From Data to Diagnosis: A Roadmap for Clinically Validating cfDNA Machine Learning Models
The integration of machine learning (ML) with cell-free DNA (cfDNA) analysis holds transformative potential for non-invasive cancer detection, therapy selection, and monitoring.
From Data to Diagnosis: A Roadmap for Clinically Validating cfDNA Machine Learning Models
Abstract
The integration of machine learning (ML) with cell-free DNA (cfDNA) analysis holds transformative potential for non-invasive cancer detection, therapy selection, and monitoring. However, translating these models from research to clinical practice requires rigorous validation in real-world cohorts. This article provides a comprehensive framework for researchers and drug development professionals, covering the foundational biology of cfDNA, state-of-the-art ML methodologies, strategies for troubleshooting common pitfalls, and robust validation standards. By synthesizing current best practices and emerging trends, this guide aims to accelerate the development of reliable, clinically actionable cfDNA-based ML tools for precision oncology.
The Bedrock of cfDNA: Understanding Biology and Biomarkers for Machine Learning
Cell-free DNA (cfDNA) analysis has revolutionized non-invasive diagnostic approaches, enabling insights into human health and disease through a simple blood draw. The field of fragmentomics investigates the unique physical and molecular characteristics of these DNA fragments, leveraging the fact that their breakdown is not a random process. This guide provides a comparative analysis of three cornerstone fragmentomic features—nucleosome positioning, fragment size, and end motifs—focusing on their biological origins, measurement methodologies, and performance in clinical biomarker development. As machine learning models increasingly integrate these features for disease detection, understanding their individual and combined strengths, validated against large clinical cohorts, is paramount for researchers and drug development professionals.
Biological Foundations of cfDNA Fragmentomics
The landscape of cfDNA in the bloodstream is a mosaic of DNA fragments originating from various cell types. The composition and structure of these fragments are directly influenced by the biological processes within their cells of origin.
- Cellular Death and Chromatin Digestion: cfDNA is primarily released into the circulation during apoptotic cell death. During apoptosis, apoptotic nucleases systematically digest cellular chromatin. These enzymes preferentially cleave the linker DNA between nucleosomes, while the DNA wrapped around the histone core is protected. This process results in a population of DNA fragments whose ends and lengths carry an imprint of the nuclear architecture of the source cell [1] [2].
- Nucleosome Positioning as a Cellular Blueprint: The genomic positioning of nucleosomes is highly cell-type-specific, reflecting the unique epigenetic and transcriptional state of the cell [3] [1]. Genes that are actively transcribed or regulated by specific transcription factors exhibit distinct nucleosome occupancy patterns at their promoters and enhancers. Consequently, the nucleosome footprint recovered from cfDNA sequencing can be used to infer the relative contributions of different tissues to the circulating DNA pool, a principle foundational to "nucleosomics" [1].
- Transcription Factor Footprinting: In addition to nucleosomes, other DNA-binding proteins like transcription factors can protect DNA from nuclease digestion. This results in very short DNA fragments that footprint the binding sites of these regulatory factors, providing an additional layer of functional genomic information [3] [4].
The following diagram illustrates the journey of cfDNA, from its origin in the nucleus to its analysis in the laboratory, highlighting the key fragmentomic features covered in this guide.
Comparative Analysis of Key Fragmentomic Features
Table 1: Comparative overview of key cfDNA fragmentomic features.
| Feature | Biological Basis | Primary Measurement Method(s) | Key Clinical Performance Examples |
|---|---|---|---|
| Nucleosome Positioning | Cell-type-specific nucleosome architecture protected from nuclease digestion [3] [1]. | Window Protection Score (WPS) [5], Promoter/Enhancer Coverage [4] [6], Coverage at ATAC-seq peaks [4]. | Ovarian Cancer: AUC improvement when combined with CNA scores [2].Preterm Birth (PTerm): AUC 0.849 in validation cohorts [6]. |
| Fragment Size | DNA cleavage periodicity around nucleosomes (10.4 bp) and protection by chromatosome (~167 bp) [3] [5]. | Fragment Length Distribution, Proportion of short fragments (<150 bp) [7], DELFI score [5] [7]. | Multi-Cancer Detection (DELFI): High performance in targeted panels [7].Cancer Detection: Short fragment proportion is a key metric [7]. |
| End Motifs | Sequence-specific cleavage preferences of DNase enzymes (e.g., DNASE1L3) [4]. | Frequency of 4-mer sequences at fragment ends, Motif Diversity Score (MDS) [5] [7]. | HCC vs. Healthy: Distinct end motif patterns [5].Cancer Typing: MDS at all exons was top metric for SCLC detection [7]. |
Nucleosome Positioning
Experimental Protocol for Nucleosome Footprinting: A standard protocol for inferring nucleosome positioning from cfDNA Whole Genome Sequencing (WGS) data involves:
- LC-WGS: Perform low-coverage (e.g., 0.1x-1x) whole-genome sequencing of plasma cfDNA [6] [2].
- Read Alignment: Map sequenced reads to a reference human genome.
- Fragment Boundary Mapping: Extract the start and end coordinates of all cfDNA fragments.
- Nucleosome Score Calculation: Compare the fragment boundary profile to a reference set of known nucleosome positions (e.g., from healthy individuals) [2]. One common method is to calculate the distance from each fragment start to the nearest reference nucleosome center, generating an M-shaped distribution. Deviations from the healthy reference profile can be quantified using multinomial modeling to generate a nucleosome footprint score for each sample [2].
Fragment Size
Experimental Protocol for Fragment Size Analysis:
- High-Quality Data Generation: Sequence cfDNA (WGS or targeted) and retain only high-quality, uniquely mapped, non-duplicate reads [5].
- Fragment Length Calculation: Compute the insert size for each paired-end read.
- Genome-Wide Distribution: Plot the frequency distribution of all fragment lengths, which typically shows a peak at ~167 bp (mononucleosome) and smaller peaks at multiples thereof [3] [5].
- Feature Calculation: Calculate specific size-based metrics such as the proportion of fragments shorter than 150 bp, the ratio of long to short fragments in genomic windows, or the Shannon entropy of the size distribution in specific regions like gene exons [7].
End Motifs
Experimental Protocol for End Motif Analysis:
- Fragment End Extraction: From aligned BAM files, extract the first 4 nucleotides (4-mer) at both the 5' and 3' ends of each cfDNA fragment.
- Motif Frequency Calculation: Count the occurrence of each unique 4-mer sequence across all fragment ends in a sample.
- Motif Diversity Score (MDS): Calculate the MDS, which quantifies the heterogeneity of end motif usage. A higher MDS indicates greater diversity. This can be calculated genome-wide or within specific genomic intervals (e.g., 100 kb bins) to increase feature resolution [5].
- Differential Analysis: Identify end motifs that are significantly over- or under-represented in case samples (e.g., cancer patients) compared to healthy controls.
Table 2: Performance comparison of fragmentomic features across cancer types and detection limits.
| Feature Category | Specific Metric | Cancer Type / Condition | AUC / Performance | Detection Limit / Tumor Fraction |
|---|---|---|---|---|
| Nucleosome Positioning | Promoter Profiling (PTerm) | Preterm Birth [6] | AUC 0.849 (Validation) | N/A |
| Nucleosome Positioning | Nucleosome Footprint Score | Ovarian Cancer [2] | Improved detection when combined with CNA | Complements CNA-low tumors |
| Fragment Size | Normalized Depth (All Exons) | Multi-Cancer (Targeted Panel) [7] | Avg. AUROC 0.943-0.964 | Varies by type (e.g., NSCLC: 0.873) |
| End Motifs | MDS (All Exons) | Small Cell Lung Cancer (SCLC) [7] | AUROC 0.888 | Specific to SCLC |
| End Motifs | End Motif Frequency | Hepatocellular Carcinoma (HCC) [5] | Pattern significantly different from healthy | Data from patient plasma |
The Scientist's Toolkit: Essential Reagents and Computational Tools
Table 3: Key research reagents and computational tools for cfDNA fragmentomics.
| Item / Tool Name | Type | Primary Function in cfDNA Fragmentomics |
|---|---|---|
| TALEs (Transcription Activator-Like Effectors) [8] | Protein Reagent | Engineered to specifically bind methylated DNA sequences, enabling enrichment and detection of methylation patterns in fragmentomics. |
| DNASE1L3 [4] | Enzyme | An apoptotic nuclease whose cleavage preference is reflected in cfDNA end motifs (e.g., CCNN motif). |
| ATAC-seq Peaks [4] | Genomic Reference | Reference maps of open chromatin regions used to interpret cfDNA enrichment patterns and infer cell-of-origin. |
| FinaleToolkit [5] | Computational Tool | A fast, memory-efficient Python package for generating comprehensive fragmentation features (WPS, end motifs, MDS) from large cfDNA sequencing datasets. |
| NucPosDB [1] | Database | A curated database of in vivo nucleosome positioning and cfDNA sequencing datasets for fundamental and clinical research. |
| XGBoost [4] | Machine Learning Model | An interpretable ML algorithm used to train classifiers on cell-type-specific open chromatin features derived from cfDNA for cancer detection. |
Integration into Machine Learning Models and Clinical Validation
The true power of fragmentomic features is realized when they are integrated into machine learning models and rigorously validated in clinical cohorts.
Feature Combination Enhances Performance: Models that combine multiple fragmentomic features consistently outperform those relying on a single feature type. For instance, combining nucleosome footprint scores with copy number alteration (CNA) scores improved the pre-surgical diagnosis of invasive ovarian cancer, with nucleosome scoring being particularly effective for tumors characterized by low chromosomal instability [2]. Similarly, a comprehensive approach using normalized depth, fragment sizes, and end motifs across all exons of a targeted panel achieved high AUROCs (up to 0.964) for multi-cancer detection [7].
Interpretability and Biologically Informed Features: Using biologically informed features, such as signals from cell-type-specific open chromatin regions, not only improves cancer detection accuracy but also enhances model interpretability. This allows researchers to identify key genomic loci associated with the disease state, providing actionable biological insights beyond a simple classification output [4].
Validation in Large, Independent Cohorts: Robust validation is critical for clinical translation. The PTerm classifier for preterm birth, based on cfDNA promoter profiling, was developed and validated in a large-scale, multi-center study involving 2,590 pregnancies, achieving an AUC of 0.849 in independent validation cohorts [6]. This demonstrates the stability and generalizability of fragmentomics-based models.
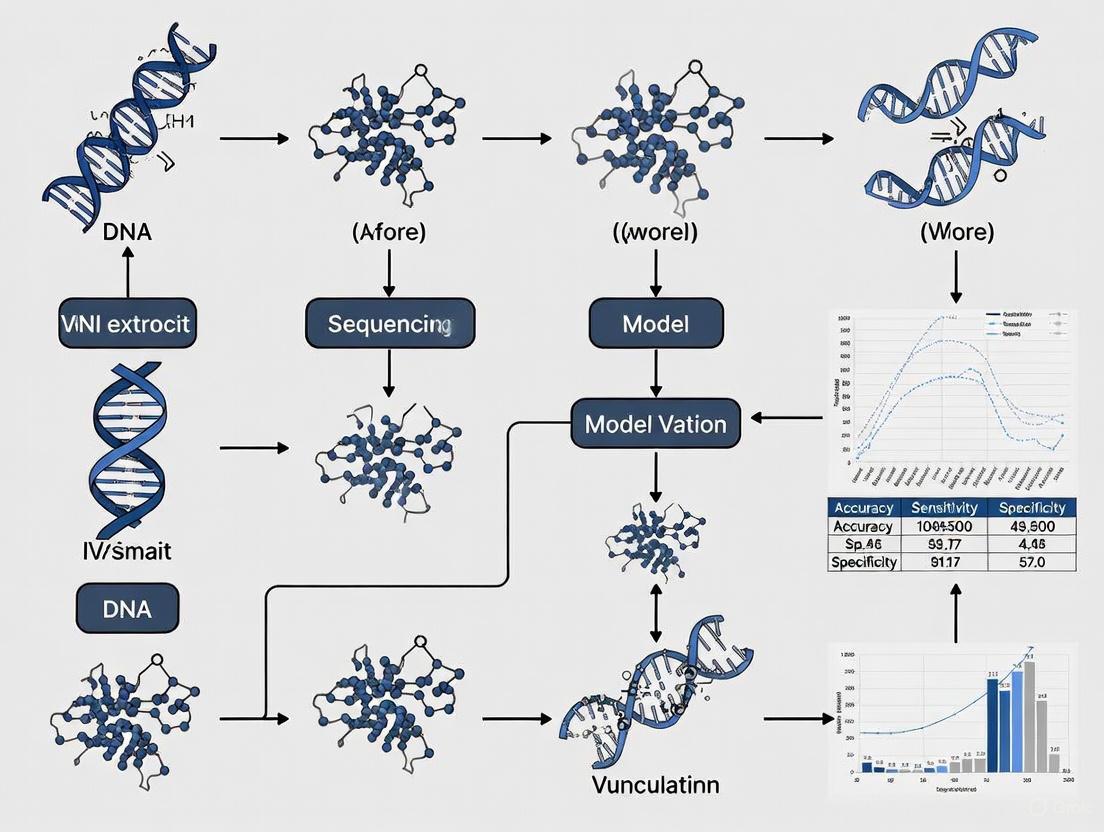
The following diagram summarizes the end-to-end workflow for building and validating a machine learning model using cfDNA fragmentomic features.
Tissue-of-origin (TOO) mapping for cell-free DNA (cfDNA) represents a transformative advancement in liquid biopsy, enabling non-invasive disease detection and monitoring. By deciphering the unique epigenetic and open chromatin signatures carried by cfDNA fragments, researchers can trace the cellular origins of these molecules, opening new frontiers in oncology, prenatal testing, and transplant monitoring. This guide provides a comprehensive comparison of the leading technological approaches in TOO mapping, focusing on their underlying mechanisms, performance characteristics, and clinical validation status. The field has evolved from genetic mutation-based analyses to sophisticated epigenetic profiling that captures the molecular footprints of active gene regulation across tissues. As these technologies mature, understanding their comparative strengths and technical requirements becomes essential for researchers and drug development professionals implementing liquid biopsy applications in clinical research and diagnostic development.
Comparative Analysis of TOO Mapping Technologies
The table below summarizes the performance characteristics and technical specifications of the primary TOO mapping approaches currently advancing in clinical research.
Table 1: Performance Comparison of Major TOO Mapping Technologies
| Technology | Biological Target | Reported Sensitivity | Reported Specificity | Key Advantages | Clinical Validation Status |
|---|---|---|---|---|---|
| Open Chromatin Footprinting (TCI Method) | TSS coverage patterns of 2,549 tissue-specific genes [9] | High accuracy in pregnancy/transplant models [9] | Established reference intervals from 460 healthy individuals [9] | Simple, cost-effective, avoids bisulfite conversion [9] | Validated in healthy cohorts and specific clinical scenarios [9] |
| cfDNA Methylation Profiling | Genome-wide methylation patterns [10] | 88.1% for GI cancers (SPOGIT assay); detects early-stage (0-II) with 83.1% sensitivity [10] | 91.2% for GI cancers (SPOGIT assay) [10] | High sensitivity for early cancer detection; detects premalignant lesions [10] | Multicenter validation (n=1,079); projected to reduce late-stage diagnoses by 92% [10] |
| Whole Genome Sequencing (WGTS) | Combined mutation features, CNVs, SVs, and mutational signatures [11] | Informs TOO diagnosis in 71% of CUP cases unresolved by clinicopathology [11] | Detects additional reportable variants in 76% of cases vs. panels [11] | Comprehensive feature detection; superior to panel sequencing [11] | Feasibility demonstrated in 73 CUP tumors; informs treatment for 79% of patients [11] |
| cfDNA Fragmentomics | Fragment size ratios, CNV, and nucleosome footprint [12] | 90.5% for RCC detection; 87.8% for stage I RCC [12] | 93.8% for RCC detection; 100% for stage IV RCC [12] | Strong performance across cancer stages and subtypes [12] | Validation in 422 participants; presented at ASCO 2025 [12] |
Table 2: Technical Requirements and Resource Considerations
| Methodology | Minimum Input DNA | Sequencing Depth | Computational Requirements | Key Tissue Coverage |
|---|---|---|---|---|
| Open Chromatin Footprinting | Not specified | Not specified | TCI algorithm; 12 reference tissues [9] | 12 human tissues [9] |
| cfDNA Methylation (SPOGIT) | <30 ng [10] | Not specified | Multi-algorithm model (Logistic Regression/Transformer/MLP/Random Forest/SGD/SVC) [10] | Focused on gastrointestinal tract cancers [10] |
| Whole Genome Sequencing | Not specified | Not specified | CUPPA algorithm; complex bioinformatics pipeline [11] | Broad cancer type coverage [11] |
| cfDNA Fragmentomics | Not specified | 5X coverage (low-pass WGS) [12] | Stacked ensemble machine learning model [12] | Renal cell carcinoma and benign renal conditions [12] |
Experimental Protocols and Methodologies
Open Chromatin Footprinting with TCI Method
The Tissue Contribution Index (TCI) method leverages the principle that cfDNA coverage near transcription start sites (TSS) of actively transcribed genes decreases due to open chromatin accessibility. The protocol involves:
Reference Atlas Development: Identify 2,549 tissue-specific, highly expressed genes across 12 human tissues using resources like GTExv8 TPM values for bulk tissues [9].
Library Preparation and Sequencing: Plasma cfDNA is extracted and prepared for whole-genome sequencing without bisulfite conversion, preserving DNA integrity.
TSS Coverage Analysis: Map sequencing reads around TSS regions (±1 kb) to generate coverage profiles, with decreased coverage indicating open chromatin regions.
TCI Calculation: Apply the TCI algorithm to quantify tissue contributions by comparing observed TSS coverage patterns against the reference tissue atlas.
Validation: Establish reference intervals using plasma cfDNA from healthy individuals (n=460) and validate in specific clinical contexts such as pregnancy and transplantation [9].
Whole Genome and Transcriptome Sequencing for CUP
For cancers of unknown primary (CUP), the WGTS approach provides comprehensive molecular profiling:
Sample Preparation: Utilize FFPE or fresh tissue samples, with FFPE samples requiring additional quality control measures due to shorter fragment lengths and higher duplication rates [11].
Sequencing: Perform whole genome sequencing at sufficient depth to detect SNVs, indels, CNVs, and SVs, complemented by whole transcriptome sequencing where RNA quality permits.
Variant Calling and Analysis: Employ specialized tools for different variant types:
- SNVs/Indels: Standard mutation calling pipelines
- CNVs: PURPLE tool with adjustment for FFPE-derived noise [11]
- SVs: Structural variant callers optimized for complex rearrangements
TOO Prediction: Apply the CUP prediction algorithm (CUPPA) trained on WGTS data of known cancer types, incorporating driver mutations, passenger mutations, and mutational signatures [11].
Clinical Interpretation: Integrate molecular features with pathological assessment to resolve tissue of origin and inform treatment options.
cfDNA Methylation Analysis for Early Cancer Detection
The SPOGIT assay for gastrointestinal cancer detection exemplifies the methylation-based approach:
Assay Development: Identify informative methylation markers from large-scale public tissue methylation data and cfDNA profiles [10].
Library Preparation: Use capture-based approaches (e.g., Twist probe cfDNA profiles) to enrich for target regions, requiring as little as <30 ng of input cfDNA [10].
Multi-Algorithm Modeling: Apply an ensemble of machine learning models (Logistic Regression, Transformer, MLP, Random Forest, SGD, SVC) to analyze methylation patterns [10].
Cancer Signal Origin Prediction: Implement a complementary CSO model to localize the primary site with 83% accuracy for colorectal cancer and 71% for gastric cancer [10].
Clinical Validation: Conduct rigorous multicenter validation focusing on early-stage cancers and precancerous lesions, with simulation analyses projecting clinical impact [10].
The Scientist's Toolkit: Essential Research Reagents and Solutions
Table 3: Key Research Reagents and Solutions for TOO Mapping
| Reagent/Solution | Function | Example Application |
|---|---|---|
| Single strand Adaptor Library Preparation (SALP-seq) | Single-stranded DNA library preparation for highly degraded DNA [13] | Esophageal cancer biomarker discovery from cfDNA [13] |
| Cell-free Reduced Representation Bisulfite Sequencing (cfRRBS) | Genome-scale methylation analysis from limited cfDNA input (6-10 ng) [14] | Early detection and monitoring of lung cancer [14] |
| Tn5 Transposase (Tagment DNA Enzyme) | Simultaneous fragmentation and tagging of DNA for ATAC-seq libraries [15] | Chromatin accessibility mapping in brain and endocrine tissues [15] |
| Boruta Feature Selection Algorithm | Random forest-based feature selection identifying all relevant predictors [16] | Cardiovascular risk prediction in diabetic patients; applicable to methylation marker selection [16] |
| Multiple Imputation by Chained Equations (MICE) | Handling missing data in clinical datasets through iterative imputation [16] | Addressing incomplete clinical variables in patient cohorts [16] |
| Illumina Unique Dual Indexes (UDIs) | Multiplexing samples while minimizing index hopping in NGS [15] | ATAC-seq library preparation for chromatin accessibility studies [15] |
Clinical Validation and Machine Learning Framework
Robust clinical validation of cfDNA-based TOO models requires addressing temporal dynamics in clinical data. A comprehensive diagnostic framework should incorporate:
Temporal Validation: Partition data from multiple years into training and validation cohorts to assess model longevity and performance consistency [17].
Drift Characterization: Monitor temporal evolution of patient characteristics, outcomes, and feature distributions that may impact model performance [17].
Feature Stability Analysis: Apply data valuation algorithms and feature importance methods (e.g., SHAP analysis) to identify stable predictors across time periods [17] [16].
Ensemble Approaches: Combine multiple algorithms to enhance robustness, as demonstrated by the SPOGIT assay's use of six different machine learning models [10].
For CUP patients, WGTS-informed treatment decisions have demonstrated clinical utility, with molecular profiling informing treatments for 79% of patients compared to 59% by panel testing [11]. This highlights the tangible clinical impact of comprehensive TOO mapping in difficult-to-diagnose cancers.
