From Code to Cure: Integrating DNA and RNA Sequencing in Modern Oncology
This article provides a comprehensive overview of the principles and clinical applications of Next-Generation Sequencing (NGS) in oncology, covering both DNA and RNA sequencing.
From Code to Cure: Integrating DNA and RNA Sequencing in Modern Oncology
Abstract
This article provides a comprehensive overview of the principles and clinical applications of Next-Generation Sequencing (NGS) in oncology, covering both DNA and RNA sequencing. It explores the foundational technology, detailing how NGS has surpassed traditional methods like Sanger sequencing. The piece delves into methodological workflows, from nucleic acid isolation to data analysis, and highlights advanced applications such as identifying expressed mutations, gene fusions, and tumor microenvironment signatures. It further addresses critical challenges in validation, troubleshooting, and optimization for clinical use. Finally, the article examines the transformative impact of integrated DNA and RNA sequencing on precision medicine, including its role in guiding tumor-agnostic therapies and improving patient outcomes through more accurate biomarker discovery and therapeutic targeting.
The Genomic Revolution: Core Principles of Next-Generation Sequencing in Cancer
The field of genomics has undergone a revolutionary transformation with the advent of Next-Generation Sequencing (NGS), moving from linear, single-fragment analysis to massively parallel processing. This technological evolution is particularly critical in oncology research, where comprehensive genomic profiling of tumors has become fundamental to understanding cancer biology and developing targeted therapies. The shift from Sanger sequencing, known as the first-generation method, to NGS represents more than just an incremental improvement—it constitutes a complete reimagining of sequencing scalability, efficiency, and application [1]. Where the Human Genome Project required 13 years and nearly $3 billion using Sanger technology, NGS can now sequence an entire human genome in approximately one week at a fraction of the cost [2] [3]. This dramatic enhancement in throughput has positioned NGS as an indispensable tool in modern oncology research, enabling scientists to decipher the complex genetic alterations that drive cancer progression, metastasis, and treatment resistance.
The fundamental distinction between these technologies lies in their core architecture: Sanger sequencing processes a single DNA fragment at a time, while NGS simultaneously sequences millions of fragments in parallel [4]. This massively parallel approach has unlocked unprecedented capabilities for comprehensive genomic analysis, from whole-genome sequencing to targeted panels of cancer-associated genes. In oncology, where tumors often harbor heterogeneous cell populations with diverse mutations, the ability to detect low-frequency variants and structural alterations across hundreds of genes in a single assay has transformed research methodologies and therapeutic development [2] [5]. This technical guide explores the throughput advantage of NGS through quantitative comparisons, experimental applications in oncology research, and detailed methodologies that highlight its transformative role in cancer genomics.
Fundamental Technological Differences: Sanger vs. NGS
Core Principles and Sequencing Chemistry
The fundamental difference between Sanger sequencing and NGS lies not in the basic biochemistry of DNA synthesis but in the scale and parallelization of the sequencing process. Both methods rely on DNA polymerase to incorporate nucleotides into a growing DNA strand complementary to the template being sequenced [4]. However, their implementation diverges significantly in how they manage this process and detect the incorporated nucleotides.
Sanger sequencing (chain-termination method) utilizes dideoxynucleoside triphosphates (ddNTPs), which lack the 3'-hydroxyl group necessary for forming a phosphodiester bond with the next nucleotide. When incorporated, these chain-terminating nucleotides halt DNA synthesis, producing DNA fragments of varying lengths [6]. In modern capillary electrophoresis implementations, each ddNTP is labeled with a distinct fluorescent dye, allowing separation by size and detection via laser excitation [6]. This process generates a single, long contiguous read (typically 500-1000 base pairs) per reaction, making it highly accurate for targeted sequencing but fundamentally limited in throughput [2] [6].
In contrast, NGS technologies employ massively parallel sequencing of millions to billions of DNA fragments simultaneously [4]. The most common approach, Sequencing by Synthesis (SBS), used by Illumina platforms, incorporates fluorescently-labeled reversible terminators that temporarily halt synthesis after each nucleotide incorporation [3]. After imaging to determine the incorporated base, the terminator is cleaved, and the process repeats [3]. This cyclical process occurs simultaneously across millions of DNA clusters on a flow cell, generating enormous volumes of data in a single run [2] [3]. Other NGS chemistries include ion semiconductor sequencing (detecting pH changes during nucleotide incorporation) and single-molecule real-time sequencing (observing incorporation in real-time) [2] [3].
Workflow Comparison: From Sample to Sequence
The experimental workflow from sample preparation to data output differs substantially between Sanger and NGS methods, with implications for throughput, scalability, and applications in oncology research.
Table 1: Comparative Workflows in Sanger Sequencing and NGS
| Workflow Step | Sanger Sequencing | Next-Generation Sequencing |
|---|---|---|
| Sample Preparation | PCR amplification of specific target regions | Fragmentation of DNA, adapter ligation, and library preparation |
| Template Amplification | Clonal amplification in bacterial vectors (historical) or PCR | Bridge amplification or emulsion PCR to create clustered DNA fragments |
| Sequencing Process | Capillary electrophoresis with fluorescent detection | Massively parallel sequencing by synthesis, ion semiconductor, or other methods |
| Data Output | Single sequence per run (up to 1,000 bp) | Millions to billions of short reads (50-600 bp) per run |
| Read Analysis | Direct sequence reading from electrophoretogram | Alignment to reference genome and variant calling through bioinformatics pipelines |
The library preparation step in NGS is particularly critical for oncology applications. DNA is fragmented into manageable pieces, and adapter sequences are attached to both ends. These adapters serve dual purposes: they enable binding to the sequencing platform and facilitate the amplification that creates clusters of identical DNA fragments [3]. For tumor samples, which often yield limited quantities of degraded DNA (especially from formalin-fixed paraffin-embedded specimens), specialized library preparation protocols have been developed to maximize data quality from suboptimal starting material [5].
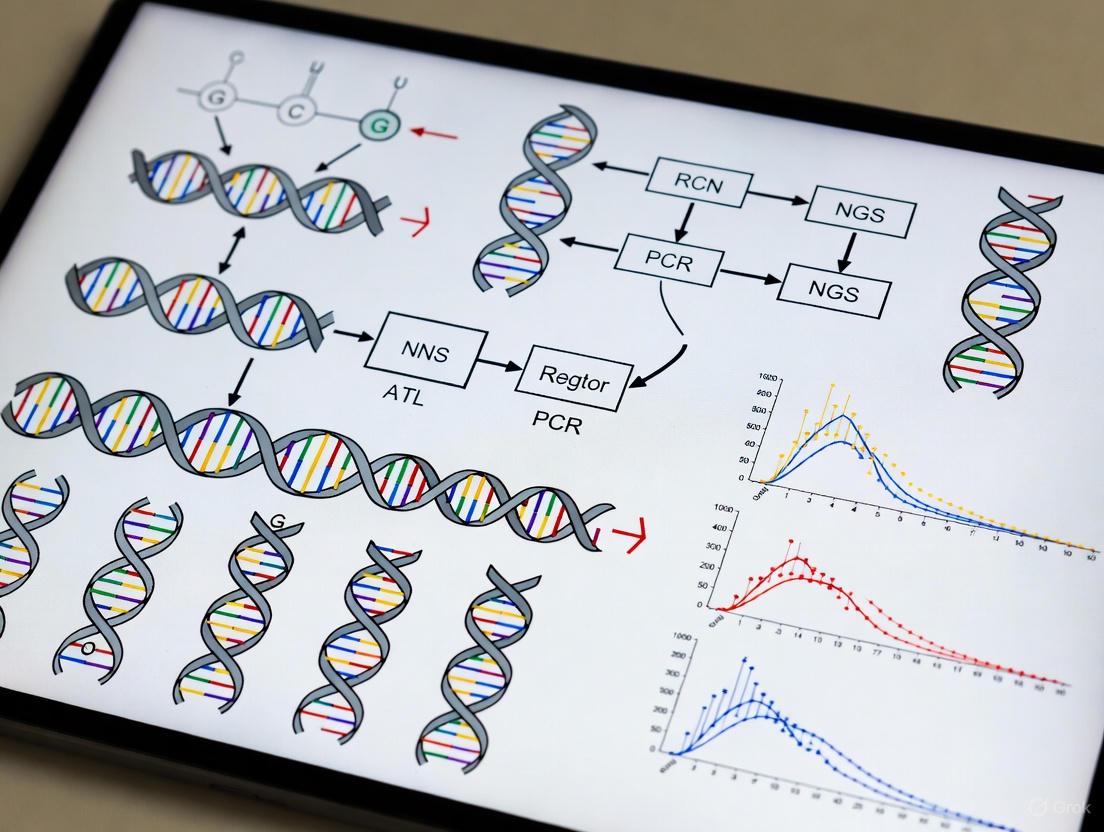
The following workflow diagram illustrates the key steps in NGS library preparation and sequencing:
NGS Library Preparation and Sequencing Workflow
Quantitative Comparison: Throughput and Performance Metrics
Throughput, Sensitivity, and Cost Analysis
The throughput advantage of NGS becomes evident when examining quantitative performance metrics across multiple parameters critical to oncology research. The massively parallel nature of NGS enables a fundamental shift in sequencing capacity that transcends simple speed comparisons.
Table 2: Performance Comparison Between Sanger Sequencing and NGS
| Parameter | Sanger Sequencing | Next-Generation Sequencing |
|---|---|---|
| Throughput | Single DNA fragment per reaction | Millions to billions of fragments simultaneously [4] |
| Sensitivity (Detection Limit) | 15-20% variant allele frequency [2] [4] | As low as 1-5% variant allele frequency [2] [7] |
| Human Genome Sequencing Time | Approximately 13 years (Human Genome Project) [3] | Approximately one week [2] |
| Cost per Human Genome | ~$3 billion (Human Genome Project) [3] | Under $1,000 [3] |
| Read Length | 500-1000 base pairs [2] [6] | 50-600 base pairs (short-read platforms) [3] |
| Applications in Oncology | Single-gene mutation confirmation | Multi-gene panels, whole exome/genome, transcriptomics, epigenomics [2] [8] |
| Variant Detection Capability | Limited to specific targeted regions | SNPs, indels, CNVs, structural variants, fusion genes [2] |
The sensitivity advantage of NGS is particularly significant in oncology applications. The ability to detect variants with ~1% variant allele frequency (VAF) compared to Sanger's 15-20% VAF enables identification of low-frequency mutations in heterogeneous tumor samples and early detection of emerging resistant clones [2] [4] [7]. This enhanced sensitivity stems from the deep sequencing capability of NGS, where each genomic region is covered hundreds to thousands of times, allowing statistical discrimination of true low-frequency variants from sequencing errors [2].
Economic and Operational Efficiency
The economic advantage of NGS emerges primarily through its massive parallelization and multiplexing capabilities. While the per-run cost of NGS is higher than Sanger sequencing, the cost per base is dramatically lower—making comprehensive genomic profiling economically feasible [6]. This economic model has enabled scaling of oncology research that would be prohibitively expensive with Sanger sequencing.
The multiplexing capability of NGS allows barcoding of hundreds of samples that can be pooled and sequenced simultaneously, further optimizing reagent use and operational efficiency [4]. For oncology drug development, where screening numerous cell lines, patient-derived xenografts, or clinical samples is routine, this multiplexing advantage significantly accelerates research timelines. The combination of higher throughput, greater sensitivity, and lower cost per base makes NGS particularly suited for the complex genomic landscape of cancer, which often requires interrogating hundreds of genes simultaneously to capture the full spectrum of clinically relevant mutations [5].
NGS Applications in Oncology Research
Comprehensive Genomic Profiling in Cancer Research
In oncology research, NGS has become the cornerstone technology for comprehensive genomic profiling of tumors, enabling a multifaceted approach to understanding cancer biology. The throughput advantage of NGS allows simultaneous assessment of multiple genomic alteration types across hundreds of cancer-associated genes, providing researchers with a complete molecular portrait of malignancy [2] [7]. This comprehensive approach has accelerated the discovery of driver mutations, fusion genes, and predictive biomarkers across diverse cancer types [2].
Targeted NGS panels specifically designed for oncology research typically focus on genes with established roles in carcinogenesis, such as KRAS, EGFR, TP53, PIK3CA, and BRCA1/2 [5]. These panels offer the advantage of deep sequencing coverage (often >500x) at lower cost compared to whole-genome approaches, making them ideal for detecting low-frequency variants in heterogeneous tumor samples [5]. The TTSH-oncopanel, a 61-gene panel described in recent research, demonstrates how targeted NGS can achieve 98.23% sensitivity for mutation detection while reducing turnaround time to just 4 days [5]. This efficiency in generating comprehensive genomic data accelerates therapeutic discovery and validation workflows.
Specialized Research Applications
The throughput advantage of NGS enables several specialized applications that are transforming oncology research:
Liquid Biopsy and Circulating Tumor DNA (ctDNA) Analysis: NGS provides the sensitivity required to detect and sequence rare ctDNA fragments in blood samples, enabling non-invasive tumor genotyping and monitoring of treatment response [2] [7]. Research applications include tracking clonal evolution, detecting minimal residual disease, and identifying emerging resistance mechanisms during targeted therapy [7].
Transcriptomic Profiling (RNA-Seq): NGS-based RNA sequencing allows comprehensive analysis of gene expression, alternative splicing, and fusion transcripts in tumor samples [9]. Recent studies demonstrate how targeted RNA-seq can complement DNA-based mutation detection by confirming expression of identified variants and detecting additional clinically relevant fusions missed by DNA sequencing alone [9].
Immuno-oncology Biomarker Discovery: The throughput of NGS enables quantification of complex biomarkers such as tumor mutational burden (TMB), microsatellite instability (MSI), and immune repertoire profiling—all critical for immunotherapy development [2] [7]. These applications require genome-wide sequencing data that would be impractical with Sanger sequencing.
Single-Cell Sequencing: Emerging NGS applications in oncology research include single-cell RNA and DNA sequencing, which reveals tumor heterogeneity and microenvironment interactions at unprecedented resolution [2]. This application exemplifies how NGS throughput enables entirely new research paradigms in cancer biology.
Experimental Design and Methodology
Implementing Targeted NGS Panels in Oncology Research
The experimental workflow for implementing targeted NGS in oncology research requires careful consideration of multiple parameters to ensure robust, reproducible results. Based on recent research validating the TTSH-oncopanel, the following methodology provides a framework for targeted NGS in cancer genomics [5]:
Sample Preparation and Quality Control:
- Input Requirement: ≥50 ng of DNA from tumor samples
- Quality Metrics: DNA integrity number (DIN) ≥4.0 for formalin-fixed paraffin-embedded (FFPE) samples
- Extraction Method: Standard column-based or magnetic bead-based protocols
- Quality Assessment: Fluorometric quantification and fragment analysis
Library Preparation Protocol:
- DNA Fragmentation: Fragment genomic DNA to ~300 bp using acoustic shearing or enzymatic fragmentation
- Adapter Ligation: Attach platform-specific adapter sequences with sample barcodes using ligase-mediated approach
- Library Amplification: Amplify ligated fragments using 6-8 cycles of PCR with high-fidelity polymerase
- Library Quantification: Assess library concentration using fluorometric methods and validate fragment size distribution
Target Enrichment:
- Method: Hybridization capture with biotinylated oligonucleotide probes
- Panel Design: Custom probes targeting 61 cancer-associated genes (or research-specific gene set)
- Hybridization: Incubate library with probe pool for 16-24 hours at 65°C
- Wash Conditions: Stringent washing to remove non-specifically bound fragments
Sequencing Parameters:
- Platform: Illumina, MGI DNBSEQ-G50RS, or comparable system
- Read Configuration: Paired-end sequencing (2×150 bp)
- Coverage Target: Minimum 250x mean coverage with >98% of targets at ≥100x
- Sample Multiplexing: 24-96 samples per flow cell lane depending on desired coverage
Bioinformatics Analysis Pipeline
The massive data output from NGS requires sophisticated bioinformatics analysis, which represents both a challenge and opportunity in oncology research:
Primary Analysis:
- Base Calling: Convert raw signal data to nucleotide sequences
- Demultiplexing: Assign reads to specific samples based on barcode sequences
- Quality Control: FastQC evaluation of read quality, adapter content, and duplication rates
Secondary Analysis:
- Read Alignment: Map sequences to reference genome (e.g., GRCh38) using BWA-MEM or similar aligner
- Variant Calling: Identify single nucleotide variants (SNVs) and small indels using Mutect2, VarDict, or LoFreq [9]
- Annotation: Annotate variants with population frequency, functional impact, and clinical significance databases
Tertiary Analysis:
- Pathway Analysis: Identify significantly mutated pathways and biological processes
- Variant Prioritization: Filter variants based on frequency, predicted impact, and relevance to cancer phenotype
- Data Visualization: Create intuitive visualizations of mutation spectra and genomic landscapes
The following diagram illustrates the bioinformatics workflow for processing NGS data in oncology research:
Bioinformatics Workflow for NGS Data in Oncology
Essential Research Reagents and Platforms
Successful implementation of NGS in oncology research requires specific reagents, platforms, and computational tools. The following table details essential components of the NGS research toolkit:
Table 3: Research Reagent Solutions for NGS in Oncology
| Category | Specific Products/Platforms | Research Application |
|---|---|---|
| Library Preparation | Illumina DNA Prep, KAPA HyperPlus, MGI EasySeq | Fragment DNA and add platform-specific adapters for sequencing |
| Target Enrichment | Sophia Genetics Oncopanel, Agilent ClearSeq, Roche Comprehensive Cancer Panel | Hybridization capture to enrich for cancer-related genes |
| Sequencing Platforms | Illumina NovaSeq, MGI DNBSEQ-G50, PacBio Sequel, Oxford Nanopore | Generate sequencing data with different read lengths and applications |
| Automation Systems | MGI SP-100RS, Hamilton NGS STAR | Automated library preparation to reduce hands-on time and variability |
| Bioinformatics Tools | BWA, GATK, Mutect2, VarDict, Sophia DDM | Align sequences, call variants, and annotate results [5] [9] |
| Reference Materials | Horizon Discovery HD701, Seraseq FFPE | Positive controls for assay validation and quality monitoring [5] |
Each component plays a critical role in the end-to-end NGS workflow. For example, automated library preparation systems like the MGI SP-100RS can improve reproducibility while reducing human error and contamination risk [5]. Bioinformatics platforms such as Sophia DDM incorporate machine learning algorithms for variant analysis and visualization, connecting molecular profiles to biological insights through specialized knowledge bases [5].
The transition from Sanger sequencing to Next-Generation Sequencing represents a fundamental shift in the scale and scope of genomic analysis possible in oncology research. The throughput advantage of NGS—enabled by massively parallel processing—has transformed cancer genomics from a gene-by-gene approach to comprehensive genomic profiling that captures the full complexity of malignant transformation. This technical evolution has accelerated therapeutic discovery, enabled personalized treatment approaches, and deepened our understanding of cancer biology.
Future developments in NGS technology continue to build upon this throughput foundation. Third-generation sequencing platforms offering long-read capabilities are addressing NGS limitations in resolving complex genomic regions [2] [3]. Single-cell sequencing methods are revealing tumor heterogeneity at unprecedented resolution [2]. Spatial transcriptomics technologies are adding morphological context to gene expression data [2]. The integration of artificial intelligence with NGS data is enhancing variant interpretation and biomarker discovery [2]. Each of these advancements extends the throughput advantage of NGS into new dimensions of genomic analysis, ensuring its continued central role in oncology research and drug development.
As NGS technologies continue to evolve, further reductions in cost and improvements in automation will make comprehensive genomic profiling increasingly accessible. However, the core principle remains: the massively parallel architecture of NGS provides a throughput advantage that has permanently transformed oncology research, enabling scientists to interrogate cancer genomes with a breadth and depth that was unimaginable with Sanger sequencing technology.
Next-generation sequencing (NGS) has revolutionized oncology research by enabling comprehensive genomic profiling of tumors, facilitating the shift toward precision medicine [8] [10]. This transformative technology allows researchers to identify genetic alterations that drive cancer progression, detect hereditary cancer syndromes, and monitor treatment response through sensitive minimal residual disease detection [8]. Unlike traditional Sanger sequencing, which processes one DNA fragment at a time, NGS employs massively parallel sequencing to simultaneously analyze millions of fragments, significantly reducing time and cost while providing unprecedented genomic resolution [8] [10]. The core NGS workflow consists of four critical stages: sample preparation, library construction, sequencing, and data analysis, each requiring meticulous execution to generate reliable results for clinical decision-making in oncology [11] [8]. This technical guide details each step of the core NGS workflow within the context of modern cancer genomics research.
Sample Preparation
Sample preparation is the foundational step in the NGS workflow, transforming nucleic acids from biological samples into sequence-ready libraries. Proper execution is crucial, as any deficiencies at this stage can compromise sequencing success and downstream analysis [11].
Nucleic Acid Extraction
The initial step involves isolating DNA or RNA from various biological samples, including tumor tissues, blood, cultured cells, or urine [11]. In oncology, samples often present challenges such as formalin-fixed paraffin-embedded (FFPE) tissue, which may yield degraded nucleic acids, or fine-needle biopsies with limited starting material [11] [12]. The quality of extracted nucleic acids directly depends on sample quality and appropriate storage conditions, with fresh material recommended but often supplemented with properly preserved specimens [11].
Essential protocols for nucleic acid extraction:
- DNA Extraction from FFPE Tissue: Using a QIAamp DNA FFPE Tissue kit (Qiagen), extract genomic DNA after manual microdissection of representative tumor areas with sufficient tumor cellularity. Quantify DNA concentration using Qubit dsDNA HS Assay kit on Qubit 3.0 Fluorometer and assess purity with NanoDrop Spectrophotometer (A260/A280 ratio 1.7-2.2) [12].
- Cell Disruption: Employ mechanical, enzymatic, or chemical methods to lyse cells and release nucleic acids while maintaining integrity.
- Purification: Remove contaminants including proteins, lipids, and carbohydrates through organic extraction or column-based methods.
- Quality Assessment: Evaluate nucleic acid quantity and quality using fluorometric methods (Qubit, PicoGreen) for precision and spectrophotometry (Nanodrop) for purity assessment (DNA: 260/280 ratio 1.8-2.0; RNA: 260/280 ratio 1.8-2.1) [11] [13].
For challenging oncology samples with limited material, amplification through polymerase chain reaction (PCR) may be necessary, though this introduces potential biases that must be minimized through specialized PCR enzymes and library complexity optimization [11].
Special Considerations for Oncology Samples
Oncology research frequently deals with heterogeneous tumor samples with varying tumor purity, requiring special considerations during sample preparation:
- Tumor Enrichment: Manual microdissection of FFPE blocks to select areas with sufficient tumor cellularity (>20% typically recommended) [12].
- Input Requirements: Minimum of 20 ng DNA for library generation, though higher amounts improve library complexity [12].
- Quality Thresholds: Samples with A260/A280 ratios outside 1.7-2.2 may indicate contamination and should be avoided [12].
- Liquid Biopsy Applications: Circulating tumor DNA (ctDNA) from blood samples requires high sensitivity to detect variants at low allele frequencies (as low as 0.5%) [14].
Library Construction
Library construction converts purified nucleic acids into formats compatible with NGS platforms through fragmentation and adapter ligation [11] [8]. This critical step determines the success of subsequent sequencing and analysis.
DNA Library Preparation
DNA library preparation involves several standardized steps to process genomic DNA for sequencing:
- Fragmentation: DNA is fragmented to desired lengths (typically 300 bp) using physical (acoustic shearing), enzymatic (transposase-based), or chemical methods. Physical methods provide more uniform fragment sizes, while enzymatic approaches offer convenience and rapid processing [11] [8].
- End Repair and A-Tailing: DNA fragment ends are repaired to create blunt ends, followed by addition of single adenosine nucleotides to facilitate adapter ligation. Efficient A-tailing prevents chimera formation during amplification [11] [13].
- Adapter Ligation: Platform-specific adapters containing sequencing primer binding sites are ligated to fragment ends. These adapters may include barcodes (indices) to enable sample multiplexing [11] [8].
- Size Selection: Libraries are size-selected to remove fragments too large or small for optimal sequencing, performed using magnetic bead-based clean-up or agarose gel electrophoresis [11].
- Amplification: PCR amplification enriches for adapter-ligated fragments, though PCR-free protocols are available to minimize amplification biases, particularly important for detecting low-frequency variants in cancer [11].
Table 1: Comparison of Nucleic Acid Fragmentation Methods
| Method | Principle | Advantages | Limitations | Best Applications |
|---|---|---|---|---|
| Physical (Sonication) | Acoustic energy shears DNA | Uniform fragment size, minimal bias | Equipment cost, sample volume requirements | Whole genome sequencing, PCR-free libraries |
| Enzymatic (Tagmentation) | Transposase simultaneously fragments and tags DNA | Rapid, cost-effective, minimal hands-on time | Sequence bias potential, optimization required | High-throughput applications, targeted sequencing |
| Chemical | divalent cations fragment DNA | Simple, inexpensive | Less control over size distribution | Basic research applications |
RNA Library Preparation
RNA sequencing library construction requires additional steps to convert RNA to sequencing-compatible DNA:
- RNA Selection: Isolate mRNA using poly-A selection or deplete ribosomal RNA to enrich for protein-coding transcripts.
- cDNA Synthesis: Reverse transcribe RNA to complementary DNA (cDNA) using reverse transcriptase, as DNA is more stable and amplifiable using DNA polymerase [11] [8].
- Library Construction: Process cDNA similarly to DNA libraries through fragmentation, end repair, adapter ligation, and amplification. Strand-specific protocols preserve transcript orientation information [11] [13].
Quality Control in Library Construction
Rigorous quality control ensures library integrity before sequencing:
- Quantification: Use qPCR or fluorometric methods for accurate library quantification, as spectrophotometry may overestimate concentration [13].
- Size Distribution: Analyze fragment size distribution using Bioanalyzer or TapeStation systems, with ideal library sizes of 250-400 bp for Illumina platforms [12].
- Adapter Dimer Check: Verify absence of primer dimers which compete with library fragments during sequencing.
- Molarity Calculation: Precisely calculate library molarity for accurate clustering during sequencing.
For oncology applications, libraries must meet stringent quality thresholds, with at least 80% of targets achieving 100x coverage, and average mean depths of 500-1000x recommended for detecting low-frequency variants in heterogeneous tumor samples [12].
Sequencing
The sequencing phase involves massive parallel sequencing of prepared libraries using NGS platforms, generating vast amounts of raw data for downstream analysis [8].
Sequencing Technologies and Platforms
Multiple NGS platforms employ different sequencing chemistries and detection methods:
- Illumina Sequencing: Utilizes sequencing-by-synthesis with fluorescently labeled nucleotides. Library fragments are immobilized on a flow cell and amplified via bridge PCR to form clusters. During each cycle, fluorescently tagged nucleotides incorporate into growing DNA strands, with imaging detecting the incorporated base at each cluster [8].
- Ion Torrent Sequencing: Employs semiconductor technology detecting hydrogen ions released during DNA polymerization rather than optical signals, enabling faster run times.
- Pacific Biosciences SMRT Sequencing: Uses single molecule real-time sequencing with zero-mode waveguides to observe polymerase activity in real time, generating long reads beneficial for resolving complex genomic regions.
- Oxford Nanopore Sequencing: Measures changes in electrical current as DNA strands pass through protein nanopores, enabling ultra-long reads and real-time analysis.
Table 2: Comparison of Major NGS Sequencing Platforms
| Platform | Technology | Read Length | Throughput | Error Rate | Primary Oncology Applications |
|---|---|---|---|---|---|
| Illumina NovaSeq | Sequencing-by-synthesis | 50-300 bp | 0.8-6.0 Tb | 0.1-0.6% | Whole genome, exome, transcriptome, targeted sequencing |
| Illumina NextSeq 550Dx | Sequencing-by-synthesis | 75-300 bp | 120-360 Gb | 0.1-0.6% | Targeted panels, clinical diagnostics [12] |
| Ion Torrent Genexus | Semiconductor sequencing | 200-400 bp | 40-500 Mb | ~1% | Rapid targeted sequencing, liquid biopsy |
| PacBio Revio | SMRT sequencing | 10-50 kb | 0.9-1.8 Tb | ~5% (random) | Structural variant detection, fusion genes, haplotype phasing |
| Oxford Nanopore PromethION | Nanopore sequencing | 10 kb-2 Mb+ | 2.5-14 Tb | 2-10% | Structural variants, epigenetics, isoform sequencing |
Sequencing Applications in Oncology
NGS enables various sequencing approaches tailored to specific oncology research questions:
- Whole Genome Sequencing (WGS): Determines the complete DNA sequence of the entire tumor genome, identifying coding and non-coding variants, structural rearrangements, and copy number alterations [11].
- Whole Exome Sequencing (WES): Targets protein-coding regions (exons), comprising ~1-2% of the genome, cost-effectively identifying coding variants responsible for cancer driver mutations [11] [8].
- Targeted Sequencing: Focuses on specific genes or genomic regions of clinical significance in cancer, using hybridization capture or amplicon-based approaches to achieve deep coverage for detecting low-frequency variants [11] [7].
