NGS Concordance Between Tissue and Liquid Biopsy: A Comprehensive Review for Precision Oncology
This article provides a comprehensive analysis of next-generation sequencing (NGS) concordance between tissue and liquid biopsy across solid tumors, with emphasis on non-small cell lung cancer.
NGS Concordance Between Tissue and Liquid Biopsy: A Comprehensive Review for Precision Oncology
Abstract
This article provides a comprehensive analysis of next-generation sequencing (NGS) concordance between tissue and liquid biopsy across solid tumors, with emphasis on non-small cell lung cancer. We examine the foundational principles of both testing modalities, methodological approaches for optimal implementation, strategies for troubleshooting discordant results, and analytical validation frameworks. For researchers and drug development professionals, we synthesize evidence from recent clinical studies demonstrating variable concordance rates (71.2%-95.7%) dependent on tumor stage, volume, and assay sensitivity. The review highlights clinical scenarios where liquid biopsy demonstrates particular utility, including when tissue is insufficient or for serial monitoring, while acknowledging limitations and optimization strategies for implementing complementary testing approaches in research and clinical development.
Fundamental Principles of Tissue and Liquid Biopsy in Precision Oncology
Tissue biopsy has long been the cornerstone of cancer diagnosis, treatment planning, and molecular profiling. However, its status as the "gold standard" is being re-evaluated in the face of significant challenges, particularly tumor spatial heterogeneity, which can limit the accuracy and comprehensiveness of the information it provides. This guide examines the technical limitations of tissue biopsy through the lens of modern oncology research, with a specific focus on implications for Next-Generation Sequencing (NGS) concordance studies between tissue and liquid biopsy.
The Spatial Heterogeneity Problem in Tissue Biopsy
Spatial heterogeneity refers to the genetic, transcriptomic, and protein expression differences that exist between distinct geographical regions of the same tumor. This phenomenon poses a fundamental challenge to the representativeness of a standard tissue biopsy, which typically samples only a small portion of the entire tumor mass.
Experimental Evidence in Esophageal Squamous Cell Carcinoma
A 2025 study on esophageal squamous cell carcinoma (ESCC) systematically quantified the impact of spatial heterogeneity on the assessment of PD-L1, a critical biomarker for immunotherapy.
- Experimental Protocol: Researchers sampled four distinct regions using endoscopic biopsy forceps from treatment-naïve ESCC patients and compared these with the largest longitudinal sections from completely resected tumors [1].
- Key Findings:
- Limited biopsy samples were insufficient to accurately determine the Combined Positive Score (CPS) for PD-L1 across the entire tumor [1].
- Spatial heterogeneity was reduced in tumors with sufficiently high CPS, suggesting that extreme negative or positive biomarker status may be more consistently assessed [1].
- A multi-region sampling approach (maximum CPS derived from three regions) provided a more accurate approximation of the bulk tumor's PD-L1 status than a single biopsy [1].
Transcriptomic Heterogeneity in Hepatocellular Carcinoma
Research in hepatocellular carcinoma (HCC) has revealed that spatial heterogeneity extends to the transcriptomic level, capturing crucial information about tumor evolution.
- Experimental Protocol: Scientists analyzed 172 multiregional transcriptomic profiles from 37 HCC patients, quantifying intra- and inter-tumor expression variation [2].
- Key Findings:
- Genes exhibiting high intra- and inter-tumoral expression variation were significantly enriched in prognostic information for HCC [2].
- This heterogeneity reflects a geospatially gradual transition from non-tumor region to tumor border and tumor core, as validated through multiregional single-cell transcriptomic profiling of 110,817 cells from 34 liver specimens [2].
Table 1: Impact of Spatial Heterogeneity on Biomarker Assessment
| Cancer Type | Biomarker | Effect of Heterogeneity | Mitigation Strategy |
|---|---|---|---|
| Esophageal Squamous Cell Carcinoma (ESCC) | PD-L1 (CPS) | Single biopsy inaccurately represents whole-tumor status [1] | Multi-region sampling (max CPS from 3 regions) [1] |
| Hepatocellular Carcinoma (HCC) | Transcriptomic Signature | Single sample misses evolutionary information [2] | Multiregional analysis captures prognostic heterogeneity [2] |
Liquid Biopsy as a Complementary Approach
Liquid biopsy has emerged as a minimally invasive alternative that can overcome some limitations of tissue biopsy by capturing tumor-derived components from bodily fluids such as blood, urine, and cerebrospinal fluid [3] [4].
Key Analytes in Liquid Biopsy
- Circulating Tumor DNA (ctDNA): Short fragments of tumor-derived DNA in circulation, representing 0.1-1.0% of total cell-free DNA. ctDNA has a short half-life, allowing for real-time monitoring of tumor dynamics [3].
- Circulating Tumor Cells (CTCs): Intact cells shed from primary and metastatic tumors into circulation. Isolating CTCs is challenging (approximately 1 CTC per 1 million leukocytes) but provides information about metastatic potential [3] [4].
- Extracellular Vesicles (EVs) and Tumor-Educated Platelets (TEPs): Other tumor-derived components that carry molecular information about the tumor [4].
Technical Platforms for Liquid Biopsy Analysis
- PCR-based methods (qPCR, ddPCR): Offer high sensitivity for detecting known mutations but limited multiplexing capability [5].
- Next-Generation Sequencing (NGS): Allows comprehensive profiling of multiple genes simultaneously, with higher sensitivity for ctDNA detection compared to ddPCR and qPCR in some settings [5].
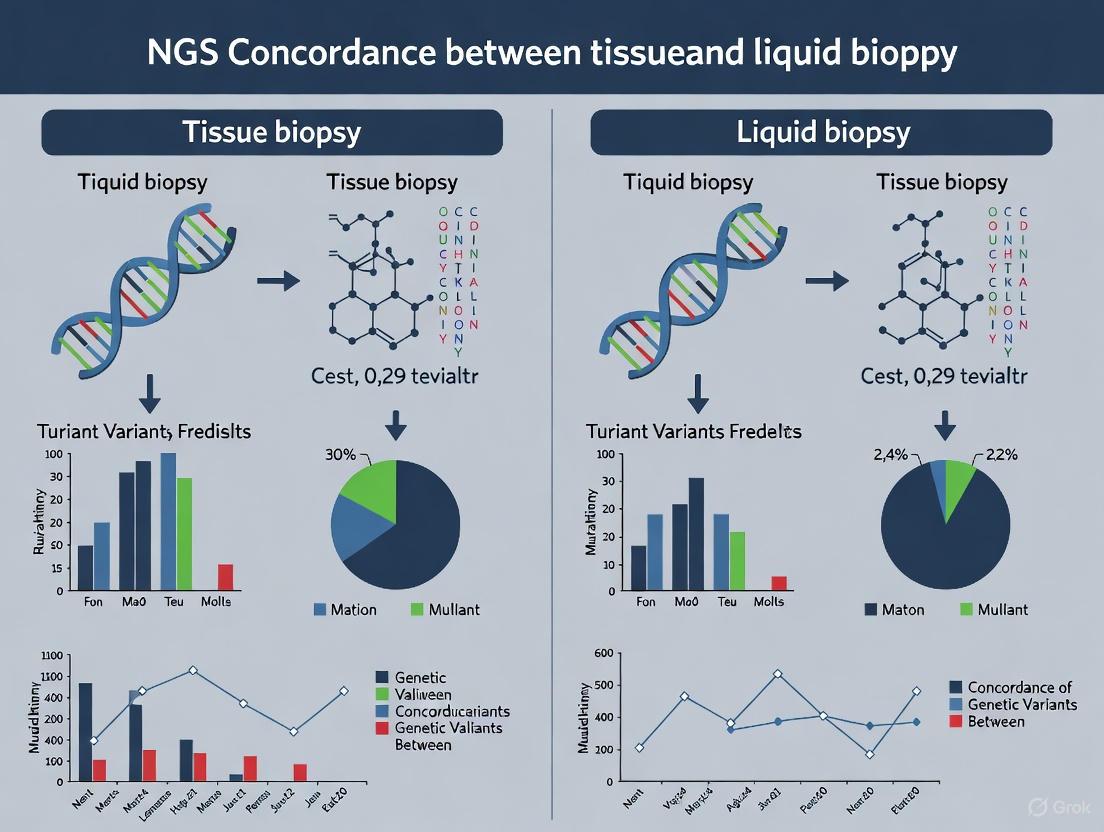
Diagram: Integrated Tissue and Liquid Biopsy Workflow for Comprehensive Tumor Profiling
NGS Concordance Between Tissue and Liquid Biopsy
The concordance between tissue and liquid biopsy NGS results has emerged as a critical factor in therapeutic decision-making, with implications for patient outcomes.
Insights from the ROME Trial
A 2025 analysis from the ROME Trial provided crucial insights into how concordance between tissue and liquid biopsy affects treatment outcomes.
- Experimental Protocol: The phase II multicenter study enrolled 1,794 patients with advanced solid tumors. NGS was performed on both tissue (FoundationOne CDx) and liquid biopsies (FoundationOne Liquid CDx). A centralized Molecular Tumor Board reviewed results to identify actionable alterations, with 400 patients randomized to tailored therapy (TT) or standard-of-care (SoC) [6].
- Concordance Definitions:
- Concordance: Detection of the same druggable alteration in both biopsy types.
- Discordance: Alteration detection in only one biopsy type [6].
- Key Findings:
- Concordance was present in 49% of cases.
- Alterations were detected exclusively in tissue (35%) or liquid (16%) biopsies [6].
- Patients in the concordant group receiving TT experienced significantly improved survival outcomes compared to SoC:
- Median OS: 11.05 vs. 7.70 months (HR 0.74)
- Median PFS: 4.93 vs. 2.80 months (HR 0.55) [6].
- The survival benefit of TT was less pronounced or absent in patients with discordant results [6].
Table 2: ROME Trial Outcomes by Biopsy Concordance Status
| Biopsy Concordance Group | Median Overall Survival (Months) | Median Progression-Free Survival (Months) | Benefit from Tailored Therapy |
|---|---|---|---|
| Concordant (T+L) | 11.05 | 4.93 | Significant improvement [6] |
| Tissue-Only | 9.93 | 3.06 | Less pronounced benefit [6] |
| Liquid-Only | 4.05 | 2.07 | Minimal to no benefit [6] |
Platform-Specific Performance in HPV-Associated Cancers
A meta-analysis of 36 studies involving 2,986 patients with HPV-associated cancers compared the diagnostic performance of different detection platforms for circulating tumor HPV DNA (ctHPVDNA).
- Experimental Protocol: Systematic review and meta-analysis assessing diagnostic accuracy of ctHPVDNA detection across cancer anatomic sites, detection platforms, and blood components [5].
- Key Findings:
- Sensitivity was greatest with NGS, followed by ddPCR and then qPCR.
- Specificity was similar across platforms.
- Plasma NGS-based testing may be the most sensitive approach for ctHPVDNA overall [5].
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Research Tools for Spatial Heterogeneity and Concordance Studies
| Research Tool | Function/Application | Example/Notes |
|---|---|---|
| FoundationOne CDx | Tissue-based comprehensive genomic profiling | Used in ROME Trial for tissue NGS [6] |
| FoundationOne Liquid CDx | Blood-based comprehensive genomic profiling | Used in ROME Trial for liquid NGS [6] |
| CellSearch System | FDA-approved CTC enumeration and analysis | Immunomagnetic separation using anti-EpCAM antibodies [3] [4] |
| ScreenCell Filtration | Label-free CTC isolation by size | Microporous membrane filter based on cell size differences [4] |
| Multi-region Sampling Protocol | Assessment of spatial heterogeneity | Sampling of 3-4 distinct tumor regions recommended [1] |
| Ultracentrifugation Methods | Extracellular vesicle isolation | >50% of EV isolation methods use preparative ultracentrifugation [7] |
Diagram: Spatial Heterogeneity Challenge and Solution Approaches
The "gold standard" status of tissue biopsy must be contextualized within its fundamental limitation: the inability to consistently overcome tumor spatial heterogeneity with single-region sampling. The evidence demonstrates that multi-region tissue sampling provides a more comprehensive tumor profile, while liquid biopsy offers a complementary approach that captures tumor-wide heterogeneity.
Crucially, NGS concordance between tissue and liquid biopsy has emerged as a significant predictor of therapeutic outcomes, with patients showing concordant results deriving the greatest benefit from tailored therapies. For researchers and drug development professionals, these findings emphasize the need for integrated diagnostic approaches that leverage the strengths of both tissue and liquid biopsy to fully characterize the complex landscape of heterogeneous tumors. Future advancements will likely focus on standardized multi-region sampling protocols, refined liquid biopsy assays with enhanced sensitivity, and AI-driven integration of multi-modal data to overcome the challenges posed by spatial heterogeneity.
Circulating tumor DNA (ctDNA) refers to fragmented DNA derived from tumor cells that circulates freely in the bloodstream alongside cell-free DNA (cfDNA) from healthy cells [8]. This biological phenomenon was first discovered in 1948, but its significance in oncology has only been fully appreciated in recent decades [3]. ctDNA originates from tumor cells through processes including apoptosis, necrosis, and active secretion, carrying tumor-specific genetic alterations that mirror the mutational profile of the tumor [8] [9]. These fragments typically measure 120-220 base pairs in length, with ctDNA fragments averaging approximately 140 bp [8]. The half-life of ctDNA in circulation is relatively short, estimated to be greater than 2 hours, enabling real-time monitoring of tumor dynamics [8].
In cancer patients, ctDNA typically constitutes less than 1% of total cfDNA, though this proportion can vary significantly based on tumor type, stage, and burden [3] [9]. The concentration of ctDNA in plasma is often elevated in cancer patients compared to healthy individuals, with studies demonstrating that plasma-free DNA levels were significantly higher in patients with advanced tumors [3]. This fundamental biological understanding provides the foundation for ctDNA's utility as a sensitive biomarker in oncology, enabling non-invasive access to tumor genetic information without the need for invasive tissue biopsies [10].
Table 1: Fundamental Biological Characteristics of cfDNA and ctDNA
| Characteristic | cfDNA | ctDNA |
|---|---|---|
| Primary Source | Apoptotic/necrotic normal cells [9] | Tumor cells (via necrosis, apoptosis, or secretion) [9] |
| Fragment Size | Predominantly 166 bp (nucleosomal) [9] | Shorter (<150 bp) + longer fragments [9] |
| Typical Concentration | 1-100 ng/mL plasma (healthy) [9] | Often <1% of total cfDNA [9] |
| Genetic Alterations | Wild-type [9] | Tumor-specific (e.g., EGFR, TP53) [9] |
| Half-Life | Variable | >2 hours [8] |
ctDNA Detection Technologies and Methodologies
Sample Collection and Pre-Analytical Processing
Proper sample collection and processing are critical for reliable ctDNA analysis due to the low abundance and fragmented nature of ctDNA. Blood collection for ctDNA analysis requires specialized approaches to preserve sample integrity. For ctDNA, blood is typically collected in specialized cell-stabilizing tubes such as Streck Cell-Free DNA BCT or Roche Cell-Free DNA collection tubes, which can maintain sample stability for up to 7 days at room temperature [11] [9] [12]. Following collection, plasma preparation involves a double-centrifugation protocol: an initial centrifugation at 1,600 × g to separate cellular components, followed by a second centrifugation of the supernatant at 16,000 × g to eliminate remaining cellular debris [9] [12]. This two-step process is essential to prevent contamination by genomic DNA from white blood cells, which could otherwise mask the rare ctDNA variants [9].
The extraction of ctDNA from plasma utilizes various methodologies, with magnetic bead-based systems demonstrating superior recovery of the short DNA fragments characteristic of ctDNA compared to traditional silica column methods [9]. Following extraction, ctDNA concentration is typically quantified using sensitive fluorescence-based methods such as the Qubit High Sensitivity dsDNA kit [12]. The entire pre-analytical workflow requires meticulous quality control measures, including assessment for hemolysis, which can significantly increase wild-type DNA background and compromise ctDNA detection sensitivity [9].
Detection Platforms and Analytical Techniques
Multiple technological platforms have been developed for ctDNA analysis, each with distinct advantages, limitations, and optimal applications. The primary detection methods include next-generation sequencing (NGS), droplet digital PCR (ddPCR), and denaturing capillary electrophoresis (DCE).
Next-Generation Sequencing (NGS) enables comprehensive profiling of multiple cancer-related genes simultaneously and can be implemented in either tumor-informed or tumor-uninformed approaches [13]. Tumor-informed NGS involves initial sequencing of tumor tissue to identify patient-specific mutations, which are then tracked in subsequent liquid biopsies [13]. This approach enhances sensitivity for detecting minimal residual disease (MRD) and monitoring treatment response. In contrast, tumor-uninformed NGS analyzes plasma samples without prior knowledge of tumor mutations, making it suitable for initial diagnosis and identifying actionable mutations [13]. Hybrid capture-based NGS methods typically achieve median deduplicated read depths of approximately 4,000x, enabling detection of variants at allele frequencies as low as 0.1% with 95% certainty when optimal DNA input (30-50 ng) is used [14] [12].
Droplet Digital PCR (ddPCR) represents an ultra-sensitive, mutation-driven approach that partitions individual DNA molecules into thousands of nanodroplets for absolute quantification of specific mutations [11]. This technology detects somatic alterations at very low frequencies (variant allele frequency of 0.01%) by dividing extracted DNA into approximately 20,000 droplets and calculating absolute quantities based on PCR-positive and negative droplets [11]. ddPCR offers significant cost advantages, with operational expenses 5-8.5-fold lower than NGS, making it particularly suitable for longitudinal monitoring of known mutations [11].
Denaturing Capillary Electrophoresis (DCE) provides a cost-effective alternative for mutation detection and monitoring, based on heteroduplex formation with subsequent electrophoretic separation to visualize mutant alleles amidst abundant wild-type DNA [13]. This method requires minimal input DNA (tens of picograms) and has been successfully applied to routine mutation detection in various solid tumors, including lung, colorectal, pancreatic, and brain cancers [13]. While less comprehensive than NGS, DCE offers a practical solution for monitoring specific mutations in tumor suppressor genes where mutations are dispersed across multiple exons, making it unsuitable for allele-specific PCR methods [13].
Table 2: Performance Comparison of Major ctDNA Detection Technologies
| Technology | Detection Sensitivity | Key Advantages | Key Limitations | Optimal DNA Input |
|---|---|---|---|---|
| NGS (Large Panels) | 0.1% VAF (with optimal input) [14] | Comprehensive profiling, detects novel variants [14] | Higher cost, complex bioinformatics [14] [13] | 30-50 ng [14] |
| ddPCR | 0.01% VAF [11] | Ultra-sensitive, absolute quantification, cost-effective [11] | Limited to known mutations, low multiplexing capability [11] | Not specified |
| DCE | Not specified | Cost-effective, applicable to dispersed mutations [13] | Limited multiplexing, lower throughput [13] | Tens of pg [13] |
Concordance Between Liquid and Tissue Biopsy
The concordance between liquid and tissue biopsy represents a critical metric for establishing the clinical validity of ctDNA-based approaches. A 2025 analysis from the ROME Trial provided significant insights into how concordance impacts patient outcomes [6]. This phase II multicenter study enrolled 1,794 patients with advanced solid tumors and performed next-generation sequencing on both tissue and liquid biopsies using FoundationOne CDx and FoundationOne Liquid CDx assays [6]. Patients with actionable alterations were randomized to tailored therapy or standard-of-care treatment.
The study revealed that concordance between tissue and liquid biopsy was present in only 49% of cases, with alterations detected exclusively in tissue (35%) or liquid (16%) biopsies in the remaining cases [6]. Most importantly, patients in the concordant group who received tailored therapy demonstrated significantly improved survival outcomes, with median overall survival of 11.05 months versus 7.70 months in the standard-of-care group, and median progression-free survival of 4.93 months versus 2.80 months [6]. In contrast, the survival benefit of tailored therapy was less pronounced or absent in patients with discordant results, with the liquid-only group showing particularly poor outcomes (median OS: 4.05 months) [6].
Another study focusing on advanced non-small cell lung cancer (NSCLC) reported a 71.2% concordance rate between standard-of-care tissue genotyping and ctDNA-NGS [12]. In 25.4% of cases, results were discordant but without direct therapeutic impact, while in 3.4% of patients, ctDNA-NGS missed an actionable driver mutation that would directly impact therapy selection [12]. This highlights both the potential and limitations of ctDNA-based genotyping, particularly in clinical contexts where identifying actionable drivers is critical for treatment decisions.
The performance of ctDNA assays is influenced by several technical and biological factors. A direct comparison of five ctDNA NGS assays revealed that detection sensitivity and reproducibility were 90% or higher when mutations were at 0.5% or 1.0% allele frequency with optimal DNA input (30 ng or 50 ng) [14]. However, performance decreased substantially when mutations were at 0.1% allele frequency and/or when lower genomic input (10 ng DNA) was used [14]. Notable differences in depth of coverage and background noise among assays profoundly impacted their performance characteristics, underscoring the importance of understanding these technical variables when selecting and implementing ctDNA testing platforms [14].