The evolving landscape of TOO mapping technologies offers researchers multiple pathways for leveraging epigenetic and open chromatin signatures in clinical liquid biopsy applications. Open chromatin footprinting provides a bisulfite-free, cost-effective approach particularly valuable for monitoring tissue damage and transplantation. Methylation-based profiling demonstrates superior sensitivity for early cancer detection and interception of premalignant progression. Whole genome sequencing offers the most comprehensive feature detection for complex diagnostic challenges like CUP, while fragmentomics emerges as a promising approach with minimal input requirements. The selection of an appropriate TOO mapping technology must consider clinical context, sample availability, and computational resources, with rigorous temporal validation essential for successful clinical implementation. As these technologies continue to mature, they hold immense potential to transform cancer diagnosis, monitoring, and personalized treatment strategies.
The analysis of cell-free DNA (cfDNA) has emerged as a cornerstone of precision oncology, enabling non-invasive access to tumor-derived genetic and epigenetic information. Circulating tumor DNA (ctDNA), the fraction of cfDNA originating from cancer cells, carries tumor-specific alterations that provide a real-time snapshot of tumor burden and heterogeneity [18] [19]. The clinical utility of cfDNA analysis spans the entire cancer care continuum, from early detection and diagnosis to therapy selection and monitoring of minimal residual disease (MRD) [20] [21]. However, the full potential of cfDNA is only realized through advanced computational approaches that can decipher the complex biological signals embedded within these fragments.
Machine learning (ML) and artificial intelligence (AI) technologies have become indispensable for integrating the high-dimensional features derived from cfDNA analysis, including genetics, epigenetics, and fragmentomics [22]. These computational approaches leverage patterns in cfDNA characteristics—such as fragment length distributions, end motifs, nucleosome positioning, and genomic distributions—to develop classifiers capable of detecting cancer, identifying its tissue of origin, monitoring treatment response, and distinguishing tumor-derived signals from confounding sources like clonal hematopoiesis [22] [23] [7]. This guide provides a comprehensive comparison of how ML-powered cfDNA analysis is addressing critical clinical needs, with a focus on performance validation across diverse clinical applications and cohorts.
Comparative Performance of cfDNA ML Models Across Clinical Applications
Table 1: Performance comparison of ML-based cfDNA models across key clinical applications
| Clinical Application | ML Approach | Key Features | Performance Metrics | Validation Cohort | Clinical Utility |
|---|---|---|---|---|---|
| Lung Cancer Detection | Fragmentome classifier | Genome-wide cfDNA fragmentation patterns | High sensitivity; Consistent across demographics/comorbidities [24] | 958 LDCT-eligible individuals (382 in validation) [24] | Blood-based adjunct to improve LDCT screening uptake [24] |
| MRD Monitoring | Tumor-informed vs. tumor-agnostic | Patient-specific mutations (informed) vs. computational ctDNA quantification (agnostic) | Tumor-informed: Higher sensitivity, especially early-stage [18] | Clinical experience across cancer types [18] | Detection of molecular relapse before clinical recurrence [18] [19] |
| Variant Origin Classification | MetaCH meta-classifier | Variant/gene embeddings, functional prediction scores, VAF, cancer type [23] | Superior auPR vs. base classifiers across 4 validation datasets [23] | External cfDNA datasets with matched WBC sequencing [23] | Distinguishes clonal hematopoiesis from true tumor variants in plasma-only samples [23] |
| Multi-Cancer Phenotyping | GLMnet elastic net | Normalized fragment read depth across exons [7] | AUROC: 0.943 (UW cohort), 0.964 (GRAIL cohort) [7] | 431 samples (UW), 198 samples (GRAIL) [7] | Accurate cancer type and subtype classification from targeted panels [7] |
Table 2: Fragmentomics metric performance for cancer phenotyping on targeted sequencing panels
| Fragmentomics Metric | UW Cohort AUROC (Range) | GRAIL Cohort AUROC (Range) | Key Strengths |
|---|---|---|---|
| Normalized depth (all exons) | 0.943 (0.873-0.986) [7] | 0.964 (0.914-1.000) [7] | Best overall performance across cancer types [7] |
| Normalized depth (E1 only) | 0.930 (0.838-0.989) [7] | N/R | Strong performance, slightly inferior to all exons [7] |
| Normalized depth (full gene) | 0.919 (0.828-0.993) [7] | N/R | Combines all exons from one gene [7] |
| End motif diversity (all exons) | Variable (Best for SCLC: 0.888) [7] | N/R | Superior for specific cancer types (e.g., SCLC) [7] |
Experimental Protocols and Methodologies
Fragmentomics Analysis for Early Cancer Detection
The DELFI-L101 study (NCT04825834) demonstrated a robust protocol for developing and validating a fragmentome-based lung cancer detection test [24]. This multicenter, prospective case-control study enrolled 958 individuals eligible for lung cancer screening according to USPSTF guidelines. The study employed a split-sample approach, with approximately 60% of subjects (n=576) used for classifier training and the remaining 40% (n=382) for independent clinical validation [24].
The experimental workflow involved: (1) collection of peripheral blood samples from all participants; (2) extraction and low-coverage whole-genome sequencing of cfDNA; (3) analysis of genome-wide cfDNA fragmentation profiles (fragmentomes); (4) training of a machine learning classifier on fragmentome features from the training set; and (5) locking the classifier model before performance assessment in the validation set [24]. This methodology specifically leveraged the fact that changes to genomic architecture in cancer cells result in abnormal genome-wide patterns of cell-free DNA in circulation, with fragmentation patterns reflective of specific chromatin configurations of the cells and tissues of origin [24].
ML Framework for Distinguishing Clonal Hematopoiesis
The MetaCH framework addresses the critical challenge of distinguishing clonal hematopoiesis (CH) variants from true tumor-derived mutations in plasma-only samples [23]. This open-source machine learning framework processes variants through three stages:
- Feature Extraction: Variants, genes, and functional impacts are numerically represented using the Mutational Enrichment Toolkit (METk), which generates: variant embeddings (E~v~) based on sequence context, associated gene, and cancer type; gene embeddings (E~g~) capturing patterns of genes with variants within individual patients; and functional prediction scores (E~f~) quantifying the impact of non-synonymous variants on gene function [23].
- Base Classifier Training: Three binary classifiers are trained: (i) a cfDNA-based classifier using features from METk plus variant allele frequencies and cancer type; (ii) sequence-based classifiers trained on public datasets of CH and somatic tumor variants to predict CH-oncogenic and CH-non-oncogenic variants [23].
- Meta-Classification: A meta-classifier applies logistic regression to combine scores from the base classifiers into a final probability that a variant originates from CH [23].
The framework was validated using cross-validation of training samples and external validation across four independent cfDNA datasets with matched white blood cell sequencing, demonstrating superior performance compared to existing approaches [23].
MetaCH Framework Workflow: This diagram illustrates the three-stage MetaCH framework for classifying variant origin in cfDNA samples without matched white blood cell sequencing.
Fragmentomic Analysis on Targeted Sequencing Panels
Recent research has demonstrated that fragmentomics analysis can be effectively performed on targeted sequencing panels commonly used in clinical settings, rather than requiring whole-genome sequencing [7]. The experimental approach involves:
- Sequencing Data Processing: Targeted panel sequencing data from cfDNA samples is processed to extract fragment-level information including size, genomic coordinates, and sequence characteristics [7].
- Multi-Metric Fragmentomics Analysis: Thirteen different fragmentomics metrics are calculated, including: (A) fragment length proportions and diversity metrics; (B) normalized fragment read depth; (C) end motif diversity score; (D) fragments overlapping transcription factor binding sites; and (E) fragments overlapping open chromatin sites [7].
- Model Training and Validation: An elastic net model (GLMnet) with 10-fold cross-validation is used to predict cancer type and subtype based on these fragmentomics features, with performance assessed using area under the receiver operating characteristic curve (AUROC) [7].
This approach has been validated across two independent cohorts—the University of Wisconsin cohort (431 samples) and the GRAIL cohort (198 samples)—demonstrating that normalized fragment read depth across all exons generally provides the best predictive performance for cancer phenotyping [7].
The Scientist's Toolkit: Essential Research Reagents and Solutions
Table 3: Key research reagents and solutions for cfDNA ML model development
| Reagent/Solution | Function | Application Examples |
|---|---|---|
| Targeted Sequencing Panels | Capture and sequence specific genomic regions of interest | FoundationOne Liquid CDx (309 genes), Guardant360 CDx (55 genes), Tempus xF (105 genes) [7] |
| Unique Molecular Identifiers (UMIs) | Tag individual DNA molecules to correct for PCR and sequencing errors | Suppression of technical artifacts in variant calling [19] [25] |
| Whole Genome Sequencing | Provide genome-wide coverage for fragmentomics analysis | DELFI approach for cancer detection and tissue of origin identification [24] |
| Methylation Atlas | Reference database for tissue-specific methylation patterns | Tissue-of-origin tracing of cfDNA; 39 cell types from 205 healthy tissue samples [22] |
| Error Correction Methods | Improve sequencing accuracy and reduce false positives | Duplex Sequencing, SaferSeqS, NanoSeq, Singleton Correction, CODEC [19] |
Technical Considerations and Implementation Challenges
Biological and Analytical Variables
The effective implementation of cfDNA-based ML models requires careful consideration of several biological and technical factors. The concentration and characteristics of cfDNA are influenced by multiple variables including age, gender, organ health, medication status, physical activity, and other individual factors [20]. Additionally, the half-life of cfDNA in circulation is estimated between 16 minutes and several hours, enabling real-time monitoring but also introducing temporal variability [19] [20].
From an analytical perspective, distinguishing true tumor-derived variants from those arising from clonal hematopoiesis remains a significant challenge. CH variants can comprise over 75% of cfDNA variants in individuals without cancer and more than 50% of variants in those with cancer [23]. Methods that rely on matched white blood cell sequencing are considered the gold standard but are often cost-prohibitive and impractical for routine clinical implementation [23].
Performance Across Commercial Panels
Fragmentomics-based cancer detection performance varies when applied to different commercial targeted sequencing panels. Research indicates that panels with larger gene content generally provide better performance, with the FoundationOne Liquid CDx panel (309 genes) outperforming smaller panels like Tempus xF (105 genes) and Guardant360 CDx (55 genes) in fragmentomics-based cancer classification [7]. However, even smaller panels maintain reasonable performance for many applications, suggesting that fragmentomics analysis can be successfully implemented across various clinical-grade panels.
cfDNA Fragmentomics Workflow: This diagram outlines the key steps in processing cfDNA samples for fragmentomics analysis, from blood draw to clinical interpretation.
Machine learning models applied to cfDNA analysis have demonstrated substantial progress in addressing critical clinical needs across the cancer care continuum. Currently, the most validated applications include cancer detection using fragmentomics patterns, particularly in lung cancer screening contexts [24], and monitoring treatment response through ctDNA dynamics [19] [21]. The discrimination of clonal hematopoiesis variants using ML approaches like MetaCH shows promising results but requires further validation in larger prospective cohorts [23].
For clinical implementation, tumor-informed MRD assays currently demonstrate superior sensitivity compared to tumor-agnostic approaches, especially in early-stage cancer settings where ctDNA fractions are minimal [18]. However, current evidence for MRD monitoring in early-stage breast cancer remains largely retrospective, highlighting the need for prospective clinical trials to establish clinical utility before routine adoption [18].
As the field advances, standardization of preanalytical steps, refinement of analysis strategies, and improved understanding of cfDNA biology will be crucial for translating these promising ML approaches into routine clinical practice. The integration of multi-omic features—including genetics, epigenetics, fragmentomics, and transcriptional data—through sophisticated machine learning models holds the potential to further enhance the sensitivity and specificity of cfDNA-based cancer management across all clinical applications.
The integration of machine learning (ML) with cell-free DNA (cfDNA) analysis represents a transformative advancement in noninvasive diagnostics for conditions such as cancer and fetal chromosomal aneuploidies [22]. As this field rapidly expands, a growing number of models with diverse architectures and objectives are being published. This surge necessitates a systematic, critical review to synthesize evidence, identify redundant research efforts, and inform the design of robust future studies [26]. This review aims to objectively compare the performance of existing ML models applied to cfDNA analysis, with a specific focus on their validation in clinical cohorts. By framing the comparison within the core requirements of Clear Objectives, Quantifiable Evaluation, and Well-Defined Extensibility [27], we provide a structured framework to guide researchers, scientists, and drug development professionals in avoiding redundancy and advancing the field through methodologically sound model development.
Methodology of the Systematic Review
This systematic review was conducted according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines [26]. The process is summarized in Figure 1.
Research Question and Eligibility Criteria
The research question was structured using the PICO framework:
- Population/Problem: Clinical cohorts and studies involving cfDNA analysis.
- Intervention/Exposure: Application of machine learning models for diagnostic or prognostic purposes.
- Comparator: Alternative ML models or standard non-ML diagnostic methods.
- Outcome: Model performance metrics (e.g., accuracy, AUC), generalizability, and clinical validity.
Inclusion criteria encompassed peer-reviewed studies involving ML models applied to human cfDNA data for disease detection, classification, or monitoring. Exclusion criteria included review articles, conference abstracts without full data, studies not published in English, and those that did not validate findings in a clinical cohort.
Search Strategy and Study Selection
A comprehensive search was executed across multiple electronic databases, including MEDLINE, Embase, and CENTRAL, tailored to each platform's specific indexing terms and search features [26]. The search strategy combined key concepts using Boolean operators: ("cell-free DNA" OR "cfDNA" OR "circulating tumor DNA" OR "ctDNA") AND ("machine learning" OR "deep learning" OR "artificial intelligence") AND ("model" OR "framework" OR "prediction") [28].
Search results were imported into a reference manager, deduplicated, and screened in a two-stage process by two independent reviewers. The initial screening was based on titles and abstracts, followed by a full-text review of potentially eligible studies. Conflicts were resolved through consensus or by a third reviewer. The study selection process is documented in the PRISMA flow diagram (Figure 1).
Figure 1: PRISMA Flow Diagram of the Systematic Review Process. This diagram visualizes the stages of study identification, screening, eligibility assessment, and final inclusion [28].
Data Extraction and Quality Assessment
Data from included studies were extracted in duplicate using a standardized template. Key extracted information included: study author and year, clinical context (e.g., cancer type), model objective, ML algorithm used, input features (e.g., fragmentomics, epigenetics), cohort size, key performance metrics, and stated limitations.
The risk of bias in included studies was assessed using appropriate tools, such as the Cochrane Risk of Bias Tool for randomized trials or the QUADAS-2 for diagnostic studies [28]. The focus was on evaluating potential biases in patient selection, index test, reference standard, and flow and timing.
Core Principles for Evaluating cfDNA Machine Learning Models
To meaningfully compare models and avoid redundant research, evaluation must extend beyond simple performance metrics. The following principles provide a framework for critical appraisal.
Clear Objectives
A model's purpose must be precisely defined, as this dictates the choice of architecture and evaluation criteria [27]. In cfDNA analysis, common objectives include:
- Disease Detection: Differentiating cancer patients from healthy individuals using features like cfDNA fragmentation patterns [22] [4].
- Tissue of Origin Mapping: Pinpointing the origin of cfDNA, which is crucial for cancers of unknown primary [22].
- Deduction of Fetal/Tumor Fraction: Estimating the proportion of fetal or tumor-derived cfDNA in a sample, a critical factor for test sensitivity [22].
Quantifiable Evaluation
Performance metrics must be robust, statistically sound, and comparable across studies. This involves:
- Statistical Significance Testing: Using null hypothesis testing or paired t-tests to ensure performance differences between models are not due to random chance [29].
- Resampling Methods: Employing ten-fold cross-validation to assess model performance on different data splits and reduce overfitting [30] [29].
- Analysis of Learning Curves: Plotting training and validation error over time to diagnose overfitting (validation error increases while training error decreases) and identify the optimal stopping point [29].
Well-Defined Extensibility
A model's utility is determined by its performance beyond the initial training data. Extensibility involves:
- Generalization: Applying the model to independent, external validation cohorts to test its robustness [27].
- Knowledge Transfer: Assessing the model's ability to maintain performance when applied to related but distinct tasks, such as different cancer types or patient demographics [27].
Comparative Analysis of Machine Learning Approaches in cfDNA Research
The following tables synthesize experimental data and methodologies from key studies applying ML to cfDNA analysis, highlighting how different approaches address the core principles.
Table 1: Comparison of ML Model Objectives and Architectures in cfDNA Studies
| Clinical Context | Model Objective | ML Algorithm(s) | Input Features | Key Findings |
|---|---|---|---|---|
| Breast & Pancreatic Cancer Detection [4] | Cancer detection using chromatin features | XGBoost | Nucleosome enrichment at cell-type-specific open chromatin regions | Improved cancer prediction accuracy by leveraging open chromatin signals from both tumor and immune (CD4+ T-cell) cells. |
| Noninvasive Prenatal Testing (NIPT) & Cancer Liquid Biopsy [22] | Fetal DNA fraction deduction; Plasma DNA tissue mapping; Cancer detection & localization | Various ML/AI approaches (Review) | cfDNA genetics, epigenetics, transcriptomics, fragmentomics | ML can integrate high-dimensional cfDNA features to deduce tissue of origin and detect pathological states. |
| General Subject Classification [30] | Comparison of classification performance | RF, SVM (RBF kernel), LDA, kNN | Simulated data with varying features, sample size, correlation | For smaller, correlated feature sets, LDA outperforms others. SVM excels with larger feature sets and adequate sample size. |
Table 2: Experimental Protocols and Performance Metrics from Key Studies
| Study Context | Experimental Protocol Summary | Cohort Size (Training/Validation) | Key Performance Metrics | Extensibility Assessment |
|---|---|---|---|---|
| Breast Cancer cfDNA Analysis [4] | 1. cfDNA isolated from patient plasma and cancer cell lines. 2. Sequencing libraries prepared and sequenced. 3. Nucleosome enrichment patterns analyzed at ATAC-seq peaks. 4. XGBoost trained on cell-type-specific open chromatin features. | 5 breast cancer patients, 6 healthy donors (cfDNA); Cell lines (T47D, KPL-1) | Model showed distinct improvement in cancer prediction accuracy for breast and pancreatic cancer. | Model identified key contributing genomic loci, providing interpretable, biologically grounded insights. |
| Model Comparison Study [30] | 1. Large-scale simulation of data with controlled factors (features, sample size, noise, etc.). 2. Models (RF, SVM, LDA, kNN) trained and evaluated using leave-one-out cross-validation. 3. Generalization errors compared across factor combinations. | Massive simulation study using high-performance computing | LDA: Best for small, correlated features. SVM (RBF): Superior for large feature sets (sample size ≥20). kNN: Improved with more features unless high data variability. | Performance guidelines provided for varying data characteristics, aiding model selection for new, specific problems. |
The data in these tables demonstrate that model performance is highly context-dependent. For instance, the choice between a simpler model like LDA and a more complex one like SVM depends on the dimensionality of the cfDNA feature set [30]. Furthermore, successful models increasingly leverage biologically informed features, such as open chromatin profiles, which not only boost accuracy but also enhance interpretability—a key consideration for clinical translation [4]. The experimental protocol for such analyses typically follows a workflow from sample collection to model interpretation, as shown in Figure 2.
Figure 2: General Workflow for cfDNA Machine Learning Studies. This diagram outlines the common steps from biological sample collection to the generation of clinically actionable insights [22] [4].
Successful development and validation of ML models for cfDNA analysis rely on a suite of wet-lab and computational tools.
Table 3: Research Reagent Solutions and Key Resources for cfDNA ML Studies
| Item / Resource | Function / Application | Examples / Notes |
|---|---|---|
| Plasma/Serum Samples | Source of cell-free DNA. | Requires careful collection and processing to avoid cellular DNA contamination [22]. |
| cfDNA Extraction Kits | Isolation of high-quality cfDNA from biofluids. | Critical for obtaining representative fragment size distributions [4]. |
| Library Prep Kits | Preparation of sequencing libraries from cfDNA. | Must be optimized for short, fragmented DNA; compatible with dual-indexing to reduce batch effects. |
| ATAC-seq/Specific Antibodies | Defining cell-type-specific open chromatin or histone modification maps. | Used to create reference feature sets for model training (e.g., cancer-specific enhancers) [4]. |
| High-Performance Computing (HPC) | Training complex models and processing large-scale sequencing data. | Essential for running large-scale simulations and hyperparameter optimization [30]. |
| Experiment Tracking Tools | Logging parameters, code, data versions, and metrics for reproducibility. | Neptune.ai, TensorBoard; vital for comparing multiple parallel ML experiments [29]. |
| Reference Databases | Providing annotated genomes, methylation atlas, and variant databases. | High-resolution methylome atlases (e.g., [22]) are key for tissue-of-origin analysis. |
This systematic review underscores that avoiding redundancy in cfDNA ML model development requires a principled approach centered on clear objectives, quantifiable and statistically robust evaluation, and rigorous testing of extensibility. The comparative analysis reveals that there is no single best algorithm; the optimal choice depends on the specific clinical question, the nature and dimensionality of the cfDNA feature data, and the available sample size. Future work should prioritize the development of standardized, publicly available benchmark datasets to facilitate fair model comparisons [27]. Furthermore, the field will benefit from a stronger emphasis on interpretable ML and the integration of diverse biological features, which together will build the trustworthiness needed for these powerful models to transition into routine clinical practice.
Building the Model: Machine Learning Approaches and Feature Engineering for cfDNA Data
The analysis of cell-free DNA (cfDNA) via liquid biopsy has emerged as a transformative, non-invasive approach in oncology, enabling early cancer detection, treatment selection, and disease monitoring [31]. Machine learning (ML) models are pivotal for interpreting the complex, multi-dimensional features derived from cfDNA, such as fragmentomics patterns, copy number variations (CNVs), and nucleosome positioning [32]. The selection of an appropriate ML algorithm—from classical ensembles like XGBoost and Random Forests to sophisticated deep learning architectures—directly impacts the clinical utility of these models. However, given the high stakes of medical diagnostics, this selection cannot be based on performance metrics alone; it must be grounded in rigorous validation frameworks specific to clinical cohorts to ensure reliability, generalizability, and ultimately, patient safety [33] [34]. This guide provides an objective comparison of ML algorithms in the context of cfDNA analysis, supported by experimental data and detailed methodologies, to inform researchers and drug development professionals.