- RNA Sequencing: Profiles the transcriptome to identify gene expression changes, fusion genes, alternative splicing, and mutation effects on transcription [11].
- Methylation Sequencing: Uses bisulfite treatment to detect DNA methylation patterns, revealing epigenetic modifications in cancer development [11].
Each application requires specialized library preparation methods, with targeted approaches particularly valuable in clinical oncology for focusing on established cancer-associated genes with high sensitivity [11] [7].
Data Analysis
NGS data analysis converts raw sequencing data into biologically meaningful information through complex computational workflows, representing a critical bottleneck in oncology genomics [8] [15].
Primary Data Analysis
The initial analysis phase processes raw instrument data into sequence reads:
- Base Calling: Converts raw signal data (fluorescence or ion potential) into nucleotide sequences, assigning quality scores (Phred scores) to each base.
- Demultiplexing: Separates pooled samples using barcode sequences added during library preparation, generating individual sequence files for each sample.
- Quality Assessment: Evaluates read quality using tools like FastQC to identify potential issues with sequencing runs, adapter contamination, or poor-quality regions.
Sequence Alignment and Processing
Processed reads are aligned to reference genomes to identify genomic variants:
- Read Alignment/Mapping: Maps sequence reads to reference genomes (e.g., GRCh38) using aligners like BWA, Bowtie2, or Novoalign, identifying genomic positions for each read [15].
- Post-Alignment Processing: Refines alignments through duplicate marking, base quality score recalibration, and local realignment around indels to improve variant detection accuracy.
- Variant Calling: Identifies genomic variants (single nucleotide variants, insertions/deletions, copy number variations, structural variants) using specialized algorithms:
Table 3: Bioinformatics Tools for NGS Data Analysis in Oncology
| Analysis Step | Common Tools | Key Features | Oncology Considerations |
|---|---|---|---|
| Read Alignment | BWA, Bowtie2, Novoalign | Efficient mapping to reference genomes | Optimal for detecting somatic variants with high specificity [15] |
| SNV/Indel Calling | Mutect2, VarScan, Strelka2 | High sensitivity for low-frequency variants | Detection limit typically 2-5% VAF; lower for ultrasensitive applications [15] [12] |
| Copy Number Analysis | ASCATNGS, CNVkit | Resolves tumor purity and ploidy | Essential for identifying oncogene amplifications and tumor suppressor deletions [16] [12] |
| Structural Variant Calling | LUMPY, Delly | Detects rearrangements, fusions | Critical for identifying targetable fusions (e.g., RET, ALK, ROS1) [12] |
| Annotation | SnpEff, VEP | Functional consequence prediction | Annotates variants with clinical databases (ClinVar, COSMIC) [12] |
Variant Interpretation and Clinical Reporting
In oncology research, identified variants require careful interpretation to determine clinical significance:
- Variant Annotation: Annotates variants using tools like SnpEff or Variant Effect Predictor with functional predictions (SIFT, PolyPhen, CADD), population frequencies, and clinical databases (ClinVar, COSMIC) [17] [12].
- Tier Classification: Classifies variants according to standardized guidelines (e.g., Association for Molecular Pathology):
- Tier I: Variants of strong clinical significance (FDA-approved or professional guidelines)
- Tier II: Variants of potential clinical significance (different tumor types or investigational therapies)
- Tier III: Variants of unknown clinical significance
- Tier IV: Benign or likely benign variants [12]
- Actionability Assessment: Determines therapeutic implications based on evidence levels, including FDA-approved therapies, clinical trials, and preclinical evidence.
- Report Generation: Creates comprehensive reports documenting methodology, variants identified, clinical interpretations, and therapeutic recommendations.
Workflow Visualization
The Scientist's Toolkit
Table 4: Essential Research Reagents and Solutions for NGS in Oncology
| Reagent/Solution | Function | Application Notes | Representative Products |
|---|---|---|---|
| Nucleic Acid Extraction Kits | Isolate DNA/RNA from various sample types | Critical for FFPE samples; ensure high purity with 260/280 ratio 1.7-2.2 | QIAamp DNA FFPE Tissue Kit [12] |
| DNA Quantitation Assays | Precisely measure DNA concentration | Fluorometric methods preferred over spectrophotometry for accuracy | Qubit dsDNA HS Assay Kit [12] |
| Library Preparation Kits | Convert nucleic acids to sequenceable libraries | Select based on application (WGS, WES, targeted, RNA-seq) | Illumina DNA Prep, Agilent SureSelectXT [12] |
| Target Enrichment Systems | Enrich specific genomic regions | Hybridization capture provides uniform coverage; amplicon-based offers simplicity | Agilent SureSelect (hybridization capture) [12] |
| Quality Control Instruments | Assess library quality and quantity | Essential for determining fragment size distribution and molarity | Agilent Bioanalyzer, TapeStation [12] |
| Sequencing Chemistries | Enable base detection during sequencing | Platform-specific reagents for cluster generation and sequencing | Illumina sequencing reagents, Ion Torrent supplies |
| Variant Calling Software | Identify genomic alterations from sequence data | Multiple algorithms recommended for comprehensive variant detection | GATK Mutect2, VarScan, Strelka2 [15] [12] |
| Bioinformatics Pipelines | Integrated analysis workflows | Combine mapping, variant calling, and annotation in reproducible workflows | GATK Best Practices, custom pipeline scripts [15] [17] |
The core NGS workflow represents a transformative technology in oncology research, enabling comprehensive molecular profiling that drives precision medicine approaches. From sample preparation through data analysis, each step requires meticulous execution and quality control to generate clinically actionable results. The integration of robust laboratory protocols with sophisticated bioinformatics pipelines allows researchers to detect diverse genomic alterations in cancer, including single nucleotide variants, insertions/deletions, copy number variations, and structural rearrangements. As NGS technologies continue to evolve with advancements in single-cell sequencing, liquid biopsies, and long-read sequencing, the workflow will further refine our understanding of tumor heterogeneity and treatment resistance mechanisms. Standardization of procedures, validation of bioinformatics pipelines, and interdisciplinary collaboration remain essential for maximizing the potential of NGS in advancing oncology research and improving patient outcomes through molecularly-guided therapies.
In the field of modern oncology research, next-generation sequencing (NGS) has revolutionized our approach to understanding and treating cancer. DNA sequencing (DNA-seq) and RNA sequencing (RNA-seq) stand as two foundational technologies that provide complementary views of the molecular machinery driving carcinogenesis. While DNA-seq reveals the hereditary blueprint and acquired mutations within the tumor genome, RNA-seq illuminates the functional transcriptome activity, revealing which genetic instructions are actively being executed [8] [18]. The integration of both data types creates a more complete picture of cancer biology, enabling researchers and clinicians to move beyond static genetic maps to dynamic functional understanding. This technical guide explores the principles, methodologies, and synergistic applications of DNA and RNA sequencing within oncology research, providing scientists and drug development professionals with a framework for leveraging these technologies to advance precision medicine.
Fundamental Principles and Technological Comparisons
Core Objectives and Molecular Targets
DNA and RNA sequencing are designed to answer fundamentally different biological questions. DNA-seq aims to determine the precise order of nucleotides (A, T, C, G) within DNA molecules, thereby characterizing the genetic blueprint of an organism or tumor. This includes identifying genetic variations such as single nucleotide variants (SNVs), insertions and deletions (indels), copy number variations (CNVs), and structural rearrangements [18]. In oncology, this enables the discovery of inherited cancer predispositions, somatic driver mutations, and tumor-specific genetic alterations that may serve as therapeutic targets.
In contrast, RNA-seq analyzes the transcriptome—the complete set of RNA transcripts produced by the genome at a specific point in time. This technology captures dynamic gene expression patterns, revealing which genes are actively transcribed into RNA, and at what levels [18]. Beyond quantifying expression, RNA-seq provides critical insights into alternative splicing events, gene fusions, post-transcriptional modifications, and non-coding RNA species. This functional dimension is particularly valuable in cancer research for understanding how genetic alterations manifest as transcriptional changes that drive tumor behavior and therapeutic responses.
Technical Workflows and Methodological Considerations
The fundamental workflow differences between DNA and RNA sequencing begin at the sample preparation stage. For DNA-seq, extracted genomic DNA is fragmented, and adapters are ligated to create a sequencing library [8]. For RNA-seq, the process is more complex due to RNA's inherent instability; extracted RNA must first be reverse-transcribed into complementary DNA (cDNA) before library construction, requiring careful handling to prevent degradation [18]. Most sequencing platforms (e.g., Illumina, Ion Torrent, PacBio, Oxford Nanopore) can be used for both DNA and RNA sequencing, though platform selection depends on the specific research goals, required read length, and desired throughput [18] [19].
Table 1: Key Technical Differences Between DNA and RNA Sequencing
| Feature | DNA Sequencing | RNA Sequencing |
|---|---|---|
| Molecular Target | Genomic DNA | RNA transcripts (converted to cDNA) |
| Primary Information | Genetic sequence, mutations, structural variants | Gene expression levels, splice variants, fusion transcripts |
| Sample Stability | Relatively stable, degrades slowly | Labile, degrades rapidly, requires careful preservation |
| Library Preparation | DNA fragmentation, adapter ligation | RNA extraction, reverse transcription to cDNA, fragmentation |
| Key Applications in Oncology | Identifying somatic mutations, CNVs, SNVs, hereditary risk | Detecting gene fusions, expression profiling, alternative splicing |
| Common Analysis Tools | BWA, Bowtie, GATK, Samtools | STAR, HISAT2, DESeq2, EdgeR |
Detection Capabilities for Oncogenic Alterations
The complementary strengths of DNA and RNA sequencing become particularly evident when assessing their capabilities to detect different classes of oncogenic alterations. DNA-seq excels at identifying single nucleotide variants, small insertions/deletions, and copy number alterations across the entire genome or targeted regions [8] [18]. However, it has significant limitations in detecting gene fusions, as the breakpoints often occur within long intronic regions containing repetitive sequences that are difficult to sequence and map [18].
RNA-seq proves superior for fusion detection because it sequences the transcribed mRNA, effectively skipping over intronic regions and providing direct evidence of expressed fusion events [18]. This capability has profound clinical implications, as numerous targeted therapies are now approved for cancers harboring fusions in genes such as ALK, ROS1, RET, and NTRK [20]. A study of 1,211 non-small cell lung cancer specimens found that approximately 10% of cases required reflex RNA sequencing to identify clinically actionable fusions that were missed by initial amplicon-based DNA testing [20].
Table 2: Detection Capabilities for Key Cancer Genomic Alterations
| Alteration Type | DNA-Seq Performance | RNA-Seq Performance |
|---|---|---|
| Single Nucleotide Variants (SNVs) | Excellent (Gold Standard) | Good, but limited to expressed mutations [21] |
| Insertions/Deletions (Indels) | Excellent | Good for expressed indels [18] |
| Copy Number Variations (CNVs) | Excellent | Limited to inferring from expression levels |
| Gene Fusions | Limited due to intronic breakpoints [18] | Excellent, detects expressed fusion transcripts [18] [20] |
| Alternative Splicing | Cannot detect directly | Excellent, captures different transcript isoforms [18] |
| Gene Expression | Not applicable | Primary application, quantitative measurement |
Experimental Design and Implementation
Integrated Sequencing Approaches in Oncology Research
Sophisticated research protocols increasingly leverage both DNA and RNA sequencing to maximize molecular insights. A prominent approach involves using DNA-seq as a comprehensive discovery tool for genetic variants, followed by RNA-seq to validate functional expression and biological relevance of these alterations [21]. This integrated strategy is particularly valuable for distinguishing driver mutations that are actively transcribed from passenger mutations that may not contribute to the oncogenic phenotype.
Real-world evidence supports this combined approach. A 2025 study on clinical utility of targeted RNA-seq analyzed 2,310 neoplasms and demonstrated that RNA-seq provided valuable molecular data for 87% of patients, including revised diagnoses and identification of clinically actionable alterations that led to treatment changes [22]. Similarly, research on reference samples showed that RNA-seq can uniquely identify variants with significant pathological relevance that were missed by DNA-seq, while also confirming expression of DNA-identified variants [21].
The Scientist's Toolkit: Essential Research Reagent Solutions
Successful implementation of DNA and RNA sequencing protocols requires carefully selected reagents and tools. The following table outlines essential components for integrated sequencing experiments in oncology research.
Table 3: Essential Research Reagent Solutions for Integrated Sequencing
| Reagent/Tool Category | Specific Examples | Function & Application Notes |
|---|---|---|
| Nucleic Acid Extraction Kits | AllPrep DNA/RNA/miRNA Universal Kit [23] | Simultaneous purification of gDNA and total RNA from limited samples, crucial for paired analysis |
| Target Enrichment Systems | Agilent Clear-seq; Roche Comprehensive Cancer panels [21] | Hybridization-capture baits for focused sequencing of cancer-related genes; variable probe lengths affect coverage |
| Library Preparation Chemistry | Illumina TruSeq; Ion Torrent Oncomine | Platform-specific reagents for NGS library construction; impact compatibility and multiplexing capabilities |
| RNA-Seq Specific Tools | Ribosomal RNA depletion kits; Reverse transcriptases | Remove abundant rRNA to enhance mRNA sequencing depth; critical for transcriptome analysis |
| Quality Control Assays | Bioanalyzer RNA integrity assessment; Fluorometric DNA/RNA quantification | Essential for evaluating sample quality pre-sequencing, particularly for FFPE-derived material |
| Hybridization Capture Reagents | Biotinylated probes; Strepavidin beads [20] | Enable targeted enrichment for fusion detection, especially valuable for novel fusion discovery |
Addressing Technical Challenges in Sequencing Workflows
Oncology researchers must navigate several technical challenges when implementing DNA and RNA sequencing. For RNA-seq, sample quality is paramount due to RNA's lability, particularly in formalin-fixed paraffin-embedded (FFPE) clinical specimens where RNA degradation can occur [22]. Implementing rigorous quality control measures, such as RNA Integrity Number (RIN) assessment, is essential for generating reliable data. For DNA-seq, achieving sufficient sequencing depth in tumor samples with low purity or high stromal contamination requires careful experimental design and bioinformatic correction.
The choice between whole transcriptome sequencing and targeted RNA-seq represents another key consideration. While whole transcriptome approaches provide comprehensive expression profiling, targeted RNA-seq panels offer deeper coverage of clinically relevant genes and can improve detection of low-abundance transcripts [21]. Research demonstrates that targeted approaches are particularly valuable for detecting expressed mutations with higher accuracy and reliability, especially for rare alleles and evolving mutant clones [21].
Applications in Precision Oncology and Drug Development
Enhancing Therapeutic Target Discovery and Validation
The complementary nature of DNA and RNA sequencing creates powerful synergies for identifying and validating novel therapeutic targets in oncology. DNA-seq can comprehensively catalog all genetic alterations present in a tumor, while RNA-seq determines which of these alterations are actively transcribed and likely to contribute to the oncogenic phenotype. This integrated approach is particularly valuable for prioritizing targets for drug development, as it helps distinguish functionally relevant driver mutations from biologically inert passenger mutations [21].
In clinical practice, this combined methodology directly impacts patient care. Studies have demonstrated that RNA-seq identifies clinically actionable fusions in lung adenocarcinomas that had no mitogenic driver alteration detected by DNA sequencing alone [24] [22]. Furthermore, RNA-seq provides critical functional characterization of variants of uncertain significance (VUS) identified through DNA sequencing, enabling more accurate interpretation of their clinical relevance and guiding appropriate targeted therapy selection [21].
Advancing Biomarker Development and Clinical Trial Design
In drug development, integrating DNA and RNA sequencing enables more sophisticated biomarker strategies and patient stratification approaches. By capturing both genetic alterations and their functional consequences, researchers can develop composite biomarkers that better predict treatment response. This is particularly relevant for immuno-oncology, where RNA-seq-derived gene expression signatures can identify tumors with immunologically "hot" microenvironments that may respond better to checkpoint inhibitors.
Clinical trials increasingly incorporate both DNA and RNA sequencing in biomarker-informed designs. The use of RNA-seq to detect neoantigens for personalized cancer vaccines represents a cutting-edge application, where expressed mutations identified through RNA sequencing are prioritized for vaccine development [21]. This approach ensures that therapeutic interventions target immunogenic peptides that are actually presented on the tumor cell surface, increasing the likelihood of clinical efficacy.
Emerging Technologies and Methodological Innovations
The field of cancer genomics continues to evolve rapidly, with several emerging technologies poised to enhance the complementary roles of DNA and RNA sequencing. Single-cell sequencing approaches now enable simultaneous DNA and RNA profiling at the individual cell level, revealing tumor heterogeneity and clonal evolution with unprecedented resolution. Long-read sequencing technologies from PacBio and Oxford Nanopore facilitate more accurate detection of complex structural variants and full-length transcript isoforms, addressing limitations of short-read sequencing for characterizing gene fusions and alternative splicing events [19].
Methodologically, integrated bioinformatics pipelines are being developed to jointly analyze DNA and RNA sequencing data from the same samples, providing more powerful approaches for linking genetic alterations to their functional consequences. These tools are particularly valuable for identifying expressed neoantigens for personalized cancer immunotherapy and elucidating non-coding drivers of oncogenesis through their effects on gene expression [21].
DNA and RNA sequencing represent complementary rather than competing technologies in oncology research and clinical practice. While DNA-seq provides a comprehensive catalog of genetic alterations, RNA-seq adds the crucial dimension of functional activity, revealing which alterations are actively transcribed and likely to drive cancer pathogenesis. The integration of both data types creates a more complete understanding of tumor biology, enabling more accurate diagnosis, prognostic stratification, and therapeutic target identification.
As sequencing technologies continue to advance and become more accessible, the routine implementation of both DNA and RNA sequencing in cancer research and clinical diagnostics will maximize our ability to decipher the complex molecular mechanisms driving malignancy. This integrated approach represents the foundation of precision oncology, ensuring that patients receive targeted therapies matched to the specific genetic and functional characteristics of their tumors. For researchers and drug development professionals, leveraging the complementary strengths of both technologies provides the most powerful approach for advancing our understanding and treatment of cancer.
The advent of next-generation sequencing (NGS) has fundamentally transformed oncology research and clinical practice, enabling a shift from histology-based to molecularly-driven cancer classification. This whitepaper provides a comprehensive technical overview of four cornerstone sequencing technologies: whole-exome sequencing (WES), whole-genome sequencing (WGS), targeted gene panels, and RNA sequencing (RNA-Seq). We examine the technical principles, clinical applications, advantages, and limitations of each method, supported by recent comparative data. Within the framework of precision oncology, we demonstrate how these technologies facilitate the identification of actionable biomarkers—including single nucleotide variants (SNVs), insertions/deletions (indels), copy number variations (CNVs), structural variants (SVs), gene fusions, and tumor mutational burden (TMB)—that inform therapeutic decision-making. Detailed experimental protocols and workflow visualizations are provided to guide researchers in technology selection and implementation. The integration of these multidimensional genomic and transcriptomic data is paving the way for increasingly personalized cancer diagnostics and treatment strategies.
Precision oncology represents a paradigm shift in cancer care, moving from blanket treatment approaches to strategies tailored to the individual molecular profile of a patient's tumor [25] [26]. This approach is predicated on comprehensive molecular characterization to identify targetable alterations driving tumorigenesis. DNA and RNA sequencing technologies form the foundational toolkit enabling this transformation, each offering distinct insights into tumor biology.
The three principal forms of NGS include whole genome sequencing (WGS), whole exome sequencing (WES), and targeted sequencing (TS) or panel sequencing [27]. WGS provides the most comprehensive coverage of the entire ~3.2 billion base pair human genome, encompassing both coding and non-coding regions, while WES targets the ~1-2% of the genome that encodes proteins [26] [28]. In contrast, targeted panels focus on a curated set of genes known to be involved in tumorigenesis, allowing for deeper sequencing at lower cost and complexity [27]. RNA sequencing (RNA-Seq) complements DNA-based methods by capturing the dynamic transcriptome, revealing gene expression levels, fusion events, and splice variants [26] [29].
The clinical utility of these technologies is evidenced by their ability to identify biomarkers such as microsatellite instability (MSI), tumor mutational burden (TMB), and homologous recombination deficiency (HRD), which predict response to targeted therapies and immunotherapies [30] [26]. As the diagnostic landscape evolves, understanding the technical specifications, applications, and trade-offs of each method becomes imperative for researchers and drug development professionals aiming to advance personalized cancer care.
Technology Comparison and Clinical Applications
Technical Specifications and Performance Characteristics
The selection of an appropriate sequencing methodology depends heavily on the research question, available resources, and desired clinical applications. Each platform offers distinct advantages and limitations in coverage, resolution, and cost-effectiveness.
Table 1: Comparative Analysis of Sequencing Technologies in Oncology
| Feature | Targeted Panels | Whole Exome Sequencing (WES) | Whole Genome Sequencing (WGS) | RNA Sequencing (RNA-Seq) |
|---|---|---|---|---|
| Genomic Coverage | Selected genes (dozens to ~500) | Protein-coding exons (~1-2% of genome) | Entire genome (~3.2 billion bp) | Full transcriptome (coding and non-coding RNA) |
| Primary Detectable Alterations | SNVs, indels, CNVs, specific fusions | SNVs, indels, CNVs | SNVs, indels, CNVs, SVs, non-coding variants | Gene expression, fusions, splice variants, allele-specific expression |
| Sequencing Depth | Very high (500–1000x or higher) | High (100–200x) | Moderate (30–60x) | Variable (depends on application) |
| Relative Cost | Low | Moderate | High | Moderate |
| Key Advantages | Cost-effective, high sensitivity for low-frequency variants, faster turnaround, simpler data analysis | Balances cost with comprehensive coverage of coding regions where most known disease variants reside | Most comprehensive; detects all variant types including structural variants and non-coding alterations; gold standard for germline | Functional view of biology; identifies expressed mutations, fusions, and immune context; crucial for resolving ambiguous cases |
| Major Limitations | Limited to known genes; may miss novel biomarkers and complex alterations | Misses non-coding and regulatory variants; may miss complex structural variants | Higher cost and data burden; may require greater computational resources | Does not directly detect DNA alterations; requires high-quality RNA |
Targeted panels, such as the TruSight Oncology 500, focus on a pre-defined set of genes with known clinical or functional significance in cancer, enabling deep sequencing (1000x or higher) that is ideal for detecting low-frequency variants in challenging samples like circulating tumor DNA (ctDNA) or formalin-fixed paraffin-embedded (FFPE) tissue [27]. WES provides a broader view, capturing approximately 95% of the exonic regions where an estimated 85% of disease-causing variants are located, making it a powerful tool for novel gene discovery while remaining more cost-effective than WGS [28]. In contrast, WGS interrrogates the entire genome, providing an unbiased platform for detecting the full spectrum of genomic alterations, including those in non-coding regulatory regions, and is considered the gold standard for identifying germline predisposition variants and complex structural rearrangements [26] [28].
RNA-Seq delivers a dynamic snapshot of gene expression, capturing the biologically relevant subset of DNA alterations that are actively transcribed [29]. It is particularly superior for detecting gene fusions and splice variants, as it sequences the actual transcript products, often revealing clinically actionable alterations that may be missed by DNA-only approaches [26] [29]. Emerging applications like single-cell RNA-Seq (scRNA-seq) and spatial transcriptomics further resolve tumor heterogeneity and cellular interactions within the tumor microenvironment [25] [29].
Clinical Utility and Biomarker Discovery
The translation of genomic findings into clinical action is the central tenet of precision oncology. Different sequencing technologies contribute uniquely to biomarker discovery and patient stratification.
Table 2: Clinical Applications and Key Biomarkers by Sequencing Technology
| Technology | Exemplary Clinical Applications | Key Biomarkers Detected | Impact on Therapy Recommendations |
|---|---|---|---|
| Targeted Panels | Routine molecular profiling for common solid tumors (e.g., NSCLC, CRC); therapy selection | SNVs/indels in EGFR, BRAF, KRAS; CNVs in HER2; MSI, TMB | Directs use of corresponding targeted therapies (e.g., EGFR inhibitors, BRAF inhibitors) |
| WES | Broad screening for rare cancers; identification of novel driver mutations; pediatric cancers | Somatic driver mutations (e.g., PIK3CA, BRCA1/2); CNVs; MSI, TMB | Expands therapeutic options beyond standard panels; identifies clinical trial eligibility |
| WGS | Hereditary cancer predisposition; complex structural variants; cases with ambiguous findings | Germline variants (e.g., Lynch syndrome); SVs, chromothripsis; HRD scores | Informs targeted therapy and immunotherapy; identifies familial risk |
| RNA-Seq | Diagnosis of fusion-driven cancers (e.g., sarcomas, lymphomas); resolving equivocal IHC/FISH | Gene fusions (e.g., ALK, ROS1, NTRK, RET); gene expression signatures (e.g., OncoPrism) | Critical for selecting fusion-targeted therapies (e.g., TRK inhibitors); improves ICI response prediction |
A direct comparative study of WES/WGS/TS and panel sequencing in 20 patients with rare or advanced tumors found that WES/WGS ± transcriptome sequencing (TS) generated a median of 3.5 therapy recommendations per patient, compared to 2.5 for the gene panel [30]. Crucially, approximately one-third of the therapy recommendations from WES/WGS ± TS relied on biomarkers not covered by the panel, and two out of ten implemented therapies were based on these additional findings, highlighting the potential for expanded clinical benefit with more comprehensive profiling [30].
From an economic perspective, comprehensive profiling can be cost-effective. In advanced non-small cell lung cancer (NSCLC), a model-based analysis found that using WES/WTS reduced costs by $14,602 per patient compared to sequential single-gene testing while also improving survival outcomes by better identifying patients eligible for targeted therapies and clinical trials [31]. RNA-Seq further enhances this value; in scenarios where RNA fusion prevalence ranges from 2.5% to 14%, adding RNA to DNA sequencing reduced costs by $400–$1,724 per patient and increased the identification of actionable alterations by 2.3%–13.0% [31].
Experimental Protocols and Workflows
Protocol for Comparative Sequencing Analysis
The following detailed methodology outlines a approach for comparing sequencing outputs from different platforms, as referenced in recent studies [30].
1. Sample Selection and Nucleic Acid Extraction:
- Select fresh-frozen or FFPE tumor tissue samples with matched normal tissue (e.g., blood, saliva) for germline comparison.
- Extract high-molecular-weight DNA and high-integrity RNA from the same tumor tissue block using standardized kits. Quantify and qualify nucleic acids using fluorometry (e.g., Qubit) and fragment analyzers (e.g., Bioanalyzer). For FFPE samples, prioritize RNA extraction protocols designed for degraded samples.
2. Library Preparation and Sequencing:
- WES Library: Use a hybridization-based capture kit (e.g., Illumina Nexome) to enrich for exonic regions. Fragment DNA, ligate adapters, and perform hybrid capture with biotinylated probes targeting the human exome.
- WGS Library: Utilize a PCR-free library preparation kit (e.g., Illumina DNA PCR-Free Prep) to minimize bias. Fragment DNA, repair ends, adenylate, and ligate with indexing adapters.
- Targeted Panel Library: Employ commercially available kits (e.g., Illumina TSO500) that use hybrid capture or amplicon-based approaches for a predefined gene set.
- RNA-Seq Library: For whole transcriptome, use kits with ribosomal RNA depletion (e.g., Illumina TruSeq Stranded Total RNA). For 3'-end counting from FFPE samples, use targeted methods like QuantSeq FPE [29]. Perform poly(A) selection for mRNA enrichment.
- Sequence all libraries on an appropriate NGS platform (e.g., Illumina NovaSeq) to a desired median depth: WES (100–200x), WGS (30–60x), Panels (500–1000x), RNA-Seq (50–100 million reads).
3. Bioinformatic Analysis and Variant Calling:
- Data Preprocessing: Align sequence reads to a reference genome (e.g., GRCh38) using aligners like BWA-MEM (for DNA) or STAR (for RNA).
- Variant Calling:
- SNVs/Indels: Use callers like GATK Mutect2 (somatic) and HaplotypeCaller (germline) for WES/WGS. Use panel-specific pipelines (e.g., Dragen) for targeted data.
- CNVs/SVs: Utilize tools like Control-FREEC (CNVs), Manta (SVs) for WES/WGS.
- RNA Fusions: Implement fusion callers such as Arriba and STAR-Fusion on RNA-Seq data [30] [26].
- Biomarkers: Calculate TMB (mutations/Mb), MSI from DNA data, and gene expression signatures from RNA data.
4. Clinical Interpretation and Actionability Assessment:
- Annotate variants using databases like ClinVar, COSMIC, and OncoKB.
- Curbate molecular findings and assess clinical relevance based on evidence levels (e.g., ESMO Scale for Clinical Actionability).
- Present comprehensive report in a molecular tumor board to formulate integrated therapy recommendations.
Diagram 1: Integrated sequencing and analysis workflow for precision oncology.