Experimental Protocols for ctDNA Analysis
NGS-Based ctDNA Analysis Protocol
The following protocol outlines a comprehensive approach for targeted NGS of ctDNA, based on methodologies described in recent literature [12]:
Sample Preparation and DNA Extraction:
- Collect peripheral blood in cell-stabilizing tubes (e.g., Roche Cell-Free DNA collection tubes)
- Process samples within five days of blood draw
- Perform double-centrifugation: 10 min at 1,600 × g followed by 10 min at 16,000 × g
- Isolate ctDNA from plasma using QIAamp Circulating Nucleic Acid kit
- Elute in 50 µL elution buffer
- Quantify DNA concentration using Qubit High Sensitivity dsDNA kit
Library Preparation and Sequencing:
- Use Twist Library Preparation Kit for library construction
- Incorporate xGEN dual index unique molecular identifiers (UMIs) adaptors
- Use custom probe set (e.g., 117 kb panel covering hotspot regions of 45 genes)
- Perform hybrid capture according to manufacturer's specifications
- Sequence on NovaSeq6000 system with 2 × 150 bp paired-end reads
- Achieve median deduplicated read depth of approximately 4,000×
Bioinformatic Analysis:
- Map reads to reference genome (Hg19)
- Perform deduplication using tools such as Fgbio
- Retain only reads with UMI family size of ≥ 2
- Perform variant detection using GATK Mutect2
- Apply stringent filtering:
- Exclude variants outside exons and splice site regions (-8/+8)
- Remove synonymous variants (unless in splice sites)
- Filter variants with population frequency > 0.1% in ExAC database
- Require minimum of five variant reads
- Exclude variants with exclusively alternative reads on forward or reverse strand
- Apply Mutect2 quality filter
- Require variant allele frequency (VAF) > 20 times higher than average VAF of healthy controls
- Manual curation using Alamut Visual Plus
- Classify variants using five-tier ACMG/AMP guidelines
ddPCR vs. NGS Comparison Protocol
A recent study directly compared ddPCR and NGS for ctDNA detection in localized rectal cancer, providing a robust experimental framework for technology comparison [11]:
Patient Cohort and Sample Collection:
- Development group: 41 patients with non-metastatic rectal cancer
- Validation group: 26 patients from SYNCOPE clinical trial (NCT04842006)
- Collect pre-therapy plasma and tumor samples
- Collect follow-up plasma samples 12 months after surgery
Tissue DNA Analysis:
- Perform primary tumor DNA sequencing using Ion AmpliSeq Cancer Hotspot Panel v2
- Cover >2800 COSMIC variants from 50 oncogene and tumor suppressor gene hotspots
- Achieve theoretical coverage of 99% in rectal patients
- Maintain average 2000× coverage with 154 bp amplicon length
ctDNA Detection with ddPCR:
- Design one to two predesigned probes based on highest VAF mutations in matched tumor
- Divide 2-9 μL extracted DNA into 20,000 droplets
- Calculate absolute quantity of targeted cfDNA based on PCR-positive/negative droplets
ctDNA Detection with NGS:
- Perform same panel sequencing as for primary tumors
- Optimize for ctDNA detection with lowered variant calling threshold
- Set detection threshold for somatic alterations at 0.01% VAF
Statistical Analysis:
- Use two-tailed Fisher's exact test for categorical variables
- Apply Shapiro-Wilk test for normality assessment
- Use Mann-Whitney test for non-normally distributed continuous variables
- Apply T-test for normally distributed continuous variables
- Use Kruskal-Wallis test for differences between cancer stages
Research Reagent Solutions for ctDNA Studies
Table 3: Essential Research Reagents and Kits for ctDNA Analysis
| Reagent/Kits | Primary Function | Key Features | Representative Examples |
|---|---|---|---|
| Blood Collection Tubes | Cellular preservation and ctDNA stabilization | Prevents leukocyte lysis, enables room temperature storage | Streck Cell-Free DNA BCT [11], Roche Cell-Free DNA Collection Tubes [12] |
| Nucleic Acid Extraction Kits | Isolation of high-quality ctDNA from plasma | Optimized for short fragment recovery, magnetic bead technology | QIAamp Circulating Nucleic Acid Kit [12], MagMAX kits [9] |
| Library Preparation Kits | NGS library construction from low-input ctDNA | Incorporates UMIs, compatible with fragmented DNA | Twist Library Preparation Kit [12] |
| Target Enrichment Panels | Hybrid capture of cancer-relevant genes | Comprehensive coverage, designed for ctDNA applications | Custom panels (e.g., 45-gene NSCLC panel) [12] |
| ddPCR Assays | Absolute quantification of specific mutations | Ultra-sensitive detection, rare allele detection | Bio-Rad ddPCR mutation assays [11] |
| Quality Control Kits | Assessment of DNA quantity and quality | High sensitivity, broad dynamic range | Qubit HS dsDNA Kit [12] |
ctDNA analysis represents a transformative approach in cancer management, providing a non-invasive means to access tumor genetic information throughout the disease course. The biological foundations of ctDNA, including its fragmentary nature, short half-life, and low abundance relative to total cfDNA, present both challenges and opportunities for analytical technologies. Current detection platforms, including NGS, ddPCR, and DCE, offer complementary strengths with NGS providing comprehensive profiling capability, ddPCR delivering ultra-sensitive quantification of known mutations, and DCE representing a cost-effective alternative for specific applications.
The concordance between liquid and tissue biopsies, while imperfect, provides valuable insights for clinical decision-making, with evidence suggesting that patients exhibiting concordant results derive greater benefit from tailored therapies. As technological advancements continue to enhance detection sensitivity and standardization, and as clinical validation accumulates across diverse cancer types and stages, ctDNA analysis is poised to play an increasingly central role in cancer diagnosis, monitoring, and personalized treatment selection.
Next-generation sequencing (NGS) has fundamentally transformed cancer care by enabling comprehensive genomic profiling of tumors, thereby facilitating precision oncology approaches. Clinical guidelines from leading oncology organizations provide critical frameworks for implementing NGS testing to match patients with optimal targeted therapies. The National Comprehensive Cancer Network (NCCN), American Society of Clinical Oncology (ASCO), and European Society for Medical Oncology (ESMO) have each developed recommendations to standardize the use of NGS technologies in clinical practice. These guidelines address key aspects including test selection, analytical validation, interpretation of results, and clinical actionability, while increasingly recognizing the importance of integrating both tissue and liquid biopsy approaches to overcome tumor heterogeneity and improve patient selection. The evolving landscape of NGS concordance between tissue and liquid biopsy represents a critical area of research with significant implications for therapeutic decision-making and clinical trial design [15] [16].
Comparative Analysis of Major Guideline Frameworks
NCCN (National Comprehensive Cancer Network) Guidelines
The NCCN guidelines provide tumor-specific recommendations for NGS testing across more than 60 cancer types. A distinctive feature of NCCN guidelines is their detailed, evidence-based categorization of treatment regimens into "preferred," "other recommended," and "useful in certain circumstances" classifications. Recent updates emphasize the critical role of NGS testing for identifying actionable biomarkers for targeted therapies. For example, the 2025 updates specify that "every patient with differentiated thyroid cancer who is going to get systemic therapy should have next-generation sequencing testing done" to identify potential targets like NTRK and RET gene fusions for specific inhibitors [17]. Similarly, guidelines for bladder cancer have been updated to include new biomarker-directed therapies such as fam-trastuzumab deruxtecan-nxki (T-DXd) for HER2-positive (IHC 3+) advanced disease [17].
The NCCN framework strongly supports the use of NGS to guide treatment selection in advanced cancers, particularly when standard therapy options have been exhausted. The guidelines acknowledge the growing importance of both tissue and liquid biopsy approaches, with recent updates reflecting an increasing number of biomarker-directed therapies across multiple tumor types [17].
ESMO (European Society for Medical Oncology) Frameworks
ESMO has developed two complementary tools for evaluating genomic targets and associated therapies: the ESMO Scale for Clinical Actionability of Molecular Targets (ESCAT) and the ESMO-Magnitude of Clinical Benefit Scale (ESMO-MCBS). The ESCAT framework categorizes genomic alterations into tiers of decreasing clinical evidence, with tier I representing alterations ready for routine clinical use [18]. The ESMO-MCBS grades the magnitude of clinical benefit (grades 1-5 for non-curative intent) based on efficacy, toxicity, and quality-of-life metrics [18].
A 2024 cross-sectional study analyzing NCCN-recommended genome-targeted therapies found that when these frameworks were applied, only 12% (32/267) of trials demonstrated substantial clinical benefit (ESMO-MCBS grades 4-5), while 45% (121/267) showed promising but unproven benefit (grade 3) [18]. This highlights ESMO's more conservative, benefit-centered approach compared to NCCN guidelines, with greater emphasis on overall survival and quality-of-life endpoints over surrogate markers.
ASCO (American Society of Clinical Oncology) Perspectives
While the search results provide less specific detail on ASCO's standalone NGS recommendations, ASCO has contributed significantly to molecular testing guidelines through its collaboration with the College of American Pathologists (CAP) and Association for Molecular Pathology (AMP). These joint guidelines establish standards for NGS test validation and bioinformatics pipelines to ensure analytical accuracy and clinical utility [15].
ASCO's approach typically emphasizes the integration of NGS testing within broader diagnostic and treatment pathways, focusing on clinical utility and patient outcomes. The organization has supported the development of quality assurance programs through partnerships with CAP and CLIA (Clinical Laboratory Improvement Amendments) to standardize NGS testing across laboratories [15].
Table 1: Comparison of Guideline Approaches to NGS Testing
| Aspect | NCCN | ESMO | ASCO/Collaborative |
|---|---|---|---|
| Primary Focus | Tumor-specific testing recommendations | Clinical benefit assessment of targets/therapies | Test validation & quality assurance |
| Evidence Grading | Levels (1, 2A, 2B) & preference categories | ESCAT tiers & MCBS grades | Standards for analytical validation |
| Biopsy Approach | Increasing incorporation of both tissue & liquid | Evidence-based for clinical actionability | Emphasis on test validation for both types |
| Key Tools/Frameworks | Drug-specific recommendations with evidence levels | ESCAT for targets, MCBS for therapies | CAP/ASHI standards for laboratory testing |
Tissue and Liquid Biopsy Concordance: Evidence from the ROME Trial
Study Methodology and Experimental Protocol
The phase II ROME trial provides critical insights into the concordance between tissue and liquid biopsy for detecting actionable mutations. This multicenter study enrolled 1,794 patients with advanced solid tumors who had received second- or third-line treatment. The experimental protocol involved:
- Centralized NGS Testing: Both tissue and liquid biopsies were analyzed using FoundationOne CDx and FoundationOne Liquid CDx tests respectively [6] [16].
- Molecular Tumor Board Review: A centralized board reviewed results to identify actionable alterations [6].
- Patient Randomization: 400 patients with actionable alterations were randomized to receive either tailored therapy (TT) or standard of care (SoC) [6].
- Concordance Assessment: Concordance was defined as detection of the same druggable alteration in both biopsy types, while discordance indicated detection in only one type [6].
This robust methodology allowed for direct comparison of the clinical utility of tissue versus liquid biopsy approaches, with survival outcomes as primary endpoints.
Key Findings on Concordance Rates and Survival Outcomes
The ROME trial revealed a 49% concordance rate between tissue and liquid biopsies for detecting actionable alterations. Notably, alterations were detected exclusively in tissue in 35% of cases and exclusively in liquid biopsy in 16% of cases [6] [16]. This demonstrates the complementary nature of both approaches, with combined testing increasing the detection of actionable alterations by over 60% compared to either method alone [16].
Most significantly, patients with concordant findings who received tailored therapy showed substantially improved survival outcomes:
- Median Overall Survival: 11.05 months with TT vs. 7.70 months with SoC (HR 0.74; 95% CI: 0.51-1.07) [6]
- Median Progression-Free Survival: 4.93 months with TT vs. 2.80 months with SoC (HR 0.55; 95% CI: 0.40-0.76) [6]
In contrast, the survival benefit of tailored therapy was "less pronounced or absent" in patients with discordant results, with the liquid-biopsy-only group showing particularly poor outcomes (median OS: 4.05 months) [6]. These findings strongly suggest that concordance between biopsy methods may identify patients with disease biology more amenable to targeted interventions.
Table 2: ROME Trial Survival Outcomes by Biopsy Concordance Group
| Biopsy Group | Median Overall Survival (Months) | Median Progression-Free Survival (Months) | Tailored Therapy Benefit |
|---|---|---|---|
| Tissue + Liquid (Concordant) | 11.05 | 4.93 | Significant improvement |
| Tissue Only | 9.93 | 3.06 | Moderate improvement |
| Liquid Only | 4.05 | 2.07 | Minimal to no improvement |
| Standard of Care (Reference) | 7.70 | 2.80 | - |
Analytical Performance of NGS Platforms
Key Performance Metrics for Clinical NGS
Clinical application of NGS requires rigorous validation of analytical performance across multiple parameters:
- Depth of Coverage: Higher sequencing depth (e.g., 1,000×) improves sensitivity for detecting low-frequency variants [19].
- Variant Allele Frequency (VAF) Sensitivity: The limit of detection for VAF is critical, especially for liquid biopsy assays [20].
- Variant Types Detected: Comprehensive tests should identify single nucleotide variants (SNVs), insertions/deletions (indels), copy number variations (CNVs), and structural variants (SVs) [19].
- Genomic Signatures: Assessment of tumor mutational burden (TMB) and microsatellite instability (MSI) is increasingly important for immunotherapy selection [19].
Comparison of Commercial NGS Platforms
Commercially available NGS platforms demonstrate variable performance characteristics:
- FoundationOne CDx: Tissue-based test analyzing 324 genes with median turnaround time of 8 days; FDA-approved as companion diagnostic for 35+ targeted therapies [21].
- FoundationOne Liquid CDx: Blood-based test analyzing 324 genes with median turnaround time of 7 days; FDA-approved as companion diagnostic for 15+ targeted therapies [21].
- Northstar Select: Recently validated liquid biopsy assay demonstrating improved sensitivity with 95% limit of detection at 0.15% VAF for SNV/Indels, detecting 51% more pathogenic SNV/indels and 109% more CNVs compared to on-market CGP assays [20].
Technological advancements are particularly evident in liquid biopsy performance, with newer assays significantly reducing null reports (no actionable findings) by 45%, primarily through enhanced detection of variants below 0.5% VAF [20].
Technical Standards and Quality Control
Regulatory and Quality Assurance Frameworks
Multiple organizations have established standards for NGS testing in clinical laboratories:
- ACMG (American College of Medical Genetics and Genomics): Developed comprehensive guidelines covering interpretation and reporting of variants, with technical standards revised in 2021 to reflect technological advancements [15].
- CAP/CLIA: Establish standards for laboratory quality assurance, proficiency testing, and analytical validation [15].
- ISO Standards: ISO 15189 provides requirements for quality and competence in medical laboratories [15].
- GA4GH (Global Alliance for Genomics and Health): Develops international standards for data sharing and interoperability [15].
These frameworks address the entire NGS workflow from sample preparation to data analysis and interpretation, emphasizing the importance of analytical validation, bioinformatics pipeline standardization, and clinical reporting consistency.
NGS Workflow and Quality Control Metrics
The following diagram illustrates the key stages and quality control checkpoints in a comprehensive clinical NGS workflow:
Diagram 1: Clinical NGS Workflow with QC Checkpoints
The Scientist's Toolkit: Essential Research Reagents and Solutions
Table 3: Key Research Reagent Solutions for NGS Concordance Studies
| Reagent/Resource | Function | Example Applications |
|---|---|---|
| FFPE Tissue Samples | Preserves tissue architecture and nucleic acids for histological correlation | Tissue-based NGS; gold standard reference [21] |
| Cell-Free DNA Collection Tubes | Stabilizes blood samples for ctDNA analysis | Liquid biopsy; enables centralized testing [21] |
| Hybrid Capture Probes | Enriches genomic regions of interest | Targeted sequencing; improves coverage of relevant genes [22] |
| Barcoded Adapters | Enables sample multiplexing | Cost reduction; batch processing of samples [22] |
| Reference Standard Materials | Provides known variants for validation | Assay performance assessment; quality control [15] |
| Bioinformatics Pipelines | Analyzes raw sequencing data | Variant calling; annotation; interpretation [22] |
The evolving guidelines from NCCN, ASCO, and ESMO reflect a growing consensus on the importance of comprehensive genomic profiling in advanced cancer, while demonstrating distinct approaches to evaluating evidence and clinical utility. The ROME trial data provides compelling evidence that integrating both tissue and liquid biopsy modalities significantly enhances the detection of actionable alterations and may identify patient populations most likely to benefit from tailored therapies. The observed survival benefit in concordant cases (11.05 vs. 7.70 months median OS) underscores the potential of combined profiling approaches to refine precision oncology strategies [6] [16].
For researchers and drug development professionals, these findings highlight the importance of considering both biopsy modalities in clinical trial design and biomarker strategy. Future directions should focus on standardizing concordance assessment, improving liquid biopsy sensitivity for low-shedding tumors, and developing integrated reporting frameworks that synthesize information from both tissue and liquid biopsies to optimize therapeutic decision-making.
In the validation of diagnostic tests, particularly when comparing new methodologies to established ones, Positive Percent Agreement (PPA) and Negative Percent Agreement (NPA) are the fundamental metrics used to quantify concordance. These statistics are essential in contexts where a perfect "gold standard" test may not exist [23] [24].
- Positive Percent Agreement (PPA) is the proportion of subjects known to be positive for a condition via a comparator method that are correctly identified as positive by the new test. It answers the question: "If a subject truly has the condition, how likely is the new test to detect it?" [25]. Its formula is identical to that of sensitivity: PPA = True Positives / (True Positives + False Negatives) [25].
- Negative Percent Agreement (NPA) is the proportion of subjects known to be negative for a condition via a comparator method that are correctly identified as negative by the new test [25]. Its formula is identical to that of specificity: NPA = True Negatives / (True Negatives + False Positives) [25].
It is critical to distinguish PPA and NPA from sensitivity and specificity. While the calculations are identical, sensitivity and specificity require comparison to a known "Ground Truth" [24]. In contrast, PPA and NPA are used when the reference method itself is an imperfect comparator, acknowledging that some discrepancies may be due to inaccuracies in the reference rather than the new test [23] [24]. Using PPA/NPA terminology more accurately frames the results as a measure of agreement between two tests, rather than absolute accuracy [23].
Article 2: Quantitative Data on NGS Concordance in Liquid vs. Tissue Biopsy
The concordance between liquid biopsy (circulating tumor DNA, or ctDNA) and traditional tissue biopsy in Next-Generation Sequencing (NGS) is a central focus in oncology research. The following tables summarize PPA and NPA from recent clinical studies across various cancer types, highlighting key influencing factors.
Table 1: Concordance Metrics for Key Genes and Alterations in Colorectal Cancer (CRC)
| Cancer Type | Genes/Alterations | Positive Percent Agreement (PPA) | Negative Percent Agreement (NPA) | Key Influencing Factor | Citation |
|---|---|---|---|---|---|
| Colorectal Cancer (CRC) | All short variants (MSAF >0) | 79% (overall); 95% (<90 days); 100% (<30 days) | Not Reported | Time between tissue and liquid biopsy | [26] |
| Colorectal Cancer (CRC) | KRAS G12X | 93% | 100% | Time between biopsies (<270 days) | [26] |
| Colorectal Cancer (CRC) | KRAS, NRAS, BRAF short variants | 80% (overall); 90% (<270 days) | Not Reported | Time between biopsies | [26] |
Table 2: Concordance Metrics Across Different Cancer Types and Platforms
| Cancer Type | Genes/Alterations | Positive Percent Agreement (PPA) | Negative Percent Agreement (NPA) | Key Influencing Factor | Citation |
|---|---|---|---|---|---|
| Pan-Cancer (20+ types) | SNVs & Indels (clinically actionable genes) | >95% | Not Reported | Analytical performance of NGS assay | [27] |
| Pan-Cancer (20+ types) | Copy Number Alterations (CNAs) | 80-83% | Not Reported | Analytical performance of NGS assay | [27] |
| Metastatic Prostate Cancer | BRCA1/2 alterations | 50% | 85% | Tumor heterogeneity; long time between samples (median 132 weeks) | [28] |
| Stage IV NSCLC | EGFR, BRAF, KRAS, etc. | 99.20% | 99.46% | Cancer stage (late-stage shows higher concordance) | [29] |
| Stage III NSCLC | EGFR, BRAF, KRAS, etc. | 28.57% | 99.20% | Cancer stage (early-stage shows lower concordance) | [29] |
Article 3: Experimental Protocols for Concordance Studies
A standard protocol for determining PPA and NPA in NGS concordance studies involves a multi-step process from sample collection to bioinformatic analysis, with rigorous quality control at each stage.
Sample Collection and Processing
The typical workflow begins with the collection of matched tissue and blood samples. Tissue is often processed into Formalin-Fixed Paraffin-Embedded (FFPE) blocks, while blood samples are collected in specialized tubes (e.g., Streck Cell-Free DNA BCT) to preserve ctDNA [27] [29]. For liquid biopsy, plasma is separated via a two-step centrifugation protocol to isolate the cell-free DNA (cfDNA) fraction [29]. The amount of input cfDNA is a critical parameter, with studies often requiring a minimum of 20 ng for library preparation [29].
Next-Generation Sequencing and Bioinformatics
The isolated DNA undergoes library preparation, which is tailored for the specific NGS panel used (e.g., Illumina TruSight Oncology 500, FoundationACT, or PGDx elio) [30] [26] [27]. These panels use hybrid capture-based chemistry to enrich for target genes of clinical interest. Sequencing is then performed on platforms such as the Illumina NextSeq [27].
Following sequencing, a robust bioinformatic pipeline is employed. Key steps include:
- Read Alignment: Mapping raw sequencing reads to a human reference genome (e.g., GRCh37) [29].
- Variant Calling: Using specialized tools (e.g., GATK, VarScan) to identify somatic alterations [29].
- Filtering and Annotation: Removing potential germline variants and artifacts by cross-referencing population databases (e.g., dbSNP, ExAC) and annotating the functional impact of variants [27] [29].
Determining Tumor Fraction and Quality Control
For liquid biopsy, the Maximum Somatic Allele Frequency (MSAF) is a crucial metric, serving as a proxy for the ctDNA fraction in the sample [26]. Samples with an MSAF of 0 are considered to have no detectable ctDNA and are often excluded from PPA calculations [26]. Stringent quality control metrics are applied, including minimum coverage depth (e.g., >1400x mean effective depth) and thresholds for variant calling (e.g., a 0.2% variant allele frequency cutoff) [29].
Statistical Analysis
Finally, the identified alterations from the two sample types (e.g., liquid and tissue) are compared at the coordinate level for sequence variants and the gene level for copy number alterations [26]. The outcomes are tabulated into true positives, false positives, true negatives, and false negatives, which are then used to calculate the final PPA and NPA values [26].
Article 4: Visualization of Factors Influencing Concordance
The concordance between liquid and tissue biopsies is not a fixed value but is influenced by a network of interrelated biological and technical factors. The following diagram maps these key factors and their logical relationships.
Article 5: The Scientist's Toolkit
Successful execution of NGS concordance studies requires a suite of specialized reagents, kits, and analytical tools. The following table details essential components of the research pipeline.
Table 3: Essential Research Reagents and Solutions for NGS Concordance Studies
| Item Name | Function/Application | Relevant Context & Examples |
|---|---|---|
| Cell-Free DNA BCT Tubes (e.g., Streck) | Stabilizes blood samples for ctDNA analysis by preventing white blood cell lysis and genomic DNA contamination, crucial for preserving sample integrity between draw and processing. | Used in liquid biopsy workflows to ensure accurate representation of the in vivo ctDNA profile [29]. |
| Nucleic Acid Extraction Kits | Isolate and purify high-quality DNA from different sample types (e.g., cfDNA from plasma, gDNA from FFPE tissue) for downstream sequencing. | A critical first step in all NGS protocols; specific kits are optimized for different sample matrices [29]. |
| Targeted NGS Panels (e.g., Illumina TSO 500, Guardant360, PGDx elio) | Hybrid capture-based kits designed to enrich for a predefined set of cancer-related genes, enabling comprehensive genomic profiling from limited input material. | Enable detection of SNVs, indels, CNVs, fusions, and genomic signatures like TMB and MSI [30] [27] [28]. |
| ddPCR Assays | Provides an orthogonal, highly sensitive method for validating specific mutations (e.g., in EGFR, KRAS) identified by NGS, confirming variant calls. | Used as a reference standard to validate the detection accuracy of NGS platforms in clinical samples [29]. |
| Bioinformatic Pipelines & Databases (e.g., GATK, Annovar, dbSNP, ExAC) | Software suites and population databases for sequence alignment, variant calling, filtering out germline polymorphisms, and functional annotation of somatic variants. | Essential for transforming raw sequencing data into clinically interpretable results [27] [29]. |
Article 6: Critical Factors Influencing Agreement
The observed PPA and NPA between liquid and tissue biopsies are not intrinsic properties of the tests alone but are heavily modulated by a confluence of factors.
