Machine Learning vs. Deep Learning for Cancer Detection: A Comparative Analysis for Researchers and Drug Developers
This article provides a comprehensive comparative analysis of Machine Learning (ML) and Deep Learning (DL) methodologies for cancer detection, tailored for researchers, scientists, and drug development professionals.
Machine Learning vs. Deep Learning for Cancer Detection: A Comparative Analysis for Researchers and Drug Developers
Abstract
This article provides a comprehensive comparative analysis of Machine Learning (ML) and Deep Learning (DL) methodologies for cancer detection, tailored for researchers, scientists, and drug development professionals. It explores the foundational principles of both approaches, detailing their application across diverse data modalities including medical imaging, genomics, and clinical records. The scope extends to methodological implementation, troubleshooting common challenges like data scarcity and model interpretability, and rigorous validation frameworks. By synthesizing current evidence and performance benchmarks, this analysis aims to guide the selection and optimization of AI tools to accelerate oncological research and the development of precise diagnostic solutions.
Core Concepts and Data Landscapes: Understanding ML and DL in Oncology
In the field of oncology, the choice between classical Machine Learning (ML) and Deep Learning (DL) architectures is pivotal for developing effective cancer detection tools. Classical ML relies on human-engineered features and often requires less computational power, making it suitable for smaller datasets. In contrast, DL models autonomously learn hierarchical features from raw data, typically achieving superior performance with large-scale, complex data but at a greater computational cost. This guide provides an objective, data-driven comparison of these paradigms to inform researchers and developers in selecting the appropriate tool for their specific cancer detection projects [1] [2].
Performance Comparison at a Glance
The table below summarizes key performance metrics and characteristics of classical ML and DL models as reported in recent cancer detection studies.
Table 1: Comparative Performance of ML and DL Models in Cancer Detection
| Cancer Type | Model Category | Best Performing Model(s) | Reported Accuracy | Key Strengths / Weaknesses |
|---|---|---|---|---|
| Multi-Cancer (7 types) [3] | Deep Learning | DenseNet121 | 99.94% | Highest accuracy; low loss (0.0017) and RMSE [3]. |
| Brain Tumor [1] | Deep Learning | ResNet18 (CNN) | 99.77% (mean) | Best overall performance and cross-domain generalization (95% accuracy) [1]. |
| Brain Tumor [1] | Deep Learning | Vision Transformer (ViT-B/16) | 97.36% (mean) | Strong performance; captures long-range spatial features [1]. |
| Brain Tumor [1] | Deep Learning | SimCLR (Self-Supervised) | 97.29% (mean) | Effective with limited labeled data; 2-stage training [1]. |
| Brain Tumor [1] | Classical ML | SVM with HOG features | 96.51% (mean) | Competitive on original data; poor cross-domain generalization (80% accuracy) [1]. |
| Lung & Colon [4] | Hybrid (Fusion) | EfficientNetB0 + Handcrafted Features | 99.87% | Combines DL with LBP, GLCM; excellent generalizability [4]. |
| Cancer Risk Prediction (Structured Data) [5] | Classical ML | CatBoost (Ensemble) | 98.75% | Effective on tabular genetic/lifestyle data; handles complex interactions [5]. |
Detailed Experimental Protocols
Understanding the methodology behind these performance metrics is crucial for replication and critical assessment.
This study offers a direct comparison of four distinct model paradigms.
- Objective: To classify brain MRIs into "tumor" or "no tumor" and evaluate model robustness.
- Dataset: 2,870 T1-weighted brain MRIs from Figshare (4 classes: glioma, meningioma, pituitary, no tumor). A separate cross-dataset was used for generalization testing [1].
- Models & Training:
- SVM+HOG: Represented classical ML. HOG features were extracted and fed into a linear SVM classifier [1].
- ResNet18: A standard CNN. The model was fine-tuned with frozen initial layers and used heavy data augmentation (affine transformations, flipping, Gaussian blur) [1].
- Vision Transformer (ViT-B/16): Leveraged self-attention mechanisms. It was pretrained and fine-tuned on the medical image dataset [1].
- SimCLR: A self-supervised learning model. It first learns representations from unlabeled data via contrastive learning, then is fine-tuned on a smaller labeled dataset [1].
- Evaluation: Models were evaluated on a hold-out test set from the primary dataset (within-domain) and a completely separate cross-dataset to assess generalization [1].
This research evaluated multiple advanced DL architectures across seven cancer types.
- Objective: To automate cancer detection and classify seven cancer types from histopathology images.
- Dataset: Publicly available image datasets for brain, oral, breast, kidney, Acute Lymphocytic Leukemia (ALL), lung and colon, and cervical cancer [3].
- Models & Training: Ten pre-trained CNN models (including DenseNet121, DenseNet201, Xception, InceptionV3, VGG19, ResNet152V2) were compared using transfer learning [3].
- Image Preprocessing: A significant part of the methodology involved advanced image segmentation techniques, including grayscale conversion, Otsu binarization, noise removal, and watershed transformation. Contour features (perimeter, area) were also extracted to enhance region identification [3].
- Evaluation: Models were evaluated based on accuracy, precision, recall, F1-score, and Root Mean Square Error (RMSE) [3].
This study demonstrates a state-of-the-art approach that integrates classical and deep learning.
- Objective: To improve classification of lung and colon cancer histopathology images.
- Dataset: LC25000 dataset, with external validation on NCT-CRC-HE-100K and HMU-GC-HE-30K [4].
- Models & Training:
- Deep Features: Extracted using an extended EfficientNetB0 model [4].
- Classical Features: Handcrafted features were extracted in parallel, including:
- Fusion & Training: A transformer-based attention mechanism was used to fuse the classical and deep features dynamically. The model was trained using an adaptive incremental learning strategy to prevent catastrophic forgetting as new data was introduced [4].
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Materials and Tools for Cancer Detection Research
| Item / Solution | Function / Description | Relevance in Cancer Detection |
|---|---|---|
| Whole Slide Imaging (WSI) [6] | High-resolution digital scans of entire histology slides. | Enables digital analysis of tissue morphology; foundational for DL-based pathology. |
| The Cancer Genome Atlas (TCGA) [7] | A public repository of cancer genomics and imaging data. | Provides comprehensive, multi-modal datasets for training and validating ML/DL models. |
| LC25000 Dataset [4] | A balanced dataset of 25,000 images for lung and colon cancer. | A standard benchmark for developing and testing histopathology image classification models. |
| Clustering-constrained Attention Multiple Instance Learning (CLAM) [6] | A weakly-supervised deep learning method. | Analyzes gigapixel WSI scans without dense, pixel-level annotations, streamlining workflow. |
| Explainable AI (XAI) Tools [7] [8] | Techniques to interpret model decisions (e.g., saliency maps). | Critical for building clinical trust by visualizing regions of interest identified by "black box" models. |
| Generative Adversarial Networks (GANs) [7] [2] | Neural networks that generate synthetic data. | Used for data augmentation to balance classes and improve model robustness with limited data. |
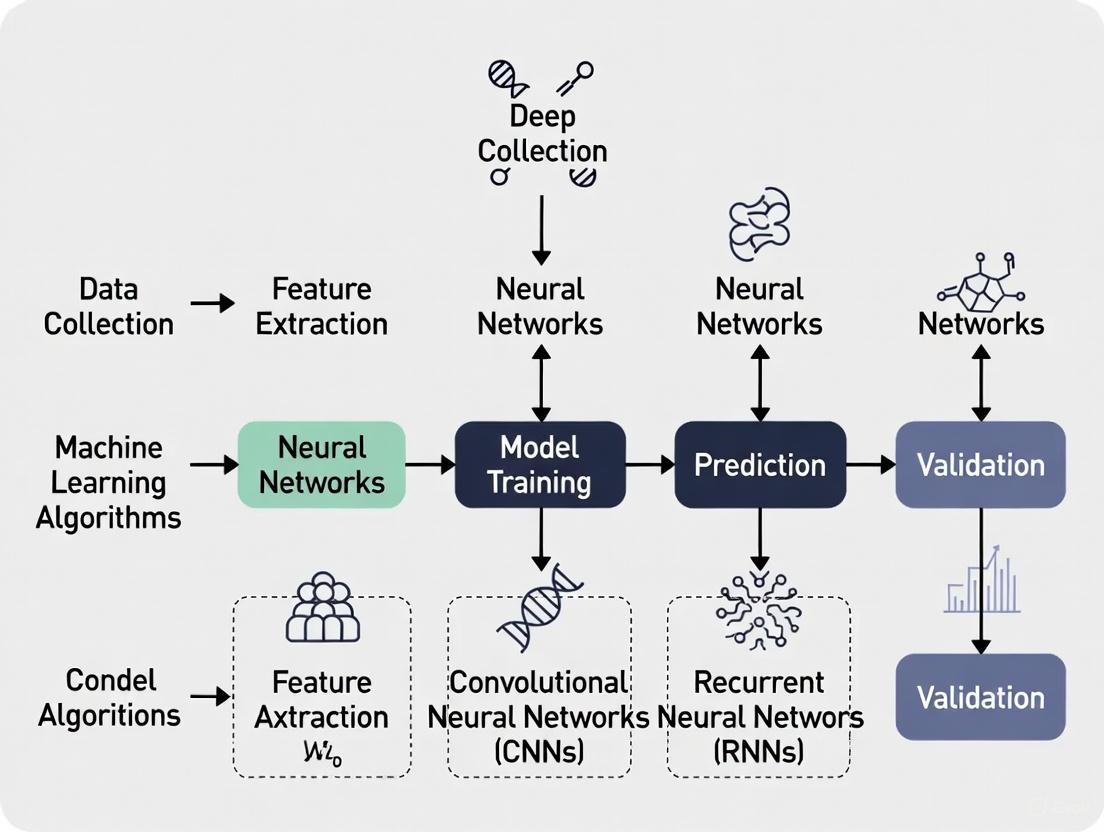
Workflow and Logical Diagrams
The diagrams below illustrate the core architectural and procedural differences between the two paradigms.
Key Selection Guidelines
The optimal model choice depends on the specific research context, driven by data, resources, and project goals.
Choose Classical ML When:
- Working with small to medium-sized datasets (n < 10,000 samples) [1].
- The data is structured or tabular (e.g., patient records with genetic risk, lifestyle factors) [5].
- Computational resources are limited, and model interpretability is a primary concern [1].
- Domain knowledge is strong, allowing for effective manual feature engineering (e.g., using HOG, GLCM) [4].
Choose Deep Learning When:
- Dealing with large-scale, complex data (e.g., high-resolution images, genomic sequences) [3] [2].
- The problem requires automatic feature extraction from raw data, minimizing the need for domain-specific feature engineering [2].
- Maximum predictive accuracy is the critical goal, and sufficient computational resources (e.g., GPUs) are available [3].
- Using pre-trained models with transfer learning can be effectively applied, even if the original labeled dataset is not massive [3] [8].
Consider Hybrid or Advanced Approaches When:
- Aiming for state-of-the-art performance on histopathology images, where fusing classical and deep features has proven highly effective [4].
- Labeled data is scarce, where self-supervised learning (SSL) methods like SimCLR can reduce annotation costs [1].
- Working with multi-modal data (e.g., imaging + genomics), requiring sophisticated fusion strategies [2].
Cancer remains a devastating global health challenge, with nearly 20 million new cases and 9.7 million deaths reported in 2022 alone [9]. The timely and accurate detection of cancer is crucial for improving patient survival rates and treatment outcomes. In contemporary oncology practice, three primary data modalities have emerged as fundamental to cancer detection: medical imaging, genomic data, and clinical records. The integration of artificial intelligence, particularly machine learning (ML) and deep learning (DL), is revolutionizing how these data modalities are analyzed to detect cancer earlier and with greater precision.
This guide provides a comparative analysis of how ML and DL approaches leverage imaging, genomics, and clinical records for cancer detection. By examining the performance characteristics, implementation requirements, and clinical applications of each modality, we aim to inform researchers, scientists, and drug development professionals about the current landscape and future directions in oncologic AI.
Comparative Analysis of Data Modalities
The table below provides a systematic comparison of the three primary data modalities used in ML/DL approaches for cancer detection.
Table 1: Performance Comparison of Data Modalities in Cancer Detection
| Data Modality | Key ML/DL Applications | Reported Performance Metrics | Strengths | Limitations |
|---|---|---|---|---|
| Medical Imaging [7] [10] | CNNs, Vision Transformers (ViTs) for classification & segmentation | ViTs: 99.92% accuracy (mammography) [10]; CNN/Ensemble models: >97% accuracy [11] [12] | Non-invasive, rich spatial data, enables early detection | Domain shift across institutions, annotation cost, model interpretability |
| Genomics [7] [9] [13] | ML for biomarker discovery; DL for sequencing analysis | Imaging genomics models predict molecular subtypes, therapeutic efficacy [9] | Reveals molecular mechanisms, enables personalized treatment | High cost, complex data integration, tissue heterogeneity |
| Clinical Records [14] [15] | NLP for data extraction; ML for risk stratification & outcome prediction | NLP-derived features outperformed genomic data or stage alone in survival prediction [14] | Real-world data, comprehensive patient context, widely available | Unstructured data, privacy concerns, requires extensive preprocessing |
Detailed Experimental Protocols and Workflows
Medical Imaging Analysis with Deep Learning
Experimental Protocol: A standard workflow for applying DL to medical imaging for cancer detection involves multiple stages of data processing and model development [10].
- Data Acquisition and Preprocessing: Collect large datasets of medical images (e.g., mammograms, MRI, whole-slide images). Apply preprocessing techniques including normalization, resizing, and data augmentation using Generative Adversarial Networks (GANs) to address class imbalance [10].
- Model Training: Implement Convolutional Neural Networks (CNNs) such as ResNet or DenseNet for feature extraction. Alternatively, employ Vision Transformers (ViTs) which divide images into patches and use self-attention mechanisms to capture global contextual information [10]. Transfer learning is commonly used by fine-tuning models pre-trained on large datasets like ImageNet.
- Validation: Perform rigorous internal validation using k-fold cross-validation (e.g., stratified k-fold) and external validation on independent datasets from different institutions to assess generalizability [10] [11]. Metrics such as accuracy, AUC, sensitivity, and specificity are reported.
The following diagram illustrates a typical deep learning workflow for medical image analysis in cancer detection.
Integrating Imaging and Genomics (Radiogenomics)
Experimental Protocol: Imaging genomics, or radiogenomics, aims to establish relationships between radiological features and genomic biomarkers [9].
- Data Collection: Acquire matched pairs of medical images (CT, MRI, etc.) and genomic data (from tissue samples or liquid biopsies) from the same patient cohort.
- Feature Extraction: Extract handcrafted radiomic features (e.g., texture, shape) or deep learning-based features from the images. In parallel, process genomic data to identify mutations, gene expression signatures, or other relevant biomarkers.
- Association Mapping and Model Building: Use statistical methods and ML algorithms (e.g., random forests, linear models) to identify significant correlations between imaging features and genomic markers. Build predictive models that can infer genomic status directly from imaging data, which can be less invasive than repeated biopsies [9].
Table 2: Research Reagents and Computational Tools for Radiogenomics
| Item/Tool | Function | Application Context |
|---|---|---|
| PyRadiomics [9] | Open-source platform for extraction of handcrafted radiomic features from medical images. | Standardized feature extraction for association studies with genomic data. |
| The Cancer Genome Atlas (TCGA) [7] | Public repository containing matched clinical, imaging, and genomic data. | Provides a foundational dataset for training and validating radiogenomic models. |
| CNN-based Feature Extractors [9] | Deep learning models that automatically learn relevant features from images. | Used as an alternative to handcrafted features for radiogenomic analysis. |
| Statistical/Machine Learning Models (e.g., Random Forest, Linear Regression) [9] | Algorithms to identify and model correlations between imaging features and genomic data. | Building the core predictive maps linking phenotypes (imaging) to genotypes. |
Leveraging Clinical Records with NLP and Machine Learning
Experimental Protocol: Harnessing real-world data from clinical records requires processing unstructured text and integrating it with structured data [14].
- Data Integration and Harmonization: Combine structured data (medications, demographics, tumor registry) with unstructured free-text from clinician notes, radiology, and pathology reports into a unified dataset (e.g., MSK-CHORD) [14].
- Automatic Annotation with NLP: Train and validate transformer-based NLP models to automatically annotate key features from text. These features include cancer progression, tumor sites, receptor status (e.g., HER2), and smoking history. Rule-based models can be used for more structured information [14].
- Predictive Modeling for Outcomes: Use the annotated, multimodal dataset to train ML models for predicting clinical outcomes like overall survival. Models incorporating NLP-derived features have been shown to outperform those based solely on genomic data or cancer stage [14].
The workflow for building predictive models from clinical records using NLP is shown below.
Discussion and Future Directions
The comparative analysis reveals that each data modality offers distinct advantages and faces unique challenges. Medical imaging is unparalleled for non-invasive, early detection but requires sophisticated DL models to achieve high accuracy. Genomic data provides fundamental insights into disease mechanisms and enables personalized therapy, though integration with other modalities remains complex. Clinical records offer a rich, real-world context that significantly enhances outcome prediction when processed with advanced NLP techniques.
The future of cancer detection lies not in using these modalities in isolation, but in their strategic integration. Multimodal AI, which combines imaging, genomics, and clinical data, holds the greatest promise for building comprehensive and accurate predictive models [7] [14]. Key areas for future development include improving model interpretability through Explainable AI (XAI) [7] [12], addressing data bias to ensure equitable performance across diverse populations [16] [10], and establishing standardized protocols for the clinical validation and deployment of these advanced AI tools [7] [13].
The Rise of Deep Learning in Analyzing Complex Cancer Datasets
The intricate and heterogeneous nature of cancer has long demanded sophisticated analytical approaches. The field of artificial intelligence (AI) has responded with two powerful subsets: classical Machine Learning (ML) and Deep Learning (DL). While ML has established a strong foundation in cancer informatics, DL is now rising to the forefront, demonstrating a remarkable capacity to analyze complex, high-dimensional datasets. This guide provides a comparative analysis of ML and DL models as research tools in cancer detection, framing them within the broader thesis of their respective roles in computational oncology. We objectively compare their performance across various cancer types, detail experimental protocols from key studies, and provide visualizations of core workflows to equip researchers, scientists, and drug development professionals with the data needed to select appropriate methodologies for their work.
The fundamental distinction lies in their approach to feature handling. ML models typically require domain expertise for manual feature extraction and engineering, such as calculating specific morphological or texture descriptors from images or selecting relevant genomic markers [17]. In contrast, DL models, particularly deep neural networks, autonomously learn hierarchical feature representations directly from raw data, such as whole images or genomic sequences [18] [3]. This capability allows DL to identify subtle, complex patterns often imperceptible to human experts or traditional ML algorithms.
To objectively evaluate the landscape, the table below synthesizes experimental performance data for ML and DL models across several cancer types, as reported in recent literature.
Table 1: Comparative Performance of ML and DL Models in Cancer Detection
| Cancer Type | Best Performing ML Model | Reported ML Accuracy | Best Performing DL Model | Reported DL Accuracy | Key Dataset(s) / Notes |
|---|---|---|---|---|---|
| Lung Cancer | Gradient-Boosted Trees [15] | 90.0% | Single-Hidden-Layer Neural Network [15] | 92.86% | Kaggle patient symptom & lifestyle data [15] |
| Multi-Cancer Image Classification | Not Applicable (Benchmark) | N/A | DenseNet121 [3] | 99.94% | Combined dataset of 7 cancer types (Brain, Oral, Breast, etc.) [3] |
| Breast Cancer (Mammography) | Not Directly Compared | N/A | Deep Learning Model (Model B) [19] | AUC: 0.93 | 129,434 screening exams from BreastScreen Norway [19] |
| Leukemia (Microarray Gene Data) | Not Directly Compared | N/A | Weighted CNN with Feature Selection [18] | 99.9% | Microarray gene data; highlights genomic application [18] |
| General Cancer Prediction | Random Forest / Ensemble Methods [17] | Varies (Review) | Convolutional Neural Networks (CNNs) [17] | Generally Higher (Review) | Survey of 191 studies (2018-2023) [17] |
The performance advantage of DL is evident, particularly in tasks involving image and genomic data. The Norwegian breast cancer screening study, a large-scale real-world validation, demonstrated that DL models could identify 93.7% of screen-detected cancers while correctly localizing the lesions [19]. Furthermore, DL excels in multi-cancer classification, with models like DenseNet121 achieving near-perfect accuracy on a complex 7-class image dataset [3]. In genomics, the integration of DL with feature selection techniques has enabled the analysis of tens of thousands of genes, achieving exceptional diagnostic precision for leukemia [18].
Experimental Protocols and Methodologies
Protocol 1: Multi-Cancer Image Classification with Transfer Learning
A 2024 study in Scientific Reports provides a robust protocol for using DL to classify seven cancer types from histopathology and radiology images [3].
A. Workflow Overview The following diagram illustrates the end-to-end experimental workflow.
B. Detailed Methodology
- Data Acquisition and Preprocessing: Publicly available image datasets for seven cancer types (brain, oral, breast, kidney, Acute Lymphocytic Leukemia (ALL), lung & colon, and cervical) were collected. Images underwent grayscale conversion and noise removal to standardize quality [3].
- Segmentation and Feature Extraction: The preprocessed images were segmented using Otsu binarization and watershed transformation techniques. Subsequently, contour features—including perimeter, area, and epsilon—were computationally extracted from the identified cancer regions to provide quantitative descriptors for the models [3].
- Model Selection and Training: Ten pre-trained CNN models, including DenseNet121, DenseNet201, Xception, and VGG19, were selected for a transfer learning approach. These models, already trained on large general image datasets like ImageNet, were fine-tuned on the multi-cancer dataset [3].
- Evaluation: Model performance was rigorously evaluated using metrics such as accuracy, loss, precision, recall, F1-score, and Root Mean Square Error (RMSE). DenseNet121 emerged as the most effective model, achieving a validation accuracy of 99.94% and the lowest RMSE values [3].
