Medical Image Denoising: A Comprehensive Guide to Techniques, Validation, and Clinical Application for Researchers
This article provides a comprehensive analysis of data denoising techniques for medical images, tailored for researchers, scientists, and drug development professionals.
Medical Image Denoising: A Comprehensive Guide to Techniques, Validation, and Clinical Application for Researchers
Abstract
This article provides a comprehensive analysis of data denoising techniques for medical images, tailored for researchers, scientists, and drug development professionals. It explores the fundamental challenge of balancing noise reduction with the preservation of critical diagnostic features in modalities like MRI and CT. The scope ranges from foundational concepts and a detailed examination of traditional, deep learning, and generative AI methodologies to practical troubleshooting for common pitfalls like over-smoothing and computational bottlenecks. A strong emphasis is placed on rigorous validation, comparing performance using quantitative metrics and clinical evaluation to guide the selection of optimal denoising strategies for precision-critical biomedical research.
The Critical Foundation: Why Medical Image Denoising is a Lifesaving Challenge
The Impact of Noise on Diagnostic Accuracy and Treatment Planning
Troubleshooting Guides
FAQ 1: How does image noise quantitatively impact the accuracy of key diagnostic measurements?
Image noise introduces significant inaccuracies in the quantification of physiological parameters, which can compromise clinical decisions. The impact is particularly pronounced in functional imaging techniques like CT perfusion (CTp), where precise blood flow (BF) measurement is critical.
Observed Impact on CT Perfusion Blood Flow [1]:
- Phantom Study Findings: In a controlled study using Digital Perfusion Phantoms (DPPs), the introduction of Gaussian noise (standard deviation of 25 HU) caused a substantial deviation in blood flow measurements.
- Quantitative Data: The table below summarizes the effect of noise and subsequent correction on BF measurements.
| Condition | Pancreatic Parenchyma BF (ml/100 ml/min) | PDAC* BF (ml/100 ml/min) | Contrast-to-Noise Ratio (CNR) |
|---|---|---|---|
| Ground Truth | 225.0 ± 120.0 | 37.5 ± 20.2 | - |
| With Noise Impact | 218.0 ± 112.0 | 62.1 ± 11.5 | 2.52 |
| After Noise Correction | 224.0 ± 119.0 | 39.7 ± 21.9 | 2.66 |
*PDAC: Pancreatic Ductal Adenocarcinoma.
The data shows that noise can lead to a 65.6% overestimation of blood flow in tumor tissue (PDAC), severely distorting the perceived physiological state. A model-based noise correction algorithm successfully reduced the absolute noise error from 18.8 ml/100 ml/min to 3.6 ml/100 ml/min [1].
FAQ 2: What denoising methods are available for structural MRI and how is their performance validated?
For structural MRI, denoising algorithms based on deep learning have been developed to enhance image quality without compromising critical anatomical details.
Solution: Smart Noise Reduction in MRI [2] This method uses residual convolutional neural networks trained via supervised learning to remove noise while preserving image contrast. The system offers different neural networks and adjustable denoising levels to balance noise removal and detail preservation.
Performance Evaluation Metrics: Validation relies on quantitative metrics comparing denoised images to a reference or low-noise "ground truth" [2]:
- Peak Signal-to-Noise Ratio (PSNR): Higher values indicate better noise removal.
- Structural SIMilarity (SSIM) Index: Measures perceptual image quality and structural preservation (1 indicates perfect similarity).
The table below shows the performance of three different neural networks on a test dataset with two noise levels [2]:
| Noise Level | Metric | Network: Quick | Network: Strong | Network: Large |
|---|---|---|---|---|
| Std. 0.05 | PSNR | 37.272 | 38.592 | 39.152 |
| SSIM | 0.9439 | 0.9657 | 0.9711 | |
| Std. 0.1 | PSNR | 34.239 | 35.380 | 35.939 |
| SSIM | 0.9332 | 0.9483 | 0.9531 |
Methodology for Validation:
- A denoised 3D MRI dataset is used as a high-quality reference (ground truth).
- Two levels of simulated Gaussian noise (Standard Deviation 0.05 and 0.1) are added to this reference to create noisy input data.
- The noisy data is reconstructed using the three denoising networks ("Quick," "Strong," and "Large").
- PSNR and SSIM are computed between the denoised outputs and the original ground truth to quantify performance [2].
FAQ 3: How can I implement a noise-resistant deep learning model for point-of-care image classification?
Point-of-care imaging devices are often limited by environmental noise and require lightweight, robust models.
Solution: A Lightweight, Noise-Resistant Student Model [3] This approach uses a knowledge distillation framework where a compact "student" model learns from one or more powerful "teacher" models.
Experimental Protocol for Model Development:
- Model Design: A lightweight student model is built using a Shift MLP-based structure on its residual branches. This design captures multi-scale spatial features while reducing parameters and computational complexity.
- Multi-Teacher Distillation:
- An Auxiliary Teacher model uses unlabeled, noisy data for adaptive learning, enhancing the student model's robustness.
- A Global Teacher model transfers deep-feature knowledge to improve the student's classification accuracy.
- Training: The student model is trained to mimic the outputs and feature representations of both teachers, inheriting both robustness and accuracy.
Performance Outcomes [3]: The resulting model achieved a 38-fold reduction in parameters and an 11-fold reduction in computational complexity compared to traditional models, with an inference time of only 18.94 ms on a CPU. It maintained an average AUC of 83.00% in noisy environments, making it suitable for deployment on resource-constrained point-of-care devices.
Experimental Workflows
Workflow 1: Development and Validation of a Model-Based Noise Correction Algorithm
This workflow outlines the process for creating and testing a noise correction algorithm for quantitative CT perfusion, as described in the research [1].
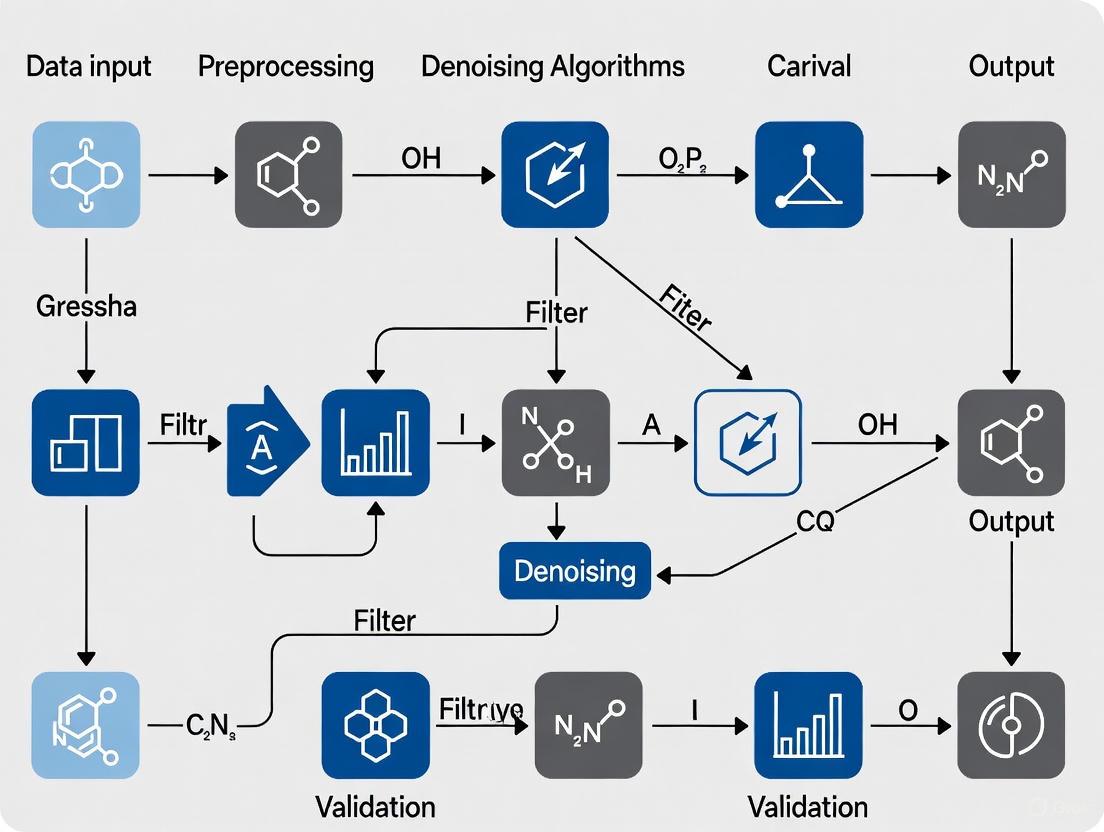
Workflow 2: Deep Learning-Based Medical Image Analysis Pipeline
This workflow illustrates a common pipeline for applying deep learning to medical image analysis, incorporating denoising and segmentation steps as referenced in the literature [4] [3].
The Scientist's Toolkit: Research Reagent Solutions
The following table details key computational tools and materials used in modern medical image denoising research.
| Item Name | Function & Explanation |
|---|---|
| Digital Perfusion Phantoms (DPPs) [1] | Computer-generated models that simulate biological tissues and perfusion parameters. They provide a known ground-truth for quantitatively evaluating denoising algorithms without the ethical and practical constraints of patient data. |
| Convolutional Neural Networks (CNNs) [2] [4] | A class of deep learning models particularly effective for image data. They are used in denoising (e.g., Smart Noise Reduction) and segmentation tasks by learning to identify and extract relevant spatial features from noisy images. |
| Fully Convolutional Neural Networks (FCNNs) [4] | A variant of CNNs designed for dense prediction tasks like pixel-wise image segmentation. They can outperform traditional methods in accurately delineating anatomical structures (e.g., femur in DXA images) even in the presence of noise. |
| Knowledge Distillation Framework [3] | A training strategy where a compact, "lightweight" model (the student) is trained to mimic the behavior of a larger, more accurate model or ensemble of models (the teachers). This is crucial for developing noise-resistant models deployable on point-of-care devices. |
| Peak Signal-to-Noise Ratio (PSNR) & Structural SIMilarity (SSIM) [2] | Two standard quantitative metrics for objectively evaluating the performance of denoising algorithms. PSNR measures the noise reduction level, while SSIM assesses the perceptual quality and structural integrity of the denoised image. |
In medical imaging research, the presence of noise is an unavoidable factor that significantly impacts quantitative analysis and diagnostic accuracy. A proper understanding of the fundamental noise types—Gaussian, Rician, and Poisson—is essential for developing effective denoising techniques and ensuring the reliability of experimental results. This guide provides a structured technical resource to help researchers troubleshoot common issues related to noise in medical images, framed within the context of advanced data denoising research.
Noise Characteristics and Identification
The table below summarizes the core characteristics, primary sources, and affected imaging modalities for the three common noise types.
| Noise Type | Probability Distribution | Primary Sources in Imaging | Commonly Affected Modalities | Key Characteristics |
|---|---|---|---|---|
| Gaussian [5] [6] | Normal (Bell-curve) distribution | Electronic circuit noise, sensor heat [6] | CT, MRI (high SNR) [5] [6] | Additive; constant variance independent of signal intensity. |
| Rician [7] [8] | Non-Gaussian; derived from Gaussian complex data [7] | Inherent to MRI magnitude reconstruction from complex (real/imaginary) data [7] [9] | MRI (especially low SNR images like DWI) [8] | Signal-dependent; causes a positive bias in low-intensity regions (e.g., background) [7]. |
| Poisson [6] [10] | Poisson distribution | Quantum (photon) noise due to statistical nature of photon detection [6] [10] | X-ray, PET, SPECT, Scintigraphy [6] [10] | Signal-dependent; variance equals the mean signal intensity [10]. |
Experimental Protocols for Noise Handling and Denoising
Protocol: Bias Correction for Rician Noise in MRI Magnitude Data
This protocol addresses the non-zero mean and signal-dependent bias introduced by Rician noise, which is critical for accurate quantitative analysis in MRI [7].
- Application Context: Preprocessing of magnitude MRI data, particularly in low-SNR conditions (e.g., diffusion tensor imaging, functional MRI).
- Step-by-Step Methodology:
- Noise Power Estimation: Estimate the noise standard deviation (σ) from a background region of the magnitude image using the relationship derived from the Rayleigh distribution:
σ = mean(background) / √(π/2)[7]. - Bias Correction: Apply a correction to the entire image using the formula:
 = √(M² - σ²), whereMis the measured magnitude value andÂis the corrected amplitude [7]. - Validation: Validate the correction by checking that the mean intensity in the background region approaches zero and that the signal distribution in homogeneous tissue regions becomes more symmetric.
- Noise Power Estimation: Estimate the noise standard deviation (σ) from a background region of the magnitude image using the relationship derived from the Rayleigh distribution:
Protocol: Denoising MRI with Pre-Smoothing Non-Local Means (PSNLM) Filter
This method effectively handles Rician noise by transforming it into additive noise, making it amenable to powerful filters like NLM [9].
- Application Context: Denoising brain MR images for improved segmentation, registration, or classification.
- Step-by-Step Methodology [9]:
- Transformation: Transform the noisy magnitude MRI (
M) using the Squared Magnitude method (M²) or a Variance-Stabilizing Transformation (VST) to make the noise approximately additive. - Pre-Smoothing: Apply a conventional spatial filter (e.g., a Gaussian filter) to the transformed image to create a "pre-smoothed" version for weight calculation.
- NLM Filtering: Apply the Non-Local Means filter to the transformed image, but compute the patch similarity weights using the pre-smoothed image from the previous step. This leads to more robust weight estimation.
- Inverse Transformation: Apply the inverse transformation (e.g., square root for the squared magnitude method) to the denoised data to obtain the final, unbiased denoised image.
- Transformation: Transform the noisy magnitude MRI (
Protocol: Handling Poisson Noise in Scintigraphic Images with SHINE
The Statistical and HEuristic Image Noise Extraction (SHINE) procedure is designed to reduce Poisson noise while preserving resolution and contrast [10].
- Application Context: Denoising low-count photon images in planar scintigraphy, SPECT, and PET.
- Step-by-Step Methodology [10]:
- Block Division: Divide the input image into small blocks (e.g., 4x4 pixels).
- Correspondence Analysis: Perform a correspondence analysis (a multivariate statistical technique) on these blocks.
- Factor Selection: For each block, reconstruct it using only its own "significant factors," which are selected using a statistical variance test designed to separate signal from noise.
- Image Reconstruction: Reassemble the denoised blocks to create the final output image. This method can improve the signal-to-noise ratio to a level comparable to an image acquired with twice the counts [10].
Research Workflows and Relationships
The following diagram illustrates the logical workflow for identifying and addressing different noise types in medical images.
The Researcher's Toolkit: Essential Denoising Algorithms
The table below catalogs key algorithms and their applications for mitigating different noise types in medical images.
| Tool/Algorithm | Primary Noise Target | Function and Mechanism | Key Considerations |
|---|---|---|---|
| BM3D (Block-Matching 3D) [5] | Gaussian | Groups similar 2D image patches into 3D arrays for collaborative filtering in the transform domain. | Considered state-of-the-art for Gaussian noise; can be computationally intensive [5]. |
| Non-Local Means (NLM) [9] | Additive (Gaussian) | Averages pixels based on the similarity of their surrounding patches across the entire image, not just local neighborhood. | Excellent edge preservation; requires modification (e.g., PSNLM) for Rician noise [9]. |
| Variance-Stabilizing Transform (VST) [9] | Rician, Poisson | Transforms data so that the noise variance becomes constant (stabilized), allowing application of filters designed for additive Gaussian noise. | Critical pre-processing step for handling signal-dependent noise; must be followed by an inverse transform [9]. |
| SHINE [10] | Poisson | Uses statistical factor analysis on image blocks to separate and extract noise while preserving signal texture and contrast. | Specifically designed for low-count scintigraphic images; helps reduce acquisition time or dose [10]. |
| DnCNN [5] | Gaussian (general) | A deep learning model that learns to predict the noise residual from a noisy image. | Effective for various noise levels; performance depends on training data [5]. |
| Bias Correction (M² - σ²) [7] | Rician | Simple algebraic correction to reduce the bias in magnitude MRI data, as described in Protocol 2.1. | Simple and effective for quantitative MRI; requires accurate estimation of σ [7]. |
Frequently Asked Questions (FAQs) and Troubleshooting
Q1: My MRI segmentation algorithm performs poorly in low-signal regions. Could noise be the cause?
- A: Yes, this is a classic issue. In MRI magnitude images, noise is Rician, not Gaussian. In low-signal regions, this creates a positive bias, meaning the measured intensity is higher than the true signal. This bias can cause segmentation algorithms to misclassify background or dark tissue regions [7]. Troubleshooting Tip: Implement the simple bias correction protocol (
 = √(M² - σ²)) as a preprocessing step and reevaluate your segmentation performance [7].
- A: Yes, this is a classic issue. In MRI magnitude images, noise is Rician, not Gaussian. In low-signal regions, this creates a positive bias, meaning the measured intensity is higher than the true signal. This bias can cause segmentation algorithms to misclassify background or dark tissue regions [7]. Troubleshooting Tip: Implement the simple bias correction protocol (
Q2: Why does my denoising model, trained on one scanner, perform poorly on data from another institution?
- A: This is often a problem of generalization. Different scanner models and acquisition parameters introduce variations that can be viewed as a form of "noise" by an AI model. If the model was only trained on clean, homogeneous data from one source, it will fail when presented with these new variations [11]. Troubleshooting Tip: Use data augmentation during training. Deliberately adding Gaussian noise and other artifacts to your training data can teach the model to focus on essential diagnostic features and ignore irrelevant scanner-specific variations, making it more robust [11] [12].
Q3: Is the noise in my CT/X-ray images Gaussian or Poisson?
- A: It is typically a combination of both, known as Poisson-Gaussian noise. The dominant source is Poisson (quantum) noise, which is signal-dependent. However, the readout noise from the electronic sensors is often Gaussian and additive [13] [6]. Troubleshooting Tip: For effective denoising, you need methods specifically designed for this mixed-noise scenario. Look for algorithms that incorporate a Poisson-Gaussian model or use a Variance-Stabilizing Transform (VST) to convert the noise to be approximately Gaussian before applying a standard denoiser [13].
Q4: I am working with diffusion-weighted MRI (DWI). Why is denoising so challenging?
- A: DWI often has a very low signal-to-noise ratio (SNR), which magnifies the problems of Rician noise. Furthermore, noise in modern multi-coil systems can be spatially variable, meaning its power is not uniform across the image. Applying a single denoising parameter to the entire image is therefore ineffective [8]. Troubleshooting Tip: Employ a denoising algorithm that accounts for spatially variable noise. These methods estimate and correct for noise on a voxel-by-voxel basis, which is crucial for accurate signal recovery in low-SNR applications like DWI [8].
Troubleshooting Guides
Troubleshooting Common Denoising Problems
Issue 1: Over-smoothing and Loss of Fine Details
- Problem: After denoising, the image appears blurry, and fine textures or subtle anatomical structures are lost.
- Cause: This is often caused by using denoising algorithms with overly aggressive filtering parameters or algorithms that are not designed to preserve high-frequency details, which constitute edges and textures [5].
- Solution:
- Switch Algorithm: Consider moving from simple spatial filters (e.g., Gaussian, median) to more advanced non-local or deep learning-based methods. For instance, Non-Local Means (NLM) excels at preserving repetitive structures and edges by comparing patches from across the entire image [14].
- Adjust Parameters: Reduce the strength of the denoising filter or adjust the threshold parameters. For transform-domain methods, carefully tune thresholding parameters to preserve more high-frequency components [5].
- Validate with Metrics: Use the Structural Similarity Index (SSIM) to quantitatively ensure structural information is being maintained post-denoising [5] [15].
Issue 2: Inadequate Noise Removal
- Problem: Significant noise remains in the image after processing, hindering diagnostic clarity.
- Cause: The denoising algorithm may be too weak for the noise level, or the parameters are not optimized for the specific noise characteristics of your imaging modality [5] [15].
- Solution:
- Re-evaluate Noise Level: Accurately estimate the global noise level in your image. Some advanced methods, like the one using the Marchenko-Pastur law, can automate this process for Gaussian noise [14].
- Choose a Stronger Algorithm: For moderate to high noise levels, BM3D has been shown to consistently outperform other algorithms, achieving high PSNR and SSIM [5]. For very high noise levels, deep learning methods like DnCNN may be more robust [5].
- Pre-process Input: For deep learning models, integrating preprocessing steps like image sharpening and K-means clustering can improve noise identification and lead to more effective denoising [16].
Issue 3: Introduction of Artifacts or Unrealistic Textures
- Problem: The denoised image contains new patterns, blurring, or textures that were not present in the original data.
- Cause: This is a known challenge with some deep learning models, which may "hallucinate" features learned from training data or create a "cartoon-like" appearance when over-trained [17] [15].
- Solution:
- Inspect a Validation Set: Always visually inspect denoising results on a subset of your data. Artifacts are often easily spotted by a trained eye.
- Use a Hybrid Approach: Implement a hybrid framework that combines different techniques. For example, a method using adaptive clustering followed by PCA thresholding and a final NLM refinement can balance noise removal with natural texture preservation [14].
- Employ Perceptual Metrics: Use no-reference image quality metrics like Naturalness Image Quality Evaluator (NIQE) and Blind/Referenceless Image Spatial Quality Evaluator (BRISQUE) to detect unrealistic outputs [5].
Issue 4: Poor Generalization Across Modalities or Anatomies
- Problem: A model trained on one type of medical image (e.g., brain MRI) performs poorly on another (e.g., liver CT).
- Cause: The model has learned features specific to its training dataset and lacks generalizability, a common issue with deep learning models [17] [15].
- Solution:
- Use Diverse Training Data: Train models on large, diverse datasets encompassing multiple imaging modalities, anatomies, and noise levels [15].
- Fine-tune Models: Transfer learning can be used to adapt a pre-trained model to a new, specific imaging domain with a smaller amount of data [17].
- Leverage Modality-Agnostic Algorithms: For some applications, high-performance traditional algorithms like BM3D can be effective across different modalities without retraining [5].
Frequently Asked Questions (FAQs)
Q1: What are the most critical metrics for evaluating denoising performance in medical images? While Peak Signal-to-Noise Ratio (PSNR) is a common metric for quantifying error, it does not always correlate with diagnostic quality [5] [15]. The most critical evaluation should combine:
- Structural Similarity Index (SSIM): Measures perceptual image quality and structural preservation [5] [15].
- Visual Inspection by Experts: Essential for identifying the preservation of clinically relevant details and the absence of artifacts.
- Task-based Assessment: The ultimate test is whether the denoised image improves performance in downstream tasks like tumor segmentation or classification.
Q2: How do I choose between traditional and deep learning-based denoising methods? The choice involves a trade-off between performance, computational cost, and data availability.
- Traditional Methods (e.g., NLM, BM3D, Wavelet): Are often less computationally intensive and do not require training data. They are well-understood and can be a good choice for projects with limited data or computational resources [5] [17]. BM3D is often a dependable choice for low-to-moderate noise levels [5].
- Deep Learning Methods (e.g., DnCNN, GANs): Typically offer state-of-the-art performance and can better handle complex noise patterns [5] [17]. However, they require large, high-quality labeled datasets for training and significant computational power. They also risk poor generalization if not trained on representative data [17] [15].
Q3: My dataset is small. What denoising strategies can I use? Deep learning models generally require large datasets, but several strategies can help:
- Pre-trained Models: Use models pre-trained on large natural or medical image datasets and fine-tune them on your small dataset.
- Data Augmentation: Artificially expand your dataset using rotations, flips, and other transformations.
- Self-Supervised Learning: Employ techniques that learn from a single noisy image or generate training pairs from noisy data alone, reducing the need for clean ground-truth data [5] [14].
- Robust Traditional Algorithms: Opt for high-performing traditional algorithms like BM3D or hybrid methods that do not require extensive training data [5] [18].
Q4: How can I ensure my denoising process is reproducible for my research?
- Document Parameters: Meticulously record all algorithm parameters, including filter sizes, threshold values, and noise level estimates.
- Version Control: Use version control for any custom code and for the specific implementation of the denoising algorithms you use.
- Standardize Workflows: Establish a standard operating procedure (SOP) for image preprocessing and denoising in your lab.
- Use Public Datasets for Benchmarking: Validate your denoising pipeline on public benchmark datasets to allow for direct comparison with other methods.
Experimental Protocols & Data
Detailed Methodology: Hybrid Adaptive Clustering and Non-Local Means
This protocol is based on a state-of-the-art approach for detail-preserving denoising of CT and MRI images [14].
1. Objective: To effectively remove Gaussian noise while preserving fine textures and structural boundaries in medical images.
2. Step-by-Step Workflow: 1. Noise Level Estimation: Analyze the statistical distribution of eigenvalues from matrices of randomly sampled image patches. Use the Marchenko-Pastur law from random matrix theory to accurately estimate the global Gaussian noise variance. 2. Adaptive Patch Clustering: Extract small, overlapping patches from the noisy image. Use an adaptive clustering technique to group these patches based on texture and edge features. This step creates clusters of similar patches for localized processing. 3. Cluster-wise PCA Thresholding: For each cluster: * Arrange the similar patches into a matrix. * Perform Singular Value Decomposition (SVD) on this matrix. * Apply hard thresholding to the singular values based on the MP law to obtain a low-rank approximation, removing noise-dominated components. * Use a Linear Minimum Mean Square Error estimator on the PCA coefficients to further suppress residual noise. 4. Image Reconstruction: Reconstruct the denoised patches from each cluster and aggregate them back into a full image, handling overlapping regions by averaging. 5. Non-Local Means Refinement: Apply a final Non-Local Means (NLM) filter to the reconstructed image. The NLM computes a weighted average of pixels across the entire image, giving higher weight to pixels in similar neighborhoods, which enhances noise reduction and preserves edges and textures.
The following workflow diagram illustrates this multi-stage denoising process:
Quantitative Performance Comparison of Denoising Algorithms
The following table summarizes objective metrics for various denoising algorithms as reported in comparative studies [5] [18] [16]. These metrics are crucial for evaluating the trade-off between noise reduction (PSNR) and structural preservation (SSIM).
