Multimodal Data Fusion in Oncology: Transforming Cancer Diagnosis Through AI Integration
This article provides a comprehensive exploration of multimodal data fusion and its transformative impact on cancer diagnosis and personalized oncology.
Multimodal Data Fusion in Oncology: Transforming Cancer Diagnosis Through AI Integration
Abstract
This article provides a comprehensive exploration of multimodal data fusion and its transformative impact on cancer diagnosis and personalized oncology. Tailored for researchers, scientists, and drug development professionals, it systematically covers the foundational principles, diverse methodological approaches, and practical applications of integrating heterogeneous data types such as genomics, digital pathology, radiomics, and clinical records. The content further addresses critical challenges in implementation, including data heterogeneity and model interpretability, and offers a rigorous comparative analysis of fusion techniques and their validation. By synthesizing evidence from recent advancements and clinical case studies, this review serves as a strategic resource for developing robust, clinically applicable AI tools that enhance diagnostic accuracy, improve patient stratification, and accelerate precision medicine.
The Foundation of Multimodal Oncology: Unraveling Data Types and Clinical Imperatives
Defining Multimodal Data Fusion in the Cancer Diagnostic Ecosystem
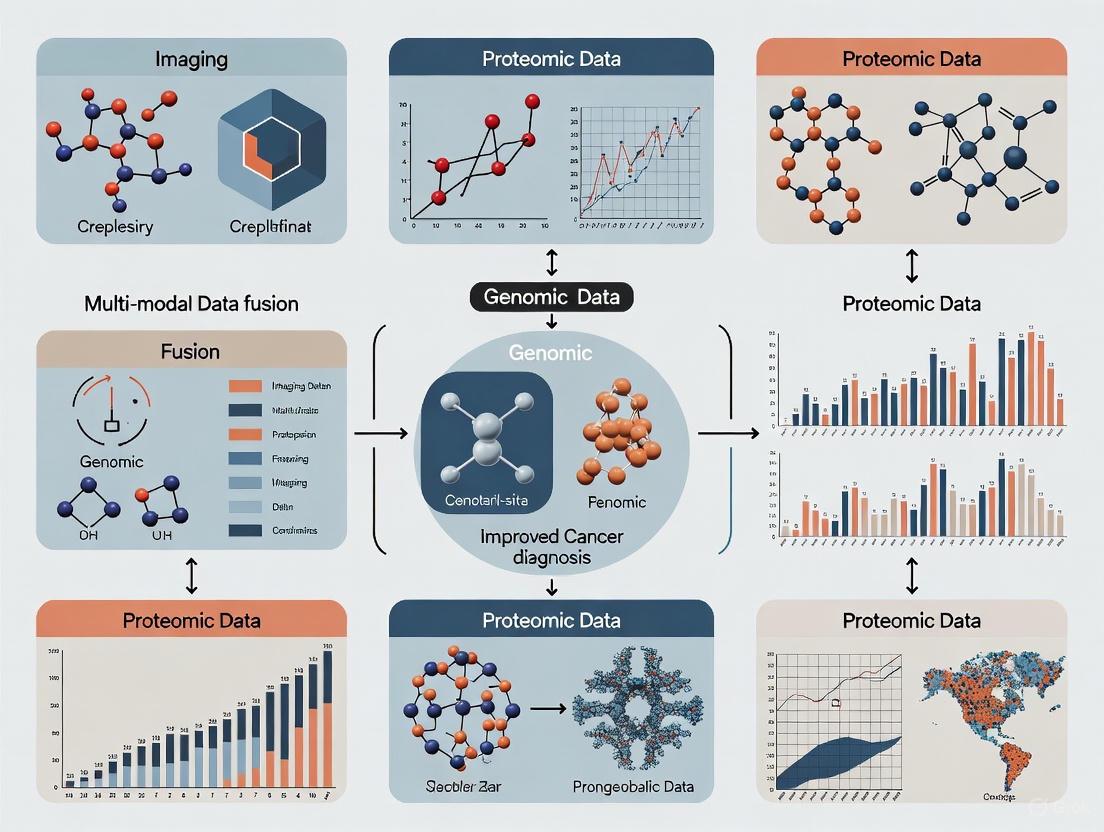
Multimodal data fusion represents a paradigm shift in oncology diagnostics, moving beyond the limitations of single-data-type analysis. It is defined as the process of integrating information from multiple, heterogeneous data types—such as genomic, histopathological, radiological, and clinical data—to create a richer, more comprehensive representation of a patient's disease status [1] [2]. The core principle is that orthogonal data modalities provide complementary information; by combining them, the resulting model can capture a more holistic view of the complex biological processes in cancer, leading to improved inference accuracy and clinical decision-making [1] [3]. This integrated approach is foundational for advancing precision oncology, as it enables a multi-scale understanding of cancer, from molecular alterations and cellular morphology to tissue organization and clinical phenotype [3].
The clinical imperative for this integration is stark. Cancer manifests across multiple biological scales, and predictive models relying on a single data modality fail to capture this multiscale heterogeneity, limiting their generalizability and clinical utility [3]. In contrast, multimodal artificial intelligence (MMAI) models that contextualize molecular features within anatomical and clinical frameworks yield a more comprehensive and mechanistically plausible representation of the disease [3]. By converting multimodal complexity into clinically actionable insights, this approach is poised to improve patient outcomes across the entire cancer care continuum, from prevention and early diagnosis to prognosis, treatment selection, and outcome assessment [3] [4].
Current Applications and Quantitative Outcomes
Multimodal fusion techniques have been successfully applied to various diagnostic challenges in oncology, demonstrating superior performance compared to unimodal approaches. The following table summarizes key applications and their documented performance metrics from recent studies.
Table 1: Performance Metrics of Selected Multimodal Data Fusion Applications in Cancer Diagnosis
| Cancer Type | Data Modalities Fused | AI Architecture / Model | Key Performance Metrics | Primary Application |
|---|---|---|---|---|
| Breast Cancer [5] | B-mode Ultrasound, Color Doppler, Elastography | HXM-Net (Hybrid CNN-Transformer) | Accuracy: 94.20%Sensitivity: 92.80%Specificity: 95.70%F1-Score: 91.00%AUC-ROC: 0.97 | Tumor classification (Benign vs. Malignant) |
| Lung Cancer [6] | CT Images, Clinical Data (24 features) | CNN (for images) + ANN (for clinical data) | Image Classification Accuracy: 92%Severity Prediction Accuracy: 99% | Histological subtype classification & cancer severity prediction |
| Melanoma [3] | Not Specified (Multimodal integration) | MUSK (Transformer-based) | AUC-ROC: 0.833 (5-year relapse prediction) | Relapse and immunotherapy response prediction |
| Glioma & Renal Cell Carcinoma [3] | Histology, Genomics | Pathomic Fusion | Outperformed WHO 2021 classification | Risk stratification |
The success of these models hinges on their ability to leverage complementary information. For instance, in breast ultrasound, B-mode images provide morphological details of a lesion, while Doppler images capture vascularity features; their fusion creates a more discriminative feature representation for classification [5]. Similarly, in lung cancer, combining the spatial patterns from CT scans with contextual clinical features like demographic, symptomatic, and genetic factors allows for both precise tissue classification and accurate severity assessment [6]. These examples underscore that fusion models reduce ambiguity and provide richer context, leading to more accurate and robust predictions than any single modality can achieve [2].
Core Technical Fusion Strategies and Protocols
The technical implementation of multimodal data fusion can be categorized into several core strategies, which determine when in the analytical pipeline the different data streams are integrated. The choice of strategy is critical and depends on factors such as data alignment, heterogeneity, and the specific clinical task.
Fusion Strategy Protocol
The three primary fusion strategies are early, intermediate, and late fusion, each with distinct advantages and implementation protocols.
Table 2: Protocols for Core Multimodal Data Fusion Strategies
| Fusion Strategy | Definition & Protocol | Advantages | Limitations | Ideal Use Case |
|---|---|---|---|---|
| Early Fusion (Feature-Level) [2] [4] | Protocol: Raw or minimally processed data from multiple modalities are combined into a single input vector before being fed into a model.Technical Note: Requires data to be synchronized and spatially aligned, often necessitating extensive preprocessing. | Allows the model to learn complex, low-level interactions between modalities directly from the data. | Highly sensitive to data alignment and noise; difficult to handle heterogeneous data rates/formats. | Fusing co-registered imaging data from the same patient (e.g., different MRI sequences). |
| Intermediate Fusion (Hybrid) [2] [4] | Protocol: Modalities are processed separately in initial layers to extract high-level features. These modality-specific features are then combined at an intermediate layer of the model for joint learning.Technical Note: Employs architectures like cross-attention transformers to dynamically weight features. | Balances modality-specific processing with joint representation learning; captures interactions at a meaningful feature level. | More complex model architecture and training; requires careful design of fusion layer. | Integrating inherently different data types (e.g., images and genomic vectors) where alignment is not trivial. |
| Late Fusion (Decision-Level) [2] [4] | Protocol: Each modality is processed by a separate model to yield an independent prediction or decision. These decisions are then combined via weighted averaging, voting, or another meta-classifier.Technical Note: The weighting of each modality's vote can be learned or heuristic. | Highly flexible; can handle asynchronous data and missing modalities easily. | Cannot model cross-modal interactions or dependencies; may miss synergistic information. | Integrating predictions from pre-trained, single-modality models or when data streams are inherently asynchronous. |
Workflow Visualization
The following diagram illustrates the logical workflow and the architectural differences between the three primary fusion strategies.
Detailed Experimental Protocol: HXM-Net for Breast Ultrasound
The following section provides a detailed, replicable protocol for implementing a state-of-the-art multimodal fusion model, HXM-Net, designed for breast cancer diagnosis using multi-modal ultrasound [5]. This can serve as a template for researchers developing similar pipelines.
Aim and Principle
To improve the accuracy of breast tumor classification (benign vs. malignant) by synergistically combining morphological information from B-mode ultrasound, vascular features from Color Doppler, and tissue stiffness information from Elastography [5]. The principle is that a hybrid CNN-Transformer architecture can optimally extract and fuse these complementary features to create a more informative and discriminative representation than any single modality provides.
Table 3: Research Reagent Solutions and Essential Materials for HXM-Net Protocol
| Item / Solution | Function / Specification | Handling & Notes |
|---|---|---|
| Class-balanced Breast Ultrasound Dataset | Contains paired B-mode, Color Doppler, and Elastography images for each lesion. | Essential to mitigate class imbalance. Ensure patient identifiers are removed for privacy. |
| Image Preprocessing Library (e.g., OpenCV, SciKit-Image) | For image resizing, normalization, and data augmentation (rotation, flipping, etc.). | Augmentation is crucial for model generalizability across different patient populations and imaging machines. |
| Deep Learning Framework (e.g., PyTorch, TensorFlow) | To implement and train the HXM-Net architecture. | Must support both CNN and Transformer modules. |
| High-Performance Computing Unit (GPU with >8GB VRAM) | To handle the computational load of training complex deep learning models. | Necessary for efficient training and hyperparameter optimization. |
| Gradient-weighted Class Activation Mapping (Grad-CAM) | To generate visual explanations for the model's predictions, enhancing clinical interpretability. | A key component for Explainable AI (XAI), helping to build clinician trust. |
Step-by-Step Procedure
Data Curation and Preprocessing:
- Data Sourcing: Obtain a dataset of breast ultrasound cases where each lesion has corresponding B-mode, Color Doppler, and Elastography images. The dataset should be annotated with ground-truth labels (benign/malignant) confirmed by biopsy.
- Image Cleaning and Standardization: Resize all images to a uniform spatial resolution (e.g., 224x224 pixels). Normalize pixel intensities to a [0, 1] range.
- Data Augmentation: Apply random data augmentation techniques to the training set, including rotation (±15°), horizontal and vertical flipping, and slight brightness/contrast adjustments, to improve model robustness.
Model Architecture Implementation (HXM-Net):
- Feature Extraction Backbone: Implement a multi-stream Convolutional Neural Network (CNN). Each stream—one for each ultrasound modality—uses a CNN (e.g., a ResNet-50 backbone, pre-trained on ImageNet and fine-tuned) to extract high-level spatial features.
- Transformer-based Fusion Module: Flatten the feature maps from each CNN stream and project them into a sequence of embedding vectors. Feed the concatenated embeddings from all modalities into a Transformer encoder.
- The Self-Attention Mechanism within the Transformer is calculated as
Attention(Q, K, V) = softmax((QK^T) / √d_k) V, where Q (Query), K (Key), and V (Value) are matrices derived from the input embeddings [5]. This mechanism allows the model to dynamically weight the importance of features both within and across the different modalities. - Classification Head: Use the [CLS] token output or the mean-pooled output of the Transformer encoder, and pass it through a final fully connected layer with a softmax activation function to generate the final classification (benign or malignant).
Model Training and Validation:
- Loss Function and Optimizer: Use a binary cross-entropy loss function and an Adam optimizer.
- Training Regimen: Train the model using a k-fold cross-validation strategy (e.g., k=5 or k=10) to ensure robustness and reduce overfitting. Monitor performance on a held-out validation set.
- Explainability Analysis: After training, apply Grad-CAM to the model's CNN streams to generate heatmaps highlighting the image regions most influential in the prediction. This provides critical, human-interpretable insights for clinical validation.
HXM-Net Architecture Visualization
The following diagram details the core architecture of the HXM-Net model as described in the protocol.
The Scientist's Toolkit: Key Reagents and Models
This section provides a consolidated reference table of key computational tools and data types essential for research in multimodal data fusion for cancer diagnostics.
Table 4: Essential Research Toolkit for Multimodal Fusion in Cancer Diagnostics
| Tool / Reagent Category | Specific Examples & Notes | Primary Function in Workflow |
|---|---|---|
| Data Modalities | Multi-omics: Genomic (mutations), Transcriptomic (RNA-seq), Proteomic, Metabolomic [1] [4].Medical Imaging: Histopathology slides, CT, MRI, Ultrasound (B-mode, Doppler, Elastography) [1] [5].Clinical Data: Electronic Health Records (EHRs), patient demographics, symptoms, lab results [1] [6]. | Provide the raw, orthogonal data streams that contain complementary information about the disease state. |
| AI/Model Architectures | Convolutional Neural Networks (CNNs): For spatial feature extraction from images [5] [6].Transformers: For cross-modal fusion and capturing long-range dependencies via self-attention [5].Artificial Neural Networks (ANNs): For processing structured, non-image data (e.g., clinical features) [6]. | Serve as the core computational engines for feature extraction, fusion, and prediction. |
| Fusion Frameworks | Early/Intermediate Fusion: Simple operations (concatenation, weighted sum) or attention-based fusion [4].Late Fusion: Weighted averaging or meta-classifiers on model outputs [2] [4].Advanced Methods: Multimodal embeddings, graph-based fusion [4] [7]. | Define the strategy and algorithmic approach for integrating information from different modalities. |
| Explainability (XAI) Tools | Gradient-weighted Class Activation Mapping (Grad-CAM): For visualizing salient regions in images [6].SHapley Additive exPlanations (SHAP): For interpreting feature importance in any model, including ANNs [6]. | Provide interpretability and transparency for model decisions, which is critical for clinical adoption. |
| Computational Infrastructure | GPU-Accelerated Computing: (e.g., NVIDIA).Deep Learning Frameworks: PyTorch, TensorFlow.Medical Imaging Platforms: MONAI (Medical Open Network for AI) [3]. | Provide the necessary hardware and software environment for developing and training complex models. |
Technological advancements have ushered in an era of high-throughput biomedical data, enabling the comprehensive study of biological systems through different "omics" layers [8]. In oncology, the integration of these modalities—genomics, transcriptomics, proteomics, and metabolomics—is transforming cancer research by providing unprecedented insights into tumour biology [9] [10]. Each omics layer offers a unique perspective: genomics provides the blueprint of hereditary and acquired mutations, transcriptomics reveals dynamic gene expression patterns, proteomics identifies functional effectors and their modifications, and metabolomics captures the functional readout of cellular biochemical activity [11] [12]. Multi-modal data fusion leverages these complementary perspectives to create a more holistic understanding of cancer development, progression, and treatment response, ultimately advancing precision oncology [13] [1].
Table 1: Core Omics Modalities: Definitions and Molecular Targets
| Omics Modality | Core Definition | Primary Molecular Target | Key Analytical Technologies |
|---|---|---|---|
| Genomics | Study of the complete set of DNA, including all genes, their sequences, interactions, and functions [11] [14]. | DNA (Deoxyribonucleic Acid) | Next-Generation Sequencing (NGS), Sanger Sequencing, Microarrays [8] [9] |
| Transcriptomics | Analysis of the complete set of RNA transcripts produced by the genome under specific circumstances [9] [12]. | RNA (Ribonucleic Acid), including mRNA | RNA Sequencing (RNA-Seq), Microarrays [8] [1] |
| Proteomics | Study of the structure, function, and interactions of the complete set of proteins (the proteome) in a cell or organism [9] [12]. | Proteins and their post-translational modifications | Mass Spectrometry (MS), Protein Microarrays [10] [12] |
| Metabolomics | Comprehensive analysis of the complete set of small-molecule metabolites within a biological sample [9] [11]. | Metabolites (e.g., lipids, amino acids, carbohydrates) | Mass Spectrometry (MS), Nuclear Magnetic Resonance (NMR) Spectroscopy [9] [14] |
Application Notes in Oncology
Genomics and Genetic Variations in Cancer
Genomics investigates the complete set of DNA in an organism, providing a foundational understanding of genetic predispositions and somatic mutations that drive oncogenesis [8] [11]. In cancer, genomic analyses focus on identifying key variations, including driver mutations that confer growth advantage, copy number variations (CNVs) that alter gene dosage, and single-nucleotide polymorphisms (SNPs) that may influence cancer risk and therapeutic response [9]. For instance, the amplification of the HER2 gene is a critical genomic event in approximately 20% of breast cancers, leading to aggressive tumour behaviour and serving as a target for therapies like trastuzumab [9]. Similarly, mutations in the TP53 tumour suppressor gene are found in about half of all human cancers [9].
Transcriptomics for Gene Expression Profiling
Transcriptomics captures the dynamic expression of all RNA transcripts, reflecting the active genes in a cell at a specific time and under specific conditions [11] [12]. This modality is crucial for understanding how genomic blueprints are executed and how they change in disease states. In cancer research, transcriptomics enables the classification of molecular subtypes with distinct clinical outcomes, as exemplified by the PAM50 gene signature for breast cancer [1]. It can also reveal mechanisms of drug resistance and immune activation within the tumour microenvironment [1]. Tests based on transcriptomic profiles, such as Oncotype DX, are used in the clinic to assess recurrence risk and guide chemotherapy decisions [1].
Proteomics for Functional Analysis
Proteomics moves beyond the genetic code to study the proteins that execute cellular functions, offering a more direct view of cellular activities and signalling pathways [12]. The proteome is highly dynamic and influenced by post-translational modifications, which are not visible at the genomic or transcriptomic levels [9]. In cancer, proteomic profiling can identify functional protein biomarkers for diagnosis, elucidate dysregulated signalling pathways for targeted therapy, and characterize the immune context of tumours to predict response to immunotherapy [10] [1]. Proteomics can be approached through expression proteomics (quantifying protein levels), structural proteomics (mapping protein locations), and functional proteomics (determining protein interactions and roles) [12].
Metabolomics as a Phenotypic Readout
Metabolomics studies the complete set of small-molecule metabolites, representing the ultimate downstream product of genomic, transcriptomic, and proteomic activity [11]. As such, it provides a snapshot of the physiological state of a cell and is considered a close link to the phenotype [9] [11]. Cancer cells often exhibit reprogrammed metabolic pathways to support rapid growth and proliferation. Metabolomics can uncover these alterations, revealing potential biomarkers for early detection and novel therapeutic targets [9]. It is increasingly used to study a range of conditions, including obesity, diabetes, cardiovascular diseases, and various cancers, and to understand individual responses to environmental factors and drugs [12].
Table 2: Omics Applications in Cancer Diagnosis and Prognosis
| Omics Modality | Representative Cancer Applications | Strengths | Limitations & Challenges |
|---|---|---|---|
| Genomics | - Identification of driver mutations (e.g., TP53) [9]- HER2 amplification testing in breast cancer [9]- Risk assessment via SNPs (e.g., BRCA1/2) [9] | - Foundation for personalized medicine [9]- Comprehensive view of genetic variation [9] | - Does not account for gene expression or environmental influence [9]- Large data volume and complexity [9] |
| Transcriptomics | - Molecular subtyping (e.g., PAM50 for breast cancer) [1]- Prognostic tests (e.g., Oncotype DX) [1]- Analysis of tumour microenvironment [1] | - Captures dynamic gene expression changes [9]- Reveals regulatory mechanisms [9] | - RNA is less stable than DNA [9]- Provides a snapshot view, not long-term [9] |
| Proteomics | - Biomarker discovery for diagnosis [10]- Drug target identification [9]- Analysis of post-translational modifications [9] | - Directly measures functional effectors [9]- Links genotype to phenotype [9] | - Proteome is complex and has a large dynamic range [9]- Difficult quantification and standardization [9] |
| Metabolomics | - Discovery of metabolic biomarkers for early detection [9]- Investigating metabolic rewiring in cancer [12]- Monitoring treatment response [12] | - Direct link to phenotype [9]- Can capture real-time physiological status [9] | - Metabolome is highly dynamic [9]- Limited reference databases [9] |
Experimental Protocols
Protocol 1: Multi-Omic Data Generation from Tumour Tissue
This protocol outlines the steps for generating genomics, transcriptomics, proteomics, and metabolomics data from a single tumour tissue sample, a common approach in studies like The Cancer Genome Atlas (TCGA) [10].
I. Sample Collection and Preparation
- Tissue Acquisition: Obtain fresh tumour tissue via biopsy or surgical resection. Immediately snap-freeze a portion of the tissue in liquid nitrogen and store at -80°C to preserve nucleic acids, proteins, and metabolites.
- Sectioning: Cryosection the frozen tissue into multiple sequential slices (e.g., 10-20 μm thickness).
- Nucleic Acid Extraction: Use one section for simultaneous DNA and RNA extraction using a commercial kit that ensures high purity and integrity. Assess DNA and RNA quality using spectrophotometry (e.g., Nanodrop) and bioanalyzer (e.g., Agilent Bioanalyzer for RNA Integrity Number, RIN).
- Protein and Metabolite Extraction: From a parallel section, homogenize the tissue. Split the homogenate:
- For proteomics, lyse the tissue in an appropriate buffer (e.g., RIPA with protease and phosphatase inhibitors). Centrifuge to clear debris.
- For metabolomics, extract metabolites using a solvent system like methanol:acetonitrile:water to precipitate proteins and recover a wide range of polar and non-polar metabolites.
II. Data Generation
- Genomics (Whole Exome Sequencing - WES):
- Library Prep: Fragment genomic DNA and perform hybrid capture-based enrichment of exonic regions using a kit (e.g., Illumina Nextera Flex for Enrichment).
- Sequencing: Sequence the libraries on a high-throughput platform (e.g., Illumina NovaSeq) to a minimum depth of 100x.
- Transcriptomics (RNA Sequencing - RNA-Seq):
- Library Prep: Deplete ribosomal RNA or enrich for poly-adenylated RNA from total RNA. Prepare sequencing libraries (e.g., Illumina TruSeq Stranded mRNA kit).
- Sequencing: Sequence on a platform like Illumina HiSeq or NovaSeq to generate at least 30 million paired-end reads per sample.
- Proteomics (Data-Independent Acquisition Mass Spectrometry - DIA-MS):
- Digestion: Digest proteins from the lysate with trypsin.
- Liquid Chromatography-Mass Spectrometry (LC-MS/MS): Separate peptides by liquid chromatography and analyze using a DIA method on a high-resolution mass spectrometer (e.g., Thermo Scientific Orbitrap Exploris 480).
- Metabolomics (Liquid Chromatography-Mass Spectrometry - LC-MS):
- Analysis: Separate the metabolite extract using reversed-phase or HILIC chromatography coupled to a high-resolution mass spectrometer (e.g., Thermo Scientific Q-Exactive).
- Polarity: Run the analysis in both positive and negative ionization modes to maximize metabolite coverage.
Protocol 2: A Basic Computational Workflow for Multi-Omic Data Integration
This protocol describes a foundational bioinformatics pipeline for integrating the generated data, inspired by machine learning approaches for survival prediction [13] [1].
I. Preprocessing and Quality Control (Per Modality)
- Genomics:
- Variant Calling: Align sequencing reads to a reference genome (e.g., GRCh38) using a tool like BWA-MEM. Call somatic variants (SNVs, indels) using GATK Best Practices or a tool like MuTect2 [1].
- Transcriptomics:
- Quantification: Align RNA-Seq reads with a splice-aware aligner (e.g., STAR) and quantify gene-level counts using featureCounts.
- Normalization: Perform normalization (e.g., TPM, DESeq2's median of ratios) and, if needed, batch correction (e.g., using ComBat).
- Proteomics:
- Quantification: Process DIA-MS data using software like Spectronaut or DIA-NN to obtain protein abundance values.
- Normalization: Normalize abundances (e.g., by median) and log2-transform.
- Metabolomics:
- Peak Picking and Annotation: Use software like XCMS or MS-DIAL for peak picking, alignment, and annotation against metabolite databases (e.g., HMDB).
- Normalization: Normalize peak intensities (e.g., by sum, PQN) and log-transform.
II. Feature Extraction and Fusion
- Dimensionality Reduction: For each preprocessed omics matrix, perform dimensionality reduction to mitigate the "curse of dimensionality" and reduce noise [13] [1].
- Data Fusion Strategy: Employ a "late fusion" or "model-level fusion" strategy, which is effective when dealing with high-dimensional data and limited samples [13].
- Step 1: Train Single-Modality Models. Train a predictive model (e.g., a Cox proportional hazards model or a Random Survival Forest) for each omics modality using the extracted features.
- Step 2: Fuse Predictions. Combine the predictions from each single-modality model (e.g., by averaging or using a stacked ensemble) to generate a final, integrated prediction [13].
Visualization of Multi-Omic Integration for Cancer Research
Diagram 1: Multi-Omic Data Integration Workflow for Clinical Insight
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Research Reagents and Kits for Omics Technologies
| Item Name | Function / Application | Specific Example / Vendor |
|---|---|---|
| Next-Generation Sequencer | High-throughput parallel sequencing of DNA and RNA libraries. | Illumina NovaSeq 6000 System; PacBio Sequel IIe System [8] [10] |
| High-Resolution Mass Spectrometer | Precise identification and quantification of proteins and metabolites. | Thermo Scientific Orbitrap Exploris Series; Sciex TripleTOF Systems [10] [1] |
| Nucleic Acid Extraction Kit | Isolation of high-purity, intact genomic DNA and total RNA from tissue. | Qiagen AllPrep DNA/RNA/miRNA Universal Kit; Zymo Research Quick-DNA/RNA Miniprep Kit |
| Protein Lysis Buffer | Efficient extraction of proteins from tissue/cells while maintaining stability. | RIPA Lysis Buffer (with protease and phosphatase inhibitors) [1] |
| Metabolite Extraction Solvent | Comprehensive extraction of polar and non-polar metabolites for LC-MS. | Methanol:Acetonitrile:Water (e.g., 40:40:20) solvent system [1] |
| Library Prep Kit for WES | Preparation of sequencing libraries with enrichment for exonic regions. | Illumina Nextera Flex for Enrichment; Agilent SureSelect XT HS2 [8] |
| Library Prep Kit for RNA-Seq | Preparation of stranded RNA-Seq libraries, often with mRNA enrichment. | Illumina TruSeq Stranded mRNA Kit; NEBnext Ultra II Directional RNA Library Prep Kit |
| Trypsin, Sequencing Grade | Proteolytic enzyme for specific digestion of proteins into peptides for MS. | Trypsin, Sequencing Grade (e.g., from Promega or Roche) [1] |
Technological advances now make it possible to study a patient from multiple angles with high-dimensional, high-throughput multi-scale biomedical data [10]. In oncology, massive amounts of data are being generated ranging from molecular, histopathology, radiology to clinical records [10]. The introduction of deep learning has significantly advanced the analysis of biomedical data, yet most approaches focus on single data modalities, leading to slow progress in methods to integrate complementary data types [10]. Development of effective multimodal fusion approaches is becoming increasingly important as a single modality might not be consistent and sufficient to capture the heterogeneity of complex diseases like cancer to tailor medical care and improve personalised medicine [10].
Multi-modal data fusion technology integrates information from different modality imaging, which can be comprehensively analyzed by imaging fusion systems [15]. This approach provides more imaging information of tumors from different dimensions and angles, offering strong technical support for the implementation of precision oncology [15]. The integration of data modalities that cover different scales of a patient has the potential to capture synergistic signals that identify both intra- and inter-patient heterogeneity critical for clinical predictions [10]. For example, the 2016 WHO classification of tumours of the central nervous system (CNS) revisited the guidelines to classify diffuse gliomas recommending histopathological diagnosis in combination with molecular markers [10].
Medical Imaging Modalities: Technical Foundations and Applications
Digital Pathology and Whole Slide Imaging (WSI)
Digital pathology, the process of "digitising" conventional glass slides to virtual images, has many practical advantages over more traditional approaches, including speed, more straightforward data storage and management, remote access and shareability, and highly accurate, objective, and consistent readouts [10]. Whole slide images (WSIs) are critical for cancer diagnosis but pose computational challenges due to their gigapixel resolution [16]. These large (~1 GB) images, containing gigapixels of data, pose significant challenges for deep learning pipelines—not because of model design limitations, but due to the substantial computational demands they impose, including memory usage, I/O throughput, and GPU processing capabilities [16].
Fine-tuning pre-trained models or using multiple-instance learning (MIL) are common approaches, especially when only WSI-level labels are available [16]. ROIs are defined using expert annotations, pre-trained segmentation models, or image features, and MIL aggregates patch information for supervision [16]. Several MIL-based methods have been developed for WSI classification, including ABMIL, ACMIL, TransMIL, and DSMI, each addressing traditional MIL limitations [16].
Radiological Imaging: CT and MRI
Computed Tomography (CT) and Magnetic Resonance Imaging (MRI) scans are useful for generating 3D images of (pre)malignant lesions [10]. CT is based on anatomical imaging while MRI has higher soft-tissue resolution than CT and causes no radiation damage [15]. Radiomics refers to the field focusing on the quantitative analysis of radiological digital images with the aim of extracting quantitative features that can be used for clinical decision-making [10]. This extraction used to be done with standard statistical methods, but more advanced deep learning (DL) frameworks like convolutional neural networks (CNN), deep autoencoders (DAN) and vision transformers (ViTs) are now available for automated, high-throughput feature extraction [10].
Radiomics and Feature Extraction
The concept of radiomics was first formally introduced by Lambin et al. in 2012, and later further refined and expanded in 2017 [17]. Radiomics utilizes computational algorithms to extract a wide range of high-dimensional, quantifiable features from medical imaging, such as shape, texture, intensity distribution, and contrast, which can reflect the tumor's microstructure and biological behavior, and subsequently assist in disease diagnosis and treatment [17]. Traditional radiomics methods typically rely on two-dimensional imaging data and predefined feature extraction techniques, which may overlook the full spatial heterogeneity of the tumor [17].
Table 1: Comparison of Medical Imaging Modalities in Oncology
| Modality | Primary Applications | Key Advantages | Technical Limitations | Data Characteristics |
|---|---|---|---|---|
| Digital Pathology (WSI) | Cancer diagnosis, subtype classification, tissue architecture analysis | Detailed cellular and morphological information; gold standard for diagnosis | Gigapixel resolution requires patch-based processing; computational demands | Whole slide images (1GB+); requires multiple-instance learning |
| CT (Computed Tomography) | Tumor localization, staging, radiotherapy planning | Fast acquisition; excellent spatial resolution; 3D reconstruction | Ionizing radiation; limited soft-tissue contrast | Anatomical imaging; quantitative texture/shape features |
| MRI (Magnetic Resonance) | Soft-tissue characterization, treatment response assessment | Superior soft-tissue contrast; multi-parametric imaging; no radiation | Longer acquisition times; more expensive | Functional and metabolic information; multi-sequence data |
| Radiomics | Prognostic prediction, biomarker discovery, heterogeneity quantification | High-dimensional feature extraction; captures tumor heterogeneity | Dependency on image quality; requires standardization | 1000+ quantitative features; shape, texture, intensity patterns |
Multi-Modal Fusion Architectures and Methodologies
Fusion Strategies and Technical Approaches
Multimodal feature fusion strategies mainly include early fusion, late fusion, and hybrid fusion [18]. Early fusion concatenates features from multiple modalities at the shallow layers (or input layers) of the model, followed by a cascaded deep network structure, and ultimately connects to the classifier or other models [18]. Early fusion learns the correlations between the low-level features of each modality. As it only requires training a single unified model, its complexity is manageable. However, early fusion faces challenges in feature concatenation due to the different sources of data from multiple modalities [18].
Late fusion involves independently training multiple models for each modality, where each modality undergoes feature extraction through separate models [18]. The extracted features are then fused and connected to a classifier for final classification [18]. Hybrid fusion combines the principles of both early and late fusion [18]. Since early fusion integrates multiple modalities at the shallow layers or input layers, it is suitable for cases with minimal differences between the modalities [18].
Multi-Modal Fusion Implementation Workflow
Application Notes: Experimental Results and Performance Metrics
Multi-Modal Fusion Performance Across Cancer Types
Multiple studies have demonstrated the superior performance of multimodal approaches compared to unimodal models across various cancer types. The integration of complementary data sources consistently enhances predictive accuracy for diagnosis, prognosis, and treatment response assessment.
