Navigating the Landscape: How Waddington's Epigenetic Model is Revolutionizing Cancer Reversion Strategies
This article explores the Waddington epigenetic landscape as a foundational framework for understanding and inducing cancer reversion.
Navigating the Landscape: How Waddington's Epigenetic Model is Revolutionizing Cancer Reversion Strategies
Abstract
This article explores the Waddington epigenetic landscape as a foundational framework for understanding and inducing cancer reversion. We provide a comprehensive analysis spanning from the core concepts of cellular plasticity and attractor states to the latest methodological approaches, including epigenetic reprogramming and differentiation therapy. The content addresses critical challenges in the field, such as stability and specificity, and validates progress through comparative analysis of emerging therapeutic strategies. Designed for researchers and drug development professionals, this synthesis aims to bridge theoretical models with translational applications for next-generation oncology.
The Conceptual Landscape: Understanding Waddington's Metaphor in Cancer Biology
Introduction The conceptual framework of Conrad H. Waddington's epigenetic landscape, originally proposed to visualize cell fate decisions during embryonic development, has found a profound modern application in oncology. This whitepaper re-examines this metaphor through the lens of current systems biology, framing cancer as a disease of disrupted epigenetic topography where cells become trapped in aberrant, proliferative "valleys." The thesis herein posits that understanding the molecular gradients and canalizing forces that shape this landscape is critical for pioneering cancer reversion therapies—strategies aimed not at killing malignant cells, but at coaxing them back onto differentiation pathways toward benign states.
The Modern Molecular Landscape: From Metaphor to Mechanism Waddington’s pictorial metaphor is now underpinned by quantifiable molecular determinants. The landscape's topography is sculpted by three primary interacting forces: transcriptional networks, chromatin remodeling complexes, and signaling pathway activity. Key developmental pathways, repurposed in cancer, serve as the dominant "gravitational" forces.
Table 1: Core Molecular Determinants of the Oncogenic Landscape
| Determinant | Role in Landscape Sculpting | Exemplary Components | Association with Cancer Reversion |
|---|---|---|---|
| Chromatin Modifiers | Alter slope and depth of valleys; define epigenetic plasticity. | DNMTs, HDACs, EZH2 (PRC2), SWI/SNF complexes. | Inhibition can flatten malignant valleys, allowing cellular re-routing (e.g., DNMT inhibitors in AML). |
| Transcription Factors (TFs) & Pioneer Factors | Define attractor states (valleys); stabilize cell fate. | OCT4, SOX2, NANOG (pluripotency); p53, MYC. | Ectopic expression can reprogram cells (e.g., OSKM in iPSCs; GATA1 in erythroleukemia). |
| Signaling Pathways | Provide extracellular cues that bias downhill trajectories. | WNT, Hedgehog, Notch, TGF-β. | Modulation can redirect differentiation (e.g., BMPs in glioma stem cells). |
| Non-Coding RNAs | Fine-tune gradients and barrier heights. | miR-145, miR-34 (tumor suppressors); HOTAIR, XIST. | Delivery of tumor-suppressive miRNAs can promote differentiation. |
Experimental Paradigms for Mapping and Manipulating the Landscape 1. Mapping Landscape Topography with Single-Cell Multi-Omics Protocol: Single-Cell ATAC-seq + RNA-seq Integration
- Cell Preparation: Generate a single-cell suspension from tumor or differentiating model system (viability >80%).
- Nuclei Isolation & Tagmentation: Isolate nuclei using a gentle lysis buffer. Use engineered Tn5 transposase to simultaneously fragment accessible chromatin and insert sequencing adapters (10x Genomics Chromium Next GEM Chip).
- Post-Labeling & Sequencing: Perform a two-step PCR to add sample indices and sequencing handles. For scRNA-seq from the same cells, partition cells into droplets with barcoded beads. Generate paired-end sequencing libraries.
- Data Analysis: Align ATAC-seq reads to a reference genome (e.g., using Cell Ranger ARC). Call peaks. Use tools like Seurat or ArchR to perform joint clustering, construct trajectories (via Monocle3 or PAGA), and infer transcription factor regulon activity (using SCENIC). Chromatin accessibility dynamics along pseudotime define landscape valleys and ridges.
2. Forcing Landscape Reversion: Epigenetic and Differentiation Therapy Protocol: Combinatorial Epigenetic Intervention in Glioblastoma Stem Cells (GSCs)
- Objective: Induce astrocytic differentiation by co-targeting histone methylation and DNA methylation.
- Materials: Patient-derived GSCs cultured in stem-permissive media (Neurobasal-A, B27, EGF, FGF). Small-molecule inhibitors: GSK343 (EZH2 inhibitor) and 5-Azacytidine (DNMT inhibitor).
- Procedure:
- Plate GSCs in 96-well plates (5,000 cells/well).
- Treat with DMSO (control), GSK343 (5µM), 5-Azacytidine (1µM), or combination for 7-14 days, with media/drug replenishment every 48h.
- Assessment: Quantify differentiation via:
- Immunofluorescence for GFAP (astrocyte marker) and β-III-tubulin (neuronal marker).
- Flow cytometry for cell surface marker CD44 (stem) vs. CD105 (differentiation).
- RNA-seq to assess global transcriptional shift and pathway enrichment.
- Perform in vivo validation in orthotopic xenograft models, monitoring tumor growth (IVIS) and histology post-treatment.
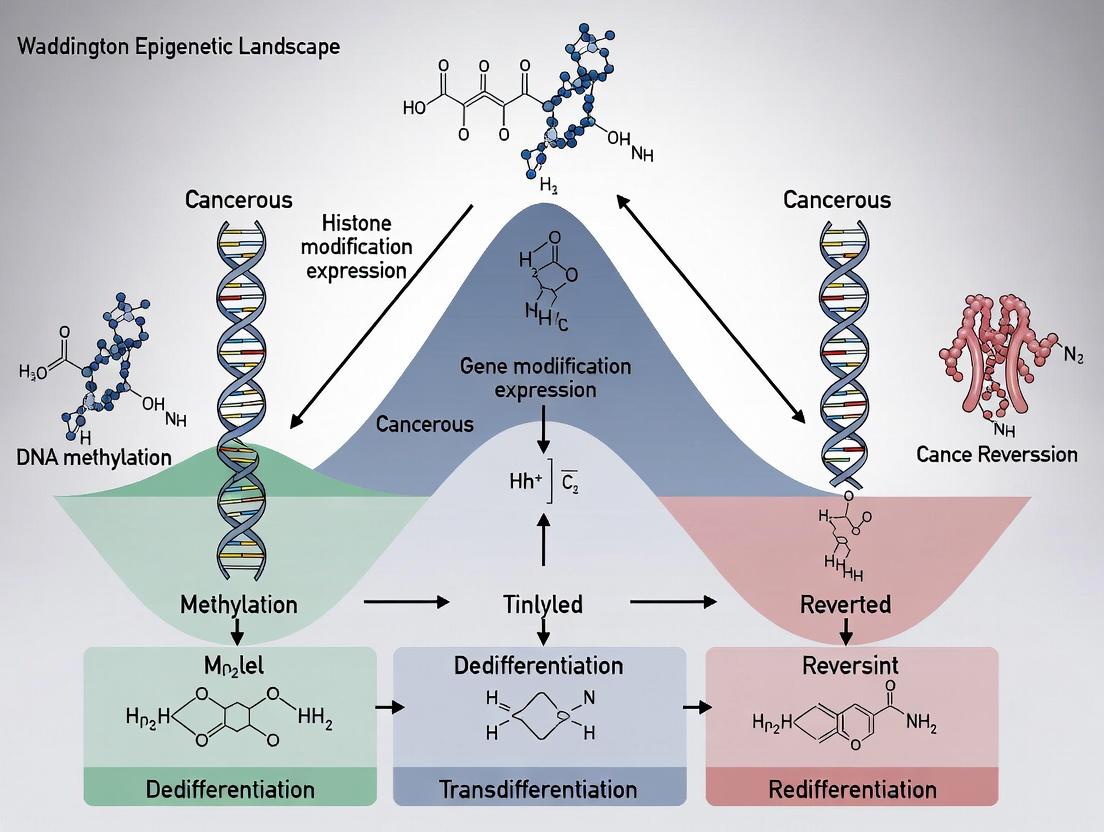
Visualizing Key Concepts and Pathways
Title: Cell Fate Decisions on the Epigenetic Landscape
Title: WNT Pathway Dysregulation and Therapeutic Intervention
The Scientist's Toolkit: Research Reagent Solutions
| Reagent Type | Specific Example(s) | Function in Landscape Research |
|---|---|---|
| Epigenetic Modulators | Trichostatin A (HDACi); Decitabine (DNMTi); GSK126 (EZH2i). | Probe the plasticity of the landscape; test reversion hypotheses by erasing epigenetic barriers. |
| Morphogens/Cytokines | Recombinant BMP4, TGF-β, Retinoic Acid. | Act as exogenous "slope modifiers" to push cells down specific differentiation valleys. |
| CRISPR-based Tools | dCas9-KRAB (CRISPRi); dCas9-p300 (CRISPRa); dCas9-DNMT3A. | Precisely rewire transcriptional networks and modify local chromatin state to reshape valleys. |
| Lineage Tracing Dyes | CellTrace Violet; CFSE. | Track cell division and fate outcomes over time in heterogeneous populations. |
| Barcoded Viral Vectors | Lentiviral barcode libraries (ClonTracer). | Quantify clonal dynamics and competitive fitness of subpopulations navigating the landscape. |
| Live-Cell Biosensors | FUCCI (cell cycle); GFP reporters for pathway activity (e.g., TCF/LEF-GFP). | Monitor real-time cell state transitions and responses to perturbations. |
Quantitative Data: Landscape Dynamics in Cancer Reversion
Table 2: Efficacy Metrics in Preclinical Reversion Studies
| Cancer Model | Reversion Agent(s) | Key Outcome Measure | Quantitative Result (vs. Control) | Reference (Ex.) |
|---|---|---|---|---|
| AML Cell Line | All-Trans Retinoic Acid (ATRA) | % CD11b+ Differentiated Cells | 65% vs. 8% | Blood, 2022 |
| Glioblastoma Stem Cells | BMP4 + Temozolomide | Tumor Sphere Formation | Reduction of 85% | Cell Stem Cell, 2023 |
| Colorectal Cancer Organoids | Tankyrase Inhibitor (XAV939) | LGR5- (Stem) / KRT20+ (Diff.) Ratio | 0.15 vs. 1.2 | Nat. Comm., 2023 |
| Pancreatic Cancer (PDX) | BET Inhibitor (JQ1) + HDACi | Median Survival Increase | 42 days vs. 28 days | Sci. Adv., 2022 |
Conclusion and Future Perspectives Revisiting Waddington’s landscape provides a powerful integrative framework for oncology. The future lies in the quantitative mapping of this terrain at single-cell resolution in patient samples and the development of sophisticated combinatorial perturbations (epigenetic, differentiation, immune) to engineer reversion. The ultimate goal is to translate this understanding into "topographic therapeutics"—drugs that remodel the oncogenic landscape itself, offering a durable and less toxic alternative to traditional cytotoxic approaches. This aligns with the core thesis that cancer reversibility is encoded within the latent regulative capacities of the epigenome, waiting to be therapeutically unlocked.
Cancer development is conceptualized within the framework of Waddington's epigenetic landscape as a series of transitions between distinct cellular attractor states. Normal, pre-malignant, and malignant phenotypes represent stable valleys of varying depth and stability. The malignant attractor is characterized by a deep, resilient basin that maintains aberrant gene expression patterns despite perturbations. Recent research into cancer reversion—the forced return of a malignant cell to a non-malignant attractor—validates this dynamical systems perspective, offering novel therapeutic paradigms focused on state transitions rather than solely on cytotoxic elimination.
Core Concepts: Attractor States in Cancer
Cellular attractors are high-dimensional stable states in gene expression space, maintained by complex regulatory networks. The transition from a normal to a malignant attractor involves traversing an epigenetic and genetic barrier, often passing through a pre-malignant, or "metastable," attractor state.
Table 1: Characteristics of Cellular Attractor States in Carcinogenesis
| Attractor State | Network Stability | Epigenetic Flexibility | Transcriptional Noise | Response to Perturbation | Typical Hallmarks Present |
|---|---|---|---|---|---|
| Normal | High | Low | Low | Elastic (returns to baseline) | 0-2 |
| Pre-Malignant | Intermediate (Metastable) | High | High | Plastic (may shift to adjacent state) | 2-4 |
| Malignant | High (Deep Basin) | Low (Locked-in) | Intermediate | Resilient (resists change) | 5+ |
Quantitative analyses of single-cell RNA-seq data reveal attractor landscapes. A 2023 study by Gupta et al. in Nature Cancer quantified the depth of malignant attractors in pancreatic ductal adenocarcinoma (PDAC) models, showing an average increase of 60-80% in relative attractor basin depth compared to pre-malignant (PanIN) states, calculated via Lyapunov function analysis.
Experimental Protocol: Mapping Attractor Landscapes with Single-Cell Multi-Omics
Objective: To delineate the gene regulatory network (GRN) structure and associated attractor landscape of a cell population transitioning from normal to malignant.
Materials & Workflow:
- Sample Collection: Isolate cells from matched normal, pre-malignant (e.g., field carcinogenesis), and malignant tissue from the same patient or genetically engineered model.
- Single-Cell Sequencing: Perform scRNA-seq (10x Genomics Chromium) and scATAC-seq in parallel on aliquots from the same sample.
- Data Integration: Use a tool like Seurat v5 or SCENIC+ to integrate transcriptomic and chromatin accessibility data to infer active GRNs.
- State Space Reconstruction: Apply dimensionality reduction (UMAP, PHATE) on the integrated data. Cell density in this reduced space estimates the "walls" and "valleys" of the landscape.
- Attractor Inference: Employ computational methods like Cell Fate Attractor (CFA) analysis or energy landscape reconstruction using Potts/Pseudo-potential models to identify stable states and transition probabilities.
Diagram 1: Single-cell multi-omic attractor mapping workflow.
The Scientist's Toolkit: Key Reagents for Attractor Research
Table 2: Essential Research Reagent Solutions
| Reagent / Tool | Category | Primary Function in Attractor Research | Example Product/Assay |
|---|---|---|---|
| Chromium Single Cell Multiome ATAC + Gene Exp. | Sequencing Kit | Simultaneous profiling of chromatin accessibility and transcriptome in single cells to infer GRN dynamics. | 10x Genomics, Cat# 1000285 |
| CUT&Tag Assay Kits | Epigenetic Profiling | High-sensitivity, low-background mapping of histone modifications/TF binding in limited cell numbers (e.g., pre-malignant foci). | Cell Signaling Technology, #86652S |
| Perturb-seq Compatible Guides/Vectors | Functional Genomics | For pooled CRISPR screens with single-cell RNA-seq readout to measure network perturbation effects. | Addgene, lentiGuide-Puro (52963) & Cas9 |
| Live-Cell Dyes for Cell State (e.g., ROS, Metabolism) | Cell Staining | Functional phenotyping to correlate metabolic attractors with transcriptomic states. | CellROX Green (Thermo Fisher, C10444) |
| Epigenetic Modulator Inhibitors | Small Molecules | Probe attractor stability by targeting "landscape architects" (HDACs, DNMTs, BET proteins). | Trichostatin A (HDACi), JQ1 (BETi) |
Signaling Pathways Governing Attractor Stability
The depth and stability of an attractor are governed by key signaling pathways that form positive feedback loops and cross-inhibitory modules. The RAS/RAF/MEK/ERK and PI3K/AKT/mTOR pathways often act as "stabilizers" of the malignant attractor, while TGF-β signaling can play dual roles, acting as a tumor suppressor in pre-malignant states and a promoter of invasion in late malignant states.
Diagram 2: Core signaling network stabilizing malignant attractor.
Experimental Protocol: Testing Attractor Stability via Pharmacological Perturbation
Objective: To measure the resilience of malignant vs. pre-malignant attractors by applying network perturbations and monitoring state reversion.
Detailed Methodology:
- Cell Lines/Organoids: Use isogenic cell lines or patient-derived organoids representing normal, pre-malignant, and malignant states (e.g., colon: Normal colonocyte, adenoma organoid, carcinoma organoid).
- Perturbation: Treat cells with a panel of inhibitors targeting key nodes in the stabilizing pathways (e.g., MEKi: Trametinib; AKTi: MK-2206; BETi: JQ1; HDACi: Panobinostat). Use a range of doses and exposure times (e.g., 72-hour pulse).
- Wash-Out & Recovery: Remove the inhibitor and allow cells to recover in standard media for 7-14 days.
- Phenotypic Readouts:
- Clonogenic Assays: Quantify the ability to form colonies post-perturbation. Malignant cells typically show high resilience (colony re-formation).
- Single-Cell RNA-seq: Profile cells at recovery endpoint. Use trajectory analysis (e.g., Monocle3) to see if malignant cells remain in their original attractor or regress towards a pre-malignant/normal state.
- Functional Metrics: Measure re-acquisition of contact inhibition, normalized metabolism (Seahorse), and structured growth in 3D Matrigel.
- Analysis: Quantify the percentage of cells that undergo state reversion. Calculate the "attractor strength" as the inverse of the reversion rate following a standardized perturbation.
Cancer Reversion: Forcing Exit from the Malignant Attractor
Cancer reversion research provides proof-of-concept for attractor theory. Successful reversion strategies often involve overriding the main stabilizing feedback loops.
Table 3: Documented Cancer Reversion Strategies and Outcomes
| Reversion Strategy | Target/Mechanism | Model System | Quantitative Reversion Metric | Key Finding (2022-2024) |
|---|---|---|---|---|
| Differentiation Therapy | Epigenetic reprogramming (e.g., targeting PML-RARα, IDH1) | Acute Promyelocytic Leukemia (APL) | >90% clinical remission rate. | ATRA/ATO combination directly reshapes the epigenetic landscape, pushing cells into a differentiation attractor. |
| Transcriptional Override | Forced expression of master regulators (e.g., GATA6 in PDAC) | Pancreatic Cancer Cell Lines | 40-60% of cells re-express differentiation markers and reduce proliferation in vitro. | Ectopic transcription factor expression can computationally rewire the GRN to a prior attractor state. |
| Network-Drug Combinations | Concurrent inhibition of major stabilizing pathways (e.g., MEK + PI3K) | BRAF-mutant Colorectal Cancer Organoids | 30% reduction in tumor organoid size post-treatment; 15% show sustained normalized gland morphology. | Synergistic perturbation lowers the barrier for exiting the malignant attractor. |
| Senescence Induction | CDK4/6 inhibition + epigenetic modulation | ER+ Breast Cancer Models | Senescence-Associated β-galactosidase (SA-β-gal) positive cells increase from <5% to >35%. | Therapy-induced senescence represents a distinct, non-malignant attractor that can be stably entered. |
The attractor landscape model provides a powerful quantitative framework for understanding carcinogenesis as a series of state transitions. Defining the precise topology of these landscapes—through single-cell multi-omics and perturbation biology—is crucial. The future of cancer therapy lies not only in killing malignant cells but in deliberately engineering transitions out of the malignant attractor, leveraging combinations of epigenetic, transcriptional, and signaling modifiers to lower the energy barriers to reversion. This requires a shift towards dynamical biomarkers that measure network stability and trajectory, rather than static snapshot markers.
Cancer has long been conceptualized as a genetic disease driven by sequential mutations in oncogenes and tumor suppressors. However, the burgeoning field of cancer epigenetics reveals that malignant transformation and progression are equally governed by reversible, heritable alterations in gene expression without changes in DNA sequence. This whitepaper reframes the classic Hanahan and Weinberg hallmarks of cancer through an epigenetic perspective, contextualized within Waddington's epigenetic landscape model. We posit that cancer represents a stabilized, aberrant epigenetic state—a "locked" valley—that can potentially be reverted through epigenetic reprogramming. This document provides a technical guide for researchers, detailing mechanisms, experimental protocols, and therapeutic implications.
Conrad Waddington's metaphor of an epigenetic landscape, where a cell's fate rolls down a valleyscape of increasing differentiation, provides a powerful framework for understanding carcinogenesis. In this model, cancer is not merely a series of genetic gatekeeper failures but represents an alternative, stable attractor state within the landscape. Genetic mutations can deepen and fortify this malignant valley, but the initial diversion and maintenance are often epigenetic. The hallmarks of cancer—sustaining proliferative signaling, evading growth suppressors, resisting cell death, enabling replicative immortality, inducing angiogenesis, and activating invasion and metastasis—are all enabled and orchestrated by epigenetic mechanisms.
Epigenetic Mechanisms: Writers, Readers, Erasers, and Remodelers
The epigenetic code is regulated by four principal classes of proteins:
- Writers: Deposit covalent marks (e.g., DNMTs for DNA methylation, HATs/KATs for histone acetylation).
- Erasers: Remove these marks (e.g., TETs for DNA demethylation, HDACs for deacetylation).
- Readers: Interpret the marks (e.g., proteins with bromodomains, chromodomains).
- Remodelers: Reposition nucleosomes (e.g., SWI/SNF complexes).
Dysregulation of these actors leads to genome-wide epigenetic instability, a hallmark of cancer.
