Next-Generation Sequencing in Precision Oncology: A Comprehensive Review of Technologies, Clinical Applications, and Future Directions
Next-generation sequencing (NGS) has fundamentally transformed precision oncology by enabling comprehensive genomic profiling of tumors, thus guiding diagnosis, prognostication, and personalized treatment selection.
Next-Generation Sequencing in Precision Oncology: A Comprehensive Review of Technologies, Clinical Applications, and Future Directions
Abstract
Next-generation sequencing (NGS) has fundamentally transformed precision oncology by enabling comprehensive genomic profiling of tumors, thus guiding diagnosis, prognostication, and personalized treatment selection. This review synthesizes current evidence on NGS technologies, including short- and long-read platforms, and their clinical applications in identifying actionable mutations, immunotherapy biomarkers, and resistance mechanisms. We detail the implementation of tissue-based and liquid biopsy approaches, discuss challenges in data interpretation and clinical integration, and provide a comparative analysis of sequencing methodologies and bioinformatics tools. For researchers and drug development professionals, this article outlines the critical role of NGS in advancing biomarker discovery, clinical trial design, and the development of targeted therapies, while also addressing future directions such as the integration of multi-omics data and artificial intelligence.
The Genomic Revolution: Core Principles and Technological Evolution of NGS in Oncology
The field of cancer genomics has undergone a revolutionary transformation, driven by a fundamental shift in sequencing technologies. This paradigm moved from first-generation Sanger sequencing to massively parallel next-generation sequencing (NGS), also known as high-throughput sequencing [1] [2]. This technological evolution has enabled the comprehensive molecular profiling of tumors, revealing the complex genetic alterations that drive cancer initiation and progression [3]. The rapid decrease in sequencing costs and the concurrent increase in throughput have made NGS increasingly accessible, allowing it to replace most other methods for precision cancer diagnostics [2]. This shift has been instrumental in realizing precision cancer medicine, where treatment decisions are guided by the specific genetic alterations present in an individual's tumor [4] [2]. This technical guide explores the core principles of this sequencing revolution, its clinical applications, and the practical methodologies that underpin modern genomic oncology.
A Technical Comparison of Sequencing Generations
Sanger Sequencing: The Chain Termination Method
Sanger sequencing, developed by Frederick Sanger in 1977, is known as the "chain termination method" and served as the foundational technology for DNA sequencing for decades [5]. Its principle involves using a DNA primer, DNA polymerase, normal deoxynucleotide triphosphates (dNTPs), and modified dideoxynucleotide triphosphates (ddNTPs) that lack a 3'-OH group, which is necessary for DNA strand elongation [5]. When a ddNTP is incorporated into the growing DNA strand, synthesis terminates, producing DNA fragments of varying lengths. These fragments are separated by capillary electrophoresis, and the sequence is determined by detecting the fluorescent labels attached to the terminating ddNTPs [5]. Sanger sequencing provides long read lengths (800-1000 base pairs) and high base accuracy (99.99%), making it the historical "gold standard" for validating DNA sequences [5].
Next-Generation Sequencing: The Principle of Massively Parallel Sequencing
Next-generation sequencing (NGS) represents a fundamental departure from Sanger's linear approach. Also termed massively parallel sequencing, NGS allows for the simultaneous sequencing of millions to billions of DNA fragments [1] [6]. The core principle involves fragmenting DNA into a library of small pieces, attaching adapters to these fragments, immobilizing them on a solid surface or in emulsion, and performing cyclic sequencing reactions that generate detectable signals [3] [6]. Unlike Sanger sequencing, which processes a single DNA fragment at a time, NGS technologies detect the incorporation of nucleotides in thousands to millions of parallel reactions, generating enormous volumes of sequence data in a single run [3].
Table 1: Comparative Analysis of Sanger Sequencing vs. Next-Generation Sequencing
| Feature | Sanger Sequencing | Next-Generation Sequencing |
|---|---|---|
| Sequencing Principle | Chain termination with ddNTPs and electrophoretic separation [5] | Massive parallel sequencing of clonally amplified or single DNA molecules [3] [6] |
| Throughput | Low; processes one sequence at a time [3] | Very high; processes millions of sequences simultaneously [3] [1] |
| Read Length | Long (800-1000 bases) [5] | Short to long (50-400 bases for short-read; 10,000+ for long-read) [6] |
| Cost-Effectiveness | Lower for sequencing single genes or small projects [5] | Higher for large-scale projects and genomic profiling [3] [5] |
| Speed | Relatively slow for large projects [5] | Rapid; entire human genome in days [3] |
| Primary Applications | Sequencing single genes, validating mutations, cloned inserts [5] | Whole genomes, exomes, transcriptomes, gene panels, epigenomics [3] [2] |
| Variant Detection Sensitivity | Lower sensitivity for mutations present at low allele frequency (<10-20%) [7] | High sensitivity, capable of detecting low-frequency mutations [7] |
The NGS Workflow: From Sample to Data
The standard NGS workflow involves a series of critical, interconnected steps to convert a biological sample into interpretable genomic data.
Sample Preparation and Library Construction
The initial step involves extracting and quantifying DNA or RNA from patient samples, typically formalin-fixed paraffin-embedded (FFPE) tumor tissue or blood [3] [7]. The quality of the input nucleic acids is critical for successful sequencing. For DNA sequencing, the extracted genomic DNA is fragmented, either physically, enzymatically, or chemically, to a size of around 300 base pairs [3]. Adapters—short, synthetic oligonucleotides with known sequences—are then ligated to the fragmented DNA ends. These adapters are essential for attaching the DNA fragments to the sequencing platform (e.g., a flow cell) and for subsequent amplification steps [3]. The resulting product is a "sequencing library." Depending on the application, libraries can be constructed for whole-genome, whole-exome, or targeted sequencing. For targeted approaches, an enrichment step using hybridization probes or PCR with specific primers is performed to isolate genomic regions of interest [3] [7].
Template Amplification and Clonal Cluster Generation
To generate a detectable signal, most NGS platforms require the amplification of single DNA molecules from the library. The two primary methods are:
- Emulsion PCR (emPCR): Used by platforms like Ion Torrent. Single-stranded DNA library fragments are bound to beads, and each bead is encapsulated in a water-in-oil emulsion droplet, creating a microreactor for clonal amplification via PCR [6].
- Bridge Amplification: Used by Illumina platforms. The single-stranded library is loaded into a flow cell where fragments hybridize to complementary surface-bound oligonucleotides. Through repeated cycles of denaturation and polymerase extension, each fragment is amplified into a clonal cluster, locally concentrated to yield a strong signal [3] [6].
Sequencing Reaction and Data Generation
The core sequencing reaction involves the cyclic addition of nucleotides and imaging. The most common chemistry is Sequencing by Synthesis (SBS) with reversible terminators, used by Illumina [3] [6]. In this process, the flow cell is flooded with fluorescently labeled nucleotides that also act as reversible terminators. In each cycle, a single complementary nucleotide is incorporated into each growing DNA strand, the fluorescence is imaged to identify the base, and then the terminator is chemically cleaved to allow the next incorporation cycle [3]. Other chemistries include pyrosequencing (454/Roche) and semiconductor sequencing (Ion Torrent), which detects hydrogen ions released during nucleotide incorporation [6].
Data Analysis and Bioinformatics
The final and most complex stage is bioinformatic analysis of the massive datasets generated [3]. The process typically involves:
- Base Calling: Translating raw signal data (images or pH changes) into nucleotide sequences (reads).
- Alignment/Mapping: Assembling short reads by aligning them to a reference human genome (e.g., hg19/GRCh38).
- Variant Calling: Using specialized algorithms to identify differences between the sequenced sample and the reference genome, including single nucleotide variants (SNVs), small insertions/deletions (indels), and copy number variations (CNVs) [3].
- Annotation and Interpretation: Determining the functional and clinical impact of identified variants (e.g., missense, nonsense), their frequency in population databases, and, crucially, their known or potential actionability as therapeutic targets or resistance markers [4].
Table 2: Essential Research Reagents and Platforms for NGS in Cancer Genomics
| Item Category | Specific Examples | Function in Workflow |
|---|---|---|
| Nucleic Acid Extraction | QIAamp DNA Mini Kit [7] | Isolation of high-quality genomic DNA from tissue or blood samples. |
| Target Enrichment | Ion AmpliSeq Panels [7] | Multiplex PCR-based amplification of a targeted set of cancer-related genes. |
| Library Prep Kits | Ion AmpliSeq Library Kit [7] | Preparation of fragmented and adapter-ligated DNA for sequencing. |
| Sequencing Platforms | Illumina MiSeq, HiSeq, NovaSeq; Ion Torrent PGM/Proton [7] [6] | Instruments performing massively parallel sequencing. |
| Bioinformatics Tools | Torrent Suite Software, Variant Caller [7] | Software for base calling, alignment, and variant identification. |
| Clinical Databases | OncoKB, MyCancerGenome, COSMIC [4] | Curated knowledgebases for interpreting the clinical significance of somatic variants. |
Clinical Applications and Experimental Design in Precision Oncology
The implementation of NGS in oncology has moved beyond research into routine clinical practice, enabling a wide range of applications that guide patient care.
Comprehensive Genomic Profiling
NGS enables simultaneous assessment of a multitude of genomic biomarkers, which is essential given the molecular heterogeneity of cancer. This is primarily achieved through:
- Targeted Gene Panels: Focused panels sequencing dozens to hundreds of cancer-associated genes. They offer high sequencing depth, making them cost-effective and ideal for detecting low-level mutations in samples with limited tumor content [7] [2]. They are widely used to identify actionable mutations for therapy selection in cancers like lung adenocarcinoma and melanoma [2].
- Whole Exome Sequencing (WES): Captures the protein-coding regions of the genome (~1-2%), where most known disease-causing variants reside. It provides a broader view than panels but less data than WGS [3] [2].
- Whole Genome Sequencing (WGS): Interrogates the entire genome, including non-coding regions. It provides the most comprehensive view, enabling detection of SNVs, indels, CNVs, and structural variants (SVs) like gene fusions from a single assay [3] [2]. It is increasingly used for pediatric cancers and rare malignancies to uncover novel drivers [2].
Monitoring Treatment Response and Residual Disease
NGS provides a highly sensitive tool for longitudinal monitoring of tumor dynamics. By tracking specific mutations in cell-free DNA (cfDNA) from patient blood plasma—a "liquid biopsy"—clinicians can monitor treatment response, detect emerging resistance mechanisms, and identify minimal residual disease (MRD) long before it becomes clinically apparent [3] [2]. This requires deep sequencing (high coverage) to detect mutations present at very low allele frequencies, enabling timely intervention and treatment adjustment [2].
A Practical Experimental Protocol: Targeted NGS for Solid Tumors
The following protocol, derived from a breast cancer study [7], outlines a typical workflow for targeted NGS using a semiconductor sequencer.
Aim: To identify somatic mutations in the PIK3CA gene and other cancer-related genes in 186 primary breast carcinomas. Methods:
- Sample Selection and DNA Extraction: Select FFPE tumor samples with at least 30% tumor cell content. Macro- or micro-dissect the marked tumor area. Extract genomic DNA using a commercial kit (e.g., QIAamp DNA Mini Kit) and quantify using a fluorometer (e.g., Qubit) [7].
- Library Preparation: Use 10 ng of genomic DNA. Prepare the sequencing library using a targeted panel (e.g., a custom 154-amplicon panel covering 48 genes) and a library preparation kit (e.g., Ion AmpliSeq Library Kit 2.0). Amplify the target regions via multiplex PCR [7].
- Template Preparation and Sequencing: Clonally amplify the library using emulsion PCR (e.g., with the Ion OneTouch system). Enrich template-positive beads and load onto a semiconductor sequencing chip (e.g., Ion 318 chip). Sequence on the appropriate platform (e.g., Ion Torrent PGM) [7].
- Data Analysis: Perform base calling and alignment to the reference genome (hg19) using the platform's software suite (e.g., Torrent Suite). Call variants with a built-in algorithm (e.g., Torrent Variant Caller), applying appropriate filters for quality and strand bias [7].
- Validation: Confirm a subset of mutations, especially those with low allele frequency or clinical significance, using an independent method like Sanger sequencing [7].
Translating Genomic Data into Clinical Action
Interpreting NGS data and translating it into a therapeutic strategy is a critical challenge in precision oncology. The process requires sophisticated tools and multidisciplinary expertise.
The Role of Precision Oncology Platforms
To aid clinicians, several curated knowledgebases have been developed. These platforms consolidate genomic data and clinical evidence into standardized, accessible formats [4]. When an NGS report lists a set of somatic variants, clinicians and molecular pathologists can query these databases to determine the clinical significance of each alteration. Key platforms include:
- OncoKB: A precision oncology database that annotates the therapeutic and prognostic implications of individual gene alterations, with levels of evidence ranging from standard-of-care to investigational therapies [4].
- MyCancerGenome: Provides detailed information on genomic alterations in cancer, focusing on their potential clinical implications and linking mutations to relevant clinical trials and targeted therapies [4].
- CIViC (Clinical Interpretation of Variants in Cancer): A community-driven resource that crowdsources clinical evidence for the interpretation of variants in cancer [4].
Molecular Tumor Boards
The final interpretation often occurs within a Molecular Tumor Board (MTB), a multidisciplinary team comprising oncologists, molecular pathologists, genetic counselors, bioinformaticians, and clinical geneticists [8] [4]. The MTB reviews the NGS findings in the context of the patient's clinical history, pathology, and evidence from precision oncology platforms to formulate a personalized treatment recommendation, which may include approved targeted therapies, clinical trial enrollment, or analysis of potential hereditary cancer risk [8].
The shift from Sanger to massively parallel sequencing represents a true paradigm shift, fundamentally altering the approach to cancer diagnosis, classification, and treatment. NGS has provided an unprecedented, comprehensive view of the cancer genome, forming the bedrock of precision oncology [2]. As the technology continues to evolve, future developments promise to further refine this field. These include the clinical integration of single-cell sequencing to resolve tumor heterogeneity [3], the expanded use of liquid biopsies for non-invasive monitoring [2], the application of long-read sequencing (e.g., PacBio, Oxford Nanopore) to resolve complex genomic regions, and the integration of artificial intelligence to improve variant interpretation and predict therapeutic responses [4]. The ongoing challenge lies not in generating data, but in robustly interpreting it and translating these insights into improved patient outcomes through equitable and clinically validated interventions.
Next-generation sequencing (NGS) has revolutionized molecular biology and oncology by fundamentally redefining approaches to disease research and clinical diagnostics [9]. Since its widespread adoption, NGS has progressively displaced traditional Sanger sequencing, becoming integral to contemporary genomic medicine and precision oncology [9]. This transformative technology enables comprehensive genomic profiling of tumors, facilitating the identification of driver mutations, fusion genes, and predictive biomarkers across diverse cancer types [9]. The capacity of NGS to simultaneously interrogate hundreds to thousands of genetic targets has made it indispensable for personalized cancer therapy, clinical trial design, and biomarker discovery [10] [11].
In precision oncology, NGS provides clinically actionable molecular insights that guide diagnosis, prognostication, therapeutic selection, and monitoring of treatment response [9]. The fundamental principles of throughput, sensitivity, and scalability define its operational capabilities and determine its appropriate application in both research and clinical settings. This technical guide examines these core principles in detail, providing researchers and drug development professionals with a comprehensive framework for understanding NGS capabilities within precision oncology.
Core Principles of NGS Technology
Throughput: Massively Parallel Sequencing Architecture
The defining attribute of NGS is its massively parallel sequencing architecture, which enables the concurrent analysis of millions of DNA fragments in a single run [9]. This represents a fundamental departure from Sanger sequencing, which processes one DNA fragment at a time, making it laborious, costly, and time-consuming for large-scale analysis [9]. The massively parallel approach allows NGS to simultaneously evaluate hundreds to thousands of genes in a single assay, offering a comprehensive genomic landscape rather than the fragmented approach inherent to Sanger sequencing [9].
Throughput capabilities vary significantly across NGS platforms. Second-generation platforms (e.g., Illumina) typically generate short reads (75-300 base pairs) with exceptionally high throughput and low error rates (typically 0.1-0.6%) [9]. Third-generation technologies (e.g., PacBio, Oxford Nanopore) offer longer read lengths (up to 100,000+ base pairs) through single-molecule real-time sequencing, providing advantages for resolving complex genomic regions and structural variations [9]. This parallel architecture provides markedly increased sequencing depth and sensitivity, detecting low-frequency variants down to ~1% variant allele frequency, and shortens turnaround times—an entire human genome can be sequenced in approximately one week, compared with years using Sanger technology [9].
Table 1: Throughput Comparison Between Sanger and NGS Technologies
| Aspect | Sanger Sequencing | Next-Generation Sequencing (NGS) |
|---|---|---|
| Throughput | Single DNA fragment at a time | Massively parallel; millions of fragments simultaneously |
| Sensitivity (detection limit) | Low (~15–20%) | High (down to 1% for low-frequency variants) |
| Cost-effectiveness | Cost-effective for 1–20 targets, high for large regions | Cost-effective for high sample volumes/many targets |
| Discovery power | Limited; interrogates a gene of interest | High; detects novel or rare variants with deep sequencing |
| Read length | Typically, up to 1000 base pairs | Short (75–300 bp) to Ultra-long (100,000+ bp) |
| Turnaround time | Years for the whole genome | About a week for the whole genome |
| Variant detection capability | Limited to specific regions; single gene analysis | Single-base resolution; detects SNPs, indels, CNVs, SVs, and large chromosomal rearrangements |
Sensitivity: Detection of Low-Frequency Variants
Sensitivity in NGS refers to the technology's ability to detect low-frequency genetic variants present in a minor subset of cells within a heterogeneous sample. NGS demonstrates significantly enhanced sensitivity compared to traditional methods, with detection limits reaching approximately 1% variant allele frequency (VAF) for low-frequency variants, a substantial improvement over Sanger sequencing's ~15-20% detection limit [9]. This heightened sensitivity is particularly crucial in oncology applications for detecting minimal residual disease (MRD), monitoring treatment resistance, and identifying emerging subclones during tumor evolution [12].
The sensitivity of NGS is directly influenced by sequencing depth (coverage), which refers to the number of times a specific nucleotide is read during sequencing. Higher sequencing depths increase confidence in variant calling, particularly for heterogeneous tumor samples where mutant alleles may be present at low frequencies. In practice, targeted NGS panels achieve significantly higher sequencing depths (often >500x) compared to whole-genome sequencing, enabling more reliable detection of low-frequency somatic mutations [10]. This enhanced sensitivity allows NGS to identify novel or rare variants, structural rearrangements, and large chromosomal abnormalities at single-nucleotide resolution [9].
Scalability: Flexible Experimental Design
Scalability represents a third fundamental principle of NGS technology, encompassing its adaptability to various experimental designs and throughput requirements. NGS platforms offer remarkable flexibility, supporting applications ranging from targeted gene panels (dozens to hundreds of genes) to whole-exome sequencing (approximately 1% of the human genome) and whole-genome sequencing (entire genomic content) [10]. This scalability enables researchers to tailor sequencing approaches to specific research questions while optimizing resources and costs.
In clinical oncology practice, targeted panel sequencing represents the most commonly used NGS application, typically interrogating dozens or hundreds of cancer-relevant genes [10]. Compared to whole-genome sequencing, targeted panels provide substantially greater sequencing depth for the same sequencing effort, which is necessary to detect mutations with varying allelic frequencies in tumor samples [10]. The scalable nature of NGS also facilitates sample multiplexing, allowing multiple samples to be sequenced simultaneously in a single run through barcoding strategies, thereby increasing throughput and reducing per-sample costs [9].
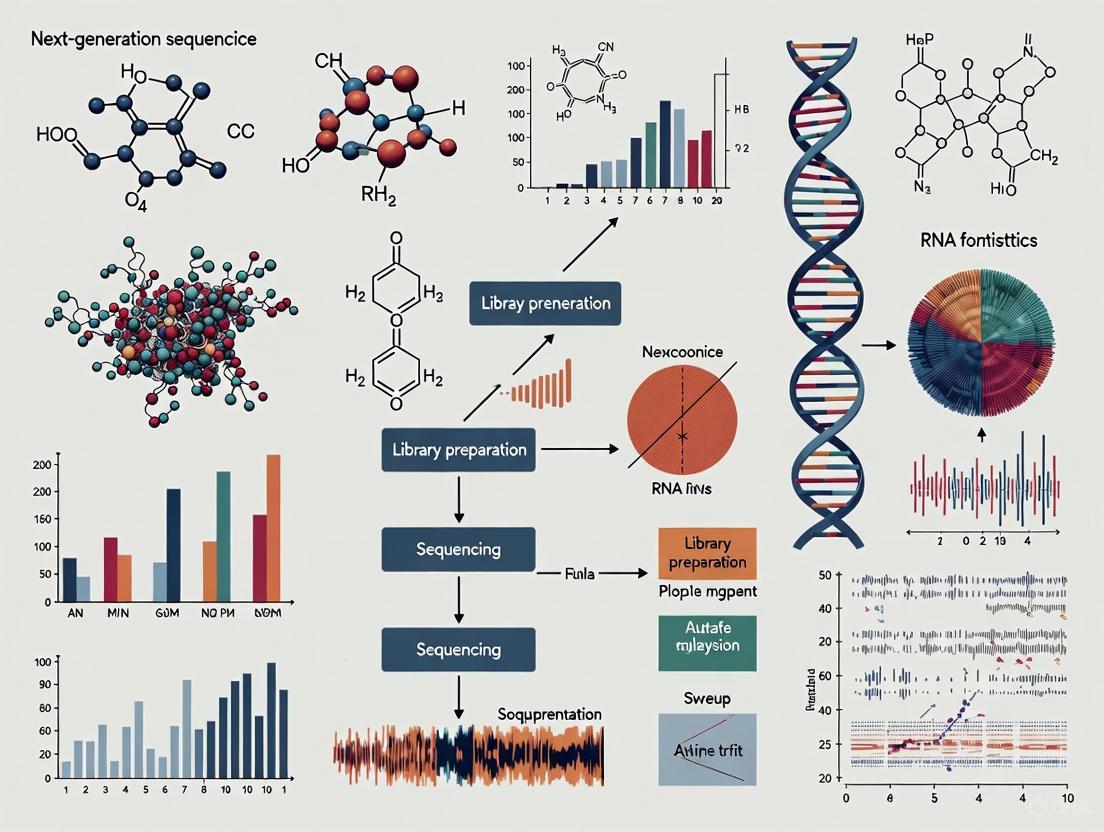
Figure 1: NGS Workflow from Sample to Result. The process begins with sample preparation and proceeds through nucleic acid extraction, library preparation, massively parallel sequencing, bioinformatics analysis, and final clinical interpretation.
NGS Workflow and Methodologies
Experimental Workflow
The standard NGS workflow involves multiple interconnected steps, each critical to achieving accurate and reproducible results. The process begins with DNA fragmentation, where targeted DNA is broken into short segments (typically 100-300 bp in length) using mechanical methods, enzymatic digestion, or other fragmentation techniques [10]. For targeted sequencing approaches, relevant segments are isolated using either hybridization capture (using specific complementary probes) or amplicon-based approaches (using PCR amplification with multiple primer pairs) [10].
Library preparation follows fragmentation, wherein DNA segments are modified to include sample-specific indices (barcodes) and sequencing adaptors [10]. This process enables sample multiplexing and allows sequencing primers to bind to all DNA fragments, facilitating the massively parallel sequencing step. The prepared libraries are then loaded onto sequencing matrices (e.g., flow cells for Illumina platforms, sequencing chips for Ion Torrent) for the massive parallel sequencing reaction, where millions to billions of DNA fragments are simultaneously sequenced [10].
Following sequencing, bioinformatics analysis processes the raw data through base calling, read alignment, variant identification, and variant annotation [10]. During this computational phase, sequence information is compared to a human reference genome to identify variants, and information from each sequenced segment is pieced together to generate final sequencing results for the full length of the targeted DNA [10]. The final annotation and interpretation phase identifies each variant and assesses its potential biological and clinical significance, a particularly crucial step for precision oncology applications [10].
Platform Technologies
The choice of NGS platform represents a strategic decision that directly influences the feasibility and success of research or clinical projects, as each technology excels in different applications. Illumina sequencing dominates second-generation NGS due to its exceptionally high throughput, low error rates, and attractive cost per base [9]. It employs sequencing-by-synthesis chemistry, enabling millions of DNA fragments to be sequenced in parallel on a flow cell, with established bioinformatics pipelines well-optimized for Illumina data [9].
Oxford Nanopore Technologies (ONT) utilizes a distinctive approach involving direct reading of single DNA molecules as they traverse protein nanopores [9]. This technology provides ultra-long read lengths, real-time data analysis, and portability, though with generally higher error rates compared to Illumina platforms. Pacific Biosciences (PacBio) offers single-molecule real-time sequencing that generates long reads with minimal bias, advantageous for resolving complex genomic regions, detecting structural variants, and performing de novo assemblies [9].
Table 2: Comparison of Major NGS Platform Types
| Characteristic | Second-Generation (Short-Read) | Third-Generation (Long-Read) |
|---|---|---|
| Representative Platforms | Illumina | Oxford Nanopore, Pacific Biosciences |
| Read Length | Short (75-300 bp) | Long (10,000-100,000+ bp) |
| Error Rates | Low (0.1-0.6%) | Higher (1-15% depending on technology) |
| Primary Strengths | High accuracy, low cost per base, established protocols | Detection of structural variants, resolution of repetitive regions, haplotype phasing |
| Primary Applications | Variant detection, transcriptome profiling, targeted sequencing | De novo assembly, complex variant detection, epigenetics |
| Throughput | Very high | Moderate to high |
| Run Time | Hours to days | Minutes to days |
The Researcher's Toolkit: Essential Reagents and Materials
Successful implementation of NGS workflows requires specific reagents and materials optimized for each procedural step. The following table details essential components for establishing a robust NGS pipeline in a research or clinical setting:
Table 3: Essential Research Reagents and Materials for NGS Workflows
| Reagent/Material | Function | Application Notes |
|---|---|---|
| Nucleic Acid Extraction Kits (e.g., QIAamp DNA FFPE Tissue Kit) | Isolation of high-quality DNA from various sample types including FFPE tissue [13]. | Critical for obtaining sufficient quality/quantity; FFPE extraction requires specialized protocols to address cross-linking and fragmentation. |
| DNA Quantification Assays (e.g., Qubit dsDNA HS Assay) | Accurate quantification of DNA concentration [13]. | Fluorometric methods preferred over spectrophotometry for better accuracy with fragmented DNA. |
| Library Preparation Kits (e.g., Agilent SureSelectXT) | Fragmentation, adapter ligation, and target enrichment [13]. | Choice between hybridization capture vs. amplicon-based depends on panel design and application requirements. |
| Target Enrichment Panels | Selection of genomic regions of interest | Custom or commercial panels available; pan-cancer designs typically cover hundreds of cancer-relevant genes. |
| Sequenceing Flow Cells/Chips | Platform-specific matrix for sequencing reactions | Capacity and configuration vary by platform; determines maximum throughput per run. |
| Bioinformatics Pipelines | Base calling, alignment, variant calling, and annotation [9] | Critical for data interpretation; requires specialized computational expertise and resources. |
Applications in Precision Oncology and Drug Development
Comprehensive Genomic Profiling in Cancer Care
NGS enables comprehensive genomic profiling (CGP) of tumors, simultaneously evaluating multiple variant types including small variants (substitutions, insertions, deletions), copy number alterations, and rearrangements (fusions and splice variants) [14]. This comprehensive approach provides a tumor-agnostic method to detect similar molecular alterations across histologies, supporting targeted therapy selection, immunotherapy response prediction, and clinical trial matching [14]. The capacity to identify novel and emerging biomarkers has become increasingly important with FDA approvals for tumor mutational burden (TMB) and microsatellite instability (MSI) as genomic biomarkers of response to immune checkpoint inhibitors [14].
In clinical practice, CGP by NGS demonstrates significant utility for guiding treatment decisions. A 2025 systematic review and meta-analysis of NGS applications in childhood and adolescent/young adult solid tumors found a pooled proportion of 57.9% actionable alterations across studies, with 22.8% impacting clinical decision-making [15]. Real-world implementation studies at tertiary care centers have demonstrated that approximately 26% of patients harbor tier I variants (strong clinical significance), with 13.7% of these patients receiving NGS-based therapy based on novel information provided by sequencing [13].
Liquid Biopsy and Circulating Tumor DNA
Liquid biopsy approaches utilizing circulating tumor DNA (ctDNA) represent a rapidly advancing application of NGS in oncology [9]. These minimally invasive tests enable real-time monitoring of tumor dynamics, assessment of molecular heterogeneity, and detection of emerging resistance mechanisms [9]. In translational research and drug development, ctDNA monitoring provides valuable tools for evaluating changes in tumor burden over time, assessing dose selection in early-phase clinical trials, and monitoring individual variants to identify acquired resistance across hundreds of genes [11].
The scalability and sensitivity of NGS platforms make them ideally suited for liquid biopsy applications, where genetic material is often limited and variant allele frequencies can be extremely low. Advanced NGS approaches can quantify ctDNA tumor fraction, a biomarker that incorporates multi-omic information to improve sensitivity while maintaining high specificity for monitoring ctDNA levels [11]. These capabilities position liquid biopsy as a complementary approach to tissue-based profiling, particularly when tissue is insufficient or serial monitoring is required.
Figure 2: Interrelationship of NGS Core Principles and Their Applications in Oncology. Throughput, sensitivity, and scalability collectively enable diverse applications in precision oncology, with each principle contributing differently to specific applications.
The fundamental principles of throughput, sensitivity, and scalability establish NGS as an indispensable technology in precision oncology and drug development. The massively parallel sequencing architecture of NGS platforms enables unprecedented throughput, allowing comprehensive genomic assessment that was previously impractical with sequential testing approaches. Enhanced sensitivity permits detection of low-frequency variants critical for understanding tumor heterogeneity, monitoring minimal residual disease, and identifying emerging resistance mechanisms. Remarkable scalability provides flexibility in experimental design, supporting applications ranging from focused targeted panels to genome-wide sequencing approaches.
For researchers and drug development professionals, understanding these core principles is essential for appropriate technology selection, experimental design, and data interpretation. As NGS continues to evolve, integration with artificial intelligence, single-cell sequencing, spatial transcriptomics, multi-omics, and nanotechnology promises to overcome current limitations and advance personalized treatment strategies [9]. Standardization of workflows, cost reduction, and improved bioinformatics expertise will be critical for the full clinical integration of these advances [9]. The ongoing refinement of NGS technologies ensures their continuing centrality in precision oncology, enabling increasingly sophisticated molecularly driven cancer care and therapeutic development.
Next-generation sequencing (NGS) has revolutionized precision oncology by enabling comprehensive genomic profiling of tumors, which is fundamental for understanding cancer development, progression, and treatment response. These technologies allow researchers and clinicians to identify specific genetic mutations, structural variations, and epigenetic modifications that drive oncogenesis [16]. The transition from first-generation Sanger sequencing to NGS has compressed research timelines from years to days, making large-scale genomic studies feasible and transforming cancer care toward a more personalized approach [16]. The global NGS market, valued at USD 15.53 billion in 2025, reflects this transformative impact, particularly in oncology applications which represent the largest market segment [17].
In precision oncology, the selection of an appropriate sequencing platform is dictated by specific research goals, including the need for particular resolution, sample availability, and the variants of interest. The three major platforms—Illumina, Oxford Nanopore Technologies (ONT), and PacBio—each offer distinct advantages and limitations for different oncology research applications [18]. This technical guide provides an in-depth comparison of these platforms, their methodologies, and their applications in precision oncology research.
Platform-Specific Technologies and Methodologies
Illumina: Short-Read Sequencing by Synthesis
Technology Principle: Illumina's technology is based on sequencing by synthesis (SBS) with fluorescently tagged nucleotides [16]. The process begins with library preparation where DNA is fragmented and adapters are ligated to the ends. These fragments are then bound to a flow cell and amplified through bridge amplification to create clusters of identical DNA molecules. During sequencing, fluorescently-labeled nucleotides are incorporated one at a time, with each nucleotide emitting a specific color signal that is captured by imaging systems [16].
Key Technical Specifications:
- Read Length: Typically generates short reads of 50-600 base pairs, with common outputs of 2×300 bp for paired-end sequencing [16] [18].
- Error Rate: Less than 0.1%, making it highly accurate for base calling [18].
- Output: High throughput, generating millions to billions of reads per run [16].
Illumina SBS Workflow: Library preparation, cluster generation, and sequence detection.
PacBio: Single Molecule Real-Time (SMRT) Sequencing
Technology Principle: PacBio's HiFi (High Fidelity) sequencing utilizes single molecule, real-time (SMRT) technology [19]. The system employs a SMRT cell containing millions of zero-mode waveguides (ZMWs)—nanophotonic structures that confine light to zeptoliter volumes. Within each ZMW, a single DNA polymerase enzyme is immobilized and incorporates fluorescently-labeled nucleotides onto a template DNA strand. The key innovation is the real-time detection of nucleotide incorporation events through emitted fluorescence, without the need for amplification [20] [19].
Key Technical Specifications:
- Read Length: 500 to 20,000+ bases, with typical HiFi reads of 15,000-20,000 bases [19].
- Accuracy: Q30 (99.9%) to Q33 (99.95%) for HiFi reads after circular consensus sequencing [19].
- Run Time: Approximately 24 hours for a typical run [19].
PacBio SMRT sequencing: SMRT cell, real-time detection, and HiFi read generation.
Oxford Nanopore Technologies: Nanopore Sequencing
Technology Principle: ONT sequencing is based on the measurement of electrical current changes as DNA or RNA molecules pass through protein nanopores embedded in a polymer membrane [19]. Each nucleotide base causes a characteristic disruption in the ionic current as the nucleic acid strand translocates through the nanopore. These current changes are decoded in real-time through sophisticated base-calling algorithms to determine the DNA sequence [18] [19].
Key Technical Specifications:
- Read Length: 20 bases to over 4 megabases, capable of producing ultra-long reads [19].
- Accuracy: Approximately Q20 (99%) with current chemistries and base-calling algorithms [18] [19].
- Run Time: Flexible, from minutes to 72 hours, with real-time data streaming [18] [19].
ONT nanopore sequencing: Sample preparation, membrane crossing, and signal decoding.
Comparative Performance Analysis
Technical Specifications Comparison
Table 1: Comprehensive comparison of major NGS platforms for precision oncology research
| Parameter | Illumina | PacBio HiFi | Oxford Nanopore |
|---|---|---|---|
| Read Length | 50-600 bp (short) | 500-20,000+ bp (long) | 20 bp->4 Mb (ultra-long) |
| Accuracy | >99.9% (Q30) [18] | 99.9% (Q30) [19] | ~99% (Q20) [18] [19] |
| Typical Run Time | Hours to days | ~24 hours [19] | Minutes to 72 hours [18] [19] |
| Variant Detection - SNVs | Excellent | Yes [19] | Yes [19] |
| Variant Detection - Indels | Good | Yes [19] | Limited in repeats [19] |
| Variant Detection - SVs | Limited | Yes [19] | Yes [19] |
| Epigenetic Detection | Requires bisulfite treatment | 5mC, 6mA without treatment [19] | 5mC, 5hmC, 6mA [19] |
| RNA Sequencing | Via cDNA | Via cDNA [19] | Direct RNA sequencing [19] |
| Portability | Benchtop systems | Laboratory systems | Portable (MinION) to large [19] |
| Key Oncology Applications | Tumor profiling, liquid biopsies [16] | Phased variants, complex regions [20] | Rapid diagnostics, methylation [21] |
Performance in Microbial and Metagenomic Studies
Recent comparative studies highlight platform-specific performance characteristics in microbiome analysis, which has implications for cancer microbiome research. A 2025 study comparing Illumina and ONT for 16S rRNA profiling of respiratory microbial communities found that Illumina captured greater species richness, while ONT provided improved resolution for dominant bacterial species [18]. Beta diversity differences were more pronounced in complex microbiomes, suggesting that platform effects vary by sample type.
Another 2025 study comparing all three platforms for rabbit gut microbiota analysis demonstrated that full-length 16S sequencing with PacBio and ONT offered better species-level resolution (63% and 76% respectively) compared to Illumina (48%) [22]. However, a significant limitation across all platforms was that most species-level classifications were labeled as "uncultured bacterium," indicating reference database limitations rather than technological shortcomings [22].
Experimental Design and Protocols
Sample Preparation Guidelines
DNA Quality and Quantity: For all NGS platforms in precision oncology applications, high-quality, high-molecular-weight DNA is essential. Recommended extraction methods include phenol-chloroform or commercial kits designed for long-read sequencing. DNA integrity should be verified via pulsed-field gel electrophoresis or Fragment Analyzer systems, with DNA Integrity Numbers (DIN) >7.0 considered optimal [22] [18].
Input Requirements:
- Illumina: 1-1000 ng, flexible with input due to amplification
- PacBio: 1-5 μg for standard libraries, with recommendations for >50 kb fragment sizes
- Oxford Nanopore: 100 ng-1 μg, with higher inputs improving ultra-long read yield
Library Preparation Protocols
Table 2: Comparison of library preparation methods across platforms
| Step | Illumina | PacBio | Oxford Nanopore |
|---|---|---|---|
| Fragmentation | Mechanical or enzymatic shearing | Size selection optional | Optional fragmentation |
| End Repair | Required | A-tailing | Ligation-ready |
| Adapter Ligation | Indexed adapters | SMRTbell adapters | Ligation or rapid kits |
| Size Selection | SPRI beads | BluePippin or SPRI | SPRI beads |
| PCR Amplification | Typically 4-10 cycles | Optional | Optional |
| Quality Control | Bioanalyzer, qPCR | Fragment Analyzer, Qubit | Qubit, agarose gel |
Platform-Specific Considerations:
- Illumina: Amplification can introduce biases in GC-rich regions; unique dual indexes are recommended for multiplexing to minimize index hopping [16].
- PacBio: SMRTbell library construction involves creating circular templates; shearing is minimized to preserve long fragments [20].
- Oxford Nanopore: The 16S Barcoding Kit (SQK-16S024) enables full-length 16S rRNA amplification with barcoding for multiplexing [22] [18].
Bioinformatics Processing Pipelines
Illumina Data Analysis:
- Quality Control: FastQC for read quality assessment
- Adapter Trimming: Cutadapt or Trimmomatic
- Read Alignment: BWA-MEM or Bowtie2 for reference-based alignment
- Variant Calling: GATK, Mutect2 for somatic variants
PacBio HiFi Data Analysis:
- CCS Read Generation: Circular Consensus Sequencing to produce HiFi reads
- Alignment: Minimap2 or pbmm2 for long reads
- Variant Calling: DeepVariant or pbsv for structural variants
Oxford Nanopore Data Analysis:
- Basecalling: Dorado or Guppy for converting raw signals to sequences
- Quality Control: NanoPlot for quality assessment
- Alignment: Minimap2 for long-read alignment
- Variant Calling: Clair3 or Medaka for variant detection
Applications in Precision Oncology Research
Tumor Genomic Profiling
Comprehensive Genomic Characterization: Illumina's TruSight Oncology Comprehensive test provides extensive genomic profiling for solid tumors, enabling detection of key biomarkers such as KRAS mutations that are crucial for therapy selection [23]. These tests help match patients to targeted therapies and clinical trials based on the specific molecular alterations in their tumors.
