Foundation Models for Cancer Imaging Biomarkers: A New Paradigm in Precision Oncology
Foundation models, large-scale deep learning models pre-trained on vast datasets through self-supervised learning, are revolutionizing the discovery of cancer imaging biomarkers.
Foundation Models for Cancer Imaging Biomarkers: A New Paradigm in Precision Oncology
Abstract
Foundation models, large-scale deep learning models pre-trained on vast datasets through self-supervised learning, are revolutionizing the discovery of cancer imaging biomarkers. This article explores their foundational principles, methodological applications, and transformative potential for researchers and drug development professionals. We detail how these models facilitate robust biomarker development, even with limited annotated data, for tasks ranging from lesion classification and malignancy diagnosis to prognostic outcome prediction. The content further addresses critical challenges in implementation, including data heterogeneity and model generalizability, and provides a comparative analysis of model performance and validation strategies. By synthesizing evidence from recent studies and benchmarks, this article serves as a comprehensive guide to the current state and future trajectory of foundation models in accelerating the translation of quantitative imaging biomarkers into clinical and research practice.
The Paradigm Shift: Understanding Foundation Models and Their Role in Biomarker Discovery
Defining Foundation Models and Self-Supervised Learning in Medical Imaging
Foundation Models (FMs) represent a transformative class of artificial intelligence systems characterized by their training on vast, diverse datasets using self-supervised learning (SSL) techniques, enabling them to serve as adaptable base models for numerous downstream tasks [1] [2]. In medical imaging, these models fundamentally shift the development paradigm from building task-specific models from scratch to adapting powerful pre-trained models for specialized clinical applications. Self-supervised learning provides the foundational methodology that enables this approach by learning representative features from unlabeled data, circumventing one of the most significant bottlenecks in medical AI: the scarcity of expensive, expertly annotated datasets [3] [4]. Within oncology, this technological convergence creates unprecedented opportunities for discovering and validating cancer imaging biomarkers by leveraging the rich information encoded in medical images without complete reliance on labeled datasets [4] [5].
Core Technical Principles
Architectural Foundations of Foundation Models
Foundation models in medical imaging typically leverage transformer-based architectures or convolutional networks, scaled to unprecedented sizes and trained on massive, multi-institutional datasets. The 3DINO-ViT model exemplifies this approach, implementing a vision transformer (ViT) adapted for 3D medical volumes while incorporating a 3D ViT-Adapter module to inject spatial inductive biases critical for dense prediction tasks like segmentation [3]. These architectures succeed through pre-training on extraordinarily diverse datasets; for instance, 3DINO-ViT was trained on approximately 100,000 3D scans spanning MRI, CT, and PET modalities across over 10 different organs [3] [6]. This diversity forces the model to learn robust, general-purpose representations rather than features specific to any single modality or anatomical region.
Self-Supervised Learning Methodologies
SSL methods construct learning signals directly from the structure of unlabeled data. The 3DINO framework implements a sophisticated approach combining both image-level and patch-level objectives, adapting the DINOv2 pipeline to 3D medical imaging inputs [3]. As shown in the experimental workflow, this process involves generating multiple augmented views of each 3D volume—typically two global and eight local crops—then training the model using a self-distillation objective where a student network learns to match the output of a teacher network across these different views [3]. Alternative SSL approaches include masked autoencoders, which randomly mask portions of input images and train models to reconstruct the missing content, and contrastive learning, which learns representations by maximizing agreement between differently augmented views of the same image while minimizing agreement with other images [2].
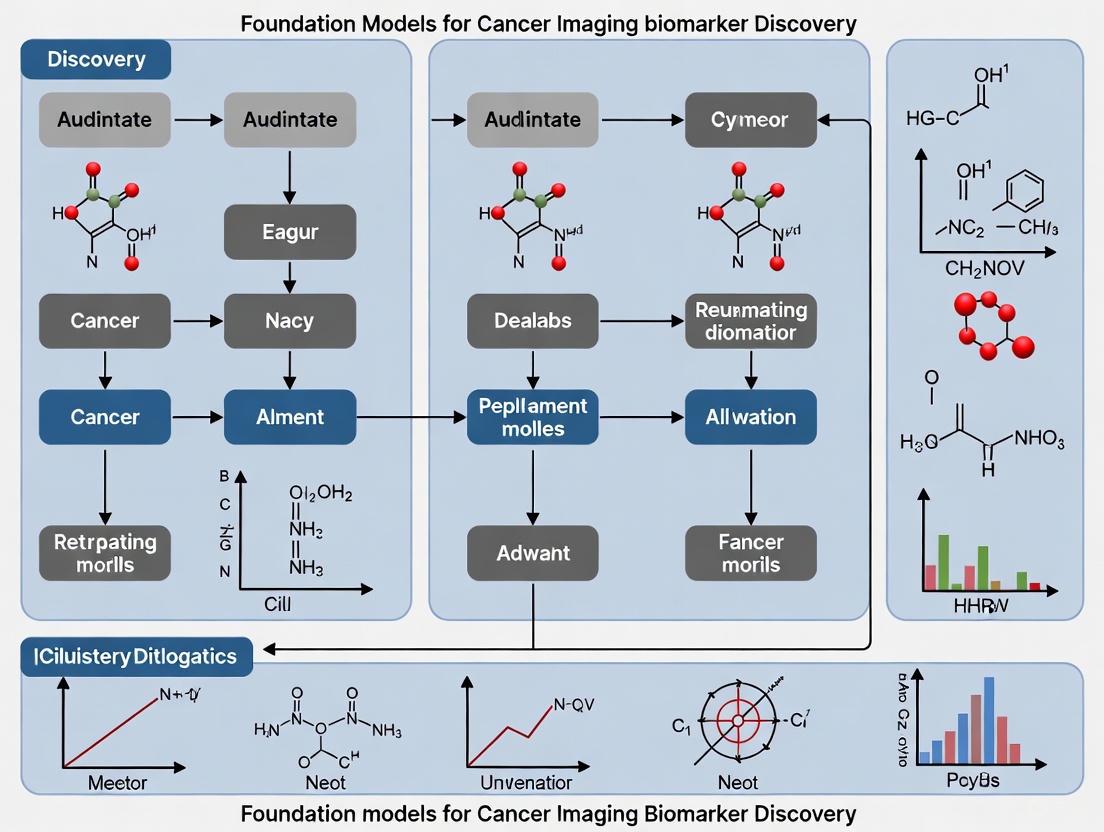
Figure 1: Self-distillation with no labels (3DINO) workflow for 3D medical imaging.
Application to Cancer Imaging Biomarker Discovery
Enhanced Biomarker Discovery with Limited Data
Foundation models demonstrate particular utility in scenarios with limited annotated data, which frequently challenges cancer biomarker discovery. In one comprehensive study, a foundation model trained on 11,467 radiographic lesions significantly outperformed conventional supervised approaches and other state-of-the-art pre-trained models, especially when training dataset sizes were severely limited [4]. The model served as a powerful feature extractor for various cancer imaging tasks, including lesion anatomical site classification (balanced accuracy: 0.804), lung nodule malignancy prediction (AUC: 0.944), and prognostic biomarker development for non-small cell lung cancer [4]. When training data was reduced to only 10% of the original dataset, the foundation model implementation showed remarkably robust performance, declining only 9% in balanced accuracy compared to significantly larger drops observed in baseline methods [4].
Quantitative Performance in Downstream Tasks
Table 1: Performance comparison of foundation models versus baseline methods on medical imaging tasks
| Task | Dataset | Foundation Model Performance | Next Best Baseline Performance | Improvement |
|---|---|---|---|---|
| Brain Tumor Segmentation | BraTS (10% data) | 0.90 Dice [3] | 0.87 Dice (Random) [3] | +3.4% [3] |
| Abdominal Organ Segmentation | BTCV (25% data) | 0.77 Dice [3] | 0.59 Dice (Random) [3] | +30.5% [3] |
| COVID-19 Classification | COVID-CT-MD | 23% higher AUC [3] | Next best baseline | Significant [3] |
| Lung Nodule Malignancy | LUNA16 | 0.944 AUC [4] | 0.917 AUC (Med3D) [4] | +2.9% [4] |
| Age Classification | ICBM | 13.4% higher AUC [3] | Next best baseline | Significant [3] |
Table 2: Impact of limited data on foundation model performance for anatomical site classification
| Training Data Percentage | Foundation Model (Features) Balanced Accuracy | Foundation Model (Fine-tuned) Balanced Accuracy | Best Baseline Balanced Accuracy |
|---|---|---|---|
| 100% | 0.779 [4] | 0.804 [4] | 0.775 (Med3D fine-tuned) [4] |
| 50% | 0.765 [4] | 0.781 [4] | 0.743 (Med3D fine-tuned) [4] |
| 20% | 0.741 [4] | 0.752 [4] | 0.692 (Med3D fine-tuned) [4] |
| 10% | 0.709 [4] | 0.698 [4] | 0.631 (Med3D fine-tuned) [4] |
Experimental Framework and Methodologies
Implementation Approaches for Downstream Tasks
Two primary implementation strategies have emerged for adapting foundation models to specific cancer imaging biomarker tasks. The feature extraction approach uses the pre-trained foundation model as a fixed feature extractor, with a simple linear classifier trained on top of these features for the specific downstream task [4]. This method offers computational efficiency and strong performance in limited-data regimes. The fine-tuning approach further trains the foundation model's weights on labeled data from the target task, typically achieving superior performance when sufficient labeled data is available but requiring more computational resources and carrying higher risk of overfitting with small datasets [4]. Research indicates that the feature extraction approach often outperforms fine-tuning in severely data-limited scenarios common to specialized cancer biomarker applications [4].
Validation Frameworks and Evaluation Metrics
Rigorous evaluation of foundation models for biomarker discovery necessitates multi-tiered validation frameworks. The AI4HI network advocates for decentralized clinical validation and continuous training frameworks to ensure model reliability across diverse populations and clinical settings [2]. Comprehensive benchmarks like those established across 11 medical datasets in the MedMNIST collection evaluate models on both in-domain performance and out-of-distribution generalization [7]. Critical evaluation metrics include area under the receiver operating characteristic curve (AUC) for classification tasks, Dice coefficient for segmentation accuracy, and balanced accuracy for multi-class problems with imbalanced distributions [3] [4]. Additionally, biomarker discovery applications require assessment of model stability through test-retest analyses and evaluation of biological relevance via correlation with genomic expression data [4].
Figure 2: Multi-dataset validation framework for foundation models in biomarker discovery.
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential computational resources for implementing foundation models in medical imaging research
| Resource Category | Specific Tools & Frameworks | Function in Research Pipeline |
|---|---|---|
| Pre-trained Models | 3DINO-ViT, Med3D, Models Genesis | Provide foundational feature extractors for downstream tasks, reducing computational requirements [3] [4] |
| SSL Frameworks | 3DINO, SimCLR, SwAV, NNCLR | Enable self-supervised pre-training on unlabeled datasets [3] [4] |
| Medical Imaging Platforms | MONAI, NVIDIA CLARA | Offer specialized implementations of medical AI algorithms and data loaders [3] |
| Model Architectures | Vision Transformer (ViT), Swin Transformer, Convolutional Encoders | Provide backbone networks for foundation models [3] [4] |
| Evaluation Benchmarks | MedMNIST+, BraTS, BTCV, LUNA16 | Standardized datasets for comparative performance assessment [3] [7] |
Challenges and Future Directions
Despite their promising performance, foundation models in medical imaging face several significant challenges. Data heterogeneity across institutions, modalities, and scanner manufacturers can limit model generalizability [2]. Limited transparency and explainability remain concerns for clinical adoption, particularly for high-stakes applications like cancer diagnosis [2] [5]. Computational requirements for training and deploying large foundation models present practical barriers for widespread implementation [3]. Additionally, models may perpetuate or amplify biases present in training data if not carefully addressed [2].
Future development directions include creating more efficient model architectures, improving explainability through techniques like attention visualization, establishing standardized validation frameworks across institutions, and developing federated learning approaches to train models on distributed data without centralization [2]. The integration of imaging biomarkers with other data modalities—including genomics, proteomics, and clinical records—represents a particularly promising direction for creating comprehensive biomarker signatures in oncology [8] [5]. As these technologies mature, foundation models are poised to significantly accelerate the discovery and validation of imaging biomarkers, ultimately enhancing precision oncology through improved diagnosis, prognosis, and treatment selection.
The development of artificial intelligence (AI) for cancer imaging represents a paradigm shift in oncology, promising enhanced diagnostic precision, prognostic stratification, and personalized treatment strategies. However, this potential is constrained by a critical bottleneck: the scarcity of large, annotated medical imaging datasets. Unlike natural image analysis where massive labeled datasets like ImageNet contain millions of images, medical imaging research faces fundamental limitations in data availability due to patient privacy concerns, the specialized expertise required for annotation, and the resource-intensive nature of data collection in clinical settings [9]. This scarcity profoundly impacts the development of robust AI models, particularly deep learning networks that typically require extensive labeled examples to generalize effectively without overfitting [9].
Within this challenging landscape, foundation models have emerged as a transformative approach. These models, characterized by large-scale architectures pretrained on vast amounts of unannotated data, can be adapted to various downstream tasks with limited task-specific labels [4] [10]. In cancer imaging biomarker discovery, foundation models pretrained through self-supervised learning (SSL) techniques demonstrate remarkable capability to overcome data scarcity constraints, enabling more accurate and efficient development of imaging biomarkers even when labeled training samples are severely limited [4]. This technical guide examines the foundational principles, methodological frameworks, and experimental evidence supporting the use of foundation models to address the critical challenge of data scarcity in cancer imaging research.
Foundation Models: A Technical Framework for Overcoming Data Scarcity
Conceptual Architecture and Core Principles
Foundation models in medical imaging are built on a core architectural principle: a single large-scale model trained on extensive diverse data serves as the foundation for various downstream tasks [4]. These models are typically pretrained using self-supervised learning (SSL), a paradigm that leverages the inherent structure and relationships within unlabeled data to learn generalized, task-agnostic representations [4]. The pretraining phase eliminates the dependency on manual annotations, thereby bypassing the primary constraint of labeled data scarcity.
The conceptual workflow follows a two-stage process:
- Pretraining Phase: A model (typically a convolutional encoder) is trained on large-scale unlabeled medical imaging datasets using SSL objectives that create supervisory signals from the data itself.
- Adaptation Phase: The pretrained model is adapted to specific clinical tasks (e.g., lesion classification, malignancy prediction) through two primary approaches:
- Feature Extraction: Using the foundation model as a fixed feature extractor with a simple linear classifier trained on top.
- Fine-tuning: Updating the weights of the pretrained model on downstream tasks with limited labeled data [4].
This approach fundamentally addresses data scarcity by transferring knowledge acquired from large unlabeled datasets to specialized tasks with limited annotations, significantly reducing the demand for labeled training samples in downstream applications [4] [10].
Self-Supervised Learning Strategies for Medical Imaging
The efficacy of foundation models hinges on selecting appropriate SSL strategies tailored to medical imaging characteristics. Research systematically comparing various pretraining approaches has revealed performance differentials critical for implementation decisions:
- Contrastive Learning Methods: A modified version of SimCLR (a contrastive framework that learns representations by maximizing agreement between differently augmented views of the same image) has demonstrated superior performance for cancer imaging tasks, achieving a balanced accuracy of 0.779 (95% CI: 0.750-0.810) in lesion anatomical site classification, significantly outperforming (p < 0.001) other approaches [4].
- Comparative Performance: In systematic evaluations, SimCLR variants surpassed other state-of-the-art SSL approaches including SwAV (a clustering-based method that enforces consistency between cluster assignments for different augmentations) and NNCLR (which uses nearest neighbors in the latent space to create positive pairs) [4].
- Baseline Comparisons: Traditional autoencoder-based pretraining (which reconstructs original images from corrupted inputs) performed worst compared to modern contrastive SSL methods, highlighting the importance of selecting contemporary approaches [4].
The table below summarizes the performance characteristics of different pretraining strategies evaluated on lesion anatomical site classification:
Table 1: Comparison of Self-Supervised Pretraining Strategies for Medical Imaging Foundation Models
| Pretraining Strategy | Balanced Accuracy | Mean Average Precision (mAP) | Key Characteristics |
|---|---|---|---|
| Modified SimCLR | 0.779 (95% CI: 0.750-0.810) | 0.847 (95% CI: 0.750-0.810) | Contrastive learning with customized augmentations for medical images |
| SimCLR | 0.696 (95% CI: 0.663-0.728) | 0.779 (95% CI: 0.749-0.811) | Standard contrastive framework with augmented views |
| SwAV | 0.652 (95% CI: 0.619-0.685) | 0.737 (95% CI: 0.705-0.769) | Online clustering with swapped assignments |
| NNCLR | 0.631 (95% CI: 0.597-0.665) | 0.719 (95% CI: 0.686-0.752) | Nearest-neighbor positive pairs in latent space |
| Autoencoder | 0.589 (95% CI: 0.554-0.624) | 0.675 (95% CI: 0.640-0.710) | Image reconstruction objective |
Experimental Evidence and Performance Benchmarks
Technical Validation: In-Distribution Task Performance
The performance advantage of foundation models becomes particularly evident in scenarios with limited labeled data. In a technical validation study classifying lesion anatomical sites (using 3,830 lesions for training/tuning and 1,221 for testing), foundation model implementations demonstrated significant superiority over conventional approaches, especially as training data decreased [4].
Table 2: Foundation Model Performance on Lesion Anatomical Site Classification Under Limited Data Scenarios
| Training Data Percentage | Foundation Model Implementation | Balanced Accuracy | Performance Advantage Over Baselines |
|---|---|---|---|
| 100% (n=3,830) | Features + Linear Classifier | 0.792 | Significant improvement over all baselines (p < 0.05) |
| 100% (n=3,830) | Fine-tuned Foundation Model | 0.804 | Outperformed all baselines (p < 0.01) |
| 50% (n=2,526) | Features + Linear Classifier | 0.773 | Significant improvement over all baselines |
| 20% (n=1,010) | Features + Linear Classifier | 0.746 | Significant improvement over all baselines |
| 10% (n=505) | Features + Linear Classifier | 0.722 | Smallest performance decline (9%) with reduced data |
Notably, the feature extraction approach demonstrated remarkable robustness, maintaining 74.2% of its maximum performance with only 10% of training data, whereas conventional supervised models exhibited substantially steeper performance degradation [4]. This stability underscores the particular value of foundation models in real-world research settings where labeled data is invariably scarce.
Clinical Application: Out-of-Distribution Generalization
The true test of foundation models lies in their generalization capability to unseen data distributions and clinical tasks. In developing a diagnostic biomarker for predicting lung nodule malignancy using the LUNA16 dataset (507 nodules for training, 170 for testing), the fine-tuned foundation model achieved an AUC of 0.944 (95% CI: 0.907-0.972) and mAP of 0.953 (95% CI: 0.915-0.979), significantly outperforming (p < 0.01) most baseline implementations [4].
For prognostic biomarker development in non-small cell lung cancer (NSCLC), foundation models demonstrated strong associations with underlying biology, particularly correlating with immune-related pathways, and exhibited enhanced stability to input variations including inter-reader differences and acquisition parameters [4] [10]. This biological relevance and robustness further validate the utility of foundation models for discovering clinically meaningful imaging biomarkers despite data limitations.
Implementation Protocols and Methodological Guidelines
Experimental Workflow for Foundation Model Development
The development and application of foundation models for cancer imaging follows a structured workflow encompassing data curation, model pretraining, and task-specific adaptation. The diagram below illustrates this comprehensive experimental pipeline:
Detailed Methodological Protocols
Data Curation and Preprocessing Protocol
Effective foundation models require diverse, large-scale medical imaging data for pretraining. The referenced research utilized 11,467 radiographic lesions from computed tomography (CT) scans encompassing diverse lesion types including lung nodules, cysts, and breast lesions [4] [10]. The preprocessing protocol involves:
- Volumetric Processing: Handling 3D CT volumes with consistent spatial normalization
- Intensity Standardization: Normalizing Hounsfield units across different scanner types
- Data Augmentation: Applying specialized transformations appropriate for medical images including:
- Controlled random cropping and resizing
- Rotation and flipping with anatomical constraints
- Noise injection and contrast variation within clinically plausible ranges
- Quality Control: Implementing rigorous exclusion criteria for corrupted or low-quality scans [4]
Self-Supervised Pretraining Implementation
The modified SimCLR framework implemented for cancer imaging foundation models includes these critical components:
- Positive Pair Generation: Creating multiple augmented views of the same lesion instance
- Encoder Network: Training a convolutional encoder (e.g., ResNet-50) to extract representations
- Projection Head: Mapping representations to a latent space where contrastive loss is applied
- Contrastive Loss Function: Using normalized temperature-scaled cross entropy (NT-Xent) to maximize agreement between positive pairs while repelling negative pairs
- Training Configuration: Optimizing with LARS optimizer, cosine learning rate decay, and global batch normalization [4]
Downstream Task Adaptation Methods
For applying pretrained foundation models to specific cancer imaging tasks, two primary adaptation strategies were systematically evaluated:
Feature Extraction Approach:
- Keeping the foundation model weights frozen
- Extracting feature representations from the penultimate layer
- Training a linear classifier (typically logistic regression or linear SVM) on these features
- Advantages: Computational efficiency, stability with very small datasets (<100 samples)
Fine-tuning Approach:
- Initializing task-specific models with foundation model weights
- Updating all parameters or only later layers using task-specific labels
- Employing reduced learning rates and early stopping to prevent catastrophic forgetting
- Advantages: Potential for higher peak performance with adequate data [4]
Successful implementation of foundation models for cancer imaging biomarker discovery requires access to specialized computational resources, datasets, and software frameworks. The table below details essential research reagents referenced in the foundational studies:
Table 3: Essential Research Reagents for Foundation Model Development in Cancer Imaging
| Resource Category | Specific Resource | Function and Application | Access Information |
|---|---|---|---|
| Primary Datasets | DeepLesion (11,467 lesions) | Foundation model pretraining; lesion anatomical site classification | Publicly available [4] [11] |
| Validation Datasets | LUNA16 | Lung nodule malignancy prediction (diagnostic biomarker) | Publicly available [4] [11] |
| Validation Datasets | LUNG1 & RADIO | Prognostic biomarker validation in NSCLC | Publicly available [4] [11] |
| Software Framework | MHub.ai | Containerized implementation for clinical deployment | Platform access [11] |
| Code Repository | GitHub (AIM Program) | Data preprocessing, model training, inference replication | Open source [11] |
| Benchmarking Tools | TumorImagingBench | Standardized evaluation across 6 datasets (3,244 scans) | Publicly released [12] |
| Radiomics Datasets | RadiomicsHub | 29 curated datasets (10,354 patients) for multi-center validation | Public repository [13] |
Comparative Analysis and Implementation Decision Framework
Performance Under Varying Data Constraints
The relative advantage of foundation models compared to conventional supervised approaches is inversely proportional to the amount of available labeled data. The diagram below illustrates this critical relationship and the recommended implementation decisions:
Integration with Existing Radiomics Workflows
Foundation models can be effectively integrated with traditional radiomics pipelines to enhance biomarker discovery:
- Complementary Feature Extraction: Deep learning features from foundation models can supplement hand-crafted radiomics features (shape, texture, intensity statistics) to create more comprehensive tumor profiles [13] [5].
- Multi-Modal Data Fusion: Foundation model embeddings can be combined with genomic, transcriptomic, and clinical data for multi-omics biomarker discovery, providing more holistic tumor characterization [5].
- Transfer Across Imaging Modalities: While typically pretrained on CT, foundation models can be adapted to MRI, PET, and multi-parametric imaging through transfer learning techniques [13].
- Standardized Validation Frameworks: Resources like TumorImagingBench enable systematic evaluation of foundation models across diverse cancer types and imaging protocols [12].
The critical challenge of scarce labeled medical datasets represents a fundamental constraint in cancer imaging biomarker discovery. Foundation models, pretrained through self-supervised learning on large-scale unlabeled imaging data, offer a transformative solution by significantly reducing the demand for annotated samples in downstream applications. Experimental evidence demonstrates that these models not only maintain robust performance in limited data scenarios but also enhance model stability, biological interpretability, and generalizability across clinical tasks.
The methodological frameworks, experimental protocols, and implementation guidelines presented in this technical guide provide researchers with practical resources to leverage foundation models in overcoming data scarcity constraints. As the field advances, the integration of these approaches with multi-institutional collaborations, standardized benchmarking, and explainable AI frameworks will accelerate the translation of imaging biomarkers into clinical practice, ultimately enhancing precision oncology and patient care.
How Foundation Models Learn Generalizable Representations from Unannotated Data
Foundation models represent a paradigm shift in artificial intelligence, characterized by their training on vast, diverse datasets through self-supervised learning (SSL) to acquire generalizable representations that adapt efficiently to various downstream tasks [14]. In cancer imaging biomarker discovery, these models directly address the critical bottleneck of annotated data scarcity by learning robust, transferable features directly from unannotated medical images [4] [15]. The capacity to learn from data without expensive, time-consuming manual labeling enables more rapid development of imaging biomarkers that can inform cancer diagnosis, prognosis, and treatment response assessment.
These models fundamentally differ from conventional supervised approaches by leveraging the inherent structure and information within the data itself through pretext tasks, creating representations that capture underlying biological patterns rather than merely memorizing labeled examples [15] [14]. This technical guide explores the mechanisms through which foundation models achieve this capability, with specific emphasis on their application in cancer imaging research, providing researchers with both theoretical understanding and practical implementation frameworks.
Core Learning Mechanisms
Self-Supervised Learning Paradigms
Foundation models circumvent the need for manual annotations by employing self-supervised learning objectives that create supervisory signals directly from the data [14]. In medical imaging, this typically involves training models to solve pretext tasks that force the network to learn meaningful representations without human intervention. Common approaches include:
- Image Reconstruction: Training models to reconstruct missing or corrupted portions of medical images, forcing the network to learn anatomical and pathological priors to complete the task successfully [4] [14].
- Contrastive Learning: Learning representations by maximizing agreement between differently augmented views of the same image while minimizing agreement with other images in the dataset [4] [15]. This approach, exemplified by frameworks like SimCLR and its derivatives, has demonstrated particular effectiveness in medical imaging domains.
- Masked Image Modeling: Randomly masking portions of input images and training the model to predict the missing content, effectively learning contextual relationships within anatomical structures [14].
The learned representations capture fundamental characteristics of medical images that transcend specific diagnostic tasks, creating a foundation that can be efficiently adapted to various downstream applications with minimal labeled examples [4].
Architectural Foundations
The architectural implementations of foundation models for medical imaging typically employ:
- Convolutional Encoders: Traditional convolutional neural networks that process local spatial relationships effectively, particularly suited for the textural patterns found in medical images [4] [16].
- Vision Transformers: Self-attention based architectures that capture long-range dependencies in image data, potentially beneficial for understanding relationships between distant anatomical structures [15] [14].
- Multimodal Architectures: Models that process multiple data types simultaneously, such as combining imaging data with clinical notes or genomic information through cross-attention mechanisms [15] [14].
These architectures create representation spaces where semantically similar images (and image regions) are positioned proximally, enabling efficient knowledge transfer to new tasks through fine-tuning or linear probing approaches [4] [15].
Table 1: Common Self-Supervised Learning Approaches in Medical Imaging Foundation Models
| Method Category | Key Mechanism | Representative Architectures | Advantages in Medical Imaging |
|---|---|---|---|
| Contrastive Learning | Maximizes similarity between augmented views of same image | SimCLR, NNCLR, SwAV | Effective with diverse lesion appearances; robust to acquisition variations |
| Masked Modeling | Predicts masked image regions based on context | Masked Autoencoders (MAE), Vision Transformers | Learns anatomical context; strong spatial reasoning |
| Reconstruction-based | Reconstructs original input from transformed version | Autoencoders, Denoising Autoencoders | Learns complete anatomical representations; stable training |
Technical Implementation in Cancer Imaging
Experimental Framework for Cancer Biomarker Discovery
The implementation of foundation models for cancer imaging biomarker discovery follows a structured pipeline that leverages self-supervised pre-training followed by task-specific adaptation:
Phase 1: Large-Scale Pre-training In this foundational phase, models are trained on extensive, diverse datasets of unannotated medical images. For example, one cancer imaging foundation model was pre-trained on 11,467 radiographic lesions from 2,312 unique patients, encompassing multiple lesion types including lung nodules, cysts, and breast lesions [4]. The training employs a task-agnostic contrastive learning strategy that learns invariant features by maximizing agreement between differently augmented views of the same lesion.
Phase 2: Downstream Task Adaptation The pre-trained foundation model is then adapted to specific clinical tasks through:
- Linear Probing: Training a simple linear classifier on top of frozen features extracted from the foundation model, requiring minimal labeled data and computational resources [4].
- Fine-Tuning: Updating all or subset of the foundation model's weights using task-specific labeled data, typically achieving higher performance but requiring more resources [4] [17].
This approach was experimentally validated across multiple clinically relevant applications, including lesion anatomical site classification (technical validation), lung nodule malignancy prediction (diagnostic biomarker), and non-small cell lung cancer prognosis (prognostic biomarker) [4].
Quantitative Performance Evidence
Empirical studies demonstrate the effectiveness of foundation models in cancer imaging applications. In lesion anatomical site classification, a foundation model approach achieved a balanced accuracy of 0.804 (95% CI: 0.775–0.835) and mean average precision (mAP) of 0.857 (95% CI: 0.828–0.886), significantly outperforming conventional supervised approaches and other pre-training methods [4]. The advantage was particularly pronounced in limited data scenarios, with the foundation model maintaining robust performance even when training data was reduced to 10% of the original size [4].
In lung nodule malignancy prediction, foundation model fine-tuning achieved an area under the curve (AUC) of 0.944 (95% CI: 0.907–0.972) and mAP of 0.953 (95% CI: 0.915–0.979), demonstrating strong generalization to out-of-distribution tasks [4]. Recent benchmarking studies evaluating ten different foundation models across six cancer imaging datasets further confirmed these findings, with top-performing models like FMCIB, ModelsGenesis, and VISTA3D showing consistent performance across diagnostic and prognostic tasks [17].
