Liquid Biopsy and Circulating Tumor DNA: A Revolutionary Tool for Cancer Detection and Monitoring
This article provides a comprehensive overview of the transformative role of liquid biopsy and circulating tumor DNA (ctDNA) analysis in modern oncology.
Liquid Biopsy and Circulating Tumor DNA: A Revolutionary Tool for Cancer Detection and Monitoring
Abstract
This article provides a comprehensive overview of the transformative role of liquid biopsy and circulating tumor DNA (ctDNA) analysis in modern oncology. Tailored for researchers, scientists, and drug development professionals, it explores the foundational biology of ctDNA, cutting-edge detection methodologies like NGS and dPCR, and their clinical applications in multi-cancer early detection (MCED), minimal residual disease (MRD) monitoring, and guiding targeted therapies. The content also critically addresses current technical challenges, optimization strategies, and the robust validation framework from clinical trials that is cementing ctDNA's utility in precision medicine, shaping the future of cancer diagnostics and treatment.
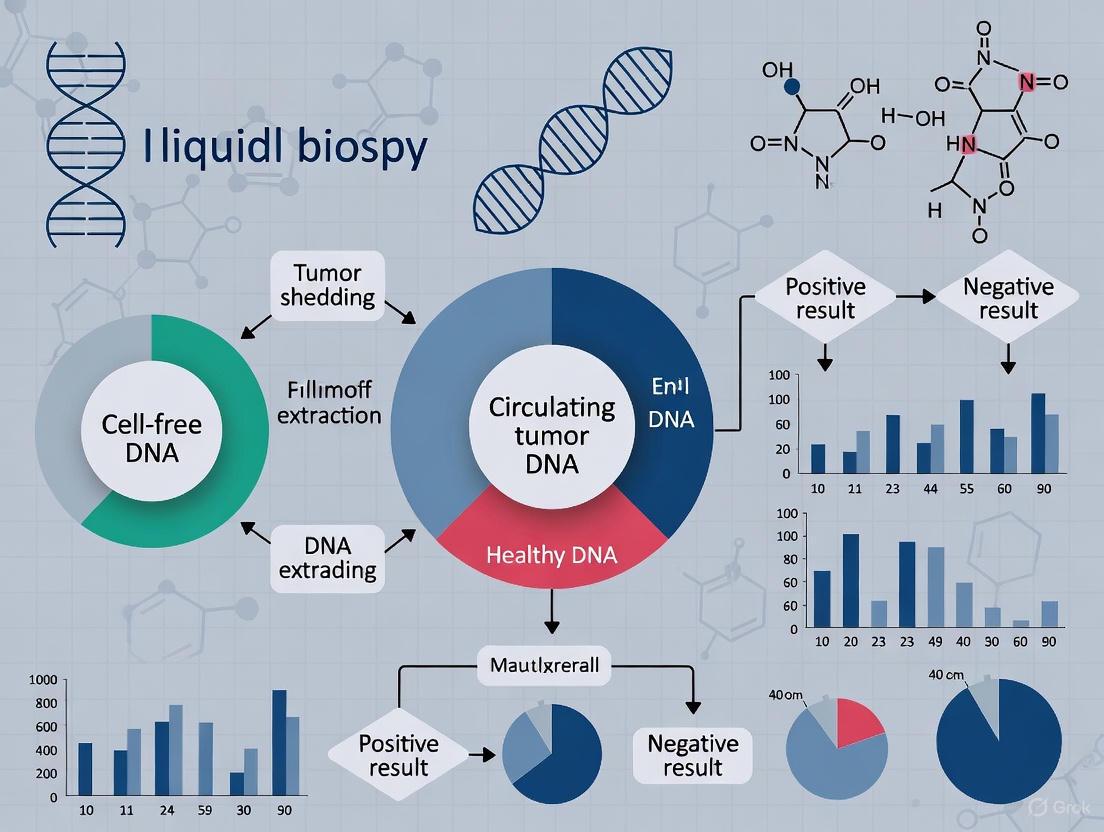
The Biology and Rising Significance of Circulating Tumor DNA
Circulating tumor DNA (ctDNA) refers to fragmented DNA released from tumor cells into the bloodstream and other bodily fluids [1] [2]. As a component of cell-free DNA (cfDNA), ctDNA carries tumor-specific genetic and epigenetic alterations, making it a critical analyte in liquid biopsies for cancer detection, monitoring, and management [3] [4]. The analysis of ctDNA provides a non-invasive means to assess tumor dynamics, genomic heterogeneity, and treatment response, representing a paradigm shift in precision oncology [5] [6]. This technical guide examines the fundamental biological characteristics of ctDNA, its mechanisms of release and clearance, and the advanced methodologies employed in its detection, providing a scientific foundation for its application in cancer research and drug development.
Biological Origins and Mechanisms of Release
ctDNA originates through several biological processes, with contributions from various cellular compartments within the tumor ecosystem. The diagram below illustrates the primary mechanisms of ctDNA release into the bloodstream.
The primary sources of ctDNA include:
Apoptotic Tumor Cells: This is considered a major source of ctDNA [1]. Apoptosis produces characteristic DNA fragments of approximately 166 base pairs, corresponding to mono-nucleosomes, which display a "ladder-like" distribution upon electrophoresis [1] [7]. During programmed cell death, cellular DNA is cleaved by endonucleases, and the resulting fragments are packaged into apoptotic bodies that may be cleared by phagocytes or released into circulation [1].
Necrotic Tumor Cells: Cells undergoing necrotic death due to hypoxia or metabolic stress release DNA in a more random, non-specific fragmentation pattern, often producing longer DNA fragments [1] [7]. Patients with advanced cancer and substantial tumor necrosis often demonstrate higher plasma ctDNA levels [1].
Active Secretion from Living Tumor Cells: Evidence suggests that viable tumor cells can actively release DNA and DNA-protein complexes through secretion mechanisms independent of cell death [1] [7]. One in vitro study found that ctDNA release from cultured cancer cells correlated with the percentage of cells in G1 phase rather than apoptosis or necrosis levels [7].
Circulating Tumor Cells (CTCs): CTCs that have detached from the primary tumor and entered circulation can release DNA directly into the bloodstream [1]. However, given the relatively low abundance of CTCs compared to the total tumor cell burden, this is unlikely to be the primary source of ctDNA [7].
The relative contribution of each mechanism varies depending on tumor type, location, disease stage, and treatments administered [7].
ctDNA in Metastasis: The Genometastasis Hypothesis
Beyond its role as a passive biomarker, experimental evidence suggests ctDNA may actively participate in cancer progression through the "genometastasis" hypothesis [1]. This proposes that ctDNA fragments containing oncogenes might be taken up by susceptible normal cells in distant organs, leading to their oncogenic transformation and potentially contributing to metastasis formation [1]. Studies have demonstrated that plasma from tumor-bearing rats and supernatants from human cancer cells can transform normal cells in vitro, an effect abolished when DNA is removed from these fluids [1]. While intriguing, this hypothesis requires further validation, particularly through in vivo clinical studies [1].
Physical and Molecular Characteristics
Quantitative and Structural Properties
ctDNA exhibits distinct physical and molecular characteristics that differentiate it from non-tumor cfDNA and inform detection methodologies.
Table 1: Physical and Molecular Characteristics of ctDNA
| Characteristic | Description | Research Significance |
|---|---|---|
| Size Distribution | Typically shorter fragments (90-150 bp) than non-tumor cfDNA; some studies report both extremely long and short fragments in cancer patients [1] [5]. | Enables size-selection enrichment strategies; short fragment enrichment can increase variant allele frequency in sequencing libraries [5]. |
| Molecular Form | Primarily double-stranded DNA, existing as mono- and oligonucleosomes, or within extracellular vesicles (1-10 µm) [1] [7]. | Influences isolation methods; vesicle-associated DNA may be protected from degradation [7]. |
| Concentration Range | Highly variable (0.01% to >90% of total cfDNA); correlates with tumor burden, stage, and metabolic activity [7] [4]. | Early-stage/low-shedding tumors present detection challenges; requires highly sensitive techniques [5] [4]. |
| Half-Life | Short half-life, estimated between 16 minutes to several hours [4]. | Enables real-time monitoring of tumor dynamics and treatment response [4]. |
| Genetic Features | Harbors tumor-specific alterations: point mutations, copy number variations, chromosomal rearrangements, methylation changes, and viral sequences [1] [3]. | Provides markers for detection, monitoring, and therapeutic targeting [1] [6]. |
The half-life of ctDNA is particularly noteworthy for its clinical applications. The brief circulation time, estimated between 16 minutes and several hours, reflects efficient clearance mechanisms primarily by the liver, kidneys, and nuclease activity in the blood [4]. This rapid turnover enables ctDNA levels to reflect real-time tumor dynamics, making it a valuable biomarker for monitoring treatment response and disease progression [4].
Comparative Analysis: ctDNA vs. General cfDNA
Understanding the differences between ctDNA and total cfDNA is fundamental for assay development.
Table 2: Key Differences Between ctDNA and General cfDNA
| Parameter | Circulating Tumor DNA (ctDNA) | General Cell-Free DNA (cfDNA) |
|---|---|---|
| Origin | Exclusively derived from tumor cells [1] [2]. | Derived from apoptosis/necrosis of normal cells, primarily hematopoietic lineages (e.g., white blood cells, erythrocyte progenitors) [7] [8]. |
| Genetic Content | Contains tumor-specific somatic mutations, copy number alterations, methylation changes, and rearrangements [1] [5]. | Reflects germline genome of the individual without tumor-specific alterations [2]. |
| Typical Fragment Size | Often shorter fragments; can show more diverse fragmentation patterns [1] [5] [3]. | More uniform fragment distribution, with a peak around 166 bp [8]. |
| Proportion in Blood | Can vary from <0.01% in early-stage disease to >90% in advanced metastatic cancer [5] [4]. | Comprises the majority of cell-free DNA in plasma, even in cancer patients [8]. |
| Clinical Utility | Biomarker for cancer detection, prognosis, treatment response, MRD, and resistance mutation identification [5] [6] [2]. | Useful in non-oncology applications (e.g., non-invasive prenatal testing, transplant rejection) [6] [8]. |
Advanced Detection Methodologies and Protocols
The low abundance of ctDNA in total cfDNA, particularly in early-stage cancers or minimal residual disease (MRD), demands highly sensitive and specific detection technologies [5] [6]. The following workflow outlines a generalized protocol for ctDNA analysis, from sample collection to data interpretation.
Critical Experimental Steps and Considerations
Sample Collection and Processing: Blood samples are collected in stabilizing tubes (e.g., Streck Cell-Free DNA BCT) to prevent genomic DNA contamination from white blood cell lysis [5]. Plasma is separated from whole blood via a two-step centrifugation process within hours of collection to ensure sample integrity [5] [4].
cfDNA Extraction and Quantification: cfDNA is isolated from plasma using specialized kits optimized for short fragments, such as magnetic bead-based technologies (e.g., MagMAX Cell-Free DNA Isolation Kit) [5] [8]. The extracted DNA is then quantified using fluorometric methods sensitive to low concentrations.
Library Preparation and Enhancement:
- Size Selection: Libraries can be enriched for shorter fragments (90-150 bp) to increase the relative abundance of tumor-derived DNA, improving the detection of low-frequency variants [5].
- Unique Molecular Identifiers (UMIs): Short nucleotide barcodes are added to individual DNA molecules before amplification. This allows bioinformatic correction of PCR amplification errors and sequencing artifacts, significantly improving detection sensitivity and specificity [4].
Analysis and Detection:
- PCR-Based Methods: Digital PCR (dPCR) and droplet digital PCR (ddPCR) enable absolute quantification of known mutations with high sensitivity (down to ~0.1% variant allele frequency) and rapid turnaround, suitable for monitoring specific mutations like ESR1 in breast cancer or KRAS in colorectal cancer [3] [4].
- Next-Generation Sequencing (NGS):
- Targeted NGS Panels: Methods like CAPP-Seq (Cancer Personalized Profiling by Deep Sequencing) and TEC-Seq (Targeted Error Correction Sequencing) focus on specific genomic regions of interest, allowing for deep sequencing and detection of rare variants down to ~0.01% VAF [5] [4].
- Structural Variant (SV) Analysis: Identifying tumor-specific chromosomal rearrangements (e.g., translocations) can achieve parts-per-million sensitivity, as these breakpoints are virtually absent in non-tumor DNA [5].
- Whole-Genome Sequencing (WGS): Low-coverage WGS can assess copy number alterations and fragmentation patterns (fragmentomics) to infer the presence of cancer, even without prior knowledge of specific mutations [3] [4].
Emerging Sensing Technologies: Nanomaterial-based electrochemical biosensors are under development for rapid, sensitive ctDNA detection. These platforms use graphene, molybdenum disulfide (MoS₂), or magnetic nano-electrodes to transduce DNA hybridization events into electrical signals, achieving attomolar sensitivity in some cases [5].
Essential Research Reagents and Solutions
Successful ctDNA analysis requires a suite of specialized reagents and instruments throughout the workflow.
Table 3: Essential Research Reagents and Solutions for ctDNA Analysis
| Reagent/Solution Category | Specific Examples | Primary Function |
|---|---|---|
| Blood Collection Tubes | Streck Cell-Free DNA BCT, PAXgene Blood ccfDNA Tubes | Stabilize nucleated blood cells to prevent lysis and preserve cfDNA profile post-phlebotomy. |
| Nucleic Acid Extraction Kits | MagMAX Cell-Free DNA Isolation Kit, QIAamp Circulating Nucleic Acid Kit | Isolation and purification of short-fragment cfDNA from plasma/serum with high efficiency and reproducibility. |
| Library Preparation Kits | KAPA HyperPrep Kit, Illumina DNA Prep Kit | Convert fragmented, double-stranded cfDNA into sequencing-ready libraries via end-repair, A-tailing, and adapter ligation. |
| Target Enrichment Probes | IDT xGen Lockdown Probes, Twist Pan-Cancer Panel | Hybridization-based capture of genomic regions of interest (e.g., cancer gene panels) from complex sequencing libraries. |
| Unique Molecular Identifiers (UMIs) | IDT UMI Adapters, Twist UMI Adapters | Molecular barcoding of original DNA molecules pre-amplification to enable accurate error correction and quantification. |
| PCR Reagents | ddPCR Supermix, Q5 High-Fidelity DNA Polymerase | Amplification of target sequences with high specificity and fidelity for detection (ddPCR) or library generation (NGS). |
| Sequence Capture Beads | MyOne Streptavidin T1 Beads, AMPure XP Beads | Magnetic bead-based purification and size selection of nucleic acids during library preparation and target enrichment. |
ctDNA is a dynamically informative biomarker with defined biological origins, distinct physical characteristics, and a short half-life that enables real-time monitoring of cancer [1] [4]. Its detection relies on sophisticated technologies capable of discriminating rare tumor-derived fragments against a background of normal cfDNA [5] [6]. As research continues to refine detection methodologies and validate clinical applications, ctDNA analysis is poised to become an increasingly integral component of precision oncology, offering a non-invasive window into tumor evolution, treatment response, and resistance mechanisms [9] [6] [4]. Future directions will focus on standardizing protocols, validating clinical utility in large-scale trials, and integrating multi-omic data to fully realize the potential of liquid biopsies in cancer management.
Circulating tumor DNA (ctDNA), comprising small fragments of DNA shed from tumor cells into the bloodstream, has emerged as a pivotal biomarker in oncology [3]. Its analysis, a core component of liquid biopsy technologies, represents a paradigm shift from traditional tissue biopsies by offering a non-invasive method for cancer detection, treatment monitoring, and prognosis [10]. The global market for ctDNA technologies is experiencing explosive growth, propelled by advances in precision oncology, rising cancer prevalence, and increasing demand for minimally invasive diagnostic tools [11]. This trajectory is underpinned by a rapidly expanding evidence base from clinical trials, demonstrating the utility of ctDNA assays in everything from early cancer detection to guiding therapy in advanced disease [9]. This whitepaper provides an in-depth analysis of the projected market growth, key technological drivers, and the experimental frameworks establishing the clinical validity of ctDNA analysis.
Global Market Size and Projections
The circulating tumor DNA (ctDNA) market is on a steep growth curve, transforming from a niche research area into a multi-billion-dollar clinical industry. The market expansion is quantified by a robust Compound Annual Growth Rate (CAGR), reflecting widespread adoption and continued innovation [11].
Table 1: Global ctDNA Market Size Projections (2025-2034)
| Year | Market Size (USD Billion) | Notes |
|---|---|---|
| 2025 | 7.96 | Calculated base year [11] |
| 2026 | 9.14 | [11] |
| 2034 | 27.67 | Projected value [11] |
| CAGR (2025-2034) | 14.85% | [11] |
This growth is not uniformly distributed geographically. Current dominance and future hotspots are clear:
- North America dominated the market in 2024, holding a 51% share [11]. The U.S. market alone is projected to grow from USD 3.09 billion in 2025 to approximately USD 10.90 billion by 2034, at a slightly higher CAGR of 15.02% [11].
- Asia-Pacific is identified as the fastest-growing region from 2025 to 2034, driven by expanding healthcare infrastructure, rising cancer incidence, and growing investment in precision medicine [11].
Key Market Drivers and Segment Analysis
The market's expansion is fueled by several interconnected factors. The rising global prevalence of cancer is a primary driver, creating an urgent need for better diagnostic and monitoring tools [11] [12]. Concurrently, there is a growing clinical and patient demand for non-invasive diagnostics to overcome the limitations of invasive tissue biopsies, such as procedural risks, sampling bias due to tumor heterogeneity, and inability to perform frequent monitoring [10] [13]. Furthermore, advancements in sequencing technologies and the broader growth of precision oncology, which relies on detailed genetic profiling to select targeted therapies, are fundamental enablers of the ctDNA market [11].
The market can be segmented to provide a clearer picture of its dynamics and leading applications.
Table 2: Key Market Segments and Leading Applications
| Segment | Leading Sub-Segment and Share | Fastest-Growing Sub-Segment |
|---|---|---|
| Technology | Next-Generation Sequencing (NGS) (48% share in 2024) [11] | PCR-based assays [11] |
| Application | Cancer Diagnosis and Screening (53% share in 2024) [11] | Minimal Residual Disease (MRD) Monitoring [11] |
| Sample Test | Blood (82% share in 2024) [11] | Urine [11] |
| End-User | Clinical Laboratories & Diagnostic Centers (51% share in 2024) [11] | Biopharma Companies [11] |
The dominance of NGS is due to its ability to analyze multiple genetic alterations simultaneously without prior knowledge of the tumor's mutation profile, making it ideal for comprehensive genomic profiling [3] [11]. Meanwhile, PCR-based assays are growing rapidly due to their cost-effectiveness, high sensitivity for detecting known mutations, and faster turnaround times, making them suitable for targeted applications like monitoring specific mutations [3] [11]. The leadership of the cancer diagnosis and screening segment underscores the critical role of ctDNA in early detection. However, the MRD monitoring segment's rapid growth highlights a pivotal application: using ctDNA to detect trace amounts of cancer cells after curative-intent therapy (surgery or chemo/radiation), often months before clinical or radiological recurrence [3] [14] [12].
Market Growth Drivers and Key Segments
Technological Foundations and Experimental Protocols
The clinical utility of ctDNA is made possible by highly sensitive analytical methods capable of detecting rare mutant DNA molecules in a vast background of wild-type cell-free DNA (cfDNA) derived from normal cells [3] [10].
Core Detection Technologies
- Next-Generation Sequencing (NGS): This is the workhorse for comprehensive ctDNA profiling. Methods include:
- Targeted Error Correction Sequencing (TEC-Seq): An ultra-deep, highly multiplexed sequencing method that uses redundant sequencing and unique molecular identifiers (UMIs) to distinguish true low-frequency mutations from errors introduced during PCR and sequencing [3].
- CAncer Personalized Profiling by deep Sequencing (CAPP-Seq): A method that uses selector probes to enrich for genomic regions that are frequently mutated in a particular cancer type, allowing for efficient and sensitive monitoring of tumor-derived DNA [3].
- Whole-Genome Sequencing (WGS) & Whole-Exome Sequencing (WES): Used for hypothesis-free discovery of mutations, though their use in ctDNA is sometimes limited by cost and the need for high sequencing depth to achieve good sensitivity [3].
- PCR-Based Methods: These are highly sensitive for detecting pre-specified mutations.
- Digital Droplet PCR (ddPCR): Partitions a sample into thousands of nanoliter-sized droplets, so that each droplet contains either zero or one target DNA molecule. After PCR amplification, the droplets are counted as positive or negative, allowing for absolute quantification of the mutant allele with very high sensitivity [3].
- BEAMing (Beads, Emulsion, Amplification, and Magnetics): Similar in principle to ddPCR, it uses emulsion PCR on magnetic beads to isolate and amplify single DNA molecules, which are then detected via flow cytometry [3] [10].
- Emerging Approaches:
- Methylomics: Analyzes the DNA methylation patterns on ctDNA, which are highly cell-type specific. Methods include whole-genome bisulfite sequencing (WGBS) to identify cancer-specific methylation signatures that can be used for early detection and cancer typing [3] [10].
- Fragmentomics: Analyzes the patterns of cfDNA fragmentation, such as fragment size and end motifs, which differ between non-cancer and cancer-derived DNA. The DELFI (DNA evaluation of fragments for early interception) method uses machine learning on low-coverage WGS data to detect cancer based on these fragmentation profiles [3].
Detailed Experimental Protocol: Tumor-Informed ctDNA MRD Detection
The following protocol, as used in studies like the VICTORI trial for colorectal cancer, details the gold-standard approach for detecting Minimal Residual Disease (MRD) with high sensitivity [14].
Objective: To detect the presence of ctDNA in plasma following curative-intent surgery to identify patients with MRD who are at high risk of relapse.
Workflow:
Tumor-Informed MRD Detection Workflow
- Tumor Whole Exome/Genome Sequencing: DNA is extracted from the patient's resected primary tumor tissue and matched normal sample (e.g., buffy coat from blood). Whole exome or genome sequencing is performed to identify a set of somatic mutations unique to the patient's tumor [14].
- Personalized Panel Design: A custom sequencing panel is computationally designed for the patient, targeting up to 1,800 somatic single nucleotide variants (SNVs) and small insertions/deletions (indels) identified in step 1. This patient-specific "fingerprint" is what allows for ultra-sensitive tracking [14].
- Longitudinal Plasma Collection: Blood samples are collected at defined timepoints:
- Pre-operatively (to confirm baseline ctDNA detectability).
- Post-operatively every 2 weeks for the first 8 weeks (a critical window for adjuvant therapy decisions).
- Thereafter, every 3 months for long-term monitoring (e.g., 3 years) [14].
- Plasma Processing and cfDNA Extraction: Blood samples are processed to isolate plasma. Cell-free DNA (cfDNA) is then extracted from the plasma using commercial kits based on magnetic bead-based technology, which maximizes recovery of short, fragmented DNA [14] [13].
- Library Preparation and Sequencing: Sequencing libraries are prepared from the extracted cfDNA using the personalized panel for target enrichment. The libraries are then sequenced on a high-throughput NGS platform [14].
- Bioinformatic Analysis and Variant Calling: The NGS data is processed through a customized bioinformatics pipeline. This pipeline performs alignment, UMI-aware deduplication, and ultra-sensitive variant calling to detect the patient-specific mutations in the plasma. Sensitivity can reach levels as low as 2 parts per million (ppm), enabling the detection of minute amounts of ctDNA [14].
- Interpretation: A sample is called "ctDNA positive" if a statistically significant number of patient-specific variants are detected above the background noise level.
Key Findings from this Protocol (VICTORI Interim Analysis):
- ctDNA was detected 198 days earlier than imaging on average, with one case detected 416 days prior to clinical recurrence [14].
- 87% of patients who later had a clinical recurrence were ctDNA-positive within the first 8 weeks after surgery [14].
- Higher ctDNA levels at first detection correlated with a shorter time to clinical relapse, providing prognostic value [14].
The Scientist's Toolkit: Essential Research Reagent Solutions
Successful ctDNA research and assay development relies on a suite of specialized reagents and tools. The following table details key solutions and their critical functions in the experimental workflow.
Table 3: Essential Research Reagent Solutions for ctDNA Analysis
| Research Solution | Critical Function | Technical Notes |
|---|---|---|
| cfDNA Extraction Kits (Magnetic Bead-Based) | Isolation of high-quality, short-fragmented cfDNA from plasma/serum while inhibiting nucleases. Maximizes yield from limited samples (<1 mL plasma) [13]. | Superior recovery of short fragments vs. traditional column-based methods. Automation-compatible for high-throughput processing and consistency [13]. |
| Unique Molecular Identifier (UMI) Adapters | Tagging of individual DNA molecules pre-amplification to enable bioinformatic error correction and accurate quantification. Essential for distinguishing low-frequency mutations from sequencing artifacts [3]. | Reduces background noise, enabling ultra-sensitive detection down to <0.1% variant allele frequency (VAF). |
| Multiplex PCR Panels & Hybridization Capture Probes | Target enrichment for NGS. Panels amplify specific genes; probes hybridize to and pull down regions of interest from complex genomic libraries [3] [15]. | Allows focused, deep sequencing of cancer-associated genes (e.g., 33-gene pan-cancer panel [15]) or patient-specific mutations. |
| Digital PCR Master Mixes & Assays | Absolute quantification of known mutations without the need for NGS. Provides high sensitivity and specificity in a rapid workflow [3]. | Ideal for longitudinal monitoring of specific mutations (e.g., ESR1 in breast cancer [9]) after they have been identified. |
| Bisulfite Conversion Reagents | Chemical modification of unmethylated cytosines to uracils, allowing for subsequent PCR-based discrimination of methylated DNA. Foundational for methylomic analysis [3]. | Enables study of DNA methylation biomarkers. Bisulfite-free methods (e.g., MeDIP-Seq) are emerging to avoid DNA degradation [3]. |
| Automated Nucleic Acid Purification Systems | High-throughput, hands-free purification of cfDNA from large sample volumes. Reduces manual labor and inter-sample variability [13]. | Critical for reproducible processing in large-scale clinical trials and commercial testing laboratories. |
Clinical Trial Evidence and Current Challenges
Recent clinical trials presented in 2025 have significantly advanced the evidence base for ctDNA, moving from prognostic validation to demonstrations of clinical utility.
- SERENA-6 Trial (Advanced Breast Cancer): This landmark study demonstrated that switching therapy based on ctDNA findings improves patient outcomes. Patients with advanced HR+/HER2- breast cancer receiving first-line aromatase inhibitor and CDK4/6 inhibitor therapy were monitored with ctDNA for emerging ESR1 mutations. Those with ESR1 mutation detected without radiological progression were randomized to switch to camizestrant (a SERD) or continue aromatase inhibitor. The study met its primary endpoint, showing a statistically significant improvement in Progression-Free Survival (PFS) and Quality of Life (QoL) for the group that switched therapy, establishing the utility of ctDNA to guide therapy in advanced disease [9].
- DYNAMIC-III Trial (Stage III Colon Cancer): This was the first prospective randomized study of ctDNA-informed management in resected stage III colon cancer. While ctDNA positivity after surgery was confirmed as a strong prognostic marker for recurrence, the primary analysis showed that treatment escalation based on ctDNA status did not improve Recurrence Free Survival (RFS). This highlights a critical challenge: while ctDNA is excellent for identifying risk, the effectiveness of the strategy depends on having therapies capable of eradicating MRD. The results suggest limitations in the available chemotherapy escalation regimens (FOLFOXIRI vs. doublet) rather than in the ctDNA assay itself [9].
- Real-World Evidence: A large retrospective study from Memorial Sloane Kettering, analyzing a real-world cohort of over 4,900 patients with advanced breast cancer, found that early on-treatment ctDNA dynamics were associated with time to next treatment, reinforcing the potential of ctDNA as a dynamic biomarker for treatment efficacy in routine practice [9].
Despite the progress, challenges remain. In early cancer detection, the limited sensitivity of non-tumor-informed ctDNA assays for early-stage cancers (due to very low ctDNA levels) is a key hurdle [9]. There is also a lack of standardization in sample collection, analysis, and clinical interpretation across platforms [3]. Furthermore, confounding factors from non-cancerous conditions (e.g., chronic inflammatory diseases) can release cfDNA and potentially interfere with tests [3]. Finally, as seen in DYNAMIC-III, the clinical utility of ctDNA-driven interventions is contingent on the availability of effective treatments for MRD-positive patients [9].
The global market trajectory for ctDNA is one of robust, sustained growth, firmly rooted in technological advancement and mounting clinical evidence. The market's projected expansion to over USD 27 billion by 2034 is driven by the critical convergence of clinical need, technological innovation (particularly in NGS and PCR), and the demonstrated utility of ctDNA in managing cancer, especially in the realms of MRD monitoring and therapy selection in advanced disease. For researchers, scientists, and drug developers, the focus is now shifting from validating ctDNA as a prognostic tool to designing and executing prospective interventional trials that definitively prove its ability to improve patient outcomes. Overcoming challenges related to sensitivity in early detection, standardization, and integration with effective therapies will be the key to fully realizing the potential of this transformative technology in precision oncology.
Circulating tumor DNA (ctDNA) refers to fragmented, tumor-derived DNA circulating in the bloodstream, representing a subset of cell-free DNA (cfDNA). Liquid biopsy is the minimally invasive technique that analyzes ctDNA from blood samples to provide real-time molecular information about a patient's cancer. This paradigm has emerged as a transformative alternative to traditional tissue biopsies, offering a dynamic window into tumor biology through a simple blood draw. The fundamental distinction lies in ctDNA's origin from apoptotic or necrotic tumor cells, carrying the same genetic alterations as the tumor tissue from which it was shed.
The clinical and research relevance of ctDNA stems from its ability to overcome critical limitations inherent to traditional tissue sampling. Tissue biopsies provide a static, geographically limited snapshot of tumor heterogeneity, are invasive with associated procedural risks, and cannot be frequently repeated for monitoring purposes. In contrast, ctDNA captures contributions from all tumor sites, including primary and metastatic lesions, providing a more comprehensive representation of the tumor's genetic landscape. This capability for frequent serial monitoring enables researchers and clinicians to track molecular evolution, treatment response, and resistance mechanisms in real time, establishing ctDNA as a cornerstone of modern precision oncology.
Technical Advantages of ctDNA Analysis
Comprehensive Assessment of Tumor Heterogeneity
Traditional tissue biopsies are limited by tumor spatial heterogeneity. A single biopsy may not capture the complete genomic landscape of a tumor, especially in cancers with significant regional genetic variation or multiple metastatic sites. ctDNA, however, is released into the bloodstream from tumor cells throughout the body, effectively providing a composite molecular profile. Studies have demonstrated that ctDNA analysis can detect mutations present in different tumor regions that are missed by a single tissue biopsy [5] [16]. This is critically important for understanding the full spectrum of therapeutic targets and resistance mechanisms.
Dynamic and Real-Time Monitoring Capability
The short half-life of ctDNA, estimated between 16 minutes and several hours, makes it an exceptionally dynamic biomarker [4]. Changes in tumor burden or cell death in response to therapy are rapidly reflected in ctDNA levels, allowing for near real-time assessment of treatment efficacy. This enables researchers to:
- Monitor treatment response much earlier than radiographic imaging, often within days or weeks of treatment initiation [5] [17].
- Detect the emergence of resistance by identifying new molecular alterations (e.g., resistance mutations like EGFR T790M in NSCLC) weeks or months before clinical progression is evident [5] [4].
- Guide adaptive therapy, allowing for treatment modifications based on molecular response rather than waiting for anatomical changes.
Superior Sensitivity for Minimal Residual Disease (MRD)
The detection of Minimal Residual Disease (MRD)—the presence of microscopic tumor cells after curative-intent therapy—is a paramount challenge in oncology. Traditional imaging lacks the sensitivity to detect MRD, leading to late diagnosis of relapse. Ultrasensitive ctDNA assays can identify MRD at variant allele frequencies (VAF) as low as 0.001%, predicting recurrence many months before it becomes clinically or radiographically apparent [5] [18]. In diffuse large B-cell lymphoma (DLBCL), for example, a positive ctDNA test at the end of treatment is a powerful predictor of relapse, even when PET scans are negative [18].
Practical and Logistical Benefits
From a practical standpoint, liquid biopsy offers significant advantages:
- Minimally Invasive: A standard blood draw poses minimal risk and discomfort compared to surgical or core needle biopsies, improving patient compliance for serial sampling [4] [17].
- Rapid Turnaround Time: Some platforms, like digital PCR and electrochemical sensors, can provide results within hours, facilitating quicker clinical decision-making [5].
- Overcoming Tissue Limitations: ctDNA analysis is viable when tissue is insufficient, unavailable, or when a biopsy is medically contraindicated [19] [16].
Table 1: Core Advantages of ctDNA over Traditional Tissue Biopsies
| Feature | Traditional Tissue Biopsy | ctDNA Liquid Biopsy |
|---|---|---|
| Invasiveness | High (surgical/surgical) | Low (blood draw) |
| Spatial Representation | Limited to sampled site | Composite, systemic |
| Temporal Resolution | Static, single time point | Dynamic, enables serial monitoring |
| Turnaround Time | Days to weeks | Hours to days |
| Sensitivity for MRD | Very low | Very high (down to 0.001% VAF) |
| Ability to Capture Heterogeneity | Low | High |
| Feasibility for Serial Sampling | Low | High |
Advanced Detection Technologies and Methodologies
The accurate detection of ctDNA is technically challenging due to its low abundance in a high background of wild-type cfDNA, especially in early-stage disease or MRD settings. This has driven the development of highly sensitive and specific analytical platforms.
Next-Generation Sequencing (NGS) Approaches
NGS-based methods allow for broad profiling of multiple genomic alterations across many genes.
- Hybrid-Capture Methods: Techniques like CAPP-Seq (Cancer Personalized Profiling by deep Sequencing) use biotinylated oligonucleotide probes to enrich for genomic regions of interest before sequencing. This allows for sensitive detection of mutations, indels, and structural variants across hundreds of kilobases [4].
- Phased Variant Enrichment: Methods like PhasED-Seq (Phased Variant Enrichment and Detection Sequencing) significantly improve sensitivity by targeting multiple mutations occurring on the same DNA molecule (phased variants), making them easier to distinguish from background sequencing errors [5].
- Error-Corrected Sequencing: To overcome PCR and sequencing errors, techniques employ Unique Molecular Identifiers (UMIs). Each original DNA molecule is tagged with a unique barcode before amplification. Bioinformatic consensus building allows for the filtering of errors that are not present in the original molecule. Duplex Sequencing further improves accuracy by sequencing both strands of the DNA duplex and requiring mutations to be present on both strands [4].
Table 2: Key NGS-Based ctDNA Detection Technologies
| Technology | Core Principle | Key Advantage | Reported Sensitivity |
|---|---|---|---|
| CAPP-Seq [4] | Hybrid-capture with bioinformatic suppression | Broad, personalized profiling of mutations and SVs | ~0.01% VAF |
| PhasED-Seq [5] | Detection of multiple mutations on a single DNA fragment | Ultra-sensitive detection for low-concentration ctDNA | Parts-per-million level |
| TEC-Seq [4] | Targeted error correction with deep sequencing | High-depth, multi-gene panel with error suppression | ~0.01% VAF |
| Safe-SeqS [4] | Assignment of UMIs to each original DNA molecule | Distinguishes true mutations from PCR/sequencing errors | High (specific % not stated) |
| Duplex Sequencing [4] | Sequencing both strands of DNA duplex for error correction | Extremely high accuracy; considered a gold standard | 1000-fold higher accuracy than NGS |
PCR-Based and Other Ultrasensitive Platforms
For applications requiring rapid, highly sensitive detection of a limited set of known mutations, non-NGS platforms are highly effective.