Structural Variant Detection: PacBio HiFi sequencing excels in identifying complex structural variants in cancer genomes, including gene fusions, amplifications, and rearrangements that are challenging to detect with short-read technologies [20]. This capability is particularly valuable in pediatric cancers and hematological malignancies where structural variants are common drivers.
Epigenetic Analysis in Cancer
Methylation Profiling: Both PacBio and Oxford Nanopore technologies can detect DNA methylation natively without bisulfite conversion [19]. ONT has been used to develop the Acute Leukemia Methylome Atlas from over 3,000 leukemia samples, demonstrating how long-read sequencing combined with machine learning can predict AML subtypes and patient outcomes with high accuracy [21].
Chromatin Accessibility: The combination of long-read sequencing with epigenetic assays enables phased epigenomic profiling, allowing researchers to determine how epigenetic marks are distributed across parental chromosomes—a crucial consideration in cancer imprinting and allele-specific expression.
Transcriptomics and Isoform Sequencing
Alternative Splicing Analysis: PacBio HiFi sequencing has enabled the creation of the first single-cell splicing atlas of human CD8⁺ T cells, capturing dynamic isoform programs across activation and subset differentiation [20]. This research revealed that approximately 50% of differentially expressed isoforms showed isoform-specific regulation without corresponding changes in overall gene expression, highlighting the importance of isoform-resolution analysis in cancer immunology.
Direct RNA Sequencing: Oxford Nanopore's capability for direct RNA sequencing without cDNA conversion preserves RNA modifications and provides full-length transcript information, enabling the discovery of novel isoforms and fusion transcripts in cancer cells [19].
Liquid Biopsies and Minimal Residual Disease
Circulating Tumor DNA Analysis: Illumina's short-read platforms are widely used for liquid biopsy applications due to their high accuracy and sensitivity for detecting low-frequency variants in circulating tumor DNA [16]. This approach enables non-invasive monitoring of treatment response and detection of minimal residual disease.
Comprehensive Liquid Biopsy: Long-read technologies are emerging for liquid biopsy applications, particularly for detecting structural variants and epigenetic modifications in circulating DNA that may provide additional information about tumor evolution and heterogeneity.
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Key research reagents and materials for NGS in precision oncology
| Reagent/Material | Function | Platform Compatibility |
|---|---|---|
| DNeasy PowerSoil Kit | DNA extraction from challenging samples | All platforms [22] |
| QIAseq 16S/ITS Region Panel | Targeted 16S/ITS amplification | Illumina [18] |
| SMRTbell Express Template Prep Kit | Library preparation for SMRT sequencing | PacBio [22] |
| ONT 16S Barcoding Kit | Full-length 16S amplification and barcoding | Oxford Nanopore [22] [18] |
| Nextera XT Index Kit | Dual indexing for multiplexing | Illumina [22] |
| Circulomics Nanobind DNA Extraction | HMW DNA extraction for long reads | PacBio, ONT |
| SPRIselect Beads | Size selection and clean-up | All platforms |
| Qubit dsDNA HS Assay | Accurate DNA quantification | All platforms |
Future Directions in Precision Oncology Sequencing
The NGS landscape continues to evolve with emerging trends that will further enhance precision oncology research. Single-cell sequencing enables the analysis of individual cells within tumor ecosystems, revealing heterogeneity and rare cell populations [17]. Multi-omic integration approaches combine genomic, epigenomic, and transcriptomic data from the same samples, providing comprehensive views of cancer biology [24]. The integration of AI and machine learning with NGS data analysis is improving variant interpretation and clinical decision support [17].
Recent regulatory approvals, such as the first clinical long-read sequencing system in China (PacBio's Sequel II CNDx) for thalassemia testing, signal the transition of long-read technologies from research to clinical applications in oncology [25]. As these technologies continue to mature, they will increasingly enable researchers and clinicians to unravel the complex genomic architecture of cancer and develop more effective, personalized treatment strategies.
The Global Cancer Burden and the Imperative for Precision Diagnostics
The global burden of cancer continues to grow, with projections indicating a dramatic increase to over 35 million new cases annually by 2050, representing a 77% rise from 2022 estimates [26]. This escalating burden, characterized by significant health disparities and economic impacts, necessitates a paradigm shift from traditional one-size-fits-all treatment approaches toward precision diagnostics. Next-generation sequencing (NGS) has emerged as a transformative technology in this landscape, enabling comprehensive genomic profiling that guides targeted therapeutic interventions. This technical review examines the current global cancer epidemiology, details the experimental frameworks and clinical applications of precision diagnostics, and explores the emerging trends and persistent challenges in implementing these advanced technologies across diverse healthcare systems. The integration of NGS into routine oncology practice represents a critical pathway to mitigating the growing cancer burden through earlier detection, personalized treatment strategies, and improved survival outcomes.
The Escalating Global Cancer Burden
Current Epidemiology and Projections
Current global cancer statistics reveal a substantial and growing health challenge worldwide. In 2022, there were an estimated 20 million new cancer cases and 9.7 million cancer deaths globally, with approximately 53.5 million people living within five years of a cancer diagnosis [26]. The burden is unevenly distributed, with striking disparities based on socioeconomic development levels as measured by the Human Development Index (HDI).
Table 1: Global Cancer Incidence and Mortality for Major Cancer Types (2022)
| Cancer Type | New Cases | Percentage of Total Cases | Deaths | Percentage of Total Deaths |
|---|---|---|---|---|
| Lung | 2.5 million | 12.4% | 1.8 million | 18.7% |
| Female Breast | 2.3 million | 11.6% | 670,000 | 6.9% |
| Colorectal | 1.9 million | 9.6% | 900,000 | 9.3% |
| Prostate | 1.5 million | 7.3% | - | - |
| Stomach | 970,000 | 4.9% | 660,000 | 6.8% |
| Liver | - | - | 760,000 | 7.8% |
Projections for 2050 indicate a dramatic 77% increase in global cancer incidence, with an estimated 35 million new cases anticipated [26]. This growth reflects both population aging and growth, alongside changes in exposure to risk factors. The proportional increase in incidence is most striking in low HDI countries (142% increase) and medium HDI countries (99%), highlighting the disproportionate future burden on healthcare systems with the fewest resources.
In the United States, the American Cancer Society projects 2,041,910 new cancer cases and 618,120 cancer deaths to occur in 2025 [27]. While cancer mortality rates have continued to decline through 2022, averting nearly 4.5 million deaths since 1991, alarming disparities persist. Native American people bear the highest cancer mortality, including rates that are two to three times those in White people for kidney, liver, stomach, and cervical cancers [27].
Disparities in Cancer Burden and Care Delivery
Significant inequities in cancer burden and access to services exist across the development spectrum. For breast cancer, women in countries with a very high HDI have a 1 in 12 lifetime risk of diagnosis, with 1 in 71 dying from the disease. In contrast, women in low HDI countries have only a 1 in 27 lifetime risk of diagnosis but a 1 in 48 chance of dying from it [26]. This disparity underscores how women in lower HDI countries are 50% less likely to be diagnosed with breast cancer yet face a much higher risk of mortality due to late diagnosis and inadequate access to quality treatment.
A WHO survey of 115 countries examining universal health coverage for cancer reveals major inequalities in service availability [26]. Only 39% of participating countries covered the basics of cancer management as part of their financed core health services for all citizens. Lung cancer-related services were 4-7 times more likely to be included in health benefit packages in high-income versus lower-income countries. The most significant disparity was observed in stem-cell transplantation, which was 12 times more likely to be covered in high-income countries [26].
Foundations of Precision Diagnostics in Oncology
Next-Generation Sequencing Technologies
Next-generation sequencing has revolutionized molecular diagnostics by enabling comprehensive genomic profiling of tumors. NGS employs massively parallel sequencing architecture that allows simultaneous analysis of millions of DNA fragments, a fundamental advancement over traditional Sanger sequencing which processes only one DNA fragment at a time [9]. This high-throughput capacity enables concurrent evaluation of hundreds to thousands of genes in a single assay, providing a complete genomic landscape rather than the fragmented approach inherent to earlier technologies.
Table 2: Comparison of Genomic Analysis Technologies
| Aspect | Sanger Sequencing | Next-Generation Sequencing |
|---|---|---|
| Throughput | Single DNA fragment at a time | Massively parallel; millions of fragments simultaneously |
| Sensitivity (Detection Limit) | Low (~15-20%) | High (down to 1% for low-frequency variants) |
| Cost-Effectiveness | Cost-effective for 1-20 targets | Cost-effective for high sample volumes/many targets |
| Discovery Power | Limited; interrogates a gene of interest | High; detects novel or rare variants with deep sequencing |
| Variant Detection Capability | Limited to specific regions | Single-base resolution; detects SNPs, indels, CNVs, and structural variants |
| Primary Use | Validation of NGS results, single gene analysis | Comprehensive genomic profiling, discovery, and large-scale studies |
The major NGS platforms include Illumina sequencing, which dominates second-generation NGS with exceptionally high throughput and low error rates (typically 0.1-0.6%), and third-generation technologies such as Oxford Nanopore Technologies (ONT) and Pacific Biosciences (PacBio) [9]. Illumina uses sequencing-by-synthesis chemistry, enabling millions of DNA fragments to be sequenced in parallel on a flow cell, producing short reads (75-300 bp) that provide high coverage and precision suitable for variant calling. ONT has introduced a distinctive approach with nanopore sequencing that directly reads single DNA molecules as they traverse a protein nanopore, enabling long-read sequencing capabilities.
Experimental Frameworks for Genomic Profiling
Comprehensive Genomic Profiling (CGP)
Comprehensive Genomic Profiling represents a significant advancement in molecular diagnostics, leveraging NGS technologies to analyze a broad array of genetic alterations across multiple genes in a single, efficient test [28]. CGP offers advantages over traditional methods by requiring smaller tissue samples and reducing the time needed to test for various biomarkers. Enhancements to CGP, such as RNA fusion assays and liquid biopsies, extend its capabilities beyond genomic DNA analyses, enabling identification of gene fusions and splicing variants that provide a more complete picture of a tumor's genetic landscape.
The typical CGP workflow involves several critical steps: nucleic acid extraction from tumor tissue or liquid biopsy samples, library preparation through either amplification-based or hybrid capture-based target enrichment, sequencing on NGS platforms, bioinformatic analysis for variant calling and annotation, and clinical interpretation using curated knowledgebases [28] [29]. This integrated approach allows for simultaneous assessment of multiple biomarker classes including single nucleotide variants (SNVs), insertions/deletions (indels), copy number variations (CNVs), gene fusions, tumor mutational burden (TMB), and microsatellite instability (MSI) status.
Liquid Biopsy and Circulating Tumor DNA Analysis
Liquid biopsy refers to the non-invasive analysis of tumor-derived material, such as circulating tumor DNA (ctDNA), circulating tumor cells (CTCs), RNA, and exosomes present in bodily fluids like blood, urine, or cerebrospinal fluid [28]. This approach offers a dynamic snapshot of cancer's genetic landscape, enabling real-time assessment of tumor evolution, resistance mechanisms, and treatment efficacy. The variability in ctDNA levels across cancer types is critical for understanding its utility as a biomarker. ctDNA is detected in more than 75% of patients with advanced stages of pancreatic, colorectal, gastroesophageal, hepatocellular, bladder, ovarian, breast, head & neck cancers, or melanoma, but is less frequent (fewer than 50% of cases) in patients with primary brain, prostate, thyroid, and renal cancers [28].
Figure 1: Liquid Biopsy and ctDNA Analysis Workflow
Variant Allele Frequency (VAF) in ctDNA has emerged as a promising biomarker with significant clinical applications [28]. VAF measures genetic variation that can be assessed from both genomic (DNA) and transcriptomic (RNA) sequencing data as the encoded and expressed allele frequencies, respectively. This metric provides insights into tumor burden, treatment efficacy, and the dynamics of tumor evolution and resistance mechanisms, serving as a surrogate for mutation clonality and a tool to evaluate genomic heterogeneity.
Clinical Implementation and Therapeutic Impact
Matching Therapies to Genomic Alterations
The fundamental goal of precision oncology is to match patients with therapies that target the specific molecular alterations driving their cancer. Several studies have demonstrated the utility of this approach. In Tsimberidou et al.'s Phase I study, advanced cancer patients given treatment matched to their tumor mutations showed significantly improved overall response rate (27% vs. 5%), time to treatment failure (median of 5.2 vs. 2.2 months), and survival (median of 13.4 vs. 9.0 months) compared to patients who did not receive sequencing-matched therapy [30]. Similarly, Radovich et al. reported that progression-free survival of patients with treatments matched to their DNA mutations, copy number variations, or mRNA levels was significantly higher than that of patients receiving non-matched therapy (86 vs. 49 days) [30].
The National Cancer Institute's Molecular Analysis for Therapy Choice (NCI-MATCH) trial represents one of the most ambitious precision medicine initiatives, using NGS to screen patients for actionable mutations and assigning targeted therapies based on these molecular alterations regardless of tumor histology [29]. This basket trial approach has demonstrated that matching therapies to genomic alterations can yield clinical benefits across multiple cancer types, supporting the histology-agnostic use of targeted agents.
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Research Reagent Solutions for Precision Oncology
| Reagent/Category | Function/Application | Technical Considerations |
|---|---|---|
| Hybrid Capture Probes | Enrich specific genomic regions by hybridization | Provide greater library complexity and uniformity; suitable for DNA and RNA templates for fusion detection |
| Amplification Primers | PCR-based enrichment of specific genomic regions | Lower input requirement and faster turn-around times; uses RNA template for fusion identification |
| Cell-free DNA Extraction Kits | Isolation of ctDNA from liquid biopsy samples | Critical for liquid biopsy applications; yield and purity affect downstream analysis sensitivity |
| NGS Library Preparation Kits | Prepare nucleic acids for sequencing | Include fragmentation, end-repair, adapter ligation, and amplification steps; impact library complexity |
| Matched Germline DNA | DNA from peripheral blood mononuclear cells | Allows unequivocal assignment of variants as somatic versus germline; enables accurate TMB calculation |
| Tumor Enrichment Tools | Macro- or microdissection tools | Enrich tumor cellularity to at least 20% to mitigate false negative results in variant calling |
Variant Interpretation and Reporting Frameworks
A significant challenge in clinical NGS implementation is the annotation and clinical interpretation of identified variants. For single nucleotide variants (SNVs) and insertions/deletions (indels), many laboratories use a "hotspot"-based approach to identify actionable variants at recurrent positions known from databases like the Catalog of Somatic Mutations in Cancer (COSMIC) to definitively affect protein function [29]. Activating alterations in oncogenes such as EGFRL858R, BRAFV600E, and KRASG12D are well suited to this approach.
To supplement hotspot-based approaches, clinical NGS assays use analysis pipelines that identify alterations predicted to result in protein truncation through termination codons or frameshift mutations. Such alterations in tumor suppressor genes are generally considered deleterious. However, interpreting missense alterations remains challenging, with in silico prediction algorithms like SIFT and PolyPhen having limited specificity [29].
Guidelines for the interpretation and reporting of cancer-related variants were published in 2017 by a joint working group of the Association of Molecular Pathology (AMP), American Society of Clinical Oncology (ASCO), and College of American Pathologists (CAP) [29]. These guidelines establish standards for variant classification, clinical actionability assessment, and report content. Additionally, curated knowledgebases including OncoKB, MyCancerGenome, CIViC, and Cancer Genome Interpreter provide "levels of evidence" to support targeted therapy use for specific variants.
Figure 2: Variant Interpretation and Clinical Reporting Pipeline
Emerging Trends and Future Perspectives
Advanced Technologies Shaping Precision Oncology
The field of precision oncology continues to evolve with several emerging technologies enhancing diagnostic capabilities:
Single-Cell Multiomics: Single-cell sequencing technologies can reveal the specific effect of individual cellular components, overcoming limitations of bulk methods that mask cellular differences [31]. Since the first report of single-cell genome-wide mRNA sequencing in 2009, various methods have been developed including single-cell DNA sequencing, single-cell DNA methylome sequencing, single-cell ATAC-seq, single-cell proteomics, and single-cell metabolomics. The emerging trend is to integrate multimodal omics data within single cells to generate a holistic picture of cellular processes.
Spatial Transcriptomics and Multiomics: These technologies preserve the spatial context of cellular interactions within tissues, providing critical insights into tumor microenvironment heterogeneity and cellular ecosystems that drive cancer progression and therapy resistance [31].
Artificial Intelligence in Biomarker Discovery: AI and machine learning algorithms are being deployed to analyze complex multi-omics datasets, identify novel biomarkers, predict treatment responses, and optimize clinical trial designs [32]. For instance, ConcertAI reported that its AI-powered platform screened oncology patients for trial eligibility more than three times faster than manual review without loss of accuracy [32].
Ultra-Rapid Whole Genome Sequencing: Advances in sequencing technologies have dramatically reduced turnaround times. A landmark study demonstrated that a cloud-distributed nanopore sequencing workflow could deliver a genetic diagnosis in just 7 hours and 18 minutes, enabling timely diagnoses in critically ill patients [32].
Implementation Challenges and Barriers
Despite the demonstrated benefits of precision diagnostics, significant challenges remain in widespread clinical implementation:
Economic and Access Barriers: The cost-benefit balance and widespread accessibility present major hurdles, particularly in low- and middle-income countries [28]. Concerns about how NGS can be properly implemented for all cancer patients remain substantial, with issues of tissue sample quality and preservation, and health technology assessment frameworks varying across healthcare systems.
Interpretative Challenges: Variants of uncertain significance (VUS) pose ongoing difficulties in clinical decision-making [9]. The absence of standardized interpretation frameworks across laboratories can lead to inconsistent reporting and treatment recommendations. Additionally, the determination of "actionable mutations" lacks universal standards, with different laboratories and studies applying varying criteria [30].
Regulatory and Reimbursement Landscape: The regulatory environment for NGS tests continues to evolve, with reimbursement remaining a subject of continuing debate [29]. While a clearer regulatory path has emerged, disparities in insurance coverage for NGS testing and sequencing-matched therapies create inequities in patient access.
Clinical Trial Access: Even when actionable mutations are identified, access to matched therapies remains challenging. Data from Japan indicate that while 44% of patients are recommended new forms of therapy following comprehensive genomic profiling testing, fewer than 10% actually receive these recommended treatments [28]. This gap between molecular identification and treatment delivery represents a critical implementation challenge.
The growing global cancer burden, projected to reach 35 million new cases annually by 2050, demands transformative approaches to cancer diagnosis and treatment. Precision diagnostics, anchored by next-generation sequencing technologies, represents a paradigm shift from histology-based to genomics-driven cancer care. The integration of comprehensive genomic profiling, liquid biopsies, and advanced computational analysis enables matching of targeted therapies to individual molecular alterations, improving patient outcomes.
However, realizing the full potential of precision oncology requires addressing significant implementation challenges, including economic barriers, interpretative standardization, and equitable access across diverse healthcare settings. Emerging technologies such as single-cell multiomics, spatial transcriptomics, and artificial intelligence promise to further refine diagnostic precision. The continued evolution of precision diagnostics offers the most promising pathway to mitigating the escalating global cancer burden through earlier detection, personalized treatment strategies, and improved survival outcomes across all populations.
Cancer is fundamentally a genetic disease driven by the accumulation of genomic alterations that enable uncontrolled cell growth and proliferation. The comprehensive characterization of these alterations has become a cornerstone of precision oncology, enabling molecularly driven cancer diagnosis, prognosis, and treatment selection [3] [33]. Next-generation sequencing (NGS) has revolutionized this field by providing powerful tools to detect diverse genomic variants across entire cancer genomes, transcriptomes, and epigenomes [33]. These technologies have revealed that cancer genomes harbor several major classes of genomic alterations, each with distinct biological consequences and clinical implications. The most significant categories include single nucleotide polymorphisms (SNPs), insertions and deletions (Indels), copy number variations (CNVs), and structural variants (SVs) [34]. Understanding the nature, detection methods, and functional impact of these variant classes is essential for researchers, scientists, and drug development professionals working to advance cancer therapeutics and diagnostic approaches within the framework of precision medicine.
Classification and Definitions of Genomic Alterations
Genomic alterations in cancer span orders of magnitude in size and complexity, from single nucleotide changes to massive chromosomal rearrangements. The following table summarizes the key characteristics of the four major variant classes discussed in this whitepaper.
Table 1: Classification of Key Genomic Alterations in Cancer
| Variant Type | Size Range | Molecular Consequence | Detection Methods | Clinical/Research Significance |
|---|---|---|---|---|
| SNPs (Single Nucleotide Polymorphisms) | Single base pair | Base substitution | NGS, Sanger sequencing | Driver mutations, therapeutic targets, prognostic markers [33] |
| Indels (Insertions/Deletions) | 1-50 bp | Frameshift or in-frame alteration | NGS, PCR-based methods | Gene disruption, altered protein function [35] |
| CNVs (Copy Number Variations) | >1 kb | Gene dosage changes (gains/losses) | SNP arrays, NGS, CMA | Oncogene amplification, tumor suppressor loss [36] [37] |
| Structural Variants | >50 bp | Chromosomal rearrangements | Karyotyping, FISH, OGM, NGS | Gene fusions, chromothripsis, complex rearrangements [38] [34] |
Single Nucleotide Polymorphisms (SNPs) and Small Insertions/Deletions (Indels)
Single nucleotide polymorphisms (SNPs) represent the smallest type of genetic variation, involving the substitution of a single nucleotide at a specific genomic position. In cancer, somatic SNPs can act as driver mutations that directly promote tumorigenesis by activating oncogenes or inactivating tumor suppressor genes [35]. Insertions and deletions (Indels), typically defined as variations involving fewer than 50 base pairs, can cause frameshift mutations that disrupt the reading frame of protein-coding genes, leading to truncated or nonfunctional proteins [35]. Both SNPs and Indels are considered "small variants" and are frequently detected using targeted NGS panels, whole exome sequencing, or whole genome sequencing approaches [13]. The identification of specific SNPs and Indels has become crucial for therapeutic decision-making, as exemplified by mutations in genes such as EGFR, KRAS, and BRAF, which now have matched targeted therapies [33] [13].
Copy Number Variations (CNVs) and Structural Variants (SVs)
Copy number variations (CNVs) are defined as DNA segments larger than 1 kilobase that exhibit variable copy number compared to a reference genome [36]. In cancer, CNVs typically manifest as amplifications (gains) of oncogenes or deletions (losses) of tumor suppressor genes, leading to altered gene dosage that promotes malignant growth [37]. For example, MYCN amplification in neuroblastoma is a well-established marker of aggressive disease and poor prognosis [37].
Structural variants (SVs) encompass larger genomic rearrangements (typically >50 bp) that alter the chromosomal architecture, including translocations, inversions, insertions, and complex rearrangements [34]. Balanced SVs (e.g., inversions, translocations) do not change copy number but can create novel gene fusions or disrupt regulatory elements, while unbalanced SVs result in copy number changes [34]. Catastrophic one-step genomic events such as chromothripsis (chromosomal shattering) and chromoplexy (interconnected rearrangements) represent particularly complex SVs that can drive rapid genomic evolution in cancer [38] [34]. These complex rearrangements have been identified across cancer subtypes and are associated with aggressive tumor behavior [38].
Detection Methodologies and Experimental Protocols
The accurate detection of genomic alterations requires sophisticated technologies and carefully optimized experimental protocols. The evolution of these methods has progressively enhanced our ability to resolve increasingly complex variants.
Next-Generation Sequencing Approaches
Next-generation sequencing has become the cornerstone technology for comprehensive genomic profiling in cancer research and clinical diagnostics [3] [33]. The fundamental NGS workflow involves: (1) library preparation through fragmentation of genomic DNA and adapter ligation; (2) cluster generation and parallel sequencing using sequencing-by-synthesis chemistry; and (3) bioinformatic analysis of the resulting reads through alignment to reference genomes and variant calling [3]. Different NGS approaches provide complementary advantages: whole-genome sequencing (WGS) enables genome-wide detection of all variant types; whole-exome sequencing (WES) focuses on protein-coding regions; and targeted panels allow deep sequencing of clinically relevant genes with lower costs and faster turnaround times [3] [37] [13].
Table 2: Comparison of Major NGS Platforms and Their Applications in Oncology
| Platform/Technology | Sequencing Chemistry | Read Length | Accuracy | Primary Applications in Oncology |
|---|---|---|---|---|
| Illumina | Sequencing-by-synthesis | Short-read (75-300 bp) | Q30 (99.9%) | SNV/Indel detection, CNV analysis, gene expression profiling [33] |
| Element AVITI | Avidite Base Chemistry | Short-read | Q40 (99.99%) | Rare variant detection, liquid biopsy, low-frequency mutation calling [39] |
| Pacific Biosciences | Single-molecule real-time (SMRT) | Long-read | ~Q20-Q30 | Structural variant detection, phased variants, complex regions [33] |
| Oxford Nanopore | Nanopore sensing | Long-read | ~Q20-Q30 | Structural variant detection, real-time sequencing [33] |
The following diagram illustrates the core workflow for NGS-based detection of genomic alterations in cancer research:
Advanced Methods for Structural Variant Detection
While short-read NGS platforms excel at detecting SNPs and small Indels, more specialized approaches are often required for comprehensive structural variant detection. Optical Genome Mapping (OGM) has emerged as a powerful cytogenomic technology that visualizes ultra-long DNA molecules labeled at specific sequence motifs, providing a genome-wide view of large-scale structural changes with resolution down to approximately 500 bp [38]. OGM can detect translocations, inversions, insertions, deletions, duplications, and complex rearrangements such as chromothripsis without the need for cell culture, offering superior resolution compared to traditional cytogenetic methods [38].
For the detection of copy number variations, the Parliament2 pipeline provides a consensus approach that integrates multiple bioinformatics tools (CNVnator, Lumpy, and Delly) to improve detection accuracy from whole-genome sequencing data [36]. This multi-tool strategy helps reduce false positives and enhances the reliability of SV calling, which is particularly valuable for detecting CNVs in complex cancer genomes.
The following workflow illustrates the integrated approach for structural variant detection using multiple technologies:
The Scientist's Toolkit: Essential Research Reagents and Solutions
The experimental workflows for genomic alteration analysis depend on specialized reagents and laboratory materials that ensure sample quality and analytical precision. The following table catalogues key research reagents and their applications in cancer genomics studies.
Table 3: Essential Research Reagents and Materials for Genomic Alteration Analysis
| Reagent/Material | Manufacturer/Example | Function in Workflow | Technical Considerations |
|---|---|---|---|
| DNA Extraction Kits | QIAamp DNA FFPE Tissue Kit (Qiagen) | Isolation of high-quality DNA from formalin-fixed paraffin-embedded (FFPE) tissue | DNA concentration >20 ng/μL, A260/A280 ratio 1.7-2.2 [13] |
| DNA Quantification Assays | Qubit dsDNA HS Assay Kit (Invitrogen) | Fluorometric quantification of double-stranded DNA | More accurate for NGS than spectrophotometric methods [13] |
| Library Prep Kits | Agilent SureSelectXT Target Enrichment | Target enrichment via hybrid capture for targeted sequencing | Compatible with Illumina platforms, enables custom panel design [13] |
| NGS Library QC | Agilent High Sensitivity DNA Kit | Assessment of library fragment size distribution | Optimal size range: 250-400 bp [13] |
| Direct Labeling Enzyme | DLE-1 (Bionano) | Sequence-specific fluorescent labeling for OGM | Labels at CTTAAG motifs for optical mapping [38] |
| UHMW DNA Isolation | Bionano Prep SP BMA DNA Isolation | Isolation of ultra-high molecular weight DNA for OGM | Critical for long DNA fragments (>150 kbp N50) [38] |
Functional Impact and Clinical Applications in Precision Oncology
Genomic alterations drive oncogenesis through diverse mechanisms that disrupt normal cellular functions. Understanding these functional consequences is essential for translating genomic findings into clinical applications.
Biological Consequences of Genomic Alterations
The functional impact of genomic alterations in cancer spans multiple levels of cellular organization. SNPs and Indels can directly alter protein function by introducing amino acid substitutions, creating premature stop codons, or causing frameshifts that disrupt protein structure [35]. These changes can lead to constitutive activation of oncogenic signaling pathways or inactivation of tumor suppressor genes. CNVs affect gene dosage, potentially leading to overexpression of oncogenes through amplification or loss of tumor suppressor function through heterozygous or homozygous deletions [36] [37].
Structural variants can have particularly complex consequences, including the creation of novel gene fusion events that generate chimeric proteins with oncogenic properties, such as the BCR-ABL1 fusion in chronic myeloid leukemia [34]. SVs can also disrupt the three-dimensional organization of the genome by altering topologically associating domains (TADs), leading to inappropriate gene regulation through the repositioning of enhancers and other regulatory elements [34]. Catastrophic events like chromothripsis can cause massive genomic rearrangements that simultaneously affect dozens of genes, driving rapid tumor evolution [38] [34].
Clinical Translation and Therapeutic Targeting
The identification of genomic alterations has become fundamental to precision oncology, enabling molecularly guided treatment strategies. Several key applications include:
Therapeutic Target Identification: Specific genomic alterations serve as direct targets for matched therapies, such as EGFR inhibitors for EGFR-mutant lung cancer or PARP inhibitors for tumors with homologous recombination deficiencies [33] [13].
Diagnostic and Prognostic Biomarkers: Certain genomic alterations provide critical diagnostic information (e.g., gene fusions defining specific sarcoma subtypes) or prognostic information (e.g., MYCN amplification in neuroblastoma) that guides clinical management [37] [13].
Immunotherapy Biomarkers: Tumor mutational burden (TMB) and microsatellite instability (MSI) status, both derived from NGS profiling, help identify patients most likely to benefit from immune checkpoint inhibitors [13].
Liquid Biopsy Applications: Analysis of circulating tumor DNA (ctDNA) enables non-invasive detection of genomic alterations, monitoring of treatment response, and early detection of resistance mechanisms [37].
Drug Resistance Monitoring: Serial genomic profiling can identify emerging resistance mutations, such as secondary mutations in kinase genes that confer resistance to targeted therapies, enabling timely treatment adjustments [33].
Emerging Technologies and Future Directions
The field of cancer genomics continues to evolve rapidly with technological innovations that enhance our ability to detect and interpret genomic alterations. Single-cell sequencing technologies, including the novel Uni-C (Uniform Chromosome Conformation Capture) method, enable the profiling of 3D chromatin architecture and genomic alterations at single-cell resolution, revealing cellular heterogeneity and clonal evolution within tumors [35]. Ultra-high-accuracy sequencing platforms achieving Q40 (99.99% accuracy) and beyond significantly improve rare variant detection while reducing sequencing depth requirements, potentially lowering costs by 30-50% for applications such as liquid biopsy and minimal residual disease monitoring [39].
The integration of artificial intelligence with multi-omics data represents another promising frontier, potentially enabling more accurate variant interpretation, prediction of functional impact, and identification of novel therapeutic vulnerabilities [40]. As these technologies mature and become more accessible, they will further advance precision oncology by providing increasingly comprehensive views of the complex genomic alterations that drive cancer pathogenesis.
From Lab to Clinic: Methodological Approaches and Translational Applications of NGS
Comprehensive Genomic Profiling (CGP) via Next-Generation Sequencing (NGS) has become the cornerstone of precision oncology, enabling the systematic discovery of actionable mutations and biomarkers that guide therapeutic decisions. This technical guide examines the foundational methodologies, analytical frameworks, and clinical applications of CGP, detailing its role in identifying targetable genomic alterations across diverse malignancies. By integrating DNA and RNA sequencing, CGP facilitates a multi-omics approach that informs targeted therapy selection, immunotherapeutic strategy, and diagnostic reclassification, ultimately advancing personalized cancer treatment and drug development.
Comprehensive Genomic Profiling represents a paradigm shift in cancer diagnostics, moving beyond single-gene assays to simultaneous interrogation of hundreds of cancer-related genes. CGP employs NGS technologies to detect multiple alteration types—including single nucleotide variants (SNVs), insertions/deletions (indels), copy number alterations (CNAs), gene fusions, and genomic signatures—from minimal tissue or liquid biopsy samples [41] [42]. The integration of CGP into clinical workflows has transformed oncology, with over 90% of advanced solid tumor samples now found to harbor therapeutically actionable alterations when broad profiling is applied [41]. This comprehensive approach is particularly valuable for rare cancers, cancers of unknown primary (CUP), and tumors with complex resistance patterns, where it unveils therapeutic opportunities that would remain undetected with conventional testing methods [43] [44].
The clinical utility of CGP extends beyond simple biomarker detection to encompass diagnostic verification and refinement. Recent evidence demonstrates that CGP results can prompt diagnostic re-evaluation, leading to tumor reclassification or refinement in significant cases [43]. In one study of 28 cases where CGP findings conflicted with initial diagnoses, integrated pathological review resulted in diagnostic changes that unveiled new targeted therapy options across multiple cancer types, highlighting CGP's role as a complementary diagnostic tool [43]. This capacity to refine cancer classification and expand treatment options underscores why major oncology guidelines from NCCN, ASCO, and ESMO now recommend CGP for patients with advanced solid tumors [44].
Technological Foundations of CGP
Next-Generation Sequencing Platforms
CGP leverages both second- and third-generation NGS platforms, each with distinct advantages for clinical cancer genomics. Illumina's sequencing-by-synthesis technology dominates clinical applications due to its high throughput, low error rates (0.1-0.6%), and cost-effectiveness for large-scale projects [9]. Short-read technologies (75-300 bp) provide excellent coverage uniformity and variant detection sensitivity, making them ideal for identifying SNVs and indels. In contrast, Oxford Nanopore Technologies (ONT) and Pacific Biosciences (PacBio) offer long-read capabilities that enable direct reading of single DNA molecules, providing advantages for detecting structural variants, resolving complex genomic regions, and characterizing fusion events [9]. The selection of an appropriate NGS platform depends on the specific clinical or research question, with considerations including required sensitivity, turnaround time, and the types of variants being targeted.
Comparative Technical Capabilities
The evolution from Sanger sequencing to NGS has dramatically improved the scale and efficiency of genomic analysis. Unlike Sanger sequencing, which processes one DNA fragment at a time, NGS employs massively parallel sequencing to simultaneously analyze millions of fragments, enabling comprehensive genomic coverage with significantly improved sensitivity for detecting low-frequency variants [9]. This parallel architecture allows NGS to detect variants down to ~1% variant allele frequency (VAF), compared to Sanger's 15-20% detection limit, making it far superior for identifying subclonal populations in heterogeneous tumor samples [9]. Additionally, NGS provides single-base resolution across hundreds to thousands of genes in a single assay, delivering a complete molecular portrait of a tumor that guides therapeutic decision-making.
Table 1: Comparison of Sequencing Technologies
| Aspect | Sanger Sequencing | Next-Generation Sequencing (NGS) |
|---|---|---|
| Throughput | Single DNA fragment at a time | Massively parallel; millions of fragments simultaneously |
| Sensitivity (Detection Limit) | Low (~15-20%) | High (down to ~1% for low-frequency variants) |
| Cost-Effectiveness | Cost-effective for 1-20 targets, high for large regions | Cost-effective for high sample volumes/many targets |
| Discovery Power | Limited; interrogates a gene of interest | High; detects novel or rare variants with deep sequencing |
| Variant Detection Capability | Limited to specific regions; single gene analysis | Single-base resolution; detects SNPs, indels, CNVs, SVs, and large chromosomal rearrangements |
| Primary Use | Validation of NGS results, single gene analysis | Comprehensive genomic profiling, discovery, and large-scale studies |
CGP Methodologies and Workflows
Specimen Collection and Processing
The CGP workflow begins with appropriate specimen collection and processing, which critically impacts assay performance. Formalin-fixed, paraffin-embedded (FFPE) tissue remains the most common source material, though CGP can also be performed on fresh frozen tissue, liquid biopsy samples (blood, pleural effusion, ascites), and fine-needle aspirates [42]. For FFPE specimens, pathologist-guided macrodissection or microdissection ensures adequate tumor content, with most validated CGP assays requiring ≥20% tumor nuclei for optimal performance. The extraction of high-quality nucleic acids is paramount, with simultaneous isolation of both DNA and RNA enabling complementary genomic and transcriptomic analyses. For tumor-normal sequencing, matched normal tissue (typically from blood or saliva) is collected to distinguish somatic from germline variants, reducing false positives and enabling accurate calculation of tumor mutational burden [41].
Library Preparation and Sequencing
Library preparation involves fragmenting nucleic acids, attaching platform-specific adapters, and amplifying target regions. Hybridization capture-based methods are preferred for CGP as they enable efficient targeting of large gene panels (500+ genes) or entire exomes while maintaining uniform coverage [41]. These methods use biotinylated oligonucleotide baits to capture genomic regions of interest from fragmented DNA libraries, followed by PCR amplification to create sequencing-ready libraries. For whole transcriptome sequencing, RNA is converted to cDNA before library preparation, enabling detection of fusion genes, alternative splicing events, and gene expression profiles. The prepared libraries are then sequenced on NGS platforms, with sequencing depth tailored to clinical requirements—≥500x median coverage is standard for tissue-based CGP to reliably detect low-VAF variants, while liquid biopsy assays often require ≥10,000x coverage to identify rare circulating tumor DNA fragments [41].
Bioinformatics Analysis Pipeline
The bioinformatics pipeline for CGP involves multiple computational steps to transform raw sequencing data into clinically actionable information. Read alignment to reference genomes (e.g., GRCh38) is performed using optimized aligners like BWA-MEM or STAR, followed by duplicate marking, base quality recalibration, and local realignment around indels [9]. Somatic variant calling utilizes specialized algorithms (e.g., MuTect2, VarScan) to identify SNVs and indels, while additional tools detect CNAs (CONTRA, ADTEx), structural variants (Manta, DELLY), and gene fusions (STAR-Fusion, Arriba) [41]. Critical quality control metrics including coverage uniformity, base quality scores, and contamination estimates are assessed at each step. The final variant annotation incorporates information from curated databases (OncoKB, CIViC, ClinVar) to classify alterations by clinical actionability, therapeutic associations, and functional impact, generating a comprehensive molecular profile for clinical interpretation [44].
Actionable Alterations and Biomarker Detection
Landscape of Therapeutically Actionable Alterations
CGP reveals a complex landscape of genomic alterations across cancer types, with recent large-scale analyses demonstrating that 92.0% of patient samples harbor therapeutically actionable alterations when comprehensive profiling is applied [41]. Among these, single nucleotide variants (SNVs) represent the most frequent alteration type, present in 85.3% of samples, followed by copy number variant amplifications (20.2%) and deletions (6.6%) [41]. Indels, gene fusions, and alternative transcripts occur at lower frequencies (6.1%, 3.9%, and 0.6% respectively) but often have profound clinical implications, particularly for rare cancers and tumors of unknown origin [41]. The distribution of alteration types varies significantly by cancer lineage, with prostate cancers showing lower SNV prevalence but higher fusion frequencies (e.g., TMPRSS2-ERG in 42.0% of cases), while breast cancers demonstrate elevated CNA amplification rates [41].
