Optimizing Pharmacophore Model Sensitivity: A Comprehensive Guide for Enhanced Virtual Screening
This article provides a systematic guide for researchers and drug development professionals on optimizing pharmacophore model sensitivity—a critical parameter for successful virtual screening.
Optimizing Pharmacophore Model Sensitivity: A Comprehensive Guide for Enhanced Virtual Screening
Abstract
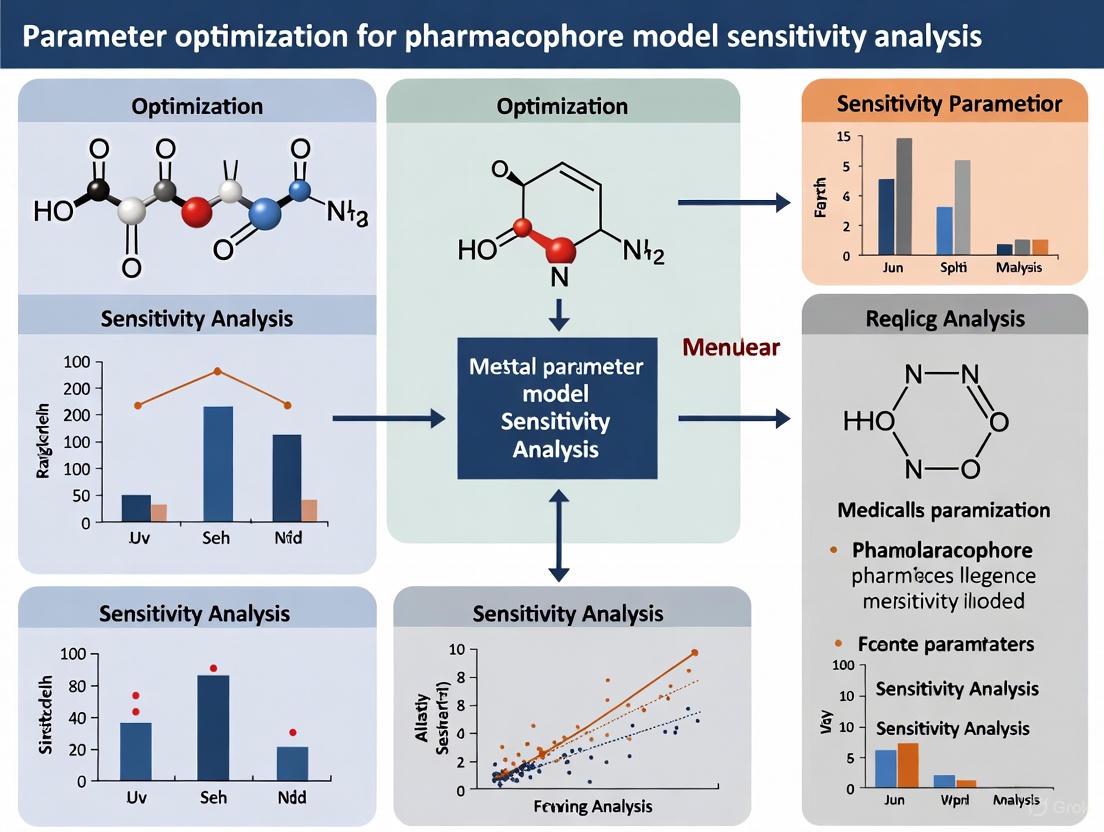
This article provides a systematic guide for researchers and drug development professionals on optimizing pharmacophore model sensitivity—a critical parameter for successful virtual screening. We explore the foundational principles of pharmacophore features and their direct impact on a model's ability to correctly identify active compounds. The content covers established and emerging methodological approaches, including structure-based and ligand-based modeling, alongside advanced AI-driven techniques. A dedicated section addresses common pitfalls and provides actionable strategies for parameter tuning to maximize sensitivity without compromising specificity. Finally, we detail rigorous validation protocols using statistical metrics like enrichment factor and GH score, supplemented by case studies from recent kinase inhibitor campaigns. This holistic framework aims to equip scientists with the knowledge to build highly sensitive, robust pharmacophore models that significantly improve hit rates in drug discovery.
Understanding Pharmacophore Sensitivity: Core Concepts and Key Features
Defining Sensitivity and Specificity in Pharmacophore Modeling
Frequently Asked Questions (FAQs)
FAQ 1: What is the fundamental difference between sensitivity and specificity in the context of pharmacophore-based virtual screening?
Sensitivity, often measured by the true positive rate, reflects a pharmacophore model's ability to correctly identify known active compounds from a database. Specificity, measured by the true negative rate, indicates the model's ability to correctly reject inactive compounds or decoys. A high-quality model must balance both; an overly sensitive model may retrieve many actives but with numerous false positives, while an overly specific model might miss potential actives. The goal of parameter optimization is to achieve a model with high sensitivity without compromising specificity [1].
FAQ 2: Which quantitative metrics should I use to formally evaluate the sensitivity and specificity of my pharmacophore model?
The primary metric for evaluating sensitivity and specificity is the Enrichment Factor (EF) [1]. The EF represents the model's ability to identify true positive active inhibitors compared to a random selection. It is calculated as the ratio of the active inhibitors in the screened subgroup over the ratio of active inhibitors in the entire database. A higher EF indicates better model performance. Additionally, the fitness score of a model, which evaluates the alignment between a ligand's conformation and the pharmacophore model, is a critical internal metric. The Receiver Operating Characteristic (ROC) curve and the area under it (AUC) provide a comprehensive view of the model's true positive rate (sensitivity) against its false positive rate (1-specificity) across all classification thresholds [1] [2].
FAQ 3: My model has high enrichment but a low fitness score for known actives. What parameters should I investigate?
This discrepancy often points to an overly restrictive model. We recommend investigating the following parameters:
- Feature Tolerance: Increase the distance tolerance (e.g., from 1.0 Å to 1.5 Å or 2.0 Å) for pharmacophore features like hydrogen bond donors/acceptors or hydrophobic centers. This makes the model more forgiving of minor spatial deviations [1].
- Exclusion Volumes: Review the number and size of exclusion spheres. An excess of restrictive volumes may sterically block valid active compounds from matching. Consider removing or reducing the radii of exclusion volumes in non-critical regions [2].
- Feature Weighting: If your software allows, adjust the weights of individual pharmacophore features. A model might be overly dependent on one particular feature that is not essential for biological activity.
FAQ 4: How can I use molecular dynamics (MD) simulations to improve the real-world reliability of my pharmacophore models?
Relying on a single, static crystal structure can lead to models that are not representative of dynamic binding interactions. Using MD simulations to generate an ensemble of protein-ligand conformations allows for the creation of multiple pharmacophore models [3]. You can then:
- Use a consensus approach (like the Common Hits Approach) across all models for virtual screening, which makes the process less sensitive to any single, poorly-performing model [3].
- Create a Hierarchical Graph Representation of Pharmacophore Models (HGPM) to visualize all unique models and their relationships. This tool helps you strategically select a diverse and representative set of models for virtual screening, rather than relying on a single "best" model, especially when active/inactive compound data is scarce [3].
FAQ 5: What are the best practices for creating a benchmark dataset to test my model's sensitivity and specificity?
A robust validation dataset is crucial for unbiased evaluation. Best practices include:
- Using established benchmark libraries like the Directory of Useful Decoys (DUD-e), which provides a curated set of active molecules and property-matched decoys for specific protein targets [1].
- Ensuring your dataset includes a diverse set of actives and decoys. Diversity can be assessed via chemical fingerprints (e.g., ECFP4) and clustering methods to avoid bias [3].
- Comparing the physicochemical properties (e.g., Molecular Weight, logP, Total Polar Surface Area) of the actives and decoys screened by your model using statistical tests like the Student's t-test. A good model will show no significant difference in these properties between the screened actives and decoys, indicating it is selecting actives based on pharmacophoric features rather than simple physicochemical properties [1].
Troubleshooting Guides
Issue 1: Low Sensitivity (Poor Recall of Known Actives)
Problem: Your pharmacophore model fails to retrieve a significant number of known active compounds during virtual screening.
| Possible Cause | Diagnostic Steps | Solution |
|---|---|---|
| Overly restrictive features | Check the fitness scores of known actives. If they are consistently just below the cutoff, the tolerance may be too tight. | Relax the distance and angle tolerances for key pharmacophore features. |
| Incorrect feature types | Re-evaluate the protein-ligand interaction patterns. Ensure critical features like metal coordination or halogen bonds are included if present. | Add missing essential pharmacophore features based on a detailed analysis of the binding site. |
| Excessive exclusion volumes | Temporarily disable exclusion volumes and re-run the screening. If sensitivity improves significantly, the volumes are too restrictive. | Strategically remove or reduce the radius of exclusion volumes that are not in direct conflict with the ligand binding mode. |
Issue 2: Low Specificity (High False Positive Rate)
Problem: Your model retrieves a large number of compounds, but most are confirmed to be inactive (decoys).
| Possible Cause | Diagnostic Steps | Solution |
|---|---|---|
| Too few defining features | Count the number of features in your model. A model with fewer than 3-4 features is often not selective enough. | Add more specific features from the binding site, such as a unique vector-based feature (e.g., hydrogen bond directionality). |
| Features are too generic | Analyze if features are located in common, non-specific regions of the binding site. | Incorporate rare or unique chemical features specific to your target, such as a cationic or anionic center. |
| Insufficient geometric constraints | The model may be matching features in the wrong spatial context. | Add exclusion volumes to define the shape of the binding pocket more accurately and prevent unrealistic matches. |
Experimental Protocols for Model Validation
Protocol 1: Validation Using the DUD-e Benchmark Set
Objective: To quantitatively assess the sensitivity and specificity of a pharmacophore model using a standardized dataset of actives and decoys.
- Dataset Preparation: Download the relevant target dataset (e.g., HIV-1 protease, acetylcholinesterase, cyclin-dependent kinase 2) from the DUD-e website [1].
- Pharmacophore Screening: Use your pharmacophore model as a query to screen the entire DUD-e dataset for your target in a virtual screening platform (e.g., Pharmit) [1].
- Result Analysis: From the screening results, count the number of true positives (TP, retrieved actives), false positives (FP, retrieved decoys), true negatives (TN, correctly rejected decoys), and false negatives (FN, missed actives).
- Metric Calculation:
- Sensitivity (Recall)= TP / (TP + FN)
- Specificity = TN / (TN + FP)
- Enrichment Factor (EF) = (TP / N) / (A / D), where N is the total number of compounds selected, A is the total number of actives in the database, and D is the total database size [1].
Protocol 2: Generating a Consensus Model from MD Simulations
Objective: To create a more robust and sensitive pharmacophore model by integrating information from molecular dynamics simulations.
- MD Simulation: Run a molecular dynamics simulation (e.g., 100-300 ns) of the protein-ligand complex using software like AMBER or GROMACS [3].
- Snapshot Extraction: Extract snapshots from the stabilized trajectory at regular intervals (e.g., every 1 ns).
- Pharmacophore Generation: For each snapshot, generate a structure-based pharmacophore model using software such as LigandScout [3].
- Model Consolidation: Instead of picking one model, use all models in a consensus screening approach, or use a tool like the Hierarchical Graph Representation (HGPM) to analyze the feature hierarchy and relationships, and then select a representative subset of models that capture the essential, persistent interactions for your virtual screening campaign [3].
Table 1: Performance Metrics of Pharmacophore Modeling Tools on DUD-e Benchmark
The following table summarizes typical performance metrics for various tools as reported in the literature, illustrating the trade-off between sensitivity and specificity [1].
| Tool / Method | Target (Family) | Sensitivity (Recall) | Specificity | Enrichment Factor (EF) |
|---|---|---|---|---|
| ELIXIR-A | HIVPR (Protease) | 0.85 | 0.92 | 25.4 |
| ELIXIR-A | ACES (Esterase) | 0.78 | 0.95 | 21.7 |
| ELIXIR-A | CDK2 (Kinase) | 0.81 | 0.89 | 19.5 |
| LigandScout | HIVPR (Protease) | 0.80 | 0.90 | 22.1 |
| Schrödinger Phase | HIVPR (Protease) | 0.82 | 0.88 | 20.8 |
Table 2: Key Research Reagent Solutions for Pharmacophore Modeling
This table lists essential software tools and datasets that function as key "research reagents" in this field [1] [2] [3].
| Item Name | Type | Function/Brief Explanation |
|---|---|---|
| DUD-e | Dataset | A benchmark database containing known active molecules and property-matched decoys for unbiased validation of virtual screening methods. |
| Pharmit | Software | An interactive online tool for pharmacophore-based and shape-based virtual screening of large compound libraries. |
| LigandScout | Software | A software application for creating structure-based and ligand-based pharmacophore models and performing virtual screening. |
| ELIXIR-A | Software | An open-source, Python-based pharmacophore refinement tool that helps unify interaction data from multiple pharmacophore models. |
| DiffPhore | Software | A knowledge-guided diffusion AI model that generates 3D ligand conformations to maximally map onto a given pharmacophore model. |
| CpxPhoreSet & LigPhoreSet | Dataset | High-quality datasets of 3D ligand-pharmacophore pairs used for training and refining AI-based pharmacophore models like DiffPhore. |
Workflow and Relationship Diagrams
Pharmacophore Validation Workflow
Sensitivity vs. Specificity Relationship
FAQ: Fundamental Concepts and Applications
Q1: What are the essential pharmacophoric features and their roles in molecular recognition? The four essential pharmacophoric features are Hydrogen Bond Donor (HBD), Hydrogen Bond Acceptor (HBA), Hydrophobic (H), and Aromatic (Ar). They represent the key steric and electronic features necessary for optimal supramolecular interactions with a biological target [4]. The table below details their roles.
Table 1: Essential Pharmacophoric Features and Their Functions in Molecular Recognition
| Feature | Abbreviation | Role in Molecular Recognition & Binding |
|---|---|---|
| Hydrogen Bond Donor | HBD | Forms a hydrogen bond by donating a hydrogen atom to a hydrogen bond acceptor on the target, often from groups like O-H or N-H [5]. |
| Hydrogen Bond Acceptor | HBA | Forms a hydrogen bond by accepting a hydrogen atom from a donor on the target, typically through electronegative atoms like oxygen or nitrogen [5] [6]. |
| Hydrophobic | H | Drives binding via van der Waals forces and the hydrophobic effect, often with non-polar aliphatic or aromatic regions of the target [5] [7]. |
| Aromatic | Ar | Engages in π-π stacking, cation-π, or polar-π interactions with aromatic residues in the binding pocket [5]. |
Q2: What is the difference between structure-based and ligand-based pharmacophore modeling? The choice of approach depends on the available input data [4].
- Structure-Based Pharmacophore Modeling: This method relies on the three-dimensional structure of a macromolecular target, often from sources like the Protein Data Bank (PDB). The model is generated by extracting the interaction pattern from a protein-ligand complex or by analyzing the topology of an empty binding site to define complementary features [8] [4].
- Ligand-Based Pharmacophore Modeling: This approach is used when the 3D structure of the target is unknown. It involves aligning the 3D structures of multiple known active molecules to identify the common pharmacophore features shared among them that are responsible for their biological activity [8] [4].
Q3: How can molecular dynamics (MD) simulations improve my pharmacophore model? Traditional structure-based models derived from a single crystal structure can be sensitive to the specific coordinates and may include transient features or miss others due to protein flexibility. MD simulations generate multiple snapshots of the protein-ligand complex over time, capturing its dynamic behavior. This information can be used to:
- Evaluate Feature Stability: Identify which pharmacophore features from the crystal structure are stable throughout the simulation and which appear only rarely (potentially as artifacts) [9].
- Create a Consensus Model: Derive a merged pharmacophore model that incorporates all features present in either the initial structure or any of the simulation snapshots, providing a more comprehensive representation of the binding interactions [9].
- Prioritize Features: The frequency with which a feature appears during the simulation can be used to rank its importance for inclusion in the final model [9].
Troubleshooting Guide: Sensitivity and Specificity
Table 2: Common Issues and Solutions in Pharmacophore Model Optimization
| Problem | Potential Causes | Solutions & Troubleshooting Steps |
|---|---|---|
| Low Sensitivity (Poor recall of known actives) | Model is too restrictive; features are too specific or numerous. | 1. Review Feature Selection: Define some features as "optional" in your pharmacophore query.2. Adjust Tolerances: Slightly increase the radius (tolerance) of feature spheres.3. Reduce Features: Remove features that are not critical for binding, especially those with low stability in MD simulations [9]. |
| Low Specificity (High recall of decoys/inactives) | Model is too permissive; lacks essential discriminatory features. | 1. Add Critical Features: Incorporate a key interaction proven by mutagenesis studies or present in all highly active ligands.2. Use Exclusion Volumes: Add exclusion volumes (XVols) to represent the protein's steric constraints and prevent the mapping of clashing compounds [8] [4].3. Refine Geometry: Adjust the spatial arrangement of features to better match the bioactive conformation. |
| Model fails to identify novel active chemotypes | Model may be over-fitted to the chemical scaffold of the training set. | 1. Use Diverse Training Set: For ligand-based models, ensure the training set contains structurally diverse molecules with a common binding mode [8].2. Employ a Structure-Based Approach: If possible, create a model directly from the protein-ligand complex to abstract away from specific ligand scaffolds [8]. |
Experimental Protocols for Model Validation
Protocol: Validation of a Pharmacophore Model Using a Decoy Set This protocol is essential for evaluating the performance of a pharmacophore model before its use in prospective virtual screening [10].
Prepare Validation Sets:
- Actives: Compile a set of known active compounds for your target. The direct interaction should be experimentally proven (e.g., by receptor binding or enzyme activity assays). Cell-based assay data should be avoided due to confounding factors like pharmacokinetics [8]. Public repositories like ChEMBL [8] are excellent sources.
- Decoys: Obtain a set of decoy molecules (assumed inactives) with similar 1D properties (e.g., molecular weight, logP, number of HBD/HBA) but different 2D topologies compared to the actives. The DUD-E website (http://dude.docking.org) can automatically generate optimized decoys for your active set [8] [10]. A ratio of 50 decoys per active is recommended [8].
Perform Virtual Screening:
- Screen the combined library of actives and decoys using your pharmacophore model as a query.
Calculate Validation Metrics:
- Analyze the screening results to calculate the following key metrics [8] [10]:
- Sensitivity (True Positive Rate) = (Ha / A) × 100
- Ha: Number of active compounds retrieved (hits).
- A: Total number of active compounds in the database.
- Specificity = (1 - (Hd / D)) × 100
- Hd: Number of decoy compounds retrieved.
- D: Total number of decoy compounds in the database.
- Enrichment Factor (EF): Measures how much better the model is at identifying actives compared to random selection [8].
- Goodness of Hit (GH) Score: A composite metric that balances the recall of actives with the false positive rate [10].
- Sensitivity (True Positive Rate) = (Ha / A) × 100
- Analyze the screening results to calculate the following key metrics [8] [10]:
Protocol: Assessing Pharmacophore Feature Stability via MD Simulations This protocol helps refine a structure-based pharmacophore by incorporating protein-ligand dynamics [9].
System Setup:
- Start with the high-resolution protein-ligand complex structure (e.g., from PDB).
- Solvate the complex in a water box, add counterions to neutralize the system, and assign appropriate force field parameters to both the protein and the ligand.
Simulation and Analysis:
- Run an all-atom molecular dynamics simulation (e.g., for 20-200 ns, depending on the system) [9] [5].
- Save snapshots of the trajectory at regular intervals (e.g., every 100 ps).
- For each saved snapshot, generate a structure-based pharmacophore model.
- Create a merged pharmacophore model that contains every unique feature observed in the initial crystal structure and across all analyzed snapshots.
Feature Prioritization:
- Calculate the frequency of occurrence for each pharmacophore feature across the entire simulation trajectory.
- Use this frequency data to rank features. Features present in the crystal structure but with a low occurrence frequency (<10%) during the simulation may be artifacts and considered for removal. Conversely, features that consistently appear (>90%) are likely critical for binding [9].
Key Research Reagents and Computational Tools
Table 3: Essential Resources for Pharmacophore Modeling and Validation
| Resource/Solution | Type | Function & Application in Research |
|---|---|---|
| Protein Data Bank (PDB) | Database | Primary repository for experimentally determined 3D structures of proteins and nucleic acids, serving as the foundational input for structure-based pharmacophore modeling [8] [4]. |
| ChEMBL / DrugBank | Database | Public compound repositories providing curated bioactivity data (e.g., IC50, Ki) for known active molecules, essential for building ligand training sets and validation decoy sets [8]. |
| DUD-E (Directory of Useful Decoys, Enhanced) | Online Tool | Generates optimized decoy molecules for a given list of actives, which are crucial for the theoretical validation of pharmacophore models to avoid over-optimistic performance estimates [8] [10]. |
| LigandScout | Software | A leading program for both structure-based and ligand-based pharmacophore model generation, analysis, and virtual screening [9] [5]. |
| ZINCPharmer / Pharmit | Online Tool | Web-based platforms that allow for the virtual screening of large chemical libraries (e.g., ZINC) using a pharmacophore model as a query [10] [5]. |
| Molecular Dynamics Software (e.g., GROMACS, AMBER) | Software | Packages used to run MD simulations to assess the stability of pharmacophore features and incorporate protein flexibility into the models [11] [9] [10]. |
Workflow and Relationship Visualizations
Diagram 1: Pharmacophore Model Development and Optimization Workflow
Diagram 2: Relationship Between Core Features and Optimization Strategies
The Impact of Exclusion Volumes (XVols) on Model Selectivity
Frequently Asked Questions (FAQs)
1. What are Exclusion Volumes (XVols) and what is their primary function? Exclusion Volumes (XVols) are steric constraints in a pharmacophore model that represent regions in the binding pocket occupied by the protein structure itself. Their primary function is to prevent the mapping of compounds that would be inactive due to steric clashes with the protein surface, thereby improving the model's selectivity [4] [8].
2. How do XVols improve the results of a virtual screening? By simulating the physical boundaries of the binding site, XVols filter out molecules whose atoms would occupy forbidden space. This enhances the "enrichment factor" – the model's ability to prioritize active compounds over inactive ones – and increases the hit rate of prospective virtual screening campaigns, which can typically range from 5% to 40% [8] [12].
3. When should I consider manually adding or removing XVols? Manual adjustment is crucial when the automated placement of XVols is insufficient. This includes refining the model based on a deeper analysis of the binding site residues to better represent its shape, or deleting automatically generated XVols that might be too restrictive and incorrectly exclude potentially active compounds with slightly different binding modes [13] [14].
4. Can a model with too many XVols be detrimental? Yes. An excessive number of XVols can make a model overly restrictive, leading to an undesirable drop in sensitivity. An overtuned model might incorrectly reject true active compounds, a problem known as "over-fitting." The goal is to balance selectivity (finding actives) with sensitivity (not missing actives) [14].
Troubleshooting Guides
Problem: Poor Selectivity – Model Retrieves Too Many Inactive Compounds
- Symptoms: Virtual screening hit lists are large, but the experimentally confirmed hit rate is very low. The model retrieves compounds that fit the feature pattern but are sterically incompatible with the target.
- Potential Causes & Solutions:
- Cause 1: Missing or insufficient exclusion volume definition.
- Solution: Generate a receptor-based excluded volumes shell. Most modern pharmacophore modeling software (e.g., Schrödinger's Phase, LigandScout) can automatically add XVols based on the 3D protein structure [13].
- Cause 2: XVols are too small or their tolerance is too high.
- Cause 1: Missing or insufficient exclusion volume definition.
Problem: Over-Restrictive Model – Model Misses Known Active Compounds
- Symptoms: The model fails to recognize known active compounds from a validation test set, or virtual screening returns an exceptionally small number of hits.
- Potential Causes & Solutions:
- Cause 1: Excessively large or inaccurately placed XVols.
- Solution: Systematically review and remove XVols that are not critical for defining the binding site's steric constraints. Focus on preserving XVols that correspond to backbone atoms or large, inflexible side chains [14].
- Cause 2: The model does not account for protein flexibility or minor ligand adjustments.
- Solution: Slightly reduce the radius of XVols in areas where side chains are known to have some rotational freedom. Use multiple protein conformations (e.g., from molecular dynamics simulations) to create a more averaged XVols definition [15].
- Cause 1: Excessively large or inaccurately placed XVols.
Problem: Inconsistent Performance Across Different Software
- Symptoms: A model validated in one software platform performs poorly when used for screening in another.