- Droplet Digital PCR (ddPCR): The sample is partitioned into thousands of nanoliter-sized droplets, and PCR is performed in each droplet individually. This allows for absolute quantification of mutant alleles with high sensitivity and specificity without the need for standard curves. It is prized for its rapid turnaround and cost-effectiveness for serial monitoring [4] [17].
- Beads, Emulsion, Amplification, and Magnetics (BEAMing): This technique combines ddPCR with flow cytometry. DNA templates are bound to magnetic beads and amplified within emulsion droplets, followed by fluorescent hybridization and detection via flow cytometry, enabling highly sensitive detection [4].
- Electrochemical Biosensors: Emerging platforms use nanomaterials (e.g., magnetic nanoparticles with gold coatings, graphene) to capture ctDNA. Binding events are transduced into measurable electrical signals (e.g., changes in impedance), achieving attomolar sensitivity within minutes, showing great promise for point-of-care applications [5].
Specialized Library Preparation and Bioinformatic Techniques
- Fragment Size Selection: ctDNA fragments are typically shorter (90-150 bp) than non-tumor cfDNA. Library preparation methods that intentionally enrich for these shorter fragments can significantly increase the tumor fraction in the sequencing library, thereby improving the detection of low-frequency variants [5].
- Methylation Analysis: Analyzing the ctDNA methylome provides an orthogonal layer of tumor-specific information. Tumor cells exhibit distinct hypermethylation and hypomethylation patterns in promoter regions, which can be used for cancer detection, classification, and monitoring [5] [16].
- Bioinformatic Error Suppression: Proprietary algorithms, such as the High-Quality unique Sequence (HQS) technology used in the AlphaLiquid100 assay, leverage context-specific background error models and advanced UMI handling to further enhance variant calling accuracy and specificity [19].
The following diagram illustrates the core workflow for NGS-based ctDNA analysis, highlighting key steps from sample collection to data interpretation.
Key Experimental Protocols in ctDNA Research
Protocol for Longitudinal MRD Monitoring
Objective: To detect Minimal Residual Disease and predict relapse after curative-intent therapy in colorectal cancer.
Methodology:
- Pre-Treatment Baseline: Perform whole-exome or deep-panel sequencing of the primary tumor tissue to identify patient-specific somatic mutations (single nucleotide variants, insertions/deletions, and/or structural variants).
- Assay Design: Create a personalized, tumor-informed multiplex PCR or hybrid-capture panel targeting 16-50 identified clonal mutations.
- Blood Collection and Processing: Collect peripheral blood in cfDNA-stabilizing tubes (e.g., Streck Cell-Free DNA BCT). Within 4-6 hours, centrifuge at 1600 ×g for 15 minutes to separate plasma. Perform a second centrifugation at 16,000 ×g for 10 minutes to remove residual cells. Extract cfDNA from 2-4 mL of plasma using a commercial kit (e.g., Maxwell RSC cfDNA Plasma Kit).
- Library Preparation and Sequencing: Construct sequencing libraries with the addition of Unique Molecular Identifiers (UMIs) to each original DNA fragment. Enrich for target regions using the custom panel. Sequence on a high-throughput platform (e.g., Illumina NovaSeq) to a minimum depth of 50,000x.
- Bioinformatic Analysis: Process raw data through a pipeline including: demultiplexing, alignment to reference genome (GRCh38), UMI family consensus building to generate error-corrected reads, and variant calling. The assay's limit of detection is determined using synthetic controls, typically aiming for a VAF sensitivity of 0.01% or lower.
- Longitudinal Sampling and Analysis: Schedule blood draws at defined time points: post-surgery (baseline), after adjuvant chemotherapy (End-of-Treatment), and every 3-6 months during surveillance. For each sample, calculate the mean variant allele frequency across all tracked mutations. A sample is classified as MRD-positive if ctDNA is detected above the assay's predefined significance threshold.
Application: This protocol has demonstrated in studies that ctDNA positivity at the end of treatment is highly predictive of recurrence, with a lead time of over 1 year compared to standard imaging [5] [4].
Protocol for Monitoring Targeted Therapy Response
Objective: To assess molecular response to Tyrosine Kinase Inhibitors (TKIs) in advanced Non-Small Cell Lung Cancer (NSCLC) with EGFR mutations.
Methodology:
- Baseline Genotyping: Identify an actionable driver mutation (e.g., EGFR L858R) in plasma ctDNA using a validated NGS panel (e.g., AlphaLiquid100) or ddPCR assay.
- Treatment Initiation: Begin therapy with a relevant TKI (e.g., Osimertinib).
- Serial Blood Collection: Collect blood at predefined intervals: pre-treatment (Day 0), early on-treatment (Week 3-4), and late on-treatment (Week 7-10). Use consistent collection and processing protocols as in 4.1.
- Quantitative ctDNA Analysis: For each time point, quantify the VAF of the EGFR L858R mutation using ddPCR for rapid, absolute quantification. Simultaneously, a broader NGS panel can be used to monitor for the emergence of resistance mutations (e.g., EGFR T790M, C797S).
- Define Molecular Response (MR): Apply predefined thresholds to categorize response:
- MR Deep Response: ≥90% decrease in mutant allele concentration from baseline.
- MR Clearance: ctDNA becomes undetectable.
- Correlation with Outcome: Correlate molecular response at the early (Week 3-4) and late (Week 7-10) time points with standard clinical endpoints such as Progression-Free Survival (PFS) and Overall Survival (OS).
Application: The ctMoniTR project aggregated data from multiple trials using this approach, establishing that early ctDNA clearance in TKI-treated NSCLC patients is strongly associated with superior PFS and OS, supporting its use as an early endpoint in clinical trials [20] [17].
The Scientist's Toolkit: Essential Reagents and Materials
Successful ctDNA analysis requires a suite of specialized reagents and tools to ensure sensitivity, specificity, and reproducibility.
Table 3: Key Research Reagent Solutions for ctDNA Analysis
| Reagent/Material | Function | Example Products / Notes |
|---|---|---|
| cfDNA Blood Collection Tubes | Stabilizes nucleated blood cells to prevent genomic DNA release, preserving the native cfDNA profile. | Streck Cell-Free DNA BCT, PAXgene Blood ccfDNA Tube |
| cfDNA Extraction Kits | Isolate and purify short-fragment cfDNA from plasma with high efficiency and low contamination. | Maxwell RSC cfDNA Plasma Kit (Promega), QIAamp Circulating Nucleic Acid Kit (Qiagen) |
| Library Prep Kits | Prepare sequencing libraries from low-input, fragmented cfDNA; often include UMI integration. | Kits from Illumina, Swift Biosciences, Integrated DNA Technologies (IDT) |
| Target Enrichment Panels | Hybrid-capture or multiplex PCR panels to enrich for cancer-relevant genomic regions. | Custom tumor-informed panels (e.g., from Natera, Personalis); Fixed panels (e.g., Guardant360, FoundationOne Liquid CDx) |
| Unique Molecular Identifiers (UMIs) | Short random nucleotide sequences ligated to each DNA fragment to enable error correction. | Integrated into modern library prep kits. Critical for distinguishing true low-VAF variants from artifacts. |
| Positive Control Reference Materials | Synthetic or cell-line derived cfDNA spikes with known mutations at defined VAFs for assay validation and QC. | Seraseq ctDNA Mutation Mix (LGC Clinical Diagnostics), Horizon Multiplex I cfDNA Reference Standard |
| ddPCR/Rare Mutation Assays | Probe-based assays for ultra-sensitive detection and absolute quantification of specific mutations. | Bio-Rad ddPCR Mutation Assays, Thermo Fisher Scientific QuantStudio Absolute Q Digital PCR Assays |
Clinical and Research Applications with Supporting Data
The utility of ctDNA spans the entire cancer care continuum, from diagnosis to advanced disease management. The following table summarizes key clinical applications supported by robust data.
Table 4: Clinical Applications and Validation Data for ctDNA
| Application | Cancer Type(s) | Key Supporting Data / Performance Metrics |
|---|---|---|
| Minimal Residual Disease (MRD) & Recurrence | Colorectal, Breast, DLBCL [5] [18] | DLBCL: EOT ctDNA positivity: HR for progression=13.69 [18].CRC: ctDNA detects recurrence >1 year before imaging [5]. |
| Monitoring Targeted Therapy Response | NSCLC (EGFR-mutant) [19] [20] [17] | NSCLC: ctDNA clearance on TKIs associated with improved OS & PFS (Aggregate analysis of 8 trials) [17]. Assays detect VAF as low as 0.02% [19]. |
| Guiding Immunotherapy | NSCLC, Urothelial Cancer [20] [21] | Urothelial Cancer: On-treatment increase in ctDNA fraction associated with poorer response (18.7% vs 76.1%) and shorter PFS (2.8 vs 9.8 months) [21]. |
| Identifying Resistance Mechanisms | NSCLC, Breast Cancer [5] [4] | NSCLC: Detection of EGFR T790M resistance mutation in plasma allows for timely switch to 3rd-gen TKIs [5]. Breast Cancer: ESR1 mutations conferring resistance to aromatase inhibitors can be detected in ctDNA [4]. |
| Prognostic Stratification | DLBCL, various solid tumors [5] [18] | DLBCL: High baseline ctDNA concentration associated with increased risk of progression (HR: 2.50) and worse OS (HR: 2.67) [18]. |
Challenges and Future Directions
Despite its promise, the widespread clinical adoption of ctDNA analysis faces several hurdles. Pre-analytical variability in blood collection, processing, and storage can significantly impact results, necessitating standardized protocols [5] [17]. Analytical variability exists between different technology platforms, making it difficult to compare results across studies or labs; efforts to harmonize and validate assays are ongoing [5] [19]. The high cost of advanced technologies like NGS and digital PCR can limit access, particularly in resource-limited settings [22]. Biological confounders like Clonal Hematopoiesis of Indeterminate Potential (CHIP), where blood cells acquire mutations unrelated to the cancer, can lead to false-positive results if not properly accounted for bioinformatically [19] [16].
Future research is focused on overcoming these challenges and expanding applications. Key areas include:
- Standardization: Initiatives like the ctMoniTR project are working to define optimal time points and molecular response criteria for use in clinical trials [20] [17].
- Novel Technologies: Integration of CRISPR-based detection, microfluidic point-of-care devices, and AI-based error suppression methods aim to enhance sensitivity, speed, and accessibility [5].
- Multi-Modal Liquid Biopsies: Combining ctDNA with other analytes like methylation patterns, fragmentomics (fragmentation patterns), and circulating tumor cells (CTCs) will provide a more comprehensive view of the tumor [5] [4] [23].
- Clinical Trial Endpoints: As evidence mounts, ctDNA-based metrics like Molecular Response and MRD detection are increasingly being validated as surrogate endpoints for accelerated drug approval [20] [17].
ctDNA analysis has unequivocally established itself as a dynamic, sensitive, and minimally invasive biomarker that surpasses traditional tissue biopsies in its ability to provide a comprehensive, real-time view of tumor dynamics. Its core advantages—capturing tumor heterogeneity, enabling serial monitoring, and detecting minimal residual disease with high sensitivity—are revolutionizing both clinical oncology and cancer research. As technologies continue to evolve towards even greater sensitivity and as the field moves towards standardized, validated protocols, ctDNA is poised to become an integral component of precision oncology, enabling more personalized, proactive, and effective cancer management.
Liquid biopsy represents a transformative approach in oncology, enabling the minimally invasive detection and analysis of tumor-derived components from bodily fluids such as blood, urine, and cerebrospinal fluid [24] [10]. This paradigm shift from traditional tissue biopsy addresses critical limitations including invasiveness, sampling constraints, and inability to serially monitor tumor evolution [24] [10]. As tumors continuously undergo evolutionary changes influenced by therapy and progression, liquid biopsy provides a dynamic window into tumor heterogeneity and clonal evolution [24]. The analytical focus of liquid biopsy centers on three principal categories of biomarkers: circulating tumor DNA (ctDNA), circulating tumor cells (CTCs), and extracellular vesicles (EVs), each offering complementary biological information and clinical applications [25] [26]. This technical guide examines these key analytes within the broader context of advancing cancer detection research, with particular emphasis on their roles in precision medicine, treatment monitoring, and the identification of therapeutic resistance markers [24].
The clinical adoption of liquid biopsy has accelerated rapidly, with recent annual meetings of prominent oncology organizations like the American Association for Cancer Research (AACR) and American Society of Clinical Oncology (ASCO) dedicating significant sessions to liquid biopsy research, highlighting its expanding role across the cancer care continuum [27] [28]. This review provides an in-depth technical comparison of ctDNA, CTCs, and EVs, summarizing their distinct characteristics, detection methodologies, and applications to guide researchers and drug development professionals in selecting appropriate analytical approaches for specific research objectives.
Circulating Tumor DNA (ctDNA): Biology, Detection, and Applications
Biological Characteristics and Origin
Circulating tumor DNA comprises fragmented DNA molecules released into the bloodstream through processes including apoptosis, necrosis, and active secretion by tumor cells [10]. These fragments typically range from 160 to 200 base pairs in length and represent a subset of total cell-free DNA (cfDNA), with ctDNA proportion (tumor fraction) varying from 0.01% to 90% depending on tumor burden and cancer type [29]. A critical advantage of ctDNA is its short half-life of approximately 15 minutes to 2.5 hours, which enables real-time monitoring of tumor dynamics and treatment response [29]. Compared to protein biomarkers that may persist for weeks, this transient nature allows for nearly contemporaneous assessment of tumor status [29].
ctDNA carries the complete mutational signature of tumors, including point mutations, copy number alterations, gene fusions, and epigenetic modifications such as DNA methylation patterns [24] [10]. The fragmentomic pattern of ctDNA—its size distribution and fragmentation characteristics—also provides distinctive information that can differentiate cancer patients from healthy individuals, with recent studies demonstrating that ctDNA fragments in cancer patients are typically shorter than non-tumor cfDNA fragments [10].
Detection Methodologies and Platforms
The detection of ctDNA requires highly sensitive technologies capable of identifying rare mutant alleles against a background of wild-type DNA. Current methodologies primarily leverage PCR-based and next-generation sequencing (NGS) approaches, each with distinct advantages for specific applications.
Table 1: Key Platforms for ctDNA Detection and Analysis
| Platform/Assay | Technology Base | Key Features | Detectable Alterations | Primary Applications |
|---|---|---|---|---|
| Guardant360 CDx [29] | NGS | Analyzes over 800 genomic targets; 15 Mb epigenomic targets | SNVs, indels, CNVs, fusions, methylation | Therapy selection, treatment monitoring, resistance detection |
| FoundationOne Liquid CDx [29] | NGS | Comprehensive genomic profiling of ctDNA | SNVs, indels, CNVs, rearrangements | Personalized treatment decisions, resistance monitoring |
| Signatera [29] | PCR/NGS | Patient-specific custom assay | Tumor-informed mutations | MRD detection, recurrence monitoring |
| UltraSEEK Lung Panel [26] | MassARRAY System | Multiplex PCR followed by single base extension | 74 hot-spot mutations in 5 NSCLC genes | Targeted mutation detection in lung cancer |
| MUTE-Seq [27] | CRISPR-Cas9 enriched NGS | Engineered FnCas9-AF2 variant selectively eliminates wild-type DNA | Low-frequency cancer-associated mutations | Ultrasensitive MRD detection |
| ddPCR [27] | PCR | Absolute quantification without standards | Known point mutations | MRD monitoring, especially in low TF samples |
For optimal ctDNA analysis, preanalytical steps are critical. The Liquid IQ panel assesses preanalytical parameters including long DNA templates from cell necrosis, white blood cell contamination, and amplifiable ctDNA copies to calculate optimal input amounts [26]. Ultrasensitive detection methods like MUTE-Seq (Mutation tagging by CRISPR-based Ultra-precise Targeted Elimination in Sequencing) have demonstrated significant improvements in detecting low-frequency cancer-associated mutant alleles, enabling more sensitive minimal residual disease (MRD) evaluation in non-small cell lung cancer and pancreatic cancer [27].
Research and Clinical Applications
ctDNA analysis has demonstrated substantial utility across multiple cancer management domains:
Early Cancer Detection and Screening: Multi-cancer early detection (MCED) platforms utilize ctDNA methylation patterns and fragmentomics to identify cancer signals and predict tissue of origin. Recent studies report specificities exceeding 98.5% with overall sensitivities around 59.7%, improving to 84.2% in late-stage tumors [27]. The Vanguard Study, part of the NCI Cancer Screening Research Network, confirmed the feasibility of implementing MCED tests in real-world settings across diverse populations [27].
Minimal Residual Disease (MRD) Monitoring: The high sensitivity of ctDNA detection enables identification of molecular residual disease following curative-intent treatment. In the VICTORI study on colorectal cancer, 87% of recurrences were preceded by ctDNA positivity, while no ctDNA-negative patients relapsed [27]. Similar findings have been reported across multiple cancer types, establishing ctDNA as a predictive biomarker for recurrence.
Treatment Response Monitoring and Resistance Identification: Dynamic changes in ctDNA levels and mutation profiles provide early indicators of treatment efficacy and emerging resistance mechanisms. Studies have demonstrated that ctDNA monitoring can predict treatment response weeks to months before radiographic imaging [27] [29].
Therapeutic Target Identification: ctDNA analysis identifies actionable mutations guiding treatment selection, such as EGFR mutations in non-small cell lung cancer and PIK3CA mutations in breast cancer [10] [29]. The combination of tissue and liquid biopsy has been shown to increase detection of actionable alterations, leading to improved survival outcomes [27].
Circulating Tumor Cells (CTCs): Biology, Detection, and Applications
Biological Characteristics and Origin
Circulating tumor cells are intact cancer cells that detach from primary tumors or metastatic deposits and enter the circulation, where they represent a fundamental mechanism of cancer dissemination [30] [25]. These cells are exceptionally rare, with approximately 1 CTC found per 1 million leukocytes in peripheral blood, creating significant technical challenges for their isolation and detection [30] [10]. Most CTCs undergo rapid apoptosis within 1-2.5 hours in circulation, though a small subset possesses the capacity to initiate metastatic colonies at distant sites [10].
CTCs exhibit considerable heterogeneity in size, morphology, molecular phenotype, and metastatic potential [25]. They can exist as single cells or clusters, with the latter demonstrating enhanced metastatic potential [30]. The molecular characterization of CTCs has revealed substantial plasticity, including epithelial-to-mesenchymal transition (EMT) states that may facilitate intravasation and extravasation [30] [25]. Unlike ctDNA, which provides a snapshot of tumor genetics, CTCs represent a more comprehensive biological entity containing DNA, RNA, proteins, and functional capabilities that can be investigated through in vitro culture and functional assays [25].
Detection Methodologies and Platforms
CTC isolation and detection strategies leverage both physical properties (size, density, deformability) and biological characteristics (surface protein expression) to overcome the challenge of extreme rarity in blood samples.
Table 2: Comparison of Major CTC Detection Technologies
| Technology | Principle | Advantages | Limitations | Capture Efficiency/Performance |
|---|---|---|---|---|
| CellSearch System [25] [29] [26] | Immunomagnetic separation targeting EpCAM | FDA-approved, standardized, high specificity | Limited to EpCAM-positive CTCs, may miss heterogeneous populations | Standardized for metastatic breast, prostate, and colorectal cancer |
| Parsortix PC1 System [29] | Microfluidic size-based separation | Label-free, preserves cell viability, enables downstream molecular analysis | Potential loss of smaller CTCs | Captures broader CTC phenotypes including EpCAM-low cells |
| Microfluidic CTC-iChip [30] | Integrated inertial focusing & immunomagnetic separation | High throughput, combines multiple separation principles | Complex design, higher cost | High purity and viability maintained |
| IsoFlux [30] | Immunomagnetic capture with flow control | High sensitivity, compatible with downstream analysis | Limited to antigen-positive cells | Efficient isolation for molecular characterization |
| DEPArray [30] | Dielectrophoretic cell manipulation | Enables single-cell isolation, high purity | Low throughput, complex operation | 100%-pure CTC clusters isolated |
| 3D Printed CTC Chip [30] | Microfluidic immunoaffinity capture | Enhanced surface area, customizable design | Requires specific antibodies | 87-92% capture efficiency for various cancer cell lines |
Recent advancements in CTC detection have incorporated machine learning algorithms to improve identification and classification. ML-powered image analysis automates CTC enumeration, reducing human error and enhancing reproducibility [30]. Convolutional neural networks (CNNs) can learn distinctive features of CTCs autonomously, improving classification accuracy particularly for rare and heterogeneous cell populations [30].
Research and Clinical Applications
CTCs provide unique insights into cancer biology and clinical management:
Prognostic Stratification: Numerous studies have established that CTC enumeration provides independent prognostic information. In metastatic breast, prostate, and colorectal cancers, elevated CTC counts correlate with reduced progression-free and overall survival [10] [29]. The CellSearch system received FDA clearance for prognostic use in these malignancies based on robust clinical validation [29].
Treatment Response Monitoring: Dynamic changes in CTC counts during therapy provide early indicators of treatment efficacy. Studies have demonstrated that persistent CTC detection during therapy predicts poor response and earlier progression [29].
Molecular Characterization and Biomarker Discovery: Comprehensive analysis of CTCs at the genomic, transcriptomic, and proteomic levels reveals heterogeneity and identifies potentially targetable alterations. In metastatic prostate cancer, morphological evaluation of chromosomal instability in CTCs (CTC-CIN) has predicted taxane resistance and treatment benefit [27].
Understanding Metastatic Biology: Functional studies of CTCs, including in vitro culture and patient-derived xenograft models, provide insights into the metastatic cascade and mechanisms of treatment resistance [25]. The detection of CTC clusters has been associated with enhanced metastatic potential and worse clinical outcomes [30].
Extracellular Vesicles (EVs): Biology, Detection, and Applications
Biological Characteristics and Origin
Extracellular vesicles are lipid bilayer-enclosed nanoparticles released by virtually all cell types, including cancer cells, through multiple biogenesis pathways [31] [32]. Tumors actively secrete EVs, which participate in intercellular communication within the tumor microenvironment and systemically [25] [31]. EVs are categorized based on size and biogenesis mechanism: exosomes (30-150 nm) originate from multivesicular bodies, microvesicles (100-1000 nm) bud directly from the plasma membrane, and apoptotic bodies (1-5 μm) are released during programmed cell death [31].
The molecular cargo of tumor-derived EVs mirrors the composition of parent cells, containing proteins, lipids, DNA, mRNA, microRNA, long non-coding RNA, and metabolites [25] [32]. This cargo is protected from degradation by the lipid bilayer, enhancing stability in circulation compared to non-vesicular biomarkers [32]. EVs play functional roles in cancer progression by facilitating primary tumor growth, immune suppression, angiogenesis, preparation of metastatic niches, and drug resistance [25] [31].
Detection Methodologies and Platforms
EV isolation and analysis present technical challenges due to their nanoscale size and heterogeneity. Current approaches exploit physical properties and surface characteristics for separation:
Ultracentrifugation: The most widely used method, involving sequential centrifugation steps at increasing forces (up to 100,000-200,000 × g) to pellet EVs based on density and size. Differential, isopycnic, and moving zone ultracentrifugation techniques can reduce EV loss and improve purity [24].
Precipitation-Based Methods: Chemical polymers (e.g., polyethylene glycol) or commercial kits (e.g., Total Exosome Precipitation Reagent) that reduce EV solubility and facilitate low-speed pelleting [26] [32].
Size-Based Chromatography and Filtration: Size exclusion chromatography (SEC) separates EVs from smaller contaminants based on hydrodynamic radius, while nanomembrane ultrafiltration concentrators offer a promising approach for gentle EV concentration [24].
Immunoaffinity Capture: Antibodies against EV surface proteins (e.g., CD9, CD63, CD81, tumor-specific antigens) enable selective isolation of subpopulations. Microfluidic devices with antibody-functionalized surfaces enhance capture efficiency [30] [31].
Microfluidic Technologies: Lab-on-a-chip devices that integrate multiple separation principles (immunoaffinity, size, acoustic, electrophoretic) for high-purity EV isolation with minimal sample requirements [30] [32].
Analytical approaches for EV characterization include nanoparticle tracking analysis (NTA), tunable resistive pulse sensing (TRPS), flow cytometry, transmission electron microscopy (TEM), and Western blot for size distribution, concentration, and marker validation [31]. Molecular profiling of EV cargo employs proteomics, transcriptomics, lipidomics, and metabolomics to identify disease-specific signatures [32].
Research and Clinical Applications
EV-based liquid biopsy applications are rapidly expanding:
Early Cancer Detection: EV biomarkers show promise for early cancer identification. In liver cancer, EV-based analyses distinguished cirrhosis and hepatocellular carcinoma from healthy states with high accuracy (AUC=0.92) [27]. Proteomic analyses of EVs have identified specific protein signatures associated with cancer risk [27].
Prognostic Stratification: EV characteristics correlate with clinical outcomes. In metastatic non-small cell lung cancer, high concentrations of PD-L1-positive small EVs were significantly correlated with overall survival, and when combined with CTC detection, identified patients with particularly poor prognosis [26]. In neuroblastoma, EV concentration and nucleolin expression were elevated in high-risk patients, suggesting utility for risk stratification [27].
Therapy Response Prediction: EV biomarkers may predict treatment efficacy and toxicity. In trastuzumab deruxtecan-treated patients, elevated inflammatory proteins in EVs (notably CXCL11) were associated with impending interstitial lung disease/pneumonitis [27].
Mechanistic Insights into Cancer Biology: EV analysis provides windows into tumor-stroma interactions, immune modulation, and metabolic reprogramming in the tumor microenvironment [31] [32].
Advanced computational approaches like the MWENA (Meta-Weight Elastic Net Algorithm) address challenges in EV omics data analysis, including high dimensionality, small sample sizes, and class imbalance, improving classification performance for disease diagnosis, staging, and subtyping [32].
Comparative Analysis and Integrative Approaches
Technical and Biological Comparison
Table 3: Comprehensive Comparison of Key Liquid Biopsy Analytes
| Parameter | ctDNA | CTCs | Extracellular Vesicles |
|---|---|---|---|
| Biological Nature | Cell-free nucleic acids | Intact tumor cells | Lipid bilayer-enclosed particles |
| Size Range | 160-200 bp (fragments) | 10-30 μm (cells) | 30-1000 nm (vesicles) |
| Abundance in Blood | 0.1-10% of total cfDNA | 1-10 cells per 10 mL blood | 10^8-10^12 particles per mL |
| Half-Life | 15 min - 2.5 hours | 1-2.5 hours | Hours to days |
| Cargo Information | Genetic & epigenetic alterations | Whole genome, transcriptome, proteome, functional properties | Proteins, nucleic acids, lipids, metabolites |
| Sensitivity Challenges | Low tumor fraction, clonal hematopoiesis | Extreme rarity, heterogeneity | Heterogeneity, non-tumor background |
| Key Isolation Methods | Silica membrane columns, magnetic beads | Immunomagnetic, microfluidic, filtration | Ultracentrifugation, precipitation, size exclusion |
| Primary Analysis Platforms | ddPCR, NGS, MassARRAY | CellSearch, Parsortix, microfluidics | NTA, TEM, flow cytometry, omics |
| Clinical Applications | MRD, treatment monitoring, target identification | Prognosis, treatment monitoring, metastasis research | Early detection, prognosis, mechanism studies |
| Regulatory Status | FDA-approved for EGFR in NSCLC | FDA-approved for prognosis in breast, prostate, colorectal cancer | Research use, early commercial development |
Integrated Multi-Analyte Approaches
Emerging evidence suggests that combining multiple liquid biopsy analytes provides complementary information that enhances clinical utility. In metastatic NSCLC, the combination of CTC detection and high PD-L1-positive sEV concentration identified patients with significantly worse prognosis (HR=7.65, 95% CI=3.11-18.83, P<0.001) compared to either analyte alone [26]. Similarly, studies have demonstrated that combining EV RNA analysis with ctDNA mutation detection increases the sensitivity for identifying EGFR mutations in plasma samples from NSCLC patients [26].
The ROME trial exploratory analysis revealed that despite only 49% concordance between tissue and liquid biopsies in detecting actionable alterations, combining both modalities significantly increased overall detection of actionable alterations and led to improved survival outcomes in patients receiving tailored therapy [27]. This highlights the importance of integrated approaches in precision oncology.
Multi-analyte liquid biopsy panels that simultaneously interrogate ctDNA mutations, CTC phenotypes, and EV cargo may provide a more comprehensive assessment of tumor burden, heterogeneity, and evolving molecular characteristics throughout the disease course and treatment continuum.
The Scientist's Toolkit: Essential Research Reagents and Platforms
Table 4: Key Research Reagent Solutions for Liquid Biopsy Applications
| Category | Specific Product/Platform | Primary Function | Application Notes |
|---|---|---|---|
| Blood Collection Tubes | CellSave Preservative Tubes [26] | Stabilizes CTCs for up to 96 hours | Required for CellSearch system |
| Streck Cell-Free DNA BCT [29] | Stabilizes nucleated blood cells and cfDNA | Prevents dilution from white blood cell lysis | |
| Nucleic Acid Extraction | Circulating Nucleic Acid Kit (Qiagen) [26] | Isolation of ctDNA from plasma | Maintains fragment integrity |
| CTC Enrichment | CellSearch CTC Kit [26] | Immunomagnetic CTC enrichment | FDA-approved for prognostic use |
| Parsortix PC1 System [29] | Size-based microfluidic CTC capture | Enables downstream molecular analysis | |
| ctDNA Analysis | Guardant360 CDx [29] | Comprehensive ctDNA NGS panel | FDA-approved for therapy selection |
| FoundationOne Liquid CDx [29] | ctDNA-based genomic profiling | Identifies FDA-approved biomarkers | |
| Signatera [29] | Tumor-informed MRD assay | Customized for individual patients | |
| EV Isolation | Total Exosome Precipitation Reagent [26] | Chemical precipitation of EVs | Compatible with downstream analyses |
| Detection Reagents | Liquid IQ Panel [26] | Preanalytical ctDNA quality control | Assesses amplifiable ctDNA copies |
| UltraSEEK Lung Panel [26] | Multiplex mutation detection | MassARRAY-based platform | |
| Analysis Software | MWENA Algorithm [32] | EV omics data classification | Handles high-dimensional, imbalanced data |
The comparative analysis of ctDNA, CTCs, and extracellular vesicles reveals distinct advantages and limitations for each class of biomarker, highlighting their complementary roles in cancer detection and monitoring. ctDNA offers superior sensitivity for detecting genetic alterations and monitoring minimal residual disease, with relatively straightforward analytical workflows and growing regulatory acceptance. CTCs provide unique insights into metastatic biology and tumor heterogeneity, with functional capabilities that enable deeper investigation of mechanisms underlying cancer dissemination and treatment resistance. Extracellular vesicles offer stable, information-rich packages of tumor-derived molecules, with emerging applications in early detection and unique windows into tumor-stroma interactions.
Future directions in liquid biopsy research will likely focus on standardizing preanalytical protocols, enhancing sensitivity for early detection applications, developing multi-analyte integration algorithms, and validating clinical utility in prospective interventional trials. The rapid pace of technological innovation, particularly in microfluidics, single-cell analysis, and computational methods, continues to expand the potential applications of liquid biopsy across the cancer care continuum. As these technologies mature and validation evidence accumulates, liquid biopsy is poised to transform cancer management through increasingly precise, dynamic, and minimally invasive assessment of tumor biology.
Cutting-Edge Technologies and Clinical Applications in Oncology
The analysis of circulating tumor DNA (ctDNA) in liquid biopsies has become a cornerstone of modern precision oncology, enabling non-invasive genomic profiling to guide cancer diagnosis, treatment selection, and disease monitoring [33] [34]. Two technological platforms form the foundational pillars of this field: Next-Generation Sequencing (NGS) and Polymerase Chain Reaction (PCR)-based assays. NGS provides comprehensive, hypothesis-free genomic analysis capable of detecting multiple variant types across hundreds of genes simultaneously, while PCR-based methods offer exceptional sensitivity for detecting specific, known mutations with minimal input DNA requirements [35] [36]. The complementary strengths of these platforms address the fundamental challenges of liquid biopsy analysis, where ctDNA often represents a tiny fraction (<0.1% to >10%) of the total cell-free DNA in circulation [34]. This technical guide examines the principles, methodologies, and applications of both NGS and PCR platforms within the context of ctDNA analysis, providing researchers and drug development professionals with the experimental protocols and technical specifications essential for implementing these technologies in cancer research.
Next-Generation Sequencing (NGS) Technology
Fundamental Principles and Platform Comparisons
Next-Generation Sequencing (NGS) represents a paradigm shift from first-generation Sanger sequencing, employing massively parallel sequencing to simultaneously decode millions to billions of DNA fragments [35] [37]. This high-throughput approach has reduced the cost of sequencing a human genome from billions of dollars to under $1,000 and decreased processing time from years to hours [37]. The core principle underlying NGS involves fragmenting DNA samples, attaching oligonucleotide adapters, and performing sequential cycles of nucleotide incorporation and detection across millions of clusters in a flow cell [35]. The most prevalent method, Sequencing by Synthesis (SBS) utilized by Illumina platforms, employs fluorescently-labeled reversible terminator nucleotides that are imaged after each incorporation cycle to determine sequence identity [35] [38].
Table 1: Comparison of Major NGS Platform Technologies
| Platform/Technology | Sequencing Principle | Read Length | Key Advantages | Primary Limitations | Common Applications in Liquid Biopsy |
|---|---|---|---|---|---|
| Illumina SBS | Sequencing by Synthesis with reversible dye-terminators | Short-read (50-300 bp) | High accuracy (>99.9%), low cost per base | Short reads struggle with repetitive regions | Targeted panels, whole exome, whole genome sequencing [35] |
| Ion Torrent | Semiconductor sequencing detecting H+ ions | Short-read (200-400 bp) | Fast run times, no optical detection | Homopolymer error rates | Targeted gene panels, tumor sequencing [35] |
| PacBio SMRT | Single Molecule Real-Time sequencing | Long-read (10,000-25,000 bp average) | Extremely long reads, detects epigenetics | Higher cost, lower throughput | Structural variant detection, complex rearrangement analysis [35] |
| Oxford Nanopore | Nanopore electrical signal detection | Long-read (10,000-30,000 bp average) | Real-time sequencing, portability | Higher error rate (~15%) | Metagenomics, structural variants, transcriptomics [35] |
The selection of appropriate NGS platforms depends on research objectives, with short-read technologies (Illumina, Ion Torrent) dominating clinical applications requiring high accuracy for single nucleotide variant detection, while long-read platforms (PacBio, Oxford Nanopore) address challenges in characterizing structural variants, complex genomic regions, and epigenetic modifications [35] [37].
Key NGS Applications in Liquid Biopsy and ctDNA Analysis
In liquid biopsy applications, NGS enables comprehensive genomic profiling of ctDNA through several targeted approaches:
Targeted Gene Panels: Focused panels (e.g., 50-500 genes) provide deep sequencing coverage (500-10,000x) to detect low-frequency variants with variant allele frequencies (VAF) as low as 0.1-0.5% in ctDNA [33] [34]. These panels optimize cost-effectiveness while maintaining sensitivity for clinically actionable mutations in cancer-related genes.
Whole Exome Sequencing (WES): Captures coding regions of ~20,000 genes, providing broad coverage of protein-altering variants without the cost of whole genome sequencing. In liquid biopsy, WES enables hypothesis-free exploration of tumor evolution and heterogeneity [39].
Whole Genome Sequencing (WGS): Provides complete genomic coverage, enabling detection of structural variants, copy number alterations, and genomic rearrangements across the entire genome, though with less sensitivity for low VAF variants in ctDNA due to distributed sequencing coverage [39].
