Harnessing Bioinformatics for Novel Anticancer Target Discovery: A Guide for Researchers and Drug Developers
This article provides a comprehensive overview for researchers and drug development professionals on leveraging bioinformatics to discover novel anticancer drug targets.
Harnessing Bioinformatics for Novel Anticancer Target Discovery: A Guide for Researchers and Drug Developers
Abstract
This article provides a comprehensive overview for researchers and drug development professionals on leveraging bioinformatics to discover novel anticancer drug targets. It explores the foundational role of multi-omics data from resources like TCGA and bioinformatics databases in identifying potential targets. The piece details advanced computational methodologies, including molecular docking, dynamics simulations, and AI-driven network biology, for target validation and drug screening. It further addresses critical challenges in data integration and computational demands, offering optimization strategies. Finally, the article covers the essential transition from computational prediction to experimental and clinical validation, highlighting successful case studies and the integration of real-world data to bridge research and clinical practice in precision oncology.
The Bioinformatics Foundation: Mining Multi-Omics Data for Target Discovery
The discovery of novel anticancer drug targets now heavily relies on the systematic analysis of large-scale genomic datasets. Among the most critical resources enabling this research are The Cancer Genome Atlas (TCGA), the International Cancer Genome Consortium (ICGC), and the Catalogue of Somatic Mutations in Cancer (COSMIC). These complementary platforms provide researchers with comprehensive molecular characterizations of thousands of tumor samples across cancer types, creating unprecedented opportunities for identifying oncogenic drivers and therapeutic vulnerabilities. TCGA, a landmark project jointly managed by the National Cancer Institute (NCI) and the National Human Genome Research Institute (NHGRI), molecularly characterized over 20,000 primary cancer and matched normal samples spanning 33 cancer types, generating over 2.5 petabytes of multi-omics data [1] [2]. ICGC complements this effort with international data contributions, while COSMIC serves as the world's largest expert-curated knowledgebase of somatic mutations, integrating data from TCGA, ICGC, and over 29,000 peer-reviewed publications [3] [4]. Together, these resources provide the foundational data necessary for advancing precision oncology through bioinformatics-driven approaches.
Table 1: Overview of Major Cancer Genomics Resources
| Resource | Primary Focus | Data Scale | Key Features | Primary Applications in Drug Discovery |
|---|---|---|---|---|
| TCGA | Multi-omics profiling of primary cancers | 20,000+ cases; 33 cancer types; 2.5 PB data | Genomic, epigenomic, transcriptomic, proteomic data; matched normal samples | Identifying dysregulated pathways, molecular subtypes, and candidate therapeutic targets |
| ICGC | International genomic data collaboration | 1,600,000+ samples (in COSMIC) | Pan-cancer data from international cohorts; genomic and transcriptomic data | Cross-population validation of targets; expanding diversity of genomic insights |
| COSMIC | Somatic mutation curation and interpretation | 29,000,000+ variants; 1,600,000+ samples | Expert-curated mutations; therapeutic actionability; cancer gene census | Mutation pathogenicity assessment; clinical actionability prediction; resistance mutation identification |
Resource-Specific Profiles and Applications
The Cancer Genome Atlas (TCGA)
TCGA represents one of the most comprehensive cancer genomics initiatives, generating data through a highly organized research network structure. The project employed multiple molecular characterization platforms including next-generation sequencing for genome and transcriptome analysis, microarray technologies for nucleic acid and protein testing, and proteomic characterization techniques [2]. The data generation workflow involved Tissue Source Sites for biospecimen collection, Biospecimen Core Resources for sample processing, Genome Characterization Centers for molecular analysis, and Genome Sequencing Centers for high-throughput sequencing [2]. This coordinated approach ensured standardized data generation across participating institutions.
TCGA data encompasses multiple molecular levels, including genomic (somatic mutations, copy number alterations), epigenomic (DNA methylation), transcriptomic (gene expression, non-coding RNA), and proteomic (protein expression) data [5]. The program studied specific cancers based on criteria including poor prognosis, public health impact, and sample availability meeting standards for patient consent, quality, and quantity [6]. Many rare cancers were also included with support from patients, patient advocacy groups, and clinicians [6].
For drug target discovery, TCGA data enables researchers to identify dysregulated pathways, molecular subtypes within cancer types, and co-occurring genomic alterations that may inform combination therapy strategies. The rich clinical dataset associated with molecular profiles allows for correlation of molecular features with treatment response and survival outcomes [7] [8].
Catalogue of Somatic Mutations in Cancer (COSMIC)
COSMIC is the world's largest and most comprehensive resource for somatic mutations in cancer, manually curated by experts to provide highly standardized data. The knowledgebase contains over 29 million genomic variants across more than 1.6 million samples, including single nucleotide variants (SNVs), insertions and deletions, structural variants, copy number variations, and gene fusions [3] [4]. COSMIC integrates data from genome-wide screens and targeted analyses, enabling robust insights into cancer genomics.
The platform offers several specialized modules designed to support different aspects of cancer research and drug discovery. The COSMIC Gene Census identifies and ranks over 750 genes with documented roles in cancer, classifying them into Tier 1 (strong evidence) and Tier 2 (emerging evidence) categories [3]. The Mutation Census tracks coding mutations and differentiates between driver and passenger mutations based on pathogenicity and frequency [3]. The COSMIC Signatures module catalogues mutational patterns across different mutation types, helping identify underlying mutational processes [3].
For therapeutic development, the Actionability module provides data on available therapies and clinical trials for specific mutations, while the Resistance module curates mutations known to confer resistance to cancer treatments [3]. The COSMIC 3D module offers structural insights into protein mutations, enabling visualization of how mutations alter protein-drug interactions [3].
Table 2: COSMIC Database Content by Variant Type and Sample Source
| Variant Type | Count in COSMIC | Sample Source | Count in COSMIC |
|---|---|---|---|
| SNV | 23,000,000 | Solid Cancers | 1,150,000 |
| Insertions & Deletions | 2,000,000 | Blood & Lymphatic Cancers | 444,000 |
| Structural & Copy Number | 4,300,000 | Circulating Tumor DNA | 6,000 |
| Fusions | 20,000 | Most Prevalent Cancers (WHO) | |
| Trachea, bronchus, lung | 217,049 | ||
| Colorectum | 216,352 | ||
| Breast | 62,902 | ||
| Stomach | 29,858 | ||
| Prostate | 26,103 |
Data Integration and Complementary Strengths
While each resource has distinct strengths, their integration provides powerful insights for drug target discovery. TCGA offers deep multi-omics profiling of carefully selected primary tumors with matched normal controls, enabling comprehensive molecular characterization of specific cancer types [1] [8]. ICGC provides international diversity and additional cases that expand the scope beyond TCGA's primary focus. COSMIC delivers expert curation and integration of somatic mutation data from both large-scale projects and targeted studies, creating a comprehensive knowledgebase of cancer genomic alterations [3] [4].
The integration of these resources enables researchers to move from single-omics analyses to multi-omics integration, providing a more complete understanding of cancer biology. For example, combining genomic mutation data from COSMIC with transcriptomic and proteomic data from TCGA can reveal how mutations impact gene expression and protein function [8]. This integrated approach helps distinguish between passenger mutations that accumulate in cancer cells and driver mutations that directly contribute to oncogenesis, thereby prioritizing the most promising therapeutic targets.
Practical Access and Analytical Methodologies
Data Access Protocols
TCGA Data Access via Genomic Data Commons (GDC)
The primary hub for accessing TCGA data is the Genomic Data Commons (GDC) Data Portal, which provides harmonized data aligned to the GRCh38 reference genome [5]. The GDC workflow involves:
- Cohort Building: Using the "Cohort Builder" to select cases of interest based on project, disease type, demographic, or clinical criteria
- Data Selection: Filtering files in the "Repository" by data type (e.g., gene expression, mutations, methylation)
- Data Download: Downloading files directly for small datasets (<5GB) or using the GDC Data Transfer Tool for larger datasets [5]
Researchers should note that TCGA data is categorized as either open-access or controlled-access. Controlled data includes individual germline variants, primary sequence files (.bam), and clinical free text, requiring dbGaP authorization [5]. For programmatic access, the GDC API provides a powerful interface for querying and retrieving data [5].
Alternative TCGA Data Access Points
Several specialized portals offer alternative access to TCGA data with enhanced analytical capabilities:
- cBioPortal: Provides intuitive visualization of genetic alterations across cancer samples, including mutation rates, copy number alterations, and mRNA expression z-scores, coupled with survival analysis capabilities [9]
- Broad Institute's GDAC Firehose: Offers merged, analysis-ready files from TCGA, with pre-processed data structures suitable for R-based analysis [9]
- University of California Santa Cruz Xena: Enables integrated analysis of TCGA data with other genomic and phenotypic data through interactive visualizations
COSMIC Data Access and Utilization
COSMIC provides both web-based query interfaces and downloadable data sets for approved users. The typical workflow for leveraging COSMIC in target discovery involves:
- Gene Search: Querying specific genes of interest to retrieve mutation frequency, distribution, and functional impact data
- Tissue-Specific Analysis: Examining mutation patterns across different cancer types to identify tissue-specific versus pan-cancer mutations
- Pathogenicity Assessment: Using the Mutation Census to evaluate the likely functional impact of mutations
- Clinical Actionability Review: Consulting the Actionability and Resistance modules to understand therapeutic implications
Analytical Workflows for Target Discovery
The following diagram illustrates a representative integrated workflow for anticancer drug target discovery using public genomics resources:
Integrated Workflow for Cancer Target Discovery
Transcriptomics-Based Target Identification Protocol
A proven methodology for identifying novel therapeutic targets involves integrated analysis of transcriptomics data from TCGA with mutation information from COSMIC [7]:
- Sample Selection: Identify tumor and matched normal samples for the cancer type of interest using TCGA's clinical annotations
- Differential Expression Analysis: Calculate significantly upregulated genes in tumors compared to normal tissues using RNA-seq data
- Tissue-Specificity Filtering: Filter results to exclude genes with high expression in vital normal organs (e.g., heart, lungs, liver, kidney)
- Mutation Enrichment Analysis: Cross-reference upregulated genes with COSMIC mutation data to identify frequently mutated candidates
- Functional Annotation: Classify candidates using COSMIC's Gene Census and assess mutation impact using COSMIC 3D
- Survival Correlation: Evaluate the correlation between candidate gene expression and patient survival using clinical data
- Experimental Validation: Perform functional validation using RNA interference or CRISPR/Cas9 systems in relevant cancer cell models
This approach successfully identified several promising drug targets, including MELK (maternal embryonic leucine zipper kinase), TOPK (T-lymphokine-activated killer cell-originated protein kinase), and BIG3 (brefeldin A-inhibited guanine nucleotide-exchange protein 3) in breast cancer [7].
Pan-Cancer Analysis Protocol
For identifying targets across multiple cancer types:
- Data Compilation: Aggregate mutation data from TCGA and ICGC via COSMIC's integrated dataset
- Mutational Significance Analysis: Identify genes with mutation rates significantly above background using mutational burden calculations
- Functional Impact Prediction: Filter mutations based on predicted functional consequences (e.g., missense vs. truncating)
- Pathway Enrichment: Map frequently mutated genes to signaling pathways using pathway databases
- Druggability Assessment: Evaluate the biochemical druggability of candidate targets using structural information
The Scientist's Toolkit: Essential Research Reagents and Platforms
Table 3: Essential Research Reagents and Platforms for Cancer Genomics
| Category | Specific Tools/Platforms | Function in Research | Application in Target Discovery |
|---|---|---|---|
| Data Access Portals | GDC Data Portal; ICGC Data Portal; COSMIC Website | Centralized access to genomic data and annotations | Initial data retrieval and cohort selection |
| Analysis Platforms | cBioPortal; Firebrowse; TANRIC; MEXPRESS | Interactive analysis and visualization of cancer genomics data | Rapid hypothesis testing and data exploration |
| Bioinformatics Tools | GDC Data Transfer Tool; BigQuery; R/Bioconductor | Large-scale data processing and statistical analysis | Advanced computational analysis and integration |
| Experimental Validation | CRISPR/Cas9; RNAi; Organoid culture | Functional validation of candidate targets | Confirmation of target essentiality in disease models |
| Specialized Databases | COSMIC Gene Census; Cancer Proteome Atlas (TCPA) | Curated information on cancer genes and proteins | Target prioritization based on biological evidence |
The integration of TCGA, ICGC, and COSMIC resources provides an unprecedented foundation for anticancer drug target discovery. By leveraging the multi-omics data from TCGA, international diversity from ICGC, and expert-curated mutation information from COSMIC, researchers can identify and prioritize novel therapeutic targets with greater efficiency and confidence. The practical protocols and resources outlined in this whitepaper provide a roadmap for harnessing these powerful platforms to advance the development of targeted cancer therapies. As these resources continue to expand and improve, they will undoubtedly play an increasingly vital role in translating cancer genomics discoveries into clinical applications that improve patient outcomes.
The discovery of novel anticancer drug targets is a cornerstone in the fight against cancer, a disease that remains a leading cause of mortality worldwide [10] [11]. Traditional drug discovery processes are notoriously lengthy, expensive, and carry high failure rates in clinical trials [12] [13]. Bioinformatics has emerged as a transformative discipline, leveraging computational power and biological data to accelerate the identification and validation of new therapeutic targets. By integrating genomic, transcriptomic, proteomic, and pharmacological data, bioinformatics resources enable researchers to prioritize candidate genes and proteins with higher precision and efficiency [12] [14]. Among the plethora of available tools, three databases—cBioPortal, GEPIA2, and canSAR—have become indispensable for modern cancer research and drug development. This whitepaper provides an in-depth technical guide to these core resources, detailing their functionalities, integrated application in experimental workflows, and their pivotal role in advancing anticancer drug discovery.
Database Profiles and Key Features
This section details the core characteristics, data sources, and primary functions of cBioPortal, GEPIA2, and canSAR, summarizing their key attributes for easy comparison.
Table 1: Core Features of cBioPortal, GEPIA2, and canSAR
| Feature | cBioPortal | GEPIA2 (Gene Expression Profiling Interactive Analysis) | canSAR |
|---|---|---|---|
| Primary Focus | Multidimensional cancer genomics data and clinical outcomes [15] | Gene expression profiling and interactive analysis [16] | Integrated translational research and drug discovery knowledgebase [17] |
| Core Data Types | Somatic mutations, DNA copy-number alterations, mRNA expression, DNA methylation, clinical data [15] | RNA-seq expression data from TCGA tumors and GTEx normal tissues [16] [18] | Genomic, protein, pharmacological, drug, chemical, structural biology, protein network, and druggability data [17] |
| Key Functionality | Visualize genetic alterations; query genes across samples; survival analysis; group comparison [15] | Differential expression analysis, profiling plotting, correlation, patient survival analysis, similar gene detection, dimensionality reduction [16] | Provides drug target prioritization, druggability assessment, and compound screening based on integrated data [17] |
| Unique Strengths | Intuitive visualization of complex genomic data in a clinical context; supports multi-gene queries [15] | Addresses the imbalance between tumor and normal samples by incorporating GTEx data; customizable analyses [16] | Multidisciplinary data integration; uses 3D structural information to assess protein druggability [17] |
cBioPortal for Cancer Genomics
cBioPortal is an open-access platform for the interactive exploration of multidimensional cancer genomics datasets [15]. It effectively translates complex genomic data into biologically and clinically actionable insights, making it particularly valuable for generating initial hypotheses about potential driver genes in specific cancer types.
GEPIA2 for Gene Expression Analysis
GEPIA2 was developed to fill the gap between cancer genomics big data and the delivery of integrated information to end users, utilizing standardized RNA-seq data from TCGA and GTEx projects [16]. A key innovation of GEPIA2 is its mitigation of sample imbalance by incorporating data from the GTEx project, providing a much larger set of normal tissue samples for robust comparison [16]. Its features allow for the identification of tumor-specific genes, which are often pursued as candidate drug targets [16].
canSAR for Drug Discovery
canSAR is a publicly available, multidisciplinary knowledgebase designed explicitly to support cancer translational research and drug discovery [17]. It stands out for its integration of diverse data types, including structural biology and druggability information, which are critical for assessing the potential of a protein to be modulated by a small-molecule drug or biologic [17].
Integrated Workflow for Target Discovery
The power of these resources is maximized when they are used in a coordinated, sequential workflow for target identification and validation. The following diagram and protocol outline a standard operational pipeline.
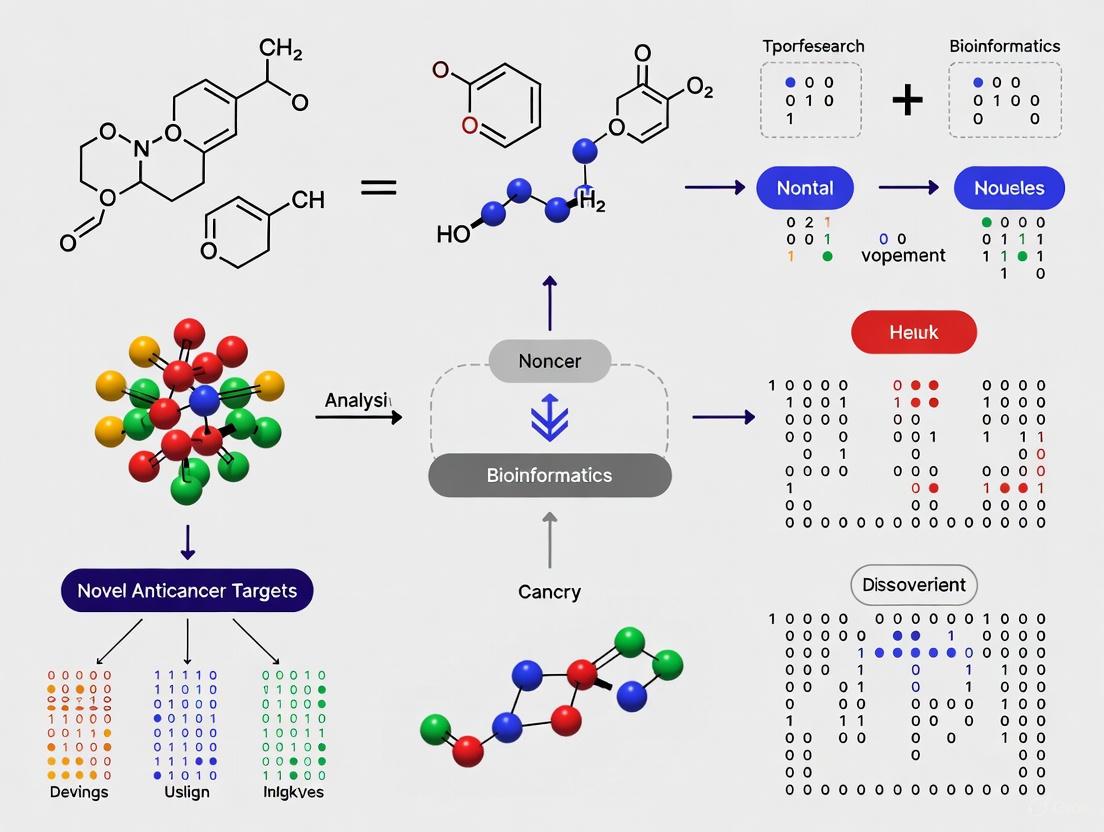
Figure 1: Integrated bioinformatics workflow for anticancer target discovery.
Protocol: A Multi-Database Target Screening Pipeline
This protocol describes a systematic approach to screen for and prioritize novel anticancer drug targets using cBioPortal, GEPIA2, and canSAR.
Step 1: Genetic Alteration Screening with cBioPortal
- Objective: Identify genes frequently altered in a cancer type of interest.
- Method:
- Access cBioPortal (https://www.cbioportal.org/).
- Select a cancer study (e.g., "Pancreatic Cancer (TCGA, PanCancer Atlas)").
- In the "Query" tab, enter a gene list or query a single gene.
- Execute the query and navigate to the "Cancer Types Summary" and "OncoPrint" tabs to visualize the frequency and types of genomic alterations (mutations, copy-number alterations) across the cohort.
- Output: A list of genes with high alteration frequencies, which are potential drivers of oncogenesis [15].
Step 2: Expression and Prognostic Validation with GEPIA2
- Objective: Validate the expression profile and clinical relevance of prioritized genes.
- Method:
- Access GEPIA2 (http://gepia.cancer-pku.cn/).
- For differential expression analysis, use the "Expression DIY" Boxplot function. Input the gene symbol, select the relevant cancer dataset (e.g., TCGA tumor vs. GTEx normal), and generate a plot to confirm tumor-specific overexpression.
- For clinical relevance, use the "Survival" function. Select the cancer type and generate Overall Survival or Disease-Free Survival plots using the log-rank test. A significant p-value (< 0.05) indicates prognostic value [16].
- Output: Genes that are differentially expressed in tumors and have a significant impact on patient survival.
Step 3: Druggability Assessment with canSAR
- Objective: Evaluate the potential of the validated gene products as druggable targets.
- Method:
- Access canSAR (http://cansar.icr.ac.uk).
- Search for the protein encoded by the validated gene.
- Review the integrated information, including the presence of known bioactive compounds, 3D protein structures, and predicted druggable pockets. A target with existing chemical probes or favorable structural features is more tractable [17].
- Output: A shortlist of high-confidence, druggable target proteins for experimental follow-up.
Successful execution of the bioinformatics workflow and subsequent experimental validation relies on a suite of key reagents and data resources.
Table 2: Key Research Reagent Solutions for Target Discovery
| Item | Function in Research | Example Sources / Identifiers |
|---|---|---|
| RNA-seq Datasets | Provide the foundational gene expression data for analysis in GEPIA2 and cBioPortal. | TCGA (The Cancer Genome Atlas), GTEx (Genotype-Tissue Expression) [16] |
| Clinical Annotation Data | Links molecular data to patient outcomes, enabling survival and correlation analyses. | TCGA clinical data files [16] |
| Drug-Target Interaction Databases | Provide information on known drug-target relationships for druggability assessment. | DrugBank [15], ChEMBL [17] |
| Protein Structure Data | Essential for canSAR's structure-based druggability predictions and molecular docking. | Protein Data Bank (PDB) [17] [14] |
| Protein-Protein Interaction (PPI) Data | Allows for network-level analysis to identify critical nodes as potential targets. | STRING database [14] |
The integration of bioinformatics databases like cBioPortal, GEPIA2, and canSAR has created a powerful, data-driven paradigm for anticancer drug target discovery. cBioPortal illuminates the genomic landscape of cancer, GEPIA2 validates the transcriptional and clinical relevance of candidate genes, and canSAR provides the critical translational bridge by assessing druggability. The structured workflow and toolkit presented in this whitepaper provide researchers with a clear, actionable strategy to navigate the complexity of cancer biology and efficiently prioritize the most promising targets for further experimental development, ultimately accelerating the journey toward novel cancer therapies.
The complexity of cancer biology, driven by tumor heterogeneity, diverse resistance mechanisms, and intricate microenvironment interactions, necessitates a systems-level approach to therapeutic discovery. Multi-omics integration represents a transformative paradigm in bioinformatics research that enables a comprehensive functional understanding of biological systems by combining data from multiple molecular layers [19]. This approach systematically integrates multidimensional data derived from genomics, transcriptomics, proteomics, metabolomics, and additional omics layers to develop a comprehensive atlas of tumor biological systems [20]. Unlike traditional single-omics analyses that provide limited insights, integrated multi-omics effectively captures cascade regulatory relationships across molecular hierarchies, thereby elucidating network-based mechanisms underlying drug resistance and identifying novel therapeutic vulnerabilities [20] [19].
In the context of anticancer drug target discovery, multi-omics technologies demonstrate distinct advantages by providing unprecedented insights into the molecular drivers of tumorigenesis and treatment resistance [20]. For instance, through the integration of transcriptomic and proteomic approaches, researchers can elucidate how neoplastic cells evade pharmacological interventions by modifying gene expression profiles and altering protein functional states [20]. The systematic integration of metabolomic datasets with systems biology modeling enables comprehensive delineation of molecular pathways underlying therapeutic resistance [20]. This holistic perspective is critical for addressing the fundamental challenge in contemporary oncology where tumor cells intricately regulate complex biological networks to circumvent drug-induced cytotoxic effects [20].
Omics Layers and Their Contributions
A comprehensive multi-omics approach encompasses several core molecular layers, each providing unique insights into cancer biology:
Genomics explores the composition, structure, function, and variations of the genetic material DNA, focusing on mutations, single nucleotide polymorphisms (SNPs), and structural variations including copy-number variations (CNVs) that may initiate oncogenic processes [19] [21]. Technologies include whole-genome sequencing (WGS) and whole-exome sequencing (WES), with functional genomics employing RNA interference, siRNA, shRNA, and CRISPR-based screening to validate gene-disease associations [19] [22].
Transcriptomics studies gene transcription and transcriptional regulation at the cellular level, revealing spatiotemporal differences in gene expression through technologies including RNA sequencing (RNA-seq), long non-coding RNA (lncRNA) sequencing, and single-cell RNA sequencing (scRNA-seq) [19] [21]. This layer helps identify genes significantly upregulated or downregulated in tumor tissues, providing candidate targets for targeted therapy [19].
Proteomics enables the identification and quantification of proteins and their post-translational modifications (phosphorylation, glycosylation, ubiquitination), offering direct functional insights into cellular processes and signaling pathways [21]. Mass spectrometry-based methods, affinity proteomics, and protein chips are widely used, with phosphoproteomics revealing novel disease mechanisms [21].
Metabolomics focuses on studying small molecule metabolites (carbohydrates, fatty acids, amino acids) that immediately reflect dynamic changes in cell physiology and metabolic vulnerabilities in tumors [21]. Both untargeted and targeted metabolomics approaches are employed to elucidate mechanisms of disease progression [21].
Public Data Repositories for Multi-Omics Research
Table 1: Major Public Data Repositories for Multi-Omics Cancer Research
| Repository Name | Data Types Available | Cancer Focus | URL |
|---|---|---|---|
| The Cancer Genome Atlas (TCGA) | RNA-Seq, DNA-Seq, miRNA-Seq, SNV, CNV, DNA methylation, RPPA | >33 cancer types, 20,000+ tumor samples | https://cancergenome.nih.gov/ |
| Clinical Proteomic Tumor Analysis Consortium (CPTAC) | Proteomics data corresponding to TCGA cohorts | Various cancer types | https://cptac-data-portal.georgetown.edu/cptacPublic/ |
| International Cancer Genomics Consortium (ICGC) | Whole genome sequencing, somatic and germline mutations | 76 cancer projects, 20,383 donors | https://icgc.org/ |
| Cancer Cell Line Encyclopedia (CCLE) | Gene expression, copy number, sequencing, drug response | 947 human cancer cell lines, 36 tumor types | https://portals.broadinstitute.org/ccle |
| Omics Discovery Index (OmicsDI) | Consolidated genomics, transcriptomics, proteomics, metabolomics | Multiple diseases from 11 repositories | https://www.omicsdi.org |
These repositories provide comprehensive molecular profiling data from thousands of tumor samples and cell lines, enabling researchers to access large-scale multi-omics datasets without conducting expensive, time-consuming experimental profiling [23]. The TCGA alone houses one of the largest collections of multi-omics data sets for more than 33 different types of cancer from over 20,000 individual tumor samples, providing rich molecular and genetic profiles that have enabled numerous discoveries about cancer progression, manifestation, and treatment [23].
Methodologies for Multi-Omics Data Integration
Computational Integration Strategies
Integration of multi-omics data presents significant computational challenges due to differences in data scale, noise ratios, preprocessing requirements, and the incomplete correlation between molecular layers [24]. Several computational strategies have been developed to address these challenges:
Matched (Vertical) Integration: Combines different omics data profiled from the same cells or samples, using the cell itself as an anchor for integration. This approach includes matrix factorization methods (MOFA+), neural network-based methods (scMVAE, DCCA, DeepMAPS), and network-based methods (cite-Fuse, Seurat v4) [24].
Unmatched (Diagonal) Integration: Integrates omics data drawn from distinct populations or cells by projecting cells into a co-embedded space to find commonality. Methods include Graph-Linked Unified Embedding (GLUE), which uses graph variational autoencoders to learn how to anchor features using prior biological knowledge [24].
Mosaic Integration: Employed when experimental designs have various combinations of omics that create sufficient overlap. Tools include COBOLT and MultiVI for integrating mRNA and chromatin accessibility data, and StabMap and bridge integration for more complex integrations [24].
Spatial Integration: Addresses the increasing development of spatial multi-omics methods that capture omics data within the confines of a cell or 'spot,' which serves as the integration anchor. Tools like ArchR have been successfully deployed for spatial integration [24].
Analytical Frameworks for Target Discovery
Several specialized analytical frameworks have been developed specifically for drug target identification using multi-omics data:
Transcriptome-Wide Association Studies (TWAS): Integrates GWAS and gene expression data to identify genes contributing to traits or diseases. The FUSION tool establishes precomputed predictive models to test associations throughout the transcriptome [25].
Proteome-Wide Association Studies (PWAS): Adapts the TWAS framework to analyze circulating proteins, identifying proteomic associations with cancer risk [25].
Summary-data-based Mendelian Randomization (SMR): Tests whether the effect of SNPs on cancers is mediated through gene expression, prioritizing causal genes for tumorigenesis. The heterogeneity in dependent instruments (HEIDI) test further determines if associations are attributable to linkage [25].
Bayesian Colocalization: Determines whether genetic associations with both identified genes and cancers share single causal variants, with a posterior probability of H4 (PP.H4) > 0.8 indicating strong colocalization [25].
These methods can be systematically combined into an integrated analytical pipeline for robust target identification, as demonstrated in recent studies that identified 24 genes (18 transcriptomic, 1 proteomic and 5 druggable genetic) showing significant associations with cancer risk [25].
Multi-Omics Data Integration Workflow
Experimental Design and Protocols
Integrated Multi-Omics Analysis Protocol
A comprehensive protocol for integrative multi-omics analysis in anticancer drug target discovery involves multiple coordinated steps:
Step 1: Sample Preparation and Data Generation
- Collect tumor and matched normal tissues from patient cohorts or appropriate cancer cell lines
- Extract DNA for whole-genome or whole-exome sequencing to identify genetic variants
- Isolate RNA for transcriptome sequencing (RNA-seq) to profile gene expression patterns
- Prepare protein lysates for mass spectrometry-based proteomic analysis
- Extract metabolites for metabolomic profiling via LC-MS or GC-MS platforms
- Ensure consistent sample processing across all omics platforms to minimize technical variability [21]
Step 2: Data Preprocessing and Quality Control
- Process genomic data: alignment to reference genome, variant calling, annotation of SNPs, indels, and CNVs
- Process transcriptomic data: read alignment, quantification of gene expression, normalization
- Process proteomic data: peptide identification, quantification, normalization
- Process metabolomic data: peak detection, compound identification, quantification
- Implement rigorous quality control measures specific to each data type [21] [24]
Step 3: Individual Omics Analysis
- Conduct differential expression/abundance analysis for each omics layer
- Perform pathway enrichment analysis on significantly altered molecules
- Identify molecular signatures associated with disease phenotypes or treatment response [25]
Step 4: Multi-Omics Data Integration
- Apply appropriate integration strategy based on data structure
- Implement computational tools for integrated analysis
- Identify concordant and discordant patterns across omics layers [24] [25]
Step 5: Target Prioritization and Validation
- Prioritize candidate targets based on multi-omics evidence
- Validate targets using experimental models (cell lines, organoids, animal models)
- Confirm mechanistic role through functional studies [20] [25]
The Scientist's Toolkit: Essential Research Reagents and Platforms
Table 2: Essential Research Reagents and Platforms for Multi-Omics Studies
| Category | Specific Tools/Reagents | Function in Multi-Omics Research |
|---|---|---|
| Sequencing Platforms | Illumina NovaSeq, PacBio Sequel, Oxford Nanopore | Generate genomic and transcriptomic data at various resolutions and applications |
| Proteomics Platforms | Thermo Fisher Orbitrap mass spectrometers, Bruker timSTOF | Enable high-throughput protein identification and quantification |
| Metabolomics Platforms | Agilent LC/Q-TOF, Sciex Triple Quad systems | Facilitate comprehensive profiling of small molecule metabolites |
| Single-Cell Technologies | 10x Genomics Chromium, BD Rhapsody | Enable single-cell transcriptomic, proteomic, and multi-omic profiling |
| Spatial Omics Technologies | 10x Genomics Visium, NanoString GeoMx | Provide spatial context for transcriptomic and proteomic data |
| CRISPR Screening | Whole-genome CRISPR libraries | Enable functional validation of candidate targets in high-throughput |
| Bioinformatics Tools | Seurat, MOFA+, GLUE, FUSION | Perform data integration, visualization, and analysis across omics layers |
Case Studies in Anti-Cancer Drug Target Discovery
Successful Applications of Multi-Omics Integration
Several recent studies demonstrate the power of multi-omics integration for identifying novel anticancer drug targets:
CLDN18.2 in Gastrointestinal Cancers: Integrative analyses combining pharmaco-omics with genomic and transcriptomic datasets revealed that elevated expression of CLDN18.2 is significantly associated with poor prognosis in bladder cancer (BLCA), esophageal carcinoma (ESCA), and pancreatic adenocarcinoma (PAAD). This comprehensive elucidation of CLDN18.2's biological functions and clinical relevance offered novel insights for the development of targeted therapies [20].