Protocol 2: Lung Cancer Prediction from Symptomatic and Lifestyle Data
A 2025 study offered a direct comparison of ML and DL for lung cancer prediction using non-image data, highlighting the importance of feature engineering for ML [15].
A. Workflow Overview The diagram below contrasts the parallel paths for ML and DL model development.
B. Detailed Methodology
- Data Preparation: A lung cancer dataset from Kaggle containing patient symptoms and lifestyle factors was used. The data was preprocessed through outlier removal and normalization [15].
- Critical Feature Selection: Pearson’s correlation was applied to identify and select the most relevant predictive features from the dataset. This step was noted as crucial for enhancing the accuracy of both ML and DL models, but it was especially critical for the performance of traditional ML algorithms [15].
- Model Training and Comparison: Multiple ML classifiers (Random Forest, SVM, Logistic Regression, etc.) were implemented and compared against neural networks with 1, 2, and 3 hidden layers. The models were evaluated using k-fold cross-validation and an 80/20 train/test split [15].
- Results: The single-hidden-layer neural network, trained for 800 epochs, achieved the highest prediction accuracy of 92.86%, outperforming all the tested traditional ML models [15].
For researchers aiming to replicate or build upon these studies, the following table details key computational reagents and resources.
Table 2: Key Research Reagents and Computational Tools for DL in Cancer Detection
| Resource / Tool | Type | Primary Function in Research | Example in Context |
|---|---|---|---|
| Pre-trained CNN Models (DenseNet, VGG, ResNet) | Deep Learning Architecture | Feature extraction and image classification; enables transfer learning, reducing data and computational needs. | DenseNet121 for multi-cancer image classification [3]. |
| The Cancer Genome Atlas (TCGA) | Data Repository | Provides large-scale, standardized multi-omics (genomic, epigenomic, transcriptomic) and clinical data for model training and validation. | Used as a primary data source in many genomic studies reviewed in [7] [18]. |
| Federated Learning Frameworks | Privacy-Preserving Technique | Enables training ML/DL models across multiple decentralized data sources (e.g., different hospitals) without sharing raw data. | Emerging solution to data privacy and siloing challenges in clinical deployment [7] [18]. |
| Explainable AI (XAI) Methods (e.g., SHAP) | Interpretation Tool | Provides post-hoc explanations for "black-box" model predictions, increasing transparency and trust for clinicians. | SHAP used to explain a hybrid CNN-RF model for breast cancer detection [20]. |
| Generative Adversarial Networks (GANs) | Deep Learning Model | Generates synthetic medical data to augment training datasets, helping to address class imbalance and data scarcity. | Used for data augmentation in breast cancer imaging studies [10]. |
The comparative analysis clearly indicates that while classical ML remains a valuable tool, particularly for structured data with expert-derived features, DL has demonstrated superior performance in analyzing the complex, high-dimensional datasets prevalent in modern oncology. Its ability to autonomously learn discriminative features from raw images and genomic sequences has resulted in groundbreaking accuracy in detection and classification tasks.
The future of DL in cancer research hinges on addressing key challenges, including the need for large, diverse, and well-annotated datasets to mitigate bias and improve generalizability [10] [18]. Furthermore, the integration of Explainable AI (XAI) is paramount for translating these powerful "black-box" models into trusted clinical tools [20]. Finally, the emergence of multimodal DL models that can seamlessly integrate imaging, genomic, and clinical data promises to unlock a new era of holistic cancer diagnostics and personalized treatment planning, ultimately advancing the fight against this complex disease [7] [18] [21].
Strengths and Inherent Limitations of ML and DL Approaches
The integration of artificial intelligence (AI) into oncology represents a paradigm shift in cancer detection, offering unprecedented opportunities to improve diagnostic accuracy, speed, and accessibility [7]. Within the AI landscape, machine learning (ML) and deep learning (DL) have emerged as pivotal technologies, each with distinct capabilities and limitations for cancer research applications. ML refers to algorithms that automatically learn and adapt from data without explicit programming, while DL is a specialized subset that mimics the human brain using multi-layered neural networks to process complex information [22] [23]. This comparative analysis examines the respective strengths and limitations of ML and DL approaches within cancer detection research, providing researchers, scientists, and drug development professionals with evidence-based insights for selecting appropriate methodologies based on specific research contexts and constraints. The framework established in this guide aims to inform strategic decisions in algorithm development and experimental design for oncological applications.
Fundamental Technical Distinctions
ML and DL differ fundamentally in their data processing approaches, architectural complexity, and feature engineering requirements. These technical distinctions directly influence their applicability to different cancer detection scenarios.
Architecture and Feature Engineering: Traditional ML relies on structured data and requires significant human intervention for feature selection and extraction [24]. In contrast, DL operates with deep neural networks that learn directly from raw, often unstructured data, automatically determining relevant features through multiple processing layers [25]. This architectural difference makes DL particularly suited for complex data types like medical images where meaningful features may be difficult to define manually.
Data Requirements and Processing: ML algorithms typically perform well with organized, structured data represented in well-defined variables and can achieve meaningful results with smaller datasets [24]. DL models require substantially larger volumes of data for training but can process and find patterns in unstructured data formats including images, audio, and text without extensive preprocessing [25]. The scalability of DL comes at the cost of computational intensity, typically demanding robust GPU-powered infrastructures not always required for ML implementations [24].
Table: Fundamental Differences Between ML and DL Approaches
| Characteristic | Machine Learning (ML) | Deep Learning (DL) |
|---|---|---|
| Data Requirements | Moderate amounts of structured data | Large volumes of unstructured data |
| Feature Engineering | Manual feature extraction required | Automatic feature learning |
| Computational Demand | Lower, can run on CPU systems | High, typically requires GPU acceleration |
| Interpretability | More transparent and explainable | "Black box" nature, less interpretable |
| Infrastructure Needs | Lighter, distributed computing environments | Robust architectures with parallel processing |
Performance Analysis in Cancer Detection
Quantitative Performance Metrics
Rigorous evaluation of ML and DL performance across various cancer types reveals distinct patterns in their detection capabilities. A comprehensive analysis of 130 research studies published between 2018-2023 demonstrated that both approaches can achieve high accuracy, with DL techniques reaching up to 100% accuracy in optimal conditions, while ML techniques achieved a maximum of 99.89% accuracy [26]. However, the lowest accuracy reported for DL was 70%, compared to 75.48% for ML, indicating potentially more significant performance variations in DL applications [26].
For multi-cancer image classification, a 2024 study evaluating ten DL architectures on seven cancer types (brain, oral, breast, kidney, Acute Lymphocytic Leukemia, lung and colon, and cervical cancer) found DenseNet121 achieving the highest validation accuracy at 99.94% with a loss of 0.0017 [3]. The Root Mean Square Error (RMSE) values were 0.036056 for training and 0.045826 for validation, demonstrating exceptional performance in classifying diverse cancer imagery [3].
Table: Performance Comparison Across Cancer Types
| Cancer Type | Best Performing ML Model | Accuracy | Best Performing DL Model | Accuracy | Key Challenges |
|---|---|---|---|---|---|
| Breast Cancer | Multiple ML Algorithms | 99.89% [26] | DenseNet121 | 99.94% [3] | Intraclass variability, high similarity between malignant and benign cases [27] |
| Skin Cancer | Ensemble Methods | 99.2% [26] | CNN Architectures | 100% [26] | Bias in training data for darker skin tones, equipment variability [22] |
| Brain Tumor | Traditional SVM | 98.5% [26] | Custom CNN | 99.1% [26] | Tumor segmentation complexity, image quality variations |
| Lung Cancer | Random Forest | 97.8% [26] | CNN with CT scans | 98.7% [26] | Nodule detection accuracy, false positive reduction |
Analysis of Performance Patterns
The performance differential between ML and DL approaches varies significantly by data type and complexity. For structured genomic data, ML algorithms often achieve comparable performance to DL with greater efficiency and interpretability [2]. In contrast, DL consistently outperforms ML for image-based cancer detection, particularly with complex unstructured data like histopathology images and CT scans [3]. This performance advantage comes with substantial computational costs and data requirements that must be factored into research planning.
The Mammography Screening with Artificial Intelligence (MASAI) randomized controlled trial demonstrated the real-world impact of these technologies, where an AI system used for triage increased cancer detection rates by 20% while reducing radiologists' workload by half [22]. This illustrates how DL integration can enhance both efficiency and effectiveness in clinical screening scenarios.
Experimental Protocols and Methodologies
Typical DL Experimental Protocol for Image Analysis
Dataset Preparation and Preprocessing: DL experiments typically begin with extensive data collection and augmentation. A standard protocol involves gathering large datasets of medical images, such as the 129,450 biopsy-proven photographic images used in a seminal dermatology study [22]. Images undergo preprocessing including grayscale conversion, Otsu binarization, noise removal, and watershed transformation for segmentation [3]. Contour feature extraction follows, with parameters such as perimeter, area, and epsilon computed to enhance cancer region identification.
Model Architecture and Training: Convolutional Neural Networks (CNNs) represent the most prevalent DL architecture in cancer detection research [2]. The convolution operation follows the mathematical formula: (f ∗ g)(t) = ∫f(τ)g(t-τ)dτ, where f denotes the input image and g represents the filter [2]. Pooling operations, including Max Pooling and Average Pooling, reduce feature map dimensionality while preserving salient features [2]. Transfer learning approaches utilizing pre-trained models like DenseNet121, InceptionV3, and ResNet152V2 have demonstrated particular effectiveness, especially with limited datasets [3].
Validation and Interpretation: Rigorous validation follows training, typically employing k-fold cross-validation and hold-out test sets. Performance metrics including precision, accuracy, F1 score, RMSE, and recall are calculated [3]. For clinical applicability, techniques like Grad-CAM and other explainable AI (XAI) methods provide visual explanations of model decisions, addressing the "black box" limitation inherent in DL approaches [7].
Typical ML Experimental Protocol for Genomic Analysis
Feature Extraction and Selection: ML protocols for genomic cancer detection begin with identifying relevant genetic markers and variations. For whole genome data, researchers often apply effect functions to mutations with location-specific weights, quantified as ∑w_i * f(m_i), where w_i represents the weight of the mutation location and f(m_i) denotes the effect function of the mutation [2]. Feature selection algorithms then identify the most discriminative genetic markers, reducing dimensionality to enhance model performance and interpretability.
Model Training and Optimization: Following feature selection, researchers implement and compare multiple ML algorithms, typically including Support Vector Machines (SVM), Random Forests, and gradient boosting methods. Regularization techniques prevent overfitting by limiting the weight models assign to specific variables, making results more generalizable and accurate [25]. This is particularly crucial with genomic data where the number of features often exceeds sample sizes.
Validation and Clinical Correlation: ML models undergo rigorous validation using techniques like bootstrapping and cross-validation. Performance is assessed through standard metrics with particular attention to clinical applicability. Models are correlated with known clinical outcomes and biological pathways to ensure translational relevance, with mutation signatures in genes like BRCA1 and BRCA2 linked to specific cancer risks and treatment responses [2].
Research Reagent Solutions
The implementation of ML and DL approaches in cancer detection relies on specialized computational tools and datasets. The following table details essential research reagents and their functions in developing and validating cancer detection models.
Table: Essential Research Reagent Solutions for ML/DL Cancer Detection
| Research Reagent | Type | Function | Example Applications |
|---|---|---|---|
| Convolutional Neural Networks (CNNs) | Algorithm Architecture | Automatically extracts features from medical images | Analysis of CT scans for lung nodules, mammogram interpretation [2] [22] |
| Whole Slide Images (WSI) | Data Type | Digital pathology slides for model training | Histopathological cancer classification [7] |
| The Cancer Genome Atlas (TCGA) | Dataset | Comprehensive genomic database | Identifying mutation patterns across cancer types [7] |
| Generative Adversarial Networks (GANs) | Algorithm Architecture | Generates synthetic data to address class imbalance | Augmenting rare cancer subtype datasets [7] [27] |
| Explainable AI (XAI) Tools | Software Library | Provides model interpretability and decision explanations | Visualizing areas of interest in medical images [7] |
| Federated Learning Frameworks | Deployment Architecture | Enables collaborative training without data sharing | Multi-institutional models while preserving patient privacy [7] |
| Variational Autoencoders (VAE) | Algorithm Architecture | Learns efficient data encodings for dimensionality reduction | Processing high-dimensional genomic data [7] |
Strengths and Limitations Analysis
Machine Learning Strengths and Limitations
Key Strengths:
- Data Efficiency: ML algorithms achieve meaningful results with moderate-sized datasets, making them suitable for rare cancer types where large datasets are unavailable [24]
- Computational Efficiency: ML models require less computational power and can often run on standard CPU-based systems, reducing infrastructure costs [25]
- Interpretability: ML models, particularly those like decision trees and linear models, offer greater transparency in decision-making, which is crucial for clinical adoption and regulatory approval [24]
- Structured Data Excellence: ML excels with structured data types, including genomic sequences and electronic health records, where features can be clearly defined [25]
Inherent Limitations:
- Feature Engineering Dependency: ML performance heavily depends on manual feature engineering and domain expertise to identify relevant variables [24]
- Limited Complex Pattern Recognition: ML struggles with unstructured data like medical images where patterns may be subtle and hierarchical [25]
- Performance Plateau: With complex data types, ML algorithms often reach performance ceilings below what DL can achieve [3]
Deep Learning Strengths and Limitations
Key Strengths:
- Automatic Feature Learning: DL eliminates the need for manual feature engineering by automatically learning relevant features directly from raw data [3]
- Superior Complex Pattern Recognition: DL excels at identifying subtle, hierarchical patterns in unstructured data like histopathology images and CT scans [22]
- State-of-the-Art Performance: For most image-based cancer detection tasks, DL has demonstrated superior performance compared to traditional ML approaches [3]
- Scalability: DL models can improve with more data and benefit from transfer learning approaches that leverage pre-trained models [25]
Inherent Limitations:
- Data Hunger: DL requires large volumes of labeled training data, which can be challenging for rare cancer types or in resource-limited settings [2]
- Computational Intensity: Training complex DL models demands substantial computational resources, typically requiring GPU acceleration [24]
- Black Box Nature: The complexity of DL models makes them difficult to interpret, raising challenges for clinical trust and regulatory approval [7]
- Generalization Challenges: DL models may suffer from performance degradation when applied to data from different institutions or demographic groups [22]
Emerging Solutions and Future Directions
Several innovative approaches are emerging to address the inherent limitations of both ML and DL approaches in cancer detection:
Federated Learning: This approach enables collaborative model training across multiple institutions without sharing sensitive patient data, addressing both data scarcity and privacy concerns [7]. By training models locally and sharing only parameter updates, federated learning facilitates the development of robust models while maintaining data confidentiality.
Explainable AI (XAI): To mitigate the "black box" problem of DL models, XAI techniques provide visual explanations and decision rationales, enhancing clinical trust and adoption [7]. These methods help clinicians understand model decisions and identify potential failure modes before clinical implementation.
Synthetic Data Generation: Generative adversarial networks (GANs) and variational autoencoders (VAEs) can create synthetic medical images to address class imbalance and data scarcity issues, particularly for rare cancer types [7] [27]. This approach enables more robust model training without compromising patient privacy.
Multimodal Data Fusion: Advanced architectures that integrate diverse data types (genomic, imaging, clinical) show promise for more comprehensive cancer detection [2]. These approaches leverage the strengths of both ML and DL for different data modalities within unified frameworks.
Transfer Learning: Leveraging pre-trained models and adapting them to specific cancer detection tasks helps address data limitations and reduces computational requirements [3]. This approach has proven particularly effective in medical imaging applications where labeled data is scarce.
The comparative analysis of ML and DL approaches for cancer detection reveals a nuanced landscape where each methodology offers distinct advantages depending on the specific research context. ML provides interpretability, computational efficiency, and effectiveness with structured data, while DL delivers superior performance with complex unstructured data at the cost of transparency and resource requirements. The optimal approach depends on multiple factors including data type and volume, computational resources, interpretability needs, and specific clinical requirements. Future research directions point toward hybrid methodologies that leverage the strengths of both approaches, with federated learning, explainable AI, and multimodal data fusion addressing current limitations. As these technologies continue to evolve, their thoughtful implementation holds significant promise for advancing cancer detection capabilities and ultimately improving patient outcomes through earlier and more accurate diagnosis.
Algorithmic Implementation and Real-World Clinical Applications
Within computational oncology, the analysis of structured, or tabular, data is a prevalent task, encompassing everything from patient clinical records to genomic data. While deep learning has revolutionized fields like image and speech processing, its superiority is not as pronounced when it comes to structured data [28]. In this domain, traditional machine learning (ML) algorithms often remain the gold standard, demonstrating equivalent or even superior performance compared to more complex deep learning models [28].
This guide provides a comparative analysis of three ML workhorses—Random Forests (RF), Support Vector Machines (SVM), and XGBoost—within the critical context of cancer detection research. For researchers, scientists, and drug development professionals, selecting the right algorithm is not merely an academic exercise; it directly impacts the accuracy of diagnostics and prognostics. We objectively compare these algorithms by synthesizing findings from recent peer-reviewed studies, presenting quantitative performance data, and detailing the experimental protocols used to generate them. The aim is to offer a clear, evidence-based resource for selecting the optimal model for structured data in oncology applications.
Algorithm Fundamentals and Comparative Mechanics
This section breaks down the core principles, strengths, and weaknesses of each algorithm to establish a foundational understanding.
Random Forest
- Core Concept: An ensemble method that constructs a "forest" of numerous decision trees during training [29]. It introduces randomness by training each tree on a different subset of the data and features, a process known as "bagging." For prediction, the outputs of all trees are aggregated—through majority voting for classification or averaging for regression [29].
- Strengths: Highly accurate and robust, resistant to overfitting due to its ensemble nature, handles missing data effectively, and can manage datasets with a wide range of features without significant performance loss [29] [30].
- Weaknesses: Can be computationally expensive with large datasets or a large number of trees, and the ensemble model operates as a "black box," making global interpretability challenging despite the interpretability of individual trees [29].
Support Vector Machine (SVM)
- Core Concept: A powerful classifier that finds the optimal hyperplane in a high-dimensional space to separate data points of different classes with the maximum possible margin [31]. It can handle non-linear relationships through the use of kernel functions, such as the Radial Basis Function (RBF) kernel.
- Strengths: Effective in high-dimensional spaces, memory efficient, and versatile due to the kernel trick. It is less prone to overfitting in high-dimensional spaces compared to other algorithms [29] [31].
- Weaknesses: Performance is highly sensitive to the choice of kernel and its parameters (e.g., penalty parameter
Cand RBF kernel parameterσ). It can be less interpretable and does not directly provide probability estimates [31]. It can also be computationally intensive for very large datasets.
XGBoost (Extreme Gradient Boosting)
- Core Concept: An advanced implementation of gradient boosting where new models are created to correct the errors of existing models in a sequential, additive manner [32]. It uses gradient descent to minimize a loss function and incorporates regularization techniques (L1 and L2) to control model complexity and prevent overfitting [29] [32].
- Strengths: Known for its high predictive accuracy and efficiency. It supports parallel processing, can automatically handle missing values, and includes built-in routines for feature importance [32].
- Weaknesses: Can be more susceptible to overfitting on noisy datasets if not properly regularized, and requires careful tuning of hyperparameters [29]. While providing feature importance, the model itself is complex and can be difficult to interpret fully.
Table 1: Fundamental Comparison of RF, SVM, and XGBoost
| Feature | Random Forest (RF) | Support Vector Machine (SVM) | XGBoost |
|---|---|---|---|
| Core Mechanism | Bagging of decision trees | Maximum-margin hyperplane | Boosting with gradient descent |
| Primary Strength | Robustness, handles missing data | Effectiveness in high-dimensional spaces | High predictive accuracy & speed |
| Key Weakness | "Black box" model, computational cost | Sensitivity to kernel parameters | Risk of overfitting without tuning |
| Interpretability | Medium (feature importance available) | Low | Medium (feature importance available) |
| Handling Non-Linearity | Inherent (tree splits) | Requires kernel function | Inherent (tree splits) |
Workflow Diagram: Model Training and Optimization
The following diagram illustrates the core training and optimization logic shared by these ML workhorses, highlighting their key differences in approach.
Performance Benchmarking in Cancer Detection
Empirical evidence from recent oncology research demonstrates the practical performance of these algorithms. The following table synthesizes results from multiple studies on different cancer types.
Table 2: Experimental Performance in Cancer Detection Studies
| Cancer Type | Algorithm | Performance Metrics | Citation |
|---|---|---|---|
| Breast Cancer | SVM (Optimized with IQI-BGWO) | Accuracy: 99.25%, Sensitivity: 98.96%, Specificity: 100% | [31] |
| Breast Cancer | KNN | High accuracy on original dataset | [33] [11] |
| Breast Cancer | XGBoost (via AutoML) | High accuracy on synthetic dataset | [33] [11] |
| Breast Cancer | Random Forest | Competitively high accuracy | [11] |
| Colorectal Cancer | Stacked RF Model | Specificity: 80.3%, Sensitivity: 65.2% (41% for Stage I) | [34] |
| Gastrointestinal Tract Cancers | Random Forest | Prediction accuracy >80% for survival rates | [30] |
| Cervical Cancer | Multiple ML Models (Pooled) | Sensitivity: 0.97, Specificity: 0.96 | [35] |
Key Insights from Benchmarking
- SVM's Peak Performance: When meticulously optimized, as with the Improved Quantum-Inspired Grey Wolf Optimizer (IQI-BGWO), SVM can achieve state-of-the-art results, as seen in breast cancer diagnosis on the MIAS dataset [31].
- Random Forest's Clinical Robustness: RF consistently demonstrates high accuracy and reliability, particularly in prognostication tasks. A systematic review of GI tract malignancies found RF models outperformed conventional statistical methods, with several studies reporting over 80% accuracy in predicting survival rates [30].
- The Power of Ensemble and Hybrid Strategies: The top-performing models often involve ensembling (like stacked RF [34]) or sophisticated optimization of base algorithms (like SVM with IQI-BGWO [31]). This underscores that model tuning and combination can be as critical as algorithm selection itself.