Table 1: Denoising Algorithm Performance Metrics
| Algorithm | Type | Key Principle | Reported PSNR (dB) | Reported SSIM | Best For |
|---|---|---|---|---|---|
| BM3D [5] | Traditional (Transform) | Collaborative filtering in 3D transform domain | High (Consistently top) | High (Consistently top) | Low-to-moderate noise; general use |
| Proposed Hybrid (AMF+MDBMF) [18] | Traditional (Hybrid Spatial) | Adaptive median filtering & decision-based recovery | Improvement up to 2.34 dB | Improvement up to 0.07 | High-density salt-and-pepper noise |
| Energy-Efficient Autoencoder [16] | Deep Learning (CNN) | Preprocessing (sharpening & clustering) before autoencoder | 28.14 (from 21.52 baseline) | 0.869 (from 0.762 baseline) | Computationally constrained environments |
| DnCNN [5] | Deep Learning (CNN) | Deep convolutional neural network learning residual noise | Competitive, especially at high noise | Competitive, especially at high noise | Handling significant noise variations |
| Non-Local Means (NLM) [14] | Traditional (Spatial) | Averages similar patches from across the image | Not Specified | Not Specified | Preserving repetitive structures & edges |
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Computational Tools for Medical Image Denoising Research
| Item / Algorithm | Function / Purpose | Key Considerations |
|---|---|---|
| BM3D (Block-Matching 3D) [5] [17] | A high-performance traditional algorithm that groups similar 2D image patches into 3D arrays for collaborative filtering. | An excellent benchmark algorithm. Does not require training data and is effective for Gaussian noise. Can be computationally heavy. |
| DnCNN (Deep Convolutional Neural Network) [5] [15] | A deep learning model trained to predict the residual noise (difference between noisy and clean image) rather than the clean image directly. | Requires a large dataset of noisy/clean image pairs for training. Often delivers state-of-the-art results but needs significant computational resources. |
| Non-Local Means (NLM) [17] [14] | Reduces noise by averaging pixels based on the similarity of their surrounding patches from the entire image, not just the local neighborhood. | Excellent at preserving fine details and textures. Computationally intensive for large images without optimization. |
| Generative Adversarial Network (GAN) [17] [15] | Uses a generator network to create denoised images and a discriminator to critique them, leading to highly realistic outputs. | Can produce very sharp images but is challenging to train and may introduce hallucinations. Used in 30% of DL-based CT denoising studies [17]. |
| Wavelet Transform [5] [17] | Decomposes an image into different frequency sub-bands. Noise is removed by thresholding the coefficients in these bands before reconstruction. | Effective for separating signal from noise. The choice of wavelet and thresholding rule is critical for performance. |
| Structural Similarity Index (SSIM) [5] [15] | A perceptual metric that compares the luminance, contrast, and structure between two images to evaluate denoising quality. | More aligned with human perception than PSNR. Essential for validating the preservation of anatomical structures. |
| Marchenko-Pastur Law [14] | A principle from random matrix theory used to accurately estimate the global noise level in an image by analyzing the eigenvalue distribution of patch matrices. | Provides a robust, data-driven method for noise estimation, which is a critical first step for many adaptive denoising algorithms. |
Frequently Asked Questions (FAQs)
Q1: What are the primary clinical risks of a noisy medical image? Noise in medical images obscures crucial anatomical details, which can directly lead to two major clinical consequences:
- Misinterpretation and Diagnostic Errors: Blurred borders, reduced contrast, and obscured minute information can hinder the detection of subtle pathologies, such as early-stage tumors or small lesions, potentially leading to missed diagnoses or misinterpretation [5].
- Increased Patient Radiation Exposure: In cases where image quality is non-diagnostic, clinicians may order additional scans to clarify findings. For modalities like CT, this results in higher cumulative radiation doses for patients [5].
Q2: My denoising algorithm is making images too soft and blurry. How can I preserve finer diagnostic details? This is a classic trade-off between noise removal and feature preservation. We recommend:
- Algorithm Selection: Choose advanced algorithms designed for detail preservation. Studies show that BM3D consistently outperforms others at low and moderate noise levels, achieving high structural similarity (SSIM) [5]. For high noise levels, deep learning-based methods like DnCNN are better suited [5].
- Advanced Architectures: Implement modern networks that use mechanisms like Optimal Attention Blocks (OAB). These blocks intelligently focus on relevant features and noise components, ensuring significant structures are highlighted while noise is minimized [19]. A Pyramidal Network structure can also help by analyzing and integrating image features across different scales, capturing both fine and coarse details [19].
Q3: I lack paired clean-noisy image data for training. Are there effective denoising solutions? Yes, several data-free and self-supervised techniques are available:
- Noise2Noise Framework: This approach trains a model using pairs of noisy images without requiring clean ground truth data [20].
- Lightweight Data-Free Models: Methods like Noise2Detail (N2D) use an innovative multistage pipeline that disrupts noise correlations and recaptures fine details directly from the noisy input, requiring no training data and minimal computational resources [20].
- Distribution-Based Schemes: Frameworks like DCDS use transfer learning and statistical modeling to distinguish between normal and noisy pixels, effectively reducing noise without large, paired datasets [21].
Q4: How can I quantitatively validate that my denoised image is fit for clinical use? Rely on a combination of objective metrics to assess different aspects of image quality:
- Peak Signal-to-Noise Ratio (PSNR): Measures the noise reduction level. A higher PSNR (e.g., improvements of 2-3 dB) generally indicates better noise suppression [19] [21].
- Structural Similarity Index (SSIM): Assesses how well the structural integrity of the original image is preserved. This is critical for ensuring diagnostic features remain intact [5] [19].
- Perceptual Quality Metrics: For a more comprehensive assessment, use metrics like NIQE, BRISQUE, and LPIPS to evaluate the visual perceptual quality of the output [5] [20].
Troubleshooting Guides
Problem: Loss of Subtle Pathologies Post-Denoising
Potential Cause: The denoising algorithm is over-smoothing the image, treating low-contrast pathological features as noise.
| Troubleshooting Step | Action/Recommendation |
|---|---|
| 1. Verify Algorithm Choice | Switch from simple filters (Gaussian, median) to more advanced, detail-preserving algorithms like BM3D or a well-designed Denoising Convolutional Neural Network (DnCNN) [5]. |
| 2. Tune Hyperparameters | Adjust the strength or weight of the denoising process. Reduce the aggression level to prevent the loss of fine, high-frequency details that may correspond to critical diagnostic information [5]. |
| 3. Implement an Attention Mechanism | Integrate an Optimal Attention Block (OAB) into your model. This mechanism uses optimization algorithms to help the network focus on important features and suppress noise more intelligently [19]. |
Problem: Inconsistent Performance Across Different Imaging Modalities
Potential Cause: The noise model your algorithm was trained on does not match the real-world noise in the target modality (e.g., applying a Gaussian denoiser to Poisson-noised images).
| Troubleshooting Step | Action/Recommendation |
|---|---|
| 1. Identify Noise Model | Determine the dominant noise type in your target modality (e.g., Rician for MRI, Poisson for CT). Artificially induce this specific noise type for model training and validation [5] [19]. |
| 2. Use a Robust Framework | Employ a flexible framework like the Distribution-Based Compressed Denoising Scheme (DCDS), which uses transfer learning and statistical analysis to adapt to different noise distributions without requiring full retraining [21]. |
| 3. Adopt a Data-Free Method | For rare modalities with no clean data, use a zero-shot method like Noise2Detail (N2D), which is trained directly on the noisy image itself and is not dependent on a pre-defined noise model [20]. |
Experimental Protocols & Methodologies
Protocol 1: Benchmarking Denoising Algorithms for Clinical Use
This protocol outlines how to compare different denoising algorithms to select the most suitable one for a specific clinical task.
1. Objective: To evaluate and compare the performance of multiple denoising algorithms on medical images using standardized quantitative metrics and qualitative assessment. 2. Materials:
- Datasets: Use standardized medical image datasets (e.g., CHASEDB1, Lumbar Spine MRI) [19].
- Algorithms for Testing: Select a range of algorithms, including BM3D, DnCNN, NLM, and WNNM [5].
- Software: Python with libraries such as PyTorch/TensorFlow for deep learning models and OpenCV for traditional algorithms.
3. Method:
- Data Preparation: Artificially introduce known types and levels of noise (Gaussian, Speckle, Poisson) into clean images to create a controlled test set [19].
- Apply Denoising: Process the noisy images with each selected algorithm.
- Quantitative Analysis: Calculate PSNR, SSIM, and perceptual metrics (NIQE, BRISQUE) between the denoised images and the original clean ground truth [5].
- Qualitative Analysis: Have clinical experts blindly rate the denoised images for diagnostic quality, feature preservation, and absence of artifacts. 4. Analysis: Compare results to determine the best-performing algorithm for your specific imaging modality and diagnostic task.
Protocol 2: Implementing a Lightweight, Data-Free Denoising Pipeline
This protocol is for scenarios where clean training data is unavailable and computational resources are limited.
1. Objective: To apply the Noise2Detail (N2D) pipeline for effective denoising using only a single noisy image. 2. Materials:
- Input: A single noisy medical image.
- Model: A pre-defined ultra-lightweight, three-layer Convolutional Neural Network (CNN) as per the N2D architecture [20].
3. Method:
- Training Phase:
- Use the Noise2Noise framework. The denoised image (or a downsampled version of the noisy input) is used as the input, and the original noisy image is set as the target.
- This unconventional setup forces the model to learn to reconstruct missing signal details rather than replicate noise [20].
- Spatial Disruption: Apply pixel-shuffle downsampling to disrupt spatial correlations in the noise patterns, creating intermediate smooth structures [20].
- Detail Refinement: The model is then refined to recapture and enhance fine anatomical details directly from the original noisy input [20]. 4. Output: A high-quality denoised image suitable for diagnostic use, generated with minimal computational overhead.
- Training Phase:
Table 1: Quantitative Performance of Denoising Algorithms on Medical Images
Table comparing PSNR (dB) and SSIM performance of various algorithms at different noise levels. Higher values are better.
| Algorithm | Type | Low Noise PSNR | Low Noise SSIM | High Noise PSNR | High Noise SSIM |
|---|---|---|---|---|---|
| BM3D | Block-Matching & Filtering | High | High | Moderate | Moderate [5] |
| DnCNN | Deep Learning | High | High | High | High [5] |
| OABPDN | Attention-based Deep Learning | ~2-3% improvement over state-of-the-art models in PSNR and SSIM [19] | |||
| DCDS | Transfer Learning / Statistical | Improves PSNR across 24-32 dB range | N/R | >82% noise reduction rate in optimal conditions [21] | |
| N2D (Noise2Detail) | Lightweight, Data-Free | Competitive with data-free techniques | Competitive with data-free techniques | High quality, detail-preserving | High quality, detail-preserving [20] |
N/R: Not explicitly reported in the provided search results.
Table 2: The Scientist's Toolkit: Essential Reagents & Materials for Denoising Research
A list of key computational "reagents" and their functions in medical image denoising experiments.
| Research Reagent / Solution | Function & Application in Denoising |
|---|---|
| BM3D (Block-Matching 3D) | A high-performance non-local algorithm that groups similar 2D image patches into 3D data arrays for collaborative filtering. Excellent for low/moderate noise [5]. |
| DnCNN (Denoising Convolutional Neural Network) | A deep learning model that uses CNN layers to learn and remove noise from images. Effective for handling significant noise variations [5]. |
| Optimal Attention Block (OAB) | A module integrated into neural networks that uses optimization algorithms (e.g., Cuckoo Search) to intelligently weight channel features, focusing the model on relevant structures and noise components [19]. |
| Noise2Noise Framework | A training paradigm that enables model learning from pairs of noisy images alone, eliminating the need for clean ground-truth data [20]. |
| Cuckoo Search Optimization (CSO) | A metaheuristic optimization algorithm used to find the optimal parameters for components like the Optimal Attention Block, improving denoising efficiency [19]. |
| Pixel-Shuffle Downsampling | An operation used in pipelines like N2D to disrupt the spatial correlation of noise, creating a smoother image that is later refined to recapture details [20]. |
Experimental and Clinical Workflow Visualization
Clinical Consequences of Noisy Medical Images
Noise2Detail Data-Free Denoising
Frequently Asked Questions (FAQs)
Q1: What are the fundamental differences between PSNR, SSIM, and perceptual quality metrics? PNSR (Peak Signal-to-Noise Ratio) and SSIM (Structural Similarity Index) are full-reference metrics that require a clean ground truth image for comparison, whereas many perceptual quality metrics are no-reference and assess image quality based on statistical properties of the image itself [22]. PSNR is a pixel-based error metric calculated as the ratio between the maximum possible power of a signal and the power of corrupting noise [15], while SSIM considers luminance, contrast, and structure to provide a more perceptually meaningful assessment [15]. Perceptual quality metrics like NIQE, BRISQUE, and PIQE evaluate quality without a reference image by assessing naturalness and statistical deviations [5].
Q2: Why might a denoising algorithm achieve high PSNR but poor performance in clinical evaluation? This discrepancy occurs because PSNR primarily measures pixel-level fidelity rather than preservation of clinically relevant features [22]. A denoising algorithm might effectively smooth away noise (improving PSNR) but simultaneously remove subtle pathological details crucial for diagnosis [5] [15]. This is particularly problematic in medical imaging where subtle textures, edges, and low-contrast features often carry critical diagnostic information that PSNR does not adequately capture [22].
Q3: How should researchers select appropriate metrics for evaluating medical image denoising? Metric selection should be guided by the specific clinical task and image modality [15]. For comprehensive evaluation, researchers should employ a multi-metric approach combining PSNR/SSIM with task-specific perceptual assessments [5] [22]. When ground truth is unavailable, no-reference metrics like NIQE and BRISQUE can provide insights, but their limitations in detecting localized anatomical errors must be considered [22]. For denoising algorithms intended to support specific clinical tasks (e.g., tumor segmentation), downstream task performance should be the ultimate validation [22].
Q4: What are the limitations of no-reference metrics for medical image evaluation? No-reference metrics exhibit significant limitations in medical contexts, particularly insensitivity to localized anatomical alterations that are clinically crucial [22]. These metrics may yield misleadingly favorable scores for images with memorized training data or mode collapse in generative models [22]. They often fail to detect distorted tumor boundaries or other morphological inaccuracies that would impact diagnostic utility, potentially creating patient safety risks if used as the sole evaluation method [22].
Q5: How can researchers implement efficient evaluation pipelines for large-scale denoising studies? Distributed evaluation frameworks can significantly accelerate metric computation for large datasets [23]. Leveraging multi-GPU configurations with optimized parallel processing (e.g., PyTorch's DistributedDataParallel) can reduce evaluation time by over 60% compared to single-GPU setups [23]. Automated scripting to compute multiple metrics simultaneously (PSNR, SSIM, perceptual metrics) across denoised image batches ensures consistent and efficient assessment [23].
Troubleshooting Guides
Issue: High PSNR/SSIM But Poor Visual Quality in Denoised Images
Problem: Denoised medical images achieve strong quantitative metrics but appear oversmoothed or lack clinically important textures.
Diagnosis and Solutions:
- Root Cause: The denoising algorithm is over-prioritizing noise removal at the expense of structural preservation, and PSNR/SSIM alone are insufficient to capture this deficiency [5] [22]
- Solution 1: Incorporate perceptual quality metrics (NIQE, BRISQUE, PIQE) that better align with human visual assessment [5]
- Solution 2: Implement task-specific validation by testing the denoised images in downstream clinical applications (e.g., segmentation accuracy, pathology detection) [22]
- Solution 3: Adjust the denoising algorithm's loss function to balance PSNR/SSIM with perceptual losses or feature preservation constraints [19]
Verification Protocol:
- Compute a comprehensive metric suite including PSNR, SSIM, and at least two perceptual metrics [5]
- Conduct a limited expert evaluation where radiologists rate image quality on a 5-point scale [22]
- Check correlation between metrics and expert scores - good algorithms should perform well across multiple assessment methods [22]
Issue: Inconsistent Metric Values Across Different Noise Levels
Problem: Metric performance varies significantly across low, moderate, and high noise conditions, making algorithm comparison difficult.
Diagnosis and Solutions:
- Root Cause: Different metrics have varying sensitivity to noise levels, and some algorithms perform better at specific noise ranges [5]
- Solution 1: Establish noise-level specific benchmarks based on your imaging modality and typical clinical scenarios [5] [15]
- Solution 2: For variable noise environments, prioritize algorithms that maintain consistent performance across noise levels rather than excelling at only one range [5]
- Solution 3: Implement adaptive denoising that selects parameters based on estimated noise level [24]
Verification Protocol:
- Artificially corrupt clean images with known noise levels (e.g., Gaussian noise with σ=10, 20, 30) [23]
- Evaluate denoising performance separately for each noise level [5]
- Calculate metric consistency as the standard deviation of performance across noise levels - lower values indicate more robust algorithms [5]
Issue: Computational Bottlenecks in Metric Evaluation
Problem: Calculating comprehensive metrics for large medical image datasets requires prohibitive computational time and resources.
Diagnosis and Solutions:
- Root Cause: Perceptual metrics and full-volume evaluations can be computationally intensive, especially for 3D medical images [23]
- Solution 1: Implement distributed evaluation using multi-GPU setups with PyTorch's DistributedDataParallel [23]
- Solution 2: Use automated mixed precision (AMP) to accelerate computations with minimal accuracy impact [23]
- Solution 3: Employ strategic sub-sampling by evaluating metrics on representative image subsets or slices rather than full datasets [22]
Verification Protocol:
- Compare metric values between full evaluation and sub-sampled approaches to ensure representativeness
- Benchmark computation time across different hardware configurations [23]
- Validate that mixed precision implementation does not significantly alter metric values (e.g., <1% difference) [23]
Quantitative Metric Comparison Tables
Table 1: Performance Metrics for Denoising Algorithms Across Modalities
| Algorithm | PSNR (dB) | SSIM | Computational Complexity (s) | Optimal Noise Level | Key Strengths |
|---|---|---|---|---|---|
| BM3D [5] | 32.1-35.8 | 0.91-0.94 | 0.8-1.2 | Low-Moderate | Excellent detail preservation |
| DnCNN [5] | 31.8-36.2 | 0.90-0.95 | 0.3-0.6 | Moderate-High | Deep learning advantage |
| Gaussian Pyramid [25] [26] | 34.2-36.8 | 0.92-0.94 | 0.004-0.006 | Various | Superior computational efficiency |
| U-Net++ [23] | 33.5-37.1 | 0.93-0.96 | 0.4-0.7 | Low-High | Enhanced structural fidelity |
| Optimal Attention Block [19] | ~2-3% improvement over baselines | ~2-3% improvement over baselines | Moderate-High | Various | Intelligent feature focusing |
Table 2: Medical Image Noise Types and Metric Sensitivity
| Noise Type | Common Sources | PSNR Sensitivity | SSIM Sensitivity | Perceptual Metric Sensitivity | Affected Modalities |
|---|---|---|---|---|---|
| Gaussian [15] | Electronic circuits, sensor heat | High | Moderate | Moderate-High | X-ray, CT, MRI |
| Rician [15] | MRI acquisition | Moderate | High | High | MRI |
| Poisson [15] | Quantum noise in photon counting | Moderate-High | Moderate | Moderate | CT, PET, low-dose X-ray |
| Salt & Pepper [15] [24] | Transmission errors, sensor faults | High | High | High | All digital modalities |
| Speckle [15] | Coherent imaging systems | Moderate | High | High | Ultrasound |
Experimental Protocols
Protocol 1: Comprehensive Denoising Algorithm Evaluation
Purpose: Systematically evaluate and compare medical image denoising algorithms using multiple quality metrics.
Materials and Setup:
- Dataset: Curated medical images with paired clean and noisy samples [23]
- Hardware: Multi-GPU workstation for distributed computation [23]
- Software: Python with PyTorch, OpenCV, scikit-image for metric computation [23]
Procedure:
- Data Preparation: Pre-process images to consistent resolution (e.g., 256×256 for 2D, 128×128×128 for 3D) [23]
- Noise Introduction: For ground truth studies, add known noise types and levels to clean images [23]
- Algorithm Application: Process noisy images through each denoising algorithm with optimized parameters [5]
- Metric Computation: Calculate PSNR, SSIM, and perceptual metrics for all output images [5] [15]
- Statistical Analysis: Perform paired t-tests or Wilcoxon signed-rank tests to determine significant differences [25] [26]
Validation Steps:
- Verify metric implementation using standardized test images with known values
- Ensure consistent intensity normalization across all images [23]
- Confirm that results are statistically significant across multiple image samples [25]
Protocol 2: Clinical Relevance Validation Framework
Purpose: Bridge the gap between quantitative metrics and clinical utility of denoised medical images.
Materials and Setup:
- Clinical Dataset: Images with verified pathological findings [22]
- Evaluation Platform: Web-based interface for expert rating [22]
- Task Pipeline: Pre-trained segmentation/classification models for downstream task evaluation [22]
Procedure:
- Expert Evaluation Setup: Prepare blinded image sets with randomized presentation of original and denoised images [22]
- Rating Protocol: Define specific evaluation criteria (diagnostic confidence, feature visibility, artifact presence) using standardized scales [22]
- Task Performance Assessment: Measure accuracy of downstream tasks (e.g., segmentation, classification) on denoised versus original images [22]
- Correlation Analysis: Compute correlation coefficients between quantitative metrics and expert ratings/task performance [22]
Validation Steps:
- Assess inter-rater reliability among multiple experts [22]
- Validate that downstream task models perform comparably on denoised versus original images [22]
- Ensure clinical evaluations are ethically approved and follow relevant guidelines [22]
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Computational Tools for Medical Image Denoising Research
| Tool/Platform | Function | Application Context | Key Features |
|---|---|---|---|
| PyTorch DDP [23] | Distributed training | Large-scale denoising experiments | Multi-GPU support, reduced training time |
| Automatic Mixed Precision [23] | Computational acceleration | Memory-intensive models | Faster computation, minimal accuracy loss |
| U-Net++ Architecture [23] | Denoising model | Medical image restoration | Nested skip connections, superior structural fidelity |
| Gaussian Pyramid [25] [26] | Multi-scale denoising | Real-world noise reduction | Multi-scale processing, computational efficiency |
| Optimal Attention Block [19] | Feature emphasis | Detail-preserving denoising | Adaptive feature weighting, cuckoo search optimization |
| BRISQUE/NIQE [5] | No-reference quality assessment | Real-world evaluation | No ground truth needed, perceptual alignment |
Metric Relationships and Evaluation Workflow
Metric Evaluation Decision Workflow
Key Experimental Design Considerations
When designing experiments for medical image denoising evaluation, several critical factors ensure meaningful and clinically relevant results:
Modality-Specific Validation: Different imaging modalities (MRI, CT, X-ray, ultrasound) have distinct noise characteristics and clinical requirements. Always validate denoising performance specifically for your target modality [15]
Clinical Task Alignment: Choose evaluation metrics that correlate with your intended clinical application. For tumor detection tasks, prioritize metrics sensitive to boundary preservation and contrast maintenance [22]
Computational Constraints: Balance metric comprehensiveness with practical computational requirements, especially for large-scale 3D medical images [23]
Statistical Robustness: Ensure adequate sample sizes and appropriate statistical tests to support claims of algorithmic superiority [25] [26]
The most effective evaluation strategy combines quantitative metrics with clinical relevance assessment, acknowledging that numerical superiority alone does not guarantee diagnostic utility [22].
From Traditional Filters to Generative AI: A Landscape of Denoising Methodologies
Troubleshooting Guide & FAQs
This guide addresses common challenges researchers face when implementing classic spatial and transform domain filters for medical image denoising. The content supports thesis research on data denoising techniques, providing clear protocols and solutions for scientists and drug development professionals.
Frequently Asked Questions
Q1: My bilateral filter is producing over-smoothed results, blurring critical diagnostic features. What could be the cause?
A1: Over-smoothing in bilateral filtering typically occurs due to improper parameter selection. The bilateral filter smoothes images while preserving edges by combining spatial (geometric) closeness and photometric similarity. Review these parameters:
- Spatial Sigma (σd): Controls the influence of neighboring pixels based on their geometric distance. A value that is too large will include too many pixels from heterogeneous regions, causing excessive blurring. For most medical images, start with a value between 1 and 3.
- Range Sigma (σr): Controls the influence of neighboring pixels based on their intensity difference. A value that is too large reduces the filter's edge-preserving capability. Start with a value proportional to the image's intensity range (e.g., 10-15% of the total range). Troubleshooting Tip: Systematically reduce σr while keeping σd small. This ensures that only pixels with very similar intensities contribute to the smoothing, thereby preserving edges. Computational complexity can be high, but this preserves edges more effectively than large kernel Gaussian filters [27] [28].
Q2: How do I select the most appropriate wavelet family and threshold function for denoising an MRI with Rician noise?
A2: Wavelet selection depends on the image characteristics and the noise properties. The denoising efficacy stems from the tendency of noise to spread across high-frequency sub-bands (LH, HL, HH), while important image structures are concentrated in the LL sub-band and strong coefficients in the detail sub-bands [29].
- Wavelet Family: For medical images like MRI, Daubechies (db4), Coiflets (coif4), or Symlets (sym4) are often preferred. These wavelets offer a good trade-off between smoothness and localization, reducing artifacts compared to simpler wavelets like Haar [29] [25].
- Threshold Function: The choice of threshold function is critical. The table below summarizes common functions [29] [30].
Table: Common Wavelet Thresholding Functions
| Threshold Name | Function | Best Use Case | ||||||
|---|---|---|---|---|---|---|---|---|
| Hard | $θ_H(x) = \begin{cases} 0 & \text{if } | x | ≤ δ \ x & \text{if } | x | > δ \end{cases}$ | Environments where strict coefficient retention is needed; can cause oscillatory artifacts [29] [30]. | ||
| Soft | $θ_S(x) = \begin{cases} 0 & \text{if } | x | ≤ δ \ \text{sgn}(x)( | x | -δ) & \text{if } | x | > δ \end{cases}$ | General-purpose denoising; can lead to edge blurring [29] [30]. |
| Smooth Garrote | $θ_{SG}(x) = \dfrac{x^{2n+1}}{x^{2n}+δ^{2n}}$ | A compromise between hard and soft thresholding, offering smoother transition [29]. |
For Rician noise in MRI, an adaptive thresholding approach that incorporates a linear prediction factor to minimize the mean squared error between the noisy and original image characteristics has shown significant improvements in metrics like PSNR and SSIM [30].
Q3: Why would I choose a transform domain method like Wavelet over a spatial method like Gaussian filtering?
A3: The choice hinges on the trade-off between noise reduction and the preservation of fine anatomical details.
- Gaussian Filtering (Spatial Domain): A linear low-pass filter that is computationally efficient and effective at suppressing high-frequency noise. Its primary limitation is that it uniformly smoothes across edges, often blurring crucial diagnostic details and reducing image sharpness [15] [27] [28].
- Wavelet Transform (Transform Domain): Provides multi-resolution analysis, capturing both coarse structures and fine details. It allows for non-linear processing (e.g., thresholding) of frequency components, which can remove noise more effectively while preserving edges and textures that are critical for diagnosis [29] [30].
In practice, a block-based Discrete Fourier Cosine Transform (DFCT) approach has been shown to consistently outperform a global DWT approach across various noise types, attributed to its localized processing strategy that adapts to local statistics without introducing global artifacts [29].
Performance Benchmarking
The following table summarizes the quantitative performance of classical denoising filters across standard medical imaging metrics, as reported in recent literature.