Tumor Burden and Cancer Stage: The amount of ctDNA shed into the bloodstream, often estimated by the Maximum Somatic Allele Frequency (MSAF), is a primary driver of PPA [26]. Late-stage cancers (Stage IV) typically have a higher tumor burden and thus higher ctDNA levels, leading to PPA often exceeding 99% [29]. In contrast, early-stage cancers (Stage III) can have much lower or undetectable ctDNA, resulting in significantly lower PPA, sometimes as low as 28.57% [29].
Temporal and Spatial Heterogeneity: The time elapsed between tissue and liquid biopsy collection is a critical and well-documented factor [26] [28]. Genomic profiles evolve over time due to selective pressure from treatments or natural disease progression (temporal heterogeneity). One study showed PPA for all variants dropped from 100% (under 30 days) to 79% overall, and another in prostate cancer reported a low 50% PPA with a median 132-week interval [26] [28]. Furthermore, a single tissue biopsy may not capture the full genomic diversity of a patient's cancer (spatial heterogeneity), whereas liquid biopsy may provide a more comprehensive profile by sampling DNA from multiple tumor sites [28].
Assay Technical Performance: The sensitivity and design of the NGS assay itself directly impact concordance metrics. Key technical parameters include the sequencing depth (coverage), the variant allele frequency (VAF) cutoff for detection, and the panel's target capture efficiency [29]. For example, detecting copy number alterations (CNAs) and gene fusions is generally more challenging than detecting single nucleotide variants (SNVs), which is reflected in their lower PPA (80-83%) even in validated pan-cancer studies [27].
The Imperfect Gold Standard: A fundamental, often overlooked factor is that the tissue biopsy comparator itself is not a perfect "Ground Truth" [23]. Tissue samples can be affected by pre-analytical variables (e.g., fixation time in formalin, which degrades DNA) and intra-tumoral heterogeneity [30]. Therefore, some observed "discrepancies" where a variant is found in liquid but not tissue may represent true biological findings rather than liquid biopsy errors, a phenomenon underscored by the use of PPA/NPA terminology instead of sensitivity/specificity [23] [24] [28].
NGS Methodologies and Clinical Application Across Cancer Types
Next-generation sequencing (NGS) has become the cornerstone of precision oncology, enabling comprehensive genomic profiling from both tissue and liquid biopsies. The concordance between these sample types is a critical focus of modern research, heavily influenced by the choice of assay design. This guide objectively compares the performance of three dominant NGS assay designs—targeted panels, hybrid capture, and unique molecular identifier (UMI) technologies—within the context of tissue and liquid biopsy concordance studies, providing the experimental data and methodologies needed for informed decision-making.
The pursuit of reliable liquid biopsy alternatives to tissue sequencing hinges on technological innovations that overcome the inherent challenges of analyzing circulating tumor DNA (ctDNA), which is often present at ultra-low concentrations in a high background of normal DNA [31].
- Targeted Panels are designed to sequence a predefined set of genes known to be relevant to a specific disease area, such as cancer. The target enrichment can be achieved through either amplicon-based or hybrid capture-based methods [32].
- Hybrid Capture-Based Enrichment uses biotinylated oligonucleotide probes to "fish out" target DNA sequences from a genomic library prior to sequencing. This method is renowned for its comprehensive profiling capabilities and flexibility [32] [33].
- Unique Molecular Identifier (UMI) Technologies involve tagging each original DNA molecule with a unique barcode before amplification. This allows bioinformatics pipelines to distinguish and group reads derived from the same original molecule, correcting for PCR and sequencing errors and significantly improving detection sensitivity [31].
Performance Comparison: Key Metrics for Liquid Biopsy
The table below summarizes the performance of these technologies based on recent experimental data, with a focus on metrics critical for liquid biopsy analysis and tissue concordance.
Table 1: Performance Comparison of Key NGS Assay Designs
| Feature | Targeted Panels (Amplicon-Based) | Hybrid Capture-Based | Hybrid Capture with UMI |
|---|---|---|---|
| Primary Use Case | Rapid, cost-effective profiling of known hotspots [32] | Broad genomic profiling, fusion detection [34] [32] | Ultra-sensitive liquid biopsy; low-frequency variant detection [31] |
| Limit of Detection (LoD) | ~2.9% VAF (for tissue) [32] | ~0.5% VAF (standard panels) [31] | ≤0.1% VAF [31] |
| Sensitivity in Liquid Biopsy | Lower; can miss >50% of alterations at 0.5% LoD [31] | Detects ~50% of alterations at 0.5% LoD [31] | Detects ~80% of alterations at 0.1% LoD [31] |
| Variant Type Flexibility | Best for SNVs/Indels; limited for fusions/CNVs [32] | Excellent for SNVs, Indels, CNVs, and fusions from a single workflow [34] | Excellent for SNVs, Indels; improved accuracy for CNVs/fusions |
| Input DNA Requirements | Can be low (e.g., ~50 ng for tissue) [32] | Requires sufficient input for library complexity (e.g., ≥60 ng for liquid biopsy) [31] | Critical; low input can make detection statistically improbable [31] |
| Key Experimental Validation | 98.23% sensitivity, 99.99% specificity in tissue [32] | 96.92% sensitivity for SNVs/Indels at 0.5% AF in reference standards [34] | Modeled >99% detection probability at 0.1% VAF with sufficient coverage [31] |
Experimental Protocols and Supporting Data
Validation of a Hybrid-Capture Pan-Cancer Tissue Panel
A 2025 study developed and validated a hybrid-capture oncopanel targeting 61 cancer-associated genes for use with solid tumour tissues [32].
- Objective: To create a sensitive, high-throughput, and rapid in-house NGS assay to reduce reliance on external labs with long turnaround times (TAT) [32].
- Methodology:
- Library Prep: Hybrid-capture-based target enrichment (Sophia Genetics) on an automated MGI SP-100RS system.
- Sequencing: MGI DNBSEQ-G50RS sequencer.
- Analysis: Variant calling with Sophia DDM software.
- Validation: 43 unique samples, including clinical tissues and reference standards, were sequenced. Performance was assessed against orthogonal methods [32].
- Key Results:
- The assay detected 794 mutations with 100% concordance for 92 known variants from other methods.
- It demonstrated a sensitivity of 98.23% and a specificity of 99.99%.
- The average turnaround time was reduced to 4 days, a significant improvement over the 3-week TAT from external providers [32].
Ultra-Broad Hybrid Capture for Pathogen Detection in Blood
Demonstrating the power of hybrid capture in liquid biopsy-type applications, a 2025 study applied it to the detection of pathogen-derived cell-free DNA (cfDNA) for diagnosing bloodstream infections [35].
- Objective: To overcome the limited detection sensitivity of traditional methods for pathogen cfDNA by developing an ultra-broad hybrid capture tNGS method [35].
- Methodology:
- Panel Design: An ultra-broad panel of 1872 pathogens with high-density probe tiling.
- Workflow: cfDNA was extracted from plasma, a pre-library was constructed, and then incubated with the capture probes.
- Sequencing: Performed on the Gene+ Seq-100 platform at a depth of 5 million reads.
- Validation: Retrospective testing on 208 suspected BSI patients, comparing tNGS to mNGS and conventional testing [35].
- Key Results:
- The diagnostic accuracy of tNGS (76.44%) was comparable to mNGS (75.00%) and significantly higher than conventional testing (45.67%).
- The method demonstrated effective enrichment and sensitivity, making it a cost-effective screening tool [35].
The Critical Role of UMIs in ctDNA Analysis
A 2025 review of the technical hurdles in ctDNA NGS analysis detailed the necessity of UMIs for achieving the sensitivity required for tissue-liquid biopsy concordance [31].
- Objective: To outline methodological improvements for ctDNA NGS, focusing on increasing sensitivity and reducing false positives [31].
- Methodology (Bioinformatic):
- UMI Deduplication: Reads from the same original DNA molecule (identified by their UMI) are grouped into a consensus, correcting for random errors.
- Variant Calling: The probability of detecting a variant is modeled as a function of sequencing depth and variant allele frequency (VAF). For example, achieving a 99% detection rate for a VAF of 0.1% requires an effective depth of coverage of approximately 10,000x after deduplication [31].
- Input DNA Consideration: The absolute number of mutant molecules is a key constraint. With a 0.1% ctDNA fraction, a 10 mL blood draw from a lung cancer patient may yield only ~8 mutant genome equivalents, making detection challenging without highly sensitive methods [31].
- Key Results & Proposal:
- Incorporating UMIs and optimizing bioinformatics pipelines are essential to lower the LoD from 0.5% to 0.1%.
- This improvement could increase the detection of true alterations in liquid biopsy from approximately 50% to 80%, thereby improving its concordance with tissue-based results [31].
Visualizing NGS Assay Workflows
The following diagrams illustrate the core workflows for hybrid capture and UMI-based NGS assays, highlighting the steps that ensure high sensitivity and specificity.
Hybrid Capture Target Enrichment Workflow
UMI-Enhanced Variant Calling Workflow
The Scientist's Toolkit: Essential Research Reagents
Successful implementation of these NGS assays requires a suite of specialized reagents and tools. The following table details key components used in the featured experiments.
Table 2: Essential Reagents and Tools for NGS Assay Development
| Item | Function | Example from Literature |
|---|---|---|
| Targeted Gene Panels | Predefined sets of probes/primers to enrich genomic regions of interest. | 61-gene pan-cancer panel [32]; 32-gene liquid biopsy panel (HP2) [34]. |
| Ultra-Broad Pathogen Panels | Extensive probe sets for detecting a wide range of microorganisms from complex samples. | Panel covering 1,872 pathogens for bloodstream infection detection [35]. |
| Hybrid Capture Probe Library | Biotinylated oligonucleotides that bind to target DNA for isolation. | 149,990-probe library targeting 663 viruses for zoonotic disease surveillance [33]. |
| Automated Library Prep System | Robotics to perform library construction, improving consistency and reducing human error. | MGI SP-100RS system used with hybrid capture kits [32]. |
| Unique Molecular Indices (UMIs) | Barcodes added to DNA molecules pre-amplification to track original molecules. | Used in ctDNA protocols to correct errors and enable ultra-deep sequencing [31]. |
| Reference Standard Materials | Samples with known mutations at defined allele frequencies for assay validation. | HD701 and other standards used for determining sensitivity and LoD [32]. |
| Specialized Analysis Software | Bioinformatics platforms for variant calling, annotation, and clinical interpretation. | Sophia DDM software with machine learning for variant analysis [32]. |
The choice of NGS assay design is a fundamental determinant in the success of tissue and liquid biopsy concordance research. Targeted panels offer a fast, cost-effective solution for profiling known genomic hotspots in tissue samples. Hybrid capture-based methods provide the broad profiling flexibility needed to detect diverse alteration types across large gene sets. For liquid biopsy, where sensitivity is paramount, the integration of UMI technologies with hybrid capture is not just an enhancement but a necessity, enabling the detection of ultra-low frequency variants and providing a more complete picture of the tumor genome.
The experimental data confirms that while each design has its place, the convergence towards hybrid capture with UMI deduplication represents the current state-of-the-art for maximizing liquid biopsy sensitivity, thereby strengthening its correlation with gold-standard tissue profiling and accelerating its adoption in precision oncology.
The integration of next-generation sequencing (NGS) into liquid biopsy represents a paradigm shift in cancer genomics, offering a minimally invasive method for tumor genotyping. However, this promise hinges on a critical technical challenge: establishing robust analytical sensitivity to detect low-frequency variants in circulating tumor DNA (ctDNA). The low abundance of ctDNA, particularly in early-stage cancers or minimal residual disease, demands exceptional assay performance. This guide objectively compares the performance of NGS against other molecular techniques in detecting genomic alterations, with a specific focus on its concordance with traditional tissue biopsy—the historical gold standard in cancer diagnostics. For researchers and drug development professionals, understanding these performance characteristics, supported by experimental data and quality metrics, is fundamental for appropriate technology selection and data interpretation in clinical studies.
Experimental Protocols for Sensitivity and Concordance Assessment
Protocol 1: Establishing LOD and Tissue-Concordance in NSCLC
A seminal study on non-small cell lung cancer (NSCLC) provides a validated protocol for establishing analytical sensitivity and validating against tissue standards [29].
- Sample Collection: Collect 14-20 mL of peripheral blood from stage III/IV NSCLC patients in Cell-Free DNA BCT tubes (Streck). Process within one week via a two-step centrifugation protocol to isolate plasma from the buffy coat. Concurrently, collect matched FFPE tissue samples where available [29].
- Nucleic Acid Extraction: Extract cfDNA from 4 mL of plasma using a specialized Nucleic Acid Extraction Kit, eluting in 52 µL of buffer. Isolate genomic DNA from FFPE tissue using the QIAamp FFPE Tissue Kit (Qiagen). Quantify cfDNA and gDNA using the Qubit dsDNA HS assay [29].
- Library Preparation and Sequencing: Construct NGS libraries from a minimum of 20 ng cfDNA using the USCI UgenDX Lung Cancer kit, a targeted 21-gene panel. Hybridize the libraries to the panel and sequence on USCISEQ-200 analyzers to generate 100 bp paired-end reads [29].
- Bioinformatic Analysis: Trim raw reads with Trimmomatic and align to the GRCh37 reference genome using BWA. Mark duplicates with Picard. Perform variant calling with GATK and VarScan, followed by annotation with ANNOVAR. Apply a 0.2% variant allele frequency (VAF) cutoff with local depth >1000x and a mean effective depth of >1400x as key quality filters [29].
- Orthogonal Validation: Validate the NGS results for specific mutations in EGFR, BRAF, and KRAS using droplet digital PCR (ddPCR). The reaction mixture includes ddPCR Supermix, mutation-specific primers and probes (FAM/HEX labeled), and 20 ng of DNA template. Perform amplification and read on a QX200 Droplet Reader, analyzing data with QuantaSoft software [29].
Protocol 2: Comparative Analysis of HPV Detection Methods
A direct comparison of NGS, ddPCR, and qPCR for detecting HPV in oropharyngeal cancer illustrates a protocol for benchmarking NGS against other PCR-based techniques [36].
- Sample Types: Utilize plasma and oral rinse samples from patients with HPV16-positive oropharyngeal cancer (HPV16-OPC) [36].
- Method Comparison: Process samples in parallel using:
- NGS: Specific library prep and sequencing methodology for HPV detection.
- ddPCR: Partition samples into nanodroplets for absolute quantification without a standard curve.
- qPCR: Use standard curve-based quantification with fluorescent probes.
- Sensitivity Calculation: Calculate and compare the sensitivity of each method for detecting HPV16 DNA in the different sample matrices [36].
Quantitative Performance Comparison Across Platforms
The analytical sensitivity of a technology defines its lowest detectable limit of a mutant allele in a wild-type background, a parameter critical for ctDNA analysis where VAF can be very low.
Sensitivity and Limit of Detection (LOD)
Table 1: Comparative Analytical Sensitivity of Molecular Detection Methods
| Method | Typical Lower Limit of Detection (Mutant Allele Frequency) | Key Strengths | Key Limitations |
|---|---|---|---|
| Quantitative PCR (qPCR) | ~10% [37] | Fast, cost-effective, accessible equipment [38] | Limited throughput, detects known sequences only [38] |
| Digital PCR (dPCR) | <0.1% [37] | High sensitivity, absolute quantification without standard curves | Limited to known targets, lower multiplexing capability |
| Targeted NGS | <1% (can reach 0.2% with optimized protocols) [29] [37] | High discovery power, high multiplexing, detects novel variants [38] | Higher cost for simple targets, complex data analysis [38] |
| Advanced NGS (with barcoding) | <0.1% [37] | Ultra-high sensitivity, reduced sequencing errors | Increased cost and protocol complexity |
NGS demonstrates a clear advantage in sensitivity over traditional qPCR. While dPCR can achieve similar or slightly better LOD for specific known mutations, NGS provides this sensitivity across hundreds to thousands of genomic regions simultaneously [38]. The establishment of a 0.2% VAF cutoff with high depth of coverage (>1400x) in the NSCLC study exemplifies the rigorous parameters required for reliable ctDNA detection in clinical research [29].
Tissue-Concordance and Stage-Dependent Performance
A critical validation of liquid biopsy NGS is its concordance with tissue-based genotyping. Data from a large cohort study reveals that concordance is highly dependent on disease stage.
Table 2: Tissue-Plasma Concordance Rates in Stage III/IV NSCLC [29]
| Clinical Stage | Positive Percentage Agreement (PPA) | Negative Percentage Agreement (NPA) |
|---|---|---|
| Stage III | 28.57% (2/7) | 99.20% (124/125) |
| Stage IV | 99.20% (124/125) | 99.46% (183/184) |
This data highlights a crucial finding: while the NPA remains excellent across stages, the PPA for Stage III is significantly lower than for Stage IV. This is biologically plausible due to the lower tumor burden and consequently lower ctDNA shed into the bloodstream in earlier-stage disease. This underscores the importance of tumor burden context when interpreting liquid biopsy results [29]. The overall high concordance in advanced disease supports the use of NGS-based liquid biopsy as a robust tool for genomic profiling when tissue is unavailable.
Essential Quality Control Metrics for NGS Liquid Biopsy
Ensuring the reliability of NGS data requires stringent quality control throughout the workflow. Key metrics established in validation studies include [29] [39]:
- Mean Effective Depth of Coverage: A minimum of >1400x is recommended for detecting low-frequency variants down to 0.2% VAF [29].
- Variant Allele Frequency (VAF) Cutoff: A 0.2% threshold is analytically validated for distinguishing true variants from background noise [29].
- Positive Percentage Agreement (PPA) & Negative Percentage Agreement (NPA): Orthogonal validation with a method like ddPCR should demonstrate >80% PPA and >95% NPA for the assay to be considered clinically reliable [29].
- Sample Quality Assessment: Pathologist review of solid tumor samples for tumor cell content is essential. For liquid biopsy, cfDNA concentration and fragment size analysis serve as initial quality checks [39].
Workflow and Pathway Visualizations
NGS Liquid Biopsy and Concordance Workflow
The following diagram illustrates the end-to-end process from sample collection to data analysis, highlighting key steps where quality metrics are critical.
Technology Selection Decision Pathway
This decision tree guides researchers in selecting the most appropriate technology based on the study's primary objective.
The Scientist's Toolkit: Essential Research Reagent Solutions
Table 3: Key Reagents and Kits for NGS Liquid Biopsy Research
| Item | Function in Workflow | Example Product / Method |
|---|---|---|
| cfDNA Collection Tubes | Stabilizes nucleated blood cells to prevent genomic DNA contamination during shipment and storage. | Cell-Free DNA BCT Tubes (Streck) [29] |
| Nucleic Acid Extraction Kit | Isulates high-quality, pure cfDNA from plasma or gDNA from FFPE tissue. | QIAamp FFPE Tissue Kit (Qiagen) [29] |
| Targeted NGS Gene Panel | Enriches for specific genomic regions of interest prior to sequencing. | USCI UgenDX Lung Cancer kit (21-gene panel) [29] |
| Orthogonal Validation Technology | Provides an independent, highly accurate method to confirm NGS-identified mutations. | Droplet Digital PCR (ddPCR) (Bio-Rad) [29] |
| Bioinformatics Pipelines | Processes raw sequencing data, aligns reads, calls variants, and filters results based on quality metrics. | BWA (alignment) + GATK (variant calling) [29] |
The establishment of rigorous analytical sensitivity parameters and quality metrics is the foundation of reliable NGS-based liquid biopsy research. As the data demonstrates, targeted NGS offers a powerful balance of high sensitivity, multiplexing capability, and discovery power, outperforming qPCR and rivaling the sensitivity of dPCR while providing a much broader genomic profile. The high concordance with tissue genotyping in advanced cancers solidifies its role in cancer genomics. For researchers and drug developers, the choice of platform must be guided by the specific study requirements—number of targets, required LOD, and the need for discovery versus confirmation—always within the context of a rigorously validated and quality-controlled workflow.
Tumor Fraction as a Critical Determinant of Liquid Biopsy Performance
Liquid biopsy, the analysis of tumor-derived components from bodily fluids such as blood, has emerged as a transformative approach in oncology, enabling non-invasive cancer detection, molecular profiling, and treatment monitoring [7] [3]. Circulating tumor DNA (ctDNA)—the tumor-derived fraction of cell-free DNA (cfDNA)—serves as a key analyte for detecting genomic alterations in circulating tumor DNA (ctDNA) [31] [3]. The performance of these assays hinges critically on one fundamental parameter: the circulating tumor DNA (ctDNA) tumor fraction (TF), defined as the proportion of ctDNA within the total cfDNA population [40] [41]. This metric serves as a primary determinant of assay sensitivity, reliability, and clinical utility.
The quantitative importance of tumor fraction becomes particularly evident in the context of Next-Generation Sequencing (NGS) concordance studies between tissue and liquid biopsy. Tissue biopsy remains the gold standard for tumor profiling, but spatial and temporal heterogeneity limits its ability to fully characterize metastatic disease [7] [42]. Liquid biopsy offers a complementary approach that captures contributions from multiple tumor sites, yet its accuracy depends substantially on the abundance of tumor-derived DNA in circulation [31] [41]. Understanding how tumor fraction influences detection sensitivity and concordance rates is thus essential for researchers, assay developers, and clinical oncologists seeking to implement liquid biopsy in precision oncology frameworks.
Technical Determinants: How Tumor Fraction Influences Assay Sensitivity
The Tumor Fraction Threshold Principle
The relationship between tumor fraction and variant detection follows fundamental statistical principles. At low tumor fractions, the number of mutant DNA molecules in a blood sample becomes limiting, requiring exceptionally high sequencing depth and sophisticated error-suppression techniques to distinguish true variants from technical noise [31]. Variant allele frequency (VAF), representing the proportion of sequencing reads harboring a specific mutation, is directly proportional to tumor fraction when the mutation is clonal and heterozygous [31] [40].
Table 1: Tumor Fraction Impact on Mutation Detection Probability
| Tumor Fraction | Variant Allele Frequency | Minimum Coverage for 99% Detection Probability | Expected Detection Rate |
|---|---|---|---|
| 1% | 0.5% | ~10,000× | ~50% |
| 0.5% | 0.25% | ~20,000× | ~30% |
| 0.1% | 0.05% | ~100,000× | <10% |
As illustrated in Table 1, achieving a 99% detection probability for variants at 0.1% VAF requires approximately 10,000× coverage, while detecting variants at 0.1% VAF necessitates approximately 100,000× coverage—demonstrating the inverse exponential relationship between required sequencing depth and tumor fraction levels [31]. This relationship explains why commercial liquid biopsy assays with reported limits of detection (LOD) around 0.5% tumor fraction achieve only approximately 50% alteration detection rates in real-world settings, while improving LOD to 0.1% could increase detection rates to approximately 80% [31].
