Integrating Radiomics and Digital Pathology: A New Paradigm for Precision Cancer Diagnostics and Drug Development
This article explores the transformative potential of integrating radiomics and digital pathology (pathomics) in oncology.
Integrating Radiomics and Digital Pathology: A New Paradigm for Precision Cancer Diagnostics and Drug Development
Abstract
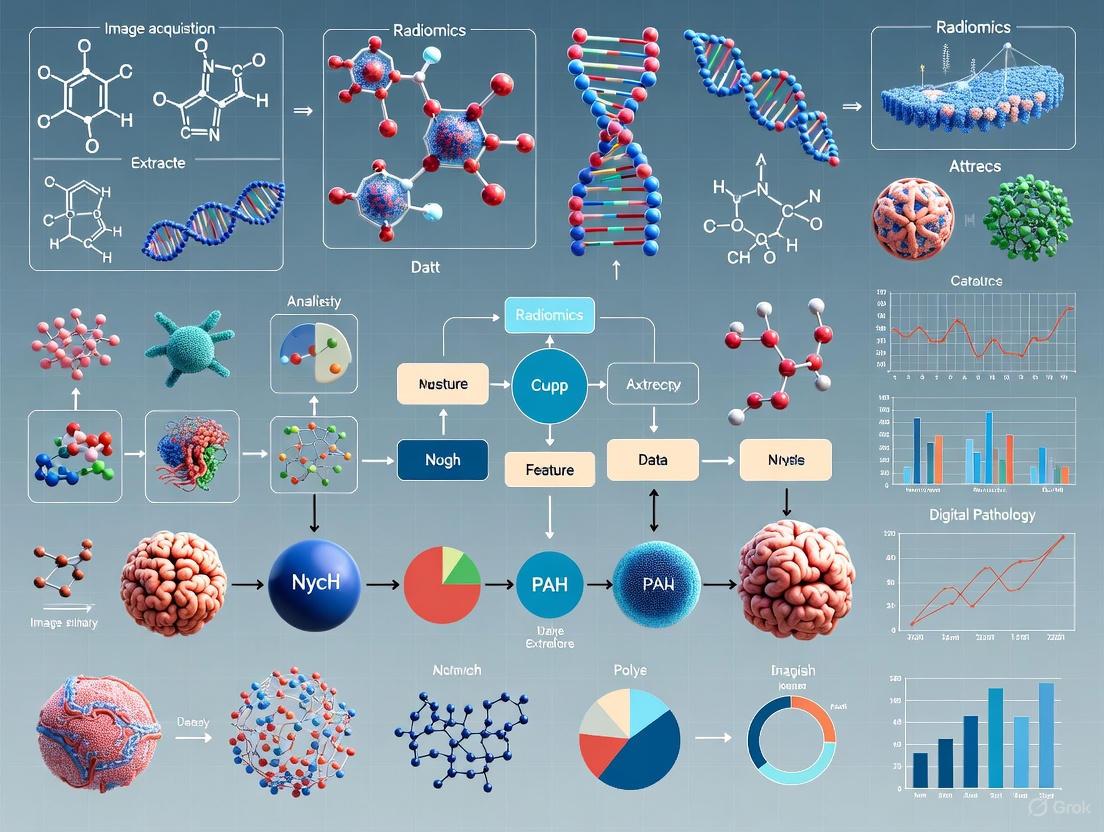
This article explores the transformative potential of integrating radiomics and digital pathology (pathomics) in oncology. Aimed at researchers, scientists, and drug development professionals, it provides a comprehensive overview of how these quantitative, AI-driven technologies are revolutionizing cancer diagnostics. We cover the foundational principles of radiomics and pathomics, detail the methodological pipelines for feature extraction and multi-omics fusion, and address key challenges in standardization and interpretability. The discussion extends to validation strategies and comparative performance analyses, highlighting how these tools enhance prognostic modeling, therapy response prediction, and biomarker discovery. By synthesizing the latest research and future directions, this article serves as a critical resource for advancing the development of robust, clinically translatable computational tools in precision oncology.
Demystifying Radiomics and Pathomics: Core Concepts and Value in Oncology
The field of oncology is undergoing a data-driven transformation, moving beyond qualitative visual assessment to the quantitative mining of medical images for prognostic and diagnostic insights. This paradigm shift is fueled by two complementary disciplines: radiomics and pathomics. Radiomics refers to the high-throughput extraction of quantitative features from radiological images, such as CT, MRI, or PET, converting images into mineable data that reveal sub-visual tissue heterogeneity [1] [2]. Pathomics applies the same principle to digitized histopathology slides, using advanced image analysis to "unlock" revealing sub-visual attributes about tumors from their morphology [3]. The core premise is that biomedical images contain information about disease-specific processes that are imperceptible to the human eye [1]. The integration of these image-based phenotypes with genomic data, known as genomics, offers a uniquely comprehensive portrait of a tumor's spatial and molecular characteristics, paving the way for more accurate assessment of disease aggressiveness in the era of precision oncology [3].
Field Definitions and Workflows
Radiomics: The Macroscopic Scale
Radiomics focuses on anatomic and functional characteristics at the macroscopic level, typically acquired through non-invasive procedures [3]. It quantifies underlying sub-visual tissue heterogeneity that is not always apparent to a human reader, allowing for the interrogation of disease regions and surrounding structures like the peri-tumoral region [3] [1]. The typical radiomics workflow involves several critical, sequential steps, as illustrated below and detailed in [1] and [2].
Pathomics: The Microscopic Scale
Pathomics, or quantitative histomorphometric analysis, is the process of extracting and mining computer-derived measurements from digitized histopathology images [3]. While pathologists visually read histopathology slides for diagnosis, pathomics can discover complex histopathological phenotypes, characterizing the spatial arrangement of tumor-infiltrating lymphocytes (TILs) and the interplay between different histological primitives [3]. This provides a comprehensive portrait of a tumor's morphologic heterogeneity from a standard hematoxylin and eosin (H&E) slide. The workflow for pathomics shares conceptual similarities with radiomics but operates on whole-slide images (WSIs) at a much higher resolution, focusing on cellular and sub-cellular features.
Detailed Methodologies and Protocols
The Radiomics Pipeline: A Step-by-Step Technical Guide
Image Acquisition and Dataset Definition
A solid radiomics study begins with a clear goal and a well-defined patient population [2]. The three cardinal rules are ensuring sufficient sample size, achieving balanced representation across patient populations, and upholding data quality. To avoid overfitting, the sample size should be at least 50 times the number of prediction classes and/or at least 10 times the number of selected features [2]. Images should ideally come from the same modality and scanner, using a consistent and standardized acquisition protocol to minimize the variability of radiomic features [2].
Image Preprocessing
Preprocessing ensures dataset uniformity and is crucial for feature repeatability and reproducibility [2]. The main steps are:
- Resampling: Altering the spatial resolution to a uniform grid (e.g., 1x1x1 mm³) to mitigate differences from varying acquisitions [1] [2].
- Intensity Discretization: Grouping pixel intensity values into a fixed number of bins or using a fixed bin width. This is critical for data with arbitrary units, like MRI [1].
- Normalization and Filtering: For CT and PET data, "range re-segmentation" excludes pixels outside a specified range. For MRI, intensity outlier filtering (e.g., excluding values outside μ ± 3σ) is common [1].
Image Segmentation
Segmentation defines the region or volume of interest (ROI/VOI). This can be done manually, semi-automatically, or fully automatically using deep learning (e.g., U-Net) [1]. Manual and semi-automated methods are time-consuming and introduce observer bias; thus, assessments of intra- and inter-observer reproducibility are essential. Automated segmentation is ideal but requires robust, generalizable algorithms [1].
Feature Extraction and Selection
Feature extraction quantifies the ROI/VOI using advanced mathematical analysis. The open-source pyRadiomics package in Python is commonly used and can extract a vast number of features [1]. These are often categorized into:
- First-Order Statistics: Describe the distribution of voxel intensities (e.g., entropy, kurtosis).
- Shape-based Features: Describe the 3D geometry of the ROI.
- Texture Features: Describe the spatial patterns of voxel intensities, often calculated from matrices like the Gray-Level Co-occurrence Matrix (GLCM) [1] [2]. Given the high dimensionality, feature selection is critical. Methods like the minimum redundancy maximum relevance (mRMR) algorithm select the most relevant features for the subsequent model building [2].
AI Model Building and Validation
The selected features are used to train machine learning models (e.g., Random Forest) for diagnostic, prognostic, or predictive tasks [2]. The dataset should be split (e.g., 70-20-10% for train-test-validation), and metrics like accuracy, F1-score, and AUC should be used for evaluation [2].
Table 1: Example Radiomics Study Workflow for Liver HCC Detection [2]
| Step | Key Question | Management in Example Study |
|---|---|---|
| Dataset Definition | Is there a sufficient sample size? | 104 patients with chronic liver disease (54 with HCC, 50 without) |
| Image Acquisition | What is the imaging modality? | 1.5 T liver MR scan with a standardized protocol |
| Image Preprocessing | Is resampling applied? | Resampling to 1x1x1 mm³ isotropic voxels |
| Segmentation | How is it performed? | Semi-automatic 3D segmentation by two radiologists in consensus |
| Feature Extraction | Which classes are extracted? | All feature classes from original and filtered images via pyRadiomics |
| Feature Selection | How is it performed? | mRMR algorithm to select 10 most relevant features from 1070 extracted |
| AI Model | Which model is chosen? | Random Forest (100 trees) with 70-20-10% train-test-validation split |
Pathomics and Multi-Omics Integration
Pathomics workflows involve digitizing H&E-stained tissue slides and using machine learning to identify and characterize various cell types, such as cancer cells, lymphocytes, and stromal cells [3] [4]. A key research focus is correlating and fusing these pathomic features with other data modalities.
- Correlating Pathomics and Genomics: This involves establishing associations between tumor morphology and large-scale genomic data to understand the inferential relationship for biomarker discovery. Methods range from classical Pearson correlation to advanced sparse canonical correlation analysis (CCA), which can identify correlated sets of genes and histomorphometrics [3]. For instance, one study correlated cellular diversity features from non-small cell lung carcinomas with bulk RNA data, finding associations with apoptotic signaling pathways [3].
- Fusion of Pathomics and Radiomics: Integrating the macroscopic view from radiology with the microscopic detail from pathology provides a multi-scale perspective on the tumor. This fusion can help understand the biological basis of specific quantitative imaging features and resolve confounding effects of tissue heterogeneity [3].
The integration of these multi-modal data offers a unique opportunity to comprehensively interrogate the cancer microenvironment, enabling a more accurate assessment of disease aggressiveness [3]. The following diagram illustrates this integrated multi-omics approach.
The Scientist's Toolkit: Essential Research Reagents & Materials
Table 2: Key Tools and Platforms for Radiomics and Pathomics Research
| Tool/Reagent | Type | Primary Function | Examples & Notes |
|---|---|---|---|
| Medical Image Scanners | Hardware | Generates primary radiological or pathological images. | MRI, CT, PET scanners; Whole Slide Imaging (WSI) scanners for pathology. |
| Image Segmentation Software | Software | Delineates Regions/Volumes of Interest (ROIs/VOIs). | 3D Slicer [1], ITK-SNAP [1], MeVisLab [1]; Deep learning models (e.g., U-Net) [1]. |
| Radiomics Feature Extraction Platforms | Software/Code Library | Extracts quantitative features from medical images. | pyRadiomics (Python) [1], LifEx [1]. |
| AI/ML Modeling Frameworks | Software/Code Library | Builds and validates diagnostic/prognostic models. | Scikit-learn (Python) for Random Forest, SVM; PyTorch, TensorFlow for deep learning. |
| Digital Pathology Standards | Data Standard | Ensures interoperability and data consistency for WSIs. | DICOM Standard Supplement 145 for WSI [5]; alternative modular architectures are under debate [6]. |
| Liquid Biopsy & AI Analysis | Wet-bench / Algorithm | Detects circulating tumor cells from blood samples. | The "RED" (Rare Event Detection) AI algorithm automates cancer cell detection in liquid biopsies [7]. |
Critical Challenges and Future Directions
Despite its promise, the field faces several significant challenges. The reproducibility of radiomic features is highly sensitive to variations in imaging scanners, acquisition parameters, and preprocessing steps [1] [2]. Initiatives like the Quantitative Imaging Biomarkers Alliance (QIBA) aim to standardize these processes [2]. Furthermore, the transition to digital pathology is hampered by interoperability hurdles and a lack of standardization, though the adoption of the DICOM standard for WSI is a positive step [5] [6]. The high cost and regulatory complexity of validating advanced diagnostic systems also limit widespread adoption, especially in resource-limited settings [8].
Future directions are focused on overcoming these hurdles. There is a strong push towards more robust and automated AI-driven tools, such as the RED algorithm for liquid biopsies, which can find rare cancer cells without human bias [7]. The market for cancer diagnostics, projected to grow from USD 65.5 billion in 2025 to USD 148.2 billion by 2035, will be driven by innovations in multi-cancer early detection (MCED) tests, liquid biopsies, and the integration of AI [8]. Ultimately, the convergence of radiomics, pathomics, and genomics into a unified analytical framework holds the key to unlocking deeper insights into cancer biology and improving patient outcomes through precision medicine.
Radiomics is a rapidly evolving field in medical imaging, particularly within oncology, that aims to extract high-dimensional quantitative data from standard-of-care images [9]. It is founded on the hypothesis that medical images contain information that reflects underlying pathophysiology and tumor heterogeneity, which may not be perceptible through visual assessment alone [10]. By converting digital images into mineable data, radiomics provides a non-invasive method to characterize tumors, potentially assisting in diagnosis, prognosis prediction, and treatment response assessment [11]. This technical guide provides a comprehensive, step-by-step overview of the radiomics pipeline, framed within cancer diagnostics research for an audience of researchers, scientists, and drug development professionals.
The Radiomics Workflow: A Step-by-Step Guide
The radiomics workflow consists of several sequential steps, each with its own methodologies and considerations. The following diagram illustrates the complete pipeline from image acquisition to final analysis.
Figure 1: Comprehensive Radiomics Pipeline Workflow. This diagram outlines the sequential steps in a standardized radiomics analysis, from initial image acquisition to final model application, including key methodological considerations at each stage.
Image Acquisition
The initial step in any radiomics study involves acquiring medical images using various imaging modalities. Each modality offers distinct advantages and captures different aspects of tumor biology [11].
Key Imaging Modalities:
- Computed Tomography (CT): Widely accessible, time-efficient, and cost-effective with highly reproducible radiomics features [11].
- Magnetic Resonance Imaging (MRI): Provides high soft-tissue contrast resolution without ionizing radiation, with functional sequences (DWI, DCE-MRI) capturing various functional states of tumors [11].
- Positron Emission Tomography (PET): Offers insight into functional and biochemical changes, though features can be influenced by variations in reconstruction parameters [11].
- Ultrasound (US): Enables real-time imaging but suffers from high operator variability, reducing reliability and reproducibility [11].
Critical Considerations: Radiomic features are highly sensitive to variations in imaging acquisition parameters, including scanner equipment, acquisition techniques, reconstruction parameters, and contrast administration [12] [2]. To ensure feature reproducibility and study quality, researchers should:
- Use consistent imaging protocols across all subjects [2]
- Minimize variations in external conditions that may influence acquisition [2]
- Report detailed acquisition parameters, including slice thickness and reconstruction kernel [12]
- Consider initiatives like the Quantitative Imaging Biomarkers Alliance (QIBA) for standardization [2]
Image Preprocessing
Preprocessing is essential to ensure dataset uniformity and consistency, thereby enhancing the robustness and reliability of subsequent analyses [2]. This step addresses variations introduced during image acquisition and prepares images for feature extraction.
Table 1: Essential Image Preprocessing Steps in Radiomics
| Step | Purpose | Common Parameters | Impact on Features |
|---|---|---|---|
| Resampling | Standardize spatial resolution; mitigate differences from acquisition devices/protocols | Establish uniform voxel grid (e.g., 1×1×1 mm³, 2×2×2 mm³) | Reduces variability due to different voxel sizes; improves comparability |
| Intensity Discretization (Binning) | Group pixel intensity values into intervals (bins) | Fixed bin width (e.g., 25) | Influences capture of small intensity variations; affects texture features |
| Normalization | Standardize intensity values across images | Various scaling methods (MinMax, standard, robust) | Ensures consistent intensity ranges; reduces scanner-specific biases |
The specific preprocessing approach should be tailored to the study objectives, anatomical structures under analysis, and imaging techniques employed [2]. For instance, the optimal resampling strategy for PET images (which may use larger voxel sizes for statistical reasons) differs from that for high-resolution CT studies examining subtle bone structures [2].
Image Segmentation
Segmentation involves delineating regions of interest (ROIs), typically tumors or other pathologies, from which radiomic features will be extracted. This critical step directly influences feature values and requires careful execution.
Segmentation Methods:
- Manual Segmentation: Performed by expert readers (e.g., radiologists), considered gold standard but time-consuming and subject to inter-observer variability [10] [12].
- Semi-automated Segmentation: Combines algorithmic approaches with human supervision, improving efficiency while maintaining accuracy [10] [2].
- Fully Automated Segmentation: Utilizes deep learning algorithms for complete automation, offering high reproducibility but requiring extensive training data [10] [13].
Best Practices: Current trends show increased reporting of human supervision in segmentation to ensure accuracy [12]. For 3D analysis, full volumetric segmentation is preferred over 2D approaches as it captures complete spatial information [2]. Researchers should clearly document segmentation methodology, including the software tools used and whether inter- or intra-observer variability was assessed [12].
Feature Extraction
Feature extraction involves computing quantitative, mathematically defined features from the segmented ROIs. These features aim to characterize tissue properties at multiple levels.
Table 2: Major Classes of Radiomic Features and Their Characteristics
| Feature Class | Description | Representative Features | Biological Correlation |
|---|---|---|---|
| First-Order Statistics | Describe distribution of voxel intensities without spatial relationships | Mean, median, minimum, maximum, variance, skewness, kurtosis, entropy [10] [14] | Overall tumor intensity patterns; simple heterogeneity measures |
| Shape-Based Features | Capture geometric properties of ROI in 2D or 3D | Volume, surface area, sphericity, elongation, flatness [10] | Tumor morphology and gross structural characteristics |
| Second-Order Texture Features | Quantify spatial relationships between voxel pairs | GLCM: Contrast, entropy, energy, homogeneity [10] [14] | Intra-tumor heterogeneity; spatial patterns of intensity variation |
| Higher-Order Texture Features | Capture complex patterns through filter applications or specialized matrices | GLRLM, GLSZM, NGTDM, GLDM [10] [14] | Fine-textured patterns, heterogeneity at multiple scales |
Feature extraction is typically performed using standardized software packages like PyRadiomics (Python-based) [10] or through in-house solutions developed in platforms such as Matlab [10]. The Image Biomarker Standardization Initiative has established guidelines to promote feature standardization across studies [14].
Feature Selection and Analysis
Following feature extraction, the typically large number of features (often hundreds per ROI) must be reduced to avoid overfitting and identify the most biologically relevant features.
Feature Selection Methods:
- Filter Methods: Select features based on statistical measures (e.g., correlation with outcome) [15]
- Wrapper Methods: Use machine learning model performance to select features (e.g., recursive feature elimination) [15]
- Embedded Methods: Incorporate feature selection during model training (e.g., LASSO, random forest importance) [15]
Dimensionality Reduction Techniques:
- Principal Component Analysis (PCA)
- Minimum Redundancy Maximum Relevance (mRMR) [15]
The "curse of dimensionality" is particularly relevant in radiomics, where the number of features often far exceeds the number of samples [10] [15]. To mitigate overfitting, studies should maintain appropriate sample-to-feature ratios, with recommendations suggesting at least 10 samples per feature [2].
Model Building and Validation
The final pipeline stage uses selected features to build predictive models for classification, prognosis, or treatment response prediction.
Common Machine Learning Classifiers:
- Logistic Regression (LR)
- Support Vector Machines (SVM)
- Random Forests (RF)
- k-Nearest Neighbors (KNNs)
- Naive Bayes (NB)
- Adaptive Boosting (AdaBoost)
- Extreme Gradient Boosting (XGBoost) [15]
Validation Strategies: Robust validation is essential for assessing model generalizability:
- Train-Test Splits: Multiple splits (e.g., 10 iterations) mitigate selection bias inherent in single splits [15]
- Cross-Validation: k-fold cross-validation (5-fold for <100 samples, 10-fold for larger datasets) [15]
- External Validation: Testing on completely independent datasets provides the strongest evidence of generalizability [16] [12]
Performance metrics such as area under the receiver operating characteristic curve (AUC) and accuracy are commonly used for evaluation [15]. More advanced frameworks like RadiomiX systematically test classifier and feature selection combinations across multiple validations to identify optimal model configurations [15].
The Scientist's Toolkit: Essential Research Reagents and Software
Table 3: Essential Tools and Software for Radiomics Research
| Tool Category | Examples | Primary Function | Key Features |
|---|---|---|---|
| Segmentation Software | 3D Slicer, ITK-SNAP, VivoQuant, Matlab [10] | ROI delineation | Manual, semi-automated, and automated segmentation capabilities |
| Feature Extraction Platforms | PyRadiomics [10], Quantitative Image Feature Pipeline (QIFP) [17] | Calculate radiomic features from segmented ROIs | Standardized feature definitions; batch processing; multiple imaging modalities |
| Integrated Analysis Platforms | Orange, KNIME [17], RadiomiX [15] | End-to-end radiomics analysis | Feature selection, machine learning, visualization; workflow management |
| Data Sources | The Cancer Imaging Archive (TCIA) [17], ePAD [17] | Access to annotated imaging datasets | Publicly available datasets; standardized formats; clinical annotations |
Methodological Considerations for Experimental Design
Dataset Definition and Sample Size
A solid radiomics study begins with a clear goal and well-defined patient population [2]. Key considerations include:
- Sample Size: Adequate samples are crucial to capture complex patterns and avoid overfitting. Recommended guidelines include at least 50 times the number of prediction classes and/or at least 10 times the number of selected features [2].
- Population Balance: Datasets should have comparable sample sizes across populations. For imbalanced datasets, undersampling or oversampling techniques can be applied, each with distinct advantages and limitations [2].
- Data Quality: Consistent protocols on the same equipment under standardized conditions are essential [2].
Reproducibility and Generalizability
Reproducibility remains a significant challenge in radiomics, with sources of variation existing at each pipeline step [12]. Strategies to enhance reproducibility include:
- Standardizing imaging protocols across participating centers [16]
- Reporting detailed acquisition and reconstruction parameters [12]
- Performing test-retest analyses to assess feature stability [12]
- Using public datasets like the RIDER Lung collection for validation [12]
The radiomics quality score (RQS) provides a framework for evaluating methodological quality, though current literature shows generally low average scores, indicating room for improvement in study design and reporting [12].
The radiomics pipeline represents a comprehensive framework for converting standard medical images into mineable, high-dimensional data with potential applications across cancer diagnostics and therapeutics. While technical challenges remain—particularly regarding reproducibility, standardization, and validation—methodological advances continue to enhance the robustness of radiomics studies. For research and drug development professionals, understanding each component of this pipeline is essential for designing rigorous studies, developing reliable biomarkers, and ultimately translating radiomics into clinically valuable tools. Future directions include increased integration with pathomics and genomics data, development of more automated and standardized pipelines, and emphasis on external validation in diverse patient populations.
Pathomics, an emerging field at the intersection of digital pathology and artificial intelligence (AI), is revolutionizing cancer diagnostics and prognostics by extracting high-throughput, quantitative features from digitized histology images. This technical guide explores how pathomics uncovers critical prognostic information embedded within whole-slide images (WSIs) that eludes conventional visual assessment. Framed within the broader context of radiomics and multi-omics integration in cancer research, we detail the computational frameworks, experimental protocols, and clinical applications driving this innovative field. For researchers and drug development professionals, this whitepaper provides a comprehensive overview of current methodologies, validation strategies, and future directions for leveraging sub-visual histologic patterns to advance precision oncology.
The complex etiology and pronounced heterogeneity of malignant tumors present significant challenges in diagnosis, treatment selection, and prognosis prediction [18]. While histopathological assessment has long been the gold standard for cancer diagnosis, traditional evaluation is inherently subjective, leading to inter-observer variability and limited quantification of tumor biology [18] [19]. The advent of whole-slide imaging (WSI) has enabled the digitization of pathology, creating opportunities for computational analysis that surpass human visual capabilities.
Pathomics applies machine learning (ML) and deep learning (DL) algorithms to extract extensive datasets from WSIs, facilitating quantitative analyses that improve diagnosis, treatment planning, and prognostic prediction [18]. This approach detects subtle morphological patterns in tissue architecture and cellular organization that are imperceptible to the human eye but contain valuable prognostic information. When integrated with radiomics (which extracts quantitative features from medical images like CT and MRI) and other omics technologies, pathomics contributes to a comprehensive multi-modal understanding of tumor biology [20] [21] [22].
The clinical imperative for pathomics is particularly strong in oncology, where tumor heterogeneity influences therapeutic response and disease progression. Current biomarkers have limitations: their assessment often requires invasive tissue sampling, interpretation can be variable, and they frequently fail to capture the full spectrum of tumor heterogeneity [20]. Pathomics addresses these limitations by non-destructively mining rich information from standard histology samples, potentially serving as non-invasive biomarkers for personalized treatment strategies [11].
Technical Foundations of Pathomics
The Pathomics Workflow
The pathomics pipeline involves several critical steps that transform raw WSIs into quantifiable, clinically actionable insights [18]. The standardized workflow ensures reproducible and biologically meaningful feature extraction.
Data Acquisition and Preprocessing: Researchers use high-resolution scanning devices to digitize tissue slides, followed by standardization procedures to produce high-quality, uniform images. Stain normalization techniques, such as the Macenko method which utilizes color deconvolution, are often employed to minimize the impact of staining variations on feature computation [23].
Segmentation and Annotation: Each WSI is subdivided into smaller patches or regions of interest (ROIs) that are meticulously annotated by pathologists. This step is crucial for accurate feature extraction in subsequent stages. Advanced algorithms can automatically segment tumor regions, cellular structures, and other histological compartments [24] [19].
Feature Extraction and Selection: Quantitative analysis of tissue structures—including cellular morphology, nuclear characteristics, and tissue architecture—is performed within target regions. Features are extracted at the patch level using pretrained models and subsequently aggregated into slide-level features via attention-based weighted averaging mechanisms [18]. Common feature classes include:
- Histogram-based features: First-order statistics describing intensity distributions
- Texture features: Gray-level co-occurrence matrix (GLCM) features that capture spatial relationships between pixels
- Wavelet features: Multi-resolution texture descriptors obtained through discrete wavelet transforms
- Local Binary Patterns (LBP): Rotation-invariant texture descriptors
Model Construction and Validation: Appropriate model architectures are selected to train on the extracted features, with performance evaluation using metrics including accuracy, precision, F1 score, area under the receiver operating characteristic curve (AUROC), and decision curve analysis (DCA) [18].
Computational Architectures and Algorithms
In AI-driven pathomics studies, researchers rely on two main architectures: convolutional neural networks (CNNs) and vision transformers (ViTs) [18]. These architectures address core challenges including gigapixel-scale whole-slide images, diverse tumor patterns, and noisy clinical labels.
CNN Backbones: 50-layer ResNet or EfficientNet-B0, pretrained on ImageNet, remain fundamental for patch-level feature extraction. Slides are typically divided into 224 × 224 to 512 × 512 pixel tiles, balancing cellular detail and tissue context within typical GPU memory limits [18].
Vision Transformers: Newer pipelines introduce ViT-base transformers (12 layers) that tokenize slides into 16 × 16 or 32 × 32 pixel patches, learning relationships across distant tissue regions. This capability is particularly valuable for capturing global tissue architecture [18].
Multi-Instance Learning (MIL): Once extracted, patch features are aggregated via attention-based MIL modules. A 128-256-dimensional attention head scores each patch, patches are grouped into 3-5 clusters, and the top 10-20 scores are pooled. This mechanism downweights uninformative areas (e.g., blank space or artifacts) and amplifies diagnostically or prognostically relevant regions, yielding a robust slide-level prediction [18].
Optimization parameters typically include the Adam optimizer with weight decay (1 × 10⁻⁵ to 1 × 10⁻⁴), a learning rate of 1 × 10⁻⁴ to 1 × 10⁻⁵ (often cosine-annealed), and batch sizes of 16-32 tiles per GPU. Models generally train for 20-50 epochs with 20-50% dropout in final layers to prevent overfitting [18].
Experimental Protocols and Methodologies
Protocol for Prognostic Model Development
A representative experimental protocol for developing pathomics-based prognostic models, as demonstrated in high-grade glioma research [24], involves the following methodology:
Patient Selection and Data Collection:
- Inclusion criteria: Patients with confirmed diagnosis, no prior treatment before confirmed diagnosis, availability of postoperative histopathological findings and histological slides, and complete clinical information.
- Exclusion criteria: Patients without histopathological reports and microscopic sections, WSIs of insufficient resolution for diagnostic use, and lack of post-treatment follow-up data.
- Clinical endpoints: Progression-free survival (PFS) and overall survival (OS) collected through regular follow-up imaging and clinical evaluation.
Image Preprocessing:
- ROI delineation by experienced pathologists using annotation software (e.g., QuPath)
- WSIs segmented into 512 × 512-pixel tiles at 20× magnification
- White background removal to eliminate tiles with sparse informative content
- Color standardization/normalization across all patches
- Result: Over 12 million viable patches from 80 WSIs in the referenced glioma study [24]
Deep Learning Model Training:
- Implementation of a dual-tier prediction framework combining patch-level predictions with multi-instance learning
- Weakly supervised learning approach labeling patches based on clinical outcomes (e.g., 1-year recurrence)
- Architecture comparison (e.g., densenet121, inception_v3, resnet101) to select optimal model
- Training parameters: Adam optimizer, cross-entropy loss, appropriate learning rate scheduling
Feature Extraction and Selection:
- Development of pathological signature using radiomics-like methodology
- Combination of patch-level predictions, probability histograms, and TF-IDF features
- Removal of redundant features using Pearson's correlation analysis (correlation coefficient threshold < 0.9)
- Further feature refinement using univariate Cox regression and ranking by p-values
- Final feature set determination through LASSO-Cox regression with optimal regularization parameter λ
Model Validation:
- Performance evaluation using concordance index (C-index) for survival models
- Kaplan-Meier survival analysis between high-risk and low-risk groups
- Stratification by molecular subtypes (e.g., IDH status in gliomas)
- Internal validation through bootstrapping or cross-validation
- External validation on independent cohorts when available
Key Research Reagents and Computational Tools
Table 1: Essential Research Reagents and Computational Tools for Pathomics
| Category | Specific Tools/Platforms | Function/Purpose |
|---|---|---|
| Annotation Software | QuPath, ImageScope | ROI delineation and pathological annotation |
| AI Platforms | OnekeyAI Platform, TensorFlow, PyTorch | Deep learning model development and training |
| Feature Extraction | PyRadiomics, Custom MATLAB scripts | High-throughput feature quantification from WSIs |
| Whole Slide Imaging | Aperio, Hamamatsu, 3DHistech scanners | Digital conversion of glass slides |
| Statistical Analysis | R, Python (scikit-survival, lifelines) | Survival analysis and model validation |
| Visualization | MATLAB, Python (matplotlib, seaborn) | Feature visualization and result presentation |
Pathomics Applications in Cancer Prognostication
Cancer-Specific Implementation and Performance
Pathomics has demonstrated significant utility across multiple cancer types, with varying emphasis on clinical tasks depending on disease-specific needs [19].