Table: Denoising Algorithm Performance Comparison on Medical Images
| Denoising Method | PSNR (dB) | SSIM | MSE | Computational Efficiency | Key Strengths |
|---|---|---|---|---|---|
| Gaussian Filtering | Moderate (e.g., ~25-30) | Moderate (~0.80-0.85) | Moderate | High / Fast | Simple, fast smoothing for high-frequency noise [5] [28]. |
| Bilateral Filtering | Moderate to High | Good (~0.85-0.90) | Moderate | Moderate (slower than Gaussian) | Edge-preserving smoothing [27]. |
| Wavelet (Coiflet4) | High (e.g., ~32-35) | Good (~0.90-0.92) | Low | Moderate | Multi-resolution analysis, good detail preservation [25]. |
| Gaussian Pyramid (GP) | 36.80 | 0.94 | Low | High / 0.0046s | Multi-scale strategy, excellent balance of quality and speed [25]. |
| BM3D | High to Very High (top performer) | High (~0.95+) | Very Low | Low / Slow | Exploits non-local similarity, state-of-the-art for traditional methods [5]. |
Standard Experimental Protocols
To ensure reproducible and comparable results in your thesis research, adhere to the following standardized protocols.
Protocol 1: Implementing a Bilateral Filter for CT Image Denoising
- Image Preprocessing: Convert the CT image to grayscale if necessary and normalize pixel intensity values to a standard range (e.g., 0-1).
- Parameter Initialization: Set the diameter of the pixel neighborhood and initialize the filter parameters. Recommended starting values are spatial sigma (σd) = 2 and range sigma (σr) = 0.1 * (maxintensity - minintensity).
- Filter Application: Apply the bilateral filter to the entire image. The output pixel value is a weighted average of neighboring pixels, where the weights are based on both the spatial kernel and the intensity range kernel.
- Validation: Quantitatively, calculate PSNR and SSIM by comparing the denoised image with a clean reference image. Qualitatively, have a domain expert assess the preservation of critical structures like small lesions and vessel edges [27] [28].
Protocol 2: Wavelet-Based Denoising for Brain MRI
- Wavelet Decomposition: Select a wavelet family (e.g., Daubechies 'db4') and a decomposition level (e.g., 3). Decompose the noisy brain MRI image into wavelet coefficients, producing approximation (LL) and detail (LH, HL, HH) sub-bands at multiple resolutions. The workflow for this process is outlined below.
- Threshold Estimation & Application: Estimate a threshold (δ) for the detail coefficients (LH, HL, HH). You can use a universal threshold or a level-dependent threshold. Apply your chosen threshold function (see Table 2) to these detail coefficients to suppress noise.
- Image Reconstruction: Perform an inverse wavelet transform using the original approximation coefficients (LL) and the modified detail coefficients to reconstruct the denoised image [29] [30].
- Validation: Evaluate using PSNR, SSIM, and Mean Squared Error (MSE). For Rician noise, perceptual quality metrics like BRISQUE can also be informative [5] [30].
Method Selection Workflow
This decision diagram helps select an appropriate denoising method based on your research constraints and goals.
Research Reagent Solutions
This table outlines key computational "reagents" essential for experiments with classic denoising filters.
Table: Essential Research Reagents for Denoising Experiments
| Reagent (Algorithm/Tool) | Function in Experiment | Specifications & Notes |
|---|---|---|
| Gaussian Filter | Baseline low-pass filtering for noise suppression. | Parameters: Kernel size, Sigma (σ). A larger σ increases smoothing. Ideal for initial pre-processing or high-noise scenarios where detail loss is acceptable [15] [28]. |
| Bilateral Filter | Edge-preserving smoothing for structural integrity. | Parameters: Spatial Sigma (σd), Range Sigma (σr). Computationally more intensive than Gaussian. Use when edges and sharp features must be maintained [27]. |
| Wavelet Transform Toolbox | Multi-resolution analysis and non-linear thresholding. | Specs: Wavelet Family (Haar, Daubechies, Coiflets), Decomposition Level, Threshold Function (Soft, Hard, Adaptive). The core tool for separating signal from noise in the frequency domain [29] [30]. |
| BM3D Algorithm | High-performance benchmark for traditional denoising. | Function: Uses collaborative filtering in 3D groups of similar image patches. Considered a state-of-the-art traditional method against which to compare your results [5] [28]. |
| Quality Metrics (PSNR, SSIM) | Quantitative evaluation of denoising performance. | PSNR: Measures noise reduction level. SSIM: Assesses perceptual image integrity and structural preservation. Both typically require a clean reference image [15] [5]. |
Frequently Asked Questions (FAQs)
Q1: Under what conditions does BM3D achieve its best performance in medical imaging? BM3D consistently achieves its best performance on medical images, such as MRI and HRCT, at low to moderate noise levels [31]. Under these conditions, it reliably produces the highest Peak Signal-to-Noise Ratio (PSNR) and Structural Similarity Index (SSIM) values compared to other classical and deep learning-based algorithms like DnCNN, NLM, and Bilateral filters [31] [28]. Its effectiveness diminishes with very high noise levels, where other methods may become more competitive.
Q2: What is the primary trade-off when using BM3D for medical image denoising? The primary trade-off is between denoising quality and computational efficiency [31]. While BM3D is highly effective at noise reduction and detail preservation, it has high computational complexity, which can limit its practicality in time-sensitive clinical scenarios [31] [32]. This is especially true when processing high-noise images or large datasets.
Q3: How does BM3D's performance compare to deep learning methods like DnCNN? BM3D and DnCNN excel in different scenarios. BM3D is a dependable, high-performing choice for images with moderate noise [31]. In contrast, advanced deep learning methods like DnCNN are often better suited for handling significant noise variations and can adapt to more complex, real-world noise distributions without compromising critical diagnostic features [31] [28]. Deep learning methods, however, typically require large, annotated datasets for training.
Q4: A key challenge with BM3D is its reliance on accurate noise level estimation. How can this be addressed? Standard BM3D requires an estimate of the noise level (variance) as an input parameter. An ineffective solution is to manually tune this parameter for different image sets. A more robust and effective approach, as demonstrated in recent research, is to integrate an automatic noise estimation technique [32]. For instance, using Singular Value Decomposition (SVD) on the image to estimate the noise variance from the tail of singular values before applying BM3D has been shown to improve denoising performance and make the algorithm more adaptive to natural images with unknown noise sources [32].
Troubleshooting Guides
Issue 1: Over-Smoothing and Loss of Fine Anatomical Details
Problem: After applying BM3D, the image appears too smooth, and small but diagnostically critical features (like early-stage tumors or small lesions) are blurred or lost [31] [28].
Solution:
- Verify Noise Level Parameter: The most common cause is using an inaccurately high noise level estimate. Re-check the
noise_std(noise standard deviation) parameter provided to the algorithm. For medical images, start with a lower value and incrementally increase it until noise is reduced without noticeable detail loss [32]. - Leverage Multi-Scale Strategies: Consider using a multi-scale framework. A hybrid approach can be implemented where a heavily smoothed version of the image (using a different filter) is used to segment large, homogeneous regions, while BM3D with a lower noise parameter is applied to preserve finer structures at subsequent scales [33].
Issue 2: High Computational Time and Memory Usage
Problem: The denoising process is slow, making it unsuitable for processing large batches of high-resolution medical images or for real-time applications [31].
Solution:
- Optimize Block-Matching Parameters: Adjust the key parameters of the BM3D algorithm. Reducing the size of the reference blocks, limiting the search window for similar patches, and controlling the maximum number of patches per group can significantly speed up computation [31].
- Investigate Alternative Algorithms: For scenarios requiring faster processing, evaluate other denoising methods. Lightweight self-supervised networks (e.g., Noise2Detail) or multi-scale Gaussian pyramid approaches have been proposed to offer a better balance between processing speed and reconstruction quality [20] [25].
Issue 3: Poor Performance on Images with Very High or Complex Noise
Problem: BM3D does not effectively remove noise from images acquired with low-dose protocols or from modalities with complex, non-Gaussian noise [34] [25].
Solution:
- Pre-Estimate Noise: Use a dedicated noise estimation step before denoising. Integrating an SVD-based noise estimator, as mentioned in FAQ 4, provides BM3D with a more accurate prior, enhancing its performance on images with unknown or complex noise characteristics [32].
- Switch to a More Robust Denoiser: For inherently low-SNR images, such as hyperpolarized 129Xe MRI, unsupervised deep learning methods like Noise2Void (N2V) have demonstrated minimal bias in quantitative metrics (like Ventilation Defect Percentage) compared to supervised methods and BM3D, making them more suitable for such challenging data [34].
Experimental Performance Data
The following tables summarize quantitative performance data for the BM3D algorithm from recent studies on medical and other image types.
Table 1: Comparative Algorithm Performance on MRI and HRCT Images [31]
| Algorithm | Domain | Key Strengths | Key Limitations | Best Suited For |
|---|---|---|---|---|
| BM3D | Transform | Highest PSNR/SSIM at low-moderate noise; preserves structural integrity [31] | High computational complexity [31] | MRI/HRCT with moderate noise |
| DnCNN | Deep Learning | Handles significant noise variations; preserves diagnostic features [31] [28] | Requires large training datasets [31] | High noise levels; large available data |
| NLM | Spatial | Exploits non-local self-similarity [28] | High computational complexity; inaccurate weights with high noise [32] | Images with repetitive structures |
| Bilateral | Spatial | Preserves edges effectively [28] | Less effective against low-frequency noise [32] | Edge preservation in low-noise images |
Table 2: Denoising Performance on Acoustic and Real-World Images [25] [35]
| Image Type | Denoising Method | Performance Metrics | Key Finding |
|---|---|---|---|
| Acoustic Images | BM3D | High PSNR and SSIM vs. ground truth [35] | Demonstrated best results for denoising acoustic image data [35] |
| Real-World Images (X-ray, MRI, SIDD) | Multi-scale Gaussian Pyramid | PSNR: 36.80 dB, SSIM: 0.94, Complexity: 0.0046 s [25] | Offers an effective balance between detail preservation and computational cost [25] |
Standard Experimental Protocol for BM3D
Title: Protocol for Evaluating BM3D on Medical Images with Synthetic Gaussian Noise
1. Objective To quantitatively and qualitatively evaluate the performance of the BM3D denoising algorithm on medical images (e.g., MRI, HRCT) corrupted with additive white Gaussian noise (AWGN).
2. Materials and Reagents Table 3: Essential Research Reagent Solutions
| Item | Function/Description | Example |
|---|---|---|
| Clean Image Dataset | Serves as high-quality ground truth data. | Set12 dataset, AxFLAIR brain MRI, Cor-PD knee MRI [32] [33] |
| Noise Model | Simulates realistic image degradation for algorithm testing. | Additive White Gaussian Noise (AWGN) with mean=0 [31] [32] |
| Performance Metrics | Quantifies denoising effectiveness and image quality preservation. | PSNR, SSIM, MSE [31] [28] [35] |
| Computational Environment | Provides the hardware/software platform for algorithm execution. | MATLAB R2021a, 10-core CPU, 32GB RAM [32] |
3. Methodology
- Step 1 - Data Preparation: Select a set of clean medical images to use as ground truth. Generate noisy images by adding AWGN with a known variance (σ²) to the clean images. Common noise levels for testing include σ = 10, 15, 20, and 25 [28].
- Step 2 - Parameter Configuration: Initialize the BM3D algorithm. The critical parameter is the noise standard deviation (
noise_std), which should be set to the known σ used in Step 1. Other parameters like block size and search window can be left at defaults or optimized. - Step 3 - Algorithm Execution: Run the BM3D algorithm on the noisy images to generate the denoised outputs.
- Step 4 - Performance Analysis: Calculate quantitative metrics by comparing the denoised images against the clean ground truth images. Key metrics include:
- Peak Signal-to-Noise Ratio (PSNR): Measures the ratio between the maximum possible power of a signal and the power of corrupting noise. Higher is better [31] [35].
- Structural Similarity Index (SSIM): Assesses the perceptual similarity between two images, focusing on structural information. Closer to 1 is better [31] [35].
- Step 5 - Qualitative Assessment: Visually inspect the denoised images to ensure that critical anatomical structures and fine details have been preserved without excessive smoothing or the introduction of artifacts.
4. Expected Output The protocol yields a set of denoised images and a table of quantitative metrics (PSNR, SSIM) for each image and noise level, allowing for a comprehensive evaluation of BM3D's performance.
BM3D Algorithm Workflow
The diagram below illustrates the core stages of the BM3D denoising algorithm.
The workflow consists of two main stages. The first stage creates a basic estimate by finding similar image patches, grouping them, and applying a hard threshold in a 3D transform domain to remove noise. The second stage uses this basic estimate to guide a more refined Wiener filtering process on new groupings of patches, leading to the final high-quality denoised output [32] [35].
Troubleshooting Guides and FAQs
This section addresses common challenges researchers face when implementing deep learning models for medical image denoising, providing targeted solutions based on recent research findings.
FAQ: My denoised medical images are losing important lesion edge information, adversely clinical diagnosis. How can I better preserve these critical details?
Answer: This is a common problem when denoising networks fail to preserve structurally significant features. Based on recent research, we recommend implementing attention mechanisms that selectively focus on important anatomical structures.
Solution 1: Integrate Multi-Attention Modules. A U-Net architecture augmented with multiple attention modules has demonstrated excellent performance in preserving lesion edge information. The local attention module localizes surrounding feature map information, the multi-feature channel attention module suppresses invalid information, and the hierarchical attention module extracts extensive feature information while maintaining network lightweight [36]. An enhancement learning module stacked with convolution, batch normalization, and activation layers can further help retain detail [36].
Solution 2: Use U-Net++ Architecture. For tasks requiring high structural fidelity, U-Net++ with its nested skip connections and intermediate layers has been shown to provide superior denoising performance and enhanced structural preservation compared to standard U-Net, particularly under moderate noise levels [23].
FAQ: How do I choose between U-Net and DnCNN for my specific medical denoising task?
Answer: The choice depends on your primary objective: detail preservation versus efficient noise removal.
U-Net and its Variants (U-Net++, U-Tunnel-Net) are generally preferred when the goal is to preserve complex structures and anatomical boundaries, thanks to their encoder-decoder structure with skip connections that maintain spatial information [36] [23] [37]. They are particularly effective for medical images where structural integrity is critical for diagnosis.
DnCNN is often more effective for pure noise removal, especially when dealing with Gaussian-type noise. It uses residual learning to predict and subtract noise from the noisy input image [5] [38] [39]. A complex-valued DnCNN (ℂDnCNN) is particularly advantageous for MRI data as it processes both magnitude and phase information, unlike traditional real-valued networks [38].
Table: Comparative Analysis of Denoising Architectures
| Architecture | Strengths | Ideal Use Cases | Key Performance Metrics (Example) |
|---|---|---|---|
| U-Net with Multi-Attention | Excellent detail preservation, retains lesion edges | LDCT images, diagnostic tasks where feature preservation is critical | PSNR: 34.73, SSIM: 0.929 on QINLUNGCT [36] |
| U-Net++ | Enhanced structural fidelity, nested skip connections | Chest X-ray denoising, complex anatomical structures [23] | Competitive PSNR/SSIM, better LPIPS under low noise [23] |
| DnCNN | Efficient Gaussian noise removal, residual learning | General denoising, MRI data (when using complex-valued variant) [5] | High PSNR on Gaussian noise [5] |
| Non-blind ℂDnCNN | Handles complex-valued MRI data, preserves phase | Low-field MRI denoising, parallel imaging noise [38] | Improved SNR and visual quality for in vivo data [38] |
| U-Tunnel-Net | Superior speckle noise reduction, repositioned pooling | Ultrasound image despeckling, image restoration [37] | PSNR 30.21-39.52 on UNS dataset [37] |
FAQ: I'm experiencing extremely long training times with my 3D medical image data. What optimization strategies can I implement?
Answer: Distributed training and architectural optimization can significantly reduce training time.
Strategy 1: Implement Distributed Data Parallel (DDP) Training. Replace standard single-GPU or DataParallel training with PyTorch's DistributedDataParallel (DDP). Research shows this, combined with Automatic Mixed Precision (AMP), can reduce training time by over 60% compared to single-GPU training and outperforms standard DataParallel by over 40%, with only a minor accuracy drop [23].
Strategy 2: Optimize Model Dimensions. Avoid the "bigger is better" assumption. Systematically benchmark model dimensions (resolution stages, depth, width). For 3D data, increasing depth (D) consistently improves performance, but adding resolution stages (S) is only beneficial for high-resolution images, and increasing width (W) is most impactful for tasks with many segmentation classes [40]. Using a smaller, optimally configured model can dramatically reduce compute time without sacrificing performance.
FAQ: The noise in my MRI datasets appears to be spatially varying, and my standard denoising model performs poorly. How can I address this?
Answer: Spatially varying noise, common in parallel imaging, requires a non-blind denoising approach.
- Solution: Implement a Non-Blind Denoising Network. Use a model that incorporates a noise level map as part of its input. For example, the non-blind ℂDnCNN model estimates the noise level from the input image and feeds this information into the complex-valued network. This allows the model to adaptively handle the spatially varying noise inherent in techniques like sensitivity encoding (SENSE) or generalized autocalibrating partially parallel acquisitions (GRAPPA) [38].
Experimental Protocols & Methodologies
This section provides detailed methodologies for key experiments cited in the troubleshooting guides, enabling replication and validation of results.
Protocol: U-Net with Multi-Attention for CT Denoising
Objective: To effectively denoise Low-Dose CT (LDCT) images while preserving critical clinical lesion edge information [36].
- Dataset: QINLUNGCT and Mayo Clinic LDCT Grand Challenge datasets.
- Network Architecture:
- Backbone: U-Net encoder-decoder structure.
- Attention Modules:
- Local Attention: Localizes surrounding information of the feature map.
- Multi-feature Channel Attention: Adds different weights to each channel in the feature map, suppressing invalid information.
- Hierarchical Attention: Extracts a large amount of feature information.
- Enhancement Learning Module: Stacked multi-layer convolution, Batch Normalization (BN), and activation function layers are inserted after each attention module to increase network depth and retain detail.
- Training Configuration:
- Loss Function: Mean Squared Error (MSE) or L1 loss.
- Evaluation Metrics: Peak Signal-to-Noise Ratio (PSNR) and Structural Similarity Index (SSIM).
- Expected Outcome: On the QINLUNGCT dataset with σ=10, the model achieved a PSNR of 34.7329 and an SSIM of 0.9293 [36].
Protocol: Distributed Training for Medical Image Denoising
Objective: To accelerate the training of denoising models on large-scale datasets while incorporating a privacy-preserving noise obfuscation mechanism [23].
- Dataset: NIH ChestX-ray14 dataset (112,120 frontal-view X-rays). A subset of 15,000 radiographs is used, resized to 256x256.
- Data Preprocessing & Obfuscation:
- Additive Gaussian noise with mean 0.1 and standard deviations of 0.1, 0.2, and 0.3 is applied to clean images to create noisy inputs, simulating privacy-preserving data sharing.
- The dataset is split into training (7,499), validation (4,949), and test (2,551) sets.
- Models: U-Net and U-Net++.
- Training Configurations:
- Single-GPU: Baseline.
- Standard Multi-GPU: Using DataParallel.
- Optimized Multi-GPU: Using PyTorch's DistributedDataParallel (DDP) with Automatic Mixed Precision (AMP).
- Evaluation: Performance is evaluated using PSNR, SSIM, and training time. The optimized DDP with AMP setup reduces training time by over 60% compared to single-GPU training [23].
Protocol: Non-Blind Complex-Valued DnCNN for MRI
Objective: To denoise complex-valued MRI data while effectively handling spatially varying noise and preserving phase information [38].
- Dataset: fastMRI brain dataset (T2-weighted, post-contrast T1, T1, FLAIR).
- Noise Simulation: Complex Additive White Gaussian Noise (AWGN) with a standard deviation (σ) sampled uniformly between 0 and 0.1 is added to normalized, complex-valued, single-coil images.
- Network Architecture:
- Input: 2D complex-valued MR image concatenated with a tunable complex-valued noise level map.
- Core Network: A series of complex-valued convolution blocks. Each block consists of:
- Complex-valued convolution (ℂConv)
- Radial Batch Normalization (BN)
- Complex-valued rectified linear unit (ℂReLU)
- Output: Denoised complex image.
- Training: The model is trained to learn the mapping from a noise-corrupted image and its noise level map to the clean, ground-truth image.
- Validation: The model is tested on both simulated and in vivo low-field data, showing significant improvement in SNR and visual quality [38].
Workflow and Architecture Diagrams
U-Net with Multi-Attention for CT Denoising
Non-blind Complex-Valued DnCNN Workflow
The Scientist's Toolkit: Research Reagent Solutions
Table: Essential Materials and Resources for Medical Image Denoising Research
| Item Name | Function / Application | Example Specifications / Notes |
|---|---|---|
| Public Medical Image Datasets | Provides standardized data for training and benchmarking denoising models. | QINLUNGCT & Mayo LDCT: For CT denoising [36]. fastMRI: For complex-valued MRI denoising [38]. NIH ChestX-ray14: For X-ray denoising [23]. |
| Evaluation Metrics Suite | Quantitatively assesses denoising performance and image quality. | PSNR & SSIM: Standard metrics for reconstruction fidelity [36] [23] [5]. LPIPS: Measures perceptual image patch similarity [23]. NRMSE: Normalized Root-Mean-Square Error [38]. |
| Distributed Training Framework | Accelerates model training on large-scale datasets using multiple GPUs. | PyTorch DDP with AMP: For optimized multi-GPU training, reducing time by >60% [23]. |
| Attention Mechanism Modules | Enhances model focus on relevant features, preserving edges and structural details. | Local, Channel, & Hierarchical Attention: Dynamic weighting to suppress noise and retain critical information [36]. |
| Complex-Valued Network Layers | Processes complex medical imaging data (e.g., MRI), preserving phase information. | ℂConv, ℂReLU, Radial BN: Core components for building complex-valued CNNs like ℂDnCNN [38]. |
Technical Support Center: Troubleshooting Guides and FAQs
This technical support center addresses common challenges researchers face when implementing Denoising Diffusion Probabilistic Models (DDPMs) for generating synthetic medical images. The guidance is framed within the broader thesis of advancing data denoising techniques for medical imaging research.
Frequently Asked Questions (FAQs)
1. My generated synthetic medical images lack critical anatomical details. What should I do? This is often related to the design of the latent space or the training objective. A common solution is to adjust the compression factor of the autoencoder used in a latent diffusion model. Excessive compression can discard fine details. It is recommended to reduce the compression factor; for instance, moving from a factor of 8 to a factor of 4 has been shown to reconstruct anatomic features like subtle textures in breast MRI or lung structures in CT more accurately [41]. Furthermore, ensure your loss function balances noise prediction with the preservation of structural integrity.
2. How can I generate 3D medical volumes (e.g., MRI, CT) with DDPMs without overwhelming computational resources? Generating high-resolution 3D data directly in image space is computationally prohibitive. The established solution is to use a latent diffusion approach. This method involves training a model (like a VQ-GAN) to compress 3D images into a lower-dimensional latent space. The DDPM is then trained on these latent representations, significantly reducing computational demands while maintaining the ability to generate high-resolution 3D volumes for brain MRI or chest CT [41].
3. My diffusion model training is unstable and slow. Are there ways to improve efficiency? Yes, several strategies can stabilize and speed up training. You can reduce the number of timesteps. Modifying the variational bound loss has allowed researchers to successfully train models with only 1000 training and 50 inference timesteps, instead of 4000 and 500 respectively, which dramatically stabilizes the process, especially for 3D data [42]. Additionally, using a simplified loss function that focuses on predicting the noise component (e.g., the L2 loss between the predicted and true noise, $ \vert \vert \epsilon - \epsilon\theta(xt, t) \vert \vert^2 $ ) has been shown to lead to better-trained models [43].
4. For medical image denoising, how do DDPMs compare to established methods like BM3D or DnCNN? The performance is noise-level dependent. BM3D consistently outperforms other algorithms at low and moderate noise levels, achieving the highest PSNR and SSIM while preserving structural integrity [5]. However, for handling significant noise variations without compromising critical diagnostic features, advanced deep learning-based methods like DnCNN and DDPMs are often better suited. DDPMs, in particular, excel at generating diverse and realistic images, which makes them powerful for creating high-quality synthetic training data rather than just denoising a single image [5] [41].
5. Can I use DDPMs without paired clean and noisy medical image data? Yes. Self-supervised, data-free approaches are available. Methods like Noise2Noise and its derivatives (e.g., Noise2Detail) enable training a denoising model using only pairs of noisy images, eliminating the need for clean ground truth data. This is particularly valuable for biomedical imaging where acquiring clean reference data is challenging [20].
Troubleshooting Common Experimental Issues
Table 1: Common Issues and Proposed Solutions in DDPM Experiments
| Problem Symptom | Potential Root Cause | Diagnostic Steps | Solution & Recommendations |
|---|---|---|---|
| Blurry or over-smoothed generated images | Loss of high-frequency details in latent space; over-regularization. | Inspect VQ-GAN reconstruction quality; check compression factor. | Reduce the autoencoder's compression factor (e.g., from 8 to 4) [41]. |
| Mode collapse; low diversity in samples | Model fails to capture full data distribution (common in GANs, less so in DDPMs). | Calculate metrics like FID or assess visual variety. | Ensure DDPM uses sufficient timesteps; verify the noise schedule is appropriate [41] [43]. |
| Unrealistic anatomical structures | Model has not learned correct spatial relationships. | Perform expert radiologist review for anatomic correctness [41]. | Increase dataset size or diversity; use data augmentation; consider transfer learning. |
| Extremely long sampling/generation time | Sequential nature of the reverse diffusion process. | Profile time per sampling step. | Use fewer inference timesteps with an adjusted loss function [42]; employ latent diffusion models [41]. |
| Training instability (loss divergence) | Poorly chosen loss function or learning rate; too many timesteps. | Monitor loss curve for sharp spikes or NaN values. | Use the simplified L2 noise prediction loss [43]; reduce the number of training timesteps [42]. |
Experimental Protocols and Methodologies
This section outlines core experimental setups for DDPMs in medical imaging, as cited in the literature.
Protocol 1: DDPM as a Feature Extractor for a Downstream Task (Change Detection) This protocol demonstrates how a DDPM, pre-trained on unlabeled data, can be repurposed as a powerful feature extractor [44].
- Pre-training: Train a DDPM on a large dataset of unlabeled remote sensing images. The model learns the underlying data distribution by mastering the denoising process.
- Feature Extraction: Use the pre-trained DDPM model (without its final denoising head) to extract feature representations from the input images.
- Fine-tuning: Train a lightweight change classifier (e.g., a simple network head) on top of the frozen DDPM features, using change detection labels.
- Result: This approach significantly outperformed existing self-supervised state-of-the-art methods in F1 score, IoU, and overall accuracy, highlighting the quality of features learned by the DDPM [44].
Protocol 2: Generating 3D Medical Data with Latent Diffusion This protocol describes a method for generating high-resolution 3D medical images (CT, MRI) with manageable computational cost [41].