Table 2: Frequency of Actionable Alterations by Tumor Type
| Tumor Type | Samples with On-Label Biomarkers | Samples with Off-Label Biomarkers | Most Frequent Actionable Alterations |
|---|---|---|---|
| Non-Small Cell Lung Cancer (NSCLC) | 19.8% (EGFR) | 28.0% (collective) | EGFR (19.8%), MET exon 14 skipping, ERBB2, ALK fusions |
| Breast Cancer | 42.2% (PIK3CA in HR+/HER2-) | 31.5% (collective) | PIK3CA (42.2% in HR+/HER2-), BRCA1/2, HER2 |
| Colorectal Cancer (CRC) | 15.7% (collective) | 35.2% (collective) | KRAS, NRAS, BRAF V600E, MSI-High |
| Prostate Cancer | 22.3% (collective) | 41.8% (collective) | TMPRSS2-ERG fusion (42.0%), PTEN, BRCA2 |
| Central Nervous System (CNS) Tumors | 5.4% (collective) | 43.9% (collective) | IDH1/2, BRAF V600E, TERT promoter |
| Epithelial Ovarian Cancer | 18.9% (collective) | 33.7% (collective) | BRCA1/2 (germline and somatic), homologous recombination deficiencies |
Biomarkers for Targeted Therapy
CGP enables detection of specific biomarkers that predict response to targeted therapies, with distinct patterns emerging across cancer types. In NSCLC, CGP identifies EGFR mutations (19.8%), ALK fusions, ROS1 fusions, RET fusions, and MET exon 14 skipping events, each with matched targeted therapies [44] [45]. Similarly, in breast cancer, CGP reveals PIK3CA mutations (42.2% in HR+/HER2- disease), germline BRCA1/2 mutations, and HER2 amplifications that guide treatment with PI3K inhibitors, PARP inhibitors, and anti-HER2 agents, respectively [41] [45]. Beyond these established biomarkers, CGP uncovers rare but clinically significant alterations including NTRK fusions (<1% of solid tumors but with approved therapies) and RET fusions across multiple cancer types, enabling tissue-agnostic treatment approaches [44]. The comprehensive nature of CGP is particularly valuable for identifying concurrent alterations that may mediate resistance to targeted therapies, informing rational combination strategies.
Immunotherapy Biomarkers
CGP plays an increasingly important role in identifying biomarkers that predict response to immune checkpoint inhibitors. Tumor mutational burden (TMB), defined as the total number of somatic mutations per megabase of DNA, represents a quantifiable genomic signature that CGP measures across the entire coding genome or large gene panels [41]. High TMB (TMB-H) correlates with improved response to immunotherapy across multiple cancer types and now serves as a tissue-agnostic predictive biomarker [41]. Similarly, CGP enables detection of microsatellite instability (MSI) status through computational analysis of microsatellite regions, with MSI-high tumors demonstrating exceptional responses to PD-1/PD-L1 inhibitors [41]. Additional immunotherapy biomarkers detectable by CGP include PD-L1 amplification, POLE/POLD1 mutations associated with ultra-hypermutation, and specific mutational signatures that reflect underlying DNA repair deficiencies, collectively providing a comprehensive immunogenomic profile to guide immunotherapy decisions.
Analytical Considerations and Quality Metrics
Detection Sensitivity and Variant Allele Frequency
A critical aspect of CGP is establishing appropriate detection thresholds for variant calling, particularly for low-frequency alterations present in heterogeneous tumor samples. The limit of detection (LOD) for most validated CGP assays ranges from 1-5% variant allele frequency (VAF) for tissue samples, with lower thresholds (0.1-0.5%) achievable through unique molecular identifiers and error-suppression techniques [41]. Importantly, 13.7% of tumor samples harbor at least one clinically relevant alteration with VAF <5%, and 9.8% of hotspot alterations associated with FDA-approved therapies fall below this threshold, highlighting the importance of sensitive detection methods [41]. For liquid biopsy applications, even greater sensitivity is required to detect rare circulating tumor DNA fragments against a background of normal cell-free DNA, with LODs of 0.1% VAF now achievable using advanced error-correction methods. These technical considerations directly impact clinical utility, as subclonal alterations may drive resistance or represent emerging therapeutic targets.
Quality Assurance and Validation
Robust quality assurance measures are essential for clinical-grade CGP, encompassing pre-analytical, analytical, and post-analytical phases. Key quality metrics include DNA/RNA quality assessments (e.g., DIN for DNA, RIN for RNA), library complexity measurements, sequencing coverage uniformity, and minimum coverage thresholds (typically ≥500x for tissue, ≥10,000x for liquid biopsy) [41]. Validation of CGP assays requires establishing accuracy, precision, reproducibility, and sensitivity across all detectable variant types using reference materials and clinical samples with orthogonal verification. For clinical implementation, ongoing quality monitoring includes periodic proficiency testing, reference standard analysis, and continuous bioinformatics pipeline verification. Additionally, validation of variant interpretation and classification processes ensures consistent reporting of actionable findings, with many institutions implementing molecular tumor boards to standardize clinical recommendations based on CGP results [42].
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Key Research Reagents for Comprehensive Genomic Profiling
| Reagent/Material | Function | Application Notes |
|---|---|---|
| FFPE Tissue Sections | Preserved tumor material for DNA/RNA extraction | Standard specimen type; requires pathologist review for tumor enrichment |
| Blood Collection Tubes (cfDNA) | Stabilization of circulating cell-free DNA | Enables liquid biopsy applications; requires processing within specified timeframes |
| Hybridization Capture Baits | Sequence-specific enrichment of target regions | Designed to cover coding regions of cancer-related genes; panel size varies (500+ genes) |
| NGS Library Preparation Kits | Fragment end-repair, adapter ligation, PCR amplification | Platform-specific chemistry (Illumina, Nanopore, PacBio) |
| Unique Molecular Identifiers (UMIs) | Tagging of original DNA molecules | Reduces sequencing errors; enables accurate variant calling at low frequencies |
| Matched Normal DNA | Germline variant filtering | Blood or saliva-derived; distinguishes somatic from germline alterations |
| Reference Standard Materials | Assay validation and quality control | Characterized genomic DNA with known variants at defined allele frequencies |
| Bioinformatics Pipelines | Variant calling, annotation, and interpretation | Integrated software solutions (e.g., Illumina DRAGEN, custom workflows) |
Comprehensive Genomic Profiling has fundamentally transformed oncology research and clinical practice by providing an unprecedented comprehensive view of the molecular landscape of cancer. Through simultaneous detection of diverse alteration types—SNVs, indels, CNAs, fusions, and genomic signatures—CGP reveals therapeutic opportunities across the spectrum of human malignancies. The integration of CGP into drug development pipelines has accelerated targeted therapy development, particularly in the tissue-agnostic setting, while its implementation in clinical care has improved diagnostic accuracy, therapeutic matching, and patient outcomes. As NGS technologies continue to evolve, CGP methodologies will undoubtedly expand, incorporating single-cell analyses, spatial transcriptomics, and artificial intelligence-driven interpretation to further refine personalized cancer treatment strategies. The ongoing challenge remains to make these advanced genomic technologies accessible across diverse healthcare settings while addressing the computational and interpretative complexities inherent in comprehensive genomic analysis.
Liquid Biopsy and Circulating Tumor DNA (ctDNA) for Real-Time Monitoring
The clinical management of cancer is undergoing a transformative shift with the integration of liquid biopsy into routine practice. This approach involves the isolation and analysis of circulating tumor DNA (ctDNA)—short fragments of DNA released into the bloodstream by tumor cells through apoptosis, necrosis, or active secretion [46] [47]. As a minimally invasive tool, liquid biopsy overcomes critical limitations of traditional tissue biopsies, including invasiveness, inability to capture tumor heterogeneity, and impracticality for serial monitoring [48] [49]. Within the broader framework of next-generation sequencing (NGS) in precision oncology, ctDNA analysis provides a dynamic snapshot of tumor genetics, enabling real-time treatment selection, response monitoring, resistance detection, and assessment of minimal residual disease (MRD) [47] [50]. The half-life of ctDNA is remarkably short (estimated between 16 minutes and several hours), facilitating almost real-time tracking of tumor burden and clonal evolution [47]. This technical guide details the methodologies, analytical validation, clinical applications, and implementation frameworks for utilizing ctDNA as a pivotal biomarker in oncology research and drug development.
Core Methodologies for ctDNA Analysis
The accurate detection of ctDNA is technically challenging due to its low abundance in plasma, sometimes constituting less than 0.01% of total cell-free DNA (cfDNA), especially in early-stage cancers or low-shedding tumors [46] [47]. Consequently, highly sensitive and specific methods are required.
Polymerase Chain Reaction (PCR)-Based Methods
PCR-based techniques are widely used for targeted mutation detection due to their high sensitivity, rapid turnaround, and cost-effectiveness.
- Digital PCR (dPCR) and Droplet Digital PCR (ddPCR): These methods partition a single PCR reaction into thousands of nanoliter-sized droplets or chambers, allowing absolute quantification of mutant DNA molecules with a sensitivity of 0.1% variant allele frequency (VAF) or better. They are ideal for tracking known hotspot mutations (e.g., KRAS G12D, BRAF V600E) [47].
- BEAMing (Beads, Emulsion, Amplification, and Magnetics): This technology combines dPCR with flow cytometry to detect and enumerate specific mutant sequences, demonstrating high sensitivity in clinical studies [51].
These targeted approaches are powerful for monitoring specific driver mutations in cancers such as melanoma (BRAF), lung cancer (KRAS), and breast cancer (ESR1, PIK3CA) but are limited by the number of mutations that can be simultaneously interrogated [47].
Next-Generation Sequencing (NGS)-Based Approaches
NGS technologies provide a comprehensive landscape of genomic alterations, enabling untargeted (tumor-agnostic) or targeted (tumor-informed) profiling.
- Tumor-Informed Approaches: These require prior sequencing of the patient's tumor tissue to identify a set of patient-specific somatic mutations (e.g., 16-50 clonal single nucleotide variants). Ultra-sensitive NGS assays are then designed to track these mutations in plasma. Examples include Signatera (NGS-based) and CAPP-Seq (CAncer Personalized Profiling by deep Sequencing) [47].
- Tumor-Naïve (Agnostic) Approaches: These panels target recurrently mutated genes in cancer without prior knowledge of the patient's tumor genome. Examples include commercial panels like Guardant360 CDx, FoundationOne Liquid CDx, and Tempus xF [52] [49]. These large panels (ranging from 105 to 544 genes) can detect single nucleotide variants (SNVs), insertions/deletions (indels), copy number variants (CNVs), gene fusions, and genomic features like microsatellite instability (MSI) and tumor mutational burden (TMB) [49] [13].
A critical innovation in NGS-based ctDNA analysis is the use of Unique Molecular Identifiers (UMIs). UMIs are short random barcodes ligated to each DNA fragment prior to PCR amplification. This allows for bioinformatic correction of PCR amplification errors and sequencing artifacts, significantly improving the signal-to-noise ratio and enabling the detection of variants at frequencies as low as 0.1% [47]. Further refinements like Duplex Sequencing (tagging and sequencing both strands of the DNA duplex) and the recently developed CODEC method have pushed sequencing accuracy up to 1000-fold higher than conventional NGS [47].
Table 1: Comparison of Key ctDNA Analysis Technologies
| Technology | Key Principle | Sensitivity (Typical VAF) | Multiplexing Capability | Primary Application |
|---|---|---|---|---|
| ddPCR/dPCR | End-point quantification via sample partitioning | ~0.01% - 0.1% | Low (1- few targets) | Tracking known hotspot mutations |
| BEAMing | PCR on magnetic beads in emulsion | ~0.01% | Medium | Enumeration of specific mutant alleles |
| Tumor-Informed NGS | Tracking patient-specific mutations from tumor tissue | ~0.01% | High (16-50 variants) | MRD detection, therapy monitoring |
| Tumor-Naïve NGS Panels | Hybrid-capture of known cancer genes | ~0.1% - 0.25% | Very High (100+ genes) | Comprehensive genomic profiling |
| Whole Genome/Exome Sequencing | Sequencing all coding/whole genome regions | ~1% - 5% | Extremely High | Discovery research, novel biomarker identification |
Analytical Validation and Performance
Rigorous validation is essential before deploying ctDNA tests in clinical or research settings. Key performance parameters include sensitivity, specificity, limit of detection (LOD), and limit of quantification (LOQ).
The Tempus xF assay (a 105-gene panel) was validated using 310 samples, demonstrating an analytical sensitivity of 93.75% for SNVs at 0.25% VAF, 95.83% for indels at ≥0.5% VAF, and 100% for CNVs at ≥0.5% VAF. Its specificity was 100% for SNVs, indels, and rearrangements at ≥0.25% VAF [49]. The HPV-SEQ assay, an NGS-based method for detecting HPV16/18 DNA in oropharyngeal cancer, also demonstrated an exceptional limit of quantification and high precision in its validation [53].
A 2024 meta-analysis of ctDNA-based NGS for advanced non-small cell lung cancer (aNSCLC) reported an overall pooled sensitivity of 0.69 (95% CI: 0.63–0.74) and a specificity of 0.99 (95% CI: 0.97–1.00) compared to tissue biopsy [52]. However, sensitivity varied significantly by driver gene: 0.77 for KRAS, 0.68 for EGFR, but only 0.29 for ROS1 fusions, highlighting that alteration type and tumor shedding impact detectability [52]. A separate meta-analysis on melanoma found a pooled sensitivity of 0.73 and specificity of 0.94 for ctDNA, with an area under the SROC curve of 0.93, confirming high diagnostic accuracy [51].
Table 2: Analytical Performance of Selected ctDNA Assays from Validation Studies
| Assay / Study | Variant Type | Input | Sensitivity | Specificity | Key Metric |
|---|---|---|---|---|---|
| Tempus xF [49] | SNVs | 30 ng cfDNA | 93.75% (at 0.25% VAF) | 100% | Analytical Performance |
| Tempus xF [49] | Indels | 30 ng cfDNA | 95.83% (at ≥0.5% VAF) | 100% | Analytical Performance |
| Tempus xF [49] | CNVs | 10 ng cfDNA | 100% (at ≥0.5% VAF) | 96.2% | Analytical Performance |
| NSCLC Meta-Analysis [52] | Any mutation | Pooled | 0.69 (95% CI: 0.63–0.74) | 0.99 (95% CI: 0.97–1.00) | Clinical Concordance |
| NSCLC Meta-Analysis [52] | KRAS mutations | Pooled | 0.77 (95% CI: 0.63–0.86) | N/R | Gene-Specific Sensitivity |
| Melanoma Meta-Analysis [51] | BRAF mutations | Pooled | 0.73 (95% CI: 0.70–0.75) | 0.94 (95% CI: 0.91–0.96) | Diagnostic Accuracy |
Critical Pre-Analytical and Bioinformatics Considerations
Robust ctDNA analysis requires stringent pre-analytical protocols and sophisticated bioinformatics.
- Sample Collection and Processing: Blood must be collected in specialized tubes (e.g., Streck Cell-Free DNA BCT) that stabilize nucleated cells and prevent cfDNA background dilution. Plasma separation via double centrifugation should occur within hours of collection [48] [47].
- Germline and Clonal Hematopoiesis (CH) Contamination: A significant challenge is distinguishing true somatic tumor variants from those originating from white blood cells due to CH. The Tempus xF assay addressed this by using a Bayesian dynamic filtering method with matched normal buffy coat sequencing, which reduced false-positive calls by 11.45% [49]. Tumor-informed approaches inherently avoid this issue by focusing on mutations previously identified in the tumor tissue.
- Circulating Tumor Fraction Estimation (ctFE): The overall fraction of ctDNA in total cfDNA is a critical quality metric. The OTTER algorithm, used with the Tempus xF assay, estimates ctFE from targeted-panel sequencing data, which correlates with disease burden and improves variant calling accuracy [49].
Experimental Protocols for Key Applications
This section outlines detailed protocols for core ctDNA analyses.
Protocol: Longitudinal Therapy Monitoring using a Tumor-Informed ctDNA Assay
Purpose: To quantitatively monitor tumor burden and detect molecular relapse during and after treatment. Background: Tumor-informed assays are the gold standard for sensitivity in MRD detection and therapy monitoring [47].
Procedure:
- Baseline Tumor Sequencing: Sequence the patient's FFPE tumor tissue (e.g., using a >500-gene panel or whole exome sequencing) alongside a matched normal sample (e.g., buffy coat) to identify ~16-50 patient-specific, clonal somatic mutations.
- Custom Assay Design: Design a personalized multiplex PCR assay targeting the selected mutations.
- Baseline and Serial Blood Collection: Collect peripheral blood (e.g., 2x10 mL Streck tubes) at predefined timepoints:
- T0: Pre-treatment (baseline)
- T1-Tn: During treatment (e.g., every 2-4 cycles)
- Post-Treatment: Every 3-6 months for surveillance
- Plasma Processing and cfDNA Extraction: Isolate plasma via double centrifugation (e.g., 1600xg for 10 min, then 16,000xg for 10 min). Extract cfDNA using silica-membrane or bead-based kits. Quantify cfDNA with a fluorescent assay.
- Library Preparation and Sequencing: Construct sequencing libraries from the extracted cfDNA, incorporating UMIs. Amplify the libraries using the custom-designed primer panel. Sequence on a high-throughput instrument (e.g., Illumina NextSeq) to achieve a minimum of 100,000x raw coverage.
- Bioinformatic Analysis:
- Process raw sequencing data (demultiplexing, adapter trimming).
- Group reads by UMI to generate consensus sequences and eliminate PCR/sequencing errors.
- Align consensus reads to the reference genome.
- Detect and quantify the patient-specific mutations.
- Calculate the mean variant allele frequency across all tracked mutations to represent the ctDNA level.
- Data Interpretation: A positive ctDNA result (ctDNA detection) at any point after treatment initiation indicates the presence of MRD or progressive disease. Serial decreases in ctDNA levels (e.g., clearance) correlate with favorable treatment response, while rising levels indicate progression or emerging resistance [47] [50].
Protocol: Analytical Validation of an NGS-Based Liquid Biopsy Assay
Purpose: To determine the sensitivity, specificity, LOD, and LOQ of a laboratory-developed ctDNA test. Background: This follows guidelines from regulatory bodies (e.g., FDA, CAP/CLIA) and is essential for assay credibility [53] [49].
Procedure:
- Reference Material Preparation: Acquire or create well-characterized reference standards. These can be:
- Commercial ctDNA Reference Standards: e.g., serially diluted, fragmented DNA from cancer cell lines with known mutations in a wild-type background.
- Contrived Samples: Mix genomic DNA from cancer cell lines with known mutations into wild-type human cfDNA or sheared gDNA to simulate specific VAFs (e.g., 2%, 1%, 0.5%, 0.25%, 0.1%).
- Precision and Reproducibility Testing:
- Repeatability (Intra-assay): Process and sequence the same reference sample (e.g., at 0.5% VAF) in at least 3-5 replicates within the same sequencing run.
- Intermediate Precision (Inter-assay): Process and sequence the same reference sample across different days, by different operators, and/or on different sequencing instruments.
- Limit of Detection (LOD) Determination: Test a dilution series of reference materials (e.g., from 1% to 0.1% VAF) with 20+ replicates per level. The LOD is the lowest VAF at which ≥95% of replicates test positive.
- Accuracy and Concordance Studies:
- Orthogonal Method Comparison: Test a set of patient plasma samples (n≥40) with both the novel NGS assay and a validated orthogonal method (e.g., ddPCR or another commercial ctDNA assay). Calculate positive/negative percent agreement.
- Tumor Tissue Concordance: Test a cohort of patients (n≥50) with matched tissue and plasma samples. Compare variants detected in plasma (via the NGS assay) with those identified in tissue (the reference standard). Report positive and negative predictive values.
The Scientist's Toolkit: Essential Research Reagents & Materials
Table 3: Key Reagents and Materials for ctDNA Research
| Item | Function/Description | Example Products / Technologies |
|---|---|---|
| Blood Collection Tubes | Stabilizes nucleated cells for up to several days, preventing lysis and release of genomic DNA that dilutes ctDNA. | Streck Cell-Free DNA BCT, PAXgene Blood ccfDNA Tubes |
| Nucleic Acid Extraction Kits | Isolation of high-purity, short-fragment cfDNA from plasma. | QIAamp Circulating Nucleic Acid Kit (Qiagen), MagMAX Cell-Free DNA Isolation Kit (Thermo Fisher) |
| DNA Quantification Kits | Accurate fluorometric quantification of low-concentration, short-fragment DNA; superior to UV spectrophotometry. | Qubit dsDNA HS Assay (Thermo Fisher) |
| Library Prep Kits | Preparation of sequencing libraries from low-input cfDNA. | KAPA HyperPrep Kit (Roche), ThruPLEX Plasma-Seq Kit (Takara Bio) |
| Hybrid Capture Panels | Target enrichment for NGS; biotinylated oligonucleotide baits capture genomic regions of interest. | IDT xGen Lockdown Probes, Agilent SureSelectXT |
| Unique Molecular Indices (UMIs) | Short random barcodes ligated to each DNA fragment pre-amplification to enable error correction. | TruSeq Unique Dual Indexes (Illumina), Custom UMI Adapters |
| Reference Standards | Controls with known mutations at defined VAFs for assay validation and quality control. | Seraseq ctDNA Mutation Mix (LGC SeraCare), Horizon Multiplex I cfDNA Reference Standard |
| Bioinformatics Pipelines | Software for processing raw data, UMI consensus building, variant calling, and filtering. | Illumina Dragen, BWA-Mutect2-GATK, Custom In-House Pipelines |
Clinical Integration and Utility in Drug Development
The integration of ctDNA analysis is advancing both clinical oncology and therapeutic development.
In real-world clinical practice, NGS-based liquid biopsy successfully identifies actionable targets. A South Korean study of 990 patients with advanced solid tumors found that 26.0% harbored Tier I variants (strong clinical significance), and 13.7% of those patients subsequently received NGS-informed therapy, with 37.5% achieving a partial response [13]. Serial ctDNA monitoring dynamically guides treatment decisions. Real-world data from a precision oncology center demonstrated that ctDNA positivity indicating MRD prompted therapy escalation, while ctDNA clearance enabled safe treatment de-intensification [50].
In drug development, ctDNA serves as a pharmacodynamic biomarker for early efficacy signals, helps identify mechanisms of acquired resistance (e.g., emergent EGFR T790M mutations after first-line osimertinib therapy), and can be a potential enrichment biomarker for clinical trial recruitment [47]. The high concordance between ctDNA-matched and tissue-matched therapies in terms of progression-free survival (PFS) and overall survival (OS) further supports its utility as a surrogate endpoint in clinical trials [52].
As of early 2025, at least 20 recruiting or not-yet-recruiting clinical trials in the U.S. are actively exploring the combination of immunotherapy and liquid biopsy, highlighting its growing role in evaluating novel therapeutic combinations [48].
Liquid biopsy for ctDNA analysis has firmly established itself as an indispensable tool in the precision oncology arsenal. By providing a minimally invasive, real-time molecular portrait of tumor dynamics, it is revolutionizing cancer monitoring, treatment modification, and resistance management. The continued evolution of ultra-sensitive NGS methodologies, robust bioinformatic pipelines for error suppression, and standardized protocols will be crucial for overcoming current challenges related to sensitivity in very early-stage disease and low-shedding tumors. Future directions include the integration of multi-omic liquid biopsy data (combining ctDNA with CTCs, extracellular vesicles, and fragmentomics), its expanded application in early cancer detection and screening, and its formal validation as a surrogate endpoint in clinical trials to accelerate drug development. As evidence of its clinical utility continues to accumulate, liquid biopsy is poised to become a cornerstone of cancer management, enabling truly dynamic and personalized therapeutic strategies.
Within the framework of precision oncology, next-generation sequencing (NGS) has enabled the identification of predictive biomarkers that are crucial for personalizing cancer immunotherapy. Immune checkpoint inhibitors (ICIs) have transformed oncology, offering durable responses in malignancies such as non-small cell lung cancer (NSCLC), melanoma, and triple-negative breast cancer (TNBC) [54]. However, only a subset of patients derives clinical benefit, underscoring the critical need for robust predictive biomarkers to guide therapy selection, reduce unnecessary toxicity, and optimize clinical outcomes [54] [55]. This technical guide focuses on three cornerstone biomarkers—tumor mutational burden (TMB), microsatellite instability (MSI), and programmed death-ligand 1 (PD-L1)—detailing their biology, clinical utility, and measurement methodologies within the context of NGS-driven precision oncology.
Biomarker Fundamentals and Clinical Utility
Programmed Death-Ligand 1 (PD-L1)
Mechanism and Biology: PD-L1 is a ligand expressed on antigen-presenting cells and tumor cells. Its expression is often induced by interferon-gamma within the tumor microenvironment (TME). Binding of PD-L1 to its receptor PD-1 on T cells inhibits T-cell activation, leading to immune tolerance. ICIs targeting the PD-1/PD-L1 axis (e.g., pembrolizumab, nivolumab, atezolizumab) disrupt this interaction, restoring antitumor immunity [54].
Clinical Application and Limitations: PD-L1 is a key biomarker in NSCLC. The KEYNOTE-024 trial demonstrated that patients with PD-L1 expression ≥50% experienced improved outcomes with pembrolizumab versus chemotherapy, with a median overall survival (OS) of 30 months versus 14.2 months [54]. However, the predictive accuracy of PD-L1 is constrained by assay variability, tumor heterogeneity, and dynamic biomarker expression [54] [55]. In fact, PD-L1 demonstrates predictive value in only 28.9% of FDA approvals for ICIs, highlighting its limitation as a standalone biomarker [55].
Microsatellite Instability (MSI)
Mechanism and Biology: MSI and mismatch repair deficiency (dMMR) reflect defects in DNA repair pathways, commonly observed in colorectal cancer. This results in a high mutational burden and increased neoantigen formation, enhancing tumor immunogenicity [54].
Clinical Application and Limitations: MSI-high/dMMR status received tissue-agnostic FDA approval for pembrolizumab in 2017. Trials such as KEYNOTE-016, -164, and -158 showed MSI-high tumors had a 39.6% overall response rate with durable responses in 78% of cases [54]. MSI-H/dMMR testing is now recommended by ASCO and NCCN guidelines [54]. Its utility, while profound, is limited to a subset of patients across various cancer types [56].
Tumor Mutational Burden (TMB)
Mechanism and Biology: TMB quantifies the total number of somatic non-synonymous mutations per megabase of genomic sequence. A higher TMB is correlated with a greater likelihood of generating immunogenic neoantigens, making it a predictive biomarker for ICI response [57] [58]. The immune system can recognize these neoantigens as "non-self," triggering an anti-tumor immune response that is enhanced by ICIs [58].
Clinical Application and Limitations: Pembrolizumab received FDA approval for TMB-high (≥10 mutations/Mb) solid tumors based on the KEYNOTE-158 trial, which showed a 29% objective response rate versus 6% in low-TMB tumors [54] [57]. A meta-analysis of 26 studies involving 5,712 patients demonstrated that high-TMB groups had better overall survival and progression-free survival with ICI treatment [57]. However, standardization of TMB calculation methods and cutoff values remains a critical challenge for its clinical implementation [57] [58].
Table 1: Clinical Utility of Key Predictive Biomarkers
| Biomarker | Biological Mechanism | Key Clinical Trial Evidence | FDA-Approved Context | Major Limitations |
|---|---|---|---|---|
| PD-L1 | Ligand expressed on tumor and immune cells; binds PD-1 on T cells to suppress anti-tumor immunity [54] | KEYNOTE-024: mOS 30 mo vs 14.2 mo (chemotherapy) in NSCLC with PD-L1 ≥50% [54] | NSCLC (1st line), various other cancers [54] | Assay variability, tumor heterogeneity, dynamic expression, predictive in <30% of FDA approvals [54] [55] |
| MSI-H/dMMR | Defective DNA mismatch repair; high frameshift mutations and neoantigen load [54] | KEYNOTE-158: 39.6% ORR in MSI-H tumors; 78% durable responses [54] | Tissue-agnostic for advanced solid tumors [54] [56] | Limited to a small subset of patients across cancer types [54] |
| TMB-H | High somatic mutation count; increased immunogenic neoantigen formation [57] [58] | KEYNOTE-158: 29% ORR vs 6% in low-TMB tumors [54] [57] | Tissue-agnostic (TMB ≥10 mut/Mb) [54] [57] | Lack of standardized cutoffs, panel-based estimation variability, cost [57] [58] |
Experimental Protocols and Measurement Methodologies
PD-L1 Immunohistochemistry (IHC) Scoring
Protocol Overview: PD-L1 expression is primarily measured via immunohistochemistry (IHC) on formalin-fixed paraffin-embedded (FFPE) tumor tissue sections. The scoring methodology varies depending on the specific approved assay and antibody clone.
Detailed Methodology:
- Tissue Preparation: Cut 4-5 µm sections from FFPE tissue blocks.
- Staining: Perform IHC using validated anti-PD-L1 antibodies (e.g., clones 22C3, 28-8, SP142, SP263) on an automated staining platform according to manufacturer specifications.
- Scoring and Quantification:
- Tumor Proportion Score (TPS): Used for clones like 22C3 and 28-8. It is the percentage of viable tumor cells exhibiting partial or complete membrane staining. A TPS ≥1% or ≥50% is often used as a predictive cutoff, depending on the clinical indication [54] [59].
- Combined Positive Score (CPS): Calculated as the number of PD-L1 staining cells (tumor cells, lymphocytes, macrophages) divided by the total number of viable tumor cells, multiplied by 100. A CPS ≥10 is a common cutoff in some cancer types like gastric cancer.
- Tumor Area Scoring: The SP142 assay (for atezolizumab) focuses on the percentage of tumor area occupied by PD-L1 staining tumor-infiltrating immune cells [59].
Limitations: The lack of standardization across different antibody clones, scoring systems, and platforms contributes to inter-observer variability and complicates cross-assay comparisons [55].
MSI and dMMR Testing
Protocol Overview: MSI status can be determined either indirectly via IHC for MMR protein expression or directly via polymerase chain reaction (PCR)- or NGS-based methods for detecting instability in microsatellite regions.
Detailed Methodology:
- IHC for MMR Proteins:
- Perform IHC on FFPE sections for the four core MMR proteins: MLH1, MSH2, MSH6, and PMS2.
- Loss of nuclear expression in tumor cells, with intact staining in internal positive controls (e.g., stromal cells, lymphocytes), indicates dMMR.
- PCR-Based MSI Testing:
- Extract DNA from matched tumor and normal tissue.
- Amplify a standard panel of 5-7 mononucleotide and dinucleotide repeat markers (e.g., BAT-25, BAT-26, NR-21, NR-24, MONO-27) via fluorescently labeled PCR.
- Analyze fragment sizes by capillary electrophoresis. A shift in the size of tumor DNA alleles compared to normal DNA defines MSI.
- Tumors are classified as MSI-High (instability in ≥30-40% of markers), MSI-Low (instability in <30-40%), or Microsatellite Stable (MSS) [54] [56].
- NGS-Based MSI Testing:
- Using NGS data from comprehensive genomic profiling panels, computational algorithms compare the length distribution of microsatellite loci in the tumor sample to a reference model built from stable samples.
- This method allows for the simultaneous assessment of MSI status alongside other genomic biomarkers like TMB and single-gene alterations [9] [56].
Tumor Mutational Burden (TMB) Measurement by NGS
Protocol Overview: TMB is measured using NGS. Whole-exome sequencing (WES) is the gold standard, but targeted gene panels are widely used in clinical practice due to lower cost and faster turnaround [57] [58].
Detailed Methodology:
- DNA Extraction and Library Preparation: Extract high-quality DNA from FFPE tumor tissue and matched normal blood/saliva. Create sequencing libraries.
- Sequencing:
- For WES: Sequence the entire exome (~30-40 Mb). This provides the most comprehensive TMB assessment.
- For Targeted Panels: Sequence a defined gene set (e.g., 0.5-2.5 Mb). The panel must be sufficiently large and representative to accurately estimate whole-exome TMB [58].
- Bioinformatic Analysis:
- Alignment: Map sequencing reads to a reference human genome.
- Variant Calling: Identify somatic (tumor-specific) single-nucleotide variants (SNVs) and small insertions/deletions (indels). Filter out germline polymorphisms using the matched normal sample and population databases.
- TMB Calculation: TMB is calculated as the total number of synonymous and non-synonymous somatic mutations divided by the size of the coding region captured (in megabases). Only variants with adequate quality scores and allele frequencies above a defined threshold (e.g., ≥5%) should be included [57] [58].
- Reporting: TMB is reported as mutations per megabase (mut/Mb). The FDA-approved cutoff for pembrolizumab is TMB ≥10 mut/Mb, though this can vary [54] [57].
Critical Considerations: Panel-based TMB (psTMB) requires careful calibration against WES. Factors such as panel size, gene content, bioinformatic pipelines, and variant filtering criteria must be standardized to ensure consistent results across laboratories [57] [58].
Table 2: Technical Specifications for Biomarker Measurement
| Assay Type | Standard Specimen | Key Analytical Output | Common Platforms/Assays | Turnaround Time |
|---|---|---|---|---|
| PD-L1 IHC | FFPE tissue section | Tumor Proportion Score (TPS) or Combined Positive Score (CPS) [59] | Dako 22C3, 28-8; Ventana SP142, SP263 | 1-3 days |
| MSI-IHC | FFPE tissue section | Loss of nuclear expression of MLH1, MSH2, MSH6, PMS2 | Automated IHC platforms | 1-3 days |
| MSI-PCR | DNA from tumor and matched normal tissue | MSI-H, MSI-L, MSS classification based on marker shifts [54] | Fluorescent fragment analysis | 3-5 days |
| TMB by NGS | DNA from tumor and matched normal tissue | Somatic mutations per megabase (mut/Mb) [57] [58] | MSK-IMPACT, FoundationOne CDx, other targeted panels | 10-21 days |
| Comprehensive Genomic Profiling (CGP) | DNA and RNA from tumor tissue | Simultaneous data for TMB, MSI, gene fusions, SNVs, CNVs [9] [56] | Hybrid-capture-based NGS panels | 14-21 days |
Signaling Pathways and Logical Workflows
PD-1/PD-L1 Checkpoint Signaling Pathway
Diagram Title: PD-1/PD-L1 Immune Checkpoint Pathway
Integrated Workflow for Biomarker Analysis via NGS
Diagram Title: NGS Workflow for Comprehensive Biomarker Profiling
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Key Research Reagent Solutions for Biomarker Analysis
| Item/Tool | Primary Function | Specific Application Example |
|---|---|---|
| FFPE Tissue Sections | Preserves tissue morphology and biomolecules for long-term storage at room temperature; standard specimen for IHC and NGS [9]. | PD-L1 IHC staining; DNA extraction for NGS-based TMB and MSI analysis. |
| Validated IHC Antibody Clones | Specifically binds to target antigen (e.g., PD-L1) for visualization and quantification under a microscope [59]. | Clones 22C3 (pharmDx), SP142, SP263, 28-8 for determining PD-L1 TPS or CPS. |
| NGS Library Prep Kits | Prepares fragmented DNA/RNA for sequencing by adding platform-specific adapters and indexes [9]. | Illumina Nextera Flex, KAPA HyperPrep; used for whole-exome or targeted panel sequencing. |
| Hybrid-Capture Panels | A set of biotinylated oligonucleotide probes designed to enrich specific genomic regions of interest from a complex DNA library [9] [56]. | Pan-cancer panels (e.g., MSK-IMPACT, FoundationOne CDx) for targeted sequencing to assess TMB, MSI, and mutations. |
| Bioinformatics Pipelines | Computational workflows for processing raw sequencing data, including alignment, variant calling, and annotation [9] [58]. | BWA (alignment), GATK (variant calling), MuTect2 (somatic calls); specialized algorithms for MSI and TMB calculation from NGS data. |
| Mass Spectrometry | Directly identifies and characterizes peptides presented on the cell surface by MHC molecules [58]. | Immunopeptidomics; validation of predicted neoantigens from high-TMB tumors. |
Next-generation sequencing (NGS) has revolutionized drug discovery and development by providing high-throughput genomic tools that accelerate the identification of novel therapeutic targets and the creation of personalized treatment strategies [60]. The global NGS in drug discovery market, valued at $1.45 billion in 2024, is projected to grow at a compound annual growth rate (CAGR) of 18.3% to reach $4.27 billion by 2034, reflecting the technology's expanding role in pharmaceutical research and development [61]. This transformative technology enables researchers to comprehensively analyze genome structure, genetic variations, gene expression profiles, and epigenetic modifications, thereby facilitating breakthroughs in precision oncology, rare disease research, and infectious disease surveillance [62] [60]. The versatility of NGS platforms has expanded the scope of genomics research, allowing for studies on cancer genomics, microbiome analysis, and population genetics while enabling the development of targeted therapies and precision medicine approaches [60].
The integration of NGS into drug discovery pipelines has been accelerated by strategic partnerships between equipment manufacturers, reagent suppliers, and pharmaceutical companies. These collaborations are crucial for streamlining NGS workflows by reducing manual intervention and enhancing reproducibility [62]. By leveraging combined expertise in reagent innovation and laboratory automation, these alliances develop versatile platforms that optimize library preparation processes and lower the risk of human error, ultimately broadening access to cutting-edge sequencing tools and empowering smaller labs and emerging research centers to adopt state-of-the-art genomic technologies [62].
NGS Technologies and Platforms
Current Sequencing Technologies
Next-generation sequencing technologies have evolved significantly, with multiple platforms offering distinct advantages for various applications in drug discovery. Second-generation sequencing methods, characterized by their ability to simultaneously sequence thousands to millions of DNA fragments, have largely superseded first-generation Sanger sequencing [60]. The most prominent platforms include Illumina's sequencing-by-synthesis technology, which utilizes reversible dye terminators and bridge amplification to achieve high accuracy for short-read sequencing (36-300 bp) [60]. Other significant technologies include Ion Torrent's semiconductor sequencing that detects hydrogen ions released during DNA synthesis, and Roche's 454 pyrosequencing which measures pyrophosphate release during nucleotide incorporation [60].
Third-generation sequencing technologies have emerged to address limitations of short-read sequencing, with Pacific Biosciences' Single-Molecule Real-Time (SMRT) sequencing and Oxford Nanopore's nanopore sequencing leading this category [60]. These platforms generate significantly longer reads (averaging 10,000-30,000 bp) without requiring PCR amplification, enabling them to resolve complex genomic regions, detect epigenetic modifications, and identify structural variations that are challenging for short-read technologies [60]. The PacBio Onso system represents a recent advancement in short-read sequencing using sequencing-by-binding (SBB) chemistry, which employs native nucleotides and scarless incorporation under optimized binding and extension conditions [60].
Experimental Protocol: Targeted Gene Panel Sequencing
Targeted gene panels represent a cornerstone of clinical NGS applications in oncology, providing focused interrogation of clinically relevant cancer-related genes while conserving precious tissue samples [29]. The standard workflow encompasses:
Sample Preparation and Library Construction
- Extract DNA from tumor specimens (minimum 20-50 ng for amplification-based approaches; 100-200 ng for hybrid capture) [29]. For liquid biopsy applications, isolate cell-free DNA from blood plasma.
- Perform macro- or microdissection to enrich for tumor cells, achieving at least 20% tumor cellularity to mitigate false negative results, particularly for copy number variant detection [29].
- Fragment DNA mechanically or enzymatically to appropriate size distributions (typically 200-500 bp).
- Convert DNA to sequencing libraries through end-repair, A-tailing, and adapter ligation. Unique molecular identifiers (UMIs) may be incorporated at this stage to enable error correction and distinguish true somatic variants from PCR artifacts.
Target Enrichment Amplification-based and hybrid capture represent the two primary enrichment methodologies [29]:
- Amplification-based approaches: Utilize PCR primers to amplify specific genomic regions. Advantages include lower input requirements and faster turnaround times.
- Hybrid capture approaches: Employ biotinylated oligonucleotides to capture target regions by hybridization. This method typically provides greater library complexity and uniformity, with enhanced performance for copy number assessment.