Algorithm Performance Comparison in Clinical cfDNA Studies
Different ML algorithms exhibit distinct strengths and weaknesses when applied to cfDNA data. The table below summarizes quantitative performance data from recent clinical studies and benchmarks, highlighting how algorithm choice affects key diagnostic metrics.
Table 1: Performance Comparison of Machine Learning Algorithms in cfDNA Analysis
| Algorithm | Clinical Context | Performance Metrics | Key Advantages | Limitations |
|---|---|---|---|---|
| XGBoost | Time series forecasting [35]; Tumor type classification from genomic alterations [36] | Lower MAE & MSE vs. deep learning on stationary time series [35]; AUC 0.97 for 10-type tumor classification [36] | High performance on structured data; faster training than deep learning; handles feature importance well [35] [36] | May underperform on highly complex, non-stationary data where deep learning excels [35] |
| Random Forest (RF) | Time series forecasting [35] | Competitive performance, faster training than deep learning [35] | Robust to overfitting; provides feature importance [35] | Can be computationally heavy with many trees; may not match XGBoost's accuracy in some tasks [35] |
| Stacked Ensemble (XGBoost, GLM, DRF, Deep Learning) | Early detection of Esophageal Squamous Cell Carcinoma (ESCC) using cfDNA fragmentomics [32] | AUC: 0.995 (Training), 0.986 (Independent Validation) [32] | Leverages strengths of multiple models; highly robust and accurate; performs well in low-coverage sequencing [32] | Complex to implement and tune; computationally intensive [32] |
| Recurrent Neural Network with LSTM (RNN-LSTM) | Time series forecasting [35] | Higher MAE & MSE vs. XGBoost on stationary vehicle flow data [35] | State-of-the-art for complex sequential data with long-range dependencies [35] | Can develop "smoother" predictions on stationary data; requires large data volumes; computationally costly [35] |
| Support Vector Machine (SVM) | Time series forecasting [35]; General model validation [34] | Competitive performance on time series [35] | Effective in high-dimensional spaces; versatile for classification and regression [34] | Performance is sensitive to kernel and hyperparameter choice [35] |
Detailed Experimental Protocols from Key Studies
Protocol 1: Stacked Ensemble Model for ESCC Detection
A study by Jiao et al. (2024) developed a robust stacked ensemble model for early ESCC detection using cfDNA fragmentomics, demonstrating a rigorous validation protocol [32].
- Objective: To develop a non-invasive assay for early detection of Esophageal Squamous Cell Carcinoma (ESCC) that maintains high sensitivity and specificity, even in low-coverage whole-genome sequencing environments [32].
- Cohort Design: The study recruited 499 participants, split into a training cohort (n=207), an independent validation cohort (n=201), and an external validation cohort (n=91) to ensure generalizability [32].
- Feature Extraction: Four distinct fragmentomics features were extracted from low-pass whole-genome sequencing (5X coverage) of plasma cfDNA:
- Copy Number Variation (CNV): Identification of chromosomal arm-level gains and losses [32].
- Fragmentation Size Coverage (FSC): Analysis of genome-wide coverage patterns of cfDNA fragments [32].
- Fragmentation Size Distribution (FSD): Characterization of the length profile of cfDNA fragments [32].
- Nucleosome Positioning (NP): Mapping of nucleosome occupancy patterns, including identification of transcription factor-binding sites [32].
- Model Training and Stacking: Four base algorithms—XGBoost, Generalized Linear Model (GLM), Distributed Random Forest (DRF), and Deep Learning—were trained on the four fragmentomics features. Instead of using fixed hyperparameters, a random grid search was employed to select the top 10 best-performing base models for the stacking process. These base models' predictions were then combined to form the final stacked ensemble model [32].
- Validation: The model's performance was rigorously assessed on the independent validation and external cohorts, demonstrating consistent AUC, sensitivity, and specificity, thus confirming its robustness [32].
Protocol 2: XGBoost for Pan-Cancer Classification
A 2023 study developed an XGBoost model to classify tumor types based on somatic genomic alterations, showcasing the algorithm's power in handling large-scale, structured genomic data [36].
- Objective: To create a tool that can accurately distinguish between different cancer types based on somatic point mutations (SPMs) and copy number variations (CNVs) at the chromosome arm-level, which could aid in diagnosing cancers of unknown origin [36].
- Data Source and Transformation: Genomic data from 9,927 samples across 32 cancer types were downloaded from The Cancer Genome Atlas (TCGA) via cBioportal. A Vector Space Model (VSM) transformation was applied, converting raw mutation and CNV data into a homogeneous dataset by counting the occurrences of SPMs and CNVs in the p-arm and q-arm of each chromosome for every sample [36].
- Model Training and Addressing Class Imbalance: An XGBoost classifier was trained on the transformed data. To handle the significant class imbalance between common and rare cancers, two strategies were employed:
- Training a model on the 10 most represented tumor types.
- Grouping the 18 most represented cancers into biologically relevant categories (endocrine-related carcinomas, other carcinomas, and other cancers) and training a specific XGBoost model for each group [36].
- Performance: The model achieved a balanced accuracy (BACC) of 77% and an AUC of 0.97 for the 10-tumor-type classification, demonstrating diagnostic potential comparable to or higher than other established methods [36].
Essential Validation Frameworks for Clinical cfML Models
Robust validation is non-negotiable for cfDNA machine learning models intended for clinical application. Proper validation ensures that performance estimates are unbiased and that the model will generalize to new, unseen patient cohorts [33] [34].
Table 2: Key Model Validation Techniques and Their Application in cfDNA Research
| Validation Technique | Core Principle | Application in cfDNA Clinical Cohorts | Considerations |
|---|---|---|---|
| Train/Test Split | Randomly split data into training (e.g., 70%) and testing (e.g., 30%) sets [33]. | A basic first step for initial performance estimation. | Prone to sampling bias if the single split is not representative of the overall cohort [33]. |
| k-Fold Cross-Validation (k-Fold CV) | Data is split into k folds (e.g., 5 or 10). The model is trained on k-1 folds and tested on the left-out fold, repeated for all k folds [33]. | Provides a more robust estimate of model performance by using all data for both training and testing. | The variance of scores across folds provides insight into model stability [33]. |
| Nested Cross-Validation | Uses two layers of k-fold CV: an inner loop for hyperparameter tuning and an outer loop for unbiased performance estimation [33]. | Crucial for avoiding optimistically biased performance estimates when tuning hyperparameters is part of the workflow. | Prevents data leakage from the tuning process into the evaluation process [33]. |
| Leave-One-Group-Out Cross-Validation (LOGOCV) | Each fold corresponds to an entire group (e.g., patients from a specific clinical center) [33]. | Ideal for validating model generalizability across multiple clinical sites in a multicenter trial. | Ensures the model is not relying on site-specific technical artifacts [33]. |
| Time-Series Split | Ensures that training data chronologically precedes test data in each split [33]. | Important for longitudinal cfDNA studies monitoring disease progression or treatment response. | Prevents over-optimism by respecting the temporal nature of the data [33]. |
| Statistical Significance Testing (e.g., Wilcoxon signed-rank test) | A non-parametric test applied to the k performance scores from two models to determine if one is significantly better [33]. | Allows for a statistically grounded comparison between two candidate cfDNA models, beyond simple average metric comparison. | Helps ensure that a perceived improvement is not due to random chance [33]. |
The Scientist's Toolkit: Essential Research Reagents and Materials
Successful development and validation of cfDNA machine learning models rely on a foundation of specific wet-lab and computational tools.
Table 3: Essential Research Reagents and Materials for cfDNA ML Studies
| Item | Function/Description | Example Use Case |
|---|---|---|
| Blood Collection Tubes (e.g., Streck, EDTA) | Stabilize blood cells to prevent lysis and release of genomic DNA that could dilute cfDNA [31]. | Standardized pre-analytical sample acquisition for all subjects in a clinical cohort. |
| cfDNA Extraction Kits | Isolate and purify cfDNA from plasma. Reproducible yield and purity are critical [31]. | Generating the input material for subsequent whole-genome sequencing. |
| Low-Pass Whole-Genome Sequencing (LP-WGS) | Sequences the entire genome at low coverage (e.g., 0.1-5X), sufficient for fragmentomics and CNV analysis [32] [12]. | A cost-effective method to generate fragmentomics features (CNV, FSC, FSD, NP) for model training. |
| Targeted Sequencing Panels | Focuses sequencing on specific genes or regions of interest at very high depth to detect rare mutations [31]. | Can be used to validate findings or as an alternative feature source for mutation-based models. |
| The Cancer Genome Atlas (TCGA) | A public repository containing multi-omics data from thousands of tumor samples [36]. | Serves as a benchmark dataset for training and testing pan-cancer classification models. |
| Python ML Libraries (e.g., scikit-learn, XGBoost, TensorFlow/PyTorch) | Open-source libraries that provide implementations of ML algorithms, from XGBoost to deep learning [33]. | The computational backbone for building, training, and validating all types of models discussed. |
| SHAP (SHapley Additive exPlanations) | A game theory-based method to interpret the output of any ML model [35]. | Explainability analysis to identify which cfDNA features (e.g., specific CNVs) most influenced a model's prediction. |
The selection of a machine learning algorithm for cfDNA-based clinical research is a nuanced decision that balances performance, complexity, and interpretability. XGBoost and tree-based ensembles consistently demonstrate high accuracy and efficiency on structured genomic and fragmentomics data, often matching or surpassing the performance of more complex deep learning models in tasks like cancer classification and detection [32] [35] [36]. For the most challenging diagnostic problems, stacked ensemble models that leverage the strengths of multiple algorithms can provide superior robustness and accuracy [32]. Regardless of the algorithm chosen, the ultimate determinant of clinical success is a rigorous, multi-tiered validation strategy that includes independent and external cohorts, careful handling of data splits, and statistical testing to ensure the model is reliable, generalizable, and ready for translation into patient care [33] [34].
Multi-omics data integration represents a paradigm shift in cancer research, particularly in the realm of cell-free DNA (cfDNA) analysis for liquid biopsy applications. The simultaneous analysis of genomic, fragmentomic, and methylation data provides a multidimensional perspective on tumor biology that surpasses the capabilities of any single data type. Fragmentomics, the study of cfDNA fragmentation patterns, has emerged as a powerful approach that reflects nucleosome positioning and chromatin organization in tissue-of-origin cells [22]. When combined with methylation analysis and genomic alterations, these data layers enable sophisticated machine learning models to detect cancer, identify its tissue of origin, and monitor therapeutic response [7] [22].
The validation of such integrated models in clinical cohorts represents a critical step toward translation into routine practice. This guide objectively compares the performance of different integration strategies, wet-lab protocols, and computational methods based on recent experimental studies, providing researchers with a framework for selecting optimal approaches for their specific clinical research questions.
Comparative Performance of Multi-Omics Integration Methods
Statistical vs. Deep Learning Integration Approaches
Table 1: Performance comparison of multi-omics integration methods for cancer subtyping
| Integration Method | Cancer Type | Classification Accuracy | Key Strengths | Limitations |
|---|---|---|---|---|
| MOFA+ (Statistical) [37] | Breast Cancer | F1-score: 0.75 (nonlinear classifier) | Superior feature selection; Identified 121 relevant pathways | Unsupervised; Requires downstream analysis |
| MOFA+ (Statistical) [38] | Glioblastoma | Successful subtype identification | Revealed AP-1, SMAD3, RUNX1/RUNX2 pathways | Bulk analysis may mask cellular heterogeneity |
| MOGCN (Deep Learning) [37] | Breast Cancer | Lower than MOFA+ | Handles complex nonlinear relationships | Identified only 100 pathways; Less interpretable |
| LASSO-MOGAT [39] | Pan-Cancer (31 types) | Accuracy: 95.9% | Effective with high-dimensional data | Complex implementation; Computationally intensive |
| Correlation-based Graph [39] | Pan-Cancer | Superior to PPI networks | Identifies shared cancer-specific signatures | May miss known biological interactions |
Fragmentomics Metrics Performance in Targeted Sequencing
Table 2: Performance of fragmentomics metrics in cancer detection using targeted panels
| Fragmentomic Metric | AUROC (UW Cohort) | AUROC (GRAIL Cohort) | Best Application Context |
|---|---|---|---|
| Normalized depth (all exons) [7] | 0.943 | 0.964 | General purpose cancer detection |
| Normalized depth (E1 only) [7] | 0.930 | - | Promoter-associated changes |
| End Motif Diversity Score [7] | 0.888 (SCLC) | - | Small cell lung cancer specifically |
| TFBS entropy [7] | Variable | Variable | Transcription factor activity |
| ATAC entropy [7] | Variable | Variable | Open chromatin regions |
Experimental Protocols for Multi-Omics Data Generation
DNA Methylation Profiling Methodologies
Table 3: Comparison of DNA methylation detection methods
| Method | Resolution | DNA Input | Advantages | Limitations |
|---|---|---|---|---|
| Whole-Genome Bisulfite Sequencing (WGBS) [40] | Single-base | High | Gold standard; Comprehensive coverage | DNA degradation; High cost |
| Enzymatic Methyl-Sequencing (EM-seq) [40] | Single-base | Lower than WGBS | Preserves DNA integrity; Better for GC-rich regions | Newer method; Less established |
| Illumina EPIC Array [40] | Pre-defined CpG sites | Low | Cost-effective; Standardized processing | Limited to pre-designed sites |
| Oxford Nanopore [40] | Single-base | High (~1μg) | Long reads; No conversion needed | Higher error rate; Custom analysis |
| FinaleMe (Computational) [41] | Inference from WGS | N/A | No bisulfite conversion; Uses existing WGS | Less accurate in CpG-poor regions |
Fragmentomics Analysis from Targeted Panels
Fragmentomics analysis typically begins with cfDNA extraction from plasma samples, followed by library preparation and sequencing using either whole-genome or targeted approaches. For targeted panels, the following steps are employed:
cfDNA Extraction and Quality Control: DNA is extracted using kits such as the DNeasy Blood & Tissue Kit or specialized cfDNA extraction kits, with quantification via fluorometry and quality assessment using NanoDrop [40].
Library Preparation and Sequencing: Libraries are prepared according to panel-specific protocols, with hybridization-based capture for targeted panels. Sequencing depth varies by application - typically 3,000x for standard panels but exceeding 60,000x for ultra-sensitive applications [7].
Fragmentomic Feature Extraction: Multiple metrics are calculated from aligned BAM files:
- Fragment size distribution: Proportion of fragments in specific size bins (e.g., <150 bp) [7]
- Normalized depth: Read counts normalized by region length and sequencing depth [7]
- End motif analysis: Diversity of 4-mer sequences at fragment ends [7]
- Nucleosome positioning: Protection patterns indicating transcription factor binding [7]
Data Integration and Model Training: Features from multiple omics layers are integrated using methods like MOFA+ or deep learning approaches, with performance validation through cross-validation in independent cohorts [37] [7].
Multi-Omics Factor Analysis (MOFA+) Protocol
MOFA+ is a statistical framework for unsupervised integration of multiple omics datasets. The standard protocol includes:
Data Preprocessing: Each omics dataset is preprocessed independently. For RNA-seq, counts are transformed using variance stabilizing transformation (VST). DNA methylation data is log-transformed to approximate normality [38].
Feature Selection: To enhance model performance, the most variable features are selected - top 2% of variable CpG sites for methylation and top 50% of variable genes for expression data [38].
Model Training: The model is trained with multiple factors (typically 5-25), with the optimal number determined by the elbow method on the evidence lower bound. Models are run with slow convergence mode and appropriate likelihoods for each data type [38].
Downstream Analysis: Factors are interpreted based on their feature weights, with association to clinical variables and survival outcomes. Factors explaining >10% variance in at least one omic are typically retained for further analysis [38] [37].
Figure 1: MOFA+ Multi-Omics Integration Workflow. The statistical framework integrates diverse data types through factor analysis. [38] [37]
The Scientist's Toolkit: Essential Research Reagents and Platforms
Table 4: Key research reagents and platforms for multi-omics studies
| Category | Product/Platform | Application | Key Features |
|---|---|---|---|
| Methylation Arrays | Illumina MethylationEPIC v2 [40] | Genome-wide methylation profiling | >935,000 CpG sites; Enhanced coverage of enhancer regions |
| Targeted Panels | Guardant360 CDx [7] | Clinical cfDNA analysis | 55 genes; FDA-approved for liquid biopsy |
| Targeted Panels | FoundationOne Liquid CDx [7] | Comprehensive cfDNA profiling | 309 genes; Broad genomic coverage |
| cfDNA Isolation | ApoStream [42] | Circulating tumor cell isolation | Preserves cellular morphology for downstream analysis |
| Spatial Analysis | ArchR [43] | Spatial multi-omics integration | Links chromatin accessibility with spatial context |
| Data Integration | Seurat v5 [43] | Multi-omics data integration | Bridge integration for unmatched datasets |
Fragmentomics-Based Methylation Inference
The FinaleMe algorithm represents a breakthrough in inferring DNA methylation states from standard whole-genome sequencing of cfDNA, bypassing the need for bisulfite conversion:
Model Architecture: FinaleMe employs a non-homogeneous Hidden Markov Model (HMM) that incorporates three key features: fragment length, normalized coverage, and the distance of each CpG to the center of the DNA fragment [41].
Training and Validation: The model is trained on matched WGS and WGBS data from the same blood samples, learning the relationship between fragmentation patterns and methylation status. Performance is validated by comparing predictions with actual methylation states from WGBS [41].
Performance Characteristics: The method achieves high accuracy in CpG-rich regions (auROC=0.91 for fragments with ≥5 CpGs) but is less accurate in CpG-poor regions. It successfully predicts tissue-of-origin fractions that correlate with tumor fractions estimated by copy number variation analysis [41].
Figure 2: FinaleMe Workflow for Methylation Inference. The computational method predicts methylation states from fragmentation patterns. [41]
Validation in Clinical Cohorts
Robust validation of multi-omics models requires careful study design and appropriate cohort selection:
Cohort Characteristics: Successful studies utilize well-characterized cohorts with appropriate sample sizes. The University of Wisconsin cohort (n=431) includes multiple cancer types with subtype information, while the GRAIL cohort (n=198) provides ultra-deep sequencing data [7].
Performance Metrics: Area under the receiver operating characteristic curve (AUROC) serves as the primary metric for classification performance, with additional evaluation using precision-recall curves and confusion matrices for subtype classification [37] [7].
Clinical Association: Validation includes association with clinical variables such as tumor stage, lymph node involvement, metastasis, and survival outcomes. Genes identified through multi-omics integration should show significant association with clinical phenotypes after false discovery rate correction [37].
Low Tumor Fraction Simulation: To assess real-world applicability, studies perform in silico dilution series to evaluate performance at low tumor fractions (0.1%-5%), mimicking minimal residual disease or early cancer detection scenarios [7].
The integration of genomics, fragmentomics, and methylation data represents a powerful approach for advancing liquid biopsy applications. Performance comparisons reveal that statistical integration methods like MOFA+ currently outperform deep learning approaches for feature selection in cancer subtyping, while fragmentomics metrics based on normalized depth provide the most robust classification across cancer types. The emergence of computational methods like FinaleMe that infer methylation from fragmentation patterns further expands the potential to extract maximal information from single assays. As these technologies mature, standardized validation in diverse clinical cohorts will be essential for translation into routine clinical practice, ultimately enabling more precise cancer detection, monitoring, and treatment selection.
The application of machine learning (ML) to cell-free DNA (cfDNA) analysis represents a transformative approach in clinical cancer research. cfDNA fragments circulating in blood plasma carry rich information, including genetic, epigenetic, and fragmentomic patterns that can reveal the presence of cancer, often at early stages [22] [44]. For researchers and drug development professionals, ensuring the validity and reliability of these ML models is paramount, as decisions based on their outputs may directly impact patient care and clinical trial outcomes.
The validation of cfDNA-based ML models extends beyond conventional performance metrics, requiring specialized strategies to address the unique challenges of clinical liquid biopsy applications. These challenges include typically low tumor DNA fractions in early-stage disease (often 1% or less), biological variability in cfDNA fragmentation patterns, and the critical need for model interpretability in clinical settings [45] [46]. This guide examines hyperparameter tuning strategies within this context, providing a structured comparison of methodologies to help researchers optimize model performance while maintaining scientific rigor and clinical relevance.
Hyperparameter Tuning Fundamentals in Machine Learning
Core Concepts and Terminology
Hyperparameters are configuration variables that govern the training process of machine learning models, set before the learning process begins. Unlike model parameters, which are learned from the data, hyperparameters control aspects such as model architecture, complexity, and learning rate [47]. In clinical cfDNA analysis, where datasets are often high-dimensional and complex, appropriate hyperparameter selection is crucial for building models that can detect subtle cancer signals amidst biological noise.
Hyperparameter optimization, or tuning, is the systematic process of finding the optimal combination of hyperparameter values that results in the best model performance [47] [48]. This process involves balancing bias (the ability to connect relationships between data points for accurate predictions) and variance (the ability to process new data) to create models that generalize well to unseen clinical samples [47].
The Hyperparameter Tuning Workflow
The following diagram illustrates the standard workflow for hyperparameter optimization in machine learning projects, particularly relevant to cfDNA analysis:
Comparative Analysis of Hyperparameter Tuning Methods
Methodologies and Experimental Protocols
Grid Search
Methodology: Grid Search is a brute-force approach that systematically works through every possible combination of hyperparameters from predefined sets [48] [49]. For each combination, it trains the model and evaluates performance using cross-validation. The algorithm exhaustively explores the search space, guaranteeing finding the optimal combination within the specified grid.