Protocol for RNA-Based Biomarker Development
This protocol details the development of a gene expression classifier for predicting response to immune checkpoint inhibitors (ICIs), as demonstrated by the OncoPrism test for head and neck squamous cell carcinoma (HNSCC) [29].
1. Cohort Selection and Sample Preparation:
- Establish a retrospective cohort of patients with a specific cancer type (e.g., RM-HNSCC) treated with ICI monotherapy. Collect pre-treatment FFPE tumor biopsies and associated clinical outcome data (e.g., disease control, overall survival).
- RNA Extraction: Cut 5–10 μm sections from FFPE blocks. Deparaffinize using xylene and ethanol washes. Extract total RNA using a commercial FFPE RNA extraction kit, including a DNase digestion step. Assess RNA quality (e.g., DV200 score).
2. Targeted RNA-Seq Library Preparation and Sequencing:
- Use a 3' mRNA-Seq method (e.g., QuantSeq FPE) for library preparation from 10–100 ng of total RNA. This method is optimized for degraded FFPE RNA and involves:
- First-Strand Synthesis: Use an oligo-dT primer containing an Illumina-compatible adapter sequence.
- RNA Template Degradation: Enzymatically degrade the original RNA template.
- Second-Strand Synthesis: Use a random primer containing the second Illumina adapter sequence.
- PCR Amplification: Amplify the final library using a limited-cycle PCR with indexed primers.
- Purify the final libraries and quantify by qPCR. Pool libraries at equimolar ratios and sequence on a mid-output Illumina flow cell (e.g., NextSeq 500/550) to a depth of 5–10 million reads per sample.
3. Bioinformatics and Classifier Training:
- Expression Quantification: Trim adapter sequences and align reads to the reference transcriptome (e.g., GENCODE) using a lightweight aligner like STARsolo or Bowtie2. Quantify gene-level counts.
- Feature Selection: Perform quality control to remove low-quality samples. Using the training cohort, apply statistical methods (e.g., LASSO regression) to a predefined immune-related gene set to identify a minimal panel of features (e.g., ~60 genes) most predictive of clinical outcome.
- Model Training: Train a logistic regression model using the selected features to generate a continuous "OncoPrism Score" (0–100) predictive of disease control. The model is trained to weight the expression values of each feature to maximize predictive accuracy.
4. Clinical Validation:
- Validate the locked model in one or more independent validation cohorts.
- Stratify patients into risk groups (e.g., Low, Medium, High) based on the score threshold established in the training phase.
- Evaluate performance by calculating sensitivity, specificity, and negative/positive predictive values for predicting disease control and correlating the score with overall survival.
Essential Research Reagent Solutions
The successful implementation of sequencing protocols relies on a suite of specialized reagents and tools. The following table details key materials used in the featured experiments and the broader field.
Table 3: Key Research Reagent Solutions for Oncology Sequencing
| Reagent/Material | Function | Example Products/Kits |
|---|---|---|
| FFPE RNA Extraction Kit | Isolves and purifies degraded RNA from formalin-fixed paraffin-embedded (FFPE) tissue samples, a common clinical source. | Qiagen RNeasy FFPE Kit, Thermo Fisher RecoverAll Total Nucleic Acid Isolation Kit |
| Hybridization Capture Probes | Biotinylated oligonucleotide probes that bind to and enrich target genomic regions (exome or gene panel) during library preparation. | Illumina Nexome, IDT xGen Exome Research Panel, TruSight Oncology 500 Probes |
| 3' mRNA-Seq Library Prep Kit | Generates strand-specific RNA-Seq libraries from the 3' end of transcripts, ideal for degraded RNA and gene expression quantification. | Lexogen QuantSeq FPE, Takara Bio SMART-Seq STRT |
| PCR-Free WGS Kit | Prepares sequencing libraries for whole genome analysis without PCR amplification steps, reducing bias and improving uniformity. | Illumina DNA PCR-Free Prep, TruSeq DNA PCR-Free |
| Bioinformatic Pipelines | Software suites for aligning sequencing reads, calling genetic variants, and performing quality control. | GATK, Dragen, STAR, Arriba, Control-FREEC |
The expanding diagnostic toolbox in oncology, comprising targeted panels, WES, WGS, and RNA-Seq, provides researchers and clinicians with a powerful, multi-faceted approach to deciphering cancer complexity. While targeted panels offer a cost-effective and efficient method for routine screening of established biomarkers, comprehensive approaches like WES, WGS, and RNA-Seq are indispensable for uncovering the full spectrum of molecular alterations, especially in rare cancers or cases with inconclusive findings. The integration of DNA and RNA sequencing, in particular, maximizes the identification of clinically actionable alterations, improves diagnostic yield, and has been shown to be economically viable by better matching patients to effective therapies.
Future advancements will be driven by the continued reduction in sequencing costs, the maturation of bioinformatic tools and artificial intelligence for data interpretation, and the development of even more sophisticated single-cell and spatial multiomics technologies. As the list of biomarker-driven therapies grows, the strategic selection and integration of these core sequencing technologies will remain the cornerstone of accelerating translational cancer research and delivering on the promise of personalized medicine.
From Lab to Clinical Report: Methodological Workflows and Translational Applications
In modern oncology research, the quality of sequencing data is profoundly influenced by the initial sample input. The choice between formalin-fixed paraffin-embedded (FFPE), fresh-frozen (FF), and liquid biopsy specimens represents a critical juncture in experimental design, with each source presenting unique advantages, challenges, and technical requirements. Within the broader principles of DNA and RNA sequencing, proper sample handling and preparation are not merely preliminary steps but fundamental determinants of data reliability and biological insight. This guide provides a comprehensive framework for navigating sample input decisions, offering best practices tailored to the distinct characteristics of each sample type to empower researchers in generating robust, reproducible sequencing data for cancer research and drug development.
Section 1: Formalin-Fixed Paraffin-Embedded (FFPE) Samples
Characteristics and Applications
FFPE tissues represent one of the most accessible biological resources in both research and clinical settings due to their widespread use in pathology for preserving tissue morphology. However, the process of formalin fixation and paraffin embedding introduces significant challenges for molecular analyses. FFPE-derived RNA is often fragmented, chemically modified, and degraded, making it suboptimal for gene expression profiling. The chemical crosslinks formed during fixation and continued degradation over time result in RNA of lower quality compared to fresh-frozen alternatives. Despite these limitations, the ubiquity of FFPE tissue specimens in tissue banks and pathology laboratories worldwide makes them an invaluable resource for translational research, particularly for biomarker discovery and validation studies [32] [33].
Technical Considerations and Best Practices
Successful sequencing from FFPE samples requires careful attention to multiple technical factors. RNA integrity is typically assessed using the DV200 metric (percentage of RNA fragments >200 nucleotides), with values above 30% generally indicating samples are usable for RNA-seq protocols. For library preparation, specialized stranded RNA-seq kits designed specifically for FFPE material are essential. A recent 2025 comparative analysis evaluated two prominent approaches: the TaKaRa SMARTer Stranded Total RNA-Seq Kit v2 (Kit A) and the Illumina Stranded Total RNA Prep Ligation with Ribo-Zero Plus (Kit B). The study revealed that Kit A achieved comparable gene expression quantification to Kit B while requiring 20-fold less RNA input, a crucial advantage for limited samples, albeit with increased sequencing depth requirements. Kit B demonstrated superior performance in ribosomal RNA depletion (0.1% vs. 17.45% rRNA content) and lower duplication rates (10.73% vs. 28.48%) [32].
For data analysis, specialized normalization methods are recommended to address the unique characteristics of FFPE data. MIXnorm has been specifically developed for FFPE RNA-seq data to handle its prominent sparsity (excessive zero or small counts) caused by RNA degradation. This method employs a two-component mixture model that models non-expressed genes using zero-inflated Poisson distributions and expressed genes using truncated normal distributions, outperforming conventional normalization methods designed for fresh-frozen samples [33].
Table 1: Performance Comparison of FFPE-Compatible RNA-Seq Library Prep Kits
| Parameter | TaKaRa SMARTer Stranded Total RNA-Seq Kit v2 | Illumina Stranded Total RNA Prep Ligation with Ribo-Zero Plus |
|---|---|---|
| Minimum RNA Input | Low (20-fold less than Kit B) | Standard |
| rRNA Depletion Efficiency | 17.45% rRNA content | 0.1% rRNA content |
| Duplication Rate | 28.48% | 10.73% |
| Reads Mapping to Intronic Regions | 35.18% | 61.65% |
| Key Advantage | Superior for low-input samples | Better rRNA depletion and lower duplication |
| Sequencing Depth Recommendation | Higher | Standard |
Section 2: Fresh-Frozen (FF) Samples
Characteristics and Applications
Fresh-frozen tissues are considered the gold standard for molecular analysis as freezing rapidly preserves RNA, proteins, and DNA in a state closer to their native condition. FF tissues are well-suited for gene expression measurements and provide high-quality nucleic acids for a wide range of sequencing applications. The integrity of molecular components in FF samples makes them particularly valuable for comprehensive transcriptome analyses, including alternative splicing detection, novel transcript identification, and fusion gene discovery [33] [34].
Technical Considerations and Best Practices
The critical factor for FF sample quality is immediate preservation after collection. Cellular degradation and enzymatic activity begin immediately upon tissue excision, compromising sample integrity. According to Nature Protocols, tissue samples should be frozen within 30 minutes of excision to preserve RNA, protein, and DNA quality. Before freezing, samples should be kept on ice or at 4°C to prevent heat damage or accelerated degradation (pre-cooling) [34].
Snap-freezing in liquid nitrogen or on dry ice is the most effective preservation method for fresh-frozen tissue. This technique ensures rapid cooling, preventing the formation of ice crystals that could disrupt cellular structures. For optimal results, researchers should submerge tissue directly in liquid nitrogen or use a dry ice and isopentane bath. Slow freezing should be avoided as it allows ice crystal formation that causes significant tissue damage, particularly to delicate samples like brain or skeletal muscle [34].
Long-term storage of FF tissues should be at -80°C or lower in dedicated ultra-low temperature freezers. Liquid nitrogen storage provides an alternative for long-term preservation. To minimize degradation, researchers should avoid multiple freeze-thaw cycles by aliquoting tissues during initial processing. During transportation, maintaining an unbroken cold chain is essential, using dry ice or liquid nitrogen dry shippers with temperature data loggers to monitor conditions throughout the shipping process [34].
Table 2: Fresh-Frozen Tissue Handling Guidelines
| Processing Stage | Key Practice | Technical Specification |
|---|---|---|
| Preservation Timing | Immediate freezing | Within 30 minutes of excision |
| Freezing Method | Snap-freezing | Liquid nitrogen submersion or dry ice-isopentane bath |
| Storage Temperature | Ultra-low temperature | -80°C or lower |
| Freeze-Thaw Cycles | Minimize | Aliquot during processing |
| Transport | Maintain cold chain | Dry ice with temperature monitoring |
Section 3: Liquid Biopsy Samples
Characteristics and Applications
Liquid biopsy represents a minimally invasive approach to cancer molecular profiling that analyzes tumor-derived materials from various body fluids, primarily blood. This methodology provides several advantages over traditional tissue biopsies, including the ability to perform serial sampling for monitoring disease progression and treatment response, capturing tumor heterogeneity, and profiling tumors that are difficult to access physically. Liquid biopsy is particularly valuable for patients unfit for invasive tissue biopsy procedures and for real-time monitoring of clonal evolution during treatment [35] [36].
The analytes used in liquid biopsy include circulating tumor cells (CTCs), circulating tumor DNA (ctDNA), extracellular vesicles (EVs), and cell-free RNA (cfRNA). Each of these components offers unique biological information and presents distinct technical challenges for isolation and analysis. CTCs are rare cells shed from tumors into circulation (approximately 1 CTC per million leukocytes) with a short half-life of 1-2.5 hours in peripheral blood. ctDNA consists of short DNA fragments (20-50 base pairs) that constitute approximately 0.1-1.0% of total cell-free DNA in cancer patients [35].
Technical Considerations and Best Practices
For CTC analysis, the CellSearch system remains the only FDA-cleared method for enumerating CTCs in blood samples. Detection methods typically exploit either biological properties (e.g., EpCAM expression) or physical characteristics (size, deformability) for isolation. ctDNA analysis requires careful handling to avoid contamination with genomic DNA from blood cells and specialized protocols to account for its short fragment length. The National Comprehensive Cancer Network (NCCN) has included liquid biopsy testing, preferably by NGS methodology, in their guidelines for when tissue testing is unavailable or insufficient [35] [36].
The concordance between liquid biopsy and tissue-based genotyping has been well-established, with studies showing high agreement for actionable mutations. Liquid biopsy offers the advantage of a faster turnaround time compared to tissue biopsy, enabling more rapid treatment decisions. However, limitations remain, including the inability to establish a primary histopathologic diagnosis and potential false negatives in cases with low tumor shedding [36].
Table 3: Liquid Biopsy Analytes and Their Characteristics
| Analyte | Key Characteristics | Primary Applications | Technical Challenges |
|---|---|---|---|
| Circulating Tumor Cells (CTCs) | Whole cells shed from tumors; ~1 per million leukocytes; 1-2.5 hour half-life | Prognostic assessment; drug resistance studies | Extremely low abundance; requires enrichment techniques |
| Circulating Tumor DNA (ctDNA) | Short fragments (20-50 bp); 0.1-1.0% of total cfDNA | Mutation detection; treatment monitoring; minimal residual disease | Low abundance; requires highly sensitive detection methods |
| Extracellular Vesicles (EVs) | Membrane-bound particles containing proteins, nucleic acids | Biomarker discovery; cell-cell communication | Isolation purity; standardization of methods |
| Cell-Free RNA (cfRNA) | Various RNA species protected in vesicles or complexes | Gene expression profiling; fusion detection | RNA stability; requires specialized preservation |
Section 4: The Scientist's Toolkit
Research Reagent Solutions
Table 4: Essential Research Reagents and Kits for Sample Processing
| Reagent/Kit | Function | Application Notes |
|---|---|---|
| TaKaRa SMARTer Stranded Total RNA-Seq Kit v2 | Library preparation from low-input RNA | Ideal for FFPE with limited material; 20-fold lower input requirements |
| Illumina Stranded Total RNA Prep Ligation with Ribo-Zero Plus | Library preparation with ribosomal RNA depletion | Superior rRNA removal (0.1% content); better for preserved samples |
| RNase Inhibitors | Protect RNA from degradation during processing | Critical for challenging samples (0.4-1U/μl concentration) |
| CellSearch System | CTC enumeration and isolation | FDA-cleared; prognostic value in multiple cancers |
| MIXnorm Algorithm | Normalization for FFPE RNA-seq data | Specifically handles excess zeros from degradation |
| DV200 Quality Metric | RNA quality assessment for FFPE samples | Values >30% indicate usability for RNA-seq |
Section 5: Integrated Experimental Design
Sample Selection Framework
Choosing the appropriate sample type requires careful consideration of research objectives, sample availability, and analytical priorities. FFPE samples offer unparalleled access to annotated clinical specimens with extensive follow-up data but require specialized protocols to overcome nucleic acid degradation. Fresh-frozen tissues provide optimal molecular integrity but present logistical challenges for collection, storage, and transportation. Liquid biopsies enable longitudinal monitoring and capture tumor heterogeneity but may lack sensitivity for early-stage disease or tumors with low shedding rates [32] [35] [34].
The research question should drive sample selection. For discovery-phase studies requiring high-quality transcriptome data, fresh-frozen tissues are preferable. For validation studies leveraging large clinical cohorts, FFPE compatibility is essential. For monitoring dynamic processes such as treatment response or resistance development, liquid biopsies offer unique advantages. In many cases, a complementary approach utilizing multiple sample types provides the most comprehensive insights [36] [37].
Emerging Technologies and Future Directions
RNA sequencing technologies continue to evolve rapidly, with recent advances including single-cell RNA sequencing (scRNA-seq) and spatial transcriptomics. These technologies offer unprecedented resolution for characterizing tumor heterogeneity and the tumor microenvironment but present additional challenges for sample preparation. For single-cell analyses, cell viability exceeding 90% is recommended, with minimal debris and careful handling to prevent shear stress during preparation. For frozen tissues, nuclei sequencing rather than whole-cell sequencing is required [38] [39] [37].
The field is moving toward integrated molecular profiling that combines DNA and RNA sequencing from multiple sample types, including matched tissue and liquid biopsies. This approach provides a more comprehensive view of cancer biology and evolution. As technologies advance, standardization of protocols across platforms and laboratories remains essential for generating comparable data and advancing precision oncology [38] [37].
The landscape of sample input options for oncology sequencing provides researchers with multiple pathways to biological insight, each with distinct advantages and limitations. FFPE samples offer clinical relevance and accessibility but require specialized handling and analysis methods. Fresh-frozen tissues deliver superior molecular integrity but present practical challenges for collection and storage. Liquid biopsies enable minimally invasive serial monitoring but have limitations in sensitivity and diagnostic capability. By understanding the technical requirements and optimized protocols for each sample type, researchers can make informed decisions that align with their experimental goals, ultimately advancing cancer research and therapeutic development through more reliable and informative sequencing data.
The adoption of next-generation sequencing (NGS) in oncology has transformed cancer research and clinical practice, enabling the identification of molecular targets for personalized treatment strategies [40]. Bioinformatics pipelines serve as the critical computational infrastructure that translates raw sequencing data into biologically meaningful and clinically actionable insights. These pipelines manage the immense complexity of genomic data through a series of coordinated steps—alignment, variant calling, and specialized detection modules—each requiring specific analytical strategies and tools [41]. In precision oncology, the accurate detection of genomic variants, including single nucleotide variations (SNVs), insertions/deletions (indels), copy number variations (CNVs), and gene fusions, is fundamental for diagnosis, prognosis, and treatment selection [41]. The principles of DNA sequencing reveal the mutational landscape of tumors, while RNA sequencing provides functional context by revealing expressed mutations and fusion events [42]. This technical guide examines the core components of bioinformatics pipelines, detailing current strategies and methodologies for aligning sequences, calling variants, and detecting gene fusions within the framework of modern oncology research.
Core Bioinformatics Workflow: From Raw Data to Biological Insight
The journey from raw sequencing data to biological interpretation follows a structured pathway. The following diagram illustrates the major stages of a typical bioinformatics pipeline in oncology genomics:
Figure 1: Core bioinformatics workflow for NGS data analysis in oncology, showing the progression from raw data to biological insights.
Alignment and Preprocessing: Foundational Steps for Accurate Analysis
The initial phase of any bioinformatics pipeline transforms raw sequencing data into aligned reads suitable for downstream analysis. This process begins with quality assessment of raw FASTQ files using tools like FastQC to evaluate sequence quality, GC content, adapter contamination, and other potential issues [41]. Following quality control, reads are aligned to a reference genome (e.g., GRCh38) using specialized alignment software.
For DNA sequencing data, BWA-Mem has emerged as a widely adopted aligner, efficiently mapping sequencing reads to the reference genome [43]. For RNA-Seq data, STAR (Spliced Transcripts Alignment to a Reference) is particularly valuable as it accounts for spliced transcripts across exon junctions, a critical consideration for transcriptome analysis [42]. The output of this alignment step is typically stored in BAM (Binary Alignment/Map) or CRAM (Compressed Reference-oriented Alignment/Map) format, compressed binary formats that efficiently store sequence alignment data [41].
Post-alignment processing includes several refinement steps. Duplicate marking identifies and flags PCR artifacts using tools like Picard or Sambamba, preventing over-representation of identical DNA fragments [43]. The Genome Analysis Toolkit (GATK) Best Practices workflow further recommends base quality score recalibration (BQSR), which empirically adjusts base quality scores to account for systematic technical errors, and local realignment around indels to correct alignment artifacts [41] [43]. These preprocessing steps collectively produce "analysis-ready" BAM files that serve as the input for subsequent variant detection phases.
Variant Calling Strategies and Methodologies
Variant calling represents the core analytical phase where genomic alterations are identified from aligned sequencing data. This process employs diverse algorithms tailored to specific variant types and biological contexts.
Variant Calling Approaches by Data Type and Context
Table 1: Variant Calling Tools and Their Applications in Oncology
| Variant Type | Biological Context | Recommended Tools | Key Advantages | Performance Metrics |
|---|---|---|---|---|
| SNVs/Indels | Germline | GATK HaplotypeCaller, Platypus | High accuracy (F-scores >0.99), handles diploid genomes effectively [43] | Excellent sensitivity/specificity for inherited variants |
| SNVs/Indels | Somatic (Tumor) | Mutect2, VarRNA | Distinguishes somatic from germline variants; VarRNA uses RNA-Seq specific classification [42] [43] | VarRNA identifies 50% of exome sequencing variants plus unique RNA variants [42] |
| Structural Variants | DNA-Level | Multiple specialized callers | Detects large-scale genomic rearrangements | Varies by tool and cancer type |
| Complex Biomarkers | Tumor Burden | Custom algorithms | Calculates TMB, MSI, HRD from combination of variant calls | Requires specialized analytical approaches [41] |
Experimental Protocol: Somatic Variant Calling from RNA-Seq Data
The VarRNA pipeline exemplifies a sophisticated modern approach to variant calling that leverages RNA-Seq data specifically for oncology applications [42]. Below is a detailed methodological overview:
Step 1: RNA-Seq Alignment and Preprocessing
- Raw RNA-Seq reads in FASTQ format are aligned to the GRCh38 reference genome using STAR two-pass alignment [42].
- Post-alignment processing includes adding read groups, splitting reads with N in CIGAR strings (indicating spliced alignments), and base quality score recalibration using known sites from dbSNP [42].
- Alignment metrics should be assessed: typical experiments yield 70-400 million total reads, with 70-96% alignment rates to the reference and <10% ribosomal RNA mapping, indicating effective ribosomal depletion [42].
Step 2: Initial Variant Calling
- GATK HaplotypeCaller is executed with specific parameters for RNA data: "do-not-use-soft-clipped-bases" set to true, "standard-min-confidence-threshold-for-calling" set to 20, and "max-reads-per-alignment-start" set to 0 to disable read down-sampling [42].
- This initial calling generates a comprehensive set of candidate variants without distinguishing between germline, somatic, or artifact events.
Step 3: Machine Learning-Based Classification
- VarRNA employs two XGBoost machine learning models trained on pediatric cancer samples with paired tumor-normal exome sequencing data as ground truth [42].
- The first model classifies variants as true variants versus artifacts, addressing the high false-positive rate typical of RNA variant calling.
- The second model distinguishes germline from somatic variants in the absence of matched normal tissue, a significant innovation for RNA-Seq analysis [42].
Step 4: Validation and Functional Interpretation
- The resulting variants are annotated and filtered based on functional impact.
- Strikingly, application of VarRNA reveals that in cancer-driving genes, variant allele frequencies in RNA-Seq data often significantly exceed those in exome sequencing, suggesting allele-specific expression patterns relevant to oncogenesis [42].
This protocol demonstrates how integrating multiple computational approaches—traditional variant calling combined with machine learning classification—enhances the accuracy and biological relevance of mutation detection from transcriptomic data.
Fusion Detection Strategies in Cancer Genomics
Gene fusions resulting from genomic rearrangements represent critical oncogenic drivers in many cancer types. Their detection requires specialized approaches that differ from standard variant calling.
Computational Frameworks for Fusion Identification
Fusion detection algorithms must account for the complex nature of chromosomal rearrangements and their transcriptomic consequences. FusionCatcher represents one such tool designed for sensitive fusion detection in RNA-Seq data, capable of identifying both coding and non-coding fusion events [44]. For DNA-based fusion detection, FindDNAFusion implements a combinatorial approach integrating multiple software tools (JuLI, Factera, GeneFuse) to improve detection accuracy to 98% in intron-tiled genes when RNA is unavailable [45].
The following diagram illustrates a validation workflow that integrates RNA-Seq and whole genome sequencing (WGS) data to distinguish true positive fusions from false positives:
Figure 2: Integrated workflow for validating fusion transcripts using matched RNA-Seq and whole genome sequencing data, followed by machine learning classifier development.
Experimental Protocol: Validation of Fusion Transcripts
Research by BMC Genomics demonstrates a robust methodology for validating fusion transcripts using matched WGS data [44]:
Step 1: Fusion Prediction from RNA-Seq Data
- Process RNA-Seq data from cancer samples (e.g., TCGA datasets across 11 cancer types) using FusionCatcher for sensitive fusion detection [44].
- Apply initial filtering to remove fusion transcripts flagged as likely false positives through the tool's built-in filters, reducing millions of initial predictions to hundreds of thousands of putative fusions [44].
Step 2: DNA-Level Validation with WGS Data
- Develop a bioinformatic pipeline to extract, filter, and process discordant read pairs in matched WGS data that support fusion transcripts identified in RNA-Seq [44].
- Search for nearby reads with high-quality soft-clipped ends and locally align these to the region of the other fusion partner containing discordant reads [44].
- Consider fusion transcripts validated when supported by both discordant read pairs and at least one identified genomic breakpoint [44].
Step 3: Machine Learning Classifier Development
- Utilize the validated fusions as true positive events to train a machine learning classifier that predicts true and false positive fusion transcripts from RNA-Seq data alone [44].
- The final classifier achieved precision and recall metrics of 0.74 and 0.71, respectively, in an independent breast cancer dataset [44].
- This approach facilitates the identification of potentially targetable kinase fusions without requiring WGS data for all samples [44].
This validation strategy addresses the fundamental challenge in fusion detection—the high false positive rate of prediction algorithms—by integrating orthogonal data types and applying machine learning for classification.
Advanced Computational Approaches and Quality Assurance
Artificial Intelligence and Deep Learning in Variant Detection
Deep learning architectures have emerged as transformative approaches for improving variant calling accuracy in cancer genomics. Convolutional Neural Networks (CNNs) and graph-based models now achieve state-of-the-art performance in variant calling and tumor stratification [46]. For example, DeepVariant employs a CNN architecture that learns read-level error context, achieving 99.1% SNV accuracy and reducing INDEL false positives compared to traditional methods [46].
These approaches demonstrate particular utility in resolving genomic discrepancies that plague conventional pipelines. DL models reduce false-negative rates by 30-40% in somatic variant detection and can prioritize pathogenic variants with high accuracy (e.g., MAGPIE at 92% accuracy) [46]. The integration of multimodal data—combining WES, transcriptome, and phenotype information—through attention-based neural networks further enhances variant prioritization and interpretation [46].
Quality Assurance and Benchmarking Frameworks
Robust quality assurance is essential for clinical-grade variant detection. ONCOLINER represents a recently developed solution for monitoring, improving, and harmonizing somatic variant calling across genomic oncology centers [47]. This framework addresses the critical challenge of analysis heterogeneity across institutions, which can affect diagnostic consistency and data sharing capabilities.
Benchmarking against reference datasets provides essential validation for variant calling pipelines. Resources such as the Genome in a Bottle (GIAB) consortium and Platinum Genomes provide "ground truth" variant calls for reference samples, enabling objective performance assessment [43]. These benchmarks are particularly important for optimizing the balance between sensitivity (minimizing false negatives) and specificity (minimizing false positives) in clinical settings.
Essential Research Reagents and Computational Tools
Table 2: Key Bioinformatics Tools and Resources for Oncology Sequencing Pipelines
| Tool Category | Specific Tools | Primary Function | Application Context |
|---|---|---|---|
| Alignment | BWA-Mem, STAR | Map sequencing reads to reference genome | DNA (BWA) and RNA (STAR) sequencing data [42] [43] |
| Variant Callers | GATK HaplotypeCaller, Mutect2, VarRNA | Detect SNVs and indels | Germline (HaplotypeCaller), somatic (Mutect2), RNA-Seq (VarRNA) [42] [43] |
| Fusion Detection | FusionCatcher, FindDNAFusion, JuLI | Identify gene fusions | RNA (FusionCatcher) and DNA (FindDNAFusion) approaches [45] [44] |
| Quality Control | FastQC, Picard, Sambamba | Assess data quality, mark duplicates | All sequencing modalities [41] [43] |
| Benchmarking | GIAB, ONCOLINER | Validate pipeline performance | Quality assurance and harmonization [47] [43] |
| Machine Learning | XGBoost, DeepVariant | Classify variants, reduce false positives | Variant filtering and prioritization [42] [46] |
Bioinformatics pipelines for alignment, variant calling, and fusion detection constitute the analytical backbone of modern oncology research. The integration of sophisticated computational methods—from established alignment algorithms to emerging deep learning approaches—has dramatically improved our ability to detect clinically relevant genomic alterations in cancer. The strategic combination of multiple data types, particularly the integration of DNA and RNA sequencing information, provides a more comprehensive view of tumor biology and enables the identification of targetable oncogenic events. As these pipelines continue to evolve, emphasis on standardization, benchmarking, and quality assurance will be essential for translating genomic discoveries into validated clinical applications that advance precision oncology and ultimately improve patient outcomes.
In precision oncology, the central dogma of molecular biology—the flow of genetic information from DNA to RNA to protein—presents a significant diagnostic challenge. While DNA-based assays are the current standard for detecting somatic mutations in tumor specimens, they primarily determine the presence or absence of genetic variants without revealing their functional consequences at the transcript level [9]. This creates a "DNA-to-protein divide" in clinical decision-making, as most cancer therapeutics target proteins, not DNA sequences themselves [9]. The critical transformative steps of transcription and translation must occur before mutated genes can influence cellular machinery and drive malignancy.