Sequencing and Data Analysis
- Sequence enriched libraries on appropriate NGS platforms (Illumina predominates for clinical applications). Achieve minimum coverage of 500x-1000x for tumor samples and 300x-500x for matched germline specimens to ensure sensitive variant detection.
- Process raw sequencing data through a bioinformatics pipeline encompassing:
- Demultiplexing and quality control (FastQC)
- Alignment to reference genome (BWA, Bowtie2)
- Variant calling (GATK, VarScan, MuTect2)
- Annotation (ANNOVAR, SnpEff, VEP)
- For liquid biopsy applications, implement specialized variant callers optimized for low variant allele fractions (0.1%-1%).
Figure 1: NGS Workflow for Targeted Gene Panel Sequencing in Clinical Oncology
Research Reagent Solutions
Table 1: Essential Research Reagents for NGS-Based Drug Discovery
| Reagent Category | Specific Examples | Function in Workflow |
|---|---|---|
| Library Preparation Kits | Illumina Nextera Flex, Twist Bioscience Library Prep Kit, Watchmaker Genomics Custom Enzymes | Fragment DNA/RNA, add adapter sequences, and prepare libraries for sequencing [62] |
| Target Enrichment Panels | FoundationOne CDx (324 genes), MSK-IMPACT (468 genes), Thermo Fisher Oncomine Dx Target Test | Capture and enrich specific genomic regions of clinical relevance through hybrid capture or amplification [63] [29] |
| Automation Reagents | Beckman Coulter Biomek NGeniuS System Reagents | Enable automated liquid handling for library preparation, reducing hands-on time and improving reproducibility [62] |
| Sequencing Consumables | Illumina NovaSeq X Series Flow Cells, PacBio SMRT Cells, Oxford Nanopore Flow Cells | Platform-specific consumables that enable the actual sequencing process [60] [64] |
| Quality Control Kits | Agilent Bioanalyzer Kits, Qubit dsDNA Assay Kits | Assess DNA/RNA quality, quantity, and fragment size distribution prior to library preparation [29] |
NGS in Target Identification and Validation
Genomic Approaches to Target Discovery
Next-generation sequencing has transformed early drug discovery by enabling comprehensive genomic profiling to identify novel therapeutic targets. Targeted sequencing dominates this application space, accounting for approximately 39.6% of the NGS technology market share in drug discovery due to its cost-effective, high-precision analysis of specific genes or regions [61]. The drug target identification segment holds the largest revenue share at 37.2%, reflecting its critical role in early-stage drug discovery where NGS pinpoints genetic drivers and molecular pathways of diseases [61].
Whole genome sequencing (WGS) provides an unbiased approach for discovering novel cancer drivers and non-coding alterations, while whole exome sequencing (WES) offers a more focused analysis of protein-coding regions at higher coverage depths [60]. RNA sequencing (RNA-seq) enables transcriptome-wide analysis of gene expression, alternative splicing, and fusion transcripts, while specialized applications like ChIP-seq identifies transcription factor binding sites and epigenetic modifications [61]. Each approach offers complementary insights into cancer biology, with the optimal strategy dependent on the specific research question, sample availability, and budget constraints.
Experimental Protocol: Whole Exome Sequencing for Target Discovery
Sample Selection and Preparation
- Select matched tumor-normal pairs (fresh frozen or FFPE tissue) to distinguish somatic from germline variants. Minimum recommended tumor cellularity is 30% for optimal variant detection.
- Extract high-quality DNA using kits optimized for formalin-fixed specimens if using FFPE material. Assess DNA quality via fluorometry and fragment analyzer.
- Prepare sequencing libraries using kits designed for whole exome capture (Illumina Nextera, Agilent SureSelect, Twist Bioscience Human Core Exome). Input requirements typically range from 50-200 ng.
Exome Capture and Sequencing
- Enrich exonic regions using manufacturer-recommended protocols. Hybrid capture-based methods generally provide more uniform coverage than amplification-based approaches.
- Pool captured libraries in equimolar ratios after quality assessment. Sequence on appropriate platforms (Illumina NovaSeq for high-throughput applications) to achieve minimum 100x mean coverage for tumor samples and 50x for matched normals.
Bioinformatic Analysis for Target Identification
- Process sequencing data through standardized pipelines: BWA-MEM for alignment, GATK for base quality recalibration and variant calling, VarScan2 or MuTect for somatic mutation detection.
- Annotate variants using resources like ClinVar, COSMIC, and gnomAD. Prioritize putative drivers using algorithms that consider functional impact (SIFT, PolyPhen), recurrence in cancer databases, and pathway context.
- Validate candidate targets through orthogonal methods (Sanger sequencing, digital PCR) in independent cohorts before proceeding to functional studies.
Figure 2: Target Identification Workflow Using Whole Exome Sequencing
Clinical Applications and Companion Diagnostics
Companion Diagnostics in Precision Oncology
Companion diagnostics (CDx) represent a critical application of NGS in clinical oncology, providing essential information for the safe and effective use of corresponding targeted therapies [63]. These FDA-approved tests undergo extensive validation to accurately identify patients most likely to benefit from specific therapeutic products [63]. Foundation Medicine's FDA-approved tests, FoundationOne CDx (tissue-based) and FoundationOne Liquid CDx (blood-based), exemplify this category, each analyzing 324 cancer-related genes and collectively encompassing over 55 FDA-approved companion diagnostic indications [63].
The clinical utility of NGS-based companion diagnostics was demonstrated in the August 2025 FDA approval of the Oncomine Dx Target Test as a companion diagnostic for zongertinib in HER2-mutant non-small cell lung cancer (NSCLC) [65]. This NGS-based test enables identification of patients with HER2 tyrosine kinase domain activating mutations who may benefit from this targeted therapy, highlighting the growing role of comprehensive genomic profiling in matching patients to appropriate treatments [65]. The integration of NGS into companion diagnostics has accelerated in recent years, with the FDA expanding approvals of NGS-based tests for use with immunotherapy treatments in oncology [61].
Experimental Protocol: Validation of NGS-Based Companion Diagnostics
Analytical Validation
- Establish analytical sensitivity and specificity for all variant types (SNVs, indels, CNVs, fusions) using well-characterized reference materials (Horizon Discovery, SeraCare).
- Determine limit of detection for key biomarkers using dilution series of positive controls. For liquid biopsy applications, validate detection of variants at low allele frequencies (0.1%-1%).
- Assess reproducibility through inter-run, inter-operator, and inter-lot testing. Include at least three replicates over multiple days.
- Verify performance across sample types (FFPE, fresh frozen, liquid biopsy) and input ranges.
Clinical Validation
- Conduct retrospective analysis of archived samples from clinical trials that established drug efficacy.
- For zongertinib example, demonstrate that the NGS test identifies HER2 TKD mutations in patients who responded to treatment in the Beamion LUNG-1 trial [65].
- Establish clinical sensitivity and specificity compared to established standard methods.
- For pan-cancer panels, validate performance separately for different tumor types when possible.
Regulatory Submission
- Compile analytical and clinical validation data in accordance with FDA guidelines for in vitro companion diagnostic devices.
- Include detailed information on the device description, performance characteristics, and manufacturing processes.
- For laboratory-developed tests, establish compliance with CLIA regulations and CAP accreditation requirements.
Table 2: Selected FDA-Approved NGS-Based Companion Diagnostics
| Companion Diagnostic | Manufacturer | Therapeutic Agent | Indication | Year Approved |
|---|---|---|---|---|
| FoundationOne CDx | Foundation Medicine | Multiple targeted therapies | Solid tumors with specific genomic alterations | 2017 (initial approval) [63] |
| FoundationOne Liquid CDx | Foundation Medicine | Multiple targeted therapies | Solid tumors via liquid biopsy | 2020 (initial approval) [63] |
| Oncomine Dx Target Test | Thermo Fisher Scientific | Zongertinib | HER2-mutant NSCLC | 2025 [65] |
| Oncomine Dx Target Test | Thermo Fisher Scientific | Multiple targeted therapies | NSCLC, cholangiocarcinoma, thyroid cancers | 2017 (initial approval) [65] |
Emerging Trends and Future Directions
Advanced Applications in Drug Development
The integration of artificial intelligence and machine learning with NGS data represents a transformative trend in drug discovery. Machine learning algorithms can now assist in predicting gene-drug interactions and potential mutation consequences more rapidly than traditional bioinformatics methods, ultimately improving target identification and enabling more precise personalized medicines [61]. In 2022, the NIH established the Bridge2AI program with $130 million in funding intended for NGS development within the AI domain, creating AI-ready datasets to improve AI-assisted decision making in genomics [61].
Real-time monitoring of treatment response in clinical trials using NGS technologies represents another significant advancement. In 2025, researchers demonstrated the use of circulating tumor DNA sequencing to monitor treatment effectiveness adaptively, detecting treatment resistance mutations weeks before clinical symptoms manifested [61]. This approach reduced total drug development timelines considerably by allowing early termination of ineffective treatment arms, highlighting the potential of NGS to accelerate oncology drug development.
Cloud-based NGS data analysis has become increasingly essential for managing massive genomic datasets. In 2023, NIH-funded institutions began leveraging hybrid cloud systems for faster genomic interpretation and AI-based analysis [61]. Pharmaceutical firms are utilizing cloud-enabled bioinformatics pipelines to reduce development cycles by up to 20%, enabling global collaboration while ensuring regulatory compliance through secure data sharing frameworks [61].
Market Outlook and Strategic Considerations
The United States NGS market is projected to grow from $3.88 billion in 2024 to $16.57 billion by 2033, representing a robust CAGR of 17.5% [64]. This growth is fueled by increasing demand for personalized medicine, expanding research applications in environmental and agricultural sciences, and continuous advances in automation and data analysis [64]. The consumables segment dominates product categories with a 48.5% revenue share in 2024, reflecting recurring demand for reagents, kits, and cartridges required for each sequencing run [61].
Strategic partnerships continue to drive innovation in the NGS landscape. Collaborations between pharmaceutical companies, sequencing platform firms, and research institutions are increasing the potential for innovation in how drugs are discovered [61]. These alliances are particularly valuable for developing automated library preparation systems that streamline workflows and enhance sequencing performance, as demonstrated by Beckman Coulter's partnerships with Illumina, Pillar Biosciences, and Watchmaker Genomics [62].
Standardization of clinical reporting has emerged as a critical need as NGS becomes more integrated into routine cancer care. In response, the Precision Medicine Working Group of the European Society of Medical Oncology has developed recommendations for presenting NGS results to support clinical decision-making in patients with solid cancers [66]. These guidelines provide detailed guidance on structuring NGS reports and adapt to various laboratory and clinical settings through priority-based recommendations, promising to enhance the clarity and utility of NGS clinical reports and ultimately improve patient outcomes [66].
Next-generation sequencing has fundamentally transformed the landscape of drug discovery and development, enabling a systematic approach from initial target identification through companion diagnostic development. The integration of NGS technologies throughout the pharmaceutical R&D pipeline has accelerated precision oncology by providing comprehensive molecular profiling capabilities that match targeted therapies to specific patient populations. As sequencing costs continue to decline and analytical capabilities advance through AI integration and automation, NGS is poised to become even more deeply embedded in drug development paradigms. The ongoing challenges of data interpretation, regulatory alignment, and clinical implementation are being addressed through international collaborations and standardization efforts, ensuring that the full potential of NGS in delivering personalized cancer therapies will be realized in the coming years.
The paradigm of oncology has undergone a fundamental transformation with the emergence of tissue-agnostic therapeutics, which target molecular drivers regardless of tumor histology or anatomical origin. This approach represents a significant departure from traditional organ-based cancer classifications, moving toward a precision oncology model grounded in the genetic basis of malignancy. Next-generation sequencing (NGS) serves as the critical enabling technology for this shift, providing comprehensive genomic profiling that identifies actionable biomarkers across diverse cancer types [9] [44] [67].
The concept of tissue-agnostic therapy gained formal recognition in 2017 with the first U.S. Food and Drug Administration (FDA) approval of pembrolizumab for microsatellite instability-high (MSI-H) or mismatch repair-deficient (dMMR) solid tumors [68]. This milestone established a new framework for oncology drug development, leading to subsequent approvals for targets including NTRK fusions, BRAF V600E mutations, and RET fusions [69] [68]. These approvals demonstrate that molecularly defined cancers can respond to targeted therapies irrespective of their tissue of origin, validating a tumor-agnostic approach to treatment.
This technical guide provides an in-depth examination of three key tissue-agnostic biomarkers—NTRK fusions, RET fusions, and BRAF V600E mutations—within the context of NGS-driven precision oncology. We explore their molecular mechanisms, clinical detection methodologies, corresponding therapeutic agents, and the real-world evidence supporting their clinical utility, providing researchers and drug development professionals with a comprehensive resource for understanding and implementing tumor-agnostic strategies.
Biomarker Profiles and Clinical Trial Data
Established Tissue-Agnostic Biomarkers: Molecular Characteristics and Prevalence
NTRK fusions result from rearrangements involving the NTRK1, NTRK2, or NTRK3 genes, which encode the TRK family of tyrosine receptor kinases. These fusions produce chimeric proteins with constitutive kinase activity that serve as primary oncogenic drivers [70]. While individually rare across most cancer types, they occur with high frequency in certain rare malignancies, including infantile fibrosarcoma (where they are highly enriched), secretory breast cancer, and mammary analog secretory carcinoma [70] [68].
The BRAF V600E mutation represents a specific valine-to-glutamate substitution at codon 600 in the BRAF gene, resulting in constitutive activation of the MAPK signaling pathway. This alteration is most prevalent in melanoma, but also occurs across diverse tumor types, with a real-world prevalence of approximately 6.5% across solid tumors [71].
RET fusions involve rearrangements of the RET proto-oncogene, producing fusion proteins with ligand-independent dimerization and constitutive kinase activity. These fusions are driver alterations in approximately 1-2% of non-small cell lung cancers and 10-20% of papillary thyroid cancers, but occur at much lower frequencies (<0.6%) across other solid tumor types [44] [71].
Clinical Trial Evidence and Response Data
Table 1: FDA-Approved Therapies for Tissue-Agnostic Biomarkers
| Biomarker | Drug | Mechanism of Action | Trial | ORR (95% CI) | mDOR (months) | mPFS (months) |
|---|---|---|---|---|---|---|
| NTRK Fusion | Larotrectinib | TRK inhibitor | LOXO-TRK-14001, SCOUT, NAVIGATE (N=180) | 57% (50-65%) | 43.3 (29.2-NE) | 24.6 (11.3-34.5) |
| Entrectinib | TRK, ROS1, ALK inhibitor | ALKA-372-001, STARTRK-1, STARTRK-2 (N=150) | 61.3% (53.2-69.2%) | 20.0 (13.2-31.1) | 13.8 (10.1-20.0) | |
| Repotrectinib | Next-gen TRK inhibitor | TRIDENT-1 (N=88) | TKI-naïve: 58% (41-73%)TKI-pretreated: 50% (35-65%) | TKI-naïve: NETKI-pretreated: 9.9 (7.4-13.0) | NA | |
| BRAF V600E | Dabrafenib + Trametinib | RAF inhibitor + MEK inhibitor | ROAR, NCI-MATCH (N=131) | 41% (33-50%) | NA | NA |
| RET Fusion | Selpercatinib | RET kinase inhibitor | LIBRETTO-001 (N=52) | 44.2% (30.5-58.7%) | 37.2 (13.3-NE) | 13.2 (5.6-26.2) |
| Pralsetinib | RET kinase inhibitor | NA | 57% (35-77%) | NA | NA |
ORR: Objective Response Rate; mDOR: median Duration of Response; mPFS: median Progression-Free Survival; NE: Not Estimable; NA: Not Available
Table 2: Real-World Evidence for Tissue-Agnostic Therapies (KISMET Study)
| Biomarker | Prevalence | GMT ORR | Non-GMT ORR | GMT mPFS (months) | Non-GMT mPFS (months) |
|---|---|---|---|---|---|
| BRAF V600E | 6.5% (662/10,158) | 51% | 17.6% | 9.2 | 4.2 |
| TMB-H | 11.2% (265/2369) | 57.6% | 9.5% | 7.9 | 3.7 |
| RET Fusion | 0.6% (42/7105) | 75% | 0% | 15.0 | NA |
GMT: Genomically Matched Therapy; TMB-H: Tumor Mutational Burden-High [71]
The Children's Oncology Group ADVL1823 trial demonstrated larotrectinib's remarkable efficacy in pediatric patients with NTRK fusion-positive tumors, showing an overall response rate (ORR) of 94% for infantile fibrosarcoma and approximately 60% for other tumor histologies. The 2-year event-free survival was 82.2% for infantile fibrosarcoma and 80% for other tumors, while 2-year overall survival reached 93.8% and 93.3%, respectively [70].
Real-world evidence from the KISMET study further validates the clinical benefit of tissue-agnostic approaches. This analysis of 10,893 molecularly profiled tumors demonstrated significantly improved outcomes with genomically matched therapies across all three biomarker classes, with an overall response rate of 55.6% for matched therapies versus 12.8% for non-matched therapies, and progression-free survival of 9.6 months versus 3.7 months, respectively [71].
Detection Methodologies and Experimental Protocols
Next-Generation Sequencing Platforms and Workflows
Next-generation sequencing represents the gold standard for detecting tissue-agnostic biomarkers due to its comprehensive genomic coverage, high sensitivity, and ability to identify novel fusion partners and rare mutations [9] [44]. NGS platforms employ massively parallel sequencing, enabling simultaneous analysis of millions of DNA fragments and providing significantly higher throughput compared to traditional Sanger sequencing [9].
Key NGS Platforms for Comprehensive Genomic Profiling:
- Illumina: Short-read sequencing with high accuracy (error rate: 0.1-0.6%) ideal for detecting single nucleotide variants, indels, and copy number variations [9]
- Oxford Nanopore Technologies (ONT): Long-read sequencing enabling direct RNA sequencing and detection of complex structural variants [9]
- Pacific Biosciences (PacBio): Long-read technology with high consensus accuracy suitable for phasing mutations and resolving complex genomic regions [9]
Table 3: Essential Research Reagent Solutions for Biomarker Detection
| Reagent/Category | Specific Examples | Function/Application |
|---|---|---|
| NGS Panels | Ion AmpliSeq Comprehensive Cancer Panel (409 genes) | Comprehensive mutation profiling across oncogenes and tumor suppressor genes [72] |
| DNA Extraction Kits | Qiagen columns (QIAamp DNA FFPE Tissue Kit) | High-quality DNA extraction from formalin-fixed paraffin-embedded (FFPE) tissue [72] |
| Library Prep Systems | Illumina Nextera Flex | Preparation of sequencing libraries from low-input and degraded DNA samples |
| RNA Fusion Detection | Archer FusionPlex, Illumina TruSight Tumor 170 | Targeted RNA sequencing for fusion gene detection |
| Validation Assays | AutoGenomics INFINITI, Biocartis Idylla | Orthogonal validation of NGS-identified mutations [72] |
Detailed Experimental Protocol for Comprehensive Genomic Profiling
Sample Preparation and DNA Extraction
- Tissue Processing: Cut 20-25 sections of 4µm thickness from FFPE tumor tissue blocks with ≥90% tumor cellularity [72]
- DNA Extraction: Use Qiagen columns with proteinase K digestion (40 mg/ml) overnight at 56°C, followed by alcohol precipitation and purification according to manufacturer protocols [72]
- DNA Quantification: Assess DNA concentration using fluorometric methods (Qubit) and quality control via spectrophotometry (A260/A280 ratio) or fragment analyzer [72]
Library Preparation and Sequencing
- Library Construction: Utilize 20ng of genomic DNA for sequencing library preparation with targeted panels (e.g., Ion AmpliSeq CCP) following manufacturer specifications [72]
- Target Enrichment: Employ multiplex PCR amplification to enrich for cancer-relevant genes (e.g., 409 oncogenes and tumor suppressor genes in CCP panel) [72]
- Sequencing: Process libraries on high-throughput sequencing systems (Ion Proton, Illumina NovaSeq) with minimum coverage of 500x for tissue and 1000x for liquid biopsies [9]
Data Analysis and Interpretation
- Variant Calling: Process raw sequencing data through bioinformatic pipelines (BWA, GATK, STAR) for alignment, variant calling, and annotation [9]
- Fusion Detection: Implement specialized algorithms (Archer, STAR-Fusion) to identify fusion events from both DNA and RNA sequencing data [44]
- Clinical Annotation: Use precision oncology decision support systems to classify variants according to clinical actionability and interpret therapeutic implications [71]
Orthogonal Validation Methods
While NGS serves as the primary detection method, orthogonal validation is often employed for confirmatory testing:
- Sanger Sequencing: PCR amplification of target regions (e.g., BRAF exon 15) followed by capillary electrophoresis for mutation confirmation [72]
- RT-PCR: Quantitative reverse transcription PCR for validating fusion transcripts and expression levels
- Immunohistochemistry: Screening for protein expression patterns (e.g., pan-TRK staining for NTRK fusions) though with limited specificity
Signaling Pathways and Therapeutic Targeting
NTRK Fusion Signaling Pathway and Inhibition
NTRK Fusion Oncogenic Signaling and Therapeutic Inhibition
NTRK fusions function as primary oncogenic drivers through ligand-independent dimerization and constitutive activation of tropomyosin receptor kinase (TRK) signaling. This leads to downstream activation of multiple pro-survival pathways including MAPK, PI3K-AKT, and PLCγ, ultimately driving uncontrolled cell proliferation and survival [70]. First-generation TRK inhibitors (larotrectinib, entrectinib) and next-generation agents (repotrectinib) competitively bind to the ATP-binding pocket of TRK kinases, effectively blocking downstream signaling and inducing tumor regression across diverse tumor types [70] [69].
BRAF V600E Mutational Signaling and Combination Therapy
BRAF V600E Signaling and Combination Inhibition Strategy
The BRAF V600E mutation results in constitutive activation of the BRAF kinase, which signals as a monomer independent of RAS activation. This leads to continuous signaling through the MAPK pathway, promoting uncontrolled cellular proliferation and survival [71]. Combination therapy with dabrafenib (RAF inhibitor) and trametinib (MEK inhibitor) provides synergistic inhibition of this hyperactive pathway, overcoming potential feedback activation mechanisms and demonstrating efficacy across multiple tumor types [69] [71]. Notably, colorectal cancers with BRAF V600E mutations exhibit inherent resistance to BRAF inhibitor monotherapy due to EGFR-mediated pathway reactivation, requiring the addition of anti-EGFR agents for effective targeting [68].
Implementation Challenges and Future Directions
Despite the compelling clinical evidence supporting tissue-agnostic therapies, significant implementation challenges persist. Current analyses indicate that only approximately one-third of eligible patients with rare tumor-agnostic indications, such as NTRK fusions, actually receive appropriate targeted therapy [68]. This implementation gap stems from multiple factors, including unequal access to comprehensive genomic testing, healthcare systems structured around traditional organ-based classifications, and insufficient awareness of tissue-agnostic indications among clinicians.
The future of tissue-agnostic drug development requires several key advancements:
- Universal Genomic Testing: Implementation of comprehensive NGS profiling for all cancer patients at diagnosis, not just after standard therapies fail [68]
- Innovative Trial Designs: Expansion of basket trials and master protocols that evaluate targeted therapies across multiple molecularly defined populations simultaneously [44] [68]
- Earlier Intervention: Investigation of tissue-agnostic therapies in earlier treatment lines where targeted approaches may demonstrate enhanced efficacy [68]
- Combination Strategies: Development of rational combination therapies to address context-specific resistance mechanisms, as exemplified by the addition of EGFR inhibition for BRAF V600E colorectal cancers [68]
The integration of artificial intelligence and multi-omic approaches promises to identify additional tissue-agnostic targets and optimize patient selection. As the field evolves, the ongoing collection of real-world evidence will be crucial for refining our understanding of how these therapies perform across diverse patient populations and tumor types [68] [67].
Tissue-agnostic biomarkers and their corresponding therapies represent a paradigm shift in oncology, moving treatment decisions from histology-based to molecular-based approaches. NTRK fusions, RET fusions, and BRAF V600E mutations have been validated as predictive biomarkers for targeted therapies that demonstrate significant clinical efficacy across diverse tumor types. Next-generation sequencing serves as the essential enabling technology for detecting these alterations and implementing precision oncology in clinical practice.
While challenges remain in ensuring widespread access and appropriate implementation, the tissue-agnostic approach fundamentally advances cancer care by providing effective targeted options for patients with rare malignancies and molecular subtypes. As comprehensive genomic profiling becomes increasingly integrated into routine oncology practice, and as drug development continues to evolve beyond organ-based classifications, tissue-agnostic therapies will play an expanding role in delivering personalized cancer treatment based on the molecular drivers of disease rather than anatomical origin.
Guidance for Targeted Therapy Selection and Clinical Trial Enrollment
Next-generation sequencing (NGS) has fundamentally transformed the paradigm of cancer care, enabling a shift from histology-based to genomics-driven treatment strategies. This massive parallel sequencing technology allows for the comprehensive genomic profiling of tumors, identifying actionable mutations that guide targeted therapy selection and clinical trial enrollment [9]. The clinical implementation of NGS represents a cornerstone of precision oncology, facilitating the delivery of molecularly matched therapies to appropriate patient populations [13].
The global precision oncology market reflects this transformative impact, projected to reach $98 billion, underscoring the growing investment in personalized medicine approaches [73]. The technology's capacity to analyze millions of DNA fragments simultaneously has led to a 96% decrease in cost-per-genome, democratizing access to comprehensive genomic information that was previously cost-prohibitive [74]. This economic shift, combined with demonstrated clinical utility, has positioned NGS as an essential tool in modern oncology research and practice.
Technological Foundations of NGS
Core Principles and Comparative Advantages
NGS technologies operate on the principle of massive parallelism, simultaneously sequencing millions to billions of DNA fragments, a fundamental departure from traditional Sanger sequencing which processes single fragments sequentially [9] [74]. This high-throughput architecture enables comprehensive genomic analysis across entire genomes, exomes, or targeted gene panels with unprecedented speed and decreasing cost.
Table 1: Comparison of Sequencing Technologies
| Aspect | Sanger Sequencing | Next-Generation Sequencing (NGS) |
|---|---|---|
| Throughput | Single DNA fragment per reaction | Millions to billions of fragments simultaneously |
| Cost-effectiveness | Cost-effective for 1-20 targets; expensive for large regions | Highly cost-effective for large gene panels and whole genomes |
| Sensitivity | ~15-20% variant detection limit | Detects variants down to 1% allele frequency |
| Turnaround Time | Days for individual genes | Whole genomes in days; targeted panels in hours |
| Variant Detection | Limited to specific regions | Comprehensive detection of SNPs, indels, CNVs, and structural variants |
| Primary Application | Validation of known variants | Discovery, comprehensive profiling, and clinical testing |
The enhanced sensitivity of NGS enables detection of low-frequency variants critical for cancer diagnostics, including subclonal populations and minimal residual disease monitoring [9]. The technology's scalability allows researchers to tailor approaches from focused panels to whole genomes based on specific research questions and clinical requirements.
Major NGS Platforms and Methodologies
The NGS landscape is dominated by several platform technologies, each with distinct strengths and applications in oncology research. Second-generation platforms, particularly Illumina's sequencing-by-synthesis technology, provide high-throughput capabilities with low error rates (0.1-0.6%), making them well-suited for clinical applications requiring high accuracy [9]. Third-generation technologies from Pacific Biosciences and Oxford Nanopore offer long-read sequencing capabilities that excel in resolving complex structural variations and repetitive regions challenging for short-read platforms.
Library preparation methodologies include hybrid capture-based and amplicon-based approaches, with each offering distinct advantages for specific applications. Hybrid capture utilizes biotinylated probes to enrich target regions, providing uniform coverage and superior capability for detecting novel variants, while amplicon approaches use PCR to amplify targeted regions, offering simpler workflows with lower input requirements [74]. The selection between these approaches depends on research goals, including the number of targets, sample quality, and desired coverage uniformity.
NGS Workflow: From Sample to Report
Experimental Protocol and Methodologies
The standard NGS workflow encompasses three critical phases: sample preparation, sequencing, and data analysis, each requiring rigorous quality control measures. The initial sample preparation phase begins with DNA extraction from tumor specimens, typically formalin-fixed paraffin-embedded (FFPE) tissue, with careful quantification and quality assessment to ensure input material suitability [13]. Most clinical protocols require a minimum of 20ng DNA with A260/A280 ratios between 1.7-2.2, with tumor content exceeding 20% for reliable variant detection.
Library preparation involves DNA fragmentation, adapter ligation, and target enrichment. In the fragmentation step, DNA is sheared to 100-800bp fragments via sonication or enzymatic methods. Adapter ligation attaches platform-specific sequences enabling cluster amplification and sequencing. For targeted panels, hybrid capture enrichment uses biotinylated probes to isolate genomic regions of interest, typically achieving >80% coverage at 100x depth, with mean coverage depths exceeding 500x for reliable variant calling [13].
Sequencing occurs on platform-specific flow cells where clonal amplification creates clusters of identical DNA fragments. The Illumina sequencing-by-synthesis approach utilizes fluorescently labeled nucleotides with reversible terminators, capturing base incorporation in real-time through optical detection [74]. Quality metrics including Q30 scores (indicating 99.9% base call accuracy) are monitored throughout the run to ensure data reliability.
Bioinformatics Analysis Pipeline
The bioinformatics workflow transforms raw sequencing data into clinically actionable information through a multi-tiered analytical process. Primary analysis involves base calling, converting raw signal data into FASTQ files containing sequence reads with associated quality scores [74]. Secondary analysis aligns these reads to reference genomes (e.g., GRCh38) producing BAM files, followed by variant calling to identify mutations, copy number alterations, and structural variants, resulting in VCF files cataloging genomic alterations.
Tertiary analysis represents the most critical phase for clinical interpretation, involving variant annotation using established databases (dbSNP, gnomAD, ClinVar) and classification according to established guidelines [13]. The Association for Molecular Pathology (AMP) variant classification system categorizes alterations into four tiers:
- Tier I: Variants of strong clinical significance with FDA-approved therapies or professional guideline recommendations
- Tier II: Variants of potential clinical significance with evidence for investigational therapies
- Tier III: Variants of unknown clinical significance
- Tier IV: Benign or likely benign variants
This standardized classification system enables consistent interpretation and reporting of NGS findings across institutions, facilitating appropriate therapy selection and trial matching [13].
NGS for Targeted Therapy Selection
Actionable Biomarkers and Interpretation
The clinical utility of NGS rests in its ability to identify actionable genomic alterations that inform targeted therapy selection. In a real-world study of 990 patients with advanced solid tumors, NGS profiling identified Tier I actionable variants in 26.0% of cases, with KRAS (10.7%), EGFR (2.7%), and BRAF (1.7%) representing the most frequently altered genes [13]. These alterations directly inform treatment selection, with 13.7% of patients with Tier I variants receiving NGS-guided therapy, demonstrating significant clinical impact across multiple cancer types.
Table 2: Clinical Utility of NGS in Advanced Solid Tumors
| Cancer Type | Patients with Tier I Variants | Receiving NGS-Guided Therapy | Response Rate |
|---|---|---|---|
| Thyroid Cancer | 7 patients | 28.6% (2/7) | Data not specified |
| Skin Cancer | 8 patients | 25.0% (2/8) | Data not specified |
| Gynecologic Cancer | 65 patients | 10.8% (7/65) | Data not specified |
| Lung Cancer | 112 patients | 10.7% (12/112) | Data not specified |
| All Cancers | 257 patients | 13.7% (35/257) | 37.5% partial response |
Biomarkers beyond single-gene alterations further expand the therapeutic landscape, with microsatellite instability (MSI), tumor mutational burden (TMB), and homologous recombination deficiency (HRD) serving as biomarkers for immunotherapy response [9] [75]. The integration of artificial intelligence tools like DeepHRD demonstrates emerging capabilities to detect HRD characteristics from standard biopsy slides with three-fold greater accuracy than current genomic tests, potentially expanding patient identification for PARP inhibitor therapies [75].
Clinical Decision-Making Framework
The translation of NGS findings into treatment decisions requires a systematic approach integrating genomic evidence with clinical considerations. The following decision pathway illustrates the recommended process for leveraging NGS results in therapeutic selection:
The framework emphasizes evidence-based therapeutic selection, prioritizing FDA-approved therapies for Tier I alterations while directing patients with Tier II alterations toward appropriate clinical trials when standard options are exhausted. This approach maximizes the potential for molecularly matched treatments while maintaining rigorous clinical standards.
NGS-Enabled Clinical Trial Enrollment
Technological Solutions for Trial Matching
The integration of NGS data with clinical trial enrollment platforms represents a significant advancement in precision oncology research. Centralized screening systems, such as the Sarah Cannon Research Institute's Central Screening platform, utilize precision medicine software (e.g., Genospace) to match patient clinical and genomic data against trial inclusion/exclusion criteria, generating lists of potentially eligible patients [76]. This technology-enabled approach is enhanced by expert clinical research nurse review, ensuring patient eligibility before generating alerts to treating oncologists.
Artificial intelligence platforms are further transforming clinical trial optimization through automated patient matching, predictive analytics, and real-time monitoring [75]. Systems like HopeLLM, introduced by City of Hope in June 2025, assist physicians in summarizing patient histories, identifying trial matches, and extracting research data [75]. These AI-driven solutions address critical barriers in trial enrollment, including the complexity of modern trial protocols and the challenge of identifying eligible patients within narrow therapeutic windows.
Operational Framework for Trial Enrollment
Successful trial enrollment requires addressing operational challenges through structured workflows and multidisciplinary collaboration. The Central Screening model demonstrates an effective approach, combining technological infrastructure with human expertise to streamline enrollment [76]. Key operational components include:
- Pre-Screening Evaluation: Research nurses prescreen studies monthly to identify potential matches or monitor patients for future trial eligibility
- New Patient Assessment: Screening new patients before initial visits to facilitate first-line trial enrollment
- Progression Monitoring: Continuous monitoring of established patients for trial opportunities at disease progression
- Expert Consultation: Peer-to-peer communication between community oncologists and physician disease specialists for complex matching decisions
This operational framework addresses common enrollment barriers, including administrative burden, complex trial designs, and multi-site coordination challenges. By delivering critical information to care teams in clear, actionable formats, these systems reduce site-level burden while accelerating enrollment timelines [76].
Implementation Challenges and Solutions
Analytical and Interpretative Challenges
Despite its transformative potential, NGS implementation faces significant analytical challenges that impact clinical utility. Variants of uncertain significance (VUS) represent a particular interpretative challenge, creating clinical ambiguity without clear therapeutic implications [9]. The management of VUS rates requires rigorous variant classification systems and ongoing reclassification as evidence accumulates. Additional analytical limitations include coverage uniformity issues, sample quality requirements, and bioinformatics complexity, particularly for detecting complex structural variants and copy number alterations.
The development of provider-friendly biomarker reports addresses interpretative challenges by standardizing the presentation of complex molecular information [77]. Joint consensus recommendations from the Association for Molecular Pathology and College of American Pathologists establish standardized reporting templates that optimize information presentation for oncologists, enhancing report effectiveness and efficiency [77]. These standardization efforts facilitate appropriate interpretation of NGS results, supporting confident clinical decision-making.
Resource and Infrastructure Requirements
The implementation of NGS testing programs demands substantial infrastructure investment and specialized expertise. Economic challenges include high initial costs for sequencing instrumentation, bioinformatics infrastructure, and specialized personnel including bioinformaticians and computational biologists [9] [13]. Ongoing operational costs include reagents, data storage, and continuous bioinformatics support, creating significant financial barriers for many institutions.
Successful implementation strategies include the adoption of streamlined NGS panels that balance comprehensiveness with practical considerations. For example, Pillar Biosciences' oncoReveal panels demonstrate approaches to deliver rapid, focused genomic testing with simplified workflows [78]. The integration of AI-based variant interpretation platforms, such as Illumina's variant interpretation software, addresses bioinformatics bottlenecks by automating aspects of variant prioritization and clinical interpretation [79]. These technological innovations make complex NGS testing more accessible while maintaining analytical rigor.
The Scientist's Toolkit: Essential Research Reagents and Platforms
Table 3: Essential Research Reagents and Platforms for NGS Implementation
| Category | Product/Platform Examples | Primary Function | Application Notes |
|---|---|---|---|
| NGS Platforms | Illumina NextSeq 550Dx, MiSeq i100 | High-throughput sequencing | Clinical-grade instruments with IVD certification |
| Target Enrichment | Agilent SureSelectXT, Pillar SLIMamp | Library preparation and target capture | Hybrid capture vs. amplicon-based approaches |
| DNA Extraction | QIAamp DNA FFPE Tissue Kit | Nucleic acid isolation | Optimized for challenging FFPE samples |
| Quality Control | Qubit dsDNA HS Assay, Bioanalyzer | DNA quantification and sizing | Essential for input quality assessment |
| Variant Interpretation | Illumina Variant Interpreter, PiVAT | Bioinformatic analysis | Clinical decision support functionality |
| Trial Matching | Genospace, HopeLLM | Patient-trial matching | Integration with EHR systems |
The selection of appropriate research reagents and platforms depends on specific application requirements, including sample types, target genes, and throughput needs. Targeted panels like the SNUBH Pan-Cancer v2.0 (544 genes) provide comprehensive coverage of clinically relevant cancer genes while maintaining manageable sequencing costs and data analysis requirements [13]. Emerging solutions focus on workflow simplification through integrated systems that combine wet-bench protocols with bioinformatics analysis, reducing implementation barriers for institutions with limited genomic medicine infrastructure.
Future Directions and Emerging Innovations
The future of NGS in precision oncology points toward increased integration of multi-omics data, artificial intelligence, and novel sequencing methodologies. Spatial transcriptomics technologies enable visualization of gene expression within tissue architecture, providing critical context for the tumor microenvironment [9]. Single-cell sequencing approaches resolve intratumoral heterogeneity, identifying resistant subclones and understanding tumor evolution under therapeutic pressure.
Liquid biopsy applications represent another frontier, with technologies for detecting circulating tumor DNA enabling non-invasive tumor genotyping and monitoring of treatment response [9] [78]. The oncoReveal Essential LBx Panel demonstrates capabilities for detecting ultra-low frequency mutations in liquid biopsy samples, potentially enabling earlier detection of resistance mechanisms [78]. These minimally invasive approaches may address tissue accessibility limitations while providing dynamic insights into tumor evolution.
Artificial intelligence integration across the NGS workflow promises enhanced accuracy and efficiency, from variant detection through clinical interpretation. Deep learning tools like DeepHRD demonstrate AI's potential to extract additional clinical insights from standard NGS data, potentially expanding biomarker identification beyond conventional genomic alterations [75]. As these technologies mature, they will likely become increasingly embedded in clinical NGS workflows, enhancing analytical performance and clinical utility while reducing interpretation time.
The continued evolution of NGS technologies and their clinical implementation will further solidify the role of comprehensive genomic profiling in precision oncology. Through standardized workflows, enhanced bioinformatics solutions, and integrated trial matching platforms, NGS will continue to transform targeted therapy selection and clinical trial enrollment, ultimately advancing personalized cancer care and drug development.
Navigating Challenges: Technical Hurdles, Data Interpretation, and Optimization Strategies in NGS
Next-generation sequencing (NGS) has fundamentally transformed precision oncology by enabling comprehensive genomic profiling of tumors, guiding targeted therapy selection, and monitoring treatment response [80] [9]. However, the widespread clinical adoption of NGS remains constrained by persistent technical challenges, particularly coverage uniformity and sample quality issues [80] [9]. These limitations directly impact assay sensitivity, reproducibility, and ultimately, the reliability of clinical decisions based on sequencing results.