Table 2: Performance Comparison of Multi-Modal vs Uni-Modal Models in Oncology
| Cancer Type | Modalities Fused | Model Architecture | Primary Task | Performance (Multimodal) | Performance (Best Uni-Modal) |
|---|---|---|---|---|---|
| Pancreatic Cancer [17] | CT Radiomics + 3D Deep Learning + Clinical | Radiomics-RSF + 3D-DenseNet + Logistic Regression | Survival Prediction | AUC: 0.87 (1-y), 0.92 (2-y), 0.94 (3-y) | Radiomics AUC: 0.78 (1-y), 0.85 (2-y), 0.91 (3-y) |
| Breast Cancer [19] | Ultrasound + Radiology Reports | Image/Text Encoders + Transformation Layer | Benign/Malignant Classification | Youden Index: +6-8% over unimodal | Image-only or text-only models |
| Breast Cancer (NAT Response) [20] | Mammogram + MRI + Clinical + Histopathological | iMGrhpc + iMRrhpc with temporal embedding | pCR Prediction Post-NAT | AUROC: 0.883 (Pre-NAT), 0.889 (Mid-NAT) | Uni-modal ΔAUROC: 10.4% (p=0.003) |
| Head and Neck SCC [21] | CT + WSI + Clinical | Multimodal DL (MDLM) with Cox regression | Overall Survival Prediction | C-index: 0.745 (internal), 0.717 (external) | CT-only or WSI-only models |
| Breast Cancer [18] | Mammography + Ultrasound | Late Fusion with Multiple DL Models | Benign/Malignant Classification | AUC: 0.968, Accuracy: 93.78% | Single modality models |
| Kidney & Lung Cancer [16] | WSI + Pathology Reports | MPath-Net (MIL + Sentence-BERT) | Cancer Subtype Classification | Accuracy: 94.65%, F1-score: 0.9473 | WSI-only or text-only baselines |
Technical Protocols for Multi-Modal Implementation
Protocol 1: Radiomics-3D Deep Learning Fusion for Pancreatic Cancer
Application: Survival prediction in pancreatic cancer patients [17]
Materials and Methods:
- Patient Cohort: 880 eligible patients split into training (n=616) and testing (n=264) sets in 7:3 ratio
- Imaging Data: Portal venous phase contrast-enhanced CT images
- ROI Delineation: Two physicians independently delineated tumor regions with third expert arbitration for discrepancies
- Feature Extraction:
- Radiomics: 1,037 features extracted using 3D Slicer Radiomics plugin
- Deep Learning: 3D-DenseNet trained on ROI-based image inputs
- Model Development:
- Radiomics features reduced via PCA and LASSO regression
- Random Survival Forest for survival prediction
- Fusion with clinical variables using multiple classifiers
- Validation: Internal-external validation via train-test split; performance evaluated using ROC curves, AUC, and accuracy
Key Parameters:
- Image resampling to 3×3×3 mm³ voxel size for isotropy
- Intraclass correlation coefficient (ICC) for ROI consistency validation
- Binary classification at 1-, 2-, and 3-year survival time points
Protocol 2: Multi-Modal Breast Cancer Neoadjuvant Therapy Response Prediction
Application: Predicting pathological complete response (pCR) in breast cancer patients undergoing neoadjuvant therapy [20]
Materials and Methods:
- Patient Cohort: 3,352 patients from multiple centers with longitudinal data
- Modalities Integrated:
- Pre-NAT mammogram exams (4,802 exams)
- Longitudinal MRI exams (3,719 exams)
- Histopathological information (molecular subtype, tumor histology)
- Personal factors (age, menopausal status, genetic mutations)
- Clinical data (cTNM staging, therapy details)
- Model Architecture:
- iMGrhpc: Processes Pre-NAT mammogram + rhpc data
- iMRrhpc: Handles longitudinal MRI + rhpc data
- Cross-modal knowledge mining strategy
- Temporal information embedding for longitudinal data
- Validation: Multi-center studies and multinational reader studies comparing model performance to breast radiologists
Key Parameters:
- Handles missing modalities through flexible architecture
- Robust to different NAT settings across hospitals
- Output: pCR probability for surgical decision support
Protocol 3: Whole Slide Image and Pathology Report Fusion
Application: Cancer subtype classification for kidney and lung cancers [16]
Materials and Methods:
- Data Source: TCGA dataset (1,684 cases: 916 kidney, 768 lung)
- Modalities: WSIs and corresponding pathology reports
- Feature Extraction:
- WSI: Multiple-instance learning (MIL) for gigapixel image processing
- Text: Sentence-BERT for report encoding
- Fusion Architecture:
- 512-dimensional image and text embeddings concatenated
- Joint fine-tuning with trainable fusion layers
- End-to-end training with image encoder fine-tuned and text encoder frozen
- Validation: Comparative analysis against state-of-the-art MIL methods
Key Parameters:
- Weakly supervised learning requiring only slide-level labels
- Attention heatmaps for interpretable tumor localization
- Cross-modal alignment through joint representation learning
Table 3: Essential Research Tools for Multi-Modal Oncology Research
| Tool/Resource | Type | Primary Function | Application Examples | Key Features |
|---|---|---|---|---|
| 3D Slicer [17] | Software Platform | Medical image visualization and processing | Radiomic feature extraction; ROI delineation | Open-source; extensible architecture; radiomics plugin |
| PyTorch [16] | Deep Learning Framework | Model development and training | Implementing MIL algorithms; custom fusion architectures | GPU acceleration; dynamic computation graphs |
| YOLOv8 [18] | Object Detection Model | Automated tumor region localization | Preprocessing ultrasound images for analysis | Real-time processing; high accuracy |
| Sentence-BERT [16] | NLP Framework | Text embedding generation | Processing pathology reports for multimodal fusion | Semantic similarity preservation; medical text optimization |
| TransMIL [16] | Multiple Instance Learning | WSI classification and analysis | Cancer subtype classification from whole slides | Transformer-based; attention mechanisms |
| TCGA [10] [16] | Data Repository | Multi-modal cancer datasets | Access to matched imaging, genomic, clinical data | 33 cancer types; standardized data formats |
| ResNet/3D-DenseNet [17] | Deep Learning Architecture | Feature extraction from images | 3D tumor characterization from CT volumes | Spatial context preservation; hierarchical feature learning |
Multimodal data fusion represents a paradigm shift in cancer diagnostics and research methodology. The integration of digital pathology, radiological imaging (CT, MRI), and radiomics features has consistently demonstrated superior performance compared to single-modality approaches across various cancer types [10] [15]. Technical implementations including early, late, and hybrid fusion strategies provide flexible frameworks for combining complementary data sources, while advanced deep learning architectures enable effective feature extraction and alignment across modalities [18].
The experimental protocols and application notes detailed in this document provide researchers with practical methodologies for implementing multi-modal fusion in oncological research. As the field advances, key challenges remain including handling missing data, improving model interpretability, and ensuring generalizability across diverse patient populations and imaging protocols [22]. Future directions will likely focus on standardized data acquisition protocols, federated learning approaches for multi-institutional collaboration, and the development of more biologically-informed fusion architectures that better capture the complex relationships between imaging features and underlying tumor biology [20] [21].
The integration of Electronic Health Records (EHRs) with other data modalities represents a transformative opportunity in cancer research. EHRs provide comprehensive clinical data on patient history, treatments, and outcomes, while patient-generated health data offers real-world insights into symptoms and quality of life. When fused with genomic, proteomic, and imaging data, these clinical and real-world data sources enable a more holistic understanding of cancer biology and patient experience. However, significant challenges exist in harnessing these data effectively. Current EHR systems often fragment information across multiple platforms, with one study reporting that 92% of gynecological oncology professionals routinely access multiple EHR systems, and 17% spend over half their clinical time searching for patient information [23]. Furthermore, data heterogeneity, lack of interoperability, and inconsistent documentation practices create substantial barriers to multimodal data integration [24] [25]. This application note details methodologies and protocols to overcome these challenges and leverage EHR data within multimodal cancer research frameworks.
Key Challenges in EHR Data Utilization for Cancer Research
Data Fragmentation and Interoperability
EHR data in oncology is typically scattered across multiple systems including clinical trials data, pathology reports, laboratory results, and symptom tracking platforms [24]. This fragmentation is particularly problematic in cancer care characterized by complex, multidisciplinary coordination over extended periods [23]. The lack of standardization across systems and institutions leads to incompatible formats and terminologies, hampering collaborative research efforts [24].
Table 1: Key Challenges in EHR Utilization for Multimodal Cancer Research
| Challenge Category | Specific Issues | Impact on Research |
|---|---|---|
| Data Fragmentation | Information scattered across multiple systems (29% of professionals use ≥5 systems) [23] | Incomplete patient journey mapping; missing critical data points |
| Interoperability | Lack of standardized formats and terminologies across institutions [24] | Difficulties in data exchange and collaborative research |
| Data Quality | Unstructured formats; high degree of missingness [13] [24] | Skewed analysis; compromised model performance |
| Workflow Integration | 17% of clinicians spend >50% of time searching for information [23] | Reduced efficiency; limited time for research activities |
Data Completeness and Quality Issues
Cancer research databases frequently suffer from incomplete clinical data, with key information such as cancer staging, biomarkers, and survival time often missing [24]. In structured oncology data platforms, critical elements like staging and molecular data may be absent in up to 50% of patient records [24]. This missingness can systematically skew survival analyses and other outcomes research [24]. Additionally, EHR data often contains unstructured elements that require expensive manual abstraction and curation [24].
Methodologies for EHR Data Processing and Integration
Data Standardization and Harmonization
The ICGC ARGO Data Dictionary provides a robust framework for standardizing global cancer clinical data collection. This framework employs an event-based data model that captures clinical relationships and supports longitudinal data collection [24]. The dictionary defines:
- Core Fields: Mandatory clinical parameters required for each cancer patient
- Extended Fields: Optional elements for specific research questions
- Conditional Fields: Required only when specific conditions are met [24]
This approach ensures consistent high-quality clinical data collection across diverse cancer types and geographical regions while maintaining interoperability with other standards like Minimal Common Oncology Data Elements (mCODE) [24].
Natural Language Processing for Unstructured Data
Natural Language Processing (NLP) techniques enable transformation of unstructured clinical notes, diagnostic reports, and other text-based EHR elements into structured, analyzable data [26]. NLP has been successfully applied to automate extraction of patient outcomes, progression-free survival data, and other tumor features from clinical narratives [26]. Implementation protocols for NLP in oncology EHR data include:
- Clinical Note Processing: Extraction of genomic and surgical information from free-text records [23]
- Symptom Data Abstraction: Processing of electronic patient-reported outcome measures (ePROs) for symptom monitoring [27]
- Outcome Automation: Gathering progression-free survival and other temporal metrics from clinical documentation [26]
Transformer-Based Patient Embedding
Advanced representation learning methods enable powerful patient stratification from longitudinal EHR data. The transformer-based embedding approach processes high-dimensional EHR data at the patient level to characterize heterogeneity in complex diseases [28]. This methodology involves:
- Vocabulary Embedding: Creating embeddings of medical codes (diagnoses, procedures) using variational autoencoder neural network architecture
- Sequence Processing: Feeding embedded codes to a transformer model that represents each patient's longitudinal visits as sequences
- Patient Vector Generation: Implementing sentence-BERT architecture to transform 2-D vector outputs into 1-D patient embedding vectors [28]
This approach has demonstrated strong predictive performance for future disease onset (median AUROC = 0.87 within one year) and effectively reveals diverse comorbidity profiles and disease progression patterns [28].
Experimental Protocols for Multimodal Data Integration
Protocol: Late Fusion for Survival Prediction
Application Note: This protocol describes a late fusion strategy for integrating multimodal data to predict overall survival in cancer patients, particularly effective with high-dimensional omics data and limited sample sizes [13].
Materials and Reagents:
- Table 2: Research Reagent Solutions for Multimodal Data Fusion
| Reagent/Resource | Function/Application | Specifications |
|---|---|---|
| AZ-AI Multimodal Pipeline | Python library for multimodal feature integration and survival prediction [13] | Includes preprocessing, dimensionality reduction, and model training modules |
| TCGA Data | Provides transcripts, proteins, metabolites, and clinical factors for model training [13] | Includes lung, breast, and pan-cancer datasets |
| Feature Selection Methods | Pearson/Spearman correlation for high-dimensional omics data [13] | Addresses challenges of low signal-to-noise ratio |
| Ensemble Survival Models | Gradient boosting, random forests for survival prediction [13] | Outperforms single models in multimodal settings |
Procedure:
- Data Preprocessing:
- Apply modality-specific preprocessing to address missingness and batch effects
- Normalize each data modality separately (transcripts, proteins, metabolites, clinical factors)
Feature Extraction:
- Perform dimensionality reduction on each modality independently
- Apply linear or monotonic feature selection methods (Pearson/Spearman correlation) suitable for high-dimensional omics data [13]
Unimodal Model Training:
- Train separate survival models for each data modality
- Utilize ensemble methods (gradient boosting, random forests) that outperform deep neural networks on tabular multi-omics data [13]
Late Fusion Integration:
- Combine predictions from unimodal models rather than raw features
- Weight each modality based on its informativeness for survival prediction [13]
Model Evaluation:
- Implement rigorous evaluation with multiple training-test splits
- Report C-indices with confidence intervals to account for uncertainty [13]
Validation: Late fusion models consistently outperformed single-modality approaches in TCGA lung, breast, and pan-cancer datasets, offering higher accuracy and robustness for survival prediction [13].
Protocol: Clinical Decision Support Integration
Application Note: This protocol details the integration of Clinical Decision Support (CDS) systems into EHR workflows for precision symptom management in cancer patients [27].
Procedure:
- Algorithm Development:
- Create symptom management algorithms for key cancer symptoms (e.g., pain, fatigue, nausea)
- Program algorithms into CDS platform using application programming interfaces and interoperable data standards
EHR Integration:
- Integrate CDS into existing EHR systems using interoperable data standards
- Generate individually tailored symptom management recommendations based on EHR and patient-reported data
Validation and Testing:
- Test system using test patients that reflect real-world patient experiences
- Have clinicians verify critical elements to assure accuracy and safety of recommendations [27]
Implementation Framework and Future Directions
Co-Design of Integrated Informatics Platforms
A human-centered design approach involving healthcare professionals, data engineers, and informatics experts is essential for developing effective EHR-integrated research platforms [23]. This methodology includes:
- Multidisciplinary Collaboration: Engaging end-users throughout development to ensure workflow compatibility
- Data Pipeline Validation: Clinicians validating extracted data against original clinical system sources
- Unified Visualization: Consolidating disparate patient data from different EHR systems into a single visual display to support clinical decision-making [23]
Emerging Technologies and Methodologies
Future advancements in EHR-based cancer research will leverage:
- Federated Learning: Enabling model training across institutions without sharing sensitive patient data [29]
- Synthetic Data Generation: Addressing data scarcity while preserving privacy [29]
- Explainable AI (XAI): Enhancing model interpretability for clinical adoption [29]
- Advanced Transformer Architectures: Improving temporal modeling of patient journeys across longer time horizons [28]
Table 3: Performance Metrics for EHR Data Integration Methods
| Methodology | Application | Performance Metrics | Reference |
|---|---|---|---|
| Transformer Patient Embedding | Disease onset prediction | Median AUROC = 0.87 (within one year) | [28] |
| Late Fusion Multimodal Integration | Cancer survival prediction | Outperformed single-modality approaches across TCGA datasets | [13] |
| Clinical Decision Support Integration | Symptom management | Improved guideline-concordant care and supportive care referrals | [27] |
The integration of EHRs and patient-generated data within multimodal cancer research frameworks requires addressing significant challenges in data standardization, processing, and interpretation. However, as the methodologies and protocols outlined herein demonstrate, overcoming these barriers enables more comprehensive cancer modeling, improved predictive accuracy, and ultimately enhanced personalized treatment strategies. The continued development of standardized frameworks, advanced computational methods, and interdisciplinary collaboration will further unlock the potential of clinical and real-world data in transforming cancer research and care.
Breast cancer diagnosis has traditionally relied on single-modality data, an approach that offers limited and one-sided information, making it difficult to capture the full complexity and diversity of the disease [30]. This limitation has driven a paradigm shift toward multi-modal data fusion, which integrates complementary information streams to generate richer, more diverse datasets, ultimately leading to greater robustness in predictive outcomes compared to single-modal approaches [30] [31]. The clinical need is particularly acute in monitoring responses to Neoadjuvant Therapy (NAT), where accurately assessing pathological complete response (pCR) is critical for patient survival but challenging to accomplish with single-source data [20]. By synthesizing information from radiological, histopathological, clinical, and personal data modalities, multi-modal fusion creates a more holistic view of the tumor microenvironment and its response to treatment, directly addressing the critical diagnostic limitations inherent in single-modality frameworks.
Quantitative Evidence of Multi-modal Superiority
Research over the past five years consistently demonstrates that multi-modal fusion models significantly outperform single-modality approaches across key diagnostic tasks in breast cancer, including diagnosis, assessment of neoadjuvant systemic therapy, prognosis prediction, and tumor segmentation [30] [31]. The following tables summarize key performance metrics from recent landmark studies.
Table 1: Performance of Multi-modal Models in Predicting Pathological Complete Response (pCR)
| Model / System | Data Modalities | AUROC | Key Comparative Improvement |
|---|---|---|---|
| MRP System (Pre-NAT phase) [20] | Mammogram, MRI, Histopathological, Clinical, Personal | 0.883 (95% CI: 0.821-0.941) | ΔAUROC of 10.4% vs. uni-modal model (p=0.003) |
| MRP System (Mid-NAT phase) [20] | Mammogram, MRI, Histopathological, Clinical, Personal | 0.889 (95% CI: 0.827-0.948) | ΔAUROC of 11% vs. uni-modal model (p=0.009) |
| HXM-Net (Diagnosis) [5] | B-mode, Doppler, Elastography Ultrasound | 0.97 | Outperformed conventional ResNet-50 and U-Net models |
Table 2: Diagnostic Accuracy of the HXM-Net Multi-modal Ultrasound Model [5]
| Metric | Performance (%) |
|---|---|
| Accuracy | 94.20% |
| Sensitivity (Recall) | 92.80% |
| Specificity | 95.70% |
| F1 Score | 91.00% |
Core Multi-modal Fusion Strategies
The success of multi-modal diagnostics hinges on the strategy used to integrate heterogeneous data. Current deep learning-based approaches can be categorized into three primary fusion techniques [30] [31]:
- Feature-Level Fusion: This strategy involves extracting features from each modality independently using dedicated neural networks (e.g., CNNs for images) and then concatenating or combining these features into a unified representation before the final classification or regression layer. This allows the model to learn complex, cross-modal interactions at an early stage.
- Decision-Level Fusion: In this approach, each modality is processed through a separate model to produce an independent prediction or decision. These individual decisions are subsequently aggregated, often via weighted averaging or voting, to form a final, consolidated output.
- Hybrid Fusion: Hybrid methods combine aspects of both feature-level and decision-level fusion to create more flexible and robust network architectures. For instance, the MRP system uses a form of hybrid fusion by independently training separate models for mammogram and MRI data and then combining their predicted probabilities [20].
The logical workflow for implementing a multi-modal fusion system, from data acquisition to clinical application, is outlined below.
Multi-modal Fusion Clinical Workflow
Experimental Protocols for Multi-modal Response Prediction
This protocol details the methodology for the Multi-modal Response Prediction (MRP) system, which predicts pathological complete response (pCR) in breast cancer patients undergoing Neoadjuvant Therapy (NAT) [20].
Data Acquisition and Curation
- Cohort Selection: Identify breast cancer patients treated with NAT. The MRP study included 3,352 eligible participants from the Netherlands Cancer Institute (2004-2020). External validation cohorts are crucial (e.g., 288 patients from Duke University, 85 from Fujian Provincial Hospital, 508 from the I-SPY2 trial) [20].
- Data Modalities:
- Imaging: Collect Pre-NAT mammograms and longitudinal MRI exams (e.g., subtracted contrast-enhanced T1-weighted imaging from pre-, mid-, and post-NAT time points) [20].
- Radiological Findings: Annotate images with standard radiological assessments.
- Histopathological Data: Collect molecular subtype, tumor histology, type, and differentiation grade.
- Personal & Clinical Data: Include patient age, weight, menopausal status, genetic mutations, and clinical TNM staging [20].
- Data Partitioning: Randomly split the internal cohort into training (80%) and testing sets. Hold out the external cohorts for final validation.
Model Architecture and Training
The MRP system comprises two independently trained models: iMGrhpc (for mammography) and iMRrhpc (for longitudinal MRI). Both integrate the rhpc non-image data [20].
- Feature Extraction:
- For images (mammogram, MRI), use a pre-trained Convolutional Neural Network (CNN) backbone to extract high-level visual features.
- For non-image data (
rhpc), process using fully connected layers to create a feature vector.
- Cross-modal Knowledge Mining: Implement a strategy to enhance visual feature learning. This allows the model to focus on imaging features that are most informative given the context of the other data modalities [20].
- Temporal Information Embedding (for
iMRrhpc): Design the model to accept longitudinal MRI sequences. Embed temporal information to handle different NAT settings and time points (Pre-, Mid-, Post-NAT) flexibly [20]. - Handling Missing Modalities: Architect the system to be robust to missing data inputs (e.g., a patient missing a mammogram or a Mid-NAT MRI), a critical feature for real-world clinical applicability [20].
- Fusion and Output: Fuse the image and non-image features (feature-level fusion). The final MRP system combines the predicted probabilities from
iMGrhpcandiMRrhpc(decision-level fusion) to produce a single pCR probability [20].
Validation and Analysis
- Performance Metrics: Evaluate the model using Area Under the Receiver Operating Characteristic curve (AUROC), Area Under the Precision-Recall Curve (AUPRC), sensitivity, specificity, Positive Predictive Value (PPV), and Negative Predictive Value (NPV) [20].
- Benchmarking: Compare the model's performance against baseline models (e.g., uni-modal
rhpcmodel,iMGrhpcalone) and, if possible, against the performance of breast radiologists in a reader study [20]. - Clinical Utility Assessment: Use Decision Curve Analysis (DCA) to evaluate the net benefit of using the model for clinical decision-making in scenarios like enrolling patients in NAT trials or de-escalating surgery [20].
The following diagram illustrates the experimental and validation workflow for the MRP system.
MRP System Experimental Workflow
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Research Materials and Computational Tools for Multi-modal Diagnostics
| Item / Resource | Function / Application | Example / Specification |
|---|---|---|
| Public Breast Cancer Datasets | Provides multi-modal, annotated data for model training and benchmarking. | Includes imaging (mammography, MRI, ultrasound), histopathology, and clinical data. |
| Convolutional Neural Network (CNN) | Backbone architecture for extracting spatial features from medical images. | Used in HXM-Net for ultrasound [5] and MRP for mammography/MRI [20]. |
| Transformer Architecture | Fuses multi-modal features using self-attention mechanisms to weight important regions. | Core component of HXM-Net's fusion module [5]. |
| Feature-wise Linear Modulation (FiLM) | Conditions the image processing pathway on non-image data (e.g., clinical text), enabling adaptive feature extraction. | Used in prompt-driven segmentation models for context-aware processing [32]. |
| Dice Loss Function | Optimizes model for single-organ or single-tumor segmentation tasks by maximizing region overlap. | Demonstrated as optimal for single-organ tasks [32]. |
| Jaccard (IoU) Loss Function | Optimizes model for complex, multi-organ segmentation tasks under cross-modality challenges. | Outperforms Dice loss in multi-organ scenarios [32]. |
The progression and treatment response of cancer are largely dictated by its heterogeneous nature, encompassing diverse cellular subpopulations with distinct genetic, transcriptional, and spatial characteristics. This complexity presents a significant challenge for accurate diagnosis and effective therapy. The emergence of multimodal data fusion—the computational integration of disparate data types—offers an unprecedented opportunity to capture a holistic view of this heterogeneity. By simultaneously analyzing genomic, transcriptomic, imaging, and clinical data, researchers can move beyond fragmented insights to develop a systems-level understanding of tumor biology, ultimately paving the way for more personalized and effective cancer interventions [33]. This article details specific protocols and applications that exemplify the power of integration in oncology research.
The field of multimodal oncology research is driven by a suite of advanced technologies, each contributing a unique piece to the puzzle of tumor heterogeneity. The table below summarizes the key characteristics of several prominent technologies and the computational methods used to integrate their data.
Table 1: Key Technologies and Integration Methods for Capturing Tumor Heterogeneity
| Technology / Method | Data Modality | Key Output | Spatial Resolution | Key Application in Heterogeneity |
|---|---|---|---|---|
| Spatial Transcriptomics (e.g., Visium) [1] | RNA | Genome-wide expression data with spatial context | 1-100 cells/spot | Tumor-immune microenvironment mapping |
| In Situ Sequencing (ISS) [34] | RNA | Targeted or untargeted RNA sequences within intact tissue | Single-cell | Subcellular RNA localization and splicing variants |
| Deep-STARmap [35] | RNA | Transcriptomic profiles of thousands of genes in 3D tissue blocks | Single-cell (in 60-200 µm thick tissues) | 3D cell typing and morphology tracing |
| Multi-contrast Laser Endoscopy (MLE) [36] | Optical Imaging | Multispectral reflectance, blood flow, and topography | ~1 Megapixel, HD video rate | In vivo enhancement of tissue chromophore and structural contrast |
| Tumoroscope [37] | Computational Fusion | Clonal proportions and their spatial distribution in ST spots | Near-single-cell | Deconvolution of clonal architecture from bulk DNA-seq and ST data |
| AZ-AI Multimodal Pipeline [13] | Computational Fusion | Integrated survival prediction model | N/A | Late fusion of multi-omics and clinical data for prognostic modeling |
| Feature-Based Image Registration [38] | Computational Fusion | Aligned multimodal images (e.g., H&E with mass spectrometry) | N/A | Correlation of tissue morphology with molecular/elemental distribution |
Detailed Experimental Protocols
Protocol 1: Mapping Clonal Architecture with Tumoroscope
This protocol details the use of the Tumoroscope probabilistic model to spatially localize cancer clones by integrating histology, bulk DNA sequencing, and spatial transcriptomics data [37].
1. Primary Data Acquisition and Preprocessing
- H&E Image Analysis: Process the H&E-stained tissue section using custom scripts in QuPath [39].
- Identify and demarcate regions containing cancer cells.
- Estimate the number of cells present within each Spatial Transcriptomics (ST) spot located in the cancerous regions.
- Bulk DNA-seq Analysis: Perform bulk whole exome sequencing on the tumor sample.
- Spatial Transcriptomics: Generate ST data from an adjacent tissue section.
- For each ST spot, obtain the count of alternative and total reads for the somatic mutations identified in the bulk DNA-seq.
- Obtain the gene expression matrix for all spots.
2. Core Tumoroscope Deconvolution Analysis
- Input Preparation: Format the preprocessed data for Tumoroscope input:
cell_count_prior: Vector of estimated cell counts per spot from H&E analysis.alternate_reads: Matrix of alternative read counts for each mutation in each spot.total_reads: Matrix of total read counts for each mutation in each spot.clone_genotypes: Scaled genotype matrix for the reconstructed clones.
- Model Execution: Run the Tumoroscope probabilistic graphical model. The model assumes each ST spot contains a mixture of clones and uses the input data to infer:
- The proportion of each clone in every spot.
- A refined estimate of the number of cells per spot.
- Output Analysis: The primary output is a spatial map of clone proportions across the tissue section, allowing for the visualization of clonal colocalization and mutual exclusion patterns.
3. Downstream Phenotypic Analysis
- Clone-Specific Gene Expression: Using the inferred clone proportions as the dependent variable and the spot-by-gene expression matrix as the independent variable, run a regression model to estimate the gene expression profile specific to each clone.
Protocol 2: 3D Spatial Transcriptomics in Thick Tissue Blocks with Deep-STARmap
This protocol describes the procedure for performing high-plex spatial transcriptomics within intact 3D tissue blocks using Deep-STARmap, enabling the correlation of molecular profiles with complex morphological structures [35].
1. Tissue Preparation, Embedding, and Clearing
- Tissue Fixation and Sectioning: Fix the fresh tissue sample (e.g., mouse brain or human skin cancer) and cut it into 60-200 µm thick sections using a vibratome.
- Hydrogel Embedding: Embed the tissue section in a hydrogel matrix. This step involves:
- Permeabilizing the tissue to allow entry of reagents.
- Anchoring RNA transcripts to the hydrogel network to preserve spatial information.
- Protein Digestion and Expansion: Digest cellular proteins with Proteinase K to clear the tissue and create a porous hydrogel-tissue hybrid. This is followed by mechanical expansion in water to physically separate biomolecules, reducing optical crowding and improving resolution.
2. In Situ Sequencing and Imaging
- Reverse Transcription and Amplification: Synthesize cDNA from RNA templates directly within the expanded hydrogel. Perform rolling circle amplification (RCA) to generate concentrated, copy-rich amplicons for each transcript.
- Sequencing by Ligation: Carry out in situ sequencing using Sequencing by Oligonucleotide Ligation and Detection (SOLiD) chemistry.
- Fluorescently labeled probes are sequentially ligated, imaged, and cleaved over multiple cycles to determine the base sequence of the amplicons.
- Multicycle Imaging: Automate cycles of probe hybridization, ligation, fluorescence imaging (using a confocal microscope), and dye cleavage to read out the nucleotide sequence for each transcript across multiple tissue sections.
3. 3D Reconstruction and Data Integration
- Image Registration and Reconstruction: Align the sequential imaging data from each thick section using computational image registration tools. Stack the aligned sections to reconstruct a 3D volume of the tissue block.
- If applicable, co-register with multicolor fluorescent protein images to correlate transcriptomic data with neuronal morphology or other structural markers.
- Data Analysis: Map the sequenced transcripts back to their 3D spatial coordinates. Perform downstream analyses such as:
- 3D molecular cell type clustering.
- Identification of spatially variable genes and expression gradients.
- Quantitative analysis of tumor-immune interactions within the 3D architecture.
Table 2: Research Reagent Solutions for Profiling Tumor Heterogeneity
| Item | Function/Description | Application Example |
|---|---|---|
| QuPath Software [37] | Open-source digital pathology platform for whole-slide image analysis and cell detection. | Automated estimation of cancer cell counts in H&E images for Spatial Transcriptomics spots. |
| Canopy Software [37] | Computational tool for reconstructing clonal populations and their phylogenies from bulk DNA-seq data. | Inferring cancer clone genotypes and frequencies as input for the Tumoroscope model. |
| Aminoallyl dUTP [34] | A modified nucleotide containing a reactive amine group, used in cDNA synthesis. | Cross-linking cDNA to the protein matrix during FISSEQ to prevent diffusion and maintain spatial fidelity. |
| Proteinase K [35] [34] | A broad-spectrum serine protease that digests proteins. | Clearing proteins in Expansion Microscopy and hydrogel-embedded tissues to enable probe access and physical expansion. |
| SOLiD (Sequencing by Oligonucleotide Ligation and Detection) Chemistry [34] | A next-generation sequencing technology based on sequential ligation of fluorescent probes. | Reading out nucleotide sequences in high-plex in situ sequencing methods like FISSEQ. |
| Custom Fiber Optic Light Guide [36] | A modified light guide for a clinical colonoscope that integrates laser illumination bundles. | Enabling multimodal imaging (MLE) during standard-of-care white light endoscopy procedures. |
The Scientist's Toolkit: Key Research Reagents and Materials
Critical advancements in capturing tumor heterogeneity rely on a core set of reagents, software, and engineered materials that enable precise spatial and molecular analysis.
The integration of multimodal data is transforming our ability to dissect the complex and heterogeneous nature of tumors. The protocols outlined herein—from computational clonal deconvolution with Tumoroscope to 3D spatial transcriptomics with Deep-STARmap—provide a tangible roadmap for researchers to implement these powerful approaches. As these technologies continue to mature and become more accessible, they hold the definitive promise to uncover novel biological insights, identify new therapeutic targets, and ultimately advance the field towards a more precise and effective paradigm of oncology care.
Fusion Techniques and Clinical Deployment: From Architectures to Real-World Impact
Modern oncology research leverages diverse data modalities, including clinical records, multi-omics data (genomics, transcriptomics, proteomics), medical imaging (histopathology, MRI, CT, ultrasound), and wearable sensor data [1]. Each modality provides unique insights into cancer biology, but their integration presents significant challenges due to data heterogeneity, varying structures, and scale differences [1]. Multimodal artificial intelligence (MMAI) approaches aim to integrate these heterogeneous datasets into cohesive analytical frameworks to achieve more accurate and personalized cancer care [3]. The fusion strategy—how these different data types are combined—critically impacts model performance, interpretability, and clinical applicability [31] [41].
Data fusion methods are broadly classified into four categories: early (data-level), late (decision-level), intermediate (feature-level), and hybrid fusion [31] [42]. Early fusion integrates raw data before model input, while late fusion combines outputs from modality-specific models. Intermediate fusion merges feature representations extracted from each modality, and hybrid approaches combine elements of the other strategies [31]. Selecting an appropriate fusion strategy requires balancing factors such as data heterogeneity, computational resources, model interpretability, and the specific clinical task [41] [13]. The following sections provide a detailed taxonomy of these fusion strategies, their applications in oncology, and practical protocols for implementation.
Theoretical Framework: Fusion Taxonomies
Table 1: Taxonomy of Multimodal Fusion Strategies in Oncology
| Fusion Type | Integration Level | Key Characteristics | Advantages | Limitations | Representative Applications in Oncology |
|---|---|---|---|---|---|
| Early Fusion | Data/Input Level | Raw data concatenated before model input; single model processes combined input [31] [42] | Simplicity of implementation; captures cross-modal correlations at raw data level [43] | Susceptible to overfitting with high-dimensional data; requires data harmonization [41] [13] | PET-CT volume fusion for segmentation [43] |
| Intermediate Fusion | Feature Level | Modality-specific features extracted then merged; shared model processes combined features [31] [43] | Balances specificity and integration; preserves modality-specific patterns [43] | Requires feature alignment; complex architecture design [43] | Anatomy-guided PET-CT fusion [43]; Multi-stage feature fusion networks [44] |
| Late Fusion | Decision/Output Level | Separate models per modality; predictions combined at decision level [31] [41] | Handles data heterogeneity; resistant to overfitting; modular implementation [41] [13] | Cannot model cross-modal correlations in early stages [43] | Survival prediction in breast cancer [41] [13]; Multi-omics integration [13] |
| Hybrid Fusion | Multiple Levels | Combines elements of early, intermediate, and/or late fusion [31] | Maximizes complementary information; highly flexible architecture [31] [5] | High computational complexity; challenging to optimize [31] | HXM-Net for ultrasound fusion [5]; PADBSRNet for multi-cancer detection [44] |
Table 2: Performance Comparison of Fusion Strategies in Oncology Applications
| Application Domain | Best Performing Fusion Strategy | Reported Performance Metrics | Modalities Combined | Reference Dataset |
|---|---|---|---|---|
| Breast Cancer Survival Prediction | Late Fusion | Highest test-set concordance indices (C-indices) across modality combinations [41] | Clinical, somatic mutations, RNA expression, CNV, miRNA, histopathology images | TCGA Breast Cancer [41] |
| PET-CT Tumor Segmentation | Intermediate Fusion | Dice score: 0.8184; HD^95: 2.31 [43] | PET and CT volumes | Head and Neck Cancer PET-CT [43] |
| Breast Cancer Diagnosis | Hybrid Fusion (HXM-Net) | Accuracy: 94.20%; Sensitivity: 92.80%; Specificity: 95.70%; AUC-ROC: 0.97 [5] | B-mode ultrasound, Doppler, elastography | Breast Ultrasound Database [5] |
| Multi-Cancer Detection | Hybrid Fusion (PADBSRNet) | Accuracy: 95.24% (brain tumors), 99.55% (lung cancer), 88.61% (skin cancer) [44] | Multi-scale imaging features | Figshare Brain Tumor, IQ-OTH/NCCD, Skin Cancer Datasets [44] |
Early Fusion (Data-Level Fusion)
Early fusion, also known as data-level fusion, involves integrating raw data from multiple modalities before model input [31] [42]. This approach concatenates or combines unprocessed data into a unified representation that serves as input to a single model. In oncology, early fusion has been applied to integrated PET-CT volumes, where PET metabolic information and CT anatomical data are combined at the voxel level [43]. The fundamental assumption is that cross-modal correlations are best learned directly from raw data.