Table 2: Pathomics Applications and Performance Across Cancer Types
| Cancer Type | Common Clinical Tasks | Key Pathomic Features | Reported Performance |
|---|---|---|---|
| Prostate Cancer | Gleason grading, risk stratification | Wavelet features, Local Binary Patterns, glandular architecture | AUC 0.97-0.99 for diagnosis; AUC 0.72-0.73 for grading [23] |
| High-Grade Glioma | Survival prediction, progression risk | Morphological, texture, and deep learning features | C-index 0.847 (train), 0.739 (test) for combined model [24] |
| Hepatocellular Carcinoma | Diagnosis, histological classification, survival prediction | Nuclear morphology, tissue texture, architectural patterns | AUROC 0.998-1.000 for tumor identification [18] |
| Breast Cancer | Diagnosis, subtyping, treatment response | Tumor-infiltrating lymphocytes, spatial arrangements | HER2+, ER+, PR+ subtyping with high accuracy [19] |
| Lung Cancer | Immunotherapy response, recurrence risk | Spatial features, shape-based descriptors | Integrated model achieved HR=8.35 for recurrence prediction [21] |
In prostate cancer, pathomics analysis has identified wavelet features and local binary pattern descriptors as particularly prominent for distinguishing high-grade from low-grade disease, while histogram-based features appear as key differentiators for diagnostic classification tasks [23]. The extremely high heterogeneity of prostate cancer makes it particularly suitable for pathomics approaches that can quantify subtle morphological patterns beyond Gleason grading.
For high-grade gliomas, pathomics models have successfully stratified patients into distinct prognostic groups. One study demonstrated that high-risk patients had a median progression-free survival of 10 months, while low-risk patients had not reached median PFS during the study period [24]. Furthermore, stratification by IDH status revealed significant PFS differences, highlighting how pathomics can enhance molecular classification.
Multi-Modal Integration: Radio-Pathomics
The integration of pathomics with radiomics represents a powerful approach for comprehensive tumor characterization, leveraging both macroscopic (imaging) and microscopic (histology) information [21] [11].
In lung cancer, integrated radio-pathomic models have significantly outperformed single-modality approaches across multiple clinical contexts:
- In early-stage NSCLC, a combined model achieved a hazard ratio of 8.35 (C-index: 0.71) for recurrence prediction, compared to HR=3.99 for radiomics alone and HR=4.83 for pathomics alone [21]
- For predicting immunotherapy response in advanced NSCLC, the integrated model showed an AUC of 0.75, representing a 2% improvement over radiomics and 8% over pathomics alone [21]
- In SCLC, the radio-pathomic model achieved an AUC of 0.78 for chemotherapy response prediction, a 5% improvement over radiomics and 22% over pathomics [21]
The most predictive features from pathomics in these integrated models often derive from spatial feature families, while radiomics contributions frequently come from Haralick entropy features [21]. This complementary information provides a more comprehensive representation of tumor heterogeneity.
Implementation Considerations and Standardization
Technical Validation and Reproducibility
The clinical translation of pathomics faces several challenges that must be addressed through rigorous validation and standardization:
Data Quality and Heterogeneity: Pathomics models are sensitive to variations in tissue processing, staining protocols, and scanning parameters. The National Cancer Institute has emphasized the need for data standardization, image quality assurance, and adoption of open standards such as DICOM for whole-slide imaging to address these challenges [25].
Model Generalizability: Many pathomics models demonstrate excellent performance on internal validation but suffer from performance degradation when applied to external datasets from different institutions. Prospective multi-center studies and the development of robust, explainable AI (XAI) are crucial to overcome this limitation [20] [18].
Regulatory Compliance: As of 2024, only three AI/ML Software as a Medical Device tools have received FDA clearance for digital pathology applications, highlighting the validation dataset gap rather than an absence of regulatory pathways [25]. Future initiatives should prioritize the enhancement of regulatory frameworks and establishment of industry-wide standardized guidelines.
Explainability and Clinical Trust
The inability to interpret extracted features and model predictions remains a major issue limiting the acceptance of AI models in clinical practice [23]. Pathomics approaches increasingly incorporate explainable AI (XAI) techniques such as SHapley Additive exPlanations (SHAP) to estimate the importance of pathomic features and their impact on prediction models [23]. This transparency helps build clinical trust and facilitates collaboration between computational scientists and pathologists.
Pathomics represents a paradigm shift in cancer diagnostics and prognostication, moving beyond qualitative histologic assessment to quantitative, data-driven analysis of tumor biology. As the field evolves, several key directions emerge:
Multi-Modal Integration: The combination of pathomics with radiomics, genomics, and clinical data will continue to provide more comprehensive tumor characterization [20] [21] [22]. Projects such as NAVIGATOR, a regional imaging biobank integrating multimodal imaging with molecular and clinical data, illustrate how research infrastructure is advancing to support these ambitions [22].
Foundation Models: Emerging pathological foundation models are revolutionizing traditional paradigms and providing a robust framework for the development of specialized pathomics models tailored to specific clinical tasks [18]. These models, pretrained on large diverse datasets, can be adapted to various cancer types with limited additional training data.
Prospective Validation: The field is moving from proof-concept retrospective studies to prospective validation in clinical trials. The integration of pathomics into cancer clinical trials will be essential for establishing its clinical utility and securing regulatory approval [25].
In conclusion, pathomics unlocks clinically valuable information embedded within routine histology samples that extends far beyond conventional assessment. For researchers and drug development professionals, these approaches offer powerful tools for biomarker discovery, patient stratification, and treatment optimization. As standardization improves and validation expands, pathomics is poised to become an integral component of precision oncology, working alongside established modalities to improve cancer care.
The contemporary paradigm of oncology is undergoing a fundamental shift, moving from isolated analyses of single data modalities to the integrated profiling of tumors through multiple, complementary lenses. This whitepaper delineates the compelling scientific and clinical rationale for creating holistic tumor profiles by integrating radiomics and digital pathology. Such a multimodal approach is paramount for addressing the profound challenge of tumor heterogeneity, both spatially and temporally, which often eludes characterization by single-scale analyses [11] [26]. The core premise is that radiological, histopathological, genomic, and clinical data provide orthogonal yet synergistic information; by computationally fusing these modalities, we can construct a more comprehensive digital representation of a tumor's state, leading to superior biomarkers for diagnosis, prognosis, and therapeutic response prediction [27]. The following sections provide a technical guide to the quantitative evidence, methodologies, and tools driving this integrative frontier in cancer research and drug development.
Quantitative Evidence for Multimodal Integration
Empirical evidence consistently demonstrates that integrated models outperform their unimodal counterparts. The enhanced performance stems from the complementary nature of the data: radiology describes gross tumor anatomy and phenotype, while histology and genomics reveal cellular and molecular characteristics [27].
Table 1: Diagnostic Performance of Single vs. Integrated Models in Cancer
| Cancer Type | Model Type | Key Modalities | Performance Metric | Value | Citation |
|---|---|---|---|---|---|
| Endometrial Cancer | Radiomics (CML) | MRI | Sensitivity / Specificity | 0.77 / 0.81 | [28] |
| Endometrial Cancer | Radiomics (DL) | MRI | Sensitivity / Specificity | 0.81 / 0.86 | [28] |
| Esophageal Cancer | Multimodal Radiomics | 18F-FDG PET, Enhanced CT, Clinical | AUSROC | Superior to single-modality | [11] |
| Rectal Cancer | Multiparameter MRI | T2, DWI, DCE | AUSROC | Superior to single-sequence | [11] |
The data in Table 1 underscores two critical trends. First, within a single modality like MRI, more advanced deep learning (DL) models can achieve higher diagnostic performance compared to conventional machine learning (CML) for tasks like detecting myometrial invasion in endometrial cancer [28]. Second, and more significantly, integrating multiple imaging modalities (e.g., PET and CT) or multiple MRI sequences consistently yields superior predictive power compared to any single source [11]. This principle extends beyond imaging; integrating macroscopic radiomic features with microscopic pathomic features—an approach termed radiopathomics—is an emerging frontier that offers innovative approaches for predicting the efficacy of neoadjuvant therapy [11].
Methodological Framework for Integrated Profiling
The workflow for creating a holistic tumor profile is a multi-stage, iterative process that requires rigorous standardization at each step.
Data Acquisition and Preprocessing
- Radiomics: Images are acquired from CT, PET, or MRI scanners. For MRI, multiparametric (mpMRI) protocols incorporating T1/T2 anatomical imaging, Diffusion-Weighted Imaging (DWI), and Dynamic Contrast-Enhanced (DCE) MRI are critical for capturing tumor heterogeneity [11]. Preprocessing includes image normalization, resampling, and noise reduction to ensure feature robustness [26].
- Pathomics: Hematoxylin and Eosin (H&E)-stained tissue sections are digitized into Whole Slide Images (WSIs) using high-resolution scanners [26]. Preprocessing may involve stain normalization to minimize inter-slide variability.
- Genomics: Data from next-generation sequencing (NGS), such as mutation status and gene expression profiles, are used [27] [26].
- Clinical Data: Patient demographics, laboratory values, treatment history, and outcomes are codified from Electronic Health Records (EHRs), often using Natural Language Processing (NLP) for unstructured text [26].
Feature Extraction and Selection
- Radiomic Feature Extraction: High-dimensional quantitative features are extracted from defined Regions of Interest (ROIs) or Volumes of Interest (VOIs). These include shape, intensity, and texture features (e.g., from Gray-Level Co-occurrence Matrix) [11]. Deep learning can also learn feature representations directly from image samples [26].
- Pathomic Feature Extraction: Features are extracted from WSIs, which can be expert-guided (e.g., quantifying Tumor-Infiltrating Lymphocytes) or deep-learning derived to capture sub-visual patterns of tissue architecture and cell morphology [27].
- Feature Selection: Given the high dimensionality of the data, feature reduction is essential. Techniques include least absolute shrinkage and selection operator (LASSO) regression, and methods that adjust for multiple testing to prevent overfitting [28] [29].
Experimental Protocol: A Systematic Review and Meta-Analysis Framework
For researchers seeking to validate the performance of integrated models, a systematic review and meta-analysis provide the highest level of evidence. The following protocol, adapted from a recent study, offers a detailed methodology [28].
- Study Registration and Protocol: Pre-register the study protocol in a prospective register like PROSPERO to ensure transparency and reduce reporting bias.
- Eligibility Criteria (PICOS):
- Participants: Patients with a specific cancer type (e.g., endometrial cancer).
- Intervention/Index Test: Radiomics-based machine learning models, with or without other data integration.
- Comparator: Standard diagnostic methods or other models.
- Outcomes: Key performance metrics (AUC, sensitivity, specificity, etc.).
- Study Design: Cohort, case-control, or cross-sectional studies.
- Information Sources and Search Strategy: Systematically search electronic databases (PubMed, Embase, Cochrane Library, Web of Science) using Medical Subject Headings (MeSH) and free-text keywords related to the cancer, radiomics, and machine learning.
- Study Selection and Data Extraction: Two independent reviewers screen titles/abstracts and then full-text articles against eligibility criteria. Data is extracted using a standardized form capturing author, year, sample size, model type, features, and performance metrics.
- Quality Assessment: Assess the risk of bias and methodological quality of included studies using the Radiomics Quality Score (RQS), a 16-item tool evaluating aspects like image protocol, feature reduction, validation, and open science [28] [29].
- Synthesis Methods: Pool performance estimates (sensitivity, specificity) using a bivariate random-effects model. Conduct subgroup analyses (e.g., CML vs. DL models) and assess publication bias.
Visualizing the Integrative Workflow
The following diagram illustrates the end-to-end pipeline for creating a holistic tumor profile, from multi-modal data acquisition to clinical application.
Successful execution of an integrated profiling study requires a suite of computational tools, data resources, and analytical techniques.
Table 2: Key Research Reagents & Solutions for Integrated Profiling
| Category | Item / Resource | Function & Application |
|---|---|---|
| Data Resources | The Cancer Imaging Archive (TCIA) | Public repository of cancer medical images (CT, MRI, etc.) for radiomics research. [30] |
| cBioPortal / GEO | Platforms for accessing and analyzing multidimensional cancer genomics data. [30] | |
| Pathway Commons / KEGG | Databases of biological pathways and networks for functional interpretation of molecular data. [31] | |
| Software & Libraries | R/Python with specialized packages (e.g., Pathview) | Statistical computing and creation of pathway visualizations integrated with genomic data. [31] |
| Cytoscape with plugins (WikiPathways, Reactome FI) | Network visualization and analysis, integrating pathways with other omics data. [31] | |
| Deep Learning Frameworks (TensorFlow, PyTorch) | Building and training complex models for feature extraction and data integration. [26] | |
| Analytical Techniques | Radiomics Quality Score (RQS) | A 16-item scoring system to ensure the methodological quality and reproducibility of radiomics studies. [28] [29] |
| Delta Radiomics | Quantifying changes in radiomic features during treatment to assess therapy response. [11] | |
| Graph Network Clustering | Identifying radiophenotypes with distinct prognoses from high-dimensional radiomic data. [30] | |
| Unbalanced Optimal Transport | A computational method used in clustering algorithms to handle datasets with complex distributions. [30] |
The integration of radiomics, pathomics, and genomics is not merely a technical exercise but a fundamental necessity for advancing precision oncology. The quantitative evidence is clear: multimodal models consistently provide a more accurate and robust characterization of tumor biology than any single data source can achieve alone. By adopting the rigorous methodologies, visual frameworks, and toolkits outlined in this guide, researchers and drug developers can systematically construct holistic tumor profiles. This approach promises to unlock deeper insights into tumor heterogeneity and therapy resistance, ultimately accelerating the development of more effective, personalized cancer therapies and improving patient outcomes. The future of cancer diagnostics and therapeutic development is unequivocally integrative.
Radiomics and digital pathology imaging artificial intelligence (AI) are revolutionizing oncology by transforming standard medical images into mineable, high-dimensional data. These fields represent a paradigm shift toward personalized, data-driven medicine, where quantitative features extracted from computed tomography (CT) scans, magnetic resonance imaging (MRI), and whole-slide images (WSI) provide insights far beyond what the human eye can detect [32] [11]. This integration of macroscopic radiological and microscopic pathological perspectives offers a comprehensive view of tumor heterogeneity—the variation in tumor cells between and within patients—which is a critical factor in diagnosis, prognosis, and treatment response [11] [33]. For researchers, scientists, and drug development professionals, understanding these technologies is essential for advancing precision oncology, developing more effective therapies, and designing smarter clinical trials that can stratify patients based on their likely treatment response.
Technical Foundations of Radiomics and Pathomics
Core Concepts and Definitions
- Radiomics: A high-throughput process that extracts large sets of quantitative features from standard-of-care medical images such as CT, PET, and MRI [34]. These features, including shape, texture, and intensity, provide a detailed description of tumor characteristics at a macroscopic level [33].
- Pathomics: The application of high-throughput image feature extraction techniques to digitized histopathology slides, especially hematoxylin–eosin–stained sections [33]. It quantifies microscopic patterns such as nuclear morphology, cellular distribution, and tissue architecture [11].
- Radiopathomics: The integration of macroscopic radiomic features with microscopic pathomic features to create a more comprehensive biomarker signature [11] [35]. This multi-scale approach aims to provide a more complete understanding of tumor biology.
The Radiomics and Pathomics Workflow
The machine learning (ML) pipeline for radiomics and pathomics generally follows a structured workflow, which can be implemented through different computational pathways [34]:
- Hand-crafted radiomics: Mathematically designed imaging features are extracted from a segmented region or volume of interest and used to build traditional statistical ML or neural network models.
- Deep radiomics: Deep learning models, particularly convolutional neural networks (CNNs), automatically learn and extract features from images.
- End-to-end deep learning: A DL model integrates the entire image processing pipeline, directly predicting outcomes from raw images without manual intervention.
The following diagram illustrates the logical relationships and pathways in a standard radiomics/pathomics analysis pipeline.
Figure 1: Radiomics and Pathomics Analysis Workflow. The pipeline processes medical images through preprocessing, segmentation, and feature extraction, followed by modeling via one of three primary pathways. CT: Computed Tomography; MRI: Magnetic Resonance Imaging; PET: Positron Emission Tomography; WSI: Whole-Slide Imaging; ROI: Region of Interest; VOI: Volume of Interest; CNN: Convolutional Neural Network.
Key Applications in Cancer Diagnostics and Staging
Tumor Characterization and Classification
Radiomics and pathomics enable refined tumor characterization by quantifying phenotypic differences that reflect underlying molecular and pathological subtypes.
- Molecular Subtype Prediction: In uterine corpus endometrial carcinoma (EC), radiomic features from Apparent Diffusion Coefficient (ADC) maps and post-contrast T1 (T1C) images show significant cross-scale correlations with pathomic features derived from histopathology images [33]. These correlations (with strengths ranging from 0.57 to 0.89 in absolute value for ADC) reflect variations in tumor aggressiveness and tissue composition, providing a non-invasive method to assess intratumoral heterogeneity [33].
- Pathomic Profiling: Quantitative analysis of digitized histopathology images in EC has revealed associations between cellular spatial patterns and radiological features, offering a bridge between in vivo imaging and ex vivo pathology [33].
Staging and Prognostication
AI-driven analysis improves the accuracy of cancer staging and provides prognostic information independent of traditional clinical factors.
- Lymph Node Metastasis Prediction: In rectal cancer, models based on multiparametric MRI (mpMRI) images taken before and after neoadjuvant therapy can predict lymph node metastasis, with combined pre- and post-treatment sequence models outperforming single-time-point models [11].
- Survival Stratification: A post hoc analysis of the CROWN trial in ALK-positive non-small cell lung cancer (NSCLC) used AI-derived early responses in brain lesions to stratify patients with baseline brain metastases into low- versus high-risk groups, with significantly longer median progression-free survival (mPFS) in the low-risk group (33.3 months versus 7.8 months in the high-risk group) [32].
Predicting Treatment Response
Methodology for Treatment Response Prediction
Predicting response to therapy, particularly to neoadjuvant treatment, is a primary application of radiomics and pathomics. The standard experimental protocol involves several key methodological considerations [11]:
- Imaging Modalities: CT, MRI, PET, and digital pathology WSI each offer distinct advantages. Multiparametric MRI, combining T2-weighted, DWI, and DCE sequences, is particularly valuable for capturing tumor heterogeneity [11].
- Timing of Imaging Examination:
- Pretreatment images capture the baseline heterogeneity of the primary tumor.
- Post-treatment images more directly reflect pathological remission status.
- Delta radiomics/pathomics analyzes changes in features during treatment, capturing dynamic tumor response patterns [11].
- Region of Interest (ROI) Selection: While most studies focus on the intratumoral region, the peritumoral region is increasingly recognized as containing valuable prognostic information about the tumor microenvironment [11].
- Outcome Evaluation: Common endpoints include pathologic complete response (pCR), overall survival (OS), progression-free survival (PFS), and RECIST-based assessments [36].
Application Across Cancer Types and Therapies
The following table summarizes key quantitative findings from recent studies on predicting treatment response across various cancers.
Table 1: Quantitative Evidence for Treatment Response Prediction Using Radiomics and Pathomics
| Cancer Type | Therapy/Context | Biomarker Type | Key Performance Metrics | Study Details |
|---|---|---|---|---|
| Metastatic Colorectal Cancer [32] | Atezolizumab + FOLFOXIRI–bevacizumab | AI-driven digital pathology biomarker | - Biomarker-high pts: Superior PFS (p=0.036) and OS (p=0.024)- Treatment-biomarker interaction for PFS (HR 0.69) and OS (HR 0.54) | AtezoTRIBE trial (N=161), validated in AVETRIC (N=48) |
| Mesothelioma [32] | Niraparib (PARP inhibitor) | AI-based imaging (ARTIMES) + genomic ITH | - PFS in ITH-high pts: HR 0.19 (p=0.003)- Pre-treatment tumor volume prognostic for OS (p=0.01) | NERO trial, CT analysis (n=85) |
| Resectable NSCLC [32] | Neoadjuvant Immunotherapy (Atezolizumab) | Radiomics ± ctDNA | - Predicted pCR: AUC 0.82 (radiomics), AUC 0.84 (+ctDNA)- Associated with event-free survival | Exploratory AEGEAN trial analysis (n=111) |
| Advanced HR+/HER2- Breast Cancer [37] | Xentuzumab, Exemestane, Everolimus | Multimodal AI/Radiomics (CT + bone scans) | - 7 of 8 imaging biomarkers predicted clinical benefit- Lower liver/overall tumor volume linked to better response | Phase Ib/II trial, retrospective analysis (n=106) |
| Advanced Gastric Cancer [35] | Immunotherapy-based combination therapy | Radiopathomics Signature (RPS) | - AUCs: 0.978 (training), 0.863 (internal validation), 0.822 (external validation) | Multicenter cohort (n=298), 7 ML approaches |
Multi-Modal Integration for Enhanced Prediction
The integration of multiple data types—radiopathomics—consistently outperforms single-modality approaches.
- Gastric Cancer Immunotherapy: A radiopathomics signature (RPS) developed from baseline CT scans and digital H&E-stained pathology images using interpretable machine learning demonstrated high predictive accuracy for treatment response (AUC of 0.978 in training) and effectively stratified survival risk [35]. Genetic analyses revealed that the high-RPS group correlated with enhanced immune regulation pathways and increased infiltration of memory B cells, providing biological plausibility [35].
- Mesothelioma: A dual AI-genomic approach combining an AI model (ARTIMES) for quantifying tumor volume from routine CT scans with genomic intratumoral heterogeneity measures helped identify patients most likely to respond to PARP inhibitors [32].
The Scientist's Toolkit: Essential Research Reagents and Platforms
Successful implementation of radiomics and pathomics research requires a suite of specialized tools and platforms for data acquisition, analysis, and validation.
Table 2: Essential Research Reagents and Platforms for Radiomics and Pathomics
| Tool Category | Specific Examples | Function and Application |
|---|---|---|
| Data Repositories & Clouds | NCI Cancer Research Data Commons (CRDC) [38], The Cancer Imaging Archive (TCIA) [33], CPTAC-UCEC [33] | Provides access to comprehensive collections of cancer research data (genomic, imaging, proteomic) for analysis and validation. |
| Visualization Software | Minerva [38], UCSC Xena [38], 3DVizSNP [38] | Light-weight browsers for multiplexed tissue images, exploration tools for multi-omic data, and 3D mutation visualization. |
| Analysis & Programming Tools | UpSetR [38], R/Python with ML libraries (e.g., Scikit-learn, PyRadiomics) [34] | R package for set intersection visualization; core programming environments for feature extraction and model building. |
| Validation Frameworks | METRICS (METhodological RadiomICs Score) [34], CLEAR checklist [36] | Critical tools for assessing the quality, robustness, and reproducibility of radiomics studies. |
| Digital Pathology Standards | DICOM for Whole-Slide Imaging (WSI) [25] | Emerging standard for digital pathology data, facilitating interoperability and data sharing in clinical trials. |
Technical Protocols for Key Experiments
Protocol: Developing a Hand-Crafted Radiomics Model
This protocol outlines the steps for building a predictive model using hand-crafted radiomic features [34].
- Image Acquisition and Preprocessing: Acquire medical images (e.g., CT, MRI) using a standardized protocol. Preprocessing may include image resampling, intensity normalization, and noise reduction to ensure feature robustness and reproducibility.
- Image Segmentation: Delineate the region of interest (ROI) or volume of interest (VOI), typically the primary tumor. This can be done manually by an expert radiologist, semi-automatically, or fully automatically. The segmentation step is critical as it directly impacts feature extraction.
- Feature Extraction: Use a dedicated software library (e.g., PyRadiomics) to extract a high-dimensional set of quantitative features from the segmented ROI/VOI. These features generally encompass:
- First-order statistics: Describe the distribution of voxel intensities (e.g., mean, median, kurtosis, skewness).
- Shape-based features: Describe the three-dimensional geometry of the tumor (e.g., volume, sphericity, surface area).
- Texture features: Describe the spatial relationship between voxels (e.g., Gray-Level Co-occurrence Matrix - GLCM, Gray-Level Run-Length Matrix - GLRLM).
- Feature Selection and Engineering: Reduce the high dimensionality of the feature set to avoid overfitting. Techniques include:
- Removal of non-informative or redundant features (e.g., low variance, high inter-feature correlation).
- Selection of the most predictive features using statistical tests (e.g., t-test, Mann-Whitney U test) or model-based importance (e.g., LASSO regression).
- Model Training and Validation: Split the dataset into training and validation cohorts. Train a machine learning model (e.g., logistic regression, random forest, support vector machine) on the training set using the selected features. Validate the model's performance on the hold-out validation set or via cross-validation. External validation on a completely independent dataset from a different institution is the gold standard to prove generalizability [36].
Protocol: Conducting a Radio-Pathomic Correlation Study
This protocol describes the methodology for correlating radiomic features with pathomic features, as exemplified in endometrial carcinoma research [33].
- Cohort Selection: Identify a patient cohort with available paired data: pre-treatment radiology images (e.g., MRI ADC maps, T1C images) and corresponding digital pathology whole-slide images (WSI) from subsequent surgical resection or biopsy. Apply inclusion/exclusion criteria based on image quality and tumor content.
- Radiomics Feature Extraction: Follow the hand-crafted radiomics protocol (Section 6.1, Steps 1-3) on the radiology images to generate a set of radiomic features.
- Pathomics Feature Extraction:
- WSI Processing: Digitize H&E-stained slides and generate cell detection maps and cell density maps at multiple resolutions.
- Feature Quantification: Extract a high-dimensional set of pathomic features characterizing cellular morphology, spatial architecture, and tissue texture from the annotated regions.
- Statistical Correlation Analysis: Perform a correlation analysis (e.g., using Spearman's rank correlation) between the extracted radiomic and pathomic features. Use additional statistical measures like Bayes Factor to assess the strength of evidence for the observed correlations. The goal is to identify significant cross-scale associations that link macroscopic imaging patterns to microscopic pathological findings.
Radiomics and digital pathology AI have established themselves as powerful tools in the oncologist's and researcher's arsenal, with demonstrated applications across the cancer care continuum—from refined diagnosis and staging to the prediction of treatment response for therapies including chemotherapy, targeted agents, and immunotherapy. The integration of these modalities into radiopathomics represents the forefront of this field, creating robust, biologically informed signatures that outperform single-modality biomarkers. However, for these technologies to transition from research tools to clinically actionable tests, the field must address challenges of standardization, reproducibility, and validation in large, multi-institutional cohorts. By adhering to rigorous methodological frameworks like METRICS, leveraging open-source data platforms, and fostering collaborative research, the scientific community can unlock the full potential of these technologies to guide precise, patient-specific treatment strategies and advance the field of precision oncology.
From Data to Decisions: Methodological Workflows and Translational Applications
The rise of computational oncology marks a shift toward data-driven cancer diagnostics. Radiomics and digital pathology (often termed pathomics) stand at the forefront of this transformation, enabling the high-throughput extraction of quantitative features from medical images and histology slides to characterize tumor heterogeneity and the microenvironment [11] [39]. These "omics" technologies move beyond qualitative visual assessment, uncovering sub-visual patterns that are intricately linked to clinical outcomes such as diagnosis, prognosis, and treatment response [39].
The technical workflows for processing this imaging data share a common, structured pipeline. This guide details the core computational procedures of image segmentation, feature extraction, and model construction, providing a foundational framework for researchers and drug development professionals aiming to build robust predictive models in oncology.
Foundational Concepts and Integrated Frameworks
Radiomics refers to the high-throughput extraction of a large number of quantitative features from standard-of-care medical images, such as CT, MRI, or PET [11] [39]. These features can capture intra-tumor heterogeneity and provide insights into the tumor microenvironment at a macroscopic level [11]. Pathomics applies a similar principle to digitized pathology whole-slide images (WSIs), providing microscopic details of the tumor from histology slides [11] [40].
While powerful as individual modalities, the integration of radiomics and pathomics into a radio-pathomic framework is an emerging and powerful area of research. This integration offers a more comprehensive view of the tumor by combining macroscopic radiological characteristics with microscopic pathological findings [11]. For instance, a 2025 study on lung cancer demonstrated that integrated radio-pathomic models significantly outperformed models based on either modality alone in predicting disease recurrence and treatment response [21]. This synergy highlights the importance of the underlying technical workflows that enable such multi-modal integration.
The Core Technical Workflow
The standard technical pipeline for radiomics and pathomics is composed of several methodically interconnected stages. The workflow progresses from data preparation through to model deployment, with each stage being critical for the development of a clinically valid and generalizable model [39].
Image Acquisition and Pre-processing
The initial stage involves acquiring medical images or pathology slides and converting them into a standardized, digital format suitable for computational analysis.
- Radiomics Imaging Modalities: Common modalities include Computed Tomography (CT), Magnetic Resonance Imaging (MRI), Positron Emission Tomography (PET), and Ultrasound (US). Each offers distinct advantages; CT features are highly reproducible, MRI offers superior soft-tissue contrast, and PET provides insight into functional and biochemical changes [11].
- Digital Pathology Creation: Glass pathology slides are digitized using whole-slide scanners to create high-resolution whole-slide images (WSIs) [40]. The quality of these images is paramount, requiring high-fidelity scanners and appropriate display monitors for pathologist review [41] [40].
- Pre-processing: This step ensures data consistency and quality. In radiomics, it may involve bias field correction (e.g., for MRI), image resampling to isotropic voxels, and intensity normalization [42]. For pathomics, it includes managing stain variation and ensuring focus across the entire WSI.
The following diagram illustrates the complete end-to-end workflow, from data input to clinical application:
Diagram 1: The core technical workflow from data to decision support.
Image Segmentation
Image segmentation is the process of delineating the Region of Interest (ROI) or Volume of Interest (VOI) from which features will be extracted. This is a critical step, as the accuracy of segmentation directly impacts the relevance of the extracted features [39].
- Segmentation Methods:
- Manual Segmentation: Performed by a radiologist or pathologist. It is considered the gold standard but is time-consuming and can suffer from inter-observer variability.
- Semi-Automatic Segmentation: The expert guides and refines an algorithm-driven segmentation, offering a balance between accuracy and efficiency.
- Fully Automatic Segmentation: Utilizes deep learning models (e.g., U-Net, Mask R-CNN) to segment the ROI without human intervention. While highly efficient, it requires large, annotated datasets for training and rigorous validation [39].
- Region of Interest (ROI): The focus is most commonly the primary tumor (intratumoral region). However, increasing evidence shows that the tissue immediately surrounding the tumor (peritumoral region) also contains biologically meaningful information, and incorporating it can improve model performance [11].
Feature Extraction
Feature extraction involves converting the segmented ROI into a set of quantitative, mineable data. These features can be broadly categorized as hand-crafted or deep learning-based.
- Hand-crafted Radiomic/Pathomic Features:
- First-order Statistics: Describe the distribution of voxel/intensities within the ROI without considering spatial relationships (e.g., mean, median, variance, skewness, kurtosis) [39].
- Second-order (Texture) Features: Describe the statistical relationships between voxel intensities and their neighbors. These are calculated from matrices like the Gray-Level Co-occurrence Matrix (GLCM) and Gray-Level Run-Length Matrix (GLRLM) [39] [21].
- Shape-based Features: Quantify the three-dimensional geometry of the ROI (e.g., volume, sphericity, surface area-to-volume ratio) [39].
- Higher-order Features: Derived from filtered images (e.g., using Wavelet, Laplacian of Gaussian, or Gabor filters) to extract repetitive or non-repetitive patterns [42].
- Deep Learning-based Features: Instead of pre-defined feature classes, convolutional neural networks (CNNs) can automatically learn a hierarchical representation of features directly from the image data. While this bypasses manual feature engineering, it often results in less interpretable "black box" models [39].