Table 2: Performance Comparison of Foundation Models vs. Traditional Approaches in Cancer Imaging Tasks
| Task Domain | Dataset | Foundation Model Performance | Traditional/Baseline Performance | Key Metric |
|---|---|---|---|---|
| Lesion Site Classification | 1,221 test lesions | 0.804 balanced accuracy | 0.696 balanced accuracy (Med3D) | Balanced Accuracy |
| Lung Nodule Malignancy | LUNA16 (170 test nodules) | 0.944 AUC | 0.917 AUC (Med3D fine-tuned) | Area Under Curve (AUC) |
| NSCLC Prognosis | NSCLC-Radiomics | 0.582 AUC (VISTA3D) | 0.449 AUC (CTClip) | Area Under Curve (AUC) |
| Renal Cancer Prognosis | C4KC-KiTS | 0.733 AUC (ModelsGenesis) | 0.463 AUC (CTFM) | Area Under Curve (AUC) |
Implementation Workflow
The following diagram illustrates the complete experimental workflow for developing and validating a foundation model for cancer imaging applications:
Foundation Model Development Workflow: The diagram illustrates the three-phase pipeline for developing cancer imaging foundation models, from self-supervised pre-training through task adaptation to clinical validation.
The Scientist's Toolkit
Table 3: Essential Research Reagents and Computational Resources for Foundation Model Development
| Resource Category | Specific Examples | Function in Workflow | Implementation Notes |
|---|---|---|---|
| Medical Imaging Datasets | 11,467 radiographic lesions [4], LUNA16 [17], NSCLC-Radiomics [17] | Pre-training and benchmarking | Diverse lesion types and anatomical sites improve model generalizability |
| Deep Learning Frameworks | TensorFlow [16], PyTorch, Caffe [16] | Model implementation and training | Open-source libraries with medical imaging extensions |
| Self-Supervised Algorithms | Modified SimCLR [4], SwAV [4], NNCLR [4] | Representation learning | Contrastive methods show superior performance in medical domains |
| Computational Infrastructure | GPU clusters, Cloud computing (AWS, GCP, Azure) | Model training and inference | Foundation models require significant computational resources for pre-training |
| Evaluation Metrics | AUC, Balanced Accuracy, Mean Average Precision [4] | Performance quantification | Multiple metrics provide comprehensive assessment of clinical utility |
Discussion and Future Directions
Foundation models represent a transformative approach to cancer imaging biomarker discovery by learning generalizable representations from unannotated data. The core innovation lies in their ability to capture fundamental patterns in medical images through self-supervised objectives, creating representations that transfer efficiently to diverse clinical tasks with minimal fine-tuning [4] [14].
The demonstrated performance advantages, particularly in limited data scenarios common in medical applications, highlight the potential of these models to accelerate the development and clinical translation of imaging biomarkers [4] [17]. Furthermore, foundation models show increased stability to input variations and stronger associations with underlying biology compared to traditional approaches [4].
Future research directions include developing more sophisticated multimodal foundation models that integrate imaging with clinical, genomic, and pathology data [15] [14], addressing challenges related to model interpretability and fairness [14], and establishing standardized benchmarking frameworks like TumorImagingBench [17] to enable reproducible comparison of foundation models across diverse cancer imaging applications. As these models continue to evolve, they hold significant promise for advancing precision oncology through more accessible, robust, and biologically-relevant imaging biomarkers.
Foundation models are revolutionizing the discovery of cancer imaging biomarkers by leveraging large-scale, self-supervised learning (SSL) on extensive unlabeled datasets. These models are characterized by their pre-training on broad data, which allows them to be adapted to a wide range of downstream tasks with minimal task-specific supervision [18]. In the context of medical imaging, where large, annotated datasets are scarce and expensive to produce, this paradigm offers a transformative approach [4] [19]. The core advantages of foundation models align perfectly with the needs of this field: they enable more efficient model development, exhibit remarkable transferability across clinical tasks and cohorts, and significantly reduce the reliance on large annotated datasets. This technical guide explores these advantages within the framework of cancer imaging biomarker research, providing evidence from recent studies, detailed methodologies, and resources for the practicing scientist.
Efficiency: Performance Gains in Data-Limited Scenarios
A primary advantage of foundation models in cancer imaging is their ability to achieve high performance with limited labeled data for downstream tasks, making the development process highly efficient.
Quantitative Evidence of Data Efficiency
Research demonstrates that foundation models maintain robust performance even when fine-tuning data is severely restricted. The following table summarizes key findings from a foundational study that developed a model trained on 11,467 radiographic lesions [4].
Table 1: Performance of a Foundation Model on Lesion Anatomical Site Classification with Limited Data [4]
| Training Data Used | Number of Lesions | Foundation Model (Balanced Accuracy) | Conventional Supervised Model (Balanced Accuracy) | Performance Drop vs. Full Data (Foundation Model) |
|---|---|---|---|---|
| 100% | 3,830 | 0.804 | 0.696 (Med3D fine-tuned) | Baseline |
| 50% | 1,915 | 0.781 | ~0.67 (estimated) | -2.9% |
| 20% | 766 | 0.752 | ~0.63 (estimated) | -6.5% |
| 10% | 383 | 0.732 | ~0.60 (estimated) | -9.0% |
In a diagnostic task for lung nodule malignancy prediction on the LUNA16 dataset, a fine-tuned foundation model achieved an Area Under the Curve (AUC) of 0.944, significantly outperforming other state-of-the-art pre-trained models [4]. This efficiency is crucial for investigating rare cancers or specific molecular subtypes where large, labeled datasets are impractical to assemble.
Experimental Protocol for Efficiency Validation
To systematically evaluate the data efficiency of a proposed foundation model, researchers typically follow this protocol:
- Foundation Model Pre-training: A convolutional encoder (e.g., ResNet) is trained using a self-supervised, task-agnostic contrastive learning strategy (e.g., a modified SimCLR framework) on a large, diverse dataset of unlabeled medical images (e.g., 11,467 CT lesions from 2,312 patients) [4] [19].
- Downstream Task Definition: Specific clinical tasks are selected, such as lesion anatomical site classification (in-distribution technical validation) or lung nodule malignancy prediction (out-of-distribution generalizability test) [4].
- Comparative Model Training:
- The foundation model is implemented in two ways: as a feature extractor with a simple linear classifier on top, and via fine-tuning the entire model.
- Baseline models are trained for comparison, including models trained from scratch in a supervised manner and other publicly available pre-trained models (e.g., Med3D, ModelsGenesis) [4] [17].
- Data Ablation Study: The downstream models are trained on progressively smaller subsets (e.g., 100%, 50%, 20%, 10%) of the available labeled data for the task.
- Performance Evaluation: Models are evaluated on a held-out test set using metrics such as balanced accuracy, mean Average Precision (mAP), and AUC. The relative performance drop for each model as training data is reduced is a key metric of efficiency [4].
Diagram 1: Workflow for Validating Foundation Model Efficiency.
Transferability: Generalizability Across Tasks and Cohorts
Transferability refers to a foundation model's ability to adapt to diverse clinical tasks, disease types, and patient populations, a critical feature for robust biomarker discovery.
Evidence of Cross-Task and Cross-Cohort Generalization
Benchmarking studies have systematically evaluated the transferability of multiple foundation models. The table below shows the performance of select models across different diagnostic and prognostic tasks [17].
Table 2: Transferability of Foundation Models Across Various Cancer Imaging Tasks [17]
| Foundation Model | LUNA16 (Diagnostic)\nAUC - Lung Nodule Malignancy | NSCLC-Radiomics (Prognostic)\nAUC - 2-Year Survival | C4KC-KiTS (Prognostic)\nAUC - 2-Year Survival (Renal) | Key Characteristics |
|---|---|---|---|---|
| FMCIB [4] | 0.886 | 0.577 | N/A | Trained on diverse CT lesions |
| ModelsGenesis | 0.806 | 0.577 | 0.733 | Self-supervised learning on CTs |
| VISTA3D | 0.711 | 0.582 | N/A | Strong in prognostic tasks |
| Voco | 0.493 | 0.526 | N/A | Lower overall performance |
The data indicates that no single model is universally superior, but models pre-trained on diverse datasets (e.g., FMCIB, ModelsGenesis) consistently rank high across tasks. For instance, FMCIB excelled in diagnostic tasks, while VISTA3D showed relative strength in prognostic tasks [17]. This demonstrates that the features learned by these models are not task-specific but capture fundamental phenotypic characteristics of disease.
Protocol for Benchmarking Transferability
To assess the transferability of a foundation model, a rigorous benchmarking framework is essential:
- Model Selection: A suite of publicly available foundation models with varied architectures (CNN vs. Transformer), pre-training strategies (contrastive, generative), and source data (CT only, multi-modal) is selected [17] [18].
- Benchmark Curation: A benchmark comprising multiple public datasets (e.g., TumorImagingBench with 3,244 scans) is assembled. These datasets should span different clinical endpoints (diagnosis, prognosis), cancer types (lung, kidney, liver), and institutions to test generalizability [17].
- Embedding Extraction & Evaluation: For each dataset, embeddings (high-dimensional feature vectors) are extracted from the images using each foundation model. A simple classifier (e.g., k-nearest neighbors or a linear model) is then trained on these embeddings to predict the clinical endpoint [17] [20].
- Multi-Dimensional Analysis: Performance is evaluated not only on endpoint prediction (AUC) but also on robustness to input variations (test-retest reliability), saliency-based interpretability, and mutual similarity of the learned embeddings across models [17].
Reduced Reliance on Annotations: The Self-Supervised Learning Core
The reduced need for manual annotation is the foundational pillar enabling the efficiency and transferability of these models. This is achieved through self-supervised learning (SSL).
The Self-Supervised Pre-training Protocol
SSL allows models to learn powerful representations from data without manual labels by defining a "pretext task" that generates its own supervision from the data's structure. The core technical steps for pre-training a foundation model for cancer imaging are as follows [4] [18]:
- Data Curation: A large dataset of medical images (e.g., 11,467 CT lesions) is assembled without the need for detailed annotations. Only weak labels, such as the presence of a lesion, may be used [4] [11].
- Pretext Task - Contrastive Learning: A popular and effective SSL method is contrastive learning. In a framework like SimCLR:
- Augmentation: Each image in a batch is randomly transformed twice (e.g., via rotation, cropping, noise addition, color distortion), creating two correlated "views."
- Encoding: Both views are passed through a convolutional encoder network.
- Projection: The resulting embeddings are mapped to a latent space via a small projection head.
- Contrastive Loss: The learning objective is to maximize the agreement (similarity) between the two views of the same image while minimizing agreement with views from other images in the same batch [4] [18].
- Model Output: After pre-training, the projection head is discarded, and the encoder is used as the feature extractor for downstream tasks.
This process forces the model to learn robust, invariant features that are relevant to the image content itself, rather than features that are specific to a narrow labeled task.
Diagram 2: Self-Supervised Pre-training via Contrastive Learning.
The Scientist's Toolkit: Research Reagent Solutions
Translating these concepts into practice requires a set of key resources. The following table details essential "research reagents" for working with foundation models in cancer imaging biomarker discovery.
Table 3: Essential Research Reagents for Foundation Model-Based Biomarker Discovery
| Resource Category | Specific Example(s) | Function and Utility |
|---|---|---|
| Pre-trained Models | FMCIB [4], ModelsGenesis [17], VISTA3D [17], CONCH (Pathology) [20] | Provides a starting point for downstream task adaptation, eliminating the need for costly pre-training from scratch. |
| Public Datasets | DeepLesion [11], LUNA16 [4], LUNG1 & RADIO [11], The Cancer Genome Atlas (TCGA) | Serves as sources for pre-training data and, more importantly, as standardized benchmarks for evaluating model performance and transferability. |
| Code & Software Platforms | Project-lighter YAML configurations [11], MHub.ai platform [11], 3D Slicer Integration [11] | Provides reproducible code for training and inference, containerized models for ease of use, and integration with clinical research workflows. |
| Benchmarking Frameworks | TumorImagingBench [17], Pathology FM Benchmark [20] | Offers a curated set of tasks and datasets for the systematic evaluation and comparison of different foundation models, guiding model selection. |
Foundation models represent a paradigm shift in quantitative cancer imaging. Their core advantages—efficiency in low-data settings, exceptional transferability across clinical tasks, and a fundamentally reduced reliance on annotations—directly address the most significant bottlenecks in traditional biomarker discovery. By leveraging self-supervised learning on large datasets, these models learn a deep, generalized representation of disease phenotypes that can be efficiently adapted with minimal fine-tuning. As benchmarking studies show, this leads to more robust and accurate imaging biomarkers. The availability of pre-trained models, public datasets, and software platforms is now empowering researchers to harness these advantages, accelerating the translation of AI-derived biomarkers from research into clinical practice and drug development.
Positioning Foundation Models within the Broader AI Landscape in Oncology
Foundation models represent a paradigm shift in artificial intelligence (AI) for oncology. These models are characterized by their training on vast, broad datasets using self-supervised learning (SSL), which enables them to serve as versatile base models for a wide array of downstream clinical tasks without requiring task-specific architectural changes [4]. In cancer care, where labeled medical data is notoriously scarce and expensive to produce, foundation models offer a transformative solution by learning generalizable, task-agnostic representations from extensive unannotated data [4] [11]. These models excel particularly in reducing the demand for large labeled datasets in downstream applications, making them exceptionally valuable for specialized oncological tasks where large annotated datasets are often unavailable [4].
The positioning of foundation models within the broader AI landscape marks a critical evolution from narrow, single-task models toward generalist AI systems capable of adapting to multiple clinical challenges. Traditional supervised deep learning approaches in oncology have typically required large labeled datasets for each specific task—such as tumor detection, classification, or prognosis prediction—limiting their applicability in data-scarce scenarios [4]. Foundation models overcome this limitation through pretraining on diverse, unlabeled datasets, capturing fundamental patterns of cancer imaging characteristics that can be efficiently transferred to various downstream applications with minimal task-specific training [4] [21]. This approach mirrors the success of foundation models in other domains, such as natural language processing, but applies these principles to the complex, multimodal world of oncology [4].
Comparative Advantages Over Traditional AI Approaches
Foundation models demonstrate significant advantages over conventional supervised learning and other pretrained models, particularly in scenarios with limited data availability. In direct performance comparisons, foundation models consistently outperform traditional approaches across multiple cancer imaging tasks [4].
Table 1: Performance Comparison of AI Approaches in Cancer Imaging Tasks
| Task Description | Model Type | Performance Metrics | Key Advantage |
|---|---|---|---|
| Lesion Anatomical Site Classification [4] | Foundation (fine-tuned) | mAP: 0.857 (95% CI 0.828-0.886) | Significantly outperformed all baseline methods (p<0.05) |
| Foundation (features) + Linear classifier | mAP: 0.847 (95% CI 0.750-0.810) | Outperformed compute-intensive supervised training | |
| Lung Nodule Malignancy Prediction [4] | Foundation (fine-tuned) | AUC: 0.944 (95% CI 0.907-0.972) | Significant superiority (p<0.01) over most baselines |
| Traditional supervised | AUC: <0.917 | Lower performance compared to foundation approaches | |
| Anatomical Site Classification with 10% Data [4] | Foundation model | Smallest performance decline (9% balanced accuracy) | Superior data efficiency and robustness in limited data scenarios |
The stability and biological relevance of foundation models further distinguish them from traditional approaches. These models demonstrate increased robustness to input variations and show strong associations with underlying biology, as validated through deep-learning attribution methods and gene expression data correlations [4]. This biological grounding enhances the clinical relevance of the derived imaging biomarkers and supports their potential for discovery of novel cancer characteristics not previously captured by handcrafted radiomic features or supervised deep learning approaches [4].
Technical Architectures and Methodological Approaches
Self-Supervised Learning Strategies for Pretraining
The effectiveness of foundation models in oncology stems from sophisticated self-supervised learning approaches that enable the model to learn meaningful representations without explicit manual annotations. Several SSL strategies have been evaluated for cancer imaging applications, with contrastive learning approaches demonstrating particular effectiveness [4].
Table 2: Self-Supervised Learning Strategies for Oncological Foundation Models
| Pretraining Strategy | Key Mechanism | Performance in Anatomical Site Classification | Relative Advantage |
|---|---|---|---|
| Modified SimCLR [4] | Contrastive learning with task-specific modifications | Balanced Accuracy: 0.779 (95% CI 0.750-0.810) | Superior to all other approaches (p<0.001) |
| Standard SimCLR [4] | Instance discrimination via contrastive loss | Balanced Accuracy: 0.696 (95% CI 0.663-0.728) | Second-best performing approach |
| SwAV [4] | Online clustering with swapped predictions | Performance lower than SimCLR variants | Moderate performance |
| NNCLR [4] | Contrastive learning with nearest-neighbor positives | Performance lower than SimCLR variants | Moderate performance |
| Autoencoder [4] | Image reconstruction | Lowest performance | Outperformed by contrastive SSL methods |
The modified SimCLR approach, which builds upon the standard SimCLR framework with domain-specific adaptations for medical imaging, has demonstrated remarkable robustness when training data is limited. When evaluated with progressively reduced training data (50%, 20%, and 10% of original dataset), this approach showed the smallest decline in performance metrics—only 9% reduction in balanced accuracy and 12% in mean average precision when reducing training data from 100% to 10% [4]. This robustness to data scarcity is particularly valuable in clinical oncology settings where collecting large annotated datasets is challenging.
Multimodal Architecture Integration
Advanced foundation models in oncology are increasingly embracing multimodal architectures that integrate diverse data types to enhance clinical utility. The Multimodal transformer with Unified maSKed modeling (MUSK) represents a cutting-edge vision-language foundation model trained on both pathology images and clinical text [22]. This model was pretrained on 50 million pathology images from 11,577 patients and one billion pathology-related text tokens using unified masked modeling, followed by additional pretraining on one million pathology image-text pairs to align visual and language features [22]. This architecture enables the model to leverage complementary information from both imaging and clinical narratives, supporting tasks ranging from image-text retrieval to biomarker prediction and outcome forecasting [22].
Diagram 1: Multimodal Foundation Model Architecture
Experimental Protocols and Validation Frameworks
Foundation Model Development Protocol
The development of a robust foundation model for cancer imaging requires a systematic approach to data curation, model training, and validation. A representative protocol, as implemented by Pai et al., involves several critical phases [4] [11]:
Phase 1: Data Curation and Preprocessing
- Collect comprehensive dataset of radiographic lesions (e.g., 11,467 lesions from 2,312 unique patients) [4]
- Include diverse lesion types: lung nodules, cysts, breast lesions, and numerous others [4]
- Implement standardized preprocessing: image normalization, resampling to consistent resolution, and data augmentation [4]
- Split data into training, validation, and test sets, ensuring patient-wise separation to prevent data leakage [11]
Phase 2: Self-Supervised Pretraining
- Implement modified SimCLR framework with domain-specific augmentations [4]
- Train convolutional encoder using contrastive learning objective
- Optimize using Adam optimizer with learning rate warmup and cosine decay
- Monitor training progress using contrastive loss and representation quality metrics
Phase 3: Downstream Task Adaptation
- Evaluate two implementation approaches: feature extraction with linear classifier and full fine-tuning [4]
- For feature extraction: freeze foundation model weights, train linear classifier on extracted features
- For fine-tuning: initialize with foundation model weights, fine-tune entire architecture on downstream task
- Compare against supervised baselines and other pretrained models (Med3D, Models Genesis) [4]
Phase 4: Comprehensive Validation
- Technical validation on in-distribution tasks (e.g., lesion anatomical site classification) [4]
- Generalizability assessment on out-of-distribution tasks (e.g., malignancy prediction on external datasets) [4]
- Robustness evaluation through test-retest and inter-reader consistency analyses [4]
- Biological relevance assessment via correlation with genomic data [4]
Benchmarking and Performance Evaluation
Rigorous benchmarking is essential for evaluating foundation models in oncology. The TumorImagingBench framework provides a standardized approach, curating multiple public datasets (3,244 scans) with varied oncological endpoints to assess model performance across diverse clinical contexts [12]. This evaluation extends beyond traditional endpoint prediction to include robustness to clinical variability, saliency-based interpretability, and comparative analysis of learned embedding representations [12].
Diagram 2: Experimental Validation Workflow
Table 3: Key Research Reagent Solutions for Oncological Foundation Models
| Resource Category | Specific Tool/Dataset | Function/Purpose | Access Information |
|---|---|---|---|
| Public Datasets | DeepLesion [11] | RECIST-bookmarked lesions for pretraining and anatomical site classification | Openly accessible |
| LUNA16 [4] [11] | Lung nodules for diagnostic biomarker development | Publicly available | |
| LUNG1 and RADIO [11] | NSCLC datasets for prognostic biomarker validation | Publicly available | |
| Computational Frameworks | MHub.ai [11] | Containerized, ready-to-use model implementation supporting various input workflows | Platform access |
| 3D Slicer Integration [11] | Clinical integration and application framework | Open source | |
| Project-lighter [11] | Training and replication via customizable YAML configurations | GitHub repository | |
| Benchmarking Tools | TumorImagingBench [12] | Curated benchmark with 3,244 scans across 6 datasets for systematic evaluation | Publicly released code and datasets |
| Model Architectures | Modified SimCLR [4] | Contrastive SSL framework optimized for medical imaging | Code available in repository |
| MUSK [22] | Vision-language foundation model for pathology | GitHub repository with model weights | |
| Validation Resources | Molecular Data Integration [4] | Gene expression correlation analysis for biological validation | Dependent on specific institutional resources |
Implementation Pathways and Clinical Translation
The translation of foundation models from research to clinical application follows multiple implementation pathways, each with distinct advantages for specific clinical scenarios. Two primary approaches have demonstrated significant utility: using the foundation model as a fixed feature extractor with a linear classifier, and full fine-tuning of the model for specific downstream tasks [4].
The feature extraction approach provides substantial computational benefits with reduced memory requirements and training time, while still achieving performance comparable to or better than compute-intensive supervised training [4]. This method is particularly valuable for rapid prototyping and applications with limited computational resources. In contrast, the fine-tuning approach typically achieves the highest performance on specific clinical tasks but requires more computational resources and careful management of training dynamics to prevent catastrophic forgetting of the pretrained representations [4].
For clinical deployment, platforms like MHub.ai provide containerized, ready-to-use implementations that support various input workflows and integration with clinical systems such as 3D Slicer [11]. This approach significantly lowers the barrier for both academic and clinical researchers to leverage foundation models without requiring deep expertise in model architecture or training procedures. The availability of these models through simple package installations and standardized APIs further accelerates their adoption in diverse research and clinical settings [11].
The demonstrated performance of foundation models in predicting clinically relevant endpoints—including lesion characterization, malignancy prediction, and cancer prognosis—combined with their robustness to input variations and association with underlying biology, positions them as powerful tools for accelerating the discovery and translation of imaging biomarkers into clinical practice [4]. As these models continue to evolve and validate across diverse patient populations and clinical contexts, they hold tremendous potential to enhance precision oncology and improve patient care through more accurate, efficient, and biologically grounded imaging biomarkers.
From Theory to Practice: Implementing Foundation Models for Oncology Biomarkers
The emergence of foundation models represents a paradigm shift in medical artificial intelligence (AI), offering unprecedented capabilities for cancer imaging biomarker discovery. These models, characterized by large-scale architectures trained on vast amounts of unannotated data, serve as versatile starting points for diverse downstream tasks through transfer learning. Within this transformative context, researchers face a critical architectural decision: convolutional encoders versus transformer-based models. This choice fundamentally influences model performance, data efficiency, computational requirements, and ultimately the clinical translation of imaging biomarkers.
Convolutional Neural Networks (CNNs) have long served as the workhorse of medical image analysis, leveraging their innate inductive biases for processing spatial hierarchies in imaging data. In contrast, Vision Transformers (ViTs) have recently emerged as powerful competitors, utilizing self-attention mechanisms to capture global contextual information. For foundation models aimed at cancer imaging biomarkers—which must extract meaningful, reproducible, and biologically relevant signatures from radiographic data—this architectural choice carries significant implications for discovery potential. This technical guide provides an in-depth analysis of both architectures within this specific research context, offering evidence-based insights, comparative evaluations, and practical implementation frameworks to inform researcher decisions.
Architectural Fundamentals and Key Properties
Convolutional Neural Networks (CNNs)
CNNs process medical images through a hierarchical series of convolutional layers, pooling operations, and nonlinear activations. The core operation is convolution, where filters slide across input images to detect local patterns through shared weights. This design incorporates strong inductive biases particularly suited to medical imagery: translation invariance, spatial locality, and hierarchical feature learning. These properties enable CNNs to efficiently recognize patterns like textures, edges, and shapes that are fundamental to radiographic interpretation [23].
The architectural properties of CNNs make them particularly well-suited for medical imaging tasks where local tissue characteristics and spatial patterns provide diagnostic value. Their parameter sharing across spatial domains confers significant computational efficiency, while their progressive receptive field expansion through layered convolutions enables learning of complex feature hierarchies from local pixels to global structures [23]. However, this localized processing approach presents limitations in capturing long-range dependencies across image regions—a potential drawback for cancer imaging contexts where relationships between distant anatomical structures or distributed tumor characteristics may carry prognostic significance.
Vision Transformers (ViTs)
Vision Transformers fundamentally reimagine image processing by treating images as sequences of patches. Unlike CNNs' local processing, ViTs utilize self-attention mechanisms that compute pairwise interactions between all patches in an image, enabling direct modeling of global dependencies. The core operation is scaled dot-product attention, which dynamically weights the influence of different image regions on each other [23].
This architecture provides several distinctive properties valuable for cancer imaging biomarker discovery. The global receptive field available from the first layer allows ViTs to capture relationships between distant anatomical structures without the progressive field expansion required in CNNs. The self-attention mechanism also enables dynamic feature weighting based on content, potentially identifying clinically relevant image regions without explicit spatial priors [24]. However, these capabilities come with substantial computational requirements and typically demand larger training datasets to reach optimal performance—a significant consideration in medical imaging domains where annotated data may be limited [23].
Table 1: Fundamental Properties of CNN and Transformer Architectures
| Property | Convolutional Encoders | Transformer-Based Models |
|---|---|---|
| Core Operation | Convolution with localized filters | Self-attention between all image patches |
| Receptive Field | Local initially, expands through depth | Global from the first layer |
| Inductive Bias | Strong (translation invariance, locality) | Weak (minimal built-in assumptions) |
| Parameter Efficiency | High (weight sharing across spatial dimensions) | Lower (attention weights scale with input) |
| Data Efficiency | Generally requires less training data | Typically requires large-scale pre-training |
| Long-Range Dependency | Limited, requires many layers | Strong, captured directly via self-attention |
| Computational Complexity | O(n) for n input pixels | O(n²) for n input patches |
Performance Comparison in Medical Imaging Tasks
Classification and Diagnostic Biomarker Development
Both architectures have demonstrated strong performance in diagnostic classification tasks, though their relative advantages depend on specific task requirements and data constraints. In cancer imaging applications, CNNs have shown particular strength in scenarios with limited training data. A foundational study developing a CNN-based foundation model for cancer imaging biomarkers achieved outstanding performance across multiple clinical tasks, including nodule malignancy prediction with an AUC of 0.944 (95% CI 0.907-0.972) on the LUNA16 dataset [4]. This model, pre-trained on 11,467 radiographic lesions through self-supervised learning, significantly outperformed conventional supervised approaches, especially when fine-tuning data was limited [4] [11].
Comparative analyses reveal a more nuanced picture of relative strengths. A 2024 systematic review noted that transformer-based models frequently achieve superior performance compared to conventional CNNs on various medical imaging tasks, though this advantage often depends on appropriate pre-training [23]. However, a 2025 comparative analysis across chest X-ray pneumonia detection, brain tumor classification, and skin cancer melanoma detection found task-specific advantages: ResNet-50 (CNN) achieved 98.37% accuracy on chest X-rays, while DeiT-Small (Transformer) excelled in brain tumor detection (92.16% accuracy), and EfficientNet-B0 (CNN) led in skin cancer classification (81.84% accuracy) [25]. This suggests that optimal architecture selection may be problem-dependent rather than universally prescribed.
Segmentation and Morphometric Biomarker Extraction
Medical image segmentation represents a critical task for cancer imaging biomarker discovery, enabling precise quantification of tumor morphology, volume, and tissue characteristics. Traditional U-Net architectures based on CNNs have dominated this domain, but recent transformer-based approaches are showing competitive or superior performance in specific contexts.
The TransUNet framework, which integrates transformers into U-Net architectures, has demonstrated significant improvements in challenging segmentation tasks. In multi-organ abdominal CT segmentation, TransUNet achieved a 1.06% average Dice improvement compared to the highly competitive nn-UNet, while showing more substantial gains (4.30% average Dice improvement) in pancreatic tumor segmentation—a particularly challenging task involving small targets [26]. The study attributed these improvements to the transformer's ability to capture global contextual relationships that help resolve ambiguous boundaries and identify small structures.
Hybrid architectures that strategically combine both approaches are emerging as particularly powerful solutions. The AD2Former network, incorporating alternate CNN and transformer blocks in the encoder alongside a dual-decoder structure, demonstrated strong performance in capturing target regions with fuzzy boundaries in multi-organ and skin lesion segmentation tasks [27]. This design allows mutual guidance between local and global feature extraction throughout the encoding process rather than simply cascading the two modalities.
Table 2: Quantitative Performance Comparison Across Medical Imaging Tasks
| Task | Dataset | Best-Performing CNN Model | Best-Performing Transformer Model | Performance Advantage |
|---|---|---|---|---|
| Nodule Malignancy Prediction | LUNA16 | Foundation CNN (AUC: 0.944) | Not specified | CNN superior [4] |
| Chest X-ray Classification | Chest X-ray | ResNet-50 (Accuracy: 98.37%) | ViT-Base (Accuracy: Not specified) | CNN superior [25] |
| Brain Tumor Classification | Brain Tumor | EfficientNet-B0 (Accuracy: Not specified) | DeiT-Small (Accuracy: 92.16%) | Transformer superior [25] |
| Multi-organ Segmentation | Synapse | nn-UNet (Dice: Baseline) | TransUNet (Dice: +1.06%) | Transformer superior [26] |
| Pancreatic Tumor Segmentation | Pancreas CT | nn-UNet (Dice: Baseline) | TransUNet (Dice: +4.30%) | Transformer superior [26] |
| TIL Level Prediction | Breast US | DenseNet121 (AUC: 0.873) | Vision Transformer (AUC: Not specified) | Comparable [28] |
Practical Implementation Considerations
Data Requirements and Pre-training Strategies
The data efficiency of architectural choices represents a critical consideration for cancer imaging biomarker discovery, where annotated datasets are typically limited. CNNs generally demonstrate superior performance in data-scarce scenarios due to their built-in inductive biases. The cancer imaging foundation model developed using a convolutional encoder maintained robust performance even when downstream training data was reduced to just 10% of the original dataset, declining by only 9% in balanced accuracy compared to significantly larger drops in other approaches [4].