IDO1 in Esophageal Squamous Cell Carcinoma: Researchers employed proteomics, genomics, and bioinformatics tools to explore the function of indoleamine 2,3-dioxygenase 1 (IDO1) within the tumor microenvironment. Findings indicated that tumor-associated macrophages (TAMs) with elevated IDO1 expression contribute to an immunosuppressive TME, thereby reducing immunotherapy effectiveness. Analysis of RNA-seq data from TCGA involving 95 patients, supplemented by clinical validation in 77 patients, demonstrated that targeting IDO1 in TAMs could serve as a viable strategy to counteract immune resistance [20].
PCK2 in Non-Small Cell Lung Cancer: Integration of transcriptomic and proteomic data revealed the role of mitochondrial PCK2 in NSCLC. Researchers found that PCK2-driven gluconeogenesis helps cancer cells evade mitochondrial apoptosis, indicating that targeting metabolic pathways like gluconeogenesis could be a strategy to combat drug resistance in nutrient-poor tumor environments [20].
NRF2 Pathway in Multiple Cancers: A comprehensive integrative analysis of transcriptomic, proteomic, druggable genetic and metabolomic association studies identified 24 genes significantly associated with cancer risk. Enrichment analysis revealed that these genes were mainly enriched in the nuclear factor erythroid 2-related factor 2 (NRF2) pathway, highlighting its importance as a therapeutic target across multiple cancer types [25].
Artificial Intelligence in Multi-Omics Target Discovery
AI and machine learning are increasingly transforming multi-omics-based drug target discovery:
Deep Learning Models: Neural networks capable of handling large, complex datasets such as histopathology images or omics data can identify patterns not discernible through traditional statistical methods [26] [22].
Target Identification: AI enables integration of multi-omics data to uncover hidden patterns and identify promising targets. For instance, ML algorithms can detect oncogenic drivers in large-scale cancer genome databases such as TCGA, while deep learning can model protein-protein interaction networks to highlight novel therapeutic vulnerabilities [26].
Drug Design and Optimization: Deep generative models, such as variational autoencoders and generative adversarial networks, can create novel chemical structures with desired pharmacological properties, significantly accelerating the drug discovery process [26].
Companies such as Insilico Medicine and Exscientia have reported AI-designed molecules reaching clinical trials in record times. Insilico developed a preclinical candidate for idiopathic pulmonary fibrosis in under 18 months, compared to the typical 3-6 years, with similar approaches being applied to oncology [26].
AI in Multi-Omics Target Discovery
Validation and Clinical Translation
Target Validation Workflows
The transition from computationally identified targets to clinically relevant therapeutics requires rigorous validation:
Experimental Validation
- Implement CRISPR-Cas9 knockout technology to quantitatively screen identified target genes individually [19]
- Use RNA interference (RNAi) approaches including small interfering RNA (siRNA) and short hairpin RNA (shRNA) for gene silencing validation [19] [22]
- Conduct functional assays to assess impact on cancer cell proliferation, invasion, metastasis, and treatment resistance
- Validate in multiple model systems including 2D cell cultures, 3D organoids, and animal models
Clinical Correlation
- Analyze target expression in patient cohorts and correlate with clinical outcomes
- Assess target prevalence across cancer subtypes and stages
- Evaluate target druggability using structural biology and chemical screening approaches
Pathway to Clinical Application
Successful translation of multi-omics discoveries to clinical applications involves:
Biomarker Development
- Develop companion diagnostics for patient stratification
- Identify predictive biomarkers of treatment response
- Discover resistance biomarkers to guide combination therapies
Therapeutic Development
- Prioritize targets with genetic support, as they demonstrate higher success rates in clinical trials [25]
- Repurpose existing drugs for new indications based on multi-omics insights
- Develop novel therapeutic modalities including small molecules, biologics, and cell therapies
The integrated approach has already yielded success stories, such as the identification of PCSK9, CCR5 and ACE2 as therapeutic targets for various diseases, highlighting the potential of genetics-driven drug development [25]. In oncology, multi-omics approaches have identified novel targets including CLDN18.2, IDO1, and components of the NRF2 pathway that are currently being evaluated in preclinical and clinical studies [20] [25].
Integrative multi-omics analysis represents a paradigm shift in anticancer drug target discovery, enabling a comprehensive understanding of the complex molecular networks driving tumorigenesis and treatment resistance. By simultaneously interrogating multiple molecular layers - genome, transcriptome, proteome, and metabolome - researchers can identify novel therapeutic vulnerabilities with higher precision and confidence. The continuing evolution of computational integration methods, coupled with advances in AI and machine learning, is further enhancing our ability to extract biologically meaningful insights from these complex datasets. As multi-omics technologies become more accessible and analytical methods more sophisticated, this approach will play an increasingly central role in precision oncology, ultimately leading to more effective, personalized cancer therapies that overcome the limitations of current treatment paradigms.
Identifying Driver Genes, Mutations, and Altered Signaling Pathways
The identification of driver genes, their mutations, and the signaling pathways they disrupt represents a cornerstone of modern precision oncology. Unlike "passenger" mutations, which occur incidentally without functional consequences, driver genetic events are causally implicated in oncogenesis, conferring a selective growth advantage that drives tumor initiation and progression [27]. The systematic discovery of these elements is fundamental to the discovery of novel anticancer drug targets, enabling the development of therapies that specifically target the molecular Achilles' heels of cancer cells [28]. This process is powered by advanced bioinformatics, which provides the computational frameworks necessary to interpret complex multi-omics data and translate genomic alterations into actionable biological insights and therapeutic strategies [29].
Fundamental Concepts and Definitions
Driver vs. Passenger Mutations
In the genomic landscape of a tumor, driver mutations are those that provide a selective advantage to the cell, promoting its proliferation and survival. These mutations are positively selected during tumor evolution. In contrast, passenger mutations do not confer a growth advantage and are merely carried along as the tumor cell divides. Distinguishing between these two classes is a primary goal of computational cancer genomics [27].
Cancer Driver Genes (CDGs) and Their Impact
Cancer driver genes are the genes harboring driver mutations. They can be further categorized as:
- Oncogenes: These genes promote cancer when mutated to become overly active or expressed. They often function in signaling pathways that stimulate cell growth and division (e.g., KRAS, BRAF). Their activity is typically likened to a stuck accelerator.
- Tumor Suppressor Genes (TSGs): These genes protect against cancer by repairing DNA, controlling cell death, or arresting cell growth. When inactivated by mutation, this protective function is lost (e.g., TP53, PTEN). Their loss is akin to a broken brake [27].
The functional deregulation of crucial molecular pathways via these driver events leads to abnormal gene expression, enabling hallmarks of cancer such as uncontrolled proliferation, resistance to cell death, and metastatic potential [27].
Data Acquisition and Preprocessing
The discovery of driver genes relies on high-throughput technologies that generate vast amounts of multi-omics data.
Sequencing Technologies and Their Applications
Table 1: Next-Generation Sequencing (NGS) Technologies for Cancer Genomics
| Technology | Generation | Key Principle | Primary Application in Driver Discovery | Advantages | Limitations |
|---|---|---|---|---|---|
| Whole Genome Sequencing (WGS) | Second / Third | Sequences the entire genome, including coding and non-coding regions. | Identification of all genetic variants (SNPs, CNVs, structural variations) [29]. | Comprehensive; detects variants in non-coding regulatory regions. | Higher cost and data burden; requires complex analysis. |
| Whole Exome Sequencing (WES) | Second | Selectively sequences protein-coding exons (~1-2% of the genome). | Discovering coding region mutations, indels, and SNPs linked to disease [29]. | Cost-effective for targeting functional regions; covers ~85% of disease-causing mutations. | Misses non-coding and regulatory mutations. |
| RNA Sequencing (RNA-seq) | Second / Third | Sequences the transcriptome to determine RNA quantity and sequence. | Analyzing gene expression, fusion genes, alternative splicing, and novel transcripts [29]. | Reveals functional consequences of genomic changes; detects expressed fusions. | Does not directly assess genomic alterations. |
Public Data Repositories
Large-scale consortium efforts have generated publicly available datasets that are invaluable for research:
- The Cancer Genome Atlas (TCGA): A comprehensive resource containing multi-omics data (genomic, transcriptomic, epigenomic, proteomic) for over 20,000 primary cancers across 33 cancer types [27] [28].
- cBioPortal for Cancer Genomics: An open-access platform that provides visualization, analysis, and download of large-scale cancer genomics data sets, including those from TCGA [27] [29].
- Genomic Data Commons (GDC): A unified data repository that enables data sharing across cancer genomic studies [29].
- OncoKB: A precision oncology knowledge base that contains information on the oncogenic effects and therapeutic implications of specific genetic alterations [27].
Computational Methodologies for Identification
A suite of bioinformatics tools and algorithms is required to process raw sequencing data and identify driver events.
Bioinformatic Workflow for Variant Discovery
The standard workflow for identifying somatic mutations from tumor sequencing data involves several key steps:
- Quality Control & Preprocessing: Assessing raw sequencing data quality using tools like FastQC and trimming adapters with Trimmomatic or Cutadapt.
- Alignment: Mapping sequencing reads to a reference genome (e.g., GRCh38) using aligners such as STAR (for RNA-seq) or BWA (for DNA-seq).
- Variant Calling: Identifying genomic variants (SNPs, indels) relative to the reference genome using tools like GATK (Genome Analysis Toolkit) or MuTect2 for somatic mutations.
- Annotation: Predicting the functional impact of identified variants using tools like ANNOVAR or SnpEff, which cross-reference variants with databases of known genes, pathways, and protein domains [29] [28].
Diagram 1: Somatic Variant Calling Workflow
Advanced Computational Frameworks
Beyond basic variant calling, sophisticated computational methods are needed to distinguish drivers from passengers and to identify genes under positive selection.
a) Frequency-Based and Signal-Based Methods: Early approaches identified driver genes based on their significant mutational frequency across patient cohorts. Newer frameworks, like the one developed by Saad et al., integrate multiple data types. This framework combines genetic mutation, chromosome copy-number, and gene expression data from thousands of tumors to pinpoint genes that drive the loss of specific chromosome arms, a common event in cancer [30].
b) Network and Graph-Based Models: These methods contextualize genes within biological interaction networks (e.g., protein-protein interaction networks) to identify modules or genes whose network properties are perturbed in cancer.
- EMOGI: Integrates multi-omics data with a PPI network using graph convolutional networks (GCNs) to predict CDGs [31].
- SEFGNN (Soft-Evidence Fused Graph Neural Network): A novel framework that treats multiple biological networks (e.g., from STRING, PCNet) as independent evidence sources. It uses GNNs to extract features from each network and employs Dempster-Shafer Theory to perform uncertainty-aware fusion at the decision level, improving the robustness of CDG identification [31].
c) Personalized Driver Prioritization Algorithms (PDPAs): These tools move beyond cohort-level analysis to identify patient-specific driver mutations, which is critical for personalized therapy. A key challenge has been validating these predictions. The TARGET-SL framework addresses this by using PDPA predictions to produce a ranked list of predicted essential genes that can be validated against ground truth data from CRISPR-knockout and drug sensitivity screens [32].
Table 2: Key Bioinformatics Tools for Driver Gene and Biomarker Discovery
| Tool Category | Example Tools | Primary Function | Application Context |
|---|---|---|---|
| Variant Callers | GATK, MuTect2, STAR | Identify genomic variants from sequenced reads versus a reference genome. | Foundational step in all WGS/WES analyses. |
| Variant Annotation | ANNOVAR, SnpEff | Annotate and predict functional impact of genetic variants. | Prioritizing mutations likely to be drivers. |
| Pathway & Network Analysis | Cytoscape, STRING, IPA, GSEA | Visualize and analyze molecular interaction networks and enriched pathways. | Understanding the functional context of driver genes. |
| Multi-Platform Portals | cBioPortal, Oncomine | Integrate, visualize, and analyze complex cancer genomics data. | Exploratory analysis and validation across datasets. |
| AI/ML Frameworks | SEFGNN, TARGET-SL, scikit-learn | Advanced prediction of driver genes and essentiality using machine learning. | Identifying novel CDGs and patient-specific vulnerabilities. |
Analyzing Altered Signaling Pathways
Once driver genes are identified, the next critical step is to map them onto the signaling pathways they disrupt.
Most Frequently Altered Pathways in Cancer
Pan-cancer analyses of thousands of tumors have revealed a consistent set of core signaling pathways that are deregulated in most cancers. A systemic analysis of TCGA data sorted the top ten most frequently mutated pathways as follows [27]:
- p53 pathway
- RTK-RAS pathway
- Lipid metabolism pathway
- PI-3-Kinase/Akt pathway
- Ubiquitination pathway
- β-catenin/Wnt pathway
- Notch pathway
- Cell cycle pathway
- Homology-directed repair (HDR) pathway
- Splicing pathway
Key Oncogenic Signaling Pathways
The p53 Pathway The TP53 gene, which encodes the p53 protein, is the most frequently altered gene in cancer [27]. p53 functions as a critical tumor suppressor, inducing cell cycle arrest, senescence, or apoptosis in response to cellular stress. Its disruption allows damaged cells to continue proliferating.
Receptor Tyrosine Kinase (RTK)-RAS Pathway This pathway is a central regulator of cell growth, proliferation, and survival. It includes upstream receptors (like EGFR, VEGFR, PDGFR) and downstream effectors such as the RAS-RAF-MAPK cascade. Dysregulation is common in cancers; for example, in hepatocellular carcinoma (HCC), targeting the VEGFR pathway with agents like bevacizumab is an established therapeutic strategy [33].
PI-3-Kinase/Akt Pathway This pathway is crucial for cell survival and metabolism. Upon activation by RTKs or other signals, PI3K phosphorylates lipids, leading to the activation of Akt, which promotes cell growth and inhibits apoptosis. Somatic mutations in components of this pathway are common in many cancers [27].
Wnt/β-catenin Pathway This pathway regulates cell fate and proliferation. In the absence of a Wnt signal, β-catenin is degraded. Oncogenic mutations, often in CTNNB1 or APC, lead to stabilized β-catenin, which translocates to the nucleus and activates transcription of proliferative genes. This is a key pathway in HCC and colorectal cancer [27] [33].
Diagram 2: Core Cancer Signaling Pathways
Table 3: Essential Research Reagents and Resources for Driver Gene Studies
| Resource Category | Specific Examples | Function and Application |
|---|---|---|
| Cell Line Models | MCF-7 (breast cancer), K562 (leukemia), A549 (lung cancer) [31] | In vitro models for functional validation of driver genes via genetic manipulation and drug screening. |
| CRISPR Screening Libraries | Genome-wide sgRNA libraries (e.g., Brunello, GeCKO) | High-throughput functional genomics to identify genes essential for cancer cell survival (gene essentiality). |
| Biological Network Databases | STRING, CPDB, PCNet, iRefIndex, Multinet [31] | Provide curated protein-protein interaction data for network-based and GNN-driven driver gene identification. |
| Validated Reference Gene Sets | COSMIC Cancer Gene Census, NCG, CGC, OncoKB [27] [32] [31] | Curated lists of known cancer genes used as gold-standard positives for training and benchmarking computational models. |
| Drug Sensitivity Databases | GDSC (Genomics of Drug Sensitivity in Cancer), CTRP (Cancer Therapeutics Response Portal) | Correlate genetic alterations with drug response data to identify predictive biomarkers and therapeutic vulnerabilities. |
Clinical Translation and Therapeutic Targeting
The ultimate goal of identifying driver genes and pathways is to translate these discoveries into effective therapies for cancer patients.
From Driver Mutation to Targeted Therapy
The paradigm of targeted therapy involves developing drugs that specifically inhibit the products of driver genes.
- EGFR mutations in non-small cell lung cancer (NSCLC) predict response to EGFR inhibitors like gefitinib [27] [29].
- BRCA1/2 mutations, which impair homology-directed repair, confer sensitivity to PARP inhibitors due to synthetic lethality [29] [28].
- BRAF V600E mutations in melanoma are targeted by BRAF inhibitors such as vemurafenib.
Pathway-Directed Immunotherapy
There is growing evidence that oncogenic signaling pathways influence the tumor immune microenvironment and response to immunotherapy. For instance, abnormal activation of the Wnt/β-catenin, p53, and PTEN pathways can promote tumor immune escape and resistance to immune checkpoint inhibitors (ICIs) like anti-PD-1/PD-L1 antibodies. Therefore, targeting these pathways in combination with immunotherapy represents a promising strategy to overcome resistance [34].
Case Study: Hepatocellular Carcinoma (HCC)
HCC treatment has been revolutionized by targeted therapies and immunotherapies aimed at specific pathways:
- VEGFR Pathway: The combination of the anti-VEGF antibody bevacizumab with the anti-PD-L1 antibody atezolizumab is a first-line standard for advanced HCC, demonstrating how targeting a driver pathway (angiogenesis) can synergize with immunotherapy [33].
- Multiple Kinase Inhibition: Sorafenib and lenvatinib are TKIs that target multiple kinases, including VEGFR, PDGFR, and RAF, effectively inhibiting several nodes in the RTK-RAS-MAPK pathway [33].
The systematic identification of driver genes, mutations, and altered signaling pathways is a fundamental pillar of anticancer drug discovery. This process, powered by ever-advancing bioinformatics tools and multi-omics data integration, has moved from a cohort-level understanding to patient-specific precision. The continued development of sophisticated computational frameworks, such as graph neural networks and personalized essentiality predictors, is dramatically accelerating the discovery of novel therapeutic targets. By mapping the intricate web of dysregulated signaling in cancer cells, researchers can design more effective combination therapies, overcome drug resistance, and ultimately deliver on the promise of precision oncology for improved patient outcomes.
The Role of Network Biology in Understanding Cancer Complexity and Dependencies
The traditional paradigm of targeting single oncogenes has yielded significant breakthroughs in cancer therapy, exemplified by drugs like Imatinib (Gleevec) for chronic myeloid leukemia and Vemurafenib (Zelboraf) for BRAF-mutant melanoma [35]. However, cancer's robust nature arises from complex, interconnected biological networks that allow tumors to adapt and develop resistance to targeted therapies. Network biology represents a paradigm shift that moves beyond this one drug–one target approach to instead model the intricate web of molecular interactions that define cancer phenotypes. By mapping these relationships systematically, researchers can now identify critical vulnerabilities that emerge from the network structure itself—dependencies that are not apparent when studying individual genes or proteins in isolation.
This whitepaper explores how network biology, powered by large-scale functional genomics and computational integration, is transforming the discovery of novel anticancer drug targets. We focus specifically on the foundational frameworks and methodologies that enable researchers to decode cancer complexity and identify therapeutically actionable dependencies within biological networks.
The Dependency Map (DepMap) Initiative: A Foundational Resource
The Cancer Dependency Map (DepMap) initiative represents a large-scale, systematic effort to identify and catalog genetic and molecular vulnerabilities across hundreds of cancer models [36]. The core premise is that the mutations driving cancer cell proliferation and survival simultaneously create unique, cancer-specific dependencies that normal cells lack [37]. These dependencies represent compelling therapeutic targets. DepMap aims to create a comprehensive "map" triangulating relationships between genomic features and these "Achilles' heels" across diverse cancer types through extensive genetic and small molecule perturbation studies [37].
This collaborative, open-science project generates genome-scale CRISPR-Cas9 knockout screens, RNAi screens, and drug sensitivity profiles across thousands of genetically characterized cancer cell lines [36]. The resulting data is made publicly available through the DepMap portal, providing researchers worldwide with an unprecedented resource for exploring cancer vulnerabilities [37]. The DepMap consortium has demonstrated feasibility for large-scale approaches to pinpoint small molecule sensitivities, working in conjunction with characterization efforts such as the Cancer Cell Line Encyclopedia (CCLE) to accelerate molecular and therapeutic discovery [36] [37].
Key Technological Platforms and Data Types
Table 1: Core Data Generation Platforms in DepMap
| Platform/Assay | Primary Function | Scale and Coverage | Key Insights Generated |
|---|---|---|---|
| CRISPR-Cas9 Screens | Genome-wide knockout to identify essential genes | Hundreds of genome-wide screens across cancer cell lines [36] | Identification of lineage-specific dependencies and pan-essential genes [36] |
| RNAi Screens | Gene knockdown using short hairpin RNAs (shRNAs) | Large-scale compendiums (e.g., Project DRIVE) [36] | Validation of CRISPR findings; identification of synthetic lethal interactions [36] |
| PRISM Drug Screening | High-throughput drug sensitivity testing in pooled cell lines | 1450 drugs across 371 diverse cancer cell lines [38] | Drug response patterns and mechanisms of action [38] |
| Molecular Characterization | Genomic, transcriptomic, and proteomic profiling | Integration with CCLE and other characterization efforts [36] [37] | Correlation of dependencies with molecular features for biomarker discovery [36] |
Computational Methodologies for Network-Based Dependency Analysis
Data Processing and Normalization Techniques
The raw data generated from dependency screens requires sophisticated computational processing before meaningful biological insights can be extracted. A critical challenge in CRISPR-Cas9 screens is correcting for copy number-associated false positives, where amplified genomic regions produce increased Cas9 cleavage activity that can be mistaken for true biological essentiality. The CERES algorithm was developed specifically to address this confounder, computationally correcting for copy number effects to improve the specificity of essentiality calls [36]. Similarly, the Chronos algorithm provides a cell population dynamics model that further refines the inference of gene fitness effects from CRISPR screening data [36].
For data analysis and exploration, tools like shinyDepMap provide user-friendly interfaces that allow researchers to identify targetable cancer genes and their functional connections without requiring advanced computational expertise [36]. These normalization methods and accessible tools collectively transform raw screening data into reliable, biologically meaningful dependency scores that accurately reflect gene essentiality across diverse cancer models.
Advanced Computational Tools for Target Discovery
Table 2: Computational Tools for Network Biology in Cancer Research
| Tool/Algorithm | Primary Function | Methodological Approach | Key Applications |
|---|---|---|---|
| DeepTarget | Predicts anti-cancer mechanisms of small molecules | Integrates genetic deletion data with drug sensitivity profiles [38] | Drug repurposing; identification of secondary targets and context-specific mechanisms [38] |
| Chronos | Models CRISPR-Cas9 screening data | Cell population dynamics model for improved fitness effect inference [36] | Correction of screen artifacts; accurate essentiality scoring [36] |
| Sparse Dictionary Learning | Identifies pleiotropic effects from fitness screens | Decomposes complex dependency patterns into interpretable components [36] | Discovery of co-functional gene modules; pathway-level analysis [36] |
| Global Computational Alignment | Maps cell line profiles to human tumors | Unsupervised alignment of transcriptional profiles [36] | Assessment of clinical relevance for identified dependencies [36] |
The recently developed DeepTarget tool exemplifies the power of integrating genetic and pharmacological data to understand network perturbations. Unlike conventional approaches that rely primarily on chemical structure and predicted binding affinity, DeepTarget leverages the principle that genetic deletion of a drug's protein target via CRISPR-Cas9 can mimic the drug's inhibitory effects [38]. By analyzing data from 1450 drugs across 371 cancer cell lines, DeepTarget infers mechanistic insights not readily apparent from structural data alone, successfully predicting both primary and secondary drug targets with high accuracy [38].
Experimental Protocols for Dependency Validation
Genome-Scale CRISPR-Cas9 Viability Screens
Objective: To identify genes essential for the proliferation and survival of specific cancer cell lines.
Methodology:
- Library Design: Employ genome-wide lentiviral sgRNA libraries (e.g., Avana or Brunello libraries) targeting ~18,000 genes with multiple sgRNAs per gene to ensure statistical robustness [36].
- Viral Transduction: Transduce cancer cell lines at low multiplicity of infection (MOI ~0.3) to ensure most cells receive a single sgRNA, followed by selection with puromycin.
- Cell Propagation: Culture transduced cells for approximately 2-3 weeks (typically 14-21 population doublings) to allow depletion of cells bearing lethal sgRNAs.
- Sample Collection: Collect genomic DNA at baseline (T0) and endpoint (Tfinal) for sgRNA abundance quantification.
- Sequencing and Analysis: Amplify integrated sgRNA sequences by PCR and sequence using high-throughput platforms. Map sequences to the reference library and quantify abundance changes using specialized algorithms (e.g., CERES or Chronos) that calculate gene-level dependency scores [36].
Key Considerations: Include negative control sgRNAs targeting non-essential genomic regions and positive controls targeting essential genes. Perform computational correction for copy number effects to minimize false positives [36].
High-Throughput Drug Sensitivity Screening (PRISM)
Objective: To profile cancer cell line sensitivities to large compound collections in a multiplexed format.
Methodology:
- Cell Line Barcoding: Label each cell line with unique DNA barcodes that can be detected via quantitative PCR or next-generation sequencing.
- Pooled Screening: Combine barcoded cell lines into pools (typically 10-50 lines per pool) and plate in multiplexed format [36].
- Compound Treatment: Treat pooled cells with individual compounds across a range of concentrations (typically 8-point, 1:3 or 1:4 serial dilutions), including DMSO vehicle controls.
- Incubation and Viability Assessment: Incubate for 3-5 cell doublings (typically 5-7 days), then harvest cells and extract genomic DNA.
- Barcode Quantification: Amplify and sequence unique barcodes to determine the relative abundance of each cell line following compound treatment.
- Data Analysis: Normalize barcode counts to vehicle controls and calculate viability metrics (e.g., AUC or IC50) for each cell line-compound combination.
Key Considerations: The PRISM method enables highly efficient screening of many cell lines against extensive compound libraries, significantly enhancing throughput compared to traditional single-line screens [36].
Visualizing Biological Networks in Cancer Research
Diagram 1: DeepTarget Computational Workflow for Network-Based Drug Target Prediction
Diagram 2: Context-Specific Drug Targeting Revealed Through Network Analysis
Research Reagent Solutions for Network Biology Studies
Table 3: Essential Research Reagents and Platforms for Cancer Dependency Studies
| Reagent/Platform | Primary Function | Key Features | Application in Network Biology |
|---|---|---|---|
| Genome-Wide CRISPR Libraries | Knockout screening for gene essentiality | Multiple guides per gene; optimized for minimal off-target effects [36] | Systematic identification of genetic dependencies across cancer models [36] |
| RNAi Libraries (shRNA) | Gene knockdown studies | Lentiviral delivery; enables stable gene suppression [36] | Validation of CRISPR findings; synthetic lethal interaction studies [36] |
| PRISM Barcoded Cell Lines | Multiplexed compound screening | Unique DNA barcodes for cell line identification in pooled assays [36] | High-throughput drug sensitivity profiling in diverse genetic backgrounds [36] |
| CCLE Molecular Characterization Data | Genomic and molecular annotation | Multi-omics data (genomic, transcriptomic, epigenomic) for cell lines [36] | Correlation of dependencies with molecular features for biomarker discovery [36] |
| Chronos Algorithm | Computational analysis of CRISPR screens | Corrects for copy number confounders and screen-specific artifacts [36] | Improved specificity in essentiality calling; accurate dependency mapping [36] |
Case Studies: Network Biology in Action
Ibrutinib Mechanism Elucidation in Lung Cancer
Ibrutinib, an established BTK inhibitor approved for blood cancers, presented a paradox when it demonstrated efficacy in lung cancer models where its canonical target BTK is largely absent. Through network biology approaches integrating dependency mapping and drug sensitivity data, DeepTarget predicted that mutant forms of the epidermal growth factor receptor (EGFR) serve as relevant targets in lung tumors [38]. This hypothesis was experimentally validated through collaborative work with Ani Deshpande's laboratory, explaining why Ibrutinib exhibits efficacy in lung cancer despite the absence of its canonical target [38]. This case exemplifies how network approaches can reveal context-specific drug mechanisms and identify novel therapeutic applications for existing drugs.
Phosphate Dysregulation in Ovarian Cancer
A network biology analysis of dependency relationships in ovarian cancer identified a novel vulnerability involving phosphate transport through the XPR1-KIDINS220 protein complex [36]. This dependency represents a non-oncogenic addiction that could be therapeutically exploited. The discovery emerged from systematic analysis of genetic dependencies across cancer lineages, followed by mechanistic studies that delineated the pathway and its critical role in specific ovarian cancer subtypes [36]. This case demonstrates how network approaches can identify non-obvious, therapeutically relevant vulnerabilities beyond traditional oncogenic drivers.
Network biology, powered by systematic dependency mapping and computational integration, is fundamentally transforming our approach to identifying novel anticancer drug targets. By modeling the complex web of molecular interactions within cancer cells, researchers can now identify critical vulnerabilities that emerge from the network structure itself. The DepMap initiative and associated computational tools like DeepTarget provide the foundational resources and methodologies needed to decode this complexity and advance therapeutic discovery.
Looking forward, several key developments will further enhance the impact of network biology in oncology. First, the expansion of dependency mapping to include more diverse cancer models, especially patient-derived organoids and in vivo models, will improve clinical translation. Second, the integration of additional data types, including proteomic, metabolomic, and spatial profiling data, will create more comprehensive network models. Finally, the development of more sophisticated computational methods, particularly artificial intelligence approaches that can predict emergent network properties, will accelerate the identification of targetable dependencies. As these advancements mature, network biology will play an increasingly central role in delivering on the promise of precision oncology by matching patients with therapies that target the specific dependency networks driving their cancer.
Computational Methodologies in Action: From In Silico Prediction to Candidate Prioritization
The discovery of novel anticancer drugs is a formidable challenge, characterized by extensive timelines, substantial financial investment, and high attrition rates [39] [12]. Traditional drug discovery approaches, heavily reliant on in vivo animal experiments and in vitro screening, are often expensive and laborious [40]. In this context, structure-based drug design (SBDD) has emerged as a transformative paradigm, leveraging computational power to streamline and enhance the drug development process [39]. SBDD utilizes the three-dimensional structural information of biological targets to design and optimize therapeutic candidates rationally [41]. Core to this approach are molecular docking and molecular dynamics (MD) simulations, which together provide a comprehensive framework for predicting how small molecules interact with target proteins and assessing the stability of these complexes [39].