- Train a VQ-GAN: First, train a Vector-Quantized Generative Adversarial Network (VQ-GAN) on 3D medical volumes. This model learns to compress a 3D image (e.g., 256x256x32) into a smaller latent representation (e.g., 64x64x8) and decode it back with high fidelity.
- Train the Diffusion Model: Train a DDPM to model the distribution of the latent codes generated by the VQ-GAN's encoder. This is done in the lower-dimensional latent space.
- Sampling: To generate a new synthetic 3D image, first sample a new latent code from the trained DDPM, then use the VQ-GAN decoder to convert it back into a high-resolution 3D image.
- Validation: Expert radiologists rated the generated images as largely realistic with only minor unrealistic areas, confirming high quality and anatomical correctness [41].
Protocol 3: Lightweight, Data-Free Denoising (Noise2Detail) This protocol is for scenarios with no clean training data and limited computational resources [20].
- Framework: Built upon the Noise2Noise training framework, which uses pairs of noisy images instead of clean targets.
- Model Architecture: Employ an ultra-lightweight, three-layer Convolutional Neural Network (CNN).
- Multistage Pipeline: Implement a two-stage inference process:
- Stage 1: Use pixel-shuffle downsampling on the noisy input to disrupt noise correlations and produce an intermediate, smooth structure.
- Stage 2: Refine this smooth structure to recapture fine details directly from the original noisy input.
- Outcome: This approach achieves a favorable balance between denoising performance and computational efficiency, making it suitable for practical clinical deployment [20].
Table 2: Quantitative Comparison of Denoising Techniques on Medical Images
| Algorithm | Key Principle | Best Use-Case | Performance Highlights |
|---|---|---|---|
| BM3D [5] | Transform-domain filtering & collaborative filtering. | Low & moderate Gaussian noise levels. | Consistently highest PSNR & SSIM; preserves structural integrity. |
| DnCNN [5] | Deep Convolutional Neural Network. | High noise levels; general denoising. | Handles significant noise variations without compromising critical features. |
| Noise2Detail (N2D) [20] | Lightweight, self-supervised pipeline. | Data-scarce environments; fast inference needed. | High-quality restoration with a fraction of computational resources. |
| Distribution-Based Compressed Denoising (DCDS) [21] | Transfer learning & pixel distribution analysis. | Gaussian-like noise in CT; resource-constrained settings. | PSNR improvement (24-32 dB); >82% noise reduction rate. |
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Tools and Metrics for DDPM Research in Medical Imaging
| Item Name | Type / Category | Brief Function & Application |
|---|---|---|
| VQ-GAN [41] | Model Architecture | Encodes 3D images into a compressed latent space for efficient diffusion training; enables high-resolution 3D medical image generation. |
| Swin-UNETR [41] | Model Architecture | A transformer-based network used for downstream tasks (e.g., segmentation); can be pre-trained using synthetic DDPM-generated data. |
| Noise Scheduler [43] | Algorithm | Defines the noise variance ($\beta_t$) schedule over timesteps for the forward and reverse diffusion processes. Critical for training stability. |
| Structural Similarity Index (SSIM) [5] | Evaluation Metric | Measures the perceptual similarity between two images, more aligned with human vision than PSNR/MSE. Used for denoising evaluation. |
| Frechet Inception Distance (FID) | Evaluation Metric | Quantifies the quality and diversity of generated images by comparing feature statistics with a real dataset. |
| Peak Signal-to-Noise Ratio (PSNR) [5] [21] | Evaluation Metric | A classic objective metric for image reconstruction quality, often reported in denoising and synthesis papers. |
| Expert Radiologist Review [41] | Evaluation Protocol | Gold-standard for assessing synthetic medical images on "realistic appearance", "anatomical correctness", and "slice consistency". |
Experimental Workflow and Signaling Pathways
The following diagrams illustrate the core workflows of DDPMs as derived from the literature.
DDPM Core Training and Sampling Workflow
DDPM for Feature Extraction & Downstream Tasks
Lightweight and Self-Supervised Approaches for Data-Scarce Scenarios
Core Concepts & Performance Metrics
This section introduces foundational architectures and quantifies the performance of lightweight, self-supervised models for medical image analysis, enabling researchers to select appropriate solutions for resource-constrained environments.
Lightweight self-supervised learning (SSL) frameworks are designed to learn transferable features from unlabeled data while minimizing computational demands, making them ideal for deployment in settings with limited data, annotation capabilities, or computing power. These models address key challenges in medical AI, such as domain shift and scanner bias, by learning robust, domain-invariant representations without relying on vast annotated datasets or GPU clusters [45]. Their efficiency stems from architectures like compact autoencoders and the use of strategies such as contrastive learning and data augmentation to create their own supervisory signals [46] [47].
Quantitative Performance of Lightweight Models
The table below summarizes the performance of recently proposed lightweight models on various medical imaging tasks.
Table 1: Performance of Lightweight Self-Supervised Models
| Model Name | Primary Task | Key Architecture/Strategy | Performance Metrics | Computational Footprint |
|---|---|---|---|---|
| HistoLite [45] | Domain Generalization (Histopathology) | Lightweight autoencoder with dual-stream contrastive learning | Modest classification accuracy; Lowest performance drop on out-of-domain data [45] | 41M parameters; Trainable on a single standard GPU [45] |
| MSL-Net [47] | Segmentation & Landmark Localization | LR-ASPP-MobileNetV3 backbone with Deeply Separable Task-Specific (DSTS) module | Dice: 93.54%; OKS: 0.803 [47] | 5.007M parameters; 0.246 GFLOPs [47] |
| FCNN with Denoising [4] | Femur Segmentation (DXA) | Fully Convolutional Neural Network with wavelet-based noise reduction filter | Segmentation Accuracy: 98.84%; BMD Correlation: 0.9928 [4] | Not Specified |
Comparative Performance of Denoising Techniques
For tasks involving image denoising, a critical preprocessing step, the following table compares the efficiency of traditional and modern methods.
Table 2: Efficiency Comparison of Image Denoising Techniques
| Denoising Method | Domain | Key Principle | Performance (PSNR/SSIM) | Computational Complexity |
|---|---|---|---|---|
| Gaussian Pyramid (GP) [25] | General & Medical Images | Multi-scale decomposition via low-pass filtering and down-sampling | PSNR: 36.80 dB; SSIM: 0.9428 [25] | 0.0046 seconds (Very Low) [25] |
| Wavelet Transforms (e.g., DB4) [25] | General & Medical Images | Transform domain thresholding | Lower than GP [25] | Higher than GP [25] |
| CNN-based Denoisers [25] | General & Medical Images | Deep learning with large-scale datasets | Competitive | High; requires significant resources [25] |
| DDPM [48] | Synthetic Contrast-Enhanced MRI | Denoising Diffusion Probabilistic Model | SSIM: 0.78 ± 0.10 [48] | Very High [48] |
Troubleshooting Guides & FAQs
This section addresses common technical challenges encountered when implementing self-supervised learning projects, providing clear, actionable solutions.
Frequently Asked Questions
Q: My model performs well on its self-supervised pre-training task but fails to generalize during fine-tuning on my downstream task. What could be wrong?
- A: This is often a problem of task misalignment. The pre-training task (e.g., solving jigsaw puzzles) may not teach the model features relevant to your target task (e.g., tumor classification). Ensure the pretext task encourages the learning of generally useful representations, such as anatomical structures. Strategies like contrastive learning (used in HistoLite) or masked image reconstruction are often more robust as they force the model to understand global and local image context [45] [46].
Q: I have very limited computational resources. What is the most resource-efficient self-supervised learning approach?
- A: Focus on lightweight architectures and efficient pre-training strategies. Models like MSL-Net (5M parameters) and HistoLite (41M parameters) are designed for this scenario [45] [47]. For pre-training, contrastive methods that do not require large batch sizes (e.g., BYOL, SimSiam) or simple autoencoders are more feasible than large diffusion models on limited hardware [46].
Q: My model's performance drops significantly when applied to data from a different hospital scanner. How can I improve its robustness?
- A: This is a domain shift problem due to scanner-specific variations. To improve generalization, incorporate data augmentation during training that simulates scanner variations (e.g., color shifts, noise, blur). Frameworks like HistoLite are explicitly designed to learn domain-invariant features by using augmentations that mimic real-world domain changes in a contrastive learning setup, which aligns features from different domains [45].
Q: What is the most effective way to incorporate denoising into my pipeline with low computational overhead?
- A: For real-time or low-power applications, Gaussian Pyramid (GP)-based denoising offers an excellent balance of performance and speed, as shown in Table 2 [25]. Alternatively, a wavelet-based filter can be used as a preprocessing step, which has been shown to improve the performance of downstream deep learning models like FCNNs without adding significant training overhead [4].
Troubleshooting Common Experimental Issues
Problem: Training is unstable and the loss diverges when using a contrastive learning framework.
- Solution: Check the following:
- Positive Pairs: Ensure that the augmentations used to create positive pairs are meaningful but not too destructive.
- Negative Pairs: If your method uses negative samples, verify that the batch size is large enough to provide a sufficient number of negatives. If not, consider using a momentum encoder with a queue (like MoCo) or a method that doesn't require negative pairs [46].
- Learning Rate: Contrastive learning can be sensitive to the learning rate. Try a lower learning rate and use a warm-up phase.
- Solution: Check the following:
Problem: The model is overfitting to the self-supervised pre-training task.
- Solution: Apply stronger regularization techniques. This includes using weight decay, dropout, and, most effectively, more diverse data augmentations during pre-training. The goal is to force the model to learn more generalized, robust features rather than "cheating" on the simple pretext task [46].
Problem: A lightweight model has lower accuracy than a large foundation model on my specific task.
- Solution: This is a classic accuracy-efficiency trade-off. To bridge the gap:
- Leverage Pre-training: Even if the foundation model is too large to use, you can use its features to distill knowledge into your smaller model.
- Architecture Tuning: Focus on optimizing the task-specific head of your network after pre-training. A slightly more complex classifier can sometimes yield significant gains without drastically increasing the overall parameter count [45] [47].
- Solution: This is a classic accuracy-efficiency trade-off. To bridge the gap:
Experimental Protocols & Methodologies
This section provides detailed, step-by-step protocols for implementing key self-supervised learning frameworks and denoising techniques.
Protocol 1: Implementing a HistoLite-like Framework for Domain Generalization
This protocol is designed for learning scanner-invariant features in histopathology or other medical imaging domains [45].
Data Preparation:
- Collect a set of unlabeled medical images (e.g., Whole Slide Image patches).
- For evaluation, curate a dataset where the same biological sample is digitized using different scanner platforms to quantify domain shift.
Model Architecture Setup:
- Implement a dual-stream autoencoder with shared weights between the two encoder networks.
- Each autoencoder should have a standard CNN-based encoder-decoder structure. The example from the search results uses an encoder that progressively increases feature maps (64, 128, 256, 384, 512) and a symmetric decoder [45].
Self-Supervised Pre-training:
- Stream 1: Pass an original image through the first autoencoder stream and compute the reconstruction loss (e.g., Mean Squared Error) between the input and output.
- Stream 2: Apply a set of strong augmentations to the original image to simulate domain shifts (e.g., stain variations, contrast changes, Gaussian noise, rotations). Pass this augmented version through the second stream.
- Contrastive Alignment: Extract the compressed representations (the bottlenecks) from both streams. Use a contrastive loss (e.g., NT-Xent) to minimize the distance between these two representations of the same image. This encourages the model to learn features that are invariant to the applied augmentations.
- The total loss is a weighted sum of the reconstruction and contrastive losses.
Downstream Fine-tuning:
- Remove the decoders from the pre-trained model.
- Attach a task-specific head (e.g., a classifier) to the encoder.
- Fine-tune the entire network end-to-end on a small set of labeled data for your target task (e.g., cancer classification).
Protocol 2: Implementing MSL-Net for Multi-Task Learning
This protocol outlines the procedure for joint segmentation and landmark localization with minimal annotations [47].
Data Preparation:
- Gather a set of sequential medical images (e.g., ultrasound video, CT slices).
- Only a sparse set of frames needs to have manual annotations for segmentation masks and landmark locations.
Self-Supervised Pre-training via Masked Reconstruction:
- Input: A sequence of unlabeled image frames.
- Process: Randomly mask a significant portion (e.g., 50-70%) of patches in the input frames.
- Objective: Train the model (encoder-decoder) to reconstruct the masked portions of the input. This task forces the model to learn meaningful spatio-temporal representations and anatomical context from the unlabeled data.
Weakly-Supervised Multi-Task Fine-tuning:
- Pseudo-label Generation: Use the sparsely annotated frames to generate pseudo-labels for the entire sequence. For example, propagate annotations to neighboring frames using linear interpolation or a simple motion model.
- Multi-Task Training:
- Use an efficient backbone like LR-ASPP-MobileNetV3 for feature extraction.
- The features are fed into a Deeply Separable Task-Specific (DSTS) module. This module contains separate, lightweight branches for segmentation and landmark localization to prevent task interference.
- Train the entire model using a combined loss function (e.g., Dice loss for segmentation and Mean Squared Error for landmark coordinates) on the pseudo-labeled dataset.
Protocol 3: Integrating Gaussian Pyramid Denoising as a Preprocessing Step
This is a highly efficient method to improve input image quality before analysis [25].
Pyramid Construction:
- Start with the original image as the base level (Level 0).
- Iteratively apply a Gaussian low-pass filter and downsample the image by a factor of 2 to create higher pyramid levels (Level 1, Level 2, etc.). A 5-layer pyramid is often sufficient.
Noise Attenuation:
- Process: Apply a simple denoising operator (e.g., a soft-thresholding function or a small, linear filter) to each level of the pyramid. Noise is more easily attenuated at the coarser, lower-resolution levels.
Image Reconstruction:
- Upsample each denoised level from the top of the pyramid (coarsest) downwards.
- Use the same Gaussian filter to smooth the upsampled images.
- Combine these levels to reconstruct the final, denoised image at the original resolution.
Workflow & Architecture Diagrams
The following diagrams visualize the core logical workflows of the methods described in this guide.
HistoLite Dual-Stream Pre-training
MSL-Net Multi-Task Learning
Gaussian Pyramid Denoising
The Scientist's Toolkit
This section catalogs essential software, datasets, and frameworks used in developing and testing lightweight self-supervised methods.
Table 3: Key Research Reagents & Resources
| Resource Name | Type | Primary Function in Research | Relevant Citation |
|---|---|---|---|
| MONAI | Open-Source Framework | Provides pre-built, optimized modules for medical AI development, including transforms, networks, and loss functions, accelerating pipeline creation. | [49] |
| EchoNet-Dynamic | Public Dataset | A large echocardiogram video dataset used for training and benchmarking models for cardiac segmentation and landmark detection. | [47] |
| SDD2020 | Public Dataset | A spine CT dataset used for cross-domain validation to test model generalization across different anatomical regions and modalities. | [47] |
| DINO/DINOv2 | SSL Algorithm | A self-supervised learning framework that uses self-distillation with no labels. It is a foundation for many state-of-the-art medical foundation models. | [45] [46] |
| Wavelet-based Filter | Preprocessing Tool | A denoising filter used to remove noise and imperfections from DXA images, improving the quality of input data for downstream deep learning models. | [4] |
FAQs: Core Concepts and Architecture Selection
1. What is the fundamental motivation for creating hybrid CNN-Transformer architectures in medical image analysis? Hybrid architectures aim to leverage the complementary strengths of Convolutional Neural Networks (CNNs) and Vision Transformers (ViTs). CNNs excel at extracting hierarchical local features and spatial patterns, which is crucial for identifying fine-grained details in medical images. In contrast, Transformers utilize self-attention mechanisms to capture long-range dependencies and global contextual information within an image. By combining them, hybrids seek to integrate precise local feature extraction with a global understanding of the image context, which is often necessary for accurate diagnosis and analysis [50] [51] [52].
2. My hybrid model is underperforming a pure CNN on a dental image segmentation task. Is this expected? Yes, this can happen, and it is supported by recent research. A 2025 study assessing architectures on dental segmentation tasks found that CNNs can significantly outperform both hybrid and pure Transformer-based models on specific medical image tasks. For instance, in tooth segmentation on panoramic radiographs, CNNs achieved a mean F1-Score of 0.89, compared to 0.86 for Hybrids and 0.83 for Transformers. The performance gap was even more pronounced in complex tasks like caries lesions segmentation [53]. This underscores that the optimal architecture is highly task-dependent and models that excel in other domains do not necessarily constitute the best choice for a given medical imaging application [53].
3. How can I improve the interpretability of my hybrid model for clinical applications? To enhance interpretability, consider an inherently interpretable-by-design hybrid architecture. One approach is to use a model that generates evidence maps as a direct part of its forward pass, rather than relying on post-hoc explanation methods. This can be achieved by using a CNN backbone as a feature extractor, a transformer module to model long-range dependencies, and a final convolutional layer with 1x1 kernels to produce a class-specific evidence map. Spatial average pooling on this evidence map then yields the final prediction, providing faithful and localized visual explanations for the model's decision [50].
4. What is a common pitfall when integrating CNNs and Transformers? A common pitfall is the inadequate design of the feature exchange between the CNN and Transformer modules. Simply stacking a Transformer on top of a CNN may not effectively leverage the strengths of both if the feature representations are not properly aligned or if the self-attention mechanism is applied to a feature map that has lost critical local spatial information. Successful integration often involves careful design choices, such as using dual-resolution self-attention mechanisms that operate on both high- and low-resolution feature maps to capture details at multiple scales [50].
Troubleshooting Guides
Issue: Model Suffers from Poor Local Feature Extraction
Symptoms: The model fails to capture fine details, edges, or small lesions in medical images. Performance on tasks requiring precise localization is subpar.
Diagnosis and Solutions:
- Check the CNN Backbone: Ensure your convolutional backbone (e.g., ResNet, BagNet) is appropriate for the task. A backbone with a larger receptive field might be necessary for capturing context, while one with a smaller receptive field is better for local details [50].
- Inspect Feature Map Resolution: Avoid over-aggressive downsampling in the initial CNN stages. Preserving a higher-resolution feature map for the Transformer module can help retain local spatial information [52].
- Consider a Hybrid Connection Strategy: Instead of a simple sequential setup, explore parallel pathways or cross-attention mechanisms that allow the Transformer to query local features from the CNN continuously [51].
Issue: Training is Unstable or Slow
Symptoms: Loss values fluctuate wildly, model convergence is slow, or performance is inconsistent across folds or runs.
Diagnosis and Solutions:
- Verify Optimizer and Learning Rate: Transformers often require different optimization hyperparameters than CNNs. Use learning rate warmup and adaptive optimizers like AdamW, which are standard for training Transformer-based models.
- Stabilize Activations: Leverage layer normalization and residual connections, which are core components of the Transformer architecture. These help stabilize the activations and mitigate the vanishing gradient problem during training [51].
- Pre-train Modules Separately: If data is limited, a effective strategy is to pre-train the CNN backbone on a related medical imaging task and then fine-tune the entire hybrid model. This can provide a more stable starting point [54].
Issue: Model Fails to Generalize to New Data
Symptoms: The model achieves high accuracy on the training set but performs poorly on the validation set or external datasets.
Diagnosis and Solutions:
- Address Overfitting: Incorporate strong regularization techniques. As demonstrated in a TensorFlow CNN example, use
Dropoutlayers (e.g., with a rate of 0.5) and data augmentation specific to medical images (e.g., rotations, flips, intensity variations) to improve generalization [55] [54]. - Analyze Data Distribution Shift: Ensure your training data is representative of the clinical setting. Performance can degrade significantly under distribution shift, and interpretable models can help diagnose this by showing if the model focuses on irrelevant features [50].
- Simplify the Architecture: For smaller datasets, a very complex hybrid model might be over-parameterized. Start with a simpler hybrid or a well-tuned CNN before scaling up complexity [53].
Experimental Protocols & Performance Data
Quantitative Performance Benchmarking
The following table summarizes key quantitative findings from recent studies comparing architectures on medical imaging tasks, providing a baseline for expected performance [53].
Table 1: Architecture Performance on Dental Image Segmentation Tasks (Mean F1-Score ± SD)
| Architecture Type | Tooth Segmentation | Tooth Structure Segmentation | Caries Lesions Segmentation |
|---|---|---|---|
| CNNs (U-Net, DeepLabV3+) | 0.89 ± 0.009 | 0.85 ± 0.008 | 0.49 ± 0.031 |
| Hybrids (SwinUNETR, UNETR) | 0.86 ± 0.015 | 0.84 ± 0.005 | 0.39 ± 0.072 |
| Transformer-based (TransDeepLab, SwinUnet) | 0.83 ± 0.022 | 0.83 ± 0.011 | 0.32 ± 0.039 |
Framework Performance for Classification
For image classification tasks, the choice of deep learning framework can impact performance and inference time. Below is a comparison from a study on blood cell image classification [56].
Table 2: Framework Comparison for Medical Image Classification (BloodMNIST)
| Framework | Key Performance Characteristic |
|---|---|
| PyTorch | Classification accuracy comparable to current benchmarks; a popular choice for research due to flexibility. |
| JAX | Classification accuracy comparable to current benchmarks; known for high-performance computing. |
| TensorFlow Keras | Performance variations can be observed; influenced by factors like image resolution and framework-specific optimizations. |
Protocol: Implementing a Basic Hybrid Model for Classification
This protocol outlines the steps to implement a simple yet effective interpretable hybrid model based on recent research [50].
- Input: Begin with a medical image (\mathbf{X} \in \mathbb{R}^{H \times W \times C}).
- CNN Feature Extraction: Pass the image through a CNN backbone (e.g., ResNet50) to extract a spatial feature representation (\mathbf{Z} = f_{\theta}(\mathbf{X}) \in \mathbb{R}^{M \times N \times D}).
- Transformer for Global Context: Feed the feature map (\mathbf{Z}) into a Transformer module that uses a convolutional window self-attention (Conv-wSA) mechanism. This module processes both the high-resolution feature map (\mathbf{Z}h = \mathbf{Z}) and a downsampled low-resolution version (\mathbf{Z}l) to model long-range dependencies and produce an enhanced attention map (\mathbf{W}).
- Generate Evidence Map: Instead of a standard fully connected classification head, use a convolutional layer with (C) (number of classes) kernels of size (1 \times 1) on the attention map (\mathbf{W}). This produces an evidence map (\mathbf{A} \in \mathbb{R}^{M \times N \times C}), where each spatial location and channel indicates evidence for a specific class.
- Classification Output: Apply global average pooling to the evidence map (\mathbf{A}) to get a vector of class logits, followed by a softmax operation to generate the final prediction (\mathbf{\hat{y}}).
- Interpretation: The evidence map (\mathbf{A}) can be visualized directly to see which image regions contributed to the classification decision for each class.
Workflow Diagram: Interpretable Hybrid Model
The following diagram illustrates the data flow and architecture of the interpretable hybrid model described in the experimental protocol [50].
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Components for Hybrid Model Development
| Item / Solution | Function / Purpose |
|---|---|
| PyTorch / TensorFlow | Primary deep learning frameworks offering flexibility (PyTorch) and production-ready deployment (TensorFlow). JAX is also emerging for high-performance computing [55] [56]. |
| CNN Backbones (ResNet, BagNet) | Pre-trained convolutional networks that serve as powerful local feature extractors. The choice affects the receptive field and the type of features captured [50]. |
| Vision Transformer (ViT) Modules | Self-attention based modules that model global dependencies and contextual relationships between extracted features [50] [51]. |
| Medical Image Datasets (e.g., BloodMNIST) | Publicly available, annotated datasets crucial for training and benchmarking model performance in a specific medical domain [56]. |
| Data Augmentation Pipelines | Techniques to artificially expand training data (e.g., rotation, flipping, elastic deformations) which are vital for improving model robustness and preventing overfitting in data-scarce medical settings. |
| Interpretability Libraries | Tools for computing saliency maps, Grad-CAM, or LRP to explain model predictions, which is critical for clinical validation and trust [50]. |
| Hybrid Architecture Blueprints | Reference designs like ConvBERT, CvT, or the interpretable hybrid from [50], which provide proven patterns for effectively combining CNNs and Transformers [51]. |
Optimizing Performance and Overcoming Common Denoising Pitfalls
Preventing Over-Smoothing and Loss of Subtle Pathologies
Frequently Asked Questions (FAQs)
Q1: Why is over-smoothing a critical problem in medical image denoising, and what causes it? Over-smoothing is critical because it removes not only noise but also fine details and subtle pathologies essential for accurate diagnosis. This is often caused by denoising algorithms that apply excessive averaging or homogeneous smoothing, which blurs edges and textures. Techniques like simple linear filters or aggressive thresholding can fail to distinguish between noise and critical diagnostic features, leading to a loss of structural integrity in the image [18] [5] [15].
Q2: What quantitative metrics can I use to monitor over-smoothing in my denoising experiments? You should use a combination of metrics to evaluate both noise reduction and feature preservation. The following table summarizes key quantitative metrics:
| Metric | Primary Function | Ideal Value Indication | Direct Indicator for Over-Smoothing |
|---|---|---|---|
| PSNR (Peak Signal-to-Noise Ratio) [5] [15] | Measures noise reduction level | Higher is better | No, but a very high PSNR can sometimes indicate over-smoothing if edges are lost. |
| SSIM (Structural Similarity Index) [18] [5] | Assesses preservation of structural information | Closer to 1.0 is better | Yes, a lower SSIM suggests image structures are being degraded. |
| MSE (Mean Squared Error) [18] [5] | Quantifies the difference between images | Lower is better | Indirectly; a very low MSE with poor SSIM can signal over-smoothing. |
| FOM (Figure of Merit) [18] | Evaluates edge preservation | Higher is better (e.g., up to 0.68 [18]) | Yes, directly measures the retention of edge information. |
| IEF (Image Enhancement Factor) [18] | Assesses the overall enhancement | Higher is better (e.g., >20% improvement [18]) | Indirectly; a high IEF confirms effective denoising without severe detail loss. |
Q3: My deep learning model removes noise effectively but makes images look too "plastic" and loses subtle textures. What can I do? This "plastic" appearance is a classic sign of over-smoothing. To address it:
- Incorporate a Perceptual Loss Function: Supplement your standard loss function (e.g., MSE) with a perceptual loss that compares feature maps from a pre-trained network. This encourages the model to preserve textures and structures that are semantically important.
- Review Your Training Data: Ensure your training set includes examples with the subtle pathologies you wish to preserve. A model trained only on "normal" tissue may remove atypical features.
- Consider a Lightweight Architecture: Overly complex models can sometimes overfit to noise. A simpler, ultra-lightweight model, like the three-layer convolutional network used in Noise2Detail, can achieve high-quality restoration by focusing on essential features and breaking noise correlations through multi-stage refinement [57].