DNA may be considered as representing "potential" rather than actualized function, as mutations must be transcribed to impact cellular phenotype [9]. While DNA mutations can be detected, measured, and reported with high accuracy and precision in a cost-effective manner, directly profiling proteins and their mutations remains challenging for high-throughput clinical applications [9]. RNA sequencing (RNA-seq) has emerged as a powerful mediator for bridging this divide, providing greater clarity and therapeutic predictability for precision medicine by revealing whether DNA mutations are actually expressed in the tumor transcriptome [9].
This technical guide explores the principles and methodologies of using RNA-seq to validate expressed mutations in oncology research, providing researchers and drug development professionals with practical frameworks for implementing these approaches in both discovery and clinical settings.
The Scientific Foundation: Why RNA Adds Essential Context
Limitations of DNA-Only Approaches
Traditional DNA sequencing approaches, including panel-based DNA sequencing (DNA-seq) and whole-exome sequencing (WES), provide essential but incomplete mutational landscapes. Several critical limitations necessitate complementary RNA analysis:
- Transcriptional Silence: DNA sequencing detects mutations regardless of whether the affected gene is expressed in the tumor tissue. A mutation in a transcriptionally silent gene may have minimal biological consequence yet be incorrectly assumed to be driving disease [9].
- Misannotation of Functional Impact: When mutations are annotated solely to reference transcripts that may not be expressed in a specific tumor type, their functional impact can be misinterpreted. A study in melanoma demonstrated that 22% (11/50) of mutation clusters were misannotated as coding mutations because the reference transcripts used for annotation were not actually expressed in those tumors [48].
- Incomplete Variant Characterization: DNA-seq alone cannot detect how mutations affect transcript expression, alternative splicing, or allele-specific expression—all critical determinants of functional impact [9].
Advantages of RNA Sequencing Integration
RNA-seq provides orthogonal data that addresses these limitations through multiple mechanisms:
- Expression Validation: RNA-seq confirms whether DNA mutations are transcribed, helping prioritize clinically relevant variants. Studies show that variants missed by RNA-seq are often not expressed or expressed at very low levels, suggesting they may be of lower clinical relevance [9].
- Fusion Detection: RNA-seq excels at identifying gene fusions resulting from chromosomal rearrangements, which are challenging to detect using DNA-based methods alone [49].
- Transcript-Specific Effects: By analyzing expressed transcripts, RNA-seq can reveal how mutations affect splicing, identify novel isoforms, and enable correct annotation of mutation consequences based on the actual transcripts expressed in the tumor [48].
- Enhanced Sensitivity: For moderate to highly expressed genes, RNA-seq can provide a stronger mutation signal for variant detection, particularly in low-purity tumor samples [9].
Table 1: Comparative Analysis of DNA-seq and RNA-seq Approaches in Cancer Genomics
| Feature | DNA Sequencing | RNA Sequencing |
|---|---|---|
| Primary Detection | Genetic variants (SNVs, INDELs, CNVs) | Expressed variants, fusion transcripts, splicing events |
| Functional Insight | Limited (presence/absence) | High (expression level, transcript consequences) |
| Variant Prioritization | Based on predicted effect | Based on actual expression and transcript context |
| Fusion Detection | Limited to breakpoint identification | Direct detection of fusion transcripts |
| Clinical Utility | Foundation for variant detection | Validation of expressed, actionable targets |
| Tumor Purity Challenges | Sensitivity decreases with lower purity | Can enhance signal for expressed variants in low-purity samples |
Methodological Framework: Experimental Design and Protocols
Integrated DNA and RNA Sequencing Workflow
Implementing a robust integrated sequencing approach requires careful experimental design from sample collection through data analysis. The following workflow visualization outlines the key steps in a validated combined RNA and DNA exome sequencing approach applied in large-scale cancer studies [49]:
Sample Preparation and Quality Control
Proper sample preparation is foundational to generating reliable sequencing data. The following protocols are adapted from validated clinical sequencing approaches [49]:
Nucleic Acid Isolation Protocol:
- Sample Types: Process fresh frozen (FF) solid tumors, formalin-fixed paraffin-embedded (FFPE) tissues, or normal control tissues (whole blood, PBMCs, saliva)
- Extraction Methods:
- FF tumors: Use AllPrep DNA/RNA Mini Kit (Qiagen) for simultaneous DNA/RNA extraction
- FFPE tumors: Use AllPrep DNA/RNA FFPE Kit (Qiagen) with modifications for degraded samples
- Normal tissues: Use QIAmp DNA Blood Mini Kit (Qiagen) or Maxwell RSC Stabilized Saliva DNA Kit (Promega)
- Quality Assessment:
- Quantify using Qubit 2.0 Fluorometer (Thermo Fisher Scientific)
- Assess purity via NanoDrop OneC Spectrophotometer (Thermo Fisher Scientific)
- Determine structural integrity with TapeStation 4200 (Agilent Technologies)
- Minimum Quality Thresholds: DNA/RNA concentration ≥10 ng/μL, A260/A280 ratio 1.8-2.0, RIN ≥7.0 for RNA
Library Preparation Protocol:
- Input Requirements: 10-200 ng of extracted DNA or RNA
- RNA Library Construction:
- FF tissue: TruSeq stranded mRNA kit (Illumina)
- FFPE tissue: SureSelect XTHS2 RNA kit (Agilent Technologies)
- DNA Library Construction: SureSelect XTHS2 DNA kit (Agilent Technologies)
- Hybridization Capture:
- RNA: SureSelect Human All Exon V7 + UTR exome probe (Agilent Technologies)
- DNA: SureSelect Human All Exon V7 exome probe (Agilent Technologies)
- Library QC: Assess concentration, size distribution, and adapter contamination before sequencing
Sequencing and Bioinformatics Analysis
Sequencing Parameters:
- Platform: NovaSeq 6000 (Illumina)
- Read Configuration: Paired-end sequencing (2×101 bp recommended)
- Quality Metrics: Q30 >90%, PF >80% [49]
Bioinformatics Pipeline:
- Alignment:
- DNA-seq: BWA aligner v.0.7.17 against hg38 reference genome
- RNA-seq: STAR aligner v2.4.2 against hg38 with default parameters
- Quality Control:
- DNA-seq: fastQC v0.11.9, FastqScreen v0.14.0, Picard v2.20.7 MarkDuplicates
- RNA-seq: RSeQC v3.0.1 for strand-specificity and DNA contamination assessment
- Variant Calling:
- DNA variants: Strelka v2.9.10 for somatic SNVs/INDELs with tumor/normal pairing
- RNA variants: Pisces v5.2.10.49 for expressed mutation detection
- Filtering: Apply thresholds for depth (tumor DP≥10, normal DP≥20), VAF (tumor VAF≥0.05), and strand bias [49]
Analytical Validation: Performance Metrics and Benchmarking
Validation Using Reference Standards
Comprehensive validation of integrated RNA-DNA sequencing requires rigorous benchmarking against established standards. One large-scale study employed exome-wide somatic reference standards containing 3,042 SNVs and 47,466 CNVs across multiple sequencing runs of cell lines at varying tumor purities [49]. The table below summarizes key performance metrics from analytical validation studies:
Table 2: Analytical Performance Metrics for Integrated DNA and RNA Sequencing
| Parameter | DNA Sequencing Performance | RNA Sequencing Performance | Validation Method |
|---|---|---|---|
| Sensitivity (SNVs) | >99% for VAF ≥5% | >95% for expressed variants | Reference standards with 3,042 SNVs |
| Specificity | >99.9% after filtering | >98% with optimized filters | Known positive/negative variants |
| VAF Precision | ±2.5% across replicates | ±5.0% for moderately expressed genes | Multiple sequencing runs |
| Fusion Detection | Limited to genomic breakpoints | >99% sensitivity for known fusions | Orthogonal validation |
| Coverage Uniformity | >90% of target bases at 100x | Variable by expression level | Coverage metrics across targets |
| Limit of Detection | 5% VAF for SNVs | Dependent on expression level | Dilution series with cell lines |
Orthogonal Confirmation in Clinical Samples
Beyond synthetic references, validation with clinical samples provides essential real-world performance data:
- Sample Cohort: 2,230 clinical tumor samples representing multiple cancer types
- Orthogonal Methods: PCR-based assays, immunohistochemistry, and independent sequencing platforms
- Key Findings:
- Integrated assay enabled detection of clinically actionable alterations in 98% of cases
- RNA-seq recovered variants missed by DNA-only testing, particularly in low-purity samples
- Direct correlation of somatic alterations with gene expression patterns revealed allele-specific expression
- Complex genomic rearrangements identified through RNA data would have remained undetected by DNA-seq alone [49]
Practical Implementation: Variant Detection Strategies
Two Complementary Approaches for Variant Detection
Research supports two primary strategies for implementing RNA-seq in mutation detection workflows, each with distinct applications and considerations:
Scenario 1: RNA-seq to Verify and Prioritize DNA Variants When DNA-seq is available, RNA-seq serves as a validation and prioritization tool. This approach:
- Uses DNA-seq as a high-sensitivity baseline for variant detection
- Employs RNA-seq to confirm expression of DNA-identified variants
- Prioritizes clinically relevant mutations based on transcriptional evidence
- Filters out silent mutations in non-expressed genes that may have minimal functional impact [9]
Scenario 2: Independent RNA-seq Variant Detection In cases where DNA-seq is unavailable or insufficient, RNA-seq can function as a primary detection method:
- Requires stringent false positive rate (FPR) control through optimized bioinformatics parameters
- Leverages targeted RNA-seq panels for deeper coverage of genes of interest
- Identifies expressed variants independently of DNA-based findings
- Particularly valuable for fusion detection and expressed mutation profiling in moderate to highly expressed genes [9]
Mutation Reannotation Based on Expressed Transcripts
A critical application of integrated sequencing is the correction of mutation annotations based on actually expressed transcripts rather than default reference transcripts. This process can be visualized as follows:
This reannotation process has revealed significant misclassification in cancer genomics. In melanoma, 22% (11/50) of mutation clusters were misannotated as coding mutations because the reference transcripts used for annotation were not expressed in the tumor tissue [48]. For example, mutations previously annotated as KNSTRN c.71C>T (p.Ser24Phe) and BCL2L12 (p.Phe17=) were actually non-coding mutations targeting promoter regions that affected expression of interferon regulatory factor 3 (IRF3) and BCL2L12, ultimately influencing tumor protein p53 (TP53) expression and immunotherapy response [48].
Successful implementation of integrated DNA-RNA sequencing approaches requires specific laboratory and computational resources. The following table details key research reagent solutions and their applications:
Table 3: Essential Research Reagent Solutions for Integrated DNA-RNA Sequencing
| Category | Specific Product | Manufacturer | Primary Application | Key Features |
|---|---|---|---|---|
| Nucleic Acid Extraction | AllPrep DNA/RNA Mini Kit | Qiagen | Simultaneous DNA/RNA from FF tissue | Preserves nucleic acid integrity |
| FFPE Extraction | AllPrep DNA/RNA FFPE Kit | Qiagen | Nucleic acids from archived samples | Optimized for cross-linked material |
| RNA Library Prep | TruSeq stranded mRNA kit | Illumina | Library construction from FF tissue | Strand-specificity, mRNA enrichment |
| FFPE Library Prep | SureSelect XTHS2 RNA kit | Agilent Technologies | RNA library from FFPE | Designed for degraded RNA |
| DNA Library Prep | SureSelect XTHS2 DNA kit | Agilent Technologies | DNA library construction | Compatible with FF/FFPE samples |
| Exome Capture | SureSelect Human All Exon V7 | Agilent Technologies | Target enrichment | Comprehensive exome coverage |
| Sequencing | NovaSeq 6000 | Illumina | High-throughput sequencing | Scalable output, high quality |
| Quality Control | TapeStation 4200 | Agilent Technologies | Nucleic acid integrity | RIN scores for RNA quality |
Clinical Applications and Impact on Patient Care
Therapeutic Decision-Making
The integration of RNA-seq with DNA sequencing directly impacts clinical management in oncology through multiple mechanisms:
- Identification of Actionable Fusions: RNA-seq significantly improves detection of targetable gene fusions compared to DNA-based methods alone. In one large cohort study, combined testing uncovered clinically actionable alterations in 98% of cases, with RNA essential for fusion identification [49].
- Expression-Based Therapy Selection: Confirming mutation expression helps prioritize treatments targeting specific pathways. For example, a mutation in the KRAS gene may be technically present by DNA testing but clinically irrelevant if not expressed in the tumor [9].
- Immunotherapy Guidance: Gene expression signatures derived from RNA-seq data can predict response to immune checkpoint inhibitors, enabling more precise patient selection for immunotherapy [49].
- Neoantigen Discovery: For novel mRNA-based individualized neoantigen therapies (e.g., mRNA-4157/V940), RNA-seq verification and prioritization of amino acid candidates is essential for developing personalized cancer vaccines [9].
Prognostic and Diagnostic Applications
Beyond therapeutic selection, integrated sequencing provides critical diagnostic and prognostic information:
- Mutation Significance Assessment: RNA-seq helps distinguish driver mutations from passenger mutations by confirming their expression and potential functional impact [9].
- Tumor Subtyping: Expression patterns from RNA-seq enable more precise molecular classification of tumors, which can influence prognosis and treatment approach.
- Promoter Mutation Detection: As demonstrated in melanoma, proper annotation of promoter mutations affecting genes like IRF3 and BCL2L12 reveals mechanisms of tumor progression and treatment resistance [48].
Future Directions and Implementation Considerations
Emerging Technologies and Methodological Advances
The field of integrated genomic profiling continues to evolve with several promising developments:
- Single-Cell Sequencing: Advances in single-cell RNA and DNA sequencing will enable resolution of tumor heterogeneity and mutation expression at the cellular level [8].
- Liquid Biopsies: Application of integrated sequencing principles to circulating tumor DNA and RNA could provide non-invasive approaches for monitoring treatment response and resistance [8].
- Standardized Validation Frameworks: Development of comprehensive guidelines for validating integrated RNA and DNA sequencing assays will support broader clinical adoption [49].
- Automated Reannotation Pipelines: Implementation of automated methods using tools like Salmon and Ensembl Variant Effect Predictor (VEP) to annotate mutations based on expressed transcripts rather than default references [48].
Implementation Challenges and Solutions
Successful implementation of integrated DNA-RNA sequencing in research and clinical settings requires addressing several practical considerations:
- Bioinformatics Expertise: The complex data analysis demands robust bioinformatics support and computational infrastructure. Collaborations with bioinformatics core facilities or investment in internal expertise is essential.
- Cost Management: While sequencing costs have decreased, integrated approaches still represent a significant investment. Strategic panel design and targeted approaches can optimize cost-effectiveness.
- Sample Quality Requirements: RNA sequencing demands high-quality nucleic acids, presenting challenges for FFPE samples. Protocol modifications and specialized kits can address degradation issues.
- Data Interpretation Framework: Developing standardized approaches for interpreting and reporting integrated findings ensures consistent application across research programs and clinical settings.
Integrating RNA-seq with DNA sequencing represents a fundamental advancement in precision oncology that directly addresses the critical "DNA-to-protein divide." By validating which mutations are actually expressed in tumors, researchers and clinicians can prioritize biologically relevant variants, correct misannotations, and make more informed therapeutic decisions. The methodological frameworks, validation approaches, and implementation strategies outlined in this technical guide provide a roadmap for effectively leveraging these complementary technologies. As the field evolves, continued refinement of integrated sequencing approaches will further enhance our understanding of cancer biology and improve patient outcomes through more precise molecularly-guided treatments.
The advent of next-generation sequencing (NGS) has fundamentally transformed oncology research and clinical practice, enabling a shift from traditional histopathological classification to molecular-driven precision medicine. The core thesis of modern oncology research is that comprehensive genomic profiling of tumors, through the synergistic use of both DNA and RNA sequencing, provides a more complete molecular portrait to identify actionable alterations for therapeutic targeting. By moving beyond DNA-only analysis, researchers can overcome the limitations of single-modality sequencing and uncover critical biomarkers that would otherwise remain undetected. The integration of DNA and RNA sequencing data creates a powerful framework for detecting key genomic and transcriptomic alterations—including gene fusions, microsatellite instability (MSI), tumor mutational burden (TMB), and copy number variations (CNVs)—that inform treatment selection, predict therapy response, and ultimately improve patient outcomes.
This technical guide examines the principles and methodologies behind detecting these crucial biomarkers through case studies that highlight both their clinical utility and the technical considerations for their accurate identification. As the field progresses toward multi-omics approaches, the combination of DNA and RNA sequencing has demonstrated significant advantages. Research shows that integrating RNA sequencing with whole exome sequencing (WES) substantially improves the detection of clinically relevant alterations, particularly for gene fusions, and enables direct correlation of somatic alterations with gene expression profiles [49]. The following sections provide an in-depth examination of the experimental protocols, analytical frameworks, and clinical applications of these essential genomic biomarkers in cancer research.
Biomarker Detection Methodologies and Clinical Applications
Gene Fusion Detection through Integrated RNA Sequencing
Gene fusions, resulting from chromosomal rearrangements that join two previously separate genes, represent critical therapeutic targets and diagnostic markers in multiple cancer types. While DNA-based sequencing can detect genomic breakpoints, RNA sequencing provides direct evidence of expressed fusion transcripts, offering enhanced sensitivity and functional validation.
Experimental Protocol for Fusion Detection: The standard methodology for fusion detection begins with RNA extraction from tumor samples (fresh frozen or FFPE), followed by assessment of RNA integrity. Library preparation is typically performed using either enrichment-based approaches (e.g., SureSelect XTHS2 RNA kit) or amplicon-based methods [49] [50]. For targeted RNA sequencing, panels focusing on genes with known fusion partners (e.g., 31-gene fusion panel) provide cost-effective solutions, while whole transcriptome sequencing enables novel fusion discovery. Sequencing is conducted on platforms such as Illumina NovaSeq 6000, with a minimum of 20,000 total mapped reads recommended for reliable detection [50]. Bioinformatics analysis utilizes specialized aligners like STAR for splice-aware mapping, followed by fusion-specific detection tools that identify chimeric transcripts through discordant read pairs and split reads.
Case Study Evidence: The critical advantage of RNA sequencing for fusion detection is demonstrated in a comparative study of two comprehensive genomic profiling platforms. In a case of KIAA1549-BRAF fusion-positive astrocytoma, the fusion event was not detected by DNA-only testing but was successfully identified through RNA sequencing. This detection had direct clinical implications, as the patient subsequently exhibited clinical benefit from MEK inhibitor treatment [50]. This case highlights how RNA analysis can uncover therapeutically actionable targets that would be missed by DNA-only approaches, particularly for fusions involving complex rearrangements or occurring in intronic regions.
Microsatellite Instability (MSI) Assessment by NGS
Microsatellite instability serves as an important predictive biomarker for immunotherapy response across multiple cancer types. While immunohistochemistry (IHC) and PCR-based methods have traditionally been used for MSI detection, NGS-based approaches offer expanded coverage of microsatellite loci and improved analytical performance.
Experimental Protocol for MSI Detection: Next-generation sequencing methods for MSI analysis employ targeted gene panels that include multiple microsatellite loci. One developed approach, MSIDRL, initially selects hundreds of robust noncoding MS loci and designs capture probes targeting these regions [51]. After sequencing, the algorithm defines a "diacritical repeat length" (DRL) for each locus, which maximizes the cumulative read count difference between MSI-H and MSI-L/MSS samples. Reads are then classified as "stable" or "unstable" based on whether their length exceeds the DRL. The background noise for each locus is calculated from MSI-L/MSS samples, and binomial testing determines whether the proportion of unstable reads in a test sample significantly exceeds this background [51]. The final classification is based on the unstable locus count (ULC), with thresholds established through validation studies (e.g., ULC >10 for MSI-H).
Analytical and Clinical Validation: Large-scale retrospective analyses of pan-cancer cases have demonstrated the robustness of NGS-based MSI detection. In a study of 35,563 Chinese pan-cancer cases, the prevalence of MSI-H varied significantly across cancer types, with the highest frequencies observed in endometrial (UTNP), gastric (GACA), and colorectal (BWCA) cancers [51]. These cancer types collectively contributed approximately 80% of all MSI-H cases. The study also identified a specific deletion in the ACVR2A gene (chr2:g.148683686del) that was present in 66.6% of MSI-H cases, highlighting the association between specific mutational signatures and MSI status [51]. Such large-scale analyses enable the refinement of locus panels and classification algorithms for optimal performance across diverse cancer types.
Tumor Mutational Burden (TMB) Quantification
Tumor mutational burden, defined as the number of somatic mutations per megabase of DNA, has emerged as a significant biomarker for predicting response to immune checkpoint inhibitors. While targeted panels have been used for TMB estimation, whole exome sequencing provides a more comprehensive and accurate assessment.
Experimental Protocol for TMB Calculation: The standard methodology for TMB assessment begins with whole exome sequencing of matched tumor-normal sample pairs. After alignment to the reference genome (hg38), somatic variant calling is performed using tools such as Strelka2, with filtering to remove potential germline variants and sequencing artifacts [49]. The TMB is calculated by counting all coding somatic mutations, including synonymous and nonsynonymous variants, across the entire exome. The final TMB value is expressed as mutations per megabase (mut/Mb), with thresholds commonly used for clinical interpretation (e.g., ≥7.5-10 mut/Mb for TMB-High) [50]. Quality control measures, including minimum coverage depth (typically >100x) and tumor purity assessment (>30%), are essential for reliable TMB estimation.
Analytical Considerations: A key advantage of whole exome sequencing over targeted panels for TMB calculation is the avoidance of panel-specific biases and the ability to assess mutational burden across a more comprehensive genomic landscape [49]. Additionally, integrated RNA and DNA analysis enables correlation between high TMB and specific gene expression profiles, potentially providing insights into the functional immune consequences of elevated mutation burden.
Copy Number Variation (CNV) Analysis
Copy number alterations, comprising amplifications and deletions of genomic regions, drive oncogenesis across diverse cancer types. Accurate detection of these alterations is essential for identifying therapeutic targets and understanding disease mechanisms.
Experimental Protocol for CNV Detection: CNV analysis from NGS data typically employs read depth-based approaches. After alignment and quality control, tools such as ONCOCNV or ADTEx analyze sequencing coverage across the genome, normalized to a control set of samples with known neutral copy number [50]. For targeted panels, baseline correction and tumor purity estimation utilize the change ratio of all loss of heterozygosity (LOH) and allelic-specific copy number alterations in pooled single nucleotide polymorphism data. Copy number amplification is typically defined as CN ≥ 6, gains as CN = 4 or 5, while homozygous and heterozygous deletions are defined as CN = 0 and CN = 1, respectively [50]. For reliable CNV calling, especially for copy number losses, tumor purity >30% is recommended.
Concordance Across Platforms: Comparative studies of different genomic profiling platforms have demonstrated variable concordance for CNV detection. In a head-to-head comparison of FoundationOne CDx and ACTOnco+ assays, copy number gains showed 76.9% concordance, while copy number losses demonstrated 66.7% concordance [50]. These findings highlight the technical challenges in CNV detection, particularly for heterozygous deletions, and underscore the importance of platform-specific validation.
Table 1: Comparison of Key Genomic Biomarkers in Cancer Research
| Biomarker | Detection Method | Primary Clinical Utility | Technical Considerations |
|---|---|---|---|
| Gene Fusions | RNA sequencing with fusion-specific panels | Identifies targetable drivers (e.g., KIAA1549-BRAF) | RNA quality critical (RIN score); requires specialized alignment |
| Microsatellite Instability (MSI) | NGS panels with multiple microsatellite loci | Predicts response to immunotherapy | Pan-cancer locus panels outperform cancer-specific ones |
| Tumor Mutational Burden (TMB) | Whole exome sequencing | Predicts response to immune checkpoint inhibitors | Requires matched normal; tumor purity >30% recommended |
| Copy Number Variations (CNV) | Read depth analysis from DNA sequencing | Identifies gene amplifications (targetable) and deletions | Challenging in low-purity samples; platform concordance variable |
Comparative Analysis of Genomic Profiling Platforms
The selection of appropriate genomic profiling platforms is crucial for comprehensive biomarker detection in cancer research. Comparative studies provide valuable insights into the performance characteristics of different assays.
Methodology for Platform Comparison: Head-to-head comparisons of genomic profiling platforms typically involve analyzing the same patient samples across different assays. Such studies evaluate concordance for various alteration types, including single nucleotide variants (SNVs), insertions-deletions (indels), CNVs, gene fusions, MSI, and TMB. The analysis encompasses both technical performance (sensitivity, specificity) and clinical utility (identification of actionable alterations).
Key Findings from Comparative Studies: In a study comparing FoundationOne CDx (324 genes) and ACTOnco+ (440 genes for DNA, 31 genes for RNA), the overall positive agreement for reported sequence alterations in clinically actionable genes was 82.8% [50]. This comprehensive evaluation demonstrated that integrated DNA and RNA analysis, as implemented in ACTOnco+, enabled detection of therapeutically relevant fusions missed by DNA-only approaches. For TMB and MSI, the assays demonstrated high concordance across various cancer types, supporting the robustness of these biomarkers when measured using different NGS-based approaches [50].
Table 2: Performance Metrics of Genomic Profiling Platforms
| Parameter | FoundationOne CDx | ACTOnco+ | Concordance |
|---|---|---|---|
| Genes Covered | 324 genes (DNA) | 440 genes (DNA) + 31 genes (RNA) | N/A |
| SNVs/Indels | Proprietary pipeline | Ion Proton sequencing with minimum 25 variant reads | 82.8% positive agreement |
| Copy Number Alterations | Proprietary algorithm | ONCOCNV with ADTEx for purity estimation | 76.9% (gains), 66.7% (losses) |
| Gene Fusions | DNA-based rearrangement detection | RNA-based fusion assay | Higher sensitivity with RNA |
| TMB Assessment | Comprehensive genomic profile | Sequenced regions of ACTOnco+ | High concordance |
| MSI Classification | Proprietary algorithm | Machine learning using >400 loci | High concordance |
Essential Research Reagents and Computational Tools
The accurate detection of actionable alterations in cancer genomics relies on a suite of specialized research reagents and bioinformatics tools that form the foundation of reliable genomic analysis.
Laboratory Reagents and Kits: Nucleic acid isolation represents the critical first step, with specialized kits required for different sample types. The AllPrep DNA/RNA Mini Kit is used for fresh frozen tumors, while the AllPrep DNA/RNA FFPE Kit is optimized for formalin-fixed paraffin-embedded tissue [49]. Library preparation employs specialized kits such as the TruSeq stranded mRNA kit for RNA from fresh tissue and SureSelect XTHS2 kits for both DNA and RNA from FFPE samples [49]. For hybridization-based capture, the SureSelect Human All Exon V7 + UTR exome probe is used for RNA, while the SureSelect Human All Exon V7 exome probe is used for DNA [49].
Bioinformatics Tools: The computational analysis of sequencing data requires a sophisticated pipeline of bioinformatics tools. Alignment of sequencing reads typically utilizes BWA for DNA and STAR for RNA-seq data [49]. Variant calling for SNVs and indels employs optimized versions of Strelka2, while fusion detection requires specialized algorithms. For CNV analysis, tools such as ONCOCNV and ADTEx provide robust detection of copy number alterations, with correction for tumor purity and ploidy [50]. Quality control metrics are essential throughout the pipeline, with tools such as FastQC, Picard, and RSeQC providing standardized quality assessment [49].
Integrated Workflows for Comprehensive Genomic Analysis
The integration of multiple data types into unified analytical workflows represents the cutting edge of cancer genomics, enabling a systems-level understanding of oncogenic mechanisms.
Data Integration Framework: Comprehensive genomic analysis requires the synthesis of diverse data types, including somatic mutations, copy number alterations, gene fusions, and gene expression profiles. This integrated approach enables the identification of complex biomarkers such as TMB and MSI, while also facilitating the correlation of genomic alterations with their functional transcriptional consequences. The bioinformatics infrastructure for such integration must accommodate diverse data types while ensuring reproducibility and scalability.
Visualization of Integrated Analysis Workflow:
Diagram 1: Integrated DNA and RNA Analysis Workflow
Validation Frameworks: Rigorous validation is essential for clinical implementation of integrated genomic workflows. This process includes three key components: (1) analytical validation using custom reference samples containing thousands of variants; (2) orthogonal testing in patient samples using established methodologies; and (3) assessment of clinical utility in real-world cases [49]. Such comprehensive validation ensures the reliability and clinical applicability of the genomic findings, enabling informed treatment decisions based on the identified alterations.
The integration of DNA and RNA sequencing technologies represents a paradigm shift in cancer genomics, enabling comprehensive detection of actionable alterations across multiple biomarker classes. This technical guide has detailed the methodologies and analytical frameworks for identifying key genomic biomarkers—gene fusions, MSI, TMB, and CNVs—that drive precision oncology initiatives. The case studies presented demonstrate that combined DNA and RNA analysis significantly enhances the detection of therapeutically relevant alterations compared to DNA-only approaches, with RNA sequencing proving particularly valuable for fusion detection and functional validation of genomic findings.