Reframing the Hallmarks: An Epigenetic Perspective
Table 1: Epigenetic Drivers of Cancer Hallmarks
| Hallmark of Cancer | Key Epigenetic Mechanisms | Exemplary Alterations | Quantitative Impact (Example) |
|---|---|---|---|
| Sustaining Proliferative Signaling | Promoter hypermethylation silencing negative regulators; H3K27me3 repression. | CDKN2A (p16) silencing via methylation in >40% of cancers. Hypermethylation in ~90% of colorectal cancers. | |
| Evading Growth Suppressors | Polycomb Repressive Complex 2 (PRC2)-mediated silencing of tumor suppressor genes. | RB1, p16 pathways silenced by EZH2 (PRC2) overexpression/H3K27me3. EZH2 overexpressed in >60% of metastatic prostate cancer. | |
| Resisting Cell Death | Promoter hypermethylation of pro-apoptotic genes; histone deacetylation. | CASP8, APAF1 methylation. CASP8 methylated in ~40% of medulloblastomas. | |
| Enabling Replicative Immortality | Dysregulation of telomere maintenance via chromatin states; ALT activation. | H3K9me3/H4K20me3 loss at telomeres promoting alternative lengthening. | |
| Inducing Angiogenesis | Hypoxia-inducible factor (HIF) pathway regulation via histone demethylases. | JMD1A/JMD2B demethylases activate HIF1α targets. | |
| Activating Invasion & Metastasis | Epithelial-Mesenchymal Transition (EMT) driven by chromatin modifiers; metastable epigenetic states. | SNAI1/SLUG repression by DNMTs/HDACs; EZH2 promotes metastasis. EZH2 high expression correlates with poor prognosis in >20 cancer types. | |
| Emerging Hallmark: Avoiding Immune Destruction | Silencing of tumor antigen presentation and immune chemokines via DNA methylation. | MHC Class I genes and CXCL9/10 methylated in melanoma, NSCLC. | |
| Enabling Characteristic: Genome Instability | Global DNA hypomethylation promoting chromosomal instability; H3K9me loss. | 20-60% global hypomethylation in tumors vs. normal tissue. |
Experimental Protocols for Epigenetic Cancer Research
Protocol 1: Genome-wide DNA Methylation Profiling (Oxidative Bisulfite Sequencing) Objective: To map 5-methylcytosine (5mC) and 5-hydroxymethylcytosine (5hmC) at single-base resolution. Procedure:
- DNA Extraction & Quality Control: Isolate high-molecular-weight DNA. Assess integrity via agarose gel or Bioanalyzer (RIN > 7).
- Oxidative Bisulfite Conversion:
- Treat 100-500ng DNA with recombinant TET1 enzyme (or potassium perruthenate, KRuO₄) to convert 5mC to 5-carboxylcytosine (5caC).
- Perform standard bisulfite conversion using a commercial kit (e.g., EZ DNA Methylation-Lightning Kit) to convert unmodified C to U, while 5caC (from 5mC) and 5hmC (if protected) are also converted to U.
- A parallel sample undergoes only bisulfite conversion (maps 5mC+5hmC). Comparison yields 5hmC maps.
- Library Preparation & Sequencing: Build sequencing libraries from converted DNA using adaptors compatible with bisulfite-treated DNA. Amplify and sequence on an Illumina platform (PE150).
- Bioinformatic Analysis: Align reads to a bisulfite-converted reference genome (e.g., using Bismark). Calculate methylation percentages per cytosine.
Protocol 2: Assessing Chromatin Accessibility (ATAC-seq) in Cancer Cells Objective: Identify open chromatin regions and infer transcription factor occupancy. Procedure:
- Cell Nuclei Preparation: Harvest 50,000-100,000 viable cells. Lyse with cold lysis buffer (10 mM Tris-HCl, pH 7.4, 10 mM NaCl, 3 mM MgCl₂, 0.1% IGEPAL CA-630). Pellet nuclei.
- Transposition Reaction: Resuspend nuclei in transposition mix (25 μL 2x TD Buffer, 2.5 μL Tn5 Transposase, 22.5 μL nuclease-free water). Incubate at 37°C for 30 min. Purify DNA using a MinElute PCR Purification Kit.
- Library Amplification & Purification: Amplify transposed DNA with 12-15 PCR cycles using indexed primers. Size-select libraries using SPRI beads (e.g., 0.5x to 1.5x ratio) to remove large fragments and primer dimers.
- Sequencing & Analysis: Sequence on Illumina NextSeq. Process reads (align, remove duplicates, call peaks) using pipeline (e.g., FASTQC, Bowtie2, MACS2).
Visualization of Key Epigenetic Pathways in Cancer
Title: Genetic and Epigenetic Inputs to Cancer Hallmarks
Title: Cancer as a Locked Attractor State in Waddington's Landscape
The Scientist's Toolkit: Key Research Reagent Solutions
Table 2: Essential Reagents for Epigenetic Cancer Research
| Reagent / Material | Function / Application | Key Considerations |
|---|---|---|
| SGI-1027 | Small-molecule inhibitor of DNMT1, DNMT3A/3B. Used to induce DNA demethylation in vitro/in vivo. | Can induce degradation of DNMT1; may have off-target effects. Monitor global & locus-specific 5mC loss. |
| GSK126 / EPZ-6438 (Tazemetostat) | Potent, selective inhibitors of EZH2 (PRC2 catalytic subunit). Target H3K27me3-dependent silencing. | Tazemetostat is FDA-approved for epithelioid sarcoma. Check cell line sensitivity and H3K27me3 reduction by WB. |
| Trichostatin A (TSA) / Vorinostat (SAHA) | Pan-HDAC inhibitors. Increase histone acetylation, reactivate silenced genes. | TSA for in vitro use; SAHA for clinical models. Can induce cell cycle arrest & apoptosis broadly. |
| JQ1 / I-BET762 | BET bromodomain inhibitors. Displace readers (e.g., BRD4) from acetylated histones, disrupting oncogenic transcription. | Particularly effective in hematological cancers (e.g., AML). Monitor c-MYC downregulation. |
| Recombinant TET1/CD Protein | Catalytic domain of TET dioxygenase for in vitro oxidation of 5mC to 5hmC/5caC. Essential for oxidative bisulfite sequencing protocols. | Requires Fe(II) and α-KG as cofactors. Activity is sequence-context dependent. |
| KAPA HiFi HotStart Uracil+ ReadyMix | Polymerase mix engineered for efficient PCR amplification of bisulfite-converted DNA (uracil-rich). | Critical for whole-genome bisulfite sequencing library prep. Reduces amplification bias. |
| Tn5 Transposase (Illumina or homemade) | Enzyme for Tagmentation in ATAC-seq. Simultaneously fragments DNA and adds sequencing adaptors. | Activity varies by batch. Titration is crucial for optimal fragment length distribution. |
| M.SssI CpG Methyltransferase | Bacterial enzyme that methylates all CpG dinucleotides in vitro. Used for creating fully methylated control DNA. | Essential control for methylation-sensitive assays (e.g., MS-PCR, HELP-seq). |
| H3K27me3 / H3K9me3 / H3K4me3 Specific Antibodies | For ChIP-seq to map repressive (H3K27me3, H3K9me3) or active (H3K4me3) histone marks. | Validation using knockout/knockdown cells is critical for specificity. Use spike-in controls for quantitation. |
| 5-hmC / 5-mC Specific Antibodies | For immunoprecipitation-based enrichment (hMeDIP, MeDIP) or immunofluorescence detection of modified cytosines. | Cross-reactivity can be an issue. Confirm findings with bisulfite-based methods. |
Therapeutic Implications and Future Directions: Reverting the Landscape
The epigenetic lens reveals cancer as a disease of cellular identity and plasticity. This offers a profound therapeutic opportunity: reversion. Unlike genetic mutations, epigenetic marks are pharmacologically reversible.
- Epigenetic Drugs: DNMT inhibitors (Azacitidine, Decitabine) and HDAC inhibitors are approved for hematological malignancies. Next-generation agents target writers (EZH2), readers (BET), and erasers (LSD1) with increasing specificity.
- Epigenetic Reprogramming: Inspired by Yamanaka factors, controlled epigenetic reprogramming—without full dedifferentiation—aims to push cells out of the malignant attractor state and towards normalcy. Combinatorial approaches targeting multiple epigenetic axes and leveraging immune recognition ("epigenetic immunotherapy") represent the frontier.
The challenge lies in manipulating this complex, interconnected system with precision to reset the malignant landscape without erasing essential cellular identity or inducing new pathologies. Understanding the epigenetic hallmarks provides the roadmap for this next generation of cancer therapy.
Cancer has long been viewed as a disease of uncontrolled proliferation driven by genetic mutations. However, the conceptual framework provided by Conrad Waddington's epigenetic landscape offers a powerful alternative perspective, where cell fate is visualized as a ball rolling down a hillside of bifurcating valleys, each representing a distinct developmental pathway. Within this model, carcinogenesis can be seen as the ball escaping its normal valley (a differentiated state) and becoming trapped in an aberrant, undifferentiated basin (a malignant state). Cancer reversion is the process of pushing the "ball" back into a normal valley, thereby restoring differentiation and ceasing malignant behavior. This whitepaper explores the three core cellular processes underlying this reversion: differentiation, dedifferentiation, and transdifferentiation, framing them within contemporary research aimed at therapeutic intervention.
Core Concepts and Mechanisms
Differentiation Therapy: The forced induction of terminal differentiation in cancer cells, rendering them post-mitotic and functionally normal. The paradigm is all-trans retinoic acid (ATRA) in Acute Promyelocytic Leukemia (APL).
Dedifferentiation: The reversion of a specialized cell to a less specialized, often stem-like progenitor within its own lineage. This process is a hallmark of tumor initiation and plasticity, often driven by oncogenic pathways.
Transdifferentiation (Lineage Reprogramming): The direct conversion of one differentiated cell type into another, bypassing a pluripotent intermediate. In cancer, this can contribute to heterogeneity and metastasis but also represents a potential therapeutic pathway to convert malignant cells into benign ones.
Key Signaling Pathways and Molecular Regulators
The following table summarizes major pathways and their roles in cell fate decisions relevant to cancer reversion.
Table 1: Key Pathways in Cell Fate and Cancer Reversion
| Pathway/Regulator | Role in Normal Development | Role in Cancer | Potential for Reversion Therapy |
|---|---|---|---|
| Wnt/β-catenin | Stem cell maintenance, cell fate specification. | Often constitutively active; promotes stemness and dedifferentiation. | Inhibition can reduce stemness; context-dependent activation may promote differentiation. |
| Notch | Cell fate decisions, lateral inhibition. | Acts as oncogene or tumor suppressor depending on context. | Agonists or inhibitors can be used to push cells toward differentiation. |
| Hedgehog (Hh) | Patterning, stem cell niche maintenance. | Aberrant activation promotes tumor growth and stemness. | Inhibition (e.g., vismodegib) can deplete cancer stem cells. |
| BMP (Bone Morphogenetic Protein) | Promotes differentiation in many lineages. | Often silenced in cancer; loss leads to stemness. | Recombinant BMPs can induce differentiation and suppress tumors. |
| MYC | Regulates growth, proliferation, metabolism. | Frequently amplified/overexpressed; drives proliferation and dedifferentiation. | Transient inhibition can promote differentiation. |
| p53 | Guardian of the genome; cell cycle arrest, apoptosis. | Most frequently mutated gene in cancer; loss enables plasticity. | Reactivation of wild-type p53 function can induce senescence/differentiation. |
| Epigenetic Modifiers (DNMTs, HDACs, PRC2) | Establish and maintain cell type-specific gene expression. | Globally dysregulated, locking cells in a de-differentiated state. | Epigenetic drugs (e.g., Azacitidine, HDACi) can unlock differentiation programs. |
Title: Signaling Network in Cancer Dedifferentiation and Reversion
Experimental Protocols for Studying Cancer Reversion
Protocol 1: In Vitro Differentiation Assay Using Soluble Factors Aim: To induce differentiation in cancer cell lines.
- Culture Cells: Maintain target cancer cell line (e.g., HL-60 for APL, glioblastoma stem cells) in appropriate growth medium.
- Factor Treatment: Seed cells at low density. Replace medium with serum-containing or defined differentiation medium supplemented with the inducing agent (e.g., 1µM ATRA, 100ng/mL BMP-4, 10nM Phorbol ester (PMA)).
- Control: Include a vehicle control (e.g., DMSO).
- Incubation: Culture for 3-7 days, refreshing medium + factors every 2-3 days.
- Assessment:
- Morphology: Daily visual analysis via phase-contrast microscopy for neurite extension, adherence, vacuolization, etc.
- Surface Markers: Analyze by Flow Cytometry for differentiation antigens (e.g., CD11b, CD14 for myeloid lines).
- Functional Assays: Perform nitroblue tetrazolium (NBT) reduction assay for myeloid differentiation (generation of superoxide).
- Proliferation: Count cells daily or use MTT assay at endpoint.
Protocol 2: Lineage Tracing and Transdifferentiation In Vivo Aim: To track cell fate and conversion in a living organism.
- Animal Model: Use an immunocompromised mouse (NSG) or a genetically engineered mouse model (GEMM) of cancer.
- Labeling: Introduce a heritable genetic label into specific cell populations.
- Method A (Cre-Lox): Cross mice carrying a Cre recombinase under a cell-type-specific promoter (e.g., Alb-Cre for hepatocytes) with reporter mice (e.g., Rosa26-LSL-tdTomato). Spontaneous or induced tumors will have labeled cells of origin.
- Method B (Lentiviral Barcoding): Infect primary tumor cells with a lentiviral library expressing unique genetic barcodes and fluorescent proteins prior to transplantation.
- Intervention: Administer a putative reversion therapy (drug, gene therapy) or allow tumor progression.
- Analysis: At endpoint, harvest tumors and process for:
- Flow Cytometry/Sorting: Isolate labeled and unlabeled cell populations.
- Single-Cell RNA Sequencing (scRNA-seq): Profile the transcriptomes of labeled cells to identify their identity (original vs. transdifferentiated).
- Immunohistochemistry: Co-stain tissue sections for the lineage label and markers of alternate lineages to visualize transdifferentiation events.
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Reagents for Cancer Reversion Research
| Reagent / Material | Function / Application | Example Product/Catalog |
|---|---|---|
| All-trans Retinoic Acid (ATRA) | Gold-standard differentiating agent; induces granulocytic differentiation in APL cells. | Sigma-Aldrich, R2625 |
| Recombinant Human BMP-4 | Potent differentiation factor for mesenchymal and other lineages; can suppress cancer stemness. | R&D Systems, 314-BP |
| 5-Azacytidine / Decitabine | DNA methyltransferase inhibitors; reverse hypermethylation and reactivate silenced differentiation genes. | Selleckchem, A2385 / S1202 |
| Trichostatin A (TSA) / Vorinostat (SAHA) | Histone deacetylase inhibitors; increase histone acetylation, opening chromatin for differentiation programs. | Cayman Chemical, 89730 / Selleckchem, S1030 |
| Doxycycline-inducible Gene Expression Systems | For controlled overexpression or knockdown of fate-determining transcription factors (e.g., SOX2, C/EBPα). | Tet-On 3G System (Clontech, 631168) |
| Lentiviral shRNA/miRNA Libraries | For high-throughput screening of genes regulating differentiation and stemness. | Mission shRNA Library (Sigma) |
| CellTrace Proliferation & CFSE Dyes | To track and quantify cell division arrest associated with differentiation. | Thermo Fisher, C34554 / C1157 |
| Annexin V / Propidium Iodide Apoptosis Kit | To distinguish true differentiation from cytotoxic or apoptotic effects of treatments. | BioLegend, 640914 |
| Single-Cell RNA-seq Kit (10x Genomics) | To deconvolute heterogeneous tumor populations and identify novel differentiation states. | Chromium Next GEM Single Cell 3' Kit v3.1 |
| Organoid Culture Matrices (e.g., Matrigel) | Provides a 3D microenvironment to study differentiation and reversion in a more physiologically relevant context. | Corning, 356231 |
Title: Core Experimental Workflow for Reversion Studies
Table 3: Selected Preclinical and Clinical Data on Differentiation Therapies
| Agent / Strategy | Cancer Model | Key Metrics & Results | Proposed Mechanism |
|---|---|---|---|
| ATRA + Arsenic Trioxide (ATO) | APL (Clinical) | CR rate >95%; 5-yr OS >90%. Synergistically target PML-RARα fusion. | Degradation of oncoprotein, release of differentiation block. |
| BMP-4 Treatment | Glioblastoma Stem Cells (GSC) In Vitro | Reduced sphere formation by 60-80%; increased GFAP+ astrocytes by 3-5 fold. | SMAD pathway activation, induction of astroglial differentiation. |
| 5-Azacytidine | AML/MDS (Clinical) | Overall response rate ~10-20%; superior to conventional care in elderly AML. | Global DNA hypomethylation, reactivation of tumor suppressors. |
| CDK8/19 Inhibitor (Senexin B) | Colon Cancer In Vitro | Reduced tumorsphere formation by 70%; induced enterocyte markers (Villin, CDX2). | Downregulation of Wnt/β-catenin stemness signature. |
| SOX2 Eradication (via shRNA) | Lung Adenocarcinoma (GEMM) | Tumor regression; lineage tracing showed conversion to dormant, post-mitotic cells. | Depletion of core stemness factor, allowing default differentiation. |
The Waddington landscape provides an enduring metaphor for understanding cancer not just as a genetic disease, but as a disorder of cell fate. Therapeutic reversion—pushing cells back onto paths of differentiation—represents a promising non-cytotoxic paradigm. Future research must focus on identifying lineage-specific master regulators, understanding the permissive epigenetic context for reversion, and developing delivery systems for reprogramming factors in vivo. The integration of single-cell omics and advanced lineage-tracing models will be crucial for mapping the precise routes back from malignancy to normalcy, ultimately turning the concept of cancer reversion into a broad clinical reality.
The conceptual framework of Waddington's epigenetic landscape provides a powerful metaphor for understanding cellular differentiation and lineage commitment. In this model, a pluripotent stem cell, represented by a ball at the top of a ridged hill, rolls down valleys representing distinct lineage paths, ultimately arriving at a terminally differentiated state. The rigidity and depth of these valleys are sculpted and maintained by stable epigenetic modifications. Conversely, in cancer, cells undergo a process of dedifferentiation or transdifferentiation, effectively climbing back up or crossing between valleys—a phenomenon central to cancer reversion research. This whitepaper details the core molecular machinery—DNA methylation, histone modifications, and chromatin remodelers—that carve these developmental pathways and whose dysregulation is implicated in oncogenesis.
DNA Methylation: The Stable Lock on Cell Identity
DNA methylation involves the covalent addition of a methyl group to the 5-carbon of cytosine, primarily in CpG dinucleotides, catalyzed by DNA methyltransferases (DNMTs). This modification is associated with long-term transcriptional silencing, crucial for locking in cell fate decisions.
Key Enzymes and Functions:
- DNMT1: Maintenance methyltransferase; copies methylation patterns during DNA replication.
- DNMT3A & DNMT3B: De novo methyltransferases; establish new methylation patterns during development.
- TET Family (TET1/2/3): Demethylation initiators; oxidize 5-methylcytosine (5mC) to 5-hydroxymethylcytosine (5hmC) and further products, facilitating active DNA demethylation.
Role in Lineage Commitment: During differentiation, de novo methylation silences pluripotency gene promoters (e.g., OCT4, NANOG), while lineage-specific gene promoters are often hypomethylated. In cancer, global hypomethylation coincides with locus-specific hypermethylation of tumor suppressor genes.
Table 1: DNA Methylation Patterns in Lineage Commitment vs. Cancer
| Genomic Context | Normal Lineage Commitment | Cancer State | Quantitative Change |
|---|---|---|---|
| Pluripotency Gene Promoters | Hypermethylated (Silenced) | Frequently Hypomethylated (Re-activated) | ~70-90% methylation in committed cells vs. <10% in some cancers |
| Tissue-Specific Gene Promoters | Hypomethylated (Active) | Often Hypermethylated (Silenced) | <20% methylation in normal tissue vs. >60% in tumors |
| CpG Island Shores | Dynamic, tissue-specific methylation | Aberrantly methylated | Highly variable; used as diagnostic biomarkers |
| Repetitive Elements | Heavily methylated (Genome stability) | Globally hypomethylated (Genomic instability) | Loss of 20-60% methylation compared to normal tissue |
| 5hmC Levels | High in stem cells, reduces upon differentiation | Globally depleted | >10-fold reduction in many solid tumors |
Experimental Protocol: Whole-Genome Bisulfite Sequencing (WGBS) for Methylome Analysis
Objective: To generate a base-pair resolution map of 5-methylcytosine across the genome. Procedure:
- DNA Extraction & Fragmentation: Isolate high-molecular-weight genomic DNA and shear to ~200-300bp via sonication or enzymatic digestion.
- Bisulfite Conversion: Treat fragmented DNA with sodium bisulfite using a kit (e.g., EZ DNA Methylation Kit). This converts unmethylated cytosines to uracil, while methylated cytosines remain unchanged.
- Desalting & Clean-up: Purify the converted DNA using column-based purification.
- Library Preparation: Repair ends, add adapters with unique molecular identifiers (UMIs), and amplify via PCR. Use polymerases resistant to uracil (e.g., KAPA HiFi Uracil+).
- High-Throughput Sequencing: Perform paired-end sequencing on an Illumina platform.
- Bioinformatic Analysis:
- Alignment: Map reads to a bisulfite-converted reference genome using tools like Bismark or BS-Seeker2.
- Methylation Calling: Calculate methylation percentage per cytosine as (#C reads / (#C reads + #T reads)).
- Differential Analysis: Identify differentially methylated regions (DMRs) using tools like methylKit or DSS.
Histone Modifications: The Dynamic Signaling Layer
Histone post-translational modifications (PTMs) on N-terminal tails—including acetylation, methylation, phosphorylation, and ubiquitination—create a dynamic "histone code" that regulates chromatin accessibility and transcription.
Key Modifications in Fate Decisions:
- H3K4me3: Associated with active transcription start sites. Marks poised and active developmental genes.
- H3K27me3: Repressive mark deposited by Polycomb Repressive Complex 2 (PRC2). Maintains genes in a silenced but poised state (bivalent domains with H3K4me3 in stem cells).
- H3K9me3: Constitutive heterochromatin mark; involved in long-term silencing.
- H3K27ac & H3K9ac: Marks active enhancers and promoters, facilitating transcription.
- H3K36me3: Associated with actively transcribed gene bodies.
Role in Lineage Commitment: Resolution of bivalent domains (loss of either H3K4me3 or H3K27me3) is a key step in lineage specification. Enhancer activation (marked by H3K27ac) is highly cell-type-specific.
Table 2: Key Histone Modifications in Stem Cells vs. Differentiated Lineages
| Histone Mark | Enzyme (Writer) | Enzyme (Eraser) | Function in Pluripotency | Change Upon Lineage Commitment |
|---|---|---|---|---|
| H3K4me3 | COMPASS family (MLL1-4, SET1A/B) | KDM5 family | Marks active/poised promoters | Resolved: retained on lineage-active genes, lost on others |
| H3K27me3 | PRC2 (EZH2) | KDM6 family (UTX, JMJD3) | Silences developmental regulators in bivalent domains | Resolved: gained on silenced lineage genes, lost on activated ones |
| H3K27ac | p300/CBP | HDAC1/2/3, SIRT1 | Marks active enhancers | Dramatic redistribution to lineage-specific enhancers |
| H3K9me3 | SUV39H1/2, SETDB1 | KDM4 family | Silences repetitive elements, facultative heterochromatin | Generally stable; can spread in cancer |
| H3K36me3 | SETD2 | KDM2A/B, KDM4A | Transcription elongation | Increases on highly expressed lineage-specific genes |
Diagram 1: Histone Mark Dynamics During Fate Choice
Chromatin Remodelers: The Architectural Engineers
ATP-dependent chromatin remodeling complexes use ATP hydrolysis to slide, evict, or restructure nucleosomes, directly controlling physical access to DNA.