Input DNA and Biological Limitations
The absolute number of mutant DNA molecules present in a sample represents another critical constraint. A 10mL blood draw from a lung cancer patient might yield only approximately 8,000 haploid genome equivalents (GEs), with a tumor fraction of 0.1% providing a mere 8 mutant GEs for analysis—making detection statistically improbable. The same volume from a high-shedding liver cancer patient could yield approximately 80,000 GEs, providing 80 mutant GEs at the same tumor fraction and substantially improving detection probability [31]. This biological variability in ctDNA shedding across tumor types and individuals introduces significant challenges for developing universally applicable liquid biopsy assays.
Technological Innovations in Low-Tumor Fraction Detection
Several advanced technological approaches have been developed to enhance detection sensitivity at low tumor fractions:
Unique Molecular Identifiers (UMIs) are short nucleotide sequences added to DNA fragments during library preparation that enable bioinformatic distinction between true variants and amplification artifacts [31]. Following sequencing, reads with identical UMIs are grouped and consensus sequences are generated, significantly reducing false positive calls. However, this process typically results in a 10-fold reduction in usable reads after deduplication, necessitating higher initial sequencing depth [31].
Error-Suppression Techniques such as the MUTE-Seq assay leverage engineered advanced-fidelity FnCas9 to selectively eliminate wild-type DNA molecules, thereby enriching for mutant alleles and improving signal-to-noise ratios [43]. This approach has demonstrated significant improvements in detecting low-frequency cancer-associated mutations for minimal residual disease (MRD) monitoring in non-small cell lung cancer (NSCLC) and pancreatic cancer [43].
Fragmentomics and Multi-Analyte Approaches integrate multiple features of ctDNA beyond simple mutation detection, including fragment size patterns, epigenetic markers, and proteomic signatures [43]. For example, cfDNA fragmentome analysis has demonstrated high accuracy (AUC = 0.92) in identifying liver cirrhosis and facilitating hepatocellular carcinoma surveillance, potentially offering enhanced sensitivity in low-tumor fraction scenarios [43].
Tumor Fraction and Clinical Concordance: Evidence Across Malignancies
Concordance Rates in Solid Tumors
Multiple studies have evaluated the concordance between tissue and liquid biopsy genomic profiling across various tumor types, with tumor fraction consistently emerging as a primary determinant of agreement rates.
Table 2: Tissue-Liquid Biopsy Concordance Across Tumor Types
| Tumor Type | Study/Reference | Overall Concordance | Concordance at TF ≥1% | Key Findings |
|---|---|---|---|---|
| Multiple Solid Tumors (n=430) | Community Health Network [42] | 88% (oncogenic mutations) | N/R | 11% had actionable mutations detected only in liquid biopsy |
| Advanced NSCLC | LUNG-MAP Study [44] | N/R | Significantly improved | Elevated TF associated with worse overall survival |
| Metastatic Breast Cancer | Real-world study [40] | Variable by TF | High at TF ≥10% | TF >10% associated with significantly worse survival |
| Pancreatic Cancer | CHAMP Study [45] | High for relevant alterations | N/R | TF prognostic in palliative setting, not adjuvant |
A comprehensive analysis of 874 patients with various cancer types demonstrated that despite a wide range of cfDNA concentrations (0.50 to 1132.9 ng/mL) across 21 tumor types, matched tumor and blood specimens (n = 430 patients) revealed high concordance for coding (median = 97%) and clinical oncogenic mutations (median = 88% concordance) [42]. Importantly, this study identified an additional 48 patients (11%) with therapeutically actionable mutations detected only in liquid biopsy, highlighting the ability of ctDNA analysis to capture tumor heterogeneity that might be missed by single-site tissue biopsy [42].
Tumor Fraction Thresholds for Clinical Decision-Making
Based on accumulating evidence, specific tumor fraction thresholds have been established to guide clinical interpretation of liquid biopsy results:
The 1% tumor fraction threshold has emerged as a critical cutpoint for determining result reliability. Foundation Medicine's FoundationOne Liquid CDx assay utilizes this threshold, with samples exceeding 1% tumor fraction considered to have "high ctDNA tumor fraction," providing greater confidence in negative results for short variants and rearrangements [41]. When tumor fraction falls below this threshold, negative results should be interpreted with caution, and follow-up tissue biopsy should be considered if clinically indicated [41].
The 10% tumor fraction threshold has demonstrated significant prognostic value across multiple studies. In metastatic triple-negative breast cancer, patients with tumor fraction >10% had significantly lower survival probability compared to those with tumor fraction <10% [40]. Similarly, in a pan-cancer cohort of metastatic breast cancer patients, tumor fraction >10% was associated with worse survival outcomes, with prognostic value maintained across cutoff points ranging from 1% to 20% [40].
Analytical Frameworks for Tumor Fraction Assessment
Methodological Approaches to Tumor Fraction Quantification
Several methodological approaches have been developed to quantify tumor fraction, each with distinct advantages, limitations, and optimal applications in research and clinical settings.
Table 3: Comparison of Tumor Fraction Assessment Methods
| Method | Principle | Limit of Detection | Key Applications | Advantages/Limitations |
|---|---|---|---|---|
| Ultra-low Pass Whole Genome Sequencing (ULP-WGS) | Shallow whole-genome sequencing to detect copy number alterations | ~1-3% | Metastatic setting, cost-effective screening | Low cost (<$100/sample), uses minimal sample, but limited sensitivity |
| Variant Allele Frequency (VAF) Approach | Calculation based on fraction of mutation-bearing reads | Varies with sequencing depth | Targeted therapy selection | Directly measures specific mutations, requires prior knowledge of mutations |
| Personalized Assays | Patient-specific mutation tracking | 0.01% or lower | MRD monitoring, early relapse detection | High sensitivity, but requires tumor tissue for assay design |
| Aneuploidy-based Approaches | Genome-wide copy number alteration analysis | ~0.5% | Commercial assays (e.g., FoundationOne Liquid CDx) | Tumor-agnostic, comprehensive genomic coverage |
Each method offers distinct trade-offs between sensitivity, cost, throughput, and required sample input. ULP-WGS provides a cost-effective approach for tumor fraction estimation in advanced cancers but lacks sensitivity for minimal residual disease detection [40]. In contrast, personalized assays tracking patient-specific mutations can achieve sensitivities of 0.01% or lower, making them suitable for MRD monitoring but requiring initial tumor tissue profiling for assay design [40].
Integrated Tumor Fraction Calculation in Commercial Assays
Advanced commercial assays have developed sophisticated integrated approaches to tumor fraction calculation. Foundation Medicine's ctDNA tumor fraction determination accounts for multiple orthogonal data types, including aneuploidy, variant allele frequency, fragment length information, clonal hematopoiesis predictions, and known tumor-associated alterations [41]. This multi-parameter approach enhances the robustness of tumor fraction estimates and improves confidence in clinical interpretation, particularly for negative results.
Tumor Fraction in Clinical Applications: Evidence from Recent Studies
Prognostic and Predictive Utility
Recent evidence has firmly established tumor fraction as both a prognostic biomarker and potential predictor of treatment response across multiple cancer types:
In the LUNG-MAP study involving patients with advanced non-small cell lung cancer, elevated ctDNA tumor fraction (≥1%) was associated with improved mutation detection but worse overall survival, demonstrating its independent prognostic value [44]. This large-scale analysis confirmed that tumor fraction provides clinical information beyond simply enabling variant detection.
In metastatic breast cancer, patients with low tumor fraction (<1%) demonstrated significantly improved real-world overall survival compared to those with intermediate (1-10%) or high tumor fraction (>10%) [40]. Notably, tumor fraction remained prognostic even in patients with bone-only metastases, who sometimes exhibit lower ctDNA shedding [40] [44].
For treatment response monitoring, serial assessment of tumor fraction dynamics has shown considerable promise. Research from the MyPathway trial demonstrated that serial monitoring of ctDNA tumor fraction levels can effectively assess treatment response to immune checkpoint inhibitors in a pan-tumor patient cohort [44]. Similarly, the NIMBUS trial revealed that changes in ctDNA tumor fraction were associated with clinical benefit in breast cancer patients receiving dual immune checkpoint blockade [44].
Tumor Fraction in Minimal Residual Disease (MRD) Detection
The most technically demanding application of liquid biopsy involves detecting minimal residual disease following curative-intent treatment, where tumor fractions are typically extremely low (<0.1%):
In the VICTORI study of colorectal cancer patients, ctDNA analysis using the neXT Personal MRD detection assay demonstrated that 87% of recurrences were preceded by ctDNA positivity, while no ctDNA-negative patient relapsed [43]. This highlights the potential clinical utility of sensitive MRD detection, though it requires specialized approaches given the low tumor fractions involved.
In bladder cancer, uRARE-seq—a high-throughput cell-free RNA (cfRNA)-based workflow applied to urine samples—achieved 94% sensitivity for MRD assessment with a limit of detection (LOD95) of 0.05% [43]. This approach demonstrated higher sensitivity in patients with more advanced stages and was associated with shorter high-grade recurrence-free survival.
Experimental Design and Methodological Considerations
Key Experimental Protocols for Tumor Fraction Analysis
For researchers designing studies involving tumor fraction assessment, several methodological considerations are critical:
Blood Collection and Processing Protocols must be optimized to prevent genomic DNA contamination and preserve ctDNA integrity. The CHAMP study protocol specifies collection of whole blood in EDTA tubes, incubation at room temperature for 30 minutes, followed by centrifugation at 2,000 × g for 10 minutes for plasma isolation [45]. A second centrifugation at 14,000 × g is then performed to minimize genomic DNA contamination before plasma storage at -80°C [45].
cfDNA Extraction Methods significantly impact assay performance. The QIAamp Circulating Nucleic Acid kit (Qiagen) with elution in 40 µl EB buffer without carrier RNA represents one validated approach [45]. Post-extraction, cfDNA concentration should be determined using fluorescent assays (e.g., Qubit dsDNA HS assay), and fragment size distribution should be verified using high-sensitivity electrophoretic methods (e.g., Agilent Cell-free DNA ScreenTape) to ensure minimal genomic DNA contamination [45].
Sequencing Library Preparation requires careful optimization for low-input cfDNA. The KAPA HyperPlus kit (Roche) with adjusted fragmentation times can achieve average fragment lengths of approximately 400 bp [45]. Incorporation of unique molecular identifiers (UMIs) during library preparation is essential for distinguishing true low-frequency variants from amplification artifacts [31].
The Researcher's Toolkit: Essential Reagents and Platforms
Table 4: Essential Research Reagents and Platforms for Tumor Fraction Studies
| Category | Specific Examples | Key Function | Considerations |
|---|---|---|---|
| Blood Collection Tubes | EDTA tubes | Stabilize blood components for plasma isolation | Standardized volume (e.g., 4 × 6 mL tubes) ensures sufficient plasma yield |
| cfDNA Extraction Kits | QIAamp Circulating Nucleic Acid Kit (Qiagen) | Isolation of high-quality cfDNA from plasma | Carrier RNA omission reduces background interference in downstream assays |
| Library Preparation | KAPA HyperPlus Kit (Roche) | Construction of sequencing libraries from cfDNA | Fragmentation time optimization critical for cfDNA |
| Target Enrichment | Customized pan-cancer panels (e.g., TWIST Bioscience) | Hybridization capture of genomic regions of interest | Panel size (e.g., 2.4 Mb) balances coverage and cost |
| Sequencing Platforms | Illumina NovaSeq 6000 | High-throughput sequencing | Enables ultra-deep sequencing (≥10,000× coverage) |
| Bioinformatics Pipelines | Autoseq, UMI-based deduplication | Variant calling, tumor fraction calculation | Specialized expertise required for optimal implementation |
Visualizing the Tumor Fraction Analysis Workflow
Figure 1: Integrated Workflow for Tumor Fraction Analysis in Liquid Biopsy. This diagram illustrates the sequential steps from blood collection through clinical interpretation, highlighting critical pre-analytical and analytical phases that impact tumor fraction quantification accuracy.
Tumor fraction represents a fundamental determinant of liquid biopsy performance, influencing variant detection sensitivity, tissue concordance rates, and clinical utility across diverse applications. The established 1% tumor fraction threshold provides a validated benchmark for interpreting liquid biopsy results with confidence, particularly for negative findings. Ongoing technological innovations continue to push detection limits lower, enabling new applications in minimal residual disease monitoring and early cancer detection.
Future research directions should focus on standardizing tumor fraction quantification methods across platforms, validating clinical cutoffs in prospective trials, and integrating multi-analyte approaches to enhance sensitivity in low-shedding tumors. As evidence accumulates, tumor fraction is poised to evolve from a technical quality metric to a clinically actionable biomarker guiding treatment decisions and improving patient outcomes across the cancer care continuum.
The emergence of precision oncology has transformed cancer care, shifting the paradigm from a one-size-fits-all approach to biomarker-driven treatment strategies. Central to this transformation is the detection of actionable mutations—genomic alterations with potential therapeutic implications—through comprehensive molecular profiling. Next-generation sequencing (NGS) technologies enable this profiling by simultaneously assessing hundreds of cancer-related genes from various sample types, primarily tissue biopsies (TBx) and liquid biopsies (LBx).
The concordance between these two biopsy modalities has become a critical area of investigation, as it directly impacts clinical decision-making and therapeutic outcomes. While tissue biopsy has long been the gold standard for tumor genotyping, liquid biopsy analyzing circulating tumor DNA (ctDNA) offers a minimally invasive alternative that captures tumor heterogeneity more comprehensively. This guide objectively compares the performance of these approaches in detecting actionable mutations and their subsequent influence on biomarker-driven therapy selection, synthesizing evidence from recent clinical studies and trials to inform researchers, scientists, and drug development professionals.
Methodological Approaches in NGS Testing
Tissue and Liquid Biopsy NGS Methodologies
The analytical performance of NGS assays for detecting genomic variants varies significantly between tissue and liquid biopsy approaches, each with distinct methodological considerations.
Tissue Biopsy NGS Protocols typically utilize formalin-fixed, paraffin-embedded (FFPE) tumor specimens. The laboratory workflow involves DNA extraction, library preparation using hybrid capture-based chemistry, and sequencing on platforms such as Illumina NextSeq. Bioinformatic analysis follows, employing tools like Mutect2 for detecting single-nucleotide variants (SNVs) and small insertions/deletions (INDELs), CNVkit for copy number variations (CNVs), and LUMPY for gene fusions. Critical quality control metrics include minimum coverage across exonic regions (often >80% at 100× coverage), with average mean depths typically around 677.8× for targeted panels. Variant calling usually applies a variant allele frequency (VAF) threshold ≥2% to ensure specificity [46].
Liquid Biopsy NGS Protocols focus on circulating tumor DNA (ctDNA) isolated from blood plasma. The process involves blood collection in specialized tubes, plasma separation, cell-free DNA extraction, and library preparation. Due to the low abundance of ctDNA in total cell-free DNA (approximately 0.1-1.0%), liquid biopsy assays require enhanced sensitivity, often employing unique molecular identifiers (UMIs) and error suppression techniques to detect variants at VAFs as low as 0.1%. The average read depth for LBx is typically higher (approximately 5,589×) to compensate for low ctDNA fraction [47].
Analytical Concordance Between Testing Platforms
Comparative studies have evaluated the performance of different NGS platforms when applied to both tissue and liquid biopsies. A rigorous comparison between the PGDx elio tissue complete assay and FoundationOne CDx demonstrated high overall concordance for various variant types [27].
Table 1: Analytical Performance Comparison Between NGS Assays
| Variant Type | Positive Percentage Agreement | Key Observations |
|---|---|---|
| Single Nucleotide Variants (SNVs) | >95% | Higher concordance for clinically actionable genes |
| Insertions/Deletions (Indels) | >95% | Consistent performance across tumor types |
| Copy Number Alterations (CNAs) | 80-83% | Lower concordance due to analytical differences |
| Gene Translocations | 80-83% | Affected by breakpoint location and read depth |
| Tumor Mutational Burden (TMB) | High concordance | Consistent across mutation load range |
| Microsatellite Instability (MSI) | High concordance | Comparable classification (MSI-H vs. MSS) |
This comparison highlights that while SNVs and indels show excellent concordance between platforms, structural variants like CNAs and translocations present greater technical challenges, regardless of the sample type used [27].
Comparative Performance of Tissue and Liquid Biopsy
Detection Rates and Concordance Patterns
The ROME trial, a phase II multicenter study enrolling 1,794 patients with advanced solid tumors, provides compelling evidence regarding the concordance between tissue and liquid biopsy for actionable mutations. The trial performed NGS using FoundationOne CDx (tissue) and FoundationOne Liquid CDx (liquid) and randomized 400 patients to tailored therapy (TT) or standard-of-care (SoC) based on the findings [6].
The study revealed that concordance—defined as detection of the same druggable alteration in both biopsy types—was present in only 49% of cases. Discordance showed distinct patterns: 35% of alterations were detected exclusively in tissue, while 16% were found only in liquid biopsy [6].
This discordance reflects the complementary biological information captured by each approach. Tissue biopsies may detect alterations present in the primary tumor site but not shed sufficiently into circulation, while liquid biopsies can identify mutations from metastatic sites not sampled by tissue biopsy, effectively capturing spatial tumor heterogeneity [47].
Tumor Heterogeneity and Mutation Capture
Liquid biopsy's ability to capture comprehensive tumor heterogeneity represents one of its significant advantages. A detailed study analyzing 56 postmortem tissue samples from eight cancer patients compared against pre-mortem liquid biopsies revealed the complex relationship between these modalities [47].
The research demonstrated substantial genetic diversity across metastatic lesions, with 4-12 mutations per patient and variant allele frequencies (VAFs) ranging from 1.5% to 71.4% in tissue samples. Liquid biopsies identified 51 variants (4-17 per patient) with VAFs of 0.2-31.1%, showing overlapping mutations with tissue samples ranging from 33% to 92% across patients [47].
Notably, 22 tissue variants were absent in matched liquid biopsies, while 18 liquid biopsy-exclusive variants were detected (VAFs: 0.2-2.8%). The mutations exclusively detected in tissue had significantly lower VAFs (mean: 15.4%) compared to all tissue-detected alterations (mean VAF: 24.5%), suggesting they represented subclonal populations not sufficiently shed into circulation [47].
Table 2: Mutation Distribution Across Biopsy Modalities in Metastatic Cancer
| Parameter | Tissue Biopsy Only | Liquid Biopsy Only | Overlapping Mutations |
|---|---|---|---|
| Number of Mutations | 22 variants across all patients | 18 variants across all patients | 33-92% overlap per patient |
| Mean VAF Range | 1.5-71.4% | 0.2-2.8% | 0.2-31.1% |
| Representation | Primarily subclonal mutations with lower VAFs | Very low VAF mutations; some potentially from CHIP | Clonal, well-shed mutations |
| Clinical Implications | May miss spatially separated metastases | Potential false positives from CHIP; lower sensitivity | Most reliable for treatment decisions |
The following diagram illustrates how tissue and liquid biopsies capture different aspects of tumor heterogeneity:
Clinical Utility and Therapeutic Outcomes
Impact on Survival Outcomes
The ROME trial provides the most direct evidence linking biopsy concordance with therapeutic outcomes. The study demonstrated that patients in the concordant group (those with the same druggable alteration detected in both tissue and liquid biopsy) who received tailored therapy experienced significantly improved survival outcomes compared to those receiving standard of care [6].
Table 3: Survival Outcomes Based on Biopsy Concordance in the ROME Trial
| Patient Group | Biopsy Type for Detection | Median Overall Survival (Months) | Median Progression-Free Survival (Months) | Hazard Ratio (TT vs. SoC) |
|---|---|---|---|---|
| Concordant | Tissue + Liquid | 11.05 vs. 7.70 (SoC) | 4.93 vs. 2.80 (SoC) | OS: HR 0.74 (0.51-1.07)\nPFS: HR 0.55 (0.40-0.76) |
| Discordant - Tissue Only | Tissue Only | 9.93 | 3.06 | Limited benefit of TT |
| Discordant - Liquid Only | Liquid Only | 4.05 | 2.07 | Minimal benefit of TT |
These findings suggest that concordant results may indicate well-shed, clonal alterations more likely to respond to targeted therapies, whereas discordant results might represent subclonal alterations or limitations in detection sensitivity that diminish therapeutic efficacy [6].
Real-World Clinical Utility Across Tumor Types
Real-world evidence supports the clinical utility of NGS profiling while highlighting limitations in certain populations. A study of 990 patients with advanced solid tumors demonstrated that 26.0% harbored tier I variants (strong clinical significance), and 13.7% of these received NGS-based therapy, with varying response rates across cancer types [46].
Of 32 patients with measurable lesions who received NGS-based therapy, 12 (37.5%) achieved partial response, and 11 (34.4%) achieved stable disease, with a median treatment duration of 6.4 months. However, a separate study in adolescent and young adult (AYA) patients with sarcoma showed more limited benefit, with only 5 of 108 patients (4.6%) deriving clinical benefit from NGS-directed therapy, highlighting that clinical utility varies significantly by cancer type [48].
Practical Implementation and Research Applications
The Scientist's Toolkit: Essential Research Reagents
Implementing NGS testing for actionable mutation detection requires specific reagents and platforms. The following table details key solutions used in the studies cited in this guide:
Table 4: Essential Research Reagents for NGS-Based Actionable Mutation Detection
| Research Reagent | Manufacturer/Provider | Primary Function | Application Context |
|---|---|---|---|
| FoundationOne CDx | Foundation Medicine | Comprehensive genomic profiling from FFPE tissue | Detection of SNVs, Indels, CNAs, fusions, TMB, MSI from tissue |
| FoundationOne Liquid CDx | Foundation Medicine | Comprehensive genomic profiling from blood | Detection of SNVs, Indels, CNAs, fusions, TMB, MSI from blood |
| PGDx elio tissue complete | Personal Genome Diagnostics | Comprehensive DNA-to-report kitted NGS solution | In-house NGS testing for SNVs, Indels, CNAs, fusions, TMB, MSI |
| SNUBH Pan-Cancer v2.0 Panel | Seoul National University Bundang Hospital | Targeted sequencing platform (544 genes) | Institutional NGS testing for advanced solid tumors |
| QIAamp DNA FFPE Tissue Kit | Qiagen | DNA extraction from FFPE tissue | Nucleic acid isolation from archival tissue samples |
| Agilent SureSelectXT Target Enrichment | Agilent Technologies | Library preparation and target enrichment | Sequence capture for targeted NGS approaches |
Biomarker-Driven Clinical Trial Designs
The integration of NGS profiling into clinical trial designs has created new paradigms for drug development. Several biomarker-driven trial designs have emerged, each with distinct advantages and applications [49]:
Enrichment Design: Enrolls only biomarker-positive participants, optimal for therapies with strong mechanistic rationale linked to a specific biomarker. Example: EGFR mutations (e.g., T790m) in NSCLC.