- Context-Dependent Performance: No single algorithm is universally superior. For example, in one breast cancer study, KNN performed best on the original dataset, while an AutoML approach based on XGBoost excelled on synthetic data [11], highlighting the importance of data characteristics.
Experimental Protocols in Detail
To ensure the reproducibility of results and provide a template for future research, this section details the methodologies from two key studies cited in the benchmarks.
Protocol 1: Optimized SVM for Breast Cancer Diagnosis
This protocol outlines the methodology from the study achieving 99.25% accuracy in breast cancer classification [31].
- 1. Objective: To enhance breast cancer classification accuracy by determining the optimal SVM parameters (RBF kernel parameter
σand error penaltyC) using an improved optimization algorithm. - 2. Dataset: The Mammographic Image Analysis Society (MIAS) dataset was used.
- 3. Preprocessing: Regions of Interest (ROI) were extracted from mammography images. Feature extraction was performed to characterize textures and patterns.
- 4. Optimization Algorithm: An Improved Quantum-Inspired Binary Grey Wolf Optimizer (IQI-BGWO) was developed. This algorithm combines the social hierarchy and hunting behavior of grey wolves with quantum computing concepts (e.g., qubit representation) to improve search capabilities and escape local optima.
- 5. Model Training & Validation: The IQI-BGWO was hybridized with the SVM (IQI-BGWO-SVM). The optimizer's role was to find the optimal (
C,σ) pair that maximized classification performance. The model was evaluated using a 10-fold cross-validation scheme to ensure robustness and avoid overfitting. - 6. Evaluation Metrics: Performance was assessed using mean accuracy, sensitivity, and specificity calculated across the validation folds.
Protocol 2: Stacked Random Forest for Colorectal Cancer Detection
This protocol details the approach used to develop a low-cost, blood-based screening model for colorectal cancer (CRC) [34].
- 1. Objective: To develop a robust machine learning model using Complete Blood Count (CBC) data to predict CRC risk and help prioritize colonoscopy referrals.
- 2. Study Design & Data Collection: A multicenter study was conducted with participants who underwent CBC testing within three months before a colonoscopy. The dataset included 1,795 CRC cases and 26,380 cancer-free individuals.
- 3. Feature Set: The model used 24 CBC features and 5 combined CBC components derived from hematology analyzer data.
- 4. Model Architecture: A stacking ensemble machine learning model was employed. While the core learner was Random Forest, stacking combines multiple base models (e.g., RF, SVM, etc.) using a meta-learner to generate final predictions, potentially capturing complementary patterns.
- 5. Validation: The model underwent external validation, meaning it was tested on data from a different source than it was trained on. This is a rigorous method to evaluate real-world generalizability.
- 6. Evaluation Metrics: Performance was reported using the Area Under the Curve (AUC), specificity, and sensitivity, with a focus on detecting early-stage (Stage I) cancer.
Diagram: Experimental Workflow for Cancer Detection
The following diagram generalizes the experimental workflow common to the detailed protocols, providing a blueprint for developing ML models in cancer detection.
The Scientist's Toolkit: Essential Research Reagents
Success in ML-driven oncology research relies on a suite of "research reagents"—both data and software. Below is a curated list of essential resources.
Table 3: Essential Research Reagents for ML in Cancer Detection
| Item Name | Type | Function & Application | Example / Source |
|---|---|---|---|
| Public Cancer Datasets | Data | Provide standardized, annotated data for model training and benchmarking. | MIAS (Mammography) [31] [36], DDSM/CBIS-DDSM (Mammography) [36], INBreast [36], UCI Breast Cancer [11] |
| Synthetic Data Generators | Data/Software | Augment limited datasets and improve model generalizability by creating realistic synthetic data. | Gaussian Copula (GC), Tabular Variational Autoencoder (TVAE) [11] |
| Optimization Algorithms | Software | Automate the tuning of model hyperparameters to maximize predictive performance. | Improved Quantum-Inspired Grey Wolf Optimizer (IQI-BGWO) [31], Grid Search, Random Search [29] |
| AutoML Frameworks | Software | Automate the end-to-end ML process, from model selection to tuning, reducing manual effort. | H2O AutoML [11], Auto-SKlearn, TPOT [11] |
| Model Interpretation Tools | Software | Provide insights into model decisions, enhancing trust and facilitating clinical adoption. | LIME (Local Interpretable Model-agnostic Explanations) [29], SHAP, built-in Feature Importance (XGBoost, RF) |
The comparative analysis presented in this guide demonstrates that Random Forests, SVMs, and XGBoost are formidable algorithms for analyzing structured data in cancer research. Their performance is not absolute but is highly dependent on the specific context—the type of cancer, the nature of the data, and, crucially, the rigor of the experimental design and optimization.
- Random Forest stands out for its robustness, ease of use, and consistent high performance, especially in clinical prognostic studies [30].
- SVM remains a powerful choice, capable of achieving top-tier accuracy when its parameters are meticulously optimized, as demonstrated in medical image-based diagnosis [31].
- XGBoost is a highly accurate and efficient algorithm that excels in structured data tasks and is often a key component in winning solutions in data science competitions [32] [11].
The future of ML in oncology lies not in seeking a single dominant algorithm, but in the intelligent application, optimization, and combination of these workhorses. Integrating tools for explainability (XAI) and leveraging synthetic data will be key to translating these powerful models from research benchmarks into trusted tools in clinical practice, ultimately aiding in the early detection and effective treatment of cancer.
In the field of deep learning, Convolutional Neural Networks (CNNs) and Transformers represent two dominant architectural paradigms, each with distinct inductive biases that make them particularly suited for different types of data. CNNs process information through a hierarchical structure that emphasizes local relationships and translation invariance, making them exceptionally powerful for image analysis and computer vision tasks [37] [38]. In contrast, Transformers utilize self-attention mechanisms to capture global dependencies across entire sequences, establishing themselves as the architecture of choice for sequential data processing, including natural language processing (NLP) and time-series analysis [39] [40]. This architectural divergence creates a natural specialization that has significant implications for applied research, particularly in critical domains such as cancer detection where both imaging data (e.g., histopathology, radiology) and sequential data (e.g., genomic sequences, temporal patient records) play crucial roles.
Understanding the fundamental operational principles of these architectures is essential for selecting the appropriate tool for a given research problem. The comparative analysis of these deep learning powerhouses within cancer research enables more informed model selection, potentially leading to improved diagnostic accuracy, prognostic stratification, and therapeutic discovery. This guide provides an objective comparison of CNN and Transformer architectures, with supporting experimental data and methodological protocols to assist researchers in leveraging these technologies effectively.
Architectural Breakdown: Core Components and Workflows
CNN Architecture for Image Analysis
Convolutional Neural Networks are specifically designed to process data with a grid-like topology, such as images, through a series of convolutional, pooling, and fully-connected layers [41] [38]. The architecture operates on the principle of hierarchical feature learning, where early layers detect simple patterns (edges, colors, textures) and subsequent layers combine these into increasingly complex structures (shapes, objects) [41].
The CNN workflow typically follows this sequence:
- Input Layer: Receives raw pixel values of the image.
- Convolutional Layers: Apply learnable filters that slide across the input, computing dot products to create feature maps that highlight relevant patterns [41] [38]. These layers exploit two key principles: parameter sharing (using the same filter across all spatial positions) and sparse connectivity (each neuron connects only to a local region).
- Activation Functions: Introduce non-linearity to the system, typically using Rectified Linear Units (ReLU) [41].
- Pooling Layers: Perform downsampling operations (e.g., max pooling, average pooling) to reduce spatial dimensions, control overfitting, and provide translational invariance [41] [38].
- Fully-Connected Layers: Integrate extracted features for final classification or regression tasks, often using softmax activation for multi-class prediction [41].
Transformer Architecture for Sequential Data
Transformers process sequential data using an encoder-decoder structure built around self-attention mechanisms, which compute relevance scores between all elements in a sequence regardless of their positional distance [39] [40]. This global receptive field from the start allows Transformers to capture long-range dependencies more effectively than previous sequential models like RNNs and LSTMs.
The key components of the Transformer architecture include:
- Input Embedding and Positional Encoding: Convert input tokens to vectors and inject information about their position in the sequence, essential since Transformers lack inherent recurrence or convolution [39] [40].
- Multi-Head Self-Attention: The core innovation that allows the model to jointly attend to information from different representation subspaces at different positions, calculating weighted sums where weights are determined by compatibility between elements [39] [40].
- Feed-Forward Networks: Apply pointwise fully-connected transformations with non-linear activation to each position separately and identically [39].
- Layer Normalization and Residual Connections: Stabilize training and facilitate gradient flow through deep networks [39].
- Output Layer: Generates probabilities for next-token prediction or sequence classification [39].
Performance Comparison: Quantitative Analysis
Benchmark Performance Across Domains
Table 1: Performance comparison of CNN and Transformer models on standard benchmarks
| Model Architecture | ImageNet Accuracy (Top-1) | GLUE Score (NLP) | Training Efficiency (Image) | Inference Latency | Data Efficiency |
|---|---|---|---|---|---|
| CNN (ResNet-50) | 76.0-80.0% [42] | N/A | High [37] | Low [37] | High [37] |
| Vision Transformer (ViT-L/16) | 85.0-91.0% [37] [42] | N/A | Medium [37] | Medium [37] | Low [37] |
| BERT (Transformer) | N/A | 80.5-82.2 [39] | N/A | Medium [40] | Low [43] |
| Hybrid (ConvNeXt) | 87.0-90.0% [37] [42] | N/A | Medium-High [37] | Low-Medium [37] | Medium [37] |
Performance in Data-Constrained Environments
Table 2: Performance comparison with limited training data (critical for medical applications)
| Model Type | <100 Samples | ~1,000 Samples | ~10,000 Samples | >100,000 Samples |
|---|---|---|---|---|
| CNN | Moderate[cite:10] | Good[cite:10] | Excellent[cite:1] | Excellent[cite:1] |
| Transformer | Poor[cite:10] | Moderate[cite:10] | Very Good[cite:1] | State-of-the-Art[cite:1] |
The performance characteristics reveal a clear trade-off: CNNs demonstrate superior data efficiency and computational performance with limited data, while Transformers achieve higher asymptotic performance with sufficient data and compute resources [37] [43]. This has direct implications for medical imaging applications, where large, annotated datasets are often difficult to acquire. A 2023 study on radiology report classification found that Transformers required approximately 1,000 training samples to match or surpass the performance of traditional machine learning methods and CNNs [43].
Experimental Protocols for Cancer Detection Research
CNN Protocol for Histopathology Image Analysis
Objective: Classify tumor histology from whole slide images (WSIs) of tissue samples.
Dataset Preparation:
- Collect and annotate WSIs according to standardized cancer grading systems (e.g., Gleason score for prostate cancer, Nottingham grade for breast cancer).
- Perform data augmentation including rotation, flipping, color jittering, and elastic deformations to increase dataset size and improve model robustness.
- Extract patches of 512×512 pixels at 10×-20× magnification, ensuring representative sampling of tumor and normal regions.
Model Training:
- Utilize a pre-trained ResNet-50 or EfficientNet architecture with ImageNet weights.
- Replace the final classification layer with number of classes specific to your cancer grading system.
- Employ progressive training: first freeze backbone and train only classifier, then fine-tune entire network with reduced learning rate.
- Use cross-entropy loss with class weighting for imbalanced datasets.
- Optimize with SGD with momentum (0.9) or AdamW, with learning rate scheduling (cosine annealing).
Evaluation Metrics:
- Calculate accuracy, precision, recall, F1-score, and area under ROC curve (AUC).
- Perform statistical significance testing using McNemar's test or bootstrapped confidence intervals.
- Conduct attention visualization using Grad-CAM to highlight discriminative regions.
Transformer Protocol for Genomic Sequence Analysis
Objective: Predict cancer type or subtype from DNA/RNA sequencing data.
Data Preprocessing:
- Obtain genomic sequences from sources like TCGA (The Cancer Genome Atlas) or ICGC (International Cancer Genome Consortium).
- Convert nucleotide sequences to tokenized representations (k-mers of length 3-6).
- Add special tokens for sequence start ([CLS]) and separation ([SEP]) following established practices [43].
- Implement padding/truncation to handle variable sequence lengths.
Model Configuration:
- Initialize with domain-specific pre-trained weights (e.g., DNABERT, BioBERT [43]).
- Configure model dimensions: hidden size (768), number of layers (12), attention heads (12).
- Apply dropout (0.1) and layer normalization for regularization.
- Use masked language modeling (MLM) for pre-training if domain adaptation is needed.
Training Procedure:
- Use cross-entropy loss for classification tasks.
- Optimize with AdamW (learning rate: 5e-5) with linear warmup and decay.
- Train with mixed-precision (FP16) to reduce memory usage.
- Implement gradient accumulation for effective batch size adjustment.
Validation Approach:
- Perform k-fold cross-validation (k=5) to account for dataset variability.
- Conduct ablation studies to measure contribution of different components.
- Use t-SNE or UMAP to visualize learned representations.
Research Reagent Solutions: Essential Tools for Implementation
Table 3: Essential research reagents and computational tools for CNN and Transformer experiments
| Category | Specific Tools | Function | Application Context |
|---|---|---|---|
| Deep Learning Frameworks | PyTorch, TensorFlow, JAX | Model implementation, training, and inference | Both CNN and Transformer |
| Computer Vision Libraries | OpenCV, scikit-image | Image preprocessing, augmentation, and transformation | Primarily CNN |
| NLP Processing Libraries | Hugging Face Transformers, NLTK, spaCy | Tokenization, text preprocessing, model hub | Primarily Transformer |
| Medical Imaging Tools | ITK, MONAI, PyDicom | Medical image I/O, domain-specific transforms | Primarily CNN |
| Genomic Data Tools | Biopython, BEDTools, SAMtools | Genomic sequence processing and analysis | Primarily Transformer |
| Model Visualization | TensorBoard, Weights & Biases | Experiment tracking, metric visualization | Both CNN and Transformer |
| Interpretability Tools | Grad-CAM, SHAP, LIME | Model decision explanation and validation | Both CNN and Transformer |
Hybrid Architectures: Combining Strengths for Enhanced Performance
The distinction between CNNs and Transformers is increasingly blurred by hybrid architectures that leverage the strengths of both approaches. Models such as ConvNeXt modernize CNN designs by incorporating Transformer-inspired elements [37], while Vision Transformers like DaViT (Dual Attention Vision Transformer) integrate both spatial and channel attention mechanisms [42]. These hybrids demonstrate state-of-the-art performance across multiple benchmarks while maintaining favorable computational characteristics.
In cancer detection research, hybrid approaches show particular promise for multimodal data integration. For instance, a hybrid architecture could use CNN-based encoders for histopathology images alongside Transformer encoders for clinical notes or genomic data, with cross-attention mechanisms enabling information exchange between modalities. This approach captures both local morphological features critical for cancer diagnosis and global contextual relationships that inform prognosis and treatment planning.
The comparative analysis reveals that CNNs and Transformers are complementary rather than competing technologies, with optimal application depending on data characteristics and research objectives. For cancer detection research, the following guidelines emerge:
Select CNNs when working primarily with imaging data (histopathology, radiology), with limited training samples, or under computational constraints. Their inductive biases for spatial locality and translation invariance align well with visual patterns in medical images [37] [38].
Choose Transformers when processing sequential data (genomic sequences, temporal records), when global context is critical, or when large-scale pretraining can be leveraged. Their ability to capture long-range dependencies makes them valuable for integrative analysis [39] [40].
Consider hybrid approaches for multimodal data integration or when seeking state-of-the-art performance without prohibitive computational costs [37] [42].
As deep learning methodologies continue to evolve, the strategic selection and implementation of these architectural paradigms will play an increasingly important role in advancing cancer detection, prognosis prediction, and therapeutic development. Researchers should consider both current performance characteristics and emerging trends when building their analytical pipelines for maximum impact in oncological applications.
Lung cancer remains a leading cause of global cancer mortality, with early detection being critical for improving patient survival rates [15]. The application of artificial intelligence (AI), particularly machine learning (ML) and deep learning (DL), has emerged as a transformative approach for early lung cancer prediction using symptomatic and lifestyle data [15] [44]. While ML models have traditionally been used for such predictive tasks, the potential of DL models to automatically learn complex patterns from raw data presents a compelling alternative [45] [46].
This case study provides a systematic comparison of ML and DL approaches for lung cancer prediction based on symptomatic and lifestyle features. We examine their relative performance, optimal application scenarios, and implementation requirements to guide researchers and clinicians in selecting appropriate methodologies for lung cancer risk assessment.
Experimental Protocols and Performance Comparison
Dataset Characteristics and Preprocessing
The foundational dataset for this analysis was sourced from Kaggle and contained patient symptom and lifestyle factors [15]. Prior to model development, rigorous data preprocessing was employed, including:
- Feature selection using Pearson's correlation to identify the most predictive variables
- Outlier removal to enhance data quality
- Normalization to ensure features were on comparable scales [15]
This preprocessing pipeline ensured optimal model training and performance evaluation across both ML and DL approaches.
Machine Learning Implementation
Multiple traditional ML classifiers were implemented using Weka software, including:
- Decision Trees (DT)
- K-Nearest Neighbors (KNN)
- Random Forest (RF)
- Naïve Bayes (NB)
- AdaBoost
- Logistic Regression (LR)
- Support Vector Machines (SVM) [15]
These models were evaluated using K-fold cross-validation and an 80/20 train/test split to ensure robust performance assessment [15].
Deep Learning Implementation
Neural network models with 1, 2, and 3 hidden layers were developed in Python within a Jupyter Notebook environment [15]. These architectures were designed to automatically learn feature representations from the input data without extensive manual feature engineering.
Performance Comparison
Table 1: Performance Comparison of ML and DL Models for Lung Cancer Prediction
| Model Type | Specific Model | Accuracy | Key Strengths | Limitations |
|---|---|---|---|---|
| Deep Learning | Single-hidden-layer NN (800 epochs) | 92.86% | Superior accuracy with symptomatic/lifestyle data [15] | Requires careful parameter tuning [15] |
| Machine Learning | Stacking Ensemble | 88.7% AUC | Excellent for questionnaire data [47] | Lower accuracy than DL in symptomatic analysis [15] |
| Machine Learning | LightGBM | 88.4% AUC | Handles mixed-type data well [47] | Performance varies with data type [47] |
| Machine Learning | XGBoost, Logistic Regression | ~100% (staging) | Excellent for cancer level classification [48] | Specialized to staging task [48] |
| Deep Learning | 3D CNN (CT scans) | 86% AUROC | Superior with imaging data [45] | Requires volumetric data [45] |
| Deep Learning | 2D CNN (CT scans) | 79% AUROC | Good performance with 2D slices [45] | Lower performance than 3D models [45] |
Key Findings and Interpretation
Performance Analysis
The comparative analysis revealed that a single-hidden-layer neural network trained for 800 epochs achieved the highest prediction accuracy of 92.86% using symptomatic and lifestyle data [15]. This DL model outperformed all traditional ML approaches implemented in the study, demonstrating the advantage of neural networks in capturing complex relationships between patient features and cancer risk [15].
However, the superiority of DL models is context-dependent. In lung cancer staging tasks, traditional ML models like XGBoost and Logistic Regression achieved nearly perfect classification accuracy (approximately 100%), outperforming DL approaches [48]. This suggests that for well-structured clinical data with clear feature relationships, traditional ML models can provide exceptional performance without the complexity of DL architectures.
Impact of Feature Selection
The study highlighted the critical importance of feature selection for enhancing model accuracy across both ML and DL approaches [15]. By employing Pearson's correlation for feature selection before model training, researchers significantly improved predictive performance, underscoring the value of thoughtful feature engineering even in DL approaches.
Data Modality Considerations
The optimal model choice depends heavily on data modality:
- Symptomatic and lifestyle data: DL models showed superior performance [15]
- Structured epidemiological questionnaires: Ensemble ML methods excelled [47]
- CT scan data: 3D DL models outperformed 2D variants [45]
Methodology and Workflow
Experimental Workflow
The following diagram illustrates the comprehensive experimental workflow for comparing ML and DL models in lung cancer prediction:
Model Architecture Comparison
The structural differences between ML and DL approaches significantly impact their application and performance:
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Research Tools for ML/DL Lung Cancer Prediction
| Tool/Resource | Type | Function | Application Context |
|---|---|---|---|
| Weka | Software Platform | Implementation of traditional ML algorithms [15] | Comparative ML model development |
| Python with Jupyter Notebook | Programming Environment | DL model development and experimentation [15] | Neural network implementation |
| Kaggle Lung Cancer Dataset | Data Resource | Symptomatic and lifestyle features for prediction [15] | Model training and validation |
| NLST (National Lung Screening Trial) Dataset | Data Resource | CT scans and clinical data [45] | Imaging-based model development |
| MATLAB R2024b | Software Platform | Image processing and ML pipeline development [49] [50] | Medical image analysis |
| Scikit-learn Library | Code Library | ML model implementation and hyperparameter tuning [47] | Traditional model development |
This case study demonstrates that both ML and DL approaches offer distinct advantages for lung cancer prediction from symptomatic data. The single-hidden-layer neural network achieved superior performance (92.86% accuracy) compared to traditional ML models, highlighting DL's capability to discern complex patterns in symptomatic and lifestyle data [15]. However, traditional ML models, particularly ensemble methods, remain highly competitive for structured clinical data and cancer staging tasks [48] [47].
The selection between ML and DL approaches should be guided by data characteristics, available computational resources, and specific clinical objectives. DL models show particular promise for complex pattern recognition in heterogeneous symptomatic data, while carefully tuned ML models provide excellent performance for structured clinical variables with greater interpretability. Future research should focus on developing hybrid approaches that leverage the strengths of both methodologies while enhancing model transparency for clinical adoption.
The integration of artificial intelligence (AI), particularly deep learning (DL), into oncology represents a paradigm shift in cancer detection and diagnosis. This case study focuses on the application of DL-driven detection in breast cancer imaging and pathology, situating it within the broader thesis of comparing machine learning (ML) with DL for cancer detection research. While traditional ML models often rely on handcrafted features and can struggle with the complexity and high dimensionality of medical images, DL models, with their hierarchical learning structure, can automatically extract relevant features from raw data, offering a significant performance advantage for complex visual tasks [51]. This analysis will objectively compare the performance of various DL architectures against traditional methods and other alternatives, supported by experimental data and detailed methodologies.