Table 1: Categories of Hand-Crafted Features in Radiomics and Pathomics
| Feature Category | Description | Example Features | Biological Correlation |
|---|---|---|---|
| First-Order Statistics | Distribution of voxel/pixel intensities | Mean, Median, Entropy, Energy, Kurtosis | Cellular density, Necrosis |
| Shape & Size | 3D geometry and morphology of the ROI | Volume, Surface Area, Sphericity, Compactness | Tumor growth pattern, Aggressiveness |
| Texture Features | Intra-tumor spatial heterogeneity | Contrast, Correlation, Homogeneity, Entropy (from GLCM, GLRLM) | Tumor heterogeneity, Treatment resistance |
| Transform-based Features | Patterns from filtered image domains | Wavelet, Gabor, Laplacian of Gaussian (LoG) | Underlying textural patterns at multiple scales |
Feature Selection and Model Construction
After extracting a high-dimensional set of features (often exceeding 1,000 per ROI), feature selection is a pivotal step to reduce dimensionality, mitigate overfitting, and improve model generalizability [39] [42].
- Feature Selection Methods:
- Filter Methods (e.g., mRMRe, ReliefF): Select features based on univariate statistical tests (e.g., Wilcoxon rank-sum) or correlation with the outcome, independent of the classifier.
- Wrapper Methods (e.g., Boruta, Recursive Feature Elimination - RFE): Use a predictive model's performance as the criterion to evaluate and select feature subsets. They are computationally intensive but can yield high-performing feature sets.
- Embedded Methods (e.g., LASSO, Random Forest variable importance): Perform feature selection as an inherent part of the model construction process [42].
- Model Construction and Validation: The selected features are used to train a machine learning model for a specific clinical task (e.g., classification, regression, survival analysis). Common algorithms include Support Vector Machines (SVM), Random Forests (RF), and regularized linear models (e.g., LASSO) [42]. Model performance must be rigorously evaluated using appropriate metrics (e.g., AUC, C-index, sensitivity, specificity) and validation techniques, preferably on an independent, external dataset [11] [39].
Table 2: Common Feature Selection Methods and Their Characteristics
| Method | Type | Mechanism | Advantages |
|---|---|---|---|
| LASSO (L1) | Embedded | Performs variable selection and regularization via L1-penalty | Creates sparse, interpretable models; Handles multicollinearity |
| Boruta | Wrapper | Compares original features with "shadow" features using Random Forest | Robust; Selects all relevant features, not just non-redundant ones |
| Recursive Feature Elimination (RFE) | Wrapper | Iteratively removes the weakest feature(s) based on model weights | Effective at finding high-performing feature subsets |
| mRMRe | Filter | Selects features with Max-Relevance and Min-Redundancy | Balances predictive power and feature independence |
| ReliefF | Filter | Weights features based on ability to distinguish nearest neighbors | Non-parametric; Effective for binary and multi-class problems |
The following diagram details the iterative process of feature selection and model building:
Diagram 2: The iterative process of feature selection and model construction.
Advanced Methodologies and Experimental Protocols
Delta-Radiomics/Pathomics
A powerful advanced methodology is delta-radiomics/pathomics, which involves analyzing the change in features over time. Instead of relying solely on a single pre-treatment scan, serial images are acquired (e.g., during or after therapy). Models are then built on the temporal changes (delta) of the features, which can more directly reflect tumor treatment sensitivity and pathological remission status [11]. Studies in esophageal and gastric cancers have shown that delta-radiomics models can achieve higher predictive performance for pathological response than models based only on pre-treatment images [11].
Detailed Experimental Protocol: Building a Radio-Pathomic Model
The following protocol is adapted from a 2025 study that integrated CT-based radiomics and H&E-based pathomics to predict outcomes in lung cancer [21].
- Objective: To develop an integrated radio-pathomic model for predicting disease recurrence in early-stage Non-Small Cell Lung Cancer (NSCLC).
- Cohort: 194 patients with early-stage NSCLC.
- Image Acquisition:
- Radiomics: Pre-treatment CT scans were collected. A standard clinical protocol (e.g., slice thickness ≤ 1.5 mm, standard kernel) should be used and documented.
- Pathomics: Digitized H&E-stained whole-slide images from diagnostic biopsies or surgical resections were obtained using a high-resolution slide scanner.
- Image Segmentation:
- Radiomics: The primary tumor was manually segmented on each CT slice by an experienced radiologist to define the 3D VOI.
- Pathomics: The tumor region on each H&E WSI was annotated by a certified pathologist.
- Feature Extraction:
- Radiomics: 1218 radiomic features were extracted from the CT VOIs using the PyRadiomics library in Python. Features included shape, first-order statistics, and texture features (e.g., Haralick, Gabor, Laws).
- Pathomics: Pathomic features were extracted from the annotated WSI regions, focusing on spatial architecture and cellular morphology (e.g., using the SPATIL feature family).
- Feature Selection & Model Construction:
- Individual Models: Separate radiomic (ES-MR) and pathomic (ES-MP) risk scores were built using the LASSO Cox regression model for feature selection and model building on the training set.
- Integrated Model: The top-selected radiomic and pathomic features were combined to create a radio-pathomic signature (RPRS). The combined ES-MRP model was built using the same LASSO Cox method.
- Validation: Models were evaluated on a held-out validation set using the Harrell's Concordance-index (C-index) and Kaplan-Meier analysis with log-rank test for recurrence-free survival.
- Key Result: The integrated radio-pathomic model (ES-MRP) significantly outperformed the individual models, with a C-index of 0.71 compared to 0.68 (radiomics alone) and 0.65 (pathomics alone) [21].
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Key Software, Hardware, and Computational Tools for Radiomics and Pathomics Research
| Item | Function/Role | Examples & Notes |
|---|---|---|
| Whole Slide Scanners | Digitizes glass pathology slides into whole-slide images (WSIs) for pathomics analysis. | KFBIO scanners, Aperio (Leica Biosystems), Axio Scan (ZEISS). Key specs: scan speed, resolution (e.g., 0.25 μm/pixel), and stability [41] [40]. |
| Medical Image Archives | Source of standard medical images (CT, MRI, etc.) for radiomics. Includes PACS systems and public datasets. | Institutional PACS, The Cancer Imaging Archive (TCIA). Must ensure data de-identification and compliance with ethics. |
| Image Analysis Software | Platforms for viewing, segmenting, and managing digital images. | AISight (PathAI), KFBIO Remote Diagnosis Platform, Vendor-agnostic viewers supporting DICOM standards [43] [41] [40]. |
| Feature Extraction Engines | Software libraries to compute hand-crafted radiomic/pathomic features from ROIs. | PyRadiomics (Python), MaZda, IBEX. PyRadiomics is a widely used, open-source option that is compliant with the Image Biomarker Standardisation Initiative (IBSI) [42]. |
| AI/ML Development Frameworks | Programming environments for building deep learning models and implementing machine learning classifiers. | Python (with TensorFlow, PyTorch, Scikit-learn), R. Essential for custom model construction, feature selection, and validation [42]. |
| High-Performance Computing (HPC) | Infrastructure for handling computationally intensive tasks like WSI analysis and deep learning model training. | Cloud computing (AWS, GCP, Azure) or local GPU clusters. Necessary due to the large size of WSIs and complexity of 3D radiomic analysis [40]. |
The technical workflows of image segmentation, feature extraction, and model construction form the backbone of modern radiomics and pathomics research in oncology. Adherence to rigorous and reproducible methodologies at each stage—from high-quality image acquisition and precise segmentation to robust feature selection and external model validation—is critical for translating these computational approaches into clinically actionable tools. The integration of multi-modal data, such as radio-pathomics, represents the future of this field, promising a more holistic and powerful paradigm for personalized cancer diagnosis and treatment.
Radiopathomics represents a cutting-edge frontier in cancer diagnostics, defined by the integration of quantitative features extracted from digital pathology images (pathomics) and radiographic medical images (radiomics). This multi-modal data fusion paradigm addresses a critical limitation in oncology: the inherent insufficiency of any single data type to fully capture the complex heterogeneity of cancer. Technological advances now make it possible to study patients from multiple angles with high-dimensional, high-throughput multiscale biomedical data, ranging from molecular and histopathology to radiology and clinical records [44] [45]. The introduction of deep learning has significantly advanced the analysis of these biomedical data modalities, yet most approaches have traditionally focused on single modalities, leading to slow progress in methods that integrate complementary data types [45].
The fundamental premise of radiopathomics is that these disparate modalities provide complementary, redundant, and harmonious information that, when combined, enables better stratification of patient populations and provides more individualized care [45]. Digital pathology with whole slide imaging (WSI) provides data about cellular and morphological architecture in a visual format for pathologists to interpret, offering key information about the spatial heterogeneity of the tumor microenvironment [45]. Conversely, radiographic images like MRI or CT scans provide visual data of tissue morphology and 3D structure [45]. Where radiology offers a macroscopic, in vivo perspective of entire tumors and their surroundings, pathology delivers microscopic, ex vivo insights into cellular and subcellular structures. The fusion of these perspectives creates a more comprehensive understanding of tumor biology that neither modality can achieve alone.
The Scientific and Clinical Rationale
Limitations of Single-Modality Approaches
Cancer prognosis remains challenging despite significant investments in research, partly because predictive models based on single modalities offer a limited view of disease heterogeneity and may not provide sufficient information to stratify patients and capture the full range of events that occur in response to treatments [45]. Molecular data, while crucial for precision medicine, inherently discard tissue architecture, spatial, and morphological information [45]. Similarly, radiographic images alone lack the cellular resolution necessary for detailed genomic profiling, and pathology images alone cannot provide the longitudinal, in vivo monitoring capability of radiology.
The tumor microenvironment (TME) exemplifies this challenge, as its cellular composition dynamically evolves with tumor progression and in response to anticancer treatments [45]. Various TME elements play roles in both tumor development and therapeutic response, particularly for immunotherapeutic approaches like antibody-drug conjugates and adoptive cell therapy, where response rates vary dramatically depending on tumor subtype and TME characteristics [45]. The increasing application of immunotherapy underscores the need for both a deeper understanding of the TME and multimodal approaches that allow longitudinal TME monitoring during disease progression and therapeutic intervention [45].
Synergistic Potential of Multi-Modal Integration
Integrating data modalities that cover different biological scales has the potential to capture synergistic signals that identify both intra- and inter-patient heterogeneity critical for clinical predictions [45]. This integration enhances our understanding of cancer biology while paving the way for precision medicine that promises individualized diagnosis, prognosis, treatment, and care [44] [45]. A prominent example of this paradigm shift occurred in the 2016 WHO classification of tumors of the central nervous system, where revised guidelines recommended histopathological diagnosis in combination with molecular markers, establishing a precedent for integrated diagnostic approaches [44].
The radiopathomics approach is particularly valuable for discovering both prognostic and predictive biomarkers. While prognostic biomarkers provide information on patient diagnosis and overall outcome, predictive biomarkers inform treatment decisions and responses [45]. By combining spatial and morphological information from pathology with longitudinal, volumetric data from radiology, radiopathomics can identify biomarkers that more accurately reflect tumor behavior and treatment sensitivity.
Technical Methodology and Workflow
Data Acquisition and Preprocessing
The radiopathomics workflow begins with the acquisition of multi-modal data, each requiring specific processing approaches:
Digital Pathology Processing: Whole slide imaging (WSI) facilitates the "digitizing" of conventional glass slides to virtual images, offering practical advantages including speed, simplified data storage and management, remote access and shareability, and highly accurate, objective, and consistent readouts [45]. For AI applications, these gigapixel-sized WSIs are typically divided into smaller patches for analysis, often using convolutional neural networks or vision transformers for feature extraction [45].
Radiomics Feature Extraction: Radiomics refers to the field focusing on the quantitative analysis of radiological digital images to extract quantitative features for clinical decision-making [46]. This extraction can be performed using traditional handcrafted feature methods or deep learning frameworks [45]. The radiomics pipeline involves image acquisition, segmentation, feature extraction, and analysis [47]. Standardization initiatives like the Image Biomarker Standardization Initiative (IBSI) provide guidelines for reproducible feature extraction [46].
Table 1: Core Data Modalities in Radiopathomics Integration
| Data Modality | Spatial Resolution | Temporal Capability | Key Information Captured | Primary Clinical Use |
|---|---|---|---|---|
| Digital Pathology | Cellular/Subcellular (microns) | Single time point (typically) | Cellular morphology, tissue architecture, tumor microenvironment | Diagnosis, grading, biomarker assessment |
| CT Imaging | Macroscopic (millimeters) | Multiple time points | 3D tumor volume, density, shape, spatial relationships | Staging, treatment response monitoring |
| MRI Imaging | Macroscopic (submillimeter to millimeters) | Multiple time points | Soft tissue contrast, functional information, vascularity | Diagnosis, surgical planning, response assessment |
| Molecular Data | Molecular scale | Single or multiple time points | Genomic alterations, protein expression, metabolic activity | Targeted therapy selection, prognosis |
Multi-Modal Data Fusion Strategies
Data fusion in radiopathomics can be implemented at different levels of abstraction:
Early Fusion: This approach involves combining raw or minimally processed data from different modalities before feature extraction. While theoretically powerful, early fusion presents significant technical challenges due to the disparate nature of radiology and pathology data structures and resolutions.
Intermediate Fusion: This method integrates features extracted separately from each modality before final analysis. This represents a practical balance, allowing domain-specific processing while enabling cross-modal information exchange.
Late Fusion: This strategy involves processing each modality independently through separate models and combining the results at the decision level. This approach offers flexibility but may miss important cross-modal interactions.
Hybrid Approaches: Advanced deep learning architectures now enable end-to-end learning from multiple modalities, with cross-attention mechanisms and transformer architectures particularly well-suited for capturing relationships across disparate data types.
Experimental Protocols and Validation
Representative Study Design
A robust radiopathomics study requires careful experimental design to ensure clinically meaningful findings. The following protocol outlines key methodological considerations:
Cohort Selection: Retrospective collection of paired radiology and pathology samples from clinically annotated patients, with explicit inclusion/exclusion criteria. Sample size should be justified by power calculations based on preliminary data or literature estimates [46]. For example, a liver metastases study enrolled 47 patients with hepatic metastatic colorectal cancer confirmed by histopathology [46].
Image Acquisition Protocol: Standardized acquisition parameters for each modality. For CT: slice thickness of 1.5mm, axial reconstruction, standardized tube voltage and current modulation, consistent reconstruction kernel [46]. For digital pathology: whole slide scanning at appropriate magnification (typically 20x or 40x) with consistent staining protocols.
Segmentation Methodology: Manual or semi-automated segmentation of regions of interest using validated software platforms (e.g., MITK Workbench for radiology, specialized tools for pathology) [46]. Multiple annotators with appropriate expertise should segment subsets of cases to assess inter-rater reliability.
Feature Extraction: Calculation of radiomics features using standardized platforms (e.g., pyradiomics) following IBSI guidelines, including gray-level discretization with fixed bin width, image resampling to isotropic voxel size, and appropriate mask processing [46]. Pathomics features may include cellular morphology, tissue architecture, and spatial arrangement metrics.
Validation Framework: Implementation of appropriate validation strategies, including data partitioning to prevent information leakage, internal validation through bootstrapping or cross-validation, and external validation on independent cohorts when possible [47].
Quality Assessment and Standardization
The complex multi-step radiopathomics pipeline requires rigorous quality assessment to ensure reproducible and clinically translatable results. Recent initiatives have developed specialized tools for this purpose:
Radiomics Quality Score (RQS): Introduced in 2017, this methodological assessment tool evaluates 16 items across the entire lifecycle of radiomics research, with a total raw score ranging from -8 to +36 [47]. Despite widespread adoption, limitations include unclear rationale for assigned scores and scaling methodological questions [47].
METRICS (METhodological RadiomICs Score): A newer consensus guideline including 30 items across five conditions, designed to accommodate traditional handcrafted methods and advanced deep-learning computer vision models [47]. Developed through a modified Delphi method with international panel input, METRICS addresses limitations of previous tools and includes an online calculator for final quality scores [47].
Table 2: Comparative Analysis of Radiopathomics Study Quality Assessment Tools
| Assessment Domain | RQS (Radiomics Quality Score) | METRICS (Methodological Radiomics Score) |
|---|---|---|
| Number of Items | 16 items | 30 items |
| Score Range | -8 to +36 | Percentage-based (0-100%) |
| Development Method | Expert consensus | Modified Delphi method with international panel |
| Key Strengths | Historical adoption, comprehensive scope | Detailed methodological assessment, conditionality consideration |
| Notable Limitations | Unclear scoring rationale, scaling methodological questions | Newer tool with less established track record |
| Coverage of Pathomics | Limited | Limited, primarily radiomics-focused |
| Recommended Use | Historical comparison | Primary assessment for new studies |
Visualization and Computational Tools
Radiopathomics Integration Workflow
The following diagram illustrates the comprehensive workflow for radiopathomics data integration, from multi-modal data acquisition to clinical decision support:
Radiopathomics Multi-Modal Fusion Workflow
Feature Map Analysis Pipeline
The visualization of radiomics and pathomics features through parameter maps enables enhanced detection and characterization of lesions. The following diagram details the feature map analysis pipeline specifically applied to liver metastases detection:
Feature Map Analysis for Liver Metastases
The Scientist's Toolkit: Essential Research Reagents and Platforms
Table 3: Essential Research Reagents and Computational Platforms for Radiopathomics
| Tool Category | Specific Tools/Platforms | Primary Function | Key Applications |
|---|---|---|---|
| Image Analysis Platforms | MITK Workbench, 3D Slicer, QuPath | Medical image visualization, processing, and segmentation | Manual/automated ROI segmentation, image registration, visualization |
| Radiomics Extraction | PyRadiomics, MaZda, IBEX | Standardized extraction of quantitative features from medical images | Feature calculation following IBSI guidelines, feature map generation |
| Digital Pathology Analysis | HALO, Visiopharm, Indica Labs | Whole slide image analysis, cellular segmentation, spatial analysis | Tumor microenvironment quantification, cellular feature extraction |
| Deep Learning Frameworks | TensorFlow, PyTorch, MONAI | Development and training of neural network models | Multi-modal data fusion, predictive model development, feature learning |
| Statistical Analysis | R Statistics, Python (SciPy, scikit-learn), MATLAB | Statistical testing, model development, data visualization | Feature selection, model validation, statistical inference |
| Containerization | Docker, Singularity | Computational environment reproducibility | Creating portable, reproducible analysis pipelines |
| Quality Assessment | METRICS calculator, RQS checklist | Methodological quality scoring | Study quality evaluation, standardization assessment |
Clinical Applications and Evidence
Colorectal Cancer and Liver Metastases
Radiopathomics approaches have shown particular promise in colorectal cancer (CRC), a major global health burden responsible for roughly 10% of all cancer diagnoses and deaths worldwide [48]. The detection and characterization of liver metastases represents a critical clinical challenge where radiopathomics provides significant value. Studies have demonstrated that selected radiomics feature maps, particularly first-order RootMeanSquared features, can increase the visual contrast of faintly demarcated liver metastases compared with standard CT reconstructions, potentially improving detectability [46]. In one study of 47 patients with hepatic metastatic colorectal cancer, the firstorder_RootMeanSquared feature map demonstrated superior performance for visual contrast enhancement compared to other feature classes, achieving very high visual contrast ratings in 57.4% of cases compared to 41.0% in standard reconstructions [46].
Microsatellite Instability Prediction
In colorectal cancer, a major genomic alteration is microsatellite instability (MSI), which results from defects in the mismatch-repair pathway and is found in about 5-20% of tumors [48]. Deep-learning models applied to routine H&E whole-slide images can infer MSI status by capturing morphologic signatures of mismatch-repair deficiency, with studies demonstrating impressive performance across multi-institutional cohorts [48]. Kather et al. developed the first automated, end-to-end deep-learning model for MSI/deficient mismatch repair detection in 2019, achieving an area under the curve (AUC) of 0.84 within The Cancer Genome Atlas cohort [48]. Subsequent studies utilizing improved methodologies have shown even better performance, with AUC values ranging from 0.78 to 0.98 [48]. These advances culminated in 2022 with the first deep-learning biomarker detector, MSIntuit, receiving approval for routine clinical use in Europe [48].
Computer-Aided Detection in Colonoscopy
Computer-aided detection (CADe) systems represent a successful clinical application of AI in CRC endoscopy, providing real-time assistance during colonoscopy by automatically flagging polyps [48]. Meta-analyses of randomized controlled trials demonstrate that CADe increases adenoma detection rates from 36.7% to 44.7% and raises adenomas per colonoscopy from 0.78 to 0.98 [48]. In tandem colonoscopy designs, CADe significantly reduces the adenoma miss rate from 35.3% to 16.1% [48]. These systems leverage convolutional neural networks for frame-by-frame inference at clinical frame rates, localizing diminutive and flat lesions without interrupting workflow [48].
Challenges and Future Directions
Despite the promising potential of radiopathomics, several significant challenges remain that must be addressed for successful clinical translation:
Data Quality and Standardization: The lack of standardization in key stages of the complex multi-step radiomic and pathomic pipelines presents a major barrier to clinical integration [47]. Variations in imaging protocols, segmentation methodologies, and feature calculation algorithms can significantly impact results and reproducibility.
Computational and Infrastructure Requirements: Radiopathomics analyses demand substantial computational resources for processing large-volume imaging data, particularly whole slide images that can reach several gigabytes per slide. Storage, processing power, and specialized software requirements can present practical implementation barriers.
Interpretability and Trust: The "black-box" nature of some complex deep learning models limits interpretability, trust, and regulatory acceptance [48]. Developing methods to explain model decisions and provide clinical understandable justifications remains an active research area.
Regulatory and Validation Frameworks: The FDA has recognized the need for specialized regulatory frameworks for AI/ML-based software as a medical device, highlighting considerations for data inclusion, relevance to clinical problems, consistent data acquisition, appropriate dataset definition, and algorithm transparency [45]. Prospective validation in diverse clinical settings remains essential.
Integration with Clinical Workflows: Successful implementation requires seamless integration with existing clinical workflows rather than disruptive additions. The clinician remains the ultimate evaluator, and adoption depends on usability, clear return on investment, and demonstrated performance improvement [48].
Future developments in radiopathomics will likely focus on addressing these challenges through improved standardization initiatives, more efficient computational methods, enhanced interpretability techniques, and prospective validation studies. As the field matures, radiopathomics promises to evolve into a dependable infrastructure that improves cancer outcomes through more precise detection, characterization, and monitoring of malignant diseases.
Predictive Modeling for Neoadjuvant Therapy Efficacy and Pathological Complete Response (pCR)
Pathological complete response (pCR) has emerged as a critical prognostic indicator in oncology, strongly correlated with improved long-term survival across multiple cancer types, including breast, esophageal, and bladder cancers [11] [49] [50]. The ability to accurately predict which patients will achieve pCR following neoadjuvant therapy remains a significant challenge in clinical oncology, primarily due to substantial tumor heterogeneity and the complex interplay between tumor biology and treatment modalities [49] [51]. Within the broader context of radiomics and digital pathology research, advanced computational approaches are now enabling unprecedented capabilities to decode this complexity through quantitative feature extraction from medical images and pathological specimens [11] [52].
The emergence of artificial intelligence (AI), particularly deep learning and multimodal integration, represents a paradigm shift in predictive oncology [53] [52]. These technologies can identify subtle patterns within complex datasets that escape human observation, thereby providing more accurate and personalized predictions of treatment response [53] [54]. This technical guide comprehensively examines state-of-the-art methodologies, performance metrics, and implementation frameworks for developing predictive models of neoadjuvant therapy efficacy, with particular emphasis on the integration of radiomics and pathomics data within a multimodal AI framework.
Multimodal Approaches for pCR Prediction
Data Modalities and Integration Strategies
Table 1: Data Modalities in Predictive Modeling for Neoadjuvant Therapy
| Modality | Data Sources | Extracted Features | Biological Significance |
|---|---|---|---|
| Radiomics | CT, MRI, PET, US [11] [52] | Shape, first-order statistics, texture features [10] | Macroscopic tumor heterogeneity, spatial characteristics [11] |
| Pathomics | Whole-slide images (WSIs) of H&E-stained specimens [55] [56] | Cellular morphology, tissue architecture, nuclear features [55] | Microscopic tumor microenvironment, cellular patterns [11] |
| Genomics | RNA sequencing, microarray data [56] | Gene expression profiles, molecular signatures [51] [56] | Molecular subtypes, therapeutic targets, resistance mechanisms [49] [51] |
| Clinical | Electronic health records, laboratory values [50] | Inflammatory markers (NLR, PLR, SIRI), demographic data [50] | Systemic inflammatory response, patient-specific factors [50] |
Multimodal AI approaches consistently demonstrate superior performance compared to unimodal models across various cancer types. In esophageal cancer, a multimodal model integrating CT radiomics, pathomics, and clinical features achieved an AUC of 0.89 for predicting pCR following neoadjuvant chemoimmunotherapy, significantly outperforming single-modality models (radiomics AUC: 0.70; pathomics AUC: 0.77; clinical AUC: 0.63) [55]. Similarly, in muscle-invasive bladder cancer, a Graph-based Multimodal Late Fusion (GMLF) framework integrating histopathology images with gene expression profiles achieved a mean AUC of 0.74, surpassing unimodal approaches using either data type alone [56].
Performance Comparison of Modeling Approaches
Table 2: Performance Comparison of Predictive Modeling Approaches Across Cancer Types
| Cancer Type | Model Architecture | Data Modalities | Performance (AUC) | Sample Size |
|---|---|---|---|---|
| Breast Cancer [54] | Multimodal DL (Various CNN) | MRI + Clinical + DP | Median AUC: 0.88 | 51 studies (median 281 patients) |
| Breast Cancer [54] | Unimodal DL | MRI only | Median AUC: 0.83 | 51 studies (median 281 patients) |
| Esophageal Cancer [55] | SVM | CT Radiomics + Pathomics + Clinical | AUC: 0.89 | 80 patients |
| Bladder Cancer [56] | GMLF | WSI + Gene Expression | AUC: 0.74 | 180 patients |
| Bladder Cancer [56] | SlideGraph+ | WSI only | AUC: 0.67 | 180 patients |
The integration of longitudinal imaging data significantly enhances predictive performance compared to single-timepoint analysis. In breast cancer, models incorporating dynamic changes in radiomic features throughout treatment (delta radiomics) achieved a median AUC of 0.91, substantially higher than models using only baseline imaging (median AUC: 0.82) [54]. This temporal analysis captures tumor phenotypic changes during treatment, providing critical insights into therapeutic sensitivity [11].
Experimental Protocols and Methodologies
Radiomics Feature Extraction Pipeline
Protocol 1: CT/MRI Radiomics Feature Extraction
Image Acquisition and Preprocessing
Tumor Segmentation
Feature Extraction
Feature Selection and Normalization
Pathomics Feature Extraction from Whole-Slide Images
Protocol 2: Digital Pathomics Feature Extraction
Slide Preparation and Digitization
Image Preprocessing and Tiling
- Convert WSIs from RGB to grayscale and apply thresholding to segment tissue regions [55]
- Perform color normalization using Vahadane Method or similar to address staining variations [55]
- Subdivide tumor regions into non-overlapping 224×224 pixel tiles at 20× equivalent magnification [55]
- Exclude tiles with less than 50% tissue content [55]
Deep Feature Extraction
Feature Selection
Multimodal Model Development
Protocol 3: Multimodal Integration Framework
Data Partitioning
Unimodal Model Development
Multimodal Integration
- Implement late fusion architecture:
- Alternative: Employ graph-based fusion (GMLF) for integrating WSI and genomic data [56]
Model Validation
The Scientist's Toolkit
Table 3: Essential Research Reagent Solutions for Predictive Modeling
| Category | Item/Software | Specification/Function | Application Notes |
|---|---|---|---|
| Image Analysis | ITK-SNAP | Open-source software for medical image segmentation | Manual delineation of ROIs on CT/MRI images [55] |
| Radiomics Extraction | PyRadiomics | Python package for extraction of radiomic features | Standardized feature extraction from medical images [55] [10] |
| Digital Pathology | ASAP | Open-source software for WSI annotation | Tumor region annotation on whole-slide images [55] |
| Deep Learning | ResNet-50 | Pre-trained CNN for feature extraction | Transfer learning for pathomics feature extraction [55] |
| Model Interpretation | SHAP | Framework for explaining model predictions | Identify influential features in multimodal models [56] |
| Statistical Analysis | R/Python | Programming languages for statistical computing | Feature selection, model development, and validation [55] |
Visualizing Multimodal Integration Workflows
Figure 1: Multimodal AI Integration Workflow. This architecture illustrates the late fusion approach for combining multiple data modalities, where unimodal models are trained separately before integration [56] [54].
Figure 2: Radiomics Analysis Pipeline. Standardized workflow for radiomic feature extraction and model development, applicable to both clinical and preclinical studies [11] [10].
Predictive modeling for neoadjuvant therapy efficacy represents a rapidly advancing field with significant clinical implications. The integration of multimodal data through sophisticated AI architectures has consistently demonstrated superior performance compared to traditional unimodal approaches [55] [56] [54]. As these technologies mature, several key challenges must be addressed to facilitate clinical translation, including limited sample sizes, methodological heterogeneity, and the need for improved interpretability [53] [54].
Future research directions should prioritize prospective validation studies, standardization of feature extraction protocols, development of explainable AI frameworks, and integration of emerging data modalities such as liquid biopsies and spatial transcriptomics [52] [54]. Furthermore, the exploration of temporal feature dynamics through delta-radiomics and treatment-response adaptation represents a promising avenue for enhancing predictive accuracy [11]. As these technologies evolve, they hold immense potential to transform oncology practice by enabling truly personalized treatment selection and improving patient outcomes through more precise prediction of neoadjuvant therapy efficacy.
The integration of quantitative imaging features with molecular data represents a paradigm shift in cancer diagnostics and research. This field, known as radiomics, extracts high-dimensional data from medical images to create mineable databases, while digital pathology imaging (DPI) enables whole-slide image analysis through artificial intelligence (AI) [57] [25]. When correlated with genomic information, these image phenotypes can reveal critical insights into underlying molecular drivers of cancer, enabling advancements in precision oncology [57] [58]. This technical guide outlines the methodologies, analytical frameworks, and practical implementations for establishing robust correlations between image-derived features and cancer genotypes, with particular relevance for researchers, scientists, and drug development professionals working within this emerging interdisciplinary domain.
Core Concepts and Definitions
Image Phenotypes: Quantitative Feature Extraction
Image phenotypes refer to quantitative features extracted from medical images that characterize tumor heterogeneity, morphology, and texture. In both radiology and digital pathology, these features are computationally derived and categorized as follows [57] [25]:
- First-order statistics: Describe the distribution of pixel intensities within the image without considering spatial relationships (e.g., mean, median, variance, skewness, kurtosis).
- Shape-based features: Quantify three-dimensional tumor geometry (e.g., volume, surface area, sphericity, compactness).
- Texture features: Capture spatial patterns of pixel intensities through mathematical matrices:
- Gray-level co-occurrence matrix (GLCM)
- Gray-level run length matrix (GLRLM)
- Gray-level size zone matrix (GLSZM)
- Neighboring gray-tone difference matrix (NGTDM)
- Wavelet-transformed features: Decompose images into frequency components to extract features at different spatial scales.
Molecular Genotypes: Driver Genes and Pathways
Cancer genotypes encompass the genetic alterations that drive oncogenesis and progression. A critical distinction exists between driver genes and phenotypic genes [59]:
- Driver genes: Genes whose mutations confer a selective growth advantage and are causally implicated in oncogenesis (e.g., genes cataloged in the COSMIC Cancer Gene Census).
- Phenotypic genes: Genes that influence observable cancer traits (e.g., invasion, metastasis) but whose targeting alone may not lead to tumor regression.