Stratified Randomization: Enrolls all patients but randomizes within biomarker subgroups, removing confounding when biomarkers are prognostic. Example: PD-L1 expression in NSCLC.
All-Comers Design: Enrolls both biomarker-positive and negative patients without stratification, used for hypothesis generation when biomarker effect is uncertain.
Tumor-Agnostic Basket Trials: Enrolls patients with biomarker-positive tumors across different cancer types into separate study arms. Example: BRAF V600 mutations across multiple solid tumors.
The following diagram illustrates the decision pathway for selecting appropriate biomarker-driven trial designs:
The comparative analysis of tissue and liquid biopsy for actionable mutation detection reveals a complementary relationship rather than a competitive one. Evidence from clinical trials and real-world studies indicates that while tissue biopsy remains essential for initial diagnosis and captures spatially restricted alterations, liquid biopsy provides a more comprehensive view of tumor heterogeneity and evolving genomic landscape under therapeutic pressure.
The concordance between these modalities itself carries prognostic significance, with concordant patients demonstrating superior outcomes from tailored therapies. This suggests that dual-testing approaches may be optimal for selecting patients most likely to benefit from biomarker-driven treatments, particularly in advanced malignancies where tumor heterogeneity is pronounced.
For researchers and drug development professionals, these findings underscore the importance of incorporating both tissue and liquid biopsy strategies into clinical trial designs, especially in later-phase studies where understanding treatment effects across molecularly defined populations is critical. As NGS technologies continue to evolve and become more accessible, their integration into standardized oncology care pathways will be essential for realizing the full potential of precision medicine in improving cancer outcomes.
Addressing Discordance and Optimizing NGS Testing Strategies
In precision oncology, next-generation sequencing (NGS) of tumor tissue and liquid biopsies (circulating tumor DNA, ctDNA) are fundamental for guiding treatment. However, the genomic results from these two methods are not always identical, leading to potential challenges in clinical interpretation. Discordance between liquid and tissue biopsies arises from two distinct categories: biological discordance, rooted in the tumor's physiology and heterogeneity, and technical discordance, stemming from the limitations of the testing platforms and methodologies themselves [50] [51]. Understanding the distinction between these two sources is critical for researchers, scientists, and drug development professionals to accurately interpret NGS data, design robust clinical trials, and develop effective diagnostic protocols. This guide objectively compares the performance of tissue and liquid biopsies by examining the frameworks for interpreting biological and technical discordance, supported by experimental data.
Defining Biological and Technical Discordance
Biological Discordance
Biological discordance occurs when the genomic differences between liquid and tissue biopsies reflect real, underlying biological phenomena. A primary cause is tumor heterogeneity, where different regions of a tumor or metastatic sites harbor distinct genetic profiles. A tissue biopsy, being localized, may capture only a subclone of the tumor, while a liquid biopsy, which samples ctDNA shed from multiple tumor sites, can provide a more comprehensive view of the overall mutational landscape [50]. Furthermore, biological factors such as the shedding rate of ctDNA can influence discordance; some tumors, like pancreatic cancers, release less DNA into the bloodstream, making mutation detection in liquid biopsies less sensitive [50]. At the time of disease progression, biological discordance becomes particularly pronounced as new, treatment-resistant subclones emerge that may not be present in the original tissue sample [51].
Technical Discordance
Technical discordance, in contrast, results from limitations inherent to the testing technologies and laboratory processes. Key factors include:
- Sample Quality: The use of formalin-fixed, paraffin-embedded (FFPE) tissue can lead to DNA damage and false-positive variant calls, while the low abundance of ctDNA in plasma presents a challenge for liquid biopsy assays [50] [27].
- Assay Sensitivity and Specificity: Different NGS platforms have varying limits of detection (LOD) for variant allele frequency (VAF). The technical error rate of NGS, though computationally suppressible, can confound the detection of low-frequency variants [52].
- Wet-lab and Bioinformatic Protocols: Variations in DNA extraction methods, target enrichment (e.g., amplicon-based vs. hybrid capture-based), sequencing depth, and the bioinformatic pipelines used for variant calling can all contribute to technical discrepancies between tests, and even between laboratories using the same kit [27] [50].
The following diagram illustrates the distinct causes and pathways leading to each type of discordance.
Quantitative Comparison of Discordance
Data from multiple clinical studies reveals consistent patterns in the rates and nature of discordance between tissue and liquid biopsy NGS.
Table 1: Key Metrics of Tissue and Liquid Biopsy Discordance from Clinical Studies
| Study / Cancer Type | Concordance Rate | Notes on Discordance | Clinical Impact |
|---|---|---|---|
| ROME Trial (Various Advanced Solid Tumors) [6] | 49% | 35% alterations exclusive to tissue; 16% exclusive to liquid. | Patients with concordant results had improved survival with tailored therapy (HR for PFS: 0.55). |
| Lung Adenocarcinoma (Diagnosis) [51] | ~80% | Tissue-NGS identified significantly more clinically relevant mutations. | A negative liquid biopsy result may require confirmation with tissue. |
| Lung Adenocarcinoma (Progression) [51] | ~40% | Steep decline in concordance at progression. | Either test alone is insufficient to identify resistance mutations. |
| Pancreatic Cancer Study [50] | N/A | Tissue found relevant variants in 87% vs. liquid 25%; Liquid missed common mutation in 29% of cases. | Tissue biopsy provided more accurate results for this cancer type. |
| Various Cancers [50] | 22% (Mutation Overlap) | Only 10 of 45 total mutations were detected by both methods. | Only 25% (9/36) of drug recommendations were concordant. |
Table 2: Analytical Performance Comparison of Two Commercial NGS Assays [27]
| Variant Type | Positive Percentage Agreement (PPA) | Notes |
|---|---|---|
| Single Nucleotide Variants (SNVs) & Indels | >95% | In clinically actionable genes. |
| Copy Number Alterations (CNAs) | 80% - 83% | - |
| Gene Translocations | 80% - 83% | - |
| Tumor Mutation Burden (TMB) | High Concordance | Across a range of mutation loads. |
| Microsatellite Instability (MSI) | High Concordance | - |
Experimental Protocols for Discordance Analysis
To generate the comparative data cited in this guide, researchers employ rigorous experimental protocols. A typical workflow for a concordance validation study, as described by [27], involves the following detailed methodology:
Sample Cohort Selection
- Cohort Size and Type: Studies often use retrospective cohorts of 100-150 unique patient specimens. For example, a key study utilized 147 formalin-fixed, paraffin-embedded (FFPE) tissue blocks from over 20 tumor types [27]. Another study on lung adenocarcinoma included 100 sequential patients [53].
- Patient Status: Cohorts should include a mix of newly diagnosed patients and those with disease progression on treatment to assess discordance in different clinical contexts [53].
Laboratory Testing Methodology
- Tissue NGS: The FFPE tissue sections are subjected to DNA extraction. For comprehensive genomic profiling, a targeted hybrid capture-based NGS approach is used, covering a panel of 500+ genes. Library preparation is performed, followed by sequencing on platforms such as the Illumina NextSeq or NovaSeq [27] [52].
- Liquid Biopsy NGS: Plasma is separated from patient blood draws. Cell-free DNA (cfDNA) is extracted, and libraries are prepared using a commercially available liquid biopsy kit designed to target a similar gene panel. Sequencing is performed on the same or a comparable NGS platform to ensure technical comparability [54] [53].
Bioinformatic and Statistical Analysis
- Variant Calling: Automated bioinformatic pipelines specific to each assay are used to call sequence variants (SNVs, indels), copy number alterations (CNAs), gene rearrangements, and genomic signatures like TMB and MSI [27].
- Concordance Calculation: Positive Percentage Agreement (PPA) is a common metric, calculated as (Number of variants detected by both assays / Number of variants detected by the reference assay) * 100 [27].
- Error Analysis: To account for technical noise, studies may perform deep sequencing and error profiling, measuring site-specific substitution error rates to establish a limit of detection for true low-frequency variants [52].
The workflow for such a comparative study is summarized below.
Interpretation Frameworks and Clinical Decision-Making
Navigating discordant results requires a structured framework that integrates biological and technical considerations. The American College of Medical Genetics and Genomics (ACMG) and the Clinical Genome Resource (ClinGen) have developed evidence-based, semi-quantitative scoring frameworks for interpreting the pathogenicity of copy number variants (CNVs) [55]. While designed for constitutional variants, the principles of this framework can be adapted for somatic cancer testing: it emphasizes the systematic evaluation of genomic content, overlap with clinically relevant genes, and evidence from population databases and functional studies.
The Role of the Molecular Tumor Board (MTB)
The complexity of NGS data interpretation often necessitates multidisciplinary review. Studies show that treatment recommendations from an MTB can differ from those in the initial NGS report in up to 49% of cases, primarily due to judgments on the level of evidence supporting a specific drug-variant match [56]. This highlights that discordance is not only between tests but also in the clinical interpretation of the results, reinforcing the utility of MTBs in translating complex genomic data into effective patient care.
A Framework for Action
When faced with discordant tissue and liquid biopsy results, the following integrated approach is recommended:
- Prioritize Tissue-Based Findings for Diagnosis: If a tumor is easily accessible, tissue biopsy remains the gold standard for initial diagnosis and biomarker identification, as it provides higher sensitivity and architectural context [53].
- Utilize Liquid Biopsies for Dynamic Monitoring: Liquid biopsies are superior for tracking tumor evolution, monitoring treatment response, and detecting minimal residual disease due to their non-invasive nature and ability to capture spatial heterogeneity [54] [50].
- Combine Modalities at Critical Junctures: At disease progression, where biological discordance is high, pursuing both tissue and liquid biopsy maximizes the likelihood of identifying targetable resistance mechanisms [51]. The ROME trial insight confirms that patients with alterations detected in both tissue and liquid biopsies (the concordant group) derived the greatest benefit from tailored therapy [6].
- Account for Technical Performance: Understand the validated limits of detection, variant calling capabilities, and potential artifacts of the specific NGS assays being used. A negative result in a liquid biopsy, particularly in a cancer type with low ctDNA shed, should be interpreted with caution [50].
The Scientist's Toolkit: Key Research Reagent Solutions
The following reagents and kits are essential for conducting the experiments cited in the comparison studies above.
Table 3: Essential Research Reagents for NGS Concordance Studies
| Reagent / Kit | Primary Function | Application in Discordance Research |
|---|---|---|
| cfDNA Extraction Kit [50] | Isolation of cell-free DNA from blood plasma or serum. | Provides the input material for liquid biopsy NGS; kit sensitivity is critical for recovering low-abundance ctDNA. |
| Magnetic Beads [50] | Solid-phase reversible immobilization for nucleic acid purification. | Used in automated and manual extraction protocols to purify cfDNA or genomic DNA from FFPE tissue. |
| Hybrid Capture Probes [27] | Sequence-specific baits to enrich target genomic regions. | Essential for comprehensive genomic profiling assays to ensure uniform coverage of hundreds of cancer-related genes. |
| PCR Purification Kit [50] | Removal of enzymes, salts, and short fragments post-amplification. | Increases the quality of NGS libraries by purifying amplicons before sequencing, reducing noise. |
| Multiplex PCR Assay Kit | Amplification of numerous target genes simultaneously. | Used in amplicon-based NGS workflows for focused gene panels; different polymerase fidelity (e.g., Q5 vs. Kapa) can influence error rates [52]. |
| External Control DNA [27] | Reference DNA with known mutations. | Used in each sequencing run to monitor assay performance, accuracy, and to calibrate variant calling. |
Tumor Heterogeneity, Clonal Hematopoiesis, and Sampling Limitations
Next-generation sequencing (NGS) has become the cornerstone of precision oncology, guiding therapeutic decisions for patients with advanced cancers. However, the critical question of concordance—the degree of molecular agreement between different sampling methods—remains a central challenge in clinical practice and drug development. This guide objectively compares the performance of two primary NGS sampling approaches: tissue biopsy (TBx), long considered the diagnostic gold standard, and liquid biopsy (LBx), a minimally invasive alternative that analyzes circulating tumor DNA (ctDNA) from blood.
The interpretation of NGS data from these methods is profoundly complicated by two biological phenomena: tumor heterogeneity, the genetic and phenotypic diversity within and across tumor sites, and clonal hematopoiesis (CH), the age-related acquisition of somatic mutations in blood cells that can masquerade as tumor-derived variants in LBx. A precise understanding of the technical performance, limitations, and optimal use cases for each method is essential for researchers designing clinical trials, scientists validating genomic assays, and drug developers interpreting biomarker data.
Performance Comparison: Tissue vs. Liquid Biopsy
The following tables summarize the core performance characteristics and clinical operational profiles of tissue and liquid biopsy based on current literature.
Table 1: Performance Characteristics of Tissue and Liquid Biopsy
| Parameter | Tissue Biopsy (TBx) | Liquid Biopsy (LBx) | Supporting Data |
|---|---|---|---|
| Analytical Sensitivity | High (Gold Standard) | Variable; lower for early-stage/low-shed tumors | Tissue-NGS identified 74 mutations vs. 41 by plasma-NGS in a lung cancer study (sensitivity 94.8% vs 52.6%) [53]. |
| Spatial Heterogeneity Capture | Limited (single-site snapshot) | Comprehensive (captures shed DNA from multiple sites) | LBx detected mutations overlooked by single-site TBx, identifying resistance mutations absent in matched tissue in up to 78% of GI cancer cases [47]. |
| Temporal Heterogeneity Capture | Low (requires repeated invasive procedures) | High (enables real-time monitoring of evolution) | LBx allows for real-time monitoring of tumor dynamics and emerging resistance [57] [47]. |
| Influence of Clonal Hematopoiesis (CH) | None | High confounder; requires specialized bioinformatics | In one study, 51.8% of patients had LBx-only mutations in TP53/DDR genes; a subset was confirmed as CH in matched whole blood [58]. |
| Limit of Detection (LOD) | Not applicable (direct tissue analysis) | Limited by low ctDNA abundance, especially in early stages | A major challenge is the low abundance of ctDNA in blood samples, particularly in early-stage cancers [57]. |
Table 2: Operational and Clinical Utility Comparison
| Parameter | Tissue Biopsy (TBx) | Liquid Biopsy (LBx) | Supporting Data |
|---|---|---|---|
| Invasiveness & Turnaround Time | High (surgical procedure); longer | Low (blood draw); short turnaround [58] | LBx is minimally invasive and easily repeatable, enabling serial monitoring of tumor evolution [57] [58]. |
| Representative Patient Populations | Patients with accessible lesions; may exclude those with high procedural risk | Broadly applicable, including patients with inaccessible tumors or contraindications to tissue biopsy | LBx is useful when tissue biopsy is unavailable, has failed, or is contraindicated due to patient health or tumor location [58]. |
| Optimal Use Case | Initial molecular diagnosis, capturing architectural context | Monitoring treatment response, identifying resistance mechanisms, tracking clonal evolution | LBx is transformative for real-time monitoring and early detection of resistance mutations [57] [47]. |
| Key Limitation | May miss inter-/ intra-lesional heterogeneity; cannot frequently repeat | Low sensitivity in low-shed tumors; false positives from CH | Spatial tumor heterogeneity may not be fully reflected, as LBx primarily captures DNA from accessible tumor sites [57]. |
Experimental Protocols for Key Studies
To critically appraise the comparative data, understanding the underlying methodologies from key cited studies is essential.
Protocol 1: Postmortem Tissue-Liquid Biopsy Concordance Study
This study directly compared the genetic profiles from multiple metastatic lesions with those from pre-mortem liquid biopsies to evaluate how well LBx captures spatial tumor heterogeneity [47].
- Objective: To determine the efficacy of LBx in capturing inter- and intra-tumor heterogeneity by comparing it with the comprehensive mutational landscape from multi-site tissue sampling.
- Patient Cohort: Seven patients with various advanced solid tumors (including lung, colorectal, and pancreatic cancers) from the Augsburger Longitudinal Plasma Study.
- Sample Collection:
- Tissue: 56 postmortem tissue samples were collected from multiple metastatic sites (e.g., lung, liver, lymph nodes).
- Liquid: Pre-mortem blood samples were collected between 6 and 74 days prior to death.
- Sequencing & Analysis: Both tissue and circulating-free DNA from plasma were sequenced using NGS. The mutational profiles, including variants and variant allele frequencies (VAFs), from multiple tissue lesions were compared against the single LBx profile for each patient.
Protocol 2: Liquid Biopsy-Only Mutations and CH Validation
This study aimed to characterize mutations found in liquid biopsy that were not confirmed in matched tissue, with a focus on distinguishing true tumor signals from CH [58].
- Objective: To describe the characteristics and biological origin of "liquid biopsy-only" mutations, particularly in TP53 and DNA damage response (DDR) genes.
- Patient Cohort: 542 patients with advanced solid cancer from the STING protocol (Gustave Roussy).
- Sample Collection & Sequencing: All patients had paired cfDNA-based (FoundationOne Liquid CDx) and tissue-based (FoundationOne CDx) NGS analysis.
- Mutation Classification:
- Liquid biopsy-only: Mutations identified in cfDNA but not in the paired tissue.
- Concordant: Mutations found in both matrices.
- Tissue biopsy-only: Mutations found only in tissue.
- CH Validation: For a subset of 37 patients, LBx-only mutations were tested against whole blood DNA to confirm their hematopoietic origin.
Visualizing Critical Workflows and Relationships
Origin and Challenge of cfDNA Variants
AI Model for Classifying CH Variants
The Scientist's Toolkit: Essential Research Reagents & Platforms
Table 3: Key Reagents and Platforms for NGS Concordance Research
| Tool / Reagent | Primary Function | Research Context |
|---|---|---|
| FoundationOne CDx | Tissue-based NGS CGP (comprehensive genomic profiling) | Used as the tissue reference standard in comparative studies to identify tissue-concordant and liquid-biopsy-only mutations [58]. |
| FoundationOne Liquid CDx | Plasma-based NGS CGP from cfDNA | FDA-approved liquid biopsy panel used in clinical studies to detect ctDNA variants and assess concordance with tissue-based results [58]. |
| Peripheral Blood Mononuclear Cells (PBMCs) | Source of germline and hematopoietic DNA | Critical control sample for distinguishing true somatic tumor variants from clonal hematopoiesis (CH) by sequencing matched white blood cells [58] [59]. |
| MetaCH (Machine Learning Framework) | Bioinformatic classification of variant origin (CH vs. Tumor) | Open-source ML tool that uses variant features (gene, sequence context, VAF) to predict the origin of ambiguous cfDNA variants in the absence of matched WBC sequencing [59]. |
| Mutect2 & VarDict | Somatic variant callers for NGS data | Used in consensus pipelines for sensitive detection of low-frequency somatic mutations, including CH-associated variants, from blood and tissue sequencing data [60]. |
The adoption of next-generation sequencing (NGS) for genomic profiling has become a cornerstone of precision oncology, enabling the identification of actionable mutations that guide targeted therapy. A critical decision in this process is the choice between tissue biopsy, long considered the diagnostic gold standard, and the less invasive liquid biopsy, which analyzes circulating tumor DNA (ctDNA). However, the performance of these methods is not uniform across disease stages. This guide provides an objective comparison of tissue and liquid biopsy performance, focusing on their stage-dependent concordance and optimization for clinical and research applications in early versus advanced solid tumors. Evidence indicates that key factors such as tumor burden, ctDNA shed, and anatomic site accessibility profoundly influence the diagnostic yield of each method [61]. Understanding this performance gradient is essential for researchers and drug development professionals designing clinical trials or diagnostic protocols.
Performance Data & Concordance Analysis
Quantitative Concordance and Clinical Impact
Data from prospective trials and comparative studies consistently demonstrate that the concordance between tissue and liquid biopsy is imperfect and is significantly influenced by disease stage and tumor type.
Table 1: Concordance Rates and Detection Patterns from Key Clinical Studies
| Study / Trial (Cancer Type) | Concordance Rate | Tissue-Only Detection | Liquid-Only Detection | Key Findings & Clinical Impact |
|---|---|---|---|---|
| ROME Trial (Pan-cancer) [6] | 49% | 35% | 16% | Patients with concordant results receiving tailored therapy (TT) showed superior median OS (11.05 vs. 7.70 mo) and PFS (4.93 vs. 2.80 mo) vs. standard of care (SoC). |
| Precision Oncology Program (NSCLC) [61] | Variable (TF-dependent) | - | - | For actionable mutations, Positive Percent Agreement (PPA) was 100% when ctDNA Tumor Fraction (TF) was high (>1%) vs. 47.5% when TF was low. |
| K-MASTER Project (Multi-cancer) [62] | Variable (gene-dependent) | - | - | NGS showed high sensitivity/specificity for EGFR (86.2%/97.5%) and ALK fusion (100%) in NSCLC, but lower for ERBB2 amplification in breast/gastric cancers (53.7-62.5% sensitivity). |
| PIK3CA Method Comparison (Breast Cancer) [63] | κ = 0.09 (Slight) | - | - | Targeted NGS was more reliable than RT-PCR for mutation detection on archival FFPE samples, especially with low DNA quality/quantity. |
A primary insight from these studies is that discordance is not merely a technical artifact but has direct clinical consequences. The ROME trial revealed that the survival benefit from tailored therapy was most pronounced in the concordant group, whereas patients whose druggable alterations were found only in liquid biopsy had markedly worse outcomes (median OS of 4.05 months), suggesting this group may represent a distinct, more aggressive disease biology [6].
The Impact of Tumor Fraction and Stage
The stage of disease is a major driver of liquid biopsy performance, primarily through its correlation with ctDNA shed and tumor fraction (TF).
Table 2: Liquid Biopsy Performance in Advanced vs. Early-Stage Disease
| Metric | Advanced-Stage Disease (High Tumor Burden) | Early-Stage Disease (Low Tumor Burden) |
|---|---|---|
| ctDNA Tumor Fraction | Typically higher [61] | Typically lower, often below 1% [61] |
| Sensitivity for Actionable Mutations | High (PPA up to 100% with TF >1%) [61] | Lower (PPA 47.5% with TF <1%) [61] |
| Tumor Mutational Burden (TMB) Correlation | Strong correlation between blood TMB (bTMB) and tissue TMB (tTMB) (Correlation: 0.71) [61] | Weaker correlation between bTMB and tTMB (Correlation: 0.13) [61] |
| Clinical Utility | Reliable for guiding therapy when TF is high; may obviate need for invasive tissue biopsy [61] | Tissue biopsy remains the more reliable source for comprehensive genomic profiling [61] |
The data indicates that in advanced disease, where TF is often high, liquid biopsy can be a highly accurate and practical alternative to tissue biopsy. In contrast, for early-stage disease, the lower sensitivity of liquid biopsy makes tissue sequencing the more dependable choice when material is available [61].