Performance Comparison: Deep Learning vs. Alternatives
Deep learning models have demonstrated remarkable accuracy in breast cancer detection across multiple imaging modalities, often surpassing both traditional machine learning methods and human expert performance.
Performance Across Imaging Modalities
Table 1: Performance of DL Models in Breast Cancer Detection Across Different Modalities
| Imaging Modality | Deep Learning Model | Reported Performance | Comparative Context |
|---|---|---|---|
| Mammography | Convolutional Neural Network (CNN) | Accuracy: 99.96% [52] | Surpasses traditional mammography sensitivity (77-95%) and specificity (92-95%) [52]. |
| Ultrasound | Convolutional Neural Network (CNN) | Accuracy: 100% [52] | Higher sensitivity than standard ultrasound (67.2%) [10]. |
| Histopathology | Vision Transformer (ViT) | Accuracy: 99.99% [10] | Exceeds the accuracy of many ML-based pathomics models. |
| Multimodal (Mammography + Ultrasound) | Deep Learning-based Multimodal Model | AUC: 0.968, Specificity: 96.41% [53] | Outperforms single-modal models in specificity, accuracy, and precision [53]. |
| Thermal Imaging | Optimized Deep Learning Models | Diagnostic Accuracy: 97-100% [52] | Presents a cost-effective, less hazardous screening option. |
Deep Learning vs. Traditional Machine Learning
The performance gap between DL and traditional ML is evident not only in raw accuracy but also in the scope of application. For instance, a comprehensive review noted that deep learning models achieve 90–99% accuracy across various breast imaging modalities, whereas traditional ML models like XGBoost, while powerful for structured data, are typically applied to risk prediction from clinical data, achieving high accuracy (99.12%) in that specific domain [52]. The key differentiator is DL's ability to process raw, high-dimensional image data end-to-end, eliminating the need for manual feature engineering which is a bottleneck and limitation of traditional ML [51].
In the context of image analysis, traditional ML pipelines involve distinct steps of image acquisition, tumor segmentation, feature extraction, and model training. In contrast, DL models, particularly CNNs, process entire image sequences in an end-to-end manner, automatically learning to extract hierarchical features directly from pixels, which enables them to identify more complex patterns [54].
Detailed Experimental Protocols and Methodologies
Protocol for a Multimodal Deep Learning Model
A study exploring a multimodal model using mammography and ultrasound images provides a robust experimental framework for comparison [53].
Data Acquisition and Preprocessing: The study collected data from 790 patients, including 2,235 mammography images and 1,348 ultrasound images.
- Tumor Localization in Ultrasound: The YOLOv8 object detection model was employed to autonomously localize and crop tumor regions in ultrasound images, eliminating irrelevant interference like text and artifacts.
- Grayscale Normalization: The min-max normalization method was applied to standardize grayscale levels across all images, mitigating variations due to equipment differences.
- Data Augmentation: To address data imbalance and scarcity, techniques including random horizontal flipping, random vertical flipping, and elastic deformation were used to increase sample diversity and quantity.
Model Construction and Training:
- Baseline Model Selection: Six deep learning models (ResNet-18, ResNet-50, ResNext-50, Inception v3, VGG16, GoogleNet) were compared to identify the best-performing architecture for each image modality.
- Fusion Strategy: A late fusion strategy was adopted. This involves training separate models for mammography and ultrasound images. The features extracted from each modality are then fused and fed into a final classifier. This approach is suitable when significant differences exist between the modalities.
- Transfer Learning: Models were pre-trained on the ImageNet dataset of natural images, with subsequent fine-tuning on the medical image datasets, a method proven superior to training from scratch.
Diagram 1: Workflow of a Multimodal Deep Learning Model for Breast Cancer Classification
Protocol for a Novel AI Pathology Model (SMMILe)
The SMMILe model represents a significant advancement in computational pathology by addressing the trade-off between whole-slide image classification and spatial quantification [55].
- Mathematical Foundation: The research team mathematically proved that models using instance-level aggregation could achieve superior spatial quantification without compromising the performance of whole-slide image prediction.
- Model Architecture: SMMILe (Super-patch based Measurable Multi-Instance Learning) was introduced as a novel weak supervision algorithm.
- Training and Evaluation:
- Data: The model was evaluated on 8 datasets comprising 3,850 whole-slide images across 6 cancer types, including breast cancer.
- Task: It was tested on three highly diverse classification tasks.
- Comparison: SMMILe was systematically compared against nine existing mainstream computational pathology methods using two different image encoders.
- Outcome: Without any manual spatial annotations, SMMILe could accurately generate a spatial map of tumors, pinpointing their location, boundaries, and the distribution of different subtypes. It matched or exceeded state-of-the-art performance in whole-slide image classification while excelling in spatial quantification, especially in complex multi-label tasks. The model drastically reduced analysis time from 20 minutes for a human to about 1 minute per slide.
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 2: Key Research Reagent Solutions for DL-Driven Cancer Detection
| Item / Solution | Function in Research | Exemplars / Standards |
|---|---|---|
| Annotated Medical Image Datasets | Serves as the foundational training and validation data for developing and testing deep learning models. | BreakHis dataset [10]; In-house datasets with expert radiologist/pathologist annotations. |
| Pre-trained Deep Learning Models | Provides a robust starting point for model development via transfer learning, improving performance and reducing data requirements. | Models pre-trained on ImageNet (e.g., ResNet, VGG) [53]; Pathology-specific foundation models [55]. |
| Radiomics/Pathomics Feature Extraction Tools | Enables quantitative feature extraction from medical images for use in traditional ML or hybrid models. | PyRadiomics Python package [56]. |
| Feature Selection Algorithms | Identifies the most relevant and non-redundant features from extracted radiomics/pathomics data to improve model generalizability. | LASSO (Least Absolute Shrinkage and Selection Operator) [56]. |
| Computational Hardware | Accelerates the computationally intensive training process of deep neural networks. | GPUs (Graphics Processing Units). |
| Model Interpretation Frameworks | Provides insights into model decision-making, enhancing trust and clinical translatability (Explainable AI - XAI). | Grad-CAM, SHAP [52]. |
Critical Analysis and Future Directions
Despite the impressive performance metrics, several challenges persist in the clinical implementation of DL models for breast cancer detection. Key issues include data variability, model interpretability (the "black-box" problem), and the risk of diminished performance on external datasets from different institutions due to domain shift [52] [10]. Ethical, privacy, and regulatory constraints also present significant barriers to widespread adoption [10].
Future research and development priorities, as identified across the literature, include:
- Multi-modal Data Integration: Combining imaging with clinicopathological and genomic data for individualized risk stratification [10] [57].
- Prospective Validation: Conducting large-scale, multi-site prospective trials to validate model efficacy in real-world clinical settings [58] [57].
- Federated Learning: Utilizing this privacy-preserving technique to train models on decentralized data without sharing sensitive patient information [57].
- Explainable AI (XAI): Advancing techniques like Grad-CAM and SHAP to make model decisions more transparent and trustworthy for clinicians [52].
In conclusion, deep learning has undeniably set a new benchmark for accuracy in breast cancer detection across imaging and pathology, outperforming traditional machine learning and, in many cases, human experts. However, the transition from a powerful research tool to a fully integrated clinical asset hinges on overcoming challenges related to generalizability, interpretability, and implementation. The future of the field lies not in replacing clinicians, but in developing robust, transparent, and augmentative AI systems that can be seamlessly woven into the clinical workflow to improve patient outcomes.
The integration of artificial intelligence (AI) into oncology represents a paradigm shift in cancer care, moving from siloed data analysis to holistic, multi-faceted approaches. Two technological frontiers are particularly transformative: multimodal artificial intelligence (MMAI) and large language models (LLMs). While both leverage advanced AI, they differ fundamentally in architecture, application, and data requirements. Multimodal AI specializes in processing and interpreting diverse, complementary data types—such as genomics, medical imaging, and clinical records—to generate clinically actionable insights for diagnosis, prognosis, and treatment planning [59] [60]. In contrast, LLMs excel at parsing, generating, and understanding complex human language, showing great potential for tasks such as clinical documentation, trial matching, and decoding various types of clinical data to support decision-making [61]. This guide provides a comparative analysis of these approaches, focusing on their performance, experimental protocols, and practical implementation for cancer research and drug development.
Comparative Performance Analysis
The table below summarizes the core characteristics and documented performance of MMAI and LLM approaches in oncology applications.
Table 1: Performance and Characteristics of MMAI and LLMs in Oncology
| Feature | Multimodal AI (MMAI) | Large Language Models (LLMs) |
|---|---|---|
| Core Function | Integrates diverse data types (imaging, genomics, clinical) for comprehensive analysis [59] [60]. | Processes and generates human language from textual or structured inputs [61]. |
| Primary Applications | Early detection, tumor characterization, prognosis, personalized treatment planning [59] [62]. | Clinical documentation, trial matching, information extraction from records, patient communication [61]. |
| Key Performance Metrics | Sensitivity, Specificity, AUC (Area Under the Curve) [59] [63]. | Accuracy, Precision, Recall on language-based tasks [61]. |
| Sample Performance Data | - OncoSeek (MCED test): AUC 0.829, 58.4% sensitivity, 92.0% specificity across 14 cancer types [63].- Sybil AI (Lung Cancer): Up to 0.92 ROC–AUC for lung cancer risk prediction [59].- Anti-HER2 Therapy: AUC=0.91 for predicting therapy response [60]. | Performance highly task-dependent; active research area for clinical application [61]. |
| Data Requirements | Large, curated, multimodal datasets (histopathology, genomics, radiomics, clinical data) [59] [3]. | Large-scale textual corpora (clinical notes, scientific literature, EHRs) [61]. |
| Key Challenge | Data standardization, computational complexity, model interpretability [59] [60]. | "Hallucinations" (generating incorrect information), ethical issues, data privacy [61]. |
Experimental Protocols and Methodologies
Multimodal AI for Multi-Cancer Early Detection
Objective: To develop and validate a blood-based test (OncoSeek) for Multi-Cancer Early Detection (MCED) using AI to analyze protein tumor markers (PTMs) and clinical data [63].
Methodology:
- Sample Collection: A large-scale, multi-centre study was conducted, ultimately involving 15,122 participants (3,029 cancer patients, 12,093 non-cancer individuals) from seven centres across three countries [63].
- Biomarker Analysis: The study integrated a panel of seven selected protein tumour markers (PTMs), analyzed from blood samples (both plasma and serum) [63].
- Platform Integration: Analyses were performed across four different quantification platforms (including Roche Cobas e411/e601 and Bio-Rad Bio-Plex 200) to test for consistency [63].
- AI Integration & Statistical Analysis: An AI algorithm was applied to integrate the quantitative PTM data with individual clinical information (e.g., age, gender). The output was a cancer probability score used to classify samples [63].
- Validation: Performance was evaluated in a blinded, prospective cohort and a symptomatic patient cohort to assess real-world diagnostic potential. The primary outcomes were sensitivity (ability to correctly identify cancer) and specificity (ability to correctly rule out cancer) [63].
Deep Learning for Multi-Cancer Image Classification
Objective: To automate cancer detection and classify seven cancer types (brain, oral, breast, kidney, leukemia, lung/colon, cervical) from histopathology images using deep learning models [3].
Methodology:
- Data Acquisition & Preprocessing: Publicly available image datasets for the seven cancer types were collected. Images underwent preprocessing, including grayscale conversion and noise removal [3].
- Image Segmentation & Feature Extraction: Advanced segmentation techniques, such as Otsu binarization and watershed transformation, were applied. Contour feature extraction was then performed, computing parameters like perimeter, area, and epsilon to enhance cancer region identification [3].
- Model Training and Evaluation: Ten different pre-trained convolutional neural networks (CNNs)—including DenseNet121, DenseNet201, Xception, and InceptionV3—were used as the core deep learning architectures. These models were evaluated using metrics such as accuracy, precision, recall, F1-score, and Root Mean Square Error (RMSE) [3].
- Results: DenseNet121 achieved the highest validation accuracy of 99.94% with a loss of 0.0017, demonstrating the capability of deep learning for highly accurate cancer image classification [3].
Workflow and Pathway Diagrams
Multimodal AI Data Integration Workflow
LLM Processing Pathway in Oncology
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Research Tools for AI-Driven Oncology
| Tool / Resource | Function in Research | Application Context |
|---|---|---|
| Protein Tumour Markers (PTMs) | Biomarkers measured in blood for early cancer detection; used as input features for AI models like OncoSeek [63]. | Multimodal AI for MCED |
| Digital Pathology Whole-Slide Images (WSIs) | High-resolution digitized histopathology slides; the raw data for training deep learning models in cancer diagnosis [59] [3]. | MMAI & Deep Learning |
| Open-Source AI Frameworks (e.g., Project MONAI) | Provides pre-trained models and tools specifically designed for medical imaging AI, built on PyTorch [59]. | MMAI for Medical Imaging |
| Circulating Tumor DNA (ctDNA) | Genetic material from tumors found in blood; analyzed by AI for early detection, monitoring treatment response, and identifying resistance mutations [64] [65]. | MMAI for Liquid Biopsy |
| Clinical Trial Matching Engines (e.g., HopeLLM) | LLM-powered platforms that parse patient records to identify eligible clinical trials, automating a traditionally manual screening process [66] [61]. | LLMs for Trial Optimization |
| Spatial Transcriptomics Data | Provides gene expression data within the context of tissue architecture; integrated with histology images by MMAI to characterize the tumor microenvironment [60]. | MMAI for Tumor Biology |
The comparative analysis reveals that Multimodal AI and Large Language Models are highly complementary technologies with distinct strengths in the oncology landscape. Multimodal AI demonstrates superior performance in clinical tasks requiring the synthesis of complex, heterogeneous biological data, achieving high accuracy in concrete endpoints like cancer diagnosis, subtyping, and therapy response prediction [59] [60] [63]. LLMs, while still emerging in direct clinical application, show immense potential for optimizing workflows, extracting information from textual data, and improving the efficiency of clinical and research operations [61]. The future of AI in oncology likely lies not in choosing one over the other, but in strategically deploying both to create a more comprehensive, efficient, and personalized cancer care ecosystem. Researchers and drug developers should select the tool based on the specific question at hand: MMAI for deep biological insight and clinical prediction, and LLMs for enhancing data management and operational efficiency.
Navigating Development Hurdles and Enhancing Model Performance
Data scarcity presents a significant bottleneck in medical research, particularly in the development of machine learning (ML) and deep learning (DL) models for cancer detection. Small, imbalanced datasets can lead to models that perform poorly and fail to generalize across diverse patient populations and clinical institutions. To combat this, two innovative technologies have emerged: Federated Learning (FL), which enables collaborative model training without sharing sensitive patient data, and synthetic data generation using Generative Adversarial Networks (GANs), which creates artificial datasets to augment real-world data [7] [67]. This guide provides a comparative analysis of these approaches, focusing on their implementation, performance, and practical application for researchers and drug development professionals in oncology.
Core Technologies and Experimental Approaches
Federated Learning Explained
Federated Learning is a decentralized machine learning paradigm. Instead of pooling sensitive patient data into a central server, a global model is trained by aggregating model updates (e.g., weights and gradients) from multiple clients, each with their own local dataset. The raw data never leaves its original institution, thereby preserving privacy and complying with regulations like GDPR and HIPAA [68].
The most common FL algorithm is Federated Averaging (FedAvg), where the central server averages the model parameters received from clients to update the global model [69]. Variants like FedProx build upon FedAvg by introducing a proximal term to the local loss function, which helps to stabilize training when data is non-Independent and Identically Distributed (non-IID) across clients [69].
GANs for Synthetic Data Generation
Generative Adversarial Networks (GANs) are a class of DL models designed to generate new data that resembles a given training set. A typical GAN consists of two neural networks:
- Generator: Learns to create synthetic data from random noise.
- Discriminator: Learns to distinguish between real data and synthetic data produced by the generator.
These two networks are trained in an adversarial process until the generator produces highly realistic synthetic data [69]. In medical imaging, Deep Convolutional GANs (DCGANs) are often used for their stability and effectiveness in generating high-quality images [69]. For tabular clinical data, models like Conditional Tabular GAN (CTGAN) are more appropriate [67].
Integrated Workflow: Combining FL and GANs
The synergy of FL and GANs creates a powerful framework for addressing data scarcity while maintaining privacy. The typical integrated workflow is illustrated below and involves both centralized synthetic data creation and decentralized model training.
Diagram 1: Integrated FL and GAN Workflow for Collaborative Cancer Detection
Performance Comparison and Experimental Data
The integration of FL and GANs has been empirically validated across various cancer types and data modalities. The table below summarizes key performance metrics from recent studies.
Table 1: Performance Comparison of Federated Learning Frameworks Integrated with GANs
| Cancer Type / Modality | Proposed Framework | Key Methodology | Comparative Performance (Accuracy / AUC) | Key Challenge Addressed |
|---|---|---|---|---|
| Breast Cancer (Ultrasound) [69] | Federated Learning with DCGAN Augmentation | FedAvg/FedProx with class-specific DCGANs for synthetic image sharing. | FedProx + GAN: AUC 0.9538 vs FedProx alone: AUC 0.9429. Excessive synthetic data reduced performance. | Data scarcity, non-IID data across institutions. |
| Lung, Prostate, Breast Cancer (EMR Data) [70] | FedCSCD-GAN | FL + Cramer GAN with quasi-identifier anonymization and f-differential privacy. | Diagnosis Accuracy: Lung: 97.80%, Prostate: 96.95%, Breast: 97%. | Data privacy, security, and collaboration. |
| Acute Myeloid Leukemia (Tabular Data) [67] | Horizontal FL with CTGAN & FedTabDiff | Evaluated fidelity-privacy trade-off of federating SDG models. | Fidelity statistically significant deterioration up to 21% (CTGAN) and 62% (FedTabDiff). Privacy was maintained. | Data scarcity and dispersion in a rare disease. |
| Brain Tumor (MRI) [68] | FedHG (Federated High-Generalization) | VAT-integrated 3D U-Net with novel aggregation. | Dice Score: 2.2% improvement over baseline FL, within 3% of centralized training. | Limited annotated data, data imbalance, non-IID data. |
The data reveals several critical insights. First, integrating GANs with FL consistently improves model performance (e.g., AUC and accuracy) compared to standalone FL, by mitigating data scarcity and imbalance [69] [70]. Second, the quality and quantity of synthetic data are crucial; excessive or low-fidelity synthetic data can degrade model performance, highlighting the need for careful calibration [69] [67]. Finally, advanced FL aggregation strategies, like those used in FedHG, can significantly bridge the performance gap with centralized training, making FL a more viable and robust option [68].
Detailed Experimental Protocols
Federated Breast Cancer Detection with DCGAN Augmentation
This experiment provides a clear protocol for integrating GAN-based augmentation into an FL pipeline for medical imaging [69].
- Objective: To improve breast ultrasound image classification in a federated setting by augmenting local datasets with synthetic images.
- Datasets: BUSI, BUS-BRA, and UDIAT public breast ultrasound datasets.
- FL Setup: A realistic FL environment with data split across multiple clients to simulate multi-institutional collaboration.
- Synthetic Data Generation:
- Two class-specific DCGANs (for benign and malignant lesions) were trained centrally using combined training and validation data.
- The generator network mapped a random noise vector, concatenated with a lesion mask, to a grayscale ultrasound image.
- The discriminator was trained to differentiate between real and synthetic images.
- Federated Training:
- A suitable number of synthetic images were distributed to clients.
- Local models were trained on a combination of real local data and the distributed synthetic data.
- Model updates were aggregated using FedAvg or FedProx.
- Key Finding: A balanced ratio of real to synthetic data was critical. The optimal setup improved FedProx's average AUC from 0.9429 to 0.9538.
FedCSCD-GAN for Multi-Cancer Diagnosis
This framework emphasizes security and privacy while leveraging synthetic data for improved cancer diagnosis [70].
- Objective: To create a secure and collaborative framework for clinical cancer diagnosis using FL and GANs.
- Data Preprocessing and Privacy:
- Attribute Segmentation: Identified Quasi-Identifiers (QIden - e.g., age, gender) and Confidential Information (CI - e.g., diagnosis) in Electronic Health Records (EHRs).
- Anonymization: Applied f-differential privacy anonymization to QIden attributes before mixing them with CI.
- Synthetic Data Generation: Trained a Cramer GAN on the anonymized data. The Cramer distance was used for improved training stability and efficiency.
- Federated Training:
- Each edge-based hospital (client) trained its local discriminator and GAN generator.
- Only the trained variables were uploaded to a cloud server for aggregation, creating a global GAN model.
- Key Finding: The framework achieved high diagnostic accuracy (up to 97.8%) for lung, prostate, and breast cancer while ensuring robust patient data privacy.
The Scientist's Toolkit: Essential Research Reagents and Materials
For researchers aiming to implement the methodologies described, the following table details key computational "reagents" and their functions.
Table 2: Key Research Reagents and Computational Tools
| Tool / Component | Category | Primary Function | Exemplar Use Case |
|---|---|---|---|
| FedAvg / FedProx [69] | Federated Learning Algorithm | Aggregates local model updates from clients to form a global model. | Baseline FL aggregation; FedProx handles statistical heterogeneity better. |
| DCGAN (Deep Convolutional GAN) [69] | Generative Model | Generates synthetic images using convolutional layers for stability and quality. | Creating synthetic breast ultrasound images for data augmentation. |
| Cramer GAN [70] | Generative Model | Uses Cramer distance to improve training stability and quality of generated data. | Generating synthetic electronic health record (EHR) data. |
| Conditional Tabular GAN (CTGAN) [67] | Generative Model | Specialized for generating synthetic tabular data, handling mixed data types. | Augmenting clinical tabular data for rare diseases like Acute Myeloid Leukemia. |
| Differential Privacy (DP) [70] [67] | Privacy-Enhancing Technology | Provides mathematical privacy guarantees by adding calibrated noise to data or models. | Anonymizing quasi-identifiers in EHRs before GAN training. |
| 3D U-Net [68] | Deep Learning Architecture | Volumetric segmentation of medical images (e.g., MRI, CT). | Segmenting brain tumors from MRI scans in a federated setting. |
The logical relationships and data flow between these core components in a typical secure federated learning setup are visualized in the following diagram.