Q4: For traditional non-deep learning methods, which algorithms best balance noise removal and detail preservation? Based on comparative studies, the following algorithms are recommended:
| Algorithm | Key Principle | Performance against Over-Smoothing |
|---|---|---|
| BM3D (Block-Matching and 3D Filtering) [5] | Groups similar 2D image patches into 3D arrays for collaborative filtering. | Consistently outperforms others at low/moderate noise, achieving high PSNR and SSIM while preserving structural integrity [5]. |
| Hybrid AMF & MDBMF [18] | Combines Adaptive Median Filter (dynamic window sizing) with a Modified Decision-Based Median Filter (selective pixel recovery). | Specifically designed to preserve edges by only filtering corrupted pixels. Shows up to 2.34 dB PSNR improvement and high FOM scores [18]. |
| Wavelet-Based Techniques [58] | Processes images in the frequency domain, applying thresholds to wavelet coefficients. | Effective at preserving features if using advanced thresholding (e.g., Soft Thresholding), but can over-smooth with large thresholds [58]. |
Q5: How can I prevent over-smoothing when I only have a single noisy image and no clean training data? Self-supervised, data-free methods are ideal for this scenario. Implement a pipeline like Noise2Detail (N2D) [57]:
- Initial Denoising: Train a compact network on two downsampled versions of your single noisy input to generate an initial, partially restored image.
- Noise Correlation Disruption: Use pixel-shuffle downsampling on the noisy input to break spatial correlations in the noise pattern. Denoise these sub-images and reassemble them.
- Detail Refinement: Fine-tune the network weights using the original noisy image to recapture critical foreground details that might have been softened in the previous step. This multi-stage approach effectively separates noise removal from detail preservation [57].
Troubleshooting Guides
Problem: Loss of Subtle Pathologies (e.g., Early-Stage Tumors, Small Lesions)
Symptoms:
- Denoised images lack fine textures and small structures.
- Low contrast between pathological and healthy tissue is further reduced.
- Quantitative metrics like SSIM and FOM are low, even if PSNR is high.
Solutions:
- Algorithm Selection: Move beyond simple spatial filters (Gaussian, Median) which are prone to over-smoothing [5]. Prioritize modern methods:
- Deep Learning: Use a Deep Convolutional Neural Network (CNN) or an Encoder-Decoder architecture, which constitute over 40% and 18% of top-performing denoising models, respectively [15]. These learn to preserve anatomical structures.
- Advanced Traditional Methods: Implement BM3D or a specialized hybrid filter like AMF+MDBMF [18] [5].
- Harmonize Your Data: If using multi-site data, batch effects can cause an algorithm to mistake scanner-specific variations for noise. Apply data harmonization techniques like histogram matching or use deep learning-based harmonization tools (e.g., MRQy, LAB-QA2GO) before denoising [59].
- Validate with Experts: Always supplement quantitative metrics with a qualitative, clinical validation by a radiologist or domain expert to confirm that subtle pathologies remain identifiable post-denoising [58].
Problem: Over-Smoothing in High-Noise Environments
Symptoms:
- Images appear blurry and lack sharp edges.
- Textural information is lost, making tissues look homogeneous.
- The denoising method struggles with high noise densities (e.g., above 70%).
Solutions:
- Leverage Deep Learning's Robustness: For high noise levels, deep learning models like DnCNN are often better suited than conventional algorithms, as they can learn to handle significant noise variations without compromising critical features as severely [5].
- Employ a Hybrid Approach: Use an adaptive filter like the Adaptive Median Filter (AMF), which dynamically adjusts its window size based on local noise density to target noisy pixels more precisely, thereby protecting intact regions [18].
- Check Computational Resources: Denoising large medical image datasets (which can be over 100 GB) requires sufficient RAM and potent GPUs. Inadequate resources can force the use of suboptimal, less computationally intensive methods that over-smooth. Ensure access to High-Performance Computing (HPC) resources for complex models [59].
Experimental Protocols for Key Cited Methods
This protocol is designed for removing high-density salt-and-pepper noise while preserving edges.
1. Objective: To effectively denoise images corrupted by impulse noise (10-90% density) while maintaining structural integrity and edge sharpness. 2. Materials:
- Input: Noisy medical images (e.g., Chest X-ray, Liver MRI) with salt-and-pepper noise.
- Software: Python (recommended) or R with standard image processing libraries (OpenCV, SciKit-Image).
3. Methodology:
- Step 1 - Noise Detection with AMF: For each pixel in the noisy image, dynamically adjust the size of the filtering window until a non-noisy pixel (value not equal to 0 or 255) is found. This adaptively identifies corrupted regions.
- Step 2 - Noise Removal with MDBMF: Replace the value of a pixel identified as noisy with the median value of the non-noisy pixels within the adaptive window. If all pixels in the window are noisy, replace the target pixel with the mean of the surrounding pixels. This selective recovery ensures intact pixels are left unchanged. 4. Validation:
- Quantitative: Calculate PSNR, SSIM, and FOM against a ground-truth clean image. Successful implementation should show an improvement in PSNR of up to 2.34 dB and an FOM value reaching up to 0.68 [18].
- Qualitative: Visually inspect the denoised image to confirm the preservation of organ boundaries and tissue textures.
This protocol is for scenarios where only a single noisy image is available and clean training data is absent.
1. Objective: To perform detail-preserving denoising using only a single noisy input image. 2. Materials:
- Input: A single noisy medical image (e.g., CT scan, fluorescence microscopy image).
- Software: Python with a deep learning framework (PyTorch/TensorFlow). A three-layer convolutional network is used.
3. Methodology:
- Step 1 - Initial Prediction: Generate two downsampled views,
D1(y)andD2(y), of the noisy inputyusing diagonal averaging kernels. Train the compact network using a symmetric loss functionL_res(Eq. 3 [57]) to predict one view from the other, producing an initial denoised image. - Step 2 - Background Refinement: Apply pixel-shuffle downsampling to the noisy input
yto create multiple sub-images. This breaks the spatial correlation of the noise. Denoise these sub-images using the pre-trained network from Step 1. Use the inverse pixel-shuffle operator to reassemble a refined image with reduced background artifacts. - Step 3 - Detail Sharpening: Fine-tune the weights of the network from Step 1 on the original noisy image
yto recapture and sharpen critical foreground details that may have been softened in Step 2. 4. Validation: - Use perceptual quality metrics like BRISQUE or NIQE [5] to evaluate the output without a clean ground truth.
- Compare the result qualitatively with the input, ensuring that fine cellular structures or pathological markers are clearly visible and not blurred.
- Step 1 - Initial Prediction: Generate two downsampled views,
Workflow Diagram
Research Reagent Solutions
| Item | Function in Denoising Research | Example / Note |
|---|---|---|
| BM3D Algorithm [5] | A high-performance non-local algorithm for removing Gaussian noise. Serves as a strong benchmark. | Dependable for moderate noise levels; available in various open-source libraries. |
| DnCNN (Deep Convolutional Neural Network) [5] [15] | A deep learning model that learns to remove noise and artifacts from training data. | The most common architecture in deep learning-based denoising (used in 40% of reviewed papers) [15]. |
| Noise2Detail (N2D) Pipeline [57] | A lightweight, self-supervised framework for denoising without clean data or explicit noise models. | Ideal for resource-constrained settings and rare imaging modalities. |
| Adaptive Median Filter (AMF) [18] | A spatial filter that dynamically adjusts window size to identify and target noisy pixels. | Core component of hybrid approaches for impulse noise. |
| SSIM (Structural Similarity Index) [18] [5] | A critical validation metric that quantifies the preservation of structural information. | More perceptually relevant than PSNR for diagnosing over-smoothing. |
| Data Harmonization Tools (e.g., MRQy) [59] | Software to identify and correct for batch effects from different scanners or sites. | Preprocessing step crucial for multi-institutional studies to prevent algorithmic errors. |
Strategies for Handling Real-World, Spatially Variant Noise
In medical image research, real-world, spatially variant noise presents a significant challenge for accurate diagnosis and quantitative analysis. Unlike simple synthetic noise, this noise is complex, non-Gaussian, and its characteristics change across different regions of an image. It arises from various physical processes during image acquisition, including sensor limitations, transmission errors, and quantum effects. This technical guide provides troubleshooting advice and methodologies for researchers and drug development professionals working to mitigate these noise artifacts in their medical imaging data.
Frequently Asked Questions (FAQs)
Q1: What distinguishes real-world, spatially variant noise from standard synthetic noise in medical images? Real-world noise in medical images is complex and non-Gaussian, often comprising a mixture of different noise types (e.g., Gaussian, Poisson) whose characteristics change across the image. This contrasts with standard synthetic noise like simple Additive White Gaussian Noise (AWGN). Real-world noise is often signal-dependent, meaning its intensity can vary with the underlying signal strength, making it spatially variant and more challenging to remove without affecting anatomical details [25].
Q2: Why do deep learning models sometimes fail to generalize on real-world medical images with spatially variant noise? Deep learning models trained on a specific noise level or type often fail to generalize due to inherent distribution shifts between the training data and the input images. If a model is trained only on images with one noise characteristic, it may perform poorly on images with different noise levels or spatial variations, leading to biased results [60]. Techniques like domain generalization are being developed to enforce the extraction of noise-level invariant features to combat this [60].
Q3: What is a key trade-off to consider when denoising medical images for diagnostic purposes? The primary trade-off is between noise reduction and the preservation of critical anatomical details. Over-smoothing an image to remove noise can lead to the loss of fine textures and edges essential for identifying subtle pathologies, such as early-stage tumors. Conversely, under-smoothing leaves noise that can obscure diagnostic information [5] [28].
Q4: How can I determine the optimal stopping point during an iterative denoising process to prevent overfitting? An entropy-based early stopping criterion can be used. This method tracks variations in image uncertainty over iterations and autonomously determines the optimal stopping point, effectively preventing overfitting without the need for external validation data [61]. Other strategies involve monitoring the estimated noise level in the image and stopping once it falls below a certain threshold [62].
Troubleshooting Guides
Problem 1: Loss of Fine Anatomical Details After Denoising
Symptoms: The denoised image appears overly smooth; edges of small structures are blurred; texture information is lost. Possible Causes & Solutions:
- Cause: The denoising algorithm is too aggressive or uses a loss function that prioritizes overall noise reduction over detail preservation.
- Solution: Employ an edge-aware loss function, such as an L1 loss or a gradient-based loss, during the training of a deep learning model. This directly penalizes the model for distorting edges and high-frequency information [61] [62].
- Solution: Utilize a multi-scale approach, such as a Gaussian Pyramid. This structure allows noise to be attenuated at coarser levels while preserving fine details at higher resolutions [25].
- Solution: For non-learning-based methods, consider switching to algorithms known for better edge preservation, like Non-Local Means (NLM) or Bilateral filtering, and carefully tune their parameters [5].
Problem 2: Model Performance Degradation on Cross-Noise Level Data
Symptoms: A model trained on one dataset performs poorly on another dataset from a different scanner, with different acquisition parameters, or different noise levels. Possible Causes & Solutions:
- Cause: Domain shift - the model has learned features specific to the noise distribution in the training data and cannot adapt to new noise characteristics.
- Solution: Implement domain generalization during training. For example, use a continuous adversarial discriminator that enforces the model to extract features that are invariant across a continuous range of noise levels. This makes the model more robust to unseen noise variances [60].
- Solution: Use native noise modeling. Instead of simulating noise with a standard distribution (e.g., Gaussian), characterize the noise directly from the target low-field or target-domain images. This "native noise" can then be used to create more realistic training data, improving model performance on the target domain [63].
Problem 3: Handling Images with Mixed Gaussian-Poisson Noise
Symptoms: Standard denoising methods designed for a single noise type leave residual noise or introduce artifacts. Possible Causes & Solutions:
- Cause: Gaussian noise is additive and signal-independent, while Poisson noise is multiplicative and signal-dependent. A single-model approach is often insufficient for this hybrid noise [61].
- Solution: Adopt a hybrid frequency-spatial domain model. Incorporate frequency-domain priors (e.g., the amplitude spectrum from a Fourier transform) along with spatial information at the input stage of a network. This dual-domain strategy helps separate noise from signal more effectively by leveraging complementary information [61].
Experimental Protocols & Methodologies
Protocol 1: Multi-Scale Denoising Using a Gaussian Pyramid
This protocol is based on a method that achieves a PSNR of 36.80 dB and an SSIM of 0.94, with low computational complexity (0.0046s) [25].
Workflow Description: The input noisy image is progressively low-pass filtered and down-sampled to create a pyramid of images at multiple resolutions (from fine to coarse). Noise is estimated and attenuated at each of these coarse levels. The processed levels are then fused together to reconstruct the final denoised image, preserving details from higher resolutions while suppressing noise from coarser levels [25].
Protocol 2: Hybrid Frequency-Spatial Domain Unsupervised Denoising
This protocol is designed for Gaussian-Poisson mixed noise and achieves a 10.7% PSNR and 17.9% SSIM gain over Deep Image Prior (DIP), reaching peak quality in just 60 iterations [61].
Workflow Description: The process begins with a noisy input image. Its Fourier Transform is computed to obtain the frequency domain representation. The amplitude spectrum is extracted and used alongside the original spatial image as a dual-domain input to a neural network. The network is trained using an edge-aware L1 loss. An entropy-based early stopping criterion monitors the process and automatically determines the optimal point to stop training, preventing overfitting [61].
Protocol 3: Iterative Joint Denoising and Motion Artifact Correction (JDAC)
This framework handles 3D brain MRIs affected by both severe noise and motion artifacts iteratively [62].
Workflow Description: The framework operates iteratively. For each iteration, the current image state is first passed to an adaptive denoising model. This model uses a novel noise level estimation strategy based on the variance of the image's gradient map. The estimated noise level conditions a U-Net to perform adaptive denoising. The denoised image is then passed to an anti-artifact model (another U-Net), which uses a gradient-based loss to remove motion artifacts while preserving brain anatomy. The process repeats for a set number of iterations or until an early stopping criterion based on the estimated noise level is met [62].
Table 1: Performance Comparison of Denoising Algorithms on Medical Images [25] [5]
| Denoising Method | Reported PSNR (dB) | Reported SSIM | Key Strengths | Computational Complexity / Speed |
|---|---|---|---|---|
| Gaussian Pyramid (GP) | 36.80 | 0.94 | Effective noise attenuation across scales, preserves details [25]. | 0.0046 s [25] |
| BM3D | Varies (Consistently High) | Varies (Consistently High) | Excellent for low/moderate noise, preserves structural integrity [5]. | High [5] |
| DnCNN | Varies (High) | Varies (High) | Handles significant noise variations, preserves diagnostic features [5]. | Moderate to High [5] |
| Wavelet Transforms | Lower than GP | Lower than GP | Moderate performance for multi-level noise [25]. | Moderate [25] |
| Non-Local Means (NLM) | Good | Good | Strong adaptability, excellent edge retention [5]. | High [5] |
Table 2: Performance of Advanced Denoising Frameworks on Specific Tasks [61] [62]
| Framework / Model | Key Innovation | Reported Improvement | Iterations to Converge |
|---|---|---|---|
| Hybrid Frequency-Spatial Model [61] | Dual-domain input (Amplitude + Spatial) | 10.7% PSNR, 17.9% SSIM gain over DIP [61] | 60 [61] |
| Joint Denoising & Artifact Correction (JDAC) [62] | Iterative learning with noise-level estimation & gradient loss | Effective on 3D MRI with simultaneous noise and motion [62] | Iterative (Early Stopping) |
| Continuous Adversarial Domain Generalization [60] | Enforces noise-level invariant features | Improved SSIM/PSNR for cross-noise level PET denoising [60] | N/A |
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Computational Tools for Medical Image Denoising Research
| Tool / Algorithm | Type | Primary Function in Denoising |
|---|---|---|
| U-Net [62] [63] | Deep Learning Architecture | Serves as a backbone for both denoising and artifact correction tasks, effective for image-to-image translation. |
| BM3D (Block-Matching and 3D Filtering) [5] | Classical Algorithm | A strong benchmark algorithm that uses collaborative filtering in a 3D transform domain for high-performance denoising. |
| Gaussian Pyramid [25] | Multi-scale Representation | Decomposes an image into multiple scales to facilitate noise removal and detail preservation at different resolutions. |
| Deep Image Prior (DIP) [61] | Unsupervised Learning Framework | Uses the structure of a CNN itself as a prior for image reconstruction, without pre-training on a large dataset. |
| Adversarial Discriminator [60] | Deep Learning Component | Used in domain generalization to ensure features learned by the model are invariant to specific noise levels. |
| Structural Similarity Index (SSIM) [25] | Evaluation Metric | Assesses the perceptual quality and structural preservation of the denoised image compared to a clean reference. |
| Peak Signal-to-Noise Ratio (PSNR) [25] | Evaluation Metric | Measures the fidelity of the denoised image by calculating the ratio between the maximum possible signal power and the corrupting noise power. |
Balancing Computational Complexity with Clinical Workflow Requirements
Troubleshooting Guides
Issue 1: Model Performance Degradation on Clinical Image Data
Problem: A denoising model, trained on benchmark datasets, shows significantly reduced Peak Signal-to-Noise Ratio (PSNR) and Structural Similarity Index (SSIM) when applied to real-world clinical images.
| Potential Cause | Diagnostic Steps | Solution |
|---|---|---|
| Domain Shift [15] | Calculate PSNR/SSIM on a sample of local clinical images; compare with training domain results. | Implement transfer learning, fine-tuning the pre-trained model with a small set of local clinical data. |
| Unexpected Noise Profile [15] | Analyze the noise distribution in the degraded images; identify if it differs from Gaussian, Poisson, or Rician noise assumed during training. | Retrain the model using data augmented with the identified noise type (e.g., Speckle, Salt-and-Pepper). |
| Insufficient Model Generalization | Perform cross-validation using data from different scanner manufacturers and protocols. | Increase model capacity or employ data augmentation strategies that mimic scanner-specific variations. |
Issue 2: Prohibitive Inference Time Disrupting Clinical Workflow
Problem: The denoising algorithm produces excellent results but is too slow for radiologists' real-time or high-volume diagnostic needs.
| Potential Cause | Diagnostic Steps | Solution |
|---|---|---|
| High Model Complexity [64] | Profile the model to identify computational bottlenecks (e.g., specific layers, operations). | Optimize the model by pruning, quantization, or knowledge distillation to create a lighter-weight version. |
| Hardware/Software Incompatibility | Verify that all required libraries (e.g., CUDA for GPU acceleration) are correctly installed and configured. | Deploy the model on optimized hardware (e.g., GPUs, TPUs) and use inference engines like TensorRT. |
| Large Input Image Size | Assess the relationship between input image resolution and inference time. | Implement a tiling strategy to process large images in smaller, manageable patches. |
Issue 3: Integration and Validation Challenges in Clinical Systems
Problem: Difficulty integrating the denoising algorithm into the existing Picture Archiving and Communication System (PACS) and obtaining clinical validation.
| Potential Cause | Diagnostic Steps | Solution |
|---|---|---|
| "Black Box" Opacity [65] [64] | The model's decision-making process is not transparent, causing distrust among clinicians. | Incorporate explainable AI (XAI) techniques, such as saliency maps, to visualize which image features the model uses. |
| Regulatory and Liability Concerns [65] | Uncertainty regarding compliance with regulations like the EU AI Act for high-risk medical devices. | Design a rigorous validation protocol that includes disparity testing across diverse patient demographics to ensure fairness and reliability [65]. |
| Alert Fatigue [65] | The system generates an excessive number of prompts or alerts, leading to user desensitization. | Calibrate alert systems to present only high-confidence, clinically critical information, reducing unnecessary interruptions. |
Frequently Asked Questions (FAQs)
Q1: What are the most common types of noise found in different medical imaging modalities? Medical images are degraded by various noise types, which are modality-specific. The table below summarizes the predominant noises as identified in recent research [15].
| Imaging Modality | Most Common Noise Type(s) | Prevalence in Research |
|---|---|---|
| X-ray | Gaussian Noise | 35% |
| CT Scan | Gaussian Noise | 35% |
| MRI | Rician Noise | 7% |
| Ultrasound | Speckle Noise | 16% |
| PET Scan | Poisson Noise | 14% |
Q2: Which deep learning architectures are most prevalent for medical image denoising? A 2024 review of 104 papers found the following distribution of architectures [15]:
- Deep Convolutional Neural Networks (CNNs): 40%
- Encoder-Decoder Architectures (e.g., U-Net): 18%
- Transformer-based Approaches: 13%
- Generative Adversarial Networks (GANs): 12%
- Other AI-based techniques: 15%
- Multilayer Perceptron (MLP): 2%
Q3: How can we balance the high computational cost of advanced models with the need for fast clinical results? A two-tiered approach is often effective. Use a lighter, faster model (like a pruned CNN) for initial, real-time previews or triage. A more complex, accurate model (like a Transformer) can then be run in the background on the server-side, with its results replacing the initial denoised image once computation is complete. This ensures workflow efficiency without sacrificing final output quality [64].
Q4: What are the key metrics for evaluating the success of a denoising technique in a clinical context? While technical metrics are crucial, clinical evaluation is multi-faceted.
- Technical Metrics [15]:
- Peak Signal-to-Noise Ratio (PSNR): Measures the quality of the denoised image compared to a clean original.
- Structural Similarity Index (SSIM): Assesses the perceptual similarity between the denoised and original images, focusing on structure.
- Clinical Metrics:
- Diagnostic Accuracy: Does the denoised image improve or preserve the radiologist's ability to make a correct diagnosis?
- Reader Confidence: Does the image increase the radiologist's confidence in their interpretation? [66]
- Workflow Efficiency: Does the tool integrate seamlessly without causing delays or disruptions? [64]
Experimental Protocol: Validating Denoising Models for Clinical Workflow
Aim: To evaluate a denoising model's performance and its impact on the clinical workflow.
1. Materials (Research Reagent Solutions)
| Item | Function |
|---|---|
| Curated Dataset | A diverse set of clinical images from multiple sources (e.g., public, synthetic [66]) with paired ground-truth or expert-annotated labels. |
| Deep Learning Model | The denoising algorithm to be tested (e.g., CNN, GAN, Diffusion Model). |
| Computational Infrastructure | Hardware (GPUs) and software frameworks (TensorFlow, PyTorch) for training and inference. |
| Evaluation Metrics Suite | Code to calculate PSNR, SSIM [15], and task-specific clinical accuracy metrics. |
| Statistical Inference Tools | Software for rigorous statistical comparison between model outputs and real data [66]. |
2. Methodology
- Phase 1: Technical Performance
- Training: Train the model on a curated dataset, using a standard loss function (e.g., L1 or L2 loss).
- Quantitative Evaluation: Calculate PSNR and SSIM on a held-out test set to establish baseline technical performance [15].
- Phase 2: Clinical Validation
- Reader Study: Engage multiple radiologists to evaluate both original and denoised images.
- Tasks: Radiologists perform diagnostic tasks (e.g., lesion detection, classification) and rate their confidence for each image.
- Statistical Analysis: Use statistical tests (e.g., ANOVA) to determine if improvements in diagnostic accuracy or confidence are significant.
- Phase 3: Workflow Impact Analysis
- Integration Testing: Deploy the model in a simulated PACS environment.
- Efficiency Measurement: Monitor inference times and system resource usage under typical clinical load.
- User Feedback: Collect qualitative feedback from radiologists and technicians on usability and integration.
The Scientist's Toolkit
| Category | Essential Materials/Tools | Brief Function |
|---|---|---|
| Data | Public/Private Medical Image Datasets (e.g., fMRI, CT) | Serves as the foundation for training and testing denoising models. |
| Synthetic Data | AI-generated images (e.g., from GANs, DDPMs) | Augments scarce data, addresses privacy concerns, and helps balance datasets [66]. |
| Software & Libraries | Python, TensorFlow/PyTorch, OpenCV, SciKit-Image | Provides the programming environment and core functions for building, training, and testing models. |
| Evaluation & Statistics | PSNR/SSIM Calculators, Statistical Inference Tools | Quantifies model performance and rigorously validates the fidelity of synthetic or denoised images [15] [66]. |
| Validation Framework | Explainable AI (XAI) Tools, Bias Detection Kits | Ensures model transparency, fairness, and reliability across diverse populations, addressing ethical and regulatory concerns [65]. |
Workflow Diagrams
Denoising Model Validation Workflow
Clinical Integration Pathway
Frequently Asked Questions (FAQs)
FAQ 1: What are the primary causes of data scarcity in rare disease research? Data scarcity in rare diseases stems from several inherent challenges. The low prevalence of each individual condition means that the number of confirmed diagnoses in any geographic area is naturally limited. This leads to small, often heterogeneous clinical trial populations, which limits the robustness of data analysis. Furthermore, data is often fragmented across different sources, and there can be inadequate natural history knowledge for many conditions. The high cost and difficulty of data annotation, combined with regulatory constraints, further exacerbate this scarcity [67] [68].
FAQ 2: How can AI help overcome small dataset sizes in pediatric rare disease studies? Artificial Intelligence offers multiple techniques to counteract data scarcity. AI can standardize and analyze unstructured data from sources like electronic health records and patient case studies. A powerful emerging approach is the generation of synthetic data or "artificial patients," which can serve as synthetic controls in studies. Furthermore, Few-Shot Learning (FSL), a subfield of AI, is specifically aimed at enabling machine learning in scenarios with a limited number of samples, making it a natural fit for rare disease identification [68] [69].
FAQ 3: What are the key challenges when using synthetic data? While synthetic data is beneficial for hypothesis generation and preliminary testing, its use comes with risks that must be recognized. A major concern is "model collapse," where AI models trained on successive generations of synthetic data begin to generate nonsense. There is also a need for robust validation against real-world data and a risk that individuals whose data was used to generate the original models could be identified, raising privacy issues. Ensuring the reliability of findings requires clear reporting standards for how synthetic data is generated [70].
FAQ 4: Beyond data size, what other data quality issues affect model performance? The challenge is not only the quantity of data but also its quality. Key issues include:
- Data Imbalance: Where one class of data is over-represented compared to others.
- Noisy Datasets: Including inaccuracies or artifacts in labels or medical images.
- Algorithmic Bias: Models may become biased and unreliable in real-world settings if not developed with measures to counteract the inherent scarcity and heterogeneity of medical data [67].
Troubleshooting Guides
Problem: My medical image data is degraded by noise, which is obscuring crucial anatomical details. Solution: Implement a deep learning-based denoising pipeline.
- 1. Diagnosis: Identify the type of noise present in your images, as different denoising strategies are effective for different noise types. Common noise in medical images includes Gaussian, Rician, and Poisson noise [15].
- 2. Model Selection: Select an appropriate model architecture. U-Net and U-Net++ have demonstrated superior performance in denoising medical images such as chest X-rays. U-Net++ often provides enhanced structural fidelity [71].
- 3. Implementation & Acceleration: To speed up training on limited data, use optimized distributed training configurations like PyTorch's DistributedDataParallel (DDP) combined with Automatic Mixed Precision (AMP). This can reduce training time by over 60% compared to single-GPU training [71].
- 4. Validation: Quantitatively evaluate the denoising performance using standard metrics like Peak Signal-to-Noise Ratio (PSNR) and the Structural Similarity Index (SSIM) to ensure both noise reduction and detail preservation [71] [15].