- Potential Causes & Solutions:
- Cause: Differences in how software algorithms handle the matching of compounds against XVols and other pharmacophore features.
- Solution: When comparing tools, ensure you understand their specific parameters for XVols tolerance. Standardize your validation protocol using a robust dataset of known active and inactive compounds to calibrate the model's performance in each software environment [16].
- Cause: Differences in how software algorithms handle the matching of compounds against XVols and other pharmacophore features.
Experimental Protocol: Optimizing XVols for Model Selectivity
The following protocol outlines a systematic method for integrating and refining XVols to maximize pharmacophore model selectivity, suitable for inclusion in a thesis methodology section.
1. Objective To construct a high-selectivity pharmacophore model by incorporating exclusion volumes (XVols) that accurately represent the steric constraints of the target protein's binding pocket.
2. Materials and Software Requirements Table: Essential Research Reagents and Solutions
| Item | Function in Protocol |
|---|---|
| Protein Data Bank (PDB) Structure | Source of the 3D atomic coordinates of the target protein, used to define the binding site and generate XVols [4]. |
| Pharmacophore Modeling Software (e.g., Schrödinger Phase, LigandScout) | Platform for hypothesis generation, manual manipulation of XVols, and performing virtual screening [13] [17]. |
| Validation Dataset (Active & Inactive Compounds/Decoys) | A pre-compiled set of molecules for theoretically assessing model quality by calculating enrichment factors and other metrics [8] [12]. |
| Directory of Useful Decoys, Enhanced (DUD-E) | Online resource for generating optimized decoy molecules with similar 1D properties but different 2D topologies compared to active molecules, used for rigorous validation [8]. |
3. Step-by-Step Methodology
Step 1: Initial Structure Preparation
- Obtain the 3D structure of your target, preferably from the PDB.
- Prepare the protein structure using a standard protein preparation workflow. This includes adding hydrogen atoms, assigning correct protonation states, and filling in missing side chains or loops [13].
Step 2: Generate a Preliminary Pharmacophore Model with XVols
- Using the prepared structure, create a structure-based pharmacophore model. If a co-crystallized ligand is present, an e-Pharmacophore method is recommended.
- In the hypothesis settings, select the option to "Create receptor-based excluded volumes shell" [13]. This will automatically populate the binding site with XVols.
Step 3: Theoretical Validation and Benchmarking
- Screen the validation dataset (containing known actives and inactives/decoys) against the initial model.
- Calculate key performance metrics:
- Record these baseline metrics for the model with automatically generated XVols.
Step 4: Manual Refinement of XVols
- Visually inspect the binding site and the generated XVols. Pay close attention to residues with flexible side chains.
- Use the software's "Manage Excluded Volumes" tool to:
- Add XVols: For critical atoms or residues that are not adequately covered, add XVols manually by selecting the specific atoms [13].
- Remove XVols: Delete XVols that are likely to be too restrictive, for example, in areas where small conformational changes could accommodate a ligand.
- The goal is to create a definition that closely matches the physical shape of the binding pocket without being overly rigid.
Step 5: Post-Refinement Validation and Iteration
- Re-run the virtual screening of the validation dataset using the refined model.
- Re-calculate the performance metrics (EF, Yield, Specificity).
- Iterate Step 4 until the model shows a strong balance, achieving high enrichment of actives while effectively excluding inactives. A successful refinement should show a significant increase in the Enrichment Factor [12].
Workflow Visualization
The following diagram illustrates the logical workflow for optimizing exclusion volumes.
Quantitative Impact of XVol Refinement
The table below summarizes real-world data from published studies demonstrating the performance improvement achieved through the systematic refinement of exclusion volumes.
Table: Impact of XVol Refinement on Model Selectivity in Published Studies
| Study Context | Model Version | Number of XVols | Active Compounds Found | Inactive/Decoys Found | Enrichment Factor (EF) | Reference |
|---|---|---|---|---|---|---|
| IKK-β Inhibitor Discovery | Initial Model (Hypo1) | Not Specified | 34 (27.4%) | 197 | 15.7 | [12] |
| Refined with XVols (Hypo1-R1) | Not Specified | 33 (26.6%) | 116 | 23.2 | [12] | |
| Refined with XVols & Shape (Hypo1-R1-S1) | Not Specified | 31 (25.0%) | 94 | 25.8 | [12] | |
| 17β-HSD2 Inhibitor Discovery | Model 1 | 54 | 8 Actives | 0 Inactives | Not Reported | [14] |
| Model 2 | Not Specified | 8 Actives | 0 Inactives | Not Reported | [14] | |
| Model 3 | 56 | 6 Actives | 0 Inactives | Not Reported | [14] |
Core Concepts and Sensitivity Profiles
The choice between structure-based and ligand-based drug design methodologies is fundamental, as each possesses distinct sensitivities, applicability domains, and performance characteristics. Understanding these differences is critical for parameter optimization and reliable model development.
Table 1: Core Characteristics and Sensitivities of Drug Design Approaches
| Feature | Structure-Based Drug Design (SBDD) | Ligand-Based Drug Design (LBDD) |
|---|---|---|
| Primary Data | 3D structure of the protein target (e.g., from X-ray, Cryo-EM, NMR) [18] [19] | Known active and inactive ligand molecules and their properties [20] [18] |
| Key Techniques | Molecular docking, Molecular Dynamics (MD), Free Energy Perturbation (FEP) [20] [18] | Quantitative Structure-Activity Relationship (QSAR), Pharmacophore modeling, Molecular similarity search [20] [18] [21] |
| Sensitivity to Data Scarcity | Less sensitive; can be applied to novel targets with little/no known ligands if a structure is available [22] | Highly sensitive; requires a sufficient number of known active compounds for model training [22] [18] |
| Sensitivity to Novel Chemotypes | Lower sensitivity; can, in principle, generate and identify novel chemotypes outside known ligand space [22] [23] | High sensitivity; models are biased towards chemical space similar to the training data, limiting novelty [22] [23] |
| Sensitivity to Protein Flexibility | Highly sensitive; static protein structures may not represent dynamic binding events [20] [18] | Not directly sensitive; implicitly captures some effects via ligand structure-activity data [20] |
| Key Sensitivity Advantage | Exploits physical principles of binding, enabling exploration of unprecedented chemistry [22] [24] | High throughput and efficiency when ample ligand data is available; excels at pattern recognition [18] [25] |
| Key Sensitivity Limitation | Accuracy depends heavily on the quality and relevance of the protein structure and scoring functions [20] [18] | Limited applicability domain; poor extrapolation to chemotypes not represented in training set [22] [18] |
Frequently Asked Questions (FAQs) and Troubleshooting
FAQ 1: My structure-based docking campaign is producing poor results. The poses look incorrect, and the scoring does not correlate with experimental activity. What are the primary parameters to optimize?
This is a common issue often rooted in the simplifications of the docking process.
Problem: Inadequate Protein Structure Preparation.
- Troubleshooting Guide: The input protein structure is critical.
- Check Protonation States: Ensure key residues (e.g., His, Asp, Glu) in the binding site have correct protonation states at physiological pH.
- Add Missing Residues: Homology models or structures with poor electron density may have missing loops or side chains that affect the pocket.
- Consider Protein Flexibility: A single rigid protein structure may not be representative. If available, use an ensemble of protein conformations (from multiple crystal structures, MD simulations, or conformational sampling) for docking to account for binding site flexibility [20] [18].
- Handle Water Molecules: Decide on the role of key water molecules in the binding site. Test docking protocols that both include (as part of the protein) and exclude specific, conserved water molecules [20].
- Troubleshooting Guide: The input protein structure is critical.
Problem: Limitations of the Scoring Function.
- Troubleshooting Guide: Scoring functions are approximations and have known limitations.
- Use Consensus Scoring: Combine rankings from multiple, different scoring functions to improve the reliability of hit identification [20] [25].
- Rescore with Advanced Methods: Take top-ranked docking poses and rescore them using more rigorous, but computationally expensive, methods like Free Energy Perturbation (FEP) or MM/GBSA [20] [18].
- Validate Your Protocol: Always perform a control docking with a known native ligand or a well-characterized inhibitor to verify that your protocol can reproduce the correct binding mode (pose validation) and rank it favorably (scoring validation) [18].
- Troubleshooting Guide: Scoring functions are approximations and have known limitations.
FAQ 2: My ligand-based QSAR model performs well on the training set but fails to predict the activity of new compound series. How can I improve its generalizability and sensitivity to novel scaffolds?
This indicates a classic case of overfitting and a model that has not learned the underlying structure-activity relationship (SAR) but has instead memorized the training data.
- Problem: Overfitting and Limited Applicability Domain.
- Troubleshooting Guide:
- Simplify the Model: Reduce the number of molecular descriptors. Use feature selection algorithms (e.g., genetic algorithms, stepwise regression) to retain only the most statistically significant and meaningful descriptors [21].
- Define the Applicability Domain: Explicitly define the chemical space where your model can make reliable predictions. This can be based on the ranges of descriptors in the training set. Flag new compounds that fall outside this domain as "unreliable" [22] [18].
- Incorporate 3D Information: If possible, move from 2D-QSAR to 3D-QSAR (e.g., CoMFA, CoMSIA). 3D-QSAR models, particularly those grounded in physics-based representations, can sometimes generalize better across diverse ligands [18].
- Data Augmentation: Incorporate data on inactive or weakly active compounds to help the model learn what features are detrimental to activity, improving its discriminatory power [20].
- Troubleshooting Guide:
FAQ 3: I have some ligand data and a protein structure. How can I combine these approaches to mitigate the sensitivity limitations of each?
A hybrid approach is often the most powerful strategy, leveraging the strengths of both methods to compensate for their individual weaknesses [20] [18] [25].
- Problem: Isolating SBDD or LBDD approaches leads to missed opportunities or high false-positive rates.
- Troubleshooting Guide: Implement a sequential or parallel workflow.
- Sequential Filtering: This is highly efficient. First, use a fast ligand-based method (e.g., 2D similarity or a QSAR model) to screen a massive virtual library and reduce it to a manageable size. Then, apply more computationally intensive structure-based methods (docking, FEP) to this pre-filtered set [18] [25]. This saves resources while applying the most powerful tools to the most promising candidates.
- Parallel Screening with Consensus: Run both ligand-based and structure-based virtual screens independently on the same compound library. You can then either:
- Take the union of the top-ranked compounds from each list to maximize the chance of finding actives (increasing sensitivity), or
- Take the intersection of the top-ranked compounds to increase confidence in the selection (increasing specificity) [25].
- Structure-Based Pharmacophore: Generate a pharmacophore model based on key interactions observed in the protein's binding site (e.g., from a crystal structure or a docked potent ligand). This pharmacophore, which embodies structure-based information, can then be used as a query for high-throughput ligand-based screening [24].
- Troubleshooting Guide: Implement a sequential or parallel workflow.
Detailed Experimental Protocols
Protocol 1: Structure-Based Virtual Screening using Molecular Docking
This protocol is used to computationally screen large compound libraries against a known protein structure to identify potential hits [20] [18].
- Objective: To identify novel small molecules that bind to a specific target protein with high predicted affinity, focusing on optimizing docking parameters for sensitivity.
Materials:
- Protein Structure: High-resolution (preferably < 2.5 Å) 3D structure from PDB (e.g., PDB ID: 7ONS for PARP1 [24]).
- Compound Library: Database of small molecules in a ready-to-dock format (e.g., SDF, MOL2).
- Software: Docking software (e.g., Glide [22], AutoDock, GOLD).
- Computing Hardware: High-performance computing (HPC) cluster or cloud computing resources.
Step-by-Step Methodology:
- Protein Preparation:
- Obtain the protein structure from the PDB. Remove any non-essential water molecules, ions, and original ligands.
- Add hydrogen atoms and assign correct protonation states to residues in the binding site using a tool like Epik or PROPKA.
- Energy minimize the protein structure to relieve any steric clashes introduced during preparation.
- Binding Site Grid Generation:
- Define the coordinates and dimensions of the binding site cavity for docking. This is typically centered on a known co-crystallized ligand or a key residue.
- Generate a grid file that the docking program will use to evaluate ligand interactions.
- Ligand Library Preparation:
- Prepare the ligand library by generating plausible 3D conformations for each molecule.
- Assign correct bond orders, charges, and protonation states at physiological pH (e.g., using LigPrep or MOE).
- Molecular Docking:
- Run the docking calculation using a validated protocol. For initial screening, standard precision (SP) mode is often used.
- Ensure the protocol is validated by re-docking the native ligand and confirming it reproduces the crystallographic pose (Root-Mean-Square Deviation, RMSD < 2.0 Å).
- Post-Docking Analysis:
- Analyze the top-ranking compounds based on docking score. Visually inspect the predicted binding poses to check for sensible interactions (e.g., hydrogen bonds, hydrophobic contacts, salt bridges).
- Apply post-docking filters, such as ADMET property prediction or interaction with key residues, to further prioritize hits.
- Protein Preparation:
Table 2: Key Research Reagent Solutions for SBDD
| Reagent / Resource | Function / Description | Example / Source |
|---|---|---|
| Protein Structure | Provides the 3D atomic coordinates of the target for docking and analysis. | Protein Data Bank (PDB) [19] |
| Homology Model | A computationally predicted 3D protein model used when an experimental structure is unavailable. | AlphaFold2, MODELLER [18] |
| Virtual Compound Library | A digital collection of compounds for in silico screening. | ZINC, ChEMBL, in-house corporate libraries [24] |
| Docking Software | Algorithm that predicts the bound pose and scores the binding affinity of a ligand. | Glide, AutoDock Vina, GOLD [22] [20] |
| Molecular Dynamics Software | Simulates the physical movements of atoms and molecules over time to study dynamics. | GROMACS, AMBER, Desmond [18] |
Protocol 2: Developing a 3D-QSAR Model using Comparative Molecular Field Analysis (CoMFA)
This protocol describes the creation of a 3D-QSAR model to understand the relationship between the molecular fields of a set of ligands and their biological activity [21].
- Objective: To build a predictive 3D-QSAR model that identifies steric and electrostatic features critical for biological activity, optimizing for model robustness and predictive power.
- Materials:
- Dataset: A series of molecules with known biological activities (e.g., IC50, Ki). A minimum of 20-30 compounds is typically required.
- Software: 3D-QSAR software (e.g., SYBYL, MOE, Open3DQSAR).
- Step-by-Step Methodology:
- Ligand Preparation and Alignment:
- This is the most critical step. Generate low-energy 3D conformations for all molecules in the dataset.
- Align the molecules to a common template or using a pharmacophore hypothesis. The alignment should reflect a presumed consistent binding mode to the target.
- Field Calculation:
- Place the aligned molecules inside a 3D grid.
- Calculate steric (Lennard-Jones) and electrostatic (Coulombic) interaction energies between a probe atom and each molecule at every grid point.
- Partial Least Squares (PLS) Analysis:
- The calculated field values (independent variables) are correlated with the biological activity data (dependent variable) using PLS regression.
- The dataset is split into a training set (to build the model) and a test set (to validate it).
- Model Validation:
- Assess the model using the cross-validated correlation coefficient (q²) from the training set. A q² > 0.5 is generally considered acceptable.
- Use the external test set to calculate the predictive correlation coefficient (r²_pred), which is the true measure of the model's predictive power [21].
- Model Interpretation:
- Visualize the results as 3D coefficient contour maps. These maps show regions where specific steric or electrostatic features are favorable or unfavorable for activity, providing a visual guide for molecular design.
- Ligand Preparation and Alignment:
Workflow and Pathway Visualizations
Diagram 1: Decision Workflow for Model Selection
Diagram 2: Sequential LB-SB Screening Workflow
Frequently Asked Questions
1. What constitutes a high-quality training set for pharmacophore model development? A high-quality training set is a balanced collection of confirmed active and inactive compounds, alongside carefully selected decoy molecules that act as negative controls. The actives should be diverse, ideally representing multiple chemical scaffolds, to prevent the model from learning narrow, scaffold-specific patterns instead of the fundamental pharmacophore [26] [27]. Inactives provide direct negative feedback, while decoys, which are property-matched to actives but are structurally distinct, help assess the model's ability to discriminate true binders from non-binders in virtual screening [28] [29].
2. My pharmacophore model has high enrichment in training but performs poorly in validation. What could be wrong? This is a classic sign of overfitting. Common causes include:
- Insufficient Data: The training set is too small or lacks chemical diversity [27].
- Data Leakage: The validation set contains compounds that are structurally too similar to those in the training set. To avoid this, split your data based on molecular scaffolds to ensure the model is validated on genuinely novel chemotypes [27].
- Inadequate Decoys: Using random compounds as decoys can make screening too easy and give a false sense of model accuracy. Decoys should be matched to actives in terms of molecular weight and other physicochemical properties to provide a rigorous test [28].
3. How can I generate meaningful decoy molecules for my target? Utilize established public databases like DUD-E (Directory of Useful Decoys: Enhanced) and its optimized version DUDE-Z [28]. These resources provide pre-generated decoys that are matched to known actives for a wide range of targets, ensuring they have similar physical properties (making them hard to distinguish based on simple filters) but different 2D topologies (making them unlikely to bind) [28] [29]. This approach is considered a best practice for benchmarking.
4. Why is sensitivity analysis important for my pharmacophore model's parameters? Sensitivity analysis helps you understand which model parameters (e.g., feature tolerances, weights) have the most significant impact on your output (e.g., enrichment factor) [30] [31]. This allows you to:
- Focus Optimization: Identify and prioritize the tuning of the most sensitive parameters, making the calibration process more efficient [31].
- Improve Robustness: Analyze how uncertainty or variability in input parameters affects model predictions, leading to more reliable and interpretable models [32] [30].
Troubleshooting Guides
Problem: Poor Virtual Screening Performance and Low Hit Rates
Issue: Your pharmacophore model fails to enrich active compounds at the top of a virtual screening ranking list.
Diagnosis and Solution:
| Step | Action | Rationale & Details |
|---|---|---|
| 1 | Audit Training Set Composition | Ensure actives cover multiple chemical series. Use Bemis-Murcko scaffold analysis to confirm diversity. A cluster of similar ligands will lead to overfitted, non-generalizable models [2] [27]. |
| 2 | Validate with Rigorous Decoys | Test model performance on a benchmark set with property-matched decoys from DUDE-Z. Low enrichment indicates poor discriminatory power, likely due to a non-robust training set [28]. |
| 3 | Apply a Sensitivity Analysis | Perform a global sensitivity analysis (GSA) to identify which pharmacophore features most influence screening outcome. Methods like Sobol' or Morris can quantify each parameter's contribution [32] [30]. |
| 4 | Optimize Critical Parameters | Use the results of the sensitivity analysis to guide parameter optimization. Techniques like Markov Chain Monte Carlo (MCMC) can be used to find the parameter set that maximizes your performance metric [31]. |
Problem: Model Fails to Generalize to New Scaffolds
Issue: The model successfully identifies actives similar to those in the training set but misses actives with novel core structures.
Diagnosis and Solution:
| Step | Action | Rationale & Details |
|---|---|---|
| 1 | Re-split Your Data | Implement a scaffold-based split for training and validation. This ensures the model is tested on chemotypes it has never seen, providing a true measure of its generalizability [27]. |
| 2 | Incorporate Inactive Compounds | Include confirmed inactive compounds in the training set. This provides the model with explicit negative examples, helping it learn which interaction patterns are not conducive to binding and refining the essential pharmacophore pattern [27]. |
| 3 | Utilize Ensemble and AI Methods | Consider advanced approaches like dyphAI, which combines multiple pharmacophore models from different ligand complexes and clusters into an ensemble. This captures a broader range of valid protein-ligand interactions and conformational dynamics [26]. Alternatively, AI methods like PharmRL use reinforcement learning to elucidate optimal pharmacophores directly from protein structures, reducing reliance on a limited set of known ligands [29]. |
Experimental Protocols for Data Set Construction and Validation
Protocol 1: Building a Robust Training Set for QSAR-Based Pharmacophore Modeling
This protocol is adapted from studies developing QSAR models for targets like Estrogen Receptor beta and Monoamine Oxidase (MAO) [33] [27].
Key Research Reagent Solutions:
| Item | Function in the Protocol |
|---|---|
| ChEMBL / BindingDB | Public databases to source bioactivity data (IC₅₀, Ki) for known active and inactive compounds [26] [27]. |
| Schrödinger Canvas / RDKit | Software tools for calculating molecular fingerprints and performing similarity clustering and Bemis-Murcko scaffold analysis [26] [27]. |
| DUD-E / DUDE-Z | Databases of property-matched decoys for rigorous virtual screening benchmarking [28] [29]. |
| ZINC Database | A public database of commercially available compounds that can be used for prospective virtual screening [26] [2]. |
Methodology:
- Data Curation: Extract compounds with reported activity (e.g., IC₅₀ ≤ 199,000 nM for actives) and explicit inactivity from reliable databases like ChEMBL or the Binding Database [26] [27].
- Structure Preparation: Generate 3D structures for all compounds using a tool like LigPrep (Schrödinger) at a physiological pH of 7.4 ± 0.2 [26].
- Clustering for Diversity: Perform structural similarity clustering using radial fingerprints and the Tanimoto metric. Determine the optimal number of clusters to balance over- and under-clustering. This ensures the final training set contains representative molecules from diverse chemical classes [26].
- Train-Test Split: Partition the data into training and test sets using a scaffold-based splitting method. This guarantees that the model is validated on chemically distinct scaffolds, providing a true test of its generalizability and pharmacophore hypothesis [27].
Protocol 2: Global Sensitivity Analysis for Pharmacophore Model Parameter Optimization
This protocol is informed by sensitivity analyses conducted in PBPK modeling and ecological model calibration [32] [31].
Methodology:
- Define Model Output: Select a key performance metric as your model output, such as Enrichment Factor (EF₁%) or the Area Under the Curve (AUC) of a receiver operating characteristic (ROC) plot.
- Identify Input Parameters: List all variable pharmacophore parameters (e.g., feature tolerances, weights, exclusion sphere radii).
- Assign Probability Distributions: Define a plausible range and distribution (e.g., uniform, normal) for each input parameter [32].
- Generate Parameter Sets: Use a sampling method (e.g., Latin Hypercube Sampling) to generate a large number of parameter sets from the defined distributions.
- Run and Analyze: Execute your pharmacophore screening for each parameter set and record the output metric. A variance-based method like Sobol' analysis can then be applied to decompose the output variance and compute sensitivity indices (Si). These indices quantify the relative contribution of each parameter (and their interactions) to the model's performance [32].
The diagram below illustrates the logical workflow of this protocol.
Diagram 1: Workflow for Global Sensitivity Analysis (GSA) in parameter optimization.
Workflow Visualization: From Data Curation to Validated Model
The following diagram summarizes the complete integrated workflow for developing a sensitive and generalizable pharmacophore model, emphasizing the critical role of high-quality training data and parameter optimization.
Diagram 2: Integrated workflow for developing a validated pharmacophore model.
Advanced Techniques for High-Sensitivity Pharmacophore Modeling
Frequently Asked Questions (FAQs)
FAQ 1: Why does my pharmacophore model perform poorly when using an AlphaFold-predicted protein structure? AlphaFold-predicted structures often represent an "apo" or unbound protein conformation, which may have binding pockets that are structurally different from the "holo" conformation adopted when a ligand is bound. Key side chains might be in unfavorable rotamer configurations, making the binding pocket appear inaccessible or incorrectly shaped for your ligand [34]. Using a dynamic docking method that can adjust the protein conformation, or sourcing a holo-structure from a high-quality curated dataset, is recommended.
FAQ 2: What are the main advantages of cryo-EM in structure-based drug design, and what are its key challenges? Cryo-electron microscopy (cryo-EM) allows you to determine the structures of large protein complexes and membrane proteins that are difficult to crystallize. A major benefit is the ability to capture multiple conformational states of a protein in a near-native environment, which is invaluable for designing drugs that target specific protein states [35]. The primary challenges involve sample preparation, which can be an iterative and time-consuming process due to issues like protein denaturation at the air-water interface. It also requires significant investment in infrastructure and specialized training for staff [35].
FAQ 3: How can I improve the selection of scoring functions for my virtual screening campaign? Instead of relying on a single scoring function, use a consensus scoring approach. The performance of individual scoring functions can be highly dependent on the target protein [36]. To enhance results, employ a feature selection-based consensus scoring (FSCS) method. This supervised approach uses docked native ligand conformations to select a set of complementary scoring functions, which has been shown to improve the enrichment of active compounds compared to using individual functions or rank-by-rank consensus [36].
