Next-Generation Sequencing in Immuno-Oncology: Unlocking Biomarker Discovery for Precision Cancer Therapies
This article provides a comprehensive overview of how Next-Generation Sequencing (NGS) is revolutionizing biomarker discovery in immuno-oncology.
Next-Generation Sequencing in Immuno-Oncology: Unlocking Biomarker Discovery for Precision Cancer Therapies
Abstract
This article provides a comprehensive overview of how Next-Generation Sequencing (NGS) is revolutionizing biomarker discovery in immuno-oncology. Tailored for researchers, scientists, and drug development professionals, it explores the foundational role of NGS in identifying critical biomarkers like tumor mutational burden (TMB) and neoantigens. The scope spans from core technological principles and multi-omics methodologies to practical challenges in assay optimization, clinical validation frameworks, and comparative analysis of emerging platforms. By synthesizing current strategies and future directions, this resource aims to equip professionals with the knowledge to advance personalized cancer immunotherapy.
The Core Biomarker Landscape: How NGS is Redefining Immuno-Oncology Targets
The advent of immune checkpoint inhibitors (ICIs) has revolutionized oncology by leveraging the host immune system to combat tumors, yet these therapies elicit beneficial responses only in a subset of patients [1] [2]. This reality has driven the urgent need for robust predictive biomarkers to guide patient selection and optimize therapeutic outcomes. Biomarkers serve as critical biological indicators that can forecast patient responsiveness to specific immunotherapeutic agents, thereby significantly enhancing the precision and efficacy of treatment [1]. In the contemporary landscape of immuno-oncology, four biomarkers have emerged as particularly actionable: Tumor Mutational Burden (TMB), Neoantigens, Microsatellite Instability (MSI), and Programmed Death-Ligand 1 (PD-L1) [1] [3] [4]. The integration of next-generation sequencing (NGS) technologies has been instrumental in discovering and validating these biomarkers, enabling a comprehensive molecular profiling approach that transcends traditional single-analyte tests [3] [5]. This technical guide delineates the biological mechanisms, assessment methodologies, clinical applications, and experimental protocols for these core biomarkers within the context of NGS-driven immuno-oncology research.
Biomarker Fundamentals and Biological Mechanisms
Tumor Mutational Burden (TMB)
Definition and Biological Rationale: Tumor Mutational Burden (TMB) is defined as the total number of somatic non-synonymous mutations within a tumor's genome, typically reported as mutations per megabase (mut/Mb) [1] [4]. The fundamental premise of TMB as a biomarker rests on the correlation between a higher mutational load and an increased likelihood of generating immunogenic neoantigens—novel peptides that can be recognized as "non-self" by the immune system, particularly T cells [1] [4]. When a tumor accumulates a high number of mutations, the probability increases that some of these alterations will be processed and presented on Major Histocompatibility Complex (MHC) molecules, enabling immune recognition and attack [4]. TMB exhibits dramatic variation across tumor types, with melanoma, non-small cell lung cancer (NSCLC), and squamous carcinomas typically demonstrating the highest levels, while leukemias and pediatric tumors show the lowest [4]. This variation reflects differing etiologies and mutagen exposures, such as UV light in melanoma and tobacco carcinogens in NSCLC [4].
Neoantigens
Definition and Sources: Neoantigens are tumor-specific peptides derived from somatic mutations that are entirely absent in the normal germline genome [1] [6]. These antigens arise from various genetic alterations, with the primary sources being:
- Single Nucleotide Variants (SNVs): Point mutations that change a single amino acid; the most extensively studied source [6] [7].
- Insertions and Deletions (INDELs): These can cause frameshift mutations, generating novel open reading frames (ORFs) and producing peptides with lower similarity to self-proteins, often conferring higher immunogenicity potential compared to SNV-derived peptides [7].
- Gene Fusions: Chimeric proteins resulting from chromosomal rearrangements that can generate entirely new amino acid sequences with high immunogenicity [7].
- Structural Variations (SVs): Large genomic alterations involving more than 50 base pairs that can fuse distinct gene regions, creating novel gene fragments [7].
The significance of neoantigens lies in their high tumor specificity, which minimizes the risk of off-target toxicity and central immune tolerance, making them ideal targets for personalized immunotherapies such as cancer vaccines and adoptive T-cell therapies [1] [6].
Microsatellite Instability (MSI)
Definition and Underlying Mechanism: Microsatellites are short, repetitive DNA sequences (1-6 nucleotide motifs repeated multiple times) scattered throughout the genome that have a higher inherent mutation rate than other regions [3]. Microsatellite Instability (MSI) occurs when the DNA mismatch repair (MMR) system is deficient (dMMR), failing to correct errors that accumulate during DNA replication in these repetitive regions [3]. This failure results in somatic changes in the length of microsatellites and a hypermutatable tumor phenotype [3]. The widespread genomic instability associated with dMMR leads to a rapid accumulation of somatic mutations, particularly insertions and deletions, which can inactivate genes in key regulatory processes and drive tumorigenesis [3]. MSI-high (MSI-H) status is determined based on the number of unstable markers in a standardized panel, with changes in two or more of the five Bethesda-recommended markers classifying a tumor as MSI-H [3].
Programmed Death-Ligand 1 (PD-L1)
Function in Immune Evasion: Programmed Death-Ligand 1 (PD-L1) is a cell surface protein expressed on tumor cells and immune cells that binds to its receptor PD-1 on T cells [2]. This ligand-receptor interaction transmits an inhibitory signal that effectively deactivates T cells, reducing their cytotoxic response and enabling tumors to evade immune surveillance—a mechanism known as immune checkpoint activation [2] [4]. PD-L1 expression has been established as a predictive biomarker for response to anti-PD-1/PD-L1 therapies, with its detection via immunohistochemistry (IHC) serving as an FDA-approved companion diagnostic for several cancer types [4]. However, its utility is limited by heterogeneous and dynamic expression patterns, diagnostic reproducibility challenges, and insufficient negative predictive value, driving the need for complementary biomarkers like TMB and MSI [4].
Table 1: Fundamental Characteristics of Actionable Immuno-Oncology Biomarkers
| Biomarker | Molecular Nature | Primary Source | Key Biological Function |
|---|---|---|---|
| TMB | Quantitative measure of non-synonymous somatic mutations | DNA-level alterations from various mutagenic processes | Proxy for neoantigen load; indicator of tumor immunogenicity |
| Neoantigens | Tumor-specific peptides presented by MHC molecules | Somatic mutations (SNVs, INDELs, fusions, SVs) | Direct targets for T-cell recognition and attack |
| MSI | Genomic hypermutability phenotype | Deficient DNA mismatch repair (dMMR) | Genome-wide indicator of high frameshift mutation burden |
| PD-L1 | Transmembrane immune checkpoint protein | Induced by inflammatory signals (e.g., IFN-γ) in TME | Suppresses T-cell activity; mediates immune evasion |
Assessment Methodologies and NGS Workflows
NGS-Based Approaches for TMB Measurement
The initial gold standard for TMB assessment was whole exome sequencing (WES), which comprehensively profiles protein-coding regions and identifies non-synonymous mutations [2] [4]. However, due to cost and analytical constraints in routine clinical practice, targeted NGS panels have been developed as a practical alternative [2]. The accuracy of TMB estimation with targeted panels is highly dependent on panel size, with research indicating that panels between 1.5 Mb and 3 Mb provide optimal performance with significantly smaller confidence intervals compared to smaller panels [2]. The wet-lab protocol for TMB assessment typically involves:
- DNA Extraction: High-quality DNA is extracted from matched tumor and normal tissues.
- Library Preparation: Sequencing libraries are prepared from both tumor and normal DNA samples.
- Hybrid Capture: For targeted panels, biotinylated probes hybridize to and enrich the genomic regions of interest.
- Sequencing: High-throughput sequencing is performed on NGS platforms.
- Bioinformatic Analysis: Sequencing data is processed through an analytical pipeline including:
- Alignment to reference genome (e.g., using BWA)
- Variant calling (somatic mutations)
- Filtering to remove germline polymorphisms
- TMB calculation: (Total non-synonymous mutations / Size of targeted region in Mb)
Critical considerations include the inclusion of both synonymous and non-synonymous mutations in targeted panels to improve sensitivity, and rigorous calibration to ensure TMB scores are comparable across different platforms [2] [4].
Integrated Neoantigen Prediction Pipeline
Neoantigen discovery requires a multi-faceted approach that integrates genomic, transcriptomic, and immunopeptidomic data [1] [6] [7]. The comprehensive workflow involves both wet-lab and computational components:
Wet-Lab Components:
- DNA/RNA Sequencing: WES or WGS on tumor-normal pairs, complemented by RNA-Seq to assess expression of mutant genes [6].
- HLA Typing: Determination of patient-specific HLA alleles using tools like HLAminer or Athlates [6].
- Immunopeptidomics: Isolation of MHC-bound peptides from tumor cells followed by liquid chromatography-tandem mass spectrometry (LC-MS/MS) to directly identify presented peptides [6].
Computational Pipeline:
- Mutation Identification: Somatic variant calling from sequencing data using tools like BWA and Genome Modeling System; annotation with Variant Effect Predictor (VEP) [6].
- Neoantigen Candidate Generation: Translation of genomic mutations into mutated protein sequences [6].
- MHC Binding Prediction: Prediction of peptide-MHC binding affinity using algorithms such as NetMHCpan, NetMHCIIpan, MixMHCpred2.2, or PRIME2.0 [1] [6].
- Immunogenicity Assessment: Evaluation of T-cell recognition potential based on predicted binding, expression levels, and sequence similarity to self-proteins [6].
- Prioritization: Ranking of candidates using integrated pipelines like pVAC-Seq, TSNAD, CloudNeo, or TIminer [6].
Advanced models are increasingly incorporating deep learning trained directly on mass spectrometry data (e.g., EDGE model) to improve prediction accuracy of genuinely presented neoantigens [6].
MSI Detection via NGS
While traditional MSI testing follows the Bethesda guidelines using capillary electrophoresis of five microsatellite markers, NGS-based approaches offer significant advantages, including higher throughput, greater reproducibility, and the ability to analyze hundreds to thousands of microsatellites simultaneously [3]. The NGS workflow for MSI assessment includes:
- Library Preparation: DNA libraries are prepared from tumor tissue.
- Sequencing: Targeted, whole exome, or whole genome sequencing is performed.
- Bioinformatic Analysis:
- Microsatellite loci are identified from sequencing data.
- Length variation is assessed by comparing tumor and normal profiles.
- MSI scoring is calculated based on the percentage of unstable loci.
- Classification: Tumors are classified as MSI-High (MSI-H), MSI-Low (MSI-L), or Microsatellite Stable (MSS) based on the scoring threshold [3].
The expanded number of markers in NGS-based assays provides a more quantitative and granular assessment of MSI status, improving sensitivity for detecting MMR deficiency across diverse cancer types [3]. Comprehensive genomic profiling panels can simultaneously assess MSI, TMB, and specific gene alterations, offering a holistic molecular characterization [2].
PD-L1 Expression Analysis
PD-L1 expression is primarily assessed through immunohistochemistry (IHC) using specific antibodies, with scoring systems that vary by assay and cancer type [8] [4]. Key methodologies include:
- IHC Staining: Formalinfixed, paraffin-embedded (FFPE) tissue sections are stained with anti-PD-L1 antibodies.
- Scoring Systems: Evaluation based on tumor proportion score (TPS) or combined positive score (CPS), which incorporate staining of tumor and immune cells.
- Digital Pathology: Emerging computational approaches for more standardized quantification.
While not primarily an NGS-based biomarker, transcriptomic profiling via RNA sequencing can provide complementary information on PD-L1 mRNA expression and the broader immune contexture of the tumor microenvironment [8].
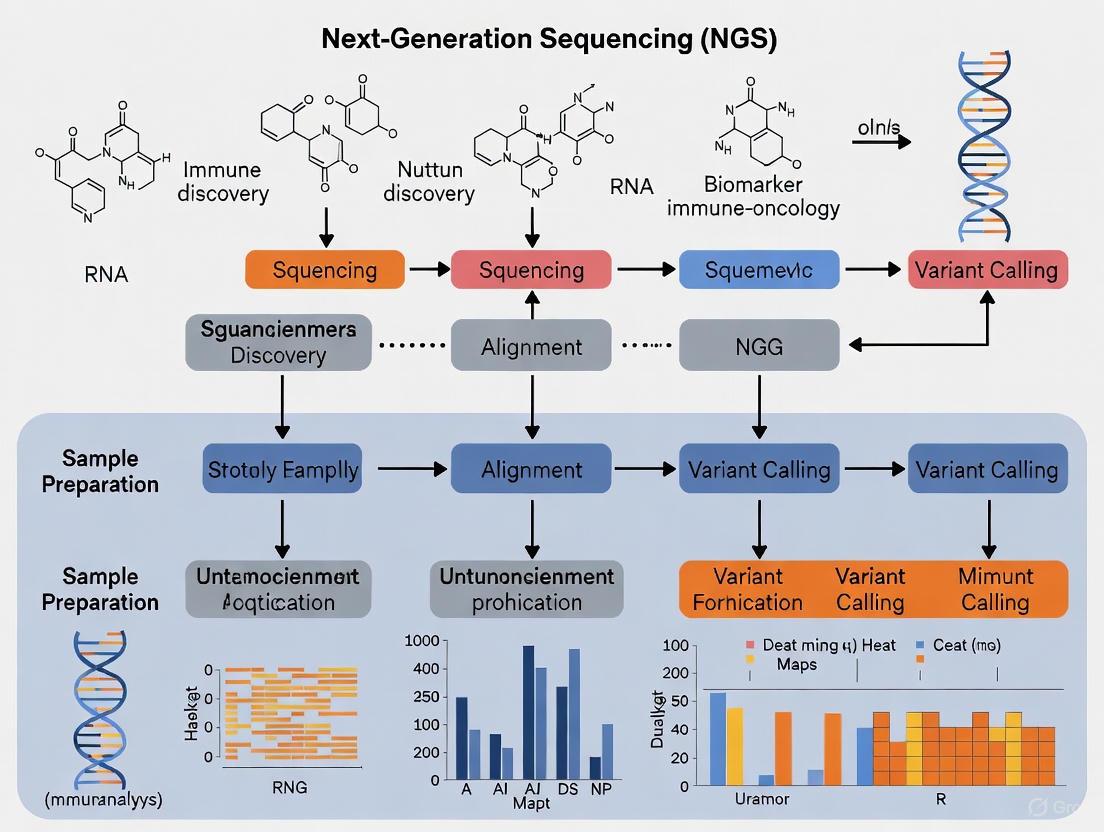
Diagram 1: NGS Workflow for Immuno-Oncology Biomarker Discovery. This diagram illustrates the integrated computational pipeline for biomarker assessment from multi-omics data inputs to clinical applications, highlighting how NGS enables comprehensive profiling.
Quantitative Data and Clinical Validation
TMB Thresholds and Clinical Outcomes
Clinical evidence has established TMB as a predictive biomarker for response to immune checkpoint inhibitors across multiple cancer types [4]. The KEYNOTE-158 trial validated TMB as a biomarker for pembrolizumab treatment across solid tumors, leading to FDA approval [5]. Proposed TMB thresholds vary by cancer type and detection method, with WES-based thresholds for lung, bladder, and head and neck cancers approximating 200 non-synonymous somatic mutations (approximately 10-20 mut/Mb depending on the coding region size) [4]. In a pan-cancer analysis, a TMB cutoff of ≥10 mutations/Mb has been used to define TMB-high (TMB-H) status for targeted NGS panels [8]. Clinical trial data has demonstrated that NSCLC patients with high TMB experienced significantly longer progression-free survival when receiving immunotherapy [2].
Table 2: TMB Thresholds and Clinical Associations Across Cancer Types
| Cancer Type | Proposed TMB Threshold (mut/Mb) | Associated Clinical Outcome | Level of Evidence |
|---|---|---|---|
| Melanoma | Varies; among highest | Improved survival with anti-CTLA-4 and anti-PD-1 | Retrospective studies [4] |
| NSCLC | ~10-20 (WES equivalent) | Significantly longer PFS with ICIs | Prospective trials [2] [4] |
| Colon Cancer | Context dependent | Sensitivity to immune checkpoint blockade | Clinical trials [2] |
| Multiple Solid Tumors | ≥10 (targeted NGS) | Objective response to pembrolizumab | Prospective trial (KEYNOTE-158) [5] |
MSI Prevalence and Therapeutic Implications
MSI-H/dMMR status represents the first tissue-agnostic biomarker approved for ICIs, with the FDA granting approval for PD-1 inhibitors regardless of cancer type [3]. The prevalence of MSI-H varies across cancers, with highest rates observed in colorectal (15%), gastric (22%), and endometrial (20-30%) cancers, while being rare in other malignancies [3]. The seminal study by Le et al. demonstrated that MMR-deficient colorectal cancers were highly sensitive to PD-1 blockade, with immune-related objective response rates of 40% and immune-related complete response rates of 10% [3]. Follow-up research on the NCI-MATCH Arm Z1D trial further validated that even within a dMMR population, NGS-based measures of microsatellite instability could serve as biomarkers of immunotherapy response, with more extensive MSI alterations associated with clinical benefit and TMB [9].
PD-L1 Expression and Predictive Value
PD-L1 expression remains an important biomarker with validated predictive value in multiple cancer types, though with limitations as a standalone biomarker [8] [4]. In a comprehensive study of anal squamous-cell carcinoma (ASCC), 64.25% of tumors expressed PD-L1, with 41.7% exhibiting high expression [8]. The PD-L1-high group treated with ICIs had significantly longer time on treatment than the PD-L1-negative group (HR 0.758, 95% CI 0.579-0.992, P = 0.044) [8]. PD-L1 expression is influenced by the tumor immune microenvironment, with PD-L1-high ASCCs showing higher infiltration of Tregs, M1 macrophages, neutrophils, CD8+ T cells, and cancer-associated fibroblasts compared to PD-L1-low tumors [8].
Integrative Biomarker Analysis
The most powerful approach for predicting immunotherapy response involves integrating multiple biomarkers [1] [2]. Research in colorectal cancer has demonstrated that combining MSI and TMB determination may better identify patients with a more active immune response [2]. Each biomarker provides complementary information:
- TMB quantifies the potential antigenic repertoire
- Neoantigens represent the actual immunogenic targets
- MSI indicates a specific hypermutational mechanism
- PD-L1 reflects an activated but suppressed immune microenvironment
This integrative approach enables more precise patient stratification and insights into resistance mechanisms.
The Scientist's Toolkit: Essential Research Reagents and Platforms
Table 3: Essential Research Reagents and Platforms for Biomarker Discovery
| Tool Category | Specific Technologies/Assays | Research Application | Key Features |
|---|---|---|---|
| Sequencing Platforms | WES, WGS, RNA-Seq, Targeted Panels | Comprehensive mutation profiling, TMB calculation, fusion detection | High-throughput, multi-analyte capability, scalable [1] [6] |
| Computational Tools | NetMHCpan, NetMHCIIpan, pVAC-Seq, TSNAD | Neoantigen prediction, MHC binding affinity estimation | Algorithmic prediction, integration of multi-omics data [1] [6] [7] |
| Immunopeptidomics | LC-MS/MS, MHC immunoprecipitation | Direct identification of presented peptides | Validation of neoantigen presentation, complement to prediction algorithms [1] [6] |
| IHC Assays | PD-L1 IHC (multiple clones) | Protein expression analysis, immune cell profiling | Spatial context, protein-level verification, standardized scoring [8] [4] |
| Multi-omics Databases | TCGA, CPTAC, DriverDBv4, GliomaDB | Data integration, biomarker validation, cross-study analysis | Annotated datasets, normalized processing, clinical correlations [5] |
Experimental Protocols for Biomarker Assessment
Comprehensive TMB and MSI Analysis via Targeted NGS Panel
Sample Requirements: FFPE tumor tissue with matched normal (blood or tissue), minimum 20% tumor content, DNA quantity ≥50ng.
Step-by-Step Protocol:
- DNA Extraction: Use commercial extraction kits following manufacturer's protocols. Assess DNA quality and quantity via fluorometry.
- Library Preparation: Fragment DNA, followed by end-repair, A-tailing, and adapter ligation. Use dual-indexed adapters for sample multiplexing.
- Hybrid Capture: Incubate libraries with biotinylated probes targeting the panel regions (ensure panel size ≥1.5Mb for TMB accuracy). Perform washing to remove non-specific binding.
- Sequencing: Amplify captured libraries and sequence on Illumina platform (minimum 100x coverage recommended).
- Bioinformatic Analysis:
- Alignment: Map sequencing reads to reference genome (hg38) using BWA-MEM.
- Variant Calling: Identify somatic mutations using paired tumor-normal variant callers (MuTect2 for SNVs, other specialized tools for INDELs).
- TMB Calculation: (Total non-synonymous somatic mutations / Panel size in Mb)
- MSI Analysis: Compare microsatellite loci in tumor vs normal using specialized tools (e.g., mSINGS, MSIsensor). Calculate percentage of unstable loci.
- Interpretation: Classify TMB-H per validated thresholds (e.g., ≥10 mut/Mb); classify MSI status based on predefined scoring thresholds.
Quality Control Metrics: Include positive and negative controls; monitor sequencing metrics (coverage uniformity, on-target rate); validate with reference materials.
Integrated Neoantigen Discovery Workflow
Sample Requirements: Matched tumor-normal DNA/RNA from fresh-frozen or high-quality FFPE tissue; viable tumor cells for immunopeptidomics.
Multi-Omics Protocol:
- Genomic Profiling:
- Perform WES on tumor-normal pairs (minimum 100x tumor, 40x normal coverage).
- Conduct RNA-Seq on tumor tissue to assess gene expression.
- Determine HLA type using specialized tools (HLAminer, OptiType).
- Variant Calling and Annotation:
- Identify somatic mutations using established pipelines.
- Annotate variants with functional impact (VEP, SnpEff).
- Filter for expressed mutations (FPKM ≥1 in RNA-Seq).
- Neoantigen Prediction:
- Generate mutant peptide sequences (typically 8-11mers).
- Predict MHC binding affinity using algorithms (NetMHCpan, MixMHCpred).
- Prioritize candidates based on binding affinity (IC50 <50nM considered strong binders), expression level, and clonality.
- Experimental Validation (Immunopeptidomics):
- Isolate MHC-peptide complexes from tumor cells by immunoprecipitation.
- Elute and fractionate peptides by liquid chromatography.
- Analyze by tandem mass spectrometry (LC-MS/MS).
- Identify peptides by searching spectra against customized databases including mutant sequences.
- Immunogenicity Assay:
- Synthesize candidate neoantigen peptides.
- Isolate peripheral blood mononuclear cells (PBMCs) from patient.
- Stimulate T-cells with peptide-pulsed antigen-presenting cells.
- Measure T-cell activation (ELISpot, intracellular cytokine staining).
- Expand reactive T-cell clones for functional validation.
Diagram 2: Biomarker Interplay in Immune Activation. This diagram illustrates the mechanistic relationships between genomic instability, neoantigen formation, T-cell recognition, and PD-L1-mediated immune regulation, explaining the biological foundation for biomarker synergy in predicting ICI response.
The integration of TMB, neoantigens, MSI, and PD-L1 represents a paradigm shift in immuno-oncology research and clinical practice. These biomarkers provide complementary information that collectively enables more precise patient stratification for immunotherapy [1] [2]. The continued evolution of NGS technologies and multi-omics integration is further refining our understanding of these biomarkers and their interactions [5]. Emerging frontiers include single-cell and spatial multi-omics technologies that resolve tumor heterogeneity at unprecedented resolution, artificial intelligence approaches that enhance neoantigen prediction accuracy, and the development of organoid and humanized models that better recapitulate human tumor-immune interactions [5] [10]. Liquid biopsy approaches for non-invasive TMB and MSI monitoring are also advancing rapidly, offering dynamic assessment of biomarker evolution during treatment [1]. As these technologies mature, the biomarker framework outlined in this guide will continue to evolve, driving further refinement of personalized immuno-oncology and expanding the benefit of immunotherapy to broader patient populations.
The Biological Mechanism of Neoantigens and TCR Recognition
Neoantigens are tumor-specific proteins arising from somatic mutations in cancer cells. These antigens are proteolytically processed and presented on the tumor cell surface by major histocompatibility complex (MHC) molecules, forming peptide-MHC (pMHC) complexes that can be recognized by T cell receptors (TCRs). This interaction represents a critical mechanism for immune-mediated tumor elimination and forms the foundation for numerous immuno-oncology approaches. The identification of neoantigens has become crucial for advancing cancer vaccines, diagnostics, and immunotherapies, with next-generation sequencing (NGS) playing an increasingly vital role in biomarker discovery for precision oncology [11] [12].
The TCR-pMHC interaction initiates anti-tumor immunity, leading to T cell activation, proliferation, and ultimately, tumor cell cytolysis. Understanding the structural and cellular determinants controlling TCR recognition of neoantigens remains a fundamental challenge in immunology, particularly given the intricate binding motifs and long-tail distribution of known binding pairs in public databases [11]. This technical guide explores the biological mechanisms underlying neoantigen formation, TCR recognition, and the integration of NGS technologies to advance biomarker discovery in immuno-oncology research.
Biological Mechanisms of Neoantigen Formation and Presentation
Origins and Classification of Neoantigens
Neoantigens originate from various genetic alterations that generate novel protein sequences not present in normal tissues:
- Missense mutations: Single nucleotide variants resulting in amino acid substitutions that create novel peptide sequences. For example, the recurrent driver mutation KRAS Q61H generates the neoantigen ILDTAGHEEY presented by HLA-A*01:01 [13].
- Frameshift mutations: Insertions or deletions that alter the reading frame, producing completely novel amino acid sequences.
- RNA splicing alterations: Cancer-specific splicing events (neojunctions) that create novel transcript variants. Recent research has identified that these neojunctions can be conserved across tumor types, with studies showing an average of 94 public neojunctions per TCGA tumor type, and 38.3% of these being translated into neopeptides verified by mass spectrometry [14].
- Genomic rearrangements: Structural variants that create fusion proteins with novel junctional epitopes.
Neoantigens can be categorized based on their structural characteristics and immunogenic properties. Group I neoantigens contain mutations in non-anchor residues and often show some cross-reactivity with wild-type peptides. In contrast, Group II neoantigens feature mutations at anchor residues that enhance MHC binding affinity and stabilize the pMHC complex, resulting in minimal cross-reactivity with wild-type peptides and resembling non-self epitopes typically generated during viral infections [15].
MHC Presentation and TCR Recognition Mechanisms
The presentation of neoantigens follows the standard antigen processing pathway. Intracellular proteins are degraded by the proteasome, transported to the endoplasmic reticulum, loaded onto MHC-I molecules, and presented on the cell surface for recognition by CD8+ T cells. The structural basis for TCR recognition of neoantigens involves highly specific molecular interactions between the TCR complementarity-determining regions (CDRs) and the pMHC complex.
Structural studies have revealed that neoantigen-specific TCRs often exhibit high functional avidity and selectivity, attributable to broad, stringent binding interfaces that enable recognition of tumor cells despite low antigen density [15]. For instance, research on the H2-Db/Hsf2 p.K72N68-76 neoantigen system demonstrated that the p.K72N mutation enhances H2-Db binding, improves cell surface presentation, and stabilizes the TCR epitope, enabling recognition by its cognate TCR (47BE7) with sub-nanomolar functional avidity (EC50 5.61 pM) [15].
Table 1: Characteristics of Neoantigen Types and Their Recognition Properties
| Neoantigen Type | Origin | MHC Binding Affinity | Cross-reactivity with WT | Example |
|---|---|---|---|---|
| Group I (Non-Anchor Mutations) | Missense mutations at non-anchor residues | Variable, often similar to WT | Moderate to high | Various private neoantigens |
| Group II (Anchor Mutations) | Missense mutations at anchor residues | Typically enhanced compared to WT | Minimal | Hsf2 p.K72N68-76 [15] |
| RNA Splicing-derived | Cancer-specific splicing events (neojunctions) | Dependent on peptide sequence | None (truly tumor-specific) | NeoARPL22, NeoAGNAS [14] |
| Oncogenic Driver-derived | Mutations in canonical oncogenes | Variable | Minimal to none | KRAS Q61H [13] |
Computational Prediction of Neoantigens and TCR Interactions
Advanced Algorithmic Approaches
Accurate prediction of pMHC binding and TCR recognition remains a significant computational challenge in immunology due to the complexity of binding motifs and the limited availability of training data. Recent advances in machine learning have led to the development of sophisticated prediction tools:
- Attention-aware differential learning: Novel frameworks like TranspMHC (for pMHC-I binding prediction) and TransTCR (for TCR-pMHC-I recognition prediction) leverage attention mechanisms to surpass existing algorithms on independent datasets at both pan-specific and allele-specific levels [11].
- Transfer learning and differential learning: TransTCR incorporates these strategies to demonstrate superior performance and enhanced generalization on independent datasets compared to existing methods [11].
- Structural affinity modeling: Approaches that incorporate molecular dynamics and structural information to predict TCR-pMHC binding affinity.
These computational tools help identify key amino acids associated with binding motifs of peptides and TCRs that facilitate pMHC-I and TCR-pMHC-I binding, indicating potential interpretability of the prediction frameworks [11].
Quantitative Performance Metrics
Table 2: Performance Metrics of Neoantigen and TCR Prediction Platforms
| Platform/Method | Prediction Target | Key Advantages | Validation Performance |
|---|---|---|---|
| TranspMHC [11] | pMHC-I binding | Attention mechanism, pan-specific and allele-specific prediction | Surpasses existing algorithms on independent datasets |
| TransTCR [11] | TCR-pMHC-I recognition | Transfer learning, differential learning strategy | Superior performance and generalization on independent datasets |
| NetMHCpan (v.4.1) [15] | Peptide-MHC binding | Wide HLA allele coverage, established performance | Used in identification of immunogenic neoantigens in B16F10 model |
| Antigen-agnostic TCR identification [13] | Tumor-specific TCRs | Comparative TCR repertoire profiling | Confirmed tumor reactivity in 3/3 validated patients |
Figure 1: Computational Workflow for Neoantigen and TCR Prediction
Experimental Methods for Validating Neoantigen-TCR Interactions
Antigen-Agnostic TCR Discovery Approach
A novel antigen-agnostic method identifies tumor-specific T-cell clonotypes by comparative high-throughput TCR repertoire profiling of tumor-infiltrating lymphocytes (TILs) and adjacent normal tissue-resident lymphocytes from surgical specimens [13]. This approach involves:
- TCRβ-chain repertoire sequencing: High-resolution sequencing of TCR repertoires from matched tumor and normal tissues.
- Clonotype selection criteria: Identification of candidate tumor-specific clonotypes based on TIL abundance and high tumor-to-nontumor frequency ratios.
- Single-cell RNA sequencing validation: Verification of tumor-specific clonotypes through gene expression signatures determined by scRNA-Seq.
- Functional validation: Testing predicted tumor-specific clonotypes for reactivity against autologous tumors.
This method successfully identified tumor-reactive TCRs in non-small cell lung cancer (NSCLC) patients, with selection validated in six of seven patients analyzed through scRNA-Seq, and experimental confirmation that predicted tumor-specific clonotypes reacted against autologous tumors in three patients [13].
TCR Functional Characterization Protocols
Comprehensive validation of neoantigen-specific TCRs requires multiple experimental approaches:
- Tetramer staining: Using pMHC tetramers to confirm direct binding between TCRs and their cognate pMHC complexes.
- Cellular activation assays: Measuring T cell activation markers (CD137, CD69) and cytokine production (IFN-γ, IL-2) following exposure to antigen-presenting cells pulsed with candidate neoantigen peptides.
- Cytotoxicity assays: Assessing the ability of TCR-engineered T cells to lyse tumor cells endogenously expressing the target neoantigen.
- Alaninescanning mutagenesis: Systematically replacing each residue in the neoantigen peptide with alanine to identify TCR contact residues and assess potential cross-reactivity with wild-type peptides [14].
For the KRAS Q61H-specific TCRs, researchers demonstrated that TCR-transduced T cells showed specific reactivity against HLA-matched NSCLC cell lines endogenously expressing the mutation, and cytotoxicity was partially blocked by HLA-I blockade, confirming TCR-mediated recognition [13].
Structural Biology Techniques
Understanding the molecular basis of TCR recognition requires structural biology approaches:
- X-ray crystallography: High-resolution structures of TCR-pMHC complexes provide atomic-level details of interaction interfaces. For example, structural studies of the TCR 47BE7 bound to H2-Db/Hsf2 p.K72N revealed how anchor-residue modifications create neoantigens that are discriminated at both MHC and TCR levels [15].
- Surface plasmon resonance (SPR): Quantitative measurement of binding kinetics and affinity between TCRs and pMHC complexes.
- Cryo-electron microscopy: Particularly useful for studying complex immune synapses and dynamic interactions.
These structural approaches have demonstrated that neoantigen-reactive TCRs often exhibit broad, stringent binding interfaces that enable high functional avidity and selectivity for mutant peptides over their wild-type counterparts [15].
Figure 2: Experimental Workflow for TCR Validation
NGS Integration in Neoantigen and TCR Research
Comprehensive Genomic Profiling for Neoantigen Discovery
Next-generation sequencing technologies have revolutionized neoantigen discovery by enabling comprehensive characterization of the tumor mutational landscape:
- Whole exome sequencing (WES): Identifies protein-altering mutations across the entire coding genome. Paired sequencing of tumor and normal tissues enables identification of somatic mutations.
- RNA sequencing: Determines mutation expression levels and identifies novel transcripts, fusion genes, and splicing variants. Studies have shown that RNA sequencing can identify cancer-specific splicing events (neojunctions) that serve as sources of shared neoantigens [14].
- Single-cell RNA sequencing: Enables simultaneous analysis of TCR sequences and transcriptional states in individual T cells, allowing identification of tumor-reactive T cell clones based on activation and exhaustion markers.
The integration of these NGS approaches provides a comprehensive view of the neoantigen landscape, informing the selection of candidate antigens for experimental validation and therapeutic development.
Automated NGS Workflows for Biomarker Discovery
Recent advancements in NGS workflow automation have significantly improved the efficiency and reproducibility of neoantigen discovery:
- Integrated automation solutions: Partnerships between companies like Integrated DNA Technologies and Hamilton Company provide complete automation-friendly solutions for NGS workflows on liquid handling systems, accelerating biomarker discovery [16].
- Rapid targeted sequencing panels: Technologies like Pillar Biosciences' oncoReveal panels enable rapid, localized NGS testing for somatic mutations, with validation studies demonstrating effective detection of actionable biomarkers in liquid biopsy samples from non-small cell lung cancer and breast cancer [17].
- Standardized bioinformatics pipelines: Robust computational workflows for variant calling, transcriptomic profiling, and neoantigen prediction from NGS data.
These technological advances make comprehensive genomic profiling more accessible and implementable in clinical research settings, supporting the broader integration of precision oncology approaches.
Table 3: NGS Applications in Neoantigen and TCR Research
| NGS Application | Technical Approach | Research Utility | Clinical Implementation |
|---|---|---|---|
| Whole Exome Sequencing | Sequencing of all protein-coding regions | Comprehensive mutation discovery | Identifying patient-specific mutations for personalized vaccines |
| RNA Sequencing | Transcriptome-wide sequencing | Determination of mutation expression, fusion genes, splicing variants | Selection of expressed neoantigens |
| Single-Cell RNA-Seq | Cell-level resolution transcriptomics | TCR sequence pairing with T cell functional states | Identification of tumor-reactive TCR clonotypes |
| TCR Repertoire Sequencing | High-throughput TCR CDR3 sequencing | Monitoring of T cell clonal dynamics | Tracking therapeutic TCR persistence |
The Scientist's Toolkit: Essential Research Reagents and Platforms
Table 4: Key Research Reagents and Platforms for Neoantigen and TCR Research
| Research Tool | Type | Function/Application | Example Platforms/Assays |
|---|---|---|---|
| NGS Library Prep Kits | Laboratory reagents | Preparation of sequencing libraries for genomic and transcriptomic profiling | IDT xGen, Archer [16] |
| Automated Liquid Handling | Laboratory equipment | Standardization and scaling of NGS workflows | Hamilton Microlab STAR, NIMBUS [16] |
| Targeted NGS Panels | Custom assay | Focused sequencing of cancer-related genes | Pillar oncoReveal panels [17] |
| pMHC Tetramers | Biochemical reagents | Detection and isolation of antigen-specific T cells | Custom tetramer production |
| TCR Reconstruction Systems | Molecular biology tools | Cloning and expression of candidate TCRs | Retroviral/Lentiviral vectors, TCR-null Jurkat76 cells [13] [14] |
| Single-Cell RNA-Seq Platforms | Instrumentation | Simultaneous analysis of gene expression and TCR sequence | 10X Genomics, Smart-seq2 |
| Cytokine Release Assays | Functional assays | Measurement of T cell activation | ELISpot, intracellular cytokine staining |
Clinical Translation and Therapeutic Applications
TCR-Based Adoptive Cell Therapies
The ultimate application of neoantigen and TCR research lies in developing effective cancer immunotherapies. Adoptive cell therapy (ACT) with TCR-engineered T cells represents a promising approach for treating advanced solid cancers [13]. Key considerations for clinical translation include:
- Target selection: Prioritizing clonal, truncal mutations that are expressed homogeneously across tumor lesions. Oncogenic driver mutations like KRAS Q61H are ideal targets due to their essential role in tumorigenesis and stable expression [13].