Vision Transformers typically require substantial pre-training to compensate for their weaker inductive biases. As noted in a comparative review, "pre-training is important for transformer applications" in medical imaging [23]. However, once adequately pre-trained, ViTs can excel in transfer learning scenarios. Self-supervised learning (SSL) has emerged as a particularly powerful strategy for both architectures in medical imaging, reducing dependency on scarce manual annotations. The convolutional foundation model for cancer imaging was pre-trained using a modified SimCLR framework, a contrastive SSL approach that significantly outperformed autoencoder and other SSL strategies [4].
Computational Requirements and Model Efficiency
Computational resources represent a practical constraint in architectural selection. CNNs generally offer greater computational efficiency, with linear scaling relative to input size versus the quadratic scaling of transformer self-attention. This difference becomes particularly significant with high-resolution 3D medical images common in oncology applications like CT and MRI [23].
Efforts to optimize transformer efficiency for medical imaging include patchified processing, hierarchical architectures, and hybrid designs. The Swin Transformer introduced a windowed attention mechanism that reduces computational complexity while maintaining global modeling capabilities [29]. Similarly, the TransUNet framework processes feature maps from a CNN backbone rather than raw image patches, improving efficiency while leveraging global context [26]. For large-scale foundation model development and deployment, these efficiency considerations directly impact feasibility, iteration speed, and clinical translation potential.
Robustness and Interpretability
Model robustness to technical variations in image acquisition is essential for clinically viable imaging biomarkers. The convolutional foundation model for cancer imaging demonstrated superior stability to input variations compared to supervised approaches [4]. Transformers may offer advantages in certain robustness metrics due to their global processing, though their performance can be more variable across domain shifts [23].
Interpretability remains challenging for both architectures, though both have established visualization techniques. CNNs typically utilize activation mapping approaches like Grad-CAM to highlight influential image regions [28]. Transformers can leverage attention weights to visualize patch interactions, though interpreting these complex interaction patterns remains an active research area [23]. For cancer biomarker discovery, biological plausibility and association with underlying pathology are crucial validation steps, with the CNN foundation model demonstrating strong associations with gene expression data [4].
Integrated Frameworks and Future Directions
Hybrid Architectures
The complementary strengths of CNNs and Transformers have motivated numerous hybrid architectures that strategically integrate both approaches. These designs aim to preserve local feature precision while incorporating global contextual understanding. The AD2Former exemplifies this trend with an alternate encoder that enables real-time interaction between local and global information, allowing both to mutually guide learning [27]. This architecture demonstrated particular strength in capturing fuzzy boundaries and small targets in challenging segmentation tasks.
Other integration strategies include parallel pathways, sequential arrangements, and attention-enhanced convolutional blocks. The TransUNet offers flexible configuration options, allowing researchers to implement transformer components in the encoder only, decoder only, or both, depending on task requirements [26]. Empirical results suggest that the encoder benefits are most pronounced for modeling interactions among multiple abdominal organs, while transformer decoders show particular strength in handling small targets like tumors [26].
Foundation Models for Cancer Imaging
Foundation models represent a particularly promising application for these architectural considerations. The successful implementation of a CNN-based foundation model for cancer imaging biomarkers demonstrates the potential of this approach [4] [11]. This model, pre-trained on 11,467 diverse radiographic lesions, facilitated efficient adaptation to multiple downstream tasks including lesion anatomical site classification, lung nodule malignancy prediction, and prognostic biomarker development for non-small cell lung cancer [4].
Ongoing benchmarking efforts like TumorImagingBench are systematically evaluating diverse foundation model architectures for quantitative cancer imaging phenotypes [12]. Such initiatives provide critical empirical evidence to guide architectural selection for specific oncological applications and imaging modalities. As the field progresses, task-specific rather than universally optimal architectural choices are likely to emerge, informed by comprehensive comparative evaluations.
Figure 1. Architectural Workflows for Cancer Imaging Foundation Models
Experimental Protocols and Methodologies
Self-Supervised Pre-training Framework
The development of foundation models for cancer imaging typically begins with self-supervised pre-training on large-scale unannotated datasets. The following protocol, adapted from successful implementations, provides a methodological framework for architectural comparison:
Data Curation and Preparation:
- Collect comprehensive dataset of radiographic lesions (e.g., 11,467 lesions from 2,312 patients)
- Ensure diversity in lesion types, anatomical locations, and imaging characteristics
- Standardize image preprocessing: resampling to consistent resolution, intensity normalization, and data augmentation (random cropping, flipping, rotation, contrast adjustment)
Self-Supervised Learning Implementation:
- For CNN architectures: Implement contrastive learning framework (e.g., modified SimCLR)
- For Transformer architectures: Consider masked autoencoding or contrastive approaches
- Train with balanced batch sampling to ensure representation of diverse lesion types
- Optimize using Adam or LAMB optimizer with cosine learning rate decay
Validation and Model Selection:
- Evaluate learned representations through linear probing on held-out validation tasks
- Assess training stability and convergence metrics
- Select optimal checkpoint based on representation quality and training efficiency
This protocol formed the basis for the successful CNN foundation model that achieved state-of-the-art performance across multiple cancer imaging tasks [4].
Downstream Task Adaptation Methodology
The true value of foundation models emerges through their adaptation to specific clinical tasks. The following experimental protocol enables systematic evaluation of architectural choices for downstream applications:
Task Formulation and Data Splitting:
- Define clinically relevant endpoints (diagnostic classification, segmentation, prognostic prediction)
- Curate task-specific datasets with appropriate ground truth annotations
- Implement rigorous train-validation-test splits with patient-level separation to prevent data leakage
- For data-scarce scenarios, create limited-data subsets (e.g., 10%, 20%, 50% of full dataset)
Transfer Learning Strategies:
- Feature Extraction Approach: Freeze foundation model weights, train linear classifier on top of extracted features
- Fine-tuning Approach: Allow partial or complete fine-tuning of foundation model with task-specific data
- Progressive Unfreezing: Systematically unfreeze layers while monitoring validation performance
Performance Evaluation:
- Employ task-appropriate metrics (AUC, accuracy, Dice coefficient, etc.)
- Assess statistical significance of performance differences between architectures
- Evaluate training efficiency: time to convergence, computational resources required
- Analyze robustness to input variations and domain shifts
This methodology enabled the comprehensive evaluation demonstrating the CNN foundation model's superiority in limited-data scenarios and its stability across input variations [4].
Figure 2. Experimental Protocol for Foundation Model Development
Table 3: Key Research Reagents and Computational Resources
| Resource Category | Specific Examples | Function in Research | Implementation Notes |
|---|---|---|---|
| Public Datasets | DeepLesion, LUNA16, LUNG1, RADIO, Synapse, ISIC2018 | Pre-training and benchmark evaluation | Curate diverse lesion types; ensure patient-level splits [4] [27] [11] |
| Deep Learning Frameworks | PyTorch, TensorFlow, MONAI | Model implementation and training | MONAI provides medical imaging-specific optimizations |
| Architecture Backbones | ResNet, DenseNet, Vision Transformer, Swin Transformer | Foundation model implementation | Select based on task requirements and data constraints [28] [25] |
| Self-Supervised Learning Methods | SimCLR, SwAV, NNCLR, Masked Autoencoding | Pre-training without manual annotations | Contrastive learning works well for CNNs; masked autoencoding for Transformers [4] |
| Evaluation Metrics | AUC, Balanced Accuracy, Dice Coefficient, mAP | Performance quantification | Use multiple metrics for comprehensive assessment [4] |
| Interpretability Tools | Grad-CAM, Attention Visualization, Saliency Maps | Model decision explanation | Critical for clinical translation and biological validation [4] [28] |
| Computational Infrastructure | High-memory GPUs (NVIDIA A100/H100), Distributed Training Frameworks | Handling large-scale medical images | Essential for transformer training and 3D processing |
The choice between convolutional encoders and transformer-based models for cancer imaging biomarker discovery involves nuanced trade-offs rather than absolute superiority. CNNs offer compelling advantages in data efficiency, computational requirements, and proven performance across multiple cancer imaging tasks, as demonstrated by state-of-the-art foundation models. Transformers provide complementary strengths in global context modeling and have shown superior performance in specific segmentation and classification tasks, particularly when adequate pre-training data is available.
Hybrid architectures that strategically integrate both approaches represent a promising direction, leveraging CNN efficiency for local feature extraction alongside transformer global modeling capabilities. For researchers embarking on foundation model development for cancer imaging biomarkers, the optimal architectural choice should be guided by specific task requirements, data availability, and computational resources. As the field advances, systematic benchmarking efforts and reproducible implementation frameworks will be essential for evidence-based architectural selection, ultimately accelerating the translation of AI-derived imaging biomarkers into clinical oncology practice.
The discovery of robust cancer imaging biomarkers is fundamental to advancing precision oncology, enabling early diagnosis, accurate prognosis, and prediction of treatment response. Foundation models—large-scale, versatile models trained on vast amounts of data—are poised to revolutionize this discovery process. These models, particularly when trained via self-supervised learning (SSL), learn generalizable representations from unlabeled medical images, which can then be tailored for specific downstream tasks with minimal labeled data. Contrastive learning, a dominant SSL paradigm, has emerged as a powerful strategy for building such foundation models in medical imaging. This technical guide focuses on SimCLR (A Simple Framework for Contrastive Learning of Visual Representations) and its modern variants, detailing their core principles, adaptations for medical data, and implementation for cancer imaging biomarker discovery.
Core Principles of SimCLR
SimCLR provides a straightforward yet effective framework for learning representations by comparing image samples [30]. Its objective is to learn an encoder network that maps input images to a latent space where similar data points (positive pairs) are pulled together, and dissimilar ones (negative pairs) are pushed apart.
The SimCLR framework operates through a systematic workflow:
- Data Augmentation: Each image in a batch is transformed twice using a stochastic data augmentation module, creating two correlated views. This generates positive pairs, ( \tilde{xi} ) and ( \tilde{xj} ), which represent the same image under different transformations.
- Base Encoder: A convolutional neural network (CNN) base encoder, ( f(\cdot) ), extracts representation vectors ( hi ) and ( hj ) from the augmented images.
- Projection Head: A small neural network, ( g(\cdot) ), maps the representations to a lower-dimensional latent space where the contrastive loss is applied, yielding ( zi ) and ( zj ).
- Contrastive Loss: The Normalized Temperature-scaled Cross Entropy (NT-Xent) loss is used to identify the positive pair ( (i, j) ) among the negative pairs in the batch.
The NT-Xent loss for a positive pair ( (i, j) ) is formally defined as: [ \ell{i,j} = -\log \frac{\exp(\text{sim}(zi, zj) / \tau)}{\sum{k=1}^{2N} \mathbb{1}{[k \neq i]} \exp(\text{sim}(zi, z_k) / \tau)} ] where ( \text{sim}(u,v) ) is the cosine similarity, ( \tau ) is a temperature parameter, and the denominator includes one positive and ( 2N-2 ) negative pairs.
Figure 1: The SimCLR framework workflow. Two augmented views of an input image are processed through a shared encoder and projection head. The contrastive loss function maximizes agreement between the latent vectors of the positive pair.
SimCLR Adaptations for Medical Imaging
Standard data augmentations used in natural image domains (e.g., color jitter) are often suboptimal for medical images, which possess unique characteristics like anatomical geometry and modality-specific contrasts. Successful adaptation of SimCLR for medical data requires domain-specific strategies.
Domain-Specific Positive Pair Formation
A critical adaptation involves redefining how positive pairs are generated to reflect clinically meaningful variations.
Counterfactual Contrastive Learning: This novel framework addresses acquisition shift, a major source of domain variation in medical imaging caused by differences in scanner vendors or protocols [31]. Instead of relying on pre-defined generic transformations, it uses deep generative models to create counterfactual images. These images answer "what-if" questions, such as simulating how a mammogram would appear if acquired on a different device. Using these realistic, domain-altered images as positive pairs forces the model to learn features that are invariant to acquisition parameters, significantly improving robustness on external datasets and reducing subgroup disparities [31].
Leveraging Native Data Structure: Some approaches move beyond image synthesis by exploiting the inherent structure of medical data. This can include using adjacent slices in 3D CT scans or multiple views of the same lesion in mammography as natural positive pairs, thereby incorporating clinical context directly into the learning process.
Optimization and Architectural Refinements
Beyond data augmentation, the core SimCLR architecture can be optimized for medical tasks.
Feature Selection with Hybrid Krill Herd Optimization (HKHO): When applying a SimCLR-pre-trained model to a specific task like cervical cancer cell classification, not all learned features are equally relevant [32]. HKHO can be integrated post-pre-training to cluster and isolate the most salient features for the target task, leading to reported performance gains and achieving accuracies as high as 97.63% [32].
Integration with Multiple Instance Learning (MIL): To apply 2D SSL models to 3D volumetric data like MRI, an SSL-MIL framework can be highly effective [33]. In this setup, a 2D SimCLR model pre-trained on individual slices serves as a feature extractor. These features are then aggregated using an attention-based MIL model to make a single prediction for the entire 3D volume, outperforming fully supervised learning in tasks like prostate cancer diagnosis in bpMRI [33].
Experimental Protocols and Performance Benchmarks
Implementation for Cancer Biomarker Discovery
The following protocol outlines the steps for developing a foundation model for cancer imaging biomarkers using SimCLR, based on successful implementations [4].
- Data Curation: Assemble a large, diverse dataset of unlabeled medical images. For a general cancer imaging model, this should include lesions from multiple anatomical sites (e.g., lung nodules, breast lesions, liver cysts) and imaging modalities (CT, MRI) [4]. A study training a foundation model used 11,467 annotated CT lesions from 2,312 patients [4].
- Self-Supervised Pre-training: Train a convolutional encoder (e.g., ResNet-50) using the SimCLR objective on the curated unlabeled dataset. Use a composition of medically relevant augmentations (e.g., random cropping, rotation, blurring, noise addition, and counterfactual generation [31]).
- Downstream Task Fine-tuning: For a specific biomarker task (e.g., malignancy classification, prognosis prediction), the pre-trained model can be used in two ways:
- Feature Extraction: Attach a linear classifier on top of the frozen pre-trained encoder and train only the classifier.
- Full Fine-tuning: Initialize the task-specific model with the pre-trained weights and fine-tune all parameters end-to-end on the labeled downstream dataset.
- Evaluation: Rigorously evaluate the model on held-out test sets, including external datasets to assess generalizability. Performance should be compared against supervised baselines and other pre-training methods.
Table 1: Performance Comparison of SimCLR-based Models on Medical Imaging Tasks
| Task | Dataset | Model | Performance | Comparison (Supervised Baseline) | Key Finding |
|---|---|---|---|---|---|
| Anatomical Site Classification | 11,467 CT Lesions [4] | SimCLR (Modified) | Balanced Accuracy: 0.78, mAP: 0.85 [4] | Superior to supervised and other SSL methods (P < 0.001) [4] | Robust performance with only 10% of training data [4] |
| Lung Nodule Malignancy | LUNA16 [4] | Foundation (Fine-tuned) | AUC: 0.94, mAP: 0.95 [4] | Significant superiority (P < 0.01) over most supervised baselines [4] | Effective for out-of-distribution tasks [4] |
| 3D Brain MRI Analysis | 11 Datasets (44,958 scans) [34] | 3D Neuro-SimCLR | Superior on 4 downstream tasks (In & Out-of-Distribution) [34] | Outperformed supervised and MAE baselines [34] | Achieved superior performance with only 20% of labels for Alzheimer's prediction [34] |
| Prostate Cancer Diagnosis (bpMRI) | 1,622 studies [33] | SSL-MIL | AUC: 0.82 [33] | Outperformed fully supervised baseline (AUC: 0.75, p=0.017) [33] | More data-efficient; attention aligned with lesion locations [33] |
| Cervical Cancer Classification | Cervical Cell Images [32] | SimCLR + HKHO | Accuracy: 97.63% [32] | Outperformed state-of-the-art methods [32] | Hybrid optimization effectively selected discriminative features [32] |
Comparative Analysis with Other Paradigms
SimCLR's performance must be contextualized against other learning strategies. A 2025 comparative analysis on small, imbalanced medical datasets found that while SSL can outperform supervised learning (SL) with large-scale pre-training, SL can sometimes surpass SSL when the downstream training sets are very small and no external data is used [35]. This underscores that the advantage of SSL is most pronounced when its pre-training scale and domain specificity are leveraged. Furthermore, when compared to other SSL architectures like Masked Autoencoders (MAE) for 3D brain MRI, a SimCLR-based model demonstrated superior performance across multiple classification tasks [34].
Table 2: Comparison of Self-Supervised Learning Paradigms in Medical Imaging
| SSL Method | Core Mechanism | Medical Imaging Applications | Advantages | Considerations |
|---|---|---|---|---|
| SimCLR & Variants | Contrastive learning via image augmentations. | Broad: CT, MRI, X-ray, histology [34] [4] [32]. | Simple framework; strong empirical results; effective with domain-specific augmentations [31] [30]. | Requires large batch sizes; performance depends on quality of augmentations. |
| Counterfactual Contrastive | Contrastive learning with generative counterfactual positive pairs. | Chest X-ray, mammography [31]. | Highly robust to acquisition shifts; improves fairness. | Requires training or access to a generative model. |
| Masked Autoencoders (MAE) | Reconstructs randomly masked patches of the input image. | 3D Brain MRI [34]. | Scalable to Vision Transformers (ViTs); high reconstruction quality. | May focus more on low-level texture than high-level semantics. |
| DINO-v2 | Self-distillation with noise-free labels using vision transformers. | Chest X-ray, brain MRI [36]. | Strong performance; generates semantically rich features. | Primarily based on ViT, which may be less intuitive for some medical domains. |
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Resources for Implementing SimCLR in Medical Imaging Research
| Resource Category | Example / Tool | Function and Application Note |
|---|---|---|
| Deep Learning Framework | PyTorch, TensorFlow | Provides the flexible backend for implementing the SimCLR model, data loaders, and training loops. |
| Compute Infrastructure | NVIDIA GPUs (e.g., A100, V100) with 16GB+ VRAM | Accelerates training of deep models on large 3D medical images. Large batch sizes benefit SimCLR performance [30]. |
| Data Augmentation Libraries | TorchIO, MONAI | Domain-specific libraries for 3D medical image transformations (e.g., elastic deformation, gamma correction, MRI bias field simulation). |
| Counterfactual Generation Model | Hierarchical VAE (e.g., from [31]) | Generates realistic positive pairs for contrastive learning by simulating domain shifts (e.g., scanner differences), improving robustness [31]. |
| Pre-trained Foundation Models | 3D-Neuro-SimCLR [34], Cancer Imaging Foundation Model [4] | Publicly released models that can be used as off-the-shelf feature extractors or fine-tuned for specific downstream tasks, reducing computational cost. |
| Optimization & Feature Selection | Hybrid Krill Herd Optimization (HKHO) [32] | A bio-inspired optimization algorithm used post-pre-training to select the most discriminative features for a specific classification task. |
SimCLR and its evolving variants represent a powerful and flexible framework for building foundation models for cancer imaging biomarker discovery. By moving beyond generic implementations to incorporate domain-specific adaptations—such as counterfactual pair generation, hybrid feature optimization, and integration with MIL—researchers can learn highly robust and generalizable representations from unlabeled data. The experimental evidence across multiple cancer types and imaging modalities consistently shows that these models not only match but often surpass supervised baselines, particularly in data-scarce scenarios and on out-of-distribution tests. As the field progresses, the fusion of realistic generative models with contrastive objectives promises to further enhance the robustness and clinical applicability of AI-derived cancer imaging biomarkers.
Foundation models, characterized by their training on vast amounts of unannotated data through self-supervised learning (SSL), represent a paradigm shift in deep learning for healthcare [37] [4]. In the domain of cancer imaging biomarker discovery, these models excel in reducing the demand for large labeled datasets, a common bottleneck in medical research [4] [38]. The implementation of these foundation models typically follows two primary pathways: feature extraction and end-to-end fine-tuning. The choice between these strategies is critical and depends on factors such as dataset size, computational resources, and the specific clinical task at hand. This guide provides a detailed technical examination of these pathways, framing them within experimental protocols and quantitative findings from recent cancer imaging research.
Core Concepts and Definitions
Feature Extraction
In this transfer learning strategy, a pre-trained foundation model is used as a fixed feature extractor [39]. The learned representations (weights) of the pre-trained model are frozen and not updated during training on the new task. A new, typically simple, classifier (e.g., a linear layer) is then trained from scratch on top of these extracted features to make predictions for the downstream task [39].
End-to-End Fine-Tuning
This approach also leverages a pre-trained model but allows for the modification of its weights to adapt to the new data [39]. In fine-tuning, some or all the layers of the pre-trained model are "unfrozen," enabling their parameters to be updated during training on the downstream task. This process often employs a lower learning rate to prevent catastrophic forgetting of the valuable features learned during pre-training [39].
The Role of Foundation Models
In cancer imaging, a foundation model is typically a convolutional encoder trained via self-supervised learning on a large corpus of unlabeled medical images, such as computed tomography (CT) scans of radiographic lesions [37] [4]. This pre-training equips the model with a generalized, task-agnostic understanding of medical image features, serving as a powerful starting point for various downstream clinical applications like diagnostic and prognostic biomarker discovery [4].
Quantitative Comparison of Implementation Pathways
The performance and applicability of feature extraction versus fine-tuning are highly dependent on the context of the downstream task. The following tables summarize key comparative data derived from experiments in cancer imaging.
Table 1: Performance comparison on an in-distribution task (Lesion Anatomical Site Classification) [4].
| Implementation Method | Balanced Accuracy (100% Data) | Mean Average Precision (100% Data) | Performance with Limited Data |
|---|---|---|---|
| Feature Extraction | 0.779 (95% CI 0.749–0.809) | 0.847 (95% CI 0.750–0.810) | Robust; smallest decline (9%) when data reduced to 10% |
| End-to-End Fine-Tuning | 0.804 (95% CI 0.773–0.834) | 0.856 (95% CI 0.828–0.886) | Larger performance drop; loses significance with ≤20% data |
| Supervised (from scratch) | 0.72 (95% CI 0.689–0.750) | 0.818 (95% CI 0.779–0.847) | Performance degrades significantly with less data |
Table 2: Performance comparison on an out-of-distribution task (Nodule Malignancy Prediction) [37] [4].
| Implementation Method | AUC | Mean Average Precision | Performance at 10% Data |
|---|---|---|---|
| Feature Extraction | Not Specified | Not Specified | Remained stable and significantly outperformed other models |
| End-to-End Fine-Tuning | 0.944 (95% CI 0.914–0.982) | 0.952 (95% CI 0.926–0.986) | Did not show significant improvement |
| Fine-Tuned Supervised Model | 0.857 (95% CI 0.806–0.918) | 0.874 (95% CI 0.822–0.936) | Performance degraded with less data |
Table 3: Strategic advantages and disadvantages of each pathway [39].
| Criterion | Feature Extraction | End-to-End Fine-Tuning |
|---|---|---|
| Required Data Size | Effective with smaller datasets [4] | Requires a larger dataset to prevent overfitting |
| Computational Cost | Lower; faster training | Higher; longer training, more resources |
| Risk of Overfitting | Reduced (fewer trainable parameters) | Increased |
| Adaptability | Limited; cannot adjust pre-trained features | High; adjusts features to fit new data |
| Best Use Case | Small datasets, tasks similar to pre-training, establishing a baseline | Large datasets, tasks differing from pre-training, maximizing performance |
Experimental Protocols in Cancer Imaging
To ensure reproducible and robust results, following a structured experimental protocol is essential. Below are detailed methodologies for implementing and evaluating both pathways, based on published research.
Protocol for Feature Extraction
This protocol is ideal for tasks with limited labeled data or for initial model validation [4].
- Model Loading: Begin by loading the weights of a foundation model pre-trained on a large-scale medical imaging dataset (e.g., a model trained on 11,467 CT lesions via contrastive SSL [4]).
- Freezing Weights: Set the
trainableparameter of the entire pre-trained base model toFalse. This ensures no gradients are computed, and the weights remain fixed during training. - Classifier Attachment: Remove the original output layer of the foundation model and attach a new, randomly initialized classification head. This often consists of a global average pooling layer followed by one or more fully connected (Dense) layers, culminating in an output layer with nodes corresponding to the number of classes in the downstream task.
- Model Compilation: Compile the new model with an appropriate optimizer (e.g., Adam) and loss function (e.g., categorical cross-entropy).
- Training: Train only the newly added classification layers on the target dataset. The foundation model acts solely as a feature extractor.
Protocol for End-to-End Fine-Tuning
This protocol is used when the goal is to achieve the highest possible performance and sufficient data is available.
- Initial Feature Extraction: It is often beneficial to first train a model using the feature extraction protocol to stabilize the training process and initialize the new classifier with sensible weights.
- Unfreezing Layers: After the classifier is trained, unfreeze a portion of the base model's layers. A common strategy is to only unfreeze and fine-tune the last few convolutional blocks of the foundation model, as these layers capture more task-specific features compared to the earlier, more general layers [39].
- Re-compilation: Re-compile the model with a significantly lower learning rate (e.g., 1e-5) than that used for feature extraction. This is critical to making small, precise updates to the pre-trained weights without distorting the previously learned features [39].
- Joint Training: Continue training the model, now updating the weights of both the unfrozen base model layers and the classification head.
Evaluation Framework
A comprehensive evaluation should extend beyond simple accuracy metrics [37] [4].
- Performance Metrics: Use metrics like Balanced Accuracy (BA), Area Under the Receiver Operating Characteristic Curve (AUC), and Mean Average Precision (mAP) on a held-out test set.
- Data Efficiency: Evaluate model performance across progressively smaller subsets of the training data (e.g., 100%, 50%, 10%) to assess robustness in limited-data scenarios [37] [4].
- Stability Analysis: Assess model performance against input variations (test-retest) and inter-reader segmentation differences to ensure clinical reliability [4].
- Biological Validation: For biomarker discovery, correlate model outputs or extracted features with underlying biological data, such as gene expression patterns, to ensure the imaging biomarkers capture relevant biology [4] [5].
Decision Framework and Experimental Workflow
The following diagram visualizes the key decision points and workflows for selecting and executing the appropriate implementation pathway.
The Scientist's Toolkit: Essential Research Reagents
The following table details key computational tools and data resources essential for implementing the described pathways in cancer imaging biomarker research.
Table 4: Key research reagents and resources for foundation model implementation.
| Item | Function & Description | Example in Cancer Imaging Research |
|---|---|---|
| Pre-trained Foundation Model | A model providing generalized image representations; the starting point for transfer learning. | A convolutional encoder pre-trained via contrastive SSL on 11,467 diverse CT lesions [37] [4]. |
| Curated Labeled Dataset | A task-specific dataset for downstream training and evaluation. | The LUNA16 dataset of lung nodules for malignancy prediction [37] [4]. |
| Self-Supervised Learning (SSL) Framework | Algorithms for pre-training models without manual labels. | Modified SimCLR (contrastive learning) for pre-training on lesion images [4]. |
| Parameter-Efficient Fine-Tuning (PEFT) | Lightweight fine-tuning methods that update a small subset of parameters. | Low-Rank Adaptation (LoRA) can be explored to fine-tune large models efficiently [40]. |
| Explainable AI (XAI) Framework | Tools to interpret model decisions and build trust. | Deep-learning attribution methods to interpret features and link them to biology [4] [5]. |
| High-Performance Computing (GPU) | Essential computational resource for training and fine-tuning deep models. | Access to GPU clusters for handling large-scale medical images and deep learning workflows [41]. |
The integration of artificial intelligence (AI), particularly foundation models, is revolutionizing the development of diagnostic biomarkers for lung nodule malignancy. Lung cancer remains a leading cause of cancer-related mortality globally, with patient prognosis critically dependent on early and accurate diagnosis [42] [43]. The challenge of differentiating benign from malignant pulmonary nodules, especially indeterminate pulmonary nodules (IPNs), represents a significant clinical hurdle, as current methods often yield high false-positive rates and unnecessary invasive procedures [44] [45]. Foundation models, characterized by their training on vast, unlabeled datasets using self-supervised learning (SSL), are emerging as a powerful paradigm. They facilitate more robust and data-efficient learning for downstream tasks, such as malignancy prediction, especially in scenarios with limited labeled data—a common challenge in medical imaging [4] [10]. This technical guide examines the evolution and current state of diagnostic biomarkers for lung nodule malignancy, framing the discussion within the transformative potential of foundation models for cancer imaging biomarker discovery.
From Classical Models to AI-Driven Biomarkers
Classical Clinical-Imaging Predictive Models
The development of risk assessment models for pulmonary nodules has evolved from statistical frameworks based on clinical and radiological features. These classical models provide a foundational benchmark against which modern AI approaches are measured.
Table 1: Classical Predictive Models for Pulmonary Nodule Malignancy
| Model Name | Key Predictors | Study Population | Reported Performance (AUC) | Notable Limitations |
|---|---|---|---|---|
| Mayo Clinic Model [45] | Age, smoking history, cancer history, nodule diameter, spiculation, upper lobe location | 629 patients (US, 1984-1986); malignancy rate: 23% | Development: 0.83; Validation: 0.80 [45] | Dated cohort; limited performance in Chinese population (AUC=0.653) [45] |
| VA Model [45] | Smoking duration, age, nodule diameter, time since smoking cessation | 375 male veterans (US); malignancy rate: 54% | 0.79 [45] | Focused on elderly males; nodules measured by X-ray [45] |
| Brock University (PanCan) Model [45] | Gender, nodule diameter, spiculation, superior lobe location | Training: 1,871 participants (PanCan); Validation: 1,090 participants (BCCA) | Not specified in results | Developed in low malignancy incidence cohorts (3.7-5.5%) [45] |
The Radiomics and Machine Learning Paradigm
The advent of radiomics—the high-throughput extraction of quantitative features from medical images—significantly advanced the field. This approach posits that medical images contain data imperceptible to the human eye that can be mined to reveal disease characteristics [42] [44].