FAQ 4: My ligand poses have high steric clashes when docked into a predicted structure. How can I resolve this? Significant clashes often occur when a rigid docking protocol is used on a protein structure that is not in a ligand-compatible state. Traditional docking methods that treat the protein as rigid are particularly prone to this [34]. Consider using a "dynamic docking" method that allows for side-chain and, in some cases, backbone adjustments upon ligand binding. Alternatively, using molecular dynamics simulations for conformational sampling can help, though this is computationally demanding [34].
FAQ 5: What can I do if my target protein has no experimentally determined structure? You have several options. The primary method is to use a deep learning-based protein structure prediction tool like AlphaFold to generate a reliable model [34] [37]. If a homologous structure exists, you can perform homology modeling [38] [37]. For an end-to-end solution that does not require a separate protein structure, emerging deep generative models can predict the protein-ligand complex structure directly from the protein sequence and ligand molecular graph [39].
Troubleshooting Guides
Troubleshooting Low-Accuracy Ligand Posing
Symptoms: Predicted ligand binding poses consistently show a high root-mean-square deviation (RMSD) when compared to a known experimental structure.
| Potential Cause | Diagnostic Steps | Recommended Solution |
|---|---|---|
| Rigid Protein Backbone | Check if your initial protein structure (e.g., from AlphaFold) has a high pocket RMSD compared to the holo reference. | Implement a dynamic docking tool like DynamicBind, which can accommodate large conformational changes in the protein from its initial state [34]. |
| Incorrect Protonation/Tautomer State | Visually inspect the ligand's functional groups in the binding site. Use software to calculate probable protonation states at physiological pH. | Use a ligand-fixing module (e.g., within the HiQBind-WF workflow) to ensure correct bond order, protonation states, and aromaticity before docking [40]. |
| Poor Quality Input Structure | Review the source of your protein structure. Check for missing residues, atoms, or severe steric clashes in the binding pocket. | Use a structure refinement workflow (e.g., HiQBind-WF) to add missing atoms and resolve clashes. Prefer high-resolution experimental structures or high-quality curated models [40]. |
| Insufficient Sampling | Check if the docking software provides multiple pose predictions and if they are all similarly inaccurate. | Increase the exhaustiveness or number of sampling runs in your docking software. For generative models, generate a larger number of candidate structures (e.g., several dozen) to improve the chance of sampling a correct pose [39]. |
Troubleshooting Feature Selection for Scoring
Symptoms: Your virtual screening fails to enrich active compounds, or the ranking of compounds by predicted affinity does not correlate with experimental data.
| Potential Cause | Diagnostic Steps | Recommended Solution |
|---|---|---|
| Target-Dependent Scoring Performance | Test individual scoring functions on a small set of known active and inactive compounds for your specific target. | Adopt a feature selection-based consensus scoring (FSCS) strategy. Use a known active ligand to select a complementary set of scoring functions before running the full screen [36]. |
| Training Data Artifacts | If using a machine learning scoring function, investigate the dataset it was trained on for known errors or biases. | Consider retraining models with a high-quality, curated dataset like HiQBind, which aims to correct structural errors and improve annotation reliability [40]. |
| Inadequate Interaction Descriptors | Analyze which molecular features (e.g., hydrogen bonds, hydrophobic contacts) are important for binding in your target. | Ensure your feature set comprehensively captures the key interactions. Use a docking program that provides a wide array of intermolecular interaction features for post-docking analysis. |
Troubleshooting Protein Structure Preparation
Symptoms: Docking or pharmacophore generation fails, or results contain unrealistic atomic distances and clashes.
| Potential Cause | Diagnostic Steps | Recommended Solution |
|---|---|---|
| Missing Heavy Atoms or Residues | Visually inspect the binding site in software like PyMol. Check the PDB file for "REMARK" sections noting missing residues. | Use a protein-fixing module (e.g., ProteinFixer in HiQBind-WF) to add missing atoms and residues in the binding site region [40]. |
| Incorrect Hydrogen Placement | Check for unrealistic bond lengths or angles involving hydrogen atoms. | Use a refinement tool that adds hydrogens to the protein and ligand in their complexed state, followed by constrained energy minimization to optimize hydrogen positions [40]. |
| Untreated Flexibility | Identify flexible loops or side chains in the binding site that could move to accommodate the ligand. | If using rigid docking, consider generating an ensemble of protein conformations from molecular dynamics simulations or using a flexible docking algorithm. |
Experimental Protocols & Data Presentation
Key Research Reagent Solutions
The following table details essential resources for conducting structure-based drug discovery, as featured in the cited research.
| Item Name | Function / Description | Example Use Case in Research |
|---|---|---|
| PDBbind Dataset | A comprehensive collection of biomolecular complexes with experimentally measured binding affinities, used for training and testing scoring functions [34] [40]. | Served as the primary training data for the DynamicBind model and is a common benchmark for docking accuracy [34]. |
| HiQBind-WF Workflow | An open-source, semi-automated workflow of algorithms for curating high-quality, non-covalent protein-ligand complex structures [40]. | Used to create the HiQBind dataset by correcting structural errors in PDBbind, such as fixing ligand bond orders and adding missing protein atoms [40]. |
| DynamicBind | A deep learning method that uses equivariant geometric diffusion networks to perform "dynamic docking," adjusting the protein conformation to a holo-like state upon ligand binding [34]. | Employed to accurately recover ligand-specific conformations from unbound (e.g., AlphaFold-predicted) protein structures, handling large conformational changes [34]. |
| GNINA / AutoDock Vina | Molecular docking software that uses scoring functions to predict ligand poses within a protein binding site [39]. | Used as baseline methods in benchmarking studies to compare the performance of new docking and complex generation tools [39]. |
| ESM-2 Protein Language Model | A deep learning model that generates informative representations from protein sequences, capturing structural and phylogenetic information [39]. | Used as a sequence input representation for end-to-end protein-ligand complex structure generation models, bypassing the need for an existing protein structure [39]. |
Performance Benchmarking Data
Table: Benchmarking Ligand Pose Prediction Accuracy (RMSD < 2 Å) on Different Test Sets. Data adapted from DynamicBind study [34].
| Method | PDBbind Test Set (Success Rate) | Major Drug Target (MDT) Set (Success Rate) |
|---|---|---|
| DynamicBind | 33% | 39% |
| DiffDock | 19% | Data Not Available |
| Traditional Docking (Vina, etc.) | <19% | <39% |
Table: Structural Improvements in a Curated Dataset (HiQBind) vs. PDBbind. Data illustrates the impact of a rigorous curation workflow [40].
| Curated Attribute | Improvement in HiQBind Workflow |
|---|---|
| Ligand Bond Order | Corrected for numerous structures |
| Protein Missing Atoms | Added for a more complete model |
| Steric Clashes | Identified and resolved |
| Hydrogen Placement | Optimized in the complexed state |
Detailed Methodology: Structure-Based Virtual Screening with Consensus Scoring
This protocol outlines a virtual screening process integrating structure-based docking and feature selection for consensus scoring, based on the method described by Teramoto et al. [36]
Protein and Ligand Library Preparation
- Protein Target: Obtain the 3D structure of your target protein. If an experimental structure is unavailable, generate a high-quality model using AlphaFold [34] or perform homology modeling with a tool like Modeller [38]. Prepare the structure by adding hydrogen atoms, assigning partial charges, and ensuring missing loops or side chains in the binding site are modeled.
- Ligand Library: Prepare a library of small molecules for screening in an appropriate format (e.g., SDF, MOL2). Generate 3D conformations and optimize the structures using tools like RDKit [34]. Apply filters for drug-likeness and other desirable properties.
Molecular Docking
- Use docking software (e.g., GNINA, AutoDock Vina) to dock each compound in your library into the binding site of the prepared protein structure [39].
- For each compound, output multiple poses (e.g., 10-20) and record the scoring function values from multiple scoring functions (e.g., F-Score, D-Score, PMF, G-Score, ChemScore) [36].
Feature Selection for Consensus Scoring (FSCS)
- Prepare Training Data: Dock a known native ligand or a small set of confirmed active compounds against your target. These will serve as the "active" reference.
- Generate Molecular Descriptors: For all docked poses (of both your test library and the known actives), calculate a comprehensive set of molecular descriptors and fingerprints using a tool like PaDEL-Descriptor [38].
- Feature Selection: Apply a supervised feature selection algorithm (e.g., based on statistical tests or model importance) to the data from the known active compounds. The goal is to identify which scoring functions and molecular descriptors best distinguish the correct pose of the active compound from decoy poses.
- Select Complementary Functions: Based on the feature selection results, choose a subset of individual scoring functions that are complementary to each other, rather than redundant.
Apply Consensus Scoring and Rank Compounds
- Apply the selected combination of scoring functions to the poses from your full virtual screening library.
- Combine the scores from the selected functions into a single consensus score for each ligand pose (e.g., by averaging ranks or using a machine learning model trained on the feature-selected data).
- Rank all compounds in the screening library based on this consensus score.
Validation
- If possible, validate the top-ranked compounds through experimental assays (e.g., binding affinity or functional assays).
Workflow Visualization
Structure-Based Drug Discovery Workflow
Troubleshooting Common Structural Challenges
FAQs and Troubleshooting Guides
Q1: My pharmacophore model matches most active compounds but also retrieves many inactive compounds during virtual screening. How can I improve its selectivity?
- Answer: This is a common issue related to model specificity. To address this:
- Incorporate Inactive Compounds: During the hypothesis generation phase, provide a set of confirmed inactive compounds. Modern tools like the approach developed by PMC can then optimize the model to match active compounds while avoiding matches to the inactives [41].
- Utilize Excluded Volumes: Generate excluded volumes from your set of inactive compounds. These volumes represent steric barriers that inactives clash with, preventing the model from matching compounds that occupy the same unfavorable space [42].
- Adjust Feature Constraints: Overly generic features can reduce selectivity. Review the types and tolerances of the pharmacophore features in your model. You may need to reduce distance tolerances or replace a common feature like a hydrogen bond acceptor with a more specific one like a negatively charged group if the data supports it.
Q2: What should I do if my active ligands are structurally diverse and will not align properly, making it difficult to identify a common pharmacophore?
- Answer: Difficult alignment is a key limitation of some traditional methods.
- Use Alignment-Free Methods: Consider tools that employ a 3D pharmacophore signature or hash representation. These methods identify common pharmacophores across a set of active compounds without requiring a prior molecular alignment step [41].
- Leverage Hierarchical Graphs: For complex data from molecular dynamics simulations, a hierarchical graph representation of pharmacophore models can help visualize the relationships between many different pharmacophores, making it easier to identify core, conserved features across diverse ligand poses [43].
- Manual Pre-alignment: If using alignment-dependent software, you can manually pre-align your ligands to a known bioactive conformation or a presumed active core using a flexible ligand alignment tool before importing them into the pharmacophore modeling workflow [42].
Q3: How can I validate my ligand-based pharmacophore model to ensure it is not random and has predictive power?
- Answer: Proper validation is crucial for trusting your model's results.
- Retrospective Screening: Perform a virtual screen of a database that contains known actives and decoys (inactive compounds). A good model should efficiently enrich the actives in the top-ranked hits [41] [43].
- Compare to 2D Methods: Compare the enrichment performance of your 3D pharmacophore model against a simple 2D fingerprint-based similarity search. A robust 3D model should offer advantages over 2D similarity alone [41].
- Check Against Crystallographic Data: If the 3D structure of a target-ligand complex is available, verify that your top pharmacophore hypothesis can match the pose of the co-crystallized ligand. This confirms the model's biological relevance [41].
Key Parameters for Pharmacophore Model Sensitivity
The sensitivity and specificity of a ligand-based pharmacophore model are highly dependent on the parameters set during its development. The table below summarizes critical parameters and their optimization strategies.
Table 1: Key Parameters for Optimizing Pharmacophore Model Sensitivity
| Parameter | Description | Optimization Guidance for Sensitivity |
|---|---|---|
| Active/Inactive Thresholds | The activity values used to categorize compounds as 'active' or 'inactive' for the model [41]. | Use consistent, stringent thresholds based on robust experimental data (e.g., pIC50 ≥ 7 for actives, ≤ 5 for inactives) to ensure clear separation between groups [41] [42]. |
| Number of Features | The range of pharmacophore features (e.g., donor, acceptor, hydrophobic) allowed in the final hypothesis [42]. | Specify a range (e.g., 4 to 6) and a preferred minimum to allow the algorithm to find the optimal balance between completeness and simplicity [42]. |
| Matching Actives Criterion | The minimum percentage or number of active compounds that the model must match [42]. | Start with a high percentage (e.g., 80%); lower it if actives are known to bind in multiple modes to avoid missing valid hypotheses [42]. |
| Excluded Volumes | Regions in space where atoms are forbidden, derived from inactive compounds or the protein structure [42]. | Generate shells from inactives to improve model selectivity and reduce false positives [42]. |
| Hypothesis Difference Criterion | The distance cutoff used to determine if two hypotheses are redundant [42]. | A smaller value (e.g., 0.5-1.0 Å) ensures returned hypotheses are distinct, providing a broader set of models for screening [42]. |
Experimental Protocol: Developing a Selective Pharmacophore Model
This protocol outlines the steps for generating a ligand-based pharmacophore model using both active and inactive compounds to optimize sensitivity and selectivity.
1. Compound Selection and Curation:
- Gather Actives: Collect a set of active compounds with consistent, potent activity against the target. A larger, structurally diverse set is preferable [41].
- Select Inactives: Curate a set of confirmed inactive compounds. These are crucial for teaching the algorithm which features to avoid [41].
- Prepare Structures: Convert all 2D structures to 3D. Generate multiple low-energy conformers for each compound to account for flexibility [41] [42].
2. Pharmacophore Hypothesis Generation:
- Input Actives and Inactives: Load the prepared compounds into a pharmacophore modeling tool (e.g., Phase, Pmapper) and define the active/inactive split based on pre-determined thresholds [41] [42].
- Set Modeling Parameters: Configure key parameters as described in Table 1. For instance, set the number of features to 5-6 and require the model to match at least 70-80% of actives initially [42].
- Run Generation Algorithm: Execute the search for common pharmacophore hypotheses. The algorithm will score hypotheses based on their ability to match actives and avoid inactives [41].
3. Model Validation and Selection:
- Review Top Hypotheses: Examine the highest-ranked hypotheses. Check the alignment of active compounds and ensure inactives show poor fits or steric clashes [42].
- Perform Retrospective Screening: Use the top models to screen a validation database spiked with known actives. Calculate enrichment factors (EF) to quantitatively assess performance [41].
- Select the Best Model: Choose the model with the best balance of high active recall (sensitivity) and low inactive matching (specificity), as confirmed by the enrichment analysis.
The following workflow diagram illustrates the key steps in this protocol.
Table 2: Key Tools and Resources for Ligand-Based Pharmacophore Modeling
| Item | Function in Research |
|---|---|
| CheMBL Database | A public repository of bioactive molecules with curated binding data. Used to source structures of active and inactive compounds for model building and validation [41] [43]. |
| Structure Curation Workflows | Standardized pipelines (e.g., via KNIME) for processing compound structures, standardizing chemistry, and filtering data to ensure high-quality input for modeling [41] [43]. |
| Conformer Generation Algorithms | Software components (e.g., idbgen in LigandScout) that generate multiple 3D conformations for each 2D molecule, essential for capturing the flexible nature of ligands [43]. |
| Free Modeling Tools (e.g., Pmapper) | Open-source software that provides access to advanced algorithms, such as alignment-free 3D pharmacophore hashing, without commercial license requirements [41]. |
| Virtual Screening Databases (e.g., ZINCPharmer) | Public platforms that allow researchers to screen millions of commercially available compounds against a custom pharmacophore query to identify potential hit molecules [44]. |
| DUD-E Library | The "Database of Useful Decoys: Enhanced." A benchmark set containing known actives and property-matched decoys, critical for rigorous validation of model selectivity and avoiding artificial enrichment [42]. |
Incorporating Protein Flexibility via Molecular Dynamics (MD) Simulations
Understanding and incorporating protein flexibility is a cornerstone of modern computational drug discovery. Proteins are highly dynamic biomolecules, and the presence of flexible regions is critical for their biological function, influencing substrate specificities, turnover rates, and pH dependency of enzymes [45]. Traditional rigid receptor docking (RRD) methods often fall short because they model the protein as a static structure, which fails to capture the true dynamic nature of biomolecular interactions [46].
Research has demonstrated that predictions incorporating protein flexibility show higher linear correlations with experimental data compared to those from RRD methods [46]. For studies focused on parameter optimization for pharmacophore model sensitivity, accounting for this flexibility is not merely an enhancement but a necessity. It ensures that the generated pharmacophore models, which are critical for virtual screening and pose prediction, accurately represent the functional conformational space of the target protein [47]. This technical support guide provides practical methodologies and troubleshooting advice to help researchers effectively integrate MD simulations into their workflows, thereby improving the sensitivity and accuracy of their pharmacophore models.
FAQs & Troubleshooting Guide
Q1: During molecular dynamics, my visualization software shows that a crucial bond in my DNA/protein ligand is missing. What is wrong?
A: This is a common visualization artifact, not necessarily an error in your simulation data.
- Root Cause: Visualization tools like VMD often guess molecular connectivity based on ideal bond lengths and atom proximity. If your initial structure has unusual bond lengths or if atoms are slightly displaced, the visual bond may not be rendered.
- Solution:
- Trust Your Topology: The definitive record of bonds in your system is the
[ bonds ]section of your topology file. Bonds cannot break or form during a classical MD simulation; they are defined at the start in the topology [48]. - Validate with an Energy-Minimized Frame: Load an energy-minimized structure (e.g., from your
em.grofile) alongside your trajectory in VMD. The minimized frame should have corrected bond geometries, allowing VMD to correctly display the bonds throughout the trajectory [48].
- Trust Your Topology: The definitive record of bonds in your system is the
Q2: When running pdb2gmx, I get the error "Residue 'XXX' not found in residue topology database". How do I resolve this?
A: This error occurs when the force field you selected does not contain a definition for the residue 'XXX' [49].
- Root Cause: The force field's residue topology database (
.rtpfile) lacks an entry for the specific molecule or residue you are trying to process. - Solution Path:
- Check Residue Naming: Ensure the residue name in your PDB file matches the name used in the force field's database. Using "HIS" for a histidine is different from "HSD".
- Obtain Topology Parameters: You cannot use
pdb2gmxfor arbitrary molecules without a database entry. Your options are:- Find a pre-existing topology file (
.itp) for your molecule and include it manually in your system's topol.top file. - Parameterize the molecule yourself using specialized tools (e.g.,
x2topor external servers). - Search the literature for published parameters compatible with your force field [49].
- Find a pre-existing topology file (
- Add Residue to Database (Advanced): For advanced users, you can create a new residue entry in the force field's
.rtpfile, defining all atom types, bonds, and interactions.
Q3: My simulation fails with an "Out of memory" error during analysis. What can I do?
A: This happens when the analysis tool requires more memory (RAM) than is available on your system [49].
- Root Cause: The memory cost of analysis scales with the number of atoms (N) and simulation length (T), sometimes as badly as N². Large systems or long trajectories can easily exhaust memory.
- Solution:
- Reduce Analysis Scope: Analyze a subset of atoms or residues instead of the entire system.
- Shorten the Trajectory: Analyze a shorter, representative segment of your trajectory to confirm the method works before processing the entire dataset.
- Check Unit Errors: Ensure you did not accidentally create a massive system due to a unit confusion (e.g., using Ångström instead of nm when defining the simulation box with
gmx solvate) [49]. - Use a High-Memory Computer: If the above are not sufficient, run the analysis on a compute node or workstation with more RAM.
Q4: The grompp command fails with "Invalid order for directive [ atomtypes ]". How do I fix the order of directives in my topology?
A: The GROMACS preprocessor (grompp) requires a specific order for directives in the topology (.top) and include (.itp) files [49].
- Root Cause: You are likely including a molecule topology (
.itpfile) that introduces new[ atomtypes ]or other[ *types ]directives after the[ moleculetype ]directive has already been declared. - Solution:
- Correct Order: All force field parameters, including atom types, must be fully defined before any molecule definitions.
- Reorganize Your Topology File: The standard order is:
[ defaults ][ atomtypes ]and other[ *types ]directives[ moleculetype ]directives for your system components.
- Ensure that the
#includestatement for your force field (e.g.,#include "oplsaa.ff/forcefield.itp") and any ligand.itpfiles that define new atom types are placed before the[ system ]and[ molecules ]directives in your main.topfile [49].
Key Experimental Protocols
Protocol: A Workflow for Studying Ligand Binding Mechanisms
This integrated protocol, adapted from a study on NF-κB inducing kinase (NIK) inhibitors, combines multiple computational techniques to understand how ligands bind to a flexible protein target [46].
- Application: Understanding the binding mechanism of tricyclic type I1/2 NIK inhibitors.
- Objective: To achieve a binding mode prediction and affinity correlation with experiment that surpasses the capabilities of rigid receptor docking.
Step-by-Step Methodology:
System Preparation:
- Protein Structures: Obtain relevant crystal structures (e.g., PDB entries: 4G3E, 5T8O, 4IDV). Use protein preparation tools (e.g., Schrödinger's Protein Preparation Wizard) to add missing loops and side chains, assign bond orders and protonation states (pH=7.0), and perform restrained energy minimization [46].
- Ligand Structures: Sketch or extract ligand structures. Prepare them using a tool like LigPrep (Schrödinger) to generate correct ionization states and tautomers at pH=7.0, and to set stereochemistry [46].
Flexible Docking:
- Go beyond simple docking by using methods that incorporate protein flexibility.
- Ensemble Docking: Perform docking calculations against an ensemble of multiple receptor conformations (MRCs) derived from different crystal structures or MD simulation snapshots [46].
- Induced-Fit Docking (IFD): Use protocols that allow side-chain or even backbone movement to accommodate the ligand.
Molecular Dynamics (MD) Simulations:
- System Setup: Solvate the protein-ligand complex in an explicit solvent box (e.g., TIP3P water model). Add ions to neutralize the system's charge.
- Equilibration: Run a two-step equilibration: first with positional restraints on heavy atoms of the protein and ligand (NVT ensemble), then with restraints only on the protein backbone (NPT ensemble).
- Production Run: Perform an unrestrained MD simulation for a time scale sufficient to capture relevant motions (e.g., 100 ns to 1 µs). Use a tool like GROMACS.
Binding Free Energy Calculation:
- Use the MM/GBSA or MM/PBSA methods on snapshots extracted from the stable portion of the MD trajectory.
- Calculate the binding free energy as: ΔGbind = Gcomplex - (Gprotein + Gligand).
Energy Decomposition:
- Decompose the total binding free energy to contributions from individual residues. This identifies "hot spot" residues critical for binding [46].
Diagram 1: Workflow for studying ligand binding mechanisms to flexible proteins.
Protocol: Generating and Optimizing Protein-Based Pharmacophore Models
This protocol details the creation of pharmacophore models directly from a protein's 3D structure, optimized to reproduce critical protein-ligand interactions, a key step for sensitive virtual screening [47].
- Application: Creating unbiased pharmacophore models for virtual screening and pose prediction.
- Objective: Generate a pharmacophore model that optimally covers known protein-ligand interaction features from a set of complex structures.
Step-by-Step Methodology:
Define the Binding Site:
- Identify and delineate the protein's binding site of interest.
Generate Molecular Interaction Fields (MIFs):
- Project a 3D grid (e.g., 0.4 Å spacing) onto the binding site.
- Compute interaction energies at each grid point using different molecular probes (hydrogen-bond donor, acceptor, hydrophobic, aromatic, ionic) with a scoring function like ChemScore [47].
Cluster Grid Points to Create Pharmacophore Elements:
- Hydrophobic Features: Apply k-means clustering over all grid points with favorable hydrophobic scores. The cluster center becomes the pharmacophore element. The number of clusters (k) is adjusted until the minimum distance between cluster centers meets a cutoff (e.g., 2.0 Å) [47].
- Specific Interactions (H-bond, Ionic, Aromatic): For each protein functional group, group grid points associated with it into a "patch." Perform k-means clustering within this patch or simply calculate the energy-weighted geometric center of the entire patch to place the pharmacophore element [47].
- Interaction Range for Pharmacophore Generation (IRFPG): Introduce distance cutoffs (min and max) to the scoring function to focus on the most relevant interaction distances and improve pharmacophore placement [47].
Add Excluded Volumes:
- Generate "forbidden" pharmacophore elements by clustering grid points that are closer than 2.0 Å to any protein heavy atom. These represent space the ligand cannot occupy.