These computational methods are particularly crucial in oncology, where the complexity and heterogeneity of cancer demand a profound understanding of disease mechanisms at the molecular level [42] [43]. Bioinformatics bridges this gap by enabling the analysis of large-scale multi-omics data—including genomics, transcriptomics, proteomics, and metabolomics—to identify novel therapeutic targets and predict new drug candidates [12] [40] [43]. The integration of SBDD with bioinformatics has already facilitated the successful development of several approved cancer therapies, such as Imatinib (Gleevec) for chronic myeloid leukemia and Vemurafenib (Zelboraf) for BRAF-mutant melanoma, demonstrating the tangible impact of these computational approaches [35]. This guide details the core methodologies and protocols of molecular docking and MD simulations, framing them within the strategic pursuit of discovering novel anticancer drug targets.
Molecular Docking: Principles and Methodologies
Molecular docking is a computational structure-based method extensively used since the early 1980s to predict the preferred orientation, conformation, and binding affinity of a small molecule (ligand) when bound to a target macromolecule (receptor) [12]. Its primary goal is molecular recognition, achieving a complementary fit at the binding site [12]. In anticancer drug discovery, docking is pivotal for virtual screening of large chemical libraries to identify potential lead compounds, thereby saving significant time and experimental resources [39] [12].
A standard molecular docking workflow involves several essential steps, as illustrated in the diagram below.
System Preparation Protocols
The accuracy of molecular docking is profoundly influenced by the careful preparation of both the protein and ligand structures [44] [45].
Protein Preparation: This critical step ensures the protein structure is optimized for docking simulations. Best practices include:
- Adding Hydrogen Atoms: The inclusion of hydrogen atoms leads to better redocking scores and more accurate predictions of binding interactions [44].
- Optimizing Hydrogen Bonds: Networks of hydrogen bonds should be optimized, which may involve flipping the side chains of asparagine, glutamine, and histidine residues to achieve optimal bonding [45].
- Removing Atomic Clashes: Minor steric clashes present in crystal structures must be resolved through restrained energy minimization [45].
- Assigning Partial Charges: The choice of charge models (e.g., Gasteiger-Marsili, MMFF94) can significantly impact docking performance and should be selected based on the force field and system requirements [44].
Ligand Preparation: Small molecules require careful preprocessing to generate accurate and relevant structures:
- Generate 3D Geometries: For ligands lacking 3D coordinates, these must be generated from 1D or 2D representations, ensuring correct stereochemistry [12].
- Assign Bond Orders: Correct bond orders are essential for representing the electronic structure of the molecule accurately [45].
- Generate Tautomers and Ionization States: At physiological pH, ligands can exist as multiple tautomers or ionization states. It is crucial to generate all accessible states, as the correct form can be a key determinant of binding [45].
Docking Execution and Parameters
The docking process consists of two main components: sampling ligand conformations and scoring the resulting poses [12]. Key parameters that influence performance include:
- Search Space Definition: The size and location of the docking search box must encompass the entire binding site. An adequately sized box is necessary for thorough sampling, but excessive size can increase computation time and false positives [44].
- Search Exhaustiveness: This parameter controls the comprehensiveness of the conformational search. Higher exhaustiveness values generally lead to more reproducible results but require greater computational resources [44].
- Ligand Flexibility: The number of rotatable bonds in the ligand directly affects the complexity of the docking simulation. Molecules with fewer torsions typically achieve more accurate docking results [44].
The performance of different docking parameter combinations can be quantitatively assessed by re-docking a known ligand and calculating the Root Mean Square Deviation (RMSD) between the predicted pose and the experimental crystal structure pose. An RMSD of less than 2.0 Å is generally considered a successful prediction [44].
Table 1: Impact of Key Preparation Parameters on Docking Performance [44] [45]
| Parameter | Protocol Option | Impact on Docking Enrichment | Recommendation |
|---|---|---|---|
| Hydrogen Atoms | Include | Improves redocking scores and interaction predictions | Always add and optimize |
| Partial Charges | Gasteiger-Marsili vs. MMFF94 | Varies by system; can significantly affect binding affinity predictions | Test multiple methods for your target |
| Ligand Tautomers | Generate accessible states | Critical for identifying correct binding pose; neglect degrades enrichment | Generate all probable states at pH 7.4 |
| Search Exhaustiveness | Low (8) vs. High (64) | Higher values improve pose recovery but increase computational time | Use ≥32 for production virtual screening |
| Binding Site Box Size | Small (15Å) vs. Large (25Å) | Oversized boxes reduce performance; appropriately sized boxes improve accuracy | Define based on known active site dimensions |
Molecular Dynamics Simulations
While molecular docking provides a static snapshot of ligand-receptor interactions, molecular dynamics (MD) simulations offer a dynamic view of the behavior and stability of the complex under near-physiological conditions [39]. MD simulations solve Newton's equations of motion for all atoms in the system, tracing their trajectories over time and enabling the study of conformational changes, binding pathways, and allosteric mechanisms that are inaccessible through static approaches [44].
Simulation Setup and Parameters
The accuracy of MD simulations depends critically on proper system setup and parameter selection, as outlined in the workflow below.
System Preparation:
- Force Field Selection: The choice of force field is fundamental, as it defines the potential energy functions and parameters governing atomic interactions. Popular choices for biomolecular systems include CHARMM, AMBER (ff14SB), and GROMOS, each with specific strengths for proteins, nucleic acids, or lipids [44].
- Solvation: The system must be hydrated using water models such as TIP3P or SPC, with the protein-ligand complex immersed in a sufficiently large water box to avoid artificial periodicity effects [44].
- Neutralization: Ions (typically Na⁺ and Cl⁻) are added to neutralize the system's net charge and achieve physiological salt concentration (e.g., 0.15 M) [44].
Equilibration and Production:
- Energy Minimization: This initial step removes any steric clashes introduced during system setup, relaxing the structure to a local energy minimum [44].
- System Equilibration: The system is gradually heated to the target temperature (e.g., 310 K) and the density is allowed to stabilize under controlled pressure conditions (e.g., 1 bar). This ensures the system reaches proper thermodynamic equilibrium before production data collection [44].
- Production Run: This is the main simulation phase where trajectory data is collected for analysis. The simulation must be sufficiently long (typically nanoseconds to microseconds) to sample the relevant biological processes. Constraints should be applied judiciously, as improper use can worsen performance rather than improve it [44].
Table 2: Key Parameters and Reagents for MD Simulations [44]
| Component | Common Options | Function | Considerations |
|---|---|---|---|
| Force Field | CHARMM, AMBER, GROMOS | Defines potential energy terms for molecular interactions | AMBER ff14SB recommended for protein accuracy |
| Water Model | TIP3P, SPC, SPC/E | Solvates the system and mediates electrostatic interactions | TIP3P widely compatible with biomolecular force fields |
| Neutralizing Ions | Na⁺, Cl⁻ | Neutralizes system charge and mimics physiological conditions | Add to 0.15M concentration for physiological relevance |
| Temperature Coupling | Berendsen, Nosé-Hoover | Maintains system at constant temperature | Nosé-Hoover provides better canonical ensemble |
| Pressure Coupling | Berendsen, Parrinello-Rahman | Maintains system at constant pressure | Parrinello-Rahman better for constant pressure simulations |
| Simulation Length | Nanoseconds to Microseconds | Determines observable biological processes | Dependent on research question and computational resources |
Integrated Workflow for Anticancer Target Discovery
The true power of computational drug discovery emerges when molecular docking and MD simulations are integrated into a cohesive workflow, complemented by bioinformatics approaches for target identification. This integrated pipeline is particularly valuable in oncology, where multi-omics data can be leveraged to identify novel, druggable targets [40] [43].
Target Identification through Bioinformatics
Bioinformatics approaches provide the foundation for identifying novel anticancer targets by analyzing large-scale biological data:
- Multi-omics Integration: Network-based algorithms analyze integrated genomics, transcriptomics, proteomics, and metabolomics data to identify indispensable proteins in cancer networks. For example, analysis of protein-protein interaction (PPI) networks using control theory has identified 56 indispensable genes across nine cancers, 46 of which were novel cancer associations [43].
- Biological Network Analysis: Methods such as shortest path analysis, module detection, and network centrality are employed to pinpoint critical nodes in cancer-associated networks. These nodes often represent potential therapeutic targets [43].
- Utilization of Specialized Databases: Cancer-specific databases like canSAR, CancerResource, and NPACT provide curated information on drug-target relationships, genomic alterations, and compound bioactivity across cancer cell lines, facilitating target prioritization and validation [12] [46].
Integrated Docking and Dynamics Pipeline
The following workflow illustrates how these components are integrated into a comprehensive drug discovery pipeline.
This integrated approach allows researchers to progress from target identification to lead optimization computationally. Virtual screening of millions of compounds through molecular docking rapidly narrows the candidate pool, which is then refined through MD simulations that assess binding stability and residence time [39]. Further computational assessments of Absorption, Distribution, Metabolism, Excretion, and Toxicity (ADMET) properties help prioritize compounds with the highest likelihood of success in experimental validation [39] [12]. This comprehensive computational pipeline significantly accelerates the discovery of novel anticancer therapies while reducing the reliance on resource-intensive experimental methods.
Successful implementation of structure-based drug design requires access to specialized computational tools, databases, and software. The following table catalogs essential resources for researchers in anticancer drug discovery.
Table 3: Essential Research Reagents and Computational Tools [44] [12] [43]
| Resource Type | Specific Tools/Databases | Function in Drug Discovery | Application in Oncology |
|---|---|---|---|
| Protein Structure Databases | PDB, World-2DPAGE | Provide experimental 3D structures of target proteins | Critical for docking against cancer targets (e.g., kinases) |
| Chemical Databases | ChEMBL, SuperNatural, NPACT | Store compound structures and bioactivity data | Source for natural and synthetic anticancer compounds |
| Cancer-Specific Databases | canSAR, CancerResource, PharmacoDB | Integrate genomic, chemical, and drug sensitivity data | Identify tumor-specific vulnerabilities and drug targets |
| Docking Software | AutoDock Vina, AutoDock-GPU, Glide | Predict ligand-binding poses and affinities | Virtual screening for novel anticancer agents |
| MD Simulation Software | AMBER, GROMACS, CHARMM | Simulate dynamic behavior of protein-ligand complexes | Assess binding stability and mechanism of action |
| Omics Data Repositories | NCBI GEO, ArrayExpress, TCGA | Store gene expression and genomic variation data | Identify dysregulated pathways in cancer for targeting |
| Bioinformatics Tools | Cytoscape, KEGG, BioCyc | Analyze biological pathways and network interactions | Contextualize targets within cancer signaling networks |
Virtual Screening and Pharmacophore Modeling for Lead Compound Identification
The discovery of novel anticancer therapeutics is a central objective in bioinformatics and pharmaceutical research. This process traditionally demands immense temporal and financial investment, often exceeding a decade and billions of dollars [47]. Modern computer-aided drug discovery (CADD) techniques have emerged as powerful tools to mitigate these burdens by accelerating the identification of promising drug candidates, thereby streamlining the transition from target validation to clinical application [48]. Within the CADD arsenal, virtual screening (VS) and pharmacophore modeling represent cornerstone methodologies for the efficient exploration of vast chemical spaces. These approaches are particularly vital in oncology, where the exploration of ultra-large chemical libraries offers unprecedented opportunities to identify novel, potent, and selective inhibitors against critical cancer targets [49] [46].
Pharmacophore modeling abstractly represents the essential steric and electronic features required for a molecule to interact with a biological target and elicit (or block) its therapeutic response [50]. The IUPAC defines it as "the ensemble of steric and electronic features that is necessary to ensure the optimal supra-molecular interactions with a specific biological target structure and to trigger (or to block) its biological response" [48] [50]. When integrated with virtual screening, these models enable the intelligent prioritization of lead compounds from millions of candidates, significantly enriching hit rates compared to random high-throughput screening [50]. This technical guide delineates the core concepts, methodologies, and applications of virtual screening and pharmacophore modeling, framing them within the context of a bioinformatics-driven discovery pipeline for novel anticancer drug targets.
Theoretical Foundations
Pharmacophore Modeling: Core Concepts and Features
A pharmacophore is not a specific molecular scaffold but an abstract depiction of functional interactions. It translates the key chemical functionalities of a bioactive molecule into a three-dimensional arrangement of generalized features [48] [50]. The most critical pharmacophore feature types are summarized in Table 1.
Table 1: Essential Pharmacophore Features and Their Descriptions
| Feature | Description | Role in Molecular Recognition |
|---|---|---|
| Hydrogen Bond Acceptor (HBA) | An atom that can accept a hydrogen bond (e.g., carbonyl oxygen). | Facilitates directional interactions with donor groups on the target protein. |
| Hydrogen Bond Donor (HBD) | A hydrogen atom covalently bound to an electronegative atom (e.g., N-H, O-H). | Forms strong, directional bonds with acceptor atoms in the binding site. |
| Hydrophobic (H) | A non-polar region of the molecule (e.g., alkyl chain). | Drives van der Waals interactions and desolvation in hydrophobic pockets. |
| Positive/Negative Ionizable (PI/NI) | Groups that can carry a formal charge under physiological conditions (e.g., carboxylate, ammonium). | Engages in strong electrostatic and charge-assisted hydrogen bonding. |
| Aromatic Ring (AR) | A planar, conjugated ring system. | Enables π-π stacking and cation-π interactions. |
| Exclusion Volume (XVOL) | A spatial constraint representing forbidden space, typically from the protein backbone. | Mimics the shape of the binding pocket, improving model selectivity by penalizing steric clashes [48] [50]. |
Structure-Based vs. Ligand-Based Approaches
Pharmacophore models are constructed using one of two primary strategies, chosen based on available structural and ligand data, as illustrated in the workflow below.
Structure-Based Pharmacophore Modeling This approach relies on the three-dimensional structure of the target, obtained from sources like the Protein Data Bank (PDB) [48] [50]. The process begins with critical protein preparation steps, including adding hydrogen atoms, assigning protonation states, and correcting any structural errors [48]. The binding site is then identified, either from a co-crystallized ligand or via computational tools like GRID or LIGANDSITE [48]. Subsequently, pharmacophore features are generated directly from the protein-ligand interactions observed in the complex or by analyzing the binding site topology to map potential interaction points (e.g., hydrogen bonding vectors, hydrophobic patches) [50] [51]. This method is highly accurate when high-resolution structural data is available, as it provides direct insight into the binding mechanics.
Ligand-Based Pharmacophore Modeling When the 3D structure of the target is unavailable, the ligand-based approach offers a powerful alternative. This method requires a set of known active molecules that bind to the target with diverse structures and measured biological activities (e.g., IC₅₀ values) [52] [50]. Multiple low-energy conformations of each active molecule are generated and then aligned to identify the 3D arrangement of chemical features common to all of them, which is presumed responsible for their biological activity [50]. The quality of the resulting model is heavily dependent on the quality, diversity, and known activity data of the training set ligands [50].
Experimental and Computational Protocols
Structure-Based Pharmacophore Modeling Protocol
The following detailed protocol, exemplified by a study targeting the X-linked inhibitor of apoptosis protein (XIAP) for anticancer therapy, outlines the key steps for structure-based model generation [51].
Protein Preparation:
- Retrieve the 3D structure of the target protein (e.g., XIAP, PDB ID: 5OQW) from the PDB.
- Prepare the protein structure by adding hydrogen atoms, assigning correct protonation states at physiological pH, and repairing any missing loops or side chains using modeling software.
- Optimize the hydrogen bonding network and perform a brief energy minimization to relieve steric clashes.
Binding Site Definition and Analysis:
- Define the binding site coordinates based on the position of a co-crystallized native ligand or through binding site prediction algorithms.
- Analyze the key residues and interaction patterns within the site. For XIAP, critical interactions were identified with residues such as THR308, ASP309, and GLU314 [51].
Pharmacophore Feature Generation:
- Using software like LigandScout or Discovery Studio, extract pharmacophore features directly from the protein-ligand complex. This includes hydrogen bond donors/acceptors, hydrophobic regions, and ionic interactions.
- Incorporate exclusion volumes (XVOLs) based on the protein structure to represent steric constraints, preventing the selection of compounds that would clash with the protein backbone [50] [51].
Model Refinement and Validation:
- Refine the initial hypothesis by selecting the most critical features for binding, potentially setting some as "optional" to allow for some chemical diversity.
- Validate the model using a test set containing known active compounds and decoy molecules (inactive compounds with similar physicochemical properties). Common validation metrics include the Enrichment Factor (EF) and the Area Under the Curve (AUC) of the Receiver Operating Characteristic (ROC) plot [50] [51]. For the XIAP model, an excellent AUC of 0.98 and an EF of 10.0 at the 1% threshold were achieved, demonstrating high predictive power [51].
Virtual Screening and Lead Identification Workflow
Once a validated pharmacophore model is obtained, it is deployed as a query to screen ultra-large chemical libraries. The integrated workflow below depicts a comprehensive virtual screening pipeline for anticancer lead identification.
Step 1: Molecular Library Preparation Chemical libraries such as ZINC (over 230 million compounds) are prepared for screening by generating 3D conformations, optimizing geometries, and standardizing formats [49] [51]. For ultra-large libraries (exceeding one billion molecules), AI-powered methods like Deep Docking are employed, which dock only a subset of the library iteratively synchronized with a ligand-based prediction of the remaining docking scores, achieving up to a 100-fold acceleration [49].
Step 2: Pharmacophore-Based Virtual Screening The validated pharmacophore model is used as a 3D query to screen the prepared chemical library. Compounds that map all or a user-defined number of the essential chemical features are retrieved as primary hits [50]. This step drastically reduces the library size, enriching the pool for molecules with a high probability of binding.
Step 3: ADMET Filtering Primary hits are subjected to in silico Absorption, Distribution, Metabolism, Excretion, and Toxicity (ADMET) profiling. This involves applying filters based on Lipinski's Rule of Five and predictive models for properties like cardiotoxicity (e.g., hERG channel inhibition) to eliminate compounds with unfavorable pharmacokinetic or toxicological profiles early in the process [52] [51].
Step 4: Molecular Docking The filtered hits are then docked into the target's binding site using programs like AutoDock Vina, Glide, or rDock [47]. Docking predicts the binding pose and estimates the binding affinity, providing a more refined ranking of compounds. For instance, in the XIAP study, the natural compound Schinilenol was identified with a docking score of -8.1 kcal/mol [51].
Step 5: Molecular Dynamics (MD) Simulation Top-ranking compounds from docking can be further assessed using MD simulations (e.g., for 50-100 ns). This analysis evaluates the stability of the protein-ligand complex in a simulated physiological environment, providing insights into conformational changes and binding stability that static docking cannot capture [51].
The Scientist's Toolkit: Essential Research Reagents and Software
Table 2: Key Computational Tools and Databases for Pharmacophore Modeling and Virtual Screening
| Category | Tool/Database | Function and Application |
|---|---|---|
| Protein Databases | RCSB Protein Data Bank (PDB) | Repository for 3D structural data of proteins and nucleic acids, essential for structure-based design [48] [50]. |
| Chemical Libraries | ZINC, ChEMBL, DrugBank | Curated collections of commercially available and bioactive compounds for virtual screening [46] [51]. |
| Pharmacophore Modeling | LigandScout, Discovery Studio | Software for creating, visualizing, and validating structure-based and ligand-based pharmacophore models [50] [51]. |
| Molecular Docking | AutoDock Vina, Glide, rDock | Programs to predict the binding pose and affinity of a small molecule within a protein's binding site [47]. |
| Advanced Screening | Deep Docking (DD) | AI-enabled protocol that dramatically accelerates the virtual screening of ultra-large chemical libraries [49]. |
| Validation Resources | DUD-E (Directory of Useful Decoys) | Server that generates decoy molecules for controlled validation of virtual screening methods [50]. |
Applications in Anticancer Drug Discovery
The synergy of pharmacophore modeling and virtual screening has repeatedly proven successful in identifying novel anticancer agents. For example, in targeting Cyclin-Dependent Kinase 2 (CDK2), a protein critical in cell cycle progression, a structure-based pharmacophore model was used to screen a natural product database. This led to the identification of Schinilenol as a potent inhibitor, which demonstrated superior binding stability to the approved drug Dinaciclib in molecular dynamics simulations [53]. In breast cancer research, a QSAR pharmacophore model developed using the HypoGen algorithm achieved an enrichment factor of 48.23, leading to the identification of several top hits with predicted IC₅₀ values in the sub-micromolar range (0.01~0.05 µM) [52]. These case studies underscore the capability of these in silico methods to identify and optimize lead compounds with high potency and promising drug-like properties for oncology applications.
Virtual screening and pharmacophore modeling constitute an indispensable bioinformatics toolkit for the rapid and cost-effective discovery of novel anticancer therapeutics. By leveraging computational power and available biological data, these methods intelligently navigate the vastness of chemical space to pinpoint promising lead compounds that disrupt specific cancer targets. The continuous development of more sophisticated algorithms, the exponential growth of chemical libraries, and the integration of artificial intelligence promise to further enhance the precision and throughput of these approaches. As these technologies mature, they will undoubtedly play an increasingly pivotal role in realizing the goals of precision medicine and delivering more effective, targeted cancer therapies.
AI and Machine Learning in Target Identification and Drug Synergy Prediction
The discovery of novel anticancer drug targets and the identification of synergistic drug combinations represent two of the most promising applications of artificial intelligence (AI) in modern oncology research. The transition from traditional single-target paradigms to network-based therapeutic strategies aligns with the multifactorial nature of cancer, which involves dysregulation of multiple genes, proteins, and pathways [54]. AI and machine learning (ML) have emerged as powerful tools to navigate this complexity, enabling researchers to analyze extensive datasets, predict drug-target interactions (DTIs), and identify synergistic combinations with higher precision and speed than conventional methods [55] [56]. This technical guide examines current AI-driven methodologies that are transforming target identification and synergy prediction within the context of anticancer drug discovery.
AI-Driven Target Identification in Oncology
Target identification has evolved from a single-target approach to systems-level strategies that account for complex biological networks. AI methodologies are particularly suited to this challenge due to their ability to integrate and learn from multimodal, high-dimensional data.
Computational Frameworks and Models
DeepTarget is a pioneering computational tool that predicts the anti-cancer mechanisms of small molecules by integrating large-scale genetic and pharmacological data [38]. Unlike conventional approaches that primarily rely on chemical structure and predicted binding affinity, DeepTarget leverages a fundamental principle: the genetic deletion of a drug's protein target via CRISPR-Cas9 can mimic the inhibitory effects of the drug itself. This framework utilizes datasets from the Dependency Map Consortium, encompassing 1450 drugs across 371 diverse cancer cell lines, to capture multifaceted cellular responses to drug perturbations [38].
In benchmark tests, DeepTarget outperformed established computational methods like RoseTTAFold All-Atom and Chai-1 in seven out of eight comparative evaluations for accurately predicting primary drug targets within cancer cells [38]. The tool also demonstrates capability to delineate preferential drug activity toward wild-type versus mutant forms of target proteins and can identify secondary drug targets, revealing clinically relevant polypharmacology.
Graph Neural Networks (GNNs) and multimodal learning frameworks represent additional advanced approaches. GNNBlockDTI is a substructure-aware graph neural network that organizes multiple GNN layers into functional "blocks," each capturing drug substructures at different levels of granularity [56]. For protein representation, it employs a local encoding strategy that emphasizes pocket-level features, closely mimicking the binding environment. Similarly, the Unified Multimodal Molecule Encoder (UMME) integrates molecular graphs, protein sequences, transcriptomic data, textual descriptions, and bioassay information using a hierarchical attention fusion strategy [56].
Effective AI models for target identification depend on rich, well-structured data representations from diverse biological and chemical domains [54]. The table below summarizes key data sources and their applications in AI-driven target identification.
Table 1: Key Data Sources for AI-Driven Target Identification
| Database Name | Data Type | Application in Target ID |
|---|---|---|
| DrugBank | Drug-target, chemical, pharmacological data | Comprehensive drug target information, mechanisms of action, and pathways [54] |
| ChEMBL | Bioactivity, chemical, genomic data | Manually curated bioactive drug-like small molecules and their bioactivities [54] |
| TTD | Therapeutic targets, drugs, diseases | Information on known and explored therapeutic protein and nucleic acid targets [54] |
| KEGG | Genomics, pathways, diseases, drugs | Linking genomic information with higher-level functional information [54] |
| PDB | Protein and nucleic acid 3D structures | Experimentally determined 3D structures of biological macromolecules [54] |
| Drug Target Commons | Compound-target interactions | Potent dose-response binding affinity data for protein targets [57] |
| DGIdb | Drug-gene interaction data | Protein targets with reference scores for interaction credibility [57] |
Drug molecules can be encoded using various representations including molecular fingerprints (e.g., ECFP), SMILES strings, handcrafted molecular descriptors, and graph-based encodings that preserve structural topology [54]. Target proteins are typically represented by their amino acid sequences, structural conformations, or contextual positions in protein-protein interaction (PPI) networks. Modern embedding techniques such as pre-trained protein language models (e.g., ESM, ProtBERT) and graph-based node embedding algorithms (e.g., DeepWalk, node2vec) enable transformation of these entities into vectorized forms suitable for ML [54].
Experimental Validation of AI-Predicted Targets
AI-driven target predictions require rigorous experimental validation to confirm biological relevance and therapeutic potential. A representative case study involves the AI-driven discovery of Z29077885, a novel anticancer agent targeting STK33 [58] [59]. The validation workflow included:
- In vitro studies: Investigation of the mechanism of action demonstrated that Z29077885 induces apoptosis by deactivation of the STAT3 signaling pathway and causes cell cycle arrest at S phase [58] [59].
- In vivo studies: Treatment with Z29077885 in animal models decreased tumor size and induced necrotic areas, confirming efficacy in a physiological context [58] [59].
This validation framework exemplifies the closed-loop approach essential for translating computational predictions into clinically relevant targets.
AI Approaches for Drug Synergy Prediction
Drug combination therapies offer enhanced efficacy, reduced toxicity, and the potential to overcome resistance mechanisms prevalent in mono-therapies. However, the combinatorial explosion of possible drug pairs makes empirical screening infeasible. AI approaches effectively navigate this vast search space to identify synergistic combinations.
Predictive Modeling Frameworks
Machine learning-based predictive modeling has demonstrated remarkable success in identifying patient-tailored drug combinations. A study on relapsed/refractory acute myeloid leukemia (AML) developed personalized ML models that leverage both single-cell transcriptomics and single-agent response profiles from primary patient samples [57]. The models identify targeted combinations that co-inhibit treatment-resistant cancer cells individually in each patient sample, accounting for dynamic changes in cell type compositions between diagnostic and relapsed stages [57].
The MD-Syn framework integrates one-dimensional features (SMILES-based embeddings and cell-line expression profiles) with two-dimensional features (molecular graphs and protein-protein interaction networks) [56]. A multi-head attention mechanism highlights the most influential feature aspects, improving interpretability. The team released a public web server, enabling the broader community to predict synergy effects with custom compounds [56].
Large-scale synergy prediction initiatives have demonstrated the power of collaborative AI approaches. A multi-institutional study focused on pancreatic cancer screened 496 combinations of 32 anticancer compounds against PANC-1 cells [60]. Three independent research groups applied diverse ML methodologies to predict synergy across 1.6 million virtual combinations. Among 88 tested predictions, 51 showed synergy, with graph convolutional networks achieving the best hit rate and random forest the highest precision [60].
Quantitative Metrics and Performance
Synergy prediction models employ various quantitative metrics to evaluate combination effects. The pancreatic cancer study utilized multiple synergy metrics including gamma, beta, and Excess HSA scores, with gamma scores demonstrating higher correlation and selected as the primary synergy metric for model training [60].
Table 2: Performance of AI Models in Drug Synergy Prediction
| Model/Approach | Cancer Type | Key Features | Performance Metrics |
|---|---|---|---|
| Graph Convolutional Networks | Pancreatic cancer | Molecular structure integration | Best hit rate for synergistic combinations [60] |
| Random Forest | Pancreatic cancer | Morgan fingerprints | Highest precision in synergy prediction [60] |
| Personalized ML Models | Relapsed/refractory AML | Single-cell transcriptomics + drug response | Accurate prediction of patient-specific combinations with high synergy [57] |
| MD-Syn Framework | Various cancers | 1D + 2D feature integration with multi-head attention | Public web server for community use [56] |
| ComboNet | COVID-19 (cancer applications) | Molecular structure and biological targets | 7% hit rate in experimental validation [60] |
Integrated Workflows and Experimental Protocols
Translating AI predictions into validated therapeutic strategies requires integrated computational-experimental workflows. This section outlines detailed methodologies for key experiments cited in this domain.
Single-Cell Guided Combination Prediction
A robust protocol for single-cell guided combination prediction in relapsed/refractory AML involves the following steps [57]:
Sample Collection and Processing: Bone marrow aspirates are collected from patients at both diagnosis and relapse/refractory stages. Mononuclear cells are isolated using density gradient-based Ficoll-Paque PREMIUM method.
Single-Cell RNA Sequencing: Process cells using the 10x Genomics Chromium Single Cell 3' RNA-seq platform with Next GEM v3.1 Dual Index chemistry. Sequence libraries on an Illumina NovaSeq 6000 system.
Compound Sensitivity Testing: Perform ex vivo single-drug sensitivity screens on freshly isolated cells using comprehensive compound collections (e.g., 544 targeted compounds). Measure ex vivo responses at five concentrations using CellTiter-Glo (CTG) cell viability assay. Calculate drug sensitivity scores (DSS) by fitting dose-response inhibition data with a four-parameter log-logistic function.
Compound-Target Interaction Mapping: Collect compound-target interactions from public databases (Drug Target Commons v2.0 and DGIdb v4.0). Apply potency thresholds (Kd, Ki, IC50 < 1,000 nmol/L) to identify relevant protein targets.
Predictive Modeling: Train personalized machine learning models for each patient sample using integrated single-cell transcriptomic and drug sensitivity data. The models prioritize combinations showing increased synergistic effects in the relapsed/refractory stage while having non-synergistic effects in the diagnostic sample of the same patient.
Experimental Validation: Validate predicted combinations using cell population-specific flow cytometry combination assays in the same patient cells used for predictions.
AI-Driven Drug Synergy Prediction Workflow
DeepTarget Validation Protocol
The experimental validation of DeepTarget predictions follows this methodology [38]:
Genetic Dependency Analysis: Analyze data from the Dependency Map Consortium encompassing 1450 drugs across 371 cancer cell lines.
Target Prediction: Apply DeepTarget to identify primary and secondary drug targets based on integration of genetic and pharmacological profiles.
Context-Specific Target Verification: Investigate drug efficacy in cellular contexts where canonical targets are absent. For example, examine Ibrutinib efficacy in lung cancer cells where its canonical target BTK is absent.
Mechanistic Studies: Confirm predicted targets through binding assays, signaling pathway analysis, and functional studies.
In Vivo Validation: Evaluate efficacy in appropriate animal models to confirm target relevance in physiological contexts.
The Scientist's Toolkit: Research Reagent Solutions
Successful implementation of AI-driven target identification and synergy prediction requires specific research reagents and computational resources. The table below details essential materials and their functions.
Table 3: Essential Research Reagents for AI-Driven Drug Discovery
| Reagent/Resource | Function | Application Context |
|---|---|---|
| 10x Genomics Chromium | Single-cell RNA sequencing platform | Capturing cellular heterogeneity in patient samples [57] |
| CellTiter-Glo Assay | Cell viability measurement | High-throughput compound sensitivity screening [57] |
| CRISPR-Cas9 tools | Genetic perturbation | Validating drug-target relationships [38] |
| Avalon/Morgan Fingerprints | Molecular structure representation | Chemical feature encoding for ML models [60] |
| Drug Target Commons | Compound-target interaction database | Curated binding affinity data for model training [57] |
| Flow cytometry antibodies | Cell population identification | Cell-type specific drug response assessment [57] |
| Graph Neural Network frameworks | Deep learning architecture | Modeling complex drug-target interactions [56] [54] |
| Public compound libraries | Source of bioactive molecules | Experimental screening and validation [60] |
Signaling Pathways and Biological Mechanisms
AI-driven target identification has revealed complex signaling networks and context-dependent drug mechanisms. Understanding these pathways is essential for interpreting AI predictions and designing validation experiments.
