotometry and ensure integrity by fragment analysis.
2. Marker Identification and Assay Setup (Diagnosis)
- Clonality Assessment: Perform PCR amplification of immunoglobulin (IG) and T-cell receptor (TCR) gene rearrangements using multiplex primers.
- Sequence Analysis: Analyze positive PCR products by Sanger sequencing to define the unique junctional regions of the clonal rearrangement.
- Primer/Probe Design: Design patient-specific allele-specific oligonucleotide (ASO) primers and fluorescent probes (e.g., TaqMan) for the identified clone.
3. Quantitative PCR (Follow-up)
- Standard Curve Generation: Create a standard curve by performing serial 10-fold dilutions of diagnostic DNA into DNA from normal mononuclear cells (e.g., from 10-1 to 10-5).
- qPCR Reaction:
- Component | Function | Volume/Role Patient DNA sample | Template for amplification | 300-500 ng ASO forward primer | Binds specifically to the patient's clonal sequence | Optimized concentration Reverse primer | Binds to a constant gene region | Optimized concentration Fluorescent probe (e.g., FAM-labeled) | Binds within the amplicon, providing fluorescence signal during amplification | Optimized concentration qPCR Master Mix (e.g., LightCycler 480 SYBR Green I Master) | Contains DNA polymerase, dNTPs, and buffer | As per manufacturer's instructions Water, Nuclease-free | Solvent | To total volume
- Cycling Conditions:
- Enzyme Activation: 95°C for 10 min
- 40-50 Cycles of:
- Denaturation: 95°C for 15 sec
- Annealing/Extension: 60°C for 1 min (probe-specific)
- Data Analysis: Use software (e.g., Bio-Rad Bio-Plex Data Pro) to determine the Cycle threshold (Cq) for each sample. Quantify MRD levels by interpolating the Cq value from the standard curve. Results are expressed as a percentage of MRD cells (e.g., 10-4 equals 0.01%) [10].
Protocol: Multiparameter Flow Cytometry for AML MRD Detection
This protocol utilizes a "different-from-normal" (DFN) approach to identify aberrant blast populations in AML [92] [93].
1. Sample Preparation and Staining
- Source: Collect bone marrow aspirates in heparin or EDTA. Process immediately or within 24-36 hours to maintain cell viability.
- Lysis and Staining:
- Use bulk lysis to remove red blood cells.
- Aliquot 1x106 nucleated cells per tube.
- Stain cells with a pre-titrated cocktail of fluorochrome-conjugated antibodies. A representative 9-color panel for AML is shown below.
- Incubate for 15-20 minutes at room temperature, protected from light.
- Wash cells twice with staining buffer (e.g., PBS with 1% FBS) to remove unbound antibody.
- Resuspend in buffer for acquisition. Fixed samples can be stored for short periods.
2. Data Acquisition
- Acquire data on a flow cytometer capable of detecting the required fluorochromes (e.g., BD FACSLyric).
- Aim to acquire a minimum of 500,000 to 1,000,000 events per tube to ensure sufficient sensitivity for low-level MRD detection [93].
3. Data Analysis via Manual Gating
- Pre-gating: Use forward and side scatter (FSC-A/SSC-A) to gate on nucleated cells, excluding debris and platelets. Use FSC-H vs. FSC-A to exclude doublets.
- Blast Identification: Identify a population of CD45dim and/or CD34+ cells, which often contain the leukemic blasts.
- DFN Analysis: Compare the immunophenotype of these cells to normal hematopoietic progenitors. Look for LAIPs, which are aberrant expressions such as:
- Overexpression of markers (e.g., CD33, CD13)
- Asynchronous antigen expression (e.g., co-expression of stem cell markers like CD117 with maturation markers)
- Antigen absence (e.g., lack of HLA-DR)
- Quantification: The percentage of cells with a confirmed LAIP among total nucleated cells is reported as the MRD level.
Methodological Workflows and Relationships
The following diagrams illustrate the core workflows and decision pathways for both qPCR and MFC.
Diagram 1: Fundamental Technological Workflow
Diagram 2: Clinical Application for MRD Detection
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Reagents and Materials for MRD Detection Workflows
| Category | Item | Function in Experiment |
|---|---|---|
| Nucleic Acid Analysis | DNA Extraction Kits (e.g., DNeasy Blood & Tissue Kit) | Isolves high-purity genomic DNA from patient bone marrow or blood samples [96]. |
| qPCR Master Mix (e.g., LightCycler 480 SYBR Green I Master) | Provides optimized buffer, enzymes, and dNTPs for efficient and specific DNA amplification in qPCR reactions [97]. | |
| TaqMan Probes | Sequence-specific fluorescent probes that enable real-time detection and quantification of the target amplicon during qPCR [10]. | |
| Cell-Based Analysis | Monoclonal Antibody Panels (e.g., CD45, CD34, CD33, CD13, CD117, CD19) | Fluorochrome-conjugated antibodies used to detect surface and intracellular proteins, defining unique immunophenotypes for cell identification [92] [93]. |
| Lysing Solution (e.g., BD FACS Lysing Solution) | Used to lyse red blood cells in whole blood or bone marrow samples, simplifying the analysis of white blood cells [91]. | |
| Flow Cytometry Staining Buffer (PBS with 1% FBS) | A buffer used to wash and resuspend cells during antibody staining procedures, helping to reduce non-specific antibody binding [91]. | |
| Data Analysis | Flow Cytometry Analysis Software (e.g., FlowJo, Infinicyt) | Specialized software for the visualization, gating, and population-based analysis of high-dimensional data generated by flow cytometers [91] [93]. |
| qPCR Analysis Software (Instrument-specific, e.g., Bio-Plex Data Pro) | Software provided with qPCR instruments to collect fluorescence data, determine Cq values, and perform quantification against standard curves [91] [97]. |
Minimal residual disease (MRD) refers to the presence of leukemic cells at levels below the detection threshold of conventional microscopy, representing a critical prognostic marker for predicting relapse in hematological malignancies [16] [17]. The detection of MRD-positive status profoundly influences clinical outcomes, with MRD-positive patients exhibiting significantly poorer 5-year disease-free survival (approximately 25%) compared to MRD-negative patients (approximately 64%) [17]. Traditionally, MRD detection has relied on multiparametric flow cytometry (MFC) and real-time quantitative polymerase chain reaction (qPCR). However, these methods present limitations in sensitivity, applicability, and standardization [16]. Next-generation sequencing (NGS) has emerged as a transformative approach, offering superior sensitivity down to 10^-6 and the unique ability to track clonal evolution, thereby reshaping MRD assessment paradigms in modern oncology [16] [98].