Model Validation and Optimization:
- Validate with Known Complexes: Use a set of protein-ligand complexes with known interactions (e.g., from the PDBbind core set). Assess how well the generated pharmacophore model "covers" the known protein-ligand contacts [47].
- Parameter Tuning: Iteratively adjust clustering cutoffs and IRFPG parameters to maximize the coverage of known native contacts. The optimized parameters are then used for generating production models [47].
Diagram 2: Workflow for generating and optimizing protein-based pharmacophore models.
Research Reagent Solutions
Table 1: Essential software tools and resources for incorporating protein flexibility in pharmacophore research.
| Category | Item Name | Function / Application |
|---|---|---|
| MD Simulation Suites | GROMACS | High-performance MD simulation package used for simulating the Newtonian motion of all atoms in a system; essential for sampling protein conformations [49]. |
| Docking & Modeling | Schrödinger Suite | Commercial software suite used for integrated protein preparation (Protein Prep Wizard), ligand preparation (LigPrep), and advanced docking protocols like Induced-Fit Docking (IFD) [46]. |
| Pharmacophore Modeling | LigandScout | Software for creating both ligand-based and structure-based pharmacophore models; used in studies for establishing validated pharmacophore models, e.g., for anti-HBV flavonols [50]. |
| Force Field Databases | GROMACS .rtp Database |
Residue Topology Database containing predefined building blocks (amino acids, nucleotides) for various force fields; critical for pdb2gmx to generate molecular topologies [49]. |
| Flexibility Analysis | ProDy | A Python package implementing Elastic Network Models (ENMs) for fast, coarse-grained normal mode analysis to predict protein collective motions and flexibility [45]. |
| Data Source | PDBbind Database | A curated database of protein-ligand complexes with binding affinities; used as a standard set for validating and optimizing computational methods, including pharmacophore generation [47]. |
Quantitative Data & Parameter Optimization
Table 2: Comparison of computational methods for quantifying and engineering protein flexibility.
| Method | Key Metrics / Outputs | Relative Computational Cost | Primary Application in Pharmacophore Research |
|---|---|---|---|
| Molecular Dynamics (MD) | Root Mean Square Fluctuation (RMSF), free energy (MM/GBSA), interaction persistence [46]. | Very High | Gold-standard for detailed sampling of conformational changes and calculating binding energetics. |
| Elastic Network Models (ENMs) | Normal modes, collective motions [45]. | Low | Rapid prediction of large-scale, collective protein motions to identify flexible regions. |
| Machine Learning Predictors (e.g., Flexpert) | Predicted B-factors or flexibility scores [45]. | Very Low | Fast, sequence-based pre-screening to identify potentially flexible regions for further investigation. |
| Rigid Receptor Docking (RRD) | Docking score, pose RMSD [46]. | Very Low | Baseline method; demonstrates the need for incorporating flexibility when results are poor. |
| Ensemble Docking | Docking score against multiple structures, consensus poses [46]. | Medium (vs. RRD) | Accounting for binding site plasticity by docking into an ensemble of pre-generated conformations. |
Frequently Asked Questions (FAQs)
FAQ 1: What is the primary advantage of using a pharmacophore-guided deep learning approach over traditional methods for molecule generation?
Pharmacophore-guided deep learning represents a paradigm shift from traditional, often inefficient, drug discovery methods. It addresses the fundamental challenge of searching vast drug-like chemical space (estimated at 10^60 molecules) by incorporating established biochemical knowledge directly into the generative model [51]. The primary advantage is its flexibility in various drug design scenarios, especially for newly discovered targets where sufficient activity data is scarce [51]. By using a pharmacophore—a set of spatially distributed chemical features essential for binding—as input, these models can generate novel molecules that satisfy critical interaction patterns, moving the process from "discovery by luck" to "discovery by design" [51] [52].
FAQ 2: My generated molecules are chemically valid but show poor binding affinity in subsequent tests. Which parameters should I investigate first?
Poor binding affinity despite chemical validity often points to issues in the pharmacophore model's sensitivity and its translation into the generative process. Key parameters to investigate include:
- Pharmacophore Feature Tolerance: Overly restrictive distance tolerances between pharmacophore features can limit the chemical space explored, leading to molecules that are theoretically correct but practically ineffective. Start by gradually adjusting distance constraints [51].
- Latent Space Sampling: In models like PGMG, which use latent variables to handle many-to-many mappings, sampling from suboptimal regions of the latent distribution can produce low-affinity molecules. Experiment with different sampling strategies from the prior distribution
p(z|c)[51] [53]. - Model Overfitting to Simple Features: Ensure your model is not over-prioritizing common features like hydrophobicity while neglecting more specific ones like hydrogen bond vectors. Review the weighting of different pharmacophore feature types in your model's objective function [2].
FAQ 3: How can I validate that my generated molecules are truly novel and not simply replicating structures from the training data?
Ensuring novelty is a critical step in the de novo design process. A robust validation protocol should include:
- Direct Database Comparison: Perform a structural similarity search (e.g., using Tanimoto coefficient) against the training dataset and public databases like ChEMBL or ZINC [51].
- Scaffold Analysis: Conduct a Bemis-Murcko scaffold analysis on the generated molecules. A high level of novel scaffolds, not present in the training data, is a strong indicator of novelty [2].
- Performance Metrics: Quantitatively, the "novelty" metric is calculated as the percentage of generated molecules not found in the training set. Models like PGMG have demonstrated a high level of novelty in their outputs [51].
FAQ 4: In a structure-based design scenario with a known protein target, what is the best method for converting the protein structure into an initial pharmacophore for the generative model?
For structure-based design, the most effective method involves a multi-step process to derive a pharmacophore directly from the protein's binding site:
- Identify Key Interactions: Analyze the 3D protein structure to identify critical amino acid residues in the binding pocket. Determine their potential for specific interactions (e.g., hydrogen bonding, ionic interactions, hydrophobic contacts) [2].
- Define Chemical Features: Translate these interaction sites into corresponding pharmacophore features, such as Hydrogen-bond Acceptors (HA), Hydrogen-bond Donors (HD), Positively Charged (PO), Negatively Charged (NE), and Hydrophobic (HY) regions [2] [54].
- Add Spatial Constraints: Map the 3D spatial relationships between these features, including distances and angles. Tools like AncPhore can be used for this purpose [2].
- Incorporate Exclusion Volumes: Add exclusion spheres to represent regions in the binding site that are sterically blocked by protein atoms, preventing the generation of molecules that would clashing with the receptor [2]. This comprehensive model then serves as the input constraint
cfor the generative model [51].
FAQ 5: What are the most common reasons for a model to fail to generate any molecules at all, and how can this be troubleshooted?
A complete failure to generate molecules typically indicates a fundamental mismatch or error at the input or model level. Troubleshoot using the following steps:
- Pharmacophore Feasibility Check: The provided pharmacophore model may be chemically impossible or overly constrained. Verify that the spatial arrangement of features (distances, angles) is physically plausible. Use software to visually inspect the pharmacophore model [54].
- Input Data Integrity: Ensure the pharmacophore graph
G_pis correctly formatted. The model expects a complete graph where each node is a pharmacophore feature and edge weights represent spatial distances. Incorrect graph construction will lead to generation failure [51] [53]. - Decoder Failure: In an autoregressive model like a transformer decoder, a corrupted initial token or an error in the conditional input
(c, z)can halt the sequence generation process immediately. Check the initialization and conditioning steps of the decoder [51].
Troubleshooting Guides
Troubleshooting Low Molecular Diversity
Problem: The generated set of molecules lacks sufficient structural and chemical diversity, limiting options for lead optimization.
Explanation: Low diversity often stems from the model collapsing to a few high-probability modes, failing to explore the full chemical space that matches the pharmacophore. This is frequently related to the handling of the many-to-many relationship between pharmacophores and molecules [51].
| Potential Cause | Diagnostic Steps | Solution & Parameter Adjustment | |
|---|---|---|---|
| Insufficient Latent Space Exploration | Analyze the variance of generated molecular scaffolds and properties (e.g., MW, LogP). | Increase the variance of the latent variable z sampled from `p(z |
c)`. Explicitly sample from diverse regions of the latent space [51] [53]. |
| Overly Restrictive Pharmacophore | Check the number and tolerance (distance constraints) of features in your pharmacophore model. | Slightly relax distance tolerances between pharmacophore features. If possible, reduce the number of mandatory features to provide the model with more flexibility [51]. | |
| Deterministic Decoding | Check if the model uses greedy decoding or beam search, which reduces variability. | Switch to stochastic decoding methods, such as sampling from the output probability distribution with a temperature parameter (T > 1.0) to increase randomness in token selection [51]. |
Troubleshooting Poor Generated Molecule Quality
Problem: Generated molecules have low validity (invalid SMILES or 3D geometry), poor drug-likeness, or undesirable physicochemical properties.
Explanation: This issue arises when the model fails to learn the underlying chemical rules and property distributions of drug-like molecules, often due to training data or model architecture limitations.
| Potential Cause | Diagnostic Steps | Solution & Parameter Adjustment |
|---|---|---|
| Training Data Bias | Compare the distribution of key properties (MW, LogP, TPSA, QED) between generated molecules and the training set. | Curate the training dataset to ensure it represents high-quality, drug-like chemical space. Consider incorporating property-based reinforcement learning to fine-tune the model [51]. |
| Weak Structural Constraints | Use tools like RDKit to check the percentage of chemically invalid SMILES strings. | For graph-based models, enforce valency checks during generation. For SMILES-based models, ensure the transformer decoder is adequately trained on canonical SMILES [51] [53]. |
| Ignoring Pharmacophore Directions | For directional features (e.g., HD, HA), check if generated molecules align their functional groups correctly. | Adopt a model like DiffPhore that explicitly encodes pharmacophore direction matching vectors N_lp during the conformation generation process, ensuring generated molecules not only have the right features but also correct orientations [2]. |
Troubleshooting Inefficient Binding Mode Mapping
Problem: Generated 2D structures match the pharmacophore, but their predicted 3D conformations do not align well with the target, leading to poor docking scores.
Explanation: This indicates a disconnect between the 2D generation process and the 3D binding requirements. The generated molecule's low-energy conformation must match the pharmacophore for effective binding [2].
Workflow for Troubleshooting 3D Binding Conformations:
Resolution Strategies:
- Integrate 3D Generation: Use a model that performs 3D generation directly, such as DiffPhore, a knowledge-guided diffusion model that generates 3D ligand conformations to maximally map a given pharmacophore "on-the-fly" [2].
- Post-processing Conformer Generation: For 2D-generative models, employ a robust conformer generation algorithm and a scoring function to select the conformer that best fits the pharmacophore hypothesis, using the fitness score as a filter [2] [54].
Experimental Protocols & Data Presentation
Core Protocol: Ligand-Based de novo Design with PGMG
This protocol details the steps for generating novel bioactive molecules using a set of known active ligands, a common scenario in early drug discovery.
Step-by-Step Methodology:
- Pharmacophore Model Creation:
- Input: A set of 3-5 known active ligands for your target.
- Software: Use tools like RDKit or PHASE to identify common chemical features and their spatial arrangements [54] [55].
- Action: Superimpose the active ligands and derive a common pharmacophore hypothesis (CPH). This hypothesis
cwill serve as the conditional input for PGMG [51].
Model Setup and Conditioning:
- Model: Load the pre-trained PGMG model. PGMG uses a graph neural network to encode the pharmacophore graph
G_pand a transformer decoder for molecule generation [51] [53]. - Action: Encode the CPH into the model. Introduce the latent variable
zby sampling from the prior distributionp(z|c)(e.g., a standard Gaussian,N(0,I)). This latent variable is key to achieving diversity [51].
- Model: Load the pre-trained PGMG model. PGMG uses a graph neural network to encode the pharmacophore graph
Molecule Generation and Sampling:
- Process: The model generates molecules autoregressively from the distribution
p(x|z, c). - Action: Generate a large library of molecules (e.g., 10,000). Use stochastic sampling with temperature tuning to balance exploration and exploitation [51].
- Process: The model generates molecules autoregressively from the distribution
Post-generation Processing and Validation:
- Validity Check: Use a cheminformatics toolkit (e.g., RDKit) to validate the chemical correctness of generated SMILES strings [51].
- Pharmacophore Fitness Scoring: Score each valid generated molecule by how well its low-energy conformations map back to the original pharmacophore model
c[2]. - Novelty & Diversity Check: Remove duplicates and assess novelty against training data and public compound libraries [51].
- Property Filtering: Filter molecules based on drug-likeness rules (e.g., QED, Lipinski's Rule of Five) and other desired physicochemical properties [51].
Key Quantitative Performance Metrics
The following table summarizes standard metrics used to evaluate the performance of pharmacophore-guided deep learning models, based on benchmarks from published studies.
Table 1: Key Performance Metrics for Generative Models
| Metric | Definition | Benchmark Value (e.g., PGMG) | Importance for Parameter Optimization |
|---|---|---|---|
| Validity | Percentage of generated molecules that are chemically valid. | > 95% [51] | Indicates model's grasp of chemical rules. Low validity requires architecture/training review. |
| Uniqueness | Percentage of valid molecules that are unique (non-duplicate). | High, comparable to top models [51] | Measures diversity of output. Low uniqueness suggests mode collapse. |
| Novelty | Percentage of unique, valid molecules not found in the training set. | High, performs best in this metric [51] | Crucial for de novo design. Ensures generation of new chemical entities. |
| Pharmacophore Fitness | Score measuring how well a generated molecule's conformation matches the input pharmacophore. | Varies by model (e.g., DiffPhore achieves high fitness) [2] | Directly measures the success of the core objective. Critical for sensitivity tuning. |
| Binding Affinity (Docking Score) | Predicted binding energy from molecular docking. | Molecules with strong docking affinities generated [51] | A functional validation metric. Correlates generated molecules with desired bioactivity. |
Research Reagent Solutions
This table lists essential computational tools, datasets, and resources for implementing and experimenting with pharmacophore-guided deep learning.
Table 2: Essential Research Reagents & Tools
| Item Name | Type | Function/Brief Explanation | Example Source/Reference |
|---|---|---|---|
| RDKit | Cheminformatics Software | Open-source toolkit for cheminformatics; used for molecule manipulation, descriptor calculation, and pharmacophore feature identification [51]. | https://www.rdkit.org |
| ChEMBL | Database | A large, open-source database of bioactive molecules with drug-like properties; commonly used for training deep learning models [51]. | https://www.ebi.ac.uk/chembl/ |
| ZINC20 | Database | A free database of commercially-available compounds for virtual screening; used for sourcing starting structures and building training sets [2]. | https://zinc20.docking.org/ |
| CpxPhoreSet & LigPhoreSet | Specialized Dataset | Datasets of 3D ligand-pharmacophore pairs for training and refining deep learning models like DiffPhore [2]. | Derived from AncPhore tool [2] |
| DeepMD-kit | Software | A deep learning framework used for developing neural network potentials, which can be integrated with molecular dynamics simulations for validation [56]. | https://github.com/deepmodeling/deepmd-kit |
| GROMACS | Software | A molecular dynamics simulation package used to study the binding stability and dynamics of generated molecules with their protein targets [54]. | https://www.gromacs.org |
| PHASE | Software | A comprehensive tool for pharmacophore modeling, hypothesis development, and 3D-QSAR studies [55]. | Schrödinger Suite |
| AutoDock Vina | Software | A widely used program for molecular docking, to predict the binding pose and affinity of generated molecules [55]. | http://vina.scripps.edu |
Frequently Asked Questions (FAQs) and Troubleshooting
FAQ 1: My virtual screening workflow has a high false-positive rate. How can I improve the specificity of my hit list?
Answer: A high false-positive rate is a common challenge. Implementing a consensus scoring strategy can significantly improve the specificity of your results. Instead of relying on a single docking program, select compounds that rank highly across multiple, independent virtual screening methods. For example, one study demonstrated that selecting HTS hits ranked in the top 2% by a specific docking program (GOLD) included 42% of the true hits while filtering out 92% of the false positives, leading to a sixfold enrichment of the hit rate [57]. Furthermore, integrating ligand-based and structure-based methods in a parallel or sequential workflow can help cancel out the individual errors of each method, leading to more reliable and confident hit selection [58].
Troubleshooting Guide:
- Symptom: Many selected compounds are inactive in follow-up biochemical assays.
- Potential Cause: Over-reliance on a single, potentially biased, scoring function.
- Solution: Re-analyze your top-ranked compounds using a different docking algorithm or a pharmacophore model. Prioritize compounds that are consensus hits across these different methods.
FAQ 2: I have a protein target but no known active ligands. Which virtual screening approach should I use?
Answer: In the absence of known active ligands, a structure-based approach is your primary option. This requires a 3D structure of your target protein, which can be obtained from the Protein Data Bank (PDB) or generated computationally using tools like AlphaFold2 [4] [10]. You can then perform molecular docking of your compound library into the binding site of the target. For initial enrichment of ultra-large libraries, consider using evolutionary algorithms like REvoLd, which efficiently search combinatorial chemical spaces with full ligand and receptor flexibility, demonstrating hit rate improvements by factors of 869 to 1622 compared to random selection [59].
Troubleshooting Guide:
- Symptom: Poor docking results or an inability to find a good binding pose.
- Potential Cause: Inaccurate binding site definition or poor protein structure preparation.
- Solution: Carefully prepare your protein structure by adding hydrogen atoms, correcting protonation states, and filling in missing residues. Use tools like GRID or LUDI to help identify the key interaction sites in the binding pocket [4].
FAQ 3: How can I effectively screen an ultra-large library of billions of compounds with limited computational resources?
- Answer: Exhaustively screening billion-compound libraries with flexible docking is computationally prohibitive. To overcome this, use advanced sampling algorithms.
- Evolutionary Algorithms: Tools like REvoLd exploit the combinatorial nature of make-on-demand libraries. They start with a random population of molecules, "dock" them, and then use "crossover" and "mutation" operations on the best-scoring individuals to generate new candidate molecules for the next generation, efficiently exploring the vast space without enumerating all compounds [59].
- Pharmacophore-Based Pre-Filtering: Before docking, use a structure-based pharmacophore model to quickly filter the ultra-large library down to a manageable set of compounds that possess the essential chemical features for binding [10] [58].
FAQ 4: What are the key steps to create and validate a robust pharmacophore model for screening?
- Answer: Creating a validated model is crucial for success. The workflow differs based on available data.
- Structure-Based Pharmacophore Modeling:
- Protein Preparation: Obtain a high-quality 3D structure (from PDB or homology modeling) and prepare it by adding hydrogens, assigning correct protonation states, and correcting any structural issues [4] [10].
- Binding Site Analysis: Identify the ligand-binding site, either from a co-crystallized ligand or using binding site detection tools [4].
- Feature Generation: Use software (e.g., Pharmit) to identify critical interaction features (e.g., HBA, HBD, hydrophobic areas) in the binding site [10].
- Model Selection: Select the most relevant features to create a hypothesis that is selective but not overly restrictive [4].
- Validation: The model must be validated before use. Use a dataset of known active compounds and decoys (inactive compounds). A good model should retrieve a high percentage of actives (high sensitivity) while rejecting most decoys (high specificity) [10]. Calculate enrichment metrics like the Enrichment Factor (EF) and Goodness of Hit (GH) to quantitatively assess performance [10].
- Structure-Based Pharmacophore Modeling:
Detailed Experimental Protocols
The following table summarizes key virtual screening protocols documented in recent literature.
| Protocol Name / Study | Core Methodology | Library Screened | Key Outcome / Enrichment |
|---|---|---|---|
| HTS/VS Consensus Screening [57] | Flexible docking (DockVision/Ludi, GOLD) of HTS hit lists. | ~18,000 compounds (NCI Diversity Set, ChemBridge DIVERSet) | 6-fold enrichment of hit rate; 42% of true hits found in top 2% of GOLD-ranked list. |
| Structure-Based FAK1 Inhibitor Identification [10] | Structure-based pharmacophore modeling with Pharmit, followed by molecular docking (AutoDock Vina, SwissDock), MD simulations, and MM/PBSA. | ZINC database | 4 novel candidate FAK1 inhibitors identified with strong binding affinity and acceptable pharmacokinetic properties. |
| REvoLd for Ultra-Large Libraries [59] | Evolutionary algorithm for flexible docking in RosettaLigand, exploring combinatorial "make-on-demand" chemical space. | Enamine REAL space (20+ billion compounds) | Hit rate improvements by factors between 869 and 1622 compared to random selection. |
| Hybrid Ligand/Structure-Based Screening [58] | Averaging predictions from a 3D-QSAR ligand-based method (QuanSA) and a structure-based method (FEP+). | Proprietary LFA-1 inhibitor series | Hybrid model achieved lower mean unsigned error (MUE) than either method alone, improving affinity prediction accuracy. |
| Step | Procedure | Technical Details & Tips |
|---|---|---|
| 1. Protein Preparation | Obtain and prepare the target protein structure. | Source a high-resolution structure from PDB. Use tools like Chimera to add missing residues and hydrogen atoms, and correct protonation states. |
| 2. Pharmacophore Modeling | Generate and validate a structure-based pharmacophore model. | Upload the protein-ligand complex to a tool like Pharmit. Select critical features (HBA, HBD, hydrophobic). Validate with a known set of actives and decoys; calculate Sensitivity, Specificity, and Enrichment Factor. |
| 3. Virtual Screening | Screen a large chemical library using the validated pharmacophore model. | Use the validated model as a query to screen a database like ZINC. This rapidly filters the library to a smaller set of candidate molecules. |
| 4. Molecular Docking | Perform docking with the pharmacophore-hit compounds. | Use docking software like AutoDock Vina for initial screening. Refine top hits with more precise docking methods (e.g., SwissDock). |
| 5. ADMET & Toxicity Filtering | Evaluate the pharmacokinetic and safety profiles of top docked hits. | Use online ADMET prediction tools to filter out compounds with poor absorption, distribution, or potential toxicity. |
| 6. Molecular Dynamics (MD) & Binding Free Energy | Assess the stability and affinity of the final protein-ligand complexes. | Run MD simulations (e.g., with GROMACS) for tens to hundreds of nanoseconds. Calculate binding free energies using methods like MM/PBSA on stable trajectory frames. |
Workflow and Signaling Pathway Visualizations
Virtual Screening Workflow
Pharmacophore Model Development
The Scientist's Toolkit: Research Reagent Solutions
| Tool / Resource Name | Type / Category | Primary Function in Virtual Screening |
|---|---|---|
| RCSB Protein Data Bank (PDB) [4] [10] | Database | Repository for experimentally determined 3D structures of proteins and nucleic acids, providing the starting point for structure-based studies. |
| Pharmit [10] | Software (Web Tool) | Enables structure-based pharmacophore model creation from receptor-ligand complexes and subsequent virtual screening of large chemical libraries. |
| ZINC Database [10] | Database | A freely available public resource of commercially available compounds for virtual screening, containing over 230 million molecules. |
| Enamine REAL Space [59] | Database | An ultra-large "make-on-demand" combinatorial library of billions of synthetically accessible compounds, designed for virtual screening. |
| AutoDock Vina [10] | Software (Docking) | A widely used, open-source molecular docking program for predicting how small molecules bind to a receptor of known 3D structure. |
| GROMACS [10] | Software (Simulation) | A molecular dynamics simulation package used to simulate the physical movements of atoms and molecules over time, assessing complex stability. |
| RosettaLigand [59] | Software (Docking) | A flexible docking protocol within the Rosetta software suite that allows for both ligand and receptor side-chain flexibility. |
| REvoLd [59] | Software (Algorithm) | An evolutionary algorithm designed to efficiently screen ultra-large make-on-demand libraries within the Rosetta framework. |
Troubleshooting Low Sensitivity and Parameter Optimization Strategies
Diagnosing Common Causes of Poor Sensitivity and High False-Negative Rates
Frequently Asked Questions
What is the difference between sensitivity and specificity in pharmacophore modeling? Sensitivity refers to a model's ability to correctly identify active compounds (true positives), while specificity indicates how well the model can exclude inactive compounds (true negatives) [60]. Poor sensitivity directly manifests as a high false-negative rate, where active compounds are incorrectly rejected by the model.
My model has good ROC-AUC but a high false-negative rate. Why? A good Area Under the Curve (AUC) of the Receiver Operating Characteristic (ROC) curve indicates overall good model performance in differentiating active from inactive compounds [60]. However, if your model is too strict—for instance, if the feature tolerances are set too narrowly or the required number of matching features is too high—it can still miss genuine actives, leading to high false-negative rates despite a respectable AUC.