Major Complexes and Functions:
- SWI/SNF (BAF) Complex: An antagonist of Polycomb, it evicts nucleosomes to create accessible chromatin. Its composition switches during differentiation (e.g., from esBAF in ESCs to lineage-specific BAF).
- ISWI Complexes: Involved in nucleosome spacing and assembly; generally promote compaction and repression.
- CHD Family: Some members (e.g., CHD1) keep chromatin open in pluripotent states, while others (e.g., CHD4 in NuRD complex) are repressive.
- INO80 Family: Facilitates exchange of histone variants (e.g., H2A.Z).
Role in Lineage Commitment: The BAF complex is particularly crucial. Its subunit exchange dictates its targeting, allowing it to activate lineage-specific genes while dismantling the pluripotency network.
Experimental Protocol: Assay for Transposase-Accessible Chromatin with Sequencing (ATAC-seq)
Objective: To map genome-wide chromatin accessibility and nucleosome positioning. Procedure:
- Cell Preparation: Harvest 50,000-100,000 viable cells. Prepare nuclei by lysis in cold lysis buffer (10mM Tris-Cl pH7.4, 10mM NaCl, 3mM MgCl2, 0.1% IGEPAL CA-630).
- Transposition: Incubate nuclei with the Tn5 transposase preloaded with sequencing adapters (commercially available kit, e.g., Nextera) at 37°C for 30 minutes. Tn5 cuts and tags accessible DNA regions.
- DNA Purification: Purify tagmented DNA using a Qiagen MinElute PCR purification column.
- Library Amplification: Amplify the purified DNA with limited-cycle PCR (typically 5-12 cycles) using indexed primers.
- Library Clean-up & Sequencing: Purify the PCR product and sequence on an Illumina platform (usually paired-end).
- Analysis:
- Alignment: Map reads to reference genome (e.g., using Bowtie2 or BWA).
- Peak Calling: Identify regions of significant enrichment (open chromatin peaks) using MACS2 or Genrich.
- Footprinting: Use tools like HINT-ATAC or TOBIAS to infer transcription factor binding sites from Tn5 cleavage patterns.
Diagram 2: Chromatin Remodeler Actions on Accessibility
Interplay in Cancer Reversion: Reprogramming the Landscape
Cancer reversion research aims to force malignant cells back into a more differentiated, less proliferative state by manipulating the epigenetic landscape. This involves reversing the dysregulated patterns of the key molecular players.
Therapeutic Strategies:
- DNMT Inhibitors (DNMTi): Azacitidine and Decitabine are hypomethylating agents used in myeloid malignancies. They integrate into DNA, trap DNMTs, and promote DNA demethylation, potentially re-expressing silenced tumor suppressors.
- Histone Methyltransferase Inhibitors: EZH2 (PRC2 catalytic subunit) inhibitors (e.g., Tazemetostat) are approved for specific sarcomas and lymphomas, aiming to derepress silenced differentiation genes.
- HDAC Inhibitors (HDACi): Vorinostat, Romidepsin. Increase histone acetylation, promoting a more open chromatin state and gene expression, but are pleiotropic.
- Combination Therapies: Co-targeting epigenetic regulators (e.g., DNMTi + HDACi) shows synergistic effects in preclinical models by more effectively re-sculpting the epigenome.
Table 3: Epigenetic Drugs in Clinical Development for Cancer Reversion
| Drug/Target | Class | Example Agents | Mechanism in Reversion | Key Trial Contexts |
|---|---|---|---|---|
| DNMT | Nucleoside Analogue | Azacitidine, Decitabine, Guadecitabine | Induce DNA demethylation, re-express silenced differentiation genes | MDS, AML, being tested in solid tumors |
| EZH2 | Competitive Inhibitor | Tazemetostat, GSK126, CPI-1205 | Inhibit H3K27me3 deposition, de-repress Polycomb-silenced targets | Follicular Lymphoma, INI1-deficient tumors |
| BET Bromodomains | BET Inhibitor | JQ1, OTX015, I-BET762 | Displace BET readers from acetylated histones, suppress oncogenic transcription | AML, NUT Midline Carcinoma |
| HDAC | Pan-/Class-Selective Inhibitor | Vorinostat, Romidepsin, Entinostat (Class I) | Increase global histone acetylation, alter gene expression programs | CTCL, PTCL, combination therapies |
| LSD1 (KDM1A) | Irreversible Inhibitor | Tranylcypromine derivatives, GSK2879552 | Block H3K4me2/H3K9me2 demethylation, induce differentiation | AML, SCLC |
The Scientist's Toolkit: Key Research Reagent Solutions
Table 4: Essential Reagents for Epigenetic Lineage Commitment Research
| Reagent Category | Specific Example(s) | Function/Application |
|---|---|---|
| DNA Methylation Analysis | EZ DNA Methylation Kit (Zymo Research), MethylCode Bisulfite Conversion Kit (Thermo Fisher) | High-efficiency bisulfite conversion of DNA for downstream sequencing or pyrosequencing. |
| HDAC Inhibitor | Trichostatin A (TSA), Sodium Butyrate, Vorinostat (SAHA) | Induces hyperacetylation of histones; used to study the role of acetylation in gene activation and differentiation. |
| DNMT Inhibitor | 5-Azacytidine, Decitabine | Incorporated into DNA, inhibits DNMT activity, leading to passive DNA demethylation. Critical for studying DNA methylation's role in fate locking. |
| EZH2/PRC2 Inhibitor | GSK126, DZNep, Tazemetostat (EPZ-6438) | Specifically inhibits H3K27 methyltransferase activity of EZH2, used to dissect Polycomb-mediated repression in stemness and differentiation. |
| ChIP-Validated Antibodies | Anti-H3K4me3 (Millipore 07-473), Anti-H3K27me3 (C36B11, Cell Signaling), Anti-H3K27ac (Abcam ab4729) | Essential for chromatin immunoprecipitation (ChIP) assays to map histone modification landscapes. Specificity and validation are critical. |
| ATAC-seq Kit | Illumina Tagment DNA TDE1 Kit, Nextera DNA Library Prep Kit | Standardized, optimized reagents for consistent and efficient ATAC-seq library preparation from low cell numbers. |
| Active Recombinant Chromatin Remodelers | Recombinant BAF complex (e.g., from Addgene co-transfection), Recombinant ACF/CHD1 (e.g., Active Motif) | For in vitro biochemical assays (e.g., ATPase, nucleosome sliding/remodeling) to study mechanistic specificity. |
| Tet-On/Off Inducible Systems | dox-inducible shRNA or cDNA expression vectors (e.g., pLKO-Tet-On, pINDUCER) | Enables controlled, inducible knockdown or overexpression of epigenetic regulators (DNMTs, TETs, EZH2) to study dynamic effects on fate. |
| Pioneer Factor Expression Constructs | Mouse/human OCT4, SOX2, KLF4 cDNAs | For forced reprogramming experiments (iPSC generation) or direct lineage conversion, studying epigenetic barrier overcoming. |
| Next-Gen Sequencing Library Prep Kits | KAPA HyperPrep Kit, NEBNext Ultra II DNA Library Prep Kit | For preparing high-quality sequencing libraries from bisulfite-converted DNA (WGBS) or ChIP/ATAC DNA. |
Reprogramming the Terrain: Experimental and Therapeutic Approaches to Induce Reversion
The conceptual framework of Waddington's epigenetic landscape, wherein a cell's fate is visualized as a ball rolling down a valley bifurcating into distinct cellular phenotypes, provides a powerful metaphor for understanding development and disease. In cancer, the ball becomes trapped in a pathological valley. Research into cancer reversion seeks to push malignant cells back up the landscape toward a more normal, controlled state. Epigenetic dysregulation—heritable changes in gene expression without altering DNA sequence—is a hallmark of this trapped state. CRISPR-dCas9 systems have emerged as precision tools for targeted chromatin modulation, allowing researchers to directly rewrite epigenetic marks and test hypotheses about manipulating the epigenetic landscape to induce therapeutic reprogramming.
Core dCas9 Effector Systems: Mechanisms and Applications
The catalytically dead Streptococcus pyogenes Cas9 (dCas9) serves as a programmable DNA-binding scaffold. Fused to epigenetic effector domains, it enables locus-specific chromatin modification.
| System Name | Effector Domain | Primary Function | Key Targeted Marks | Typical Application in Cancer Research |
|---|---|---|---|---|
| CRISPRa | VP64, p65, Rta (e.g., SunTag, VPR) | Transcriptional Activation | H3K27ac, H3K4me3 | Reactivation of tumor suppressor genes (e.g., p53, PTEN). |
| CRISPRi | KRAB, MeCP2 | Transcriptional Repression | H3K9me3, DNA methylation | Silencing of oncogenic drivers or vulnerability genes. |
| CRISPRon/off | DNA Methyltransferases (DNMT3A/3L) | DNA Methylation | 5-methylcytosine | Silencing via promoter hypermethylation. |
| CRISPRoff (v2.0) | DNMT3A + KRAB | DNA Methylation & Repression | 5mC, H3K9me3 | Durable, heritable gene silencing. |
| CRISPRon | TET1 Catalytic Domain | DNA Demethylation | 5-hydroxymethylcytosine | Reactivation of hypermethylated, silenced genes. |
| CRISPR-LSD1 | LSD1 | Histone Demethylation | H3K4me1/2 | Alteration of enhancer activity. |
| CRISPR-p300 | p300 Core | Histone Acetylation | H3K27ac, H3K18ac | Potent activation of gene expression & enhancers. |
| CRISPR-PRDM9 | PRDM9 Methyltransferase | Histone Methylation | H3K4me3, H3K36me3 | De novo establishment of activating marks. |
The performance of these systems varies based on design, delivery, and target locus. Below is a summarized comparison based on recent studies (2023-2024).
Table 1: Performance Metrics of Select dCas9-Effector Systems
| Parameter | CRISPR-p300 | CRISPR-KRAB (i) | CRISPR-DNMT3A (off) | CRISPR-TET1 (on) |
|---|---|---|---|---|
| Max Fold Change (Gene Expression) | 50-1000x activation | 5-20x repression | 10-100x repression | 2-50x activation |
| Time to Onset | 24-48 hrs | 12-24 hrs | 48-72 hrs | 48-96 hrs |
| Duration after transient transfection | 3-7 days | 5-10 days | Weeks to months (heritable) | 5-14 days |
| Typical Editing Window | -250 to +50 bp from TSS | -50 to +500 bp from TSS | Promoter/CpG Island | Methylated promoter regions |
| Off-target Epigenetic Effects | Low (localized) | Moderate (spreading) | Low-Medium (localized) | Low (highly localized) |
| Primary Delivery Method | Lentivirus, AAV, mRNA | Lentivirus, Plasmid | Lentivirus, Stable Line | mRNA, Lentivirus |
Detailed Experimental Protocol: Reactivating a Hypermethylated Tumor Suppressor Gene
Objective: Use CRISPR-TET1 and CRISPR-p300 systems to reverse epigenetic silencing of CDKN2A/p16INK4a in a glioblastoma cell line.
Workflow Diagram Title: Protocol for Epigenetic Reactivation of p16INK4a
Materials & Reagents:
- U87-MG Glioblastoma Cells: Model cell line with known p16 promoter hypermethylation.
- Lentiviral Vectors: pLV-dCas9-TET1-CD and pLV-dCas9-p300Core (Addgene #,).
- sgRNA Oligos: Designed using CRISPick or similar, targeting the p16 promoter.
- Lentiviral Packaging Mix (psPAX2, pMD2.G): For virus production in HEK293T cells.
- Polybrene (8 µg/mL): Enhances viral transduction.
- Puromycin (1-2 µg/mL): For selection of stably transduced cells.
- TRIzol Reagent: For RNA isolation and subsequent qRT-PCR.
- EZ DNA Methylation-Direct Kit: For bisulfite conversion of genomic DNA.
- Antibodies for ChIP: Anti-H3K27ac, Anti-H3K4me3, Normal Rabbit IgG control.
- Senescence β-Galactosidase Staining Kit: For functional validation of p16 reactivation.
Procedure:
- sgRNA Design & Cloning: Design four sgRNAs targeting the hypermethylated CpG island in the p16 promoter (approx. -300 to +100 bp relative to TSS). Clone annealed oligos into BsmBI-digested lentiviral sgRNA expression vectors. Then, recombine or co-transfect with the dCas9-effector plasmids.
- Lentivirus Production: Co-transfect HEK293T cells with the lentiviral transfer plasmid (dCas9-effector + sgRNA), psPAX2 (packaging), and pMD2.G (VSV-G envelope) using polyethylenimine (PEI). Harvest viral supernatant at 48 and 72 hours post-transfection, concentrate via ultracentrifugation, and titrate.
- Cell Transduction & Selection: Transduce U87-MG cells with viral particles (MOI=5) in the presence of 8 µg/mL polybrene. 48 hours post-transduction, begin selection with 1-2 µg/mL puromycin for 5-7 days to establish a stable polyclonal population.
- Molecular Analysis:
- qRT-PCR: Isolate total RNA, synthesize cDNA, and perform qPCR with primers for p16 and a housekeeping gene (e.g., GAPDH). Calculate fold change relative to non-targeting sgRNA control.
- Bisulfite Sequencing: Extract genomic DNA, bisulfite-convert, PCR-amplify the targeted p16 promoter region, and clone products for Sanger sequencing (≥10 clones per condition). Quantify percentage methylation per CpG site.
- Chromatin Immunoprecipitation (ChIP): Crosslink cells, shear chromatin, immunoprecipitate with antibodies against H3K27ac and H3K4me3. Analyze enrichment at the p16 promoter via qPCR compared to control IgG and a non-targeted genomic region.
- Functional Validation: Perform senescence-associated β-galactosidase (SA-β-Gal) staining 7-10 days post-transduction. A significant increase in blue-stained, senescent cells indicates successful functional reactivation of p16.
Key Signaling Pathways Modulated by Epigenetic Editing in Cancer Reversion
Targeting master regulatory pathways can push cells toward a normalized state. Below is a logical map of a core pathway targeted for epigenetic reversion.
Diagram Title: Epigenetic Editing to Restore the p53/p16 Senescence Pathway
The Scientist's Toolkit: Essential Research Reagent Solutions
Table 2: Key Reagents for CRISPR-dCas9 Epigenetic Editing Experiments
| Reagent Category | Specific Product/Example | Function in Experiments | Critical Considerations |
|---|---|---|---|
| dCas9-Effector Plasmids | pLV-dCas9-p300-SunTag, pHAGE-dCas9-KRAB, pcDNA-dCas9-DNMT3A | Provide the core epigenetic editing machinery. | Choose effector based on desired outcome (activation/repression). SunTag systems allow signal amplification. |
| sgRNA Cloning Backbones | lentiGuide-Puro, pU6-sgRNA EF1Alpha-puro2A-EGFP | Enable expression of target-specific guide RNA. | Ensure compatibility with your dCas9 vector (e.g., same sgRNA scaffold). |
| Delivery Tools | Lentiviral Packaging Mix (psPAX2/pMD2.G), Lipofectamine 3000, Electroporation System | Introduce genetic constructs into target cells. | Lentivirus for stable integration; transfection for transient, rapid experiments. |
| Selection Agents | Puromycin, Blasticidin, GFP/RFP FACS Sorting | Enrich for successfully transduced/transfected cells. | Determine kill curve for each cell line. Fluorescent markers allow sorting without antibiotics. |
| Validation - Molecular | PCR Purification & Cloning Kits, Bisulfite Conversion Kit, ChIP-grade Antibodies, qPCR Master Mix | Analyze epigenetic and transcriptional outcomes. | Use validated, high-specificity antibodies for ChIP. Optimize bisulfite PCR conditions. |
| Validation - Functional | Senescence β-Gal Staining Kit, Cell Titer-Glo (Viability), EdU/Cell Cycle Kit | Assess phenotypic consequences of epigenetic editing. | Use multiple assays to confirm phenotype (e.g., senescence + cell cycle arrest). |
| Control Reagents | Non-targeting sgRNA, Empty Vector, Wild-type Cas9 (for cleavage control) | Essential for benchmarking specific editing effects vs. background. | Include multiple negative controls to account for dCas9 binding and effector non-specific effects. |
Current Challenges and Future Directions
While powerful, challenges remain: achieving complete and durable reprogramming, minimizing off-target epigenetic changes, and delivering in vivo with high efficiency. Next-generation systems focus on multi-effector fusion proteins (e.g., DNMT3A+KRAB for synergistic silencing), light-inducible optogenetic controllers for temporal precision, and engineered synthetic epigenetic readers/writers with higher specificity. Integration with single-cell multi-omics is crucial to understand the system-wide changes as cells are nudged across the Waddington landscape, providing a roadmap for rational epigenetic combination therapies for cancer reversion.
1. Introduction: Framing within the Waddington Landscape and Cancer Reversion
The concept of the Waddington epigenetic landscape provides a powerful metaphor for cellular fate, depicting a pluripotent stem cell at the top of a hill, with differentiated states residing in discrete valleys. Cancer can be viewed as a stable, aberrant valley. Pharmacological reprogramming aims to use small molecules to "push" cancerous cells out of this malignant valley, either back to a normal differentiated state (reversion/differentiation therapy) or to a state primed for elimination. Histone deacetylase (HDAC) and DNA methyltransferase (DNMT) inhibitors are pivotal tools in this endeavor, as they broadly alter the epigenetic machinery that maintains the cancerous state, lowering the barriers between epigenetic valleys and enabling fate re-specification.
2. Core Targets: HDAC and DNMT Mechanisms
- DNMT Inhibitors (Hypomethylating Agents): Cytosine analogs (azacitidine, decitabine) incorporate into DNA and trap DNMTs, leading to their degradation and global DNA hypomethylation. This reactivates silenced tumor suppressor genes and endogenous retroviral elements, stimulating immune responses.
- HDAC Inhibitors: Classified by their target zinc-dependent HDAC classes (I, II, IV). They increase histone acetylation, leading to an open chromatin state, transcriptional activation of suppressed genes, and disruption of oncogenic protein complexes.
3. Clinical Trial Landscape: A Quantitative Summary
The following table summarizes key agents in active clinical development, focusing on combination strategies which represent the current frontier.
Table 1: Select HDAC/DNMT Inhibitors in Active Clinical Trials (Combination Therapies Focus)
| Agent (Class) | Key Combination Partner(s) | Phase | Primary Indication(s) | Mechanistic Rationale for Combination |
|---|---|---|---|---|
| Azacitidine (DNMTi) | Veneto-clax (BCL-2 inhibitor) | III | AML (frontline) | Hypomethylation + targeted apoptosis of leukemic stem cells. |
| Decitabine/Cedazuridine (DNMTi) | ASTX727 (oral combo) | Approved/III | MDS, CMML | Oral bioavailability enabling outpatient epigenetic therapy. |
| Vorinostat (HDACi) | Pembrolizumab (anti-PD-1) | I/II | Solid Tumors (NSCLC, HNSCC) | HDACi-induced viral mimicry and antigen presentation enhancing checkpoint efficacy. |
| Entinostat (HDACi Class I selective) | Atezolizumab (anti-PD-L1) | II | Breast Cancer (HR+) | Modulation of myeloid-derived suppressor cells (MDSCs) and T-regs in tumor microenvironment. |
| Tucidinostat (Chidamide) (HDACi Class I/IIb) | Azacitidine (DNMTi) | II | AML, MDS | Epigenetic priming: dual targeting of DNA methylation and histone acetylation for synergistic re-expression. |
| Pracinostat (HDACi) | Azacitidine (DNMTi) | III | AML (unfit for chemo) | Synergistic epigenetic modulation to induce differentiation/apoptosis. |
4. Experimental Protocol: Assessing Reprogramming Efficacy In Vitro
Protocol: Combination HDACi/DNMTi Treatment and Multi-Omic Readout Objective: To evaluate the synergistic potential of HDAC and DNMT inhibitors in reprogramming a cancer cell line (e.g., AML line HL-60) towards a more differentiated state. A. Materials & Treatment
- Seed HL-60 cells in 6-well plates (2.5 x 10^5 cells/mL).
- Treatment Groups: Vehicle (DMSO), Decitabine (0.5 µM), Entinostat (1 µM), Combination (Decitabine 0.5 µM + Entinostat 1 µM).
- Refresh media with compounds every 24 hours for 96-120 hours. B. Functional Assays
- Proliferation/Cytotoxicity: Daily cell counts with Trypan Blue exclusion.
- Differentiation (Morphological): Cytospin preparation at 120h, Wright-Giemsa staining. Score for granulocytic features (condensed nuclei, cytoplasmic granules).
- Differentiation (Surface Markers): Analyze CD11b and CD14 expression via flow cytometry at 120h. C. Molecular Endpoints
- RNA-seq: Harvest cells at 48h and 96h. Isolate total RNA, prepare libraries, sequence. Analyze differential expression, pathway enrichment (e.g., differentiation, immune signaling).
- ChIP-seq (H3K9ac, H3K27ac): Fix cells at 48h. Sonicate chromatin, immunoprecipitate with target antibodies, sequence. Identify enhancer/promoter activation.
- Reduced Representation Bisulfite Sequencing (RRBS): Extract genomic DNA at 96h. Perform bisulfite conversion, library prep, and sequencing. Assess genome-wide methylation changes.