- TCR safety profiling: Comprehensive screening for off-target reactivity against normal tissues using methods like alanine scanning mutagenesis and screening against primary human cells.
- Manufacturing optimization: Developing robust processes for TCR gene transfer, T cell expansion, and quality control.
Notably, the discovery of highly homologous or identical TCRs across multiple patients with shared HLA types and mutations enables development of "off-the-shelf" TCR therapies targeting public neoantigens, potentially overcoming the personalized nature of most neoantigen-directed approaches [13].
Clinical Impact of NGS-Guided Therapies
Meta-analyses of randomized controlled trials have demonstrated the significant clinical impact of NGS-guided targeted therapies. In advanced cancer patients who had progressed after prior systemic therapy, NGS-guided matched targeted therapies (MTTs) were associated with:
- 30-40% reduction in the risk of disease progression
- Improved overall survival when MTTs were combined with standard of care, particularly in prostate and urothelial cancers
- PFS gains without OS improvement in breast and ovarian cancers when MTTs were combined with standard of care [12]
These findings support the routine integration of genomic profiling into the management of patients with advanced or recurrent cancers and highlight the importance of neoantigen and TCR research in advancing precision oncology.
The biological mechanism of neoantigens and TCR recognition represents a rapidly advancing field with significant implications for cancer immunotherapy. Advances in NGS technologies, computational prediction tools, and experimental validation methods have accelerated the discovery and characterization of tumor-specific antigens and their cognate TCRs. The integration of comprehensive genomic profiling, automated workflows, and sophisticated functional assays enables the identification of optimal targets for TCR-based therapies. As these technologies continue to evolve, they promise to enhance the precision and effectiveness of cancer immunotherapies, ultimately improving outcomes for cancer patients.
NGS Applications in Decoding the Tumor Microenvironment (TME)
The tumor microenvironment (TME) is a complex ecosystem comprising cancer cells, immune cells, stromal cells, blood vessels, and extracellular matrix, which collectively influence tumor progression and therapeutic response [18]. Next-generation sequencing (NGS) has revolutionized our ability to deconvolute this complexity by providing high-throughput, cost-effective methods for analyzing DNA and RNA molecules at unprecedented resolution [19]. The application of NGS in immuno-oncology has been particularly transformative, enabling the discovery of predictive biomarkers and characterization of the immune components within the TME that were previously obscured by bulk sequencing approaches [18] [5].
In personalized oncology, understanding the TME is crucial for predicting patient responses to immunotherapies, such as immune checkpoint inhibitors, adoptive cell therapies, and cancer vaccines [5] [18]. Multi-omics strategies that integrate genomics, transcriptomics, proteomics, and metabolomics have revealed that the functional state and spatial distribution of TME components, rather than their mere presence or absence, serve as critical determinants of therapeutic efficacy and resistance mechanisms [5] [10].
NGS Technological Platforms for TME Analysis
Various NGS platforms offer complementary strengths for TME interrogation, ranging from short-read technologies that provide high accuracy to long-read technologies that resolve complex genomic regions and full-length transcripts.
Table 1: Comparison of NGS Platforms for TME Analysis
| Platform | Technology | Read Length | Key Applications in TME | Limitations |
|---|---|---|---|---|
| Illumina | Sequencing-by-synthesis | 36-300 bp [19] | High-throughput transcriptomics (RNA-seq), whole exome sequencing, epigenomics [19] | Potential signal overcrowding with error rates up to 1% [19] |
| Ion Torrent | Semiconductor sequencing | 200-400 bp [19] | Targeted immuno-oncology panels (TCR/BCR profiling, TMB) [20] | Homopolymer sequence errors [19] |
| PacBio SMRT | Single-molecule real-time sequencing | 10,000-25,000 bp [19] | Full-length transcript sequencing for immune receptor characterization | Higher cost per sample [19] |
| Oxford Nanopore | Nanopore sensing | 10,000-30,000 bp [19] | Real-time RNA sequencing, epitranscriptomics in immune cells | Error rates up to 15% [19] |
The versatility of these platforms has facilitated the development of specialized assays specifically designed for immuno-oncology research. For example, the Oncomine TCR Beta-SR Assay enables characterization of the immune status and detection of T-cell minimal residual disease by specifically interrogating the CDR3 region of the TCR beta chain, while the Oncomine Tumor Mutation Load Assay covers 409 cancer-related genes to quantify tumor mutational burden (TMB), an independent predictor for patient stratification for response to immunotherapy [20].
Single-Cell RNA Sequencing for TME Deconvolution
Methodological Approaches
Single-cell RNA sequencing (scRNA-seq) has emerged as a powerful tool for deciphering the cellular heterogeneity of the TME at unprecedented resolution [18]. The technology can be broadly categorized into three methodological approaches:
- Plate-based methods (e.g., SMART-Seq2): These involve sorting individual cells into separate wells via fluorescence-activated cell sorting (FACS), providing full-length transcript coverage and enabling index-sorting for protein expression quantification [18].
- Droplet-based methods (e.g., 10X Chromium, Drop-seq): These use microfluidics to capture single cells with barcode-carrying beads into droplets, allowing high-throughput processing of thousands of cells at relatively low cost but restricted to either 3' or 5' end sequencing [18].
- Combinatorial barcoding methods (e.g., SPLiT-seq, Sci-RNA-seq): These bypass physical isolation of single cells by using combinatorial barcoding, enabling fixation of cells and mitigating batch effects in longitudinal studies [18].
Experimental Protocol for scRNA-seq
A standardized workflow for scRNA-seq analysis of the TME typically involves the following steps:
- Sample Preparation: Fresh tumor tissues are dissociated into single-cell suspensions using enzymatic digestion (e.g., collagenase, dispase) with viability typically >90% [18].
- Cell Capture: Depending on the chosen platform, 500-10,000 cells are loaded onto microfluidic devices or sorted into multiwell plates [18].
- Library Preparation: This includes cell lysis, reverse transcription with cell-specific barcodes and unique molecular identifiers (UMIs), cDNA amplification, and library construction with platform-specific reagents [18].
- Sequencing: Libraries are sequenced on appropriate NGS platforms (e.g., Illumina NovaSeq for droplet-based methods) with recommended read depths of 20,000-100,000 reads per cell [18].
- Computational Analysis: Data processing includes alignment (to GRCh38 or mm10 genomes), UMI counting, quality control, normalization, clustering, and cell type annotation using reference databases [18].
Diagram: scRNA-seq Workflow for TME Analysis
Key Insights from scRNA-seq Studies
Application of scRNA-seq to various cancer types has yielded fundamental insights into TME biology. In breast carcinoma, a study profiling over 45,000 cells revealed increased heterogeneity of gene expression in intratumoral lymphoid and myeloid cells compared to normal breast tissue, reflecting adaptation to diverse environmental signals within the TME [18]. In malignant glioma, scRNA-seq demonstrated that conventional subtype distinctions are primarily accounted for by differences in non-malignant cell types within the TME, highlighting the importance of comprehensive immune profiling beyond cancer cell-intrinsic classification [18].
Spatial Transcriptomics and Multi-Omics Integration
Spatial Biology Technologies
While scRNA-seq provides detailed cellular taxonomy, it loses critical spatial context. Spatial transcriptomics and multiplex immunohistochemistry (IHC) have emerged to address this limitation by enabling in situ analysis of gene and protein expression while preserving tissue architecture [10]. These technologies allow researchers to study the TME without altering spatial relationships between cells, providing crucial information about physical proximity, cellular organization, and interaction patterns that serve as important biomarkers themselves [10].
Studies suggest that the distribution of spatial interactions, rather than simple presence or absence of specific cells, can significantly impact therapeutic response [10]. For instance, the physical distance between cytotoxic T cells and cancer cells, or the organization of immunosuppressive macrophages around tumor nests, may serve as more accurate predictors of immunotherapy efficacy than bulk expression signatures.
Multi-Omics Integration Strategies
The integration of spatial data with other molecular layers through multi-omics approaches provides a comprehensive framework for understanding cancer biology and discovering clinically actionable biomarkers [5]. Multi-omics integration can be achieved through:
- Horizontal Integration: Combining similar data types across different samples or conditions to identify consistent patterns [5].
- Vertical Integration: Combining different molecular data types (genomics, transcriptomics, proteomics, metabolomics) from the same samples to derive systems-level insights [5].
Advanced computational approaches, including machine learning and deep learning, are essential for integrating these complex datasets and extracting biologically meaningful signatures [5] [10]. For example, AI-powered platforms like BostonGene's multi-omics platform integrate genomic, transcriptomic, immune, and spatial profiling data to deliver a multidimensional view of disease biology, enabling improved patient stratification and trial design [21].
Table 2: Multi-Omics Data Types for Comprehensive TME Analysis
| Omics Layer | Technology | Key Information | Clinical Application Example |
|---|---|---|---|
| Genomics | Whole exome sequencing (WES) | Somatic mutations, copy number variations, TMB [5] | FDA approval of TMB as biomarker for pembrolizumab [5] |
| Transcriptomics | RNA-seq, scRNA-seq | Gene expression signatures, immune cell composition [5] | Oncotype DX (21-gene) for breast cancer chemotherapy decisions [5] |
| Proteomics | Mass spectrometry, reverse-phase protein arrays | Protein abundance, post-translational modifications [5] | CPTAC studies revealing functional subtypes in ovarian and breast cancers [5] |
| Epigenomics | Whole genome bisulfite sequencing, ChIP-seq | DNA methylation, histone modifications [5] | MGMT promoter methylation predicting temozolomide benefit in glioblastoma [5] |
| Metabolomics | LC-MS, gas chromatography-MS | Cellular metabolites, metabolic pathway activity [5] | 2-hydroxyglutarate as diagnostic biomarker in IDH-mutant gliomas [5] |
Diagram: Multi-omics Integration Framework for TME Analysis
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Research Reagents and Platforms for TME NGS Analysis
| Category | Product/Platform | Key Features | Application in TME Research |
|---|---|---|---|
| TCR Profiling | Oncomine TCR Beta-LR Assay [20] | Long-read sequencing for CDR1, CDR2, CDR3 regions; 10 ng RNA input | Predictive biomarker discovery, T cell characterization, variable gene polymorphism identification |
| BCR Profiling | Oncomine BCR IgH SR Assay [20] | CDR3 region interrogation from FFPE tissue; identifies somatic hypermutations | Study of clonal evolution, isotype abundance, measurable residual disease monitoring |
| Immune Monitoring | Oncomine Immune Response Research Assay [20] | Carefully selected gene panel to monitor tumor microenvironment | Biomarker identification, mechanism of action studies, combination therapy experiments |
| Tumor Mutational Burden | Oncomine Tumor Mutation Load Assay [20] | Covers 1.7 Mb across 409 genes; correlates with exome mutation counts | TMB quantification for immunotherapy patient stratification |
| Computational Analysis | ngs.plot [22] | Standalone program to visualize enrichment patterns of DNA-interacting proteins | Integrative visualization of NGS data at functional genomic regions |
| Single-Cell Analysis | Seurat, Scanpy [18] | R and Python packages for scRNA-seq data normalization and analysis | Cell clustering, trajectory inference, and population characterization in TME |
| Multi-Omics Platform | BostonGene Platform [21] | AI-powered integration of genomic, transcriptomic, immune, and spatial data | Comprehensive TME profiling for patient stratification and clinical trial optimization |
Biomarker Discovery and Clinical Translation
Analytical Workflows for Biomarker Discovery
The biomarker discovery pipeline from NGS data involves sophisticated analytical workflows that transform raw sequencing data into clinically actionable insights. For TME-focused biomarkers, key steps include:
- Quality Control and Preprocessing: Tools like FastQC and MultiQC assess read quality, followed by adapter trimming and alignment to reference genomes using STAR or HISAT2 [22].
- Feature Quantification: Expression quantification (e.g., HTSeq, featureCounts), variant calling (e.g., GATK), or epigenetic feature identification [5].
- TME-Specific Analysis: Immune cell deconvolution (e.g., CIBERSORT, MCP-counter), TCR/BCR repertoire analysis, and spatial neighborhood assessment [18] [10].
- Multi-Omics Integration: Horizontal and vertical integration strategies combine different data types using computational tools specifically designed for multi-omics data [5].
- Biomarker Validation: Cross-validation within datasets and experimental validation using orthogonal methods (e.g., flow cytometry, multiplex IHC) [10].
Clinical Applications and Validation
NGS-derived TME biomarkers have demonstrated significant clinical utility across multiple cancer types. For example, tumor mutational burden (TMB), validated in the KEYNOTE-158 trial, has received FDA approval as a predictive biomarker for pembrolizumab treatment across solid tumors [5]. Similarly, spatial biomarkers that quantify immune cell distribution within the TME have shown promise in predicting response to immunotherapy in clinical studies [10].
The Clinical Proteomic Tumor Analysis Consortium (CPTAC) studies of ovarian and breast cancers demonstrated that proteomics can identify functional subtypes and reveal druggable vulnerabilities missed by genomics alone, directly informing the discovery of protein-based biomarkers for predicting therapeutic responses [5]. These approaches are increasingly being incorporated into adaptive clinical trial designs where treatment decisions are modified based on accumulating biomarker data [10].
Next-generation sequencing technologies have fundamentally transformed our ability to decode the complex ecosystem of the tumor microenvironment. Through single-cell RNA sequencing, spatial transcriptomics, and multi-omics integration, researchers can now delineate the cellular composition, functional states, and spatial organization of the TME at unprecedented resolution. These advances have accelerated the discovery of novel biomarkers for immuno-oncology, enabling more precise patient stratification, therapeutic response prediction, and clinical trial optimization. As NGS technologies continue to evolve toward higher throughput, lower costs, and improved integration with artificial intelligence, their impact on personalized cancer care and drug development will undoubtedly expand, ultimately improving outcomes for cancer patients.
Key Genomic Alterations Driving Response to Immunotherapy
Immunotherapy has revolutionized cancer treatment, yet durable responses remain unpredictable, occurring in only a minority of patients. The clinical efficacy of immune checkpoint inhibitors (ICIs) is profoundly influenced by the complex interplay between tumor genomic features and the host immune system. This technical review synthesizes current evidence on key genomic alterations that dictate response and resistance to immunotherapy, with emphasis on their discovery through next-generation sequencing (NGS) technologies. We examine the predictive value of tumor mutational burden (TMB), neoantigen landscape, specific driver mutations, and microenvironmental factors, providing a comprehensive framework for biomarker discovery in immuno-oncology research and drug development.
The remarkable success of immune checkpoint inhibitors targeting cytotoxic T-lymphocyte-associated protein 4 (CTLA-4) and the programmed cell death 1 (PD-1)/programmed death-ligand 1 (PD-L1) axis has transformed therapeutic paradigms across multiple cancer types. However, response rates remain limited, with only 18-38% of advanced solid cancer patients achieving objective responses to single-agent ICIs [23]. This clinical heterogeneity underscores the critical need to identify molecular determinants of treatment outcome.
Immunogenomics represents an emerging field that integrates genomic data with immunologic parameters to decipher the complex tumor-immune interplay. Advances in NGS technologies have enabled comprehensive profiling of somatic alterations, neoantigen landscapes, and immune cell repertoires, revealing distinct genomic features that orchestrate anti-tumor immunity [5]. The convergence of these technologies with immunotherapy clinical trials has accelerated the discovery of predictive biomarkers essential for patient stratification and treatment personalization.
Key Genomic Biomarkers of Immunotherapy Response
Tumor Mutational Burden (TMB) and Neoantigen Landscape
Tumor mutational burden, defined as the total number of non-synonymous mutations per megabase of DNA, has emerged as a quantitative biomarker of immunotherapy response across multiple cancer types. The underlying biological rationale centers on the principle that somatic mutations can generate novel immunogenic peptides (neoantigens) that enable T-cell recognition and targeting of tumor cells [23].
Table 1: Tumor Mutational Burden as a Predictive Biomarker Across Cancers
| Cancer Type | TMB Threshold (mut/Mb) | Predictive Value | Clinical Context | Reference Study |
|---|---|---|---|---|
| Melanoma | >100 | OS advantage | Anti-CTLA-4 therapy | [23] |
| NSCLC | Varies (discovery vs validation cohorts) | PFS and response | Anti-PD-1 therapy | [23] |
| Urothelial Carcinoma | Not specified | Significant association | Anti-PD-L1 therapy | [23] |
| Small Cell Lung Cancer | Not specified | Significant association | ICI therapy | [23] |
| Diffuse Large B-Cell Lymphoma | Not specified | Correlation with neoantigen burden | Immunochemotherapy | [24] |
High TMB correlates with increased neoantigen burden, creating a more immunogenic tumor microenvironment. In diffuse large B-cell lymphoma (DLBCL), patients harboring ≥2 BCL2-derived neoantigens exhibit significantly worse overall survival (HR 5.61 for OS) following immunochemotherapy [24]. Beyond single nucleotide variants, non-SNV sources including frameshift mutations, splice variants, and gene fusions can produce more immunogenic neoantigens due to greater sequence divergence from wild-type peptides. For example, frameshift mutations in microsatellite-unstable lymphomas generate 9× more neoantigens per mutation than SNVs [24].
The predictive utility of TMB, however, shows limitations in cancers with low mutation rates, such as pediatric acute lymphoblastic leukemia (typically <20 mutations/exome), where reduced neoantigen availability limits immunogenicity [24]. Furthermore, the correlation between TMB and immunogenic neoantigen burden is imperfect (Spearman ρ = 0.55–0.56 in DLBCL), as only 1–3% of mutations yield immunogenic epitopes due to HLA-binding constraints and inefficient antigen processing [24].
Specific Genomic Alterations with Immunomodulatory Effects
Beyond quantitative mutational burden, specific genomic alterations in oncogenic pathways can actively shape the tumor immune microenvironment and modulate ICI response.
Table 2: Specific Genomic Alterations Modulating Immunotherapy Response
| Gene/Pathway | Alteration Type | Cancer Context | Effect on Immune Response | Mechanistic Insight |
|---|---|---|---|---|
| BCL2 | Somatic mutations | DLBCL | Poor survival (HR 5.61 for OS) | Neoantigen generation |
| CRMA cluster | Overexpression | Melanoma | Anti-CTLA-4 resistance | Autophagy interference affecting antigen presentation |
| HLA class I | Evolutionary divergence | Pan-cancer | Superior survival with high HED | Diverse immunopeptidomes enhancing tumor surveillance |
| MYC | Activation | Multiple cancers | Immunotherapy non-response | Negative regulation of immune response |
| RAS-like subtype | Transcriptomic signature | Thyroid cancer, SKCM | Lower immune signature scores | Immunosuppressive microenvironment |
| ARID1A | Alterations | Multiple cancers | Predictive for ICI response | Impact on tumor immunogenicity |
The eight-gene "anti-CTLA4 resistance-associated MAGEA" (CRMA) cluster demonstrates how specific gene expression patterns can mediate resistance. In melanoma patients treated with ipilimumab, CRMA expression associates with poor response, potentially through autophagy interference that disrupts antigen processing and presentation [23]. Conversely, ARID1A alterations have emerged as positive predictors of ICI response, potentially through enhancing tumor immunogenicity [25].
Transcriptomic analyses reveal that RAS-like subtypes in both skin cutaneous melanoma (SKCM) and thyroid cancer (THCA) are significantly associated with lower immune signature scores compared to other molecular subtypes, suggesting these tumors create immunosuppressive microenvironments less conducive to ICI response [26]. Similarly, MYC activation has been identified as a negative regulator of immune response, associated with immunotherapy non-response [26].
HLA Diversity and Antigen Presentation Machinery
The host germline genetics, particularly the human leukocyte antigen (HLA) system, plays a crucial role in determining immunotherapy efficacy. HLA class I evolutionary divergence (HED) quantifies physicochemical differences between HLA alleles and predicts ICI efficacy. Patients with high HED (top quartile) exhibit superior survival post-ICI, as divergent alleles present more diverse immunopeptidomes, enhancing tumor surveillance [24]. This effect persists even among fully heterozygous individuals, underscoring HED's role beyond heterozygosity [24].
Allele-specific associations also influence outcomes; for instance, HLA-B*44 supertypes correlate with prolonged survival in chronic lymphocytic leukemia (CLL) due to efficient presentation of leukemia-associated antigens [24]. These findings highlight how germline genetic factors interact with somatic alterations to ultimately determine the effectiveness of anti-tumor immunity.
Biological Mechanisms Linking Genomic Alterations to Immune Response
The relationship between genomic alterations and immunotherapy response operates through multiple interconnected biological mechanisms that collectively shape the tumor-immune microenvironment.
This framework illustrates how genomic features translate through molecular and cellular mechanisms to ultimately determine clinical outcomes to immunotherapy. High TMB increases the probability of generating immunogenic neoantigens that can be recognized by T-cells as non-self, initiating an immune response [23]. Specific driver mutations can activate oncogenic signaling pathways that create an immunosuppressive microenvironment, while defects in antigen presentation machinery can limit the visibility of tumor cells to the immune system [26] [24].
The resulting immune phenotype exists on a spectrum from "immune-hot" tumors characterized by robust T-cell infiltration and activation to "immune-cold" tumors with exclusion of immune effector cells and dominant immunosuppressive signals. Understanding where a patient's tumor falls on this spectrum based on its genomic features enables more accurate prediction of immunotherapy response.
Experimental Approaches for Profiling Immunogenomic Biomarkers
Next-Generation Sequencing Methodologies
Comprehensive genomic profiling for immunotherapy biomarkers primarily utilizes targeted NGS panels, whole exome sequencing (WES), and increasingly, whole genome sequencing (WGS). Each approach offers distinct advantages and limitations for biomarker discovery.
Targeted NGS panels (e.g., MSK-IMPACT, FoundationOne) focus on several hundred cancer-related genes with high sequencing depth (typically 500-1000×), enabling sensitive detection of somatic variants down to 5% variant allele frequency [27]. These panels are designed to identify actionable mutations across major variant classes including single nucleotide variants (SNVs), insertions/deletions (indels), copy number variants (CNVs), and structural rearrangements while conserving limited tissue samples [27]. The high depth of coverage makes targeted approaches particularly suitable for calculating TMB and detecting microsatellite instability (MSI) from limited clinical specimens.
Whole exome sequencing provides broader coverage of protein-coding regions (~1-2% of the genome) but at lower depth (typically 100-200×), resulting in reduced sensitivity for subclonal alterations [27]. While WES enables more comprehensive TMB calculation and neoantigen prediction beyond predefined gene panels, its lower sensitivity and higher DNA input requirements have limited routine clinical adoption compared to targeted approaches.
Whole genome sequencing offers the most comprehensive genomic assessment, covering both coding and non-coding regions, but remains predominantly a research tool due to higher costs, computational demands, and challenges in interpreting non-coding variants.
Immune Signature Profiling
Transcriptomic approaches enable quantification of immune cell populations and functional states within the tumor microenvironment. Bulk RNA sequencing coupled with deconvolution algorithms (CIBERSORT, xCell) can quantify relative abundances of immune cell subsets from complex tissue mixtures [26] [24]. This methodology has delineated "hot" versus "cold" tumor microenvironments, with "hot" TMEs featuring CD8+ effector T-cells and NK cells correlating with response to immunotherapy across multiple cancer types [24].
Single-cell RNA sequencing (scRNA-seq) provides higher resolution insights into cellular heterogeneity and functional states. In classical Hodgkin lymphoma, scRNA-seq revealed that responders show CD4+ memory T-cell expansion, while non-responders accumulate immunosuppressive CD163+ macrophages [24]. Similarly, in DLBCL patients receiving CD19-CAR-T therapy, pre-infusion upregulation of exhaustion genes (LAG3, TIM3, TOX, NR4A) in manufactured products associates with poor persistence and disease progression [24].
Algorithmic Approaches for Neoantigen Prediction
Computational pipelines for neoantigen prediction have become increasingly sophisticated, integrating multiple data dimensions to prioritize immunogenic candidates. Modern approaches like INTEGRATE-neo and NetMHCpan incorporate variant allele frequency, gene expression, and mutation clonality alongside HLA binding affinity to identify high-priority neoantigens [24]. These pipelines typically follow a multi-step process: (1) identification of somatic mutations from tumor-normal sequencing pairs; (2) prediction of HLA haplotypes from normal tissue sequencing; (3) in silico prediction of peptide-MHC binding affinity; (4) prioritization based on expression, clonality, and binding strength.
The integration of multi-omics data layers through machine learning approaches has demonstrated improved prediction of immunotherapy response compared to single-parameter biomarkers. For instance, the IS score (immune signature score) developed from gene expression data of patients treated with MAGE-A3 antigen-based immunotherapy successfully separated responders from non-responders with an AUC of 0.83 and also predicted response to anti-CTLA-4 therapy in independent cohorts [26].
The Scientist's Toolkit: Essential Research Reagents and Platforms
Table 3: Essential Research Solutions for Immunogenomics
| Category | Specific Tool/Platform | Application in Immunogenomics | Key Features |
|---|---|---|---|
| NGS Platforms | Illumina sequencing | Targeted panels, WES, WGS | High throughput, low error rates (0.1-0.6%) |
| Oxford Nanopore | Long-read sequencing | Real-time sequencing, structural variant detection | |
| PacBio SMRT sequencing | Long-read sequencing | High-fidelity reads, isoform sequencing | |
| Computational Tools | CIBERSORT/xCell | Immune cell deconvolution | Bulk RNA-seq to immune cell proportions |
| NetMHCpan/INTEGRATE-neo | Neoantigen prediction | HLA binding affinity, immunogenicity | |
| GATK/BWA | Variant calling | SNV, indel, CNV detection | |
| Data Resources | TCGA Pan-Cancer Atlas | Multi-omics reference dataset | 30 tumor types, clinical annotations |
| CPTAC | Proteogenomic datasets | Proteomic-phosphoproteomic integration | |
| CGGA | Glioma-specific database | Multi-omics glioma data | |
| Laboratory Assays | PD-L1 IHC | Protein expression assessment | Companion diagnostic for multiple ICIs |
| Multiplex immunofluorescence | Spatial immune profiling | Tissue context, cell-cell interactions | |
| scRNA-seq | Single-cell transcriptomics | Cellular heterogeneity, rare populations |
Clinical Translation and Trial Design Implications
The discovery of genomic determinants of immunotherapy response has catalyzed the development of novel clinical trial designs that transcend traditional histology-based approaches. Basket trials investigate the efficacy of targeted immunotherapies for molecularly-defined subsets across different tumor histologies [28]. These designs are predicated on the understanding that specific genomic alterations can drive response regardless of tissue of origin.
Umbrella trials represent a complementary approach, evaluating multiple targeted immunotherapies stratified by molecular alterations within a single cancer type [28]. This design enables efficient evaluation of multiple biomarker-drug combinations simultaneously. More recently, platform trials have emerged as adaptive designs that continuously assess several interventions against a control arm, allowing for early termination of ineffective interventions and flexibility in adding new interventions during the trial [28].
Despite these advances, the implementation of biomarker-guided combination therapies remains limited. A comprehensive analysis of clinical trials combining gene-targeted agents with immune checkpoint inhibitors revealed that only 1.3% (4/314) of such trials incorporated biomarkers for both therapeutic modalities [25]. This represents a significant missed opportunity for precision immuno-oncology, particularly as evidence mounts that dual biomarker-matched approaches can yield durable clinical benefit even in heavily pretreated patients [25].
The integration of NGS-based genomic profiling has been instrumental in deciphering the complex relationship between tumor genetics and response to immunotherapy. TMB, specific driver alterations, neoantigen quality, and HLA diversity collectively contribute to a multidimensional framework for predicting ICI outcomes. However, significant challenges remain in standardizing biomarker assessment, validating predictive models across diverse populations, and translating these insights into clinically actionable tools.
Future directions in immunogenomics will likely focus on multi-omics integration, combining genomic, transcriptomic, proteomic, and spatial data to build more comprehensive predictive models. Artificial intelligence approaches are showing promise in this domain, with systems like SCORPIO and LORIS demonstrating superior performance compared to single-biomarker methods [29]. Additionally, the emergence of single-cell and spatial multi-omics technologies is expanding the scope of biomarker discovery and deepening our understanding of tumor-immune interactions at unprecedented resolution [5].
As the field advances, the successful implementation of precision immuno-oncology will require continued collaboration between researchers, clinicians, and drug developers to ensure that genomic insights are rapidly translated into improved patient outcomes through biomarker-driven clinical trials and treatment strategies.
The integration of multi-omics data—encompassing genomics, transcriptomics, epigenomics, proteomics, and other molecular layers—has revolutionized oncology research by providing comprehensive molecular portraits of tumors. This approach is particularly crucial for biomarker discovery in immuno-oncology, where understanding the complex interactions between tumors and the immune system requires analysis across multiple biological dimensions. Next-generation sequencing (NGS) technologies serve as the foundational engine powering this revolution, enabling high-throughput characterization of the molecular features that influence immunotherapy response and resistance [30] [31]. The convergence of NGS with multi-omics data integration creates unprecedented opportunities to identify predictive biomarkers, discover novel therapeutic targets, and ultimately advance precision immuno-oncology.
Public multi-omics databases provide the essential infrastructure for storing, standardizing, and sharing the vast datasets generated by the research community. These resources have become indispensable for researchers seeking to validate findings, generate hypotheses, and leverage previously generated data to accelerate discovery. This whitepaper provides a comprehensive technical guide to the major public multi-omics databases and resources, with particular emphasis on their application to NGS-driven biomarker discovery in immuno-oncology research.
Major Public Multi-Omics Databases
The landscape of public cancer databases has expanded significantly, with several flagship projects leading the way in data aggregation, standardization, and dissemination. The table below summarizes the core characteristics of major multi-omics databases relevant to oncology research.
Table 1: Major Public Multi-Omics Databases for Oncology Research
| Database Name | Primary Focus | Key Features | Data Types | Access Method |
|---|---|---|---|---|
| The Cancer Genome Atlas (TCGA) [32] [33] | Pan-cancer molecular characterization | >20,000 primary cancer and matched normal samples across 33 cancer types | Genomic, transcriptomic, epigenomic, clinical data | Genomic Data Commons (GDC) Data Portal |
| MLOmics [34] | Machine learning-ready multi-omics data | 8,314 patient samples across 32 cancer types with four omics types; preprocessed feature versions | mRNA, miRNA, DNA methylation, copy number variations | Open access database |
| International Cancer Genome Consortium (ICGC) [32] | Global cancer genomics collaboration | Catalog of 77 million somatic mutations from >20,000 participants across 84 projects | Genomic, transcriptomic, epigenomic data | ICGC Data Portal |
| cBioPortal [32] [33] | Visualization and analysis of cancer genomics | User-friendly interface for complex genomic datasets; integration with TCGA and ICGC | Genomic, clinical, and basic protein data | Web interface and API |
| Gene Expression Omnibus (GEO) [32] [33] | Functional genomics data repository | MIAME-compliant data submissions; beyond genomics to methylation and chromatin structure | Gene expression, methylation, chromatin structure | Public data download |
| NCI Genomic Data Commons (GDC) [32] | Unified cancer genomic data management | Stores, analyzes, and shares genomic and clinical data; promotes precision medicine | Genomic, transcriptomic, clinical data | GDC Data Portal |
| Human Tumor Atlas Network (HTAN) [33] | 3D tumor atlases | Cancer Moonshot initiative; dynamic cellular, morphological, and molecular features | Multi-omics, spatial, imaging data | HTAN Data Portal |
| ProteomicsDB [33] | Multi-omics and multi-organism resource | Protein-centric interrogation with analytics section | Proteomic, transcriptomic, phenomic data | Web interface |
Beyond these comprehensive resources, specialized databases have emerged to address specific analytical needs. For instance, MLOmics represents a recent innovation specifically designed to serve the machine learning community by providing off-the-shelf, preprocessed multi-omics datasets [34]. This database addresses a critical bottleneck in bioinformatics by providing data in multiple feature versions (Original, Aligned, and Top), with the Top version containing the most significant features selected via ANOVA testing across all samples to filter out potentially noisy genes [34]. Such specialized resources significantly reduce the preprocessing burden on researchers and facilitate more rapid development of predictive models for immunotherapy response.
Standardized Experimental Methodologies
Data Generation Protocols
Robust biomarker discovery requires standardized experimental protocols to ensure data quality and reproducibility. The CIMACs-CIDC Network (Cancer Immune Monitoring and Analysis Centers-Cancer Immunologic Data Center), established by the NCI, provides a exemplary framework for standardized immuno-oncology biomarker analysis [35]. This network has harmonized a core set of assays across multiple leading institutions to reduce data variability and facilitate cross-trial analysis.
Table 2: Standardized Assay Protocols for Immuno-Oncology Biomarker Discovery
| Assay Category | Specific Technologies | Key Applications in Immuno-Oncology |
|---|---|---|
| Tissue Imaging | Multiplex immunofluorescence, Multiplex IHC, MIBI, Spatial transcriptomics (Visium, GeoMx) | Spatial analysis of immune cell infiltration, PD-L1 expression, tumor-immune interactions |
| Immune Cell Profiling | Mass Cytometry (CyTOF), EliSPOT, Single-cell RNA sequencing, CITE-seq | Comprehensive immunophenotyping, functional immune response assessment, T cell activation status |
| Sequencing Assays | RNA-seq, Whole Exome Sequencing, TCR/BCR sequencing, ATAC-seq, ctDNA analysis | Tumor mutational burden, neoantigen prediction, immune repertoire diversity, clonal evolution |
| Soluble Factor Analysis | Olink cytokine analysis, ELISA, NULISA | Systemic immune activation, cytokine profiling, biomarker quantification |
The NGS workflows for immuno-oncology research typically involve standardized library preparation methods targeting specific biological questions. For immune repertoire analysis, targeted panels like the AmpliSeq for Illumina Immune Repertoire Plus TCR beta Panel enable investigation of T cell diversity and clonal expansion by sequencing T-cell receptor beta chain rearrangements [31]. For transcriptomic analysis of the tumor microenvironment, the Illumina Stranded Total RNA Prep with RiboZero Plus provides exceptional performance for coding and noncoding RNA analysis, enabling discovery of alternative transcripts, gene fusions, and allele-specific expression [31].
Data Processing and Normalization
Raw NGS data requires sophisticated processing to generate biologically meaningful information. The MLOmics database provides a representative example of standardized processing pipelines for different omics types [34]. For transcriptomics data (mRNA and miRNA), their pipeline includes: (1) identification of transcriptomics data using "experimental_strategy" field in metadata; (2) determination of experimental platform; (3) conversion of gene-level estimates using edgeR package to generate FPKM values; (4) filtering of non-human miRNAs; (5) elimination of features with zero expression in >10% of samples; and (6) logarithmic transformation of expression values [34].
For epigenomic data (DNA methylation), standard processing includes: (1) identification of methylation regions from metadata; (2) normalization of methylation data using median-centering normalization with the limma R package to adjust for systematic biases; and (3) selection of promoters with minimum methylation for genes with multiple promoters [34]. Genomic data (copy number variations) processing involves: (1) identification of CNV alterations from metadata descriptions; (2) filtering for somatic mutations; (3) identification of recurrent alterations using the GAIA package; and (4) annotation of genomic regions using BiomaRt [34].
Following data processing, feature selection and normalization are critical for downstream analysis. The MLOmics database provides three feature versions to support different analytical needs: (1) Original features with full gene set; (2) Aligned features filtering non-overlapping genes and selecting genes shared across cancer types with z-score normalization; and (3) Top features identifying the most significant features via multi-class ANOVA with Benjamini-Hochberg correction for false discovery rate control, followed by z-score normalization [34].