Experimental Protocols & Methodologies
Protocol for Paired Tissue-Liquid Biopsy Concordance Studies
The following methodology is synthesized from the ROME trial and the Hong Kong Precision Oncology Program for NSCLC, which provide robust frameworks for assessing concordance [6] [61].
Patient Cohort Selection:
- Recruit patients with a histologically confirmed diagnosis of the solid tumor under investigation.
- For studies focusing on stage-dependence, stratify recruitment to include cohorts with early-stage (e.g., I/II) and advanced-stage (e.g., IV) disease.
- Collect paired tissue and blood samples concurrently before the initiation of a new line of therapy.
Sample Processing and Sequencing:
- Tissue Biopsy: Use Formalin-Fixed Paraffin-Embedded (FFPE) tumor tissue from either primary or metastatic sites. Extract genomic DNA and perform Comprehensive Genomic Profiling (CGP) using an FDA-approved tissue NGS panel such as FoundationOneCDx [6] [61].
- Liquid Biopsy: Collect peripheral blood in cell-stabilizing tubes. Iserve plasma via centrifugation and extract ctDNA. Perform CGP using a validated liquid NGS panel such as FoundationOneLiquid CDx [6] [61].
- Both assays should report short nucleotide variants, insertions/deletions, copy number alterations, genomic rearrangements, and genomic signatures like TMB and MSI.
Bioinformatic Analysis and Concordance Assessment:
- Variant Calling: Use the manufacturer's validated bioinformatics pipelines for each assay.
- Tumor Fraction Estimation: For liquid biopsies, calculate the TF from the NGS data using established methods [61].
- Concordance Definition: Define concordance for an actionable mutation as its detection in both paired tissue and liquid samples. Discordance is defined as detection in only one sample type [6].
- Statistical Analysis: Calculate Positive Percent Agreement (PPA) and Negative Percent Agreement (NPA) using tissue as the reference standard. Analyze clinical outcomes (e.g., Overall Survival, Progression-Free Survival) based on concordance status and treatment received [6] [61].
Workflow for Integrated Spatial Genomic Analysis
For a deeper investigation of tumor heterogeneity that underlies observed discordance, the Tumoroscope methodology integrates multi-modal data to map clones spatially [64].
Figure 1. Workflow of the Tumoroscope probabilistic model for spatial clone mapping. This diagram illustrates the integration of H&E images, bulk DNA-seq, and spatial transcriptomics data to infer the spatial distribution and phenotypic features of cancer clones within a tumor tissue section [64].
The model's output allows researchers to visualize the spatial co-localization or mutual exclusion of distinct clones and infer their specific gene expression profiles, providing a direct window into the spatial heterogeneity that complicates biopsy-based profiling [64].
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Research Tools for NGS Concordance Studies
| Tool / Reagent | Function in Research | Application Note |
|---|---|---|
| FoundationOneCDx [6] [61] | Comprehensive genomic profiling from FFPE tissue. | FDA-approved panel; used as a tissue standard in many clinical trials. |
| FoundationOneLiquid CDx [6] [61] | Comprehensive genomic profiling from ctDNA. | FDA-approved liquid panel; enables direct comparison to tissue NGS. |
| ResolveDNA (PTA) [65] | Whole-genome amplification from single cells. | Overcomes amplification bias to study heterogeneity at single-cell resolution. |
| Ion AmpliSeq / Oncomine Panels [63] [64] | Targeted NGS library preparation. | Used in custom or comprehensive panels for focused or broad mutational analysis. |
| EasyPGX PIK3CA Kit [63] | RT-PCR detection of specific mutations. | CE-IVD marked kit for detecting hotspot mutations in genes like PIK3CA. |
| PGDx elio tissue complete [27] | Distributed kitted NGS solution for in-house labs. | Provides an alternative to centralized labs; shows high concordance with FoundationOne. |
Signaling Pathways & Biological Basis of Heterogeneity
The discordance between tissue and liquid biopsies is biologically rooted in tumor heterogeneity and evolutionary processes. The clonal theory of cancer posits that tumors evolve from a single cell, accumulating mutations over time that lead to subpopulations (clones) with distinct genomic profiles [65]. This heterogeneity is spatially organized.
Figure 2. Biological basis of biopsy discordance through tumor evolution. A founding clone diverges into spatially separated subclones (e.g., in the primary tumor and a metastasis). A liquid biopsy captures a mixture of ctDNA shed from all clones, while a single tissue biopsy may only sample one geographic region, leading to potential discordance [64] [65].
This model explains why a tissue biopsy from one site might miss a resistant clone residing in another location, a clone which nonetheless sheds ctDNA into the bloodstream. This is particularly relevant in advanced, metastatic disease where spatial heterogeneity is maximized [64].
The performance of tissue and liquid biopsy is intrinsically stage-dependent. The choice between them, or the decision to use them in concert, should be a strategic one based on clinical context and research goals.
- For Advanced-Stage Disease: Liquid biopsy performs with high accuracy when the ctDNA tumor fraction is sufficient (>1%). It is an excellent tool for rapidly identifying actionable mutations, assessing TMB, and overcoming the challenges of sampling metastatic sites. A combined approach, as in the ROME trial, may yield the highest rate of actionable target identification and optimize patient selection for therapy [6] [61].
- For Early-Stage Disease and Low-TF Cancers: Tissue biopsy remains the more reliable method for comprehensive genomic profiling due to generally lower ctDNA shed. Techniques like spatial genomics and single-cell sequencing are crucial research tools for understanding the underlying heterogeneity in these cases [61] [64] [65].
- For Drug Developers: Clinical trial designs should incorporate paired tissue-liquid biopsy protocols where feasible. This not only enriches the understanding of a drug's mechanism but also helps identify biomarkers for response and resistance across different disease stages, ultimately paving the way for more effective and personalized cancer therapies.
In the era of precision oncology, comprehensive genomic profiling has become indispensable for guiding targeted therapy decisions. The historical gold standard of tissue biopsy is now complemented by the minimally invasive approach of liquid biopsy, which analyzes circulating tumor DNA (ctDNA) and other biomarkers in blood or other bodily fluids. Next-generation sequencing (NGS) enables detailed molecular characterization through both methods, yet a critical question remains regarding their concordance and optimal clinical application. Concordance between tissue and liquid biopsy is defined as the detection of the same druggable alteration in both sample types, while discordance indicates detection in only one [6]. Emerging evidence from clinical trials and real-world studies demonstrates that these approaches are not competitive but rather synergistic, with integrated testing maximizing the detection of actionable alterations and ultimately improving patient outcomes. This guide systematically compares the performance characteristics, technical protocols, and clinical utility of tissue versus liquid biopsy, providing researchers and drug development professionals with an evidence-based framework for implementing complementary testing strategies in oncology research and clinical trials.
Performance Comparison: Quantitative Data Analysis
Clinical Outcomes Based on Biopsy Concordance
Table 1: Survival Outcomes Based on Biopsy Concordance from the ROME Trial
| Biopsy Category | Median Overall Survival (Months) | Median Progression-Free Survival (Months) | Objective Response to Tailored Therapy |
|---|---|---|---|
| Concordant (T+L+) | 11.05 (TT) vs. 7.70 (SoC) (HR 0.74) | 4.93 (TT) vs. 2.80 (SoC) (HR 0.55) | Significantly improved [6] |
| Tissue-Only (T+L-) | 9.93 | 3.06 | Less pronounced benefit [6] |
| Liquid-Only (T-L+) | 4.05 | 2.07 | Minimal to no survival benefit [6] |
Data from the phase II ROME Trial (N=1,794) provides crucial insights into how concordance influences therapeutic efficacy. Patients in the concordant group receiving tailored therapy (TT) experienced significantly improved survival outcomes compared to standard-of-care (SoC), with hazard ratios favoring TT for both overall survival (HR 0.74) and progression-free survival (HR 0.55) [6]. The stark contrast in outcomes between concordant and discordant groups underscores the clinical importance of detecting actionable mutations through both modalities.
Technical Performance Metrics Across Cancer Types
Table 2: Analytical Performance Across Tumor Types
| Cancer Type | Study | Concordance Rate | Sensitivity | PPV | Key Findings |
|---|---|---|---|---|---|
| Advanced Solid Tumors | ROME Trial | 49% | N/A | N/A | 35% tissue-only; 16% liquid-only alterations [6] |
| Biliary Tract Cancer | Hwang et al. | N/A | 84.8% | 79.4% | Identified novel FGFR2-TNS1 fusion in ctDNA [66] |
| Advanced NSCLC | Memorial Cancer Institute | 94.8-100% (for guideline biomarkers) | N/A | N/A | Liquid biopsy identified biomarkers in 76.5% vs. 54.9% with tissue-first approach [67] |
The variation in performance metrics across cancer types reflects differences in tumor shedding characteristics, anatomical location, and disease burden. In advanced NSCLC, liquid biopsy demonstrates remarkably high concordance with tissue for guideline-recommended biomarkers (94.8-100%), supporting its utility as a reliable diagnostic tool [67]. The ROME Trial finding that 49% of cases showed concordance, with 35% having tissue-only alterations and 16% having liquid-only alterations, highlights the complementary nature of both approaches [6].
Operational Metrics in Clinical Practice
Table 3: Operational Comparison in NSCLC Clinical Practice
| Parameter | Tissue Biopsy | Liquid Biopsy | Statistical Significance |
|---|---|---|---|
| Median Turnaround Time | 20-36.4 days [68] [67] | 8-9.6 days [68] [67] | p<0.0001 |
| Testing Success Rate | 85.9% [68] | 100% [68] | N/A |
| Time to Treatment Decision | Significantly longer [68] | Significantly shorter [68] | p<0.0001 |
Operational efficiency represents a significant advantage for liquid biopsy, with consistently faster turnaround times (TAT) across multiple studies. In a retrospective analysis of 368 NSCLC patients, liquid biopsy NGS reduced TAT by 12 days compared to tissue biopsy (8 days vs. 20 days, p<0.0001) [68]. Similarly, another NSCLC study reported median TAT of 9.6 days for liquid biopsy versus 36.4 days for tissue (P < .0001) [67]. This accelerated diagnostic pathway enables more timely treatment initiation, which is particularly critical in aggressive malignancies.
Methodological Approaches: Experimental Protocols
Integrated Testing Workflow Protocol
The following diagram illustrates the comprehensive integrated testing workflow derived from contemporary clinical studies:
Diagram 1: Integrated Testing Workflow. This workflow illustrates the complementary diagnostic pathway implemented in clinical studies like the ROME trial [6].
Laboratory Techniques for Biomarker Analysis
Circulating Tumor DNA (ctDNA) Analysis: Current methodologies for ctDNA analysis include next-generation sequencing (NGS), real-time PCR (RT-PCR), droplet digital PCR (ddPCR), and mass spectrometry. NGS-based techniques, including targeted sequencing, whole-exome sequencing, and whole-genome sequencing, allow comprehensive analysis of tumor mutations with sensitivity up to 0.01% variant allele frequency (VAF) [69]. ddPCR provides an alternative with high sensitivity, detecting nucleotide mutations in ctDNA at concentrations as low as 0.01% while precisely quantifying DNA molecules, making it suitable for samples with limited availability or for detecting low-frequency mutations [69].
Circulating Tumor Cells (CTCs) Isolation: The CellSearch system remains the only FDA-cleared method for monitoring CTC counts in blood samples [3]. Isolation techniques include density gradient centrifugation, inertial focusing, and filtration based on biophysical properties like size and deformability. Immunological approaches using epithelial cell adhesion molecule (EpCAM), vimentin, and N-cadherin expression enable immunomagnetic separation and microfluidic device capture [3]. These methods face challenges due to the extreme rarity of CTCs (approximately 1 per 1 million leukocytes) and their short half-life in peripheral circulation (1-2.5 hours) [3].
Extracellular Vesicles (EVs) Separation: Over 50% of EV isolation methods involve preparative ultracentrifugation. Differential, isopycnic, and moving zone ultracentrifugation reduce EV loss and contamination, improving EV purity. Nanomembrane ultrafiltration concentrators represent a promising alternative approach for efficient EV separation from diverse forms of cellular waste [7].
Concordance Assessment Methodology
The ROME Trial protocol defined concordance as detection of the same druggable alteration in both tissue and liquid biopsy specimens [6]. Specimens were processed using FoundationOne CDx for tissue and FoundationOne Liquid CDx for liquid biopsies, with a centralized Molecular Tumor Board reviewing results to identify actionable alterations [6]. Similarly, in the PGDx elio tissue complete validation study, 147 unique specimens across more than 20 tumor types were compared between the PGDx assay and FoundationOne test, with analytical performance evaluated across all genomic variant types [27]. For ctDNA and tissue genomic profiling in biliary tract cancer, concordance was assessed using sensitivity and positive predictive value calculations, with targetable alterations including FGFR2 fusions, IDH1 mutations, microsatellite instability-high, ERBB2 amplifications, and other actionable genomic changes [66].
The Scientist's Toolkit: Essential Research Reagents
Table 4: Key Research Reagent Solutions for Integrated Biopsy Analysis
| Reagent Category | Specific Examples | Research Application | Technical Considerations |
|---|---|---|---|
| NGS Assay Kits | FoundationOne CDx, FoundationOne Liquid CDx, PGDx elio tissue complete | Comprehensive genomic profiling across 500+ genes | Hybrid capture-based chemistry; requires Illumina sequencing platforms [6] [27] |
| ctDNA Extraction Kits | QIAamp Circulating Nucleic Acid Kit, Maxwell RSC ccfDNA Plasma Kit | Isolation of cell-free DNA from plasma samples | Input volume 10-20ml blood; strict prevention of cellular DNA contamination [69] |
| CTC Enrichment Reagents | CellSearch CTC Kit, EpCAM-coated magnetic beads | Immunomagnetic separation of circulating tumor cells | Preservative blood collection tubes required; limited CTC stability [3] |
| EV Isolation Kits | ExoQuick, Total Exosome Isolation Reagent, ultracentrifugation kits | Separation of extracellular vesicles from biofluids | Differential centrifugation protocols; nanomembrane alternatives available [7] |
| PCR Master Mixes | ddPCR Supermix, Qubit dsDNA HS Assay Kit | Quantification and mutation detection | ddPCR offers 0.01% sensitivity for low-frequency mutations [69] |
Clinical Applications and Limitations
Optimal Use Cases for Each Modality
The integrated testing workflow demonstrates specific clinical scenarios where each modality offers distinct advantages:
Diagram 2: Clinical Decision Pathway for Biopsy Selection. This pathway guides modality selection based on specific clinical scenarios and research objectives.
Technical Limitations and Challenges
Liquid Biopsy Limitations: Sensitivity remains a significant challenge, particularly in cancers with low tumor burden such as early-stage lung cancer, pancreatic cancer, colorectal cancer, ovarian cancer, and localized prostate cancer [69]. The concentration of ctDNA in blood can be extremely low (approximately 0.1-1.0% of total cell-free DNA), creating detection challenges [3]. Tumor heterogeneity and anatomic barriers (e.g., blood-brain barrier) can limit ctDNA shedding, potentially resulting in false negatives [67]. Additionally, clonal hematopoiesis of indeterminate potential can obscure liquid biopsy results with non-tumor findings [67].
Tissue Biopsy Limitations: Invasiveness of collection procedures presents patient risks and practical constraints [7]. Tumor heterogeneity is a fundamental challenge, as a single biopsy may not represent the complete genomic landscape of a tumor [7] [3]. Tissue biopsies also face logistical challenges including insufficient sample quantities, slow turnaround times, and inability to perform serial assessments [67].
The evidence from clinical trials and real-world studies consistently demonstrates that tissue and liquid biopsies are complementary rather than competitive modalities. The ROME Trial's finding that tailored therapy significantly improves outcomes primarily in patients with concordant results (49% of cases) underscores the clinical value of detecting actionable mutations through both methods [6]. The operational advantages of liquid biopsy, including significantly faster turnaround times and higher testing success rates, position it as a valuable tool for initial testing and monitoring [68] [67]. Meanwhile, tissue biopsy remains essential for comprehensive molecular profiling, particularly for alterations that may not be adequately detected in plasma. For researchers and drug development professionals, implementing integrated testing protocols maximizes the detection of targetable alterations, enables more precise patient stratification for clinical trials, and ultimately advances the field of precision oncology. As biomarker-driven therapies continue to expand, dual-modality testing approaches will become increasingly central to both clinical practice and therapeutic development.
Analytical Validation and Real-World Performance Assessment
Next-generation sequencing (NGS) has revolutionized precision oncology, enabling the detection of molecular alterations that guide targeted therapies. The clinical application of this technology, particularly through both tissue and liquid biopsy approaches, necessitates robust assay validation frameworks to ensure analytical accuracy and clinical utility [70] [15]. These frameworks rely critically on well-characterized reference standards and carefully selected clinical specimens to establish test performance metrics. Within oncology, a key focus is understanding the concordance between tissue biopsy, long considered the diagnostic gold standard, and the less invasive liquid biopsy, which analyzes circulating tumor DNA (ctDNA) [6] [71]. This guide objectively compares validation frameworks and performance data for NGS assays, situating the analysis within the broader thesis that integrating both tissue and liquid biopsy can optimize clinical decision-making, especially when their results are concordant.
Comparison of Key Validation Frameworks and Standards
The validation of NGS assays is governed by a complex landscape of guidelines and standards developed by various organizations to ensure reliability and clinical applicability.
Core Regulatory and Professional Guidelines
A robust validation framework is built upon guidelines covering the entire testing lifecycle, from initial design to routine clinical operation. Key resources include:
- College of American Pathologists (CAP) NGS Worksheets: Developed with the Association for Molecular Pathology, these seven worksheets provide a structured approach to the entire life cycle of a clinical NGS test, focusing on germline applications. They guide laboratories through test familiarization, content design, assay optimization, validation, quality management, bioinformatics, and interpretation/reporting [72].
- CDC's Next-Generation Sequencing Quality Initiative (NGS QI): This initiative provides over 100 publicly available tools, including standard operating procedures and guidance documents, to help clinical and public health laboratories implement quality management systems for NGS. Its "Pathway to Quality-Focused Testing" and method validation tools help laboratories ensure compliance with regulatory and quality standards [70].
- International Standards: Globally, organizations like the Global Alliance for Genomics and Health (GA4GH) develop frameworks for responsible data sharing and interoperability. The International Organization for Standardization provides standards like ISO 20387:2018 for biobanking, which is critical for sample handling [15].
The Role of Reference Standards and Clinical Specimens
Reference standards and clinical specimens are the cornerstones of assay validation, serving distinct but complementary purposes.
- Engineered Reference Standards: Products like the Mimix Geni standards, developed by Revvity in collaboration with the Medical Device Innovation Consortium and the National Institute of Standards and Technology, are engineered from a "Genome-in-a-Bottle" cell line. They incorporate specific oncogenic mutations at defined allele frequencies to provide a consistent and traceable benchmark for evaluating assay performance across different NGS platforms [73]. These are vital for initial validation, quality control, and proficiency testing.
- Characterized Clinical Specimens: Validation also requires a diverse cohort of clinical samples that have been pre-characterized by orthogonal methods. These specimens reflect the real-world biological complexity that engineered standards cannot fully capture, including variations in sample collection, DNA quality, and tumor heterogeneity [34]. Using clinical samples allows laboratories to confirm assay performance in a diagnostic context.
The following diagram illustrates the typical workflow for validating an NGS assay, integrating both reference standards and clinical specimens.
Performance Comparison of NGS Assays
The performance of NGS assays, whether tissue- or liquid-based, is quantified through key analytical metrics. Direct comparisons reveal significant differences in sensitivity and variant detection capabilities.
Analytical Sensitivity and Limit of Detection
A primary goal of newer liquid biopsy assays is to improve sensitivity, particularly for detecting variants at very low allele frequencies in ctDNA.
Table 1: Comparison of Analytical Performance for Liquid Biopsy Assays
| Assay Name | Variant Types Detected | Reported Sensitivity | Limit of Detection (LOD) for SNV/Indels | Key Performance Findings |
|---|---|---|---|---|
| Northstar Select [74] | SNV/Indels, CNV, Fusions, MSI | 95% | 0.15% VAF (Confirmed by ddPCR) | Identified 51% more pathogenic SNV/Indels and 109% more CNVs vs. on-market CGP assays; 91% of additional actionable variants were below 0.5% VAF. |
| Hedera Profiling 2 (HP2) [34] | SNV/Indels, Fusions, CNV, MSI | 96.92% (SNV/Indels), 100% (Fusions) | 0.5% VAF (in reference standards) | 94% concordance for ESMO Level I variants in clinical samples vs. orthogonal methods. |
| FoundationOne Liquid CDx [6] | N/A | N/A | N/A | In the ROME trial, concordance with tissue (FoundationOne CDx) for druggable alterations was 49%. |
Abbreviations: VAF, Variant Allele Frequency; SNV, Single-Nucleotide Variant; Indel, Insertion/Deletion; CNV, Copy Number Variation; MSI, Microsatellite Instability; CGP, Comprehensive Genomic Profiling; ESMO, European Society for Medical Oncology.
Clinical Concordance and Outcomes
Beyond analytical performance, the clinical impact of NGS testing—particularly the relationship between tissue-liquid concordance and patient survival—is paramount.
- The ROME Trial Findings: This large phase II study provided critical insights into how concordance affects therapy. When tissue and liquid biopsy identified the same druggable alteration, patients receiving tailored therapy saw significantly improved outcomes: median Overall Survival of 11.05 vs. 7.70 months and median Progression-Free Survival of 4.93 vs. 2.80 months compared to standard of care [6].
- Impact of Discordance: The survival benefit from tailored therapy was less pronounced or absent when alterations were found in only one biopsy type. The group with alterations detected only in liquid biopsy had the poorest outcomes (median OS 4.05 months), potentially reflecting higher tumor burden and ctDNA shed [6].
- Tumor Fraction as a Key Variable: In NSCLC, the diagnostic accuracy of liquid biopsy is highly dependent on ctDNA tumor fraction (TF). One study found that for patients with high ctDNA TF (>1%), the positive percent agreement for detecting actionable mutations was 100%, compared to only 47.5% in the low TF group [71].
The relationship between assay detection, tumor biology, and clinical decision-making is summarized in the pathway below.
Detailed Experimental Protocols
To ensure the reproducibility of validation studies, the experimental methodologies for key assays and the specific reagents used must be clearly detailed.
Protocol for the ROME Trial
The ROME trial serves as a benchmark for large-scale concordance studies.
- Study Design: This was a phase II, multicenter study that enrolled 1,794 patients with advanced solid tumors [6].
- Sample Processing: Both tissue and liquid biopsies were collected from participants. Tissue samples were processed and analyzed using the FoundationOne CDx assay, while blood-based liquid biopsies were analyzed using the FoundationOne Liquid CDx assay [6].
- Centralized Review: A centralized Molecular Tumor Board (MTB), comprising multidisciplinary experts, reviewed all NGS results to identify actionable genomic alterations. This step is critical for standardizing the interpretation of complex genomic data [6].