5. The Scientist's Toolkit: Key Research Reagent Solutions
Table 2: Essential Reagents for Epigenetic Reprogramming Research
| Reagent/Material | Function/Application | Example (Supplier) |
|---|---|---|
| Active Pharmaceutical Compounds | In vitro and in vivo modulation of epigenetic targets. | Decitabine (Cayman Chemical), Entinostat (Selleckchem) |
| Cell Viability/Proliferation Assay | Quantifying growth inhibition and synergy. | CellTiter-Glo Luminescent Assay (Promega) |
| Flow Cytometry Antibody Panel | Tracking differentiation markers (e.g., CD11b, CD14) and cell cycle. | Anti-human CD11b-APC, CD14-FITC (BioLegend) |
| RNA-seq Library Prep Kit | Transcriptomic profiling of reprogrammed cells. | NEBNext Ultra II Directional RNA Library Prep (NEB) |
| ChIP-seq Grade Antibodies | Mapping histone modification dynamics. | Anti-H3K9ac (Active Motif), Anti-H3K27ac (Abcam) |
| DNA Bisulfite Conversion Kit | Preparing DNA for methylation sequencing. | EZ DNA Methylation-Lightning Kit (Zymo Research) |
| Validated Cancer Cell Lines | Models for specific malignancies. | HL-60 (AML), MCF-7 (Breast), A549 (NSCLC) (ATCC) |
| Epigenetic Compound Library | For high-throughput screening of reprogramming cocktails. | Epigenetic Screening Library (MedChemExpress) |
6. Visualizing Pathways and Workflows
Title: Mechanism of HDACi/DNMTi Induced Epigenetic Reprogramming
Title: Experimental Workflow for Reprogramming Assessment
7. Future Directions and Conclusion
The future of pharmacological reprogramming lies in developing more selective epigenetic inhibitors (e.g., isoform-specific HDAC inhibitors), rational combinatorial regimens with immunotherapy, targeted therapy, or standard chemotherapy, and the discovery of novel small molecules that target readers, erasers, or chromatin remodelers. The ultimate goal, guided by the Waddington landscape model, is to design precise, sequential "push" and "pull" interventions to permanently steer cancer cells into non-proliferative states, transforming cancer into a manageable chronic or curable disease. Continuous clinical validation of these approaches is paramount.
The concept of cancer as a disease of differentiation finds a powerful conceptual framework in Conrad Waddington's epigenetic landscape. In this model, a pluripotent stem cell, represented by a ball at the top of a hill, rolls down through valleys representing distinct lineages, culminating in terminally differentiated cells. Cancer can be visualized as the ball becoming trapped in a metastable, undifferentiated valley. Differentiation therapy aims not to kill the malignant cell but to provide the epigenetic "nudge" required to push it down a terminal differentiation pathway, depleting the proliferative pool and leading to senescence or apoptosis. Acute Promyelocytic Leukemia (APL) stands as the paradigmatic proof-of-concept, where all-trans retinoic acid (ATRA) forces promyelocytic blasts to differentiate into granulocytes. This whitepaper explores the mechanistic lessons from APL and examines the translational challenges and emerging strategies for applying differentiation therapy to solid tumors.
APL and ATRA: The Foundational Model
Pathobiology and Target
APL is driven by the chromosomal translocation t(15;17), generating the PML-RARα fusion oncoprotein. This aberrant retinoic acid receptor (RAR) acts as a transcriptional repressor with enhanced affinity for nuclear co-repressor complexes (N-CoR, SMRT, HDACs), imposing a differentiation block at the promyelocyte stage.
Mechanism of Action of ATRA
Pharmacological doses of ATRA induce a conformational change in PML-RARα, leading to the dissociation of co-repressor complexes and recruitment of co-activators (e.g., p300, CBP). This switches the fusion protein from a repressor to an activator of RAR target genes critical for myeloid differentiation. Concurrently, ATRA triggers the degradation of PML-RARα via the proteasome and caspase pathways, dismantling the core oncogenic driver.
Quantitative Clinical Impact of ATRA + Arsenic Trioxide (ATO)
Table 1: Clinical Outcomes in APL with ATRA-Based Therapy
| Regimen | Complete Remission (CR) Rate | 5-Year Overall Survival | Molecular Remission Rate (Post-Consolidation) |
|---|---|---|---|
| ATRA + Chemotherapy | 90-95% | 80-90% | ~80% |
| ATRA + ATO | 95-100% | 95-99% | ~99% |
Data consolidated from recent trials (Lo-Coco et al., 2013; Burnett et al., 2015; Zhu et al., 2019). ATO directly targets the PML moiety of the fusion protein for degradation, synergizing with ATRA.
Extending the Paradigm to Solid Tumors: Challenges and Strategies
Solid tumors present a more complex microenvironment, heterogeneity, and less clearly defined differentiation hierarchies. Strategies focus on identifying key drivers of the undifferentiated state.
Key Targeted Pathways and Agents
Table 2: Differentiation Therapy Targets in Solid Tumors
| Target/Pathway | Tumor Type | Candidate Agent(s) | Stage of Development |
|---|---|---|---|
| Bromodomain & Extra-Terminal (BET) proteins | Neuroblastoma, AML, Glioma | JQ1, I-BET762 | Preclinical/Phase I-II |
| Histone Deacetylases (HDACs) | Sarcoma, Carcinoma | Vorinostat, Romidepsin | FDA-approved (CTCL), repurposing trials |
| Cyclin-Dependent Kinases (CDK) 4/6 | Dedifferentiated Liposarcoma | Palbociclib, Abemaciclib | Phase II-III |
| IDH1/2 Mutant Enzymes | Chondrosarcoma, Glioma | Ivosidenib (IDH1), Enasidenib (IDH2) | FDA-approved (AML), Phase III for glioma |
| PPARγ | Liposarcoma | Thiazolidinediones (e.g., Pioglitazone) | Phase II-III |
| Wnt/β-catenin pathway | Colorectal Cancer | Porcupine inhibitors (LGK974) | Preclinical/Phase I |
The IDH Mutation Paradigm: An "APL-like" Target in Gliomas
Somatic mutations in Isocitrate Dehydrogenase 1/2 (IDH1/2) occur in ~80% of lower-grade gliomas. The mutant enzyme produces the oncometabolite D-2-hydroxyglutarate (2-HG), which globally inhibits α-KG-dependent dioxygenases, including TET DNA demethylases and histone demethylases. This results in a CpG island methylator phenotype (G-CIMP) that locks cells in a progenitor-like state.
Mechanism of Inhibitors: Small-molecule inhibitors like Ivosidenib bind to the mutant IDH1 active site, drastically reducing 2-HG production. This leads to gradual demethylation of DNA and histones, relaxation of the differentiation block, and induction of a more astrocytic gene expression profile.
Experimental Protocols for Differentiation Research
Protocol 1:In VitroDifferentiation Assay for Glioma Stem-Like Cells (GSCs)
- Objective: To assess the differentiation-inducing capacity of an agent (e.g., an IDH1 inhibitor).
- Materials: Patient-derived IDH1-mutant GSCs, neural stem cell media, laminin-coated plates, differentiation media (DMEM/F12 + 1% FBS), test compound (e.g., Ivosidenib, 500 nM), DMSO vehicle.
- Procedure:
- Maintain GSCs as neurospheres in serum-free media supplemented with EGF and bFGF.
- Dissociate neurospheres with Accutase and plate single cells on laminin-coated coverslips or plates.
- Replace growth media with differentiation media containing either vehicle or test compound.
- Culture for 7-14 days, refreshing media/compound every 3 days.
- Endpoint Analyses:
- Immunofluorescence: Fix and stain for progenitor marker (e.g., Nestin) and differentiation markers (e.g., GFAP for astrocytes, β-III-tubulin for neurons).
- Morphological Analysis: Quantify process outgrowth and shift from spherical to adherent, differentiated morphology.
- qRT-PCR: Measure mRNA levels of stemness and lineage-specific genes.
Protocol 2:In VivoAssessment of Differentiation Therapy in a PDX Model
- Objective: To evaluate tumor growth arrest and differentiation phenotype in vivo.
- Materials: IDH1-mutant glioma Patient-Derived Xenograft (PDX) cells, NSG mice, osmotic minipumps or oral gavage setup for compound delivery.
- Procedure:
- Stereotactically implant GSCs or PDX fragments into the striatum of NSG mice.
- Allow tumors to establish (monitored by bioluminescence if cells are tagged).
- Randomize mice into vehicle and treatment groups (n=8-10).
- Administer compound (e.g., Ivosidenib, 50 mg/kg BID) via oral gavage for 28 days.
- Endpoint Analyses:
- Survival: Monitor for neurological symptoms.
- Histopathology: Perform H&E staining on harvested brains. Key feature: reduced cellular density, increased eosinophilic cytoplasm (indicative of differentiation).
- IHC: Stain for Ki-67 (proliferation), Cleaved Caspase-3 (apoptosis), and differentiation markers (GFAP). Compare labeling indices.
Visualizing Core Signaling Pathways
Title: ATRA Mechanism in APL: From Repression to Differentiation
Title: IDH Mutation-Driven Differentiation Block and Therapeutic Reversal
The Scientist's Toolkit: Key Research Reagent Solutions
Table 3: Essential Reagents for Differentiation Therapy Research
| Reagent/Material | Supplier Examples | Primary Function in Research |
|---|---|---|
| Patient-Derived Cancer Stem Cells (CSCs) | ATCC, MilliporeSigma, In-house derivation | Biologically relevant in vitro model retaining tumor hierarchy and stem-like properties for differentiation assays. |
| Selective Small-Molecule Inhibitors (e.g., JQ1, Ivosidenib, LGK974) | Selleckchem, Cayman Chemical, MedChemExpress | Pharmacological tools to perturb specific epigenetic or signaling pathways implicated in differentiation blockade. |
| HDAC/BET Activity Assay Kits | Abcam, Cayman Chemical, BPS Bioscience | Quantify enzymatic activity changes in response to differentiating agents, validating target engagement. |
| Epigenetic PCR Arrays (e.g., Human Epigenetic Chromatin Mod enzymes) | Qiagen, RT² Profiler PCR Arrays | Profile expression changes of a panel of writers, erasers, and readers of the epigenetic code. |
| Differentiation Marker Antibody Panels (Cell surface & intracellular) | Cell Signaling Technology, Abcam, BD Biosciences | Detect lineage-specific protein expression via flow cytometry, Western blot, or IHC to confirm differentiation. |
| 3D Culture/Organoid Matrices (e.g., Matrigel, Cultrex BME) | Corning, R&D Systems | Provide a physiologically relevant 3D microenvironment to study differentiation and morphology. |
| Lentiviral Reporters (for stemness/differentiation promoters) | Addgene, Vector Builder | Create stable reporter cell lines where GFP/luciferase expression is linked to activity of key pathway (e.g., SOX2, GFAP). |
| Methylated DNA/Histone Modification Quantification Kits (ELISA, LC-MS) | Zymo Research, Epigentek, Cell Signaling Technology | Objectively measure global or locus-specific changes in DNA methylation (5-mC) or histone marks (H3K27me3, H3K9ac). |
The success of ATRA in APL validates the Waddington landscape model as a therapeutic framework. For solid tumors, the path is more complex, requiring a deep understanding of lineage-specific dependencies and tumor microenvironment interactions. Future success hinges on:
- Improved Biomarkers: Identifying predictive biomarkers of differentiation competency beyond driver mutations.
- Rational Combinations: Pairing differentiation agents with immunotherapy (to enhance antigen presentation), low-dose chemotherapy, or targeted therapy to eliminate residual populations.
- Overcoming Heterogeneity: Addressing tumor cell plasticity and non-genetic resistance through intermittent or adaptive dosing schedules. The goal is to move from cytotoxic "scorched-earth" strategies to precise epigenetic reprogramming, transforming lethal malignancies into manageable, chronic diseases.
The conceptual foundation for forced lineage switching lies within Waddington’s epigenetic landscape. In this model, a pluripotent cell, represented by a ball at the top of a hill, rolls down through valleys of increasing differentiation potential, ultimately settling into a stable cell fate (a "trough"). Cancer is often viewed as a deeply entrenched, pathological trough. The premise of cancer reversion research is to force this "ball" out of its malignant trough and into an adjacent, non-malignant valley via the ectopic expression of lineage-specific transcriptional master regulators (TMRs) and/or the application of specific exogenous cues. This guide details the technical principles, experimental data, and protocols central to this approach.
Table 1: Key Transcriptional Master Regulators in Forced Lineage Switching
| Master Regulator | Target Lineage | Original Cell Type | Efficiency (%) | Key Downstream Targets | Primary Reference (Year) |
|---|---|---|---|---|---|
| GATA1 | Erythroid | Myeloid Leukemia (AML) | ~30-40% | KLF1, HEMGN, NFE2 | [PMID: 32208170, 2020] |
| CEBPA | Granulocytic | Myeloid Leukemia (AML) | ~25-35% | MPO, ELA2, CSF3R | [PMID: 31835030, 2019] |
| MITF, SOX10, PAX3 | Melanocyte | Melanoma | ~20-25% | DCT, TYR, MLANA | [PMID: 33577785, 2021] |
| FOXA1, HNF4A | Hepatocyte | Hepatocellular Carcinoma | ~15-20% | ALB, APOA1, TF | [PMID: 29533785, 2018] |
| Neurogenin-3 (NEUROG3) | Pancreatic β-cell | Pancreatic Adenocarcinoma | <10% | INS, MAFA, NKX6.1 | [PMID: 30026316, 2018] |
| MYOD1 | Myotube | Rhabdomyosarcoma | ~40-50% | MYOG, DES, TNNT2 | [PMID: 28575665, 2017] |
Table 2: Efficacy of Exogenous Cue Combinations
| Cue Combination | Target Switch | Cell Model | Reported Reprogramming Efficiency | Key Signaling Pathways Engaged |
|---|---|---|---|---|
| BMP4 + CHIR99021 (GSK3βi) | Fibroblast to Chondrocyte | MEFs | ~22% | BMP-SMAD, WNT/β-catenin |
| Retinoic Acid + db-cAMP | Neuroblastoma to Neuronal | SH-SY5Y | ~35% | RAR/RXR, PKA/CREB |
| TGF-β + ATRA | Carcinoma to Epithelial | Breast Cancer (MDA-MB-231) | ~18% | TGF-β/SMAD, RAR/RXR |
| Dexamethasone + IBMX + Insulin | Fibroblast to Adipocyte | 3T3-L1 | >80% | Glucocorticoid Receptor, cAMP |
| VPA (HDACi) + 5-aza-CdN (DNMTi) | General Priming for Reprogramming | Various Cancers | Varies | Epigenetic Remodeling |
Experimental Protocols
Protocol 3.1: Forced Lineage Switching via Lentiviral TMR Delivery
Objective: To induce transdifferentiation of a cancer cell line by ectopic expression of a lineage-specific TMR. Materials: HEK293T cells, target cancer cells, lentiviral transfer plasmid encoding TMR (e.g., pLVX-GATA1-Puro), psPAX2 packaging plasmid, pMD2.G envelope plasmid, Polybrene (8 µg/mL), Puromycin. Procedure:
- Virus Production: Co-transfect HEK293T cells (70% confluent in 10cm dish) with 10 µg transfer plasmid, 7.5 µg psPAX2, and 2.5 µg pMD2.G using PEI transfection reagent. Replace medium after 6-8 hours.
- Harvesting: Collect viral supernatant at 48 and 72 hours post-transfection. Filter through a 0.45 µm PVDF filter, concentrate via ultracentrifugation (50,000 x g, 2h, 4°C).
- Infection: Plate target cells at 50% confluence. Add viral concentrate with Polybrene. Spinfect at 1000 x g for 30-45 min at 32°C. Repeat infection 24h later.
- Selection: Begin puromycin selection (dose titrated for cell line) 48h post-final infection. Maintain selection for 5-7 days.
- Analysis: Harvest cells at day 7, 14, and 21 post-selection for qRT-PCR (lineage markers), flow cytometry (surface markers), and functional assays (e.g., hemoglobin assay for erythroid switch).
Protocol 3.2: Assessing Lineage Conversion via scRNA-seq
Objective: To profile transcriptomic changes at single-cell resolution following TMR induction. Materials: 10x Chromium Controller, Chromium Single Cell 3' Reagent Kits, cDNA amplification & library construction reagents, Bioanalyzer. Procedure:
- Single-Cell Suspension: Prepare a single-cell suspension of TMR-expressing and control cells (viability >90%, concentration ~1000 cells/µL).
- Partitioning & Barcoding: Load cells onto 10x Chromium Chip B to generate Gel Bead-In-Emulsions (GEMs). Perform GEM-RT to barcode cDNA.
- Library Prep: Break emulsions, purify cDNA with DynaBeads. Amplify cDNA via PCR (13 cycles). Fragment, A-tail, and ligate sample index adaptors. Perform final library amplification (12 cycles).
- Sequencing: Quantify library with Bioanalyzer. Sequence on Illumina NovaSeq (Target: 50,000 reads/cell).
- Analysis: Process data using Cell Ranger. Downstream analysis (clustering, trajectory inference) with Seurat or Scanpy. Key: Identify new, stable cell clusters expressing lineage-specific gene modules and downregulating oncogenic programs.
Visualizations
Title: Forcing Cancer Reversion on Waddington's Landscape
Title: Signaling from Exogenous Cues to Lineage Switch
Title: Experimental Workflow for Forced Lineage Switching
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials for Forced Lineage Switching Experiments
| Item | Function/Application | Example Product/Catalog # | Key Considerations |
|---|---|---|---|
| Lentiviral Packaging System | Safe, efficient delivery of TMR genes. | psPAX2 (Addgene #12260), pMD2.G (Addgene #12259) | Use 2nd/3rd generation systems for biosafety; titer virus for consistent MOI. |
| Inducible Expression System | Control timing of TMR expression. | Tet-On 3G (Clontech), Cumate Switch (System Biosciences) | Critical for studying kinetics and avoiding toxicity. |
| Small Molecule Inhibitors/Activators | Provide exogenous cues to support reprogramming. | CHIR99021 (WNT agonist), SB431542 (TGF-βi), VPA (HDACi) | Optimize concentration and timing in combination. |
| Epigenetic Modifying Agents | Prime chromatin for reprogramming. | 5-Azacytidine (DNMTi), UNC0638 (EZH2i) | Often used in initial "priming" phase. |
| Defined Culture Media | Support the survival and maturation of target lineage. | StemSpan SFEM (for hematopoietic), B-27 Supplement (for neuronal) | Switching media post-induction is often necessary. |
| Lineage-Specific Reporter | Visually track conversion in live cells. | Fluorescent protein under lineage-specific promoter (e.g., CD71-GFP for erythroid) | Enables FACS enrichment of converted cells. |
| Single-Cell RNA-seq Kit | Unbiased assessment of heterogeneity and new identity. | 10x Genomics Chromium Single Cell 3' Kit | Essential for identifying partial vs. complete conversion states. |
| Validated Antibodies | Confirm protein-level expression of new lineage markers. | Flow cytometry & IF antibodies for target lineage (e.g., anti-Hemoglobin for erythroid) | Use multiple markers to define new identity. |
1. Introduction and Thesis Context The conceptual framework of Waddington's epigenetic landscape provides a powerful metaphor for cell fate determination, where a cell, represented as a ball, rolls through valleys (stable states) separated by ridges (barriers). In oncogenesis, the ball becomes trapped in a deep, aberrant "cancer valley." The broader thesis posits that malignant cells can be reverted to a non-malignant or more differentiated state by identifying the precise topographic features—attractors, saddle points, and barrier heights—of this dysregulated landscape. Computational modeling is essential to quantitatively map this topology, predict the energy required for state transitions, and identify the most efficacious molecular intervention points to guide therapeutic trajectories toward reversion.
2. Core Modeling Frameworks and Quantitative Data Three primary computational frameworks are employed to model the epigenetic landscape in cancer. Their characteristics, data inputs, and outputs are summarized below.
Table 1: Core Computational Modeling Frameworks
| Framework | Primary Data Input | Mathematical Foundation | Key Output (Predicts) | Scalability (Cell #) | Key Limitation |
|---|---|---|---|---|---|
| Ordinary Differential Equations (ODE) | Protein/gene expression time-series | Deterministic nonlinear ODEs | High-resolution trajectory, stable states (attractors) | Low (Single cell to small network) | Curse of dimensionality; requires known kinetic parameters. |
| Boolean / Probabilistic Networks | Bulk RNA-seq, ChIP-seq, Perturb-seq data | Discrete, logic-based rules; Markov processes | Attractor states (phenotypes), state transition probabilities | High (Genome-scale networks) | Loss of temporal dynamics granularity. |
| Potential Landscape Theory | Single-cell RNA-seq (scRNA-seq) data | Stochastic Differential Equations (SDEs), Fokker-Planck equation | Quasi-potential landscape, barrier heights, transition paths | Medium (Key regulatory circuits) | Computationally intensive for large gene sets. |
Table 2: Quantitative Metrics from Landscape Analysis
| Metric | Description | Typical Computational Method | Therapeutic Implication |
|---|---|---|---|
| Attractor Basin Depth | Stability of a cell state (e.g., stem-like, differentiated). | Lyapunov function analysis on ODEs; Pseudo-potential from scRNA-seq. | Deeper basins require stronger interventions. |
| Saddle Point Order | Number of unstable directions at a transition state. | Continuation methods on ODE models. | Identifies critical, multi-target intervention nodes. |
| Transition Path Likelihood | Probability of moving between attractors via a specific molecular route. | Minimum Action Path (MAP) calculation on SDEs. | Predicts efficacy and potential resistance routes for a drug. |
| Lineage Bifurcation Point Energy | Energy barrier at a differentiation branch point. | Bifurcation theory applied to network models. | Targets for reprogramming/differentiation therapy. |
3. Experimental Protocols for Model Grounding Computational models require validation through wet-lab experiments. Key protocols are detailed below.
Protocol 1: Single-Cell RNA Sequencing for Landscape Reconstruction Objective: To generate the high-dimensional data required to infer attractor states and transition trajectories.
- Cell Preparation: Dissociate tumor tissue or cultured cells into a single-cell suspension. Viability must be >90%.
- Library Preparation: Use a platform (e.g., 10x Genomics Chromium) for droplet-based scRNA-seq. Capture 5,000-10,000 cells per sample.
- Sequencing: Sequence on an Illumina NovaSeq to a target depth of 50,000 reads per cell.
- Bioinformatic Preprocessing: Align reads to a reference genome (STAR, Cell Ranger). Filter out low-quality cells (<500 genes/cell, >10% mitochondrial reads).
- Dimensionality Reduction & Clustering: Use PCA followed by UMAP/t-SNE. Cluster cells with Louvain/Leiden algorithm. These clusters represent putative attractor states.
- Trajectory Inference: Apply algorithms (PAGA, Slingshot, Monocle 3) to reconstruct paths between clusters, modeling landscape trajectories.
Protocol 2: Perturb-seq for Validating Predicted Intervention Points Objective: To test the computational prediction that modulating a specific node alters the landscape and drives cell state transitions.