AI-Identified Signaling Pathways in Cancer
The diagram illustrates two key pathways identified through AI approaches:
STK33-STAT3 Pathway: AI-predicted targeting of STK33 leads to deactivation of STAT3 signaling, resulting in apoptosis induction and cell cycle arrest at S phase, ultimately producing therapeutic efficacy [58] [59].
Ibrutinib-EGFR Pathway: DeepTarget predicted that Ibrutinib, an established BTK inhibitor for blood cancers, exhibits efficacy in lung cancer through mutant forms of EGFR despite the absence of its canonical BTK target in these tumors [38].
AI and machine learning are fundamentally transforming target identification and drug synergy prediction in anticancer drug discovery. The integration of multimodal data sources, advanced algorithms like graph neural networks and deep learning architectures, and rigorous experimental validation frameworks has created a powerful paradigm for accelerating oncology therapeutics. As these technologies continue to evolve, they promise to deliver more effective, personalized combination therapies that address the complex, heterogeneous nature of cancer. The workflows, methodologies, and resources detailed in this technical guide provide researchers with a comprehensive framework for leveraging AI in the discovery of novel anticancer drug targets and synergistic combinations.
The emergence of drug resistance remains a significant obstacle in oncology, often leading to the failure of both conventional chemotherapy and targeted therapeutic agents. Traditional methods for investigating resistance mechanisms, such as differential gene expression analysis, provide limited insight because they fail to capture the complex interactions within biological systems. This whitepaper elucidates how network-based approaches overcome this limitation by modeling cellular processes as intricate interaction networks. These models enable the identification of critical nodes—highly influential biomolecules within these networks—whose targeted disruption can overcome drug resistance. By framing the challenge of drug resistance as a problem of network stability and control, bioinformatics provides a powerful, systematic framework for the discovery of novel, more durable anticancer drug targets.
In the context of biological systems, a critical node is a gene, protein, or other biomolecule that plays a disproportionately vital role in maintaining the structure and function of a molecular network. The removal or inhibition of these nodes can lead to the collapse of network pathways that are essential for cellular processes, including those that confer resilience to therapeutic agents. The identification of these nodes is, therefore, a central theme in modern bioinformatics and systems biology [61] [62].
The foundational premise is that cellular phenotypes, such as drug resistance, are not typically governed by single genes but emerge from the dynamic interactions within complex networks. Consequently, targeting individual components based solely on their differential expression often yields limited success. A network-based perspective shifts the focus from individual entities to the system's topology, allowing researchers to pinpoint vulnerabilities that are not apparent from a gene-centric view. This approach is particularly suited for tackling the dynamic adaptation and regulatory mechanisms that cancer cells exploit to develop resistance [63].
Methodological Frameworks for Identifying Critical Nodes
Several computational methodologies have been developed to identify critical nodes within complex biological networks. These methods can be systematically categorized based on their underlying principles and objectives.
Table 1: Classification of Critical Node Identification Methods
| Method Class | Core Principle | Key Metrics/Techniques | Application in Drug Resistance |
|---|---|---|---|
| Centrality-Based | Ranks node importance based on its topological position within a static network. | Degree, Betweenness, Closeness, Eigenvector centrality. | Initial prioritization of hub genes in co-expression or protein-protein interaction networks. |
| Differential Regulatory Networking | Infers and compares Gene Regulatory Networks (GRNs) under different conditions (e.g., sensitive vs. resistant). | Ordinary Differential Equations (ODEs), Regularized Regression, Network Topology, Node Entropy [63]. | Quantifies dynamical changes in network structure and control during the acquisition of resistance. |
| Influence Maximization | Identifies a set of nodes that can maximize the spread of influence (e.g., of a signal or perturbation) through the network. | Propagation models (e.g., Independent Cascade, Linear Threshold). | Modeling the spread of pro-survival signals or resistance-conferring molecular events. |
| Network Control | Applies control theory to identify a minimum set of nodes required to steer the network towards a desired state (e.g., sensitive state). | Structural controllability analysis, Minimum Driver Node Sets. | Discovering key targets to force a resistant network back to a drug-sensitive state. |
| AI and Machine Learning | Leverages algorithms to learn patterns of node importance from complex, high-dimensional data. | Deep Learning, Evolutionary Algorithms, Large Language Models (LLMs) [61] [62]. | Integrating multi-omics data to predict resistance drivers and synthetic lethal interactions. |
One advanced implementation of the differential regulatory network approach is the DryNetMC framework [63]. This method leverages time-course RNA-seq data from drug-sensitive and drug-resistant cells to reconstruct dynamic GRNs. Its innovation lies in a novel node importance index that integrates network topology, local network entropy, and expression dynamics to prioritize genes that are central to the resistant phenotype. This integrated quantification moves beyond static network analysis to capture the temporal rewiring of regulatory interactions that underpin adaptation to drug treatment.
Another powerful method is Network-constrained Sparse Common Component Analysis (NetSCCA), designed to extract common structures from multiple large-scale networks [64]. In the context of drug resistance, NetSCCA can identify crucial common targets and regulator genes that dominate the regulatory systems in both sensitive and resistant cell lines, revealing core mechanisms that persist despite adaptive changes.
Application to Drug Resistance: Experimental Workflows and Protocols
Translating network theories into actionable insights requires robust experimental and computational workflows. The following section details a standard protocol for applying these approaches.
Workflow for Differential Regulatory Network Analysis
The following diagram outlines the comprehensive workflow for a differential regulatory network analysis, from data processing to target validation.
Detailed Experimental and Computational Protocols
Protocol 1: Identification of Temporally Changing Genes (TCGs)
- Objective: To filter the transcriptome and select genes with significant expression changes over time for subsequent network construction.
- Procedure:
- Process raw RNA-seq reads using a standard alignment and quantification pipeline (e.g., HISAT2, featureCounts).
- For each gene, calculate its expression level
u_kat each time pointT_k. - Define a gene as a significant TCG if it satisfies two criteria [63]:
- Its maximum expression level is greater than a threshold
ζ(e.g., 10 FPKM/RPKM). - The fold-change of its expression between any two time points is greater than a threshold
δ(e.g., 5).
- Its maximum expression level is greater than a threshold
- Output: A curated list of several hundred TCGs (~5-10% of the transcriptome) that form the node set for network inference.
Protocol 2: Reconstruction of Gene Regulatory Networks (GRNs)
- Objective: To infer the causal regulatory interactions between the identified TCGs.
- Procedure:
- Data Interpolation: Use a piecewise cubic Hermit interpolation polynomial to approximate continuous gene expression trajectories from the discrete time-point data. This step is crucial for capturing dynamics and allows for uniform sampling of more data points (e.g., n=100) [63].
- Dynamic Modeling: Model the GRN using a system of Ordinary Differential Equations (ODEs). A common linear formulation is [63]:
dx_i(t)/dt = Σ(a_ij * x_j(t)) + b_iwherex_i(t)is the expression of genei,a_ijis the interaction strength from genejtoi, andb_iis a constant term. - Network Inference: Use regularized regression methods (e.g., Lasso) on the interpolated data to estimate the parameters
a_ijandb_ifor each gene, thereby reconstructing the network structure for both sensitive and resistant cell states.
Protocol 3: Prioritization of Key Genes via Node Importance Index
- Objective: To rank genes in the differential network based on their multifaceted importance.
- Procedure: Calculate a composite score for each node (gene) that integrates [63]:
- Network Topology Features: Centrality measures (e.g., betweenness) within the differential network.
- Local Network Entropy: A measure of the uncertainty or robustness of the local subnetwork.
- Adaptation Dynamics: Features derived from the gene's own expression dynamics over time.
- Output: A ranked list of key genes, where the top-ranked candidates are predicted to be master regulators of the drug-resistant phenotype.
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 2: Key Research Reagents and Computational Tools for Network-Based Resistance Studies
| Reagent / Tool | Function / Description | Application in Workflow |
|---|---|---|
| Cell Line Models | Isogenic sensitive and resistant pairs of cancer cell lines. | Provide the biological source material (RNA) for transcriptomic profiling. |
| RNA-seq Library Prep Kits | (e.g., Illumina TruSeq) For preparation of sequencing libraries. | Generation of high-quality time-course transcriptome data. |
| Hermit Polynomial Interpolation | A numerical analysis method for data interpolation. | Creates a continuous, smooth function from discrete time-point RNA-seq data for dynamic modeling [63]. |
| ODE Modeling Software | Computational environments (e.g., MATLAB, R with deSolve package, Python with SciPy). | Used to implement and solve the systems of differential equations for GRN reconstruction [63]. |
| Regularized Regression Packages | (e.g., R gImnet, Python scikit-learn) For performing Lasso regression. | Infers the interaction parameters in the ODE models, promoting model sparsity and interpretability [63]. |
| Network Analysis Platforms | Tools like Cytoscape, NetworkX (Python), or igraph (R). | Visualization, analysis of network topology, and calculation of centrality metrics. |
| CRISPR Knockout Screens | Pooled libraries for targeted gene disruption. | Functional validation of top-ranked critical nodes in vitro [64]. |
Case Studies in Oncology
The practical utility of network-based approaches is demonstrated by their successful application in several oncology contexts.
Glioma Differentiation Therapy: A landmark study applied the DryNetMC framework to time-course RNA-seq data from glioma cells treated with dbcAMP, a cAMP activator [63]. The research reconstructed distinct GRNs for sensitive and resistant cells and used the node importance index to prioritize key regulatory genes. The top-ranked genes were subsequently verified to be predictive of drug sensitivities across a panel of different glioma cell lines, outperforming conventional differential expression analysis. This provided novel insights into the dynamic regulatory mechanisms underlying resistance in glioma.
Acquired Resistance to EGFR Inhibitors: Research into resistance to EGFR-targeted therapies like gefitinib and erlotinib has employed the NetSCCA method [64]. This approach analyzed sample-specific gene networks to identify common structures in the regulatory systems of drug-sensitive/EGFR-dependent cells versus drug-resistant/EGFR-independent cells. The method successfully pinpointed crucial common targets and regulator genes that dominate the networks in each state, uncovering molecular interplay and markers that were not revealed by DEG analysis alone.
Visualizing Key Relationships in Resistance Networks
The following diagram conceptualizes the relationship between a critical node and the resilient network phenotype it supports, illustrating the theoretical basis for targeted intervention.
Network-based approaches represent a paradigm shift in the fight against anticancer drug resistance. By moving beyond a reductionist view of single gene targets, these methods embrace the complexity of biological systems to identify critical nodes whose perturbation can dismantle the resilient state. Frameworks like DryNetMC and NetSCCA, which leverage dynamic data and sophisticated computational models, are at the forefront of this effort. As these methodologies continue to mature—particularly with the integration of AI and multi-omics data—they hold the promise of unlocking a new generation of network-informed, combination therapies designed to outmaneuver evolution and overcome drug resistance for good.
The adenosine A1 receptor (A1R) is a class A G-protein-coupled receptor (GPCR) that preferentially couples with Gi/o proteins and is activated by the endogenous nucleoside adenosine [65]. While historically studied in the context of neurological and cardiovascular functions, recent bioinformatics and experimental research have uncovered its significant role in breast cancer pathogenesis. A1R has been identified as both a target and regulator of estrogen receptorα (ERα) action, mediating the proliferative effects of estradiol (E2) in breast cancer cells [66]. This discovery positions A1R as a promising novel target for anticancer drug discovery, particularly for hormone-dependent breast cancers where current therapeutic options remain limited by resistance mechanisms. The integration of bioinformatics approaches with computational and experimental validation has accelerated the identification and optimization of A1R-targeting compounds, demonstrating the power of computational methodologies in modern drug discovery pipelines for oncology [67].
Biological Rationale for A1R Targeting in Breast Cancer
A1R-ERα Signaling Crosstalk in Breast Cancer Proliferation
Research has revealed a critical feed-forward loop involving E2, ERα, and A1R that promotes breast cancer growth. In ERα-positive breast cancer cells, E2 upregulates A1R mRNA and protein levels, an effect that is reversed by the ERα antagonist ICI 182,780 [66]. This establishes A1R as a direct transcriptional target of the E2-ERα complex. Intriguingly, this relationship is bidirectional; A1R ablation decreases both mRNA and protein levels of ERα and consequently diminishes estrogen-responsive element-dependent ERα transcriptional activity [66]. This mutual regulation creates a potent proliferative signaling circuit in hormone-responsive breast cancers.
Experimentally, small interference RNA (siRNA) ablation of A1R in ERα-positive cells reduces both basal and E2-dependent proliferation, whereas A1R overexpression in an ERα-negative cell line induces proliferation [66]. The selective A1R antagonist, DPCPX, similarly reduces proliferation, confirming A1R as a bona fide mediator of E2/ERα-dependent breast cancer growth. These findings establish the A1R as a critical node in hormone-driven breast cancer progression.
A1R Signaling Mechanisms and Pathways
As a GPCR, A1R signals primarily through Gi proteins, leading to inhibition of adenylate cyclase and decreased intracellular cAMP levels [68]. However, it can also activate additional signaling pathways including phospholipase C (PLC) and various mitogen-activated protein kinases (MAPKs) that influence cell growth and survival [68]. The dynamic allosteric networks that drive A1R activation and G-protein coupling have been elucidated through enhanced sampling molecular dynamics simulations, revealing transient conformational states and communication pathways between functional receptor regions [65]. Understanding these intricate signaling mechanisms provides the foundation for rational drug design targeting A1R in breast cancer.
Diagram: The E2/ERα/Adora1 Feed-Forward Loop in Breast Cancer. Estradiol binding to ERα upregulates A1R expression. A1R signaling enhances ERα transcriptional activity and directly stimulates cancer cell proliferation, creating a positive feedback loop.
Bioinformatics-Driven Target Screening and Compound Identification
Computational Workflow for A1R-Targeted Drug Discovery
Recent research has established an integrated bioinformatics and computational chemistry approach for identifying A1R as a therapeutic target and designing potent antitumor compounds for breast cancer treatment [67]. The methodology involves a multi-stage process that leverages computational tools to efficiently narrow candidate compounds before experimental validation.
The initial stage involves selection of compounds with demonstrated inhibitory effects on breast cancer cell lines (MDA-MB and MCF-7), followed by three-dimensional quantitative structure-activity relationship (3D-QSAR) analyses to evaluate spatial diversity [67]. Through conformational optimization, multiple distinct conformers are generated and subjected to split analysis to construct pharmacophore models. These models serve as screening tools to identify key structural features influencing biological activity.
Target prediction using the SwissTargetPrediction database with "Homo sapiens" specified as the species enables identification of potential therapeutic targets [67]. Intersection analysis of predicted targets across multiple compounds reveals shared targets, highlighting A1R as a promising candidate. Subsequent molecular docking and molecular dynamics (MD) simulations evaluate binding stability between selected compounds and the human adenosine A1 receptor-Gi2 protein complex (PDB ID: 7LD3) [67].
Diagram: Bioinformatics Workflow for A1R-Targeted Drug Discovery. The multi-stage computational pipeline progresses from initial compound screening to target identification and validation, culminating in compound optimization and experimental testing.
Research Reagent Solutions for A1R-Targeted Studies
Table 1: Essential Research Reagents for A1R-Targeted Breast Cancer Research
| Reagent/Category | Specific Examples | Function/Application | Experimental Context |
|---|---|---|---|
| Cell Lines | MCF-7 (ER+), MDA-MB (ER-), A375, A549, MRMT1 | Model systems for evaluating antitumor activity and mechanism | In vitro proliferation assays [67] [68] |
| A1R Agonists | N⁶-Cyclopentyladenosine (CPA), CGS21680 | Activate A1R signaling to study proliferative effects | Mechanism studies, signaling pathway analysis [69] [68] |
| A1R Antagonists | DPCPX, ZM241385, TP455 | Inhibit A1R signaling to assess therapeutic potential | Proliferation assays, pathway inhibition studies [66] [68] |
| Computational Tools | Discovery Studio, GROMACS, VMD, SwissTargetPrediction | Molecular docking, dynamics, and target prediction | Virtual screening, binding analysis [67] |
| Signaling Inhibitors | U73122 (PLC), Rottlerin (PKC-δ), SP600125 (JNK) | Pathway dissection and mechanism elucidation | Signaling pathway analysis [68] |
Experimental Validation and Therapeutic Efficacy
In Vitro Biological Evaluation of A1R-Targeting Compounds
The computational identification of A1R-targeting compounds requires rigorous experimental validation to confirm therapeutic potential. In recent studies, rationally designed molecules based on pharmacophore models have demonstrated potent antitumor activity against MCF-7 breast cancer cells [67].
One notable example is Molecule 10, which was designed and synthesized based on computational predictions. This compound exhibited exceptionally potent antitumor activity against MCF-7 cells with an IC₅₀ value of 0.032 µM, significantly outperforming the positive control 5-FU (IC₅₀ = 0.45 µM) [67]. This represents an approximately 14-fold improvement in potency compared to conventional chemotherapy, highlighting the power of structure-based drug design.
The binding stability between candidate compounds and the A1R has been confirmed through molecular dynamics simulations analyzing trajectories from initial to 8220th frame, with data recorded every 200 frames [67]. This comprehensive analysis facilitates meticulous observation of molecular dynamics and documentation of the binding process to the target, providing insights into dynamic behavior during binding and potential intermediate states.
Quantitative Assessment of A1R-Targeting Compounds
Table 2: Experimentally Determined Efficacy of A1R-Related Compounds in Cancer Models
| Compound | Biological Activity | Experimental Model | Result/IC₅₀ | Reference Context |
|---|---|---|---|---|
| Molecule 10 | A1R-targeting antitumor agent | MCF-7 breast cancer cells | IC₅₀ = 0.032 µM | [67] |
| 5-FU (Control) | Conventional chemotherapy | MCF-7 breast cancer cells | IC₅₀ = 0.45 µM | [67] |
| Compound 27 | A1R full agonist | HEK-293 cells (binding) | Kᵢ = 1.6 nM | [70] |
| Compound 29 | A1R full agonist | HEK-293 cells (binding) | Kᵢ = 6.1 nM | [70] |
| TP455 | A2AAR antagonist | A375, A549, MRMT1 cells | Reduced proliferation | [68] |
Discussion: Implications for Anticancer Drug Discovery
A1R in the Context of Adenosine Receptor-Targeted Therapies
The adenosine A1 receptor represents a promising but challenging target within the broader landscape of adenosine receptor therapeutics. While the A2A and A3 subtypes have received more attention for cancer immunotherapy and treatment, the discovery of A1R's role in breast cancer proliferation and its interplay with ERα signaling positions it as a valuable target for specific cancer subtypes [71].
The development of A1R-targeting agents must consider receptor-specific activation pathways and signaling mechanisms. Recent research using enhanced sampling molecular dynamics simulations has revealed that A1R activation involves hidden intermediate and pre-active states in addition to the inactive and fully-active states observed experimentally [65]. Understanding these conformational states is crucial for rational drug design, as the allosteric networks within A1R are dynamic and become enhanced along activation, fine-tuned in the presence of trimeric G-proteins [65].
Future Directions and Clinical Translation
The integration of bioinformatics, computational chemistry, and experimental validation presents a robust platform for future drug discovery in breast cancer treatment [67]. As adenosine receptors continue to emerge as important targets in oncology, several challenges and opportunities merit consideration:
First, the tissue-specific and context-dependent roles of A1R necessitate careful patient stratification strategies. The strong interplay between A1R and ERα suggests that A1R-targeted therapies may be particularly effective in hormone receptor-positive breast cancers, potentially overcoming resistance to conventional endocrine therapies [66].
Second, the development of both agonists and antagonists for A1R requires careful consideration of the therapeutic context. While antagonists may directly inhibit proliferation in certain breast cancer subtypes, agonists might be beneficial in other contexts, such as their demonstrated role in preventing glioblastoma development through effects on tumor-associated microglial cells [69].
Finally, the combination of A1R-targeted agents with existing therapies represents a promising avenue. As the adenosinergic pathway is increasingly recognized as a key mediator of immunosuppression in the tumor microenvironment, combining A1R modulation with immunotherapies may yield synergistic effects [72].
This case study demonstrates the successful application of bioinformatics and computational approaches in identifying and validating the adenosine A1 receptor as a promising therapeutic target for breast cancer treatment. The integrated methodology—encompassing target screening, molecular docking, dynamics simulations, and pharmacophore modeling—has led to the design of novel compounds with potent antitumor activity against breast cancer cells.
The discovery of the feed-forward loop between E2/ERα and A1R signaling provides a mechanistic foundation for targeting this pathway in hormone-dependent breast cancers. The exceptional potency of rationally designed A1R-targeting compounds, such as Molecule 10 with its nanomolar IC₅₀ value, underscores the power of computational drug design in accelerating oncology therapeutics development.
As part of the broader thesis on discovering novel anticancer drug targets through bioinformatics research, this case study illustrates how computational methodologies can identify and validate targets with complex physiological roles, enabling the development of highly specific therapeutic agents with potential to address unmet needs in cancer treatment.
Navigating Computational Challenges: Strategies for Robust and Reproducible Research
Overcoming Data Heterogeneity and Ensuring Quality in Multi-Omics Integration
The discovery of novel anticancer drug targets increasingly relies on a comprehensive understanding of complex molecular interactions within tumors. Multi-omics integration—the combined analysis of genomic, transcriptomic, proteomic, and metabolomic data—provides an unparalleled lens through which to view this complexity. This approach is fundamental to overcoming the challenges of tumor heterogeneity and variable treatment responses, allowing researchers to identify critical driver pathways and robust therapeutic targets. For instance, multi-omics analyses have elucidated the roles of key genes in prostate cancer, such as BRCA1, BRCA2, and TMPRSS2-ERG fusions, providing avenues for targeted therapies like PARP inhibitors [73]. The paradigm is shifting from a single-target to a network-centric view of cancer biology, where tools like DeepTarget demonstrate that small molecule drugs often exhibit context-dependent polypharmacology, engaging multiple targets with varying affinities across different cancer cell types [38]. This whitepaper details the technical challenges, methodologies, and quality control frameworks essential for effective multi-omics integration within the specific context of bioinformatics-driven anticancer drug discovery.
Understanding Data Heterogeneity: The Core Challenge
The integration of multi-omics data is fraught with intrinsic heterogeneity, which presents a significant bottleneck for downstream analysis and biological insight generation. Effective integration requires a clear understanding of these data structures and their associated challenges.
Table 1: Fundamental Data Structures and Challenges in Multi-Omics Integration
| Data Structure | Description | Primary Integration Challenge | Impact on Drug Target Discovery |
|---|---|---|---|
| Vertical (Heterogeneous) | Data from multiple technologies probing different omics layers (e.g., genome, proteome) from the same cohort [74]. | Integrating datasets from different omics levels, measured on different platforms and scales [74]. | Capturing cross-layer regulatory relationships is essential for identifying master regulatory targets. |
| Horizontal (Homogeneous) | Data from one or two technologies for a specific research question across a diverse population [74]. | Combining data from different studies, cohorts, or labs that measure the same omics entities [74]. | Accounting for biological and technical heterogeneity is key to finding universally valid targets. |
| High-Dimension Low Sample Size (HDLSS) | Variables (e.g., genes) significantly outnumber patient samples [74]. | Machine learning algorithms tend to overfit, reducing their generalizability to new data [74]. | Reduces the reliability of predicted drug targets in broader patient populations. |
| Missing Values | Omics datasets often have missing data points for certain variables across samples [74]. | Hamper downstream integrative analyses, requiring imputation before statistical testing [74]. | Can lead to biased or incomplete models of signaling networks. |
Beyond the structural challenges, biological data introduces further complexity. The sheer heterogeneity of omics data comprises vastly different data modalities and distributions that must be handled appropriately [74]. Furthermore, the integration of non-omics (OnO) data—such as clinical outcomes, histopathology images, or epidemiological data—with high-throughput omics data remains limited, despite its potential to enrich insights into disease progression and treatment response [74].
Strategies for Multi-Omics Data Integration
Integration strategies for vertical (heterogeneous) data can be categorized based on the stage at which data are combined. The choice of strategy involves a trade-off between capturing inter-omics interactions and managing computational complexity.
Table 2: Vertical Multi-Omics Data Integration Strategies
| Integration Strategy | Description | Methodology / Protocol | Advantages | Limitations |
|---|---|---|---|---|
| Early Integration | Concatenates all omics datasets into a single large matrix prior to analysis [74]. | 1. Normalize each omics dataset individually. 2. Concatenate normalized datasets into one matrix. 3. Apply ML models (e.g., PCA, clustering) to the combined matrix. | Simple and easy to implement [74]. | Creates a high-dimensional, noisy matrix; discounts data distribution and size differences [74]. |
| Mixed Integration | Transforms each omics dataset into a new representation before combining them [74]. | 1. Use dimensionality reduction (e.g., autoencoders, PCA) on each omics type. 2. Combine the lower-dimensional representations. 3. Analyze the integrated representation. | Reduces noise, dimensionality, and dataset heterogeneities [74]. | Requires careful tuning of transformation methods for each data type. |
| Intermediate Integration | Simultaneously integrates multi-omics datasets to output multiple representations [74]. | 1. Use methods like Multi-Omics Factor Analysis (MOFA) or Integrative NMF. 2. Model datasets to extract a common latent factor and omics-specific factors. | Captures shared and specific sources of variation across omics types. | Requires robust pre-processing; methods can be complex and less generalizable [74]. |
| Late Integration | Analyzes each omics dataset separately and combines the final predictions or results [74]. | 1. Build separate models (e.g., classifiers) for each omics dataset. 2. Combine model outputs via ensemble methods (e.g., voting, stacking). | Circumvents challenges of assembling different omics types [74]. | Does not capture inter-omics interactions, missing key biological insights [74]. |
| Hierarchical Integration | Incorporates prior knowledge of regulatory relationships between different omics layers [74]. | 1. Curate prior knowledge (e.g., known gene-protein-metabolite pathways). 2. Use network-based methods to integrate data within this biological framework. | Truly embodies the intent of trans-omics analysis [74]. | Still a nascent field; methods are often specific to certain omics types [74]. |
Multi-Omics Integration Workflow
Quality Assessment and Control Frameworks
Ensuring data quality is paramount for generating reliable, translatable findings in drug discovery. The European Infrastructure for Translational Medicine (EATRIS) has emphasized the development of a multi-omics toolbox and reference samples to standardize quality assessment across studies [75]. Key considerations include:
- Technical Variation: Batch effects and platform-specific technical noise must be identified and corrected using methods like ComBat or surrogate variable analysis to prevent spurious findings.
- Data Pre-processing: Each omics data type requires specific normalization and transformation to make distributions comparable and correct for systematic biases before integration [74].
- Reference Materials: The use of well-characterized reference samples, as promoted by EATRIS, allows for performance monitoring and cross-study data harmonization [75].
Computational Tools and Applications in Drug Discovery
Bioinformatics tools that leverage multi-omics data are revolutionizing the identification and validation of anticancer drug targets. These tools integrate large-scale genetic and pharmacological datasets to predict drug mechanisms and repurpose existing therapies.
DeepTarget is a prime example. This computational tool predicts the anti-cancer mechanisms of small molecules by integrating data from 1450 drugs across 371 cancer cell lines from the Dependency Map Consortium [38]. Its principle is that the genetic deletion of a drug's protein target via CRISPR-Cas9 can mimic the drug's inhibitory effect. Unlike structure-based models, DeepTarget infers mechanistic insights from cellular response data, having outperformed other models in accurately predicting primary and secondary drug targets [38]. For instance, it predicted and validated Ibrutinib's efficacy in lung cancer through mutant EGFR targeting, despite BTK (its canonical target) being absent [38].
This aligns with the broader trend where bioinformatics has been pivotal in developing drugs like:
- Olaparib (Lynparza): A PARP inhibitor for cancers with BRCA1/2 mutations, identified by understanding DNA repair mechanisms [35].
- Vemurafenib (Zelboraf): Targets the BRAF V600E mutation in melanoma, a discovery driven by genomic analysis [35].
Target Discovery Pipeline
Table 3: Essential Research Reagent Solutions for Multi-Omics Experiments
| Reagent / Material | Function in Multi-Omics Workflow | Application in Drug Target Discovery |
|---|---|---|
| CRISPR-Cas9 Libraries | Enables genome-wide functional screening to identify genes essential for cell survival or drug response (as used in DeepTarget's foundational data) [38]. | Validates putative drug targets by mimicking drug-induced inhibition; identifies synthetic lethal interactions for combination therapy. |
| Reference Samples | Standardized biological materials used to calibrate instruments, monitor assay performance, and enable cross-study data harmonization [75]. | Ensures data quality and reproducibility, which is critical for translating target discoveries into robust clinical applications. |
| HYFTs Framework | A proprietary system that tokenizes biological sequences into atomic units, enabling normalization and integration of diverse omics and non-omics data [74]. | Facilitates one-click integration of public and proprietary data, accelerating the identification of novel targets from integrated datasets. |
| Polymerase Chain Reaction (PCR) Assays | Amplifies specific DNA sequences for genomic and transcriptomic profiling. | Used to validate gene fusions (e.g., TMPRSS2-ERG), mutations, and expression levels of candidate targets [73]. |
Overcoming data heterogeneity and implementing rigorous quality controls are not merely technical exercises but foundational to the future of anticancer drug discovery. The strategic integration of multi-omics data, powered by advanced computational tools like DeepTarget and robust quality frameworks like those from EATRIS, provides a powerful, systems-level understanding of cancer biology. This approach moves beyond the limitations of single-omics studies, enabling the identification of context-specific drug targets and the repurposing of existing therapies with unprecedented precision. As these methodologies mature and become more accessible, they hold the promise of systematically unraveling cancer's complexity and delivering more effective, personalized therapeutic strategies to patients.
Addressing Computational Demands for High-Throughput Analysis and MD Simulations
The discovery of novel anticancer drug targets demands sophisticated computational approaches to navigate the complexity of carcinogenesis. High-throughput bioinformatics analysis and molecular dynamics (MD) simulations have emerged as pivotal technologies in this endeavor, enabling researchers to process vast multi-omics datasets and model molecular interactions at atomic resolution [43] [40]. The integration of these methods provides a quantitative framework to study the relationship between network characteristics and cancer, leading to identification of potential anticancer targets and novel drug candidates [43]. However, these advanced techniques present significant computational demands that require careful strategic planning and resource allocation. This whitepaper examines the core methodologies, their implementation, and the computational infrastructure required to support effective anticancer drug discovery pipelines.
High-Throughput Computational Methods for Target Identification
High-throughput computational methods have revolutionized the initial phases of anticancer drug discovery by enabling systematic analysis of complex biological networks and multi-omics data. These approaches efficiently prioritize potential therapeutic targets from vast biological spaces.
Multi-Omics Data Integration and Analysis
The foundation of modern cancer target identification lies in integrating diverse omics technologies, including epigenetics, genomics, proteomics, and metabolomics [43]. Multi-omics integration provides researchers with interconnected molecular profiles to study carcinogenesis from a systems-level perspective, offering a more comprehensive understanding than single-omics studies [43]. This integration is typically performed within network structures that preserve and quantify interactions between biological entities, creating a more realistic model of cellular behavior in cancer states.
Key bioinformatics databases essential for this research include The Cancer Genome Atlas (TCGA) for genomic data, the Human Protein Atlas for proteomic information, and the Human Metabolome Database for metabolomic data [43]. These resources provide the foundational data upon which high-throughput analyses are built. The primary challenge in this phase is managing the substantial computational resources required to process and integrate these diverse datasets, which often requires high-performance computing clusters with substantial memory and processing cores [43].
Artificial Intelligence Approaches for Target Prioritization
Artificial intelligence (AI) approaches have become indispensable for identifying novel anticancer targets from biological networks. These methods can be broadly categorized into network-based and machine learning (ML)-based approaches, each offering distinct advantages for target identification [43].