Can the alignment algorithm itself cause false negatives? Yes. Traditional alignment algorithms that optimize for minimum Root Mean Square Distance (RMSD) or maximum volume overlap can inadvertently prioritize the perfect fit of a few features over matching the maximum number of features defined by the model [61]. This can cause alignments to be discarded because the algorithm favored a lower RMSD for three features over a slightly worse RMSD that would have allowed four features to match, thereby increasing false negatives [61].
How does the source of my protein structure affect model sensitivity? Pharmacophore models are highly sensitive to the atomic coordinates of the single protein-ligand complex from which they are derived [9]. This structure is a static snapshot of a dynamic system. Features present in this snapshot might be transient or artifacts of the crystal environment. If these unstable features are included in your model, they can prevent otherwise active compounds from matching, increasing false negatives [9].
The following table lists key resources and their functions for developing and validating robust pharmacophore models.
| Resource / Tool | Function in Diagnosis & Validation |
|---|---|
| Decoy Set (e.g., DUD-E) | A set of molecules with similar physicochemical properties but different 2D topologies to known actives, used to test a model's ability to discriminate [60]. |
| Receiver Operating Characteristic (ROC) Curve | A plot of the True Positive Rate (sensitivity) against the False Positive Rate; a sharp curve that flattens indicates good performance [60]. |
| Goodness of Hit Score (GH) | A statistical metric for model performance; a score above 0.6 is generally considered a threshold for a good model [60]. |
| Enrichment Factor (EF) | Measures how much the model enriches active compounds at a given fraction of the screened database compared to a random selection [60] [62]. |
| Molecular Dynamics (MD) Simulations | Used to generate multiple protein-ligand structures to assess the stability of pharmacophore features over time and avoid artifacts from a single static structure [9]. |
Key Performance Metrics for Model Validation
When validating your pharmacophore model, calculating the following quantitative metrics will provide a clear picture of its performance, particularly its sensitivity and false-negative rate.
| Metric | Formula / Interpretation | Ideal Value |
|---|---|---|
| Sensitivity (True Positive Rate) | TPR = TP / (TP + FN) [60] | Closer to 1 |
| Specificity (True Negative Rate) | TNR = TN / (TN + FP) [60] | Closer to 1 |
| Enrichment Factor (EF) | EF = (Ha / Ht) / (A / D) [60] | Significantly > 1 |
| Goodness of Hit Score (GH) | GH = [(Ha / Ht) * ( (3A + Ht) / (4HtA) )] * (1 - (Ht - Ha) / (D - A)) [60] | > 0.6 [60] |
| ROC-AUC | Area Under the ROC Curve [60] | Closer to 1 |
Abbreviations: TP: True Positives, FN: False Negatives, TN: True Negatives, FP: False Positives, Ha: number of active hits, Ht: total number of hits, A: number of active compounds in database, D: number of compounds in database.
Troubleshooting Guide: Diagnosing Low Sensitivity
Suboptimal Model Features and Tolerances
- Problem: The model may contain an incorrect number of features, unstable features, or feature tolerances (the spatial allowed distance for a match) that are too restrictive.
- Diagnosis Protocol:
- Use Molecular Dynamics (MD) Simulations: Run a short MD simulation (e.g., 20 ns) of the protein-ligand complex. Derive a "merged" pharmacophore model that aggregates features from all simulation snapshots [9]. Compare this to your static model.
- Analyze Feature Frequency: Identify features in your static model that appear less than 5-10% of the time in the MD simulation—these are likely artifacts causing false negatives [9].
- Validation with Known Actives: Screen a small, diverse set of known active and inactive compounds. If known actives with varied scaffolds are consistently failing to match one specific feature, that feature's tolerance or necessity should be investigated.
Limitations in the Alignment Algorithm
- Problem: The algorithm used for pharmacophore alignment may be optimizing for the wrong goal (e.g., minimal RMSD) instead of maximizing the number of matched feature pairs [61].
- Diagnosis Protocol:
- Manual Inspection of Failures: Take a few false-negative compounds and manually inspect if a reasonable alignment exists that satisfies most pharmacophore features, even if the RMSD is not perfect.
- Algorithm Awareness: Be aware of the algorithm your software uses. If possible, use or switch to algorithms like Greedy 3-Point Search (G3PS), which are specifically designed to maximize the number of matching feature pairs, thereby reducing false negatives [61].
Inadequate Conformational Sampling
- Problem: The conformational ensemble generated for the database compounds may not include the bioactive conformation required to match the pharmacophore model.
- Diagnosis Protocol:
- Increase Conformer Count: Systematically increase the number of conformers generated per compound during screening and observe if the false-negative rate decreases.
- Energy Window Check: Ensure the energy window for generated conformers is sufficiently large (e.g., 10-20 kcal/mol above the ground state) to include a diverse range of plausible bioactive conformations.
Improper Validation and Decoy Set Design
- Problem: The model was validated on a dataset that is not representative or contains decoys that are too easy to distinguish from actives.
- Diagnosis Protocol:
- Use Challenging Decoys: Employ a dedicated decoy set like DUD-E, which provides decoys with similar 1D physicochemical properties (e.g., molecular weight, logP, number of H-bond donors/acceptors) but different 2D topologies to the active compounds [60] [8]. This provides a more realistic assessment of model selectivity and sensitivity.
Experimental Protocol: Improving Sensitivity with MD-Driven Feature Analysis
This protocol helps create a more robust pharmacophore model by incorporating protein-ligand dynamics, mitigating the risk of false negatives caused by static structure artifacts [9].
Objective: To generate a dynamics-informed pharmacophore model that prioritizes stable interaction features. Materials: Protein-ligand complex structure (PDB), MD simulation software (e.g., GROMACS, NAMD), structure-based pharmacophore modeling software (e.g., LigandScout, Discovery Studio). Workflow:
- System Setup: Prepare the protein-ligand complex for simulation (add hydrogens, solvate in a water box, add ions for neutrality).
- MD Simulation: Run an all-atom MD simulation of the solvated complex for a sufficient time (e.g., 20-100 ns) to capture relevant motions in the binding site. Save snapshots at regular intervals (e.g., every 10-100 ps).
- Generate Snapshots Pharmacophores: For the initial PDB structure and for each saved MD snapshot, generate a structure-based pharmacophore model.
- Build a Merged Pharmacophore Model: Combine all features from all generated pharmacophore models into a single consensus model.
- Analyze Feature Stability: Calculate the frequency of each feature—the percentage of snapshots in which it appears.
- Prune and Prioritize:
- Remove unstable features: Consider deleting features with a very low frequency (e.g., <10%).
- Assign weights: Use the frequency as a criterion to assign higher weight or priority to features that are consistently present (e.g., >90% frequency) during the simulation.
- Validate the Improved Model: Validate the refined, merged model using a decoy set and calculate the metrics in Table 2. Compare its sensitivity and false-negative rate with the original static model.
Workflow for Diagnosis and Optimization
The following diagram illustrates the logical workflow for diagnosing and remedying poor sensitivity in pharmacophore models.
How Alignment Algorithms Influence False Negatives
This diagram contrasts the outcomes of different alignment optimization goals, explaining why some algorithms inherently cause more false negatives.
Frequently Asked Questions (FAQs)
1. What is the primary risk of using too few features in a pharmacophore model? An overly permissive model with too few features lacks the specificity to distinguish between active and inactive compounds effectively. This can lead to unmanageably large numbers of false positives during virtual screening, wasting computational resources and requiring extensive experimental validation of unpromising hits [62].
2. How does an excessive number of features impact model performance? An overly restrictive model with too many features may become overly specific to the training set of compounds. It can miss valid, structurally novel active compounds (hits) that possess the core interacting features but do not match the exact geometric constraints of the model. This undermines the goal of scaffold hopping in drug discovery [63] [62].
3. What quantitative metrics can help evaluate if my feature count is balanced? You should use statistical performance measures to validate your model. Key metrics include the Receiver Operator Characteristic Area Under the Curve (ROC-AUC), with a value above 0.8 indicating good discrimination, and enrichment factors, which should be above 3 at different fractions of the screened sample. These metrics help balance sensitivity (finding actives) and specificity (rejecting inactives) [62].
4. Are certain types of features more critical for maintaining this balance? Yes. Hydrophobic (HYD) features and their spatial arrangement are often critical for binding but can easily make a model too restrictive if overused. Furthermore, the inclusion of a positive ionizable (PI) feature, often from a basic amino group, is a common cornerstone in many successful models, but its geometric tolerance with HYD regions must be carefully optimized [62] [33].
5. How can I use my model's performance to guide feature adjustment? If your model has high sensitivity but low specificity (many false positives), consider adding a critical feature or tightening distance tolerances. Conversely, if the model has high specificity but low sensitivity (missing known actives), try removing the least critical feature or loosening angular and distance constraints [62] [50].
Troubleshooting Guides
Problem: High False Positive Rate in Virtual Screening
Your model retrieves many compounds, but most are inactive when tested experimentally.
| Step | Action | Rationale & Reference |
|---|---|---|
| 1. Diagnose | Calculate the enrichment factor for the top 1% of your screening results. A low value indicates poor model specificity [62]. | Quantifies the model's ability to prioritize active compounds over random selection. |
| 2. Validate | Check if key inactives (decoys) from your validation set are incorrectly matched by the model. Analyze which superfluous feature(s) they are satisfying. | Identifying patterns in false matches reveals redundant or incorrectly defined features in the model [62]. |
| 3. Refine | Incorporate exclusion volumes (EX) to represent steric clashes from the protein binding site. This prevents the model from matching ligands that would have unfavorable atomic overlaps [64] [2]. | Directly blocks poses that occupy sterically forbidden regions of the binding site. |
| 4. Optimize | Add a directional feature (e.g., hydrogen bond donor/acceptor vector) or refine the spatial tolerances of existing hydrophobic features based on the binding site topology [62]. | Increases the stringency of the model by demanding more geometrically precise ligand interactions. |
Problem: High False Negative Rate in Virtual Screening
Your model fails to retrieve known active compounds from a validation set.
| Step | Action | Rationale & Reference |
|---|---|---|
| 1. Diagnose | Test the model against a diverse set of known actives, including those used in its creation and external ones. Identify which actives are being missed and why [50]. | Determines the scope of the problem and pinpoints specific feature constraints that are too tight. |
| 2. Validate | Manually inspect the non-matching active compounds. Check if they possess the essential interaction features but in a slightly different spatial orientation. | Confirms whether the model is overly restrictive due to minor geometric differences rather than a lack of key interactions [62]. |
| 3. Refine | Systematically remove the least conserved feature from the model or increase the distance and angle tolerances (by 0.5-1.0 Å and 10-20 degrees, respectively) for critical features [62]. | Loosens the model constraints to accommodate legitimate chemical variability while retaining core requirements. |
| 4. Optimize | Re-validate the refined model to ensure the increase in sensitivity has not led to a significant drop in specificity. Use a statistical measure like ROC-AUC to confirm overall improvement [62] [50]. | Ensures that the model optimization leads to a net gain in predictive performance and not just overfitting. |
Quantitative Data on Pharmacophore Features
The following table summarizes common pharmacophore features and their impact on model restrictiveness, based on published models and datasets [64] [2] [62].
Table 1: Common Pharmacophore Features and Their Characteristics
| Feature Type | Abbrev. | Key Interaction | Impact on Restrictiveness | Optimal Count Range* | Notes |
|---|---|---|---|---|---|
| Hydrophobic | HYD | Van der Waals | High | 2-4 | Often the most common feature; overuse is a common cause of overly restrictive models. |
| Hydrogen Bond Acceptor | HA | H-bond with donor | Medium-High | 1-3 | Directional nature increases restrictiveness. |
| Hydrogen Bond Donor | HD | H-bond with acceptor | Medium-High | 1-3 | Directional nature increases restrictiveness. |
| Positive Ionizable | PI | Ionic/Charge | High | 0-1 | Often a key anchor point; usually essential if present but not always required. |
| Aromatic Ring | AR | Pi-Pi stacking | Medium | 1-2 | Can sometimes be substituted with a HYD feature. |
| Negative Ionizable | NE | Ionic/Charge | High | 0-1 | Less common than PI; use only when critical. |
| Exclusion Volume | EX | Steric clash | Very High | Varies | Powerful for reducing false positives; overuse can make model impossibly restrictive. |
*Note: The optimal count is highly dependent on the specific target and binding site. These ranges are a general guideline for initial model building.
Experimental Protocol for Feature Count Optimization
This protocol provides a detailed methodology for systematically balancing the feature count in a structure-based pharmacophore model, adapted from recent literature [64] [62].
Objective: To develop a pharmacophore model with a balanced feature set that maximizes the enrichment of active compounds while maintaining the ability to identify structurally diverse hits.
Required Materials: See "Research Reagent Solutions" below.
Workflow:
Initial Model Generation:
- Using a crystal structure (e.g., PDB: 5HK1), use software like Discovery Studio or LigandScout to identify critical receptor-ligand interactions.
- Generate an initial model that includes all potential interaction features (hydrogen bonds, ionic interactions, hydrophobic patches) and add exclusion spheres based on the protein structure.
Creation of a Validation Dataset:
- Compile a diverse and annotated dataset of active and inactive compounds. The dataset should be large (e.g., thousands of structures) and chemically diverse to ensure a robust validation [62].
- Divide the dataset into a training set (for model generation) and a test set (for validation).
Iterative Feature Pruning and Validation:
- Run virtual screening on the validation dataset using the initial, feature-rich model.
- Calculate performance metrics: Sensitivity (true positive rate), Specificity (true negative rate), and ROC-AUC.
- Systematically remove the least conserved feature (e.g., the feature missed by the largest number of known active compounds) to create a simplified model.
- Re-run the virtual screening and re-calculate the performance metrics.
- Repeat the pruning process until a significant drop in sensitivity or ROC-AUC is observed. The model prior to this drop is considered the optimal one.
Final Model Selection and Cross-Validation:
- Select the model with the best balance of high ROC-AUC and high enrichment factor in the early stages of virtual screening.
- Perform external validation using a completely independent set of compounds not used in any previous step.
Diagram Title: Feature Count Optimization Workflow
Research Reagent Solutions
Table 2: Essential Software and Data Resources for Pharmacophore Modeling
| Item Name | Function/Description | Use Case in Optimization |
|---|---|---|
| LigandScout | Software for advanced pharmacophore model creation from protein-ligand complexes or ligand-based data [50]. | Used for initial feature identification and model generation. |
| Discovery Studio | Comprehensive modeling and simulation suite for drug discovery. | Used for protein preparation, pharmacophore generation, and model validation [62]. |
| AncPhore/Pharmit | Open-source tool for pharmacophore perception and online virtual screening [2] [50]. | Useful for generating diverse pharmacophore hypotheses and high-throughput screening. |
| CpxPhoreSet & LigPhoreSet | Public datasets of 3D ligand-pharmacophore pairs for training and testing AI models [2]. | Provides standardized data for benchmarking model performance and generalizability. |
| PDBbind Database | Curated database of protein-ligand complexes with binding affinity data. | Source of high-quality structures for structure-based model building and test sets for validation [2]. |
| ZINC20 Database | Public database of commercially available compounds for virtual screening. | Provides a large, diverse chemical library to test the practical screening performance of the model [2]. |
Refining Feature Definitions and Tolerances for Improved Hit Retrieval
A pharmacophore is defined as "the ensemble of steric and electronic features that is necessary to ensure the optimal supramolecular interactions with a specific biological target structure and to trigger (or to block) its biological response" [65]. In practical virtual screening, this abstract concept is translated into a 3D pharmacophore model consisting of features such as hydrogen-bond donors, hydrogen-bond acceptors, charged groups, hydrophobic regions, and aromatic rings, along with their spatial arrangements and tolerances [65]. The sensitivity and specificity of these models are paramount for successful hit retrieval in virtual screening campaigns. This technical guide addresses common challenges researchers face when refining feature definitions and tolerances to optimize model performance within the broader context of parameter optimization for pharmacophore sensitivity research.
Frequently Asked Questions (FAQs)
Q1: Why is my pharmacophore model retrieving too many false positives (decoys) during virtual screening?
A1: High false-positive rates typically indicate that your feature tolerances are too permissive. This often occurs with overly large tolerance radii or an insufficient number of essential features in the query. To address this, systematically reduce tolerance radii for hydrophobic and aromatic features first, as these are commonly overrepresented in compound libraries. Additionally, consider adding directional constraints to hydrogen-bond donors and acceptors to increase stringency [65] [66].
Q2: How can I improve my model's ability to identify active compounds with diverse scaffolds?
A2: To enhance scaffold hopping capability, focus on the essential interactions rather than the specific chemical structure. Ensure your model contains a minimal set of critical features (typically 4-6) that define the core interactions necessary for biological activity. Avoid over-defining the model with excessive features that might represent ligand-specific characteristics rather than target-specific requirements [65]. Using structure-based approaches that define features from receptor-ligand complexes can also help capture the fundamental interaction patterns required for binding [10] [66].
Q3: What are the best practices for setting initial tolerance radii for different feature types?
A3: Initial tolerance radii should reflect the variability of each interaction type. Hydrogen-bond donors and acceptors typically require smaller tolerances (1.0-1.5 Å) to maintain directional specificity, while hydrophobic features can often accommodate larger tolerances (1.5-2.0 Å) due to the less specific nature of these interactions. These radii should then be refined through validation against known active and decoy compounds [66].
Q4: How can I validate that my refinements actually improve model performance?
A4: Comprehensive validation requires testing your model against a curated set of known active compounds and decoys. Use statistical metrics including sensitivity, specificity, enrichment factor (EF), and goodness of hit (GH) to quantitatively assess performance improvements after each refinement iteration [10]. The Directory of Useful Decoys - Enhanced (DUD-E) provides standardized datasets for this purpose [10].
Troubleshooting Guides
Problem: Poor Enrichment in Virtual Screening
Symptoms:
- Low retrieval rate of known active compounds
- High number of decoy compounds in hit list
- Enrichment factor (EF) below acceptable thresholds
Solution Protocol:
- Verify Feature Essentiality: Re-evaluate each feature's contribution to binding using available structure-activity relationship (SAR) data. Remove non-essential features that may unnecessarily constrain the model.
- Adjust Tolerance Spheres: Gradually increase tolerance radii for critical features by 0.1-0.2 Å increments while monitoring the impact on active compound retrieval.
- Incorporate Shape Constraints: Add molecular shape constraints to prioritize compounds with similar steric properties to known actives. Tools like Pharmit allow combination of pharmacophore and shape queries [66].
- Validate with Known Actives: Test the refined model against a validation set of active compounds not used in model generation, such as those from CHEMBL [66].
Problem: Overly Restrictive Model Excluding Valid Hits
Symptoms:
- Missed known active compounds with minor structural variations
- Very small hit lists from large compound databases
- High specificity but unacceptably low sensitivity
Solution Protocol:
- Conformational Analysis: Ensure your screening database contains adequate conformational diversity. Generate multiple conformers (typically 10-20 per compound) to account for flexible ligands [66].
- Feature Criticality Assessment: Identify features that may be too restrictive. Consider converting mandatory features to optional for screening, then applying post-screening filters.
- Tolerance Optimization: Systematically increase tolerance radii, particularly for directional features like hydrogen bonds, which may require greater angular flexibility.
- Utilize Advanced Refinement Tools: Employ specialized tools like ELIXIR-A for pharmacophore refinement, which uses point cloud registration and RANSAC algorithms to optimize feature alignment across multiple active compounds [1].
Problem: Inconsistent Performance Across Different Compound Libraries
Symptoms:
- Variable enrichment factors when screening different databases
- Inconsistent retrieval of similar active compounds
- Performance dependent on library composition rather than compound activity
Solution Protocol:
- Library Standardization: Pre-process all compound libraries using consistent protocols for protonation, tautomer generation, and conformer sampling [66].
- Feature Compatibility Check: Ensure your pharmacophore features are compatible with the chemical space covered in each library. Some commercial libraries may have biases in certain feature types.
- Apply Property Filters: Implement property-based filters (molecular weight, logP, polar surface area) to normalize library composition before screening [1].
- Multi-Model Approach: Develop library-specific variations of your pharmacophore model tuned to the distinct characteristics of each database.
Experimental Protocols for Parameter Optimization
Quantitative Validation Framework for Feature Tolerance Optimization
A robust validation framework is essential for systematic parameter optimization. The following protocol establishes a quantitative approach for evaluating tolerance refinements:
Materials and Reagents:
- Set of known active compounds (10-50 compounds with measured activity)
- Curated decoy set (property-matched inactive compounds from DUD-E or similar)
- Virtual screening platform (e.g., Pharmit, LigandScout)
- Statistical analysis software (R, Python, or spreadsheet application)
Procedure:
- Prepare Validation Sets: Compile a dataset of known active compounds and decoys in appropriate file formats (SDF or SMILES). Ensure decoys are matched to actives by molecular weight and logP to reduce bias [10].
- Establish Baseline Performance: Screen the validation set using your initial pharmacophore model and record:
- Number of retrieved active compounds (True Positives)
- Number of retrieved decoy compounds (False Positives)
- Total actives and decoys in database
- Calculate Performance Metrics:
- Sensitivity = (True Positives / Total Actives) × 100
- Specificity = (True Negatives / Total Decoys) × 100
- Enrichment Factor (EF) = (True Positives / Selected Compounds) / (Total Actives / Total Database)
- Goodness of Hit (GH) = (True Positives / Selected Compounds) × (3A + Total Actives) / (4 × Total Actives × Selected Compounds); where A = Total Actives in database [10]
- Iterative Refinement: Systematically adjust feature tolerances and recalculate these metrics after each modification to identify optimal values.
Table 1: Statistical Metrics for Pharmacophore Model Validation
| Metric | Formula | Optimal Range | Interpretation |
|---|---|---|---|
| Sensitivity | (Ha / A) × 100 [10] | >70% | Ability to identify true active compounds |
| Specificity | (1 - Hd / D) × 100 [10] | >80% | Ability to reject decoy compounds |
| Enrichment Factor (EF) | (Ha / Ht) / (A / T) [1] | >10 | Improvement over random selection |
| Goodness of Hit (GH) | [(3A + Ht) / (4 × A × Ht)] × Ha [10] | 0.6-0.8 | Overall model quality balance |
Structure-Based Feature Definition Protocol
When structural information about the target is available, structure-based pharmacophore modeling provides a powerful approach for defining features with optimal tolerances:
Materials and Reagents:
- Protein Data Bank (PDB) structure of target-ligand complex
- Molecular visualization software (PyMOL, Chimera)
- Structure-based pharmacophore tool (Pharmit, LigandScout)
Procedure:
- Structure Preparation:
Interaction Analysis:
- Identify key interactions between the ligand and binding site residues.
- Classify interactions into pharmacophore feature types: hydrogen bond donors/acceptors, hydrophobic regions, charged interactions, aromatic rings.
Feature Generation:
Tolerance Setting:
- Set initial tolerances based on interaction geometry and B-factors of surrounding residues.
- Adjust tolerances to account for potential ligand flexibility and protein side-chain mobility.
Research Reagent Solutions
Table 2: Essential Tools and Platforms for Pharmacophore Optimization
| Tool/Platform | Primary Function | Application in Parameter Optimization | Access Information |
|---|---|---|---|
| Pharmit | Web-based virtual screening | Interactive screening with real-time tolerance adjustment; supports both pharmacophore and shape queries [66] | http://pharmit.csb.pitt.edu [66] |
| LigandScout | Structure & ligand-based modeling | Advanced feature definition with detailed directional constraints; shared pharmacophore refinement [1] | Commercial software (Inte:Ligand) [50] |
| ELIXIR-A | Pharmacophore refinement & alignment | Point cloud-based alignment of multiple pharmacophores; consensus feature identification [1] | Open-source Python application [1] |
| DUD-E Database | Validation compound sets | Provides curated active/decoy compounds for model validation and metric calculation [10] | http://dude.docking.org [10] |
| OpenBabel | Chemical file processing | Compound format conversion, protonation, and initial conformer generation [66] | Open-source tool [66] |
Advanced Refinement Techniques
Shape-Focused Pharmacophore Optimization
Recent advancements in pharmacophore modeling emphasize the importance of molecular shape complementarity. The O-LAP algorithm represents a novel approach for generating shape-focused pharmacophore models through graph clustering of overlapping atomic content from docked active ligands [28]. This method addresses the critical limitation of traditional docking scoring functions by prioritizing shape similarity to known active compounds.