Despite its conceptual simplicity, early fusion presents significant challenges with high-dimensional oncology data. Different modalities often exhibit heterogeneous data structures, resolutions, and dimensionalities, requiring careful normalization and alignment before integration [43]. Furthermore, early fusion is particularly susceptible to overfitting when dealing with the "curse of dimensionality"—a common scenario in oncology where patient sample sizes are often small relative to feature dimensions [41] [13]. This approach works best when modalities share similar dimensionalities and data structures, or when strong inter-modality correlations exist at the raw data level.
Intermediate Fusion (Feature-Level Fusion)
Intermediate fusion operates at the feature level, where modality-specific features are first extracted independently and subsequently merged [31] [43]. This strategy preserves modality-specific patterns while allowing the model to learn cross-modal interactions in a shared representation space. The architecture typically consists of separate feature extractors for each modality, followed by fusion layers that combine these features before final prediction.
In oncology applications, intermediate fusion has demonstrated particular success in medical imaging tasks. For PET-CT tumor segmentation, an anatomy-guided intermediate fusion approach with "zero layers" (learnable normalization) achieved superior performance by separately encoding anatomical and metabolic features followed by attentive fusion [43]. This strategy balances the preservation of modality-specific information with the learning of cross-modal relationships, making it suitable for modalities with complementary but distinct information content.
The main challenges of intermediate fusion include designing effective feature alignment mechanisms and managing computational complexity, particularly with 3D volumetric data [43]. Successful implementation requires careful consideration of how and where to integrate features within the network architecture to maximize information retention while minimizing redundancy.
Late Fusion (Decision-Level Fusion)
Late fusion, or decision-level fusion, employs separate models for each modality and combines their predictions at the decision level [31] [41]. This approach maintains complete modality independence throughout the feature extraction and modeling phases, integrating information only after each modality-specific model has generated its predictions. Common fusion methods include averaging, weighted voting, or meta-learners that combine the predictions.
In oncology, late fusion has consistently demonstrated strong performance for survival prediction tasks. For breast cancer survival prediction using multi-omics and clinical data, late fusion models outperformed early fusion approaches across all modality combinations [41]. Similarly, in a comprehensive evaluation of multimodal survival prediction, late fusion provided higher accuracy and robustness compared to single-modality approaches [13]. The success of late fusion in these contexts stems from its resistance to overfitting—particularly important with high-dimensional omics data—and its ability to handle heterogeneous data types without requiring complex alignment [41] [13].
The primary limitation of late fusion is its inability to model cross-modal correlations during feature learning, potentially missing synergistic relationships between modalities [43]. However, for many oncology applications where modalities provide complementary but independent information, this approach offers practical advantages in implementation and robustness.
Hybrid Fusion
Hybrid fusion strategies combine elements of early, intermediate, and/or late fusion to leverage their respective strengths [31]. These approaches are architecturally complex but can capture cross-modal interactions at multiple levels of abstraction. Hybrid models typically employ custom-designed fusion blocks that integrate information flexibly based on the specific characteristics of each modality and the clinical task.
In breast cancer diagnosis, HXM-Net exemplifies hybrid fusion by combining CNN-based spatial feature extraction with Transformer-based fusion of B-mode and Doppler ultrasound images [5]. This architecture captures both local morphological patterns and global contextual relationships between modalities. Similarly, PADBSRNet integrates multiple attention mechanisms, bidirectional recurrent neural networks, and cross-connections for multi-cancer detection [44]. These sophisticated fusion schemes demonstrate the potential of hybrid approaches to outperform single-strategy methods across diverse oncology applications.
The main challenges of hybrid fusion include architectural complexity, extensive hyperparameter tuning, and computational intensiveness [31] [5]. However, for clinical applications where marginal performance improvements significantly impact patient outcomes, the investment in developing tailored hybrid approaches can be justified.
Experimental Protocols and Methodologies
Protocol 1: Late Fusion for Survival Prediction in Breast Cancer
This protocol outlines the methodology for implementing late fusion in breast cancer survival prediction, based on the approach that demonstrated superior performance in comparative studies [41].
Data Acquisition and Preprocessing
- Data Sources: Utilize The Cancer Genome Atlas (TCGA) breast cancer dataset, including clinical variables, somatic mutations, RNA expression, copy number variations, miRNA expression, and histopathology images [41].
- Clinical Data Preprocessing: Process demographic data (age at diagnosis, race), tumor subtype (PAM50, OncoTree), and pathological features (stage). Apply one-hot encoding to categorical variables and impute missing values [41].
- Omics Data Processing:
- Somatic SNVs: Convert to binary sample-by-gene matrix with 1% mutation frequency threshold.
- RNA-seq: Filter to cancer-related genes using CGN MSigDB gene set.
- CNV data: Normalize to range -2 to 2 and aggregate gene-level scores.
- miRNA: Retain features altered in at least 10% of cohort.
- Imaging Data Processing: Use CLAM pipeline for tissue segmentation and patch extraction from H&E-stained whole-slide images. Encode patches into 1024-dimensional feature vectors using pretrained deep neural networks [41].
- Data Splitting: Implement rigorous validation with fixed test set (20% of samples) and 5-fold cross-validation on remaining data, maintaining balanced outcome representation [41].
Model Architecture and Training
- Unimodal Base Models: Develop separate neural networks for each modality with optimized architectures:
- Clinical data: Fully connected network with appropriate input dimension.
- Omics data: Deep networks with regularization to handle high dimensionality.
- Imaging data: CNN-based architecture for feature extraction.
- Fusion Methodology: Implement late fusion by training unimodal models independently and combining predictions through weighted averaging or meta-learner.
- Training Protocol: Use discretized survival time as outcome variable. Minimize survival-specific loss function (e.g., negative log-likelihood of discrete survival model) with early stopping and cross-validation for hyperparameter optimization [41].
- Evaluation Metrics: Assess performance using concordance index (C-index) for survival prediction, with confidence intervals estimated across multiple validation folds [41].
Protocol 2: Intermediate Fusion for PET-CT Tumor Segmentation
This protocol details the anatomy-guided intermediate fusion approach for PET-CT segmentation, which achieved state-of-the-art performance in tumor delineation [43].
Data Preprocessing and Normalization
- Input Modalities: Co-registered PET and CT volumes in 3D.
- Zero Layers Implementation: Apply learnable normalization layers separately to each modality:
- Mathematical formulation: ( Norm (\text{M}) = \lambda{\text{M}} \cdot \left( \frac{P{\text{M}} - \mu (P{\text{M}})}{\sqrt{\sigma ^2(P{\text{M}}) + \epsilon }}\right) + \delta{\text{M}} )
- Where M denotes modality (PET or CT), (PM) is convolved input, (\lambdaM) and (\deltaM) are learnable parameters [43].
- Data Augmentation: Apply spatial transformations (rotation, flipping) and intensity variations to improve model robustness.
Network Architecture
- Encoder Streams: Implement parallel squeeze-and-excited (SE) encoders for PET and CT:
- Each encoder consists of convolutional layers with decreasing filters [128, 64, 32, 16].
- SE mechanism adaptively emphasizes important feature maps for each modality [43].
- Fusion Mechanism: Design anatomy-guided attention fusion module:
- Use CT anatomical features to guide the fusion with PET metabolic features.
- Implement attentive fusion to selectively combine features based on spatial importance.
- Decoder Design: Use shared decoder with skip connections from both modality encoders to preserve spatial details.
- Output Layer: Generate binary segmentation mask with sigmoid activation.
Training and Evaluation
- Loss Function: Combine Dice loss and cross-entropy for robust segmentation performance.
- Optimization: Use Adam optimizer with learning rate scheduling.
- Evaluation Metrics: Calculate Dice similarity coefficient and 95% Hausdorff distance (HD^95) for comprehensive segmentation assessment [43].
Protocol 3: Hybrid Fusion for Breast Cancer Diagnosis using Ultrasound
This protocol describes the HXM-Net architecture for multi-modal ultrasound fusion in breast cancer diagnosis [5].
Multi-modal Ultrasound Data Preparation
- Input Modalities: Collect B-mode ultrasound, color Doppler, and elastography images of breast lesions.
- Data Preprocessing:
- Resize images to uniform dimensions while maintaining aspect ratios.
- Apply normalization appropriate for each modality.
- Implement data augmentation (rotation, flipping, contrast adjustment) to address class imbalance.
- Data Partitioning: Split data into training, validation, and test sets with balanced representation of benign and malignant cases.
HXM-Net Architecture Implementation
- Feature Extraction Backbone: Use multi-stream CNN with modality-specific encoders:
- Each stream processes one ultrasound modality.
- Employ pre-trained CNN weights (transfer learning) for initialization.
- Transformer Fusion Module: Implement multi-head self-attention to fuse features across modalities:
- Mathematical formulation: ( Attention \left(Q,K,V\right)=softmax\left(\frac{Q{K}^{T}}{\sqrt{{d}_{k}}}\right) V )
- Where Q, K, V are query, key, and value matrices derived from modality features [5].
- Classification Head: Use fully connected layers with softmax activation for benign/malignant prediction.
Model Training and Interpretation
- Training Strategy: Employ staged training—first train modality-specific encoders, then joint training of full architecture.
- Explainability Implementation: Integrate Gradient-weighted Class Activation Mapping (Grad-CAM) to visualize regions influencing predictions.
- Performance Validation: Assess using comprehensive metrics: accuracy, sensitivity, specificity, F1-score, and AUC-ROC [5].
Visualization of Fusion Strategies
Fusion Strategies Workflow: Early, intermediate, and late fusion approaches for multimodal data integration in oncology.
PET-CT Intermediate Fusion: Anatomy-guided fusion with learnable normalization for tumor segmentation.
Research Reagent Solutions
Table 3: Essential Research Resources for Multimodal Fusion in Oncology
| Resource Category | Specific Tools/Platforms | Application in Multimodal Fusion | Key Features |
|---|---|---|---|
| Data Sources | The Cancer Genome Atlas (TCGA) [41] [13] | Provides matched multi-omics, clinical, and imaging data for model development | Standardized processing pipelines; large sample sizes; multiple cancer types |
| Medical Imaging Libraries | CLAM (Whole Slide Image Processing) [41] | Feature extraction from histopathology images for integration with other modalities | Patch-based processing; multiple backbone networks; attention mechanisms |
| Deep Learning Frameworks | MONAI (Medical Open Network for AI) [3] | Domain-specific tools for medical imaging integration in multimodal pipelines | Pre-trained models; specialized transforms; 3D network architectures |
| Fusion-Specific Architectures | HXM-Net (CNN-Transformer Hybrid) [5] | Reference implementation for multi-modal ultrasound fusion | Multi-stream design; attention mechanisms; explainability features |
| Survival Analysis Tools | PySurvival, Survival Python Libraries [41] [13] | Implementation of discrete survival models for outcome prediction | Handles censored data; multiple survival models; evaluation metrics |
The taxonomy of fusion strategies—early, intermediate, late, and hybrid—provides a systematic framework for designing multimodal AI systems in oncology. Each approach offers distinct advantages and limitations, with optimal selection dependent on data characteristics, clinical task, and computational resources. Late fusion demonstrates particular strength for survival prediction with high-dimensional omics data [41] [13], while intermediate fusion excels in medical imaging applications like PET-CT segmentation [43]. Hybrid approaches show promising results in diagnostic tasks using multi-modal ultrasound [5]. As multimodal AI continues to evolve, future research should address challenges in model interpretability, data harmonization, and clinical integration to realize the full potential of these fusion strategies in oncology research and practice.
Multi-modal data fusion represents a paradigm shift in cancer diagnostics, moving beyond the limitations of single-modality analysis. By integrating diverse data sources such as medical imaging, histopathology, genomics, and clinical records, deep learning models can capture a more holistic and complementary view of cancer's complexity [31] [45]. The success of these integrative approaches critically depends on the architectural frameworks used to process and combine heterogeneous data streams. This document provides detailed application notes and experimental protocols for three foundational deep learning architectures—Convolutional Neural Networks (CNNs), Transformers, and Autoencoders—in constructing robust multi-modal fusion systems for cancer diagnosis and research, with a particular emphasis on breast cancer applications.
Core Architectures in Multi-Modal Fusion
Convolutional Neural Networks (CNNs) excel at processing spatial data through hierarchical feature learning using convolutional layers, pooling operations, and non-linear activations. In multi-modal fusion, CNNs primarily extract localized patterns from imaging modalities such as mammograms, MRI, and histopathology slides [31] [46]. Their inductive biases for translation invariance and hierarchical composition make them particularly suited for medical image analysis.
Transformers utilize self-attention mechanisms to capture long-range dependencies and global context across sequential or structured data. Vision Transformers (ViTs) adapt this architecture for image data by treating patches as sequences, enabling them to model relationships across disparate image regions [46] [47]. In multi-modal contexts, transformers facilitate cross-modal attention, allowing features from one modality to influence the processing of another.
Autoencoders are unsupervised learning frameworks composed of an encoder that compresses input data into a latent representation and a decoder that reconstructs the original input from this representation. Masked Autoencoders (MAEs) have emerged as powerful self-supervised pre-training tools that learn robust representations by reconstructing randomly masked portions of input data [47]. These architectures are particularly valuable for modality-specific feature extraction and handling missing modalities in clinical settings.
Performance Comparison in Cancer Diagnostic Tasks
Table 1: Performance comparison of deep learning architectures in multi-modal cancer diagnosis
| Architecture | Primary Function | Modalities Supported | Reported Performance | Key Advantages |
|---|---|---|---|---|
| CNN-Based Hybrids | Spatial feature extraction from images | Mammography, MRI, Histopathology | 95.2% accuracy for subtype classification [46] | Excellent spatial feature extraction, parameter efficiency |
| Vision Transformers | Global context modeling | CT, MRI, Whole Slide Images | AUC 0.80 for immunotherapy response prediction [45] | Long-range dependency capture, superior global context |
| Masked Autoencoders | Self-supervised pre-training | CT, MRI, Clinical data | ~80% accuracy for cancer stage classification [47] | Reduces annotation requirements, robust representations |
| CNN-Transformer Hybrids | Joint spatial-temporal modeling | Mammography sequences, Clinical data | 14% ΔAUROC improvement over uni-modal baselines [20] [46] | Balances local features with global context |
Experimental Protocols for Multi-Modal Fusion
Protocol 1: Implementing a CNN-Transformer Hybrid for Breast Cancer Subclassification
Objective: Develop a hybrid architecture (TransBreastNet) for simultaneous breast cancer subtype classification and temporal lesion progression analysis [46].
Materials:
- Full-field digital mammogram (FFDM) sequences
- Clinical metadata (hormone receptor status, tumor size, genetic markers)
- Computational resources: GPU cluster with ≥16GB memory
Procedure:
- Data Preprocessing:
- Extract lesion regions using a pretrained CNN segmentation model
- Normalize pixel values to [0,1] range
- For longitudinal data, align temporal sequences by registration
Spatial Feature Extraction:
- Utilize a CNN backbone (ResNet-50) pretrained on ImageNet
- Extract multi-scale feature maps from the penultimate convolutional layer
- Apply Global Average Pooling to generate fixed-size feature vectors
Temporal Modeling:
- Split feature sequences into fixed-length patches (e.g., 16×16)
- Flatten patches and project to embedding space with positional encoding
- Process through standard Transformer encoder layers
- Use multi-head self-attention with 8 heads and hidden dimension of 512
Clinical Data Fusion:
- Encode categorical clinical variables using embedding layers
- Process continuous variables through fully connected layers
- Fuse image and clinical features via concatenation or cross-attention
Multi-Task Prediction:
- Implement dual classification heads for subtype and stage prediction
- Use cross-entropy loss with class weighting for imbalance
- Jointly optimize with AdamW (lr=1e-4, weight decay=1e-2)
Validation:
- Perform 5-fold cross-validation on internal datasets
- External validation on BreaKHis and INbreast datasets
- Compare against uni-modal baselines and ablation studies
Protocol 2: Longitudinal Multi-Modal Fusion for Therapy Response Prediction
Objective: Implement the Multi-modal Response Prediction (MRP) system for predicting pathological complete response (pCR) to neoadjuvant therapy in breast cancer [20].
Materials:
- Longitudinal MRI exams (Pre-, Mid-, and Post-NAT)
- Mammogram data
- Clinical variables (molecular subtype, TNM staging, patient demographics)
Procedure:
- Multi-Modal Data Preparation:
- For MRI: Extract subtracted contrast-enhanced T1-weighted sequences
- Apply N4 bias field correction and z-score normalization
- For clinical data: One-hot encode categorical variables, standardize continuous variables
Cross-Modal Knowledge Mining:
- Implement two independently trained models: iMGrhpc and iMRrhpc
- iMGrhpc processes Pre-NAT mammograms with clinical data
- iMRrhpc processes longitudinal MRI sequences with clinical data
- Apply cross-modal attention between imaging features and clinical variables
Temporal Information Embedding:
- Encode treatment timepoints as positional embeddings
- Use sinusoidal positional encoding with dimension 64
- Implement temporal self-attention across longitudinal sequences
Handling Missing Modalities:
- Apply modality dropout during training (probability=0.2)
- Implement cross-modal imputation using knowledge distillation
- Use mean teacher framework to maintain consistency
Fusion and Prediction:
- Combine predictions from iMGrhpc and iMRrhpc via weighted averaging
- Calibrate probabilities using temperature scaling
- Output pCR probability with confidence estimation
Validation:
- Multi-center validation across ≥3 independent institutions
- Reader studies comparing against radiologist performance
- Decision curve analysis for clinical utility assessment
Protocol 3: Self-Supervised Pre-training with Masked Autoencoders
Objective: Leverage Masked Autoencoders (MAEs) for self-supervised pre-training on unannotated medical images to improve downstream cancer staging performance [47].
Materials:
- Unannotated CT or MRI scans (≥10,000 slices recommended)
- Target annotated dataset for fine-tuning
- Vision Transformer backbone (ViT-Base or larger)
Procedure:
- Data Preprocessing for MAE:
- Resize images to uniform resolution (e.g., 224×224 or 384×384)
- Normalize intensity values per dataset statistics
- Apply random augmentation: rotation, flipping, color jitter
Masking Strategy:
- Divide images into regular non-overlapping patches (e.g., 16×16)
- Apply random masking with 75-80% masking ratio
- Use uniform random masking strategy
MAE Architecture Configuration:
- Encoder: Vision Transformer processing visible patches only
- Decoder: Lightweight transformer for reconstruction
- Reconstruction target: normalized pixel values
Pre-training Protocol:
- Optimize using AdamW (lr=1.5e-4, β1=0.9, β2=0.95)
- Batch size: 2048 (distributed across GPUs)
- Training epochs: 800 with cosine learning rate decay
- Weight decay: 0.05 with gradient clipping
Fine-tuning for Downstream Tasks:
- Initialize target model with pre-trained encoder weights
- Add task-specific head (classification, segmentation)
- Fine-tune with lower learning rate (5e-5) and linear warmup
- Apply gradual unfreezing strategy
Validation:
- Linear probing on target datasets
- Few-shot learning evaluation (1%, 10% data regimes)
- Transfer learning across different cancer types and imaging modalities
Visualizing Multi-Modal Fusion Architectures
Diagram 1: Multi-modal fusion architecture integrating CNNs, Transformers, and Autoencoders for cancer diagnosis.
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential research reagents and computational tools for multi-modal cancer research
| Category | Specific Tool/Resource | Function | Application Example |
|---|---|---|---|
| Deep Learning Frameworks | PyTorch, TensorFlow | Model development and training | Implementing custom fusion architectures [46] |
| Vision Transformer Models | ViT, DeiT, BEiT, DINO | Image classification and feature extraction | Self-supervised pre-training on medical images [47] |
| CNN Backbones | ResNet, VGG, EfficientNet | Spatial feature extraction | Lesion characterization in mammograms [46] |
| Multi-Modal Datasets | TCGA, I-SPY2, Internal institutional datasets | Model training and validation | Breast cancer subtype classification [20] [16] |
| Attention Mechanisms | Cross-attention, CBAM, BAM | Feature refinement and fusion | Focusing on diagnostically relevant regions [47] |
| Explainability Tools | Grad-CAM, SHAP, LIME | Model interpretation and validation | Identifying decision-relevant features [45] [48] |
| Data Harmonization | Nested ComBat, batch correction | Multi-site data integration | Reducing scanner and protocol variability [45] |
The strategic integration of CNNs, Transformers, and Autoencoders provides a powerful foundation for advancing multi-modal cancer diagnostics. CNN architectures deliver robust spatial feature extraction from medical images, while Transformers enable effective modeling of long-range dependencies and cross-modal interactions. Autoencoders, particularly in self-supervised configurations, address critical challenges of data scarcity and missing modalities commonly encountered in clinical practice. The experimental protocols outlined herein provide reproducible methodologies for implementing these architectures in cancer diagnostic pipelines, with demonstrated efficacy in breast cancer subtype classification, therapy response prediction, and tumor staging. As the field evolves, future research directions should prioritize adaptive fusion strategies, enhanced explainability, and robust validation across diverse patient populations and clinical settings.
The integration of multimodal data represents a frontier in oncology, aiming to capture the complex molecular, morphological, and spatial heterogeneity of cancer. Traditional unimodal deep learning approaches often fail to fully leverage the complementary information available from disparate data sources such as histopathology, genomics, and clinical metadata. The Mixture-of-Experts (MoE) paradigm and Foundation Models (FMs) are emerging as two powerful architectures that address key limitations in multimodal data fusion for cancer diagnosis and research. MoE architectures dynamically route inputs to specialized neural network "experts," enabling more nuanced and sample-specific integration of multimodal data. Concurrently, large-scale FMs, pre-trained on vast datasets, provide a robust foundational representation that can be adapted for various downstream oncology tasks with limited task-specific labeling. This application note details the experimental protocols, performance benchmarks, and practical implementation guidelines for deploying these advanced fusion paradigms to advance precision oncology.
Application Notes & Experimental Protocols
Mixture-of-Experts for Adaptive Multimodal Fusion
The core principle of the MoE architecture is to replace a monolithic neural network with a set of specialized sub-networks (experts) and a gating network that dynamically weights their contributions for each input sample. This is particularly powerful in oncology, where the diagnostic relevance of different data modalities (e.g., imaging vs. genomics) can vary significantly between patients.
Protocol 1: Implementing an MoE Fusion Module for Cancer Diagnosis
- Aim: To adaptively fuse image and clinical metadata for cancer subtype classification.
- Background: Standard fusion methods like concatenation or averaging treat all samples and modalities with a fixed strategy. An MoE module personalizes fusion by selecting the most relevant experts based on individual patient characteristics [49].
- Materials:
- Software: Python 3.8+, PyTorch or TensorFlow.
- Data: Paired diagnostic images (e.g., Whole Slide Images or mammography) and clinical metadata (e.g., age, sex, anatomical site).
- Procedure:
- Feature Extraction:
- Process images through a pre-trained convolutional neural network (CNN) to extract a feature embedding vector.
- Process clinical metadata through a dense feed-forward network to obtain a metadata embedding vector.
- Expert Specialization:
- Instantiate
Nexpert networks. Each expert is a separate neural network (e.g., a multi-layer perceptron) that takes the concatenated image and metadata features as input. - In practice, experts can be encouraged to specialize implicitly through training, or explicitly by designing them for specific data types (e.g., image-centric vs. metadata-centric experts).
- Instantiate
- Gating Network:
- Implement a gating network that takes the metadata embedding as input. The choice of input is critical; patient metadata often provides a strong prior for determining the optimal fusion strategy [49].
- The gating network outputs a probability distribution over the
Nexperts (e.g., using a Softmax output layer).
- Final Fusion and Prediction:
- For a given input, the final fused representation is computed as the weighted sum of the outputs of all experts, where the weights are the probabilities from the gating network.
- Formula:
Final_Output = Σ (Gating_Probability_i * Expert_i_Output) - The final output is passed to a classification or regression head for diagnosis or survival prediction.
- Feature Extraction:
- Validation: Perform ablation studies comparing the MoE fusion against static fusion baselines. Evaluate metrics like accuracy, precision, and F1-score across different patient subgroups to verify that the model adapts effectively [49].
Table 1: Key Research Reagent Solutions for MoE Implementation
| Item Name | Function / Description | Example / Application Context |
|---|---|---|
| Gating Network | Dynamically computes weights for each expert based on the input sample. | A shallow neural network taking clinical metadata as input to personalize fusion [49]. |
| Specialized Experts | Set of sub-networks, each potentially specializing in a data pattern or modality. | Separate experts for image-dominant, metadata-dominant, or balanced diagnostic cases [49]. |
| Top-K Routing | Computational optimization that only activates the top K experts for each input. | Reduces computational cost during training and inference in large MoE systems. |
| Auxiliary Loss | A regularization loss that encourages load balancing across experts. | Prevents model collapse where the gating network favors only a few experts. |
Leveraging Foundation Models for Multimodal Oncology
Foundation Models are pre-trained on broad data at scale and can be adapted to a wide range of downstream tasks. In oncology, FMs like the Segment Anything Model (SAM) and large-scale vision transformers (ViTs) are reducing the dependency on large, annotated datasets.
Protocol 2: Unsupervised Prompting of SAM for Lesion Localization
- Aim: To generate precise lesion segmentation masks without manual pixel-level annotations.
- Background: SAM is a powerful foundation model for segmentation but requires manual prompts. This protocol automates prompt generation to leverage SAM's generalization for medical images [49].
- Materials:
- Software: Python, the SAM library (e.g.,
segment-anything), OpenCV. - Model: Pre-trained SAM model (e.g.,
vit_hcheckpoint).
- Software: Python, the SAM library (e.g.,
- Procedure:
- Dual Cross-Validation:
- Train an initial segmentation model on a public medical imaging dataset (e.g., a skin lesion dataset) to generate preliminary lesion masks.
- A second, independent model is trained to validate the first model's outputs, creating a set of high-confidence pseudo-labels.
- Automatic Prompt Generation:
- From the high-confidence pseudo-labels, derive prompts for SAM. These can be:
- Point Prompts: The centroid of the segmented lesion.
- Bounding Box Prompts: The bounding box enclosing the lesion.
- From the high-confidence pseudo-labels, derive prompts for SAM. These can be:
- SAM Inference:
- Feed the original image and the automatically generated prompts into SAM.
- SAM produces a refined, high-quality segmentation mask.
- Dual Cross-Validation:
- Validation: Compare the SAM-generated masks against a held-out test set with manual annotations using Dice coefficient and Intersection-over-Union (IoU) metrics. The unsupervised SAM-guided approach has been shown to achieve state-of-the-art performance, closely matching fully supervised methods [49].
Protocol 3: Vision Transformer (ViT) for Global Context in Survival Prediction
- Aim: To extract rich, global feature representations from histopathological whole-slide images (WSIs) for survival prediction.
- Background: CNNs have limited receptive fields. Vision Transformers, a class of FMs, model long-range dependencies across the entire tissue section, capturing crucial global context [50].
- Materials:
- Software: Python, PyTorch, Hugging Face
transformerslibrary. - Model: Pre-trained ViT model (e.g., DINOv2, Swin Transformer).
- Software: Python, PyTorch, Hugging Face
- Procedure:
- Patch Extraction and Embedding:
- Divide a WSI into smaller, non-overlapping patches (e.g., 256x256 pixels).
- Pass each patch through the pre-trained ViT to extract a feature vector. The Swin Transformer is often preferred for its hierarchical structure and efficiency with high-resolution images [50].
- Multimodal Fusion with Genomics:
- Use the genomic data (e.g., gene expression) as a query in a cross-attention mechanism to interact with the set of ViT patch features.
- This "early fusion" allows the model to learn the interaction between the morphological patterns in the image and the molecular genomic profile [50].
- Uncertainty Estimation with Evidence Theory:
- To address modal uncertainty, parameterize the class probability distribution using the fused features.
- Apply Dempster-Shafer Theory (DST) to dynamically weight the contributions of each modality based on the estimated evidence and uncertainty, leading to more reliable survival predictions [50].
- Patch Extraction and Embedding:
Integrated Workflow Diagram
The following diagram illustrates a unified experimental workflow combining MoE and Foundation Models for multimodal cancer data analysis.
Diagram 1: Integrated MoE and Foundation Model workflow for multimodal cancer data analysis.
Performance Benchmarking
Empirical evaluations demonstrate the superior performance of advanced fusion paradigms over traditional methods across various cancer types and tasks.
Table 2: Quantitative Performance of MoE and Foundation Models in Oncology Tasks
| Model / Framework | Cancer Type | Data Modalities | Key Performance Metric | Result | vs. Baseline |
|---|---|---|---|---|---|
| UnSAM-MoME [49] | Skin Cancer (ISIC) | Dermoscopy, Clinical Metadata | Accuracy | State-of-the-art | Significant improvement |
| UnSAM-MoME [49] | Breast Cancer (InBreast) | Mammography, Clinical Metadata | Accuracy | State-of-the-art | Significant improvement |
| Pathomic Fusion [51] | Glioma, Renal Cell Carcinoma | Histology, Genomics (Mutation, CNV, RNA-Seq) | C-Index (Survival) | Outperformed unimodal and late fusion | Improvement over grading/subtyping |
| M²EF-NNs [50] | Multiple Cancers (TCGA) | Histology (ViT), Genomics | C-Index, AUC | Significant improvement | Outperformed CNNs and non-evidence fusion |
| CSM-FusionNet [52] | Hepatocellular Carcinoma | Ultrasound (Multi-network) | Detection Accuracy | 95.56% | Increased from 56.11% (baseline) |
| AZ-AI Pipeline (Late Fusion) [13] | Pan-Cancer (TCGA) | Transcripts, Proteins, Metabolites, Clinical | C-Index (Survival) | Consistently superior | Outperformed single-modality and early fusion |
The Scientist's Toolkit
Table 3: Essential Research Reagents and Computational Tools
| Category | Item | Specification / Purpose |
|---|---|---|
| Foundation Models | Segment Anything Model (SAM) | For unsupervised or prompt-based lesion segmentation in medical images [49]. |
| Vision Transformer (ViT/Swin) | For extracting global contextual features from histopathology or radiology images [50]. | |
| Data Resources | The Cancer Genome Atlas (TCGA) | Provides paired multi-omics, histopathology images, and clinical data for model training [51] [13]. |
| Genomic Data Commons (GDC) | Central repository for standardized cancer genomic datasets [10]. | |
| Software & Libraries | MONAI (Medical Open Network for AI) | PyTorch-based framework providing pre-trained models and tools for medical imaging AI [3]. |
| AstraZeneca-AI (AZ-AI) Pipeline | Python library for multimodal feature integration and survival prediction, supporting various fusion strategies [13]. | |
| Fusion Techniques | Kronecker Product Fusion | Models pairwise feature interactions across modalities for tight integration [51]. |
| Dempster-Shafer Evidence Theory | Dynamically models uncertainty and adjusts modality weights for more reliable fusion [50]. |
The complex heterogeneity of solid tumors means that predictive models relying on a single data modality often fail to capture the complete biological picture, limiting their diagnostic accuracy and clinical utility [3]. Multimodal Artificial Intelligence (MMAI) addresses this fundamental limitation by integrating diverse diagnostic data streams—including histopathology, medical imaging, genomic profiling, and clinical records—into unified analytical frameworks [3] [1]. This synthesis converts multimodal complexity into clinically actionable insights, enabling more accurate detection, classification, and prognostic assessment of solid tumors [53]. The transition from unimodal to multimodal analysis represents a paradigm shift in oncological diagnostics, enabling a more comprehensive understanding of tumor biology that directly supports the advancement of precision medicine [54].
Performance of Multimodal AI in Solid Tumor Diagnosis
Multimodal AI approaches have demonstrated superior performance compared to traditional single-modality methods across various cancer types and clinical tasks. The quantitative evidence summarized in the tables below highlights the diagnostic and prognostic value of MMAI in oncology.
Table 1: Performance of MMAI in Tumor Diagnosis and Classification
| Cancer Type | MMAI Approach | Data Modalities Integrated | Performance | Clinical Application |
|---|---|---|---|---|
| Breast Cancer | Deep learning fusion model [55] | Pathology images, lncRNA data, immune-cell scores, clinical information | Superior prognostic performance vs. unimodal models | Prognostic prediction & immunotherapy candidate identification [56] |
| Breast Cancer | AI-based risk stratification [3] | Clinical metadata, mammography, trimodal ultrasound | Similar or better than pathologist-level assessment | Breast cancer risk prediction [3] |
| Multiple Solid Tumors | Digital pathology classifier [3] | Histology slides (with genomic correlation) | 96.3% sensitivity, 93.3% specificity | Tumor-type classification [3] |
| Glioma & Renal Cell Carcinoma | Pathomic Fusion [3] | Histology, genomics | Outperformed WHO 2021 classification | Risk stratification [3] |
| NSCLC | Multimodal predictor [53] | CT scans, immunohistochemistry slides, genomic alterations | Improved prediction of anti-PD-1/PD-L1 response | Immunotherapy response prediction [53] |
Table 2: MMAI for Survival and Treatment Response Prediction
| Cancer Type | MMAI Model/Platform | Data Modalities | Key Outcome | Performance Metrics |
|---|---|---|---|---|
| Pan-Cancer (15,726 patients) | Explainable AI with multimodal real-world data [3] | Multimodal real-world data | Identified 114 key prognostic markers across 38 solid tumors | Validated in external lung cancer cohort [3] |
| Metastatic NSCLC | TRIDENT machine learning model [3] | Radiomics, digital pathology, genomics | Identified patient subgroup with optimal treatment benefit | HR reduction: 0.88-0.56 (non-squamous) [3] |
| Melanoma | MUSK (Transformer-based) [3] | Not specified | Improved accuracy for relapse and immunotherapy response | ROC-AUC 0.833 for 5-year relapse prediction [3] |
| Lung, Breast, Pan-Cancer | Late Fusion Models [13] | Transcripts, proteins, metabolites, clinical factors | Consistently outperformed single-modality approaches | Higher accuracy and robustness in survival prediction [13] |
| Prostate Cancer | MMAI patient stratification [3] | Data from five Phase 3 trials | Predicted long-term clinically relevant outcomes | 9.2–14.6% improvement vs. NCCN risk stratification [3] |
Experimental Protocols for Multimodal Integration
Protocol 1: Late-Fusion Survival Prediction Pipeline
This protocol outlines the methodology for integrating multi-omics data to predict overall survival in cancer patients, based on the AstraZeneca-AI multimodal pipeline [13].
1. Data Acquisition and Preprocessing
- Obtain multi-omics datasets from sources such as The Cancer Genome Atlas (TCGA), including transcriptomic, proteomic, metabolomic, and clinical data [13].
- Perform modality-specific preprocessing: normalize gene expression data using DESeq2 or EdgeR, impute missing clinical values using appropriate statistical methods, and apply batch effect correction where necessary [13] [1].
- Address data heterogeneity by ensuring consistent patient identifiers across modalities and aligning samples.
2. Feature Selection and Dimensionality Reduction
- Apply supervised feature selection methods to handle high-dimensional data. Use Spearman correlation for nonlinear relationships or Pearson correlation for linear associations with overall survival [13].