The PAN100 panel exemplifies a hybridization capture-based NGS approach designed for liquid biopsy, targeting 101 genes with demonstrated ability to detect variants at 0.3% VAF with 73.1% positive percent agreement for single-nucleotide variants compared to tissue NGS [33]. Similarly, the Northstar Select assay demonstrates recent advancements with improved sensitivity (0.15% VAF for SNVs/indels) across 84 genes, addressing the challenge of low-shedding tumors through enhanced capture and bioinformatics methods [34].
Experimental Protocol: Hybridization Capture-Based NGS for ctDNA Analysis
The following protocol outlines the key steps for implementing hybridization capture-based NGS in liquid biopsy analysis, as validated in the PAN100 panel study [33]:
Step 1: Sample Collection and Plasma Processing
- Collect whole blood in cell-stabilization tubes (e.g., Streck Cell-Free DNA BCT) to prevent genomic DNA contamination and preserve ctDNA integrity.
- Process within 4-6 hours of collection: centrifuge at 1,600-2,000 × g for 10-20 minutes at 4°C to separate plasma from cellular components.
- Transfer plasma to microcentrifuge tubes and perform a second centrifugation at 16,000 × g for 10 minutes to remove residual cells.
- Store plasma at -80°C if not processing immediately.
Step 2: Cell-Free DNA Extraction
- Extract cell-free DNA from 4-10 mL plasma using silica membrane-based kits or magnetic bead systems specifically validated for low-abundance DNA recovery.
- Quantify extracted DNA using fluorometric methods (e.g., Qubit dsDNA HS Assay) rather than spectrophotometry to accurately measure low concentrations.
- Evaluate DNA fragment size distribution using Bioanalyzer or TapeStation; expected cfDNA peak at ~166 bp.
Step 3: NGS Library Preparation
- Repair DNA ends and adenylate 3' ends using commercial library preparation kits.
- Ligate platform-specific adapter sequences with unique molecular identifiers (UMIs) to correct for amplification errors and duplicate reads.
- Amplify libraries with 8-12 PCR cycles using high-fidelity polymerases.
- Clean up amplified libraries using magnetic beads and quantify by fluorometry.
Step 4: Target Enrichment by Hybridization Capture
- Pool libraries (typically 8-96 samples) for multiplexed hybridization.
- Hybridize with biotinylated oligonucleotide probes targeting genes of interest (e.g., 101 cancer-related genes for PAN100 panel) for 16-24 hours.
- Capture probe-bound fragments using streptavidin-coated magnetic beads.
- Wash to remove non-specifically bound DNA and amplify captured libraries with 12-16 PCR cycles.
Step 5: Sequencing and Data Analysis
- Pool enriched libraries in equimolar ratios and sequence on NGS platform (typically Illumina) with minimum 10,000x raw coverage.
- Process raw data through bioinformatics pipeline: demultiplexing, UMI consensus building, alignment to reference genome (GRCh38), and variant calling.
- Filter variants by quality metrics, population frequency, and functional prediction.
- Annotate variants using databases (COSMIC, ClinVar, OncoKB) and report clinically actionable findings.
PCR-Based Assay Technologies
Fundamental Principles and Platform Comparisons
Polymerase Chain Reaction (PCR) technology, introduced by Kary Mullis in 1985, revolutionized molecular biology by enabling exponential amplification of specific DNA sequences through repeated cycles of denaturation, annealing, and extension [36]. In liquid biopsy applications, PCR-based assays provide exceptional sensitivity for detecting known mutations in ctDNA, with digital PCR platforms capable of detecting variant alleles at frequencies as low as 0.001%-0.01% [40]. The fundamental PCR process relies on thermal cycling to denature double-stranded DNA, allow primers to anneal to complementary sequences, and extend new strands using thermostable DNA polymerase [36]. Advances in PCR technology have evolved from conventional PCR to real-time quantitative PCR (qPCR) and digital PCR (dPCR), each offering distinct advantages for ctDNA analysis.
Table 2: Comparison of PCR Technologies for Liquid Biopsy Applications
| Technology | Detection Method | Sensitivity (VAF) | Throughput | Quantification | Primary Applications in Liquid Biopsy |
|---|---|---|---|---|---|
| Conventional PCR | End-point gel electrophoresis | ~5-10% | Low | No | Target amplification prior to sequencing [36] |
| Quantitative PCR (qPCR) | Fluorescent probes during amplification | ~1-5% | Medium | Relative | Mutation detection in high-prevalence settings [36] |
| Digital PCR (dPCR) | End-point counting of positive partitions | ~0.001-0.1% | Medium | Absolute | Low-frequency mutation detection, treatment monitoring [40] |
| Multiplex PCR | Multiple primer sets in single reaction | Varies by platform | High | Varies | Simultaneous detection of multiple mutations [41] |
Multiplex PCR represents a significant advancement, enabling simultaneous amplification of multiple targets in a single reaction through optimized primer design and reaction conditions [41]. This approach conserves precious liquid biopsy samples while providing comprehensive mutation profiling, particularly valuable when sample volume is limited. The global multiplex PCR assay market, valued at USD 1.45 billion in 2024 and projected to reach USD 3.25 billion by 2034, reflects the growing adoption of this technology in clinical diagnostics and research [41].
Key PCR Applications in Liquid Biopsy and ctDNA Analysis
PCR-based assays serve critical roles in liquid biopsy applications where high sensitivity for known mutations is required:
Treatment Response Monitoring: dPCR enables precise quantification of specific mutations during therapy, allowing early detection of response or resistance with sensitivity sufficient to measure changes of 0.1% VAF or lower [40].
Minimal Residual Disease (MRD) Detection: The exceptional sensitivity of dPCR (to 0.001% VAF) makes it ideal for detecting MRD following surgery or treatment, often months before clinical or radiographic recurrence [40].
Multiplex Mutation Screening: Multiplex PCR assays facilitate simultaneous detection of dozens of hotspot mutations in key oncogenes (e.g., KRAS, NRAS, BRAF, EGFR) from limited ctDNA samples, streamlining diagnostic workflows [41].
Validation of NGS Findings: Targeted dPCR provides orthogonal validation for low-frequency variants identified by NGS, confirming mutation presence with an alternative methodology [33].
The integration of artificial intelligence with PCR technologies further enhances their utility in liquid biopsy applications. AI algorithms analyze complex amplification patterns in real-time PCR data, improving classification accuracy and reducing turnaround time for infectious disease and oncology testing [40] [41]. Machine learning approaches combined with digital PCR have demonstrated enhanced capability to distinguish true low-frequency mutations from technical artifacts, addressing a key challenge in liquid biopsy analysis [41].
Experimental Protocol: Droplet Digital PCR (ddPCR) for ctDNA Mutation Detection
The following protocol details the steps for implementing droplet digital PCR to detect and quantify low-frequency mutations in ctDNA, based on established methodologies and recent advancements [40]:
Step 1: Sample Preparation and DNA Quantification
- Extract cell-free DNA from 2-8 mL plasma using specialized cfDNA extraction kits.
- Quantify cfDNA using fluorometric methods (e.g., Qubit dsDNA HS Assay).
- Dilute cfDNA to working concentration (typically 1-10 ng/μL) in low-EDTA TE buffer.
Step 2: Assay Design and Validation
- Design TaqMan hydrolysis probes with 5' fluorescent dyes (FAM for mutant allele, HEX/VIC for wild-type allele).
- Validate assay specificity and efficiency using synthetic oligonucleotides or cell line DNA with known mutation status.
- Optimize primer and probe concentrations through titration experiments.
Step 3: Droplet Digital PCR Reaction Setup
- Prepare 20-22 μL reaction mix containing:
- 10 μL 2× ddPCR Supermix (no dUTP)
- 1-5 μL cfDNA template (1-100 ng total)
- 900 nM forward and reverse primers (final concentration)
- 250 nM FAM and HEX/VIC probes (final concentration)
- Nuclease-free water to final volume
- Load reaction mixture into DG8 cartridge followed by 70 μL droplet generation oil.
- Place cartridge in droplet generator to create 10,000-20,000 nanoliter-sized droplets per sample.
Step 4: PCR Amplification
- Transfer emulsified samples to 96-well PCR plate and seal with pierceable foil heat seal.
- Perform thermal cycling with the following profile:
- 95°C for 10 minutes (enzyme activation)
- 40 cycles of: 94°C for 30 seconds (denaturation) and 55-60°C for 60 seconds (annealing/extension)
- 98°C for 10 minutes (enzyme deactivation)
- 4°C hold (optional ramp rate of 2°C/second)
Step 5: Droplet Reading and Data Analysis
- Load PCR plate into droplet reader which sequentially analyzes each droplet.
- Measure fluorescence in two channels (FAM and HEX/VIC) for each droplet.
- Analyze data using manufacturer's software to classify droplets as mutant-positive, wild-type-positive, or negative.
- Calculate mutant allele concentration using Poisson statistics: Concentration = -ln(1 - (p/t)) × (1/v) × d Where p = mutant-positive droplets, t = total droplets, v = droplet volume, d = dilution factor
- Report results as copies/μL or variant allele frequency (mutant/(mutant + wild-type) × 100).
Research Reagent Solutions for Liquid Biopsy Applications
Table 3: Essential Research Reagents for NGS and PCR-Based Liquid Biopsy Analysis
| Reagent Category | Specific Products/Examples | Function in Workflow | Key Considerations for ctDNA Analysis |
|---|---|---|---|
| Blood Collection Tubes | Streck Cell-Free DNA BCT, PAXgene Blood cDNA Tube | Stabilize nucleated cells and prevent lysis during storage/transport | Critical for preserving ctDNA profile; determines maximum processing time [33] |
| cfDNA Extraction Kits | QIAamp Circulating Nucleic Acid Kit, MagMAX Cell-Free DNA Isolation Kit | Isolve and purify cell-free DNA from plasma | Recovery efficiency for short fragments (∼166 bp); minimal genomic DNA contamination [33] |
| Library Preparation Kits | Illumina DNA Prep Kit, KAPA HyperPrep Kit, Swift Accel Amplification Kit | Fragment DNA, add adapters, and amplify libraries | Efficiency with low-input DNA; minimal bias in representation [35] |
| Hybridization Capture Reagents | IDT xGen Lockdown Probes, Twist Target Enrichment, Agilent SureSelect | Enrich specific genomic regions of interest | Probe design covering target regions; capture efficiency; off-target rate [33] |
| PCR Master Mixes | Bio-Rad ddPCR Supermix, TaqMan Genotyping Master Mix | Provide optimized buffer and enzyme for amplification | Sensitivity, specificity, and performance with inhibited samples [40] |
| Sequence-Specific Probes/Primers | TaqMan Assays, Custom UMI Adapters, Targeted Panels | Enable specific detection of mutations or regions | Specificity for mutant vs. wild-type alleles; optimization for multiplexing [41] |
| Quality Control Reagents | Agilent High Sensitivity DNA Kit, Qubit dsDNA HS Assay | Assess DNA quantity, quality, and fragment size | Sensitivity for low-concentration samples; accurate size determination [33] |
Comparative Analysis and Future Directions
Technology Selection Guidelines for Liquid Biopsy Applications
The choice between NGS and PCR platforms for liquid biopsy applications depends on multiple factors including research objectives, mutation information priori, sample availability, and budgetary constraints. The following guidelines assist in technology selection:
Known vs. Unknown Mutations: For monitoring known specific mutations, dPCR provides superior sensitivity (0.001-0.1% VAF) and absolute quantification. For discovery of novel or unexpected mutations, NGS offers comprehensive profiling capability [40] [33].
Sample Volume and Input Requirements: dPCR typically requires less input DNA (1-10 ng) compared to targeted NGS (5-30 ng), making it preferable for samples with limited ctDNA [40] [33].
Multiplexing Capability: Modern NGS panels simultaneously interrogate dozens to hundreds of genes, while multiplex PCR assays typically target 10-50 mutations in a single reaction [41].
Turnaround Time and Cost: dPCR and qPCR provide results within hours, while NGS requires days for library preparation, sequencing, and bioinformatics analysis. However, NGS provides more comprehensive data per sample [36] [37].
Analytical Sensitivity Requirements: For detecting extremely low-frequency variants (<0.1%), dPCR offers the highest sensitivity, while NGS typically achieves 0.1-0.5% VAF detection limits with standard approaches [40] [34].
Emerging Trends and Future Directions
The field of liquid biopsy technology continues to evolve rapidly, with several emerging trends shaping future development:
Integrated Multi-omics Approaches: Combining mutation analysis with methylation profiling, fragmentomics, and protein markers in single workflows enhances diagnostic sensitivity and specificity [39].
Ultra-Sensitive NGS Methods: Novel techniques including unique molecular identifiers (UMIs), duplex sequencing, and improved error suppression algorithms are pushing NGS sensitivity toward 0.01% VAF, approaching dPCR performance [34].
Point-of-Care Testing: Miniaturized, automated systems such as the Bio-Rad QX600 ddPCR system and Oxford Nanopore portable sequencers are enabling decentralized liquid biopsy testing [40] [39].
Artificial Intelligence Integration: Machine learning algorithms are being deployed to enhance variant calling, distinguish technical artifacts from true mutations, and predict clinical outcomes from complex ctDNA profiles [40] [39].
Standardization and Validation: As liquid biopsy moves toward clinical adoption, standardized protocols, reference materials, and validation frameworks are being established to ensure reproducibility and reliability across platforms [33] [34].
The ongoing technological innovations in both NGS and PCR platforms continue to expand the applications of liquid biopsy in oncology, from early cancer detection to monitoring treatment response and guiding personalized therapeutic strategies. The complementary nature of these technologies enables researchers to address diverse biological and clinical questions, driving the field toward increasingly sensitive, comprehensive, and accessible ctDNA analysis.
Multi-Cancer Early Detection (MCED) represents a transformative approach in oncology that leverages liquid biopsy technologies to identify multiple cancer types simultaneously through a simple blood draw. These tests analyze circulating tumor DNA (ctDNA), which is released into the bloodstream by tumors, to detect cancer-specific genomic alterations. The fundamental principle underpinning MCED is that cancer cells, through their rapid turnover and death, release characteristic DNA fragments into circulation that carry cancer-specific signatures distinguishable from normal cell-free DNA (cfDNA) [42] [43].
The clinical imperative for MCED technologies is starkly evident in current cancer statistics. Despite advances in single-cancer screening methods, approximately 83% of cancer-related deaths in the United States result from cancers without recommended screening strategies [44]. Furthermore, the majority of cancers are diagnosed after symptom presentation, often at later stages when treatments are less effective and survival rates are lower [44]. MCED tests aim to shift this paradigm by enabling detection of cancers at earlier, more treatable stages, potentially significantly reducing cancer mortality rates.
This whitepaper examines the core technological principles of MCED platforms, with particular emphasis on breakthroughs presented at the American Association for Cancer Research (AACR) Annual Meeting 2025, and explores their integration into the broader liquid biopsy research landscape for cancer detection and management.
Core Technological Principles of MCED Assays
MCED tests rely on identifying minute quantities of cancer-derived DNA in blood and differentiating it from normal cfDNA through sophisticated molecular analyses. The limited abundance of ctDNA in early-stage cancer presents a significant technological challenge, necessitating highly sensitive and specific analytical approaches [42]. Four primary analytical methodologies have emerged as cornerstones of modern MCED platforms.
DNA Methylation Analysis
DNA methylation patterns represent one of the most promising biomarkers for MCED applications. Cancer cells exhibit widespread alterations in DNA methylation, including global hypomethylation and site-specific hypermethylation of promoter regions [42]. These aberrant methylation patterns are highly cancer-specific and can be detected in ctDNA. The Galleri test (GRAIL, Inc.), for example, uses targeted bisulfite sequencing to analyze methylation patterns across hundreds of thousands of genomic regions [44]. Machine learning algorithms then process this data to both detect cancer signals and predict the tissue of origin (cancer signal origin, or CSO) with high accuracy. Real-world data from over 100,000 tests demonstrated that this approach correctly predicted the CSO in 87% of diagnosed cancer cases, facilitating efficient diagnostic workups [44].
Fragmentomics
Fragmentomics analyzes the size, structure, and distribution of cfDNA fragments, which exhibit distinct patterns in cancer patients compared to healthy individuals [43] [27]. Research presented at AACR 2025 revealed that fragmentomic patterns can predict outcomes in lung cancer patients treated with immunotherapy and require only minimal blood volumes (as low as one nanogram of cfDNA) [43]. This approach is particularly valuable because it does not depend on tracking specific mutations, making it broadly applicable across cancer types. One study demonstrated that cfDNA fragmentome analysis could identify liver cirrhosis with high accuracy (AUC of 0.92), facilitating earlier intervention in high-risk populations before hepatocellular carcinoma develops [27].
Somatic Mutation Profiling
This approach involves identifying somatic mutations in ctDNA, such as single nucleotide variants, insertions, deletions, and copy number alterations. While mutation-based profiling has demonstrated utility in advanced cancers, its application in early detection remains challenging due to the low variant allele frequency of mutations in early-stage disease and the background clonal hematopoiesis mutations that can confound results [42]. Nevertheless, studies continue to refine mutation-based approaches for specific applications, with some MCED tests incorporating limited mutation profiling alongside other biomarkers.
Proteomic and Multi-Omic Integration
Emerging research presented at AACR 2025 highlighted the growing trend toward integrating multiple analyte types to improve detection sensitivity and specificity. Proteomic analyses within the European Prospective Investigation into Cancer and Nutrition (EPIC) cohort identified 19 circulating proteins associated with premenopausal breast cancer risk and three with postmenopausal risk [27]. Another multi-omics study validated a 27-plasma biomarker panel that effectively predicted cancer development in high-risk populations, including smokers with cardiovascular disease [27]. These integrated approaches demonstrate the potential of combining fragmentomics with protein biomarkers and mutation data to enhance early cancer detection.
Table 1: Core Analytical Methodologies in MCED Development
| Methodology | Analytical Target | Key Strengths | Primary Limitations |
|---|---|---|---|
| DNA Methylation | Cytosine methylation patterns in CpG islands | High tissue specificity, enables cancer signal origin prediction | Complex bioinformatics requirements |
| Fragmentomics | Size, end motifs, and genomic distribution of cfDNA fragments | Mutation-agnostic, requires minimal input material | Emerging validation framework |
| Somatic Mutation Profiling | Single nucleotide variants, indels, copy number alterations | Well-established cancer associations | Low sensitivity in early-stage, confounded by clonal hematopoiesis |
| Proteomic/Multi-omic | Protein biomarkers combined with DNA alterations | Potential for enhanced sensitivity/specificity | Increased analytical complexity and cost |
Key Advances from AACR 2025
The AACR Annual Meeting 2025 featured significant advancements in MCED technology, validation, and implementation, with several presentations highlighting improved performance metrics and novel applications.
Enhanced Sensitivity for Early-Stage Detection
A critical breakthrough presented at AACR 2025 addressed the fundamental challenge of detecting extremely low levels of ctDNA in early-stage cancers. Research from the Atherosclerosis Risk in Communities (ARIC) study demonstrated that ctDNA could be detected more than three years before clinical diagnosis in some cases [45]. The study analyzed prospectively collected serial plasma samples from 26 participants later diagnosed with cancer and 26 matched controls. In four of six participants where earlier plasma samples were available (collected 3.1 to 3.5 years prior to diagnosis), the same mutations detected at diagnosis were identifiable at significantly lower mutant allele fractions (8.6- to 79-fold lower) [45]. These findings establish benchmark sensitivity requirements for truly early cancer detection and suggest an extended temporal window for intervention.
Refined Cancer Signal Origin Prediction
Accurate prediction of the cancer signal origin is crucial for guiding diagnostic follow-up after a positive MCED test. AACR 2025 featured novel algorithms with improved CSO prediction capabilities. One research team developed a plasma-based sequencing platform that could predict the CSO across 12 different tumor types with 88.2% top prediction accuracy, increasing to 93.6% when considering the top two predictions [27]. Another study presented a methylation-based deconvolution model capable of quantifying proportions of lung cancer histology subtypes (LUAD, LSCC, SCLC) within a single blood sample with 85.1% accuracy, even at tumor fractions as low as 0.1% [27]. These advances in tissue of origin determination are critical for streamlining diagnostic pathways after a positive MCED result.
Integration with Current Screening Paradigms
Presentations at AACR 2025 emphasized the complementary role of MCED tests alongside existing screening modalities rather than as replacement. The Vanguard Study, part of the NCI Cancer Screening Research Network, established the feasibility of implementing MCED tests in real-world settings, enrolling over 6,200 participants and confirming high adherence and operational viability across diverse populations [27]. This study lays the groundwork for future large-scale randomized controlled trials of MCED assays. Additionally, real-world data from over 100,000 individuals tested with the Galleri MCED test demonstrated a cancer signal detection rate of 0.91%, consistent with clinical studies and modeled values [44]. The median time from result receipt to cancer diagnosis was 39.5 days, indicating that CSO prediction enables efficient diagnostic workup [44].
Table 2: Performance Metrics of MCED Technologies from Recent Studies
| Study | Sample Size | Specificity | Overall Sensitivity | CSO Prediction Accuracy |
|---|---|---|---|---|
| Real-world MCED Experience [44] | 111,080 | 99.09% (implied) | Not reported | 87% |
| Hybrid-Capture Methylation Assay [27] | Not specified | 98.5% | 59.7% (Overall); 84.2% (Late-stage); 73% (Cancers without screening) | Not reported |
| Novel CSO Classifier [27] | Not specified | Not reported | Not reported | 88.2% (Top prediction); 93.6% (Top two) |
| Fragmentomics for Liver Cirrhosis [27] | 724 | Not reported | Not reported | AUC 0.92 |
Figure 1: MCED Testing Workflow from Blood Draw to Clinical Report
Experimental Protocols and Methodologies
Recent studies presented at AACR 2025 featured refined experimental approaches that enhance the sensitivity and specificity of MCED assays. This section details key methodologies from prominent research presentations.
Targeted Methylation Sequencing Protocol
The Galleri test methodology, supported by real-world data from over 100,000 individuals, involves the following key steps [44]:
Sample Collection and Processing: Blood samples are collected in Streck Cell-Free DNA Blood Collection Tubes. Plasma is separated through centrifugation within specified time and temperature parameters to ensure cfDNA stability.
cfDNA Extraction and Library Preparation: cfDNA is extracted from plasma using magnetic bead-based methods. Libraries are prepared through end-repair, A-tailing, and adapter ligation, followed by bisulfite conversion to distinguish methylated from unmethylated cytosines.
Targeted Methylation Sequencing: Bisulfite-converted libraries undergo hybrid capture targeting approximately 100,000 informative methylation regions. Sequencing is performed on high-throughput platforms to achieve sufficient coverage for methylation pattern analysis.
Bioinformatic Analysis: Machine learning algorithms analyze methylation patterns to detect cancer signals and predict tissue of origin. The model is trained on reference methylation databases from cancer and normal samples.
Clinical Reporting: Results indicate "Cancer Signal Detected" or "Not Detected," and for positive results, a predicted Cancer Signal Origin (CSO) is provided to guide diagnostic evaluation.
Fragmentomics Analysis for Early Detection
A study presented at AACR 2025 detailed a fragmentomics approach for identifying liver cirrhosis and early hepatocellular carcinoma [27]:
Low-Coverage Whole Genome Sequencing: Extracted cfDNA undergoes low-coverage (0.5-1x) whole genome sequencing without bisulfite conversion or targeted enrichment.
Fragment Size Distribution Analysis: Bioinformatic tools calculate the size distribution of cfDNA fragments, with cancer-derived fragments typically shorter than those from healthy cells.
End Motif and Genomic Position Analysis: The sequences at fragment ends and their genomic distribution patterns are analyzed, as these exhibit cancer-specific characteristics.
Machine Learning Classification: A classifier trained on fragmentomic features from healthy, cirrhotic, and hepatocellular carcinoma cohorts distinguishes between these states with high accuracy (AUC 0.92).
Ultrasensitive Mutation Detection for MRD Monitoring
The VICTORI study presented at AACR 2025 utilized a personalized, tumor-informed approach for minimal residual disease (MRD) detection in colorectal cancer patients [43] [27]:
Tumor Sequencing: Whole exome or genome sequencing of tumor tissue identifies up to 1,800 somatic variants unique to the patient's cancer.
Personalized Assay Design: A custom panel is designed to target 16-50 selected clonal variants for tracking in plasma.
Plasma Analysis: cfDNA from serial blood draws is sequenced using the personalized panel with unique molecular identifiers to suppress sequencing errors.
Variant Calling and MRD Assessment: The NeXT Personal algorithm detects ctDNA fragments with the patient's specific mutations, achieving sensitivity to detect ctDNA as low as two parts per million.
This approach detected all post-resection clinical recurrences in colorectal cancer patients before imaging, with half of recurrences detected at least six months prior to radiological evidence [43].
The Scientist's Toolkit: Essential Research Reagents and Platforms
Table 3: Key Research Reagents and Platforms for MCED Development
| Reagent/Platform | Function in MCED Research | Application Notes |
|---|---|---|
| Streck Cell-Free DNA Blood Collection Tubes | Stabilizes nucleated blood cells for up to 14 days at room temperature | Prevents genomic DNA contamination and preserves cfDNA profile during transport |
| Bisulfite Conversion Reagents | Converts unmethylated cytosines to uracils while preserving methylated cytosines | Critical for methylation-based MCED assays; optimization required for minimal DNA degradation |
| Hybrid Capture Baits | Enriches targeted genomic regions for sequencing | Methylation-specific baits cover informative CpG sites; design impacts assay performance |
| Unique Molecular Identifiers (UMIs) | Tags individual DNA molecules before amplification | Reduces sequencing errors and enables accurate quantification of rare variants |
| Methylation-Aware Sequencing Enzymes | Maintains methylation patterns during amplification | Essential for library preparation in bisulfite sequencing workflows |
| Bioinformatic Pipelines | Analyzes sequencing data for cancer signals | Machine learning algorithms require training on reference datasets of cancer and normal samples |
Signaling Pathways and Molecular Mechanisms
Understanding the biological foundations of MCED biomarkers provides crucial context for test interpretation and further research development. The following diagram illustrates key molecular mechanisms that generate detectable signals in MCED assays.
Figure 2: Molecular Mechanisms Generating MCED-Detectable Signals
The field of Multi-Cancer Early Detection stands at a pivotal juncture, with technologies demonstrating significant promise in real-world settings while awaiting validation through large-scale randomized trials. MCED tests represent a paradigm shift in cancer detection, moving from organ-specific screening approaches to a comprehensive, blood-based methodology that can detect numerous cancer types simultaneously.
The research presented at AACR 2025 indicates several critical directions for the field. First, increasing sensitivity for early-stage cancers remains a primary focus, with studies demonstrating the feasibility of detecting ctDNA years before clinical diagnosis [45]. Second, the integration of multiple analytical approaches—methylation, fragmentomics, proteomics, and mutation profiling—shows potential for enhancing both sensitivity and specificity [27]. Third, addressing health disparities and ensuring equitable access to these emerging technologies will be essential for maximizing their public health impact.
As MCED technologies continue to evolve, their successful integration into clinical practice will require careful consideration of ethical implications, cost-effectiveness, and implementation pathways. The establishment of the NCI Cancer Screening Research Network and studies like Vanguard represent important steps toward generating the evidence needed to guide these implementation decisions [27]. With continued refinement and validation, MCED tests hold immense potential to transform cancer care by shifting diagnosis to earlier, more treatable stages, ultimately reducing cancer mortality worldwide.
The management of solid tumors is undergoing a transformative shift with the integration of molecular tools for detecting minimal residual disease (MRD), also termed molecular residual disease. Following curative-intent treatment in cancers such as colorectal cancer (CRC) and non-small cell lung cancer (NSCLC), conventional imaging and clinical assessments lack the sensitivity to detect microscopic disease deposits that eventually lead to recurrence. The detection of circulating tumor DNA (ctDNA), a tumor-derived fraction of cell-free DNA (cfDNA) in the bloodstream, has emerged as a powerful tool to identify MRD and predict recurrence risk long before it becomes radiologically apparent [46] [4]. This in-depth technical guide, framed within the broader thesis of liquid biopsy research, synthesizes the current evidence, methodologies, and clinical applications of ctDNA-based MRD monitoring for researchers, scientists, and drug development professionals. The procedural ease, low cost, and diminished invasiveness of liquid biopsy confer substantial promise for integration into routine clinical practice, providing a dynamic platform for personalized therapeutic interventions and quick adaptations to evolving disease states [4].
Clinical Evidence and Prognostic Value
The prognostic value of MRD status post-treatment is strongly validated across multiple large-scale studies in both colorectal and lung cancers. The consistent correlation between ctDNA detection and clinical outcomes underscores its potential as a robust biomarker for risk stratification.
Evidence in Colorectal Cancer
A landmark study presented at the 2025 ASCO Annual Meeting, which analyzed data from a phase III trial (NCCTG N0147) involving over 2,000 patients with stage III colon cancer, demonstrated the powerful prognostic capacity of the Guardant Reveal test [47]. With a median follow-up of 6.1 years, the results were striking:
- 62.6% of patients with detectable ctDNA after surgery experienced recurrence within 3 years, despite adjuvant chemotherapy.
- In contrast, only 15.4% of patients with undetectable ctDNA recurred in the same period [47].
This >4-fold difference in recurrence risk provides a clear stratification metric. Furthermore, the study indicated that the level of ctDNA, or tumor fraction, could help identify individuals less likely to clear residual disease with standard adjuvant treatment [47].
Evidence in Non-Small Cell Lung Cancer
In NSCLC, the evidence is equally compelling. A prospective, observational study by the Guangdong Lung Cancer Institute followed 261 surgically treated NSCLC patients (stages I–III) with longitudinal blood sampling. The updated analysis, with a median follow-up of 43.4 months, revealed that the negative predictive value (NPV)—the proportion of MRD-negative patients who remained relapse-free—was highly dependent on testing frequency [48]:
- With only a single post-surgical test, the NPV was 76.5% (56 of 238 MRD-negative patients relapsed).
- With longitudinal testing every 3–6 months, the NPV rose significantly to 93.2% (only 13 of 192 MRD-negative patients relapsed) [48].
This underscores that sustained MRD negativity over time defines a potentially cured population, while a single time point is insufficient. Notably, a majority of the relapses in sustained MRD-negative patients (7/13; 53.8%) occurred in the brain, highlighting a limitation of plasma ctDNA in detecting central nervous system (CNS) involvement, likely due to the blood-brain barrier [48].
Table 1: Key Prognostic Studies on MRD in Solid Tumors
| Cancer Type | Study / Trial | Patient Population | Key Finding | Clinical Implication |
|---|---|---|---|---|
| Stage III Colon Cancer | NCCTG N0147 (2025 ASCO) [47] | >2,000 patients | 3-year recurrence: 62.6% (ctDNA+) vs. 15.4% (ctDNA-) | ctDNA status post-surgery is a strong predictor of recurrence. |
| Stage II Colon Cancer | DYNAMIC Trial [48] | Patients with R0 resection | ctDNA-guided management reduced adjuvant chemo use by ~50% without compromising 5-year OS. | Supports therapeutic de-escalation in ctDNA- patients. |
| NSCLC (Stages I-III) | Guangdong Lung Cancer Institute [48] | 261 patients | NPV for relapse: 76.5% (single test) vs. 93.2% (longitudinal tests). | Longitudinal monitoring is critical to identify cured patients. |
Technical Methodologies for MRD Detection
The detection of MRD is technically challenging, as ctDNA can constitute a very small fraction (≤0.1%) of total cfDNA in early-stage cancer or post-surgical settings [46]. The assays developed to overcome this require high sensitivity and specificity, primarily leveraging two overarching approaches.
Tumor-Informed Approaches
Tumor-informed methods require prior sequencing of the patient's tumor tissue, typically via whole-exome sequencing (WES) or whole-genome sequencing (WGS), to identify patient-specific somatic mutations. A bespoke, highly sensitive assay is then designed to track these specific alterations in plasma [46].
Key Platforms:
- Signatera (Natera) & RaDaR (Inivata): Use amplicon-based targeted NGS with a limit of detection (LoD) as low as 0.001–0.02% [46].
- MRDetect (Veracyte) & NeXT Personal (Personalis): WGS-based platforms that offer broader genomic coverage and use advanced computational methods to achieve high sensitivity (LoD as low as 0.0001% tumor fraction) [46].
Advantages and Disadvantages:
- Advantages: High specificity and sensitivity, as the assay is tailored to the individual's tumor; reduced background noise from clonal hematopoiesis (CHIP) [46].
- Disadvantages: Relies on sufficient high-quality tumor tissue, involves longer assay development times (weeks), and may not capture newly emerging, therapy-relevant mutations arising from tumor heterogeneity or clonal evolution [46].
Tumor-Naïve (Agnostic) Approaches
Tumor-naïve methods do not require prior tumor sequencing. Instead, they use fixed panels targeting recurrent cancer-associated genomic or epigenomic alterations, such as common driver mutations or DNA methylation patterns [46].
Key Platforms:
- Guardant Reveal (Guardant Health): A tumor-naïve ctDNA assay that uses epigenomic (methylation) analysis for MRD detection and recurrence monitoring [47] [46].
- InVisionFirst-Lung (Inivata): An amplicon-based platform for lung cancer.
Advantages and Disadvantages:
- Advantages: Broader applicability, faster turnaround time, and lower cost as no tumor tissue is needed [46].
- Disadvantages: May be less sensitive than tumor-informed approaches for heterogeneous tumors, as patient-specific mutations may be missed; broader genomic coverage can increase background noise, necessitating advanced bioinformatic filters [46].
Emerging Multi-Omic and Enhancing Technologies
To further improve sensitivity, several emerging techniques are being investigated:
- Fragmentomics: Analysis of cfDNA fragmentation patterns, sizes, and end characteristics. Cancer patients show more diverse fragmentation patterns that can distinguish cancer from non-cancer cfDNA [3] [4]. The DELFI (DNA evaluation of fragments for early interception) method uses a machine learning model on genome-wide fragmentation profiles [3].
- Methylomics: Profiling of DNA methylation patterns, which are highly cell-type specific. Integrating epigenomic signatures has been shown to increase the sensitivity for detection of recurrence by 25–36% compared with genomic alterations alone [3] [4].
- Priming Agents: Novel in vivo approaches, such as the use of priming agents to transiently reduce the clearance of cfDNA, are being explored to overcome the challenge of low ctDNA levels in the circulation [3].
Experimental Workflows and Visualization
A standardized experimental protocol is critical for generating reliable and reproducible MRD data. The following workflow delineates the key steps from sample collection to clinical interpretation.
MRD Detection Workflow
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 2: Key Research Reagent Solutions for MRD Assay Development
| Reagent / Material | Function / Application | Key Considerations |
|---|---|---|
| cfDNA Extraction Kits | Isolation of high-quality, low-fragmentation cfDNA from plasma. | Critical for yield and purity; must minimize wild-type DNA contamination. |
| Unique Molecular Identifiers (UMIs) | Short DNA barcodes ligated to individual DNA molecules before PCR amplification. | Enables error correction and distinguishes true low-frequency variants from PCR/sequencing errors [4]. |
| Targeted NGS Panels | Custom (tumor-informed) or fixed (tumor-agnostic) panels for deep sequencing. | Panel size and design (amplicon vs. hybrid-capture) balance breadth, sensitivity, and cost. |
| Multiplex PCR Assays | Amplification of multiple target regions simultaneously for NGS library preparation. | Requires optimization to minimize amplification bias and ensure uniform coverage. |
| Bisulfite Conversion Reagents | Chemical treatment of DNA for methylation analysis; converts unmethylated cytosines to uracils. | Can cause significant DNA degradation; bisulfite-free alternatives (e.g., MeDIP-Seq) are emerging [3]. |
| Bioinformatic Pipelines | Software for alignment, UMI consensus building, variant calling, and fragmentomics analysis. | The core of MRD detection; must incorporate robust error-suppression models (e.g., SaferSeqS, CODEC) [4]. |
Clinical Integration and Future Directions
The compelling data on MRD's prognostic value is now being translated into interventional clinical trials that test its utility for guiding therapy, moving from pure risk stratification to clinical actionability.