- Core driver gene sets (CDGS): Collections of genes that broadly promote carcinogenesis across multiple cancer types, identified through methods like mutation enrichment region (geMER) analysis [60].
The Correlation Hypothesis
The fundamental premise linking image phenotypes to genotypes posits that genetic alterations induce molecular changes that manifest in tissue microstructure and organization, which can be captured through quantitative imaging analysis [57]. This creates a detectable bridge between macroscopic imaging appearances and microscopic molecular events.
Experimental Design and Methodologies
Data Collection and Cohort Establishment
Comprehensive data collection forms the foundation for robust phenotype-genotype correlation studies. The following table outlines essential datasets and their specifications:
Table 1: Essential Data Modalities for Phenotype-Genotype Correlation Studies
| Data Type | Specifications | Sample Size Considerations | Preprocessing Requirements |
|---|---|---|---|
| Imaging Data | CT, MRI, or Whole-Slide Imaging (WSI); DICOM format; slice thickness ≤1.0mm [57] [25] | Minimum 591 patients for imaging features [57] | Tumor segmentation; image normalization; quality assurance |
| Genomic Data | RNA-seq (TPM normalization); Whole Genome Sequencing (WGS); targeted panels [57] [60] | Minimum 142 patients for RNA-seq [57] | TPM normalization; variant calling; quality control (e.g., TPM >1) |
| Proteomic Data | Liquid chromatography-tandem mass spectrometry (LC-MS/MS); data-independent acquisition (DIA) mode [57] | Minimum 31 patients [57] | Relative expression values >1; selection based on abundance |
| Metabolomic Data | LC-MS/MS; positive/negative ion modes [57] | Minimum 56 patients [57] | Median relative abundance >1; database matching (HMDB, Metlin) |
| Clinical Data | 73+ factors including demographics, treatment history, outcomes [57] | Minimum 159 patients with survival data [57] | Missing value imputation; standardization |
Ethical considerations require approval from institutional review boards, informed consent, and compliance with declarations such as Helsinki [57]. Data should be de-identified following standards like those discussed in the NCI workshop on DPI [25].
Image Feature Extraction Protocol
The following workflow details the image processing and feature extraction pipeline:
Image Acquisition: Obtain preoperative contrast-enhanced abdominal CT scans using standardized protocols (e.g., Siemens SOMATOM Definition AS 64-slice CT scanner) or whole-slide images for digital pathology [57] [25].
Tumor Segmentation: Manually delineate tumor regions using software such as 3D Slicer (version 4.10.2+) with verification by at least two radiologists/pathologists [57].
Feature Extraction: Utilize specialized plugins (e.g., SlicerRadiomics, SlicerImaging) to extract 854+ imaging features encompassing:
- First-order statistics
- Shape-based features in 2D and 3D
- Texture features using GLCM, GLRLM, GLSZM, NGTDM
- Wavelet-transformed features for multi-resolution analysis [57]
Feature Preprocessing: Apply Z-score normalization, handle missing values, and perform quality checks to ensure feature reliability.
Molecular Profiling and Sequencing Analysis
Molecular data generation requires standardized wet-lab protocols:
Tissue Processing: Collect tumor and adjacent normal tissues during surgery, immediately store in liquid nitrogen [57].
RNA Extraction and Sequencing:
- Extract RNA using trizol-based methods
- Perform RNA sequencing using Illumina HiSeq PE150 platform or similar
- Process transcriptomic data to transcripts per million (TPM) values
- Filter genes based on TPM >1 and match to cancer gene databases (NCG7.0, oncogene database, TSGene, Tissue-specific Gene DataBase) [57]
Pathway Enrichment Analysis:
- Conduct using "GSVA" package with reference to KEGG, REACTOME, BIOCARTA databases
- Calculate enrichment pathway scores for 283+ cancer-relevant pathways [57]
Mutation Analysis:
Integrated Analytical Framework
The correlation between image phenotypes and genotypes employs a multi-modal analytical approach:
Statistical Correlation: Calculate Spearman correlation coefficients between imaging features and molecular entities (RNAs, proteins, metabolites, pathways) using "psych" package [57].
Differential Analysis: Identify significantly different molecules across clinical phenotypes using "DESeq2" for RNA data, "limma" for protein data, and Wilcoxon test for metabolites and imaging features [57].
Survival Analysis: Evaluate association with overall survival using Kaplan-Meier curves and Cox proportional hazards models [57].
Multi-omics Integration: Combine somatic mutations, copy number variations, transcription, DNA methylation, transcription factors, and histone modifications to elucidate mechanistic relationships [60].
Diagram 1: Multi-modal Data Integration Workflow
Computational Methods and Statistical Approaches
Correlation Analysis Framework
Establishing robust correlations between image phenotypes and genotypes requires specialized statistical approaches:
Spearman Correlation Analysis:
- Implemented via "psych" package in R
- Non-parametric measure of monotonic relationships
- Appropriate for non-normally distributed imaging and molecular data
- Formula: ρ = 1 - (6∑dᵢ²)/(n(n²-1)) where dᵢ represents the difference in ranks [57]
Multiple Testing Correction:
- Apply Benjamini-Hochberg procedure to control false discovery rate (FDR)
- Significance threshold: adjusted p-value < 0.05 [57]
Multivariate Regression Models:
- Incorporate clinical covariates (age, sex, stage)
- Address confounding factors through stratified analysis
- Utilize ridge regression or LASSO for high-dimensional data
Machine Learning for Predictive Modeling
Advanced machine learning approaches enable prediction of molecular status from imaging features:
Feature Selection:
- Recursive feature elimination to identify most predictive imaging features
- Minimum redundancy maximum relevance (mRMR) for multi-modal integration
Model Training:
- Random forests for robust feature importance estimation
- Support vector machines (SVM) with radial basis function kernels
- Deep learning architectures (CNNs) for end-to-end learning from images [58]
Validation Framework:
- K-fold cross-validation (k=5 or 10) to prevent overfitting
- Independent test set validation on held-out data
- Performance metrics: AUC, accuracy, precision, recall, F1-score
AI and Deep Learning Applications
Artificial intelligence, particularly deep learning, has demonstrated remarkable capabilities in linking images to molecular subtypes:
- DeepHRD: Deep learning tool detecting homologous recombination deficiency from standard biopsy slides with 3x greater accuracy than genomic tests [58]
- Prov-GigaPath and Owkin's models: Whole-slide image analysis frameworks predicting molecular alterations from histology [58]
- MSI-SEER: AI-powered diagnostic identifying microsatellite instability-high regions in gastrointestinal tumors [58]
Key Research Reagents and Computational Tools
Table 2: Essential Research Reagents and Computational Solutions
| Category | Specific Tools/Reagents | Function/Application | Key Features |
|---|---|---|---|
| Image Analysis | 3D Slicer with SlicerRadiomics [57] | Tumor segmentation and feature extraction | Open-source; 854+ imaging features; DICOM support |
| Genomic Analysis | geMER [60] | Identification of mutation enrichment regions | Detects drivers in coding/non-coding elements; web interface available |
| Pathway Analysis | GSVA R package [57] | Gene set variation analysis | Non-parametric; unsupervised; KEGG/REACTOME/BIOCARTA |
| Multi-omics Integration | DriverNet, DawnRank [60] | Network-based driver identification | Integrates DNA + RNA data; identifies regulatory networks |
| AI/ML Platforms | DeepHRD, Prov-GigaPath, MSI-SEER [58] | AI-based genotype prediction from images | Deep learning; high accuracy; clinical validation |
| Data Management | MIPD Database [57] | Cross-modal data exploration | 9965 genes, 5449 proteins, 1121 metabolites, 854 imaging features |
Validation Strategies and Clinical Translation
Analytical Validation
Rigorous validation ensures the reliability of phenotype-genotype correlations:
Technical Validation:
- Test-retest reliability for imaging feature extraction
- Batch effect correction for molecular data
- Inter-observer agreement for tumor segmentation (Cohen's κ > 0.8)
Biological Validation:
- Functional enrichment analysis of correlated genes
- Pathway overrepresentation analysis (GO, KEGG)
- In vitro/in vivo validation of key associations
Clinical Validation
Translating findings to clinical applications requires demonstration of:
Prognostic Value:
- Survival analysis using Kaplan-Meier curves and log-rank test
- Multivariate Cox regression adjusting for clinical covariates
- Time-dependent ROC analysis for predictive accuracy
Predictive Utility:
Regulatory Considerations
Adherence to regulatory standards facilitates clinical adoption:
- FDA Clearance: Only three AI/ML tools had received FDA clearance as of 2024, highlighting validation requirements [25]
- Standardization: Adoption of DICOM standards for digital pathology imaging [25]
- Data Quality: Implementation of quality assurance protocols for both imaging and molecular data [25]
Signaling Pathways and Biological Interpretation
The biological plausibility of image-genotype correlations is strengthened when linked to cancer hallmarks and signaling pathways:
Diagram 2: Biological Pathway Correlations with Imaging Phenotypes
Key pathway correlations established in literature include:
- MAPK and PI3K/AKT/mTOR pathways: Regulation of cell proliferation correlates with texture heterogeneity on imaging [59]
- Immune response pathways: Association with tumor-infiltrating lymphocytes visible on histopathology [60] [58]
- Angiogenesis pathways: Correlation with contrast enhancement patterns on CT/MRI [57]
- DNA repair pathways: Homologous recombination deficiency detectable through DeepHRD AI analysis [58]
Applications in Drug Development and Clinical Trials
The integration of image phenotypes with genotypes offers significant opportunities for oncology drug development:
Biomarker Development
Imaging biomarkers can serve as surrogate endpoints for molecular targeted therapies:
- Predictive Biomarkers: Identify patients likely to respond to targeted therapies (e.g., PARP inhibitors for HRD-positive tumors) [58]
- Pharmacodynamic Biomarkers: Monitor early response to targeted therapies before anatomical changes occur
- Resistance Biomarkers: Detect emerging resistance mechanisms through serial imaging
Clinical Trial Optimization
Image-genotype integration enhances clinical trial design and execution:
- Patient Stratification: Enrich trial populations with specific molecular alterations using imaging prescreening
- Endpoint Acceleration: Utilize imaging surrogates for molecular responses to accelerate trial readouts
- Adaptive Design: Inform dynamic treatment allocation based on imaging and molecular profiling
Companion Diagnostic Development
Radiomic and AI-based approaches can complement or replace invasive tissue-based molecular testing:
- Non-invasive Monitoring: Track molecular evolution during treatment through serial imaging
- Tumor Heterogeneity Assessment: Capture spatial heterogeneity that may be missed by biopsy
- Multi-regional Analysis: Enable assessment of multiple tumor sites simultaneously
The correlation of image phenotypes with molecular genotypes represents a transformative approach in cancer research and clinical practice. By establishing robust computational and statistical frameworks for multi-modal data integration, researchers can uncover biologically plausible relationships between non-invasive imaging features and underlying molecular drivers. As AI technologies advance and multi-omics datasets expand, the precision and clinical utility of these correlations will continue to improve, ultimately enabling more personalized cancer diagnostics and therapeutics.
Future developments will likely focus on standardizing analytical pipelines, validating findings across diverse populations, and integrating real-world evidence from clinical practice. The continued collaboration between radiologists, pathologists, computational biologists, and oncologists will be essential to fully realize the potential of image-genotype correlations in advancing precision oncology.
The field of oncology is undergoing a data-driven transformation, propelled by advances in artificial intelligence (AI). Within this paradigm, radiomics and digital pathology have emerged as pivotal disciplines, enabling the high-throughput extraction of minable data from standard-of-care medical images and histopathological slides, respectively [61] [25]. These quantitative features, often imperceptible to the human eye, capture critical information about tumor heterogeneity, microenvironment, and pathophysiology.
When analyzed with machine learning (ML) and deep learning (DL) algorithms, this data provides non-invasive biomarkers for cancer diagnosis, prognosis, and treatment response prediction [62] [63]. This whitepaper synthesizes the current landscape of AI applications through detailed case studies in gastric, breast, and lung cancers, framing them within the broader context of precision oncology research and drug development. The integration of these tools offers a promising path toward virtual biopsy, potentially refining patient stratification for clinical trials and enabling more personalized therapeutic interventions [61] [64].
Methodological Foundations
The experimental pipeline for AI-driven analysis in radiomics and digital pathology follows a standardized workflow, encompassing data acquisition, preprocessing, feature extraction, model development, and validation [61] [25].
Core Experimental Protocol
A typical protocol for developing an AI model in this domain involves the following key stages:
Data Acquisition & Curation: For digital pathology, formalin-fixed, paraffin-embedded (FFPE) tissue sections are stained (e.g., with Hematoxylin and Eosin - H&E) and digitized into Whole Slide Images (WSIs) using high-resolution scanners [65] [66]. For radiomics, standard medical images such as CT, PET, or MRI scans are collected [61] [63]. Cohort definition is critical, requiring clear inclusion/exclusion criteria and stratification.
Annotation & Region of Interest (ROI) Segmentation: Expert pathologists or radiologists annotate the datasets. This can involve detailed pixel-level segmentation of tumors, or slide-level or WSI-level diagnostic labels (e.g., carcinoma vs. adenoma) [65] [67]. In radiomics, 3D tumor volumes are often segmented manually, semi-automatically, or fully automatically.
Preprocessing & Stain Normalization: WSIs are often partitioned into smaller image patches (e.g., 256x256 or 512x512 pixels) to manage computational load [65]. Stain normalization techniques may be applied to minimize inter-site variability introduced by different staining protocols [25]. In radiomics, image resampling and intensity normalization are common preprocessing steps.
Feature Extraction:
- Pathomics/Deep Learning: DL models, particularly Convolutional Neural Networks (CNNs) like ResNet, Inception, or DenseNet, are trained end-to-end or used as feature extractors. They automatically learn hierarchical feature representations from the image data [66] [67].
- Radiomics/Handcrafted Features: A large number of quantitative features (e.g., shape, intensity, texture) are extracted from the segmented ROIs using standardized software such as PyRadiomics [61] [68].
- Multi-modal Integration: Features from different sources (e.g., pathomics, radiomics, clinical variables) can be fused to create a more comprehensive model [62] [68].
Model Development & Training: ML classifiers (e.g., Support Vector Machines, Random Forests) or DL architectures are trained on the extracted features. Given the large size of WSIs, Multiple Instance Learning (MIL) frameworks are frequently employed, where a slide is treated as a "bag" of instances (patches) [67]. Techniques like cross-validation are used to optimize model parameters and prevent overfitting.
Validation & Interpretation: Model performance is rigorously assessed on held-out test sets and, ideally, on independent external validation cohorts from different institutions to ensure generalizability [65] [61]. Metrics such as Area Under the Curve (AUC), accuracy, sensitivity, and specificity are reported. Explainable AI (XAI) techniques, such as Gradient-weighted Class Activation Mapping (Grad-CAM), are used to visualize which regions of an image most influenced the model's decision, building trust and providing biological insights [62] [64].
The following diagram illustrates this generalized workflow, highlighting the parallel processes for digital pathology and radiomics.
Case Study 1: Gastric Cancer
Gastric cancer (GC) is the fifth most common malignancy and a leading cause of cancer-related mortality globally [65]. The application of AI in GC focuses on improving diagnostic accuracy from biopsy specimens and predicting aggressive phenotypes.
AI for Detection and Histological Classification
A primary application is the automated classification of gastric epithelial lesions from WSIs of biopsy samples. Iizuka et al. developed a CNN-based model using the Inception-v3 architecture to classify WSIs into three categories: adenocarcinoma, adenoma, and non-neoplastic [65]. The model was trained on a large dataset of 4,128 WSIs and validated on an external set of 500 WSIs, achieving an Area Under the Curve (AUC) of 0.974 and 0.924, respectively, demonstrating robust generalizability [65]. Similarly, a study by Abe et al., which utilized a GoogLeNet-based DL system to diagnose gastric biopsies from 10 different institutes, reported an accuracy of 91.3% on a validation cohort of 3,450 samples [65]. These models highlight the potential of AI to serve as a highly sensitive screening tool, alleviating the workload of pathologists.
Table 1: Performance of Deep Learning Models in Gastric Cancer Detection and Classification from Histopathology Images
| Study (Year) | AI Model | Task | Dataset Size (WSIs) | Performance Metrics |
|---|---|---|---|---|
| Iizuka et al. (2020) [65] | Inception-v3 | Classify ADC, adenoma, non-neoplastic | 4,128 (Training) | AUC: 0.980 (Internal) |
| 500 (External) | AUC: 0.974 (External) | |||
| Abe et al. (2022) [65] | GoogLeNet (CNN) | Diagnose normal vs. carcinoma | 4,511 (Training) | Accuracy: 91.0% (Internal) |
| 3,450 (External) | Accuracy: 94.6% (External) | |||
| Fan et al. (2022) [65] | ResNet-50 | Japanese 'Group Classification' | 260 (Training) | Accuracy: 93.2%, AUC: 0.994 |
| Song et al. (2020) [65] | DeepLab v3 | Segment malignant vs. benign | 2,123 (Training) | AUC: 0.945 |
Prediction of Metastatic Potential
A critical challenge in managing advanced GC is the detection of occult peritoneal metastases, which conventional CT imaging often misses. Dong et al. developed a radiomic nomogram that integrated features from both the primary tumor and the peritoneal region on CT scans [62]. This approach, rooted in the "seed and soil" hypothesis of metastasis, achieved exceptional performance with AUCs of 0.958 in the training cohort and 0.928-0.941 in multi-center external validation cohorts [62]. Advancements include deep learning models like the Peritoneal Metastasis Network, which outperformed conventional clinicopathological factors and could identify metastases missed by radiologists [62].
Case Study 2: Breast Cancer
Breast cancer management relies heavily on accurate histopathological grading and biomarker assessment. AI is revolutionizing this space by introducing objectivity and reproducibility into these processes [66] [69].
AI in Histological Grading and Biomarker Quantification
The Nottingham Histologic Grade system is a key prognostic factor but suffers from significant inter-observer variability. AI models are now adept at deconstructing and automating its components. DL models can stratify intermediate-grade (NHG 2) tumors into groups with prognoses similar to NHG 1 and NHG 3, providing more precise risk stratification [69]. For biomarker evaluation, AI tools have been developed to predict the status of crucial markers like HER2, Estrogen Receptor (ER), and Progesterone Receptor (PR) directly from H&E-stained slides, potentially reducing the need for additional costly assays [66] [69].
Table 2: AI Applications in Breast Cancer Digital Pathology: Tasks and Performance
| Task | AI Model / Method | Key Findings / Performance | Reference |
|---|---|---|---|
| Tumor Grading | DL (DeepGrade) | Provided independent prognostic information (HR=2.94) on 1,567 patients. | [66] |
| TILs Assessment | CNN (QuPath) | TIL variables showed significant prognostic association with outcomes in 920 TNBC patients. | [66] |
| Nuclear Grade Assessment | DL | Stratified NHG 2 tumors into low/high-risk groups with prognoses mirroring NHG 1/NHG 3. | [69] |
| Mitosis Counting | DL | Demonstrated superior accuracy, precision, and sensitivity over manual methods. | [69] |
| Molecular Subtype Prediction | Deep Learning Radiomics (DLRN) | Integrated PA/US images and clinical data to predict luminal vs. non-luminal subtypes (AUC: 0.924). | [68] |
Protocol: Predicting Molecular Subtypes from Multi-Modal Imaging
A pioneering study by Lan et al. exemplifies the power of multi-modal AI. They developed a Deep Learning Radiomics integrated model to preoperatively distinguish between luminal and non-luminal breast cancer subtypes using photoacoustic/ultrasound imaging [68].
Detailed Methodology:
- Patient Cohort: 388 breast cancer patients were retrospectively enrolled, split into 271 for training and 117 for testing.
- Image Acquisition: Patients underwent PA/US examination using a handheld linear array probe (L9-3PAU) on a Resona 7 platform. PA imaging was performed at 750 nm and 830 nm to quantify oxygen saturation (SO₂).
- Feature Extraction:
- Radiomics Features: 1,309 handcrafted features were extracted from the PA/US images using PyRadiomics software.
- Deep Learning Features: 2,048 deep features were extracted using a pre-trained ResNet50 CNN.
- Feature Selection & Model Building: Independent sample t-tests, Pearson correlation analysis, and LASSO regression were used to select the most predictive features. A Deep Learning Radiomics model was built, which was subsequently combined with significant clinical features (age, menopausal status, BMI) to form the final DLRN model using multivariate logistic regression.
- Validation: The model was evaluated on the independent test set, where it significantly outperformed models based on clinical features, radiomics, or deep learning alone [68].
Case Study 3: Lung Cancer
Lung cancer, a leading cause of cancer mortality, benefits from AI applications across the entire clinical spectrum, from screening and diagnosis to treatment personalization [61] [63] [64].
AI-Enhanced Screening and Diagnostic Characterization
In screening, deep learning models have demonstrated superior performance in detecting lung nodules on low-dose CT (LDCT) scans. A model developed by Google AI analyzed current and prior CT scans, achieving an AUC of 94.4% and reducing false positives and false negatives by 11% and 5%, respectively, compared to radiologists [64]. Another model, Sybil, showed remarkable capability in predicting future lung cancer risk from a single LDCT scan, with an AUC of 0.92 for 1-year risk prediction [64].
Beyond detection, radiomics enables non-invasive genomic profiling. AI models can predict the status of key driver mutations, such as EGFR and ALK, directly from CT images, effectively acting as a "virtual biopsy" [61] [64]. This can potentially guide treatment decisions while awaiting results from invasive tissue sampling or genetic testing.
Protocol: Predicting EGFR Mutation Status from CT Images
Predicting EGFR mutation status from routine CT scans is a well-established application of radiomics in NSCLC [64].
Detailed Methodology:
- Cohort & Imaging Data: A retrospective cohort of pathologically confirmed NSCLC patients with pre-treatment CT scans and confirmed EGFR mutation status (e.g., via NGS or PCR) is assembled. The cohort is split into training and validation sets.
- Tumor Segmentation: The 3D volumetric region of interest encompassing the primary lung tumor is manually segmented by expert radiologists on the CT scans slice-by-slice. This step is critical and often a major source of variability.
- Radiomic Feature Extraction: Thousands of quantitative features describing tumor intensity, shape, and texture (e.g., Gray-Level Co-occurrence Matrix features) are extracted from the segmented volume using a standardized software platform like PyRadiomics.
- Model Development and Validation:
- Handcrafted Radiomics: After feature reduction (using methods like LASSO), an ML classifier (e.g., Random Forest or SVM) is trained to predict EGFR mutation status.
- Deep Learning: Alternatively, an end-to-end CNN or a multiple-instance learning framework can be trained directly on the image patches or segments to predict the genetic alteration.
- Performance & Interpretation: The model's performance is evaluated using AUC, sensitivity, and specificity on the hold-out test set. Grad-CAM techniques can be applied to visualize the regions within the tumor that the model found most predictive, which may correspond to areas of specific histopathological features associated with the mutation [64].
Table 3: AI Applications in Lung Cancer: From Screening to Molecular Prediction
| Application Domain | Exemplar Model/Study | Data Modality | Reported Performance |
|---|---|---|---|
| Nodule Detection/Screening | Google AI Model [64] | LDCT (with prior scans) | AUC: 94.4%, reduced FPs/FNs |
| Future Risk Prediction | Sybil [64] | Single LDCT Scan | 1-year AUC: 0.92; 6-year AUC: 0.75 |
| Histology Subtype Classification | Radiomics/CNN [61] | CT Scan | Differentiate adenocarcinoma vs. squamous cell carcinoma |
| EGFR Mutation Prediction | Radiomics/DL Models [64] | CT Scan | High predictive accuracy (AUC >0.8 in multiple studies) |
| PD-L1 Expression Prediction | Radiomics/Pathomics [64] | CT Scan / H&E Slide | Guides immunotherapy decisions |
The Scientist's Toolkit: Essential Research Reagents & Materials
The following table details key reagents, software, and platforms essential for conducting research in AI-based radiomics and digital pathology.
Table 4: Essential Research Reagents and Solutions for AI in Cancer Diagnostics
| Category | Item / Solution | Specific Example / Vendor | Critical Function in Research |
|---|---|---|---|
| Tissue Processing & Staining | H&E Staining Kit | Various (e.g., Sigma-Aldrich) | Standard histological staining for morphological assessment on WSIs. |
| IHC Staining Kit / Antibodies | Dako, Roche Ventana | Detection of protein biomarkers (e.g., HER2, PD-L1). | |
| Digital Pathology Hardware | Whole Slide Scanner | Philips Ultrafast, Leica Aperio, Hamamatsu NanoZoomer | Converts glass slides into high-resolution digital WSIs for analysis. |
| Image Analysis Software | Digital Image Analysis Platform | QuPath, Halo, Visiopharm | Open-source/commercial software for manual annotation and automated analysis. |
| Radiomics Feature Extraction | Standardized Feature Extraction Software | PyRadiomics | Open-source Python library for extracting a large set of handcrafted radiomic features. |
| AI/ML Development | Deep Learning Frameworks | TensorFlow, PyTorch | Open-source libraries for developing and training custom CNN and DL models. |
| Pre-trained CNN Models | ResNet50, Inception-v3, VGG-16 | Models for transfer learning, used as feature extractors or fine-tuned for specific tasks. | |
| Data & Compute | Cloud Computing Platform | AWS, Google Cloud, Azure | Provides scalable GPU resources for training complex DL models on large datasets. |
| Publicly Available Datasets | The Cancer Genome Atlas (TCGA) | Provides large, often annotated, multi-omics datasets for model training and validation. |
The case studies in gastric, breast, and lung cancers underscore a consistent theme: AI-powered radiomics and digital pathology are transitioning from research curiosities to indispensable tools in oncological research and drug development. These technologies provide a robust, quantitative framework for deciphering tumor biology from routine data, enabling tasks ranging from precise histological classification and grading to non-invasive prediction of molecular features.
The future of this field lies in the development of multi-modal, explainable AI systems that can seamlessly integrate pathomic, radiomic, genomic, and clinical data. This integrated approach will provide a holistic view of the tumor, crucial for advancing precision oncology. However, for this potential to be fully realized, challenges such as data standardization, model generalizability across diverse populations, and seamless integration into clinical and research workflows must be addressed through large-scale, multi-institutional collaborative efforts [62] [25] [64].
Navigating the Challenges: Technical Hurdles and Optimization Strategies
The integration of radiomics and digital pathology into cancer diagnostics represents a paradigm shift in precision oncology. However, the clinical translation of these promising technologies is significantly hampered by data heterogeneity, which undermines the robustness and reproducibility of quantitative imaging biomarkers. This technical review examines the multifaceted nature of data heterogeneity across imaging protocols, segmentation variability, feature extraction methodologies, and statistical modeling approaches. We synthesize current evidence on reproducibility challenges and present standardized frameworks, experimental protocols, and computational strategies to enhance reliability across multi-institutional studies. Within the broader thesis of advancing cancer diagnostics, this review provides researchers, scientists, and drug development professionals with practical methodologies to overcome critical bottlenecks in biomarker validation and clinical implementation.
Radiomics, defined as the high-throughput extraction of quantitative features from medical images, converts standard medical images into mineable data by applying numerous automated feature-characterization algorithms [70]. This approach aims to uncover tumor characteristics that may not be visually apparent, serving as non-invasive biomarkers for clinical decision-making in cancer diagnostics. Similarly, digital pathology enables quantitative analysis of tissue morphology through whole-slide imaging and computational approaches. The convergence of these fields with artificial intelligence (AI) analytics promises to transform cancer research by providing multidimensional views of tumor biology that capture both morphological nuances and molecular heterogeneity [71].
Despite remarkable potential, both fields face a significant challenge: the robustness and reproducibility of extracted features are substantially impacted by data heterogeneity arising from multiple sources. In radiomics, this includes variations in imaging parameters, reconstruction algorithms, segmentation methodologies, and feature calculation techniques [70] [72] [73]. This variability is particularly problematic in high-dimensional datasets where the number of features vastly exceeds the number of samples, increasing the risk of identifying spurious patterns and producing false-positive results [70]. Similar challenges affect digital pathology, where staining protocols, scanner variations, and tissue processing introduce pre-analytical variability that impacts downstream AI analysis.
Addressing these challenges is crucial for clinical translation. As noted in recent assessments, "radiomics is impeded by imaging and statistical reproducibility issues" that limit the interpretability and clinical utility of predictive models [70]. This review systematically addresses these challenges by providing experimental frameworks and methodological standards to enhance robustness across the entire analytical pipeline.
Imaging Acquisition and Reconstruction Variability
Medical imaging data are inherently heterogeneous due to differences in acquisition protocols, scanner manufacturers, and reconstruction parameters. This variability directly impacts radiomic feature stability through multiple mechanisms:
Scanner and Protocol Differences: Variations in CT tube current, reconstruction kernels, magnetic resonance imaging (MRI) sequence parameters, and positron emission tomography (PET) reconstruction algorithms introduce significant variability in feature measurements [70] [73]. Studies have demonstrated that inconsistent signal-to-noise ratio (SNR) and unintended outliers can dramatically alter first-order radiomic features by changing histogram distributions [72].
Reconstruction Parameter Effects: The choice of reconstruction algorithm substantially influences feature reliability. In brain PET imaging, reblurred Van Cittert (RVC) and Richardson-Lucy (RL) methods demonstrated the best reproducibility, with over 60% of features maintaining coefficient of variation (COV) < 25% and intraclass correlation coefficient (ICC) ≥ 0.75, while multi-target correction (MTC) and parallel level set (PLS) methods resulted in the highest variability [74].
Voxel Size and Spatial Resolution: The reconstructed voxel size and spatial resolution of different cameras critically affect higher-order radiomic features, with conventional indices like SUVpeak and SUVmean proving most reliable (CV < 10%) across different devices [75].
Segmentation and Preprocessing Inconsistencies
Region of interest (ROI) segmentation represents another major source of variability through both inter- and intra-rater delineation differences. The manual segmentation process is inherently subjective, with studies demonstrating that even expert delineations can vary substantially, directly impacting extracted feature values [70]. Additionally, preprocessing approaches—including image normalization, discretization parameters, and filtering operations—significantly influence feature stability:
Discretization Parameters: Variations in quantization range and bin number alter probability distributions in texture matrices (GLCM, GLRLM), consequently affecting derived feature values [72]. One study found that with high SNR and no outliers, all first-order radiomic features showed acceptable reliability, whereas inconsistent SNR and outlier conditions dramatically reduced reliability [72].
Filtering Operations: The application of preprocessing filters (e.g., wavelet, Laplacian of Gaussian) introduces additional variability, particularly when different parameter settings are employed across institutions [76]. The non-linear effects of these operations can render radiomic features highly non-reproducible across sites [70].
Table 1: Impact of Imaging Parameters on Radiomic Feature Robustness
| Parameter Category | Specific Parameters | Impact on Feature Robustness | Most Affected Feature Classes |
|---|---|---|---|
| Acquisition | Tube current (CT), sequence parameters (MRI), SNR | High impact; low SNR increases feature variability | First-order statistics, GLRLM features |
| Reconstruction | Algorithm, voxel size, kernel | Algorithm choice significantly affects reproducibility | Higher-order texture features |
| Segmentation | Inter-observer variability, method (manual vs. auto) | Major impact; different segmentations yield different features | Shape features, all texture classes |
| Preprocessing | Discretization (bin number), normalization, filtering | Moderate to high impact depending on parameters | GLCM, GLSZM, NGTDM features |
Quantitative Assessment of Feature Reproducibility
Metrics for Evaluating Robustness
Systematic assessment of feature reproducibility requires standardized metrics that can quantify different aspects of robustness:
Intraclass Correlation Coefficient (ICC): Measures agreement or consistency between repeated measurements, with ICC ≥ 0.75 typically indicating acceptable reliability [72] [74]. In brain PET studies, ICC values varied significantly across brain regions, with cerebellum and lingual gyrus showing highest reproducibility (ICC ≥ 0.9) while fusiform gyrus and brainstem showed poor reproducibility (ICC < 0.5) [74].