- Randomization: Out of the overall cohort, 400 patients with identified actionable alterations were randomized to receive either Molecular Tumor Board-guided tailored therapy or standard-of-care therapy [6].
- Concordance Definition: Concordance was strictly defined as the detection of the identical druggable alteration in both the tissue and liquid biopsy specimens. Discordance was declared if an alteration was detected in only one of the two biopsy types [6].
Validation of a High-Sensitivity Liquid Biopsy Assay
The validation of the Northstar Select assay exemplifies a rigorous analytical and clinical validation protocol.
- Sample Cohorts: The validation involved a retrospective analysis of 674 patient samples from routine care and a prospective, head-to-head comparison study of 182 patients [74].
- Analytical Validation: The limit of detection was established for different variant classes. For SNVs and Indels, a 95% LOD of 0.15% VAF was determined using digital droplet PCR for confirmation. For CNVs, the LOD was established at 2.11 copies for amplifications and 1.80 copies for losses. The LOD for gene fusions was 0.30% VAF [74].
- Comparative Performance: In the prospective study, the Northstar Select assay was directly compared to other commercially available CGP liquid biopsy assays. The primary metrics for comparison were the number of pathogenic variants detected and the reduction in "null" reports (those with no pathogenic or actionable findings) [74].
The Scientist's Toolkit: Essential Research Reagents
Table 2: Key Reagents and Materials for NGS Assay Validation
| Item | Function in Validation | Example(s) |
|---|---|---|
| Engineered Reference Standards | Provide a genetically defined, reproducible material for determining LOD, sensitivity, specificity, and cross-platform performance. | Mimix Geni standards from Revvity [73]; Cell lines from Genome in a Bottle (GIAB) [15]. |
| Pre-Characterized Clinical Specimens | Assess assay performance against a known benchmark in a biologically relevant matrix; used for concordance studies. | Clinical samples characterized by orthogonal methods (e.g., ddPCR, other validated NGS assays) [34] [74]. |
| Orthogonal Validation Assays | Serve as a reference method to confirm the accuracy of variant calls from the NGS assay under validation. | Digital droplet PCR (ddPCR) [74]. |
| Hybrid Capture-Based NGS Panels | Enable targeted sequencing of specific genes associated with cancer from both tissue and liquid biopsy DNA. | FoundationOne CDx, FoundationOne Liquid CDx [6]; Hedera Profiling 2 (HP2) [34]. |
| Bioinformatics Pipelines | Process raw sequencing data into aligned sequences and interpret variants; must be validated for clinical use. | Pipelines validated per CAP/AMP guidelines [72] [15]. |
The validation of NGS assays is a multifaceted process underpinned by sophisticated frameworks from organizations like CAP, CDC, and CLSI. The consistent use of high-quality reference standards and well-characterized clinical specimens is non-negotiable for establishing the accuracy and reliability of these complex tests. Data from recent studies clearly demonstrate that liquid biopsy assays are achieving new heights of sensitivity, with some tests like Northstar Select reliably detecting variants below 0.2% VAF [74]. The critical insights from the ROME trial cement the clinical relevance of these technical advancements, showing that concordance between tissue and liquid biopsy is not merely a metric of analytical performance but a potent predictor of patient response to tailored therapy [6]. The future of precision oncology lies not in choosing one biopsy modality over the other, but in strategically integrating both to maximize the chances of identifying actionable alterations and, ultimately, improving patient outcomes.
Next-generation sequencing (NGS) has revolutionized genomic profiling in oncology, enabling personalized cancer treatment. Traditionally, this profiling relies on tissue biopsy (TB), the long-standing gold standard. However, the emergence of liquid biopsy (LB), which analyzes circulating tumor DNA (ctDNA) from blood, presents a minimally invasive alternative. This guide objectively compares the performance of these two methodologies across multiple scientific studies, focusing on their diagnostic accuracy, clinical utility, and practical application within the framework of NGS concordance research. Understanding their complementary strengths and limitations is crucial for researchers and drug development professionals aiming to optimize diagnostic strategies for precision medicine.
Performance Metrics and Clinical Validity
Extensive research has directly compared the performance of tissue and liquid biopsy across various cancer types, particularly non-small cell lung cancer (NSCLC). The data reveals a complex landscape where each method excels in different parameters.
Diagnostic Accuracy and Concordance
A systematic review and meta-analysis encompassing 32 studies and 6,210 lung cancer patients provides high-level evidence on diagnostic performance. The analysis found that liquid biopsy has a pooled sensitivity of 0.78 (95% CI: 0.72-0.83) and a pooled specificity of 0.93 (95% CI: 0.89-0.96) when tissue biopsy is used as the reference standard. The overall diagnostic odds ratio (DOR) was 45.3 (95% CI: 28.1-73.0) [75]. This indicates that while liquid biopsy is highly specific, its sensitivity is moderate, meaning a positive result is very reliable, but a negative result cannot definitively rule out the presence of a mutation.
Concordance rates between the two methods vary significantly by gene, reflecting biological and technical factors. The same meta-analysis reported the following mutation-specific concordance rates [75]:
- EGFR: 85%
- ALK: 78%
- KRAS: 65%
- ROS1: 59%
A separate retrospective study of 170 metastatic NSCLC patients highlighted that a "liquid-first" testing approach identified guideline-recommended biomarkers in 76.5% of patients, compared to 54.9% with a "tissue-first" approach. This study also reported that for established biomarkers, liquid biopsy was 94.8% to 100% concordant with tissue results [67].
Table 1: Summary of Key Performance Metrics from Recent Studies
| Performance Metric | Liquid Biopsy (LB) Findings | Tissue Biopsy (TB) Findings | Context / Study |
|---|---|---|---|
| Pooled Sensitivity | 0.78 (95% CI: 0.72-0.83) [75] | (Reference Standard) | Meta-analysis of 32 studies (n=6,210) in lung cancer [75] |
| Pooled Specificity | 0.93 (95% CI: 0.89-0.96) [75] | (Reference Standard) | Meta-analysis of 32 studies (n=6,210) in lung cancer [75] |
| Diagnostic Odds Ratio | 45.3 (95% CI: 28.1-73.0) [75] | N/A | Meta-analysis of 32 studies (n=6,210) in lung cancer [75] |
| Testing Success Rate | Higher [67] | Lower (insufficient tissue) [67] | Retrospective study in mNSCLC (n=170) [67] |
| Median Turnaround Time | 9.6 days [67] | 36.4 days [67] | Retrospective study in mNSCLC (n=170); P < .0001 [67] |
| Biomarker Detection (1st-line) | 76.5% of patients [67] | 54.9% of patients [67] | "Liquid-first" vs. "Tissue-first" approach in mNSCLC [67] |
Impact of Concordance on Clinical Outcomes
The phase II ROME trial offers critical insights into how the concordance between tissue and liquid biopsy directly influences patient survival. This large study enrolled 1,794 patients with advanced solid tumors and performed centralized NGS on both tissue and liquid biopsies [6] [16].
The trial reported an overall concordance rate of 49% for the detection of druggable alterations. Actionable alterations were found exclusively in tissue in 35% of cases and exclusively in liquid in 16% of cases [6] [16]. This demonstrates that each method can capture unique molecular information missed by the other.
Most importantly, patients whose tailored therapy was based on a druggable alteration detected in both biopsy types (the concordant group) experienced significantly improved outcomes. Their median overall survival was 11.05 months versus 7.70 months in the standard-of-care group (HR 0.74), and median progression-free survival was 4.93 months versus 2.80 months (HR 0.55) [6]. In contrast, the survival benefit from tailored therapy was less pronounced or absent when biopsy results were discordant [6] [16].
Table 2: Survival Outcomes Based on Biopsy Concordance from the ROME Trial
| Biopsy Result Group | Median Overall Survival (Months) | Median Progression-Free Survival (Months) | Tailored Therapy Benefit |
|---|---|---|---|
| Alteration in T+L (Concordant) | 11.05 [6] | 4.93 [6] | Significant improvement [6] [16] |
| Alteration in Tissue Only | 9.93 [6] | 3.06 [6] | Less pronounced or absent [6] [16] |
| Alteration in Liquid Only | 4.05 [6] | 2.07 [6] | Less pronounced or absent [6] [16] |
Experimental Protocols and Methodologies
To critically appraise comparative study data, understanding the underlying experimental protocols is essential. The following outlines methodologies commonly cited in the literature.
The ROME Trial Protocol
The ROME trial is a phase II multicenter study designed to evaluate the impact of integrated biopsy analysis on treatment outcomes [6] [16].
- Patient Population: Enrolled 1,794 patients with advanced solid tumors who had progressed on their second- or third-line of treatment.
- Biopsy Collection: Both tissue and liquid biopsy samples were collected from each participant at study enrollment.
- Sequencing Methodology: Centralized, high-quality NGS was performed using two commercially available, CLIA-certified assays:
- Tissue: FoundationOne CDx
- Liquid: FoundationOne Liquid CDx
- Analysis Workflow: A centralized Molecular Tumor Board (MTB), comprising multidisciplinary experts, reviewed all NGS results to identify actionable genomic alterations suitable for tailored therapy.
- Randomization: Out of the screened population, 400 patients with identifiable actionable alterations were randomized to receive either tailored therapy (TT) or standard-of-care (SoC) treatment.
- Concordance Definition: Concordance was strictly defined as the detection of the same druggable alteration in both tissue and liquid biopsy types. Discordance indicated detection in only one type.
This rigorous protocol ensures the comparability of data and the reliability of the survival outcomes associated with biopsy concordance [6] [16].
Standard NGS-Based Comparison Study Protocol
Many retrospective studies comparing biopsy methods follow a similar core protocol, exemplified by the NSCLC study by and colleagues [67].
- Study Design: Retrospective analysis of patients who received both tissue and liquid biopsy NGS as part of routine clinical care.
- Sample Processing:
- Liquid Biopsy: Blood samples are collected in specialized tubes (e.g., Streck Cell-Free DNA BCT) to preserve ctDNA. Plasma is separated via centrifugation, and cell-free DNA is extracted before NGS library preparation.
- Tissue Biopsy: Formalin-fixed paraffin-embedded (FFPE) tumor tissue samples are macrodissected to enrich tumor content. DNA is then extracted from the tissue sections.
- Sequencing & Analysis: Both extracted DNA samples undergo NGS using validated, commercially available panels (e.g., Guardant360 for liquid, Oncomine for tissue). Bioinformatic pipelines identify somatic mutations, with careful filtering for clonal hematopoiesis in liquid biopsies.
- Primary Endpoints: Typically include testing success rate, turnaround time (TAT), detection rate of guideline-recommended biomarkers, and concordance between platforms.
Technological and Biological Factors Influencing Performance
The observed differences in performance and concordance between tissue and liquid biopsy are not arbitrary; they stem from fundamental technological and biological factors.
A nuanced understanding of why the two methods sometimes disagree is critical for data interpretation.
- Tumor Heterogeneity: Tissue biopsy provides a snapshot of a single tumor site at a single point in time. It may miss spatial heterogeneity within a primary tumor or temporal heterogeneity as a tumor evolves. Liquid biopsy, by capturing ctDNA shed from multiple tumor sites, can offer a more comprehensive view of the overall disease burden, potentially explaining some discordances [3] [50].
- Tumor Shed and ctDNA Fraction: The sensitivity of liquid biopsy is directly dependent on the amount of ctDNA shed into the bloodstream. Factors such as low tumor burden, specific metastatic locations (e.g., brain), or indolent tumor biology can result in low ctDNA levels, leading to false negatives [67] [76]. One study noted the specificity of LB is near 100%, but sensitivity is around 80%, making a negative LB result difficult to interpret [76].
- Clonal Hematopoiesis: A key challenge for liquid biopsy is distinguishing somatic tumor-derived mutations from those originating from clonal hematopoiesis of indeterminate potential (CHIP), a common age-related phenomenon where blood cells acquire mutations. Bioinformatic filtering is required to avoid false positives [67].
- Technical Failures: Tissue biopsies can suffer from insufficient tumor cell content or tissue degradation (e.g., due to formalin fixation) [50] [67]. Liquid biopsies require adequate blood volume and proper sample handling to prevent white blood cell lysis, which can contaminate the sample with germline DNA.
The ROME trial analysis found that the PI3K/PTEN/AKT/mTOR and ERBB2 pathways had particularly high discordance rates, suggesting that biological mechanisms of ctDNA shedding may vary by altered pathway [16].
The Scientist's Toolkit: Key Research Reagents and Materials
Successful execution of comparative NGS studies requires a suite of specialized reagents and tools. The following table details essential components used in the featured research.
Table 3: Essential Research Reagents and Kits for NGS-Based Biopsy Studies
| Item / Solution | Primary Function | Application Context |
|---|---|---|
| Cell-Free DNA Blood Collection Tubes (e.g., Streck BCT) | Stabilizes nucleated blood cells to prevent lysis and preserve cfDNA profile for up to several days at room temperature. | Liquid biopsy sample collection and transport; critical for pre-analytical sample integrity [7]. |
| cfDNA Extraction Kits (Magnetic Bead-Based) | Isolate and purify short-fragment cfDNA from plasma with high efficiency and sensitivity, often from less than 1 mL of plasma. | Liquid biopsy workflow; superior recovery of cfDNA is crucial for downstream NGS sensitivity [50]. |
| Formalin-Fixed Paraffin-Embedded (FFPE) Tissue Kits | Extract DNA from archived FFPE tissue blocks, often involving steps to reverse formaldehyde-induced cross-links and fragmentation. | Tissue biopsy workflow; dealing with degraded DNA from FFPE is a major technical challenge [50]. |
| Next-Generation Sequencing Panels | Targeted panels (e.g., FoundationOne CDx, FoundationOne Liquid CDx, Guardant360) for multiplexed sequencing of cancer-associated genes. | Mutation detection in both tissue and liquid DNA; panels must be validated for each specimen type [6] [67]. |
| PCR Purification Kits | Remove enzymes, salts, primers, and other impurities from amplified DNA libraries to increase sequencing quality and reliability. | Post-library preparation clean-up in NGS workflow for both tissue and liquid biopsies [50]. |
Integrated Analysis and Future Directions
The collective evidence strongly supports a complementary, rather than competitive, relationship between tissue and liquid biopsy in molecular profiling.
The Complementary Role: The high specificity and faster turnaround time of liquid biopsy make it an excellent tool for initial rapid screening and for monitoring treatment response and resistance mechanisms over time [75] [67]. However, tissue biopsy remains indispensable for initial tumor diagnosis, histologic subtyping, and providing a comprehensive genomic landscape, especially when liquid biopsy is negative despite clinical suspicion of disease [76]. As one expert commentary notes, many institutions are adopting a parallel testing approach at initial diagnosis to maximize the chance of detecting actionable alterations [76].
Future Outlook: Future advancements will focus on improving the sensitivity of liquid biopsy assays through better ctDNA capture and more sophisticated error-corrected NGS technologies. Standardizing assay protocols and analytical pipelines across laboratories is another critical goal [75] [3]. Furthermore, research is expanding into other liquid biopsy biomarkers, such as methylation patterns in ctDNA, circulating tumor cells (CTCs), and tumor-derived extracellular vesicles (EVs), which may provide additional layers of information for early detection and monitoring [3] [7].
In conclusion, the decision between tissue and liquid biopsy is not a binary choice. The most effective precision oncology strategies, as demonstrated by the ROME trial, leverage the integrated findings from both modalities to guide therapeutic decisions, ultimately leading to improved patient survival outcomes [6] [16].
Real-world evidence (RWE) has emerged as a transformative force in healthcare, particularly in evaluating diagnostic technologies and their influence on clinical decision-making. Within precision oncology, a critical application of RWE lies in assessing the concordance between next-generation sequencing (NGS) methodologies—specifically, tissue versus liquid biopsy. While randomized controlled trials establish the efficacy of these technologies under ideal conditions, RWE provides crucial insights into their performance, yield, and impact on treatment decisions in diverse, routine clinical settings. This real-world validation is especially vital as regulatory bodies increasingly recognize RWE to support drug approvals and post-market surveillance [77] [78]. This guide objectively compares the diagnostic yield of tissue and liquid biopsy NGS and evaluates their subsequent impact on treatment selection, drawing on recent real-world studies to inform researchers, scientists, and drug development professionals.
Comparative Diagnostic Yield of Tissue and Liquid Biopsy
The diagnostic yield of a testing modality—its ability to successfully generate actionable results—is a primary determinant of its clinical utility. Real-world studies directly compare how tissue and plasma-based liquid biopsies perform in detecting guideline-recommended biomarkers.
Key Metrics from Real-World Analyses
A 2023 retrospective analysis of 170 new NSCLC patients treated at two cancer centers provides compelling real-world data on this front. The study implemented both tissue and liquid biopsy NGS as standard care and found that a liquid-first approach identified guideline-recommended biomarkers in 76.5% of patients, compared to 54.9% with a tissue-first approach [54]. This substantial difference in success rate highlights one of the key practical advantages of liquid biopsy.
Furthermore, the same study reported that liquid biopsy NGS returned results on average 26.8 days faster than tissue biopsy [54]. This dramatically shorter turnaround time (TAT) can be critical in advanced cancer settings where rapid treatment initiation is essential.
Stage-Dependent Performance
A 2025 real-world study of 522 Chinese patients with stage III or IV NSCLC provided a more nuanced view of liquid biopsy performance, revealing a significant stage-dependent variation in its sensitivity [29].
Table 1: Diagnostic Yield of Liquid vs. Tissue Biopsy by Cancer Stage
| Cancer Stage | Positive Percentage Agreement (PPA) | Negative Percentage Agreement (NPA) |
|---|---|---|
| Stage III | 28.57% (2/7) | 99.20% (124/125) |
| Stage IV | 99.20% (124/125) | 99.46% (183/184) |
This data indicates that while liquid biopsy has high specificity (as shown by the high NPA) across stages, its sensitivity for detecting mutations in Stage III disease is significantly lower than in Stage IV disease. This is likely attributable to lower levels of circulating tumor DNA (ctDNA) shed by less advanced tumors [29]. Consequently, a negative liquid biopsy result in a stage III patient may require confirmation via tissue biopsy, as suggested by clinical guidelines [29].
Impact on Treatment Decisions and Patient Outcomes
Beyond analytical performance, the ultimate test of a diagnostic method is its influence on clinical management. Real-world evidence demonstrates that liquid biopsy is not just a supplementary tool but is increasingly central to therapeutic decision-making.
Real-World Prescribing Patterns
In the 170-patient retrospective study, physicians based the majority of their treatment decisions (73.5%) on liquid biopsy results, compared to 25.9% based on tissue biopsy [54]. This clear preference in a real-world setting was driven by the combination of high biomarker concordance, faster turnaround time, and higher testing success rate of liquid biopsy.
Clinical Utility and Patient Outcomes
Critically, the adoption of liquid biopsy has not compromised patient outcomes. The same study found no significant difference in time-to-treatment, overall survival, or progression-free survival between patients whose treatment was guided by liquid versus tissue biopsy results [54]. This RWE confirms that the clinical utility of liquid biopsy is equivalent to the traditional tissue-based approach in metastatic NSCLC.
Table 2: Impact of Liquid Biopsy on Clinical Decision-Making and Outcomes
| Metric | Liquid Biopsy | Tissue Biopsy |
|---|---|---|
| Physician Reliance for Front-Line Therapy | 73.5% | 25.9% |
| Average Turnaround Time (TAT) | Faster (Specific reduction of 26.8 days) | Slower |
| Testing Success Rate | Higher | Lower |
| Overall Survival | No Significant Difference | No Significant Difference |
| Progression-Free Survival | No Significant Difference | No Significant Difference |
Experimental Protocols and Methodologies
The robustness of RWE depends on the rigor of the underlying experimental protocols. The studies cited here employed detailed, validated methodologies for head-to-head comparison.
Sample Collection and Processing
In the 2025 cohort study, blood samples were collected in 10 mL Cell-Free DNA BCT tubes (Streck) and processed within one week using a two-step centrifugation protocol to separate plasma and buffy coat. Cell-free DNA (cfDNA) was isolated from 4 mL of plasma using a specialized Nucleic Acid Extraction Kit. For tissue comparison, genomic DNA was extracted from Formalin-Fixed Paraffin-Embedded (FFPE) tumor tissue using the QIAmp FFPE Tissue Kit (Qiagen) [29].
Sequencing and Analysis
The core NGS protocol involved:
- Library Preparation: Generating sequencing libraries from a minimum of 20 ng of cfDNA.
- Target Capture: Hybridizing libraries to a customized 21-gene panel (e.g., USCI UgenDX Lung Cancer kit) designed to detect SNVs, insertions/deletions (InDels), and copy number variants (CNVs) in key NSCLC driver genes like EGFR, BRAF, and KRAS.
- Sequencing: Performing high-depth sequencing (mean effective depth >1400x) on platforms such as USCISEQ-200 analyzers.
- Bioinformatic Analysis: A standardized pipeline was used, including read alignment (Burrows-Wheeler Aligner), variant calling (Genome Analysis Tool Kit, VarScan), and annotation (ANNOVAR). A variant allele frequency (VAF) cutoff of 0.2% was established to ensure high sensitivity and specificity [29].
Validation and Concordance Testing
Methodological rigor was ensured through orthogonal validation. Droplet digital PCR (ddPCR) was used as a reference standard to validate the NGS assay's performance. The 2025 study established that with a 0.2% VAF cutoff and >1400x mean effective depth, their NGS assay demonstrated >80% Positive Percentage Agreement (PPA) and >95% Negative Percentage Agreement (NPA) with ddPCR results [29]. This level of validation is critical for generating trustworthy RWE.
Visualizing the Liquid Biopsy Clinical Workflow
The following diagram illustrates the integrated clinical workflow for liquid biopsy analysis, from sample collection to clinical decision, as implemented in the cited real-world studies.
The Scientist's Toolkit: Essential Reagents and Materials
Successful implementation of liquid biopsy NGS in a real-world setting relies on a suite of specialized research reagents and platforms. The table below details key solutions used in the featured studies.