MRD-Guided Therapeutic Decisions
The paradigm is shifting towards using MRD status to personalize adjuvant therapy. The successful DYNAMIC trial in stage II colon cancer demonstrated that a ctDNA-guided strategy could reduce adjuvant chemotherapy use by approximately half without compromising 5-year overall survival [48]. This provides a blueprint for therapy de-escalation in MRD-negative patients, sparing them unnecessary toxicity. Conversely, MRD positivity is being used to identify patients for therapy escalation or enrollment in clinical trials evaluating novel agents in the MRD-positive setting, such as the MERMAID-1 trial in NSCLC and the IMvigor011 trial in bladder cancer [49].
Ongoing Challenges and Research Frontiers
Despite rapid progress, several challenges remain before MRD monitoring becomes routine practice globally:
- Standardization: A lack of standardized protocols for sample collection, analysis, and interpretation across laboratories exists [3].
- Low-Shedding Tumors and CNS Relapse: Some tumors release minimal ctDNA, leading to false-negative results. Furthermore, CNS relapses are often not detected in plasma, requiring alternative approaches like cerebrospinal fluid analysis [48].
- Regulatory and Reimbursement Hurdles: While the FDA's Biomarker Qualification Program (BQP) exists, its impact has been limited, with long development timelines and few qualified biomarkers to date [50]. Outside the US, ESMO guidelines remain cautious, pending more robust evidence [49].
- Defining Clinical Utility: Critical questions remain, including whether intervening based on MRD positivity improves survival more than waiting for radiographic relapse and how to best integrate MRD into composite endpoints for clinical trials [51] [52].
Future efforts will focus on validating MRD as a surrogate endpoint for drug approval, optimizing multi-omic assays, and conducting large prospective trials to firmly establish the clinical utility of MRD-guided treatment strategies across cancer types and stages.
Guiding Targeted Therapy and Monitoring Treatment Response in Metastatic Disease
The management of metastatic cancer is being transformed by the use of liquid biopsies, particularly those analyzing circulating tumor DNA (ctDNA). This non-invasive approach provides real-time insights into tumor genetics, enabling clinicians to guide targeted therapy selection and monitor treatment response with unprecedented precision. Unlike traditional tissue biopsies, which provide a single snapshot in time, liquid biopsies allow for serial monitoring of tumor evolution and emerging resistance mechanisms [3]. In metastatic disease, where tumor heterogeneity and adaptation present significant treatment challenges, the ability to repeatedly assess tumor genetics through a simple blood draw represents a paradigm shift in personalized oncology. This technical guide explores the methodologies, clinical applications, and experimental protocols underpinning the use of ctDNA analysis in metastatic cancer management, with a focus on implementing these approaches in research and drug development settings.
Methodologies for ctDNA Analysis
The detection and analysis of ctDNA require highly sensitive technologies capable of identifying rare tumor-specific mutations against a background of normal cell-free DNA. The choice of methodology depends on the clinical or research question, with a fundamental distinction between tumor-informed and tumor-agnostic approaches.
PCR-Based Methods
Digital Droplet PCR (ddPCR) and BEAMing (Beads, Emulsion, Amplification, and Magnetics) technologies enable highly sensitive detection of known, predefined mutations. These methods partition individual DNA molecules into thousands to millions of separate reactions, allowing for absolute quantification of mutant alleles with sensitivity down to 0.01%-0.1% variant allele frequency (VAF). These approaches are ideal for tracking specific resistance mutations during therapy monitoring, such as emerging ESR1 mutations in breast cancer or KRAS mutations in colorectal cancer [3].
Next-Generation Sequencing (NGS) Approaches
NGS-based methods provide comprehensive genomic profiling and can detect both known and novel mutations:
- Targeted NGS panels focus on genes with known clinical significance in specific cancers, offering deep sequencing coverage (>10,000x) to detect low-frequency variants.
- Whole exome sequencing (WES) and whole genome sequencing (WGS) provide broader genomic coverage but with lower sensitivity for rare variants.
- Tagged-amplicon deep sequencing (TAm-Seq), CAncer Personalized Profiling by deep Sequencing (CAPP-Seq), and targeted error correction sequencing (TEC-Seq) incorporate molecular barcoding and error-correction algorithms to improve detection sensitivity and specificity [3].
Emerging Analytical Dimensions
Beyond mutation detection, several advanced analytical approaches are enhancing the utility of ctDNA:
- Methylation analysis using bisulfite conversion or bisulfite-free methods (ChIP-Seq, MeDIP-Seq) identifies cancer-specific methylation patterns.
- Fragmentomics analyzes cfDNA fragmentation patterns, size distribution, and end characteristics, with approaches like the DELFI (DNA evaluation of fragments for early interception) method using machine learning to distinguish cancer from non-cancer fragmentation profiles with 91% sensitivity [3].
- Multimodal analysis integrates genomic, epigenomic, and fragmentomic data to improve detection sensitivity and provide complementary biological insights [3].
Table 1: Comparison of Major ctDNA Analysis Technologies
| Technology | Analytical Sensitivity | Genomic Coverage | Turnaround Time | Primary Applications |
|---|---|---|---|---|
| ddPCR/BEAMing | 0.01%-0.1% VAF | Single to few mutations | 1-2 days | Monitoring known resistance mutations |
| Targeted NGS | 0.1% VAF | 10-500 genes | 7-14 days | Comprehensive genomic profiling, MRD detection |
| Whole Genome Sequencing | 1-5% VAF | Genome-wide | 2-4 weeks | Discovery research, novel biomarker identification |
| Methylation Analysis | Varies by method | Hundreds to thousands of CpG sites | 1-3 weeks | Cancer origin detection, early detection |
| Fragmentomics | N/A (pattern-based) | Genome-wide | 3-7 days | Cancer detection, tissue of origin identification |
Clinical Applications in Metastatic Disease
Guiding Targeted Therapy Selection
ctDNA analysis enables comprehensive molecular profiling to match metastatic patients with appropriate targeted therapies. In colorectal cancer, guidelines recommend testing RAS (KRAS/NRAS), BRAF V600E, and mismatch repair status in all metastatic cases, with HER2 amplification and NTRK fusions assessed for clinical trial eligibility [53]. The SERENA-6 trial demonstrated the power of ctDNA to dynamically guide therapy switches, where detection of emerging ESR1 mutations prompted a change to camizestrant in HR+/HER2- metastatic breast cancer, significantly improving progression-free survival [9] [54].
Monitoring Treatment Response and Resistance
Serial ctDNA monitoring provides early insights into treatment efficacy and emerging resistance mechanisms:
- In the VICTORI study of resectable colorectal cancer, ctDNA detection preceded radiographic recurrence by a median of 198 days, with one case detecting recurrence 416 days earlier [14].
- A real-world study of 4,910 metastatic breast cancer patients found that early on-treatment ctDNA dynamics strongly correlated with time to next treatment [9].
- The VERITAC-2 trial showed that ctDNA identification of ESR1 mutations could select patients most likely to benefit from the PROTAC degrader vepdegestrant, who demonstrated doubled progression-free survival compared to those receiving standard fulvestrant (5 months vs. 2.1 months) [54].
Assessing Tumor Burden and Heterogeneity
Quantitative ctDNA levels correlate with metastatic burden and disease activity. In the VICTORI study, ctDNA levels at first detection ranged from 2 parts per million (ppm) to 111,120 ppm, with higher levels predicting shorter time to clinical relapse [14]. The ability to sequence ctDNA from multiple time points provides insights into clonal evolution and tumor heterogeneity under therapeutic pressure, enabling more informed treatment decisions.
Experimental Protocols and Workflows
Blood Collection and Plasma Processing Protocol
Proper pre-analytical processing is critical for reliable ctDNA analysis:
- Blood Collection: Collect 20-30mL of whole blood into cell-stabilizing tubes (e.g., Streck, PAXgene).
- Processing Timeline: Process within 4-6 hours of collection (or according to tube manufacturer specifications).
- Centrifugation: First centrifugation at 800-1600×g for 10-20 minutes at 4°C to separate plasma from cellular components.
- Plasma Transfer: Carefully transfer supernatant to microcentrifuge tubes without disturbing buffy coat.
- Second Centrifugation: High-speed centrifugation at 16,000×g for 10 minutes to remove remaining cellular debris.
- Storage: Aliquot cleared plasma and store at -80°C until DNA extraction.
- cfDNA Extraction: Use commercially available cfDNA extraction kits following manufacturer protocols.
- Quality Control: Quantify cfDNA using fluorometric methods (e.g., Qubit) and assess fragment size distribution (e.g., Bioanalyzer, TapeStation) [3] [14].
Tumor-Informed MRD Detection Workflow (VICTORI Study Protocol)
The VICTORI study implemented a highly sensitive personalized ctDNA detection approach:
- Tissue Sequencing: Perform whole genome or exome sequencing of tumor tissue to identify patient-specific somatic variants.
- Panel Design: Create a personalized panel targeting up to 1,800 somatic variants for each patient.
- Longitudinal Sampling: Collect liquid biopsies at predefined intervals (pre-surgery, every 2 weeks for 8 weeks post-surgery, then every 3 months).
- Library Preparation: Use hybrid capture-based NGS with unique molecular identifiers.
- Sequencing: Perform ultra-deep sequencing (>100,000x raw coverage).
- Bioinformatic Analysis: Implement custom pipelines (e.g., NeXT Personal assay) for error suppression and variant calling.
- Result Interpretation: Classify samples as positive or negative based on statistical significance of detected variants [14].
Dynamic Therapy Switching Protocol (SERENA-6 Model)
The SERENA-6 trial established a paradigm for ctDNA-guided treatment adaptation:
- Baseline Assessment: Enroll patients with HR+/HER2- metastatic breast cancer on first-line aromatase inhibitor + CDK4/6 inhibitor therapy.
- Serial Monitoring: Perform ctDNA testing every 2-3 months using a targeted NGS panel covering ESR1 and other relevant genes.
- Mutation Detection: Identify emerging ESR1 mutations in ctDNA in the absence of radiographic progression.
- Randomization: Randomize patients with detected ESR1 mutations to continue current therapy or switch to experimental arm (camizestrant + CDK4/6 inhibitor).
- Endpoint Assessment: Evaluate progression-free survival, toxicity, and quality of life [9] [54].
Diagram 1: SERENA-6 ctDNA-Guided Therapy Switching Protocol
Signaling Pathways and Resistance Mechanisms
Understanding the molecular pathways targeted by therapies and their resistance mechanisms is essential for interpreting ctDNA results. Key pathways in metastatic disease include estrogen receptor signaling in breast cancer, EGFR signaling in lung cancer, and MAPK signaling across multiple tumor types.
Estrogen Receptor Signaling andESR1Mutations
In hormone receptor-positive breast cancer, the estrogen receptor (ER) functions as a ligand-dependent transcription factor. Prolonged endocrine therapy pressure selects for ESR1 mutations in the ligand-binding domain, which confer constitutive ER activation independent of estrogen. These mutations include Y537S, Y537N, Y537C, and D538G, which reduce the efficacy of aromatase inhibitors but remain sensitive to newer selective estrogen receptor degraders (SERDs) like camizestrant and proteolysis-targeting chimeras (PROTACs) like vepdegestrant [54].
EGFR Resistance Mechanisms in NSCLC
Epidermal growth factor receptor (EGFR)-mutant non-small cell lung cancer develops diverse resistance mechanisms to tyrosine kinase inhibitors (TKIs):
- Secondary EGFR mutations (e.g., T790M, C797S) that alter drug binding.
- Bypass track activation through MET, HER2, or KRAS amplification.
- Histologic transformation to small cell or squamous cell carcinoma.
- The FLAURA2 trial demonstrated that combining osimertinib with chemotherapy can overcome some resistance mechanisms, extending median survival to 47.5 months versus 37.6 months with osimertinib alone [55].
Diagram 2: ESR1 Mutation Signaling and Therapeutic Implications
The Scientist's Toolkit: Essential Research Reagents
Table 2: Essential Research Reagents for ctDNA Studies
| Reagent/Category | Specific Examples | Research Function | Technical Considerations |
|---|---|---|---|
| Blood Collection Tubes | Cell-free DNA BCT (Streck), PAXgene Blood cDNA Tube | Preserves nucleated blood cell integrity and prevents lysis during storage/transport | Critical for pre-analytical standardization; different stabilizers affect downstream analysis |
| cfDNA Extraction Kits | QIAamp Circulating Nucleic Acid Kit, MagMAX Cell-Free DNA Isolation Kit | Isolation of high-quality cfDNA from plasma | Yield and purity vary by kit; consider fragment size distribution in QC |
| Library Prep Kits | KAPA HyperPrep, Illumina DNA Prep | NGS library construction from low-input cfDNA | Molecular barcoding essential for error correction; capture-based vs. amplicon-based approaches |
| Target Enrichment Panels | CAPP-Seq selector, Signatera custom panels, commercial panels (Guardant, FoundationOne Liquid) | Hybrid capture or amplicon-based targeting of cancer-relevant genes | Tumor-informed panels offer higher sensitivity than fixed panels |
| PCR Reagents | ddPCR Supermix, BEAMing reagents | Absolute quantification of specific mutations | Extremely sensitive for tracking known mutations; limited to few variants per reaction |
| Bisulfite Conversion Kits | EZ DNA Methylation kits | Conversion of unmethylated cytosines to uracils for methylation analysis | Causes DNA degradation; bisulfite-free alternatives emerging (MeDIP-seq, TAPS) |
| Bioinformatic Tools | FastQC, BWA-MEM, GATK, custom error-suppression algorithms | Raw data processing, alignment, variant calling, and interpretation | Error-suppression algorithms critical for low VAF detection; machine learning approaches gaining traction |
Current Limitations and Future Directions
Despite significant advances, ctDNA analysis in metastatic disease faces several challenges that require further research and standardization. The low abundance of ctDNA, particularly in early-stage disease or low-shedding tumors, remains a technical hurdle, though approaches like priming agents to transiently reduce cfDNA clearance show promise for enhancing detection [3]. The lack of standardized protocols for sample collection, processing, and analysis complicates cross-study comparisons and clinical implementation [3].
The DYNAMIC-III trial in stage III colon cancer demonstrated that while ctDNA detection effectively identifies high-risk patients, current escalation strategies (FOLFOXIRI vs. doublet chemotherapy) may not sufficiently improve outcomes, highlighting the need for more effective consolidation therapies for MRD-positive patients [9]. Future directions include combining ctDNA analysis with other liquid biopsy components (CTC, exosomes), developing novel therapies specifically for MRD eradication, and advancing bioinformatic tools for multi-omic integration.
Liquid biopsy and ctDNA analysis have matured into powerful tools for guiding targeted therapy and monitoring treatment response in metastatic disease. The methodologies outlined in this guide provide researchers and drug development professionals with a framework for implementing these approaches in both clinical trials and translational research settings. As the field evolves, standardization of pre-analytical and analytical processes, validation of clinical utility through randomized trials, and development of novel therapies targeting ctDNA-identified resistance mechanisms will be essential for fully realizing the potential of liquid biopsies to transform metastatic cancer management.
The field of liquid biopsy is undergoing a transformative shift from single-analyte approaches to integrated multi-omic strategies that provide a more comprehensive view of cancer biology. Among the most promising developments is the convergence of cell-free DNA (cfDNA) fragmentomics and DNA methylation profiling, two powerful approaches that capture complementary aspects of tumor characteristics. Fragmentomics analyzes the patterns of cfDNA fragmentation, including fragment size distributions, end motifs, and genomic positioning, which reflect nucleosome positioning and gene regulatory landscapes [56]. DNA methylation profiling detects epigenetic modifications that frequently occur early in carcinogenesis and regulate gene expression without altering the DNA sequence itself [57]. When integrated, these approaches create a synergistic diagnostic system that enhances the sensitivity and specificity of cancer detection, particularly in early-stage disease where tumor DNA in circulation is minimal.
The clinical imperative for such advanced approaches is clear. Global cancer incidence continues to rise, with the International Agency for Research on Cancer predicting over 35 million new diagnoses by 2050 [57]. Gastrointestinal cancers alone account for approximately 4.8 million new cases annually, representing nearly a quarter of all cancer cases worldwide [58]. These malignancies are frequently diagnosed at advanced stages when treatment options are limited, creating an urgent need for sensitive early detection methods. The integration of fragmentomics and methylation profiling represents a technological response to this clinical challenge, leveraging the inherent stability of DNA methylation patterns and the rich biological information encoded in fragmentation profiles to overcome the limitations of traditional single-marker approaches [57] [56].
Scientific Foundations: Core Concepts and Biological Rationale
DNA Methylation in Cancer
DNA methylation involves the addition of a methyl group to the 5' position of cytosine, typically at CpG dinucleotides, resulting in 5-methylcytosine. This epigenetic modification regulates gene expression and chromatin structure without altering the underlying DNA sequence [57]. In cancer, DNA methylation patterns are frequently altered through both genome-wide hypomethylation, which can induce chromosomal instability, and hypermethylation of CpG-rich gene promoters, which is commonly associated with silencing of tumor suppressor genes [57]. These methylation alterations often emerge early in tumorigenesis and remain stable throughout tumor evolution, making them ideal biomarkers for cancer detection [57].
The inherent stability of the DNA double helix provides additional protection compared to single-stranded nucleic acid-based biomarkers, offering practical advantages during sample collection, storage, and processing [57]. Furthermore, DNA methylation appears to impact cfDNA fragmentation, as nucleosome interactions help protect methylated DNA from nuclease degradation, resulting in relative enrichment of methylated DNA fragments within the cfDNA pool [57]. This relationship between methylation status and fragmentation stability creates a natural connection between the two analytical approaches.
cfDNA Fragmentomics
Cell-free DNA fragmentomics refers to the study of fragmentation patterns of circulating DNA molecules, which provide a window into nuclear organization and cell death processes [56]. The most frequent size of cfDNA fragments observed in blood is approximately 167 base pairs, corresponding to the length of DNA wrapped around a single nucleosome complex [59]. The fragmentation process is not random but reflects underlying biological processes, with cleavage patterns influenced by transcription factor binding, gene expression, and chromatin accessibility [59].
Multiple fragmentomic features can be quantified for cancer detection, including:
- Fragment size distributions: The proportional representation of different fragment lengths
- End motifs: The nucleotide sequences at fragment termini
- Nucleosome positioning: Patterns reflecting chromatin organization
- Genomic coverage densities: Regional variations in fragment abundance
These fragmentation patterns are influenced by genomic organization and cell death mechanisms, positioning fragmentomics at the intersection of multiple aspects of cancer biology, including epigenetic dysregulation, transcriptomic alterations, and aberrant cellular turnover [56]. Cancer cells exhibit distinct fragmentomic profiles compared to normal cells, enabling discrimination of tumor-derived cfDNA even at low variant allele frequencies.
Integrated Methodologies: Technical Approaches and Workflows
Analytical Techniques for Multi-Omic Profiling
The successful integration of fragmentomics and methylation profiling requires specialized wet-lab methodologies and bioinformatic approaches. Key technologies include:
Table 1: Core Methodologies for Integrated Fragmentomics and Methylation Analysis
| Method Category | Specific Techniques | Key Applications | Advantages | Limitations |
|---|---|---|---|---|
| Methylation Profiling | Reduced Representation Bisulfite Sequencing (RRBS) [58] | Genome-wide methylome discovery | Balanced coverage and cost | Limited to CpG-rich regions |
| Targeted Bisulfite Sequencing [60] [58] | Clinical validation and application | Focused on informative markers | Requires prior knowledge of key markers | |
| Enzymatic Methyl-Sequencing (EM-seq) [57] | Comprehensive methylation profiling | Better DNA preservation than bisulfite | Less established protocol | |
| Fragmentomics Analysis | Whole Genome Sequencing (WGS) [59] | Discovery of genome-wide fragmentation patterns | Unbiased coverage | Costly for clinical application |
| Targeted Exon Sequencing [59] | Clinical cancer phenotyping | Cost-effective, high-depth | Limited genomic coverage | |
| End Motif Analysis [59] | Cancer detection and subtyping | Requires minimal sequencing | Biological significance not fully understood | |
| Multi-Omic Integration | Targeted Panels with UMI [58] | Combined methylation and fragmentomics | Single-assay multi-omic data | Complex assay design |
| Computational Integration [61] | Combining separate methylation and fragmentomics datasets | Flexible approach | Batch effects and normalization challenges |
The GutSeer Assay: An Integrated Workflow
The GutSeer assay exemplifies an optimized integrated approach for gastrointestinal cancer detection [60] [58]. This targeted sequencing panel was developed through genome-wide methylome profiling that identified 1,656 markers specific to five major GI cancers (colorectal, esophageal, gastric, liver, and pancreatic) and their tissues of origin. The assay employs a streamlined workflow:
- Sample Collection: Blood is collected in cfDNA BCT tubes (Streck) to preserve fragment integrity
- Plasma Separation: Double centrifugation (1,600g followed by 16,000g) to isolate cell-free plasma
- cfDNA Extraction: Using QIAamp Circulating Nucleic Acid kit with modified lysis incubation
- Bisulfite Conversion: Using MethylCode Bisulfite Conversion Kit
- Library Preparation: Bisulfite-converted DNA is dephosphorylated and ligated to randomized 6N splint adapters with unique molecular identifiers (UMIs)
- Semi-targeted Amplification: Captures one fragment end within targeted regions while preserving natural cfDNA ends on the opposite side
- Sequencing: Illumina NextSeq 6000 in paired-end 150-bp mode, minimum 40 million reads per sample
This approach enables simultaneous capture of both methylation information (via bisulfite conversion) and fragmentomic features (including regional fragment densities and end motifs) from the same DNA molecules [58].
Computational Integration and AI Approaches
Advanced computational methods are essential for integrating fragmentomic and methylation data. Machine learning and deep learning algorithms have significantly improved the accuracy of multi-omic liquid biopsy applications [61]. These approaches typically involve:
- Feature Extraction: Deriving quantitative metrics from raw sequencing data
- Feature Selection: Identifying the most informative methylation markers and fragmentomic features
- Model Training: Using elastic net models, random forests, or neural networks to integrate features
- Validation: Rigorous testing in independent cohorts to ensure generalizability
In the GutSeer assay, the integrated model combining methylation and fragmentomics outperformed models based on either approach alone, as well as whole-genome sequencing-based fragmentomics [58]. Similarly, fragmentomics analyses of targeted panels have demonstrated that normalized fragment read depth across all exons provides superior performance for cancer detection compared to size-based metrics or end motif analyses alone [59].
Performance Metrics and Clinical Validation
Diagnostic Performance in Clinical Studies
Integrated fragmentomics and methylation approaches have demonstrated remarkable performance in large-scale clinical validation studies. The GutSeer assay was evaluated in a prospective cohort study (GUIDE) involving 3,318 participants across five medical centers [60] [58]. The results demonstrate the robust diagnostic capability of this integrated approach:
Table 2: Performance of Integrated Fragmentomics and Methylation Assays in Clinical Validation
| Cancer Type | Sensitivity (Stage I/II) | Overall Sensitivity | Specificity | AUC | Study/Assay |
|---|---|---|---|---|---|
| All GI Cancers | 81.5% | 82.8% | 94.4% | 0.950 | GutSeer [60] [58] |
| Colorectal | 92.2% | 92.2% | - | - | GutSeer [60] |
| Esophageal | 75.5% | 75.5% | - | - | GutSeer [60] |
| Gastric | 65.3% | 65.3% | - | - | GutSeer [60] |
| Liver | 92.9% | 92.9% | - | - | GutSeer [60] |
| Pancreatic | 88.6% | 88.6% | - | - | GutSeer [60] |
| Advanced Precancerous Lesions | 63.0% (Detection Rate) | - | - | - | GutSeer [60] |
| Multiple Cancer Types | - | - | - | 0.943 (Average) | UW Cohort Fragmentomics [59] |
Notably, the GutSeer assay demonstrated 81.5% sensitivity for early-stage (I/II) GI cancers while maintaining 94.4% specificity in an independent test cohort [58]. The assay also detected 63 advanced precancerous lesions in the colorectum, esophagus, and stomach, highlighting its potential for cancer interception before malignant progression [60].
Comparison to Single-Modality Approaches
Direct comparisons between integrated approaches and single-modality methods consistently demonstrate the superiority of multi-omic integration. In the GutSeer development, the combined model outperformed both methylation-only and fragmentomics-only models, as well as whole-genome sequencing-based fragmentomics approaches [58]. Similarly, fragmentomics analyses of targeted panels have shown that integrated features provide better cancer classification than individual fragmentomic metrics alone [59].
The performance advantage of integrated approaches is particularly evident in early-stage disease and low-shedding tumors, where ctDNA fractions may be extremely low (below 1% of total cfDNA) [4]. In these challenging scenarios, the combination of highly specific methylation markers with sensitive fragmentomic patterns creates a synergistic effect that enhances diagnostic accuracy beyond what either approach could achieve independently.
Essential Research Reagents and Materials
Successful implementation of integrated fragmentomics and methylation analyses requires specific reagents and materials optimized for cfDNA work. The following table details key components used in established protocols:
Table 3: Essential Research Reagents for Integrated Fragmentomics-Methylation Studies
| Reagent/Material | Specific Product Examples | Function | Critical Features |
|---|---|---|---|
| Blood Collection Tubes | cfDNA BCT Tubes (Streck) [58] | Stabilize nucleosomal DNA | Preserves fragmentomics patterns by preventing white blood cell lysis |
| DNA Extraction Kit | QIAamp Circulating Nucleic Acid Kit (QIAGEN) [58] | Isolate cfDNA from plasma | Optimized for low-concentration samples, maintains fragment integrity |
| Bisulfite Conversion Kit | MethylCode Bisulfite Conversion Kit (ThermoFisher) [58] | Convert unmethylated cytosines to uracils | High conversion efficiency while minimizing DNA degradation |
| Library Prep Enzymes | KAPA Library Quantification Kit (KAPA) [58] | Amplify bisulfite-converted DNA | Bias-free amplification of converted DNA |
| Target Capture Panels | Custom-designed probes [58] | Enrich target regions | Covers informative methylation sites and fragmentomic regions |
| UMI Adapters | Randomized 6N splint adapters [58] | Unique molecular identifiers | Enable error correction and accurate fragment counting |
| Sequencing Platform | Illumina NextSeq/NovaSeq [58] | High-throughput sequencing | Paired-end 150bp reads for fragmentomics |
These specialized reagents address the unique challenges of cfDNA analysis, particularly the need to preserve native fragmentation patterns while enabling sensitive detection of methylation modifications. The use of cell-stabilizing blood collection tubes is especially critical for fragmentomic analyses, as conventional EDTA tubes can yield genomic DNA contamination from lysed blood cells, altering fragmentation profiles [57] [58].
Technical Considerations and Implementation Challenges
Preanalytical Variables and Standardization
The accuracy of integrated fragmentomics and methylation analyses is highly dependent on rigorous control of preanalytical variables. Blood sample processing requires particular attention, as delays in plasma separation can result in white blood cell lysis and contamination of cfDNA with genomic DNA [57]. Standardized double-centrifugation protocols (initial 1,600g followed by 16,000g) are essential to remove cellular debris while preserving cfDNA integrity [58]. The use of specialized blood collection tubes containing cell-stabilizing preservatives is recommended for multicenter studies where processing delays may occur [58].
DNA extraction methods must balance yield with fragment representation. Silica membrane-based methods like the QIAamp Circulating Nucleic Acid Kit have demonstrated consistent performance across diverse sample types [58]. Input DNA quantities typically range from 10-20ng of cfDNA, requiring optimized library preparation protocols to maintain complexity while enabling adequate sequencing depth [58].
Bioinformatics and Data Integration Challenges
The integration of fragmentomic and methylation data presents substantial bioinformatic challenges. Key considerations include:
- Data Normalization: Accounting for technical variability in sequencing depth and efficiency
- Feature Selection: Identifying the most informative methylation markers and fragmentomic features from high-dimensional datasets
- Model Optimization: Balancing model complexity with generalizability to avoid overfitting
- Batch Effect Correction: Mitigating technical artifacts across different processing batches
Computational methods that have shown success include elastic net regularization for feature selection, cross-validation strategies for model tuning, and ensemble approaches that combine multiple algorithmic strategies [61] [59]. The implementation of unique molecular identifiers (UMIs) is particularly valuable for both fragmentomics and methylation analyses, as they enable distinction of true biological fragments from PCR duplicates and sequencing errors [58].
Future Directions and Emerging Applications
The integration of fragmentomics and methylation profiling continues to evolve with several promising directions emerging. Artificial intelligence approaches, particularly deep learning, are being increasingly applied to extract subtle patterns from multi-omic liquid biopsy data that may not be captured by conventional analytical methods [61]. These AI-powered models can integrate fragmentomic and methylation features with other data types, including protein biomarkers and clinical variables, to further enhance diagnostic accuracy [61] [62].
Another significant frontier is the application of these integrated approaches to cancer monitoring and treatment response assessment. Studies have demonstrated that fragmentome profiles can track response to therapy, with changing fragmentation patterns reflecting tumor cell death and treatment effectiveness [56] [62]. The combination of fragment dynamics with methylation-based tumor fraction estimates provides a multifaceted view of treatment response that may surpass conventional imaging-based assessment [4].
Spatial multi-omic approaches represent another exciting direction, integrating single-cell transcriptomic, mutational, and spatial data from tumor tissues with ctDNA analyses from liquid biopsies [63]. This integration enables mapping of ctDNA release at single-cell resolution, potentially identifying which tumor subclones contribute most significantly to circulating DNA and how tumor spatial organization influences DNA shedding patterns [63].
As these technologies mature, key challenges remain in standardization, regulatory approval, and clinical implementation. However, the remarkable progress in integrating fragmentomics and methylation profiling suggests that these multi-omic approaches will play an increasingly central role in cancer detection, monitoring, and personalized treatment selection in the coming years.
Navigating Technical Challenges and Analytical Hurdles
The analysis of circulating tumor DNA (ctDNA) has emerged as a paradigm-shifting approach in oncology, enabling non-invasive assessment of tumor burden, genetic heterogeneity, and therapeutic response [4]. This liquid biopsy methodology provides a compelling alternative to conventional tissue biopsies by capturing tumor-derived DNA fragments circulating in bloodstream and other biofluids. However, the clinical application of ctDNA analysis, particularly for early-stage disease detection, confronts a fundamental limitation: the vanishingly low abundance of ctDNA in circulation during initial disease stages [42] [5].
In early-stage malignancies, ctDNA often constitutes less than 0.1% of the total circulating cell-free DNA (cfDNA), which is predominantly derived from hematopoietic and other normal cells through physiological apoptosis [5] [10]. This minimal presence creates a significant sensitivity barrier for reliable detection, as the signal from genuine tumor-derived fragments must be distinguished from both background wild-type DNA and technical artifacts introduced during analysis [5]. The clinical implications of overcoming this barrier are substantial, as approximately 50% of lung cancer cases are detected at stage 4 when curative treatment is no longer an option, with 5-year survival rates plummeting to approximately 15% [42]. This review examines the technological innovations and methodological refinements aimed at breaching the sensitivity barrier in early-stage ctDNA detection.
The Biological and Technical Dimensions of the Sensitivity Barrier
The sensitivity challenge in ctDNA detection stems from interconnected biological and technical factors. Biologically, early-stage tumors exhibit lower tumor burden and reduced cell turnover, resulting in diminished ctDNA shedding into circulation [4]. The half-life of ctDNA is estimated between 16 minutes and several hours, enabling real-time monitoring but requiring highly sensitive detection methods to capture these transient signals [4].
From a technical perspective, the limitations of current detection technologies become pronounced at low variant allele frequencies (VAF). Traditional sequencing approaches encounter significant background noise from sequencing errors and PCR amplification artifacts that can obscure true low-frequency variants [5]. The pre-analytical variables including blood collection methods, sample processing techniques, and DNA extraction efficiency further contribute to variability in ctDNA recovery and detection sensitivity [5].
The blood-brain barrier presents an additional biological constraint for central nervous system tumors, restricting ctDNA release into peripheral circulation [64]. Research indicates that cerebrospinal fluid (CSF), due to its proximity to the brain, contains elevated amounts of ctDNA relative to plasma, particularly in CNS cancers [64]. This observation highlights how tumor location and anatomical barriers further modulate the sensitivity challenge.
Table 1: Factors Contributing to the Sensitivity Barrier in Early-Stage ctDNA Detection
| Factor Category | Specific Factor | Impact on Detection Sensitivity |
|---|---|---|
| Biological Factors | Low tumor burden in early-stage disease | Reduces absolute ctDNA concentration in blood |
| Anatomical barriers (e.g., blood-brain barrier) | Limits ctDNA release into peripheral circulation | |
| Variable tumor shedding rates | Creates heterogeneity in ctDNA availability | |
| Clonal hematopoiesis | Introduces confounding non-tumor mutations | |
| Technical Factors | Sequencing depth and coverage | Limits ability to detect rare variants |
| PCR amplification errors | Generates background noise masking true signals | |
| Sample processing variability | Affects ctDNA recovery and integrity | |
| DNA input requirements | May exceed available ctDNA in early-stage disease |
Technological Innovations Overcoming Detection Limitations
Advanced Sequencing Methodologies
Significant innovation in sequencing technologies has focused on enhancing sensitivity for low-abundance ctDNA. Tumor-informed approaches leverage prior knowledge of tumor-specific mutations to create personalized panels that track hundreds to thousands of somatic variants. The NeXT Personal platform exemplifies this strategy, utilizing whole-genome sequencing of tumor and matched normal DNA to design bespoke panels targeting approximately 1,800 patient-specific somatic variants, predominantly from non-coding regions [65]. This approach achieves an unprecedented limit of detection of 1-3 parts per million (ppm) with 99.9% specificity, enabling detection of ctDNA in 81% of patients with early-stage lung adenocarcinoma, including 53% of those with stage I disease [65].
Structural variant (SV)-based assays represent another technological advancement, identifying karyotype-specific rearrangements with breakpoint sequences unique to the tumor. These assays mitigate challenges associated with single nucleotide variant detection by targeting translocations, insertions, or deletions that are essentially absent from normal cells [5]. In early-stage breast cancer, SV-based ctDNA assays detected ctDNA in 96% (91/95) of participants at baseline with a median variant allele frequency of 0.15%, with 10% (9/91) having a variant allele frequency of < 0.01% [5].
Error-correction methodologies have also substantially improved detection fidelity. Techniques employing unique molecular identifiers (UMIs) tag DNA fragments before PCR amplification, enabling bioinformatic filtering of true mutations from sequencing artifacts [4]. Advanced methods like Duplex Sequencing tag and sequence both strands of DNA duplexes, requiring mutation concordance between strands for verification [4]. The recently developed CODEC (Concatenating Original Duplex for Error Correction) method achieves 1000-fold higher accuracy than conventional NGS while using up to 100-fold fewer reads than duplex sequencing [4].
Nanomaterial-Based Sensing Platforms
Convergence of nanotechnology with molecular diagnostics has yielded innovative sensing platforms with attomolar sensitivity. Magnetic nano-electrode systems harness superparamagnetic Fe₃O₄–Au core–shell particles for both PCR substrates and electrochemical detection, achieving signal detection within 7 minutes of PCR initiation at three attomolar sensitivity [5]. Similarly, electrochemical biosensors utilize graphene or molybdenum disulfide (MoS₂) to facilitate label-free sensing methods, whereby ctDNA hybridization is detected through impedance changes or current-voltage characteristics [5].