- Employ information-theoretic approaches to identify features most relevant to survival outcomes.
- Apply principal component analysis (PCA) to genomic data to capture primary axes of variation [1].
- Generate predefined gene signatures (e.g., PAM50 for breast cancer) associated with specific biological states or clinical phenotypes [1].
3. Model Training with Late Fusion
- Train separate predictive models for each data modality using survival modeling approaches such as gradient boosting or random forests, which have demonstrated success with multi-omics tabular data [13].
- Combine modality-specific predictions using late fusion strategies, such as weighted averaging or meta-learners, to generate a final survival prediction [13].
- Implement rigorous cross-validation with multiple training-test splits to account for uncertainty and avoid overfitting, which is critical with low sample-size-to-feature ratios [13].
4. Model Evaluation and Interpretation
- Evaluate model performance using concordance index (C-index) for survival prediction with confidence intervals reported over multiple data splits [13].
- Compare multimodal models against unimodal benchmarks to validate the added value of integration.
- Employ explainable AI techniques to interpret model predictions and identify key biomarkers contributing to survival outcomes [3].
Protocol 2: Deep Learning for Multimodal Breast Cancer Subtyping
This protocol details the methodology for developing deep learning models that integrate pathological images, genomic data, and clinical information for breast cancer classification and prognostication [56] [55].
1. Data Preparation and Feature Extraction
- Collect whole-slide histopathology images, genomic data (e.g., lncRNA expression), immune-cell scores, and clinical information [56].
- For image data: extract regions of interest (ROI) and apply data augmentation techniques to address limited dataset sizes [55].
- For genomic data: process lncRNA expression data using unsupervised clustering to identify distinct expression patterns associated with treatment response [56].
- Calculate immune-cell scores using single-sample gene set enrichment analysis (ssGSEA) to quantify tumor microenvironment composition [56].
2. Deep Learning Model Architecture
- Implement a convolutional neural network (CNN) with a modified ResNet50 architecture and attention-gated mechanisms for pathology image analysis [56].
- Train the CNN to predict immune-metabolic subtypes directly from histopathology slides.
- For genomic data, employ deep neural networks to extract meaningful features from lncRNA expression and immune-cell scores [56] [55].
3. Multimodal Fusion and Classification
- Develop a multimodal fusion model (e.g., DeepClinMed-PGM) that integrates features from all modalities [56].
- Apply feature-level fusion to combine deep learning-derived features from different data sources.
- Use the fused representation to predict breast cancer subtypes (e.g., immune-active, immune-exclusion, immune-dysfunctional, immune-desert) and prognostic outcomes [56].
4. Validation and Clinical Application
- Validate model performance using independent datasets from multiple institutions [56].
- Assess the model's ability to predict immunotherapy response based on the identified subtypes.
- Perform gene set enrichment analysis (GSEA) to uncover metabolic pathways (fatty acid, amino acid, glucose, folate metabolism) associated with each subtype [56].
Technical Implementation of Multimodal Fusion
Fusion Strategies for Multimodal Data
The successful integration of heterogeneous data modalities requires careful selection of fusion strategies, each with distinct advantages and limitations.
Feature-Level Fusion (Early Fusion)
- This approach combines raw data or extracted features from different modalities before model training [55].
- Advantages: Preserves correlations between modalities; allows for complex cross-modal interactions [55].
- Challenges: Requires data alignment; susceptible to overfitting with high-dimensional data [13].
- Applications: Particularly effective when modalities have similar dimensionalities and sufficient sample sizes [13].
Decision-Level Fusion (Late Fusion)
- This method trains separate models for each modality and combines their predictions [13] [55].
- Advantages: Resistant to overfitting; naturally handles data heterogeneity; allows modality-specific weighting [13].
- Applications: Particularly effective for multi-omics data with low sample-size-to-feature ratios, as demonstrated in TCGA analysis [13].
Hybrid Fusion
- This strategy combines elements of both feature-level and decision-level fusion for increased flexibility [55].
- Advantages: Captures both intermediate and final decision-level interactions; adaptable to specific data characteristics [55].
- Applications: Emerging as a promising approach for complex multimodal tasks in medical imaging and genomics [55].
Research Reagent Solutions for Multimodal Oncology Research
Table 3: Essential Research Reagents and Platforms for Multimodal Cancer Studies
| Category | Specific Tools/Platforms | Primary Function | Application in MMAI |
|---|---|---|---|
| Genomic Analysis | GATK [1], MuTect [1], VarScan [1] | Detection of mutations and structural variants | Genomic feature extraction for integration with other modalities |
| Transcriptomic Analysis | DESeq2 [1], EdgeR [1] | Quantification of gene expression and differential expression | Identification of expression patterns associated with tumor subtypes |
| Pathway Analysis | KEGG [1], Reactome [1] | Mapping gene expression changes to biological pathways | Functional interpretation of multimodal findings |
| Single-Cell & Spatial Technologies | 10x Genomics Visium [1], scRNA-seq [1] | High-resolution analysis of tumor heterogeneity | Characterization of tumor microenvironment for multimodal integration |
| AI Frameworks | MONAI (Medical Open Network for AI) [3], PyTorch [3] | Pre-trained models and tools for medical AI | Development of multimodal fusion architectures |
| Multimodal Pipelines | AstraZeneca-AI Multimodal Pipeline [13] | Preprocessing, feature integration, and survival modeling | Benchmarking and implementation of multimodal fusion strategies |
Multimodal AI represents a transformative approach to solid tumor diagnosis, enabling a comprehensive understanding of cancer biology that transcends the limitations of single-modality analysis. By integrating diverse data streams—including medical imaging, genomic profiling, digital pathology, and clinical information—MMAI models achieve superior performance in tumor classification, risk stratification, and outcome prediction [3] [13]. The experimental protocols and technical implementations outlined in this document provide researchers with practical frameworks for developing and validating multimodal approaches in oncological research. As the field advances, addressing challenges related to data standardization, computational infrastructure, and model interpretability will be crucial for translating multimodal AI from research environments into routine clinical practice, ultimately advancing the goals of precision oncology and personalized cancer care [54] [53].
Technological advancements of the past decade have transformed cancer research, significantly improving patient survival predictions through high-throughput genotyping and multimodal data analysis [13]. Comprehensive integrated analysis of multi-omics data enables discovery of the complex mechanisms underlying cancer development and progression [13]. Training predictive models using complementary information from multiple sources—including genomic, transcriptomic, proteomic, clinical, and imaging data—leads to substantially improved model predictions and more robust clinical decision-making tools [13]. This document provides detailed application notes and experimental protocols for implementing multimodal data fusion approaches in cancer prognosis, specifically focusing on predicting treatment response and survival outcomes.
Performance Comparison of Machine Learning Algorithms in Ovarian Cancer
Table 1: Performance metrics of machine learning and radiomics models for predicting treatment response and survival in ovarian cancer, synthesized from a systematic review of 13 studies [57].
| Prediction Task | Number of Studies | Common Algorithms | Median AUC | Median Accuracy | Performance Notes |
|---|---|---|---|---|---|
| Response to Neoadjuvant Chemotherapy | 7 | Random Forest, Neural Networks, Support Vector Machines | 0.77 (Range: 0.72-0.93) | 73% (Range: 66-98%) | Higher performance than traditional statistics |
| Optimal/Complete Cytoreduction | 6 | Random Forest, Neural Networks, Support Vector Machines | 0.82 (Range: 0.77-0.89) | 73% (Range: 66-98%) | Assists surgical decision-making |
| 5-Year Survival | 1 | XGBoost vs. Linear Regression | Not Reported | XGBoost: 80.9%, Linear Regression: 79% | XGBoost outperformed linear regression |
| 12-Month Progression-Free Survival | 1 | Random Forest vs. Linear Regression | Not Reported | Random Forest: 93.7%, Linear Regression: 82% | Superior performance in platinum-resistant setting |
Multimodal Data Fusion Performance Across Cancer Types
Table 2: Performance improvements of multimodal fusion models over unimodal approaches for survival prediction across different cancer datasets, as reported in large-scale studies [13] [58].
| Model Type | Cancer Type/Dataset | Key Data Modalities | Performance (C-index) | Improvement Over Unimodal |
|---|---|---|---|---|
| Late Fusion Model | TCGA Lung Cancer | Transcripts, Proteins, Metabolites, Clinical | Details in [13] | Consistent outperformance |
| Late Fusion Model | TCGA Breast Cancer | Transcripts, Proteins, Metabolites, Clinical | Details in [13] | Consistent outperformance |
| Late Fusion Model | TCGA Pan-Cancer | Transcripts, Proteins, Metabolites, Clinical | Details in [13] | Consistent outperformance |
| MICE Foundation Model | Pan-Cancer (30 types) | Pathology Images, Clinical Reports, Genomics | 3.8% to 11.2% improvement on internal cohorts | Substantial improvement in generalizability |
| MICE Foundation Model | Independent Cohorts | Pathology Images, Clinical Reports, Genomics | 5.8% to 8.8% improvement on external cohorts | Enhanced data efficiency |
Experimental Protocols
Protocol: Multimodal Data Fusion Pipeline for Survival Prediction
This protocol outlines the procedure for implementing the AZ-AI multimodal pipeline for survival prediction in cancer patients, adapted from the AstraZeneca Oncology Data Science Team [13].
Materials and Equipment
- Hardware: High-performance computing cluster with minimum 64GB RAM
- Software: Python 3.8+, AZ-AI Multimodal Pipeline library
- Data: Multi-omics data (transcripts, proteins, metabolites) and clinical data from sources like TCGA
Procedure
Data Preprocessing and Imputation
- Load multimodal datasets (transcripts, proteins, metabolites, clinical factors)
- Apply appropriate preprocessing for each modality:
- Perform batch normalization for gene expression data
- Address high degrees of missingness in clinical data using pipeline imputation options
- Handle sparsity of signal in mutation data
- Validate data integrity across modalities
Dimensionality Reduction
- Apply feature selection methods to handle high-dimensional data:
- Utilize linear (Pearson correlation) or monotonic (Spearman correlation) feature selection methods
- Select top features based on correlation with overall survival time
- Adjust parameters to manage low sample size to feature space ratios
- Apply feature selection methods to handle high-dimensional data:
Modality Integration via Late Fusion
- Implement late fusion strategy (prediction-level fusion):
- Train separate survival models for each data modality
- Combine predictions from each modality using weighted averaging
- Optimize weights based on modality informativeness
- Implement late fusion strategy (prediction-level fusion):
Survival Model Training
- Configure ensemble survival models (gradient boosting or random forests)
- Set training parameters with 5-fold cross-validation
- Train models using overall survival as the primary endpoint
Model Evaluation
- Evaluate model performance using C-index with confidence intervals
- Compare against unimodal approaches across multiple training-test splits
- Perform statistical significance testing on performance differences
Timing
- Complete procedure requires approximately 72 hours for a typical TCGA dataset
- Dimensionality reduction: 8-12 hours
- Model training and validation: 48-60 hours
Protocol: MICE Foundation Model for Pan-Cancer Prognosis
This protocol details the methodology for implementing the Multimodal data Integration via Collaborative Experts (MICE) foundation model for pan-cancer prognosis prediction [58].
Materials and Equipment
- Hardware: GPU-accelerated computing environment (NVIDIA A100 or equivalent)
- Software: PyTorch or TensorFlow deep learning frameworks
- Data: Curated multimodal dataset from 11,799 patients across 30 cancer types
Procedure
Multimodal Data Preparation
- Collect and align three data modalities:
- Histopathology whole slide images
- Clinical reports and structured electronic health record data
- Genomic profiling data (mutations, copy number variations)
- Implement data harmonization across different cancer types
- Collect and align three data modalities:
Model Architecture Configuration
- Initialize MICE framework with multiple functionally diverse experts:
- Configure cross-cancer experts to capture pan-cancer patterns
- Configure cancer-specific experts to capture type-specific insights
- Implement collaborative learning between expert modules
- Initialize MICE framework with multiple functionally diverse experts:
Multi-Task Learning Optimization
- Couple contrastive learning with supervised learning:
- Apply contrastive learning to enhance representation learning
- Implement supervised learning for direct survival prediction
- Balance loss functions between multiple objectives
- Couple contrastive learning with supervised learning:
Training and Validation
- Train model on multi-institutional dataset
- Validate on held-out internal cohorts
- Test generalizability on independent external cohorts
Data Efficiency Assessment
- Evaluate model performance with progressively reduced training data
- Measure C-index degradation compared to baseline models
- Establish minimum data requirements for clinical application
Timing
- Model training requires approximately 1-2 weeks depending on dataset size
- Data preparation and preprocessing: 3-5 days
- Model validation and testing: 2-3 days
Workflow Visualizations
Multimodal Data Fusion Strategy Workflow
MICE Foundation Model Architecture
Research Reagent Solutions
Table 3: Essential research reagents, computational tools, and datasets for implementing multimodal data fusion in cancer prognosis research.
| Category | Item | Specification/Version | Function/Purpose |
|---|---|---|---|
| Computational Libraries | AZ-AI Multimodal Pipeline | Python Library | Comprehensive pipeline for multimodal feature integration and survival prediction [13] |
| XGBoost | Gradient Boosting Framework | Ensemble survival modeling for tabular multi-omics data [57] | |
| Random Forest | Ensemble Algorithm | Robust survival prediction handling high-dimensional data [57] | |
| Data Resources | The Cancer Genome Atlas (TCGA) | Multi-omics Dataset | Primary data source containing transcripts, proteins, metabolites, and clinical data [13] |
| Curated Pan-Cancer Dataset | 11,799 patients, 30 cancer types | Training and validation data for foundation models [58] | |
| Feature Selection Tools | Pearson Correlation | Linear Correlation Method | Feature selection for modalities with linear relationships to survival [13] |
| Spearman Correlation | Monotonic Correlation Method | Feature selection for modalities with nonlinear but monotonic relationships [13] | |
| Model Evaluation Metrics | Concordance Index (C-index) | Survival Model Metric | Primary performance metric for survival prediction models [13] [58] |
| Area Under Curve (AUC) | Classification Metric | Performance assessment for treatment response prediction [57] |
The discovery of predictive molecular signatures is fundamental to advancing precision oncology. Traditional approaches, which often rely on a single data type (e.g., genomics alone), offer a limited view of cancer's profound heterogeneity. Consequently, they may lack the robustness required for accurate prognosis and treatment selection. The integration, or fusion, of multiple data modalities—including molecular, histopathological, radiological, and clinical information—provides a synergistic and more comprehensive profile of a tumor. This multimodal data fusion paradigm captures complementary biological signals, enabling the identification of more reliable and powerful predictive biomarkers that can accurately stratify patients and forecast therapeutic responses [59] [10] [60]. This Application Note provides a detailed protocol for implementing a multimodal fusion approach to discover and validate predictive molecular signatures for cancer patient survival.
The following table summarizes the key data modalities utilized in modern multimodal biomarker discovery, their content, and their specific value in creating a holistic cancer profile.
Table 1: Summary of Key Data Modalities in Cancer Biomarker Discovery
| Data Modality | Example Data Types | Biological/Clinical Insight Provided | Role in Predictive Signature |
|---|---|---|---|
| Molecular Data [10] [13] | Genomics (DNA mutations), Transcriptomics (RNA expression), Proteomics, Metabolomics | Driver mutations, gene expression programs, protein signaling pathways, metabolic activity | Reveals fundamental molecular mechanisms of oncogenesis, progression, and potential drug targets. |
| Digital Pathology [10] [60] | Whole Slide Images (WSIs), Pathomics features | Tissue architecture, cellular morphology, tumor microenvironment (TME), spatial heterogeneity | Provides contextual information on tumor structure and immune cell infiltration, complementing molecular findings. |
| Radiographic Images [10] [60] | CT, MRI, PET scans, Radiomics features | 3D tumor morphology, lesion location, texture, and heterogeneity beyond visual perception | Offers non-invasive, longitudinal monitoring capability and captures intra-tumoral variation. |
| Clinical Records [10] [13] | Electronic Health Records (EHR), Patient demographics, Treatment history, Lab values | Patient overall health, comorbidities, prior treatment responses, performance status | Informs on clinical context, enabling the adjustment of predictions based on patient-specific factors. |
Experimental Protocol: A Machine Learning Pipeline for Multimodal Fusion
This protocol outlines a robust computational pipeline for integrating multimodal data to predict patient overall survival (OS), based on established frameworks applied to datasets like The Cancer Genome Atlas (TCGA) [13].
Data Acquisition and Preprocessing
- Data Collection: Assemble patient cohorts with matched data across multiple modalities. Public resources like TCGA provide curated datasets encompassing transcripts, proteins, metabolites, and clinical data [13].
- Molecular Data Preprocessing:
- Genomics/Transcriptomics: Perform standard normalization (e.g., TPM for RNA-Seq, VAF for mutations), batch effect correction, and gene annotation.
- Missing Data Imputation: Apply appropriate imputation methods (e.g., k-nearest neighbors, multivariate imputation) for missing clinical or molecular data points [13].
- Image Data Preprocessing:
- Digital Pathology: Utilize whole slide images (WSIs). Employ deep learning models (e.g., Convolutional Neural Networks or Vision Transformers) for automated feature extraction from tissue regions [10] [60].
- Radiology: Extract radiomic features from tumor volumes segmented on CT or MRI scans. Alternatively, use deep learning for end-to-end feature learning from image patches [10].
- Data Partitioning: Split the complete dataset into training, validation, and hold-out test sets (e.g., 70/15/15), ensuring stratification by the event of interest (e.g., death) to preserve outcome distribution.
Dimensionality Reduction and Feature Selection
Given the high dimensionality of omics data, feature reduction is critical to avoid overfitting.
- Per-Modality Processing: Apply feature selection methods independently to each data modality.
- Selection Techniques: Use linear (Pearson correlation) or monotonic (Spearman correlation) methods due to their performance in high-dimensional, low-sample-size settings [13]. For survival outcomes, univariate Cox regression can also be used.
- Feature Extraction: Alternatively, employ unsupervised methods like Principal Component Analysis (PCA) or autoencoders to create a lower-dimensional representation of the original features [13].
Multimodal Data Fusion and Model Training
The core of the protocol involves integrating the processed modalities. Late fusion (prediction-level fusion) is recommended for its robustness with high-dimensional data [13].
- Late Fusion Strategy:
- Step 1: Train separate, single-modality survival prediction models on the training set for each data type (e.g., one model on genomic data, another on pathomic data).
- Step 2: Use these trained models to generate prediction scores (e.g., risk scores) for each patient in the validation and test sets.
- Step 3: Combine these per-modality prediction scores into a final feature set. This can be done using a simple linear weighted average or by training a meta-learner (a second-level model) on these scores to produce the final, fused prediction [13].
- Model Selection:
- For the base models and the meta-learner, use ensemble methods like Gradient Boosting (e.g., XGBoost) or Random Survival Forests, which have been shown to outperform deep learning and linear models on tabular biomedica data [13].
- Compare the late fusion model's performance against unimodal benchmarks.
The following diagram illustrates the logical workflow and data flow of this late fusion protocol:
Model Validation and Interpretation
- Performance Evaluation: Validate the model on the held-out test set. Use the Concordance-Index (C-index) to evaluate the model's ability to rank patient survival times correctly. Report confidence intervals from multiple data splits to ensure statistical robustness [13].
- Interpretability: Employ model-agnostic interpretation tools (e.g., SHAP values) to determine the contribution of each input modality and specific features to the final prediction, thereby generating biologically interpretable insights [59] [13].
The Scientist's Toolkit: Essential Research Reagents and Solutions
Table 2: Key Research Reagent Solutions for Multimodal Biomarker Discovery
| Item/Category | Function/Application | Specific Examples / Notes |
|---|---|---|
| Next-Generation Sequencing (NGS) | Comprehensive genomic, transcriptomic, and epigenomic profiling for molecular biomarker identification. | Foundation for molecular data modality. Panels for multi-target companion diagnostics (CDx) are becoming prevalent [10] [61]. |
| Liquid Biopsy Assays | Non-invasive sampling for biomarker discovery and longitudinal monitoring via circulating tumor DNA (ctDNA) and circulating tumor cells (CTCs). | Enables real-time tracking of tumor evolution and treatment response. Critical for biomarkers like KRAS, EGFR mutations [62] [61]. |
| Automated Sample Prep Systems | Ensures consistent, high-quality, and reproducible extraction of biomolecules (DNA, RNA, proteins) for downstream analysis. | Standardized sample prep (e.g., via automated homogenizers) reduces variability, forming a reliable foundation for AI/ML analysis [62]. |
| Multiplex Immunoassays | Simultaneous measurement of multiple protein biomarkers from a single sample to understand signaling pathways. | Used for proteomic profiling and validating protein-based signatures (e.g., OVA1 test) [61]. |
| AI/ML Software Libraries | Provides algorithms for data fusion, feature reduction, and predictive survival modeling. | Python libraries (e.g., Scikit-survival, XGBoost, PyTorch) and specialized multimodal pipelines (e.g., AZ-AI pipeline) are essential [13]. |
| Digital Pathology Scanners & Software | Digitizes glass slides for quantitative analysis and deep learning-based feature extraction (pathomics). | Whole Slide Imaging (WSI) systems are the gateway to extracting spatial and morphological information from tissue [10] [60]. |
Visualization of the Multimodal Fusion Conceptual Framework
The following diagram summarizes the overarching conceptual framework of multimodal data fusion for biomarker discovery, showing how disparate data sources are integrated to improve clinical decision-making.
The integration of multi-modal data through advanced artificial intelligence (AI) is revolutionizing oncology, moving the field beyond traditional single-modality diagnostics. By fusing diverse data types—including medical imaging, genomic profiles, and clinical information—researchers can capture a more comprehensive view of cancer heterogeneity, leading to significant improvements in detection, prognostication, and risk stratification [31] [10]. This application note presents success stories across breast, lung, and skin cancers, highlighting the practical protocols, performance gains, and reagent tools that are driving the success of multi-modal data fusion in modern cancer research and drug development.
Breast Cancer: Multi-modal Fusion for Recurrence Risk Prediction
A 2025 retrospective study developed a Multimodal Deep Learning (MDL) model to stratify recurrence risk in non-metastatic invasive breast cancer, achieving a high-performance benchmark superior to single-modality approaches [63]. The model integrated multi-sequence MRI (T2WI, DWI, DCE-MRI) with clinicopathologic characteristics, demonstrating that fused data provides a more robust prediction of patient outcomes than any single data source alone.
Quantitative Performance
Table 1: Performance Metrics of the Breast Cancer MDL Model [63]
| Metric | Testing Cohort Result | Validation Cohort Result | Clinical Significance |
|---|---|---|---|
| Area Under Curve (AUC) | 0.8448 - 0.9856 | Up to 0.956 | Accurate recurrence risk stratification |
| Concordance-index (C-index) | 0.803 | Not reported | Superior prognostic model discrimination |
| 5-Year RFS AUC | 0.836 | 0.936 | Accurate long-term survival prediction |
| 7-Year RFS AUC | 0.783 | 0.956 | Accurate long-term survival prediction |
RFS: Recurrence-Free Survival.
Experimental Protocol
1. Patient Cohort and Data Collection:
- Cohort: Enroll 574 patients with non-metastatic invasive breast cancer from multiple institutions, divided into training (n=285), validation (n=123), and testing (n=166) cohorts [63].
- Clinical Data: Extract clinicopathologic features including age, menopausal status, tumor stage, surgery type, and treatment history (neoadjuvant chemotherapy, radiotherapy, endocrine therapy) [63].
- Follow-up: Define recurrence-free survival (RFS) as the time from primary treatment to tumor recurrence or death. Conduct follow-up via telephone or outpatient visits [63].
2. Multi-sequence MRI Acquisition and Preprocessing:
- Imaging: Perform breast MRI using a 3.0 T scanner with the following sequences: T2-weighted imaging (T2WI), diffusion-weighted imaging (DWI), and dynamic contrast-enhanced MRI (DCE-MRI). Use gadopentetate dimeglumine (Gd-DTPA) as the contrast agent [63].
- Segmentation: Manually outline the region of interest (ROI) of the tumor on all MRI sequences using software (e.g., 3D Slicer). For multifocal tumors, select the largest lesion. Resolve annotation discrepancies through a senior radiologist [63].
- 2.5D Dataset Construction: For each MRI sequence, select the largest cross-sectional slice and six adjacent slices (±1, ±2, ±4) to create a 2.5D dataset. Combine the three sequences (DWI, T2WI, DCE-MRI) to form a three-channel input for the model [63].
3. Model Development and Fusion Strategy:
- Architecture: Employ a ResNet18 deep learning architecture within a multi-instance learning (MIL) framework [63].
- Fusion: Implement an intermediate fusion strategy. The model extracts features from the 2.5D MRI data and fuses them with the clinicopathologic features before the final prediction layer. This allows for interaction between imaging and clinical data at the feature level [63].
- Output: The model predicts a continuous recurrence risk score, which is then used to stratify patients into high- and low-risk groups [63].
4. Validation and Correlation Analysis:
- Performance Evaluation: Assess the model using ROC curves, calibration curves, and decision curve analysis. Perform survival analysis with Kaplan-Meier curves [63].
- Biological Correlation: Conduct enrichment analysis to correlate the model's deep-learning radiographic features with the expression of known prognostic genes from the Oncotype DX assay [63].
Diagram 1: Breast cancer multi-modal workflow.
Lung Cancer: Enhancing Diagnostic Accuracy with MFDNN
A 2024 study introduced a Multimodal Fusion Deep Neural Network (MFDNN) that integrated medical imaging, genomic data, and clinical records to significantly improve lung cancer classification accuracy. The approach demonstrated that synergistic information from disparate modalities can overcome the limitations of unimodal analysis [64].
Quantitative Performance
Table 2: Performance Metrics of the Lung Cancer MFDNN Model [64]
| Metric | MFDNN Performance | Compared to Established Methods (e.g., CNN, ResNet) | Clinical Impact |
|---|---|---|---|
| Accuracy | 92.5% | Superior | More reliable diagnosis |
| Precision | 87.4% | Superior | Reduced false positives |
| Recall (Sensitivity) | 86.4% | Superior | Reduced false negatives |
| F1-Score | 86.2% | Superior | Balanced performance |
Experimental Protocol
1. Data Acquisition and Curation:
- Data Types: Collect three primary data modalities:
- Medical Images: Radiological scans (e.g., CT, MRI) and histopathological slides [64].
- Genomic Data: Obtain genomic profiling data (e.g., from next-generation sequencing) relevant to lung cancer [64].
- Clinical Data: Extract structured data from Electronic Health Records (EHR), including patient demographics, smoking history, and laboratory results [64].
2. Modality-Specific Preprocessing and Feature Engineering:
- Imaging Data: Utilize pre-trained convolutional neural networks (CNNs) such as VGG-16 or ResNet-50 to extract high-level, informative features from the medical images [65].
- Genomic Data: Apply appropriate normalization and employ feature selection techniques (e.g., based on Spearman correlation or mutual information) to manage high dimensionality and select the most predictive genomic features [13].
- Clinical Data: Preprocess structured clinical data by handling missing values and normalizing numerical features. Categorical variables can be encoded using one-hot encoding [13].
3. Multimodal Fusion and Classification:
- Fusion Strategy: The MFDNN implements a feature-level (early) fusion strategy. The extracted feature vectors from each modality are concatenated into a unified, high-dimensional feature representation [64].
- Model Architecture: The fused feature vector is fed into a deep neural network classifier comprising multiple fully connected layers. The model is trained end-to-end to optimize classification performance [64].
- Output: The final layer uses a softmax activation function to generate probabilities for each diagnostic class (e.g., benign vs. malignant lung nodules) [64].
Skin Cancer: Multi-modal Data Fusion for Accessible Diagnosis
Research in skin cancer diagnosis has successfully demonstrated that combining dermoscopic images with patient clinical data significantly improves the performance of intelligent diagnostic systems. The MDFNet framework addressed the challenge of establishing internal relationships between heterogeneous data types, moving beyond simple concatenation [66].
Quantitative Performance
Table 3: Performance Comparison of Skin Cancer Fusion Models
| Model / Approach | Data Modalities Used | Accuracy | Key Advancement |
|---|---|---|---|
| MDFNet [66] | Clinical skin images & patient clinical data | 80.42% | Establishes mapping between heterogeneous features |
| EViT-Dens169 [67] | Dermoscopic images (Hybrid ViT & CNN) | 97.1% | Fuses global (ViT) and local (CNN) image features |
| Uni-modal Baseline [66] | Clinical skin images only | ~71% | Benchmark for performance improvement |
Experimental Protocol
1. Patient Data and Image Collection:
- Clinical Data: Collect relevant patient clinical information, which may include skin type, age, gender, lesion location, and personal/family history of skin cancer. Encode this data into a discrete feature vector using one-hot encoding [66].
- Skin Images: Acquire clinical or dermoscopic images of skin lesions. Utilize standard datasets like the ISIC archive for benchmarking [66] [67].
2. Feature Extraction and Fusion with MDFNet:
- Image Feature Extraction: Pass the skin images through a feature extractor based on a pre-trained CNN (e.g., VGGNet, ResNet, DenseNet) to obtain an image feature vector [66].
- Clinical Data Processing: Expand the dimension of the encoded clinical feature vector to match that of the image features, facilitating subsequent fusion operations [66].
- Fusion Strategy: Implement a hybrid fusion strategy inspired by gating mechanisms in LSTM networks. Perform various fusion operations (e.g., cascade, weight scaling, filtering) to allow cross-modal interaction and feature recalibration, rather than simple concatenation [66].
3. Model Training and Evaluation:
- Classification: The fused feature vector is fed into a final classification layer (e.g., a fully connected layer with softmax) to distinguish between benign and malignant skin lesions or to classify different cancer subtypes [66].
- Evaluation: Use standard metrics such as accuracy, sensitivity, specificity, and AUC on a held-out test set to evaluate model performance and generalizability [66] [67].
Diagram 2: Multi-modal fusion strategy types.
The Scientist's Toolkit: Essential Research Reagents & Materials
Table 4: Key Research Reagent Solutions for Multi-modal Cancer Studies
| Item / Resource | Function / Application | Example Use in Featured Studies |
|---|---|---|
| TCGA (The Cancer Genome Atlas) | Provides standardised, multi-modal patient data (genomic, transcriptomic, clinical) for model training and benchmarking. | Used as a primary data source for developing and validating multi-omics survival prediction models [10] [13]. |
| ISIC (International Skin Imaging Collaboration) Archive | Provides a large, public repository of dermoscopic images and metadata for developing skin AI algorithms. | Served as the source of skin lesion images for training the EViT-Dens169 and MDFNet models [66] [67]. |
| PyRadiomics | An open-source Python package for extracting a large number of quantitative features from medical images. | Used to extract handcrafted radiomics features from mammograms or other medical images for fusion with deep learning features [68]. |
| Pre-trained Deep Learning Models (VGG, ResNet, DenseNet) | Act as powerful feature extractors from images. Transfer learning from models pre-trained on natural images is highly effective for medical imaging tasks. | ResNet18 was used for breast MRI feature extraction; VGG/ResNet were used as backbones for skin and lung cancer image analysis [66] [63] [68]. |
| 3D Slicer | An open-source software platform for medical image informatics, image processing, and three-dimensional visualization. | Used for manual segmentation of tumors on breast MRI scans to define the region of interest (ROI) [63]. |
| Federated Learning Frameworks (e.g., PMM-FL) | Enable collaborative training of ML models across multiple institutions without sharing raw patient data, addressing privacy and data siloing. | Proposed for skin cancer diagnosis to leverage distributed multi-modal data while preserving patient confidentiality [69]. |
Navigating Implementation Challenges: Data, Model, and Clinical Hurdles
Addressing Data Heterogeneity, Sparsity, and High Dimensionality
Core Challenges in Multi-Modal Cancer Data
The integration of multi-modal data is pivotal for advancing cancer diagnosis research, yet it is fraught with significant technical challenges. The table below summarizes the three primary obstacles and their impact on model development.
Table 1: Core Data Challenges in Multi-Modal Cancer Research
| Challenge | Description | Impact on Model Performance |
|---|---|---|
| Data Heterogeneity | Disparate data sources (e.g., genomic, imaging, clinical records) with different formats, structures, and scales [10] [70]. | Hinders data integration, leads to information silos, and complicates the training of unified models [70] [71]. |
| Data Sparsity | A large number of features have zero values (e.g., in genomic data or one-hot encoded clinical data), distinct from missing data [72]. | Increases model complexity and storage needs, lengthens processing times, and can obscure important predictive signals [72]. |
| High Dimensionality | The number of features ((p)) is comparable to or vastly exceeds the number of observations ((n)) [73]. | Leads to the "curse of dimensionality," noise accumulation, model overfitting, and breakdowns in classical statistical methods [72] [73]. |
Experimental Protocols for Data Integration and Analysis
Protocol: Managing Data Heterogeneity via Ontology-Driven Standardization
The following protocol outlines a method for integrating heterogeneous data sources using formal ontologies, which provide a structured, machine-readable framework for data harmonization [74].
- Objective: To integrate disparate multi-modal cancer data (e.g., radiology reports, genomic variants, pathology images) into a coherent schema for downstream analysis.
- Materials:
- Data Sources: Raw data from EHRs, genomic sequencers, digital pathology scanners, and radiographic imaging systems [10].
- Tools: Ontology development tools (e.g., Protégé), data processing scripts (Python/R), and a triple store or graph database.
- Reference Resources: Domain-specific ontologies (e.g., NCI Thesaurus, Disease Ontology) and authority files (e.g., Geonames, VIAF) [74].
- Procedure:
- Domain Scoping & Ontology Selection: Define the scope of the integration project and identify relevant pre-existing ontologies. For a pan-cancer study, this might include ontologies for anatomy, diseases, and cell types.
- Schema Mapping: Map the schema of each source dataset to the concepts and relationships defined in the chosen ontologies. This creates a unified conceptual model.
- Data Value Standardization: Process individual data points (values) using controlled vocabularies and thesauri (e.g., HUGO gene names) to ensure consistency [74].
- RDF Conversion: Transform the mapped and standardized data into Resource Description Framework (RDF) triples (subject-predicate-object).
- Data Fusion & Querying: Load the RDF data into a graph database. Perform integrative queries using SPARQL to retrieve connected information across all original modalities.
- Troubleshooting:
- If an ontology lacks necessary concepts, extend it judiciously rather than creating a new one from scratch.
- For legacy data with poor provenance, manual curation may be required before automated processing.
Protocol: Dimensionality Reduction for Sparse and High-Dimensional Genomic Data
This protocol uses Principal Component Analysis (PCA) to mitigate the challenges of sparsity and high dimensionality in genomic feature sets, such as gene expression data [72].
- Objective: To reduce the dimensionality of a sparse, high-dimensional genomic dataset while retaining the maximum amount of informative variance.
- Materials:
- Dataset: A gene expression matrix (e.g., from RNA-Seq) with dimensions (n) (samples) x (p) (genes), where (p >> n) [73].
- Software: Python with scikit-learn, NumPy, and SciPy libraries.
- Procedure:
- Data Preprocessing: Perform log-transformation and standardization (z-score normalization) on the raw gene expression counts.