As the field advances, standardized validation frameworks for integrated assays will be crucial for widespread clinical adoption. The continuing evolution of sequencing technologies, bioinformatics algorithms, and multi-omics integration approaches promises to further refine our understanding of cancer biology and expand the repertoire of actionable alterations for therapeutic targeting. By embracing these integrated approaches, researchers and clinicians can unlock the full potential of precision oncology, ultimately improving outcomes for cancer patients through more personalized and effective treatment strategies.
The longstanding view of cancer as purely a genetic disease, driven by the cumulative acquisition of somatic mutations, has been fundamentally challenged by recent research. While carcinogenesis undoubtedly involves mutations in key driver genes, the tumor microenvironment (TME) has emerged as a critical orchestrator of tumor behavior, therapeutic response, and clinical outcomes [52]. The TME encompasses not only cancer cells but also the complex ecosystem in which they reside—including immune cells, cancer-associated fibroblasts (CAFs), blood vessels, lymphatic vessels, neurons, adipocytes, and the extracellular matrix (ECM) [52]. This intricate network engages in a continuous, dynamic cross-talk with transformed cells, capable of rewiring their epigenetic landscape and dictating their morphogenetic course without additional genetic alterations [52].
The clinical importance of this paradigm is underscored by puzzling observations: cancer cells with high mutational burdens can contribute to normal, tumor-free tissues when developing within healthy embryonic environments [52]. Conversely, adult tissue cells expressing only one or few oncogenes can, in specific contexts, generate highly aggressive tumors [52]. Furthermore, the remarkable disparity in mutation counts between pediatric and adult cancers—despite comparable aggressiveness—suggests that non-genetic factors are potent drivers of malignancy [52]. This technical guide explores how integrating DNA and RNA sequencing technologies with sophisticated computational analyses enables researchers to decode the complex language of the TME, providing unprecedented insights for diagnostic, prognostic, and therapeutic applications in modern oncology.
The Biology of the Tumor Microenvironment and Its Clinical Impact
Components and Functions of the TME
The TME represents a complex society of cellular and non-cellular components that collectively influence tumor progression. Key constituents include:
- Immune Cells: A diverse population of adaptive and innate immune cells, including T lymphocytes, B lymphocytes, natural killer (NK) cells, macrophages, and dendritic cells. Their functional polarization (e.g., M1 vs. M2 macrophages) significantly impacts tumor control or promotion [52] [53].
- Cancer-Associated Fibroblasts (CAFs): Activated fibroblasts that deposit and remodel the extracellular matrix, create physical barriers to drug delivery, and secrete growth factors and cytokines that support cancer cell survival and proliferation [52].
- Vasculature and Lymphatics: The tumor vasculature, often abnormal and leaky, regulates nutrient delivery, oxygen availability, and waste removal while serving as conduits for metastatic dissemination [52].
- Extracellular Matrix (ECM): The non-cellular scaffold that provides structural and biochemical support to surrounding cells. Remodeling of the ECM influences tumor stiffness, mechanotransduction, and invasion [52].
These components collectively establish biophysical forces, metabolic constraints, and signaling networks that can either suppress tumor development or foster its aggressive progression.
Environmental Cues in Malignant Transformation
Seminal studies have demonstrated that environmental context fundamentally determines whether an oncogenically transformed cell will initiate tumorigenesis or behave normally [52]. For instance, skin from chickens infected with Rous sarcoma virus or from mice transgenic for transforming growth factor-α (TGFα) exhibited no overt phenotype until wounded, after which tumors developed specifically along the wound site [52]. This demonstrates that secreted factors like TGFα and TGFβ can exert paracrine transforming functions without necessitating additional genetic alterations [52].
Similarly, the phenomenon of cell competition, wherein "fitter" transformed cells must outcompete their healthy neighbors to avoid death and extrusion, highlights how cell-cell interactions within the tissue architecture determine the fate of pre-malignant cells [52]. Live imaging studies have documented the out-competition of transformed cells by healthy neighbors within both hair follicles and pancreatic ductal regions [52] [54].
Table 1: Environmental Triggers and Their Impact on Tumor Development
| Environmental Trigger | Impact on Tumor Development | Key Molecular Mediators |
|---|---|---|
| Chronic Inflammation | Promotes tumor initiation and progression; creates immunosuppressive microenvironment | TGFβ, IL-1β, TNF-α [52] |
| Tissue Injury/Wounding | Triggers tumor formation at wound sites | TGFα, TGFβ [52] |
| Obesity | Creates chronic inflammatory state; paradoxical better response to treatment | Leptin, inflammatory cytokines [52] |
| Dietary Effects | Modifies tumor formation and progression | Metabolites, hormones [52] |
Decoding the TME: Sequencing Technologies and Methodologies
Advanced Sequencing Platforms for TME Analysis
The resolution required to dissect the TME necessitates sequencing technologies with exceptional accuracy and sensitivity. Recent advancements have introduced Q40 sequencing (99.99% accuracy), representing a significant leap over standard Q30 platforms (99.9% accuracy) [55]. This enhanced precision has profound implications for TME research:
- Cost Efficiency: Q40 data achieves accuracy comparable to Q30 data at only 66.6% of the relative coverage, translating to estimated per-sample cost savings of 30-50% [55].
- Rare Variant Detection: The improved base-level accuracy enables highly confident detection of low-frequency somatic mutations within heterogeneous tumor samples, which is critical for identifying rare subclones that may influence therapeutic resistance [55].
- Liquid Biopsy Applications: For circulating tumor DNA (ctDNA) analysis, where variant allele frequencies can be at or below 0.1%, Q40 sequencing reduces the sequencing depth required for reliable detection, enhancing the scalability of liquid biopsy applications in clinical research [55].
Complementing these accuracy improvements, platforms like the DNBSEQ-T1+ system provide cost-effective, scalable sequencing across applications ranging from whole exome to single-cell studies, while the DNBSEQ-G99RS* flow cells extend throughput flexibility from 40 million to 400 million reads per run [56].
Single-Cell RNA Sequencing for TME Deconvolution
Single-cell RNA sequencing (scRNA-seq) has revolutionized our ability to characterize cellular heterogeneity within the TME. This technology provides detailed RNA transcript profiles at the individual cell level, overcoming the limitations of bulk tumor sequencing which masks critical differences between cell types [57] [58].
A representative analytical workflow for scRNA-seq data includes:
- Data Preprocessing: Raw sequencing data undergoes quality control, excluding low-quality cells and doublets based on gene expression thresholds and mitochondrial gene content [57].
- Data Integration: Integration algorithms like those implemented in the Seurat pipeline address batch effects and combine datasets from different sources, enabling robust comparative analyses [57] [58].
- Cell Type Identification: Unsupervised clustering coupled with marker gene expression allows annotation of distinct cell populations within the TME (e.g., immune cells, fibroblasts, endothelial cells, malignant cells) [57] [53].
- Differential Expression Analysis: Identification of differentially expressed genes (DEGs) between conditions (e.g., normal vs. tumor, different TME subtypes) reveals molecular signatures associated with specific biological states [57] [54].
Single-Cell RNA Sequencing Workflow for TME Analysis
Analytical Frameworks for TME Characterization
Identifying TME-Associated Gene Expression Signatures
The integration of scRNA-seq data with bulk transcriptomic profiles enables the identification of robust gene expression signatures that reflect specific TME states. A representative study in bladder cancer (BLCA) exemplifies this approach [57]:
- Data Acquisition: scRNA-seq data from normal and tumor bladder cells were obtained from public repositories (GEO accession GSE129845), complemented by tumor cell data from additional sources.
- Differential Expression Analysis: Comparison of normal versus tumor cells identified 403 differentially expressed genes (DEGs) with significant alterations in transcription.
- Prognostic Modeling: LASSO Cox regression and multivariate Cox regression analyses pinpointed eight genes with strong prognostic value (CD74, AMIGO2, IGF2, EVPL, TM4SF1, MRFAP1L1, P4HB, and DDX39B).
- Model Validation: The resulting prognostic model demonstrated reliable prediction of patient outcomes across multiple validation cohorts (GSE31684, GSE13507, GSE32894), with area under the curve (AUC) values of 0.74, 0.74, and 0.72 for 1-, 2-, and 3-year survival, respectively [57].
In colorectal cancer (CRC), a similar approach identified a "Signature associated with FOLFIRI resistant and Microenvironment" (SFM) consisting of 250 unique genes that discriminate both TME composition and drug sensitivity [54]. Unsupervised clustering using this signature revealed six distinct SFM subtypes (A-F) with characteristic clinical, molecular, and phenotypic features:
- SFM-C: Characterized by microsatellite instability (MSI) and hypermutation, responsive to immunotherapy
- SFM-F: Exhibits high stromal fraction with epithelial-to-mesenchymal transition phenotype
- SFM-A, -B, -C: Responsive to EGFR inhibitors
- SFM-D, -E, -F: Sensitive to FOLFIRI and FOLFOX chemotherapy [54]
Computational Tools for TME Subclassification
Multiple computational approaches have been developed to classify TME phenotypes based on transcriptomic data:
- Gene Set Variation Analysis (GSVA): A non-parametric, unsupervised method that estimates the enrichment of predefined gene sets in sample populations, allowing characterization of specific biological processes [53] [58].
- CIBERSORT/xCell: Algorithms that leverage signature gene matrices to infer immune cell composition from bulk transcriptomic data, providing insights into immune infiltration patterns [57] [53].
- Unsupervised Clustering: Methods like consensus clustering identify stable TME subtypes based on patterns of immune gene expression, typically categorizing samples into inflamed, intermediate, and non-inflamed phenotypes [58].
Table 2: Representative TME Classification Systems Across Cancers
| Cancer Type | Classification System | Subtypes | Clinical Associations |
|---|---|---|---|
| Colorectal Cancer | SFM Subtypes [54] | SFM-A to SFM-F | Distinct chemotherapy responses, survival outcomes |
| Pan-Cancer | Inflamed/Non-inflamed [58] | Inflamed, Intermediate, Non-inflamed | Immunotherapy response, overall survival |
| Lung Cancer (Never Smokers) | Sherlock-Lung Subtypes [59] | Piano, Mezzo-forte, Forte | Growth rate, treatment strategies |
| Osteosarcoma | TME Clusters [53] | Cluster 1, Cluster 2 | Immune infiltration, drug sensitivity |
Signaling Pathways Linking TME and Cancer Progression
The bidirectional communication between cancer cells and their microenvironment is mediated by numerous signaling pathways that collectively drive tumor progression and therapeutic resistance.
Signaling Pathways in TME-Mediated Malignant Progression
Key pathways implicated in TME-mediated tumor progression include:
- TGF-β Signaling: Functions as a tumor suppressor during early carcinogenesis but transforms into a tumor promoter in advanced stages as cancer cells develop resistance to its growth-inhibitory effects [60]. In the TME, active TGFβ from pro-tumorigenic immune cells drives invasion and associates with the perivascular niche [52].
- PPAR Signaling: Suppression of PPAR signaling pathways has been associated with immunotherapy resistance in inflamed TMEs, suggesting its role in maintaining effective anti-tumor immunity [58].
- APOBEC Mutagenesis: APOBEC3 enzymes, initially protective against viral infections, can inadvertently mutate host DNA following a specific pattern observed in multiple tumor types [59]. This process represents a link between inflammatory microenvironments and mutagenesis.
- Interleukin Signaling: Upregulation of interleukin signaling pathways characterizes inflamed microenvironments and correlates with response to immunotherapy in some tumor types [58].
The Scientist's Toolkit: Essential Research Reagent Solutions
Table 3: Essential Research Reagents and Platforms for TME Characterization
| Research Tool | Function/Application | Key Features |
|---|---|---|
| DNBSEQ-T1+ System [56] | Scalable sequencing for WES, single-cell studies, oncology research | Cost-effective, flexible throughput, supports MSK-IMPACT and MSK-ACCESS assays |
| AVITI System with Q40 Chemistry [55] | High-accuracy DNA/RNA sequencing | 99.99% base accuracy, enhanced rare variant detection, reduced sequencing depth requirements |
| OmicsNest Bioinformatics Platform [56] | End-to-end analysis for microbial identification and genome assembly | Docker-based deployment, ZLIMS/PaaZ integration, streamlined bioinformatics workflows |
| Seurat Pipeline [57] [58] | Single-cell RNA sequencing data analysis | Data integration, clustering, visualization, differential expression testing |
| CIBERSORT/xCell [57] [53] | Immune cell infiltration estimation from bulk RNA data | Deconvolution algorithms, signature-based cell type quantification |
| mSigPortal [59] | Mutational signature analysis | Curated signature database, association with etiologies, tissue specificity analysis |
| IMAPR Pipeline [61] | Somatic mutation detection from RNA-seq data | Machine learning-based variant filtering, reduced false positives, RNA editing detection |
The characterization of tumor microenvironment and gene expression signatures represents a fundamental advancement in cancer research that transcends the traditional mutation-centric view of oncology. The integration of high-accuracy sequencing technologies with sophisticated computational frameworks has enabled researchers to decode the complex language of cellular ecosystems that govern tumor behavior. As these approaches continue to evolve, several promising directions emerge:
The field is moving toward multi-omics integration, combining information from genomics, transcriptomics, proteomics, and epigenomics to capture a more comprehensive view of molecular changes in the TME [60]. Additionally, machine learning and deep learning techniques show tremendous promise for identifying complex patterns and interactions within large-scale omics datasets, potentially improving the accuracy and reproducibility of gene signature identification [60]. There is also growing emphasis on spatial transcriptomics technologies that preserve the architectural context of cells within tissues, providing critical insights into the spatial organization of the TME and cellular neighborhoods that influence tumor progression.
As these technologies mature, standardized protocols, benchmarking exercises, and open science practices will be essential for enhancing the reproducibility and clinical translation of TME-based biomarkers [60]. The ongoing refinement of these approaches promises to accelerate the development of more effective, personalized cancer therapies that target not only cancer cells but also their supportive microenvironmental niches.
Navigating Technical Challenges and Optimizing Sequencing Assays
In modern oncology research, the principles of DNA and RNA sequencing are foundational to personalized cancer treatment. However, the integrity of molecular data is fundamentally constrained by the quality of the starting biological material. Formalin-fixed paraffin-embedded (FFPE) tissues, the most widely available clinical specimens, present significant challenges due to nucleic acid degradation and fragmentation caused by formalin-induced cross-linking. Compounding this issue, tumor samples often exhibit low purity, with tumor content frequently below 40% [62]. These factors directly impact variant detection sensitivity, particularly for low allele fraction variants that may drive treatment resistance. This guide details established methodologies to overcome these limitations, ensuring reliable genomic data from even the most challenging clinical samples.
Quantitative Landscape of Tumor Purity and Low-Allele-Fraction Variants
Understanding the prevalence and impact of sample quality issues is the first step in addressing them. Large-scale genomic studies provide a clear picture of the challenges inherent in real-world samples.
Table 1: Prevalence of Low VAF Variants and Tumor Purity Across Common Cancers [62]
| Tumor Type | Patients with ≥1 VAF ≤10% Variant | Median Tumor Purity | Samples with Purity <40% |
|---|---|---|---|
| Pancreatic Cancer | 37% | 19% | 68% |
| Non-Small Cell Lung Cancer | 35% | 23% | 57% |
| Colorectal Cancer | 29% | 26% | 41% |
| Prostate Cancer | 24% | 26% | 36% |
| Breast Cancer | 23% | 29% | 30% |
| All Solid Tumors (Cohort Median) | 29% | 43% | 44% |
A comprehensive analysis of 331,503 tumors revealed that nearly one-third of patients harbored at least one somatic variant with a variant allele fraction (VAF) of 10% or lower [62]. These low VAF variants are critically important, as they can represent emerging resistance mechanisms or subclonal driver alterations. The data show that samples across tumor types from the real-world clinical setting tend to be of relatively low tumor purity, which, along with tumor heterogeneity, contributes to the high proportion of low VAF variants [62]. This underscores the necessity of optimized workflows capable of detecting these clinically relevant, low-frequency variants.
Optimized Wet-Lab Protocols for Nucleic Acid Extraction and Library Preparation
Pathologist-Assisted Tissue Selection and Macrodissection
The first and most critical step is ensuring the analyzed tissue region is enriched for tumor content. A recommended protocol involves:
- Histological Staining and Review: Perform Hematoxylin and Eosin (H&E) staining on FFPE sections. A pathologist then marks selected regions enriched for tumor content [63] [32].
- Targeted Macrodissection: Instead of bulk tissue scraping, use precise macrodissection or microdissection to isolate the marked tumor-rich regions from the slides (see Figure 1). This excludes non-tumor parenchyma and mitigates the effects of intratumoral heterogeneity, significantly improving the yield and quality of tumor-derived nucleic acids [63] [32].
- DNA/RNA Co-Extraction: For DNA and RNA extraction from the same dissected region, specialized kits like the AllPrep DNA/RNA FFPE Kit (Qiagen) are recommended. Some protocols allow for both DNA and RNA extraction from the same FFPE section, while others may require two distinct blocks from the same specimen [49] [32].
Enhanced Extraction and Library Construction for FFPE and Low-Input Samples
Standard protocols often fail with suboptimal FFPE samples. The following modifications are critical for success:
- Deparaffinization and Digestion: Replace toxic xylene with a heat-based deparaffinization protocol. Heat tissue sections in digestion buffer at 90°C for 3 minutes, followed by centrifugation and manual removal of the solidified paraffin ring. This reduces toxicity and does not compromise DNA recovery [63].
- Automated Nucleic Acid Extraction: Automated systems, such as the Sonication STAR automated method, significantly improve reliability and throughput. This approach has been shown to increase fully reported tumor profiles for patients by 16% by reducing "Quantity Not Sufficient" (QNS) rates and improving sequencing performance [64].
- Low-Input Library Preparation for RNA-seq: When RNA is limited, the TaKaRa SMARTer Stranded Total RNA-Seq Kit v2 (Kit A) achieves performance comparable to the Illumina Stranded Total RNA Prep (Kit B) with 20-fold less RNA input [32]. This is crucial for small biopsies. For DNA library prep from FFPE-derived, low molecular weight DNA, using a ligation sequencing kit with optimized bead-to-sample ratios and extended incubation times (30 min DNA repair, 40 min adapter ligation) improves library yield and sequencing success [63].
Advanced Analytical and Computational Methods
Integrated RNA and DNA Sequencing
Relying on DNA sequencing alone can miss clinically significant alterations. Combining whole exome sequencing (WES) with RNA sequencing (RNA-seq) from a single sample substantially improves detection.
- Clinical Validation: One study validated an integrated WES and RNA-seq assay on 2230 clinical tumor samples. This combined approach enabled the direct correlation of somatic alterations with gene expression, recovered variants missed by DNA-only testing, and improved the detection of gene fusions, uncovering clinically actionable alterations in 98% of cases [49].
- Variant Calling from RNA-seq: Implementing an RNA-seq variant-calling framework (e.g., using Pisces software) can improve the detection of low-coverage hotspot variants, providing an orthogonal method to confirm DNA findings [49].
Comprehensive Genomic Profiling and Whole-Genome Sequencing
Targeted panels are standard in clinics, but broader sequencing approaches offer advantages for low-purity tumors.
- Superior Feature Detection: Compared to a 523-gene panel (FoundationOneCDx), Whole Genome Sequencing (WGS) detected 95% of somatic single nucleotide variants, 90% of insertions/deletions, and 76% of amplifications in FFPE samples. Crucially, nearly all structural variants (98%) and most copy number variants (62%) were detected only by WGS, providing a more complete genomic portrait [65] [66].
- Computational Tools for Structural Variation: New computational tools like BACDAC help visualize elusive genomic patterns in low-purity or low-coverage samples. This tool detects signs of genomic instability, such as whole-genome doubling, which is often linked to aggressive behavior and treatment resistance [67].
Table 2: Comparison of Genomic Profiling Methods for FFPE/Low-Purity Tumors
| Methodology | Key Advantage | Ideal Use Case | Considerations |
|---|---|---|---|
| Targeted NGS Panels (e.g., F1CDx) | High depth (>500x); validated for clinical actionability | Routine clinical care; focused therapeutic biomarker identification | Limited to panel genes; may miss complex structural variants |
| Integrated WES + RNA-seq | 98% actionable alteration rate; detects fusions & expression | Research & advanced diagnostics; cases where fusions/expression are critical | More complex workflow and analysis; higher cost than targeted panels |
| Whole Genome Sequencing (WGS) | Detects 98% of SVs and 62% of CNVs missed by panels; reveals mutational signatures | Cancer of unknown primary; complex cases; comprehensive biomarker discovery | Higher data storage and computational burden; requires sophisticated bioinformatics |
| Automated Extraction & CGP | 16% increase in fully reported patient profiles | High-throughput clinical labs; standardizing sample processing | Requires initial investment in automation equipment |
The Scientist's Toolkit: Essential Research Reagents and Solutions
Table 3: Key Reagents for Managing FFPE and Low-Purity Tumor Samples
| Item | Function | Example Products/Citations |
|---|---|---|
| Automated NA Extraction System | Standardizes and improves yield from FFPE | Sonication STAR (Hamilton, Covaris, Labcorp) [64] |
| FFPE RNA-seq Kit (Low Input) | Library prep from minimal RNA | TaKaRa SMARTer Stranded Total RNA-Seq Kit v2 [32] |
| FFPE DNA-seq Kit (Low Input) | Library prep from fragmented DNA | Ligation Sequencing Kit (ONT LSK114) with modified protocol [63] |
| Tumor Enrichment Reagents | Pathologist-guided macrodissection | H&E Staining Kits [63] [32] |
| DNA/RNA Co-Extraction Kit | Isolates both nucleic acids from one sample | AllPrep DNA/RNA FFPE Kit (Qiagen) [49] |
| Computational Tool for Ploidy | Analyzes chromosomal instability in low-purity samples | BACDAC [67] |
| Bioinformatic Classifier | Methylation-based tumor classification | Sturgeon classifier for Oxford Nanopore data [63] |
Navigating the challenges of FFPE degradation and low tumor purity is not merely a technical obstacle but a fundamental aspect of modern oncology research. As the data show, failing to address these issues means overlooking a substantial fraction of clinically relevant genomic alterations. By implementing a holistic strategy that combines pathologist-guided sample selection, optimized wet-lab protocols for low-input and degraded materials, integrated multi-omic sequencing, and advanced computational tools, researchers can significantly enhance the quality and clinical utility of genomic data. This rigorous approach ensures that the principles of sequencing are fully realized, enabling more accurate diagnostics, revealing resistant subclones, and ultimately guiding more effective, personalized cancer therapies.
In the evolving paradigm of precision medicine, the identification of somatic mutations is fundamental for characterizing the cancer genome and guiding therapeutic decisions [61]. While DNA sequencing (DNA-seq) has been the standard method for detecting mutations, it primarily reveals the potential for pathogenic changes without confirming their functional transcription into proteins, the actual targets of most cancer drugs [9]. RNA sequencing (RNA-seq) bridges this "DNA to protein divide" by detecting mutations present in the transcribed genome, thereby providing functional evidence of a variant's biological activity [9] [61]. This capability makes RNA-seq an invaluable complement to DNA-based assays.
However, detecting somatic mutations from RNA-seq data presents unique bioinformatic challenges that, if unaddressed, lead to an unacceptably high rate of false positives. Sources of these errors include alignment inaccuracies near splice junctions, RNA editing sites misinterpreted as DNA variants, uneven gene expression leading to non-uniform read depth, and contamination from highly expressed but clinically irrelevant genes [9] [61]. Early studies revealed that without sophisticated filtering, only about 10% of variants called from RNA-seq data could be validated by whole exome sequencing (WXS) [61]. This technical note provides an in-depth guide to the bioinformatic strategies and experimental protocols developed to control false positives, ensuring the reliability of somatic mutation detection in oncology research.
Core Bioinformatics Strategies for False Positive Control
Specialized Filtering Pipelines for RNA-Seq Data
A primary defense against false discoveries is the implementation of filters specifically designed for RNA-seq idiosyncrasies. One prominent pipeline, the Integrated Mutation Analysis Pipeline for RNA-seq data (IMAPR), employs eighteen distinct mutation filters, ten of which are tailored for RNA-seq data [61]. The application of these filters can drastically reduce false discoveries.
Table 1: Key Filters in the IMAPR Pipeline and Their Efficacy
| Filter Type | Description | Impact on Candidate Variants |
|---|---|---|
| Dual Variant Calling | Requires variants to be called by multiple, independent variant callers. | Rejected 31.8% of candidates [61] |
| Low Mutated Reads | Filters variants supported by an insufficient number of alternative allele reads. | Rejected 20.1% of candidates [61] |
| Dual Alignment | Requires variants to be consistently identified using two different sequence alignment tools. | Rejected 12.6% of candidates [61] |
| RNA Editing | Removes known RNA editing sites (e.g., A-to-I deamination sites). | Significantly reduces T>C transitions, a hallmark of RNA editing [61] |
Machine Learning Classification
Filtering alone may not be sufficient to distinguish true somatic mutations from RNA-specific artifacts. Supervised machine learning models offer a powerful solution. In the IMAPR pipeline, a Stacking model that integrates three top-performing classifiers—Random Forest, XGBoost, and Multiplayer Perceptron—was developed to differentiate true somatic mutations from false positives arising from processes like RNA editing [61]. This model, based on a logistic regression meta-classifier, achieved a high ROC-AUC of 0.950 and a precision-recall AUC of 0.991 on a validation cohort, drastically reducing the portion of RNA-only mutations from 14.9% to 6.2% while maintaining a sensitivity of 0.650 [61].
Leveraging Long-Read Single-Cell RNA-Seq
The emergence of long-read (LR) single-cell RNA sequencing (scRNA-seq) provides new opportunities and methods for variant detection. The LongSom workflow leverages high-quality LR scRNA-seq to call somatic single-nucleotide variants (SNVs), mitochondrial SNVs (mtSNVs), copy number alterations (CNAs), and gene fusions de novo without matched normal samples [68]. A critical innovation in LongSom is its mutational profile-based cell type reannotation. The workflow first calls a set of "high-confidence cancer variants" and then reannotates cells based on their mutational burden, which corrects for misannotation arising from ambiguous gene expression markers. This step is crucial because even a low percentage of cancer cells misannotated as noncancer can lead to true somatic variants being incorrectly filtered out as germline [68]. LongSom applies extensive sets of hard filters and statistical tests—10 steps for nuclear SNVs and 5 steps for mtSNVs—to distinguish somatic variants from noise and germline polymorphisms.
Experimental Protocols for Validation
Protocol: Validation of RNA-Detected Somatic Mutations Using DNA-Seq
Purpose: To confirm that somatic mutations identified via RNA-seq are genuine genomic alterations and not transcriptional or technical artifacts. Materials: Paired tumor RNA and DNA samples from the same patient. Methods:
- Parallel Sequencing: Perform targeted DNA-seq (e.g., using comprehensive cancer panels like Agilent Clear-seq or Roche Comprehensive Cancer panels) and RNA-seq on the same tumor specimen [9].
- Independent Variant Calling: Call somatic variants from the DNA-seq and RNA-seq data using independent, optimized bioinformatic pipelines for each data type. For RNA-seq, employ a pipeline like IMAPR that includes RNA-specific filters and a machine learning classifier [61].
- Intersection Analysis: Compare the final, high-confidence mutation sets from both DNA-seq and RNA-seq. A mutation detected by both platforms is considered robustly validated. Validation Metrics: Calculate the validation rate, defined as the percentage of RNA-seq-called mutations that are also present in the DNA-seq data. High-performing pipelines can achieve validation rates exceeding 77.6% with WXS and 86.8% with high-coverage whole-genome sequencing (WGS) [61].
Protocol: De Novo Somatic Mutation Calling from scRNA-Seq Data
Purpose: To identify somatic mutations and reconstruct clonal heterogeneity from single-cell RNA-seq data in the absence of a matched normal DNA sample. Materials: LR scRNA-seq data (e.g., from PacBio platform) from a tumor biopsy containing both cancer and microenvironment cells [68]. Methods:
- Cell Type Reannotation:
- Perform initial cell type annotation based on standard marker gene expression.
- Call a set of high-confidence cancer variants (SNVs, mtSNVs, fusions) from the initial data.
- Reannotate cells as "cancer" or "noncancer" based on their mutational burden, correcting for initial expression-based misannotations [68].
- Variant Calling on Reannotated Data:
- For nuclear SNVs, apply a multi-step filter including hard filters (e.g., for read depth, allele frequency) and statistical tests against the reannotated noncancer cells to distinguish somatic from germline variants [68].
- For mtSNVs, apply a separate 5-step filtering process that accounts for high levels of ambient mitochondrial RNA.
- Clonal Reconstruction: Use the detected somatic SNVs, mtSNVs, and fusions as input for a Bayesian clustering method (e.g., BnpC) to infer the clonal substructure of the tumor [68]. Validation: Validate clinically relevant somatic SNVs against matched DNA samples from the same patient where available [68].