Key Experimental Protocol in Radiomics: A seminal study on the National Lung Screening Trial (NLST) data exemplifies the radiomics methodology [44]:
- Data Curation: A subset of 479 participants (244 training, 235 testing) from the NLST was curated, including incident lung cancers and nodule-positive controls.
- Image Segmentation & Feature Extraction: Nodules were segmented in 3D, and 219 quantitative features were extracted. These were categorized into:
- C1: Size and Shape (e.g., volume, sphericity)
- C2: Location and Context (e.g., border to lung, relative volume airspace)
- C3: Texture (e.g., wavelet-based features, co-occurrence matrices)
- Feature Selection & Model Building: An exhaustive search identified optimal, non-redundant 4-feature sets. Linear classifiers were constructed and validated on the independent test set.
Findings: The study demonstrated that non-size-based radiomic features (C2) achieved an AUROC of 0.85 in the training cohort and 0.88 in the test set, outperforming models based solely on size and shape (AUROC 0.80 train, 0.86 test) [44]. This underscored that malignancy risk is encoded in texture and context, not just size.
The Emergence of Deep Learning and Foundation Models
Deep learning (DL), particularly convolutional neural networks (CNNs), further advanced the field by automatically learning hierarchical feature representations directly from images, moving beyond handcrafted radiomic features [42] [43]. Foundation models represent the next evolutionary step, trained on vast, diverse datasets via SSL to serve as a base for various downstream tasks with minimal task-specific data [4].
Experimental Protocol for a Cancer Imaging Foundation Model: A landmark study by Pai et al. (2024) detailed the development and validation of such a model [4] [11] [10].
- Pretraining Data: A foundation model (a convolutional encoder) was pretrained using a modified SimCLR contrastive SSL strategy on a comprehensive dataset of 11,467 diverse radiographic lesions from 2,312 unique patients (DeepLesion dataset) [4] [11].
- Downstream Task Application: The model was evaluated on three distinct use cases:
- Technical Validation: Lesion anatomical site classification (in-distribution task).
- Diagnostic Biomarker: Predicting malignancy of lung nodules in the LUNA16 dataset (out-of-distribution task).
- Prognostic Biomarker: Predicting survival in non-small cell lung cancer (NSCLC).
- Implementation Approaches: For each downstream task, two implementation methods were compared:
- Feature Extraction: Using the pretrained foundation model as a fixed feature extractor, with a linear classifier trained on top.
- Fine-Tuning: Updating the weights of the entire foundation model for the specific task (transfer learning).
The following diagram illustrates this foundational model's workflow and its application to downstream tasks like lung nodule malignancy prediction.
Findings for Malignancy Prediction (Use Case 2): For the task of predicting lung nodule malignancy on the LUNA16 dataset, the fine-tuned foundation model (Foundation (fine-tuned)) achieved an AUC of 0.944, significantly outperforming most baseline supervised and pretrained models. This demonstrates the model's efficacy as a powerful diagnostic biomarker [4].
Comparative Performance of Diagnostic Biomarkers
The performance of AI-driven biomarkers, particularly those leveraging foundation models, shows marked improvement over traditional approaches, especially in challenging, data-limited scenarios.
Table 2: Comparative Performance of AI-Based Diagnostic Biomarkers for Lung Nodule Malignancy
| Model / Approach | Data Modality | Dataset Details | Performance (AUC) | Key Advantage |
|---|---|---|---|---|
| Radiomics Linear Classifier [44] | CT | NLST subset; 479 participants | 0.88 (Test Set) | Uses handcrafted, interpretable non-size features |
| Deep Learning (Google) [43] | CT | 6,716 NLST cases | 0.944 | Analyzes current and prior CTs; outperformed 6 radiologists |
| Ensemble GBDT Model [46] | Clinical & CT Features | 830 patients (internal), 330 (external test) | Internal: 0.873; External: 0.726 | Integrates clinical and imaging features |
| Foundation Model (Fine-tuned) [4] | CT | LUNA16 dataset; 507 nodules (train), 170 (test) | 0.944 | Superior generalizability and data efficiency |
| Foundation Model (Features) [4] | CT | LUNA16 dataset | ~0.92 (estimated from graph) | Fast, computationally efficient; strong with linear classifier |
The stability of foundation models is a critical asset. The same study reported that these models demonstrated greater robustness to input variations and stronger associations with underlying biology, particularly immune-related pathways, enhancing their value as trustworthy biomarkers [4] [10].
The Scientist's Toolkit: Research Reagent Solutions
For researchers aiming to replicate or build upon these methodologies, the following table details key resources and their functions.
Table 3: Essential Research Reagents and Resources for Imaging Biomarker Development
| Resource / Reagent | Type | Function in Research | Example / Source |
|---|---|---|---|
| Annotated Public Datasets | Data | Training, validation, and benchmarking of models | DeepLesion [4], LUNA16 [4], NLST [44], LUNG1, RADIOMICS [11] |
| Foundation Model Weights | Software | Transfer learning and feature extraction for new tasks; reduces need for large labeled sets | Pretrained model from Pai et al. (available via pip package) [11] |
| Computational Framework | Software | Standardizes and simplifies training, inference, and evaluation pipelines | Project-lighter (YAML configuration) [11], MHub.ai platform [11] |
| SSL Pre-training Algorithm | Algorithm | Enables model to learn generalizable representations from unlabeled data | Modified SimCLR, SwAV, NNCLR [4] |
| Model Interpretation Tool | Software | Provides explainability by identifying image regions influential to predictions | Deep-learning attribution methods (e.g., Saliency maps) [4] [12] |
The workflow for developing a diagnostic biomarker using a foundation model, from data preparation to clinical application, involves multiple critical stages as shown in the diagram below.
The journey of diagnostic biomarkers for lung nodule malignancy from classical statistical models to AI-driven foundation models marks a paradigm shift in cancer imaging. Foundation models, pretrained on vast datasets through self-supervised learning, address the critical bottleneck of labeled data scarcity in medicine. They enable the development of highly accurate, robust, and data-efficient biomarkers for malignancy prediction, as evidenced by state-of-the-art performance on benchmark datasets [4]. The demonstrated stability of these models and their association with underlying biology further bolster their potential for clinical translation [10]. Future work must focus on multi-center prospective validation, standardization of imaging protocols to mitigate model bias, and the development of secure, scalable systems to integrate these powerful tools into routine clinical workflows, ultimately paving the way for personalized and early diagnosis of lung cancer.
The management of non-small cell lung cancer (NSCLC) has been revolutionized by precision medicine, wherein prognostic biomarkers play a critical role in stratifying patients, guiding therapeutic decisions, and predicting disease outcomes. Prognostic biomarkers provide insights into the likely course of cancer independent of therapeutic interventions, distinguishing them from predictive biomarkers that forecast response to specific treatments [5]. The evolving landscape of NSCLC treatment, marked by the integration of targeted therapies and immunotherapies, has heightened the need for robust biomarkers that can enhance prognostic accuracy [47] [48]. Traditional factors such as tumor stage, histological subtype, and patient performance status remain foundational; however, advances in molecular profiling, radiomics, and artificial intelligence (AI) are enabling the development of multi-parameter biomarkers with superior prognostic performance.
The emergence of foundation models in medical imaging represents a transformative advancement for cancer imaging biomarker discovery. These large-scale AI models, pretrained on vast datasets through self-supervised learning, facilitate more accurate and efficient identification of prognostic patterns from conventional imaging like computed tomography (CT) [4] [10]. This technical guide explores current prognostic biomarkers in NSCLC, with a specific focus on the integration of multiomic approaches and foundation models to refine prognostic assessment, providing methodologies and resources to support research and clinical translation.
Current Prognostic Biomarkers in Clinical Practice
Prognostic assessment in NSCLC routinely incorporates clinical, pathological, molecular, and inflammatory biomarkers. The table below summarizes key biomarkers and their prognostic utility.
Table 1: Established and Emerging Prognostic Biomarkers in NSCLC
| Biomarker Category | Specific Biomarker | Prognostic Significance | Clinical Application Context |
|---|---|---|---|
| Clinical/Pathological | Oligometastatic Disease (≤5 lesions) | Improved median OS (25.9 vs 18.7 months; HR 0.60, p<0.001) [49] | Patient selection for aggressive local therapy |
| Molecular | KRAS mutations | Increased 3-month mortality (23.5% vs 17.7%) [50] | General prognostic stratification |
| Molecular | EGFR mutations | More frequent in polymetastatic disease (33.1% vs 21.4%) [49] | More common in never-smokers; associated with metastasis pattern |
| Molecular | PI3K pathway alterations | Higher incidence in oligometastatic disease (24.3% vs 14.7%) [49] | Defines a distinct biological subtype with limited metastatic spread |
| Inflammatory | Neutrophil-to-Lymphocyte Ratio (NLR) | Higher levels correlate with poorer overall survival [51] | Easily derived from routine complete blood count |
| Inflammatory | Systemic Immune-inflammation Index (SII) | Higher levels correlate with poorer overall survival [51] | Composite index reflecting neutrophil, platelet, and lymphocyte counts |
| Tumor Burden | Longest Tumor Diameter at Baseline | Incorporated into multiomic prognostic models [50] | Standard radiological measurement |
| Tumor Biology | PD-L1 Expression | Imperfect predictor; 40-50% response in high-PD-L1 tumors to anti-PD-1 [50] | Primarily predictive, but associated with overall prognosis |
Molecular profiling has uncovered distinct genomic landscapes associated with metastatic patterns. Oligometastatic disease (≤5 metastases), which carries a better prognosis, is genetically distinct from polymetastatic disease. Oligometastatic NSCLC shows enrichment for alterations in the PI3K pathway and LRP1B, while polymetastatic disease is associated with higher incidence of EGFR and ALK alterations [49]. Pathway analysis further reveals that polymetastatic tumors are enriched for biological processes related to motility and epithelial-mesenchymal transition, including WNT and TGFB signaling [49].
Inflammatory biomarkers, derived from routine complete blood counts, provide accessible prognostic information. These include the Neutrophil-to-Lymphocyte Ratio (NLR), Platelet-to-Lymphocyte Ratio (PLR), Monocyte-to-Lymphocyte Ratio (MLR), Systemic Immune-inflammation Index (SII), and Systemic Inflammation Response Index (SIRI). In studies excluding the indolent adenocarcinoma in situ (AIS) to avoid confounding, elevated levels of these biomarkers consistently correlate with significantly poorer long-term overall survival [51]. However, multivariate analyses indicate that while these biomarkers hold short-term prognostic value, traditional factors like age, tumor stage, and differentiation often remain independent predictors of long-term outcome [51].
Foundation Models for Imaging Biomarker Discovery
Concept and Workflow
Foundation models are large deep learning models trained on extensive, broad datasets using self-supervised learning (SSL). This approach allows the model to learn generalizable, task-agnostic representations from data without the need for manual annotations. In medical imaging, once a foundation model is pretrained, it can be adapted to specific downstream tasks with limited labeled data, addressing a significant bottleneck in biomedical AI research [4] [11].
Diagram: Workflow for Developing and Applying an Imaging Foundation Model
Technical Validation and Performance
One foundation model for cancer imaging was pretrained on a diverse dataset of 11,467 annotated lesions from CT scans from 2,312 unique patients [4] [11]. Its performance was validated across several tasks. In a technical validation task (lesion anatomical site classification), the model achieved a balanced accuracy of 0.804 and mean average precision (mAP) of 0.857, significantly outperforming baseline methods [4]. For a prognostic task in NSCLC, the foundation model, when used as a feature extractor, demonstrated superior performance, especially in limited-data scenarios that are typical in biomarker development [4].
These models show remarkable stability to input variations and their derived patterns demonstrate strong associations with underlying biology, particularly immune-related pathways, suggesting they capture biologically relevant tumor phenotypes [10].
Multiomic Integration for Enhanced Prognostication
Methodology and Model Architecture
A multiomic approach integrates data from multiple sources to create a more comprehensive prognostic signature. One developed methodology combines radiomic, radiological, pathological, and clinical variables into a single prognostic model [50].
The process involves:
- Radiomic Feature Extraction: Using standardized software (e.g., Cancer Phenomics Toolkit - CapTk) to extract high-dimensional features from baseline CT imaging.
- Data Harmonization: Applying a nested ComBat technique to mitigate heterogeneity from different image acquisition parameters.
- Radiomic Phenotyping: Using unsupervised hierarchical clustering on radiomic features to identify distinct phenotypic signatures.
- Graph-Based Multiomic Integration: Constructing a novel multiomic graph by combining constituent graphs built from radiomic, radiological (SUVmax, tumor diameter), and pathological (PD-L1, STK11, KRAS) data. The edges in this graph represent patient similarities based on each data modality.
- Final Model Combination: The multiomic phenotypes identified from the graph are then integrated with clinical variables (e.g., smoking status, BMI) into a final prognostic model [50].
Diagram: Multiomic Biomarker Development Workflow
Comparative Performance of Multiomic Models
The prognostic performance of a multiomic graph clinical model was evaluated for predicting progression-free survival (PFS) in advanced NSCLC patients treated with first-line immunotherapy.
Table 2: Performance Comparison of Prognostic Models for PFS
| Prognostic Model | C-statistic (95% CI) | Akaike Information Criterion (AIC) |
|---|---|---|
| Clinical Model | 0.58 (0.52–0.61) [50] | 1289.6 [50] |
| Combination Clinical Model | 0.68 (0.58–0.69) [50] | 1284.1 [50] |
| Multiomic Graph Clinical Model | 0.71 (0.61–0.72) [50] | 1278.4 [50] |
The multiomic graph clinical model demonstrated the best prognostic performance, evidenced by the highest c-statistic and the lowest AIC value, indicating a superior fit to the data compared to a model built by simple concatenation of variables or a clinical-only model [50]. This underscores the value of sophisticated integration methods for multi-source data.
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Resources for NSCLC Prognostic Biomarker Research
| Resource / Reagent | Function / Application | Example / Specification |
|---|---|---|
| Foundation Model Weights | Pretrained model for feature extraction or fine-tuning on imaging data. Enables research with limited datasets. | Publicly available via pip package and code repository [11]. |
| Standardized Radiomics Software | Extracts reproducible, IBSI-compliant radiomic features from medical images. | Cancer Phenomics Toolkit (CapTk) [50]. |
| Nested ComBat Harmonization | Algorithm for mitigating batch effects and technical variation in multi-site radiomic studies. | Corrects for multiple scanner and acquisition parameters [50]. |
| Graph-Based Integration Tools | Computational methods for integrating multiple data types (e.g., radiomics, pathology) into a unified model. | Custom scripts for constructing multiomic graphs [50]. |
| Curated Public Datasets | Benchmark datasets for training and validating prognostic models. | DeepLesion, LUNA16, LUNG1, RADIO [11]. |
| Containerized Implementation | Ensures reproducible deployment and easy application of complex models in diverse research environments. | Available through MHub.ai platform and 3D Slicer integration [11]. |
Experimental Protocols for Key Methodologies
Protocol 1: Self-Supervised Pretraining of a Foundation Model
This protocol outlines the procedure for pretraining a foundation model for cancer imaging, as described in [4].
- Data Curation: Assemble a large, diverse dataset of radiographic findings. The foundational study used 11,467 annotated lesions (including lung nodules, cysts, etc.) from CT scans of 2,312 patients.
- Preprocessing: Standardize all input images. This typically involves resampling to a uniform voxel spacing, intensity normalization, and cropping volumes of interest around the lesions.
- Self-Supervised Pretraining: Train a convolutional encoder using a contrastive self-supervised learning strategy. The specific method used was a modified version of SimCLR.
- Augmentation: Generate multiple augmented views for each training image through random transformations (e.g., cropping, rotation, blurring, noise addition).
- Contrastive Loss: The model is trained to maximize the similarity between representations of different augmented views of the same image (positive pairs) while minimizing the similarity with views from different images (negative pairs).
- Model Output: The final output is a pretrained foundation model that can serve as a generic feature extractor for various downstream prognostic tasks.
Protocol 2: Developing and Validating a Multiomic Prognostic Model
This protocol details the steps for creating a multiomic biomarker for PFS, based on [50].
Cohort Definition:
- Identify a retrospective cohort of stage IV NSCLC patients (e.g., n=243) uniformly treated with first-line anti-PD-1/PD-L1 therapy.
- Ensure availability of baseline contrast-enhanced CT scans, radiological measurements (SUVmax, longest tumor diameter), pathological data (PD-L1, KRAS, STK11 status), and clinical variables (smoking status, BMI).
Radiomic Processing:
- Segmentation: Manually or semi-automatically segment the primary tumor volumes on baseline CT scans.
- Feature Extraction: Use standardized software (e.g., CapTk) to extract a comprehensive set of radiomic features (shape, intensity, texture) from each segmentation, complying with the IBSI guidelines.
- Harmonization: Apply nested ComBat harmonization to correct for inter-scanner and acquisition protocol variability.
Phenotype Identification:
- Perform unsupervised hierarchical clustering on the harmonized radiomic features to identify significant radiomic phenotypes.
- Construct a multiomic graph where patients are nodes. Connect patients based on similarity within each data layer (radiomics, radiology, pathology), then combine these layers into a single graph.
- Identify distinct multiomic phenotypes from this integrated graph.
Model Building and Validation:
- Integrate the multiomic phenotypes with key clinical variables into a Cox proportional-hazards model for PFS.
- Evaluate model performance using the concordance index (C-statistic) and compare it against simpler models (e.g., clinical-only or simply concatenated models) using Akaike Information Criterion (AIC).
- Perform internal validation via bootstrapping or cross-validation to assess robustness.
The field of prognostic biomarkers in NSCLC is rapidly advancing beyond single-modality approaches. The integration of radiomics, pathological data, and clinical variables into multiomic models has demonstrated superior prognostic performance over traditional models [50]. Furthermore, the emergence of foundation models presents a paradigm shift, enabling the discovery of robust, biologically associated imaging biomarkers even in data-limited settings [4] [10]. These AI-driven approaches show tremendous potential for translation into clinical practice, promising to enhance patient stratification, refine prognostication, and ultimately personalize management strategies in NSCLC. Future efforts should focus on the external validation of these models and their integration into prospective clinical trials to firmly establish their utility in improving patient outcomes.
Within the paradigm of foundation model development for cancer imaging biomarker discovery, technical validation on in-distribution tasks is a critical first step. It establishes that the model has learned generalized, transferable representations from its vast pre-training dataset before being applied to downstream clinical problems. The task of anatomical site classification—categorizing a radiographic lesion by its location in the body—serves as a robust and necessary benchmark for this purpose. A foundation model's proficiency in this task demonstrates its fundamental understanding of medical image anatomy, paving the way for its reliable application in diagnostic and prognostic biomarker development [4] [11].
This guide details the methodologies, performance benchmarks, and implementation protocols for using anatomical site classification as a technical validation step for a cancer imaging foundation model, providing a framework for researchers and drug development professionals to evaluate model readiness.
The Role of Anatomical Site Classification in Model Validation
Technical validation ensures a foundation model has effectively encoded relevant features from its pre-training data without overfitting to specific, narrow tasks. Anatomical site classification is exceptionally well-suited for this role for several reasons. First, it is an "in-distribution" task when the foundation model is pre-trained on a broad dataset of radiographic lesions, meaning the validation data is drawn from the same population as the pre-training data [4]. This allows researchers to directly assess what the model has learned from its initial training.
Second, the anatomical context of a lesion is a fundamental piece of information that often correlates with pathology and is crucial for accurate diagnosis and treatment planning. A model that can accurately identify anatomical location has demonstrably learned meaningful visual features representative of different human anatomies [52] [53]. This capability is a prerequisite for more complex tasks, such as distinguishing between benign and malignant lesions or predicting patient outcomes, where anatomical context can be a decisive factor [4] [54].
Foundation Model Pre-training and Validation Strategy
Foundation Model Pre-training
The foundational step involves self-supervised learning (SSL) on a large, diverse dataset of unannotated medical images. The core objective is to train a convolutional encoder to learn generalized, task-agnostic representations of radiographic lesions.
- Dataset: A comprehensive dataset, such as the one used in the study by Pai et al., comprising 11,467 annotated radiographic lesions from computed tomography (CT) scans of 2,312 unique patients. The lesions should be diverse, including lung nodules, cysts, and breast lesions, among others [4] [11].
- Pre-training Strategy: A contrastive SSL strategy, such as a modified version of SimCLR, has been shown to outperform other methods like auto-encoders, SwAV, and NNCLR. This approach learns by maximizing agreement between differently augmented views of the same image while distinguishing them from other images in the dataset [4].
- Output: A pre-trained foundation model (convolutional encoder) that can serve as a feature extractor or a starting point for transfer learning on a wide range of downstream tasks [4] [11].
Technical Validation via Anatomical Site Classification
Once pre-trained, the model is validated on the task of anatomical site classification. The workflow for this validation is outlined below.
Experimental Protocol and Performance Benchmarking
Experimental Setup for Validation
To quantitatively validate the foundation model, a structured experiment on a dataset of lesions with known anatomical sites is required.
- Dataset for Validation: The study by Pai et al. used a dataset of 3,830 lesions for training and tuning, with a separate held-out test set of 1,221 lesions. The sites should cover multiple anatomical regions [4].
- Benchmarking Models: The foundation model's performance should be compared against relevant baselines:
- Supervised: A model trained from scratch with supervised learning on the classification task.
- Other Pre-trained Models: Models initialized with weights from other public medical imaging pre-training efforts (e.g., Med3D, Models Genesis) [4].
- Implementation Modes: Two primary methods for applying the foundation model:
- Feature Extraction: The foundation model's weights are frozen, and it acts as a fixed feature extractor. A simple linear classifier (e.g., a linear layer) is then trained on top of these extracted features.
- Fine-Tuning: The entire foundation model, or a majority of its layers, is unfrozen and fine-tuned end-to-end on the anatomical site classification task alongside a new classifier head [4].
- Evaluation Metrics: Performance is evaluated using Balanced Accuracy (to account for class imbalance) and mean Average Precision (mAP) [4].
Quantitative Performance Benchmarks
The following tables summarize the expected performance outcomes based on the cited research, providing a benchmark for successful technical validation.
Table 1: Overall performance comparison on the anatomical site classification test set (n=1,221 lesions).
| Model Implementation | Balanced Accuracy | Mean Average Precision (mAP) |
|---|---|---|
| Foundation (Fine-tuned) | 0.804 (0.775 - 0.835) | 0.857 (0.828 - 0.886) |
| Foundation (Features) | 0.779 (0.750 - 0.810) | 0.847 (0.819 - 0.875) |
| Med3D (Fine-tuned) | 0.791 | 0.840 |
| Supervised (from scratch) | 0.759 (0.729 - 0.789) | 0.819 (0.791 - 0.847) |
| Models Genesis (Features) | 0.699 (0.667 - 0.731) | 0.778 (0.748 - 0.808) |
Table 2: Performance in limited-data scenarios, showing the balanced accuracy of the Foundation (Features) model as training data is reduced.
| Training Data Percentage | Number of Lesions | Foundation (Features) Balanced Accuracy |
|---|---|---|
| 100% | 3,830 | 0.779 |
| 50% | 2,526 | 0.773 |
| 20% | 1,010 | 0.743 |
| 10% | 505 | 0.709 |
Interpretation of Benchmarking Results
- Superior Performance: A successfully pre-trained foundation model should achieve superior balanced accuracy and mAP compared to supervised training from scratch and other pre-training baselines. The fine-tuning approach often yields the highest absolute performance [4].
- Strength in Limited Data: A key indicator of a powerful foundation model is its performance when labeled data is scarce. As shown in Table 2, the feature extraction approach should see only a minimal drop in performance even when 90% of the training data is removed, significantly outperforming other methods in these constrained scenarios [4].
- Feature Quality: The fact that a simple linear classifier on top of frozen features performs nearly as well as a fine-tuned model indicates that the foundation model has learned rich, discriminative features that are linearly separable for anatomical site classification. This is a hallmark of a high-quality representation learner [4].
The Scientist's Toolkit: Research Reagent Solutions
The following table details key resources required to replicate this technical validation.
Table 3: Essential research reagents and computational tools for anatomical site classification experiments.
| Item | Function / Description | Example / Specification |
|---|---|---|
| Curated CT Lesion Dataset | Serves as the pre-training corpus for the foundation model. Requires expert annotation. | DeepLesion dataset; ~11,5k lesions with RECIST marks [4] [11]. |
| Annotated Anatomical Site Dataset | Used for technical validation and benchmarking. Requires pixel-level or lesion-level anatomical labels. | In-house dataset or public datasets with anatomical site labels [4] [53]. |
| Deep Learning Framework | Provides the environment for building, training, and evaluating complex models. | TensorFlow, PyTorch, Python-based libraries [53]. |
| Pre-trained Model Weights | Enables transfer learning and benchmarking against established baselines. | Model weights from Med3D, Models Genesis, or published foundation models [4]. |
| Compute Infrastructure | Supports the intensive computational demands of training large foundation models. | High-performance GPU clusters (e.g., NVIDIA Titan Xp) [53]. |
Technical validation through anatomical site classification is a critical milestone in the development of foundation models for cancer imaging. It rigorously tests the model's foundational understanding of medical image anatomy on an in-distribution task, ensuring it has learned robust and generalizable features. The demonstrated performance, particularly in data-scarce environments, provides the confidence needed to proceed with applying the model to downstream diagnostic and prognostic biomarker tasks, such as lung nodule malignancy classification or treatment outcome prediction. A model that successfully passes this validation is a potent tool, poised to accelerate the discovery and translation of imaging biomarkers into clinical and drug development pipelines.
Cancer research is increasingly driven by the integration of diverse data modalities, spanning from genomics and proteomics to medical imaging and clinical factors [55]. However, extracting actionable insights from these vast and heterogeneous datasets remains a key challenge. The rise of foundation models (FMs)—large deep-learning models pretrained on extensive amounts of data serving as a backbone for a wide range of downstream tasks—offers new avenues for discovering biomarkers, improving diagnosis, and personalizing treatment [55]. Foundation models represent a paradigm shift in deep learning wherein a single model trained on vast amounts of unannotated data can serve as the foundation for various downstream tasks [56]. In medical applications, these models are generally trained using self-supervised learning (SSL) and excel in reducing the demand for training samples in downstream applications, which is especially important in medicine where large labeled datasets are often scarce [4] [56].
The integration of multimodal data is particularly crucial for comprehensive cancer characterization. Biological variability manifests differently across domains, and integrating data from sources like clinical imaging, pathology, and next-generation sequencing (NGS) requires careful consideration to ensure that observed patterns are genuine and not artifacts of the integration process [57]. Furthermore, differences in data resolutions present significant hurdles—while imaging data might possess high spatial resolution, molecular data may operate at the genomic level. Integrating datasets with varying resolutions necessitates meticulous consideration to prevent loss of information or misinterpretation [57]. This whitepaper provides a technical framework for multimodal data integration specifically within the context of cancer imaging biomarker discovery, detailing methodologies, experimental protocols, and implementation strategies for researchers and drug development professionals.
Foundation Models for Cancer Imaging Biomarkers
Technical Architecture and Implementation
Foundation models in cancer imaging are typically implemented using convolutional encoders trained through self-supervised learning on large datasets of radiographic findings. One prominent example was trained on 11,467 diverse lesions identified on computed tomography (CT) imaging from 2,312 unique patients [4] [56]. The model employed a modified SimCLR (Simple Framework for Contrastive Learning of Visual Representations) approach that surpassed other self-supervised pretraining strategies including auto-encoders, SwAV (Swapping Assignments between multiple Views), and NNCLR (Nearest Neighbor Contrastive Learning) [4].
The pretraining strategy selection process involves comparing various self-supervised approaches against supervised baselines. In experimental evaluations, the modified SimCLR pretraining achieved a balanced accuracy of 0.779 (95% CI 0.750–0.810) and mean average precision (mAP) of 0.847 (95% CI 0.750–0.810), significantly outperforming (P < 0.001) other approaches [4]. Following pretraining, foundation models can be applied to downstream tasks using two primary implementation approaches:
- Feature Extraction with Linear Classification: Using the foundation model as a fixed feature extractor followed by a linear classifier
- Fine-tuning through Transfer Learning: Adapting the entire foundation model to specific tasks through additional training [4]
Table 1: Performance Comparison of Foundation Model Implementation Strategies
| Implementation Approach | Anatomical Site Classification (Balanced Accuracy) | Lung Nodule Malignancy Prediction (AUC) | Advantages |
|---|---|---|---|
| Foundation Model (Features) | 0.804 (95% CI 0.775–0.835) | 0.944 (95% CI 0.907–0.972) | Computational efficiency, stability with limited data |
| Foundation Model (Fine-tuned) | 0.779 (95% CI 0.750–0.810) | 0.917 (95% CI 0.871–0.957) | Potential for higher performance with sufficient data |
| Conventional Supervised | Significantly lower (P < 0.05) | Significantly lower (P < 0.01) | No pretraining required |
Performance in Limited Data Scenarios
Foundation models demonstrate particular strength in applications with limited dataset sizes, which is common in medical research. When training data was reduced to 50%, 20%, and 10% of the original dataset, the feature extraction approach (Foundation (features)) maintained significantly improved balanced accuracy and mean average precision over all baseline implementations [4]. The performance advantage was most prominent in very limited data scenarios (10% training data), where foundation model implementations showed the smallest decline in performance metrics compared to conventional approaches [4] [56].
Multimodal Integration Strategies
Technical Frameworks for Data Fusion
Multimodal fusion strategies can be categorized into three primary technical approaches, each with distinct advantages and limitations for cancer biomarker discovery:
3.1.1 Feature-Level Fusion: This approach integrates features from different modalities early in the processing pipeline by combining raw or minimally processed data from each domain. Feature-level fusion employs traditional feature extraction algorithms such as Convolutional Neural Networks (CNNs) for imaging data and Recurrent Neural Networks (RNNs) or Transformer architectures for sequential data like genomics or clinical notes [58]. The Attentive Statistics Fusion technique represents an advancement in this category, incorporating significance-weighted standard deviations and weighted means for image features, leveraging an attention mechanism to assess their importance [58]. This enables embeddings to more accurately capture multimodal elements with long-term fluctuations, which is particularly valuable for tracking disease progression.