Coefficient of Variation (COV): Quantifies the ratio of standard deviation to mean, with COV < 15-25% typically considered acceptable depending on application [72] [74]. However, one phantom study noted that low COV values do not necessarily indicate robust parameters but may instead reflect insensitive radiomic indices [75].
Concordance Correlation Coefficient (CCC): Assesses agreement between two measures of the same variable, often used in test-retest scenarios [77].
Jaccard Index (JI) and Dice-Sorensen Index (DSI): Evaluate stability of feature selection methods by measuring overlap between selected feature sets [76].
Reproducibility Profiles Across Feature Classes
Different classes of radiomic features exhibit distinct reproducibility characteristics under varying imaging conditions:
Table 2: Feature Class Reproducibility Across Imaging Modalities
| Feature Class | CT Reproducibility | PET Reproducibility | Most Stable Subtypes | Key Influencing Factors |
|---|---|---|---|---|
| First-Order Statistics | High (with optimal SNR) | Moderate | Mean, entropy | SNR, outlier inclusion, quantization |
| GLCM | Moderate to high | High in brain PET | Contrast, homogeneity, entropy | Bin number, quantization range |
| GLRLM | Moderate | Variable | Short-run emphasis | Reconstruction method, SNR |
| GLDM | Limited data | High in brain PET | Dependence entropy | PVC method, region anatomy |
| Shape Features | High | Limited applicability | Volume, sphericity | Segmentation consistency |
| NGTDM | Moderate | Low in brain PET | Coarseness | Noise levels, reconstruction |
Evidence suggests that Gray Level Co-occurrence Matrix (GLCM) and Gray Level Dependence Matrix (GLDM) features tend to be the most stable across different imaging conditions, while First Order and Neighborhood Gray Tone Difference Matrix (NGTDM) features are generally most variable [74]. The robustness of specific features is highly dependent on anatomical region, with cerebellum and lingual gyrus demonstrating highest reproducibility in brain PET studies [74].
Methodological Frameworks for Enhanced Reproducibility
Standardized Image Acquisition and Harmonization
Implementing standardized imaging protocols across institutions is fundamental for reducing variability. When protocol standardization is not feasible, computational harmonization techniques can mitigate batch effects:
Protocol Standardization: Establishing consensus guidelines for image acquisition parameters, reconstruction algorithms, and quality control procedures minimizes technical variability. The Image Biomarker Standardisation Initiative (IBSI) provides standardized definitions for radiomic feature calculation to ensure consistency across software platforms [76] [76].
ComBat Harmonization: This empirical Bayes method effectively removes inter-site variability by adjusting for batch effects, though it requires access to raw imaging data and can be challenging to implement in multi-institutional settings [76].
Phantom-Based Harmonization: Using physical phantoms with reproducible uptake patterns, such as the "activity painting" phantom technique, enables cross-scanner calibration and validation of radiomic feature stability [75].
Advanced Feature Selection Strategies
Conventional feature selection methods often yield unstable feature sets when applied across different preprocessing settings or cross-validation splits. Recent advances address this limitation:
Graph-Based Feature Selection (Graph-FS): This novel approach constructs a feature similarity graph where nodes represent radiomic features and edges encode statistical similarities (e.g., Pearson correlation). Features are grouped into connected components, with the most representative nodes selected using centrality measures such as betweenness centrality [76]. In multi-institutional validation, Graph-FS achieved significantly higher stability (JI = 0.46, DSI = 0.62) compared to conventional methods like Boruta (JI = 0.005), Lasso (JI = 0.010), RFE (JI = 0.006), and mRMR (JI = 0.014) [76].
Stability-Enhanced Selection: Integrating feature stability metrics directly into the selection process improves generalizability. Methods such as Kendall's W can identify and retain consistently performing features across different parameter configurations [76].
Graph-FS Methodology: A graph-based approach to stable feature selection
Experimental Design for Reproducibility Assessment
Robust evaluation of methodological stability requires carefully designed experimental protocols:
Test-Retest Studies: Acquiring repeated images of the same subject under identical conditions assesses intrinsic feature variability. For practical reasons, nearby image slices can simulate test-retest scenarios when true rescanning is not feasible [77].
Multi-Parameter Configuration Testing: Systematically varying preprocessing parameters (e.g., normalization scales, discretized gray levels, outlier removal thresholds) evaluates feature stability across technically diverse conditions [76]. One comprehensive study applied 36 different radiomics parameter configurations to simulate real-world variability [76].
Phantom Validation: Using physical phantoms with known ground truth patterns, such as the "activity painting" approach in radioactive environments, enables precise assessment of how imaging parameters affect radiomic feature values [75].
Table 3: Essential Resources for Reproducible Radiomics Research
| Resource Category | Specific Tools/Standards | Function/Purpose | Implementation Considerations |
|---|---|---|---|
| Feature Standardization | IBSI Reference Manual | Standardized feature definitions | Verify software compliance with IBSI standards |
| Feature Extraction | PyRadiomics (v3.0+) | Open-source feature extraction | IBSI-compliant, Python integration |
| Phantom Systems | "Activity painting" phantoms | Scanner harmonization | Customizable heterogeneity patterns |
| Harmonization Tools | ComBat, GFSIR Package | Multi-site batch effect correction | Requires raw data access for ComBat |
| Quality Metrics | ICC, COV, Jaccard Index | Reproducibility quantification | Context-dependent threshold selection |
| Reporting Guidelines | CLEAR, METRICS | Methodological quality assessment | Ensure comprehensive study reporting |
Rethinking Reproducibility: Beyond Individual Feature Stability
Conventional approaches to reproducibility focus heavily on the stability of individual features, but emerging evidence suggests this perspective may be limited. A provocative hypothesis proposes that "nonreproducible features can contribute significantly to predictive performance" when considered collectively within multivariate models [77]. This concept draws an analogy to the parable of blind men examining an elephant - each perceives only a part of the whole reality.
Experimental evidence demonstrates that removing features classified as "nonreproducible" based on test-retest assessment can sometimes decrease model accuracy rather than improve it [77]. In one experiment using four different radiomics datasets, nonreproducible features actually outperformed reproducible ones for certain cancer types, particularly at specific reproducibility thresholds [77]. This suggests that predictive information may be distributed across multiple features rather than confined to individually stable ones.
This paradigm shift has important implications for radiomic research:
- Holistic Assessment: Rather than filtering features based solely on individual stability, researchers should consider how feature ensembles collectively capture biological information.
- Model-Level Reproducibility: The ultimate metric should be the reproducibility of clinical predictions rather than individual feature stability.
- Dynamic Thresholds: Reproducibility thresholds should be context-dependent rather than universally applied.
Reproducibility Paradigms: Comparing traditional and ensemble approaches
Ensuring robustness and reproducibility in radiomics and digital pathology requires a systematic, multifaceted approach that addresses data heterogeneity throughout the entire analytical pipeline. Key strategies include standardizing image acquisition protocols, implementing advanced feature selection methods like Graph-FS, conducting comprehensive reproducibility assessments using appropriate metrics, and adopting a more nuanced perspective on feature stability that considers ensemble performance rather than individual feature reproducibility.
The integration of computational harmonization techniques, phantom validation systems, and standardized reporting frameworks will accelerate the translation of radiomic biomarkers into clinical practice. As these fields evolve within the broader context of cancer diagnostics, maintaining rigorous methodological standards while embracing innovative analytical approaches will be essential for realizing the full potential of quantitative imaging biomarkers in precision oncology.
Future efforts should focus on developing more sophisticated stability metrics that account for feature interactions, establishing larger multi-institutional datasets with standardized imaging protocols, and creating validated reference standards for cross-platform harmonization. Through collaborative efforts across institutions and disciplines, the field can overcome current reproducibility challenges and deliver on the promise of robust, clinically impactful imaging biomarkers.
In the rapidly evolving fields of radiomics and digital pathology, high-dimensional data extracted from medical images and tissue samples presents both unprecedented opportunities and significant challenges for cancer diagnostics research. The curse of dimensionality—where an excessive number of features hampers model performance—manifests through data sparsity, distance metric instability, and heightened risk of overfitting, particularly problematic in preclinical studies with limited sample sizes. This technical guide examines the theoretical foundations of dimensionality challenges and provides validated methodologies for feature selection and regularization tailored to oncological research. By integrating experimental protocols from recent studies and presenting quantitative comparisons of technique efficacy, this review serves as an essential resource for researchers and drug development professionals navigating high-dimensional data landscapes in cancer diagnostics.
The Curse of Dimensionality: Theoretical Foundations
The "curse of dimensionality," a term first coined by Richard E. Bellman in the 1960s, refers to the various phenomena that arise when analyzing and organizing data in high-dimensional spaces that do not occur in low-dimensional settings [78]. In oncology research, this curse manifests when the number of features (dimensions) becomes excessively large relative to the number of observations (patient samples), leading to fundamental challenges in data analysis and model development.
The core issue stems from the exponential growth of available space as dimensions increase. In high-dimensional spaces, data points become sparse and dissimilar in many dimensions, making it difficult to find meaningful patterns [79]. This sparsity negatively impacts machine learning algorithms that rely on distance metrics, as the concept of proximity becomes less meaningful. In radiomics, where hundreds of quantitative features can be extracted from a single medical image, and in digital pathology, where whole-slide images generate millions of data points, these challenges are particularly acute [80] [48].
Context in Radiomics and Digital Pathology
Radiomics involves extracting mineable, high-dimensional data from medical images such as CT, MRI, PET, and SPECT scans, converting images into quantitative features that can be correlated with clinical outcomes [80]. Similarly, digital pathology leverages whole-slide imaging and AI tools to analyze tissue samples at scale, detecting patterns that may elude human observation [48] [81]. Both fields generate extensive feature sets that far exceed typical sample sizes, especially in preclinical studies where animal cohorts are often limited.
The bias-variance tradeoff becomes critically important in these contexts. As model complexity increases with additional features, models may achieve perfect fit on training data but fail to generalize to unseen data—a phenomenon known as overfitting [80]. This is especially problematic in medical research, where models must maintain diagnostic or prognostic accuracy when applied to new patient populations or imaging protocols.
Manifestations in Radiomics and Digital Pathology
Data Sparsity and Distance Metric Instability
In high-dimensional spaces, data points become increasingly isolated, residing sparsely within the vast feature space. This sparsity undermines the fundamental assumptions of many machine learning algorithms. For distance-based algorithms like k-nearest neighbors, the concept of "nearest" neighbors becomes less meaningful as all pairwise distances converge to similar values [78]. Research demonstrates that as dimensionality increases, the difference between maximum and average distances diminishes significantly, with the normalized difference approaching zero in very high dimensions [78].
This distance convergence has direct implications for cancer research. In radiomics, tumor subtyping based on feature similarity becomes less reliable. In digital pathology, content-based image retrieval systems that identify similar histopathological patterns struggle as discrimination between tissue classes diminishes. The table below quantifies this phenomenon through simulated distance metrics across increasing dimensions:
Table 1: Distance Metric Behavior Across Dimensions (Simulated Data from 500 Points in [0,1]^d Hypercube)
| Dimensions | Mean Pairwise Distance | Std Dev Pairwise Distance | Normalized Difference (Max-Mean)/Max |
|---|---|---|---|
| 3 | 0.52 | 0.15 | 0.38 |
| 10 | 1.25 | 0.17 | 0.22 |
| 50 | 2.89 | 0.18 | 0.09 |
| 100 | 4.08 | 0.18 | 0.05 |
Overfitting in Preclinical Radiomics Studies
Preclinical radiomics research faces particular challenges with dimensionality due to limited animal cohort sizes combined with extensive feature extraction. A review of preclinical radiomics studies revealed sample sizes ranging from just 1 to 91 animals, while the number of extracted radiomic features often exceeds 100 [80]. This creates a dimensionality ratio that strongly predisposes models to overfitting.
The problem is exacerbated by the multiple timepoints often collected in longitudinal studies, further increasing feature dimensionality without proportionally increasing independent samples. One study investigating texture features in mouse liver tumor growth used 10 mice across 5 timepoints, effectively creating 50 data points [80]. However, temporal correlation between measurements from the same animal violates the assumption of independence, effectively reducing the true sample size and worsening the dimensionality problem.
Diagram 1: High dimensionality leads to overfitting
Methodologies for Dimensionality Reduction and Feature Selection
Conventional Feature Selection Techniques
Feature selection methods identify and retain the most informative features while discarding redundant or irrelevant ones, directly reducing dimensionality without transforming the original feature space. Multiple approaches have been validated in radiomics and digital pathology contexts:
Filter Methods employ statistical measures to rank features according to their correlation with outcomes, independent of any specific model. Common techniques include variance thresholding (removing constant or near-constant features), univariate statistical tests (SelectKBest with f_classif), and correlation-based feature selection [82]. These methods are computationally efficient but may miss feature interactions.
Wrapper Methods evaluate feature subsets using model performance as the evaluation metric. Examples include recursive feature elimination and forward/backward selection. While potentially more accurate than filter methods, they are computationally intensive, especially with high-dimensional starting points [83].
Embedded Methods integrate feature selection within the model training process. Regularization techniques like Lasso (L1) and Ridge (L2) regression automatically perform feature selection by penalizing coefficient magnitudes, driving less important feature weights toward zero [79]. Tree-based methods like Random Forests provide intrinsic feature importance measures.
Feature Extraction Approaches
Feature extraction techniques transform original features into a lower-dimensional space while preserving essential information. Unlike feature selection, these methods create new features that are combinations of the original ones:
Principal Component Analysis (PCA) is the most widely used linear dimensionality reduction technique. PCA identifies orthogonal axes of maximum variance in the data, projecting features onto a reduced set of uncorrelated principal components [84]. Studies demonstrate that PCA can improve model accuracy while significantly reducing computational demands; one analysis showed accuracy improvement from 0.8745 to 0.9236 after applying PCA to a high-dimensional dataset [82].
Nonlinear Techniques including t-distributed Stochastic Neighbor Embedding (t-SNE) and Uniform Manifold Approximation and Projection (UMAP) are particularly valuable for visualizing high-dimensional pathology data in two or three dimensions while preserving local structure [85]. These methods can reveal clusters and patterns that might inform biological insights.
Domain-Specific Selection Methods
Genomics-Informed Feature Selection represents an innovative approach that leverages biological knowledge to guide radiomics feature selection. In a study on esophageal squamous cell carcinoma (ESCC), researchers used differentially expressed genes between patients with and without relapse to select radiomic features correlated with these genomic markers [86]. This methodology produced a more robust prognostic model than purely data-driven selection, with the genomics-informed radiomic signature achieving areas under the curve of 0.912, 0.852, and 0.769 in training, internal test, and external test sets, respectively [86].
Heuristic Radiomics Feature Selection represents another specialized approach. One study proposed a method based on frequency iteration and multi-supervised training that decomposed all features layer by layer to select optimal features for each layer, then fused them to form a local optimal group [83]. This approach reduced the number of required features from approximately ten to three while maintaining or improving classification accuracy [83].
Table 2: Performance Comparison of Feature Selection Methods in Cancer Research
| Method | Application Context | Features Before | Features After | Performance Metric | Result |
|---|---|---|---|---|---|
| Genomics-Informed [86] | ESCC Prognosis | 100+ | Not specified | AUC (5-year DFS) | 0.769-0.912 |
| Heuristic Frequency Iteration [83] | General Radiomics | ~10 | ~3 | Classification Accuracy | Maintained/Improved |
| PCA + Random Forest [82] | Semiconductor Manufacturing | 50+ | 10 | Accuracy | 0.8745→0.9236 |
| L1 Regularization [79] | General High-Dimensional Data | 1000+ | Varies | Generalization Error | Significant Reduction |
Experimental Protocols and Workflows
Integrated Radiomics Pipeline with Dimensionality Control
A standardized radiomics pipeline incorporates multiple stages where dimensionality considerations are critical. The following workflow represents current best practices in preclinical and clinical radiomics research:
Diagram 2: Radiomics pipeline with dimensionality risk
Image Acquisition and Preprocessing: Standardized imaging protocols are essential to minimize technical variation. Preprocessing steps include artifact correction, image registration for multi-modal studies, intensity normalization, and noise reduction [80]. These steps reduce non-biological variance that could otherwise be captured as spurious features.
Region of Interest (ROI) Segmentation: Manual, semi-automated, or fully automated segmentation delineates tumors or pathologies. Common tools include 3D Slicer, ITK-SNAP, and deep learning-based algorithms [80]. Multiple segmentations by different radiologists with intra-class correlation coefficient (ICC) calculation helps assess feature robustness.
Feature Extraction: Using standardized software like PyRadiomics (Python-based) ensures consistency and reproducibility [80]. Features typically include shape-based descriptors (tumor sphericity, surface area), first-order statistics (intensity histogram features), and texture features (capturing heterogeneity patterns).
Dimensionality Reduction and Analysis: The critical stage where feature selection and extraction methods are applied prior to model building. Studies should report specific parameters for reproducibility, including binning methods, normalization approaches, and selection criteria.
Digital Pathology AI Workflow
In digital pathology, whole-slide images are processed through a multi-stage pipeline:
Tissue Preparation and Scanning: Standardized tissue processing and staining followed by high-resolution slide scanning creates digital whole-slide images.
Patch Extraction and Feature Learning: Due to the enormous size of whole-slide images (gigapixels), images are typically divided into smaller patches. Convolutional neural networks (CNNs) then extract relevant features from these patches, either through predefined architectures or deep learning [48].
Feature Selection and Aggregation: Patch-level features are aggregated to slide-level predictions. Dimensionality reduction is often necessary at this stage to create manageable feature sets for classification tasks.
Integration with Multi-Omics Data: Advanced workflows integrate pathology features with genomic, transcriptomic, and clinical data, requiring careful dimensionality management across modalities [81].
Research Reagents and Computational Tools
Implementing effective dimensionality reduction strategies requires both computational tools and methodological frameworks. The following table summarizes key resources mentioned in recent literature:
Table 3: Essential Research Reagents and Computational Tools
| Tool/Resource | Type | Primary Function | Application Context |
|---|---|---|---|
| PyRadiomics [80] | Open-source Python package | Standardized radiomic feature extraction | Clinical and preclinical radiomics |
| 3D Slicer [80] | Open-source software platform | Image visualization and segmentation | Multi-modal imaging data |
| ITK-SNAP [80] | Specialized software | Manual and semi-automated segmentation | ROI delineation in 3D images |
| Scikit-learn [82] | Python library | Feature selection and dimensionality reduction | General machine learning applications |
| ComBat [86] | Statistical method | Batch effect correction and feature harmonization | Multi-center study normalization |
| MSIntuit [48] | AI software | MSI detection from H&E slides | Digital pathology biomarker discovery |
| GI Genius [48] | CADe system | Real-time polyp detection during colonoscopy | Colorectal cancer screening |
Discussion and Future Directions
The integration of biological knowledge into feature selection processes represents a promising direction for addressing dimensionality challenges in cancer research. Genomics-informed radiomics feature selection has demonstrated that leveraging domain knowledge can produce more robust and interpretable models than purely data-driven approaches [86]. Similarly, in digital pathology, connecting morphological features with molecular subtypes creates opportunities for biologically grounded dimensionality reduction.
Future methodological developments should focus on hybrid approaches that combine the strengths of filter, wrapper, and embedded methods while incorporating biological constraints. As deep learning continues to advance, attention must be paid to the unique dimensionality challenges in these models, particularly in transfer learning and domain adaptation scenarios common in medical applications where labeled data is scarce.
For the research community, standardization of radiomics and digital pathology pipelines remains crucial for reproducibility. Reporting of feature selection parameters, preprocessing steps, and validation protocols should follow established guidelines to enable proper evaluation and comparison across studies. Only through rigorous attention to dimensionality challenges can we fully realize the potential of high-dimensional data in advancing cancer diagnostics and therapeutics.
In the fields of radiomics and digital pathology for cancer diagnostics, the tension between methodological ambition and data availability represents a fundamental challenge. The development of robust, generalizable predictive models is intrinsically linked to sample size, a resource often scarce in medical research. Radiomics, which involves extracting high-dimensional quantitative features from medical images for predictive modeling, particularly suffers from what statisticians call the "small n-to-p" problem—where the number of predictors (p) far exceeds the number of independent samples (n) [87]. This phenomenon introduces critical challenges including data sparsity, overfitting, and inflated false-positive rates, ultimately compromising model generalizability.
The generalizability of a study refers to whether its results can be reliably applied to different settings or populations, a quality also known as external validity [87]. In contrast, reproducibility—encompassing imaging data, segmentation, and computational processes—forms the foundation of internal validity [87]. Without addressing both reproducibility and sufficient sample size, even the most sophisticated radiomics or digital pathology models will fail in real-world clinical implementation, limiting their utility in drug development and clinical decision-making.
Quantitative Assessment of the Sample Size Problem
Systematic reviews of the prediction model literature reveal a pervasive neglect of sample size considerations across medical research. The data demonstrates that most studies are developed with insufficient samples, fundamentally limiting their reliability and generalizability.
Table 1: Sample Size Deficits in Prediction Model Studies
| Study Focus | Studies with Sample Size Justification | Studies Meeting Minimum Sample Requirements | Median Deficit in Events | Key References |
|---|---|---|---|---|
| Oncology ML Prediction Models | 1/36 (2.8%) | 5/17 (29.4%) able to calculate requirements | 302 participants with the event | [88] |
| Binary Outcome Prediction Models | 9/119 (7.6%) | 27% (of 94 studies that could be calculated) | 75 events | [89] |
The magnitude of this problem becomes particularly evident when examining the performance gap between models developed with adequate versus inadequate samples. Research on breast cancer gene signatures demonstrates that increasing sample sizes directly corresponds to improved stability, better concordance in outcome prediction, and enhanced prediction accuracy [90]. For instance, the overlap between independently developed prognostic gene signatures increased from approximately 1.33% with 100 samples to 16.56% with 600 samples, while prediction concordance rose to 96.52% with 500 training samples [90].
Methodological Approaches to Enhance Generalizability
Formal Sample Size Calculation and Study Design
The foundation of generalizable research begins with appropriate sample size planning. Riley et al. provide formal methodological guidance for calculating minimum sample size requirements for prediction models [89]. These calculations should ensure: (1) small overfitting with expected shrinkage of predictor effects by 10% or less; (2) small absolute difference (0.05) in the model's apparent and adjusted R² value; and (3) precise estimation (within ±0.05) of the average outcome risk in the population [89]. Researchers should justify, perform, and report these sample size calculations during study design rather than as post hoc justification.
The traditional rule of thumb of 10 events per variable (EPV) has been widely cautioned against in prediction model research as it disregards methodological advancements and has been shown to have no rational evidence base [89]. For machine learning studies in oncology, sample size calculations for regression-based models provide a suitable lower bound, though ML models almost certainly require larger samples [88].
Virtual Sample Generation and Data Augmentation
Virtual Sample Generation (VSG) represents a promising computational approach to address small sample size problems by artificially expanding datasets. This technique significantly improves learning and classification performance when working with small samples [91]. Several methodological approaches have been developed:
- Mega Trend Diffusion (MTD): Uses fuzzy theories and a general diffusion function to scatter data across the whole dataset, though it can complicate calculations [91].
- Functional Virtual Population (FVP): Operates through data domain expansion methods (left, right, and both sides) for small datasets, though it has limitations with nominal variables or high variance between stages [91].
- Multivariate Normal Synthesis (MVN): Utilizes multivariate covariance dependencies among basic samples while maintaining ingrained noise of samples [91].
- Genetic Algorithm-Based VSG: Determines appropriate data ranges using MTD functions, then applies genetic algorithms to generate optimal virtual samples [91].
- Cycle-Consistent Adversarial Networks (CycleGAN): A style transfer technique that can decrease inter-institutional image heterogeneity while preserving predictive information, improving model generalizability across institutions [92].
Table 2: Virtual Sample Generation Techniques and Applications
| Method | Mechanism | Advantages | Limitations | Reported Efficacy |
|---|---|---|---|---|
| Genetic Algorithm-Based VSG | Determines data ranges via MTD, then uses genetic algorithms | Superior to original training data without virtual samples | Complexity in implementation | Enhanced diagnostic accuracy from 84% to 95% with 5 actual samples [91] |
| CycleGAN | Unpaired image-to-image translation using adversarial networks | Decreases inter-institutional heterogeneity, preserves predictive information | Requires technical expertise in deep learning | Increased AUC from 0.77 to 0.83 in meningioma grading [92] |
| Bootstrap Methods | Resampling with replacement from original dataset | Simple implementation, well-established | Limited innovation for complex patterns | Improved radiotherapy outcome prediction from 55% to 85% [91] |
Advanced Machine Learning Strategies
Several advanced machine learning approaches can enhance model performance even with limited data:
Transfer and Few-Shot Learning: Transfer learning adapts AI models pre-trained on large-scale datasets to new clinical tasks, while few-shot learning enables robust performance with minimal labeled data [93]. Both methods substantially enhance performance and stability across multiple clinical scenarios.
Subtype-Specific Analysis: Focusing on more homogeneous patient subgroups can improve prediction accuracy. Research on breast cancer demonstrates that estrogen receptor-positive-specific analysis produced lower error rates (35.92%) compared to analysis using both ER-positive and ER-negative samples (38.71%) [90].
Penalized Regression Methods: Techniques like LASSO, Ridge regression, and elastic nets can help control overfitting, though they don't eliminate the need for adequate samples as their shrinkage parameters are estimated with uncertainty when sample size is small [89].
Image Harmonization and Domain Adaptation
The inter-institutional heterogeneity of medical imaging protocols represents a major barrier to generalizability. Image harmonization techniques can mitigate variations across different scanners and imaging protocols [93]. CycleGAN has demonstrated particular promise in converting heterogeneous MRIs, improving radiomics model performance on external validation by transferring the style of external validation images to match the training set distribution while preserving semantic information [92].
Experimental Protocols for Enhanced Generalizability
Protocol for Virtual Sample Generation Using Genetic Algorithms
Purpose: To generate synthetic samples that expand training datasets while preserving the statistical properties of original data. Materials: Original dataset, computing environment with genetic algorithm libraries. Procedure:
- Determine the appropriate data range using MTD functions to establish boundaries for virtual sample generation.
- Initialize a population of potential virtual samples with random values within the established boundaries.
- Evaluate the fitness of each virtual sample based on discriminative power and maintenance of original data relationships.
- Apply selection, crossover, and mutation operations to generate new candidate virtual samples.
- Iterate the process until convergence criteria are met, selecting the most appropriate virtual samples.
- Validate the approach by comparing model performance with and without virtual samples on a holdout test set [91].
Protocol for Image Harmonization Using CycleGAN
Purpose: To reduce inter-institutional image heterogeneity while preserving predictive information for improved model generalizability. Materials: Source and target domain images, deep learning framework with CycleGAN implementation. Procedure:
- Prepare unpaired institutional training and external validation datasets, resizing images to standardized dimensions.
- Configure CycleGAN architecture with two generators (G1, G2) and two discriminators (D1, D2).
- Train the first generator (G1) to convert images from the external validation dataset to the institutional training dataset domain.
- Train the first discriminator (D1) to distinguish between real institutional images and those generated by G1.
- Train the second generator (G2) to convert synthetic images from G1 back to the original external validation domain.
- Train the second discriminator (D2) to distinguish between real external validation images and those generated by G2.
- Apply cycle consistency loss to ensure meaningful translations that preserve content.
- Use quantitative metrics (e.g., Fréchet Inception Distance) to validate reduction in inter-institutional heterogeneity [92].
Protocol for Multi-Cohort Validation
Purpose: To assess model generalizability across diverse clinical settings and populations. Materials: Developed prediction model, multiple independent validation cohorts representing different clinical settings. Procedure:
- Identify distinct clinical settings relevant to the model's intended use (e.g., screening-detected, incidental, and biopsied pulmonary nodules).
- Acquire independent validation cohorts for each clinical setting, ensuring adequate sample sizes for meaningful evaluation.
- Apply the model to each cohort without retraining to assess baseline generalizability.
- Evaluate performance metrics (AUC, accuracy, sensitivity, specificity) separately for each cohort.
- Implement fine-tuning approaches for cohorts with poor performance, adjusting models using local data.
- Compare performance patterns across cohorts to identify specific settings where the model maintains adequate performance [93].
The Scientist's Toolkit: Essential Research Reagents and Solutions
Table 3: Key Research Reagent Solutions for Enhancing Generalizability
| Tool/Reagent | Function | Application Context | Technical Notes |
|---|---|---|---|
| pmsampsize R/Stata Package | Calculates minimum sample size for prediction models | Study design phase for clinical prediction models | Implements Riley et al. method; requires outcome proportion, candidate predictors, and anticipated R² [89] |
| CycleGAN Framework | Image domain adaptation for heterogeneity reduction | Multi-institutional radiomics studies | Requires unpaired datasets; preserves semantic information while transferring style [92] |
| PyRadiomics (v3.0+) | Standardized radiomic feature extraction | Radiomics model development | Adheres to Image Biomarker Standardization Initiative standards; ensures reproducible feature calculation [92] |
| Virtual Sample Generation Algorithms | Artificially expands training datasets | Studies with limited sample availability | Includes MTD, FVP, MVN, and genetic algorithm approaches; selection depends on data characteristics [91] |
| Advanced Normalization Tools (ANTs) | Image registration and preprocessing | Multi-scanner, multi-protocol imaging studies | Enables spatial normalization and intensity correction; critical for handling dataset variability [92] |
Visualizing Workflows for Enhanced Generalizability
Virtual Sample Generation for Radiomics
Domain Adaptation for Multi-Institutional Generalizability
Overcoming limited sample sizes in preclinical and clinical studies requires a multifaceted approach that addresses both quantitative deficiencies and qualitative heterogeneity. The strategies outlined—ranging from rigorous sample size calculation and virtual sample generation to advanced domain adaptation techniques—provide a roadmap for developing more generalizable models in radiomics and digital pathology. As these fields continue to evolve, emphasis must shift from simply developing predictive models to creating robust, translatable tools that maintain performance across diverse clinical settings and patient populations. By adopting these methodologies, researchers and drug development professionals can enhance the real-world impact of their work, ultimately contributing to more personalized and effective cancer diagnostics and therapeutics.
The integration of artificial intelligence (AI), particularly machine learning (ML) and deep learning (DL) models, into cancer diagnostics represents a paradigm shift in radiology and pathology. However, the "black-box" nature of these complex models—where internal workings and decision-making processes are opaque—poses a significant barrier to clinical adoption [94] [95]. In mission-critical domains like oncology, where decisions directly impact patient survival, understanding the why behind a model's prediction is as crucial as the prediction itself [96]. This whitepaper examines the foundational concepts of interpretability and transparency, frames them within the context of radiomics and digital pathology for cancer diagnostics, and provides a technical roadmap for developing biologically plausible, trustworthy AI systems.
The black-box problem is particularly acute in medical image analysis. Highly complex models, including deep neural networks (DNNs), achieve state-of-the-art performance but derive predictions from intricate, non-linear statistical models with innumerable parameters, inherently compromising transparency [94] [95]. Explainable AI (XAI) has therefore emerged as a critical field of study, seeking to develop AI systems that provide both accurate predictions and explicit, interpretable explanations for their decisions, thereby fostering trust and enabling clinical validation [94].
Foundations of Interpretability and Transparency
Defining the Core Concepts
While often used interchangeably, interpretability and transparency represent distinct but complementary concepts in AI:
- Transparency describes the degree to which appropriate information about a machine learning-enabled medical device (MLMD)—including its intended use, development, performance, and logic—is clearly communicated to relevant audiences [97]. It is a broader concept encompassing the entire system lifecycle.