Analytical Frameworks and Computational Tools
Bioinformatics Workflows for Biomarker Discovery
The integration of multi-omics data requires sophisticated computational approaches. A typical biomarker discovery workflow in immuno-oncology incorporates data from multiple molecular layers to identify signatures predictive of immunotherapy response. The following diagram illustrates a standardized analytical framework:
NGS-Based Biomarker Discovery Workflow for Immuno-Oncology
This workflow highlights how different NGS data types feed into established immuno-oncology biomarkers. Tumor Mutational Burden (TMB) is calculated from whole exome sequencing data by counting the number of somatic mutations per megabase of genome sequenced [30] [31]. Neoantigen prediction combines somatic variant information with HLA typing and binding affinity algorithms to identify tumor-specific antigens that could trigger T-cell responses [30]. Immune gene expression signatures are derived from RNA sequencing data to quantify the inflammatory state of the tumor microenvironment [31]. T-cell receptor (TCR) and B-cell receptor (BCR) repertoire sequencing provides measures of immune clonality and diversity that correlate with antigen-specific immune responses [20] [31].
Machine Learning Approaches
Machine learning frameworks have shown significant promise in multi-omics analysis for cancer research [34]. These approaches can integrate complex, high-dimensional multi-omics data to predict therapeutic response, identify novel subtypes, and discover biomarkers. The MLOmics database supports this development by providing 20 task-ready datasets for machine learning models ranging from pan-cancer classification and cancer subtype clustering to omics data imputation [34].
For pan-cancer and gold-standard cancer subtype classification tasks, established baselines include both classical machine learning methods (XGBoost, Support Vector Machines, Random Forest, Logistic Regression) and deep learning approaches (Subtype-GAN, DCAP, XOmiVAE, CustOmics, DeepCC) [34]. Evaluation metrics for these tasks typically include precision, recall, F1-score, normalized mutual information (NMI), and adjusted rand index (ARI) to assess agreement between clustering results and true labels [34].
Essential Research Reagents and Platforms
The experimental workflows described previously depend on specialized reagents and platforms designed for multi-omics analysis. The table below catalogues key research solutions cited in the literature:
Table 3: Research Reagent Solutions for Multi-Omics Oncology Research
| Category | Product/Platform | Key Features and Applications |
|---|---|---|
| Targeted NGS Panels | Oncomine TCR Beta-SR Assay [20] | Interrogates CDR3 region of TCR beta chain; enables immune status characterization and MRD detection |
| Oncomine Tumor Mutation Load Assay [20] | Covers 1.7 Mb across 409 genes; correlates with exome mutation counts for TMB assessment | |
| Ion Torrent Oncomine Immune Response Panel [20] | Monitors tumor microenvironment; identifies biomarkers and studies mechanism of action | |
| Library Prep Technologies | AmpliSeq for Illumina Immune Repertoire Plus [31] | Targeted RNA panel for T-cell receptor beta chain rearrangements; assesses diversity and clonal expansion |
| Illumina Stranded Total RNA Prep with RiboZero Plus [31] | Analysis of coding and noncoding RNA; discovers alternative transcripts, fusions, allele-specific expression | |
| Sequencing Platforms | NovaSeq X Series [31] | Extreme data output for production-scale sequencing of large cohorts or multiple omics datasets |
| NextSeq 1000/2000 Systems [31] | Mid-throughput flexibility for targeted panels, transcriptomics, and immune repertoire sequencing | |
| Analysis Software | BaseSpace Sequence Hub [31] | Cloud-based NGS data analysis environment with specialized apps for immuno-oncology |
| cBioPortal [32] [33] | Open-access platform for visualization, analysis, and exploration of cancer genomics datasets |
These research tools enable the comprehensive profiling required for immuno-oncology biomarker discovery. For example, the Oncomine TCR Beta-LR Assay utilizes long-read sequencing technology to efficiently capture all three complementarity-determining regions of the TCR beta chain (CDR1, CDR2, CDR3), enabling applications in predictive biomarker discovery, T-cell characterization, and identification of variable gene polymorphisms [20]. Such specialized assays provide the granular data needed to understand the dynamics of immune-tumor interactions.
Data Integration and Cross-Study Analysis
A critical challenge in immuno-oncology biomarker discovery is the integration of data across multiple studies to increase statistical power and validate findings. The CIMACs-CIDC Network addresses this through a centralized database that collects clinical and biomarker data from multiple immunotherapy trials, enabling cross-trial analysis [35]. This approach helps overcome the limitations of small cohort sizes in individual trials and facilitates the identification of robust biomarkers across different cancer types and therapeutic regimens.
The FAIRness principle (Findable, Accessible, Interoperable, and Reusable) provides a framework for evaluating database utility [32]. Databases that are easily discoverable through web browsers, allow free access, provide statistical analysis functions, and enable data download maximize their value to the research community [32]. The growing trend of creating smaller, user-friendly databases derived from larger resources (such as cBioPortal's interface to TCGA data) enhances accessibility for researchers without extensive bioinformatics support [32].
Emerging resources like the Human Tumor Atlas Network (HTAN) represent the next generation of cancer databases, constructing three-dimensional atlases of dynamic cellular, morphological, and molecular features of human cancers as they evolve from precancerous lesions to advanced disease [33]. These comprehensive resources will further enable the study of tumor-immune interactions across space and time, providing unprecedented insights into the dynamics of immunotherapy response and resistance.
Public multi-omics databases have become indispensable infrastructure for advancing biomarker discovery in immuno-oncology research. The integration of diverse molecular data types through NGS technologies provides a comprehensive view of the complex interactions between tumors and the immune system. As these resources continue to grow in scale and sophistication, and as analytical methods become increasingly powerful, researchers are better positioned than ever to identify robust biomarkers that can guide immunotherapy development and clinical application. The continued expansion of standardized, well-annotated multi-omics resources will be essential for realizing the full potential of precision immuno-oncology.
From Data to Insights: NGS Workflows and Multi-Omic Integration Strategies
Next-generation sequencing (NGS) has fundamentally transformed the landscape of immuno-oncology research by enabling comprehensive molecular profiling of tumors and their microenvironment. These technologies provide researchers with powerful tools to decipher the complex genomic, transcriptomic, and epigenomic alterations that dictate cancer immunogenicity, T-cell recognition, and response to immunotherapies. The integration of diverse NGS approaches—including whole-genome sequencing (WGS), whole-exome sequencing (WES), RNA sequencing (RNA-Seq), and targeted panels—has accelerated the discovery and validation of novel biomarkers essential for predicting treatment response, understanding resistance mechanisms, and developing personalized cancer immunotherapies. As the field of immuno-oncology advances, each NGS platform offers distinct advantages and limitations that researchers must strategically leverage to address specific biological questions within the constraints of resources, sample availability, and clinical applicability.
Comparative Analysis of NGS Platforms
The selection of an appropriate NGS platform represents a critical strategic decision in immuno-oncology research, with each approach offering distinct advantages for biomarker discovery. Whole-genome sequencing (WGS) provides the most comprehensive analysis by sequencing the entire genome—approximately 3 billion base pairs—enabling the detection of genetic variants in both coding and noncoding regions, including intergenic and regulatory elements, intron sequences, and regions corresponding to noncoding RNAs [36]. This breadth makes WGS particularly valuable for discovering novel biomarkers in noncoding regions and identifying complex structural variants that may influence cancer immunogenicity. In contrast, whole-exome sequencing (WES) focuses primarily on protein-coding regions (approximately 1-2% of the genome), offering a more cost-effective approach for identifying mutations in known functional elements while achieving higher sequencing depth in targeted regions [36].
Targeted gene panels represent a precision-focused approach, sequencing a predefined set of genes or genomic regions with known relevance to cancer biology or immunotherapy response [37]. These panels streamline the identification of actionable genetic mutations, biomarkers, and therapeutic targets, offering the highest sensitivity for detecting low-frequency variants while minimizing data complexity [38]. RNA sequencing (RNA-Seq) complements DNA-based approaches by profiling the transcriptome, enabling researchers to analyze gene expression patterns, alternative splicing, fusion transcripts, and immune repertoire characteristics within the tumor microenvironment [5]. Each platform serves distinct but complementary roles in immuno-oncology biomarker discovery, with the optimal choice dependent on research goals, sample characteristics, and resource constraints.
Table 1: Technical Specifications and Applications of Major NGS Platforms
| Platform | Genomic Coverage | Primary Applications in Immuno-Oncology | Key Advantages | Typical Sequencing Depth |
|---|---|---|---|---|
| WGS | Entire genome (~3 billion base pairs) [36] | Discovery of novel variants in noncoding regions, structural variant detection, comprehensive biomarker identification [39] | Unbiased genome-wide coverage, detection of regulatory elements | 30x (standard) to 22x (with advanced platforms) [40] |
| WES | Protein-coding exons (~1-2% of genome) [36] | Mutation profiling in functional elements, identification of neoantigens, tumor mutational burden calculation | Cost-effective for coding regions, higher depth in targeted areas | 100x and above [40] |
| Targeted Panels | Predefined cancer-associated genes (dozens to hundreds) | High-sensitivity detection of actionable mutations, therapy selection, minimal residual disease monitoring [38] [37] | Highest sensitivity for low-frequency variants, fast turnaround, cost-efficient | 500x-1000x+ (ultra-deep sequencing) |
| RNA-Seq | Entire transcriptome | Gene expression profiling, fusion gene detection, immune cell infiltration analysis, biomarker validation [5] | Direct measurement of gene expression, reveals functional consequences | Varies by application |
Table 2: Performance Characteristics and Practical Considerations
| Parameter | WGS | WES | Targeted Panels | RNA-Seq |
|---|---|---|---|---|
| DNA Input Requirements | Varies by platform | ≥50 ng recommended [38] | Can work with lower inputs (including ctDNA) [37] | Dependent on RNA quality and yield |
| Variant Detection Sensitivity | High for structural variants, moderate for SNVs | High for coding SNVs/indels | Very high for targeted regions (VAF detection down to 2.9%) [38] | High for expressed variants |
| Turnaround Time | Weeks | 1-2 weeks | 4 days (in-house panels) [38] to 1 week | 1-2 weeks |
| Cost per Sample | Highest | Moderate | Lower (focused resources) | Moderate to high |
| Data Storage Requirements | Very high (hundreds of GB/sample) | High (tens of GB/sample) | Low (focused data output) | Moderate to high |
| Bioinformatics Complexity | Very high | High | Moderate | High (specialized tools needed) |
Experimental Workflows and Methodologies
Sample Preparation and Quality Control
Robust sample preparation represents the foundational step in any NGS workflow for immuno-oncology research. The selection of appropriate sample types is guided by research objectives, with tissue biopsies providing comprehensive tumor genomic information, while liquid biopsies containing circulating tumor DNA (ctDNA) enable non-invasive monitoring of tumor dynamics and treatment response [37]. For DNA-based approaches (WGS, WES, targeted panels), high-quality genomic DNA extraction is essential, with recommended inputs of ≥50 ng for optimal library preparation and target capture [38]. For RNA-Seq applications, special attention must be paid to RNA integrity, as transcript degradation can significantly impact data quality and interpretation. In liquid biopsy applications, specialized collection tubes are employed to stabilize ctDNA during transport and processing, overcoming the challenge of low nucleic acid yield in plasma samples [37].
Quality control steps implemented throughout the workflow include spectrophotometric and fluorometric quantification to ensure adequate DNA/RNA concentration and purity, followed by fragment analysis to assess nucleic acid integrity. For formalin-fixed paraffin-embedded (FFPE) samples—common in clinical oncology research—additional quality metrics are necessary to account for potential DNA cross-linking and fragmentation. Recent advances in automated liquid handling systems, such as Hamilton's Microlab STAR and NIMBUS platforms, have improved the reproducibility and throughput of these initial sample processing steps, reducing human error and contamination risk while increasing processing consistency [41].
Library Preparation and Target Enrichment
Library preparation converts isolated nucleic acids into sequencing-compatible formats while incorporating sample-specific barcodes to enable multiplexing. For WGS, library preparation involves DNA fragmentation, end-repair, adapter ligation, and PCR amplification without target enrichment, preserving representation across the entire genome [40]. For WES and targeted panels, target enrichment follows initial library preparation using either hybrid capture or amplicon-based approaches. Hybrid capture methodologies employ biotinylated probes complementary to target regions (exonic regions for WES, specific gene panels for targeted sequencing) to "pull down" sequences of interest [36] [37]. This approach offers superior coverage uniformity and flexibility in panel design. Amplicon-based enrichment utilizes target-specific primers to amplify regions of interest through PCR, providing a more streamlined workflow suitable for analyzing limited sample material [38].
The selection between enrichment strategies involves important trade-offs: hybrid capture provides more uniform coverage and better performance in GC-rich regions, while amplicon approaches typically require less input DNA and involve simpler workflows. Recent innovations in automated library preparation systems, such as the MGI SP-100RS platform, have significantly improved reproducibility while reducing hands-on time and potential contamination [38]. For RNA-Seq applications, library preparation typically includes mRNA enrichment using poly-A selection or ribosomal RNA depletion, followed by cDNA synthesis, fragmentation, and adapter ligation. Specialized RNA-Seq protocols enable specific applications in immuno-oncology, such as immune repertoire sequencing and single-cell transcriptome analysis.
Sequencing Platforms and Data Generation
Multiple sequencing platforms are available for generating NGS data, each with distinct technical characteristics that influence their application in immuno-oncology research. Illumina platforms dominate the sequencing landscape, employing sequencing-by-synthesis chemistry with reversible terminators to achieve high accuracy (error rates typically 0.1-0.6%) and massive parallel sequencing capabilities [42]. The MGI DNBSEQ-G50RS platform utilizes combinatorial Probe-Anchor Synthesis (cPAS) technology and DNA nanoball (DNB) generation to deliver high-quality data with reduced sequencing artifacts [38]. Ion Torrent systems (Thermo Fisher Scientific) employ semiconductor-based detection of hydrogen ions released during DNA polymerization, offering rapid turnaround times ideal for targeted applications [37]. Emerging third-generation platforms such as Pacific Biosciences (PacBio) and Oxford Nanopore Technologies enable long-read sequencing, facilitating the resolution of complex genomic regions and structural variants that are particularly relevant in cancer genomics.
Platform selection involves careful consideration of multiple factors, including read length, error profiles, throughput requirements, and cost constraints. For biomarker discovery applications in immuno-oncology, different platforms may be optimally deployed at various stages of research: benchtop systems like Illumina's MiSeq or Thermo Fisher's Ion GeneStudio S5 for targeted validation studies, and high-throughput systems like Illumina's NovaSeq 6000 or MGI's DNBSEQ-G400 for large-scale discovery projects. Performance benchmarking studies have demonstrated that platforms such as the GeneMind GenoLab M can achieve accuracy comparable to established Illumina systems at reduced sequencing depth (22x versus standard 30x for WGS), offering potential cost savings for large-scale studies [40].
NGS Platforms for Immuno-Oncology Biomarker Discovery
Biomarker Classes and Their Clinical Applications
NGS technologies have enabled the discovery and validation of diverse biomarker classes with significant implications for immuno-oncology. Tumor mutational burden (TMB), quantified through WES or comprehensive targeted panels, measures the total number of mutations per megabase of DNA and has been validated as a predictive biomarker for immune checkpoint inhibitor response across multiple cancer types [5]. Microsatellite instability (MSI), detected through specialized NGS panels or WES, results from defective DNA mismatch repair and predicts response to PD-1/PD-L1 inhibitors [39]. Neoantigens, arising from somatic tumor mutations, can be identified through integrated WES and RNA-Seq analysis, with neoantigen burden correlating with improved immunotherapy outcomes.
Gene expression signatures quantified through RNA-Seq provide insights into the tumor immune microenvironment, with specific profiles such as interferon-gamma signaling, T-cell inflammation, and immune cell infiltration patterns predicting response to immunotherapies [5]. Immune repertoire sequencing through specialized RNA-Seq approaches characterizes the diversity and clonality of T-cell and B-cell receptors, serving as biomarkers for antitumor immune responses and monitoring treatment efficacy. Each biomarker class requires specific NGS approaches for optimal detection and quantification, with multi-omics integration providing the most comprehensive immunogenomic profiling for predictive biomarker development.
Table 3: Key Biomarkers in Immuno-Oncology and Their NGS Detection Platforms
| Biomarker Category | Specific Biomarkers | Primary NGS Detection Method | Clinical/Research Utility |
|---|---|---|---|
| Mutational Burden | Tumor mutational burden (TMB) [5] | WES, Large targeted panels | Predicts response to immune checkpoint inhibitors |
| Genomic Instability | Microsatellite instability (MSI) [39] | WES, Targeted panels (including NTRK, HRD) | Biomarker for PD-1 blockade sensitivity |
| Viral Sequences | Oncogenic viruses | RNA-Seq, Targeted panels | Indicates viral-induced cancers amenable to immunotherapy |
| Immune Microenvironment | PD-L1 expression, T-cell infiltration signatures [5] | RNA-Seq, Digital spatial profiling | Quantifies immune contexture and inhibitory pathways |
| Oncometabolites | IDH1/2 mutations (2-HG production) [5] | WES, Targeted panels | Diagnostic and mechanistic biomarkers |
| Epigenetic Alterations | MGMT promoter methylation [5] | Targeted bisulfite sequencing | Predicts temozolomide response in glioblastoma |
Multi-Omics Integration for Comprehensive Biomarker Discovery
The integration of multiple NGS data types through multi-omics strategies has revolutionized biomarker discovery in immuno-oncology by providing a systems-level view of tumor biology and immune interactions. Horizontal integration combines data from the same omics type across different samples or timepoints, enabling the identification of conserved immuno-oncology signatures across patient populations. Vertical integration simultaneously analyzes different molecular layers (genome, transcriptome, epigenome, proteome) from the same sample, revealing the functional consequences of genomic alterations and their impact on antitumor immunity [5]. Multi-omics integration has proven particularly powerful for identifying composite biomarkers that combine genomic, transcriptomic, and immunologic features to improve prediction accuracy for immunotherapy response.
Computational approaches for multi-omics integration include matrix factorization methods that identify shared patterns across data types, network-based approaches that model molecular interactions within the tumor microenvironment, and machine learning algorithms that leverage diverse molecular features to predict treatment response. These integrated analyses have revealed that response to immunotherapies is influenced by complex interactions between tumor-intrinsic factors (mutational burden, neoantigen quality, oncogenic signaling pathways) and tumor-extrinsic factors (immune cell composition, cytokine expression, immunosuppressive mechanisms). The continued refinement of multi-omics integration frameworks will be essential for developing next-generation biomarkers that capture this complexity and improve patient stratification for immuno-oncology therapies.
The Scientist's Toolkit: Essential Reagents and Technologies
Table 4: Essential Research Reagent Solutions for NGS in Immuno-Oncology
| Reagent/Technology | Function | Example Products/Platforms | Application Notes |
|---|---|---|---|
| Hybridization Capture Probes | Enrich target genomic regions for WES and targeted sequencing | xGen (IDT), SureSelect (Agilent) | Biotinylated oligonucleotides complementary to regions of interest; critical for panel sensitivity and uniformity [41] |
| Library Preparation Kits | Convert nucleic acids to sequencing-ready libraries | KAPA HyperPrep (Roche), TruSeq Nano (Illumina) | Include enzymes for fragmentation, end-repair, A-tailing, and adapter ligation; optimized for input type (FFPE, ctDNA) |
| Automated Liquid Handling | Standardize and scale library preparation processes | Hamilton Microlab STAR, Hamilton NIMBUS | Improve reproducibility, reduce contamination risk, increase throughput [41] |
| Targeted Gene Panels | Simultaneously interrogate multiple cancer-associated genes | TSO500 (Illumina), TST170 (Illumina), Oncopanels | Can be pre-designed or customized; focus on clinically actionable targets (e.g., KRAS, EGFR, PIK3CA) [38] |
| Sequence Analysis Software | Variant calling, annotation, and interpretation | Sophia DDM, Sentieon, GATK | Incorporate machine learning for variant filtration; link molecular profiles to clinical insights [38] |
| ctDNA Stabilization Tubes | Preserve circulating tumor DNA in blood samples | Cell-free DNA BCT tubes (Streck) | Prevent white blood cell lysis and genomic DNA contamination; essential for liquid biopsy applications |
Implementation Considerations for Immuno-Oncology Research
Platform Selection Guidelines
Strategic selection of NGS platforms for immuno-oncology research depends on multiple factors, including research objectives, sample characteristics, and resource constraints. Targeted panels offer the most practical solution for clinical trial screening and therapeutic decision-making, providing rapid turnaround times (as short as 4 days for in-house panels) [38] and high sensitivity for detecting actionable mutations in limited sample material. The TruSight Oncology 500 and similar comprehensive panels simultaneously assess multiple biomarker classes—including TMB, MSI, and specific mutations—from minimal DNA input, facilitating streamlined patient stratification for immunotherapy trials [39].
WES provides an optimal balance between comprehensiveness and cost for discovery-phase research, enabling the identification of novel neoantigens and mutation signatures while maintaining focus on protein-coding regions most likely to generate immunogenic peptides. WGS remains the gold standard for comprehensive genomic characterization, detecting variants in noncoding regulatory elements, complex structural rearrangements, and viral integration events that may influence cancer immunogenicity [39]. RNA-Seq is indispensable for characterizing the immune microenvironment, quantifying immune cell populations, identifying expressed neoantigens, and detecting fusion transcripts with immunotherapeutic implications. For multi-institutional collaborative studies, standardized processing protocols and automated workflows—such as the integrated solutions from IDT and Hamilton—enhance reproducibility and facilitate data integration across sites [41].
Analytical Validation and Quality Assurance
Robust analytical validation is essential for generating reliable NGS data for immuno-oncology biomarker discovery. Key performance parameters include sensitivity (ability to detect true variants), specificity (ability to exclude false positives), precision (reproducibility across replicates), and accuracy (concordance with orthogonal methods). For targeted panels, validation studies should establish minimum DNA input requirements (typically ≥50 ng), limit of detection for variant allele frequency (as low as 2.9% for established panels) [38], and performance with challenging sample types such as FFPE tissue and liquid biopsies.
Quality control metrics must be monitored throughout the NGS workflow, including pre-sequencing metrics (DNA/RNA quantity and quality), sequencing performance indicators (cluster density, Q-scores, duplication rates), and post-sequencing parameters (on-target rates, coverage uniformity, molecular duplication). For immuno-oncology applications, special attention should be paid to metrics that influence biomarker quantification, such as uniformity of coverage for TMB calculation and minimal sequencing depth for confident variant detection. Computational pipelines should incorporate best practices for alignment, variant calling, and artifact filtering, with regular updates to maintain compatibility with evolving reference databases and analysis methods.
NGS technologies have become indispensable tools for biomarker discovery in immuno-oncology, with each platform—WGS, WES, RNA-Seq, and targeted panels—offering complementary strengths for elucidating the complex interactions between tumors and the immune system. The strategic integration of these approaches through multi-omics frameworks provides the most comprehensive understanding of determinants of immunotherapy response and resistance. As the field advances, developments in single-cell sequencing, spatial transcriptomics, artificial intelligence, and automated workflows will further enhance our ability to discover, validate, and implement novel biomarkers for immuno-oncology. By strategically leveraging the appropriate NGS platforms for specific research questions, scientists can accelerate the development of more effective immunotherapies and biomarkers to guide their application, ultimately improving outcomes for cancer patients.
Immunopeptidomics, the large-scale study of peptides presented by Major Histocompatibility Complex (MHC) molecules, has emerged as a critical bridge between genomic discoveries and clinically actionable immunotherapies. Within the context of next-generation sequencing (NGS) for biomarker discovery in immuno-oncology, immunopeptidomics provides the essential functional validation that predicted neoantigens are actually presented on the cell surface [43]. While NGS approaches can identify thousands of potential tumor-specific mutations through whole-exome and whole-genome sequencing, mass spectrometry (MS) remains the only method that provides direct proof of actual peptide presentation on living cells [44] [43]. This direct validation is crucial for developing epitope-specific cancer immunotherapies, including therapeutic vaccines and T-cell receptor-transgenic T cells, where confirmation of surface presentation strongly correlates with therapeutic success [43].
The integration of NGS and immunopeptidomics creates a powerful pipeline for translational research. NGS technologies define the initial "search space" of potential antigens by identifying somatic mutations, alternative splicing events, RNA editing, and other genomic alterations [43] [45]. However, genomic data alone cannot predict which peptides will successfully navigate the complex antigen processing and presentation pathway, including proteasomal cleavage, TAP transport, and HLA binding [43]. Immunopeptidomics closes this critical validation gap by experimentally confirming which predicted neoantigens are genuinely presented on tumor cells, thereby prioritizing the most promising candidates for further therapeutic development [44] [43].
Core Immunopeptidomics Workflow: From Cells to Peptide Identification
The standard immunopeptidomics workflow involves multiple precisely executed stages to isolate, identify, and validate MHC-presented peptides. The process begins with cell line or tissue samples, including cancerous and infected cells, and typically requires 2-3 days to complete [46] [47].
MHC-Peptide Complex Isolation and Peptide Extraction
Two primary methods exist for isolating MHC-peptide complexes: immunoprecipitation (IP) and mild acid elution (MAE). Immunoprecipitation has become the preferred method due to its higher specificity and yield, despite being more technically complex [43] [48]. The IP approach uses antibodies (typically pan-specific anti-HLA antibodies like clone W6/32) crosslinked to protein A or G beads to specifically capture HLA-peptide complexes from cell lysates [44]. Following capture, peptides are dissociated from HLA molecules through acid denaturation using conditions such as citric acid buffer at pH 3-3.3 [46] [48]. In contrast, mild acid elution uses brief acidic treatment of viable cells to release MHC class I-bound peptides while maintaining cell viability, but this method may co-purify non-HLA associated peptides and is ineffective for MHC class II peptides due to their greater stability under acidic conditions [48].
Peptide Separation and Mass Spectrometry Analysis
Following extraction, the peptide cargo undergoes fractionation by high-performance liquid chromatography (HPLC) to reduce sample complexity [46]. The fractions are then analyzed using nano-ultra-performance liquid chromatography coupled to high-resolution tandem mass spectrometry (nUPLC-MS/MS) [46] [47]. For MS analysis, two primary acquisition methods are employed:
- Data-Dependent Acquisition (DDA): Unbiased discovery approach that selects the most abundant ions for fragmentation [44]
- Data-Independent Acquisition (DIA): Fragments all ions within predefined mass windows, providing more comprehensive coverage but with greater computational complexity [44]
Advanced MS instrumentation, particularly Orbitrap-based mass spectrometers, provide the exceptional sensitivity and dynamic range needed to detect low-abundance neoantigens amid highly abundant self-peptides [49]. The resulting MS/MS spectra are then computationally matched to peptide sequences using database search engines, with the "search space" typically informed by NGS data from the same sample [43] [45].
Table 1: Key Mass Spectrometry Instrumentation for Immunopeptidomics
| Platform | Technology | Key Applications | Strengths |
|---|---|---|---|
| Orbitrap Astral MS [49] | High-resolution accurate mass | Comprehensive immunopeptide discovery | Exceptional sensitivity and dynamic range for low-abundance antigens |
| Orbitrap Ascend Tribrid [49] | High-resolution Orbitrap + sensitive linear ion trap | Simultaneous Quantitation and Discovery (SQUAD) | Combines untargeted discovery with targeted PRM quantification |
| Orbitrap Exploris 480 [49] | High-resolution accurate mass | Targeted quantitation (SureQuant) | Dynamic control of targeted acquisition using internal standards |
| Stellar Mass Spectrometer [49] | PRM with MS3 capabilities | High-throughput targeted screening | Absolute quantitation with reduced noise; sensitivity down to 1 amol |
The following diagram illustrates the core immunopeptidomics workflow from sample preparation through peptide identification:
Advanced Methodologies for Enhanced Neoantigen Detection
Targeted Mass Spectrometry Approaches
While untargeted DDA and DIA methods provide comprehensive immunopeptidome profiling, their sensitivity limitations often miss clinically relevant low-abundance neoantigens. To address this challenge, targeted MS approaches have been developed that focus specifically on predefined peptide sets, offering significantly enhanced sensitivity [44]. These include:
- Parallel Reaction Monitoring (PRM): Targeted detection of specific peptides with high sensitivity and selectivity, enabling quantification of known neoantigens [49] [44]
- optiPRM: An advanced targeted workflow that employs per-peptide collision energy optimization to maximize detection sensitivity, enabling identification of neoepitopes from as little as 2.5 × 10^6 cells [44]
- SureQuant: A targeted workflow that uses internal standards to trigger acquisition specifically when target peptides are eluting, maximizing sensitivity for precious clinical samples [49]
The optiPRM methodology is particularly noteworthy for clinical applications where sample material is limited. By systematically optimizing MS parameters for each individual target peptide through direct infusion experiments, this approach achieves ultra-high sensitivity that enables detection of mutation-derived neoepitopes from small patient tumor samples that would be undetectable with standard parameters [44].
Functional Genetic Screening Platforms
Complementing MS-based approaches, functional genetics platforms like EpiScan provide high-throughput screening for MHC class I ligands [50]. EpiScan uses surface MHC class I levels as a readout for whether a genetically encoded peptide is an MHC class I ligand. In TAP-deficient cells, MHC class I surface expression is dramatically reduced unless a high-affinity peptide ligand is introduced into the endoplasmic reticulum [50]. This system allows screening of predetermined pools composed of >100,000 peptides designed using oligonucleotide synthesis, permitting large-scale MHC class I ligand discovery without the limitations of synthetic peptide production [50].
Addressing Search Space Challenges with Proteogenomics
A significant challenge in immunopeptidomics is the exponentially large search space of potential peptides, particularly when considering non-canonical reading frames, proteasomal splicing, and other unconventional peptide sources. Automated workflows like Sequoia and SPIsnake have been developed to address this complexity [45]. Sequoia builds RNA-seq-informed and exhaustive sequence search spaces for various non-canonical peptide origins, while SPIsnake uses MS data to pre-filter these search spaces before database searching, thereby improving sensitivity in peptide identification [45].
Integration with NGS-Based Biomarker Discovery
The integration of immunopeptidomics with NGS-based biomarker discovery creates a powerful iterative feedback loop for neoantigen validation. NGS technologies, including whole-genome sequencing, whole-exome sequencing, and RNA sequencing, define the initial "search space" of potential tumor antigens by identifying somatic mutations, gene fusions, indels, and non-canonical alterations [43] [16]. However, as studies have consistently demonstrated, there is poor correlation between source protein abundance and epitope presentation, meaning that highly expressed proteins may yield few presented peptides while low-abundance proteins can be rich sources of epitopes [43].
This disconnect necessitates direct experimental validation through immunopeptidomics. The following diagram illustrates how NGS and immunopeptidomics integrate in the biomarker discovery pipeline:
This integrative approach is particularly valuable for identifying non-canonical tumor antigens that arise from sources not predictable by standard genomic analysis alone, including:
- Alternative mRNA splicing and intron retention [43]
- RNA editing events [43]
- Usage of alternative transcription start sites or reading frames [43]
- Proteasome-catalyzed peptide splicing (PCPS) creating spliced peptides [45]
- Peptides with post-translational modifications [43]
Advanced proteogenomic approaches that leverage ribosome profiling (Ribo-seq) data can further refine the search space by identifying transcripts undergoing active translation, enabling generation of sample-specific de novo reference proteomes that include previously unannotated open reading frames [43].
The Scientist's Toolkit: Essential Research Reagents and Materials
Successful immunopeptidomics studies require specialized reagents and materials optimized for working with low-abundance peptides from often limited clinical samples. The following table details key components of the immunopeptidomics toolkit:
Table 2: Essential Research Reagents for Immunopeptidomics Studies
| Reagent/Material | Function | Examples/Specifications |
|---|---|---|
| HLA Antibodies [44] | Immunoaffinity capture of HLA-peptide complexes | Clone W6/32 for pan-HLA class I capture; allele-specific antibodies for restricted studies |
| Protein A/G Beads [44] | Solid support for antibody immobilization | Protein A Sepharose 4B; GammaBind Plus Sepharose beads |
| Lysis Buffer [44] | Solubilization of membrane-bound HLA complexes | 1% NOG, 0.25% SDC, protease inhibitors in PBS |
| Solid Phase Extraction [44] | Peptide cleanup and concentration | C18 cartridges or plates for desalting and concentration |
| HPLC Columns [49] | Peptide separation prior to MS | Nanoflow to high microflow UHPLC columns; Vanquish Neo UHPLC systems |
| Synthetic Peptide Standards [49] | Targeted assay development and quantification | Heavy isotope-labeled AQUA peptides for absolute quantitation |
| Cell Culture Materials [44] | Expansion of cell lines for immunopeptidomics | Appropriate media and supplements for target cells; IFNγ for immunoproteasome induction |
Experimental Protocols: Key Methodologies for Immunopeptidomics
Standard Immunoprecipitation Protocol for HLA-Peptide Complexes
Based on established protocols with recent optimizations [44], the standard IP method includes these critical steps:
Cell Lysis: Use 1 ml lysis buffer (1% N-octyl-β-D glucopyranoside, 0.25% sodium deoxycholate, protease inhibitors in PBS) per 1 × 10^8 cells. For tissue samples, homogenize 100 mg tissue in 1 ml lysis buffer using an Ultra Turrax homogenizer on ice with 3-5 short intervals of 5 seconds at maximum speed [44].
Clarification: Centrifuge lysates at 40,000g at 4°C for 30 minutes to remove insoluble material [44].
Immunoprecipitation: Incubate clarified lysate with W6/32 antibody crosslinked to protein A or G beads (125 μg antibody/50 μl beads; 170 μl 50:50 beads suspension per 1 × 10^8 cells) for 4 hours at 4°C with constant mixing [44].
Washing: Pellet beads (3200g, 3 minutes, room temperature) and wash 3 times with ice-cold 20 mM Tris-HCl (pH 8) containing 150 mM NaCl, followed by 3 washes with ice-cold 20 mM Tris-HCl (pH 8) alone [44].
Peptide Elution: Elute peptides from HLA molecules using 1% trifluoroacetic acid or 0.2% formic acid [44].
Peptide Cleanup: Desalt using C18 solid-phase extraction cartridges or StageTips [44].
optiPRM Workflow for Sensitive Neoantigen Detection
For targeted validation of specific neoantigens, the optiPRM workflow provides optimized sensitivity [44]:
Peptide Selection: Define target peptides based on NGS data and in silico predictions.
Synthetic Standards: Obtain heavy isotope-labeled versions of target peptides for retention time alignment and quantification.
Parameter Optimization: For each target peptide, systematically optimize collision energy (CE) using direct infusion experiments to determine the CE that maximizes fragmentation and detection sensitivity.
LC-MS Method Development: Create a targeted MS method incorporating peptide-specific optimized CE values and scheduled retention time windows.
Sample Analysis: Run samples using the optimized PRM method, with heavy isotope-labeled peptides spiked in as internal standards for retention time alignment and quantification.
Data Analysis: Process data using Skyline or similar software, confirming peptide identity based on co-elution with standards, matching MS/MS spectra, and accurate mass measurement.
Immunopeptidomics has evolved from a specialized technique to an essential component of the immuno-oncology toolkit, providing the critical link between genomic discoveries and clinically actionable immunotherapies. As precision medicine advances toward increasingly personalized cancer treatments, the integration of NGS-based biomarker discovery with mass spectrometric validation of MHC-presented peptides will continue to grow in importance. The ongoing development of more sensitive instrumentation, advanced targeted workflows like optiPRM, and integrated computational pipelines promises to further enhance our ability to identify therapeutically relevant neoantigens from ever-smaller clinical samples. This progress reinforces the essential role of immunopeptidomics in translating NGS-derived biomarkers into effective cancer immunotherapies, ultimately enabling the development of truly personalized cancer treatments targeting each patient's unique immunopeptidome.
Single-Cell and Spatial Transcriptomics for Tumor Heterogeneity
In the field of immuno-oncology research, next-generation sequencing (NGS) has revolutionized our capacity to discover and validate novel biomarkers. Single-cell RNA sequencing (scRNA-seq) and spatial transcriptomics (ST) represent two of the most transformative advancements in this domain, enabling researchers to dissect tumor heterogeneity with unprecedented resolution. While conventional bulk sequencing approaches average signals across heterogeneous cell populations, obscuring clinically relevant rare cellular subsets [51], single-cell technologies resolve the cellular composition of complex tissues and characterize previously inaccessible cell subsets. Spatial transcriptomics further enhances this capability by preserving the geographical context of gene expression, revealing how cellular positioning within the tumor microenvironment (TME) influences immune responses and therapeutic outcomes [52]. The integration of these approaches within NGS biomarker discovery pipelines is providing critical insights into tumor evolution, immune escape mechanisms, and treatment resistance, thereby advancing the development of personalized cancer immunotherapies [51].