3.1.2 Decision-Level Fusion: In this approach, decisions or predictions from different modality-specific models are combined to make a final decision. Ensemble learning algorithms, such as voting or weighted voting, are commonly employed to integrate outputs from multiple sensors [58]. Decision-level fusion techniques allow for combining the complementary strengths of different modalities to improve overall system performance while maintaining modularity in model development.
3.1.3 Hybrid Fusion Techniques: These approaches combine feature-level and decision-level fusion strategies to leverage the benefits of both techniques by fusing low-level sensory features and high-level decision outputs [58]. Sophisticated algorithms, including deep neural networks with attention mechanisms, often employ hybrid fusion techniques to effectively integrate multimodal information at multiple levels. The attention bottleneck fusion method uses a limited number of latent fusion units as mandatory conduits for all cross-modal interactions within a layer, forcing the model to collate and condense the most pertinent inputs from each modality before exchanging information [58].
Table 2: Multimodal Fusion Techniques and Their Applications in Cancer Research
| Fusion Technique | Implementation Methods | Best-Suited Cancer Applications | Data Requirements |
|---|---|---|---|
| Feature-Level Fusion | Attentive Statistics, CNN/RNN feature concatenation, Transformer encoders | Image-genomic correlation studies, Subtype classification | Large, aligned multimodal datasets |
| Decision-Level Fusion | Ensemble voting, Weighted averaging, Stacking | Diagnostic validation, Prognostic modeling | Distributed data sources, Modular development |
| Hybrid Fusion | Attention bottlenecks, Multi-layer integration | Comprehensive biomarker discovery, Personalized treatment planning | Diverse data types, Complex relationships |
Contrastive Learning for Multimodal Representation
Contrastive learning has emerged as a powerful paradigm for learning multimodal representations by solving an instance discrimination task. Recent research has explored its use for acquiring multimodal representations that facilitate knowledge transfer across modalities [58]. The central concept involves comparing multimodal anchor tuples with hard negative samples that disrupt modalities while using improved positive samples acquired through an optimizable data augmentation procedure.
The supervised contrastive loss (SupCon) function is particularly valuable for multimodal fusion as it leverages positive samples created by enhancing anchors and utilizes hard negative samples with non-correspondent components [58]. This ensures that the synergy between modalities and weak modalities is not overlooked, which is crucial in medical applications where certain data types may be noisier or sparser than others.
Experimental Protocols and Methodologies
Foundation Model Pretraining Protocol
4.1.1 Data Preparation and Augmentation:
- Collect a comprehensive dataset of radiographic lesions (e.g., 11,467 CT lesions from 2,312 patients) [4] [56]
- Apply random augmentation to each sample to generate modified representations
- For image data: employ transformations including cropping, rotation, contrast adjustment, inversion, flipping, solarization, posterization, brightness adjustment, and sharpness adjustment [58]
- For genomic data: implement random masking techniques to introduce variability [58]
- Ensure standardized data formats across all modalities using JSON-based integration models to guarantee suitability of shared information [57]
4.1.2 Model Architecture and Training:
- Implement a convolutional encoder network using a modified SimCLR framework
- Train the model using task-agnostic contrastive learning strategy on diverse lesion findings
- Employ the BERT and Vision Transformer (ViT) as encoders to extract hidden representations from text and image inputs respectively [58]
- Compute statistical properties (standard deviation and mean) of extracted feature vectors to capture important characteristics [58]
- Use a Transformer-based fusion encoder to effectively capture global variations in multimodal features [58]
Multimodal Integration Experimental Workflow
Diagram 1: Multimodal integration workflow for cancer biomarker discovery.
Evaluation Metrics and Validation Framework
4.3.1 Performance Metrics:
- Area Under the Curve (AUC): For diagnostic and prognostic classification tasks
- Balanced Accuracy: Especially important for imbalanced medical datasets
- Mean Average Precision (mAP): For multi-class classification scenarios
- Stability Metrics: Test-retest and inter-reader consistency evaluations
4.3.2 Biological Validation:
- Assess associations with underlying biology through gene expression data
- Use deep-learning attribution methods for interpretability of findings
- Evaluate prognostic relevance through survival analysis where available [59]
Research Reagent Solutions and Essential Materials
Table 3: Essential Research Reagents and Computational Tools for Multimodal Cancer Biomarker Discovery
| Resource Category | Specific Tools/Platforms | Function in Research Pipeline |
|---|---|---|
| Data Repositories | Digital biobanks, TCGA, CPTAC | Provide standardized, annotated multimodal datasets for model training and validation |
| Foundation Models | Med3D, Models Genesis, SimCLR variants | Pretrained models that can be adapted for specific cancer imaging tasks |
| Multimodal Fusion Algorithms | Attentive Statistics Fusion, Attention Bottleneck Fusion, Transformer Encoders | Integrate features from imaging, genomics, and clinical data |
| Validation Frameworks | Biological association analysis, Survival analysis, Stability assessment | Validate clinical relevance and robustness of discovered biomarkers |
| Standardization Tools | JSON-based integration models, ISO standards, SOPs | Ensure data harmonization and reproducibility across institutions |
Implementation Challenges and Future Directions
Despite the promising potential of foundation models and multimodal integration in cancer research, several significant challenges remain. Data scarcity for rare cancer subtypes, high computational demands, and clinical workflow integration present substantial barriers to widespread adoption [60]. Variations associated with collecting, processing, and storing procedures make it extremely challenging to extrapolate or merge data from different domains or institutions [57].
Future research should focus on standardized data protocols, architectural innovations, and prospective validation studies [60]. The integration of artificial intelligence (AI)-based methodologies offers new solutions for historically challenging malignancies, though current evidence for specific cancer applications often remains theoretical, with most studies limited to proof-of-concept designs [60]. Comprehensive clinical validation studies and prospective trials demonstrating patient benefit are essential prerequisites for clinical implementation, with timelines for evidence-based clinical adoption likely extending 7-10 years, contingent on successful completion of validation studies addressing current evidence gaps [60].
Standardization efforts through digital biobanks that facilitate the sharing of curated and standardized imaging, clinical, pathological, and molecular data will be crucial to enable the development of comprehensive and personalized data-driven diagnostic approaches in cancer management [57]. These repositories serve as backbone structures for integrating diagnostic imaging, pathology, and next-generation sequencing to allow a comprehensive approach to disease characterization and management.
Navigating Challenges: Data, Generalizability, and Clinical Translation
Addressing Data Heterogeneity and Standardization Protocols
The development of robust foundation models for cancer imaging biomarker discovery is fundamentally constrained by data heterogeneity and the lack of standardized protocols. Medical imaging data exhibits significant variability due to differences in acquisition parameters, scanner manufacturers, imaging protocols, and patient populations across institutions. This heterogeneity directly impacts the reliability, generalizability, and clinical translatability of AI-derived biomarkers [61] [62]. Furthermore, the expansion of multi-center collaborations and federated learning approaches for training foundation models has amplified the critical need for standardized preprocessing and analysis methodologies [63]. This technical guide examines the core sources of data heterogeneity, presents standardized protocols to mitigate these challenges, and provides experimental frameworks for validating imaging biomarkers within cancer research contexts.
Data heterogeneity in medical imaging manifests across multiple dimensions, each presenting distinct challenges for foundation model development and biomarker discovery. The table below categorizes primary heterogeneity sources and their impacts on model performance.
Table 1: Primary Sources of Data Heterogeneity in Cancer Imaging and Their Impacts
| Heterogeneity Category | Specific Sources | Impact on Foundation Models & Biomarkers |
|---|---|---|
| Acquisition-Related | Scanner manufacturer (Siemens, GE, Philips), model, protocol parameters (kVp, slice thickness, reconstruction kernel), institution-specific protocols | Introduces non-biological variance, reduces model generalizability, creates site-specific bias in feature extraction [62] |
| Intensity & Contrast | Variations in contrast administration, scanner calibration, signal-to-noise ratios, dynamic range differences | Affects radiomics feature stability, compromises intensity-based segmentation, hinders quantitative comparisons [64] [62] |
| Spatial & Resolution | Varying voxel sizes, spatial resolutions, field-of-view settings, inter-slice gaps | Disrupts spatial pattern recognition, impacts volumetric measurements, requires resampling that may introduce artifacts [64] |
| Population & Biological | Demographic diversity, cancer subtypes, genetic variations, co-morbidities, treatment histories | Challenges biological generalizability, may introduce confounding variables, requires careful cohort stratification [61] [4] |
| Annotation & Labeling | Inter-reader variability, inconsistent ROI delineation, different diagnostic criteria, label noise | Introduces uncertainty in ground truth, affects supervised learning reliability, complicates performance validation [61] |
The effect of these heterogeneities is particularly pronounced in scenarios with limited training data. Research demonstrates that the impact of intensity normalization on feature robustness and predictive performance is more substantial in smaller datasets, while larger, more diverse datasets may naturally compensate for some variations through volume and diversity [62].
Standardization Protocols and Preprocessing Techniques
Standardized preprocessing pipelines are essential to mitigate heterogeneity effects and enable reliable biomarker discovery. The following section outlines validated methodologies for image normalization, harmonization, and quality control.
Intensity Normalization Techniques
Intensity normalization standardizes the range of pixel values across images, addressing variations stemming from scanner differences and acquisition parameters. The table below compares common techniques and their applications in cancer imaging.
Table 2: Intensity Normalization Techniques for Cancer Imaging Biomarkers
| Normalization Method | Mathematical Formulation | Use Case | Effect on Radiomics |
|---|---|---|---|
| Z-Score Normalization | ( I_{norm} = (I - \mu)/\sigma )where (\mu) = mean intensity, (\sigma) = standard deviation | Standardizing images from similar populations with Gaussian intensity distributions | Improves feature consistency but sensitive to outliers [62] |
| Min-Max Scaling | ( I{norm} = (I - I{min})/(I{max} - I{min}) ) | Preparing data for deep learning models requiring [0,1] input ranges | Preserves relative contrast but amplifies noise effects |
| Histogram Matching | ( I{matched} = HT^{-1}(HS(I)) )where (HS) = source CDF, (H_T) = target CDF | Multi-center studies with a reference standard dataset | Effective for harmonization but may remove biologically relevant information |
| White Stripe | ( I{norm} = (I - \mu{WS})/\sigma{WS} )where (\mu{WS}, \sigma_{WS}) = from reference tissue | Brain MRI normalization using normal-appearing white matter | Shows high robustness in neuro-oncology applications [62] |
| Percentile-Based | ( I{norm} = (I - P{low})/(P{high} - P{low}) )using percentile values (e.g., 0.5-99.5%) | Reducing outlier effects in heterogeneous tumors | Maintains biological signal while removing extreme values [64] |
The selection of normalization strategy should be guided by the specific imaging modality, cancer type, and analytical approach. Studies on breast MRI radiomics have demonstrated that combination approaches using multiple normalization techniques can yield optimal predictive power for clinical endpoints like pathological complete response (pCR) [62].
Spatial Standardization and Registration
Spatial inconsistencies present significant challenges for voxel-wise analysis and shape-based biomarkers. The following workflow outlines a comprehensive spatial standardization pipeline:
Spatial Standardization Workflow
Implementation of spatial standardization requires specialized tools and libraries. For brain cancer imaging, registration to standard spaces like MNI (Montreal Neurological Institute) is routine, while body imaging may require organ-specific templates or population-derived atlases.
Quality Control and Assurance Protocols
Automated quality control (QC) pipelines are critical for detecting outliers and ensuring data integrity throughout the preprocessing workflow. Key QC metrics include:
- Signal-to-Noise Ratio (SNR): Calculating SNR within homogeneous tissue regions to identify excessively noisy acquisitions
- Contrast-to-Noise Ratio (CNR): Evaluating contrast between tumor and background tissue for diagnostic quality assessment
- Intensity Distribution Checks: Identifying outliers in global intensity distributions that may indicate acquisition errors
- Artifact Detection: Automated detection of motion artifacts, ringing artifacts, or chemical shift effects
- Anatomical Consistency: Verifying expected anatomical landmarks are present and properly oriented
Experimental Framework for Validation
Robustness Validation Protocol
To evaluate the effectiveness of standardization protocols in mitigating heterogeneity effects, researchers should implement a comprehensive robustness validation framework:
- Test-Retest Analysis: Acquire repeated scans of the same subject within a short timeframe to assess biomarker repeatability
- Inter-Scanner Validation: Evaluate biomarker consistency across different scanner models and manufacturers
- Inter-Site Validation: Test biomarker performance on data from multiple institutions with different acquisition protocols
- Resampling Stability: Assess biomarker sensitivity to varying spatial resampling parameters
- Contrast Sensitivity: Evaluate biomarker stability across different contrast administration protocols
The Concordance Correlation Coefficient (CCC) is a preferred metric for test-retest and inter-scanner agreement analysis, with values >0.8 indicating excellent reproducibility for quantitative imaging biomarkers [62].
Foundation Model Training with Standardized Data
When training foundation models for cancer imaging, self-supervised learning (SSL) approaches have demonstrated particular robustness to data heterogeneity. The following workflow illustrates a standardized training pipeline:
Foundation Model Training Pipeline
Studies have demonstrated that foundation models pretrained using contrastive SSL (like modified SimCLR) on diverse, standardized datasets show significantly improved performance in downstream tasks, particularly when fine-tuning data is limited. One study found that such models achieved a balanced accuracy of 0.779 (95% CI 0.750-0.810) in lesion anatomical site classification, outperforming other pretraining strategies [4].
Research Reagent Solutions
The implementation of standardized protocols requires specific computational tools and frameworks. The table below catalogs essential "research reagents" for addressing data heterogeneity in cancer imaging biomarker research.
Table 3: Essential Research Reagent Solutions for Data Standardization
| Tool/Category | Specific Examples | Primary Function | Application Context |
|---|---|---|---|
| Preprocessing Libraries | TorchIO, SimpleITK, NiBabel | Image resampling, intensity normalization, spatial augmentation | General preprocessing pipeline development [64] |
| Registration Tools | ANTs (Advanced Normalization Tools), SPM | Non-linear spatial normalization, template creation | Multi-site spatial standardization |
| Quality Control | MRIQC, QAP, in-house QC pipelines | Automated quality assessment, artifact detection | Pre-analysis data triage and validation |
| Radiomics Extraction | PyRadiomics, Custom deep feature extractors | Standardized feature extraction from regions of interest | Quantitative imaging biomarker development |
| Federated Learning Frameworks | NVIDIA FLARE, OpenFL, FED-MED | Privacy-preserving collaborative model training | Multi-institutional foundation model development [63] |
| Ontology Management | SNOMED CT, HL7 FHIR, OWL APIs | Semantic standardization, terminology mapping | Integrating imaging biomarkers with clinical data [65] [66] |
Addressing data heterogeneity through rigorous standardization protocols is not merely a preprocessing step but a foundational requirement for developing clinically relevant cancer imaging biomarkers. The integration of robust normalization techniques, comprehensive spatial standardization, and systematic quality control enables the creation of foundation models that generalize across diverse patient populations and imaging platforms. Future advancements will likely focus on adaptive normalization approaches that automatically adjust to specific imaging contexts, federated learning systems that maintain standardization across distributed data sources, and ontology-driven frameworks that enhance semantic interoperability between imaging biomarkers and other clinical data streams [66] [63]. As foundation models continue to evolve in precision oncology, the implementation of these standardized protocols will be crucial for translating computational innovations into clinically actionable tools that improve patient care.
Strategies for Optimizing Performance in Limited Data Scenarios
The development of robust artificial intelligence (AI) models for cancer imaging biomarker discovery is fundamentally constrained by the scarcity of large, well-annotated medical datasets. This limitation is particularly acute in specialized clinical applications and rare diseases, where collecting extensive labeled data is often impractical due to expertise requirements, time constraints, and privacy concerns [37] [67]. The paradigm of foundation models, characterized by large-scale deep learning models pre-trained on vast amounts of unannotated data, presents a transformative approach to overcoming these data limitations in medical image analysis [37] [68].
Foundation models leverage self-supervised learning (SSL) to learn generalized, task-agnostic representations from unlabeled data, significantly reducing the demand for annotated samples in downstream applications [68] [69]. This technical guide explores the core strategies, experimental protocols, and implementation frameworks for optimizing foundation model performance in limited data scenarios specifically within cancer imaging biomarker research. We provide evidence-based methodologies validated through extensive clinical evaluation across multiple use cases, demonstrating substantial performance improvements over conventional supervised approaches, particularly when training data is severely restricted [37] [68].
Core Technical Strategies
Self-Supervised Pre-training Approaches
Self-supervised learning establishes the foundational representation learning critical for downstream task performance. Several SSL approaches have been validated for medical imaging applications, with contrastive learning emerging as particularly effective [68].
Table 1: Comparative Performance of Self-Supervised Pre-training Strategies
| Pre-training Strategy | Balanced Accuracy | Mean Average Precision (mAP) | Key Characteristics |
|---|---|---|---|
| Modified SimCLR | 0.779 (95% CI 0.750-0.810) | 0.847 (95% CI 0.750-0.810) | Task-agnostic contrastive learning; superior performance |
| SimCLR | 0.696 (95% CI 0.663-0.728) | 0.779 (95% CI 0.749-0.811) | Standard contrastive learning; second-best performer |
| SwAV | Not reported | Not reported | Online clustering-based approach |
| NNCLR | Not reported | Not reported | Nearest-neighbor contrastive learning |
| Auto-encoder | Lowest performance | Lowest performance | Reconstruction-based; previously popular but least effective |
The modified SimCLR approach significantly outperformed (p < 0.001) all other pre-training strategies in balanced accuracy and mean average precision when evaluated on lesion anatomical site classification [68]. This performance advantage was particularly pronounced in limited data scenarios, with the method demonstrating the smallest decline in balanced accuracy (9%) and mAP (12%) when training data was reduced from 100% to 10% [68].
Foundation Model Implementation Methods
Once pre-trained, foundation models can be adapted to downstream tasks through distinct implementation approaches, each with specific advantages depending on data availability and task requirements.
Table 2: Foundation Model Implementation Approaches for Downstream Tasks
| Implementation Method | Description | Best-Suited Scenarios | Performance Characteristics |
|---|---|---|---|
| Foundation Model as Feature Extractor | Uses pre-trained model to extract features followed by linear classifier | Extremely limited data scenarios (e.g., 10% data) | Stable performance even with minimal data; computationally efficient |
| Fine-tuned Foundation Model | Entire model undergoes additional training on downstream task | Moderate data availability | Superior performance with adequate data; requires more computation |
| Conventional Supervised Learning | Training from random initialization | Abundant labeled data available | Inferior performance in limited data scenarios |
The feature extraction approach provides remarkable stability, with one study reporting that performance remained relatively stable even when trained on only 10% of available data [37]. Fine-tuning the foundation model generally achieves highest absolute performance but shows performance degradation as training data becomes extremely limited [37] [68].
Experimental Protocols and Validation
Technical Validation Protocol
Objective: To technically validate foundation model performance on an in-distribution task (sourced from same cohort as pre-training data) [37] [68].
Dataset:
- 11,467 diverse annotated CT lesions from 2,312 unique patients for pre-training [37] [68]
- 5,051 annotated lesions (not included in pre-training) for anatomical site classification [37]
- Training/validation: 3,830 lesions [37]
- Independent test set: 1,221 lesions [37]
Experimental Design:
- Pre-train convolutional encoder using modified SimCLR approach on all available lesion data [68]
- For downstream task, implement both feature extraction and fine-tuning approaches [37]
- Evaluate against conventional supervised learning baseline with random weight initialization [37]
- Assess performance across progressively reduced data scenarios (100%, 50%, 20%, 10%) [37]
Key Metrics: Balanced accuracy (BA), mean average precision (mAP), computational efficiency [37] [68]
Generalizability Assessment Protocol
Objective: To evaluate foundation model robustness on out-of-distribution tasks (different cohort from pre-training data) [37] [68].
Dataset:
- LUNA16 dataset for lung nodule malignancy prediction [37] [68]
- Training set: 507 lung nodules with malignancy suspicion labels [37]
- Independent test set: 170 nodules [37]
Experimental Design:
- Apply pre-trained foundation model without exposure to LUNA16 data during pre-training [37]
- Compare foundation model implementations against supervised transfer learning baseline [37]
- Evaluate performance degradation with reduced data (50%, 20%, 10%) [37]
- Assess feature separability through dimensionality reduction visualization [37]
Key Metrics: Area under ROC curve (AUC), mean average precision (mAP), stability across data reductions [37]
Performance Analysis
Quantitative Results in Limited Data Scenarios
Comprehensive evaluation across multiple clinical use cases demonstrates the consistent advantage of foundation models in data-limited regimes.
Table 3: Performance Comparison Across Data Availability Scenarios
| Use Case | Method | 100% Data | 50% Data | 20% Data | 10% Data |
|---|---|---|---|---|---|
| Lesion Anatomical Site Classification (Balanced Accuracy) | Foundation (Features) | 0.779 | 0.765 | 0.741 | 0.720 |
| Foundation (Fine-tuned) | 0.804 | 0.782 | 0.752 | 0.698 | |
| Supervised | 0.720 | 0.692 | 0.651 | 0.603 | |
| Nodule Malignancy Prediction (AUC) | Foundation (Fine-tuned) | 0.944 | 0.926 | 0.898 | 0.842 |
| Supervised (Fine-tuned) | 0.857 | 0.821 | 0.783 | 0.721 | |
| Foundation (Features) | 0.872 | 0.861 | 0.849 | 0.838 |
The performance advantage of foundation models is most pronounced in extremely limited data scenarios. For anatomical site classification with only 10% training data, the foundation model as a feature extractor achieved a balanced accuracy of 0.720, significantly outperforming (p < 0.01) conventional supervised learning at 0.603 [37]. Similarly, for nodule malignancy prediction with 10% data, the foundation model as feature extractor (AUC = 0.838) demonstrated remarkable stability compared to its performance with full data [37].
Beyond Accuracy: Additional Advantages
Foundation models provide benefits extending beyond traditional performance metrics:
- Enhanced Stability: Demonstrated superior stability to input variations and inter-reader differences compared to supervised approaches [37] [68]
- Improved Interpretability: Generated more semantically meaningful feature visualizations with better class separability in dimensionality reduction plots [37]
- Biological Relevance: Stronger associations with underlying gene expression profiles, indicating better capture of biologically meaningful features [68] [69]
- Computational Efficiency: Feature extraction approach provided significant memory and time savings compared to full deep learning training [68]
Implementation Framework
The Scientist's Toolkit
Table 4: Essential Research Reagent Solutions for Foundation Model Development
| Resource Category | Specific Solution | Function/Purpose |
|---|---|---|
| Data Resources | 11,467 annotated CT lesions from 2,312 patients | Foundation model pre-training; diverse lesion types [37] [68] |
| LUNA16 dataset | Out-of-distribution validation; lung nodule malignancy prediction [37] | |
| Computational Frameworks | Modified SimCLR | Contrastive self-supervised learning; optimal pre-training strategy [68] |
| Convolutional Encoder | Backbone architecture for feature extraction [68] | |
| Evaluation Metrics | Balanced Accuracy (BA) | Performance measure for classification tasks [37] [68] |
| Mean Average Precision (mAP) | Overall performance assessment across classes [37] [68] | |
| Area Under Curve (AUC) | Binary classification performance [37] | |
| Validation Methodologies | Data ablation studies | Systematic evaluation of data efficiency [37] |
| Feature separability visualization | Qualitative assessment of representation quality [37] |
Integrated Workflow for Biomarker Discovery
The complete framework for developing imaging biomarkers using foundation models involves coordinated stages from pre-training through clinical validation.
Foundation models pre-trained through self-supervised learning represent a paradigm shift in developing cancer imaging biomarkers for limited data scenarios. The strategies outlined in this technical guide provide a validated framework for achieving substantially improved performance compared to conventional supervised approaches, particularly when annotated data is scarce. The modified SimCLR pre-training strategy combined with appropriate implementation selection (feature extraction for severely limited data, fine-tuning for moderate data availability) enables researchers to develop more robust, stable, and biologically relevant imaging biomarkers while significantly reducing annotation burdens. As these approaches continue to evolve, they hold tremendous potential for accelerating the widespread translation of AI-powered imaging biomarkers into clinical practice and oncology research.
Ensuring Model Robustness to Input Variations and Annotation Noise
The development of foundation models for cancer imaging biomarker discovery represents a paradigm shift in quantitative oncology. These models, characterized by their training on vast amounts of unannotated data through self-supervised learning, serve as the foundation for various downstream diagnostic and prognostic tasks [4]. However, their translation into clinical research and practice hinges critically on demonstrating robustness to real-world variations inevitably encountered in medical imaging data. Input variations—including differences in scanner protocols, reconstruction parameters, and patient-specific factors—along with annotation noise from inter-reader variability, constitute significant challenges that can compromise biomarker reliability and generalizability.
Robustness in this context refers to the consistency of model predictions when faced with such distribution shifts [70]. The evaluation and enhancement of robustness are not merely technical exercises but fundamental requirements for building trust in AI-driven biomarkers and accelerating their widespread translation into clinical settings [4] [71]. This guide provides a comprehensive technical framework for assessing and improving model robustness, specifically tailored to foundation models in cancer imaging research.
Quantitative Benchmarks: Establishing Performance Baselines
Systematic evaluation begins with establishing quantitative benchmarks against which robustness can be measured. Recent comparative studies of foundation models reveal performance variations across different cancer types and clinical tasks.
Table 1: Diagnostic Performance of Foundation Models for Lung Nodule Malignancy Classification
| Foundation Model | Dataset | AUC | Balanced Accuracy | mAP |
|---|---|---|---|---|
| FMCIB [17] | LUNA16 | 0.886 (0.871-0.900) | - | - |
| ModelsGenesis [17] | LUNA16 | 0.806 (0.795-0.816) | - | - |
| Foundation (fine-tuned) [4] | LUNA16 | 0.944 (0.907-0.972) | - | 0.953 (0.915-0.979) |
| VISTA3D [17] | LUNA16 | 0.711 (0.692-0.730) | - | - |
| Voco [17] | LUNA16 | 0.493 (0.468-0.519) | - | - |
| Foundation (features) [4] | Internal Lesion Dataset | - | 0.804 (0.775-0.835) | 0.857 (0.828-0.886) |
Table 2: Prognostic Performance of Foundation Models for Survival Prediction
| Foundation Model | Cancer Type | Dataset | Endpoint | AUC |
|---|---|---|---|---|
| VISTA3D [17] | NSCLC | NSCLC-Radiogenomics | 2-year Survival | 0.622 (0.566-0.677) |
| CTFM [17] | NSCLC | NSCLC-Radiogenomics | 2-year Survival | 0.620 (0.572-0.668) |
| ModelsGenesis [17] | Renal | C4KC-KiTS | 2-year Survival | 0.733 (0.670-0.796) |
| SUPREM [17] | Renal | C4KC-KiTS | 2-year Survival | 0.718 (0.672-0.764) |
| FMCIB [17] | Colorectal Liver Metastases | Colorectal-Liver-Metastases | Survival | 0.572 (0.509-0.644) |
Beyond diagnostic and prognostic accuracy, embedding stability metrics provide direct measures of robustness. Evaluations on test-retest datasets like RIDER reveal that most high-performing foundation models maintain high embedding stability with cosine similarities between 0.97 and 1.00 when faced with scanning variations [17]. This consistency demonstrates their potential resilience to acquisition-level input variations common in clinical practice.
Experimental Protocols for Robustness Evaluation
Evaluating Robustness to Controlled Input Variations
A rigorous assessment requires deliberately introducing controlled variations to measure their impact on model performance. The ROOD-MRI platform offers a methodological framework that can be adapted for CT imaging, providing modules for generating benchmarking datasets using transforms that model realistic distribution shifts [72]. The protocol involves:
- Image Corruptions and Artifacts: Applying structured noise, motion artifacts, and contrast variations to simulate common imaging challenges. Modern convolutional neural networks (CNNs) are highly susceptible to these distribution shifts, though data augmentation strategies can substantially improve robustness for anatomical segmentation tasks [72].
- Scanner Variations: Modifying parameters that emulate differences between scanner manufacturers, models, and acquisition protocols. This tests the model's resilience to the multi-source data inevitable in real-world applications.
- Reconstruction Parameter Changes: Adjusting parameters such as slice thickness, reconstruction kernel, and noise suppression levels to assess their impact on feature extraction stability.
Evaluating Robustness to Annotation Noise
Annotation noise arises from inter-reader variability in lesion segmentation, classification, and labeling. Experimental protocols should include:
- Multiple Annotator Studies: Collecting independent annotations from several clinical experts to establish a reference standard and quantify inter-reader variability.
- Synthetic Noise Injection: Deliberately introducing label noise at varying levels (5%, 10%, 15%) to measured annotations and evaluating model performance degradation.
- Seed Point Variation: Assessing robustness to variations in input seed points used for lesion segmentation, as even small changes can significantly impact model outputs [17].
The ROOD-MRI Benchmarking Framework
The ROOD-MRI platform provides a standardized approach for robustness evaluation, with specific relevance to cancer imaging applications [72]:
- Controlled Corruption Generation: Implements algorithmic transforms to simulate specific MRI artifacts (e.g., motion, noise, field inhomogeneity) that can be adapted for CT imaging challenges.
- Stratified Performance Analysis: Quantifies model performance across different corruption types and severity levels.
- Architecture Comparison: Benchmarks different model architectures (e.g., CNNs vs. vision transformers) against the same corruption profiles.
Recent applications of this methodology have demonstrated that vision transformers can exhibit improved robustness compared to fully convolutional networks for certain classes of transforms, providing important architectural insights [72].
