Navigating Bioinformatics Challenges in Clinical NGS: A Roadmap for Robust Implementation in Research and Diagnostics
The integration of next-generation sequencing (NGS) into clinical practice and drug development research is fraught with complex bioinformatics challenges that impact data accuracy, reproducibility, and clinical utility.
Navigating Bioinformatics Challenges in Clinical NGS: A Roadmap for Robust Implementation in Research and Diagnostics
Abstract
The integration of next-generation sequencing (NGS) into clinical practice and drug development research is fraught with complex bioinformatics challenges that impact data accuracy, reproducibility, and clinical utility. This article provides a comprehensive analysis for researchers, scientists, and drug development professionals, addressing the foundational, methodological, troubleshooting, and validation hurdles. Drawing on current guidelines and multi-center studies, we outline standardized bioinformatics practices, optimization strategies for scalable workflows, and robust validation frameworks essential for ensuring reliable NGS results in clinical implementation and therapeutic discovery.
The Core Hurdles: Understanding Foundational Bioinformatics Barriers in Clinical NGS
Next-Generation Sequencing (NGS) has revolutionized clinical diagnostics and public health surveillance, but its implementation faces a critical human resources challenge. Specialized NGS personnel require unique expertise spanning laboratory techniques, bioinformatics, and data interpretation, yet retaining these skilled professionals has become a substantial obstacle for laboratories. Current data indicates that testing personnel in these specialized roles often hold their positions for less than four years on average [1] [2]. Furthermore, a 2021 survey by the Association of Public Health Laboratories (APHL) revealed that 30% of surveyed public health laboratory staff indicated an intent to leave the workforce within the next five years [1] [2]. This impending workforce crisis threatens the sustainability and quality of NGS operations in clinical and public health settings, creating vulnerabilities in our public health infrastructure precisely when genomic capabilities are most needed for pandemic preparedness and personalized medicine.
The problem extends beyond mere retention statistics. The specialized knowledge required for NGS operations creates significant hiring and qualification challenges, particularly under regulations such as the Clinical Laboratory Improvement Amendments of 1988 (CLIA) and state hiring statutes [1] [2]. The combination of high expertise requirements and relatively short tenure creates a perpetual cycle of training and knowledge loss that undermines laboratory efficiency and test reliability. This article examines these workforce challenges within the broader context of bioinformatics challenges in clinical NGS implementation research, providing actionable frameworks and troubleshooting guidance to help institutions address these critical gaps.
Table 1: Statistical Overview of NGS Workforce Challenges
| Metric | Finding | Source |
|---|---|---|
| Average Position Tenure | <4 years for testing personnel | Akkari et al. [1] [2] |
| Projected Workforce Attrition | 30% of public health laboratory staff intend to leave within 5 years | APHL 2021 Survey [1] [2] |
| Primary Retention Barriers | Specialized knowledge requirements, compensation costs, regulatory qualifications | NGS Quality Initiative Assessment [1] [2] |
Tiered Expertise Distribution Framework
NGS operations require diverse expertise distributed across different laboratory levels. The Global Emerging Infections Surveillance (GEIS) program has implemented a tiered framework that illustrates how specialized NGS personnel are distributed across different levels of laboratory operations [3]. This framework is particularly valuable for understanding how expertise gaps at any level can disrupt the entire sequencing workflow.
Diagram 1: NGS Expertise Distribution Across Laboratory Tiers. This framework illustrates how specialized personnel are distributed across different laboratory levels and the specific retention challenges at each tier.
Technical Support Center: NGS Workforce Troubleshooting Guides and FAQs
Frequently Asked Questions: Workforce and Expertise Gaps
Q1: What are the primary factors contributing to high turnover among specialized NGS personnel?
Multiple factors create retention challenges in the NGS workforce. Specialized NGS personnel require unique expertise that commands competitive compensation, increasing operational costs [1] [2]. The CLIA regulations and state hiring statutes create additional qualification barriers that limit the pool of eligible candidates [1] [2]. Furthermore, the rapid evolution of NGS technologies requires continuous training, creating burnout among personnel who must constantly update their skills while maintaining production workloads. This is particularly challenging in public health laboratories where budget constraints may limit competitive compensation and professional development opportunities.
Q2: How can laboratories document expertise and standardize procedures to mitigate knowledge loss when staff depart?
The Next-Generation Sequencing Quality Initiative (NGS QI) has developed specific tools to address this challenge. Laboratories should implement the "Identifying and Monitoring NGS Key Performance Indicators SOP" and "Bioinformatician Competency Assessment SOP" to objectively document staff capabilities and performance standards [1] [2]. These resources help create standardized benchmarks that survive individual staff transitions. Additionally, the NGS Method Validation Plan and Validation SOP provide templates for consistently documenting laboratory procedures, ensuring that institutional knowledge remains accessible when personnel depart [1] [2]. These tools collectively help laboratories maintain quality standards despite staff turnover.
Q3: What training resources are available for building NGS workforce capabilities?
The NGS QI has published 25 tools specifically for personnel management, including the "Bioinformatics Employee Training SOP" [1] [2]. These resources provide frameworks for structured training programs that can accelerate the development of new staff. Additionally, the GEIS program's tiered framework employs a "train-the-trainer" approach where tier 3 laboratories provide training to tier 2 personnel, who then train tier 1 staff [3]. This cascading training model efficiently distributes expertise across the network while building regional training capabilities. Laboratories should also participate in the online trainings hosted by NGS QI partners to access current best practices [1] [2].
Q4: How do workforce gaps specifically impact NGS quality and operations?
Workforce instability directly impacts NGS quality through several mechanisms. First, inexperienced staff are more likely to make errors during library preparation that lead to sequencing failures, such as inaccurate fragmentation, poor ligation efficiency, or overly aggressive purification [4]. Second, high turnover creates inconsistency in bioinformatic analyses, as different analysts may employ varying methodologies or quality thresholds. Third, the constant need to train new staff diverts resources from quality improvement initiatives. The NGS QI addresses these challenges through its QMS Assessment Tool, which helps laboratories maintain quality standards despite personnel changes [1] [2].
Q5: What strategies help distribute expertise across different laboratory tiers?
The GEIS program's 3-tiered framework provides a model for strategically distributing expertise [3]. In this model, tier 1 laboratories (field/point-of-care) focus on rapid pathogen identification using portable sequencers like the Oxford Nanopore MinION or Illumina iSeq. Tier 2 laboratories (regional support centers) conduct more comprehensive strain-level analysis and serve as regional training hubs. Tier 3 laboratories (core reference labs) perform advanced genetic characterization and develop new methods. This framework ensures that each level maintains appropriate expertise while having clear pathways for technical support and consultation from higher tiers [3].
Workforce-Dependent Technical Issues: Troubleshooting Guide
Table 2: Common NGS Technical Issues Linked to Workforce Experience Gaps
| Technical Problem | Workforce-Related Causes | Corrective Actions | Preventive Strategies |
|---|---|---|---|
| Low library yield | Inconsistent sample quantification; Poor technique in purification steps; Inadequate monitoring of reagent quality [4] | Re-purify input samples; Verify quantification with fluorometric methods; Calibrate pipettes [4] | Implement "Bioinformatician Competency Assessment SOP" [1] [2]; Use master mixes to reduce pipetting errors [4] |
| High duplication rates | Overamplification due to inexperience with optimization; Poor quantification leading to excessive PCR cycles [4] | Repeat amplification from leftover ligation product; Optimize PCR cycle number [4] | Standardize protocols using NGS QI templates [1] [2]; Create technician checklists for critical steps [4] |
| Adapter dimer contamination | Improper adapter-to-insert ratios; Inefficient cleanup techniques; Inconsistent size selection [4] | Titrate adapter:insert ratios; Optimize bead-based cleanup parameters [4] | Implement "Identifying and Monitoring NGS Key Performance Indicators SOP" [1] [2]; Use two-step indexing protocols [4] |
| Inconsistent bioinformatic results | High analyst turnover with varying methodologies; Insufficient documentation of analysis parameters; Lack of standardized quality thresholds | Cross-train personnel between wet lab and bioinformatics [3]; Implement version-controlled analysis pipelines | Use "Bioinformatics Employee Training SOP" [1] [2]; Establish clear analysis protocols with tiered review [3] |
Essential Research Reagent Solutions for NGS Workflows
Table 3: Key Research Reagents and Their Functions in NGS workflows
| Reagent Category | Specific Examples | Primary Function | Workforce Considerations |
|---|---|---|---|
| Fragmentation Reagents | Enzymatic fragmentation mixes; Acoustic shearing reagents | Prepare nucleic acids for library construction by reducing fragment size | Inconsistent technique affects fragment distribution; requires trained personnel [4] |
| Library Preparation Kits | Illumina Nextera; ONT Rapid Kits; Element Biosciences AVITI | Convert nucleic acid fragments to sequencing-ready libraries | Commercial kits reduce but don't eliminate expertise requirements [1] [4] |
| Quantification Reagents | Qubit dsDNA HS Assay; qPCR quantification mixes | Accurately measure library concentration for loading calculations | Technique-sensitive; requires consistent training and competency assessment [4] |
| Cleanup & Size Selection | SPRI beads; Agarose gel extraction | Remove unwanted fragments and select optimal size ranges | Highly technique-dependent; common source of cross-operator variability [4] |
Addressing workforce and expertise gaps in NGS operations requires systematic approaches that combine standardized tools, structured training, and strategic workforce planning. The NGS Quality Initiative provides essential resources for standardizing procedures and documenting expertise, while the tiered framework exemplified by the GEIS program offers a model for distributing expertise across laboratory networks [1] [2] [3]. As NGS technologies continue evolving with platforms from Oxford Nanopore Technologies, Element Biosciences, and others offering improved accuracy and lower costs, the human expertise required to implement these technologies remains the critical factor in successful clinical implementation [1] [2]. Laboratories that proactively address workforce challenges through standardized quality management systems, competitive compensation structures, and strategic training investments will be best positioned to maintain robust NGS capabilities despite the broader industry challenges. The frameworks and troubleshooting guides presented here provide actionable starting points for institutions seeking to stabilize their NGS workforce while maintaining quality standards in clinical and public health applications.
Frequently Asked Questions (FAQs)
Q: What are the respective roles of CMS, FDA, and CDC in the CLIA program? Three federal agencies administer the Clinical Laboratory Improvement Amendments (CLIA) program, each with a distinct role [5]:
- Centers for Medicare & Medicaid Services (CMS): Issues laboratory certificates, conducts inspections, enforces regulatory compliance, and monitors laboratory performance of Proficiency Testing (PT).
- Food and Drug Administration (FDA): Categorizes tests based on complexity and reviews requests for CLIA Waiver by Application.
- Centers for Disease Control and Prevention (CDC): Provides analysis, research, technical assistance, and develops technical standards and laboratory practice guidelines.
Q: What are the key 2025 changes to CLIA personnel qualifications? Recent CLIA updates revised personnel qualification standards effective in 2025 [6] [7]. Key changes include:
- Degree Requirements: Permitted degrees now explicitly include chemical, biological, clinical, or medical laboratory science, or medical technology. "Physical science" has been removed as a qualifying degree.
- Equivalency Pathways: Updated pathways allow qualifying with specific credit hours (e.g., 120 semester hours with specific science coursework) as equivalent to a bachelor's degree for several positions.
- Grandfathering: Personnel who met qualifications before December 28, 2024, and remain in their roles continuously are generally permitted to continue under prior criteria.
- Laboratory Director CE: Directors qualifying as MD or DO now need at least 20 continuing education hours in laboratory practice.
Q: What are the major bioinformatic challenges when implementing NGS in a clinical setting? Implementing NGS in clinical settings poses unique bioinformatics challenges that impede the translation of genomic data into interpretable information [8] [9]:
- Sample Quality: Suboptimal samples (e.g., FFPE tissues with low DNA quality, low-abundance cell-free DNA in liquid biopsy) complicate variant detection and elevate false positives.
- Computational Complexity: The massive data output from NGS requires sophisticated algorithms and significant computing power for assembly and analysis [10].
- Variant Calling Precision: Detecting variants with low allele frequency (e.g., in CHIP or ctDNA) requires rigorous parameter settings, often forcing a trade-off between sensitivity and specificity [8].
- Data Interpretation: The volume and complexity of generated data make processing, storage, management, and clinical interpretation particularly challenging [9].
Q: What resources are available to help laboratories establish a quality management system for NGS? The CDC and APHL collaborated to form the Next-Generation Sequencing Quality Initiative (NGS QI), which develops publicly available tools to help laboratories implement NGS and build a robust Quality Management System (QMS) [2]. Their most widely used documents include the QMS Assessment Tool, SOP for Identifying and Monitoring NGS Key Performance Indicators, NGS Method Validation Plan, and NGS Method Validation SOP.
Troubleshooting Guides
Issue: Failing Proficiency Testing (PT) for Hemoglobin A1C
Problem Laboratory results for Hemoglobin A1C proficiency testing fall outside the newly defined acceptable performance ranges.
Solution
- Verify Performance Criteria: Ensure you are using the correct 2025 performance threshold for your PT provider [7]:
- CMS: ±8% accuracy range
- College of American Pathologists (CAP): ±6% accuracy threshold
- Implement Corrective Actions: For results outside limits, immediately begin root cause analysis and document all corrective actions taken.
- Review Personnel Qualifications: Confirm testing personnel meet updated 2025 CLIA qualifications, as inadequate training can contribute to PT failures [6] [7].
Issue: NGS Assay Validation Failure
Problem NGS assay validation cannot meet stringent CLIA quality control criteria and performance standards.
Solution
- Utilize NGS QI Resources: Follow the "Pathway to Quality-Focused Testing" and use the NGS Method Validation Plan template from the NGS Quality Initiative to structure your validation [2].
- Lock Down Workflow: Once validated, ensure the entire NGS workflow—including library preparation, sequencing, and bioinformatic pipeline—is locked down to maintain integrity [2].
- Monitor Key Performance Indicators (KPIs): Implement the NGS QI's "Identifying and Monitoring NGS Key Performance Indicators SOP" to track metrics like coverage uniformity, sensitivity, and specificity during validation [2].
Issue: Navigating Personnel Qualification Changes
Problem Laboratory personnel (new hires or existing staff) do not clearly meet updated 2025 CLIA qualification pathways.
Solution
- Consult Updated Definitions: Refer to the 2025 CLIA definitions for "doctoral degree," "laboratory training or experience," and "experience directing or supervising" [6].
- Explore Equivalency Pathways: For bachelor's degree requirements, investigate the new equivalency option of 120 semester hours with specific science coursework (48 semester hours in specific science/medical laboratory technology courses) [6].
- Apply Grandfathering Clause: For personnel employed before December 28, 2024, confirm they meet previous qualifications and maintain continuous employment to qualify for grandfathering [6].
Regulatory Relationships and NGS Validation Workflow
CLIA Regulatory Structure for NGS
NGS Assay Validation Process
Essential Research Reagents and Materials
Table 1: Key Research Reagent Solutions for Clinical NGS Implementation
| Reagent/Material | Function in Clinical NGS | Key Considerations |
|---|---|---|
| NGS Library Prep Kits | Fragments DNA/RNA and adds platform-specific adapters for sequencing. | Select kits designed for specific sample types (e.g., FFPE, liquid biopsy) to address input quality challenges [8]. |
| Targeted Enrichment Panels | Selectively captures genomic regions of clinical interest (e.g., cancer genes). | Panels must be clinically validated; performance affected by sample quality and intratumor heterogeneity [8]. |
| Bioinformatic Pipelines | Software for sequence alignment, variant calling, and annotation. | Pipelines require extensive validation and locking; sensitivity/specificity trade-offs are critical for low-frequency variants [2] [8]. |
| Proficiency Testing (PT) Materials | External quality control samples to verify assay performance and personnel competency. | Must use approved PT providers for regulated analytes (e.g., Hemoglobin A1C) and meet 2025 performance criteria [7]. |
| Reference Standards | Samples with known variants used for assay validation and quality control. | Essential for establishing accuracy, precision, and limit of detection during NGS method validation [2]. |
Troubleshooting Guides and FAQs
Frequently Asked Questions
Q1: Our data storage costs are escalating rapidly with increasing NGS data. What are the most effective strategies for cost-effective, scalable storage?
A1: A combination of storage tiering and hybrid cloud solutions is the most effective strategy for managing scalable storage.
- Implement Tiered Storage: Utilize high-performance storage for active analysis and cheaper, cooler storage for archived data. Automated data lifecycle management policies can transition data between these tiers to optimize costs [11].
- Adopt a Hybrid Cloud Model: Hybrid cloud platforms provide elastic storage that can be scaled up or down with demand, reducing the overhead of maintaining large on-premise infrastructure [12]. For sensitive data, a federated analysis model can be employed, where analytical workflows are sent to the data's secure location instead of moving the data itself [11].
- Use Advanced Data Compression: Apply modern compression techniques to reduce file sizes without compromising data integrity, easing the burden on storage and network bandwidth [12].
Q2: We struggle with workflow reproducibility and portability between different computing environments. How can we standardize our bioinformatics analyses?
A2: Reproducibility is a cornerstone of scientific research and can be achieved through containerization and workflow management systems.
- Containerize Tools: Use containerization technologies like Docker or Singularity to package software, libraries, and dependencies into a single, portable unit. This eliminates the "it works on my machine" problem and ensures a consistent environment across different systems [11].
- Utilize Workflow Management Systems: Employ workflow languages like Nextflow to define complex, multi-step pipelines. These systems manage software versions, execute steps in a predefined order, and provide a complete audit trail for every analysis run [11]. Leveraging version-controlled, community-validated pipelines from repositories like nf-core can further enhance standardization [11].
- Choose a Bioinformatics Platform: Consider an integrated bioinformatics platform that provides a unified environment for data management, workflow orchestration, and analysis, often described as a "single pane of glass" for your research ecosystem [11].
Q3: What are the best practices for ensuring the security and privacy of sensitive clinical genomic data?
A3: Protecting patient data requires a multi-layered security approach.
- Implement Robust Access Controls: Enforce granular, role-based access controls (RBAC) to ensure researchers can only access the data necessary for their work. Comprehensive audit trails should log every data access and analysis action [11].
- Employ Advanced Encryption: Use end-to-end encryption to protect data both when it is stored (at rest) and when it is being transmitted (in transit) [13].
- Explore Federated Learning: For collaborative projects, federated learning allows you to train AI models across multiple institutions without centralizing or sharing the underlying raw data. The model is sent to the data, and only the aggregated results are returned [14].
Q4: The computational demands for AI-driven NGS analysis are straining our resources. How can we manage this surge in compute demand?
A4: The exponential growth in AI compute demand is a industry-wide challenge that requires strategic planning.
- Leverage Cloud and HPC Resources: Cloud platforms offer scalable, on-demand access to high-performance computing (HPC) resources, including GPUs essential for training AI models. National and institutional HPC centers are also expanding capacity to support AI and genomics research [15].