- Handle Sparsity: The input matrix is typically sparse. The PCA implementation in scikit-learn can efficiently handle sparse matrix inputs.
- PCA Implementation:
- Variance Assessment: Examine the explained variance ratio to determine the proportion of total variance captured by the selected components.
- Downstream Application: Use the transformed dataset (
X_reduced) for tasks like patient stratification, survival analysis, or as input for a classifier.
- Troubleshooting:
- If the reduced features lack interpretability, use factor loadings to identify which original genes contribute most to each principal component.
- For non-linear relationships in the data, consider non-linear methods like UMAP after initial PCA densification [72].
Protocol: Feature Selection using LASSO Regression for Predictive Biomarker Discovery
LASSO (Least Absolute Shrinkage and Selection Operator) regression is a powerful technique for feature selection in high-dimensional spaces, such as identifying key genomic biomarkers from a large panel of candidates [72] [73].
- Objective: To identify a sparse set of non-redundant genomic features predictive of a clinical outcome (e.g., treatment response) and build an interpretable model.
- Materials:
- Dataset: A matrix of genomic features (e.g., SNP arrays, protein expressions) and a corresponding vector of clinical outcomes (e.g., binary response status).
- Software: Python with scikit-learn or R with the
glmnetpackage.
- Procedure:
- Data Preparation: Split the data into training and testing sets (e.g., 70/30 split). Ensure the outcome variable is correctly encoded.
- Model Training: Fit a LASSO logistic regression model on the training data. LASSO applies an L1 penalty that shrinks the coefficients of irrelevant features to exactly zero.
- Feature Selection: Extract the features whose coefficients are non-zero after the model has been trained.
- Model Validation: Assess the model's performance on the held-out test set using metrics like AUC (Area Under the ROC Curve) and examine the selected features for biological plausibility.
- Troubleshooting:
- If the model is too sparse (too many features eliminated), adjust the regularization parameter
C(inverse of regularization strength) to a less stringent value. - For highly correlated features, LASSO may arbitrarily select one. Use Elastic Net (a combination of L1 and L2 penalty) to encourage group selection.
- If the model is too sparse (too many features eliminated), adjust the regularization parameter
Workflow Visualization
The following diagram illustrates the logical flow for addressing the three core challenges, from raw data to a validated integrated model.
Fig 1. Multi-modal data integration workflow.
The Scientist's Toolkit: Research Reagent Solutions
The table below lists essential computational tools and resources for implementing the protocols described in this document.
Table 2: Key Research Reagents and Computational Tools
| Item Name | Function/Brief Explanation | Example Use Case |
|---|---|---|
| Formal Ontologies (e.g., NCI Thesaurus) | Standardized, machine-readable vocabularies for describing biomedical concepts and relationships [74]. | Mapping heterogeneous clinical trial data from multiple sites to a unified schema. |
| scikit-learn Library | A comprehensive Python library offering implementations of PCA, LASSO, and other machine learning algorithms [72]. | Performing dimensionality reduction and feature selection on genomic data. |
| Controlled Thesauri (e.g., HUGO Gene Nomenclature) | Curated lists of controlled terminologies for specific domains to standardize data values [74]. | Ensuring consistent use of gene names across genomic and transcriptomic datasets. |
| UMAP (Uniform Manifold Approximation and Projection) | A dimensionality reduction technique particularly effective for visualizing complex structures in high-dimensional data [72]. | Visualizing patient subpopulations in integrated multi-omics data. |
| TensorFlow/PyTorch with Deep Learning Architectures (CNNs, RNNs, GNNs) | Frameworks for building complex models that can learn directly from raw data, such as images or sequences [10] [75]. | Fusing features from histopathology images (CNNs) and genomic sequences (RNNs) for prognostic prediction. |
Application Notes
Note on Multi-Modal Fusion Strategies in Breast Cancer Research
In breast cancer research, multi-modal fusion strategies are typically categorized into three levels, each with distinct advantages [55]:
- Feature-Level Fusion: This method involves combining raw or extracted features from different modalities (e.g., MRI radiomics and genomic pathway scores) into a single feature vector before input into a machine learning model. The primary advantage is the model's ability to learn from complex, cross-modal interactions. However, this approach requires careful normalization and alignment of features and is sensitive to noise in any single modality.
- Decision-Level Fusion: Here, separate models are trained on each data modality independently. Their predictions (e.g., probabilities of malignancy) are then combined, often by averaging or using a meta-classifier. This strategy is more robust to missing modalities and easier to implement, but it cannot capture fine-grained, non-linear interactions between the different data types.
- Hybrid Fusion: This advanced strategy seeks to leverage the strengths of both aforementioned methods. For instance, intermediate features from modality-specific deep learning models can be fused in a shared latent space. This is increasingly used with flexible deep learning architectures to achieve state-of-the-art performance in tasks like pathological complete response (pCR) prediction.
Note on Data Scarcity and Augmentation
A significant bottleneck in multi-modal cancer research is the scarcity of large, annotated datasets, which is exacerbated by privacy concerns and the labor-intensive nature of labeling medical data [10] [75]. To address this, researchers are turning to techniques such as:
- Synthetic Data Generation: Using Generative Adversarial Networks (GANs) or Variational Autoencoders (VAEs) to generate realistic, synthetic patient data that can augment training sets without compromising real patient privacy [29].
- Transfer Learning: A pre-trained model (e.g., a CNN trained on natural images or a large public genomic dataset) is fine-tuned on a smaller, target cancer dataset. This reduces the reliance on massive, task-specific labeled data [75].
- Federated Learning: This paradigm allows for model training across multiple decentralized institutions (e.g., hospitals) without sharing the raw data. Instead, only model updates are exchanged, thus preserving data privacy and enabling the use of larger, more diverse datasets [29].
Strategies for Handling Missing Modalities and Incomplete Data
In the field of multimodal data fusion for cancer diagnosis, the integration of diverse data types—such as histopathological images, genomic features, clinical notes, and radiological scans—has demonstrated significant potential to improve diagnostic accuracy and prognostic predictions beyond what is possible with single-modality approaches [76] [13] [53]. However, a fundamental challenge consistently arises in real-world clinical settings: the prevalence of missing modalities and incomplete data [76] [77] [78]. In contrast to controlled research environments, patient data in clinical practice are often incomplete due to factors such as cost constraints, variations in clinical protocols, equipment availability, and patient-specific considerations [77] [78]. Consequently, developing robust strategies to handle missing data has become a critical frontier in advancing multimodal learning for oncology applications [76] [78].
The problem of missing data manifests in two primary forms: random missing values within a modality and the complete absence of an entire modality for a given patient [78]. Traditional approaches that simply discard samples with missing modalities lead to significant information loss, reduced statistical power, and increased risk of model overfitting [76]. Moreover, such approaches limit the clinical applicability of models, as they cannot generate predictions for patients with incomplete data [77]. This paper synthesizes current methodologies and provides detailed protocols for addressing these challenges, with a specific focus on applications in cancer research and clinical oncology.
Classification of Fusion Strategies for Handling Missing Data
Multimodal fusion strategies for handling missing data can be categorized based on when the integration of different modalities occurs and how missingness is addressed. The following table summarizes the primary fusion categories, their descriptions, advantages, and limitations.
Table 1: Classification of Fusion Strategies for Incomplete Multimodal Data
| Fusion Category | Description | Advantages | Limitations |
|---|---|---|---|
| Early Fusion | Raw data from modalities are combined directly or missing data are imputed before feature extraction [78]. | Simplicity; allows direct feature interaction; can use statistical imputation methods. | Highly susceptible to noise and sparsity; imputation may introduce bias; requires complete data for training [78]. |
| Intermediate Fusion | Features are extracted from each modality first, then fused in a shared latent space, often using architectures that tolerate missing inputs [76] [77]. | Flexibility to handle arbitrary missing patterns; learns complex cross-modal interactions. | Complex model architecture; requires careful training procedures [76]. |
| Late Fusion | Models are trained separately on each modality, and their predictions are combined, e.g., via weighted averaging [13] [78]. | Naturally handles missing modalities; modular and easier to implement. | Cannot model complex, fine-grained interactions between modalities [13]. |
Detailed Experimental Protocols
Protocol 1: Intermediate Fusion with Latent Representation Learning
This protocol, adapted from multi-modal learning architectures for cancer grade classification, leverages a latent representation that is robust to missing modalities [76].
Research Reagent Solutions
Table 2: Essential Materials for Intermediate Fusion Protocol
| Item | Function/Description |
|---|---|
| TCGA-GBM/LGG Datasets | Publicly available datasets containing matched pathological images and genomic features for glioma patients [76]. |
| VGG-19 Network | Pre-trained convolutional neural network used for feature extraction from histopathological image patches [76]. |
| Graph Convolutional Network (GCN) | Neural network model for processing cell graph data constructed from tissue images to capture cell-to-cell interactions [76]. |
| Self-Normalizing Network (SNN) | A fully connected network designed to mitigate overfitting when learning from high-dimensional genomic data [76]. |
| CPM-Nets Fusion Framework | A fusion module that learns a common latent representation from multiple modalities and can handle missingness via reconstruction loss [76]. |
Step-by-Step Procedure
Data Preprocessing and Feature Extraction:
- Histopathological Images: For each Whole Slide Image (WSI), extract multiple 512x512 pixel patches. Use a pre-trained VGG-19 network to extract deep feature vectors (e.g., length 32) from each patch [76].
- Cell Graph Construction: From the WSIs, segment nuclei and construct a cell graph where nodes represent nuclei and edges represent cellular interactions. Process this graph using a GCN to obtain a structured feature vector [76].
- Genomic Data: Select informative genomic features (e.g., 79 copy number variation features and mutation status). Process these using an SNN to obtain a compact genomic feature vector [76].
Multi-Modal Fusion with Missing Modality Handling:
- Input Paired Features: For a patient with complete data, input the triple set of feature vectors (CNN image features, GCN graph features, SNN genomic features) [76].
- Latent Representation Learning: The CPM-Nets framework maps all available modalities of a sample into a structured hidden representation,
H[76]. - Reconstruction Loss: For each modality, train a decoder network that attempts to reconstruct the original feature vector from the shared representation
H. This is only computed for available modalities [76]. - Classification Loss: A clustering-like classification loss is applied to the latent representation
Hto ensure it is discriminative for the task (e.g., glioma grade classification) [76].
Training with Missing Data:
- During training, simulate real-world missingness by randomly discarding a percentage (e.g., n=25%, 50%) of one modality (image or genomic) in the training samples [76].
- For a sample with a missing modality, the reconstruction loss is computed only on the available modalities. The shared representation
His updated based on the available data, learning to encode comprehensive information from variable inputs [76].
Inference:
- During testing, the model accepts input with any combination of missing modalities. The shared representation
His generated from the available data via the trained model, and classification proceeds based on this representation [76].
- During testing, the model accepts input with any combination of missing modalities. The shared representation
The following diagram illustrates the workflow for this protocol, highlighting the flow of data and the pivotal role of the latent representation H in handling missing modalities.
Protocol 2: Transformer-Based Tri-Modal Fusion with Multivariate Loss
This protocol details a method for fusing three heterogeneous modalities (image, text, tabular) and is designed to be robust to missing modalities during inference, as demonstrated in chest pathology applications [77].
Research Reagent Solutions
Table 3: Essential Materials for Transformer-Based Fusion Protocol
| Item | Function/Description |
|---|---|
| MIMIC-IV & MIMIC-CXR | Public datasets containing chest radiographs, corresponding radiology reports, and structured tabular data (demographics, lab tests) [77]. |
| Transformer Encoder | Neural network architecture used as the core building block for the bi-modal fusion modules, effective at capturing complex relationships [77]. |
| Feature Embedding Networks | Separate neural networks (e.g., CNNs for images, BERT-like models for text, MLPs for tabular data) to convert raw inputs into feature vectors [77]. |
| Multivariate Loss Function | A composite loss function incorporating cross-entropy and reconstruction terms to enhance robustness [77]. |
Step-by-Step Procedure
Modality-Specific Feature Embedding:
- Image Modality: Use a CNN (e.g., ResNet) pre-trained on medical images to extract feature embeddings from radiographs.
- Text Modality: Use a clinical language model (e.g., ClinicalBERT) to encode radiology reports into a feature vector.
- Tabular Modality: Use a simple multi-layer perceptron (MLP) to process structured data (e.g., patient demographics, lab results) [77].
Bi-Modal Fusion Module Design:
- Construct three separate Transformer-based fusion modules, one for each possible pair of modalities: Image-Text, Image-Tabular, and Text-Tabular [77].
- Each bi-modal fusion module takes the feature embeddings from its two respective modalities and uses cross-attention mechanisms to learn their interactions, outputting a fused representation [77].
Tri-Modal Fusion Architecture:
- The outputs from the three bi-modal fusion modules are combined (e.g., via concatenation or weighted averaging) to form a comprehensive tri-modal representation [77].
Training with Multivariate Loss:
- The model is trained using a multivariate loss function, ( L{total} = L{task} + \lambda L{recon} ), where:
- ( L{task} ) is the primary task loss (e.g., cross-entropy for disease classification).
- ( L_{recon} ) is an auxiliary reconstruction loss that encourages the model to reconstruct the original feature embeddings of available modalities from the fused representation, improving robustness [77].
- ( \lambda ) is a weighting hyperparameter.
- The model is trained using a multivariate loss function, ( L{total} = L{task} + \lambda L{recon} ), where:
Inference with Missing Modalities:
- If one modality is missing at inference time (e.g., no radiology report), the corresponding bi-modal fusion modules are disabled. The final prediction is made by combining the outputs of the remaining active bi-modal modules [77].
- The model demonstrates strong performance even when one or more modalities are absent, as the training process with the multivariate loss encourages the learning of complementary representations [77].
The logical structure of this transformer-based approach is outlined below.
The strategies and protocols outlined herein address a critical impediment in translational oncology research: the reliable fusion of multimodal data under realistic conditions of incompleteness. While simple imputation or discarding of samples offers a straightforward baseline, advanced methods like intermediate fusion that learn modality-invariant representations [76] and Transformer-based architectures with robust loss functions [77] represent the state-of-the-art, demonstrating that models can be designed to explicitly leverage all available data without being crippled by what is missing.
The choice of an optimal strategy is highly context-dependent. Key considerations include:
- The Pattern of Missingness: Whether modalities are Missing Completely At Random (MCAR) or if the missingness is systematic.
- The Number and Heterogeneity of Modalities: Late fusion may be more practical for integrating many very different data types [13].
- Computational Resources and Model Complexity: Simpler methods may be preferred when data is scarce or computational budget is limited.
Future directions in this field point towards the development of Medical Multimodal Foundation Models (MMFMs) pre-trained on large-scale datasets, which could possess inherent robustness to missing data and be adapted to specific clinical tasks with limited fine-tuning [79]. Furthermore, improving model interpretability is crucial for clinical adoption, helping to build trust by allowing clinicians to understand how predictions are made from the available multimodal inputs [53] [79].
In conclusion, effectively handling missing modalities is not merely a technical pre-processing step but a foundational component of building clinically viable AI tools for cancer diagnosis and treatment planning. The continued development and refinement of these strategies are essential for bridging the gap between research prototypes and tools that can function reliably in the complex and data-incomplete environment of real-world clinical oncology.
Mitigating Overfitting in High-Dimension, Low-Sample-Size Settings
In the field of oncology research, the emergence of high-throughput technologies has facilitated the collection of rich, multimodal data, encompassing genomics, transcriptomics, proteomics, digital pathology, radiology, and clinical records [3] [10] [1]. The integration of these diverse modalities through multimodal artificial intelligence (MMAI) holds significant promise for revolutionizing cancer diagnosis, prognosis, and therapeutic decision-making [3] [53]. However, a pervasive and critical challenge in developing such predictive models is the high-dimension, low-sample-size (HDLSS) scenario, where the number of features (dimensions) vastly exceeds the number of patient samples [13]. This data structure inherently predisposes models to overfitting, a phenomenon where a model learns not only the underlying signal but also the noise and random fluctuations specific to the training dataset [80]. An overfitted model typically exhibits excellent performance on the training data but fails to generalize its predictions to new, unseen data, such as independent patient cohorts or clinical trial populations [80] [81]. This lack of generalizability poses a substantial barrier to the clinical translation of MMAI models, as it can lead to unreliable predictions and potentially harmful patient care decisions [82]. Therefore, developing robust strategies to mitigate overfitting is a cornerstone of building trustworthy and clinically applicable AI tools in oncology. This document outlines specific application notes and experimental protocols to address this challenge within the context of multimodal data fusion for cancer research.
Background & Key Concepts
The Overfitting Problem in HDLSS Settings
Overfitting occurs when a statistical machine learning model becomes excessively complex, tailoring itself too closely to the training data. In HDLSS settings, common in oncology due to the cost and complexity of patient data acquisition, the risk is magnified [13]. Models with millions of parameters can easily "memorize" the small training set rather than learning the generalizable patterns. The curse of dimensionality exacerbates this issue, as the data becomes sparse, making it difficult for the model to infer robust relationships [83]. The consequences are not merely technical; they can manifest as irreproducible research findings, misguided clinical decisions, and an erosion of trust in AI-based tools for healthcare [82] [81].
Multimodal Data Fusion Strategies
A foundational decision in MMAI is choosing when to integrate different data modalities. The choice of fusion strategy significantly impacts a model's susceptibility to overfitting, especially when samples are limited [1] [13].
Table 1: Multimodal Data Fusion Strategies and Their Suitability for HDLSS Settings
| Fusion Strategy | Description | Advantages | Disadvantages for HDLSS | Suitability for HDLSS |
|---|---|---|---|---|
| Early Fusion (Data-Level) | Raw data from different modalities are concatenated into a single input vector before being fed into a model. | Model can learn complex, cross-modal interactions from the raw data. | Creates an extremely high-dimensional feature space, dramatically increasing overfitting risk [13]. | Low |
| Intermediate Fusion (Model-Level) | Modalities are processed separately in initial layers, with features fused in intermediate model layers. | Balances the learning of intra-modal and inter-modal relationships. | Still requires a complex, high-capacity model (e.g., deep neural network), prone to overfitting with small samples [13]. | Medium |
| Late Fusion (Decision-Level) | Separate models are trained on each modality independently, and their predictions are combined (e.g., by averaging or stacking). | Isolates modality-specific learning, reducing the feature space for any single model. More resistant to overfitting [13]. | Cannot learn complex, fine-grained interactions between raw data modalities. | High [13] |
The following workflow diagram illustrates the decision process for selecting a fusion strategy in an HDLSS context, emphasizing the relative safety of late fusion approaches.
Application Notes: Core Mitigation Strategies
Dimensionality Reduction and Feature Selection
Reducing the number of input features is the most direct defense against the curse of dimensionality. This can be achieved through feature selection (choosing a subset of original features) or feature extraction (creating a new, smaller set of derived features) [83] [13].
Table 2: Dimensionality Reduction Techniques for HDLSS Omics Data
| Technique | Type | Mechanism | Key Considerations |
|---|---|---|---|
| Principal Component Analysis (PCA) | Feature Extraction | Unsupervised. Finds orthogonal axes of maximum variance in the data. | Preserves global structure; is unsupervised and may not be relevant to the outcome [1]. |
| LASSO (L1 Regularization) | Feature Selection | Supervised. Adds a penalty equal to the absolute value of coefficient magnitude, driving less important coefficients to zero. | Enforces sparsity; effective for selecting a small number of features from a large pool [13]. |
| Spearman Correlation | Feature Selection | Supervised. Ranks features based on monotonic relationship with the outcome. | Non-parametric; robust to outliers; computationally efficient for initial filtering [13]. |
| Mutual Information | Feature Selection | Supervised. Measures the dependency between each feature and the outcome based on information theory. | Can capture non-linear relationships; more computationally intensive than correlation [13]. |
| Hybrid Metaheuristics (TMGWO, BBPSO) | Feature Selection | Supervised. Uses evolutionary algorithms to search for an optimal feature subset that maximizes prediction accuracy. | Can be highly effective but computationally expensive; requires careful validation [83]. |
Model Regularization and Algorithm Selection
Regularization techniques explicitly modify the learning algorithm to discourage complexity, thereby preventing the model from fitting the noise in the training data [80] [81].
- L1 (Lasso) & L2 (Ridge) Regularization: These techniques add a penalty term to the model's loss function. L1 regularization tends to produce sparse models (good for feature selection), while L2 regularization shrinks all coefficients proportionally [81].
- Dropout: Primarily used in deep learning, dropout randomly "drops" a proportion of units in a neural network layer during training, preventing complex co-adaptations on training data and effectively training an ensemble of networks [80].
- Algorithm Choice with Built-in Regularization: For HDLSS tabular data (common with multi-omics), ensemble methods like Random Forests and Gradient Boosting Machines (e.g., XGBoost) often outperform very complex deep learning models. They possess strong inductive biases for regularization and have been shown to achieve state-of-the-art results in multi-omics survival prediction tasks [13].
Robust Validation and Evaluation Practices
Robust validation is non-negotiable in HDLSS settings to obtain unbiased performance estimates and detect overfitting [80] [13].
- Stratified K-Fold Cross-Validation: The dataset is split into K folds, ensuring each fold preserves the same proportion of outcome classes (e.g., cancer subtypes). The model is trained K times, each time using K-1 folds for training and the remaining fold for validation. This maximizes the use of limited data for both training and validation. A minimum of K=5 or K=10 is recommended.
- Nested Cross-Validation: An outer loop estimates the generalization error, while an inner loop is used for hyperparameter tuning. This prevents optimistic bias in performance estimates that occurs when tuning and evaluating on the same data splits.
- Reporting with Confidence Intervals: Performance metrics (e.g., C-index, AUC) should be reported as the mean and 95% confidence interval across all cross-validation folds, providing a measure of estimation uncertainty [13].
- Comparison to Unimodal Baselines: Any multimodal model must be rigorously compared against models trained on single modalities to confirm that integration provides a genuine performance boost and is not an artifact of overfitting [13].
Experimental Protocols
Protocol: A Late-Fusion Pipeline for Survival Prediction
This protocol provides a step-by-step methodology for building a robust, late-fusion model to predict overall survival in cancer patients using multimodal data, designed to mitigate overfitting [13].
1. Objective: To integrate transcriptomic, proteomic, and clinical data to predict patient overall survival without overfitting the limited training data.
2. Research Reagent Solutions & Computational Tools: Table 3: Essential Tools and Materials for the Survival Prediction Pipeline
| Item / Tool | Function / Description | Application Note |
|---|---|---|
| Python AZ-AI Pipeline | A custom Python library for multimodal feature integration and survival prediction [13]. | Provides a standardized framework for preprocessing, fusion, and evaluation. |
| The Cancer Genome Atlas (TCGA) | A public repository of multimodal cancer patient data, including genomics, imaging, and clinical data [10]. | A primary source for benchmark datasets. |
| Scikit-learn | A Python library for machine learning, providing feature selection, regression, and classification algorithms. | Used for implementing preprocessing, feature selection, and base learners. |
| XGBoost | An optimized distributed gradient boosting library. | An effective algorithm for tabular data; often used as a base model in late fusion [13]. |
| Cox Proportional-Hazards Model | A regression model commonly used in medical research for investigating the association between variables and survival time. | A standard baseline for survival analysis. |
3. Procedure:
Step 1: Data Preprocessing and Imputation. For each modality (e.g., RNA-seq, proteomics, clinical), perform modality-specific normalization. Handle missing data using appropriate imputation methods (e.g., mean/median for continuous variables, mode for categorical). Split the entire dataset into training (e.g., 80%) and hold-out test (e.g., 20%) sets, stratifying on the survival event indicator. The hold-out test set must only be used for the final evaluation.
Step 2: Unimodal Feature Selection. Within the training set only, perform feature selection for each modality independently to avoid data leakage. Use a supervised method like univariate Cox regression or Spearman correlation with the survival time/event. Select the top N features (e.g., top 100) from each modality based on the strength of their association with the outcome.
Step 3: Train Unimodal Survival Models. Train a separate survival prediction model (e.g., Cox model with Lasso penalty, Random Survival Forest, or XGBoost) on the selected features of each modality. Tune the hyperparameters of each unimodal model using 5-fold cross-validation on the training set.
Step 4: Generate Unimodal Predictions. Use each tuned unimodal model to generate out-of-fold predictions on the training set and predictions on the hold-out test set. These predictions (e.g., risk scores) become the new features for the fusion model.
Step 5: Fuse Predictions with a Meta-Learner. Train a final "meta-learner" (a linear model like logistic regression or a simple ensemble method like averaging) on the out-of-fold predictions from Step 4. This model learns the optimal way to combine the predictions from each unimodal model.
Step 6: Final Evaluation and Interpretation. Use the trained meta-learner to generate final predictions on the hold-out test set. Evaluate performance using the C-index and plot calibration curves. Perform error analysis and interpret the contribution of each modality through the meta-learner's coefficients.
The following Graphviz diagram maps this protocol's logical flow and key decision points.
Protocol: Benchmarking Fusion Strategies
This protocol describes a comparative experiment to evaluate the performance and overfitting resistance of different fusion strategies on a fixed multimodal dataset.
1. Objective: To systematically compare early, intermediate, and late fusion strategies on a common benchmark, assessing both performance and robustness.
2. Procedure:
Step 1: Dataset Curation. Select a publicly available multimodal cancer dataset (e.g., from TCGA) with a defined prediction task (e.g., cancer subtype classification, survival prediction). Ensure the sample size is characteristic of an HDLSS setting (e.g., 200-500 samples).
Step 2: Implement Fusion Strategies.
- Early Fusion: Concatenate all features from all modalities after preprocessing and feature selection (e.g., top 50 features per modality). Train a single model (e.g., an MLP or XGBoost) on this concatenated vector.
- Intermediate Fusion: Implement a neural network architecture with separate input branches for each modality, merging the branches in a hidden layer. Use regularization techniques like dropout and L2 weight decay.
- Late Fusion: Follow the protocol outlined in Section 4.1.
Step 3: Rigorous Evaluation. Evaluate all models using a consistent 5x5 nested cross-validation scheme (5 outer folds, 5 inner folds for tuning). For each outer fold, record the performance on the validation set.
Step 4: Analysis. Compare the mean C-index (or AUC) and the 95% confidence intervals across the three strategies. A model with a higher mean performance and a narrower confidence interval is preferred. Critically, compare the performance of the multimodal models against unimodal baselines to confirm the value of integration.
The Scientist's Toolkit
Table 4: Key Reagents, Tools, and Software for MMAI in HDLSS Contexts
| Category | Item | Function / Utility |
|---|---|---|
| Data Sources | The Cancer Genome Atlas (TCGA) | Provides standardized, multi-platform molecular data and clinical information for various cancer types [10]. |
| UK Biobank | A large-scale biomedical database containing in-depth genetic and health information from half a million UK participants [3]. | |
| Software & Libraries | Scikit-learn | Essential for feature selection (SelectKBest), dimensionality reduction (PCA), and implementing traditional ML models with regularization [81]. |
| MONAI (Medical Open Network for AI) | A PyTorch-based framework for deep learning in healthcare imaging, providing pre-trained models and domain-specific tools [3]. | |
| AstraZeneca's AZ-AI Pipeline | A Python library specifically designed for multimodal feature integration and survival prediction, as used in published research [13]. | |
| Computational Methods | Two-phase Mutation Grey Wolf Optimization (TMGWO) | A hybrid feature selection algorithm that can identify significant features for classification in high-dimensional data [83]. |
| Late Fusion | A decision-level fusion strategy that is particularly robust to overfitting in HDLSS settings [13]. | |
| Nested Cross-Validation | A gold-standard validation technique for providing an almost unbiased estimate of the true generalization error of a model [13]. |
Ensuring Model Interpretability and Explainability for Clinical Trust
The integration of Multimodal Artificial Intelligence (MMAI) into oncology represents a paradigm shift, enabling more accurate diagnostics, personalized treatment strategies, and enhanced patient monitoring by combining diverse data sources such as medical imaging, genomics, and electronic health records (EHRs) [3] [54]. However, the "black-box" nature of many complex AI models poses a fundamental obstacle to their clinical adoption, as understanding the reasoning behind a diagnosis is as crucial as the decision itself in high-stakes medical domains [84]. Explainable AI (XAI) has emerged as an essential discipline to bridge this gap, providing transparency and fostering trust among healthcare professionals (HCPs) [85]. This application note outlines the critical challenges, methodologies, and validation protocols for ensuring model interpretability within the context of multimodal data fusion for cancer diagnosis, providing researchers and drug development professionals with a framework for developing clinically trustworthy AI systems.
The Imperative for Explainability in Clinical Oncology
The Trust Gap in Medical AI
Despite their demonstrated precision, traditional machine learning models, especially deep neural networks, face a critical limitation: their opaque decision-making process. This lack of transparency hinders trust and acceptance among clinicians, who require understanding not just the "what" but the "why" behind AI-generated insights [84]. A systematic review of HCP perspectives found that explainability and integrability are two key technical factors influencing their acceptance and use of AI-based decision support systems [85]. The clinical oncology domain is particularly sensitive to this trust gap, given the life-altering consequences of diagnostic and treatment decisions.
The Multimodal Complexity Challenge
MMAI systems in oncology integrate heterogeneous datasets spanning multiple biological scales—from molecular alterations and cellular morphology to tissue organization and clinical phenotype [3]. This multi-scale heterogeneity, while providing a more comprehensive representation of disease, introduces significant interpretability challenges. Each data modality—including cancer multiomics, histopathology, medical imaging, and clinical records—possesses distinct structural characteristics and requires specialized processing before fusion and analysis [1]. Converting this multimodal complexity into clinically actionable insights demands sophisticated XAI approaches that can articulate not just predictions but the inter-scale relationships and biologically meaningful patterns driving those predictions [3].
Table 1: Key Challenges in Multimodal Explainable AI for Oncology
| Challenge Category | Specific Issues | Impact on Clinical Trust |
|---|---|---|
| Technical Complexity | Data heterogeneity, synchronization across modalities, computational demands | Increases opacity and limits clinical validation |
| Explanation Diversity | Varying explanation needs across clinical specialties, multiple explanation formats | Creates confusion and inconsistent adoption |
| Clinical Workflow | Integration with existing EHRs, workflow disruption, time constraints | Reduces usability and increases resistance |
| Validation Gaps | Lack of standardized evaluation metrics, limited clinical validation studies | Undermines evidence-based trust building |
Explainability Techniques for Multimodal Oncology AI
Technical Approaches to XAI
XAI techniques can be broadly categorized into model-specific and model-agnostic approaches, each with distinct advantages for clinical applications. For multimodal oncology AI, hybrid approaches that combine multiple explanation methods often prove most effective.
Model-Agnostic Explanation Methods: Techniques such as SHAP (SHapley Additive exPlanations) and LIME (Local Interpretable Model-agnostic Explanations) provide post-hoc interpretability without requiring access to the model's internal architecture [84]. These methods generate feature importance scores and local explanations that help clinicians understand which input variables most significantly influenced a particular prediction. For example, in a hybrid ML-XAI framework for disease prediction, SHAP and LIME provided transparent insights into the features contributing to predictions for conditions including diabetes, anemia, and heart disease, achieving 99.2% accuracy while maintaining interpretability [84].
Model-Specific Explanation Methods: These include attention mechanisms in transformer architectures and prototype-based models that classify images by comparing them to representative parts of images from the training set [86]. One study adapted a prototype-based XAI model for gestational age estimation from fetal ultrasound, providing explanations similar to how a clinician might reason: "this fetus is 30 weeks of gestation because it looks like a 30-week fetus I have seen before" [86].
Multimodal Fusion Explanations: Advanced MMAI architectures require explanation techniques that can articulate how information from different modalities interacts to produce predictions. Techniques such as cross-modal attention maps and integrated gradients can visualize which features across different data types (e.g., genomic, imaging, clinical) contributed to a diagnosis or treatment recommendation [3].
Quantitative Comparison of XAI Techniques
Table 2: Performance Comparison of Explainable AI Techniques in Healthcare Applications
| XAI Technique | Application Context | Performance Metrics | Clinical Benefits | Limitations |
|---|---|---|---|---|
| Prototype-Based Models [86] | Gestational age estimation from ultrasound | Reduced MAE from 23.5 to 14.3 days with explanations | Intuitive case-based reasoning; aligns with clinical cognition | Variable impact across users; some clinicians performed worse with explanations |
| SHAP + LIME with Ensemble Models [84] | Multi-disease risk prediction | 99.2% accuracy with feature attribution | High transparency for feature importance; model-agnostic | Computational intensity; complex explanations for non-technical users |
| Pathomic Fusion [3] | Glioma and renal cell carcinoma stratification | Outperformed WHO 2021 classification for risk stratification | Integrates histology and genomics; biologically plausible insights | Requires specialized multimodal data alignment |
| Transformer-Based Explainers(e.g., MUSK) [3] | Melanoma relapse prediction | ROC-AUC 0.833 for 5-year relapse prediction | Captures long-range dependencies; superior to unimodal approaches | Computationally intensive; requires large datasets |
Experimental Protocols for Validating Explainability
Protocol 1: Clinical Reader Studies for XAI Validation
Objective: To evaluate the impact of model explanations on clinician performance, trust, and reliance in a controlled setting.
Materials:
- Curated dataset with ground truth labels
- AI model with integrated explainability interface
- Cohort of clinical domain experts
- Pre- and post-study questionnaires
Procedure:
- Baseline Assessment: Participants review cases without AI assistance to establish baseline performance.
- Model Prediction Phase: Participants review the same cases with model predictions but without explanations.
- Explanation Phase: Participants review cases with both model predictions and explanations.
- Data Collection: Record diagnostic accuracy, time per case, trust ratings, and reliance metrics at each phase.
- Appropriate Reliance Analysis: Categorize participant responses as appropriate reliance, under-reliance, or over-reliance based on model performance.
Validation Metrics:
- Diagnostic accuracy (sensitivity, specificity)
- Mean Absolute Error (MAE) for continuous outcomes
- Trust scales (self-reported)
- Reliance indices (behavioral measures)
This protocol, adapted from a gestational age estimation study [86], revealed that while model predictions significantly reduced clinician MAE (from 23.5 to 15.7 days), the addition of explanations had a variable impact—some clinicians improved further while others performed worse, highlighting the importance of personalized approaches to XAI presentation [86].
Protocol 2: Multimodal Fusion Interpretability Assessment
Objective: To validate the interpretability of MMAI systems integrating histopathology, genomics, and clinical data for cancer diagnosis and prognosis.
Materials:
- Paired histopathology images and genomic sequencing data
- Clinical variables and outcomes data
- Multimodal fusion AI architecture
- XAI visualization tools (heatmaps, feature attribution maps)
Procedure:
- Data Preprocessing: Standardize histopathology images, normalize genomic expression data, and structure clinical variables.
- Model Training: Implement cross-modal attention mechanisms to enable inherent interpretability.
- Explanation Generation: Apply post-hoc explanation methods (SHAP, LIME) to quantify feature importance across modalities.
- Clinical Correlation: Validate explanations against known biological pathways and clinical outcomes.