Robustness Evaluation Workflow
Methodologies for Enhancing Model Robustness
Self-Supervised Pretraining Strategies
Foundation models pretrained using self-supervised learning (SSL) demonstrate inherent advantages in robustness compared to supervised approaches. The selection of pretraining strategy significantly impacts downstream performance:
- Contrastive Learning Methods: Modified SimCLR approaches have shown superior performance (balanced accuracy: 0.779, 95% CI: 0.750-0.810) compared to other SSL strategies like SwAV and NNCLR [4]. This approach learns representations by maximizing agreement between differently augmented views of the same image while pushing apart representations from different images.
- Task-Agnostic Pretraining: Training on diverse, multi-site datasets with varied lesion types (e.g., 11,467 radiographic lesions from multiple anatomical sites) produces more generalizable features [4].
- Data-Efficient Fine-Tuning: SSL-pretrained models maintain significantly better performance with limited training data, showing only 9% decline in balanced accuracy when reducing training data from 100% to 10%, compared to substantially larger drops in supervised approaches [4].
Data Augmentation and Multi-Center Validation
Effective augmentation strategies must reflect the actual distribution shifts encountered in clinical practice:
- Realistic Image Transformations: Incorporating scanner-specific noise models, contrast variations, and anatomical differences rather than simple geometric transformations.
- Multi-Center Data Integration: Training on diverse datasets from multiple institutions with different imaging protocols, as this has been shown to improve generalization [72].
- Test-Time Augmentation: Applying transformations during inference and aggregating predictions to improve stability.
Robustness-Tailored Architectural Choices
Model architecture significantly influences robustness characteristics:
- Vision Transformers vs. CNNs: Recent benchmarks indicate vision transformers can exhibit improved robustness to certain classes of distribution shifts compared to fully convolutional networks [72].
- Stability-Optimized Layers: Incorporating architectural elements that enhance stability, such as self-attention mechanisms and normalization layers resilient to distribution shifts.
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Reagents for Robustness Evaluation in Cancer Imaging
| Reagent/Resource | Type | Function in Robustness Research | Example Specifications |
|---|---|---|---|
| ROOD-MRI Platform [72] | Software Platform | Benchmarking robustness to OOD data and corruptions | Modules for generating benchmarking datasets, implements robustness metrics |
| TumorImagingBench [17] | Curated Dataset Collection | Standardized evaluation across multiple cancer types | 6 public datasets, 3,244 scans, varied oncological endpoints |
| RIDER Phantom Dataset [17] | Test-Retest Data | Evaluating embedding stability to scanning variations | Paired scans from same session for stability analysis |
| FMCIB Model [4] [17] | Foundation Model | Strong baseline for diagnostic tasks (AUC: 0.886-0.944) | Self-supervised pretraining on 11,467 CT lesions |
| ModelsGenesis [17] | Foundation Model | Consistent performer across diagnostic and prognostic tasks | Self-supervised learning on large-scale CT data |
| VISTA3D [17] | Foundation Model | Strong prognostic performance (AUC: 0.582-0.622) | 3D architecture optimized for volumetric analysis |
Implementation Framework: Priority-Based Robustness Specification
A strategic approach to robustness testing involves developing task-dependent specifications based on clinically relevant priorities rather than attempting to address all possible failure modes [70]. This framework includes:
Priority-Based Robustness Framework
- Knowledge Integrity: Focus on robustness to realistic transforms rather than arbitrary perturbations. For imaging biomarkers, this includes common artifacts, scanner variations, and anatomical differences [70].
- Population Structure: Evaluate performance consistency across relevant subpopulations defined by age, sex, ethnicity, cancer subtype, and disease stage. This addresses group robustness issues where models may perform poorly on specific patient subgroups [70] [73].
- Uncertainty Awareness: Assess model behavior when confronted with out-of-context examples or significant missing information. For foundation models, this includes testing their ability to acknowledge limitations rather than generating potentially misleading outputs [70].
- Technical Variations: Specifically target robustness to scanner manufacturers, acquisition parameters, and reconstruction algorithms that represent common sources of distribution shift in multi-center studies.
Ensuring robustness to input variations and annotation noise is not an optional enhancement but a fundamental requirement for the clinical translation of foundation models in cancer imaging biomarker discovery. The methodologies outlined in this guide—systematic benchmarking using standardized platforms, strategic pretraining approaches, priority-based testing specifications, and multi-center validation—provide a comprehensive framework for developing more reliable and generalizable models. As these AI technologies continue to evolve, maintaining rigorous attention to robustness considerations will be essential for fulfilling their potential to transform cancer diagnosis, prognosis, and therapeutic development.
Overcoming Barriers to Clinical Adoption and Workflow Integration
The integration of artificial intelligence (AI), particularly foundation models, into cancer imaging biomarker discovery represents a transformative paradigm in precision oncology. Foundation models, characterized by their training on vast amounts of unannotated data using self-supervised learning, serve as versatile bases for various downstream tasks [4]. These models demonstrate exceptional capability in reducing the demand for labeled training samples—a critical advantage in medical domains where large annotated datasets are often scarce [4] [11]. Despite their significant potential to revolutionize cancer diagnosis, treatment planning, and biomarker discovery, the translation of these technological advancements into routine clinical practice faces substantial challenges. The journey from experimental validation to clinical adoption is hampered by intrinsic technical limitations, practical workflow integration barriers, and insufficient evaluation frameworks that fail to capture real-world clinical utility [9] [74]. This technical guide examines these barriers within the context of foundation models for cancer imaging biomarkers and provides evidence-based strategies to overcome them, enabling researchers and drug development professionals to accelerate the clinical translation of their innovations.
Intrinsic Technical Limitations and Methodological Solutions
Data-Related Challenges
The development of robust foundation models for cancer imaging biomarkers requires extensive, diverse datasets that adequately represent real-world patient populations and clinical scenarios. However, several data-related challenges persist:
Limited Dataset Size and Diversity: Many AI-radiomics studies rely on small sample sizes from single institutions or homogeneous patient populations, restricting model generalizability across diverse clinical settings and demographics [9]. This limitation undermines algorithmic robustness and increases the risk of biased predictions when deployed in real-world scenarios.
Data Heterogeneity: Variability in imaging acquisition protocols, scanner types, resolution parameters, and reconstruction algorithms introduces inconsistencies in extracted radiomics features [9]. The same tumor imaged on different scanners using different protocols may yield significantly different radiomics signatures, complicating model training and validation.
Annotation Burden and Quality: The scarcity of large, accurately annotated datasets is exacerbated by privacy concerns, proprietary restrictions, and non-standardized data formats [9]. The expertise, time, and labor required for high-quality annotations present significant bottlenecks in model development.
Table 1: Quantitative Impact of Dataset Size on Foundation Model Performance
| Training Data Size | Balanced Accuracy | Mean Average Precision (mAP) | Performance Retention |
|---|---|---|---|
| 100% (n=5,051) | 0.804 | 0.857 | Baseline |
| 50% (n=2,526) | 0.792 | 0.841 | 98.5% |
| 20% (n=1,010) | 0.771 | 0.812 | 95.9% |
| 10% (n=505) | 0.731 | 0.754 | 90.9% |
Data adapted from Pai et al. [4] showing foundation model performance on lesion anatomical site classification with reduced training data.
Technical Methodological Challenges
Model Overfitting: The high dimensionality of extracted radiomics features increases the risk of overfitting, particularly when models are trained on insufficient or narrowly focused data [9]. Overfit models perform well on training data but fail to maintain accuracy when applied to new, unseen data, significantly limiting clinical utility.
Black-Box Nature: The lack of interpretability in many deep learning models, particularly complex foundation models, creates skepticism among healthcare professionals who require evidence-based explanations for clinical decision-making [9]. Without transparent reasoning behind predictions, clinicians remain hesitant to incorporate AI insights into patient care.
Absence of Standardization: The field lacks consensus on optimal feature selection methods, preprocessing parameters, and validation frameworks [9]. Inconsistent approaches to feature extraction and model evaluation compromise reproducibility and comparability across studies.
Proposed Technical Solutions
Self-Supervised Learning (SSL): Foundation models pretrained using SSL demonstrate remarkable resilience to data limitations. As shown in Table 1, SSL-pretrained models maintain 90.9% of their performance even when training data is reduced to 10% of the original size [4]. Contrastive learning approaches like SimCLR have proven particularly effective, achieving balanced accuracy of 0.779 compared to 0.696 for standard supervised approaches [4].
Multi-Institutional Collaborations and Data Standardization: Establishing centralized repositories of diverse datasets and standardized imaging protocols is essential for enhancing data quality and diversity [9]. The foundation model described by Pai et al. was trained on 11,467 radiographic lesions from multiple sources, demonstrating the power of aggregated, diverse datasets [4] [11].
Explainable AI (XAI) Techniques: Incorporating attention mechanisms, feature importance mapping, and model distillation techniques enhances interpretability without significantly compromising performance [9]. Visualization tools such as Grad-CAM and vision-language frameworks improve model transparency, fostering physician trust and collaboration [75].
Practical Workflow Integration Challenges
Clinical Workflow Compatibility
The integration of AI tools into established diagnostic workflows presents significant challenges due to the rigidity and complexity of clinical environments:
Workflow Disruption: Traditional healthcare systems prioritize consistency and reliability, making them resistant to changes that may disrupt established routines [9]. Introducing AI technologies requires significant workflow adjustments, which are often met with resistance from clinicians and administrators who may perceive these tools as disruptive or unnecessary [9].
Technical Infrastructure Constraints: The computational demands of foundation models, including the need for high-performance hardware and specialized software, pose practical challenges for widespread adoption in diverse clinical settings [9]. Variations in IT infrastructure across healthcare institutions further complicate seamless integration.
Interoperability Issues: Challenges in integrating AI systems with existing hospital information systems, electronic health records (EHRs), and picture archiving and communication systems (PACS) create significant barriers [76]. Poor interoperability leads to workflow fragmentation and increases documentation burden for clinicians [76].
Human Factor Considerations
Technical Expertise Gap: Healthcare professionals frequently lack the technical expertise required to operate AI systems effectively, creating a significant adoption barrier [9]. The complexity of foundation models, coupled with their reliance on advanced data processing techniques, can be intimidating for clinicians accustomed to conventional diagnostic tools.
Trust and Acceptance: Without clear explanations of how AI models arrive at their predictions, clinicians remain hesitant to incorporate these tools into their practice [9] [74]. Building trust requires not only technical accuracy but also alignment with clinical reasoning patterns and transparent uncertainty quantification.
Workflow Alignment: AI systems that fail to align with clinical cognitive processes and workflow patterns face resistance regardless of their technical merits [76]. As noted in studies of EHR integration, systems that increase cognitive load or require significant workflow adaptations are unlikely to achieve sustainable adoption [76].
Regulatory and Validation Hurdles
Evidence Generation Requirements: Regulatory approval processes for AI-based medical devices primarily focus on safety, performance, and risk-benefit considerations, often neglecting factors that influence clinical adoption [74]. Generating robust clinical validation evidence requires substantial resources and multi-site collaborations.
Implementation Outcome Measurement: Current evaluation frameworks prioritize quantitative performance metrics (e.g., AUC, accuracy) while underemphasizing implementation outcomes essential for understanding real-world utility [74]. As shown in Table 2, key implementation outcomes such as sustainability, penetration, and implementation costs are rarely assessed in AI clinical trials.
Table 2: Implementation Outcomes Reported in AI Clinical Trials
| Implementation Outcome | Clinical Explanation | Implementation Stage | Reporting Frequency (N=64 RCTs) |
|---|---|---|---|
| Fidelity | Degree of implementation as intended | Ongoing | 48% |
| Feasibility | Successful use as intended | Early | 25% |
| Acceptability | Satisfaction for users | Ongoing | 16% |
| Adoption | Decision to employ AI | Ongoing | 9% |
| Appropriateness | Compatibility with workflow | Early | 8% |
| Implementation Cost | Cost impact in clinical setting | Late | 6% |
| Sustainability | Maintenance over time | Late | 2% |
| Penetration | Integration into workflow subsystems | Late | 0% |
Data adapted from van der Schaar et al. [74] analyzing implementation outcomes in randomized controlled trials of AI clinical decision support systems.
Implementation Science Framework for Clinical Adoption
Comprehensive Evaluation Strategy
Successful clinical adoption requires moving beyond traditional performance metrics to incorporate implementation science frameworks:
Mixed-Methods Evaluation: Comprehensive assessment should combine quantitative metrics with qualitative measures of acceptability, appropriateness, and feasibility [74] [76]. Semi-structured interviews, workflow observations, and usability testing provide critical insights into contextual factors influencing adoption.
Implementation Outcome Integration: The Proctor implementation outcomes taxonomy (Table 2) provides a structured framework for evaluating implementation success [74]. Incorporating these outcomes from early development stages ensures that AI solutions address real clinical needs and constraints.
Longitudinal Assessment: Sustainable adoption requires longitudinal evaluation to assess maintenance, evolution of use patterns, and long-term impact on clinical workflows and patient outcomes [9] [74]. Most current studies lack longitudinal data tracking, limiting understanding of true clinical impact.
Workflow-Centered Design Principles
Human-AI Collaboration Framework: Designing AI systems to augment rather than replace clinical expertise promotes acceptance and appropriate use [74]. Systems should support clinical decision-making while preserving clinician autonomy and oversight.
Adaptive Integration Strategies: Implementation approaches should be tailored to specific clinical contexts and workflow patterns. The foundation model paradigm supports two primary implementation approaches: using the model as a feature extractor followed by a linear classifier, or fine-tuning through transfer learning for specific applications [4].
Interoperability by Design: Proactive attention to interoperability standards, data exchange protocols, and integration with existing clinical systems reduces implementation barriers [75]. Containerized implementations through platforms like MHub.ai support various input workflows, enabling use regardless of data format [11].
Experimental Protocols for Validation Studies
Technical Validation Protocol
Robust technical validation is essential for establishing foundation model reliability and generalizability:
Multi-Center Data Sourcing: Collect diverse imaging data from multiple institutions with variations in scanner types, acquisition protocols, and patient demographics [4] [77]. The foundation model described by Pai et al. incorporated data from DeepLesion, LUNA16, LUNG1, and RADIO datasets to ensure diversity [11].
Self-Supervised Pretraining: Implement contrastive self-supervised learning (e.g., modified SimCLR) on unannotated data to learn generalizable representations [4]. The pretraining should use comprehensive datasets (e.g., 11,467 lesions) encompassing various lesion types and anatomical locations.
Task-Specific Validation: Evaluate model performance on both in-distribution tasks (e.g., lesion anatomical site classification) and out-of-distribution tasks (e.g., lung nodule malignancy prediction) to assess generalizability [4].
Limited Data Scenario Testing: Systematically evaluate model performance with progressively reduced training data (100%, 50%, 20%, 10%) to quantify resilience to data limitations [4].
Comparative Analysis: Benchmark foundation model performance against conventional supervised approaches and other state-of-the-art pretrained models using standardized metrics (balanced accuracy, mAP, AUC) [4].
Clinical Validation Protocol
Clinical validation must establish both efficacy and practical utility:
Prospective Validation Studies: Conduct studies evaluating model performance in real clinical settings with appropriate control groups and blinding procedures [74].
Workflow Impact Assessment: Quantify effects on clinical workflow efficiency, including time-to-decision, documentation burden, and cognitive load using both objective measures (time-motion studies) and subjective assessments (usability surveys) [76].
Clinical Outcome Correlation: Establish correlations between model predictions and clinically relevant endpoints, including diagnostic accuracy, treatment response prediction, and patient outcomes [9] [78].
Robustness Evaluation: Assess model stability to input variations through test-retest and inter-reader analyses, particularly important for quantitative imaging biomarkers [4].
Biological Relevance Assessment: Investigate associations between imaging features identified by the model and underlying biology through correlation with genomic data or histopathological findings [4] [78].
Table 3: Essential Research Resources for Foundation Model Development
| Resource Category | Specific Tools/Solutions | Function/Purpose |
|---|---|---|
| Data Resources | DeepLesion, LUNA16, LUNG1, RADIO datasets | Diverse, annotated imaging data for training and validation |
| Software Frameworks | Project-lighter, MHub.ai, 3D Slicer integration | Streamlined model development, containerized deployment |
| Pretraining Approaches | Modified SimCLR, SwAV, NNCLR contrastive learning | Self-supervised representation learning from unannotated data |
| Implementation Platforms | Federated learning frameworks, TinyViT, MedSAM | Privacy-preserving collaboration, computational efficiency |
| Evaluation Tools | Proctor implementation outcomes taxonomy, Consolidated Framework for Implementation Research (CFIR) | Comprehensive assessment of implementation success |
| Interpretability Methods | Grad-CAM, attention mechanisms, feature importance mapping | Model transparency and explainability for clinical trust |
The clinical adoption of foundation models for cancer imaging biomarkers faces significant but surmountable barriers. Intrinsic technical challenges including data limitations, model generalizability, and interpretability require methodological solutions such as self-supervised learning, multi-institutional collaboration, and explainable AI techniques. Practical workflow integration barriers necessitate comprehensive implementation science approaches that address human factors, workflow compatibility, and contextual adaptation. By adopting the experimental protocols, validation frameworks, and resource strategies outlined in this technical guide, researchers and drug development professionals can accelerate the translation of foundation models from research tools to clinically impactful solutions. The future of cancer imaging biomarkers lies in models that combine technical excellence with practical clinical utility, ultimately advancing precision oncology through trustworthy, integrated AI systems.
The integration of artificial intelligence (AI), particularly deep learning, into cancer research is transforming the paradigm of biomarker discovery. This is especially true in the field of cancer imaging, where foundation models—large-scale models pretrained on vast amounts of unannotated data—are demonstrating tremendous potential for identifying robust radiographic phenotypes [4]. However, the superior predictive performance of these complex "black box" models often comes at the cost of transparency, creating a significant barrier to their clinical translation [79] [80]. Explainable AI (XAI) has thus emerged as a critical discipline, aiming to make the decision-making processes of AI models transparent, interpretable, and trustworthy [81]. Within the context of a broader thesis on foundation models for cancer imaging biomarker discovery, this whitepaper argues that XAI is not merely a supplementary feature but an imperative. It is the crucial bridge that transforms opaque predictions into interpretable, biologically plausible, and clinically actionable biomarker insights, thereby accelerating the widespread translation of AI-driven discoveries into precision oncology.
The Rise of Foundation Models in Cancer Imaging
Foundation models are characterized by their training on extensive datasets using self-supervised learning (SSL), which reduces the dependency on large, manually labeled datasets—a frequent bottleneck in medical research [4]. Once pretrained, these models can be adapted to various downstream tasks through fine-tuning or by using their extracted features in simpler classifiers.
A prime example is the development of a foundation model for cancer imaging biomarkers, which was pretrained on a comprehensive dataset of 11,467 radiographic lesions from computed tomography (CT) scans [4]. This model was technically validated on an in-distribution task of lesion anatomical site classification and further evaluated on clinically relevant out-of-distribution tasks, including lung nodule malignancy prediction and prognosis forecasting for non-small cell lung cancer (NSCLC). The model's effectiveness was particularly pronounced in scenarios with limited training data, a common challenge in medical research [4]. The expanding application of these models necessitates rigorous benchmarking. The TumorImagingBench, a curated benchmark comprising six public datasets (3,244 scans), has been introduced to systematically evaluate the performance of various medical imaging foundation models across diverse oncological endpoints [17]. Such initiatives are vital for guiding the selection of optimal models for specific quantitative imaging tasks in cancer research.
The Critical Need for Explainability in Biomarker Discovery
The "black-box" nature of sophisticated AI models poses a fundamental challenge to their adoption in safety-critical fields like oncology. Without explanations, clinicians and researchers are unable to validate whether a model's prediction is based on biologically credible image features or spurious, confounding correlations [82] [80]. This lack of transparency undermines trust and hinders the model's utility for generating new biological hypotheses.
The need for interpretability in machine learning for medical imaging (MLMI) arises from a mismatch between the objective of predictive performance and the real-world requirements for clinical deployment [82]. These requirements can be formalized into five core elements:
- Localization: The ability to identify which regions in an image contributed to the prediction.
- Visual Recognizability: The explanations should align with features recognizable to a human expert, such as specific texture or shape.
- Physical Attribution: The explanation must connect the prediction to the physical reality of the tissue sample, avoiding reliance on scanner-specific artifacts [82].
- Model Transparency: Understanding the internal mechanics of the model itself.
- Actionability: The insights must be sufficient to inform clinical decisions or guide further research.
XAI addresses these needs by providing a suite of techniques that make AI models interrogable. This is indispensable for building trust, ensuring regulatory compliance, validating the biological plausibility of discovered biomarkers, and ultimately, generating actionable insights for drug development and personalized treatment strategies [79] [80].
Key XAI Methods and Experimental Protocols
A range of XAI methodologies has been developed to peel back the layers of complex AI models. The selection of a specific method often depends on the model architecture, the data modality, and the primary interpretability goal (e.g., local vs. global explanations).
Prominent XAI Techniques
- SHapley Additive exPlanations (SHAP): A game theory-based approach that calculates the marginal contribution of each input feature (e.g., a pixel or an imaging feature) to the final prediction. It is model-agnostic and provides both local and global interpretability [83] [79]. For instance, SHAP has been effectively used to identify cystatin C as a primary contributor in machine learning models predicting biological age and frailty from blood-based biomarkers [83].
- Local Interpretable Model-agnostic Explanations (LIME): This method approximates any complex model locally with a simpler, interpretable model (e.g., a linear classifier) to explain individual predictions [79] [81].
- Gradient-weighted Class Activation Mapping (Grad-CAM): A technique specifically for convolutional neural networks that uses gradient information flowing into the final convolutional layer to produce a coarse localization map, highlighting important regions in the image for a particular prediction [79].
- Concept-based Interpretability Frameworks: Moving beyond feature attribution, newer frameworks aim to discover and validate human-understandable concepts (e.g., biological pathways) within the model's latent space. For example, a novel framework for single-cell RNA-seq models uses sparse dictionary learning and counterfactual perturbations to identify genes that influence concept activation, moving beyond mere correlation [84].
Protocol for Interpreting a Cancer Imaging Foundation Model
The following workflow outlines a standardized protocol for applying XAI to a foundation model in cancer imaging, from training to biological validation [4] [17] [79].
Quantitative Performance and Benchmarking
Systematic benchmarking is essential to understand the performance and robustness of different foundation models when applied to cancer imaging tasks. The following tables summarize key findings from large-scale evaluations, providing a comparative view of model efficacy.
Table 1: Diagnostic Performance of Foundation Model Embeddings on the LUNA16 Dataset (Lung Nodule Malignancy) [17]
| Foundation Model | Architecture & Pre-training Strategy | AUC (95% CI) |
|---|---|---|
| FMCIB [4] | Convolutional; Contrastive SSL on CT lesions | 0.886 (0.871-0.900) |
| ModelsGenesis | Convolutional; Generative on CT | 0.806 (0.795-0.816) |
| VISTA3D | Vision Transformer; Supervised on CT+MRI | 0.711 (0.692-0.730) |
| Voco | Vision Transformer; Masked Autoencoding | 0.493 (0.468-0.519) |
Table 2: Prognostic Performance of Foundation Models Across Cancer Types (2-Year Overall Survival Prediction) [17]
| Cancer Type / Dataset | Top-Performing Model | AUC (95% CI) | Other Notable Models |
|---|---|---|---|
| NSCLC (Radiomics) | VISTA3D | 0.582 (0.545-0.620) | FMCIB, ModelsGenesis (AUC ~0.577) |
| Renal Cancer (C4KC-KiTS) | ModelsGenesis | 0.733 (0.670-0.796) | SUPREM (AUC = 0.718) |
| Colorectal Liver Metastases | FMCIB | 0.572 (0.509-0.644) | ModelsGenesis (AUC = 0.530) |
The data reveals that no single foundation model is universally superior. Performance is highly task-dependent, with models like FMCIB excelling in diagnostic tasks, while others like VISTA3D show relative strength in prognostic tasks [17]. Furthermore, the stability of model embeddings to input variations (e.g., test-retest) is a critical factor for clinical reliability, with most models demonstrating high robustness in such analyses [17].
The Scientist's Toolkit: Research Reagents & Essential Materials
Translating foundation models and XAI into tangible biomarker discoveries requires a suite of computational "research reagents."
Table 3: Essential Research Reagents for XAI-based Cancer Imaging Biomarker Discovery
| Item / Resource | Function & Explanation | Example Instances |
|---|---|---|
| Curated Public Datasets | Serve as standardized benchmarks for training and evaluating foundation models and XAI methods. | TumorImagingBench [17], LUNA16 [4] [17], NSCLC-Radiomics [17] |
| Pre-trained Foundation Models | Provide a starting point for transfer learning, significantly reducing computational cost and data requirements for downstream tasks. | FMCIB [4], ModelsGenesis [17], VISTA3D [17] |
| XAI Software Libraries | Open-source packages that implement popular explanation algorithms, enabling researchers to interpret their models. | SHAP [83] [81], LIME [79] [81], Captum (for PyTorch) |
| Biological Knowledge Bases | Used to validate whether features identified by XAI align with known cancer biology, lending plausibility to discoveries. | Gene Ontology, TCGA, ImmPort (for immunology) [84] [79] |
| Visualization & Interaction Tools | Critical for exploring concept-based explanations and saliency maps, facilitating collaboration between data scientists and domain experts. | Interactive interfaces for concept exploration [84], TensorBoard, medical image viewers |
The journey from a radiographic image to a clinically actionable cancer biomarker is complex. Foundation models offer a powerful vehicle for this journey, capable of navigating the high-dimensional landscape of medical images to uncover subtle phenotypic signatures. However, without interpretability, the destination remains uncertain. Explainable AI provides the essential map and compass, revealing the "why" behind the model's predictions. By integrating XAI methodologies—from feature attribution techniques like SHAP to emerging concept-based frameworks—researchers can transform foundation models from black-box predictors into engines for hypothesis generation and biological discovery. This synergy between performance and interpretability is the cornerstone for building trust, ensuring validation, and ultimately achieving the promise of precision oncology, where AI-derived biomarkers can reliably guide drug development and personalize patient care.
Ethical Considerations and Algorithmic Transparency in High-Stakes Settings
The integration of artificial intelligence (AI), particularly foundation models, into high-stakes healthcare settings like cancer imaging biomarker discovery represents a paradigm shift in medical research and clinical practice. These models, characterized by their training on vast amounts of unannotated data using self-supervised learning (SSL), demonstrate remarkable capability in reducing the demand for large labeled datasets in downstream applications [4] [10]. However, their increasing adoption necessitates rigorous examination of the ethical implications and transparency mechanisms required for trustworthy deployment. This technical guide examines these considerations within the specific context of foundation models for cancer imaging biomarkers, addressing the critical needs of researchers, scientists, and drug development professionals working at this frontier.
Foundation models in medical imaging leverage architectures such as convolutional encoders trained through SSL on comprehensive datasets of radiographic lesions [4] [11]. The resulting models serve as foundational platforms for various downstream tasks including lesion classification, malignancy prediction, and prognostic assessment [4]. While these models demonstrate superior performance, especially in data-limited scenarios, their "black-box" nature and potential impact on human decision-making create compelling ethical challenges that must be addressed through technical and governance frameworks [85] [86].
Technical Foundations of Imaging Foundation Models
Architecture and Pretraining Methodologies
Cancer imaging foundation models typically employ convolutional encoder architectures pretrained using self-supervised learning on diverse datasets of radiographic lesions [4]. The pretraining process utilizes a modified contrastive learning strategy (adapted from SimCLR) that has demonstrated superiority over other approaches including autoencoders, SwAV, and NNCLR in balanced accuracy and mean average precision [4].
Table 1: Comparative Performance of SSL Pretraining Strategies for Lesion Anatomical Site Classification
| Pretraining Strategy | Balanced Accuracy | Mean Average Precision | Performance Decline with 10% Data |
|---|---|---|---|
| Modified SimCLR (Proposed) | 0.779 | 0.847 | 9% (accuracy), 12% (mAP) |
| Standard SimCLR | 0.696 | 0.779 | Not Reported |
| SwAV | Not Reported | Not Reported | Not Reported |
| NNCLR | Not Reported | Not Reported | Not Reported |
| Autoencoder | Lowest Performance | Lowest Performance | Highest Performance Decline |
The technical validation of these models typically involves multiple use cases: (1) technical validation through in-distribution tasks like lesion anatomical site classification; (2) diagnostic biomarker development for applications like lung nodule malignancy prediction; and (3) prognostic biomarker development for outcomes such as overall survival in non-small cell lung cancer [4]. This multi-stage evaluation framework ensures robust assessment of model capabilities across clinically relevant scenarios.
Implementation Approaches for Downstream Tasks
Two primary implementation approaches are employed when adapting foundation models to specific clinical tasks:
- Feature Extraction with Linear Classification: The pretrained foundation model serves as a fixed feature extractor, with a simple linear classifier trained on top of the extracted features. This approach offers computational efficiency and stability, particularly in limited data scenarios [4].
- End-to-End Fine-Tuning: The entire foundation model undergoes additional training (fine-tuning) on task-specific data. While potentially offering higher performance with sufficient data, this method requires more computational resources and may exhibit greater performance degradation with limited training samples [4].
Experimental evidence indicates that the feature extraction approach often outperforms fine-tuning and conventional supervised learning when training data is severely limited (e.g., 10% of total data), highlighting the particular value of foundation models in specialized medical applications where large annotated datasets are unavailable [4].