Diagram 2: Core Components and Secure Data Flow in Federated Learning with GANs
Federated Learning and GAN-based synthetic data generation are not mutually exclusive but are highly complementary technologies in the fight against data scarcity in oncology research. The experimental data and protocols outlined in this guide demonstrate that their integrated use can significantly enhance the performance and generalizability of ML/DL models for cancer detection while rigorously protecting patient privacy. For researchers, the choice of specific FL algorithms and GAN architectures should be guided by the data modality and the specific clinical challenge. As these technologies continue to mature, they hold the promise of accelerating the development of robust, equitable, and clinically impactful AI tools for cancer diagnostics and drug development.
Combating Bias and Ensuring Generalizability Across Diverse Populations
The application of Artificial Intelligence (AI) in cancer detection represents one of the most promising advancements in modern oncology, with both machine learning (ML) and deep learning (DL) approaches demonstrating remarkable diagnostic capabilities. However, the transition from research environments to widespread clinical implementation faces a significant hurdle: combating bias and ensuring generalizability across diverse patient populations [71]. The performance of AI models can be substantially compromised when applied to demographics, imaging equipment, or healthcare systems not represented in their training data, potentially leading to disparities in diagnostic accuracy [2].
This challenge stems from multiple factors. Medical data is often sourced from single institutions or specific geographic regions, resulting in datasets that lack the ethnic, genetic, and environmental diversity of global populations [2]. Furthermore, variations in medical imaging equipment, protocols, and sample processing techniques introduce technical heterogeneity that can impair model performance when deployed in new clinical settings [71]. The "black box" nature of many complex DL models further complicates this issue, as it obstructs the identification of when and why models might fail on unfamiliar data [2].
Addressing these limitations requires concerted efforts across the research community, including the development of more robust validation methodologies, the creation of diverse multicenter datasets, and the implementation of technical solutions that enhance model transparency and fairness [71]. This analysis examines the comparative strengths and limitations of ML and DL approaches in achieving these critical objectives, providing researchers with a framework for developing more generalizable cancer detection systems.
Performance Comparison: ML vs. DL Across Cancer Types
Table 1: Comparative Performance of ML and DL Models in Cancer Detection
| Cancer Type | Best Performing ML Model | ML Accuracy | Best Performing DL Model | DL Accuracy | Generalizability Challenges Documented |
|---|---|---|---|---|---|
| Breast Cancer | Logistic Regression [72] | 98.1% [72] | DenseNet121 [3] | 99.94% [3] | Model performance variance across different mammography devices and patient demographics [73] |
| Lung Cancer | DAELGNN Framework [74] | 99.7% [74] | Custom CNN [26] | 99.5% (Approx.) [26] | Sensitivity to CT scan parameters and reconstruction algorithms [73] |
| Brain Tumor | Random Forest [73] | 99.3% (Approx.) [73] | Hybrid DNN with Fuzzy Clustering [3] | 99.2% (Approx.) [3] | Contrast and resolution variations in MRI across clinical centers [71] |
| Skin Cancer | SVM [26] | 99.89% [26] | CNN Ensemble [26] | 100% [26] | Accuracy differences of up to 28.8% reported between model performances [26] |
| Colorectal Cancer | XGBoost with SimCSE [74] | 75% [74] | CNN with Genomic Data [74] | 73% (Approx.) [74] | Limited diversity in genomic datasets [74] |
The performance comparison between ML and DL approaches reveals a complex landscape where accuracy metrics alone are insufficient indicators of real-world applicability. While DL models frequently achieve superior accuracy rates in controlled environments—reaching up to 100% for specific cancer detection tasks—this performance often comes with increased vulnerability to data distribution shifts [26]. The substantial accuracy variance observed in skin cancer detection (up to 28.8% difference between highest and lowest performing models) highlights the sensitivity of these systems to variations in input data characteristics [26].
Traditional ML models such as Logistic Regression and Support Vector Machines demonstrate strong performance for specific cancer types, with the advantage of typically being more interpretable than their DL counterparts [72]. This interpretability facilitates the identification of potential bias sources, as feature importance can be more readily analyzed and understood. However, ML models generally require careful manual feature engineering, which may inadvertently introduce human bias or miss subtle patterns detectable by DL systems [74].
The generalization gap becomes most apparent when comparing reported accuracy on benchmark datasets versus real-world performance. For instance, while lung cancer detection models achieve exceptional results (up to 99.7% for ML and 99.5% for DL), their sensitivity to variations in CT scanning protocols presents significant deployment challenges [74]. Similarly, the relatively lower performance of both approaches on colorectal cancer (75% for ML and 73% for DL) underscores the difficulties in managing heterogeneous genomic data, which exhibits substantial diversity across populations [74].
Experimental Protocols for Bias Assessment
Multicenter Validation Frameworks
Rigorous experimental design is essential for quantifying and addressing bias in cancer detection models. The most effective protocols incorporate multicenter validation using datasets collected from geographically distinct institutions with diverse patient demographics [2]. This approach involves intentionally recruiting participants from varying ethnic backgrounds, age groups, and socioeconomic statuses to create a representative sample. Researchers should implement stratified sampling techniques to ensure adequate representation of minority populations that are often underrepresented in medical datasets [71].
The validation protocol must maintain strict separation between training, validation, and test sets, with patients from each clinical site distributed across all three sets to prevent data leakage. Performance metrics should be calculated not only overall but also disaggregated by demographic subgroups, imaging device manufacturers, and clinical protocols to identify specific failure modes [2]. Model calibration should be assessed across subgroups to ensure prediction confidence aligns with accuracy across populations.
Data Augmentation and Normalization Techniques
Technical standardization procedures are critical for controlling variability introduced by differing medical equipment and protocols. For imaging data, these include implementing normalization algorithms that adjust for variations in contrast, resolution, and staining protocols [3]. Data augmentation techniques such as random rotations, flips, and color space adjustments can improve robustness, though they must be applied consistently across training and validation phases [2].
For genomic data, batch effect correction methods must be employed to address technical variations between sequencing platforms and laboratories [74]. Cross-platform normalization algorithms should be applied to ensure feature compatibility, particularly when integrating data from multiple sources. The experimental protocol should include ablation studies to quantify the individual contribution of each normalization technique to overall model robustness.
Technical Approaches to Enhance Generalizability
Multimodal Data Integration
Table 2: Technical Strategies for Improving Model Generalizability
| Technical Approach | Implementation Method | Applicable Cancer Types | Documented Efficacy | Limitations |
|---|---|---|---|---|
| Multimodal Learning | Combining imaging, genomic, and clinical data using autoencoders or late fusion [71] | Breast, Brain, Lung [2] | Improves accuracy by 5-15% compared to single-mode models [71] | Increased complexity; requires aligned multimodal datasets [2] |
| Explainable AI (XAI) | Saliency maps, attention mechanisms, SHAP values [71] | All types, particularly high-stakes diagnoses [71] | Enables identification of spurious correlations and bias sources [71] | May reduce model performance; adds computational overhead [2] |
| Transfer Learning | Pretraining on natural images followed by medical domain adaptation [3] | Skin, Breast, Lung [3] | Reduces data requirements by 30-50% while maintaining accuracy [3] | Risk of transferring irrelevant features from source domain [2] |
| Federated Learning | Training models across institutions without data sharing [2] | All types, particularly rare cancers [2] | Improves generalization while preserving patient privacy [2] | Computational complexity; communication bottlenecks [2] |
| Domain Adaptation | Adversarial training to learn domain-invariant features [71] | Types with significant technical variability (e.g., histopathology) [71] | Redures performance drop across domains by 10-25% [71] | Requires representative target domain data [71] |
Integrating diverse data modalities represents one of the most promising approaches for creating robust cancer detection systems. Multimodal learning frameworks combine complementary data types—such as histopathological images with genomic sequencing data—to develop more comprehensive representations of cancer biology [71]. This approach enables models to learn invariant features that remain predictive across different populations and technical platforms.
Implementation typically involves using autoencoder architectures to create meaningful representations of each data modality, followed by fusion layers that integrate these representations into a unified feature space [71]. For example, graph convolutional neural networks (GCNNs) can incorporate protein-protein interaction networks with genomic data to leverage known biological relationships, thereby enhancing both performance and biological plausibility [71]. Similarly, combining CT imaging with clinical data has been shown to improve lung cancer detection accuracy while reducing false positives across diverse patient populations [2].
Explainable AI and Model Interpretation
The "black box" problem in DL represents a significant barrier to clinical adoption, particularly for models intended for use across diverse populations. Explainable AI (XAI) methods address this limitation by providing visibility into model decision processes, enabling researchers to identify when models rely on spurious correlations or biologically implausible features [71]. Saliency maps, attention mechanisms, and feature importance scores allow clinicians to verify that models focus on clinically relevant image regions or genomic markers [71].
Technical approaches include post-hoc explanation methods such as SHAP (SHapley Additive exPlanations) and LIME (Local Interpretable Model-agnostic Explanations), which estimate feature importance for individual predictions [71]. Alternatively, inherently interpretable architectures such as attention-based transformers provide built-in explanations by highlighting which parts of an input sequence or image region contributed most to the final prediction [2]. These explanations facilitate the detection of dataset bias by revealing when models inappropriately rely on technical artifacts or demographic proxies rather than genuine cancer signatures.
Figure 1: Comprehensive Framework for Developing Generalizable Cancer Detection Models
Table 3: Essential Research Resources for Bias-Resistant Cancer Detection
| Resource Category | Specific Tools & Databases | Primary Application | Key Features for Generalizability |
|---|---|---|---|
| Public Genomic Databases | TCGA [71], ICGC [71], GEO [71] | Model training and validation | Multicenter design with associated clinical data |
| Medical Imaging Archives | LIDC-IDRI [74], JSRT [74], ChestX-ray14 [74] | Algorithm development and testing | Multiple institution contributions with varied equipment |
| Data Processing Tools | CUDA [3], TensorFlow [3], PyTorch [3] | Model implementation and training | Support for multimodal data structures |
| Explainability Libraries | SHAP [71], LIME [71], Captum [71] | Model interpretation and bias detection | Feature importance visualization across subgroups |
| Federated Learning Platforms | NVIDIA FLARE [2], OpenFL [2] | Privacy-preserving collaborative training | Enables model development across institutions without data sharing |
| Biomedical Knowledge Graphs | STRING [71], Reactome [71] | Biological prior integration | Protein-protein interactions and pathway information |
The experimental resources required for developing generalizable cancer detection systems extend beyond conventional laboratory reagents to encompass specialized computational tools and data resources. Public genomic databases such as The Cancer Genome Atlas (TCGA) and International Cancer Genome Consortium (ICGC) provide comprehensively characterized cancer datasets that serve as benchmarks for initial model development [71]. These resources offer multidimensional data including genomic, transcriptomic, and clinical information from thousands of patients, though researchers should note their limitations in demographic diversity.
For medical imaging analysis, archives such as the Lung Image Database Consortium (LIDC-IDRI) and ChestX-ray14 provide curated image collections with expert annotations, enabling standardized comparison across different algorithms [74]. Computational frameworks including TensorFlow and PyTorch offer implementations of advanced architectures specifically designed for handling heterogeneous medical data, while specialized libraries such as SHAP and LIME facilitate model interpretation and bias detection [71].
Emerging platforms for federated learning represent particularly valuable tools for addressing data scarcity while preserving patient privacy. These systems enable model training across multiple institutions without transferring sensitive patient data, thereby facilitating the inclusion of more diverse populations while complying with data protection regulations [2]. Integration of biomedical knowledge graphs such as STRING provides prior biological knowledge that can constrain models to more physiologically plausible decision pathways, enhancing both interpretability and generalizability [71].
The comparative analysis of ML and DL approaches for cancer detection reveals that while both methodologies offer substantial diagnostic capabilities, their real-world utility ultimately depends on overcoming critical challenges in bias and generalizability. DL models typically achieve higher peak performance on benchmark datasets but demonstrate greater vulnerability to data distribution shifts and technical variations across clinical settings [26] [3]. Traditional ML approaches offer advantages in interpretability and data efficiency but may lack the capacity to detect subtle patterns in complex multimodal data [72] [74].
The path forward requires a methodological shift from simply maximizing accuracy on isolated datasets to optimizing robustness across diverse populations and clinical environments. This transition necessitates increased emphasis on comprehensive validation protocols including subgroup analysis, external validation, and bias auditing [2]. Technical innovations in explainable AI, multimodal learning, and federated systems will play crucial roles in developing more transparent and equitable cancer detection systems [71].
Future research should prioritize the creation of more diverse and representative datasets, the development of standardized evaluation frameworks for assessing generalizability, and the establishment of interdisciplinary collaborations between computer scientists, oncologists, and epidemiologists. Only through these concerted efforts can we realize the full potential of AI in delivering accurate, equitable cancer detection across all patient populations.
The integration of Artificial Intelligence (AI) into clinical cancer detection represents a paradigm shift in diagnostic medicine, offering unprecedented enhancements in accuracy, speed, and accessibility [7]. Deep Learning (DL) and Machine Learning (ML) models, particularly sophisticated convolutional neural networks (CNNs) like DenseNet121 and VGG16, have demonstrated remarkable performance, achieving validation accuracies upwards of 99% in classifying various cancers from histopathology and radiological images [3] [75]. However, a significant barrier impedes their widespread clinical adoption: the "black box" problem [76]. This term refers to the characteristic of many complex AI models, especially deep neural networks, which provide predictions or classifications without offering human-comprehensible insights into their internal decision-making processes [77] [78]. In high-stakes domains like oncology, where clinicians must justify decisions and ensure patient safety, this opacity is a substantial drawback [79].
The ethical and clinical ramifications of this opacity are profound. Physicians are understandably reluctant to trust and act upon recommendations from systems they do not understand, particularly when these decisions directly impact patient lives and treatment pathways [76] [78]. This reluctance is not merely a matter of technophobia; it is rooted in core principles of medical ethics. The "do no harm" principle obligates physicians to consider the potential harms from AI misdiagnoses, which may be more serious than those from human doctors due to the enigmatic nature of the error [76]. Furthermore, in patient-centered care, physicians are obligated to provide adequate information to patients for shared decision-making. The unexplainability of AI systems can thus limit patient autonomy by making it impossible for clinicians to articulate the rationale behind an AI-influenced diagnosis or treatment plan [76].
Explainable AI (XAI) has emerged as a critical subfield of AI aimed at bridging this trust gap. XAI encompasses a suite of techniques designed to make the behavior and predictions of AI systems understandable and trustworthy to human users [77]. The push for XAI is not merely technical; it is increasingly a legal and regulatory necessity. Frameworks like the European Union's General Data Protection Regulation (GDPR) emphasize a "right to explanation," and regulatory bodies such as the U.S. Food and Drug Administration (FDA) are stressing the need for transparency and accountability in AI-based medical devices [77] [78]. By providing insights into which features influence a model's decision, XAI supports informed consent, enables model debugging, helps identify biases, and fosters the human-AI collaboration essential for the future of clinical care [77] [79].
Comparative Analysis: Performance and Explainability of ML and DL in Cancer Detection
The debate between ML and DL for cancer detection often involves a trade-off between raw predictive performance and inherent interpretability. This section provides a comparative analysis, complete with quantitative data, to delineate the strengths and limitations of each approach.
Performance Metrics and Quantitative Comparison
Traditional ML models often rely on handcrafted features (e.g., texture, morphology) extracted from medical images, which are then used by classifiers like Support Vector Machines (SVM) or Random Forests. In contrast, DL models, particularly CNNs, autonomously learn hierarchical feature representations directly from raw pixel data. The table below summarizes the performance ranges of ML and DL models across several cancer types, based on a comprehensive review of recent literature (2018-2023) [26].
Table 1: Performance Comparison of ML and DL Models in Cancer Detection (2018-2023)
| Cancer Type | Best Performing ML Model | ML Accuracy Range | Best Performing DL Model | DL Accuracy Range |
|---|---|---|---|---|
| Brain Cancer | Support Vector Machine (SVM) | 87.5% - 95.2% | Custom CNN / DenseNet | 94.8% - 99.9% |
| Breast Cancer | Random Forest | 89.1% - 97.1% | Fusion Model (VGG16, DenseNet121) | 95.3% - 97.0% |
| Lung Cancer | Gradient-Boosted Trees | 85.0% - 90.0% | Single-Hidden-Layer Neural Network | 92.9% - 99.1% |
| Skin Cancer | Ensemble Classifier | 89.5% - 99.9% | InceptionV3 / ResNet152V2 | 70.0% - 100% |
The data reveals that DL models frequently achieve the highest reported accuracies, sometimes reaching perfect classification on specific datasets [26]. For instance, a study utilizing DenseNet121 for multi-cancer image classification reported a validation accuracy of 99.94% with an exceptionally low loss of 0.0017 [3]. Similarly, a fused DL model integrating VGG16, DenseNet121, and Xception for breast cancer detection achieved an accuracy of 97%, which was approximately 13% higher than the performance of any of the individual constituent models [75].
However, DL's performance advantage is not absolute. For some cancers, like skin cancer, top-tier traditional ML models can compete with or even surpass the performance of some DL approaches, as evidenced by the 99.89% accuracy for ML versus a low of 70% for a DL model [26]. This highlights the significant variability in DL model performance and the critical importance of architecture selection and training protocols.
The Explainability Divide
While DL often leads in performance, traditional ML models typically hold a strong advantage in inherent interpretability.
- Inherently Interpretable ML Models: Models like linear regression, decision trees, and logistic regression are often considered "glass-box" or ante hoc interpretable. Their logic is transparent: linear models show coefficient weights, and decision trees display a clear pathway of if-then rules. This allows clinicians to easily trace how input features (e.g., patient age, smoking status, tumor size) lead to a specific prediction [79] [15].
- Black-Box DL Models: The internal workings of deep neural networks, with their millions of parameters and complex, non-linear interactions, are not intuitively understandable to humans. This makes them opaque by design [77] [75]. Consequently, explaining their decisions requires post hoc XAI techniques—external methods applied after the model has made a prediction to approximate its reasoning.
Table 2: Comparison of Explainability Characteristics between ML and DL
| Characteristic | Traditional ML Models | Deep Learning Models |
|---|---|---|
| Interpretability Type | Often inherently interpretable (ante hoc) | Typically opaque, require post hoc explanation |
| Explanation Clarity | High; direct feature weights or decision paths | Approximate; highlights influential regions or features |
| Best for | Tabular data, structured clinical data | Image, text, and complex unstructured data |
| Trust Building | Via transparency of internal logic | Via visualization and validation of outputs |
Key XAI Methodologies and Experimental Protocols
To address the black-box nature of high-performing DL models, researchers have developed a rich toolkit of XAI methods. These techniques can be broadly categorized by their scope and approach.
Taxonomy of XAI Techniques
- Model-Agnostic vs. Model-Specific: Model-agnostic methods like LIME and SHAP can explain any ML model, whereas model-specific methods like Grad-CAM are designed for particular architectures like CNNs [77] [79].
- Global vs. Local Explanation: Global explanations aim to summarize the overall behavior of the model across the entire dataset. Local explanations, which are often more critical in clinical settings, focus on justifying a single prediction for a specific patient [79].
- Explanation Types: The three primary types of post hoc explanations are:
- Influence-based: Quantify the contribution of each input feature to the prediction (e.g., SHAP, LIME, Saliency Maps) [77] [79].
- Example-based: Explain predictions by referencing similar instances from the training data (e.g., Case-Based Reasoning) [79].
- Simplification-based: Use a simpler, interpretable model to approximate the complex model's predictions in a local region (e.g., LIME) [79].
Detailed Experimental Protocol for an XAI-Enabled DL System
The implementation of a robust, explainable cancer detection system involves a multi-stage pipeline. The following workflow, exemplified by a breast cancer detection study [75], details the key experimental steps.
XAI-Enabled Cancer Detection Workflow
1. Data Preprocessing & Model Training [3] [75]:
- Input Data: The study used a benchmark Breast Ultrasound Image Dataset. A similar multi-cancer study [3] utilized public datasets for seven cancer types (e.g., brain, breast, lung, kidney), applying rigorous segmentation techniques including grayscale conversion, Otsu binarization, noise removal, and watershed transformation.
- Model Architecture (Fusion): Instead of a single model, three pre-trained CNN architectures—DenseNet121, Xception, and VGG16—were employed. These models were not ensembled at the output level; rather, they were fused at an intermediate layer. This intermediate fusion strategy involves extracting partial feature maps from each model, concatenating them, and then passing the combined feature set through a final fully-connected layer for classification. This leverages the complementary strengths of each architecture for richer feature representation.
- Training Protocol: The models are trained using a large set of annotated images. Performance is evaluated using standard metrics: accuracy, precision, recall, F1-score, and Root Mean Square Error (RMSE). The fused model in [75] achieved a top accuracy of 97%.
2. Explainability & Clinical Validation [75]:
- XAI Technique Application: To explain the fused model's predictions, the study employed Grad-CAM++. This is a model-specific technique for CNNs that produces visual explanations.
- Generating Explanations: For a given input image and the model's prediction (e.g., "malignant"), Grad-CAM++ uses the gradients of the target concept (malignancy) flowing into the final convolutional layer to create a heatmap (saliency map). This heatmap is superimposed on the original image, highlighting regions that were most influential in the model's decision. The authors noted that Grad-CAM++ highlighted "multiple lesions with finer edges," providing sharper localization than its predecessor, Grad-CAM.
- Clinical Validation: The critical final step involves presenting the image, the prediction, and the Grad-CAM++ heatmap to radiologists or clinical experts. They then correlate the highlighted regions with their clinical knowledge (e.g., BI-RADS criteria for ultrasound) to determine if the model's "reasoning" is clinically plausible. This process is essential for calibrating trust and validating the model for real-world use.