- Expert Evaluation: Engage domain experts to assess clinical plausibility of explanations.
Validation Metrics:
- Explanation faithfulness (how accurately explanations represent model reasoning)
- Biological plausibility (alignment with established cancer biology)
- Clinical utility (usefulness for diagnostic or treatment decisions)
This approach is exemplified by Pathomic Fusion, which combined histology and genomics in glioma and clear-cell renal-cell carcinoma datasets, outperforming the World Health Organization 2021 classification for risk stratification [3].
Implementation Framework for Clinical Integration
Workflow Integration Strategy
Successful integration of explainable MMAI into clinical oncology requires meticulous attention to workflow compatibility. A systematic review of HCP perspectives identified workflow adaptation, system compatibility with EHRs, and ease of use as primary conditions for real-world adoption [85]. The following dot code provides a visualization of the optimal integration workflow:
The Scientist's Toolkit: Essential Research Reagents
Table 3: Essential Research Reagents and Computational Tools for Multimodal XAI in Oncology
| Tool/Reagent | Function | Application Context |
|---|---|---|
| SHAP (SHapley Additive exPlanations) | Model-agnostic feature importance calculation | Quantifies contribution of individual features to model predictions across all data modalities |
| LIME (Local Interpretable Model-agnostic Explanations) | Local explanation generation | Creates interpretable approximations of model behavior for specific cases or predictions |
| MONAI (Medical Open Network for AI) | Domain-specific AI framework for healthcare imaging | Provides pre-trained models and specialized processing for medical image data within multimodal pipelines |
| 10x Genomics Visium/Xenium | Spatial transcriptomics platform | Enables correlation of histological features with gene expression patterns in tissue sections |
| Pathomics Feature Extractors | Quantitative characterization of histopathology images | Extracts morphometric and texture features from digitized slides for integration with other modalities |
| Prototype-Based Networks | Case-based reasoning for image data | Provides similarity-based explanations comparing new cases to prototypical examples from training data |
The path to clinical trust in multimodal AI systems for oncology requires rigorous attention to explainability throughout the development lifecycle. By implementing validated explanation techniques, conducting thorough clinical reader studies, and ensuring seamless workflow integration, researchers can build MMAI systems that not only achieve high predictive accuracy but also earn the trust of healthcare professionals. The future of AI in clinical oncology depends on this crucial balance between technological sophistication and clinical interpretability—a balance that will ultimately determine the successful translation of algorithmic insights into improved patient outcomes.
Computational and Infrastructure Demands for Large-Scale Data
The integration of multimodal data represents a prevailing trend in artificial intelligence and is essential for advancing health management and cancer care [87]. For complex systems like modern oncology, high-value characteristics necessitate the fusion of diverse data modalities, including video surveillance, internal sensors, genomic data, medical imaging, and digital twins [87] [88]. This multimodal approach offers increased information amount and diversity compared to single-modal data, making it particularly suitable for cancer diagnosis research [87]. However, effective utilization of these datasets presents significant computational and infrastructure challenges that must be addressed to realize their potential for improved cancer diagnostics and treatment.
The core challenge in multimodal data fusion lies in calculating correlations among different modalities with inherent multi-source heterogeneity and substantial timing discrepancies [87]. The primary objective is to project information from various modalities into a shared low-dimensional space for unified processing, thereby avoiding the curse of dimensionality while preserving critical diagnostic information [87]. For cancer research, this involves simultaneous analysis of genomic, imaging, clinical, and sensor data to enable precise, efficient, and personalized patient management [88].
Computational Challenges in Multimodal Data Fusion
Data Heterogeneity and Temporal Inconsistencies
Multimodal health data exhibits significant variations in temporal characteristics and structural properties across different modalities. A fundamental challenge involves addressing inconsistencies arising from varying temporal lengths across different data streams [87]. In response, researchers have developed global monotonicity calculation methods and time series data augmentation techniques to synchronize and align these disparate data sources for effective fusion [87].
The health condition estimation can be regarded as a regression problem where for a certain complex system, the distribution of its health condition can be described as X = (x₁, ..., xk, ..., xp) ∈ R^(N × p), where p is the number of modalities, xk represents the data set of the kth modality, and N is the sample number of each modality [87]. The multimodal health condition estimation establishes a many-to-one mapping relationship between multimodal information and health status as expressed in Equation 1:
Y(t) = f(X(t)) = f(f₁(x₁(t)), ..., fk(xk(t)), ..., fp(xp(t))) (1)
where fk represents the conversion function for the kth modality [87]. Since the dimensions and characteristics of different modalities are different, each modality requires a dedicated conversion function to enable meaningful fusion and analysis.
Representation Learning and Correlation Calculation
A common approach for handling multimodal heterogeneity is to project information from various modalities into a shared low-dimensional space for unified processing [87]. Correlation calculation methods include canonical correlation analysis (CCA) and maximum mean discrepancy (MMD), with CCA being widely applied in dimensionality reduction, classification, and aggregation of multimodal data [87]. The linear nature of traditional CCA limits its effectiveness for handling nonlinear mappings common in cancer data, leading to the development of nonlinear variants such as Kernel CCA (KCCA) and deep CCA (DCCA) [87].
Recent advances have explored the combination of Generative Adversarial Networks (GAN) with deep CCA, enabling discriminators to distinguish between generated and original data through DCCA transformations, thus enhancing multimodal data learning and generation [87]. These approaches have shown particular promise in addressing the unique challenges of cancer data fusion, where capturing complex, nonlinear relationships between genomic, imaging, and clinical modalities is essential for accurate diagnosis and prognosis.
Table 1: Computational Challenges in Multimodal Data Fusion for Cancer Research
| Challenge Category | Specific Technical Hurdles | Potential Solutions |
|---|---|---|
| Data Heterogeneity | Varying temporal lengths across modalities; Structural differences between data types | Global monotonicity calculation; Time series data augmentation; Dedicated conversion functions per modality [87] |
| Representation Learning | Nonlinear relationships between modalities; High-dimensional feature spaces | Kernel CCA (KCCA); Deep CCA (DCCA); Shared low-dimensional space projection [87] |
| Model Architecture | Limited single-modal learning; Inefficient correlation capture | Multi-source GAN (Ms-GAN); Many-to-many transfer training; Fast sequential learning networks [87] |
| Computational Complexity | Processing large-scale multimodal datasets; Training complex fusion models | Transfer learning; Dimensionality reduction; Sequential learning architectures [87] |
Infrastructure Requirements for Large-Scale Data
Computational Architecture for Multimodal Fusion
Effective multimodal data fusion requires specialized computational architectures designed to handle the substantial infrastructure demands of large-scale cancer datasets. The proposed solutions include fast sequential learning network architectures along with time series generative data structures to address the need for efficient time series fusion [87]. These architectures must simultaneously process both static characteristics (affected by current multimodal health condition information at time t) and dynamic characteristics (affected by multimodal information before time t) [87].
Time series data mining methods such as recurrent neural networks (RNN) can simultaneously consider the impact of the data from current time t and before time t, dynamically adjusting the degree of preference for current information and early information through different activation functions or corresponding thresholds [87]. This capability is particularly valuable in cancer research, where both historical trends and current measurements contribute to accurate diagnosis and prognosis predictions.
Storage and Processing Infrastructure
The infrastructure for large-scale multimodal cancer data must accommodate diverse data types ranging from high-resolution medical images to genomic sequences and clinical records. The classification of multimodal health condition information relevant to cancer research includes:
- Observation-Based Multimedia Information: Video footage, images, and auditory data captured by external instruments [87].
- Sensor-Based Condition Information: Diverse types of health condition data acquired during operation via internal or external sensors [87].
- Knowledge-Based Experience Information: Empirical formulas alongside subjective estimation provided by users as well as actual historical data [87].
- Digital Twins-Based Homologous Information: Pertinent historical records associated with similar cancer cases; derivative outputs generated by digital twins and fitting models [87].
Each category presents unique storage and processing requirements, necessitating scalable infrastructure solutions that can handle both structured and unstructured data while maintaining accessibility for analysis and model training.
Experimental Protocols for Multimodal Data Fusion
Protocol 1: Multimodal Timing Alignment Algorithm
Purpose: To address inconsistencies in timing lengths across different modalities in cancer data streams.
Materials and Equipment:
- Multimodal cancer dataset (genomic, imaging, clinical)
- Computational environment with Python 3.8+
- Deep learning framework (PyTorch or TensorFlow)
- High-performance computing cluster with GPU acceleration
Procedure:
- Data Preprocessing: For each modality, extract time series features and normalize using z-score normalization.
- Monotonicity Calculation: Apply global monotonicity calculation method to establish temporal relationships across modalities [87].
- Time Series Augmentation: Implement time series data augmentation technique to address temporal inconsistencies [87].
- Alignment Verification: Validate alignment quality through cross-correlation analysis between modality pairs.
- Performance Assessment: Evaluate alignment effectiveness using downstream task performance (e.g., classification accuracy).
Troubleshooting Tips:
- For highly asynchronous data, consider dynamic time warping as an alternative alignment approach.
- When dealing with missing temporal markers, implement probabilistic alignment methods.
Protocol 2: Many-to-Many Transfer Training with Ms-GAN
Purpose: To implement a many-to-many transfer training approach that culminates in the formation of a Multi-source Generative Adversarial Network (Ms-GAN) for cancer data fusion [87].
Materials and Equipment:
- Aligned multimodal cancer dataset
- Computational environment with high-performance GPUs (≥ 16GB memory)
- Specialized libraries: NumPy, SciPy, Scikit-learn
- Implementation of KCCA for loss function calculation
Procedure:
- Network Initialization: Initialize generator and discriminator networks for each data modality.
- KCCA Loss Configuration: Implement Kernel CCA as the basis for the loss function to capture overall correlation between generated data and multimodal real data [87].
- Pre-training Phase: Pre-training key parameters through transfer learning architecture [87].
- Adversarial Training: Alternate between generator and discriminator training using many-to-many transfer approach.
- Fusion Validation: Evaluate fusion quality through correlation analysis and downstream task performance.
Troubleshooting Tips:
- For unstable training, consider modifying learning rates or implementing gradient penalty.
- If mode collapse occurs, add diversity terms to the loss function.
Visualization of Multimodal Data Fusion Workflows
Multimodal Fusion Architecture Diagram
Multi-source GAN (Ms-GAN) Training Workflow
Table 2: Essential Research Reagents and Computational Solutions for Multimodal Cancer Data Fusion
| Category | Item/Technology | Specification/Function |
|---|---|---|
| Data Types | Genomic Sequencing Data | NGS-based diagnostics analyzing somatic mutations, single-nucleotide variants, insertions, deletions [88] |
| Medical Imaging Data | CT, MRI, PET, ultrasound, digital pathology images for spatial analysis [88] | |
| Clinical & EHR Data | Unstructured clinical notes, diagnostic reports, procedural data [88] | |
| Sensor Data | Internal/external sensor monitoring data from clinical equipment [87] | |
| Computational Frameworks | Deep Learning Models | CNNs (image data), RNNs/LSTMs (sequential data), GNNs (relational data) [88] |
| Fusion Algorithms | Multi-source GAN (Ms-GAN), Deep CCA (DCCA), Kernel CCA (KCCA) [87] | |
| Pre-trained Models | BERT/BioBERT/ClinicalBERT for NLP tasks, Vision Transformers for image analysis [88] | |
| Analysis Tools | Correlation Analysis | Canonical Correlation Analysis (CCA), Maximum Mean Discrepancy (MMD) [87] |
| Temporal Alignment | Global monotonicity calculation, Time series data augmentation techniques [87] | |
| Representation Learning | Transfer learning, Self-supervised learning, Multi-task learning approaches [88] | |
| Evaluation Metrics | Performance Measures | AUROC, Accuracy, Sensitivity, Specificity, F1-score [88] |
| Survival Analysis | Kaplan-Meier, C-index for time-to-event predictions [88] | |
| Fusion Quality | Correlation metrics, Downstream task performance, Visualization quality |
The computational and infrastructure demands for large-scale multimodal data in cancer research present significant but addressable challenges. Through specialized architectures like Multi-source GANs, advanced correlation calculation methods like Kernel CCA, and robust temporal alignment algorithms, researchers can effectively fuse diverse data modalities to enhance cancer diagnosis and treatment planning. The experimental protocols and visualization workflows provided in this document offer practical guidance for implementing these approaches in research settings.
As cancer care continues to evolve toward more personalized, data-driven approaches [89], the ability to effectively integrate and analyze multimodal data will become increasingly critical. The methods outlined here provide a foundation for addressing the computational challenges inherent in this integration, potentially leading to more precise diagnostics and improved patient outcomes in oncology.
Within the framework of multi-modal data fusion for enhanced cancer diagnosis, managing high-dimensionality and preventing model overfitting are paramount challenges. Technological advancements have transformed oncology research, generating vast amounts of data from modalities like genomics, transcriptomics, proteomics, metabolomics, and clinical records [13] [25]. However, this wealth of data introduces significant computational and statistical hurdles, including the "curse of dimensionality," data heterogeneity, and the risk of models learning noise instead of underlying biological signals [13] [45]. Optimization techniques, specifically dimensionality reduction and regularization, are therefore critical for constructing robust, generalizable, and clinically actionable diagnostic models. These techniques ensure that the integration of multiple data modalities leads to genuine performance improvements, ultimately supporting more informed clinical decisions in precision oncology [13] [45] [25].
Dimensionality Reduction in Multi-Modal Oncology
Dimensionality reduction techniques are essential for simplifying complex, high-dimensional multi-omics data sets, which typically have a very low ratio of patient samples to the number of measured features [13]. The primary goal is to protect survival and diagnostic models from overfitting by reducing the feature space to a manageable set of informative components.
Core Techniques and Comparative Analysis
The following table summarizes the key dimensionality reduction methods and their application contexts in cancer research.
Table 1: Dimensionality Reduction Techniques for Multi-Modal Cancer Data
| Technique | Category | Key Principle | Example Application in Oncology | Advantages | Limitations |
|---|---|---|---|---|---|
| Principal Component Analysis (PCA) [90] [25] | Linear Feature Extraction | Finds orthogonal axes of maximum variance in the data. | Capturing primary transcriptional variation to identify molecular cancer subtypes [25]. | Computationally efficient; simple to interpret. | Limited to capturing linear relationships. |
| Kernel PCA (KPCA) [90] | Non-linear Feature Extraction | Uses kernel functions to perform PCA in a high-dimensional feature space. | Effective non-linear mapping for complex agroecosystem data; KPCA-poly offered best cluster definition [90]. | Captures complex non-linear structures. | Higher computational cost; kernel selection is critical. |
| t-SNE [90] | Manifold Learning | Preserves local neighborhoods and similarities between data points. | Applied for visual insights in data exploration [90]. | Excellent for visualizing high-dimensional data in 2D/3D. | Computationally intensive; results can be sensitive to parameters. |
| UMAP [90] | Manifold Learning | Preserves both local and most of the global structure. | Used for visual insights alongside t-SNE [90]. | Better preservation of global structure than t-SNE; faster. | Can also be sensitive to parameter choices. |
| Autoencoders [13] [91] | Deep Learning | Neural network trained to reconstruct its input through a compressed bottleneck layer. | Learning condensed item representations in recommender systems [91]; used in unsupervised feature extraction for omics data [13]. | Highly flexible; can learn complex, non-linear representations. | Requires large data volumes; risk of learning identity function. |
| Supervised Feature Selection (e.g., Spearman Correlation) [13] | Feature Selection | Selects features based on their statistical correlation with the outcome. | Used in cancer survival prediction pipelines to account for nonlinear correlations with overall survival time [13]. | Incorporates outcome labels for more relevant feature selection. | Univariate methods ignore feature interactions. |
Protocol: Implementing Dimensionality Reduction for Multi-Omic Fusion
This protocol outlines a standardized pipeline for applying dimensionality reduction to multi-omic data, such as transcriptomic, proteomic, and metabolomic data, prior to fusion and model training.
- Objective: To reduce the dimensionality of individual omics modalities to mitigate overfitting and enhance the performance of a downstream diagnostic or prognostic model.
- Inputs: Matrices of normalized and scaled omics data (e.g., gene expression, protein abundance) where rows are patient samples and columns are features.
- Software: Python libraries including scikit-learn, and specialized packages for non-linear methods (e.g., UMAP).
Step-by-Step Procedure:
- Data Preprocessing and Modality-Specific Cleaning:
- Perform quality control and normalization specific to each data type (e.g., DESeq2 for RNA-seq data, batch correction using tools like Nested ComBat) [45] [25].
- Handle missing values using appropriate imputation methods (e.g., k-nearest neighbors) or removal.
- Standardize or scale features so they have a mean of zero and a standard deviation of one, which is critical for distance-based methods like PCA.
Unimodal Dimensionality Reduction:
- Apply the chosen dimensionality reduction technique independently to each omics modality.
- For PCA:
- Instantiate the PCA class from scikit-learn, specifying the number of components (
n_components) to retain. This can be a fixed number (e.g., 50) or determined by the fraction of variance explained (e.g., 95%). - Fit the PCA model to the training data for one modality using
fit(). - Transform both the training and test data using
transform().
- Instantiate the PCA class from scikit-learn, specifying the number of components (
- For UMAP:
- Instantiate the UMAP class, specifying key parameters like
n_components,n_neighbors, andmin_dist. - Fit the model on the training data and transform both training and test sets.
- Instantiate the UMAP class, specifying key parameters like
Fusion of Reduced Modalities:
- Concatenate the reduced-dimension representations (e.g., the principal components from each modality) along the feature axis to create a unified, lower-dimensional dataset for model training [13].
- Alternatively, proceed with a late fusion strategy where models are trained on each reduced modality separately and their predictions are combined [13].
Validation and Iteration:
- Train a predictive model (e.g., a Cox model for survival or a classifier for diagnosis) on the fused training data.
- Evaluate model performance on the held-out test set using appropriate metrics (e.g., C-index, AUC). The process of selecting the dimensionality reduction method and number of components may be iterated based on validation performance.
Diagram: Dimensionality Reduction Workflow for Multi-Omic Data
Regularization Strategies for Robust Multi-Modal Models
Regularization techniques are employed to constrain model complexity, prevent overfitting to training data, and ensure that no single modality dominates the learning process unfairly—a phenomenon known as modality competition [92].
Advanced Regularization Frameworks
Table 2: Regularization Techniques for Multi-Modal Fusion in Cancer Analysis
| Technique | Category | Key Principle | Application Context | Impact |
|---|---|---|---|---|
| L1 / L2 Regularization [13] [92] | Parameter Penalization | Adds a penalty on the size of model coefficients (L1 for sparsity, L2 for small weights). | Training multivariate Cox PH models with Lasso (L1) to impose sparsity in survival prediction [13]. | Prevents overfitting; L1 encourages feature selection. |
| Multi-Loss Training [92] | Auxiliary Task | Introduces additional unimodal task losses alongside the main multimodal loss. | A baseline method to ensure each modality learns meaningful representations [92]. | Encourages unimodal competency; can be difficult to balance. |
| Gradient Modulation (e.g., OGM [92]) | Gradient-based | Modulates gradients for each modality based on their performance relative to others. | Used to mitigate competition where one modality dominates and suppresses others [92]. | Dynamically balances modality influence during training. |
| Multimodal Competition Regularizer (MCR) [92] | Game-Theoretic & Info-Theoretic | Uses a mutual information decomposition to balance unique and shared information from each modality. | Framed modality interaction as a game to automatically balance contributions; outperformed ensemble baselines [92]. | Theoretically grounded; ensures all modalities contribute informatively. |
Protocol: Applying Game-Theoretic Regularization with MCR
This protocol details the implementation of the Multimodal Competition Regularizer (MCR), a novel method designed to balance modality contributions during training.
- Objective: To regularize a multi-modal deep learning model such that all modalities are sufficiently trained and their unique and shared information is effectively leveraged, thereby improving generalization.
- Inputs: Encoded latent representations from multiple modalities (e.g., ( Z1 ) for histopathology features, ( Z2 ) for genomic features).
- Software: PyTorch or TensorFlow, and the custom MCR loss component.
Step-by-Step Procedure:
- Model and Encoder Setup:
- Define unimodal encoders (( f1, f2, ... )) for each data modality, which project raw input data into latent representations (( Z1, Z2, ... )).
- Define a fusion network (( f_c )) that takes the concatenated latent representations and produces a final prediction.
Loss Function Construction:
- Calculate the standard task loss (e.g., Cross-Entropy for classification or Negative Log-Likelihood for survival analysis) between the model's predictions and the true labels. Denote this as ( \mathcal{L}_{task} ).
- Calculate the MCR loss component (( \mathcal{L}_{MCR} )) as defined in Kontras et al. [92]. This involves:
- Decomposing Mutual Information (MI): The regularizer refines bounds for the MI between each latent representation and the target, promoting task-relevant information.
- Game-Theoretic Balancing: The framework treats modalities as players, encouraging each to maximize its informative role without being suppressed by others.
- Efficient Estimation: Use proposed latent space permutations to estimate conditional MI, avoiding computationally expensive full-model passes.
- Construct the total loss function: ( \mathcal{L}{total} = \mathcal{L}{task} + \lambda \mathcal{L}_{MCR} ), where ( \lambda ) is a hyperparameter controlling the strength of the regularization.
Model Training:
- During each training iteration, perform a forward pass to compute both ( \mathcal{L}{task} ) and ( \mathcal{L}{MCR} ).
- Perform backpropagation to compute gradients from the combined ( \mathcal{L}_{total} ) and update model parameters.
- Monitor the performance of the fused model and, if possible, the unimodal streams on a validation set to ensure balanced learning.
Hyperparameter Tuning:
- The regularization weight ( \lambda ) is a critical hyperparameter. Perform a grid search over a validation set (e.g., values like 0.1, 0.5, 1.0) to identify the value that yields the best performance without degrading training.
Diagram: MCR Integration in a Multi-Modal Learning Loop
The Scientist's Toolkit: Key Research Reagents and Materials
The following table catalogues essential computational tools and data resources for implementing the described optimization techniques in multi-modal cancer research.
Table 3: Research Reagent Solutions for Multi-Modal Oncology Analysis
| Item Name | Type | Function / Application | Relevance to Protocols |
|---|---|---|---|
| TCGA (The Cancer Genome Atlas) [13] [45] | Data Repository | Provides comprehensive, multi-modal patient data including genomics, transcriptomics, proteomics, and clinical information. | Primary source of data for benchmarking fusion pipelines and survival prediction models. |
| scikit-learn [90] | Software Library | Provides standardized implementations of PCA, KPCA, and other ML algorithms for preprocessing and modeling. | Used for dimensionality reduction (Protocol 2.2) and baseline model training. |
| UMAP [90] | Software Library | Specialized package for performing UMAP non-linear dimensionality reduction. | Applied for visual insights and non-linear feature extraction in Protocol 2.2. |
| PyTorch / TensorFlow [92] | Deep Learning Framework | Flexible platforms for building and training custom neural network architectures, including autoencoders and fusion models. | Essential for implementing the MCR regularizer and other complex fusion models (Protocol 3.2). |
| AstraZeneca-AI (AZ-AI) Pipeline [13] | Software Pipeline | A Python library for multimodal feature integration and survival prediction, includes preprocessing and various fusion strategies. | Serves as a reusable framework for replicating and extending advanced multi-modal analysis. |
| SHAP / LIME [45] [48] | Explainable AI (XAI) Library | Post-hoc interpretation tools to explain model predictions and link them to input features (e.g., genes, image regions). | Critical for validating model decisions and ensuring biological plausibility in clinical applications. |
Achieving Generalizability and Robustness Across Diverse Patient Cohorts
Performance Benchmarks for Multi-Modal Cancer Models
Multi-modal artificial intelligence (MMAI) models have demonstrated significant performance improvements across various oncology tasks. The following table summarizes quantitative benchmarks for key clinical applications, highlighting the enhanced generalizability achieved through multi-modal data fusion.
Table 1: Performance Benchmarks of Multi-Modal AI Models in Oncology
| Clinical Application | Cancer Type | Data Modalities | Performance Metric | Result | Reference |
|---|---|---|---|---|---|
| Neoadjuvant Therapy Response Prediction | Breast Cancer | Mammogram, MRI, Histopathology, Clinical data | AUROC | 0.883 (Pre-NAT) | [20] |
| In-Hospital Mortality Prediction | Mixed (Critical Care) | Chest X-ray, Clinical notes, Tabular data | AUROC/AUPRC | 0.886 / 0.459 | [93] |
| Early Detection & Risk Stratification | Lung Cancer | Low-dose CT, Demographic data | ROC-AUC | Up to 0.92 | [3] |
| Melanoma Relapse Prediction | Melanoma | Histology, Genomics, Clinical data | ROC-AUC (5-year) | 0.833 | [3] |
| Breast Cancer Risk Stratification | Breast Cancer | Clinical metadata, Mammography, Ultrasound | Performance | Similar or better than pathologist | [3] |
| Clinical Deterioration Prediction | Mixed (Ward Patients) | Structured EHR, Clinical notes | AUROC | 0.870 | [94] |
Experimental Protocols for Robust Model Development
Protocol: Handling Missing Modalities with Knowledge Distillation
Background: A fundamental challenge in real-world clinical deployment is the frequent unavailability of all data modalities for every patient due to variations in clinical protocols, resource constraints, or patient-specific factors [93].
Objective: To develop an MMAI model that maintains robust performance even when one or more input modalities are missing.
Materials:
- Multi-modal dataset (e.g., chest X-rays, clinical notes, tabular laboratory/demographic data)
- Computational framework supporting deep learning (e.g., PyTorch, TensorFlow)
Methods:
- Model Architecture: Implement a multi-branch neural network where each branch processes a specific modality (image, text, tabular).
- Fusion Module: Integrate the modality-specific features using a Pooled Bottleneck (PB) attention mechanism. This module learns to weigh the importance of different features dynamically [93].
- Knowledge Distillation (Training Phase):
- Train a complete "teacher" model with access to all modalities.
- Simultaneously, train a "student" model that learns to mimic the teacher's predictions, even when provided with only a subset of modalities.
- This process forces the student model to develop robust representations that do not over-rely on any single modality [93].
- Gradient Modulation: Apply a Gradient Modulation (GM) method during training to balance the optimization process across modalities, preventing one dominant modality from hindering the learning of others [93].
- Validation: Evaluate the final model on a test set containing samples with complete and intentionally ablated modalities.
Protocol: Longitudinal Multi-Modal Integration for Therapy Response
Background: Accurately predicting a patient's response to Neoadjuvant Therapy (NAT) in breast cancer requires integrating multi-modal data collected at different timepoints throughout the treatment journey [20].
Objective: To create a predictive system that integrates longitudinal multi-modal data to predict Pathological Complete Response (pCR) in breast cancer patients undergoing NAT.
Materials:
- Multi-modal, longitudinal datasets including:
- Radiological Images: Pre-NAT mammograms, longitudinal MRI exams (Pre-, Mid-, Post-NAT).
- Clinical & Histopathological Data: Molecular subtype, tumor histology, patient demographics, clinical TNM staging [20].
- Access to computational resources for deep learning model development.
Methods:
- Data Preprocessing: Standardize and curate data from all sources. For imaging, this may involve region-of-interest (ROI) extraction and normalization [31] [20].
- Model Design (MRP System):
- Implement two independently trained models:
- iMGrhpc: Processes Pre-NAT mammograms combined with radiological, histopathological, personal, and clinical (rhpc) data.
- iMRrhpc: Processes longitudinal MRI sequences with embedded temporal information and rhpc data [20].
- Implement two independently trained models:
- Cross-Modal Knowledge Mining: Enhance the image feature extraction by allowing the model to mine and leverage contextual information from the non-image modalities (e.g., clinical notes) during training [20].
- Temporal Information Embedding: Design the model to explicitly incorporate the timing of examinations (e.g., Pre-, Mid-, Post-NAT) to capture the dynamic nature of treatment response [20].
- Robust Inference: Architect the system to function effectively even with missing data inputs, mimicking real-world clinical scenarios where not all exams or data points are available for every patient [20].
Protocol: Multi-Modal Fusion for Generalizable Biomarker Discovery
Background: Tumor biology is complex and manifests across multiple biological scales. MMAI can integrate heterogeneous datasets to discover robust, generalizable biomarkers that are not apparent from single-modality analysis [3] [1].
Objective: To identify and validate key predictive biomarkers across multiple solid tumors by integrating real-world multi-modal data.
Materials:
- Multi-modal real-world data (imaging, histology, genomics, clinical records) from large patient cohorts.
- Explainable AI (XAI) tools (e.g., SHAP, LIME) for model interpretation.
- Independent external validation cohort.
Methods:
- Data Harmonization: Preprocess and align diverse data modalities. For genomics, use tools like GATK for mutation detection and DESeq2 for differential expression analysis. For histopathology, leverage deep learning models like CNNs to extract morphological features [1] [45].
- Multi-Modal Fusion: Employ a fusion strategy (e.g., feature-level or hybrid fusion) to combine the processed unimodal data into a cohesive representation [31] [45].
- Pan-Tumor Analysis: Train an explainable AI model on the integrated dataset to identify features that are predictive of outcomes (e.g., treatment response, survival) across multiple cancer types [3] [45].
- Biomarker Identification: Use XAI techniques to extract and rank the importance of features (markers) from the trained model. This links model predictions to biologically and clinically plausible features [45].
- External Validation: Validate the identified biomarker signature on a completely independent, external cohort (e.g., a cohort with a specific cancer type like lung cancer) to confirm generalizability [3].
Visualizing the Multi-Modal Fusion Workflow for Robust Models
The following diagram illustrates the core workflow for developing a generalizable and robust multi-modal model, incorporating strategies to handle real-world challenges like missing data and longitudinal analysis.
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Computational Tools and Frameworks for Multi-Modal Oncology Research
| Tool/Reagent | Type | Primary Function | Application in Protocol |
|---|---|---|---|
| MONAI (Medical Open Network for AI) [3] | Open-source Framework | Provides AI tools and pre-trained models for medical imaging. | Medical image analysis and segmentation (Sections 2.1, 2.2). |
| Apache cTAKES [94] | Natural Language Processing Tool | Extracts medical concepts (CUIs) from unstructured clinical notes. | Processing clinical notes for fusion with structured data (Section 2.1). |
| SHAP/LIME [45] | Explainable AI (XAI) Library | Provides post-hoc interpretations of model predictions, highlighting important features. | Biomarker identification and model explanation (Section 2.3). |
| PyTorch/TensorFlow | Deep Learning Framework | Core infrastructure for building and training neural networks. | Implementing all model architectures and training loops (All Sections). |
| Model Context Protocol (MCP) [95] | Interoperability Protocol | Standardizes communication and data alignment between different AI models and data modalities in distributed environments. | Federated learning setups and schema-driven data fusion (Background). |
| GATK/DESeq2 [1] | Genomic Analysis Toolbox | Processes genomic data for variant calling and differential expression analysis. | Unimodal processing of genomics data (Section 2.3). |
Benchmarking Performance and Clinical Validation of Fusion Models
In the field of oncology research, the integration of multi-modal data—including genomic, histopathological, radiological, and clinical information—has emerged as a transformative approach for improving cancer diagnosis, prognosis, and treatment planning [4]. The development of artificial intelligence (AI) models that can effectively fuse these diverse data modalities requires robust evaluation frameworks to assess their clinical utility and reliability [48]. Key performance metrics, including Area Under the Receiver Operating Characteristic Curve (AUC), Concordance Index (C-index), Accuracy, and F1-Score, provide distinct perspectives on model performance and are essential for validating predictive models in translational cancer research.
Multi-modal data fusion enables a more comprehensive understanding of complex biological processes in cancer by combining orthogonal information from different data types [1]. However, the heterogeneity of these data sources—varying in format, structure, and scale—presents significant challenges for model development and evaluation [96]. Performance metrics serve as critical tools for comparing different fusion strategies, optimizing model architectures, and ultimately ensuring that predictive models can generalize across diverse patient populations and clinical settings [31]. The selection of appropriate metrics is particularly important in clinical applications, where the consequences of false positives and false negatives can significantly impact patient care and treatment decisions [97].
Metric Definitions and Clinical Interpretations
Core Metric Definitions
Area Under the ROC Curve (AUC): The AUC represents the probability that a classifier will rank a randomly chosen positive instance higher than a randomly chosen negative instance. It provides an aggregate measure of performance across all possible classification thresholds, with values ranging from 0 to 1 (where 1 indicates perfect classification and 0.5 represents random guessing) [20]. In cancer diagnostics, AUC is widely used for binary classification tasks such as distinguishing malignant from benign tumors or predicting treatment response [20].
Concordance Index (C-index): The C-index measures the discriminative power of survival models by evaluating whether the model correctly ranks survival times for pairs of patients. It calculates the proportion of comparable pairs in which the predicted survival times are correctly ordered, with values ranging from 0 to 1 (where 1 indicates perfect concordance) [96] [50]. This metric is particularly valuable for assessing prognostic models in oncology, where time-to-event outcomes such as overall survival and progression-free survival are common endpoints [96].
Accuracy: Accuracy represents the proportion of correct predictions (both true positives and true negatives) among the total number of cases examined. It is calculated as (TP + TN) / (TP + TN + FP + FN), where TP = True Positives, TN = True Negatives, FP = False Positives, and FN = False Negatives [97]. While intuitively simple, accuracy can be misleading in imbalanced datasets where one class significantly outweighs the other [97].
F1-Score: The F1-score is the harmonic mean of precision and recall, providing a balanced measure that accounts for both false positives and false negatives. It is calculated as 2 × (Precision × Recall) / (Precision + Recall), with values ranging from 0 to 1 (where 1 indicates perfect precision and recall) [97]. This metric is particularly useful when dealing with class imbalance, as it gives equal weight to both precision and recall rather than combining them arithmetically [97].
Table 1: Key Performance Metrics for Classification Models in Cancer Diagnostics
| Metric | Calculation | Range | Optimal Value | Primary Use Case |
|---|---|---|---|---|
| AUC | Area under ROC curve | 0-1 | 1.0 | Binary classification performance across thresholds |
| C-index | Proportion of concordant pairs | 0-1 | 1.0 | Survival model discrimination |
| Accuracy | (TP + TN) / (TP + TN + FP + FN) | 0-1 | 1.0 | Overall classification correctness |
| F1-Score | 2 × (Precision × Recall) / (Precision + Recall) | 0-1 | 1.0 | Balanced measure of precision and recall |
Clinical Interpretation and Contextual Considerations
The interpretation of these metrics must be contextualized within specific clinical scenarios and research objectives. In cancer detection applications, such as identifying malignant tumors from histopathological images or radiologic scans, high sensitivity (recall) is often prioritized to minimize false negatives that could lead to delayed diagnosis and treatment [97]. Conversely, for cancer subtype classification or molecular characterization, high specificity may be more important to ensure accurate treatment selection [4].
The F1-score offers particular utility in scenarios where both false positives and false negatives carry significant clinical consequences. For instance, in cancer detection models, a false negative (missing a cancer diagnosis) could delay critical treatment, while a false positive (incorrectly diagnosing cancer) may lead to unnecessary invasive procedures and patient anxiety [97]. The harmonic mean calculation of the F1-score ensures that neither metric is optimized at the extreme expense of the other, creating a balanced evaluation framework [97].