In oncology applications, coverage uniformity refers to the consistency of sequencing depth across targeted genomic regions, while sample quality encompasses factors related to nucleic acid integrity, tumor purity, and the absence of inhibitors that may interfere with library preparation or sequencing [81] [82]. Both factors critically influence the detection of somatic variants, especially low-frequency mutations that may have significant clinical implications [82]. This technical guide examines the root causes of these limitations and provides evidence-based strategies to overcome them, with a specific focus on applications within precision oncology.
Understanding Coverage Uniformity Challenges
Coverage uniformity is a critical performance parameter in NGS that measures the variation in read depth across targeted genomic regions. Inconsistent coverage can lead to false negatives in variant detection, particularly for clinically important genomic regions with inherently poor coverage [81] [82].
Technical Root Causes
Several factors contribute to coverage unevenness in NGS workflows. Library preparation method significantly influences uniformity, with hybrid capture-based approaches generally providing more even coverage compared to amplicon-based methods, though the latter often deliver higher depth in specifically targeted regions [82] [83]. GC bias represents another major challenge, as regions with extremely high or low GC content typically demonstrate reduced coverage due to fragmentation biases and amplification inefficiencies [84]. Probe or primer design limitations also contribute substantially to coverage gaps, particularly in regions with complex genomic architecture or repetitive elements [82].
The choice of NGS technology further impacts uniformity. Second-generation short-read platforms (e.g., Illumina) typically provide more uniform coverage across exonic regions compared to third-generation long-read technologies (e.g., PacBio, Oxford Nanopore), though the latter offer advantages for resolving structural variants and complex genomic regions [9].
Table 1: Factors Affecting Coverage Uniformity in NGS Workflows
| Factor | Impact on Uniformity | Potential Solutions |
|---|---|---|
| Library Preparation Method | Hybrid capture generally provides more uniform coverage than amplicon-based approaches [82] [83] | Method selection based on application requirements; hybrid capture for uniform coverage |
| GC Content | Extreme GC regions (>70% or <30%) show significant coverage drop-offs [84] | GC-balanced PCR protocols; specialized library prep kits |
| Probe/Primer Design | Poorly designed probes/primers lead to coverage gaps in specific genomic regions [82] | Improved bioinformatic design tools; overlapping probe designs |
| Sequencing Technology | Short-read platforms generally provide more uniform coverage than long-read technologies [9] | Platform selection based on application; hybrid approaches |
Impact on Variant Detection
The minimum recommended coverage for clinical NGS assays typically ranges from 100× to 500×, with higher depth required for detecting low-frequency variants [82]. In regions with poor coverage, the effective variant allele frequency (VAF) detection limit increases substantially, potentially missing clinically relevant subclonal populations [81]. For example, at 100× coverage, the theoretical detection limit for a heterozygous variant is approximately 10-15%, while 500× coverage enables reliable detection of variants at 1-5% VAF [82]. This sensitivity is particularly crucial in precision oncology for several applications: detecting minimal residual disease, identifying early resistance mutations, and analyzing samples with low tumor purity [80] [9].
Addressing Sample Quality Limitations
Sample quality issues represent perhaps the most significant challenge in clinical NGS implementation, particularly for solid tumors where formalin-fixed paraffin-embedded (FFPE) tissue represents the most widely available specimen type [82] [83].
FFPE-Derived DNA Challenges
The FFPE preservation process introduces multiple molecular artifacts that directly impact NGS data quality. DNA fragmentation occurs through cross-linking and chemical damage, resulting in short fragment lengths that complicate library preparation and reduce mapping efficiency [82]. Sequence artifacts include cytosine deamination leading to C>T and G>A transitions, which can be misinterpreted as true somatic variants if not properly accounted for [83]. These artifacts particularly affect precision oncology applications where single-nucleotide variants (SNVs) serve as critical biomarkers for therapy selection [82].
The age of FFPE blocks correlates strongly with DNA quality, with older samples (>3 years) typically exhibiting greater degradation and higher artifact rates [83]. Pre-analytical factors including fixation time, fixative type, and storage conditions further influence sample quality and subsequent NGS performance [82].
Tumor Purity and Cellularity
Tumor purity—the percentage of tumor cells in a sample—directly affects variant detection sensitivity [81] [82]. The relationship between tumor purity and minimum detectable VAF follows the formula: Minimum VAF ≈ (1/Purity) × (1/Coverage). For example, in a sample with 30% tumor purity and 300× coverage, the theoretical detection limit for a heterozygous variant is approximately 1.7% [82]. This has profound implications for precision oncology, where low-purity samples may fail to detect clinically actionable mutations.
Pathological assessment of tumor cellularity through manual microdissection represents a critical pre-sequencing step to enrich tumor content and improve variant detection [82]. Additionally, computational methods for purity estimation from sequencing data itself provide orthogonal validation of histopathological assessment [81].
Strategic Solutions and Methodological Approaches
Wet-Lab Optimization Strategies
Several methodological improvements can substantially mitigate coverage uniformity and sample quality issues. Library preparation method selection should be guided by application requirements: hybrid capture-based methods demonstrate superiority for assessing copy number variations and achieving uniform coverage, while amplicon-based approaches may be preferable for analyzing small genomic regions where maximum depth is required [82] [83].
FFPE-specific protocol modifications include uracil-DNA glycosylase (UDG) treatment to reduce artifacts from cytosine deamination, specialized repair enzymes to address DNA fragmentation, and optimized fragmentation protocols that account for pre-existing DNA damage [83]. Input quality control measures must be implemented, including DNA quantification methods that accurately assess amplifiable DNA (e.g., qPCR-based approaches) rather than total DNA, and RNA integrity number (RIN) assessment for transcriptome sequencing [82].
Table 2: Experimental Protocols for Addressing Technical Limitations
| Protocol | Key Steps | Application Context |
|---|---|---|
| Hybrid Capture-Based NGS | 1. DNA fragmentation (mechanical or enzymatic)2. Adapter ligation3. Hybridization with biotinylated probes4. Target enrichment with streptavidin beads5. Library amplification [82] | Comprehensive genomic profiling; copy number variation analysis; fusion detection [82] [83] |
| Amplicon-Based NGS | 1. DNA fragmentation2. PCR with target-specific primers3. Adapter ligation or incorporation4. Library purification and normalization5. Pooling and sequencing [82] | Hotspot mutation screening; low-input samples; rapid turnaround applications [83] |
| FFPE DNA Restoration | 1. DNA extraction with xylene/ethanol deparaffinization2. Proteinase K digestion3. UDG treatment to reduce deamination artifacts4. DNA repair enzyme incubation5. Quality assessment by fluorometry and qPCR [82] [83] | FFPE-derived DNA; archived samples; historically valuable specimens |
Bioinformatic Compensation Methods
Advanced bioinformatic approaches can compensate for wet-lab limitations. Coverage normalization algorithms, including GC-content correction and bin-based normalization, significantly improve coverage uniformity and facilitate more accurate copy number calling [84]. Variant calling algorithms specifically designed for FFPE artifacts implement duplex sequencing approaches, strand bias filters, and statistical models that account for damage patterns characteristic of FFPE-derived DNA [83].
Tumor purity estimation from sequencing data itself provides orthogonal validation of histopathological assessment and enables more accurate variant calling in mixed samples [81]. Tools such as ggcoverage offer specialized visualization capabilities that help identify coverage gaps, GC biases, and other technical artifacts that may impact variant interpretation [84].
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Research Reagents and Materials for NGS Quality Improvement
| Reagent/Material | Function | Application Notes |
|---|---|---|
| UDG (Uracil-DNA Glycosylase) | Removes uracil residues resulting from cytosine deamination in FFPE DNA | Critical for reducing false positive C>T mutations in archival samples [83] |
| DNA Repair Enzyme Mixes | Repairs abasic sites, nicks, and other damage in FFPE-derived DNA | Improves library complexity and sequencing quality of compromised samples [82] |
| Hybrid Capture Probes | Solution-based biotinylated oligonucleotides for target enrichment | Longer probes tolerate mismatches better, reducing allele dropout; design impacts coverage uniformity [82] |
| Multiplexing Barcodes | Unique oligonucleotide sequences that label DNA fragments from specific samples | Enable sample pooling and reduce batch effects; crucial for cost-effective sequencing [81] |
| Targeted Gene Panels | Pre-designed probe sets for clinically relevant cancer genes | Cost-effective for focused applications; better coverage uniformity for included regions compared to WGS [82] [83] |
Quality Control and Validation Frameworks
Rigorous quality control measures throughout the NGS workflow are essential for reliable results in precision oncology applications. Pre-sequencing QC should include tumor purity assessment by pathological review, DNA quality metrics (e.g., DV200 for FFPE samples), and quantitation of amplifiable DNA [82]. The College of American Pathologists recommends minimum standards including at least 20% tumor cellularity for most applications, though lower purity samples can be analyzed with appropriate depth and validation [82].
Post-sequencing QC must encompass coverage uniformity metrics (e.g., >80% of targets with ≥100× coverage), base quality scores (Q30>70%), and mapping rates (>90%) [82]. The Association of Molecular Pathology guidelines recommend an error-based validation approach that identifies potential sources of errors throughout the analytical process and addresses these through test design and quality controls [82].
For clinical implementation, ongoing quality monitoring should include reference materials with known variant allele frequencies to ensure continued sensitivity for low-frequency variants, and regular proficiency testing to maintain analytical performance [82].
Visualizing NGS Workflow Challenges and Solutions
The following workflow diagrams illustrate the key challenges and strategic solutions for coverage uniformity and sample quality issues in NGS for precision oncology.
Coverage uniformity and sample quality issues remain significant technical challenges in implementing robust NGS workflows for precision oncology. Addressing these limitations requires a comprehensive approach spanning pre-analytical sample assessment, optimized wet-lab methodologies, and sophisticated bioinformatic processing. The strategic solutions outlined in this guide—including library preparation method selection, FFPE-specific protocol modifications, coverage normalization algorithms, and rigorous quality control frameworks—provide a pathway toward more reliable and clinically actionable genomic profiling.
As precision oncology continues to evolve, emerging technologies such as single-cell sequencing, spatial transcriptomics, and artificial intelligence-enhanced bioinformatics promise to further overcome current limitations [80] [85]. However, the fundamental principles of quality management and technical optimization detailed in this guide will remain essential for translating NGS data into improved cancer patient care.
Managing Variants of Uncertain Significance (VUS) and Complex Data Output
The integration of Next-Generation Sequencing (NGS) into routine clinical practice has fundamentally transformed the diagnostic and therapeutic landscape of precision oncology, enabling comprehensive genomic profiling that identifies targetable alterations to guide personalized treatment strategies [3] [33]. However, this technological advancement has concurrently generated a significant interpretive challenge: the management of variants of uncertain significance (VUS). These genetic alterations, for which the clinical and functional implications are currently unknown, represent a critical bottleneck in the path from genomic data to actionable clinical insights [86] [87].
The scale of this challenge is substantial. Recent analyses reveal that more than 70% of all unique variants in the ClinVar database are classified as VUS, with the rate of VUS identification continuing to grow over time [86]. In clinical practice, VUS account for approximately 48% of variant annotations provided to oncologists, creating considerable uncertainty in therapeutic decision-making [87]. The burden of VUS is not uniformly distributed across patient populations; studies demonstrate that the number of reported VUS relative to pathogenic variants can vary by over 14-fold depending on the primary indication for genetic testing and 3-fold depending on self-reported race, highlighting important disparities in genomic medicine [86].
This technical guide provides a comprehensive framework for managing VUS and complex NGS data outputs within precision oncology, offering detailed methodologies for classification, functional validation, and clinical interpretation to advance molecularly driven cancer care.
VUS Classification and Actionability Frameworks
Standardized Classification Systems
The consistent categorization of genomic variants is fundamental to reproducible and clinically actionable NGS reporting. The established standard for variant interpretation in oncology is the four-tiered system developed through a joint consensus recommendation by the Association for Molecular Pathology, American Society of Clinical Oncology, and College of American Pathologists [13] [87].
Table 1: Standardized Tier System for Variant Classification in Cancer
| Tier | Classification | Description | Clinical Utility |
|---|---|---|---|
| Tier I | Strong Clinical Significance | Variants with FDA-approved therapies or professional guideline recommendations | Directs clinically actionable treatment decisions |
| Tier II | Potential Clinical Significance | Variants with evidence from clinical trials or different tumor types | Identifies candidates for investigational therapies |
| Tier III | Unknown Significance (VUS) | Variants without established evidence for clinical impact | Requires further investigation; not diagnostic |
| Tier IV | Benign or Likely Benign | Variants known to have no clinical impact | Not considered for clinical decision-making |
In real-world clinical implementation, this classification system enables stratification of patient populations for targeted therapies. A 2024 study of 990 patients with advanced solid tumors found that 26.0% harbored Tier I variants, while 86.8% carried Tier II variants, demonstrating the prevalence of potentially actionable findings in combination with VUS in clinical cohorts [13].
Actionability Assessment for VUS
Beyond standardized tiering, specialized frameworks have been developed to further refine the actionability potential of VUS. The MD Anderson Precision Oncology Decision Support (PODS) team has established a rule-based actionability classification scheme that subcategorizes VUS as either "Unknown" or "Potentially" actionable based on specific molecular characteristics [87].
Key Criteria for "Potentially Actionable" VUS Classification:
- Location within functional protein domains known to harbor oncogenic mutations
- Close proximity to known oncogenic variants (within 1-2 amino acids)
- Truncating mutations in tumor suppressor genes where loss-of-function is driving
- Presence in functional hotspots with established therapeutic implications
The clinical utility of this refined classification is significant. Functional genomics validation has demonstrated that variants categorized as "Potentially actionable" are substantially more likely to be oncogenic (37%) compared to those classified as "Unknown" (13%), with an odds ratio of 3.94 (p = 4.08e-09) [87]. This approach enables prioritization of VUS for functional validation and identifies patients more likely to benefit from genomically matched therapies.
Diagram: VUS Actionability Classification Workflow. This decision framework outlines the systematic process for categorizing Variants of Uncertain Significance based on therapeutic actionability and functional characteristics.
Functional Validation of VUS: Experimental Approaches
Functional Genomics Platform
Determining the oncogenic potential of VUS requires robust functional validation. The MD Anderson functional genomics platform employs a standardized methodology to assess the impact of variants on cell viability, a key indicator of oncogenic transformation [87].
Experimental Protocol:
- Mutant Generation: Site-directed mutagenesis is used to introduce specific VUS into wild-type cDNA constructs of the gene of interest.
- Cell Line Models: Constructs are expressed in two distinct cell line models:
- MCF10A: Immortalized, non-transformed human mammary epithelial cells
- Ba/F3: Murine pro-B cells dependent on IL-3 for growth
- Viability Assays: Transfected cells are cultured under growth factor-independent conditions to assess:
- Anchorage-independent growth in MCF10A cells (hallmark of transformation)
- Factor-independent proliferation in Ba/F3 cells (indicator of oncogenic signaling)
- Quantitative Analysis: Cell viability is measured and compared to wild-type controls and known oncogenic variants.
Interpretation Criteria:
- Oncogenic: Significant increase in viability in at least one cell line
- Not Oncogenic: No difference from wild-type or decreased viability
- Conflicting: Opposing effects in the two cell lines (requires further investigation)
This platform has demonstrated that approximately 24% of VUS in actionable genes (106 of 438 variants tested) exhibit oncogenic potential in functional assays, providing critical evidence for therapeutic targeting [87].
High-Throughput Functional Characterization
Advanced approaches for VUS functionalization are emerging to address the scale of the classification challenge. High-throughput pipelines enable parallel assessment of hundreds of variants, dramatically accelerating the characterization process [87].
Key Methodological Considerations:
- Deep Mutational Scanning: Systematic introduction of all possible amino acid substitutions within clinically relevant domains
- Multiplexed Assays: Pooled variant expression with barcode-based tracking of cellular fitness
- Diverse Cellular Contexts: Evaluation across multiple cell lines to identify context-specific functional effects
- Therapeutic Sensitivity Profiling: Assessment of variant-specific responses to targeted therapies
While these high-throughput approaches generate invaluable data for VUS interpretation, they currently face implementation challenges for real-time clinical decision support due to throughput limitations and turnaround times [87].
Computational and Bioinformatic Strategies
AI-Enhanced Variant Prioritization
Artificial intelligence and machine learning approaches are increasingly deployed to address the challenge of VUS interpretation in NGS data analysis. Modern bioinformatics platforms incorporate specialized algorithms that significantly enhance variant classification efficiency [88].
AI-Driven Classification Capabilities:
- Oncogenicity Prediction: Proprietary AI algorithms achieve significant accuracy improvements in predicting variant oncogenic potential through integrative analysis of molecular features and clinical annotations [88].
- Variant Prioritization: Advanced computational methods enable up to 90% reduction in variants requiring manual review by filtering based on functional impact, population frequency, and predictive biomarkers [88].
- Push-Button Workflows: Streamlined bioinformatics pipelines automate comprehensive genomic profiling, including assessment of tumor mutational burden (TMB), microsatellite instability (MSI), and complex biomarkers from NGS data [88].
Integrated Multi-Omic Data Analysis
The interpretation of VUS is enhanced through integration of diverse molecular data types beyond genomic sequencing alone [67].
Multi-Omic Integration Framework:
- Transcriptomic Correlates: RNA sequencing to assess variant impact on gene expression, splicing alterations, and fusion gene formation
- Epigenetic Context: Chromatin accessibility and methylation profiling to evaluate variant location in regulatory regions
- Proteomic Validation: Mass spectrometry-based verification of variant expression at the protein level
- Spatial Validation: Spatial transcriptomics and proteomics to confirm variant expression within tumor microenvironments
These integrated approaches facilitate a more comprehensive understanding of VUS functional impact, moving beyond singular genomic evidence to multi-dimensional assessment [67].
Clinical Implementation and Reporting
NGS Workflow Optimization
The successful clinical implementation of VUS management strategies requires optimization of the complete NGS workflow, from sample preparation to final reporting [13] [89].
Table 2: Key Quality Metrics for NGS Implementation in Clinical Practice
| Workflow Stage | Quality Parameter | Threshold | Clinical Impact |
|---|---|---|---|
| Sample Preparation | Tumor Cellularity | >20% | Reduces false negatives |
| DNA Quantity | ≥20 ng | Ensures library complexity | |
| DNA Purity (A260/A280) | 1.7-2.2 | Prevents sequencing artifacts | |
| Library Preparation | Fragment Size | 250-400 bp | Optimizes sequencing efficiency |
| Library Concentration | ≥2 nM | Ensures adequate cluster density | |
| Sequencing | Mean Depth | >500× | Enables sensitive variant detection |
| Coverage Uniformity | >80% at 100× | Reduces coverage gaps | |
| Variant Calling | Variant Allele Frequency | ≥2% | Balances sensitivity/specificity |
| Read Depth | ≥200 | Ensures variant calling confidence |
Real-world data from clinical implementation demonstrates that optimized NGS workflows achieve a technical success rate of 97.6% (990/1014 tests) with a mean sequencing depth of 677.8×, enabling reliable detection of clinically actionable variants [13].
VUS Reporting and Reclassification Systems
The dynamic nature of genomic evidence necessitates systems for ongoing VUS reclassification and updated reporting. Current assessments reveal significant gaps in these processes [86].
Reclassification Challenges:
- Communication Gaps: At least 1.6% of variant classifications used in electronic health records are outdated based on current ClinVar annotations [86].
- Systemic Limitations: Documented cases include 26 instances where testing laboratories updated ClinVar classifications but these reclassifications were never communicated to patients or providers [86].
- Liability Concerns: Ambiguity regarding responsibility for initiating patient re-contact after variant reclassification [86].
Recommended Best Practices:
- Systematic Re-evaluation: Establish protocols for periodic review of VUS classifications based on emerging evidence
- Automated Alert Systems: Implement computational tools to flag updated variant classifications in public databases
- Clear Re-contact Policies: Develop institutional guidelines for provider and patient notification of clinically significant reclassifications
- EHR Integration: Ensure seamless incorporation of updated variant interpretations into clinical documentation systems
Diagram: VUS Reclassification and Reporting Pathway. This workflow illustrates the continuous process of evidence accumulation, variant reassessment, and communication required for effective VUS management.
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Essential Research Reagents for VUS Functional Validation
| Reagent/Material | Specification | Application | Key Considerations |
|---|---|---|---|
| Nucleic Acid Extraction | QIAamp DNA FFPE Tissue Kit (Qiagen) | Isolation of high-quality DNA from archival specimens | Maintains DNA integrity from degraded samples [13] |
| Library Preparation | Agilent SureSelectXT Target Enrichment | Hybrid capture-based target enrichment | Enables focused sequencing of relevant genomic regions [13] |
| Sequencing Platform | Illumina NextSeq 550Dx | Clinical-grade sequencing system | Provides high accuracy (99.9%) and validated workflow [13] |
| Functional Validation | MCF10A Cell Line | Non-transformed mammary epithelial cells | Assesses transforming potential in relevant cellular context [87] |
| Functional Validation | Ba/F3 Cell Line | IL-3-dependent murine pro-B cells | Evaluates factor-independent growth signaling [87] |
| Variant Calling | MuTect2 | Somatic variant detection | Sensitive identification of low-frequency variants [13] |
| Variant Annotation | SnpEff | Genomic variant annotation | Functional prediction of coding sequence alterations [13] |
| CNV Detection | CNVkit | Copy number variation analysis | Identifies gene amplifications/deletions from NGS data [13] |
| Fusion Detection | LUMPY | Structural variant calling | Comprehensive detection of gene fusions [13] |
Emerging Technologies and Approaches
The evolving landscape of genomic medicine promises enhanced strategies for VUS resolution through technological innovations and collaborative frameworks.
Advanced Functional Genomics:
- Single-Cell Sequencing: Enables assessment of variant impact at cellular resolution within heterogeneous tumor populations [33].
- Spatial Transcriptomics: Contextualizes variant expression within tissue architecture and tumor microenvironments [67].
- CRISPR-Based Screening: High-throughput functional characterization of variants using genome editing technologies [87].
Data Integration and Collaboration:
- Global Knowledgebases: Federated data sharing platforms aggregate evidence for variant interpretation across institutions [86].
- Standardized Reporting: Harmonized classification frameworks facilitate consistent variant interpretation across clinical laboratories [86] [87].
- AI-Powered Prediction: Advanced machine learning models integrate multi-omic data to predict variant pathogenicity with increasing accuracy [88].
The effective management of Variants of Uncertain Significance represents both a critical challenge and significant opportunity in precision oncology. Through the implementation of standardized classification frameworks, robust functional validation methodologies, computational prioritization strategies, and systematic reclassification processes, the clinical utility of NGS testing can be maximized. As these approaches continue to evolve and integrate with emerging technologies, the resolution of VUS will increasingly enable personalized therapeutic strategies, ultimately advancing the core mission of precision oncology: to deliver molecularly informed cancer care tailored to the individual genetic landscape of each patient's malignancy.
Economic and Reimbursement Challenges in Widespread Clinical Adoption
Next-generation sequencing (NGS) has fundamentally transformed precision oncology by enabling comprehensive genomic profiling that guides targeted therapy selection, clinical trial enrollment, and personalized treatment strategies [9] [44]. The technology's capacity to simultaneously analyze hundreds of cancer-related genes from both tissue and liquid biopsy samples has positioned it as an essential component in modern cancer care [9]. Major oncology guideline bodies, including the National Comprehensive Cancer Network (NCCN), American Society of Clinical Oncology (ASCO), and European Society for Medical Oncology (ESMO), now recommend NGS-based molecular profiling for patients with advanced solid tumors [90] [44]. Despite this professional consensus and demonstrated clinical utility, significant economic and reimbursement barriers continue to hinder the widespread clinical adoption of NGS technologies [90] [91] [92]. These challenges create disparities in patient access to precision oncology and limit the realization of personalized cancer care across diverse healthcare settings. This technical guide examines the multifaceted reimbursement landscape, presents quantitative data on economic barriers, and explores emerging solutions aimed at expanding appropriate access to NGS-based testing in oncology.
Current Reimbursement Landscape for NGS Testing
The reimbursement environment for NGS-based cancer testing is characterized by complexity, variability, and ongoing evolution. In the United States, the Centers for Medicare & Medicaid Services (CMS) established a National Coverage Determination (NCD) for NGS in 2018, which was subsequently amended in 2020 to include germline testing for breast and ovarian cancer risk assessment [92]. This regulatory framework was intended to create consistency in coverage policies; however, evidence suggests that uncertainty persists regarding coverage boundaries. A recent analysis of Medicare claims data revealed that more than 20% of cancer-related NGS claims were denied between 2016 and 2021, with denial rates actually increasing following NCD implementation from 16.8% before the NCD to 27.4% after the NCD was amended [92].
Key Payer Challenges and Knowledge Gaps
Table 1: Primary Payer-Identified Barriers to NGS Coverage
| Barrier Category | Specific Challenge | Prevalence Among Payers |
|---|---|---|
| Clinical Guidelines | Lack of clear clinical guidelines | 74% (ranked in top 3 barriers) |
| Internal Payer Processes | Lack of internal consensus on which NGS tests to cover | 45% |
| Expertise Gaps | Absence of internal expertise on NGS | 39% |
| Guideline Awareness | Unfamiliarity with current NCCN biomarker testing recommendations | 33% |
Source: Multi-stakeholder survey data adapted from [90]
Payer decision-making regarding NGS coverage is complicated by several factors. A multi-stakeholder survey revealed that approximately one-third (33%) of payers were not aware of the current somatic biomarker testing recommendations from NCCN guidelines [90]. This knowledge gap contributes to inconsistent coverage policies and creates barriers to appropriate test utilization. Additionally, payers identified the lack of clear clinical guidelines (74% ranked this as a top three barrier), absence of internal consensus on which NGS tests to cover (45%), and lack of internal NGS expertise (39%) as primary hurdles for broader NGS access [90].
Quantitative Analysis of Economic Barriers
Physician-Reported Reimbursement Challenges
Table 2: Physician-Reported Barriers to NGS Implementation
| Barrier Type | Specific Challenge | Prevalence Among Physicians |
|---|---|---|
| Reimbursement Challenges | Prior authorization requirements | 72.0% |
| Reimbursement Challenges | Knowledge of new fee codes for reimbursement | 68.0% |
| Reimbursement Challenges | Paperwork/administrative duties | 67.5% |
| Knowledge Gaps | Lack of knowledge of NGS testing methodologies | 81.0% |
| Evidence Gaps | Lack of clinical utility evidence | 80.0% |
Source: U.S. Physician-based survey data adapted from [91] [93]
A comprehensive survey of 200 U.S. physicians (including oncologists/hematologists, surgeons, and pathologists) demonstrated that 99.5% reported concerns or barriers regarding NGS testing, with reimbursement challenges being the most frequently cited issue (87.5%) [91] [93]. The most common reimbursement-specific challenges included prior authorization requirements (72.0%), knowledge of new fee codes for reimbursement or corresponding therapy (68.0%), and paperwork/administrative duties (67.5%) [91]. These administrative burdens consume significant clinical resources and may discourage providers from ordering appropriate NGS testing for their patients.
Additional physician-identified barriers included lack of knowledge regarding NGS testing methodologies (81.0%) and insufficient evidence of clinical utility (80.0%) [91]. Surgeons were more likely to encounter challenges in using NGS testing compared to other physician specialties, potentially reflecting unique workflow or reimbursement considerations in surgical oncology [91] [93].
Site-Specific Variations in Claim Denials
Analysis of Medicare claims data demonstrates significant variation in NGS claim denials based on testing site. Claims were more likely to be denied if performed at independent laboratories (odds ratio [OR] = 2.76; 95% confidence interval [CI] = 2.58–2.95) or other non-hospital sites (OR = 2.55; 95% CI = 2.12–3.07) compared to hospital-based laboratories [92]. Additionally, claims for large-panel tests (≥50 genes) for solid tumors were more likely to be denied (OR = 1.32; 95% CI = 1.23–1.43) than smaller panels [92]. These findings suggest that both testing location and test complexity significantly influence reimbursement outcomes.
Methodological Approaches to Reimbursement Research
Multi-Stakeholder Survey Methodology
Understanding the economic challenges in NGS adoption requires robust research methodologies. A recent multi-stakeholder study employed quantitative online surveys with United States-based medical oncologists (n=109), nurses and physician assistants (n=50), lab directors and pathologists (n=40), payers (n=31), and patients diagnosed with metastatic breast cancer (n=137) [90]. The survey design incorporated several methodological safeguards:
- Preliminary Qualitative Research: Sixty-minute double-blinded phone-based interviews informed the development of the quantitative survey instrument, ensuring relevance of content domains including reimbursement, coverage, tissue sample sufficiency, turnaround time, and NGS testing behavior [90].
- Survey Validation: Beta-testing with representative stakeholders ensured appropriate question and answer options, question clarity, neutrally framed questions, and overall survey flow [90].
- Bias Mitigation: Invitations were distributed across diverse clinical settings, clinical laboratories, payer types, and US geographies with stratification quotas to limit oversampling of any individual demographic. Multiple recruitment channels were utilized, including two major market research vendors supplemented with an internally developed database of healthcare professionals [90].
- Anonymity Protection: The survey was designed to be fully anonymous to reduce participation barriers and social desirability bias, encouraging honest and complete responses [90].
Claims Data Analysis Methodology
A cohort study examining Medicare claim denials for cancer-related NGS testing employed a rigorous analytical approach [92]:
- Data Source: A 20% random sample of Medicare claims data for cancer-related NGS testing from January 1, 2016, to December 31, 2021.
- Sample Size: 29,919 total cancer-related NGS claims among 24,443 Medicare beneficiaries.
- Time Period Analysis: Claim denial rates were assessed across three time periods: before NCD implementation, after initial NCD implementation, and after the NCD was amended in January 2020.
- Statistical Analysis: Multivariate analysis identified factors associated with claim denials, including testing site and test characteristics, with results expressed as odds ratios with 95% confidence intervals.
Visualization of NGS Reimbursement Barrier Pathways
The following diagram illustrates the complex relationships between different stakeholders and the primary economic and reimbursement challenges in NGS adoption:
Figure 1: Interrelationships between stakeholders, economic barriers, and clinical impacts in NGS adoption. This systems map illustrates how challenges experienced by different stakeholders (payers, providers, patients, and laboratories) collectively contribute to suboptimal testing utilization, ultimately affecting treatment quality and equity in cancer care.
Emerging Solutions and Innovative Approaches
Technological Innovations to Reduce Barriers
Recent technological advances aim to address both economic and accessibility challenges in NGS implementation:
Decentralized Testing Models: New FDA-approved NGS systems enable rapid, automated testing in local hospital settings rather than centralized reference laboratories, potentially reducing turnaround times from weeks to as little as 24 hours with approximately 20 minutes of hands-on time [94] [95]. This decentralization expands access to precision oncology for community-based hospitals and reduces logistical barriers.
Automated Workflows: Integrated systems with end-to-end automation streamline previously labor-intensive processes, reducing specialized technical expertise requirements and associated operational costs [94] [95]. These improvements make NGS implementation feasible in a broader range of clinical settings without significant investments in specialized personnel.
Legislative and Policy Initiatives
Policy approaches are emerging to address coverage disparities and expand access to biomarker testing:
State-Level Biomarker Testing Legislation: As of 2024, 16 states have passed legislation to align coverage of biomarker testing with evidence-based guidelines, with ongoing efforts in additional states [96]. These laws aim to ensure more consistent coverage across insurance types.
Federal Legislative Activity: Congressional attention to laboratory test pricing, coverage, and reimbursement includes oversight of Medicare Advantage and Managed Care Organizations, with proposed legislation to reform prior authorization processes, enhance pricing transparency, and increase coverage for innovative tests [96].
Coding Improvements: The American Medical Association CPT coding system has implemented new genomic testing code paradigms to enhance clarity and specificity for NGS tests, while Proprietary Laboratory Analysis (PLA) codes provide unique identifiers for specific advanced diagnostic laboratory tests [96].
Evidence Generation Strategies
Addressing evidence gaps regarding clinical utility remains critical for sustainable reimbursement:
Advanced Diagnostic Laboratory Tests (ADLTs): The ADLT designation recognizes innovative tests that provide new clinical diagnostic information unavailable from other testing approaches [96]. Evidence generation for ADLTs focuses not only on clinical validity but also on demonstrating how test results change treatment pathways and whether these changes improve outcomes while reducing overall healthcare costs [96].
Multi-Stakeholder Education: Targeted education for payers and providers addressing identified knowledge gaps, particularly regarding current clinical guidelines and NGS methodologies, may reduce implementation barriers [90] [91].
The Scientist's Toolkit: Essential Research Reagent Solutions
Table 3: Key Research Reagents and Platforms for NGS Implementation
| Tool Category | Specific Technology/Reagent | Primary Function in NGS Workflow |
|---|---|---|
| Sequencing Platform | Ion Torrent Genexus Dx System | Fully automated NGS system enabling decentralized testing with minimal hands-on time [95] |
| Test Kit | Oncomine Dx Target Test | First distributable FDA-approved NGS-based companion diagnostic for multiple genes and cancer types [95] |
| Test Kit | Oncomine Dx Express Test | FDA-approved test for CDx and tumor profiling with 24-hour turnaround time [95] |
| Automation Technology | Proprietary automated library prep and template preparation | Reduces manual processing time and technical expertise requirements [94] [95] |
| Bioinformatics | Integrated data analysis pipelines | Automated variant calling and interpretation following sequencing [94] |
The research reagents and platforms listed in Table 3 represent critical components for implementing NGS in clinical settings. These technologies address previous barriers through automation, regulatory clearance, and integration, potentially reducing economic challenges associated with specialized personnel requirements and test validation.
Economic and reimbursement challenges continue to significantly impact the widespread clinical adoption of NGS in precision oncology despite its demonstrated clinical value and inclusion in major professional guidelines. The complex interplay of payer policy inconsistencies, administrative burdens, coverage uncertainties, and varying stakeholder knowledge creates substantial barriers to optimal implementation. Recent technological innovations in decentralized testing, automated workflows, and policy initiatives aimed at standardizing coverage show promise in addressing these challenges. Future success in achieving equitable access to precision oncology will depend on continued evidence generation regarding clinical utility, multi-stakeholder education, and policy reforms that align reimbursement structures with the value of comprehensive genomic profiling in cancer care.
Standardizing Bioinformatics Pipelines and Quality Control Measures
The adoption of next-generation sequencing (NGS) has fundamentally transformed precision oncology by enabling comprehensive genomic profiling of tumors, which guides targeted therapy selection, improves patient outcomes, and advances drug development [97] [9]. However, the complexity of NGS workflows—spanning wet-lab procedures and sophisticated bioinformatics analysis—introduces significant challenges in ensuring the accuracy, reproducibility, and reliability of results across different laboratories and platforms [98] [99]. The clinical utility of NGS-derived data is paramount; it informs critical treatment decisions, such as identifying actionable mutations in genes like EGFR in non-small cell lung cancer (NSCLC) or BRAF V600E in melanoma [97] [9]. Consequently, standardizing bioinformatics pipelines and implementing robust quality control (QC) measures are not merely technical exercises but essential prerequisites for generating clinically actionable genomic data that can be trusted to guide patient care in oncology [100] [99]. This guide provides a detailed framework for achieving this standardization, directly supporting the broader thesis that NGS is a cornerstone of modern precision oncology.
Foundational Principles of NGS and Quality Management
NGS Technology and Its Clinical Application
Next-Generation Sequencing represents a paradigm shift from traditional Sanger sequencing, offering massively parallel analysis that allows for the simultaneous interrogation of millions of DNA fragments [9]. This high-throughput capability is critical in oncology, where tumors are driven by diverse and complex genomic alterations. NGS provides the capacity to detect a wide variety of genomic variants—including single nucleotide polymorphisms (SNPs), insertions/deletions (indels), copy number variations (CNVs), and structural variants—at a significantly lower cost per base and with greater sensitivity than earlier technologies [9]. The clinical application of NGS in precision oncology primarily involves identifying "actionable mutations"—genomic alterations that can be targeted with specific therapies or that have prognostic or diagnostic significance [97]. For instance, the identification of microsatellite instability (MSI) status via NGS has become a critical biomarker for predicting response to immunotherapy across multiple cancer types [101].
The Quality Management System (QMS) Framework
A robust Quality Management System (QMS) provides the foundational structure for ensuring the quality and consistency of NGS data. The Clinical & Laboratory Standards Institute (CLSI) framework of 12 Quality System Essentials (QSEs) is widely adopted as the standard for clinical and public health laboratories [100] [99]. These QSEs are coordinated activities that direct and control an organization with regard to quality, covering all aspects of laboratory operations from personnel and equipment to process management and information management [100]. The U.S. Centers for Disease Control and Prevention (CDC) and the Association of Public Health Laboratories (APHL) have launched the NGS Quality Initiative, which provides more than 100 free, customizable guidance documents and Standard Operating Procedures (SOPs) tailored to NGS workflows, helping laboratories implement or enhance their QMS [100]. A risk-based approach is recommended for implementation, initially prioritizing the QSEs of Personnel, Equipment, and Process Management, as these pose the most immediate risk to NGS data quality [99].
Table 1: Core Quality System Essentials (QSEs) for NGS Workflows
| Quality System Essential (QSE) | Key Challenges in NGS | Recommended Mitigation Strategies |
|---|---|---|
| Personnel | Complex technology requiring substantial training; mismatch between existing and needed skill sets [99]. | Develop standardized training SOPs; implement competency assessments for wet-lab and bioinformatics staff [99]. |
| Equipment | Specific physical environment requirements; frequent software/hardware updates; need for preventive maintenance [99]. | Use pre-installation checklists; establish preventive maintenance schedules and logs; validate all software updates [99]. |
| Process Management | Multistep workflow with multiple error sources; use of expensive reagents; complex bioinformatic analysis [99]. | Implement QC checks at each stage (pre-analytic, analytic, post-analytic); validate entire NGS workflow [99]. |
The following diagram illustrates the core components of a QMS for NGS, highlighting the interconnected nature of the essential quality systems:
Figure 1: A Quality Management System (QMS) Framework for NGS. The system is built on coordinated activities (Quality System Essentials) that ensure the production of reliable data [100] [99].
Standardizing Bioinformatics Pipelines: Performance and Selection
Comparative Evaluation of Bioinformatics Pipelines
The selection of a bioinformatics pipeline is a critical decision that directly impacts the accuracy and reliability of genomic results. A comparative study evaluated four open-source pipelines—dshiver (a Dockerized version of shiver), SmaltAlign, viral-ngs, and V-Pipe—for assembling full-length viral genomes from NGS data, providing a model for pipeline assessment that is applicable in oncology [98]. The performance of these pipelines was assessed using both simulated and real-world HIV-1 paired-end short-read datasets under default settings. The study found that all four pipelines produced high-quality consensus genome assemblies when the reference sequence used for assembly was highly similar to the analyzed sample. Key performance metrics included genome fraction recovery, mismatch and indel rates, and variant calling F1 scores [98]. However, performance varied significantly when the reference sequence was divergent from the sample. Under these more challenging conditions, shiver and SmaltAlign demonstrated robust performance, whereas viral-ngs and V-Pipe did not [98]. This underscores that the choice of a reference sequence is a critical parameter in pipeline standardization.