Comparative Analysis of MRD Detection Methods
Technical Performance Metrics
The evolution of MRD detection technologies has progressively enhanced sensitivity and specificity. The following table summarizes the key characteristics of current methodologies:
Table 1: Comparison of MRD Detection Methodologies
| Method | Sensitivity | Key Advantages | Major Limitations |
|---|---|---|---|
| Multiparametric Flow Cytometry (MFC) | 10^-4 to 10^-5 [17] | Fast, widely applicable, relatively cheap, standardized [16] | Antigenic modulation leading to false negatives, reliance on operator skill, influenced by immunotherapy [16] |
| qPCR for Fusion Genes | ~10^-5 [17] | High sensitivity, relatively simple, no patient-specific primers needed [16] | Limited applicability (<50% of cases have fusion genes), cannot detect clonal evolution [16] |
| qPCR for IG/TCR Rearrangements | ~10^-5 [17] | High sensitivity, standardized within EuroMRD Consortium [16] | Requires patient-specific primers, time-consuming (3-4 weeks), costly, cannot accurately quantify very low disease burden [16] |
| Next-Generation Sequencing (NGS) | 10^-6 [16] [17] | Ultra-high sensitivity, universal primer sets, detects clonal evolution and subclones, tracks immune repertoire [16] [98] | High cost, requires sophisticated bioinformatics, standardization in progress [16] |
Clinical Performance and Concordance
Studies directly comparing NGS with established qPCR methods demonstrate both strong correlation and important advantages for NGS-based approaches. In a comprehensive study of 432 pediatric B-cell precursor acute lymphoblastic leukemia (ALL) patients, NGS and qPCR showed 81.9% concordance across 780 immunoglobulin (IG) and T-cell receptor (TR) markers [99]. Notably, NGS provided more specific results by eliminating false-positive qPCR findings, which accounted for 13.3% of markers that were positive only by qPCR [99]. This enhanced specificity directly impacted risk stratification, with 19% of patients appropriately assigned to a lower risk group by NGS compared to qPCR-based assessment [99].
Tracking Clonal Evolution with NGS
Understanding Clonal Dynamics
The ability to monitor clonal evolution represents a paradigm shift enabled by NGS-based MRD detection. Clonal evolution refers to the process whereby cancer cells acquire new mutations over time, leading to the emergence of subclones with distinct genetic profiles [100] [98]. This process is a major driver of treatment resistance and disease relapse. Traditional MRD methods like qPCR target a single, predefined marker, making them vulnerable to false negatives if the dominant clone shifts or evolves [16]. In contrast, NGS comprehensively profiles the entire repertoire of IG/TR rearrangements or multiple mutations simultaneously, enabling detection of emerging subclones even at very low frequencies [98].
Clinical Evidence and Applications
Single-cell DNA sequencing studies in acute myeloid leukemia (AML) have vividly demonstrated the clinical relevance of tracking clonal architecture. In one patient with AML relapse following bone marrow transplantation, single-cell NGS revealed the exclusive expansion of a TP53-mutated oncogenic clone, which increased from 9% at pre-transplant to nearly 70% at relapse [100]. This clonal dynamic was undetectable by conventional morphological assessment [100]. Similarly, NGS enables monitoring of challenging mutations like FLT3-ITDs in AML, which are difficult to detect reliably with PCR-based methods due to their variable size and sequence complexity [98]. The comprehensive genomic profiling provided by NGS reveals mechanisms of resistance and informs subsequent targeted therapy decisions.
Experimental Protocols for NGS-Based MRD Detection
NGS MRD Workflow for IG/TR Rearrangements
Table 2: Step-by-Step Protocol for NGS-Based MRD Detection
| Step | Procedure | Key Considerations | Quality Control |
|---|---|---|---|
| 1. Sample Preparation | - Obtain bone marrow aspirates in EDTA tubes- Isolate genomic DNA using automated extraction systems (e.g., Maxwell RSC Instrument, Promega) [101] | - Ideally use two independent marrow pulls [101]- Minimum DNA input: 650 ng (for 10^-5 sensitivity) [101] | - Assess DNA quality via NanoDrop [101]- Quantify using Qubit dsDNA BR Assay [101] |
| 2. Library Preparation | - Use multiplex PCR primers targeting IG/TR framework regions (e.g., LymphoTrack IGH Panel, EuroClonality-NGS protocol) [16] [99] [101]- Include unique molecular barcodes | - Universal primer sets applicable to all patients [16]- Incorporate spike-in control cells (e.g., 100 clonal B-cells) for absolute quantification [101] | - Purify libraries with AMPure XP beads [101]- Assess library quality with TapeStation [101] |
| 3. Sequencing | - Sequence on NGS platforms (e.g., MiSeq, Ion Torrent) [102] [101]- Aim for ~1 million reads per sample [101] | - Use v3 reagent kits for 2×251 bp paired-end sequencing [101] | - Validate with control samples in each run- Minimum 20,000 total reads for valid result [101] |
| 4. Data Analysis | - Process FastQ files with specialized software (e.g., LymphoTrack MRD Analysis, ARResT/Interrogate) [99] [101]- Identify clonotypic sequences from diagnostic sample- Track these sequences in follow-up samples | - Minimum of 3 identical reads required for positivity [99]- Normalize results based on spike-in controls and total DNA input [99] | - Exclude markers with insufficient specificity- Verify against polyclonal background |
NGS MRD Workflow Visualization
NGS MRD Detection Workflow
Research Reagent Solutions for NGS-Based MRD
Table 3: Essential Research Reagents and Platforms for NGS-MRD
| Category | Product/Platform Examples | Key Features | Applications |
|---|---|---|---|
| Targeted NGS Panels | - LymphoTrack IGH Panels (Invivoscribe) [101]- SureSeq Myeloid MRD Panel (OGT) [98]- EuroClonality-NGS Protocols [16] [99] | - Target IG/TR rearrangements or myeloid mutations- Designed for MRD sensitivity- Standardized protocols | - B-cell and T-cell malignancies [101]- AML monitoring [98]- Multi-center studies [16] |
| Sequencing Platforms | - Illumina MiSeq [101]- Ion Torrent Platforms [102] | - Moderate throughput suitable for MRD- Fast turnaround times- Semiconductor sequencing | - Amplicon sequencing [102]- Library validation [101] |
| Analysis Tools | - ARResT/Interrogate Pipeline [99]- LymphoTrack MRD Analysis Software [101]- Vidjil [101] | - Clonotype identification and tracking- MRD quantification- Visualization capabilities | - Clinical research [99]- Minimal residual disease monitoring [101] |
| Control Materials | - Spike-in control cells [101]- Polyclonal normal controls [99] | - Enable absolute quantification- Assess assay specificity- Monitor technical variability | - Quality assurance [101]- Specificity validation [99] |
Clinical Implications and Future Directions
The enhanced sensitivity and specificity of NGS-based MRD detection directly impacts clinical decision-making. In treatment protocols, NGS-MRD status provides robust stratification, with negative patients exhibiting superior event-free survival (EFS) and overall survival (OS) compared to MRD-positive patients [16]. The technology is particularly valuable for predicting outcomes following hematopoietic stem cell transplantation and CAR-T cell therapy [16]. Furthermore, regulatory agencies including the FDA and EMA have begun recognizing MRD as an exploratory endpoint in clinical trials, accelerating drug development for hematological malignancies [98].
Despite these advances, challenges remain in standardizing NGS-MRD protocols across laboratories and reducing costs for widespread implementation [16]. The EuroClonality-NGS consortium is actively addressing these issues by developing standardized guidelines for data analysis and interpretation [16]. As the field evolves, the combination of NGS with other technologies like next-generation flow cytometry may offer complementary advantages, providing a comprehensive approach to MRD assessment that leverages the unique strengths of each methodology [16] [101].