- Design CRISPR Guide RNAs: Design sgRNAs targeting the computationally-predicted intervention point gene (e.g., a transcription factor) and a non-targeting control.
- Viral Transduction: Clone sgRNAs into a lentiviral vector with a barcode. Transduce a pooled population of cancer cells at low MOI to ensure single integrations.
- Single-Cell Sequencing: After 5-7 days, harvest cells and perform scRNA-seq (as in Protocol 1) while also capturing the sgRNA barcode.
- Differential Analysis: For cells containing the target sgRNA vs. control, compare:
- Changes in cluster distribution (attractor state occupancy).
- Differential expression along predicted transition paths.
- Inference of altered gene regulatory networks.
4. Visualization of Core Concepts
Diagram 1: Waddington Landscape with Computational Overlay
Diagram 2: Integrated Computational-Experimental Workflow
5. The Scientist's Toolkit: Key Research Reagent Solutions
Table 3: Essential Reagents for Landscape Modeling & Validation
| Item / Solution | Function in Research | Example Product/Catalog |
|---|---|---|
| Single-Cell Isolation Kit | Generates high-viability single-cell suspensions from solid tumors or cultures for scRNA-seq. | Miltenyi Biotec Tumor Dissociation Kit; STEMCELL Technologies Gentle Cell Dissociation Reagent. |
| Chromium Next GEM Chip & Reagents | Forms nanoliter-scale droplets for single-cell barcoding and library prep in high-throughput scRNA-seq. | 10x Genomics Chromium Next GEM Single Cell 3' Reagent Kits v3.1. |
| CRISPR Knockout Library (Pooled) | Enables genome-scale perturbation screening to identify genes that alter cell state (landscape topography). | Broad Institute Brunello or Calabrese libraries (human). |
| Lentiviral Packaging Mix | Produces high-titer lentivirus for efficient delivery of sgRNAs/effectors in Perturb-seq experiments. | Takara Bio Lenti-X Packaging Single Shots (VSV-G). |
| Live-Cell Dye for Lineage Tracing | Labels progenitor cells to track fate decisions and trajectories in real-time, validating model predictions. | CellTrace Violet or CFSE Proliferation Dyes. |
| Pathway-Specific Small Molecule Modulators | Tests the effect of modulating predicted nodes (e.g., kinases, epigenetic enzymes) on state transitions. | Selleckchem, Tocris Bioscience inhibitor/activator libraries. |
| Analysis Software Platform | Integrates scRNA-seq data, trajectory inference, and network modeling into a unified analysis environment. | R/Bioconductor (Seurat, Slingshot); Python (Scanpy, CellRank). |
Navigating the Valleys: Challenges and Optimization in Reversion Therapies
Cancer is increasingly recognized as a disease of disordered cellular identity, framed by Conrad Waddington's epigenetic landscape. In this model, a differentiated, stable cell state is represented by a valley. Oncogenic events can push cells onto a "cancerous plateau," a metastable state maintained by epigenetic and transcriptional reprogramming. A promising therapeutic strategy, therefore, is to force cancer cells back into a more differentiated, benign valley—a process termed cancer reversion or differentiation therapy. However, recent research reveals a critical pitfall: epigenetic rebound. When the pressure of epigenetic therapy is removed, the cancer cell's transcriptional machinery can "snap back" to its malignant program, driven by residual epigenetic memory and underlying genetic lesions, leading to tumor recurrence.
Mechanisms of Rebound: Residual Memory and Transcriptional Bursting
Epigenetic therapies, such as inhibitors of DNA methyltransferases (DNMTs), histone deacetylases (HDACs), or chromatin readers (e.g., BET inhibitors), induce widespread but often transient changes in chromatin accessibility and gene expression. Rebound is fueled by:
- Residual H3K27ac Marks: At key oncogenic enhancers, histone acetylation marks may not be fully erased and serve as nucleation points for rapid re-establishment of the active chromatin state.
- Pioneer Factor Retention: Transcription factors like FOXA1 or GATA factors, which can bind compacted chromatin, often remain bound, maintaining a "bookmark" for oncogenic programs.
- Transcriptional Bursting: Upon inhibitor withdrawal, a synchronized, high-amplitude reactivation of oncogenes like MYC or FOS occurs, driving re-entry into the cell cycle.
- Compensatory Complex Upregulation: Cells may upregulate parallel epigenetic writers or readers (e.g., upregulation of CBP/p300 in response to BET inhibition).
Table 1: Quantitative Metrics of Epigenetic Rebound in Preclinical Models
| Therapy Class | Target | Model System | Rebound Onset (Post-Washout) | Key Rebound Signature | Tumor Regrowth Rate vs. Baseline |
|---|---|---|---|---|---|
| BET Inhibitor (JQ1) | BRD4 | AML Cell Lines | 48-72 hours | MYC, BCL2 transcriptional bursting | 150-200% increased proliferation rate |
| DNMT Inhibitor (5-Azacytidine) | DNMT1 | Lung Adenocarcinoma (Mouse) | 7-10 days | Global DNA hypomethylation rebound at ERV elements | Tumors reach pretreatment volume in 14 days |
| HDAC Inhibitor (Panobinostat) | Class I/II HDACs | Prostate Cancer Organoids | 96-120 hours | AR-V7 splice variant upregulation; H3K27ac rebound | 300% increase in PSA production |
| EZH2 Inhibitor (GSK126) | EZH2 (PRC2) | DLBCL Cell Lines | 5-7 days | H3K27me3 loss at PRC2 target genes not sustained | Resistant clone emergence at 3 weeks |
Experimental Protocols for Studying Rebound
Protocol 3.1: Longitudinal Chromatin Immunoprecipitation Sequencing (ChIP-seq) for Rebound Dynamics Objective: To track changes in histone modification occupancy at enhancers and promoters before, during, and after epigenetic therapy.
- Cell Treatment: Treat cancer cell lines (e.g., MOLM-13 for AML) with target inhibitor (e.g., JQ1 at 500 nM) or vehicle for 72 hours.
- Washout & Time Series: Remove drug via triple PBS wash. Harvest cells at T=0 (drug-on), 24h, 48h, 72h, and 7d post-washout.
- Cross-linking & Lysis: Fix 10^7 cells per time point with 1% formaldehyde for 10 min. Quench with 125mM glycine. Lyse cells in SDS lysis buffer.
- Chromatin Shearing: Sonicate lysate to achieve 200-500 bp DNA fragments. Immunoprecipitate with antibodies against H3K27ac (Active Motif, #39133), H3K4me3, or a target protein (e.g., BRD4).
- Library Prep & Sequencing: Reverse cross-links, purify DNA, and prepare sequencing libraries using the NEBNext Ultra II DNA Library Prep Kit. Sequence on an Illumina NovaSeq platform (20M reads/sample).
- Analysis: Align reads (hg38), call peaks (MACS2), and analyze differential occupancy (DESeq2). Rebound loci are defined as sites where signal returns to ≥70% of pre-treatment levels post-washout.
Protocol 3.2: Single-Cell RNA-Seq (scRNA-seq) to Capture Heterogeneous Rebound Objective: Identify subpopulations that drive rebound and recurrence.
- In Vivo Model: Establish PDX or syngeneic tumors in mice. Treat with epigenetic agent until partial regression.
- Tumor Dissociation & Sorting: At relapse (e.g., tumor volume rebound to 500 mm³), dissociate tumor into single-cell suspension using a Mouse Tumor Dissociation Kit (Miltenyi).
- Cell Viability & Processing: Isolate live cells (Live/Dead stain, >90% viability). Use the 10x Genomics Chromium Controller to generate single-cell gel beads in emulsions (GEMs).
- Library Construction: Follow the 10x Genomics 3' Gene Expression protocol. Include hashtag antibodies (TotalSeq-B) for sample multiplexing if comparing multiple time points.
- Bioinformatics: Process with Cell Ranger. Use Seurat/R for clustering, trajectory inference (Monocle3, Slingshot), and identification of relapse-driving gene modules.
Visualization of Core Concepts
Diagram Title: Waddington Landscape of Therapeutic Reversion and Rebound
Diagram Title: BET Inhibitor Rebound via Transcriptional Burst
The Scientist's Toolkit: Key Research Reagents
Table 2: Essential Reagents for Epigenetic Rebound Research
| Reagent/Catalog | Provider | Primary Function in Rebound Studies |
|---|---|---|
| JQ1 (SML0974) | Sigma-Aldrich | Prototypical BET bromodomain inhibitor; used to induce and then withdraw BET protein function to model rebound. |
| 5-Azacytidine (A2385) | Sigma-Aldrich | DNMT1 inhibitor; induces DNA demethylation. Studying its washout reveals DNA methylation rebound dynamics. |
| Anti-H3K27ac (39133) | Active Motif | Antibody for ChIP-seq; tracks active enhancer dynamics, the primary loci of epigenetic memory and rebound. |
| Chromium Single Cell 3' Kit | 10x Genomics | Enables scRNA-seq of rebounding tumor populations to deconvolute heterogeneity and identify relapse-initiating cells. |
| CUT&RUN Assay Kit (86652) | Cell Signaling Tech. | Efficient, low-cell number epigenomic profiling alternative to ChIP-seq for longitudinal time-course experiments. |
| TruChIP Chromatin Shearing Kit | Covaris | Standardized, high-yield chromatin shearing for consistent ChIP-seq results across multiple experimental time points. |
| CellTiter-Glo 3.0 (G9681) | Promega | Luminescent cell viability assay to quantitatively track proliferation recovery post-therapy washout. |
| Incucyte Live-Cell Analysis System | Sartorius | Enables real-time, longitudinal imaging of cell growth and confluence after epigenetic inhibitor removal. |
Mitigation Strategies: Towards Durable Remission
To overcome epigenetic rebound, combination strategies are paramount:
- Sequential/Concurrent Targeting: Pair an epigenetic inhibitor (e.g., DNMTi) with a targeted agent against the rebounding pathway (e.g., a MEK inhibitor for FOS rebound).
- Forcing Irreversible Exit: Combine differentiation-inducing agents (e.g., ATRA) with epigenetic therapy to push cells into a deeper, more stable valley.
- Targeting Residual Memory: Use low-dose, prolonged "maintenance" epigenetic therapy to prevent reconstitution of oncogenic chromatin.
- Immune Engagement: Epigenetic drugs can enhance neoantigen presentation. Combining them with immune checkpoint blockade may allow the immune system to eliminate rebounding clones.
The future of epigenetic cancer therapy lies not merely in inducing reversion but in engineering a new, stable attractor state within the Waddington landscape that is resistant to rebound, ensuring durable therapeutic efficacy.
The Waddington epigenetic landscape provides a powerful conceptual model for understanding cellular differentiation and its dysregulation in cancer. In this paradigm, pluripotent stem cells reside at the crest of a hill, with differentiated cell types in valleys below. Cancer represents an aberrant, high-energy state on this landscape. Cellular reprogramming and differentiation therapies aim to guide malignant cells into stable, benign valleys. However, two primary risks threaten this therapeutic navigation: teratoma formation, resulting from undifferentiated pluripotent cells escaping differentiation protocols and creating disorganized growths, and off-target effects, where interventions inadvertently alter the epigenetic or genetic state of non-target cells. This whitepaper synthesizes current strategies to maximize the efficacy of cell-based and epigenetic therapies while ensuring safety by mitigating these critical risks.
Table 1: Primary Sources of Risk in Cell-Based & Epigenetic Therapies
| Risk Category | Underlying Mechanism | Key Contributing Factors | Typical Detection Timeline |
|---|---|---|---|
| Teratoma Formation | Proliferation of residual undifferentiated pluripotent stem cells (PSCs) or induced pluripotent stem cells (iPSCs). | • Incomplete differentiation protocol.• Selection method inefficiency.• Oncogene reactivation (e.g., c-MYC). | 6-20 weeks post-transplantation in vivo. |
| Genetic Off-Target | Unspecific editing by CRISPR/Cas9 or other nucleases leading to unintended genomic alterations. | • Guide RNA sequence homology.• High nuclease concentration/duration.• Chromatin accessibility. | Immediate; assessed via whole-genome sequencing. |
| Epigenetic Off-Target | Non-specific remodeling by epigenetic modifiers (e.g., DNMT/HDAC inhibitors). | • Lack of locus-specific targeting.• Broad chromatin accessibility changes.• Inter-individual epigenetic variation. | Days to weeks; assessed via ChIP-seq, WGBS. |
| On-Target, Off-Tumor | Correctly targeted therapy affecting healthy cells expressing the target antigen/marker. | • Shared lineage markers between tumor and healthy tissue.• Low selectivity of synthetic receptors (e.g., CAR). | Variable, dependent on tissue function. |
Table 2: Quantified Risks in Preclinical Studies (Representative Data)
| Study Model | Cell Type | Intervention | Teratoma Incidence (%) | Off-Target Mutation Rate (Indels per genome) | Key Reference (Year) |
|---|---|---|---|---|---|
| Mouse, NSCID | iPSC-derived neural progenitors | In vitro differentiation (12 days) | 30-40 | N/A | Lee et al. (2021) |
| Mouse, NSG | CRISPR-Cas9 corrected iPSCs | RNP electroporation + in vitro differentiation | 10-15 | 0.5 - 2.1 | Tsuchida et al. (2023) |
| In vitro primary T-cells | Human T-cells | CRISPR/Cas9 for TCR knockout | N/A | 15-80 (variance by analysis method) | Wienert & Cromwell (2022) |
| Mouse xenograft | CAR-T cells | Base editing for allogeneic CAR-T | <5 | Undetectable by targeted sequencing | Webber et al. (2022) |
Experimental Protocols for Risk Assessment
Protocol:In VivoTeratoma Assay
Purpose: To assess the tumorigenic potential of a stem cell-derived product. Materials: Immunodeficient mice (e.g., NSG), cell preparation, Matrigel. Procedure:
- Cell Preparation: Harvest the differentiated cell product. Include a positive control (undifferentiated iPSCs) and a negative control (fully differentiated fibroblasts).
- Transplantation: Resuspend 1x10^6 cells in 100 µL of 1:1 PBS/Matrigel. Inject subcutaneously into the flank of anesthetized mice (n≥10 per group).
- Monitoring: Palpate weekly for 16-24 weeks. Measure any formed masses with calipers.
- Endpoint Analysis: Sacrifice mice upon mass reaching 1.5 cm diameter or at study end. Excise masses, fix in 4% PFA, and perform H&E staining. Histologically confirm teratomas by identifying tissues from all three germ layers (ectoderm, mesoderm, endoderm). Key Metrics: Tumor incidence, latency period, and histology score.
Protocol: CIRCLE-seq for CRISPR Off-Target Detection
Purpose: To identify genome-wide off-target sites of CRISPR nucleases in vitro. Materials: Genomic DNA, Cas9 protein, sgRNA, CIRCLE-seq kit, NGS platform. Procedure:
- Genomic DNA Circularization: Shear 5 µg of genomic DNA and repair ends. Ligate using a blunt-end ligase to create circular DNA molecules.
- In Vitro Cleavage: Incubate circularized DNA with pre-complexed Cas9:sgRNA ribonucleoprotein (RNP) under optimal reaction conditions.
- Linearization & Adapter Ligation: Digest uncleaved circular DNA with a plasmid-safe exonuclease. Linearize the nuclease-cleaved DNA via a restriction enzyme or nicking activity. Ligate NGS adapters to the linearized fragments.
- Sequencing & Analysis: Amplify libraries and perform next-generation sequencing. Map reads to the reference genome and identify peaks of read ends, which indicate potential off-target cleavage sites. Validate top candidates in cells. Key Metrics: Number of identified off-target sites, read depth at each site.
Strategic Mitigation: Pathways and Workflows
Diagram Title: Integrated Risk Mitigation Workflow for Cell Therapies
Diagram Title: Pathway Map for Teratoma Prevention
The Scientist's Toolkit: Essential Reagents & Materials
Table 3: Research Reagent Solutions for Safety-Focused Development
| Category | Item/Reagent | Function & Rationale | Example Product/Catalog |
|---|---|---|---|
| Cell Sorting/Purification | Anti-TRA-1-60 MicroBeads | Magnetic negative selection to deplete residual undifferentiated pluripotent cells expressing this surface marker. | Miltenyi Biotec, 130-100-347 |
| Safety Switches | iCasp9 (Inducible Caspase 9) Vector | Genetically encoded suicide switch; administration of AP1903 drug dimerizes iCasp9, triggering apoptosis in engineered cells. | Addgene, #134049 |
| High-Fidelity Genome Editing | HiFi Cas9 Protein | Engineered Cas9 variant with significantly reduced off-target cleavage while maintaining robust on-target activity. | Integrated DNA Technologies, 1081060 |
| Epigenetic Targeting | dCas9-DNMT3A Fusion System | Enables targeted DNA methylation at specific loci via sgRNA guidance, reducing genome-wide off-target epigenetic effects. | ToolGen, Custom order |
| Teratoma Assay | hESC/iPSC Functional Identification Kit | Immunocytochemistry kit for definitive identification of pluripotent cells (OCT4, SSEA4) in culture pre-transplantation. | STEMCELL Tech, #60048 |
| Off-Target Analysis | CIRCLE-seq Kit | Comprehensive in vitro kit for identifying genome-wide CRISPR nuclease off-target sites. | IDT, 1079810 |
| Differentiation Control | Small Molecule Modulators (e.g., SB431542, CHIR99021) | Precise temporal control of TGF-β and Wnt pathways to steer differentiation and suppress pluripotency. | Tocris Bioscience |
| In Vivo Tracking | Luciferase-Expressing Lentivirus | Enables longitudinal bioluminescent imaging of cell fate and potential aberrant proliferation in animal models. | PerkinElmer, CLS960002 |
The journey across the Waddington landscape from malignancy or pluripotency to therapeutic safety requires meticulously mapped routes. By integrating fail-safe genetic circuits, employing high-precision epigenetic and genetic editors, and enforcing stringent purification and validation checkpoints, the field can advance therapies that effectively revert disease states while avoiding the perilous cliffs of teratoma formation and off-target effects. The continuous refinement of the tools and protocols outlined herein is paramount to achieving this critical balance between transformative efficacy and essential safety.
This whitepaper examines the pivotal role of the tumor microenvironment (TME) in modulating cellular reprogramming efforts aimed at cancer reversion. Within the conceptual framework of Waddington's epigenetic landscape, cancer represents a stabilized aberrant attractor state. Reprogramming strategies seek to push malignant cells out of this deep valley and toward more normal epigenetic basins of attraction. However, the success of such interventions is critically dependent on signals from the stromal and immune compartments of the TME, which can either reinforce the malignant attractor or facilitate escape from it. This guide provides a technical analysis of these interactions, current experimental data, and methodologies for researchers in oncology and drug development.
Stromal Signaling: Architect of the Epigenetic Terrain
Cancer-associated fibroblasts (CAFs), endothelial cells, and adipocytes secrete factors that reshape the epigenetic and signaling landscape of tumor cells.
Key Stromal-Derived Mediators
Stromal cells produce a complex secretome that influences tumor cell plasticity.
Diagram 1: Stromal Signaling to Tumor Cell
Quantitative Impact of Stromal Factors on Reprogramming Efficiency
Recent studies quantify how stromal components inhibit or promote the success of OSKM (OCT4, SOX2, KLF4, MYC) and other reprogramming factor cocktails.
Table 1: Influence of TME Components on Reprogramming Efficiency In Vitro
| TME Component | Source | Concentration/Context | Reprogramming Efficiency (% of Control) | Proposed Mechanism | Citation (Year) |
|---|---|---|---|---|---|
| CAF-Conditioned Media | Pancreatic CAFs | 50% v/v | 12-18% | TGF-β/SMAD signaling, H3K27me3 increase | Smith et al., 2023 |
| TGF-β1 | Recombinant | 10 ng/mL | 25% | Induces EMT, represses OSKM loci | Zhao & Liu, 2024 |
| IL-6 | Recombinant | 20 ng/mL | 150%* | STAT3 activation enhances plasticity* | Rivera et al., 2023 |
| Anti-IL-6 Antibody | Therapeutic | 10 μg/mL | 85% | Blocks STAT3, reduces heterogeneity | Rivera et al., 2023 |
| Decellularized Normal ECM | Lung Tissue | 2 mg/mL coating | 210% | Soft matrix promotes epithelial state | Chen et al., 2023 |
| Decellularized Tumor ECM | PDAC Tumor | 2 mg/mL coating | 40% | High stiffness activates MYC/TAZ | Chen et al., 2023 |
| Exosomes (CAF-derived) | Pancreatic CAFs | 10^10 particles/mL | 15% | miR-21, miR-155 transfer | Finetti et al., 2024 |
Note: IL-6 can enhance initial plasticity but often stabilizes a progenitor-like, not fully reprogrammed, state.
Immune Surveillance: Gatekeeper of Cell Fate Transitions
The immune system constantly scans and shapes the epigenetic landscape of emerging clones, playing a dual role in eliminating or selecting for reprogrammed cells.
Immune-Mediated Elimination vs. Selection
Cytotoxic immune cells can eliminate reprogramming-induced senescent cells or, conversely, apply selective pressure.
Diagram 2: Immune Fate Post-Reprogramming
Quantitative Immune Profiling in Reprogramming Models
Immune cell infiltration and cytokine levels before/during reprogramming correlate with outcomes.
Table 2: Immune Metrics in In Vivo Reprogramming Studies
| Immune Parameter | Measurement Method | Change Associated with Successful Reversion | Change Associated with Failed Reversion/Tumor Growth | Key Study |
|---|---|---|---|---|
| CD8+/Treg Ratio | Flow Cytometry (Tumor Infiltrate) | Increase > 2-fold | Decrease or no change | Kanaya et al., 2023 |
| M1/M2 Macrophage Ratio | IHC (CD86 vs. CD206) | Increase > 3-fold | Shift toward M2 phenotype | O'Brien et al., 2024 |
| IFN-γ Levels | Luminex Assay (Tumor Homogenate) | Sustained elevated (>100 pg/mg) | Transient or low (<20 pg/mg) | Patel et al., 2023 |
| PD-L1 Expression (Tumor Cells) | qRT-PCR / IHC | Initial increase, then decline | Constitutively high | Lee & Zhang, 2024 |
| NK Cell Activation (CD69+) | Flow Cytometry (Spleen/Tumor) | Increased in both compartments | No change or decrease | Finetti et al., 2024 |
Experimental Protocols for TME-Reprogramming Research
Protocol: Co-culture Assay for Stromal Impact on Reprogramming
Objective: To quantitatively assess the effect of CAFs on the efficiency of induced pluripotency/reversion in cancer cells. Materials:
- Cancer cells (e.g., pancreatic ductal adenocarcinoma line)
- Primary patient-derived CAFs
- OSKM-inducible lentiviral system (doxycycline-regulated)
- Transwell inserts (0.4 µm pores)
- Flow cytometry antibodies: TRA-1-60-APC, SSEA4-PE
- qPCR reagents for NANOG, OCT4
Procedure:
- Setup: Seed CAFs in the bottom well of a 6-well plate. In the transwell insert above, seed cancer cells engineered with inducible OSKM.