Experimental Protocol:
- Define a grid of hyperparameter values (e.g., for a random forest: nestimators = [50, 100, 150], maxdepth = [None, 10, 20])
- For each combination in the grid, train the model with k-fold cross-validation (typically 3-5 folds)
- Calculate the average performance metric across all folds for each combination
- Select the combination with the highest average performance [48]
Implementation Example (from cfDNA research):
This grid with 6 hyperparameters would require training 3×4×3×3×3×2 = 648 different models, each with k-fold cross-validation [49].
Random Search
Methodology: Random Search randomly samples hyperparameter combinations from specified distributions over a fixed number of iterations [48] [49]. Instead of exhaustive search, it explores the parameter space stochastically, which can be more efficient in high-dimensional spaces where only a few parameters significantly impact performance.
Experimental Protocol:
- Define distributions for each hyperparameter (e.g., n_estimators = randint(10, 200))
- Set the number of iterations (n_iter) based on computational budget
- For each iteration, randomly sample one value from each distribution
- Train and evaluate the model with cross-validation
- After all iterations, select the best-performing combination [48]
Implementation Example:
Bayesian Optimization
Methodology: Bayesian Optimization builds a probabilistic model (surrogate function) that maps hyperparameters to performance metrics, then uses this model to select the most promising hyperparameters to evaluate in the next iteration [47] [48]. It balances exploration (trying uncertain regions) and exploitation (focusing on known promising regions).
Experimental Protocol:
- Build a prior distribution over the objective function (performance metric)
- For several iterations:
- Select the next hyperparameter combination by optimizing an acquisition function
- Evaluate the objective function at the selected point
- Update the surrogate model with the new results
- Return the best-performing hyperparameter combination
Common surrogate models include Gaussian Processes, Random Forest Regression, and Tree-structured Parzen Estimators (TPE) [48].
Performance Comparison and Experimental Data
Table 1: Comparative Analysis of Hyperparameter Tuning Methods
| Method | Computational Efficiency | Best For | Advantages | Limitations | cfDNA Application Context |
|---|---|---|---|---|---|
| Grid Search | Low - tests all combinations [49] | Small parameter spaces (≤4 parameters) [49] | Guaranteed optimal in grid; Simple implementation [48] | Exponential complexity; Wasted computation [48] | Limited utility; Suitable for final fine-tuning of 2-3 key parameters |
| Random Search | Medium - fixed number of samples [49] | Medium to large spaces; When some parameters unimportant [49] | More efficient for high dimensions; Better resource allocation [48] [49] | May miss optimum; No convergence guarantee [48] | Preferred for initial exploration of fragmentomic feature spaces |
| Bayesian Optimization | High - learns from previous trials [47] [48] | Complex spaces; Limited computational budget [48] | Requires fewer evaluations; Informed search strategy [47] [48] | Complex implementation; Overhead in model maintenance [48] | Ideal for clinical cfDNA models with constrained sample availability |
Table 2: Empirical Performance in Clinical cfDNA Studies
| Study Reference | Application | Tuning Method | Performance Metrics | Clinical Impact |
|---|---|---|---|---|
| SPOGIT Study [10] | GI cancer detection (multi-model) | Not specified (multiple algorithms) | 88.1% sensitivity, 91.2% specificity in multicenter validation (n=1,079) | Projected 92% reduction in late-stage diagnoses |
| DECIPHER-RCC [46] | Renal cell carcinoma detection | Stacked ensemble with automated tuning | AUC: 0.966 (validation), 0.952 (external) | High sensitivity for early-stage RCC with 92.9% specificity |
| Open Chromatin Guide [45] | Breast/pancreatic cancer detection | XGBoost with hyperparameter optimization | Improved accuracy using chromatin features | Identified key genomic loci associated with disease |
| Theoretical Comparison [49] | Breast cancer classification | Grid vs Random Search | Similar best scores (≈96.4%) with 60x fewer evaluations for random search | Significant computational savings without performance loss |
Domain-Specific Validation Strategies for cfDNA ML Models
Addressing Unique Challenges in cfDNA Analysis
Clinical cfDNA analysis presents distinctive challenges that necessitate specialized validation approaches beyond standard ML practices. These include low tumor fraction in early-stage disease (often 1-3% as reported in breast cancer studies [45]), biological variability in fragmentation patterns, and the multi-factorial nature of cfDNA signatures encompassing genetic, epigenetic, and fragmentomic features [22] [44].
Critical Validation Practices for Robust Clinical Models
Stratified Performance Reporting
Merely reporting aggregate performance metrics across an entire test set can mask critical performance variations across clinically relevant subgroups. As demonstrated in protein function prediction studies, models achieving 95% overall accuracy may perform below 50% on challenging "twilight zone" cases that lack obvious parallels in the training data [50]. In cfDNA analysis, stratification should consider:
- Tumor fraction levels: Model performance should be evaluated across different tumor fraction ranges, particularly at low fractions (<1%) relevant for early detection
- Cancer stages and subtypes: Separate reporting for early-stage (I/II) versus late-stage (III/IV) cancers, and across histological subtypes
- Sample characteristics: Performance across different sample collection protocols, processing delays, and DNA yield categories
Challenge-Based Validation Set Design
Curating validation sets that represent "worthwhile learning points" is essential for meaningful model assessment [50]. This involves deliberately including challenging cases that probe the model's ability to make clinically subtle distinctions:
- Hard negatives: Benign conditions with similar cfDNA profiles to malignancies (e.g., inflammatory conditions vs. cancer)
- Early-stage cases: Samples with low tumor fraction that represent the intended use case for screening
- Biologically similar classes: Different cancer types with overlapping cfDNA features to test classification specificity
The following diagram illustrates a comprehensive validation workflow for cfDNA machine learning models:
Essential Research Reagents and Computational Tools
Table 3: Research Reagent Solutions for cfDNA ML Studies
| Category | Specific Solution | Function/Application | Implementation Example |
|---|---|---|---|
| Wet Lab Reagents | Plasma collection tubes (e.g., Streck, EDTA) | Cell-free DNA stabilization | 600 μL human plasma used in breast cancer study [45] |
| DNA Extraction Kits | Commercial cfDNA isolation kits | Recovery of short DNA fragments | Extraction within 24h of plasma arrival for RCC study [46] |
| Library Prep | PCR-free library preparation | Minimizing amplification bias | Used in DECIPHER-RCC study to preserve fragmentomics [46] |
| Sequencing | Low-pass whole genome sequencing | Cost-effective fragmentomic analysis | Uniform 5× coverage on DNBSEQ-T7 platform [46] |
| Computational Tools | Hyperparameter optimization libraries (scikit-learn, Optuna, HyperOpt) | Automated parameter tuning | GridSearchCV/RandomizedSearchCV for model optimization [47] [48] |
| ML Frameworks | XGBoost, Random Forest, Deep Learning | Model implementation | XGBoost for open chromatin-guided classification [45] |
| Validation Platforms | Custom cross-validation pipelines | Performance assessment | 5-fold cross-validation in ensemble models [46] |
Based on the comparative analysis of hyperparameter tuning methods and their application in clinical cfDNA research, the following best practices emerge:
Method Selection Strategy: Begin with Random Search for initial exploration of large parameter spaces, particularly when working with high-dimensional cfDNA feature sets (fragmentomics, methylomics, nucleosomics). Reserve Grid Search for final fine-tuning of 2-3 most critical parameters, and consider Bayesian Optimization when computational resources are limited relative to model complexity [47] [48] [49].
Clinical Validation Rigor: Implement comprehensive validation strategies that include independent multicenter cohorts, stratification by clinical variables (cancer stage, subtype, tumor fraction), and challenge sets containing diagnostically difficult cases [10] [50]. The SPOGIT study exemplifies this approach with validation across 1,079 participants from multiple centers [10].
Performance Interpretation Context: Always interpret hyperparameter tuning results within the context of clinical utility rather than purely statistical metrics. A model with slightly lower overall accuracy but consistent performance across early-stage cancers and low tumor fractions may have greater clinical value than a high-performing model that fails on these critical cases [50] [46].
Computational-Clinical Balance: Strike a balance between computational efficiency and clinical robustness. While Random Search may efficiently identify good parameters, the final model selection should prioritize clinical reliability across diverse patient subgroups and challenging clinical scenarios [50].
The integration of sophisticated hyperparameter tuning strategies with domain-specific validation approaches will continue to enhance the development of robust, clinically applicable cfDNA-based machine learning models, ultimately advancing their translation into cancer diagnostics and drug development pipelines.
Validating machine learning (ML) models for cell-free DNA (cfDNA) analysis in clinical cohorts presents unique data challenges. A significant hurdle is managing censored observations—where a patient's outcome remains unknown at the end of the study—and competing risks—where alternative events precludes the occurrence of the primary event of interest. For instance, in a study of cfDNA's ability to detect cancer relapse, death from an unrelated cause is a competing risk that prevents the observation of a relapse. Traditional survival analysis methods, like the Kaplan-Meier estimator, can produce biased results in these scenarios by inappropriately treating competing events as simple censoring. This guide objectively compares the performance of modern statistical and machine learning methods designed to handle these complexities, providing a framework for robust clinical model validation.
Foundational Concepts in Competing Risks Analysis
In standard survival analysis with a single event of interest, subjects who experience a different event are typically treated as censored. However, this approach relies on an assumption of independent censoring, which is unverifiable and often invalid in the presence of competing risks. Analyzing such data requires a shift in perspective and methodology [51].
The two principal measures for competing risks data are:
- Cause-Specific Hazard (CSH): The instantaneous rate of occurrence of the primary event in subjects who are still event-free. This approach treats competing events as censored and answers the question, "What is the risk of the event among those who have not yet experienced any event?" [51] [52].
- Cumulative Incidence Function (CIF): The marginal probability of experiencing the primary event over time, in the presence of competing events. It does not assume independence between events and provides a more direct and interpretable estimate of the actual risk [51].
Consequently, two primary regression models have been developed, each tied to one of these measures:
- Cause-Specific Hazards (CSH) Model: Models the hazard for the primary event, treating competing events as censored. It is ideal for etiologic research questions aimed at understanding the direct biological effect of a variable (e.g., a biomarker) on the event itself [52].
- Fine-Gray (Subdistribution Hazards) Model: Models the hazard of the CIF. It keeps subjects who experience a competing event in the risk set, thereby estimating the total effect of a variable, which includes both its direct effect and any indirect effects mediated through the competing event [51] [52]. This is often more relevant for public health interventions, but can be misleading for understanding direct biological mechanisms.
Comparative Performance of Modern Analytical Methods
A recent comparative review evaluated multiple modern methods in high-dimensional settings, assessing them on variable selection, estimation accuracy, discrimination, and calibration. The table below summarizes the key findings from this extensive simulation study [53].
Table 1: Performance Comparison of Competing Risks Methods in High-Dimensional Settings
| Method Category | Specific Methods | Key Performance Findings | Strengths | Weaknesses |
|---|---|---|---|---|
| Penalized Regression | LASSO, SCAD, MCP | SCAD and MCP provided superior calibration in specific scenarios. | Provides variable selection and stable estimation. | Performance can vary depending on the penalty function. |
| Likelihood-Based Boosting | CoxBoost (CB) | Achieved the best variable selection, estimation stability, and discriminative ability, particularly in high-dimensional settings. | Highly stable and accurate for variable selection and prediction. | - |
| Random Forest | Random Survival Forest (RF) | Captured nonlinear effects but exhibited instability, with high false discovery rates. | Capable of modeling complex, nonlinear relationships. | High false discovery rate; can be unstable. |
| Deep Learning | DeepHit (DH) | Captured nonlinear effects but suffered from poor calibration. | Flexible architecture for complex pattern recognition. | Poor calibration; can be computationally intensive. |
Furthermore, when data originates from multiple clinical centers, introducing a cluster structure, standard competing risks methods may be inadequate. A 2023 simulation study found that a Fine-Gray model extension by Katsahian et al., which uses a specific weighting technique, showed the best performance in terms of bias, the square root of the mean squared error, and power in nearly all clustered scenarios [54].
Essential Experimental Protocols for Model Validation
Protocol 1: Benchmarking ML Models with Multiple Data Splits
A robust comparison of ML models, including those for competing risks, requires accounting for variance in performance estimates. A flawed evaluation can lead to selecting a suboptimal model for deployment [55] [29].
Detailed Methodology:
- Multiple Random Splits: Instead of a single train-test split, generate multiple (e.g., 20-100) random splits of the dataset. Vary the ratios (e.g., 70/30, 80/20) to assess stability [55] [29].
- Ten-Fold Cross-Validation: Within the training set of each split, perform 10-fold cross-validation for hyperparameter tuning and initial performance estimation. Use consistent random seeds for initialization and data ordering across model comparisons to ensure fairness [29].
- Statistical Testing: On the held-out test sets, use statistical tests to determine if performance differences between models are meaningful. For metrics like the C-index or AUC, a Student's paired t-test can be applied across the multiple test splits to assess significance [29].
- Learning Curves: Plot training and validation learning curves for all models. The optimal model typically shows a "sweet spot" where the validation error is minimized before the training error continues to decrease alone—a sign of overfitting [29].
Protocol 2: Applying the Katsahian Method for Clustered Data
For multi-center clinical trial data with competing events, the following workflow is recommended based on the superior performance of the Katsahian method [54].
Detailed Methodology:
- Data Preparation: Structure the data to include time-to-event, event type indicator (e.g., 0: censored, 1: primary event, 2: competing event), treatment/exposure group, and a cluster identifier (e.g., center ID).
- Model Specification: Implement the Fine-Gray subdistribution hazards model while incorporating the cluster structure. This is achieved using a specific weighting technique where individuals who have experienced a competing event remain in the risk set but are weighted [54].
- Parameter Estimation & Effect Estimation: Use the alternative estimation method proposed by Katsahian et al. to fit the model and obtain the regression coefficients for the treatment effect. This method allows for unbiased effect estimation while accounting for both the competing events and the correlation of outcomes within clusters [54].
- Variance Assessment: Calculate the confidence intervals for the hazard ratios, ensuring the model has correctly accounted for the within-cluster correlation to avoid underestimating the variance [54].
The following diagram illustrates the logical workflow and key decision points for selecting an appropriate analytical method.
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Materials and Analytical Tools for cfDNA and Competing Risks Analysis
| Item Name | Function/Brief Explanation | Example Application in Protocol |
|---|---|---|
| Plasma Samples (EDTA Tubes) | Collection and stabilization of peripheral blood for cfDNA isolation. | The foundational biological material for all downstream analysis [56]. |
| Magnetic Bead-based cfDNA Kits | Isolation and purification of cfDNA from plasma samples. | Used to extract high-quality cfDNA prior to sequencing or qPCR [56]. |
| Bisulfite Conversion Kit | Chemical treatment that converts unmethylated cytosine to uracil, allowing for methylation analysis. | Critical for preparing cfDNA for methylation-based biomarker assays [56]. |
| LASSO / Boruta Algorithm | Machine learning feature selection methods to identify the most relevant biomarkers from a high-dimensional set. | Filters thousands of potential methylation sites or fragmentomics features to a panel with the highest predictive power for the event of interest [56]. |
| CoxBoost (Likelihood-Based Boosting) | A high-dimensional competing risks method for variable selection and prediction. | Building a robust prognostic model from high-dimensional genomic data (e.g., >47,000 gene expressions) while accounting for competing events like non-cancer mortality [53]. |
R glmnet & Boruta Packages |
Software implementations for performing LASSO and Boruta feature selection, respectively. | Used in the model development workflow to select the best-performing variables from a candidate set [56]. |
| Fine-Gray Model Extension | A statistical model for competing risks that accounts for cluster correlations. | Analyzing time-to-relapse data from a multi-center clinical trial, where death from other causes is a competing event [54]. |
| Stacked Ensemble ML Model | A machine learning model that combines multiple base models to improve predictive performance. | Integrating predictions from several different models (e.g., RF, GLM) to improve the sensitivity and specificity of a liquid biopsy assay for early cancer detection [12]. |
Discussion and Concluding Remarks
The choice between cause-specific and Fine-Gray models is not one of superiority but of aligning the analytical method with the research question. For etiologic studies seeking a direct biological effect—common in early-stage biomarker and drug mechanism validation—the cause-specific hazards model is often the most appropriate as it isolates the effect on the disease process itself [52]. In contrast, for predicting the overall real-world benefit of an intervention where the risk of competing events is part of the clinical context, the Fine-Gray model provides a more comprehensive estimate [51] [52].
For high-dimensional settings typical of cfDNA studies (e.g., involving methylation sites or fragmentomics features), CoxBoost (CB) has demonstrated top-tier performance in variable selection and discriminative ability, outperforming other complex methods like random forests and deep learning, which, despite their flexibility, can suffer from instability and poor calibration [53]. Finally, researchers must be vigilant of the data structure; ignoring clustering from multi-center studies can lead to underestimated variances, making the extended Fine-Gray model by Katsahian et al. a critical tool for maintaining statistical integrity in modern clinical research [54].
Navigating Real-World Hurdles: Technical and Analytical Challenges in cfDNA ML
The accurate detection of circulating tumor DNA (ctDNA) in early-stage disease represents a significant challenge in oncology diagnostics. The primary obstacle is the low tumor fraction (TF), the proportion of tumor-derived DNA in the total cell-free DNA (cfDNA) pool, which often falls below the detection limits of conventional methods. This limitation critically impedes applications in cancer early detection, minimal residual disease (MRD) monitoring, and treatment response assessment. Researchers and drug developers are now advancing a new generation of sophisticated analytical techniques designed to enhance detection sensitivity. This guide objectively compares the performance of three innovative strategic approaches—methylation-based deconvolution, fragmentomics, and multimodal integration—against traditional methods, providing a detailed analysis of their experimental protocols and validation data for clinical cohort research.
Comparative Performance of Advanced Detection Methods
The following table summarizes key performance metrics of emerging strategies as validated in recent studies, highlighting their effectiveness in overcoming the low TF challenge.
Table 1: Performance Comparison of Advanced ctDNA Detection Methods for Early-Stage Disease
| Methodology | Reported Sensitivity in Early-Stage Cancers | Specificity | Key Cancer Types Validated In | Primary Technological Approach |
|---|---|---|---|---|
| Methylation-Based Deconvolution (SRFD-Bayes) [57] | 86.1% | 94.7% | Pan-Cancer (Breast, Colon, Lung, Liver, Prostate) | Machine learning on cfDNA methylation signatures from WGBS data. |
| Fragmentomics (NMF on Fragment Length) [58] | AUC = 0.96 (for early-stage cancers) | Not Explicitly Stated | Prostate Cancer, various other early-stage cancers | Shallow Whole-Genome Sequencing (sWGS) and Non-negative Matrix Factorization. |
| Tumor-Naïve Multimodal Profiling [59] | 54.5% (Breast Cancer); 80.0% (Colorectal Cancer) | 98.8% (Breast Cancer); 100% (Colorectal Cancer) | Breast Cancer, Colorectal Cancer | Integration of mutation, copy number alteration (CNA), and fragmentomics. |
| Traditional Mutation-Only (qPCR/ddPCR) [60] | Limited by VAF (~5% LOD for cobas EGFR test) | High | NSCLC (for EGFR mutations) | Reverse Transcription-PCR or digital PCR. |
Detailed Experimental Protocols and Methodologies
Methylation-Based Deconvolution Using SRFD-Bayes
This approach leverages the distinct methylation patterns of tumor-derived DNA, which persist even at low concentrations.
Workflow Overview:
The following diagram illustrates the key stages of the SRFD-Bayes diagnostic approach:
Key Experimental Steps [57]:
- Data Collection: Utilize single-end or paired-end Whole Genome Bisulfite Sequencing (WGBS) data of plasma cfDNA from both healthy individuals and cancer patients.
- Informative Methylation Marker Selection: Apply a custom informative score based on matrix norm to identify type-discriminative (TD) and type-specific (TS) methylation markers from hundreds of thousands of sites.
- Semi-Reference-Free Deconvolution (SRFD): Instead of relying on a pre-defined tissue methylation atlas, implement the SRFD algorithm to automatically learn a reference database directly from the mixed plasma cfDNA methylation data. Class labels provide structural constraints for the decomposition.
- Bayesian Diagnostic Model Construction:
- Use the learned reference database to deconvolve training samples (from late-stage patients and healthy controls) into source fraction vectors.
- Fit each tumor component to an independent Beta distribution.
- Train a Support Vector Machine (SVM) classifier on the original methylation profiles to create a pre-diagnostic model.
- For testing, fuse the SVM's diagnostic prior with the conditional probability from the Beta distributions to make a final SRFD-Bayes decision.
Unsupervised Fragmentomics via Non-Negative Matrix Factorization (NMF)
This method exploits the differences in fragment length patterns and genomic distributions between ctDNA and non-tumor cfDNA.
Workflow Overview:
The NMF-based fragmentomics workflow for unsupervised cancer detection is shown below:
Key Experimental Steps [58]:
- Sample Preparation and Sequencing: Perform shallow Whole-Genome Sequencing (sWGS) of plasma cfDNA. A mean coverage of 0.60X is sufficient, making this a cost-effective approach.
- Bioinformatic Processing: Align paired-end reads to the human reference genome. Using the resulting BAM files, compute a fragment length histogram for each sample, typically focusing on fragments between 50 bp and 350 bp.
- Data Matrix Construction: Compile the individual histograms into a single sample-by-fragment-length matrix. Normalize each row (sample) so that the counts sum to one, converting them to frequencies.
- Non-Negative Matrix Factorization (NMF): Apply NMF to the normalized frequency matrix. This unsupervised algorithm decomposes the matrix into two smaller, non-negative matrices:
- Signature Matrix: Represents the characteristic fragment length distributions of the underlying cfDNA sources (e.g., tumor vs. non-tumor).
- Weight Matrix: Represents the contribution (weight) of each signature to each sample. The weight of the tumor signature strongly correlates with the ctDNA fraction (r=0.75 in validation studies).
Tumor-Naïve Multimodal Profiling
This strategy enhances sensitivity by integrating signals from multiple orthogonal genomic and epigenetic features, without requiring prior tumor tissue sequencing.