The Scientist's Toolkit: Essential Research Reagents and Tools
Table 2: Key Reagents and Computational Tools for RNA-Seq Somatic Mutation Detection
| Item Name | Type | Function in Workflow |
|---|---|---|
| Targeted RNA-seq Panels (e.g., Afirma Xpression Atlas) | Wet-bench Reagent | Enriches sequencing coverage for genes of interest, improving detection accuracy for rare alleles and low-abundant mutant clones [9]. |
| Mutect2 | Computational Tool | A widely used variant caller that can be applied to RNA-seq data; often used as part of a larger, multi-tool pipeline [9] [61]. |
| IMAPR Pipeline | Computational Workflow | An integrated pipeline employing 18 filters and a machine learning Stacking model to significantly reduce false positives in bulk RNA-seq data [61]. |
| LongSom Workflow | Computational Workflow | A workflow for de novo somatic variant detection and clonal reconstruction from long-read scRNA-seq data [68]. |
| VarDict & LoFreq | Computational Tool | Additional variant callers used in ensemble approaches to improve call robustness [9]. |
Diagram: Integrated Workflow for False Positive Control
The following diagram illustrates the logical relationships and sequential stages of a comprehensive bioinformatics strategy that integrates the methods discussed above to control false positives in RNA-seq somatic mutation detection.
The integration of RNA-seq into somatic mutation detection portfolios represents a significant advancement for precision oncology, enabling the discovery of expressed, functionally relevant variants. However, the path to reliable detection is paved with technical challenges that manifest as false positives. Addressing these requires a multi-faceted bioinformatic strategy that includes specialized filtering pipelines for RNA-seq artifacts, sophisticated machine learning models to classify variants, and robust experimental protocols for orthogonal validation with DNA-seq. Furthermore, emerging technologies like long-read single-cell RNA-seq offer novel computational workflows for de novo variant calling and clonal reconstruction. By adhering to these rigorous strategies, researchers and drug developers can harness the full potential of RNA-seq to build a more accurate and clinically actionable mutational landscape of cancer, ultimately guiding the development of more effective targeted therapies and improving patient outcomes.
In the precision medicine era, targeted next-generation sequencing (NGS) panels have become indispensable tools in oncology research and clinical diagnostics, enabling focused analysis of cancer-associated genes with high sensitivity and cost-efficiency [69]. The performance of these panels hinges critically on the biochemical properties of the oligonucleotide probes used to capture genomic regions of interest. Probe design parameters—particularly length and specificity—directly determine key assay metrics including sensitivity, specificity, uniformity, and ultimately, the reliability of variant detection [9] [70]. As targeted panels evolve from DNA-based mutation detection to integrated RNA-seq applications for analyzing expressed mutations and fusion transcripts [9] [20], optimizing these fundamental parameters becomes increasingly critical for accurate molecular profiling in cancer research and drug development.
This technical guide examines the experimental evidence and practical considerations for probe design optimization within the broader context of DNA and RNA sequencing principles in oncology. We synthesize recent benchmarking studies, analyze performance trade-offs, and provide detailed methodologies for validating probe specificity, equipping researchers with the knowledge to develop robust, reliable targeted sequencing assays.
Core Principles of Probe Design
Probe Length: Balancing Specificity and Hybridization Efficiency
Probe length fundamentally influences hybridization kinetics, specificity, and practical implementation in target enrichment. Longer probes generally exhibit higher thermal stability and better tolerance to minor sequence variations, while shorter probes provide greater specificity but reduced hybridization efficiency, particularly for challenging genomic regions.
Table 1: Impact of Probe Length on Assay Performance
| Probe Length | Technical Considerations | Optimal Use Cases | Performance Implications |
|---|---|---|---|
| Short Probes (~70-100 bp) | • Higher specificity for distinguishing homologous sequences• Reduced hybridization efficiency• More affected by sequence mismatches | • Distinguishing highly homologous genes (e.g., gene families)• RNA panels targeting specific isoforms | • ROCR panels: Fewer false positives/uncharacterized calls [9] |
| Long Probes (~120 bp) | • Increased hybridization efficiency and coverage uniformity• Greater tolerance for sequence variations• Higher risk of off-target binding | • Comprehensive cancer panels• Targeting genomic regions with common SNPs | • AGLR panels: Higher coverage but more false positives [9] |
| Very Short Probes (40 bp, e.g., Xenium) | • Maximum specificity for single transcript detection• Requires sophisticated in situ detection chemistry• Highly susceptible to off-target binding | • Spatial transcriptomics with padlock probes• Single-cell imaging applications | • Critical dependence on perfect sequence matching; 21/280 genes showed off-target binding [70] |
Experimental evidence demonstrates that length optimization must be context-dependent. In targeted RNA-seq applications, Agilent panels with 120 bp probes reported significant false positives and uncharacterized calls when lenient bioinformatic parameters were applied, whereas Roche panels with shorter probes (~70-100 bp) demonstrated substantially fewer such artifacts despite similar target regions [9]. This highlights the critical interplay between probe length and data analysis stringency.
Probe Specificity: The Determinant of Assay Accuracy
Probe specificity—the ability to uniquely bind intended target sequences—is paramount for accurate variant calling and expression quantification. Non-specific binding generates false positives, compromises detection sensitivity, and distorts biological interpretations [70] [71].
Spatial transcriptomics platforms like the 10x Genomics Xenium system exemplify the critical importance of perfect specificity. A recent evaluation of the Xenium v1 Human Breast Gene Expression Panel revealed that at least 21 of 280 genes were impacted by off-target binding to protein-coding genes [70]. For these genes, observed expression patterns reflected aggregate signal from both intended targets and off-target genes, fundamentally compromising data interpretation. This phenomenon was validated through orthogonal comparisons with Visium CytAssist and single-cell RNA-seq data from the same tumor blocks [70].
In molecular diagnostics, specificity failures can have direct clinical implications. Evaluation of the LEISH-1/LEISH-2 primer pair with TaqMan MGB probe for visceral leishmaniasis diagnosis demonstrated unexpected amplification in all serologically negative samples, revealing critical specificity flaws primarily associated with the probe design [71]. Subsequent in silico analyses confirmed structural incompatibilities and low sequence selectivity, necessitating redesign of the oligonucleotide set.
Experimental Evidence and Performance Benchmarking
Systematic Comparisons of Commercial Platforms
Recent benchmarking studies provide quantitative insights into how probe design choices impact practical performance across platforms. A systematic evaluation of four high-throughput spatial transcriptomics platforms with subcellular resolution revealed substantial differences in sensitivity and specificity attributable to underlying technology and probe design [72].
Table 2: Platform Performance Comparison in Spatial Transcriptomics
| Platform | Technology Type | Gene Panel Size | Key Performance Findings | Implications for Probe Design |
|---|---|---|---|---|
| Xenium 5K | Imaging-based (iST) | 5,001 genes | • Superior sensitivity for multiple marker genes• Strong correlation with scRNA-seq (r=0.89)• High transcript capture efficiency | • Optimized probe chemistry enables high sensitivity despite large panel size |
| CosMx 6K | Imaging-based (iST) | 6,175 genes | • Higher total transcripts than Xenium but lower correlation with scRNA-seq (r=0.68)• Substantial deviation from reference data | • Probe performance variability affects quantitative accuracy despite larger panel |
| Visium HD FFPE | Sequencing-based (sST) | 18,085 genes | • High correlation with scRNA-seq (r=0.86)• Competitive sensitivity for marker genes | • Poly(dT) capture provides unbiased profiling but with lower spatial resolution |
| Stereo-seq v1.3 | Sequencing-based (sST) | Whole transcriptome | • High correlation with scRNA-seq (r=0.85)• Comparable performance to Visium HD | • High-density spatial barcoding compensates for non-targeted approach |
This comprehensive analysis demonstrated that while all platforms could detect established marker genes like EPCAM, their quantitative performance varied significantly [72]. Xenium 5K consistently showed superior sensitivity, underscoring the effectiveness of its optimized probe chemistry, while CosMx 6K's discordance with reference scRNA-seq data suggested potential issues with probe performance uniformity across its extensive panel.
Impact on Variant Detection in Oncology
In clinical oncology, probe design directly influences mutation detection capability and therapeutic decision-making. A study evaluating targeted RNA-seq for detecting expressed mutations found that RNA sequencing uniquely identified variants with significant pathological relevance that were missed by DNA-seq alone [9]. This demonstrates RNA probes' ability to bridge the "DNA to protein divide" by confirming which mutations are actually transcribed.
Similarly, in non-small cell lung cancer (NSCLC), a testing algorithm using amplicon-based DNA/RNA sequencing followed by reflex hybridization-capture-based RNA sequencing identified actionable oncogenic fusions in approximately 10% of cases that were missed by the initial test [20]. The hybridization-capture approach—which relies on probe-based enrichment—detected clinically relevant fusions in ALK, BRAF, NRG1, NTRK3, ROS1, and RET genes, maximizing patient eligibility for targeted therapies [20].
Methodologies for Probe Validation
In Silico Specificity Analysis
Computational assessment represents the foundational step in probe validation. The Off-target Probe Tracker (OPT) tool exemplifies a rigorous approach to predicting potential cross-hybridization [70]. OPT employs the following workflow:
- Sequence Alignment: Probe sequences are aligned to reference transcriptomes using nucmer with adjustable stringency parameters (mismatch tolerance, indel penalties)
- Multi-Annotation Comparison: Analyses are performed against multiple annotation databases (GENCODE, RefSeq, CHESS) to account for annotation discrepancies
- Protein-Coding Focus: Filtering to identify off-target binding to expressed protein-coding genes rather than pseudogenes or non-coding RNAs
- Impact Assessment: Integration with orthogonal expression data to validate predicted off-target effects
Application of OPT to the Xenium v1 Human Breast Gene Expression Panel identified 180 probe sequences across 45 genes with perfect-sequence homology to off-target transcripts [70]. When restricted to protein-coding genes with potential clinical relevance, 21 genes remained affected by off-target binding.
Experimental Validation of Specificity
Wet-lab confirmation remains essential for verifying computational predictions. The systematic benchmarking approach used for spatial transcriptomics platforms provides a robust template [72]:
- Orthogonal Technology Comparison: Profiling serial sections from the same tumor block with different technologies (e.g., Xenium, Visium, scRNA-seq, CODEX)
- Structural Alignment: Using tools like STalign to spatially register datasets from adjacent sections
- Pattern Correlation: Assessing whether expression patterns match the intended target or represent aggregate signal from multiple genes
- Cross-Platform Concordance: Evaluating correlation of gene expression measurements with established reference methods
For qPCR assays, comprehensive specificity testing should include:
- Evaluation against negative control samples from the same species
- Testing against closely related organisms or gene family members
- Assessment under varying stringency conditions (temperature, Mg²⁺ concentration)
- Comparison with alternative detection methods or probe sets [71]
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Reagents for Probe-Based Targeted Sequencing
| Reagent Category | Specific Examples | Function in Workflow | Technical Considerations |
|---|---|---|---|
| Target Enrichment Systems | • Agilent Clear-seq Custom Cancer Panels• Roche Comprehensive Cancer Panels• 10x Genomics Xenium Panels | Selective capture of genomic regions of interest through hybridization | • Probe length design (70-120 bp)• Inclusion of exon-junction spanning probes for RNA |
| NGS Library Prep Kits | • Sophia Genetics Library Kit (compatible with MGI SP-100RS)• Illumina DNA/RNA Library Prep | Convert nucleic acids to sequencer-compatible formats with adapter ligation | • Compatibility with automation platforms• Input DNA/RNA requirements (≥50 ng) |
| Sequencing Platforms | • MGI DNBSEQ-G50RS (cPAS technology)• Illumina NovaSeq• Oxford Nanopore | High-throughput sequencing of enriched libraries | • Read length, error profiles, and throughput vary• Impact on variant calling accuracy |
| Bioinformatics Tools | • OPT (Off-target Probe Tracker)• Sophia DDM• GATK/Mutect2 | Analyze sequencing data, call variants, and predict/probe performance | • Machine learning integration• Database connectivity (OncoPortal, ClinVar) |
Visualizing Probe Design and Optimization Workflows
Probe Design and Validation Workflow
Diagram 1: Comprehensive workflow for probe design and validation, emphasizing computational prediction and experimental confirmation.
Targeted Sequencing Wet-Lab Process
Diagram 2: End-to-end workflow for targeted sequencing experiments, from sample preparation to data analysis.
Probe design remains both an art and science in targeted sequencing panel development. The experimental evidence clearly demonstrates that probe length and specificity are non-negotiable parameters that directly determine assay performance in oncogenomics. While longer probes (~120 bp) offer practical advantages in hybridization efficiency and coverage uniformity, shorter probes (~70-100 bp) provide superior specificity with appropriate bioinformatic stringency [9]. The optimal balance depends on the specific application—whether comprehensive mutation screening, fusion detection, or spatial transcriptomics.
Future directions in probe design will likely incorporate artificial intelligence and machine learning approaches to predict hybridization behavior and optimize sequences in silico before experimental validation [73]. As oncology research increasingly relies on multi-omic profiling integrating DNA and RNA sequencing [9] [74] [20], the development of dual-purpose probes capable of capturing both genomic and transcriptomic information from limited clinical samples represents an exciting frontier. Through continued rigorous benchmarking and validation—as demonstrated in recent spatial transcriptomics evaluations [72]—probe design will remain foundational to advancing precision oncology and enabling more personalized cancer therapeutics.
Next-generation sequencing (NGS) has fundamentally transformed oncology research, enabling comprehensive molecular profiling of cancers at unprecedented resolution. However, the inherent complexity of NGS methodologies, from wet-lab procedures to bioinformatic analysis, introduces substantial variability that can compromise data integrity and research reproducibility. Achieving robustness in sequencing outputs demands rigorous, standardized quality control (QC) metrics throughout the entire workflow. Within oncology, where findings directly influence understanding of tumorigenesis, drug discovery, and personalized treatment strategies, this robustness is not merely beneficial—it is essential. Imperfections in sequencing data can lead to false positives, obscuring true driver mutations, or false negatives, missing critical therapeutic targets. This technical guide provides an in-depth examination of QC metrics and procedures, framed within the context of DNA and RNA sequencing for oncology research. It details a comprehensive framework for monitoring quality from initial sample preparation through final variant calling, equipping researchers and drug development professionals with the methodologies needed to ensure data reliability, enhance cross-study comparability, and ultimately, advance robust precision medicine.
Three-Stage Quality Control Framework for Sequencing Data
Quality control for sequencing data is not a single checkpoint but a continuous process applied at multiple stages. A robust framework divides QC into three critical stages: raw data, alignment, and variant calling. Monitoring QC metrics at each stage provides unique, independent evaluations of data quality from differing perspectives, ensuring that issues undetected at one stage can be captured at another [75].
Stage 1: Raw Data QC. This initial quality assessment acts as a quick screening to flag samples with fundamental issues. It is performed on the raw FASTQ files generated by the sequencer. Key parameters include:
- Base Quality Scores: The median Phred quality score (Q-score) should typically remain above 30 across the length of the reads, indicating a base call accuracy of 99.9%. A significant drop in quality at the ends of reads is common and may require trimming [75].
- Nucleotide Distribution: The proportion of each base (A, T, C, G) should remain relatively stable across sequencing cycles for whole-genome and exome sequencing. Major deviations can indicate contamination or fluidics issues during the run [75].
- GC Content: The overall GC percentage should align with the expected biological norm for the species and genomic region (e.g., ~38-39% for human whole-genome sequencing). Abnormal deviations may suggest contamination [75].
- Sequence Duplication Levels: A high rate of duplicate reads can indicate PCR over-amplification during library preparation or low input material, which may reduce effective coverage.
Tools such as FastQC, FASTX-Toolkit, and NGS QC Toolkit are routinely used for this stage. While essential, passing raw data QC does not guarantee a sample will pass subsequent stages. Conversely, a sample with some raw data issues might still be salvageable for further analysis after appropriate filtering or trimming [75].
Stage 2: Alignment QC. After raw reads are aligned to a reference genome, QC focuses on the quality and characteristics of the alignment, contained within BAM or SAM files. This stage helps identify issues not apparent in the raw data. Critical metrics include:
- Alignment Rate: The percentage of reads that successfully map to the reference genome. A low rate can indicate contamination or poor-quality libraries.
- Coverage Uniformity: In target enrichment approaches (e.g., exome sequencing), this measures how evenly reads cover the targeted regions. High variability can lead to gaps in variant detection.
- Insert Size Metrics: The distribution of fragment sizes in paired-end sequencing should be consistent with the library preparation protocol. Aberrations can hint at degradation or preparation artifacts.
- Duplication Rate: The proportion of aligned reads that are PCR duplicates. High duplication rates reduce effective sequencing depth and can confound variant calling.
Stage 3: Variant Calling QC. This final stage is the last opportunity to identify sample-level issues and filter out false-positive variant calls. It is crucial for ensuring the accuracy of the final research results.
- Transition/Transversion (Ti/Tv) Ratio: In human exomes, the expected Ti/Tv ratio is typically around 2.5-3.0. Significant deviations from this range can indicate systematic errors in sequencing or variant calling.
- Variant Call Quality Scores: Metrics such as QUAL and QD in GATK outputs help filter low-confidence calls.
- Variant Allele Frequency (VAF) Distribution: The distribution of VAFs for heterozygous SNPs in a diploid sample should cluster around 0.5. Skewed distributions may suggest sample contamination or copy number alterations.
Table 1: Key Quality Control Metrics and Their Interpretations
| QC Stage | Metric | Target / Normal Range | Interpretation of Deviation |
|---|---|---|---|
| Raw Data | Median Base Quality (Phred Q-score) | > 30 (Q30) across reads | General loss of sequencing accuracy; consider trimming. |
| Nucleotide Distribution per Cycle | Stable proportions of A,T,C,G | Contamination, fluidics problems, or low-quality DNA. | |
| GC Content | Species/region specific (e.g., ~38% human WGS) | Potential contamination. | |
| Raw Read Yield | Project-dependent | Improper library pooling or sequencing failure. | |
| Alignment | Alignment Rate | > 90-95% (context-dependent) | High contamination or poor reference specificity. |
| Duplication Rate | As low as possible | PCR over-amplification; low input material. | |
| Mean Depth of Coverage | Project-dependent (e.g., >100x for WGS) | Inadequate sequencing depth for confident variant calling. | |
| Variant Calling | Ti/Tv Ratio (Exome) | ~2.5 - 3.0 | Systematic sequencing or variant calling errors. |
| Heterozygous SNP VAF Distribution | Peak at ~0.5 | Sample contamination or aneuploidy. |
Wet-Lab Protocols and Their Impact on Data Quality
The fidelity of sequencing data is profoundly influenced by the wet-lab procedures employed before sequencing even begins. Variations in library preparation kits, DNA extraction methods, and input material quality can introduce significant artifacts and inter-laboratory variability, challenging the reproducibility of oncogenomic studies.
Interlaboratory Variability in Wet-Lab Protocols
A 2023 interlaboratory study on whole-genome sequencing of bacterial pathogens, highly relevant to standardized cancer genomics, demonstrated that while Illumina raw data quality was generally high with little overall variability, one specific library preparation kit was identified as an outlier [76]. Furthermore, the variability of Ion Torrent data was consistently higher across the investigated species, independent of the participating laboratory [76]. This underscores that the choice of sequencing technology and specific reagents can be a major source of technical bias. The study also found that for certain species like Campylobacter, a minority of isolate data showed higher divergence in sequence type and core genome MLST (cgMLST) analysis, indicating that the impact of wet-lab protocols can be species- or sample-specific [76]. Such findings highlight that robust, cross-institutional studies, such as those in consortia, require rigorous standardization of wet-lab protocols to ensure data comparability.
Analytical Validation of Targeted NGS for Precision Oncology
The National Cancer Institute's Molecular Analysis for Therapy Choice (NCI-MATCH) trial provides a seminal example of rigorous validation of a wet-lab and analysis pipeline for clinical-grade sequencing. The trial utilized a targeted NGS panel (Oncomine Cancer Panel) across four CLIA-certified laboratories. The validation established key performance metrics for the entire workflow, from biopsy to report [77]:
- Overall Sensitivity and Specificity: The assay achieved 96.98% sensitivity for 265 known mutations and 99.99% specificity.
- Reproducibility: A 99.99% mean inter-operator pairwise concordance was observed across the four laboratories.
- Limit of Detection (LOD): The LOD was established for different variant types: 2.8% for single-nucleotide variants (SNVs), 10.5% for small insertions/deletions (indels), 6.8% for large indels, and four copies for gene amplification [77].
This multi-laboratory validation demonstrates that high reproducibility of a complex NGS assay is achievable through strict standard operating procedures (SOPs) and a locked data analysis pipeline, providing a template for robust assay development in oncology research.
Quality Control for RNA-Sequencing in Cancer Transcriptomics
RNA-sequencing (RNA-seq) is a powerful tool in oncology for measuring gene expression, identifying fusion transcripts, and characterizing the tumor microenvironment. However, as a relatively new and complex technology, it lacks standardization, and the choice of methodology can significantly impact the robustness and reproducibility of results [78].
Robustness of Differential Gene Expression Analysis
A study investigating the robustness of five differential gene expression (DGE) models (DESeq2, voom + limma, edgeR, EBSeq, NOISeq) found that their performance varied [78]. Patterns of relative model robustness were dataset-agnostic with sufficiently large sample sizes. Overall, the non-parametric method NOISeq was identified as the most robust, followed by edgeR, voom, EBSeq, and DESeq2 [78]. This research highlights that the selection of a DGE tool is a critical analytical decision that influences the stability of research findings, especially in a clinical translation context.
Integrated QC Systems for RNA-Seq
To address the multifaceted nature of RNA-seq QC, integrated systems like QuaCRS (Quality Control for RNA-Seq) have been developed. QuaCRS simplifies the execution of multiple open-source QC tools (FastQC, RNA-SeQC, and RSeQC), aggregates their output, and allows for meta-analyses of QC metrics across large numbers of samples [79]. This comprehensive approach provides a more complete view of sample data quality than any single tool. Key motivations for such systems include the need to identify diverse systematic errors (e.g., from library preparation protocols, sample degradation, or batch effects) and to prevent the costly analysis of unreliable data, which can mask underlying biological effects [79].
Table 2: Essential Research Reagent Solutions for Sequencing QC
| Reagent / Kit | Function / Application | Key Considerations |
|---|---|---|
| Formalin-Fixed, Paraffin-Embedded (FFPE) Tissue | Common source of archival clinical cancer samples. | DNA/RNA can be fragmented and cross-linked; requires specialized extraction and library prep protocols [77]. |
| Targeted NGS Panels (e.g., Oncomine Cancer Panel) | Focused sequencing of known cancer-related genes. | Increases depth of coverage for cost; performance must be validated for sensitivity/specificity/LOD [77]. |
| Exome Capture Kits (e.g., Agilent SureSelect) | Enrichment for protein-coding regions. | Performance varies; QC must assess uniformity of coverage and on-target rate [75]. |
| Library Preparation Kits | Prepare nucleic acids for sequencing. | Kit choice significantly impacts data quality and can be a major source of inter-laboratory variability [76]. |
| Reference Standard Materials | Samples with known mutations. | Essential for analytical validation, determining sensitivity, specificity, and limit of detection [77]. |
Visualization of the End-to-End QC Workflow
The following diagram illustrates the integrated, three-stage quality control workflow for next-generation sequencing data, from wet-lab procedures to final analytical output, highlighting key checkpoints and metrics at each stage.
Sequencing Data QC Workflow
The path to robust, reliable sequencing data in oncology research is underpinned by a commitment to rigorous, multi-stage quality control. This guide has outlined a comprehensive framework, from standardizing wet-lab protocols to mitigate inter-laboratory variability, to implementing sequential QC checks at the raw data, alignment, and variant calling stages. The selection of analytical tools, such as DGE models, further influences the stability of biological conclusions. As sequencing technologies evolve and their application in precision medicine expands, the principles of thorough validation and continuous quality monitoring remain paramount. By adhering to these practices, researchers and drug development professionals can ensure that their genomic findings are accurate, reproducible, and capable of confidently guiding the next generation of cancer discoveries and therapies.
Ensuring Clinical Rigor: Validation Frameworks and Comparative Utility
In the field of oncology research, the analytical validation of next-generation sequencing (NGS) assays is a critical gateway to generating reliable, clinically actionable data. It provides the foundational evidence that a test consistently and accurately detects the intended genomic alterations. Framed within the broader principles of DNA and RNA sequencing for cancer, the process of analytical validation ensures that the complex data informing personalized treatment strategies are robust and reproducible. Two methodologies form the cornerstone of this process: the use of well-characterized reference standards and the systematic application of cell line dilutions. These tools work in tandem to empirically establish key performance metrics such as sensitivity, specificity, and limit of detection (LoD) across different variant types and sample conditions. This guide details the protocols and strategic application of these resources, providing a technical roadmap for researchers and drug development professionals tasked with implementing rigorous validation frameworks for integrated genomic assays.
Core Principles and Strategic Application
Reference standards and cell line dilutions serve complementary, yet distinct, roles in a comprehensive validation strategy. Reference standards, which are often commercially available and synthetic, provide a known truth set for a wide array of pre-defined variants. They are instrumental in initial assay optimization and establishing baseline performance for detecting single nucleotide variants (SNVs), insertions/deletions (indels), copy number alterations (CNAs), and gene fusions [80] [81]. For instance, the AcroMetrix Oncology Hotspot Control contains over 500 mutations from the COSMIC database across 53 genes, while SeraSeq reference materials are engineered with specific fusion and mutation mixes [80].
Conversely, cell line dilutions are used to simulate a critical real-world variable: tumor purity. By mixing DNA or RNA from well-characterized cancer cell lines with that from normal (germline) cell lines or samples, researchers can create a series of samples with precisely known tumor fractions [82] [49]. This process is vital for determining an assay's LoD—the lowest variant allele frequency (VAF) or tumor purity at which an alteration can be reliably detected—and for understanding how declining tumor cellularity impacts performance, especially for CNAs and low-frequency variants [83]. A combined approach, using reference standards to confirm variant calling accuracy and cell line dilutions to assess performance across a spectrum of purity, creates a robust and holistic validation framework.
Quantitative Performance Data from Validation Studies
The following tables summarize key analytical performance metrics achieved in recent validation studies employing these materials.
Table 1: Performance Metrics for DNA-Based Variant Detection from Recent Studies
| Variant Type | Sensitivity | Specificity/PPV | Limit of Detection | Study Context |
|---|---|---|---|---|
| SNVs | 96.92% - 100% [14] [84] | 99.67% - >99.9% [14] [81] | ≥ 0.5% Allele Frequency [84] | Liquid biopsy (ctDNA) [14] [84] |
| Indels | 95.83% - 100% [14] [85] | >99.9% [81] | 0.1% Allele Frequency [85] | Liquid biopsy (ctDNA) [14] [85] |
| Copy Number Alterations (CNA) | 91.67% (for Fusions at 0.5% VAF) [85] | N/R | Empirically determined [85] | Solid tumor profiling (TST170 panel) [80] |
Table 2: Performance Metrics for RNA and Complex Biomarkers from Recent Studies
| Analytical Target | Sensitivity | Specificity/PPV | Key Material Used | Study Context |
|---|---|---|---|---|
| Gene Fusions | 100% [14] | N/R | SeraSeq Fusion RNA Mix [80] | Integrated DNA/RNA panel [80] |
| Tumor Mutational Burden (TMB) | High concordance in orthogonal testing [81] | N/R | Clinical FFPE samples & cell lines [81] | Whole exome sequencing [81] |
| Microsatellite Instability (MSI) | High concordance in orthogonal testing [81] | N/R | Clinical FFPE samples [81] | Whole exome sequencing [81] |
Detailed Experimental Protocols
Protocol for Analytical Validation Using Reference Standards
This protocol outlines the steps for using commercial reference standards to validate an NGS assay, as demonstrated in studies of assays like the TruSight Tumor 170 (TST170) and various liquid biopsy panels [84] [80].
- Standard Selection and Acquisition: Procure commercially available reference standards (e.g., from Horizon Discovery or SeraCare). These standards are engineered to contain a wide range of variant types, including SNVs, indels, CNAs, and fusions, fragmented to ~160 bp to mimic circulating tumor DNA (ctDNA) or derived from characterized cell lines [84] [80].
- Nucleic Acid Extraction and QC: Isolate DNA and/or RNA from the reference materials according to the manufacturer's protocol. Quantify the nucleic acid concentration using a fluorescence-based method (e.g., Qubit) and assess quality using an instrument such as the Agilent TapeStation or Bioanalyzer. For FFPE-derived standards, a DNA Integrity Number (DIN) or DV200 value is typically required to be ≥20-50% [80].
- Library Preparation and Sequencing: Process the reference standard nucleic acids through the entire NGS workflow. This includes library preparation (using either hybrid-capture or amplicon-based approaches), target enrichment, and sequencing on a platform such as an Illumina NovaSeq to a pre-defined target coverage (e.g., 400x mean coverage for tumor DNA) [49] [81].