- Optimize AI Models and Infrastructure: Invest in efficient AI model architectures and utilize specialized hardware from providers like Nvidia, whose data-center GPU sales have surged due to AI demand [15]. The industry is responding with massive infrastructure investments, forecast to reach $2.8 trillion in AI-related spending by 2029 [15].
Common Computational Bottlenecks and Solutions
| Bottleneck | Symptoms | Proposed Solutions |
|---|---|---|
| Insufficient Storage Capacity & Cost | - Inability to store new datasets- Rapidly increasing infrastructure costs- Long data retrieval times | - Implement tiered storage (hot, cold, archive) [11]- Deploy data compression techniques [12]- Adopt a hybrid-cloud strategy for elastic scaling [12] |
| Long Workflow Runtimes & Lack of Reproducibility | - Analysis pipelines take days/weeks to complete- Inability to replicate results on a different system- "Software dependency hell" | - Use containerization (Docker/Singularity) for software environments [11]- Implement workflow managers (Nextflow) for portable, scalable execution [11]- Choose validated, version-controlled pipelines (e.g., nf-core) [11] |
| Data Security & Privacy Concerns | - Difficulty complying with regulations (HIPAA, GDPR)- Concerns over sharing data with collaborators- Risk of sensitive data exposure | - Enforce role-based access controls (RBAC) and audit trails [11]- Utilize end-to-end encryption for data at rest and in transit [13]- Apply federated learning models for privacy-preserving analysis [14] |
| High AI Compute Demand | - Inability to run complex AI/ML models- Long queue times for job scheduling- High cloud compute costs | - Leverage scalable cloud HPC and GPU resources [15]- Explore access to new supercomputers dedicated to life sciences (e.g., Isambard-AI, Doudna) [15] |
Experimental Protocols and Workflows
Protocol 1: Implementing a Reproducible NGS Analysis Pipeline
This methodology outlines the steps for setting up a containerized, reproducible RNA-Seq analysis pipeline using Nextflow.
1. Requirements and Setup:
- Software Dependencies: Install Nextflow, Docker (or Singularity), and a Git client.
- Compute Infrastructure: Access to a high-performance computing (HPC) cluster, cloud environment, or a powerful local server.
- Reference Data: Download the appropriate reference genome (e.g., GRCh38) and annotation file (GTF).
2. Pipeline Configuration:
- Select a pre-validated pipeline from the nf-core community (e.g.,
nf-core/rnaseq). - Create a nextflow.config file to define:
- Path to your input data (e.g., FASTQ files)
- Path to reference genome and annotation
- Execution profile (e.g.,
dockerfor containerization,slurmfor HPC execution) - All parameters must be explicitly declared and versioned [11].
3. Pipeline Execution and Provenance Tracking:
- Launch the pipeline with a command like:
nextflow run nf-core/rnaseq -profile docker,sge -c nextflow.config. - The workflow system automatically handles parallelization, software execution via containers, and failure recovery.
- Upon completion, the platform generates a detailed report including software versions, parameters, and an execution timeline, creating an immutable audit trail for full provenance [11].
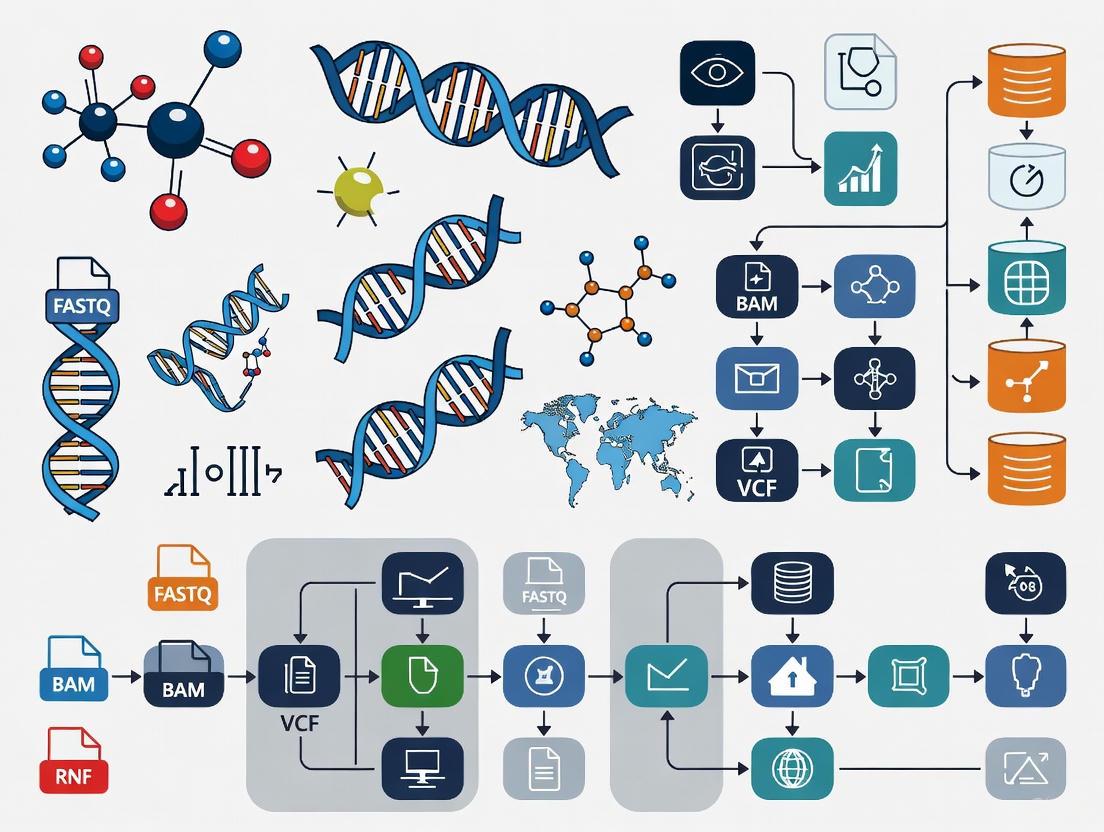
Workflow Visualization: From Wet Lab to Analysis
The following diagram illustrates the integrated, AI-enhanced workflow for NGS data generation and analysis, covering pre-wet-lab, wet-lab, and post-wet-lab phases [16].
The Scientist's Toolkit: Essential Research Reagents & Solutions
The following table details key resources for managing NGS data and computational infrastructure.
| Item | Category | Function & Application |
|---|---|---|
| Docker / Singularity | Containerization Platform | Packages bioinformatics software, dependencies, and environment into a portable, reproducible unit, ensuring consistent operation across different systems [11]. |
| Nextflow | Workflow Management System | Defines and executes scalable, portable data analysis pipelines across diverse computing infrastructures (cloud, HPC), enabling reproducibility [11]. |
| nf-core | Pipeline Repository | A curated collection of community-built, peer-reviewed bioinformatics pipelines that follow best practices for reproducibility and standardization [11]. |
| Galaxy Filament | Data Access Framework | Unifies access to reference genomic data from multiple public repositories, allowing seamless combination with user data for analysis without massive downloads [17]. |
| Federated Learning Platform | Privacy-Preserving AI | Enables training AI models on data distributed across multiple secure locations (e.g., different hospitals) without moving or sharing the raw, sensitive data [14]. |
| Hybrid Cloud Storage | Data Storage Infrastructure | Provides elastic, scalable storage by combining on-premise resources with cloud storage, allowing labs to adjust capacity with demand and control costs [12]. |
| Role-Based Access Control (RBAC) | Security & Governance | Manages data security by granting users permissions based on their role, ensuring researchers only access the data necessary for their specific tasks [11]. |
| AI-Assisted Variant Caller (e.g., DeepVariant) | Analysis Tool | Uses a deep neural network to call genetic variants from sequencing data, achieving higher accuracy than traditional heuristic methods [16]. |
Troubleshooting Guides
Sample Quality & FFPE Handling
Problem: Poor sequencing efficiency from FFPE samples
- Root Cause: Formalin fixation causes DNA damage including crosslinks, nucleotide oxidation, and fragmentation. Archival storage time exacerbates these effects [18].
- Detection: Implement PCR-based QC assays using incremental amplicon sizes (e.g., 105bp and 236bp). A QC ratio below 0.20 compared to control DNA indicates poor quality [18].
- Solution: Increase DNA input during library preparation for moderately degraded samples. For severely degraded samples (QC ratio <0.20), consider alternative specimens or targeted panels optimized for low-quality DNA [18].
Problem: Inconsistent variant calling in low GC-content regions
- Root Cause: Sample quality and GC content independently affect sequencing depth, with worst performance in low GC-content regions like KRAS in suboptimal samples [18].
- Detection: Monitor coverage uniformity across genomic regions with varying GC content.
- Solution: Increase sequencing depth for low GC-content regions when using suboptimal samples and utilize hybridization-capture techniques that perform better in these challenging regions [18].
Tumor Purity Assessment
Problem: Discrepant purity estimates between methods
- Root Cause: Different purity estimation methods (pathological, genomic, transcriptomic) measure different components of the tumor microenvironment and show poor concordance [19].
- Detection: Compare estimates from multiple methods (e.g., ESTIMATE, ABSOLUTE, LUMP, pathology) noting significant inter-method variation [20] [19].
- Solution: Parameterize genomic analyses with tumor purity estimated from the matched molecular analyte being analyzed. For DNA sequencing, use DNA-based purity estimates; for RNA sequencing, use RNA-based estimates [19].
Problem: Failed purity estimation in "quiet" genomes
- Root Cause: DNA-based purity estimation methods (ASCAT, CLONET, ABSOLUTE) may fail in tumors with low numbers of somatic single nucleotide variants, particularly in prostate cancer and other malignancies with quiet genomes [19].
- Detection: Monitor failure rates of DNA-based purity estimation methods; samples with failed estimates typically exhibit low SNV counts [19].
- Solution: Implement RNA-based purity estimation methods (DeMix, ISOpure-R) as alternatives for tumors with quiet genomes, or utilize multi-method consensus approaches [19].
Library Preparation
Problem: Biased library representation
- Root Cause: Nearly all library preparation steps introduce bias, especially in RNA-seq. Fragmentation methods, enzymatic manipulations, and PCR amplification can skew sequence representation [21].
- Detection: Analyze coverage uniformity and examine GC bias in sequencing results.
- Solution: Optimize fragmentation conditions, minimize PCR cycles, use high-fidelity polymerases, and consider PCR-free methods for appropriate sample types [22] [21].
Problem: Low library conversion efficiency
- Root Cause: Insfficient adapter ligation, residual contaminants, or suboptimal end repair and A-tailing reactions reduce the fraction of input fragments that become sequencing-competent molecules [22].
- Detection: Assess library concentration and size distribution using methods like qPCR, fluorometry, Bioanalyzer, or TapeStation [22].
- Solution: Optimize adapter concentration, use clean-up methods (magnetic beads, gel extraction) to remove adapter dimers, and ensure proper end repair and A-tailing reactions [22].
Frequently Asked Questions (FAQs)
Q: What is the minimal acceptable tumor purity for reliable NGS analysis? A: While TCGA initially used 80% tumor nuclei as a quality threshold, this was later reduced to 60%. However, purity requirements depend on your specific application and detection sensitivity needs. Samples with purity below 60% may still be analyzable but require specialized methods and careful interpretation [20].
Q: How does FFPE storage time impact sequencing success? A: FFPE storage time significantly correlates with sequencing efficiency metrics including depth of coverage, alignment rate, insert size, and read quality. Older samples generally show degraded performance, but successful sequencing can be achieved with samples over 20 years old when proper QC and protocol adjustments are implemented [18].
Q: What are the key differences between mechanical and enzymatic fragmentation? A: The table below compares these fragmentation methods:
| Factor | Mechanical Shearing | Enzymatic Fragmentation |
|---|---|---|
| Sequence Bias | Minimal sequence bias, more random | Potential bias in GC or motif regions |
| Input Requirements | Higher input requirements | Accommodates lower input DNA |
| Equipment Needs | Requires specialized equipment (e.g., Covaris) | Lower equipment cost, reagent-based |
| Throughput | Lower throughput, scaling challenges | Automation-friendly, high-throughput |
| Insert Size Flexibility | Better for long inserts (>1kb) | Smaller dynamic range of insert sizes |
Q: How should we handle discrepancies between pathological and molecular tumor purity estimates? A: Discrepancies are common due to tumor heterogeneity and methodological differences. Pathological estimates represent a specific section while molecular estimates reflect the entire sample used for extraction. When discrepancies occur, trust the estimate from the analyte being sequenced (DNA-based for DNA sequencing, RNA-based for RNA sequencing) and consider the molecular estimate more representative for genomic analyses [19].
Q: What QC metrics are most critical for NGS library preparation? A: Essential QC metrics include:
- Concentration assessment (qPCR, fluorometry)
- Size distribution (Bioanalyzer, TapeStation)
- Adapter-dimer contamination levels
- Molar concentration verification
- Conversion efficiency calculation [22]
Impact of Pre-analytical Variables on Sequencing Efficiency
| Variable | Impact Level | Correlation with Sequencing Metrics | Recommended Threshold |
|---|---|---|---|
| FFPE Storage Time | Significant | Negative correlation with coverage depth, alignment rate, insert size, read quality | Use PCR QC ratio >0.20 regardless of age |
| PCR-based QC Ratio | Critical | Directly correlates with all sequencing efficiency parameters | Ratio >0.20 indicates favorable quality |
| DNA Input Amount | Significant | Affects library complexity and coverage uniformity | Follow manufacturer's recommendations based on QC ratio |
| Tumor Purity | Variable by cancer type | Affects variant calling sensitivity and expression profiling | Minimum 60% for most applications; lower may require specialized methods |
Tumor Purity Estimation Method Comparison
| Method | Principle | Average Purity Estimate | Advantages | Limitations |
|---|---|---|---|---|
| Pathology Review | Visual estimation of tumor nuclei | 75.7% ± 21.2% | Direct assessment, clinically established | Subjective, intra- and inter-observer variability |
| ESTIMATE | Gene expression of 141 immune + 141 stromal genes | 81.1% ± 13.9% | RNA-based, accounts for microenvironment | Indirect measure, affected by expression patterns |
| ABSOLUTE | Somatic copy-number variation | 62.3% ± 19.9% | Direct measure of tumor cells | Requires copy number changes, fails in quiet genomes |
| LUMP | 44 non-methylated immune-specific CpG sites | 76.1% ± 16.1% | Methylation-based, reproducible | Measures immune infiltration specifically |
Experimental Protocols
PCR-Based DNA Quality Control Assay for FFPE Samples
Purpose: Determine DNA quality and recommend appropriate DNA input for library preparation [18].
Materials:
- 10ng DNA sample
- Two independent primer pairs generating 105bp and 236bp amplicons
- Control DNA from non-degraded source (e.g., A549 cell line)
- Agilent 2200 TapeStation or equivalent fragment analyzer
Procedure:
- Amplify 10ng of each DNA sample with both primer pairs
- Run PCR products on fragment analyzer for yield and fragmentation assessment
- Calculate QC ratio by dividing band quantification for each sample by respective band in positive control
- Average the ratios from both amplicons
- Interpret results: QC ratio >0.20 indicates favorable quality; <0.20 suggests moderate or poor quality
Application: Use this QC ratio to guide DNA input amount in subsequent library preparation steps [18].
Consensus Purity Estimation Methodology
Purpose: Generate robust tumor purity estimates by combining multiple estimation methods [20] [19].
Materials:
- Tumor sample with matched molecular data (DNA, RNA, methylation)
- Multiple purity estimation tools (ESTIMATE, ABSOLUTE, LUMP, etc.)
- IHC estimates if available
Procedure:
- Generate purity estimates using at least three different methods (e.g., DNA-based, RNA-based, and pathology)
- Normalize all estimates to have equal means and standard deviations
- Calculate Consensus Measurement of Purity Estimations (CPE) as the median of normalized values
- Use CPE for downstream analyses instead of individual method estimates
Note: This approach mitigates limitations of individual methods and provides more robust purity assessment [20].
Workflow Diagrams
Pre-analytical Factors Impact on NGS Data Quality
Tumor Purity Estimation Landscape
Research Reagent Solutions
| Reagent/Kit | Function | Application Context |
|---|---|---|
| Maxwell 16 FFPE Plus LEV DNA Purification Kit | Automated DNA extraction from FFPE samples | Standardized nucleic acid extraction from challenging FFPE samples [18] |
| Agilent Haloplex Target Enrichment System | Targeted gene capture using restriction enzymes | Custom panel design for specific gene sets; uses restriction digestion rather than sonication [18] |
| HostZERO Microbial DNA Kit | Reduces host DNA background in microbiome samples | Microbiome studies from host-associated samples where microbial DNA is a small fraction [23] |
| RiboFree rRNA Depletion Kit | Removes ribosomal RNA from RNA samples | Metatranscriptomics studies to enrich for messenger RNA and improve functional insights [23] |
| AMPure XP Beads | Magnetic bead-based purification and size selection | Library cleanup and size selection to remove adapter dimers and short fragments [22] |
| Quant-iT High-Sensitivity DNA Assay Kit | Accurate quantification of DNA concentration | Precise measurement of low-concentration DNA samples prior to library preparation [18] |
Building Robust Pipelines: Standardized Methods and Applications for Clinical NGS
This technical support center addresses the key challenges researchers and clinicians face when implementing robust, clinical-grade next-generation sequencing (NGS) workflows. The following guides and FAQs provide direct solutions to specific issues encountered during the bioinformatics pipeline.
What are the key stages in the NGS bioinformatics workflow?
The bioinformatics workflow for Illumina sequencing involves a multi-step process to transform raw data from the sequencer into annotated, clinically actionable variants. The journey begins with Binary Base Call (BCL) files, the raw data output containing base calls and quality scores from the sequencing run [24]. These are converted into FASTQ files, which store the sequence data and its corresponding quality scores in a text-based format, making it the standard starting point for most downstream analysis tools [24] [25]. The subsequent secondary analysis entails aligning these reads to a reference genome, resulting in BAM files (Binary Alignment Map), and then identifying variants to generate VCF files (Variant Call Format) [26] [27]. The final tertiary analysis involves annotating the VCF with biological and clinical information to aid in interpretation [28].
What are the most common policy barriers to clinical NGS implementation?
A multi-stakeholder Delphi study identified four critical policy challenges hindering the clinical adoption of NGS [29]:
- Payer variation in evidence standards: Different health plans use different criteria for assessing clinical utility, leading to inconsistent coverage policies.
- Proprietary databases: Companies maintaining private databases of variants slow down the collective understanding of variant clinical significance.
- Lack of standardized reporting: Inconsistent formats and content for reporting NGS test results to clinicians and patients.
- Uncertain regulatory role: Ongoing debate about the appropriate role of the FDA in overseeing NGS-based laboratory-developed tests (LDTs).
Troubleshooting Common Workflow Failures
FAQ 1: BCL to FASTQ Conversion Issues
Q: My BCL conversion is failing or producing empty FASTQ files. What should I check?