Core Technologies and Methodological Frameworks
Single-Cell RNA Sequencing: Technical Foundations
Single-cell RNA sequencing enables the unbiased characterization of gene expression programs at the single-cell level. The fundamental workflow begins with the efficient and accurate isolation of individual cells from tumor tissues, which can be achieved through several advanced strategies including fluorescence-activated cell sorting (FACS), magnetic-activated cell sorting (MACS), microfluidic technologies, and laser capture microdissection (LCM) [51]. Following cell isolation, a critical step involves the reverse transcription of mRNA from individual cells into cDNA, with subsequent amplification to generate sufficient material for sequencing. Modern scRNA-seq protocols incorporate unique molecular identifiers (UMIs) and cell-specific barcodes to minimize technical noise and enable high-throughput analysis [51]. Platforms such as 10x Genomics Chromium and BD Rhapsody have dramatically expanded the scalability and precision of scRNA-seq, allowing researchers to profile hundreds to thousands of cells simultaneously and detect rare cell populations that drive tumor progression and therapy resistance [51].
The analytical outputs of scRNA-seq provide multidimensional insights into tumor biology. Beyond simply quantifying gene expression, scRNA-seq data enable the identification of distinct cell subpopulations, characterization of intermediate cell states, and reconstruction of developmental trajectories across diverse biological contexts [51]. Sophisticated computational methods have been developed for lineage tracing, RNA velocity analysis, and cell-cell communication inference, further enhancing the utility of scRNA-seq data in mapping the cellular ecosystem of tumors [51].
Figure 1: scRNA-seq Workflow from Sample to Analysis
Spatial Transcriptomics: Preserving Geographical Context
Spatial transcriptomics complements scRNA-seq by mapping gene expression patterns within the architectural context of intact tumor tissues. This approach maintains the original spatial coordinates of cells, enabling researchers to determine how cellular interactions and local environmental niches influence tumor behavior and immune evasion [52]. Technologies such as Visium spatial gene expression platforms from 10x Genomics allow comprehensive transcriptome-wide mapping while preserving tissue morphology through histological staining compatibility [53]. The integration of ST with multiplexed imaging techniques, such as co-detection by indexing (CODEX), further enhances spatial profiling by simultaneously localizing numerous proteins within the tissue architecture, providing a multidimensional view of the tumor ecosystem [53].
The analytical framework for spatial transcriptomics involves several key steps. First, histological hematoxylin and eosin (H&E) staining and transcriptional profiles are used to identify spatially distinct cancer cell clusters separated by stromal areas, which researchers have termed "tumor microregions" [53]. Computational toolsets such as Morph are then employed to refine tumor boundaries, determine distances of spots from these boundaries, and construct layers of spots that index their depths relative to tumor margins [53]. This spatial mapping enables the characterization of variable T cell infiltrations within microregions and the identification of macrophage populations predominantly residing at tumor boundaries - patterns that would be obscured in dissociated single-cell analyses [53].
Integrated Multi-Omic Approaches
The convergence of scRNA-seq, spatial transcriptomics, and other molecular profiling technologies creates a powerful multi-omic framework for comprehensive tumor characterization. Single-cell multi-omics technologies encompass genomics, transcriptomics, epigenomics, proteomics, and spatial omics, significantly enhancing our ability to dissect tumor heterogeneity at single-cell resolution with multilayered depth [51]. For instance, single-cell DNA sequencing (scDNA-seq) provides complementary information by directly profiling the genomic landscape of individual cells, enabling researchers to identify mutations such as copy number variations and single nucleotide variants with cellular precision [51].
Similarly, single-cell epigenomic technologies offer crucial insights into the gene regulatory landscape governing cellular identity and plasticity. Approaches such as single-cell assay for transposase-accessible chromatin sequencing (scATAC-seq) enable high-resolution mapping of chromatin accessibility, while bisulfite sequencing and enzyme-based conversion strategies facilitate single-cell methylome profiling [51]. The integration of these multidimensional datasets reveals how genetic alterations, epigenetic states, and transcriptional programs collectively shape tumor heterogeneity and influence responses to immunotherapy.
Applications in Tumor Heterogeneity and Biomarker Discovery
Dissecting Intra-tumoral Heterogeneity
Single-cell and spatial transcriptomic approaches have revealed remarkable heterogeneity within individual tumors, with significant implications for biomarker discovery and therapeutic targeting. A recent study applying scRNA-seq to seven palbociclib-naïve luminal breast cancer cell lines and their palbociclib-resistant derivatives demonstrated that established biomarkers and pathways related to CDK4/6 inhibitor resistance present marked intra- and inter-cell-line heterogeneity [54]. Transcriptional features of resistance could already be observed in naïve cells, correlating with levels of sensitivity (IC50) to palbociclib, while resistant derivatives showed transcriptional clusters that significantly varied for proliferative, estrogen response signatures, or MYC targets [54].
This heterogeneity extends to the clinical setting, as validated in the FELINE trial where, compared to sensitive ones, ribociclib-resistant tumors developed higher clonal diversity at the genetic level and showed greater transcriptional variability for genes associated with resistance [54]. The study inferred a potential signature of resistance from cell-line models that was positively enriched for MYC targets and negatively enriched for estrogen response markers. When probed on the FELINE trial, this signature separated sensitive from resistant tumors and revealed higher heterogeneity in resistant versus sensitive cells [54]. These findings suggest that heterogeneity for CDK4/6 inhibitor resistant markers might facilitate the development of resistance and challenge the validation of clinical biomarkers.
Table 1: Key Biomarkers of CDK4/6 Inhibitor Resistance Identified via scRNA-seq
| Biomarker | Expression Change in Resistance | Heterogeneity Pattern | Potential Clinical Utility |
|---|---|---|---|
| CCNE1 | Significantly increased | Higher in CCNE1-amplified models (TamR PDR, BT474 PDR) | Predictive marker for resistance |
| RB1 | Significantly decreased | Lower in RB1-deleted models (T47D PDR, MDAMB361 PDR) | Marker of resistance mechanisms |
| CDK6 | Upregulated in MCF7, EDR, ZR751, MDAMB361 | Not consistently altered across all models | Potential therapeutic target |
| FAT1 | Downregulated in MCF7, TamR, ZR751, MDAMB361 | Heterogeneous across cell types | Emerging resistance biomarker |
| FGFR1 | Upregulated in T47D, downregulated in others | Highly context-dependent | Combination therapy target |
| Interferon Signaling | Increased in MCF7, EDR, T47D, MDAMB361 | Decreased in ZR751 | Predictive signature development |
Spatial Architecture of Tumor Microenvironments
Spatial transcriptomics has uncovered fundamental principles of tumor organization that directly impact immune responses and therapy efficacy. A comprehensive analysis of 131 tumor sections across six cancer types (breast cancer, colorectal carcinoma, pancreatic ductal adenocarcinoma, renal cell carcinoma, uterine corpus endometrial carcinoma, and cholangiocarcinoma) revealed that tumors are organized into discrete "tumor microregions" - spatially distinct cancer cell clusters separated by stromal components [53]. These microregions varied considerably in size and density among cancer types, with the largest microregions observed in metastatic samples [53]. Researchers further grouped microregions with shared genetic alterations into "spatial subclones," with 35 tumor sections exhibiting such subclonal structures [53].
The spatial organization of these microregions has profound functional implications. Analysis revealed increased metabolic activity at the center and enhanced antigen presentation along the leading edges of microregions [53]. Additionally, variable T cell infiltrations were observed within microregions, while macrophages predominantly resided at tumor boundaries [53]. Three-dimensional reconstruction of tumor structures from serial spatial transcriptomics sections provided further insights into the spatial organization and heterogeneity of tumors, revealing immune hot and cold neighborhoods and enhanced immune exhaustion markers surrounding 3D subclones [53].
Table 2: Tumor Microregion Characteristics Across Cancer Types
| Cancer Type | Average Microregion Depth (Layers) | Tumor Fraction | Microregion Size Distribution | Notable Spatial Features |
|---|---|---|---|---|
| Colorectal Carcinoma (CRC) | 2.9 | Moderate | Larger microregions | Deeper structures with complex organization |
| Breast Cancer (BRCA) | 2.1 | Variable | More small microregions | Heterogeneous immune infiltration |
| Pancreatic Ductal Adenocarcinoma (PDAC) | 2.37 | Lowest | Smaller microregions | High stromal content, limited immune access |
| Renal Cell Carcinoma (RCC) | Not specified | Highest | Not specified | Dense tumor regions |
| Primary Tumors (Overall) | 1.9 | Variable | 66.3% small | More constrained growth pattern |
| Metastases (Overall) | 3.4 | Variable | 43.2% medium, 16.3% large | Expanded, deeper microregions |
Computational Methods for Heterogeneity Analysis
The complexity of single-cell and spatial transcriptomics data necessitates advanced computational approaches for meaningful biological interpretation. A recently developed statistical method called generalized binary covariance decomposition (GBCD) addresses the challenge of strong intertumor heterogeneity obscuring subtle patterns shared across tumors [55]. This approach can decompose transcriptional heterogeneity into interpretable components—including patient-specific, dataset-specific, and shared components relevant to disease subtypes [55]. When applied to pancreatic ductal adenocarcinoma data, GBCD produced a refined characterization of existing tumor subtypes and identified a gene expression program prognostic of poor survival independent of tumor stage and subtype [55]. This gene expression program was enriched for genes involved in stress responses, suggesting a role for the integrated stress response in pancreatic cancer progression [55].
Other computational frameworks enable the integration of multimodal single-cell data, connecting molecular alterations to their functional consequences in the tumor ecosystem [51]. These approaches help bridge the gap between tumor heterogeneity and personalized immunotherapy by identifying immune cell subsets and states associated with immune evasion and therapy resistance [51]. Integrative analysis of multimodal single-cell data has accelerated the discovery of predictive biomarkers and enhanced our mechanistic understanding of treatment responses, thereby paving the way for personalized immunotherapeutic strategies [53] [56].
Figure 2: Computational Analysis of Transcriptional Heterogeneity
Experimental Protocols and Technical Considerations
Standardized Workflow for Single-Cell RNA Sequencing
A robust scRNA-seq protocol involves multiple critical steps to ensure high-quality data generation:
Sample Collection and Preparation: Obtain fresh tumor tissues through surgical resection or biopsy. Immediately place tissue in appropriate preservation medium (e.g., RNAlater) or process immediately for single-cell isolation. Mechanical dissociation and enzymatic digestion (using collagenase/hyaluronidase cocktails) are employed to create single-cell suspensions while preserving cell viability [51].
Cell Viability and Quality Assessment: Assess cell viability using trypan blue exclusion or fluorescent viability dyes. Only preparations with >80% viability should proceed to sequencing. Cell count and concentration are adjusted according to platform specifications [51].
Single-Cell Partitioning and Barcoding: Load cells into appropriate partitioning systems such as the 10x Genomics Chromium controller, which encapsulates individual cells into droplets with barcoded beads. Each bead contains oligonucleotides with poly(dT) sequences for mRNA capture, unique molecular identifiers (UMIs) to quantify individual transcripts, and cell barcodes to identify each cell [51].
Library Preparation and Sequencing: Reverse transcribe captured mRNA within droplets, followed by cDNA amplification and library construction with platform-specific adapters. Quality control assessments including fragment analysis and quantitative PCR ensure library integrity before sequencing on Illumina platforms with sufficient depth (typically 20,000-50,000 reads per cell) [51] [57].
Spatial Transcriptomics Processing Pipeline
Spatial transcriptomics requires specialized wet-lab and computational procedures:
Tissue Preparation and Sectioning: Flash-freeze fresh tumor tissues in optimal cutting temperature (OCT) compound or preserve through formalin-fixation and paraffin-embedding (FFPE). Section tissues at appropriate thickness (typically 5-10μm) and transfer onto Visium spatial gene expression slides [53].
Histological Staining and Imaging: H&E stain sections to visualize tissue morphology and identify regions of interest. Acquire high-resolution brightfield images for spatial reference and downstream analysis [53].
Permeabilization and cDNA Synthesis: Optimize permeabilization conditions to release RNA from tissue sections while maintaining spatial localization. Allow released RNA to bind to spatially barcoded oligonucleotides on the slide surface. Perform reverse transcription to generate cDNA with spatial barcodes [53].
Library Construction and Sequencing: Harvest cDNA, followed by second strand synthesis, adapter ligation, and PCR amplification to create sequencing libraries. Sequence on Illumina platforms with paired-end reads to capture both transcript sequences and spatial coordinates [53].
Spatial Data Integration: Align sequencing reads to a reference genome, assign them to spatial barcodes, and create expression matrices mapped to tissue positions. Integrate with H&E images using computational alignment tools [53].
Quality Control Metrics and Validation
Rigorous quality control is essential for both single-cell and spatial transcriptomic studies:
Single-Cell QC Parameters: Exclude cells with fewer than 2000 detected genes or excessively high mitochondrial gene percentage (>20%), indicating poor viability or damaged cells [54]. Require minimum sequencing saturation >70% and median genes per cell >3000 for robust detection [54].
Spatial Transcriptomics QC: Assess RNA integrity number (RIN) >7 for fresh-frozen samples. Require minimum spot detection of >1000 genes per spot and >50,000 reads per spot. Verify spatial barcode uniqueness and tissue alignment accuracy [53].
Technical Validation: Employ orthogonal validation methods including fluorescence in situ hybridization (FISH), immunohistochemistry (IHC), or CODEX multiplexed imaging to confirm key findings from transcriptomic analyses [53].
Essential Research Reagents and Computational Tools
Table 3: Research Reagent Solutions for Single-Cell and Spatial Transcriptomics
| Category | Specific Products/Platforms | Key Function | Technical Considerations |
|---|---|---|---|
| Single-Cell Partitioning | 10x Genomics Chromium, BD Rhapsody, Drop-seq | Partitioning cells into nanoliter reactors with barcoded beads | Throughput, cell recovery rate, multiplet rate |
| Spatial Capture | 10x Genomics Visium, Slide-seq, DBiT-seq | Capturing RNA while preserving spatial information | Resolution (55μm vs 10μm spots), RNA capture efficiency |
| Tissue Dissociation | Miltenyi Tumor Dissociation Kits, Worthington Enzymes | Generating single-cell suspensions from tumor tissues | Viability preservation, cell type bias, stress responses |
| Cell Viability Stains | Propidium Iodide, DAPI, Calcein AM, 7-AAD | Distinguishing live vs dead cells | Compatibility with downstream sequencing, cytotoxicity |
| Library Prep Kits | Illumina Nextera, SMART-Seq v4, NEB Next | Preparing sequencing libraries from small RNA inputs | Amplification bias, transcript coverage, UMI incorporation |
| Sequencing Platforms | Illumina NovaSeq, NextSeq, PacBio, Oxford Nanopore | High-throughput DNA sequencing | Read length, error rates, cost per million reads |
| Bioinformatics Tools | Seurat, Scanpy, Cell Ranger, Space Ranger, GBCD | Processing, analyzing, and visualizing single-cell/spatial data | Algorithm sensitivity, computational resources, usability |
| Multiplexed Imaging | CODEX, CosMx, MERFISH | Protein and RNA validation in spatial context | Multiplexing capacity, resolution, tissue compatibility |
Computational Pipelines for Neoantigen Prediction (pVAC-Seq, NetMHC)
The advent of Next-Generation Sequencing (NGS) has fundamentally transformed biomarker discovery in immuno-oncology, enabling the identification of tumor-specific neoantigens—novel peptides arising from somatic mutations that can elicit T-cell-mediated anti-tumor responses. These neoantigens represent ideal biomarkers and therapeutic targets for personalized cancer vaccines and immunotherapies due to their tumor-specific expression and absence in normal tissues. Computational pipelines that integrate genomic, transcriptomic, and immunologic data are critical for systematically prioritizing neoantigen candidates from the thousands of somatic mutations typically detected in tumor samples. Among these, pVAC-Seq and NetMHC have emerged as foundational components in a rapidly evolving ecosystem that bridges bioinformatics analysis with clinical application, framing a new paradigm in precision immuno-oncology.
Core Computational Frameworks and Tools
pVAC-Seq: A Genome-Guided In Silico Approach
pVAC-Seq (Personalized Variant Antigens by Cancer Sequencing) provides an integrated computational workflow that identifies tumor neoantigens through systematic analysis of DNA and RNA sequencing data. The pipeline processes somatic variants, incorporates patient-specific HLA typing information, and implements epitope prediction algorithms to prioritize candidate neoantigens [58]. This open-source tool, available through GitHub, has been successfully applied in both preclinical models and clinical trials to identify neoantigens for dendritic cell-based personalized vaccines [58].
The pVAC-Seq framework has evolved into the comprehensive pVACtools suite, which extends neoantigen prediction capabilities beyond single nucleotide variants to include gene fusions, splice variants, and indels [59] [60]. This expansion addresses the growing recognition that diverse genomic alterations can generate immunogenic neoantigens, thereby broadening the targetable mutational landscape for cancer immunotherapy.
NetMHC and NetMHCpan: Epitope Binding Prediction Algorithms
NetMHC and its pan-specific counterpart NetMHCpan represent core binding prediction engines utilized within neoantigen discovery pipelines. These artificial neural network-based algorithms predict peptide-MHC class I binding affinity by training on extensive datasets of known MHC ligands and eluted peptides [58] [61]. NetMHCpan extends this capability to a wider range of HLA alleles through its pan-specific training approach, making it particularly valuable for diverse patient populations [61].
The pVACtools suite supports an ensemble of eight MHC Class I prediction algorithms, including NetMHCpan, NetMHC, NetMHCcons, PickPocket, SMM, SMMPMBEC, MHCflurry, and MHCnuggets, providing researchers with flexibility in prediction methodologies [59]. This multi-algorithm approach enhances prediction robustness through consensus methods, mitigating limitations inherent to individual prediction tools.
Table 1: Key Computational Pipelines for Neoantigen Discovery
| Pipeline Name | Primary Input | Core Features | Supported Alterations | Clinical Application |
|---|---|---|---|---|
| pVACseq/pVACtools | VCF files | Integrates DNA & RNA sequencing; Multiple prediction algorithms; Vaccine design support | SNVs, indels, gene fusions | Personalized cancer vaccines [58] [59] |
| PGV Pipeline | Tumor/Normal exome + RNA | Modular design; Expression-weighted ranking; RNA-supported coding sequences | SNVs, indels | PGV-001 vaccine trial [61] |
| NeoPredPipe | VCF files | Multi-region sample support; TCR recognition potential; ITH assessment | SNVs, indels | Tumor heterogeneity studies [62] |
Integrated Workflow for Neoantigen Identification
Data Acquisition and Pre-processing
The neoantigen discovery pipeline begins with comprehensive genomic profiling of matched tumor-normal samples. For optimal results, fresh frozen tumor tissue is preferred over FFPE samples due to superior RNA preservation and variant detection accuracy [61]. DNA sequencing should achieve minimum coverage of 150× for normal samples and 300× for tumor samples (assuming 50% tumor purity), while RNA sequencing should utilize sufficient read length (≥125bp) to enable accurate variant phasing across candidate epitopes [61].
Alignment typically employs BWA-MEM for DNA sequencing data and STAR for RNA-Seq data, followed by GATK Best Practices processing [61]. For neoantigen prediction, somatic variant calling combines multiple callers such as MuTect and Strelka to maximize sensitivity, with union approaches increasing candidate neoantigen yield [61].
HLA Typing and Neoantigen Prediction
Patient-specific HLA haplotypes are prerequisite for accurate neoantigen prediction. While clinical genotyping provides the gold standard, in silico methods such as HLAminer (for WGS data) and Athlates (for exome data) demonstrate >85% concordance with experimental methods [58]. Alternatively, tools like seq2HLA can determine HLA types directly from tumor RNA sequencing data [61].
The core prediction phase translates somatic variants into mutant peptide sequences, typically 8-11mers for MHC class I and 13-25mers for MHC class II. pVACtools generates wild-type and mutant peptide sequences, incorporating proximal phased variants when available [59]. These sequences undergo binding affinity prediction against the patient's HLA alleles using the ensemble of algorithms described previously.
Table 2: Essential Research Reagents and Computational Tools
| Resource Category | Specific Tools/Reagents | Function in Pipeline |
|---|---|---|
| Variant Calling | MuTect, Strelka, VarScan2 | Identify somatic mutations from tumor-normal pairs |
| HLA Typing | HLAminer, Athlates, seq2HLA | Determine patient-specific HLA alleles from sequencing data |
| Epitope Prediction | NetMHCpan, NetMHC, MHCflurry | Predict peptide-MHC binding affinity |
| Variant Effect | VEP, Varcode, ANNOVAR | Annotate functional consequence of mutations |
| Expression Support | Isovar, RSEM, Kallisto | Determine mutant allele expression from RNA-Seq |
| Vaccine Design | pVACvector, Vaxrank | Prioritize and format candidates for vaccine formulation |
Candidate Prioritization and Filtering
Following epitope prediction, multi-parameter prioritization filters candidates based on both immunogenic potential and tumor prevalence. The pVACseq ranking system incorporates binding affinity (B), mutant versus wild-type fold change (F), mutant allele expression (M), and DNA variant allele fraction (VAF) into a composite score: B + F + (M*2) + (D/2) [59]. This expression-weighted approach prioritizes highly expressed mutations with strong binding affinity.
Additional filtering incorporates transcript-level evidence, with recent pVACtools versions prioritizing MANE Select and canonical transcripts while filtering out incomplete transcripts [60]. Agretopicity—the differential binding between mutant and wild-type peptides—provides further refinement, though most pipelines avoid strict filtering based solely on this metric since T-cell recognition often depends on TCR contact residues rather than anchor positions [59].
Advanced Applications and Integration with Therapeutic Modalities
Integration with Radiotherapy and Other Combinatorial Approaches
Emerging evidence supports synergistic relationships between neoantigen-directed therapies and conventional cancer treatments. Radiotherapy, in particular, demonstrates capability to enhance neoantigen presentation by upregulating expression of genes containing immunogenic mutations [63]. In murine triple-negative breast cancer models, radiation significantly increased expression of mutated genes including Dhx58, Cand1, and Adgrf5, whose encoded neoantigens elicited both CD8+ and CD4+ T-cell responses that improved therapeutic efficacy when combined with vaccination [63]. This combination approach demonstrates how conventional therapies can modulate the tumor-immune microenvironment to enhance neoantigen-directed treatment efficacy.
Multi-Omics Integration and Emerging Technologies
The integration of multi-omics data represents the next frontier in neoantigen discovery, combining genomic, transcriptomic, proteomic, and epigenomic layers to refine prediction accuracy. Mass spectrometry-based immunopeptidomics directly identifies peptides presented by MHC molecules, providing empirical validation of in silico predictions [5]. Spatial biology technologies, including spatial transcriptomics and multiplex immunohistochemistry, reveal the topographic distribution of neoantigen expression within tumor microenvironments, informing both heterogeneity and immune context [10]. Artificial intelligence and machine learning approaches are increasingly deployed to identify subtle patterns in high-dimensional multi-omics data that escape conventional analytical methods [10].
Experimental Protocols and Validation
In Vitro Binding Validation
Candidate neoantigens prioritized by computational pipelines require experimental validation to confirm immunogenicity. MHC binding assays represent the initial validation step, typically employing T2 cell-based MHC stabilization assays or direct binding measurements [63]. For example, in the 4T1 breast cancer model, candidate peptides including CAND1 and DHX58 demonstrated strong binding to H2-Kd and H2-Ld respectively, with complex half-lives exceeding 6 hours—a key determinant of immunogenicity [63]. These assays provide critical confirmation of computational binding predictions before proceeding to more resource-intensive functional assays.
T-Cell Immunogenicity Assays
Functional immunogenicity represents the ultimate validation metric for predicted neoantigens. Standard approaches include vaccinating naive mice with candidate peptides, followed by ex vivo restimulation of lymph node and splenic T-cells with corresponding neoantigens [63]. Intracellular cytokine staining for IFN-γ and TNF-α identifies antigen-specific T-cell responses, with polyfunctional responses (simultaneous production of multiple cytokines) indicating higher-quality immune responses [63]. In the 4T1 model, this approach confirmed that DHX58 and CAND1 stimulated polyfunctional CD8+ T-cell responses, while an ADGRF5-derived peptide elicited CD4+ T-cell responses [63].
In Vivo Therapeutic Efficacy
Therapeutic validation requires demonstrating that neoantigen-specific responses impart anti-tumor effects. In murine models, this typically involves vaccination followed by tumor challenge, or treatment of established tumors, with tumor growth monitoring over time [63]. For neoantigens identified through pVACseq and similar pipelines, successful therapeutic efficacy often depends on combination approaches—as demonstrated by the requirement for radiotherapy to uncover the full therapeutic potential of DHX58 and CAND1 neoantigens in the 4T1 model [63]. These combinatorial approaches more accurately reflect the clinical reality where neoantigen-directed therapies will be deployed alongside standard cancer treatments.
Computational pipelines for neoantigen prediction represent a transformative advancement in immuno-oncology, bridging NGS-based biomarker discovery with personalized cancer therapy. The integrated workflows of pVAC-Seq, NetMHC, and related tools provide systematic approaches to identify and prioritize tumor-specific antigens from complex genomic datasets. As these pipelines evolve to incorporate multi-omics data, AI-driven analytics, and empirical validation, they continue to enhance the precision and efficacy of cancer immunotherapies. The ongoing refinement of neoantigen prediction methodologies promises to accelerate the development of personalized cancer vaccines and biomarker-driven treatment strategies, ultimately improving outcomes for cancer patients across diverse malignancies.
AI and Machine Learning for Multi-Omics Data Integration and Biomarker Prioritization
The integration of artificial intelligence (AI) and machine learning (ML) with multi-omics data represents a transformative paradigm in immuno-oncology research. This synergy is addressing one of the most significant challenges in modern cancer biology: deciphering the complex molecular interactions within the tumor microenvironment (TME) to identify robust biomarkers that predict response to immunotherapy [20]. Next-generation sequencing (NGS) technologies have enabled the high-throughput generation of genomic, transcriptomic, epigenomic, and proteomic data at unprecedented scales [64]. However, the volume, variability, and high-dimensional nature of these multi-omics datasets have surpassed the capabilities of traditional analytical methods.
AI and ML algorithms are uniquely positioned to parse these complex biological datasets, identify nonlinear patterns, and extract clinically actionable insights [65] [66]. In the context of immuno-oncology, this capability is crucial for understanding cancer-immune cell interactions, mechanisms of therapy resistance, and identifying patient subgroups most likely to benefit from specific immunotherapies [67]. The AI-driven multi-omics approach is moving the field beyond single-biomarker paradigms toward comprehensive molecular signatures that more accurately reflect the biological complexity of cancer-immune system interactions [68].
The Multi-Omics Landscape in Immuno-Oncology
Multi-omics approaches provide complementary layers of biological information that collectively enable a systems-level understanding of the tumor microenvironment and anti-tumor immune responses. In immuno-oncology, several omics layers are particularly informative for biomarker discovery.
- Genomics: Identifies somatic mutations, including tumor mutational burden (TMB), which has emerged as an independent predictor for response to immune checkpoint inhibitors [20]. Specific mutational signatures can also predict response to immunotherapies.
- Transcriptomics: Reveals gene expression patterns of immune cell populations within the TME, enabling immune cell profiling and quantification of immune checkpoint gene expression [69] [20].
- Epigenomics: Characterizes DNA methylation patterns and chromatin accessibility that regulate gene expression in both tumor and immune cells, influencing therapy response [65].
- Proteomics: Identifies and quantifies protein expression and post-translational modifications that directly reflect functional immune processes and signaling pathways [69].
- Metabolomics: Profiles metabolic pathways that shape the immunosuppressive TME and impact immune cell function [69].
The integration of these diverse data layers through AI-powered approaches enables the identification of complex biomarker signatures that more accurately predict therapeutic responses than any single data type alone [65] [66].
Table 1: Key Omics Data Types in Immuno-Oncology Biomarker Discovery
| Omics Layer | Analytical Focus | Relevant Biomarkers in Immuno-Oncology |
|---|---|---|
| Genomics | DNA sequences, mutations, structural variations | Tumor Mutational Burden (TMB), Microsatellite Instability (MSI), Homologous Recombination Deficiency (HRD) |
| Transcriptomics | RNA expression, alternative splicing, gene fusions | Immune cell gene signatures, PD-L1 expression, T-cell inflamed signature |
| Epigenomics | DNA methylation, histone modifications, chromatin accessibility | Promoter methylation of immunomodulatory genes, epigenetic regulators of T-cell exhaustion |
| Proteomics | Protein expression, post-translational modifications, protein-protein interactions | Immune checkpoint protein levels, signaling pathway activity, cytokine profiles |
| Metabolomics | Metabolic pathways, small molecule metabolites | Metabolites associated with T-cell function, nutrient availability in TME |
AI and ML Methodologies for Multi-Omics Integration
Machine Learning Approaches
ML algorithms can be categorized into supervised, unsupervised, and semi-supervised approaches, each with distinct applications in multi-omics data analysis for biomarker discovery.
- Supervised Learning: Trains models on labeled datasets to predict outcomes such as therapy response or patient survival. Random Forest and Support Vector Machines have been successfully applied to classify patients based on their immunotherapy response using integrated genomic and transcriptomic features [66].
- Unsupervised Learning: Discovers inherent patterns or clusters within data without pre-existing labels. Techniques such as clustering and dimensionality reduction can identify novel patient subtypes based on integrated multi-omics profiles that may correlate with distinct clinical outcomes [66].
- Deep Learning: Utilizes multi-layered neural networks to model complex nonlinear relationships in high-dimensional data. Convolutional Neural Networks (CNNs) excel at processing spatial omics data, while Recurrent Neural Networks (RNNs) effectively model sequential data such as DNA or protein sequences [65] [64].
Multi-Omics Data Integration Strategies
The integration of diverse omics datasets presents significant computational challenges. Several AI-driven strategies have been developed to address these challenges:
- Early Integration: Combines raw data from multiple omics layers into a single matrix for analysis. This approach requires extensive normalization to address technical variations between platforms [66].
- Intermediate Integration: Analyzes each omics dataset separately then combines the analyses. This preserves data-specific characteristics while enabling cross-omics validation [65].
- Late Integration: Analyzes each data type independently and integrates the results at the decision level. This approach often employs ensemble methods that combine predictions from multiple models [66].
Experimental Workflows and Protocols
NGS-Based Biomarker Discovery Pipeline
A robust experimental workflow for AI-driven biomarker discovery from multi-omics data involves sample processing, sequencing, and computational analysis.
Step 1: Sample Collection and Preparation
- Collect tumor tissue, blood (for liquid biopsy), or other relevant specimens.
- Process samples for various omics analyses: extract DNA for genomics, RNA for transcriptomics, protein for proteomics [20].
- For single-cell analyses, dissociate tissue into single-cell suspensions while preserving cell viability.
- Quality control assessments: measure DNA/RNA integrity, protein concentration, and cell viability.
Step 2: Library Preparation and Sequencing
- Prepare sequencing libraries using targeted panels (e.g., Oncomine TCR Beta Assay for immune repertoire) or whole-genome/transcriptome approaches [20].
- For multi-omics integration, use platforms that enable coordinated analysis of multiple molecular layers from the same sample.
- Sequence using NGS platforms such as Illumina or Oxford Nanopore, ensuring sufficient depth for variant detection and expression quantification [64].
Step 3: Data Processing and Quality Control
- Process raw sequencing data: demultiplex, trim adapters, and assess quality metrics.
- Align sequences to reference genomes using optimized aligners.
- For AI-ready data preparation, perform normalization, batch effect correction, and feature selection.
Step 4: AI-Driven Multi-Omics Integration and Biomarker Prioritization
- Apply integration algorithms to combine multi-omics datasets.
- Use supervised ML for predictive biomarker identification or unsupervised approaches for novel subtype discovery.
- Prioritize biomarkers based on statistical significance, biological relevance, and clinical applicability.
The Scientist's Toolkit: Essential Research Reagents and Platforms
Table 2: Essential Research Tools for AI-Driven Multi-Omics in Immuno-Oncology
| Tool Category | Specific Examples | Key Applications in Immuno-Oncology |
|---|---|---|
| NGS Assays | Oncomine TCR Beta Assay, Oncomine BCR IgH Assay, Oncomine Immune Response Assay, Oncomine Tumor Mutation Load Assay [20] | Immune repertoire analysis, tumor mutational burden quantification, tumor microenvironment monitoring |
| Single-Cell Technologies | 10x Genomics, Single-cell RNA-seq, ATAC-seq | Immune cell heterogeneity, T-cell clonality, tumor microenvironment characterization [67] |
| Spatial Omics Platforms | Spatial transcriptomics, Digital pathology with AI [67] | Spatial organization of immune cells, tumor-immune interactions within tissue architecture |
| AI/ML Platforms | DeepVariant, CRISPResso2, Ion Reporter Software [64] | Variant calling, genome editing analysis, integrated multi-omics data interpretation |
| Cell Culture Models | Patient-derived organoids, Explant models [67] | Preclinical testing of immunotherapies, hypothesis validation before clinical studies |
Case Studies and Applications in Immuno-Oncology
Predictive Biomarkers for Immunotherapy Response
AI-driven multi-omics approaches have identified several clinically relevant biomarkers for immuno-oncology:
DeepHRD: A deep learning tool that detects homologous recombination deficiency (HRD) characteristics in tumors using standard biopsy slides. This AI approach is reported to be up to three times more accurate in detecting HRD-positive cancers compared to traditional genomic tests and has a negligible failure rate versus the 20-30% failure rates of current tests [70]. HRD status helps identify patients who may benefit from PARP inhibitors and platinum-based chemotherapy.
MSI-SEER: An AI-powered diagnostic tool developed at Vanderbilt University Medical Center that identifies microsatellite instability-high (MSI-H) regions in tumors, which are often missed by traditional testing. This technology enables more gastrointestinal cancer patients to benefit from immunotherapy [70].
TMB Quantification: The Oncomine Tumor Mutation Load Assay uses NGS to assess TMB across 409 cancer-related genes, providing a standardized approach for identifying patients likely to respond to immune checkpoint inhibitors [20].
AI-Enhanced Clinical Trial Optimization
The application of AI extends to optimizing clinical trial design and patient recruitment in immuno-oncology:
- HopeLLM: An AI platform introduced by City of Hope in June 2025 that assists physicians in summarizing patient histories, identifying trial matches, and extracting data for research [70].
- Automated Patient Matching: AI-powered tools streamline the identification of eligible patients for immuno-oncology trials by analyzing electronic health records, molecular profiles, and trial criteria [70].
- Predictive Analytics: ML models forecast patient responses to investigational immunotherapies based on integrated multi-omics profiles, enabling more efficient trial designs [68].
Table 3: Quantitative Impact of AI on Biomarker Discovery and Clinical Applications
| Application Area | Traditional Approach | AI-Enhanced Approach | Performance Improvement |
|---|---|---|---|
| HRD Detection | Genomic tests (20-30% failure rate) | DeepHRD (deep learning) | 3x higher accuracy, negligible failure rate [70] |
| Variant Calling | Heuristic-based methods | DeepVariant (deep neural networks) | Significant accuracy improvement, especially in challenging genomic regions [64] |
| Tumor Microenvironment Analysis | Single-parameter biomarkers (e.g., PD-L1 IHC) | Multi-omics integration with AI | Comprehensive immune profiling, identification of novel resistance mechanisms [67] |
| Clinical Trial Recruitment | Manual patient screening | AI-powered automated matching (e.g., HopeLLM) | Reduced screening time, improved trial accrual rates [70] |
Validation and Clinical Translation
Analytical Validation Frameworks
The translation of AI-discovered biomarkers to clinical applications requires rigorous validation:
- Technical Validation: Assess assay reproducibility, sensitivity, specificity, and robustness across sample types and processing conditions [68].
- Biological Validation: Confirm functional relevance of biomarkers using experimental models such as patient-derived organoids and explant models [67].
- Clinical Validation: Establish association between biomarkers and clinical endpoints (response, survival) in well-characterized patient cohorts [68].
Regulatory Considerations
As AI-derived biomarkers advance toward clinical implementation, several regulatory aspects must be addressed:
- Standardization: Development of standardized protocols for biomarker validation to enhance reproducibility and reliability across studies [68].