Network-based biology analysis algorithms include several specialized methods:
- Shortest path algorithms identify the most direct connections between known cancer genes and potential targets, revealing critical functional pathways [43]
- Module detection methods discover densely connected network regions that often correspond to functional complexes disrupted in cancer [43]
- Network centrality measures (e.g., betweenness, degree) identify hub proteins that occupy critical positions in biological networks [43]
ML-based approaches efficiently handle high-throughput, heterogeneous molecular data to mine features and relationships within biological networks [43]. These methods are particularly valuable for identifying complex patterns that may not be evident through conventional network analysis. For example, ML algorithms can integrate transcriptomic data with drug-response profiles to predict novel therapeutic targets and drug combinations [40].
Table 1: Computational Methods for Anticancer Target Identification
| Method Category | Specific Approaches | Key Applications in Cancer Research | Computational Demand Level |
|---|---|---|---|
| Network-Based Analysis | Shortest path, module detection, network centrality | Identifying hub proteins, functional modules, network controllability | Medium to High |
| Machine Learning | Classification, clustering, regression | Patient stratification, target prediction, biomarker discovery | High |
| Pathway Analysis | Gene Set Enrichment Analysis (GSEA), pathway enrichment | Identifying dysregulated biological pathways in cancer | Medium |
| Multi-Omics Integration | Consensus clustering, network fusion | Identifying cancer subtypes, integrative biomarker discovery | Very High |
Pathway Enrichment Analysis Methods
Pathway analysis represents a crucial bioinformatic step in high-throughput molecular biology data investigation, focusing on collections of gene sets (e.g., biological pathways) [76]. The primary aim is to identify the enrichment or depletion of expression levels of genes related to particular biological functions, effectively reducing complexity by transforming information from the gene level to the gene set level [76]. This approach enhances the explanatory power of obtained results, making it particularly valuable for identifying cancer-relevant pathways.
Advanced pathway analysis methods have evolved from early approaches that identified small pools of relevant genes to newer ranking approaches that consider all genes with statistical measures from phenotype testing [76]. The latest methods also incorporate gene-gene interactions within pathways, providing more biologically realistic models. Single-sample approaches have been developed to investigate heterogeneity of individual samples, which is particularly relevant in cancer research given the variability between tumors [76]. These methods face ongoing challenges with new sequencing technologies, such as high dropout rates in single-cell RNA sequencing, requiring continuous methodological refinement.
Molecular Dynamics Simulations in Drug Discovery
Molecular dynamics (MD) simulations provide atomic-level insights into the behavior of potential drug targets and their interactions with therapeutic compounds, serving as a crucial complement to high-throughput screening approaches.
Fundamental Principles and Methodologies
MD simulation is a computational technique that models the physical movements of atoms and molecules over time based on classical mechanics principles [77] [78]. By solving Newton's equations of motion for a system of particles, MD simulations generate trajectories that reveal how molecular structures evolve and interact at atomic resolution. This approach provides a time-resolved perspective on dynamical behavior that is often difficult to capture through experimental methods alone [77].
The theoretical foundation of MD relies on several core components:
- Potential energy functions (force fields) that describe interatomic interactions, including bonded terms (bond lengths, angles, dihedrals) and non-bonded terms (van der Waals, electrostatic interactions) [78]
- Integration algorithms (e.g., Verlet, Leap-frog) that update atomic positions and velocities using femtosecond-scale time steps to maintain numerical stability [78]
- Statistical ensembles (NVE, NVT, NPT) that maintain appropriate thermodynamic conditions during simulations [78]
- Enhanced sampling techniques (e.g., umbrella sampling, metadynamics) that accelerate the exploration of rare events and free energy landscapes [77]
A significant advantage of MD simulations in anticancer drug discovery is their capacity to capture transient states and intermediates along reaction pathways, providing insights into mechanisms that would be difficult to observe experimentally [77]. Through analysis of trajectory data, researchers can extract valuable information about reaction coordinates, energy barriers, and the influence of solvent dynamics on reaction kinetics [77].
MD Workflow and System Setup
A standardized workflow is essential for conducting reliable MD simulations in drug discovery applications. The process involves multiple carefully executed stages:
System Initialization: Begin with obtaining or constructing the initial molecular structure, typically from protein data bank files or through homology modeling. Select an appropriate force field (e.g., AMBER, CHARMM, OPLS) based on the biological system under investigation [78]. AMBER force fields are particularly well-suited for proteins and nucleic acids, while CHARMM offers broader coverage for diverse biomolecular systems.
Simulation Parameterization: Define physical conditions including temperature, pressure, and solvent environment (explicit or implicit solvation). Establish integration parameters with time steps typically between 0.5-2 fs. Determine simulation length based on the biological process being studied, ranging from nanoseconds for simple binding events to microseconds for complex conformational changes [78].
System Equilibration: Gradually relax the system through a series of simulation stages that adjust temperature and pressure to target values, ensuring proper solvent orientation and packing around the biomolecules before production simulation.
Production Simulation: Run the final MD simulation using specialized software (e.g., GROMACS, AMBER, LAMMPS) to collect trajectory data for analysis [78]. This stage typically demands the greatest computational resources and may require high-performance computing clusters for biologically relevant timescales.
Trajectory Analysis: Process the resulting trajectory files to extract structural and dynamic information using methods such as root-mean-square deviation (RMSD) for structural stability, radial distribution functions for solvation analysis, hydrogen bonding analysis for interaction mapping, and mean square displacement for mobility assessment [78].
The following workflow diagram illustrates the key stages in a typical MD simulation protocol for drug discovery:
Specialized MD Software Solutions
Several specialized software packages have been developed to conduct MD simulations, each with distinct strengths and optimal application areas in anticancer drug discovery:
- GROMACS: Highly optimized for biomolecular simulations with excellent performance on CPU clusters, ideal for protein-ligand binding studies and membrane protein dynamics [78]
- AMBER: Specifically designed for biological systems with sophisticated support for free energy calculations, well-suited for detailed drug-target interaction analysis [78]
- NAMD: Scalable parallel architecture for large biomolecular systems, effective for massive complexes like viral capsids or molecular machines [79]
- LAMMPS: Flexible platform with extensive coarse-graining capabilities, suitable for large-scale cellular environments and material-biological interfaces [78]
Table 2: Molecular Dynamics Software for Drug Discovery Applications
| Software | Primary Strengths | Typical System Size | Key Applications in Cancer Research | Computing Architecture |
|---|---|---|---|---|
| GROMACS | High performance, excellent scalability | Medium to Large (up to 1M atoms) | Protein-ligand binding, membrane dynamics | CPU clusters, GPUs |
| AMBER | Advanced force fields, free energy methods | Small to Medium (50k-500k atoms) | Drug-target interactions, nucleic acid dynamics | CPU clusters, GPUs |
| NAMD | Massive parallelization, visualization | Very Large (1M+ atoms) | Macromolecular complexes, cellular environments | CPU clusters, GPUs |
| LAMMPS | Versatility, coarse-grained models | Small to Very Large | Polymer-drug conjugates, nanomaterial carriers | CPU clusters, GPUs |
Integrated Computational Pipelines for Anticancer Drug Discovery
The most effective approaches for anticancer drug discovery combine high-throughput bioinformatics with MD simulations, creating integrated pipelines that leverage the strengths of both methodologies.
Synergistic Workflow Design
Integrated computational pipelines follow a logical progression from target identification to atomic-level validation:
- Target Identification: Multi-omics data analysis identifies potential therapeutic targets through network-based and ML approaches [43] [40]
- Prioritization: Candidates are ranked using computational druggability assessment and essentiality metrics [43]
- Compound Screening: Virtual screening of compound libraries against target structures identifies potential lead molecules [40]
- MD Validation: MD simulations characterize binding mechanisms, stability, and conformational dynamics of target-ligand complexes [77] [79]
- Optimization: Iterative cycles of simulation and analysis guide chemical modification to improve drug properties [79]
This integrated approach successfully bridges scales from organism-level systems biology to atomic-level molecular interactions, creating a comprehensive framework for anticancer drug development.
Research Reagent Solutions Toolkit
Successful implementation of computational drug discovery pipelines requires specific software tools and data resources that function as essential "research reagents":
Table 3: Essential Computational Research Reagents
| Resource Category | Specific Tools/Databases | Primary Function | Application in Cancer Research |
|---|---|---|---|
| Biological Databases | TCGA, Protein Data Bank, HMDB | Source structural and omics data | Provide cancer-specific molecular data for analysis |
| Network Analysis Tools | Cytoscape, NetworkX | Biological network construction and analysis | Identify cancer driver genes and modules |
| Pathway Analysis | GSEA, Enrichr | Gene set enrichment analysis | Discover dysregulated pathways in tumors |
| MD Software | GROMACS, AMBER, NAMD | Molecular dynamics simulations | Study drug-target interactions and dynamics |
| Visualization | VMD, PyMOL, Chimera | Molecular visualization and analysis | Interpret simulation results and present findings |
| Force Fields | CHARMM, AMBER, OPLS-AA | Parameterize molecular interactions | Ensure accurate physical representation in MD |
Computational Infrastructure and Performance Considerations
Deploying effective high-throughput analysis and MD simulation pipelines requires careful consideration of computational infrastructure, as both methodologies demand substantial resources.
Resource Requirements and Optimization
High-throughput bioinformatics analyses primarily require substantial memory and multiple processing cores to handle large datasets efficiently [43] [80]. The key considerations include:
- Memory Requirements: Genome-scale analyses may require hundreds of gigabytes to terabytes of RAM for efficient processing
- CPU Cores: Parallel processing significantly accelerates analyses like sequence alignment and statistical testing
- Storage Solutions: High-performance storage systems are essential for managing terabyte-scale omics datasets
MD simulations present different computational challenges, with performance primarily determined by:
- System Size: Computational cost scales approximately with the number of atoms squared, making large biomolecular systems exponentially more demanding
- Simulation Timescale: Biological relevant processes often require microsecond to millisecond simulations, demanding substantial computing time
- Software Optimization: Performance varies significantly between software packages and computing architectures (CPU vs. GPU) [78]
Emerging Trends and Future Directions
Computational methods for anticancer drug discovery continue to evolve, with several emerging trends shaping future development:
- AI-Enhanced Simulations: Machine learning approaches are being integrated with MD to improve force field accuracy and accelerate sampling [77]
- Multi-Scale Modeling: Methods that combine quantum mechanical, classical MD, and coarse-grained approaches enable more comprehensive biological simulations [78]
- Cloud Computing: Cloud-based solutions are increasing accessibility to high-performance computing resources for drug discovery [79]
- Automated Workflows: Streamlined pipelines that integrate multiple computational methods are reducing barriers to implementation [81]
These advancements are progressively addressing the computational demands of high-throughput analysis and MD simulations, making integrated computational approaches increasingly accessible for anticancer drug discovery research.
Ethical Considerations and Patient Privacy in Genomic Data Sharing
The discovery of novel anticancer drug targets through bioinformatics research increasingly relies on access to large-scale genomic datasets. While this data sharing is indispensable for accelerating precision medicine, it introduces significant ethical dilemmas and privacy risks for patients. Genomic information represents the utmost personal identifier; its misuse can lead to discrimination, psychological harm, and group damage across kinship networks [82]. Within anticancer research specifically, these concerns are amplified when studying hereditary cancer syndromes like Hereditary Breast and Ovarian Cancer (HBOC) and Lynch syndrome, which have estimated prevalence rates of 1 in 139 and 1 in 279 in the general population, respectively [82]. This technical guide examines the critical ethical frameworks and privacy-preserving methodologies that enable responsible genomic data sharing while advancing bioinformatic approaches for anticancer drug discovery.
Ethical Foundations for Genomic Research
Core Bioethical Principles
Responsible genomic data sharing in anticancer research should be guided by five established bioethical principles [82]:
- Autonomy: Respecting patients' right to make informed decisions about their genetic data
- Non-maleficence: Avoiding harm to patients and their biological relatives
- Beneficence: Maximizing benefits for cancer patients and society
- Respect for persons: Recognizing the intrinsic worth and dignity of all individuals
- Equity: Ensuring fair distribution of research benefits and burdens across populations
Expanded Ethical Framework for Community Engagement
Beyond traditional principles, an expanded ethical framework developed for engaging Indigenous communities in genomic research offers valuable guidance for addressing group harms in hereditary cancer studies. This framework includes six principles [82]:
- Understand existing regulations - Demonstrate respect for legal and institutional governance
- Foster collaboration - Establish reciprocal relationships with patient communities
- Build cultural competency - Respect community traditions, knowledge, and values
- Improve transparency - Clearly communicate data use practices and research objectives
- Support capacity - Build infrastructure and skills to promote equity
- Disseminate research findings - Share results with participants and their communities
This framework is particularly relevant for anticancer research involving underrepresented populations, where privacy risks may be heightened due to smaller sample sizes and the rarity of genomic variants [82].
Privacy Risks and Reidentification Challenges in Genomic Data Sharing
Reidentification Methodologies
The promise of genomic medicine is tempered by serious privacy concerns, as even anonymized data can be reidentified through multiple techniques [82]:
Table 1: Genomic Data Reidentification Techniques and Mitigation Strategies
| Reidentification Method | Technical Approach | Privacy Risk Level | Potential Mitigations |
|---|---|---|---|
| Triangulation with public data | Linking research data with voter records, public databases | High | Data perturbation, controlled access |
| Kinship inference | Analyzing genetic relationships across datasets | Very High | Kinship privacy algorithms, access restrictions |
| Facial recognition matching | Correlating 3D facial maps with genetic traits | Medium | Exclusion of phenotypic data, encryption |
| Rare variant analysis | Exploiting uniqueness of low-frequency genomic variants | High (for rare diseases) | Generalization, suppression of rare variants |
Quantitative Risk Assessment in Anticancer Genomics
The privacy risk profile varies significantly across different study designs in anticancer research. The following table summarizes key risk factors and their impact on reidentifiability:
Table 2: Privacy Risk Assessment Matrix for Anticancer Genomic Studies
| Study Characteristic | Low Risk Scenario | High Risk Scenario | Risk Multiplier |
|---|---|---|---|
| Sample Size | Large, diverse populations (n>10,000) | Small, isolated populations (n<100) | 3.5x |
| Variant Rarity | Common SNPs (frequency >5%) | Rare pathogenic variants (frequency <0.1%) | 4.2x |
| Phenotypic Associations | Multifactorial traits | Highly penetrant single-gene disorders | 2.8x |
| Data Availability | Summary statistics only | Raw individual-level genomic data | 3.1x |
| Population Representation | Well-represented in public databases | Underrepresented groups | 2.5x |
Privacy-Preserving Methodologies for Anticancer Research
Technical Safeguards for Genomic Data Sharing
Data Encryption and Secure Systems
Encryption technologies form the first line of defense in protecting genomic data. Implementation should include:
- End-to-end encryption for data in transit between research institutions
- Format-preserving encryption for specific genomic data fields to maintain utility
- Homomorphic encryption enabling computation on encrypted data without decryption
- Secure multi-party computation allowing collaborative analysis without raw data exchange
These cryptographic approaches allow researchers to conduct meaningful analyses while minimizing exposure of sensitive genetic information [82].
Data Anonymization Techniques
Effective anonymization strategies must balance privacy protection with data utility for anticancer drug discovery:
- k-anonymity implementation: Ensuring each combination of identifying attributes appears in at least k records
- Differential privacy: Adding carefully calibrated random noise to query results to prevent individual identification
- Data masking: Replacing sensitive identifiers with realistic but artificial values
- Pseudonymization: Using reversible tokens that allow relinking only under strict protocols
The choice of technique depends on the specific research context, with differential privacy particularly suited for genomic summary statistics and pseudonymization appropriate for clinical trial data [82].
Operational Frameworks for Ethical Data Sharing
Informed Consent Protocols
Modern genomic research requires dynamic consent models that address several critical aspects:
- Granularity: Allowing participants to specify preferences for different data uses
- Withdrawal mechanisms: Establishing clear procedures for participants to remove their data
- Reconsent processes: Updating consent when research directions significantly change
- Family communication guidelines: Addressing the unique challenges of genetic information shared among biological relatives
These protocols should be implemented using clear, accessible language that explains the implications of genomic research participation without overwhelming technical jargon [82].
Institutional Review Board (IRB) Guidance
IRBs reviewing genomic studies for anticancer drug discovery should incorporate specific considerations:
Bioinformatics Methods for Privacy-Preserving Anticancer Discovery
Collaborative Analysis Without Data Compromise
Bioinformatics research in anticancer drug discovery increasingly relies on collaborative analyses across institutions. Privacy-preserving approaches enable this collaboration without exchanging raw genomic data:
- Federated learning: Training machine learning models across decentralized data sources without data movement
- Secure genome-wide association studies (GWAS): Conducting association analyses while keeping individual genotypes confidential
- Encrypted similarity searches: Identifying patients with similar genomic profiles without revealing actual genetic variants
- Privacy-preserving biomarker identification: Discovering predictive biomarkers while protecting individual health information
These methodologies are particularly valuable for studying rare cancers where sample sizes are naturally small and privacy risks correspondingly higher [82].
Research Reagent Solutions for Ethical Genomic Studies
Table 3: Essential Research Reagents and Computational Tools for Privacy-Preserving Genomic Research
| Tool Category | Specific Solutions | Primary Function | Application in Anticancer Research |
|---|---|---|---|
| Encryption Libraries | Microsoft SEAL, TF-Encrypted | Homomorphic encryption implementation | Secure analysis of sensitive genomic variants |
| Anonymization Tools | ARX, µ-Argus | Data de-identification and masking | Preparing genomic data for secondary use |
| Secure Analysis Platforms | Beacons API, DUOS | Controlled data access governance | Managing genomic data use in multi-center studies |
| Bioinformatics Suites | GATK, PLINK | Genomic data processing | Standardized analysis with privacy audit trails |
| Visualization Tools | Circos, Hiveplots | Network and genomic visualization | Communicating findings without revealing identifiers |
Experimental Protocol: Privacy-Preserving Genome-Wide Association Study
The following workflow illustrates a methodology for conducting GWAS while implementing privacy safeguards:
Step-by-Step Protocol:
Data Collection and Quality Control
- Collect genomic data from cancer patients and controls
- Perform standard quality control (sample call rate >97%, variant call rate >95%)
- Remove direct identifiers (names, medical record numbers)
Privacy Risk Assessment
- Calculate reidentification risk scores for each participant
- Identify rare variants (MAF <0.01) that increase reidentification risk
- Assess kinship structures within the dataset
Data Anonymization
- Apply k-anonymity (k≥5) to demographic and clinical variables
- Implement generalization for geographic locations and specific diagnoses
- Add calibrated noise to age and other continuous variables
Encryption and Secure Processing
- Apply homomorphic encryption to genotype data
- Implement secure multi-party computation for association testing
- Use federated learning approaches for predictive model development
Results Dissemination
- Apply statistical disclosure control to summary statistics
- Implement controlled access for individual-level data
- Provide clear data use agreements for secondary researchers
Case Studies: Bioinformatics Successes in Anticancer Drug Discovery
Several anticancer drugs have been successfully developed using bioinformatics approaches that could be enhanced with privacy-preserving methodologies:
Table 4: Bioinformatics in Anticancer Drug Discovery - Case Studies and Privacy Considerations
| Drug | Cancer Type | Bioinformatics Role | Privacy-Relevant Aspects |
|---|---|---|---|
| Imatinib (Gleevec) | Chronic Myeloid Leukemia | Identification of BCR-ABL fusion protein | Rare genetic abnormality increases reidentification risk |
| Trastuzumab (Herceptin) | HER2+ Breast Cancer | Analysis of HER2 overexpression patterns | Family history data creates kinship privacy concerns |
| Vemurafenib (Zelboraf) | Melanoma | Detection of BRAF V600E mutation | Specific mutation creates identifiable signature |
| Olaparib (Lynparza) | BRCA-mutated Cancers | Study of DNA repair mechanisms | Highly penetrant mutations affect biological relatives |
| Palbociclib (Ibrance) | HR+ Breast Cancer | Cell cycle regulation analysis | Treatment response data could be commercially sensitive |
Emerging Technologies and Ethical Implications
The future of privacy-preserving genomic research for anticancer drug discovery will be shaped by several emerging technologies:
- Blockchain for consent management: Creating immutable audit trails of data use permissions
- Federated learning at scale: Enabling collaborative model training across global research networks without centralizing sensitive data
- AI-powered risk assessment: Developing machine learning models that dynamically predict reidentification risks
- Quantum-resistant cryptography: Preparing for future computational threats to current encryption standards
Implementation Roadmap for Research Institutions
Research institutions should prioritize the following actions to enhance ethical genomic data sharing:
Short-term (0-6 months): Conduct privacy risk assessments for existing genomic datasets; implement staff training on ethical data handling; establish clear protocols for kinship communication in hereditary cancer studies
Medium-term (6-18 months): Adopt privacy-preserving technologies for collaborative research; develop dynamic consent platforms; create patient-friendly materials explaining genomic privacy concepts
Long-term (18+ months): Participate in development of international standards for genomic privacy; implement advanced cryptographic methods; establish transparent benefit-sharing models for research participants
Genomic data sharing presents both unprecedented opportunities for anticancer drug discovery and serious ethical challenges regarding patient privacy. By implementing robust ethical frameworks, adopting privacy-preserving technologies, and maintaining transparent engagement with research participants, the bioinformatics community can advance precision oncology while respecting individual rights and minimizing group harms. The integration of these approaches will be essential for maintaining public trust and realizing the full potential of genomic medicine in the fight against cancer.
The discovery of novel anticancer drug targets represents one of the most pressing challenges in modern biomedical research. Addressing this challenge requires deep integration of biological expertise with advanced computational methodologies. This whitepaper examines the critical intersection between biology and data science, outlining established protocols, resource frameworks, and collaborative models that have demonstrated success in precision oncology. By examining cutting-edge approaches like the DeepTarget platform and machine learning-driven biomarker discovery, we provide a roadmap for fostering productive collaborations that accelerate the translation of molecular insights into therapeutic interventions. The frameworks presented here emphasize practical implementation, with structured data presentation, experimental protocols, and visualization tools designed for immediate application by research teams.
Cancer remains a leading cause of mortality worldwide, characterized by immense genetic and molecular heterogeneity that complicates therapeutic intervention [83]. Traditional drug discovery approaches, predominantly based on in vivo animal experiments and in vitro drug screening, have proven expensive, laborious, and increasingly insufficient for addressing the complexity of cancer biology [40]. The advent of high-throughput technologies has generated massive multi-omics datasets encompassing genomics, transcriptomics, proteomics, and metabolomics, creating both unprecedented opportunities and substantial analytical challenges [84].
This data explosion necessitates sophisticated computational approaches that transcend traditional biological methodologies. However, effectively leveraging these approaches requires more than mere technical capability; it demands deep, structural collaboration between biologists with domain expertise and data scientists with computational proficiency. Network biology has emerged as a particularly promising framework for this integration, emphasizing interactions between molecular entities and providing systems-level understanding of disease mechanisms [85]. This whitepaper examines successful collaborative frameworks, provides detailed methodological protocols, and identifies essential resources to bridge disciplinary gaps in anticancer drug discovery.
Foundational Concepts and Frameworks
Network Medicine as an Integrative Paradigm
Network medicine represents an extension of network biology with focused goals related to understanding disease etiology, identifying biomarkers, and designing therapeutic interventions [84]. This approach conceptualizes biological systems as complex networks of interacting molecular entities, providing a mathematical framework for analyzing system perturbations. The fundamental premise is that cellular function emerges from these interactions rather than from individual molecules in isolation, making network analysis particularly suited to complex diseases like cancer.
Key Network Archetypes in Biomedical Research:
- Protein-Protein Interaction (PPI) Networks: Map physical interactions between proteins, often derived from yeast two-hybrid assays (Y2H) and co-immunoprecipitation followed by mass spectrometry (AP/MS) [85]
- Gene Regulatory Networks (GRNs): Represent regulatory relationships between transcription factors and their target genes
- Expression-Based Networks: Constructed from correlation patterns in gene expression data across diverse conditions
- Drug-Target Networks: Map interactions between pharmaceutical compounds and their biological targets
Quantitative Data Analysis Fundamentals
Effective collaboration requires shared understanding of data types and appropriate analytical approaches. Quantitative data analysis transforms numerical data into meaningful insights through mathematical, statistical, and computational techniques [86].
Table 1: Quantitative Data Analysis Methods in Cancer Research
| Method Category | Key Techniques | Applications in Drug Discovery |
|---|---|---|
| Descriptive Statistics | Measures of central tendency (mean, median, mode), measures of dispersion (range, variance, standard deviation) | Characterizing baseline molecular profiles across cancer cell lines |
| Inferential Statistics | Hypothesis testing, T-tests, ANOVA, regression analysis, correlation analysis | Determining significant differences between treatment groups, predicting drug response |
| Cross-Tabulation | Contingency table analysis | Analyzing relationships between categorical variables (e.g., mutation status and drug sensitivity) |
| MaxDiff Analysis | Preference measurement through choice tasks | Prioritizing drug targets based on multiple efficacy parameters |
| Gap Analysis | Actual vs. potential performance comparison | Identifying disparities between current and desired therapeutic outcomes |
Computational Methodologies for Drug Target Discovery
DeepTarget: Integrating Genetic and Pharmacological Data
The DeepTarget platform exemplifies successful integration of biological and computational approaches. Developed by researchers at Sanford Burnham Prebys Medical Discovery Institute, this computational tool predicts anti-cancer mechanisms of small molecule drugs by integrating large-scale genetic and pharmacological data [38]. Unlike conventional approaches that rely primarily on chemical structure and predicted binding affinity, DeepTarget leverages an extensive dataset derived from genetic and drug screening experiments encompassing 1450 drugs across 371 diverse cancer cell lines from the Dependency Map (DepMap) Consortium [38] [87].
The foundational principle of DeepTarget is that genetic deletion of a drug's protein target via CRISPR-Cas9 can mimic the inhibitory effects of the drug itself [38]. This approach captures multifaceted cellular responses to drug perturbations, enabling inference of mechanistic insights not readily apparent from structural data alone. In benchmark tests, DeepTarget outperformed state-of-the-art computational methods like RoseTTAFold All-Atom and Chai-1 in seven out of eight comparative evaluations for accurately predicting primary drug targets [38].
Machine Learning-Driven Multi-Target Therapies
Machine learning (ML) approaches have demonstrated remarkable success in identifying multi-target therapies for complex cancers. A recent study on colon cancer (CC) integrated biomarker signatures from high-dimensional gene expression, mutation data, and protein interaction networks [88]. The methodology employed Adaptive Bacterial Foraging (ABF) optimization to refine search parameters, maximizing predictive accuracy of therapeutic outcomes, while the CatBoost algorithm classified patients based on molecular profiles and predicted drug responses [88].
This ABF-CatBoost integration achieved exceptional performance metrics (accuracy: 98.6%, specificity: 0.984, sensitivity: 0.979, F1-score: 0.978), outperforming traditional ML models like Support Vector Machine and Random Forest [88]. The model successfully predicts toxicity risks, metabolism pathways, and drug efficacy profiles, enabling safer and more effective treatment strategies while addressing drug resistance through analysis of mutation patterns, adaptive resistance mechanisms, and conserved binding sites.
Perturbation-Theory Machine Learning (PTML)
PTML has emerged as a cutting-edge approach for multi-target small molecule anticancer discovery [89]. This methodology overcomes limitations of conventional computational approaches that often use limited structural information through homogeneous datasets, predict activity against single targets, and lack interpretability. PTML modeling enables the discovery of versatile anticancer agents with multi-target modes of action and multi-cell inhibition versatility, which can translate into more efficacious and safer chemotherapeutic treatments [89].
Experimental Protocols and Workflows
Protocol: Network-Based Drug Target Identification
This protocol outlines a standardized approach for identifying novel drug targets through integration of multi-omics data using network biology principles.
Materials and Reagents:
- Multi-omics data (genomic, transcriptomic, proteomic)
- Protein-protein interaction databases (STRING, BioGRID)
- Pathway annotation resources (KEGG, Reactome)
- Computational infrastructure for large-scale data analysis
Procedure:
- Data Acquisition and Preprocessing:
- Collect disease-specific molecular profiling data from sources like TCGA (Transcriptome, mutations, copy number variations)
- Obtain normal tissue reference data from GTEx or similar resources
- Perform quality control, normalization, and batch effect correction
Differential Expression Analysis:
- Identify significantly dysregulated genes/proteins using appropriate statistical tests (e.g., moderated t-tests with multiple testing correction)
- Calculate fold-change values for all molecular entities
Network Construction:
- Retrieve physical and functional interactions from curated databases
- Construct context-specific networks by integrating expression data
- Apply confidence scores to interactions based on supporting evidence
Module Detection:
- Identify densely connected network regions using community detection algorithms
- Score modules based on collective dysregulation using methods like jActiveModules or Heinz
- Annotate significant modules with functional enrichment analysis (GO, KEGG)
Target Prioritization:
- Apply network-based metrics (centrality, betweenness) to identify key regulators
- Integrate essentiality data from CRISPR screens (DepMap)
- Evaluate druggability using databases like DrugBank and ChEMBL
Experimental Validation:
- Design functional assays for top candidates
- Test target engagement using appropriate biochemical methods
- Evaluate phenotypic effects in disease-relevant models
Protocol: Cross-Disciplinary Model Validation
Rigorous validation is essential for translating computational predictions into biological insights.
Procedure:
- Computational Validation:
- Perform cross-validation using held-out data
- Compare against known biological benchmarks
- Apply perturbation analyses to test model robustness
Experimental Case Studies:
- Select top predictions for empirical testing
- Design appropriate biological assays (e.g., cell viability, target engagement)
- Include relevant controls and counter-screens
Clinical Correlation:
- Assess association with clinical outcomes using patient data
- Evaluate predictive value in independent cohorts
- Analyze relationship with established biomarkers
Table 2: Research Reagent Solutions for Collaborative Drug Discovery
| Reagent/Resource | Function | Example Sources |
|---|---|---|
| Cancer Cell Line Panels | Model systems for high-throughput drug screening | DepMap Consortium, CCLE |
| CRISPR-Cas9 Libraries | Genome-wide functional genomics screening | Broad Institute, Addgene |
| Multi-omics Datasets | Molecular profiling of cancers and model systems | TCGA, GTEx, ENCODE |
| PPI Network Databases | Maps of physical and functional interactions between proteins | STRING, BioGRID, HINT |
| Drug Response Data | Pharmacological profiles of compounds across models | GDSC, CTRP, LINCS |
| Structural Bioinformatics Tools | Prediction of drug-target interactions | RoseTTAFold, Chai-1, AlphaFold |
Case Study: DeepTarget Implementation and Validation
Ibrutinib Repurposing for Lung Cancer
A compelling validation of the DeepTarget approach emerged from studies on Ibrutinib, an FDA-approved BTK inhibitor for blood cancers [87]. Prior clinical research showed that Ibrutinib could treat lung cancer despite the absence of its canonical target (BTK) in lung tumors. DeepTarget analysis predicted that mutant forms of the epidermal growth factor receptor (EGFR) served as relevant targets in lung cancer contexts [38] [87].
Experimental Validation: Researchers compared Ibrutinib's effects on cancer cells with and without the cancerous mutant EGFR [87]. Cells harboring the mutant form demonstrated significantly greater sensitivity to the drug, validating EGFR as a context-specific target of Ibrutinib. This finding explained the drug's efficacy in lung cancer despite BTK absence and demonstrated DeepTarget's ability to identify clinically relevant secondary targets that vary by cellular context [87].
Performance Benchmarking
DeepTarget's performance was rigorously evaluated against established computational methods. In seven out of eight comparative tests, it outperformed state-of-the-art tools including RoseTTAFold All-Atom and Chai-1 in accurately predicting primary drug targets within cancer cells [38] [87]. The tool also demonstrated proficiency in predicting secondary targets when evaluated against existing data on 64 cancer drugs known to have more than one target [87].