- A: This initial step is critical. Ensure the Illumina
bcl2fastqconversion software is correctly configured. Verify the run directory structure is intact and that you have provided the correct sample sheet. Confirm that the BCL files are not corrupted and that you have sufficient storage space, as BCL files are very large (>225 GB) and are often only stored for a short period (e.g., 3 months) [25].
FAQ 2: Poor Sequence Quality or Low Yield
Q: My FASTQ files have low-quality scores or low yield. What are the potential causes?
- A: Poor data quality often originates in the wet lab. Use a tool like FastQC to visualize quality metrics [27]. Common issues and their solutions are listed below.
Table: Troubleshooting Low-Quality FASTQ Data
| Problem Symptom | Potential Root Cause | Corrective Action |
|---|---|---|
| Low Q-scores, high error rate | Over-clustered flow cell, degraded reagents | Check cluster density metrics; use fresh PhiX control; ensure proper sequencer maintenance [27]. |
| High adapter contamination | Inefficient adapter ligation, inaccurate fragmentation | Optimize fragmentation parameters; titrate adapter-to-insert molar ratio; use trimming tools (Trimmomatic, Cutadapt) [4] [27]. |
| Low library complexity, high duplication | Insufficient input DNA, over-amplification | Re-quantify input DNA using fluorometry (Qubit); reduce PCR cycles during library prep [4]. |
| Abnormal GC bias | PCR artifacts, sequence-specific bias | Use PCR inhibitors; employ unique molecular identifiers (UMIs) to correct for amplification duplicates [27]. |
FAQ 3: Low Mapping Rates in BAM Files
Q: A high percentage of my reads are failing to align to the reference genome. How can I fix this?
- A: Low mapping rates can stem from several issues. First, ensure you are using the correct version of the reference genome (e.g., GRCh38/hg38 for human) and that it is properly indexed for your aligner (e.g., BWA, Bowtie2) [30] [27]. Second, review the quality of your FASTQ files—high levels of adapter content or poor base quality will hinder alignment and should be addressed by more stringent read cleanup. Finally, consider the sample origin; high contamination levels or the presence of large, complex variants not well-represented in the reference can also cause low mapping rates.
FAQ 4: VCF Normalization and Annotation Errors
Q: Why do my variants not match known databases, and how can I ensure accurate annotation?
- A: A primary reason for this discrepancy is that a single line in a VCF file can describe multiple alternative alleles at a single locus, a process that can "hijack" simple variants and make them difficult to match against standardized databases [31]. To ensure accurate annotation, you must pre-process your VCF file by splitting multi-allelic sites and left-normalizing indels [31].
The recommended command-line solution using bcftools is:
bcftools norm -m-both -o output.step1.vcf input.vcf.gz(Splits multi-allelic sites)bcftools norm -f reference_genome.fasta -o output.step2.vcf output.step1.vcf(Left-normalizes variants) [31].
After this pre-processing, annotation with tools like ANNOVAR or Ensembl VEP will be more reliable, as they can correctly match your variants to left-normalized database records [31] [28].
The Scientist's Toolkit: Essential Research Reagents & Software
Table: Key Tools and Resources for the BCL to VCF Pipeline
| Item Name | Function/Application | Technical Notes |
|---|---|---|
| bcl2fastq / bcl-convert | Converts raw BCL files from the sequencer into demultiplexed FASTQ files. | Illumina-provided software; essential first step for most data analysis pipelines [24] [26]. |
| FastQC | Provides quality control metrics for raw FASTQ data. | Visualizes per-base quality, adapter contamination, GC content, etc.; used for QC check pre-alignment [27]. |
| Trimmomatic / Cutadapt | Trims adapter sequences and low-quality bases from reads. | Critical for "cleaning" FASTQ files before alignment to improve mapping rates [27]. |
| BWA / Bowtie2 | Aligns (maps) sequencing reads to a reference genome. | Industry-standard aligners; output is in SAM/BAM format [24] [27]. |
| SAMtools / Picard | Manipulates and processes alignment files (BAM/SAM). | Used for sorting, indexing, marking duplicates, and extracting metrics [27]. |
| GATK / VarScan | Calls sequence variants (SNPs, indels) from aligned reads. | Identifies differences between the sample and the reference genome; generates a raw VCF [28]. |
| bcftools | Manipulates and normalizes VCF files. | Used for filtering, splitting, normalizing, and validating VCFs [31]. |
| VEP / ANNOVAR | Annotates variants with functional, population, and clinical data. | Adds context to variants (e.g., gene effect, frequency in 1000 Genomes, ClinSig) for interpretation [31] [28]. |
| GRCh38 Reference Genome | The standard reference sequence for human alignment and variant calling. | Always use the correct, consistently labeled version; available from GENCODE or GATK resource bundle [27]. |
Implementing a Quality Management System
For clinical implementation, simply having a workflow is insufficient. Laboratories must establish a robust Quality Management System (QMS). The Next-Generation Sequencing Quality Initiative (NGS QI) provides tools to help laboratories navigate CLIA requirements and other complex regulatory environments [2]. Key recommendations include:
- Workflow Lockdown: Once validated, the entire bioinformatic workflow (including software versions and parameters) must be locked down to ensure reproducibility [2].
- Personnel Competency: Ensure staff receive ongoing training and competency assessments, as specialized bioinformatics knowledge is critical and staff turnover can be a significant barrier [2].
- Standardized Validation: Use available validation tools and templates (e.g., the NGS QI's Method Validation Plan) to ensure compliance with quality and regulatory standards [2].
Frequently Asked Questions
Q1: Why is it recommended to use different specialized callers for different variant types, and what are the top choices? Using a single, universal variant caller is not optimal because the distinct biological signatures and genomic patterns of different variant types require specialized algorithmic approaches. A "jack of all trades" caller is often a "master of none," making the consolidation of calls from multiple best-in-class tools the preferred strategy for comprehensive variant detection [32]. The table below summarizes recommended tools for key variant types.
Table: Recommended Variant Calling Tools by Variant Type
| Variant Type | Recommended Tools | Key Considerations |
|---|---|---|
| Germline SNVs/Indels | GATK HaplotypeCaller [33] [34], Platypus [33] [34], FreeBayes [34], BCFtools [34] | Combining two orthogonal callers (e.g., HaplotypeCaller and Platypus) can offer a slight sensitivity advantage [33]. |
| Somatic SNVs/Indels | MuTect2 [34], Strelka2 [34], VarScan2 [34], VarDict [34] | Tumor heterogeneity and subclonal populations require callers specifically designed for somatic variants [32]. |
| Structural Variants (SVs) | Manta [34], DELLY [34], Lumpy [34] | SV callers rely on patterns like discordant read pairs, split reads, and read depth changes [32]. |
| Copy Number Variants (CNVs) | ExomeDepth [34], XHMM [34] | CNV detection from exome and panel data is possible, but whole-genome sequencing is superior [33]. |
Q2: What are the essential data pre-processing steps required before variant calling to ensure accuracy? A robust pre-processing workflow is critical to avoid the "garbage in, garbage out" problem. The primary goal is to generate an analysis-ready BAM file [32]. Key steps include:
- Read Alignment: Map raw sequencing reads (FASTQ) to a reference genome using an aligner like BWA-MEM [33] [34]. Initially, prioritize sensitivity over specificity to avoid overlooking true variants [32].
- Duplicate Marking: Identify and mark PCR duplicate reads using tools like Picard or Sambamba to prevent over-counting of the same original DNA fragment [33] [34].
- Base Quality Score Recalibration (BQSR): This step, part of the GATK Best Practices, uses an empirical error model to adjust base quality scores. Note that evaluations show marginal improvements, and it is computationally expensive, making it somewhat optional [33] [34].
- Quality Control (QC): Perform routine QC on the BAM file to evaluate sequencing metrics, verify sufficient coverage, and check for sample contamination using tools like BEDTools, Picard, and VerifyBamID [33] [34].
The following diagram illustrates the standard pre-processing workflow.
Q3: How does the choice of sequencing strategy (Panel, Exome, Genome) impact my ability to detect different variants? The choice of sequencing strategy involves a trade-off between the breadth of the genome interrogated, the average depth of sequencing achieved, and cost. Each strategy has distinct strengths and weaknesses for detecting various variant types [33] [32].
Table: Impact of Sequencing Strategy on Variant Detection
| Sequencing Strategy | Target Space | Average Depth | SNV/Indel | CNV | SV | Low VAF/Variant |
|---|---|---|---|---|---|---|
| Targeted Panel | ~0.5 - 5 Mbp | 500 - 1000x | Outstanding (++) | Good (+) | Poor (-) | Excellent for low VAF |
| Whole Exome (WES) | ~50 Mbp | 100 - 150x | Outstanding (++) | Good (+) | Poor (-) | Good |
| Whole Genome (WGS) | ~3200 Mbp | 30 - 60x | Outstanding (++) | Outstanding (++) | Good (+) | Good |
Q4: What publicly available benchmark resources should I use to validate my variant calling pipeline's performance? To objectively evaluate the sensitivity and specificity of a variant calling pipeline, it is essential to use benchmark datasets where the "ground truth" variants are known [33]. The following are key resources:
- Genome in a Bottle (GIAB): Provides high-confidence consensus variant calls for several human samples, along with defined high-confidence genomic regions. It is one of the most widely used benchmarks for germline small variants [33] [34].
- Platinum Genomes: Another benchmark set for the NA12878 sample, offering a high-quality set of truth variants [33] [34].
- Synthetic Diploid (Syndip): A benchmark derived from long-read assemblies of two homozygous cell lines. It is less biased than consensus-based resources and is particularly valuable for assessing accuracy in challenging genomic regions, such as segmental duplications [33].
Q5: My pipeline crashed during SV benchmarking. What are the common pre-processing steps required for structural variant VCFs? SV benchmarking often fails due to inconsistent VCF formatting across different callers. A standardization and normalization workflow is required to homogenize the test and truth VCF files for an accurate comparison [35]. Key steps include:
- Reformatting: Use tools like
svyncto reformat VCFs from different SV callers into a consistent structure [35]. - Standardization & Decomposition: Tools like
SVTK standardizeandrtgtools svdecomposeare used to standardize SV types to breakends (BND) and decompose complex SVs [35]. - Normalization: Use
bcftools normto split multi-allelic variants, deduplicate variants, and left-align indels. This ensures all variants are represented in a canonical form [35].
The logic for troubleshooting a failed SV benchmarking run is outlined below.
The Scientist's Toolkit
This table lists essential reagents, software, and reference materials critical for setting up a standardized variant detection workflow.
Table: Key Research Reagent Solutions for Core Variant Calling
| Item Name | Function / Explanation |
|---|---|
| SureSeq FFPE DNA Repair Mix | Enzyme mix designed to repair a broad range of DNA damage in formalin-fixed paraffin-embedded (FFPE) samples, helping to reduce formalin-induced artifacts and increase confidence in variant calls from degraded samples [32]. |
| SureSeq CLL + CNV Panel | An example of a targeted gene panel that provides comprehensive coverage of key genes and regions for a specific disease (Chronic Lymphocytic Leukemia), enabling simultaneous detection of SNVs, Indels, and exon-level CNVs in a single workflow [32]. |
| OGT Interpret NGS Analysis Software | Automated data analysis software that provides predefined settings for calling SNVs, indels, and structural aberrations (like ITDs, CNVs), minimizing user intervention and maximizing consistency [32]. |
| Illumina BaseSpace Sequence Hub / DNAnexus | Cloud-based platforms that provide user-friendly, AI-powered bioinformatics analysis without requiring advanced programming skills, facilitating variant calling and interpretation [16]. |
| Genome in a Bottle (GIAB) Reference Materials | Publicly available reference DNA samples and associated "ground truth" variant datasets used to benchmark, validate, and optimize the performance of variant calling pipelines for clinical implementation [33]. |
Implementing Quality System Essentials (QSE) for Clinical Bioinformatics
Clinical bioinformatics represents a critical bridge between raw next-generation sequencing (NGS) data and clinically actionable information. Within diagnostic laboratories, implementing robust Quality System Essentials (QSE) ensures the accuracy, reliability, and reproducibility of genomic data analysis. The Next-Generation Sequencing Quality Initiative (NGS QI), established by the CDC and Association of Public Health Laboratories (APHL), provides a structured framework based on twelve Quality System Essentials adapted from the Clinical & Laboratory Standards Institute (CLSI) [2] [36]. This framework addresses the entire testing lifecycle, from personnel qualifications and equipment management to process control and data management, creating a foundation for clinical-grade bioinformatics operations.
As NGS technologies evolve with new platforms, improved chemistries, and advanced bioinformatic analyses, the complexity of validation and quality management increases significantly [2]. Clinical bioinformatics now demands production-scale operations that differ substantially from research-oriented core facilities, requiring standardized practices, rigorous validation, and comprehensive documentation [37]. The dynamic nature of this field presents ongoing challenges for quality management, particularly with the introduction of targeted sequencing approaches, metagenomic applications, and increasingly sophisticated bioinformatics pipelines [2] [38].
Troubleshooting Guides & FAQs
Common NGS Bioinformatics Challenges: Q&A
Q: Our clinical NGS assay failed to detect variants present in reference materials at expected allele frequencies. What are the primary causes?
A: Variant detection failures typically stem from several technical issues:
- Assay incompatibility: Verify that your assay's target regions actually include the variant positions. Review manufacturer Target Region GTF files and variant coordinates carefully, as not all assays cover all variants in a gene [39].
- Insufficient sequencing depth: Low coverage dramatically reduces variant detection sensitivity. Modeled data shows that 500 reads for a 10% variant yields a 95% confidence interval of approximately 7.2-13.0%, while 2000 reads narrows this to 8.7-11.4% [39].
- Low library complexity: Inadequate input DNA or over-amplification can reduce library complexity. For ctDNA applications with typical 165bp fragments, 120-160bp amplicons will capture only 3-27% of input molecules, potentially dropping effective input below 15ng [39].
- Amplicon size limitations: Larger amplicons in fragmented DNA (e.g., ctDNA) show reduced efficiency. Variants requiring larger amplicons may be undetectable while those with smaller amplicons are reliably detected [39].
Table 1: Troubleshooting Variant Detection Issues
| Problem | Root Cause | Corrective Action |
|---|---|---|
| Variants in reference materials not detected | Assay target region doesn't cover variant | Verify variant coordinates in assay design files |
| Low variant allele frequency precision | Insufficient sequencing depth | Increase coverage to manufacturer recommendations |
| Inconsistent variant detection across samples | Low library complexity from inadequate input | Optimize input DNA quantity; avoid over-amplification |
| Specific variants consistently missed | Amplicon size inefficiencies for fragmented DNA | Redesign assays with smaller amplicons for fragmented DNA |
Q: Our bioinformatics pipeline produces inconsistent variant calls across sequencing runs. How can we improve reproducibility?
A: Inconsistent variant calling typically indicates issues with pipeline stability, documentation, or validation:
- Implement containerization: Use Docker or Singularity containers to encapsulate software environments, ensuring consistent tool versions and dependencies across executions [37].
- Establish version control: Maintain all code, documentation, and configurations in a git-tracked system with strict change control procedures [37].
- Standardize analysis parameters: Adopt hg38 as reference genome and define a standard analysis set including SNV, CNV, SV, STR, and LOH analyses [37].
- Enhance validation practices: Supplement standard truth sets (GIAB for germline, SEQC2 for somatic) with recall testing of previously validated clinical samples [37].
Q: We're experiencing high personnel turnover in our clinical bioinformatics unit. How can we maintain quality despite staffing changes?
A: Workforce stability challenges are common in clinical genomics, with surveys indicating some personnel holding positions for <4 years on average, and 30% of public health laboratory staff planning to leave within 5 years [2]. Address this through:
- Comprehensive documentation: Develop detailed SOPs covering all analytical processes. The NGS QI offers over 100 free guidance documents and templates for customization [2] [36].
- Structured competency assessment: Implement regular competency evaluations using tools like the Bioinformatician Competency Assessment SOP from NGS QI [2].
- Cross-training programs: Ensure multiple team members understand each component of the bioinformatics workflow to maintain operations during transitions.
Experimental Protocols for Key Validation Experiments
Protocol: Bioinformatics Pipeline Validation for Clinical WGS
Purpose: Establish analytical validity of clinical whole genome sequencing bioinformatics pipelines according to regulatory standards [37].
Materials:
- Reference materials: Genome in a Bottle (GIAB) for germline variants, SEQC2 for somatic variants
- Previously characterized clinical samples with orthogonal validation
- High-performance computing infrastructure
- Containerization software (Docker/Singularity)
Procedure:
- Unit Testing: Validate individual pipeline components (alignment, variant calling, annotation) using synthetic datasets with known variants.
- Integration Testing: Assess component interactions using intermediate file formats (BAM, VCF) from reference materials.
- System Testing: Execute end-to-end analysis on GIAB reference materials with predefined acceptance criteria for sensitivity (>99%), specificity (>99.5%), and reproducibility (100% concordance).
- Performance Validation: Test pipeline on 25-30 previously characterized clinical samples representing intended use cases.
- Sample Identity Verification: Implement genetic fingerprinting checks including sex chromosome concordance and relatedness estimation between serial samples [37].
Validation Criteria:
- Sensitivity: >99% for SNVs/indels in covered regions
- Specificity: >99.5% for all variant types
- Reproducibility: 100% concordance between replicate analyses
- Sample identity: Zero mismatches in genetic fingerprinting
Table 2: Required Bioinformatics Team Competencies
| Skill Domain | Essential Competencies | Quality Documentation |
|---|---|---|
| Software Development | Version control, testing, containerization | Git repositories, test logs, container manifests |
| Data Management | Secure transfer, integrity verification, backup | Checksum logs, access controls, backup logs |
| Quality Assurance | Validation protocols, change control, audit trails | Validation reports, SOPs, audit reports |
| Domain Knowledge | Human genetics, variant interpretation, regulatory standards | Training records, competency assessments, CME documentation |
Workflow Visualization
Clinical Bioinformatics QSE Workflow
The Scientist's Toolkit
Table 3: Essential Research Reagents & Resources for Clinical Bioinformatics
| Resource Category | Specific Products/Tools | Function & Application |
|---|---|---|
| Reference Materials | Genome in a Bottle (GIAB), SEQC2, Seraseq Reference Materials | Benchmark variant calling accuracy; validate assay performance across variant types [37] [39] |
| Bioinformatics Containers | Docker, Singularity, Bioconda | Reproducible software environments; version-controlled dependencies [37] |
| Quality Control Tools | FastQC, MultiQC, Qualimap | Monitor sequencing quality metrics; identify pre-analytical errors [4] [38] |
| Variant Calling Tools | Multiple complementary tools for SNV, CNV, SV detection | Comprehensive variant detection; reduce false positives/negatives through tool combination [37] |
| Validation Resources | NGS QI Validation Plan Template, Method Validation SOP | Standardized validation protocols; regulatory compliance documentation [2] [36] |
Implementing robust Quality System Essentials in clinical bioinformatics requires both technical solutions and organizational commitment. As the field continues to evolve with platforms offering increasing accuracy and new applications like metagenomic pathogen detection, the QSE framework provides the necessary foundation for maintaining quality amidst rapid change [2]. The NGS Quality Initiative offers laboratories a valuable starting point with customizable tools that can be adapted to specific laboratory needs while maintaining compliance with regulatory requirements [36]. Success ultimately depends on integrating quality management into each step of the bioinformatics workflow, from sample to clinical report, while maintaining the flexibility to incorporate technological advancements that benefit patient care.