The landscape of clinical diagnostics has been fundamentally transformed by the advent of molecular technologies, with quantitative polymerase chain reaction (qPCR) and next-generation sequencing (NGS) emerging as cornerstone methodologies. While qPCR has served as the long-standing gold standard for targeted molecular detection, NGS provides a powerful, high-throughput platform for comprehensive genomic analysis [103] [104]. In the specific context of minimal residual disease (MRD) detection—a critical independent prognostic factor in acute lymphoblastic leukemia (ALL) and other hematological malignancies—these technologies are not mutually exclusive but rather form a complementary alliance [10] [12]. MRD monitoring requires the detection of rare leukemic cells among a large population of normal cells, often at sensitivities of 10⁻⁴ to 10⁻⁵, making technological choice paramount [10].
The growing demand for personalized diagnostics drives the need for integrated approaches. The personalized medicine market is projected to grow at a compound annual growth rate of 10.8%, reaching nearly $590 billion by 2028, underscoring the shift toward patient-specific therapeutic strategies [103]. This review examines the synergistic application of qPCR and NGS in clinical diagnostics, with a particular emphasis on MRD detection workflows, providing structured comparisons and detailed protocols to guide researchers and drug development professionals.
Technology Comparison: qPCR versus NGS
Fundamental Characteristics and Workflows
qPCR and NGS differ fundamentally in their operational principles, capabilities, and optimal applications. qPCR operates by amplifying specific DNA targets using predefined primers and fluorescent probes, allowing for the precise quantification of known sequences. In contrast, NGS employs massive parallel sequencing to simultaneously decode millions of DNA fragments, enabling the detection of both known and novel variants without prior sequence knowledge [105].
The NGS workflow involves multiple intricate steps: nucleic acid extraction, library preparation (fragmentation and adapter ligation), massive parallel sequencing, and sophisticated bioinformatics analysis for base calling, read alignment, and variant identification [104] [106]. qPCR workflows are significantly more straightforward, requiring only sample preparation, primer/probe design, and amplification with real-time fluorescence detection [103]. This fundamental difference in complexity directly influences their respective applications in clinical diagnostics, particularly for MRD monitoring where speed, sensitivity, and specificity are critical.
Comparative Performance in Diagnostic Applications
The table below provides a structured comparison of the technical and performance characteristics of qPCR and NGS in clinical diagnostics, with special consideration for MRD detection:
Table 1: Comprehensive Comparison of qPCR and NGS for Clinical Diagnostics
| Parameter | qPCR | NGS |
|---|---|---|
| Discovery Power | Limited to known, predefined targets; cannot identify novel variants [105] | Hypothesis-free; detects both known and novel variants, including single nucleotide variants (SNVs), insertions/deletions (indels), and structural variations [105] |
| Throughput | Low to medium; optimal for ≤ 20 targets [105] | Very high; capable of profiling >1000 target regions in a single assay [105] |
| Sensitivity | High (can detect 1 mutant cell in 10,000-100,000 normal cells) [10] | High to very high (detection down to 1% with targeted approaches; can be optimized further) [105] |
| Turnaround Time | Fast (hours to 1-2 days for limited targets) [107] | Moderate to long (days to weeks depending on scale and workflow) [107] |
| Cost Effectiveness | Highly cost-effective for limited target numbers [103] [105] | Cost-effective for multi-target analyses; higher initial investment [104] |
| Quantitative Capability | Excellent; relative or absolute quantification with standard curves [103] | Digital counting of reads enables absolute quantification [105] |
| Data Complexity | Low; straightforward interpretation | High; requires specialized bioinformatics expertise [104] [108] |
| Ideal Clinical Use Case | Rapid detection of known mutations, routine pathogen detection, initial MRD screening [103] [10] | Comprehensive genomic profiling, novel variant discovery, heterogeneous mutation detection, refined MRD monitoring [10] [106] |
In MRD detection for ALL, qPCR of immunoglobulin (IG) and T-cell receptor (TCR) gene rearrangements has been the gold standard, offering sensitivities of up to 10⁻⁵ [10]. However, this approach requires careful primer design specific to the patient's clonal rearrangement identified at diagnosis, a process that can take 3-4 weeks [10]. Additionally, qPCR struggles with clonal evolution, where the emergence of new clones during therapy can lead to false-negative results [10]. NGS-based MRD methods overcome this limitation by simultaneously tracking multiple clonal sequences, providing a more comprehensive assessment of residual disease [10].
Integrated Workflow for MRD Detection
The complementary strengths of qPCR and NGS can be leveraged in a unified workflow for comprehensive MRD assessment. The following diagram illustrates this integrated approach:
Diagnostic Marker Identification Phase
At diagnosis, comprehensive genomic profiling establishes the baseline genetic landscape of the leukemia. NGS plays a crucial role in this initial phase by identifying multiple potential MRD targets, including:
- IG/TCR gene rearrangements: NGS enables highly multiplexed amplification and sequencing of IG/TCR gene rearrangements, providing a sensitive and specific marker for clonal tracking [10]. This approach can identify multiple rearrangements simultaneously, creating a "fingerprint" of the leukemic clone that guards against false negatives due to clonal evolution.
- Fusion transcripts: Chromosomal translocations generating chimeric transcripts (e.g., BCR-ABL1, ETV6-RUNX1) serve as stable, clone-specific markers present in all leukemic cells [10]. RNA-Seq using NGS can comprehensively identify these and other novel fusion events.
- Somatic mutations: NGS panels can identify recurrent mutations in genes like TP53, NOTCH1, and others that may serve as additional MRD markers, particularly in cases with limited IG/TCR repertoire [104] [106].
While NGS provides comprehensive marker discovery, qPCR offers rapid assessment of known, clinically actionable mutations. For example, in B-ALL, qPCR can quickly detect the Philadelphia chromosome (BCR-ABL1 fusion), enabling immediate tyrosine kinase inhibitor therapy while broader NGS profiling continues [10].
Longitudinal MRD Monitoring Phase
During treatment, the integrated approach leverages the strengths of both technologies:
- qPCR for high-frequency monitoring: The speed and cost-effectiveness of qPCR make it ideal for frequent MRD assessments at predetermined timepoints (e.g., post-induction, post-consolidation) [10]. When targeting well-characterized markers identified at diagnosis, qPCR provides rapid, sensitive quantification of MRD levels, with results available within hours [10].
- NGS for comprehensive assessment: At critical decision points or when qPCR results are discordant with clinical presentation, NGS provides a more comprehensive MRD assessment. NGS can monitor multiple clones simultaneously, detecting emerging resistant subclones that might be missed by targeted qPCR approaches [10]. This is particularly valuable in cases with clonal evolution, where the dominant clone at relapse may differ from the diagnostic clone [10].
This integrated approach combines the speed and accessibility of qPCR with the comprehensive nature of NGS, providing both rapid turnaround for clinical decision-making and deep genomic insight for complex cases.
Detailed Experimental Protocols
qPCR Protocol for MRD Detection in ALL
This protocol details the quantitative PCR method for detecting minimal residual disease in acute lymphoblastic leukemia using patient-specific IG/TCR rearrangements.
Sample Requirements and Preparation
- Sample Type: Bone marrow aspirate is the preferred specimen for MRD assessment in ALL, as MRD levels in peripheral blood are typically 1-3 logs lower [10].
- DNA Extraction: Use validated extraction kits (e.g., QIAamp DNA Blood Mini Kit) to obtain high-quality genomic DNA. Assess DNA concentration using fluorometry and quality via spectrophotometry (A260/A280 ratio ~1.8-2.0).