Table 2: Comparative Performance of Open-Source Bioinformatics Pipelines
| Pipeline | Performance with Matched Reference | Performance with Divergent Reference | Runtime | Key Applicability Notes |
|---|---|---|---|---|
| dshiver | High quality metrics [98] | Robust performance [98] | Longer runtime [98] | Dockerized version offers ease of use and robustness [98]. |
| SmaltAlign | High quality metrics [98] | Robust performance [98] | Shorter runtime [98] | Combines user-friendliness with robust performance [98]. |
| viral-ngs | High quality metrics [98] | Lowered performance [98] | Shorter runtime [98] | Requires less computational resources [98]. |
| V-Pipe | High quality metrics [98] | Lowered performance [98] | Longer runtime [98] | Provides the broadest range of functionalities [98]. |
Experimental Protocol for Pipeline Benchmarking
To ensure a standardized and fair comparison of different bioinformatics pipelines, the following detailed methodology, adapted from Zsichla et al., is recommended [98]:
- Dataset Curation: Utilize both simulated and empirical NGS datasets. Simulated datasets, generated from a known reference sequence, allow for precise calculation of accuracy metrics (e.g., sensitivity, specificity). Empirical datasets (real-world data) with a known or consensus truth set are crucial for validating performance under real laboratory conditions.
- Performance Metrics: Define and calculate a core set of quantitative metrics for evaluation:
- Genome Fraction: The percentage of the reference genome covered by the assembly.
- Mismatch Rate (Substitutions/base): The number of incorrect base calls per base in the consensus.
- Indel Rate (Indels/base): The number of insertions or deletions per base in the consensus.
- Variant Calling F1 Score: The harmonic mean of precision and recall for identifying true variants.
- Runtime and Computational Resource Usage: Measure the wall-clock time and memory/CPU consumption.
- Reference Sequence Divergence: Test pipeline performance using reference sequences with varying degrees of similarity to the sample (e.g., same subtype, different subtype) to assess robustness.
- Containerization: Employ containerization technologies like Docker (as demonstrated with dshiver) to package the entire pipeline, including all software dependencies and version-specific configurations. This guarantees a consistent computational environment, eliminating "it works on my machine" problems and enhancing reproducibility [98].
Quality Control Measures Across the NGS Workflow
A Phase-Based QC Strategy
Quality control must be integrated throughout the entire NGS workflow, which is broadly divided into three phases: pre-analytic, analytic, and post-analytic. Each phase presents unique risks that must be managed through specific QC checks [99].
- Pre-analytic Phase: This phase involves sample collection, nucleic acid extraction, and library preparation. Key QC measures here include:
- Sample Quality Assessment: Quantifying DNA/RNA using fluorometric methods and assessing purity (e.g., A260/280 ratio). For formalin-fixed paraffin-embedded (FFPE) tissues, evaluating DNA fragmentation is critical.
- Library QC: Using fluorometry or capillary electrophoresis to quantify the final library and ensure the correct fragment size distribution before sequencing.
- Analytic Phase: This is the sequencing run itself. QC measures include:
- Sequencing Metrics: Monitoring instrument performance data, such as cluster density (for Illumina platforms), output data yield, and quality scores (e.g., Q30 score, which indicates a base call accuracy of 99.9%).
- Internal Controls: Using spike-in controls to detect contamination or failures in library preparation and sequencing.
- Post-analytic Phase: This encompasses bioinformatics analysis and data interpretation. QC measures include:
- Raw Data QC: Assessing metrics like per-base sequence quality, adapter content, and overall read quality using tools like FastQC.
- Alignment Metrics: Evaluating the percentage of reads aligned to the target region, mean depth of coverage, and uniformity of coverage.
- Variant Calling QC: Monitoring metrics such as the transition/transversion (Ti/Tv) ratio, which should fall within an expected range for human exome or genome data, and the number of variants in databases like dbSNP.
The following workflow diagram maps the key QC checkpoints from sample to result:
Figure 2: NGS Workflow with Key QC Checkpoints. Integrated quality control at each phase is essential to ensure final data integrity [99].
Case Study: QC in MSI Detection via NGS
The detection of Microsatellite Instability (MSI) using NGS (NGS-MSI) exemplifies the need for specialized algorithms and rigorous QC. A large-scale 2025 study of 35,563 pan-cancer cases developed a novel NGS-based MSI detector, MSIDRL, which analyzes length changes at microsatellite loci [101]. The experimental protocol for developing and validating such an assay involves:
- Algorithm Development: The MSIDRL algorithm selected 100 highly sensitive and specific noncoding microsatellite loci not used in traditional PCR-based tests. For each locus, a "diacritical repeat length" (DRL) was defined to distinguish stable from unstable reads based on sample data with known MSI status [101].
- Threshold Determination: The unstable locus count (ULC) for each sample was calculated. A pan-cancer ULC cutoff of 11 was established based on the bimodal distribution of ULCs across a massive dataset, clearly separating Microsatellite Stable (MSS) from MSI-High (MSI-H) cases [101].
- Validation and Concordance Testing: The NGS-MSI results were compared against gold-standard methods (IHC or PCR). The study noted that while concordance is very high in colorectal cancers, discordance can occur in non-colorectal cancers, highlighting the need for rigorous, cancer-type-specific validation [101].
The Scientist's Toolkit: Essential Research Reagents and Materials
The following table catalogs key reagents, technologies, and computational tools referenced in contemporary NGS studies, which are essential for building and standardizing oncology-focused genomic workflows.
Table 3: Research Reagent Solutions for NGS in Precision Oncology
| Category / Item | Specific Examples | Function / Application |
|---|---|---|
| Targeted NGS Panels | oncoReveal Myeloid Panel, oncoReveal MPN Panel, oncoReveal Essential LBx Panel (Pillar Biosciences) [78] | Focused sequencing for rapid, cost-effective detection of somatic mutations and fusions in specific cancer types (e.g., leukemias, solid tumors) and liquid biopsies. |
| Proprietary NGS Chemistry | SLIMamp, PiVAT (Pillar Biosciences) [78] | Proprietary technologies designed to improve amplification efficiency and variant calling accuracy, streamlining the NGS workflow and localizing testing. |
| Sequencing Platforms | Illumina MiSeq i100, Illumina MiSeq [78] [99] | Benchtop sequencers for rapid, high-quality targeted sequencing in clinical research settings. |
| Containerization Software | Docker [98] | Creates isolated, reproducible computational environments for bioinformatics pipelines (e.g., dshiver), ensuring consistent results across different systems. |
| Open-Source Pipelines | shiver, SmaltAlign, viral-ngs, V-Pipe [98] | Provide standardized, community-vetted workflows for tasks like viral or pathogen genome assembly, serving as models for pipeline development in oncology. |
| QC & Analysis Tools | MSIsensor, MSI-ColonCore [101]; Bioinformatics QC workflows (CDC) [99] | Specialized tools for assessing specific genomic features (e.g., MSI) and for performing general quality control on NGS data. |
The standardization of bioinformatics pipelines and the implementation of comprehensive quality control measures are non-negotiable components of robust NGS applications in precision oncology. As the field evolves, several emerging trends will shape the future of standardization. The integration of artificial intelligence (AI) and machine learning (ML) is poised to enhance variant interpretation, prioritize findings, and even predict treatment responses by uncovering complex patterns in large genomic datasets [75] [97]. Furthermore, the convergence of NGS with other advanced technologies like single-cell sequencing, spatial transcriptomics, and multi-omics will generate even more complex data types, necessitating new standards and integrative bioinformatics pipelines [9] [102]. To fully realize the potential of precision oncology, the community must continue to collaborate on developing and adopting these standards, investing in the necessary bioinformatics infrastructure, and ensuring that equitable access to high-quality genomic testing becomes a global reality [97] [9].
Addressing Disparities in Access and Ensuring Equitable Implementation
Next-Generation Sequencing (NGS) has fundamentally transformed oncology, enabling comprehensive genomic profiling that guides targeted therapy selection, identifies clinical trial opportunities, and informs prognostic assessment [9]. The clinical utility of this approach is well-established, with studies demonstrating that treatment adjustments based on NGS findings can significantly improve patient outcomes. Real-world data from the Middle East and North Africa (MENA) region shows a promising trend toward improved progression-free survival (5.32 vs. 3.28 months, p=0.023) when NGS-guided treatment adjustments are implemented [103]. However, the implementation of this transformative technology has been markedly uneven, creating significant disparities in access and outcomes across racial, ethnic, socioeconomic, and geographic lines [104] [105].
The fundamental thesis of this technical guide is that equitable implementation of NGS in precision oncology requires a multifaceted approach addressing both technical and systemic barriers. Without concerted intervention, the very technologies designed to personalize cancer treatment risk exacerbating existing health disparities as advances continue to outpace equitable implementation [104]. This whitepaper provides researchers, scientists, and drug development professionals with a comprehensive analysis of the current disparities landscape, evidence-based quantitative assessments, and practical methodologies for advancing equity in precision oncology research and implementation.
Quantitative Assessment of Current Disparities
Disparities in precision oncology manifest across multiple dimensions, including biomarker testing rates, genomic data diversity, and clinical trial representation. The following tables synthesize key quantitative findings from recent studies that document these inequities.
Table 1: Disparities in Biomarker Testing and Clinical Trial Representation
| Disparity Dimension | Study Population | Findings | Source |
|---|---|---|---|
| NGS Testing Rates | Non-squamous NSCLC patients | 36.6% of White patients vs. 29.9% of Black patients received NGS before first-line therapy | [106] |
| ctDNA Testing Utilization | Hispanic breast cancer patients | Observed-to-expected testing ratio of 0.80 (CI 0.77-0.83) | [105] |
| Clinical Trial Representation | FDA oncology trial participants (2014-2018) | Black patients represented only 7.44% of participants | [105] |
| Treatment Access | Metastatic breast cancer patients | Lower rates of genotype-matched therapy in racially/ethnically underrepresented groups | [105] |
Table 2: Survival Outcomes from Real-World NGS Implementation in MENA Region
| Outcome Measure | NBTA Group (n=40) | Non-NBTA Group (n=140) | Statistical Significance |
|---|---|---|---|
| Median Overall Survival | 59 months | 23 months | p = 0.096 |
| Median Progression-Free Survival | 5.32 months | 3.28 months | p = 0.023 |
| Stage IV Disease at Diagnosis | 58.3% of total cohort | 58.3% of total cohort | N/A |
The data from the MENA region study is particularly instructive as it demonstrates both the potential benefits of NGS-guided treatment and the challenges of late-stage implementation, with 78.9% of patients undergoing profiling only after disease progression [103]. Furthermore, among patients with identified actionable mutations, 15.9% (14/88) could not access recommended treatments due to barriers including cost, unavailability, or patient refusal [103].
Root Cause Analysis: Technical and Systemic Barriers
Biological and Genomic Variability
Emerging research reveals significant differences in mutational profiles across racial and ethnic groups that have implications for assay performance and treatment matching. In metastatic breast cancer, Black patients show higher frequencies of specific single-nucleotide variants in CDKN2 (OR 5.37), GATA3 (OR 1.99), and PTPN11 (OR 7.96), along with distinct pathway-level alteration patterns compared to White patients [105]. These differences extend to pan-cancer analyses, with Black patients demonstrating higher TP53 mutation frequencies and lower PI3K pathway alterations [105].
Biological factors also influence ctDNA assay performance. Patients of African ancestry show significantly higher ctDNA positivity rates and levels even after adjusting for disease stage, suggesting ancestry-related biological differences in ctDNA shedding and clearance mechanisms [105]. These differences can affect minimal residual disease detection sensitivity and require population-specific validation of ctDNA assays.
Structural and Implementation Barriers
The implementation gap for NGS technologies stems from interconnected structural barriers that disproportionately affect underserved populations:
Infrastructure and Cost Barriers: Deploying NGS requires significant institutional investment in equipment, bioinformatics infrastructure, and specialized staff training [104]. Community oncology settings, which deliver approximately 80% of U.S. cancer care, often lack these resources [104]. Economic disparities are particularly pronounced in low- and middle-income countries and underserved regions where reimbursement frameworks may not exist [107] [103].
Workforce and Education Gaps: Community oncologists face challenges staying current with rapidly evolving NGS technologies and their applications across multiple tumor types [104]. Interpretation of complex genomic reports requires specialized expertise that may be concentrated at academic centers [104] [106].
Data Diversity Deficits: Genomic databases suffer from significant representation gaps, with over-representation of populations of European ancestry [104] [108]. As one expert noted, "China and India are the two most populated countries in Asia, and they look nothing alike, yet they're often lumped into the same 1% category in our data sets" [104]. This lack of diversity limits the generalizability of biomarkers and algorithms across populations.
The following diagram illustrates the interconnected nature of these barriers and their impact on equitable implementation:
Diagram: Interconnected Technical and Systemic Barriers to Equitable NGS Implementation. The diagram illustrates how biological factors and data diversity deficits (technical barriers) interact with infrastructure, economic, workforce, and educational challenges (systemic barriers) to perpetuate disparities.
Methodologies for Equity-Focused Research
Protocol for Diverse Cohort Recruitment and Retention
Objective: Establish methodological framework for recruiting and retaining diverse populations in clinicogenomic research.
Materials:
- Multilingual consent forms (reading level ≤8th grade)
- Cultural navigation support
- Community advisory board
- Federated data governance tools
- Trusted Exchange Framework and Common Agreement (TEFCA)-aligned infrastructure
Procedure:
- Community Engagement Phase: Establish community advisory board with representative stakeholders; co-develop research protocols and consent processes [108].
- Infrastructure Setup: Implement federated data systems with privacy-preserving technologies (encryption, blockchain-based governance) that enable data sharing while maintaining patient agency [108].
- Recruitment: Deploy multi-channel recruitment strategy including community health centers, patient advocacy groups, and trusted clinical settings; offer linguistic and literacy-appropriate materials [104] [105].
- Data Collection: Collect comprehensive demographic, clinical, genomic, and social determinant data using standardized instruments; implement liquid biopsy protocols to overcome tissue access barriers [105] [106].
- Retention: Maintain ongoing engagement through patient portals, result return programs, and community updates; employ digital tools for longitudinal follow-up [108].
Validation Metrics: Track recruitment yields by racial/ethnic group, retention rates at 6/12 months, data completeness, and participant satisfaction scores.
Protocol for Population-Specific Assay Validation
Objective: Validate ctDNA assays across diverse ancestral populations to ensure equitable performance characteristics.
Materials:
- Matched tumor tissue and blood samples from diverse participants
- NGS platforms (Illumina, Oxford Nanopore, or PacBio)
- Digital PCR systems
- Bioinformatics pipelines for variant calling
- Computational resources for statistical analysis
Procedure:
- Sample Collection: Recruit participants across diverse ancestral backgrounds with matched tumor tissue (FFPE blocks) and blood samples (cfDNA) [105] [103].
- Sequencing: Perform whole exome or targeted sequencing of tumor tissue; sequence cfDNA using both tumor-informed and tumor-agnostic approaches [105].
- Assay Performance Assessment:
- Calculate sensitivity/specificity for MRD detection within and across ancestral groups
- Compare variant allele frequency distributions
- Assess ctDNA shedding rates by tumor type and ancestry
- Evaluate tumor fraction correlations with clinical outcomes [105]
- Bioinformatic Analysis:
- Implement ancestry-informed reference panels
- Assess variant calling accuracy across genomic regions with differing linkage disequilibrium patterns
- Evaluate the impact of population-specific germline variants on somatic mutation calling [105]
Analytical Methods: Use generalized linear mixed models to assess the impact of ancestry on ctDNA detection after adjusting for clinical covariates including stage, histology, and treatment history.
Research Reagent Solutions for Equity-Focused Studies
Table 3: Essential Research Materials for Equity-Focused Genomic Studies
| Reagent/Material | Specification | Application in Equity Research |
|---|---|---|
| Diverse Reference Standards | Commercially available cell lines or synthetic controls representing multiple ancestral backgrounds | Validation of assay performance across populations; identification of ancestry-specific technical artifacts |
| Liquid Biopsy Collection Kits | Cell-free DNA blood collection tubes (e.g., Streck, PAXgene) | Non-invasive sampling in settings with limited tissue availability; serial monitoring in underserved communities |
| Multiplex PCR Assays | Customizable panels covering population-specific variants | Cost-effective targeted sequencing; validation of findings from large-scale sequencing studies |
| Bioinformatic Pipelines | Ancestry-informed variant calling algorithms (e.g., GATK with diverse reference panels) | Improved accuracy in variant detection across diverse populations; reduction in false positives/negatives |
| Federated Learning Platforms | Privacy-preserving distributed analysis tools (e.g., blockchain-based governance) | Multi-site collaboration without data transfer; inclusion of underrepresented centers with data sovereignty |
Implementation Framework and Pathway Analysis
A multi-level implementation framework is essential for translating equity-focused research into clinical practice. The following pathway outlines key intervention points from basic research to equitable implementation:
Diagram: Pathway from Equity-Focused Research to Implementation. This framework emphasizes continuous feedback between implementation outcomes and research priorities to iteratively improve equity in precision oncology.
Critical success factors for implementation include:
Workforce Development: Training "precision medicine stewards" to assist patients and providers in navigating complex testing processes, particularly in underserved settings [106]. These specialized navigators can address language barriers, health literacy challenges, and insurance navigation.
Clinical Decision Support: Integrating equity-focused tools into electronic health records to surface digestible insights at point-of-care [109]. Systems like Flatiron Assist have demonstrated 44% reduction in care variation through standardized pathway implementation [109].
Policy Interventions: Advocating for comprehensive insurance coverage of NGS testing across diverse practice settings; developing reimbursement models that support appropriate testing in community oncology [104] [106].
Data Governance Models: Implementing patient-centric data sharing frameworks that maintain privacy while enabling broad research participation [108]. Federated learning approaches and blockchain-based smart contracts can help balance these competing priorities [108].
Addressing disparities in NGS implementation requires concerted effort across the research and clinical spectrum. Technical advances must be coupled with deliberate strategies to ensure equitable access and benefit. Key priorities include: (1) expanding diversity in genomic research cohorts and databases; (2) validating technologies across diverse populations; (3) developing implementation strategies that address structural barriers; and (4) creating policy environments that support equitable access.
Without systematic attention to these equity dimensions, the tremendous promise of precision oncology may remain unfulfilled for significant segments of the population. Researchers and drug development professionals have both scientific and ethical imperatives to ensure that NGS technologies benefit all patients, regardless of race, ethnicity, geography, or socioeconomic status.
The Role of Molecular Tumor Boards (MTBs) in Complex Case Interpretation
Molecular Tumor Boards (MTBs) represent a critical interdisciplinary framework for interpreting complex genomic data and guiding personalized treatment strategies in oncology. As the adoption of comprehensive genomic profiling (CGP) expands, MTBs have evolved from academic initiatives to essential components of precision oncology programs worldwide. This technical guide examines the operational workflows, analytical methodologies, and clinical impact of MTBs, with particular focus on their role in translating next-generation sequencing (NGS) findings into actionable therapeutic recommendations. Evidence from recent real-world studies demonstrates that MTBs successfully identify actionable biomarkers in 59-81% of advanced cancer patients and facilitate matched therapy implementation for 17-23% of discussed cases, underscoring their growing importance in modern cancer care.
The foundation of precision oncology rests on the premise that genomic biomarkers enable tailored treatment recommendations for individual cancer patients [110]. Molecular Tumor Boards (MTBs) have emerged as multidisciplinary conferences where experts interpret complex genomic results to guide therapy selection for patients who have exhausted standard treatment options [110] [111]. The dramatic increase in clinically actionable biomarkers and targeted therapies over the past decade has necessitated this collaborative approach to data interpretation [112] [29]. MTBs serve as the critical interface between complex molecular data and clinical application, addressing the challenge that while over 30% of cancer patients may benefit from molecularly driven therapy, the interpretation of genomic results requires specialized expertise [112] [29].
MTB Composition and Operational Workflows
Interdisciplinary Team Structure
MTBs bring together diverse specialists essential for comprehensive case interpretation:
- Molecular pathologists and bioinformaticians who analyze and interpret genomic variants
- Oncologists (medical, hematological, radiation) who contextualize clinical implications
- Genetic counselors who assess potential germline implications
- Molecular biologists who provide functional insights
- Additional specialists (radiologists, pharmacists, surgeons) recruited based on specific cases [110] [111]
This collaborative model represents "genomic expertise in action," integrating domain-specific knowledge to translate molecular findings into clinical recommendations [113].
Standardized MTB Workflow
The MTB process follows a structured pathway from case selection to therapy implementation, with digital tools increasingly integrated to enhance efficiency [110] [111]. The following diagram illustrates the core workflow:
Figure 1: Molecular Tumor Board Clinical Workflow. The standardized process from patient identification through therapy implementation, highlighting key stages where digital tools provide critical support.
Global Operational Models
MTB operational structures vary globally, reflecting regional healthcare systems and reimbursement frameworks:
Table 1: International MTB Operational Characteristics
| Country | Structure | Remuneration | Evidence Levels | Meeting Frequency |
|---|---|---|---|---|
| Germany | Integrated into healthcare system | Statutory health insurance, flat rates per case | NCT levels (Heidelberg, Augsburg) | Weekly [110] |
| USA | Decentralized, variable by institution | Private insurance, various models ($100-500/session) | Varies by institution | Bi-monthly [110] |
| Japan | Centralized, in large hospitals | National health insurance, fixed fees (¥5,000-10,000/session) | C-CAT levels | Weekly [110] |
| Czech Republic | Single institutional | Mixed insurance reimbursement | AMP Tier system | Weekly [112] |
| UK | National network + local MTBs | Public NHS funding | ESCAT, OncoKB | Variable [113] |
| Belgium | National network across 9 labs | Research and healthcare funding | AMP Tier system | Weekly [114] |
Comprehensive Genomic Profiling: Technical Methodologies
Next-Generation Sequencing Platforms
MTBs rely on Comprehensive Genomic Profiling (CGP) using NGS technologies that have become the standard for precision oncology. The TruSight Oncology 500 (Illumina) platform exemplifies the integrated approach required for MTB-level analysis, combining DNA and RNA sequencing to detect multiple variant classes simultaneously [112]. Successful CGP implementation requires careful consideration of platform selection based on clinical needs and tissue availability.
Table 2: Comprehensive Genomic Profiling Methodologies
| Methodological Component | Technical Specifications | Genomic Targets | Clinical Applications |
|---|---|---|---|
| Hybrid Capture NGS | 523-gene DNA panel, 55-gene RNA panel | SNVs, indels, CNVs, fusions | Primary solid tumor profiling |
| Tumor Mutational Burden (TMB) | Algorithmic calculation from NGS panel | Total coding mutations | Immunotherapy response prediction |
| Microsatellite Instability (MSI) | Analysis of specific microsatellite loci | Mononucleotide repeats | Immunotherapy biomarker |
| Homologous Recombination Deficiency (HRD) | Genomic scar analysis | Genome-wide patterns | PARP inhibitor sensitivity |
| Programmed Death-Ligand 1 (PD-L1) | Immunohistochemistry (22C3 antibody) | Protein expression | Immune checkpoint inhibitor selection |
Analytical Validation and Bioinformatics
The bioinformatic pipeline represents a critical component in the MTB workflow. Following sequencing, data undergoes:
- Alignment to reference genome (GRCh37.p13)
- Variant calling with minimum 5% variant allele frequency threshold
- Annotation using databases (ClinVar, COSMIC, dbSNP, gnomAD)
- Tertiary analysis using platforms like Clinical Genomics Workspace (PierianDx) [112]
Validation studies demonstrate high concordance between NGS and traditional methods like FISH for detecting copy number variations, though challenges remain in low tumor cellularity samples [29].
Variant Interpretation Framework
Variant classification follows standardized frameworks such as the AMP/ASCO/CAP tier system:
- Tier IA/B: Variants with strong clinical significance (FDA-approved, professional guidelines)
- Tier IIC/D: Variants with potential clinical significance (off-label evidence, preclinical data) [112]
Knowledge bases including OncoKB, ClinGen, CIViC, and Cancer Genome Interpreter provide curated evidence levels to support therapeutic matching [29]. The integration of these resources enables consistent interpretation across different MTB settings.
MTB Clinical Impact: Quantitative Outcomes
Actionability and Therapy Implementation
Recent real-world evidence demonstrates the substantial impact of MTBs on clinical decision-making:
Table 3: Real-World MTB Outcomes Across Healthcare Systems
| Study Cohort | Patients Discussed | Actionable Findings | Therapy Recommended | Therapy Implemented | Clinical Benefit |
|---|---|---|---|---|---|
| University Hospital Brno (Czech Republic) | 553 | 59.0% (326/553) | 59.0% (326/553) | 17.4% (96/553) | 41.4% PFS ratio ≥1.3 [112] |
| BALLETT Study (Belgium) | 756 | 81.0% (616/756) | 69.0% (522/756) | 23.0% (174/756) | Under evaluation [114] |
| MTB Freiburg (Germany) | 1,400 (2015-2020) | 53.0% (742/1400) | 53.0% (742/1400) | Not specified | Not specified [110] |
The BALLETT study notably demonstrated that CGP identified actionable markers in 81% of patients, substantially higher than the 21% actionability rate achievable with nationally reimbursed small panels [114].
Therapy Recommendation Patterns
Analysis of therapy recommendations from the Brno MTB cohort reveals distinct patterns in targeted therapy selection:
- Immunotherapy: 29.7% (162/545 recommendations)
- Tyrosine kinase inhibitors: 25.7% (140/545)
- PARP inhibitors: 11.6% (63/545) [112]
These findings reflect the growing importance of immunotherapy biomarkers (TMB, MSI) alongside traditional targeted therapies in modern MTB recommendations.
Digital Support Systems and Visualization Tools
Integrated Software Platforms
Digital support tools have become essential for managing the complexity of MTB workflows. The cBioPortal has emerged as a leading platform for visualizing and analyzing cancer genomics data, with implementations at multiple institutions including Freiburg, Augsburg, and Heidelberg [110] [111]. These systems provide:
- Automated variant annotation and knowledge base integration
- Structured data presentation for clinical decision-making
- Visualization of clinical timelines with molecular events
- Therapy matching to clinical trials [110] [111]
Implementation studies show that these tools reduce preparation time and improve the quality of therapy suggestions compared to manual processes [111].
Patient-Reported Outcome Integration
Emerging research focuses on integrating Patient-Reported Outcome Measures (PROMs) into MTB workflows. The German PM4Onco project has developed specialized visualizations within cBioPortal to display PROMs data alongside genomic and clinical information [115]. This integration includes:
- Timeline view displaying PROMs scores alongside clinical events
- Trend indicators and line graphs for symptom progression
- Customizable displays for different MTB stakeholder needs [115]
Usability evaluations of these visualizations yielded a System Usability Scale (SUS) score of 67, indicating acceptable usability with opportunities for refinement [115].
Implementation Challenges and Optimization Strategies
Operational Barriers
Despite demonstrated efficacy, MTBs face significant implementation challenges:
- Reimbursement complexity: Varying insurance coverage for targeted therapies across healthcare systems [112]
- Workflow integration: Difficulty embedding MTB recommendations into standard oncology practice [111]
- Turnaround time: Median of 29 days from consent to MTB report in the BALLETT study [114]
- Sample quality: 7% screen failure rate due to insufficient tissue in the Brno cohort [112]
Survey data from UK MTB participants indicates that one-third of healthcare professionals encounter challenges attending MTBs regularly due to clinical workload [113].
Educational and Collaborative Value
Beyond immediate clinical impact, MTBs provide significant educational benefits:
- 97.7% of UK respondents reported increased awareness of clinical trials matching genomic alterations
- 84% felt more confident interpreting genomic data after MTB participation
- 95.4% valued MTBs as educational opportunities for training healthcare professionals [113]
These findings highlight the role of MTBs in building genomic literacy across oncology practice.
Molecular Tumor Boards represent an essential infrastructure component for modern precision oncology, transforming complex genomic data into actionable clinical recommendations. As the field evolves, key areas for development include:
- Enhanced digital integration through user-centered design of support tools [111]
- Standardized evidence frameworks for variant interpretation across institutions [110] [112]
- Expanded biomarker scope incorporating transcriptomic, proteomic, and patient-reported data [115] [114]
- Operational efficiency improvements to reduce turnaround times and increase accessibility [113]
The continued evolution of MTBs will be critical for realizing the full potential of precision oncology and ensuring that advances in genomic science translate to improved patient outcomes across diverse healthcare settings.
Benchmarking NGS: Comparative Analyses, Clinical Validation, and Concordance Studies
Next-generation sequencing (NGS) has become the cornerstone of precision oncology, enabling comprehensive genomic profiling that guides diagnosis, prognostication, and therapeutic selection. The transition from traditional Sanger sequencing to modern NGS platforms represents a paradigm shift, driven by the ability to perform massively parallel sequencing, which allows for the concurrent analysis of millions of DNA fragments and the interrogation of hundreds to thousands of genes in a single assay [9]. This technological evolution supports the core tenets of precision medicine by facilitating the identification of actionable mutations, immunotherapy biomarkers, and complex genomic alterations across diverse cancer types [9]. The clinical oncology NGS market, valued at hundreds of millions of USD, is a testament to this adoption, with projections indicating a compound annual growth rate (CAGR) of over 16%, potentially reaching a multi-billion dollar market by 2034 [116] [117] [118].
This whitepaper provides a comparative analysis of the major sequencing platforms, focusing on the critical parameters of accuracy, cost, and clinical utility within oncology. We summarize quantitative performance data in structured tables, detail experimental protocols for platform validation, and visualize key workflows to equip researchers and drug development professionals with the information necessary to select and implement appropriate sequencing technologies.
Platform Technologies and Performance Comparison
The landscape of sequencing technologies is broadly divided into second-generation (short-read) and third-generation (long-read) platforms, each with distinct advantages and limitations for clinical oncology applications [9].
Table 1: Comparative Analysis of Major NGS Platform Technologies
| Feature | Illumina (Short-Read) | Pacific Biosciences (PacBio) (Long-Read) | Oxford Nanopore (ONT) (Long-Read) | Element Biosciences (Short-Read) |
|---|---|---|---|---|
| Technology Principle | Sequencing-by-synthesis on a flow cell [9] | Single-molecule real-time (SMRT) sequencing [9] | Nanopore-based electronic signal detection [9] | Avidity sequencing chemistry [39] |
| Typical Read Length | Short (75-300 bp) [9] | Long (10,000+ bp) [9] | Ultra-long (100,000+ bp) [9] | Short-read [39] |
| Defining Strength | High throughput, low per-base cost, high accuracy [9] | High accuracy for long reads (>99.9%) [119] | Real-time sequencing, portability, ultra-long reads [9] | Ultra-high raw read accuracy (Q40, 99.99%) [39] |
| Primary Clinical Utility in Oncology | Targeted panels, whole exome/genome, liquid biopsy [116] | Detection of complex structural variants, phasing [120] | Rapid diagnosis, structural variants, repeat expansions [120] | Superior rare variant detection, reduced sequencing depth required [39] |
Accuracy and Error Profiles
Accuracy is a paramount consideration, especially for detecting low-frequency somatic variants. The standard metric for sequencing accuracy is the Phred quality score (Q-score). A Q30 score represents a 1 in 1,000 error rate (99.9% accuracy), which has been the benchmark for platforms like Illumina [39]. Emerging technologies are pushing this boundary further; for instance, Element Biosciences' AVITI system with Q40 accuracy (99.99% accuracy) demonstrates that higher raw read accuracy can significantly enhance the detection of rare variants and reduce the sequencing depth required to achieve confidence equivalent to Q30 data, leading to an estimated 30-50% cost savings per sample [39].
Long-read platforms have historically been associated with higher error rates. However, recent advances have substantially improved their fidelity. PacBio's circular consensus sequencing (CCS) model can achieve accuracies exceeding 99.9% by making multiple passes of the same DNA molecule [119]. Similarly, Oxford Nanopore's latest chemistry and flow cells (e.g., R10.4.1) coupled with improved base-calling algorithms have increased base accuracy to over 99% [119] [120]. A clinical validation study of an ONT-based pipeline reported an analytical sensitivity of 98.87% and a specificity exceeding 99.99% for detecting single nucleotide variants (SNVs) and indels [120].
Cost and Throughput Considerations
The cost-effectiveness of NGS is a critical driver for its clinical integration. While the upfront investment in NGS infrastructure can be high, the cost per base has plummeted over time [116] [17]. Targeted sequencing panels currently dominate the clinical oncology market due to their lower cost per sample, faster turnaround times, and higher depth of coverage for detecting rare variants, making them ideal for guiding therapy selection [116] [118]. Whole genome sequencing (WGS), while more expensive, is experiencing the fastest growth rate as its comprehensive nature becomes more valuable for discovering novel variants and non-coding drivers [116] [17].
Table 2: Cost and Application Analysis by Sequencing Strategy
| Sequencing Strategy | Dominant Market Share (2024) | Key Strengths | Estimated Cost & Turnaround Time (TAT) | Typical Applications in Oncology |
|---|---|---|---|---|
| Targeted Sequencing & Resequencing | Largest share (~48.6%) [117] | Cost-effective, fast TAT, high sensitivity for known targets [118] | Lower cost; TAT as low as 4 days [121] | Therapy selection, companion diagnostics, tumor profiling [116] |
| Whole Genome Sequencing (WGS) | Fastest growing segment [116] | Comprehensive view, discovers novel/rare variants and complex SVs [116] | Higher cost; TAT of several days to a week [9] | Discovery research, complex cases, comprehensive genomic profiling [17] |
| Extended Whole-Exome Sequencing (WES) | Niche, but growing | Cost-effective middle ground, covers non-coding regions near exons [122] | Cost comparable to conventional WES [122] | Increasing diagnostic yield by detecting deep intronic and UTR variants without WGS [122] |
Experimental Protocols for Platform Validation
Implementing a robust NGS assay in a clinical or research setting requires rigorous validation. The following protocol, synthesized from recent studies, outlines a comprehensive approach for validating a targeted sequencing panel for solid tumor profiling.
Protocol: Validation of a Targeted NGS Panel for Solid Tumors [121]
1. Objective: To develop and validate a custom, hybridization-capture-based NGS panel (e.g., targeting 61 cancer-associated genes) for sensitive and specific detection of somatic mutations in formalin-fixed paraffin-embedded (FFPE) tumor samples and reference controls.
2. Sample Selection and DNA Extraction:
- Sample Types: Collect a validation set comprising clinical FFPE tissues, external quality assessment (EQA) samples, and commercially available reference controls (e.g., HD701, NA12878) [121].
- DNA Extraction: Purify DNA using standardized kits (e.g., Qiagen DNeasy Blood & Tissue Kit). Quantify DNA using a fluorometric method (e.g., Qubit) and assess quality via agarose gel electrophoresis or a fragment analyzer [121].
3. Library Preparation and Sequencing:
- Library Construction: Use an automated library preparation system (e.g., MGI SP-100RS) with hybridization-based capture probes to ensure consistency and reduce contamination risk. A minimum of 50 ng of input DNA is recommended [121].
- Sequencing: Perform sequencing on a benchtop platform (e.g., MGI DNBSEQ-G50RS or Illumina MiSeq) to generate high-quality data. Target a median read coverage of >500x to ensure sensitivity for low-frequency variants [121].
4. Bioinformatic Analysis and Validation Metrics:
- Primary Analysis: Use integrated software (e.g., Sophia DDM) for base calling, alignment, and variant calling. Apply a machine learning-based approach to filter and prioritize variants.
- Performance Metrics Calculation:
- Sensitivity:
True Positives (TP) / [TP + False Negatives (FN)]- Aim for >98% [121]. - Specificity:
True Negatives (TN) / [TN + False Positives (FP)]- Aim for >99.99% [121]. - Precision:
TP / [TP + FP]- Aim for >97% [121]. - Accuracy:
[TP + TN] / [TP + TN + FP + FN]- Aim for >99.99% [121]. - Limit of Detection (LoD): Establish the lowest variant allele frequency (VAF) detectable with high confidence; typically ~3% for SNVs and indels from FFPE samples [121].
- Reproducibility/Repeatability: Assess by running replicate samples across different batches and operators, targeting >99.9% concordance [121].
- Sensitivity:
NGS Clinical Validation Workflow
The Scientist's Toolkit: Essential Research Reagents & Materials
A successful NGS experiment relies on a suite of high-quality reagents and materials. The following table details key components used in the validation protocol and broader NGS workflows.
Table 3: Essential Reagents and Materials for NGS in Oncology Research
| Item | Function/Description | Example Product/Citation |
|---|---|---|
| DNA Extraction Kit | Purifies high-quality genomic DNA from diverse sample types (FFPE, blood, buffy coat). | Qiagen DNeasy Blood & Tissue Kit [120] [121] |
| Hybridization Capture Probes | Biotinylated oligonucleotides designed to enrich specific genomic regions of interest. | Custom probes (e.g., from Twist Bioscience) [122] [121] |
| Library Preparation Kit | Prepares DNA fragments for sequencing by adding adapters and barcodes. | Twist Library Preparation EF Kit [122] |
| Automated Library Prep System | Automates library preparation steps to improve throughput, consistency, and reduce error. | MGI SP-100RS System [121] |
| Reference Control DNA | Well-characterized genomic DNA from reference cell lines for benchmarking platform performance. | NIST RM 8398, HG001/NA12878, HG002/NA24385 [122] [120] |
| Positive Control DNA | Contains known mutations at defined allele frequencies for assay validation and quality control. | HD701 Reference Standard [121] |
Clinical Utility and Application in Precision Oncology
The ultimate value of a sequencing platform is determined by its ability to answer clinically relevant questions and improve patient outcomes.
- Comprehensive Genomic Profiling (CGP): NGS enables simultaneous assessment of a broad spectrum of genomic alterations—including SNVs, indels, copy number variations (CNVs), gene fusions, and tumor mutational burden (TMB)—from a single test, which is crucial for matching patients with targeted therapies [9] [118].
- Resolving Technically Challenging Variants: Long-read sequencing is uniquely positioned to identify variants that are difficult or impossible to detect with short reads. A clinical study demonstrated 99.4% concordance in detecting 167 challenging, clinically relevant variants, including repeat expansions, structural variants (SVs), and variants in genes with highly homologous pseudogenes (e.g., PMS2, NF1) [120].
- Liquid Biopsy and Minimal Residual Disease (MRD): The high sensitivity of modern platforms, particularly when combined with unique molecular identifiers (UMIs), is foundational for analyzing circulating tumor DNA (ctDNA). This allows for non-invasive tumor genotyping, monitoring treatment response, and detecting MRD and emerging resistance mechanisms [9] [116] [39].
Platform Strengths Drive Clinical Applications
The NGS landscape continues to evolve rapidly. Key trends shaping its future in precision oncology include the integration of artificial intelligence (AI) and machine learning to enhance variant calling, interpretation, and drug response prediction [116] [17] [117]. The rise of single-cell and spatial sequencing technologies promises to unravel tumor heterogeneity and the tumor microenvironment with unprecedented resolution [9]. Furthermore, the ongoing reduction in costs and the development of more portable, accessible platforms like the MinION are set to democratize genomic testing, expanding its reach into resource-limited settings [118].
In conclusion, the choice of a sequencing platform is a strategic decision that balances accuracy, cost, and the specific clinical or research question at hand. Short-read platforms remain the workhorse for high-throughput, targeted applications, while long-read technologies are indispensable for resolving complex genomic regions. The emergence of ultra-high-accuracy short-read sequencing offers a compelling path for enhancing sensitivity while reducing costs. As these technologies mature and integrate with advanced computational tools, they will collectively propel precision oncology forward, enabling more personalized and effective cancer care.