Problem: I need to identify rare disease cases from a large set of unstructured clinical notes. Solution: Employ a Natural Language Processing (NLP) pipeline that combines semi-supervised and supervised techniques.
- 1. Initial Case Detection: Use a semi-supervised, keyphrase-based system to perform an initial detection of mentions of rare diseases. This method uses domain-specific keyphrases and external knowledge sources (like the Orphanet Rare Disease Ontology) and does not rely on extensive labeled datasets [69].
- 2. Expert Validation & Dataset Creation: The initial detections must be validated and refined by clinical experts to build a high-quality, consolidated dataset for model training [69].
- 3. Supervised Classification: Use the validated dataset to train state-of-the-art supervised models. Recent studies show that such models (including discriminative and generative Large Language Models) can improve the performance of the initial semi-supervised system by over 10% (e.g., from 67.37% to 78.74% in F-Measure) [69].
- 4. Handling Linguistic Variation: Account for inconsistent disease naming (e.g., "Ehlers-Danlos syndrome" might also be referred to as "cutis laxa") by incorporating synonyms and leveraging ontologies during the keyphrase-matching and model training stages [69].
Quantitative Data on Denoising Techniques
The table below summarizes the prevalence of different deep learning models and noise types in medical image denoising research, based on an analysis of 104 relevant papers [15].
Table 1: Prevalence of Deep Learning Models in Medical Image Denoising
| Model Type | Percentage of Use | Key Characteristics |
|---|---|---|
| Deep Convolutional Neural Networks (CNNs) | 40% | Widely adopted for effective image feature learning. |
| Encoder-Decoder Architectures | 18% | Often used for pixel-wise prediction tasks. |
| Transformer-based Approaches | 13% | Leverages attention mechanisms for global context. |
| Generative Adversarial Networks (GANs) | 12% | Useful for generating clean images from noisy inputs. |
| Other AI-based Techniques | 15% | Includes methods like Deep Image Prior (DIP). |
| Multilayer Perceptron (MLP) | 2% | Less commonly used for this task. |
Table 2: Prevalence of Noise Types in Medical Image Denoising Studies
| Noise Type | Percentage of Studies | Commonly Affected Modalities |
|---|---|---|
| Gaussian Noise | 35% | A common model for various acquisition noises. |
| Speckle Noise | 16% | Frequently found in ultrasound imaging. |
| Poisson Noise | 14% | Often present in X-ray and PET scans. |
| Artifacts | 10% | Can occur in CT, MRI, etc., from motion or equipment. |
| Rician Noise | 7% | Characteristic of MRI images. |
| Salt-pepper Noise | 6% | Can affect various modalities. |
| Impulse Noise | 3% | Can affect various modalities. |
| Other | 9% | Various other noise types. |
Experimental Protocols
Protocol 1: Synthetic Data Generation for Augmenting Rare Disease Cohorts
Purpose: To create artificial patient data that mimics the statistical properties of a real, small rare disease cohort, enabling preliminary testing and hypothesis generation when real data is scarce [70]. Materials: A source of real-world data (e.g., a small, anonymized patient registry), computational resources, and a synthetic data generation algorithm. Methodology:
- Data Preparation: Start with a carefully curated set of real-world data. Ensure all patient identifiers are removed and ethical guidelines are followed.
- Model Selection and Training: Choose a generative model, such as a Generative Adversarial Network (GAN). Train the model on the real-world dataset to learn its underlying statistical distributions and correlations between variables (e.g., genotype, phenotype, lab results).
- Data Generation: Use the trained model to generate new, synthetic patient records.
- Validation and Reporting: Critically, the synthetic data must be validated. This involves:
- Comparing the statistical properties of the synthetic data with the original data.
- As real-world data may be scarce, researchers should thoroughly document and report the algorithm, parameters, and assumptions used to generate the synthetic data so that other groups can attempt to validate the results [70].
Protocol 2: NLP-Based Rare Disease Detection in Clinical Notes
Purpose: To automatically detect and classify mentions of rare diseases in unstructured clinical reports, such as those from primary care [69]. Materials: A corpus of clinical notes (e.g., electronic health records), a list of rare disease terms and synonyms (e.g., from the Orphanet ORDO ontology), and computational NLP tools. Methodology:
- Keyphrase-Based Detection (Semi-Supervised):
- Develop a set of keyphrases and patterns associated with target rare diseases, incorporating official names and known synonyms.
- Apply this keyphrase system to the raw clinical texts to perform an initial detection of disease mentions.
- Expert Validation and Dataset Curation:
- The outputs from the previous step are validated and refined by clinical experts. This step is crucial for building a high-quality, annotated dataset.
- Supervised Model Training:
- Use the expert-validated dataset to train a state-of-the-art supervised model, such as a transformer-based Large Language Model (LLM), for the task of rare disease classification.
- Evaluation:
- Evaluate the final model's performance using standard metrics (e.g., F-Measure) and compare its performance against the initial semi-supervised system [69].
Research Reagent Solutions
Table 3: Essential Tools and Platforms for Data-Scarce Research
| Item Name | Function / Application | Specific Examples / Notes |
|---|---|---|
| Orphanet (ORDO) | International knowledge base providing standardized nomenclature for rare diseases and genes. | Essential for creating keyphrase lists for NLP and for standardizing data [69]. |
| Human Phenotype Ontology (HPO) | A standardized vocabulary of phenotypic abnormalities encountered in human disease. | Used for phenotype-genotype matching in AI diagnostic tools [72]. |
| U-Net/U-Net++ Architectures | Deep learning model architectures particularly effective for image denoising tasks. | U-Net++ has been shown to deliver superior denoising performance on chest X-rays [71]. |
| DistributedDataParallel (DDP) | A PyTorch library for distributed multi-GPU training. | Significantly accelerates model training, reducing time by over 60% [71]. |
| Large Language Models (LLMs) | Can be fine-tuned for tasks such as rare disease concept normalization and classification in clinical text. | Models like Llama 2 can be fine-tuned with domain-specific corpora from HPO [69]. |
| Synthetic Data Generators | Algorithms that create artificial data with statistical properties similar to real data. | Can be used to create "artificial patients" as synthetic controls in studies with limited data [68] [70]. |
Workflow Diagrams
Synthetic Data Pipeline
NLP Clinical Text Analysis
Parameter Tuning and Adaptive Clustering for Heterogeneous Image Regions
FAQs: Core Concepts and Configuration
Q1: What is the primary purpose of using adaptive clustering in medical image denoising?
Adaptive clustering is used to group similar image patches based on underlying features such as textures and edges within heterogeneous medical images. This enables localized denoising operations that are tailored to specific image regions. Unlike global denoising, this approach prevents over-smoothing of fine details in complex areas while effectively suppressing noise in more homogeneous regions, thereby preserving critical anatomical structures for diagnosis [14].
Q2: How can I automatically determine the optimal number of clusters (k) without manual intervention?
You can employ frameworks like SONSC (Separation-Optimized Number of Smart Clusters), which are designed to automatically infer the optimal number of clusters. SONSC iteratively maximizes a novel internal validity metric called the Improved Separation Index (ISI) that jointly evaluates intra-cluster compactness and inter-cluster separability. This parameter-free approach eliminates the need for pre-defining k and is particularly robust for high-dimensional and noisy biomedical data [73].
Q3: Our denoising algorithm is losing subtle textures in MRI scans. How can we better preserve these details?
The loss of subtle textures often indicates an imbalance between noise removal and detail preservation. Consider implementing a two-stage denoising process within each cluster:
- Initial Denoising: Apply hard thresholding in the SVD domain, guided by the Marchenko-Pastur (MP) law, to obtain a low-rank approximation that removes noise-dominated components [14].
- Detail Refinement: Use a non-local means (NLM) algorithm afterward. The NLM computes weighted averages of pixel intensities based on neighborhood similarity, which is highly effective at preserving edges and fine textures that are spatially repeated within the image [14].
Q4: What is a reliable method for estimating the global noise level in a corrupted image for parameter initialization?
You can analyze the statistical distribution of eigenvalues from noisy image patch matrices. By leveraging the Marchenko-Pastur (MP) law from random matrix theory, you can accurately determine the Gaussian noise variance by examining the distribution of eigenvalues in the covariance matrix of these patches. This provides a robust, data-driven estimate of the global noise level, which can then guide subsequent thresholding operations [14].
Troubleshooting Guides
Problem: Over-Smoothing in Homogeneous Image Regions
- Symptoms: Loss of fine texture, blurred tissue boundaries, and an artificially "plastic" appearance in areas like soft tissue or large organ regions.
- Potential Causes:
- Excessively high threshold values in the PCA or SVD domain.
- Too few clusters, causing diverse textures to be grouped together and processed with inappropriate parameters.
- Over-aggressive filtering in the non-local means step.
- Solutions:
- Re-calibrate Thresholds: Revisit the MP law-based thresholding. Ensure the hard thresholding step removes only components definitively identified as noise. A lower, more conservative threshold may be necessary [14].
- Optimize Clustering: Verify that your adaptive clustering algorithm is correctly distinguishing between different tissue types. Increasing the number of clusters might allow for more granular parameter tuning in homogeneous areas [14] [73].
- Adjust NLM Parameters: Tune the filtering parameter
hin the non-local means algorithm. A lowerhvalue will result in less aggressive averaging and better texture preservation [14].
Problem: High Computational Time and Memory Usage
- Symptoms: Experiment runtime is prohibitively long, especially on high-resolution CT or MRI volumes.
- Potential Causes:
- A very high value for
k(number of clusters) in the adaptive clustering stage. - Large patch sizes for the clustering and NLM steps.
- Computationally expensive similarity searches in the NLM algorithm.
- A very high value for
- Solutions:
- Cluster Efficiency: Implement an efficient clustering framework like SONSC, which is designed for scalability. Alternatively, use a Silhouette analysis or the ISI metric to find the smallest sufficient number of clusters that maintains performance [73].
- Explore Lightweight Models: For a less resource-intensive alternative, consider a lightweight, data-free model like Noise2Detail (N2D). This method uses a very small CNN and a self-supervised training scheme, offering a favorable balance between speed and denoising quality [20].
- Patch Size & Search Window: Reduce the patch size and limit the search window for similar patches in the NLM algorithm, as these are primary drivers of computational cost [14].
Problem: Inconsistent Denoising Performance Across Different Modalities
- Symptoms: An algorithm tuned for CT images performs poorly on MRI data, or vice versa.
- Potential Causes:
- Fixed parameters that do not adapt to the different noise statistics or textural properties of each modality.
- Assumption of a single, global noise distribution.
- Solutions:
- Modality-Specific Noise Estimation: Always perform a modality-specific noise level estimation using the MP law or other techniques at the beginning of your pipeline. Do not reuse the same noise variance value across different modalities or scan protocols [14].
- Re-tune Cluster Parameters: The optimal settings for patch size and cluster count may differ between MRI (which often has Rician noise) and CT (which may have Gaussian or Poisson noise). Perform separate validation for each modality [5].
Experimental Protocols and Methodologies
Protocol 1: Benchmarking Denoising Performance
This protocol outlines how to quantitatively compare your adaptive clustering method against established algorithms.
- 1. Dataset Preparation: Use a publicly available dataset of medical images (e.g., a chest X-ray or MRI dataset). Corrupt the clean images with synthetic additive white Gaussian noise (AWGN) at multiple standard deviation levels (e.g., σ = 15, 25, 50) to create a ground-truth benchmark [5].
- 2. Algorithm Comparison: Run the following algorithms on the noisy datasets:
- 3. Quantitative Evaluation: Calculate the following metrics between the denoised images and the clean ground truth:
- Peak Signal-to-Noise Ratio (PSNR): Measures the ratio between the maximum possible power of a signal and the power of corrupting noise [5].
- Structural Similarity Index (SSIM): Assesses the perceived quality by measuring structural similarity [5].
- Mean Squared Error (MSE): Measures the average squared difference between the estimated and actual values [5].
Table 1: Example Benchmark Results (PSNR in dB) on a Synthetic MRI Dataset with Gaussian Noise (σ=25)
| Denoising Algorithm | PSNR | SSIM | Computation Time (s) |
|---|---|---|---|
| Noisy Image | 20.2 | 0.45 | - |
| Proposed Adaptive Clustering [14] | 33.5 | 0.92 | 45.1 |
| BM3D [5] | 32.1 | 0.89 | 12.3 |
| DnCNN (supervised) [5] | 31.8 | 0.90 | 0.5 |
| NLM [5] | 29.4 | 0.83 | 65.8 |
| WNNM [5] | 32.5 | 0.91 | 28.9 |
Protocol 2: Validating Clinical Coherence of Clusters
This protocol ensures that the clusters generated by your algorithm align with clinically relevant features.
- 1. Expert Annotation: Collaborate with a radiologist or clinical expert to manually annotate regions of interest (ROIs) in a set of images. These ROIs should correspond to key anatomical structures or pathologies (e.g., lung nodules, white matter lesions, bone fractures).
- 2. Unsupervised Clustering: Run your adaptive clustering algorithm (e.g., SONSC [73]) on the same set of images without using the expert annotations.
- 3. Quantitative Alignment: Calculate metrics like Normalized Mutual Information (NMI) to measure the agreement between the machine-generated clusters and the expert-defined ROIs. A high NMI score indicates that the algorithm is discovering clinically meaningful structures without supervision [73].
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Computational Tools for Adaptive Clustering Denoising Research
| Item / Tool | Function / Purpose |
|---|---|
| Marchenko-Pastur (MP) Law | A principle from random matrix theory used to estimate global noise levels and guide hard thresholding in the PCA domain by analyzing the eigenvalue distribution of noisy data matrices [14]. |
| Improved Separation Index (ISI) | A novel internal cluster validity metric that jointly optimizes intra-cluster compactness and inter-cluster separation, used to automatically determine the optimal number of clusters without manual tuning [73]. |
| Non-Local Means (NLM) Algorithm | A refinement filter that reduces noise by averaging pixels across the entire image based on the similarity of their surrounding patches, thereby effectively preserving edges and repeated textures [14]. |
| Peak Signal-to-Noise Ratio (PSNR) & Structural Similarity Index (SSIM) | Standard objective image quality metrics used to quantitatively evaluate the performance of denoising algorithms against a known ground truth [5]. |
| Noise2Detail (N2D) | An example of a lightweight, self-supervised denoising model that can serve as a computationally efficient baseline or alternative for specific applications where data and resources are limited [20]. |
Workflow Visualization
The diagram below illustrates the integrated workflow of a denoising framework that combines adaptive clustering with multi-stage filtering, as described in the troubleshooting guides and FAQs.
Integrated Denoising Workflow
Benchmarks and Validation: Ensuring Clinical Reliability and Trust
Troubleshooting Guides and FAQs
Frequently Asked Questions
Q1: My denoising model outputs a high PSNR value (>35 dB), but the resulting image appears blurry and loses critical anatomical details. What could be the cause? A high PSNR indicates low pixel-wise error but does not guarantee the preservation of structural information or perceptual quality. Blurring often occurs when the model over-prioritizes mean squared error (MSE) reduction at the cost of high-frequency details essential for diagnosis [5]. It is recommended to use SSIM in conjunction with PSNR, as SSIM better assesses structural preservation [74]. For a more comprehensive evaluation, consider incorporating perceptual metrics such as the Learned Perceptual Image Patch Similarity (LPIPS) [23].
Q2: I am getting inconsistent SSIM values when evaluating the same model on different medical image modalities (e.g., MRI vs. X-ray). Why does this happen? A common cause is the improper handling of image intensity ranges. The SSIM metric is designed for strictly positive intensity values [75]. Medical image formats, such as Hounsfield Units (HU) in CT scans or z-score normalized images, often contain negative values. Using SSIM on such data introduces a downward bias, making scores non-comparable across modalities [75]. Ensure images are scaled to a positive dynamic range before computation and consistently report the range used.
Q3: What is a "good" PSNR or SSIM value for medical image denoising tasks? Acceptable values are context-dependent and vary by modality, noise level, and anatomical region. As a general reference, on chest X-ray datasets with synthetic noise, advanced deep learning models like U-Net++ can achieve PSNR values around 24.07 dB and SSIM values of 0.85 or higher [23] [76]. For 12-bit medical images, a PSNR value exceeding 60 dB is typically considered high quality [77]. Establishing a baseline with state-of-the-art methods on your specific dataset is crucial for meaningful comparison.
Q4: Should I use 2D or 3D SSIM for evaluating denoising performance on volumetric medical data? For volumetric data like MRI or CT, 3D SSIM is more appropriate. When a 2D SSIM is computed slice-by-slice, it can overestimate the quality by ignoring inter-slice discontinuities that are typical of 2D synthesis methods [75]. A 3D SSIM calculation, which accounts for correlations between adjacent slices, provides a more robust and accurate assessment of the overall image quality.
Troubleshooting Common Problems
Problem: Drastic performance drop when a model trained on natural images is applied to medical images.
- Potential Cause 1: Domain shift. The noise characteristics in medical images (e.g., Rician in MRI, Poisson in CT) are fundamentally different from the additive white Gaussian noise (AWGN) common in natural image benchmarks [5] [25].
- Solution: Fine-tune pre-trained models on medical datasets with realistic noise profiles. Alternatively, employ domain adaptation techniques or use self-supervised methods like Noise2Noise that can learn directly from noisy medical data [20].
Problem: Significant variation in metric scores when using different implementations of PSNR or SSIM.
- Potential Cause: Inconsistent parameter settings. Different libraries may use default parameters for the SSIM window size and Gaussian kernel weights.
- Solution: Standardize the evaluation protocol. Explicitly define and report all parameters, such as the dynamic range (
MAX_I) for PSNR and the window function, data range, and weights for SSIM [77] [74]. Use the same codebase for all comparative evaluations.
Experimental Protocols and Benchmarking Data
Standardized Experimental Methodology
To ensure reproducible and comparable benchmarking, follow this structured protocol:
Dataset Selection and Preparation:
Synthetic Noise Injection:
- To simulate a controlled denoising task, additive Gaussian noise is a common and lightweight obfuscation technique [23].
- For a reference protocol, use a fixed mean (e.g., 0.1) and varying standard deviations (e.g., 0.1, 0.2, 0.3) to generate different noise levels (10%, 20%, 30%) [23]. The noisy images serve as input, and the clean originals are the reconstruction targets.
Model Training and Evaluation:
- Implement standard baseline models like U-Net and U-Net++ due to their proven effectiveness in medical image tasks [23].
- Train models using a loss function that aligns with the evaluation metric, often a combination of L1/L2 loss.
- Run evaluation on the held-out test set. Report both PSNR and SSIM as primary metrics. For a more complete picture, consider including perceptual metrics like LPIPS [23].
Quantitative Benchmarking Table
The following table summarizes the performance of various denoising techniques as reported in recent literature, providing a reference for expected results on standardized tasks.
Table 1: Performance Benchmark of Denoising Algorithms on Medical Images
| Denoising Method | Dataset / Modality | PSNR (dB) | SSIM | Key Findings |
|---|---|---|---|---|
| U-Net++ [23] | NIH ChestX-ray14 (X-ray) | Competitive PSNR (exact value not specified in context) | Superior SSIM (exact value not specified in context) | Consistently delivers superior denoising performance with enhanced structural fidelity [23]. |
| Stacked Convolutional Autoencoder (SCAE) [76] | Heterogeneous Medical Datasets | 24.07 | 0.85 | Provides good denoising results across small, heterogeneous medical datasets [76]. |
| BM3D [5] | MRI & HRCT | Highest at low/moderate noise | Highest at low/moderate noise | Consistently outperforms other algorithms at low and moderate noise levels [5]. |
| Optimal Attention Block-based Pyramid Denoising Network (OABPDN) [19] | CHASEDB1, MRI, Lumbar Spine | ~2-3% improvement over baselines | ~2-3% improvement over baselines | Shows approximate 2-3% improvement in PSNR and SSIM over existing state-of-art models [19]. |
| Gaussian Pyramid (GP) [25] | X-ray, MRI, SIDD | 36.80 | 0.94 | Achieves high PSNR/SSIM with low computational complexity (0.0046s), suitable for real-world applications [25]. |
Workflow and Metric Visualization
Experimental Workflow for Benchmarking
The diagram below outlines a standard workflow for training and evaluating a medical image denoising model, from data preparation to quantitative assessment.
Relationship between Denoising Metrics
This diagram illustrates the relationship between core quantitative metrics and the aspects of image quality they evaluate, highlighting their role in comprehensive benchmarking.
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Tools and Materials for Medical Image Denoising Research
| Item Name | Function / Explanation | Example Use Case |
|---|---|---|
| Standardized Public Datasets | Provides a common benchmark for fair comparison of different algorithms. | NIH ChestX-ray14 [23]: A large-scale dataset of chest X-rays used for training and evaluating denoising models. |
| Deep Learning Architectures | Pre-defined model structures known to perform well on image-to-image tasks. | U-Net & U-Net++ [23]: Encoder-decoder CNNs with skip connections, effective for preserving fine anatomical details in denoising. |
| Synthetic Noise Models | Allows for controlled experimentation by adding known noise to clean images. | Additive Gaussian Noise [23]: A simple model to simulate noise for obfuscation and algorithm testing. |
| Distributed Training Frameworks | Libraries that enable faster training across multiple GPUs, crucial for large models and datasets. | PyTorch DDP with AMP [23]: Reduces training time by over 60% compared to single-GPU setups, accelerating research cycles. |
| Evaluation Metric Libraries | Code packages that provide standardized implementations of PSNR, SSIM, and other metrics. | JuliaImages/ImageDistances, Python libraries [74]: Ensures consistent and accurate calculation of quantitative benchmarks. |
| Self-supervised Training Frameworks | Methods that enable training without clean target data, overcoming data scarcity. | Noise2Noise/Noise2Detail [20]: Learns to denoise from noisy data alone, useful for modalities where clean images are hard to acquire. |
Frequently Asked Questions (FAQs)
1. What are the limitations of traditional metrics like PSNR and SSIM for evaluating denoised medical images? While Peak Signal-to-Noise Ratio (PSNR) and Structural Similarity Index (SSIM) are widely used, they have significant drawbacks for medical imaging. They can be insensitive to specific, clinically relevant distortions and may not correlate well with human perceptual quality, potentially underestimating issues like blurriness that can obscure diagnostic details [78]. Relying solely on them provides an incomplete picture of image quality.
2. What alternative metrics should I use for a more comprehensive evaluation? A robust evaluation strategy uses a combination of metrics:
- Perceptual Quality Metrics: Incorporate no-reference (blind) metrics like NIQE, BRISQUE, and PIQE to assess the naturalness and perceptual quality of images without a clean reference [5]. These are particularly useful for detecting over-smoothing.
- Task-Based Metrics: For image-to-image translation tasks (e.g., synthetic contrast generation), validate your results using metrics from a downstream task, such as segmentation accuracy. This ensures the denoised images are useful for clinical analysis [78].
- Reference-based Metrics: Continue using SSIM and PSNR, but supplement them with other reference-based metrics that may be more sensitive to specific MR artifacts [78].
3. My denoising model performs well on my internal dataset but fails on data from a different hospital. What is wrong? This is a classic generalizability issue. Models can overfit to the specific noise characteristics, scanner protocols, and patient population of their training data. To ensure reliability, you must perform external validation on datasets from multiple, independent institutions that were not used in training [79] [80].
4. What does "clinical validation" entail beyond good metric scores? Technical performance (good metric scores) is only the first step. Clinical validation demonstrates that the use of your denoised images leads to a clinically meaningful impact. This is often assessed through reader studies where radiologists, often in a prospective, randomized controlled trial, diagnose images with and without the AI model's assistance to see if it improves their performance or workflow [79].
5. How can I validate an AI denoising model without compromising patient data privacy? Frameworks like ClinValAI advocate for a "Model to Data" (MTD) paradigm. Instead of sharing sensitive patient data, the AI model is packaged into a Docker container and deployed within the hospital's secure cloud environment. The model is run on the private data behind the firewall, and only the outputs (e.g., the denoised images and metrics) are shared, preserving patient confidentiality and the developer's intellectual property [80].
Troubleshooting Guides
Problem: Denoising algorithm removes noise but also smooths out fine anatomical details, making small lesions harder to detect.
This is a critical problem of over-smoothing where the algorithm fails to preserve the high-frequency details essential for diagnosis.
| Troubleshooting Step | Action and Rationale |
|---|---|
| 1. Evaluate with Perceptual Metrics | Calculate no-reference metrics like NIQE and BRISQUE on the output. A worsening score compared to the noisy input quantitatively confirms the loss of natural image texture and detail [5]. |
| 2. Inspect for Specific Distortions | Systematically check for blurring and texture loss in regions of clinical interest. Use the guide in the table below to identify and quantify the issue [78]. |
| 3. Compare Advanced Algorithms | Benchmark your model against state-of-the-art methods known for detail preservation. The following table summarizes the performance of various algorithms, which can serve as a baseline for your own work [5]. |
| 4. Tune Algorithm Parameters | If using a traditional algorithm like BM3D or a bilateral filter, adjust parameters that control the degree of smoothing versus edge preservation. This often involves reducing the filter strength or kernel size. |
Problem: Inconsistent metric performance; my denoised images have high PSNR but low scores on perceptual metrics like NIQE, or vice-versa.
This discrepancy arises because these metrics capture different aspects of image quality. High PSNR indicates low overall error but does not guarantee that the image looks natural or perceptually high-quality to a human expert [78].
| Troubleshooting Step | Action and Rationale |
|---|---|
| 1. Normalize Image Intensities | Ensure all images (input, output, and reference) are normalized consistently before calculating metrics. Different normalization methods (e.g., min-max, z-score) can drastically affect metric values [78]. |
| 2. Adopt a Multi-Metric Portfolio | Do not rely on a single metric. Establish a portfolio of metrics (e.g., PSNR, SSIM, and at least one perceptual metric like NIQE) and track all of them. A robust model should perform well across this portfolio. |
| 3. Correlate with Radiologist Feedback | Perform a small reader study. If radiologists consistently prefer images that have a certain combination of metric scores, you can use this finding to weight your metrics accordingly for future development. |
Protocol 1: Comprehensive Denoising Algorithm Evaluation This protocol is adapted from a recent review to benchmark denoising algorithms across multiple metrics [5].
- Dataset Curation: Use a dataset of medical images (e.g., MRI or HRCT) with known pathologies. Include data from multiple scanners and institutions if possible.
- Synthetic Noise Addition: For a controlled experiment, add synthetic noise (e.g., Gaussian, Rician) to clean images at varying levels (low, moderate, high) to create standardized noisy inputs.
- Algorithm Application: Apply a suite of denoising algorithms to the noisy images. The suite should include:
- Traditional Methods: BM3D, Non-Local Means (NLM), Bilateral Filter.
- Deep Learning Methods: DnCNN, or other relevant CNN architectures.
- Multi-Metric Assessment: Calculate the following metrics for all outputs against the clean reference images:
- Reference-based: PSNR, SSIM.