These platforms offer potential for point-of-care applications due to their minimal processing requirements and compact form factors. Their rapid assay times (e.g., 20 minutes for some platforms) and compatibility with small sample volumes address practical limitations of conventional sequencing approaches, particularly for serial monitoring applications [5].
Fragmentomic and Epigenetic Approaches
Beyond sequence-based detection, innovative methods leveraging the physical and chemical properties of ctDNA have emerged. Fragmentomics exploits the distinct size distribution of tumor-derived DNA, which typically fragments to lengths of 90-150 base pairs, whereas DNA derived from nontumor cells tends to be longer [5]. Bead-based or enzymatic size selection of cfDNA specifically enriching shorter fragments can increase the fractional abundance of tumor-derived sequences by several folds within sequencing libraries [5].
Methylation profiling analyzes tumor-specific DNA methylation patterns, providing an orthogonal layer of tumor-specific information independent of mutational status [5]. Tumor-agnostic hypermethylated gene promoter panels can detect and quantify tumor development in patients with early-stage gastroesophageal cancer, achieving greater concordance with tumor tissues than mutation-based approaches alone [5]. The combination of mutational and methylation analyses in cell-free DNA may enable more sensitive pan-cancer screening initiatives [5].
Table 2: Comparison of Advanced ctDNA Detection Technologies
| Technology | Mechanism of Action | Limit of Detection | Key Advantages | Representative Applications |
|---|---|---|---|---|
| Tumor-informed WGS (NeXT Personal) | Personalized panels targeting ~1,800 somatic variants from whole-genome sequencing | 1-3 ppm | Exceptional sensitivity for MRD and early-stage disease | Preoperative ctDNA detection in 53% of stage I lung adenocarcinoma [65] |
| SV-based assays | Detection of structural variants (translocations, insertions, deletions) | <0.01% VAF | Avoids sequencing artifacts; tumor-specific | Baseline ctDNA detection in 96% of early-stage breast cancer [5] |
| Nanomaterial sensors | Electrochemical detection using conductive nanomaterials | Attomolar | Rapid results (20 min); point-of-care potential | Not yet widely implemented in clinical practice [5] |
| Methylation profiling | Analysis of tumor-specific DNA methylation patterns | Varies by platform | Epigenetic marker; tissue-of-origin identification | Improved detection in gastroesophageal cancer [5] |
| Fragment enrichment | Size selection of shorter ctDNA fragments | Improves sensitivity 2-5 fold | Low-cost enhancement to existing methods | MRD detection with reduced sequencing depth [5] |
Experimental Protocols for Ultrasensitive ctDNA Detection
NeXT Personal Workflow for Ultrasensitive Detection
The NeXT Personal platform exemplifies a rigorously optimized protocol for detecting minimal ctDNA concentrations. The methodology begins with whole-genome sequencing of tumor tissue (80X coverage) and matched normal DNA (40X coverage) to identify approximately 1,800 patient-specific somatic variants prioritized by signal-to-noise ratio [65]. A bespoke hybridization capture panel is designed against these variants, with ~98% originating from non-coding regions to maximize discriminatory power [65].
For plasma analysis, cell-free DNA is extracted from patient blood samples, with a median input of 23.5 ng reported in validation studies [65]. Following library preparation, hybridization-based enrichment is performed using the patient-specific panel, followed by ultradeep sequencing. The bioinformatic pipeline employs molecular consensus to identify independent sequence reads arising from a common founder molecule, grouping these reads into unique molecule families to distinguish true signals from technical noise [65].
This integrated approach achieves a median predicted limit of detection of 1.33 ppm (range: 0.85-4.45 ppm), substantially improving upon earlier methods that detected ctDNA in only 14% of pathological stage I lung adenocarcinomas [65]. The protocol demonstrates that clinically meaningful prognostic information can be obtained from ctDNA levels below 80 ppm, with patients exhibiting <80 ppm preoperative ctDNA levels experiencing reduced overall survival compared with ctDNA-negative patients [65].
Fragment-Enriched Library Preparation Protocol
Size-based selection of ctDNA fragments represents a complementary approach to enhance detection sensitivity. The protocol begins with extraction of cell-free DNA from plasma using standardized kits (e.g., QIAamp Circulating Nucleic Acid Kit) [5] [66]. Following quantification, libraries are prepared with specific attention to preserving shorter fragments.
Bead-based purification systems with optimized size cutoffs selectively enrich fragments in the 90-150 base pair range characteristic of tumor-derived DNA [5]. Enzymatic methods employing nucleases with size-specific activity provide an alternative approach for fragment selection. The enriched libraries then undergo error-corrected next-generation sequencing with unique molecular identifiers to distinguish true mutations from amplification artifacts [5].
This methodology increases the fractional abundance of tumor-derived sequences in the sequencing library, thereby enhancing the signal-to-noise ratio for variant calling. The approach can be particularly valuable for minimal residual disease detection, where shorter fragment enrichment reduces the required sequencing depth, improving cost-effectiveness [5].
Diagram 1: Fragment-Enriched ctDNA Analysis Workflow. This workflow illustrates the process of size-based selection to enrich for tumor-derived DNA fragments, which are typically shorter (90-150 bp) than non-tumor circulating DNA.
The Scientist's Toolkit: Essential Research Reagents and Platforms
Successful implementation of sensitive ctDNA detection requires carefully selected reagents and platforms optimized for low-abundance targets. The following table details essential components of the methodological toolkit for researchers addressing the sensitivity barrier.
Table 3: Essential Research Reagents and Platforms for Sensitive ctDNA Detection
| Reagent/Platform | Function | Key Characteristics | Representative Examples |
|---|---|---|---|
| Cell-free DNA Preservation Tubes | Stabilize blood samples to prevent white blood cell lysis and background DNA release | Maintains integrity of ctDNA profile for up to several days post-phlebotomy | Streck Cell-Free DNA BCT tubes [66] |
| cfDNA Extraction Kits | Isolate cell-free DNA from plasma/serum | Optimized for recovery of low-concentration, short-fragment DNA | QIAamp Circulating Nucleic Acid Kit [66] |
| Unique Molecular Identifiers (UMIs) | Tag individual DNA molecules before amplification | Enables error correction and distinction of true mutations from PCR artifacts | Various commercial UMI systems [4] |
| Hybridization Capture Panels | Enrich target sequences before sequencing | Tumor-informed panels provide highest sensitivity; fixed panels offer convenience | NeXT Personal bespoke panels [65] |
| Digital PCR Systems | Absolute quantification of rare variants | High sensitivity for known mutations; minimal hands-on time | Droplet digital PCR (ddPCR) [66] [4] |
| Next-Generation Sequencers | High-throughput sequencing of ctDNA libraries | Ultra-deep sequencing capabilities (>10,000X coverage) | Illumina, Element Biosciences platforms [4] |
| Magnetic Nanoparticles | Capture and concentrate target DNA sequences | Enable electrochemical detection; facilitate sample preparation | Fe₃O₄–Au core–shell particles [5] |
Analytical Validation and Clinical Correlation
Establishing robust analytical validation frameworks is essential for translating sensitive ctDNA detection into clinically actionable information. The NeXT Personal platform underwent comprehensive validation demonstrating 99.9% specificity while maintaining sensitivity at 1-3 ppm, representing a significant advancement over earlier methodologies [65]. This level of performance enables detection of molecular residual disease and recurrence risk stratification even in patients with low disease burden.
Clinical validation studies have demonstrated the prognostic significance of these ultrasensitive detection methods. In lung adenocarcinoma, preoperative ctDNA detection using NeXT Personal predicted worse clinical outcome, with ctDNA-negative patients showing 100% 5-year overall survival compared to 61.4% in ctDNA-low patients and 48.8% in ctDNA-high patients [65]. Notably, even ctDNA levels below 80 ppm—previously undetectable—remained prognostic for poor overall survival (HR = 12.33) and relapse-free survival (HR = 18.07) [65].
In metastatic breast cancer monitoring, rational thresholding approaches have established that ctDNA levels below 10 mutant allele copies/ml provide high negative predictive value (88%), while levels above 100 copies/ml detected 64% of progressions 10 weeks earlier than standard of care [66]. These findings underscore the clinical value of establishing validated thresholds for ctDNA interpretation across different cancer types and clinical scenarios.
Diagram 2: Clinically Validated ctDNA Thresholds in Metastatic Breast Cancer. This decision pathway illustrates risk stratification based on validated ctDNA thresholds, demonstrating how quantitative ctDNA monitoring can guide clinical management.
The field of ctDNA analysis continues to evolve with several promising directions emerging. Multi-modal approaches integrating fragmentomics, methylation patterns, and protein biomarkers may further enhance sensitivity and specificity for early cancer detection [5] [4]. The emerging application of artificial intelligence for error suppression and pattern recognition holds potential for extracting maximal information from limited ctDNA signals [5].
The clinical implementation of these sensitive detection methods faces ongoing challenges, including pre-analytical technique variability, analytical platform standardization, and the necessity of large-scale prospective validation trials [5]. Additionally, the detection of mutations associated with clonal hematopoiesis of indeterminate potential represents a confounding factor that requires careful interpretation [16].
In conclusion, overcoming the sensitivity barrier in early-stage ctDNA detection requires sophisticated methodological approaches that address both biological and technical limitations. The integration of tumor-informed sequencing, fragmentomic analysis, and nanotechnology-based sensing platforms has progressively lowered the detection limits, enabling new applications in cancer early detection, minimal residual disease monitoring, and treatment response assessment. As these technologies mature and undergo clinical validation, they hold immense potential to transform cancer management through liquid biopsy-based approaches that provide real-time, comprehensive assessment of tumor dynamics.
The analysis of circulating tumor DNA (ctDNA) has emerged as a revolutionary, non-invasive approach in oncology, offering potential for early cancer detection, monitoring treatment response, and profiling tumor heterogeneity [3] [10]. However, a significant challenge complicating ctDNA analysis is the presence of clonal hematopoiesis of indeterminate potential (CHIP), an age-related condition where hematopoietic stem cells acquire somatic mutations, leading to expanded clones in peripheral blood without overt hematologic malignancy [67] [68]. These CHIP mutations can be detected in blood and, when present in tumor-infiltrating immune cells, can be sequestered in tumor tissue and subsequently shed into circulation, creating false positive signals that mimic tumor-derived mutations [67]. This whitepaper examines the specificity concerns at the intersection of liquid biopsy and CHIP, detailing the mechanisms, prevalence, and sophisticated methodologies required to distinguish true tumor signals from confounding hematologic noise.
CHIP Biology and Its Interference with Tumor Detection
Defining Clonal Hematopoiesis of Indeterminate Potential
CHIP is characterized by somatic mutations in leukemia-associated driver genes occurring in hematopoietic stem cells, with a variant allele frequency (VAF) of at least 2% in blood or bone marrow, in the absence of definitive hematologic neoplasia [68]. The prevalence of CHIP increases dramatically with age, affecting approximately 10% of individuals over 65 years old but only 1% of those under 50 [68]. Environmental factors such as smoking, obesity, and prior chemotherapy exposure further promote CHIP through increased oxidative stress and inflammatory microenvironments that provide a selective advantage to mutated clones [68].
The most frequently mutated genes in CHIP include DNMT3A (approximately 50% of cases), TET2 (20-25%), ASXL1 (10%), and JAK2 (3-5%) [69] [68]. These epigenetic regulators and signaling molecules play critical roles in hematopoietic differentiation and inflammatory responses. When mutated, they establish a proinflammatory state characterized by elevated interleukin (IL)-1β, IL-6, and tumor necrosis factor-α (TNF-α) secretion, which contributes to both cardiovascular disease progression and solid tumor microenvironments [69] [68].
Tumor-Infiltrating Clonal Hematopoiesis (TI-CH)
A particularly challenging phenomenon occurs when CHIP-mutated immune cells infiltrate tumor tissues. Recent research has identified this as tumor-infiltrating clonal hematopoiesis (TI-CH), where CHIP mutations with high variant allele frequencies are detected within tumors themselves [67]. This is not merely a theoretical concern; in non-small cell lung cancer (NSCLC), 42% of patients with CHIP exhibited TI-CH, and across solid tumors, 26% of CHIP patients showed evidence of TI-CH [67].
The clinical significance of TI-CH is profound. In NSCLC, TI-CH independently predicted the risk of death or recurrence with an adjusted hazard ratio of 1.80 compared to absence of CHIP, and 1.62 compared to CHIP without TI-CH [67]. Across solid tumors, TI-CH conferred a 1.17 greater risk of all-cause mortality compared to CHIP without TI-CH [67]. Mechanistically, TET2-mutant CHIP has been shown to enhance monocyte migration to lung tumor cells, fuel a myeloid-rich tumor microenvironment in mouse models, and promote tumor organoid growth [67].
Quantitative Assessment of the Problem
Prevalence and Distribution of CHIP Mutations
Table 1: Prevalence of CHIP and TI-CH Across Cancer Types
| Cancer Type | CHIP Prevalence | TI-CH Prevalence (among CHIP+ patients) | Most Frequent CHIP Genes |
|---|---|---|---|
| Non-Small Cell Lung Cancer (TRACERx) | 34% (143/421) | 42% (60/143) | DNMT3A, TET2, ASXL1 |
| Pan-Cancer (MSK-IMPACT) | 35% (917/2,602) | 36% (333/917) | DNMT3A, TET2, ASXL1 |
| Solid Tumors (Overall) | Varies by age | 26% | DNMT3A, TET2, ASXL1 |
Table 2: Clinical Impact of TI-CH on Patient Outcomes
| Patient Cohort | Comparison | Hazard Ratio | 95% Confidence Interval | Endpoint |
|---|---|---|---|---|
| NSCLC (TRACERx) | TI-CH vs. No CHIP | 1.80 | 1.23-2.66 | Death or Recurrence |
| NSCLC (TRACERx) | TI-CH vs. CHIP (no TI-CH) | 1.62 | 1.02-2.56 | Death or Recurrence |
| Solid Tumors (MSK-IMPACT) | TI-CH vs. CHIP (no TI-CH) | 1.17 | 1.06-1.29 | All-Cause Mortality |
Multi-Cancer Early Detection Test Performance
The Galleri test, a commercially available multi-cancer early detection (MCED) test, demonstrates the current state-of-the-art in liquid biopsy performance, achieving 99.6% specificity in validation studies [70]. This exceptionally high specificity is crucial for population-level screening, as it translates to a false positive rate of just 0.4%, meaning approximately 1 in 250 individuals without cancer will receive a false positive result [70]. The test's positive predictive value (PPV) of 61.6% indicates that 6 out of 10 patients with a positive test result will be diagnosed with cancer [70].
Table 3: Performance Characteristics of MCED Testing
| Performance Metric | Value | Context/Implication |
|---|---|---|
| Specificity | 99.6% | Proportion of people without cancer who received No Cancer Signal results |
| False Positive Rate | 0.4% | Approximately 1 in 250 individuals without cancer receive false positive |
| Positive Predictive Value | 61.6% | 6 out of 10 patients with positive result are diagnosed with cancer |
| Cancer Signal Origin Accuracy | 93.4% | Predicts tissue of origin in confirmed cancer cases |
| Overall Sensitivity (all cancers, all stages) | 51.5% | Provides opportunity to detect additional cancers when added to standard screening |
Methodological Approaches for Discrimination
Experimental Design and Bioinformatic Strategies
Distinguishing true tumor-derived mutations from CHIP variants requires multi-faceted experimental approaches:
Paired Sequencing of Tumor and Normal Samples: The most critical methodological control involves sequencing both the cell-free DNA (cfDNA) from plasma and matched peripheral blood mononuclear cells (PBMCs) or buffy coat from the same individual [67] [71]. This enables direct identification of hematopoietic-derived mutations present in both compartments.
Variant Allele Frequency Analysis: CHIP mutations typically demonstrate VAFs below 10% in plasma, while tumor-derived mutations may show more variable VAFs depending on tumor burden and shedding [67]. In the TRACERx study, CHIP mutations in blood showed a median VAF of 5% (IQR: 2.9-11%) [67].
Fragmentomic Profiling: Circulating tumor DNA fragments typically are shorter (20-50 base pairs) than non-tumor cfDNA fragments [3] [10]. Techniques like the DELFI (DNA evaluation of fragments for early interception) method utilize machine learning to analyze genome-wide fragmentation patterns, achieving 91% sensitivity in cancer detection [3].
Methylation-Based Approaches: Multi-cancer early detection tests like Galleri utilize targeted methylation sequencing of cfDNA, analyzing approximately 100,000 informative methylation regions [70]. This epigenetic signature is more specific to tissue of origin than mutation-based approaches alone.
Phylogenetic Inference: For circulating tumor cell (CTC) clusters, sophisticated computational methods like CTC-SCITE (a Bayesian phylogenetic tree inference model) can deconvolve aggregate read count profiles of CTC clusters and infer genealogical relationships of constituent cells [71].
Research Reagent Solutions for CHIP Discrimination
Table 4: Essential Research Tools for CHIP-Tumor Discrimination Studies
| Research Tool | Function/Application | Example Implementation |
|---|---|---|
| Matched PBMC Collection | Provides hematopoietic reference genome | Blood collection in EDTA or Streck tubes with subsequent density gradient centrifugation |
| UMI (Unique Molecular Identifier) Adapters | Reduces sequencing artifacts and enables error correction | TruSight Oncology UMI Reagents for detection of low-frequency variants |
| Targeted Methylation Panels | Detects cancer-specific epigenetic signatures | Galleri test targeting ~100,000 methylation regions |
| Microfluidic CTC Capture Platforms | Isolates circulating tumor cells for single-cell analysis | Parsortix FDA-approved platform for CTC enrichment |
| Multiplex IMC Panels | Spatial phenotyping of tumor immune microenvironment | 40+ metal-tagged antibody panels for imaging mass cytometry |
Signaling Pathways and Biological Mechanisms
The molecular mechanisms by which CHIP mutations influence cancer progression are becoming increasingly elucidated. DNMT3A and TET2 mutations, the most common CHIP drivers, alter epigenetic programs in hematopoietic cells, skewing myelopoiesis and increasing proinflammatory cytokine production [69] [68]. This creates a chronic inflammatory state that remodels tumor microenvironments.
Figure 1: Signaling Pathways Linking CHIP to Tumor Progression. CHIP mutations initiate epigenetic dysregulation, driving inflammatory signaling and cytokine release that promotes monocyte recruitment and TI-CH formation, ultimately accelerating tumor progression through fibroblast activation and direct microenvironment modulation.
DNMT3A inactivation in macrophages intensifies interactions with cardiac fibroblasts and increases cardiac fibrosis through amplified release of heparin-binding epidermal growth factor-like growth factor (HB-EGF), facilitating fibroblast activation via the epidermal growth factor receptor (EGFR) axis [69]. Similarly, TET2 deficiency augments NLRP3 inflammasome activation in macrophages, leading to elevated secretion of IL-1β and IL-6, which exacerbates systemic inflammatory responses [68]. These mechanisms explain how minor clones of CHIP-mutated cells (with VAF as low as 2%) can exert disproportionate effects on tumor progression and patient outcomes.
Advanced Experimental Workflows
Comprehensive Discrimination Protocol
Figure 2: Bioinformatic Workflow for CHIP-Tumor Discrimination. Integrated experimental and computational pipeline for distinguishing tumor-derived mutations from CHIP variants in liquid biopsy analyses, emphasizing the critical importance of matched PBMC sequencing.
Single-Cell and Phylogenetic Analysis
For circulating tumor cell clusters, sophisticated single-cell approaches are required to determine clonal architecture:
Microfluidic CTC Capture: Utilizing FDA-approved platforms like Parsortix, CTCs are enriched from peripheral blood based on size and deformability [71].
Robotic Micromanipulation: Individual CTCs and CTC clusters are harvested using micromanipulation and transferred into individual tubes for genomic analysis [71].
Whole-Exome Sequencing: Captured cells undergo low-input whole-exome sequencing to obtain mutation profiles [71].
Bayesian Phylogenetic Inference: The CTC-SCITE algorithm deconvolves aggregate read count profiles of CTC clusters, placing constituent cells in the most likely configuration on phylogenetic trees and inferring genotypes even when cells cannot be physically dissociated [71].
This approach has revealed that 73% of patient-derived CTC clusters show evidence of branching evolution, indicating oligoclonal composition with significant implications for understanding metastatic seeding [71].
Future Directions and Clinical Implications
The growing recognition of CHIP as a confounder in liquid biopsy assays necessitates continued refinement of discrimination strategies. Emerging approaches include:
Integrated Genomic-Epigenomic Analysis: Combining mutation detection with methylation profiling and fragmentomic patterns to improve specificity [3] [70].
Longitudinal Monitoring: Tracking variant dynamics over time, as CHIP mutations typically remain stable while tumor-derived mutations may fluctuate with treatment response [67].
Single-Cell Multi-omics: Applying simultaneous genomic and transcriptomic analysis to individual cells to definitively assign mutation origin [71].
Machine Learning Classifiers: Developing sophisticated algorithms that integrate multiple features (VAF, fragment size, methylation status, chromatin accessibility) to probabilistically assign mutation origin [3] [70].
As liquid biopsy technologies evolve toward earlier cancer detection and minimal residual disease monitoring, the challenge of distinguishing true tumor signals from CHIP-associated mutations will only intensify. Research and clinical laboratories must implement robust paired sequencing protocols and bioinformatic filters to ensure accurate variant interpretation. Furthermore, recognizing that CHIP and TI-CH are not merely confounders but biologically significant phenomena with direct impacts on tumor progression and patient outcomes opens new avenues for therapeutic intervention targeting the inflammatory interface between hematopoiesis and cancer biology [67] [69] [68].
The analysis of circulating tumor DNA (ctDNA) has emerged as a transformative approach in oncology, enabling non-invasive tumor genotyping, monitoring of treatment response, and detection of minimal residual disease. Despite its considerable promise, the field faces a fundamental challenge: substantial inter-assay variability that threatens the reproducibility and clinical translation of ctDNA findings. This variability stems from multiple technical and biological sources across the entire liquid biopsy workflow, from blood collection to bioinformatic analysis. Recognizing and addressing these sources of variability is not merely a technical exercise but a critical prerequisite for integrating liquid biopsies into mainstream cancer management and regulatory decision-making.
The clinical implications of unaddressed variability are profound. Studies have demonstrated that in the absence of therapeutic intervention, ctDNA levels in patients with advanced EGFR-mutant non-small cell lung cancer (NSCLC) can show spontaneous fluctuations, including ≥20% reductions in 18.9-23.5% of patients and even ≥50% reductions in 9.1-10.1% of patients when measured between paired pretreatment samples [72]. Such background variability constitutes biological "noise" that can confound the interpretation of treatment effects, particularly when using molecular response definitions based on specific percentage decreases in ctDNA levels [72]. This technical whitepaper examines the sources of inter-assay variability in ctDNA analysis, provides standardized experimental frameworks for validation, and proposes pathways toward enhanced reproducibility for research and clinical applications.
Biological and Pre-Analytical Variability
Biological variability and pre-analytical factors constitute significant sources of inconsistency in ctDNA measurements. Biological fluctuations in ctDNA levels occur independently of treatment, influenced by factors such as circadian rhythms, physical activity, and inflammatory states [72]. The physical characteristics of ctDNA itself further complicate analysis; ctDNA is highly fragmented and unstable, with rapid clearance from the bloodstream (half-lives ranging from minutes to a few hours) making sample timing and processing critical variables [57].
Pre-analytical conditions introduce additional variability. The choice of liquid biopsy source significantly impacts biomarker concentration and background noise. While blood plasma is the most common source, local fluids like urine, cerebrospinal fluid, and bile often offer higher biomarker concentration for cancers in proximate anatomical locations [57]. Even within blood collection, sample processing protocols vary substantially; studies comparing ctDNA assays have found variation in DNA extraction efficiency, with some assays demonstrating efficiencies as low as 16% for plasma samples [73]. The interval between sample collection and processing, blood tube additives, and centrifugation protocols all contribute to pre-analytical variability that can impact downstream results.
Analytical and Technical Variability
At the analytical level, multiple technical factors introduce variability into ctDNA measurement. The efficiency of ctDNA extraction and quantification varies significantly between platforms, directly impacting sensitivity [73]. Input DNA quantity represents another critical variable, with lower inputs (<20 ng) generally associated with reduced sensitivity and reproducibility across platforms [73]. Sequencing depth and on-target rates further contribute to variability, with different assays demonstrating substantial differences in these parameters even when analyzing identical samples [73].
The limit of detection (LOD) varies considerably between platforms, typically ranging from 0.1% to 0.5% variant allele frequency (VAF) [74]. This technical variability directly impacts clinical sensitivity, particularly for low-frequency variants. Assays with higher sensitivity can detect variants at lower VAFs (0.15% for some newer assays compared to >0.5% for others), enabling identification of more clinically actionable alterations and reducing null reports with no pathogenic findings [34]. The variant calling and bioinformatic pipelines employed also significantly influence results, with differences in filtering algorithms affecting both sensitivity and specificity [75].
Post-Analytical and Bioinformatics Variability
The bioinformatic analysis of ctDNA sequencing data introduces another layer of variability. Distinguishing true somatic variants from background artifacts, germline polymorphisms, and clonal hematopoiesis of indeterminate potential (CHIP) remains challenging. Dynamic filtering methods that incorporate matched normal samples can significantly reduce false positives by identifying CHIP-derived variants [75]. The specific algorithms and thresholds used for variant calling, as well as methods for calculating ctDNA levels (e.g., mean VAF versus maximum VAF), further contribute to inter-assay differences [72] [74].
Table 1: Key Sources of Variability in ctDNA Analysis
| Variability Category | Specific Sources | Impact on Results |
|---|---|---|
| Biological | Circadian fluctuations, physical activity, inflammatory states, tumor heterogeneity | Background ctDNA variation unrelated to treatment |
| Pre-analytical | Sample type (plasma vs. serum), collection tubes, processing time, extraction efficiency | DNA yield and quality, false negatives/positives |
| Analytical | Input DNA quantity, sequencing depth, on-target rate, limit of detection | Sensitivity, particularly for low-frequency variants |
| Post-analytical | Variant calling algorithms, CHIP filtering, molecular response definitions | Specificity, false positive rates, response classification |
Standardized Experimental Protocols for Validation
Reference Material Design and Validation Framework
Robust validation of ctDNA assays requires carefully designed reference materials that mimic clinical samples while enabling precise evaluation of performance characteristics. A comprehensive approach utilizes multiple sample types, including diluted cell-free DNA and contrived plasma samples, spanning a range of clinically relevant variant allele frequencies (e.g., 0.1-2.5%) and input quantities (e.g., 10-50 ng) [73]. These materials should incorporate multiple variant types—single nucleotide variants (SNVs), insertions/deletions (Indels), copy number variants (CNVs), and structural variants (SVs)—across cancer-relevant genes to assess differential performance across alteration types [73].
The validation framework should systematically evaluate key analytical performance metrics including:
- Sensitivity: Detection rate for known variants across different VAFs and input amounts
- Specificity: False positive rate in wild-type samples
- Reproducibility: Intra-assay and inter-assay concordance across replicates
- Accuracy: Comparison with orthogonal methods (ddPCR, reference assays)
This approach enables comprehensive characterization of assay performance across clinically relevant conditions, identifying limitations particularly at low VAFs and input amounts where variability is most pronounced [73].
Orthogonal Method Comparison and Verification
Establishing assay accuracy requires comparison with validated orthogonal methods across multiple platforms. Digital droplet PCR (ddPCR) provides highly sensitive and quantitative verification for specific hotspot mutations (e.g., KRAS G12D, TP53 R273H), with high correlation (R² = 0.892) observed between NGS VAF and ddPCR measurements [75]. Additionally, comparison with tissue-based sequencing using matched samples enables evaluation of clinical concordance while controlling for tumor heterogeneity. Such comparisons typically reveal moderate sensitivity (68.18% for SNVs/indels; 57.89% for CNVs) for liquid versus tissue biopsies, reflecting both biological and technical factors [75].
For comprehensive assay evaluation, cross-platform comparisons with other validated ctDNA assays (e.g., Roche AVENIO ctDNA Expanded Kit) provide benchmarking against established standards. These comparisons should assess performance across variant types and concentrations, with particular attention to variants near the limit of detection where discordance is most likely [75] [73]. Verification studies should also specifically evaluate the assay's ability to distinguish tumor-derived variants from CHIP, utilizing white blood cell or matched normal sequencing to identify hematopoietic-derived mutations [75].
Analytical Frameworks for Assessing Performance
Quantitative Performance Metrics Across Platforms
Systematic evaluation of ctDNA assays reveals substantial variability in key performance parameters. The following table summarizes analytical performance characteristics across different assay types based on multi-platform studies:
Table 2: Analytical Performance Comparison of ctDNA Assays
| Performance Metric | Small Panels (<1 Mb) | Large Panels (>1 Mb) | High-Sensitivity Assays |
|---|---|---|---|
| SNV Sensitivity at 0.5% VAF | ~95% (at >20 ng input) | Variable (68-95%) | >95% (LOD: 0.15% VAF) |
| Indel Sensitivity | >90% (at ≥0.5% VAF) | Variable | >95% (LOD: 0.15% VAF) |
| CNV Detection | Limited to specific genes | Variable sensitivity (≈58%) | Sensitive (2.11 copies for gains) |
| Fusion Detection | Limited to specific rearrangements | Variable | High (LOD: 0.30% VAF) |
| Input DNA Requirements | 10-50 ng (sensitivity input-dependent) | 20-50 ng (larger inputs preferred) | 20-50 ng (optimized for low input) |
| Sequencing Depth | High (>10,000×) | Moderate (<5,000×) | Variable (technology-dependent) |
Data synthesized from [75] [73] [34]
Performance varies substantially based on input DNA quantity, with assays generally demonstrating optimal sensitivity at inputs >20 ng [73]. At very low inputs (<20 ng), sensitivity decreases significantly, particularly for low-frequency variants (<0.5% VAF). This input-dependent performance highlights the importance of standardizing input requirements and quality control metrics.
Molecular Response Definitions and Clinical Correlations
Defining molecular response (MR) based on ctDNA dynamics requires standardization to ensure consistent interpretation across studies. Analysis of clinical trials has evaluated multiple MR thresholds:
Table 3: Molecular Response Definitions and Clinical Correlations in Advanced NSCLC
| Molecular Response Definition | Association with OS in Anti-PD(L)1 Therapy | Association with OS in Chemotherapy | Optimal Timing for Assessment |
|---|---|---|---|
| ≥50% decrease in ctDNA | Significant association at both T1 and T2 | Weaker association at T1, stronger at T2 | T2 (7-13 weeks) marginally stronger |
| ≥90% decrease in ctDNA | Significant association at both T1 and T2 | More pronounced at T2 than T1 | T2 preferred for both modalities |
| 100% clearance (undetectable) | Strongest association with improved OS | Association present but variable | T2 shows more consistent association |
Data synthesized from [74]
The timing of ctDNA assessment significantly impacts the association with clinical outcomes. Early assessment (T1, up to 7 weeks post-treatment) and later assessment (T2, 7-13 weeks post-treatment) both show significant associations with overall survival (OS), with T2 demonstrating marginally stronger associations in some contexts [74]. These relationships also vary by treatment modality, highlighting the need for modality-specific response definitions and timing considerations.
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 4: Essential Research Reagents and Materials for ctDNA Analysis
| Reagent/Material | Function/Application | Technical Considerations |
|---|---|---|
| Cell-free DNA Blood Collection Tubes | Stabilizes nucleated blood cells and preserves ctDNA | Critical for pre-analytical standardization; different preservatives affect DNA yield |
| ctDNA Extraction Kits | Isolation of high-quality ctDNA from plasma | Efficiency varies (16-100% reported); impacts downstream sensitivity |
| Reference Standard Materials | Assay validation and quality control | Synthetic cfDNA with predetermined variants; cell line-derived controls |
| Targeted Hybridization Capture Panels | Enrichment of cancer-relevant genomic regions | Panel size (74-500 genes) affects coverage and depth; design impacts variant detection |
| ddPCR Assays | Orthogonal validation of specific variants | High sensitivity for hotspot mutations; quantitative VAF measurement |
| Unique Molecular Identifiers (UMIs) | Error suppression and accurate quantification | Reduces PCR and sequencing errors; essential for low-frequency variant detection |
| Methylation Control DNA | Analysis of epigenetic alterations in ctDNA | Bisulfite conversion controls; enriches cancer-derived signals |
Strategies for Enhancing Reproducibility and Standardization
Pre-Analytical and Analytical Standardization
Standardization begins at the pre-analytical phase, where implementation of uniform protocols for blood collection, processing, and storage can significantly reduce variability. The use of standardized blood collection tubes with cellular stabilizers, defined centrifugation protocols (time, force, temperature), and strict timelines from collection to plasma separation (preferably within 2-4 hours) minimizes white blood cell lysis and preserves ctDNA integrity [57]. Plasma, rather than serum, is recommended as the preferred sample type due to higher ctDNA enrichment and reduced genomic DNA contamination [57].
DNA extraction methodologies represent another critical area for standardization. Protocols should be optimized for efficient recovery of short-fragment DNA, with quantification methods that specifically target adapter-ligated molecules rather than total DNA [76]. Input DNA normalization should be based on read count distribution rather than fluorometry alone, as this better predicts sequencing performance by specifically quantifying molecules that will contribute to sequencing data [76]. For targeted sequencing, maintaining consistent input amounts (optimally >20 ng) and implementing quality thresholds for DNA fragment size distribution improves inter-assay reproducibility [73].
Bioinformatics and Reporting Standards
Bioinformatic standardization is equally crucial for reducing inter-assay variability. The implementation of optimized normalization methods that account for read count distribution significantly improves data consistency in high-throughput sequencing [76]. For RNA-seq data, which is sometimes analyzed alongside ctDNA, appropriate normalization methods (CPM, FPKM, TPM, TMM) must be selected based on the specific comparison being made—within sample, between samples, or across datasets [77].
Dynamic filtering approaches that incorporate matched normal samples substantially improve specificity by removing germline variants and CHIP-related mutations [75]. These methods can reduce discordance between liquid and tissue biopsies by over 11% [75]. Standardized reporting metrics for ctDNA assays should include DNA input quantity, deduplicated sequencing depth, on-target rate, limit of detection for each variant type, and circulating tumor fraction estimates. The development of consensus bioinformatic pipelines and quality thresholds will further enhance reproducibility across laboratories and platforms.
The standardization of ctDNA analysis represents an ongoing challenge requiring coordinated effort across multiple stakeholders. The substantial inter-assay variability observed in current platforms necessitates comprehensive validation using standardized reference materials and orthogonal verification methods. As the field progresses toward using ctDNA as a regulatory endpoint in clinical trials, consensus must be reached on critical parameters including molecular response definitions, optimal timing for assessment, and analytical performance requirements.
Future developments should focus on establishing harmonized protocols across pre-analytical, analytical, and bioinformatic phases. Reference standards, proficiency testing programs, and open-source bioinformatic pipelines will be essential tools for enhancing reproducibility. Only through such rigorous standardization can the full potential of liquid biopsies be realized, enabling reliable detection of residual disease, accurate monitoring of treatment response, and ultimately, improved patient outcomes through more personalized cancer management.
Optimizing Sample Collection and Bioinformatic Analysis for Reliable Results
Liquid biopsy, particularly the analysis of circulating tumor DNA (ctDNA), has emerged as a transformative paradigm in precision oncology. This non-invasive approach enables real-time assessment of tumor burden, genetic heterogeneity, and therapeutic response, offering a dynamic alternative to traditional tissue biopsies [5] [4]. The analysis of ctDNA—a small subset of total cell-free DNA (cfDNA) that originates specifically from tumor cells—holds significant promise for early cancer detection, monitoring treatment response, identifying minimal residual disease (MRD), and tracking the emergence of therapy resistance [78] [79].