Implementation Framework for Cross-Disciplinary Collaboration
Organizational Structures for Team Science
Successful collaboration requires intentional organizational design that bridges cultural, methodological, and communication divides between disciplines.
Key Elements:
- Integrated Team Structure: Combine biologists and data scientists in unified teams with shared goals and metrics rather than siloed departments
- Cross-Training Programs: Establish regular knowledge-sharing sessions where each discipline educates the other on fundamental concepts, methodologies, and constraints
- Joint Project Ownership: Ensure both biological and computational team members have equal stake in project outcomes from conception through execution
- Unified Data Management: Implement shared data repositories with standardized formats, metadata requirements, and access protocols
Communication Protocols
Effective interdisciplinary collaboration requires structured communication frameworks that translate concepts across domain boundaries.
Best Practices:
- Glossary Development: Create and maintain shared vocabulary definitions to ensure precise understanding of technical terms
- Visualization Standards: Establish conventions for data presentation that are interpretable by both biological and computational team members
- Regular Sync Meetings: Implement frequent checkpoints with structured agendas that address both experimental progress and analytical developments
- Documentation Protocols: Maintain detailed, accessible records of both wet-lab and computational procedures using standardized templates
The integration of biological expertise with computational methodologies represents a paradigm shift in anticancer drug discovery. Approaches like DeepTarget, PTML, and network medicine demonstrate the powerful insights that emerge when these disciplines collaborate as equal partners. The protocols, resources, and frameworks outlined in this whitepaper provide practical guidance for research teams seeking to implement these collaborative models.
Looking forward, the field is poised for further transformation through several emerging trends. First, the integration of single-cell multi-omics data will enable unprecedented resolution of cellular heterogeneity in tumors. Second, the application of artificial intelligence for de novo drug design promises to expand the therapeutic landscape beyond existing chemical space. Finally, the increasing availability of real-world evidence from clinical practice creates opportunities for continuous model refinement and validation.
As these developments unfold, the imperative for deep, structural collaboration between biologists and data scientists will only intensify. By embracing the frameworks presented here, research organizations can position themselves at the forefront of innovative cancer therapeutics discovery, ultimately accelerating the delivery of effective treatments to patients.
Best Practices for Standardization, Validation, and Avoiding Analytical Pitfalls
The discovery of novel anticancer drug targets through bioinformatics represents a frontier in modern therapeutic development. However, the transition from computational prediction to validated target requires rigorous analytical frameworks to ensure success. Standardization and validation of analytical methods are not merely regulatory checkboxes but fundamental scientific practices that determine the reliability, reproducibility, and ultimate clinical relevance of research findings. In the high-stakes domain of oncology drug discovery, where biological complexity meets urgent medical need, systematic approaches to method validation and standardization become particularly crucial. This technical guide provides a comprehensive framework for establishing robust analytical practices specifically contextualized within anticancer drug target discovery, addressing both established best practices and emerging challenges in the field.
The integration of bioinformatics has dramatically expanded the landscape of potential oncology targets, with computational approaches now capable of scoring proteins for "druggability" based on multiple features including network properties, tissue specificity, and essentiality [90]. However, these computational predictions require subsequent experimental validation using rigorously standardized wet-lab methodologies to translate digital insights into tangible therapeutic candidates. The analytical journey from target identification to confirmation demands meticulous attention to each phase of experimentation—from sample preparation and quenching to data analysis and interpretation—each with its own specific pitfalls and standardization requirements [91].
Foundational Principles of Analytical Method Validation
Analytical method validation provides the foundational framework for establishing that a particular method is suitable for its intended purpose in the drug discovery pipeline. According to regulatory guidelines and best practices, method validation systematically evaluates multiple performance parameters to ensure reliability [92].
Core Validation Parameters and Acceptance Criteria
The following parameters represent the essential components of method validation, each addressing a specific aspect of analytical performance:
- Accuracy: Defined as the closeness of agreement between measured and true values, accuracy is typically assessed by spiking known amounts of analyte into sample matrix and calculating recovery percentages [92]. For drug target validation, this might involve spiking known concentrations of a metabolite or protein of interest into cellular lysates.
- Precision: This parameter measures the closeness of agreement between replicate measurements and is expressed as relative standard deviation (RSD) or coefficient of variation (CV) [92]. Precision should be evaluated at multiple levels: repeatability (within-day), intermediate precision (different days, analysts, instruments), and reproducibility (between laboratories).
- Linearity: The ability of a method to produce results proportional to analyte concentration within a given range, linearity is demonstrated by preparing and analyzing standards at multiple concentrations [92]. For oncology drug discovery applications, the range should adequately cover expected physiological and pathological concentrations.
- Limit of Detection (LOD) and Limit of Quantitation (LOQ): LOD represents the lowest detectable concentration, while LOQ is the lowest quantitatively measurable concentration with acceptable precision and accuracy [92]. These parameters are particularly critical when measuring low-abundance targets or biomarkers.
- Specificity: The ability to measure the analyte accurately in the presence of other components, specificity is especially important in complex biological matrices like cell lysates, plasma, or tissue homogenates [92].
Table 1: Method Validation Parameters and Typical Acceptance Criteria for Oncology Drug Discovery Applications
| Parameter | Definition | Recommended Acceptance Criteria | Considerations for Oncology Applications |
|---|---|---|---|
| Accuracy | Closeness to true value | 85-115% recovery | Matrix effects from cell culture conditions |
| Precision | Agreement between replicates | <15% RSD | Biological variability in tumor models |
| Linearity | Proportionality of response | R² > 0.99 | Adequate range for pathway analysis |
| LOD | Lowest detectable concentration | Signal-to-noise ≥ 3 | Critical for low-abundance targets |
| LOQ | Lowest quantifiable concentration | Signal-to-noise ≥ 10, precision <20% RSD | Essential for biomarker quantification |
| Specificity | Ability to distinguish analyte | No interference ≥ 20% | Complex biological matrices |
Experimental Design for Robust Validation
Proper experimental design is fundamental to obtaining meaningful validation data. Key principles include [92]:
- Randomization: Analyzing samples in random order to minimize bias from instrument drift or environmental factors.
- Replication: Performing sufficient replicate measurements (typically n≥6 for precision assessments) to obtain reliable estimates of variability.
- Blocking: Grouping similar samples together to reduce variability from sample preparation.
A well-designed validation experiment follows a logical progression from definition of requirements through final method qualification, as illustrated below:
Diagram 1: Method Validation Workflow
Standardization Approaches Across the Analytical Workflow
Standardization encompasses the comprehensive set of practices, procedures, and protocols that ensure consistency and reliability throughout the analytical process. In anticancer drug discovery, standardization is particularly challenging due to the complexity of biological systems and the frequent need to measure low-abundance analytes in the presence of complex matrices.
Pre-analytical Standardization: Sample Collection and Preparation
The pre-analytical phase represents the most vulnerable stage for introducing variability, with studies indicating that 46-68% of total laboratory errors originate in this phase [93]. For cellular studies in oncology research, proper quenching of metabolism is especially critical when analyzing metabolites that turn over rapidly (e.g., ATP, glucose 6-phosphate) [91].
Best Practices for Metabolic Quenching
Effective quenching requires immediate termination of enzymatic activity to preserve the in vivo metabolic state. Recommended approaches include [91]:
- Cold Acidic Solvent: For many mammalian cell systems, cold acidic acetonitrile:methanol:water with 0.1 M formic acid effectively denatures enzymes while minimizing metabolite interconversion.
- Fast Filtration: For suspension cultures, fast filtration followed by immediate immersion in quenching solvent provides rapid separation from media.
- Acidic Conditions: Addition of 0.1 M formic acid (approximately 0.5% v/v) prevents interconversion of metabolites during quenching, as demonstrated by reduced transformation of 3-phosphoglycerate to phosphoenolpyruvate and ATP to ADP [91].
- Neutralization: After quenching with acidic solvent, neutralization with ammonium bicarbonate avoids acid-catalyzed degradation in the resulting extract.
Sample Preparation and Extraction
The goal of extraction is quantitative recovery of metabolites with minimal artifactual production or degradation. Key considerations include [91]:
- Pulverization: Tissue samples should be pulverized into fine powders using cryomills at liquid nitrogen temperature to ensure homogeneous extraction.
- Serial Extraction: Studies show that 20-40% of total metabolites may be recovered in a second extraction, suggesting that single extraction protocols may significantly underestimate total metabolite levels [91].
- Matrix Considerations: The choice of extraction solvent should be optimized for the specific analyte classes of interest, with different solvents required for water-soluble versus insoluble compounds.
Table 2: Research Reagent Solutions for Analytical Standardization in Drug Discovery
| Reagent/Category | Specific Examples | Function/Purpose | Key Considerations |
|---|---|---|---|
| Quenching Solvents | Cold acidic acetonitrile:methanol:water | Immediate termination of enzymatic activity | Acid concentration critical; neutralize after quenching |
| Certified Reference Materials | NIST standard reference materials | Method calibration and accuracy verification | Traceability to international standards |
| Isotopic Internal Standards | 13C or 15N labeled metabolites | Absolute quantitation and correction for losses | Account for incomplete labeling in cells |
| Protein Assay Standards | BSA for Bradford/Lowry assays | Protein quantification for normalization | Compatibility with detergents in lysis buffers |
| Chromatography Standards | Retention time markers | LC-MS system performance monitoring | Stable under analytical conditions |
Analytical Standardization: Instrumentation and Measurement
Standardization of the analytical phase ensures that instrument performance remains consistent over time and across platforms. For the bioinformatics-driven oncology research, several platforms are particularly relevant:
Liquid Chromatography-Mass Spectrometry (LC-MS)
LC-MS has become a cornerstone technology for untargeted metabolomics and proteomics in drug discovery. Standardization considerations include [94]:
- System Suitability Testing: Regular analysis of standardized mixtures to verify chromatographic retention, peak shape, mass accuracy, and sensitivity.
- Quality Control Samples: Pooled quality control (QC) samples analyzed throughout the batch to monitor system stability.
- Blank Injections: Solvent blanks to monitor carryover and system contamination.
Standardization Through Automation
Automation of sample preparation represents a powerful approach to standardization by reducing manual variability. Recent advances include [95]:
- Robotic Platforms: Automated systems for preparing stable and homogeneous nanomaterial suspensions, applicable to techniques like DLS, SAXS, FFF, and sp-ICP-MS.
- Air-Liquid Interface Systems: For exposure of biological samples to nanomaterial-containing aerosols under reproducible conditions.
- High-Throughput Automation: Robot platforms enabling autonomous optimization of experimental conditions (e.g., concentration, temperature).
The following diagram illustrates an automated, standardized workflow for sample preparation and analysis:
Diagram 2: Automated Sample Preparation Workflow
Bioinformatics Integration in Analytical Validation
The integration of bioinformatics and analytical chemistry creates a powerful synergy for anticancer drug target discovery. Computational approaches can guide analytical validation by identifying critical parameters and potential interference specific to oncology targets.
Machine Learning for Target Prioritization
Machine learning approaches can score proteins according to their similarity to approved drug targets, incorporating features such as [90]:
- Network Centrality Measures: Drug targets tend to have higher degree, betweenness, and closeness centrality in protein-protein interaction networks.
- Protein Essentiality: Targets are more likely to be essential based on knockout studies.
- Tissue Specificity: Cancer drug targets often show specific expression patterns in relevant tissues.
- Structural Features: Membrane localization, enzyme classification, and post-translational modifications.
Statistical analysis reveals that these features show significant differences between drug targets and non-targets (p < 2.2×10⁻¹⁶ for network measures) [90]. This computational prioritization allows researchers to focus analytical validation efforts on the most promising candidates.
Experimental Validation of Computational Predictions
The transition from computational prediction to experimentally validated target requires carefully designed analytical workflows:
- Orthogonal Validation: Important findings should be validated using orthogonal methods when possible. For example, targets identified through computational approaches should be confirmed using both proteomic and genetic techniques.
- Dose-Response Relationships: Establishing appropriate concentration ranges for compound testing based on target affinity and cellular permeability.
- Pathway Analysis: Confirming that target modulation produces the expected effects on downstream pathways.
Common Analytical Pitfalls and Corrective Strategies
Despite careful planning, analytical workflows in drug discovery are susceptible to specific pitfalls that can compromise data quality and lead to erroneous conclusions.
Pre-analytical Pitfalls
Incomplete Quenching: Slow or incomplete quenching of metabolism can lead to dramatic changes in metabolite levels. For example, residual enolase activity can convert 3-phosphoglycerate to phosphoenolpyruvate during quenching [91].
- Solution: Implement rapid quenching methods with acidic solvent and verify effectiveness through spiking experiments.
Inadequate Sample Size: Untargeted metabolomics requires sufficient biological replicates (typically 5-10 per group) to achieve statistical power [94].
- Solution: Perform power analysis using pilot data or public datasets to determine appropriate sample sizes.
Improper Sample Handling: Clinical biochemistry data shows that preanalytical errors account for significant sample rejection, with insufficient volume (34%), clotted specimens (24%), and hemolysis (8%) as major contributors [93].
- Solution: Implement standardized protocols for sample collection, handling, and processing with regular training for personnel.
Analytical and Post-analytical Pitfalls
Insufficient Method Validation: Failure to adequately validate methods for their intended purpose leads to unreliable data [92].
- Solution: Follow established validation protocols with predefined acceptance criteria for all relevant parameters.
Incorrect Data Normalization: Improper normalization can introduce systematic errors or obscure biological effects [91].
- Solution: Use appropriate normalization strategies (e.g., based on protein content, cell number, or internal standards) validated for the specific application.
Failure to Account for Matrix Effects: Ion suppression or enhancement in MS-based methods can significantly impact quantitation accuracy [94].
- Solution: Use stable isotope-labeled internal standards, standard addition methods, or matrix-matched calibration curves.
Regulatory Compliance and Documentation
Adherence to regulatory guidelines ensures that analytical data will support regulatory submissions and facilitates collaboration across institutions. Key considerations include:
Regulatory Framework
- ICH Guidelines: ICH Q2(R1) provides validation methodology for analytical procedures [92].
- FDA Guidance: Bioanalytical Method Validation guidance outlines expectations for regulated studies [92].
- ISO Standards: ISO/IEC 17025 outlines general requirements for laboratory competence [96].
Documentation Practices
Comprehensive documentation creates an auditable trail and supports data integrity:
- Validation Protocols and Reports: Document all validation activities with raw data and deviations from the protocol [92].
- Standard Operating Procedures (SOPs): Detailed, step-by-step protocols for all critical procedures.
- Data Management: Implementation of FAIR (Findable, Accessible, Interoperable, Reusable) data principles [95].
Standardization, validation, and avoidance of analytical pitfalls form an inseparable triad in the successful discovery and development of novel anticancer drug targets. As bioinformatics approaches continue to expand the universe of potential targets, rigorous analytical practices become increasingly critical for distinguishing genuine therapeutic opportunities from computational artifacts. By implementing the systematic approaches outlined in this guide—from robust method validation and standardized sample preparation to bioinformatics integration and comprehensive documentation—researchers can significantly enhance the reliability, reproducibility, and translational potential of their findings. In the challenging landscape of oncology drug discovery, where biological complexity meets urgent clinical need, analytical rigor provides the foundation upon which successful therapeutic development is built.
From In Silico to In Vivo: Validating Targets and Benchmarking Tools
Transitioning from Computational Prediction to Experimental Validation
The discovery of novel anticancer drug targets represents one of the most significant challenges in modern oncology research. With cancer causing approximately one in six deaths globally [97] and traditional drug development requiring an average of 12 years and $2.7 billion USD per approved drug [98], the pharmaceutical industry urgently needs more efficient discovery pipelines. Bioinformatics and computational methods have emerged as powerful technologies that can significantly reduce the cost and time required for initial target identification while improving the success rate of experimental validation. This technical guide outlines a comprehensive framework for transitioning from computational prediction to experimental validation in the context of anticancer drug target discovery, providing researchers with detailed methodologies and practical considerations for building a robust discovery pipeline.
The fundamental premise of integrated computational-experimental approaches lies in their ability to systematically prioritize the most promising targets from thousands of potential candidates. While the human genome contains approximately 30,000 genes, only about 6,000-8,000 are estimated as potential pharmacological targets, and fewer than 400 encoded proteins have been successfully exploited for drug development [98]. Computational methods provide the necessary triage mechanism to navigate this vast biological complexity and focus experimental resources on targets with the highest therapeutic potential. This guide examines the complete workflow from initial bioinformatic analysis through experimental confirmation, with special emphasis on technical protocols, validation methodologies, and practical implementation considerations for research teams.
Computational Prediction Phase
Target Identification and Prioritization
The initial stage of target discovery relies on comprehensive bioinformatic analyses to identify molecular targets with compelling connections to cancer pathophysiology. Several complementary approaches have proven effective for this purpose:
Differential Expression Analysis: Identify genes significantly upregulated in cancer cells versus normal tissues. For example, in triple-negative breast cancer (TNBC), bioinformatics-driven analysis identified syndecan-1 (SDC1) as a differentially expressed gene with high expression levels correlating with poorer overall survival [99].
Network Pharmacology Modeling: Analyze protein-protein interaction networks to understand how ligand-receptor interactions influence signaling pathways. The CHANCE framework exemplifies this approach, utilizing molecular signaling pathways and protein-protein interaction networks derived from cancer genomes to associate potential driver genes in cancer samples with drug targets [100].
Pathway Activation Analysis: Tools like OncoFinder calculate Pathway Activation Strength (PAS) scores to quantitatively estimate the degree of pathway activation in cancer samples relative to controls. This approach has identified molecular pathways correlated with sensitivity to targeted therapies like Pazopanib, Sorafenib, Sunitinib, and Temsirolimus [101].
Multi-Omics Data Integration: Combine genomic, transcriptomic, epigenomic, and proteomic data to build comprehensive molecular profiles. The CHANCE model successfully integrates coding and non-coding mutations, network proximity metrics, drug target information, and tissue of origin features to predict drug responses [100].
Table 1: Computational Tools for Anticancer Target Identification
| Tool/Method | Primary Function | Application in Cancer Research |
|---|---|---|
| SwissTargetPrediction | Predicts protein targets of small molecules | Identifies potential targets for compounds with anti-cancer activity [67] |
| OncoFinder | Calculates Pathway Activation Strength (PAS) | Links pathway activation with drug sensitivity [101] |
| CHANCE | Predicts anticancer activities of non-oncology drugs | Repurposes approved drugs for oncology applications [100] |
| Molecular Docking | Predicts ligand-receptor binding interactions | Virtual screening of compound libraries against cancer targets [98] |
Compound Screening and Optimization
Once promising targets are identified, computational methods facilitate the discovery and optimization of compounds that modulate these targets:
Structure-Based Virtual Screening (SBVS): Utilizes known structural information of target proteins to screen large compound libraries. Molecular docking, a cornerstone SBVS method, predicts binding patterns and interaction affinities between ligands and receptor biomolecules [98]. Both rigid docking (fast, considering static geometrical complementarity) and flexible docking (accounting for ligand flexibility and induced-fit theory) approaches are employed depending on screening scale and accuracy requirements [98].
Ligand-Based Virtual Screening: Employs pharmacophore modeling and quantitative structure-activity relationship (QSAR) analyses based on compounds with known activity. In breast cancer drug discovery, researchers have successfully generated pharmacophore models from active compounds and used them for virtual screening of additional candidates [67].
Deep Learning Approaches: Neural network models have demonstrated promising results in predicting cancer response to drug treatments. Recent analyses have identified 61 deep learning-based models for drug response prediction, with TensorFlow/Keras and PyTorch emerging as the most popular frameworks [102]. These models typically use the formulation r = f(d, c), where the model f predicts the response r of cancer c to treatment with drug d [102].
ADMET and Toxicity Prediction
Before proceeding to experimental validation, computational assessment of absorption, distribution, metabolism, excretion, and toxicity (ADMET) properties helps prioritize compounds with favorable pharmacological profiles:
- Quantitative Structure-Property Relationship (QSPR): Models the relationship between structural descriptors and pharmacokinetic properties.
- Physiologically Based Pharmacokinetic (PBPK) Modeling: Simulates drug disposition in virtual human populations.
- In silico Toxicity Prediction: Identifies potential toxicophores and off-target effects early in the discovery process [103].
Experimental Validation Phase
In Vitro Validation Protocols
The transition from computational prediction to experimental validation begins with rigorously designed in vitro assays that assess compound efficacy and selectivity.
Cell Viability and Cytotoxicity Assays
Objective: Determine the concentration-dependent effects of candidate compounds on cancer cell viability and prioritize candidates based on their potency and selectivity.
Protocol Details:
- Cell Line Selection: Utilize relevant cancer cell lines representing specific cancer types. For breast cancer research, estrogen receptor-positive (ER+) MCF-7 cells and triple-negative MDA-MB-231 cells are commonly used [67]. Include multiple cell lines to account for tumor heterogeneity.
- Compound Treatment: Prepare serial dilutions of candidate compounds in appropriate vehicle controls. Include standard chemotherapeutic agents (e.g., 5-fluorouracil) as positive controls for comparison.
- Viability Assessment: Incubate cells with compounds for 48-72 hours, then measure viability using standardized assays:
- SRB Assay: Measures cellular protein content following fixation.
- MTT Assay: Quantifies metabolic activity through tetrazolium salt reduction [104].
- Data Analysis: Calculate half-maximal inhibitory concentration (IC50) values using non-linear regression analysis of dose-response curves. For enhanced predictive value, calculate selectivity indices by dividing IC50 values in non-malignant cells by IC50 values in cancer cells [104].
Table 2: Key Reagents for Cell-Based Validation assays
| Reagent/Cell Line | Application | Experimental Role |
|---|---|---|
| MCF-7 cells | Breast cancer research | Model estrogen receptor-positive breast cancer [67] |
| MDA-MB-231 cells | Breast cancer research | Model triple-negative breast cancer [67] |
| SRB assay reagent | Cell viability testing | Quantifies cellular protein content [104] |
| MTT assay reagent | Metabolic activity measurement | Assesses mitochondrial function [104] |
| 5-Fluorouracil | Positive control | Reference chemotherapeutic agent [67] |
Selectivity Assessment Using Non-Malignant Cells
Objective: Evaluate the therapeutic window of candidate compounds by comparing their effects on cancer cells versus non-malignant cells.
Protocol Details:
- Cell Panel Design: Include multiple non-malignant cell types from various tissues, with particular emphasis on cells from the same tissue origin as the cancer cells being studied [104].
- Experimental Conditions: Maintain identical culture and treatment conditions for both malignant and non-malignant cells to enable direct comparison.
- Selectivity Calculation: Determine selectivity indices for each compound by dividing IC50 values in non-malignant cells by IC50 values in cancer cells. Compare these indices with those of standard anticancer drugs to assess relative therapeutic potential [104].
In Vivo Validation Protocols
After establishing efficacy and selectivity in vitro, promising candidates advance to animal models for pharmacokinetic and efficacy assessment.
Xenograft Mouse Models
Objective: Evaluate the antitumor activity of candidate compounds in a physiologically relevant context.
Protocol Details:
- Model Establishment: Implant human cancer cells or patient-derived xenografts (PDXs) into immunocompromised mice (e.g., NOD scid gamma mice).
- Treatment Protocol: Once tumors reach a predetermined volume (typically 100-200 mm³), randomize animals into treatment groups including vehicle control, candidate compound, and standard-of-care arms.
- Compound Administration: Administer compounds via appropriate routes (oral, intraperitoneal, or intravenous) at predetermined schedules based on pharmacokinetic properties.
- Endpoint Monitoring: Regularly measure tumor dimensions and calculate volumes using the formula: V = (length × width²)/2. Monitor body weight and clinical signs for toxicity assessment.
- Data Analysis: Compare tumor growth inhibition between treatment groups and calculate treated-to-control ratios (T/C). Statistical significance is typically determined using ANOVA with post-hoc tests [67].
Advanced In Vivo Models
For more clinically predictive assessment, consider these refined approaches:
- Orthotopic Models: Implant cancer cells into their organ or tissue of origin to better mimic the tumor microenvironment.
- Genetically Engineered Models: Utilize transgenic mice that develop spontaneous tumors to assess prevention or treatment in immunocompetent hosts.
- Metastasis Models: Evaluate compound effects on metastatic dissemination using tail vein injection or spontaneous metastasis assays.
Case Study: Integrated Discovery of a Breast Cancer Therapeutic
A recent study exemplifies the seamless integration of computational prediction and experimental validation for breast cancer therapy development [67]. This case study illustrates the practical application of the principles outlined in this guide.
Computational Phase
Researchers began by selecting 23 compounds with documented inhibitory effects on MDA-MB and MCF-7 breast cancer cell lines from published literature. They performed 3D quantitative structure-activity relationship (3D-QSAR) analyses, generating 249 distinct conformers and constructing five pharmacophore models with significant spatial diversity [67]. Through SwissTargetPrediction analysis of the most potent compounds from each pharmacophore category, they identified potential protein targets, highlighting the adenosine A1 receptor as a promising candidate [67]. Molecular docking simulations against the human adenosine A1 receptor-Gi2 protein complex (PDB ID: 7LD3) identified Compound 5 with stable binding characteristics, which was further confirmed through molecular dynamics simulations [67].
Experimental Validation
The researchers synthesized a novel molecule (Molecule 10) based on their computational predictions and evaluated its anticancer activity against MCF-7 breast cancer cells [67]. The experimentally determined IC50 value of 0.032 µM significantly outperformed the positive control 5-fluorouracil (IC50 = 0.45 µM), demonstrating the successful translation of computational predictions into a potent therapeutic candidate [67]. This case study exemplifies the power of integrated computational-experimental approaches for accelerating anticancer drug discovery.
Integrated Drug Discovery Workflow
Technical Considerations and Best Practices
Experimental Design Principles
Robust experimental design is critical for generating clinically relevant validation data:
Patient-Oriented Testing: Design experiments that address actual patient needs rather than purely academic questions. Focus on whether candidate treatments improve upon standard therapies rather than just demonstrating standalone activity [104].
Species Considerations: Use human cells for in vitro selectivity assessment to avoid artifacts caused by species differences in drug sensitivity. Rodent cells may show dramatically different sensitivity profiles compared to human cells for certain compound classes, such as the extreme resistance of rodent cells to cardiac glycosides [104].
Relevant Controls: Always include appropriate controls:
- Positive controls (standard-of-care treatments)
- Vehicle controls (matching compound formulation)
- Untreated controls (baseline measurements)
Data Analysis and Interpretation
Proper data analysis and interpretation ensure meaningful conclusions:
Selectivity Over Potency: Prioritize compounds with high selectivity indices over those with mere potency against cancer cells. A compound that kills cancer cells at low concentrations but also affects normal cells at similar concentrations will have limited clinical utility due to dose-limiting toxicity [104].
Pathway-Centric Analysis: Interpret results in the context of pathway activation rather than individual gene effects. Pathway Activation Strength (PAS) values provide more stable biomarkers compared to expression of individual genes [101].
Multi-parameter Assessment: Evaluate multiple parameters beyond IC50 values, including IC90, LC50, and area under the dose-response curve (AUC) to capture the full pharmacological profile [104] [100].
The integration of computational prediction with rigorous experimental validation represents a paradigm shift in anticancer drug discovery. This approach leverages the strengths of both worlds: the scalability and hypothesis-generating power of bioinformatics with the physiological relevance and confirmatory strength of experimental biology. As computational methods continue to advance, particularly in artificial intelligence and deep learning, their predictive accuracy will further improve, enhancing the efficiency of the entire drug discovery pipeline. However, computational predictions will always require experimental validation in biologically relevant systems to translate virtual hits into clinical candidates. The framework outlined in this guide provides a structured pathway for researchers to navigate this complex process, ultimately accelerating the development of novel therapeutics for cancer patients.
In Vitro and In Vivo Models for Assessing Target Efficacy and Drug Candidate Potency
The journey of an anticancer drug from discovery to clinical application is a complex, multi-stage process, and its success is heavily reliant on the biological relevance of the preclinical models used to assess target efficacy and compound potency [105] [106]. Preclinical studies are designed to evaluate the safety and efficacy of a drug candidate before it can be tested in humans, and they fundamentally rely on two categories of models: in vitro (Latin for "within the glass") and in vivo (Latin for "within the living") [105]. In vitro studies utilize cell cultures grown outside their natural biological context, typically in Petri dishes or test tubes, while in vivo studies are conducted within living organisms, which, in the preclinical phase, are animal subjects [105].
The integration of these models is crucial within the modern paradigm of anticancer drug discovery, which is increasingly driven by bioinformatics. The identification of novel drug targets through computational analysis of genetic, proteomic, and clinical datasets must be followed by rigorous experimental validation in biological systems that faithfully represent human disease [38]. This guide provides an in-depth technical overview of the established and emerging in vitro and in vivo models, detailing their applications, methodologies, and integration into the workflow of discovering and validating novel anticancer drug targets.
In Vitro Models: From Simple Monolayers to Complex Microphysiological Systems
Two-Dimensional (2D) Cell Cultures
2.1.1 Overview and Applications Two-dimensional cell cultures represent the most traditional and widely used in vitro system. In this model, cells grow as a monolayer on a flat, rigid plastic or glass surface [107]. These models are a cornerstone of initial drug screening due to their ease of handling, high reproducibility, low cost, and suitability for high-throughput screening (HTS) campaigns [106] [107]. They are primarily used for the initial assessment of compound cytotoxicity, target engagement, and mechanism of action studies [107].
2.1.2 Limitations and Considerations Despite their utility, 2D cultures possess significant limitations in predicting clinical efficacy [107]. Growing on a flat plastic substrate, tumor cells have equal and unlimited access to nutrients and oxygen and are uniformly exposed to drug treatment. This artificial environment fails to recapitulate the three-dimensional architecture, cell-cell interactions, and nutrient gradients found in in vivo tumors [107]. Consequently, processes such as diffusion-limited drug penetration are lost, often resulting in higher proliferation rates and drug sensitivity compared to in vivo cancer cells, which can impair the predictive power of 2D models for anticancer drug efficacy [107].
Three-Dimensional (3D) Cell Cultures
2.2.1 The Shift Towards Greater Physiological Relevance To bridge the gap between 2D cultures and in vivo tumors, three-dimensional cell culture models have been developed. These models are regarded as a promising alternative, due to their ability to mimic several features of in vivo tumors such as natural tumor architecture, cell-cell interactions, nutrient and oxygen gradients, drug penetration and resistance, and, with a varying degree of faithfulness, the tumor microenvironment (TME) [107]. The adoption of 3D systems is considered a step toward improving the success rate in drug discovery [108].
2.2.2 Types of 3D Models and Generation Techniques 3D in vitro cancer models are broadly categorized into scaffold-free and scaffold-based systems [107].
Scaffold-free models rely on cellular self-assembly to form natural cell-matrix interactions. Key techniques include:
- Liquid Overlay: Cells are seeded in low-adhesion surface plates to prevent attachment and promote aggregation into spheroids [107].
- Hanging Drop: Cell-laden liquid drops are suspended on a lid; surface tension and gravity induce cell aggregation within the drop [107].
- Agitation-based: Cells aggregate under continuous stirring to avoid adherence to surfaces [107].
- Magnetic Levitation: Cells are magnetized with nanoparticles and levitated under magnetic forces to form aggregates [107].
Scaffold-based models use exogenous structures to support 3D growth and mimic the extracellular matrix (ECM).
- Hydrogels (e.g., Matrigel): 3D polymer networks with high water content, similar in bioactivity and mechanical properties to native ECM [107].
- Decellularized Scaffolds: ECM obtained from native tissue by removing cellular components, providing a natural biological scaffold [107].
- 3D Bioprinting: Automated deposition of cells and bio-inks to create precise, complex 3D structures [107].