Concordance in Pathogenicity and Actionability Assessment Across Annotation Services
The implementation of next-generation sequencing (NGS) in precision oncology has revolutionized cancer care by enabling comprehensive genomic profiling of tumors. However, the interpretation of genomic alterations represents a significant bottleneck for realizing precision medicine [123]. The intricate results of NGS assays present numerous somatic genetic variants, many characterized as variants of unknown significance, whose implications remain poorly defined [123]. This complexity is further compounded by intratumoral genetic heterogeneity [123].
Annotation services have emerged as essential tools to assist with data curation, providing interpretations regarding the likelihood of tumorigenicity and drug actionability [123]. Multiple professional societies, including AMP/ASCO/CAP and ESMO, have established classification guidelines to standardize variant interpretation [124]. Despite these efforts, significant challenges remain in achieving consistent variant classification across different annotation platforms, creating uncertainty in clinical decision-making and impacting patient management in precision oncology.
Quantitative Evidence of Annotation Discordance
Key Studies Demonstrating Variability
Substantial evidence reveals concerning discrepancies in variant classification across annotation services. A 2020 study examining the Veterans Affairs National Precision Oncology Program analyzed 1,388 unique variants from 1,227 NGS results and found wide-ranging agreement in pathogenicity assessment [123]. For pathogenic and likely pathogenic variants, concordance was only 30% between Watson for Genomics (WfG) and N-of-One (kappa, -0.26), 76% between WfG and OncoKB (kappa, 0.22), and 42% between N-of-One and OncoKB (kappa, -0.07) [123].
For level 1 drug actionability of gene variant-diagnosis combinations, moderate agreement was observed between WfG and OncoKB (96.9%; kappa, 0.44), with 27 combinations identified as level 1 by both services, 58 by WfG alone, and 6 variants by OncoKB alone [123].
A more recent 2024 study analyzing 80 pan-cancer cases revealed striking differences in tier classifications across four annotation software solutions: navify Mutation Profiler (Roche), SOPHIA DDM (SOPHiA GENETICS), QIAGEN Clinical Insights Interpret, and Franklin (Genoox) [124]. The investigation focused on Tiers I and II variants according to AMP/ASCO/CAP guidelines, which hold the highest clinical relevance [124].
Table 1: Pathogenicity Concordance Across Annotation Services (2020 Study)
| Comparison | Percentage Agreement | Cohen's Kappa Statistic | Interpretation |
|---|---|---|---|
| WfG vs. NoO | 30% | -0.26 | Poor agreement |
| WfG vs. OncoKB | 76% | 0.22 | Fair agreement |
| NoO vs. OncoKB | 42% | -0.07 | Poor agreement |
Table 2: Therapeutic Actionability Concordance (2020 Study)
| Evidence Level | Service Agreement | Shared Calls | Unique to WfG | Unique to OncoKB |
|---|---|---|---|---|
| Level 1 | 96.9% (kappa: 0.44) | 27 combinations | 58 combinations | 6 combinations |
Factors Contributing to Annotation Discordance
Multiple technical and methodological factors contribute to the observed variability in annotation results:
- Subjectivity in Guidelines: The AMP/ASCO/CAP and other professional guidelines contain inherent subjectivity that allows for different interpretations [124]
- Threshold Variations: Differing settings for variant allele frequencies (VAF) and population allele frequencies significantly impact variant classification [124]
- Disease Ontology Differences: Variation in disease ontologies and tumor type classifications affect actionability predictions [124]
- Content Source Variation: Annotators utilize different knowledge bases and update them at varying frequencies, leading to discrepancies in the underlying evidence [124]
- Input Requirements: Annotation tools have different requirements for input files and data types, which can influence the completeness of analysis [124]
Experimental Protocols for Annotation Comparison
Methodology for Multi-Service Concordance Analysis
The 2020 study employed a systematic approach to evaluate annotation concordance [123]. Unique gene variants were generated from NGS gene panel results using two sequencing services. For each unique gene variant, annotations were provided through three sources: N-of-One (commercial annotation service used by sequencing vendors), IBM Watson for Genomics (cloud-based cognitive computing system), and OncoKB (evidence source from Memorial Sloan Kettering Cancer Center) [123].
Annotations for pathogenicity from all three sources and actionability from WfG and OncoKB were examined for concordance. Cohen's kappa statistic was calculated to measure agreement between annotation services, with variants categorized as pathogenic, likely pathogenic, or other [123]. For actionability, WfG used levels of evidence (level 1, 2A, 2B, 3A, 3B, 4, or R1) while OncoKB employed a four-tier system, with level 1 representing the highest evidence for FDA-approved therapies [123].
Protocol for Software Solution Comparison
The 2024 study established a rigorous methodology for comparing four annotation software solutions using 80 pan-cancer cases [124]. Formalin-fixed paraffin-embedded (FFPE) tumor samples underwent processing using the TruSight Oncology 500 (TSO500) assay, a targeted panel comprising 523 DNA genes and 55 RNA genes with cancer relevance [124].
The resulting sequencing files were analyzed using four different commercial software annotators: navify Mutation Profiler (v. 2.3.2.c090e09), SOPHIA DDM (v. 5.10.42.1), QIAGEN Clinical Insight Interpret (v. 9.2.1.20231012), and Franklin (v. 2023.7) [124]. Each annotator had specific requirements for input data, all representing the hg19 genome build. To ensure consistency between the secondary analysis pipeline of SOPHIA and TSO500 variant calls, a Python script was employed for variant comparison, achieving a per-case SNP match rate average of 93.604% [124].
Diagram 1: Annotation comparison experimental workflow
Annotation Services and Software Solutions
Major Annotation Platforms
Recent studies have evaluated numerous annotation platforms with diverse approaches to variant interpretation:
- OncoKB: A precision oncology knowledge base developed by Memorial Sloan Kettering Cancer Center that contains information on the clinical actionability for somatic gene variants organized by indication and four-tier levels of evidence [123]
- Watson for Genomics (WfG): A cloud-based service that uses computerized models to simulate human thought to analyze large volumes of genome data and generate evidence-based guidelines [123]
- N-of-One: A commercial annotation service that provides therapeutic and biomarker interpretations for precision medicine [123]
- navify Mutation Profiler (Roche): Interprets genomic variants following AMP/ASCO/CAP guidelines, utilizing VCF files plus combined variant output files as input [124]
- SOPHIA DDM: Serves as both secondary and tertiary analysis software, taking processed FASTQ files as input and generating its own quality metrics [124]
- QIAGEN Clinical Insight Interpret: Employs VCF files, copy number variants files, fusions files, and splice variants files for comprehensive analysis [124]
- Franklin (Genoox): A publicly available annotator that uses VCF files as input and classifies variants into Tiers I-IV with a broad evidence framework [124]
Table 3: Annotation Software Solutions and Key Characteristics
| Software Solution | Input Requirements | Tiering System | Special Features |
|---|---|---|---|
| navify Mutation Profiler | VCF + combined variant output | AMP/ASCO/CAP (IA, IB, IIC, IID, III) | Incorporates copy number amplification data & TMB |
| SOPHIA DDM | Processed FASTQ files | AMP/ASCO/CAP (IA, IB, IIC, IID) | Integrated secondary and tertiary analysis |
| QIAGEN Clinical Insight | VCF, CNV, fusions, splice variants | AMP/ASCO/CAP (IA, IB, IIC, IID) | Comprehensive alteration analysis |
| Franklin | VCF files | Tiers I-IV (broad evidence framework) | Free publicly available annotator |
Emerging Solutions and Validation Approaches
Recent feasibility studies demonstrate the emergence of validated in-house solutions, particularly for specific populations. The TumorSecTM bioinformatics pipeline, developed for Latin and Hispanic populations, showed 80.5% concordance with validated laboratory results and ~94% concordance between hybridization capture-based and amplicon-based library preparation methods for actionable variants in colorectal cancer samples [83]. This approach represents a cost-effective strategy for implementing precision oncology in resource-limited settings by focusing on relevant population-specific variants.
The Scientist's Toolkit: Research Reagent Solutions
Table 4: Essential Research Reagents and Platforms for Annotation Studies
| Research Reagent/Pipeline | Function/Application | Key Features |
|---|---|---|
| TruSight Oncology 500 (TSO500) | Targeted NGS panel for comprehensive genomic profiling | 523 DNA genes + 55 RNA genes; detects SNVs, CNVs, fusions, TMB, MSI |
| TumorSecTM Custom Panel | Targeted sequencing for Latin American populations | 25 genes relevant for approved oncological drugs in Latin America |
| Illumina AmpliSeq v2 Hotspot Panel | Amplicon-based targeted sequencing | Hotspot regions of 50 cancer-related genes |
| Hybridization Capture-Based Method | Library preparation using sequence-specific probes | Custom panel of probes; compatible with KAPA HyperPlus kit |
| Sophia DDM Software | Variant analysis with machine learning | Uses machine learning for rapid variant analysis and visualization |
| Oncomine Precision Assay | Targeted NGS testing platform | 50 key genes including DNA mutation analysis, fusion detection, CNV identification |
Annotation Decision Pathway and Clinical Impact
The variability in annotation services has direct implications for clinical decision-making in precision oncology. Understanding the annotation decision pathway is essential for interpreting discordant results.
Diagram 2: Annotation decision pathway and discordance sources
Substantial variability exists in pathogenicity and clinical actionability assessment across annotation services, with concordance rates for pathogenic variants ranging from 30% to 76% between different services [123]. This discordance stems from multiple factors including subjectivity in professional guidelines, varying threshold settings for variant allele frequencies and population allele frequencies, differences in disease ontologies, and variation in the underlying evidence bases and their update cycles [124].
The implications for precision oncology are significant, as these discrepancies can directly impact therapy selection, clinical trial eligibility, and ultimately patient outcomes. Future directions should focus on improved standardization of annotation processes, harmonization of classification guidelines, and the development of consensus approaches for variant interpretation. Regular reconciliation of knowledge bases and validation of annotation outputs through molecular tumor boards remain essential for ensuring the accuracy and clinical utility of NGS-based genomic profiling in oncology.
The adoption of next-generation sequencing (NGS) has fundamentally transformed precision oncology, enabling molecular-guided treatment strategies that improve patient outcomes [30] [125]. However, the optimal choice of genomic sequencing platform remains a critical consideration for researchers and clinicians. The decision primarily centers on three approaches: targeted gene panels, whole-exome sequencing (WES), and whole-genome sequencing (WGS), each with distinct advantages and limitations [2] [126].
Targeted panels focus on a predefined set of genes with known clinical or research relevance, while WES sequences all protein-coding regions (~1-2% of the genome), and WGS provides a truly comprehensive view of the entire ~3.2 billion base pair genome [125] [127]. This technical guide provides an in-depth, evidence-based comparison of these methodologies, focusing on their analytical performance, clinical utility, and practical implementation in precision oncology research and drug development.
Technical Specifications and Methodological Comparison
Fundamental Technological Differences
The core distinction between sequencing methods lies in their genomic coverage and enrichment strategies. Targeted panels use hybrid capture or amplicon-based methods to enrich specific genomic regions of interest, typically covering from dozens to hundreds of cancer-associated genes [121] [127]. This focused approach allows for extremely high sequencing depth (often 500-2000x or higher), enabling detection of low-frequency variants in heterogeneous tumor samples [127] [126].
WES employs capture probes to enrich all protein-coding exons, covering approximately 37 million bases, while WGS sequences the entire genome without enrichment, providing uniform coverage across both coding and non-coding regions [128]. The comprehensive nature of WGS comes with substantially higher data output—approximately 100 GB per sample compared to 5-15 GB for WES and even less for targeted panels—creating significant computational and storage challenges [128] [126].
Detection Capabilities by Alteration Type
Each sequencing method exhibits distinct strengths in detecting different classes of genomic alterations:
Single Nucleotide Variants (SNVs) and Small Indels: Targeted panels and WES demonstrate high sensitivity for detecting SNVs and small insertions/deletions within their covered regions, with panels achieving superior sensitivity for low-frequency variants due to higher sequencing depth [121] [127]. WGS provides the most comprehensive detection across the entire genome but at generally lower depth for the same sequencing cost [129].
Copy Number Variations (CNVs): WGS provides the most accurate CNV detection due to uniform coverage and absence of hybridization biases [125] [128]. Targeted panels can detect CNAs in selected genes but may miss events outside targeted regions [121].
Structural Variants (SVs) and Gene Fusions: WGS excels at detecting complex structural variants, translocations, and rearrangements regardless of genomic location [125]. RNA-based panels or whole-transcriptome sequencing (WTS) are particularly valuable for detecting expressed gene fusions [125] [2].
Complex Biomarkers: WGS enables comprehensive assessment of complex biomarkers including tumor mutational burden (TMB), microsatellite instability (MSI), mutational signatures, and homologous recombination deficiency (HRD) [130] [128]. Targeted panels can estimate these biomarkers but with limitations in accuracy and standardization [128].
Table 1: Comparative Analysis of Sequencing Method Capabilities
| Parameter | Targeted Panels | Whole Exome Sequencing (WES) | Whole Genome Sequencing (WGS) |
|---|---|---|---|
| Genomic Coverage | 0.016 - 5 Mb [128] | ~37 Mb (exonic regions) [128] | ~3,200 Mb (entire genome) [125] |
| Typical Sequencing Depth | 500-2000x [126] | 100-200x [126] | 30-100x [128] |
| SNV/Indel Detection | Excellent in targeted regions [121] | Good in exonic regions [128] | Comprehensive but at lower depth [129] |
| CNV Detection | Limited to panel genes [121] | Moderate with biases [128] | Excellent, genome-wide [125] |
| Structural Variants | Limited unless specifically targeted | Limited to breakpoints in exons [128] | Comprehensive detection [125] |
| TMB Estimation | Possible but platform-dependent [128] | Good, correlates with WGS [128] | Gold standard [128] |
| Turnaround Time | 2-5 days [121] [127] | 1-2 weeks | 2-4 weeks |
| Data Volume per Sample | 0.5-5 GB [127] | 5-15 GB [126] | 80-120 GB [126] |
Diagram 1: Experimental workflow for sequencing methodologies
Clinical and Research Utility in Precision Oncology
Biomarker Detection and Therapy Matching
Direct comparative studies reveal significant differences in clinical actionability between sequencing approaches. A 2025 study comparing WES/WGS with transcriptome sequencing to targeted panel sequencing (TruSight Oncology 500) found that while panel sequencing identified a median of 2.5 treatment recommendations per patient, WES/WGS ± TS identified a median of 3.5 recommendations [130]. Approximately half of the therapy recommendations were identical across platforms, while one-third of WES/WGS-based recommendations relied on biomarkers not covered by the panel [130].
Notably, in a study of 20 patients with rare or advanced tumors, 8 of 10 molecularly informed therapy implementations were supported by the panel, while the remaining two were based exclusively on biomarkers detectable only through WGS/TS approaches [130]. This demonstrates the potential for comprehensive sequencing to identify additional clinical options, particularly for patients with rare cancers or limited treatment options.
Detection of Complex Biomarkers
Complex biomarkers such as TMB, MSI, and HRD represent critical predictors of response to immunotherapy and targeted therapies, with significant variability in their accurate measurement across platforms:
Tumor Mutational Burden (TMB): WGS provides the most comprehensive TMB assessment but correlates well with WES when calculated consistently. TMB estimates from targeted panels show good correlation with WGS but demonstrate platform-specific variability in absolute values, necessitating method-specific thresholds [128].
Microsatellite Instability (MSI): WGS enables genome-wide assessment of microsatellite regions, while targeted panels estimate MSI from a limited set of loci. Studies show that classification concordance between methods is high (>90%), but absolute scores vary significantly [128].
Homologous Recombination Deficiency (HRD): WGS provides the most robust HRD assessment through detection of specific mutational signatures (e.g., signature 3) and genomic scarring patterns [125]. Targeted approaches have limited ability to assess these complex genomic patterns.
Table 2: Clinical Validation Studies Comparing Sequencing Approaches
| Study | Sample Size | Key Findings | Clinical Implications |
|---|---|---|---|
| Translational Comparison (npj Precision Oncology, 2025) [130] | 20 patients | WES/WGS ± TS provided 1.0 additional therapy recommendation per patient compared to panels; 30% of WGS recommendations relied on biomarkers absent from panels | Comprehensive sequencing identifies additional actionable targets, particularly in rare cancers |
| In Silico Downsampling Study (ESMO Open, 2022) [128] | 726 tumors across 10 cancer types | Comprehensive panels detected most FDA-approved biomarkers; WGS identified more biomarkers for treatments in clinical trials (investigational therapies) | WGS provides greater opportunities for experimental therapeutic matching |
| Target-Enhanced WGS Validation (Cancer Research and Treatment, 2025) [129] | 49 patients | TE-WGS detected 100% of variants identified by TSO500 panel; additionally identified germline origins of 44.8% of variants and provided accurate CNV/fusion calls | WGS matches panel detection for core targets while providing additional clinical insights |
| Targeted Panel Implementation (Scientific Reports, 2025) [121] | 43 samples | Custom 61-gene panel achieved 99.99% reproducibility, 98.23% sensitivity; reduced turnaround time to 4 days vs. 3 weeks for external testing | Optimized panels provide rapid, cost-effective clinical testing for established biomarkers |
Practical Considerations for Implementation
Sample Requirements and Quality
Sample quality and type significantly impact sequencing success. Targeted panels demonstrate superior performance with suboptimal samples, including formalin-fixed paraffin-embedded (FFPE) tissue and liquid biopsy specimens with low tumor content or degraded DNA [121] [127]. WGS typically requires high-quality DNA from fresh-frozen tissue, posing challenges for routine clinical implementation where FFPE remains the standard [126].
The input DNA requirements also vary substantially: targeted panels can generate reliable data with as little as 1-10 ng of DNA, while WES typically requires 50-100 ng, and WGS performs best with 100-1000 ng of high-quality DNA [121] [126].
Turnaround Time and Computational Infrastructure
Targeted panels offer significantly faster turnaround times (2-5 days) compared to comprehensive sequencing approaches (2-4 weeks), making them particularly valuable for time-sensitive clinical decisions [121] [127]. The streamlined data analysis for panels requires less computational infrastructure compared to WES and WGS, which generate massive datasets requiring sophisticated bioinformatics pipelines and storage solutions [2] [126].
Cost Considerations
While sequencing costs have decreased dramatically, total cost of ownership extends beyond sequencing alone. Targeted panels have lower direct sequencing costs and more manageable data storage requirements. WGS has higher direct costs and requires significant investment in computational infrastructure, bioinformatics expertise, and interpretation resources [126]. One study noted that shifting from external panel testing to an in-house targeted panel reduced costs and decreased turnaround time from 3 weeks to 4 days [121].
Experimental Design and Methodologies
Key Experimental Protocols
Targeted Panel Sequencing Methodology
The standard workflow for targeted panel sequencing involves:
Sample Collection and DNA Extraction: DNA is extracted from tumor samples (tissue, blood, or liquid biopsy) using column-based or magnetic bead methods, with quality control measures including quantification and fragmentation analysis [121] [127].
Library Preparation: For hybridization capture-based panels (such as TruSight Oncology 500), DNA is fragmented, adapters are ligated, and target regions are enriched using biotinylated probes [121]. For the TTSH-oncopanel (61 genes), researchers used a hybridization-capture method with library kits from Sophia Genetics, compatible with automated library preparation systems to reduce human error and contamination risk [121].
Sequencing: Libraries are sequenced on platforms such as Illumina NovaSeq or MGI DNBSEQ-G50RS to achieve high depth coverage (typically 500-2000x) [121]. The TTSH-oncopanel validation achieved median coverage of 1671x with 98% of target regions covered at ≥100x [121].
Bioinformatic Analysis: Raw sequencing data is processed through pipelines including base calling, alignment to reference genomes, variant calling, and annotation using tools like GATK or Mutect2 [127]. For the TTSH-oncopanel, Sophia DDM software with machine learning algorithms was used for variant analysis and visualization [121].
Whole Genome/Exome Sequencing Methodology
Comprehensive sequencing approaches follow these key steps:
Sample Preparation: Matched tumor-normal pairs are typically sequenced to distinguish somatic from germline variants. DNA quality is critically important, with fresh-frozen tissue preferred over FFPE for WGS [128] [126].
Library Preparation and Sequencing: WGS library preparation typically uses fragmentation and adapter ligation without target enrichment. The MASTER program employs WGS (30-60x coverage) and whole-transcriptome sequencing with paired germline sequencing for somatic variant identification [130].
Bioinformatic Processing: WGS data analysis involves alignment, somatic variant calling (SNVs/indels), copy number analysis, structural variant detection, and mutational signature analysis [130] [128]. The MASTER program uses specialized pipelines including Arriba for fusion detection and assesses complex biomarkers including TMB, MSI, and HRD scores [130].
Diagram 2: Decision pathway for sequencing methodology selection
The Scientist's Toolkit: Essential Research Reagents and Platforms
Table 3: Key Research Reagent Solutions for Sequencing Studies
| Category | Specific Examples | Function and Application |
|---|---|---|
| Commercial Panels | TruSight Oncology 500 (TSO500) [130], TruSight Tumor 170 (TST170) [130], TTSH-oncopanel (61 genes) [121] | Standardized targeted sequencing with validated content and analysis pipelines |
| Library Prep Kits | Sophia Genetics library kits [121], TruSeq DNA Nano [128] | Prepare sequencing libraries with appropriate adapters and barcodes for multiplexing |
| Automation Systems | MGI SP-100RS automated library preparation system [121] | Reduce human error, increase throughput, and maintain consistency in library prep |
| Sequencing Platforms | Illumina NovaSeq [128], MGI DNBSEQ-G50RS [121] | High-throughput sequencing with different read lengths and output characteristics |
| Bioinformatics Tools | Sophia DDM with machine learning [121], GATK [128], Arriba (fusion detection) [130] | Variant calling, annotation, and interpretation with clinical relevance scoring |
| Reference Materials | HD701 reference standard [121] | Assay validation, quality control, and detection limit determination |
The choice between targeted panels, WES, and WGS represents a strategic balance between clinical practicality and comprehensive genomic assessment. Targeted panels provide a cost-effective, rapid solution for focused clinical questions with limited samples, while WES and WGS offer increasingly comprehensive genomic characterization at higher resource costs [130] [121] [126].
For clinical trials and drug development, this comparison suggests a tiered approach: targeted panels for large-scale patient screening and biomarker stratification, with comprehensive sequencing reserved for exploratory endpoints, resistance mechanism studies, and rare cancer populations [130] [128]. As sequencing costs continue to decline and bioinformatic tools become more sophisticated, the integration of comprehensive genomic profiling into routine research and clinical care will accelerate, further advancing precision oncology approaches across diverse cancer types [125] [2].
Future directions include the development of target-enhanced WGS approaches that combine the comprehensive nature of WGS with focused analysis pipelines [129], the standardization of complex biomarker assessment across platforms [128], and the integration of multi-omic data for more complete tumor characterization [125]. These advances will continue to blur the distinctions between sequencing approaches while enhancing their collective value in precision oncology research and therapeutic development.
Next-generation sequencing (NGS) has become a cornerstone of precision oncology, enabling comprehensive genomic profiling that guides targeted therapy and improves patient outcomes [9] [44]. The transition of NGS from research to clinical diagnostics necessitates rigorous validation to ensure reliable and accurate results. This process verifies that an assay consistently performs to predefined specifications for its intended use, providing clinicians with the confidence needed for therapeutic decision-making. Within the broader context of precision oncology, establishing robust validation frameworks for NGS assays is fundamental to realizing the promise of molecularly driven cancer care. This guide details the core performance metrics—sensitivity, specificity, and reproducibility—and outlines the experimental protocols essential for the analytical validation of NGS assays in clinical settings.
Core Analytical Performance Metrics
Analytical validation establishes the performance characteristics of a test under defined conditions. For clinical NGS assays, key metrics must be quantified using validated reference materials and well-designed experiments. The table below summarizes the performance targets for different variant types based on recent studies.
Table 1: Key Analytical Performance Metrics for NGS Assays
| Performance Metric | Variant Type | Target Performance | Key Influencing Factors |
|---|---|---|---|
| Sensitivity (Limit of Detection) | SNVs/Indels [131] [121] [132] | ≥95% at 0.15%-0.5% VAF [131] [132] | Sequencing depth, base quality, bioinformatic pipelines |
| Gene Fusions [131] [133] | 100% at 0.30% Tumor Fraction [131] | RNA input quantity, capture efficiency, intronic coverage | |
| Copy Number Variations (CNVs) [131] [132] | 2.11 copies (amplification), 1.80 copies (loss) [131] | Tumor fraction, coverage uniformity, background noise | |
| Microsatellite Instability (MSI) [131] [132] | 100% at 0.07% Tumor Fraction [131] | Panel size, number of loci, baseline stability | |
| Specificity | SNVs/Indels [134] [121] | >99.99% [134] [121] | Unique molecular identifiers (UMIs), error suppression |
| Fusions & CNVs [131] | >99.9% [131] | Bioinformatic filters against artifactual calls | |
| Reproducibility | All Variants [121] | >99.9% inter-run and intra-run precision [121] | Standardized protocols, reagent lots, personnel |
Sensitivity and Limit of Detection
Sensitivity defines the lowest value at which a variant can be reliably detected. The Limit of Detection (LOD) is the lowest variant allele frequency (VAF) or tumor fraction at which a variant is detected with ≥95% probability [131]. For example, the Northstar Select liquid biopsy assay demonstrated a 95% LOD of 0.15% VAF for SNVs/Indels, allowing it to identify 51% more pathogenic variants than comparator assays, with 91% of these additional actionable variants found below 0.5% VAF [131]. Technological advancements, such as Q40 sequencing (99.99% base accuracy), can enhance sensitivity for rare variant detection while reducing required sequencing depth by an estimated 30-50%, lowering overall costs [39].
Specificity
Specificity is the probability that the test will not generate a false positive result when a true variant is absent. It is measured as the proportion of true negative calls among all non-variant positions. High specificity (>99.9%) is critical for avoiding incorrect treatment recommendations [134] [131] [121]. Specificity is maintained through wet-lab techniques like using Unique Molecular Identifiers (UMIs) to tag original DNA molecules and bioinformatic tools that filter out sequencing errors and artifacts related to clonal hematopoiesis [131] [132].
Reproducibility
Reproducibility, or precision, ensures the assay yields consistent results across multiple runs of the same sample. This includes intra-run (within a single run), inter-run (across different runs), and inter-operator precision. A validated NGS assay should demonstrate >99.9% reproducibility for all variant types [121]. Long-term reproducibility is monitored by repeatedly testing a positive control, such as the HD701 reference standard, which should show a coefficient of variation of less than 0.1x for detected variants [121].
Experimental Protocols for Validation
A robust validation framework requires carefully designed experiments to measure the metrics above.
Establishing Sensitivity and LOD
Materials:
- Serially diluted, commercially available reference standards with known VAFs (e.g., Tru-Q, S800, OncoSpan) [121] [132].
- For liquid biopsy: Contrived samples spiked with cell-free DNA from characterized cell lines.
Method:
- Titration Series: Sequence a dilution series of the reference standard covering a range of VAFs (e.g., from 0.06% to 0.35%) [131].
- Variant Calling: Process the data through the standard bioinformatics pipeline.
- Calculate LOD: For each VAF level, calculate the detection rate. The LOD95 is the lowest VAF at which ≥95% of expected variants are detected. This can be confirmed orthogonally with digital droplet PCR (ddPCR) [131].
- Input DNA/RNA Titration: Repeat the assay with decreasing input amounts of nucleic acids (e.g., from 100 ng to 10 ng) to determine the minimum required input. A study established that ≥50 ng of DNA input was necessary for reliable performance of their 61-gene panel [121].
Determining Specificity
Materials:
- Wild-type reference standards (e.g., Tru-Q0) [132].
- Confirmed negative clinical samples.
Method:
- Sequence Negative Samples: Process multiple wild-type and negative samples through the entire workflow.
- Analyze False Positives: The number of false positive calls is divided by the total number of bases or positions interrogated to calculate the false positive rate. Specificity is calculated as: (Number of True Negatives) / (True Negatives + False Positives) [121] [132].
Assessing Reproducibility
Materials:
- A set of well-characterized positive samples, including FFPE and liquid biopsy specimens.
Method:
- Replicate Testing: Prepare and sequence multiple replicates (n≥3) of each sample. This should include:
- Intra-run: Multiple libraries from the same sample within a single sequencing run.
- Inter-run: The same sample across different runs, on different days, and by different operators [132].
- Variant Concordance Analysis: Compare the variant calls (presence/absence and VAF) across all replicates. The percentage of variants that are consistently detected in all replicates is the measure of reproducibility [121] [133]. The FoundationOneRNA assay, for instance, demonstrated 100% reproducibility for 10 pre-defined fusions [133].
The Scientist's Toolkit: Essential Research Reagents
Successful validation relies on high-quality, traceable materials. The following table lists key reagents and their functions.
Table 2: Essential Research Reagents for NGS Assay Validation
| Reagent / Material | Function in Validation | Examples & Key Features |
|---|---|---|
| Reference Standards | Benchmarking sensitivity, specificity, and LOD; quality control. | - Mimix Geni (Revvity): Contains 7 clinically relevant oncogenic mutations; cross-platform compatible [135]. - OncoSpan (Horizon Discovery): 386 variants across 152 cancer genes; includes 52 variants at ≤20% AF for LOD determination [132]. |
| Library Prep Kits | Preparing sequencing libraries from input nucleic acids. | - Hybridization-capture based kits (e.g., Sophia Genetics): Offer high specificity and uniform coverage [121]. - Automated systems (e.g., MGI SP-100RS): Reduce human error and increase consistency [121]. |
| Bioinformatic Pipelines | Variant calling, filtering artifacts, and generating reports. | - Sophia DDM: Uses machine learning for rapid variant analysis and clinical interpretation [121]. - Custom pipelines: Designed to improve sensitivity and reduce noise, especially for CNVs in liquid biopsy [131]. |
Signaling Pathways and Workflow in NGS-Based Therapy Selection
NGS identifies actionable genomic alterations that drive cancer progression through specific signaling pathways, enabling targeted therapy. Two prominent examples in precision oncology are the NTRK and RET signaling pathways, which are oncogenic drivers across multiple cancer types (tumor-agnostic) [44].
The diagram below illustrates the core workflow from sample processing to therapy selection, highlighting how NGS identifies targets within these pathways.
Diagram 1: NGS Clinical Testing Workflow and Targeted Pathways. The process begins with sample acquisition and proceeds through sequencing and analysis to a clinical report. This report can identify actionable genomic alterations, such as NTRK fusions, which drive oncogenic signaling and are targeted by specific inhibitors (e.g., Larotrectinib) [44].
The rigorous analytical validation of NGS assays is a non-negotiable prerequisite for their reliable application in clinical oncology. By systematically establishing and monitoring sensitivity, specificity, and reproducibility using standardized reference materials and protocols, laboratories can ensure the generation of accurate data that clinicians can trust. As the field evolves with longer-read technologies, multi-omic integrations, and more sophisticated bioinformatics, the principles of robust validation will remain the foundation upon which precision oncology advances, ultimately ensuring that patients receive the most informed and effective treatments possible.
Assessing Clinical Actionability with Frameworks like ESMO ESCAT
The ESMO Scale for Clinical Actionability of molecular Targets (ESCAT) is a systematic framework developed by the ESMO Translational Research and Precision Medicine Working Group to rank genomic alterations based on clinical evidence supporting their value as therapeutic targets [136] [137]. This evidence-based classification system addresses the critical need in precision oncology to harmonize the interpretation of genomic data and prioritize molecular alterations for targeted therapies [136]. ESCAT provides a standardized approach that enables researchers, clinicians, and drug development professionals to communicate using a common language, thereby facilitating more equitable and consistent implementation of precision medicine across different healthcare systems and geographical regions [137].
The fundamental concept underpinning ESCAT is clinical actionability – the demonstrated potential of a genomic alteration to serve as a reliable biomarker for selecting patients who would benefit from a specific targeted therapy [137]. Unlike classification systems based on regional drug approval status, ESCAT ranks alterations solely according to scientific evidence, making it particularly valuable for global research collaboration and drug development efforts [137].
The ESCAT Tier System: Definition and Classification Criteria
The ESCAT framework categorizes molecular targets into a hierarchical structure of six main tiers, with clinical evidence strength decreasing from top to bottom [136] [137]. This tiered system enables systematic prioritization of genomic alterations for therapeutic targeting in both research and clinical settings.
Tier I: Ready for Routine Clinical Implementation
Tier I represents genomic alterations with the strongest evidence base, considered ready for implementation in routine clinical practice [136]. This tier is subdivided into three categories based on study design and evidence level:
- Tier I-A: Alteration-drug combinations supported by evidence from randomized clinical trials demonstrating statistically significant and clinically relevant improvements in survival endpoints [138]. Examples include EGFR exon 19 mutations in non-small cell lung cancer (NSCLC) treatable with tyrosine kinase inhibitors [137] [56].
- Tier I-B: Supported by evidence from prospective single-arm clinical trials [138].
- Tier I-C: Supported by evidence from basket trials [138].
Tier II: Investigational Targets
Tier II includes investigational targets that likely define patient populations benefiting from targeted drugs but require additional data for full validation [136]. This tier includes:
- Tier II-A: Evidence derived from retrospective clinical trials [138].
- Tier II-B: Evidence from prospective clinical trials demonstrating increased response rates but without documented survival benefits [138].
Tier III: Clinical Benefit in Other Contexts
Tier III encompasses targets with demonstrated clinical benefit in different tumor types or for similar molecular targets [136]. Subcategories include:
- Tier III-A: Relevant in other tumor entities [138].
- Tier III-B: Located in the same pathway as other actionable alterations but without direct clinical evidence for the specific alteration [138].
Additional Tiers
Tier IV includes targets with preclinical evidence of actionability (IV-A: in vitro or in vivo models; IV-B: in silico models) [138]. Tier V contains alterations with evidence supporting co-targeting approaches that improve objective response rates [138]. Tier X includes alterations with no current evidence for actionability, which should not guide treatment decisions [136] [138].
Table 1: ESCAT Tier Classification System and Clinical Implications
| ESCAT Tier | Level of Evidence | Clinical Implications | Examples |
|---|---|---|---|
| I-A | Randomized clinical trials with survival benefit | Ready for routine clinical implementation; standard of care | PIK3CA mutations in breast cancer; EGFR exon 19 mutations in NSCLC [56] [138] |
| I-B | Prospective single-arm trials | Ready for routine clinical implementation | Uncommon EGFR mutations (G719X-exon-18, L861Q-exon-21) [138] |
| I-C | Basket trials | Ready for routine clinical implementation | - |
| II-A | Retrospective clinical trials | Potential clinical relevance; additional evidence needed | BRCA1/2 somatic mutations in breast cancer; ERBB2 mutations [56] |
| II-B | Prospective trials without survival benefit | Potential clinical relevance; additional evidence needed | - |
| III-A | Clinical benefit in other tumor types | Potential relevance in different context | - |
| III-B | Same pathway as actionable alterations | Hypothetical actionability | - |
| IV-A/B | Preclinical models (in vitro/vivo or in silico) | Early research evidence | - |
| V | Co-targeting approaches | Combination therapy strategies | - |
| X | No evidence for actionability | Not recommended for treatment decisions | - |
Methodological Framework for ESCAT Implementation
Comprehensive Genomic Profiling in Research Settings
Implementing ESCAT in research requires robust comprehensive genomic profiling (CGP) methodologies. The foundational step involves next-generation sequencing (NGS) of tumor samples using targeted multigene panels that cover established and emerging biomarkers [56]. The analytical workflow encompasses:
DNA and RNA Extraction: Simultaneous isolation of both DNA and RNA from tumor tissue samples (fresh-frozen or FFPE) or liquid biopsies [56]. DNA analysis identifies single nucleotide variants (SNVs), insertions/deletions (indels), and copy number variations (CNVs), while RNA sequencing detects gene fusions and expression outliers [56].
Library Preparation and Sequencing: Target enrichment using hybrid capture-based methods followed by NGS on platforms such as Illumina or Ion Torrent. The recommended sequencing depth is >500x for tumor samples and >100x for matched normal samples to ensure high sensitivity for variant detection [56].
Bioinformatic Analysis: Pipeline processing includes quality control, alignment to reference genome (GRCh38), variant calling, and annotation. Critical steps include tumor mutation burden (TMB) calculation, microsatellite instability (MSI) status determination, and homologous recombination deficiency (HRD) assessment using established algorithms [56].
Variant Interpretation and ESCAT Classification: Identified genomic alterations are interpreted through the ESCAT framework by cross-referencing with clinical trial databases, drug approval labels, and literature evidence. This process requires specialized bioinformatics tools and expert curation to assign appropriate tiers based on tumor type and alteration specificity [138].
Biomarker Detection Methodologies
ESCAT implementation requires specific methodological approaches for detecting different biomarker classes:
Tumor Mutational Burden (TMB) Assessment: Calculated as the total number of nonsynonymous mutations per megabase of sequenced genome. TMB-high status is typically defined as ≥10 mutations/Mb, making patients eligible for immune checkpoint inhibitors [56].
Microsatellite Instability (MSI) Analysis: Detected through NGS-based evaluation of mononucleotide repeat markers or computational analysis of sequencing data. MSI-high status indicates deficiency in DNA mismatch repair systems [56].
Gene Fusion Detection: Requires RNA sequencing to identify expressed fusion transcripts, particularly for targets such as NTRK, RET, and ALK fusions [56].
Homologous Recombination Deficiency (HRD) Assessment: Determined through genomic scar analysis (loss of heterozygosity, telomeric allelic imbalance, large-scale transitions) or direct sequencing of HR pathway genes (BRCA1/2, ATM, RAD51) [56].
Research Applications and Clinical Validation of ESCAT
Evidence from Real-World Studies
Recent research has validated the clinical utility of ESCAT in various cancer types. A 2025 pan-cancer study of 1,166 Asian patient samples demonstrated the distribution of ESCAT-tiered alterations across diverse malignancies [56]:
Table 2: ESCAT Tier Distribution in Real-World Pan-Cancer Study (n=1,166)
| Cancer Type | Tier I Alterations | Tier II Alterations | Tumor-Agnostic Biomarkers | HRD Prevalence |
|---|---|---|---|---|
| Breast Cancer | 39.0% (PIK3CA mutations) | 23.0% (BRCA1/2 somatic mutations) | Not specified | 50.0% |
| Non-Small Cell Lung Cancer | 29 cases (EGFR exon 19 mutations) | Not specified | 16.8% (TMB-high, MSI-high, fusions) | 44.2% |
| Prostate Cancer | 22 cases (BRCA1/2 alterations) | 17 cases (PTEN alterations) | Not specified | Not specified |
| Ovarian Cancer | Not specified | Not specified | Not specified | 40.0% |
| All Cancers Combined | 12.7% | 6.0% | 8.4% | 34.9% |
The study further identified tumor-agnostic biomarkers in 8.4% of samples across 26 cancer types, including MSI-high (1.4%), TMB-high (6.6%), NTRK fusions (0.3%), RET fusions (0.2%), and BRAF V600E mutations (1.3%) [56]. These findings underscore the importance of comprehensive genomic profiling for identifying patients eligible for tissue-agnostic therapies.