- No-reference/Perceptual: NIQE, BRISQUE, PIQE.
- Statistical Analysis: Perform statistical testing to determine if performance differences between algorithms are significant.
Summary of Denoising Algorithm Performance [5] Table: Example quantitative results for denoising algorithms on medical images. Higher values are better for PSNR and SSIM; lower values are better for NIQE, BRISQUE, and PIQE.
| Algorithm | PSNR (dB) | SSIM | NIQE | BRISQUE | PIQE |
|---|---|---|---|---|---|
| BM3D | 38.5 | 0.96 | 3.8 | 25.1 | 24.5 |
| DnCNN | 37.8 | 0.94 | 3.5 | 22.3 | 21.0 |
| NLM | 35.2 | 0.91 | 4.5 | 30.7 | 32.1 |
| Bilateral Filter | 33.1 | 0.89 | 5.1 | 35.2 | 38.9 |
| Noisy Image | 20.0 | 0.45 | 7.2 | 45.0 | 50.0 |
Protocol 2: Clinical Validation Workflow for an AI Denoiser This protocol is based on frameworks for robust clinical validation [79] [80].
- Internal Validation: Train and perform initial technical validation on your internal dataset.
- External Validation: Partner with at least one independent clinical site. Use a "Model-to-Data" framework (e.g., ClinValAI) to deploy your model securely on their data.
- Reader Study Design: Conduct a prospective, randomized study. Radiologists should read cases in two arms: with and without the AI-denoised images.
- Outcome Measurement: Measure clinically relevant outcomes such as diagnostic accuracy (sensitivity, specificity), confidence scores, and reading time.
- Bias and Generalizability Analysis: Stratify results by patient subgroups (e.g., age, sex, disease severity, scanner type) to identify any latent biases.
The Scientist's Toolkit: Research Reagent Solutions
Table: Essential components for developing and validating medical image denoising models.
| Item | Function / Explanation |
|---|---|
| BM3D Algorithm | A high-performance traditional denoising algorithm that serves as a strong baseline for comparison against new methods [5]. |
| DnCNN | A deep learning-based denoising model that learns to remove noise from data. Represents the class of supervised CNN denoisers [5]. |
| Noise2Noise Framework | A self-supervised training framework that enables learning denoising from pairs of noisy images, eliminating the need for clean ground truth data [81] [20]. |
| ClinValAI Framework | An open-source, cloud-agnostic framework designed to establish robust infrastructures for the clinical validation of AI models while preserving data privacy [80]. |
| Structural Similarity (SSIM) Index | A popular reference-based metric for predicting the perceived quality of an image by comparing it to a pristine reference [78]. |
| Natural Image Quality Evaluator (NIQE) | A perceptual, no-reference metric that assesses image quality based on deviations from a statistical model built from natural, high-quality images [5]. |
Workflow Visualization
Medical Image Denoising Validation Workflow
Troubleshooting Over-smoothing
Quantitative Performance Comparison
The table below summarizes the core performance characteristics of BM3D, DnCNN, and DDPM-based models as established by current research.
| Algorithm | Typical PSNR (dB) | Typical SSIM | Key Strengths | Key Limitations |
|---|---|---|---|---|
| BM3D (Traditional) [5] [28] | High (at low-moderate noise) | High (at low-moderate noise) | Excellent detail preservation; Strong performance on Gaussian noise; Well-established [5]. | Performance can drop with high/complex noise; Computationally complex [5]. |
| DnCNN (Deep Learning) [5] | Competitive across various levels | Competitive across various levels | Handles significant noise variations; Preserves critical diagnostic features [5]. | Requires large, high-quality training datasets [28]. |
| DDPM (Generative) [82] | High (e.g., 39.9 PSNR reported) [83] | High | Superior image diversity & fidelity; Less artifacts than GANs; High-quality synthesis [82]. | Very high computational cost; Slow sampling/speed [82] [83]. |
| cDDGAN (Hybrid) [83] | High (e.g., 39.9 PSNR reported) [83] | Information Missing | Speed: ~74x faster than cDDPM; Maintains cDDPM-level accuracy [83]. | Still slower than some pure GANs [83]. |
Frequently Asked Questions & Troubleshooting
Algorithm Selection
Q: Which denoising algorithm should I choose for MRI/HRCT images with moderate Gaussian noise? A: For this scenario, BM3D is a dependable and high-performing choice [5]. It consistently outperforms other algorithms at low and moderate noise levels, achieving the highest PSNR and SSIM values while preserving structural integrity [5]. Deep learning methods like DnCNN also show strong results, but BM3D remains a robust benchmark.
Q: My application requires high-speed inference. Are DDPMs suitable? A: No, standard Denoising Diffusion Probabilarial Models (DDPMs) are not suitable for real-time or rapid processing tasks [82] [83]. Their main drawback is the significant time required for image sampling, running into thousands of seconds [83]. Consider a faster deep learning model like DnCNN or explore hybrid models like cDDGAN, which was designed specifically to reduce sampling time by orders of magnitude while maintaining performance [83].
Performance & Output Issues
Q: After denoising with a deep learning model, the output appears oversmoothed and has lost subtle textures. What might be the cause? A: This is a classic trade-off in denoising. The model may be over-prioritizing noise removal at the expense of feature preservation [5]. To troubleshoot:
- Check your training data: Ensure your training dataset includes high-quality examples where the subtle textures you wish to preserve are clearly defined.
- Adjust the loss function: Incorporate a loss component that penalizes structural distortion, such as the Structural Similarity Index (SSIM) [5].
- Validate subjectively: Quantitative metrics like PSNR are not perfect [84]. Always include a qualitative visual assessment by experts, as their preference may not always align with the highest PSNR value [84].
Q: The synthetic medical images generated by my model lack diversity and show repetitive features. What is happening? A: This issue, known as mode collapse, is a known limitation of Generative Adversarial Networks (GANs) [82]. A study found that GAN-generated fundoscopy images sometimes exhibited two optical discs, an error not seen in real images or those generated by Diffusion Models [82].
- Solution: Consider switching to a Denoising Diffusion Probabilistic Model (DDPM). Research has demonstrated that DDPMs significantly outperform GANs in terms of diversity (Recall) across multiple medical image domains, including fundoscopy, radiographs, and histopathology [82].
Q: My denoising algorithm performs well on test datasets but poorly on my real-world clinical images. Why? A: This is often due to a domain shift. Most classic algorithms and many deep learning models are developed and trained for specific, often simpler, noise models like Additive White Gaussian Noise (AWGN) [25] [85]. Real-world noise is complex, signal-dependent, and non-Gaussian [25].
- Solution: Implement a multi-scale denoising approach like the Gaussian Pyramid (GP), which has shown better adaptability to real-world noise profiles compared to wavelet transforms [25]. Alternatively, ensure your deep learning model is trained or fine-tuned on datasets that accurately reflect the noise characteristics of your specific clinical imaging equipment and protocols.
Experimental Setup
Q: What are the essential metrics for a comprehensive evaluation of a denoising algorithm in a medical context? A: A robust evaluation uses a combination of metrics:
- Pixel-based Fidelity: Peak Signal-to-Noise Ratio (PSNR) and Mean Squared Error (MSE) [5] [85].
- Structural Preservation: Structural Similarity Index (SSIM) and Multiscale SSIM (MS-SSIM) [5] [82].
- Perceptual Quality: Natural Image Quality Evaluator (NIQE), BRISQUE, and PIQE [5].
- Task-specific Performance: For generative tasks, use Fréchet Inception Distance (FID) and Precision/Recall to measure realism and diversity [82]. Ultimately, the most critical validation is qualitative assessment by clinical experts [84].
Experimental Protocols
Protocol for Benchmarking Denoising Algorithms
This protocol provides a standard methodology for comparing the performance of different denoising algorithms on a common dataset [5] [85].
Objective: To quantitatively and qualitatively compare the performance of BM3D, DnCNN, and a DDPM on a set of medical images corrupted with Gaussian noise.
Materials:
- A public dataset of clean medical images (e.g., a subset of the CheXpert dataset for radiographs [82] or a brain MRI dataset).
- High-performance computing hardware with GPUs (essential for training and running deep learning and diffusion models).
Methodology:
- Data Preparation: Split your dataset into training, validation, and test sets. For a fair comparison, all algorithms should be evaluated on the same test set.
- Noise Introduction: To the test set images, add AWGN with varying standard deviations (σ) to simulate low (e.g., σ=25), moderate (e.g., σ=35), and high (σ=50) noise levels [5] [85].
- Algorithm Implementation:
- BM3D: Use a standard implementation with its default parameters.
- DnCNN: Train the network from scratch or use a pre-trained model on your training dataset. The network should be trained to predict the noise residual.
- DDPM: Train the diffusion model on your training dataset, or use a pre-trained model if available. The sampling process should be run for a sufficient number of timesteps (e.g., 1000).
- Evaluation: Run the denoising algorithms on the noisy test set. Calculate PSNR, SSIM, and perceptual quality metrics (NIQE, BRISQUE) for all outputs. Visually inspect the results for qualitative assessment.
Protocol for Training a Deep Learning Denoiser (DnCNN)
Objective: To train a DnCNN model to remove AWGN from medical images.
Materials:
- A large dataset of clean medical images (e.g., the DIV2K or LSDIR datasets used in benchmarks [85]).
- A deep learning framework like PyTorch or TensorFlow.
Methodology:
- Data Preparation: Use clean images as ground truth. Generate training pairs by adding AWGN to these clean images. The noise level can be fixed or varied during training to improve robustness.
- Network Architecture: Implement the DnCNN architecture, which typically consists of convolutional layers with residual learning (predicting the noise rather than the clean image).
- Training Procedure:
- Loss Function: Use Mean Squared Error (MSE) loss between the predicted noise and the actual added noise.
- Optimizer: Use Adam or SGD with momentum.
- Training: Train the network until the validation loss converges.
Diagram 1: DnCNN training uses residual learning to predict and subtract noise.
The Scientist's Toolkit: Research Reagent Solutions
| Item / Resource | Function / Description |
|---|---|
| Public Datasets (DIV2K, LSDIR) [85] | High-resolution, general-image datasets commonly used for training and benchmarking denoising algorithms. |
| Medical Imaging Datasets (CheXpert, AIROGS) [82] | Domain-specific public datasets containing fundoscopy and chest radiograph images for developing and validating medical image denoisers. |
| PSNR / SSIM Metrics [5] [85] | Standard quantitative metrics for evaluating the pixel-level accuracy and structural fidelity of denoised images. |
| FID / Precision-Recall Metrics [82] | Metrics used specifically for evaluating generative models (like DDPMs), measuring the realism and diversity of generated images. |
| Pre-trained Models (e.g., Medfusion) [82] | Publicly available, pre-trained models that can be used for inference or fine-tuned on specific datasets, reducing development time and computational cost. |
| BM3D Implementation [5] [28] | A well-established, non-deep-learning benchmark algorithm that is highly effective for Gaussian denoising and useful for baseline comparisons. |
Troubleshooting Guides
Troubleshooting Guide 1: Addressing Domain Gap in Synthetic Images
Problem: My AI model, trained on synthetic medical images, performs poorly on real clinical data due to the domain gap.
Explanation: The domain gap is the disparity between synthetic and real datasets, encompassing both appearance (e.g., color, texture, lighting) and content (e.g., scene layout) differences. This gap can significantly impact the performance of deep learning models when deployed in real-world scenarios [86].
Solution:
- Quantify the Fidelity: Implement a multi-faceted fidelity assessment. Calculate separate scores for local texture (using Local Binary Patterns - LBP), global texture (using Grey Level Co-occurrence Matrix - GLCM and Haralick metrics), and frequency features (using Discrete Cosine Transform - DCT) [86].
- Fuse the Scores: Use a multi-criteria approach, such as evidence theory, to merge these individual scores into a final global fidelity score. This method also quantifies uncertainty and conflict between the different metrics, providing a more comprehensive assessment [86].
- Iterate and Validate: Use this global score to guide improvements in your image generation process. Continuously validate your AI model's performance on a held-out set of real clinical images.
Troubleshooting Guide 2: Handling Low Signal-to-Noise Ratio (SNR) in Synthetic Images
Problem: The synthetic medical images I've generated have a low Signal-to-Noise Ratio (SNR), which is impairing their diagnostic utility and quantitative analysis.
Explanation: Low SNR can obscure crucial anatomical details and lead to biased measurements, such as inaccurate Ventilation Defect Percentage (VDP) in lung MRI or Apparent Diffusion Coefficient (ADC) values [34]. This is a critical issue in medical imaging where precision is paramount.
Solution:
- Apply Denoising Algorithms: Integrate a post-processing denoising step into your synthetic data pipeline.
- Choose the Right Denoiser:
- For moderate noise levels, use BM3D (Block-Matching and 3D Filtering), which consistently outperforms other algorithms in preserving structural integrity and perceptual quality [5].
- For significant noise variations, consider deep learning-based methods like DnCNN (Deep Convolutional Neural Network) or unsupervised methods like Noise2Void (N2V) which require only single noisy images [5] [34].
- Validate Metrics: After denoising, ensure that key quantitative biomarkers (e.g., VDP, ADC) show minimal bias compared to ground-truth or high-quality real images [34].
Troubleshooting Guide 3: Detecting and Preventing AI-Generated Image Fraud
Problem: I need to ensure the integrity of my research by verifying that synthetic images have not been inappropriately used or generated to misrepresent scientific evidence.
Explanation: Advanced generative models can create highly realistic fake scientific images, which can be used for fabrication, falsification, or plagiarism. These fakes can be difficult to detect by visual inspection alone, potentially threatening academic integrity [87].
Solution:
- Leverage Forensic Detection Tools: Utilize specialized detection frameworks. Spatial-domain analysis methods use CNNs to identify texture irregularities and unnatural edge formations in pixel-level data [88]. Fingerprint-based analysis examines unique, model-specific artifacts left in the generated images [88].
- Implement a Multi-Modal Framework: For greater robustness, employ a hybrid approach that combines:
- Frequency-domain analysis to spot anomalies not visible in the spatial domain.
- Multimodal reasoning-based models that use vision-language models to check for semantic inconsistencies [88].
- Promote Transparency: Maintain detailed records of your image generation process, including the model used and its parameters. Where possible, use synthetic image detectors as part of the peer-review workflow [87].
Frequently Asked Questions (FAQs)
FAQ 1: What are the most relevant metrics for evaluating the fidelity of synthetic medical images beyond simple visual inspection?
While metrics like PSNR and SSIM are common, a robust evaluation for medical images should also include:
- Haralick Texture Metrics: A set of 14 metrics derived from the Grey Level Co-occurrence Matrix (GLCM) to assess statistical texture properties and spatial relationships between pixels [86].
- Local Binary Pattern (LBP): Provides a localized texture analysis, complementing the global view of GLCM [86].
- Noise-to-Signal Ratio (NSR) and Sharpness: Critical for quantifying the clarity and diagnostic quality of the image, directly impacting the measurement of clinical biomarkers [34].
- Task-based Functional Fidelity: The ultimate test is whether the synthetic data leads to the same clinical outcome (e.g., biomarker quantification, segmentation accuracy) as real data [84] [34].
FAQ 2: My deep learning model is overfitting on my synthetic medical image dataset. How can I improve generalization?
Overfitting to synthetic data often indicates a realism gap. Address this by:
- Enhancing Data Diversity: Ensure your synthetic dataset covers the entire Operating Design Domain (ODD), including various anatomical variations, pathological presentations, and imaging artifacts [86].
- Employing Domain Adaptation: Use techniques like Conditional Alignment and Reweighting (CARE) to explicitly reduce the gap between the synthetic (source) and real (target) domains during training [86].
- Incorporating Real Data: Even a small amount of real data, used in conjunction with synthetic data, can significantly improve model generalization and performance on real-world tasks.
FAQ 3: How can I statistically validate that my set of synthetic images is a representative sample of the real-world data distribution?
Statistical rigor is key for validation:
- Move Beyond P-values: Do not rely solely on p-values. Always report effect sizes and confidence intervals to provide a measure of the magnitude and uncertainty of any differences [89].
- Use Multiple Hypothesis Testing Corrections: When comparing multiple image features or metrics, apply corrections (e.g., Bonferroni) to control the family-wise error rate.
- Leverage Reproducibility Frameworks: Ensure your validation is reproducible by thoroughly documenting preprocessing steps, model architectures, and training conditions. Adhere to reporting guidelines like CONSORT-AI or TRIPOD-AI where applicable [89].
Experimental Protocols & Data
Table 1: Comparison of Denoising Algorithm Performance on Medical Images
This table summarizes the performance of various denoising algorithms as evaluated in experimental studies, highlighting their suitability for different scenarios [5] [34].
| Algorithm | Core Methodology | Best Use Case | Key Strength | Key Limitation |
|---|---|---|---|---|
| BM3D | Transform-domain processing & collaborative filtering [5] | Moderate noise levels [5] | High PSNR/SSIM; preserves structural & perceptual quality [5] | Less effective on very high noise; can be computationally complex [5] |
| DnCNN | Deep Convolutional Neural Network [5] | Significant noise variations [5] | Handles strong noise without compromising critical features [5] | Requires paired training data (supervised) [5] |
| Noise2Noise (N2N) | Deep Learning with multiple noisy image realizations [34] | When clean targets are unavailable [34] | Reduces need for clean ground-truth data [34] | Requires multiple noisy acquisitions of the same scene [34] |
| Noise2Void (N2V) | Unsupervised Deep Learning [34] | Single, noisy images [34] | Trains on single noisy images; no repeated scans needed [34] | Performance may be lower than supervised methods [34] |
Table 2: Fidelity Evaluation Scores for Synthetic Images Under Different Conditions
This table outlines the core components of a multi-criteria fidelity assessment framework for synthetic images, as proposed in recent research [86].
| Fidelity Score | Method / Feature Used | What It Measures | Application in Adverse Conditions |
|---|---|---|---|
| Local Texture Score | Local Binary Pattern (LBP) [86] | Localized texture patterns and micro-structures | Evaluates preservation of fine details in rain/fog |
| Global Texture Score | Grey Level Co-occurrence Matrix (GLCM) & Haralick Metrics [86] | Global image structural properties and spatial relationships between pixels | Assesses overall structural integrity in poor visibility |
| Frequency Score | Discrete Cosine Transform (DCT) [86] | High-frequency information and patterns | Analyzes retention of edge information and sharpness |
| Final Global Score | Evidence Theory-based Fusion [86] | Unified fidelity score with uncertainty quantification | Provides a robust overall assessment across all conditions |
Experimental Protocol 1: Multi-Feature Fidelity Assessment
Objective: To quantitatively evaluate the fidelity of a set of synthetic medical images by analyzing multiple feature domains and producing a unified score [86].
Methodology:
- Dataset Curation: Gather paired real and synthetic image datasets covering the target medical domain (e.g., brain MRI, chest CT) and various conditions (e.g., clear, noisy).
- Feature Extraction:
- Local Texture: Compute the Local Binary Pattern (LBP) for each image to capture local texture statistics.
- Global Texture: Calculate the Grey Level Co-occurrence Matrix (GLCM) and derive a subset of the 14 Haralick metrics (e.g., contrast, correlation, energy, homogeneity).
- Frequency Analysis: Apply the Discrete Cosine Transform (DCT) to analyze the distribution of frequency components.
- Score Calculation: Use a pre-trained Convolutional Neural Network (CNN) or a statistical distance measure (e.g., Frechet Distance) to compute a fidelity score for each feature type by comparing the distributions of real vs. synthetic features.
- Score Fusion: Fuse the individual scores using a multi-criteria method based on Dempster-Shafer evidence theory. This generates a final global fidelity score along with measures of uncertainty and conflict.
<100chars> Workflow for Multi-Feature Fidelity Assessment
Experimental Protocol 2: Validation of Denoising Techniques for Low-SNR Synthetic Images
Objective: To compare the performance of supervised and unsupervised denoising algorithms on low-SNR synthetic medical images and evaluate their impact on clinically relevant quantitative metrics [34].
Methodology:
- Data Preparation: Use a dataset of synthetic medical images (e.g., 129Xe MRI) where a ground-truth or high-SNR reference is available. Artificially add noise to create a test set if necessary.
- Algorithm Application: Apply a suite of denoising algorithms to the low-SNR images. This should include:
- A traditional benchmark (e.g., BM3D).
- Supervised DL methods (e.g., DnCNN, Noise2Noise if paired data exists).
- Unsupervised DL methods (e.g., Noise2Void).
- Quantitative Evaluation: Calculate standard image quality metrics:
- Clinical Metric Validation: For denoised images, compute key clinical biomarkers (e.g., Ventilation Defect Percentage (VDP), Apparent Diffusion Coefficient (ADC)) and compare them to values derived from the high-SNR reference to assess bias [34].
<100chars> Workflow for Denoising Algorithm Validation
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Tools for Synthetic Medical Image Analysis
| Tool / Reagent | Function | Application Example |
|---|---|---|
| Grey Level Co-occurrence Matrix (GLCM) | Quantifies statistical texture by analyzing the spatial relationship of pixel intensities [86]. | Measuring the global structural fidelity of a synthetic CT scan compared to a real one. |
| Haralick Metrics | A set of 14 statistical features (e.g., Contrast, Correlation, Energy) derived from the GLCM to describe texture [86]. | Providing quantitative scores for different aspects of synthetic image texture in a fidelity assessment framework [86]. |
| Local Binary Pattern (LBP) | A visual descriptor for classifying textures based on the local neighborhood of each pixel [86]. | Analyzing fine-grained, local texture patterns in synthetic skin lesion images. |
| Discrete Cosine Transform (DCT) | Converts image data from the spatial domain into frequency components [86]. | Evaluating how well high-frequency details (like edges) are preserved in a synthetic MRI. |
| Evidence Theory (Dempster-Shafer) | A framework for reasoning under uncertainty and combining evidence from multiple, potentially conflicting, sources [86]. | Merging local, global, and frequency fidelity scores into a single, robust global score with confidence measures [86]. |
| BM3D Denoising Algorithm | A state-of-the-art image denoising algorithm that uses collaborative filtering in 3D transform groups [5]. | Improving the SNR of a noisy synthetic ultrasound image as a post-processing step. |
| Noise2Void (N2V) | An unsupervised deep learning denoiser that can be trained using only single noisy images [34]. | Denoising synthetic medical images when clean reference targets are unavailable for training. |
The NTIRE 2025 challenges have established new state-of-the-art benchmarks in fundamental image processing tasks, with profound implications for medical image analysis. This technical support center translates the winning methodologies from these competitive benchmarks into practical, actionable guidance for researchers and scientists developing data denoising techniques for medical images. The core insight from NTIRE 2025 is that advanced architectures incorporating attention mechanisms and multi-scale feature extraction are consistently pushing performance boundaries, which can directly enhance diagnostic accuracy and the reliability of downstream analysis in drug development pipelines [85] [19].
Troubleshooting Guide: Common Experimental Challenges in Image Denoising
1. Problem: Model Fails to Generalize to Clinical Image Data
- Question: "I trained a denoising model with a high PSNR on a standard dataset, but performance drops significantly on my clinical MRI/CT scans. What is the issue?"
- Diagnosis: This is typically a domain shift problem. The noise distribution or image characteristics in your clinical data differ from the model's training data.
- Solution:
- Adaptation Training: Follow the approach used by top NTIRE teams: fine-tune your pre-trained model on a small, representative sample of your clinical data. This allows the model to adapt its parameters to the new noise distribution.
- Data Synthesis: If real noisy-clean clinical pairs are unavailable, synthesize training data by adding noise to your clean medical images. The NTIRE 2025 Denoising Challenge used Additive White Gaussian Noise (AWGN) with σ=50 as a standard benchmark [85]. For medical imaging, you may need to experiment with Poisson or Speckle noise models to better match the physics of your imaging modality [19].
2. Problem: Denoised Images Appear Over-Smoothed and Lack Textural Detail
- Question: "My model achieves a good PSNR, but the output images look blurry and have lost fine, clinically important textures."
- Diagnosis: The loss function is overly weighted towards pixel-wise accuracy (PSNR), which can penalize sharp, high-frequency details that are critical for diagnosis.
- Solution:
- Hybrid Loss Functions: Incorporate perceptual loss functions, as seen in the NTIRE 2025 Super-Resolution challenge's "Perceptual Track," which used a blend of LPIPS, DISTS, and NIQA to better align with human visual perception and preserve realism [90] [91].
- Architectural Enhancements: Integrate an Optimal Attention Block (OAB). As demonstrated in medical image denoising research, an OAB helps the network intelligently focus on preserving critical structural features while suppressing noise, preventing important details from being washed out [19].
3. Problem: Training is Unstable or Model Convergence is Poor
- Question: "The training loss fluctuates wildly and the model doesn't seem to converge to a good solution."
- Diagnosis: This can be caused by an unstable optimization process, often related to the choice of optimizer, learning rate, or complex model architecture.
- Solution:
- Advanced Optimizers: Move beyond basic optimizers. Recent methods, including those using Cuckoo Search Optimization (CSO) for parameter tuning, have shown more robust convergence in complex denoising tasks by helping to escape local minima [19].
- Pyramidal Processing: Employ a multi-scale pyramidal network architecture. This design, used by the winning solutions, processes images at multiple scales, which stabilizes training by allowing the network to learn both coarse and fine-grained features progressively [85] [19].
Performance Benchmarks: Quantitative Results from NTIRE 2025
The following tables summarize the top-performing methods from the NTIRE 2025 challenges, providing a benchmark against which medical imaging solutions can be measured.
Table 1: Top Teams from NTIRE 2025 Image Denoising Challenge (σ=50) This challenge focused on restoring images corrupted by Additive White Gaussian Noise, a common benchmark for fundamental denoising capability [85].
| Team Name | Rank | PSNR (dB) | SSIM |
|---|---|---|---|
| SRC-B | 1 | 31.20 | 0.8884 |
| SNUCV | 2 | 29.95 | 0.8676 |
| BuptMM | 3 | 29.89 | 0.8664 |
| HMiDenoise | 4 | 29.84 | 0.8653 |
| Pixel Purifiers | 5 | 29.83 | 0.8652 |
Table 2: Key Metrics for Medical Image Denoising Evaluation Beyond standard benchmarks, these metrics are critical for evaluating performance in a medical context [19].
| Metric | Description | Importance in Medical Imaging |
|---|---|---|
| PSNR (Peak Signal-to-Noise Ratio) | Measures pixel-wise fidelity and reconstruction accuracy. | A high value indicates good general noise removal, but can be misleading if textures are lost. |
| SSIM (Structural Similarity Index) | Measures the perceived change in structural information. | Crucial for ensuring that anatomical structures are preserved after denoising. |
| LPIPS (Learned Perceptual Image Patch Similarity) | Measures perceptual similarity using a deep neural network. | Correlates well with radiologists' assessment of image quality and diagnostic utility. |
Experimental Protocols: Detailed Methodologies
1. Standardized Benchmarking Protocol (Based on NTIRE 2025 Denoising Challenge) This protocol provides a fair and reproducible framework for comparing denoising algorithms [85] [92].