The two most common types of 3D models are spheroids and organoids. Spheroids are self-assembled aggregates of cells that can be generated from immortalized cell lines [107]. Organoids are more complex structures that are typically derived from patient tumor tissue (patient-derived organoids, PDOs) and can recapitulate the heterogeneity and some architectural features of the original tumor [107].
Table 1: Comparison of Primary In Vitro Models Used in Cancer Research
| Feature | 2D Monolayers | 3D Spheroids | 3D Organoids |
|---|---|---|---|
| Complexity | Low | Medium | High |
| Physiological Relevance | Low | Medium-High | High |
| Throughput | High | Medium | Low-Medium |
| Cost | Low | Medium | High |
| Key Applications | High-throughput initial drug screening, target engagement | Drug penetration studies, hypoxia, intermediate throughput screening | Personalized medicine, tumor heterogeneity studies, biomarker discovery |
| Limitations | Lacks TME, no gradients, poor clinical predictivity | Limited TME complexity, may not fully capture tumor heterogeneity | Technically challenging, expensive, variable success rate in establishment |
Experimental Protocols for Key In Vitro Models
2.3.1 Protocol: High-Throughput Drug Combination Screening in 2D/3D Cultures This protocol is adapted from methodologies used to discover promising anti-cancer drug combinations by maximizing a therapeutic index (TI) [109].
- Cell Seeding: Seed cancer cell lines (e.g., HCT116 for colorectal carcinoma) and normal cell models (e.g., CCD 841 CoN) in 384-well plates. For 3D spheroids, use ultra-low attachment plates and culture for 7 days to allow for spheroid formation [109].
- Compound Preparation: Prepare stock solutions of drug candidates in PBS or DMSO. Use a liquid handling robot (e.g., Beckman Coulter Biomek) for accurate, high-throughput "cherry picking" and combinatorial dilution [109].
- Drug Treatment: Treat cells with single agents or combinations at various concentrations. The IC~20~ (concentration for 20% growth inhibition) is often a useful starting point for combination studies [109].
- Viability Assessment: After a defined incubation period (e.g., 72 hours), measure cell viability. For 2D cultures, use assays like the Fluorometric Microculture Cytotoxicity Assay (FMCA) [109]. For 3D spheroids, metrics like mean spheroid GFP fluorescence can be used if fluorescently labeled cells are employed [109].
- Data Analysis: Calculate the Therapeutic Index (TI). A commonly used in vitro TI is the difference in cytotoxicity between the target cancer model and the adverse side effect model (e.g., a normal cell line) [109]. Iterative algorithms like MACS (Medicinal Algorithmic Combinatorial Screen) can be used to search for optimal combinations that maximize this TI [109].
In Vivo Models: Assessing Systemic Efficacy and Toxicity
The Role of Animal Models in the Preclinical Pipeline
In vivo studies address the major limitation of in vitro systems by demonstrating the impact of a pharmaceutical on the body as a whole [105]. This allows researchers to visualize complex pharmacokinetic and pharmacodynamic interactions, providing better predictions of safety, toxicity, and overall efficacy [105] [106]. For anticancer drugs, positive results from in vivo models are typically a prerequisite for progression to human clinical trials.
Common In Vivo Models in Oncology
The most prevalent in vivo models are murine xenografts [107].
- Ectopic Xenografts: Human cancer cells are inoculated subcutaneously into immunocompromised mice. This is the most popular model due to the ease of monitoring tumor growth by caliper measurement [107].
- Orthotopic Xenografts: Cancer cells are implanted into the organ or tissue of origin in the mouse (e.g., liver cancer cells into the liver). This model provides a more relevant microenvironment for tumor growth and metastasis [107].
- Patient-Derived Xenografts (PDX): Fragments of a patient's tumor are directly implanted into mice. PDX models are believed to better preserve the heterogeneity and stromal components of the original human tumor and are increasingly used in co-clinical trials [107].
Experimental Protocol: Efficacy Study in a Xenograft Model
- Model Establishment: Inoculate immunocompromised mice (e.g., NOD/SCID) subcutaneously with a suspension of human cancer cells or a fragment of a patient-derived tumor.
- Randomization and Dosing: Once tumors reach a predetermined volume (e.g., 100-150 mm³), randomize animals into treatment and control groups. Administer the drug candidate, a vehicle (placebo), and/or a positive control compound according to the planned schedule (e.g., daily oral gavage, intraperitoneal injection).
- Efficacy Monitoring: Monitor tumor volume and body weight regularly (e.g., 2-3 times per week). Tumor volume is calculated from caliper measurements using the formula: V = (length × width²) / 2.
- Endpoint Analysis: The study typically concludes when tumors in the control group reach a maximum allowable size. Efficacy is assessed by metrics such as:
- Tumor Growth Inhibition (TGI): % TGI = [1 - (ΔT/ΔC)] × 100, where ΔT and ΔC are the mean change in tumor volume for the treatment and control groups, respectively.
- Tumor Growth Delay: The difference in time taken for tumors in treated and control groups to reach a specific volume.
- Pharmacokinetic/Pharmacodynamic (PK/PD) Analysis: Terminal blood and tissue samples can be collected to measure drug concentration (PK) and the effect on the target pathway (e.g., phosphorylation status by Western blot) [107].
The Scientist's Toolkit: Essential Research Reagent Solutions
Table 2: Key Reagents and Materials for Preclinical Efficacy Models
| Reagent / Material | Function and Application in Research |
|---|---|
| Caco-2 Cell Line | A human colorectal adenocarcinoma cell line that spontaneously differentiates into enterocyte-like cells. It is the gold standard in vitro model for predicting oral drug absorption and permeability [106]. |
| Calu-3 Cell Line | A human lung adenocarcinoma cell line grown on an air-liquid interface (ALI). It is the model of choice for in vitro permeation studies related to pulmonary drug delivery [106]. |
| Matrigel | A solubilized basement membrane preparation extracted from the Engelbreth-Holm-Swarm (EHS) mouse sarcoma. It is used as a hydrogel scaffold to support the growth and differentiation of 3D organoids and for establishing xenograft models [107]. |
| Crystal Violet / MTT / FMCA | These are common assays for measuring cell viability and proliferation in 2D and 3D cultures. The Fluorometric Microculture Cytotoxicity Assay (FMCA) measures the activity of esterases in living cells, providing a fluorescence readout of viability [109]. |
| Transwell Inserts | Permeable supports used for cell culture to study transport, migration, and invasion. They are central to co-culture models and assessing drug permeation across cellular barriers [106]. |
| Liquid Handling Robot | Automated systems (e.g., Beckman Coulter Biomek) enable high-throughput, precise compound dispensing and combinatorial liquid handling for large-scale drug screening efforts [109]. |
Integration with Bioinformatics and Future Perspectives
The field of preclinical modeling is being transformed by the integration of bioinformatics and computational biology. Tools like DeepTarget exemplify this trend by predicting the anti-cancer mechanisms of small molecules through the integration of large-scale genetic (e.g., CRISPR-Cas9 screens) and pharmacological data across hundreds of cancer cell lines [38]. This approach moves beyond the traditional "one drug-one target" dogma, embracing the context-dependent nature of drug-target interactions and accelerating the repurposing of existing drugs [38].
Furthermore, the drive to adhere to the 3Rs principle (Replacement, Reduction, and Refinement of animal experiments) is a major impetus for innovation [106] [107]. Advanced 3D models, particularly patient-derived organoids and organ-on-a-chip microphysiological systems, are poised to play a pivotal role in this transition, potentially replacing certain animal studies and improving the clinical predictivity of preclinical research [107]. The future of assessing target efficacy and drug potency lies in the intelligent combination of computational predictions, high-fidelity in vitro models, and targeted, hypothesis-driven in vivo validation.
Visualizing Workflows and Signaling Pathways
Diagram: Preclinical Drug Discovery and Validation Workflow
Preclinical Drug Discovery Workflow
Diagram: Optimizing Drug Combinations via Therapeutic Index
Therapeutic Index Optimization Loop
The integration of bioinformatics into oncology drug discovery has fundamentally transformed the landscape of cancer therapy, shifting the paradigm from traditional cytotoxic agents to precision medicine. This whitepaper examines the pivotal role of bioinformatics methodologies in identifying novel anticancer drug targets and accelerating the development of approved therapeutics. By leveraging multi-omics data, computational modeling, and artificial intelligence, researchers can now decipher the complex molecular mechanisms driving carcinogenesis and identify precision interventions with unprecedented efficiency. Through detailed case studies and methodological breakdowns, this review demonstrates how bioinformatics-driven approaches have successfully bridged the gap between genomic insights and clinically effective cancer treatments, while also exploring emerging trends and future directions in the field.
Cancer remains a leading cause of mortality worldwide, with complex pathogenesis rooted in genetic and epigenetic alterations that drive uncontrolled cellular proliferation [97]. The traditional drug discovery pipeline has historically been lengthy, expensive, and fraught with high failure rates, often requiring over a decade and substantial financial investment to bring a single drug to market [12] [46]. Bioinformatics has emerged as a transformative discipline within anticancer drug discovery, leveraging computational approaches to analyze vast biological datasets and identify therapeutic targets with higher precision and efficiency [12] [40].
The completion of the Human Genome Project in 2003 marked a pivotal moment, providing the foundational data that catalyzed the development of bioinformatics tools for drug discovery [12] [46]. This review examines how bioinformatics approaches—including omics integration, molecular docking, network pharmacology, and AI-driven prediction models—have contributed to the successful development of clinically approved anticancer drugs. By analyzing specific success stories and methodological frameworks, we aim to provide researchers and drug development professionals with a comprehensive technical guide to bioinformatics-driven drug discovery in oncology.
Methodological Framework: Bioinformatics Approaches in Drug Discovery
Omics Data Integration and Target Identification
The bioinformatics-driven drug discovery pipeline begins with comprehensive omics data integration from genomics, transcriptomics, proteomics, and metabolomics [12] [110]. These high-throughput technologies generate massive datasets that require sophisticated computational tools for meaningful analysis and target identification.
Genomics approaches identify disease-associated genes through techniques including DNA microarrays and next-generation sequencing (NGS) [110]. Transcriptomics analyses, utilizing databases such as NCBI GEO and ArrayExpress, reveal differentially expressed genes in cancer cells compared to normal tissues [46]. Proteomics focuses on protein structures and functions, while metabolomics studies small molecule metabolites to identify critical cancer pathways [110]. The integration of these multi-omics data provides a systems-level understanding of carcinogenesis and enables the identification of novel druggable targets.
Table 1: Key Biological Databases for Anti-cancer Drug Discovery
| Database Name | Type | Primary Application | Reference |
|---|---|---|---|
| NCBI RefSeq | Genomic | Genome sequence data storage and analysis | [46] |
| UniProtKB/Swiss-Prot | Protein | Protein sequence and functional information | [46] |
| NCBI GEO | Transcriptomic | Gene expression data repository | [46] |
| KEGG | Pathway | Biomarker and pathway analysis | [46] |
| canSAR | Integrated | Druggability assessment and target validation | [46] |
| CancerResource | Integrated | Drug-target relationships and sensitivity data | [46] |
| PharmacoDB | Pharmacogenomic | Cancer datasets, tissues, cell lines, compounds | [46] |
Computational Modeling and Virtual Screening
Once potential targets are identified, structure-based drug design (SBDD) approaches, particularly molecular docking, are employed to screen compound libraries against target structures [12] [46]. Molecular docking predicts the binding orientation and affinity of small molecules to protein targets, enabling virtual screening of thousands to millions of compounds [12]. This approach significantly accelerates the hit identification process compared to traditional high-throughput screening alone.
Quantitative structure-activity relationship (QSAR) modeling represents another critical bioinformatics tool, predicting compound activity and toxicity based on chemical structures [97]. When combined with molecular dynamics simulations, which analyze atomic-level movements and binding stability, researchers can optimize lead compounds with improved efficacy and pharmacokinetic properties [97] [110].
Figure 1: Bioinformatics Drug Discovery Workflow. This diagram illustrates the sequential process from omics data analysis to experimental validation.
Network Pharmacology and Systems Biology Approaches
Network pharmacology represents a paradigm shift from the traditional "one drug-one target" model to a systems-level understanding of drug action [110]. By constructing and analyzing protein-protein interaction networks, drug-target networks, and disease-gene networks, researchers can identify multi-target therapeutic strategies that address cancer complexity and heterogeneity [40]. This approach is particularly valuable for understanding polypharmacology—where drugs interact with multiple targets—and for designing combination therapies that overcome drug resistance [38] [110].
Success Stories: Clinically Approved Drugs
Ibrutinib: Drug Repurposing Through Context-Specific Targeting
Ibrutinib, an established Bruton's tyrosine kinase (BTK) inhibitor approved for blood cancers, exemplifies how bioinformatics tools can reveal novel therapeutic applications through drug repurposing [38]. DeepTarget, a computational tool that integrates large-scale genetic and pharmacological data, predicted Ibrutinib's efficacy in lung cancer models where its canonical target BTK is absent [38].
The methodology involved analyzing data from 1450 drugs across 371 diverse cancer cell lines from the Dependency Map Consortium [38]. DeepTarget leveraged the principle that genetic deletion of a drug's protein target via CRISPR-Cas9 can mimic the drug's inhibitory effects [38]. The tool predicted that mutant forms of the epidermal growth factor receptor (EGFR) serve as relevant targets for Ibrutinib in lung tumors, a hypothesis subsequently validated through experimental studies [38]. This discovery explains Ibrutinib's efficacy in lung cancer despite the absence of its primary target, highlighting the importance of context-specific drug action.
Figure 2: Ibrutinib Repurposing Mechanism. This diagram shows how bioinformatics revealed Ibrutinib's novel target in lung cancer.
Natural Product-Derived Therapeutics: Vinca Alkaloids to Betulinic Acid
Natural products have contributed significantly to anticancer drug discovery, with approximately 34% of newly approved drugs originating from natural products or their derivatives [12] [46]. Vinca alkaloids (vincristine and vinblastine) represent early success stories, derived from the Madagascar periwinkle plant and used in managing leukemia and Hodgkin's disease [97]. These discoveries began with traditional medicinal knowledge and were subsequently optimized through modern computational and experimental approaches.
Contemporary research continues this tradition with compounds like betulinic acid and withaferin A, which have progressed from computational identification to experimental validation [97]. The bioinformatics pipeline for natural product drug discovery typically involves:
- Virtual screening of natural compound libraries against specific cancer targets
- Molecular docking to predict binding modes and affinities
- ADME (absorption, distribution, metabolism, excretion) property prediction
- Network pharmacology analysis to understand multi-target effects
- Experimental validation through in vitro and in vivo studies [97]
Table 2: Clinically Approved Anti-cancer Drugs Discovered Through Bioinformatics-Assisted Approaches
| Drug Name | Cancer Indications | Primary Target | Bioinformatics Approach | Reference |
|---|---|---|---|---|
| Ibrutinib | Blood cancers, Lung cancer | BTK, mutant EGFR | Genetic-pharmacological data integration (DeepTarget) | [38] |
| Vincristine/Vinblastine | Leukemia, Hodgkin's disease | Tubulin | Natural product screening and optimization | [97] |
| Drugs targeting mutant EGFR | Lung cancer | EGFR | Genomic analysis and molecular docking | [38] |
| Proteasome inhibitors | Pancreatic cancer | Proteasome subunits | Structure-based virtual screening | [111] |
Essential Research Reagents and Computational Tools
The successful application of bioinformatics in anticancer drug discovery relies on a sophisticated toolkit of research reagents, computational resources, and experimental systems. These tools enable researchers to transition from computational predictions to validated therapeutic candidates.
Table 3: Research Reagent Solutions for Bioinformatics-Driven Drug Discovery
| Reagent/Tool Category | Specific Examples | Function in Drug Discovery | Reference |
|---|---|---|---|
| Genomic Editing Tools | CRISPR-Cas9 | Target validation through genetic deletion | [38] [110] |
| Microarray Platforms | Affymetrix Human Genome U133 Plus 2.0 | Gene expression profiling in tumor vs. normal tissues | [111] |
| Protein Structure Databases | AlphaFold Protein Structure Database | Access to predicted protein structures for molecular docking | [111] |
| Molecular Docking Servers | DockThor Server | Prediction of ligand-protein interactions and binding affinity | [111] |
| Cell Line Resources | Cancer Cell Line Encyclopedia (CCLE) | In vitro models for validating drug sensitivity predictions | [38] |
| Compound Libraries | MCULE database | Source of potential therapeutic compounds for virtual screening | [111] |
| Pathway Analysis Tools | Gene Set Enrichment Analysis (GSEA) | Identification of significantly enriched pathways in cancer | [111] |
Experimental Protocols and Methodologies
Transcriptional Meta-Analysis Pipeline for Target Identification
A robust protocol for identifying novel gastric cancer targets demonstrates the practical application of bioinformatics in target discovery [111]:
Data Acquisition: Collect Minimum Information About a Microarray Experiment (MIAME)-compliant microarray studies from the Gene Expression Omnibus (GEO) database based on predefined inclusion criteria (human tissue samples, GPL570 platform, tumor and normal samples) [111].
Data Processing and Normalization: Process raw .cel files using R packages (GEOquery, affy). Normalize data using frozen Robust Multiarray Averaging (fRMA) method, which uses pre-calculated probe drifts to normalize raw microarray data and outperforms traditional RMA for pooled analyses [111].
Metadata Construction and Batch Effect Correction: Merge normalized datasets from multiple studies. Identify batch effects using Uniform Manifold Approximation and Projection (UMAP) and remove them using ComBat algorithm within the SVA package [111].
Differential Expression Analysis: Perform analysis using the limma package in R. Filter genes based on expression variation (75th percentile) and collapse redundant probes to corresponding human gene symbols. Apply thresholds of |LogFC| ≥ 1.0 and false discovery rate (FDR) < 0.01 for significance [111].
Validation Using Independent Databases: Confirm findings using data from The Cancer Genome Atlas (TCGA) database through tools like Gene Expression Profiling Interactive Analysis (GEPIA) for differential expression and survival analysis [111].
Structure-Based Virtual Screening (SBVS) Protocol
For identified targets, the following SBVS protocol enables efficient lead compound identification [111]:
Target Preparation: Retrieve 3D protein structures from Protein Data Bank (PDB) or predicted structures from AlphaFold Database. Prepare structures by adding hydrogen atoms, assigning partial charges, and defining binding sites.
Compound Library Preparation: Curate libraries from databases like MCULE, applying chemical filters for drug-likeness and removing compounds with undesirable structural features.
Molecular Docking: Perform high-throughput docking using programs like DockThor server. Generate multiple binding poses and rank compounds based on scoring functions that estimate binding affinity.
Binding Analysis and Selection: Analyze top-ranking compounds for specific interactions with key residues in the binding pocket. Select candidates based on binding mode, affinity predictions, and chemical tractability.
Pharmacokinetic and Toxicological Prediction: Evaluate selected compounds using in silico ADMET prediction tools to assess potential absorption, distribution, metabolism, excretion, and toxicity properties before experimental testing.
Emerging Trends and Future Perspectives
The field of bioinformatics-driven anticancer drug discovery continues to evolve rapidly, with several emerging trends shaping its future trajectory. Artificial intelligence and deep learning algorithms are increasingly being integrated with traditional computational methods to enhance prediction accuracy and explore vast chemical spaces more efficiently [97] [112]. Tools like AlphaFold have revolutionized protein structure prediction, enabling more reliable structure-based drug design for targets without experimental structures [112].
Another significant trend involves the movement toward multi-target therapies and drug repurposing, facilitated by tools like DeepTarget that embrace the complexity of drug-target interactions rather than treating off-target effects as mere liabilities [38]. This approach acknowledges the context-dependent nature of drug action and enables identification of novel therapeutic applications for existing compounds, significantly reducing development time and costs [38] [110].
Future developments will likely focus on improved multimodal data integration, AI-driven high-throughput screening, and the establishment of standardized platforms to address challenges related to data heterogeneity and reproducibility [110]. As these technologies mature, bioinformatics will play an increasingly central role in realizing the vision of personalized cancer therapy tailored to individual molecular profiles.
Bioinformatics has fundamentally transformed anticancer drug discovery, providing powerful computational methodologies that complement and enhance traditional experimental approaches. Through integrated analysis of multi-omics data, structure-based virtual screening, and network pharmacology, bioinformatics enables more efficient identification of novel targets and therapeutic candidates with higher precision. The success stories of drugs like Ibrutinib in new indications and natural product-derived therapies demonstrate the tangible impact of these approaches on clinical oncology.
As the field advances, the integration of artificial intelligence, deep learning, and increasingly sophisticated computational models promises to further accelerate and refine the drug discovery process. By embracing biological complexity and leveraging large-scale datasets, bioinformatics-driven approaches will continue to bridge the gap between genomic insights and effective cancer therapies, ultimately advancing the goal of personalized precision medicine for cancer patients worldwide.
Comparative Analysis of Bioinformatics Tools and Platforms for Different Research Goals
The discovery of novel anticancer drug targets represents one of the most critical challenges in modern oncology research. With cancer's extensive heterogeneity and complex molecular mechanisms, traditional experimental approaches alone are insufficient for comprehensively unraveling the disease complexity. Bioinformatics has emerged as a transformative discipline, providing the computational frameworks and analytical capabilities necessary to navigate the vast landscape of cancer genomics and identify therapeutic vulnerabilities [113]. The integration of bioinformatics tools into oncology research has catalyzed a paradigm shift from generalized cancer treatment to precision oncology, enabling the development of targeted therapies tailored to individual molecular profiles [114].
This technical guide provides a comprehensive comparative analysis of contemporary bioinformatics tools and platforms specifically contextualized within anticancer drug target discovery. We present a detailed examination of tool functionalities, experimental methodologies, and practical workflows to assist researchers, scientists, and drug development professionals in selecting appropriate computational strategies for their specific research objectives. By synthesizing current capabilities and emerging innovations in the field, this review aims to equip investigators with the knowledge to leverage bioinformatics most effectively in the quest for novel anticancer therapeutics.
Comprehensive Tool and Platform Landscape
Major Multi-Omics Data Repositories and Platforms
The foundation of cancer bioinformatics research rests upon access to comprehensive, well-annotated datasets. Several large-scale consortia and data platforms have been established to aggregate and standardize cancer multi-omics data, serving as indispensable resources for the research community.
Table 1: Major Multi-Omics Data Repositories for Cancer Research
| Name | Primary Focus | Key Features | Data Types | Access Method |
|---|---|---|---|---|
| TCGA [115] [29] | Pan-cancer atlas | >20,000 samples across 33 cancer types | Genomics, epigenomics, proteomics, clinical data | GDC Portal, Broad GDAC Firehose |
| ICGC [115] | Global genetic abnormalities | 77 million somatic mutations from 20,000+ participants | Somatic mutations, molecular profiles | ICGC Data Portal |
| COSMIC [115] | Somatic mutations | Expert manually curated mutations | CNA, methylation, gene fusions, SNPs | Web interface |
| CPTAC [115] | Clinical proteomics | Proteogenomic correlations | Genomic, transcriptomic, proteomic, clinical data | CPTAC Data Portal |
These resources provide the essential raw data required for cancer bioinformatics analyses. TCGA stands as the most comprehensive pan-cancer multi-omics dataset, while COSMIC offers expertly curated somatic mutation information critical for understanding cancer-driving genetic alterations [115]. The integration of proteomic data through CPTAC adds a crucial functional dimension to genomic discoveries, enabling researchers to connect genetic alterations with their protein-level consequences [115].
Analysis and Visualization Platforms
Beyond data repositories, numerous platforms have been developed to facilitate interactive exploration and analysis of cancer genomic data, significantly lowering the barrier for researchers without extensive computational backgrounds.
Table 2: Analysis and Visualization Platforms for Cancer Genomics
| Platform | Primary Functionality | Strengths | Integration Capabilities |
|---|---|---|---|
| cBioPortal [115] | Interactive exploration | Mutation visualization, clinical correlation | TCGA, ICGC, user datasets |
| UCSC Xena [115] | Public/private data analysis | Survival analysis, genomic signatures | TCGA, GTEx, user datasets |
| GEPIA2 [115] | Expression profiling | Differential expression, patient survival | TCGA, GTEx normal tissues |
| GSCA [115] | Gene set analysis | Multi-omics at gene set level | Expression, mutation, drug sensitivity |
These platforms address different analytical needs within the drug discovery pipeline. cBioPortal excels in visualizing molecular alterations across patient samples and identifying correlated genomic events [115]. GEPIA2 provides robust differential expression analysis between tumor and normal tissues, crucial for identifying overexpressed oncogenes or underexpressed tumor suppressors [115]. GSCA offers the unique capability of analyzing gene sets as unified entities rather than individual genes, enabling pathway-centric approaches to target discovery [115].
Specialized Tools for Key Research Goals
Tools for Drug Targeting and Repurposing
The emerging frontier of computational drug discovery has yielded sophisticated tools that leverage large-scale genetic and pharmacological data to predict drug-target interactions with increasing accuracy.
DeepTarget represents a groundbreaking approach that diverges from traditional structure-based prediction methods. Instead of relying primarily on chemical structure and binding affinity, DeepTarget integrates large-scale drug and genetic knockdown viability screens from resources like the Dependency Map (DepMap) Consortium, which encompasses data for 1,450 drugs across 371 cancer cell lines [38] [116]. This tool operates on the principle that genetic deletion of a drug's protein target via CRISPR-Cas9 should mimic the drug's inhibitory effect, enabling more biologically contextual prediction of drug mechanisms [38].
In benchmark testing, DeepTarget outperformed established tools like RoseTTAFold All-Atom and Chai-1 in 7 out of 8 drug-target test pairs, demonstrating particular strength in predicting both primary and secondary targets [116] [87]. This capability is critically important because many FDA-approved drugs and investigational agents exert their effects through polypharmacology [38]. The tool successfully predicted context-specific targeting, such as identifying mutant EGFR as a secondary target of Ibrutinib in BTK-negative solid tumors, which was subsequently validated experimentally [116] [87].
Molecular docking tools continue to play a vital role in structure-based drug design. The standard docking workflow involves: (1) preparation of three-dimensional structures of target macromolecules and small molecules; (2) identification of binding sites through computational tools or experimental data; (3) docking simulations; and (4) analysis of results with selection of highest-scoring binding modes [12]. These approaches are particularly valuable for virtual screening of compound libraries and lead optimization, significantly reducing the time and cost associated with experimental high-throughput screening [12].
Tools for Biomarker Discovery and Tumor Heterogeneity
Bioinformatics tools for genomic biomarker discovery employ sophisticated pipelines that process next-generation sequencing data to identify genetic variants with clinical relevance. The standard workflow begins with quality control and trimming of raw sequencing data, followed by alignment to reference genomes, duplicate marking, base quality score recalibration, variant calling, and functional annotation [114] [29].
Single-cell bioinformatics has emerged as a transformative approach for resolving tumor heterogeneity, a major challenge in oncology. Single-cell RNA sequencing (scRNA-seq) enables researchers to deconstruct the cellular complexity of tumors, identifying distinct subpopulations and their unique genetic signatures [113]. This granular resolution allows for tracking clonal evolution, profiling immune cells within the tumor microenvironment, and pinpointing cellular populations responsible for metastasis or drug resistance [113]. International initiatives like the Human Tumor Atlas Network (HTAN) are generating comprehensive single-cell atlases across multiple tumor types, providing unprecedented insights into intratumoral heterogeneity [114].
Tools for immune repertoire analysis play a specialized role in immuno-oncology by characterizing the diverse landscape of T-cell and B-cell receptors within the tumor microenvironment. These analyses help identify neoantigens—unique tumor antigens arising from somatic mutations—that can be targeted with personalized cancer vaccines [113]. By analyzing tumor mutational profiles, bioinformatics algorithms can predict which neoantigens are most likely to be presented on major histocompatibility complex molecules and elicit robust immune responses [113].
Experimental Protocols and Workflows
Genomics-Based Drug Selection Protocol
The genomics-based drug selection workflow represents a foundational protocol for precision oncology, enabling the identification of clinically actionable genetic alterations that can guide targeted therapy.
Diagram 1: Genomics-Based Drug Selection Workflow
Step 1: Sample Preparation and Sequencing
- Collect matched tumor and normal samples from patients
- Extract DNA and perform quality assessment
- Prepare sequencing libraries using targeted panels, whole-exome (WES), or whole-genome sequencing (WGS) approaches [114]
- Sequence using next-generation sequencing platforms (Illumina, Ion Torrent, etc.)
Step 2: Data Processing and Quality Control
- Perform initial quality control using FastQC or similar tools
- Trim adapter sequences and low-quality bases using Trimmomatic or Cutadapt
- Align sequences to reference genome using BWA-MEM or STAR aligner [114]
- Process aligned reads: mark duplicates, perform local realignment around indels, and apply base quality score recalibration following GATK Best Practices [114]
Step 3: Variant Calling and Annotation
- Call somatic variants (single nucleotide variants, small insertions/deletions) using Mutect2, VarScan, or similar tools [114]
- Identify copy number variations (CNVs) using CONTRA, ADTEx, or other CNV callers
- Detect structural variants (translocations, inversions) using BreakDancer, Delly, or similar tools
- Annotate variants using ANNOVAR, VEP, or similar annotation tools to predict functional consequences [29]
- Filter variants based on population frequency, functional impact, and clinical relevance
Step 4: Clinical Interpretation and Therapy Matching
- Prioritize variants based on known cancer associations (COSMIC, CIViC, OncoKB)
- Match genetic alterations to targeted therapies using drug-gene interaction databases (DGIdb)
- Interpret results in context of clinical guidelines and clinical trial eligibility
- Generate comprehensive molecular reports for clinical decision-making
Transcriptomics Analysis for Target Identification Protocol
RNA sequencing analysis provides critical insights into gene expression patterns, alternative splicing, and fusion events that may reveal therapeutic vulnerabilities.
Diagram 2: Transcriptomics Analysis Workflow
Step 1: Library Preparation and Sequencing
- Extract high-quality RNA from tumor samples (RIN > 7)
- Prepare stranded RNA-seq libraries using poly-A selection or rRNA depletion
- Sequence on appropriate platform (Illumina NovaSeq, HiSeq, etc.) to sufficient depth (typically 30-100 million reads per sample)
Step 2: Data Processing and Quantification
- Perform quality control using FastQC, MultiQC
- Trim adapter sequences and low-quality bases
- Align reads to reference genome/transcriptome using STAR, HISAT2, or similar aligners
- Quantify gene-level expression using featureCounts, HTSeq, or Salmon
Step 3: Differential Expression and Pathway Analysis
- Identify differentially expressed genes between sample groups using DESeq2, edgeR, or limma-voom
- Perform gene set enrichment analysis (GSEA) or pathway analysis using IPA, GSEA, or clusterProfiler [29]
- Construct co-expression networks using WGCNA or similar approaches
- Identify alternatively spliced transcripts using rMATS, DEXSeq, or similar tools
- Detect fusion transcripts using STAR-Fusion, Arriba, or FusionCatcher
Step 4: Target Prioritization and Validation
- Integrate expression data with genomic alterations to identify candidate targets
- Prioritize targets based on differential expression, essentiality scores (from DepMap), and druggability
- Validate candidate targets experimentally using CRISPR screens, siRNA knockdown, or small molecule inhibition
Essential Research Reagent Solutions
Successful implementation of bioinformatics workflows requires not only computational tools but also well-characterized research reagents and resources that ensure analytical reproducibility and biological relevance.