The Scientist's Toolkit: Key Research Reagents and Solutions
Implementing XAI-enabled cancer detection systems requires a suite of computational and data resources. The table below details essential components.
Table 3: Research Reagent Solutions for XAI in Cancer Detection
| Tool/Resource | Type | Primary Function | Example Use Case |
|---|---|---|---|
| DenseNet121 / VGG16 | Deep Learning Model | Feature extraction and image classification. Acts as a backbone architecture. | Used in fused model [75] and multi-cancer study [3] for high-accuracy classification. |
| Grad-CAM++ | Explainability Tool (Model-Specific) | Generates visual explanations for CNN predictions by highlighting discriminative regions. | Provided heatmaps for breast ultrasound images, showing foci of malignancy [75]. |
| SHAP / LIME | Explainability Tool (Model-Agnostic) | Quantifies the contribution of each input feature to a single prediction. | Explains risk predictions based on symptomatic and lifestyle data [77] [15]. |
| Benchmark Datasets (e.g., Breast Ultrasound Image Dataset) | Data Resource | Provides standardized, annotated medical images for training and fair evaluation of models. | Served as the input data for model training and validation in [75]. |
| Python (Libraries: TensorFlow, PyTorch) | Programming Framework | Provides the computational environment for building, training, and explaining DL models. | The standard platform for implementing the majority of cited studies [3] [75] [15]. |
Critical Gaps and Future Research Directions
Despite significant progress, the field of XAI for clinical trust faces several persistent challenges that dictate future research directions.
- The Accuracy-Explainability Trade-Off: A key challenge is the perceived trade-off between model performance and explainability. The most accurate models (e.g., very deep neural networks) are often the hardest to explain [78]. While some argue that in healthcare, accuracy should be paramount—"the proof is in the pudding"—the counter-argument is that without explainability, trust and adoption will remain low, and critical errors may go unnoticed [78]. Future work must continue to develop high-performing yet inherently interpretable models or highly faithful post-hoc explanations.
- Lack of Standardized Evaluation: There is a notable absence of standardized metrics to evaluate the quality and usefulness of XAI explanations [77] [79]. What constitutes a "good explanation" can be subjective, varying by clinical context and the user's expertise. Developing and adopting standardized, task-specific evaluation frameworks is crucial for the rigorous comparison of XAI methods.
- User-Centered Design and Workflow Integration: Many XAI solutions are developed from a technical perspective without sufficient input from end-user clinicians [79]. This leads to a mismatch between the explanations provided and the information clinicians actually need to make decisions. As one review notes, effective XAI must be the product of a "user-centered design" process, co-designed with clinicians and seamlessly integrated into existing clinical workflows, such as Electronic Health Record (EHR) systems, without causing disruption [77] [79].
- Psychological Trust and Human-AI Collaboration: The ultimate goal of XAI is not just to provide an explanation but to foster appropriate trust—a calibrated understanding of when the AI is likely to be correct or wrong. Future research needs to explore the psychological aspects of how clinicians perceive and interact with AI explanations, viewing the combination as a "joint cognitive system" where cognitive work is distributed between the human and the artificial agent [79].
The journey toward fully trustworthy AI in clinical cancer detection is a balancing act between the formidable predictive power of black-box deep learning models and the non-negotiable ethical and clinical requirement for transparency. As the comparative analysis shows, DL models frequently push the boundaries of diagnostic accuracy, with models like DenseNet121 achieving near-perfect classification on specific tasks [3]. However, this performance is moot if clinicians cannot trust or understand the output.
Explainable AI is the essential bridge to this gap. Techniques like Grad-CAM++, SHAP, and LIME provide a window into the model's decision-making process, transforming an opaque prediction into an interpretable and actionable insight [77] [75]. The implementation of these techniques, as detailed in the experimental protocols, involves a structured pipeline from data preparation and model fusion to clinical validation of the generated explanations.
Moving forward, the focus must shift from purely technical XAI solutions to human-centered, clinically integrated systems. The solution is not just better algorithms, but better collaborations—between computer scientists and clinicians, and between the clinician and the AI, forming a joint cognitive system dedicated to improving patient outcomes. By systematically addressing the black box problem through rigorous XAI implementation, the field can unlock the full potential of AI, ushering in an era of enhanced, equitable, and trustworthy cancer care.
In the competitive landscape of medical artificial intelligence, the choice of optimization strategy can significantly influence the performance and clinical applicability of machine learning (ML) and deep learning (DL) models for cancer detection. As these models increasingly support diagnostic decisions, understanding the empirical performance of different optimization approaches becomes crucial for researchers and drug development professionals. This guide provides a comparative analysis of three fundamental optimization paradigms—feature selection, transfer learning, and hyperparameter tuning—within the context of cancer detection research. We objectively evaluate these strategies through synthesized experimental data from recent studies, enabling informed decisions for model development in oncology applications.
Comparative Performance Analysis of Optimization Strategies
The table below summarizes quantitative performance data for various optimization approaches applied to cancer detection tasks, highlighting the efficacy of each method across different cancer types.
Table 1: Performance Comparison of Optimization Strategies in Cancer Detection
| Optimization Strategy | Specific Algorithm/Approach | Cancer Type | Performance Metrics | Key Comparative Findings |
|---|---|---|---|---|
| Feature Selection | Binary Al-Biruni Earth Radius (bABER) [80] | Multiple Cancers | Significantly outperformed 8 other metaheuristic algorithms | Superior accuracy in selecting relevant features from medical datasets |
| Feature Selection | IG-GPSO (Info Gain + Grouped PSO) [81] | Multiple Cancers | Average Accuracy: 98.50% [81] | Better accuracy and smaller feature scale vs. traditional feature selection algorithms |
| Transfer Learning | DenseNet121 [3] | Multi-Cancer Classification | Accuracy: 99.94%, Loss: 0.0017, RMSE: 0.036 [3] | Highest accuracy among 10 evaluated CNN architectures |
| Transfer Learning | Inception V3 [82] | Lymphoma (CLL vs FL) | Accuracy: 97.5%, RMSE: 0.393 [82] | Best performance for histopathological image classification |
| Transfer Learning | Vision Transformers (ViTs) [10] | Breast Cancer | Accuracy up to 99.99% on BreakHis dataset [10] | Effective for histopathology analysis; captures global image context |
| Hybrid Optimization | HHO-LOA + DCNN-LSTM [83] | Lung Cancer | Accuracy: 98.75% [83] | Combines feature optimization with architectural tuning |
Experimental Protocols and Methodologies
Feature Selection Implementation
Feature selection algorithms play a critical role in handling high-dimensional genomic and medical imaging data by eliminating redundant or irrelevant features that can degrade model performance.
IG-GPSO Hybrid Algorithm Protocol [81]: The Information Gain-Grouped Particle Swarm Optimization (IG-GPSO) algorithm follows a structured workflow to identify optimal feature subsets. The process begins with calculating information gain values for all features in the dataset, which are then ranked in descending order. These ranked features are grouped based on their information gain indices, ensuring features with similar values are clustered. The algorithm then employs a grouped Particle Swarm Optimization to search for optimal feature subsets, evaluating selections through both in-group and out-group assessment methods. Validation is performed using Support Vector Machines (SVM) on gene expression datasets including Prostate-GE, TOX-171, GLIOMA, and Lung-discrete, characterized by large feature sets (3,325-5,966 genes) and small sample sizes (50-171 samples) [81].
Binary Al-Biruni Earth Radius (bABER) Protocol [80]: The bABER algorithm represents a novel metaheuristic approach for feature selection. The methodology involves intelligent removal of unnecessary data through a binary optimization process. Researchers evaluated bABER against eight established binary metaheuristic algorithms (bSC, bPSO, bWAO, bGWO, bMVO, bSBO, bFA, and bGA) across seven medical datasets. The experimental protocol included rigorous statistical validation using ANOVA and Wilcoxon signed-rank tests to ensure robust performance assessment [80].
Transfer Learning Implementation
Transfer learning addresses data scarcity in medical applications by leveraging knowledge from pre-trained models, significantly reducing training time and computational resources.
Histopathological Image Classification Protocol [82] [3]: For lymphoma classification, researchers implemented a comprehensive transfer learning framework evaluating six CNN architectures: VGG-16, VGG-19, MobileNetV2, ResNet50, DenseNet161, and Inception V3. The experimental setup involved training on a dataset of 4,500 histopathological images of Chronic Lymphocytic Leukemia (CLL) and Follicular Lymphoma (FL). Models were pre-trained on ImageNet and fine-tuned with histopathology-specific data. The protocol included four data thresholds (0.05 to 0.2) to evaluate performance with limited data. For multi-cancer classification, ten transfer learning models were evaluated on seven cancer types using histopathology images, incorporating advanced preprocessing with grayscale conversion, Otsu binarization, noise removal, and watershed transformation for segmentation [3].
Vision Transformers for Breast Cancer Protocol [10]: The implementation of Vision Transformers (ViTs) for breast cancer imaging involved dividing images into patches and processing them as sequences using self-attention mechanisms. Researchers employed self-supervised learning to pre-train models on large unlabeled medical image datasets before fine-tuning on annotated mammography and histopathology images. Hybrid models combining CNNs for local feature extraction with ViTs for capturing long-range dependencies were developed to address challenging cases involving dense breast tissue and multifocal tumors [10].
Hyperparameter Optimization and Hybrid Approaches
HHO-LOA Optimization Protocol [83]: The hybrid Horse Herd Optimization (HHO) and Lion Optimization Algorithm (LOA) approach was designed to balance global search and local optimization capabilities. This method was integrated with a Deep Convolutional Neural Network and Long Short-Term Memory (DCNN-LSTM) hybrid architecture for lung cancer classification from CT images. The optimizer automatically tracked accuracy to identify optimal parameters during training, addressing underfitting issues caused by dataset limitations through refined feature dimensions [83].
Workflow Visualization of Optimization Strategies
The following diagram illustrates the integrated workflow for implementing feature selection, transfer learning, and hyperparameter tuning in cancer detection models.
Figure 1: Integrated Workflow for Cancer Detection Optimization
Research Reagent Solutions for Experimental Implementation
The table below details essential computational tools and datasets that form the foundational "research reagents" for implementing these optimization strategies in cancer detection research.
Table 2: Essential Research Reagent Solutions for Cancer Detection Optimization
| Resource Category | Specific Resource | Function in Research | Application Context |
|---|---|---|---|
| Public Genomic Datasets | TCGA (The Cancer Genome Atlas) [2] | Provides genomic and clinical data for model training and validation | Pan-cancer analysis; genomic feature selection |
| Public Genomic Datasets | Prostate-GE, TOX-171, GLIOMA [81] | Gene expression data for evaluating feature selection algorithms | High-dimensional data with small sample sizes |
| Medical Image Datasets | BreakHis [10] | Histopathological images for breast cancer classification | Transfer learning evaluation |
| Medical Image Datasets | Lymphoma Histopathological Images [82] | CLL and FL images for subtype classification | Transfer learning model comparison |
| Computational Frameworks | Simulated Federated Learning [82] | Privacy-preserving model training across institutions | Decentralized data scenarios |
| Computational Frameworks | Grouped Particle Swarm Optimization [81] | Efficient search for optimal feature subsets | High-dimensional feature selection |
| Pre-trained Models | ImageNet Pre-trained CNNs [82] [3] | Foundation models for transfer learning | Medical image feature extraction |
| Validation Tools | Statistical Tests (ANOVA, Wilcoxon) [80] | Robust performance comparison of algorithms | Methodological validation |
Discussion and Strategic Recommendations
Based on the comparative analysis of experimental results, each optimization strategy demonstrates distinct advantages for specific scenarios in cancer detection research.
Feature Selection Strategy Application: Feature selection algorithms, particularly advanced metaheuristic approaches like bABER and IG-GPSO, show exceptional performance for high-dimensional genomic data [80] [81]. These methods significantly improve model accuracy while reducing computational complexity by eliminating redundant features. IG-GPSO achieves 98.50% accuracy by combining information gain filtering with grouped particle swarm optimization, effectively addressing the challenge of high feature redundancy in gene expression data [81]. These approaches are particularly valuable for biomarker discovery and development of interpretable diagnostic models where feature importance must be transparent.
Transfer Learning Strategy Application: Transfer learning consistently delivers superior performance across various medical imaging modalities, with DenseNet121 achieving remarkable 99.94% accuracy in multi-cancer classification [3]. The approach demonstrates particular effectiveness for histopathological image analysis, where pre-trained CNNs and Vision Transformers extract meaningful patterns despite limited annotated medical data [10] [82]. Vision Transformers show exceptional capability in capturing global contextual information in breast histopathology, achieving up to 99.99% accuracy on the BreakHis dataset [10]. Transfer learning represents the optimal choice for image-based cancer detection where data scarcity poses a significant challenge.
Implementation Considerations: For genomic data with high dimensionality and small sample sizes, feature selection strategies are indispensable. In contrast, for image-based diagnosis with moderate dataset sizes, transfer learning provides the most robust performance. Hybrid approaches combining HHO-LOA optimization with DCNN-LSTM architectures demonstrate that strategic integration of multiple optimization techniques can achieve superior results (98.75% accuracy for lung cancer classification) [83]. Emerging strategies like federated learning address critical data privacy concerns while maintaining model performance, making them particularly relevant for multi-institutional research collaborations [82].
The choice of optimization strategy should align with data characteristics, computational resources, and clinical requirements. Feature selection enhances interpretability for genomic applications, while transfer learning excels in image-based diagnosis with limited data. Future research directions should focus on standardized benchmarking, improved model interpretability, and integration of multimodal data to further advance cancer detection capabilities.
Benchmarking Performance and Pathways to Clinical Translation
In the high-stakes field of cancer detection, establishing rigorous validation frameworks is not merely an academic exercise but a fundamental requirement for clinical translation. Machine Learning (ML) and Deep Learning (DL) models show transformative potential in oncology, with DL models demonstrating remarkable accuracy in tasks ranging from image classification to genomic analysis [7] [23]. However, these sophisticated algorithms are susceptible to overfitting, where models learn patterns specific to training data but fail to generalize to new datasets [84]. This challenge is particularly acute in medical imaging, where limited dataset sizes, imbalanced classes, and institutional variations in data collection can significantly impact model performance [3] [84]. The validation frameworks discussed herein provide methodological guardrails against overoptimism, enabling researchers to develop models that maintain diagnostic accuracy in diverse clinical environments.
The comparative analysis between ML and DL approaches extends beyond raw performance metrics to encompass their respective relationships with validation protocols. Traditional ML models often rely on handcrafted features and may demonstrate more predictable behavior across datasets, while DL models can automatically learn hierarchical feature representations but typically require larger datasets and more sophisticated validation approaches due to their increased complexity and parameter count [85] [23]. Cross-validation methodologies serve as critical tools for estimating true generalization performance, guiding algorithm selection, and optimizing hyperparameters when large external test sets are unavailable [84]. This article systematically examines these frameworks, providing researchers with structured approaches for validating cancer detection models across the development lifecycle.
Comparative Performance of ML and DL in Cancer Detection
Quantitative Performance Metrics
Rigorous comparison between ML and DL approaches for cancer detection requires examination across multiple cancer types and imaging modalities. The following tables summarize key performance indicators from recent studies, highlighting accuracy, model architecture, and validation approaches.
Table 1: Deep Learning Performance Across Cancer Types
| Cancer Type | Model Architecture | Accuracy | Dataset Size | Reference |
|---|---|---|---|---|
| Multi-Cancer Classification | DenseNet121 | 99.94% | 7 cancer types [3] | |
| Brain Tumor Detection | YOLOv7 with CBAM attention | 99.5% | 10,288 images [86] | |
| Brain Tumor Classification | VGG16-based CNN | 99.24% | 17,136 images [87] | |
| Brain Tumor Classification | Ensemble Model | 99.94% | BraTS2020 dataset [85] |
Table 2: Traditional Machine Learning Performance in Cancer Detection
| Cancer Type | Model Approach | Accuracy | Key Features | Reference |
|---|---|---|---|---|
| Brain MRI Classification | SVM with Wavelet Transform | 65% | 17,689 feature vectors [85] | |
| Brain Tumor Detection | SVM with ICA | 98% | Spectral distance technique [85] | |
| Brain Tumor Classification | SVM with Discrete Wavelet Transform | 100% | Limited sample size (32 test images) [85] |
The performance differential between ML and DL approaches evident in these studies reflects both model capacity and feature engineering requirements. Traditional ML models depend heavily on manual feature extraction techniques such as wavelet transforms, intensity features, and texture analysis [85]. In contrast, DL models automatically learn relevant features directly from data, enabling them to capture subtle patterns that may be overlooked in manual feature engineering [3] [87]. This distinction becomes particularly significant in complex cancer detection tasks where discriminative features may not be intuitively apparent to human researchers.
Methodological Considerations in Performance Comparison
Interpreting these performance metrics requires careful consideration of methodological factors. Dataset size emerges as a critical variable, with DL models typically requiring larger training sets to achieve optimal performance [3] [87]. Studies employing extensive data augmentation demonstrate improved generalization, with one brain tumor classification study expanding their dataset from 5,712 to 17,136 images through augmentation techniques [87]. Additionally, model architecture choices significantly impact performance, with integrated attention mechanisms such as CBAM (Convolutional Block Attention Module) showing improved feature extraction capabilities for tumor localization [86].
The validation methodology employed also substantially influences reported performance metrics. Studies using simple holdout validation with limited samples may report optimistic accuracy that doesn't generalize to broader populations [84]. For instance, while one study reported 100% accuracy using SVM with discrete wavelet transform, this was achieved on only 32 test images [85]. In comparison, DL studies typically employ more rigorous cross-validation approaches, with one multi-cancer classification implementing comprehensive evaluation across seven cancer types [3]. These methodological differences underscore the importance of standardized validation frameworks when comparing ML and DL approaches.
Cross-Validation Protocols for Robust Validation
Core Cross-Validation Methodologies
Cross-validation (CV) represents a fundamental component of rigorous validation frameworks, enabling reliable performance estimation when large external datasets are unavailable. CV methods repeatedly partition available data into independent training and testing cohorts, with final performance metrics representing averages across partitions [84]. The selection of appropriate CV strategies depends on multiple factors including dataset size, class distribution, and the specific validation task.
Table 3: Cross-Validation Techniques and Applications
| Method | Procedure | Advantages | Limitations | Ideal Use Cases |
|---|---|---|---|---|
| Holdout Validation | Single split into training/validation/test sets | Simple implementation; computationally efficient | Vulnerable to sampling bias; unstable with small datasets | Very large datasets with representative distributions |
| K-Fold CV | Partition data into k folds; each fold serves as test set once | Reduced variance; more reliable performance estimation | Computational intensity increases with k | Medium-sized datasets; algorithm comparison |
| Stratified K-Fold | K-fold with preserved class distribution in each fold | Maintains class balance; better for imbalanced datasets | Same computational cost as standard k-fold | Imbalanced classification tasks |
| Nested CV | Outer loop for performance estimation; inner loop for hyperparameter tuning | Unbiased performance estimation with hyperparameter optimization | High computational cost | Small to medium datasets requiring hyperparameter tuning |
The experimental protocol for implementing k-fold CV, one of the most widely used approaches, involves several methodical steps. First, the dataset is randomly partitioned into k mutually exclusive folds of approximately equal size. For each iteration i (where i ranges from 1 to k), fold i is designated as the validation set, while the remaining k-1 folds constitute the training set. The model is trained on the training set and evaluated on the validation set, with performance metrics recorded. This process repeats until each fold has served as the validation set exactly once. The final performance estimate represents the average across all k iterations [84]. For stratified k-fold variants, the partitioning process maintains consistent class distribution across all folds to prevent skewed performance estimates in imbalanced datasets.
Advanced Cross-Validation Considerations
Beyond basic implementation, several advanced considerations significantly impact CV reliability in cancer detection applications. First, data partitioning must occur at the patient level rather than the image level, particularly when multiple images derive from single patients, to prevent artificially inflated performance estimates [84]. This approach ensures the model's ability to generalize to new patients rather than simply recognizing images from previously seen patients.
Second, the challenge of hidden subclasses necessitates careful experimental design. Unlike known subclasses (e.g., specific cancer subtypes), hidden subclasses represent unknown groupings within datasets that share unique characteristics potentially affecting prediction difficulty [84]. For example, a brain tumor dataset might contain hidden subclasses based on imaging device manufacturers or acquisition protocols. The impact of hidden subclasses diminishes with larger dataset sizes, emphasizing the importance of multi-institutional collaborations in cancer detection research [84].
Finally, nested cross-validation protocols provide robust frameworks for both hyperparameter optimization and final performance estimation. In this approach, an outer k-fold loop estimates generalization performance, while an inner loop performs hyperparameter tuning exclusively on training folds [84]. This separation prevents information leakage from the test set into model development, addressing the pervasive pitfall of unintentionally tuning models to specific test sets, which generates overoptimistic performance expectations [84].
Implementation Framework: Visualization and Workflows
Cross-Validation Workflow
The following diagram illustrates the systematic workflow for implementing k-fold cross-validation, highlighting the iterative training and validation process essential for reliable performance estimation:
Model Development and Validation Pipeline
The comprehensive pipeline for cancer detection model development integrates multiple validation stages to ensure clinical reliability:
Essential Research Reagents and Computational Tools
Research Reagent Solutions for Cancer Detection Research
Table 4: Essential Research Materials and Their Applications
| Reagent/Resource | Function | Application in Cancer Detection |
|---|---|---|
| Public Datasets (BraTS, TCGA) | Benchmarking and comparative analysis | Provides standardized datasets for model development and validation [7] [86] |
| Attention Mechanisms (CBAM) | Feature enhancement and localization | Improves model focus on salient tumor regions [86] |
| Data Augmentation Tools | Dataset expansion and regularization | Increases effective dataset size; reduces overfitting [86] [87] |
| Preprocessing Frameworks | Image quality enhancement | Guided filtering, anisotropic Gaussian side windows for improved clarity [85] |
| Feature Extraction Modules | Automated feature learning | CNNs for hierarchical feature extraction from medical images [3] [87] |
Machine Learning Frameworks for Cancer Detection
The selection of appropriate computational frameworks significantly influences implementation efficiency and model performance in cancer detection research.