However, the reliable detection and analysis of ctDNA present substantial technical challenges. In early-stage cancers or MRD settings, ctDNA can exist at vanishingly low concentrations, sometimes constituting less than 0.1% of total cfDNA [5]. This biological rarity, combined with pre-analytical variables and technical artifacts, demands optimized approaches across the entire workflow—from sample collection to computational analysis. This technical guide provides a comprehensive framework for optimizing these processes to generate robust, clinically actionable data from liquid biopsy specimens.
Pre-Analytical Phase: Sample Collection and Processing
The pre-analytical phase is arguably the most critical determinant of success in ctDNA analysis, as errors introduced at this stage cannot be remedied by subsequent bioinformatic corrections.
Blood Collection and Plasma Separation
- Tube Selection: Use specialized blood collection tubes designed for stabilizing cfDNA, such as those containing EDTA or specific preservatives. Proper stabilization prevents the release of genomic DNA from white blood cells, which can dilute the ctDNA fraction [80].
- Processing Timeline: Process blood samples within 1-2 hours of collection if using EDTA tubes, or within up to 72 hours if using commercial cfDNA preservation tubes. Immediate processing minimizes background wild-type DNA contamination from hematopoietic cell lysis [4].
- Centrifugation Protocol: Implement a double-centrifugation protocol:
- Plasma Storage: Aliquot purified plasma to avoid freeze-thaw cycles and store at -80°C until DNA extraction.
cfDNA Extraction and Quality Control
Extract cfDNA using silica-membrane columns or magnetic beads specifically optimized for recovering short DNA fragments. Quantify cfDNA using fluorometric methods (e.g., Qubit) rather than spectrophotometry, as the latter is less accurate for low-concentration, fragmented DNA [33]. Assess fragment size distribution using bioanalyzer systems; authentic ctDNA typically shows a peak at 160-180 bp, corresponding to mononucleosomal fragments [78] [5].
Table 1: Critical Pre-Analytical Parameters for ctDNA Analysis
| Parameter | Optimal Specification | Impact on Assay Performance |
|---|---|---|
| Blood Collection Tube | EDTA or dedicated cfDNA tubes | Preuces genomic DNA contamination |
| Processing Time | 1-2 hours (EDTA); up to 72 hours (preservative tubes) | Maintains cfDNA integrity and prevents dilution |
| Centrifugation | Double-spin protocol | Removes cellular contaminants |
| Plasma Volume | 4-10 mL | Ensures sufficient DNA yield for analysis |
| cfDNA Extraction | Fragment-size optimized kits | Enriches for ctDNA (160-180 bp fragments) |
| Storage Condition | -80°C in aliquots | Preserves DNA integrity |
Analytical Phase: ctDNA Enrichment and Sequencing Strategies
Overcoming the challenge of low ctDNA abundance requires specialized wet-lab methodologies that enhance detection sensitivity and specificity.
Fragment Size Selection
Tumor-derived ctDNA fragments are typically shorter (90-150 bp) than those from non-tumor cells. Employing bead-based or enzymatic size selection to enrich for these shorter fragments can increase the fractional abundance of ctDNA in sequencing libraries by several folds, significantly improving the detection of low-frequency variants [5]. This approach is particularly valuable for minimal residual disease detection, where it can reduce the required sequencing depth, enhancing both efficiency and cost-effectiveness [5].
Unique Molecular Identifiers (UMIs)
UMIs (also called molecular barcodes) are short random nucleotide sequences added to individual DNA molecules during library preparation [78] [80]. Each original DNA molecule receives a unique barcode before PCR amplification, enabling precise tracking of amplification duplicates and distinguishing true somatic mutations from artifacts introduced during library preparation and sequencing [78]. UMI-based error correction strategies can improve detection sensitivity to variant allele frequencies below 0.1% [78] [33].
Diagram 1: UMI Workflow for Error Correction. Unique molecular identifiers (UMIs) tag original DNA molecules before PCR amplification, enabling bioinformatic distinction between true variants and technical artifacts during data analysis.
Targeted Sequencing Approaches
While whole-genome and whole-exome sequencing are valuable for discovery research, targeted sequencing panels focusing on clinically relevant genes provide the depth required for sensitive ctDNA detection. Hybridization capture-based panels targeting 100-200 genes allow for sequencing depths of 10,000x or more, enabling detection of variants at allele frequencies as low as 0.1% [33] [81]. These panels can be further enhanced by incorporating tumor-informed approaches, where patient-specific mutations identified in tissue biopsies are prioritized for monitoring in plasma [4].
Bioinformatic Analysis for ctDNA Detection
Advanced computational methods are essential for distinguishing true tumor-derived signals from technical noise and biological background in ctDNA sequencing data.
Bioinformatics Tools for UMI Processing
Dedicated bioinformatics tools have been developed specifically for processing UMI-tagged sequencing data:
- UMI-tools: Identifies PCR duplicates based on UMI sequences and genomic coordinates, improving quantification accuracy by correcting for amplification biases [78].
- MAGERI: Provides an efficient analysis pipeline for UMI-encoded data, enabling sensitive variant calling by constructing consensus sequences from reads sharing the same UMI [78].
- Duplex Sequencing: The gold-standard for high-accuracy sequencing, this method tags and sequences each strand of a DNA duplex, requiring that true mutations appear on both strands to significantly reduce false positives [4].
Somatic Variant Calling
Variant calling in ctDNA presents unique challenges due to low variant allele frequencies. Specialized callers that incorporate error models accounting for sequencing artifacts, base quality scores, and UMI information are essential. These tools typically apply statistical models that calculate the probability of observed variants being true somatic mutations versus technical errors, with sensitivity down to 0.01% variant allele frequency for optimized workflows [78] [5].
Copy Number Alteration Analysis
Detecting copy number variations (CNVs) in ctDNA requires specialized algorithms that account for the non-uniform fragmentation of cfDNA and the shallow allele fractions typical of plasma DNA. Key tools include:
- QDNAseq: Simultaneously corrects for GC content and mappability biases, which are particularly problematic in cfDNA data [78].
- CNVkit: Utilizes both on-target and off-target reads to infer copy number changes, improving sensitivity for detecting focal amplifications and deletions [78].
Methylation Analysis
Tumor-specific methylation patterns in ctDNA provide an orthogonal approach to mutation-based detection. Bioinformatics tools for methylation analysis must account for bisulfite conversion efficiency and map converted reads to reference genomes. Methods such as CancerLocator can simultaneously infer the proportion and tissue of origin of ctDNA based on methylation signatures [78].
Table 2: Essential Bioinformatics Tools for ctDNA Analysis
| Analysis Type | Software Tools | Key Features | Performance Considerations |
|---|---|---|---|
| UMI Processing | UMI-tools, MAGERI | PCR duplicate removal, consensus building | Enables variant detection <0.1% VAF |
| Variant Calling | VarScan, custom error-suppression methods | Low-frequency variant detection, error modeling | Sensitivity to 0.01% VAF with sufficient depth |
| Copy Number Variation | QDNAseq, CNVkit, BIC-seq2 | GC/mappability correction, off-target read utilization | Requires appropriate matched normal reference |
| Methylation Analysis | CancerLocator, Bismark | Bisulfite read alignment, tissue-of-origin prediction | Dependent on bisulfite conversion efficiency |
Specialized Applications and Methodologies
Tumor Mutation Burden (TMB) Analysis
Tumor mutation burden (TMB) has emerged as an important biomarker for predicting response to immune checkpoint inhibitors. Accurate TMB measurement from ctDNA requires specific considerations:
- Panel Size: Large genomic regions (typically >1 Mb) are necessary for precise TMB estimation. Smaller panels suffer from higher variability and less accurate TMB quantification [81].
- Algorithm Optimization: For tumor-only sequencing (without matched normal), specialized algorithms like Somatic-Germline-Zygosity (SGZ) must be optimized for specific populations. Recent studies have shown that the optimal TMB cut-off for predicting immunotherapy response in East Asian lung cancer patients may be 7 mutations/Mb rather than the 10 mutations/Mb established in Western populations [82].
- Analytical Validation: TMB algorithms require thorough validation using reference materials with known mutation counts across the targeted genomic region [82] [81].
Structural Variant (SV) Detection
Structural variants (translocations, insertions, deletions) offer advantages for ctDNA detection because their breakpoint sequences are unique to the tumor and unlikely to occur as technical artifacts. SV-based assays can achieve parts-per-million sensitivity, with one study in early-stage breast cancer detecting ctDNA in 96% of participants at baseline with median variant allele frequency of 0.15% [5]. Personalized hybrid-capture probes targeting individual-specific breakpoints can further enhance sensitivity for minimal residual disease monitoring.
Multimodal Integration
The most advanced ctDNA analysis approaches integrate multiple genomic features—including mutations, copy number alterations, methylation patterns, and fragmentation profiles—to improve sensitivity and specificity. Machine learning algorithms that combine these orthogonal signals can detect ctDNA at lower concentrations than any single approach alone [5] [4].
Diagram 2: Multi-Omic Approach to ctDNA Analysis. Integrating multiple molecular features and detection methods through machine learning significantly enhances the sensitivity and specificity of ctDNA detection compared to single-modality approaches.
Essential Research Reagent Solutions
Table 3: Key Research Reagents and Platforms for ctDNA Analysis
| Reagent/Platform | Function | Application in ctDNA Workflow |
|---|---|---|
| Commercial cfDNA Blood Collection Tubes (e.g., Streck, PAXgene) | Cellular component stabilization | Preserves blood sample integrity during transport and storage |
| Size-selection Beads (e.g., SPRI, AMPure) | Fragment size selection | Enriches for shorter ctDNA fragments (90-150 bp) |
| UMI Adapter Kits (commercially available) | Molecular barcoding | Tags individual DNA molecules for error correction |
| Hybrid Capture Panels (e.g., PAN100, Oncomine Precision) | Target enrichment | Focuses sequencing on clinically relevant genomic regions |
| Methylation Conversion Kits | Bisulfite treatment | Converts unmethylated cytosines to uracils for methylation analysis |
| Reference Standards (e.g., Seraseq ctDNA) | Analytical validation | Provides known mutation controls for assay qualification |
Optimizing sample collection and bioinformatic analysis for ctDNA detection requires a comprehensive, integrated approach that addresses challenges across the entire workflow. From proper blood collection and processing to fragment size selection, molecular barcoding, and advanced computational analysis, each step must be meticulously controlled and validated. The implementation of UMI-based error correction, multimodal data integration, and population-specific bioinformatic algorithms has significantly enhanced the sensitivity and specificity of ctDNA analysis, enabling detection at variant allele frequencies below 0.01% in some applications.
As the field continues to evolve, emerging technologies such as multiplexed CRISPR-Cas ctDNA assays, nanomaterial-based biosensors, and artificial intelligence-driven error suppression methods promise to further push the boundaries of detection sensitivity [5]. However, standardization of pre-analytical protocols, analytical workflows, and computational pipelines remains essential for translating these technological advances into clinically validated applications. By adhering to the optimized methods outlined in this guide, researchers can generate more reliable, reproducible ctDNA data that ultimately advances precision oncology and improves patient care.
The convergence of artificial intelligence (AI) with liquid biopsy technologies represents a paradigm shift in cancer detection. Liquid biopsy, which involves the analysis of circulating tumor DNA (ctDNA) and other biomarkers in blood, offers a minimally invasive window into tumor genetics and dynamics [4]. However, the inherent complexity and low abundance of these biomarkers present significant analytical challenges. AI and machine learning (ML) are emerging as powerful tools to overcome these hurdles, enhancing the sensitivity, specificity, and overall accuracy of cancer detection. This technical guide explores the cutting-edge methodologies and future directions of AI-driven liquid biopsy, providing a framework for researchers and drug development professionals working at the intersection of computational biology and precision oncology.
AI Methodologies Revolutionizing Liquid Biopsy Analysis
The application of AI in liquid biopsy spans diverse computational techniques, each tailored to address specific analytical challenges. The selection of an AI model is primarily dictated by the data modality and the clinical objective [83] [84].
Machine Learning (ML) models, including logistic regression and ensemble methods, are effectively applied to structured data such as genomic biomarkers and clinical lab values for tasks like survival prediction or therapy response assessment [83] [84]. Deep Learning (DL) architectures, particularly Convolutional Neural Networks (CNNs), are the cornerstone for analyzing imaging data from histopathology and radiology, enabling tasks like tumor detection, segmentation, and grading [83] [84]. For sequential data, such as genomic sequences or clinical notes, Recurrent Neural Networks (RNNs) and Transformers are employed to model long-range dependencies, facilitating biomarker discovery and in-depth mining of electronic health records (EHRs) [83]. The recent advent of Large Language Models (LLMs) further enhances the ability to extract knowledge from vast scientific literature and clinical text, accelerating hypothesis generation in cancer research [83].
A key innovation is the use of AI for "needle-in-a-haystack" problems. For instance, the Rare Event Detection (RED) algorithm uses a deep learning approach to identify rare cancer cells among millions of normal blood cells without requiring pre-defined features of the target cell. Instead, it ranks cells by rarity, allowing the most unusual findings to rise to the top for review [85]. Another advanced approach uses machine learning to identify complex patterns of DNA fragments in the blood, combining the analysis of fragmentation profiles and repeating genome patterns linked to tumors, which has proven particularly effective for detecting cancers like brain cancer that were previously difficult to identify via liquid biopsy [86].
Table 1: Overview of AI Models Used in Liquid Biopsy Applications
| AI Model Category | Primary Data Modalities | Key Applications in Liquid Biopsy | Examples |
|---|---|---|---|
| Classical Machine Learning | Structured genomic data, lab values, clinical parameters | Therapy response prediction, survival analysis, risk stratification | Logistic Regression, Ensemble Methods [83] |
| Deep Learning (CNNs) | Imaging data (histopathology, radiology) | Tumor detection, segmentation, and grading from medical images | Convolutional Neural Networks (CNNs) [83] [84] |
| Sequential Models (RNNs, Transformers) | Genomic sequences, clinical notes (EHR) | Biomarker discovery, EHR mining, longitudinal data analysis | Recurrent Neural Networks (RNNs), Transformers [83] |
| Large Language Models (LLMs) | Scientific literature, clinical text | Hypothesis generation, knowledge extraction from unstructured data | GPT-5 [83] |
Quantitative Performance of AI-Enhanced Detection
AI-powered liquid biopsy has demonstrated significant improvements in detection accuracy across multiple cancer types. The following table summarizes key performance metrics from recent studies, highlighting the quantitative advances enabled by machine learning and deep learning approaches.
Table 2: Performance Metrics of AI-Enhanced Liquid Biopsy in Cancer Detection
| Cancer Type | AI Approach / Tool | Detection Sensitivity | Key Performance Highlights | Study Details |
|---|---|---|---|---|
| Multiple Cancers (Liquid Biopsy) | RED (Rare Event Detection) Algorithm | 99% for added epithelial cancer cells; 97% for added endothelial cells | Reduced data for human review by 1,000-fold; found twice as many "interesting" cells vs. old approach [85] | Tested on advanced breast cancer patients and spiked normal blood samples [85] |
| Brain Cancer | Next-gen AI liquid biopsy (DNA fragments + immune cell changes) | ~75% (in a cohort of 505 patients) | Significant improvement over previous liquid biopsy approaches (<10% detection) [86] | Multi-national cohorts (US, South Korea, Poland); validated in a second set of ~95 patients [86] |
| Breast Cancer | AI for Mammography Interpretation | +9.4% reduction in false negatives (US data); +2.7% (UK data) vs. radiologists [87] | AUC: 0.889 (UK), 0.8107 (US); outperformed radiologists in clinically relevant task [84] | Trained on 25,856 women (UK), tested on 3,097 women (US) [84] |
| Gastrointestinal Cancers | AI-powered ctDNA analysis (methylation, fragmentomics) | Superior sensitivity/specificity for early detection vs. traditional methods [61] | AI enables high-throughput biomarker discovery and multi-omics integration [61] | Review of AI/ML for enhancing liquid biopsy accuracy in GICs [61] |
Detailed Experimental Protocols for AI-Powered Liquid Biopsy
To ensure reproducibility and facilitate adoption of these advanced techniques, this section outlines detailed methodological workflows for key experiments in AI-enhanced liquid biopsy.
Protocol: AI-Assisted Rare Cell Detection in Liquid Biopsy
This protocol is based on the RED (Rare Event Detection) algorithm, which automates the detection of rare cancer cells in blood samples [85].
Sample Preparation and Imaging:
- Collect peripheral blood samples from patients in EDTA-containing tubes.
- Process samples to isolate peripheral blood mononuclear cells (PBMCs) using density gradient centrifugation.
- Stain cells with fluorescently labeled antibodies targeting epithelial (e.g., EpCAM) and other relevant cancer-specific surface markers.
- Prepare microscopic slides and perform high-resolution, high-throughput scanning to generate digital images of millions of cells.
Data Preprocessing and Augmentation:
- Use image processing software to segment individual cells from the background.
- Extract image patches centered on each segmented cell.
- Apply data augmentation techniques (e.g., rotation, flipping, minor color shifts) to the training dataset to increase robustness and reduce overfitting.
AI Model Training and Execution:
- Architecture: Employ a deep learning-based rare event detection model. The RED algorithm, for instance, does not rely on pre-defined cellular features but instead uses an unsupervised or self-supervised approach to identify anomalous patterns.
- Training: Train the model on a large dataset of pre-annotated cell images, or using a self-supervised learning paradigm where the model learns to identify outliers without explicit labels for every cancer cell.
- Inference: Input new, unseen cell images into the trained model. The algorithm analyzes and ranks cells based on their "rarity" or deviation from the majority of normal blood cells.
- Output: Generate a prioritized list of the most "unusual" cells for expert pathologist review, drastically reducing the number of cells a human needs to examine.
Protocol: AI-Driven ctDNA Analysis for Brain Tumor Detection
This protocol details the method developed by Johns Hopkins researchers, which combines ctDNA fragmentomics and immune profiling for detecting brain cancers [86].
Blood Collection and Plasma Separation:
- Draw blood from patients into cell-free DNA blood collection tubes.
- Centrifuge samples within a defined post-collection window (e.g., within 2-6 hours) to separate plasma from blood cells.
- Perform a second, high-speed centrifugation of the plasma to remove any residual cells or debris.
- Aliquot and store the purified plasma at -80°C until DNA extraction.
Cell-free DNA (cfDNA) Extraction and Sequencing:
- Extract total cfDNA from plasma using a commercial cfDNA extraction kit, ensuring high recovery of short DNA fragments.
- Prepare sequencing libraries from the purified cfDNA. If using a targeted approach, hybridize the libraries to a panel of cancer-associated genes.
- Perform high-throughput, deep next-generation sequencing (NGS) on the libraries to achieve high coverage (e.g., >10,000x).
Multi-Feature Data Generation:
- Variant Calling: Use bioinformatics pipelines to identify somatic mutations (single nucleotide variants, indels) in the cfDNA, comparing them to a matched white blood cell (germline) control if available.
- Fragmentomics Analysis: Calculate the size distribution of all cfDNA fragments. Tumor-derived ctDNA fragments often have a characteristic size profile that differs from non-tumor cfDNA.
- Immune Profile Inference: Analyze the fragmentation patterns and sequencing data to infer the relative proportions of different immune cell types (e.g., neutrophils, lymphocytes) in the blood, as brain tumors can cause systemic immune suppression.
Machine Learning-Based Classification:
- Feature Vector Construction: Compile a feature vector for each patient sample that includes data on mutations, fragment size distributions, and inferred immune cell proportions.
- Model Training: Train a machine learning classifier (e.g., a random forest or support vector machine) on a labeled dataset from known cancer patients and healthy controls.
- Validation: Validate the trained model on an independent, held-out cohort of patients to assess its real-world performance in detecting brain cancer.
The Scientist's Toolkit: Essential Reagents and Research Solutions
Successful implementation of AI-powered liquid biopsy requires a combination of wet-lab reagents and dry-lab computational tools. The following table details key components of the research pipeline.
Table 3: Essential Research Reagent Solutions for AI-Powered Liquid Biopsy
| Tool / Reagent | Function / Application | Key Considerations |
|---|---|---|
| Cell-free DNA Blood Collection Tubes | Stabilizes blood cells to prevent genomic DNA contamination and preserve ctDNA profile during transport and storage. | Critical for pre-analytical sample integrity; enables longer processing windows [86] [88]. |
| cfDNA Extraction Kits | Isolate high-quality, short-fragment cfDNA from plasma with high yield and minimal contamination. | Recovery efficiency and fragment size bias can impact downstream analysis and sensitivity [4] [88]. |
| Targeted NGS Panels | Multi-gene panels for deep sequencing of cancer-associated mutations from low-input cfDNA. | Panels must be designed for high coverage and should incorporate unique molecular identifiers (UMIs) for error correction [4] [88]. |
| Unique Molecular Identifiers (UMIs) | Short DNA barcodes ligated to each DNA fragment before PCR amplification to correct for sequencing errors and PCR duplicates. | Essential for accurately detecting low-frequency variants; gold-standard methods include Duplex Sequencing and SaferSeqS [4]. |
| AI/ML Software Frameworks | Open-source libraries (e.g., TensorFlow, PyTorch) for developing and training custom deep learning models. | Requires expertise in computational biology; model performance depends on quality and size of training datasets [83] [84]. |
| Bioinformatics Pipelines | Custom or commercial software for processing raw NGS data, including alignment, variant calling, and fragmentomics analysis. | Must be optimized for ctDNA's low variant allele frequency and characteristic fragmentation patterns [4] [61]. |
The integration of AI and machine learning with liquid biopsy is fundamentally enhancing the accuracy of cancer detection. By leveraging sophisticated algorithms to analyze complex, multi-modal data from ctDNA, circulating cells, and fragmentomics, researchers are overcoming traditional limitations of sensitivity and specificity. Future progress will depend on addressing key challenges such as algorithmic bias, data standardization, and the need for robust validation in large, diverse patient populations. The implementation of fairness-aware AI models, federated learning to leverage data across institutions while preserving privacy, and strong regulatory frameworks will be critical for translating these technologies into equitable and effective clinical tools [89]. As these technologies mature, AI-powered liquid biopsy is poised to become an indispensable component of precision oncology, enabling earlier diagnosis, dynamic monitoring of treatment response, and improved outcomes for cancer patients.
Clinical Trial Evidence and Comparative Performance Analysis
Circulating tumor DNA (ctDNA) has emerged as a transformative biomarker in oncology, representing a fragment of cell-free DNA (cfDNA) shed into the bloodstream from tumor cells. This minimally invasive "liquid biopsy" enables real-time monitoring of tumor dynamics, overcoming limitations of traditional tissue biopsies, including invasiveness, tumor heterogeneity, and inability to serial monitor [90]. The clinical utility of ctDNA spans cancer detection, molecular profiling, therapy selection, and monitoring treatment response. Most notably, in the adjuvant setting for solid tumors, ctDNA detection after curative-intent surgery identifies Molecular Residual Disease (MRD), predicting recurrence much earlier than standard imaging and creating a window for therapeutic intervention [91] [14]. This whitepaper examines three pivotal studies—DYNAMIC-III, PEGASUS, and VICTORI—that are shaping the clinical application of ctDNA-guided strategies in colorectal cancer (CRC), highlighting their methodologies, findings, and implications for drug development and clinical practice.
The following tables summarize the designs and primary results from the DYNAMIC-III, PEGASUS, and VICTORI trials.
Table 1: Key Design Elements of the Featured Clinical Trials
| Trial Aspect | DYNAMIC-III [92] | PEGASUS [92] [93] | VICTORI (Interim) [14] |
|---|---|---|---|
| Study Phase | Phase III Randomized | Phase II Investigator-Initiated | Prospective Observational (Interim) |
| Patient Population | 702 patients with Stage III colon cancer post-resection | 135 patients with Stage III/high-risk Stage II colon cancer | 71 patients with resectable CRC (Stages I-IV) |
| Primary Objective | Establish non-inferiority of ctDNA-guided management for 3-year RFS | Assess feasibility of ctDNA-guided therapy (2-year DFS in ctDNA-negative) | Identify optimal post-surgical timepoint for ctDNA detection to predict recurrence |
| ctDNA Assay | SaferSeqS targeted CRC panel | Guardant Reveal | NeXT Personal (tumor-informed, up to 1,800 variants) |
| Intervention | ctDNA-negative results prompted de-escalated adjuvant chemo | Dynamic therapy escalation/de-escalation based on serial ctDNA results | Observational; serial ctDNA monitoring without intervention |
Table 2: Key Efficacy and Safety Outcomes
| Outcome Measure | DYNAMIC-III [92] | PEGASUS [92] [93] | VICTORI (Interim) [14] |
|---|---|---|---|
| Primary Endpoint Result | 3-yr RFS: 85.3% (ctDNA) vs 88.1% (Standard); non-inferiority not met | 12 relapses in 100 ctDNA-neg pts; feasibility threshold not met | 87% of pts with clinical recurrence were ctDNA+ by 8 weeks post-surgery |
| Recurrence Prediction | N/A | HR for DFS (ctDNA+ vs ctDNA-): 2.71 (p=0.0036) | ctDNA detected recurrence a median of 198 days earlier than imaging |
| Chemotherapy Use | Oxaliplatin use reduced from 88.6% to 34.8% (p<0.001) | Enabled dynamic treatment modulation | N/A (Observational study) |
| Toxicity Impact | Grade ≥3 adverse events: 6.2% vs 10.6% (p=0.037) | Potential for reduced overtreatment, though not quantified in results | N/A (Observational study) |
| ctDNA Level at Detection | N/A | N/A | Median: 24.4 ppm (Range: 2 ppm - 111,120 ppm) |
Detailed Experimental Protocols and Methodologies
DYNAMIC-III Trial Protocol
DYNAMIC-III employed a pragmatic, prospective randomized design. After curative resection for Stage III colon cancer, 702 patients who were ctDNA-negative at 5-6 weeks post-surgery were randomized to either standard management or ctDNA-guided management [92]. Prior to randomization, clinicians pre-specified the standard adjuvant regimen they would typically prescribe based on clinicopathological factors. In the experimental arm, a negative ctDNA result triggered a pre-defined de-escalation strategy: for instance, switching from a planned 6-month oxaliplatin-based regimen to 3 months of the same regimen or a fluoropyrimidine (FP) alone, or from single-agent FP to no chemotherapy [92]. The primary endpoint was 3-year Recurrence-Free Survival (RFS), with a statistical non-inferiority margin of -7.5% [92]. ctDNA analysis was performed using the SaferSeqS assay, a tumor-informed platform designed for high-sensitivity detection of MRD [92].
PEGASUS Trial Protocol
The PEGASUS trial implemented a more complex, dynamic adaptive protocol based on serial liquid biopsies. Patients underwent initial ctDNA testing 2-4 weeks post-surgery using the Guardant Reveal assay [93]. Those testing positive (LB+) received 3 months of CAPOX, while those testing negative (LB-) received 6 months of capecitabine (CAPE) [93]. A second liquid biopsy was performed after one cycle of CAPE for LB- patients, with treatment escalation to CAPOX if the test turned positive. A final liquid biopsy at the end of adjuvant therapy guided further decisions: CAPOX-treated patients who were ctDNA-positive switched to FOLFIRI, while those who were negative de-escalated to CAPE. CAPE-treated patients who were positive switched to CAPOX, while those who were negative entered standard follow-up [93]. This design tested the feasibility of using real-time ctDNA dynamics to personalize therapy intensity.
VICTORI Study Protocol
VICTORI is a prospective, observational study focusing on the technical and temporal aspects of MRD detection. Its unique protocol involves creating a personalized, tumor-informed panel (NeXT Personal) for each patient, sequencing tumor tissue to select up to 1,800 somatic variants for tracking in plasma [14]. Blood samples are collected with high frequency: pre-operatively, every two weeks for the first eight weeks post-surgery, and then every three months for up to three years [14]. This intensive schedule aims to pinpoint the earliest and most reliable post-operative timepoint for ctDNA detection. The study's interim analysis confirmed the utility of this approach, demonstrating that ctDNA can be detected as early as two weeks after surgery, though four weeks is suggested as a more clinically robust timepoint to avoid dilution by normal cfDNA released from surgical trauma [14].
Visualizing ctDNA Workflows and Trial Logic
The following diagrams illustrate the core workflows and decision pathways from these trials.
Post-Surgical ctDNA-Guided Decision Pathway (DYNAMIC-III / PEGASUS)
High-Frequency Monitoring for MRD Detection (VICTORI)
The Scientist's Toolkit: Essential Research Reagents & Platforms
Table 3: Key Reagents and Platforms for ctDNA Research
| Tool / Reagent | Type | Primary Function in Research | Example Use in Trials |
|---|---|---|---|
| Guardant Reveal [93] [94] | Tissue-free, methylation-based ctDNA assay | Detects MRD and predicts recurrence without requiring tumor tissue sequencing. | Primary ctDNA detection assay in the PEGASUS trial. |
| NeXT Personal [14] | Tumor-informed, whole-genome-based MRD assay | Ultra-sensitive detection of MRD via personalized panels tracking up to 1,800 patient-specific variants. | Primary assay in the VICTORI study; enabled detection as low as 2 ppm. |
| SaferSeqS [92] | Tumor-informed, targeted ctDNA assay | High-sensitivity MRD detection focusing on a predefined set of CRC-associated mutations. | ctDNA analysis platform used in the DYNAMIC-III trial. |
| CAPOX / FOLFIRI [92] [93] | Chemotherapy Regimens | Standard cytotoxic backbones for CRC; used to test therapy modulation based on ctDNA risk. | Interventional chemotherapies in PEGASUS and DYNAMIC-III. |
| Personalized Variant Panels [14] | Bioinformatics Tool | Custom-designed NGS panels for tracking patient-specific mutations in plasma, maximizing sensitivity. | Core to the NeXT Personal assay used in VICTORI. |
Discussion and Future Directions
The DYNAMIC-III, PEGASUS, and VICTORI trials collectively represent a significant maturation of ctDNA technology, yet they also highlight the challenges in its clinical integration. DYNAMIC-III demonstrated that a ctDNA-guided strategy can significantly reduce chemotherapy use and toxicity but narrowly failed to meet its statistical non-inferiority endpoint for RFS [92]. This suggests that while current assay sensitivity is high, it may not yet be sufficient to reliably identify all patients who can safely forgo chemotherapy. This is further supported by the 12% false-negative rate observed in the PEGASUS trial [92] [93].
A critical insight from these studies is the importance of assay sensitivity and timing. The VICTORI study indicates that ultra-sensitive, tumor-informed assays can detect MRD at very low levels (parts per million) and weeks to months before radiographic recurrence [14]. Furthermore, VICTORI's data suggesting 4 weeks post-surgery as an optimal sampling timepoint provides crucial guidance for standardizing future trial designs [14].
For researchers and drug developers, these findings have several implications:
- Nov Trial Endpoints: The FDA now supports using ctDNA to enrich trial populations for high-risk patients and using ctDNA dynamics as an early signal of drug activity in early-phase trials [91].
- Assay Selection is Critical: The choice between tumor-informed (higher sensitivity, more complex) and tissue-agnostic (faster, simpler) assays carries trade-offs that directly impact trial outcomes and clinical validity [91].
- Intervention is Key: VICTORI confirms ctDNA's prognostic power, but observational data alone is insufficient. The next wave of trials must test specific interventions for ctDNA-positive patients to demonstrate improved survival [14].
Future research must focus on enhancing assay sensitivity, standardizing testing protocols, and—most importantly—demonstrating that therapeutic interventions driven by ctDNA status ultimately improve overall survival for cancer patients.
Note: This whitepaper synthesizes information from conference presentations and interim analyses, some of which are not yet published in peer-reviewed journals. The findings should be interpreted as reflecting the state of knowledge as of the ESMO 2025 Congress and the AACR Annual Meeting 2025.
Circulating tumor DNA (ctDNA) analysis has emerged as a transformative technology in oncology, providing a minimally invasive alternative to traditional diagnostic methods. This concordance analysis systematically evaluates the correlation between ctDNA profiling, tissue biopsy results, and imaging modalities across various cancer types. Evidence demonstrates that ctDNA shows high concordance with tissue biopsy for mutation detection in advanced cancers (70-100% for specific mutations), while offering superior capabilities for tracking dynamic changes and tumor heterogeneity. Compared to imaging, ctDNA provides significantly earlier detection of treatment response and disease recurrence—in some cases by more than 12 months—while also addressing critical limitations of anatomical assessments. This whitepaper provides technical protocols, methodological considerations, and clinical validation data to guide researchers and drug development professionals in implementing integrated diagnostic approaches.
The gold standard in cancer diagnosis has historically relied on tissue biopsy for tumor typing, grading, and identification of therapeutic targets, complemented by imaging techniques—primarily computed tomography (CT) and positron emission tomography (PET)—for monitoring anatomical changes according to Response Evaluation Criteria in Solid Tumors (RECIST) [3] [4]. However, these conventional approaches face significant limitations: tissue biopsies are invasive, prone to sampling bias, and impractical for repeated assessment of tumor evolution, while imaging lacks sensitivity for microscopic disease and early treatment response evaluation [3] [4] [16].
Liquid biopsy, particularly the analysis of circulating tumor DNA (ctDNA), represents a paradigm shift in cancer diagnostics and monitoring. ctDNA consists of small fragments of DNA released by tumor cells into the bloodstream and other biofluids through apoptosis, necrosis, and cellular secretion [3] [4]. As a minimally invasive approach, ctDNA analysis enables real-time assessment of tumor burden, genetic heterogeneity, and therapeutic response, capturing both primary and metastatic disease components [5] [16]. The half-life of ctDNA ranges from 16 minutes to several hours, allowing for near real-time monitoring of tumor dynamics—a significant advantage over traditional methods [4].
This technical review provides a comprehensive concordance analysis comparing ctDNA with established diagnostic modalities, with particular focus on validation methodologies, quantitative agreement metrics, and applications in drug development and clinical research.
Concordance Between ctDNA and Tissue Biopsy
Mutational Concordance Rates
Multiple studies have demonstrated variable but generally high concordance between ctDNA and tissue biopsy for detection of actionable mutations across cancer types. The concordance rate depends on tumor burden, cancer type, assay sensitivity, and the specific mutation analyzed.
Table 1: Mutational Concordance Between ctDNA and Tissue Biopsy
| Cancer Type | Gene/Mutation | Concordance Rate | Factors Influencing Concordance | Clinical Implications |
|---|---|---|---|---|
| Advanced NSCLC | EGFR mutations | 70-100% [4] [16] | Tumor burden, assay sensitivity | FDA-approved for guiding EGFR TKI therapy; alternative when tissue is unavailable |
| Colorectal Cancer | KRAS/NRAS mutations | 80-95% [4] | Tumor location, metastatic burden | Identifies resistance mutations; monitors clonal evolution |
| Breast Cancer | ESR1, PIK3CA mutations | 75-90% [4] | Tumor subtype, treatment history | Detects acquired resistance to endocrine therapy |
| Multiple Cancers | Multiple driver mutations | Varies by variant allele frequency | Technical factors, bioinformatics | Captures spatial heterogeneity missed by single-site biopsy |
The European Medicines Agency (EMA) authorized the use of ctDNA for identifying EGFR mutations in non-small cell lung cancer (NSCLC) in 2014, establishing regulatory precedent for liquid biopsy in clinical decision-making [3]. More recently, the International Association for the Study of Lung Cancer (IASLC) issued a consensus statement supporting liquid biopsy use in advanced NSCLC, particularly when tissue is insufficient or unavailable [3].