Frequently Asked Questions (FAQs)
FAQ 1: Why am I getting different TMB values from different targeted sequencing panels?
Different panels can yield different TMB values due to variations in panel size, genomic content, and bioinformatic pipelines. The confidence of TMB estimation is highly dependent on the size of the targeted sequencing panel [40]. Smaller panels are more susceptible to statistical noise and may lack the robustness of larger panels or whole-exome sequencing (WES). To troubleshoot:
- Verify Panel Size: Use panels covering at least 1.0-1.5 Mb whenever possible. Smaller panels may require specific correction factors [40].
- Check for Synonymous Mutations: Determine if the panel's bioinformatic pipeline includes synonymous mutations in its TMB calculation. Some panels include them to reduce sampling noise, while others, like MSK-IMPACT, do not [40].
- Validate with a Reference Standard: If possible, validate your panel's TMB output against a WES-derived TMB value for a set of samples to understand the concordance.
FAQ 2: How can I accurately determine MSI status from degraded FFPE samples using NGS?
FFPE-derived DNA is often fragmented and damaged, which can lead to sequencing artifacts and false-positive MSI calls.
- Use Degradation-Robust Library Prep Kits: Employ library preparation kits specifically designed for FFPE and cell-free DNA (cfDNA), which are optimized for low-input and degraded material [41].
- Incorporate Unique Molecular Identifiers (UMIs): Use kits that leverage UMIs to correct for errors introduced during amplification and sequencing, improving the accuracy of mutation calling in difficult samples [41].
- Leverage Specialized Bioinformatics: Utilize analysis software with modules specifically designed for MSI quantification from FFPE samples. These tools often include algorithms to account for sample-specific noise [41].
FAQ 3: What are the major challenges when transitioning TMB and MSI analysis to a liquid biopsy platform?
Liquid biopsy, while less invasive, presents unique challenges compared to tissue-based analysis.
- Low Abundance of ctDNA: In early-stage cancers or certain cancer types, the fraction of circulating tumor DNA (ctDNA) in the total cell-free DNA (cfDNA) can be very low, affecting detection sensitivity [42] [41].
- Tumor Heterogeneity: A liquid biopsy may not fully capture the spatial heterogeneity of the entire tumor, as ctDNA is shed from multiple tumor sites [41].
- Lack of Standardization: It is not yet fully established how TMB and MSI results from liquid biopsies compare to the gold standard of tissue biopsy, and validation against a tissue standard is currently recommended [41].
FAQ 4: My bioinformatic pipeline for MSI detection has a high false-positive rate. How can I improve its specificity?
A high false-positive rate is often due to sequencing artifacts or misclassification of polymerase slippage in homopolymer regions.
- Implement a Matched Normal: Always sequence a matched normal sample (e.g., from blood or saliva) alongside the tumor sample. This allows for the subtraction of germline polymorphisms and the identification of individual-specific sequencing artifacts [43].
- Optimize Bioinformatics Filters: Apply filters for sequencing quality, read depth, and mapping quality. For MSI, specifically, ensure the algorithm is tuned to distinguish true somatic instability from technical noise.
- Choose an Appropriate Method: Some NGS-based methods, like Archer's VARIANTPlex panels, are designed to accurately quantify MSI status without a matched normal by using a robust baseline of normal samples, which can be a viable alternative [41].
Quantitative Data Tables
Table 1: Comparison of Commercial NGS Panels for TMB and MSI Analysis
This table summarizes key features of various targeted sequencing panels used for TMB and MSI assessment in clinical research, highlighting the diversity in approach [40].
| Laboratory | Panel Name | Number of Genes | Total Region Covered (Mb) | TMB Region Covered* (Mb) | Mutation Types in TMB |
|---|---|---|---|---|---|
| Foundation Medicine | FoundationOne CDx | 324 | 2.20 | 0.80 | Non-synonymous, Synonymous |
| Memorial Sloan Kettering | MSK-IMPACT | 468 | 1.53 | 1.14 | Non-synonymous |
| Illumina | TSO500 (TruSight Oncology 500) | 523 | 1.97 | 1.33 | Non-synonymous, Synonymous |
| Thermo Fisher Scientific | Oncomine Tumor Mutation Load Assay | 409 | 1.70 | 1.20 | Non-synonymous |
| Tempus | TEMPUS Xt | 595 | 2.40 | 2.40 | Non-synonymous |
| Guardant Health | GuardantOMNI | 500 | 2.15 | 1.00 | Non-synonymous, Synonymous |
*Coding region used to estimate TMB.
Table 2: Key Biomarker Definitions and Clinical Significance
This table provides a clear overview of the biomarkers discussed, their biological basis, and their role in immunotherapy [43] [41].
| Biomarker | Full Name | Biological Mechanism | Role as Predictive Biomarker |
|---|---|---|---|
| MMRd | Mismatch Repair Deficiency | Inability of the cell to correct errors (mismatches) made during DNA replication. | Predicts response to immune checkpoint inhibitors (ICIs). Tumors with MMRd are often MSI-H and TMB-H. |
| MSI-H | Microsatellite Instability-High | A consequence of MMRd; accumulation of mutations in short, repetitive DNA sequences (microsatellites). | An established biomarker for ICI efficacy across multiple cancer types. |
| TMB-H | High Tumor Mutational Burden | A high number of mutations (typically ≥10 mut/Mb) per megabase of DNA sequenced. | Used to identify patients likely to respond to ICIs, as high mutation load can lead to more neoantigens. |
Experimental Protocols
Protocol 1: Determining MSI Status Using a Targeted NGS Panel
Methodology: This protocol uses DNA extracted from tumor tissue (ideally FFPE with a matched normal) and a targeted NGS panel covering multiple microsatellite regions.
- Library Preparation: Use a library prep kit validated for your sample type (e.g., FFPE). Kits like the xGen cfDNA & FFPE DNA Library Prep Kit are designed for degraded samples. Incorporate UMIs to improve variant calling accuracy [41].
- Target Enrichment: Enrich for the target regions (including microsatellites) using either:
- Hybridization Capture: Uses biotinylated probes to pull down regions of interest. Common for comprehensive panels.
- Amplicon-Based (e.g., AMP): Uses gene-specific primers for PCR-based enrichment. Can be effective for smaller, focused panels [41].
- Sequencing: Perform high-throughput sequencing on an NGS platform to achieve sufficient depth (e.g., >500x coverage) for accurate mutation detection.
- Bioinformatic Analysis:
- Alignment: Map sequencing reads to a reference genome.
- Variant Calling: Identify insertions and deletions (indels) within the targeted microsatellite loci.
- MSI Scoring: Compare the number and length of indels in the tumor sample to a baseline (from the matched normal or a built-in baseline of normal samples). A sample is classified as MSI-H if the instability score exceeds a predefined threshold [41].
Protocol 2: Calculating TMB from Targeted Sequencing Data
Methodology: This protocol outlines the steps to calculate TMB from the same targeted NGS data used for other somatic variant detection.
- Somatic Variant Calling: Identify somatic mutations in the tumor sample using a matched normal to filter out germline variants. Call single nucleotide variants (SNVs) and small indels.
- Mutation Filtering:
- Remove known germline polymorphisms from population databases (e.g., gnomAD).
- Filter out technical artifacts and variants in low-complexity or blacklisted genomic regions.
- TMB Calculation:
- Count the total number of somatic, coding (often non-synonymous) mutations that pass all filters.
- Divide the total number of mutations by the size of the coding region (in megabases) targeted by the panel that was effectively sequenced. For example: TMB = (Total Passed Mutations) / (Panel Size in Mb).
- Report the result as mutations per megabase (mut/Mb) [40].
- Interpretation: Classify the tumor as TMB-H based on a validated cutoff. The FDA has approved a cutoff of ≥10 mut/Mb for pembrolizumab in certain solid tumors, but optimal cutoffs can vary by cancer type [40].
Workflow and Pathway Visualizations
Diagram 1: Integrated NGS Workflow for TMB and MSI Analysis. This chart outlines the key steps from sample collection to final biomarker report, highlighting parallel bioinformatics pathways.
Diagram 2: Biological Relationship Between MMRd, MSI-H, and TMB-H. This chart shows how different molecular defects converge on a common mechanism of increased immunogenicity and response to immunotherapy.
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Research Reagents and Kits
This table lists key products and technologies used in experiments for TMB, MSI, and liquid biopsy analysis.
| Item Name | Function / Application | Key Feature |
|---|---|---|
| xGen cfDNA & FFPE DNA Library Prep Kit | Library preparation for NGS from challenging samples like cfDNA and degraded FFPE DNA. | Optimized for low-input, fragmented DNA; includes UMI adapters for error correction [41]. |
| Archer VARIANTPlex Panels | Targeted NGS panels (e.g., Solid Tumor) for variant, MSI, and TMB analysis. | Uses Anchored Multiplex PCR (AMP) chemistry; works with degraded samples; includes analysis suite [41]. |
| FoundationOne CDx | Comprehensive genomic profiling panel for solid tumors. | FDA-approved IVD test; reports TMB, MSI, and other genomic alterations from FFPE tissue [40]. |
| MSK-IMPACT | Targeted panel sequencing for tumor profiling. | FDA-authorized test; assesses TMB and mutations in 468 genes [43] [40]. |
| CellSearch System | Enumeration and isolation of Circulating Tumor Cells (CTCs) from blood. | FDA-cleared system for prognostic use in metastatic breast, prostate, and colorectal cancer [42]. |
Optimizing for Production: Troubleshooting and Scaling Clinical Bioinformatics Workflows
Troubleshooting Guides
Guide 1: Resolving Common Bioinformatics Pipeline Failures
Problem: Pipeline execution fails or produces unexpected results.
| Problem | Possible Cause | Solution |
|---|---|---|
| Pipeline fails immediately | Incorrect software version or missing dependency [44] | Use containerized environments (e.g., Docker, Singularity) to ensure consistency [45]. |
| Low-quality variant calls | Poor initial data quality or misaligned reads [46] | Check FastQC reports; re-trim reads; verify alignment metrics with SAMtools [44] [46]. |
| Pipeline runs very slowly | Computational bottlenecks; inefficient resource allocation [44] [47] | Use a workflow manager (e.g., Nextflow) for dynamic resource allocation; leverage cloud scaling [47]. |
| Results are irreproducible | Unrecorded parameters or manual intervention in workflow [46] | Implement version control (Git) for all scripts and use workflow managers for full automation [44] [46]. |
| High cloud computing costs | Misconfigured execution environment; over-provisioning resources [47] | Audit cloud configuration; right-size computing instances; use spot pricing where possible [47]. |
Guide 2: Addressing Data Quality and Preprocessing Issues
Problem: The input data is of low quality, leading to unreliable downstream analysis.
| Symptom | Diagnostic Tool | Corrective Action |
|---|---|---|
| Low Phred scores, adapter contamination | FastQC, MultiQC [44] [46] | Use Trimmomatic or Picard to trim adapters and remove low-quality bases [44] [46]. |
| Low alignment rate | Alignment tool (BWA, STAR) logs, SAMtools [44] | Verify reference genome compatibility; check for sample contamination [44] [46]. |
| Unexpected coverage depth | Qualimap, SAMtools coverage stats [46] | Re-sequence with adjusted depth; use hybrid capture methods for targeted regions [48]. |
| Batch effects in sample group | Principal Component Analysis (PCA) [46] | Include batch as a covariate in statistical models; use normalization methods like ComBat [46]. |
| Sample mislabeling or swap | Genetic fingerprinting, sex-check markers [45] | Implement barcode labeling and use LIMS for sample tracking; verify identity with genetic markers [45] [46]. |
Frequently Asked Questions (FAQs)
Q1: What is the primary goal of bioinformatics workflow optimization? The primary goal is to enhance reproducibility, efficiency, and agility in data analysis. This is crucial for managing growing dataset sizes and complexity, ensuring reliable results in clinical and research settings, and controlling computational costs [47].
Q2: When should we start optimizing our bioinformatics workflows? Optimization should begin when usage scales justify the investment. Key triggers include rising computational costs, frequent pipeline failures, difficulties in reproducing results, or the need to process significantly larger datasets. Starting early builds a strong foundation for scalability [47].
Q3: What are the most common tools for managing bioinformatics workflows? Workflow management systems like Nextflow and Snakemake are industry standards. They help automate processes, manage software dependencies, and ensure portability across different computing environments (local servers, HPC clusters, or cloud platforms) [44] [47].
Q4: How can we ensure our clinical bioinformatics pipeline is robust? Follow consensus recommendations for clinical production, which include:
- Using the latest human reference genome (GRCh38/hg38) [45].
- Implementing a standard set of analyses (SNV, INDEL, CNV, and SV calling) [45].
- Validating pipelines with standard truth sets (e.g., GIAB) and in-house data [45].
- Ensuring sample identity through genetic fingerprinting [45].
Q5: Our pipeline works but is too slow. How can we improve its speed? Address computational bottlenecks by:
- Profiling the pipeline to identify slow steps.
- Parallelizing tasks where possible using workflow managers.
- Optimizing resource allocation (CPU, memory) for each tool.
- Migrating to a cloud platform with scalable compute power for demanding tasks like metagenomics analysis [44] [47].
Q6: What are the cost implications of poor workflow optimization? Poorly optimized workflows can lead to massive and unnecessary expenses. While analyzing a single sample may be cheap, processing millions of data points with inefficient methods can cost hundreds of thousands of dollars monthly. Optimization can lead to time and cost savings of 30% to 75% [47].
Workflow Optimization Diagrams
Bioinformatics Pipeline Lifecycle
Systematic Troubleshooting Process
Optimization Impact on Cost and Time
Essential Research Reagent Solutions
| Reagent / Material | Function in NGS Workflow |
|---|---|
| DNA/RNA Extraction Kits | Purify and isolate nucleic acids from various sample types (e.g., FFPE, fresh-frozen) for sequencing [48]. |
| Library Preparation Kits | Fragment DNA and ligate adapter sequences to create a library amenable to NGS sequencing [48]. |
| Hybridization Capture Probes | Designed oligonucleotide "baits" used to enrich specific genomic regions of interest from a complex library [48]. |
| PCR Primers for Amplicon Sequencing | Flanking primers that amplify target regions for focused sequencing panels [48]. |
| Unique Dual Indexes (UDIs) | Oligonucleotide barcodes used to label individual samples during library prep, enabling sample multiplexing and de-multiplexing after sequencing [48]. |
| Positive Control DNA | A reference DNA sample with known variants, used to validate the performance and accuracy of the entire wet-lab and bioinformatics pipeline [45]. |
Addressing Tumor Heterogeneity and Low-Frequency Variant Detection
Frequently Asked Questions (FAQs)
General Principles
1. What makes tumor heterogeneity a significant challenge in cancer genomics? Tumor heterogeneity refers to the cellular diversity within a single tumor (intra-tumor) or between tumors of the same type in different patients (inter-tumor). This variation occurs at genetic, epigenetic, transcriptional, and metabolic levels. It poses a major challenge because different cellular subclones within a tumor can have varying metastatic potential and responses to treatment. This heterogeneity can lead to drug resistance, more aggressive metastasis, and disease recurrence, as subclones not targeted by therapy can survive and proliferate [49].
2. Why is detecting low-frequency variants critical in clinical NGS assays? Many clinically actionable somatic mutations are present at low variant allele frequencies (VAFs) due to factors like low tumor purity, tumor heterogeneity, or the emergence of treatment-resistant mutations. For example, in a study of 5,095 clinical samples, a significant fraction of mutations in key driver genes like EGFR, KRAS, PIK3CA, and BRAF were found at VAFs below 5%. Specifically, 24% of EGFR T790M resistance mutations were found below 5% VAF. Detecting these variants is imperative for selecting effective targeted therapies, such as osimertinib for NSCLC patients with EGFR T790M mutations [50].
Technical Troubleshooting
3. Our NGS assay is missing known low-frequency variants. What are the primary factors to check? If your assay is missing low-frequency variants, first investigate these key parameters:
- Sequencing Depth: Ensure sufficient depth. While panel sequencing often achieves ~900x mean coverage, hotspots require even higher depth (e.g., >1000x) to robustly call low-VAF variants [50].
- Variant Calling Tool: Standard variant callers struggle with VAFs below 1%. Utilize tools specifically designed for low-frequency detection. UMI-based callers generally outperform raw-reads-based callers for very low VAFs [51].
- Sample Quality: For FFPE samples, assess DNA quality and quantity. Low input DNA or high degradation can exacerbate errors and limit detection [52] [48].
- Tumor Purity: Pathological estimation of tumor cell content is crucial. Low tumor purity directly results in lower VAFs for somatic mutations, potentially pushing them below the detection limit [48].
4. We are getting a high number of false positives in our low-frequency variant calls. How can we improve specificity? A high false positive rate is a common challenge when pushing detection limits. To improve specificity:
- Utilize UMIs: Incorporate Unique Molecular Identifiers (UMIs) into your workflow. UMIs label original DNA molecules, allowing bioinformatics tools to create consensus reads for each molecule and filter out errors introduced during PCR amplification and sequencing [51].
- Employ Specialized Callers: Use variant callers validated for low-frequency detection. Benchmarking studies show that UMI-based tools like DeepSNVMiner and UMI-VarCal offer an excellent balance of high sensitivity and precision for low-VAF variants [51].
- Apply Robust Filtering: Implement a panel-of-normals (PoN) to filter out common germline variants and recurring technical artifacts. One study demonstrated that a PoN of ~400 normal samples could remove over 94% of germline variants, approaching the efficiency of a matched normal sample [50].
5. How can we effectively measure and analyze tumor heterogeneity from sequencing data?
- Single-Cell Sequencing: This is the gold standard for directly resolving cellular heterogeneity. Technologies like Primary Template directed Amplification (PTA) enable accurate detection of single nucleotide variants (SNVs) and copy number variations (CNVs) in individual cells, revealing subpopulations that bulk sequencing averages out [53].
- Computational Methods on Bulk Data: For bulk sequencing, computational techniques can quantify heterogeneity. Expression Variation Analysis (EVA) is an algorithm that performs multivariate statistical analyses of differential variation in gene sets from single-cell RNA-sequencing (scRNA-seq) data, allowing quantification of pathway-level heterogeneity between different cell groups [54].
- Tumor Mutation Burden (TMB): TMB, the total number of somatic mutations per coding area, is a related biomarker. Bioinformatics standardization is essential for reliable TMB estimation from targeted NGS panels, requiring careful pipeline selection and validation against whole-exome sequencing [52].
Troubleshooting Guides
Guide 1: Selecting a Low-Frequency Variant Caller
Problem: Inconsistent or unreliable detection of variants with VAF < 5%.