For survival prediction models, which are central to precision oncology, the C-index provides a specialized evaluation metric that accounts for censored data—cases where the event of interest (e.g., death) has not occurred during the study period [96] [50]. This capability makes it particularly valuable for assessing prognostic models that guide clinical decision-making for treatment planning and patient counseling [98].
Experimental Protocols for Metric Evaluation
General Validation Framework for Multi-modal Fusion Models
Robust evaluation of multi-modal fusion models requires a structured validation framework that accounts for data heterogeneity, sample size limitations, and potential overfitting. The following protocol outlines a comprehensive approach for evaluating model performance using the key metrics discussed:
Data Partitioning: Implement stratified splitting to ensure representative distribution of key clinical variables (e.g., cancer stage, molecular subtypes) across training (70%), validation (15%), and test (15%) sets. Stratification maintains similar event rates (for survival analysis) and class distributions (for classification) across partitions [96].
Cross-Validation: Perform k-fold cross-validation (typically k=5 or k=10) with multiple random seeds to account for variability in data splitting. This approach provides more reliable performance estimates and helps identify model stability across different data partitions [96].
Multi-modal Feature Processing: Apply modality-specific preprocessing and feature extraction techniques:
- Genomic Data: Utilize tools such as GATK for mutation detection, DESeq2 for differential expression analysis, and pathway-based approaches (KEGG, Reactome) for functional annotation [1].
- Histopathological Images: Employ stain normalization, tissue segmentation, and feature extraction using pre-trained deep learning models (e.g., Vision Transformers, Convolutional Neural Networks) [50].
- Clinical Data: Implement standardization of continuous variables, encoding of categorical variables, and handling of missing data through appropriate imputation methods [20].
Fusion Strategy Implementation: Based on research objectives and data characteristics, select and implement appropriate fusion strategies:
- Early Fusion: Combine raw data or low-level features from multiple modalities before model training [4].
- Intermediate Fusion: Integrate modality-specific representations in intermediate layers of neural networks using attention mechanisms or other feature interaction approaches [20].
- Late Fusion: Train separate models for each modality and combine their predictions through weighted averaging, stacking, or meta-learning [96] [98].
Performance Assessment: Calculate all relevant metrics (AUC, C-index, Accuracy, F1-Score) on the held-out test set following model training and hyperparameter optimization. Report confidence intervals derived from bootstrapping or repeated cross-validation to quantify estimation uncertainty [96].
Statistical Comparison: Perform formal statistical testing (e.g., DeLong's test for AUC, bootstrap tests for C-index) to compare model performances and demonstrate significant improvements over baseline approaches [20].
Explainability Analysis: Incorporate model interpretability techniques (e.g., SHAP, Grad-CAM, attention visualization) to identify influential features and validate biological relevance [48] [98].
Model Evaluation Workflow
Specialized Protocol for Survival Prediction Evaluation
Survival prediction requires specialized methodological considerations due to the presence of censored observations and time-to-event outcomes. The following protocol details the evaluation procedure for survival models:
Data Preparation:
- Compile overall survival (OS) or progression-free survival (PFS) data with appropriate time-to-event variables and censoring indicators [96].
- Ensure consistent representation of time units (e.g., days, months) across all data sources.
- Address informative censoring through appropriate statistical methods.
Feature Engineering:
- For genomic features: Apply dimensionality reduction techniques (PCA, autoencoders, or supervised feature selection) to address high dimensionality [96].
- For histopathological images: Extract features using pre-trained models (Vision Transformers or CNNs) capable of capturing morphological patterns predictive of survival [50].
- For clinical variables: Include established prognostic factors (e.g., age, stage, tumor grade) as baseline predictors.
Model Training:
- Implement appropriate survival models: Cox Proportional Hazards (with regularization), survival forests, deep survival networks, or multi-modal fusion architectures [96].
- For multi-modal integration, consider late fusion strategies that have demonstrated superior performance in survival prediction tasks [98].
- Optimize hyperparameters using cross-validation based on partial likelihood (for Cox models) or appropriate survival loss functions.
Performance Evaluation:
- Calculate the C-index on the test set to assess model discrimination [96] [50].
- Generate time-dependent ROC curves and calculate AUC at clinically relevant time points (e.g., 1-year, 3-year, 5-year survival) [20].
- Assess calibration using plots of predicted versus observed survival probabilities.
- Compare performance against established clinical benchmarks and unimodal baselines.
Validation and Interpretation:
- Perform subgroup analysis to assess performance consistency across different patient populations (e.g., by cancer subtype, stage, or treatment regimen).
- Conduct sensitivity analyses to evaluate robustness to different censoring assumptions.
- Employ explainability techniques to identify features driving predictions and validate their biological and clinical relevance [98].
Table 2: Experimental Protocol for Multi-modal Survival Prediction in Cancer
| Protocol Step | Key Considerations | Recommended Methods | Quality Controls |
|---|---|---|---|
| Data Collection | Multi-modal representation; Censoring patterns | TCGA; Institutional cohorts; Clinical trials | Data completeness audit; Censoring documentation |
| Feature Processing | Modality-specific normalization; Dimensionality reduction | PCA; Autoencoders; Pathway analysis | Batch effect correction; Feature stability assessment |
| Fusion Strategy | Data heterogeneity; Missing modalities | Late fusion; Attention mechanisms; Cross-modal learning | Modality importance weighting; Robustness to missing data |
| Model Validation | Discrimination; Calibration; Clinical utility | C-index; Time-dependent AUC; Calibration plots | Comparison against clinical benchmarks; Subgroup analysis |
Application in Multi-modal Cancer Research
Performance Benchmarking in Recent Studies
Recent advances in multi-modal fusion for cancer diagnostics have demonstrated the critical importance of comprehensive metric evaluation. In breast cancer research, a systematic review of 49 studies revealed that multi-modal models often outperformed unimodal approaches, with effect sizes varying based on validation design (cross-validation vs. external validation) and handling of missing modalities [48]. The specific metrics reported across studies provide insights into expected performance ranges for different diagnostic tasks.
For breast carcinoma diagnosis using explainable multi-modal fusion, studies have reported AUC values ranging from 0.82 to 0.94, with performance improvements of 5-15% compared to single-modality baselines [48]. The integration of imaging, clinical records, histopathology, and genomic data produced richer, more reliable predictions, though the authors noted significant variability in evaluation methodologies across studies [48].
In a specialized study predicting neoadjuvant therapy response in breast cancer, the Multi-modal Response Prediction (MRP) system achieved an AUC of 0.883 (95% CI: 0.821-0.941) in the pre-therapy phase and 0.889 (95% CI: 0.827-0.948) in the mid-therapy phase [20]. The model demonstrated a 10.4% improvement in AUC compared to uni-modal models without radiological images, highlighting the value of multi-modal integration [20].
For cancer survival prediction, multi-modal approaches have shown consistent improvements in C-index values. A comparative deep learning study on breast cancer survival reported that late fusion strategies outperformed early fusion approaches, with optimized models achieving C-index values of approximately 0.78 when integrating omics and clinical data [98]. Similarly, a multi-modal multi-instance evidence fusion neural network (M2EF-NNs) demonstrated significant improvements in overall C-index and AUC across three cancer datasets, incorporating uncertainty estimation through Dempster-Shafer evidence theory [50].
Metric Selection Guidelines for Specific Applications
The selection of appropriate performance metrics should align with the specific clinical or research objective:
Cancer Detection and Diagnosis: For binary classification tasks (e.g., malignant vs. benign), AUC provides a comprehensive assessment of model performance across all decision thresholds, while F1-score offers a balanced view of precision and recall trade-offs [97]. In applications where false negatives have severe consequences (e.g., cancer screening), recall may be prioritized, while specificity becomes more critical in confirmatory testing.
Treatment Response Prediction: AUC is widely used for evaluating models predicting pathological complete response (pCR) to neoadjuvant therapy [20]. Additionally, accuracy, sensitivity, and specificity are commonly reported to provide clinically interpretable performance measures at specific decision thresholds.
Survival Prediction: The C-index serves as the primary metric for assessing prognostic models, complemented by time-dependent AUC values at clinically relevant timepoints [96] [50]. Calibration measures should also be reported to ensure predicted probabilities align with observed outcomes.
Cancer Subtyping and Molecular Classification: For multi-class classification problems, accuracy and F1-score (both micro- and macro-averaged) provide comprehensive performance assessments. The Matthews Correlation Coefficient (MCC) may be particularly valuable for imbalanced class distributions [31].
Metric Selection Guide
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Computational Tools for Multi-modal Cancer Research
| Tool Category | Specific Solutions | Primary Function | Application Context |
|---|---|---|---|
| Genomic Analysis | GATK; MuTect; VarScan; DESeq2; EdgeR | Mutation detection; Differential expression; Variant calling | Processing genomic, transcriptomic, and epigenomic data [1] |
| Pathology Image Analysis | Vision Transformers; CNNs; Stain normalization tools | Feature extraction from histopathological images; Whole slide image analysis | Quantifying morphological patterns; Tumor microenvironment characterization [50] |
| Radiomics Processing | Custom deep learning architectures; 3D CNNs | Feature extraction from medical images (MRI, CT, mammography) | Predicting treatment response; Tumor characterization [20] |
| Multi-modal Fusion Frameworks | Attention mechanisms; Cross-modal learning; Tensor fusion | Integrating heterogeneous data modalities | Late fusion architectures; Cross-modal knowledge transfer [20] [50] |
| Survival Analysis | Cox PH models; Deep survival networks; Random survival forests | Modeling time-to-event data with censoring | Prognostic model development; Survival prediction [96] [98] |
| Model Explainability | SHAP; Grad-CAM; Attention visualization | Interpreting model predictions; Feature importance | Biological validation; Clinical trust building [48] [98] |
The evaluation of multi-modal fusion models in cancer research requires careful consideration of performance metrics that align with clinical objectives and account for the complexities of integrated data types. AUC, C-index, Accuracy, and F1-Score each provide distinct insights into model performance, with optimal metric selection depending on the specific application context—whether cancer detection, treatment response prediction, survival analysis, or molecular subtyping. As multi-modal approaches continue to evolve, robust validation methodologies and comprehensive performance reporting will be essential for translating these advanced computational frameworks into clinically actionable tools that enhance precision oncology.
Multimodal artificial intelligence (MMAI) is redefining oncology by integrating heterogeneous datasets from various diagnostic modalities into cohesive analytical frameworks, enabling more accurate and personalized cancer care [3]. This integration addresses the fundamental biological complexity of cancer, which manifests across multiple scales—from molecular alterations and cellular morphology to tissue organization and clinical phenotype [3]. Predictive models relying on a single data modality fail to capture this multiscale heterogeneity, limiting their ability to generalize across patient populations [3] [45].
The core challenge in multimodal learning lies in effectively fusing information from diverse sources such as genomics, histopathology, medical imaging, and clinical records [45] [1]. Fusion strategies are broadly categorized into three architectural paradigms: early fusion, late fusion, and hybrid fusion, each with distinct mechanisms, advantages, and limitations [18] [4]. This analysis provides a structured comparison of these fusion methodologies within the context of cancer diagnostics, offering experimental protocols and implementation frameworks to guide researchers and drug development professionals in advancing precision oncology.
Fusion Strategy Definitions and Mechanisms
Early Fusion (Data-Level Fusion)
Early fusion, also known as data-level fusion, involves integrating raw data or low-level features from multiple modalities before model training [18] [4]. This approach concatenates features from multiple modalities at the shallow layers or input layers of the model, followed by a cascaded deep network structure that ultimately connects to the classifier [18]. The fundamental premise is learning correlations between low-level features of each modality within a single unified model [18].
Key Mechanism: In early fusion, dedicated feature extractors capture deep features from each modality—for instance, a convolutional neural network (CNN) for pathological images and a deep neural network for genomic data [53]. These features are then integrated through a fusion model to achieve predictions [53]. Early fusion is particularly suitable for cases with minimal differences between the modalities being integrated [18].
Late Fusion (Decision-Level Fusion)
Late fusion, or decision-level fusion, involves independently training separate models for each modality and combining their predictions at the output level [18]. Each modality undergoes feature extraction through separate models, and the extracted features or predictions are fused before connecting to a final classifier [18]. This approach maintains modality-specific processing pipelines until the final decision stage.
Key Mechanism: In late fusion, multiple models are trained independently on their respective modalities [18]. For example, in breast cancer detection, separate models might process mammography and ultrasound images, with their outputs combined through averaging, weighted voting, or meta-learners to produce the final classification [18]. This strategy offers robustness against modality-specific inconsistencies and data imbalances [45].
Hybrid Fusion
Hybrid fusion combines principles of both early and late fusion to leverage their complementary strengths [18] [99]. This approach integrates modalities at multiple levels of the processing pipeline, enabling both low-level feature interactions and high-level decision integrations. Advanced implementations include learned early-fusion with joint projection that enables early cross-talk between local CNN-extracted features and global Transformer-derived context [100].
Key Mechanism: Hybrid architectures often employ multi-stage fusion strategies that integrate cross-connections, multiple attention mechanisms, and bidirectional recurrent neural networks to effectively extract local-global contextual features [99]. For instance, the PADBSRNet model integrates separable and traditional convolution layers with attention mechanisms and feature fusion strategies for cancer detection [99].
Comparative Performance Analysis in Oncology Applications
Table 1: Quantitative Performance Comparison of Fusion Strategies Across Cancer Types
| Cancer Type | Fusion Strategy | Architecture | Performance Metrics | Reference |
|---|---|---|---|---|
| Breast Cancer | Multimodal (Mammography + Ultrasound) | Late Fusion with ResNet-18 | AUC: 0.968, Accuracy: 93.78%, Specificity: 96.41% | [18] |
| Breast Cancer | Hybrid Feature Fusion | Deep + Traditional features with XGBoost | Accuracy: 98.67% (Rodrigues), 97.06% (INbreast) | [101] |
| Ovarian Cancer | Learned Early-Fusion Hybrid | EfficientNet-B7 + Swin Transformer | AUC: 0.9904, Accuracy: 92.13%, Sensitivity: 92.38% | [100] |
| Breast Cancer | Model Fusion Intermediate | VGG16 + DenseNet121 + Xception | Accuracy: 97% with improved feature representation | [102] |
| NSCLC | Multimodal Integration | Radiology-Pathology-Genomics | AUC: 0.80 for immunotherapy response prediction | [45] |
| Pan-Cancer | Multimodal Deep Learning | Selective Integration (3-5 modalities) | AUC improvements of 10-15% over unimodal baselines | [45] |
Table 2: Strategic Advantages and Limitations in Clinical Oncology Settings
| Fusion Strategy | Key Advantages | Major Limitations | Optimal Use Cases |
|---|---|---|---|
| Early Fusion | Learns cross-modal correlations at feature level; Single unified model complexity | Challenges with feature concatenation from different modalities; High dimensionality requires extensive preprocessing | Modalities with minimal differences; Availability of aligned multimodal data [18] |
| Late Fusion | Robust against modality imbalances and inconsistencies; Enables modality-specific optimization | May overlook critical cross-modal interactions; Requires training multiple models | Asynchronous or incomplete data; Integration of established single-modality models [45] [18] |
| Hybrid Fusion | Captures both local and global contextual dependencies; Flexible architecture design | Increased computational complexity; More challenging to implement and train | Complex diagnostic tasks requiring comprehensive feature representation [100] [99] |
Experimental Protocols for Fusion Implementation
Protocol 1: Late Fusion for Multimodal Breast Cancer Detection
Objective: Implement late fusion for classifying breast lesions as benign or malignant using mammography and ultrasound images [18].
Materials and Datasets:
- Mammography datasets: Mini-DDSM, INbreast [101] [18]
- Ultrasound datasets: Rodrigues, BUSI [101] [18]
- Pre-trained CNN models: ResNet-18, ResNet-50, VGG16 [18]
Methodology:
- Image Preprocessing:
- Resize all images to standardized dimensions (e.g., 224×224 pixels)
- Apply grayscale normalization using min-max normalization:
x_norm = (x - x_min)/(x_max - x_min)[18] - Enhance contrast using CLAHE (Contrast Limited Adaptive Histogram Equalization) [101]
- Perform data augmentation (horizontal/vertical flipping, elastic deformation) [18]
Modality-Specific Model Training:
- Train separate CNN models on mammography and ultrasound datasets
- Apply transfer learning with ImageNet pre-trained weights [18]
- Fine-tune final layers for lesion classification
Feature Extraction and Fusion:
- Extract deep features from intermediate layers of both models
- Concatenate feature vectors using late fusion strategy
- Train meta-classifier (XGBoost, AdaBoost, or CatBoost) on fused features [101]
Validation:
- Use stratified k-fold cross-validation
- Evaluate using AUC, accuracy, sensitivity, specificity
- Generate Grad-CAM visualizations for model interpretability [102]
Protocol 2: Hybrid CNN-Transformer for Ovarian Tumor Classification
Objective: Develop hybrid CNN-Transformer model with learned early-fusion for multiclass ovarian tumor classification [100].
Materials and Datasets:
- OTU-2D dataset (1,469 2D ultrasound images across 8 classes) [100]
- EfficientNet-B7 and Swin Transformer architectures [100]
Methodology:
- Image Preprocessing:
- Resize images to 224×224 pixels
- Apply ultrasound-specific augmentations: Rayleigh-distributed speckle noise, time-gain compensation, acoustic artifacts [100]
- Address class imbalance with train-only oversampling
Hybrid Architecture Implementation:
- Implement EfficientNet-B7 for local feature extraction
- Integrate Swin Transformer for hierarchical global context
- Apply learned early-fusion with joint projection for cross-modality interaction [100]
Model Training:
- Use strong regularization (weight decay, dropout)
- Employ patient-level stratified 5-fold cross-validation
- Apply multiple independent runs with fixed seeds for statistical robustness [100]
Evaluation and Interpretation:
Workflow Visualization
Diagram 1: Architectural comparison of fusion strategies showing information flow from multimodal inputs to classification outputs.
Research Reagent Solutions for Multimodal Fusion
Table 3: Essential Research Tools and Platforms for Multimodal Fusion Implementation
| Resource Category | Specific Tools/Platforms | Primary Function | Application Context |
|---|---|---|---|
| Deep Learning Frameworks | PyTorch (MONAI), TensorFlow | Model development and training | Medical imaging with pre-trained models [3] |
| Multimodal Datasets | TCGA, OTU-2D, INbreast, BUSI | Benchmarking and validation | Pan-cancer analysis, ovarian and breast tumor classification [45] [100] |
| Feature Extraction | Pre-trained CNNs (ResNet, VGG, DenseNet) | Deep feature representation | Transfer learning for medical images [102] [18] |
| Explainability Tools | Grad-CAM++, SHAP, LIME | Model interpretability and visualization | Clinical validation and trust-building [45] [102] |
| Data Harmonization | Nested ComBat, Min-Max Normalization | Batch effect correction and standardization | Preprocessing heterogeneous multimodal data [45] [18] |
The strategic selection of fusion methodologies significantly impacts the performance and clinical applicability of multimodal AI systems in oncology. Evidence from recent studies indicates that late fusion consistently demonstrates robustness in handling heterogeneous data sources, while early fusion excels when modalities share complementary low-level features [18] [45]. Hybrid approaches represent the most advanced paradigm, offering superior performance for complex diagnostic tasks by leveraging both local feature interactions and global contextual dependencies [100] [99].
The implementation of these fusion strategies must be guided by specific clinical contexts, data availability, and performance requirements. As multimodal AI continues to evolve, the integration of explainability frameworks and standardized validation protocols will be essential for clinical translation and adoption in precision oncology workflows [45] [102]. Future research should focus on adaptive fusion mechanisms that dynamically optimize integration strategies based on data characteristics and clinical task requirements.
Benchmarking Against Unimodal Baselines and Traditional Methods
Within the broader thesis on multi-modal data fusion for improved cancer diagnosis, benchmarking against unimodal baselines and traditional clinical methods is a critical step for validating the added value of integrated approaches. Multi-modal artificial intelligence (MMAI) aims to capture the multifaceted nature of cancer by combining complementary data types, such as histology, genomics, and clinical reports [3]. However, to robustly demonstrate its superiority, MMAI must be systematically compared to established unimodal methods and clinical standards. This document provides detailed application notes and protocols for conducting such benchmarks, enabling researchers to quantitatively assess whether multi-modal fusion offers significant improvements in prognostic accuracy, risk stratification, and treatment response prediction for oncology applications.
Quantitative Benchmarking Data
A rigorous benchmark requires comparison on multiple cancer types using established quantitative metrics. The following tables summarize performance data from a state-of-the-art multimodal model, PS3, which integrates whole slide images (WSIs), transcriptomic data, and pathology reports. It is evaluated against unimodal baselines and traditional clinical staging on six TCGA cancer cohorts. The primary evaluation metric is the Concordance Index (C-Index), which measures the model's ability to correctly rank patient survival times.
Table 1: Performance Benchmarking Across Cancer Types (C-Index)
| Cancer Type | PS3 (Multimodal) | WSI Only | Transcriptomics Only | Pathology Report Only | Clinical Baseline |
|---|---|---|---|---|---|
| BRCA | 0.723 | 0.681 | 0.662 | 0.634 | 0.601 |
| LUAD | 0.705 | 0.652 | 0.643 | 0.621 | 0.588 |
| UCEC | 0.741 | 0.698 | 0.674 | 0.645 | 0.623 |
| SKCM | 0.686 | 0.641 | 0.633 | 0.602 | 0.579 |
| KIRC | 0.734 | 0.692 | 0.668 | 0.651 | 0.625 |
| GBM | 0.698 | 0.649 | 0.631 | 0.598 | 0.567 |
Table 2: Ablation Study on Fusion Strategies (Average C-Index across cohorts)
| Model Configuration | Average C-Index | Key Features |
|---|---|---|
| PS3 (Full Model) | 0.715 | Early fusion with cross-attention, all three modalities |
| Late Fusion Baseline | 0.673 | Concatenation of unimodal predictions |
| WSI + Transcriptomics | 0.691 | Ablation: Pathology reports removed |
| WSI + Pathology Reports | 0.684 | Ablation: Transcriptomics removed |
| Transcriptomics + Pathology Reports | 0.667 | Ablation: WSIs removed |
The benchmark data shows that the full PS3 model consistently outperforms all unimodal and traditional clinical baselines across all six cancer types [103]. The integration of pathology reports, an often-underutilized data source, provides complementary information that enhances models based solely on WSIs and genomics. Furthermore, the ablation studies confirm that the model's performance gain is attributable to its effective fusion strategy and the use of all three modalities, rather than the dominance of a single data type [103].
Experimental Protocols
This section outlines the core methodologies for replicating the benchmark comparisons, from data preprocessing to model training and evaluation.
Data Preprocessing and Unimodal Feature Extraction Protocol
Objective: To standardize raw input data from three modalities into compact, meaningful representations suitable for fusion.
Materials:
- WSIs: Formalin-fixed, paraffin-embedded (FFPE) tissue sections, digitized using a whole-slide scanner (e.g., at 40x magnification).
- Transcriptomic Data: RNA-Seq data (e.g., FPKM or TPM normalized counts) from repositories like TCGA.
- Pathology Reports: Text reports in unstructured or semi-structured format, typically containing diagnostic summaries, tumor grade, and stage.
Procedure:
Whole Slide Image Processing a. Tiling: Use an open-source library (e.g., OpenSlide) to partition the WSI into smaller, manageable patches (e.g., 256x256 pixels) at a specified magnification level. b. Feature Embedding: Pass each patch through a pre-trained convolutional neural network (CNN) such as ResNet50 (pre-trained on ImageNet) to extract a feature vector for each patch. c. Histological Prototyping: To overcome the gigapixel-scale of WSIs, cluster a representative sample of patch features from the training set using a Gaussian Mixture Model (GMM). The cluster centroids become the "histological prototypes," compressing the WSI into a set of key morphological patterns [103].
Transcriptomic Data Processing a. Normalization: Apply standard normalization (e.g., log2(TPM+1)) to the gene expression matrix. b. Pathway Activation Scoring: Move from gene-level to pathway-level analysis. Using a predefined database like the Cancer Hallmarks, aggregate the expression of genes within each of the 50 hallmark pathways [103]. Calculate a single activation score for each pathway (e.g., using single-sample Gene Set Enrichment Analysis - ssGSEA). These scores form the "pathway prototypes," providing a biologically meaningful and compact representation of genomic function [103].
Pathology Report Processing a. Sectioning: Divide the full text of the report into smaller, coherent segments (e.g., "Diagnosis," "Microscopic Description"). b. Feature Embedding: Use a pre-trained language model (e.g., a transformer-based model like BERT) to generate a feature vector for each text segment. c. Diagnostic Prototyping: Apply a self-attention mechanism to the text segment embeddings. This identifies and weights the most diagnostically relevant sections of the report, creating a standardized "diagnostic prototype" vector that captures critical clinical information [103].
Output: For each patient, three sets of prototype vectors: Histological, Pathway, and Diagnostic.
Multimodal Fusion and Benchmarking Protocol
Objective: To integrate the three unimodal prototype sets and train a model for survival prediction, comparing its performance against unimodal and clinical baselines.
Materials:
- Preprocessed prototype vectors for all patient samples.
- Corresponding overall survival data (survival time and event indicator).
Procedure:
Model Architecture (PS3) a. Input Layer: The prototype vectors from all three modalities are treated as tokens and fed into a transformer encoder. b. Fusion Layer: The transformer models intra-modal and cross-modal interactions using self-attention and cross-attention mechanisms. This allows the model to learn complex relationships, for example, between a specific morphological pattern in the WSI and a particular pathway activation [103]. c. Output Head: The fused representation is passed through a fully connected layer and a Cox proportional hazards layer to predict a hazard ratio for each patient.
Benchmarking and Evaluation a. Unimodal Baselines: Train separate survival prediction models using only the prototypes from a single modality (e.g., only WSI prototypes, only pathway prototypes). b. Clinical Baseline: Establish a baseline using traditional clinical variables (e.g., TNM stage, age, grade) in a Cox regression model. c. Training: Use k-fold cross-validation (e.g., 5-fold) on the cohort to ensure robust performance estimation. d. Evaluation: Calculate the Concordance Index (C-Index) for the full PS3 model and all baselines on the held-out test folds. Perform statistical significance testing (e.g., bootstrapping) to confirm that the multimodal model's improvement is not due to chance.
Signaling Pathways and Workflow Visualizations
Multimodal Fusion Workflow
Benchmarking Logic
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials and Computational Tools for Multimodal Benchmarking
| Item Name | Type | Function in Experiment |
|---|---|---|
| TCGA Datasets | Data Repository | Provides curated, clinically annotated multi-omics data, WSIs, and pathology reports for model training and validation [1]. |
| Whole-Slide Image (WSI) Scanners | Hardware | Digitizes histopathology glass slides into high-resolution digital images for computational analysis (e.g., Aperio, Hamamatsu). |
| Pre-trained Convolutional Neural Network (CNN) | Software/Model | Extracts meaningful feature representations from image patches. Models like ResNet50 (pre-trained on ImageNet) are standard [103]. |
| Pre-trained Language Model (e.g., BERT) | Software/Model | Converts unstructured text from pathology reports into numerical feature vectors, capturing semantic meaning [103]. |
| Gaussian Mixture Model (GMM) | Algorithm | Clusters similar WSI patch embeddings to generate a compact set of "histological prototypes," reducing dimensionality [103]. |
| Cancer Hallmark Gene Sets | Biological Database | Provides a curated list of 50 biological pathways that are routinely dysregulated in cancer, used to create pathway prototypes from transcriptomic data [103]. |
| Transformer Architecture | Model Architecture | The core fusion engine that models complex intra-modal and cross-modal interactions between histological, pathway, and diagnostic prototypes [103]. |
| Concordance Index (C-Index) | Statistical Metric | The primary evaluation metric for survival prediction models, measuring the model's ability to correctly rank patient survival times. |
In the field of multi-modal data fusion for cancer diagnosis, the development of robust predictive models hinges on rigorous validation frameworks. Validation frameworks are systematic methodologies used to evaluate the performance, generalizability, and clinical applicability of computational models. As artificial intelligence (AI) models increasingly integrate diverse data types—including genomic, imaging, histopathological, and clinical data—the potential for overfitting and biased performance estimates grows significantly. Cross-validation and external validation in independent cohorts represent two foundational pillars of these frameworks. Their critical importance is underscored by the fact that despite the proliferation of powerful AI models in oncology, few have achieved widespread clinical adoption, often due to inadequate validation practices [104]. This document outlines standardized protocols for implementing these validation strategies, specifically within the context of multi-modal cancer diagnostic research.
Core Concepts and Definitions
- Cross-Validation: A resampling technique used to assess how the results of a statistical analysis will generalize to an independent dataset. It is primarily used in model development and hyperparameter tuning when data is limited.
- External Validation: The process of evaluating a final, fixed model's performance on data that was not used in any part of the model development process. This data is ideally collected from a different population, institution, or timeframe.
- Internal Validation: A broader term that includes cross-validation and bootstrap methods, all performed using the original development dataset.
- Generalizability: The ability of a model to maintain its predictive performance when applied to new, unseen data from different sources.
- Overfitting: A modeling error that occurs when a model is too closely aligned to the development data, capturing its noise and random fluctuations rather than the underlying relationship, leading to poor performance on new data.
The Critical Need for Robust Validation in Multi-Modal Oncology
The integration of multiple data modalities introduces unique challenges that make rigorous validation non-negotiable. Multi-modal data fusion often suffers from a low sample size to feature space ratio, high dimensionality, data heterogeneity, and significant inter-modality correlations [13]. These factors dramatically increase the risk of model overfitting. Furthermore, the clinical imperative for safety and efficacy demands that models perform reliably across diverse patient populations and clinical settings. Studies have repeatedly shown that models achieving exceptional performance via internal validation can fail dramatically in external test cohorts, highlighting the profound gap between theoretical efficacy and practical application [104] [105]. Therefore, a robust validation framework is not merely a technical formality but a prerequisite for clinical translation.
Cross-Validation: Protocols and Application Notes
Cross-validation is employed during the model training phase to provide a robust estimate of model performance and to guide model selection without the need for a separate hold-out test set.
Standard k-Fold Cross-Validation Protocol
This is the most widely used cross-validation technique.
- Random Shuffling: Randomly shuffle the development dataset.
- Splitting: Split the development dataset into k equally sized folds (common values are k=5 or k=10).
- Iterative Training and Validation: For each unique fold:
- Designate the current fold as the validation set.
- Designate the remaining k-1 folds as the training set.
- Train the model on the training set.
- Evaluate the model on the validation set and record the performance metric(s) (e.g., AUC, accuracy).
- Performance Estimation: Calculate the average performance across all k iterations. This average is the cross-validation performance estimate.
Stratified k-Fold Cross-Validation Protocol
In cancer studies, outcome classes (e.g., responder vs. non-responder) are often imbalanced. Standard k-fold can lead to folds with no representatives of a minority class.
- Follow the standard k-fold protocol, but ensure that each fold is stratified to preserve the same percentage of samples of each target class as in the complete development dataset.
- This is the recommended default for most classification tasks in medical research.
Nested Cross-Validation Protocol
When both model selection and unbiased performance estimation are required, nested (or double) cross-validation is the gold standard.
- Outer Loop: Set up a k-fold cross-validation (e.g., 5-fold). This loop is for performance estimation.
- Inner Loop: For each training set of the outer loop, perform another, separate k-fold cross-validation (e.g., 3-fold). This inner loop is for model and hyperparameter selection.
- Process: For each outer fold, the inner loop is used to select the best model/hyperparameters using only the outer training fold. This best model is then trained on the entire outer training fold and evaluated on the outer test fold.
- Outcome: This provides an almost unbiased estimate of the performance of the model selection process.
Table 1: Comparison of Common Cross-Validation Strategies
| Strategy | Primary Use Case | Key Advantage | Key Disadvantage | Recommended k for Oncology |
|---|---|---|---|---|
| k-Fold | General performance estimation | Reduces variance compared to a single train-test split | Can be biased with imbalanced data | 5 or 10 |
| Stratified k-Fold | Classification with imbalanced classes | Preserves class distribution in folds, more reliable | Slightly more complex implementation | 5 or 10 |
| Leave-One-Out (LOO) | Very small datasets (<100 samples) | Utilizes maximum data for training | Computationally expensive; high variance | N (sample size) |
| Nested Cross-Validation | Unbiased performance estimation with hyperparameter tuning | Provides unbiased estimate for the full modeling process | Computationally very expensive | Outer: 5-6, Inner: 3-5 |
Application Notes for Multi-Modal Data
- Modality-Preserving Splits: When splitting data into folds, ensure that all data from a single patient (e.g., their MRI, genomics, pathology) are contained within the same fold. This prevents data leakage and over-optimistic performance.
- Handling Missing Modalities: Multi-modal datasets often have incomplete cases. The cross-validation strategy must be designed to handle this, for example, by training modality-specific models on available data or using imputation techniques within each training fold to avoid leakage.
External Validation: Protocols and Application Notes
External validation is the most stringent test of a model's real-world utility and is considered essential before any clinical deployment.
External Validation Protocol
- Cohort Selection: Identify one or more independent validation cohorts. These should be from:
- A different geographic location or country.
- A different hospital or healthcare system.
- A different time period (temporal validation).
- A population with different demographic or clinical characteristics.
- Model Locking: The model to be validated must be completely locked. No further tuning or retraining is allowed based on the external cohort's data.
- Data Preprocessing: Apply the same preprocessing steps (e.g., normalization, feature scaling, image resampling) that were defined on the development cohort to the external cohort.
- Performance Evaluation: Apply the locked model to the external cohort and calculate all relevant performance metrics.
- Comparison and Analysis: Compare performance between the development (internal) and external validation cohorts. A significant drop in performance indicates poor generalizability.
Application Notes and Best Practices
- Multi-Center Collaboration: Proactively plan for external validation by engaging in multi-center collaborations during the study design phase, as demonstrated in the MRP system for breast cancer NAT response prediction [20].
- Heterogeneous Cohorts: Actively seek out heterogeneous external cohorts to stress-test the model across different scanners, protocols, and patient populations. This provides a more realistic assessment of clinical applicability.
- Performance Metrics: Report a comprehensive set of metrics including discrimination (e.g., AUROC, C-index), calibration (e.g., calibration plots, E:O ratio), and clinical utility (e.g., Decision Curve Analysis) [20] [106].
- Sample Size: While larger is better, even smaller external cohorts (n > 100) can provide valuable evidence of generalizability, though confidence intervals will be wider [106].