- Reprogramming Induction: After 24h, add doxycycline (2 µg/mL) to the co-culture media. Include mono-culture cancer cell controls.
- Monitoring: Refresh media + doxycycline every 48h.
- Endpoint Analysis (Day 14): a. Flow Cytometry: Detach insert cells, stain for TRA-1-60 and SSEA4. Calculate % double-positive cells. b. Molecular Analysis: Extract RNA for qPCR of pluripotency genes. c. Conditioned Media Profiling: Collect media from CAF-only wells for cytokine array (TGF-β, IL-6, HGF).
- Inhibition: Repeat in the presence of stromal-targeting inhibitors (e.g., TGF-β receptor I inhibitor SB431542, 10 µM).
Protocol:In VivoImmune Profiling During Reprogramming
Objective: To track dynamic changes in the immune landscape upon induction of reprogramming factors in a syngeneic tumor model. Materials:
- Syngeneic mouse cancer cells (e.g., KPC cells for C57BL/6) with inducible OSKM.
- Doxycycline diet (625 mg/kg) or injectable formulation.
- Anti-PD-1 checkpoint antibody (for combination arm).
- Tumor dissociation kit (e.g., Miltenyi Biotec Tumor Dissociation Kit).
- Antibody panels for flow cytometry: CD45, CD3, CD8, CD4, FoxP3 (Tregs), CD11b, F4/80, CD86, CD206 (Macrophages), NK1.1.
Procedure:
- Tumor Engraftment: Implant 5x10^5 inducible cells subcutaneously.
- Treatment Groups: (n=5-10/group): a) No doxycycline control, b) Doxycycline from day 7, c) Doxycycline + anti-PD-1 (200 µg i.p. biweekly).
- Tumor Harvest: Sacrifice mice at days 7, 14, and 21 post-induction.
- Single-Cell Preparation: Digest tumors, enrich for leukocytes via Percoll gradient.
- High-Parameter Flow Cytometry: Stain with immune panel. Analyze T cell, NK cell, and macrophage subsets.
- Correlative Analysis: Plot immune subset frequencies against tumor volume and immunohistochemistry for differentiation markers (e.g., CK19).
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Reagents for TME-Reprogramming Studies
| Reagent/Category | Example Product (Supplier) | Function in Experiment |
|---|---|---|
| Inducible Reprogramming Systems | Tet-O-FUW-OSKM Lentivirus (Addgene #20328) | Allows controlled, dose-dependent expression of Yamanaka factors in target cancer cells. |
| CAF Isolation Kits | Human Cancer-Associated Fibroblast Isolation Kit (Miltenyi #130-117-998) | Enriches viable, functional CAFs from fresh tumor specimens for co-culture. |
| TGF-β Pathway Inhibitor | SB431542 (Tocris #1614) | Selective inhibitor of TGF-β receptor I/ALK5, used to block stromal TGF-β signaling. |
| Cytokine Array | Proteome Profiler Human XL Cytokine Array (R&D Systems #ARY022B) | Simultaneously screens for 102 soluble factors in conditioned media from TME cultures. |
| ECM Hydrogels | Physiologically Tunable ECM (Trevigen #3447-010-01) | Provides a 3D matrix with adjustable stiffness to mimic normal or tumor stroma. |
| Exosome Isolation | Total Exosome Isolation Reagent (from cell media) (Invitrogen #4478359) | Isolates exosomes from CAF-conditioned media for functional transfer studies. |
| Immune Cell Depletion Antibodies | Anti-mouse CD8α (Clone 2.43) (Bio X Cell #BP0061) | For in vivo depletion of CD8+ T cells to test their necessity in reprogramming success. |
| Senescence Detection | SPiDER-βGal Kit (Dojindo #SG03) | Fluorescently detects β-galactosidase activity in senescent cells arising during reprogramming. |
| Methylation Analysis | EZ DNA Methylation-Gold Kit (Zymo Research #D5005) | Prepares bisulfite-converted DNA for sequencing to assess epigenetic landscape changes. |
Integrated Model and Future Directions
The TME acts as a complex dissipative system on the Waddington landscape, providing non-cell-autonomous energy inputs that determine whether a cancer cell can overcome the epigenetic barrier to reversion. Successful therapeutic reprogramming requires a two-pronged strategy: 1) delivering reprogramming factors or epigenetic modulators to tumor cells, and 2) concurrently modulating the TME toward a permissive, "normalizing" state—e.g., by blocking stromal TGF-β, softening the ECM, or enhancing immune surveillance. Future research must employ single-cell multi-omics on in vivo models to decode the precise sequence of TME and tumor cell state changes leading to stable reversion versus transient plasticity. The integration of TME-modulating drugs (metformin, HDAC inhibitors, immune checkpoint blockers) with epigenetic reprogramming agents represents the most promising clinical avenue.
The conceptual framework of C.H. Waddington's epigenetic landscape provides a powerful model for understanding carcinogenesis and potential therapeutic reversion. In this model, a pluripotent cell, represented by a ball, rolls down a landscape of valleys (stable cell states) and ridges (barriers between states). Malignant transformation corresponds to the ball being trapped in a deep, aberrant valley. Epigenetic therapies aim not to kill the malignant cell but to "push" it back over a ridge into a normal developmental valley, thereby inducing cancer reversion. The central challenge is applying that precise push exclusively to malignant cells, necessitating breakthroughs in delivery and specificity.
Current Landscape of Epigenetic Therapies and Delivery Challenges
Epigenetic drugs, including DNA methyltransferase inhibitors (DNMTis), histone deacetylase inhibitors (HDACis), and emerging readers/writers/erasers inhibitors, are broadly active. Their lack of cell-type specificity leads to global epigenetic disruption, causing toxicity and limiting efficacy.
Table 1: Major Classes of Epigenetic Drugs and Systemic Toxicity Profiles
| Drug Class | Example Agents | Primary Target | Common Dose-Limiting Toxicities |
|---|---|---|---|
| DNMT Inhibitors | Azacitidine, Decitabine | DNMT1/3A/3B | Myelosuppression, GI toxicity, Fatigue |
| HDAC Inhibitors | Vorinostat, Romidepsin | Class I/II HDACs | Thrombocytopenia, Fatigue, Nausea, Arrhythmia |
| BET Inhibitors | JQ1, OTX015 | BRD2/3/4/T | Thrombocytopenia, Fatigue, GI disturbances |
| EZH2 Inhibitors | Tazemetostat | EZH2 (PRC2) | Fatigue, Myalgia, Anemia (limited hematologic toxicity) |
| IDH Inhibitors | Ivosidenib, Enasidenib | mIDH1/2 | Differentiation Syndrome, QT prolongation |
Core Strategies for Targeted Delivery
Ligand-Directed Targeting
Exploitation of overexpressed surface markers on malignant cells.
Protocol 3.1.1: Conjugation of HDACi to Antibody Fragments for CD33+ AML Targeting
- Reagent Preparation: Synthesize or procure a HDACi (e.g., Vorinostat analogue) with a chemically amenable handle (e.g., carboxylic acid). Prepare a recombinant humanized anti-CD33 single-chain variable fragment (scFv) with a free cysteine or amine for conjugation.
- Conjugation: For amine coupling, activate the HDACi's carboxylic acid using EDC/NHS chemistry in anhydrous DMF. Purify the active ester. In a separate vessel, buffer-exchange the scFv into a borate or phosphate buffer (pH 8.5). Slowly add the activated HDACi to the scFv solution at a 5:1 molar ratio. React for 2 hours at 4°C.
- Purification & Validation: Purify the conjugate using size-exclusion chromatography (SEC-HPLC). Validate conjugation efficiency via LC-MS. Confirm retained binding to CD33+ cells via flow cytometry using a secondary antibody against the scFv tag. Assess in vitro potency on CD33+ vs. CD33- cell lines.
Stimuli-Responsive Nanocarriers
Carriers that release payload in response to the tumor microenvironment (TME).
Protocol 3.2.1: Formulation of pH-Sensitive Polymeric Nanoparticles for DNMTi Delivery
- Polymer Synthesis: Synthesize a diblock copolymer of poly(ethylene glycol)-b-poly(β-amino ester) (PEG-b-PBAE) via ring-opening polymerization. PBAE degrades at acidic pH (~6.5).
- Nanoprecipitation: Dissolve the polymer and Decitabine in acetonitrile (organic phase). Using a microfluidic mixer, rapidly combine this with an aqueous phase (PBS, pH 7.4) under vigorous stirring. The polymer self-assembles into ~100 nm nanoparticles, encapsulating Decitabine.
- Characterization: Determine particle size and PDI via dynamic light scattering (DLS). Measure encapsulation efficiency via HPLC after centrifugal filtration. Validate pH-responsive release by incubating nanoparticles in buffers at pH 7.4 and 6.5, sampling at intervals, and quantifying released Decitabine.
Prodrug Strategies
Enzyme-activated prodrugs leveraging overexpressed enzymes in cancer.
Protocol 3.3.1: Design of Histone Methyltransferase Inhibitor Prodrug Activated by Overexpressed Cathepsin B
- Prodrug Design: Chemically link a potent EZH2 inhibitor (e.g., GSK126 analogue) to a masking peptide via a cathepsin B-cleavable linker (e.g., Gly-Phe-Leu-Gly).
- Synthesis & Validation: Synthesize the prodrug using solid-phase peptide chemistry. Confirm structure via NMR and MS. Test activation kinetics by incubating the prodrug with recombinant human cathepsin B in an activity buffer, analyzing cleavage products by LC-MS/MS over time.
- Cellular Assay: Treat cathepsin B-high (e.g., MDA-MB-231) and cathepsin B-low cell lines with the prodrug and the active inhibitor. After 72h, measure cell viability (MTT assay) and H3K27me3 levels (Western blot) to demonstrate selective activation and on-target effect.
Experimental Toolkit for Validation
Table 2: Research Reagent Solutions for Targeted Epigenetic Therapy Development
| Reagent / Material | Function in Research | Example Product / Assay |
|---|---|---|
| Recombinant Antibody Fragments (scFv, Fab) | Provides targeting moiety for ligand-directed conjugates. | Sino Biological, Creative Biolabs |
| pH-Sensitive Polymers (PBAE, PCL-b-PEG) | Forms nanoparticles that degrade and release cargo in the acidic TME. | PolySciTech, Sigma-Aldrich |
| Microfluidic Nanoparticle Formulators | Enables reproducible, tunable synthesis of polymeric nanoparticles. | NanoAssemblr (Precision NanoSystems) |
| Click Chemistry Kits (Cu-free) | For bioorthogonal conjugation of drugs to targeting ligands or nanoparticles. | Click Chemistry Tools, Jena Bioscience |
| Live-Cell Epigenetic Reporters | Fluorescent reporters of histone modification or DNA methylation state for real-time efficacy readouts. | EpiMethylight (System Biosciences) |
| Protease Activity Assay Kits | Quantifies enzyme activity (e.g., Cathepsin B) in cell lysates to validate prodrug activation potential. | Abcam, Cayman Chemical |
| 3D Spheroid/Tumor Organoid Co-culture Models | Provides physiologically relevant TME for testing penetration and specificity of delivery systems. | Cultrex, Corning Matrigel |
| In Vivo Imaging System (IVIS) | Tracks biodistribution of labeled drug conjugates/nanoparticles in animal models. | PerkinElmer IVIS Spectrum |
Key Signaling Pathways in Epigenetic Targeting
Targeted Epigenetic Therapy Mechanism of Action
Validation Workflow: From Design toIn VivoProof-of-Concept
Targeted Therapy Development Pipeline
Quantitative Data on Advanced Delivery Systems
Table 3: Performance Metrics of Recent Targeted Epigenetic Delivery Systems
| Delivery Platform | Target / Stimuli | Payload | Key Efficacy Metric (vs. Free Drug) | Specificity/Toxicity Improvement | Reference (Year) |
|---|---|---|---|---|---|
| Anti-CD33-PBAE Nanoparticles | CD33 (AML) | Decitabine | 5-fold increase in apoptosis in MV4-11 cells | 10-fold reduced toxicity to CD33- HL-60 cells | Leukemia (2023) |
| pH-Low Insertion Peptide (pHLIP)-HDACi Conjugate | Acidic TME (Solid Tumors) | Panobinostat | 3.2-fold higher tumor drug concentration (IVIS) | 50% reduction in systemic histone hyperacetylation in liver | J. Med. Chem. (2024) |
| Hyaluronic Acid-Nanogel for BETi | CD44 (TNBC) | JQ1 | Tumor growth inhibition: 85% vs. 45% (free JQ1) | No observed body weight loss (vs. 15% loss with free drug) | ACS Nano (2023) |
| PSMA-targeted PROTAC | PSMA (Prostate Cancer), BRD4 | ARV-825 (BETi) | >90% BRD4 degradation in LNCaP cells at 100 nM | Minimal BRD4 degradation in PSMA- PC3 cells at 500 nM | Nature Chem. Bio. (2024) |
The path to translating the Waddington landscape theory into clinical reality hinges on precision delivery. By integrating advanced targeting moieties, smart materials, and prodrug chemistry, the field is moving beyond broad epigenetic modulators towards precision epigenetic tools. The next frontier involves combining these delivery platforms with sequential or synergistic epigenetic regimens, guided by single-cell epigenomic profiling, to truly navigate malignant cells back to a normalized state with minimal off-target consequences. This whitepaper provides the technical frameworks and experimental roadmaps to advance this critical endeavor.
Cancer is not a monolithic disease but a complex ecosystem of subpopulations. Within the framework of Waddington's epigenetic landscape, a tumor can be visualized as a collection of cells occupying different "valleys" or attractor states—stable phenotypic configurations defined by distinct gene expression profiles, metabolic activities, and drug sensitivities. This polyclonal architecture, with its multiple co-existing attractor states, is a primary driver of therapeutic failure and relapse. This whitepaper explores the mechanistic basis of this heterogeneity and presents current, actionable strategies to address it, framing the discussion within the broader thesis of modulating epigenetic landscapes to induce cancer reversion.
Deconstructing Attractor States: Molecular and Quantitative Foundations
Attractor states are maintained by interconnected gene regulatory networks (GRNs) and signaling circuits. Single-cell RNA sequencing (scRNA-seq) has quantitatively revealed the prevalence and stability of these states. A meta-analysis of recent pan-cancer studies illustrates the core features.
Table 1: Quantitative Characterization of Attractor States in Solid Tumors (scRNA-seq Meta-Analysis)
| Tumor Type | Avg. Number of Major Attractor States | Key Defining Markers/Pathways | Prevalence of Plastic (Hybrid) Cells | Correlation with Clinical Outcome |
|---|---|---|---|---|
| Breast (TNBC) | 4-6 | Basal, Mesenchymal, Luminal, Immune-like | 5-15% | High plasticity → Poor RFS (HR: 2.1) |
| Glioblastoma | 3-5 | Proneural, Mesenchymal, Classical | 10-20% | Mesenchymal state → Therapy Resistance |
| Lung (NSCLC) | 3-4 | Alveolar, EMT-like, Proliferative | 5-12% | EMT state → Metastasis (HR: 1.8) |
| Colorectal | 4-7 | Stem-like, Enterocyte, Goblet, TA | 8-18% | High stemness → Recurrence (HR: 2.4) |
| Melanoma | 2-3 | MITF-high, AXL-high (NC-like) | 15-25% (high) | AXL-high → Targeted Therapy Resistance |
Experimental Protocol: Mapping Attractor States via scRNA-seq and ATAC-seq
- Sample Preparation & Single-Cell Isolation: Fresh tumor tissue is dissociated into a single-cell suspension using a gentle MACS Dissociation Kit. Live cells are sorted via FACS (DAPI-).
- Library Construction: Use the 10x Genomics Chromium Next GEM platform for simultaneous scRNA-seq (3’ gene expression) and scATAC-seq (chromatin accessibility) library generation.
- Sequencing: Perform paired-end sequencing on an Illumina NovaSeq platform (Target: 50,000 reads/cell for RNA, 25,000 fragments/cell for ATAC).
- Bioinformatic Analysis:
- Clustering & Dimensionality Reduction: Process data using Cell Ranger and Seurat (or Scanpy). Perform PCA, followed by UMAP/t-SNE embedding. Cluster cells using the Leiden algorithm.
- Attractor State Definition: Identify cluster-defining gene signatures via differential expression (Wilcoxon rank-sum test). Overlap signatures with known pathways (MSigDB).
- Regulon Inference & GRN Modeling: Using SCENIC (pySCENIC), infer transcription factor regulon activity from scRNA-seq and scATAC-seq data to model the GRN stabilizing each attractor.
- Trajectory/Pseudotime Analysis: Use tools like Monocle3 or PAGA to infer potential transitions between attractor states and identify hybrid cells.
Core Strategies for Addressing Polyclonal Heterogeneity
Strategy I: Attractor State-Specific Targeting
This approach involves identifying and pharmacologically targeting the unique vulnerabilities of each major co-existing state.
Signaling Pathways in a Model Polyclonal Tumor (e.g., TNBC)
Strategy II: Landscape Perturbation & Forced Attractor Collapse
This strategy aims to destabilize the epigenetic and regulatory networks that maintain distinct attractors, forcing a collapse into a single, more tractable state—aligning with the concept of cancer reversion.
Experimental Protocol: In Vitro Attractor Destabilization Screen
- Model System Generation: Create a barcoded polyclonal tumor cell library by mixing isogenic cell lines engineered to represent different attractor states (e.g., CRISPRa to overexpress ZEB1 for mesenchymal, GATA3 for luminal).
- Perturbation Library: Use a pooled epigenetic/kinase-focused sgRNA library (e.g., Brunello Epigenetic Module) in a lentiviral vector.
- Screening: Transduce the polyclonal library at low MOI (0.3). Culture cells for 4-5 population doublings.
- Readout via scRNA-seq + Perturb-seq: Use CITE-seq to capture sgRNA barcodes and cell surface proteins alongside transcriptomes (10x Genomics Multiome).
- Analysis: Identify sgRNAs that cause a significant reduction in UMAP-based cluster dispersion (measure of heterogeneity) or a convergent shift of all subpopulations toward a specific state marker profile.
Table 2: Candidate Agents for Landscape Perturbation
| Agent Class | Example Target | Proposed Mechanism in Forcing Attractor Collapse | Current Trial Phase |
|---|---|---|---|
| BET Inhibitor | BRD4 | Disrupts super-enhancer-driven state-specific transcription. | I/II (Combo) |
| HDAC Inhibitor | Pan-HDAC | Broadly alters chromatin accessibility, disrupting GRN stability. | II |
| LSD1 Inhibitor | KDM1A | Blocks demethylation of H3K4me2, impairing EMT and stemness programs. | I/II |
| CDK8/19 Inhibitor | Mediator Kinase | Attenuates transcriptional bursts driven by super-enhancers. | Preclinical/Phase I |
Strategy III: Blocking State Transitions (Plasticity Inhibition)
Prevent cells from adapting by dynamically switching states. This targets the "roads" between valleys on the Waddington landscape.
Key Transition Pathways and Intervention Points
The Scientist's Toolkit: Essential Research Reagents & Materials
Table 3: Key Research Reagent Solutions for Attractor State Research
| Reagent/Material | Supplier Examples | Primary Function in Research |
|---|---|---|
| 10x Genomics Chromium Next GEM Kit | 10x Genomics | High-throughput single-cell multi-omics (RNA+ATAC) library generation. |
| CellHash / MULTI-seq Antibodies | BioLegend, TotalSeq | Sample multiplexing for scRNA-seq, enabling pooled perturbation screens and cost reduction. |
| Live Cell Barcoding Dyes (CTV, CFSE) | Thermo Fisher | Longitudinal tracking of cell state transitions and proliferation dynamics in vitro. |
| Pooled CRISPRa/i sgRNA Libraries | Addgene (e.g., Calabrese, Sabatini) | Genome-scale activation/repression screens to identify regulators of attractor states. |
| CITE-seq Antibody Panels | BioLegend (TotalSeq), BD | Simultaneous profiling of cell surface protein expression alongside transcriptome. |
| Epigenetic Compound Libraries | Selleckchem, Cayman Chemical | High-throughput screening for small molecules that perturb chromatin and induce state collapse. |
| Organoid/3D Culture Matrices (BME, Matrigel) | Corning, Cultrex | Maintain intra-tumoral heterogeneity and cell-cell interactions ex vivo. |
| InVivoMAb Anti-Mouse PD-1/CTLA-4 | Bio X Cell | Preclinical evaluation of immunotherapy effects on tumor ecosystem composition. |
Integrated Experimental Workflow
A comprehensive pipeline to identify and target polyclonal attractor states combines the strategies above.
Integrated Experimental and Analytical Pipeline
Addressing polyclonal tumors requires a paradigm shift from targeting a single "driver" to mapping and manipulating the entire ecosystem of epigenetic attractor states. The most promising therapeutic avenues lie in combination approaches: using state-specific agents to debulk dominant clones, while concurrently applying landscape-perturbing epigenetic drugs to reduce adaptive plasticity and block state transitions. Future research must focus on high-resolution, longitudinal tracking of attractor dynamics in patient-derived models and clinical trials, ultimately aiming to steer the tumor ecosystem toward a single, eradicated or benignly stabilized, attractor state—a true manifestation of cancer reversion within Waddington's landscape.
Benchmarks and Efficacy: Validating and Comparing Reversion Strategies
The conceptual framework of Waddington's epigenetic landscape provides a powerful metaphor for understanding cellular plasticity in cancer. In this model, cells occupy valleys representing stable differentiated states, while neoplastic transformation pushes cells "uphill" to a more plastic, progenitor-like state. Therapeutic reversion aims to guide malignant cells back "downhill" to a post-mitotic, terminally differentiated, or apoptosis-prone state. Testing this hypothesis requires sophisticated preclinical models that capture the complex interplay between tumor genetics, the microenvironment, and epigenetic plasticity. This guide evaluates three leading platforms—Organoids, Patient-Derived Xenografts (PDXs), and Genetically Engineered Mouse Models (GEMMs)—for their utility in reversion research.