Solution: Select and validate a variant caller designed for low-frequency detection. The performance of these tools varies significantly. The table below summarizes a systematic evaluation of eight callers, based on a benchmarking study using simulated and reference datasets [51].
Table 1: Performance Comparison of Low-Frequency Variant Calling Tools
| Variant Caller | Type | Theoretical Detection Limit | Key Strengths | Key Limitations |
|---|---|---|---|---|
| DeepSNVMiner | UMI-based | Very Low (≤0.1%) | High sensitivity (88%) and precision (100%) in benchmarking [51]. | May lack a strand bias or homopolymer filter, potentially leading to FPs [51]. |
| UMI-VarCal | UMI-based | ~0.1% | High sensitivity (84%) and precision (100%); uses Poisson statistical test [51]. | - |
| MAGERI | UMI-based | ~0.1% | Fast analysis speed; uses Beta-binomial model [51]. | Can have high memory consumption [51]. |
| smCounter2 | UMI-based | 0.5%-1% | Uses Beta-Beta-binomial model [51]. | Lower detection limit; consistently slow analysis time [51]. |
| LoFreq | Raw-reads-based | ~0.05% | Calls variants based on base quality scores; effective down to low VAFs [51] [50]. | High false positive rate compared to UMI-based callers [51]. |
| SiNVICT | Raw-reads-based | ~0.5% | Good for time-series analysis; uses Poisson model [51]. | High false positive rate at very low VAFs [51]. |
| outLyzer | Raw-reads-based | ~1% | Uses Thompson Tau test to measure background noise [51]. | Fixed limit of detection is higher than other tools [51]. |
| Pisces | Raw-reads-based | - | Tuned for amplicon sequencing data [51]. | Performance varies with sequencing design. |
Recommendation: For the most critical applications requiring the highest sensitivity and specificity for VAFs below 1%, UMI-based callers like DeepSNVMiner or UMI-VarCal are recommended. If UMIs are not available, LoFreq is a capable raw-reads-based alternative, though it requires stringent post-calling filtration to manage false positives [51].
Guide 2: Designing a Robust Wet-Lab Protocol for Sensitive Detection
Problem: Even with the best bioinformatics, the wet-lab protocol introduces too much noise for reliable low-VAF detection.
Solution: Implement a rigorous laboratory workflow that minimizes artifacts. The following diagram and protocol outline key steps.
Diagram: Experimental Workflow for Reliable Low-Frequency Detection
Detailed Protocol:
Sample Quality Control (QC):
- Input: Use a minimum of 10-1000 ng of DNA, depending on the application [48].
- Tumor Purity: Before sequencing, have a pathologist estimate tumor cell purity. This is critical for interpreting VAFs. Low purity samples will require greater sequencing depth [48].
- FFPE DNA: If using FFPE-derived DNA, use quantification methods that assess quality and yield, as FFPE DNA is more prone to damage [48].
Library Preparation with UMIs:
- Unique Molecular Identifiers (UMIs): Incorporate UMIs during the library preparation step, immediately after DNA fragmentation and before amplification. This tags each original DNA molecule with a unique barcode [51].
- Amplification: Use the minimum number of PCR cycles necessary to maintain library complexity and avoid over-amplification, which can exacerbate errors and create duplicates that bioinformatic tools must correctly handle [51].
Sequencing:
- Depth: Plan for a mean coverage of at least 900x-1000x for panel sequencing. Ensure that coverage over clinically critical hotspots is even higher to confidently call low-frequency variants [50].
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Materials and Tools for Tumor Heterogeneity and Low-Variant Studies
| Item | Function / Explanation | Example / Note |
|---|---|---|
| Targeted NGS Panels | Focuses sequencing on cancer-related genes, allowing for high-depth coverage of key regions at a lower cost than WES/WGS. | Panels like the Oncomine Tumor Mutational Load (OTML) assay cover hundreds of genes (e.g., 409) for estimating TMB [52]. |
| Single-Cell Whole Genome Amplification (WGA) | Enables genomic analysis at the single-cell level to directly characterize intra-tumor heterogeneity. | Primary Template directed Amplification (PTA) is a novel WGA method that reduces artifacts and improves detection of SNVs and CNVs from single cells [53]. |
| UMI Adapter Kits | Reagents that add unique barcodes to each original DNA molecule during library prep, enabling error correction. | Various commercial kits are available. Essential for leveraging UMI-based variant callers [51]. |
| Bioinformatics Pipelines | Integrated software for aligning sequences, calling variants, and interpreting results in a clinical context. | Ion Reporter software with specialized workflows (e.g., for TMB); QCI Interpret for Oncology for clinical decision support and variant interpretation [52] [55]. |
| Reference Materials | Well-characterized cell lines or control samples used to validate assay performance and bioinformatics pipelines. | Cultured and FFPE cell lines with known MSI and mutational status can be used for validation and benchmarking [52]. |
What is a VUS and Why is it a Major Challenge in Clinical NGS?
A Variant of Uncertain Significance (VUS) is a genetic variant identified through genetic testing whose clinical significance to patient health is not known [56]. Unlike pathogenic variants (which cause disease) or benign variants (which do not), a VUS has insufficient or conflicting evidence regarding its role in disease [57]. This classification is one of the five standard categories recommended by the American College of Medical Genetics and Genomics (ACMG), which include: Pathogenic, Likely Pathogenic, VUS, Likely Benign, and Benign [57] [56].
The core challenge is that a VUS result cannot be used for clinical decision-making. It is not considered causative of a disease, nor can it be used for predictive testing in family members [57]. The prevalence of VUS is not trivial; approximately 20% of genetic tests identify a VUS, and in next-generation sequencing (NGS) for hereditary breast cancer, this figure can be as high as 35% [58]. The frequency can vary by gene; for instance, in comprehensive germline TP53 testing, a VUS rate of 0.65% has been observed, though this can differ based on the clinical criteria of the tested population [59].
The following table summarizes quantitative data on VUS prevalence from key studies.
| Context of Genetic Testing | Reported VUS Frequency | Key Findings |
|---|---|---|
| Overall Genetic Tests | ~20% [58] | A significant portion of tests results in a VUS, leaving patients and clinicians with uncertainty. |
| Hereditary Breast Cancer NGS | ~35% encounter one or more VUS [58] | Highlights the challenge in well-studied cancer genes. |
| Germline TP53 Testing (independent of clinical criteria) | 0.65% (12 VUS in 1844 patients) [59] | Demonstrates that VUS rates are gene-specific and can be influenced by testing criteria. |
How Do I Troubleshoot a VUS Finding in My Research Data?
Encountering a VUS in your data requires a systematic approach to gather evidence for its potential reclassification. The following troubleshooting guide outlines the key steps and common pitfalls.
VUS Interpretation and Troubleshooting Workflow
Detailed Troubleshooting Steps:
Step 1: Database Interrogation
- Action: Systematically query population and clinical variant databases.
- Key Resources: ClinVar, gnomAD, and disease-specific databases.
- Objective: Determine the variant's frequency in general populations (evidence for benignity if high) and review existing classifications and evidence in ClinVar [58]. Sharing your VUS findings with these databases is critical for collective learning [58].
Step 2: In Silico Analysis
- Action: Use computational tools to predict the variant's impact on the protein.
- Methodology: These tools analyze evolutionary conservation, protein structure, and splice site effects [59].
- Limitation: Predictions are computational and should not be used as standalone evidence for pathogenicity [56].
Step 3: Phenotype-Genotype Correlation
- Action: Correlate the finding with the patient's clinical presentation.
- Key Question: Is the patient's phenotype consistent with the diseases associated with the gene? The absence of a clear Li-Fraumeni syndrome (LFS) phenotype, for example, complicates the interpretation of a TP53 VUS [59].
Step 4: Functional Studies
- Action: Conduct laboratory experiments to assess the biological consequences of the variant.
- Protocols: These can range from biochemical assays to high-throughput functional screens. While powerful, they are often reserved for variants with a higher suspicion of pathogenicity due to resource requirements [56].
Step 5: Segregation Analysis
- Action: Test relevant family members to see if the variant co-segregates with the disease.
- Interpretation: If the variant is found in all affected family members and not in unaffected ones, this is strong evidence for pathogenicity. This is a primary method for "VUS resolution" [57].
Common Problems and Solutions:
Problem: "The VUS is novel and not in any database."
- Solution: Prioritize the in silico and functional evidence gathering pipeline. Report the novel VUS to ClinVar to contribute to the public knowledge base [58].
Problem: "I have conflicting evidence; a VUS is found at a frequency slightly above the threshold for disease, but a functional study suggests it is damaging."
- Solution: This is a classic scenario for a VUS. Per ACMG guidelines, conflicting evidence automatically results in a VUS classification. The solution is to gather more evidence, such as segregation analysis or additional independent functional data [57].
Problem: "My clinical team wants to act on a VUS result."
What is the ACMG/AMP Framework for Variant Classification?
The variant classification framework is a semi-quantitative system that weighs different types of evidence to place a variant into one of five categories [57]. The process involves assessing criteria for and against pathogenicity.
ACMG/AMP Variant Classification Framework
The framework is intentionally conservative to protect patients from the consequences of misclassification, embodying the principle that variants should be "uncertain until proven guilty" [57]. A VUS classification arises either from a complete lack of evidence or, critically, from conflicting evidence—when some data points toward pathogenicity and other data points toward benignity [57]. It's important to note that gene-specific modifications to the ACMG guidelines, such as those developed by the ClinGen consortium for genes like MYH7, are increasingly used to tailor the framework for specific disease contexts [57].
What are the Best Practices for Bioinformatics Pipelines to Ensure Accurate VUS Identification?
The accuracy of the initial variant call is paramount. A robust bioinformatics pipeline is the first line of defense against interpretation errors. The following table outlines essential materials and data sources that form the backbone of a clinical-grade bioinformatics operation for NGS.
| Research Reagent / Resource | Category | Function in VUS Analysis |
|---|---|---|
| Genome Reference Consortium Human Build 38 (GRCh38) [45] | Reference Genome | Provides the standard against which patient sequences are aligned; using the latest build improves mappability and variant calling accuracy. |
| Genome in a Bottle (GIAB) [45] | Standard Truth Set | A set of reference genomes with highly validated variant calls; used for accuracy validation and benchmarking of bioinformatics pipelines. |
| CLINVar [58] [56] | Clinical Variant Database | A public archive of reports of genotype-phenotype relationships; critical for comparing a VUS against existing classifications and evidence. |
| Clinical-grade High-Performance Computing (HPC) System [45] | Computing Infrastructure | Off-grid systems ensure data security and integrity for processing sensitive clinical genomic data. |
| Containerized Software Environments [45] | Software Management | Tools like Docker/Singularity ensure computational reproducibility and pipeline stability across different computing environments. |
Key Bioinformatics Protocols and Data Analysis Steps:
Primary Data Processing: The process begins with de-multiplexing pooled samples (converting BCL files to FASTQ), followed by alignment of sequencing reads to a reference genome (e.g., GRCh38) to create BAM files [45]. The Nordic Alliance for Clinical Genomics specifically recommends adopting the hg38 genome build [45].
Variant Calling: The aligned reads (BAM files) are processed to identify variants, producing a Variant Call Format (VCF) file. A comprehensive clinical pipeline should call multiple variant types [45]:
- Single Nucleotide Variants (SNVs) and small insertions/deletions (indels)
- Copy Number Variants (CNVs)
- Structural Variants (SVs), including insertions, inversions, and translocations
- Short Tandem Repeats (STRs) It is recommended to use multiple tools for structural variant calling to improve sensitivity and specificity [45].
Pipeline Validation and Quality Assurance: Pipelines must be rigorously tested for accuracy and reproducibility. This includes:
- Unit, integration, and end-to-end testing [45].
- Using standard truth sets like GIAB for germline variant calling to measure performance [45].
- Supplementing with recall testing of real human samples previously characterized by validated methods [45].
- Verifying sample identity through genetic fingerprinting and checks for sex and relatedness to prevent sample mix-ups [45].
How Should VUS Results Be Communicated in a Research or Clinical Setting?
Effective communication is critical to prevent misunderstanding and anxiety. For both researchers and clinicians, the key messages when disclosing a VUS are [58] [57]:
- A VUS is inconclusive. It is neither diagnostic nor predictive.
- Clinical management should not be based on a VUS. Patient care should be guided by personal and family medical history.
- Most VUS are eventually reclassified as benign. The majority of these variants are harmless [58].
- The interpretation may change. New evidence can lead to the VUS being reclassified in the future, which necessitates long-term monitoring and re-evaluation [58].
Engaging with genetic experts and counselors is highly recommended. They can help communicate the significance and limitations of these uncertain variants with clarity, helping to manage patient and family anxiety while empowering informed decision-making [58]. Some research explores the utility of sub-classifying VUS (e.g., "VUS-possibly pathogenic") to provide more nuance, but this is not yet standard practice in clinical reporting [57].
Transitioning bioinformatics pipelines from local servers to cloud and High-Performance Computing (HPC) environments is a critical step in clinical and public health Next-Generation Sequencing (NGS) implementation. This shift addresses the computational intensity of analyzing large cohorts, such as those in genome-phenome projects, but introduces challenges in workflow management, cost control, and ensuring reproducibility under quality standards like CLIA [2] [60]. This guide provides targeted troubleshooting and FAQs to help researchers and drug development professionals navigate this complex transition.
Frequently Asked Questions (FAQs)
1. What are the first signs that our pipeline needs to scale to cloud or HPC? You will likely notice that standard analyses, such as variant calling or phylogenetic analysis, are taking days or weeks to complete on your local machines, significantly delaying research outcomes. Other signs include an inability to process large sample batches simultaneously, frequent memory exhaustion errors, or the need to constantly delete old data to free up storage for new datasets [60].
2. How can we control costs when running pipelines in the cloud? A key strategy is to implement an automated data lifecycle management policy. This involves transitioning data through different storage tiers—from high-performance (and high-cost) active storage to low-cost archival or cold storage—based on its current need for access [11]. Furthermore, leveraging spot instances (preemptible VMs) for fault-tolerant workloads and meticulously tagging all resources to monitor spending by project are highly effective best practices.
3. Our validated clinical pipeline must be "locked down." How do we ensure reproducibility in a scalable environment? Reproducibility is ensured by using containerization (e.g., Docker, Singularity) to encapsulate the exact software environment and workflow management systems (e.g., Nextflow, Snakemake) to define the pipeline steps. These tools create an immutable, version-controlled record of the entire analysis, from the software and parameters to the input data checksums, which is essential for clinical validation and audits [11] [60].
4. What is the biggest bottleneck when moving to a scalable architecture? Often, the bottleneck is not computation but data transfer and I/O (Input/Output). Moving terabytes of raw sequencing data from on-premises storage to the cloud can be slow and expensive. Once there, poorly designed pipelines that frequently read/write small files can become I/O-bound, where processes wait for data rather than computing. Using data compression techniques and optimizing for parallel I/O can mitigate this [61].
5. We have a legacy tool (e.g., PAML) that isn't parallel. Can we still benefit from HPC? Absolutely. This is a classic use case for "embarrassingly parallel" scaling. While the tool itself runs on a single CPU, you can use a workflow manager to run hundreds of independent instances simultaneously, each processing a different gene alignment or dataset. This scatters the workload across many cores and gathers the results, drastically reducing total computation time from days to hours [60].
Troubleshooting Common Scalability Issues
Problem 1: Pipeline Fails Inconsistently on a Large Cluster
- Symptoms: Jobs crash sporadically across different compute nodes without a clear error pattern, or there are permission errors when accessing shared storage.
- Diagnosis:
- Intermittent Failures: Often caused by subtle differences in software environments across nodes. A dependency might be missing or be a different version on some nodes.
- Permission Errors: Arise from misconfigured file system permissions on network-attached or distributed storage, where worker nodes cannot read/write to a common path.
- Solution:
- Use Containers: Package your entire pipeline, including all tools and dependencies, into a Docker or Singularity container. This guarantees a consistent, portable environment regardless of the underlying node [11] [60].
- Centralize Data: Use a distributed file system (e.g., Lustre, Ceph) or cloud object storage (e.g., AWS S3) that is designed for concurrent access from multiple nodes, and verify access permissions in your job scheduler scripts [61].
Problem 2: Poor Performance Despite High Resource Allocation
- Symptoms: The pipeline runs but does not finish faster, or it takes much longer than expected even with many CPUs. Compute nodes are often idle.
- Diagnosis:
- I/O Bottlenecks: The pipeline may be waiting for data to be read from or written to disk. This is common with tools that process many small files.
- Inefficient Workflow Design: The pipeline may have long, sequential steps that block parallel execution, or tasks may be too small, causing overhead from managing thousands of tiny jobs.
- Solution:
- Optimize I/O: Use data formats optimized for parallel access (e.g., HDF5, Zarr) and leverage parallel I/O libraries. For small files, consider grouping them into larger archives [61].
- Profile and Redesign: Use monitoring tools to identify slow pipeline steps. Redesign the workflow to maximize parallelization, and adjust task sizes to balance overhead and utilization. Tools like Nextflow and Snakemake can automatically parallelize independent steps [62] [60].
Problem 3: Sky-High Cloud Bill
- Symptoms: The cloud computing costs are significantly higher than initial estimates, with storage being a major cost driver.
- Diagnosis:
- Data Left in Expensive Tiers: All data, including final results and raw files no longer needed for active analysis, is stored on high-performance storage.
- Over-Provisioning: Virtual machines are chosen that are too large for the workload, or they are left running after jobs have completed.
- Solution:
- Implement Data Lifecycle Policies: Automatically transition raw data to cool/archive storage after processing and delete temporary intermediate files. The
nf-corepipelines, for example, have built-in options to clean up intermediate files [11]. - Right-Sizing and Automation: Use instance types that match CPU and memory requirements. Leverage automated scaling groups that add or remove compute resources based on workload demand to avoid paying for idle VMs [61].
- Implement Data Lifecycle Policies: Automatically transition raw data to cool/archive storage after processing and delete temporary intermediate files. The
Problem 4: "My Pipeline Works on My Machine!" (Lack of Reproducibility)
- Symptoms: A pipeline that runs perfectly on a developer's laptop or a specific server fails when deployed to the cloud or cluster due to missing software, library conflicts, or different environment variables.
- Diagnosis: The pipeline's execution is dependent on the specific system configuration where it was developed, which is not replicated in the new environment.
- Solution:
- Adopt Containerization and Workflow Managers: This is the foundational solution. Define your pipeline with a system like Nextflow or CWL, and package all software in a container. This combination captures the complete execution environment, making it portable and reproducible across any platform that supports these standards [60].
- Use Version Control: Store your pipeline code, configuration files, and container definitions in a version-controlled repository (e.g., Git) to track all changes and enable collaboration [62].