Implementation Protocol:
- Input Preparation: Generate multiple conformations of active ligands docked into the target binding site using flexible docking software (e.g., PLANTS1.2) [28].
- Atomic Clustering: Apply distance-based graph clustering to identify consensus atomic positions across multiple active compounds.
- Model Generation: Create representative pharmacophore models from the clustered atomic features, weighting features by their frequency across active compounds.
- Performance Validation: Test the shape-focused models using the same quantitative metrics applied to traditional pharmacophore models (Table 1).
Knowledge-Guided Diffusion for Ligand-Pharmacophore Mapping
Emerging artificial intelligence approaches show promise for addressing the challenges of sparse pharmacophore feature matching. The DiffPhore framework implements a knowledge-guided diffusion model for 3D ligand-pharmacophore mapping that incorporates explicit type and directional matching rules [2]. This approach leverages large-scale training on 3D ligand-pharmacophore pairs to improve binding conformation prediction and virtual screening performance.
Application Workflow:
- Feature Encoding: Represent pharmacophore models as graphs incorporating type and directional constraints.
- Conformation Generation: Employ diffusion models to generate ligand conformations that optimally align with pharmacophore constraints.
- Virtual Screening: Apply the trained model to screen compound libraries for molecules that match the essential pharmacophore features.
Utilizing Consensus Models and Multi-Complex-Based Pharmacophores
Troubleshooting Guide: Common Issues in Pharmacophore Modeling
1. My pharmacophore model has low sensitivity and misses known active compounds. How can I improve it? This is often caused by using an insufficient number of input structures or over-relying on a single protein-ligand complex, which makes the model too specific. To improve sensitivity:
- Solution A: Implement a Consensus Model Approach. Generate multiple pharmacophore models from several high-resolution protein-ligand complexes of the same target. A compound is considered a "hit" only if it matches a majority (e.g., 2 out of 3) of your consensus models. This reduces false positives from any single, overly rigid model [10].
- Solution B: Use Multi-Complex-Based Pharmacophores. As demonstrated by the O-LAP method, you can fill the target protein cavity with multiple top-ranked docked poses from active ligands. Software like O-LAP then clusters the overlapping atoms to create a single, shape-focused model that represents a consensus of multiple binding modes, significantly improving enrichment rates [28].
2. My model retrieves too many false positives during virtual screening. What parameter should I optimize? A high false positive rate often indicates that the pharmacophore features are not specific enough to distinguish true actives from decoys.
- Solution: Optimize Feature Selection and Tolerance Settings. During model building, carefully select critical interactions and avoid including redundant or uncertain features. Validate your model's performance using a dataset of known actives and decoys. Statistical metrics like the Goodness of Hit (GH) score and Enrichment Factor (EF) are essential for this optimization. A model with high specificity will have a high GH score, indicating its ability to retrieve actives while excluding decoys [10].
3. How can I ensure my model is suitable for scaffold hopping? Traditional models based on a single ligand can be biased toward its specific chemical scaffold.
- Solution: Leverage Ligand-Based Interpretable Pharmacophore Fingerprints. Tools like TransPharmer use multi-scale, interpretable pharmacophore fingerprints that capture essential pharmaceutical features while abstracting fine-grained structural details. This approach has been validated to excel at "scaffold hopping," generating structurally distinct compounds that still maintain the core pharmacophoric constraints needed for bioactivity [67].
4. My computational hits show poor activity in wet-lab experiments. What might be wrong? This translation gap can arise from models that do not adequately represent the dynamic nature of binding or key physicochemical properties.
- Solution: Integrate Molecular Dynamics (MD) and Binding Free Energy Calculations. After screening, subject your top hits to MD simulations. This tests the stability of the protein-ligand complex over time. Subsequently, use methods like MM/PBSA (Molecular Mechanics/Poisson-Boltzmann Surface Area) to calculate binding free energies. This provides a more reliable estimate of binding affinity than docking scores alone and helps prioritize candidates with a higher probability of experimental success [10].
Experimental Protocol: Building a Multi-Complex-Based Pharmacophore with O-LAP
This protocol outlines the generation of a shape-focused pharmacophore model using the O-LAP software, which effectively creates a consensus from multiple docked ligands [28].
1. Protein and Ligand Preparation
- Protein Structure: Obtain high-resolution crystal structures of your target protein from the Protein Data Bank (PDB). Prepare the protein by adding hydrogen atoms using a tool like REDUCE and ensuring protonation states are correct.
- Active Ligands: Curate a set of known active ligands. Generate their 3D conformers and optimize their geometries using software like LIGPREP in Schrödinger's MAESTRO or similar tools. Convert the final structures to MOL2 format.
2. Flexible Molecular Docking
- Setup: Perform flexible-ligand docking using software such as PLANTS. Define the docking site based on the centroid of a co-crystallized ligand.
- Execution: Dock your set of active ligands. Generate multiple poses (e.g., 10 per ligand) to sample different binding modes.
3. O-LAP Model Input Preparation
- Pose Selection: From the docking results, extract the top 50 ranked poses of active ligands based on the docking score (e.g., ChemPLP in PLANTS).
- File Preparation: Merge the separate MOL2 files of these poses into a single input file. Remove non-polar hydrogen atoms and delete covalent bonding information from the file.
4. Graph Clustering with O-LAP
- Run O-LAP: Process the prepared input file with the O-LAP algorithm. The software performs pairwise distance-based graph clustering on the overlapping ligand atoms.
- Model Generation: O-LAP clusters atoms with matching types and generates representative centroids, creating a new, consolidated pharmacophore model that fills the protein cavity.
5. Model Validation and Optimization
- Validation Set: Use a benchmark dataset like DUD-E or PharmBench, which provides known active and decoy compounds for many targets [68] [28].
- Performance Metrics: Calculate key statistical metrics to validate your model's performance.
- Optimization (Optional): If a training set is available, use a greedy search optimization (like BR-NiB) to iteratively refine the O-LAP model for maximum enrichment [28].
The workflow is summarized in the diagram below.
Performance Validation & Quantitative Metrics
After building your pharmacophore model, it is crucial to quantitatively evaluate its performance using a benchmark dataset. The table below defines key metrics used for this validation, based on screening a library containing known active and decoy compounds [10].
Table 1: Key Statistical Metrics for Pharmacophore Model Validation
| Metric | Formula | Interpretation | Ideal Value |
|---|---|---|---|
| Sensitivity (Recall) | (Ha / A) × 100 | The model's ability to identify true active compounds. | High (Close to 100%) |
| Specificity | (Dd / D) × 100 | The model's ability to reject decoy (inactive) compounds. | High (Close to 100%) |
| Enrichment Factor (EF) | (Ha / Ht) / (A / T) | Measures how much more likely you are to find an active compound compared to a random selection. | >1 (Higher is better) |
| Goodness of Hit (GH) | Ha × (3A + Ht) / (4 × Ht × A) | A composite score balancing the recall of actives and the rejection of decoys. A score of 0.7-0.8 is good; 0.8-0.9 is excellent. | Close to 1.0 |
Where: Ha = number of found actives ("hits"); A = total number of actives in the database; Dd = number of rejected decoys; D = total number of decoys; Ht = total number of hits (actives + decoys) retrieved; T = total compounds in the database (A + D).
Table 2: Example Performance Comparison from Recent Studies
| Model / Software | Application / Target | Key Performance Result |
|---|---|---|
| TransPharmer [67] | De novo generation & scaffold hopping for PLK1 inhibitors | Generated a novel 4-(benzo[b]thiophen-7-yloxy)pyrimidine scaffold. The most potent compound (IIP0943) showed 5.1 nM activity and high selectivity. |
| O-LAP [28] | Docking rescoring for five DUDE-Z targets (e.g., NEU, AA2AR) | Showed massive improvement over default docking enrichment, proving effective in both rescoring and rigid docking scenarios. |
| Structure-Based Model [10] | Virtual screening for FAK1 inhibitors from the ZINC database | Identified a candidate (ZINC23845603) with strong binding affinity and a favorable pharmacokinetic profile for experimental testing. |
The Scientist's Toolkit: Essential Research Reagents & Software
Table 3: Key Software and Data Resources for Pharmacophore Modeling
| Item | Function / Application | Reference / Source |
|---|---|---|
| O-LAP | A C++/Qt5-based graph clustering algorithm for generating shape-focused pharmacophore models from multiple docked ligands. | GitHub (GNU GPL v3.0) [28] |
| Pharmit | A web-based tool for structure-based pharmacophore modeling, virtual screening, and creating custom chemical libraries for validation. | http://pharmit.csb.pitt.edu [10] |
| TransPharmer | A generative pre-training transformer (GPT)-based model that uses pharmacophore fingerprints for de novo molecule generation and scaffold hopping. | N/A (Research Model) [67] |
| PharmBench | A benchmark data set of 81 targets with 960 aligned ligands, providing a "gold standard" for evaluating pharmacophore elucidation methods. | http://www.moldiscovery.com/PharmBench [68] |
| DUD-E Database | Directory of Useful Decoys - Enhanced; provides property-matched decoy compounds for 102+ targets to test virtual screening specificity. | http://dude.docking.org [10] |
| PLANTS | Software for flexible molecular docking, used to generate input poses for multi-complex-based pharmacophore modeling. | http://www.tcd.uni-konstanz.de/plants_download/ [28] |
| ZINC Database | A public database of commercially available compounds for virtual screening to identify potential hit molecules. | https://zinc.docking.org/ [10] |
Integrating MD Trajectories to Create Dynamic, Consensus Pharmacophore Models
Frequently Asked Questions (FAQs)
Q1: What is the primary advantage of using MD simulations in pharmacophore modeling compared to a single crystal structure? A single crystal structure provides only a static snapshot of the protein-ligand complex, which may contain artifacts from the crystalline environment and misses the inherent dynamics of the binding site [9]. Molecular Dynamics (MD) simulations capture the flexibility of both the protein and the ligand, allowing you to observe interactions that persist over time or are transient but critical. This dynamic information helps create a consensus pharmacophore model that is more representative of the solution-state behavior, mitigating the sensitivity of the model to a single set of coordinates [9] [69].
Q2: My MD trajectory is messy, with the protein looking like it exploded. Is my simulation ruined? No, your simulation is likely fine. This visual chaos is typically caused by Periodic Boundary Conditions (PBC), a computational trick that simulates an infinite system [70]. When molecules cross the box boundaries, they reappear on the other side, making different parts of the complex appear scattered. Your trajectory needs post-processing to correct for PBC and center the protein before analysis. Tools like CPPTRAJ or MDAnalysis can fix this [70].
Q3: How do I decide which pharmacophore features from the MD trajectory are truly important? Features should be prioritized based on their stability and frequency throughout the simulation [9]. A feature present in the initial crystal structure but appearing less than 5-10% of the time during the MD may be an artifact and can potentially be discarded [9]. Conversely, a feature not seen in the crystal structure but appearing very frequently (e.g., >90% of the time) during the simulation should be considered important. This frequency information provides a quantitative criterion for feature ranking [9].
Q4: Can I create a dynamic pharmacophore model if I have multiple ligands but only one protein structure? Yes. A methodology called the Molecular dYnamics SHAred PharmacophorE (MYSHAPE) approach can be used [71]. It involves running multiple, short MD simulations of the same protein structure, each with a different ligand bound. The crucial ligand-protein interactions observed across these dynamic simulations are then used to generate a shared pharmacophore model, which has been shown to improve early enrichment in virtual screening [71].
Troubleshooting Guides
Issue 1: Handling Raw MD Trajectories for Analysis
Problem: After loading your MD trajectory into visualization software, your protein complex appears fragmented and scattered across the simulation box [70].
Diagnosis: This is a classic symptom of uncorrected Periodic Boundary Conditions (PBC). The raw coordinates from the simulation account for PBC, but visualization and analysis software need the molecules to be "re-imaged" so the complex appears intact [70].
Solution: Use trajectory processing tools to fix PBC, remove solvent, and align the frames.
Step-by-Step Protocol (Using CPPTRAJ) [70]:
- Center the system on your most stable protein domain.
- Unwrap other components (e.g., a second protein, a ligand) so they stay connected to the main domain.
- Fix the overall presentation using the
autoimagecommand. - (Optional) Strip water and ions to drastically reduce file size and speed up analysis.
- Align all frames to a reference (e.g., the protein backbone) to remove overall rotation and translation.
- Output your clean trajectory for pharmacophore analysis.
Alternative Python Solution (Using MDAnalysis) [70]:
Issue 2: Generating and Refining the Consensus Pharmacophore Model
Problem: You have generated hundreds of individual pharmacophore models from your MD snapshots, and you need a robust way to consolidate them into a single, consensus model.
Diagnosis: Manually sifting through all the models is inefficient. A systematic, algorithmic approach is required to identify the essential, persistent pharmacophore features.
Solution: Employ a refinement tool to align the pharmacophore points from multiple models and select a consensus set. The following workflow can be implemented with tools like ELIXIR-A [1].
Step-by-Step Protocol:
- Generate Individual Models: Use a structure-based pharmacophore program (e.g., LigandScout [9]) to create a model for each snapshot in your cleaned MD trajectory.
- Prepare Pharmacophore Point Clouds: Represent each pharmacophore feature as a sphere with a defined radius and type (e.g., HBA, HBD, H). Each sphere is converted into a cloud of uniformly distributed points [1].
- Align Pharmacophore Models: Use a point cloud registration algorithm to align two or more pharmacophore models. This is typically a two-step process:
- Global Registration: A rough alignment is performed using geometric descriptors (Fast Point Feature Histogram, FPFH) and the RANSAC algorithm to handle "noise" [1].
- Local Refinement: A more precise Colored Iterative Closest Point (ICP) algorithm is used, which considers both geometric and pharmacophore feature type ("color") information to achieve the best superposition [1].
- Refine and Select Consensus Features: After alignment, calculate the Euclidean distance between all pharmacophore points. Points from different models that are within a defined threshold distance are considered a single, consensus feature. Irrelevant points (those without a counterpart) are removed [1].
- Prioritize by Frequency: The final consensus model should be annotated with the frequency of each feature, which can be used for virtual screening and to understand the relative importance of specific interactions [9].
Issue 3: Validating the Dynamic Pharmacophore Model
Problem: You have built a consensus dynamic pharmacophore model, but you are unsure of its quality and performance for virtual screening.
Diagnosis: A model must be validated to ensure it can distinguish known active compounds from inactive ones (decoys). Without validation, the model's utility is unknown.
Solution: Validate the model using a dataset of known actives and decoys, and calculate standard enrichment metrics.
Step-by-Step Protocol:
- Prepare a Validation Library: Obtain a set of known active inhibitors and property-matched decoy molecules for your target. Public databases like DUD-E (Directory of Useful Decoys: Enhanced) are excellent sources for this [10] [1].
- Perform Virtual Screening: Use your dynamic pharmacophore model as a query to screen the validation library. This can be done in pharmacophore screening platforms like Pharmit [10] [1].
- Calculate Performance Metrics: After screening, calculate the following statistical metrics to quantify model performance [10]:
- Sensitivity: The fraction of known active compounds correctly identified by the model.
- Specificity: The fraction of decoy compounds correctly rejected by the model.
- Enrichment Factor (EF): Measures how much better the model is at identifying actives compared to a random selection.
Table 1: Key Statistical Metrics for Pharmacophore Model Validation [10]
| Metric | Formula | Interpretation |
|---|---|---|
| Sensitivity (Recall) | (True Positives / Total Actives) × 100 | Higher is better; indicates ability to find actives. |
| Specificity | (True Negatives / Total Decoys) × 100 | Higher is better; indicates ability to reject decoys. |
| Enrichment Factor (EF) | (Hit Rateactive / Hit Ratetotal) | Values >1 indicate enrichment over random. |
Experimental Protocols & Workflows
Detailed Methodology: Creating an MD-Derived Consensus Pharmacophore
This protocol details the process of creating a dynamic, consensus pharmacophore model, from MD simulation setup to the final validated model.
Workflow Overview:
Procedure:
System Setup:
- Obtain a high-resolution crystal structure of the target protein in complex with a ligand from the PDB [72] [10].
- Use tools like CHARMM-GUI's Membrane Builder (for membrane proteins) or a standard solvation tool to embed the complex in a water box, add ions to neutralize the system, and set up the simulation parameters [72].
MD Simulation:
Trajectory Preprocessing:
- Follow the Troubleshooting Guide 1 to correct for PBC, center the protein, remove solvent, and align all frames to a reference structure. This yields an analysis-ready trajectory [70].
Pharmacophore Generation and Consensus Building:
- For each saved snapshot, generate a structure-based pharmacophore model using software such as LigandScout [9] or Pharmit [10]. This will result in hundreds of individual models.
- Use a tool like ELIXIR-A to align and refine these models [1]. The tool will output a consensus model containing only the pharmacophore features that are geometrically consistent across multiple snapshots.
Frequency Analysis and Final Model Creation:
- Annotate each feature in the consensus model with its frequency of occurrence across the entire MD simulation. This provides a measure of its stability and importance [9].
- The final dynamic pharmacophore model is this frequency-annotated consensus model.
Model Validation:
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Software and Resources for Dynamic Pharmacophore Modeling
| Tool / Resource | Type | Primary Function | Key Application in Workflow |
|---|---|---|---|
| NAMD / GROMACS [72] | MD Engine | Runs molecular dynamics simulations. | Simulating the dynamic behavior of the protein-ligand complex in a solvated environment. |
| CPPTRAJ / MDAnalysis [70] | Trajectory Analysis | Processes and analyzes MD trajectories. | Fixing PBC, aligning frames, stripping solvent to create clean trajectories for analysis. |
| LigandScout [72] [9] | Pharmacophore Modeling | Generates structure-based and ligand-based pharmacophore models. | Creating an individual pharmacophore model from each MD snapshot. |
| ELIXIR-A [1] | Pharmacophore Refinement | Aligns and refines multiple pharmacophore models. | Generating the final consensus model from hundreds of individual snapshot-derived models. |
| Pharmit [10] [1] | Virtual Screening | Screens large compound libraries using pharmacophore queries. | Validating the consensus model by screening actives/decoys from DUD-E. |
| DUD-E Database [10] | Benchmarking Set | Provides sets of known active and decoy molecules for various targets. | Validating the pharmacophore model's enrichment performance. |
Robust Validation and Performance Benchmarking of Optimized Models
Frequently Asked Questions
1. What do the ROC-AUC, EF, and GH scores actually tell me about my pharmacophore model's performance? These metrics evaluate your model's performance from complementary angles. The ROC-AUC (Receiver Operating Characteristic - Area Under the Curve) summarizes the model's overall ability to discriminate between active and inactive compounds across all possible classification thresholds, with a score of 1.0 representing perfect discrimination and 0.5 representing a random classifier [73] [74]. The Enrichment Factor (EF) measures the model's effectiveness specifically in the early stage of virtual screening by calculating the concentration of active compounds found within a small, top-ranked fraction of the screened database compared to a random selection [75] [76]. The Goodness of Hit (GH) Score is a composite metric that balances the model's ability to identify a high proportion of active compounds (recall) with the relative size of the hit list it produces, penalizing models that retrieve too many compounds to be practically useful [75] [77].
2. My model has a high ROC-AUC but a low EF. What does this mean and how can I fix it? This is a common scenario indicating that while your model is generally good at ranking actives above inactivates overall, it performs poorly in the critically important early retrieval phase—the top of your ranked list is not enriched with actives [76]. To address this:
- Optimize Feature Selection: The pharmacophore features might be too generic. Re-evaluate your hypothesis to ensure it captures features unique to potent actives.
- Incorporate Shape Constraints: Add inclusive shape constraints based on your most active ligand to improve the steric fit of top-ranked compounds [78] [28].
- Adjust Scoring Weights: If your screening software allows, increase the weight of specific, critical interactions over more common hydrophobic features.
3. How do I know if my EF or GH score is "good"? There are standard benchmarks for these metrics. The table below summarizes the typical calculations and interpretations.
Table 1: Interpretation of EF and GH Scores
| Metric | Calculation Formula | Interpretation |
|---|---|---|
| Enrichment Factor (EF) | (\text{EF} = \frac{\text{Hits}{\text{sampled}} / N{\text{sampled}}}{\text{Hits}{\text{total}} / N{\text{total}}}) | An EF of 1 indicates no enrichment over random. A higher EF is better. It is often reported at a specific cutoff (e.g., EF1% for the top 1% of the database) [76] [77]. |
| Goodness of Hit (GH) Score | (\text{GH} = \left( \frac{\text{Hits}{\text{sampled}}}{3 \times \text{Hits}{\text{total}}} \right) \times \left( \frac{\text{Hits}{\text{total}} + \left( N{\text{total}} - N{\text{sampled}} \right)}{N{\text{sampled}}} \right)) | The score ranges from 0 to 1, where 1 represents an ideal model. A score >0.7 is considered to indicate a good model, while <0.5 suggests a poor one [75] [77]. |
4. During validation with a decoy set, my model's ROC curve is below the diagonal (AUC < 0.5). What went wrong? An AUC below 0.5 indicates that your model is performing worse than random chance [73] [74]. This is a critical error that requires revisiting your fundamental model.
- Check for Feature Reversal: The most common cause is that the model's definition of "active" is inverted. For a binary classifier, reversing the predictions (swapping the positive and negative class labels) can immediately transform a worse-than-random model into a better-than-random one without retraining [73].
- Re-examine the Training Set: Ensure your set of known active compounds is correct and that the model's pharmacophore features are indeed representative of true bioactivity and not an artifact of a small or biased training set.
- Verify Decoy Quality: Confirm that the decoy (presumably inactive) compounds in your validation set are truly inactive and are property-matched to your actives to avoid artificial inflation of difficulty [28].
Experimental Protocols for Metric Calculation
Protocol 1: Validating a Pharmacophore Model Using a Decoy Set This protocol is essential for establishing the predictive power of your pharmacophore model before its use in large-scale virtual screening [75] [79].
- Prepare the Validation Database: Compile a database containing a known set of active compounds and a larger set of decoy (presumably inactive) compounds. The decoys should be property-matched (e.g., similar molecular weight, logP) to the actives to ensure a realistic screening challenge [28].
- Run the Virtual Screen: Use your pharmacophore model as a query to screen the entire validation database.
- Rank the Results: Rank all compounds in the database based on their fit value or similarity score to the pharmacophore query.
- Calculate the Metrics:
- ROC-AUC: At multiple threshold values of the fit score, calculate the True Positive Rate (TPR = TP / (TP + FN)) and False Positive Rate (FPR = FP / (FP + TN)). Plot TPR vs. FPR to generate the ROC curve and calculate the area underneath it [75] [74].
- EF and GH: Define a cutoff (e.g., the top 1% of the ranked database). Count the number of active compounds found within this cutoff to calculate the EF and GH score using the formulas provided in Table 1 [75].
Protocol 2: Structure-Based Pharmacophore Generation and Optimization This protocol outlines a method for creating a pharmacophore model directly from a protein structure, which is particularly useful when known active ligands are scarce [80] [77].
- Protein Preparation: Obtain the 3D structure of your target protein (e.g., from PDB). Prepare the structure by adding hydrogen atoms, assigning correct protonation states, and removing unwanted water molecules [4].
- Identify the Binding Site: Define the binding site cavity, either from the location of a co-crystallized ligand or using a binding site detection algorithm [4] [80].
- Generate Pharmacophore Features: Use molecular interaction fields or fragment-based methods to map potential interaction points (hydrogen bond donors/acceptors, hydrophobic areas, ionizable groups) within the binding site. Software like LigandScout or Discovery Studio can automate this [4] [79].
- Select Key Features: From all generated features, select a subset that represents interactions critical for binding, often by removing redundant features or those with weak energetic contributions [4] [77].
- Validate and Optimize: Validate the initial model using Protocol 1. To optimize for high early enrichment (EF), you can use an enrichment-driven brute-force optimization (e.g., BR-NiB) to iteratively adjust the model's features and their weights [28].
Relationship and Calculation of Key Metrics
The following diagram illustrates the workflow for calculating and interpreting the key validation metrics, showing how they relate to the virtual screening process.
Diagram 1: Metric Calculation Workflow.
The Scientist's Toolkit: Essential Research Reagents & Software
The following table lists key computational tools and their functions used in pharmacophore modeling and validation as discussed in the search results.