Workflow Overview:
The tumor-naïve method integrates multiple data types from a single blood draw as depicted below:
Key Experimental Steps [59]:
- Comprehensive Library Preparation: Extract cfDNA and prepare sequencing libraries using a kit that incorporates Unique Molecular Identifiers (UMIs) to correct for amplification and sequencing errors.
- Parallel Multi-Assay Sequencing:
- Mutation Detection: Sequence the libraries using two complementary methods: a) Hybridization capture with a custom panel (e.g., 22 genes), and b) Multiplex PCR (mPCR) with an ultra-deep amplicon sequencing panel (e.g., 500 hotspots) to capture low-frequency variants.
- Non-Mutation Feature Profiling: Subject a portion of the libraries to shallow Whole-Genome Sequencing (sWGS) at low coverage (~0.5x) to obtain genome-wide data for Copy Number Alteration (CNA) analysis and fragmentomics (fragment length and end-motif analysis).
- Bioinformatic Analysis and Integration:
- Call variants from both hybridization and mPCR data, and filter out germline and clonal hematopoiesis (CHIP) variants using matched white blood cell DNA.
- Calculate CNA-based TF using the ichorCNA tool from sWGS data.
- Convert fragment length features into a quantitative score (NMFFLEN) using Non-negative Matrix Factorization.
- Determine the sample's final TF: if mutations are detected, TF is the mean Variant Allele Frequency (VAF); if not, TF is derived from the highest signal among the CNA or NMFFLEN scores.
The Scientist's Toolkit: Essential Research Reagents & Solutions
The following table catalogs key reagents, assays, and software tools essential for implementing the described methodologies.
Table 2: Essential Research Tools for Advanced ctDNA Analysis
| Tool Name | Type | Primary Function in Research | Example Use Case |
|---|---|---|---|
| xGen cfDNA Library Prep Kit [59] | Library Prep Kit | Prepares NGS libraries from low-input cfDNA; incorporates UMIs for error correction. | Foundation step for tumor-naïve multimodal and methylation sequencing workflows. |
| PredicineCARE Assay [61] | Targeted NGS Panel | Detects genomic alterations (SNVs, indels, fusions, CNVs) in blood/urine cfDNA. | Used in clinical trials (e.g., INAVO120, FIGHT-207) for patient selection and genomic profiling. |
| cobas EGFR Mutation Test v2 [62] [60] | FDA-Approved CDx | Detects specific EGFR mutations in plasma or tissue by RT-PCR. | Standard for detecting EGFR T790M and other mutations in NSCLC; comparator for novel assays. |
| BEAMing PCR [63] | Digital PCR Method | Ultra-sensitive quantification of mutant alleles in a wild-type background via emulsion PCR. | Detecting low-VAF EGFR mutations in ctDNA for NSCLC patient monitoring. |
| ichorCNA [59] [58] | Bioinformatics Algorithm | Estimates tumor fraction from low-coverage whole-genome sequencing data using CNA signals. | Critical component in fragmentomics and multimodal workflows for TF estimation. |
| Non-negative Matrix Factorization (NMF) [59] [58] | Computational Algorithm | Unsupervised decomposition of fragment length distributions to infer tumor-specific signatures and weights. | Core of the fragmentomics approach for cancer detection and TF estimation. |
The relentless challenge of low tumor fraction in early-stage cancer is being met with a new wave of sophisticated diagnostic strategies. Methylation-based deconvolution, unsupervised fragmentomics, and tumor-naïve multimodal profiling each offer distinct mechanisms to enhance detection sensitivity far beyond the capabilities of traditional mutation-based assays. While methylation profiling provides high sensitivity and critical tumor localization data, fragmentomics offers a cost-effective and entirely unsupervised alternative. The multimodal approach, by integrating several orthogonal signals, promises robustness and high performance, particularly in cancers with higher ctDNA shedding. The choice of methodology for clinical cohort validation will depend on the specific research objectives, required sensitivity, budget, and computational resources. The ongoing development and refinement of these platforms, as evidenced by the advancing reagent and software toolkit, are poised to solidify the role of liquid biopsy in early cancer detection and personalized medicine.
Managing Missing Data and Ensuring Representative Cohort Selection
The validation of cell-free DNA (cfDNA) machine learning models for clinical cancer phenotyping represents a frontier in liquid biopsy research. The analytical performance of these models—whether for cancer detection, tissue-of-origin mapping, or therapy monitoring—depends fundamentally on two pillars: robust handling of missing data and selective recruitment of representative patient cohorts. cfDNA fragmentomics analyzes population-level patterns in DNA fragmentation, such as fragment length distributions, end motifs, and nucleosomal positioning, to infer epigenetic and transcriptional information from tumor cells [7]. These patterns serve as inputs for machine learning classifiers that must perform reliably across diverse clinical settings and patient populations.
Missing data poses a particular challenge in cfDNA analyses, where technical artifacts from sample collection, processing, or sequencing can introduce systematic gaps in fragmentomic metrics. The handling of these missing values directly influences model accuracy and clinical applicability. Simultaneously, cohort selection strategies determine whether developed models can generalize beyond the development dataset to broader populations. This guide systematically compares current methodologies for addressing these interconnected challenges, providing experimental data and frameworks to guide researchers in developing clinically translatable cfDNA models.
Understanding Missing Data Mechanisms in Clinical Studies
The statistical literature classifies missing data into three primary mechanisms, each with distinct implications for analytical approaches and potential biases [64] [65].
- Missing Completely at Random (MCAR): The absence of data values is unrelated to both observed and unobserved variables. Examples include sample processing errors, random tube labeling mistakes, or instrument failures affecting measurements unpredictably. Under MCAR, the complete cases remain representative of the original sample [65].
- Missing at Random (MAR): Missingness depends on observed variables but not on unobserved values. For instance, blood sample hemolysis rates might correlate with patient body mass index (observable), but conditional on BMI, hemolysis is random regarding cfDNA concentration (potentially missing) [64] [65].
- Missing Not at Random (MNAR): The missingness mechanism depends on the unobserved values themselves. For example, very low cfDNA concentrations might fall below assay detection limits, resulting in missing fragmentomic metrics that systematically differ from observed values [64] [65].
Table 1: Missing Data Mechanisms and Their Impact on cfDNA Studies
| Mechanism | Definition | cfDNA Example | Potential Bias |
|---|---|---|---|
| MCAR | Missingness independent of all data | Sample lost due to freezer malfunction | Minimal with sufficient sample size |
| MAR | Missingness depends on observed variables | Sequencing depth variation by clinical site | Correctable with appropriate methods |
| MNAR | Missingness depends on unobserved values | Undetectable short fragments in low-tumor fraction samples | Significant and difficult to correct |
Comparative Analysis of Missing Data Handling Methods
Traditional and Modern Imputation Approaches
Multiple methodologies exist for handling missing data, ranging from simple deletion to sophisticated machine learning-based imputation [64] [65] [66].
Complete Case Analysis (CCA), also known as list-wise deletion, removes any observation with one or more missing values. While traditionally discouraged in statistical analysis except for negligible missingness under MCAR, recent evidence suggests CCA performs comparably to multiple imputation in supervised machine learning contexts, even with substantial missingness (up to 75%) under MAR and MNAR mechanisms [66].
Imputation methods replace missing values with estimated substitutes:
- Simple imputation uses mean, median, or mode substitution, potentially distorting distributions and relationships [65].
- Regression imputation predicts missing values based on relationships with observed variables in complete cases [65].
- Multiple Imputation (MI) creates several complete datasets with different imputed values, analyzes each separately, and pools results [66].
- Machine learning approaches include k-nearest neighbors (KNN), random forest methods (e.g., missForest), and deep learning models that capture complex, nonlinear relationships among variables [65] [67].
Experimental Comparison of Handling Methods
A comprehensive 2024 study evaluated five missing data methods (CCA, mean imputation, hot deck imputation, regression imputation, and multiple imputation) across ten real-world datasets with intentionally introduced missingness ranging 5-75% under MCAR, MAR, and MNAR mechanisms [66]. The research focused specifically on supervised machine learning applications, measuring classification accuracy and computational efficiency.
Table 2: Performance Comparison of Missing Data Handling Methods in Supervised Machine Learning
| Method | Computational Efficiency | MCAR Performance | MAR Performance | MNAR Performance | Optimal Use Case |
|---|---|---|---|---|---|
| Complete Case Analysis | Highest | Comparable to MI | Comparable to MI | Comparable to MI | Large datasets, computational constraints |
| Mean Imputation | High | Moderate | Poor | Poor | Minimal missingness, exploratory analysis |
| Hot Deck Imputation | Moderate | Moderate | Moderate | Moderate | Mixed data types, small to moderate datasets |
| Regression Imputation | Moderate | Good | Good | Moderate | Strong correlations among variables |
| Multiple Imputation | Lowest | Best | Best | Best | Final analysis, small to moderate datasets |
The investigation revealed that "in nearly all scenarios, CCA performs comparably to MI, even with substantial levels of missingness under the MAR and MNAR conditions and with missingness in the output variable for regression problems" [66]. Given MI's considerable computational demands, the study recommends CCA for supervised machine learning in big-data environments.
Specialized Machine Learning Approaches
Advanced machine learning methods offer distinct advantages for high-dimensional cfDNA data:
- Cross-Fit Double Machine Learning (DM): A semiparametric approach that uses flexible machine learning models to estimate nuisance functions (propensity scores and outcome models) while employing cross-fitting to reduce overfitting bias. DM maintains double robustness—remaining consistent if either the propensity score or outcome model is correctly specified [67].
- XGBoost and Random Forest: Tree-based ensemble methods naturally handle missing values through surrogate splits in decision trees, often performing well without explicit imputation [68] [67].
- Deep Neural Networks: Can learn complex missingness patterns and implement sophisticated imputation strategies, such as denoising autoencoders, particularly beneficial for high-dimensional fragmentomics data [67].
Cohort Selection and Representation Frameworks
Multi-Cohort Validation Strategies
Robust model development requires intentional cohort selection and validation across diverse populations. The 2025 multi-center rheumatoid arthritis metabolomics study established a comprehensive framework applicable to cfDNA research, employing seven cohorts across five medical centers with distinct geographical distributions [69]. This design included:
- Exploratory cohort (n=90) for initial biomarker discovery
- Discovery cohort (n=1,350) for model development
- Five independent validation cohorts (n=1,423 total) from geographically distinct locations
This strategy ensures that developed models maintain performance across diverse clinical settings and patient populations, a critical requirement for clinically applicable tests [69].
Temporal Validation in Dynamic Clinical Environments
Clinical environments evolve rapidly due to changing medical practices, technologies, and patient characteristics. A 2025 diagnostic framework for temporal validation addresses this challenge through four stages [70]:
- Temporal partitioning - Splitting data by time period rather than randomly
- Characterization of evolution - Tracking how patient outcomes and characteristics change over time
- Longevity analysis - Exploring trade-offs between data quantity and recency
- Feature importance monitoring - Identifying shifting variable relevance across time periods
When applied to predicting acute care utilization in cancer patients, this framework revealed moderate temporal drift, underscoring the importance of temporal considerations when validating machine learning models for clinical deployment [70].
Consortium-Based Cohort Development
Large-scale consortium cohorts provide statistical power and diversity for developing generalizable models. The NCI Cohort Consortium includes investigators responsible for more than 77 high-quality cohorts studying large and diverse populations [71]. Membership eligibility requires:
- Minimum enrollment thresholds (5,000+ participants for cancer incidence endpoints; 400+ cancer diagnoses for survival outcomes)
- Willingness to share data and actively participate in consortium activities
- Adherence to standardized bylaws governing data quality and governance [71]
Such consortia enable validation across diverse demographic groups and healthcare systems, strengthening evidence for clinical applicability.
Integrated Workflow for Managing Missing Data and Cohort Selection
The following workflow diagram illustrates a comprehensive approach to managing missing data and cohort selection throughout the model development lifecycle, integrating methods discussed in this guide:
Experimental Protocols for Method Validation
Protocol for Evaluating Missing Data Handling Methods
To validate missing data approaches specifically for cfDNA fragmentomics, implement this experimental protocol:
Data Preparation: Begin with a complete cfDNA dataset (e.g., from a targeted sequencing panel) with comprehensive fragmentomic metrics including fragment size distributions, end motif diversity, and nucleosomal positioning patterns [7].
Missingness Introduction: Systematically introduce missing values under controlled mechanisms:
- MCAR: Randomly remove values across all variables
- MAR: Remove values in specific variables based on observed values in other variables (e.g., remove fragment length data when GC content is extreme)
- MNAR: Remove values based on thresholds in the variable itself (e.g., remove very short fragments <100bp that might be undetectable in low-quality samples)
Method Application: Apply each handling method (CCA, MI, KNN, etc.) to the datasets with introduced missingness.
Performance Assessment: Compare each method's performance using:
- Model Accuracy: AUC, sensitivity, specificity for classification tasks
- Parameter Recovery: Bias in effect size estimates for key variables
- Computational Efficiency: Processing time and resource requirements [66]
Protocol for Multi-Cohort Validation Studies
To establish generalizable cfDNA models, implement this cohort validation protocol:
Cohort Selection: Identify multiple independent cohorts representing:
- Different geographic regions
- Diverse healthcare settings (academic, community)
- Varied demographic compositions
- Different sample collection and processing protocols [69]
Standardized Data Collection: Implement consistent:
Model Training and Validation:
- Train initial models on discovery cohorts
- Validate performance across independent cohorts
- Assess performance consistency across patient subgroups
- Evaluate temporal stability in longitudinal cohorts [70]
Research Reagent Solutions for cfDNA Studies
Table 3: Essential Research Reagents and Platforms for cfDNA Fragmentomics
| Reagent/Platform | Function | Application in cfDNA Studies |
|---|---|---|
| Streck Cell-Free DNA BCT Tubes | Blood collection tube with preservatives | Maintains cfDNA stability during transport |
| QIAamp Circulating Nucleic Acid Kit | Nucleic acid extraction | Isolates cfDNA from plasma samples |
| Targeted Sequencing Panels (e.g., Tempus xF, Guardant360, FoundationOne Liquid CDx) | Gene capture and sequencing | Enables focused fragmentomic analysis of cancer-related genes |
| UHPLC Systems (e.g., Vanquish UHPLC) | Liquid chromatography separation | Separates metabolites in untargeted metabolomics |
| Orbitrap Mass Spectrometers | High-resolution mass detection | Identifies and quantifies metabolites |
| Custom Targeted Panels (e.g., 508-822 gene panels) | Hypothesis-driven sequencing | Balances coverage with practical constraints |
Effective management of missing data and strategic cohort selection are interdependent components in developing clinically valid cfDNA machine learning models. The experimental evidence presented demonstrates that complete case analysis remains a competitive approach for supervised learning problems, even under high missingness rates and non-random mechanisms. This challenges conventional statistical wisdom but offers practical advantages for computational efficiency in big-data environments.
Simultaneously, multi-cohort validation strategies that incorporate temporal monitoring and diverse population representation provide the necessary foundation for generalizable models. The integration of these approaches—through the workflow and protocols outlined—enables researchers to develop cfDNA fragmentomics models that maintain performance across varied clinical settings and patient populations, accelerating the translation of liquid biopsy technologies into clinical practice.
Mitigating Algorithmic Bias and Promoting Model Fairness Across Demographics
Ensuring algorithmic fairness is a critical challenge in the development and deployment of machine learning models for clinical applications. In the context of validating cell-free DNA (cfDNA) machine learning models for cancer detection, mitigating bias is not just an ethical imperative but a prerequisite for clinical utility. This guide compares predominant bias mitigation strategies, provides detailed experimental protocols, and outlines essential tools for researchers developing equitable clinical models.
Comparison of Algorithmic Bias Mitigation Techniques
Bias mitigation strategies are categorized by their point of intervention in the machine learning lifecycle. The following table summarizes the core approaches, their methodologies, and key performance trade-offs.
Table 1: Comparison of Algorithmic Bias Mitigation Approaches
| Mitigation Category | Core Methodology | Key Advantages | Key Limitations & Trade-offs | Exemplary Performance in Healthcare |
|---|---|---|---|---|
| Pre-processing [73] [74] | Adjusts training data to remove biases before model training. Techniques include resampling, reweighting, and relabeling data points. | Addresses the root cause of bias in data. Does not require modifying model architecture. | Can be computationally expensive to gather new data; effects on downstream model bias lack theoretical guarantees [73]. | Performance varies highly with dataset quality; can improve model accuracy for underrepresented groups if data is representative [74]. |
| In-processing [73] | Modifies the model training algorithm itself to incorporate fairness constraints or adversarial debiasing. | Can provide provable guarantees on bias mitigation; allows for a tunable trade-off between fairness and accuracy [73]. | Requires access to model training process; computationally intensive, often requiring models to be trained from scratch [73]. | Effectiveness is model-specific; can enforce statistical fairness metrics like Equalized Odds during learning [75]. |
| Post-processing [76] [73] | Adjusts model outputs after training. Methods include threshold adjustment, reject option classification, and calibration. | Computationally efficient; does not require retraining model; ideal for "off-the-shelf" or commercial models [76]. | May require group membership for threshold adjustment; can involve direct trade-offs with overall accuracy [76] [73]. | Threshold adjustment reduced bias in 8/9 trials [76]. Reject option classification and calibration reduced bias in ~50% of trials (5/8 and 4/8, respectively) [76]. |
Detailed Experimental Protocols for Bias Mitigation
For researchers validating cfDNA models, implementing and testing these mitigation strategies requires rigorous, reproducible protocols.
Protocol for Post-Processing via Threshold Adjustment
This protocol is based on methods that demonstrated significant bias reduction in healthcare algorithms [76].
- 1. Model Training & Baseline Assessment: Train a binary classification model (e.g., cancer vs. healthy) using your standard protocol. Calculate performance metrics (Sensitivity, Specificity, AUC) and group fairness metrics (e.g., Equal Opportunity Difference, Demographic Parity) across relevant demographic groups (e.g., sex, race) [76] [75].
- 2. Group-Specific Threshold Calibration: Instead of a single global decision threshold, determine optimal thresholds for each demographic subgroup. This can be done by optimizing for a fairness metric (e.g., equalizing True Positive Rates) on a held-out validation set.
- 3. Threshold Application & Validation: Apply the group-specific thresholds to the model's outputs on a separate test set. Re-calculate all performance and fairness metrics to quantify the change in bias and any associated impact on overall accuracy. Studies note that accuracy loss is typically "low" or "negligible" [76].
Protocol for Fairness-Aware Model Validation in Clinical Cohorts
This protocol expands on principles from the IEEE 7003-2024 standard and clinical AI validation studies [10] [77].
- 1. Bias Profile Creation: Before validation, document a "bias profile" for the model. This includes the intended use, known limitations, and a priori identified protected attributes (e.g., age, genetic ancestry) and potential proxies in the data [77].
- 2. Stratified Performance Analysis: Validate the model on a hold-out clinical cohort. Report performance metrics not just as aggregates, but stratified by all protected attributes defined in the bias profile. For example, a cfDNA cancer detection model should report sensitivity for early-stage cancers separately for different demographic groups [10].
- 3. Continuous Monitoring for Drift: Implement systems to monitor for "data drift" (changes in the input data distribution) and "concept drift" (changes in the relationship between input and output) post-deployment, as these can introduce or exacerbate bias over time [77].
Workflow: Bias Mitigation in Clinical cfDNA Model Development
The following diagram illustrates a comprehensive workflow for integrating bias mitigation throughout the development and validation of a clinical cfDNA model.
Successful development of fair cfDNA models relies on a suite of computational tools, datasets, and regulatory frameworks.
Table 2: Research Reagent Solutions for Fairness in cfML
| Tool/Resource Name | Type | Primary Function in Fairness R&D |
|---|---|---|
| FHIBE (Fair Human-Centric Image Benchmark) [78] | Benchmark Dataset | Provides a consensually-sourced, globally diverse image dataset for evaluating bias in computer vision tasks; a model for ethical data collection. |
| SPOGIT/CSO Model [10] | Clinical Validation Framework | A multi-algorithm model (Logistic Regression, Transformer, etc.) for early GI cancer detection via cfDNA methylation; exemplifies rigorous multi-center clinical validation. |
| IEEE 7003-2024 Standard [77] | Regulatory & Process Framework | Provides a structured process for defining, measuring, and mitigating algorithmic bias throughout the AI system lifecycle, promoting transparency and accountability. |
| XGBoost [4] | Machine Learning Algorithm | An interpretable machine learning model effective for cfDNA-based cancer detection; allows for feature importance analysis to understand model drivers. |
| Software Libraries for Bias Mitigation [76] | Computational Tool | Various open-source libraries (e.g., AIF360, Fairlearn) provide implemented algorithms for pre-, in-, and post-processing bias mitigation. |
| Demographic Parity & Equalized Odds [75] | Fairness Metric | Core statistical definitions used to quantify algorithmic fairness, enabling objective comparison of model performance across groups. |
The integration of machine learning (ML) into clinical diagnostics, particularly with cell-free DNA (cfDNA) analysis, represents a transformative shift in medical research and practice. However, the "black box" nature of many complex models poses a significant barrier to clinical adoption [79]. Clinicians and regulatory bodies require not just high performance, but also understandable justifications for model-based decisions to ensure safety, fairness, and correctness [80]. In high-stakes fields like healthcare, where algorithmic decisions can have significant consequences, understanding machine learning mechanisms ensures decision fairness and minimizes systemic errors [81]. This guide objectively compares approaches to achieving explainability and interpretability in cfDNA ML models, framing the comparison within the critical context of clinical validation for research and drug development.
The terms "explainability" and "interpretability," while often used interchangeably, have distinct nuances crucial for clinical settings. Interpretability is the inherent ability to understand the decision-making process of an AI system, focusing on the inner logic and mechanics—the "how" [79] [81]. An interpretable model allows researchers to see the correlations between input variables and output results. Explainability, meanwhile, concerns the ability to communicate the decision-making process in accessible ways to the end user, answering the "why" behind a specific decision or prediction [79] [81]. For a cfDNA model, interpretability might involve understanding how specific fragmentation features contribute to a cancer risk score, while explainability would describe why a particular blood sample was flagged as high-risk.