Comparison of Scalability Solutions
The table below summarizes the core approaches to scaling bioinformatics pipelines, helping you select the right model for your needs.
| Feature | High-Performance Computing (HPC) Cluster | Cloud Computing | Hybrid Model |
|---|---|---|---|
| Primary Use Case | Fixed, predictable workloads; large, single-site projects [61] | Dynamic, variable workloads; collaborative, multi-institutional projects [60] | Bursting from a local cluster to the cloud for peak demands [60] |
| Cost Model | High capital expenditure (CapEx) for hardware | Operational expenditure (OpEx) - pay-as-you-go | Mix of CapEx and OpEx |
| Data Management | Local or distributed file systems (e.g., Lustre) [61] | Cloud object storage & databases; potential egress fees | Data resides on-prem; compute can burst to cloud |
| Key Advantage | High-performance interconnects; full control | Infinite, on-demand scalability; rich managed services (AI, databases) | Flexibility; cost-control for predictable base loads |
| Best for Clinical NGS | Large, centralized public health labs with stable workflows [2] | Rapidly scaling projects, clinical trials, integrating new tools like AI [13] | Labs with existing HPC investment needing to handle periodic large analyses |
The Scientist's Toolkit: Key Technologies for Scalable Pipelines
| Tool Category | Examples | Function in Scalable Pipelines |
|---|---|---|
| Workflow Management Systems | Nextflow, Snakemake, CWL [62] [60] | Orchestrate complex, multi-step pipelines across different compute infrastructures, ensuring portability and reproducibility. |
| Containerization Platforms | Docker, Singularity [11] [60] | Package software and dependencies into isolated, consistent environments that run identically on any system. |
| Cluster & Job Schedulers | SLURM, Kubernetes [62] [61] | Manage and schedule computational workloads across a pool of resources (nodes), ensuring efficient utilization. |
| Distributed File Systems | Lustre, Hadoop (HDFS) [61] | Provide high-speed, parallel access to large datasets from multiple compute nodes simultaneously. |
| Cloud Platforms | AWS, Google Cloud, Microsoft Azure [61] | Provide on-demand, scalable computing, storage, and specialized services (e.g., AI) without maintaining physical hardware. |
Experimental Protocol: Implementing a Scalable Clinical NGS Pipeline
This methodology outlines the key steps for deploying a validated clinical NGS analysis pipeline, such as a variant caller, into a scalable cloud or HPC environment.
1. Environment Setup and Containerization:
- Create a Container: Write a
Dockerfilethat defines the base operating system, installs all necessary bioinformatics tools (e.g., BWA, GATK), and sets the correct environment variables. Build this into a container image [60]. - Define the Workflow: Script the analytical steps (quality control, alignment, variant calling, annotation) using a workflow language like Nextflow. The workflow definition should specify inputs, outputs, processes, and the container image to use for each step.
2. Configuration for Scalability:
- Specify Compute Profiles: Within your workflow configuration (e.g.,
nextflow.config), create profiles for different execution platforms (e.g.,local,cluster,cloud). Define parameters like the job scheduler (SLURM, AWS Batch), queue names, memory/CPU requirements per task, and auto-scaling policies [62] [60]. - Configure Data Access: Set up secure access to reference genomes and input data, which may be on a distributed file system, object storage, or a hosted database. Ensure all compute nodes have the necessary permissions.
3. Execution, Monitoring, and Validation:
- Launch with Parameters: Execute the workflow using a command that specifies the correct profile and any runtime parameters (e.g.,
nextflow run main.nf -profile cluster --input /project/data/*.fastq). - Monitor Resources: Use the HPC's job scheduler (e.g., SLURM) or the cloud provider's monitoring console (e.g., AWS CloudWatch) to track job status, resource utilization, and spot any failures [61].
- Validate Outputs: Before using results in a clinical context, run the scaled pipeline on a dataset with known expected outcomes (a positive control) to ensure the scaled deployment produces identical results to the validated local version. Adhere to NGS QI validation guidelines for clinical settings [2].
Scalable Pipeline Implementation Workflow
The diagram below illustrates the logical flow and key decision points for transitioning a bioinformatics pipeline to a scalable architecture.
Ensuring Accuracy: Validation, Benchmarking, and Comparative Analysis of NGS Methods
The implementation of Next-Generation Sequencing (NGS) in clinical diagnostics has revolutionized genetic testing, enabling comprehensive analysis from single genes to entire genomes. However, the complexity of bioinformatics pipelines presents significant challenges for clinical adoption, where accuracy and reproducibility are paramount. Pipeline validation serves as the foundation for ensuring reliable clinical results, protecting patient safety, and maintaining regulatory compliance. As the field moves toward large-scale clinical production, standardized bioinformatics practices have emerged as an urgent necessity to ensure consensus, accuracy, and comparability across laboratories [37] [45].
The validation framework for clinical bioinformatics pipelines encompasses multiple testing levels, each with distinct objectives and methodologies. Unit testing verifies the functionality of individual pipeline components, integration testing ensures these components work together correctly, and end-to-end (E2E) testing validates the entire workflow from raw data to final variant calls. According to recent consensus recommendations from the Nordic Alliance for Clinical Genomics (NACG), pipelines must be documented and tested for accuracy and reproducibility, minimally covering unit, integration, and end-to-end testing to meet clinical standards [37] [45].
Table: Testing Levels for Clinical Bioinformatics Pipeline Validation
| Testing Level | Scope | Validation Focus | Key Metrics |
|---|---|---|---|
| Unit Testing | Individual software components | Algorithm accuracy, boundary conditions | Precision, recall for specific variant types |
| Integration Testing | Interfaces between pipeline components | Data handoff, file format compatibility | Process completion rates, error handling |
| End-to-End Testing | Complete workflow from FASTQ to VCF | Overall diagnostic accuracy, reproducibility | Sensitivity, specificity, precision, accuracy |
Essential Testing Protocols and Experimental Designs
Unit Testing for Discrete Pipeline Components
Unit testing forms the foundational layer of pipeline validation, focusing on individual components and algorithms. This testing level isolates specific tools to verify their performance characteristics under controlled conditions.
Variant Caller Validation Protocol:
- Test Data Preparation: Curate benchmark datasets with known variant positions and types, including SNVs, indels, and structural variants. The Genome in a Bottle (GIAB) consortium provides extensively characterized reference materials ideal for this purpose [37] [45].
- Execution Parameters: Run each variant caller with standardized parameters across multiple replicates to assess consistency.
- Output Analysis: Compare identified variants against known truth sets, calculating performance metrics for each variant type separately.
- Boundary Testing: Evaluate performance with challenging variants, such as those in low-complexity regions, high-GC content areas, or near indels.
For example, in the validation of a long-read sequencing pipeline, researchers employed eight different variant callers to comprehensively detect diverse genomic alterations, achieving 98.87% analytical sensitivity and exceeding 99.99% specificity against NIST benchmarked samples [63]. This approach demonstrates how multiple specialized tools can be integrated to overcome the limitations of any single algorithm.
Integration Testing for Pipeline Workflows
Integration testing verifies that individual pipeline components function together correctly, with particular attention to data handoffs and compatibility.
Data Flow Validation Protocol:
- Interface Verification: Confirm each stage produces output in the expected format for the subsequent stage (e.g., BAM to VCF conversion).
- Error Handling: Introduce corrupted or malformed files at each pipeline stage to verify robust error detection and reporting.
- Resource Management: Monitor computational resources (memory, CPU) during pipeline execution to identify bottlenecks or memory leaks.
- Metadata Integrity: Track sample identifiers and metadata throughout the entire workflow to prevent sample swapping or data misassignment.
The NACG recommendations emphasize that clinical bioinformatics should operate at standards similar to ISO 15189, utilizing strict version control and containerized software environments to ensure consistency across pipeline executions [37] [45]. This standardization is particularly crucial for integration testing, where environmental variables can significantly impact performance.
End-to-End Testing for Clinical Validity
End-to-end (E2E) testing validates the complete pipeline from raw sequencing data to final variant calls, simulating real-world clinical usage. E2E testing is defined as a software testing methodology that validates an application's entire workflow to ensure all components and integrations work together correctly [64].
Comprehensive E2E Validation Protocol:
- Sample Selection: Assay well-characterized reference samples (e.g., GIAB) alongside previously tested clinical samples with known variants. The NACG recommends supplementing standard truth sets with recall testing of real human samples previously tested using validated methods [37] [45].
- Whole Workflow Execution: Process samples through the complete pipeline, from raw data (FASTQ) through alignment, variant calling, and annotation.
- Performance Assessment: Calculate sensitivity, specificity, precision, and accuracy for each variant type against established truth sets.
- Reproducibility Testing: Execute multiple replicates across different sequencing runs, operators, and timepoints to establish precision.
In a recent validation of a targeted NGS panel for solid tumours, researchers employed comprehensive E2E testing across 43 unique samples, demonstrating 99.99% repeatability and 99.98% reproducibility while detecting all 92 known variants from orthogonal methods [65]. This approach highlights how E2E testing provides the final validation of clinical readiness.
Table: Performance Metrics from Published Pipeline Validations
| Study | Pipeline Type | Sensitivity | Specificity | Precision | Accuracy | Sample Size |
|---|---|---|---|---|---|---|
| Long-Read Sequencing Pipeline [63] | Germline variant detection | 98.87% | >99.99% | N/R | N/R | 72 clinical samples |
| Targeted Oncology Panel [65] | Somatic variant detection | 98.23% | 99.99% | 97.14% | 99.99% | 43 unique samples |
| NACG Recommendations [37] [45] | Clinical WGS | Target: >99% | Target: >99% | Target: >99% | Target: >99% | GIAB + clinical samples |
Troubleshooting Guide: Common Validation Challenges and Solutions
FAQ: Addressing Frequent Validation Issues
Q1: Our pipeline shows excellent performance with GIAB reference materials but performs poorly with our in-house clinical samples. What could explain this discrepancy?
A1: This common issue often stems from differences in sample quality or variant types not well-represented in reference sets.
- Solution: Supplement standard truth sets with in-house data from previously validated methods. The NACG specifically recommends this approach to ensure pipeline performance across the variant types relevant to your specific clinical applications [37] [45]. Additionally, review sample preparation protocols and quality metrics to identify potential pre-analytical variables affecting performance.
Q2: We observe decreasing pipeline performance over time despite no intentional changes to the workflow. How should we investigate this?
A2: This "performance drift" typically results from undocumented environmental changes or software updates.
- Solution: Implement strict version control for all software components, including dependencies. Use containerized environments (Docker, Singularity) to ensure consistency [37] [45]. Establish regular monitoring of key performance indicators and automated alerts for performance degradation. Maintain a sample repository for continuous quality monitoring across pipeline versions.
Q3: Our validation shows high sensitivity for SNVs but poor performance for structural variants and indels. What strategies can improve detection of complex variants?
A3: Variant type-specific performance differences indicate a need for specialized tools and validation approaches.
- Solution: Implement multiple complementary tools for structural variant calling, as recommended by the NACG consensus guidelines [37] [45]. For indel detection, ensure validation includes samples with indels of various sizes and contexts. In the long-read sequencing pipeline validation, researchers used a combination of eight variant callers to achieve comprehensive variant detection [63].
Q4: How can we verify sample identity throughout the pipeline to prevent sample swapping or contamination?
A4: Sample identification errors can compromise entire clinical datasets.
- Solution: Implement genetic fingerprinting checks by comparing genetically inferred identification markers (sex, common SNPs) against expected values [37] [45]. Verify sample relatedness when processing family cohorts. Use file hashing (MD5, SHA-1) to ensure data integrity throughout processing steps.
Table: Key Resources for Clinical NGS Pipeline Validation
| Resource Category | Specific Examples | Purpose in Validation | Key Characteristics |
|---|---|---|---|
| Reference Materials | GIAB samples (e.g., NA12878) [63] | Gold standard for benchmarking | Extensively characterized variants across technologies |
| SEQC2 reference samples [37] [45] | Somatic variant calling validation | Designed for cancer sequencing benchmarks | |
| In-House Samples | Previously tested clinical samples [37] [45] | Real-world performance assessment | Variants of clinical relevance to specific applications |
| External Quality Assessment (EQA) samples [65] | Independent performance verification | Blinded samples for objective assessment | |
| Bioinformatics Tools | Multiple variant callers [63] [37] | Comprehensive variant detection | Tool-specific strengths for different variant types |
| Containerization software (Docker/Singularity) [37] [45] | Computational reproducibility | Environment consistency across executions | |
| Quality Metrics | File hashing (MD5, SHA-1) [37] [45] | Data integrity verification | Detection of corruption or unintended changes |
| Genetically inferred identifiers [37] [45] | Sample identity confirmation | Sex chromosomes, common SNPs for fingerprinting |
Comprehensive pipeline validation through unit, integration, and end-to-end testing is not merely a technical formality but a fundamental requirement for clinical NGS implementation. The consensus emerging from leading clinical genomics organizations emphasizes standardized practices, containerized environments, and multi-faceted testing approaches [37] [45]. By adopting these structured validation methodologies, clinical laboratories can ensure their bioinformatics pipelines generate reliable, reproducible results suitable for patient care decisions.
The integration of standardized reference materials with in-house clinical samples creates a validation framework that balances general benchmarking with application-specific performance assessment. Furthermore, the implementation of continuous monitoring and version control practices ensures that initially validated performance remains stable throughout the pipeline's operational lifetime. As NGS technologies continue evolving and playing increasingly prominent roles in clinical diagnostics, rigorous validation approaches will remain essential for translating technological advances into improved patient outcomes.
What are GIAB and SEQC2, and why are they critical for clinical NGS?
The Genome in a Bottle (GIAB) Consortium, hosted by the National Institute of Standards and Technology (NIST), develops widely characterized reference genomes and benchmark variant calls to enable translation of whole human genome sequencing to clinical practice [66]. The Sequencing Quality Control Phase 2 (SEQC2) consortium (also known as MAQC-III), an FDA-led international effort, builds upon this foundation to establish best practices and standards for specific sequencing applications, including oncopanels, ctDNA, and epigenomics [67] [68]. Together, these initiatives provide the essential infrastructure to validate the analytical performance of NGS workflows, a fundamental requirement for clinical implementation.
How do benchmarking standards address bioinformatics challenges in clinical NGS?
Clinical NGS workflows are prone to specific, context-dependent errors. Common challenges include:
- False positives/negatives in difficult genomic regions: Areas with low complexity, high GC content, or segmental duplications can lead to mapping errors and variant calling inaccuracies [69] [70].
- Inconsistent detection of complex variants: Large indels, structural variants (SVs), and variants in tandem repeats are frequently missed by standard short-read NGS bioinformatic pipelines [71] [70].
- Inter-laboratory reproducibility: Differences in protocols, reagents, and bioinformatic tools can lead to conflicting results for the same sample [67] [68].
GIAB and SEQC2 resources allow laboratories to measure their performance against a known truth set, identifying and correcting these specific weaknesses before implementing tests for patient care.
Troubleshooting Guides and FAQs
FAQ: How do I select the appropriate GIAB reference sample for my assay validation?
Answer: The choice depends on your assay's intended use and the population you serve. GIAB has characterized multiple samples, including the well-known NA12878 (HG001) and two parent-child trios of Ashkenazi Jewish (HG002-HG004) and Han Chinese (HG005-HG007) ancestry, all consented for commercial redistribution [66]. For comprehensive testing, using multiple samples is advised to capture a wider range of genetic diversity and variant types.
Answer: This is a common issue, as indels are an order of magnitude more challenging to detect than SNVs [71]. Follow this troubleshooting pathway:
First, sequence a GIAB sample (e.g., HG002) and run your variant calling pipeline. Next, use GIAB's benchmark indel calls and genomic stratifications to compare your results. The stratifications will show if the problem is universal or confined to specific challenging contexts like homopolymers or tandem repeats [69]. If errors are concentrated in difficult regions, your short-read technology or standard aligner may be insufficient, suggesting a need for complementary long-read sequencing or specialized algorithms [70].
FAQ: My targeted oncopanel shows high sensitivity but also a high false positive rate. What best practices can I implement from SEQC2?
Answer: The SEQC2 Oncopanel Sequencing Working Group specifically addressed this trade-off. Their key recommendation is to restrict analysis to a Consensus Targeted Region (CTR) [68]. This region is rigorously defined and has known positive variants and millions of confirmed negative positions. By limiting variant calling to the CTR and applying a validated VAF threshold (e.g., 5%), you can dramatically reduce false positives with minimal impact on sensitivity.
Troubleshooting Guide: Inconsistent Methylation Results Across Replicates
Problem: In epigenomic studies, DNA methylation levels are inconsistent between technical replicates prepared using the same WGBS kit.
Investigation and Resolution:
- Check Conversion Efficiency: Use the lambda phage DNA spike-in control. A non-conversion rate significantly above 0% in the CHH and CHG contexts indicates inefficient bisulfite treatment, a major source of bias [72].
- Review Mapping Metrics: Use the SEQC2 EpiQC study data for comparison. For example, if using TruSeq, expect a higher PCR duplicate rate and GC bias [72]. High duplication can reduce effective coverage and increase variance.
- Verify Spike-in Controls: Check the methylation levels of completely methylated (e.g., pUC19) and unmethylated (lambda) controls. Deviations from 100% and 0%, respectively, indicate problems with the conversion or sequencing process itself [72].
FAQ: A large fraction of my NGS data is unmapped or poorly aligned. What are the potential causes?
Answer: Low mapping efficiency can stem from several pre-analytical and analytical factors. The SEQC2 EpiQC study showed that mapping rates are highly protocol-specific, with methods like Swift Accel-NGS MethylSeq having high primary mapping rates, while others like SPLAT have a higher fraction of unmapped reads [72]. Use the following table to diagnose the issue:
Table: Troubleshooting Low Mapping Rates in NGS Data
| Observation | Potential Cause | Corrective Action |
|---|---|---|
| High adapter content in FastQC | Adapter dimer in library; short fragment length | Use tools like CutAdapt or Trimmomatic to remove adapters [73]. |
| Low base quality scores, especially at 3' end | General degradation of library quality; sequencing cycle errors | Trim low-quality bases. Check sequencer performance and flow cell quality [73]. |
| High duplication rate | Insufficient input DNA; over-amplification during PCR | Optimize input DNA quantity; use PCR-free library prep kits where possible. |
| Consistent low mapping across samples | Incorrect reference genome version or index | Ensure the reference genome (GRCh37, GRCh38, T2T-CHM13) matches the annotation used and is properly indexed for your aligner [30]. |
Experimental Protocols and Methodologies
Protocol: Benchmarking a Germline Small Variant Calling Pipeline
This protocol uses GIAB resources to calculate the sensitivity and precision of your SNV and indel calling.
1. Resource Acquisition:
- Sample: Obtain DNA from a GIAB cell line (e.g., HG002) from Coriell [66].
- Benchmark Calls: Download the high-confidence small variant benchmark (VCF) for your chosen sample and reference genome (GRCh37/38) from the GIAB FTP site [66] [74].
- Stratification BED files: Download the genomic stratifications from the GIAB GitHub repository [69].
2. Sequencing and Analysis:
- Sequence the GIAB sample using your standard laboratory WGS or WES protocol.
- Process the raw data through your bioinformatic pipeline (alignment and variant calling).