Impact on Clinical Outcomes
Research has demonstrated that ESCAT-guided therapy selection significantly improves patient outcomes. A 2022 study in cholangiocarcinoma patients revealed that those with ESCAT tier I-II alterations receiving matched targeted therapy achieved significantly longer median overall survival compared to patients with tier III-IV alterations or no ESCAT alterations (22.6 months versus 14.3 months) [139]. Additionally, progression-free survival was substantially longer in patients with tier I-II alterations treated with targeted therapy (5.0 months versus 1.9 months for tier III-IV alterations) [139].
These findings confirm that the ESCAT framework effectively identifies genomic alterations with clinically meaningful therapeutic implications, validating its utility in both research and clinical decision-making.
Integration with Other ESMO Tools and Molecular Tumor Boards
Synergy with ESMO-Magnitude of Clinical Benefit Scale (MCBS)
ESCAT is designed to complement the ESMO-Magnitude of Clinical Benefit Scale (MCBS), which quantitatively assesses the clinical benefit of new oncological therapies based on clinical trial outcomes [138]. While ESCAT ranks genomic alterations according to clinical actionability evidence, ESMO-MCBS evaluates the magnitude of benefit provided by targeted therapies [138]. This dual assessment framework enables more comprehensive evaluation of targeted therapy options in research and clinical practice.
The ESMO-MCBS assigns scores of 5 or 4 (palliative setting) or A or B (curative setting) to therapies considered clinically relevant, providing critical context for interpreting the potential value of ESCAT-tiered alterations [138]. Joint application of both scales offers a standardized methodology for evaluating both the strength of evidence linking a genomic alteration to a targeted therapy and the demonstrated clinical benefit of that therapeutic approach.
Application in Molecular Tumor Boards
Molecular Tumor Boards (MTBs) represent the practical implementation venue for ESCAT in research and clinical care [138]. These multidisciplinary teams include molecular pathologists, clinical geneticists, bioinformaticians, oncologists, and bioethicists who collaboratively interpret complex genomic data and generate evidence-based treatment recommendations [138].
The optimal MTB workflow incorporates ESCAT as follows:
- Pre-MTB Preparation: NGS data analysis and preliminary ESCAT tier assignment for detected alterations
- MTB Discussion: Review of ESCAT tiers in context of individual patient factors, disease history, and treatment options
- Therapy Recommendation: Selection of targeted therapies based on ESCAT tier, ESMO-MCBS score, and patient-specific considerations
- Documentation and Follow-up: Recording of ESCAT-based decisions and outcomes for continuous learning
Research indicates that patients receiving MTB-recommended regimens based on frameworks like ESCAT experience significantly longer overall survival and progression-free survival compared to those treated with physician-choice regimens [138].
Essential Research Reagents and Platforms for ESCAT Implementation
Table 3: Research Reagent Solutions for ESCAT Implementation
| Research Tool Category | Specific Examples | Research Application |
|---|---|---|
| Comprehensive Genomic Profiling Panels | UNITED DNA/RNA multigene panel [56] | Simultaneous detection of SNVs, indels, CNVs, fusions, and expression outliers across cancer-related genes |
| Nucleic Acid Extraction Kits | DNA/RNA co-extraction kits | High-quality nucleic acid isolation from FFPE tissues, fresh-frozen samples, and liquid biopsies |
| Library Preparation Reagents | Hybrid capture-based target enrichment systems | Efficient target capture with uniform coverage and minimal off-target sequencing |
| Sequencing Platforms | Illumina NovaSeq, Illumina NextSeq, Ion Torrent Genexus | High-throughput NGS with rapid turnaround times for clinical research applications |
| Bioinformatic Analysis Pipelines | Custom analysis workflows for TMB, MSI, HRD calculation | Standardized variant calling, annotation, and biomarker assessment |
| Variant Interpretation Databases | MyCancerGenome, CIViC, OncoKB | Evidence-based interpretation of variant clinical significance and therapy matching |
| ESCAT Classification Tools | Custom bioinformatic implementations for automated tier suggestion | Streamlined ESCAT tier assignment based on current literature and clinical trial evidence |
The ESMO Scale for Clinical Actionability of molecular Targets represents a critical methodological framework for advancing precision oncology research and clinical practice. By providing an evidence-based, standardized system for ranking genomic alterations according to clinical actionability, ESCAT enables more systematic and reproducible interpretation of complex genomic data across diverse research settings. The tiered classification system facilitates prioritization of therapeutic targets, guides clinical trial design, and supports regulatory evaluation of biomarker-directed therapies.
Research validation has demonstrated that ESCAT implementation significantly improves patient outcomes when used to guide therapy selection, particularly for malignancies with established targeted therapy options. The framework's compatibility with other ESMO tools, especially the Magnitude of Clinical Benefit Scale, creates a comprehensive ecosystem for evaluating both the biological rationale and clinical impact of targeted therapeutic approaches.
As precision oncology continues to evolve, ESCAT provides a dynamic framework that accommodates emerging evidence while maintaining methodological rigor. Its application in molecular tumor boards and research consortia standardizes the interpretation of genomic findings and promotes equitable access to targeted therapies based on scientific evidence rather than geographical location or healthcare system variations. For researchers and drug development professionals, ESCAT represents an indispensable tool for translating genomic discoveries into clinically meaningful therapeutic strategies.
The Impact of Sequencing Accuracy (Q40 and Beyond) on Rare Variant Detection
In precision oncology, the detection of rare somatic variants is paramount for understanding tumor heterogeneity, tracking disease evolution, and monitoring emergent resistance mechanisms. Next-generation sequencing (NGS) has become the cornerstone of this endeavor, with its effectiveness fundamentally dependent on sequencing accuracy. The Phred quality score (Q-score) provides a logarithmic measure of base-calling confidence, where Q30 denotes a 1 in 1,000 error probability (99.9% accuracy) that has long represented the industry standard [140]. Advances in sequencing chemistry and analysis are now pushing accuracy to Q40 (99.99% accuracy, 1 in 10,000 error rate) and beyond, representing a transformative leap for identifying low-frequency variants crucial in cancer research and clinical diagnostics [39].
This enhanced accuracy is particularly critical for applications like minimal residual disease (MRD) monitoring and liquid biopsy, where detecting tumor-derived DNA fragments requires identifying mutant molecules present at frequencies of 0.1% or lower against a background of normal DNA [39] [2]. As oncology applications increasingly target these minute variant allele frequencies, the limitations of standard Q30 sequencing become apparent, necessitating either extremely high sequencing depths with associated cost increases or improved base-calling accuracy to maintain sensitivity while controlling costs [39]. This technical guide explores how Q40 and higher accuracy sequencing reshapes rare variant detection, providing methodologies, performance benchmarks, and clinical implications for researchers and drug development professionals working at the forefront of precision oncology.
Technical Foundations: From Q30 to Q40 and Beyond
Understanding Q-Scores and Error Rate Reduction
The Phred quality score is mathematically defined as Q = -10 × log₁₀(P), where P is the probability of an incorrect base call [140]. This logarithmic relationship means that incremental increases in Q-score represent substantial reductions in error rates:
Table 1: Q-Score Accuracy Specifications
| Phred Quality Score | Base Calling Accuracy | Error Probability | Key Applications |
|---|---|---|---|
| Q30 | 99.9% | 1 in 1,000 | Standard germline variant calling, routine RNA-seq |
| Q40 | 99.99% | 1 in 10,000 | Rare somatic variant detection, liquid biopsy |
| Q50 | 99.999% | 1 in 100,000 | Emerging applications with UltraQ chemistry |
The transition from Q30 to Q40 represents a tenfold reduction in sequencing error rates, directly impacting the signal-to-noise ratio in variant detection [39]. This improvement is especially crucial for distinguishing true low-frequency variants from sequencing artifacts in challenging but clinically vital applications like detecting resistance mutations emerging under therapeutic selective pressure [39] [2].
Technology Enablers of High-Accuracy Sequencing
Multiple technological advancements have converged to enable routine Q40+ sequencing:
Advanced Sequencing Chemistries: The implementation of XLEAP-SBS chemistry on Illumina's NovaSeq X and NextSeq 1000/2000 platforms has enabled ≥85% of bases to achieve Q40 quality, a significant improvement over previous generations [140]. Similarly, Element Biosciences' Avidity Base Chemistry powers the AVITI system to consistently deliver Q40 data [39].
Enhanced Base-Calling Algorithms: Improved calibration workflows and error modeling allow quality scores to more accurately reflect empirical error rates, ensuring that reported Q-scores faithfully represent true accuracy [140].
PCR-Free Library Preparation: By minimizing amplification errors during library preparation, PCR-free methods enable quality score calibration that more closely represents sequencer performance rather than preparation artifacts [140].
These technological advances collectively address multiple sources of error in NGS workflows, including sample extraction, library preparation, sequencing biochemistry, and imaging [140].
Experimental Evidence: Benchmarking Q40 Performance
Comparative Study Design and Methodology
A comprehensive preprint study from Fudan University provides one of the most direct comparisons of Q40 versus Q30 performance for both DNA and RNA sequencing applications [39]. The experimental design employed validated reference standards to ensure rigorous benchmarking:
Germline Variant Calling: Assessed using whole exome sequencing of the NIST RM 8398 standard and Mendelian consistency evaluation with the Quartet control set [39].
RNA Quantification Analysis: Measured using bulk RNA-seq data from well-characterized RNA controls, including MAQC samples and ERCC synthetic spike-in pools [39].
Somatic Variant Detection: Analyzed using the HCC1295/BL mixed reference sample designed to model low-frequency mutations [39].
Platform Comparison: The same samples were sequenced on Element AVITI (generating Q40 data) and Illumina NovaSeq 6000 systems, with all datasets downsampled as needed to achieve comparable coverage levels for fair performance comparison [39].
This robust experimental design enabled direct assessment of how increased raw read accuracy impacts downstream analytical precision across multiple genomic applications relevant to oncology research.
Key Performance Findings
Table 2: Quantitative Performance Comparison of Q30 vs. Q40 Sequencing
| Performance Metric | Q30 Performance | Q40 Performance | Improvement/Impact |
|---|---|---|---|
| Germline SNV/InDel accuracy at equivalent coverage | Baseline reference | Equivalent accuracy achieved at 66.6% of coverage | 30-50% cost savings per sample [39] |
| Somatic CNV detection sensitivity | Baseline at full coverage | Improved detection at reduced coverage | Enables accurate CNV analysis with less sequencing [39] |
| Duplication rate | Higher duplication rate | Lower duplication rate with AVITI | More efficient library complexity utilization [39] |
| Rare variant detection confidence | Requires high depth for low VAF | Higher confidence at equivalent depth | Improved signal-to-noise for variants <1% VAF [39] |
The most significant finding was that AVITI Q40 data consistently achieved accuracy comparable to Illumina Q30 data at only 66.6% of the relative coverage across multiple applications [39]. This efficiency gain translates directly into substantial cost savings, with researchers estimating 30-50% reduction in per-sample sequencing costs while maintaining equivalent analytical performance [39].
Figure 1: Experimental workflow for benchmarking Q40 versus Q30 sequencing performance, utilizing reference standards and comparative analysis across multiple genomic applications.
Methodological Implementation in Oncology Research
Enhanced Rare Variant Detection Strategies
The improved raw read accuracy of Q40 sequencing creates new opportunities for detecting rare variants in oncology applications through several mechanisms:
Reduced Reliance on Duplicate Sequencing: The characteristic lower duplication rate of AVITI systems with Avidity Base Chemistry means more unique reads are obtained per sequencing run, improving the efficiency of rare variant detection without requiring excessive sequencing depth [39].
Improved Unique Molecular Identifier (UMI) Efficiency: Current methods for detecting very low-frequency variants (<0.1%) rely heavily on UMIs to suppress sequencing noise. With higher base-level accuracy, highly confident consensus sequences can be generated with far fewer reads per UMI, reducing total sequencing requirements and overall costs [39].
Enhanced Copy Number Variant (CNV) Detection: The Fudan University study observed notable improvements in CNV detection at reduced coverage levels with Q40 sequencing, important for identifying gene amplifications and deletions driving oncogenesis [39].
These methodological advantages position Q40 sequencing as a key enabler for transitioning liquid biopsy applications from research settings into routine clinical testing, particularly for monitoring tumor evolution and early detection of resistance mutations [39].
Research Reagent Solutions for High-Accuracy Sequencing
Table 3: Essential Research Tools for High-Accuracy Sequencing Applications
| Reagent/Tool Category | Specific Examples | Function in Rare Variant Detection |
|---|---|---|
| Targeted Amplicon Panels | CleanPlex OncoZoom Cancer Hotspot Panel, CleanPlex TMB 500 Gene Panel [141] | Ultra-sensitive multiplex PCR-based targeted sequencing for low-input samples and low-frequency mutations |
| UMI Adapter Systems | CleanPlex UMI Technology [141] | Molecular barcoding for error correction and accurate detection of low-frequency variants |
| Comprehensive Genomic Profiling Panels | UNITED DNA/RNA multigene panel [56] | Simultaneous detection of SNVs, indels, CNVs, fusions, TMB, and MSI across cancer-related genes |
| Library Preparation Kits | AVITI-compatible reagents, XLEAP-SBS chemistry kits [39] [140] | Optimized library construction for specific platforms to maintain sequencing accuracy |
| Hybrid Capture Systems | Various solid-phase hybridization capture systems | Alternative to amplicon-based approaches for comprehensive genomic profiling |
Each solution addresses specific challenges in rare variant detection. For example, amplicon-based approaches like the CleanPlex technology offer advantages for samples with limited DNA input or high levels of normal DNA contamination, common challenges in liquid biopsy and FFPE samples [141]. The incorporation of UMIs is particularly crucial for distinguishing true low-frequency variants from PCR and sequencing errors, with the effectiveness of these molecular barcodes being enhanced when coupled with higher base-calling accuracy [39] [141].
Clinical Applications in Precision Oncology
Liquid Biopsy and Minimal Residual Disease Monitoring
The impact of Q40 sequencing is perhaps most transformative in liquid biopsy applications, where the detection of circulating tumor DNA (ctDNA) requires identifying extremely rare variants against a background of predominantly wild-type DNA [39]. The inherent signal-to-noise challenges of these applications have traditionally required massive sequencing depths (often >10,000x coverage) to reliably detect variants at frequencies near 0.1% [39] [2].
With Q40 accuracy, the fundamental error rate of sequencing more closely approaches the variant frequency threshold of clinical interest, enabling several advantages:
Reduced Input Requirements: Higher accuracy decreases the amount of starting material needed for confident variant calling, critical when dealing with limited ctDNA samples [39].
Earlier Detection Capability: The improved signal-to-noise ratio may enable detection of emerging resistance mutations or residual disease at earlier timepoints or lower variant frequencies [2].
Cost-Effective Monitoring: The ability to achieve equivalent sensitivity with less sequencing depth makes longitudinal monitoring more economically feasible for clinical research applications [39].
These advantages position Q40 sequencing as a key enabler for the transition of liquid biopsy from research applications to routine clinical monitoring tools in oncology [39].
Tumor-Agnostic Therapy Selection
Comprehensive genomic profiling using NGS has enabled tumor-agnostic treatment approaches, where therapies target specific molecular alterations regardless of tumor histology [44] [56]. The detection of rare but therapeutically relevant biomarkers benefits substantially from improved sequencing accuracy:
Gene Fusion Detection: Identifying low-prevalence but highly actionable fusions in NTRK (1.2, and 3), RET, and other kinase genes requires high specificity to avoid false positives while maintaining sensitivity across diverse cancer types [44] [56].
Microsatellite Instability (MSI) Assessment: MSI status, a tumor-agnostic biomarker for immunotherapy response, can be challenging to determine accurately in samples with low tumor purity or limited material [56].
Tumor Mutational Burden (TMB) Calculation: Accurate TMB quantification depends on precise distinction between true somatic mutations and sequencing artifacts, particularly in cancers with moderate mutation rates [141] [56].
Recent real-world evidence demonstrates the clinical utility of comprehensive genomic profiling, with one Asian cohort study identifying actionable biomarkers in 62.3% of samples and tumor-agnostic biomarkers in 8.4% of cases across 26 cancer types [56]. The reliability of such findings depends fundamentally on the accuracy of the underlying sequencing data.
Figure 2: Clinical applications of Q40 sequencing in precision oncology, highlighting how enhanced accuracy improves detection of key biomarkers across multiple use cases.
Emerging Technologies and Future Directions
Beyond Q40: The Path to Q50 and Higher Accuracy
Sequencing technology continues to evolve beyond current Q40 capabilities. Element Biosciences has recently introduced UltraQ chemistry, which enables Q50+ sequencing performance (99.999% accuracy, 1 in 100,000 error rate) [39]. This further order-of-magnitude improvement in accuracy may unlock new applications in precision oncology, particularly for detecting ultra-rare variants in early cancer detection and monitoring scenarios.
The pursuit of higher accuracy must balance with other sequencing parameters, including read length, throughput, and cost. Different technological approaches offer complementary strengths:
Short-Read High-Accuracy Platforms: Illumina's XLEAP-SBS chemistry and Element Biosciences' AVITI system provide exceptional accuracy within the short-read paradigm, ideal for variant detection applications [39] [140].
Long-Read Sequencing Technologies: PacBio HiFi sequencing and Oxford Nanopore Technologies offer longer read lengths that excel at detecting structural variants and resolving complex genomic regions, with accuracy now approaching Q30-Q40 levels [142].
Integrated Multi-Modal Approaches: Combining short-read Q40+ accuracy with long-read structural variant detection may provide the most comprehensive view of cancer genomics, though cost and complexity remain implementation challenges [142].
Computational and Analytical Innovations
The full potential of Q40+ sequencing data can only be realized through parallel advances in bioinformatics and analytical methods:
Enhanced Variant Calling Algorithms: Traditional variant callers designed for Q30 data may not fully leverage the improved signal in Q40+ data, necessitating development of specialized algorithms optimized for high-accuracy datasets [140].
Error Profile Characterization: As sequencer error rates decrease, the relative contribution of sample preparation artifacts increases, highlighting the need for improved error correction methods targeting these non-sequencing errors [140].
Integrated Quality Metrics: New quality control frameworks are needed to validate and monitor the performance of Q40+ sequencing in clinical research settings, ensuring consistent performance across samples and batches.
These computational advances will be essential for translating the theoretical benefits of Q40+ sequencing into practical improvements in diagnostic yield and reliability for precision oncology applications.
The transition from Q30 to Q40 sequencing accuracy represents a fundamental advancement with profound implications for rare variant detection in precision oncology research. This technical guide has demonstrated how a tenfold reduction in error rates enables more sensitive detection of low-frequency somatic variants, enhances the efficiency of liquid biopsy applications, and improves the cost-effectiveness of comprehensive genomic profiling.
The experimental evidence clearly indicates that Q40 sequencing achieves equivalent accuracy to Q30 methods with approximately 66.6% of the sequencing coverage, translating to substantial cost savings while maintaining or improving analytical performance [39]. This efficiency gain makes resource-intensive applications like longitudinal monitoring of treatment response and minimal residual disease detection more feasible for widespread research implementation.
As sequencing technology continues to evolve toward Q50 and beyond, and as computational methods adapt to leverage these high-accuracy datasets, researchers and drug development professionals can expect further improvements in detecting clinically relevant rare variants. The ongoing integration of these technological advances into oncology research workflows will accelerate the development of more effective targeted therapies and enable more precise monitoring of treatment response, ultimately advancing the goals of precision oncology to deliver the right treatment to the right patient at the right time.
Conclusion
Next-generation sequencing has irrevocably established itself as a cornerstone of precision oncology, providing unprecedented insights into the molecular underpinnings of cancer and enabling more personalized treatment approaches. The integration of comprehensive genomic profiling, liquid biopsies, and sophisticated bioinformatics has improved patient stratification, therapy selection, and disease monitoring. However, challenges related to data interpretation, cost, and equitable access remain significant hurdles. Future progress hinges on the standardization of workflows, reduction of costs, improved bioinformatics expertise, and the integration of NGS with emerging technologies such as artificial intelligence, single-cell sequencing, and multi-omics approaches. For researchers and drug developers, these advances will be critical for discovering novel therapeutic targets, validating biomarkers, and designing innovative, molecularly informed clinical trials that ultimately improve outcomes for cancer patients.
References
- 1. Massively parallel sequencing — Knowledge Hub [https://www.genomicseducation.hee.nhs.uk/genotes/knowledge-hub/massively-parallel-sequencing/]
- 2. Current and emerging sequencing-based tools for ... [https://www.sciencedirect.com/science/article/abs/pii/S0098299724000098]
- 3. Next-generation sequencing in cancer diagnosis and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12009796/]
- 4. Precision oncology platforms: practical strategies for genomic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11566986/]
- 5. Sanger Sequencing: Introduction, Principle, and Protocol [https://www.cd-genomics.com/blog/sanger-sequencing-introduction-principle-and-protocol/]
- 6. Massive parallel sequencing [https://en.wikipedia.org/wiki/Massive_parallel_sequencing]
- 7. Comparison of targeted next-generation sequencing and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4652376/]
- 8. Precision oncology: lessons learned and challenges for the ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6698584/]
- 9. Next-Generation Sequencing: A Review of Its Transformative ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12523276/]
- 10. Next-generation sequencing and its clinical application [https://pmc.ncbi.nlm.nih.gov/articles/PMC6528456/]
- 11. Biomarker Discovery & Translational Research [https://www.foundationmedicine.com/service/discovery-and-translational-research]
- 12. Tracking NGS Adoption in Oncology: Insights from ... [https://www.decibio.com/insights/tracking-ngs-adoption-in-oncology-insights-from-oncologists-pathologists-and-industry-leaders-webinar]
- 13. Clinical implementation of next-generation sequencing ... [https://www.nature.com/articles/s41598-024-84909-9]
- 14. A scalable high-throughput targeted next-generation ... [https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0260089]
- 15. The Clinical Utility of Next-Generation Sequencing in ... [https://www.mdpi.com/2072-6694/17/8/1292]
- 16. Next-generation sequencing: 2025 Revolution [https://lifebit.ai/blog/next-generation-sequencing/]
- 17. Next Generation Sequencing Market Size 2025 to 2034 [https://www.precedenceresearch.com/next-generation-sequencing-market]
- 18. Comparative analysis of illumina and oxford nanopore ... [https://www.nature.com/articles/s41598-025-18768-3]
- 19. Comparing long-read sequencing technologies [https://www.pacb.com/blog/sequencing-101-comparing-long-read-sequencing-technologies/]
- 20. Powered by PacBio:Selected publications from September ... [https://www.pacb.com/blog/powered-by-pacbioselected-publications-from-september-2025/]
- 21. Oxford Nanopore at AMP 2025 [https://nanoporetech.com/about/events/conferences/amp-2025]
- 22. Comparative analysis of Illumina, PacBio, and nanopore ... [https://www.frontiersin.org/journals/microbiomes/articles/10.3389/frmbi.2025.1587712/full]
- 23. Illumina advances personalized cancer care with new ... [https://www.illumina.com/company/news-center/press-releases/2025/cafb84d4-ffe1-431b-ab7c-712a24857022.html]
- 24. Precision Medicine World Conference 2025 (PMWC 25) [https://nanoporetech.com/about/events/conferences/precision-medicine-world-conference-pmwc-2025]
- 25. PacBio Supports Berry Genomics in Achieving First ... [https://www.pacb.com/press_releases/pacbio-supports-berry-genomics-in-achieving-first-regulatory-approval-for-clinical-long-read-sequencing-in-china/]
- 26. Global cancer burden growing, amidst mounting need for ... [https://www.who.int/news/item/01-02-2024-global-cancer-burden-growing--amidst-mounting-need-for-services]
- 27. Cancer statistics, 2025 [https://pubmed.ncbi.nlm.nih.gov/39817679/]
- 28. Next-generation sequencing impact on cancer care [https://www.frontiersin.org/journals/genetics/articles/10.3389/fgene.2024.1420190/full]
- 29. Clinical Applications of Next-Generation Sequencing in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6658137/]
- 30. The Role of Next-Generation Sequencing in Precision ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6164147/]
- 31. Precision Oncology: Current Landscape, Emerging Trends ... [https://www.mdpi.com/2073-4409/14/22/1804]
- 32. Top five scientific trends shaping precision medicine in 2025 [https://sanogenetics.com/resources/blog/top-five-scientific-trends-shaping-precision-medicine-in-2025]
- 33. Next-Generation Sequencing: A Review of Its ... [https://www.mdpi.com/2075-4418/15/19/2425]
- 34. Structural Variants: Mechanisms, Mapping, and Interpretation ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12385565/]
- 35. Identification of multiple genomic alterations and prediction ... [https://www.nature.com/articles/s41467-025-62215-w]
- 36. Detection and functional assessment of structural variants ... [https://www.nature.com/articles/s41598-025-14139-0]
- 37. Comparative analysis of whole-genome sequencing ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12081241/]
- 38. Case Report: Unraveling complex genomic alterations in a ... [https://www.frontiersin.org/journals/oncology/articles/10.3389/fonc.2025.1639849/full]
- 39. Q40 sequencing reshapes precision oncology research [https://www.elementbiosciences.com/blog/q40-sequencing-reshapes-precision-oncology-research]
- 40. Precision oncology through next generation sequencing in ... [https://www.sciencedirect.com/science/article/pii/S2405844025004347]
- 41. Comprehensive genomic profiling of over 10,000 advanced ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12406462/]
- 42. Integrating comprehensive genomic profiling in the ... [https://www.sciencedirect.com/science/article/pii/S2319417025000253]
- 43. Tumor diagnosis recharacterization enabled by ... [https://www.nature.com/articles/s41698-025-00942-5]
- 44. Next-Generation Sequencing in Oncology—A Guiding ... [https://www.mdpi.com/1422-0067/26/7/3123]
- 45. NGS Streamlines Biomarker Testing in Solid Tumors [https://www.oncnursingnews.com/view/ngs-streamlines-biomarker-testing-in-solid-tumors]
- 46. Circulating tumor DNA: a promising biomarker in the liquid ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5217053/]
- 47. Circulating tumor DNA to monitor treatment response in ... [https://www.nature.com/articles/s41698-025-00876-y]
- 48. Liquid biopsy – a narrative review with an update on current ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12333414/]
- 49. of a Validation assay with molecular and liquid ... biopsy clinical [https://www.nature.com/articles/s41698-021-00202-2?error=cookies_not_supported&code=28ba77af-b7db-4623-a851-412be9870ef7]
- 50. Liquid biopsy- A pivotal test to help navigate clinical ... [https://www.sciencedirect.com/science/article/pii/S2950195425000396]
- 51. A Systematic Review and Meta-Analysis - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC9581609/]
- 52. Clinical Validity and Utility of Circulating Tumor DNA (ctDNA ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11349784/]
- 53. Analytical and clinical performance validation of HPV-SEQ, a novel... [https://pubmed.ncbi.nlm.nih.gov/40578243/]
- 54. Predictive Biomarkers in Cancer Immunotherapy [https://pmc.ncbi.nlm.nih.gov/articles/PMC12289453/]
- 55. Predictive models for immune checkpoint inhibitor ... [https://www.sciencedirect.com/science/article/pii/S1040842825003683]
- 56. High clinical actionability of a pan-cancer tissue-based ... [https://www.nature.com/articles/s41698-025-01126-x]
- 57. TMB as a predictive biomarker for ICI response in TNBC [https://pmc.ncbi.nlm.nih.gov/articles/PMC12628467/]
- 58. The role of neoantigens and tumor mutational burden in ... [https://jhoonline.biomedcentral.com/articles/10.1186/s13045-025-01732-z]
- 59. Prediction of checkpoint inhibitor immunotherapy efficacy ... [https://www.nature.com/articles/s41591-024-03398-5]
- 60. Next-Generation Sequencing Technology: Current Trends ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10376292/]
- 61. Next-Generation Sequencing in Drug Discovery Market ... [https://www.cervicornconsulting.com/next-generation-sequencing-in-drug-discovery-market]
- 62. NGS is evolving: collaboration and tech lead the way [https://www.drugtargetreview.com/article/168383/ngs-is-evolving-collaboration-and-tech-lead-the-way/]
- 63. Companion Diagnostics Explained [https://www.foundationmedicine.com/blog/companion-diagnostics-explained-their-critical-role-cancer-care-and-our-latest-approvals]
- 64. United States Next Generation Sequencing (NGS) Market ... [https://crisprmedicinenews.com/press-release-service/card/united-states-next-generation-sequencing-ngs-market-research-2025-2033-personalized-medicine-res/]
- 65. FDA Approves NGS-Based Companion Diagnostic for ... [https://www.cancernetwork.com/view/fda-approves-ngs-based-companion-diagnostic-for-zongertinib-in-nsclc]
- 66. New guidelines on how to report clinical sequencing data ... [https://news.ki.se/new-guidelines-on-how-to-report-clinical-sequencing-data-help-doctors-make-decisions-about-cancer-treatment]
- 67. Editorial: Next generation sequencing and cancer [https://www.frontiersin.org/journals/genetics/articles/10.3389/fgene.2025.1675753/full]
- 68. Tissue-agnostic cancer therapies: promise, reality, and the ... [https://www.nature.com/articles/s41467-025-60369-1]
- 69. Tissue-agnostic biomarkers in solid tumors - PubMed Central [https://pmc.ncbi.nlm.nih.gov/articles/PMC12204918/]
- 70. Advancing the treatment of NTRK-fused pediatric solid ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12597198/]
- 71. Clinical outcomes of tumor-agnostic targeting of BRAF, tumor ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12167085/]
- 72. BRAF mutations and targeted therapy in unclassified pericytic ... [https://bmccancer.biomedcentral.com/articles/10.1186/s12885-025-14595-x]
- 73. Clinical Trial Trends & Insights for 2025 [https://cms.centerwatch.com/insights/clinical-trial-trends-insights-2025/]
- 74. Next Generation Sequence Testing: Essential 2025 Guide [https://lifebit.ai/blog/next-generation-sequence-testing/]
- 75. Top Oncology Innovations That Shaped the First Half of 2025 [https://binaytara.org/cancernews/article/top-oncology-innovations-that-shaped-the-first-half-of-2025]
- 76. Integrating Technology With Expert Oversight Can Simplify ... [https://www.targetedonc.com/view/integrating-technology-with-expert-oversight-can-simplify-clinical-trial-enrollment]
- 77. Developing Consensus for a More Provider-Friendly Next ... [https://www.sciencedirect.com/science/article/abs/pii/S1525157825002247]
- 78. Pillar Biosciences to Showcase NGS Research Insights at ... [https://www.pillarbiosci.com/2025/10/22/pillar-biosciences-to-showcase-ngs-research-insights-at-2025-amp-meeting/]
- 79. The future of precision oncology: Scaling NGS with smarter ... [https://www.illumina.com/content/illumina-marketing/amr/en_US/events/webinar/2025/future-precision-oncology-scaling-ngs-smarter-variant-interpretation-obrador-gao.html]
- 80. A Review of Its Transformative Impact on Cancer Diagnosis ... [https://pubmed.ncbi.nlm.nih.gov/41095644/]
- 81. A clinician's guide to bioinformatics for next-generation ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9870988/]
- 82. Guidelines for Validation of Next-Generation Sequencing– ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6941185/]
- 83. A Feasibility Study of NGS-Based Variant Analysis of FFPE ... [https://www.mdpi.com/1467-3045/47/8/599]
- 84. ggcoverage: an R package to visualize and annotate genome ... [https://bmcbioinformatics.biomedcentral.com/articles/10.1186/s12859-023-05438-2]
- 85. Integrating next-generation sequencing and artificial ... [https://www.frontiersin.org/journals/oncology/articles/10.3389/fonc.2025.1568205/full]
- 86. Systematic gaps in reporting variants of uncertain ... [https://www.sciencedirect.com/science/article/pii/S1098360025001480]
- 87. Actionability classification of variants of unknown ... [https://www.nature.com/articles/s41698-023-00420-w]
- 88. Illumina AI and informatics are driving research to make ... [https://www.illumina.com/content/illumina-marketing/amr/en_US/events/webinar/2025/illumina-ai-and-informatics-make-personalized-cancer-care-more-a.html]
- 89. Next Generation Sequencing Platform: Ultimate Guide 2025 [https://lifebit.ai/blog/next-generation-sequencing-platform/]
- 90. Perceived Barriers to NGS-Based Molecular Profiling ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12564138/]
- 91. Potential barriers to implementation of next-generation ... [https://pubmed.ncbi.nlm.nih.gov/39606845/]
- 92. Medicare Claim Denials for Cancer-Related NGS Testing ... [https://ascopost.com/news/april-2025/claim-denials-for-medicare-cancer-related-ngs-testing-show-uncertainty-of-coverage/]
- 93. Potential barriers to implementation of next-generation ... [https://www.openhealthgroup.com/publication-library/potential-barriers-to-implementation-of-next-generation-sequencing-in-cancer-management-a-u-s-physician-based-survey/]
- 94. Rapid NGS Technology Accelerates Clinical Trial ... [https://clpmag.com/diagnostic-technologies/molecular-diagnostics/rapid-ngs-technology-accelerates-clinical-trial-breakthroughs-in-oncology/]
- 95. Decentralizing precision oncology: How CDx are moving ... [https://www.fiercepharma.com/pharma/decentralizing-precision-oncology-how-cdx-are-moving-closer-patient]
- 96. Emerging Trends in Coverage and Reimbursement for ... [https://www.nextgenerationdx.com/24/reimbursement-diagnostics]
- 97. Advances in personalized medicine: translating genomic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12106117/]
- 98. Comparative Evaluation of Open-Source Bioinformatics ... [https://pubmed.ncbi.nlm.nih.gov/39772134/]
- 99. Practical Guidance to Implementing Quality Management ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6663893/]
- 100. The Next Generation Sequencing Quality Initiative [https://www.cdc.gov/lab-quality/php/ngs-quality-initiative/index.html]
- 101. Applying next-generation sequencing to detect ... [https://www.nature.com/articles/s41698-025-01096-0]
- 102. Experts Forecast Cancer Research and Treatment ... [https://www.aacr.org/blog/2025/01/10/experts-forecast-cancer-research-and-treatment-advances-in-2025/]
- 103. Real-World Data: Implementation and Outcomes of Next- ... [https://www.mdpi.com/2075-4418/15/10/1183]
- 104. From Innovation to Access: Addressing Disparities in ... [https://oncpracticemanagement.com/issues/2025/july-2025-vol-15-no-7/from-innovation-to-access-addressing-disparities-in-precision-oncology]
- 105. ctDNA, genomics, and equity in breast cancer care [https://www.nature.com/articles/s41523-025-00811-1]
- 106. Achieving Health Equity in Oncology with Precision ... [https://www.accc-cancer.org/acccbuzz/blog-post-template/accc-buzz/2023/04/20/achieving-health-equity-in-oncology-with-precision-medicine-stewards]
- 107. Implementing next-generation sequencing and public ... [https://www.sciencedirect.com/science/article/abs/pii/S1040842824001768]
- 108. Health equity innovation in precision medicine: data ... [https://health-policy-systems.biomedcentral.com/articles/10.1186/s12961-024-01258-9]
- 109. Ensuring equity: Expanding precision medicine in cancer ... [https://resources.flatiron.com/point-of-care/ensuring-equity-expanding-precision-medicine-in-cancer-care]
- 110. Unveiling the Digital Evolution of Molecular Tumor Boards [https://pmc.ncbi.nlm.nih.gov/articles/PMC11762447/]
- 111. Empowering personalized oncology: evolution of digital ... [https://bmcmedinformdecismak.biomedcentral.com/articles/10.1186/s12911-024-02821-8]
- 112. Real‐World Data From a Molecular Tumor Board‐Assisted ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12319421/]
- 113. Real-world experience of Molecular Tumour Boards for ... [https://www.nature.com/articles/s41698-025-00863-3]
- 114. A nationwide comprehensive genomic profiling and ... [https://www.nature.com/articles/s41698-025-00858-0]
- 115. User-centered design approach to visualize PROMs for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12325938/]
- 116. Clinical Oncology Next Generation Sequencing Market ... [https://www.novaoneadvisor.com/report/clinical-oncology-next-generation-sequencing-market]
- 117. Global Clinical Oncology NGS: Poised for a Decade of ... [https://www.linkedin.com/pulse/global-clinical-oncology-ngs-poised-decade-double-digit-growth-l2llf]
- 118. Clinical Oncology Next Generation Sequencing Market [https://www.maximizemarketresearch.com/market-report/clinical-oncology-next-generation-sequencing-market/100383/]
- 119. Comparative evaluation of sequencing platforms [https://pmc.ncbi.nlm.nih.gov/articles/PMC12365774/]
- 120. Validation of a comprehensive long-read sequencing ... [https://www.frontiersin.org/journals/genetics/articles/10.3389/fgene.2025.1499456/full]
- 121. A targeted next-generation sequencing panel for ... [https://www.nature.com/articles/s41598-025-08039-6]
- 122. Augmenting cost-effectiveness in clinical diagnosis using ... [https://www.nature.com/articles/s10038-025-01403-4]
- 123. Comparison of Annotation Services for Next-Generation ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7446349/]
- 124. Comparing Classifications from Multiple Variant Annotation ... [https://www.mdpi.com/2673-5261/5/1/6]
- 125. Advances in Precision Oncology: From Molecular Profiling to ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12607717/]
- 126. Whole genome, whole exome or panel sequencing in ... [https://frontlinegenomics.com/whole-genome-whole-exome-or-panel-sequencing-in-precision-oncology-clinical-trials/]
- 127. Targeted Gene Panels: Revolutionizing Genomic Testing ... [https://blog.crownbio.com/targeted-gene-panels-genomic-testing-oncology]
- 128. Comparison of actionable events detected in cancer ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9463385/]
- 129. Target-Enhanced Whole-Genome Sequencing Shows ... [https://pubmed.ncbi.nlm.nih.gov/39300929/]
- 130. Translational and clinical comparison of whole genome ... [https://www.nature.com/articles/s41698-024-00788-3]
- 131. Validation of a liquid biopsy assay with increased sensitivity ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12447423/]
- 132. Comprehensive Evaluation of a 1021-Gene Panel in FFPE ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12249698/]
- 133. Analytical validation (accuracy, reproducibility, limit of ... [https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0329697]
- 134. Analytical Validation of a Pan-Cancer NGS Assay for In- ... [https://www.sciencedirect.com/science/article/pii/S152515782500220X]
- 135. New Somatic Cancer Reference Standards Aim To ... [https://www.labmanager.com/new-somatic-cancer-reference-standards-may-strengthen-ngs-diagnostic-accuracy-34640]
- 136. the ESMO Scale for Clinical Actionability of molecular Targets ... [https://pubmed.ncbi.nlm.nih.gov/30137196/]
- 137. ESCAT: ESMO Scale for Clinical Actionability of molecular ... [https://www.oncopedia.wiki/contributions/escat-esmo-scale-for-clinical-actionability-of-molecular-targets]
- 138. Applicability of ESMO-MCBS and ESCAT for molecular ... [https://link.springer.com/article/10.1007/s12254-022-00800-1]
- 139. Matched targeted treatment based on ESCAT actionable ... [https://ecancer.org/en/news/21493-matched-targeted-treatment-based-on-escat-actionable-genomic-alterations-associates-with-improved-prognosis-of-cholangiocarcinoma-patients]
- 140. XLEAP-SBS chemistry enables Q40 and above data ... [https://www.illumina.com/science/genomics-research/articles/data-quality-q-scores.html]
- 141. CleanPlex NGS Amplicon Panels for Oncology [https://www.paragongenomics.com/applications/oncology/]
- 142. Long-Read Sequencing and Structural Variant Detection [https://pmc.ncbi.nlm.nih.gov/articles/PMC12293859/]