Technical and Biological Factors Affecting Concordance
Several pre-analytical and biological factors contribute to discordance between ctDNA and tissue biopsy results:
- Tumor heterogeneity: Tissue biopsies provide a snapshot of a single anatomical site, while ctDNA potentially represents the entire tumor burden, including metastatic deposits [4] [16]. This difference enables ctDNA to capture spatial heterogeneity that may be missed by single-site biopsies.
- Tumor shedding and ctDNA fraction: The proportion of tumor-derived DNA in total cell-free DNA varies significantly (0.01% to >90%) depending on cancer type, stage, and tumor biology [5] [4]. Low-shedding tumors and early-stage disease present detection challenges.
- Temporal evolution: Treatment-selective pressure drives clonal evolution, creating discrepancies between baseline tissue genotype and subsequent ctDNA profiles that reflect emerging resistance mechanisms [4] [16].
Advantages of ctDNA Over Tissue Biopsy
ctDNA analysis offers distinct advantages for drug development and clinical research:
- Longitudinal monitoring: Enables real-time assessment of tumor dynamics and acquisition of resistance mutations during treatment [4] [16].
- Comprehensive profiling: Captures heterogeneity across multiple tumor sites simultaneously [16].
- Practical feasibility: Less invasive, with faster turnaround times and applicability when tissue biopsy is contraindicated or impractical [5] [4].
Concordance Between ctDNA and Imaging Modalities
Temporal Relationships in Disease Monitoring
Imaging modalities including CT, PET, and magnetic resonance imaging (MRI) provide anatomical assessment of tumor burden based on RECIST criteria, but lack sensitivity for microscopic disease and early treatment response evaluation [4]. Substantial evidence demonstrates that ctDNA analysis can detect molecular response and recurrence significantly earlier than radiographic imaging.
Table 2: Temporal Comparison of ctDNA vs. Imaging for Disease Detection
| Clinical Scenario | Cancer Type | Lead Time of ctDNA | Performance Metrics | Study Details |
|---|---|---|---|---|
| Post-operative MRD detection | Colorectal Cancer | ≥6 months in 50% of cases; up to >1 year in some cases [43] | 100% sensitivity for future recurrence [43] | VICTORI study; NeXT Personal assay |
| Treatment response assessment | NSCLC | Weeks before radiographic changes [5] [4] | Better prediction of PFS than imaging [5] | Correlation with tumor burden |
| End-of-treatment assessment | DLBCL | N/A (complementary) | 90.8% specificity for relapse in PET-negative patients [18] | Meta-analysis of 53 studies |
| Early relapse detection post-CAR T | Lymphoid cancers | Variable (1-3 months) | More sensitive than PET/CT for molecular relapse [5] [18] | PhasED-Seq and SV-based assays |
In the VICTORI study, an ultrasensitive tumor-informed ctDNA assay (NeXT Personal) detected all post-resection recurrences in colorectal cancer patients before radiographic evidence, with half of recurrences detected at least six months earlier than imaging [43]. This early detection window provides critical opportunities for intervention before macroscopic disease progression.
Complementary Roles in Clinical Management
While ctDNA demonstrates superior sensitivity for minimal residual disease (MRD) detection, imaging and ctDNA provide complementary information in clinical management:
- End-of-treatment assessment in DLBCL: A meta-analysis of 53 studies demonstrated that in patients with negative end-of-treatment PET scans, positive ctDNA was highly specific (90.8%) for subsequent relapse [18]. Conversely, in patients with positive PET scans, negative ctDNA decreased relapse risk (negative likelihood ratio: 0.15) [18], suggesting that combined assessment improves prognostic stratification.
- Response monitoring in NSCLC: Declines in ctDNA levels during treatment predicted radiographic response more accurately than follow-up imaging and correlated better with progression-free survival [5] [4].
- Discordance resolution: In cases where ctDNA and imaging results disagree, the combination provides more nuanced clinical information than either modality alone. For instance, positive imaging with negative ctDNA may indicate non-malignant processes or low-shedding tumors, while positive ctDNA with negative imaging defines molecular relapse [18] [43].
Methodological Considerations for Concordance Studies
ctDNA Detection Technologies
Multiple technological platforms with varying sensitivities and applications have been developed for ctDNA analysis:
PCR-based methods including digital droplet PCR (ddPCR) and BEAMing (beads, emulsion, amplification, magnetics) offer high sensitivity for detecting single or few well-characterized mutations, with rapid turnaround times suitable for tracking known mutations during treatment [3] [4].
Next-generation sequencing (NGS) approaches including whole-exome sequencing (WES), whole-genome sequencing (WGS), and targeted methods (CAPP-Seq, TAm-Seq, Safe-SeqS, TEC-Seq) enable broad genomic profiling and detection of novel alterations [3] [4]. These methods utilize unique molecular identifiers (UMIs) to distinguish true low-frequency variants from sequencing artifacts [4].
Emerging approaches fragmentomics analysis examines cfDNA fragmentation patterns, end motifs, and size distributions to distinguish tumor-derived DNA without relying on specific mutations [3] [43]. Machine learning approaches like DELFI (DNA evaluation of fragments for early interception) achieve 91% sensitivity for cancer detection by analyzing genome-wide fragmentation profiles [3]. Methylation analysis identifies cancer-specific epigenetic patterns that can improve tissue-of-origin determination and detection sensitivity [5] [57].
Ultrasensitive Detection Technologies
Recent technological advances have dramatically improved ctDNA detection sensitivity, enabling applications in minimal residual disease monitoring and early-stage cancer detection:
- Structural variant (SV)-based assays: These assays identify tumor-specific chromosomal rearrangements (translocations, insertions, deletions) with breakpoint sequences unique to the tumor, achieving parts-per-million sensitivity [5]. In early-stage breast cancer, SV-based assays detected ctDNA in 96% of patients at baseline with median variant allele frequency of 0.15%, with 10% of positive cases having variant allele frequency <0.01% [5].
- Phased variant approaches: Techniques like PhasED-Seq improve sensitivity by targeting multiple single-nucleotide variants on the same DNA fragment [5].
- Nanomaterial-based biosensors: Electrochemical sensors utilizing magnetic nanoparticles coated with gold and conjugated with complementary DNA probes can achieve attomolar detection limits within 20 minutes [5].
- Fragment enrichment methods: Size-based selection of short DNA fragments (90-150 bp) characteristic of tumor-derived DNA can increase the fractional abundance of ctDNA in sequencing libraries by several folds [5].
Essential Research Reagents and Platforms
Table 3: Research Reagent Solutions for ctDNA Analysis
| Reagent/Platform | Function | Application in Concordance Studies |
|---|---|---|
| Streck cfDNA BCT tubes | Preserve blood samples by preventing white blood cell lysis | Maintain sample integrity for up to 7 days at room temperature [95] |
| Unique Molecular Identifiers (UMIs) | Molecular barcodes for error correction | Distinguish true mutations from sequencing artifacts in NGS [4] |
| Hybrid-capture probes | Enrich target genomic regions | Tumor-informed panels for MRD detection (e.g., NeXT Personal, Signatera) [18] [43] |
| Methylation-specific panels | Detect cancer-specific epigenetic changes | Tissue-of-origin determination; increased detection sensitivity [5] [57] |
| Magnetic nanoparticles | Target capture and signal amplification | Attomolar sensitivity in electrochemical biosensors [5] |
Experimental Protocols for Validation Studies
Protocol 1: Concordance Study Between ctDNA and Tissue Biopsy
Objective: To determine the agreement rate for specific mutations between ctDNA and matched tissue samples in treatment-naïve patients.
Sample Collection:
- Collect 2×10 mL blood in cell-free DNA collection tubes (e.g., Streck cfDNA BCT)
- Process within recommended timeframe (varies by tube type: 2-6 hours for EDTA tubes; up to 7 days for specialized BCTs) [95]
- Isolate plasma using double centrifugation (first spin: 800-1600×g for 10 min; second spin: 16,000×g for 10 min) [95]
- Extract cfDNA using silica-membrane or magnetic bead-based methods
- Obtain matched formalin-fixed paraffin-embedded (FFPE) tumor tissue with >20% tumor content
Mutation Analysis:
- For tissue: Perform targeted NGS using validated panels (e.g., Oncomine, FoundationOne)
- For ctDNA: Use matching NGS panel or ddPCR for specific mutations
- Sequence at appropriate depth: >10,000X for ctDNA; >500X for tissue [4]
Concordance Calculation:
- Calculate positive percent agreement (sensitivity) and negative percent agreement (specificity)
- Report overall percent agreement with 95% confidence intervals
- Stratify by mutation type, variant allele frequency, and tumor content
Protocol 2: Temporal Lead Time Analysis Compared to Imaging
Objective: To determine how early ctDNA detection predicts radiographic recurrence in the adjuvant setting.
Study Design:
- Enroll patients with curative-intent resection of solid tumors
- Collect serial blood samples at predefined intervals (e.g., 4 weeks post-operatively, then every 3 months for 2 years) [43]
- Perform radiographic imaging (CT/PET) per standard guidelines (e.g., every 6 months)
ctDNA Analysis:
- Use tumor-informed, personalized ctDNA assays for maximum sensitivity [43]
- For each timepoint, classify samples as ctDNA-positive or ctDNA-negative
- For ctDNA-positive samples, quantify variant allele frequency
Statistical Analysis:
- Calculate lead time as interval between first ctDNA-positive sample and radiographic recurrence
- Use Kaplan-Meier method to compare recurrence-free survival between ctDNA-positive and ctDNA-negative groups
- Calculate hazard ratios for recurrence based on ctDNA status
Protocol 3: Integrated Response Assessment
Objective: To evaluate combined ctDNA and imaging for treatment response monitoring in metastatic disease.
Study Design:
- Enroll patients initiating new systemic therapy for advanced cancer
- Collect blood samples at baseline, early on-treatment (2-4 weeks), and at time of routine imaging
- Perform imaging (CT/PET) at baseline and every 8-12 weeks per standard protocols
Response Classification:
- ctDNA response: >50% decrease in variant allele frequency from baseline
- Radiographic response: RECIST 1.1 criteria
- Concordant response: Both modalities show response or progression
- Discordant response: Disagreement between modalities
Statistical Analysis:
- Calculate concordance rate using Cohen's kappa statistic
- Compare progression-free survival between different response categories
- Assess time to ctDNA response versus time to radiographic response
Implications for Drug Development and Clinical Research
The integration of ctDNA analysis into oncology drug development offers significant opportunities to accelerate and improve clinical trials:
- Early efficacy signals: ctDNA dynamics can provide early readouts of drug activity weeks to months before radiographic assessments, enabling go/no-go decisions earlier in development [4].
- Patient enrichment: ctDNA-based biomarkers can identify high-risk patients for adjuvant trials or those with specific resistance mechanisms for targeted therapy trials [16] [43].
- Biomarker-driven trial designs: Novel adaptive trial designs using ctDNA for patient selection and response assessment are emerging, particularly in the minimal residual disease setting [16].
- Treatment monitoring: Longitudinal ctDNA analysis provides insights into therapeutic resistance mechanisms and tumor evolution under treatment pressure [4] [16].
Recent trials demonstrate the transformative potential of ctDNA-guided approaches. The IMvigor011 trial in muscle-invasive bladder cancer showed that ctDNA-guided adjuvant treatment with atezolizumab resulted in a 41% improvement in overall survival [96]. A phase II study presented at AACR 2025 demonstrated that ctDNA-guided immunotherapy with pembrolizumab in mismatch repair-deficient solid tumors resulted in 86.4% of ctDNA-positive patients clearing their disease and remaining recurrence-free at two years [43].
Concordance analysis reveals that ctDNA shows strong agreement with tissue biopsy for mutation detection in advanced cancers while offering substantial advantages for longitudinal monitoring and assessment of tumor heterogeneity. Compared to imaging, ctDNA provides significantly earlier detection of treatment response and disease recurrence, with lead times of months in many cases. However, these modalities are increasingly recognized as complementary rather than competitive, with integrated approaches providing the most comprehensive assessment of tumor dynamics.
For researchers and drug development professionals, ctDNA technologies offer powerful tools for accelerating oncology trials, identifying responsive patient populations, and understanding therapeutic resistance mechanisms. As ultrasensitive detection methods continue to evolve and standardization improves, ctDNA analysis is poised to become an integral component of cancer diagnostics, monitoring, and drug development.
Circulating tumor DNA (ctDNA) has emerged as a transformative biomarker in oncology, offering a non-invasive method to detect tumor-specific genetic alterations in blood. This liquid biopsy approach provides real-time insights into tumor dynamics, heterogeneity, and treatment response. The integration of ctDNA into randomized controlled trials (RCTs) represents a paradigm shift in cancer drug development, enabling more precise patient stratification, early response assessment, and adaptive trial designs [4] [97]. As the field evolves from observational correlation to interventional guidance, ctDNA is increasingly being deployed to direct therapeutic decisions in clinical trials, particularly in the adjuvant setting where it shows exceptional promise for detecting minimal residual disease (MRD) and informing treatment intensity [98] [99].
The clinical appeal of ctDNA lies in its biological characteristics: with a short half-life of approximately 2 hours, it provides a nearly real-time snapshot of tumor burden and evolution [12]. Compared to traditional protein biomarkers like carcinoembryonic antigen (CEA), ctDNA demonstrates higher cancer specificity and sensitivity, particularly in detecting residual disease and early recurrence [12]. Technologically, advances in next-generation sequencing (NGS) and digital PCR (dPCR) have enabled the detection of ctDNA at variant allele frequencies as low as 0.001%, making MRD assessment feasible even in early-stage cancers [100]. This technical evolution, coupled with growing evidence from prospective studies, has positioned ctDNA as a robust biomarker for guiding intervention strategies across multiple cancer types, with particular prominence in colorectal, breast, and lung cancers [98] [4].
Current Landscape of ctDNA-Guided Clinical Trials
Proliferation of Trial Activity
The clinical trial landscape for ctDNA-guided interventions has expanded significantly in recent years. A comprehensive review published in 2025 identified 57 phase II/III trials focusing on ctDNA for MRD detection, with a notable acceleration in trial initiation [98]. These trials predominantly target stage II or III colon/colorectal cancer (CRC), followed by breast cancer and non-small cell lung cancer (NSCLC) [98]. The growth in ctDNA-focused trials mirrors the increasing global prevalence of CRC and other solid tumors, highlighting the urgent need for more precise adjuvant treatment strategies [12].
Table 1: Ongoing Phase II/III ctDNA-Guided Trials in Major Cancer Types
| Cancer Type | Number of Trials | Primary Focus | Common Interventions |
|---|---|---|---|
| Colorectal Cancer | ~24 | MRD detection, adjuvant therapy escalation/de-escalation | Chemotherapy intensification (FOLFIRINOX) vs. standard (FOLFOX/CAPOX) |
| Breast Cancer | ~12 | MRD detection, therapy selection | Extended endocrine therapy, CDK4/6 inhibitors |
| Non-Small Cell Lung Cancer | ~9 | Adjuvant treatment guidance | Immunotherapy, targeted therapy |
| Other Solid Tumors | ~12 | MRD detection and monitoring | Various cancer-specific regimens |
Data synthesized from [98]
The United States and China lead in ctDNA trial publications, with 555 and 306 papers respectively, reflecting significant research investment in this field [12]. This geographical distribution aligns with the market dynamics of the ctDNA sector, which is projected to grow from USD 7.96 billion in 2025 to approximately USD 27.67 billion by 2034, at a compound annual growth rate of 14.85% [11].
Key Trial Design Paradigms
Current ctDNA-guided trials predominantly follow two complementary design philosophies:
Treatment Escalation for ctDNA-Positive Patients: Most trials focus on intensifying treatment for patients with detectable ctDNA post-surgery, who demonstrate high recurrence risk [98]. For example, in colorectal cancer, ctDNA-positive patients may be randomized between standard-of-care adjuvant chemotherapy versus intensified regimens [98] [99].
Treatment De-escalation for ctDNA-Negative Patients: A parallel approach involves reducing treatment intensity for patients without detectable ctDNA, who generally have favorable outcomes [98] [99]. This strategy aims to spare patients from unnecessary treatment toxicity while maintaining efficacy.
The NRG-GI008/"CIRCULATE-NORTH AMERICA" study exemplifies this dual approach, assigning resected colon cancer patients to different pathways based on ctDNA status [99]. ctDNA-negative patients are randomized to receive either standard adjuvant chemotherapy (mFOLFOX6/CAPOX) or active surveillance with serial ctDNA testing, while ctDNA-positive patients are randomized to standard chemotherapy versus intensified regimen (mFOLFIRINOX) [99].
Methodological Framework for ctDNA-Guided Trials
Core Analytical Technologies
The reliability of ctDNA-guided trials depends on sophisticated detection technologies capable of identifying minute quantities of tumor-derived DNA amidst normal cell-free DNA. The main technological approaches include:
Next-Generation Sequencing (NGS) - This dominates the ctDNA landscape with 48% market share [11]. Targeted NGS panels enable simultaneous assessment of multiple mutations across various genes. Key methodologies include:
- TAm-Seq (Tagged-Amplicon Deep Sequencing): Uses PCR amplicons with tags to detect low-frequency variants [4].
- CAPP-Seq (CAncer Personalized Profiling by deep Sequencing): A hybrid capture-based approach that combines optimized library preparation with bioinformatic suppression of background noise [4].
- Safe-SeqS (Safe-Sequencing System): Employs unique molecular identifiers (UMIs) to distinguish true mutations from PCR/sequencing errors [4].
PCR-Based Methods - While less comprehensive than NGS, PCR-based assays offer advantages in cost, turnaround time, and sensitivity for known mutations [11] [4]. Digital PCR (dPCR) and BEAMing (beads, emulsion, amplification, and magnetics) provide highly sensitive quantification of specific mutations [4].
Emerging Approaches - Fragmentomics analysis, which examines ctDNA fragmentation patterns and end motifs, shows promise for distinguishing tumor-derived DNA from normal cfDNA [4]. Low-pass whole genome sequencing (LP-WGS) detects copy number alterations across the genome without deep sequencing [97].
Figure 1: ctDNA Analysis Workflow for Clinical Trials - This diagram illustrates the three-phase process for ctDNA analysis, from sample collection through data interpretation, highlighting both tumor-informed and tumor-naïve approaches.
Tumor-Informed vs. Tumor-Naïve Approaches
A critical methodological consideration in trial design is the choice between tumor-informed and tumor-naïve approaches:
Tumor-Informed Assays require sequencing of the primary tumor tissue (typically via whole exome sequencing) to identify patient-specific mutations, followed by design of personalized panels to track these alterations in plasma [100]. This approach offers superior sensitivity (limit of detection ~0.001% variant allele frequency) by reducing background noise but requires longer turnaround time (2-3 weeks) and more resources [100].
Tumor-Naïve Assays use fixed panels of common cancer mutations without prior knowledge of the tumor's genomic profile [100]. While less sensitive than tumor-informed approaches, they offer faster turnaround (approximately 1 week) and don't require tumor tissue, making them more practical for certain trial contexts [100].
Table 2: Comparison of ctDNA Assay Approaches for Clinical Trials
| Parameter | Tumor-Informed | Tumor-Naïve |
|---|---|---|
| Sensitivity (LOD) | 0.001% VAF (RaDaR) to 0.01% VAF (Signatera) | 0.01% VAF (Guardant Reveal) to 0.1% VAF (AVENIO) |
| Turnaround Time | 3-5 weeks total (includes tumor sequencing + assay design) | 1-2 weeks |
| Tissue Requirement | Mandatory (FFPE tumor tissue) | Not required |
| Multiplexing Capacity | High (tracks 16-50 mutations per patient) | Fixed (50-100 gene panels) |
| Cost Considerations | Higher (personalized assay development) | Lower (standardized panels) |
| Ideal Use Case | MRD detection in adjuvant setting | Molecular profiling in advanced cancer |
Data synthesized from [100]
Essential Research Reagents and Platforms
Table 3: Key Research Reagent Solutions for ctDNA Analysis
| Reagent/Platform | Function | Key Features |
|---|---|---|
| Unique Molecular Identifiers (UMIs) | Molecular barcodes that tag individual DNA molecules before amplification | Distinguishes true mutations from PCR/sequencing errors; enables error-corrected sequencing [4] |
| Hybrid Capture Probes | Oligonucleotide baits for target enrichment in NGS | Enables sequencing of thousands of genomic regions simultaneously; compatible with complex mutation profiles [100] |
| Multiplex PCR Panels | Amplification of multiple genomic targets in parallel | Cost-effective for known mutation hotspots; rapid turnaround time [4] |
| Methylation-Specific Reagents | Chemicals or enzymes that detect DNA methylation patterns | Identifies epigenetic alterations; useful for cancer origin determination [97] |
| Fragment Size Selection Kits | Size-based separation of DNA fragments | Enriches for ctDNA (90-150 bp) over normal cfDNA (166 bp) [100] |
Key Clinical Trial Designs and Implementation Strategies
Phase I Trial Integration
The implementation of ctDNA in Phase I trials is evolving from traditional "all-comers" approaches to more enriched, biomarker-driven populations [97]. This paradigm shift enables better patient selection, dose optimization, and early signals of molecular response. In Phase I settings, ctDNA assessment provides three key advantages:
Patient Stratification: Baseline tumor fraction (TF) assessment identifies patients with varying risks of progression, enabling integration of TF as a confounding factor in analysis or prospective patient selection [97]. Recent prospective analysis confirms that high TF is associated with significantly worse overall survival, making it a strong prognostic factor for Phase I trial entry [97].
Dose Optimization: Rather than focusing solely on maximum tolerated dose (MTD), Phase I trials can use ctDNA kinetics to identify biologically effective doses, particularly for targeted therapies and immunotherapies that may have target saturation limits below MTDs [97]. The FDA's Project Optimus initiative emphasizes this need for better dose optimization prior to registration trials [97].
Early Response Assessment: Changes in TF can indicate molecular responses to investigational drugs before imaging or clinical outcomes are evident. Studies have demonstrated that ctDNA dynamics can predict treatment response across various tumor types and therapies [97].
Adjuvant Therapy Trial Designs
The most advanced application of ctDNA guidance is in adjuvant therapy trials, where it directly informs treatment intensity decisions based on MRD detection:
Figure 2: ctDNA-Guided Adjuvant Therapy Trial Design - This diagram illustrates the dual-pathway approach for ctDNA-guided adjuvant therapy trials, featuring separate randomization strategies for ctDNA-negative and ctDNA-positive patients.
The NRG-GI008/"CIRCULATE-NORTH AMERICA" study exemplifies this design in stage III colon cancer [99]. This trial incorporates distinct primary endpoints for different trial phases and patient cohorts:
- For Phase II (ctDNA-negative cohort): Primary endpoint is time to ctDNA-positive status comparing immediate versus delayed chemotherapy [99].
- For Phase III (ctDNA-negative cohort): Primary endpoint is time to disease-free survival (DFS) event [99].
- For ctDNA-positive cohort: Primary endpoint is time to DFS event following resection treated with adjuvant chemotherapy [99].
This endpoint structure acknowledges that ctDNA conversion may serve as a earlier, more sensitive endpoint than traditional DFS in lower-risk populations, while maintaining DFS as the definitive clinical outcome measure for higher-risk groups.
Analytical Validation and Quality Assurance
Robust ctDNA-guided trials require rigorous analytical validation with attention to several key parameters:
Limit of Detection (LOD): Defined as the lowest variant allele frequency at which a mutation can be reliably detected. For MRD applications, LOD typically ranges from 0.001% to 0.1% VAF depending on the technology [100].
Analytical Sensitivity: The probability of detecting ctDNA when present, which depends on tumor fraction, number of mutations tracked, and sequencing depth [100]. Tumor-informed assays typically achieve >95% sensitivity for tumor fractions ≥0.01% [100].
Specificity: The probability of a negative result when ctDNA is absent. High specificity (>99%) is crucial to avoid false-positive results that could lead to overtreatment [100].
Precision: Repeatability and reproducibility of ctDNA measurements across different runs, operators, and laboratories [100].
Quality control measures should include:
- Standardized blood collection tubes (e.g., Streck Cell-Free DNA BCT)
- Processing within specified timeframes (typically <48-72 hours)
- Input cfDNA quantification and quality assessment
- Control samples in each run (positive, negative, environmental)
- Blinded analysis to prevent interpretation bias
Challenges and Future Directions
Methodological and Implementation Challenges
Despite the promising trajectory of ctDNA-guided trials, several challenges remain:
Technical Standardization: The lack of standardized protocols across platforms creates variability in sensitivity, specificity, and result interpretation [4]. Efforts to harmonize pre-analytical (blood collection, processing), analytical (sequencing protocols), and post-analytical (bioinformatic pipelines) steps are needed.
Tumor Heterogeneity and Shedding: Not all tumors shed DNA equally into circulation. Low-shedding tumors (e.g., some gliomas, renal cell carcinomas) present detection challenges, particularly in early-stage disease [4]. The use of multi-mutation tracking in tumor-informed approaches helps mitigate this issue.
Clonal Hematopoiesis: Age-related mutations in blood cells can create false-positive results if not properly distinguished from tumor-derived mutations [100]. Sequencing of paired white blood cells or using genomic features like fragmentomics can help filter these false positives.
Clinical Utility Evidence Gap: While analytical validity and prognostic value are established, evidence demonstrating that ctDNA-guided management improves overall survival or quality of life remains limited [98]. Ongoing RCTs like CIRCULATE-NORTH AMERICA aim to address this gap.
Ethical Considerations in Trial Design
ctDNA-guided trials present unique ethical challenges that require careful consideration:
Equipoise Justification: Randomizing ctDNA-positive patients to less intensive therapy (or surveillance) requires careful ethical justification, given the established poor prognosis associated with ctDNA positivity [98]. Similarly, de-escalation in ctDNA-negative patients must be supported by robust observational data showing their favorable outcomes.
Blinding and Disclosure: Decisions about whether to disclose ctDNA results to patients and physicians during the trial involve balancing patient autonomy against potential bias in outcome assessment [98].
Access and Equity: The high cost of ctDNA testing and geographic variability in availability could limit patient access to biomarker-driven trials, potentially exacerbating health disparities [97].
Emerging Applications and Future Evolution
The future trajectory of ctDNA in clinical trials includes several promising directions:
Novel Biofluids: Beyond blood, urine, cerebrospinal fluid, and other biofluids offer potential for ctDNA detection in cancers with limited blood shedding [11] [4]. The urine segment is expected to grow at the highest CAGR in the ctDNA market between 2025 and 2034 [11].
Multi-Omic Integration: Combining mutation analysis with fragmentomics, methylation patterns, and other molecular features may enhance sensitivity and provide additional biological insights [4] [97].
Artificial Intelligence Enhancement: Machine learning approaches applied to ctDNA data may improve early cancer detection, resistance prediction, and outcome forecasting [11].
Earlier Disease Stage Applications: While current focus is predominantly on stage II-III cancers, future applications may extend to earlier detection and prevention trials in high-risk populations.
As the field matures, ctDNA is poised to become an integral component of cancer clinical trials, potentially serving as a primary endpoint for drug approval in specific contexts. The continued refinement of trial designs, coupled with technological advances and accumulating evidence from ongoing studies, will solidify the role of liquid biopsies in precision oncology drug development.
Minimal Residual Disease (MRD) refers to the small number of cancer cells that persist in the body after treatment, remaining under the threshold of microscopic detection [101] [102]. In hematological malignancies and increasingly in solid tumors, MRD represents a latent reservoir of disease that can lead to clinical relapse if not properly addressed [102]. The detection and monitoring of MRD have emerged as critical components for assessing treatment efficacy, predicting relapse risk, and guiding therapeutic decisions in precision oncology [102] [103]. The clinical significance of MRD kinetics is well established, with numerous studies demonstrating that MRD levels during chemotherapy are strongly associated with relapse risk, particularly in acute lymphoblastic leukemia (ALL) and acute myeloid leukemia (AML) [101].
The emergence of liquid biopsy platforms, particularly those analyzing circulating tumor DNA (ctDNA), has revolutionized MRD monitoring by providing a minimally invasive method for serial assessment of tumor burden [4] [24]. ctDNA consists of small fragments of tumor-derived DNA circulating in the bloodstream, carrying tumor-specific genetic alterations that distinguish it from normal cell-free DNA [4]. With a half-life between 16 minutes and several hours, ctDNA enables real-time monitoring of tumor dynamics and treatment response [4]. The fraction of ctDNA in total cell-free DNA correlates with tumor burden, ranging from below 1% in early-stage cancer to over 90% in advanced disease [4]. Among the various technologies available for ctDNA-based MRD detection, droplet digital PCR (ddPCR) and next-generation sequencing (NGS) have emerged as leading platforms, each with distinct technical characteristics, performance metrics, and clinical applications.
Technical Principles of ddPCR and NGS
Droplet Digital PCR (ddPCR) Technology
Droplet digital PCR is an advanced form of PCR that enables absolute quantification of nucleic acid targets without the need for standard curves [101]. The technology works by partitioning a PCR reaction into thousands to millions of nanoliter-sized droplets, effectively creating individual reaction chambers [104]. Each droplet undergoes traditional PCR amplification, and after thermal cycling, the droplets are analyzed one by one using a droplet reader to determine the fraction of positive reactions [104]. The fundamental principle is that through massive sample partitioning, the number of target DNA molecules in the original sample can be directly counted using Poisson statistics, providing absolute quantification rather than relative measurement [104].
For MRD detection, ddPCR typically targets known tumor-specific single nucleotide variants (SNVs) or other mutations identified through prior tumor profiling [101]. The method uses mutation-specific probes designed to distinguish mutant from wild-type sequences with high specificity. The partitioning step is particularly crucial for MRD applications as it enables the detection of rare mutant alleles present at very low frequencies by effectively enriching them in individual droplets, thereby overcoming the background of wild-type DNA [101]. A key advantage of ddPCR is its ability to provide precise quantification without requiring external standards, making it particularly suitable for monitoring dynamic changes in mutation abundance during treatment and follow-up [101] [105].
Next-Generation Sequencing (NGS) Technology
Next-generation sequencing represents a fundamentally different approach that enables simultaneous analysis of millions of DNA fragments across multiple genomic regions [102] [4]. Unlike ddPCR's targeted approach, NGS-based MRD detection can encompass broad panels of genes, including those commonly mutated in specific cancers, or can even employ whole-exome or whole-genome sequencing approaches [4]. The technology involves fragmenting DNA, attaching adapters, clonal amplification, and sequential sequencing using various platforms (e.g., Illumina, Ion Torrent) [4].
For MRD applications, NGS methods have evolved significantly to address the challenge of detecting rare tumor-derived mutations amidst abundant wild-type DNA [4]. Key technological advancements include the implementation of unique molecular identifiers (UMIs), which are molecular barcodes attached to individual DNA fragments before amplification [4]. These barcodes enable differentiation between true somatic mutations and PCR or sequencing errors by requiring multiple reads with the same UMI to confirm a mutation [4]. Further refinements like Duplex Sequencing tag and sequence both strands of DNA duplexes, providing even higher accuracy by requiring mutation confirmation on both strands [4]. More recent innovations such as SaferSeqS, NanoSeq, and CODEC (Concatenating Original Duplex for Error Correction) have pushed the sensitivity boundaries while improving efficiency [4]. The CODEC method, for instance, reportedly achieves 1000-fold higher accuracy than conventional NGS while using up to 100-fold fewer reads than duplex sequencing [4].
Performance Comparison: Sensitivity, Specificity, and Applicability
Quantitative Performance Metrics
The performance characteristics of ddPCR and NGS for MRD detection have been systematically evaluated across multiple studies, revealing distinct strengths and limitations for each technology. The table below summarizes the key performance metrics based on current literature:
Table 1: Performance Comparison of ddPCR and NGS for MRD Detection
| Parameter | ddPCR | NGS |
|---|---|---|
| Sensitivity | Up to 1E-4 to 1E-5 [101] | 10^-2 to 10^-6, typically 10^-5 to 10^-6 with error correction [102] [4] |
| Specificity | High for known mutations [104] | High with UMI error correction [4] |
| Quantitative Capability | Absolute quantification without standards [101] [105] | Relative quantification, requires bioinformatic analysis [102] |
| Multiplexing Capacity | Limited (typically 1-4 targets per reaction) [104] | High (dozens to hundreds of targets simultaneously) [102] [4] |
| Turnaround Time | Rapid (hours to 1-2 days) [102] | Longer (several days to weeks) [102] |
| Input DNA Requirements | Low (nanograms) [101] | Variable, typically higher for broader panels [4] |
| Cost per Sample | Lower for limited targets [104] | Higher, especially for comprehensive panels [102] |
A direct comparative study in rectal cancer demonstrated that ddPCR detected ctDNA in 58.5% (24/41) of baseline plasma samples compared to 36.6% (15/41) for NGS panel sequencing (p = 0.00075) [104]. This significant difference highlights ddPCR's potential advantage in detection rate for specific applications, though the study noted that NGS provides broader genomic coverage [104].
In the context of hematological malignancies, ddPCR has shown superior quantification capabilities compared to real-time quantitative PCR (RQ-PCR), another established MRD detection method. One study reported that ddPCR significantly reduced the proportion of positive but not quantifiable samples—2.6% versus 14% (P = 0.003)—and allowed disease quantifiability in 6.6% of RQ-PCR-negative samples [105]. This improved quantification translated to better clinical stratification, with ddPCR successfully identifying patients at risk of relapse who were classified as negative or not quantifiable by RQ-PCR [105].
Applicability and Limitations
The applicability of each technology varies significantly based on clinical context and information needs. ddPCR is particularly suitable when a limited set of known, well-characterized mutations need to be tracked with high sensitivity and rapid turnaround [101] [104]. Its absolute quantification capability makes it ideal for monitoring mutation abundance over time without the need for standard curves [105]. However, ddPCR's major limitation is its inability to detect unexpected or novel mutations that weren't predefined in the assay design [104].
NGS offers the distinct advantage of detecting a broad spectrum of genetic alterations without prior knowledge of specific mutations [102] [4]. This makes it particularly valuable for heterogeneous tumors or when monitoring for clonal evolution during treatment [4]. The comprehensive nature of NGS also enables detection of various alteration types including single nucleotide variants, insertions/deletions, copy number alterations, and structural variants in a single assay [4]. The main limitations of NGS include higher cost, longer turnaround time, greater bioinformatic complexity, and generally higher DNA input requirements compared to ddPCR [102].
Table 2: Applicability and Clinical Utility of ddPCR vs. NGS for MRD Detection
| Application Scenario | Recommended Technology | Rationale |
|---|---|---|
| Tracking known mutations | ddPCR | Superior sensitivity and quantification for predefined targets [101] [105] |
| Detection of novel/unknown mutations | NGS | Comprehensive coverage without need for prior mutation knowledge [102] [4] |
| Monitoring clonal evolution | NGS | Ability to detect emerging resistance mutations not initially present [4] |
| Rapid treatment response assessment | ddPCR | Faster turnaround time enables more timely clinical decisions [104] |
| Low tumor mutational burden | ddPCR | More cost-effective for monitoring limited number of mutations [104] |
| High tumor heterogeneity | NGS | Broader coverage better captures heterogeneous subclones [4] |
Experimental Protocols and Methodologies
ddPCR-MRD Detection Protocol
The following detailed methodology for ddPCR-based MRD detection is adapted from published studies in hematological malignancies [101]:
Step 1: Sample Collection and DNA Extraction
- Collect bone marrow or peripheral blood samples in appropriate anticoagulant tubes.
- Extract genomic DNA using commercial kits (e.g., QIAamp DNA Mini kit or GeneRead DNA FFPE kit for formalin-fixed samples).
- Quantify DNA concentration using fluorometric methods and assess quality via spectrophotometry or gel electrophoresis.