- Interpretability refers to the ability to understand and provide meaning to model operations, often by explaining how a specific output was reached or the basis for a particular decision [97]. It is frequently concerned with local, prediction-level explanations.
- Explainability is the degree to which a model's logic can be explained in a way that a human can understand, making it a key aspect of transparency [97].
From a regulatory perspective, agencies like the U.S. FDA, Health Canada, and the UK's MHRA emphasize that transparency is not merely a technical feature but a fundamental requirement for patient-centered care, safety, and effectiveness. It enables the identification and evaluation of device risks and benefits, helps ensure devices are used safely and effectively, and promotes health equity by helping to identify bias [97].
The Radiomics Pipeline and Its Reproducibility Challenges
Radiomics, the high-throughput extraction of quantitative features from medical images, aims to convert imaging data into a mineable feature space that can serve as a surrogate for biomarkers [98] [99]. The standard radiomics pipeline involves several sequential steps, each introducing potential variability that can compromise both reproducibility and interpretability.
Figure 1: The Radiomics Pipeline with Critical Challenge Points. Yellow nodes highlight steps prone to imaging reproducibility issues; red nodes indicate steps with statistical reproducibility challenges.
This pipeline faces two major reproducibility crises that directly impact interpretability:
- Imaging Reproducibility: Variations in imaging parameters, scanner vendors, reconstruction techniques, and voxel sizes significantly impact extracted radiomic features [99]. Furthermore, manual or semi-automated tumor segmentation is sensitive to intra- and inter-rater variability, making features partially non-reproducible before modeling even begins [99].
- Statistical Reproducibility: Radiomics typically generates hundreds to thousands of highly correlated features from limited patient samples, creating high-dimensional datasets [99]. This "needle in a haystack" problem increases the risk of identifying spurious patterns and false-positive results, complicating training and validation [99]. The feature selection methods themselves vary in complexity and robustness, adding another layer of variability [99].
Technical Approaches for Interpretable AI in Cancer Diagnostics
Model-Specific vs. Model-Agnostic Interpretation Techniques
Interpretability methods can be broadly categorized based on their relationship to the underlying model.
- Model-Specific Interpretability: These techniques are intrinsically linked to the architecture of a specific model class. Examples include analyzing the weights of a linear regression model or the feature importance in a decision tree. While often highly precise, their applicability is limited to their specific model class.
- Model-Agnostic Interpretability: These methods treat the ML model as a true black box and can be applied to any model. They interpret predictions by analyzing the relationship between input data and output predictions. A prominent example is LIME (Local Interpretable Model-agnostic Explanations), which approximates a complex model locally around a specific prediction with a simpler, interpretable model (e.g., linear classifier) to generate explanations [95]. Another common method is SHAP (SHapley Additive exPlanations), which is based on cooperative game theory to assign each feature an importance value for a particular prediction [94].
The Critical Role of Human-Centered Design
Achieving true transparency is not solely a computational challenge; it is a human-factor challenge. According to a systematic review, current transparent ML development is dominated by computational feasibility and barely considers end-users [96]. This is a critical oversight because transparency is not a property of the ML model but an affordance—a relationship between the algorithm and its users [96].
The INTRPRT guideline proposes a human-centered design (HCD) process for transparent ML in medical imaging [96]. This involves:
- Formative User Research: Understanding user needs and domain requirements before model construction.
- Iterative Prototyping and Validation: Involving clinical stakeholders throughout design and development to ensure the explanations provided are relevant, comprehensible, and actionable within the clinical workflow [96] [97].
For a medical device, HCD means providing the appropriate level of detail for the intended audience (e.g., a clinician versus a patient) and using plain language where appropriate to ensure understanding and usability [97].
A Case Study in Pathology-Interpretable Radiomics
A 2025 study on osteosarcoma provides a seminal example of moving beyond a black-box radiomic model by linking it directly to underlying pathobiology [98]. The study's methodology offers a template for developing interpretable models in cancer diagnostics.
Experimental Protocol and Workflow
The research developed an MRI-based radiomic model to predict disease-free survival (DFS) in osteosarcoma patients [98]. The interpretability protocol was integrated into the core of the study design.
Figure 2: Workflow for Pathology-Interpretable Radiomic Modeling
Key Experimental Steps [98]:
- Cohort and Imaging: A multicenter retrospective study of 270 patients with osteosarcoma was conducted. Baseline contrast-enhanced MRI scans were acquired 1-2 weeks prior to treatment.
- Radiomic Model Development:
- Segmentation: Tumors were segmented on MRI.
- Feature Extraction: 1130 radiomic features were extracted.
- Modeling: After dimensionality reduction, a final model comprising 12 features was developed to predict DFS.
- Pathological Correlation for Interpretation:
- H&E Analysis: Ten types of nuclear morphological features were extracted from every nucleus in H&E-stained whole slide images (WSIs) and aggregated into 150 patient-level features.
- Immunohistochemistry (IHC) Analysis: IHC for immune (CD3, CD8, CD68, FOXP3) and hypoxia (CAIX) biomarkers was quantitatively analyzed from WSIs.
- Statistical Correlation: Spearman correlation analysis, with false discovery rate control, was used to link radiomic features to histopathologic markers.
Quantitative Results and Biological Validation
The study successfully linked its radiomic model to underlying tumor biology, providing a critical layer of interpretability.
Table 1: Correlation Between Radiomic Features and Histopathologic Markers [98]
| Histopathologic Marker Type | Specific Marker | Correlation with Radiomic Features (Number of Features, Correlation Coefficient Range) | Biological Interpretation |
|---|---|---|---|
| Immune-related IHC Biomarkers | CD3 | 4 features, r = 0.50–0.75 | Indicates model features capture tumor-infiltrating T-lymphocytes. |
| CD8 | 2 features, r = 0.46 and 0.60 | Reflects presence of cytotoxic T-cells within the tumor microenvironment. | |
| CD8/FOXP3 Ratio | 3 features, r = 0.69–0.81 | Suggests features are associated with the balance between cytotoxic and regulatory T-cells, a known prognostic factor. | |
| Nuclear Morphological Features from H&E | 10 nuclear features aggregated to patient level | 9 radiomic features correlated with 17 cellular features (32 pairs total) | Demonstrates a moderate link between imaging features and cellular architecture. |
The findings revealed that while radiomic features showed only moderate associations with H&E-derived nuclear morphology, they exhibited higher correlations with key immune-related biomarkers [98]. This suggests that the predictive power of the MRI-based radiomic model was significantly driven by its ability to non-invasively characterize the immune tumor microenvironment, a crucial determinant of cancer prognosis and therapy response.
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 2: Key Research Reagents and Solutions for Interpretable Radiomics
| Item/Reagent | Function in the Experimental Workflow |
|---|---|
| Contrast-enhanced MRI Data | Provides the primary imaging data for radiomic feature extraction. Essential for capturing tumor morphology and heterogeneity. |
| H&E-Stained Whole Slide Images | The gold standard for pathological diagnosis. Used to extract quantitative data on tissue architecture and cellular morphology (e.g., nuclear size, shape). |
| IHC Stains (CD3, CD8, CD68, FOXP3, CAIX) | Antibody-based stains used to identify and quantify specific immune cell populations (T-cells, macrophages) and hypoxia markers within the tumor tissue. |
| Digital Pathology Scanner | High-resolution scanner used to digitize glass slides, creating whole slide images for computational analysis. |
| Image Biomarker Standardisation Initiative (IBSI) Compliant Software | Standardized software for radiomic feature extraction, critical for ensuring reproducibility and cross-study comparisons [99]. |
| Statistical Software (R, Python with scikit-learn, PyRadiomics) | Platforms for feature selection, model development, and performing correlation analyses (e.g., Spearman correlation) to link radiomic and pathologic data. |
Visualization and Communication of Interpretable Data
Effective communication of model outputs and explanations is a final, critical step in achieving transparency. The choice of visualization must be guided by the nature of the quantitative data and the needs of the audience.
Best Practices for Quantitative Data Visualization
- Selecting Appropriate Charts: Use bar charts for comparing categories, line charts for tracking trends over time, scatter plots for analyzing relationships between two variables, and heatmaps for representing data density or intensity (e.g., gene expression, regional cancer incidence) [100] [101].
- Color Integrity: Color is a powerful tool but is often misused. Employ color-blind friendly palettes and perceptually uniform gradients to ensure accurate and inclusive data representation [102] [103]. Tools like Viz Palette can be used to test color accessibility for individuals with color vision deficiencies (CVD) [102].
- Providing Context: Clear labeling, annotations, and titles are essential to guide the audience's interpretation and prevent misunderstanding [100].
The journey beyond black-box models in cancer diagnostics requires a multidisciplinary commitment to interpretability and transparency. This involves the development of robust technical methods like model-agnostic explanations, a human-centered design philosophy that engages end-users throughout the process, and biological validation, as demonstrated in the osteosarcoma case study, to ground AI predictions in known pathophysiology. By adhering to these principles and the regulatory guidelines taking shape globally, researchers and clinicians can build AI systems that are not only accurate but also trustworthy, reliable, and ultimately, transformative for patient care.
The field of oncology is witnessing a paradigm shift with the integration of high-throughput computational methods into diagnostic and prognostic workflows. Radiomics, the science of extracting mineable data from medical images, and digital pathology are at the forefront of this transformation [104] [105]. By converting standard-of-care images into rich, quantitative datasets, these disciplines unlock sub-visual information related to tumor heterogeneity, morphology, and pathophysiology. This whitepaper details the core advanced techniques—Delta-Radiomics, Multi-Modal Imaging, and sophisticated Machine Learning (ML) algorithms—that are refining these data into clinically actionable insights. When framed within cancer diagnostics research, these optimization techniques are pivotal for developing robust, interpretable, and predictive models that can accelerate drug development and usher in a new era of precision oncology.
Core Techniques and Theoretical Foundations
Delta-Radiomics: Capturing Temporal Dynamics
Delta-Radiomics refers to the analysis of changes in radiomic features over time or between different treatment time points. This longitudinal approach captures the dynamic response of a tumor to therapy or its natural progression, offering a more powerful prognostic tool than single-time-point analysis [106] [107].
- Fundamental Principle: It is predicated on comparing medical imaging data at disparate time points to identify the characteristics of imaging changes before and after treatment, thereby unveiling the tumor's response and dynamic evolution [106]. This is crucial because cancer is a dynamic disease, and a static snapshot often fails to capture its evolving biology.
- Key Advantage: The primary benefit over conventional radiomics lies in its capacity to discern temporal alterations within the tumor microenvironment in response to therapeutic interventions. This allows for a more precise assessment of treatment outcome and can reveal early indicators of response or resistance that are not apparent from size-based metrics alone [106].
Multi-Modal Imaging Data Fusion
Multi-Modal Artificial Intelligence (MMAI) involves integrating heterogeneous datasets from various diagnostic modalities into a cohesive analytical framework [108]. This fusion is essential because cancer manifests across multiple biological scales, and predictive models relying on a single data modality fail to capture this multiscale heterogeneity.
- Data Modalities: MMAI in oncology typically integrates information from:
- Medical Imaging: CT, MRI (T1, T2, DWI), PET, and SPECT scans provide anatomical, functional, and metabolic information [109] [110].
- Digital Pathology: Whole-slide images (WSI) of tissue samples offer cellular and morphological detail [25].
- Genomics and Molecular Data: Gene expression, mutation status, and other molecular markers elucidate the underlying biological drivers [108].
- Clinical Records: Electronic Health Records (EHRs) provide patient history, treatment context, and outcomes [104].
- Enhanced Predictive Power: MMAI approaches enhance predictive accuracy and robustness by contextualizing molecular features within anatomical and clinical frameworks. Models that integrate histology and genomics, for instance, have been shown to outperform standard pathological classifications for risk stratification [108].
Advanced Machine Learning Algorithms
The high-dimensional data produced by radiomics and multi-modal fusion necessitates the use of advanced ML algorithms for feature selection, dimensionality reduction, and model building.
- Feature Selection and Regularization: The "curse of dimensionality" is a significant challenge, given the vast number of features extracted from often limited samples. The Least Absolute Shrinkage and Selection Operator (LASSO) is a widely used algorithm for feature selection. It applies an L1 penalty to the regression model, forcing the coefficients of non-informative features to zero, thereby retaining only the most prognostic features [106] [109]. This is critical for building parsimonious and generalizable models.
- Model Construction and Validation: Selected features are used to construct predictive models, often using logistic regression or cox regression for survival outcomes [106] [109]. Model performance is rigorously evaluated using metrics like the Area Under the Curve (AUC) of the Receiver Operating Characteristic (ROC) curve and validated in independent cohorts to ensure clinical applicability [106] [109].
- Interpretability Frameworks: For clinical adoption, model decisions must be interpretable. SHapley Additive exPlanations (SHAP) is a game-theoretic approach that quantifies the contribution of each feature to an individual prediction, providing a clear, human-understandable explanation for the model's output [107].
Experimental Protocols and Methodologies
A Standardized Radiomics Pipeline
A robust radiomics pipeline, whether for clinical or preclinical research, involves several sequential steps to ensure reproducibility and validity [10]. The following workflow diagram outlines this standardized process, which is foundational to both delta-radiomics and multi-modal studies.
Detailed Protocol Steps:
- Image Acquisition: Medical images are acquired using one or more modalities (e.g., CT, MRI, US). Consistent, standardized imaging protocols are critical to minimize variability and ensure feature robustness [10]. Parameters such as slice thickness, resolution, and contrast timing must be documented.
- Image Preprocessing: Raw images are processed to improve quality and standardize data. This includes:
- Resampling: Images are resampled to a uniform voxel size (e.g., 1×1×1 mm³) [109].
- Intensity Normalization: Gray-level values are normalized (e.g., Z-score normalization or histogram-based normalization) to reduce inter-scanner and inter-protocol differences [106] [10].
- Artifact Correction: Correcting for motion artifacts or other acquisition-related noise.
- Region of Interest (ROI) Segmentation: The tumor or pathology is delineated to create a binary mask. This can be performed:
- Feature Extraction: High-throughput extraction of quantitative features from the ROI is performed using open-source software like PyRadiomics [10]. Features are broadly categorized into:
- Shape-based: Describe the 3D geometry of the tumor (e.g., volume, sphericity, surface area).
- First-order Statistics: Describe the distribution of voxel intensities within the ROI (e.g., mean, median, kurtosis, entropy) without considering spatial relationships.
- Second-order/Texture Features: Quantify the spatial heterogeneity of voxel intensities using matrices like the Gray-Level Co-Occurrence Matrix (GLCM), Gray-Level Run-Length Matrix (GLRLM), and Gray-Level Size Zone Matrix (GLSZM) [109] [10].
- Data Analysis & Modeling: The extracted features are analyzed using statistical and machine learning methods. This involves feature selection (e.g., using LASSO) to reduce dimensionality and avoid overfitting, followed by model construction (e.g., logistic regression, random forest) and rigorous validation in training and independent validation cohorts [106] [109] [10].
Implementing a Delta-Radiomics Study
The following diagram illustrates the specific workflow for a delta-radiomics study, which builds upon the standard radiomics pipeline by incorporating serial imaging.
Detailed Delta-Radiomics Protocol:
- Serial Image Acquisition: Images are acquired at two or more defined time points (e.g., pre-treatment and post-treatment after 2 cycles of neoadjuvant therapy) [106]. The imaging protocol must be consistent across time points.
- Image Co-registration: The post-treatment image is rigorously aligned with the pre-treatment image to ensure the same anatomical frame of reference. This is a critical step for accurate comparison [109].
- ROI Segmentation and Feature Extraction: The tumor is segmented on both co-registered images, and radiomic features are extracted from each timepoint independently.
- Delta Feature Calculation: The delta radiomics feature (ΔFeature) is defined as the absolute or relative change between the feature values at the two timepoints. A common formula is:
ΔFeature = (Feature_Time2 - Feature_Time1)or(Feature_Time2 - Feature_Time1) / Feature_Time1[106]. - Model Building and Validation: The delta features are used as inputs for predictive model development, following the same feature selection and validation principles outlined in the standard pipeline.
Protocol for Multi-Modal Radiomics Integration
Integrating data from multiple modalities, such as CT and MRI, follows a structured process to leverage complementary information.
Detailed Multi-Modal Integration Protocol:
- Multi-Modal Data Collection: Patients undergo multiple imaging scans within a close timeframe to minimize biological changes. For example, a study on Esophageal Squamous Cell Carcinoma (ESCC) acquired both CT and MRI (T2WI-FS sequence) simulations before treatment [109].
- Modality-Specific Feature Extraction: The standard radiomics pipeline (preprocessing, segmentation, extraction) is applied to each imaging modality separately. In the ESCC study, 547 features were extracted from both CT and MRI, resulting in a total of 1094 features [109].
- Feature Pooling and Selection: Features from all modalities are pooled into a single, large feature set. Dimensionality reduction is then performed across this combined set. The LASSO algorithm is highly effective for this, as it identifies the most predictive features from the entire multi-modal pool [109].
- Combined Model Construction: A single predictive model (e.g., a Cox regression model) is built using the selected features from all modalities. Research has demonstrated that this hybrid model often outperforms models based on any single modality alone [109].
Quantitative Data and Performance Metrics
The efficacy of these optimization techniques is demonstrated through quantitative improvements in predictive performance across various cancer types. The tables below summarize key findings from recent studies.
Table 1: Performance of Delta-Radiomics Models in Predictive Oncology
| Cancer Type | Study Focus | Imaging Modality | Key Predictive Features | Model Performance (AUC) | Citation |
|---|---|---|---|---|---|
| Triple-Negative Breast Cancer (TNBC) | Predicting Pathologic Complete Response (pCR) to Neoadjuvant Therapy | Ultrasound | 9 Delta radiomics features, change rate of tumor size (delta size), Adler grade | Training: 0.850Validation: 0.787 | [106] |
| Infertility Treatment (SVBT) | Predicting Live Birth Outcome | Ultrasound | Delta radiomics features from gestational sac (6th vs. 8th week), Maternal age | Training: 0.883Testing: 0.747 | [107] |
Table 2: Performance of Multi-Modal Radiomics Models in Prognostic Oncology
| Cancer Type | Study Focus | Integrated Modalities | Key Findings | Model Performance (AUC for 2-year OS) | Citation |
|---|---|---|---|---|---|
| Esophageal Squamous Cell Carcinoma (ESCC) | Predicting 2-Year Overall Survival (OS) after Chemoradiotherapy | CT & MRI (T2WI-FS) | The hybrid model demonstrated superior performance compared to single-modality models. | CT-only: 0.654 (Validation)MRI-only: 0.686 (Validation)Hybrid (CT+MRI): 0.715 (Validation) | [109] |
| Pan-Cancer (Multiple Tumors) | Risk Stratification & Treatment Response | Histology, Genomics, Clinical Data | Pathomic Fusion model outperformed WHO 2021 classification for risk stratification in glioma and renal cell carcinoma. | N/A (Outperformed standard classification) | [108] |
Table 3: Key Machine Learning Algorithms and Their Applications in Optimized Radiomics
| Algorithm | Main Function | Application in Radiomics | Key Advantage | Citation |
|---|---|---|---|---|
| LASSO (Least Absolute Shrinkage and Selection Operator) | Feature Selection & Regularization | Identifies the most prognostic features from high-dimensional data by applying an L1 penalty. | Prevents overfitting, creates parsimonious and interpretable models. | [106] [109] |
| SHAP (SHapley Additive exPlanations) | Model Interpretability | Quantifies the contribution of each input feature to an individual prediction. | Enhances model transparency and trust for clinical adoption. | [107] |
| Logistic / Cox Regression | Model Construction | Builds the final predictive model for classification or survival outcomes using selected features. | Provides a statistical foundation and is widely accepted in clinical research. | [106] [109] |
| Convolutional Neural Networks (CNNs) | Automated Feature Learning | Directly learns relevant patterns from images for tasks like segmentation or classification. | Reduces reliance on hand-crafted features; can discover novel imaging biomarkers. | [104] [105] |
Successful implementation of the described protocols requires a suite of software tools and data resources. The following table details key components of the research toolkit.
Table 4: Essential Research Toolkit for Advanced Radiomics Studies
| Tool/Resource | Category | Primary Function | Application in Current Context |
|---|---|---|---|
| PyRadiomics | Software Library | Open-source platform for standardized extraction of radiomic features from medical images. | Core feature extraction engine in both delta-radiomics and multi-modal studies. [106] [10] |
| 3D Slicer / ITK-SNAP | Software Application | Open-source platforms for visualization, segmentation, and analysis of medical images. | Used for manual or semi-automatic delineation of Regions of Interest (ROI). [106] [10] |
| LASSO Regression | Analytical Algorithm | A regression method that performs variable selection and regularization to enhance prediction accuracy. | Critical for feature selection from high-dimensional delta-radiomics and multi-modal feature pools. [106] [109] |
| SHAP | Interpretability Framework | A game-theoretic approach to explain the output of any machine learning model. | Provides post-hoc interpretability for "black box" models, clarifying feature contributions to predictions. [107] |
| DICOM Standard | Data Standard | A standard for storing and transmitting medical images and associated metadata. | Ensures interoperability and data consistency across imaging devices and software, crucial for multi-center studies. [25] |
| MONAI (Medical Open Network for AI) | AI Framework | A PyTorch-based, open-source framework for deep learning in healthcare imaging. | Provides pre-trained models and tools for tasks like segmentation, enhancing efficiency in AI-aided workflows. [108] |
The optimization techniques of Delta-Radiomics, Multi-Modal Imaging, and Advanced ML Algorithms represent a significant leap forward for cancer diagnostics research and drug development. By moving beyond static, single-modality analyses to dynamic, integrated, and computationally robust models, these methods provide a more comprehensive and nuanced understanding of tumor biology. They enable the prediction of treatment response and patient prognosis with unprecedented accuracy, as evidenced by the quantitative data from recent studies. For researchers and drug development professionals, the adoption of these techniques, supported by the standardized protocols and tools outlined in this whitepaper, is critical for developing the next generation of predictive biomarkers and personalized cancer therapies. The future of oncology lies in the intelligent integration of multi-scale data, and these optimization techniques are the key to unlocking its full potential.
Benchmarking Performance: Validation Frameworks and Comparative Analysis
The integration of advanced computational methods like radiomics and digital pathology into cancer diagnostics research represents a paradigm shift in oncology. These technologies offer unprecedented capabilities to extract quantitative, sub-visual data from medical images and pathology slides, revealing novel biomarkers for cancer detection, characterization, and treatment response prediction [11] [111]. However, the promising performance of these models in development environments often fails to translate into clinical practice, primarily due to inadequate validation methodologies [111]. A comprehensive survey revealed that approximately only 10% of published papers on pathology-based lung cancer detection models reported external validation, highlighting a critical gap in the field [111]. Without rigorous validation across multiple cohorts, these tools remain research curiosities rather than clinically actionable assets. This whitepaper establishes a framework for implementing a tripartite validation strategy—encompassing internal, external, and prospective cohorts—to ensure the development of robust, generalizable, and clinically translatable models in cancer diagnostics.
Defining the Validation Spectrum
Internal Validation
Internal validation assesses model performance using data derived from the same source population as the training data, typically through resampling methods. It provides an initial estimate of model performance and helps prevent overfitting during the development phase.
Key Methodologies:
- K-fold Cross-validation: The dataset is partitioned into k equally sized folds. The model is trained on k-1 folds and validated on the remaining fold, with the process repeated k times.
- Bootstrap Resampling: Multiple samples are drawn with replacement from the original dataset to create training sets, with the out-of-bag samples used for validation.
- Hold-out Validation: A simple split of the data into training and testing sets, though this approach is less robust for small datasets.
External Validation
External validation evaluates model performance on completely independent datasets collected from different institutions, populations, or using different protocols [112] [111]. This critical step tests the model's generalizability beyond the development context. The study by [112] on HER2 positivity in gastric cancer exemplifies rigorous external validation, where a model developed on conventional CT scans was successfully validated on dual-energy CT (DECT) datasets from different time periods and scanners, demonstrating true generalizability.
Prospective Validation
Prospective validation represents the highest standard of validation, where the model is applied to new patients in a real-world clinical setting according to a predefined study protocol. This approach evaluates not only algorithmic performance but also practical implementation factors including workflow integration, interoperability with clinical systems, and usability. The Beta-CORRECT study referenced in [113], which validated the Oncodetect test for molecular residual disease in colorectal cancer across multiple timepoints, exemplifies a well-designed prospective validation study with clear clinical utility.
Table 1: Comparative Analysis of Validation Types
| Validation Type | Primary Objective | Dataset Characteristics | Key Statistical Measures | Limitations |
|---|---|---|---|---|
| Internal | Optimize model parameters and prevent overfitting | Resampled from original population | AUC, accuracy, precision, recall computed across resamples | Limited assessment of generalizability |
| External | Assess generalizability across populations and settings | Independently collected from different sources | Performance degradation analysis, calibration metrics | May not reflect real-world clinical workflow |
| Prospective | Evaluate real-world clinical utility and impact | New patients enrolled according to protocol | Clinical utility measures, change in patient management | Resource-intensive, time-consuming |
Methodological Framework for Cohort Establishment
Internal Validation Cohort Design
The internal validation process begins with appropriate cohort partitioning. For radiomics studies, the workflow typically involves image acquisition, tumor segmentation, feature extraction, feature selection, and model building [11] [112]. The dataset should be randomly split into training and testing sets while preserving the distribution of key clinical variables (e.g., cancer stage, biomarker status). For the gastric cancer radiomics study by [112], 388 patients were assigned to a training cohort for model development. Techniques such as stratification ensure balanced representation of important characteristics across splits. Internal validation performance metrics should be interpreted as the best-case scenario, with an expected performance decrease in external validation.
External Validation Cohort Implementation
External validation requires meticulously selected independent cohorts that test specific aspects of generalizability. Key considerations include:
- Multi-institutional participation: Sourcing data from multiple institutions with different patient demographics, equipment, and protocols [111].
- Temporal validation: Using data collected from the same institution but during different time periods, as demonstrated in [112] where an internal validation cohort (August 2019 to July 2020) and external validation cohort (December 2011 to July 2020) were established.
- Technical variability: Incorporating images from different scanner manufacturers, acquisition parameters, and reconstruction algorithms.
- Protocol differences: Including data from different imaging protocols, such as validating conventional CT-based models on dual-energy CT datasets [112].
The digital pathology review [111] identified that most external validation studies used restricted datasets from limited centers, highlighting a common methodological weakness. Optimal external validation should include diverse, representative datasets that reflect real-world clinical variability.
Prospective Validation Cohort Execution
Prospective validation follows a predefined protocol with clearly defined endpoints. The Beta-CORRECT study [113] provides an exemplary framework with these key elements:
- Clear inclusion/exclusion criteria: Well-defined patient population (stage II-IV colorectal cancer).
- Pre-specified endpoints: Primary endpoints defined before study initiation (recurrence prediction).
- Standardized procedures: Consistent timing of sample collection and processing across sites.
- Clinical outcome correlation: Association of model outputs with clinically relevant endpoints (recurrence risk).
Sample size calculation for prospective studies should be based on the minimum acceptable performance and expected effect size, rather than convenience sampling.
Diagram 1: Prospective validation workflow
Experimental Protocols and Technical Considerations
Radiomics-Specific Validation Methodology
The radiomics workflow introduces specific technical considerations for validation [11] [112]:
Image Acquisition and Preprocessing:
- Standardize acquisition parameters across validation cohorts where possible
- Implement resampling to common voxel spacing (e.g., 1×1×1 mm) to minimize resolution differences [112]
- Account for variations in reconstruction kernels and slice thickness
Tumor Segmentation:
- Employ multiple segmentation methods (manual, semi-automated, automated) with inter-observer variability assessment
- Document segmentation protocols thoroughly for replication
- For external validation, consider segmentations performed by different radiologists
Feature Extraction and Reproducibility:
- Extract features from original and filtered images (Laplacian of Gaussian, wavelet) [112]
- Calculate intra-class correlation coefficients (ICC) for feature reproducibility, retaining only features with ICC > 0.75 [112]
- Remove low-variance features (variance < 1.0) and handle missing values appropriately
Model Building and Feature Selection:
- Apply robust feature selection methods (correlation analysis, tree-based importance ranking) [112]
- Use appropriate algorithms (SVM, random forests, neural networks) with hyperparameter optimization
- Implement cross-validation strictly on the training set to avoid data leakage
Digital Pathology Validation Considerations
Digital pathology validation presents unique challenges [111]:
Whole Slide Image (WSI) Variability:
- Account for differences in tissue preparation, staining protocols, and scanner characteristics
- Implement color normalization techniques to handle staining variability
- Consider multiple magnification levels and region selection methods
Annotation and Ground Truth:
- Establish consensus protocols for pathologist annotations
- Document inter-observer variability among pathologists
- For external validation, include WSIs from different institutions with local ground truth
Algorithm Validation:
- Test models on different WSI formats and compression levels
- Validate across different tissue types (biopsies, resection specimens)
- Assess performance at both slide-level and patch-level predictions
Table 2: Essential Research Reagents and Computational Tools
| Category | Specific Tools/Reagents | Function in Validation | Implementation Considerations |
|---|---|---|---|
| Image Analysis | ITK-SNAP [112], PyRadiomics [112], QuPath | Tumor segmentation, feature extraction | Standardize versions, parameters across sites |
| Machine Learning | Scikit-learn, TensorFlow, PyTorch, SVM [112], GBDT [112] | Model development, validation | Fix random seeds for reproducibility |
| Statistical Analysis | R, Python (statsmodels, scipy) | Performance evaluation, statistical testing | Predefine all statistical tests in protocol |
| Data Management | REDCap, XNAT, OMERO | Data curation, version control | Implement data anonymization procedures |
| Pathology Platforms | Whole Slide Scanners (Aperio, Hamamatsu), Digital pathology APIs [111] | Slide digitization, analysis | Control for scanner-specific characteristics |
Quantitative Assessment and Performance Metrics
Comprehensive Metric Reporting
Each validation stage requires comprehensive metric reporting to enable meaningful interpretation and comparison:
Discrimination Metrics:
- Area Under the Curve (AUC) with confidence intervals
- Sensitivity, specificity, positive and negative predictive values
- Accuracy balanced with prevalence considerations
Calibration Metrics:
- Calibration curves and intercept
- Hosmer-Lemeshow test [11]
- Brier score for probabilistic predictions
Clinical Utility Assessment:
- Decision curve analysis (DCA) to evaluate net benefit [11] [112]
- Net reclassification improvement
- Clinical impact curves
Performance Across Validation Stages
Performance typically decreases across validation stages, and documenting this degradation provides crucial information about model robustness:
- Internal-External Performance Gap: The difference between internal and external performance indicates overfitting to development data characteristics
- Temporal Performance Drift: Performance variation across time periods reveals model stability
- Cross-institutional Variability: Performance differences across institutions highlight population or technical biases
The gastric cancer radiomics study [112] demonstrated modest but consistent performance across validation cohorts with AUCs of 0.732 (training), 0.703 (internal validation), and 0.711 (external validation), indicating robust generalizability.