3. Performance Assessment:
- Use the GA4GH benchmarking tool
hap.py(available on GitHub) to compare your pipeline's variant calls (VCF) against the GIAB benchmark VCF. - Run the comparison with and without the stratification BED files to understand performance in different genomic contexts.
4. Interpretation:
- Review the summary metrics for whole-genome sensitivity (recall) and precision.
- Use the stratification-specific metrics to identify weak spots. For example, you may find that precision for indels in homopolymer regions is unacceptably low, guiding pipeline improvements [69].
Protocol: Validating an Oncopanel Using SEQC2 Reference Samples
This protocol is based on the SEQC2 Oncopanel Sequencing Working Group's best practices [68].
1. Resource Acquisition:
- Reference Sample: Obtain the SEQC2 reference sample from Agilent Technologies. This is a pooled DNA sample from ten cancer cell lines (Sample A), which can be diluted into a normal background (Sample B) to create variants with low VAF [68].
- Truth Set: Download the known positive variants and negative positions for the reference sample.
2. Experimental Design:
- Process the reference samples (e.g., Sample A, B, and mixtures) in at least four technical replicates across multiple labs or sequencing runs to assess reproducibility.
3. Sequencing and Variant Calling:
- Sequence the samples using your targeted oncopanel according to the manufacturer's protocol.
- Call somatic variants using your standard bioinformatics pipeline.
4. Analytical Performance Calculation:
- Sensitivity: Calculate as (True Positives) / (True Positives + False Negatives). True Positives are known variants in the truth set that you detected.
- False Positive Rate: Calculate as (False Positives) / (False Positives + True Negatives). False Positives are variants you called that are not in the truth set. Report this as false positives per megabase.
- Reproducibility: Calculate the concordance of variant calls between replicates.
5. Implementation:
- Restrict your clinical reporting to the validated Consensus Targeted Region (CTR) and apply the optimized VAF threshold determined from your validation [68].
The Scientist's Toolkit: Key Research Reagent Solutions
Table: Essential Reference Materials for NGS Benchmarking
| Resource Name | Source | Function in Experimentation |
|---|---|---|
| GIAB Reference Genomes (e.g., HG001-HG007) | NIST / Coriell Institute [66] | Provides genetically diverse, well-characterized genomic DNA for germline assay development and validation. |
| GIAB Benchmark Variant Calls | GIAB FTP Site [66] [69] | Serves as a "truth set" to calculate sensitivity and precision for SNVs, indels, and SVs. |
| GIAB Genomic Stratifications | GIAB GitHub Repository [69] | Defines challenging genomic regions (e.g., low-mappability, high-GC), enabling context-specific performance analysis. |
| SEQC2 Reference Sample for Oncopanels | Agilent Technologies [68] | A multiplexed cancer cell line DNA sample with a dense set of known low-VAF variants, ideal for somatic mutation assay validation. |
| SEQC2 Methylation Reference Data | EpiQC Study / Genome Biology [72] | Provides a cross-platform benchmark for evaluating methylation sequencing methods (WGBS, EMseq, Nanopore) across seven cell lines. |
| Synthetic Plasmid Controls | Commercially available (e.g., from SeraCare) [70] | Contains specific, challenging variants (e.g., large indels, homopolymer variants) spiked into a background genome to test specific bioinformatic capabilities. |
Advanced Topics: Navigating Difficult Genomic Regions
Understanding and Using Genomic Stratifications
GIAB's genomic stratifications are BED files that partition the genome into categories based on functional context and technical challenge [69]. They are critical for a realistic performance assessment because a pipeline may perform well in easy regions but fail in difficult ones. Key stratifications include:
- Low Mappability Regions: Areas where short reads cannot be uniquely aligned.
- High GC Content and Low GC Content: Regions where sequencing coverage is often non-uniform.
- Segmental Duplications: Genomic regions with highly similar, nearly identical sequences that cause mapping ambiguity.
- Tandem Repeats and Homopolymers: Contexts that induce systematic errors in certain sequencing technologies.
A study found that one in seven pathogenic variants fall into such technically challenging categories, affecting 556 of 1,217 genes commonly tested clinically [70]. This underscores why using stratifications is not optional for clinical-grade assay validation.
The Impact of the Evolving Reference Genome
The new Telomere-to-Telomere (T2T) CHM13 reference genome adds ~200 million bases, including centromeric DNA and other highly repetitive regions previously absent from GRCh38 [69]. GIAB has now extended its stratifications to CHM13. Benchmarking on CHM13 reveals a performance penalty due to these new, difficult-to-sequence regions, providing a more rigorous and complete assessment of your pipeline's capabilities [69]. As the field moves toward pangenome references, benchmarking practices will continue to evolve.
### Frequently Asked Questions (FAQs)
Q: What are the key sources of non-reproducible results in multi-center NGS studies? A: Non-reproducibility in multi-center NGS studies often stems from several technical and bioinformatic sources. A key issue is methylation-related basecalling errors when sequencing native bacterial DNA, which can lead to incorrect allele calls in genotyping [75]. Other major sources include a lack of standardized bioinformatics protocols across sites, differences in sequencing platforms and library prep chemistries, and variable data analysis pipelines [75] [37]. Ensuring reproducibility requires strict standardization, validation using truth sets, and containerized software environments to guarantee consistent bioinformatic analysis across all participating centers [37].
Q: What minimum bioinformatics standards are recommended for clinical NGS operations? A: For clinical NGS, operating under standards similar to ISO 15189 is recommended. Key bioinformatics standards include [37]:
- Genome Build: Using hg38 as the reference genome for alignment.
- Variant Calling: Employing a standard set of analyses, including SNV, CNV, and SV detection. For structural variants, using multiple tools in combination is advised.
- Validation: Pipelines must be validated for accuracy and reproducibility using standard truth sets (e.g., GIAB for germline, SEQC2 for somatic variants), supplemented by recall tests on real clinical samples.
- Data Integrity: Ensuring data integrity through file hashing and verifying sample identity via fingerprinting and relatedness checks.
- Reproducibility: Using containerized software (e.g., Docker, Conda) and strict version control (git) for all code and documentation.
Q: What experimental strategies can improve the reproducibility of nanopore sequencing for bacterial typing? A: A multi-center study identified several strategies to significantly improve the reproducibility of nanopore sequencing-based bacterial genotyping [75]:
- PCR Preamplification: Using PCR during library preparation can remove basecalling errors associated with native DNA methylation.
- Updated Basecalling Models: Employing the latest basecalling models and sequencing chemistry (e.g., Dorado basecaller, 400 bp/s sequencing speed) reduces errors.
- Optimized Polishing Strategies: Implementing improved bioinformatic polishing strategies for the sequenced data diminishes non-reproducible typing results.
Q: What is the demonstrated real-world interlaboratory concordance for in-house NGS testing? A: Multi-center studies demonstrate that well-standardized in-house NGS testing can achieve high interlaboratory concordance. A study focusing on non-small-cell lung cancer (NSCLC) biomarker testing across multiple institutions reported a 95.2% interlaboratory concordance for variant detection and a 99.2% sequencing success rate for DNA samples in a prospective validation phase [76].
Q: How can I troubleshoot low concordance rates between centers in a sequencing study? A: Low concordance often points to a lack of standardization. Focus on these areas:
- Re-agenting: Ensure all centers use the same validated library prep kits, chemistries (e.g., ONT's V14 chemistry), and flow cells (e.g., R10.4.1) [75].
- Protocol Synchronization: Standardize every laboratory step from DNA extraction and quantification to library preparation and sequencing run parameters [75].
- Bioinformatic Unification: Implement a single, containerized bioinformatics pipeline across all sites for basecalling, alignment, and variant calling to eliminate software-related discrepancies [37].
- Control Samples: Include shared control samples with expected results in each sequencing run to identify lab-specific deviation [76].
### Troubleshooting Guides
### Guide 1: Troubleshooting Inter-Laboratory Variant Calling Discrepancies
Problem: Different centers in a multi-center study report different variant calls for the same sample.
Investigation and Resolution:
| Step | Investigation Action | Common Causes | Corrective Action |
|---|---|---|---|
| 1 | Verify wet-lab protocol uniformity. | Differences in DNA extraction methods, library prep kits, or sequencing platforms/chemistries. | Audit and align all laboratory Standard Operating Procedures (SOPs). Mandate the use of identical validated kits and platforms [75]. |
| 2 | Check for systematic sequencing errors. | Methylation motifs in native DNA causing basecalling errors (specific to nanopore sequencing) [75]. | Switch to a PCR-based library prep protocol for the affected samples or use the latest bacterial methylation-aware basecalling models [75]. |
| 3 | Validate the bioinformatics pipeline. | Different software versions, parameters, or reference genomes used for alignment and variant calling [37]. | Implement a single, version-controlled pipeline in a containerized environment (e.g., Docker/Singularity). Enforce the use of the hg38 genome build [37]. |
| 4 | Interrogate the specific variant. | Low allele fraction, variant located in a low-complexity region, or near an indel. | Manually inspect the BAM files for alignment artifacts at the locus. Use an orthogonal method (e.g., Sanger sequencing) to confirm the variant [76]. |
### Guide 2: Addressing Low Sequencing Concordance with Orthogonal Methods
Problem: NGS results from multiple centers show poor concordance with an orthogonal, gold-standard method.
Investigation and Resolution:
| Step | Investigation Action | Common Causes | Corrective Action |
|---|---|---|---|
| 1 | Re-inspect the raw data quality. | Low sequencing depth or coverage in the target regions for the NGS method. | Re-sequence the sample to achieve a higher uniform depth of coverage, ensuring it meets the minimum requirement for the assay (e.g., >500x) [76]. |
| 2 | Cross-validate the orthogonal method. | The "gold-standard" method may have lower sensitivity or specificity for certain variant types. | Use a validated commercial reference standard with known truth sets to benchmark the performance of both the NGS and orthogonal methods [37]. |
| 3 | Reconcile sample integrity issues. | Sample degradation or cross-contamination occurring at one or more sites. | Implement a centralized quality control (QC) point for all samples before analysis, using a standardized metric like DIN (DNA Integrity Number) for DNA [76]. |
| 4 | Recalibrate the variant filtering strategy. | Overly stringent or lenient variant filtering parameters in the bioinformatic pipeline. | Use a standardized set of truth samples to recalibrate and harmonize the variant filtering thresholds (e.g., VAF cutoff, depth) across all centers [37]. |
### Experimental Protocols & Data
### Quantitative Data from Multi-Center NGS Studies
Table 1: Performance Metrics from a Multi-Center NGS Study in NSCLC [76]
| Metric | Retrospective Phase (21 samples) | Prospective Phase (262 samples) |
|---|---|---|
| Sequencing Success Rate (DNA) | 100% | 99.2% |
| Sequencing Success Rate (RNA) | 100% | 98% |
| Interlaboratory Concordance | 95.2% | Not Applicable |
| Median Turnaround Time | Not Specified | 4 days |
Table 2: Impact of Protocol Modifications on Nanopore Sequencing Error Rates [75]
| Experimental Condition | Effect on Typing Errors in Bacterial cgMLST |
|---|---|
| Standard Protocol (Native DNA) | Highly strain-specific typing errors observed across all participating laboratories. |
| PCR Preamplification | Notably diminished non-reproducible typing. |
| Updated Basecalling Models | Significantly reduced error rates. |
| Optimized Polishing Strategy | Diminished non-reproducible typing. |
### Key Research Reagent Solutions
Table 3: Essential Materials for Standardized Multi-Center Sequencing
| Item | Function in Multi-Center Studies |
|---|---|
| Native Barcoding Kit (e.g., SQK-NBD114.24) | Allows for multiplexed sequencing of samples, standardizing library preparation across labs using ligation-based protocols [75]. |
| R10.4.1 Flow Cells | The latest nanopore flow cell version, which, combined with V14 chemistry, provides higher raw read accuracy, which is critical for reducing inter-lab variability [75]. |
| Q20+ Chemistry | Provides very high raw read accuracy (>99%), minimizing a fundamental source of platform-based variation between sequencing runs and centers [75]. |
| Control Ion Sphere Particles | Used in Ion Torrent systems to monitor chip loading and sequencing performance, serving as a critical quality control reagent to ensure run success and data comparability [77]. |
| Thermo Fisher Scientific NGS Panels | Targeted gene panels (e.g., for 50 genes in NSCLC) provide a standardized set of assays for all centers, ensuring uniform coverage and variant calling across the same genomic regions [76]. |
### Methodology for a Multi-Center Reproducibility Study
The following workflow outlines a generalized protocol for conducting a multi-center study to assess the reproducibility of a sequencing platform, based on methodologies used in the cited literature [75] [76].
Phase 1: Retrospective Inter-laboratory Testing
- Centralized Material Preparation: A central coordinating laboratory selects a panel of characterized samples (e.g., 18-20 bacterial isolates or tumor samples) [75].
- DNA Distribution: Identical aliquots of high-quality, extracted DNA are distributed to all participating laboratories under blinded conditions [75] [76].
- Standardized Sequencing: All labs process the DNA using an identical, pre-defined sequencing protocol, including the same library prep kit, flow cell type, and sequencing platform [75].
Phase 2: Prospective Intra-laboratory Testing
- Local Material Preparation: Participating laboratories receive pure cultures or tissue samples and perform local DNA extraction using a standardized method [75] [76].
- In-house Sequencing: Labs sequence the locally prepared DNA using the established protocol from Phase 1, mimicking real-world implementation.
Data Analysis and Concordance Assessment
- Centralized Bioinformatic Processing: All raw sequencing data (FASTQ files) are collected and processed through a single, containerized bioinformatics pipeline to eliminate analysis variability [37].
- Performance Metric Calculation: Key metrics are calculated, including:
- Inter-laboratory Concordance: Percentage agreement on primary variant calls or allele types between all labs in Phase 1 [76].
- Sequencing Success Rate: Percentage of samples that passed QC in each lab [76].
- Variant Allele Fraction (VAF) Correlation: Correlation between observed and expected VAF for known variants [76].
- Reproducibility Rate: The consistency of results for the same sample processed in different labs in Phase 2 [75].
### Technical Diagrams
### NGS Reproducibility Challenge Map
The following diagram categorizes the primary sources of non-reproducibility in multi-center NGS studies and their relationships, based on findings from the literature [75] [37] [76].
Proficiency Testing and Quality Assurance for Continuous Monitoring
Proficiency Testing (PT) is a fundamental component of the quality management system for clinical Next-Generation Sequencing (NGS), serving as an external quality assessment tool to verify the accuracy and reliability of test results. In the context of clinical bioinformatics, PT provides objective evidence that laboratory testing processes—from wet bench analysis to bioinformatic interpretation—produce clinically valid data that can be trusted for patient care decisions. The Clinical Laboratory Improvement Amendments (CLIA) of 1988 mandate PT participation for microbiology subspecialties, creating uniform quality standards for all laboratory testing to ensure accuracy, reliability, and timeliness of patient results regardless of where testing is performed [78].
For clinical NGS implementation, PT transcends mere regulatory compliance, offering laboratories a mechanism to benchmark their performance against peers, identify potential weaknesses in analytical or bioinformatic workflows, and demonstrate competency to accrediting bodies. The complex nature of NGS technologies, with their multi-step processes involving both wet laboratory and computational components, makes comprehensive quality assurance particularly challenging yet critically important [2] [79]. This technical support guide addresses the specific proficiency testing and quality assurance challenges laboratories face when implementing clinical NGS, providing practical troubleshooting guidance for maintaining continuous quality monitoring.
Regulatory Framework and Quality Management Systems
Key Regulatory Requirements
Clinical NGS laboratories must navigate a complex regulatory landscape encompassing multiple accrediting and standard-setting organizations. The Centers for Disease Control and Prevention (CDC), in collaboration with the Association of Public Health Laboratories (APHL), established the Next Generation Sequencing Quality Initiative (NGS QI) to address challenges associated with implementing NGS in clinical and public health settings [2]. This initiative provides laboratories with over 100 free guidance documents and standard operating procedures (SOPs) to support high-quality sequencing data and adherence to standards [38].
Table: Core Organizations Governing Clinical NGS Quality
| Organization | Primary Focus Area | Key Contributions |
|---|---|---|
| CDC/APHL NGS QI | Quality Management Systems | Provides free guidance documents, SOPs, and validation templates for NGS implementation [2] |
| College of American Pathologists (CAP) | Comprehensive Laboratory Standards | QC metrics for clinical diagnostics; emphasis on pre-analytical, analytical, and post-analytical validation [38] |
| Clinical Laboratory Improvement Amendments (CLIA) | Regulatory Compliance | Standards for sample quality, test validation, and proficiency testing in U.S. clinical laboratories [78] [38] |
| Global Alliance for Genomics and Health (GA4GH) | Data Standards & Interoperability | International standards for responsibly collecting, storing, analyzing, and sharing genomic data [38] |
| American College of Medical Genetics (ACMG) | Variant Interpretation & Reporting | Technical standards for clinical NGS laboratories, including variant classification and reporting guidelines [38] |
Quality Management System Essentials
A robust Quality Management System (QMS) enables continual improvement and proper document management in laboratories performing NGS. The NGS QI crosswalks its documents with regulatory, accreditation, and professional bodies to ensure they provide current and compliant guidance on Quality System Essentials [2]. These QMS elements must be able to adapt to an ever-changing environment, including improvements in software and chemistry, which can affect how validated NGS assays, pipelines, and results are developed, performed, and reported [2].
Quality Management System for Clinical NGS
Proficiency Testing Implementation Guide
CLIA Proficiency Testing Requirements
For clinical NGS, PT requirements follow the CLIA framework for high-complexity testing. CLIA mandates that all laboratories performing non-waived testing participate in a PT program approved by the Centers for Medicare & Medicaid Services (CMS) [78]. Key requirements include:
- Enrollment in a CMS-approved PT program for each specialty and subspecialty
- Analysis of at least five PT samples per testing event
- Achieving a minimum 80% correct score on each testing event for satisfactory performance
- Satisfactory performance on two out of three testing events for successful annual performance
- Testing PT samples in the same manner as patient specimens [78]
Laboratories must not engage in inter-laboratory communication pertaining to PT until after the due date for reporting results to the PT program, and must not send PT samples or portions of samples to another laboratory for analysis [78].
PT Process Implementation
Table: Proficiency Testing Process Steps
| Process Step | Key Activities | Common Challenges |
|---|---|---|
| Enrollment | Select appropriate PT programs for test menu; Ensure enrollment covers all specialties/subspecialties | Navigating multiple PT providers; Changing programs requires one-year participation before switching [78] |
| Sample Processing | Reconstitute lyophilized samples per manufacturer instructions; Process using routine methods | Lyophilized microorganisms may have different properties than live counterparts; Sample preparation errors [78] |
| Testing & Analysis | Test PT samples same as patient specimens; Rotate testing among all technical staff | PT samples may not resemble actual specimens; Method limitations when samples differ from patient specimens [78] |
| Result Reporting | Report results as for patient specimens; Follow established reporting protocols | Inconsistent reporting practices; Interpretation challenges with atypical results |
| Performance Assessment | Review grading reports; Investigate unsatisfactory results; Implement corrective actions | Determining root cause of failures; Distinguishing systematic vs. random errors |
Troubleshooting Guides and FAQs
Pre-Analytical and Analytical Phase Troubleshooting
FAQ: Our laboratory consistently fails to achieve adequate coverage uniformity in our NGS runs. What factors should we investigate?