Comparative Analysis of Explainability Methodologies
Various technical approaches exist to make ML models more transparent. The choice of method often involves a trade-off between model performance (often higher in complex models) and transparency (higher in simpler models) [79]. The following table summarizes the core methodologies relevant to cfDNA model development.
Table 1: Comparison of Explainability and Interpretability Approaches for Clinical cfDNA Models
| Method Category | Core Principle | Best Suited Model Types | Key Advantages | Key Limitations for Clinical Use |
|---|---|---|---|---|
| Intrinsically Interpretable Models [79] | Model structure itself is simple and understandable (e.g., linear regression, decision trees). | Linear/Logistic Regression, Decision Trees | High transparency; No need for post-hoc analysis; Easily audited. | Often lower predictive power on complex datasets like cfDNA fragmentomes; May oversimplify biology. |
| Post-hoc Explainability Methods [81] | Apply techniques after a prediction to explain it. | Complex models (e.g., Deep Neural Networks, Ensemble Methods) | Can be applied to high-performance black-box models; Flexible. | Explanation is separate from the model, may not reflect true inner workings; "How" and "why" can be obscured. |
| Model Visualization [81] | Use graphical tools to represent model decisions and feature importance. | All model types, especially those with high-dimensional input | Intuitive for human understanding; Helps identify key predictive features. | Can become complex with many features; May not provide causal certainty. |
| Example-Based Explanations [81] | Provide similar cases from the training set to justify a new prediction. | All model types | Intuitively understandable for clinicians; Builds trust through familiarity. | Requires a large, well-curated database of reference cases; Privacy considerations. |
A critical consideration is that a model can be interpretable but not explainable. For instance, a linear regression model is interpretable because its internal workings are transparent, but it may not be explainable if the input features themselves are not understandable or clinically meaningful [79]. The selection of a method must align with the clinical question and the required level of accountability.
Experimental Protocols for Validating Explainable cfDNA Models
Robust validation is paramount. The following experimental protocols are essential for establishing trust in an explainable cfDNA model, moving beyond mere metric performance to clinical utility.
Protocol: Clinical Cohort Design and Model Training
This protocol is foundational for ensuring that the model and its explanations are valid across diverse populations.
- Objective: To train and validate a cfDNA classifier on a cohort that reflects the intended-use population, ensuring explanations are biologically and clinically plausible.
- Methodology: A prospective, multicenter, case-control study design is the gold standard, as demonstrated in the DELFI-Lung Cancer Training Study (L101) [24].
- Cohort Recruitment: Participants should be enrolled based on clear, pre-specified clinical eligibility criteria (e.g., USPSTF guidelines for lung cancer screening) [24]. This ensures the model is validated on a clinically relevant population.
- Data Splitting: A split-sample approach is used, where the cohort is divided into a training set (e.g., ~60%) for classifier development and a held-out validation set (e.g., ~40%) for independent performance assessment [24]. This prevents over-optimistic performance estimates.
- Model Training: A machine learning classifier is trained on fragmentome features from the training set. The model can range from intrinsically interpretable (e.g., logistic regression) to complex (e.g., deep learning), with appropriate explainability techniques applied.
- Key Measurements: Demographic and clinical characteristics of the training and validation sets to ensure representativeness and balance across age, sex, race, and comorbid conditions [24].
Protocol: Performance and Explanation Benchmarking
This protocol assesses both the model's predictive power and the quality of its explanations.
- Objective: To quantitatively compare the model against existing alternatives and ablate the importance of its explanations.
- Methodology:
- Performance Metrics: Standard classification metrics must be reported on the held-out validation set. These include Accuracy, Sensitivity (Recall), Specificity, and Precision [82] [83]. For imbalanced datasets common in medicine, the F1-score (harmonic mean of precision and recall) and Area Under the Receiver Operating Characteristic Curve (AUC-ROC) are particularly informative [82] [83].
- Statistical Testing: To claim superiority over an existing model, statistical tests like the paired t-test or 10-fold cross-validation followed by a hypothesis test should be deployed to validate if the differences in metrics are statistically significant and not due to random noise [29] [82].
- Explanation Ablation: The contribution of features highlighted by the explainability method (e.g., SHAP values) is validated by systematically removing them and observing the drop in model performance. This tests whether the explanations point to features truly important for the prediction.
- Key Measurements: The values of all performance metrics for the new model and comparator models, along with p-values from statistical tests establishing significance [82].
Protocol: Clinical Utility and Bias Assessment
This protocol tests the real-world impact of the model and its explanations.
- Objective: To ensure the model's explanations are actionable for clinicians and that the model performs fairly across demographic subgroups.
- Methodology:
- Analyst-Blinded Review: Clinical researchers are provided with model predictions accompanied by explanations (e.g., "sample flagged as high-risk due to abnormal fragmentation patterns on chromosomes X and Y") and without. Their diagnostic accuracy and confidence with and without the explanation are measured.
- Subgroup Analysis: Model performance (sensitivity, specificity) and explanations are rigorously analyzed across subgroups defined by age, sex, race, and ethnicity to identify any performance disparities or reliance on spurious correlated features [24] [80].
- Key Measurements: Diagnostic accuracy of clinical researchers; consistency of performance metrics (e.g., sensitivity, specificity) across demographic groups [24].
The workflow below visualizes the integration of these protocols into a coherent validation pipeline.
Diagram 1: Model validation workflow.
The Scientist's Toolkit: Essential Research Reagents & Materials
Success in developing explainable clinical ML models relies on a suite of computational and data resources.
Table 2: Key Research Reagent Solutions for Explainable cfDNA ML
| Tool Category | Specific Examples | Function in Workflow |
|---|---|---|
| Explainability Software Libraries | SHAP, LIME [79] [81] | Post-hoc explanation methods that quantify the contribution of each input feature to a single prediction, making complex models locally interpretable. |
| Model Evaluation Frameworks | Scikit-learn, PyTorch, TensorFlow [83] | Provide built-in functions for calculating performance metrics (accuracy, precision, recall, F1) and generating confusion matrices. |
| Cloud Computing Platforms | Google Cloud Genomics, Amazon Web Services (AWS) [84] | Provide scalable infrastructure to store, process, and analyze vast cfDNA sequencing datasets (often terabytes), enabling global collaboration. |
| Variant Calling & Bioinformatic Tools | DeepVariant [84] | AI-powered tools for accurately identifying genetic variants from sequencing data, forming a reliable foundation for downstream ML models. |
| Statistical Testing Tools | R, Python (SciPy, StatsModels) | Enable performance of rigorous statistical tests (e.g., t-tests, ANOVA) to validate that performance differences between models are statistically significant. |
The transition of cfDNA ML models from research tools to clinical assets hinges on demonstrating not just high accuracy, but also robust explainability. As shown, this requires a multi-faceted approach: selecting appropriate interpretability methods, rigorously validating models on representative clinical cohorts, and thoroughly assessing their clinical utility and fairness. By systematically comparing and applying the methodologies and protocols outlined in this guide, researchers and drug developers can build the transparent, trustworthy AI systems necessary to advance precision medicine and gain the confidence of the clinical community. The future of AI in clinical research is not merely predictive, but also understandable and actionable.
Proving Clinical Utility: Robust Validation Frameworks and Benchmarking
In the field of clinical cancer research, machine learning models developed using cell-free DNA (cfDNA) data hold transformative potential for non-invasive cancer detection, subtype classification, and early interception strategies. The analytical promise of these models, as demonstrated in studies on colorectal, breast, and lung cancers, must be underpinned by robust internal validation to ensure their performance estimates are reliable and generalizable [85] [86] [24]. Internal validation techniques, primarily bootstrapping and cross-validation, serve as foundational statistical procedures to quantify model performance, mitigate overoptimism, and provide confidence intervals for performance metrics such as sensitivity, specificity, and AUC-ROC. Without these techniques, a model's apparent accuracy may reflect mere data-specific fitting rather than true predictive power, potentially leading to flawed clinical interpretations. This guide objectively compares bootstrapping and cross-validation methodologies, providing a framework for their application in clinical cfDNA research to help scientists and drug development professionals select the most appropriate validation strategy for their specific context.
Core Concepts and Definitions
What is Cross-Validation?
Cross-validation (CV) is a resampling technique used to assess how the results of a statistical analysis will generalize to an independent dataset. It is primarily used in settings where the goal is to estimate the predictive performance of a model and to mitigate the over-optimistic bias that results from using the same data for both training and evaluation [87]. The most common implementation is K-Fold Cross-Validation, which operates through a systematic process:
- The entire dataset is randomly split into k approximately equal-sized folds or partitions.
- For each of the k iterations, a single fold is retained as the validation data, and the remaining k-1 folds are used as training data.
- The model is trained on the training set and its performance is evaluated on the validation fold.
- The final performance estimate is calculated as the average of the k individual performance scores [88].
This process ensures that every observation in the dataset is used for both training and validation exactly once, providing a more stable estimate of out-of-sample performance than a single train-test split.
What is Bootstrapping?
Bootstrapping is a powerful resampling technique that estimates the sampling distribution of a statistic by repeatedly drawing new samples from the original data with replacement. In the context of model validation, the bootstrap is used to estimate the variability and potential bias of performance metrics. The most straightforward application is the Out-of-Bag Bootstrap:
- From a dataset of size n, a bootstrap sample is created by randomly selecting n observations with replacement. This sample, which contains approximately 63.2% of the original data, serves as the training set.
- The model is trained on this bootstrap sample.
- The model is evaluated on the observations not included in the bootstrap sample (the "out-of-bag" or OOB samples), which constitute about 36.8% of the data [89].
- This process is repeated many times (typically B = 500-2000), and the OOB performance metrics are averaged to produce a final estimate.
Advanced variants like the .632 Bootstrap and .632+ Bootstrap were developed to correct the pessimistic bias inherent in the simple OOB estimate, particularly in settings with high variance learners or small sample sizes [89].
Performance Comparison and Experimental Data
Quantitative Comparison of Techniques
The table below summarizes the core operational characteristics and typical performance of each method, synthesizing findings from simulation studies and methodological comparisons.
Table 1: Operational and Performance Comparison of Validation Techniques
| Feature | K-Fold Cross-Validation | Bootstrapping (OOB) | Bootstrapping (.632+) |
|---|---|---|---|
| Core Mechanism | Partitioning without replacement | Resampling with replacement | Resampling with replacement, with bias correction |
| Typical Number of Iterations | k = 5 or 10 | B = 500 - 2000 | B = 500 - 2000 |
| Data Usage (Training) | (k-1)/k of data (e.g., 80% for k=5) | ~63.2% of data per sample | ~63.2% of data per sample |
| Primary Use Case | Generalization error estimation | Estimating performance variance and creating confidence intervals | Reducing bias in high-variance settings |
| Computational Cost | Low to Moderate (k model fits) | High (B model fits) | High (B model fits) |
| Bias of Estimate | Generally low, but can be slightly pessimistic with small k | Can be pessimistic | Designed to be low |
| Variance of Estimate | Can be higher, especially with small k | Lower than CV | Lower than CV |
| Stability | Moderate (depends on k) | High | High |
Empirical Findings from Comparative Studies
Simulation studies have provided nuanced insights into the performance of these methods under various conditions. Overall, no single method is superior in all scenarios, but clear recommendations exist for specific use cases:
- General Performance: Repeated 5- or 10-fold cross-validation and the .632+ bootstrap are often recommended as they generally provide a good balance between bias and variance [89].
- Small Sample Scenarios: The .632+ bootstrap estimator tends to perform relatively well under small sample settings, except when regularized estimation methods are used [89].
- High-Dimensional Data (p >> n): The optimism bootstrap (Efron-Gong method) may perform worse than repeated 10-fold cross-validation when there are more predictors than samples [89].
- Computational Efficiency: For comparing models, the bootstrap is often faster than obtaining a precise estimate from cross-validation, as one may need to repeat 10-fold CV 50-100 times to achieve sufficient precision, whereas the bootstrap might require 300-1000 repetitions, which can be more computationally efficient for complex models [89].
Experimental Protocols for cfDNA Model Validation
Protocol 1: K-Fold Cross-Validation for a cfDNA Classifier
This protocol outlines the steps for implementing k-fold cross-validation to evaluate a machine learning model designed for cancer detection using cfDNA fragmentation profiles, as seen in studies like the DELFI approach for lung cancer screening [24].
- Data Preparation: Assemble a cohort of cfDNA samples from both cancer patients and healthy controls. For each sample, extract relevant features such as fragment length distributions, nucleosome protection patterns, and genomic coverage profiles. Ensure the dataset is properly labeled with ground truth diagnoses (e.g., cancer vs. healthy, or specific cancer subtypes).
- Stratification: Given the class imbalance typical in clinical cohorts (e.g., more controls than cases), use stratified k-fold splitting. This ensures each fold maintains the same proportion of cancer and control samples as the full dataset.
- Model Training and Validation: For each of the k folds (commonly k=5 or 10):
- Hold out one fold as the validation set.
- Use the remaining k-1 folds to train the classifier (e.g., a random forest or logistic regression model).
- Use the trained model to predict the labels of the held-out validation fold.
- Calculate performance metrics (e.g., Sensitivity, Specificity, AUC-ROC) based on the predictions for the held-out fold.
- Performance Aggregation: After iterating through all k folds, compute the final performance estimates by averaging the metrics from each fold. Report the mean and standard deviation to convey both central tendency and variability. For example: "The classifier achieved a mean cross-validated AUC of 0.94 ± 0.03."
Figure 1: K-Fold Cross-Validation Workflow for cfDNA Models
Protocol 2: Bootstrap Validation for a cfDNA Methylation Model
This protocol describes how to apply bootstrap validation to assess the stability and confidence intervals of performance metrics for a multi-model assay, such as the SPOGIT assay for gastrointestinal cancer screening which combines Logistic Regression, Transformer, and Random Forest models [10].
- Bootstrap Sampling: From the original dataset of n cfDNA samples, draw B bootstrap samples (e.g., B = 1000). Each bootstrap sample is created by randomly selecting n samples with replacement.
- Model Training and Out-of-Bag Testing: For each bootstrap sample b:
- Train the model(s) on the bootstrap sample.
- Identify the out-of-bag (OOB) samples—those not included in bootstrap sample b.
- Use the trained model to generate predictions for the OOB samples.
- Calculate the desired performance metric (e.g., Sensitivity, Specificity) based on the OOB predictions.
- Performance Distribution: After all B iterations, you will have a distribution for each performance metric (e.g., 1000 sensitivity estimates). The mean of this distribution provides the overall bootstrap performance estimate.
- Confidence Interval Construction: To construct a 95% confidence interval for a metric, use the percentile method: identify the 2.5th and 97.5th percentiles of the bootstrap distribution. This interval quantifies the uncertainty of your model's performance. For instance: "The bootstrap-estimated sensitivity was 88.1% (95% CI: 85.8% - 90.3%)."
Figure 2: Bootstrap Validation Workflow for cfDNA Models
Application in Clinical cfDNA Research: Case Examples
The selection between bootstrapping and cross-validation is not merely theoretical; it has practical implications in clinical cfDNA research, as evidenced by its application in recent high-impact studies.
Table 2: Validation Methods in Published cfDNA Clinical Studies
| Study (Example) | Cancer Type | Primary Validation Method | Reported Performance | Implied Rationale for Method Choice |
|---|---|---|---|---|
| SPOGIT Assay [10] | Gastrointestinal | Hold-out Validation (Split-sample) | Sensitivity: 88.1%, Specificity: 91.2% (Multicenter cohort, n=1,079) | Standard for clinical assay locking and independent validation |
| DELFI-L101 [24] | Lung | Hold-out Validation (Split-sample) | High sensitivity demonstrated in validation set (n=382) | Regulatory alignment and clear separation of training/validation |
| Griffin Framework [86] | Breast Cancer (ER Subtyping) | Not explicitly stated, common practice is CV | AUC = 0.89 (n=139), validated in independent cohort (AUC=0.96) | Model development and feature selection phase |
| cfDNA Q&S Study [85] | Colorectal, Breast, etc. | Age Resampling (to control for confounder) | AUC=0.98 for MNR in stage IV CRC vs healthy | Addressing specific covariate imbalance rather than overall performance |
The prevalence of the simple hold-out method (splitting into training and validation sets) in the final validation stages of clinical studies like SPOGIT and DELFI-L101 is noteworthy. This approach is often mandated for regulatory approval processes, as it uses a completely independent, locked-down model to evaluate a held-out cohort, providing the least biased estimate of real-world performance. However, cross-validation and bootstrapping remain critical during the model development and algorithm selection phase, which often precedes the final hold-out validation. For instance, when determining the optimal set of cfDNA quantitative parameters (like nuclear DNA concentration or mitochondrial-to-nuclear ratio) or selecting a classifier, these internal validation methods allow researchers to efficiently compare options without exhausting the test set [85].
Successfully implementing these validation techniques requires both wet-lab reagents for generating cfDNA data and dry-lab computational tools for analysis.
Table 3: Essential Research Reagent Solutions and Computational Tools
| Category | Item / Tool | Critical Function in cfDNA Model Validation |
|---|---|---|
| Wet-Lab Reagents & Kits | Blood Collection Tubes (e.g., Streck, EDTA) | Stabilizes nucleosomes and prevents white blood cell lysis, ensuring accurate fragmentation profiles. |
| cfDNA Extraction Kits (e.g., QIAamp, MagMAX) | Isulates high-quality, non-degraded cfDNA, which is fundamental for all downstream analyses. | |
| Library Prep Kits for WGS/ULP-WGS | Prepares sequencing libraries from low-input cfDNA (<30 ng), enabling fragmentomic analysis [10]. | |
| Bisulfite Conversion Kits | For methylation-based assays like SPOGIT, enabling the detection of epigenetic cancer signals [10]. | |
| Computational Tools & Languages | R or Python (Scikit-learn) | Provides statistical computing environment and libraries for implementing k-fold CV and bootstrap (e.g., cross_val_score, custom bootstrap scripts) [88]. |
| Whole Genome Sequencing Aligner (e.g., BWA-MEM) | Aligns sequencing reads to a reference genome, the first step in generating fragmentation profiles. | |
| Fragmentomics Analysis Pipelines (e.g., Griffin) | Computational frameworks for GC correction and nucleosome profiling from cfDNA WGS data [86]. | |
| Tumor Fraction Estimators (e.g., ichorCNA) | Estimates the proportion of tumor-derived cfDNA, used to correlate with nucleosome accessibility features [86]. |
The choice between bootstrapping and cross-validation for internal validation of clinical cfDNA models is not a matter of which is universally better, but which is more appropriate for the specific research context.
- Use K-Fold Cross-Validation when: Your primary goal is to obtain an accurate, low-bias estimate of the model's generalization error, particularly during the model development and feature selection phase. It is computationally more efficient than bootstrapping for a comparable number of iterations and is highly effective for comparing multiple modeling algorithms.
- Use Bootstrapping when: Your goal is to understand the stability and variance of your performance metrics or to construct confidence intervals. It is particularly valuable for assessing the reliability of a chosen model's performance in smaller sample sizes, with the .632+ variant being recommended for high-variance models.
Ultimately, for the final validation of a model intended for clinical application, these internal validation methods should be viewed as complementary to, not a replacement for, a final evaluation on a completely held-out test set or a prospective multi-center validation cohort, as demonstrated by the leading studies in the field. A robust validation strategy often employs cross-validation or bootstrapping during internal development, followed by a rigorous hold-out test on an independent population to provide the definitive performance estimate required for clinical translation.
The integration of machine learning (ML) with cell-free DNA (cfDNA) analysis represents a frontier in clinical cancer research, promising non-invasive methods for early detection, prognosis, and monitoring. However, the path from a promising algorithm to a clinically valid tool requires rigorous validation, with external validation standing as the definitive assessment of a model's generalizability. External validation evaluates a model's performance on data completely separate from its development cohort, testing its robustness across different populations, clinical settings, and sample processing protocols. For researchers, scientists, and drug development professionals, understanding and implementing rigorous external validation is not merely a methodological formality but a fundamental requirement for establishing clinical credibility and ensuring that predictive models perform reliably in the diverse, real-world settings where they are intended to be deployed.
Comparative Performance of Externally Validated cfDNA Models
The true measure of a cfDNA-based ML model is its performance when applied to entirely new patient cohorts. The following tables summarize the published external validation results of recent high-impact studies, providing a benchmark for model generalizability across different cancer types.
Table 1: External Validation Performance of cfDNA Models for Cancer Detection
| Cancer Type | Model Name/ Approach | Validation Cohort (n) | Key Features Analyzed | Sensitivity (Early-Stage) | Specificity | AUC |
|---|---|---|---|---|---|---|
| Lung Cancer [24] | Fragmentome Classifier | 382 cases/controls | Genome-wide cfDNA fragmentation profiles | High sensitivity reported (consistency across demos) | -- | -- |
| Pancreatic Cancer [90] | PCM Score (Combined Model) | External Val. 1 (n=129); External Val. 2 (n=139) | End motif, fragmentation, NF, CNA | -- | -- | 0.992 (Cohort 1); 0.986 (Cohort 2) |
| Esophageal SCC [91] | EMMA (Multimodal) | External Val. Cohort (n=30 ESCC); Precancerous Cohort (n=50 IEN) | Methylation (50 DMRs), CNVs, Fragmentation (FSRs) | 87% (ESCC); 62% (Precancerous) | >95% | 0.89 (ESCC); 0.87 (Precancerous) |
| GI Cancers [10] | SPOGIT | Multicenter Val. (386 cancers/113 controls/580 precancers) | cfDNA Methylation | 88.1% (All); 83.1% (Stage 0-II) | 91.2% | -- |
| Clonal Hematopoiesis [23] | MetaCH | Four independent external cfDNA datasets | Variant, gene embeddings, functional scores | -- | -- | Superior auPR/auROC vs. baselines |
Table 2: Performance on Precancerous and Early-Stage Lesions
| Model | Target Condition | Lesion Type | Sensitivity | Specificity |
|---|---|---|---|---|
| SPOGIT [10] | GI Precancers | Advanced Adenomas (AA) | 56.5% | -- |
| SPOGIT [10] | Gastric Precancers | High-risk preGC | 62.4% | -- |
| EMMA [91] | Esophageal Precursors | Intraepithelial Neoplasia (IEN) | 62% | >95% |
| EMMA [91] | Early-Stage ESCC | Stage I/II Cancer | -- | -- |
Experimental Protocols for Key Validation Studies
The reliability of external validation data is contingent on the rigorous methodologies employed. Below are detailed protocols for the core experiments cited in the performance tables.