Experimental Protocols and Validation Frameworks
Foundation Model Pretraining Protocol
The foundational protocol for developing cancer imaging foundation models involves several methodical stages:
Data Curation and Preprocessing:
- Source diverse radiographic lesions from publicly available datasets (e.g., DeepLesion) and institutional collections [4] [11]
- Implement rigorous quality control and standardization procedures across multi-institutional data
- Apply appropriate data augmentation techniques tailored to medical imaging characteristics
Self-Supervised Pretraining:
- Implement modified contrastive learning framework (adapted from SimCLR) [4]
- Train convolutional encoder on large-scale unannotated lesion dataset (n=11,467 lesions) [4]
- Optimize model parameters to maximize representation learning without task-specific labels
Validation and Benchmarking:
- Evaluate learned representations on technical validation tasks (e.g., anatomical site classification)
- Compare against established baseline models (Med3D, Models Genesis) and supervised approaches
- Assess data efficiency by measuring performance degradation with progressively limited training data
Performance Benchmarking Methodology
Rigorous benchmarking of foundation models against established baselines follows a structured experimental design:
Table 2: Downstream Task Performance Comparison Across Implementation Approaches
| Implementation Approach | Anatomical Site Classification (mAP) | Lung Nodule Malignancy Prediction (AUC) | Performance with Limited Data |
|---|---|---|---|
| Foundation Model (Features) | 0.847 | Not Reported | Minimal performance degradation (9-12% with 10% data) |
| Foundation Model (Fine-tuned) | 0.857 | 0.944 | Significant performance degradation with ≤20% data |
| Med3D (Fine-tuned) | 0.779 (Balanced Accuracy) | 0.917 | Not Reported |
| Supervised Baseline | Lower than foundation approaches | Lower than foundation approaches | Substantial performance degradation |
Evaluation Metrics and Statistical Analysis:
- Utilize domain-appropriate metrics including balanced accuracy, mean average precision (mAP), and area under the curve (AUC) [4]
- Implement statistical significance testing (p<0.05 threshold) for performance comparisons
- Assess robustness through test-retest reliability and inter-reader variability analyses
- Evaluate biological plausibility through association studies with genomic data [4]
Limited Data Scenario Testing:
- Systematically reduce training data (100%, 50%, 20%, 10%) to evaluate data efficiency
- Compare performance degradation across implementation approaches
- Identify optimal approach selection based on available annotated data resources
Ethical Framework for High-Stakes Deployment
Core Ethical Principles and Implementation Challenges
The deployment of foundation models in cancer imaging must adhere to established ethical principles while addressing domain-specific challenges:
Autonomy and Informed Consent:
- Ensure patients understand the role of AI in their diagnostic process
- Develop transparent consent processes that communicate AI limitations and uncertainties
- Establish protocols for handling incidental findings identified by AI systems
Beneficence and Non-Maleficence:
- Rigorously validate model performance across diverse patient populations
- Implement safeguards against automation bias in clinical interpretation
- Establish monitoring systems for performance degradation over time
Justice and Equity:
- Proactively address algorithmic bias through diverse training data and bias testing
- Ensure equitable access to AI-enhanced diagnostics across socioeconomic groups
- Regularly audit model performance across demographic subgroups
Transparency and Explainability:
- Develop interpretability methods tailored to imaging foundation models
- Create standardized reporting frameworks for AI-assisted diagnoses
- Enable traceability from model outputs to contributing image regions
Recent research highlights the particular risk that AI assistance can degrade human performance in high-stakes settings when predictions are incorrect. Studies with nursing professionals demonstrated that while accurate AI predictions improved performance by 53-67%, misleading AI predictions caused performance degradation of 96-120% compared to unaided assessment [85]. This underscores the critical importance of transparency and appropriate human-AI collaboration frameworks.
Accountability and Liability Frameworks
As AI systems become more autonomous in healthcare decision-making, assigning responsibility for errors grows increasingly complex [86]. Legal frameworks must evolve to address:
- Liability Distribution: Clarifying responsibilities among clinicians, developers, healthcare institutions, and regulatory bodies [86] [87]
- Performance Standards: Establishing appropriate standards of care for AI-assisted diagnosis
- Regulatory Compliance: Navigating evolving regulatory landscapes including the EU AI Act, FDA guidelines, and GDPR requirements [88]
The EU AI Act classifies healthcare AI systems as high-risk, imposing specific regulatory obligations including transparency requirements, human oversight provisions, and robust accuracy standards [88]. Similar regulatory developments are emerging globally, creating a complex compliance landscape for researchers and developers.
Algorithmic Transparency and Explainability
Technical Approaches to Model Interpretability
Explainable AI (XAI) techniques are essential for building trust and facilitating clinical adoption of foundation models:
Saliency and Attribution Methods:
- Implement gradient-based attribution techniques to identify image regions influencing predictions
- Develop class activation mapping tailored to foundation model architectures
- Validate attribution plausibility through clinician assessment and correlation with known imaging biomarkers
Feature Analysis and Representation Interpretation:
- Analyze learned representations for biological plausibility using gene expression correlation studies [4]
- Assess feature stability across acquisition parameters and inter-reader variations
- Identify potential confounding factors embedded in model representations
Uncertainty Quantification:
- Implement calibration techniques to ensure prediction confidence aligns with accuracy
- Develop uncertainty estimation methods to flag potentially unreliable predictions
- Create confidence communication protocols for clinical reporting
Research demonstrates that foundation models for cancer imaging can learn biologically meaningful representations, with identified patterns showing strong associations with immune-related pathways [4] [10]. This biological plausibility provides important validation of model interpretability and clinical relevance.
Human-AI Collaboration Design
Effective human-AI collaboration requires careful design of interaction paradigms:
Collaboration Models:
- Human-in-the-Loop: Clinicians maintain primary decision authority with AI support
- Human-on-the-Loop: AI generates primary decisions with human oversight and override capability
- Human-out-of-the-Loop: Fully autonomous operation for well-defined, validated tasks with appropriate safeguards
Studies indicate that the optimal collaboration model depends on task complexity, AI reliability, and clinical context. Joint Activity Testing—which evaluates human and AI performance together across a range of challenging scenarios—has emerged as a critical methodology for identifying potential collaboration failures before clinical deployment [85].
Essential Research Tools and Platforms
Table 3: Key Research Reagents and Computational Resources for Cancer Imaging Foundation Models
| Resource Category | Specific Tools/Platforms | Primary Function | Access Method |
|---|---|---|---|
| Public Datasets | DeepLesion, LUNA16, LUNG1, RADIO | Model training and validation | Publicly available downloads [11] |
| Code Repositories | GitHub with project-lighter integration | Data preprocessing, model training, inference | Public repository with YAML configurations [11] |
| Model Platforms | MHub.ai with 3D Slicer integration | Containerized model deployment | Pip package installation [11] |
| Benchmarking Suites | TumorImagingBench (6 datasets, 3,244 scans) | Standardized model evaluation | Publicly released code and curated datasets [12] |
| Explainability Tools | SHAP, LIME, custom attribution methods | Model interpretation and transparency | Open-source libraries and custom implementations |
Implementation and Deployment Considerations
Successful implementation of foundation models in research settings requires attention to several practical considerations:
Computational Infrastructure:
- GPU memory and processing time requirements vary significantly between feature extraction and fine-tuning approaches [4]
- Model serving infrastructure must support clinical workflow integration and real-time inference
- Data storage and management systems must handle large-scale imaging data with appropriate privacy protections
Regulatory Compliance:
- Implement data privacy safeguards compliant with HIPAA, GDPR, and other applicable regulations [86] [88]
- Maintain comprehensive documentation for model development, validation, and monitoring
- Establish quality management systems aligned with medical device regulatory requirements
Interoperability Standards:
- Adopt standard imaging formats (DICOM) and healthcare data standards (FHIR)
- Implement APIs for seamless integration with clinical picture archiving and communication systems (PACS)
- Develop vendor-neutral architecture solutions to ensure platform flexibility
Foundation models for cancer imaging biomarker discovery represent a transformative advancement with significant potential to improve early detection, diagnosis, and prognosis in oncology. However, their ethical deployment in high-stakes clinical settings requires robust technical validation, comprehensive transparency measures, and thoughtful human-AI collaboration frameworks. The experimental protocols and implementation considerations outlined in this guide provide researchers and developers with practical approaches to address these critical challenges.
As the field evolves, continued attention to algorithmic fairness, regulatory compliance, and real-world performance validation will be essential to realizing the full potential of these technologies while maintaining the trust of both clinicians and patients. Through rigorous ethical practice and technical excellence, foundation models can fulfill their promise as powerful tools in the fight against cancer.
Benchmarking Success: Performance, Validation, and Comparative Analysis
Systematic benchmarking is a critical methodology in the validation of foundation models for cancer imaging biomarker discovery, ensuring these complex algorithms perform robustly across diverse patient populations and clinical scenarios. As artificial intelligence (AI) transforms oncology research, the ability to objectively evaluate model performance through standardized, comprehensive benchmarking protocols has become essential for clinical translation. Foundation models, characterized by their large-scale architecture and pre-training on vast datasets, show particular promise in addressing the perennial challenge of limited annotated data in medical applications [4] [10]. However, their complexity and potential variability necessitate rigorous evaluation frameworks that can accurately assess performance across different cancer types, imaging modalities, and patient demographics.
This technical guide examines the core principles, methodologies, and practical implementations of systematic benchmarking for cancer imaging foundation models, with emphasis on their application within biomarker discovery research. We present standardized experimental protocols, quantitative performance comparisons across leading platforms, and visual workflows to assist researchers, scientists, and drug development professionals in designing robust validation strategies. By establishing comprehensive benchmarking frameworks that account for technical performance, biological relevance, and clinical utility, the oncology research community can accelerate the development of reliable, generalizable AI tools that ultimately improve patient care through more accurate diagnosis, prognosis, and treatment selection.
Foundational Concepts in Benchmarking Cancer Imaging Models
Systematic benchmarking of foundation models for cancer imaging extends beyond conventional performance metrics to encompass several specialized dimensions critical for clinical applicability. Technical validation establishes baseline model performance on defined tasks using standardized datasets, while clinical validation assesses performance in real-world scenarios with diverse patient populations and imaging protocols [12]. Biological plausibility evaluation ensures that model predictions align with established cancer biology, often through correlation with molecular pathways or genomic data [4] [10]. The emerging paradigm of multi-modal benchmarking evaluates how effectively models integrate imaging data with complementary omics datasets, including genomics, transcriptomics, and proteomics [89] [79].
Foundation models pre-trained using self-supervised learning on extensive datasets have demonstrated particular utility in cancer imaging applications, significantly reducing the demand for labeled data in downstream tasks [4] [11]. These models typically employ contrastive learning frameworks that learn robust representations by maximizing agreement between differently augmented views of the same image while distinguishing them from other images in the dataset [4]. This pre-training approach has shown superior performance compared to traditional supervised learning, especially in limited-data scenarios common in specialized oncology applications [4].
Table 1: Key Evaluation Dimensions for Cancer Imaging Foundation Models
| Dimension | Core Metrics | Applications | Data Requirements |
|---|---|---|---|
| Technical Performance | AUC, balanced accuracy, mAP, sensitivity, specificity | Lesion classification, malignancy prediction | Curated benchmark datasets with expert annotations |
| Clinical Utility | Hazard ratios, decision curve analysis, clinical net benefit | Prognostic stratification, treatment response prediction | Annotated clinical cohorts with outcome data |
| Biological Relevance | Pathway enrichment, correlation with molecular subtypes | Biomarker discovery, mechanism interpretation | Multi-omics data with paired imaging |
| Robustness | Performance stability across sites, scanners, populations | Generalizability assessment, fairness evaluation | Multi-center datasets with diverse demographics |
Experimental Frameworks for Benchmarking Studies
Standardized Benchmarking Protocols
Implementing robust benchmarking protocols for cancer imaging foundation models requires meticulous experimental design with standardized workflows. The TumorImagingBench framework exemplifies this approach, providing a curated benchmark comprising multiple public datasets (3,244 scans) with varied oncological endpoints [12]. This framework facilitates comprehensive evaluation of foundation models across diverse architectures and pre-training strategies, assessing not only endpoint prediction performance but also robustness to clinical variability and interpretability of results [12].
A critical component of effective benchmarking is the establishment of appropriate data curation protocols. These should include: (1) multi-center dataset collection with intentional variability in scanner manufacturers, acquisition parameters, and patient populations; (2) comprehensive annotation by multiple clinical experts with documentation of inter-reader variability; (3) stratified sampling across cancer types, stages, and demographic factors to ensure representative evaluation; and (4) standardized pre-processing pipelines to minimize technical confounders while maintaining biological relevance [4] [12]. For foundation models specifically, benchmarking should include both in-distribution tasks (sourced from the same cohort as pre-training) and out-of-distribution tasks (belonging to different cohorts) to thoroughly assess generalizability [4].
Performance Metrics and Statistical Evaluation
Comprehensive benchmarking requires multi-dimensional assessment using both standard and domain-specific metrics. For classification tasks (e.g., malignancy prediction, site classification), area under the curve (AUC), balanced accuracy, and mean average precision (mAP) provide robust evaluation of discriminatory performance [4]. For prognostic applications, time-dependent AUC and concordance index evaluate survival prediction capability, while hazard ratios in multivariable Cox models assess independent predictive value [4].
Statistical evaluation should include confidence interval estimation through appropriate resampling methods (e.g., bootstrapping), comparative testing between models using paired statistical tests, and subgroup analysis to identify performance variations across patient demographics, cancer subtypes, and imaging modalities [4] [12]. For clinical translation, decision curve analysis provides assessment of clinical utility by quantifying net benefit across different probability thresholds [4].
Quantitative Benchmarking of Spatial Transcriptomics Platforms
Recent systematic benchmarking of imaging spatial transcriptomics (iST) platforms in FFPE tissues provides a compelling case study in comprehensive technology evaluation. A 2025 Nature Communications study directly compared three commercial iST platforms—10X Xenium, Vizgen MERSCOPE, and Nanostring CosMx—using serial sections from tissue microarrays containing 17 tumor and 16 normal tissue types [90]. This rigorous analysis employed matched samples and gene panels where possible, with careful attention to experimental standardization across platforms.
The benchmarking revealed significant differences in platform performance characteristics. Xenium consistently generated higher transcript counts per gene without sacrificing specificity, while both Xenium and CosMx demonstrated RNA transcript measurements in strong concordance with orthogonal single-cell transcriptomics data [90]. All three platforms successfully performed spatially resolved cell typing, but with varying sub-clustering capabilities—Xenium and CosMx identified slightly more clusters than MERSCOPE, though with different false discovery rates and cell segmentation error frequencies [90]. These nuanced performance differences highlight the importance of application-specific platform selection, where factors such as target gene panel, required spatial resolution, and sample quality must be balanced against technical performance characteristics.
Table 2: Performance Benchmarking of Commercial Spatial Transcriptomics Platforms
| Platform | Transcript Detection Sensitivity | Concordance with scRNA-seq | Cell Segmentation Accuracy | Cell Clustering Resolution | Best Application Context |
|---|---|---|---|---|---|
| 10X Xenium | Highest transcripts per gene | High concordance | Moderate segmentation accuracy | High cluster resolution | High-plex targeted studies |
| Nanostring CosMx | High transcript detection | High concordance | Variable segmentation | High cluster resolution | Large gene panel applications |
| Vizgen MERSCOPE | Moderate sensitivity | Lower concordance | Varies with sample | Moderate clustering | Standard gene panels |
Multi-Modal Integration Benchmarking
The integration of imaging data with complementary multi-omics datasets represents a particularly challenging dimension of benchmarking for cancer foundation models. Effective multi-modal integration requires sophisticated computational strategies that can harmonize heterogeneous data types while preserving biological meaning. Benchmarking studies typically evaluate three primary fusion approaches: early fusion (feature-level integration), late fusion (decision-level integration), and hybrid fusion strategies that combine elements of both [79] [91].
Evidence from recent multi-modal oncology reviews indicates that selective integration of 3-5 core modalities often yields optimal predictive performance, with AUC improvements of 10-15% over unimodal baselines [79]. For example, in non-small cell lung cancer (NSCLC), the integration of radiology, pathology, and genomics data achieved an AUC of 0.80 for immunotherapy response prediction [79]. The emerging paradigm of immunology-informed integration specifically focuses on connecting predictive signatures to tumor-immune microenvironment dynamics, enhancing biomarker discovery and immunotherapy stratification [79].
Benchmarking multi-modal foundation models requires specialized evaluation protocols that assess both integration effectiveness and biological coherence. Explainable AI (XAI) techniques, including SHAP (SHapley Additive exPlanations) and LIME (Local Interpretable Model-agnostic Explanations), provide critical insights into model behavior by identifying which modalities contribute most significantly to specific predictions [79]. Additionally, specialized metrics such as cross-modal attention consistency and modality ablation impact help quantify the effectiveness of integration strategies [79] [91].
The Scientist's Toolkit: Essential Research Reagents and Platforms
Implementing robust benchmarking studies for cancer imaging foundation models requires access to specialized computational resources, datasets, and analytical tools. The table below summarizes key research reagent solutions essential for conducting comprehensive model evaluations.
Table 3: Essential Research Reagents and Platforms for Benchmarking Studies
| Resource Category | Specific Solutions | Primary Applications | Key Features |
|---|---|---|---|
| Spatial Transcriptomics Platforms | 10X Xenium, Nanostring CosMx, Vizgen MERSCOPE | Spatial biomarker discovery, tumor microenvironment analysis | Single-cell resolution, FFPE compatibility, targeted gene panels [90] |
| Public Benchmark Datasets | TumorImagingBench, DeepLesion, LUNA16, TCIA | Model training and validation | Curated datasets with expert annotations, multiple cancer types [4] [12] |
| Multi-Omics Databases | TCGA, CPTAC, DriverDBv4, GliomaDB | Multi-modal integration studies | Integrated genomic, transcriptomic, proteomic data [89] |
| Foundation Model Implementations | MHub.ai, GitHub repositories | Feature extraction, transfer learning | Pre-trained weights, containerized deployment [11] |
| Explainable AI Tools | SHAP, LIME, Grad-CAM | Model interpretation, biological validation | Feature attribution, visual explanations [79] |
Systematic benchmarking represents a foundational component in the development and validation of cancer imaging foundation models, providing the rigorous evaluation framework necessary for clinical translation. As demonstrated through spatial transcriptomics platform comparisons and multi-modal integration studies, comprehensive benchmarking must encompass technical performance, biological plausibility, and clinical utility across diverse patient cohorts. The standardized protocols, quantitative metrics, and visual workflows presented in this guide provide researchers with practical frameworks for implementing robust model evaluation strategies. Continued refinement of benchmarking methodologies, with particular emphasis on reproducibility, generalizability, and biological interpretation, will accelerate the development of clinically impactful AI tools that advance precision oncology and improve patient outcomes.
Performance Metrics in Diagnostic vs. Prognostic Tasks
Within oncology, the accurate evaluation of artificial intelligence (AI) models, particularly foundation models for cancer imaging biomarker discovery, hinges on the precise application of task-specific performance metrics. Diagnostic tasks focus on identifying the presence or type of cancer, whereas prognostic tasks predict future patient outcomes such as survival or therapy response. This guide details the core metrics, experimental protocols, and computational tools required to rigorously validate foundation models in each context. Adherence to these principles is paramount for translating algorithmic discoveries into clinically actionable biomarkers that can improve patient care.
The advent of foundation models—large-scale deep learning models trained on vast amounts of unannotated data—heralds a new era in cancer imaging biomarker discovery [4] [92]. These models, typically trained using self-supervised learning (SSL), serve as a versatile foundation for various downstream tasks, significantly reducing the demand for large, labeled datasets [4]. A critical aspect of their development and validation involves the rigorous application of performance metrics tailored to the task's specific clinical objective. In oncology, a fundamental distinction exists between diagnostic biomarkers, which ascertain the presence or type of disease, and prognostic biomarkers, which forecast the likely course of a disease, including survival and response to treatment, independent of or in response to therapy [5] [93]. This whitepaper provides an in-depth technical guide for researchers and drug development professionals on the performance metrics, experimental methodologies, and validation frameworks essential for evaluating foundation models in diagnostic versus prognostic contexts within cancer imaging.
Core Conceptual Framework: Diagnostic vs. Prognostic Tasks
Diagnostic Tasks
Diagnostic tasks in cancer imaging are centered on the contemporaneous assessment of a patient's condition. The primary question is: "Does the patient have cancer, or what specific type of cancer is present?" For instance, a foundation model might be fine-tuned to classify lesions from computed tomography (CT) scans as benign or malignant [4] or to subtype non-small cell lung cancer (NSCLC) into adenocarcinoma (LUAD) and squamous cell carcinoma (LUSC) from histopathological whole slide images (WSIs) [92]. The output is typically a classification or a probability pertaining to the current disease state.
Prognostic Tasks
Prognostic tasks are inherently forward-looking, aiming to predict a future patient outcome. The central question is: "What is the likely outcome for this patient?" Common endpoints include overall survival (OS), disease-free survival (DFS), disease-specific survival (DSS), and response to adjuvant chemotherapy [94] [92]. For example, an AI model can be developed to predict survival outcomes from histopathology slides of gastrointestinal cancers, subsequently stratifying patients into high-risk and low-risk groups [94]. The output is often a risk score or a time-to-event prediction.
The logical relationship and primary metrics for these two tasks are summarized in the diagram below.
Performance Metrics: A Comparative Analysis
Metrics for Diagnostic Tasks
Diagnostic tests yield binary, categorical, or continuous results that require interpretation against a gold standard (e.g., pathology confirmation). Metrics for these tasks evaluate the model's discriminative and classification abilities at a single point in time.
- Area Under the Receiver Operating Characteristic Curve (AUC/ROC): The ROC curve plots the true positive rate (sensitivity) against the false positive rate (1 - specificity) across all possible classification thresholds. The AUC provides a single scalar value representing the model's ability to distinguish between classes [95] [96]. An AUC of 0.5 indicates performance no better than chance, while 1.0 represents perfect discrimination [95]. The following table provides a standard interpretation guide for AUC values [95]:
Table 1: Interpretation of AUC Values in Diagnostic Tasks
| AUC Value | Interpretation Suggestion |
|---|---|
| 0.9 ≤ AUC | Excellent |
| 0.8 ≤ AUC < 0.9 | Considerable |
| 0.7 ≤ AUC < 0.8 | Fair |
| 0.6 ≤ AUC < 0.7 | Poor |
| 0.5 ≤ AUC < 0.6 | Fail |
- Sensitivity and Specificity: Sensitivity (or recall) is the proportion of actual positives correctly identified. Specificity is the proportion of actual negatives correctly identified [95] [96]. These metrics are interdependent and should be reported alongside the AUC.
- Balanced Accuracy: Particularly useful in imbalanced datasets, it is the arithmetic mean of sensitivity and specificity [4].
- Mean Average Precision (mAP): Crucial for multi-class classification, mAP summarizes the precision-recall curve across all classes and is a key metric for complex diagnostic tasks like lesion anatomical site classification [4].
Metrics for Prognostic Tasks
Prognostic models predict the time until a specific event (e.g., death, recurrence), necessitating metrics that account for censored data (where the event has not occurred for some patients during the study period).
- Concordance Index (C-index): The most critical metric for prognostic models, the C-index measures the model's ability to provide a correct ranking of individuals based on their survival times. It is the fraction of all pairs of patients whose predicted survival order is concordant with their observed order. A C-index of 0.5 is random prediction, and 1.0 is perfect concordance [94] [92]. In practice, values above 0.7 are considered clinically useful.
- Hazard Ratio (HR): Derived from Cox proportional hazards models, the HR quantifies the effect size of a predictive variable (e.g., a high-risk vs. low-risk score from an AI model). An HR greater than 1 indicates increased risk of the event [94].
- Kaplan-Meier Survival Analysis and Log-Rank Test: This non-parametric statistic is used to visualize and compare the survival curves of different risk groups (e.g., high-risk vs. low-risk) stratified by the model's output. The log-rank test determines if the observed differences between these curves are statistically significant [94] [97].
The following table offers a consolidated comparison of these core metrics.
Table 2: Core Performance Metrics for Diagnostic vs. Prognostic Tasks
| Aspect | Diagnostic Tasks | Prognostic Tasks |
|---|---|---|
| Primary Objective | Identify current disease state | Predict future patient outcome |
| Core Metrics | AUC/ROC, Sensitivity, Specificity, Balanced Accuracy, mAP | Concordance Index (C-index), Hazard Ratio (HR), Kaplan-Meier Analysis |
| Key Interpretation | AUC: 0.5 (chance) to 1.0 (perfect) [95] | C-index: 0.5 (chance) to 1.0 (perfect) [94] |
| Clinical Benchmark | AUC > 0.80 generally considered clinically useful [95] | C-index > 0.70 generally considered clinically useful |
| Statistical Test for Comparison | DeLong's test (for comparing AUCs) [95] | Log-rank test (for comparing survival curves) |
Experimental Protocols and Methodologies
A Protocol for Diagnostic Biomarker Development
A typical experimental workflow for validating a foundation model on a diagnostic task, such as distinguishing malignant from benign lung nodules, involves the following steps [4]:
- Foundation Model Pretraining: A convolutional encoder is pretrained on a large, diverse dataset of unlabeled images (e.g., 11,467 radiographic lesions from CT scans) using a self-supervised learning strategy like contrastive learning (e.g., SimCLR) [4].
- Downstream Fine-Tuning/Feature Extraction:
- Feature Extraction Approach: The pretrained foundation model is used as a fixed feature extractor. A simple linear classifier (e.g., logistic regression) is then trained on these extracted features using the labeled diagnostic dataset.
- Fine-Tuning Approach: The weights of the foundation model are further updated (fine-tuned) end-to-end on the labeled diagnostic dataset.
- Performance Evaluation: The model's predictions on a held-out test set are compared against the histopathology-confirmed gold standard. Performance is reported using AUC, balanced accuracy, sensitivity, and specificity, along with 95% confidence intervals.
- Robustness and Data Efficiency Analysis: Model performance is evaluated across progressively smaller training subsets (e.g., 100%, 50%, 10% of data) to demonstrate its data efficiency—a key advantage of foundation models [4].
- Statistical Comparison: The model's AUC is compared against baseline supervised models and other pretrained models using statistical tests like the DeLong test [95].
A Protocol for Prognostic Biomarker Development
For a prognostic task, such as predicting overall survival from histopathological images of gastric cancer, the protocol differs [94] [92]:
- Foundation Model Pretraining: A foundation model (e.g., BEPH) is pretrained on a massive corpus of unlabeled histopathological images (e.g., 11 million patches from The Cancer Genome Atlas) using self-supervised learning like masked image modeling (MIM) [92].
- WSI-Level Representation Learning: For whole-slide images, a multiple instance learning (MIL) framework is often employed. The WSI is divided into patches, and the foundation model encodes each patch. These patch-level features are aggregated to form a single WSI-level representation.
- Prognostic Model Training: A survival model, such as a Cox proportional hazards model, is trained on the WSI-level representations to predict a continuous risk score.
- Risk Stratification: Patients are dichotomized into high-risk and low-risk groups based on the median risk score or an optimized cutoff.
- Performance Validation:
- The C-index is calculated to evaluate the model's ranking accuracy.
- Kaplan-Meier curves are plotted for the risk groups, and a log-rank test is performed to assess the significance of the survival difference.
- Multivariable Cox regression is used to determine if the AI-derived risk score is an independent prognostic factor after adjusting for clinical variables like stage and age [94].
- Predictive Biomarker Analysis: To assess if the biomarker can predict treatment benefit, a formal test for interaction between the risk score and adjuvant chemotherapy treatment is performed in a multivariate model [94].
The workflow for developing and validating these models is illustrated below.
The Scientist's Toolkit: Essential Research Reagents and Materials
The development and validation of imaging biomarkers via foundation models rely on a suite of computational and data resources.
Table 3: Essential Research Reagents and Computational Tools
| Item / Resource | Function / Description | Example in Context |
|---|---|---|
| Foundation Model Architecture | A large, pre-trained model serving as a base for feature extraction or fine-tuning. | Convolutional encoder (e.g., ResNet) pretrained with SimCLR on CT lesions [4]; Vision Transformer (ViT) pretrained with MIM on histopathology patches [92]. |
| Self-Supervised Learning (SSL) Algorithm | Algorithm for learning representations from unlabeled data. | Contrastive learning (SimCLR, NNCLR) [4]; Masked Image Modeling (MAE, BEiT) [92]. |
| Curated Medical Imaging Datasets | Large-scale, often public, datasets for pre-training and benchmarking. | The Cancer Genome Atlas (TCGA) for histopathology [92]; LUNA16 for lung nodules [4]. |
| Multiple Instance Learning (MIL) Framework | A method for learning from weakly labeled data (e.g., a label for a whole slide but not its patches). | Used to aggregate patch-level features from a WSI into a slide-level representation for prognosis [92]. |
| Statistical Software / Libraries | Tools for computing performance metrics and conducting statistical tests. | R packages (survival for C-index, KM curves; pROC for AUC); Python (scikit-learn, lifelines, PySuvival). |
| Explainable AI (XAI) Tools | Techniques to interpret model predictions and ensure clinical transparency. | SHAP, attention mechanisms to visualize regions of the image influencing the diagnosis or prognosis [92] [97]. |
The rigorous distinction between diagnostic and prognostic tasks, and the correct application of their associated performance metrics, is non-negotiable in the development of robust, clinically relevant cancer imaging biomarkers. Foundation models, with their data efficiency and strong transfer learning capabilities, offer a powerful platform for both endeavors. By adhering to the detailed experimental protocols and validation frameworks outlined in this guide—employing AUC and sensitivity/specificity for diagnostic questions, and the C-index and Kaplan-Meier analysis for prognostic inquiries—researchers can accelerate the translation of these advanced AI models from bench to bedside, ultimately enhancing precision oncology.
Cancer imaging biomarker discovery is a cornerstone of precision oncology, enabling non-invasive characterization of tumor phenotypes for improved diagnosis, prognosis, and treatment evaluation. Traditionally, this field has been dominated by two methodological paradigms: traditional radiomics, which relies on handcrafted feature engineering, and supervised deep learning, which learns features directly from data. However, both approaches face significant limitations in clinical translation, including dependency on large annotated datasets and poor generalizability across diverse patient populations and imaging protocols.
The emergence of foundation models represents a paradigm shift in medical image analysis. These models, pre-trained on vast amounts of unlabeled data through self-supervised learning (SSL), can be adapted to various downstream tasks with minimal task-specific data [4] [98]. This technical review provides a comprehensive comparative analysis of these three methodologies within the context of cancer imaging biomarker discovery, focusing on their technical foundations, performance characteristics, and implementation considerations.
Methodological Fundamentals
Traditional Radiomics
Traditional radiomics follows a standardized pipeline that converts medical images into mineable quantitative data. The process begins with image acquisition and preprocessing, followed by manual or semi-automated segmentation of regions of interest (ROIs). From these ROIs, hundreds of handcrafted features are mathematically extracted [99] [9].