Table 2: Key Research Reagents & Software Solutions
| Tool / Resource Name | Type | Primary Function in Research |
|---|---|---|
| LigandScout [75] [4] | Software | Advanced software for creating and validating both structure-based and ligand-based 3D pharmacophore models. |
| Decoy Set (DUD-E/Z) [76] [28] | Database | A publicly available database of property-matched decoy molecules used to rigorously test a model's ability to discriminate actives from inactives. |
| ROC Curve Analysis [73] [74] | Analytical Method | A graphical plot and associated AUC metric used to evaluate the overall diagnostic ability of a classifier across all thresholds. |
| Pharmacophore Fit Value | Scoring Metric | An algorithm-generated score quantifying how well a compound from a database aligns with the spatial and chemical constraints of the pharmacophore query. |
| O-LAP [28] | Software | A specialized algorithm for generating shape-focused pharmacophore models via graph clustering to improve docking enrichment. |
| MCSS-based Protocols [77] | Computational Method | A method for placing functional group fragments in a protein's active site to generate structure-based pharmacophores, useful for targets with few known ligands. |
Benchmarking Against Known Actives and Decoys from DUD-E Database
This technical support guide provides essential information for researchers using the Directory of Useful Decoys, Enhanced (DUD-E) database to benchmark virtual screening methods, with particular emphasis on pharmacophore model development. Proper use of this benchmarking set is crucial for evaluating the sensitivity and specificity of computational approaches in drug discovery pipelines.
Frequently Asked Questions (FAQs)
What is the DUD-E database and why is it used for benchmarking?
The DUD-E database is an enhanced benchmarking set designed for rigorous evaluation of molecular docking and virtual screening methods. It addresses limitations of the original DUD set by providing improved chemical diversity and more challenging decoys. DUD-E contains 102 targets with 22,886 clustered ligands drawn from ChEMBL, each with 50 property-matched decoys drawn from ZINC [81]. Researchers use DUD-E to assess how well their methods can separate known active compounds from decoys, providing a standardized way to measure enrichment performance.
How are decoys in DUD-E different from random compounds?
DUD-E decoys are carefully designed to be "difficult but fair" by matching key physicochemical properties of known actives while ensuring topological dissimilarity. The decoys are property-matched to ligands by molecular weight, calculated logP, number of rotatable bonds, hydrogen bond donors, and acceptors [81]. Additionally, net formal charge was added as a matching property in DUD-E to address imbalances present in the original DUD, where 42% of ligands were charged versus only 15% of decoys [81]. This design ensures that enrichment reflects true method performance rather than simple property-based discrimination.
What are common pitfalls when using DUD-E for pharmacophore model validation?
Common issues include analogue bias, where models perform well simply by recognizing overrepresented chemotypes rather than true pharmacophore patterns. DUD-E addresses this by clustering each target's ligands by their Bemis-Murcko atomic frameworks to ensure chemotype diversity [81]. Additionally, researchers should verify that their pharmacophore features don't accidentally leverage residual property imbalances between actives and decoys rather than capturing genuine binding interactions.
How can I assess if my pharmacophore model is performing well on DUD-E?
Strong performance is indicated by good early enrichment, meaning active compounds rank highly within the top 1-5% of screened compounds. The area under the receiver operating characteristic curve (AUROC) and enrichment factors (EF) are standard metrics. However, be cautious of artificial enrichment that can occur if your method inadvertently exploits subtle differences in simple molecular properties rather than recognizing true binding pharmacophores [82].
Troubleshooting Guides
Issue: Poor Enrichment in DUD-E Benchmarking
Problem: Your pharmacophore model shows low enrichment when screening DUD-E actives versus decoys.
Solution Steps:
- Verify your model isn't overly specific - ensure it captures essential rather than exhaustive interaction features
- Check for feature conflicts with decoy properties using DUD-E's property analysis tools
- Implement scaffold-hopping validation by testing performance across different molecular frameworks within the actives
- Consider hybrid approaches that combine pharmacophore matching with complementary methods like shape similarity [28]
Prevention: During model development, use cross-validation with multiple target classes and monitor for overfitting to specific chemotypes.
Issue: Analogue Bias in Screening Results
Problem: Your model successfully identifies actives from certain chemical classes but misses structurally distinct actives.
Solution Steps:
- Analyze your hit distribution across different Bemis-Murcko scaffolds in the actives
- Implement the unsupervised distance analysis method described in DUD-E publications using the G(t) and F(t) spatial distribution functions [82]
- Apply cluster-based evaluation where actives are grouped by scaffold and performance is assessed across clusters
- Consider using the Unbiased Ligand Set (ULS) methodology which explicitly addresses this bias [82]
Expected Outcome: More consistent performance across diverse chemotypes and reduced overoptimistic enrichment metrics.
Issue: Computational Bottlenecks in Large-Scale Screening
Problem: Screening millions of compounds from DUD-E with complex pharmacophore models becomes computationally prohibitive.
Solution Steps:
- Implement a tiered screening approach using rapid filters before detailed pharmacophore matching
- Utilize ultra-large-scale screening tools like PharmacoNet that leverage deep learning for pharmacophore modeling [83]
- Consider shape-focused pre-screening using methods like O-LAP to rapidly eliminate obvious mismatches [28]
- Explore cloud-based distributed computing options for embarrassingly parallel screening tasks
Performance Gain: Modern deep learning pharmacophore tools like PharmacoNet demonstrate ~3000x speedup compared to conventional docking while maintaining competitive accuracy [83].
Experimental Protocols
Standard DUD-E Benchmarking Protocol for Pharmacophore Models
Purpose: To evaluate pharmacophore model performance using the DUD-E benchmark set.
Materials:
- DUD-E database (freely available from http://dude.docking.org)
- Pharmacophore modeling software (e.g., LigandScout, MOE, or custom implementations)
- Computing resources appropriate for screening ~1 million compounds
Procedure:
- Target Selection: Choose relevant protein targets from DUD-E's 102 options based on your research focus
- Data Preparation: Download actives and decoys for selected targets, preserving the predefined groupings
- Pharmacophore Screening: Screen all actives and decoys against your pharmacophore model
- Score Ranking: Rank compounds based on pharmacophore fit scores or compatibility metrics
- Performance Calculation:
- Generate enrichment curves (ROC curves)
- Calculate enrichment factors (EF) at 1%, 5%, and 10% of the screened database
- Compute BEDROC metrics with appropriate alpha values [83]
- Bias Assessment: Perform spatial distribution analysis to check for analogue bias [82]
Troubleshooting Notes: If performance is significantly worse than literature values, verify your pharmacophore features correspond to known binding interactions rather than incidental molecular properties.
Protocol for Building Unbiased Benchmarking Sets
Purpose: To create custom benchmarking sets following DUD-E principles for targets not covered in standard DUD-E.
Materials:
- Known active compounds with binding affinity data
- Large compound database (e.g., ZINC) for decoy generation
- Automated decoy generation tools (available at http://decoys.docking.org)
Procedure:
- Ligand Curation: Collect and curate known actives with verified binding data
- Scaffold Clustering: Cluster actives by Bemis-Murcko frameworks to ensure chemotype diversity
- Decoy Generation:
- Match decoys to actives by molecular weight, logP, rotatable bonds, HBD, HBA, and net charge
- Ensure minimum topological similarity to all actives
- Apply synthetic feasibility filters
- Set Validation:
- Verify decoys are property-matched but topologically dissimilar
- Check for spatial random distribution using G(t) and F(t) functions [82]
- Performance Testing: Validate the set with standard methods before research use
Data Presentation
Key DUD-E Database Specifications
Table 1: DUD-E Database Composition
| Parameter | Specification | Notes |
|---|---|---|
| Number of targets | 102 | Covers diverse protein families |
| Target categories | 26 kinases, 15 proteases, 11 nuclear receptors, 5 GPCRs, 2 ion channels, 2 cytochrome P450s, 36 other enzymes, 5 miscellaneous proteins | Broad coverage [81] |
| Total ligands | 22,886 clustered ligands | Average of 224 ligands per target |
| Ligand source | ChEMBL with measured affinities | Literature-supported data |
| Decoys per ligand | 50 property-matched | ~1.4 million total decoys |
| Property matching | MW, logP, rotatable bonds, HBD, HBA, net charge | Improved over original DUD |
| Decoy source | ZINC database | Commercially available compounds |
Performance Metrics for Benchmarking
Table 2: Essential Metrics for DUD-E Evaluation
| Metric | Calculation | Interpretation |
|---|---|---|
| Enrichment Factor (EF) | (Hitssampled/Nsampled)/(Hitstotal/Ntotal) | Measures concentration of actives in top ranked compounds |
| Area Under ROC Curve (AUROC) | Area under receiver operating characteristic curve | Overall ranking quality |
| BEDROC | Boltzmann-enhanced discrimination of ROC | Early enrichment emphasis |
| PRAUC | Area under precision-recall curve | Useful for imbalanced datasets |
| Robust Initial Enhancement (RIE) | Metric emphasizing early enrichment | Similar to BEDROC with different weighting |
Research Reagent Solutions
Table 3: Essential Resources for DUD-E Benchmarking
| Resource | Function | Availability |
|---|---|---|
| DUD-E database | Primary benchmarking set | http://dude.docking.org [81] |
| DecoyFinder | Tool for building target-specific decoy sets | Open source [82] |
| PharmacoNet | Deep learning-guided pharmacophore modeling | Academic use [83] |
| O-LAP | Shape-focused pharmacophore modeling | GNU GPL v3.0 [28] |
| DiffPhore | Knowledge-guided diffusion for 3D pharmacophore mapping | Research use [84] |
| DEKOIS 2.0 | Alternative benchmarking sets | Academic use [83] |
Workflow Visualization
DUD-E Benchmarking Workflow
Troubleshooting Decision Framework
This technical support center addresses common challenges researchers face during campaigns to discover and optimize Focal Adhesion Kinase 1 (FAK1) inhibitors. FAK1 is a non-receptor tyrosine kinase that is a promising target for cancer therapy due to its role in regulating cell migration, survival, and tumor progression [85] [10]. The guidance below is framed within a thesis investigating parameter optimization for enhancing pharmacophore model sensitivity in structure-based drug design.
Frequently Asked Questions (FAQs)
Q1: Our virtual screening hits show excellent predicted binding affinity for FAK1 but poor cellular activity. What could be the cause?
This common issue often stems from poor physicochemical properties or off-target binding.
- Troubleshooting Steps:
- Check Selectivity: FAK1 shares high homology with PYK2 (Proline-rich tyrosine kinase 2). Use counter-screening to ensure your compounds are not promiscuous kinase inhibitors. A selectivity ratio (FAK IC50 / PYK2 IC50) of >5 is generally desirable [86].
- Analyze ADMET Properties: Early integration of Absorption, Distribution, Metabolism, Excretion, and Toxicity (ADMET) predictions is crucial. Use tools like SwissADME or admetSAR to evaluate key parameters:
- Permeability: The Blood-Brain Barrier (BBB) permeability can be a positive or negative attribute depending on the target cancer. For glioblastoma, a high BBB score (e.g., Pe > 40) is beneficial, as demonstrated by the macrocyclic inhibitor GZD-257 [86].
- Solubility and Metabolic Stability: Ensure compounds have adequate aqueous solubility and are not predicted to be rapid substrates for CYP450 enzymes.
- Consider FAK's Scaffold Function: Traditional kinase inhibitors only block enzymatic activity. FAK also has kinase-independent "scaffold" functions that promote cancer progression. If cellular activity is lacking despite good kinase inhibition, consider employing Proteolysis-Targeting Chimeras (PROTACs) like BI-0319, which degrade the entire FAK protein and disrupt both functions [87] [88].
Q2: How can we improve the sensitivity and specificity of our pharmacophore model for virtual screening?
A poorly validated pharmacophore model can yield too many false positives or miss promising hits.
- Troubleshooting Steps:
- Use a Validated Set of Actives and Decoys: Build a robust validation set from databases like DUD-E (Directory of Useful Decoys: Enhanced). For FAK1, one study used 114 known active compounds and 571 decoys to validate their model [85] [10].
- Calculate Statistical Metrics: After screening the validation set, calculate standard metrics to assess model performance.
- Incorporate Key Protein-Ligand Interactions: Ensure your model includes features critical for FAK1 binding, typically derived from a high-resolution co-crystal structure (e.g., PDB ID: 6YOJ). Essential interactions often include hydrogen bonds with the hinge region residue Cys502 and hydrophobic interactions with the gatekeeper Met499 and other residues like Leu553 and Ile428 [87] [85].
Q3: Our lead compound has low selectivity for FAK1 over other kinases. How can we improve it?
Lack of selectivity can lead to off-target toxicities.
- Troubleshooting Steps:
- Analyze the Binding Mode: Examine the molecular docking pose. The chlorine atom at the C-5 position of a pyrimidine-based inhibitor can penetrate near the gatekeeper Met499 residue. Optimizing groups that interact with unique residues in the FAK1 ATP-binding pocket can enhance selectivity [87].
- Explore Macrocyclization: This strategy can constrain the compound in a bioactive conformation, improving both potency and selectivity. The macrocyclic FAK inhibitor GZD-257 showed a 4.77-fold selectivity for FAK over PYK2 [86].
- Target Allosteric Sites: Instead of the highly conserved ATP-binding site, consider developing inhibitors that target protein-protein interactions (PPIs) involving the FERM or FAT domains, which may offer greater selectivity [87].
Experimental Protocols & Data Presentation
Protocol: Structure-Based Pharmacophore Modeling and Validation for FAK1
This methodology is critical for achieving high sensitivity in virtual screening [85] [10].
Protein Structure Preparation:
- Obtain the co-crystal structure of the FAK1 kinase domain (e.g., PDB ID: 6YOJ, resolution 1.36 Å).
- Use software like MODELLER via a Chimera interface to model any missing residues (e.g., residues 570–583 and 687–689 in 6YOJ). Select the model with the lowest zDOPE score.
Pharmacophore Model Generation:
- Upload the prepared FAK1-ligand complex to the Pharmit server.
- Identify critical pharmacophoric features (e.g., hydrogen bond donors/acceptors, hydrophobic regions, aromatic rings). The software may detect ~8 initial features.
- Generate multiple pharmacophore models (e.g., 6 models), each containing 5-6 key features.
Model Validation:
- Download a set of known FAK1 active compounds (e.g., 114 actives) and decoys (e.g., 571 decoys) from the DUD-E database.
- Screen this combined set against each of your generated pharmacophore models.
- Calculate sensitivity, specificity, and enrichment factor (EF) for each model.
- Select the model with the highest validation performance (best balance of sensitivity and specificity) for virtual screening.
Quantitative Data on Representative FAK1 Inhibitors
Table 1: Key Characteristics of Selected FAK1 Inhibitors from Literature
| Compound / ID | Type / Core Structure | FAK1 IC50 (nM) | Key Features / Issues | Clinical Status |
|---|---|---|---|---|
| TAE226 [87] | 2,4-Diaminopyrimidine | 5.5 | Dual FAK/IGF-1R inhibitor; severe toxic side effects. | Preclinical (Not advanced) |
| Defactinib (VS-6063) [87] [85] | 2,4-Diaminopyrimidine | Not Specified | ATP-competitive; tested in solid tumors and mesothelioma. | Phase III / II |
| CT-707 (Contertinib) [87] | 2,4-Diaminopyrimidine | Not Specified | Multi-target inhibitor (FAK/ALK/FRK). | Phase III |
| BI-853520 [87] [85] | 2,4-Diaminopyrimidine | Not Specified | Highly selective; issues with bioavailability and clearance. | Clinical Trials |
| GZD-257 [86] | Macrocyclic | 14.3 | Good BBB penetration (Pe=43.85); 4.77x selective over PYK2. | Preclinical |
| P4N [85] [10] | Pyrimidine-based | Not Specified | Binds ATP-pocket; used as a reference in computational studies. | Preclinical |
| PROTAC-FAK (BI-0319) [88] | PROTAC Degrader | N/A (Degrader) | Abrogates both kinase and scaffold functions; reduces H3K9ac. | Preclinical |
Table 2: Computationally Identified FAK1 Inhibitor Candidates from Virtual Screening
| ZINC ID | Docking Score (kcal/mol) | Binding Free Energy (MM/PBSA) | Key Interactions | ADMET Profile |
|---|---|---|---|---|
| ZINC23845603 [85] [10] | Low (Favorable) | Favorable | Similar to known ligand P4N; stable in MD simulations. | Acceptable; Low predicted toxicity |
| ZINC44851809 [85] [10] | Low (Favorable) | Favorable | Strong binding in the kinase domain. | Acceptable; Low predicted toxicity |
| CID24601203 [89] | -10.4 | Not Specified | Identified via ligand-based pharmacophore model. | Effective; Nontoxic |
Visualization of Workflows and Pathways
FAK1 Signaling Pathway and Inhibitor Mechanisms
Diagram: FAK1 Signaling and Inhibitor Mechanisms. This diagram shows how extracellular matrix (ECM) and growth factors activate FAK1, leading to downstream signaling that promotes tumor cell survival, proliferation, and migration. The points of intervention for different inhibitor types are highlighted.
Computational Workflow for Sensitivity Optimization
Diagram: FAK1 Inhibitor Computational Discovery Workflow. This flowchart outlines the key steps for a sensitivity-optimized computational campaign, highlighting critical validation and filtering stages.
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Research Tools for a FAK1 Inhibitor Campaign
| Item / Reagent | Function / Role | Example Product / Source |
|---|---|---|
| FAK1 Kinase Domain Structure | Template for structure-based design; resolving key ligand interactions. | Protein Data Bank (PDB ID: 6YOJ) [85] [10] |
| Validated Pharmacophore Model | Virtual screening query to identify novel hit compounds from large databases. | Generated via Pharmit [85] [10] or Ligand Scout [89] |
| Small Molecule Database | Source of commercially available compounds for virtual screening. | ZINC Database [85] [10] |
| Docking & Simulation Software | Predicting binding poses, affinity, and complex stability. | PyRx/AutoDock Vina, SwissDock, GROMACS (for MD) [85] [10] |
| Reference Kinase Inhibitor | Positive control for enzymatic and cellular assays. | TAE226 (IC50 = 5.5 nM) [87] [86] |
| PROTAC FAK Degrader | Tool compound to investigate kinase-independent (scaffold) functions of FAK. | BI-0319 (from Boehringer Ingelheim opnMe) [88] |
| FAK1 siRNA / esiRNA | Genetic validation of pharmacological effects on viability, invasion, etc. | Commercially available from various suppliers [88] |
| ADMET Prediction Tool | Early assessment of compound drug-likeness and toxicity risks. | SwissADME, admetSAR, pkCSM [85] [89] |
Comparative Analysis of Different Modeling Software and Algorithms
Frequently Asked Questions (FAQs)
Q1: What is the fundamental difference between structure-based and ligand-based pharmacophore modeling? The choice between a structure-based or ligand-based approach is the first critical parameter in model generation and depends entirely on the available input data [4].
- Structure-Based Pharmacophore Modeling: This method requires the three-dimensional (3D) structure of the macromolecular target (e.g., a protein receptor or enzyme). The model is generated by analyzing the binding site to identify key interaction points—such as hydrogen bond donors/acceptors and hydrophobic areas—that a ligand must satisfy for optimal binding [4]. This approach is ideal when a high-resolution protein structure, often from the Protein Data Bank (PDB), is available.
- Ligand-Based Pharmacophore Modeling: This approach is used when the 3D structure of the target is unknown. It develops a model by identifying the common steric and electronic features shared by a set of known active ligands. This model hypothesizes the essential features responsible for the biological activity [4] [90].
Q2: How can I improve the sensitivity and hit rates of my pharmacophore virtual screening? Optimizing sensitivity—the ability to correctly identify active compounds—often involves a multi-faceted strategy:
- Integrate Machine Learning (ML): Employ ML models to predict docking scores, which can accelerate virtual screening by up to 1000 times compared to classical docking. This allows for the rapid prioritization of compounds from ultra-large libraries [27].
- Combine Pharmacophore and Docking: Use pharmacophore models as a pre-filter to reduce the number of compounds before subjecting them to more computationally intensive molecular docking simulations. This hybrid approach enhances virtual screening efficiency [91] [92].
- Utilize Prepared Commercial Libraries: Leverage fully prepared, curated databases of purchasable compounds (e.g., from Enamine, MilliporeSigma) to ensure high-quality, relevant chemical matter for screening, which improves the likelihood of identifying viable hits [90].
Q3: My pharmacophore model is retrieving too many false positives. How can I enhance its specificity? To enhance specificity—the ability to reject inactive compounds—consider these parameter adjustments:
- Add Exclusion Volumes: Incorporate exclusion volumes (XVOL) into your model to represent the steric boundaries of the binding pocket. This prevents the selection of compounds that have favorable pharmacophore features but are too bulky to fit [4].
- Refine Feature Selection: A common mistake is including too many features. Manually refine the model to retain only the features that are essential for bioactivity, often informed by analyzing conserved interactions in protein-ligand complexes [4].
- Apply Tautomeric and Ionization States: Use software capabilities to rapidly and thoroughly sample conformational, ionization, and tautomeric states during database creation. This ensures a more accurate representation of the compounds being screened [90].
Q4: What role do modern generative models play in pharmacophore-based drug discovery? Generative models like TransPharmer represent a cutting-edge advancement. They integrate interpretable pharmacophore fingerprints with generative AI (e.g., a GPT-based framework) for de novo molecule generation [67]. This facilitates scaffold hopping, producing structurally novel compounds that still conform to the desired pharmacophoric constraints, thereby expanding the chemical space explored in a discovery campaign [67].
Troubleshooting Common Experimental Issues
Issue 1: Poor Correlation Between Pharmacophore Screening Hits and Experimental Activity
| Potential Cause | Diagnostic Steps | Solution |
|---|---|---|
| Inadequate Conformational Sampling | Check if the software's conformational search method (e.g., within MOE or Phase) adequately covers the low-energy states of your query ligands and database compounds. | Increase the thoroughness of conformational analysis. Use software with best-in-class force fields (e.g., OPLS4 in Phase) to generate more biologically relevant conformers [90]. |
| Low-Quality Input Structure | For structure-based models, validate the protein structure's resolution, check for missing loops/atoms, and verify protonation states of key residues. | Critically evaluate and prepare the input structure before modeling. Use tools for protein structure refinement or consider homology modeling if the experimental structure is poor [4]. |
| Overly General Pharmacophore Model | Analyze if the model lacks specific geometric constraints or key chemical features. Test the model against a small set of known inactive compounds. | Manually edit the hypothesis to include critical features and adjust tolerance radii. Incorporate exclusion volumes to define the binding site shape more accurately [4]. |
Issue 2: Software Performance and Workflow Integration Bottlenecks
| Potential Cause | Diagnostic Steps | Solution |
|---|---|---|
| Handling Ultra-Large Libraries | Monitor screening times for databases containing millions to billions of compounds. | Employ GPU-accelerated screening (e.g., with GPU Shape) [90] or machine learning models that predict docking scores to pre-emptively rank compounds [27]. |
| Incompatibility Between Tool Outputs | Ensure file formats (e.g., SDF, MOL2, PDB) are correctly specified and interpreted when transferring data between software (e.g., from a pharmacophore tool to a docking program). | Use platforms that support a wide range of data formats or offer integrated suites of applications (e.g., Discovery Studio, MOE) to streamline the workflow from pharmacophore modeling to docking [92] [93]. |
Experimental Protocols for Parameter Optimization
Protocol for Developing a Sensitive Ligand-Based Pharmacophore Model
This protocol is optimized for creating a model with high sensitivity to identify novel active chemotypes, using tools like LigandScout or Phase [50] [90].
- Ligand Set Curation: Assemble a set of 8-15 known active compounds with diverse scaffolds but similar high potency. Including diverse actives helps the model generalize and improves sensitivity for scaffold hopping [50].
- Conformational Expansion: For each ligand, generate a representative set of low-energy conformations. Use software like ConfGen with a force field (e.g., OPLS4) to ensure comprehensive coverage [90].
- Common Pharmacophore Perception: Run the common pharmacophore perception algorithm. The software will propose multiple hypotheses—arrangements of features like H-bond donors/acceptors (HBD/HBA), hydrophobic areas (H), and aromatic rings (AR) [90].
- Hypothesis Selection Based on Sensitivity:
- Score Hypotheses: Rank the generated hypotheses based on their alignment scores to the active ligand set.
- Validate with Decoys: Screen a small validation set containing known actives and inactives (decoys). Select the hypothesis that retrieves the highest percentage of true actives (high sensitivity) while minimizing the retrieval of inactives [50].
- Model Refinement: Manually inspect the top hypothesis. Remove redundant features that are not critical for activity to prevent over-constraining the model and reducing sensitivity.
Protocol for Structure-Based Model Generation and Validation
This protocol is for when a protein target structure is available, using software such as MOE or Discovery Studio [94] [4].