DELFI-L101: Fragmentome-Based Lung Cancer Detection
- Study Design: A prospective, multicenter, case-control study (NCT04825834) across 47 centers in the United States [24].
- Cohort: 958 individuals eligible for lung cancer screening per USPSTF guidelines. The cohort was split into a training set (n=576) and a held-out, independent clinical validation set (n=382) [24].
- cfDNA Analysis: Low-pass whole-genome sequencing (lp-WGS) was performed on plasma cfDNA. The analysis focused on genome-wide cfDNA fragmentation profiles (the "fragmentome"), which reflect genomic and chromatin characteristics of lung cancer cells [24].
- ML & Validation: A machine learning classifier was trained on fragmentome features from the training set. The locked model was then applied to the held-out validation set without further modification to assess its real-world performance and consistency across demographic groups [24].
EMMA: Multimodal Analysis for Esophageal Cancer
- Framework: The Expanded Multi-Modal Analysis (EMMA) framework was designed to simultaneously extract multiple feature types from a single whole-genome bisulfite sequencing (WGBS) cfDNA dataset [91].
- Feature Extraction:
- Methylation: Identified 50 optimal differentially methylated regions (DMRs) to compute an "ESCC-cfMeth" score [91].
- Copy Number Variants (CNVs): Analyzed from the same WGBS data [91].
- Fragmentation: Calculated fragment size ratios (FSRs) based on the tendency for tumor-derived fragments to be shorter [91].
- Model Training & Validation: A random forest model was trained using a combination of DMRs, CNVs, and FSRs. The model was independently validated on an external cohort from a different hospital (n=30 ESCC) and a precancerous cohort (n=50 with IEN) [91].
SPOGIT: Multi-Algorithm Model for GI Cancer Screening
- Model Development: SPOGIT is a multi-algorithm ensemble model that incorporates Logistic Regression, Transformer, MLP, Random Forest, SGD, and SVC. It was developed using large-scale public tissue methylation data and cfDNA profiles [10].
- Validation Strategy: The model underwent a two-tiered validation process:
MetaCH: Machine Learning for Variant Origin Classification
- Problem: To distinguish clonal hematopoiesis (CH) variants from true tumor-derived variants in plasma-only cfDNA samples without matched white blood cell sequencing [23].
- ML Framework: A three-stage metaclassifier:
- Stage 1 (Feature Extraction): Numerical representation of variants, genes, and functional impact using the Mutational Enrichment Toolkit (METk) [23].
- Stage 2 (Base Classifiers): Three classifiers were trained on different data types—a cfDNA-based classifier and two sequence-based classifiers using large public datasets of tumor and blood-derived variants [23].
- Stage 3 (Meta-Classifier): A logistic regression model combined the scores from the base classifiers into a final CH-likelihood score [23].
- Validation: Performance was rigorously evaluated using cross-validation and four independent external cfDNA validation datasets with matched WBC sequencing as a ground truth reference [23].
Diagram 1: External validation workflow.
Visualizing Key Analytical Workflows
Understanding the logical flow of these complex analytical methods is crucial for their implementation and critical evaluation.
Diagram 2: Multimodal cfDNA analysis framework.
The Scientist's Toolkit: Essential Reagents and Materials
Successful execution of cfDNA ML studies depends on a suite of specialized reagents and analytical tools. The following table details key solutions required for these investigations.
Table 3: Essential Research Reagent Solutions for cfDNA ML Studies
| Reagent / Solution | Primary Function | Application Notes |
|---|---|---|
| cfDNA Blood Collection Tubes | Stabilizes nucleated blood cells to prevent genomic DNA contamination and preserves cfDNA profile [92]. | Critical for standardized pre-analytics. Tubes containing cell-stabilizing agents are preferred. |
| cfDNA Extraction Kits | Isolves and purifies short-fragment cfDNA from plasma with high efficiency and low shearing [92]. | Yield and purity are paramount. Manual column-based or automated magnetic bead-based kits are standard. |
| Library Prep Kits for lp-WGS | Prepares sequencing libraries from low-input, low-concentration cfDNA for fragmentome analysis [24]. | Must be optimized for short fragments. Kits with dual-strand sequencing adapters reduce bias. |
| Whole-Genome Bisulfite Conversion Kits | Converts unmethylated cytosines to uracils while preserving methylated cytosines for methylation sequencing [91]. | Conversion efficiency (>99%) must be rigorously quantified to ensure data quality. |
| Multiplex PCR Assays | Enables targeted amplification of specific genomic regions for focused mutation panels [92]. | Used in targeted approaches for variant detection or dd-cfDNA analysis. |
| Unique Molecular Identifiers (UMIs) | Tags individual DNA molecules pre-amplification to correct for PCR duplicates and sequencing errors [92]. | Essential for achieving high sensitivity and accurate quantification, especially for low-VAF variants. |
External validation remains the non-negotiable standard for demonstrating the generalizability and clinical potential of cfDNA-based machine learning models. As evidenced by the performance data and detailed methodologies presented, models that succeed in independent, multicenter validation cohorts—particularly those detecting early-stage and precancerous lesions—represent the most promising candidates for translation into clinical practice. The field's progression will be guided by increasingly rigorous validation standards, transparent reporting as outlined in initiatives like the "Model Facts" label [93], and the adoption of comprehensive multimodal approaches that leverage the full spectrum of information embedded in cfDNA.
In the field of clinical genomics, particularly in the development of cell-free DNA (cfDNA) machine learning models for cancer detection, the Area Under the Receiver Operating Characteristic Curve (AUC) has long been the dominant metric for evaluating model performance. While AUC provides valuable information about a model's overall discriminatory power, it offers an incomplete picture of real-world clinical utility. A model with high AUC may still be poorly calibrated, producing risk estimates that don't align with observed outcomes, or may lack clinical net benefit despite strong discriminatory performance [94].
The limitation of relying solely on AUC has become increasingly apparent as cfDNA-based liquid biopsies transition from research settings to clinical applications. For instance, the SPOGIT multi-model cfDNA methylation assay for gastrointestinal cancer screening demonstrated 88.1% sensitivity and 91.2% specificity in a multicenter validation, but its true clinical value lies in its projected ability to reduce late-stage diagnoses by 92% and boost 5-year survival rates by 27.02-30.47% [10]. These clinical impact measures transcend what AUC alone can communicate.
This guide examines the essential performance metrics beyond AUC that researchers must consider when validating cfDNA machine learning models, with particular focus on calibration assessment and clinical utility quantification. By adopting a more comprehensive validation framework, researchers and clinicians can better evaluate which models are truly ready for integration into clinical care pathways.
Essential Performance Metrics Beyond AUC
Calibration Metrics
Calibration measures how well a model's predicted probabilities match observed outcomes. Perfect calibration exists when a model predicting 70% risk for a group of patients corresponds to exactly 70% of those patients experiencing the event. Poor calibration can persist even in models with excellent AUC, potentially leading to clinical harm through overestimation or underestimation of risk [94].
The most robust approach to assessing calibration involves creating a calibration plot that compares predicted probabilities to observed event rates across risk strata. Statistical measures include:
- Calibration-in-the-large: Compares the average predicted risk to the overall event rate in the population.
- Calibration slope: Evaluates whether the relationship between predicted and observed risk is appropriately scaled, with ideal values close to 1.
- Brier score: Measures the overall mean squared difference between predicted probabilities and actual outcomes, combining both discrimination and calibration aspects.
For cfDNA models, calibration is particularly important in cancer screening contexts where accurate risk stratification determines subsequent diagnostic pathways. A well-calibrated model enables clinicians to make informed decisions about proceeding to more invasive diagnostic procedures based on cfDNA test results.
Clinical Utility Metrics
Clinical utility metrics evaluate whether using a model improves patient outcomes compared to standard practice or alternative approaches. These metrics are increasingly recognized as essential for clinical implementation [94].
Decision Curve Analysis (DCAA) provides a framework for evaluating the clinical value of prediction models by quantifying net benefit across different probability thresholds. Unlike AUC, which evaluates model performance across all possible thresholds simultaneously, decision curve analysis specifically assesses net benefit at clinically relevant decision thresholds where test results would change clinical management.
Sensitivity and Specificity at clinically relevant thresholds offer more actionable information than AUC alone. For example, a pancreatic cancer detection model achieved sensitivities ranging from 57% to >99% across cancer types at 98% specificity, with an overall AUC of 0.94 [95]. The selection of optimal thresholds involves trade-offs between false positives and false negatives that must be calibrated to the specific clinical context.
Net Reclassification Improvement (NRIAA) quantifies how well a new model reclassifies patients into more appropriate risk categories compared to an existing standard. This is particularly relevant when evaluating incremental improvements to established cfDNA assays.
Table 1: Key Performance Metrics Beyond AUC for cfDNA Model Validation
| Metric Category | Specific Metrics | Interpretation | Clinical Relevance |
|---|---|---|---|
| Calibration | Calibration slope | Ideal value = 1.0 | Ensures predicted probabilities match observed event rates |
| Calibration-in-the-large | Compares average predicted risk to overall event rate | Identifies systematically overconfident or underconfident predictions | |
| Brier score | Range 0-1, lower is better | Combined measure of discrimination and calibration | |
| Clinical Utility | Decision Curve Analysis | Net benefit across decision thresholds | Quantifies clinical value at relevant probability thresholds |
| Sensitivity/Specificity | Performance at clinically chosen thresholds | Reflects real-world test performance | |
| Net Reclassification Improvement | Improved risk categorization | Measures value added over existing standards |
Comparative Performance Data: Calibration and Clinical Utility in Practice
Recent studies of cfDNA-based machine learning models demonstrate how comprehensive evaluation beyond AUC provides deeper insights into clinical applicability.
The SPOGIT cfDNA methylation assay for gastrointestinal cancers exemplifies robust validation, reporting not only sensitivity and specificity but also projected clinical impact metrics including potential reduction in late-stage diagnoses and improvements in 5-year survival rates [10]. This comprehensive reporting facilitates better assessment of real-world clinical value compared to models reporting only discrimination metrics.
In pancreatic cancer detection, a multi-feature cfDNA model incorporating fragmentation patterns, end motifs, nucleosome footprint, and copy number alterations demonstrated exceptional discrimination (AUC 0.975-0.992 across cohorts) but also showed strong performance in clinically challenging scenarios including distinguishing pancreatic cancer from benign pancreatic tumors (AUC 0.886) and detecting CA19-9 negative cancers (AUC 0.990) [96]. This specificity in difficult diagnostic situations represents crucial clinical utility information beyond overall discrimination.
Comparative studies between machine learning approaches and conventional risk scores further highlight the importance of comprehensive metrics. A meta-analysis of models predicting major adverse cardiovascular and cerebrovascular events after percutaneous coronary intervention found that machine learning models (AUC 0.88) outperformed conventional risk scores (AUC 0.79), but the authors emphasized the need for assessment of calibration and clinical utility before widespread implementation [97].
Table 2: Comparative Performance of Recent cfDNA Machine Learning Models
| Study/Model | Cancer Type | AUC | Calibration Assessment | Clinical Utility Evidence |
|---|---|---|---|---|
| SPOGIT [10] | Gastrointestinal | Not specified | Not explicitly reported | Projected 92% reduction in late-stage diagnosis, 27-30% 5-year survival improvement |
| Pancreatic Cancer Model [96] | Pancreatic | 0.975-0.992 | Not explicitly reported | AUC 0.886 for distinguishing cancer from benign tumors, detects CA19-9 negative cancers |
| DELFI [95] | Multiple | 0.94 | Not explicitly reported | Sensitivities 57->99% at 98% specificity, tissue of origin identification in 91% of cases |
| XGBoost with chromatin features [4] | Breast & Pancreatic | Improved with chromatin features | Not explicitly reported | Identified key genomic loci associated with disease state |
Diagram 1: Comprehensive model evaluation workflow extending beyond AUC assessment
Experimental Protocols for Metric Assessment
Calibration Assessment Methodology
Proper evaluation of model calibration requires specific experimental approaches:
Calibration Plot Generation:
- Stratify the validation cohort into quantiles based on predicted probabilities (typically deciles)
- Calculate the mean predicted probability and observed event rate for each stratum
- Plot observed event rates (y-axis) against mean predicted probabilities (x-axis)
- Add a reference line representing perfect calibration (slope=1, intercept=0)
- Assess deviation from the ideal line, with particular attention to clinically relevant probability ranges
Statistical Calibration Measures:
- Calculate calibration-in-the-large as the difference between mean predicted probability and overall event rate
- Estimate calibration slope via logistic regression of observed outcomes on log-odds of predicted probabilities
- Compute Brier score as the mean squared difference between predicted probabilities and observed outcomes
- For large datasets, consider using flexible calibration curves rather than quantile-based approaches
The TRIPOD+AI reporting guideline provides comprehensive recommendations for transparent reporting of prediction model studies, including calibration assessment [94].
Decision Curve Analysis Protocol
Decision curve analysis evaluates the clinical net benefit of a prediction model across a range of clinically reasonable probability thresholds:
- Define Threshold Probabilities: Identify the range of probability thresholds at which clinical decisions would change (e.g., thresholds for recommending additional testing or intervention)
- Calculate Net Benefit: For each threshold probability (Pt), compute net benefit using the formula: Net Benefit = (True Positives / N) - (False Positives / N) × (Pt / (1 - Pt)) where N is the total number of patients
- Compare Strategies: Plot net benefit for the model against default strategies of "treat all" and "treat none"
- Interpret Results: The strategy with highest net benefit at clinically relevant thresholds is preferred
This methodology explicitly incorporates the clinical consequences of false positives and false negatives, which vary across clinical contexts and patient populations.
Research Reagent Solutions for cfDNA Model Development
Table 3: Essential Research Reagents for cfDNA Machine Learning Studies
| Reagent/Category | Specific Examples | Function in Workflow |
|---|---|---|
| cfDNA Extraction Kits | QIAamp Circulating Nucleic Acid Kit, Maxwell RSC ccfDNA Plasma Kit | Isolation of high-quality cfDNA from plasma samples with minimal contamination |
| Library Preparation | ThruPLEX Plasma-seq, NEBNext Ultra II DNA Library Prep | Preparation of sequencing libraries from low-input cfDNA samples |
| Bisulfite Conversion | EZ DNA Methylation Lightning Kit, Premium Bisulfite Kit | Conversion of unmethylated cytosines for methylation-based assays |
| Target Enrichment | Twist Human Methylation Panel, IDT xGen Pan-Cancer Panel | Hybridization capture for targeted sequencing approaches |
| Sequencing Platforms | Illumina NovaSeq, NextSeq | High-throughput sequencing for cfDNA fragment analysis |
| Quality Control | Agilent Bioanalyzer, TapeStation, Qubit fluorometer | Assessment of cfDNA quality, quantity, and fragment size distribution |
Comprehensive evaluation of cfDNA machine learning models requires moving beyond AUC to include rigorous assessment of calibration and clinical utility. As these models increasingly influence clinical decision-making in oncology, researchers must adopt validation frameworks that more accurately predict real-world performance and clinical impact.
The field is moving toward standardized reporting guidelines like TRIPOD+AI that emphasize complete model evaluation [94]. Future development should prioritize prospective validation studies that assess both statistical performance and actual impact on clinical outcomes and patient management. By embracing these comprehensive evaluation standards, the research community can accelerate the translation of promising cfDNA technologies into clinically valuable tools that improve cancer detection and patient outcomes.
The integration of circulating tumor DNA (ctDNA) analysis into clinical oncology represents a paradigm shift in cancer management, enabling non-invasive assessment of tumor burden, genetic heterogeneity, and therapeutic response. However, the transition of ctDNA assays from research tools to clinically actionable diagnostics necessitates rigorous validation against established standards. Head-to-head comparison studies provide the critical evidence base required for researchers and drug development professionals to evaluate the analytical and clinical performance of emerging technologies. Such comparisons are particularly vital in the context of ctDNA analysis, where pre-analytical variables, analytical sensitivity, and the ability to detect low-frequency variants in early-stage disease or minimal residual disease (MRD) settings present significant technical challenges [98]. As the field progresses toward liquid biopsy-based screening and therapy monitoring, understanding the relative strengths and limitations of available platforms becomes essential for advancing personalized oncology and designing robust clinical trials.
This guide synthesizes evidence from recent comparative studies to objectively benchmark the performance of various ctDNA detection platforms, with a focus on their application in clinical cohorts. We examine technologies ranging from tumor-informed and tumor-agnostic approaches to fragmentomics-based machine learning models, providing detailed experimental protocols and performance metrics to inform research and development decisions in the field of liquid biopsy.
Comparative Performance of ctDNA Detection Methodologies
Multi-Assay Comparison in Early Breast Cancer
A comprehensive 2025 study directly compared four tumor-agnostic ctDNA detection methods in patients with triple-negative or luminal B breast cancer before neoadjuvant chemotherapy. The research evaluated their ability to detect ctDNA at baseline using the same patient cohort, providing a unique direct comparison of analytical sensitivity [99].
Table 1: Comparison of Tumor-Agnostic ctDNA Detection Methods in Early Breast Cancer
| Assay Method | Detection Principle | Patients Detected | Detection Rate | Key Features |
|---|---|---|---|---|
| Oncomine Breast cfDNA Panel | Targeted SNV hotspots in 10 genes | 3/24 | 12.5% | 150 SNV hotspots; 20,000x read depth |
| mFAST-SeqS | LINE-1 sequencing for CNV detection | 5/40 | 12.5% | Genome-wide aneuploidy score |
| Shallow Whole Genome Sequencing | Copy number variation detection | 3/40 | 7.7% | Low-pass whole genome sequencing |
| MeD-Seq | Genome-wide methylation profiling | 23/40 | 57.5% | Methylation patterns at CpG sites |
| Combined All Methods | Multi-modal approach | 26/40 | 65.0% | Complementary detection approaches |
The study revealed substantial variability in detection rates among tumor-agnostic methods, with MeD-Seq (57.5%) significantly outperforming mutation-based (Oncomine: 12.5%) and CNV-based (mFAST-SeqS: 12.5%; sWGS: 7.7%) approaches. Notably, the combined application of all methods increased the overall detection rate to 65%, highlighting the complementary nature of different biological signals and the potential advantage of multi-modal approaches [99].
The superior performance of MeD-Seq in this comparison aligns with the understanding that methylation alterations are early events in tumorigenesis and may be more abundantly represented in early-stage disease compared to specific genetic alterations. However, the study concluded that further optimization is still needed for tumor-agnostic methods to reach the sensitivity levels currently demonstrated by tumor-informed approaches, which have reported detection rates of 73-100% in similar clinical settings [99].
Prospective Validation of Ultrasensitive Liquid Biopsy Assays
A landmark prospective head-to-head comparison study evaluated the performance of Northstar Select, a single-molecule next-generation sequencing (smNGS) liquid biopsy assay, against six commercially available liquid biopsy assays from four CLIA/CAP laboratories. The study enrolled 182 patients with more than 17 solid tumor types from six community oncology clinics and one large hospital across the United States [100].
Table 2: Performance Comparison of Northstar Select vs. Other Commercial Liquid Biopsy Assays
| Performance Metric | Northstar Select | Comparator Assays (Range) | Improvement |
|---|---|---|---|
| Pathogenic SNV/Indel Detection | 51% more alterations | Baseline | 51% increase |
| Copy Number Variant Detection | 109% more CNVs | Baseline | 109% increase |
| Null Reports | 45% fewer | Baseline | 45% reduction |
| CNS Cancer Detection | 87% | 27-55% | Substantial improvement |
| VAF Detection Threshold | <0.5% | Typically >0.5% | Enhanced low-VAF sensitivity |
| Specificity | >99.9% | Variable | Industry standard |
| LOD₉₅ for SNVs | 0.15% VAF | Higher than 0.15% | Superior sensitivity |
| LOD₉₅ for CNV Amplifications | 2.1 copies | 2.46-3.83 copies | Improved detection |
| LOD₉₅ for CNV Losses | 1.8 copies | ≥20-30.4% tumor fraction | Dramatic improvement |
The study demonstrated that Northstar Select's enhanced sensitivity was particularly evident for variants below 0.5% variant allele frequency (VAF), where 91% of the additional clinically actionable variants were detected. Orthogonal validation with digital droplet PCR confirmed 98% concordance with Northstar Select results, verifying that the additional alterations represented true positives rather than false positives. Importantly, the enhanced sensitivity was not attributed to increased detection of clonal hematopoiesis variants, which were identified at similar rates in both Northstar Select and comparator assays [100].
A key advantage of Northstar Select is its ability to differentiate focal copy number changes from aneuploidies, addressing a significant limitation of many existing assays that cannot reliably distinguish clinically actionable focal "driver" amplifications from broad chromosomal aneuploidies that lack specific therapeutic targets. This capability, combined with its patented Quantitative Counting Templates (QCT) technology, enables more precise genomic profiling for treatment selection [100].