- DNA Quantity: Use 1-2 μg of DNA per reaction to ensure adequate representation of the cellular population and achieve desired sensitivity.
Patient-Specific Primer and Probe Design
- Target Identification: Sequence IG/TCR gene rearrangements (e.g., IGH, IGK, TCRB, TCRG) from diagnostic DNA using NGS or Sanger sequencing.
- Junctional Region Mapping: Identify unique nucleotide sequences in the V-N-J or V-J junctional regions of rearranged genes.
- ASO Primer Design: Design patient-specific allele-specific oligonucleotide (ASO) primers complementary to the junctional region sequences. The 3'-end should align with the patient-specific nucleotides.
- Probe Design: Design TaqMan probes with a 5' fluorescent reporter (e.g., FAM) and 3' quencher (e.g., TAMRA). Position the probe to span conserved framework or gene segments adjacent to the junctional region.
qPCR Reaction Setup
Table 2: qPCR Reaction Components for MRD Detection
| Component | Volume per Reaction | Final Concentration |
|---|---|---|
| 2× qPCR Master Mix | 12.5 μL | 1× |
| Patient-Specific Forward Primer | 0.5 μL | 200 nM |
| Conserved Reverse Primer | 0.5 μL | 200 nM |
| TaqMan Probe | 0.5 μL | 100 nM |
| Template DNA | 5 μL | 100-200 ng/μL |
| Nuclease-Free Water | to 25 μL | - |
Thermal Cycling Conditions
- Initial Denaturation: 95°C for 10 minutes
- Amplification (45 cycles):
- Denature: 95°C for 15 seconds
- Anneal/Extend: 60°C for 60 seconds (acquire fluorescence)
- Hold: 4°C forever
Standard Curve and Quantification
- Limiting Dilution Series: Prepare a standard curve by serially diluting diagnostic DNA (with known leukemic cell percentage) in normal mononuclear cell DNA across a 4-5 log range.
- Quantification: Use the standard curve to interpolate MRD levels in follow-up samples. Include no-template controls and negative controls (polyclonal DNA) in each run.
- Sensitivity Validation: Establish the quantitative limit of detection for each patient-specific assay through dilution experiments.
Quality Control and Interpretation
- EuroMRD Guidelines: Follow established guidelines for data analysis and interpretation [10].
- Quality Metrics: Assay sensitivity should be validated to at least 10⁻⁴, with optimal assays reaching 10⁻⁵.
- Result Reporting: Report MRD levels as quantitative values when above the quantitative limit; classify as "positive not quantifiable" (PNQ) for results below the quantitative limit but above the detection limit [10].
Targeted NGS Protocol for MRD Detection
This protocol describes an NGS-based method for MRD monitoring using IG/TCR sequencing, which addresses several limitations of the qPCR approach.
Library Preparation
- DNA Fragmentation: Fragment 50-100 ng of genomic DNA to 150-300 bp fragments using mechanical shearing or enzymatic fragmentation.
- Library Construction: Use commercially available MRD-specific NGS kits (e.g., LymphoTrack, ClonoSEQ) that employ multiplex PCR to amplify IG/TCR loci. These kits contain predefined primer sets covering multiple V and J gene segments.
- Adapter Ligation: Attach dual-indexed adapters containing sample barcodes to enable sample multiplexing.
- Library Quantification: Quantify libraries using fluorometric methods (e.g., Qubit) and assess size distribution using capillary electrophoresis (e.g., Bioanalyzer).
Sequencing
- Platform Selection: Use benchtop NGS systems (e.g., MiSeq, Ion GeneStudio S5) suitable for targeted sequencing.
- Sequencing Depth: Aim for minimum coverage of 100,000 reads per sample to achieve sensitivity of 10⁻⁵. Increase depth for higher sensitivity.
- Run Parameters: Use 2×150 bp paired-end sequencing to adequately cover rearrangement junctions.
Bioinformatics Analysis
Data Processing Pipeline:
- Demultiplexing: Separate sequences by sample barcodes.
- Quality Filtering: Remove low-quality reads and adaptor sequences.
- Alignment: Map sequences to reference V, D, J, and C gene databases.
- Clonotype Identification: Group sequences with identical V-J combinations and junctional sequences.
- Quantification: Calculate the frequency of each clonotype as a percentage of total productive sequences.
MRD Assessment:
- Compare follow-up samples to the diagnostic clonotype profile.
- Track multiple dominant clonotypes simultaneously to detect clonal evolution.
- Report MRD levels based on the aggregate frequency of all leukemia-associated sequences.
Research Reagent Solutions
The table below details essential reagents and kits for implementing integrated qPCR and NGS approaches in MRD research:
Table 3: Essential Research Reagents for MRD Detection Workflows
| Reagent/Kits | Technology | Primary Function | Key Features |
|---|---|---|---|
| dUTP Master Mixes | qPCR | Prevents carryover contamination in high-throughput settings | Contains dUTP and uracil-N-glycosylase (UNG) to degrade PCR products from previous amplifications [103] |
| Lyo-Ready Master Mixes | qPCR | Enables ambient-temperature stable assay formulation | Ready for lyophilization; maintains stability without cold chain [103] |
| Glycerol-Free Enzymes | qPCR/NGS | High-concentration enzymes for specialized applications | Compatible with lyophilization; ideal for high-throughput workflows [103] |
| NGS Library Preparation Kits | NGS | Targeted sequencing of IG/TCR loci | Multiplex PCR-based; covers major IG/TCR genes; optimized for MRD detection [10] |
| Hybridization Capture Kits | NGS | Target enrichment for comprehensive mutation profiling | Probe-based capture; suitable for custom gene panels; better uniformity [104] |
| TaqMan Gene Expression Assays | qPCR | Validation of fusion transcripts and expression markers | Predesigned assays for known targets; high specificity and sensitivity [107] |
Analytical Considerations and Data Interpretation
Sensitivity and Specificity Parameters
Achieving optimal sensitivity and specificity requires careful consideration of several analytical parameters:
- Sample Quality: Degraded DNA or RNA significantly impacts assay sensitivity. Implement rigorous quality control measures, including DNA integrity number (DIN) or RNA integrity number (RIN) assessment.
- Input Material: Higher DNA input increases sensitivity but may be limited by sample availability. For qPCR, 1-2 μg DNA enables detection at 10⁻⁵ sensitivity. For NGS, 50-100 ng DNA is typically sufficient due to the digital counting nature of the technology.
- Background Estimation: In NGS-based MRD, distinguish true clonal sequences from PCR and sequencing errors using error-correcting algorithms and statistical thresholds (typically 2-5 identical sequences required to call a clonotype).
- Clonal Evolution: NGS offers significant advantages in detecting clonal evolution by simultaneously tracking multiple sequences. Implement strategies to identify emerging clones that differ from the dominant diagnostic clone.
Clinical Correlation and Thresholds
MRD levels must be interpreted in the context of clinical timelines and established prognostic thresholds:
- Timepoint Dependency: The prognostic significance of MRD varies with treatment phase. Early MRD assessment (during induction) identifies rapid responders, while persistent MRD at later timepoints (end of consolidation) carries poorer prognosis [10].
- Quantitative Thresholds: Established risk stratification typically uses thresholds of ≥10⁻⁴ for high-risk and <10⁻⁴ for standard-risk in B-ALL [10].
- Trend Analysis: Sequential monitoring provides more prognostic information than single timepoint assessments. Rising MRD levels, even below established thresholds, may indicate emerging resistance.