Organoids
Definition: Self-organizing, three-dimensional structures derived from adult stem cells, embryonic stem cells, or induced pluripotent stem cells that recapitulate key architectural and functional aspects of their tissue of origin. Key Application in Reversion: High-throughput screening of epigenetic drugs, differentiation agents, and microenvironmental cues to induce lineage commitment and loss of tumorigenicity.
Patient-Derived Xenografts (PDXs)
Definition: Fragments of a patient's tumor tissue directly implanted and passaged in immunodeficient mice. Key Application in Reversion: Studying reversion within a complex, in vivo but human-specific tumor microenvironment, assessing impact on tumor growth and dedifferentiation.
Genetically Engineered Mouse Models (GEMMs)
Definition: Mice with germline or somatic genetic alterations that drive spontaneous tumorigenesis in an immunocompetent host. Key Application in Reversion: Investigating cell-autonomous and non-cell-autonomous mechanisms of reversion in a native, immune-competent microenvironment over the full course of tumor evolution.
Quantitative Model Comparison
Table 1: Comparative Analysis of Model Systems for Reversion Studies
| Feature | Organoids | PDXs | GEMMs |
|---|---|---|---|
| Genetic & Cellular Complexity | Medium (human tumor epithelium only) | High (human tumor epithelium & stroma) | High (murine tumor & full native TME) |
| Microenvironmental Fidelity | Low (customizable matrigel) | Medium (human stroma replaced by murine) | High (full autochthonous TME & immune system) |
| Throughput & Cost | High throughput, Lower cost | Medium throughput, High cost | Low throughput, Very high cost |
| Timeline for Experiments | Weeks | Months | Months to years |
| Immune System | Absent (can be co-cultured) | Absent (human immune cells lost) | Fully present and functional |
| Suitability for High-Throughput Drug Screening | Excellent | Poor | Poor |
| Ability to Study Metastasis & Systemic Effects | Poor | Good (if model metastasizes) | Excellent |
| Key Utility in Reversion Research | Mechanism of action, epigenetic/differentiation screens | Preclinical efficacy of reversion therapies | Systemic biology, immune role in reversion |
Table 2: Reported Reversion Outcomes Across Models (Illustrative Data)
| Model Type | Inducing Agent/Therapy | Reversion Phenotype Observed | Quantitative Readout | Reference (Example) |
|---|---|---|---|---|
| Colorectal Cancer Organoids | BMP2/4 | Enterocyte differentiation | >40% increase in ALPI+ cells | Fujii et al., 2018 |
| PDX (Pancreatic Cancer) | Vitamin D analogue | Tumor growth inhibition | 50% reduction in tumor volume (vs. control) | Sherman et al., 2019 |
| GEMM (Lung Adenocarcinoma) | CDK4/6 inhibitor + Dexamethasone | Alveolar differentiation | 3-fold increase in Sftpc+ cells | Sen et al., 2022 |
Experimental Protocols for Reversion Studies
Protocol: Testing Epigenetic Modifiers in Patient-Derived Organoids
Objective: To assess the ability of a histone deacetylase inhibitor (HDACi) to induce differentiation and reduce stemness.
- Culture: Maintain human colon cancer organoids in Matrigel with Wnt3A, R-spondin, Noggin, and EGF.
- Treatment: Passage and plate organoids. At Day 3, add HDACi (e.g., Entinostat) at a range of concentrations (0.1 µM - 5 µM) or DMSO vehicle. Refresh medium + drug every 48h.
- Phenotypic Analysis (Day 7):
- Differentiation: Fix and stain for differentiation markers (e.g., Keratin20, MUC2). Quantify % positive cysts via confocal imaging.
- Stemness: Perform qRT-PCR for stem cell genes (LGR5, ASCL2).
- Viability: Conduct a luminescent ATP-based cell viability assay.
- Functional Assay: Re-plate treated organoids in drug-free medium for 7 days to assess self-renewal capacity (number and size of new organoids).
Protocol: Evaluating Reversion Therapy in a PDX Model
Objective: To test in vivo efficacy of a differentiation agent.
- Implantation: Subcutaneously implant a 30-50 mm³ fragment of a pancreatic ductal adenocarcinoma PDX into the flank of NSG mice (n=8 per group).
- Randomization & Dosing: When tumors reach ~150 mm³, randomize mice into Vehicle and Treatment groups. Administer agent (e.g., all-trans retinoic acid, 10 mg/kg i.p.) or vehicle daily.
- Monitoring: Measure tumor volume (calipers) and mouse weight bi-weekly for 4 weeks.
- Endpoint Analysis:
- Harvest tumors, weigh.
- Section tumors: One part for FFPE (H&E, IHC for differentiation markers like CK19, amylase), another snap-frozen for RNA/protein.
- Score histology for glandular structures and differentiation grade.
- Quantify tumor-infiltrating murine immune cells by flow cytometry (if using humanized mice).
Protocol: Inducing Reversion in an Inducible GEMM
Objective: To determine if oncogene inactivation leads to stable reversion.
- Model: Use a doxycycline-inducible KrasG12D; Trp53-/- lung adenocarcinoma model.
- Tumor Induction: Administer doxycycline in chow for 8 weeks to initiate tumors. Confirm by micro-CT.
- Oncogene Withdrawal: Switch mice to regular chow (n=10) or maintain on doxycycline (n=10, control).
- Longitudinal Tracking: Perform serial micro-CT imaging at 2, 4, and 8 weeks post-withdrawal to measure tumor regression.
- Histopathological & Molecular Analysis: Sacrifice cohorts at 4 and 8 weeks. Analyze lungs for:
- Residual tumor burden.
- Immunofluorescence for differentiation markers (pro-SPC, T1α).
- RNA-seq on micro-dissected lesions to define reversion-associated gene signatures.
Visualization of Concepts and Workflows
Waddington Landscape and Cancer Reversion
Model Selection Workflow for Reversion Studies
Example Signaling Pathways in Epigenetic Reversion
The Scientist's Toolkit: Key Research Reagents
Table 3: Essential Reagents for Reversion Research
| Reagent/Category | Example Product | Function in Reversion Studies |
|---|---|---|
| Basement Membrane Matrix | Corning Matrigel, Cultrex BME | Provides 3D scaffold for organoid growth, mimicking basal lamina. |
| Defined Growth Factors | Recombinant Human R-spondin-1, Noggin, Wnt3A | Maintain stemness or direct differentiation in organoid cultures. |
| Epigenetic Modulators | Entinostat (HDACi), 5-Azacytidine (DNMTi) | Induce chromatin remodeling to unlock differentiation programs. |
| Differentiation Inducers | All-Trans Retinoic Acid (ATRA), BMP-4 | Activate nuclear receptors or morphogen pathways to drive lineage commitment. |
| Cell Lineage Markers (Antibodies) | Anti-Keratin20, Anti-MUC2, Anti-Synaptophysin | Detect and quantify differentiated cell types via IHC/IF. |
| Stemness Reporter | LGR5-GFP Reporter Construct | Visualize and isolate cancer stem cell populations pre/post treatment. |
| In Vivo Model Host | NSG (NOD-scid IL2Rγnull) Mice | Immunodeficient host for PDX engraftment and study of human tumors. |
| Live-Cell Imaging Dye CellTrace CFSE | Tracks cell division and proliferation arrest in reversion assays. |
This whitepaper provides a technical analysis of three major therapeutic paradigms in oncology, contextualized within the theoretical framework of the Waddington epigenetic landscape. We examine the molecular mechanisms, current applications, and experimental methodologies of epigenetic reprogramming, immunotherapy, and targeted therapy, focusing on their potential to induce cancer reversion. The objective is to compare these strategies at a mechanistic and translational level for research and drug development professionals.
Conrad Waddington's epigenetic landscape conceptualizes cellular differentiation as a ball rolling down a valley, with stable cell types represented by low points. Cancer can be viewed as a "diseased attractor state"—a deep, aberrant valley. Therapeutic interventions aim to either eradicate cells in this state or push them back to a healthier landscape. This paper analyzes three strategies: Targeted Therapy (precise targeting of oncogenic drivers), Immunotherapy (empowering the immune system to eliminate the diseased state), and Epigenetic Reprogramming (directly remodeling the epigenetic landscape to revert the state).
Core Mechanistic Analysis
Epigenetic Reprogramming
This strategy aims to reverse the epigenetic dysregulation that maintains the cancerous attractor state. It involves forcibly resetting the epigenetic landscape to promote differentiation or senescence.
Key Targets & Agents:
- DNA Methyltransferase Inhibitors (DNMTi): Azacitidine, Decitabine. Inhibit DNMTs, leading to DNA demethylation and reactivation of silenced tumor suppressor genes.
- Histone Deacetylase Inhibitors (HDACi): Vorinostat, Romidepsin. Increase histone acetylation, promoting a more open chromatin state and gene expression.
- Enhancer Reprogramming: Small molecules or genetic tools targeting oncogenic transcription factors (e.g., MYC) or pioneer factors (e.g., OCT4, SOX2) to alter super-enhancer activity.
- Combination Epigenetic Therapy: Concurrent use of DNMTi and HDACi shows synergistic reactivation of genes.
Therapeutic Goal: Epigenetic "shock" to destabilize the cancer cell identity, pushing it towards a less malignant or more immunogenic state, potentially enabling combination with immunotherapy.
Immunotherapy
Immunotherapy does not directly target the cancer cell's landscape but empowers the immune system (T cells, NK cells) to recognize and eliminate the "diseased valley."
Key Modalities:
- Immune Checkpoint Inhibitors (ICIs): Monoclonal antibodies against PD-1 (Pembrolizumab), PD-L1 (Atezolizumab), CTLA-4 (Ipilimumab). Block inhibitory signals, releasing T-cell activity.
- CAR-T Cell Therapy: Autologous T cells engineered to express a Chimeric Antigen Receptor (CAR) targeting specific tumor-associated antigens (e.g., CD19, BCMA).
- Cancer Vaccines & Neoantigen Targeting: Strategies to prime the immune system against tumor-specific antigens.
- Oncolytic Viruses: Engineered viruses that selectively replicate in and lyse tumor cells, stimulating systemic anti-tumor immunity.
Therapeutic Goal: Enhance immune surveillance and cytotoxic clearance of the cancer attractor state.
Targeted Therapy
Targeted therapy uses small molecules or antibodies to specifically inhibit oncoproteins that are essential for maintaining the cancerous state, effectively "drying up" the diseased valley.
Key Classes:
- Tyrosine Kinase Inhibitors (TKIs): Imatinib (BCR-ABL), Erlotinib (EGFR), Dabrafenib (BRAF V600E). Competitively inhibit ATP-binding or function of mutant kinases.
- Monoclonal Antibodies: Trastuzumab (HER2), Cetuximab (EGFR). Bind extracellular domains, blocking signaling and inducing antibody-dependent cellular cytotoxicity (ADCC).
- Proteasome Inhibitors: Bortezomib. Disrupt protein degradation, leading to endoplasmic reticulum stress and apoptosis in cells with high protein synthesis.
- PARP Inhibitors: Olaparib. Exploit synthetic lethality in homologous recombination-deficient (e.g., BRCA-mutant) cancers.
Therapeutic Goal: Selective inhibition of critical oncogenic driver pathways.
Quantitative Data Comparison
Table 1: Clinical & Mechanistic Comparison of Therapeutic Paradigms
| Parameter | Epigenetic Reprogramming | Immunotherapy | Targeted Therapy |
|---|---|---|---|
| Primary Target | Epigenetic machinery (DNMTs, HDACs, chromatin readers) | Immune cells/checkpoints (T-cells, PD-1, CTLA-4) | Oncogenic proteins (Kinases, growth factor receptors) |
| Therapeutic Goal | Alter transcriptional program, induce differentiation/senescence | Enable immune-mediated tumor clearance | Inhibit specific driver signaling pathway |
| Typical Response Time | Slow (weeks-months, due to cell cycle-dependent effects) | Can be delayed (pseudo-progression possible) | Rapid (days-weeks) |
| Durability of Response | Variable; can be transient without continuous treatment | Potential for long-term "immune memory" | Often limited by acquired resistance (months-years) |
| Major Toxicity Concerns | Myelosuppression, gastrointestinal effects | Immune-related adverse events (irAEs: colitis, pneumonitis) | Off-target kinase effects, specific organ toxicities |
| Biomarker Dependency | Emerging (e.g., TET2/IDH mutations, specific methylation signatures) | High (PD-L1 expression, TMB, MSI-H/dMMR) | Essential (requires specific genetic alteration) |
| Approx. Avg. ORR* in Approved Indications | 15-30% (as monotherapy in myeloid malignancies) | 20-60% (varies greatly by cancer type & biomarker) | 50-80% (in biomarker-selected populations) |
| Combination Potential | High with immunotherapy & targeted therapy | High with chemo, targeted, epigenetic therapy | High with chemo, other targeted agents, immunotherapy |
*ORR: Objective Response Rate
Table 2: Common Experimental Readouts & Assays
| Assay Type | Epigenetic Reprogramming | Immunotherapy | Targeted Therapy |
|---|---|---|---|
| In Vitro Primary | RNA-seq, ChIP-seq, WGBS, proliferation/differentiation assays | T-cell activation/cytotoxicity assays, cytokine profiling (ELISA/MSD) | Cell viability (MTT/CTG), phospho-protein flow cytometry/WB, apoptosis assays |
| In Vivo Models | Patient-derived xenografts (PDXs), genetically engineered mouse models (GEMMs) | Immunocompetent syngeneic models, humanized mouse models | PDX models, cell-line derived xenografts (CDX), GEMMs |
| Clinical Biomarkers | DNA methylation arrays, histone modification ChIP-seq from biopsies | PD-L1 IHC, Tumor Mutational Burden (TMB), immune cell infiltrate profiling | Genomic sequencing (NGS), RT-PCR for fusion genes, IHC for protein expression |
Detailed Experimental Protocols
Protocol: Assessing Epigenetic Reprogramming via Combined DNMTi/HDACi Treatment
Aim: To evaluate synergistic gene reactivation and anti-proliferative effects. Materials: Cultured cancer cell line (e.g., AML line), Azacitidine (DNMTi), Romidepsin (HDACi), DMSO (vehicle). Method:
- Treatment: Seed cells in 6-well plates. After 24h, treat in triplicate: (i) Vehicle, (ii) Azacitidine (0.5 µM), (iii) Romidepsin (10 nM), (iv) Combination.
- Media Change: Replace drug-containing media every 24h for 96-120 hours.
- Harvest: Collect cells at 72h (molecular analysis) and 120h (phenotypic analysis).
- DNA Methylation Analysis: (72h sample) Extract genomic DNA. Perform Reduced Representation Bisulfite Sequencing (RRBS) or pyrosequencing of candidate gene promoters (e.g., p15/INK4B).
- Gene Expression Analysis: (72h sample) Extract total RNA. Perform RT-qPCR for reactivated genes (e.g., p15, NY-ESO-1) and RNA-seq for global profiling.
- Phenotypic Assay: (120h sample) Perform Cell Titer-Glo assay to quantify viability. Prepare cytospins for Wright-Giemsa staining to assess morphological differentiation.
Protocol: In Vitro T-cell Cytotoxicity Assay for Immunotherapy Screening
Aim: To measure antigen-specific T-cell killing of tumor cells post-checkpoint blockade. Materials: Target tumor cell line (expressing target antigen, e.g., MART-1), MART-1-specific CD8+ T-cell clone, anti-PD-1 antibody, control IgG. Method:
- Labeling: Label 1e5 target tumor cells with Calcein-AM fluorescent dye for 30 min. Wash twice.
- Co-culture: Seed labeled targets in a 96-well U-bottom plate. Add T-cells at various Effector:Target (E:T) ratios (e.g., 1:1, 5:1, 10:1). Add anti-PD-1 (10 µg/mL) or control.
- Incubation: Centrifuge plate briefly to initiate contact. Incubate at 37°C, 5% CO2 for 4-6 hours.
- Measurement: Centrifuge plate, transfer 100 µL supernatant to a black plate. Measure fluorescence (Ex/Em ~494/517nm) on a plate reader.
- Calculation: Calculate % Specific Lysis = [(Experimental Release – Spontaneous Release) / (Maximum Release – Spontaneous Release)] * 100. Maximum release from targets lysed with 1% Triton X-100.
Protocol: Target Inhibition & Signaling Pathway Analysis for TKI
Aim: To validate on-target effect and map downstream signaling inhibition of a novel TKI. Materials: Cancer cell line with known TKI-sensitive mutation (e.g., EGFR-mutant NSCLC line), novel EGFR TKI, Erlotinib (control), Phospho-EGFR (Tyr1068) antibody. Method:
- Dose-Response: Seed cells in 96-well plates. Next day, treat with 10-point serial dilution of TKI (e.g., 10 µM to 0.1 nM) for 72h. Assess viability via CellTiter-Glo to generate IC50.
- Short-Term Stimulation/Inhibition: Serum-starve cells overnight. Pre-treat with IC90 concentration of TKI or DMSO for 2h. Stimulate with EGF (100 ng/mL) for 15 minutes.
- Cell Lysis: Immediately lyse cells in RIPA buffer with protease/phosphatase inhibitors.
- Western Blot: Run 30 µg lysate per lane on SDS-PAGE, transfer to PVDF membrane. Probe with antibodies against: p-EGFR (Y1068), total EGFR, p-AKT (S473), p-ERK1/2 (T202/Y204), and corresponding total proteins. Use β-actin as loading control.
- Analysis: Quantify band intensity to demonstrate specific phospho-target inhibition and downstream pathway suppression.
Visualizations
Diagram: Core Signaling Pathways in Cancer Therapy
Diagram Title: Core Cancer Pathways and Therapeutic Intervention Points
Diagram: Experimental Workflow for Epigenetic-Immunotherapy Combo
Diagram Title: Combo Epigenetic-Immunotherapy Study Workflow
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Reagent Solutions for Featured Experiments
| Reagent Category | Specific Example(s) | Function in Experiment |
|---|---|---|
| Epigenetic Modulators | 5-Azacytidine (Azacitidine), Romidepsin, GSK126 (EZH2 inhibitor) | Induce DNA demethylation, histone hyperacetylation, or inhibit specific chromatin modifiers to test reprogramming. |
| Immune Checkpoint Reagents | Recombinant anti-mouse/human PD-1, PD-L1, CTLA-4 antibodies (functional grade, low endotoxin), Recombinant PD-L1 protein | Block checkpoint interactions in vitro/vivo or use as binding controls in flow cytometry. |
| Tyrosine Kinase Inhibitors | Erlotinib (EGFRi), Dabrafenib (BRAFi), Sapitinib (pan-ERBBi) | Positive controls for targeted pathway inhibition in viability and phospho-signaling assays. |
| Cell Viability/Proliferation Assays | CellTiter-Glo 3D, MTS/PMS, Calcein-AM | Quantify metabolic activity or live cells for dose-response and cytotoxicity experiments. |
| Phospho-Specific Antibodies | Anti-p-EGFR (Y1068), p-AKT (S473), p-ERK1/2 (T202/Y204) (validated for WB/Flow) | Detect acute changes in pathway activation upon targeted therapy. |
| Epigenetic Analysis Kits | EZ DNA Methylation-Lightning Kit, EpiQuik Histone Methyltransferase Assay Kit, ChIP-grade antibodies (H3K27ac, H3K9me3) | Enable bisulfite conversion, enzyme activity measurement, and chromatin state analysis. |
| Immune Cell Isolation Kits | Pan T Cell Isolation Kit (human/mouse, magnetic beads), CD8+ T Cell Negative Selection Kit | Isulate specific immune cell populations from tumors or spleen for functional assays. |
| Cytokine Detection | LegendPlex/LEGENDplex bead-based array, ELISA MAX Deluxe kits (IFN-γ, TNF-α) | Multiplex or single-plex quantification of immune cytokines from cell culture supernatants. |
| In Vivo Models | C57BL/6J mice (for syngeneic models), NOG/NSG mice (for PDX/humanized models), Matrigel | Provide immunocompetent or humanized systems for testing therapies in a physiological context. |
| Next-Gen Sequencing Library Preps | TruSeq RNA Library Prep Kit, Accel-NGS Methyl-Seq DNA Library Kit | Prepare high-quality libraries for transcriptomic and epigenomic profiling. |
Within the conceptual framework of Waddington's epigenetic landscape, cancer represents a stabilized aberrant attractor state. Reversion therapy aims to push malignant cells "uphill" toward more differentiated, functional, and non-proliferative states. This whitepaper details the biomarkers and methodologies required to measure this critical transition, providing a technical guide for researchers and drug developers in the field of differentiation therapy and cancer reversion.
Core Biomarker Categories for Reversion
Successful reversion is multidimensional, requiring assessment of differentiation, proliferation arrest, and functional restoration.
Table 1: Core Biomarker Categories for Assessing Reversion
| Category | Purpose | Example Biomarkers | Quantitative Readout |
|---|---|---|---|
| Epigenetic Remodeling | Measure global & locus-specific chromatin reconfiguration. | 5-hmC, H3K9ac, H3K27me3, DNA methylation at promoters of tumor suppressors. | % methylation (bisulfite-seq), ChIP-seq peak density, immunofluorescence intensity. |
| Differentiation Status | Assess reactivation of lineage-specific programs. | Cytokeratins (epithelial), CD14/CD68 (macrophage), Thy-1 (stromal), β-III tubulin (neuronal). | qPCR (fold-change), flow cytometry (% positive cells), IHC scoring (0-3+). |
| Proliferation Arrest | Confirm exit from cell cycle, not just cytostasis. | Ki-67 index, phospho-histone H3, EdU incorporation, p21CIP1/p27KIP1 expression. | % Ki-67+ cells (IHC/flow), EdU+ cells per field, Western blot densitometry. |
| Senescence & Apoptosis | Distinguish beneficial arrest from cell death. | SA-β-Gal activity, p16INK4A, Lamin B1 loss, Annexin V/PI. | SA-β-Gal+ cells (%), Annexin V+ PI- early apoptotic cells (%). |
| Functional Restoration | Demonstrate recovered tissue-specific function. | Albumin secretion (hepatocytes), contractile force (cardiomyocytes), TER (epithelial barriers), phagocytosis (macrophages). | µg/mL/day, mN/mm², Ω·cm², % phagocytosis of fluorescent beads. |
| Metabolic Reprogramming | Shift from aerobic glycolysis (Warburg) to oxidative phosphorylation. | Lactate production, OCR/ECAR ratio (Seahorse), GLUT1 vs. PDH expression. | pmol/min/µg (lactate), Basal OCR (pmol/min). |
Detailed Experimental Protocols
Protocol: Integrated Epigenomic and Transcriptomic Profiling
Objective: To correlate chromatin accessibility/state changes with gene expression during reversion.