Diagram 2: Validation metrics progression
Challenges and Mitigation Strategies
Common Methodological Pitfalls
The literature reveals recurrent challenges in validation methodology [11] [111]:
- Dataset Shift: Differences in data distribution between development and deployment environments significantly impact performance
- Spectrum Bias: Non-representative patient spectra in development cohorts limit generalizability
- Insufficient Sample Size: Underpowered validation studies unable to detect clinically relevant performance differences
- Heterogeneous Ground Truth: Variability in reference standard determination across institutions
- Technical Heterogeneity: Differences in imaging protocols, scanner manufacturers, and reconstruction algorithms
Mitigation Approaches
- Proactive Cohort Design: Anticipate sources of heterogeneity and deliberately include them in external validation cohorts
- Stratified Analysis: Report performance across clinically relevant subgroups (e.g., by cancer stage, demographic factors)
- Multiple External Cohorts: Include several independent external cohorts to assess consistency of performance
- Comprehensive Reporting: Document all technical parameters, inclusion/exclusion criteria, and patient characteristics
- Failure Analysis: Systematically investigate cases where model performance fails to identify potential limitations
The establishment of rigorous validation methodologies encompassing internal, external, and prospective cohorts is not merely an academic exercise but a fundamental requirement for translating radiomics and digital pathology models from research environments to clinical practice. The tripartite validation framework presented here provides a structured approach to building evidentiary support for model robustness, generalizability, and clinical utility. As the field progresses toward more complex multi-omics integration [11] and foundation models [111], the validation standards must evolve correspondingly. By implementing these comprehensive validation strategies, researchers can accelerate the development of clinically impactful tools that ultimately improve cancer diagnosis, treatment selection, and patient outcomes.
Within oncology, the emergence of high-throughput computational methods, particularly radiomics and digital pathology, has revolutionized the approach to cancer diagnostics and prognostics. Radiomics converts standard-of-care medical images into mineable, high-dimensional data by extracting many quantitative features, thereby uncovering tumor characteristics that are invisible to the human eye [114]. Similarly, digital pathology applies analogous computational techniques to whole-slide images, quantifying cellular and tissue-level patterns. The diagnostic and prognostic models built from this data hold immense promise for personalized medicine, but their real-world utility depends entirely on the rigorous and appropriate evaluation of their accuracy [115]. This guide provides a technical framework for researchers and drug development professionals to evaluate the performance of these advanced tools.
Core Performance Metrics for Model Evaluation
The evaluation of diagnostic and prognostic models requires a multi-faceted approach, assessing different aspects of model performance using standardized metrics.
Table 1: Core Performance Metrics for Diagnostic and Prognostic Models
| Metric Category | Specific Metric | Interpretation and Use Case |
|---|---|---|
| Overall Performance | Brier Score (BS) / Integrated Brier Score (IBS) | Measures the average squared difference between predicted probabilities and actual outcomes. Lower values (closer to 0) indicate better overall accuracy [116]. |
| Discrimination | Concordance Index (C-index) | For prognostic models with time-to-event data (e.g., overall survival), the C-index quantifies the model's ability to correctly rank order individuals by their survival time. A value of 0.5 is no better than chance, 1.0 is perfect discrimination [116]. |
| Area Under the ROC Curve (AUC) | For diagnostic models, the AUC measures the ability to distinguish between two classes (e.g., benign vs. malignant). Values range from 0.5 (useless) to 1.0 (perfect) [117]. | |
| Calibration | Calibration Plots | A visual and statistical assessment of the agreement between predicted probabilities and observed frequencies. A perfectly calibrated model has predictions that fall along the 45-degree line [115]. |
The Brier Score provides a straightforward measure of a model's overall accuracy. In prognostic research, the C-index is the gold standard for assessing a model's ability to discriminate between high-risk and low-risk patients. For instance, a study developing machine learning models for prostate cancer survival reported C-indices ranging from 0.779 to 0.782, outperforming traditional Cox regression (C-index: 0.770) [116]. For diagnostic tasks, the AUC is the most commonly reported metric. A large meta-analysis of deep learning in medical imaging found AUCs for detecting diseases like diabetic retinopathy and lung cancer typically ranged from 0.864 to 1.000, demonstrating high discriminatory power [117]. However, high discrimination is meaningless without good calibration; a model can be perfectly discriminative but systematically over- or under-estimate risk. Calibration plots are therefore essential for a complete performance picture [115].
Methodological Framework for Technical Evaluation
Robust evaluation requires more than just calculating final metrics; it necessitates a rigorous methodology from study design through validation.
Study Design and Data Considerations
Before model development begins, a study protocol should be registered to ensure transparency and reduce selective reporting [115]. The data used for development and evaluation must be representative of the target population and clinical setting where the model is intended to be used. A critical, yet often overlooked, step is conducting a sample size calculation to ensure the dataset is sufficiently large to develop a stable model and obtain reliable performance estimates, thereby minimizing overfitting [115]. Furthermore, researchers must have a clear plan for handling missing data, as simply excluding cases with incomplete information can introduce significant bias [115].
Model Validation Strategies
A model's performance on its training data is an overly optimistic estimate of its real-world performance. Rigorous validation is therefore non-negotiable.
- Internal Validation: Techniques like bootstrapping or cross-validation use resampling methods on the development data to provide a more realistic assessment of model performance and correct for overoptimism [115].
- External Validation: The strongest evidence for a model's generalizability comes from external validation—testing its performance on entirely new data collected from different institutions, scanners, or patient populations [115] [117]. The failure to perform external validation is a major barrier to clinical adoption.
Evaluation of Clinical Utility
Finally, evaluating a model's statistical performance is insufficient. Its clinical utility must be assessed by determining whether it leads to better decision-making compared to standard practice. This is often evaluated using decision curve analysis to calculate the "net benefit" of using the model across a range of probability thresholds [115].
Experimental Protocols for Radiomics and Digital Pathology Studies
The development and evaluation of radiomics-based biomarkers follow a standardized pipeline. The following workflow outlines the key stages from image acquisition to clinical application.
Diagram 1: Biomarker Development Workflow
Image Acquisition and Preprocessing
The initial stage involves acquiring high-quality, standardized images. For radiomics, this typically involves CT, MRI, or PET scans [114] [10]. For digital pathology, it involves whole-slide imaging of biopsy or resection specimens [118]. Preprocessing is critical to minimize technical variation and includes:
- Artifact Correction: Addressing motion, noise, or scanner-specific artifacts [10].
- Intensity Normalization: Standardizing pixel or voxel values across different images and scanners to ensure feature comparability [10].
- Image Registration: For multi-modal studies (e.g., PET-MRI), aligning images to a common coordinate system is necessary [10].
Image Segmentation and Feature Extraction
This step defines the region of interest (ROI) for analysis.
- Segmentation: The tumor or pathology is delineated manually, semi-automatically, or using fully automated tools (e.g., 3D Slicer, ITK-SNAP, or deep learning algorithms) [10]. Accurate segmentation is vital, as features are extracted from this defined region.
- Feature Extraction: From the segmented ROI, hundreds of quantitative radiomic or pathomic features are calculated [114] [10]. These can be categorized as:
- Shape-based: Describe the 3D geometry of the ROI (e.g., sphericity, surface area).
- First-order Statistics: Describe the distribution of pixel/voxel intensities without considering spatial relationships (e.g., mean, median, kurtosis).
- Second-order and Higher-order Texture Features: Quantify the spatial interrelationships between pixels/voxels using matrices like the Gray-Level Co-occurrence Matrix (GLCM) and Gray-Level Run Length Matrix (GLRLM) [114] [10].
Statistical Analysis and Model Development
The final stage involves linking the extracted features to clinical or biological endpoints.
- Feature Selection: Given the high number of features relative to sample size, dimensionality reduction (e.g., using LASSO regularization) is essential to prevent overfitting [115] [10].
- Model Building: Machine learning algorithms (e.g., random forests, gradient boosting, neural networks) are trained to classify phenotypes (Use Case 2) or predict risk (Use Case 3) based on the selected features [119] [116].
- Performance Evaluation: The model is then subjected to the rigorous validation process and evaluated using the metrics described in Section 2 [115].
The Scientist's Toolkit: Essential Research Reagents and Solutions
The following table details key tools and solutions required for conducting rigorous radiomics and digital pathology research.
Table 2: Essential Research Toolkit for Radiomics and Digital Pathology
| Tool / Solution | Function | Examples & Notes |
|---|---|---|
| Image Analysis Software | Segmentation of regions of interest (ROIs) such as tumors. | 3D Slicer, ITK-SNAP, VivoQuant; deep learning-based segmentation tools [10]. |
| Feature Extraction Platform | High-throughput calculation of quantitative features from images. | PyRadiomics (open-source Python package), in-house pipelines using Matlab [10]. |
| Statistical Computing Environment | Data analysis, model development, and calculation of performance metrics. | R, Python (with scikit-survival, SHAP libraries) [116]. |
| Biomarker Validation Framework | Structured process for transitioning from discovery to clinical application. | QIBA (Quantitative Imaging Biomarker Alliance) profiles; Phased approach (Discovery, Development, Validation, Clinical Utility) [119] [120]. |
The transformative potential of radiomics and digital pathology in oncology is contingent upon a rigorous and standardized approach to evaluating diagnostic and prognostic accuracy. This involves a comprehensive assessment that moves beyond simple discrimination metrics like AUC to include calibration and clinical utility. By adhering to robust methodological principles—including prospective protocol registration, appropriate sample size planning, diligent handling of missing data, and thorough internal and external validation—researchers can develop trustworthy models. Ultimately, this rigorous framework is the foundation for translating computational biomarkers from research tools into clinically actionable solutions that can personalize cancer therapy and improve patient outcomes.
The burgeoning field of quantitative image analysis in oncology has given rise to two predominant paradigms: single-modality radiomics or pathomics and the emerging integrated approach of radiopathomics. Radiomics extracts high-dimensional data from medical images such as computed tomography (CT), magnetic resonance imaging (MRI), and ultrasound to decode tumor phenotype [121] [122]. Similarly, pathomics applies analogous computational techniques to digital pathology images, often Hematoxylin and Eosin (H&E) stained whole-slide images (WSIs), to quantify cellular and tissue features [25] [48]. While these single-modality approaches have demonstrated significant promise, they offer a fragmented view of the complex tumor microenvironment. Radiopathomics, defined as the integration of radiographic and digital pathology images via artificial intelligence (AI), emerges as a transformative methodology to capture hidden correlations between cancer phenotypes and treatment responses [121]. This integrative framework is propelled by the convergence of data science, AI, and precision medicine, aiming to provide a more holistic characterization of tumor heterogeneity for improved diagnosis, prognosis, and therapeutic decision-making [121] [25]. This technical guide, framed within a broader thesis on radiomics and digital pathology in cancer diagnostics, delineates the comparative advantages of radiopathomics over single-modality approaches, providing researchers and drug development professionals with structured data, experimental protocols, and essential toolkits for its implementation.
Technical Foundations and Methodologies
Single-Modality Approaches: Core Concepts and Limitations
Radiomics transforms standard-of-care medical images into mineable, high-dimensional data via an automated extraction process [122]. The standard workflow encompasses image acquisition, region of interest (ROI) segmentation, feature extraction, and model building linked to clinical outcomes [121] [123]. Extracted features are typically categorized into intensity, shape, texture, and wavelet features [122]. A key strength of radiomics is its non-invasive nature and ability to capture intra-tumoral heterogeneity that may elude visual assessment [123]. However, its limitations are notable. Feature reproducibility is highly sensitive to variations in imaging protocols, scanner manufacturers, and segmentation methodologies [122]. Furthermore, radiomic features are inherently macroscopic and indirect, reflecting phenotypic manifestations rather than the underlying microcellular environment.
Pathomics (Digital Pathology AI) applies similar computational principles to histopathological images. The process involves WSI acquisition, tissue segmentation, patch-level analysis, and feature extraction to identify cellular and nuclear morphology, spatial relationships, and tissue architecture patterns [121] [25]. Deep learning (DL) models, particularly convolutional neural networks (CNNs), have shown remarkable proficiency in tasks such as cancer subtyping and predicting genomic alterations, like microsatellite instability (MSI), directly from H&E slides [48]. A landmark study by Kather et al. achieved an area under the curve (AUC) of 0.84 for MSI prediction, demonstrating the power of pathomics [48]. The primary limitation of pathomics is its invasive requirement for tissue biopsy, which may not capture spatial heterogeneity across the entire tumor and is subject to sampling bias [121].
Radiopathomics: An Integrative Framework
Radiopathomics is founded on the premise that radiographic and pathologic images offer complementary biological information. The fusion of these data streams creates a more complete model of the tumor ecosystem. The core methodology involves:
- Independent Feature Extraction: Quantitative features are harvested separately from matched radiological scans (e.g., MRI, CT) and digital pathology WSIs.
- Data Integration and Modeling: The extracted features are integrated using fusion strategies, such as early fusion (feature concatenation) or late fusion (model stacking), to build predictive or prognostic models [121].
- Validation and Interpretation: The integrated model is rigorously validated, and techniques like Shapley Additive exPlanations (SHAP) are employed to interpret the contribution of features from each modality [124].
This approach hypothesizes that the combination of non-invasive macroscopic tumor phenotypes (from radiomics) with high-resolution microscopic cellular data (from pathomics) will yield a more robust and biologically informative signature than either can provide alone.
Quantitative Comparative Analysis
The theoretical advantages of radiopathomics are substantiated by empirical evidence demonstrating its superior performance in key prognostic and predictive tasks across multiple cancer types.
Table 1: Performance Comparison of Single-Modality vs. Radiopathomics Models
| Cancer Type | Predictive Task | Single-Modality Approach (Performance) | Radiopathomics / Multi-Modal Approach (Performance) | Citation |
|---|---|---|---|---|
| Breast Cancer | Differentiating Benign vs. Malignant Lesions | Traditional B-mode Ultrasound Radiomics (AUC: Not specified) | Dual-modal (BUS + CEUS) Deep Learning Radiomics (AUC: 0.825) [124] | [124] |
| Breast Cancer | Predicting Pathologic Complete Response (pCR) | Radiomics model (AUC range: 0.707–0.858) [125] | Inferred potential for enhancement via integration with pathology | [125] |
| Colorectal Cancer | Predicting Microsatellite Instability (MSI) | Deep Learning on H&E WSIs (AUC range: 0.78 - 0.98) [48] | Radiopathomics proposed to enrich model biological context | [48] |
| Non-Small Cell Lung Cancer (NSCLC) | Clustering for Overall Survival | Radiomic model based on pre-treatment CT | Immune pathology-informed model integrating histopathology (IHC for PD-L1, TILs) and radiomics [121] | [121] |
Table 2: Impact of AI Assistance on Radiologist Diagnostic Performance in Breast Cancer
| Study Round | Diagnostic Entity | Average Radiologist Performance (AUC) | Performance with AI Assistance (AUC) | Performance Gain (ΔAUC) |
|---|---|---|---|---|
| Round 1 | Integrated DL Model vs. Radiologists | 0.701 - 0.824 | Model itself achieved 0.825 [124] | Model outperformed all radiologists |
| Round 2 | AI-Assisted Radiologists | Baseline: 0.718 - 0.811 | 0.748 - 0.869 [124] | +0.030 to +0.058 [124] |
The data reveals a consistent theme: integrative models consistently match or surpass the performance of single-modality baselines. For instance, in breast cancer diagnosis, a dual-modal ultrasound radiomics model outperformed radiologists in a reader study and subsequently enhanced their diagnostic accuracy when provided as a decision-support tool [124]. This demonstrates the direct clinical value of multi-modal AI assistance. Furthermore, the ability of pathomics to predict molecular alterations like MSI from routine H&E slides [48] opens a pathway for radiopathomics to serve as a non-invasive bridge for probing the tumor immune microenvironment, a critical factor in the era of immunotherapy.
Experimental Protocols for Radiopathomics
Implementing a radiopathomics study requires a meticulous, multi-stage protocol to ensure robust and reproducible results.
Protocol 1: Multi-Center Data Curation and Preprocessing
Objective: To assemble a cohort of matched, pre-processed radiological and pathological images from multiple institutions to ensure generalizability.
- Patient Selection: Identify patients with confirmed cancer diagnoses who have undergone both target imaging (e.g., preoperative MRI/CT) and subsequent surgical resection with available pathology specimens. Adhere to strict inclusion/exclusion criteria (e.g., no prior treatment) [124].
- Multi-Center Data Collection: Collect data from several hospitals to mitigate center-specific bias. A center-split design is recommended, where data from one institution serves as the training set and data from others form an independent testing set [124].
- Image Acquisition Standardization:
- Radiology: Follow standardized imaging protocols for each modality (e.g., MRI sequences, CT parameters). Document scanner manufacturers and acquisition parameters meticulously [126].
- Pathology: Convert histology glass slides into Whole-Slide Images (WSIs) using digital scanners. Adopt the DICOM standard for pathology to ensure interoperability and data consistency [25].
- Image Preprocessing:
- Radiology: Normalize voxel sizes and intensity ranges. Co-register different imaging sequences if necessary.
- Pathology: Perform stain normalization to minimize inter-slide color variation caused by different staining batches [25].
Protocol 2: Feature Extraction and Model Integration
Objective: To extract quantitative features from both modalities and construct an integrated radiopathomics model.
- Region of Interest (ROI) Segmentation:
- Radiology: Delineate the 3D tumor volume on the medical images. This can be done manually by experienced radiologists, with subsequent review for consistency, or by employing automated deep learning models like nnU-Net for improved reproducibility [122].
- Pathology: Annotate the corresponding tumor region on the WSI. This may involve outlining the tumor area and sampling representative patches for analysis [121].
- High-Throughput Feature Extraction:
- Radiomics: Use standardized software like PyRadiomics to extract a comprehensive set of features (e.g., shape, first-order statistics, texture features like Gray Level Co-occurrence Matrix) [124]. Adhere to the Image Biomarker Standardisation Initiative (IBSI) guidelines to ensure compliance [127].
- Pathomics: Extract features from WSIs, which can range from hand-crafted morphometric features (nuclear shape, size, density) to deep learning features automatically learned by CNNs [121] [48].
- Feature Selection and Integration:
- Feature Selection: Apply algorithms to reduce dimensionality and select the most informative and non-redundant features from each modality. Common methods include minimum Redundancy Maximum Relevance (mRMR) and Least Absolute Shrinkage and Selection Operator (LASSO) [125] [122].
- Data Fusion: Integrate the selected radiomic and pathomic features into a single dataset. This "early fusion" concatenates features for input into a final machine learning model.
- Model Building and Validation:
- Model Training: Train a classifier (e.g., Support Vector Machine, Random Forest, or a mixed-stacked ensemble model) on the integrated feature set to predict the clinical endpoint of interest (e.g., survival, treatment response) [127].
- Validation: Rigorously validate the model using the held-out independent testing set. Perform statistical analysis including receiver operating characteristic (ROC) curves, calibration plots, and decision curve analysis (DCA) to evaluate predictive performance and clinical utility [124].
Diagram 1: Radiopathomics analysis workflow.
The Scientist's Toolkit: Key Research Reagents and Solutions
Successful execution of radiopathomics research requires a suite of specialized software tools and platforms for image processing, feature extraction, and model development.
Table 3: Essential Research Toolkit for Radiopathomics
| Tool Category | Representative Solutions | Primary Function | Key Application in Radiopathomics |
|---|---|---|---|
| Radiomics Feature Extraction | PyRadiomics, LIFEx | Standardized extraction of quantitative features from medical images. | Converts ROIs from CT, MRI, or PET into mineable data, adhering to IBSI standards [124] [126]. |
| Digital Pathology & AI | QuPath, HistoQC, MSIntuit CRC | Whole-slide image analysis, quality control, and AI-based biomarker detection. | Enables WSI visualization, annotation, stain normalization, and deep learning-based feature extraction or endpoint prediction (e.g., MSI status) [48]. |
| Image Segmentation | ITK-SNAP, 3D Slicer, nnU-Net | Manual, semi-automated, or fully automated delineation of regions of interest. | Critical for defining tumor boundaries in both radiological images and pathology slides. Deep learning models (U-Net, nnU-Net) enhance reproducibility [124] [122]. |
| Machine Learning & Statistical Computing | Python (scikit-learn, PyTorch), R | Environment for feature selection, model building, and statistical validation. | Implements algorithms for mRMR, LASSO, and classifiers (SVM, Random Forest). Used for data fusion and model interpretation (e.g., SHAP) [124] [125]. |
| Data Management & Standardization | DICOM Standard for Pathology, Cloud Platforms | Standardized data formats and scalable storage for multi-modal data. | Ensures interoperability between radiology and pathology imaging systems. Facilitates multi-center data sharing and analysis [25]. |
Discussion and Future Directions
The evidence consolidated in this guide compellingly argues that radiopathomics holds a distinct comparative advantage over single-modality approaches. Its capacity to fuse macroscopic tumor phenotypes with microscopic cellular detail provides a more comprehensive lens through which to view tumor biology and heterogeneity [121]. This is particularly crucial for drug development, where understanding the complex interplay between tumor structure, microenvironment, and therapeutic response can de-risk clinical trials and identify predictive biomarkers.
However, the path to widespread clinical and research adoption is fraught with challenges. Data standardization remains a primary hurdle; variability in image acquisition protocols, reconstruction algorithms, and staining processes across institutions can drastically alter feature values, impeding reproducibility [126] [122]. Technical and computational complexity is significant, requiring interdisciplinary collaboration between radiologists, pathologists, and data scientists. Furthermore, the "black box" nature of complex AI models necessitates the use of explainable AI (XAI) techniques to build clinical trust and provide biological insights [48].
Future efforts must prioritize multi-center prospective validation of radiopathomics models to demonstrate generalizability and clinical utility [25] [48]. The field will also benefit from the development of automated, end-to-end software platforms that streamline the radiopathomics workflow, making it more accessible. Finally, extending integration beyond radiology and pathology to include genomic, transcriptomic, and proteomic data—creating true multi-omic models—represents the next frontier in personalized oncology [122]. By collectively addressing these challenges, the research community can fully unlock the potential of radiopathomics to refine cancer diagnostics, prognostication, and therapeutic strategies.
Decision Curve Analysis (DCA) has emerged as a crucial methodology for evaluating the clinical utility of predictive models in healthcare, addressing significant limitations of traditional statistical metrics. Unlike accuracy measures such as sensitivity, specificity, or area under the curve (AUC), which do not directly inform clinical value, DCA incorporates the clinical consequences of decisions made based on a model or test [128] [129]. This approach is particularly valuable in emerging fields like radiomics and digital pathology, where complex artificial intelligence models generate predictions requiring translation into clinically actionable insights [130] [131].
The foundational principle of DCA is the net benefit, a metric that balances the relative harms of false positives (e.g., unnecessary treatments or procedures) and false negatives (e.g., missed diseases) across a range of clinically reasonable probability thresholds [128] [132]. This methodology enables researchers and clinicians to determine whether using a prediction model—such as one derived from CT radiomics features or digital pathology images—would improve patient outcomes compared to default strategies of treating all or no patients [133] [129]. As radiomics and digital pathology continue to revolutionize cancer diagnostics by extracting high-dimensional data from medical images and whole slide images, DCA provides the critical framework for establishing their practical clinical value beyond statistical performance [130] [131].
Theoretical Foundations of Decision Curve Analysis
The Net Benefit Concept
The core calculation in DCA is the net benefit, which quantifies the relative value of true positives against the cost of false positives, scaled by the odds of the probability threshold. The standard formula for net benefit is:
Net Benefit = True Positives / n - False Positives / n × [pt / (1 - pt)]
Where:
- n is the total number of patients in the study
- pt is the threshold probability
- True Positives and False Positives are counts determined by classifying patients as test-positive if their predicted probability equals or exceeds pt [128] [132]
This calculation effectively converts the trade-off between true and false positives into a single clinical utility metric that can be compared across different strategies. The threshold probability (pt) represents the minimum probability of disease at which a patient or clinician would opt for intervention, reflecting their personal valuation of the relative harms of false-positive versus false-negative results [132] [129].
Key Theoretical Components
Table 1: Key Components of Decision Curve Analysis
| Component | Definition | Clinical Interpretation |
|---|---|---|
| Threshold Probability (pt) | The minimum probability of disease at which intervention is warranted | Determined by the ratio of harm of false positives to false negatives; reflects patient preferences and clinical context |
| Net Benefit | Weighted difference between true and false positive rates | Quantifies clinical value by accounting for the consequences of decisions |
| Default Strategies | "Treat all" and "Treat none" approaches | Reference points representing clinical alternatives to using a model |
| Test Positivity Criteria | Definition of a positive result based on predicted probability ≥ pt | Links model outputs to clinical decisions across threshold probabilities |
The mathematical derivation of DCA stems from decision theory, where the goal is to maximize expected utility. The threshold probability embodies the clinical decision point where the expected utility of treatment equals that of no treatment. For a given threshold probability, the harm of a false positive relative to a true positive can be expressed as pt / (1 - pt) [128] [129]. This theoretical foundation connects statistical predictions to clinical decision-making by explicitly incorporating the relative values of different outcomes.
Methodological Framework and Protocols
Core DCA Protocol for Binary Outcomes
The standard protocol for performing DCA for binary outcomes (e.g., cancer present/absent) involves these methodical steps:
Select a threshold probability (pt): Choose a specific probability value that represents the minimum risk level at which a patient would opt for intervention [128]
Define test positivity: For the model or test under study, classify patients as test-positive if their predicted probability equals or exceeds the selected pt [128] [132]
Calculate classification metrics: Determine the number of true positives and false positives based on this classification [128]
Compute net benefit: Apply the net benefit formula using the counts of true positives, false positives, total sample size, and threshold probability [128] [132]
Iterate across thresholds: Repeat steps 1-4 across a clinically relevant range of threshold probabilities (e.g., 1%-35% for cancer diagnostics) [132]
Compare strategies: Calculate net benefit for the strategies of treating all patients and treating no patients for the same range of thresholds [132] [129]
This protocol can be applied to various predictor types, including binary tests, continuous markers converted to probabilities via logistic regression, or outputs from multivariable prediction models [128] [132].
Experimental Design for Radiomics Studies
Table 2: Key Methodological Components in Radiomics and Digital Pathology Studies
| Component | Function | Implementation Example |
|---|---|---|
| Image Segmentation | Define region of interest for feature extraction | Manual delineation of tumor boundaries on CT scans by experienced radiologists [130] [131] |
| Feature Extraction | Convert images into quantifiable data | Extraction of 1046 radiomics features (morphological, histogram, texture) using PyRadiomics [130] |
| Feature Selection | Identify most predictive features while reducing dimensionality | Statistical selection methods applied to reduce 1834 radiomic features to 6 most predictive features [131] |
| Model Construction | Build predictive algorithm using selected features | Logistic regression, support vector machines, or other machine learning algorithms [130] [131] |
| Validation | Assess model performance on independent data | Split-sample validation (70:30) with performance evaluation in training and testing cohorts [130] |
In a typical radiomics study, such as one predicting International Neuroblastoma Pathology Classification (INPC) from CT images, researchers retrospectively enroll patients, divide them into training and testing cohorts, and extract radiomics features from segmented tumor regions [130]. After feature reduction and model construction using methods like logistic regression, the model is validated in both cohorts using ROC curve analysis and calibration curves, with DCA finally applied to assess clinical utility across different risk thresholds [130].
Advanced Methodological Extensions
Several methodological extensions enhance DCA's applicability to complex research scenarios:
Correction for overfitting: Methods like repeated 10-fold cross-validation can correct decision curves for model overfit, preventing overly optimistic evaluations [128]
Confidence intervals: Statistical techniques can generate confidence intervals around decision curves to quantify uncertainty [128]
Application to censored data: DCA can be extended to time-to-event outcomes, including competing risk scenarios [128]
Polytomous outcomes: For multi-category outcomes, extensions like Weighted Area Under the Standardized Net Benefit Curve (wAUCsNB) can synthesize binary measures into a single utility value [134]
These advanced methods broaden DCA's applicability to diverse research contexts common in cancer diagnostics.
Applications in Radiomics and Digital Pathology
Radiomics for Neuroblastoma Classification
In a study evaluating CT-based radiomics for predicting International Neuroblastoma Pathology Classification (INPC) in neuroblastoma, researchers developed a radiomics model using 17 selected features [130]. The model demonstrated acceptable discrimination with an AUC of 0.851 (95% CI: 0.805-0.897) in the training cohort and 0.816 (95% CI: 0.725-0.906) in the testing cohort [130]. While these statistical measures indicated reasonable accuracy, the critical evidence for clinical implementation came from DCA.
The decision curve analysis demonstrated that the radiomics model provided superior net benefit compared to alternative strategies across a range of clinically relevant threshold probabilities for classifying neuroblastoma as favorable or unfavorable histology [130]. This finding confirmed the model's potential clinical utility despite not having the highest possible AUC, highlighting how DCA provides different information than traditional accuracy measures alone.
Radiopathomics Integration for Gastric Cancer Staging
A groundbreaking study developed a radiopathomics model combining preoperative CT scans and postoperative hematoxylin-eosin (HE) stained whole slide images to discriminate between Stage I-II and Stage III gastric cancer [131]. This integrated approach extracted 311 pathological features from HE images and 1,834 radiomic features from CT scans, ultimately constructing a support vector machine model with 17 selected features [131].
The radiopathomics model demonstrated superior discrimination (AUC: training cohort=0.953; validation cohort=0.851) compared to models using either pathology or radiomics features alone [131]. Most importantly, DCA confirmed the enhanced clinical utility of this integrated approach, showing greater net benefit across threshold probabilities compared to single-modality models or default strategies [131]. This exemplifies how DCA can validate the value of combining digital pathology with radiomics for improved cancer staging.
Net Benefit Regression for Economic Evaluation
In addition to diagnostic applications, the net benefit framework extends to economic evaluations through net benefit regression. This approach, particularly valuable in cancer trials, uses regression analysis to evaluate cost-effectiveness by computing net benefit as:
NB = WTP × Effect - Cost
Where WTP represents the willingness-to-pay threshold for a unit of health effect [135]. Net benefit regression facilitates analysis of patient-level cost-effectiveness data, allowing adjustment for confounders, identification of subgroups, and handling of scenarios where more effective treatments might be cost-saving [135]. This framework was applied in the Canadian Cancer Trials Group CO.17 study of cetuximab in advanced colorectal cancer, demonstrating how net benefit analysis extends beyond diagnostic utility to therapeutic economic evaluation [135].
Comparative Performance Assessment
Quantitative Comparison of Model Performance
Table 3: Performance Metrics of Predictive Models in Cancer Diagnostics
| Study/Model | Clinical Context | Discrimination (AUC) | DCA Findings |
|---|---|---|---|
| Radiomics Model for Neuroblastoma [130] | INPC classification from CT images | Training: 0.851 (95% CI: 0.805-0.897)Testing: 0.816 (95% CI: 0.725-0.906) | Positive net benefit across relevant thresholds compared to treat-all or treat-none strategies |
| Radiopathomics Model for Gastric Cancer [131] | Stage I-II vs. Stage III gastric cancer | Training: 0.953Validation: 0.851 | Superior net benefit versus single-modality models or default strategies |
| Mortality Prediction in Dementia [136] | 1-year mortality in older women with dementia | 75.1% (95% CI: 72.7%-77.5%) | Net benefit across probability thresholds from 0.24 to 0.88 |
| Pediatric Appendicitis Predictors [133] | Suspected appendicitis in pediatric patients | PAS and leukocyte count: "acceptable" AUCs | Decision curves revealed substantially different net benefit profiles despite similar AUCs |
These comparative data demonstrate that statistical discrimination (AUC) and clinical utility (net benefit) provide complementary information. In the pediatric appendicitis study, for example, PAS and leukocyte count achieved similar AUCs but substantially different net benefit profiles, while serum sodium with poor discrimination provided no meaningful benefit across thresholds [133]. This underscores why DCA is essential for comprehensive model evaluation.
Advantages Over Traditional Metrics
DCA addresses critical limitations of traditional evaluation metrics:
Clinical relevance: Unlike sensitivity or specificity, DCA directly incorporates clinical consequences of decisions [128] [129]
Threshold continuum: DCA evaluates performance across all reasonable threshold probabilities rather than at a single arbitrary cutoff [132]
Comparative framework: Net benefit enables direct comparison of multiple strategies, including simple defaults [132] [129]
Intuitive interpretation: When properly labeled with "benefit" and "preference," decision curves are readily interpretable by clinical audiences [129]
These advantages make DCA particularly valuable for complex radiomics and digital pathology models, where demonstrating practical clinical impact is essential for adoption.