The following diagram illustrates the decision pathway for MRD assessment and therapeutic stratification:
The integration of qPCR and NGS technologies represents a powerful paradigm for modern clinical diagnostics, particularly in the challenging domain of MRD detection. Rather than existing as competing methodologies, these technologies form a complementary alliance that leverages the speed, sensitivity, and accessibility of qPCR with the comprehensive, unbiased nature of NGS. The protocols and analytical frameworks presented here provide researchers and drug development professionals with practical guidance for implementing these integrated approaches.
As precision medicine continues to evolve, the synergy between qPCR and NGS will become increasingly important. Emerging approaches, such as liquid biopsy and single-cell sequencing, will further enhance our ability to detect and characterize minimal residual disease. However, the fundamental principle of leveraging complementary technologies to achieve both breadth and depth in molecular analysis will remain relevant. Through thoughtful integration of these powerful technologies, clinicians and researchers can advance toward more personalized, effective therapeutic strategies for cancer patients.
In minimal residual disease (MRD) detection research, the reproducibility of findings is a cornerstone of the scientific method. The reliability of quantitative PCR (qPCR) data, crucial for clinical decision-making in oncology, strongly depends on the transparency of the analytical process. Historically, reproducibility depended on detailed method descriptions in research papers. However, with the increasing complexity of molecular research, the availability of reproducible analysis code has become equally important [109]. Reviews estimate that of papers that share code and data, only a fraction is fully reproducible, with estimates ranging widely between 17% and 82% [109]. In the specific context of qPCR for MRD, where results can directly influence patient treatment pathways, ensuring that raw data and analysis code are shared is not merely a scientific ideal but an ethical imperative. This practice allows for the independent verification of results, facilitates the reanalysis of data with updated methods, and accelerates collective progress in the field.
The growing use of high-dimensional data and recent methodological advances mean that research reproducibility is now inextricably linked to the code used for data preprocessing, derivation of analytical datasets, and statistical analysis [109]. Despite this, code is rarely made available and is often only partly reproducible. Adopting transparent practices benefits individual researchers by enhancing efficiency and impact, as well-documented code can be easily reused in new studies. Furthermore, preliminary findings from other disciplines suggest that papers with shared code and data may accumulate citations faster, ultimately creating a scientific ecosystem where researchers can build directly upon prior work [109].
The Critical Role of Data and Code Sharing in MRD Research
Enhancing Reproducibility and Validating Clinical Relevance
For MRD detection, the clinical implications of qPCR findings are significant. Sharing raw qPCR data—including amplification plots, baseline and threshold settings, and quantification cycle (Cq) values—allows other researchers to verify the accuracy of reported results. This is particularly vital when developing new assays or establishing diagnostic thresholds. A key part of this process is the transparent reporting of the Cq value, which is a relative measure of the concentration of the target in the PCR reaction [110]. The accurate determination of this value is sensitive to background fluorescence and requires precise baseline correction and threshold setting [111]. When raw data is available, others can confirm that baseline periods were set correctly—typically using the fluorescence intensity from early cycles (e.g., 5 to 15) to define the linear component of background fluorescence, avoiding the initial cycles (1-5) which may contain reaction stabilization artifacts [111]. Without this level of transparency, minor, unreported adjustments in data analysis can lead to substantially different results and conclusions [109].
Enabling Secondary Analysis and Methodological Advancement
Sharing full datasets and code enables the scientific community to perform secondary analyses, such as applying new normalization methods or testing different statistical models on existing data. This maximizes the value of each meticulously generated dataset. In qPCR, the method of quantification is a major consideration. While absolute quantification determines the exact copy number of a target, relative quantification—which compares the expression of a target gene to a reference gene—is one of the most common techniques [110]. The availability of raw data allows other researchers to apply alternative quantification methods, such as the Pfaffl method, which accounts for differences in PCR efficiency between the target and reference genes, rather than assuming an ideal efficiency [110]. This is crucial for advancing the technical standards of MRD detection assays.
Practical Framework for Transparent qPCR Research
Five Key Recommendations for Reproducible Practices
Based on an analysis of practices in epidemiological research, the following five recommendations provide a practical starting point for enhancing reproducibility in qPCR-based MRD studies [109].
- Make Reproducibility a Priority: Actively allocate time and resources for organizing data, annotating code, and preparing materials for sharing. This is a societal responsibility for publicly funded research and is increasingly required by journals and funding agencies [109].
- Implement Systematic Code Review: Introduce a process where analytical code is examined by peers. This improves code quality, helps identify bugs, and fosters discussion on analytical choices. Using quality checks like unit tests for custom functions can make this review more efficient [109].
- Write Comprehensible Code: Write code with the explicit goal of enabling a third party to understand its logic. This involves using a clear structure with headings, a
ReadMefile explaining the workflow, consistent naming for variables, and a data dictionary describing the variables in detail [109]. - Report Decisions Transparently: Document all key decisions made during the analytical process directly within the code or an accompanying log. For qPCR, this includes the specific cycles used for baseline correction, the chosen threshold level, the method of Cq determination, and the rationale for excluding any outliers [109].
- Focus on Accessibility of Code and Data: Share code and, when possible, data via an open repository managed by the researcher's institution or a general repository like Zenodo. This makes the research discoverable and usable by everyone [109].
Essential Elements for Sharing
To be truly useful for independent verification, shared materials for a qPCR-based MRD study should include the items listed in the table below.
Table 1: Essential Components of a Transparent qPCR Data Submission
| Component | Description | Importance for Reproducibility |
|---|---|---|
| Raw Fluorescence Data | The output file from the qPCR instrument containing fluorescence values for every well at every cycle. | Allows for independent re-analysis with different baseline and threshold settings. |
| Annotated Analysis Code | Scripts (e.g., in R or Python) for data preprocessing, Cq calculation, and statistical analysis, with comments explaining each step. | Makes the analytical workflow transparent and executable. |
| Sample Metadata | A table linking sample IDs to experimental groups, sample types, and any other relevant covariates. | Ensures the biological context is clear for re-analysis. |
| Data Dictionary | A document defining all variables, units, and abbreviations used in the dataset and code. | Prevents misinterpretation of data columns and analysis outputs. |
| PCR Efficiency Data | The standard curve data, including dilution factors and corresponding Cq values, used to calculate amplification efficiency. | Enables others to verify the quantitative performance of the assay. |
| qPCR Assay Details | Information on primers, probes, and reference genes used, including sequences and concentrations. | Allows for technical replication of the experimental setup. |
Experimental Protocol for Transparent qPCR Data Analysis
The following protocol provides a detailed methodology for analyzing and reporting qPCR data in a transparent and reproducible manner, suitable for MRD detection studies.
Protocol: Reproducible qPCR Data Analysis Workflow
I. Pre-analysis Phase: Data Export and Organization
- Export the raw fluorescence data (Rn or R values per cycle for all wells) from the qPCR instrument in a standard, machine-readable format (e.g.,
.csv). - Create a structured project directory with separate folders for
raw_data,scripts,metadata, andoutputs. - Document all sample information and experimental groups in a sample metadata file (
sample_metadata.csv).