- Cell Treatment: Apply reversion-inducing agent (e.g., all-trans retinoic acid, HDAC inhibitor) to cancer cell line for 7-14 days. Include DMSO/vehicle control.
- Nuclei Isolation: Harvest cells, lyse in NP-40 buffer, pellet nuclei.
- Assay for Transposase-Accessible Chromatin with sequencing (ATAC-seq): Use 50,000 nuclei. Treat with Tn5 transposase (Illumina). Purify DNA, amplify with indexed primers (5-7 PCR cycles).
- RNA Sequencing: In parallel, extract total RNA (TRIzol). Prepare poly-A selected libraries (Illumina TruSeq).
- Bioinformatics: Align ATAC-seq reads (Bowtie2), call peaks (MACS2). Align RNA-seq reads (STAR), quantify gene expression (featureCounts, DESeq2). Integrate using tools like HOMER or R/Bioconductor packages (ChIPseeker, clusterProfiler).
Protocol: Functional Assessment of Re-epithelialization
Objective: To measure restoration of epithelial barrier integrity.
- Culture on Transwells: Seed reverted and control cells on collagen-coated polyester membrane inserts (0.4 µm pore) at confluence.
- Transepithelial Electrical Resistance (TER): Measure daily using volt-ohm meter. Apply chopstick electrodes to apical and basolateral chambers. Calculate TER (Ω·cm²): (Resistancesample - Resistanceblank) * Membrane area.
- Paracellular Permeability Assay: On day of peak TER, add FITC-dextran (4 kDa) to apical chamber. Sample from basolateral chamber after 2 hours. Quantify fluorescence (Ex/Em: 485/535 nm). Compare flux rates.
- Immunofluorescence for Tight Junctions: Fix cells on inserts, stain for ZO-1, Occludin, and E-cadherin. Confocal imaging and line-scan analysis for junctional continuity.
Protocol: In Vivo Lineage Tracing and Clonal Analysis
Objective: To track the fate and longevity of reverted cells in vivo.
- Cell Labeling: Stably transduce cancer cells with a tamoxifen-inducible Cre recombinase and a Cre-reporting allele (e.g., Rosa26-LSL-tdTomato).
- Tumor Formation & Reversion Induction: Inject labeled cells into immunocompromised mice. Allow tumors to reach 100 mm³. Initiate reversion therapy. Administer tamoxifen to pulse-label a subset of cells.
- Longitudinal Tracking: Image tumors weekly via fluorescence tomography. Harvest cohorts at 2, 4, 8 weeks.
- Tissue Analysis: Process for frozen sectioning. Image tdTomato+ clones. Co-stain for differentiation (cell-type-specific markers) and proliferation (Ki-67). Quantify clone size and composition.
Visualization of Key Pathways and Workflows
Title: Molecular Pathway to Reversion from Malignancy
Title: Experimental Workflow for Reversion Biomarker Discovery
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Reagents for Reversion Biomarker Research
| Reagent/Tool | Supplier Examples | Primary Function in Reversion Studies |
|---|---|---|
| HDAC Inhibitors (e.g., Trichostatin A, Vorinostat) | Cayman Chemical, Selleckchem | Induce histone acetylation, open chromatin, and promote differentiation gene expression. |
| DNA Demethylating Agents (e.g., 5-Azacytidine, Decitabine) | Sigma-Aldrich, MedChemExpress | Inhibit DNMTs, reduce promoter hypermethylation of tumor suppressors and differentiation factors. |
| All-Trans Retinoic Acid (ATRA) | Tocris, Sigma-Aldrich | Canonical differentiation agent; ligand for RAR nuclear receptors, drives granulocytic differentiation. |
| Recombinant Human BMP-2/4 | PeproTech, R&D Systems | Bone Morphogenetic Proteins; activate SMAD pathway, induce mesenchymal differentiation and growth arrest. |
| Click-iT EdU Proliferation Kits | Thermo Fisher Scientific | Superior alternative to BrdU for quantifying DNA synthesis and proliferation rates without harsh denaturation. |
| Seahorse XF Cell Mito Stress Test Kit | Agilent Technologies | Measures OCR and ECAR to quantify the metabolic shift from glycolysis to oxidative phosphorylation. |
| CellTrace Proliferation & Division Trackers | Thermo Fisher Scientific | Fluorescent cytoplasmic dyes that dilute with each division, enabling tracking of proliferation history via flow cytometry. |
| MethylFlash Global DNA Methylation (5-mC) ELISA Kit | Epigentek | Quantifies global 5-methylcytosine levels as a readout of epigenetic reprogramming efficiency. |
| Senescence β-Galactosidase Staining Kit | Cell Signaling Technology | Detects lysosomal SA-β-Gal activity, a hallmark of senescence, at pH 6.0. |
| Human Cytokeratin Pan-Type Antibody Cocktail | Abcam, MilliporeSigma | IHC/IF reagent to detect re-expression of epithelial cytoskeletal markers indicating re-differentiation. |
| TruSeq ATAC Library Prep Kit | Illumina | Standardized kit for preparing sequencing libraries from transposed chromatin to map open chromatin regions. |
| Live-Cell Reporter Lines (e.g., p21CIP1-GFP) | Generated via CRISPR or lentiviral transduction | Enables real-time tracking of cell cycle exit and senescence induction in live cells. |
The conceptual framework of Waddington's epigenetic landscape provides a powerful metaphor for understanding tumorigenesis and potential therapeutic reversion. In this model, a differentiated cell resides in a stable "valley." Oncogenic events push the cell up toward a pluripotent, proliferative "ridge" of malignancy. The goal of reversion therapy is to guide the cell back to a stable, differentiated state. This whitepaper evaluates experimental models of neuroblastoma, sarcoma, and carcinoma through this lens, assessing their utility in probing the landscape and testing reprogramming strategies.
Neuroblastoma Models: Differentiation and Dormancy
Neuroblastoma (NB), an embryonal tumor of the sympathetic nervous system, exhibits unique biology amenable to landscape modeling, including spontaneous regression and differentiation.
Successes
In vitro models using all-trans retinoic acid (ATRA) have successfully demonstrated differentiation of NB cell lines (e.g., SH-SY5Y, SK-N-BE(2)) into neuron-like cells, validating the reversion concept. In vivo, the TH-MYCN transgenic mouse faithfully recapitulates high-risk NB and has shown that MYCN downregulation can trigger differentiation and tumor regression.
Limitations
Many NB cell lines are derived from aggressive, late-stage metastases and may have lost plasticity. The stochastic nature of spontaneous regression in humans is not fully captured in genetically engineered mouse models (GEMMs).
Table 1: Key Quantitative Findings in Neuroblastoma Models
| Model System | Intervention/Feature | Key Metric | Result | Implication for Reversion |
|---|---|---|---|---|
| SH-SY5Y Cell Line | 10µM ATRA, 5 days | % Neurite-bearing cells | ~70% increase | Confirms differentiation capacity |
| TH-MYCN Mouse | MYCN shutdown | Tumor volume reduction | >80% at 4 weeks | Oncogene addiction & plasticity |
| Patient-Derived Xenograft (PDX) | CDK4/6 inhibition | Survival prolongation | Median 42 vs 28 days (control) | Cyclin D-CDK4/6 maintains stemness |
Protocol: ATRA-Induced Differentiation of SH-SY5Y Cells
- Culture: Maintain SH-SY5Y cells in Dulbecco's Modified Eagle Medium (DMEM)/F-12 with 10% FBS.
- Seed: Plate cells at 5x10^4 cells/cm² on poly-L-lysine-coated plates.
- Treat: 24h post-seeding, replace medium with serum-free DMEM/F-12 containing 10µM ATRA (from a 10mM stock in DMSO). Include vehicle control (0.1% DMSO).
- Maintain: Refresh treatment medium every 48 hours.
- Assess: At day 5-7, fix cells and stain for β-III-tubulin. Quantify neurite length and branching per cell via image analysis (e.g., ImageJ).
Title: ATRA-Induced Differentiation Pathway in Neuroblastoma
Sarcoma Models: Reprogramming Mesenchymal Lineages
Sarcomas, derived from mesenchymal stem cells (MSCs), offer insights into disrupting core regulatory circuitries (CRCs) to force lineage exit.
Successes
For Ewing sarcoma, driven by EWSR1-ETS fusions (e.g., EWS-FLI1), RNAi-mediated oncogene knockdown in cell lines leads to re-expression of mesenchymal differentiation programs. Osteosarcoma GEMMs (e.g., Trp53+/-) have demonstrated that bone morphogenetic protein (BMP) signaling can redirect tumors toward osteoblastic differentiation.
Limitations
The undifferentiated, stem-like nature of many sarcomas makes identifying a "target" differentiated state challenging. The tumor microenvironment (TME), critical in sarcoma progression, is often simplified in vitro.
Table 2: Key Quantitative Findings in Sarcoma Models
| Model System | Intervention/Feature | Key Metric | Result | Implication for Reversion |
|---|---|---|---|---|
| Ewing Sarcoma Cell Line (A673) | EWS-FLI1 siRNA | Expression of MSC marker CD105 | 5.2-fold increase | Oncogene maintains de-differentiated state |
| Osteosarcoma PDX | BMP-2 protein delivery | Tumor Mineralization (µCT density) | 2.3-fold increase | Can push toward terminal differentiation |
| Trp53+/-; Rb1+/- Mouse Model | TGF-β pathway inhibition | Metastatic incidence | Reduced from 60% to 20% | TGF-β maintains landscape instability |
Protocol: Chick Chorioallantoic Membrane (CAM) Assay for Sarcoma Invasion & Drug Testing
- Fertilized Eggs: Incubate at 37.5°C, 60% humidity for 8 days.
- Window Preparation: On embryonic day 8 (E8), use a hobby drill to create a 1cm² window over the air sac. Gently drop the CAM away from the shell membrane.
- Tumor Implantation: At E9, place a 1mm³ fragment of sarcoma PDX or 2x10^6 cells in Matrigel (50% v/v) onto a major blood vessel.
- Treatment: At E11, apply treatment (e.g., small molecule in PBS) directly onto the tumor daily.
- Harvest & Analyze: At E16, resect the tumor. Measure volume, weight, and process for IHC (Ki67, cleaved caspase-3) or RNA-seq.
Title: Ewing Sarcoma De-Differentiation and Reversion Logic
Carcinoma Models: Targeting Epithelial Plasticity
Carcinomas exploit epithelial-to-mesenchymal transition (EMT) and its reverse (MET) for plasticity. Reversion strategies often aim to induce MET or stable differentiation.
Successes
In basal cell carcinoma (BCC), Smoothened inhibitors (e.g., vismodegib) force differentiation by inhibiting Sonic Hedgehog signaling. In hepatocellular carcinoma (HCC), histone deacetylase inhibitors (HDACi) like panobinostat have shown efficacy in restoring hepatocyte gene networks in vitro.
Limitations
Inducing reversion in advanced carcinomas with numerous mutations is complex. The TME, including cancer-associated fibroblasts (CAFs), can antagonize reversion signals. Models often fail to capture adaptive resistance mechanisms.
Table 3: Key Quantitative Findings in Carcinoma Models
| Model System | Intervention/Feature | Key Metric | Result | Implication for Reversion |
|---|---|---|---|---|
| BCC (Ptch1+/- Mouse) | Vismodegib (Smo inhibitor) | Tumor area regression | 90% reduction at 28 days | Pathway inhibition forces lineage commitment |
| HCC Organoid | 50nM Panobinostat (HDACi) | Albumin secretion | 4.5-fold increase | Epigenetic remodeling restores function |
| Pancreatic Ductal Adenocarcinoma (PDAC) GEMM | TGF-β + MEK inhibition | % Epithelial (E-cadherin+) cells | Increased from 15% to 45% | Co-inhibition promotes MET |
Protocol: 3D Matrigel Culture for Mammary Carcinoma Organoid Differentiation
- Base Layer: Add 40µL of growth factor-reduced Matrigel to each well of a 96-well plate. Polymerize for 30 min at 37°C.
- Cell Suspension: Trypsinize cells (e.g., MCF-7, T47D). Mix with assay medium (DMEM/F-12, B27, 10ng/mL FGF-10) and 2% Matrigel.
- Seed: Plate 5000 cells in 100µL suspension on top of the base layer.
- Differentiate: After 3 days for formation, switch to differentiation medium (assay medium + 5µM dexamethasone, 5µg/mL prolactin, 1µM aldosterone). Refresh every 2 days.
- Analyze: At day 10, image organoids for acinar structure formation. Fix and stain for β-casein and ZO-1.
Research Reagent Solutions Toolkit
| Reagent/Material | Function in Reversion Studies | Example Use Case |
|---|---|---|
| All-trans Retinoic Acid (ATRA) | Ligand for retinoic acid receptors (RARs); induces differentiation gene programs. | Neuroblastoma cell differentiation. |
| Recombinant Human BMP-2 | Morphogen promoting osteogenic differentiation of mesenchymal cells. | Osteosarcoma reversion assay. |
| Vismodegib (SMO Inhibitor) | Small molecule inhibitor of Smoothened, blocking Hedgehog signaling. | Basal cell carcinoma differentiation therapy. |
| Panobinostat (LBH589) | Pan-histone deacetylase inhibitor (HDACi); modulates chromatin state. | HCC organoid epigenetic reprogramming. |
| Growth Factor-Reduced Matrigel | Basement membrane matrix for 3D organoid culture, providing structural and biochemical cues. | Mammary carcinoma acinar differentiation assay. |
| Chick Embryos (for CAM) | In vivo model with rich vasculature for studying tumor invasion and drug response in a semi-immunocompetent setting. | Sarcoma PDX growth and treatment study. |
| siRNA against EWS-FLI1 | RNA interference to specifically knock down the driving oncogene fusion. | Probing Ewing sarcoma oncogene addiction. |
The conceptual framework of Waddington's epigenetic landscape provides a powerful metaphor for understanding cell fate decisions. In this model, a pluripotent cell is depicted as a ball rolling down a valley bifurcating into distinct canals, representing differentiation into specific lineages. Cancer has been described as a pathological "attractor state" within this landscape—a stable, but diseased, cellular phenotype. The emerging field of cancer reversion seeks to identify the molecular levers that can push malignant cells out of this cancerous attractor and back onto trajectories toward normalized or benign states. This whitepaper details the integration of single-cell multi-omics technologies to map these complex reversion trajectories, providing a high-resolution atlas of the epigenetic and transcriptional reprogramming required for therapeutic reversion.
Foundational Technologies & Principles
Single-Cell RNA Sequencing (scRNA-seq)
ScRNA-seq enables the quantification of gene expression in individual cells, revealing transcriptional heterogeneity within populations. This is critical for identifying rare subpopulations of cells that may be initiating reversion or occupying intermediate states.
Assay for Transposase-Accessible Chromatin (ATAC-seq) at Single-Cell Resolution
scATAC-seq maps regions of open chromatin genome-wide in single cells. Accessible chromatin is a hallmark of active regulatory elements (enhancers, promoters), providing a direct readout of the cell's epigenetic state and regulatory potential.
The Power of Integration
Neither modality alone is sufficient to define a trajectory. Integrated analysis correlates transcriptional outputs (scRNA-seq) with underlying regulatory architecture (scATAC-seq), allowing causal inference of transcription factor (TF) activity, identification of key regulatory elements, and reconstruction of the gene regulatory networks (GRNs) that drive fate transitions.
Experimental Protocols for Mapping Reversion
Paired scRNA-seq and scATAC-seq from the Same Cell
Protocol (Based on 10x Genomics Multiome ATAC + Gene Expression):
- Cell Preparation: Generate a single-cell suspension from in vitro reversion models (e.g., drug-treated cancer cell lines) or in vivo samples (e.g., tumors from mice treated with differentiation therapy). Viability must be >90%. Cell number: 5,000–100,000.
- Nuclei Isolation & Tagmentation: Isolate nuclei using a gentle lysis buffer. Incubate nuclei with engineered Tn5 transposase loaded with sequencing adapters. The Tn5 inserts adapters into accessible chromatin regions.
- GEM Generation & Barcoding: Co-encapsulate single nuclei, Gel Beads with cell-barcode oligonucleotides, and the transposase reaction mixture in a droplet. Within each droplet, the transposed chromatin fragments and poly-adenylated mRNA molecules from the same nucleus are tagged with a unique cellular barcode and a unique molecular identifier (UMI).
- Library Construction & Sequencing: Post-emulsion, two separate libraries are constructed: a gene expression library (from the mRNA-derived cDNA) and an ATAC library (from the transposed DNA fragments). Libraries are sequenced on a platform like Illumina NovaSeq (Recommended: ≥20,000 read pairs per cell for ATAC; ≥10,000 read pairs per cell for RNA).
Time-Course Experimental Design for Trajectory Inference
To capture dynamics, samples are collected at multiple time points during a reversion-inducing intervention (e.g., T0: untreated cancer, T6h, T24h, T72h, T1week). Cells from all time points are multiplexed using sample barcoding (e.g., CellPlex), processed together in a single Multiome run to minimize batch effects, and demultiplexed bioinformatically.
Integrated Computational Analysis Workflow
The core analytical pipeline transforms raw sequencing data into a model of the reversion trajectory.
Diagram Title: Computational Pipeline for Multi-omic Trajectory Mapping
Key Analytical Steps:
- Preprocessing: scRNA-seq data is aligned (e.g., STARsolo) and quantified. scATAC-seq data is aligned (e.g., CellRanger-ATAC) and a peak-by-cell matrix is generated.
- Integration: A Weighted Nearest Neighbors (WNN) approach is used to learn a joint representation of each cell, balancing information from RNA and ATAC modalities.
- Trajectory Inference: Algorithms like Slingshot are applied to the integrated cell embedding to order cells along inferred paths from the cancerous state to reverted states.
- Gene Regulatory Network (GRN) Inference: Tools like SCENIC+ leverage paired data to identify transcription factors (TFs) whose motif accessibility (from ATAC) predicts target gene expression (from RNA), defining active GRNs for each state in the trajectory.
Key Signaling Pathways in Reversion
Reversion often involves reactivation of developmental or differentiation pathways suppressed in cancer.
Diagram Title: Core Pathways Driving Cellular Reversion
Quantitative Data from Key Studies
Table 1: Multi-omic Profiling Reveals Reversion Dynamics in Acute Myeloid Leukemia (AML)
| Study Feature | Metric | Findings |
|---|---|---|
| Model System | Cell Line / Treatment | HL-60 cells treated with all-trans retinoic acid (ATRA) |
| Time Points Analyzed | Number | 5 time points (0, 12, 24, 48, 96 hours) |
| Cells Profiled (Multiome) | Cell Count | ~12,000 high-quality nuclei |
| Key Regulated TFs | Number Identified | 42 TFs with dynamic motif accessibility & expression |
| Critical GRN Module | Key Regulator | PU.1 (SPI1) network reactivation preceded phenotypic change |
| % Cells in Terminal State | At 96h | 78% showed granulocytic differentiation signature |
Table 2: Integrated -Omics Identifies Barriers to Solid Tumor Reversion
| Analysis | Method | Key Insight for Therapeutic Design |
|---|---|---|
| Heterogeneity Mapping | Latent Dirichlet Allocation (LDA) | Found 3 distinct epigenetic "resistance programs" coexisting pre-treatment. |
| Regulator Prioritization | SCENIC+ & Perturb-seq | Ranked TFs by their centrality in the reversion GRN; top 5 were non-druggable. |
| Cistromic Drivers | Motif Enrichment in Dynamic Peaks | AP-1 motif accessibility was the primary barrier; its inhibition accelerated reversion in models. |
| Clinical Correlation | Survival Analysis (TCGA) | High activity of the reversion GRN signature correlated with improved patient survival (HR = 0.65, p<0.01). |
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Reagent Solutions for scMulti-ome Reversion Studies
| Reagent / Kit | Provider Examples | Critical Function |
|---|---|---|
| Chromium Next GEM Single Cell Multiome ATAC + Gene Expression | 10x Genomics | Gold-standard kit for generating paired scRNA-seq and scATAC-seq libraries from the same single nucleus. |
| Cell-Plex / Feature Barcoding Kits | 10x Genomics, BioLegend | Enables sample multiplexing. Different samples are tagged with oligonucleotide-conjugated antibodies prior to pooling, allowing cost-effective time-course experiments. |
| Nuclei Isolation Kits | Miltenyi Biotec, Sigma-Aldrich | Gentle, optimized reagents for liberating intact nuclei from diverse tissue types (especially critical for solid tumors). |
| Tn5 Transposase (Custom Loaded) | Illumina, Diagenode | Engineered transposase pre-loaded with sequencing adapters. The core enzyme for tagmentation in ATAC-seq. Custom loading allows unique sample indexing. |
| Viability Stains (DAPI, Propidium Iodide) | Thermo Fisher, Bio-Rad | Essential for assessing nuclei/cell health and viability via flow cytometry prior to loading on the Chromium chip. |
| Magnetic Bead-Based Library Cleanup Kits | SPRIselect (Beckman), KAPA Pure Beads (Roche) | Used at multiple steps for size selection and purification of ATAC and cDNA libraries. |
| Dual Index Kit TS Set A | 10x Genomics | Provides the unique dual indexes required for sequencing the combined Multiome libraries on Illumina platforms. |
Conclusion
The Waddington epigenetic landscape provides a powerful and evolving paradigm for conceptualizing cancer not as a point of no return, but as a maladaptive cellular state within a plastic developmental field. This article has synthesized foundational principles, methodological advances, persistent challenges, and validation frameworks, highlighting a paradigm shift from cytotoxic elimination to cellular reprogramming. The future of cancer reversion lies in integrating multi-omics data for personalized landscape mapping, developing next-generation epigenetic editors with enhanced precision, and designing combination therapies that synergistically push cells into stable, therapeutic attractors. For biomedical research and clinical translation, this approach promises a new class of interventions aimed at co-opting the body's inherent programs for tissue homeostasis to combat malignancy.