- Explainability: Implementation of explainable AI (XAI) approaches to enhance transparency and build clinical trust in model predictions [65].
- Real-World Evidence: Growing regulatory acceptance of real-world evidence for evaluating biomarker performance in diverse patient populations [68].
Future Perspectives and Challenges
The field of AI-driven multi-omics integration for biomarker discovery faces several important challenges and opportunities:
- Data Quality and Heterogeneity: Variations in sample processing, platform technologies, and data analysis pipelines can introduce biases that affect model performance [64].
- Interpretability and Explainability: The "black box" nature of some complex AI models remains a barrier to clinical adoption, driving the need for explainable AI approaches [65].
- Data Privacy and Security: Federated learning approaches that train algorithms across decentralized data sources without exchanging raw data are emerging as promising solutions [64].
- Integration of Novel Data Types: The inclusion of emerging data types such as digital pathology, spatial transcriptomics, and real-world evidence will further enhance multi-omics biomarker discovery [67] [71].
The continued advancement of AI and ML technologies for multi-omics data integration holds tremendous promise for advancing immuno-oncology research. By enabling more comprehensive analysis of the complex interactions between tumors and the immune system, these approaches are accelerating the discovery of robust biomarkers that can guide personalized immunotherapy strategies, ultimately improving outcomes for cancer patients.
Navigating Technical Hurdles: From Tumor Heterogeneity to Clinical Implementation
Addressing Tumor Heterogeneity and Clonal Evolution
Tumor heterogeneity describes the cellular diversity within a single tumor or between a primary tumor and its metastatic lesions, arising from Darwinian and non-Darwinian evolutionary trajectories [72]. This heterogeneity manifests at multiple levels, including copy number variations, epigenetic alterations, and somatic mutations, which collectively drive cancer progression and therapeutic resistance [72]. Clonal evolution refers to the dynamic process through which tumor cells acquire sequential mutations and undergo subclonal selection, resulting in tumors composed of multiple genetically distinct cell populations known as clones [73]. Understanding and reconstructing this clonal architecture is essential for deciphering how tumors respond to treatments, identifying mutations that drive cancer progression or cause therapeutic resistance, and informing the design of more effective therapeutic strategies [73].
In the context of immuno-oncology research, resolving tumor heterogeneity is particularly crucial for biomarker discovery. The complex interaction between evolving tumor clones and the immune microenvironment directly impacts treatment efficacy, especially for immunotherapies [74]. Next-generation sequencing (NGS) technologies provide the high-throughput data necessary to unravel this complexity, enabling researchers to correlate cellular activity, spatial context, and genomic alterations for a more complete picture of the immune response over time [74].
Computational Frameworks for Clonal Reconstruction
Core Principles and Definitions
Clonal reconstruction from bulk sequencing data involves inferring the clonal composition of a tumor, including the number of clones, the set of mutations each clone contains, and the cancer cell fraction (CCF) of each mutation [73]. The cancer cell fraction (CCF) of a mutation represents the proportion of tumor cells carrying that mutation. Mutations with similar CCFs are clustered together, suggesting they belong to the same clone [73]. Sequencing provides variant allele frequencies (VAFs), defined as the ratio of mutant allele reads to total reads at a given locus. Accurate clonal reconstruction requires integrating VAF data with copy number information from the mutation loci [73].
The MyClone Method
MyClone represents a significant advancement in probabilistic methods for clonal reconstruction. This method processes read counts and copy number information of single nucleotide variants from deep sequencing data to determine the mutational composition of clones and their CCFs [73]. The mathematical foundation of MyClone calculates VAF based on the average number of mutant alleles per cell and tumor purity. For a mutation belonging to clone k in sample j, the VAF is calculated as:
VAF = (Average mutant alleles per cell × CCF of clone k) / (Average copy number at locus × Tumor purity)
MyClone utilizes Bayesian inference to deduce clonal architecture, outputting the inferred clones, their CCFs in each sequencing sample, and mutation-cluster assignments [73]. The method's workflow consists of four specialized modules:
- Basic Clustering Module: Performs initial clustering without considering copy number alterations.
- Clonal Segmentation Module: Isolates mutations affected by copy number alterations.
- Tumor Purity Correction Module: Infers or corrects tumor purity estimates.
- Clonal Merging Module: Assigns CNA-affected mutations to correct clusters using their copy number information [73].
MyClone demonstrates superior performance for deeply sequenced data, particularly on targeted sequencing data commonly used in clinical settings due to lower costs and higher sequencing depth [73]. When validated against simulated and real clinical datasets, MyClone outperformed existing methods including PyClone-VI, PhyloWGS, FastClone, Pairtree, CONIPHER, DeCiFer, Sclust, CALDER, and CSR in both clustering accuracy and computational speed [73].
Quantitative Performance Comparison of Clonal Reconstruction Methods
Table 1: Performance comparison of clonal reconstruction methods on simulated targeted sequencing data
| Method | Clustering Accuracy | CCF Prediction Accuracy | Computational Speed | Data Compatibility |
|---|---|---|---|---|
| MyClone | Superior | Superior | Fastest | Targeted sequencing, Bulk tumor |
| PyClone-VI | Moderate | Moderate | Slow | Bulk tumor |
| PhyloWGS | Moderate | Moderate | Slow | Bulk tumor |
| FastClone | Moderate | Moderate | Moderate | Single-sample only |
| cfdna-wgs | Lower | Lower | Moderate | ctDNA sequencing |
Single-Cell Resolution for Unraveling Heterogeneity
Integrated Single-Cell DNA Sequencing Approach
While bulk sequencing provides a broad view of tumoral complexity, single-cell analysis is essential for identifying rare subclones that may drive chemotherapy resistance [75]. A recent study on core-binding factor acute myeloid leukemia (CBF AML) demonstrated an integrated approach combining bulk and single-cell DNA sequencing (scDNA-seq) to resolve intra-tumor heterogeneity with unprecedented resolution [75]. The methodology included:
- Sample Collection: Analysis of diagnosis, complete remission, and relapse samples
- Sequencing Techniques: Whole exome sequencing, targeted sequencing, and nanopore sequencing
- Single-Cell DNA Sequencing: Custom panels covering patient-specific somatic variants, somatic copy-number alterations (SCNAs), and CBF fusions [75]
This approach enabled researchers to sequence a median of 4,103 cells per sample with a mean coverage of 106 reads per amplicon per cell, achieving high concordance between bulk and scDNA-seq variants [75].
Two-Step Approach for SCNA Integration
A key innovation in this study was the development of a 2-step approach for assigning copy-number profiles to inferred tumor phylogenies, allowing identification of subclonal SCNAs that were not supported by single nucleotide variants (SNVs) and missed using existing computational methods [75]. This method integrated subclonal SCNAs into phylogenetic tree analysis and validated results with karyotype data, detecting subclonal SCNAs that conventional bulk sequencing methods had missed [75].
Experimental Protocol for Single-Cell Clonal Evolution Analysis
Sample Preparation and Sequencing:
- Collect matched tumor samples from multiple time points (diagnosis, remission, relapse)
- Perform bulk whole exome sequencing to identify somatic variants and SCNAs
- Design custom single-cell DNA sequencing panels covering patient-specific mutations, SCNAs, and fusion genes
- Process cells through scDNA-seq platform (e.g., Mission Bio Tapestri) with a target of 4,000+ cells per sample
- Achieve mean coverage of >100 reads per amplicon per cell with allele dropout (ADO) rates <25% [75]
Data Analysis and Phylogenetic Reconstruction:
- Generate single-cell variant calling matrices (cells x mutations)
- Infer tumor phylogenies using tools like COMPASS, incorporating reference and alternative counts without genotype or zygosity information
- Apply 2-step approach to integrate SCNAs into phylogenetic trees
- Assign individual cells to clones based on mutation profiles
- Track clonal dynamics across time points to reconstruct evolutionary trajectories [75]
Key Findings from CBF AML Study:
- Identification of 3-11 distinct AML clones per patient at diagnosis
- CBF fusion genes (RUNX1::RUNX1T1 or CBFB::MYH11) were among the earliest events in leukemogenesis
- Detection of residual tumor cells (0.16%-1.54%) in all complete remission samples
- Relapse often involved both loss of diagnosis-specific clones and acquisition of new mutations [75]
Integrated Workflows for Biomarker Discovery
Multi-Technology Integration in Immuno-Oncology
Resolving tumor heterogeneity in immuno-oncology requires integrating multiple analytical techniques to capture the full complexity of the tumor and its evolving immune microenvironment [74]. No single platform can fully capture the complexity of the immune response, which is why leading laboratories combine:
- Flow Cytometry (FCM): Rapidly profiles a patient's immune system by analyzing surface and intracellular markers, enabling functional immune analysis and precise immunophenotyping [74].
- Immunohistochemistry (IHC): Provides spatial context through antibody-mediated screening that profiles tissue samples, enabling biomarker detection, immune cell localization, and structural information about the tumor microenvironment [74].
- Next-Generation Sequencing (NGS): Reveals underlying genetic drivers by simultaneously sequencing millions of DNA fragments, enabling comprehensive profiling of tumor mutational burden, microsatellite instability, and immune repertoire [74].
This integrated approach allows researchers to correlate cellular activity (FCM), spatial distribution (IHC), and genomic alterations (NGS), creating a more complete picture of the immune response over time and enabling more reliable predictions of therapeutic efficacy and safety [74].
Visualizing the Integrated Multi-Technology Workflow
Essential Research Reagent Solutions
Table 2: Key research reagents and materials for clonal evolution studies
| Reagent/Material | Function | Application Example |
|---|---|---|
| Custom scDNA-seq Panels | Target patient-specific mutations, SCNAs, and fusions | CBF AML study: panels covering 232 variants, 7 SCNAs, fusion breakpoints [75] |
| Validated IHC Biomarkers | Spatial profiling of immune cell infiltration | >250 validated IHC biomarkers including multiple PD-L1 clones [74] |
| Flow Cytometry Multiplex Panels | High-dimensional immune phenotyping | Standardized protocols for T-cell exhaustion, macrophage polarization markers [74] |
| NGS Assays for Solid/Hematologic Tumors | Comprehensive genomic profiling | Detection of TMB, MSI, dMMR, TCR/BCR repertoire [74] |
| CRISPR/Cas9 GEMM Systems | In vivo modeling of clonal evolution | Lineage tracing in intestinal adenomas using Lgr5+ stem cell markers [72] |
Visualizing Clonal Reconstruction and Experimental Design
Computational Workflow for Clonal Reconstruction
Experimental Design for Longitudinal Clonal Evolution Studies
Addressing tumor heterogeneity and clonal evolution requires sophisticated integration of computational methods, single-cell technologies, and multi-platform biomarker assessment. Computational frameworks like MyClone enable rapid and precise clonal reconstruction from deep sequencing data, while single-cell DNA sequencing provides unprecedented resolution of intra-tumor heterogeneity and clonal dynamics. The integration of flow cytometry, immunohistochemistry, and next-generation sequencing creates a comprehensive picture of tumor-immune interactions essential for immuno-oncology research. As these technologies continue to evolve, they will increasingly enable researchers to identify therapeutic targets, understand mechanisms of resistance, and develop more effective personalized cancer therapies.
Overcoming Challenges in Low-Abundance Neoantigen Detection
The success of cancer immunotherapy often hinges on the immune system's ability to recognize and eliminate tumor cells, a process primarily mediated by T cells targeting neoantigens—tumor-specific peptides derived from somatic mutations. These neoantigens are ideal targets for personalized cancer vaccines and adoptive T-cell therapies due to their high tumor specificity and minimal risk of off-target toxicity against healthy tissues [6] [76]. However, a significant challenge persists in reliably identifying low-abundance neoantigens, which often exist in scarce quantities within the complex tumor microenvironment but may possess high immunogenic potential [77].
The accurate detection of these rare targets is technically demanding, as they frequently evade conventional discovery methods. Mass spectrometry (MS)-based immunopeptidomics, while capable of directly identifying human leukocyte antigen (HLA)-presented peptides, faces sensitivity limitations in detecting low-abundance neoantigens [6] [76]. Simultaneously, next-generation sequencing (NGS)-based computational predictions, though comprehensive, generate numerous candidates with poor immunogenic predictive value, as only approximately 1% of somatic mutations induce spontaneous T-cell responses [77]. This article examines the technical hurdles in low-abundance neoantigen detection and explores integrated multi-omics solutions that enhance sensitivity and reliability for advancing immuno-oncology research and therapeutic development.
Technical Challenges in Detection
Fundamental Biological and Technical Barriers
The journey from tumor mutation to T-cell-mediated immune response involves multiple sequential steps, each presenting efficiency bottlenecks that limit the final abundance of immunogenic peptides. Neoantigens must first be generated through somatic mutations such as single nucleotide variants (SNVs), insertions/deletions (INDELs), gene fusions, or splice variants [6] [76]. The resulting mutant proteins undergo proteasomal processing into peptides, which are then transported to the endoplasmic reticulum, where they bind to HLA molecules for presentation on the tumor cell surface [6]. Each step in this pathway represents a potential attenuation point where low-abundance neoantigens may be lost before becoming visible to immune surveillance.
Mass spectrometry, the gold standard for direct detection of HLA-presented peptides, encounters specific sensitivity limitations when targeting low-abundance neoantigens. The stochastic nature of data-dependent acquisition (DDA) methods, combined with signal interference from highly abundant housekeeping peptides, often obscures rare neoantigens from detection [77]. Additionally, technical variability in sample processing, limited starting material from clinical biopsies, and the inherent inefficiency of immunoprecipitation protocols further compound these sensitivity challenges [6] [76].
Tumor Heterogeneity and Immune Evasion Mechanisms
Tumor heterogeneity presents another substantial obstacle to consistent neoantigen detection. Spatial and temporal variations in mutation profiles across different tumor regions and metastatic sites lead to inconsistent neoantigen expression [76]. This heterogeneity is further complicated by immune editing pressures, where tumor cells with highly immunogenic neoantigens are eliminated, leaving behind clones that express less immunogenic or lower-abundance targets [78]. Additionally, some tumor cells develop defects in their antigen processing and presentation machinery (APPM), including mutations in HLA genes or components of the interferon signaling pathway, effectively reducing neoantigen presentation regardless of source protein abundance [76].
Table 1: Key Challenges in Low-Abundance Neoantigen Detection
| Challenge Category | Specific Limitations | Impact on Detection |
|---|---|---|
| Technical Sensitivity | Limited MS sensitivity for rare peptides; Signal interference from high-abundance peptides; Stochastic DDA sampling | Failure to detect neoantigens present at low concentrations |
| Sample Constraints | Limited tumor biopsy material; Low neoantigen abundance relative to total immunopeptidome; Sample processing losses | Reduced input for analysis leading to missed identifications |
| Tumor Biology | Spatial and temporal heterogeneity; Immune editing; Antigen presentation machinery defects | Inconsistent neoantigen expression and presentation |
| Computational Prediction | High false-positive rates; Over-reliance on binding affinity predictions; Poor immunogenicity forecasting | Inaccurate prioritization of candidates for validation |
Advanced Wet-Lab Methodologies
Enhanced Mass Spectrometry Acquisition
Innovative mass spectrometry acquisition strategies have emerged to specifically address the sensitivity limitations in low-abundance neoantigen detection. Targeted-DDA hybrid methods, such as NeoDiscMS, leverage next-generation sequencing data to create inclusion lists of candidate neoantigens, which then guide real-time spectral acquisition [77]. This approach uses mutanome-informed filters to trigger high-sensitivity MS2 scans specifically for precursors matching predicted neoantigens, dramatically improving detection capabilities for low-abundance targets while maintaining global immunopeptidome coverage.
The NeoDiscMS workflow implements a priority-based acquisition system with three sequential levels: MS1 scans followed by targeted branch scans, and finally discovery (DDA) branch scans. When a precursor mass matches an entry in the inclusion list, the system first acquires a rapid scouting MS2 (sMS2) scan. Real-time cross-correlation analysis against predicted spectra determines whether to trigger a subsequent time-intensive, high-sensitivity MS2 (hMS2) scan with increased AGC target, extended maximum injection time, and stepped collision energies [77]. This targeted approach, free from dynamic exclusion restrictions, enables multiple MS/MS spectra collection for the same precursor, significantly boosting identification confidence for low-abundance neoantigens.
Immunopeptidome Enrichment and Sample Preparation
Optimized sample preparation protocols are equally critical for enhancing neoantigen detection sensitivity. Efficient immunoprecipitation of HLA complexes with high-purity antibodies maximizes peptide recovery while minimizing co-purification contaminants. The use of HLA-null cell lines (e.g., K562) stably transfected with specific HLA alleles helps validate antibody specificity and presentation patterns [6]. For limited clinical samples, miniaturized processing workflows and capillary-scale chromatography systems reduce sample losses, while chemical labeling techniques can enhance ionization efficiency for specific peptide classes.
Wide isolation windows (3.2 Th) during DDA acquisition, coupled with advanced chimeric spectrum deconvolution algorithms, have demonstrated significant improvements in identification rates. When processed with tools like MSFragger's DDA+ mode, this approach increases the fraction of scans yielding confident peptide-to-spectrum matches by 7-9%, effectively leveraging co-isolated precursors to boost detection depth without compromising specificity [77]. These sample processing and acquisition innovations collectively address the fundamental sensitivity barriers that have traditionally limited low-abundance neoantigen discovery.
Integrated Multi-Omics Computational Strategies
Bioinformatics Pipelines for Neoantigen Prioritization
Sophisticated bioinformatics pipelines form the computational backbone of effective low-abundance neoantigen discovery. These workflows integrate genomic, transcriptomic, and proteomic data to prioritize candidate neoantigens for experimental validation. The standard process begins with quality assessment of raw sequencing data using tools like FastQC and adapter trimming with cutadapt or trimmomatic [79]. Processed reads are then aligned to reference genomes using optimized aligners such as BWA, followed by variant calling with tools like MuTect2 and HaplotypeCaller to identify somatic mutations [80] [79].
Following mutation identification, pipelines such as pVAC-Seq, TSNAD, and CloudNeo predict HLA binding affinities using algorithms including NetMHC and NetMHCpan, while simultaneously incorporating RNA expression data to filter for mutations with sufficient transcript-level support [6] [76]. Advanced pipelines now employ machine learning classifiers that integrate multiple features beyond binding affinity, including peptide processing probabilities, residue exposure patterns, and sequence similarity to known immunogenic epitopes [6]. These computational prioritization steps are essential for enriching candidate lists with higher-probability targets before resource-intensive experimental validation.
Artificial Intelligence and Advanced Modeling
Machine learning and deep learning approaches have substantially improved neoantigen prediction accuracy by capturing complex patterns within multi-omics data that traditional methods frequently miss. Models such as EDGE are trained directly on mass spectrometry-identified peptides rather than traditional binding affinity measurements, better capturing the biological reality of antigen presentation [6] [76]. Similarly, the SHERPA framework systematically combines monoallelic and multiallelic immunopeptidomics samples to emulate native antigen presentation more accurately, enhancing model generalizability across diverse HLA backgrounds.
These AI-driven approaches excel at integrating features from proteogenomic sources, including peptide cleavage signatures, transporter associated with antigen processing (TAP) binding affinity, and HLA-peptide complex stability. Emerging models also incorporate T-cell receptor (TCR) recognition probabilities using tools like TEIM-Res, providing a more comprehensive immunogenicity assessment beyond mere presentation [6] [76]. By leveraging increasingly large and diverse training datasets, these computational models continue to close the sensitivity gap in neoantigen prediction, particularly for low-abundance targets that challenge conventional detection methods.
Table 2: Computational Tools for Enhanced Neoantigen Discovery
| Tool Name | Primary Function | Key Features | Advantages for Low-Abundance Detection |
|---|---|---|---|
| NeoDiscMS | Targeted immunopeptidomics | Real-time spectral matching; Targeted-DDA hybrid | 20% improved tumor-associated antigen detection; Enhanced confidence |
| MSFragger-DDA+ | Chimeric spectrum deconvolution | Wide isolation windows (3.2Th); Open search strategy | 7-9% increase in PSM yield; Better low-abundance peptide identification |
| EDGE | Neoantigen prediction | MS-trained model; Direct immunopeptidome learning | Reduced false positives; Better presentation prediction |
| SHERPA | HLA presentation modeling | Monoallelic & multiallelic integration; K562 HLA-null line | Improved native presentation emulation |
| pVAC-Seq | Neoantigen prioritization | Integration of expression and binding affinity | Multi-parameter candidate filtering |
Experimental Protocols for Validation
NeoDiscMS Workflow Implementation
The NeoDiscMS protocol represents a cutting-edge methodology for sensitive neoantigen discovery, specifically designed to address low-abundance challenges. The process begins with nucleic acid extraction from tumor and matched normal tissue, followed by whole exome sequencing and RNA sequencing to identify somatic mutations and confirm their expression [77]. Bioinformatic preprocessing includes quality control with FastQC, adapter trimming, read alignment with BWA, and variant calling using designated callers. The resulting mutations are translated into candidate peptides and filtered through HLA binding prediction algorithms to generate a prioritized neoantigen list.
For mass spectrometry analysis, HLA-peptide complexes are immunoprecipitated from tumor tissue or cell lines using HLA-specific antibodies. Eluted peptides are then separated via liquid chromatography and analyzed on a tribrid mass spectrometer capable of real-time spectral matching. The NeoDiscMS method divides acquisition into 3-second cycles, beginning with MS1 scans, followed by targeted branch scans for inclusion list matches, and concluding with discovery branch scans using wide isolation windows (3.2Th) to maximize coverage [77]. Raw data processing with MSFragger-DDA+ enables chimeric spectrum deconvolution, significantly enhancing peptide identification rates particularly for lower-abundance species.
T-Cell Immunogenicity Assays
Functional validation of predicted neoantigens remains essential for confirming their therapeutic relevance, particularly for low-abundance candidates where presentation may be transient or context-dependent. T-cell recognition assays typically involve co-culturing candidate peptide-pulsed antigen-presenting cells with autologous or HLA-matched T cells, followed by measurement of activation markers (CD137, CD134) via flow cytometry [6] [76]. For higher-sensitivity detection, enzyme-linked immunospot (ELISpot) assays quantify interferon-gamma release in response to peptide stimulation, capable of detecting T-cell responses even to minimally presented antigens.
To address the challenge of low precursor frequency for neoantigen-specific T cells, researchers may employ in vitro priming protocols using dendritic cells loaded with candidate peptides or tandem minigene constructs. These expanded T-cell populations can then be tested for specific recognition of tumor cells endogenously presenting the target neoantigen, providing functional confirmation of both presentation and immunogenicity [6]. For the most challenging low-abundance neoantigens, TCR sequencing of tumor-infiltrating lymphocytes before and after expansion can reveal clonal expansion indicative of successful antigen recognition, even when direct functional readouts remain equivocal.
The Scientist's Toolkit
Table 3: Essential Research Reagent Solutions for Neoantigen Discovery
| Reagent/Category | Specific Examples | Function in Workflow |
|---|---|---|
| HLA Antibodies | W6/32 (anti-HLA class I), HLA-DR antibodies | Immunoprecipitation of peptide-HLA complexes for MS analysis |
| Cell Lines | HLA-null K562; JY B-cells; RA957 | System validation; Positive controls; HLA transfections |
| MS Instruments | Tribrid mass spectrometers (Orbitrap Fusion Lumos) | High-sensitivity peptide identification; Real-time targeted acquisition |
| Chromatography | Nano-flow LC systems; Capillary columns | Peptide separation prior to MS analysis |
| NGS Platforms | Illumina (short-read); Oxford Nanopore (long-read) | Mutation identification; HLA typing; Expression validation |
| Bioinformatics Tools | MSFragger; NeoDisc; pVAC-Seq | Data analysis; Neoantigen prediction; Prioritization |
Visualizing Workflows and Signaling Pathways
Neoantigen Discovery and Validation Workflow
Diagram 1: Neoantigen Discovery and Validation Workflow. This diagram illustrates the integrated multi-omics approach for identifying and validating neoantigens, highlighting the convergence of different data sources and technologies. SNVs: Single Nucleotide Variants; INDELs: Insertions and Deletions; NGS: Next-Generation Sequencing; WES: Whole Exome Sequencing; HLA: Human Leukocyte Antigen.
NeoDiscMS Targeted Acquisition Methodology
Diagram 2: NeoDiscMS Targeted Acquisition Methodology. This workflow demonstrates the real-time mutanome-guided immunopeptidomics approach that enhances sensitivity for low-abundance neoantigens through prioritized acquisition. MS: Mass Spectrometry; DDA: Data-Dependent Acquisition; Th: Thomson; RTSf: Real-Time Spectral Matching Filters.
The reliable detection of low-abundance neoantigens represents a critical frontier in precision immuno-oncology, with significant implications for therapeutic development. While technical challenges persist, integrated approaches that combine enhanced mass spectrometry acquisition, optimized sample preparation, and advanced computational prediction are progressively overcoming these limitations. The field continues to evolve toward more sensitive and clinically feasible workflows, with technologies like NeoDiscMS demonstrating that mutanome-guided immunopeptidomics can significantly improve detection confidence for rare but therapeutically relevant targets.
Future advancements will likely emerge from several promising directions. Single-cell multi-omics technologies offer unprecedented resolution for characterizing tumor heterogeneity and identifying neoantigens expressed in specific cellular subpopulations [5]. Spatial transcriptomics and proteomics will further contextualize neoantigen presentation within the architectural framework of the tumor microenvironment [5]. Artificially intelligent algorithms, trained on expanding multi-omics datasets, will continue to improve prediction accuracy for both antigen presentation and T-cell recognition. As these technologies mature and converge, they will undoubtedly unlock new opportunities for targeting the complete spectrum of tumor neoantigens, ultimately expanding the reach and efficacy of personalized cancer immunotherapies.
Optimizing Wet-Lab Protocols for FFPE and Low-Input Samples
Formalin-fixed paraffin-embedded (FFPE) samples represent an invaluable resource for oncology research, with estimates suggesting over a billion such samples exist in hospitals and tissue banks worldwide [81]. These archives, frequently paired with detailed clinical documentation, provide an unparalleled opportunity for both retrospective and prospective studies in immuno-oncology. However, the very processing that preserves tissue morphology for pathology induces significant chemical modifications that challenge molecular analysis, complicating their use in next-generation sequencing (NGS) for biomarker discovery.
Within immuno-oncology research, understanding the tumor microenvironment (TME) is fundamental for deciphering the complex relationship between the immune system and tumor biology [82]. The TME is a dynamic system comprising tumor-infiltrating leukocytes (TILs), cancer-associated fibroblasts, blood vessels, and other stromal components that intrinsically affect tumor development and pharmacology [83]. Comprehensive molecular profiling of FFPE specimens enables researchers to characterize this microenvironment, identify predictive biomarkers for therapy response, and discover novel therapeutic targets for modalities like checkpoint inhibitors, CAR T-cell therapy, and cancer vaccines [82] [84].
Understanding FFPE-Derived Nucleic Acid Challenges
The chemical crosslinking that makes FFPE samples so stable for storage also creates substantial obstacles for molecular analysis. The fixation process causes multiple types of damage that impact downstream sequencing results.
Molecular Damage Mechanisms
- Cross-linkage: Formalin creates covalent cross-links between DNA and proteins, between DNA molecules, and between DNA and RNA [81]. These crosslinks impede enzyme access during library preparation, reducing polymerase efficiency and amplification rates.
- Nucleotide Damage: The most frequent chemical alteration is the spontaneous deamination of cytosine and 5'methyl-cytosine to form uracil and thymine, respectively [81]. This process induces sequencing artifacts that can increase false-positive mutation calls, particularly problematic for detecting low allelic frequency variants.
- Fragmentation: FFPE DNA experiences backbone breakage, resulting in highly fragmented nucleic acids [81]. This fragmentation reduces the amount of amplifiable template and limits library insert sizes, which can affect sequencing economy and data quality.
- RNA Integrity Issues: RNA from FFPE samples is particularly challenging due to its single-stranded composition, susceptibility to RNases, and vulnerability to heat degradation during deparaffinization [81]. This degradation can reduce cDNA synthesis yields, limit gene detection, and introduce artifacts.
Impact on NGS Library Preparation
The cumulative effect of these damages manifests in several operational challenges during NGS workflow. Libraries prepared from FFPE-derived nucleic acids typically exhibit:
- Higher duplication rates due to reduced library complexity
- Smaller insert sizes that may not align with optimal sequencing read lengths
- Less uniform coverage across the genome or transcriptome
- Reduced library yields from lower conversion rates of damaged template
- Potential false-positive variant calls from deamination artifacts [81]
Optimized Wet-Lab Protocols for FFPE Samples
Successful NGS from FFPE samples requires optimized protocols at every stage, from extraction through library preparation, with special considerations for the unique challenges of these valuable specimens.
Pre-Analytical Quality Control and Extraction
Robust quality assessment of input material is crucial for predicting library preparation success and interpreting subsequent results.
Recommended QC Methods:
- Electrophoretic Methods: Techniques like TapeStation or BioAnalyzer provide information about DNA fragmentation levels but offer limited insight into chemical damage [85].
- qPCR-Based Quality Scores: Quantitative PCR methods that measure amplifiable DNA are superior predictors of FFPE library prep outcomes, as they reflect the utilizable fraction of DNA despite chemical modifications [85].
- RNA Integrity Number (RIN): For transcriptomic applications, RIN ≥7 is recommended for successful library construction [83].
Optimized Extraction Protocols:
- Gentle Deparaffinization: Implement overnight deparaffinization processes combining heat and oil to preserve nucleic acid integrity, avoiding excessive temperatures that can cause additional damage [81].
- Specialized Buffers: Use extraction buffers specifically formulated to reverse macromolecular cross-linkage, thereby increasing yield and quality of nucleic acids [81].
- Magnetic Bead-Based Purification: This technology enables efficient recovery of fragmented nucleic acids while removing inhibitors that may interfere with downstream applications [81].
Table 1: Quality Control Metrics for FFPE-Derived Nucleic Acids
| Metric | DNA (Recommended) | RNA (Recommended) | Assessment Method |
|---|---|---|---|
| Quantity | >1μg total | >1μg total | Fluorometric assays (Qubit) |
| Concentration | >20 ng/μL | >20 ng/μL | Spectrophotometry (NanoDrop) |
| Purity | OD260/280 = 1.8-2.0, OD260/230 ≥ 2.0 | OD260/280 = 1.8-2.0, OD260/230 ≥ 2.0 | Spectrophotometry |
| Integrity | DIN ≥ 4 (if applicable) | RIN ≥ 7 | Electrophoresis (BioAnalyzer/TapeStation) |
| Functionality | qPCR Ct value within acceptable range | Amplifiable mRNA detected | qPCR-based quality scores |
DNA Library Preparation Optimization
Traditional sonication-based fragmentation approaches present specific challenges for FFPE samples, including significant material loss (up to 44% of input DNA) and introduction of sequencing artifacts [85]. Enzymatic fragmentation strategies offer compelling advantages.
Watchmaker DNA Library Prep Kit with Fragmentation Protocol:
- Input DNA: 50-200 ng of FFPE DNA, with increased input compensating for lower quality samples [85]
- Fragmentation Condition: 3 minutes at 30°C using a specialized enzyme cocktail [85]
- Single-Tube Protocol: Minimizes sample loss through reduced tube transfers and facilitates automation [85]
- Post-Ligation Cleanup: SPRI ratio adjustment (0.5X-0.8X) to selectively retain longer fragments and tailor insert size to sequencing read length [85]
Size Selection Strategies: For highly fragmented FFPE samples, eliminating the fragmentation step entirely during library preparation can improve success rates by preserving the already limited fragment length [81]. Adjusting SPRI cleanup ratios provides control over final library properties:
- 0.8X ratio: Standard yield and size distribution
- 0.65X ratio: Favors longer fragments with moderate yield reduction
- 0.5X ratio: Maximizes fragment length with significant yield trade-offs [85]
RNA Library Preparation for Immune Transcriptomics
Transcriptomic analysis of FFPE samples enables quantitative evaluation of immune cell markers, checkpoint pathways, and cytokine signaling within the tumor microenvironment. Targeted NGS approaches offer significant advantages for degraded RNA specimens.
Oncomine Immune Response Research Assay Protocol:
- Input RNA: As little as 10 ng total RNA from FFPE samples [86]
- Technology: Multiplex PCR-based target enrichment (Ion AmpliSeq Technology)
- Content: 395 genes across 36 functional annotation groups relevant to immuno-oncology [86]
- Applications: Tumor microenvironment characterization, predictive biomarker identification, immunotherapy mechanism studies
Key Functional Annotation Groups in Immune Response Panels:
- Immune Cell Lineages: B-cell (11 genes), T-cell (multiple subsets), dendritic cell (7 genes), macrophage (5 genes), neutrophil (5 genes) markers [86]
- Checkpoint Pathways: 30 genes covering inhibitory and stimulatory immune checkpoints [86]
- Cytokine Signaling: 15 genes involved in interleukins, interferons, and related signaling pathways [86]
- Antigen Processing and Presentation: 19 genes critical for neoantigen recognition and immune activation [86]
Bulk RNA-Seq Considerations: For whole transcriptome approaches, eliminating the fragmentation step during library preparation can improve success rates with degraded FFPE RNA [81]. While expression profiles from FFPE samples show high correlation with matched fresh-frozen tissues (r > 0.89-0.95), FFPE-derived RNA typically exhibits:
- Higher mapping to intronic regions due to fragmentation
- Reduced transcript integrity numbers
- Slight shifts in GC content [81]
Table 2: Comparison of NGS Approaches for FFPE-Derived Nucleic Acids
| Parameter | Whole Genome/Exome Sequencing | Targeted DNA Sequencing | Bulk RNA Sequencing | Targeted RNA Sequencing |
|---|---|---|---|---|
| Recommended Input | 50-200 ng DNA | 10-50 ng DNA | 10-100 ng RNA | 10 ng RNA |
| Optimal Fragment Size | >150 bp | N/A (targeted) | >100 bp | N/A (targeted) |
| Key QC Metrics | qPCR quality score, fragment distribution | qPCR quality score | RIN ≥ 7, DV200 > 30% | RIN ≥ 7, amplifiable mRNA |
| Primary Applications | Mutation discovery, CNV analysis | Hotspot validation, focused panels | Differential expression, splicing | Immune profiling, pathway analysis |
| FFPE-Specific Challenges | High duplication rates, uneven coverage | Artifact management, low input | 3' bias, reduced complexity | Sensitivity for low-expressed genes |
| Best Use Cases | Discovery studies with high-quality FFPE | Clinical validation, limited samples | Biomarker discovery, whole transcriptome | Immuno-oncology, tumor microenvironment |
Advanced Applications: Single-Cell and Spatial Profiling of FFPE Samples
Recent technological advances have expanded the applications of FFPE samples to single-cell resolution and spatial transcriptomics, opening new possibilities for retrospective studies of the tumor microenvironment.
Single-Cell RNA Sequencing of FFPE Samples
The Chromium Single Cell Gene Expression Flex workflow (10x Genomics) enables single-cell profiling of fixed tissues, including FFPE specimens, using a probe-based system to target the whole transcriptome [81]. This approach overcomes traditional limitations in single-cell analysis of archived samples.
Key Advantages for FFPE Samples:
- Probe-Based Detection: Unlike traditional oligo(dT) capture methods that require intact polyA tails, the Flex assay uses gene-specific probes that can bind to fragmented RNA [81].
- Enhanced Sensitivity: Studies demonstrate approximately 2x higher transcript detection compared to traditional 3' single-cell kits when working with degraded material [81].
- Integration with Spatial Data: Shared probe sets between Flex and Visium Spatial assays enable correlation of single-cell data with spatial tissue context [81].
Performance Characteristics: Investigations comparing patient-matched fresh, cryopreserved, and archival FFPE tissues show robust preservation of clinically relevant cell type information in FFPE specimens, with high correlations in clinically relevant signaling pathways between matched tissues [81]. This enables both retrospective and prospective analysis of the tumor microenvironment at single-cell resolution.
Spatial Transcriptomics in Archival Tissues
The integration of single-cell and spatial gene expression datasets represents a powerful approach for investigating the tumor microenvironment [81]. By leveraging shared probe sets between single-cell and spatial platforms, researchers can accurately deconvolute cell type information within the spatial context of tumor architecture.