II. Baseline Correction and Threshold Setting
- Baseline Correction: In your analysis code, explicitly define the cycles used for baseline calculation. Typically, the baseline is set using the fluorescence intensity from cycles 5-15 to establish a constant, linear background. Avoid using the first few cycles (1-5) due to potential reaction stabilization artifacts [111]. The baseline should be set at the limit of detection for the qPCR machine, where measurements would be inaccurate [110].
- Threshold Setting: Programmatically set a fixed threshold for all samples to be compared. The threshold must be set sufficiently above the baseline, within the exponential phase of all amplification plots where they are parallel [111]. Visually inspect a plot of the log(fluorescence) versus cycle number to confirm the threshold is within the parallel, linear phase of the plots. Document the final threshold value used in the analysis.
III. Cq Determination and Efficiency Calculation
- Cq Calculation: Use the algorithm in your code to calculate the Cq value for each well as the intersection between the amplification curve and the fixed threshold.
- PCR Efficiency: Calculate PCR efficiency using a standard curve with serial dilutions.
- Prepare a minimum of 3 serial dilutions of a known template, running each in triplicate.
- Plot the average Cq value against the logarithm of the dilution factor.
- Calculate the slope of the standard curve and then the efficiency using the formula: Efficiency (%) = (10^(-1/slope) - 1) * 100 [110].
- An acceptable efficiency is typically between 85% and 110%. Report the slope, R², and calculated efficiency.
IV. Quantification and Statistical Analysis
- For MRD research, choose the appropriate quantification method.
- Absolute Quantification: Use the standard curve to determine the exact copy number in unknown samples.
- Relative Quantification (e.g., ΔΔCq method): Normalize the Cq of the target gene to a stable reference gene (ΔCq = Cqtarget - Cqreference). Then, compare this to the control group (ΔΔCq = ΔCqtreatment - ΔΔCqcontrol). The fold-change is calculated as 2^(-ΔΔCq) [110].
- Perform statistical tests as required by the experimental design. Ensure the code for statistical testing is fully annotated, indicating the choice of test and the rationale.
V. Reporting and Sharing
- Generate a final report that includes key results, plots (amplification curves, standard curve), and statistical summaries.
- Bundle the raw data, annotated analysis code, sample metadata, and a detailed
ReadMefile for public sharing in a repository.
Workflow and Data Sharing Visualization
The following diagram illustrates the integrated workflow for conducting a transparent qPCR experiment, from data generation to sharing.
Diagram 1: Transparent qPCR data workflow.
The decision-making process for selecting the appropriate quantification method in qPCR analysis is critical and must be documented.
Diagram 2: qPCR quantification decision tree.
The Scientist's Toolkit: Research Reagent Solutions
The following table details key reagents and materials essential for conducting robust and reproducible qPCR experiments for MRD detection.
Table 2: Essential Research Reagents for qPCR-based MRD Detection
| Reagent/Material | Function | Critical Considerations for Reproducibility |
|---|---|---|
| Sequence-Specific Primers/Probes | To specifically amplify and detect the target gene of interest (e.g., a leukemia-specific fusion transcript). | Sequences and concentrations must be documented and shared. Purity (HPLC-purified) is critical for high efficiency and specificity. |
| Reverse Transcriptase (for RT-qPCR) | To synthesize complementary DNA (cDNA) from RNA templates. | The specific enzyme and protocol used can impact cDNA yield and quality, affecting downstream Cq values. Must be reported. |
| qPCR Master Mix | Contains DNA polymerase, dNTPs, buffer, and salts necessary for the PCR reaction. Often includes a passive reference dye (ROX). | The commercial brand and formulation can influence amplification efficiency. The lot number should be recorded. |
| Nuclease-Free Water | The solvent for preparing reagent mixes. | Ensures the reaction is not degraded by RNases or DNases, which could lead to variable results. |
| Standard Curve Template | A known quantity of the target sequence (e.g., gBlock, plasmid) used in serial dilutions to generate a standard curve. | Essential for calculating PCR efficiency and for absolute quantification. The source and preparation method must be detailed. |
| Reference Gene Assay | Primers and probes for a stably expressed gene (e.g., ABL, GUSB) used for normalization in relative quantification. | The gene must be validated as stable across all test conditions. The choice of reference gene is a key methodological detail. |
Conclusion
qPCR remains a powerful, cost-effective cornerstone for MRD detection, with its clinical utility firmly established in hematologic malignancies. The key to unlocking its full potential lies in meticulous protocol optimization, rigorous validation of reference genes, and strict adherence to MIQE guidelines to ensure data integrity. While next-generation sequencing offers enhanced sensitivity and the ability to track clonal evolution, qPCR continues to provide a rapid and accessible alternative. The future of MRD monitoring will likely involve integrated, multi-method approaches, combining the strengths of qPCR, flow cytometry, and NGS. For researchers and clinicians, embracing transparency, standardized reporting, and continuous methodological refinement is paramount for advancing personalized treatment strategies and improving patient outcomes.
References
- 1. Measurable Residual Disease Testing in Acute Leukemia: Technology and Clinical Significance - Leukemia - NCBI Bookshelf [https://www.ncbi.nlm.nih.gov/books/NBK586210/]
- 2. Minimal Residual Disease Detection: Implications for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12079024/]
- 3. testing in haematological and solid cancers | Leukemia [https://www.nature.com/articles/s41375-024-02252-4]
- 4. ADVANCING THE MRD CONCEPT IN ACUTE MYELOID LEUKEMIA - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC4484880/]
- 5. Sensitive detection of minimal residual disease and ... [https://jeccr.biomedcentral.com/articles/10.1186/s13046-025-03481-w]
- 6. Detection of minimal residual disease in circulating cell ... [https://www.nature.com/articles/s41598-025-20589-3]
- 7. Universal SYBR Green qPCR Protocol [https://www.sigmaaldrich.com/US/en/technical-documents/protocol/genomics/qpcr/sybr-green-qpcr?srsltid=AfmBOoqpCARM3U18Plw9yRn2azYz2Bhf5nR6sYdPJ169LIoqpiw5uram]
- 8. Basic principles of real-time quantitative PCR [https://pubmed.ncbi.nlm.nih.gov/15833050/]
- 9. A survey of tools for the analysis of quantitative PCR ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5129434/]
- 10. Minimal residual disease in acute lymphoblastic leukemia [https://pmc.ncbi.nlm.nih.gov/articles/PMC7386891/]
- 11. qPCR Steps: Creating a Successful Experiment | IDT [https://www.idtdna.com/page/support-and-education/decoded-plus/successful-qpcr/]