Table 2: Key Considerations for External Validation Cohorts in Multi-Modal Cancer Studies
| Consideration | Description | Example from Literature |
|---|---|---|
| Geographic Diversity | Testing model on populations from different continents or healthcare systems. | MRP system tested on cohorts from the Netherlands, US (Duke), and China [20]. |
| Temporal Validation | Using data from a future time period to validate a model developed on historical data. | The QCancer algorithm was validated on data from subsequent years [105]. |
| Protocol Variability | Ensuring cohorts include data from different imaging devices, sequencing machines, or laboratory protocols. | The PDxBR digital prognostic test was validated in an independent Dutch cohort, demonstrating scalability [106]. |
| Demographic Shifts | Validating across populations with different ethnicities, age distributions, or socioeconomic statuses. | Large-scale cancer prediction algorithms were validated across subgroups defined by ethnicity and age [105]. |
Integrated Validation Workflow for Multi-Modal Fusion
A comprehensive validation framework for a multi-modal cancer diagnostic model should integrate both internal and external validation. The following diagram illustrates this end-to-end workflow.
Workflow for Multi-Modal Model Validation
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Tools and Resources for Multi-Modal Validation
| Tool / Resource | Type | Function in Validation | Example / Note |
|---|---|---|---|
| Scikit-learn | Software Library | Provides implementations for k-fold, stratified k-fold, and other cross-validation splitters. | Standard for classical ML models; StratifiedKFold, cross_val_score. |
| PyTorch / TensorFlow | Deep Learning Framework | Facilitates custom data loaders and training loops that respect patient-level splits for multi-modal data. | Crucial for handling complex neural network architectures on image and genomic data. |
| The Cancer Genome Atlas (TCGA) | Data Resource | Provides public multi-modal data (genomics, images, clinical) for initial development and as a source for external cohorts. | Used in [13] [107]; requires careful splitting to simulate external validation. |
| AstraZeneca-AI (AZ-AI) Pipeline | Software Library | A Python library for multimodal feature integration and survival prediction, includes rigorous evaluation methods [13]. | Manages challenges like high dimensionality, small sample sizes, and data heterogeneity. |
| Segment Anything Model (SAM) | Foundation Model | Used for unsupervised lesion localization in images, reducing dependency on costly manual annotations during preprocessing [108]. | Improves generalizability by standardizing ROI extraction across different institutions. |
| SHAP / LIME | Software Library | Explainable AI (XAI) tools used post-validation to interpret model predictions and ensure biological/clinical plausibility [45]. | Helps build trust in the validated model by linking predictions to known biomarkers. |
| Federated Learning Platforms | Framework | Enables model training and validation across multiple institutions without sharing raw data, addressing privacy concerns [45]. | Emerging solution for creating large, diverse external validation sets. |
Multimodal Artificial Intelligence (MMAI) is redefining oncology by integrating heterogeneous datasets from diverse diagnostic modalities into cohesive analytical frameworks, enabling more accurate and personalized cancer care [3]. Cancer manifests across multiple biological scales, from molecular alterations and cellular morphology to tissue organization and clinical phenotype [3]. Predictive models relying on a single data modality fail to capture this multiscale heterogeneity, significantly limiting their ability to generalize across patient populations [3]. MMAI approaches systematically integrate information from diverse sources, including cancer multiomics (genomics, proteomics, metabolomics), histopathology, medical imaging, and clinical records, enabling models to exploit biologically meaningful inter-scale relationships [3] [109]. By contextualizing molecular features within anatomical and clinical frameworks, MMAI enhances predictive accuracy, robustness, and clinical relevance, ultimately providing a more comprehensive representation of disease [3]. This technical analysis examines three pioneering MMAI frameworks—TRIDENT, ABACO, and MONAI—that are advancing oncology research and clinical practice through sophisticated multimodal data fusion.
Framework-Specific Application Notes
TRIDENT (Translational Integration of Data in Oncology)
Overview and Purpose: TRIDENT is a machine learning multimodal model designed to integrate radiomics, digital pathology, and genomics data to optimize treatment personalization in oncology, particularly for metastatic non-small cell lung cancer (NSCLC) [3] [109]. Developed based on data from the Phase 3 POSEIDON study, TRIDENT addresses the critical clinical challenge of identifying patient subgroups most likely to benefit from specific therapeutic combinations [3].
Technical Architecture: The framework employs a multimodal fusion strategy that processes imaging data (CT scans), digitized histopathology slides, and genomic sequencing data through specialized feature extraction pipelines [3]. These extracted features are then integrated using machine learning algorithms to generate predictive signatures for treatment response [3].
Key Performance Metrics: In validation studies, TRIDENT identified a patient signature in >50% of the population that would obtain optimal benefit from a particular treatment strategy, demonstrating significant hazard ratio reductions: 0.88-0.56 in the non-squamous histology population and 0.88-0.75 in the intention-to-treat population [3]. This represents a substantial improvement over conventional patient stratification methods.
Table 1: TRIDENT Framework Performance Metrics
| Metric Category | Specific Outcome | Clinical Impact |
|---|---|---|
| Patient Selection | Identified >50% of population as optimal treatment responders | Enables precision targeting of therapies |
| Risk Reduction (Non-squamous) | HR: 0.88-0.56 | Significant survival benefit in specific histology |
| Risk Reduction (Overall) | HR: 0.88-0.75 | Meaningful improvement across broader population |
| Data Integration | Combines radiomics, digital pathology, genomics | Comprehensive tumor profiling |
ABACO (AI-Based Analytics for Cancer Oncology)
Overview and Purpose: ABACO is a pilot real-world evidence (RWE) platform utilizing MMAI to identify predictive biomarkers for targeted treatment selection, optimize therapy response predictions, and improve patient stratification in hormone receptor-positive (HR+) metastatic breast cancer [3] [109]. The platform dynamically links treatment outcomes to AI-driven insights for enhanced patient management [3].
Technical Architecture: ABACO incorporates multimodal integration of remote patient monitoring data and conventional data streams, capturing complementary physiological and contextual information [3] [109]. The platform leverages real-world data from electronic health records, wearable sensors, and patient-reported outcomes, processed through machine learning algorithms to generate continuous insights for clinical decision-making [3].
Key Performance Metrics: While specific quantitative performance metrics for ABACO are not explicitly detailed in the available literature, the platform has demonstrated capability in improving predictive performance for therapy response and enabling dynamic adjustment of treatment strategies based on near real-time feedback loops [3]. Its RWE approach facilitates more efficient and precise drug trials based on real-world evidence rather than strictly controlled clinical trial data [3].
Implementation Advantages: ABACO's continuous monitoring capability allows oncologists to proactively adjust treatment and management plans specific to each patient, potentially minimizing adverse events and optimizing therapeutic efficacy throughout the treatment journey [3].
MONAI (Medical Open Network for AI)
Overview and Purpose: Project MONAI is an open-source, PyTorch-based framework providing a comprehensive suite of AI tools and pre-trained models for medical imaging applications [3]. Co-founded by NVIDIA, MONAI specifically targets care pathway optimization through enhanced medical image analysis across multiple cancer types [3].
Technical Architecture: MONAI provides specialized deep-learning capabilities for various imaging modalities including digital mammograms, CT scans, and magnetic resonance imaging [3]. The framework includes domain-specific implementations for precise organ delineation, tumor detection, and feature extraction from medical images [3].
Key Performance Metrics: MONAI-based models have demonstrated significant clinical utility across multiple cancer types. In breast cancer screening, these models enable precise delineation of the breast area in digital mammograms, improving both accuracy and efficiency of screening programs [3]. For ovarian cancer, deep learning models developed with MONAI enhance diagnostic accuracy on CT and MRI scans [3]. In lung cancer applications, MONAI facilitates integration of radiomics and patient demographic data within deep learning models, leading to improved risk assessment and screening outcome accuracy compared with standard Lung Imaging Reporting and Data System (Lung-RADS) classification [3].
Table 2: MONAI Framework Clinical Applications
| Cancer Type | Application | Performance Outcome |
|---|---|---|
| Breast Cancer | Precise breast area delineation in mammograms | Improved screening accuracy and efficiency |
| Ovarian Cancer | Diagnostic accuracy on CT and MRI scans | Enhanced detection and classification |
| Lung Cancer | Risk assessment integrating radiomics and demographics | Superior to Lung-RADS classification |
| Multiple Cancers | Open-source pre-trained models | Accelerated development of imaging AI |
Experimental Protocols for Multimodal Integration
Protocol 1: TRIDENT Multimodal Predictive Modeling
Objective: To develop and validate a multimodal machine learning model integrating radiomics, digital pathology, and genomics for predicting treatment response in metastatic NSCLC.
Materials and Reagents:
- High-resolution CT scans (radiomics data)
- Digitized histopathology slides (H&E staining)
- Genomic sequencing data (whole exome or targeted panels)
- Clinical outcome data (treatment response, progression-free survival)
- Computational infrastructure (GPU-accelerated workstations)
Methodology:
- Data Preprocessing Phase:
- Perform image normalization and quality control for CT scans
- Execute tissue segmentation and annotation on histopathology slides
- Conduct variant calling and normalization for genomic data
- Implement clinical data harmonization using OMOP CDM standards
Feature Extraction Phase:
- Extract radiomic features (shape, texture, intensity) from CT volumes
- Compute histomorphometric features from digitized pathology slides
- Identify genomic alterations (mutations, copy number variations)
- Derive clinical variables (stage, performance status, prior treatments)
Multimodal Integration Phase:
- Apply dimensionality reduction techniques to each modality
- Implement cross-modal attention mechanisms for feature alignment
- Train ensemble classifiers on integrated feature representations
- Validate model performance using cross-validation and hold-out testing
Clinical Validation Phase:
- Assess model performance using ROC-AUC for response prediction
- Evaluate survival discrimination using Kaplan-Meier analysis
- Compare against unimodal benchmarks and standard clinical criteria
Quality Control Measures: Implement batch effect correction, address missing data through appropriate imputation methods, and ensure reproducibility through version control of analysis pipelines.
Protocol 2: ABACO Real-World Evidence Generation
Objective: To create continuous learning pipelines from multimodal real-world data for dynamic treatment optimization in metastatic breast cancer.
Materials and Reagents:
- Structured EHR data (laboratory values, medication records)
- Unstructured clinical notes (processed with NLP)
- Patient-generated health data (wearables, symptom trackers)
- Molecular profiling data (when available)
- Cloud computing infrastructure with appropriate security protocols
Methodology:
- Data Ingestion and Harmonization:
- Extract and transform EHR data to OMOP Common Data Model
- Process clinical notes using natural language processing for concept extraction
- Normalize temporal patterns in patient-generated health data
- Implement de-identification procedures for privacy protection
Multimodal Feature Engineering:
- Construct traditional features from structured EHR data
- Generate novel features from unstructured text using transformer models
- Derive behavioral patterns from continuous sensor data
- Create integrated patient representations across all modalities
Longitudinal Modeling:
- Develop time-to-event models for treatment effectiveness
- Train reinforcement learning algorithms for dynamic treatment optimization
- Implement counterfactual reasoning frameworks for causal inference
- Create early warning systems for adverse event prediction
Validation and Deployment:
- Perform temporal validation using forward-chaining approaches
- Conduct prospective pilot studies in clinical settings
- Establish continuous model monitoring and updating procedures
- Implement explainability interfaces for clinical interpretation
Ethical Considerations: Establish federated learning capabilities to minimize data movement, implement strict access controls, and ensure compliance with regional data protection regulations.
Visualization of Multimodal Integration Workflows
TRIDENT Multimodal Data Integration
ABACO Real-World Evidence Pipeline
Research Reagent Solutions for Multimodal Oncology
Table 3: Essential Research Reagents and Computational Tools
| Reagent/Tool | Function | Application Context |
|---|---|---|
| MONAI Framework | Open-source medical AI imaging tools | Pre-processing, segmentation, and analysis of medical images |
| PyTorch/TensorFlow | Deep learning model development | Custom neural network architecture for multimodal fusion |
| OMOP CDM | Standardized data model for observational data | Harmonization of real-world evidence from multiple sources |
| Hugging Face Transformers | Natural language processing capabilities | Extraction of concepts from unstructured clinical notes |
| Digital Slide Scanner | Conversion of glass slides to digital images | Creation of digital pathology datasets for analysis |
| Genomic Sequencing Platforms | Generation of molecular profiling data | Identification of genomic alterations for integration |
| GPU Acceleration | High-performance computing resources | Training and inference of computationally intensive models |
| Federated Learning Infrastructure | Privacy-preserving distributed learning | Multi-institutional collaboration without data sharing |
Discussion and Future Directions
The integration of multimodal data through frameworks like TRIDENT, ABACO, and MONAI represents a paradigm shift in oncology research and clinical practice. These platforms demonstrate that combining complementary data types—imaging, pathology, genomics, and clinical records—produces more accurate predictive models than any single modality alone [3] [109]. The documented performance improvements, such as TRIDENT's significant hazard ratio reductions in NSCLC and MONAI's enhanced screening accuracy across multiple cancer types, provide compelling evidence for the value of multimodal integration [3].
Future development should focus on several critical areas. First, enhancing interoperability through standardized data formats and APIs will facilitate broader adoption and integration. Second, addressing ethical considerations and potential biases through rigorous validation across diverse patient populations is essential for equitable implementation [109]. Third, advancing explainability methods will build clinician trust and support translation into routine practice. Finally, establishing comprehensive regulatory frameworks specifically tailored for MMAI in healthcare will ensure patient safety while encouraging innovation [3] [109].
As these frameworks evolve, they hold tremendous potential to reshape the oncology ecosystem—from drug discovery and clinical trial optimization to personalized treatment selection and dynamic therapy adjustment—ultimately improving outcomes for cancer patients worldwide through more precise, data-driven care.
The integration of multimodal data fusion into clinical practice represents a paradigm shift in oncology, enabling a more comprehensive characterization of tumor biology. This approach combines diverse data sources—such as medical images, genomic profiles, and electronic health records—to improve diagnostic accuracy and personalized treatment planning [110]. However, the path to clinical translation requires robust validation and regulatory approval. Real-world evidence has emerged as a critical component in this pathway, providing clinical evidence derived from the analysis of real-world data collected during routine patient care [111] [112]. This document outlines application notes and protocols for generating regulatory-grade evidence for multimodal cancer diagnostic tools.
Regulatory Framework for Real-World Evidence
Definitions and Key Concepts
- Real-World Data (RWD): Data relating to patient health status and/or the delivery of health care routinely collected from a variety of sources [111]. Examples include electronic health records (EHRs), medical claims data, product or disease registries, and data from digital health technologies [111] [112].
- Real-World Evidence (RWE): Clinical evidence derived from the analysis of RWD regarding the usage, potential benefits, and risks of a medical product [111] [112].
The U.S. Food and Drug Administration (FDA) has established a framework for evaluating the potential use of RWE in regulatory decision-making, as mandated by the 21st Century Cures Act [113]. Regulatory bodies are increasingly incorporating RWE to support drug approvals, label expansions, and post-marketing surveillance [112].
RWE Applications in the Product Lifecycle
Table 1: Applications of Real-World Evidence in the Medical Product Lifecycle
| Product Stage | RWE Application | Regulatory Purpose |
|---|---|---|
| Preclinical | Enhancing safety and efficacy assessment [112] | Informing trial design; historical controls |
| Clinical Development | Supporting patient recruitment and retention [112] | Identifying eligible populations; enriching trials |
| Regulatory Submission | Demonstrating effectiveness in broader populations [113] | Supporting new drug applications; supplemental indications |
| Post-Marketing | Long-term safety monitoring and pharmacovigilance [111] [112] | Fulfilling post-approval study requirements; risk management |
Application Note: Multimodal Fusion for Breast Cancer Diagnosis
The HXM-Net model exemplifies the successful application of deep learning for multimodal fusion in cancer diagnosis. This architecture combines Convolutional Neural Networks for spatial feature extraction with a Transformer-based fusion module to optimally integrate information from B-mode and Doppler ultrasound images [5]. The model captures both morphological and vascular features of breast lesions, creating a more discriminative feature representation for classifying benign and malignant tumors [5].
Performance Metrics and Validation
Table 2: Quantitative Performance of the HXM-Net Model for Breast Cancer Diagnosis
| Performance Metric | Result | Comparative Advantage |
|---|---|---|
| Accuracy | 94.20% | Established superiority over conventional models (e.g., ResNet-50, U-Net) [5] |
| Sensitivity (Recall) | 92.80% | Enhanced detection of malignant cases [5] |
| Specificity | 95.70% | Improved ability to correctly identify benign tumors [5] |
| F1 Score | 91.00% | Balanced precision and recall performance [5] |
| AUC-ROC | 0.97 | Excellent discriminatory capacity [5] |
The model incorporated multi-scale feature learning and data augmentation to ensure generalizability across different lesion types and patient populations [5]. Furthermore, the inclusion of explainable AI methods provided clinically meaningful insights into the decision-making process, fostering trust among healthcare professionals [5].
Experimental Protocols
Protocol 1: Generating RWE for Algorithm Validation
Objective: To validate the clinical performance of a multimodal fusion algorithm for cancer diagnosis using real-world data.
Study Design:
- Data Source: Federated network of electronic health records from multiple institutions [111].
- Population: Patients with suspected breast lesions undergoing standard ultrasound imaging.
- Inclusion Criteria: Adult patients (≥18 years) with complete clinical, imaging, and pathological data.
- Exclusion Criteria: Incomplete follow-up or missing key variables.
Methodology:
- Data Extraction: Retrospective extraction of structured and unstructured data from EHRs.
- Data Curation:
- Image Processing: Standardize ultrasound images (B-mode and Doppler) to a common resolution.
- Feature Engineering: Extract radiomic features from regions of interest.
- Data Labeling: Use pathological diagnosis as ground truth.
- Model Validation:
- Apply the pre-trained HXM-Net model to the retrospective cohort.
- Compare algorithm predictions with histopathological outcomes.
- Assess performance across predefined subgroups (e.g., age, lesion size).
Statistical Analysis:
- Calculate sensitivity, specificity, accuracy, and area under the receiver operating characteristic curve.
- Perform 95% confidence interval estimation for all performance metrics.
- Conduct subgroup analyses to evaluate model consistency.
Protocol 2: Prospective Validation Study Design
Objective: To prospectively validate the clinical utility of a multimodal fusion algorithm in a real-world setting.
Study Design:
- Design: Multicenter, prospective, observational cohort study.
- Duration: 24-month recruitment with 12-month follow-up.
- Sites: 5-10 academic and community hospitals.
Methodology:
- Patient Recruitment: Consecutive enrollment of eligible patients.
- Data Collection:
- Collect multimodal data (ultrasound images, clinical variables, patient-reported outcomes).
- Ensure data quality through standardized operating procedures.
- Intervention:
- Apply the multimodal algorithm to patient data.
- Record algorithm predictions and confidence scores.
- Outcome Measures:
- Primary Endpoint: Diagnostic accuracy compared to histopathology.
- Secondary Endpoints: Time to diagnosis, physician agreement rates, change in clinical management.
Regulatory Considerations:
- Obtain IRB approval at all participating sites.
- Implement data privacy protections in compliance with HIPAA/GDPR [112].
- Pre-specify statistical analysis plan and success criteria.
Visualization of Workflows
RWE Generation Pathway for Multimodal Tools
Multimodal Fusion Architecture
The Scientist's Toolkit
Table 3: Essential Research Reagents and Materials for Multimodal Cancer Diagnostics
| Item | Function/Application | Example/Notes |
|---|---|---|
| Medical Imaging Devices | Acquisition of anatomical and functional data | Ultrasound systems with B-mode and Doppler capabilities [5] |
| Feature Extraction Software | Automated analysis of medical images | Convolutional Neural Networks for spatial feature extraction [5] [114] |
| Data Fusion Frameworks | Integration of heterogeneous data modalities | Transformer-based fusion modules for optimal information concatenation [5] [114] |
| Electronic Health Record Systems | Source of real-world clinical data | Provide comprehensive patient histories and outcomes data [111] [112] |
| Statistical Analysis Tools | Validation of model performance | Software for calculating sensitivity, specificity, AUC-ROC [5] |
The successful clinical translation of multimodal data fusion technologies for cancer diagnosis hinges on generating robust real-world evidence that meets regulatory standards. The frameworks and protocols outlined herein provide a pathway for developers and researchers to validate their algorithms in real-world settings and navigate the evolving regulatory landscape. As multimodal AI continues to advance, its integration with RWE will play an increasingly vital role in bringing innovative diagnostic tools to patients, ultimately improving early detection and personalized treatment in oncology.
Conclusion
Multimodal data fusion represents a paradigm shift in cancer diagnosis, moving beyond the limitations of single-data-type analysis to a holistic, AI-powered approach. The synthesis of insights across foundational principles, diverse methodologies, troubleshooting of implementation barriers, and rigorous validation underscores its unparalleled potential to capture the true complexity of cancer. By integrating complementary information from genomics, imaging, and clinical data, these models achieve superior accuracy in diagnosis, prognosis, and biomarker discovery, directly advancing the goals of precision oncology. Future progress hinges on developing more adaptive and robust fusion architectures, creating large-scale, high-quality public datasets, and establishing standardized frameworks for clinical validation and regulatory approval. The continued evolution of this field is poised to fundamentally reshape clinical decision-making and unlock new frontiers in personalized cancer care.
References
- 1. Multimodal integration strategies for clinical application in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12405423/]
- 2. Multimodal Data Fusion: Key Techniques, Challenges & ... [https://www.sapien.io/blog/mastering-multimodal-data-fusion]
- 3. The AI revolution: how multimodal intelligence will reshape ... [https://www.nature.com/articles/s44387-025-00044-4]
- 4. Application of deep learning-based multimodal fusion ... [https://www.sciencedirect.com/science/article/abs/pii/S0952197624021316]
- 5. Multimodal fusion of ultrasound images using HXM net for ... [https://www.nature.com/articles/s41598-025-23912-0]
- 6. Multimodal AI framework for lung cancer diagnosis [https://pubmed.ncbi.nlm.nih.gov/40449048/]
- 7. MULTI-MODAL DATA FUSION SCHEMES FOR ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4335721/]
- 8. Genome, transcriptome and proteome: the rise of omics data ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6018996/]
- 9. Navigating Cancer Complexity: Integrative Multi-Omics ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12553891/]
- 10. Multimodal data fusion for cancer biomarker discovery with ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10484010/]
- 11. 'Omics' Sciences: Genomics, Proteomics, and Metabolomics [https://www.isaaa.org/resources/publications/pocketk/15/default.asp]
- 12. The Big 'Omics: Genomics, Transcriptomics, Proteomics, & ... [https://www.medreport.foundation/post/the-big-omics-genomics-transcriptomics-proteomics-metabolomics]
- 13. A machine learning approach for multimodal data fusion ... [https://www.nature.com/articles/s41698-025-00917-6]
- 14. Integrating Omics Data and AI for Cancer Diagnosis and ... [https://www.mdpi.com/2072-6694/16/13/2448]
- 15. Application of Multimodality Imaging Fusion Technology in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5198535/]
- 16. Multimodal Data for Whole-Slide Histopathology Image... Fusion [https://link.springer.com/article/10.1007/s41666-025-00212-w]
- 17. Development of a radiomics-3D deep learning fusion ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12539123/]
- 18. A deep learning-based multimodal medical imaging model ... [https://www.nature.com/articles/s41598-025-99535-2]
- 19. Multimodal deep learning for enhanced breast cancer ... [https://www.sciencedirect.com/science/article/pii/S0010482525008170]
- 20. An explainable longitudinal multi-modal fusion model for ... [https://www.nature.com/articles/s41467-024-53450-8]
- 21. Multimodal fusion model for prognostic prediction and ... [https://www.nature.com/articles/s41746-025-01712-0]
- 22. Deep learning-based multimodal data fusion in bone tumor ... [https://www.sciencedirect.com/science/article/pii/S2950261625000378]
- 23. Understanding and Addressing Challenges ... - JMIR Cancer [https://cancer.jmir.org/2025/1/e58657]
- 24. The ICGC ARGO data dictionary for standardizing global ... [https://www.nature.com/articles/s41597-025-06068-4]
- 25. Multimodal integration strategies for clinical application in ... [https://www.frontiersin.org/journals/pharmacology/articles/10.3389/fphar.2025.1609079/full]
- 26. Current AI technologies in cancer diagnostics and treatment [https://molecular-cancer.biomedcentral.com/articles/10.1186/s12943-025-02369-9]
- 27. Using Data-driven Clinical Decision Support to Integrate ... [https://pubmed.ncbi.nlm.nih.gov/40675875/]
- 28. Transformer patient embedding using electronic health ... [https://www.nature.com/articles/s41746-025-01872-z]
- 29. Deep Learning Applications in Clinical Cancer Detection [https://www.sciencedirect.com/science/article/pii/S2949761225000604]
- 30. Deep learning in multi-modal breast cancer data fusion [https://pubmed.ncbi.nlm.nih.gov/41209219/]
- 31. Deep learning in multi-modal breast cancer data fusion [https://pmc.ncbi.nlm.nih.gov/articles/PMC12591796/]
- 32. Prompt-Driven Multimodal Segmentation with Dynamic ... [https://www.mdpi.com/2072-6694/17/22/3691]
- 33. Tumor heterogeneity: preclinical models, emerging ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10175698/]
- 34. Multiplexed spatial transcriptomics methods and the ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11298486/]
- 35. Scalable spatial single-cell transcriptomics and ... [https://www.nature.com/articles/s41592-025-02867-0]
- 36. Multi-contrast laser endoscopy for in vivo gastrointestinal ... [https://arxiv.org/html/2505.10492v1]
- 37. Integrative spatial and genomic analysis of tumor ... [https://www.nature.com/articles/s41467-024-53374-3]
- 38. Novel feature-based method for multi-modal biomedical ... [https://www.nature.com/articles/s41598-025-12862-2]
- 39. New Endoscopic Imaging Technology Based on MEMS ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6190023/]
- 40. Deformable multi-modal image registration for the ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11167953/]
- 41. Multimodal fusion strategies for survival prediction in breast ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12595345/]
- 42. A review of cancer data fusion methods based on deep ... [https://www.sciencedirect.com/science/article/abs/pii/S1566253524001398]
- 43. Anatomy guided modality fusion for cancer segmentation in ... [https://www.nature.com/articles/s41598-025-95757-6]
- 44. A multi-stage fusion deep learning framework merging ... [https://pubmed.ncbi.nlm.nih.gov/40054172/]
- 45. Explainable Artificial Intelligence for Multi-Modal Cancer ... [https://www.sciencedirect.com/science/article/pii/S1040842825004287]
- 46. TransBreastNet a CNN transformer hybrid deep learning ... [https://www.nature.com/articles/s41598-025-19173-6]
- 47. Multimodal Deep Learning for Stage Classification of Head ... [https://www.mdpi.com/2072-6694/17/13/2115]
- 48. Explainable multimodal fusion for breast carcinoma ... [https://www.sciencedirect.com/science/article/pii/S0169260725005681]
- 49. Unsupervised SAM-Guided Mixture-of-Multimodal-Experts ... [https://www.sciencedirect.com/science/article/pii/S0893608025012298]
- 50. Multimodal multi-instance evidence fusion neural networks ... [https://www.nature.com/articles/s41598-025-93770-3]
- 51. Pathomic Fusion: An Integrated Framework for Fusing ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10339462/]
- 52. Mixture of Expert-Based SoftMax-Weighted Box Fusion for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11899514/]
- 53. Multimodal Integration in Health Care: Development With ... [https://www.jmir.org/2025/1/e76557]
- 54. Multimodal AI (MMAI) for Next-Generation Healthcare [https://www.sciencedirect.com/science/article/pii/S2468451125000571]
- 55. Deep learning in multi-modal breast cancer data fusion [https://qims.amegroups.org/article/view/143128/html]
- 56. Multimodal data fusion AI model uncovers tumor ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11635117/]
- 57. Predicting Response to Treatment and Survival in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11815807/]
- 58. [2509.12600] A Multimodal Foundation Model to Enhance ... [https://arxiv.org/abs/2509.12600]
- 59. Multimodal data fusion for cancer biomarker discovery with deep learning - PubMed [https://pubmed.ncbi.nlm.nih.gov/37693852/]
- 60. Multimodal data fusion for cancer biomarker discovery with deep learning | Nature Machine Intelligence [https://www.nature.com/articles/s42256-023-00633-5]
- 61. Cancer Biomarkers: Reflection on Recent Progress, Emerging ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12468363/]
- 62. What Are Biomarkers? Definition, Applications and ... [https://blog.omni-inc.com/blog/what-are-biomarkers-and-whats-new-in-2025]
- 63. Multimodal deep learning model for prediction of breast ... [https://breast-cancer-research.biomedcentral.com/articles/10.1186/s13058-025-02129-z]
- 64. An enhanced multimodal fusion deep learning neural ... [https://www.sciencedirect.com/science/article/pii/S2772941923000212]
- 65. Towards improved breast cancer detection via multi-modal ... [https://www.sciencedirect.com/science/article/pii/S295036392400019X]
- 66. MDFNet: application of multimodal fusion method based on ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11796586/]
- 67. Enhanced early skin cancer detection through fusion of ... [https://www.nature.com/articles/s41598-025-18570-1]
- 68. Enhanced Breast Cancer Diagnosis Using Multimodal ... [https://www.mdpi.com/2075-4418/15/17/2170]
- 69. A Personalized Multimodal Federated Learning Framework ... [https://www.mdpi.com/2079-9292/14/14/2880]
- 70. Heterogeneous data integration: Challenges and ... [https://www.sciencedirect.com/science/article/pii/S2352340924008175]
- 71. Solutions to help you deal with heterogeneous data sources [https://www.bi-kring.nl/101-business-intelligence-archief/1252-solutions-to-help-you-deal-with-heterogeneous-data-sources1]
- 72. Handling Sparse and High-Dimensional Data in Machine ... [https://medium.com/@siddharthapramanik771/handling-sparse-and-high-dimensional-data-in-machine-learning-strategies-and-techniques-for-34516e88efff]
- 73. Sparse High Dimensional Models in Economics - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC3196636/]
- 74. Data Heterogeneity Solutions - Parthenos training [https://training.parthenos-project.eu/sample-page/formal-ontologies-a-complete-novices-guide/data-heterogeneity-solutions/]
- 75. Deep Learning for Cancer Detection Based on Genomic and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12459622/]
- 76. Multi-modal Learning with Missing Data for Cancer ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9605813/]
- 77. Missing-modality enabled multi-modal fusion architecture ... [https://www.sciencedirect.com/science/article/abs/pii/S1532046425000255]
- 78. Multimodal missing data in healthcare: A comprehensive ... [https://www.sciencedirect.com/science/article/abs/pii/S1574013724001035]
- 79. Medical multimodal foundation models in clinical diagnosis ... [https://www.sciencedirect.com/science/article/abs/pii/S0933365725002003]
- 80. Overfitting, Model Tuning, and Evaluation of Prediction ... - NCBI [https://www.ncbi.nlm.nih.gov/books/NBK583970/]
- 81. Overfitting In Academic Research [https://www.meegle.com/en_us/topics/overfitting/overfitting-in-academic-research]
- 82. Importance of sample size on the quality and utility of AI ... [https://www.sciencedirect.com/science/article/pii/S2589750025000214]
- 83. Optimizing high dimensional data classification with a ... [https://www.nature.com/articles/s41598-025-08699-4]
- 84. integrating explainable AI (XAI) with machine learning ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12465982/]
- 85. Improving Explainability and Integrability of Medical AI to ... [https://www.jmir.org/2025/1/e73374]
- 86. The human factor in explainable artificial intelligence [https://www.nature.com/articles/s41746-025-02023-0]
- 87. Multimodal data generative fusion method for complex ... [https://www.nature.com/articles/s41598-025-04985-3]
- 88. Current AI technologies in cancer and treatment - PMC diagnostics [https://pmc.ncbi.nlm.nih.gov/articles/PMC12128506/]
- 89. Frontiers | The data scientist as a mainstay of the tumor board: global... [https://www.frontiersin.org/journals/digital-health/articles/10.3389/fdgth.2025.1535018/full]
- 90. Data Fusion and Dimensionality Reduction for Pest ... [https://www.mdpi.com/2079-3197/13/6/137]
- 91. Shrinking for success: Multimodal dimensionality reduction ... [https://www.sciencedirect.com/science/article/pii/S0957417425025461]
- 92. Balancing Multimodal Training Through Game-Theoretic ... [https://arxiv.org/html/2411.07335]
- 93. Robust multi-modal fusion architecture for medical data ... [https://pubmed.ncbi.nlm.nih.gov/39709743]
- 94. Comparison of Multimodal Deep Learning Approaches for ... [https://www.jmir.org/2025/1/e75340]
- 95. Secure Multi-Modal Data Fusion in Federated Digital ... [https://arxiv.org/html/2510.01780v1]
- 96. A machine learning approach for multimodal data fusion ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12053085/]
- 97. F1 Score in Machine Learning Explained [https://encord.com/blog/f1-score-in-machine-learning/]
- 98. Multimodal Fusion Strategies for Survival Prediction in ... [https://www.sciencedirect.com/science/article/pii/S2001037025004404]
- 99. A multi-stage fusion deep learning framework merging ... [https://www.sciencedirect.com/science/article/abs/pii/S0010482525002677]
- 100. Early-fusion hybrid CNN-transformer models for multiclass ... [https://www.frontiersin.org/journals/artificial-intelligence/articles/10.3389/frai.2025.1679310/full]
- 101. HyFusion-X: hybrid deep and traditional feature fusion with ... [https://www.nature.com/articles/s41598-025-22262-1]
- 102. Explainable AI-enabled hybrid deep learning architecture for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12531632/]
- 103. PS3: A Multimodal Transformer Integrating Pathology Reports with... [https://arxiv.org/html/2509.20022v1]
- 104. Artificial Intelligence for the Diagnosis and Management of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12587170/]
- 105. Development and external of... | Nature Communications validation [https://www.nature.com/articles/s41467-025-57990-5?error=cookies_not_supported&code=c5f9b59d-ed96-4c5e-a59c-53b71c94c209]
- 106. of precisebreast, a digital prognostic External for... validation test [https://breast-cancer-research.biomedcentral.com/articles/10.1186/s13058-025-02104-8]
- 107. Multimodal Cancer Modeling in the Age of Foundation ... [https://arxiv.org/html/2505.07683v3]
- 108. Unsupervised SAM-Guided Mixture-of-Multimodal-Experts ... [https://www.sciencedirect.com/science/article/abs/pii/S0893608025012298]
- 109. The AI Revolution: How Multimodal Intelligence Will ... [https://www.sophiagenetics.com/resource/the-ai-revolution-how-multimodal-intelligence-will-reshape-the-oncology-ecosystem/]
- 110. Multimodal Integration in Health Care - PubMed Central - NIH [https://pmc.ncbi.nlm.nih.gov/articles/PMC12370271/]
- 111. Real‐World Data and Real‐World Evidence in Regulatory ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11897686/]
- 112. A Guide to Real-World Evidence in Clinical Trials [https://www.quanticate.com/blog/real-world-evidence-in-clinical-drug-development]
- 113. Considerations for the Use of Real-World Data and ... [https://www.fda.gov/regulatory-information/search-fda-guidance-documents/considerations-use-real-world-data-and-real-world-evidence-support-regulatory-decision-making-drug]
- 114. Multimodal Alignment and Fusion: A Survey [https://arxiv.org/html/2411.17040v1]