The Scientist's Toolkit: Essential Reagents and Solutions
Table 3: Essential Research Reagents for FFPE and Low-Input NGS Workflows
| Product/Technology | Manufacturer/Provider | Key Function | FFPE-Specific Benefits |
|---|---|---|---|
| Watchmaker DNA Library Prep Kit with Fragmentation | Watchmaker Genomics | Enzymatic fragmentation-based library prep | Consistent insert sizes independent of input amount or FFPE quality; minimal molecular artifacts [85] |
| Oncomine Immune Response Research Assay | Thermo Fisher Scientific | Targeted NGS gene expression for immuno-oncology | Enables analysis of 395 immune-related genes from as little as 10 ng FFPE RNA [86] |
| Chromium Single Cell Gene Expression Flex | 10x Genomics | Single-cell RNA sequencing of fixed tissues | Probe-based system works with fragmented FFPE RNA; enables single-cell analysis of archived samples [81] |
| RNeasy Mini Kit | QIAGEN | RNA extraction and purification | Provides high-quality RNA with OD260/280 = 1.8-2.0, suitable for demanding NGS applications [83] |
| AMPure XP Beads | Beckman Coulter | SPRI-based size selection and cleanup | Adjustable ratios (0.5X-0.8X) enable optimization of library insert sizes for FFPE samples [85] [83] |
| PanCancer Mouse IO 360 Panel | NanoString | Mouse immuno-oncology transcript profiling | Microarray-based profiling of 770 immune-related genes in mouse models; useful for preclinical studies [83] |
FFPE samples represent a vast, clinically annotated resource that continues to drive innovation in immuno-oncology research. While these specimens present well-characterized challenges for molecular analysis, optimized wet-lab protocols can successfully overcome these limitations to yield high-quality NGS data. The key to success lies in implementing tailored approaches at each step: from gentle extraction methods that preserve already-fragmented nucleic acids, through library preparation protocols that minimize additional damage and maximize information capture from limited input.
The ongoing development of specialized technologies—including enzymatic fragmentation, targeted enrichment panels, and single-cell methods adapted for fixed tissues—continues to expand the utility of FFPE archives. These advances enable increasingly sophisticated analyses of the tumor microenvironment, allowing researchers to extract maximal biological insight from these precious clinical resources. As the field progresses, the integration of multi-omics approaches applied to well-characterized FFPE cohorts will undoubtedly accelerate the discovery and validation of next-generation biomarkers for immuno-oncology, ultimately improving patient stratification and therapeutic outcomes.
Computational Challenges and Bioinformatics Pipeline Standardization
The adoption of Next-Generation Sequencing (NGS) has become fundamental to biomarker discovery in immuno-oncology, enabling the comprehensive genomic profiling essential for developing immunotherapies [87] [88]. However, the analytical journey from raw sequencing data to clinically actionable insights is fraught with computational challenges that can compromise data integrity, reproducibility, and clinical validity. Bioinformatic pipelines form the analytical backbone of modern immuno-oncology research, transforming terabytes of raw sequence data into identifiable biomarkers—such as tumor mutational burden (TMB), microsatellite instability (MSI), and homologous recombination deficiency (HRD)—that predict response to immune checkpoint inhibitors [89] [70]. The standardization of these pipelines is not merely a technical exercise but a critical prerequisite for generating reliable, comparable results across research institutions and clinical trials, ultimately accelerating the development of novel immunotherapies [89].
This technical guide examines the core computational challenges in NGS data analysis for immuno-oncology and presents a standardized framework for bioinformatic pipelines, complete with detailed protocols, essential toolkits, and visualization to support robust biomarker discovery.
Core Computational Challenges in NGS Data Analysis
The analysis of NGS data for immuno-oncology introduces several distinct computational hurdles that must be addressed to ensure accurate biomarker identification.
- Data Volume and Complexity: A single whole-genome sequencing run can generate multiple terabytes of data [90]. The computational burden is compounded in immuno-oncology by the need to distinguish subtle tumor-specific mutations from the background of normal genetic variation and sequencing artifacts, a process that demands immense processing power and sophisticated algorithms [87] [91].
- Data Heterogeneity and Integration: Immuno-oncology research increasingly relies on multi-modal data fusion, integrating genomic, transcriptomic, proteomic, and clinical data to build a comprehensive view of the tumor-immune microenvironment [87] [91]. The heterogeneity in data types, formats, and scales presents significant challenges for computational integration and analysis.
- Analytical Reproducibility: Variations in bioinformatic tools, reference genomes, and parameter settings can lead to dramatically different results from the same raw data [89]. A study might utilize dozens of software tools, each with its own dependencies and versioning, making it exceptionally difficult to replicate an analysis exactly without strict containerization and version control [89] [92].
- Reference Genome Biases: The reliance on reference genomes like GRCh38 (hg38) is essential for alignment; however, these references are not genetically representative of global populations [92]. This can introduce biases in variant calling, particularly in regions of the genome that are highly polymorphic or structurally diverse, potentially leading to missed biomarkers in underrepresented groups [92].
A Standardized Bioinformatics Framework for Immuno-Oncology
To overcome these challenges, a consensus framework for clinical bioinformatics operations has emerged, championed by initiatives like the Nordic Alliance for Clinical Genomics (NACG) [89]. The following workflow delineates the critical stages and decision points in a standardized NGS pipeline for immuno-oncology.
Standardized NGS Bioinformatics Pipeline for Immuno-Oncology
Key Recommendations for Pipeline Standardization
The framework above is operationalized through the following technical recommendations, which are critical for production-scale clinical bioinformatics [89]:
- Adopt the hg38 Genome Build: The GRCh38 (hg38) reference genome offers improved coverage of complex regions and is recommended as the current standard over older builds like hg19 [89].
- Implement a Core Set of Analyses: Clinical production pipelines should comprehensively call different variant types, including single nucleotide variants (SNVs), small insertions and deletions (indels), copy number variants (CNVs), and structural variants (SVs) [89]. For immuno-oncology, this must be extended to specific biomarkers like TMB, MSI, and HRD.
- Ensure Reproducibility through Containerization: All software should be run in containerized environments (e.g., Docker, Singularity) to encapsulate dependencies and guarantee consistent execution across different computing systems [89].
- Rigorous Pipeline Testing and Validation: Pipelines must be subjected to a multi-tiered testing strategy, including unit, integration, and end-to-end testing. Accuracy and reproducibility should be validated using standard truth sets from the Genome in a Bottle (GIAB) consortium and the SEQC2 project, supplemented with in-house data from previously tested clinical samples [89].
- Maintain Data Integrity and Sample Identity: Data integrity must be verified using file hashing, while sample identity should be confirmed through genetic fingerprinting and checks for genetically inferred sex and relatedness to prevent sample mix-ups [89].
Detailed Experimental Protocols for Key IO Biomarkers
Tumor Mutational Burden (TMB) Calculation
TMB quantifies the total number of somatic mutations per megabase (Mb) of the genome and is a validated predictor of response to immune checkpoint inhibitors [89] [70].
Methodology:
- Variant Calling: Perform somatic variant calling (SNVs and indels) from matched tumor-normal sample pairs using a validated tool like MuTect2 or VarScan2. The panel or exome capture region must be well-defined [89].
- Filtering: Apply strict filters to remove known germline polymorphisms (using population frequency databases like gnomAD), driver mutations, and synonymous (silent) mutations. Only non-synonymous (missense, nonsense, frameshift) mutations in the coding regions are typically counted [89].
- Calculation: The TMB is calculated using the formula: ( TMB = \frac{Total\ Number\ of\ Qualified\ Somatic\ Mutations}{Size\ of\ Analyzed\ Genomic\ Region\ (in\ Mb)} ) For whole-exome sequencing (WES), the region is ~35-40 Mb. For targeted panels, the size of the panel's coding region is used, and calibration to WES-equivalent values may be necessary [89].
Microsatellite Instability (MSI) Analysis
MSI analysis detects hypermutation in microsatellite regions caused by deficient DNA mismatch repair (dMMR), a key biomarker for immunotherapy [89] [70].
Methodology:
- Locus Selection: Identify a set of homopolymer or dinucleotide repeat loci (typically 10-20 loci) within the sequencing target region. These can be included in a targeted panel or assessed from WES data [89].
- Variant Calling: Use a specialized tool or an algorithm sensitive to small indels within these repetitive regions. The analysis compares the length distribution of microsatellite sequences in the tumor DNA to that of the matched normal DNA [89].
- Instability Scoring: For each locus, instability is called if the tumor sample shows a significant shift in the length distribution compared to the normal. The MSI score is often reported as the percentage of unstable loci or as a binary classification (MSI-High vs. MSI-Stable/MSS) based on a predefined threshold (e.g., >30-40% unstable loci) [89].
Homologous Recombination Deficiency (HRD) Genomic Scarring
HRD signifies a tumor's inability to repair double-strand DNA breaks effectively. "Genomic scarring" assays measure the accumulated mutational patterns caused by this deficiency [70].
Methodology (Using NGS Data):
- Whole-Genome Data: Calculate three key metrics from whole-genome sequencing data of the tumor:
- Loss of Heterozygosity (LOH): The number of genomic regions with LOH events.
- Telomeric Allelic Imbalance (TAI): The number of regions with allelic imbalance that extend to the telomere.
- Large-Scale State Transitions (LST): The number of chromosomal breaks between adjacent regions of at least 10 Mb.
- HRD Score Calculation: The composite HRD score is the sum of the LOH, TAI, and LST scores. A score above a validated threshold (e.g., 42) is indicative of HRD positivity, suggesting potential benefit from PARP inhibitors [70].
- AI-Assisted Detection: Emerging deep-learning tools like DeepHRD can now detect HRD characteristics directly from standard hematoxylin and eosin (H&E)-stained biopsy slides, potentially offering a more accessible alternative to genomic tests with reported higher accuracy [70].
The Scientist's Toolkit: Essential Research Reagents and Materials
The following table details key reagents, materials, and software solutions essential for implementing a standardized NGS pipeline for immuno-oncology research.
Table 1: Essential Toolkit for NGS-Based IO Biomarker Research
| Item Category | Specific Tool/Reagent | Function and Application Notes |
|---|---|---|
| Wet-Lab Reagents | NGS Library Prep Kits (e.g., Illumina, Thermo Fisher) | Convert extracted nucleic acids into sequencing-ready libraries. Selection depends on sample type (DNA/RNA), input quantity, and application (WGS, targeted panels) [90]. |
| Targeted Panels for IO (e.g., Oncomine, TSO) | Multiplexed PCR or hybrid-capture-based panels designed to enrich for genes relevant to cancer and immuno-oncology, enabling focused, cost-effective sequencing [88]. | |
| DNA/RNA Extraction Kits | Isolate high-quality, high-purity nucleic acids. Quality (A260/A280 ~1.8-2.0) and integrity (RIN >7 for RNA) are critical for library success [93]. | |
| Bioinformatics Software | Quality Control Tools (FastQC, Trimmomatic, Cutadapt) | Assess raw read quality, detect adapter contamination, and trim low-quality bases. Essential first step in any pipeline [93] [94]. |
| Alignment Tools (BWA-MEM, STAR) | Map sequencing reads to the reference genome (hg38). BWA-MEM is standard for DNA-Seq; STAR is optimized for RNA-Seq [89] [94]. | |
| Variant Callers (MuTect2, Strelka2, DeepVariant) | Identify somatic mutations from tumor-normal pairs. DeepVariant, an AI-based tool, has demonstrated superior accuracy in benchmark studies [92]. | |
| Annotation & IO Tools (ANNOVAR, VEP, MSIsensor) | Annotate variants with functional predictions and population frequencies. Specialized tools (MSIsensor) calculate specific IO biomarkers [89]. | |
| Computational Infrastructure | High-Performance Computing (HPC) or Cloud (AWS, Google Cloud) | Off-grid clinical-grade computing systems are necessary to manage the intensive data processing, storage, and analysis demands of NGS [89] [92]. |
| Containerization Software (Docker, Singularity) | Package software and all its dependencies into a portable, reproducible unit, ensuring consistent analysis results across different environments [89]. | |
| Workflow Management Systems (Nextflow, Snakemake) | Orchestrate complex, multi-step bioinformatics pipelines, enabling scalability, portability, and robust execution [90]. |
Quantitative Data and Performance Metrics
Standardized pipelines must be validated against known performance benchmarks. The following table summarizes key quality control and performance metrics that should be monitored.
Table 2: Key NGS Quality Control and Performance Metrics
| Metric | Target Value/Range | Importance and Interpretation |
|---|---|---|
| Q-score | >30 (Q30) | Probability of an incorrect base call is 1 in 1000. A Q30 score of >80% of bases is a common quality threshold [93]. |
| Read Depth (Coverage) | >100x for WGS; >500x for targeted panels | Ensures sufficient sampling to detect heterozygous variants with high confidence. Higher depth is required for liquid biopsies [88]. |
| Alignment Rate | >95% | Indicates the percentage of reads that successfully map to the reference genome. A low rate may suggest contamination or poor-quality library [94]. |
| Duplication Rate | Variable, but <20% often acceptable | High duplication rates can indicate PCR over-amplification during library prep, reducing effective coverage [93]. |
| TMB Accuracy | High correlation with WES-based truth sets | Validated against standardized samples to ensure calls are consistent with gold-standard methods [89]. |
| MSI/HRD Sensitivity | >95% for established biomarkers | The pipeline must reliably detect these biomarkers against validated clinical test results [89] [70]. |
The path to reliable biomarker discovery in immuno-oncology is inextricably linked to the rigor and standardization of the underlying bioinformatics pipelines. By adopting a consensus framework that addresses data volume, reproducibility, and analytical validity—supported by detailed experimental protocols, a curated toolkit, and continuous performance monitoring—research institutions and drug developers can significantly enhance the quality and translational potential of their findings. As NGS technologies evolve and AI-powered tools become more integrated, the principles of standardization outlined here will form the critical foundation upon which the next generation of cancer immunotherapies is built.
Bridging the Adoption Gap Between Academic and Community Settings
Next-generation sequencing (NGS) has revolutionized biomarker discovery in immuno-oncology, enabling comprehensive profiling of the tumor microenvironment, identification of predictive biomarkers for immunotherapy response, and characterization of the immune repertoire. However, a significant adoption gap persists between academic research centers and community oncology settings, creating disparities in patient access to precision medicine. This technical guide examines the root causes of this divide and provides evidence-based strategies, standardized protocols, and implementation frameworks to bridge this gap, thereby accelerating the translation of NGS-based biomarker research into widespread clinical practice.
Research demonstrates that insurance type is a key contributor to inequity in NGS testing. Patients with metastatic non-small cell lung cancer (mNSCLC) who have commercial insurance have significantly higher odds of receiving NGS testing compared to those with Medicare, Medicaid, or other insurance types [95]. This disparity is particularly problematic in community settings where the effect of insurance type on NGS testing is most pronounced [95]. When all patients receive equitable access to NGS testing, a positive downstream effect enables more equitable access to targeted therapy, highlighting the critical importance of addressing this adoption gap [95].
Root Causes of the NGS Adoption Gap
Technical and Operational Challenges
The implementation of NGS in community settings faces significant technical hurdles that contribute to the adoption gap. Community practices often lack the specialized expertise and infrastructure required for NGS-based biomarker testing, which involves complex workflows from sample preparation to data interpretation [96]. The bioinformatics pipeline presents a particularly substantial barrier, as community settings typically don't have access to bioinformaticians and computational resources needed for variant calling, annotation, and interpretation [97].
Equipment requirements and reagent costs further exacerbate this divide. Academic centers often benefit from institutional funding, research grants, and economies of scale that allow them to absorb the substantial startup and operational costs of NGS implementation [96]. In contrast, community practices face prohibitive costs for equipment, reagents, and specialized personnel, creating significant financial barriers to adoption [95].
Regulatory and compliance complexity presents another substantial challenge. Navigating the Clinical Laboratory Improvement Amendments (CLIA) certification, College of American Pathologists (CAP) accreditation, and FDA regulatory pathways for laboratory-developed tests (LDTs) requires specialized expertise that may not be available in community settings [96]. This regulatory burden disproportionately affects smaller community practices with limited administrative support structures.
Economic and Reimbursement Barriers
Economic factors constitute a primary driver of the NGS adoption gap, with significant disparities in reimbursement creating financial disincentives for community implementation.
Table 1: Economic Barriers to NGS Adoption in Community Settings
| Barrier Category | Academic Setting | Community Setting | Impact on Adoption |
|---|---|---|---|
| Testing Reimbursement | Higher rates for technical components; often supplemented by research funding | Lower reimbursement rates; heavily dependent on payer mix | Reduced financial viability in community practices [95] |
| Infrastructure Investment | Cross-subsidized by institutional funds and research grants | Must demonstrate direct return on investment | Prohibitive startup costs for community practices [96] |
| Personnel Costs | Access to specialized expertise through academic appointments | Requires competitive recruitment for specialized staff | Challenges in attracting/retaining bioinformaticians [96] |
| Payer Coverage Variability | More consistent coverage across complex cases | High variability based on insurance type; prior authorization burdens | Creates uncertainty and administrative burden [95] |
The economic data reveals that insurance type significantly influences NGS testing rates. Patients with commercial insurance have markedly higher odds of receiving NGS testing compared to those with Medicare or Medicaid, with this effect being particularly pronounced in community settings [95]. This reimbursement disparity creates a financial disincentive for community practices to invest in NGS capabilities, especially those serving predominantly publicly insured populations.
Integrated Technical Strategies for Bridging the Gap
Standardized NGS Wet-Lab Protocols
Implementation of robust, standardized protocols is essential for ensuring reproducible NGS biomarker results across diverse laboratory settings. The following technical protocols address the most critical aspects of NGS workflow standardization for immuno-oncology applications.
DNA Extraction and Quality Control for Immuno-Oncology Biomarkers
Proper nucleic acid extraction is foundational for successful NGS biomarker profiling. The following protocol ensures high-quality DNA suitable for comprehensive immune biomarker analysis:
- Sample Requirements: Formalin-fixed paraffin-embedded (FFPE) tissue sections (5-10 μm thickness) with ≥20% tumor content or peripheral blood samples (8-10 mL) in EDTA tubes for circulating tumor DNA (ctDNA) analysis [98]
- Extraction Method: Use of silica-membrane based kits with optimized deparaffinization steps for FFPE or magnetic bead-based extraction for blood samples
- DNA Quantification: Fluorometric methods (Qubit dsDNA HS Assay) with minimum yield of 50 ng for FFPE, 30 ng for liquid biopsies
- Quality Metrics: DNA integrity number (DIN) ≥4.0 for FFPE, fragment size distribution analysis showing predominant peak at ~165-200 bp for ctDNA [98]
- QC Failure Criteria: Degraded samples with DIN <3.0 or concentration <10 ng/μL should be excluded from sequencing
Hybrid Capture-Based Library Preparation for Comprehensive Immune Profiling
Hybrid capture methods provide superior performance for heterogeneous immuno-oncology biomarkers compared to amplicon-based approaches:
- DNA Fragmentation: Covaris shearing to 150-200 bp fragment size with settings optimized for input DNA quality
- Library Preparation: Dual-indexed adapter ligation with unique molecular identifiers (UMIs) to mitigate PCR duplication artifacts and enable accurate variant allele frequency quantification [97]
- Hybrid Capture: Pooled RNA baits targeting 300-500 immune-related genes including T-cell receptor loci, immune checkpoint genes, cytokine signaling pathways, and tumor mutational burden (TMB) calculation regions [98]
- Capture Conditions: 16-24 hour hybridization at 65°C with stringent post-capture washes to remove non-specific binding
- Library Amplification: 8-10 cycle PCR with polymerase optimized for GC-rich regions to minimize bias in immune gene coverage [96]
Bioinformatic Pipeline Standardization
A standardized bioinformatics workflow is crucial for consistent identification and interpretation of immuno-oncology biomarkers across settings with varying computational resources.
NGS Bioinformatics Pipeline for Immuno-Oncology
The computational workflow encompasses specific tools and parameters optimized for immuno-oncology biomarkers:
- Quality Control: FastQC (v0.11.9) with adapter contamination check and quality threshold Q≥30; sample exclusion for <80% bases ≥Q30
- Sequence Alignment: BWA-MEM (v0.7.17) for DNA sequencing with GRCh38 reference genome including decoy sequences; STAR (v2.7.10a) for RNA sequencing with GENCODE v38 annotation
- Variant Calling: Mutect2 (GATK v4.2.6.1) for somatic SNVs/indels with panel of normals; minimum base quality Q20, mapping quality Q30; VarScan2 (v2.4.4) for consensus calling with minimum variant allele frequency 0.05 for ctDNA, 0.02 for tissue
- Immuno-Oncology Biomarkers: TMB calculation using nonsynonymous mutations per megabase with ≥5% VAF; microsatellite instability (MSI) analysis using MANTIS with ≥30% instability threshold; T-cell receptor repertoire analysis using MIXCR (v3.0.13) [99]
Implementation Framework for Community Settings
Collaborative Operational Models
Successful implementation of NGS in community settings requires innovative operational models that address both technical and economic barriers.
Collaborative NGS Implementation Model
The Genomics Organisation for Academic Laboratories (GOAL) initiative demonstrates an effective collaborative model where 29 academic centers share probe resources and technical expertise to reduce costs and standardize NGS testing [96]. This model can be adapted for academic-community partnerships through several key components:
- Reagent and Technology Sharing: Pooled purchasing of NGS reagents and shared access to sequencing instrumentation through hub-and-spoke models, reducing costs by 30-50% compared to individual implementation [96]
- Centralized Bioinformatics: Cloud-based bioinformatic analysis with standardized pipelines, eliminating the need for local computational infrastructure and specialized personnel in community settings [99]
- Telepathology Integration: Digital pathology consultation for sample adequacy assessment and tumor content evaluation prior to NGS testing, ensuring appropriate test utilization [71]
- Professional Development: Structured training programs for community laboratory personnel including hands-on workshops for pre-analytical sample processing and basic result interpretation
Essential Research Reagent Solutions
Successful implementation of NGS-based biomarker discovery requires access to high-quality, standardized reagents optimized for immuno-oncology applications.
Table 2: Essential Research Reagent Solutions for NGS in Immuno-Oncology
| Reagent Category | Specific Product Examples | Key Functions | Implementation Considerations |
|---|---|---|---|
| Nucleic Acid Extraction Kits | QIAamp DNA FFPE Tissue Kit, MagMAX Cell-Free DNA Isolation Kit | High-quality DNA extraction from FFPE and liquid biopsy samples; preservation of low-abundance variants | Automation compatibility; minimal cross-contamination; suitable for low-input samples [98] |
| Library Preparation Kits | Illumina DNA Prep with Enrichment, KAPA HyperPlus with UMI adapters | Fragmentation, end-repair, adapter ligation; incorporation of unique molecular identifiers | PCR duplicate removal; GC-bias minimization; compatibility with degraded samples [97] |
| Hybrid Capture Panels | GOAL collaborative panels, FoundationOne CDx, SureSelect XT HS2 | Target enrichment for cancer-relevant genes; comprehensive immune profiling | Coverage uniformity; inclusion of immuno-oncology biomarkers; TMB calculation capability [96] [98] |
| Sequencing Reagents | Illumina NovaSeq 6000 S-Prime kits, Ion Torrent Ion 550 Chip | Cluster generation and sequencing-by-synthesis; semiconductor sequencing | Output flexibility; read length options; cost-per-sample optimization [19] |
| Quality Control Reagents | Agilent D1000 ScreenTape, Qubit dsDNA HS Assay | Fragment size distribution analysis; accurate DNA quantification | Integration with automated electrophoresis systems; low sample consumption [97] |
Validation and Quality Assurance Protocols
Analytical Validation Framework
Rigorous analytical validation is essential for implementing NGS biomarkers in community settings. The following protocol outlines a comprehensive validation approach:
- Precision and Reproducibility: Intra-run, inter-run, and inter-operator precision testing using commercial reference standards with variants at 5%, 10%, and 15% allele frequencies; ≥95% concordance for variant calls at ≥5% VAF [97]
- Accuracy and Concordance: Comparison to orthogonal methods (Sanger sequencing, digital PCR) for 50-100 known positive samples; ≥99% positive percentage agreement and ≥99% negative percentage agreement for variants at ≥10% VAF
- Limit of Detection: Serial dilutions of characterized cell lines or synthetic controls to establish minimum variant allele frequency detection; typical LOD of 2-5% for DNA from FFPE, 0.5-1% for ctDNA [98]
- Specificity and Interference: Testing for potential interferents including hemoglobin, bilirubin, excess non-human DNA; acceptable performance with ≥80% tumor content and ≤10% contamination
- Reportable Range: Verification of performance across entire targeted region including difficult-to-sequence areas with high GC content; ≥95% of targets with ≥100x coverage [96]
Quality Control and Proficiency Testing
Ongoing quality assurance is critical for maintaining NGS testing quality across diverse implementation settings:
- Internal Quality Controls: Incorporation of positive and negative control materials in each sequencing run; monitoring of key metrics including library complexity, on-target rate, and uniformity of coverage
- External Proficiency Testing: Participation in CAP NGS surveys or equivalent external proficiency testing programs at least twice annually; investigation and corrective action for any unsuccessful results
- Data Quality Monitoring: Continuous assessment of quality metrics including average coverage depth (>300x for tissue, >10,000x for liquid biopsy), duplication rates (<20% for DNA sequencing), and base quality scores (≥90% bases ≥Q30) [97]
- Variant Curation and Classification: Regular review of variant classifications according to AMP/ASCO/CAP guidelines; documentation of evidence supporting therapeutic, prognostic, or diagnostic interpretations
Bridging the adoption gap between academic and community settings requires a multifaceted approach addressing technical, operational, and economic barriers. The standardized protocols, collaborative implementation models, and quality assurance frameworks presented in this guide provide a roadmap for expanding access to NGS-based biomarker discovery in immuno-oncology. By adopting these strategies, the oncology community can work toward eliminating disparities in precision medicine access and accelerating the translation of biomarker research into improved patient outcomes across all care settings. Future success will depend on continued collaboration, technological innovation, and commitment to equitable implementation of genomic medicine.
Bench to Bedside: Analytical Validation and Comparative Platform Analysis
Frameworks for Clinical NGS Assay Validation and Regulatory Compliance
The integration of Next-Generation Sequencing (NGS) into immuno-oncology has fundamentally transformed biomarker discovery and therapeutic stratification, enabling the identification of complex molecular signatures such as tumor mutational burden (TMB), microsatellite instability (MSI), and novel fusion genes that predict response to immunotherapy [5] [100]. However, the inherent complexity of NGS workflows—spanning wet-lab procedures, sophisticated bioinformatics pipelines, and nuanced clinical interpretation—poses significant challenges for ensuring reproducible and clinically actionable results [101] [102]. The global NGS market is projected to grow from USD 9 billion to USD 27 billion between 2024 and 2032, underscoring the urgent need for robust validation frameworks and standardized quality management systems [102]. This technical guide provides a comprehensive overview of the core principles, experimental protocols, and regulatory requirements for validating clinical NGS assays, with a specific focus on applications within immuno-oncology research and drug development. By establishing a rigorous validation framework, researchers and clinicians can ensure that NGS-derived biomarkers reliably inform patient stratification, therapeutic decision-making, and clinical trial endpoints, thereby advancing the field of precision oncology.
Regulatory Frameworks and Quality Management
A robust Quality Management System (QMS) is the cornerstone of clinical NGS testing, providing the structural framework for all pre-analytical, analytical, and post-analytical processes. The Centers for Disease Control and Prevention (CDC), in collaboration with the Association of Public Health Laboratories (APHL), launched the Next-Generation Sequencing Quality Initiative (NGS QI) to address the unique challenges of implementing NGS in clinical settings [101] [102]. This initiative offers over 100 freely available guidance documents and Standard Operating Procedures (SOPs) tailored to NGS workflows, built upon the Clinical & Laboratory Standards Institute’s (CLSI) 12 Quality System Essentials (QSEs) [101]. These resources cover critical areas such as personnel competency, method validation, equipment management, and bioinformatics pipeline monitoring, enabling laboratories to build a compliant QMS that adapts to rapidly evolving sequencing technologies and analytical methods [101].
Navigating the global regulatory landscape is essential for laboratories developing NGS-based assays. Regulatory requirements vary by region but share a common emphasis on analytical validation, clinical utility, and ongoing quality assurance.
Table 1: Key Regulatory and Professional Guidelines for Clinical NGS Assays
| Organization/Regulation | Region | Primary Focus & Requirements |
|---|---|---|
| FDA NGS-Based IVD Guidance [103] | United States | Analytical validation standards for germline NGS tests; flexibility for novel technologies while ensuring safety/effectiveness. |
| NY State CLEP Guidelines [104] | United States | Stringent analytical validation, clinical validation, and pre-approval for lab-developed tests (LDTs); considered a national benchmark. |
| In Vitro Diagnostic Regulation (IVDR) [105] | European Union | Stricter clinical evidence, risk classification (Class C for large panels), post-market performance follow-up (PMPF), and state-of-the-art compliance. |
| Clinical Laboratory Improvement Amendments (CLIA) [102] | United States | Quality standards for all clinical laboratory testing, including personnel qualifications, proficiency testing, and quality control. |
| College of American Pathologists (CAP) [102] | International (Accreditation) | Comprehensive laboratory accreditation standards, including specific NGS checklist requirements for analytical and bioinformatics processes. |
For complex NGS assays, particularly large multi-gene panels for immuno-oncology, a risk-based approach to validation is critical. Under IVDR, manufacturers must define a clear and specific Intended Purpose, which dictates the scope of clinical evidence required [105]. This includes detailing the specific genes, variant types (SNVs, indels, CNVs, fusions), sample types (FFPE, liquid biopsy), and clinical claims (diagnosis, therapy selection). A proactive Post-Market Performance Follow-up (PMPF) plan is mandatory to monitor real-world performance, address emerging evidence, and update variant classifications as scientific knowledge and clinical practice evolve [105].
Diagram 1: NGS Quality & Regulatory Framework
Analytical Validation: Core Principles and Protocols
Analytical validation establishes the performance characteristics of an NGS assay, providing objective evidence that the test consistently and reliably detects the intended variants with a high degree of accuracy and precision. The New York State Department of Health's Clinical Laboratory Evaluation Program (NYS CLEP) guidelines are widely recognized as a national standard for analytical validation, mandating rigorous assessment of accuracy, precision, reproducibility, and analytical sensitivity/specificity [104]. The fundamental principle is assay locking, whereby upon successful validation, the entire workflow—including wet-lab protocols, bioinformatics pipelines, and all versioned reagents—must be formally locked down to ensure future results are comparable to the validation data [101].
A comprehensive analytical validation study must evaluate all variant types and sample types specified in the assay's intended use. For an immuno-oncology panel, this typically includes:
- Single Nucleotide Variants (SNVs) and Insertions/Deletions (Indels)
- Copy Number Variations (CNVs)
- Gene Fusions/Rearrangements
- Microsatellite Instability (MSI) Status
- Tumor Mutational Burden (TMB)
Table 2: Key Analytical Performance Metrics and Target Values for NGS Assay Validation
| Performance Characteristic | Experimental Approach | Target Acceptance Criteria |
|---|---|---|
| Accuracy/Concordance | Comparison to orthogonal method (e.g., Sanger sequencing, digital PCR) or reference materials. | ≥99% for SNVs/Indels; ≥95% for CNVs/Fusions [104]. |
| Precision (Repeatability & Reproducibility) | Intra-run, inter-run, inter-operator, and inter-instrument replication. | 100% concordance for variant calls; ≥95% for key QC metrics (e.g., coverage) [104]. |
| Analytical Sensitivity (Limit of Detection) | Serial dilution of positive samples in negative background; determines minimum Variant Allele Frequency (VAF). | ≥95% detection rate at established VAF cutoff (e.g., 5% for tissue; 1-2% for ctDNA) [105]. |
| Analytical Specificity | Analysis of known negative samples. | ≥99.5% (fewer than 0.5% false positives) [105]. |
| Reportable Range | Assessment of all genomic regions targeted by the panel. | Uniform coverage (e.g., ≥500x for tissue; ≥3000x for ctDNA) for ≥95% of target regions [104]. |
Experimental Protocol for Validation Studies
The following protocol, adapted from the NYS CLEP-compliant validation of the Rapid Pan-Heme (RPPH) assay, provides a template for designing a robust analytical validation study for an immuno-oncology NGS panel [104].
1. Sample Selection and Quality Control (QC):
- Procure well-characterized reference samples from commercial sources (e.g., Genome in a Bottle from NIST) or in-house cell lines.
- For tumor testing, establish a minimum neoplastic cell content threshold (e.g., 20%) to ensure analytical sensitivity. Assess tumor content by pathology review [104].
- Extract nucleic acids using standardized kits. For DNA, quantify using fluorometry (e.g., Qubit dsDNA HS Assay) and assess quality/fragment size (e.g., Agilent TapeStation). Input material must meet pre-defined QC thresholds (e.g., DNA Integrity Number >7 for WGS).
2. Library Preparation and Sequencing:
- For DNA-based panels (SNVs, Indels, CNVs), use hybridization capture or amplicon-based methods (e.g., Archer AMP chemistry) for target enrichment [106] [104].
- For RNA-based fusion detection, use targeted methods like the Archer FusionPlex, which is optimized for degraded FFPE RNA and can identify novel fusions without prior knowledge of the partner gene [106] [104].
- Incorporate Unique Molecular Indices (UMIs) during library preparation to enable error correction and accurate quantification of variant allele frequency [106].
- Perform sequencing on an appropriate NGS platform (e.g., Illumina NextSeq) to achieve a minimum mean depth of coverage commensurate with the intended use (see Table 2).
3. Bioinformatics Analysis:
- Use a locked, version-controlled bioinformatics pipeline for demultiplexing, UMI consensus building, alignment, and variant calling.
- Establish and document all variant filtering parameters and quality thresholds (e.g., minimum read depth, VAF cutoff, quality scores).
4. Data Analysis and Acceptance Criteria:
- Calculate performance metrics (see Table 2) by comparing NGS results to expected values from orthogonal methods or reference materials.
- The assay is considered validated only if all pre-defined acceptance criteria for accuracy, precision, sensitivity, and specificity are met.
Diagram 2: Analytical Validation Workflow
Clinical Validation and Biomarker Application in Immuno-Oncology
While analytical validation confirms an assay measures variants correctly, clinical validation demonstrates that the test results are meaningfully associated with specific clinical endpoints, such as diagnosis, prognosis, or prediction of treatment response [107] [104]. In immuno-oncology, this is paramount for ensuring that NGS-derived biomarkers can reliably guide therapeutic decisions, particularly for immunotherapy.
Distinguishing Prognostic and Predictive Biomarkers
The clinical validation strategy depends fundamentally on whether the biomarker is intended to be prognostic or predictive [107].
Prognostic Biomarkers provide information about the patient's overall cancer outcome, regardless of therapy. They can be identified through retrospective analysis of a cohort representing the target population. An example is the STK11 mutation, which is associated with poorer outcomes in non-squamous non-small cell lung cancer (NSCLC) [107]. Validation involves testing the main effect of the biomarker on a clinical outcome (e.g., overall survival) in a statistical model.
Predictive Biomarkers inform the likely benefit from a specific therapy. They must be identified through an interaction test between the treatment and the biomarker in the context of a randomized controlled trial (RCT) [107]. The IPASS study is a classic example, which established that EGFR mutation status predicts superior progression-free survival with gefitinib versus chemotherapy in NSCLC [107].
Statistical Considerations for Biomarker Validation
Robust clinical validation requires careful statistical planning to avoid bias and overstatement of a biomarker's utility [107].
- Avoiding Bias: Implement randomization (to control for batch effects in testing) and blinding (so those generating biomarker data are unaware of clinical outcomes) during study design [107].
- Statistical Metrics: The appropriate metrics depend on the biomarker's application. Common metrics include sensitivity, specificity, positive/negative predictive values, and measures of discrimination such as the Area Under the Receiver Operating Characteristic Curve (AUC) [107].
- Biomarker Panels: Combining multiple biomarkers into a panel often yields better performance than a single marker. Using continuous data (rather than dichotomized values) retains more information during model development. Methods to control for false discovery (e.g., False Discovery Rate) are essential when evaluating high-dimensional omics data [107].
Application in Immuno-Oncology
Multi-omics strategies, which integrate genomics, transcriptomics, and proteomics, are revolutionizing biomarker discovery in immuno-oncology by providing a comprehensive view of the tumor and its microenvironment [5] [100]. Key clinically validated NGS-based biomarkers include:
- Tumor Mutational Burden (TMB): A high number of mutations per megabase, as validated in the KEYNOTE-158 trial, is an FDA-approved predictive biomarker for response to pembrolizumab across multiple solid tumors [5].