Table 3: Essential Research Reagent Solutions for Liquid Biopsy NGS
| Reagent / Solution | Primary Function | Example Product (from studies) |
|---|---|---|
| cfDNA Blood Collection Tubes | Preserves cell-free DNA in blood samples for transport and storage, preventing white blood cell lysis and genomic DNA contamination. | Cell-Free DNA BCT tubes (Streck) [29] |
| Nucleic Acid Extraction Kit | Isulates and purifies high-quality cfDNA from plasma samples; critical for achieving sufficient yield and purity for NGS. | Nucleic Acid Extraction Kit (Beijing USCI Medical Devices Co., Ltd., TQ003) [29] |
| NGS Library Prep Kit | Prepares sequencing libraries from low-input cfDNA, often with unique molecular identifiers to reduce artifacts and improve accuracy. | USCI UgenDX Lung Cancer Kit [29] |
| Targeted Gene Panel | A set of probes designed to capture and sequence specific genes of clinical relevance in the disease of interest (e.g., NSCLC). | 21-gene NGS Panel (covers EGFR, BRAF, KRAS, etc.) [29] |
| Orthogonal Validation Assay | An independent technology used to confirm the accuracy and specificity of NGS findings, ensuring result reliability. | Droplet Digital PCR (ddPCR) (Bio-Rad) [29] |
Real-world evidence solidly positions liquid biopsy NGS as a clinically valid and impactful complement to tissue biopsy in advanced NSCLC. The high concordance for actionable biomarkers, faster turnaround time, and superior testing success rate have already led to its predominant use in guiding first-line treatment decisions in real-world practice [54]. However, RWE also clarifies its limitations, notably the stage-dependent sensitivity, which necessitates a complementary rather than a purely replacement role for tissue biopsy in some clinical scenarios [29]. For researchers and drug developers, these findings underscore the power of RWE to validate diagnostic technologies in heterogenous patient populations and to illuminate their true integrated role in the clinical care pathway.
In the era of precision oncology, comprehensive genomic profiling is indispensable for guiding targeted therapy and immunotherapy. While tissue biopsy has long been the gold standard for molecular analysis, liquid biopsy—the analysis of circulating tumor DNA (ctDNA) from blood plasma—has emerged as a transformative diagnostic tool. Liquid biopsy addresses critical limitations of tissue sampling, including invasiveness, tumor heterogeneity, and insufficient material, while providing a more complete representation of the tumor landscape [79] [80]. The clinical utility of liquid biopsy has been recognized through its incorporation into professional guidelines for several cancer types, including non-small cell lung cancer (NSCLC), breast cancer, metastatic colorectal cancer, and prostate cancer [80].
This comparison guide evaluates the performance of various liquid biopsy assays in detecting three emerging biomarkers essential for modern oncology: tumor mutational burden (TMB), microsatellite instability (MSI), and copy number variations (CNVs). These biomarkers provide critical insights for both targeted therapy and immunotherapy selection. We frame this evaluation within the broader thesis of Next-Generation Sequencing (NGS) concordance between tissue and liquid biopsy, examining how technological advancements are bridging historical sensitivity gaps and establishing liquid biopsy as a reliable standalone or complementary diagnostic approach.
Performance Comparison of Liquid Biopsy Assays
The landscape of liquid biopsy assays varies significantly in terms of gene coverage, sensitivity, and specific capabilities for biomarker detection. The following tables provide a structured comparison of different assay performances based on recent validation studies.
Table 1: Overview of Liquid Biopsy Assays and Key Capabilities
| Assay Name | Gene Coverage | Sample Input | Key Biomarkers Detected | Special Features |
|---|---|---|---|---|
| 1021-Gene Panel [79] | 1021 genes | 50-200 ng DNA | SNVs, Indels, CNVs, Fusions, TMB, MSI | Validated for both FFPE tissue and liquid biopsy; analyzes MSI and TMB |
| Northstar Select [80] | 84 genes | Not Specified | SNVs/Indels, CNVs, Fusions, MSI | Tissue-naive; proprietary QCT technology for enhanced sensitivity |
| TruSight Oncology 500 ctDNA [81] | 523 genes | 5-30 ng cfDNA | SNVs, Indels, Fusions | Performance optimized at 30 ng input and VAF ≥0.5% |
| Caris Assure [82] | Whole Exome/Transcriptome (720 genes at high depth) | Not Specified | SNVs, INDELs, CNVs, TMB, MSI, Fusions, Expression | AI-enabled; couples WES and WTS; uses CHIP subtraction |
Table 2: Analytical Performance Metrics for Key Biomarkers Across Assays
| Assay & Study | SNV/Indel Sensitivity (LOD) | CNV Detection Sensitivity | MSI Detection Sensitivity | Concordance with Tissue |
|---|---|---|---|---|
| 1021-Gene Panel [79] | 85-100% (VAF 0.5-2%) | Detected in validation | Detected in validation | Actionable alterations in >50% of cases; 70% detection in liquid |
| Northstar Select [80] | 95% LOD at 0.15% VAF | 2.11 copies (amplification); 1.8 copies (loss) | LOD: 0.07% Tumor Fraction | 51% more pathogenic SNVs/indels and 109% more CNVs vs. other CGPs |
| TruSight Oncology 500 ctDNA [81] | High sensitivity at VAF ≥0.5% | Not Specified | Not Specified | VAFs highly concordant with ddPCR |
| Caris Assure [82] | PPA 93.8% (with CHIP subtraction) | Detected in validation | Detected in validation | High PPV of 96.8% for driver mutations |
Experimental Protocols and Methodologies
Assay Validation and Workflow
The fundamental workflow for liquid biopsy involves sample collection, plasma separation, cell-free DNA (cfDNA) extraction, library preparation, target enrichment or whole exome/transcriptome sequencing, and bioinformatic analysis. However, each assay employs specific protocols to optimize performance.
The 1021-Gene Panel utilizes Unique Molecular Identifiers (UMIs) to achieve high sensitivity. Validation required mean sequencing coverages of 500× and 2000×, generating 5 GB and 17 GB of data, respectively. The assay maintained >99% of target bases covered at ≥50× depth, with a base quality score (Q30) of 94.7%, ensuring data reliability [79].
Northstar Select employs a proprietary Quantitative Counting Template (QCT) technology that enhances cfDNA extraction and target enrichment, minimizing errors. Its custom bioinformatic pipelines are designed to reduce noise, which is particularly crucial for CNV analysis. The assay's validation involved a head-to-head comparison study where blood draws for Northstar Select and comparator assays were taken simultaneously from the same venipuncture [80].
The Caris Assure assay demonstrates a more integrated approach. It performs simultaneous whole exome and whole transcriptome sequencing on plasma cfDNA and cfRNA in a single run using a hybridization capture methodology. A critical step is the separate sequencing of matched buffy coat nucleic acids to identify and subtract variants arising from clonal hematopoiesis (CHIP), thereby reducing false positives. The platform further leverages machine learning models (ABCDai) built on multiple "pillars" or feature sets (e.g., Mutationome, Fragmentome, Transcriptome) to enhance detection accuracy across its applications [82].
The following diagram illustrates a generalized workflow for NGS-based liquid biopsy, integrating key steps that are enhanced in the specific assays discussed.
The Scientist's Toolkit: Essential Research Reagents and Materials
Successful implementation of liquid biopsy assays relies on a suite of specialized reagents and materials. The following table details key components used in the featured experiments.
Table 3: Key Research Reagent Solutions for Liquid Biopsy Analysis
| Reagent / Material | Function / Application | Example Assay & Details |
|---|---|---|
| Reference Standards | Analytical validation; determining LOD, sensitivity, and specificity. | S800-1/S800-2 & OncoSpan [79]: Contain predefined variants at specific VAFs (e.g., 0.5%, 2%). Tru-Q 7 [79]: Used for lower limit of detection calculations. |
| Unique Molecular Identifiers (UMIs) | Tagging original DNA molecules to correct for PCR errors and sequencing artifacts, improving sensitivity. | 1021-Gene Panel [79]: Employs UMIs to achieve accurate sequencing down to 0.5% VAF. |
| Hybridization Capture Panels | Enriching target genomic regions prior to sequencing. | Caris Assure [82]: Uses custom baits to enrich for 720 clinically relevant genes at high coverage and >20,000 genes at lower depth. |
| cfDNA/cfTNA Extraction Kits | Isolving cell-free total nucleic acids from plasma with high yield and integrity. | Caris Assure [82]: Uses a customized, automated method from the DSP Virus/Pathogen Midi kit (Qiagen). |
| Library Preparation Kits | Preparing sequencing-ready libraries from low-input cfDNA. | TruSight 500 [81]: Optimized for 30 ng cfDNA input. Caris Assure [82]: Uses HyperPrep kits (KAPA/Roche) for gDNA libraries. |
| Clonal Hematopoiesis Subtraction | Differentiating true tumor-derived variants from those originating from blood cells. | Caris Assure [82]: Sequenced matched buffy coat is used to identify and subtract CHIP variants. |
Discussion and Clinical Implications
Concordance with Tissue Biopsy and Clinical Utility
The overarching goal in liquid biopsy development is to achieve high concordance with tissue biopsy, the traditional gold standard. A retrospective analysis of 170 NSCLC patients demonstrated that liquid biopsy could inform the majority (73.5%) of front-line therapy decisions and was, on average, 26.8 days faster than tissue biopsy. For guideline-recommended biomarkers, liquid biopsy was 94.8% to 100% concordant with tissue. Critically, there was no significant difference in time-to-treatment or survival outcomes between patients guided by liquid versus tissue biopsy results [54].
The 1021-gene panel study further supports this, revealing actionable alterations in over 50% of profiled solid tumor cases. The combined analysis of FFPE tissue and plasma samples was noted to provide complementary information, increasing the actionability of results [79]. This demonstrates that liquid biopsy is not merely a substitute for tissue but can be a complementary tool that provides a more comprehensive biological overview of the tumor.
Advancements in Detecting Challenging Biomarkers
Technological innovations are particularly evident in the detection of historically challenging biomarkers in liquid biopsy, such as CNVs and low-frequency variants.
Copy Number Variant (CNV) Detection: CNV detection has been a major challenge due to the background noise in ctDNA samples. The Northstar Select assay addresses this with a reported LOD of 2.11 copies for amplifications and 1.80 copies for losses [80]. In a head-to-head study, it identified 109% more CNVs than comparator on-market CGP assays [80]. This is a significant advancement, as focal CNVs are often key drivers of oncogenesis.
Sensitivity at Low VAF: The limit of detection for SNVs and Indels is crucial, as many clinically actionable variants are present at low frequencies. The Northstar Select assay's LOD of 0.15% VAF represents a substantial improvement over many existing assays [80]. This enhanced sensitivity is clinically relevant, as studies show that over 25% of somatic mutations in NSCLC are detected below 0.2% VAF [80], and variants at low VAF can be equally actionable [80].
Overcoming Clonal Hematopoiesis (CHIP): The Caris Assure assay tackles the problem of false positives from CHIP by sequencing the matched buffy coat and bioinformatically subtracting hematopoietic-derived variants. This process contributes to its high positive predictive value (PPV) of 96.8% for driver mutations when compared to matched tumor tissue [82].
The collective evidence from recent studies firmly establishes that liquid biopsy is a robust and clinically valid method for detecting key biomarkers like TMB, MSI, and CNVs. The performance of modern assays, driven by innovations in UMIs, proprietary capture technologies, sophisticated bioinformatics, and AI, now rivals and in some aspects surpasses that of tissue-based profiling, particularly in turnaround time and capturing tumor heterogeneity.
While tissue biopsy remains a vital tool, the data supports the use of liquid biopsy as a first-line test or in concordance with tissue to guide treatment decisions in cancer patients. For researchers and drug development professionals, the choice of assay depends on the specific application: large panels for maximum genomic coverage, sensitive targeted panels for low-VAF variant detection, or AI-enabled whole exome/transcriptome platforms for a multi-faceted view of the tumor genome and transcriptome. As technology continues to evolve, liquid biopsy is poised to become an even more integral component of precision oncology, from therapy selection to monitoring and early detection.
Conclusion
The evidence demonstrates that NGS concordance between tissue and liquid biopsy is influenced by multiple factors including cancer type, disease stage, assay sensitivity, and tumor fraction. While tissue remains the gold standard, liquid biopsy shows high concordance for actionable mutations in advanced disease (85.3%-99.2% PPA for EGFR) and offers advantages in speed, accessibility, and overcoming tumor heterogeneity. The future of precision oncology lies in complementary use of both modalities—liquid biopsy for initial testing and monitoring, with tissue confirmation when negative. For researchers and drug developers, this integrated approach enables more comprehensive molecular profiling, accelerates clinical trial enrollment, and supports the development of novel biomarkers. Future directions should focus on standardizing assays, improving detection of fusion variants and copy number alterations in liquid biopsy, and validating liquid biopsy for minimal residual disease monitoring across cancer types.
References
- 1. Spatial heterogeneity of PD-L1 expression influence its ... [https://www.sciencedirect.com/science/article/pii/S1936523325001731]
- 2. Spatial heterogeneity reveals an evolutionary signature ... [https://www.frontiersin.org/journals/bioinformatics/articles/10.3389/fbinf.2025.1669236/full]
- 3. Liquid biopsy in cancer: current status, challenges and ... [https://www.nature.com/articles/s41392-024-02021-w]
- 4. Liquid Biopsy: The Challenges of a Revolutionary ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12154446/]
- 5. Comparing the Diagnostic Performance of Quantitative ... [https://www.sciencedirect.com/science/article/pii/S1525157823002921]
- 6. The Impact of Concordance Between Liquid and Tissue ... [https://pubmed.ncbi.nlm.nih.gov/40833744/]
- 7. Liquid biopsy – a narrative review with an update on current ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12333414/]
- 8. Liquid biopsy: Comprehensive overview of circulating tumor ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11420644/]
- 9. Comparative Overview of cfDNA and ctDNA: Biology, Utility ... [https://www.cd-genomics.com/resource-cfdna-ctdna-key-differences-applications-extraction-considerations.html]
- 10. Liquid biopsy in cancer management: Integrating ... [https://www.sciencedirect.com/science/article/pii/S2352551724000921]
- 11. Performance Comparison of Droplet Digital PCR and Next ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12062871/]
- 12. Clinical utility of liquid biopsy next-generation sequencing ... [https://www.nature.com/articles/s41598-025-13667-z]
- 13. Detection and Quantification of ctDNA for Longitudinal ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9274771/]
- 14. Direct comparison of circulating tumor DNA sequencing ... [https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0266889]
- 15. Evolving Standards in Clinical NGS (updated) [https://www.euformatics.com/blog-post/evolving-standards-in-clinical-ngs]
- 16. Survival Outcomes May Improve When Treatment Is ... [https://ascopost.com/news/april-2025/survival-outcomes-may-improve-when-treatment-is-guided-by-using-both-tissue-and-liquid-biopsies]
- 17. NCCN Clinical Practice Guidelines in Oncology: 2025 ... [https://ascopost.com/issues/may-25-2025/nccn-clinical-practice-guidelines-in-oncology-2025-updates/]
- 18. Clinical value of guideline recommended molecular targets ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11333991/]
- 19. Key Elements in Comparing Different Next-Generation ... [https://canaryonco.com/blog/key-elements-in-comparing-different-next-generation-sequencing-ngs-tests/]
- 20. Validation of a liquid biopsy assay with increased ... [https://www.sciencedirect.com/science/article/pii/S2950195425000384]
- 21. Compare Our Tests [https://www.foundationmedicine.com/portfolio]
- 22. ACMG clinical laboratory standards for next-generation ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4098820/]
- 23. The effect of uncertainty in patient classification on ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6530857/]
- 24. Diagnostic accuracy (sensitivity/specificity) versus ... [https://analyse-it.com/blog/2020/4/diagnostic-accuracy-sensitivity-specificity-versus-agreement-ppa-npa-statistics]
- 25. Understanding PPA and NPA: Key Metrics in Diagnostic ... [https://www.linkedin.com/pulse/understanding-ppa-npa-key-metrics-diagnostic-test-norm-ramiento-md-qgyjc]
- 26. Genomic profiling of cell-free circulating tumor DNA in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6776816/]
- 27. Next-Generation Sequencing Concordance Analysis of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8567158/]
- 28. Feasibility of Next-generation Sequencing of Liquid Biopsy ... [https://www.sciencedirect.com/science/article/pii/S2405456924000439]
- 29. Implementing liquid biopsy NGS in stage III/IV NSCLC [https://pmc.ncbi.nlm.nih.gov/articles/PMC12619507/]
- 30. Comparison of next‑generation sequencing quality metrics ... [https://pubmed.ncbi.nlm.nih.gov/39991725/]
- 31. Real-World Technical Hurdles of ctDNA NGS Analysis [https://pmc.ncbi.nlm.nih.gov/articles/PMC12564474/]
- 32. A targeted next-generation sequencing panel for ... [https://www.nature.com/articles/s41598-025-08039-6]
- 33. Hybrid Capture-Based Sequencing Enables Highly ... [https://www.mdpi.com/2076-0817/14/3/264]
- 34. Analytical Validation of a Pan-Cancer NGS Assay for In- ... [https://www.sciencedirect.com/science/article/pii/S152515782500220X]
- 35. Ultra-broad hybrid capture-based targeted next-generation ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12576977/]
- 36. Comparison of next generation sequencing, droplet ... - PubMed [https://pubmed.ncbi.nlm.nih.gov/35334415/]
- 37. Next-generation sequencing in liquid biopsy - Human Genomics [https://humgenomics.biomedcentral.com/articles/10.1186/s40246-019-0220-8]
- 38. NGS vs qPCR [https://www.illumina.com/science/technology/next-generation-sequencing/beginners/advantages/ngs-vs-qpcr.html]
- 39. Guidelines for Validation of Next-Generation Sequencing– ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6941185/]
- 40. Circulating DNA tumor fraction as a biomarker for ... [https://www.frontiersin.org/journals/oncology/articles/10.3389/fonc.2025.1655415/full]
- 41. ctDNA Tumor Fraction Matters When Interpreting Liquid ... [https://www.foundationmedicine.com/resources/knowledge-center/ctdna-tumor-fraction-matters-when-interpreting-liquid-biopsy-test-results]
- 42. Cell-Free DNA, Tumor Molecular Concordance, and ... [https://www.sciencedirect.com/science/article/pii/S1525157825001412]
- 43. Cancer in a Drop: Liquid biopsy insights from AACR 2025 [https://pmc.ncbi.nlm.nih.gov/articles/PMC12223554/]
- 44. Demonstrating the Clinical Utility of Foundation Medicine's ... [https://www.foundationmedicine.com/blog/q3-research-recap-blog?utm_source=linkedin&utm_medium=organic-social&utm_campaign=q3-research-recap&utm_content=corporate]
- 45. Reliable on-treatment prognostication and target ... [https://www.nature.com/articles/s41598-025-22369-5]
- 46. Clinical implementation of next-generation sequencing ... [https://www.nature.com/articles/s41598-024-84909-9]
- 47. Dissecting Tumor Heterogeneity by Liquid Biopsy—A ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12347833/]
- 48. Real-World Clinical Utility of Tumor Next-Generation ... [https://pubmed.ncbi.nlm.nih.gov/40601894/]
- 49. Biomarker-Driven Clinical Trials in Oncology [https://www.precisionformedicine.com/blog/biomarker-driven-clinical-trials-in-oncology-enrichment-stratification-all-comers-basket-when-to-use-what-and-why]
- 50. A Tale of Two Biopsies: Liquid Biopsy vs Tissue Biopsy [https://www.biochain.com/blog/a-tale-of-two-biopsies-liquid-biopsy-vs-tissue-biopsy/]
- 51. Discordance Between Liquid and Tissue Biopsy-Based ... [https://www.sciencedirect.com/science/article/pii/S1525730423000050]
- 52. Analysis of error profiles in deep next-generation sequencing ... [https://genomebiology.biomedcentral.com/articles/10.1186/s13059-019-1659-6]
- 53. Comparison of solid tissue sequencing and liquid biopsy ... [https://www.sciencedirect.com/science/article/pii/S0893395222003775]
- 54. Liquid Biopsy Versus Tissue Biopsy to Determine Front ... [https://pubmed.ncbi.nlm.nih.gov/36585341/]
- 55. Technical standards for the interpretation and reporting of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7313390/]
- 56. Discordance in Recommendation Between Next ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10954076/]
- 57. Challenges and limitations of liquid biopsy in precision ... [https://www.sciencedirect.com/science/article/pii/B9780443274961000038]
- 58. Genomic landscape of liquid biopsy mutations in TP53 and ... [https://www.nature.com/articles/s41698-024-00544-7]
- 59. An artificial intelligence-based model for prediction of ... [https://www.nature.com/articles/s41698-025-00921-w]
- 60. Germline genetic variation impacts clonal hematopoiesis ... [https://www.nature.com/articles/s41588-025-02250-x]
- 61. The diagnostic accuracy of next-generation sequencing in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12409309/]
- 62. Comparison of the Data of a Next-Generation Sequencing ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8756135/]
- 63. Breast Cancer - PubMed Central [https://pmc.ncbi.nlm.nih.gov/articles/PMC9688837/]
- 64. Integrative spatial and genomic analysis of tumor ... [https://www.nature.com/articles/s41467-024-53374-3]
- 65. Cancer Heterogeneity Extended [https://www.bioskryb.com/cancer-heterogeneity-entended/]
- 66. Concordance of ctDNA and tissue genomic profiling in ... [https://pubmed.ncbi.nlm.nih.gov/39442892/]
- 67. Liquid Biopsy Versus Tissue Biopsy to Determine Front ... [https://www.sciencedirect.com/science/article/abs/pii/S1525730422002650]
- 68. P2.06.75 Liquid Biopsy NGS Accelerating Treatment ... [https://www.sciencedirect.com/science/article/pii/S1556086425016594]
- 69. The prospects and limitations of liquid biopsy utilization for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11937291/]
- 70. The Next-Generation Sequencing Quality Initiative and ... [https://wwwnc.cdc.gov/eid/article/31/13/24-1175_article]
- 71. The Diagnostic Accuracy of Next-Generation Sequencing ... [https://www.sciencedirect.com/science/article/pii/S2950195425000414]
- 72. Next Generation Sequencing (NGS) Worksheets [https://www.cap.org/member-resources/precision-medicine/next-generation-sequencing-ngs-worksheets]
- 73. New Somatic Cancer Reference Standards Aim To ... [https://www.labmanager.com/new-somatic-cancer-reference-standards-may-strengthen-ngs-diagnostic-accuracy-34640]
- 74. Validation of a liquid biopsy assay with increased ... [https://pubmed.ncbi.nlm.nih.gov/40980342/]
- 75. Diagnostic Performance of Liquid Biopsy Compared to ... [https://jchr.org/index.php/JCHR/article/view/10903]
- 76. Dr Hirsch on the Benefits of Tissue vs Liquid Biopsy in ... [https://www.onclive.com/view/dr-hirsch-on-the-benefits-of-tissue-vs-liquid-biopsy-in-nsclc]
- 77. Regulatory Submissions with Real-World Evidence ... [https://www.fda.gov/news-events/speeches-fda-officials/regulatory-submissions-real-world-evidence-successes-challenges-and-lessons-learned-09232025]
- 78. RWE as the Top Trend in 2025 [https://www.iqvia.com/blogs/2025/01/rwe-as-the-top-trend-in-2025]
- 79. Comprehensive Evaluation of a 1021-Gene Panel in FFPE ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12249698/]
- 80. Validation of a liquid biopsy assay with increased sensitivity ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12447423/]
- 81. Analytical Performance Evaluation of a 523-Gene ... [https://www.sciencedirect.com/science/article/pii/S1525157823002441]
- 82. Validation of an AI-enabled exome/transcriptome liquid ... [https://www.nature.com/articles/s41598-025-08986-0]