- 12. A New View on Minimal Residual Disease Quantification in ... [https://www.sciencedirect.com/science/article/pii/S1525157822001453]
- 13. rtpcr: a package for statistical analysis and graphical ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12530193/]
- 14. How To Interpret RT-qPCR Results [https://www.goldbio.com/blogs/articles/how-to-interpret-rt-qpcr-results?srsltid=AfmBOoqx_AZr8EjY55RBd7CFl1_NLCG8YTjzqT4JgOAkkdyGd5X4hav3]
- 15. Basic Principles of RT-qPCR [https://www.thermofisher.com/us/en/home/brands/thermo-scientific/molecular-biology/molecular-biology-learning-center/molecular-biology-resource-library/spotlight-articles/basic-principles-rt-qpcr.html]
- 16. The emerging role of next-generation sequencing in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12052730/]
- 17. Breaking Research: MRD Positive Status Predicts ... [https://globalrph.com/2025/10/breaking-research-mrd-positive-status-predicts-leukemia-outcomes/]
- 18. Analysis of measurable residual disease by IG/TR gene ... [https://www.nature.com/articles/s41375-024-02272-0]
- 19. Clinical and analytical validation of a combined RNA ... [https://www.nature.com/articles/s43856-025-00934-3]
- 20. MIQE 2.0 and the Urgent Need to Rethink qPCR Standards [https://pmc.ncbi.nlm.nih.gov/articles/PMC12154065/]
- 21. Measurable residual disease in hematologic malignancies [https://pmc.ncbi.nlm.nih.gov/articles/PMC12257026/]
- 22. Myriad Genetics Announces Precise MRD Clinical Data ... [https://investor.myriad.com/news-releases/news-release-detail/26656/]
- 23. 2148 MRD Study Reaches Milestone With First Patient In ... [https://www.eortc.org/blog/2025/08/04/2148-mrd-study-first-patient-in/]
- 24. Fig. 1, [ddPCR MRD quantification - Immunogenetics - NCBI [https://www.ncbi.nlm.nih.gov/books/NBK586952/figure/ch5.Fig1/]
- 25. qPCR Troubleshooting: How to Ensure Successful ... [https://dispendix.com/blog/qpcr-troubleshooting]
- 26. Optimizing Molecular Minimal Residual Disease Analysis in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9856386/]
- 27. Comprehensive Protocol to Sample and Process Bone ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5931431/]
- 28. Bone Marrow Cytology Meets qPCR in a Pilot Study ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12472918/]
- 29. Whole Blood Samples for Faster Real-Time PCR Analysis of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9470097/]
- 30. Impact of different stabilization methods on RT-qPCR ... [https://www.nature.com/articles/s41598-020-60618-x]
- 31. Quantitative PCR (qPCR) Data Analysis [https://www.thermofisher.com/us/en/home/life-science/pcr/real-time-pcr/real-time-pcr-learning-center/gene-expression-analysis-real-time-pcr-information/precision-qpcr.html]
- 32. Quantitative PCR validation for research scientists: Part 1 of 2 [https://virologyresearchservices.com/2023/01/13/quantitative-pcr-validation-part-1-of-2/]
- 33. Consensus guidelines for the validation of qRT-PCR ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8792405/]
- 34. A PCR-based quantitative assay for the evaluation of mRNA ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6006387/]
- 35. How to optimize qPCR in 9 steps? [https://westburg.eu/knowledge/pcr_qpcr/hate_optimizing_qpcr]
- 36. Rules and Tips for PCR & qPCR Primer Design | IDT [https://www.idtdna.com/page/support-and-education/decoded-plus/how-to-design-primers-and-probes-for-pcr-and-qpcr/]
- 37. Analysis of qPCR Data: From PCR Efficiency to Absolute ... [https://www.preprints.org/manuscript/202510.2485]
- 38. Understanding qPCR Efficiency and Why It Exceeds 100% [https://biosistemika.com/blog/qpcr-efficiency-over-100/]
- 39. Introduction to Quantitative PCR (qPCR) Gene Expression ... [https://www.thermofisher.com/us/en/home/life-science/pcr/real-time-pcr/real-time-pcr-learning-center/gene-expression-analysis-real-time-pcr-information/introduction-gene-expression.html]
- 40. Predicting sequence-specific amplification efficiency in ... [https://www.nature.com/articles/s41467-025-64221-4]
- 41. Real-time PCR probe optimization using design of ... [https://www.sciencedirect.com/science/article/pii/S2214753515300139]
- 42. Read This Before You Design Those qPCR Primers [https://bitesizebio.com/2504/read-this-before-you-design-those-qpcr-primers/]
- 43. From RNA to results: the essential guide to RT-PCR [https://www.integra-biosciences.com/united-states/en/blog/article/rna-results-essential-guide-rt-pcr]
- 44. Universal SYBR Green qPCR Protocol [https://www.sigmaaldrich.com/US/en/technical-documents/protocol/genomics/qpcr/sybr-green-qpcr?srsltid=AfmBOooyHE7y4hGtY4R71aHFu89ec7SlDbctU4UIIbV8dD3hhy6c9aiL]
- 45. Guidelines for RNA Analysis by Reverse Transcription ... [https://pubmed.ncbi.nlm.nih.gov/40699418/]
- 46. Insights into qPCR: Protocol, Detection Methods, and Analysis [https://www.the-scientist.com/insights-into-qpcr-protocol-detection-methods-and-analysis-71478]
- 47. Level Up Your qPCR Game: Mastering Probes and Dyes [https://krakensense.com/blog/level-up-your-qpcr-game-mastering-probes-and-dyes]
- 48. Real-Time PCR (qPCR) Basics [https://www.thermofisher.com/us/en/home/life-science/pcr/real-time-pcr/real-time-pcr-learning-center/real-time-pcr-basics.html]
- 49. A stable combination of non-stable genes outperforms ... [https://www.nature.com/articles/s41598-024-82651-w]
- 50. qPCR Double Delta Ct Analysis in 4 Easy Steps [https://bitesizebio.com/24894/4-easy-steps-to-analyze-your-qpcr-data-using-double-delta-ct-analysis/]
- 51. qPCRtools: An R package for qPCR data processing and ... [https://www.frontiersin.org/journals/genetics/articles/10.3389/fgene.2022.1002704/full]
- 52. How To Interpret RT-qPCR Results [https://www.goldbio.com/blogs/articles/how-to-interpret-rt-qpcr-results?srsltid=AfmBOoq9HTvmzSb8WY38ik0O66MbRJAUoTiis5h31Dic7JbPRYoSteBn]
- 53. Learn about the importance of the qPCR standard curve [https://bitesizebio.com/31470/obligate-qpcr-standard-curve/]
- 54. RQdeltaCT: an open-source R package for relative ... [https://www.nature.com/articles/s41598-025-11822-0]
- 55. Designing standard curves for qPCR | IDT [https://www.idtdna.com/page/support-and-education/decoded-plus/easily-designed-standard-curves-for-qpcr/]
- 56. Multivariable Linear Models Outperform 2−ΔΔCT for qPCR ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11844642/]
- 57. RealTimeDesign qPCR Assay Design Software [https://oligos.biosearchtech.com/tools/realtimedesign-software]
- 58. MIQE 2.0: Revision of the Minimum Information for ... [https://pubmed.ncbi.nlm.nih.gov/40272429/]
- 59. How to Select Endogenous Controls for Real-Time PCR [https://www.thermofisher.com/us/en/home/life-science/pcr/real-time-pcr/real-time-pcr-learning-center/gene-expression-analysis-real-time-pcr-information/choosing-endogenous-control-gene-expression-analysis-real-time-pcr.html]
- 60. PCR/qPCR Data Analysis [https://www.sigmaaldrich.com/US/en/technical-documents/technical-article/genomics/qpcr/data-analysis?srsltid=AfmBOopq3F9yg1QhTCAvSL7QC81lXj1pjDGegZMrHeNAICepku_xLa4-]