Poor coverage uniformity can result from multiple pre-analytical and analytical factors. Implement the following troubleshooting protocol:
DNA Quality Assessment: Verify DNA integrity using the KAPA hgDNA Quantification and QC Kit or similar. Samples must have a Q129/Q41 ratio ≥0.4 [79]. Degraded DNA will yield non-uniform coverage.
Library Preparation QC: Ensure library quantification shows ≥100 pM concentration. Use multiple quantification methods if inconsistent results are obtained [79].
Template Preparation: Verify that post-emulsification PCR shows templated ISPs between 10-30%. Outside this range, adjust template dilution factors [79].
Sequencing Run Metrics: Monitor chip loading (>70%), usable sequences (>55%), and polyclonality (<35%) during sequencing [79].
FAQ: We are encountering elevated false positives in our ctDNA liquid biopsy assays. How can we optimize our bioinformatic parameters?
Liquid biopsy analysis presents unique bioinformatic challenges due to highly fragmented ctDNA with low abundance. Implement these strategies:
Unique Molecular Identifiers (UMIs): Incorporate UMIs during library preparation to distinguish true low-frequency variants from amplification artifacts [8].
Strand Bias Analysis: Implement rigorous strand bias filters (approximately 0.40-0.59) to eliminate technical artifacts [79].
Integrated Error Suppression: Use duplicate read removal and position-specific error modeling to reduce false positives in low variant allele frequency detection [8].
Limit of Detection Validation: Establish and validate assay-specific limits of detection for low-frequency variants using contrived reference materials with known variant allele frequencies [8].
Proficiency Testing and Quality Monitoring Troubleshooting
FAQ: Our laboratory received unsatisfactory scores on a recent PT event for variant classification. What steps should we take?
Unsatisfactory PT performance requires systematic investigation and corrective action:
Immediate Response:
- Remove affected test system from service until problem resolution
- Notify testing personnel and laboratory director
- Begin documented investigation within 30 days of result notification
Root Cause Analysis:
- Review all analytical steps from nucleic acid extraction through variant interpretation
- Verify bioinformatics pipeline version and parameters against validated specifications
- Assess personnel competency and training records for involved staff
- Examine equipment maintenance and calibration records
Corrective Actions:
- Retrain staff if competency issues identified
- Implement additional QC checks at identified failure points
- Verify reference database versions and annotation sources
- Consider secondary confirmation method for challenging variant types
Documentation:
- Complete comprehensive corrective action report
- Submit required documentation to accrediting bodies
- Monitor subsequent PT performance for effectiveness of corrections
FAQ: How often should we review and update our NGS quality management system?
The NGS QI recommends that all QMS documents undergo a review period every 3 years to ensure they remain current with technology, standard practices, and regulatory changes [2]. However, more frequent reviews may be necessary when:
- Implementing new sequencing platforms or major chemistry changes
- Adopting significant bioinformatics pipeline updates
- Incorporating new test methodologies or expanding test menus
- Responding to regulatory changes or accreditation requirements
Quality Control Metrics and Performance Monitoring
Essential QC Metrics for Clinical NGS
Implementing comprehensive quality control checkpoints throughout the NGS workflow is essential for ensuring reliable results. The following table summarizes critical QC metrics established through clinical implementation:
Table: Essential Quality Control Checkpoints for Clinical NGS
| QC Checkpoint | Quality Metric | Acceptance Criteria | Clinical Impact |
|---|---|---|---|
| Pre-DNA Extraction (QC1) | Tumor content assessment | ≥10% tumor content (established during validation) [79] | Prevents false negatives due to insufficient tumor representation |
| DNA Quantification (QC2) | DNA concentration | ≥1.7 ng/μL [79] | Ensures sufficient input material for library preparation |
| DNA Quality (QC3) | DNA integrity | Q129/Q41 ratio ≥0.4 (KAPA hgDNA QC Kit) [79] | Degraded DNA affects library complexity and coverage uniformity |
| Library Quantification (QC4) | Library concentration | ≥100 pM [79] | Insufficient library quantity leads to poor sequencing performance |
| Template Preparation (QC5) | Templated ISPs | 10-30% [79] | Outside this range indicates suboptimal emulsion PCR efficiency |
| Sequencing Run (QC6) | Chip loading | >70% [79] | Affects overall data yield and cost efficiency |
| Sample-Level (QC6) | On-target reads | >90% [79] | Low on-target rate indicates poor capture efficiency |
| Variant-Level (QC6) | Coverage depth | ≥500× with ≥95% amplicons covered [79] | Insufficient coverage reduces variant detection sensitivity |
Key Performance Indicators for Continuous Monitoring
Establishing and monitoring Key Performance Indicators (KPIs) enables laboratories to track quality trends over time. The NGS QI recommends monitoring these essential KPIs:
- Analytical Sensitivity: Ability to detect true positive variants
- Analytical Specificity: Ability to correctly identify true negative samples
- Reproducibility: Consistency of results across operators, instruments, and time
- Turnaround Time: From sample receipt to final report issuance
- Assay Failure Rate: Percentage of samples failing quality metrics
Laboratories should establish baseline performance for each KPI during validation and monitor continuously, investigating trends that deviate from established baselines [2].
Research Reagent Solutions and Essential Materials
Table: Essential Research Reagents for NGS Quality Assurance
| Reagent/Material | Function | Application in Quality Assurance |
|---|---|---|
| FFPE QC Cell Lines (e.g., Horizon Diagnostics) | Process control for entire workflow | Detects deficiencies in analytical process; monitors reagent lot changes and instrument performance [79] |
| KAPA hgDNA Quantification and QC Kit | DNA quality and quantity assessment | Determines DNA integrity via Q129/Q41 ratio; establishes sample suitability for sequencing [79] |
| CLIA-Certified PT Samples | External quality assessment | Verifies analytical and interpretative performance; satisfies regulatory requirements [78] |
| NIST Genome in a Bottle Reference Materials | Benchmarking variant detection accuracy | Provides reference genomes for validating analytical accuracy of variant calling [38] |
| Multiplex Reference Standards | Assessing multi-sample reproducibility | Evaluates performance across sample batches and different operators |
Proficiency testing and quality assurance for continuous monitoring represent foundational elements for successful clinical NGS implementation. As NGS technologies evolve with the introduction of new platforms, improved chemistries, and advanced bioinformatic analyses, quality management systems must remain agile and responsive [2]. The integration of comprehensive PT programs, robust quality control metrics, and systematic troubleshooting approaches enables laboratories to navigate the complexities of clinical genomics while ensuring result reliability.
Future directions in NGS quality assurance will likely involve greater harmonization of international standards, development of PT programs for emerging applications like liquid biopsy and direct RNA sequencing, and increased integration of artificial intelligence for quality monitoring. By establishing and maintaining rigorous proficiency testing and quality assurance programs, clinical laboratories can ensure that NGS technologies fulfill their promise to advance precision medicine while maintaining the highest standards of patient care.
Conclusion
Successful implementation of NGS in clinical and research settings hinges on overcoming interconnected bioinformatics challenges through standardized methodologies, rigorous validation, and continuous optimization. The path forward requires embracing evolving standards like the hg38 genome build, containerized environments for reproducibility, and participation in external quality assessment programs. As technologies advance with long-read sequencing and AI-based basecalling, bioinformatics frameworks must remain agile. Future directions include integrating real-world data from initiatives like precisionFDA, developing clinical decision support tools, and establishing robust data-sharing frameworks to accelerate therapeutic discovery and personalized medicine applications. For researchers and drug developers, mastering these bioinformatics fundamentals is no longer optional but essential for generating clinically actionable insights from genomic data.
References
- 1. The Next-Generation Sequencing Quality Initiative and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12078536/]
- 2. The Next-Generation Sequencing Quality Initiative and ... [https://wwwnc.cdc.gov/eid/article/31/13/24-1175_article]
- 3. Next-Generation Sequencing and Bioinformatics ... [https://wwwnc.cdc.gov/eid/article/30/14/24-0306_article]
- 4. How to Troubleshoot Sequencing Preparation Errors (NGS ... [https://www.cd-genomics.com/resource-sequencing-preparation-troubleshooting.html]
- 5. Clinical Laboratory Improvement Amendments (CLIA) [https://www.fda.gov/medical-devices/ivd-regulatory-assistance/clinical-laboratory-improvement-amendments-clia]
- 6. CMS Enacts New CLIA Regulations Effective January 2025 [https://www.bakerdonelson.com/cms-enacts-new-clia-regulations-effective-january-2025]
- 7. 2025 Changes to Point-of-Care Testing Regulatory ... [https://myadlm.org/education/point-of-care-testing-professional-certification/the-point/articles/2025/may]
- 8. Clinical Genome Sequencing: Bioinformatics Challenges ... [https://www.frontiersin.org/research-topics/19897/clinical-genome-sequencing-bioinformatics-challenges-and-key-considerations/magazine]
- 9. Challenges in clinical interpretation of next-generation ... [https://www.sciencedirect.com/science/article/pii/S2590123023005480?dgcid=rss_sd_all&]
- 10. Next-generation sequencing: 2025 Revolution [https://lifebit.ai/blog/next-generation-sequencing/]
- 11. Bioinformatics Platform: Unlock Insights 2025 [https://lifebit.ai/blog/bioinformatics-platform-best-practices-2025/]
- 12. Managing the Data Deluge: 2025's Breakthroughs in Lab ... [https://labhorizons.co.uk/2024/12/managing-the-data-deluge-2025s-breakthroughs-in-lab-data-storage-and-analysis/]
- 13. The 2025 Bioinformatics Toolkit: From Sample Prep to AI- ... [https://blog.omni-inc.com/blog/the-2025-bioinformatics-toolkit-from-sample-prep-to-ai-driven-analysis]
- 14. Molecular biology in the exabyte era: Taming the data ... [https://www.sciencedirect.com/science/article/abs/pii/S1476927125001951]
- 15. AI Compute Demand in Biotech: 2025 Report & Statistics [https://intuitionlabs.ai/articles/ai-compute-demand-biotech]
- 16. Integrating Artificial Intelligence in Next-Generation Sequencing [https://pmc.ncbi.nlm.nih.gov/articles/PMC12191491/]
- 17. Galaxy at Genome Informatics 2025 [https://galaxyproject.org/news/2025-11-07-genome-informatics2025/]
- 18. Impact of Pre-Analytical Variables on Cancer Targeted ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4659597/]
- 19. Systematic Assessment of Tumor Purity and Its Clinical ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7529507/]
- 20. Systematic pan-cancer analysis of tumour purity [https://www.nature.com/articles/ncomms9971]
- 21. methods for next-generation sequencing: tone... Library preparation [https://pubmed.ncbi.nlm.nih.gov/24440557/]
- 22. : Proven Ways to Optimize... - CD Genomics NGS Library Preparation [https://www.cd-genomics.com/resource-library-preparation-for-ngs.html]
- 23. How to Master the Microbiome: Library for Preparation NGS [https://www.zymoresearch.de/blogs/blog/how-to-master-the-microbiome-library-preparation-for-ngs]
- 24. Sequence File Formats | FASTQ & BCL ... [https://www.illumina.com/informatics/sequencing-data-analysis/sequence-file-formats.html]
- 25. NGS Data Storage Policy | Iowa Institute of Human Genetics [https://humangenetics.medicine.uiowa.edu/genomics-division/genome-sequencing/ngs-data-storage-policy]
- 26. Automating Clinical Workflows: Part I - The Golden Helix Blog [https://www.goldenhelix.com/blog/automating-clinical-workflows-part-1/]
- 27. NGS Data Analysis for Illumina Platform—Overview and ... [https://www.thermofisher.com/mx/en/home/life-science/cloning/cloning-learning-center/invitrogen-school-of-molecular-biology/next-generation-sequencing/ngs-data-analysis-illumina.html]
- 28. File Format: VCF - GDC Docs - National Cancer Institute [https://docs.gdc.cancer.gov/Data/File_Formats/VCF_Format/]
- 29. Barriers to clinical adoption of next-generation sequencing [https://pmc.ncbi.nlm.nih.gov/articles/PMC5722256/]
- 30. Troubleshooting Your First NGS Dataset [https://genomebeans.com/blog/troubleshooting-your-first-ngs-dataset-how-genomebeans-simplifies-it]
- 31. VCF Processing Guide - ANNOVAR Documentation [https://annovar.openbioinformatics.org/en/latest/articles/VCF/]
- 32. Summoning insights: NGS variant calling best practice [https://www.ogt.com/ca/resources/ngs-resources-and-support/ngs-resources/summoning-insights-ngs-variant-calling-best-practices/]
- 33. Best practices for variant calling in clinical sequencing [https://genomemedicine.biomedcentral.com/articles/10.1186/s13073-020-00791-w]
- 34. Best practices for variant calling in clinical sequencing - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC7586657/]
- 35. variantbenchmarking: Introduction [https://nf-co.re/variantbenchmarking/dev/]
- 36. The Next Generation Sequencing Quality Initiative [https://www.cdc.gov/lab-quality/php/ngs-quality-initiative/index.html]
- 37. Recommendations for bioinformatics in clinical practice - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC12535132/]
- 38. Evolving Standards in Clinical NGS (updated) [https://www.euformatics.com/blog-post/evolving-standards-in-clinical-ngs]
- 39. FAQ: What to do when your NGS assay fails to detect a ... [https://blog.seracare.com/ngs/faq-what-to-do-when-your-ngs-assay-fails-to-detect-a-variant-contained-in-seraseq-reference-materials]
- 40. Tumor Mutational Burden (TMB) as a Predictive Biomarker ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7710563/]
- 41. Tumor Mutational Burden & Microsatellite Instability | IDT [https://www.idtdna.com/pages/research-area/cancer/cancer-research/tumor-mutational-burden-(tmb)-microsatellite-instability-(msi)]
- 42. Liquid Biopsy: The Challenges of a Revolutionary ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12154446/]
- 43. MMRd, MSI-H, and TMB-H Tumors: What They Are and ... [https://www.mskcc.org/cancer-care/diagnosis-treatment/cancer-treatments/immunotherapy/mmrd-msi-h-and-tmb-h-tumors]
- 44. Bioinformatics Pipeline Troubleshooting [https://www.meegle.com/en_us/topics/bioinformatics-pipeline/bioinformatics-pipeline-troubleshooting]
- 45. Recommendations for bioinformatics in clinical practice [https://genomemedicine.biomedcentral.com/articles/10.1186/s13073-025-01543-4]
- 46. Garbage In, Garbage Out: Dealing with Data Errors ... [https://blog.omni-inc.com/blog/garbage-in-garbage-out-dealing-with-data-errors-bioinformatics]
- 47. Optimizing Bioinformatics Workflows: Why It Matters & ... [https://ardigen.com/optimizing-bioinformatics-workflows-why-it-matters-and-when-to-start-thinking-about-it/]
- 48. A clinician's guide to bioinformatics for next-generation ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9870988/]
- 49. Tumor heterogeneity: preclinical models, emerging ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10175698/]
- 50. Prevalence and detection of low-allele-fraction variants in ... [https://www.nature.com/articles/s41467-017-01470-y]
- 51. Evaluating the performance of low-frequency variant ... [https://www.nature.com/articles/s41598-023-47135-3]
- 52. Challenges in bioinformatics approaches to tumor mutation ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8161416/]
- 53. Cancer Heterogeneity [https://www.bioskryb.com/cancer-heterogeneity/]
- 54. Differential variation analysis enables detection of tumor ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6844448/]
- 55. Advancing Clinical NGS: An integrated bioinformatics ... [https://digitalinsights.qiagen.com/news/blog/clinical/advancing-clinical-ngs-cancer-genome-and-exome-sequencing/]
- 56. - Wikipedia Variant of uncertain significance [https://en.wikipedia.org/wiki/Variant_of_uncertain_significance]
- 57. Variants of Uncertain Significance: Should We Revisit How ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5999032/]
- 58. Handling variants of uncertain significance (VUS) in clinical ... [https://sanogenetics.com/resources/blog/handling-variants-of-uncertain-significance-vus-in-clinical-trials]
- 59. TP53 variants : increasing of in... uncertain significance challenges [https://pubmed.ncbi.nlm.nih.gov/31321604/]
- 60. Scalable Workflows and Reproducible Data Analysis for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7613310/]
- 61. 12.7 High-performance computing in bioinformatics [https://fiveable.me/bioinformatics/unit-12/high-performance-computing-bioinformatics/study-guide/x2snkNO92bsfb4KZ]
- 62. Bioinformatics Pipeline For High-Performance Computing [https://www.meegle.com/en_us/topics/bioinformatics-pipeline/bioinformatics-pipeline-for-high-performance-computing]
- 63. Validation of a comprehensive long-read sequencing ... [https://www.frontiersin.org/journals/genetics/articles/10.3389/fgene.2025.1499456/full]
- 64. End-to-End Testing in 2025: Complete Beginner's Guide [https://www.bunnyshell.com/blog/introduction-to-end-to-end-testing-everything-you-/]
- 65. A targeted next-generation sequencing panel for ... [https://www.nature.com/articles/s41598-025-08039-6]
- 66. Genome in a Bottle | NIST [https://www.nist.gov/programs-projects/genome-bottle]
- 67. The Sequencing Quality Control 2 study - Genome Biology [https://genomebiology.biomedcentral.com/articles/10.1186/s13059-021-02528-3]
- 68. FDA-led consortium studies advance quality control of ... [https://pcm.amegroups.org/article/view/6609/html]
- 69. The GIAB genomic stratifications resource for human ... [https://www.nature.com/articles/s41467-024-53260-y]
- 70. One in seven pathogenic variants can be challenging to ... [https://www.nature.com/articles/s41436-021-01187-w]
- 71. Challenges of Accuracy in Germline Clinical Sequencing ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9969524/]
- 72. The SEQC2 epigenomics quality control (EpiQC) study [https://genomebiology.biomedcentral.com/articles/10.1186/s13059-021-02529-2]
- 73. How-to: NGS Quality Control [https://frontlinegenomics.com/how-to-ngs-quality-control/]
- 74. Genomic variant benchmark: if you cannot measure it, you ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10552390/]
- 75. A multicenter study on accuracy and reproducibility of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11389150/]
- 76. Impact and Reproducibility of In-House Targeted Next ... [https://www.sciencedirect.com/science/article/pii/S152515782500042X]
- 77. NGS Sequencing Support-Troubleshooting [https://www.thermofisher.com/us/en/home/technical-resources/technical-reference-library/next-generation-sequencing-support-center/ngs-support/ngs-support-troubleshooting.html]
- 78. Use of Proficiency Testing as a Tool to Improve Quality in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4696484/]
- 79. Effective quality management practices in routine clinical ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5506542/]