Experimental Protocols and Methodologies
Protocol for Multi-Assay ctDNA Detection Comparison
The comparative study of four ctDNA assays followed a standardized protocol for sample processing and analysis [99]:
Patient Cohort and Sample Collection:
- 40 patients with triple-negative or luminal B breast cancer scheduled for neoadjuvant chemotherapy
- Plasma blood samples collected before first chemotherapy cycle using EDTA, CellSave, or Streck tubes
- Plasma isolation within 4 hours (EDTA) or 96 hours (CellSave/Streck) via two centrifugation steps (10 min at 1711 g at room temperature followed by 10 min at 12,000 g at 4°C)
- Plasma stored at -80°C until cfDNA extraction
cfDNA Extraction and Quantification:
- cfDNA extracted using QiaAmp kit (Qiagen) according to manufacturer's instructions
- Concentration estimated using Quant-IT dsDNA high-sensitivity Assay (Invitrogen) and Qubit Fluorometer (Thermo Fischer Scientific)
- DNA stored at -30°C until analysis
Assay-Specific Protocols:
- Oncomine Breast cfDNA Panel: 10 ng cfDNA input; 1.9 kb panel covering 150 hotspots in 10 genes (AKT1, EGFR, ERBB2, ERBB3, ESR1, FBXW7, KRAS, PIK3CA, SF3B1, TP53); median 20,000x read depth
- mFAST-SeqS: 1 ng cfDNA input; LINE-1 sequence amplification with single primer pair; sequencing to ≥90,000 reads per sample on MiSeq system; genome-wide aneuploidy score ≥5 considered positive
- Shallow Whole Genome Sequencing: Low-pass whole genome sequencing for CNV detection
- MeD-Seq: 10 ng cfDNA digested with LpnPI (New England Biolabs) yielding 32 bp fragments around methylated CpG sites; ligation to dual-indexed adaptors; multiplexed sequencing; initial sequencing to ~2M reads with extension to ~20M reads for positive samples
This standardized protocol ensured comparable analysis across platforms while maintaining assay-specific optimization, enabling a direct comparison of detection capabilities in the same patient cohort.
Fragmentomics Workflow for Early Cancer Detection
Fragmentomics-based approaches leverage the distinctive fragmentation patterns of ctDNA to enable cancer detection and classification. The following protocol outlines a standardized workflow for fragmentomics analysis, as implemented in multiple recent studies [12] [101]:
Sample Preparation and Sequencing:
- Plasma collection and cfDNA extraction following standardized protocols (as above)
- Low-pass whole genome sequencing at 5X coverage for fragmentomics analysis
- Capture of multiple fragmentomics features: copy number variation, fragment size ratio, and nucleosome footprint
Fragmentomics Feature Extraction:
- Fragment Size Distribution: Analysis of cfDNA fragment lengths with particular attention to the prevalence of shorter fragments (90-150 bp) characteristic of tumor-derived DNA
- Nucleosome Positioning: Mapping of fragment ends to infer nucleosome occupancy and positioning patterns across the genome
- End Motif Analysis: Examination of 4-mer sequences at fragment ends to identify cancer-associated cleavage patterns
- Copy Number Variation Profiling: Identification of chromosomal gains and losses from shallow whole-genome sequencing data
Machine Learning Integration:
- Stacked ensemble model training on multiple fragmentomics features
- Model validation on independent cohorts with strict separation of training and validation sets
- Performance assessment using AUC, sensitivity, and specificity metrics
This fragmentomics workflow has demonstrated remarkable performance across multiple cancer types, achieving an AUC of 0.96 for renal cell carcinoma detection with 90.5% sensitivity and 93.8% specificity [12], and an AUC of 0.926 for colorectal cancer detection with 91.3% sensitivity and 82.3% specificity [101].
Advanced Detection Modalities and Integrated Approaches
Fragmentomics Performance Across Cancer Types
Fragmentomics-based liquid biopsy approaches have demonstrated exceptional performance in early cancer detection across multiple malignancies, as evidenced by recent rigorous validation studies:
Table 3: Fragmentomics Assay Performance Across Cancer Types
| Cancer Type | Study Cohort | AUC | Sensitivity | Specificity | Key Fragmentomics Features |
|---|---|---|---|---|---|
| Renal Cell Carcinoma | 223 RCC vs 219 controls [12] | 0.96 | 90.5% | 93.8% | CNV, fragment size ratio, nucleosome footprint |
| Colorectal Cancer | 167 CRC vs 227 benign conditions [101] | 0.926 | 91.3% | 82.3% | Multi-feature integration |
| Stage I CRC | Subset of above cohort [101] | - | 94.4% | - | Consistent early-stage performance |
| Advanced Colorectal Adenomas | 31 advCRA vs benign [101] | 0.846 | 67.7% | - | Superior to traditional blood tests |
| Gastrointestinal Cancers | 386 cancers/113 controls/580 precancers [10] | - | 88.1% | 91.2% | Methylation-based multi-algorithm model |
The performance of fragmentomics assays in detecting precancerous lesions represents a particular advancement, as traditional blood-based biomarkers have historically shown poor sensitivity for these entities. The SPOGIT assay demonstrated 56.5% sensitivity for advanced adenomas and up to 62.4% for gastric precancerous lesions, substantially higher than the 11.2-13.2% sensitivity reported for methylated SEPT9 DNA tests [10] [101].
Notably, fragmentomics approaches maintain robust performance across early cancer stages, with one study reporting 87.8% specificity for stage I renal cell carcinoma and 100% for stage IV disease [12]. This consistent performance across stages highlights the potential of fragmentomics to address a critical gap in cancer screening and early detection.
Integration with Targeted Sequencing Panels
A significant innovation in fragmentomics analysis involves the adaptation of these approaches to targeted sequencing panels already in clinical use for variant detection. A 2025 comprehensive analysis demonstrated that fragmentomics metrics could be effectively extracted from commercial targeted panels, enabling combined variant calling and cancer phenotyping from the same sequencing data [7].
The study evaluated 13 different fragmentomics metrics across two independent cohorts (University of Wisconsin cohort with 431 samples and GRAIL cohort with 198 samples), comparing their performance for cancer type and subtype classification. Key findings included:
- Normalized fragment read depth across all exons provided the best overall performance for predicting cancer types and subtypes (average AUROC of 0.943 in UW cohort and 0.964 in GRAIL cohort)
- Multi-metric approaches generally outperformed single-metric models
- Commercial panel compatibility was demonstrated for Tempus xF (105 genes), Guardant360 CDx (55 genes), and FoundationOne Liquid CDx (309 genes) panels
- FoundationOne Liquid CDx panel genes yielded the best performance among commercial panels tested
This integration enables the extraction of additional layers of information from existing clinical sequencing data without requiring additional sequencing costs or sample material, representing a significant advancement in the cost-effectiveness of comprehensive liquid biopsy analysis [7].
The Scientist's Toolkit: Essential Research Reagents and Platforms
Table 4: Essential Research Reagents and Platforms for ctDNA Analysis
| Category | Specific Products/Platforms | Research Application | Key Features |
|---|---|---|---|
| Blood Collection Tubes | EDTA, CellSave, Streck | Sample stabilization | Varied stability windows (4h-96h) |
| cfDNA Extraction Kits | QiaAmp Kit (Qiagen) | Nucleic acid isolation | Standardized yield across sample types |
| Quantification Assays | Quant-IT dsDNA HS Assay (Invitrogen) | DNA quantification | High sensitivity for low-concentration samples |
| Targeted Sequencing Panels | Oncomine Breast cfDNA Panel | Mutation detection | 150 SNV hotspots in 10 breast cancer genes |
| Methylation Analysis | MeD-Seq | Genome-wide methylation profiling | LpnPI digestion for CpG site analysis |
| CNV Detection Assays | mFAST-SeqS | Aneuploidy detection | LINE-1 amplification for genome-wide CNV |
| Whole Genome Sequencing | Shallow WGS (5X coverage) | Fragmentomics analysis | Cost-effective genome-wide profiling |
| Ultrasensitive Platforms | Northstar Select (smNGS) | Low-VAF variant detection | 0.15% LOD₉₅ for SNVs; QCT technology |
| Computational Tools | XGBoost, GLMnet elastic net | Machine learning modeling | Fragmentomics feature integration |
The landscape of ctDNA analysis is rapidly evolving, with head-to-head comparisons providing essential validation for emerging technologies. The evidence synthesized in this guide demonstrates that while tumor-informed approaches remain the sensitivity gold standard for many applications, tumor-agnostic methods—particularly those leveraging methylation patterns and fragmentomics—are achieving increasingly competitive performance. The integration of machine learning models with multi-analyte approaches represents the most promising direction for advancing liquid biopsy applications in early cancer detection, minimal residual disease monitoring, and comprehensive genomic profiling.
For researchers and drug development professionals, selection of appropriate ctDNA platforms must be guided by the specific clinical or research context. Ultrasensitive mutation-based assays like Northstar Select offer clear advantages for therapy selection in advanced cancers, while fragmentomics and methylation-based approaches show particular promise for early detection applications. The demonstrated compatibility of fragmentomics analysis with targeted sequencing panels suggests a near-term future where combined variant calling and cancer phenotyping from single liquid biopsies becomes clinically feasible across multiple cancer types.
As validation studies continue to demonstrate the superior performance of these advanced platforms across diverse clinical scenarios, the implementation of standardized comparison methodologies and reporting standards will be essential for translating these technological advances into improved patient outcomes through more precise cancer detection and monitoring.
Conclusion
The successful clinical validation of cfDNA machine learning models hinges on a multidisciplinary approach that integrates a deep understanding of cfDNA biology with rigorous data science and a steadfast focus on clinical relevance. Key takeaways include the necessity of using biologically informed features, such as fragmentomics and open chromatin patterns, the critical importance of external validation in diverse cohorts to ensure generalizability, and the need for explainable and equitable models. Future progress depends on collaborative efforts to create large, standardized, multi-omics datasets, the development of guidelines for robust model reporting, and the implementation of post-deployment monitoring systems. By adhering to these principles, the field can fully realize the potential of cfDNA and ML to usher in a new era of precise, non-invasive cancer diagnostics and monitoring.
References
- 1. NucPosDB: a database of nucleosome positioning in vivo and nucleosomics of cell-free DNA | Chromosoma [https://link.springer.com/article/10.1007/s00412-021-00766-9]
- 2. Nucleosome footprinting in plasma cell-free DNA for the pre-surgical diagnosis of ovarian cancer | npj Genomic Medicine [https://www.nature.com/articles/s41525-022-00300-5]
- 3. Cell-free DNA Comprises an In Vivo Nucleosome Footprint that Informs Its Tissues-Of-Origin - PubMed [https://pubmed.ncbi.nlm.nih.gov/26771485/]
- 4. Open chromatin-guided interpretable machine learning ... [https://www.nature.com/articles/s42003-025-08920-0]
- 5. FinaleToolkit: accelerating cell-free DNA fragmentation ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12597888/]
- 6. Genome-wide nucleosome footprints of plasma cfDNA predict ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11999135/]
- 7. Analysis of cfDNA fragmentomics metrics and commercial ... [https://www.nature.com/articles/s41467-025-64153-z]
- 8. Ultrasensitive TALEs-mediated electrochemical sensor for ... [https://www.sciencedirect.com/science/article/abs/pii/S0003267025004829]
- 9. Tracing the tissue origin of cell-free DNA through open ... [https://www.nature.com/articles/s42003-025-09232-z]
- 10. Clinical validation of a multi-model blood cfDNA ... [https://www.sciencedirect.com/science/article/pii/S209012322500832X]
- 11. Whole genome sequencing improves tissue-of-origin ... [https://www.nature.com/articles/s41467-025-59661-x]
- 12. Can a Liquid Biopsy Detect Early-Stage RCC? [https://www.cancernursingtoday.com/post/fragmentomics-liquid-biopsy-accurately-detects-early-rcc]
- 13. Finding new cancer epigenetic and genetic biomarkers from ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7387736/]
- 14. Clinical cancer epigenetics [https://clinicalepigeneticsjournal.biomedcentral.com/articles/10.1186/s13148-025-01948-3]
- 15. Tissue-Specific Chromatin Accessibility Regions and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12433345/]
- 16. Development and validation of a machine learning model ... [https://www.nature.com/articles/s41598-025-18443-7]
- 17. Diagnostic framework to validate clinical machine learning ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12219301/]
- 18. How MRD Is Being Used to Guide Treatment Decisions [https://www.targetedonc.com/view/how-mrd-is-being-used-to-guide-treatment-decisions]
- 19. Circulating tumor DNA to monitor treatment response in ... [https://www.nature.com/articles/s41698-025-00876-y]
- 20. The emerging role of cell-free DNA as a molecular marker ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6425120/]
- 21. Clinical applications of cell-free DNA-based liquid biopsy ... [https://www.sciencedirect.com/science/article/pii/S1936523325002505]
- 22. Artificial intelligence and machine learning in cell-free-DNA ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11789496/]
- 23. An artificial intelligence-based model for prediction of ... [https://www.nature.com/articles/s41698-025-00921-w]
- 24. Clinical Validation of a Cell-Free DNA Fragmentome Assay for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11528203/]
- 25. A machine learning approach to optimizing cell-free DNA ... [https://bmccancer.biomedcentral.com/articles/10.1186/s12885-020-07318-x]
- 26. Writing a Systematic Review and Meta-analysis: A Step-by ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12402582/]
- 27. Perspective: Machine learning in experimental solid ... [https://www.sciencedirect.com/science/article/abs/pii/S0022509623000352]
- 28. Steps of a Systematic Review - Research Guides [https://lib.guides.umd.edu/SR/steps]
- 29. How to Compare Machine Learning Models and Algorithms [https://neptune.ai/blog/how-to-compare-machine-learning-models-and-algorithms]
- 30. A comparison of machine learning methods for classification ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5081132/]
- 31. Cell-free DNA analysis in current cancer clinical trials [https://www.nature.com/articles/s41416-021-01696-0]
- 32. Leveraging cfDNA fragmentomic features in a stacked ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11384130/]
- 33. Validating your Machine Learning Model [https://maartengrootendorst.com/blog/validate/]
- 34. Model validation in machine learning: How to do it [https://www.leewayhertz.com/model-validation-in-machine-learning/]
- 35. A comparison between machine and deep learning models ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11339414/]
- 36. Classification of tumor types using XGBoost machine learning ... [https://translational-medicine.biomedcentral.com/articles/10.1186/s12967-023-04720-4]
- 37. Comparative analysis of statistical and deep learning-based ... [https://translational-medicine.biomedcentral.com/articles/10.1186/s12967-025-06662-5]
- 38. Multi‐omic integration of DNA methylation and gene ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10483606/]
- 39. Comparative Analysis of Multi-Omics Integration Using ... [https://pubmed.ncbi.nlm.nih.gov/40123934/]
- 40. Comparison of current methods for genome-wide DNA ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12376410/]
- 41. FinaleMe: Predicting DNA methylation by the fragmentation ... [https://www.nature.com/articles/s41467-024-47196-6]
- 42. Lost in Translation: Turning Multi-omic Chaos into Clinical ... [https://www.precisionformedicine.com/blog/lost-in-translation-turning-multi-omics-chaos-into-clinical-clarity]
- 43. A Guide to Multi-omics Integration Strategies [https://frontlinegenomics.com/a-guide-to-multi-omics-integration-strategies/]
- 44. Bridging biological cfDNA features and machine learning ... [https://www.sciencedirect.com/science/article/pii/S0168952523000197]
- 45. Open chromatin-guided interpretable machine learning ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12612109/]
- 46. a novel cell-free DNA fragmentomics-based liquid biopsy assay [https://pmc.ncbi.nlm.nih.gov/articles/PMC12221767/]
- 47. A Beginner's Guide to Hyperparameter Optimization in ... [https://www.coursera.org/articles/hyperparameter-optimization]
- 48. Hyperparameter Tuning [https://www.geeksforgeeks.org/machine-learning/hyperparameter-tuning/]
- 49. Grid Search vs Random Search: Which One Should You ... [https://www.blog.trainindata.com/grid-search-vs-random-search-which-one-should-you-use/]
- 50. Ten quick tips for ensuring machine learning model validity [https://pmc.ncbi.nlm.nih.gov/articles/PMC11412509/]
- 51. Competing Risk Analysis [https://www.publichealth.columbia.edu/research/population-health-methods/competing-risk-analysis]
- 52. A practical guide to handling competing events in etiologic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10446108/]
- 53. Comparative Review of Modern Competing Risk Methods ... [https://arxiv.org/html/2503.12824v1]
- 54. Systematic comparison of approaches to analyze clustered ... [https://bmcmedresmethodol.biomedcentral.com/articles/10.1186/s12874-023-01908-6]
- 55. How to Properly Compare Machine Learning Models - Devansh [https://machine-learning-made-simple.medium.com/how-to-properly-compare-machine-learning-models-b283c0abb3e3]
- 56. A prediction model based on cfDNA concentration and ... [https://www.nature.com/articles/s41598-025-15273-5]
- 57. Tumor fractions deciphered from circulating cell-free DNA ... [https://www.nature.com/articles/s41467-022-35320-3]
- 58. Unsupervised detection of fragment length signatures ... [https://elifesciences.org/articles/71569]
- 59. Tumor-naïve multimodal profiling of circulating tumor DNA ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12627382/]
- 60. Clinical utility of liquid biopsy-based companion ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9630093/]
- 61. FDA Approval Is Sought for PredicineCARE Assay as ... [https://www.onclive.com/view/fda-approval-is-sought-for-predicinecare-assay-as-companion-diagnostic-in-bladder-cancer]
- 62. List of Cleared or Approved Companion Diagnostic Devices [https://www.fda.gov/medical-devices/in-vitro-diagnostics/list-cleared-or-approved-companion-diagnostic-devices-in-vitro-and-imaging-tools]
- 63. Comparative analysis of EGFR mutations in circulating ... [https://www.nature.com/articles/s41598-025-85160-6]
- 64. A Comprehensive Review of Handling Missing Data: Exploring Special Missing Mechanisms [https://arxiv.org/html/2404.04905v1]
- 65. A survey on missing data in machine learning - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC8549433/]
- 66. Effective and efficient handling of missing data in supervised machine learning - ScienceDirect [https://www.sciencedirect.com/science/article/pii/S2666764924000663]
- 67. On the use of machine learning methods for missing data problems - ScienceDirect [https://www.sciencedirect.com/science/chapter/handbook/abs/pii/S0169716125000689]
- 68. Development and multi-cohort validation of a machine ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12357463/]
- 69. Development and multi-center validation of machine learning ... [https://translational-medicine.biomedcentral.com/articles/10.1186/s12967-025-07265-w]
- 70. Diagnostic framework to validate clinical machine learning ... [https://www.nature.com/articles/s43856-025-00965-w]
- 71. NCI Cohort Consortium Membership | EGRP/DCCPS/NCI/NIH [https://epi.grants.cancer.gov/cohort-consortium/members/]
- 72. A Novel Cell-Free DNA Fragmentomic Assay and Its ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12606779/]
- 73. Building AI Fairness by Reducing Algorithmic Bias [https://tepperspectives.cmu.edu/all-articles/building-ai-fairness-by-reducing-algorithmic-bias/]
- 74. Bias in AI | Examples, Causes & Mitigation Strategies 2025 [https://kodexolabs.com/bias-in-ai/]
- 75. Deep Dive: Bias & Fairness in AI Models [https://research.contrary.com/deep-dive/bias-fairness]
- 76. Post-processing methods for mitigating algorithmic bias in ... [https://bmcdigitalhealth.biomedcentral.com/articles/10.1186/s44247-025-00166-4]
- 77. Landmark AI framework sets new standard for tackling ... [https://www.dlapiper.com/en/insights/publications/ai-outlook/2025/landmark-ai-framework-sets-new-standard-for-tackling-algorithmic-bias]
- 78. Groundbreaking Fairness Evaluation Dataset From ... [https://ai.sony/articles/Groundbreaking-Fairness-Evaluation-Dataset-From-Sony%20AI%20/]
- 79. Explainable vs. Interpretable Artificial Intelligence [https://www.splunk.com/en_us/blog/learn/explainability-vs-interpretability.html]
- 80. 2 Interpretability – Interpretable Machine Learning [https://christophm.github.io/interpretable-ml-book/interpretability.html]
- 81. Interpretability vs explainability: understanding the ... [https://www.xcally.com/news/interpretability-vs-explainability-understanding-the-importance-in-artificial-intelligence/]
- 82. Evaluation metrics and statistical tests for machine learning [https://www.nature.com/articles/s41598-024-56706-x]
- 83. What Is Model Performance in Machine Learning? [https://www.ibm.com/think/topics/model-performance]
- 84. 2025 and Beyond: The Future of Genomic Data Analysis ... [https://blog.crownbio.com/2025-and-beyond-the-future-of-genomic-data-analysis-and-innovations-in-genomics-services]
- 85. Machine Learning‐Assisted Evaluation of Circulating DNA ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7509651/]
- 86. A framework for clinical cancer subtyping from nucleosome ... [https://www.nature.com/articles/s41467-022-35076-w]
- 87. Bootstrapping the Cross-Validation Estimate [https://arxiv.org/html/2307.00260v2]
- 88. Evaluating Machine Learning Models: A Guide to Cross ... [https://christianbernecker.medium.com/evaluating-machine-learning-models-a-guide-to-cross-validation-and-performance-metrics-19c5641af014]
- 89. Bootstrap vs Crossvalidation for assessing the predictive ... [https://stats.stackexchange.com/questions/656710/bootstrap-vs-crossvalidation-for-assessing-the-predictive-performance-of-a-machi]
- 90. Cell-free DNA testing for the detection and prognosis ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12274360/]
- 91. Multimodal analysis of cfDNA methylomes for early ... [https://www.nature.com/articles/s41467-024-47886-1]
- 92. Technical Advances in Circulating Cell-Free DNA ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11048502/]
- 93. Presenting machine learning model information to clinical ... [https://www.nature.com/articles/s41746-020-0253-3]
- 94. Clinical prediction models using machine learning in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12506039/]
- 95. Novel technologies in cfDNA analysis and potential utility in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8742177/]
- 96. Cell-free DNA testing for the detection and prognosis ... [https://www.nature.com/articles/s41467-025-61890-z]
- 97. Comparing the Performance of Machine Learning Models ... [https://www.jmir.org/2025/1/e76215]
- 98. Monitoring and Assessment of Circulating Tumor DNA in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12550271/]
- 99. A comparative study of four cell-free DNA assays for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12217890/]
- 100. BillionToOne's Northstar Select® Demonstrates Superior ... [https://www.northstaronc.com/news/billiontoones-northstar-select-r-demonstrates-superior-sensitivity-in-prospective-head-to-head-validation-study-publication]
- 101. A multi-center study for colorectal cancer early detection in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12574013/]