Table 5: Machine Learning Framework Comparison
| Framework | Primary Language | Strengths | Limitations | Cancer Detection Applications |
|---|---|---|---|---|
| TensorFlow | Python, C++ | Production deployment; extensive libraries | Steep learning curve; complex debugging | End-to-end model development and deployment [88] [89] |
| PyTorch | Python | Research flexibility; dynamic graphs | Smaller deployment ecosystem | Rapid prototyping; academic research [88] [89] |
| Scikit-learn | Python | Simple API; traditional ML algorithms | Limited deep learning support | Traditional ML models for cancer prediction [88] [89] |
| Keras | Python | User-friendly; high-level abstraction | Less granular control | Quick prototyping of deep learning models [88] |
The establishment of rigorous validation frameworks represents a critical pathway toward clinically viable AI tools for cancer detection. This comparative analysis demonstrates that while DL models generally achieve higher accuracy rates for complex image classification tasks, their superior performance is contingent upon appropriate validation protocols that account for dataset limitations, potential biases, and generalization requirements. The cross-validation methodologies, performance metrics, and implementation workflows detailed herein provide researchers with structured approaches for developing models that maintain diagnostic accuracy across diverse clinical settings.
Future advancements in cancer detection validation will likely incorporate several emerging trends. Federated learning approaches show promise for multi-institutional collaboration while addressing data privacy concerns [7]. Explainable AI (XAI) techniques are becoming increasingly important for enhancing model interpretability and clinical trust [7]. Additionally, integration of multimodal data sources, including genomic information alongside medical images, may enable more comprehensive cancer detection platforms [7] [23]. As these technical capabilities advance, maintaining methodological rigor through robust validation frameworks will remain essential for translating algorithmic potential into improved patient outcomes in oncology.
The integration of artificial intelligence (AI) in oncology represents a paradigm shift in cancer detection, offering unprecedented opportunities for improving diagnostic accuracy and patient outcomes. Within the AI domain, a critical methodological distinction exists between traditional machine learning (ML) and deep learning (DL) approaches. ML models typically rely on handcrafted feature extraction and statistical learning algorithms, whereas DL models utilize complex neural networks to autonomously learn hierarchical feature representations directly from raw data. This comparative analysis objectively evaluates the performance of these two methodological frameworks across key metrics—accuracy, sensitivity, specificity, and Area Under the Curve (AUC)—within the context of cancer detection. Understanding their relative strengths and limitations provides crucial guidance for researchers, scientists, and drug development professionals seeking to implement AI solutions in oncological research and clinical practice.
Performance Metrics Comparison
The quantitative performance of ML and DL models varies significantly across different cancer types and data modalities. The following tables summarize comparative performance data extracted from recent studies, providing a comprehensive overview of their capabilities in specific diagnostic contexts.
Table 1: Performance Comparison of ML and DL Models in Brain Tumor Detection using MRI
| Model Type | Specific Model | Accuracy (%) | Sensitivity (%) | Specificity (%) | AUC | Dataset |
|---|---|---|---|---|---|---|
| DL | Automated Deep Learning Framework [85] | 99.94 | - | - | - | BraTS2020 |
| DL | Automated Deep Learning Framework [85] | 99.67 | - | - | - | Figshare |
| DL | Refined YOLOv7 [86] | 99.5 | - | - | - | Curated Dataset |
| ML | SVM with Wavelet Transform [85] | 65.0 | - | - | - | 60 Images |
| ML | SVM with ICA [85] | 98.0 | - | - | - | 60 Images |
| ML | DWT with SVM [85] | 100 | - | - | - | 80 Images |
Table 2: Performance of DL Models in Melanoma Prognosis using Dermatoscopy
| Prediction Task | Model Architecture | Performance | Value | Additional Context |
|---|---|---|---|---|
| Metastasis Prediction | Foundation Model | AUC | 0.96 (95% CI: 0.93-0.99) | Comparable to tumor prognostic factors [90] |
| Metastasis Prediction | Pre-trained ResNet50 | Accuracy | Comparable to tumor prognostic factors | - [90] |
| Breslow Thickness | Various MLAs | Substantial accuracy in binary tasks | - | Particularly with semi-supervised learning [90] |
Table 3: Performance Overview Across Multiple Cancers using AI
| Cancer Type | Model Approach | Imaging Modality | Key Performance Highlights |
|---|---|---|---|
| Breast Cancer | Radiomics-guided DL/ML [56] | Ultrasound, DCE-MRI | Remarkable precision in distinguishing malignant vs. benign tumors |
| Various Cancers | AI-based Models [91] | Multimodal | Improved accuracy and efficiency in cancer identification, classification, and treatment assessment |
| Various Cancers | Deep Learning [2] | Genomic and Imaging data | Enhanced early detection accuracy by autonomously extracting complex features |
Detailed Experimental Protocols
Deep Learning Protocol for Brain Tumor Classification
The high-performance deep learning framework for brain tumor classification [85] follows a sophisticated multi-stage pipeline:
Image Preprocessing: Image clarity is enhanced through a combination of guided filtering techniques with anisotropic Gaussian side windows (AGSW) to improve signal-to-noise ratio while preserving tumor boundary information.
Morphological Analysis: Prior to segmentation, morphological operations are conducted to exclude non-tumor regions from the enhanced MRI images, reducing false positives.
Deep Learning Segmentation: Deep neural networks segment the processed images, extracting high-quality regions of interest (ROIs) and multiscale features that capture texture, shape, and intensity characteristics.
Attention Mechanism: An attention module isolates distinctive features while eliminating irrelevant information, allowing the model to focus on diagnostically significant regions.
Ensemble Classification: An ensemble model integrates predictions from multiple architectures to classify brain tumors into distinct categories (e.g., glioma, meningioma, pituitary), leveraging complementary strengths of different network architectures.
This protocol demonstrates the data-intensive, computationally complex nature of DL approaches, requiring substantial computational resources but achieving exceptional accuracy through automated feature learning.
Machine Learning Protocol for Brain Tumor Detection
Traditional machine learning approaches follow a fundamentally different, feature-engineering-intensive pipeline [85]:
Preprocessing: Standard image normalization and noise reduction techniques are applied to MRI scans.
Feature Extraction: Handcrafted features are explicitly engineered using:
- Local feature extraction: Techniques including wavelet transform, symmetry analysis, texture descriptors, intensity statistics, Gabor features, and shape characteristics.
- Global feature extraction: Methods such as scale-invariant feature transformation (SIFT), fisher vector (FV), and bag of words (BoW) to capture broader image representations.
- Statistical features: Calculation of mean, standard deviation, skewness, and grey level co-occurrence matrix (GLCM) properties.
Feature Selection/Reduction: Techniques like principal component analysis (PCA) and linear discriminant analysis (LDA) reduce dimensionality and mitigate overfitting.
Classification: The curated feature sets are fed into traditional classifiers including support vector machines (SVM), Naive Bayes, random forest, or artificial neural networks for final tumor classification.
This protocol highlights the human expertise-dependent nature of ML approaches, where diagnostic performance heavily relies on the quality and relevance of manually engineered features.
Workflow Visualization
The Scientist's Toolkit: Essential Research Reagents and Solutions
Table 4: Key Research Reagents and Computational Tools for AI-Driven Cancer Detection
| Tool/Reagent | Type/Category | Primary Function | Example Applications |
|---|---|---|---|
| MRI Datasets | Data | Model training and validation | Brain tumor classification (BraTS2020, Figshare) [85] |
| Dermatoscopic Images | Data | Preoperative melanoma assessment | Metastasis prediction, Breslow thickness estimation [90] |
| Radiomics Software | Computational Tool | Quantitative feature extraction from medical images | Breast cancer tumor characterization [56] |
| PyRadiomics Python Package | Computational Library | Standardized radiomic feature extraction | Breast cancer detection from multiple imaging modalities [56] |
| Convolutional Neural Networks | Algorithm | Automatic feature learning from images | Brain tumor classification in MRI [85] |
| ResNet, VGG, DenseNet | Model Architectures | Deep feature extraction for classification | Breast cancer diagnosis [56] |
| Support Vector Machines | Algorithm | Classification based on handcrafted features | Traditional brain tumor detection [85] |
| Attention Mechanisms | Algorithm | Focus model on salient image regions | Brain tumor classification (CBAM) [86] |
| Data Augmentation Techniques | Method | Expand training dataset diversity | Address limited medical data [86] |
| Ensemble Learning | Method | Combine multiple models for improved accuracy | Brain tumor classification [85] |
Comparative Analysis and Performance Interpretation
The performance data reveals a consistent pattern where DL approaches generally outperform ML models in scenarios with sufficient training data, particularly in complex visual pattern recognition tasks like tumor detection in medical images. The superior performance of DL models (achieving up to 99.94% accuracy in brain tumor classification [85]) stems from their ability to automatically learn relevant features directly from raw image data, capturing subtle patterns that may be overlooked in manual feature engineering processes.
However, this performance advantage comes with significant trade-offs. DL models require substantial computational resources, large annotated datasets, and lack inherent interpretability—a critical concern in clinical settings where understanding model decision-making processes is essential [91] [2]. In contrast, ML models offer greater transparency and computational efficiency, performing adequately in situations with limited data where DL models would typically overfit.
The choice between ML and DL approaches depends on multiple factors including available data quantity, computational resources, interpretability requirements, and specific clinical application. While DL currently demonstrates superior quantitative performance metrics, ML approaches remain valuable in resource-constrained environments or when model interpretability is prioritized. Future directions likely involve hybrid approaches that leverage the strengths of both methodologies, along with increased focus on model interpretability and clinical validation to facilitate translation from research to clinical practice [91] [2] [65].
The Critical Role of External Validation and Multi-Center Trials
The integration of artificial intelligence (AI) into oncology represents a paradigm shift in cancer detection and diagnosis. However, the transition from experimental algorithms to clinically valuable tools faces a significant hurdle: proving that these models perform reliably across diverse, real-world clinical settings, not just on the data used to create them. This challenge separates academically interesting models from clinically useful ones. External validation—evaluating an AI model on data entirely separate from its development dataset—and multi-center trials are the fundamental processes that bridge this gap. They test a model's robustness against variations in patient populations, imaging equipment, and clinical protocols. Within this framework, a critical examination of both machine learning (ML) and deep learning (DL) approaches reveals distinct strengths, limitations, and pathways toward clinical adoption. This guide provides a comparative analysis of these approaches, focusing on their performance and validation in the critical domain of cancer detection.
Performance Comparison: ML vs. DL in Validated Studies
Quantitative data from externally validated studies provide the most meaningful comparison of model performance. The following tables synthesize evidence from recent rigorous validation efforts across various cancer types and clinical tasks.
Table 1: Performance of Externally Validated Deep Learning Models in Cancer Detection
| Cancer Type | Imaging Modality | Task | Model Architecture | Key Performance Metric | Result | Study Details |
|---|---|---|---|---|---|---|
| Ovarian Cancer [92] | Ultrasound | Benign vs. Malignant Classification | Transformer-based | F1 Score | 83.50% (outperformed human experts) | 17,119 images; 20 centers; 8 countries |
| Lung Cancer [93] | Digital Pathology | Subtyping (Adeno. vs. Squamous) | Various DL | Average AUC Range | 0.746 - 0.999 | Review of 22 external validation studies |
| Breast Cancer [94] | DCE-MRI | Tumor Segmentation | nnU-Net | Dice Similarity (Baseline) | (Pre-trained model provided) | 1,506 cases; multi-center dataset for benchmarking |
| Pan-Cancer [95] | Various Radiologic Images | Diagnostic Classification | CNN (mostly ResNet) | Performance Drop in External Validation | ~81% of models showed a decrease; ~24% showed a substantial decrease (≥0.10) | Systematic review of 86 externally validated algorithms |
Table 2: Comparison of ML and Conventional Models vs. Deep Learning
| Model Category | Typical Algorithms | Application Context | Comparative Performance | Key Strengths & Weaknesses |
|---|---|---|---|---|
| Machine Learning (ML) | Random Forest, XGBoost, Logistic Regression [96] [97] | Predicting MACCEs* after PCI in AMI patients [96] | AUC: 0.88 (ML) vs. AUC: 0.79 (Conventional scores) [96] | Superior to conventional scores Handles non-linear relationships [96] Requires large datasets [96] |
| Conventional Models | GRACE, TIMI Risk Scores [96] | Predicting MACCEs* after PCI in AMI patients [96] | AUC: 0.79 [96] | Established, easy to apply [96] Cannot capture complex variable interplay [96] |
| Deep Learning (DL) | CNNs, Transformers | Image-based cancer diagnosis & segmentation [92] [94] | Variable; can surpass human experts [92] | High accuracy on complex image data [92] Performance can drop substantially in external validation [95] |
MACCEs: Major Adverse Cardiovascular and Cerebrovascular Events; PCI: Percutaneous Coronary Intervention; AMI: Acute Myocardial Infarction.
The data demonstrates that both advanced ML and DL models can significantly outperform traditional clinical tools. The standout DL models, particularly those validated in large multi-center settings like the ovarian cancer study, achieve diagnostic performance at or beyond human expert levels [92]. However, the systematic review of radiology AI models sounds a strong note of caution, indicating that performance degradation upon external validation is a common challenge for DL, underscoring why it is a critical step in the evaluation process [95].
Experimental Protocols for Robust Validation
To achieve the level of evidence shown in the highest-performing studies, rigorous experimental methodologies are essential. Below are detailed protocols for key validation designs cited in this guide.
Leave-One-Center-Out Cross-Validation (LOCO-CV)
This protocol was used effectively in the large-scale ovarian cancer study to ensure generalizability across clinical centers [92].
- Objective: To train and validate a model in a way that explicitly tests its performance on data from previously unseen hospitals or clinical sites.
- Procedure:
- Data Collection: Aggregate a dataset comprising patient data from multiple (N) independent clinical centers. The ovarian cancer study, for instance, used data from 20 centers across 8 countries [92].
- Iterative Training and Testing: For each of N iterations:
- Hold-Out Set: Designate the data from one entire center as the test set.
- Training Set: Combine the data from the remaining N-1 centers to form the training dataset.
- Model Training: Train a new instance of the model from scratch using only the data from the N-1 training centers.
- Model Testing: Evaluate the trained model's performance on the held-out center's data.
- Performance Aggregation: The final performance metrics are calculated by aggregating the results from all N iterations, providing a robust estimate of how the model will perform at a new, unseen center.
External Validation Using Blinded Biobank Reference Sets
This protocol, employed by the NCI's Cancer Screening Research Network for evaluating multi-cancer detection (MCD) assays, is the gold standard for objective performance assessment [98].
- Objective: To impartially evaluate the performance of a developed assay on a curated, blinded set of biological specimens.
- Procedure:
- Assay Lock-Down: The developer finalizes the assay ("locks it down") before evaluation on the reference set. No further changes are permitted based on these results [98].
- Blinded Specimen Distribution: A trusted third party (e.g., the Alliance for Clinical Trials in Oncology) provides a reference set of blinded specimens to the developer. This set includes samples from cancer patients and non-cancer controls, with the ground truth known only to the evaluator [98].
- Assay Execution: The developer runs their locked assay on the provided specimens and returns the predictions (e.g., cancer/no cancer, tissue of origin) to the evaluating body.
- Independent Statistical Analysis: The evaluating body unblinds the results and performs an independent analysis of key performance metrics, such as sensitivity, specificity, and tissue-of-origin accuracy [98].
Workflow for Multi-Cancer Detection Assay Validation
The following diagram illustrates the rigorous, multi-stage pathway used by the National Cancer Institute (NCI) to select and validate multi-cancer detection (MCD) assays for large-scale clinical trials, as detailed in [98].
The Scientist's Toolkit: Essential Research Reagents & Materials
Successful development and validation of AI models for cancer detection rely on a foundation of high-quality, well-characterized resources. The table below details key solutions and materials used in the featured studies.
Table 3: Key Research Reagent Solutions for AI in Cancer Detection
| Item Name | Function & Application | Example from Search Results |
|---|---|---|
| Annotated Multi-Center Datasets | Serves as the benchmark for training and testing AI models, ensuring they learn from diverse, real-world data. | The MAMA-MIA dataset: 1,506 breast DCE-MRI cases with expert segmentations from 4 collections [94]. |
| Blinded Biobank Reference Sets | Provides an objective, standardized resource for the external validation of diagnostic assays on blinded specimens. | The Alliance Reference Set: A biospecimen set specifically designed for validating Multi-Cancer Detection (MCD) assays [98]. |
| Pre-trained Baseline Models | Accelerates research by providing a starting point for model development and a benchmark for performance comparison. | The MAMA-MIA dataset includes pre-trained weights for a baseline nnU-Net segmentation model [94]. |
| Stain Normalization Algorithms | (Digital Pathology) Reduces technical variability in Whole Slide Images caused by differences in staining protocols across labs, improving model generalizability [93]. | Used in several lung cancer pathology AI studies to minimize inter-site image variability [93]. |
| Radiomics Feature Extraction Software | Enables the quantitative characterization of tumor phenotypes from medical images, which can be used as input for ML models [97]. | Central to radiomic pipelines that link imaging features to clinical outcomes in oncology [97]. |
Analysis of Critical Factors for Clinical Adoption
Beyond raw performance metrics, the pathway to integrating an AI tool into clinical workflow depends on several factors solidified during rigorous validation.
Impact on Clinical Workflow and Decision-Making
The ultimate value of an AI tool is measured by its ability to improve patient care and streamline clinical processes. The ovarian cancer study demonstrated that an AI-driven triage system could reduce referrals to experts by 63% while simultaneously surpassing the diagnostic performance of current practice, directly addressing the critical shortage of expert ultrasound examiners [92]. Similarly, a scoping review of oncology ML models found that clinical utility assessments, involving 499 clinicians, indicated improved clinician performance with AI assistance and superior outcomes compared to standard clinical systems [97].
Common Pitfalls and Methodological Limitations
Despite promising results, the literature consistently highlights recurring limitations that hinder clinical adoption:
- High Risk of Bias: A systematic review of AI in lung cancer pathology found a high or unclear risk of bias in most studies, particularly in the "Participant selection/study design" domain (86% of studies) [93].
- Retrospective and Case-Control Designs: The vast majority of validation studies are retrospective, with a significant number using case-control designs which can overestimate performance compared to real-world, prospective cohorts [95] [93].
- Small and Non-Representative Datasets: External validation is often performed on small, non-representative datasets that do not fully capture the heterogeneity of clinical practice [97] [93].
- Inconsistent Reporting: There is a persistent lack of consistent reporting of calibration metrics and insufficient detail on validation methodologies, which hinders reliable model comparison and clinical trust [97] [95].
Performance Generalization Across Domains
The following diagram synthesizes findings from systematic reviews to illustrate the typical performance trajectory of AI models from internal development to external validation, highlighting the critical importance of multi-center trials [92] [95] [93].
The comparative analysis of ML and DL for cancer detection unequivocally demonstrates that sophisticated model architectures are capable of achieving diagnostic performance that meets or exceeds human expertise and conventional tools. However, this performance is context-dependent. External validation and multi-center trials are not merely supplementary checks; they are the definitive processes that separate robust, clinically generalizable models from those that are academically proficient but clinically fragile. The evidence shows that models validated on large, diverse, multi-center datasets, such as the transformer-based ovarian cancer classifier, show the most promise for real-world impact [92]. Conversely, models lacking this level of rigorous validation, a common issue in digital pathology AI for lung cancer, face significant barriers to clinical trust and integration [93]. The future of AI in oncology therefore hinges on a committed shift toward larger, prospective, multi-center trials, standardized reporting, and a relentless focus on clinical utility, not just algorithmic performance.
The integration of artificial intelligence (AI), particularly machine learning (ML) and deep learning (DL), into oncology represents a paradigm shift in cancer detection, offering the potential for enhanced diagnostic accuracy and workflow efficiency [17] [99]. These technologies are being applied across multiple cancer types, including lung, breast, and brain cancers, to assist in tasks ranging from medical image interpretation to risk prediction based on symptomatic and lifestyle data [100] [11] [15]. However, the transition from research validation to routine clinical use has been markedly slow [101]. This guide objectively compares the performance of ML and DL models in cancer detection and analyzes the primary barriers—regulatory hurdles, ethical concerns, and workflow integration challenges—that impede their widespread clinical adoption. Understanding these barriers is crucial for researchers, scientists, and drug development professionals working to translate promising algorithms into tools that improve patient outcomes.
Performance Comparison: ML versus DL in Cancer Detection
The comparative performance of ML and DL models is highly context-dependent, varying with the cancer type, data modality, and specific clinical task. The following tables summarize experimental results from recent studies, providing a quantitative basis for comparison.
Table 1: Comparative Performance of ML and DL Models Across Different Cancers
| Cancer Type | Data Modality | Best Performing ML Model | ML Performance (%) | Best Performing DL Model | DL Performance (%) | Key Study Finding |
|---|---|---|---|---|---|---|
| Brain Tumor [100] | MRI (BraTS 2024) | Random Forest | Accuracy: 87.00 | EfficientNet | Accuracy: 70.00 | Traditional ML (Random Forest) significantly outperformed all DL models evaluated. |
| Lung Cancer [15] | Symptom & Lifestyle Data | Not Specified | Accuracy: <92.86 | Single-hidden-layer Neural Network | Accuracy: 92.86 | A simple DL architecture outperformed several traditional ML classifiers. |
| Breast Cancer [11] | Clinical & Synthetic Data | K-Nearest Neighbors (KNN) | High Accuracy* | AutoML (H2OXGBoost) | High Accuracy* | Traditional ML (KNN) and AutoML demonstrated high effectiveness, with performance boosted using synthetic data. |
| Brain Tumor [102] | MRI | - | - | YOLOv9 | High Precision/Recall | YOLOv9 outperformed other DL models like YOLOv8 and Faster R-CNN in detection tasks. |
*The specific accuracy value was not detailed in the provided summary.