- Bioinformatic Analysis and Variant Calling: Process the raw sequencing data through the established bioinformatics pipeline. This involves alignment to a reference genome (e.g., hg38), duplicate read marking, and variant calling using specialized algorithms (e.g., Strelka2 for somatic SNVs/indels, Manta for structural variants) [49].
- Performance Calculation: Compare the assay's variant calls to the manufacturer's provided "ground truth" data for the reference standard. Calculate key performance metrics:
- Positive Percent Agreement (Sensitivity): (True Positives / (True Positives + False Negatives)) * 100
- Positive Predictive Value (PPV): (True Positives / (True Positives + False Positives)) * 100
- Specificity: (True Negatives / (True Negatives + False Positives)) * 100 [80]
Protocol for Determining Limit of Detection via Cell Line Dilutions
This protocol describes the use of serially diluted cell lines to establish the lowest detectable VAF and the impact of tumor purity, a method used in the validation of combined RNA/DNA exome assays [82] [49].
- Cell Line Culture and Nucleic Acid Extraction: Culture characterized cancer cell lines (e.g., GM24385, NCI-H596) and normal cell lines. Extract high-quality DNA and/or RNA from both using standardized kits (e.g., AllPrep DNA/RNA FFPE Kit) [80].
- Quantification and Qualification: Precisely quantify the nucleic acids and ensure they meet quality thresholds (e.g., A260/280 ratio of 1.8-2.0, DV200 ≥20% for RNA).
- Series Dilution: Create a dilution series by mixing the cancer cell line DNA/RNA with the normal cell line DNA/RNA in defined ratios. This simulates a range of tumor purities (e.g., 50%, 25%, 10%, 5%, 1%) and corresponding expected VAFs for heterozygous variants [82] [49].
- Library Prep and Sequencing: Subject each dilution point in the series to the full NGS workflow, ensuring consistent library preparation and sequencing depth across all samples.
- Data Analysis and LoD Determination: Analyze the sequencing data to determine at which dilution point known variants from the cancer cell line can no longer be reliably detected. The LoD is defined as the lowest VAF or tumor purity at which the assay maintains a predetermined sensitivity (e.g., ≥95%) and specificity [83]. This is particularly crucial for establishing performance for CNAs and fusions, which are highly purity-dependent [83].
Experimental Workflow and Logical Relationships
The following diagram illustrates the integrated workflow for analytical validation, highlighting the parallel and complementary paths of using reference standards and cell line dilutions.
The Scientist's Toolkit: Essential Research Reagents
Successful analytical validation relies on a suite of essential reagents and materials. The table below details key components of this "toolkit," as referenced in recent validation studies.
Table 3: Essential Research Reagents for Analytical Validation
| Tool/Reagent | Primary Function in Validation | Specific Examples & Use Cases |
|---|---|---|
| Commercial Reference Standards | Provides a "ground truth" set of variants for accuracy and reproducibility testing. | Horizon Discovery Multiplex cfDNA Reference Standard; SeraSeq ctDNA Mutation Mix; AcroMetrix Oncology Hotspot Control [84] [80]. |
| Characterized Cell Lines | Serves as a source of known genomic material for creating purity dilutions and validating rare alterations. | GM24385; NCI-H596; Coriell Cell Line Pools [82] [80]. |
| Nucleic Acid Extraction Kits | Iserts high-quality, pure DNA and RNA from various sample types, including challenging FFPE tissue. | AllPrep DNA/RNA FFPE Kit (Qiagen); AVENIO cfDNA Extraction Kit (Roche) [49] [84]. |
| Target Enrichment & Library Prep Kits | Prepares sequencing libraries from input nucleic acids, defining the genomic regions to be analyzed. | TruSeq Tumor 170 Kit (Illumina); AVENIO ctDNA Library Prep Kit (Roche); SureSelect Hybrid Capture (Agilent) [49] [84] [80]. |
| Orthogonal Assay Technologies | Provides an independent method for confirming variant calls and validating NGS results. | Droplet Digital PCR (ddPCR); allele-specific PCR (AS-PCR); cobas EGFR Mutation Test v2 [84] [85] [81]. |
The rigorous application of reference standards and cell line dilutions is non-negotiable for establishing the analytical validity of NGS assays in oncology. These materials empower researchers to move beyond theoretical performance and generate empirical data on how their assays function under controlled conditions that mimic real-world challenges. As the field advances towards ever more complex integrated DNA/RNA analyses and liquid biopsy applications, the principles outlined in this guide will continue to form the bedrock of robust genomic research and reliable clinical translation. By adhering to these detailed protocols and leveraging the described toolkit, scientists and drug developers can ensure the generation of high-quality, trustworthy genomic data that ultimately fuels the advancement of precision medicine.
The integration of RNA sequencing (RNA-seq) with whole exome sequencing (WES) represents a transformative approach in precision oncology, enabling comprehensive detection of clinically relevant alterations. However, the clinical adoption of this integrated methodology has been limited by the absence of standardized validation frameworks. This whitepaper delineates a rigorous three-step validation framework—encompassing technical benchmarking, orthogonal verification, and real-world clinical assessment—for combined RNA and DNA testing. Drawing upon validation data from 2,230 clinical tumor samples, we demonstrate that this approach achieves detection of actionable alterations in 98% of cases, improves fusion detection, and recovers variants missed by DNA-only analysis. The provided guidelines, experimental protocols, and performance metrics offer a validated roadmap for implementing integrated genomic assays in clinical and translational oncology research.
Advances in cancer genomics have revealed that comprehensive molecular profiling is essential for understanding tumor heterogeneity and developing personalized treatment strategies. While next-generation sequencing (NGS) has become a cornerstone of cancer research, most clinical NGS assays rely primarily on DNA sequencing with targeted gene panels, leaving many clinically relevant transcriptional events undetected [49]. The integration of RNA sequencing with whole exome sequencing enables a more complete molecular portrait by simultaneously assessing gene expression, somatic mutations, gene fusions, copy number variations, and tumor microenvironment signatures from a single sample [49] [86].
Despite its potential, routine clinical implementation of integrated RNA-DNA sequencing has been hampered by significant validation challenges. The complexity of these assays, particularly the absence of robust reference standards for somatic variant calling and the lack of comprehensive validation guidelines, has limited their adoption in regulated clinical environments [49] [86]. This whitepaper addresses these challenges by presenting a rigorously validated three-step framework for integrated assay validation, developed within the context of a CLIA-certified, CAP-accredited laboratory [86].
The Three-Step Validation Framework
A robust validation framework for integrated RNA and DNA assays must establish analytical performance, verify clinical concordance, and demonstrate real-world utility. The following three-step approach provides a comprehensive validation pathway.
Step 1: Analytical Validation Using Reference Standards
Objective: Establish the fundamental analytical performance characteristics of the integrated assay using well-characterized reference materials.
Experimental Protocol: Analytical validation requires the development of exome-wide somatic reference standards generated from multiple cell lines sequenced at varying tumor purities [49]. These reference materials should encompass a comprehensive spectrum of genomic alterations:
- Variant Types: 3,042 small mutations (SNVs/INDELs) and 47,466 copy number variations (CNVs) across five cell lines [49] [86]
- Tumor Purity Range: 20-100% to assess detection sensitivity across clinically relevant purity levels
- Replication: Multiple sequencing runs to establish reproducibility
Performance Metrics:
- Sensitivity and specificity for SNV/INDEL detection
- Precision in CNV calling across genomic regions
- Accuracy of gene expression quantification (correlation coefficient = 0.97) [86]
- Reproducibility of fusion detection (<3.6% coefficient of variation at 1 TPM) [86]
Table 1: Analytical Performance Metrics for Integrated RNA-seq and WES Assay
| Analytical Parameter | Performance Metric | Acceptance Criterion |
|---|---|---|
| SNV/INDEL Sensitivity | >99% at 5% VAF | ≥95% |
| CNV Concordance | >95% for amplifications/deletions | ≥90% |
| Gene Expression Accuracy | R² = 0.97 vs. reference | ≥0.95 |
| Expression Reproducibility | <3.6% CV at 1 TPM | ≤5% |
| Fusion Detection Sensitivity | >98% for known fusions | ≥95% |
Step 2: Orthogonal Verification with Patient Samples
Objective: Verify assay performance against established clinical methods using patient-derived samples.
Experimental Protocol: Orthogonal validation requires parallel testing of clinical specimens using both the integrated assay and established reference methods [49] [86]. The protocol includes:
- Sample Selection: 40-60 patient samples with known molecular alterations across different cancer types [87]
- Reference Methods:
- DNA-level alterations: FDA-approved targeted panels or PCR-based methods
- RNA-level alterations: RT-PCR, Nanostring, or microarray technologies
- Fusion detection: FISH or RT-PCR for known fusion events
- Testing Conditions: Independent sample preparation and analysis across multiple days to assess inter-run reproducibility
Data Analysis: Method comparison statistics including:
- Percent positive agreement (sensitivity) and percent negative agreement (specificity)
- Deming regression for quantitative comparisons [87]
- Bland-Altman analysis to assess bias across the measurement range [87]
Step 3: Clinical Utility Assessment in Real-World Cohorts
Objective: Demonstrate the clinical value and practical implementation of the integrated assay in a real-world setting.
Experimental Protocol: Clinical validation involves applying the fully optimized assay to a large cohort of clinical samples representing diverse cancer types [49]. The protocol includes:
- Cohort Design: 2,230 clinical tumor samples with matched normal tissue [49] [86]
- Analysis Pipeline:
- Somatic variant calling with optimized filters (tumor depth ≥10 reads, normal depth ≥20 reads, normal VAF ≤0.05) [49]
- RNA-seq variant calling to recover low-coverage DNA variants
- Integrated fusion detection combining DNA and RNA evidence
- Tumor microenvironment analysis from gene expression signatures
- Clinical Annotation: Association of molecular findings with therapeutic implications and clinical outcomes
Validation Metrics:
- Actionable alteration rate (percentage of cases with clinically relevant findings)
- Variant recovery rate (additional alterations detected through RNA-seq)
- Fusion detection improvement compared to DNA-only approaches
- Turnaround time and failure rate in clinical workflow
Table 2: Clinical Validation Results from 2,230 Patient Samples
| Clinical Performance Measure | Result | Clinical Impact |
|---|---|---|
| Cases with Actionable Alterations | 98% | Guides personalized treatment strategies |
| ADC Target Overexpression | 89% | Identifies candidates for antibody-drug conjugates |
| Variants Recovered by RNA-seq | Up to 50% of protein-coding mutations | Enhances detection of clinically relevant mutations |
| Fusion Detection Improvement | Significant vs. DNA-only | Identifies additional therapeutic targets |
| Complex Rearrangements Detected | Multiple cases | Reveals oncogenic mechanisms missed by single-modality testing |
Experimental Methodologies
Laboratory Procedures
Nucleic Acid Isolation
- Sample Types: Fresh frozen (FF) solid tumors, FFPE tissue, normal tissue (blood, PBMCs, saliva) [49]
- Extraction Methods:
- FF tumors: AllPrep DNA/RNA Mini Kit (Qiagen)
- Normal tissue: QIAmp DNA Blood Mini Kit (Qiagen)
- FFPE tumors: AllPrep DNA/RNA FFPE Kit (Qiagen)
- Quality Control: Qubit 2.0 for quantification, NanoDrop OneC for purity, TapeStation 4200 for integrity [49]
Library Preparation and Sequencing
- Input Requirements: 10-200 ng of DNA or RNA [49]
- Library Construction:
- FF tissue RNA: TruSeq stranded mRNA kit (Illumina)
- FFPE tissue: SureSelect XTHS2 DNA and RNA kits (Agilent)
- Exome Capture:
- DNA: SureSelect Human All Exon V7 (Agilent)
- RNA: SureSelect Human All Exon V7 + UTR (Agilent)
- Sequencing Platform: NovaSeq 6000 (Illumina) with Q30 >90% and PF >80% [49]
Bioinformatics Analysis
Alignment and Quantification
- DNA Alignment: BWA aligner v.0.7.17 to hg38 with GATK duplicate marking [49]
- RNA Alignment: STAR aligner v2.4.2 to hg38 [49]
- Expression Quantification: Kallisto v0.43.0 with default parameters [49]
Variant Calling and Filtration
- Somatic SNVs/INDELs: Strelka v2.9.10 with tumor VAF ≥0.05 and complex quality filters [49]
- RNA Variants: Pisces v5.2.10.49 [49]
- Filtration Parameters:
- Basic filter: tumor depth ≥10 reads, normal depth ≥20 reads, normal VAF ≤0.05
- Advanced filter: Combined QSS and EVS scores via logistic regression [49]
Integrated Assay Workflow
The Scientist's Toolkit: Essential Research Reagents and Materials
Successful implementation of integrated RNA and DNA sequencing requires carefully selected reagents and computational tools. The following table outlines essential components of the validation workflow.
Table 3: Essential Research Reagents and Materials for Integrated Assay Validation
| Category | Specific Product/Platform | Function in Validation Workflow |
|---|---|---|
| Nucleic Acid Extraction | AllPrep DNA/RNA Mini Kit (Qiagen) | Simultaneous DNA/RNA extraction from single sample [49] |
| Library Preparation | SureSelect XTHS2 DNA/RNA (Agilent) | Target enrichment for exome sequencing [49] |
| Sequencing Platform | NovaSeq 6000 (Illumina) | High-throughput sequencing [49] |
| Reference Materials | Custom cell line mixtures | Analytical validation with known variants [49] [86] |
| Alignment Software | BWA (DNA), STAR (RNA) | Sequence alignment to reference genome [49] |
| Variant Caller | Strelka v2.9.10 | Somatic SNV/INDEL detection [49] |
| Expression Quantification | Kallisto v0.43.0 | Transcript-level quantification [49] |
| Validation Software | EP Evaluator, Analyse-it | Statistical analysis of validation data [87] |
Analytical Considerations for Validation
Establishing Performance Limits
Validation of integrated assays requires establishing a priori performance limits based on intended use. Key parameters include:
- Precision: Total observed variance should not exceed 33% of total allowable error in 20×2×2 replication studies [87]
- Bias: Mean bias should not typically exceed half of the total allowable error in method comparison studies [87]
- Linearity: Verification across the analytical measurement range using patient-derived sample pools [87]
Quality Control Metrics
Implementation requires rigorous quality control at each processing stage:
- DNA/RNA Quality: RIN scores, DV200, concentration, and purity measurements [49]
- Library Preparation: Fragment size distribution, adapter contamination assessment [88]
- Sequencing: Q30 scores >90%, cluster density optimization [49]
- Bioinformatics: Mapping rates, duplication rates, coverage uniformity [49]
Three-Phase Validation Logic
The three-step validation framework presented herein provides a comprehensive roadmap for implementing integrated RNA and DNA sequencing assays in clinical research and diagnostic settings. By addressing analytical validation, orthogonal verification, and clinical utility assessment, this approach establishes the rigorous foundation necessary for reliable tumor profiling. The demonstrated performance across 2,230 clinical samples confirms that integrated RNA-seq and WES significantly enhances the detection of actionable alterations compared to DNA-only approaches, with 98% of cases exhibiting clinically relevant findings.
As precision oncology continues to evolve, the ability to simultaneously assess genomic and transcriptomic alterations from a single sample will become increasingly crucial for drug development and therapeutic selection. The validation framework, experimental protocols, and performance metrics outlined in this whitepaper provide researchers and drug development professionals with practical guidelines for implementing these powerful technologies while maintaining the rigorous standards required for clinical application.
Within the framework of modern oncology research, the principles of DNA and RNA sequencing serve as foundational pillars for unraveling the molecular complexities of cancer. DNA sequencing (DNA-Seq) provides a static blueprint of the genetic code, identifying the potential for pathogenic mutations that may drive tumorigenesis. In contrast, RNA sequencing (RNA-Seq) delivers a dynamic snapshot of the actively transcribed genome, revealing the functional expression of those mutations and other transcriptional alterations. This technical guide provides an in-depth comparative analysis of these two technologies, focusing on their performance in detecting clinically actionable variants. The integration of DNA and RNA sequencing is reshaping precision oncology by bridging the gap between genetic potential and functional protein expression, thereby offering a more robust platform for diagnostic, prognostic, and therapeutic decision-making [9] [74].
Technical Performance and Detection Capabilities
The comparative analysis of DNA-Seq and RNA-Seq reveals distinct and complementary strengths in variant detection. A comprehensive understanding of their capabilities is essential for designing effective genomic testing strategies.
Table 1: Comparative Variant Detection Capabilities of DNA-Seq and RNA-Seq
| Variant Type | DNA-Seq Performance | RNA-Seq Performance | Key Differentiating Factors |
|---|---|---|---|
| Single Nucleotide Variants (SNVs) & Indels | High sensitivity and accuracy for identifying genomic alterations [9]. | Detects transcribed variants, confirming expression and functional relevance; may miss non-expressed or lowly expressed mutations [9] [82]. | RNA-Seq filters out non-expressed mutations, prioritizing biologically relevant changes [74]. |
| Gene Fusions | Limited to detecting DNA breakpoints; may miss novel or complex rearrangements [89]. | Superior detection capability; directly identifies expressed fusion transcripts, making it 1.8x more common in pediatric cancers [82] [90]. | RNA-Seq directly sequences the fusion transcript, avoiding reliance on predictive DNA-based methods [29]. |
| Splice Variants | Indirect prediction via algorithms (e.g., SpliceAI); high rate of false positives or uncertainties [91]. | Directly profiles splicing consequences (e.g., exon skipping, intron retention), empirically validating predicted effects [9] [91]. | RNA-Seq provides functional evidence, resolving variants of uncertain significance (VUS) [91]. |
| Copy Number Variations (CNVs) | High accuracy in detecting genomic amplifications and deletions [82]. | Infers CNVs from expression outliers; can be confounded by transcriptional regulation [91]. | DNA-Seq is the gold standard; RNA-Seq can provide correlative functional evidence. |
| Neoantigens | Identifies a wide array of somatic mutations as potential neoantigen sources [74]. | Confirms transcription of mutations, detects novel isoforms/fusions, and provides expression data for immunogenicity ranking [74]. | RNA-Seq narrows the candidate list to expressed, clinically relevant targets, improving vaccine design [74]. |
A validation study of a combined RNA and DNA exome assay across 2,230 clinical tumor samples demonstrated that the integrated approach enhances the detection of actionable alterations. It allowed for direct correlation of somatic alterations with gene expression, recovered variants missed by DNA-only testing, and improved the detection of gene fusions and complex genomic rearrangements [82]. In clinical practice, targeted RNA-Seq has been shown to detect clinically actionable alterations in 87% of tumors, offering decisive results when DNA sequencing is inconclusive [90].
Methodologies for Integrated Sequencing Analysis
Implementing a robust integrated DNA-RNA sequencing workflow requires stringent protocols from sample collection through data analysis to ensure data quality and reliability.
Sample Preparation and Quality Control
The preanalytical phase is critical, especially for RNA-Seq, where sample quality significantly impacts results.
- Sample Collection: For RNA-Seq from blood, collection in PAXgene Blood RNA tubes is standard. Tissues are often snap-frozen or preserved as FFPE (Formalin-Fixed Paraffin-Embedded) blocks [91] [29].
- RNA Extraction and QC: RNA is extracted using dedicated kits (e.g., PAXgene Blood RNA kit). A key quality control step is assessing RNA Integrity Number (RIN). Contaminating genomic DNA is removed with a DNase treatment step, which has been shown to significantly reduce intergenic read alignment [92].
- Library Preparation: Several methods are available:
- Whole Transcriptome (WTS): Provides the most comprehensive view, ideal for novel transcript discovery.
- Targeted RNA-Seq: Uses panels (e.g., Afirma Xpression Atlas) to enrich for specific genes of interest, providing deeper coverage and higher sensitivity for low-abundance transcripts [9].
- 3' mRNA-Seq (e.g., QuantSeq): A streamlined method focusing on the 3' end of transcripts, efficient for gene expression quantification, especially from degraded FFPE samples [74] [29].
Table 2: Essential Research Reagents and Kits for Sequencing Workflows
| Item | Function | Example Product/Brand |
|---|---|---|
| RNA Stabilization Tubes | Preserves RNA integrity at the point of sample collection. | PAXgene Blood RNA Tubes [92] [91] |
| RNA Extraction Kit | Isolves high-quality total RNA from samples. | PAXgene Blood RNA Kit [91] |
| Globin & rRNA Depletion Kit | Removes highly abundant non-informative RNAs from blood samples to increase coverage of relevant transcripts. | NEBNext Globin and rRNA Depletion Kit [91] |
| RNA Library Prep Kit | Converts RNA into a sequencing-ready library. | NEBNext Ultra Directional RNA Library Prep Kit [91] |
| Targeted Sequencing Panels | Enriches sequencing coverage on a predefined set of genes. | Agilent Clear-seq, Roche Comprehensive Cancer panels [9] |
Bioinformatics and Data Analysis Pipelines
A multi-step bioinformatics pipeline is required to translate raw sequencing data into actionable variants.
- Alignment: RNA-Seq reads are aligned to a reference genome using splice-aware aligners like STAR (Spliced Transcripts Alignment to a Reference) [91].
- Variant Calling: For DNA-Seq, tools like Mutect2 and LoFreq are standard. For RNA-Seq, specialized callers such as VarDict are often used in conjunction with DNA callers in pipelines like SomaticSeq to improve accuracy [9].
- Expression & Splicing Analysis: Tools like the DROP pipeline are used to identify aberrant expression (AE) and aberrant splicing (AS) outliers, which are crucial for diagnosing rare diseases and interpreting splice-altering variants [91].
- Machine Learning Integration: Support Vector Machines (SVM) and other classifiers have demonstrated high accuracy (up to 99.87%) in classifying cancer types based on RNA-Seq gene expression data, facilitating biomarker discovery [93].
The following diagram illustrates the core bioinformatics workflow for processing and integrating DNA and RNA sequencing data.
Clinical Applications and Actionability
The integration of DNA and RNA sequencing has demonstrated significant clinical utility across multiple domains in oncology and rare disease diagnostics, directly impacting patient management.
Resolving Variants of Uncertain Significance (VUS)
In rare disease diagnostics, where approximately 60% of cases remain unsolved after exome/genome sequencing, RNA-Seq proves invaluable. A study of 121 unsolved cases used blood RNA-Seq to resolve splicing VUS, providing a 60% (6/10) diagnostic uplift in cases with pre-existing candidate VUS. It also achieved a 2.7% (3/111) diagnostic uplift in cases with no prior candidate variants by enabling an RNA-driven discovery approach [91]. RNA-Seq provides functional evidence that can reclassify VUS as either pathogenic or benign, directly informing clinical diagnosis.
Enhancing Neoantigen Discovery and Cancer Immunotherapy
The development of personalized cancer vaccines relies on identifying tumor-specific neoantigens. DNA-Seq identifies a large pool of somatic mutations, but only a fraction are transcribed and presented as neoantigens. RNA-Seq is critical for filtering and prioritizing by confirming mutation expression and detecting neoantigens from novel RNA-derived sources like alternative splicing and gene fusions. Studies show that integrating RNA-Seq with DNA-Seq allows for the selection of neoantigen candidates with higher immunogenic potential, significantly improving the design of personalized cancer immunotherapies [74]. The following diagram outlines this integrated neoantigen discovery pipeline.
Informing Targeted Therapy and Patient Stratification
RNA-Seq-based classifiers are increasingly used to predict patient responses to therapy, such as immune checkpoint inhibitors (ICIs). For example, the OncoPrism test uses RNA-Seq and machine learning to stratify patients with head and neck squamous cell carcinoma into groups based on their likelihood of responding to anti-PD-1 therapy. This RNA-based multi-analyte biomarker has demonstrated higher sensitivity and specificity compared to traditional PD-L1 immunohistochemistry, leading to more accurate patient selection for immunotherapy and avoiding unnecessary chemotherapy [29]. In a real-world assessment, among 104 patients considered for targeted therapy based on RNA-Seq findings, 94 received matched treatment, most commonly with MAPK pathway inhibitors, tyrosine kinase inhibitors, and immune checkpoint therapies [90].
DNA and RNA sequencing are not mutually exclusive technologies but rather synergistic components of a comprehensive genomic profiling strategy. DNA-Seq excels at providing a complete catalog of genomic alterations, while RNA-Seq adds the crucial dimension of functional validation and activity, effectively bridging the "DNA to protein divide" [9]. The integration of both data types enhances diagnostic accuracy, improves the detection of fusions and splice variants, refines neoantigen prediction for immunotherapy, and ultimately enables more personalized and effective treatment strategies for cancer patients. As standardized validation frameworks and end-to-end quality control protocols continue to develop [92] [82], the routine clinical adoption of integrated RNA and DNA sequencing is poised to become the cornerstone of precision oncology.
The integration of DNA and RNA sequencing technologies represents a paradigm shift in the diagnosis and treatment of pediatric and rare cancers. For these malignancies, which are often characterized by low mutational burdens but driven by specific structural variants and gene fusions, traditional chemotherapy approaches frequently yield suboptimal outcomes. Next-generation sequencing (NGS) technologies now enable comprehensive molecular profiling that reveals actionable alterations, guiding targeted therapeutic interventions. Major precision medicine platforms worldwide have demonstrated that comprehensive genomic profiling is not only feasible but delivers clinically meaningful benefits, particularly for patients with relapsed, refractory, or high-risk disease [94]. This technical review examines the evidence establishing clinical utility, details experimental methodologies, and explores implementation frameworks that translate genomic insights into improved survival outcomes.
Quantitative Evidence of Clinical Impact
Actionable Alterations and Therapeutic Impact Across Studies
Large-scale collaborative studies have consistently demonstrated that molecular profiling identifies actionable targets in a significant majority of pediatric and rare cancer patients. The evidence for this comes from multiple major precision medicine initiatives conducted globally, which have systematically reported their findings.
Table 1: Evidence of Actionable Findings from Major Precision Oncology Trials
| Study/Platform | Patient Population | Sequencing Approach | Actionable Alteration Rate | PGT Uptake Rate | Reported Clinical Benefit |
|---|---|---|---|---|---|
| MAPPYACTS (Europe) | Children/adolescents with relapsed/refractory cancers | WES, RNA-seq, panel sequencing | 69% (432/624 patients) | 30% (107/356 with follow-up) | ORR 17% (38% for "ready for routine use" recommendations) [94] |
| GAIN/iCat2 (USA) | ≤30 years with relapsed/refractory or high-risk extracranial solid tumors | Targeted DNA/RNA NGS panels (FFPE) | 70% (240/345 patients) | 12% (29/240 with actionable targets) | ORR 17%; overall clinical benefit 24% [94] |
| INFORM (Germany, multinational) | Pediatric patients with high-risk cancers | WES, low-coverage WGS, RNA-seq, DNA methylation | 8% with very high-level evidence targets | 28% (147/519) | Significant PFS and OS improvement for ALK, BRAF, NTRK inhibitors (p=0.012, p=0.036) [94] |
| ZERO Childhood Cancer (Australia) | Children with high-risk cancers (<30% expected cure) | WGS (tumor-germline), RNA-seq, DNA methylation | 67% (256/384) | 43% (110/256 with recommendations) | Significant event-free and overall survival benefit [94] |
RNA Sequencing Enhances Detection of Actionable Alterations
Targeted RNA sequencing has demonstrated particular value as both a complementary and stand-alone tool in cancer molecular diagnostics. In a substantial real-world clinical experience involving 2,310 solid, central nervous system, and hematopoietic neoplasms from patients aged 0-90 years, RNA-seq provided valuable molecular data for 87% of patients despite most samples being formalin-fixed and paraffin-embedded (FFPE) [22]. The assay identified diagnostic alterations that revised diagnoses and detected clinically actionable alterations that changed treatment decisions, including administration of targeted therapies. With a failure rate of only 4.8%, this approach demonstrated reliability comparable to DNA-based diagnostics while minimizing cost, tissue requirements, and turnaround time [22].
RNA sequencing bridges the critical "DNA to protein divide" in precision medicine by confirming which mutations are actually expressed and therefore more likely to be functionally relevant. While DNA-based assays determine variant presence, they cannot distinguish expressed mutations from silent ones. Research shows that incorporating RNA-seq helps verify and prioritize DNA variants based on expression, with one study finding that up to 18% of somatic single nucleotide variants detected by DNA sequencing were not transcribed, suggesting limited clinical relevance [9]. This functional validation is particularly crucial for fusion detection and characterizing splice site mutations, where RNA-seq provides superior analytical capability compared to DNA-based approaches alone [22].