- 1. Dataset Curation:
- Training Data: Use the DIV2K (800 images) and LSDIR (84,991 images) datasets for model development.
- Validation & Test Data: Use the separate 100-image validation and 100-image test splits from the DIV2K dataset, plus the 1000-image test split from LSDIR.
- 2. Noise Simulation:
- For each clean image
I_cleanin the dataset, generate a noisy counterpartI_noisyby adding synthetic AWGN:I_noisy = I_clean + N, whereN ~ Gaussian(0, σ)and the noise level is set to σ = 50.
- For each clean image
- 3. Model Training & Evaluation:
- Train the model to predict
I_cleanfromI_noisy. - Use PSNR and SSIM as the primary evaluation metrics on the hidden test set.
- The final score is the average PSNR/SSIM across all test images (200 in total).
- Train the model to predict
2. Medical Image Denoising with an Optimal Attention Block (OAB) This protocol is adapted from a state-of-the-art medical denoising study and can be integrated into a thesis methodology [19].
- 1. Network Architecture (OABPDN):
- Optimal Pre-processing Block (OPB): An initial block to prepare input features.
- Multi-scale Pyramidal Network with OAB: The core denoising unit. The pyramid captures features at multiple scales. The OAB uses an optimization algorithm (e.g., Cuckoo Search) to estimate optimal weights for blending channel-wise features, directing attention to the most relevant information for noise removal.
- Pyramidal Feature Selection Block (PFSB): A block that fuses the multi-scale features from the pyramid to produce the final denoised output.
- 2. Experimental Setup:
- Platform: Google Colab with GPU acceleration.
- Training: 100 epochs with an input image size of 256x256 pixels.
- Datasets: CHASEDB1 (retinal images), MRI, and Lumbar Spine datasets.
- Noise Types: Gaussian, Speckle, and Poisson noise should be evaluated to simulate different medical imaging modalities.
The workflow for this advanced denoising network can be visualized as follows:
Table 3: Key Resources for Advanced Image Denoising Research
| Resource / Solution | Type | Function in Research | Example/Note |
|---|---|---|---|
| DIV2K & LSDIR Datasets | Dataset | High-resolution benchmark datasets for training and evaluation. | Provided as standard in NTIRE challenges [85]. |
| Peak Signal-to-Noise Ratio (PSNR) | Metric | Quantifies pixel-level reconstruction accuracy. | Primary metric for the NTIRE Denoising restoration track [85]. |
| Structural Similarity Index (SSIM) | Metric | Assesses perceptual image quality and structural preservation. | Critical for medical imaging fidelity [85] [19]. |
| Optimal Attention Block (OAB) | Algorithm | Dynamically highlights important features and suppresses noise. | Can improve PSNR/SSIM by 2-3% in medical images [19]. |
| Cuckoo Search Optimization (CSO) | Algorithm | A metaheuristic algorithm for optimizing complex parameters. | Used to find optimal coefficients in attention blocks [19]. |
| Pyramidal Network Architecture | Model Architecture | Captures image features and context at multiple scales. | Enables robust denoising of both fine and coarse structures [85] [19]. |
| LPIPS / DISTS / NIQA | Metric Suite | Evaluate perceptual quality and visual realism. | Used in the NTIRE Super-Resolution perceptual track [90] [91]. |
Frequently Asked Questions (FAQs)
Q1: For a medical imaging thesis, should I prioritize PSNR or perceptual quality metrics? A1: The choice depends on your research goal. For tasks requiring quantitative measurement from images (e.g., tumor volume), a high PSNR is crucial for pixel-level accuracy. For diagnostic tasks where a radiologist's interpretation is key, perceptual metrics (SSIM, LPIPS) and qualitative evaluation are equally, if not more, important, as they better correlate with human perception. The dual-track design of NTIRE 2025 (Restoration vs. Perceptual) underscores this distinction [90] [91].
Q2: How can I validate that my denoising model does not remove clinically significant information? A2: Beyond quantitative metrics, a task-based evaluation is essential. This involves:
- Expert Review: Have clinical experts (e.g., radiologists) perform a blinded assessment of denoised versus original images.
- Downstream Analysis: Use the denoised images as input for a downstream task (e.g., a segmentation or classification algorithm for a specific pathology) and measure if performance improves or is maintained.
Q3: The top NTIRE models are large and complex. How can I adapt them for resource-constrained clinical environments? A3: This is a key translational challenge. Consider the following strategies:
- Model Distillation: Train a smaller, more efficient "student" model to mimic the performance of a large, winning "teacher" model.
- Pruning: Remove redundant neurons or filters from a large pre-trained model to reduce its size with minimal performance loss.
- Focus on Efficiency: While the main NTIRE 2025 Denoising Challenge had no complexity constraints, other NTIRE challenges (e.g., "Efficient Super-Resolution") are dedicated to this specific problem, and their methodologies can be highly informative [93].
Troubleshooting Guide: Common Denoising Challenges and Solutions
This guide addresses frequent challenges researchers encounter when applying denoising techniques to medical images, with a focus on preserving diagnostically critical information.
1. Problem: Over-smoothing and Loss of Fine Textures
- Challenge: Aggressive noise removal erases subtle textures, such as those in lung parenchyma on HRCT or early-stage tumor regions, which are essential for diagnosis [5].
- Solution: Implement a hybrid denoising approach. Start with an algorithm like BM3D, which is known for high performance at moderate noise levels, as it preserves structural integrity better than many conventional filters [5]. For higher noise levels, consider deep learning-based methods like DnCNN, which are trained to handle significant noise variations while preserving critical features [5].
2. Problem: Blurred Edges and Lesion Boundaries
- Challenge: Denoising algorithms fail to maintain sharp boundaries around lesions or organ margins, complicating accurate segmentation and size measurements [5].
- Solution: Utilize algorithms that incorporate edge-preserving properties. The Non-Local Means (NLM) filter or a Bilateral filter are suitable options, as they smooth homogeneous regions while respecting strong edges by giving lower weights to pixels that differ significantly in intensity [5].
3. Problem: Inconsistent Performance Across Different Noise Levels
- Challenge: An algorithm performs well on one dataset but fails on another with a different noise variance, leading to unreliable results [5].
- Solution: Employ an adaptive algorithm that can adjust its parameters based on local or global noise estimation. The hybrid algorithm combining Adaptive Median Filter (AMF) and Modified Decision-Based Median Filter (MDBMF) dynamically adjusts to noise density, effectively reducing high-density salt-and-pepper noise without affecting intact regions [18].
4. Problem: Suboptimal Tissue or Cell Segmentation After Denoising
- Challenge: The output of the denoising step leads to errors in downstream tasks like tissue or cell segmentation, manifesting as incomplete coverage or inclusion of non-target regions [94].
- Solution: If automatic segmentation is sub-optimal, use interactive editing tools in platforms like StereoMap for local refinements. For large-scale errors, leverage third-party tools like Cellpose, DeepCell, or QuPath to generate new, corrected masks based on the denoised images and import them into your analysis pipeline [94].
5. Problem: Algorithm Introduces Artifacts or Unnatural Textures
- Challenge: The denoising process introduces new, unnatural patterns or artifacts that were not present in the original noisy image, potentially leading to misinterpretation [5].
- Solution: Evaluate the denoised image using perceptual quality metrics like Natural Image Quality Evaluator (NIQE), Blind/Referenceless Image Spatial Quality Evaluator (BRISQUE), and Perception-based Image Quality Evaluator (PIQE) in addition to standard metrics like PSNR and SSIM. A rise in these metric scores often correlates with more natural-looking results and can help identify artifact-introducing methods [5].
Frequently Asked Questions (FAQs)
Q1: What is the most important trade-off in medical image denoising? The primary trade-off is between noise reduction and the preservation of critical diagnostic features. Over-smoothing an image to remove noise can erase subtle textures and blur edges of small lesions, while under-smoothing leaves noise that can obscure crucial information. The key is to find a balance that suppresses noise without compromising the fine structural details essential for identifying pathologies [5].
Q2: Which denoising algorithm should I choose for my medical imaging data? There is no single best algorithm for all scenarios. The choice depends on your specific data and goal [5]. The table below summarizes the performance of various algorithms based on a recent comparative study.
- For moderate noise levels: BM3D is a dependable choice, offering high PSNR and SSIM while preserving structural integrity [5].
- For high noise levels or when handling complex noise patterns: Deep learning-based methods like DnCNN are often better suited [5].
- For impulse (salt-and-pepper) noise: A hybrid approach using Adaptive Median Filter (AMF) and Modified Decision-Based Median Filter (MDBMF) has shown superior performance [18].
Q3: How can I quantitatively evaluate if my denoising method preserves edges and structures? While Peak Signal-to-Noise Ratio (PSNR) is common, it does not always correlate well with perceived image quality. A more robust metric is the Structural Similarity Index (SSIM), which measures the perceptual difference between two images. A higher SSIM value indicates better preservation of structural information, including edges and textures [18] [5]. The Figure of Merit (FOM) metric is also specifically designed to evaluate edge preservation [18].
Q4: What are some common pitfalls in developing and testing denoising algorithms for medical use? A major pitfall is dataset bias, where an algorithm is trained and tested on data that does not represent the full clinical population or range of imaging devices. This can lead to models that perform well in benchmarks but fail in real-world scenarios. To mitigate this, use datasets from multiple sources and critically evaluate them for hidden subgroups or labeling errors [95]. Another pitfall is focusing only on benchmark performance, where minor algorithmic improvements can be smaller than the inherent evaluation noise [95].
Q5: Can I use the same denoising approach for MRI and CT images? Not always. Different imaging modalities are characterized by different noise distributions (e.g., Rician noise in MRI vs. Poisson noise in CT). While some advanced algorithms like DnCNN can be trained to handle various noise types, it is crucial to select or train a method that is appropriate for the specific noise characteristics of your modality to achieve optimal results [5].
Experimental Data and Performance Comparison
Table 1: Quantitative Performance of Denoising Algorithms on Medical Images
This table summarizes the performance of various algorithms as reported in experimental analyses, providing a comparison based on key metrics [18] [5].
| Algorithm | Best For | PSNR (dB) | SSIM | Key Strengths | Key Limitations |
|---|---|---|---|---|---|
| BM3D | Moderate Gaussian noise | High (Consistently top) | High (Consistently top) | Preserves structural integrity and perceptual quality. | Performance may drop at very high noise levels. |
| Hybrid AMF-MDBMF | High-density salt-and-pepper noise | Up to 2.34 dB improvement over others | Improvement up to 0.07 | Dynamically adjusts to noise; preserves edges effectively. | Primarily focused on impulse noise. |
| DnCNN | High noise variations, various noise types | Competitive at high noise levels | Competitive at high noise levels | Handles significant noise without compromising features. | Requires training data; computational complexity. |
| EPLL | Homogeneous areas, fine texture | Competitive | Competitive | Preserves fine texture. | Computationally complex. |
| WNNM | Homogeneous areas | Competitive | Competitive | Effective in homogeneous regions. | Computationally complex. |
A list of key platforms, tools, and frameworks used in modern medical image analysis and denoising research [94] [96].
| Tool Name | Type/Category | Primary Function in Research |
|---|---|---|
| SAW & StereoMap | Analysis Platform | Central platform for spatial transcriptomics analysis; allows manual correction of image registration and segmentation [94]. |
| Cellpose / DeepCell | Segmentation Tool | Deep learning-based software for generating accurate cell segmentation masks, which can be imported into analysis pipelines [94]. |
| QuPath | Segmentation Tool | Open-source software for bioimage analysis, used for both classic thresholding-based and deep learning-based segmentation [94]. |
| TensorFlow / PyTorch | Deep Learning Framework | Foundational frameworks for building and training custom deep learning models, including denoising CNNs [96]. |
| OpenCV | Computer Vision Library | Provides a vast collection of functions for image processing, including traditional denoising filters and preprocessing tasks [96]. |
| Aidoc / RapidAI | Clinical AI Software | FDA-cleared platforms that demonstrate the clinical application of AI for analyzing medical images and triaging critical findings [96]. |
Experimental Protocol: Comparing Denoising Algorithms
Objective: To systematically evaluate and compare the performance of different denoising algorithms on medical images in terms of noise reduction and feature preservation.
Methodology:
- Dataset Preparation: Use a benchmark dataset of medical images (e.g., chest CT, brain MRI). A "ground truth" clean image is ideal. To simulate real conditions, synthetically add known types and levels of noise (e.g., Gaussian, Rician, salt-and-pepper) to the clean images [5].
- Algorithm Selection: Choose a set of algorithms representing different approaches (e.g., BM3D, DnCNN, NLM, a hybrid AMF-MDBMF, and a simple Gaussian filter for baseline comparison) [18] [5].
- Parameter Optimization: For each algorithm and noise level, perform a parameter sweep to find the optimal settings that maximize PSNR and SSIM.
- Execution: Apply each optimized algorithm to the noisy test images.
- Quantitative Evaluation: Calculate performance metrics for all outputs against the ground truth. Key metrics include [18] [5]:
- Peak Signal-to-Noise Ratio (PSIR): Measures the ratio between the maximum possible power of a signal and the power of corrupting noise.
- Structural Similarity Index (SSIM): Assesses the perceptual impact of denoising on structural information.
- Figure of Merit (FOM): Specifically evaluates the preservation of edges.
- Qualitative Evaluation: Conduct a visual assessment by radiologists or experienced researchers to rank the results based on the clarity of critical features and the absence of artifacts.
Diagram: Experimental Workflow for Denoising Evaluation
Decision Framework for Selecting a Denoising Algorithm
The following flowchart provides a logical pathway for researchers to select an appropriate denoising strategy based on their specific data characteristics and goals.
Diagram: Denoising Algorithm Selection Guide
Conclusion
The field of medical image denoising is advancing beyond simple noise removal toward intelligent, detail-aware restoration. The synthesis of current research indicates that while traditional algorithms like BM3D remain robust for moderate noise levels, deep learning and generative models offer superior handling of complex, real-world noise. The critical takeaway is that no single algorithm is universally superior; the choice depends on a careful balance of noise level, imaging modality, required detail preservation, and computational constraints. Future directions point toward more lightweight, self-supervised models that operate without clean training data, the rigorous statistical validation of synthetic images to overcome data scarcity, and the development of standardized, clinically-relevant benchmarking frameworks. For biomedical research, these advancements promise enhanced reliability of image-based biomarkers, improved power for clinical trials, and ultimately, more precise diagnostic tools that can be trusted in life-or-death decision-making.
References
- 1. Model based noise correction enhances the accuracy of ... [https://www.nature.com/articles/s41598-025-24482-x]
- 2. in structural MRI Noise reduction methods imaging [https://www.news-medical.net/whitepaper/20250114/Improving-noise-reduction-methods-in-structural-MRI-imaging.aspx]
- 3. A lightweight and noise-resistant student model for point-of ... [https://www.sciencedirect.com/science/article/abs/pii/S0957417425007675]
- 4. Exploring the Impact of Noise and Image Quality on Deep ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11240833/]
- 5. A Review and Experimental Analysis of Denoising ... [https://openneuroimagingjournal.com/VOLUME/18/ELOCATOR/e18744400404813/FULLTEXT/]
- 6. learning from noise and context for medical image denoising [https://arxiv.org/html/2507.19035v1]
- 7. The Rician Distribution of Noisy MRI Data - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC2254141/]
- 8. Spatially variable Rician noise in magnetic resonance ... [https://www.sciencedirect.com/science/article/abs/pii/S1361841511001721]
- 9. Brain MR image denoising for Rician noise using pre-smooth ... [https://biomedical-engineering-online.biomedcentral.com/articles/10.1186/1475-925X-14-2]
- 10. Statistical and heuristic image noise extraction (SHINE) [https://pubmed.ncbi.nlm.nih.gov/12539975/]
- 11. Gaussian Noise and Smarter Medical AI [https://www.cloudfactory.com/blog/gaussian-noise-medical-ai]
- 12. The effect of Gaussian noise on pneumonia detection ... [https://www.sciencedirect.com/science/article/pii/S1078817422001444]
- 13. Denoising method for X-ray images with poisson-Gaussian ... [https://www.sciencedirect.com/science/article/pii/S1687850724002589]
- 14. Detail-preserving denoising of CT and MRI images via ... [https://www.nature.com/articles/s41598-025-08034-x]
- 15. Recent developments in denoising medical images using ... [https://www.sciencedirect.com/science/article/abs/pii/S0968432824000325]
- 16. Energy-Efficient Machine Learning Based Denoising ... [https://pubmed.ncbi.nlm.nih.gov/41052129/?utm_source=FeedFetcher&utm_medium=rss&utm_campaign=None&utm_content=14mzXgUgXxOhz72eR8oGB-fhcdG9zbPCC1041iU1Zt22GVtQAD&fc=None&ff=20251024010210&v=2.18.0.post22+67771e2]
- 17. CT image denoising methods for image quality improvement ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10860577/]
- 18. A new hybrid image denoising algorithm using adaptive ... [https://www.nature.com/articles/s41598-025-92283-3]
- 19. Medical image denoising using optimal attention block ... [https://www.sciencedirect.com/science/article/abs/pii/S1746809425003052]
- 20. Lightweight Data-Free Denoising for Detail-Preserving ... [https://papers.miccai.org/miccai-2025/0500-Paper3959.html]
- 21. A Distribution-Based Compressed Denoising Scheme ... [https://pubmed.ncbi.nlm.nih.gov/40968426/]
- 22. Evaluating Image Quality Metrics for Medical ... [https://arxiv.org/html/2505.07175v1]
- 23. Distributed Deep Learning for Medical Image Denoising ... [https://arxiv.org/html/2511.06006v1]
- 24. A new hybrid image denoising algorithm using adaptive ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11910666/]
- 25. Efficient real-world image denoising using multi-scale ... [https://www.nature.com/articles/s41598-025-23942-8]
- 26. Efficient real-world image denoising using multi-scale ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12623492/]
- 27. Overview of Research on Digital Image Denoising Methods [https://pmc.ncbi.nlm.nih.gov/articles/PMC12031399/]
- 28. A Survey on MRI and HRCT Image Denoising Methods [https://biomedpharmajournal.org/vol18no3/from-spatial-domain-to-learning-based-methods-a-survey-on-mri-and-hrct-image-denoising-methods/]
- 29. Comparative study of Wavelet transform and Fourier ... [https://arxiv.org/html/2509.26608v1]
- 30. Noise reduction in brain magnetic resonance imaging using ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11757293/]
- 31. A Review and Experimental Analysis of Denoising ... [https://openneuroimagingjournal.com/VOLUME/18/ELOCATOR/e18744400404813]
- 32. BM3D optical image denoising algorithm based on SVD ... [https://www.sciencedirect.com/science/article/abs/pii/S0030402625001378]
- 33. an image denoising method using layer wise medical ... [https://arxiv.org/html/2503.08094v1]
- 34. Comparative Evaluation of Supervised and Unsupervised ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12370284/]
- 35. Block-matching and 3D filtering-based denoising of ... [https://www.sciencedirect.com/science/article/pii/S0003682X23006412]
- 36. A novel denoising method for CT images based on U-net ... [https://www.sciencedirect.com/science/article/abs/pii/S0010482522010952]
- 37. An effective image despeckling and reconstruction ... [https://www.nature.com/articles/s41598-025-10220-w]
- 38. MRI denoising with a non‐blind deep complex‐valued ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11605166/]
- 39. Research on Seismic Signal Denoising Model Based ... [https://www.mdpi.com/2076-3417/15/4/2083]
- 40. Revisiting model scaling with a U-net benchmark for 3D ... [https://www.nature.com/articles/s41598-025-15617-1]
- 41. Denoising diffusion probabilistic models for 3D medical ... [https://www.nature.com/articles/s41598-023-34341-2]
- 42. shaoyanpan/2D-Medical-Denoising-Diffusion-Probabilistic- ... [https://github.com/shaoyanpan/2D-Medical-Denoising-Diffusion-Probabilistic-Model-]
- 43. Denoising Diffusion Probabilistic Models (DDPM) [https://medium.com/@mathparracho/denoising-diffusion-probabilistic-models-ddpm-generative-intuition-practice-ef6b10d232a2]
- 44. WACV Open Access Repository [https://openaccess.thecvf.com/content/WACV2025/html/Bandara_DDPM-CD_Denoising_Diffusion_Probabilistic_Models_as_Feature_Extractors_for_Remote_WACV_2025_paper.html]
- 45. Lightweight self supervised learning framework for domain ... [https://www.nature.com/articles/s41598-025-20411-0]
- 46. Self-supervised learning for medical image classification [https://www.nature.com/articles/s41746-023-00811-0]
- 47. A lightweight self-supervised multi-task framework for IoMT ... [https://www.sciencedirect.com/science/article/abs/pii/S2542660525002239]
- 48. Denoising Diffusion Probabilistic Model to Simulate ... [https://www.sciencedirect.com/science/article/abs/pii/S1076633225001278]
- 49. Project-MONAI/tutorials [https://github.com/Project-MONAI/tutorials]
- 50. A Hybrid Fully Convolutional CNN-Transformer Model for ... [https://arxiv.org/html/2504.08481v1]
- 51. The Transformer Architecture with Hybrid Models [https://medium.com/@bijit211987/the-transformer-architecture-with-hybrid-models-eca885e12056]
- 52. Systematic Review of Hybrid Vision Transformer Architectures ... [https://pubmed.ncbi.nlm.nih.gov/39871042/]
- 53. Assessment of CNNs, transformers, and hybrid ... [https://www.sciencedirect.com/science/article/pii/S0300571225001137]
- 54. Medical image analysis using deep learning algorithms - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC10662291/]
- 55. PyTorch vs TensorFlow for Image Classification | by Ненавин [https://medium.com/@natsunoyuki/pytorch-vs-tensorflow-for-image-classification-ce11f19d877b]
- 56. Performance comparison of medical image classification ... [https://arxiv.org/abs/2507.14587]
- 57. Lightweight Data-Free Denoising for Detail-Preserving ... [https://arxiv.org/html/2510.15611v1]
- 58. A Review of Denoising Medical Images Using Machine ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6225344/]
- 59. Ten quick tips for computational analysis of medical images [https://pmc.ncbi.nlm.nih.gov/articles/PMC9815662/]
- 60. TR&D 2 Projects < Yale Biomedical Imaging Institute [https://medicine.yale.edu/biomedical-imaging-institute/training/cmitt/research-projects/tr-d-2/]
- 61. A hybrid frequency-spatial domain unsupervised denoising ... [https://www.sciencedirect.com/science/article/abs/pii/S0010482525007255]
- 62. Iterative Learning for Joint Image Denoising and Motion ... [https://www.sciencedirect.com/science/article/pii/S1361841525004189?dgcid=rss_sd_all]
- 63. Denoising very low-field magnetic resonance images using ... [https://www.frontiersin.org/journals/neuroimaging/articles/10.3389/fnimg.2025.1501801/full]
- 64. Navigating the AI revolution: will radiology sink or soar? - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC12479635/]
- 65. Predictive techniques in medical imaging [https://www.nature.com/articles/s41746-025-01791-z]
- 66. Making medical images make sense - W&M News [https://news.wm.edu/2025/10/22/making-medical-images-make-sense/]
- 67. A review and systematic guide to counteracting medical ... [https://www.sciencedirect.com/science/article/pii/S266699002500045X]
- 68. Insights From ISPOR 2025: Breaking the Data Barrier in ... [https://petauri.com/insights/ispor-2025-rare-disease-data-ai/]
- 69. An integrated approach for rare disease detection and ... [https://www.nature.com/articles/s41598-025-21827-4]
- 70. Synthetic data can benefit medical research — but risks ... [https://www.nature.com/articles/d41586-025-02869-0]
- 71. Distributed Deep Learning for Medical Image Denoising ... [https://arxiv.org/abs/2511.06006]
- 72. Artificial Intelligence in the Diagnosis of Pediatric Rare Diseases [https://pmc.ncbi.nlm.nih.gov/articles/PMC12470782/]
- 73. Adaptive clustering for medical image analysis using the ... [https://www.nature.com/articles/s41598-025-13670-4]
- 74. Structural Similarity Index, Peak Signal-to-Noise Ratio [https://juliaimages.org/latest/examples/image_quality_and_benchmarks/structural_similarity_index/]
- 75. On the proper use of structural similarity for the robust ... [https://pubmed.ncbi.nlm.nih.gov/35106778/]
- 76. Medical image denoising system based on stacked ... [https://www.sciencedirect.com/science/article/abs/pii/S1746809421004390]
- 77. Peak signal-to-noise ratio [https://en.wikipedia.org/wiki/Peak_signal-to-noise_ratio]
- 78. Similarity and quality metrics for MR image-to- ... [https://www.nature.com/articles/s41598-025-87358-0]
- 79. Clinical Validation [https://aimi.stanford.edu/research/focal-areas/clinical-validation]
- 80. ClinValAI: A framework for developing Cloud-based ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12240695/]
- 81. Lightweight Data-Free Denoising for Detail-Preserving ... [https://arxiv.org/abs/2510.15611]
- 82. A multimodal comparison of latent denoising diffusion ... [https://www.nature.com/articles/s41598-023-39278-0]
- 83. Conditional Denoising Diffusion Generative Adversarial ... [https://jnm.snmjournals.org/content/65/supplement_2/241626]
- 84. Advancements in biomedical rendering: A survey on AI ... [https://www.sciencedirect.com/science/article/pii/S0010482525013319]
- 85. The Tenth NTIRE 2025 Image Denoising Challenge Report [https://arxiv.org/html/2504.12276v1]
- 86. Fidelity assessment of synthetic images with multi-criteria ... [https://www.nature.com/articles/s41598-025-15480-0]
- 87. AI-enabled image fraud in scientific publications - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC9278510/]
- 88. Methods and Trends in Detecting AI-Generated Images [https://arxiv.org/html/2502.15176v2]
- 89. Statistical Rigor and Reproducibility in the AI Era - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC12402953/]
- 90. NTIRE 2025 Challenge on Image Super-Resolution ... [https://arxiv.org/abs/2504.14582]
- 91. zhengchen1999/NTIRE2025_ImageSR_x4 [https://github.com/zhengchen1999/NTIRE2025_ImageSR_x4]
- 92. The Tenth NTIRE 2025 Image Denoising Challenge Report [https://openaccess.thecvf.com/content/CVPR2025W/NTIRE/html/Sun_The_Tenth_NTIRE_2025_Image_Denoising_Challenge_Report_CVPRW_2025_paper.html]
- 93. New Trends in Image Restoration and Enhancement workshop [https://cvlai.net/ntire/2025/]
- 94. Stereo-seq Image Processing: Troubleshooting Common Analysis ... [https://en.stomics.tech/resources/stomics-blog/1137.html]
- 95. Machine learning for medical imaging: methodological ... [https://www.nature.com/articles/s41746-022-00592-y]
- 96. Medical Image Software: Techniques, Value & Stats Analysis [https://www.itransition.com/healthcare/image-analysis]