- Protein Preparation:
- Obtain the 3D structure from the PDB (e.g., 2Z5Y for MAO-A) [27].
- Add hydrogen atoms, correct protonation states of residues (especially in the binding site), and remove crystallographic water molecules unless they are crucial for binding.
- Binding Site Analysis and Feature Mapping:
- Define the binding site, either from the co-crystallized ligand or using a binding site detection tool (e.g., GRID, LUDI) [4].
- Generate a set of pharmacophore features that a ligand would need to interact with key residues in the pocket.
- Feature Selection and Exclusion Volume Application:
- Validation via Virtual Screening:
- Use the model to screen a database of compounds.
- Take the top-ranking hits and subject them to molecular docking studies (e.g., with Glide or AutoDock Vina) to assess binding pose and affinity [94].
- The model's sensitivity and specificity are optimized when it successfully identifies hits that also show strong, pose-predictable binding in docking simulations [91] [94].
Experimental Workflow and Logical Pathway Visualizations
Pharmacophore Modeling Decision Workflow
Sensitivity vs. Specificity Optimization Logic
Research Reagent Solutions: Essential Software and Tools
The following table details key software tools used in advanced pharmacophore modeling, as identified in recent literature.
| Software Name | Primary Function | Key Features Relevant to Sensitivity | Application in Cited Research |
|---|---|---|---|
| MOE (Molecular Operating Environment) [92] [94] | Comprehensive molecular modeling and simulation. | Structured-Based Design, 3D Query Editor, virtual screening, and molecular docking. | Used for structure-based pharmacophore modeling, virtual screening, and MD simulations to identify LpxH inhibitors against Salmonella Typhi [94]. |
| LigandScout [92] [50] | Advanced pharmacophore modeling and virtual screening. | Intuitive interface for creating 3D pharmacophore models from protein-ligand complexes or ligand sets. | Used to establish a flavonol-based pharmacophore model for identifying anti-HBV compounds [50]. |
| Schrödinger Phase [92] [90] | Ligand- and structure-based pharmacophore modeling. | Unique common pharmacophore perception; can create hypotheses from ligands, complexes, or apo proteins. | Recommended for scaffold hopping and creating hypotheses in the absence of a protein structure [90]. |
| Discovery Studio [92] [93] | Life science modeling and simulation suite. | Integrated suite for pharmacophore modeling, QSAR, protein-ligand docking, and simulation. | Contains tools for bioinformatics, molecular modeling, and simulation, supporting a full drug discovery workflow [92] [93]. |
| TransPharmer [67] | Pharmacophore-informed generative model. | GPT-based framework using pharmacophore fingerprints for de novo molecule generation and scaffold hopping. | Generated novel PLK1 inhibitors with a new scaffold, demonstrating potent activity (5.1 nM) [67]. |
Troubleshooting Guide: FAQs on Pharmacophore Model Validation
This section addresses common challenges researchers face during the prospective validation of pharmacophore models, from virtual screening to experimental confirmation of hits.
FAQ 1: Why do my virtual hits show excellent computed potency but fail in initial experimental assays?
This common issue often stems from a disconnect between the computational model and the biological reality. Key troubleshooting steps include:
- Re-evaluate Model Specificity: Your pharmacophore model may be insufficiently selective, retrieving compounds that fit the model but are promiscuous binders or subject to off-target effects. Refine the model by incorporating known inactive compounds to define exclusion volumes or features.
- Verify Assay Conditions: Ensure your in silico conditions (e.g., protonation states, tautomers) match the experimental bioassay's buffer chemistry and pH. A mismatch can lead to a false negative.
- Check for Artifact Compounds: Screen hits for chemical structures known to cause assay interference, such as compounds that act as fluorescent quenchers, aggregators, or reactive chemical groups (e.g., pan-assay interference compounds, or PAINS).
FAQ 2: How can I improve the structural novelty of hits generated from a pharmacophore model?
A major goal of pharmacophore-based screening is scaffold hopping. If your model consistently produces analogs of known actives, consider the following:
- Use Fuzzy Pharmacophore Features: Instead of relying on precise geometric constraints, employ "fuzzy" or tolerance-based features that allow for greater chemical diversity while maintaining critical interactions. Methodologies like the TransPharmer model use multi-scale, interpretable pharmacophore fingerprints to enable scaffold hopping by focusing on pharmaceutical features rather than exact scaffolds [67].
- Incorporate Ligand-Based Information: If the model is structure-based, augment it with ligand-based information from diverse known actives. This can help the model generalize the essential features required for binding.
- Optimize the Screening Library: Curate your virtual screening library to include a higher proportion of diverse, lead-like compounds with under-represented scaffolds to increase the probability of novel discoveries.
FAQ 3: What are the critical parameters to optimize for enhancing pharmacophore model sensitivity during virtual screening?
Parameter optimization is crucial for balancing sensitivity (finding true actives) and specificity (excluding inactives). Focus on these key parameters:
- Feature Tolerances: The distance and angle tolerances for pharmacophore features (e.g., hydrogen bond donors/acceptors, hydrophobic regions) are paramount. Overly strict tolerances reduce sensitivity, while overly loose ones reduce specificity.
- Weighting of Features: Not all pharmacophore features contribute equally to binding. Assign higher weights to features known from mutagenesis studies or structural data to be critical for biological activity.
- Conformational Sampling: The method and exhaustiveness of conformational analysis for both the model and the database molecules significantly impact results. Ensure the sampling protocol is robust enough to represent bioactive conformers without being computationally prohibitive.
FAQ 4: My model successfully identifies active compounds, but they exhibit poor solubility or cytotoxicity. How can this be addressed earlier in the workflow?
This indicates a need to integrate Absorption, Distribution, Metabolism, Excretion, and Toxicity (ADMET) profiling earlier in the virtual screening process.
- Implement Parallel ADMET Filtering: During or immediately after the pharmacophore screen, apply computational filters for key drug-like properties. This includes predicting solubility, cytochrome P450 inhibition, and human ether-a-go-go related gene (hERG) channel binding.
- Use Multi-Parameter Optimization: Rather than selecting hits based solely on pharmacophore fit score, employ a scoring function that balances fit with predicted ADMET properties. This ensures that prioritized compounds have a higher probability of progressing through the drug discovery pipeline.
Experimental Protocols for Validation
This section provides detailed methodologies for key experiments cited in successful prospective validation studies.
Case Study: Prospective Discovery of PLK1 Inhibitors using TransPharmer
The following protocol is adapted from the workflow that led to the identification of a novel, potent PLK1 inhibitor (IIP0943) with a 4-(benzo[b]thiophen-7-yloxy)pyrimidine scaffold [67].
1. Pharmacophore-Informed In Silico Screening
- Objective: To generate novel chemical structures conforming to target pharmacophores derived from known bioactive ligands.
- Methodology:
- Model Setup: Employ a generative pre-training transformer (GPT)-based framework (e.g., TransPharmer) conditioned on multi-scale, interpretable pharmacophore fingerprints [67].
- Generation: Run the model in a "scaffold-hopping" exploration mode to generate new molecular structures (in SMILES format) that satisfy the pharmacophoric constraints of a reference active compound but are structurally distinct.
- Evaluation of Generated Molecules: Assess the output using two primary metrics against the target pharmacophore:
- Dcount: The average difference in the number of individual pharmacophoric features.
- Spharma: The pharmacophoric similarity, measured by the Tanimoto coefficient of ErG fingerprints or similar pharmacophore fingerprints [67].
- Expected Outcome: A library of generated molecules with high pharmacophoric similarity (
Spharma) to the target and a low deviation in feature counts (Dcount).
2. In Vitro Kinase Inhibition Assay
- Objective: To experimentally determine the half-maximal inhibitory concentration (IC₅₀) of synthesized hits against the target kinase (e.g., PLK1).
- Methodology:
- Assay Format: Conduct a homogenous time-resolved fluorescence (HTRF) kinase assay or a similar validated biochemical assay.
- Procedure: Incubate the target kinase with its substrate and ATP in the presence of a serial dilution of the test compound. Measure the product formation using HTRF reagents.
- Data Analysis: Plot the inhibition percentage against the logarithm of compound concentration. Fit the data to a four-parameter logistic model to calculate the IC₅₀ value.
- Expected Outcome: Dose-response curves and IC₅₀ values for all tested compounds. A successful hit, like IIP0943, demonstrated a potency of 5.1 nM in the published study [67].
3. Cellular Proliferation Assay
- Objective: To evaluate the functional efficacy of the inhibitor in a cellular context.
- Methodology:
- Cell Line: Use a relevant cancer cell line, such as HCT116 colon carcinoma cells.
- Procedure: Seed cells in 96-well plates and treat them with a range of concentrations of the test compound. After an incubation period (e.g., 72 hours), measure cell viability using a method like the CellTiter-Glo luminescent assay.
- Data Analysis: Calculate the half-maximal growth inhibitory concentration (GI₅₀) from the dose-response curve.
- Expected Outcome: Determination of the compound's potency in cells. IIP0943 showed submicromolar activity in inhibiting HCT116 cell proliferation [67].
4. Selectivity Profiling
- Objective: To ensure the compound is selective for the intended target over closely related targets.
- Methodology:
- Panel Testing: Screen the compound against a panel of related kinases (e.g., other Plk family members like PLK2 and PLK3) at a single concentration (e.g., 1 µM) or perform full IC₅₀ determinations.
- Data Analysis: Calculate the selectivity index (e.g., IC₅₀(off-target) / IC₅₀(target)).
- Expected Outcome: A selectivity profile. IIP0943 was reported to have high selectivity for PLK1 over other Plks [67].
The quantitative results from the prospective PLK1 case study are summarized in the table below.
Table 1: Experimental Validation Data for a Novel PLK1 Inhibitor (IIP0943)
| Assay Type | Target | Result | Interpretation / Benchmark |
|---|---|---|---|
| Biochemical IC₅₀ | PLK1 Kinase | 5.1 nM | High potency; comparable to reference inhibitor (4.8 nM) [67]. |
| Cellular GI₅₀ | HCT116 Cells | Submicromolar | Confirmed functional activity in a cellular context [67]. |
| Selectivity Screening | PLK2, PLK3 | High Selectivity | Reduced potential for off-target side effects [67]. |
| Scaffold Analysis | Chemical Structure | 4-(benzo[b]thiophen-7-yloxy)pyrimidine | Novel scaffold, distinct from known inhibitors [67]. |
Workflow Visualization
The following diagram illustrates the integrated computational and experimental workflow for the prospective validation of pharmacophore-generated hits, leading from model creation to a confirmed lead compound.
The Scientist's Toolkit: Research Reagent Solutions
This table details key reagents, software, and databases essential for conducting prospective validation of pharmacophore models.
Table 2: Essential Research Reagents and Tools for Prospective Validation
| Item / Resource | Function / Description | Example Use Case |
|---|---|---|
| Generative Model (TransPharmer) | A GPT-based framework conditioned on pharmacophore fingerprints for de novo molecule generation and scaffold hopping [67]. | Generating novel chemical structures that fulfill specific pharmacophoric constraints derived from known actives. |
| Pharmacophore Modeling Software | Software (e.g., MOE, LigandScout, Schrödinger Phase) used to create and validate the 3D pharmacophore hypothesis from structural or ligand data [94]. | Defining the essential features and their spatial arrangement for virtual screening. |
| Virtual Compound Library | A curated database of purchasable or synthesizable compounds (e.g., ZINC, Enamine) or a database for in silico generation. | Serves as the chemical space for virtual screening or as a benchmark for generative models. |
| HTRF Kinase Assay Kit | A homogenous, immunoassay-based kit for measuring kinase activity by detecting phosphorylation of a substrate [67]. | Performing initial high-throughput biochemical screening of synthesized hits for target inhibition (IC₅₀). |
| Cell Viability Assay Reagent | A luminescent or colorimetric reagent (e.g., CellTiter-Glo) that quantifies the number of metabolically active cells in culture. | Determining the functional anti-proliferative effect (GI₅₀) of compounds in relevant cell lines. |
| ADMET Prediction Software | In silico tools that predict key drug properties like solubility, metabolic stability, and toxicity. | Filtering virtual hits to prioritize compounds with a higher probability of favorable drug-like properties. |
Conclusion
Optimizing pharmacophore model sensitivity is a multifaceted process that requires a deep understanding of fundamental concepts, application of advanced modeling techniques, careful parameter tuning, and rigorous validation. By systematically addressing feature selection, incorporating dynamic protein data from MD simulations, and leveraging AI-driven methods, researchers can significantly enhance model performance. The ultimate goal is to develop sensitive and specific models that reliably enrich active compounds in virtual screening, thereby accelerating the discovery of novel bioactive molecules. Future directions point towards the deeper integration of AI and machine learning for automated parameter optimization, the increased use of ensemble and dynamic models to capture full target flexibility, and the application of these refined models in complex areas like drug repurposing and safety profiling. These advances promise to further solidify pharmacophore modeling as an indispensable, high-yield tool in modern computational drug discovery.
References
- 1. ELIXIR-A: An Interactive Visualization Tool for Multi-Target ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9025992/]
- 2. Knowledge-guided diffusion model for 3D ligand ... [https://www.nature.com/articles/s41467-025-57485-3]
- 3. Hierarchical Graph Representation of Pharmacophore ... [https://www.frontiersin.org/journals/molecular-biosciences/articles/10.3389/fmolb.2020.599059/full]
- 4. Drug Design by Pharmacophore and Virtual Screening ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9145410/]
- 5. Structure‐based pharmacophore modeling for precision ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11299079/]
- 6. Pharmacophore-Based Virtual Screening, Quantum ... [https://www.mdpi.com/1420-3049/26/16/4961]
- 7. Pharmacophore modeling: advances, limitations, and ... [https://www.dovepress.com/pharmacophore-modeling-advances-limitations-and-current-utility-in-dru-peer-reviewed-fulltext-article-JRLCR]
- 8. Concepts and Applications Exemplified on Hydroxysteroid ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6332202/]
- 9. Evaluating the stability of pharmacophore features using ... [https://www.sciencedirect.com/science/article/abs/pii/S0006291X1630081X]
- 10. Structure-based identification of novel FAK1 inhibitors ... [https://www.nature.com/articles/s41598-025-23203-8]
- 11. Water-Based Pharmacophore Modeling in Kinase Inhibitor ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12458683/]
- 12. Discovery of a novel IKK-β inhibitor by ligand-based virtual ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3013379/]
- 13. Schrodinger-Notes—Target-based Pharmacophore Modeling [https://blog.jiangshen.org/2024/schrodinger-notes-target-based-pharmacophore-modeling/]
- 14. Ligand-Based Pharmacophore Modeling and Virtual ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4111740/]
- 15. μ Opioid receptor: novel antagonists and structural modeling [https://www.nature.com/articles/srep21548]
- 16. Prospective performance evaluation of selected common ... [https://www.sciencedirect.com/science/article/pii/S0223523415002664]
- 17. Pharmacophore Modeling of Janus Kinase Inhibitors [https://www.mdpi.com/1420-3049/30/10/2183]
- 18. Leveraging ligand-based and structure-based approaches ... [https://www.iptonline.com/articles/leveraging-ligand-based-and-structure-based-approaches-for-advan]
- 19. The power of structure-based drug design [https://www.drugdiscoverynews.com/structure-based-drug-design-15997]
- 20. Merging Ligand-Based and Structure-Based Methods in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7587536/]
- 21. Integration of Ligand-Based and Structure-Based Methods ... [https://www.mdpi.com/1420-3049/27/13/4026]
- 22. Comparison of structure- and ligand-based scoring functions ... [https://jcheminf.biomedcentral.com/articles/10.1186/s13321-021-00516-0]
- 23. Integrating structure-based approaches in generative ... [https://www.sciencedirect.com/science/article/pii/S0959440X23000337]
- 24. A structure-based framework for selective inhibitor design ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11903766/]
- 25. Structure-based and ligand-based drug discovery [https://optibrium.com/knowledge-base/leveraging-structure-based-and-ligand-based-drug-discovery/]
- 26. dyphAI dynamic pharmacophore modeling with AI: a tool ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11865752/]
- 27. Machine learning accelerates pharmacophore-based ... [https://www.nature.com/articles/s41598-024-58122-7]
- 28. Building shape-focused pharmacophore models for effective ... [https://jcheminf.biomedcentral.com/articles/10.1186/s13321-024-00857-6]
- 29. PharmRL: pharmacophore elucidation with deep geometric ... [https://bmcbiol.biomedcentral.com/articles/10.1186/s12915-024-02096-5]
- 30. Global parameter optimisation and sensitivity analysis of ... [https://www.sciencedirect.com/science/article/pii/S0041010123001927]
- 31. Parameter Optimization of the 3PG Model Based on ... [https://www.mdpi.com/1999-4907/11/12/1369]
- 32. Global sensitivity analysis of Open Systems Pharmacology ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11646943/]
- 33. Identification of pharmacophore synergism for optimization ... [https://www.sciencedirect.com/science/article/pii/S266702242500060X]
- 34. DynamicBind: predicting ligand-specific protein ... [https://www.nature.com/articles/s41467-024-45461-2]
- 35. Cryo-EM Structure Based Drug Design (SBDD) [https://www.nanoimagingservices.com/about/blog/three-common-challenges-to-adopting-cryo-em-in-your-drug-discovery-program-and-how-to-overcome-them]
- 36. Consensus scoring with feature selection for structure- ... [https://pubmed.ncbi.nlm.nih.gov/18229906/]
- 37. A Guide to In Silico Drug Design - PMC - PubMed Central [https://pmc.ncbi.nlm.nih.gov/articles/PMC9867171/]
- 38. Structure based drug design and machine learning ... [https://www.nature.com/articles/s41598-025-17708-5]
- 39. End-to-end protein–ligand complex structure generation ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10240776/]
- 40. A workflow to create a high-quality protein–ligand binding ... [https://pubs.rsc.org/en/content/articlehtml/2025/dd/d4dd00357h]
- 41. Ligand-Based Pharmacophore Modeling Using Novel 3D ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6321403/]
- 42. Schrödinger Notes—Ligand-based Pharmacophore Modeling [https://blog.jiangshen.org/2024/schrodinger-notes-ligand-based-pharmacophore-modeling/]
- 43. Hierarchical Graph Representation of Pharmacophore ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7793842/]
- 44. Ligand-based pharmacophore modeling targeting the ... [https://www.sciencedirect.com/science/article/pii/S2950363924000218]
- 45. Learning to engineer protein flexibility [https://arxiv.org/html/2412.18275v1]
- 46. Importance of Incorporating Protein Flexibility in Molecule ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6465739/]
- 47. Exploring the potential of protein-based pharmacophore ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3725268/]
- 48. DNA molecular dynamic trouble - GROMACS forums [https://gromacs.bioexcel.eu/t/dna-molecular-dynamic-trouble/7557]
- 49. Common errors when using GROMACS [https://manual.gromacs.org/2024.4/user-guide/run-time-errors.html]
- 50. Pharmacophore modeling and QSAR analysis of anti-HBV ... [https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0316765]
- 51. A pharmacophore-guided deep learning approach for ... [https://www.nature.com/articles/s41467-023-41454-9]
- 52. How AI Is Irrevocably Altering the DNA of Drug Development [https://www.drugpatentwatch.com/blog/how-ai-is-already-changing-drug-development/?srsltid=AfmBOoqbDU_2DtW_p4HbK1YwnTjuWaHZH0yg1DsRtWq9GHMmKCQoptZS]
- 53. PGMG: A Pharmacophore-Guided Deep Learning ... [https://arxiv.org/abs/2207.00821]
- 54. Target screening and optimization of candidate ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12098522/]
- 55. A beginner's approach to deep learning applied to VS and MD ... [https://jcheminf.biomedcentral.com/articles/10.1186/s13321-025-00985-7]
- 56. Overview — DP-GEN documentation [https://docs.deepmodeling.com/projects/dpgen/en/latest/overview/overview.html]
- 57. Virtual screening to enrich hit lists from high-throughput ... [https://pubmed.ncbi.nlm.nih.gov/12471601/]
- 58. Combining Ligand- and Structure-Based Methods for More ... [https://www.genengnews.com/topics/drug-discovery/combining-ligand-and-structure-based-methods-for-more-effective-virtual-screening/]
- 59. Ultra-large library screening with an evolutionary algorithm ... [https://www.nature.com/articles/s42004-025-01758-x]
- 60. 2.1.2. Pharmacophore model validation [https://bio-protocol.org/exchange/minidetail?type=30&id=9385508]
- 61. Greedy 3-Point Search (G3PS)—A Novel Algorithm for Pharmacophore Alignment [https://www.mdpi.com/1420-3049/26/23/7201]
- 62. A New Pharmacophore Model for the Design of Sigma-1 ... [https://www.frontiersin.org/journals/pharmacology/articles/10.3389/fphar.2019.00519/full]
- 63. Recent advances in molecular representation methods and ... [https://www.nature.com/articles/s44386-025-00017-2]
- 64. Pharmacophore-based virtual screening and in silico ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12009819/]
- 65. Strategies for 3D pharmacophore-based virtual screening [https://www.sciencedirect.com/science/article/abs/pii/S1740674910000375]
- 66. Pharmit: interactive exploration of chemical space - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC4987880/]
- 67. Accelerating discovery of bioactive ligands with ... [https://www.nature.com/articles/s41467-025-56349-0]
- 68. PharmBench, a benchmark data set for evaluating ... [https://pubmed.ncbi.nlm.nih.gov/22970854/]
- 69. The quest for a consensus dynamic pharmacophore [https://www.sciencedirect.com/science/article/pii/S1093326314000485]
- 70. A guide to fixing broken AMBER MD trajectory files and ... [https://www.blopig.com/blog/2025/09/a-guide-to-fixing-broken-amber-md-trajectory-files-and-visualisations/]
- 71. A Molecular Dynamics-Shared Pharmacophore Approach ... [https://pubmed.ncbi.nlm.nih.gov/28135036/]
- 72. Molecular Dynamics-Derived Pharmacophore Model ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8396485/]
- 73. Classification: ROC and AUC | Machine Learning [https://developers.google.com/machine-learning/crash-course/classification/roc-and-auc]
- 74. How to explain the ROC curve and ROC AUC score? [https://www.evidentlyai.com/classification-metrics/explain-roc-curve]
- 75. Pharmacophore model, docking, QSAR, and molecular ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8047494/]
- 76. Ligand-Based Virtual Screening Approach Using a New ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3405195/]
- 77. Structure-based pharmacophore modeling 1. Automated ... [https://www.sciencedirect.com/science/article/abs/pii/S109332632300027X]
- 78. interactive exploration of chemical space [https://pharmit.csb.pitt.edu/help.html]
- 79. Pharmacophore Modeling, Virtual Screening, and ... [https://www.medsci.org/v10p0265.htm]
- 80. Structure-Based Pharmacophore Modeling, Virtual ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8777599/]
- 81. Directory of Useful Decoys, Enhanced (DUD-E) [https://pmc.ncbi.nlm.nih.gov/articles/PMC3405771/]
- 82. An Unbiased Method To Build Benchmarking Sets for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4038372/]
- 83. deep learning-guided pharmacophore modeling for ultra-large ... [https://pubs.rsc.org/en/content/articlehtml/2024/sc/d4sc04854g]
- 84. Knowledge-guided diffusion model for 3D ligand ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11885826/]
- 85. Structure-based identification of novel FAK1 inhibitors using ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12606203/]
- 86. Discovery of a macrocyclic FAK inhibitor GZD-257 for ... [https://www.sciencedirect.com/science/article/abs/pii/S0960894X25003336]
- 87. Recent advances in focal adhesion kinase (FAK)-targeting ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12180522/]
- 88. FAK inhibition disrupts tumor growth, apoptosis, and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12358824/]
- 89. Integrative Ligand-Based Pharmacophore Modeling ... [https://www.mdpi.com/1424-8247/16/1/120]
- 90. Phase - Schrödinger [https://www.schrodinger.com/platform/products/phase/]
- 91. Pharmacophore modeling in drug design [https://pubmed.ncbi.nlm.nih.gov/40175047/]
- 92. A Comprehensive Guide to the Top 8 Pharmacophore ... [https://parssilico.com/blogs/79-top-8-pharmacophore-modeling-software]
- 93. Comparison of software for molecular mechanics modeling [https://en.wikipedia.org/wiki/Comparison_of_software_for_molecular_mechanics_modeling]
- 94. Pharmacophore-based approach for the identification of ... [https://www.sciencedirect.com/science/article/pii/S266702242500012X]