- Microsatellite Instability (MSI): A genomic signature of defective DNA mismatch repair, MSI is a strong predictor of response to immune checkpoint inhibitors [108].
- Gene Expression Profiles (GEPs): RNA sequencing can quantify the expression of immune-related genes to define "hot" vs. "cold" tumor microenvironments, predicting ICI responsiveness [100].
Implementation and Ongoing Quality Assurance
Successfully deploying a validated NGS assay in a clinical or research setting requires meticulous attention to personnel training, ongoing quality monitoring, and post-market surveillance to maintain compliance and performance standards.
Personnel and Training
The complex nature of NGS necessitates a highly specialized workforce. However, retaining proficient personnel is a known challenge, with some positions averaging less than four years of tenure [101]. The NGS QI addresses this by providing tools for personnel management, including SOPs for bioinformatics employee training and competency assessment, which are critical for meeting CLIA and other regulatory personnel requirements [101].
Quality Control and Continuous Monitoring
A locked assay requires continuous performance monitoring using Key Performance Indicators (KPIs). The NGS QI's "Identifying and Monitoring NGS Key Performance Indicators SOP" is a widely used resource for this purpose [101]. Essential KPIs to track per sequencing run include:
- Mean Depth of Coverage and the percentage of targets achieving minimum coverage (e.g., ≥500x).
- Base Quality Scores (e.g., percentage of bases ≥Q30).
- Library Insert Size distribution.
- On-Target Rate (specificity of capture).
- Performance of positive and negative controls.
Deviations from established KPI baselines must be investigated as part of the laboratory's quality management system.
Post-Market Surveillance and PMPF
For IVDR compliance, a Post-Market Performance Follow-up (PMPF) plan is mandatory [105]. This proactive process involves:
- Continuously monitoring the scientific literature and clinical guidelines for changes impacting the test's biomarkers.
- Tracking real-world performance data to identify any discrepancies.
- Planning for and executing re-validation when changes to the locked assay are necessary (e.g., adding a new biomarker, updating the bioinformatics pipeline).
The Scientist's Toolkit: Essential Research Reagent Solutions
The following table details key reagents and technologies referenced in the validation frameworks discussed in this guide.
Table 3: Essential Research Reagent Solutions for NGS Assay Validation
| Reagent/Technology | Primary Function | Key Features & Applications |
|---|---|---|
| Archer NGS Assays (AMP Chemistry) [106] | Targeted library preparation for DNA and RNA. | Enables fusion discovery without prior partner knowledge; flexible panel design; optimized for FFPE and low-input samples. |
| Unique Molecular Indices (UMIs) [106] | Molecular barcoding of nucleic acid molecules. | Error correction for accurate variant calling; reduces false positives; enables quantification of variant allele frequency. |
| NIST Genome in a Bottle (GIAB) Reference Materials [102] | Benchmark reference genomes. | Provides gold-standard variants for assessing assay accuracy during validation. |
| Hybridization Capture Kits (e.g., Agilent Magnis) [104] | Target enrichment for DNA-based panels. | Captures large genomic regions; suitable for comprehensive panels detecting SNVs, Indels, and CNVs. |
| Qiagen Nucleic Acid Extraction Kits [104] | Isolation of DNA and RNA from clinical samples. | Standardized purification from diverse sample types (blood, FFPE, bone marrow); ensures high-quality input material. |
| Integrative Bioinformatics Tools (e.g., IntegrAO, NMFProfiler) [100] | Multi-omics data integration and analysis. | Classifies patient samples using incomplete datasets; identifies biologically relevant signatures across omics layers. |
The establishment of a rigorous framework for clinical NGS assay validation and regulatory compliance is a non-negotiable prerequisite for generating reliable data in immuno-oncology research and drug development. This process, grounded in a robust Quality Management System and adherence to evolving global standards from bodies like the FDA, NYS CLEP, and EU IVDR, ensures that complex NGS assays perform with the accuracy, precision, and reliability required for clinical decision-making. As multi-omics approaches continue to uncover novel biomarkers, the principles outlined in this guide—comprehensive analytical and clinical validation, stringent ongoing quality control, and adaptive post-market surveillance—will remain fundamental. By implementing these frameworks, researchers and drug developers can confidently translate NGS data into actionable insights, ultimately accelerating the delivery of personalized immunotherapies to patients.
Comparing NGS Platforms and Assays for Sensitivity and Specificity
Next-generation sequencing (NGS) has become an indispensable tool in immuno-oncology research, enabling comprehensive profiling of tumor genomes, transcriptomes, and the immune microenvironment. The selection of appropriate NGS platforms and assay configurations directly impacts the sensitivity and specificity of biomarker detection, which in turn influences patient stratification, therapeutic targeting, and clinical trial outcomes. Metagenomic NGS (mNGS) and targeted NGS (tNGS) represent two fundamental approaches with complementary strengths and limitations within the biomarker discovery pipeline [109] [110]. This technical guide provides a detailed comparison of NGS methodologies, focusing on their performance characteristics and applications in immuno-oncology research and drug development.
Metagenomic NGS (mNGS) employs a hypothesis-free approach that sequences all nucleic acids in a sample without prior targeting. This method enables simultaneous detection of diverse pathogens and host genetic material, making it particularly valuable for identifying novel, rare, or unexpected biomarkers [109]. In infectious disease diagnostics, mNGS has demonstrated diagnostic yields as high as 63% in central nervous system infections, compared to less than 30% for conventional approaches [109]. The untargeted nature of mNGS allows researchers to discover previously uncharacterized biomarkers and microbial influences on cancer immunity.
Targeted NGS (tNGS) focuses sequencing capacity on predefined genomic regions of interest using either amplification-based or capture-based enrichment techniques [110] [37]. Amplification-based tNGS uses multiplex PCR to amplify specific targets, while capture-based tNGS employs probes to hybridize and enrich for regions of interest. Targeted panels are meticulously designed to include genes with known clinical or research relevance in cancer, such as those implicated in specific pathways, mutations, or immunotherapy resistance mechanisms [37]. This focused approach significantly reduces data noise and computational burden compared to mNGS.
Table 1: Fundamental Characteristics of mNGS versus tNGS
| Feature | Metagenomic NGS (mNGS) | Targeted NGS (tNGS) |
|---|---|---|
| Sequencing Approach | Untargeted, hypothesis-free | Targeted, hypothesis-driven |
| Target Enrichment | No specific enrichment; may include host DNA depletion | Amplification-based or capture-based methods |
| Advantages | Detects novel/rare pathogens and biomarkers; comprehensive profile | Higher sensitivity for known targets; cost-effective; faster turnaround |
| Limitations | Higher cost; longer turnaround; complex bioinformatics | Limited to predefined genes; may miss novel biomarkers |
| Primary Applications | Discovery-phase research; unknown etiology cases | Clinical validation; therapeutic monitoring; routine diagnostics |
Performance Comparison: Sensitivity and Specificity Metrics
Diagnostic Performance in Clinical Settings
Recent comparative studies have elucidated the distinct performance profiles of different NGS approaches. A 2025 study comparing mNGS with two tNGS methods for lower respiratory infections found that capture-based tNGS demonstrated significantly higher diagnostic accuracy (93.17%) and sensitivity (99.43%) compared to mNGS when benchmarked against comprehensive clinical diagnosis [110]. Meanwhile, amplification-based tNGS showed lower sensitivity for both gram-positive (40.23%) and gram-negative bacteria (71.74%) but higher specificity for DNA virus identification (98.25%) compared to capture-based tNGS (74.78%) [110].
A meta-analysis focusing on periprosthetic joint infection reported pooled sensitivity and specificity of 0.89 and 0.92 for mNGS, compared to 0.84 and 0.97 for tNGS, respectively [111]. The higher specificity of tNGS makes it particularly valuable for confirming infections when false-positive results could lead to unnecessary treatments.
In oncology applications, a systematic review and meta-analysis evaluating NGS for actionable mutations in advanced non-small cell lung cancer (NSCLC) demonstrated that tissue-based NGS achieved 93% sensitivity and 97% specificity for EGFR mutations, and 99% sensitivity and 98% specificity for ALK rearrangements [112]. Liquid biopsy NGS showed strong performance for EGFR, BRAF V600E, KRAS G12C, and HER2 mutations (sensitivity: 80%, specificity: 99%) but exhibited limited sensitivity for fusion detection including ALK, ROS1, RET, and NTRK rearrangements [112].
Table 2: Comparative Performance Metrics Across NGS Applications
| Application & Platform | Sensitivity (%) | Specificity (%) | Area Under Curve (AUC) | Reference |
|---|---|---|---|---|
| Lower Respiratory Infection (2025) | [110] | |||
| ⋄ Metagenomic NGS (mNGS) | Not specified | Not specified | Not specified | |
| ⋄ Capture-based tNGS | 99.43 | Not specified | 93.17 (Accuracy) | |
| ⋄ Amplification-based tNGS | 40.23 (G+ bacteria) | 98.25 (DNA virus) | Not specified | |
| Periprosthetic Joint Infection | [111] | |||
| ⋄ Metagenomic NGS (mNGS) | 89 | 92 | 0.935 | |
| ⋄ Targeted NGS (tNGS) | 84 | 97 | 0.911 | |
| NSCLC (Tissue-based) | [112] | |||
| ⋄ EGFR mutations | 93 | 97 | Not specified | |
| ⋄ ALK rearrangements | 99 | 98 | Not specified | |
| NSCLC (Liquid biopsy) | [112] | |||
| ⋄ EGFR, BRAF, KRAS G12C, HER2 | 80 | 99 | Not specified | |
| ⋄ ALK, ROS1, RET, NTRK fusions | Limited sensitivity reported | 99 | Not specified |
Turnaround Time and Cost Considerations
Operational parameters significantly impact the practical implementation of NGS in research and clinical settings. The same 2025 respiratory infection study reported that mNGS showed significantly higher cost ($840) and longer turnaround time (20 hours) compared to tNGS methods [110]. For advanced NSCLC, liquid biopsy NGS demonstrated a significantly shorter turnaround time (8.18 days) compared to tissue-based approaches (19.75 days; p < 0.001) [112], highlighting one of the key advantages of liquid biopsies for clinical decision-making in oncology.
Experimental Protocols for NGS-Based Biomarker Detection
Protocol 1: Capture-Based Targeted NGS for Solid Tumors
This protocol is adapted from the K-MASTER precision medicine platform and optimized for immuno-oncology biomarker discovery [113]:
Sample Collection and Preparation: Obtain tumor tissue via biopsy (minimum 10-20 mg) or liquid biopsy (10 mL blood in cell-free DNA collection tubes). For tissue samples, use formalin-fixed paraffin-embedded (FFPE) sections with >20% tumor content. For liquid biopsies, process plasma within 4 hours of collection to prevent ctDNA degradation.
Nucleic Acid Extraction: Extract DNA from FFPE sections using the QIAamp DNA FFPE Tissue Kit with extended proteinase K digestion (incubate overnight at 56°C). For liquid biopsies, isolate ctDNA using the MagPure Pathogen DNA/RNA Kit with elution in 25-50 μL TE buffer. Quantify using fluorometry (Qubit dsDNA HS Assay).
Library Preparation: Fragment 50-100 ng DNA to 200-300 bp using ultrasonication. Repair ends and ligate with Illumina-compatible adapters. Perform size selection (200-400 bp) using SPRIselect beads.
Target Enrichment: Hybridize libraries with biotinylated probes targeting a custom immuno-oncology panel (e.g., 409 cancer-related genes, immune checkpoint genes, T-cell receptor sequences, and viral integration sites). Incubate at 65°C for 16-24 hours. Capture target-probe hybrids using streptavidin-coated magnetic beads. Wash with increasing stringency buffers.
Amplification and Quality Control: Amplify captured libraries with 10-12 PCR cycles. Validate library quality using the Agilent 4200 TapeStation System (DV200 > 70%). Quantify by qPCR using the KAPA Library Quantification Kit.
Sequencing: Pool libraries in equimolar ratios. Sequence on Illumina NextSeq 550 or NovaSeq 6000 with 2×150 bp paired-end reads, targeting minimum 500x mean coverage.
Bioinformatic Analysis: Align reads to reference genome (GRCh38) using BWA-MEM. Call variants with GATK Mutect2 (somatic SNVs/indels) and CNVkit (copy number alterations). Annotate variants using Ensembl VEP. For immune profiling, use MiXCR for T-cell receptor repertoire analysis.
Protocol 2: Metagenomic NGS for Microbiome-Immune Interactions
This protocol enables comprehensive profiling of tumor-associated microbiomes and their potential immunomodulatory effects [109] [110]:
Sample Processing: Homogenize 100-200 mg tumor tissue in sterile PBS. Centrifuge at low speed (500 × g) to pellet eukaryotic cells. Collect supernatant and filter through 5 μm then 0.8 μm filters to remove host cells.
Host DNA Depletion: Treat filtrate with Benzonase (25 U/μL) and Tween20 (0.1%) at 37°C for 1 hour to degrade mammalian DNA while protecting microbial DNA with tough cell walls.
Microbial DNA Extraction: Use QIAamp UCP Pathogen DNA Kit with lysozyme (10 mg/mL) and mutanolysin (250 U/mL) pretreatment for gram-positive bacteria. Include bead-beating (0.1 mm zirconia beads) for comprehensive cell lysis.
Library Preparation: Fragment 1-10 ng microbial DNA by ultrasonication. Prepare libraries using the Ovation Ultralow System V2 with 12-14 amplification cycles. Include negative controls (sterile water) and positive controls (mock microbial community) with each batch.
Sequencing: Sequence on Illumina NextSeq 550 with 75 bp single-end reads, generating 20-50 million reads per sample.
Bioinformatic Analysis: Remove human reads by alignment to hg38 using BWA. Quality filter remaining reads with Fastp. Classify microbial reads by alignment to curated RefSeq databases using Kraken2. Perform functional annotation with HUMAnN2 for pathway analysis.
Visualizing NGS Selection Pathways for Immuno-Oncology
The following diagram illustrates the decision-making process for selecting appropriate NGS methodologies in immuno-oncology research based on project goals, sample types, and analytical requirements:
The Scientist's Toolkit: Essential Research Reagent Solutions
Table 3: Key Research Reagents for NGS-Based Biomarker Discovery
| Reagent Category | Specific Products | Function in Workflow |
|---|---|---|
| Nucleic Acid Extraction | QIAamp UCP Pathogen DNA Kit (Qiagen), MagPure Pathogen DNA/RNA Kit (Magen) | Isolate high-quality DNA/RNA while preserving integrity of target sequences |
| Host DNA Depletion | Benzonase (Qiagen), Tween20 (Sigma) | Selectively degrade mammalian DNA to improve microbial signal in low-biomass samples |
| Library Preparation | Ovation Ultralow System V2 (NuGEN), KAPA HyperPrep Kit (Roche) | Convert minimal input DNA into sequencing-ready libraries with minimal bias |
| Target Enrichment | IDT xGen Lockdown Probes, Twist Human Pan-Cancer Panel | Capture and sequence specific genomic regions of interest with high efficiency |
| Sequencing Platforms | Illumina NextSeq 550, Illumina NovaSeq 6000, Oxford Nanopore MinION | Generate high-throughput sequence data with varying read lengths and applications |
| Bioinformatics Tools | GATK, Kraken2, MiXCR, PathoScope, One Codex | Analyze sequencing data, call variants, and perform taxonomic classification |
The optimal selection of NGS platforms and assays requires careful consideration of research objectives, sample characteristics, and analytical requirements. mNGS offers unparalleled potential for novel biomarker discovery and comprehensive profiling of complex samples, while tNGS provides superior sensitivity, specificity, and cost-effectiveness for focused applications. As immuno-oncology continues to evolve, integrating these complementary approaches will accelerate the identification and validation of biomarkers that predict immunotherapy response and resistance, ultimately advancing personalized cancer care. Future developments in long-read sequencing, artificial intelligence-driven analysis, and multi-omics integration promise to further enhance the sensitivity and specificity of NGS platforms for immuno-oncology applications [109] [114].
The advent of immuno-oncology (IO) has revolutionized cancer treatment, leveraging the body's immune system to combat malignancies. Central to optimizing these therapies is the accurate and timely profiling of the tumor microenvironment and its associated biomarkers. Next-Generation Sequencing (NGS) has become an indispensable tool for this biomarker discovery, fueling the need for robust tumor sampling methods. The long-standing gold standard, tissue biopsy, is now complemented—and in some scenarios challenged—by the minimally invasive approach of liquid biopsy. This technical guide provides an in-depth comparison of liquid and tissue biopsy within the context of IO research and drug development, framing their applications, limitations, and technical protocols around the core objective of NGS-driven biomarker discovery.
Tissue Biopsy: The Incumbent Standard
Tissue biopsy involves the physical removal of a tumor tissue sample, typically via core needle, surgical, or fine-needle aspiration. Its primary strength lies in providing a rich, structural context of the tumor.
- Histopathological Context: It allows for direct visualization of tumor morphology, immune cell infiltration, and spatial relationships between tumor and stromal/immune cells within the tumor microenvironment (TME) [115]. This is critical for biomarkers like PD-L1, where expression patterns on tumor versus immune cells have clinical implications [116].
- Comprehensive Biomarker Analysis: Tissue enables a multi-omics approach from a single sample, including genomics, transcriptomics, and proteomics, which can be essential for developing comprehensive biomarker panels [5].
However, tissue biopsy has significant limitations. It is an invasive procedure with associated clinical risks, and it is not always feasible for deep-seated or inaccessible tumors. Furthermore, a single biopsy may not capture tumor heterogeneity, the complex variation within a single tumor or between primary and metastatic sites [116] [117]. This spatial and temporal heterogeneity can lead to sampling bias and an incomplete picture of the biomarker landscape, which is a critical challenge in understanding and predicting response to IO therapies [116].
Liquid Biopsy: A Minimally Invasive Window
Liquid biopsy involves the analysis of tumor-derived components from peripheral blood or other bodily fluids. The key analytes include:
- Circulating Tumor DNA (ctDNA): Short fragments of DNA shed by tumor cells into the bloodstream. It typically constitutes 0.1–1.0% of total cell-free DNA (cfDNA) [118] [117].
- Circulating Tumor Cells (CTCs): Whole cells shed from primary or metastatic tumors, present in very low frequencies (approximately 1 CTC per million leukocytes) [117] [119].
- Extracellular Vesicles (EVs): Membrane-bound particles, including exosomes, that carry proteins, nucleic acids, and lipids from their parent tumor cells [87] [117].
The primary advantages of liquid biopsy are its minimally invasive nature, which allows for serial sampling to monitor tumor evolution and treatment response in real-time, and its potential to provide a more holistic representation of tumor heterogeneity by capturing material from all tumor sites [118] [117] [119]. The main challenge is its lower analytic sensitivity, especially for early-stage disease where tumor shedding is minimal, and the need for highly sophisticated and sensitive detection technologies [120] [119].
Table 1: Core Characteristics of Tissue and Liquid Biopsy
| Feature | Tissue Biopsy | Liquid Biopsy |
|---|---|---|
| Invasiveness | Invasive surgical procedure | Minimally invasive phlebotomy |
| Sampling Feasibility | Limited by tumor accessibility | Generally feasible |
| Tumor Representation | Limited by spatial heterogeneity | Potential "whole-tumor" overview |
| Suitability for Serial Monitoring | Low (highly impractical) | High (ideal for longitudinal studies) |
| Primary Analytes | Formalin-fixed paraffin-embedded (FFPE) tissue, RNA, protein | ctDNA, CTCs, EVs |
| Turnaround Time | Longer (processing and pathology) | Shorter (streamlined workflow) |
Methodologies and Analytical Validation for NGS
The transition of a biopsy sample into robust NGS data requires meticulously validated workflows. The following protocols and validation standards are critical for generating reliable data for IO biomarker discovery.
Sample Preparation and NGS Library Construction
Tissue Biopsy Workflow: Following pathological review and macrodissection to enrich tumor content, nucleic acids are extracted. For NGS, two primary library preparation methods are used:
- Hybrid-Capture-Based: DNA is fragmented, and adapters are ligated. Biotinylated probes complementary to the genes of interest are used to capture the target regions from the entire genomic library. This method is robust for detecting a wide range of variant types, including single nucleotide variants (SNVs), insertions/deletions (indels), copy number alterations (CNAs), and gene fusions, especially when probes are designed to cover intronic regions [121].
- Amplicon-Based: PCR primers are used to amplify specific target regions directly. While highly efficient, it can be susceptible to artifacts like allele dropout [121].
Liquid Biopsy Workflow: Blood is collected in specialized tubes to stabilize nucleated cells and plasma. Plasma is separated via centrifugation, and cfDNA is extracted. Due to the low abundance of ctDNA, library preparation for liquid biopsy almost exclusively uses hybrid-capture-based methods to maximize sensitivity and specificity for detecting low-frequency variants [122]. Protocols must be optimized for shorter DNA fragment lengths characteristic of cfDNA [118].
Analytical Validation and Quality Control
For clinical-grade NGS, rigorous analytical validation is non-negotiable. The Association of Molecular Pathology (AMP) and the College of American Pathologists (CAP) provide best-practice guidelines [121]. Key performance metrics must be established:
- Positive Percentage Agreement (Sensitivity) & Positive Predictive Value (Specificity): Determined for each variant type (SNV, Indel, CNA, Fusion) using validated reference materials.
- Limit of Detection (LOD): The lowest variant allele frequency (VAF) reliably detected by the assay. For liquid biopsy, this is particularly critical, with modern assays demonstrating high sensitivity for VAFs as low as 0.5% [122].
- Precision: Both reproducibility (run-to-run) and repeatability (within-run).
For liquid biopsy assays, a recent international multicenter study of a 32-gene ctDNA panel reported a sensitivity of 96.92% and a specificity of 99.67% for SNVs/Indels at a 0.5% allele frequency, demonstrating the high performance achievable with validated NGS assays [122].
The following workflow diagram illustrates the parallel paths of sample processing for tissue and liquid biopsy in NGS-based biomarker discovery.
Application in Key Immuno-Oncology Biomarkers
The choice between liquid and tissue biopsy is often dictated by the specific biomarker in question. Below is a detailed comparison of their roles in analyzing critical IO biomarkers.
Table 2: Biopsy Modality Performance for Key IO Biomarkers
| Biomarker | Role in IO | Tissue Biopsy Application | Liquid Biopsy Application |
|---|---|---|---|
| PD-L1 Expression | Predicts response to anti-PD-1/PD-L1 therapies | Gold standard via IHC. Allows spatial assessment on tumor/immune cells. Suffers from heterogeneity and assay/platform variability [116]. | Indirect detection via mRNA or protein in EVs is exploratory. Not a validated standalone method for PD-L1 status [87]. |
| Tumor Mutational Burden (TMB) | Measures total mutations; high TMB predicts ICI response [115]. | Measured via NGS panels. Challenged by panel size, bioinformatics, and tissue heterogeneity. | Measured from ctDNA. Emerging as a reliable alternative. Requires careful calibration against tissue TMB and standardization [115] [122]. |
| Microsatellite Instability (MSI) | Pan-cancer biomarker for response to immune checkpoint inhibitors. | Standard via IHC or NGS of tumor tissue. | Can be accurately detected in ctDNA using NGS panels, showing high concordance with tissue-based results [122]. |
| Circulating Tumor Cells (CTCs) | Provide whole cells for functional studies and prognostic value. | Not applicable. | Enriched via EpCAM-based (e.g., CellSearch) or size-based microfluidic chips. Enables functional characterization, culture, and protein analysis (e.g., AR-V7 in prostate cancer) [117] [119]. |
Successful implementation of NGS-based biomarker discovery requires a suite of trusted reagents, platforms, and data resources.
Table 3: Key Research Reagent Solutions for NGS-Based Biopsy Analysis
| Tool / Reagent | Function | Specific Examples / Notes |
|---|---|---|
| NGS Library Prep Kits | Prepare nucleic acids for sequencing by adding adapters and barcodes. | Hybrid-capture kits (e.g., from Illumina, IDT) are preferred for liquid biopsy and comprehensive tissue panels. Amplicon kits (e.g., from Thermo Fisher) offer simplicity for focused panels. |
| ctDNA Extraction Kits | Isolate and purify cell-free DNA from plasma samples. | Specialized kits from QIAGEN, Roche, or Norgen Biotek are designed to maximize yield of short-fragment cfDNA/ctDNA. |
| CTC Enrichment Platforms | Islect rare CTCs from whole blood. | CellSearch: FDA-cleared, immunomagnetic (EpCAM-based) system. Microfluidic Chips (CTC-Chip): Label-free or antibody-based isolation for downstream culture/analysis [117]. |
| Reference Standards | Act as positive controls for assay validation and quality control. | Commercially available from Horizon Discovery, SeraCare, etc. Contain predefined mutations at specific allele frequencies to validate sensitivity and specificity [121]. |
| Bioinformatics Pipelines | Analyze raw NGS data to call variants, TMB, MSI, etc. | Open-source (e.g., GATK, BWA) and commercial software. Must be rigorously validated for each assay and variant type [5] [121]. |
| Multi-omics Databases | Provide context for biomarker discovery and validation. | The Cancer Genome Atlas (TCGA), MSK-IMPACT, CPTAC. Provide integrated genomic, transcriptomic, and proteomic data from thousands of tumor samples [5]. |
Integrated Perspectives and Future Directions
The future of biomarker discovery in IO lies not in choosing one biopsy modality over the other, but in their strategic integration. Tissue biopsy provides the foundational, spatial context, while liquid biopsy offers a dynamic, systemic view. Using them in tandem can provide a more complete picture of the tumor-immune dialogue.
Emerging technologies are pushing the boundaries of both methods. In liquid biopsy, the analysis of methylation patterns in ctDNA shows great promise for early cancer detection and determining the tissue of origin [87] [5]. Single-cell and spatial multi-omics technologies applied to tissue biopsies are unraveling the complex cellular interactions within the TME with unprecedented resolution, identifying novel cellular states and therapeutic targets [5] [115]. Furthermore, the application of artificial intelligence (AI) and machine learning to integrate multi-omics data from both tissue and liquid biopsies is poised to uncover novel, composite biomarkers and significantly improve predictive models for IO response [87] [5].
For researchers and drug developers, the path forward involves:
- Prioritizing Assay Validation: Adhering to established guidelines [121] to ensure data reliability.
- Embracing Standardization: Especially for liquid biopsy-based biomarkers like TMB, to ensure consistency across studies and platforms.
- Designing Studies for Integration: Prospective clinical trials should incorporate paired tissue and serial liquid biopsies to fully leverage the complementary strengths of both modalities in elucidating the mechanisms of response and resistance to immuno-oncology therapies.
Correlating NGS Biomarkers with Clinical Response to Immunotherapy
Next-generation sequencing (NGS) has fundamentally transformed the landscape of immuno-oncology by enabling the comprehensive discovery and validation of biomarkers that predict clinical response to immune checkpoint inhibitors (ICIs) and other immunotherapies. This technical guide synthesizes current evidence and methodologies for correlating NGS-derived biomarkers with immunotherapy outcomes, focusing on both validated and emerging biomarkers across major cancer types. We explore the integration of genomic, transcriptomic, and immunogenomic data to construct predictive models of therapeutic response, addressing both technical considerations and clinical applications. By providing detailed experimental protocols, analytical frameworks, and visualization of key biological pathways, this review serves as an essential resource for researchers and drug development professionals working to advance precision immuno-oncology.
The clinical development of immune checkpoint inhibitors has revealed substantial heterogeneity in treatment response, creating an urgent need for robust biomarkers to guide patient selection [123]. Next-generation sequencing technologies now provide unprecedented capabilities for profiling the complex molecular features that underlie this heterogeneity, enabling a shift from single-analyte tests to comprehensive biomarker panels. NGS facilitates simultaneous assessment of multiple biomarker classes including tumor mutational burden (TMB), microsatellite instability (MSI), genomic alterations in immunomodulatory pathways, and immune cell repertoire diversity [74]. The integration of these data layers with clinical outcomes has become fundamental to understanding the determinants of immunotherapy response and resistance.
In clinical oncology, NGS has streamlined biomarker testing by allowing simultaneous assessment of hundreds of genes from limited tissue samples [124]. This efficiency is particularly valuable in immunotherapy development, where multiple complementary biomarkers may be needed to accurately predict response. The growing adoption of NGS in both research and clinical settings has facilitated the discovery of tissue-agnostic biomarkers such as MSI-high and TMB-high, which now guide treatment decisions across multiple solid tumors [123]. This whitepaper examines the core NGS-derived biomarkers in immuno-oncology, their correlation with clinical outcomes, and the methodological frameworks for their validation and application.
Validated NGS Biomarkers and Clinical Correlations
Established Biomarkers with Clinical Utility
Several NGS-derived biomarkers have achieved validation through prospective clinical trials and are incorporated into clinical practice guidelines. The table below summarizes the key validated biomarkers, their biological significance, and associated clinical outcomes.
Table 1: Validated NGS-Derived Biomarkers for Immunotherapy Response
| Biomarker | Biological Significance | Cancer Types Validated | Clinical Response Correlation |
|---|---|---|---|
| High Tumor Mutational Burden (TMB) | Increased neoantigen load enhancing tumor immunogenicity | Multiple solid tumors (tissue-agnostic) | ORR: 29% in TMB-high (≥10 mut/Mb) vs. 6% in TMB-low in KEYNOTE-158 leading to FDA approval for pembrolizumab [123] |
| Microsatellite Instability-High (MSI-H)/Mismatch Repair Deficient (dMMR) | Defective DNA repair resulting in hypermutation and increased neoantigen formation | Colorectal, endometrial, and multiple other cancers (tissue-agnostic) | ORR: 39.6% with 78% durable responses in KEYNOTE-016/164/158 trials leading to first tissue-agnostic FDA approval for pembrolizumab [123] |
| PD-L1 Expression | Direct measure of PD-1/PD-L1 pathway activation | NSCLC, melanoma, TNBC, HNSCC | In NSCLC with PD-L1 ≥50%, median OS: 30 months with pembrolizumab vs. 14.2 months with chemotherapy (HR: 0.63) in KEYNOTE-024 [123] |
| Homologous Recombination Deficiency (HRD) | Genomic scarring indicative of defective DNA repair, increasing immunogenicity | Breast, ovarian, pancreatic | Emerging biomarker; DeepHRD AI tool improves detection; associated with response to PARP inhibitors and potentially immunotherapy [70] |
Emerging Biomarkers and Multi-Analyte Approaches
Beyond individually validated biomarkers, research increasingly supports integrated biomarker approaches that combine multiple genomic features to improve predictive accuracy. CD274 (PD-L1) amplification has been identified as a genomic biomarker associated with exceptional responses to ICIs in breast cancer and other malignancies [125]. ARID1A alterations have been correlated with enhanced immunotherapy response, potentially through effects on chromatin remodeling and tumor immunogenicity [25]. Additionally, T-cell receptor (TCR) repertoire diversity assessed through NGS of the TCR beta chain has emerged as a promising indicator of pre-existing anti-tumor immunity and capacity for immune response [74].
Multi-omics integration represents the cutting edge of biomarker development, with studies demonstrating approximately 15% improvement in predictive accuracy when combining genomic, transcriptomic, and proteomic data [123]. For instance, the Lung-MAP S1400I trial identified that high CD8⁺GZB⁺ T-cell infiltration (requiring integrated genomic and transcriptomic analysis) predicted improved response to nivolumab, while elevated IL-6 and CXCL13 levels were associated with resistance [123]. These advanced approaches require sophisticated NGS methodologies but offer substantially enhanced predictive value over single-analyte biomarkers.
Table 2: Emerging and Investigational NGS Biomarkers in Immuno-Oncology
| Biomarker | Measurement Approach | Mechanistic Rationale | Current Evidence Level |
|---|---|---|---|
| TCR Clonality/Diversity | NGS of TCR beta chain CDR3 regions | Reflects pre-existing anti-tumor T-cell response breadth and depth | Retrospective analyses across multiple cancers; prognostic in early-stage disease [125] |
| CD274 (PD-L1) Amplification | DNA-based NGS panels or WGS | Genomic driver of PD-L1 overexpression independent of transcriptional regulation | Case series and retrospective cohorts; particularly strong predictor in breast cancer [125] |
| ARID1A Mutations | DNA-based NGS panels | Alters chromatin remodeling, potentially increasing tumor immunogenicity | Retrospective analyses showing correlation with improved ICI response [25] |
| Oncogenic Pathway Alterations (e.g., MAPK, WNT) | Targeted NGS panels | Modulates tumor microenvironment and immune cell infiltration | Preclinical and early clinical evidence for resistance mechanisms [25] |
Experimental Design and Methodological Frameworks
NGS Platform Selection and Assay Design
Effective correlation of NGS biomarkers with immunotherapy response begins with appropriate platform selection. Targeted gene panels (200-500 genes) offer cost-effective TMB assessment and focused mutation profiling with high sequencing depth, ideal for clinical trial biomarker analysis [74]. Whole exome sequencing (WES) provides comprehensive mutation profiling for TMB calculation and neoantigen prediction but with lower depth and higher cost. RNA sequencing enables simultaneous evaluation of gene expression signatures, immune cell deconvolution, and fusion detection, while TCR/BCR sequencing specializes in immune repertoire analysis [5].
For biomarker discovery phases, WES provides the most unbiased approach, while targeted panels are often preferred for validation studies due to their clinical feasibility. The MSK-IMPACT assay exemplifies a successful targeted NGS approach that has identified actionable biomarkers in approximately 37% of tumors [5]. Critical design considerations include ensuring adequate coverage of key immuno-oncology genes (e.g., CD274, JAK1/2, B2M), incorporating appropriate positive and negative controls, and implementing unique molecular identifiers (UMIs) to reduce sequencing artifacts.
Integrated Multi-Technique Approaches
While NGS provides essential genomic information, its predictive value is enhanced when integrated with complementary technologies. Immunohistochemistry (IHC) validates protein expression and provides spatial context for key biomarkers like PD-L1 [74]. Flow cytometry enables detailed immunophenotyping of peripheral blood and dissociated tumor samples, quantifying immune cell populations and activation states [74]. Multiplex IHC/immunofluorescence adds spatial resolution to protein expression data, revealing critical cellular interactions within the tumor microenvironment [10].
A representative integrated workflow begins with simultaneous collection of tumor tissue (FFPE and fresh frozen) and peripheral blood at multiple timepoints (baseline, on-treatment, progression). DNA and RNA are extracted from tumor samples for NGS analysis, while peripheral blood mononuclear cells (PBMCs) are cryopreserved for flow cytometry. The same FFPE blocks used for DNA extraction are sectioned for IHC/ multiplex analysis, enabling direct correlation of genomic features with immune contexture [74].
Diagram 1: Integrated Biomarker Analysis Workflow
Analytical Approaches for Biomarker-Clinical Response Correlation
Robust statistical frameworks are essential for establishing meaningful correlations between NGS biomarkers and clinical outcomes. Time-to-event analyses (Cox proportional hazards models for progression-free survival [PFS] and overall survival [OS]) constitute the primary endpoint for most immunotherapy trials, with biomarker associations expressed as hazard ratios (HRs) and confidence intervals (CIs) [123]. Objective response rate (ORR) analysis using logistic regression models correlates biomarker status with radiographic response per RECIST criteria. Continuous biomarker optimization utilizes receiver operating characteristic (ROC) curves to establish optimal cutpoints for continuous variables like TMB [123].
Longitudinal sampling designs that incorporate on-treatment and progression biopsies enable assessment of dynamic biomarker changes and resistance mechanisms. For such analyses, circulating tumor DNA (ctDNA) monitoring provides a minimally invasive approach to track clonal evolution during therapy [123]. Studies have demonstrated that ≥50% reduction in ctDNA levels within 6-16 weeks of ICI initiation correlates with significantly improved PFS and OS across multiple tumor types [123]. This approach allows for real-time assessment of molecular response and emerging resistance mechanisms.