Table 3: Essential Research Reagent Solutions for Cancer Bioinformatics
| Reagent/Resource | Function | Application in Drug Target Discovery | Examples/Sources |
|---|---|---|---|
| Reference Genomes | Baseline for sequence alignment | Essential for variant calling and expression quantification | GRCh38 (hg38), CHM13 |
| Cell Line Models | In vitro cancer models | Provide context for validating computational predictions | CCLE, DepMap consortium |
| CRISPR Libraries | Gene knockout screening | Functional validation of candidate targets | Broad Institute, Addgene |
| Compound Libraries | Small molecule screening | Experimental therapeutic testing | Selleckchem, MedChemExpress |
| Antibody Reagents | Protein validation | Confirm protein expression of candidate targets | CST, Abcam, Proteintech |
| Clinical Data | Patient outcome correlation | Validate prognostic significance of targets | TCGA, ICGC, GEO |
Reference genomes serve as the foundational coordinate system for all genomic analyses, with GRCh38 (hg38) representing the current standard for human genome alignment [29]. Cancer cell line models from resources like the Cancer Cell Line Encyclopedia (CCLE) provide essential in vitro systems for experimentally validating computational predictions of gene essentiality and drug sensitivity [38]. CRISPR knockout libraries enable genome-wide functional screening to identify genes essential for cancer cell survival, providing powerful validation for computationally-predicted targets [38]. Compound libraries facilitate experimental testing of therapeutic hypotheses generated through computational drug repurposing analyses [12].
The landscape of bioinformatics tools for anticancer drug target discovery is both diverse and rapidly evolving. This comparative analysis demonstrates that tool selection must be guided by specific research objectives, with multi-omics data repositories serving as foundational resources, specialized analytical platforms addressing distinct methodological needs, and integrated workflows combining computational predictions with experimental validation. The emergence of advanced tools like DeepTarget highlights the increasing sophistication of approaches that leverage large-scale genetic and pharmacological datasets to transcend traditional one drug-one target paradigms [38] [116].
As the field advances, several key trends are shaping the future of bioinformatics in oncology research: the integration of artificial intelligence and machine learning for pattern recognition in complex datasets [113], the maturation of single-cell technologies to resolve tumor heterogeneity [114] [113], the incorporation of real-world evidence to complement clinical trial data [113], and the development of increasingly sophisticated in silico drug prioritization approaches [114]. By strategically leveraging the appropriate tools and platforms for their specific research goals, investigators can accelerate the discovery and validation of novel anticancer drug targets, ultimately advancing the field of precision oncology and improving patient outcomes.
Leveraging Real-World Data and Clinical Trials to Refine Predictive Models
The discovery of novel anticancer drug targets represents one of the most promising yet challenging frontiers in precision oncology. While high-throughput technologies generate vast amounts of multi-omics data, a critical translational gap remains between target identification and successful clinical application. This gap stems largely from biological complexity, tumour heterogeneity, and the limitations of preclinical models in recapitulating human cancer biology [114]. The integration of real-world data (RWD) and clinical trial data with bioinformatics pipelines offers a transformative approach to bridge this gap by continuously refining predictive models of drug response and resistance.
Real-world evidence, derived from RWD gathered during routine clinical care, provides insights into drug performance across diverse patient populations and practice settings that are often not fully represented in traditional randomized controlled trials (RCTs) [117] [118]. When strategically integrated with the controlled evidence from clinical trials, these data streams enable researchers to develop more robust, generalizable models for anticancer drug discovery. This review provides a technical framework for leveraging these complementary data sources to enhance predictive modelling throughout the drug development pipeline, with particular emphasis on overcoming tumour heterogeneity and drug resistance mechanisms.
Defining Key Data Types and Their Roles
Clinical Trial Data generated through controlled studies provide high-quality evidence regarding drug efficacy and safety under ideal conditions. These data include precisely measured patient demographics, molecular profiling data, rigorously adjudicated treatment outcomes, and adverse events [119].
Real-World Data (RWD) encompasses information collected during routine clinical care from diverse sources, including electronic health records (EHRs), insurance claims, patient registries, wearable devices, and patient-reported outcomes [118] [119]. When analyzed, RWD generates real-world evidence (RWE) that reflects drug performance in broader, more heterogeneous patient populations.
The strategic integration of these complementary data sources addresses fundamental challenges in anticancer drug discovery. RWD helps validate whether targets identified through preclinical models remain clinically relevant in human populations, while clinical trial data provides mechanistic insights that explain patterns observed in real-world settings [117] [114].
Bioinformatics Infrastructure for Data Integration
Effective integration requires specialized computational infrastructure. Biological databases form the foundation for target discovery, storing and organizing genomic, transcriptomic, proteomic, and metabolomic data [12]. Key resources include:
Table 1: Selected Biological Databases for Anticancer Drug Discovery
| Database Name | Data Type | Application in Target Discovery |
|---|---|---|
| SuperNatural | Natural compounds | Source of potential anticancer compounds with multi-dimensional information [12] |
| NPACT | Plant-derived anticancer compounds | Provides chemical structure, target protein interaction, and biological activity data [12] |
| TCMSP | Traditional Chinese medicine compounds | Contains ADMET (absorption, distribution, metabolism, excretion, toxicity) properties for natural products [12] |
| CancerHSP | Cancer herbal systems pharmacology | Facilitates study of molecular mechanisms of anticancer herbs [12] |
| COSMIC | Somatic mutations in cancer | Catalogs mutational profiles across cancer types for target identification [114] |
Molecular docking tools represent another critical component, enabling virtual screening of compound libraries against potential targets. These computational methods predict binding conformations and affinities between small molecules and target proteins, prioritizing candidates for experimental validation [12].
Technical Framework for Data Integration
Proposed Workflow for Integrated Predictive Modeling
A systematic, phased approach ensures rigorous integration of RWD with clinical trial data. The following workflow outlines key stages in developing refined predictive models:
Data Collection and Preprocessing
The initial phase involves aggregating multimodal data from diverse sources. For RWD, this includes electronic health records, genomic profiles, medical images, and pathology reports [120]. Clinical trial data encompasses structured datasets from interventional studies. Preprocessing addresses several critical challenges:
- Data Cleaning: Handling missing values, outliers, and inconsistent formatting across sources [120]
- Standardization: Applying common data models and ontologies to ensure interoperability
- Feature Selection: Identifying biologically and clinically relevant variables for modeling
- Coding of Medical Concepts: Transforming clinical narratives into structured data using standardized vocabularies like MEDRA or SNOMED CT [120]
For genomic data, additional preprocessing includes quality control, alignment to reference genomes, and variant calling using established pipelines like GATK Best Practices [114].
Predictive Modeling Approaches
Multiple algorithmic strategies can be employed depending on the research question and available data:
- Supervised Learning (Support Vector Machines, Random Forests, Logistic Regression) for classification tasks such as treatment response prediction [120] [121]
- Deep Learning (Convolutional Neural Networks, Transformers) for complex pattern recognition in imaging, omics, and clinical data [120] [122]
- Multimodal AI architectures that integrate diverse data types while handling missing modalities [122]
The Madrigal framework exemplifies advanced multimodal integration, using transformer architectures to unify structural, pathway, cell viability, and transcriptomic data for predicting drug combination effects [122].
Model Validation and Interpretation
Rigorous validation is essential for clinical translation. This includes:
- Cross-validation strategies (k-fold, leave-one-out) to assess performance on held-out data [120]
- External validation using completely independent datasets to evaluate generalizability
- Interpretability analysis using methods like SHAP (SHapley Additive exPlanations) to identify features driving predictions and provide biological insights [120]
For example, Guo et al. used SHAP analysis to identify primary tumor stage as a critical factor influencing metastasis risk in ovarian clear cell carcinoma, which correlated with drug resistance development [120].
Experimental and Clinical Validation
Computational predictions require experimental confirmation through:
- Molecular biology techniques (Western blot, RT-qPCR) to validate target expression [120]
- Cell-based assays to test drug sensitivity predictions in relevant models
- Patient-derived xenografts and organoids to assess therapeutic efficacy in more physiologically relevant systems [122]
Cai et al. exemplify this approach, using machine learning to identify RAC3 as associated with chemoresistance in bladder cancer, followed by validation through immunohistochemistry, RT-qPCR, and Western blot [120].
Experimental Protocols and Methodologies
Development and Validation of Risk Prediction Models for Adverse Drug Reactions
The following protocol outlines a methodology for developing risk prediction models for adverse drug reactions (ADRs) using integrated real-world and clinical trial data, based on a study of anlotinib-related ADRs [121]:
Objective: To identify risk factors and develop a validated prediction model for adverse drug reactions to anticancer therapies.
Data Collection:
- Collect demographic, clinical, treatment, and outcome data from EHRs of patients receiving the drug of interest
- Include variables such as age, gender, BMI, clinical stage, ECOG performance status, comorbidities, metastasis status, diagnosis, prior treatments, combination therapies, treatment lines, and cumulative dose [121]
- Document ADRs using standardized methodologies like the IHI Global Trigger Tool and establish causality using Naranjo's criteria or similar frameworks [121]
- Grade severity using CTCAE (Common Terminology Criteria for Adverse Events) criteria [121]
Statistical Analysis:
- Divide dataset into training and validation cohorts (typically 70:30 ratio) [121]
- Perform univariate analysis to identify candidate variables (p < 0.2) for multivariate analysis
- Conduct multivariate binary logistic regression to identify independent predictors (p < 0.05)
- Construct a nomogram incorporating significant predictors to visualize the model
- Assess model discrimination using area under the ROC curve (AUC) and concordance index
- Evaluate calibration using Hosmer-Lemeshow test
- Determine clinical utility through decision curve analysis (DCA) [121]
Validation:
- Internally validate using bootstrap resampling or cross-validation
- Externally validate using independent patient cohorts from different institutions [121]
Multimodal AI for Predicting Clinical Outcomes from Preclinical Data
The Madrigal framework provides a methodology for predicting clinical outcomes of drug combinations from preclinical data [122]:
Objective: To predict clinical efficacy and adverse effects of drug combinations using multimodal preclinical data.
Data Modalities:
- Drug Structure: Molecular representations (SMILES, fingerprints)
- Pathway Information: Knowledge graphs of molecular pathways
- Cell Viability: Dose-response profiles across cell lines
- Transcriptomic Data: Gene expression changes following drug treatment [122]
Model Architecture:
- Implement modality-specific encoders for each data type
- Use contrastive pretraining to align modality-specific embeddings with the structure modality
- Employ a transformer-based fusion module with bottleneck tokens to integrate multimodal information
- Generate unified embeddings for each drug, which are combined for combination predictions [122]
Training Strategy:
- Train on large-scale drug interaction datasets (e.g., TWOSIDES, DrugBank)
- Implement specialized splitting strategies (by drug pairs, by drugs) to evaluate generalizability to novel compounds
- Handle missing modalities through the model architecture rather than imputation [122]
Validation:
- Evaluate predictions against clinical outcomes from real-world evidence and clinical trials
- Test in patient-derived models (xenografts, primary samples) for personalized combination predictions [122]
Research Reagent Solutions
Successful implementation of integrated predictive modeling requires specialized computational and experimental resources:
Table 2: Essential Research Reagents and Resources for Integrated Predictive Modeling
| Resource Category | Specific Examples | Function and Application |
|---|---|---|
| Bioinformatics Databases | SuperNatural, NPACT, TCMSP, COSMIC, TCGA | Provide chemical, genomic, and clinical data for target discovery and validation [12] [114] |
| Molecular Docking Tools | AutoDock, Glide, GOLD | Predict binding interactions between potential drugs and target proteins [12] |
| AI/ML Frameworks | TensorFlow, PyTorch, Scikit-learn | Provide algorithms for developing predictive models from multimodal data [120] [122] |
| Real-World Data Platforms | Electronic Health Records, Insurance Claims, Patient Registries | Source of clinical outcomes data from diverse patient populations [117] [118] |
| Validation Assays | IHC, RT-qPCR, Western Blot, Patient-derived Xenografts | Experimental validation of computational predictions [120] |
Visualization of Drug Resistance Mechanisms and Modeling Approach
Understanding drug resistance mechanisms is critical for developing effective predictive models. The following diagram illustrates key resistance pathways and corresponding modeling strategies:
Discussion and Future Perspectives
The integration of real-world data and clinical trials represents a paradigm shift in anticancer drug discovery, enabling the development of predictive models that continuously improve through iterative learning. This approach directly addresses the challenges of tumor heterogeneity and drug resistance by incorporating evidence from diverse patient populations and clinical contexts [114].
Key advantages of this integrated framework include:
Enhanced Generalizability: Models trained on both controlled trial data and real-world evidence perform more consistently across diverse patient subgroups, including those typically underrepresented in clinical trials [117].
Accelerated Discovery: Identification of drug resistance patterns in real-world populations enables more rapid development of combination strategies and next-generation therapeutics [120].
Personalized Therapy Optimization: Integration of patient-specific molecular profiles with clinical outcomes data supports truly personalized treatment selection [122] [114].
Future developments will likely focus on standardizing RWD quality across institutions, developing more sophisticated multimodal AI architectures, and establishing regulatory pathways for model validation and clinical implementation. As these technologies mature, integrated predictive models will become increasingly central to the discovery of novel anticancer drug targets and the development of more effective, personalized cancer therapies.
Conclusion
The integration of bioinformatics into anticancer drug discovery has fundamentally shifted the paradigm from serendipitous finding to rational, data-driven design. By systematically exploring multi-omics data, applying sophisticated computational models, and rigorously validating predictions, researchers can uncover novel, druggable targets with higher efficiency. The future of the field lies in refining AI and machine learning algorithms, deepening the integration of single-cell and spatial omics data to tackle tumor heterogeneity, and strengthening the pipeline for clinical translation. As bioinformatics tools and collaborative frameworks continue to evolve, they hold the undeniable potential to accelerate the development of personalized, effective, and less toxic anticancer therapies, ultimately advancing the goals of precision oncology.
References
- 1. Program ( The ) - NCI Cancer Genome Atlas TCGA [https://www.cancer.gov/ccg/research/genome-sequencing/tcga]
- 2. ( The ): an immeasurable source of... Cancer Genome Atlas TCGA [https://pmc.ncbi.nlm.nih.gov/articles/PMC4322527/]
- 3. COSMIC Database for Somatic Cancer Mutation Insights | QIAGEN [https://digitalinsights.qiagen.com/products-overview/cosmic/]
- 4. (Catalogue Of Somatic Mutations In COSMIC ) Cancer [https://www.cosmickb.org/knowledgebase/cosmic-product/]
- 5. and Accessing - BTEP Coding Club Downloading TCGA Data [https://bioinformatics.ccr.cancer.gov/docs/btep-coding-club/CC2024/TCGA/TCGA_download/]
- 6. Selected for TCGA - NCI Cancers Study [https://www.cancer.gov/ccg/research/genome-sequencing/tcga/studied-cancers]
- 7. Functional genomics for breast cancer drug target discovery | Journal of Human Genetics [https://www.nature.com/articles/s10038-021-00962-6]
- 8. Integration of Online Omics-Data Resources for Cancer Research - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC7645150/]
- 9. to Guide TCGA data [https://www.biostars.org/p/179077/]
- 10. of Genomic Discovery and Therapeutic Candidates for Liver... Targets [https://pmc.ncbi.nlm.nih.gov/articles/PMC12024973/]
- 11. Historical Perspective and Current Trends in Anticancer Drug Development - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC11120596/]
- 12. Frontiers | The role and application of bioinformatics techniques and tools in drug discovery [https://www.frontiersin.org/journals/pharmacology/articles/10.3389/fphar.2025.1547131/full]
- 13. Computer-aided drug design in anti-cancer drug discovery: What have we learnt and what is the way forward? - ScienceDirect [https://www.sciencedirect.com/science/article/pii/S2352914823001788]
- 14. Multi-level bioinformatics resources support drug target discovery of protein–protein interactions - ScienceDirect [https://www.sciencedirect.com/science/article/abs/pii/S1359644624001041]
- 15. Frontiers | Integrated genomic analysis to identify druggable targets for... [https://www.frontiersin.org/journals/oncology/articles/10.3389/fonc.2022.989077/full]
- 16. GEPIA: a web server for cancer and normal gene expression profiling and interactive analyses - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC5570223/]
- 17. canSAR: an updated cancer research and drug discovery knowledgebase - PubMed [https://pubmed.ncbi.nlm.nih.gov/26673713/]
- 18. GEPIA (Gene Expression Profiling Interactive Analysis) [http://gepia.cancer-pku.cn/]
- 19. Advances in Integrated Multi-omics Analysis for Drug - Target ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11201992/]
- 20. Editorial: Multi - omics application in exploring potential biomarkers... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12044877/]
- 21. Applications of multi‐omics analysis in human diseases - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC10390758/]
- 22. Frontiers | Advancing precision oncology with AI-powered genomic analysis [https://www.frontiersin.org/journals/pharmacology/articles/10.3389/fphar.2025.1591696/full]
- 23. Multi-omics Data Integration, Interpretation, and Its Application - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC7003173/]
- 24. A Guide to Multi-omics Integration Strategies - Front Line Genomics [https://frontlinegenomics.com/a-guide-to-multi-omics-integration-strategies/]
- 25. Prioritization of therapeutic targets for cancers using integrative ... [https://humgenomics.biomedcentral.com/articles/10.1186/s40246-024-00571-2]
- 26. Artificial Intelligence in Cancer Drug Discovery in 2025 - OncoDaily [https://oncodaily.com/oncolibrary/artificial-intelligence-in-cancer-drug-discovery]
- 27. Targeting Oncogenic in the Era of Personalized Oncology... Pathways [https://pmc.ncbi.nlm.nih.gov/articles/PMC8833388/]
- 28. Current Bioinformatics Tools in Precision Oncology - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC12238682/]
- 29. A Comprehensive Review of Bioinformatics Tools for Genomic Biomarker Discovery Driving Precision Oncology - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC11353282/]
- 30. November 2025 : Saad: New computational framework identifies genes ... [https://safrabio.cs.tau.ac.il/ron_saad_uri_ben_david_ron_shamir_study_in_cell_reports_november2025]
- 31. Soft-Evidence Fused Graph Neural Network for Cancer ... Driver Gene [https://arxiv.org/html/2510.06290v1]
- 32. TARGET-SL: precision essential gene prediction using driver ... [https://pubmed.ncbi.nlm.nih.gov/40483544/]
- 33. Hepatocellular carcinoma: signaling and therapeutic... pathways [https://www.nature.com/articles/s41392-024-02075-w?error=cookies_not_supported&code=c0cc51b9-8149-44ff-8075-8f3711f9b54f]
- 34. From intracellular drivers to immune modulators: emerging paradigms... [https://biosignaling.biomedcentral.com/articles/10.1186/s12964-025-02465-9]
- 35. in Bioinformatics Anticancer Drug Discovery [https://www.linkedin.com/pulse/bioinformatics-anticancer-drug-discovery-drug-discovery-pro-7svzf]
- 36. The present and future of the Cancer Map Dependency [https://www.nature.com/articles/s41568-024-00763-x?error=cookies_not_supported&code=fa5cb63c-ddfb-4cf7-b964-985661848160]
- 37. Map | Broad Institute Cancer Dependency [https://www.broadinstitute.org/cancer/cancer-dependency-map]
- 38. Exploring New Frontiers in Cancer Through... Drug Targets [https://bioengineer.org/exploring-new-frontiers-in-cancer-drug-targets-through-computational-deep-dive/]
- 39. Frontiers | Editorial: Enhancing drug discovery through... [https://www.frontiersin.org/journals/drug-discovery/articles/10.3389/fddsv.2025.1632015/full]
- 40. Bioinformatics Approaches for Anti-cancer Drug Discovery - PubMed [https://pubmed.ncbi.nlm.nih.gov/31549592/]
- 41. Euro Medchem and CADD Conferences | Euro Medchem [https://medchem.pharmaceuticalconferences.com/events-list/structure-based-drug-design-and-molecular-docking]
- 42. in Recent Compounds from Marine... Advancement Anticancer [https://pmc.ncbi.nlm.nih.gov/articles/PMC9862894/]
- 43. Artificial intelligence in cancer target identification and drug discovery | Signal Transduction and Targeted Therapy [https://www.nature.com/articles/s41392-022-00994-0]
- 44. Effect of preprocessing and simulation on the... parameters [https://link.springer.com/article/10.1007/s00894-023-05637-x]
- 45. Protein and ligand preparation: parameters , protocols , and influence... [https://pubmed.ncbi.nlm.nih.gov/23579614/]
- 46. The role and application of bioinformatics techniques and tools in drug discovery - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC11865229/]
- 47. Molecular docking-based computational platform for high-throughput virtual screening - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC8754542/]
- 48. Drug Design by Pharmacophore and Virtual Screening Approach - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC9145410/]
- 49. Artificial intelligence–enabled virtual screening of ultra-large chemical libraries with deep docking | Nature Protocols [https://www.nature.com/articles/s41596-021-00659-2]
- 50. Pharmacophore Models and Pharmacophore-Based Virtual Screening: Concepts and Applications Exemplified on Hydroxysteroid Dehydrogenases - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC6332202/]
- 51. Structure based pharmacophore , modeling ... virtual screening [https://www.nature.com/articles/s41598-021-83626-x?error=cookies_not_supported&code=acfedd3a-a1a7-46a9-805c-5c3e75436165]
- 52. QSAR Pharmacophore -based Virtual , CoMFA and... | Scilit Screening [https://www.scilit.com/publications/87150844a63838f10a191dcb2f23baf3]
- 53. Structure-based pharmacophore , modeling and... virtual screening [https://pubmed.ncbi.nlm.nih.gov/34151738/]
- 54. Machine Learning for Multi-Target Drug Discovery: Challenges and Opportunities in Systems Pharmacology - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC12473769/]
- 55. Bridging technology and medicine: artificial intelligence in targeted ... [https://pubs.rsc.org/en/content/articlelanding/2025/ra/d5ra03747f]
- 56. Frontiers | Editorial: Advancing drug with discovery : AI – drug ... target [https://www.frontiersin.org/journals/pharmacology/articles/10.3389/fphar.2025.1721323/full]
- 57. A Machine Learning–Based Strategy Predicts Selective and Synergistic Drug Combinations for Relapsed Acute Myeloid Leukemia - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC12260508/]
- 58. Artificial Intelligence-Driven Innovations in Oncology Drug Discovery [https://www.dovepress.com/artificial-intelligence-driven-innovations-in-oncology-drug-discovery--peer-reviewed-fulltext-article-DDDT]
- 59. Artificial Intelligence-Driven Innovations in Oncology Drug Discovery: Transforming Traditional Pipelines and Enhancing Drug Design - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC12232943/]
- 60. -driven AI of synergistic discovery ... | Nature Communications drug [https://www.nature.com/articles/s41467-025-56818-6?error=cookies_not_supported&code=a4343ba8-50ea-4437-abef-fc8235328bb8]
- 61. in Complex Critical : A Survey Nodes Identification Networks [https://arxiv.org/abs/2507.06164]
- 62. in Complex Critical | Ali Rouhanifar Nodes Identification Networks [https://www.linkedin.com/posts/ali-rouhanifar-a08b0b139_critical-nodes-identification-in-complex-activity-7350366416874754048-NFeE]
- 63. Differential regulatory network -based quantification and prioritization of... [https://journals.plos.org/ploscompbiol/article?id=10.1371/journal.pcbi.1007435]
- 64. Uncovering Molecular Mechanisms of Drug via... Resistance [https://pubmed.ncbi.nlm.nih.gov/35073162/]
- 65. Dynamic allosteric networks drive adenosine activation... A 1 receptor [https://elifesciences.org/articles/90773]
- 66. Adenosine A1 receptor, a target and regulator of estrogen receptorα action, mediates the proliferative effects of estradiol in breast cancer | Oncogene [https://www.nature.com/articles/onc2009409]
- 67. Frontiers | Target screening and optimization of candidate compounds... [https://www.frontiersin.org/journals/pharmacology/articles/10.3389/fphar.2025.1467504/full]
- 68. Frontiers | Inhibition of A2A Adenosine Receptor Signaling in Cancer Cells Proliferation by the Novel Antagonist TP455 [https://www.frontiersin.org/journals/pharmacology/articles/10.3389/fphar.2017.00888/full]
- 69. Adenosine Receptors and Cancer - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC3598010/]
- 70. of Highly Potent Discovery Agonists... Adenosine A 1 Receptor [https://pmc.ncbi.nlm.nih.gov/articles/PMC9353746/]
- 71. Adenosine receptors and cancer - PubMed [https://pubmed.ncbi.nlm.nih.gov/20888788/]
- 72. The progress and prospects of targeting the adenosine pathway in cancer immunotherapy | Biomarker Research | Full Text [https://biomarkerres.biomedcentral.com/articles/10.1186/s40364-025-00784-0]
- 73. Molecular Medicine Reports [https://www.spandidos-publications.com/10.3892/mmr.2025.13495]
- 74. in Challenges - multi omics data integration [https://blog.biostrand.ai/challenges-in-multi-omics-data-integration]
- 75. - Multi Assessment in Personalized Medicine Through... omics Quality [https://researchportal.helsinki.fi/en/publications/multi-omics-quality-assessment-in-personalized-medicine-through-e]
- 76. and Novel Applications for Pathway... Computational Methods [https://www.frontiersin.org/research-topics/54825/computational-methods-and-novel-applications-for-pathway-analysis-using-high-throughput-biological-data/magazine]
- 77. : Unraveling the Complexities of... Molecular Dynamics Simulations [https://sciencepublishinggroup.com/article/10.11648/j.ajpa.20251303.11]
- 78. 分子动力学模拟:原理、步骤、软件、方法! | 华算科技 [https://www.huasuankeji.com/news/?p=336174]
- 79. Software in the Real World: 5 Uses... Molecular Dynamics Simulation [https://www.linkedin.com/pulse/molecular-dynamics-simulation-software-real-6faqf]
- 80. Unlocking Insights: High - Throughput Data Analysis [https://www.numberanalytics.com/blog/high-throughput-data-analysis-biostatistics]
- 81. and experimental High for... throughput computational methods [https://pubs.rsc.org/en/content/articlehtml/2025/ta/d5ta00331h]
- 82. An Ethical Approach to Genomic Preserving Technology... Privacy [https://pmc.ncbi.nlm.nih.gov/articles/PMC11976530/]
- 83. Frontiers | Innovative Machine Strategies for Therapeutic... Learning [https://www.frontiersin.org/research-topics/69087/innovative-machine-learning-strategies-for-therapeutic-target-identification-in-cancer-drug-discovery]
- 84. Network Medicine in the Age of Biomedical Big Data - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC6470635/]
- 85. Network biology methods integrating biological data for translational science - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC3404396/]
- 86. Top 6 Visualizations for Quantitative Data Analysis Methods - [https://chartexpo.com/blog/quantitative-data-analysis-methods]
- 87. DeepTarget tool uncovers primary and secondary drug across... targets [https://www.news-medical.net/news/20251118/DeepTarget-tool-uncovers-primary-and-secondary-drug-targets-across-cancer-types.aspx]
- 88. -driven multi- Machine in colon... learning targeted drug discovery [https://www.nature.com/articles/s41698-025-01058-6?error=cookies_not_supported&code=090c1595-2d32-4432-985d-0a575a2608c4]
- 89. Perturbation-Theory Machine for Multi- Learning ... Target Drug [https://pubmed.ncbi.nlm.nih.gov/40699700/]
- 90. Machine learning prediction of oncology drug targets based on protein and network properties | BMC Bioinformatics | Full Text [https://bmcbioinformatics.biomedcentral.com/articles/10.1186/s12859-020-3442-9]
- 91. Metabolite Measurement: Pitfalls to Avoid and Practices to Follow - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC5734093/]
- 92. Analytical Method Validation Best Practices [https://www.numberanalytics.com/blog/analytical-method-validation-best-practices]
- 93. Clinical biochemistry laboratory rejection rates due to various types of preanalytical errors - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC4210258/]
- 94. Promises and Pitfalls of Untargeted Metabolomics - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC5960440/]
- 95. Automation and Standardization —A Coupled Approach towards... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8838799/]
- 96. , quality control and education in Standardization analytical chemistry [https://www.academia.edu/26173597/Standardization_quality_control_and_education_in_analytical_chemistry]
- 97. Anticancer Drug Discovery Based on Natural Products: From Computational Approaches to Clinical Studies - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC10813144/]
- 98. Frontiers | Discovering Anti - Cancer via Drugs Methods Computational [https://www.frontiersin.org/journals/pharmacology/articles/10.3389/fphar.2020.00733/full]
- 99. driven in gene Bioinformatics platform for gold targeting ... anticancer [https://pubmed.ncbi.nlm.nih.gov/41209699/]
- 100. Personalized prediction of anticancer potential of non-oncology... [https://www.nature.com/articles/s41698-025-00813-z?error=cookies_not_supported&code=042d39ee-90ac-459b-843b-ab34690b2754]
- 101. Combinatorial high-throughput experimental and bioinformatic ... [https://www.oncotarget.com/article/4507/text/]
- 102. Frontiers | Deep learning methods for drug response prediction in cancer: Predominant and emerging trends [https://www.frontiersin.org/journals/medicine/articles/10.3389/fmed.2023.1086097/full]
- 103. Approaches in Computational and Precision Medicine Drug Discovery [https://www.frontiersin.org/research-topics/10839/computational-approaches-in-drug-discovery-and-precision-medicine/magazine]
- 104. Two preclinical tests to evaluate anticancer activity and to help validate drug candidates for clinical trials - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC4381701/]
- 105. vs In Preclinical Studies Vitro In Vivo [https://www.news-medical.net/life-sciences/In-Vitro-vs-In-Vivo-Preclinical-Studies.aspx]
- 106. Evaluation of Drug Permeation Enhancement by Using In Ex... Vitro and [https://pmc.ncbi.nlm.nih.gov/articles/PMC11859300/]
- 107. Replacement, Reduction, and Refinement of Animal Experiments in... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10136119/]
- 108. Using 3D in cell culture vitro in models - anti cancer drug discovery [https://pubmed.ncbi.nlm.nih.gov/33823728/]
- 109. of promising In - vitro combinations using... discovery anti cancer drug [https://www.nature.com/articles/srep14118?error=cookies_not_supported]
- 110. Frontiers | Strategies for the drug development of cancer therapeutics [https://www.frontiersin.org/journals/pharmacology/articles/10.3389/fphar.2025.1656012/full]
- 111. A Shortcut from Genome to Drug: The Employment of Bioinformatic Tools to Find New Targets for Gastric Cancer Treatment - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC10535099/]
- 112. An in-depth review of AI-powered advancements in cancer drug discovery - ScienceDirect [https://www.sciencedirect.com/science/article/abs/pii/S0925443925000250]
- 113. How Data Science and Bioinformatics Services Are Revolutionizing Oncology Research [https://blog.crownbio.com/how-data-science-and-bioinformatics-services-are-revolutionizing-oncology-research]
- 114. Bioinformatics roadmap for therapy selection in cancer genomics - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC9627786/]
- 115. Bioinformatics tools and resources for cancer and application - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC11374212/]
- 116. New Computational Tool Shows Strong Accuracy in... - The ASCO Post [https://ascopost.com/news/november-2025/new-computational-tool-shows-strong-accuracy-in-predicting-cancer-drug-targets/]
- 117. How Real - World Improves Data Research Clinical [https://www.linkedin.com/top-content/project-management/improving-clinical-trials/how-real-world-data-improves-clinical-research/]
- 118. - Real : Methodologies for World - Evidence ... Integrating Real World [https://pubmed.ncbi.nlm.nih.gov/41078689/]
- 119. with Clinical - Data (RWE) | Umbrex Integration Real World Evidence [https://umbrex.com/resources/how-to-analyze-a-biotechnology-company/clinical-data-integration-with-real-world-evidence-rwe/]
- 120. Emerging artificial intelligence-driven precision therapies in tumor drug ... [https://molecular-cancer.biomedcentral.com/articles/10.1186/s12943-025-02321-x]
- 121. Development and validation of a risk- prediction for adverse... model [https://pmc.ncbi.nlm.nih.gov/articles/PMC11946284/]
- 122. Multimodal AI predicts outcomes of clinical combinations from... drug [https://arxiv.org/html/2503.02781v1]