- 61. Identification of new reference genes with stable ... [https://www.nature.com/articles/s41598-021-98869-x]
- 62. Quantitative Evaluation of Endogenous Reference Genes ... [https://www.mdpi.com/2076-2607/13/8/1721]
- 63. Validation of reference genes for the normalization of RT ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5431254/]
- 64. PCR inhibition in qPCR, dPCR and MPS—mechanisms and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7072044/]
- 65. Inhibit inhibition: PCR inhibition and how to prevent it [https://www.bioecho.com/blog/inhibit-inhibition-pcr-inhibition-and-how-to-prevent-it]
- 66. Overcoming qPCR Inhibitors: Strategies for Reliable ... [https://www.promegaconnections.com/overcoming-qpcr-inhibitors-strategies-for-reliable-quantification/]
- 67. Have you tested the effect of inhibitors on PCR performance? [https://www.qiagen.com/us/resources/faq/818]
- 68. Low input or inhibition? Quantitative approaches to detect ... [https://www.bioecho.com/blog/low-input-or-inhibition-quantitative-approaches-to-detect-qpcr-inhibitors]
- 69. Evaluation of PCR-enhancing approaches to reduce ... [https://www.sciencedirect.com/science/article/abs/pii/S0048969724069250]
- 70. Measuring and mitigating inhibition during quantitative real ... [https://www.sciencedirect.com/science/article/abs/pii/S0043135412002850]
- 71. PCR Inhibitor Levels in Concentrates of Biosolid Samples ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3008220/]
- 72. Validation of Endogenous Control Genes by Real-Time ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10887733/]
- 73. Validation of Reference Genes for Normalization ... [https://www.nature.com/articles/s41598-019-49247-1]
- 74. Stability of PCR Targets for Monitoring Minimal Residual ... [https://www.sciencedirect.com/science/article/pii/S1525157811003187]
- 75. Normalization of Gene Expression by Quantitative RT-PCR ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6308757/]
- 76. Efficiency of Real-Time PCR [https://www.thermofisher.com/us/en/home/life-science/pcr/real-time-pcr/real-time-pcr-learning-center/real-time-pcr-basics/efficiency-real-time-pcr-qpcr.html]
- 77. What is a Ct Value and does it differ from qPCR Cq Values? [https://bitesizebio.com/24581/what-is-a-ct-value/]
- 78. What to do when the qPCR results are weird? - Yeasen [https://www.yeasenbio.com/blogs/molecular-biology/what-to-do-when-the-qpcr-results-are-weird]
- 79. Understanding Ct Values in Real-Time PCR [https://www.thermofisher.com/blog/behindthebench/understanding-ct-values/]
- 80. Advancing qPCR with highly reproducible results [https://www.qiagen.com/us/applications/pcr/reproducibility-with-qpcr]
- 81. Analyzing qPCR data: Better practices to facilitate rigor and ... [https://www.sciencedirect.com/science/article/pii/S2405580825004431]
- 82. How To Interpret RT-qPCR Results [https://www.goldbio.com/blogs/articles/how-to-interpret-rt-qpcr-results?srsltid=AfmBOooSx0cGs7B0qacOPpdvkV9sphGgHpJpTQfFcqBwxQX0rTms4V54]
- 83. PCR/qPCR Data Analysis [https://www.sigmaaldrich.com/US/en/technical-documents/technical-article/genomics/qpcr/data-analysis?srsltid=AfmBOoq95Ky0tytcP2R3ReyJtRS9Ho3KxQChbY3fF3DEsashiL0jm5vu]
- 84. Preventing False Positive and False Negative PCR Results [https://www.clinicallab.com/preventing-false-positive-and-false-negative-pcr-results-26261]
- 85. Avoiding false positives with PCR | IDT [https://www.idtdna.com/page/support-and-education/decoded-plus/how-to-avoid-false-positives-in-pcr-and-what-to-do-if-you-get-them/]
- 86. PCR/qPCR Plates and Tubes Troubleshooting Guide [https://www.thermofisher.com/us/en/home/life-science/cloning/cloning-learning-center/invitrogen-school-of-molecular-biology/pcr-education/pcr-qpcr-plastics/pcr-qpcr-plastics-troubleshooting.html]
- 87. Real-Time Quantitative PCR: Primer Design, Reference ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10384377/]
- 88. Minimizing errors in RT-PCR detection and quantification ... [https://www.sciencedirect.com/science/article/pii/S0048969721049524]
- 89. Pitfalls in PCR troubleshooting: Expect the unexpected? [https://pmc.ncbi.nlm.nih.gov/articles/PMC4822207/]
- 90. Methods to determine limit of detection and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5496743/]
- 91. Correlation Between Chimeric Antigen Receptor T‐Cell ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12445920/]
- 92. Applications of machine learning for immunophenotypic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12093103/]
- 93. A machine learning approach for the rapid identification of ... [https://haematologica.org/article/view/11964]
- 94. Application of droplet digital PCR in minimal residual ... [https://www.nature.com/articles/s41598-024-57016-y]
- 95. Digital PCR Improves Sensitivity and Quantification in ... [https://www.sciencedirect.com/science/article/pii/S2666636723024119]
- 96. Inter-laboratory comparison of eleven quantitative or digital ... [https://bmcvetres.biomedcentral.com/articles/10.1186/s12917-024-04228-z]
- 97. Comparison of Analytic Methods for Quantitative Real-Time ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4642823/]
- 98. How NGS-Based MRD Is Reshaping Hematological ... [https://clpmag.com/diagnostic-technologies/molecular-diagnostics/sequencing-systems/how-ngs-based-mrd-is-reshaping-hematological-malignancy-management/]
- 99. NGS better discriminates true MRD positivity for the risk ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10651772/]
- 100. Clonal Evolution and Changes in Two AML Patients ... [https://www.nature.com/articles/s41598-019-47297-z]
- 101. Comparison of next-generation sequencing (NGS) and ... [https://www.nature.com/articles/s41408-020-00377-0]
- 102. Targeted, Amplicon-Based, Next-Generation Sequencing ... [https://pubmed.ncbi.nlm.nih.gov/30941718/]
- 103. The Growing Demand for Personalized Diagnostics [https://www.meridianbioscience.com/lifescience-blog/the-growing-demand-for-personalized-diagnostics-navigating-the-benefits-and-limits-of-qpcr-vs-ngs/]
- 104. Next-generation sequencing and its clinical application [https://pmc.ncbi.nlm.nih.gov/articles/PMC6528456/]
- 105. NGS vs qPCR [https://www.illumina.com/science/technology/next-generation-sequencing/beginners/advantages/ngs-vs-qpcr.html]
- 106. Next-generation sequencing in cancer diagnosis and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12009796/]
- 107. Real-Time PCR (qPCR) and Whole-Transcriptome NGS [https://www.thermofisher.com/us/en/home/life-science/pcr/real-time-pcr/ngs-comparison.html]
- 108. NGS Approaches in Clinical Diagnostics: From Workflow to ... [https://www.mdpi.com/1422-0067/26/19/9597]
- 109. Improving reproducibility of data analysis and code in medical ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12496075/]
- 110. How To Interpret RT-qPCR Results [https://www.goldbio.com/blogs/articles/how-to-interpret-rt-qpcr-results?srsltid=AfmBOoqEbPYkUc1O0NZah3icCGWqC3VZdLP8AzDwVquk4r-_YNHrziav]
- 111. PCR/qPCR Data Analysis [https://www.sigmaaldrich.com/US/en/technical-documents/technical-article/genomics/qpcr/data-analysis?srsltid=AfmBOopw-h2I8HA77TWN9gPIKtN_zuFltqnZstXbHzIID7gWG-o-NxDg]