The Scientist's Toolkit: Essential Research Reagents and Platforms
Table 3: Essential Research Reagents and Platforms for NGS Biomarker Discovery
| Category | Specific Tools/Platforms | Research Application | Key Considerations |
|---|---|---|---|
| NGS Platforms | MSK-IMPACT, FoundationOne CDx, Whole Exome Sequencing | Comprehensive genomic profiling for TMB, MSI, mutation detection | Validation status (LDT vs. FDA-approved), gene content, TMB calculation method [5] |
| RNA Sequencing | Bulk RNA-seq, Single-cell RNA-seq, Spatial transcriptomics | Immune cell deconvolution, gene expression signatures, tumor microenvironment characterization | Input requirements, cellular resolution, integration with spatial data [5] |
| Immuno-seq | TCRβ sequencing, BCR repertoire analysis | T-cell/B-cell clonality, diversity, and tracking of specific clones | Coverage depth, template bias, ability to detect rare clones [74] |
| Multi-omics Integration | DriverDBv4, HCCDBv2, custom machine learning pipelines | Horizontal and vertical integration of multi-omics data for biomarker discovery | Data harmonization methods, computational requirements, interpretability [5] |
| AI/Analytical Tools | DeepHRD, Prov-GigaPath, MSI-SEER, HopeLLM | Pattern recognition in complex datasets, prediction of HRD, MSI from standard images | Training data diversity, algorithmic transparency, regulatory considerations [70] |
| Spatial Biology | Multiplex IHC/IF, CODEX, GeoMx Digital Spatial Profiler | Spatial context of immune cell-tumor interactions, regional biomarker expression | Antibody validation, tissue preservation, data analysis complexity [10] |
Signaling Pathways and Biomarker Biology
The biological rationale for NGS biomarkers in immunotherapy response centers on key signaling pathways that regulate anti-tumor immunity. Understanding these pathways provides essential context for interpreting biomarker data and developing new biomarker hypotheses.
Diagram 2: Key Pathways Linking NGS Biomarkers to Immune Response
The IFNγ signaling pathway represents a central axis connecting tumor genomics with immune recognition. Genomic alterations that increase neoantigen burden (TMB, MSI, HRD) enhance T-cell activation through increased TCR engagement, leading to IFNγ release that subsequently upregulates PD-L1 expression on tumor and immune cells [123]. This pathway creates a feedback loop where tumors with higher immunogenic potential induce their own immune suppression, explaining the correlation between TMB and PD-L1 expression in some cancer types.
The antigen presentation pathway is frequently disrupted in immunotherapy-resistant tumors, with NGS identifying genomic alterations in B2M, HLA genes, and components of the antigen processing machinery. These alterations represent adaptive resistance mechanisms that can be detected through comprehensive genomic profiling [125]. Similarly, alterations in oncogenic pathways such as WNT/β-catenin and MAPK signaling can exclude T-cells from the tumor microenvironment, creating immunologically "cold" tumors resistant to checkpoint inhibition [25].
The correlation of NGS biomarkers with clinical response to immunotherapy continues to evolve beyond single biomarkers toward integrated multi-analyte signatures. The field is moving toward dual-matched therapy approaches where both genomic targets and immune biomarkers inform treatment selection, though currently only 1.3% of clinical trials incorporate biomarkers for both targeted therapy and immunotherapy [25]. Advanced computational methods including machine learning and artificial intelligence are increasingly essential for integrating complex multi-omics data, with models demonstrating superior predictive value compared to individual biomarkers [70] [5].
Future biomarker development will leverage single-cell multi-omics and spatial transcriptomics to resolve tumor and immune heterogeneity at unprecedented resolution [5]. Longitudinal ctDNA monitoring will enable dynamic assessment of clonal evolution during therapy, potentially guiding adaptive treatment strategies [123]. As these technologies mature, the successful translation of NGS biomarkers to clinical practice will require standardized analytical frameworks, robust validation in diverse patient populations, and integration into clinical trial designs that establish both predictive utility and clinical utility for improving patient outcomes.
The integration of Next-Generation Sequencing (NGS) into clinical trial frameworks has fundamentally transformed the paradigm of patient stratification in oncology research. By enabling comprehensive molecular profiling of tumors, NGS facilitates the precise alignment of patients with investigational therapies based on the specific genetic alterations driving their disease. This approach is particularly pivotal in immuno-oncology research, where identifying predictive biomarkers is essential for selecting patients most likely to benefit from immunotherapies. The ability to simultaneously analyze hundreds of genes from limited tissue or liquid biopsy samples allows researchers to stratify patient populations with unprecedented accuracy, thereby enhancing clinical trial efficiency and accelerating the development of targeted treatments [126] [127]. This technical guide explores the foundational methodologies, biomarker applications, and practical implementations of NGS for patient stratification within clinical trials, providing a framework for researchers and drug development professionals operating at the intersection of genomics and therapeutic development.
The shift from histology-based to genomics-driven trial eligibility represents a cornerstone of precision oncology. By 2025, NGS has become embedded in routine practice, with its ability to detect actionable mutations enabling patients to receive targeted therapies sooner, often with better outcomes [126]. The technology's capacity to interrogate diverse molecular features—from single nucleotide variants to complex immune repertoire signatures—provides a multi-dimensional view of the tumor and its microenvironment. This comprehensive profiling is indispensable for identifying patient subpopulations that may exhibit differential responses to immunotherapeutic agents, thereby addressing the critical challenge of patient selection in an era of increasingly mechanism-driven cancer therapies [31] [127].
Foundational Biomarkers for Immuno-Oncology Stratification
Tumor Mutational Burden and Neoantigen Prediction
Tumor Mutational Burden (TMB), defined as the total number of somatic mutations per megabase of DNA, has emerged as a critical independent predictor for patient stratification for response to immunotherapy. Tumors with high TMB are more likely to express neoantigens—novel peptide sequences that are recognized by the immune system as foreign, thereby triggering a robust T-cell response. NGS enables researchers to quantify TMB and predict neoantigen burden through comprehensive genomic and transcriptomic analysis, providing a biomarker for identifying patients most likely to respond to immune checkpoint inhibitors [31] [128].
The analytical workflow for TMB assessment typically involves whole exome sequencing or targeted NGS panels specifically designed to cover coding regions with sufficient breadth to accurately estimate total mutational load. Following variant calling, bioinformatics pipelines filter and annotate somatic mutations, with particular emphasis on non-synonymous mutations that have the highest potential for neoantigen generation. Advanced algorithms then predict which mutated peptides are likely to be presented by major histocompatibility complex (MHC) molecules and potentially recognized by T-cell receptors. This multi-step process, powered by NGS, allows clinical trial designs to stratify patients based on their likelihood of immunotherapy response, ultimately enriching for responders and improving trial success rates [31].
Immune Repertoire Profiling
The T-cell receptor (TCR) repertoire represents the collective diversity of T-cell clones within the tumor microenvironment and peripheral blood, serving as a dynamic indicator of anti-tumor immune activity. NGS-based immune repertoire sequencing provides a powerful tool for characterizing the clonality and diversity of TCR populations, with specific TCR convergence patterns—wherein multiple T-cell clones recognize the same antigen—correlating with effective anti-tumor immunity and positive responses to immunotherapy [31] [128].
Targeted NGS approaches for TCR profiling typically amplify the hypervariable complementarity-determining region 3 (CDR3) of TCR β-chain genes using multiplex PCR systems. The AmpliSeq for Illumina Immune Repertoire Plus TCR Beta Panel is one example of a targeted RNA research panel specifically designed to investigate T-cell diversity and clonal expansion by sequencing T-cell receptor beta chain rearrangements [31]. Through deep sequencing of these regions, researchers can quantify TCR diversity, track dominant clones, and monitor clonal dynamics throughout treatment. In clinical trial settings, baseline TCR metrics and early on-treatment changes in repertoire composition serve as valuable stratification factors and pharmacodynamic biomarkers, enabling real-time assessment of immunotherapy-induced immune modulation [31].
Table 1: Key Biomarkers for NGS-Guided Patient Stratification in Immuno-Oncology Trials
| Biomarker Category | Specific Metrics | NGS Application | Clinical Utility |
|---|---|---|---|
| Tumor Mutational Burden | Mutations per megabase; Non-synonymous mutation count | Whole exome sequencing; Large targeted panels | Predicts response to immune checkpoint inhibitors |
| Neoantigen Landscape | Neoantigen quality and quantity; Clonal vs. subclonal neoantigens | Integration of DNA and RNA sequencing data | Identifies patients with immunogenic tumors; Guides neoantigen-directed therapies |
| TCR Repertoire | Clonality; Diversity; Convergence | Targeted sequencing of TCR CDR3 regions | Measures pre-existing anti-tumor immunity; Monitors immunotherapy-induced immune expansion |
| Microbiome Composition | Intratumoral and gut microbiome signatures | 16S rRNA sequencing; Metagenomic sequencing | Identifies microbiome-associated responders to immunotherapy |
| Gene Expression Profiles | Immune cell signatures; Checkpoint molecule expression | RNA sequencing; Spatial transcriptomics | Quantifies immune cell infiltration; Guides combination therapy strategies |
NGS Methodologies for Patient Stratification
Tissue and Liquid Biopsy Approaches
The application of NGS in clinical trial stratification utilizes both traditional tissue biopsies and emerging liquid biopsy approaches, each offering distinct advantages for specific trial contexts. Tissue-based NGS profiling, typically performed on Formalin-Fixed Paraffin-Embedded (FFPE) tumor specimens, provides comprehensive molecular information from the primary tumor site and remains the gold standard for initial biomarker assessment. However, the invasive nature of tissue biopsies and challenges associated with tumor heterogeneity have driven the adoption of liquid biopsy methods that analyze circulating tumor DNA (ctDNA) from blood samples [126] [129].
Liquid biopsy approaches offer the significant advantage of capturing a more comprehensive representation of tumor heterogeneity across multiple metastatic sites while enabling serial monitoring throughout treatment. In the context of clinical trial stratification, liquid biopsies facilitate real-time molecular assessment of evolving tumor genomes, including the emergence of resistance mechanisms that may inform subsequent line therapy assignments. Furthermore, for trials requiring assessment of minimal residual disease (MRD), NGS-based liquid biopsy approaches provide unprecedented sensitivity for detecting molecular relapse, enabling early intervention strategies in adjuvant settings [126] [129]. The complementary use of both tissue and liquid biopsy NGS profiling in clinical trials provides a comprehensive molecular view that enhances stratification accuracy and enables dynamic patient management throughout the trial lifecycle.
Multiomic Integration for Enhanced Stratification
Multiomic approaches that integrate genomic, transcriptomic, epigenomic, and proteomic data are increasingly advancing patient stratification beyond what can be achieved through genomic analysis alone. By combining multiple molecular data types, researchers can develop more comprehensive biomarker signatures that better capture the complexity of tumor-immune interactions and therapeutic vulnerabilities [31]. NGS serves as the foundational technology enabling these integrated analyses, with different sequencing modalities providing complementary layers of biological insight.
The integration of spatial transcriptomics with genomic data exemplifies the power of multiomic stratification. While standard RNA sequencing provides information about gene expression levels, it loses critical spatial context within the tumor architecture. Spatial transcriptomics technologies preserve this topological information, allowing researchers to map gene expression patterns directly onto tissue sections and articulate biological interactions at the cellular level. This approach enables precise characterization of immune cell localization relative to tumor nests, stromal components, and vascular structures—spatial relationships that profoundly influence immunotherapy response [31]. Similarly, the incorporation of epigenetic profiling through methods like chromatin immunoprecipitation sequencing (ChIP-Seq) and assay for transposase-accessible chromatin with sequencing (ATAC-Seq) provides insights into the regulatory mechanisms governing gene expression programs relevant to therapeutic response. The convergence of these diverse data types through integrated bioinformatics pipelines creates multidimensional biomarker signatures with enhanced predictive power for clinical trial stratification [31].
Experimental Protocols for NGS-Based Stratification
Sample Processing and Library Preparation
Robust sample processing and library preparation are critical prerequisites for generating high-quality NGS data suitable for patient stratification in clinical trials. The following protocol outlines a standardized workflow for processing FFPE tissue specimens, the most common sample type in oncology trials:
Protocol 1: FFPE DNA Extraction and Quality Control
- Deparaffinization: Incubate FFPE sections at 65°C for 10 minutes, followed by xylene treatment to remove paraffin.
- DNA Extraction: Use commercial kits (e.g., QIAamp DNA FFPE Tissue Kit) with optimized proteolytic digestion (proteinase K, 56°C overnight) to isolate high-quality DNA from tumor regions with >20% tumor cellularity.
- DNA Quantification: Assess DNA concentration using fluorometric methods (e.g., Qubit dsDNA HS Assay); verify fragment size distribution via capillary electrophoresis (e.g., TapeStation Genomic DNA ScreenTape).
- Quality Thresholds: Proceed with samples yielding ≥50ng of DNA with average fragment sizes ≥200bp; exclude degraded samples failing quality metrics [31] [129].
Protocol 2: Library Preparation for Targeted Sequencing
- DNA Shearing: Fragment 50-100ng of input DNA to ~200bp using acoustic shearing (Covaris) or enzymatic fragmentation (Illumina DNA Prep).
- Library Construction: Perform end-repair, A-tailing, and adapter ligation using commercial library preparation kits compatible with downstream hybridization capture.
- Target Enrichment: Hybridize libraries with biotinylated probes targeting specific gene panels (e.g., immuno-oncology-focused panels covering TMB-relevant genes, immune checkpoint genes, and HLA typing); use streptavidin-coated beads for capture.
- Library Amplification: Perform 8-10 cycles of PCR amplification to enrich for target-bound fragments; purify final libraries using SPRI bead-based cleanups [31].
Protocol 3: RNA Library Preparation for Immune Repertoire Sequencing
- RNA Extraction: Isolve total RNA from PAXgene-fixed or flash-frozen tissue using silica-membrane based kits with DNase I treatment.
- TCR Amplification: Use multiplex PCR systems (e.g., AmpliSeq for Illumina Immune Repertoire Plus TCR Beta Panel) with primers targeting TCR V, D, and J gene segments.
- Library Indexing: Incorporate dual indices during amplification to enable sample multiplexing; purify libraries and assess quality via capillary electrophoresis [31].
Sequencing and Data Analysis
Following library preparation, sequencing and bioinformatic analysis transform raw data into actionable stratification biomarkers:
Protocol 4: Sequencing Execution and Quality Control
- Platform Selection: Utilize Illumina NovaSeq X Series for production-scale sequencing or NextSeq 1000/2000 Systems for mid-throughput applications.
- Sequencing Configuration: Sequence targeted DNA libraries to ≥500x mean coverage with >95% of targets achieving ≥100x coverage; sequence TCR libraries to sufficient depth (>1 million reads per sample) to detect rare clones.
- QC Metrics: Monitor sequencing quality through base call quality scores (Q30 ≥80%), cluster density within optimal range, and minimal index hopping (<1%) [31].
Protocol 5: Bioinformatic Analysis for Stratification Biomarkers
- Variant Calling: Align sequencing reads to reference genome (GRCh38) using optimized aligners (BWA-MEM, STAR); call somatic variants using mutational callers (MuTect2, VarScan) with filtering against population databases (gnomAD, 1000 Genomes).
- TMB Calculation: Count coding, non-synonymous somatic mutations (excluding known drivers and germline variants); normalize by the total megabases of effectively sequenced territory.
- Neoantigen Prediction: Use computational tools (NetMHC, NetMHCpan) to predict MHC binding affinity of mutant peptides based on patient HLA type (determined from sequencing data).
- TCR Repertoire Analysis: Assemble CDR3 sequences from immune repertoire sequencing data using specialized tools (MiXCR, IMGT/HighV-QUEST); quantify clonality and diversity metrics [31] [130].
Table 2: Essential Research Reagent Solutions for NGS-Based Stratification
| Reagent Category | Specific Product Examples | Primary Function | Application in Stratification |
|---|---|---|---|
| Nucleic Acid Extraction Kits | QIAamp DNA FFPE Tissue Kit; RNeasy Mini Kit | Isolation of high-quality DNA/RNA from clinical specimens | Ensures input material quality for reliable variant calling |
| Library Preparation Kits | Illumina DNA Prep; TruSeq RNA Library Prep Kit | Conversion of nucleic acids into sequencing-ready libraries | Standardizes library construction across multiple trial sites |
| Target Enrichment Panels | AmpliSeq for Illumina Immune Repertoire Plus; TruSight Oncology 500 | Selective capture of genomic regions relevant to immunotherapy response | Enables focused sequencing of stratification biomarkers |
| Sequencing Reagents | NovaSeq X Series Reagent Kits; NextSeq 1000/2000 P3 Reagents | Template amplification and nucleotide incorporation during sequencing | Generates high-quality sequencing data for biomarker assessment |
| Bioinformatic Tools | BaseSpace Sequence Hub; Local Run Manager | Management, analysis, and interpretation of NGS data | Transforms raw sequencing data into clinical stratification decisions |
Visualizing NGS Stratification Workflows
The following diagrams illustrate key experimental and analytical workflows for NGS-guided patient stratification in clinical trials, providing visual references for implementation.
NGS Stratification Biomarker Workflow
Multiomic Data Integration for Enhanced Stratification
The strategic implementation of NGS-guided patient stratification represents a transformative advancement in clinical trial methodology, particularly within the domain of immuno-oncology research. By leveraging comprehensive molecular profiling to align patients with targeted therapies and immunomodulatory agents, researchers can significantly enhance trial efficiency, increase the probability of technical success, and accelerate the development of novel cancer treatments. The integration of multiomic data streams—encompassing genomic, transcriptomic, and immune repertoire information—provides an increasingly refined lens through which to view patient subpopulations most likely to derive clinical benefit from specific therapeutic interventions.
As NGS technologies continue to evolve, becoming more accessible, cost-effective, and analytically robust, their role in clinical trial stratification will undoubtedly expand. Future directions will likely include greater incorporation of artificial intelligence methodologies for biomarker discovery, increased utilization of liquid biopsy approaches for dynamic monitoring, and more sophisticated integration of spatial biology data to contextualize immune-tumor interactions within the tissue microenvironment [127] [131]. For researchers and drug development professionals, maintaining expertise in both the technical aspects of NGS implementation and the analytical frameworks for biomarker interpretation will be essential for harnessing the full potential of this powerful technology to advance precision oncology and deliver more effective, personalized cancer therapies to patients.
Conclusion
NGS has become an indispensable engine for biomarker discovery in immuno-oncology, fundamentally advancing our ability to decode the complex dialogue between tumors and the immune system. The integration of multi-omics data, powered by AI and sophisticated computational models, is moving the field beyond single biomarkers towards holistic, predictive signatures of treatment response. Future progress hinges on overcoming tumor heterogeneity, standardizing analytical and clinical validation pathways, and broadening access to NGS technologies. The continued evolution of NGS promises to further refine patient stratification, unlock novel therapeutic targets like shared neoantigens, and solidify a new paradigm of truly personalized cancer immunotherapy, ultimately improving outcomes for patients.
References
- 1. The role of neoantigens and tumor mutational burden in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12406617/]
- 2. Tumour Mutational Burden & Microsatellite Instability | Nonacus [https://nonacus.com/blog-tumour-mutational-burden-microsatellite-instability-markers-immunotherapy-response/]
- 3. Microsatellite Instability ( MSI ) | Thermo Fisher Scientific - SG [https://www.thermofisher.com/sg/en/home/life-science/sequencing/sequencing-learning-center/next-generation-sequencing-information/cancer-research/microsatellite-instability.html]
- 4. Development of tumor mutation burden as an immunotherapy... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6336005/]
- 5. Multi-omics strategies for biomarker discovery and application ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12638490/]
- 6. Advances and challenges in neoantigen prediction for ... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2025.1617654/full]
- 7. Computation strategies and clinical applications in neoantigen ... [https://biomarkerres.biomedcentral.com/articles/10.1186/s40364-025-00808-9]
- 8. Uncovering PD-L1 among immune cell predictive ... [https://pubmed.ncbi.nlm.nih.gov/40499464/]
- 9. Next-Generation Sequencing-Based MSI Scoring Predicts Benefit in... [https://pubmed.ncbi.nlm.nih.gov/39670863/]
- 10. Emerging Technologies in Biomarker Discovery You ... [https://blog.crownbio.com/emerging-technologies-in-biomarker-discovery-you-should-know-about]
- 11. Attention-aware differential learning for predicting peptide-MHC class... [https://pubmed.ncbi.nlm.nih.gov/39883517/]
- 12. Clinical Impact of Next-Generation Sequencing-Guided ... [https://pubmed.ncbi.nlm.nih.gov/41101085/]
- 13. Frontiers | T - cell identified by a personalized... receptors [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2025.1509855/full]
- 14. Tumoral RNA splicing: source of neoantigens for off-the-shelf therapies? [https://acir.org/weekly-digests/2025/march/tumoral-rna-splicing-source-of-neoantigens-for-off-the-shelf-therapies]
- 15. Structural basis for self-discrimination by neoantigen -specific TCRs [https://www.nature.com/articles/s41467-024-46367-9?error=cookies_not_supported&code=8eab7030-8679-4a6a-940e-65381a90733c]
- 16. Automated NGS Workflows for Biomarker Discovery | IDT [https://www.idtdna.com/pages/about/news/2025/10/01/integrated-dna-technologies-and-hamilton-company-partner-to-automate-customizable-ngs-workflows-and-accelerate-biomarker-discovery]
- 17. Pillar Biosciences to Showcase NGS Research Insights at ... [https://www.prnewswire.com/news-releases/pillar-biosciences-to-showcase-ngs-research-insights-at-2025-amp-meeting-302591939.html]
- 18. Revolutionizing cancer immunology: the power of next ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6366855/]
- 19. Next-Generation Sequencing Technology: Current Trends ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10376292/]
- 20. Next-Generation Immuno-Oncology Solutions [https://www.thermofisher.com/us/en/home/products-and-services/promotions/life-science/next-generation-immuno-oncology-solutions.html]
- 21. BostonGene Named Platinum Winner for AI Research ... [https://bostongene.com/news-and-publications/news/bostongene-named-platinum-winner-for-ai-research-innovation-at-2025-pinnacle-awards]
- 22. ngs.plot: Quick mining and visualization of next-generation ... [https://bmcgenomics.biomedcentral.com/articles/10.1186/1471-2164-15-284]
- 23. The evolving landscape of biomarkers for checkpoint inhibitor ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6705396/]
- 24. Beyond single biomarkers: multi-omics strategies to predict ... [https://link.springer.com/article/10.1007/s10238-025-01902-w]
- 25. Gene- and immune-targeted therapy combinations using ... [https://www.nature.com/articles/s41698-025-01038-w]
- 26. Genomic landscape associated with potential response to ... [https://www.nature.com/articles/s41467-017-01018-0]
- 27. Clinical Applications of Next-Generation Sequencing in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6658137/]
- 28. New clinical trial design in precision medicine [https://www.nature.com/articles/s41392-024-01760-0]
- 29. Predictive models for immune checkpoint inhibitor ... [https://www.sciencedirect.com/science/article/pii/S1040842825003683]
- 30. Immunotherapy and next-generation sequencing guided ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6934166/]
- 31. Immuno-Oncology Research | Cancer immunotherapy ... [https://www.illumina.com/areas-of-interest/cancer/research/applications/immuno-oncology-research.html]
- 32. An Updated Overview of Existing Cancer Databases and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10452211/]
- 33. Human Multi-Omic Data - Data-Driven Science (DDS) Hub - NIH [https://www.ddshub.nih.gov/data-sources/human-multiomic-data]
- 34. Cancer Multi-Omics Database for Machine Learning [https://www.nature.com/articles/s41597-025-05235-x]
- 35. CIMACs and CIDC Network - NCI [https://dctd.cancer.gov/research/networks/precision-medicine-oncology/cimac-cidc]
- 36. vs WGS vs Custom Panels WES [https://sequencing.roche.com/us/en/article-listing/wes-wgs-custom.html]
- 37. Targeted Gene Panels: Revolutionizing Genomic Testing ... [https://blog.crownbio.com/targeted-gene-panels-genomic-testing-oncology]
- 38. A targeted next-generation sequencing panel for ... [https://www.nature.com/articles/s41598-025-08039-6]
- 39. Translational and clinical comparison of whole genome ... [https://www.nature.com/articles/s41698-024-00788-3]
- 40. Accuracy benchmark of the GeneMind GenoLab M sequencing... [https://bmcgenomics.biomedcentral.com/articles/10.1186/s12864-022-08775-3]
- 41. Automated NGS Workflows for Biomarker Discovery | IDT [https://sg.idtdna.com/pages/about/news/2025/10/01/integrated-dna-technologies-and-hamilton-company-partner-to-automate-customizable-ngs-workflows-and-accelerate-biomarker-discovery]
- 42. Next-Generation Sequencing: A Review of Its ... [https://www.mdpi.com/2075-4418/15/19/2425]
- 43. Target Validation by Immunopeptidomics for Epitope-Specific ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9018990/]
- 44. optiPRM: A Targeted Immunopeptidomics LC-MS Workflow ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11405902/]
- 45. An Automated Workflow to Address Proteome Complexity ... [https://www.sciencedirect.com/science/article/pii/S1535947625001380]
- 46. Mass spectrometry–based identification of MHC-bound peptides for immunopeptidomics | Nature Protocols [https://www.nature.com/articles/s41596-019-0133-y]
- 47. Mass spectrometry-based identification of MHC-bound peptides for immunopeptidomics - PubMed [https://pubmed.ncbi.nlm.nih.gov/31092913/]
- 48. Mass Spectrometry-Based Identification of MHC-Associated Peptides - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC7139412/]
- 49. Immunopeptidomics Workflows [https://www.thermofisher.com/us/en/home/industrial/mass-spectrometry/immunopeptidomics-mass-spectrometry/workflows.html]
- 50. High-throughput, targeted MHC class I immunopeptidomics ... [https://www.nature.com/articles/s41587-022-01566-x]
- 51. Single-cell multi-omics in cancer immunotherapy: from tumor ... [https://molecular-cancer.biomedcentral.com/articles/10.1186/s12943-025-02426-3]
- 52. Decoding the Tumor Microenvironment: Insights and New ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12468534/]
- 53. Tumour evolution and microenvironment interactions in 2D ... [https://www.nature.com/articles/s41586-024-08087-4]
- 54. Single-cell transcriptomics reveals biomarker ... [https://www.nature.com/articles/s41523-025-00803-1]
- 55. Dissecting tumor transcriptional heterogeneity from single-cell ... [https://pubmed.ncbi.nlm.nih.gov/39747597/]
- 56. Frontiers | Immunotherapy biomarkers in brain metastases: insights... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2025.1600261/full]
- 57. Testing and RNA NGS : Profiling... Biomarker Biomarker Discovery [https://www.sepscience.com/ngs-biomarker-testing-and-rna-biomarker-discovery-profiling-transcriptomic-signatures-12051]
- 58. pVAC-Seq: A genome-guided in silico approach to identifying ... [https://genomemedicine.biomedcentral.com/articles/10.1186/s13073-016-0264-5]
- 59. pVACtools: a computational toolkit to identify and visualize ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7056579/]
- 60. pVACtools — pVACtools 6.0.2 documentation [https://pvactools.readthedocs.io/]
- 61. Computational Pipeline for the PGV-001 Neoantigen ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5778604/]
- 62. NeoPredPipe: high-throughput neoantigen prediction and ... [https://bmcbioinformatics.biomedcentral.com/articles/10.1186/s12859-019-2876-4]
- 63. Radiotherapy-exposed CD8+ and CD4+ neoantigens enhance tumor... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7919731/]
- 64. Artificial Intelligence in Next-Generation Sequencing... Integrating [https://pmc.ncbi.nlm.nih.gov/articles/PMC12191491/]
- 65. Machine learning enhances biomarker discovery: From multi [https://esmed.org/MRA/mra/article/view/6888]
- 66. Machine Learning: A New Prospect in Multi-Omics Data ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8829119/]
- 67. GSK's Head of Precision Medicine on Biomarker Focus ... [https://theconferenceforum.org/editorial/gsks-head-of-precision-medicine-on-biomarker-focus-and-the-use-of-next-generation-technologies]
- 68. Challenges and Future Trends in Biomarker Analysis for Clinical... [https://blog.crownbio.com/challenges-and-future-trends-in-biomarker-analysis-for-clinical-research-whats-ahead-in-2025]
- 69. The role of multi-omics in biomarker discovery, diagnosis ... [https://www.sciencedirect.com/science/article/pii/S2214031X25001196]
- 70. Top Oncology Innovations That Shaped the First Half of 2025 [https://binaytara.org/cancernews/article/top-oncology-innovations-that-shaped-the-first-half-of-2025]
- 71. Biomarkers and Precision Medicine 2025 [https://www.labcorp.com/education-events/events/biomarkers-2025]
- 72. Tumor heterogeneity: preclinical models, emerging ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10175698/]
- 73. MyClone: rapid and precise reconstruction of clonal ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12506407/]
- 74. Combining Flow Cytometry, IHC, and NGS in Immuno- ... [https://www.cerbaresearch.com/article/blog-post-combining-flow-cytometry-ihc-and-ngs-in-immuno-oncology-the-essential-trio-for-biomarker-assessment-success/]
- 75. Resolving intra-tumor heterogeneity and clonal evolution of ... [https://ehoonline.biomedcentral.com/articles/10.1186/s40164-025-00718-4]
- 76. Advances and challenges in neoantigen prediction for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12198247/]
- 77. Sensitive neoantigen discovery by real-time mutanome- ... [https://www.nature.com/articles/s41467-025-62647-4]
- 78. Immuno-oncology research overview [https://www.abcam.com/en-us/knowledge-center/oncology/immuno-oncology-research]
- 79. A Bioinformatics Toolkit for Next-Generation Sequencing in ... [https://www.mdpi.com/1467-3045/45/12/608/xml]
- 80. A Bioinformatics Toolkit for Next-Generation Sequencing in ... [https://pubmed.ncbi.nlm.nih.gov/38132454]
- 81. With Great FFPE Challenges, Comes Novel Research ... [https://www.admerahealth.com/blog/optimizations-for-ffpe-samples]
- 82. Cancer Biomarker Discovery and Verification for Immuno ... [https://www.thermofisher.com/us/en/home/life-science/cancer-research/immuno-oncology-research/cancer-biomarker-discovery-validation.html]
- 83. An NGS-based assay for accurate detection and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11104603/]
- 84. Cancer Biomarkers | NGS detection [https://www.illumina.com/areas-of-interest/cancer/ngs-in-oncology/biomarkers.html]
- 85. Optimize FFPE Library Preparation for NGS [https://www.technologynetworks.com/genomics/application-notes/optimize-ffpe-library-preparation-for-ngs-391853]
- 86. Oncomine Immune Response Research Assay [https://www.thermofisher.com/us/en/home/clinical/preclinical-companion-diagnostic-development/oncomine-oncology/oncomine-immune-response-research-assay.html]
- 87. Cancer Biomarkers: Reflection on Recent Progress, Emerging ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12468363/]
- 88. Next-generation sequencing in cancer diagnosis and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12009796/]
- 89. Recommendations for bioinformatics in clinical practice [https://genomemedicine.biomedcentral.com/articles/10.1186/s13073-025-01543-4]
- 90. Next Generation Sequencing Platform: Ultimate Guide 2025 [https://lifebit.ai/blog/next-generation-sequencing-platform/]
- 91. Applications and challenges of biomarker-based predictive ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12399543/]
- 92. The 2025 Bioinformatics Toolkit: From Sample Prep to AI- ... [https://blog.omni-inc.com/blog/the-2025-bioinformatics-toolkit-from-sample-prep-to-ai-driven-analysis]
- 93. How-to: NGS Quality Control [https://frontlinegenomics.com/how-to-ngs-quality-control/]
- 94. Best Practices for Quality Control of NGS Data [https://www.basepairtech.com/blog/best-practices-for-quality-control-and-pre-processing-of-ngs-data-a-guide-for-academic-researchers/]
- 95. bridging inequities in NGS fosters equity in targeted treatment [https://pmc.ncbi.nlm.nih.gov/articles/PMC12060717/]
- 96. GOAL: A Collaborative Approach to Next Generation ... [https://oxfordglobal.com/precision-medicine/resources/goal-a-collaborative-approach-to-next-generation-sequencing-in-oncology-and-beyond]
- 97. An NGS Workflow Blueprint for DNA Sequencing Data and Its ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4827795/]
- 98. Biomarker Discovery & Translational Research [https://www.foundationmedicine.com/service/discovery-and-translational-research]
- 99. Computational Tools for Next-Generation Sequencing ... [https://dromicslabs.com/computational-tools-for-next-generation-sequencing-analysis-a-comprehensive-guide/]
- 100. The Future of Clinical Trials: Incorporating 'Omics for ... [https://blog.crownbio.com/the-future-of-clinical-trials-incorporating-omics-for-enhanced-stratification]
- 101. Early Release - The Next-Generation Sequencing Quality Initiative and... [https://wwwnc.cdc.gov/eid/article/31/13/24-1175_article]
- 102. Evolving Standards in Clinical (updated) - Euformatics NGS [https://www.euformatics.com/blog-post/evolving-standards-in-clinical-ngs]
- 103. Considerations for Design, Development, and Analytical... | FDA [https://www.fda.gov/regulatory-information/search-fda-guidance-documents/considerations-design-development-and-analytical-validation-next-generation-sequencing-ngs-based]
- 104. A Comprehensive Guide to Achieving New York State Clinical ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12163385/]
- 105. IVDR Compliance for Next-Generation Sequencing ( NGS ): Key... [https://www.qbdgroup.com/en/blog/ivdr-compliance-large-panel-ngs]
- 106. Archer NGS Solutions & Assays | IDT [https://sg.idtdna.com/page/solutions/research-techniques/next-generation-sequencing/archer-ngs-technology/]
- 107. Biomarker Discovery and Validation: Statistical Considerations [https://pmc.ncbi.nlm.nih.gov/articles/PMC8012218/]
- 108. A Comprehensive Oncological Biomarker Framework ... [https://www.mdpi.com/2218-273X/15/9/1304]
- 109. Metagenomic Next-Generation Sequencing in Infectious ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12384723/]
- 110. Comparative diagnostic performance of metagenomic and ... [https://www.nature.com/articles/s41598-025-11834-w]
- 111. Comparative Diagnostic Accuracy of Metagenomic Next ... [https://www.sciencedirect.com/science/article/pii/S0163445325002610]
- 112. Diagnostic accuracy of next-generation sequencing (NGS) ... [https://link.springer.com/article/10.1007/s12094-025-04040-7]
- 113. Comparison of the Data of a Next-Generation Sequencing ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8756135/]
- 114. AI-driven biomarker discovery: enhancing precision in cancer ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11906928/]
- 115. Next-Generation Sequencing Applications for Preclinical ... [https://blog.championsoncology.com/blog/next-generation-sequencing-applications-for-preclinical-oncology-research]
- 116. - and Tissue -based biomarkers for immunotherapy in... liquid biopsy [https://pmc.ncbi.nlm.nih.gov/articles/PMC10070181/]
- 117. : a step closer to transform diagnosis, prognosis and... Liquid biopsy [https://molecular-cancer.biomedcentral.com/articles/10.1186/s12943-022-01543-7]
- 118. Liquid biopsy in cancer: current status, challenges and ... [https://www.nature.com/articles/s41392-024-02021-w]
- 119. Liquid biopsy – a narrative review with an update on current ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12333414/]
- 120. Emerging biomarkers for early cancer detection and diagnosis [https://eurjmedres.biomedcentral.com/articles/10.1186/s40001-025-03003-6]
- 121. Guidelines for Validation of Next-Generation Sequencing– ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6941185/]
- 122. Analytical Validation of a Pan-Cancer NGS Assay for In- ... [https://www.sciencedirect.com/science/article/pii/S152515782500220X]
- 123. Predictive Biomarkers in Cancer Immunotherapy [https://pmc.ncbi.nlm.nih.gov/articles/PMC12289453/]
- 124. NGS Streamlines Biomarker Testing in Solid Tumors [https://www.oncnursingnews.com/view/ngs-streamlines-biomarker-testing-in-solid-tumors]
- 125. Biomarkers of response and resistance to immune ... [https://www.sciencedirect.com/science/article/pii/S0960977625005624]
- 126. Oncology Next Generation Sequencing ( Clinical ) in the Real... NGS [https://www.linkedin.com/pulse/clinical-oncology-next-generation-sequencing-puoof]
- 127. Frontiers | Next Generation Sequencing ( NGS ) and Cancer: New Steps... [https://www.frontiersin.org/journals/genetics/articles/10.3389/fgene.2025.1675753/abstract]
- 128. - Immuno with Oncology | Thermo Fisher Scientific - US Research NGS [https://www.thermofisher.com/us/en/home/life-science/sequencing/sequencing-learning-center/next-generation-sequencing-information/immuno-oncology-research.html]
- 129. Minimal residual disease detection by next-generation ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9426755/]
- 130. NGS Catalog: A Database of Next Generation Sequencing ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4431973/]
- 131. Artificial intelligence for predictive biomarker in... discovery [https://pubmed.ncbi.nlm.nih.gov/37879443/]