Table 2: Performance of Deep Learning Models in Specific Diagnostic Tasks
| Cancer Type | Clinical Task | DL Model | Sensitivity (%) | Specificity (%) | AUC | Evidence Level | Ref |
|---|---|---|---|---|---|---|---|
| Colorectal Cancer | Malignancy Detection via Colonoscopy | CRCNet | 91.30 (vs. 83.80 human) | 85.30 | 0.882 | Retrospective multicohort diagnostic study with external validation | [99] |
| Breast Cancer | Screening Detection via Mammography | Ensemble of 3 DL models | +2.70 (absolute increase vs. 1st reader) | +1.20 (absolute increase vs. 1st reader) | 0.889 | Diagnostic case-control study with comparison to radiologists | [99] |
| Lung Cancer | Nodule Classification from CT scans | Multi-attention Ensemble Model | 98.73 | 98.96 | - | Advanced model demonstrating high performance | [103] |
Experimental Protocols in Cited Studies
To critically assess the performance data, understanding the underlying experimental methodology is essential. Below are the detailed protocols from key studies cited in this guide.
Brain Tumor Classification with ML and DL
- Objective: To evaluate and compare several ML and DL techniques for classifying brain tumors from MRI scans using the BraTS 2024 dataset [100].
- Data Preprocessing: The study utilized a subset of MRI modalities, specifically contrast-enhanced T1 (T1c), T2w, and T2-FLAIR images. Corresponding segmentation masks were used to extract quantitative measurements, such as tumor size, to create binary labels (high vs. low tumor burden) based on the median tumor volume [100].
- Models Evaluated:
- Deep Learning: Simple CNN, VGG16, VGG19, ResNet50, Inception-ResNetV2, and EfficientNet.
- Machine Learning: Random Forest classifier applied to features extracted from the imaging data.
- Training & Evaluation: Model performance was assessed using standard metrics including accuracy, loss, and confusion matrices. The results were visualized using ROC curves and accuracy metrics [100].
Lung Cancer Prediction Based on Symptomatic and Lifestyle Features
- Objective: To systematically evaluate and compare the predictive efficacy of ML and DL models for lung cancer prediction using patient symptom and lifestyle factor data from a Kaggle dataset [15].
- Data Preprocessing: The protocol involved rigorous data preprocessing, including feature selection using Pearson’s correlation to identify the most relevant features, outlier removal, and data normalization to prepare the dataset for modeling [15].
- Models Evaluated:
- Machine Learning: Decision Trees, K-Nearest Neighbors, Random Forest, Naïve Bayes, AdaBoost, Logistic Regression, and Support Vector Machines, implemented using Weka.
- Deep Learning: Neural network models with 1, 2, and 3 hidden layers, developed in Python within a Jupyter Notebook environment.
- Training & Evaluation: The model performance was assessed using K-fold cross-validation and an 80/20 train/test split to ensure robust evaluation and prevent overfitting [15].
Regulatory, Ethical, and Workflow Barriers to Adoption
Despite their promising performance, ML and DL models face significant roadblocks to clinical integration. These challenges extend beyond technical accuracy to encompass regulatory, ethical, and practical concerns.
Regulatory and Ethical Barriers
The regulatory landscape for AI in healthcare is complex and evolving. Key concerns include:
- Data Privacy and Protection: The most frequently reported ethical and legal concern is patient data privacy [103]. ML models require access to large volumes of sensitive patient data for training and operation, raising concerns about compliance with regulations like the Health Insurance Portability and Accountability Act (HIPAA) in the United States and the General Data Protection Regulation (GDPR) in the European Union [103] [104].
- Algorithmic Bias and Fairness: Models trained on biased or non-representative datasets can perpetuate or exacerbate health disparities [104] [105]. For instance, if a training dataset underrepresents certain demographic groups, the algorithm's predictions may be inaccurate for those populations, leading to inequitable care [103] [105].
- Transparency and Explainability: The "black-box" nature of many complex DL models poses a challenge for clinical trust and regulatory approval. Clinicians are often hesitant to rely on systems without a clear understanding of the reasoning behind a decision [103] [104].
- Liability and Accountability: A critical legal challenge is determining liability for AI-based medical errors. It remains ambiguous whether responsibility lies with the algorithm developers, the healthcare providers who use the tool, or the institutions that deploy it [103] [104].
Workflow Integration Barriers
Successfully deploying a validated model into a clinical setting requires careful planning and execution. The following diagram illustrates the key stages and critical components of a clinical AI implementation roadmap.
Clinical AI Implementation Roadmap
The implementation of AI models is a continuous lifecycle, not a one-time event [101]. Key workflow barriers include:
- Pre-Implementation: A significant barrier is the performance drop models often experience when moving from a controlled research environment to a real-world clinical setting due to factors like "dataset shift" [101]. Conducting local retrospective validation and ensuring data infrastructure compatibility with clinical systems (e.g., EHRs via FHIR APIs) are critical first steps [101].
- Peri-Implementation: A lack of clear governance structures and effective communication between IT, informatics, data science, and clinical teams can derail deployment [101]. Before full rollout, a "silent validation" (where model outputs are logged but not shown to clinicians) and a pilot study are essential to validate production data feeds and assess impact on clinical workflow without patient risk [101].
- Post-Implementation: A deployed model's performance can degrade over time due to changes in disease patterns, medical equipment, or treatment protocols [101]. Continuous performance monitoring and surveillance are necessary to detect model drift, alongside establishing clear protocols for model updating, retraining, and decommissioning [101].
The Scientist's Toolkit: Research Reagent Solutions
The following table details key computational tools and resources used in the development and validation of ML/DL models for cancer detection, as referenced in the studies analyzed.
Table 3: Essential Research Tools and Resources for AI in Cancer Detection
| Tool / Resource Name | Type / Category | Primary Function in Research | Example Use Case |
|---|---|---|---|
| BraTS Dataset [100] | Medical Imaging Dataset | Provides a standardized, multi-institutional dataset of brain MRIs with corresponding tumor segmentation masks. | Serves as a benchmark for training and evaluating brain tumor segmentation and classification models [100]. |
| Weka [15] | Machine Learning Software Suite | A comprehensive workbench for applying a wide variety of ML algorithms to datasets, facilitating data preprocessing, classification, and evaluation. | Used to implement and compare traditional ML classifiers like SVM, RF, and KNN for lung cancer prediction [15]. |
| Python with Jupyter Notebook [15] | Programming Language & Development Environment | Provides a flexible and interactive platform for developing custom DL models, performing data analysis, and visualizing results. | Used to build and train neural network models with multiple hidden layers for lung cancer prediction [15]. |
| AutoML (e.g., H2O) [11] | Automated Machine Learning Framework | Automates the process of model selection, hyperparameter tuning, and feature engineering, making ML more accessible. | Employed to create an ensemble model (H2OXGBoost) for breast cancer prediction, achieving high accuracy [11]. |
| Pre-trained CNN Models (VGG, ResNet) [100] [99] | Deep Learning Architecture | Leverages transfer learning by using models pre-trained on large image datasets (e.g., ImageNet) as a starting point for medical image analysis. | Fine-tuned on specific medical imaging tasks, such as classifying lung nodules from CT scans or detecting tumors in MRIs [100] [99]. |
| Synthetic Data Generators (Gaussian Copula, TVAE) [11] | Data Generation Model | Creates realistic, synthetic tabular data that mirrors the statistical properties of an original dataset, addressing data scarcity and privacy concerns. | Used to generate synthetic breast cancer data, which helped improve the prediction performance of ML models [11]. |
The comparative analysis of ML and DL for cancer detection reveals a nuanced landscape. While DL models often achieve state-of-the-art performance, particularly in image-based tasks like detecting lung nodules or segmenting brain tumors, traditional ML models can be highly competitive and sometimes superior, especially with structured data or smaller dataset sizes [100] [15]. The choice between ML and DL is not merely a pursuit of the highest accuracy metric but a strategic decision that must account for the broader context of clinical adoption. The most significant barriers—stringent regulatory requirements, profound ethical concerns around data privacy and algorithmic bias, and the complexities of workflow integration—often present greater challenges than the initial model development. Future progress in the field hinges on the development of more transparent and explainable models, robust and continuous multi-site validation studies, and the creation of clear regulatory pathways and governance frameworks that ensure these powerful technologies are deployed safely, equitably, and effectively to improve patient care.
Conclusion
The comparative analysis reveals that the choice between ML and DL is not a matter of superiority but of strategic application. Classical ML models, with their computational efficiency and strong performance on structured data, remain excellent choices for specific predictive tasks. In contrast, DL architectures excel at unraveling complex patterns in high-dimensional data like medical images and genomics, offering superior accuracy where data is abundant. The future of AI in cancer detection lies not in a single algorithm, but in hybrid models that leverage the strengths of both approaches, integrated within robust, explainable, and ethically sound frameworks. For biomedical and clinical research, the imperative is to move beyond isolated model development towards interdisciplinary collaboration, the creation of large, diverse, and high-quality datasets, and the implementation of rigorous, prospective validation studies to ensure these powerful tools can be translated safely and equitably into clinical practice, ultimately paving the way for more personalized and effective cancer care.
References
- 1. Trade-Off Analysis of Classical Machine Learning and Deep ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12456844/]
- 2. Deep Learning for Cancer Detection Based on Genomic and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12459622/]
- 3. Automating cancer diagnosis using advanced deep ... [https://www.nature.com/articles/s41598-024-75876-2]
- 4. Fusion of classical and deep learning features with ... [https://www.nature.com/articles/s41598-025-24734-w]
- 5. Predicting cancer risk using machine learning on lifestyle ... [https://www.nature.com/articles/s41598-025-15656-8]
- 6. Using AI for Cancer Detection: Challenges and Opportunities [https://mobidev.biz/blog/ai-cancer-detection-approaches-challenges-opportunities]
- 7. Deep Learning Applications in Clinical Cancer Detection [https://www.sciencedirect.com/science/article/pii/S2949761225000604]
- 8. Early cancer detection using deep learning and medical ... [https://www.sciencedirect.com/science/article/pii/S1040842824002713]
- 9. Imaging genomics of cancer: a bibliometric analysis and review [https://pmc.ncbi.nlm.nih.gov/articles/PMC11877899/]
- 10. Exploring AI Approaches for Breast Cancer Detection and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12553387/]
- 11. Advancing breast cancer prediction: Comparative analysis of ... [https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0326221]
- 12. Detection of breast cancer using machine learning and ... [https://www.nature.com/articles/s41598-025-12644-w]
- 13. Emerging biomarkers for early cancer detection and diagnosis [https://eurjmedres.biomedcentral.com/articles/10.1186/s40001-025-03003-6]
- 14. Automated real-world data integration improves cancer ... [https://www.nature.com/articles/s41586-024-08167-5]
- 15. Comparative Analysis of Machine Learning and Deep ... [https://www.mdpi.com/2076-3417/15/8/4507]
- 16. Cancer statistics, 2025 - PMC - PubMed Central - NIH [https://pmc.ncbi.nlm.nih.gov/articles/PMC11745215/]
- 17. Comparative analysis of machine learning and deep ... [https://www.sciencedirect.com/science/article/abs/pii/S0957417424017056]
- 18. Deep Learning Applications in Clinical Cancer Detection [https://pmc.ncbi.nlm.nih.gov/articles/PMC12351333/]
- 19. Performance of Two Deep Learning-based AI Models for ... [https://pubmed.ncbi.nlm.nih.gov/39907587/]
- 20. A Deep Learning and Explainable Artificial Intelligence ... [https://www.nature.com/articles/s41598-024-80535-7]
- 21. How Artificial Intelligence Is Transforming Cancer Care in ... [https://oncodaily.com/oncolibrary/artificial-intelligence-ai]
- 22. Uses and limitations of artificial intelligence for oncology - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC11170282/]
- 23. Machine Learning and AI in Cancer Prognosis, Prediction ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10312208/]
- 24. Machine Learning vs. Deep Learning: What Changes in Practice [https://skyone.solutions/en/blog/ia/machine_learning_and_deep_learning_in_practice/]
- 25. AI vs ML vs DL: Key Differences and Real-World ... [https://morsoftware.com/blog/ai-vs-ml-vs-dl]
- 26. A comprehensive analysis of recent advancements in cancer ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11796559/]
- 27. A comprehensive review of machine learning and deep ... [https://www.sciencedirect.com/science/article/pii/S2773186325000854]
- 28. A comprehensive benchmark of machine and deep ... [https://www.sciencedirect.com/science/article/pii/S0925231225020090]
- 29. Basic Comparison Between RandomForest, SVM, and ... [https://medium.com/@ap.nattapoj_st/basic-comparison-between-randomforest-svm-and-xgboost-0e5862871175]
- 30. The application of random forest-based models in ... [https://www.frontiersin.org/journals/artificial-intelligence/articles/10.3389/frai.2025.1517670/full]
- 31. Breast cancer diagnosis using support vector machine ... [https://www.nature.com/articles/s41598-024-61322-w]
- 32. XGBoost Explained: A Beginner's Guide [https://medium.com/low-code-for-advanced-data-science/xgboost-explained-a-beginners-guide-095464ad418f]
- 33. Comparative analysis of ML models and deep learning ... [https://pubmed.ncbi.nlm.nih.gov/40531928/]
- 34. Stacked random forest model for colorectal cancer ... [https://pubmed.ncbi.nlm.nih.gov/40755955/]
- 35. Performance evaluation of Machine Learning models in ... [https://www.sciencedirect.com/science/article/pii/S0959804925005544]
- 36. Review of Artificial Intelligence Techniques for Breast Cancer ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12561872/]
- 37. CNN vs Vision Transformer (ViT): Which Wins in 2025? [https://hiya31.medium.com/cnn-vs-vision-transformer-vit-which-wins-in-2025-e1cb2dfcb903]
- 38. Convolutional neural network [https://en.wikipedia.org/wiki/Convolutional_neural_network]
- 39. Evaluating Transformer Architectures: Metrics & Benchmarks [https://futureagi.com/blogs/evaluating-transformer-architectures-key-metrics-and-performance-benchmarks]
- 40. Comparing Natural Language Processing Techniques [https://www.kdnuggets.com/comparing-natural-language-processing-techniques-rnns-transformers-bert]
- 41. What are Convolutional Neural Networks? [https://www.ibm.com/think/topics/convolutional-neural-networks]
- 42. Image Classification: State-of-the-Art Models in 2025 [https://hiringnet.com/image-classification-state-of-the-art-models-in-2025]
- 43. Transformer versus traditional natural language processing [https://pmc.ncbi.nlm.nih.gov/articles/PMC10461267/]
- 44. The Impact of Artificial Intelligence on Lung Cancer Diagnosis ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12429163/]
- 45. A benchmark of deep learning approaches to predict lung ... [https://www.nature.com/articles/s41598-024-84193-7]
- 46. Artificial intelligence in cancer: applications, challenges, and ... [https://molecular-cancer.biomedcentral.com/articles/10.1186/s12943-025-02450-3]
- 47. Improving Lung Cancer Risk Prediction Using Machine ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12109916/]
- 48. A Comprehensive Analysis on Machine Learning based ... [https://www.sciencedirect.com/science/article/pii/S2666521225001139]
- 49. Enhancing Ishihara and educational images using ... [https://www.frontiersin.org/journals/artificial-intelligence/articles/10.3389/frai.2025.1676644/full]
- 50. Enhancing Ishihara and educational images using ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12575240/]
- 51. 人工智能在临床领域的研究进展及前景展望 [https://aammt.tmmu.edu.cn/Upload/rhtml/202112092.htm]
- 52. Advancements in Breast Cancer Detection: A Review of Global Trends, Risk Factors, Imaging Modalities, Machine Learning, and Deep Learning Approaches [https://www.mdpi.com/2673-7426/5/3/46]
- 53. A deep learning-based multimodal medical imaging model ... [https://www.nature.com/articles/s41598-025-99535-2]
- 54. 图2 内镜图像分析:ML vs DL [https://www.china-oncology.com/CN/figure/showFigure.do?fid=3869]
- 55. 新型AI病理模型,实现大规模肿瘤筛查及细粒度量化诊断 [https://m.thepaper.cn/newsDetail_forward_32004905]
- 56. Frontiers | Breast cancer diagnosis using radiomics-guided DL/ML model-systematic review and meta-analysis [https://www.frontiersin.org/journals/computer-science/articles/10.3389/fcomp.2025.1446270/full]
- 57. AI in Breast Cancer Imaging: An Update and Future Trends [https://www.sciencedirect.com/science/article/pii/S000129982500008X]
- 58. The Future of Breast Cancer Organized Screening Program Through Artificial Intelligence: A Scoping Review - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC11855082/]
- 59. The AI revolution: how multimodal intelligence will reshape ... [https://www.nature.com/articles/s44387-025-00044-4]
- 60. Multimodal Integration in Health Care - PubMed Central - NIH [https://pmc.ncbi.nlm.nih.gov/articles/PMC12370271/]
- 61. Review The potential of large language models to advance ... [https://www.sciencedirect.com/science/article/pii/S2352396425001392]
- 62. Current AI technologies in cancer diagnostics and treatment [https://molecular-cancer.biomedcentral.com/articles/10.1186/s12943-025-02369-9]
- 63. A large-scale, multi-centre validation study of an AI ... [https://www.nature.com/articles/s41698-025-01105-2]
- 64. Artificial Intelligence in Cancer Drug Discovery in 2025 [https://oncodaily.com/oncolibrary/artificial-intelligence-in-cancer-drug-discovery]
- 65. Experts Forecast Cancer Research and Treatment ... [https://www.aacr.org/blog/2025/01/10/experts-forecast-cancer-research-and-treatment-advances-in-2025/]
- 66. Top Oncology Innovations That Shaped the First Half of 2025 [https://binaytara.org/cancernews/article/top-oncology-innovations-that-shaped-the-first-half-of-2025]
- 67. Synthetic Tabular Data Generation Under Horizontal ... [https://medinform.jmir.org/2025/1/e74116]
- 68. A highly generalized federated learning algorithm for brain ... [https://www.nature.com/articles/s41598-025-05297-2]
- 69. Federated Breast Cancer Detection Enhanced by Synthetic ... [https://arxiv.org/html/2506.23334v1]
- 70. FedCSCD-GAN: A secure and collaborative framework for ... [https://www.sciencedirect.com/science/article/abs/pii/S1746809423013265]
- 71. Deep learning in cancer diagnosis, prognosis and treatment selection | Genome Medicine | Full Text [https://genomemedicine.biomedcentral.com/articles/10.1186/s13073-021-00968-x]
- 72. A Comparative Analysis of Breast Cancer Detection and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7349542/]
- 73. A review on recent developments in cancer detection using Machine Learning and Deep Learning models - ScienceDirect [https://www.sciencedirect.com/science/article/abs/pii/S1746809422008527]
- 74. A review and comparative study of cancer detection using ... [https://bmcbioinformatics.biomedcentral.com/articles/10.1186/s12859-023-05235-x]
- 75. Explainable AI-enabled hybrid deep learning architecture for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12531632/]
- 76. Medical artificial intelligence and the black box problem [https://www.sciencedirect.com/science/article/pii/S2667102623000578]
- 77. Explainable AI in Clinical Decision Support Systems [https://pmc.ncbi.nlm.nih.gov/articles/PMC12427955/]
- 78. Should AI models be explainable to clinicians? - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC11391805/]
- 79. Explainable AI for Clinical Decision Support Systems [https://www.mdpi.com/2227-9709/12/4/119]
- 80. Improved cancer detection through feature selection using ... [https://www.nature.com/articles/s41598-025-92187-2]
- 81. A hybrid feature selection algorithm combining information ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10927139/]
- 82. Enhancing lymphoma cancer detection using deep transfer ... [https://www.nature.com/articles/s41598-025-21888-5]
- 83. Enriched lung cancer classification approach using an ... [https://www.nature.com/articles/s41598-025-07322-w]
- 84. A Guide to Cross-Validation for Artificial Intelligence in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10388213/]
- 85. An automated deep learning framework for brain tumor ... [https://www.nature.com/articles/s41598-025-02209-2]
- 86. Brain Tumor Detection Based on Deep Learning Approaches ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10453020/]
- 87. Brain tumor classification using MRI images and deep ... [https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0322624]
- 88. Top 10 Machine Learning Frameworks to Use In 2025 [https://www.igmguru.com/blog/machine-learning-frameworks]
- 89. Top 10 Machine Learning Frameworks in 2025 [https://www.geeksforgeeks.org/blogs/machine-learning-frameworks/]
- 90. Machine learning algorithms using dermatoscopy for the ... [https://www.sciencedirect.com/science/article/pii/S2772611825004896]
- 91. Artificial Intelligence for the Diagnosis and Management of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12587170/]
- 92. International multicenter validation of AI-driven ultrasound detection ... [https://www.nature.com/articles/s41591-024-03329-4?error=cookies_not_supported]
- 93. Systematic scoping review of external validation studies ... [https://www.nature.com/articles/s41698-025-00940-7]
- 94. A large-scale multicenter breast cancer DCE-MRI ... [https://www.nature.com/articles/s41597-025-04707-4]
- 95. External Validation of Deep Learning Algorithms for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9152694/]
- 96. Comparing the Performance of Machine Learning Models ... [https://www.jmir.org/2025/1/e76215]
- 97. Externally validated and clinically useful machine learning ... [https://bmcmedresmethodol.biomedcentral.com/articles/10.1186/s12874-025-02463-y]
- 98. Framework to Select Multi-Cancer Detection Assays in the ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12491945/]
- 99. Artificial intelligence in cancer: applications, challenges, and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12574039/]
- 100. Comparative analysis of machine learning techniques on ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12477006/]
- 101. Implementing AI Models in Clinical Workflows: A Roadmap [https://pmc.ncbi.nlm.nih.gov/articles/PMC11666800/]
- 102. Performance comparison of deep learning models for MRI ... [https://www.aimspress.com/article/doi/10.3934/bioeng.2025001?viewType=HTML]
- 103. Ethical and legal concerns in artificial intelligence applications ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12558840/]
- 104. Ethical and regulatory challenges in machine learning- ... [https://www.sciencedirect.com/science/article/pii/S2772485925000286]
- 105. 2025 Outlook: Machine Learning Applications in Healthcare [https://kms-technology.com/blog/machine-learning-applications-in-healthcare/]