Implementation and Research Reagents
Table 4: Essential Research Reagents and Computational Tools
| Tool/Resource | Function | Application Example |
|---|---|---|
| PyRadiomics [131] | Open-source Python package for extraction of radiomics features | Feature extraction from CT images in DICOM format |
| ITK-SNAP [130] [131] | Software for manual, semi-automatic, and automatic segmentation of medical images | Defining regions of interest (ROI) around tumors on CT scans |
| QuPath [131] | Open-source digital pathology and bioimage analysis software | Annotation of tumor regions in pathological whole slide images |
| dcurves R Package [132] | R package for performing decision curve analysis | Calculation and plotting of net benefit across threshold probabilities |
| Synthetic Minority Over-sampling Technique (SMOTE) [130] | Algorithm for balancing classes in training data | Addressing class imbalance in radiomics model development |
These tools form the foundation for implementing the radiomics and digital pathology workflows that generate predictions evaluated using DCA. Their proper use requires specialized expertise in image analysis, machine learning, and clinical interpretation.
Practical Implementation Workflow
Diagram 1: Integrated Radiomics-Digital Pathology DCA Workflow illustrating the sequential process from image acquisition to clinical utility assessment, highlighting the role of DCA in the implementation decision.
Decision Curve Analysis represents a paradigm shift in how predictive models are evaluated in healthcare, moving beyond statistical accuracy to practical clinical value. For the rapidly advancing fields of radiomics and digital pathology in cancer diagnostics, DCA provides the critical framework for determining whether complex artificial intelligence and machine learning models will genuinely improve patient outcomes and clinical decision-making. By quantifying net benefit across clinically relevant threshold probabilities, DCA enables researchers to demonstrate that their models offer tangible advantages over current practice, ultimately facilitating the translation of technological innovations into routine clinical care. As these fields continue to evolve, DCA will play an increasingly vital role in validating that sophisticated diagnostic tools deliver meaningful benefits to patients and healthcare systems.
Benchmarking Against Standard Biomarkers and Pathologist Interpretation
The integration of artificial intelligence (AI) into cancer diagnostics, particularly through digital pathology and radiomics, promises to revolutionize precision medicine. However, the transition from experimental algorithms to clinically validated tools requires rigorous benchmarking against established standards—traditional biomarker assays and expert pathologist interpretation. This foundational practice ensures that new AI models meet the stringent requirements for diagnostic accuracy, reliability, and clinical utility before they can impact patient care and drug development pipelines. The gold standard for diagnosis in most solid tumors remains the histological examination by a pathologist, a 140-year-old technology now being transformed by high compute and machine learning [3] [137]. This guide provides a technical framework for researchers and drug development professionals to design and execute robust benchmarking studies that effectively evaluate AI-driven diagnostic tools against these conventional standards, thereby bridging the gap between algorithmic innovation and clinical adoption.
Performance Benchmarks in Computational Pathology and Radiomics
A critical first step in benchmarking is understanding the current performance landscape of both established standards and emerging AI technologies. The table below synthesizes key quantitative findings from recent large-scale evaluations and meta-analyses, providing reference points for model assessment.
Table 1: Performance Benchmarks for Diagnostic AI and Pathologist Standards
| Model / Standard | Task / Disease Context | Sensitivity (Mean) | Specificity (Mean) | AUROC (Mean) | Evidence Source |
|---|---|---|---|---|---|
| AI in Digital Pathology (Aggregate) | Diagnostic accuracy across multiple cancer types (100 studies) | 96.3% (CI 94.1–97.7) | 93.3% (CI 90.5–95.4) | - | Systematic Review & Meta-Analysis [138] |
| Pathology Foundation Models (CONCH) | Morphology-related tasks (5 tasks) | - | - | 0.77 | Benchmarking Study (n=6,818 patients) [139] |
| Pathology Foundation Models (CONCH) | Biomarker-related tasks (19 tasks) | - | - | 0.73 | Benchmarking Study (n=6,818 patients) [139] |
| Pathology Foundation Models (CONCH) | Prognostication-related tasks (7 tasks) | - | - | 0.63 | Benchmarking Study (n=6,818 patients) [139] |
| Human Pathologist Interpretation | Gold standard for surgical pathology | Varies by case complexity and experience | Varies by case complexity and experience | - | Established Clinical Practice [3] [137] |
These benchmarks highlight that while AI models can demonstrate high aggregate sensitivity and specificity, their performance varies significantly based on the specific task, with prognostication remaining a particular challenge. Furthermore, 99% of AI diagnostic studies were found to have at least one area at high or unclear risk of bias, often related to patient selection or use of an unclear reference standard, underscoring the need for meticulous study design [138].
Methodological Framework for Benchmarking Studies
A robust benchmarking methodology must account for data curation, model selection, and performance evaluation to ensure findings are valid and generalizable.
Cohort Selection and Dataset Curation
The foundation of any benchmarking study is a well-characterized cohort. Key considerations include:
- Data Source and Size: Studies should utilize datasets of sufficient scale; however, most current radiomics studies include cohorts smaller than 200 patients, and only 22% employ external validation cohorts, limiting their reliability [36]. Benchmarking efforts should strive for larger, multi-institutional datasets.
- Tumor and Tissue Representation: Ensure the cohort reflects the biological heterogeneity of the cancer type(s) in question. For pan-cancer models, larger cohorts are required to account for the inherent heterogeneity across tumor types [36].
- Ground Truth Definition: The "standard" against which AI is benchmarked must be unequivocally defined. This involves:
- Pathologist Interpretation: For diagnostic tasks, the ground truth is typically established by one or more board-certified pathologists. Discrepancies are resolved by consensus or a third expert. Tools like Nuclei.io facilitate this by creating a "human-in-the-loop" process where pathologists remain the final decision-makers [137].
- Standard Biomarker Assays: For molecular prediction (e.g., PD-L1, MMR status), the ground truth is defined by validated clinical assays such as immunohistochemistry (IHC), PCR, or next-generation sequencing [140] [36].
Experimental and Control Configurations
Benchmarking is a comparative process that should include several configurations:
- Ablation Studies: Compare the performance of the novel AI model against established feature sets or older model architectures.
- Human-AI Collaboration: Evaluate the "human-in-the-loop" paradigm, where AI assists pathologists. For instance, user studies with Nuclei.io showed that pathologists became significantly more efficient and reluctant to return to unassisted work [137].
- Multi-modal Integration: Test whether integrating AI with other data modalities (e.g., radiomics with genomics) outperforms either approach alone. Research shows that integrating pathomics with genomics and radiomics can provide a more comprehensive portrait of a tumor's morphologic heterogeneity and improve prognostic estimates [3].
The following workflow diagram outlines the key stages of a robust benchmarking experiment, from data preparation to performance analysis.
Technical Protocols for Key Experiments
This section details specific experimental protocols for validating AI models against standard biomarkers and pathologist interpretation.
Experiment 1: Predictive Biomarker Discovery from Histology
This experiment tests the hypothesis that AI can predict molecular biomarker status directly from H&E-stained whole slide images (WSIs), a capability known as "pathomics."
- Objective: To determine if a pathomics model can predict the status of a key biomarker (e.g., PD-L1 expression, MMR deficiency, or a specific genetic mutation) from standard H&E WSIs with performance comparable to or exceeding standard IHC or genomic assays.
- Workflow:
- Input: A cohort of WSIs with paired, clinically validated biomarker status.
- Feature Extraction: Process WSIs using a pre-trained pathology foundation model (e.g., CONCH, Virchow2) to generate feature embeddings for each image tile [139].
- Model Training: Train a multiple instance learning (MIL) classifier, such as a transformer-based aggregator, on these features to predict the binary or continuous biomarker status.
- Validation: Evaluate the model on a held-out test set, ideally from an external institution, reporting AUROC, sensitivity, specificity, and F1-score.
- Benchmarking: Compare the model's performance against the standard assay used to define the ground truth. The model's predictions should be analyzed for biological plausibility by correlating salient image regions with known histomorphological features.
Table 2: Key Reagent Solutions for Biomarker Discovery
| Research Reagent / Tool | Function in Experiment | Technical Notes |
|---|---|---|
| Pathology Foundation Models (e.g., CONCH, Virchow2) | Extracts meaningful feature representations from image tiles without task-specific labels. | Vision-language models like CONCH show strong performance on biomarker tasks. Virchow2 (vision-only) is a close competitor [139]. |
| Multiple Instance Learning (MIL) Aggregator | Aggregates tile-level features to make a slide-level or patient-level prediction. | Transformer-based aggregators slightly outperform traditional attention-based MIL (ABMIL) [139]. |
| Whole Slide Images (WSIs) with Paired Biomarker Data | Serves as the input data and ground truth for model training and validation. | Data diversity in pretraining is more critical than volume for foundation model performance [139]. |
| Digital Pathology Platform (e.g., AISight) | Manages the storage, viewing, and analysis of WSIs; facilitates AI application. | Cloud-native systems enable scalable workflow management and deployment of AI tools [43]. |
Experiment 2: AI-Assisted Pathologist Diagnostic Accuracy
This experiment evaluates a human-in-the-loop system where an AI tool assists pathologists in making a specific diagnosis, such as detecting tumor cells or quantifying tumor-infiltrating lymphocytes.
- Objective: To quantify the improvement in pathologist diagnostic accuracy, efficiency, and confidence when using an AI-assisted workflow compared to traditional, unassisted microscopy.
- Workflow:
- Selection: Recruit pathologists with varying experience levels.
- Study Design: Employ a randomized, controlled reader study. Each pathologist reviews a set of cases twice: once without AI assistance and once with AI assistance (or vice versa, with a washout period), using a tool like Nuclei.io [137].
- AI Assistance: The AI tool pre-analyzes the WSI and provides guidance, such as highlighting regions of interest (e.g., potential malignant cells or plasma cells) for the pathologist to review.
- Metrics: Measure and compare:
- Diagnostic Accuracy: Sensitivity, specificity, and agreement with a pre-defined expert consensus.
- Efficiency: Time to diagnosis (turnaround time).
- Workflow Impact: Reduction in the need for additional special stains (e.g., IHC) as reported in studies of Nuclei.io [137].
- User Confidence: Qualitative feedback via post-study surveys.
The following diagram illustrates the interactive workflow between the pathologist and the AI tool in such a study.
A Toolkit for the Modern Cancer Researcher
Successful benchmarking and development in this field rely on a suite of specialized tools and platforms that facilitate data management, AI model development, and integration into research workflows.
Table 3: Essential Research Toolkit for AI Biomarker Development
| Tool Category | Example Solutions | Primary Research Application |
|---|---|---|
| Digital Pathology Platforms | AISight (PathAI) [43], Nuclei.io [137] | Centralized management of WSIs, AI-powered analysis, and collaborative review for diagnostic validation and workflow improvement. |
| Pathology Foundation Models | CONCH, Virchow2, UNI, Phikon [139] | Pre-trained models for feature extraction from WSIs, serving as a starting point for developing downstream predictive models with limited data. |
| Radiomics & AI Biomarker Platforms | Picture Health [141] | Develops "biologically inspired radiomics" biomarkers (e.g., QVT Phenotype) for patient stratification and treatment response prediction in clinical trials. |
| Multi-omics Integration Platforms | Sapient Biosciences, Element Biosciences (AVITI24), 10x Genomics [142] | High-throughput profiling to layer genomic, transcriptomic, and proteomic data with pathomic and radiomic features for comprehensive biomarker discovery. |
| Quality & Regulatory Frameworks | CAP Quality Measures (e.g., QPP 249, QPP 491) [140], IVDR Compliance Tools [142] | Provides standardized metrics and regulatory pathways to ensure AI models and biomarkers meet clinical quality and safety standards for adoption. |
Benchmarking AI-driven tools against standard biomarkers and pathologist interpretation is a non-negotiable step in the translation of computational pathology and radiomics from research to clinical practice. This process demands meticulous methodology, including well-characterized cohorts, unambiguous ground truth, and rigorous experimental designs that evaluate both standalone AI performance and its synergistic value in a human-in-the-loop system. As the field matures, overcoming challenges related to data standardization, regulatory ambiguity, and clinical trust will be paramount. By adhering to the frameworks and protocols outlined in this guide, researchers and drug developers can generate the high-quality evidence needed to validate the next generation of cancer diagnostics, ultimately accelerating the delivery of precision medicine to patients.
Conclusion
The integration of radiomics and digital pathology marks a paradigm shift in cancer diagnostics, offering an unprecedented, multi-scale window into tumor biology. By fusing macroscopic radiological phenotypes with microscopic pathological details, this approach provides a more comprehensive and quantitative basis for assessing tumor heterogeneity, predicting treatment efficacy, and uncovering novel biomarkers. While significant challenges in standardization, reproducibility, and clinical translation remain, the continuous evolution of AI and machine learning methodologies is steadily addressing these hurdles. For researchers and drug developers, these technologies present a powerful opportunity to de-risk and accelerate the development of targeted therapies and companion diagnostics. The future of oncology lies in the intelligent fusion of multi-omics data, with integrated radiopathomic models poised to become indispensable tools for enabling truly personalized and predictive cancer care.
References
- 1. Radiomics in medical imaging—“how-to” guide and critical ... [https://insightsimaging.springeropen.com/articles/10.1186/s13244-020-00887-2]
- 2. Insights into radiomics: a comprehensive review ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12559095/]
- 3. Integrating pathomics with radiomics and genomics for cancer prognosis: A brief review - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC8580801/]
- 4. Understanding Success Criterion 1.4.3: Contrast (Minimum) [https://www.w3.org/WAI/WCAG21/Understanding/contrast-minimum.html]
- 5. Enabling the future of digital pathology with DICOM at ... [https://www.merative.com/blog/enabling-the-future-of-digital-pathology-with-dicom-at-pathology-visions-2025]
- 6. Evolving standards for a smarter digital pathology ecosystem [https://pmc.ncbi.nlm.nih.gov/articles/PMC12546968/]
- 7. Researchers Invent New AI Tool to Automate Detection ... [https://viterbischool.usc.edu/news/2025/10/researchers-invent-new-ai-tool-to-automate-detection-of-cancer-in-blood-samples/]
- 8. Cancer Diagnostics Market Size & Trends 2025 to 2035 [https://www.futuremarketinsights.com/reports/cancer-diagnostics-market]
- 9. Review Introduction to radiomics for a clinical audience [https://www.sciencedirect.com/science/article/pii/S000992602200705X]
- 10. Radiomics in preclinical imaging research: methods ... [https://www.nature.com/articles/s44303-025-00104-z]
- 11. Advances in the use of Radiomics and Pathomics for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12162063/]
- 12. Understanding Sources of Variation to Improve the ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8039446/]
- 13. How Artificial Intelligence Is Transforming Cancer Care in ... [https://oncodaily.com/oncolibrary/artificial-intelligence-ai]
- 14. Introduction to Radiomics | Journal of Nuclear Medicine [https://jnm.snmjournals.org/content/61/4/488]
- 15. RadiomiX for Radiomics Analysis: Automated Approaches ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12345906/]
- 16. Addressing the current challenges in the clinical application of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12515897/]
- 17. Quantitative imaging feature pipeline: a web-based tool for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7070161/]
- 18. Artificial intelligence-driven pathomics in hepatocellular ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12304379/]
- 19. AI in Histopathology Explorer for comprehensive analysis ... [https://www.nature.com/articles/s41746-025-01524-2]
- 20. Artificial intelligence in advanced gastric cancer [https://pmc.ncbi.nlm.nih.gov/articles/PMC12401684/]
- 21. Computationally integrating radiology and pathology ... [https://www.nature.com/articles/s41698-025-00939-0]
- 22. Radiomics, Biomarkers & Multi-Omics at RSNA 2025 [https://vestarad.com/precision-imaging-at-rsna-2025-radiomics-biomarkers-and-the-era-of-multi-omics-integration/]
- 23. Unveiling key pathomic features for automated diagnosis and ... [https://bmcmedimaging.biomedcentral.com/articles/10.1186/s12880-025-01841-8]
- 24. Deep learning and pathomics analyses predict prognosis ... [https://www.frontiersin.org/journals/neurology/articles/10.3389/fneur.2025.1614678/full]
- 25. Digital pathology imaging artificial intelligence in cancer ... [https://www.sciencedirect.com/science/article/pii/S2153353925001178]
- 26. Current AI technologies in cancer diagnostics and treatment | Molecular Cancer [https://link.springer.com/article/10.1186/s12943-025-02369-9]
- 27. Harnessing multimodal data to advance precision oncology... integration [https://pmc.ncbi.nlm.nih.gov/articles/PMC8810682/]
- 28. Journal of Medical Internet Research - Radiomics-Based Machine Learning for the Detection of Myometrial Invasion in Endometrial Cancer: Systematic Review and Meta-Analysis [https://www.jmir.org/2025/1/e78809]
- 29. Systematic review Tracking tumor biology with radiomics [https://www.sciencedirect.com/science/article/pii/S0167814018301798]
- 30. Radiomic clustering using graph network techniques ... [https://www.sciencedirect.com/science/article/pii/S2001037025004684]
- 31. Tools for visualization and analysis of molecular networks ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4461095/]
- 32. New AI-based biomarkers offer insight into treatment ... [https://dailyreporter.esmo.org/esmo-congress-2025/ai-digital-oncology/new-artificial-intelligence-based-biomarkers-offer-early-insight-into-treatment-response]
- 33. Exploratory Analysis of Radiomics and Pathomics in ... [https://www.nature.com/articles/s41598-024-78987-y]
- 34. Decoding Radiomics: A Step-by-Step Guide to Machine ... [https://www.mdpi.com/2075-4418/14/22/2473]
- 35. Multimodal radiopathomics signature for prediction of ... [https://www.sciencedirect.com/science/article/pii/S0304383525004999]
- 36. A whirl of radiomics-based biomarkers in cancer ... [https://www.nature.com/articles/s41698-024-00534-9]
- 37. Artificial Intelligence and Radiomics Biomarkers for ... [https://www.sciencedirect.com/science/article/pii/S0960977625005880]
- 38. Visualizing Data - NCI [https://www.cancer.gov/about-nci/organization/cbiit/training/learn/visualize]
- 39. Radiomics and Its Feature Selection: A Review [https://www.mdpi.com/2073-8994/15/10/1834]
- 40. Digital pathology systems enabling quality patient care - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC11265285/]
- 41. Digital Pathology Workflow: Breakthrough Innovation ... - KFBIO [https://kfbiopathology.com/2025/09/19/digital-pathology-workflow-breakthrough-innovation-in-clinical-application/]
- 42. Optimizing radiomics for prostate cancer diagnosis: feature ... [https://insightsimaging.springeropen.com/articles/10.1186/s13244-024-01783-9]
- 43. PathAI | Pathology Transformed [https://www.pathai.com/]
- 44. Multimodal data fusion for cancer biomarker discovery with ... [https://www.nature.com/articles/s42256-023-00633-5]
- 45. Multimodal data fusion for cancer biomarker discovery with ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10484010/]
- 46. Comparison of diagnostic accuracy of radiomics parameter ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11491382/]
- 47. Exploring radiomics research quality scoring tools [https://dirjournal.org/articles/exploring-radiomics-research-quality-scoring-tools-a-comparative-analysis-of-metrics-and-rqs/dir.2024.242793]
- 48. Real-Time Detection, Radiomics, and Digital Pathology [https://pmc.ncbi.nlm.nih.gov/articles/PMC12543294/]
- 49. Predictive Biomarkers of Response to Neoadjuvant ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9405974/]
- 50. Pathological complete response and prognostic predictive ... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2025.1570394/full]
- 51. Efficacy, safety, and predictive biomarkers of neoadjuvant ... [https://www.nature.com/articles/s41467-025-66667-y]
- 52. Current AI technologies in cancer diagnostics and treatment [https://molecular-cancer.biomedcentral.com/articles/10.1186/s12943-025-02369-9]
- 53. Artificial Intelligence for the Diagnosis and Management of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12587170/]
- 54. Multimodal deep learning for predicting neoadjuvant treatment ... [https://biologydirect.biomedcentral.com/articles/10.1186/s13062-025-00661-8]
- 55. A preoperative predictive model based on multi-modal ... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2025.1530279/full]
- 56. Predicting response to neoadjuvant chemotherapy in ... [https://www.nature.com/articles/s41746-025-01560-y]
- 57. MIPD: Molecules, Imagings, and Clinical Phenotype ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12010968/]
- 58. Top Oncology Innovations That Shaped the First Half of 2025 [https://binaytara.org/cancernews/article/top-oncology-innovations-that-shaped-the-first-half-of-2025]
- 59. Review Decoding driver and phenotypic genes in cancer [https://www.sciencedirect.com/science/article/pii/S0098299725000226]
- 60. A core driver gene set identified based on geMER reveals ... [https://www.nature.com/articles/s41698-025-01060-y]
- 61. Radiomics for lung cancer diagnosis, management, and ... [https://www.sciencedirect.com/science/article/pii/S000992602500131X]
- 62. Artificial intelligence in advanced gastric cancer [https://www.frontiersin.org/journals/oncology/articles/10.3389/fonc.2025.1630628/full]
- 63. Artificial Intelligence-Enhanced Liquid Biopsy and Radiomics ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12524159/]
- 64. Progress and challenges of artificial intelligence in lung ... [https://www.nature.com/articles/s41698-025-00986-7]
- 65. Applications of artificial intelligence in digital pathology for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11551048/]
- 66. Artificial Intelligence in digital pathology of breast cancer ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12626545/]
- 67. Application of deep learning models in gastric ... - BMC Cancer [https://bmccancer.biomedcentral.com/articles/10.1186/s12885-025-14662-3]
- 68. Deep learning and radiomics integration of photoacoustic ... [https://breast-cancer-research.biomedcentral.com/articles/10.1186/s13058-025-02113-7]
- 69. Advances in Breast Cancer Care: The Role of Artificial ... [https://eurjbreasthealth.com/articles/advances-in-breast-cancer-care-the-role-of-artificial-intelligence-and-digital-pathology-in-precision-medicine/ejbh.galenos.2025.2024-12-8]
- 70. Reproducibility and interpretability in radiomics: a critical ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12239541/]
- 71. A perspective on integrating digital pathology, proteomics, ... [https://pubmed.ncbi.nlm.nih.gov/40680990/]
- 72. Reliability of CT radiomic features reflecting tumour ... [https://www.nature.com/articles/s41598-020-60868-9]
- 73. The impact of the variation of imaging parameters on ... [https://www.sciencedirect.com/science/article/pii/S0010482521001943]
- 74. Toward standardization: Assessing the reproducibility of ... [https://www.sciencedirect.com/science/article/pii/S105381192500401X]
- 75. Multicentric study on the reproducibility and robustness of PET ... [https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0309540]
- 76. Graph feature selection for enhancing radiomic stability ... [https://www.nature.com/articles/s41598-025-12161-w]
- 77. Rethinking feature reproducibility in radiomics: the elephant in ... [https://eurradiolexp.springeropen.com/articles/10.1186/s41747-025-00629-3]
- 78. Curse of Dimensionality: An Intuitive Exploration [https://towardsdatascience.com/curse-of-dimensionality-an-intuitive-exploration-1fbf155e1411/]
- 79. The Relationship Between High Dimensionality and Overfitting [https://vtiya.medium.com/the-relationship-between-high-dimensionality-and-overfitting-5bca0967b60f]
- 80. Radiomics in preclinical imaging research [https://pmc.ncbi.nlm.nih.gov/articles/PMC12454655/]
- 81. AI-powered Digital Pathology Workflows Support Confident ... [https://www.diagnosticsworldnews.com/news/2025/10/10/ai-powered-digital-pathology-workflows-support-confident-cancer-diagnosis]
- 82. Curse of Dimensionality in Machine Learning [https://www.geeksforgeeks.org/machine-learning/curse-of-dimensionality-in-machine-learning/]
- 83. A Heuristic Radiomics Feature Selection Method Based on ... [https://www.sciencedirect.com/org/science/article/pii/S1546221824002819]
- 84. A Review of Dimensionality Reduction Techniques for ... [https://www.sciencedirect.com/science/article/pii/S1877050920300879]
- 85. The Curse of Dimensionality in Machine Learning [https://www.datacamp.com/blog/curse-of-dimensionality-machine-learning]
- 86. Using Genomics Feature Selection Method in Radiomics ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8124289/]
- 87. Reproducibility and Generalizability in Radiomics Modeling: Possible... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6609433/]
- 88. Larger sample sizes are needed when developing a ... [https://www.sciencedirect.com/science/article/pii/S0895435625000083]
- 89. Sample size requirements are not being considered in studies ... [https://bmcmedresmethodol.biomedcentral.com/articles/10.1186/s12874-023-02008-1]
- 90. Effects of sample size on robustness and prediction accuracy ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC2689196/]
- 91. A Novel Virtual Sample Generation Method to Overcome ... [https://www.mdpi.com/1999-4893/12/8/160]
- 92. Cycle-consistent adversarial networks improves generalizability of... [https://www.nature.com/articles/s41598-022-10956-9?error=cookies_not_supported&code=2e52b182-e756-475f-b280-39eaed418ed9]
- 93. Lung Cancer Predictive Models [https://www.rsna.org/news/2025/august/lung-cancer-predictive-models]
- 94. Interpreting Black-Box Models: A Review on Explainable ... [https://link.springer.com/article/10.1007/s12559-023-10179-8]
- 95. towards interpretable and reliable deep learning models - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC10702969/]
- 96. Explainable medical imaging AI needs human-centered ... [https://www.nature.com/articles/s41746-022-00699-2]
- 97. Guiding Principles - Transparency for Machine Learning ... [https://www.fda.gov/medical-devices/software-medical-device-samd/transparency-machine-learning-enabled-medical-devices-guiding-principles]
- 98. Pathology-interpretable radiomic model for predicting clinical ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12573972/]
- 99. Reproducibility and interpretability in radiomics: a critical ... [https://dirjournal.org/articles/reproducibility-and-interpretability-in-radiomics-a-critical-assessment/dir.2024.242719]
- 100. Visualizing Quantitative Data: Best Practices [https://ajelix.com/data/visualizing-quantitative-data-best-practices/]
- 101. 332. Examples of scientific data visualization with ... [https://medium.com/@ilakk2023/examples-of-scientific-data-visualization-with-quantitative-components-77ec53b7ce43]
- 102. Best Color Palettes for Scientific Figures and Data ... [https://www.simplifiedsciencepublishing.com/resources/best-color-palettes-for-scientific-figures-and-data-visualizations]
- 103. Navigating color integrity in data visualization [https://www.sciencedirect.com/science/article/pii/S2666389924000801]
- 104. Artificial intelligence in cancer: applications, challenges, and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12574039/]
- 105. Revolutionizing Medical Imaging: The Transformative Role of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12191749/]
- 106. A delta radiomics model based on ultrasound images ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12641098/]
- 107. An interpretable delta ultrasound radiomics model for ... [https://ovarianresearch.biomedcentral.com/articles/10.1186/s13048-025-01859-0]
- 108. The AI revolution: how multimodal intelligence will reshape ... [https://www.nature.com/articles/s44387-025-00044-4]
- 109. - Multi features to predict overall survival of locally... modal radiomics [https://pmc.ncbi.nlm.nih.gov/articles/PMC11967038/]
- 110. Multimodal imaging in cancer detection: the role of SPIONs ... [https://pubmed.ncbi.nlm.nih.gov/40531182/]
- 111. Systematic scoping review of external validation studies ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12145442/]
- 112. Development and external validation of a radiomics model for ... [https://insightsimaging.springeropen.com/articles/10.1186/s13244-022-01361-x]
- 113. Exact Sciences Announces Expanded Clinical Validation ... [https://www.exactsciences.com/newsroom/press-releases/exact-sciences-announces-expanded-clinical-validation-of-the-oncodetect-test]
- 114. Precision Digital Oncology: Emerging Role of Radiomics ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7983689/]
- 115. Clinical prediction models using machine learning in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12506039/]
- 116. Development of machine learning prognostic models for ... [https://www.nature.com/articles/s41598-023-45804-x]
- 117. Diagnostic accuracy of deep learning in medical imaging [https://www.nature.com/articles/s41746-021-00438-z]
- 118. Biologically-Inspired Radiomic Biomarker Development [https://www.decibio.com/insights/radiomics-biologically-inspired-radiomic-biomarker-development--an-interview-with-nathaniel-braman-co-founder-of-picture-health]
- 119. A Framework for Evaluating the Technical Performance of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9825639/]
- 120. A Framework for Evaluating the Technical Performance of ... [https://www.sciencedirect.com/science/article/abs/pii/S1076633222004846]
- 121. Radiomics at a Glance: A Few Lessons Learned from ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7563283/]
- 122. Radiomics-Driven Tumor Prognosis Prediction Across ... [https://www.mdpi.com/2072-6694/17/19/3121]
- 123. MRI-based radiomics for assisting diagnosis, assessment ... [https://www.sciencedirect.com/science/article/pii/S2950162825000372]
- 124. Dual-modal ultrasound-based deep learning radiomics for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12596425/]
- 125. of Comparison -based machine-learning classifiers for the... radiomics [https://pmc.ncbi.nlm.nih.gov/articles/PMC11257043/]
- 126. Paving a Path to Clinical Impact with Radiomics [https://pubmed.ncbi.nlm.nih.gov/40598943/]
- 127. Comparison of conventional and radiomics-based analysis ... [https://www.nature.com/articles/s41598-025-10515-y]
- 128. Extensions to decision curve analysis, a novel method for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC2611975/]
- 129. A simple, step-by-step guide to interpreting decision curve ... [https://diagnprognres.biomedcentral.com/articles/10.1186/s41512-019-0064-7]
- 130. of contrast-enhanced computed tomography in... Radiomics analysis [https://pmc.ncbi.nlm.nih.gov/articles/PMC10267098/]
- 131. Development and validation of a Radiopathomics model based on CT... [https://bmccancer.biomedcentral.com/articles/10.1186/s12885-024-12021-2]
- 132. Decision Curve Analysis • dcurves [https://www.danieldsjoberg.com/dcurves/articles/dca.html]
- 133. Decision Curve Analysis Explained [https://www.medrxiv.org/content/10.1101/2025.08.16.25333820v1]
- 134. Evaluating clinical utility of multi-category outcome risk ... [https://pubmed.ncbi.nlm.nih.gov/40343018/]
- 135. Advantages of the net benefit regression framework for trial ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6555934/]
- 136. Development, validation, and clinical utility of a risk ... [https://www.sciencedirect.com/science/article/pii/S0167494325001116]
- 137. AI tool gives pathologists speed, accuracy and a new way to ... [https://med.stanford.edu/news/all-news/2025/09/ai-tool-pathology.html]
- 138. a systematic review and meta-analysis of diagnostic test ... [https://www.nature.com/articles/s41746-024-01106-8]
- 139. Benchmarking foundation models as feature extractors for ... [https://www.nature.com/articles/s41551-025-01516-3]
- 140. 2025 Pathology Quality Measures [https://www.cap.org/advocacy/quality-payment-program-for-pathologists/mips-for-pathologists/2025-pathology-quality-measures]
- 141. Biologically-Inspired Radiomic Biomarker Development– ... [https://friendsofcancerresearch.org/news/decibio-radiomics-biologically-inspired-radiomic-biomarker-development-an-interview-with-nathaniel-braman-co-founder-of-picture-health/]
- 142. Insights from Biomarkers & Precision Medicine 2025 [https://www.signifyresearch.net/insights/biomarkers-billions-and-breakthroughs-insights-from-biomarkers-precision-medicine-2025/]