Step 2: Mutation Identification (Tumor-Informed Approach)
- Perform whole-exome sequencing (WES) on tumor specimens and matched normal DNA to identify tumor-specific somatic mutations.
- Library preparation: Fragment DNA to ~200bp using acoustics (Covaris), followed by library construction with combination of SureSelect HumanAll Exon Kit and KAPA Hyper Prep Kit.
- Sequencing: Execute on Illumina HiSeq 2500 in 101-bp paired-end mode.
- Bioinformatics analysis: Align reads to reference genome (GRCh37), remove PCR duplicates, perform local realignment and base quality recalibration.
- Variant calling: Use multi-sample calling with diagnostic and remission samples to detect tumor-specific mutations.
- Annotation: Utilize ANNOVAR software with databases including SIFT, Polyphen2, and CADD.
Step 3: ddPCR Assay Design and Optimization
- Design primers and mutation-specific probes for identified SNVs using appropriate software.
- Validate assay specificity and efficiency using control samples with known mutation status.
- Optimize reaction conditions including annealing temperature and primer/probe concentrations.
Step 4: ddPCR Reaction Setup
- Prepare 22μL reaction mixtures containing:
- ddPCR Supermix for Probes (No dUTP)
- Primers (final concentration 0.25μM)
- Probes (final concentration 1μM)
- Restriction enzyme Hind III (10 units)
- Genomic DNA (typically 150ng)
- Generate droplets using droplet generator.
- Perform PCR amplification with optimized thermal cycling conditions.
Step 5: Data Analysis and Interpretation
- Read droplets using QX-200 Droplet Reader.
- Analyze data with proprietary software to determine mutant and wild-type droplet counts.
- Calculate variant allele frequency (VAF) based on Poisson statistics.
- Establish threshold for positive detection based on negative controls and background signal.
This protocol has demonstrated sensitivity up to 1E-4 (1 mutant cell in 10,000 normal cells) in clinical applications [101].
NGS-MRD Detection Protocol
The following protocol outlines a typical NGS-based approach for MRD detection using tumor-informed assays [4]:
Step 1: Sample Processing and Cell-Free DNA Extraction
- Collect blood in Streck Cell-Free DNA BCT tubes or similar preservation tubes.
- Process within specified time frame (typically within 6 hours for EDTA tubes, up to 72-96 hours for specialized tubes).
- Centrifuge to separate plasma from cellular components (e.g., 1600×g for 10 minutes, then 16,000×g for 10 minutes).
- Extract cell-free DNA using commercial kits (e.g., QIAamp Circulating Nucleic Acid Kit).
- Quantify cfDNA using sensitive fluorometric methods.
Step 2: Tumor Tissue Sequencing and Mutation Selection
- Sequence tumor tissue using targeted panels, whole exome, or whole genome sequencing.
- Identify somatic mutations present in tumor with reasonable allele frequency.
- Select 16-50 mutations for tracking based on:
- High allele frequency in tumor
- Representation in different genomic regions
- Analytical performance in previous assays
Step 3: Library Preparation
- Fragment DNA (if using high molecular weight DNA) or use directly (for cfDNA).
- Repair ends and add A-overhangs.
- Ligate adapters containing unique molecular identifiers (UMIs).
- Amplify libraries with limited-cycle PCR.
- Purify and quantify libraries.
Step 4: Target Enrichment and Sequencing
- Perform hybrid capture using custom baits designed for selected mutations.
- Amplify captured libraries.
- Quantify final libraries and pool appropriately.
- Sequence on appropriate platform (e.g., Illumina NovaSeq) with sufficient depth (typically 50,000-100,000x raw coverage).
Step 5: Bioinformatic Analysis and MRD Calling
- Demultiplex sequencing data and align to reference genome.
- Group reads by UMI families to generate consensus sequences.
- Call variants using duplex or simplex error correction methods.
- Apply statistical models to distinguish true mutations from sequencing errors.
- Calculate variant allele frequencies and establish significance thresholds.
- Report MRD status based on detection of multiple mutations above background.
This approach can achieve sensitivities of 10^-5 to 10^-6 with robust error correction methods [4].
Research Reagent Solutions and Essential Materials
The following table outlines key reagents and materials essential for implementing ddPCR and NGS-based MRD detection assays:
Table 3: Essential Research Reagents for MRD Detection assays
| Reagent/Material | Function | Example Products |
|---|---|---|
| Cell-Free DNA Collection Tubes | Preserve blood samples and prevent genomic DNA contamination | Streck Cell-Free DNA BCT tubes [104] |
| Nucleic Acid Extraction Kits | Isolate high-quality DNA from various sample types | QIAamp DNA Mini kit, QIAamp Circulating Nucleic Acid Kit [101] |
| Library Preparation Kits | Prepare sequencing libraries with appropriate adapters | KAPA Hyper Prep Kit, SureSelect kits [101] |
| Target Enrichment Systems | Capture genomic regions of interest | SureSelect HumanAll Exon Kit [101] |
| ddPCR Master Mixes | Provide optimized reagents for droplet digital PCR | ddPCR Supermix for Probes (No dUTP) [101] |
| Unique Molecular Identifiers | Enable error correction and accurate variant calling | Custom UMI adapters [4] |
| Sequencing Platforms | Perform high-throughput DNA sequencing | Illumina HiSeq 2500, Illumina NovaSeq [101] [4] |
| Droplet Generation Systems | Partition samples for digital PCR | QX-200 Droplet Generator [101] |
| Bioinformatic Tools | Analyze sequencing data and call variants | ANNOVAR, custom pipelines for UMI processing [101] [4] |
Decision Framework and Implementation Pathways
The choice between ddPCR and NGS for MRD detection depends on multiple factors including clinical context, available resources, and specific research questions. The following diagram illustrates the decision pathway for selecting the appropriate technology:
Technology Selection Workflow
This decision pathway highlights scenarios where each technology excels. ddPCR is preferable when tracking a limited set of known mutations with requirements for high sensitivity, absolute quantification, and rapid turnaround [101] [104] [105]. NGS is more appropriate when comprehensive mutation profiling is needed, particularly for heterogeneous tumors or when monitoring for clonal evolution [102] [4]. In many cases, a complementary approach utilizing both technologies may provide optimal results, with NGS for broad mutation discovery and ddPCR for sensitive longitudinal monitoring of specific mutations [104].
The comparative analysis of ddPCR and NGS for MRD detection reveals a complementary rather than competitive relationship between these technologies. ddPCR offers advantages in sensitivity, quantification accuracy, and turnaround time for tracking known mutations, while NGS provides broader genomic coverage and the ability to detect unexpected genetic alterations [101] [104] [102]. The choice between them should be guided by specific clinical scenarios, available resources, and the particular mutations of interest.
Future developments in MRD detection are likely to focus on enhancing the sensitivity and specificity of both platforms while reducing costs and turnaround times [4]. For NGS, advances in error correction methods, molecular barcoding strategies, and bioinformatic pipelines continue to push detection limits lower [4]. For ddPCR, developments in multiplexing capabilities and assay design may expand its applicability [104]. The growing field of liquid biopsy and MRD detection is also witnessing the emergence of novel approaches including fragmentomics, epigenomic analyses, and multi-omic integration that may complement or enhance current mutation-based detection methods [4] [24].
As the clinical utility of MRD monitoring becomes increasingly established across cancer types, standardization of assays, validation protocols, and reporting criteria will be essential for broader adoption in clinical practice [103]. Both ddPCR and NGS are poised to play important roles in the evolving landscape of precision oncology, enabling earlier detection of treatment failure, guiding therapeutic adjustments, and ultimately improving patient outcomes through more personalized cancer management.
Liquid biopsy, particularly the analysis of circulating tumor DNA (ctDNA), represents a transformative approach in oncology that enables non-invasive detection of cancer-specific genetic and epigenetic alterations. Unlike traditional tissue biopsies, liquid biopsies analyze tumor-derived components from blood and other biofluids, offering a dynamic view of tumor heterogeneity and evolution [3]. The regulatory landscape for these technologies is rapidly evolving as evidence of their clinical utility accumulates. Current approvals primarily focus on specific mutations in advanced cancers, but the field is advancing toward earlier detection and minimal residual disease (MRD) monitoring [3] [9]. Reimbursement frameworks struggle to keep pace with technological innovation, creating disparities in patient access and uncertain sustainability for developers [106]. This whitepaper analyzes the current regulatory and reimbursement status of ctDNA-based liquid biopsies and identifies critical future needs to fully integrate these technologies into cancer care and research.
Current Regulatory Landscape
Approved Indications and Platforms
The regulatory approval of ctDNA-based liquid biopsy assays has followed a pathway from complementary to standalone diagnostics, with increasing recognition of their clinical value. The European Medicines Agency (EMA) pioneered regulatory acceptance by approving ctDNA for EGFR mutation testing in non-small cell lung cancer (NSCLC) in 2014 [3]. This established liquid biopsy as a valid alternative when tissue is unavailable. Current FDA-approved platforms include Guardant Health's Guardant360 CDx and Foundation Medicine's FoundationOne Liquid CDx, which detect genomic alterations to guide targeted therapies in advanced cancers [107].
Table 1: Currently Regulated ctDNA Assay Categories and Their Characteristics
| Assay Category | Technology Platform | Primary Indications | Regulatory Status |
|---|---|---|---|
| Single-gene PCR assays | ddPCR, BEAMing | EGFR (NSCLC), KRAS (CRC) | FDA-approved, CE-marked for specific mutations |
| Targeted NGS panels | Hybrid-capture NGS | Multi-gene profiling (e.g., Guardant360 CDx, FoundationOne Liquid CDx) | FDA-approved for advanced solid tumors |
| Methylation-based assays | Bisulfite sequencing | Multi-cancer early detection (e.g., TriOx) | Emerging; most in clinical trials [3] |
| Fragmentomic assays | Low-coverage WGS (e.g., DELFI) | Cancer detection and tissue of origin | Research use only [3] |
Regional Regulatory Variations
Significant geographic variations exist in regulatory approaches to liquid biopsy. The United States employs a dual-approval system where assays may be approved as companion diagnostics alongside specific drugs. The European Union has a more decentralized approach with CE marking indicating conformity with health and safety standards, though the new In Vitro Diagnostic Regulation (IVDR) imposes stricter requirements [106]. Many Asian countries are developing expedited pathways for innovative diagnostics, particularly for biomarkers with high unmet need. These regulatory discrepancies create challenges for global trial design and market access, potentially delaying patient benefit [108] [106].
Reimbursement Frameworks and Challenges
Current Reimbursement Models
Reimbursement for ctDNA testing varies significantly across healthcare systems, reflecting differing evidence requirements and cost considerations. Most established coverage exists for targeted mutation detection in advanced cancers where results directly inform therapy selection. For example, Medicare covers FDA-approved liquid biopsy tests for advanced cancer when they meet specific criteria, including clinical utility evidence [107]. The European systems increasingly cover ctDNA testing through diagnosis-related group (DRG) add-ons or specific fee-for-service arrangements, though with substantial country-level variation [106].
Table 2: Current Reimbursement Landscape for ctDNA Testing
| Test Type | Coverage Status | Evidence Requirements | Limitations |
|---|---|---|---|
| Therapy selection in advanced cancer | Widely covered in high-income countries | FDA/EMA approval; clinical guideline inclusion | Often restricted to specific clinical scenarios |
| Minimal residual disease (MRD) monitoring | Emerging coverage (e.g., Natera's Signatera in US) | Prospective clinical validity data (e.g., predictive of recurrence) | Limited evidence on clinical utility for intervention |
| Multi-cancer early detection | Limited to no coverage | Rigorous trials demonstrating mortality reduction | High cost; potential for false positives [9] |
| Treatment response monitoring | Mostly out-of-pocket or research context | Evidence of clinical management changes | Lack of standardized methodologies [3] |
Reimbursement Barriers
Multiple barriers impede consistent reimbursement for ctDNA assays. Evidence generation remains challenging, particularly for demonstrating improved patient outcomes rather than just analytical or clinical validity [9] [106]. The DYNAMIC-III trial in stage III colon cancer demonstrated that ctDNA could identify patients at high recurrence risk, but treatment escalation based on ctDNA findings did not improve recurrence-free survival, highlighting that detection alone is insufficient without effective intervention strategies [9]. Economic sustainability concerns payers, particularly for expensive technologies without clear cost-offset projections. The complex regulatory-pathway interactions create circular dependencies where limited evidence restricts coverage, while limited coverage impedes evidence generation through real-world clinical use [106].
Experimental Protocols and Methodologies
Sample Collection and Processing
Standardized pre-analytical protocols are critical for reliable ctDNA analysis. The following protocol outlines optimal procedures for blood-based ctDNA collection and processing:
Blood Collection: Draw whole blood into commercially available cell-stabilization tubes (e.g., Streck Cell-Free DNA BCT, Roche Cell-Free DNA Collection Tubes) to prevent genomic DNA contamination and preserve ctDNA integrity [3].
Plasma Separation: Process samples within 4-6 hours of collection. Centrifuge at 800-1600 × g for 10 minutes at room temperature to separate plasma from blood cells. Transfer supernatant to a fresh tube and perform a second centrifugation at 16,000 × g for 10 minutes to remove residual cells [3].
cfDNA Extraction: Extract cell-free DNA using validated kits (e.g., QIAamp Circulating Nucleic Acid Kit from QIAGEN, MagMAX Cell-Free DNA Isolation Kit from Thermo Fisher) according to manufacturer protocols [107]. Elute in low-EDTA TE buffer or nuclease-free water.
Quality Control: Quantify cfDNA using fluorometric methods (e.g., Qubit dsDNA HS Assay). Verify fragment size distribution (typically 160-180 bp) using bioanalyzer or TapeStation systems [3].
ctDNA Analysis Techniques
Multiple technological approaches exist for ctDNA detection, each with distinct strengths and applications:
PCR-Based Methods
- Digital Droplet PCR (ddPCR): Partition samples into ~20,000 nanodroplets; perform endpoint PCR amplification; detect mutations based on fluorescence. Optimal for tracking known mutations with sensitivity to ~0.01% variant allele frequency (VAF) [3].
- BEAMing (Beads, Emulsion, Amplification, Magnetics): Couple PCR with flow cytometry; bind cfDNA to magnetic beads; create emulsion for amplification; detect mutations via fluorescent antibodies. Sensitivity comparable to ddPCR [3].
Next-Generation Sequencing Approaches
- Targeted NGS Panels (e.g., Guardant360, FoundationOne Liquid CDx): Use hybrid capture or amplicon-based approaches to sequence cancer-related genes. Typical sequencing depth >10,000x enables detection of low VAF mutations (~0.1-0.5%) [3] [9].
- Whole-Genome Sequencing (e.g., DELFI): Perform low-coverage (~0.1-1x) WGS; analyze fragmentation patterns and genomic features using machine learning algorithms. Does not require prior knowledge of specific mutations [3].
Methylation Analysis
- Bisulfite Sequencing: Treat DNA with bisulfite to convert unmethylated cytosine to uracil; sequence converted DNA to identify methylated positions. Whole-genome bisulfite sequencing provides comprehensive methylation profiling but requires substantial sequencing depth [3].
- Bisulfite-Free Methods (e.g., MeDIP-Seq): Use antibodies or enzymes to enrich methylated DNA fragments; reduces DNA degradation compared to bisulfite conversion [3].
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Research Reagents for ctDNA Analysis
| Reagent/Category | Specific Examples | Research Function | Considerations |
|---|---|---|---|
| Blood Collection Tubes | Streck Cell-Free DNA BCT, PAXgene Blood ccfDNA Tubes | Preserve cfDNA integrity by inhibiting nucleases and preventing white blood cell lysis | Storage time and temperature affect DNA yield and quality |
| Nucleic Acid Extraction Kits | QIAamp Circulating Nucleic Acid Kit (QIAGEN), MagMAX Cell-Free DNA Isolation Kit (Thermo Fisher) | Isolve and purify cell-free DNA from plasma samples | Recovery efficiency for short fragments varies between kits |
| Library Preparation Kits | KAPA HyperPrep, Illumina DNA Prep | Prepare sequencing libraries from low-input cfDNA | Optimized protocols needed for fragmented DNA |
| Target Enrichment Panels | xGen Panels (IDT), SureSelect (Agilent) | Capture genomic regions of interest for targeted sequencing | Panel design affects coverage uniformity and off-target rates |
| Methylation Conversion Reagents | EZ DNA Methylation kits (Zymo), TrueMethyl kits | Convert unmethylated cytosines to uracils for methylation analysis | Conversion efficiency critical for accurate quantification |
| PCR Master Mixes | ddPCR Supermix (Bio-Rad), AmpliTaq Gold (Thermo Fisher) | Enable sensitive amplification of low-abundance mutations | Polymerase fidelity affects error rates in mutation detection |
| Reference Standards | Seraseq ctDNA Reference Materials, Horizon Multiplex I cfDNA Reference | Validate assay performance and quantify sensitivity | Commutable materials essential for inter-laboratory comparisons |
Future Needs and Recommendations
Regulatory Harmonization
The global regulatory landscape requires greater harmonization to accelerate patient access to validated liquid biopsy technologies. Key needs include:
Standardized Performance Metrics: Development of internationally accepted standards for analytical validation, including sensitivity, specificity, and limit of detection for different clinical contexts [3] [9].
Context-Specific Regulatory Pathways: Tailored approval pathways reflecting distinct clinical uses (e.g., companion diagnostics, cancer screening, monitoring) with appropriate evidence requirements for each context [106].
Real-World Evidence Integration: Regulatory frameworks that incorporate real-world data to complement traditional clinical trials, particularly for rapidly evolving technologies where practice may outpace evidence generation [9] [106].
Sustainable Reimbursement Models
Future reimbursement systems must balance innovation with fiscal responsibility through:
Value-Based Arrangements: Contractual models linking payment to demonstrated clinical outcomes, particularly for high-cost applications like multi-cancer early detection [106].
Staged Coverage: Limited coverage for promising technologies coupled with mandatory evidence development, enabling patient access while generating necessary outcomes data [9].
Cross-Stakeholder Collaboration: Structured dialogues between developers, payers, regulators, and patients to align on evidence requirements and establish appropriate coverage pathways early in technology development [106].
Research and Development Priorities
Advancing the field requires addressing critical evidence gaps:
Interventional Trial Designs: Prospective studies demonstrating that ctDNA-guided management improves clinically meaningful endpoints, as initiated in the SERENA-6 trial for breast cancer [9].
Standardization Initiatives: Development of reference materials, standardized protocols, and quality control frameworks to enable reproducibility across laboratories and platforms [3].
Health Economics Research: Robust cost-effectiveness analyses across diverse healthcare systems to inform appropriate resource allocation and pricing strategies [106].
The regulatory and reimbursement landscape for ctDNA-based liquid biopsies is at a critical inflection point. Current frameworks have successfully advanced these technologies from research tools to clinically validated assays for specific applications in advanced cancers. However, significant challenges remain in standardizing approvals, establishing sustainable reimbursement, and generating robust evidence of clinical utility—particularly for early detection and MRD monitoring. Addressing these challenges requires coordinated efforts among regulators, payers, industry, and researchers to create pathways that balance innovation, evidence, and equitable access. As the field evolves toward increasingly sensitive multi-modal assays, the regulatory and reimbursement frameworks must similarly evolve to ensure these promising technologies reach the patients who need them while maintaining rigorous standards for clinical validity and utility.
Conclusion
The integration of liquid biopsy and ctDNA analysis marks a paradigm shift in oncology, moving the field toward less invasive, highly dynamic, and personalized cancer management. Evidence from recent clinical trials solidifies its value for MRD detection, therapy guidance, and early cancer screening. For researchers and drug developers, the future lies in overcoming sensitivity challenges through technological innovation, validating these tools in large-scale prospective studies, and integrating multi-omic data with artificial intelligence. The ongoing convergence of advanced detection methodologies and robust clinical evidence promises not only to refine cancer care but also to open new frontiers in drug development and interceptive oncology, ultimately improving patient outcomes.
References
- 1. Circulating tumor DNA: a promising biomarker in the liquid ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5217053/]
- 2. What is circulating tumor DNA and how is it used ... [https://medlineplus.gov/genetics/understanding/testing/circulatingtumordna/]
- 3. A Review of Circulating Tumor DNA (ctDNA) and the Liquid ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12032849/]
- 4. Circulating tumor DNA to monitor treatment response in ... [https://www.nature.com/articles/s41698-025-00876-y]
- 5. Monitoring and Assessment of Circulating Tumor DNA in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12550271/]
- 6. Circulating tumor DNA: current challenges for clinical utility [https://pmc.ncbi.nlm.nih.gov/articles/PMC9197509/]
- 7. Life and death of circulating cell-free DNA - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC6606043/]
- 8. Cell-Free DNA (cfDNA) vs. Circulating Tumor DNA (ctDNA) ... [https://www.thermofisher.com/blog/life-in-the-lab/cfdna-vs-ctdna/]
- 9. Circulating tumour DNA assays in focus - Nature [https://www.nature.com/articles/s44276-025-00181-y]
- 10. Liquid biopsy in cancer: current status, challenges and ... [https://www.nature.com/articles/s41392-024-02021-w]
- 11. Circulating Tumor DNA (ctDNA) Market Size 2025 to 2034 [https://www.precedenceresearch.com/circulating-tumor-dna-market]
- 12. Research trends and prospects of Circulating tumor DNA ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12360996/]
- 13. A Tale of Two Biopsies: Liquid Biopsy vs Tissue Biopsy [https://www.biochain.com/blog/a-tale-of-two-biopsies-liquid-biopsy-vs-tissue-biopsy/]
- 14. A Liquid Biopsy-based Assay Could Detect Recurrence ... [https://www.aacr.org/about-the-aacr/newsroom/news-releases/a-liquid-biopsy-based-assay-could-detect-recurrence-prior-to-imaging-in-patients-with-resectable-colorectal-cancer/]
- 15. Validation and Clinical Utility of a Pan-Cancer Circulating ... [https://pubmed.ncbi.nlm.nih.gov/41015180/]
- 16. Clinical applications of cell-free DNA-based liquid biopsy ... [https://www.sciencedirect.com/science/article/pii/S1936523325002505]
- 17. Drug Discovery News — ctDNA monitoring is providing a ... [https://friendsofcancerresearch.org/news/drug-discovery-news-ctdna-monitoring-is-providing-a-smarter-way-to-track-and-treat-cancer/]
- 18. The prognostic and clinical utility of circulating tumor DNA ... [https://www.nature.com/articles/s41698-025-01174-3]
- 19. Analytical and Clinical Validation of a Highly Sensitive ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11261189/]
- 20. Molecular response cutoffs and ctDNA collection ... [https://pubmed.ncbi.nlm.nih.gov/40983343/]
- 21. Clinical Utility of Serial Circulating Tumor DNA Analysis as ... [https://pubmed.ncbi.nlm.nih.gov/39761498/]
- 22. GCC Liquid Biopsy Market Analysis, Growth Trends and ... [https://www.businesswire.com/news/home/20251006494713/en/GCC-Liquid-Biopsy-Market-Analysis-Growth-Trends-and-Forecast-Report-2025-2033-Rising-Cancer-Incidence-Genomics-Advancements-and-Precision-Medicine-Incentives-Drive-Growth---ResearchAndMarkets.com]
- 23. Liquid Biopsy for Early Cancer Detection and Monitoring ... [https://finance.yahoo.com/news/liquid-biopsy-early-cancer-detection-132000600.html]
- 24. Liquid biopsy – a narrative review with an update on current ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12333414/]
- 25. Research progress of CTC , ctDNA , and EVs in cancer liquid biopsy... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10850354/]
- 26. Circulating tumour cells and PD-L1-positive small extracellular ... [https://www.nature.com/articles/s41416-023-02491-9?error=cookies_not_supported&code=6c700bc8-378a-4c1b-89df-0a8b27368a1a]
- 27. Cancer in a Drop: Liquid biopsy insights from AACR 2025 [https://pmc.ncbi.nlm.nih.gov/articles/PMC12223554/]
- 28. Cancer in a drop: Liquid biopsy highlights from the ... [https://www.sciencedirect.com/science/article/pii/S2950195425000360]
- 29. Advances in CTC and ctDNA detection techniques [https://breast-cancer-research.biomedcentral.com/articles/10.1186/s13058-025-02024-7]
- 30. Advancements in Circulating Tumor Cell Detection for Early ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12024602/]
- 31. Liquid biopsy based on EV biomarkers: A new frontier for ... [https://www.sciencedirect.com/science/article/pii/S2790676025000159]
- 32. MWENA: a novel sample re-weighting-based algorithm for disease... [https://bmcgenomics.biomedcentral.com/articles/10.1186/s12864-025-12093-9]
- 33. Development and Performance Validation of a ... [https://pubmed.ncbi.nlm.nih.gov/40888113/]
- 34. Validation of a liquid biopsy assay with increased ... [https://www.sciencedirect.com/science/article/pii/S2950195425000384]
- 35. Next-Generation Sequencing Technology: Current Trends ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10376292/]
- 36. Polymerase Chain Reaction (PCR) - StatPearls - NCBI - NIH [https://www.ncbi.nlm.nih.gov/books/NBK589663/]
- 37. Next-generation sequencing: 2025 Revolution [https://lifebit.ai/blog/next-generation-sequencing/]
- 38. Next-generation Sequencing Market Size, Share [https://www.fortunebusinessinsights.com/industry-reports/next-generation-sequencing-ngs-market-101000]
- 39. Next Generation Sequencing (NGS) Market Poised to Hit ... [https://finance.yahoo.com/news/next-generation-sequencing-ngs-market-151500577.html]
- 40. PCR Technologies Market Size to Hit USD 31.39 Billion ... [https://www.precedenceresearch.com/pcr-technologies-market]
- 41. Multiplex PCR Assay Market CAGR, Segments and ... [https://www.towardshealthcare.com/insights/multiplex-pcr-assay-market-sizing]
- 42. Advances and challenges in circulating tumor DNA-based ... [https://pubmed.ncbi.nlm.nih.gov/41234819/]
- 43. Leveraging Liquid Biopsy to Improve Cancer Care | Blog [https://www.aacr.org/blog/2025/05/21/breakthroughs-in-the-blood-leveraging-liquid-biopsy-to-improve-cancer-care/]
- 44. Real-world data and clinical experience from over ... [https://www.nature.com/articles/s41467-025-64094-7]
- 45. Editors' Picks: Precision Cervical Cancer Screening and ... [https://www.aacr.org/blog/2025/09/30/editors-picks-september-2025-cervical-cancer-screening-immunotherapy-breakthroughs-metabolic-vulnerabilities-and-more/]
- 46. A comprehensive overview of minimal residual disease in ... [https://www.nature.com/articles/s41698-025-00984-9]
- 47. In Largest Molecular Residual Disease (MRD) Study ... [https://investors.guardanthealth.com/press-releases/press-releases/2025/In-Largest-Molecular-Residual-Disease-MRD-Study-in-Colon-Cancer-Guardant-Reveal-Testing-Prior-to-Chemotherapy-Provides-Robust-Stratification-for-Risk-of-Disease-Recurrence-and-Survival-to-Enable-Timely-Treatment-Decisions/default.aspx]
- 48. Molecular minimal residual disease in resected non-small cell ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12605196/]
- 49. MRD in solid tumors: The future of oncology sequencing [https://www.simon-kucher.com/en/insights/minimal-residual-disease-solid-tumors-next-big-thing-oncology-diagnostics]
- 50. Timelines and Takeaways from the Biomarker Qualification ... [https://link.springer.com/article/10.1007/s43441-025-00889-6]
- 51. Measurable residual disease in hematologic malignancies [https://pmc.ncbi.nlm.nih.gov/articles/PMC12257026/]
- 52. Looking Ahead: The Future of MRD Testing and Breast ... [https://www.onclive.com/view/looking-ahead-the-future-of-mrd-testing-and-breast-cancer-management-and-insights-from-asco-2025]
- 53. 2025 Updated version v1.0 SEOM-GEMCAD-TTD clinical ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12000258/]
- 54. ASCO 2025 Metastatic Breast Cancer Updates [https://www.bcrf.org/blog/asco-2025-metastatic-breast-cancer-updates/]
- 55. New Insights in Treating Metastatic Lung Cancer ... [https://www.lungevity.org/blogs/new-insights-in-treating-metastatic-lung-cancer-from-wclc-2025]
- 56. Review Cell-free DNA fragmentomics in cancer [https://www.sciencedirect.com/science/article/pii/S1535610825003988]
- 57. a roadmap for DNA methylation biomarkers in liquid biopsies [https://www.nature.com/articles/s41388-025-03624-5]
- 58. GUIDE: a prospective cohort study for blood-based early ... [https://molecular-cancer.biomedcentral.com/articles/10.1186/s12943-025-02367-x]
- 59. Analysis of cfDNA fragmentomics metrics and commercial ... [https://www.nature.com/articles/s41467-025-64153-z]
- 60. a prospective cohort study for blood-based early detection ... [https://pubmed.ncbi.nlm.nih.gov/PMC12139136]
- 61. AI-powered liquid biopsy for early detection of ... [https://pubmed.ncbi.nlm.nih.gov/40669686/]
- 62. Fragmentomics Platform - DELFI [https://delfidiagnostics.com/our-technology/fragmentomics/]
- 63. Multiomic spatial profiling & ctDNA to understand cancer [https://dailyreporter.esmo.org/molecular-analysis-for-precision-oncology-congress-map-2025/integrating-multiomic-spatial-profiling-and-ctdna-for-a-deeper-understanding-of-cancer-complexity]
- 64. The emerging role of circulating tumor DNA in brain tumor ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12203871/]
- 65. Ultrasensitive ctDNA detection for preoperative disease ... [https://www.nature.com/articles/s41591-024-03216-y]
- 66. Rational thresholding of circulating tumor DNA ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10937210/]
- 67. -infiltrating Tumor - PMC clonal hematopoiesis [https://pmc.ncbi.nlm.nih.gov/articles/PMC12021423/]
- 68. of indeterminate potential: a multisystem hub... Clonal hematopoiesis [https://mmrjournal.biomedcentral.com/articles/10.1186/s40779-025-00654-8]
- 69. DNMT3A clonal -driver... | Nature Communications hematopoiesis [https://www.nature.com/articles/s41467-023-43003-w?error=cookies_not_supported]
- 70. Galleri Test Sensitivity & Specificity | Galleri® for HCPs [https://www.galleri.com/hcp/galleri-test-performance]
- 71. Phylogenetic inference reveals clonal heterogeneity in ... [https://www.nature.com/articles/s41588-025-02205-2]
- 72. Variability of Circulating Tumor DNA Levels in Plasma ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12591551/]
- 73. Analytical evaluation of circulating tumor DNA sequencing ... [https://www.nature.com/articles/s41598-024-54361-w]
- 74. Molecular response cutoffs and ctDNA collection ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12458711/]
- 75. Validation of a liquid biopsy assay with molecular and ... [https://www.nature.com/articles/s41698-021-00202-2]
- 76. Maximizing the potential of high-throughput next-generation ... [https://pubmed.ncbi.nlm.nih.gov/37350611/]
- 77. RNA-Seq Normalization: Methods and Stages [https://bigomics.ch/blog/why-how-normalize-rna-seq-data/]
- 78. Bioinformatics Analysis for Circulating Cell-Free DNA in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6627444/]
- 79. Implementation of Circulating Tumor DNA (ctDNA) Testing ... [https://www.sciencedirect.com/science/article/pii/S2950195425000359]
- 80. Strategies for improving detection of circulating tumor DNA ... [https://www.sciencedirect.com/science/article/pii/S0305737223000889]
- 81. Tumor Mutational Burden | TMB NGS testing [https://www.illumina.com/areas-of-interest/cancer/ngs-in-oncology/biomarkers/tumor-mutational-burden.html]
- 82. Systematic assessment and optimizing algorithm of tumor ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9679647/]
- 83. Artificial intelligence in cancer: applications, challenges, and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12574039/]
- 84. Artificial intelligence in cancer: applications, challenges, and ... [https://molecular-cancer.biomedcentral.com/articles/10.1186/s12943-025-02450-3]
- 85. Researchers Invent New AI Tool to Automate Detection ... [https://viterbischool.usc.edu/news/2025/10/researchers-invent-new-ai-tool-to-automate-detection-of-cancer-in-blood-samples/]
- 86. AI-Based Liquid Biopsy Shows Promise for Detecting Brain ... [https://www.hopkinsmedicine.org/news/newsroom/news-releases/2025/04/ai-based-liquid-biopsy-shows-promise-for-detecting-brain-cancer]
- 87. How Artificial Intelligence Is Transforming Cancer Care in ... [https://oncodaily.com/oncolibrary/artificial-intelligence-ai]
- 88. Integrating Circulating Tumor DNA into Clinical ... [https://www.mdpi.com/2072-6694/17/15/2520]
- 89. Revolutionizing Oncology Through AI: Addressing Cancer ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12427515/]
- 90. Liquid biopsy: Comprehensive overview of circulating tumor ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11420644/]
- 91. The emerging clinical utility of ctDNA to guide adjuvant ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12173074/]
- 92. Colon cancer: ctDNA-guided adj chemo not ready for prime ... [https://dailyreporter.esmo.org/esmo-congress-2025/gastrointestinal-cancers/ctdna-guided-adjuvant-chemotherapy-in-colon-cancer-not-ready-for-prime-time]
- 93. PEGASUS Trial at ESMO 2025: Liquid Biopsy-Guided ... [https://oncodaily.com/oncolibrary/pegasus-trial-at-esmo2025]
- 94. October 15, 2025 [https://investors.guardanthealth.com/press-releases/press-releases/2025/Guardant-Health-and-Collaborators-to-Present-New-Data-Across-the-Cancer-Care-Continuum-at-ESMO-2025/default.aspx]
- 95. Improvement of the sensitivity of circulating tumor DNA- ... [https://www.explorationpub.com/Journals/etat/Article/1002333]
- 96. Liquid Biopsy | October Round-Up 2025 [https://www.decibio.com/insights/liquid-biopsy-october-round-up-2025]
- 97. A perspective review on the systematic implementation of ... [https://jeccr.biomedcentral.com/articles/10.1186/s13046-025-03328-4]
- 98. A review of trials investigating ctDNA-guided adjuvant ... [https://www.sciencedirect.com/science/article/pii/S0959804924008153]
- 99. Testing ctDNA as a Biomarker for Adjuvant Therapy ... [https://www.nrgoncology.org/Home/News/Post/testing-ctdna-as-a-biomarker-for-adjuvant-therapy-intensity-in-colon-cancer-nrg-gi008-circulate-north-america-study/]
- 100. Commercial ctDNA assays for minimal residual disease ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9016631/]
- 101. Minimal residual disease detection by mutation-specific ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10225364/]
- 102. Minimal Residual Disease Detection: Implications for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12079024/]
- 103. Understanding MRD in Clinical Trials [https://www.bloodpac.org/bloodpac-blog/mrd-clinical-trials]
- 104. Performance Comparison of Droplet Digital PCR and Next ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12062871/]
- 105. Digital Droplet PCR Is a Reliable Tool to Improve Minimal ... [https://www.sciencedirect.com/science/article/pii/S152515782200157X]
- 106. Precision cancer medicine 2025: some concerns - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC12439214/]
- 107. Liquid Biopsy Market Competitive Landscape Report 2025: [https://www.globenewswire.com/news-release/2025/11/24/3193673/0/en/Liquid-Biopsy-Market-Competitive-Landscape-Report-2025-Recent-Developments-Strategies-Sustainability-Benchmarking-Product-Analysis-Key-Persons-and-Revenue.html]
- 108. WHO publishes new R&D landscape analyses highlighting ... [https://www.who.int/news/item/22-09-2025-who-publishes-new-r-d-landscape-analyses-highlighting-gaps-and-inequities-in-cancer-research]