Methodological Approaches and Workflows
Integrated DNA-RNA Sequencing Protocol
The most comprehensive precision oncology approaches utilize paired tumor-germline sequencing with multiple analytical modalities to maximize clinical insights. The following workflow diagram illustrates a standardized protocol for integrated genomic profiling:
Essential Research Reagents and Platforms
Successful implementation of precision oncology requires carefully selected reagents and platforms optimized for clinical-grade sequencing. The following table details key solutions utilized in major studies:
Table 2: Essential Research Reagent Solutions for Precision Oncology Studies
| Reagent Category | Specific Examples | Function & Application | Considerations |
|---|---|---|---|
| Nucleic Acid Stabilization | Roche Cell-Free DNA collection tubes [95] | Cell-stabilizing blood collection tubes for ctDNA analysis | Enables room temperature transport; preserves sample integrity |
| Nucleic Acid Extraction | QIAamp Circulating Nucleic Acid kit [95] | Isolation of ctDNA from plasma | Optimized for low-concentration circulating nucleic acids |
| Target Enrichment | Twist Custom Probe Set (117kb) [95] | Hybrid-capture targeting 45 cancer-related genes | Customizable content; balanced coverage |
| Library Preparation | Twist Library Preparation Kit [95] | NGS library construction with UMI integration | Incorporates unique molecular identifiers for error correction |
| Sequencing Platforms | Illumina NovaSeq6000 [95] | Production-scale sequencing | 2×150bp paired-end reads; high throughput |
| Bioinformatic Tools | GATK Mutect2 [95], VarDict [9], LoFreq [9] | Variant calling from NGS data | Multiple callers improve sensitivity/specificity balance |
Molecular Tumor Board Operational Framework
The translation of genomic findings into clinical recommendations requires systematic interpretation through multidisciplinary molecular tumor boards (MTBs). The following diagram illustrates the decision pathway for therapeutic recommendation development:
Case Studies Demonstrating Clinical Utility
Salivary Gland Cancers: WGS for Diagnostic Clarification and Target Identification
Salivary gland cancers (SGCs) represent a compelling case study for the application of comprehensive genomic profiling in rare cancers. These malignancies comprise multiple histologic entities with limited effective treatment options in the recurrent or metastatic setting. In a study of 15 patients with recurrent/metastatic SGC who underwent tumor biopsy and blood sampling for whole-genome sequencing (WGS), quality control was acceptable in 14 cases [96].
Genomic rearrangements and fusions were present in 12 of 14 patients (85.7%). Notably, rearrangements involving MYB and/or NFIB were identified in 8 of 10 patients with adenoid cystic carcinoma, confirming a characteristic molecular driver. Critically, WGS enabled definitive histologic reclassification in several cases based on fusion identification: one patient harbored a clinically actionable FGFR1-pleomorphic adenoma gene 1 fusion and responded to fibroblast growth factor receptor-targeted therapy, while other fusions included EWSR1-ATF1 and CRTC1-MAML2, which also aided definitive histologic classification [96].
This study demonstrated that WGS in SGC is achievable in clinically relevant timeframes, providing genomic information for deeper understanding of disease pathophysiology, clarifying histologic subtype, and identifying actionable genomic targets that may be missed through routine sequencing technologies.
Pediatric Solid Tumors: Meta-Analysis of Actionable Findings
A systematic review and meta-analysis of NGS utility in childhood and adolescent/young adult (AYA) solid tumors provides comprehensive quantitative evidence of clinical impact. The analysis included 24 studies comprising 5,278 patients and 5,359 samples, with 5,207 providing usable data [97]. The pooled proportion of actionable alterations was 57.9% (95% CI: 49.0-66.5%), demonstrating that more than half of young patients with solid tumors harbor potentially targetable genomic alterations [97].
Clinical decision-making outcomes were reported in 21 studies, with a pooled proportion of 22.8% (95% CI: 16.4-29.9%), indicating that genomic findings influenced treatment decisions in nearly one quarter of cases. Germline mutation rates, reported in 11 studies, yielded a pooled proportion of 11.2% (95% CI: 8.4-14.3%), consistent with rates typically observed in childhood cancers and highlighting the dual importance of germline and somatic sequencing in pediatric oncology [97].
Implementation Considerations and Challenges
Standardization of Methodologies and Reporting
A significant challenge identified across precision oncology initiatives is substantial variability in methodological approaches, which influences interpretation and comparability of results. Heterogeneity arises from multiple aspects, including differences in sequencing techniques (targeted panels, WES, WGS, RNA sequencing, methylation profiling), tumor sampling strategies (primary vs. relapsed disease), and definitions of "actionable alterations" [97]. To maximize clinical utility, future research should emphasize standardization of sequencing methodologies, sample collection practices, and establishment of consistent, clinically meaningful reporting standards. Relevant existing guidelines from international oncology organizations (ESMO, ASCO, Children's Oncology Group) provide valuable structured frameworks that can enhance methodological consistency [97].
Tissue Considerations and FFPE Compatibility
Most real-world samples available for clinical testing are formalin-fixed and paraffin-embedded (FFPE) tissue, which presents challenges for nucleic acid integrity. However, recent studies have demonstrated that targeted RNA-seq can achieve a 4.8% failure rate despite FFPE preservation, making it feasible for routine clinical application [22]. DNA degradation during storage in FFPE tissue blocks remains a concern, but optimized extraction and library preparation methods can yield high-quality sequencing data suitable for clinical decision-making [22].
The integration of DNA and RNA sequencing technologies has unequivocally demonstrated clinical utility in pediatric and rare cancers by improving diagnostic accuracy, identifying actionable therapeutic targets, and ultimately enhancing patient outcomes. Large collaborative studies have consistently shown that comprehensive genomic profiling reveals actionable alterations in a majority of patients, with a significant subset deriving clinical benefit from matched targeted therapies. The growing body of evidence supports the systematic implementation of precision oncology approaches for children and patients with rare cancers, particularly those with high-risk, relapsed, or refractory disease. Future directions should focus on standardizing methodologies, addressing access barriers, expanding biomarker-driven clinical trials, and integrating non-genomic assays to further advance the field of precision medicine for these vulnerable populations.
Advancements in next-generation sequencing (NGS) are revolutionizing clinical oncology by enabling detailed molecular characterization of tumors. While DNA sequencing alone has been a cornerstone of precision medicine, its limitations in detecting key transcriptional events are increasingly apparent. This technical guide demonstrates that integrating RNA sequencing with whole exome sequencing from a single tumor sample substantially enhances the detection of clinically actionable alterations. We present validation data from large-scale clinical cohorts showing that this combined approach improves the identification of gene fusions, resolves ambiguous variants, and characterizes the tumor immune microenvironment, thereby expanding the scope of personalized cancer therapy.
The journey from first-generation sequencing to modern NGS platforms has fundamentally transformed cancer research and treatment [38]. The initial Sanger method, developed in 1977, provided the foundation for genomic analysis but was limited in throughput and scalability [38]. The advent of NGS technologies addressed these limitations, offering unprecedented capacity to interrogate the cancer genome with high fidelity at progressively reduced costs [38]. DNA-based sequencing approaches have successfully identified numerous somatic mutations, including single nucleotide variants (SNVs), insertions/deletions (INDELs), and copy number variations (CNVs), establishing genomic profiling as an essential component of cancer management [82] [98].
However, DNA-centric approaches provide an incomplete picture of tumor biology. They cannot capture critical transcriptional events such as gene expression changes, alternative splicing, and gene fusions—key drivers in many cancers [82]. RNA sequencing complements DNA analysis by revealing the functional output of the genome, effectively bridging the gap between genetic blueprint and cellular phenotype. Despite its potential, the clinical adoption of integrated RNA and DNA sequencing has been hampered by the absence of standardized validation frameworks and complex analytical workflows [82].
This whitepaper examines the technical and clinical validation of combined DNA/RNA assays, demonstrating through large-scale studies how this integrated approach significantly increases the detection of actionable alterations and facilitates tumor-agnostic treatment strategies that transcend traditional histopathological classifications.
Technical Validation of Combined DNA/RNA Assays
Analytical Validation Using Reference Standards
The development of clinically reliable combined assays requires rigorous validation against established standards. One comprehensive framework involves a three-step process:
- Reference Sample Validation: Custom reference materials containing 3,042 SNVs and 47,466 CNVs are used to establish analytical performance across multiple sequencing runs at varying tumor purity levels [82]. This exome-wide validation ensures sensitivity and specificity across different alteration types.
- Orthogonal Confirmation: Patient samples are tested using both the integrated assay and established independent methods to verify concordance and identify potential discrepancies [82].
- Clinical Utility Assessment: Real-world clinical cases are evaluated to demonstrate how the integrated assay impacts treatment decisions and patient management [82].
Performance Metrics in Large Cohorts
Applied to 2,230 clinical tumor samples, the combined RNA and DNA exome assay demonstrated significant advantages over DNA-only approaches [82]. The integration enabled direct correlation of somatic alterations with gene expression patterns, recovery of variants missed by DNA sequencing alone, and improved detection of gene fusions [82]. Most notably, the assay revealed complex genomic rearrangements that would likely have remained undetected without transcriptional data [82].
Table 1: Detection Rates of Actionable Alterations in Combined DNA/RNA Sequencing
| Alteration Type | Detection Method | Clinical Utility | Example Alterations |
|---|---|---|---|
| Gene Fusions | RNA-seq | Identifies targetable rearrangements | NTRK, RET fusions [98] |
| Somatic SNVs/INDELs | WES | Detects point mutations and small insertions/deletions | BRAF V600E, TP53 [82] [98] |
| Copy Number Variations | WES | Identifies gene amplifications/deletions | ERBB2 amplification [82] [98] |
| Tumor Microenvironment | RNA-seq | Characterizes immune cell infiltration | Immunotherapy response prediction [38] |
| Gene Expression | RNA-seq | Quantifies transcriptional activity | Biomarker discovery [38] |
Clinical Actionability Across Cancer Types
Comprehensive Genomic Profiling in Asian Populations
A recent pan-cancer study of 1,166 tissue samples encompassing 29 cancer types demonstrated the high clinical actionability of comprehensive genomic profiling (CGP) in an Asian cohort [98]. The research utilized an Asian-centric DNA/RNA CGP panel to identify biomarkers with therapeutic implications.
Actionable biomarkers were identified in 62.3% of samples, including 1,291 (4.7%) somatic variants potentially targetable by regulatory-approved therapies [98]. The study employed the ESMO Scale for Clinical Actionability of molecular Targets (ESCAT) to classify alterations, with 12.7% of samples harboring Tier I alterations (linked to approved standard-of-care therapies) and 6.0% harboring Tier II alterations (targets with evidence of benefit in clinical trials) [98].
Tumor-Agnostic Biomarker Detection
The combined assay approach is particularly valuable for identifying tumor-agnostic biomarkers that indicate treatment response regardless of cancer origin. In the Asian cohort study, at least one tumor-agnostic biomarker was detected in 26 cancer types (89.7%), across 98 samples (8.4%) [98]. These biomarkers are critical for matching patients with targeted therapies based on molecular characteristics rather than tumor histology.
Table 2: Prevalence of Tumor-Agnostic Biomarkers Across Major Cancer Types
| Cancer Type | TMB-High Prevalence | MSI-High Prevalence | BRAF V600E Prevalence | NTRK Fusion Prevalence |
|---|---|---|---|---|
| Lung | 15.4% | N/R | 0.2% | 0% |
| Endometrial | 11.8% | 5.9% | N/R | 0% |
| Thyroid | 30.0% | N/R | 10.0% | 0% |
| Melanoma | 22.7% | N/R | 13.6% | 0% |
| Colorectal | N/R | 2.6% | 1.7% | 0.3% |
| Pancreatic | N/R | 1.0% | 0% | 0.3% |
| Gastric | N/R | 4.7% | 0% | 0.3% |
N/R = Not reported in the study [98]
Emerging Biomarkers with Clinical Potential
Beyond established tumor-agnostic biomarkers, combined assays identified several emerging targets with significant therapeutic implications:
- Homologous Recombination Deficiency (HRD): Observed in 407 samples (34.9%) and present in approximately half of breast (50%), colon (49.0%), lung (44.2%), ovarian (42.2%), and gastric (39.5%) tumors [98]. HRD-positive tumors exhibited significantly higher TMB compared to HRD-negative tumors [98].
- ERBB2 Amplification: Identified in 42 samples (3.6%), most frequently in breast (15.0%), endometrial (11.8%), and ovarian (8.9%) tumors [98].
- High Tumor Mutational Burden (TMB-High): Found in 77 samples (6.6%), with the highest proportions in lung (15.4%), endometrial (11.8%), and esophageal (11.1%) cancers [98].
Experimental Workflows and Methodologies
Integrated DNA/RNA Sequencing Workflow
The following diagram illustrates the comprehensive workflow for combined DNA and RNA analysis from sample preparation to clinical reporting:
Computational Analysis Pipeline
The bioinformatic processing of combined sequencing data involves multiple specialized tools and analytical steps [38]:
- Quality Control and Trimming: Raw sequencing data in FASTQ format undergo quality assessment using tools like FastQC, Trimmomatic, or PRINSEQ to remove low-quality reads and adapter sequences [38].
- Read Alignment: Clean reads are mapped to reference genomes using aligners such as STAR (for RNA-seq), HISAT2, or BWA [38].
- Variant Calling and Transcript Assembly: DNA alignment files are processed for SNV, INDEL, and CNV detection, while RNA-seq data undergo transcript assembly using StringTie or Cufflinks [38].
- Expression Quantification: Transcript abundance is estimated at gene, transcript, and exon levels using FeatureCounts, HTSeq-count, or alignment-free tools like Kallisto and Salmon [38].
- Differential Expression Analysis: Statistical methods implemented in DESeq2 or edgeR identify significantly differentially expressed genes between sample groups [38].
The Scientist's Toolkit: Essential Research Reagents and Materials
Successful implementation of combined DNA/RNA sequencing assays requires carefully selected reagents and analytical tools. The following table details essential components of the integrated profiling workflow:
Table 3: Essential Research Reagents and Analytical Tools for Combined Assays
| Item Category | Specific Examples | Function in Workflow |
|---|---|---|
| Nucleic Acid Extraction Kits | DNA/RNA co-isolation or separate extraction kits | High-quality nucleic acid preservation from single tumor sample [82] |
| Library Preparation Kits | Whole exome capture panels, RNA-seq library prep | Target enrichment and sequencing library construction [82] |
| Reference Standards | Custom cell lines with known variants (3,042 SNVs, 47,466 CNVs) [82] | Analytical validation and quality control |
| Sequencing Platforms | Illumina NovaSeq, HiSeq, or similar NGS systems | High-throughput sequencing of DNA and RNA libraries [38] |
| Alignment Software | STAR, HISAT2, BWA, Bowtie2 | Mapping sequences to reference genome [38] |
| Variant Callers | Mutect2, VarScan, GATK tools | Identification of SNVs, INDELs, and CNVs [82] |
| Fusion Detection Tools | STAR-Fusion, Arriba, FusionCatcher | Identification of gene fusions from RNA-seq data [82] |
| Expression Analysis Tools | DESeq2, edgeR, Cufflinks | Differential expression and transcript quantification [38] |
Molecular Pathways in Precision Oncology
The following diagram illustrates key signaling pathways frequently altered in cancer and detectable through combined DNA/RNA profiling, highlighting therapeutic implications:
The integration of DNA and RNA sequencing technologies represents a paradigm shift in cancer genomics, moving beyond the limitations of single-modality approaches. Combined assays significantly enhance the detection of clinically actionable alterations, particularly gene fusions, expression biomarkers, and tumor microenvironment signatures that inform therapeutic decisions. Validation across large clinical cohorts demonstrates that this integrated approach identifies actionable alterations in over 98% of cases [82], potentially expanding treatment options for patients with advanced cancers.
As molecularly guided tumor-agnostic therapies continue to gain regulatory approval, comprehensive genomic profiling that simultaneously interrogates DNA and RNA will become increasingly essential for precision oncology. The future of cancer diagnostics lies in multimodal integration, where combined assays not only streamline clinical workflows but also unlock deeper insights into tumor biology, ultimately guiding more personalized and effective treatment strategies.
Conclusion
The integration of DNA and RNA sequencing represents a paradigm shift in oncology, moving beyond mere mutation detection to a functional understanding of tumor biology. The combined approach significantly enhances the detection of clinically actionable alterations, from expressed mutations and gene fusions to complex genomic rearrangements, thereby facilitating more personalized and effective treatment strategies. As evidenced by large-scale clinical validations, this integration is crucial for advancing precision medicine, particularly for cancers with low mutation burden or rare tumors. Future directions will focus on standardizing validation frameworks, refining bioinformatics tools to manage the complexity of multi-omic data, and incorporating emerging technologies like single-cell sequencing and liquid biopsies. The ongoing evolution of sequencing technologies promises to further deepen our molecular understanding of cancer, solidifying NGS as an indispensable compass for targeted therapy and drug development.
References
- 1. Next Generation Sequencing: Latent applications in clinical ... [https://www.sciencedirect.com/science/article/abs/pii/S034403382400517X]
- 2. Next-Generation Sequencing: A Review of Its Transformative ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12523276/]
- 3. Next-generation sequencing: 2025 Revolution [https://lifebit.ai/blog/next-generation-sequencing/]
- 4. NGS vs Sanger Sequencing [https://www.illumina.com/science/technology/next-generation-sequencing/beginners/advantages/ngs-vs-sanger.html]
- 5. A targeted next-generation sequencing panel for ... [https://www.nature.com/articles/s41598-025-08039-6]
- 6. Next-Generation Sequencers vs. Sanger ... [https://www.labx.com/resources/next-generation-sequencers-vs-sanger-sequencers-key-differences/5597]
- 7. Benefits of NGS in Oncology [https://www.illumina.com/areas-of-interest/cancer/ngs-in-oncology.html]
- 8. Next-generation sequencing in cancer diagnosis and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12009796/]
- 9. Augmenting precision medicine via targeted RNA-Seq ... [https://www.nature.com/articles/s41698-025-00993-8]
- 10. Next-Generation Sequencing: A Review of Its ... [https://www.mdpi.com/2075-4418/15/19/2425]
- 11. Sample Preparation for NGS – A Comprehensive Guide [https://frontlinegenomics.com/sample-preparation-for-ngs-a-comprehensive-guide/]
- 12. Clinical implementation of next-generation sequencing ... [https://www.nature.com/articles/s41598-024-84909-9]
- 13. NGS Library Construction | DNA Technologies Core - UC Davis [https://dnatech.ucdavis.edu/ngs-library-construction]
- 14. Analytical Validation of a Pan-Cancer NGS Assay for In- ... [https://www.sciencedirect.com/science/article/pii/S152515782500220X]
- 15. Detailed evaluation of cancer sequencing pipelines in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8068765/]
- 16. AscatNGS - GDC Docs - National Cancer Institute [https://docs.gdc.cancer.gov/Encyclopedia/pages/AscatNGS/]
- 17. Sharing genetic variants with the NGS pipeline is essential ... [https://www.nature.com/articles/s41598-021-82006-9]
- 18. Differences Between RNA Sequencing and DNA Sequencing [https://rna.cd-genomics.com/resource/differences-rna-seq-dna-seq.html]
- 19. Next-Generation Sequencing Technology: Current Trends ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10376292/]
- 20. Comparison of Targeted RNA-Sequencing Platforms for ... [https://www.sciencedirect.com/science/article/pii/S1525157825000649]
- 21. Augmenting precision medicine via targeted RNA-Seq ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12166063/]
- 22. Clinical utility of targeted RNA sequencing in cancer ... [https://pubmed.ncbi.nlm.nih.gov/40676318/]
- 23. Comparison of RNA- and DNA-based 16S amplicon ... [https://www.nature.com/articles/s41598-025-00969-5]
- 24. The power of RNA sequencing in molecular oncology [https://www.nature.com/articles/s41591-025-03973-4]
- 25. Precision Oncology: Current Landscape, Emerging Trends ... [https://www.mdpi.com/2073-4409/14/22/1804]
- 26. Advances in Precision Oncology: From Molecular Profiling to ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12607717/]
- 27. Targeted Sequencing Approach and Its Clinical ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9913990/]
- 28. WGS vs WES: Which Genetic Sequencing Method is Right ... [https://www.novogene.com/us-en/resources/blog/wgs-vs-wes-which-genetic-sequencing-method-is-right-for-you/]
- 29. RNA-Seq in Cancer Research: Driving Precision Medicine ... [https://www.lexogen.com/blog/how-rna-sequencing-is-revolutionizing-cancer-research-bringing-precision-medicine-to-cancer-patients/]
- 30. Translational and clinical comparison of whole genome ... [https://www.nature.com/articles/s41698-024-00788-3]
- 31. Costs and Benefits of Whole-Exome, Whole-Transcriptome ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12184969/]
- 32. Comparative analysis of library preparation approaches for ... [https://www.nature.com/articles/s41598-025-12992-7]
- 33. MIXnorm: normalizing RNA-seq data from formalin-fixed ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7267832/]
- 34. Proper Preparation of Fresh Frozen Tissue Post-Collection [https://biosampleconnect.com/resources/proper-preparation-of-fresh-frozen-tissue-post-collection]
- 35. Liquid biopsy in cancer: current status, challenges and ... [https://www.nature.com/articles/s41392-024-02021-w]
- 36. Liquid Biopsy for Guiding Treatment Decisions in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9881738/]
- 37. Changing Technologies of RNA Sequencing and Their ... [https://www.frontiersin.org/journals/oncology/articles/10.3389/fonc.2020.00447/full]
- 38. RNA sequencing: new technologies and applications in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7716291/]
- 39. Best practices for cell preparation for Illumina Single Cell ... [https://knowledge.illumina.com/library-preparation/illumina-single-cell-rna-prep/library-preparation-illumina-single-cell-rna-prep-reference_material-list/000009437]
- 40. Current Bioinformatics Tools in Precision Oncology - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC12238682/]
- 41. Bioinformatics: From NGS Data to Biological Complexity in Variant Detection and Oncological Clinical Practice - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC9495893/]
- 42. Variant calling from RNA-Seq data reveals allele-specific ... [https://www.nature.com/articles/s43856-025-00901-y]
- 43. Best practices for variant calling in clinical sequencing | Genome Medicine | Full Text [https://genomemedicine.biomedcentral.com/articles/10.1186/s13073-020-00791-w]
- 44. Improved detection of clinically relevant fusion transcripts in ... [https://bmcgenomics.biomedcentral.com/articles/10.1186/s12864-023-09889-y]
- 45. Regular article FindDNAFusion: An Analytical Pipeline with ... [https://www.sciencedirect.com/science/article/pii/S1525157823002751]
- 46. Deep learning approaches for resolving genomic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12579925/]
- 47. ONCOLINER: A new solution for monitoring, improving ... [https://www.sciencedirect.com/science/article/pii/S2666979X2400243X]
- 48. Reannotation of cancer mutations based on expressed ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12256795/]
- 49. Clinical and analytical validation of a combined RNA ... [https://www.nature.com/articles/s43856-025-00934-3]
- 50. Characterization of a novel comprehensive genomic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12342955/]
- 51. Applying next-generation sequencing to detect ... [https://www.nature.com/articles/s41698-025-01096-0]
- 52. Beyond genetics: driving cancer with the tumour microenvironment behind the wheel - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC11077468/]
- 53. Comprehensive investigation of tumor immune ... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2024.1424950/full]
- 54. A tumor microenvironment-specific gene expression signature predicts chemotherapy resistance in colorectal cancer patients | npj Precision Oncology [https://www.nature.com/articles/s41698-021-00142-x]
- 55. Q40 sequencing reshapes precision oncology research [https://www.elementbiosciences.com/blog/q40-sequencing-reshapes-precision-oncology-research]
- 56. Complete Genomics Highlights Clinical Research ... [https://www.completegenomics.com/complete-genomics-highlights-clinical-research-sequencing-solutions/]
- 57. Identification and Validation of Prognostic Model for Tumor ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11371085/]
- 58. Analysis of Gene Signatures of Tumor Microenvironment Yields Insight Into Mechanisms of Resistance to Immunotherapy - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC7263059/]
- 59. Beyond the Signature: Exposing Mutational Patterns of Cancer - NCI [https://dceg.cancer.gov/news-events/news/2021/mutational-signatures]
- 60. Gene signatures for cancer research: A 25-year ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11482671/]
- 61. Pan-cancer discovery of somatic mutations from RNA ... [https://www.nature.com/articles/s42003-024-06326-y]
- 62. Tissue-based genomic profiling of 300000 tumors ... [https://www.nature.com/articles/s41698-025-00991-w]
- 63. Brain tumor classification from FFPE samples using nanopore ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12574666/]
- 64. Fully automated extraction of high-quality total nucleic ... [https://www.sciencedirect.com/science/article/pii/S247263032500010X]
- 65. Whole genome sequencing improves tissue-of-origin ... [https://www.nature.com/articles/s41467-025-59661-x]
- 66. Integrating Formalin-Fixed, Paraffin-Embedded–Derived ... [https://www.sciencedirect.com/science/article/pii/S1525157825001345]
- 67. New Mayo Clinic tool exposes hidden cancer DNA ... [https://newsnetwork.mayoclinic.org/discussion/new-mayo-clinic-tool-exposes-hidden-cancer-dna-changes-that-may-drive-treatment-resistance/]
- 68. De novo detection of somatic variants in high-quality long- ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12047253/]
- 69. Targeted Gene Panels: Revolutionizing Genomic Testing ... [https://blog.crownbio.com/targeted-gene-panels-genomic-testing-oncology]
- 70. Evidence of off-target probe binding in the 10x Genomics ... [https://elifesciences.org/reviewed-preprints/107070]
- 71. Specificity of Primers and Probes for Molecular Diagnosis ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12566895/]
- 72. Systematic benchmarking of high-throughput subcellular ... [https://www.nature.com/articles/s41467-025-64292-3]
- 73. Advances in personalized medicine: translating genomic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12106117/]
- 74. Precision Cancer Vaccines - How RNA- and DNA-Seq ... [https://www.lexogen.com/blog/precision-cancer-vaccines-how-rna-and-dna-seq-shape-the-future-of-neoantigen-discovery/]
- 75. Three-stage quality control strategies for DNA re- ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4492405/]
- 76. Impact of wet-lab protocols on quality of whole-genome short ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10716212/]
- 77. Analytical Validation of the Next-Generation Sequencing ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5397672/]
- 78. Robustness of differential gene expression analysis ... [https://www.sciencedirect.com/science/article/pii/S200103702100221X]
- 79. Quality Control for RNA-Seq (QuaCRS) - PMC - NIH [https://pmc.ncbi.nlm.nih.gov/articles/PMC4214596/]
- 80. Frontiers | Guideline-Adherent Clinical Validation of a Comprehensive... [https://www.frontiersin.org/journals/genetics/articles/10.3389/fgene.2021.503830/full]
- 81. Analytic validation and clinical utilization of the ... [https://www.oncotarget.com/article/27945/text/]
- 82. Clinical and analytical of a combined validation and RNA exome... DNA [https://pubmed.ncbi.nlm.nih.gov/40523952/]
- 83. Guidelines for Validation of Next-Generation Sequencing– ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6941185/]
- 84. performance evaluation of a commercial next generation... Analytical [https://bmccancer.biomedcentral.com/articles/10.1186/s12885-020-07445-5]
- 85. and clinical Analytical of an amplicon-based... | PLOS One validation [https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0267389]
- 86. From Bench to Trial: Validating RNA-Seq and WES to ... [https://communities.springernature.com/posts/from-bench-to-trial-validating-rna-seq-and-wes-to-accelerate-oncology-therapeutics]
- 87. Validating a new quantitative assay [https://www.pathologyoutlines.com/topic/managementlabvalidatingnewassay.html]
- 88. RNA Sequencing | RNA-Seq methods & workflows [https://www.illumina.com/techniques/sequencing/rna-sequencing.html]
- 89. Diagnostic accuracy of next-generation sequencing (NGS) ... [https://link.springer.com/article/10.1007/s12094-025-04040-7]
- 90. RNA-seq outperforms DNA methods in detecting ... [https://acgt.co.za/rna-seq-outperforms-dna-methods-in-detecting-actionable-cancer-mutations/]
- 91. Blood RNA-seq in rare disease diagnostics: a comparative ... [https://translational-medicine.biomedcentral.com/articles/10.1186/s12967-025-06609-w]
- 92. Development of an End-to-End Total RNA Sequencing ... [https://www.sciencedirect.com/science/article/abs/pii/S1525157825001436]
- 93. Machine learning approach to identify significant genes ... [https://pubmed.ncbi.nlm.nih.gov/41142322/]
- 94. The Growing Role of Precision Medicine in Paediatric ... [https://link.springer.com/article/10.1007/s11523-025-01178-w]
- 95. Clinical utility of liquid biopsy next-generation sequencing ... [https://www.nature.com/articles/s41598-025-13667-z]
- 96. Clinical Utility of Whole-Genome Sequencing to Aid ... [https://pubmed.ncbi.nlm.nih.gov/41166678/?utm_source=SimplePie&utm_medium=rss&utm_campaign=pubmed-2&utm_content=1bAXfGTh08tVk-e1kpwuqxoVfiUn_5olMN9ewCML2bdAMGPEOD&fc=20220524054416&ff=20251030193326&v=2.18.0.post22+67771e2]
- 97. The Clinical Utility of Next-Generation Sequencing in ... [https://www.mdpi.com/2072-6694/17/8/1292]
- 98. High clinical actionability of a pan-cancer tissue-based ... [https://www.nature.com/articles/s41698-025-01126-x]