Core Feature Categories:
- Shape-based features: Describe geometric properties of ROIs (e.g., sphericity, surface area)
- First-order statistics: Quantify voxel intensity distributions (e.g., mean, median, entropy)
- Texture features: Capture spatial relationships between voxels using matrices including:
- Gray-Level Co-occurrence Matrix (GLCM)
- Gray-Level Run-Length Matrix (GLRLM)
- Gray-Level Size Zone Matrix (GLSZM) [99]
This approach requires significant domain expertise for feature selection and is susceptible to variability in imaging protocols and segmentation methods.
Supervised Deep Learning
Supervised deep learning utilizes convolutional neural networks (CNNs) to automatically learn hierarchical feature representations directly from image data. Unlike traditional radiomics, these models eliminate the need for manual feature engineering by learning relevant features end-to-end through backpropagation [100]. However, they typically require large datasets of annotated images (often thousands of labeled examples) to achieve optimal performance and generalize effectively. This substantial data requirement creates a significant bottleneck in medical imaging applications where expert annotations are scarce and costly [4] [9].
Foundation Models
Foundation models are large-scale neural networks pre-trained on extensive, diverse datasets using self-supervised learning objectives. Rather than being trained for a specific task, they learn general-purpose representations of medical images that can be efficiently adapted to various downstream applications [4] [98]. The critical innovation lies in their pre-training approach, which uses self-supervised learning to create learning signals directly from the data itself without manual annotations [98].
Two primary implementation strategies are used for downstream task adaptation:
- Feature extraction: Using the pre-trained model as a fixed feature extractor, with simple classifiers (e.g., linear models) trained on these features.
- Fine-tuning: Updating all or部分 of the pre-trained model's weights on task-specific data [4].
Table 1: Core Methodological Characteristics
| Characteristic | Traditional Radiomics | Supervised Deep Learning | Foundation Models |
|---|---|---|---|
| Feature Learning | Handcrafted mathematical features | Learned from labeled data end-to-end | Self-supervised pre-training, then adaptation |
| Data Requirements | Moderate sample size, manual segmentation | Large annotated datasets (thousands of samples) | Extensive unlabeled data for pre-training, minimal labels for adaptation |
| Domain Expertise | High (for feature selection & interpretation) | Moderate (for architecture design & training) | Lower (for adaptation to specific tasks) |
| Computational Load | Low to moderate | High | Very high for pre-training, low to moderate for adaptation |
| Key Advantages | Interpretable features, works with small samples | Automatic feature discovery, high performance with sufficient data | Strong generalization, data efficiency, multi-task capability |
Performance Comparison in Cancer Imaging Applications
Quantitative Performance Metrics
Recent studies have systematically evaluated the performance of foundation models against established benchmarks across multiple cancer imaging tasks. The following table summarizes key comparative results:
Table 2: Performance Comparison Across Methodologies
| Study/Task | Traditional Radiomics | Supervised Deep Learning | Foundation Model | Dataset Size |
|---|---|---|---|---|
| Lesion Anatomical Site Classification [4] | - | Balanced Accuracy: 0.696mAP: 0.779 | Balanced Accuracy: 0.804mAP: 0.857 | 3,830 lesions |
| Lung Nodule Malignancy Prediction [4] | - | AUC: 0.917mAP: 0.930 | AUC: 0.944mAP: 0.953 | 507 nodules |
| HCC Differentiation via Ultrasound [100] | AUC: 0.736(95% CI: 0.578-0.893) | AUC: 0.861(95% CI: 0.75-0.972) | Combined Model AUC: 0.918(95% CI: 0.836-1.0) | 224 patients |
Performance in Limited Data Scenarios
Foundation models demonstrate particular advantage in data-scarce environments, which are common in medical imaging. In one comprehensive study, a foundation model pretrained on 11,467 radiographic lesions maintained robust performance even when downstream training data was reduced to just 10% of the original dataset, showing only a 9% decline in balanced accuracy compared to significantly larger drops in supervised approaches [4]. This data efficiency stems from the rich feature representations learned during pretraining, which capture generally relevant visual concepts transferable to specialized tasks.
Generalization and Robustness
Beyond raw performance metrics, foundation models exhibit superior generalization across institutions and imaging protocols. They demonstrate increased stability to input variations, including inter-reader segmentation differences and acquisition parameter variations [4] [9]. This robustness is critical for clinical translation, where models must perform consistently across diverse healthcare settings with varying equipment and protocols.
Experimental Protocols and Methodologies
Foundation Model Pretraining Protocol
The following diagram illustrates the typical self-supervised pretraining workflow for medical imaging foundation models:
Figure 1: Foundation Model Pretraining Workflow. This diagram illustrates the self-supervised learning process where models learn from unlabeled data through pretext tasks.
Key Methodological Details:
- Architecture: Convolutional encoders (e.g., ResNet variants) or vision transformers are commonly used as backbone networks [4] [12].
- Pretraining Data: Large-scale diverse datasets like RadImageNet [101] or DeepLesion (11,467 lesions from 2,312 patients) [4] [11].
- SSL Methodology: Contrastive learning frameworks (e.g., modified SimCLR) that learn representations by maximizing agreement between differently augmented views of the same image while distinguishing them from other images [4].
- Pretext Tasks: Include instance discrimination, where the model learns to identify different augmented views of the same image as similar while contrasting them against other images [4] [98].
Downstream Task Adaptation Protocol
Once pretrained, foundation models can be adapted to specific cancer imaging tasks through two primary approaches:
Figure 2: Downstream Task Adaptation Methods. This diagram shows the two primary approaches for applying foundation models to specific clinical tasks.
Implementation Approaches:
- Feature Extraction Approach
- The foundation model backbone remains frozen
- Only a linear classifier (e.g., SVM or logistic regression) is trained on the extracted features
- Computationally efficient and less prone to overfitting with very small datasets [4]
- Fine-Tuning Approach
- All or部分 of the foundation model weights are updated on task-specific data
- Can achieve higher performance but requires more data and computational resources
- More susceptible to overfitting in extremely data-scarce scenarios [4]
Comparative Validation Framework
Rigorous evaluation of cancer imaging biomarkers requires assessment across multiple dimensions. The TumorImagingBench framework [12] provides a standardized approach for comparing models across six public datasets (3,244 scans) with varied oncological endpoints. Evaluation metrics extend beyond traditional performance measures to include:
- Robustness: Performance consistency across acquisition variations and inter-reader differences
- Interpretability: Saliency mapping and feature importance analysis
- Biological relevance: Association with genomic pathways and clinical outcomes [4] [12]
Implementation of foundation models for cancer imaging biomarker discovery requires specific computational resources and software tools:
Table 3: Essential Research Resources
| Resource Category | Specific Tools/Platforms | Application in Research |
|---|---|---|
| Pretrained Models | Radio DINO [101], AIM Foundation Model [11] | Baseline models for feature extraction or transfer learning |
| Data Repositories | DeepLesion, LUNA16, LUNG1, RADIO [11] | Sources of diverse medical imaging data for pretraining and validation |
| Feature Extraction | PyRadiomics [99], ResNet-101 [100] | Traditional radiomic feature extraction and deep learning features |
| Implementation Platforms | MHub.ai [11], 3D Slicer Integration | Containerized, ready-to-use model implementations for clinical workflows |
| Benchmarking Frameworks | TumorImagingBench [12], MedMNISTv2 [101] | Standardized evaluation across multiple datasets and tasks |
Foundation models represent a significant advancement over both traditional radiomics and supervised deep learning for cancer imaging biomarker discovery. By leveraging self-supervised learning on large-scale diverse datasets, these models address critical limitations in data efficiency, generalizability, and robustness. The demonstrated performance advantages, particularly in limited data scenarios common in medical imaging, position foundation models as transformative tools for precision oncology.
Future development should focus on enhancing model interpretability, establishing standardized validation frameworks, and improving multimodal integration capabilities. As these models continue to evolve, they hold tremendous potential to accelerate the discovery and clinical translation of imaging biomarkers, ultimately improving cancer diagnosis, prognosis, and treatment personalization.
In the field of cancer imaging biomarker discovery, the transition from traditional radiomics to foundation models (FMs) represents a paradigm shift. These models, characterized by large-scale architecture, self-supervised learning on extensive datasets, and adaptability to various downstream tasks, offer tremendous potential for identifying robust imaging biomarkers [18]. However, their clinical translation hinges on demonstrating reliability and stability—key challenges in medical imaging where acquisition parameters and reader variations can significantly impact results [17]. This technical guide examines two critical components of stability assessment for foundation models in cancer imaging: test-retest reliability, which measures consistency across repeated imaging sessions, and input perturbation analysis, which evaluates robustness to variations in input data. These assessments are fundamental for establishing foundation models as trustworthy tools for quantitative biomarker discovery in oncology.
Foundation Models in Cancer Imaging: A Primer
Foundation models in medical imaging are typically pre-trained using self-supervised learning (SSL) on large, diverse datasets of unlabeled images [18]. Unlike traditional supervised approaches that require extensive manual annotation, SSL methods leverage the inherent structure of the data itself to learn generalizable representations. For cancer imaging applications, these models are subsequently adapted to specific downstream tasks such as lesion classification, malignancy prediction, or prognosis estimation [4] [37].
A prominent example is the FM developed by Mass General Brigham researchers, trained on 11,467 radiographic lesions from computed tomography (CT) scans [4] [10] [11]. This model demonstrated exceptional performance in predicting anatomical site, lung nodule malignancy, and patient prognosis, particularly in data-scarce scenarios [4] [37]. The model's stability across input variations and strong biological associations highlight the potential of FMs to overcome limitations of traditional radiomics, including feature reproducibility and standardization issues [17].
Test-Retest Reliability Assessment
Conceptual Framework
Test-retest reliability measures the consistency of results when the same test is repeated on the same sample under similar conditions at different time points [102]. In cancer imaging, this evaluates how stable a foundation model's outputs remain when applied to images of the same lesion acquired in short-interval rescans, where biological changes are not expected [17]. High test-retest reliability indicates that a model is robust to typical variations in image acquisition, a crucial property for clinical deployment.
Experimental Protocol
A standardized protocol for assessing test-retest reliability of cancer imaging foundation models involves:
- Dataset Selection: Utilize a test-retest dataset where patients undergo repeated imaging sessions within a short timeframe (e.g., 15-30 minutes) without intervening treatment or biological change. The RIDER dataset provides such paired CT scans for reliability assessment [17].
- Image Preprocessing: Apply identical preprocessing steps to all scans, including intensity normalization, resampling to consistent resolution, and registration if necessary.
- Embedding Extraction: Process both scan pairs through the foundation model to extract embedding vectors for the same lesion.
- Similarity Calculation: Compute the cosine similarity between embedding vectors from paired scans across all test cases.
- Statistical Analysis: Calculate aggregate statistics (mean, standard deviation) of similarity scores across the dataset.
Quantitative Benchmarks
Recent benchmarking studies have evaluated the test-retest reliability of various foundation models:
Table 1: Test-Retest Reliability of Foundation Models on RIDER Dataset
| Foundation Model | Average Cosine Similarity | Interpretation |
|---|---|---|
| FMCIB [4] | 0.97-1.00 | High reliability |
| ModelsGenesis [17] | 0.97-1.00 | High reliability |
| VISTA3D [17] | 0.97-1.00 | High reliability |
| CTClip [17] | 0.93 | Moderate reliability |
| Merlin [17] | 0.81 | Lower reliability |
The high test-retest reliability (0.97-1.00 cosine similarity) observed for top-performing models like FMCIB indicates remarkable stability to scanning variations [17]. This suggests their embeddings capture consistent tumor characteristics rather than noise from acquisition differences.
Technical Workflow
The diagram below illustrates the experimental workflow for test-retest reliability assessment:
Input Perturbation Analysis
Conceptual Framework
Input perturbation analysis evaluates model robustness to controlled variations in input data, simulating real-world scenarios such as annotation variability, acquisition parameter differences, or image noise [17]. For cancer imaging foundation models, this assessment reveals how sensitive embeddings or predictions are to these perturbations, which is crucial for clinical applications where perfect standardization is impossible.
Experimental Protocol
A comprehensive input perturbation analysis for cancer imaging foundation models includes:
- Seed Point Variation: Simulate annotation variability by applying random perturbations to lesion seed points or bounding boxes and measure the stability of resulting embeddings [17].
- Image Quality Degradation: Systematically introduce noise, blur, or compression artifacts to assess performance degradation.
- Acquisition Parameter Simulation: Modify slice thickness, reconstruction kernel, or contrast levels to mimic protocol variations across institutions.
- Inter-reader Variability Simulation: Utilize multiple annotations from different radiologists for the same lesions to assess robustness to human interpretation differences.
Quantitative Benchmarks
The FMCIB foundation model demonstrated notable stability in input perturbation analyses:
Table 2: Input Perturbation Analysis of FMCIB Foundation Model
| Perturbation Type | Metric | Performance | Context |
|---|---|---|---|
| Inter-reader variations | Prediction stability | High | Model remained stable across different reader interpretations [4] |
| Acquisition differences | Prediction stability | High | Consistent despite acquisition parameter variations [4] |
| Annotation noise | Embedding similarity | High | Robust to variations in input seed points [17] |
Technical Workflow
The diagram below illustrates the experimental workflow for input perturbation analysis:
Integrated Stability Assessment Framework
Comprehensive Workflow
A complete stability assessment integrates both test-retest reliability and input perturbation analysis:
Interpretation Guidelines
When interpreting stability assessment results:
- High test-retest reliability (cosine similarity >0.95) indicates the model captures biologically stable tumor characteristics rather than imaging noise [17].
- Robustness to input perturbations suggests the model will perform consistently across different clinical settings with varying acquisition protocols and reader expertise [4].
- Combined high scores in both dimensions increase confidence for clinical deployment, as the model likely learns true tumor biology rather than artifact features.
The Scientist's Toolkit
Table 3: Essential Research Reagents for Stability Assessment Experiments
| Resource | Function in Stability Assessment | Example Implementations |
|---|---|---|
| Test-Retest Datasets | Provide paired scans for reliability testing | RIDER dataset [17] |
| Multi-reader Annotations | Enable inter-reader variability analysis | Datasets with multiple expert segmentations |
| Data Augmentation Tools | Generate controlled input perturbations | TorchIO, MONAI, Custom Python scripts |
| Similarity Metrics | Quantify embedding stability | Cosine similarity, Intra-class correlation |
| Public Foundation Models | Enable comparative benchmarking | FMCIB, ModelsGenesis, VISTA3D [17] |
| Benchmarking Frameworks | Standardize evaluation protocols | TumorImagingBench [17] |
Rigorous assessment of test-retest reliability and input perturbation stability is paramount for translating cancer imaging foundation models from research tools to clinical applications. Current evidence demonstrates that leading foundation models like FMCIB exhibit high reliability (cosine similarity 0.97-1.00) and robustness to various perturbations [4] [17]. By adopting standardized assessment protocols and benchmarking frameworks, researchers can systematically quantify these properties, accelerating the development of clinically viable imaging biomarkers that consistently capture tumor biology across diverse clinical settings.
In the evolving landscape of precision oncology, the ability to connect non-invasive imaging phenotypes to underlying molecular biology represents a paradigm shift in cancer diagnosis, prognosis, and therapeutic development. Foundation models for cancer imaging biomarker discovery are now enabling this translation at unprecedented scale and resolution [4] [11]. These large-scale models, pretrained on vast datasets of radiographic lesions through self-supervised learning, provide a powerful foundation for mapping imaging features to gene expression patterns without requiring extensive labeled datasets for each new application [4].
The clinical significance of this integration is profound. Traditional cancer characterization often relies on invasive tissue biopsies, which provide limited spatial and temporal sampling of inherently heterogeneous tumors [103]. Quantitative imaging biomarkers, when linked to genomic underpinnings, offer a non-invasive alternative for comprehensive tumor assessment, enabling continuous monitoring of treatment response and disease evolution [4] [103]. This whitepaper provides a technical framework for establishing and validating associations between imaging features and gene expression data, with emphasis on methodology, experimental design, and analytical approaches tailored for research scientists and drug development professionals.
Methodological Foundations
Foundation Models for Imaging Feature Extraction
The foundation model approach begins with self-supervised pretraining on diverse radiographic datasets. The model referenced in the search results was trained on 11,467 annotated computed tomography (CT) lesions from 2,312 unique patients, utilizing a modified SimCLR (Contrastive Learning) framework that demonstrated superiority over other self-supervised approaches [4]. This pretraining phase enables the model to learn generalized, transferable representations of imaging features without task-specific annotations.
Table 1: Foundation Model Pretraining Performance Comparison
| Pretraining Strategy | Balanced Accuracy | Mean Average Precision (mAP) | Performance with 10% Data |
|---|---|---|---|
| Modified SimCLR (Ours) | 0.779 (95% CI 0.750-0.810) | 0.847 (95% CI 0.750-0.810) | 9% decline in balanced accuracy |
| Standard SimCLR | 0.696 (95% CI 0.663-0.728) | 0.779 (95% CI 0.749-0.811) | Not specified |
| Auto-encoder | Worst performance | Worst performance | Not specified |
Following pretraining, the foundation model can be implemented in downstream tasks through two primary approaches:
- Feature Extraction: Using the pretrained model as a fixed feature extractor followed by a linear classifier.
- Fine-tuning: Adapting the pretrained model to specific tasks through additional training [4].
The feature extraction approach has demonstrated particular strength in limited-data scenarios, making it valuable for specialized applications where large annotated datasets are unavailable [4].
Multimodal Data Integration Frameworks
Integrating imaging features with genomic data requires specialized architectures capable of processing heterogeneous data types. The prevailing methodology employs dedicated feature extractors for each modality, followed by fusion models that combine these representations for predictive tasks [103].
For genomic data, trained deep neural network models extract features from gene expression profiles, while convolutional neural networks process imaging data. These multimodal features are then integrated through fusion architectures to predict molecular phenotypes or clinical endpoints [103]. This approach has been successfully applied to predict breast cancer subtypes and perform pan-cancer analyses [103].
Experimental Protocols and Workflows
Technical Validation of Imaging Features
Before linking imaging features to gene expression, rigorous technical validation is essential. The foundation model approach includes a technical validation phase using lesion anatomical site classification as an in-distribution task [4]. This validation ensures the model has learned meaningful representations of radiographic features before applying them to biological association studies.
Table 2: Experimental Parameters for Technical Validation
| Parameter | Specification | Purpose |
|---|---|---|
| Dataset | 3,830 lesions (training/tuning) 1,221 lesions (held-out test) | Technical validation of feature representations |
| Performance Metrics | Balanced accuracy, mean average precision (mAP) | Quantitative assessment of feature quality |
| Comparison Baselines | Conventional supervised models, Med3D, Models Genesis | Benchmarking against established approaches |
| Implementation | Feature extraction vs. fine-tuning | Strategy optimization for specific applications |
The performance advantage of foundation models is particularly pronounced in limited data scenarios. When training data was reduced to 10% (n=505), the feature extraction approach maintained significantly better performance compared to conventional supervised methods, demonstrating robustness crucial for specialized applications where large datasets are unavailable [4].
Associating Imaging Features with Gene Expression
The core methodology for linking imaging features to biology involves correlating deep learning-derived image embeddings with gene expression patterns. This process can be implemented at various resolutions, from whole-tumor analyses to spatially-resolved approaches.
Cross-modal prediction represents an advanced application of these associations. Studies have demonstrated that gene expression can be predicted from histopathological images of breast cancer tissue with a resolution of 100 μm [103]. Conversely, spatial transcriptomic features can better characterize breast cancer tissue sections, revealing hidden histological features not apparent through conventional analysis [103].
The Scientist's Toolkit: Essential Research Reagents
Successful implementation of imaging-genomic association studies requires carefully selected computational frameworks, data resources, and analytical tools.
Table 3: Essential Research Reagents for Imaging-Genomic Studies
| Research Reagent | Function | Example Implementations |
|---|---|---|
| Foundation Models | Pre-trained deep learning models for imaging feature extraction | Convolutional encoders trained on large-scale lesion datasets [4] |
| Curated Benchmark Datasets | Standardized evaluation of imaging-genomic associations | TumorImagingBench (3,244 scans with oncological endpoints) [12] |
| Multimodal Fusion Architectures | Integration of imaging and genomic feature representations | Dedicated feature extractors with fusion models [103] |
| Spatial Transcriptomics Technologies | High-resolution mapping of gene expression in tissue context | Technologies preserving spatial information for correlation with imaging [103] |
| Accessibility-Focused Visualization Tools | Clear presentation of complex multimodal data | Tools with keyboard navigation, screen reader support, and high contrast color schemes [104] |
Accessibility considerations are crucial for developing sustainable research tools. Implementing keyboard navigation, screen reader compatibility, and high-contrast color schemes ensures that visualization tools are usable by diverse research teams [104]. These features also improve overall usability, as demonstrated by the success of tools that provide multiple color schemes including colorblind-friendly modes [104].
Analytical Framework and Validation
Statistical Association Methods
Establishing robust associations between imaging features and gene expression requires specialized statistical approaches that account for high-dimensional data and multiple testing. Canonical correlation analysis (CCA) and regularized variants (rCCA) are widely used to identify linear relationships between multimodal data types [103]. These methods identify imaging features that covary with specific gene expression patterns while controlling for confounding factors.
More recent approaches employ multivariable linear regression models with regularization (LASSO, Ridge) to predict gene expression values from imaging features [103]. The performance of these models is typically evaluated using cross-validation techniques to ensure generalizability, with metrics including root mean square error (RMSE) for continuous outcomes and area under the curve (AUC) for classification tasks.
Biological Validation and Interpretation
Beyond statistical associations, biological validation is essential to establish clinical relevance. This includes pathway enrichment analysis to determine whether imaging-associated genes are enriched in specific biological processes, and experimental validation using in vitro or in vivo models [103].
Foundation models have demonstrated particular strength in capturing biologically relevant imaging features. Studies have shown that these models are more stable to input variations and show strong associations with underlying biology compared to conventional supervised approaches [4]. This biological relevance is crucial for ensuring that imaging biomarkers capture meaningful aspects of tumor biology rather than technical artifacts.
The integration of imaging features with gene expression data through foundation models represents a transformative approach in cancer research and drug development. The methodologies outlined in this technical guide provide a framework for establishing robust, biologically relevant associations that can advance precision oncology. As these techniques continue to evolve, they promise to unlock deeper insights into tumor biology and enable more personalized treatment approaches based on non-invasive imaging biomarkers. The field is poised for significant advancement as foundation models become more sophisticated and multimodal integration techniques more refined, ultimately accelerating the translation of imaging biomarkers into clinical practice.
Foundation models, characterized by large-scale deep learning models trained on vast amounts of unlabeled data, are emerging as transformative tools for cancer imaging biomarker discovery [4]. These models, typically trained using self-supervised learning (SSL), significantly reduce the demand for large labeled datasets in downstream applications—a critical advantage in medical imaging where annotated data is often scarce [4] [11]. However, as the number of proposed foundation models grows, independent evaluation on external cohorts and clinically relevant tasks becomes essential to guide model selection and future development.
This technical guide synthesizes key benchmark findings from recent large-scale evaluations of pathology and radiology foundation models. We present quantitative performance disparities across models, detail experimental methodologies, and identify top-performing architectures for specific clinical tasks in computational oncology.
Quantitative Benchmarking of Foundation Models
Comprehensive Histopathology Model Evaluation
A landmark study benchmarked 19 histopathology foundation models across 13 patient cohorts comprising 6,818 patients and 9,528 whole slide images [20]. Models were evaluated on 31 weakly supervised downstream tasks related to morphology, biomarkers, and prognostication. The table below summarizes the top-performing models across task categories:
Table 1: Performance of Top Pathology Foundation Models Across Task Categories
| Model | Model Type | Morphology Tasks (Mean AUROC) | Biomarker Tasks (Mean AUROC) | Prognosis Tasks (Mean AUROC) | Overall Rank |
|---|---|---|---|---|---|
| CONCH | Vision-Language | 0.77 | 0.73 | 0.63 | 1 |
| Virchow2 | Vision-Only | 0.76 | 0.73 | 0.61 | 2 |
| DinoSSLPath | Vision-Only | 0.76 | 0.69 | 0.61 | 3 |
| Prov-GigaPath | Vision-Only | 0.72 | 0.72 | 0.63 | 4 |
CONCH, a vision-language model trained on 1.17 million image-caption pairs, demonstrated the highest overall performance, achieving a mean AUROC of 0.71 across all 31 tasks [20]. Virchow2, a vision-only model trained on a substantially larger dataset of 3.1 million whole slide images, performed on par with CONCH in biomarker prediction tasks [20]. This suggests that architectural advantages (vision-language vs. vision-only) can compensate for differences in pretraining dataset size.
Performance in Limited Data Scenarios
A key claimed advantage of foundation models is their utility in data-scarce environments. Benchmark studies specifically evaluated performance with reduced training data, comparing performance with 300, 150, and 75 patients [20]. In the largest sampled cohort (n=300), Virchow2 demonstrated superior performance in 8 tasks, while with medium-sized cohorts (n=150), PRISM led in 9 tasks [20]. With the smallest cohort (n=75), performance balanced between CONCH (leading in 5 tasks), PRISM, and Virchow2 (each leading in 4 tasks) [20]. Notably, performance metrics remained relatively stable between n=75 and n=150 cohorts, demonstrating the particular value of foundation models in low-data scenarios.
Table 2: Performance Stability in Data-Scarce Environments
| Training Cohort Size | Best-Performing Model | Number of Tasks Where Model Led | Performance Drop vs. Full Dataset |
|---|---|---|---|
| 300 patients | Virchow2 | 8/31 tasks | Minimal (~2-5%) |
| 150 patients | PRISM | 9/31 tasks | Minimal (~3-6%) |
| 75 patients | CONCH | 5/31 tasks | Moderate (~5-10%) |
Experimental Protocols and Methodologies
Benchmarking Framework Design
The evaluated histopathology benchmarking study employed a standardized framework to ensure fair comparison across models [20]. The experimental workflow encompassed data curation, feature extraction, model training, and validation phases, as illustrated below:
Self-Supervised Pretraining for Radiology Foundation Models
In radiology, a separate foundation model for cancer imaging biomarkers was developed using a convolutional encoder trained on 11,467 radiographic lesions from computed tomography (CT) imaging [4] [11]. The pretraining strategy employed a modified version of SimCLR (a contrastive self-supervised learning approach) that significantly outperformed other strategies including autoencoders, SwAV, and NNCLR (P < 0.001) [4].
The critical experimental components included:
- Pretraining Data: 11,467 diverse radiographic lesions from 2,312 unique patients
- Architecture: Convolutional encoder using modified SimCLR framework
- Validation: Three distinct use cases - lesion anatomical site classification (technical validation), lung nodule malignancy prediction (diagnostic biomarker), and non-small cell lung cancer prognosis (prognostic biomarker)
- Implementation: Two approaches evaluated - using the foundation model as a feature extractor with linear classifier, and full fine-tuning of the foundation model
When evaluated on an out-of-distribution task (lung nodule malignancy prediction on the LUNA16 dataset), the fine-tuned foundation model achieved an AUC of 0.944, significantly outperforming (P < 0.01) most baseline implementations [4].
Research Reagent Solutions
Table 3: Essential Resources for Foundation Model Research in Cancer Imaging
| Resource Category | Specific Resource | Function/Application | Access Information |
|---|---|---|---|
| Public Datasets | DeepLesion | RECIST-bookmarked lesions for pretraining and validation | Openly accessible [11] |
| LUNA16 | Lung nodule malignancy prediction | Openly accessible [11] | |
| LUNG1 & RADIO | Prognostic biomarker validation | Openly accessible [11] | |
| Benchmarking Tools | TumorImagingBench | Curated benchmark for quantitative radiographic phenotypes | Six public datasets (3,244 scans) [12] |
| Model Platforms | MHub.ai | Containerized, ready-to-use model implementation | Supports various input workflows [11] |
| 3D Slicer Integration | Clinical application and adaptation | Seamless integration for diverse research settings [11] | |
| Code Repositories | GitHub Repository | Data preprocessing, model training, and inference | Includes YAML files for replication [11] |
Critical Insights and Performance Disparities
Determinants of Foundation Model Performance
Benchmarking analyses revealed several critical factors influencing model performance:
Data Diversity vs. Volume: Data diversity demonstrates a stronger correlation with downstream performance than sheer data volume [20]. This explains how CONCH, trained on fewer but more diverse image-caption pairs, can outperform models trained on larger but less diverse datasets.
Architectural Advantages: Vision-language models (e.g., CONCH) consistently outperform vision-only models on most tasks, particularly in capturing semantically meaningful features for biomarker prediction [20]. However, their superior performance is less pronounced in low-data scenarios and low-prevalence tasks.
Complementary Feature Learning: Models trained on distinct cohorts learn complementary features to predict the same labels [20]. Ensemble approaches combining CONCH and Virchow2 predictions outperformed individual models in 55% of tasks, leveraging their complementary strengths.
Performance Stability and Clinical Applicability
The radiology foundation model demonstrated remarkable stability to input variations and showed strong associations with underlying biology [4]. When using only 10% of training data (n=505), the foundation model implementation with linear classification maintained robust performance, declining only 9% in balanced accuracy and 12% in mean average precision compared to using the full dataset [4]. This stability in data-scarce environments is particularly valuable for clinical applications where labeled data is limited.
For radiology models, the feature extraction approach (using the foundation model as a fixed feature extractor with a linear classifier) proved particularly effective in limited data scenarios, significantly outperforming fine-tuning approaches when training data was reduced to 20% or less [4]. This suggests that the representations learned during self-supervised pretraining are robust and transferable even with minimal task-specific adaptation.
Comprehensive benchmarking of foundation models for cancer imaging biomarkers reveals significant performance disparities across models, tasks, and data environments. Vision-language models like CONCH and vision-only models like Virchow2 currently lead in histopathology applications, while modified contrastive learning approaches show strong performance in radiology applications. The stability of these models in data-scarce scenarios, their complementary feature representations, and their ability to capture biologically relevant patterns underscore their potential to accelerate the discovery and clinical translation of imaging biomarkers in oncology. Future work should focus on standardized benchmarking frameworks, multimodal integration, and prospective validation in diverse clinical settings.
Conclusion
Foundation models represent a transformative leap for cancer imaging biomarker discovery, demonstrating superior performance—especially in data-scarce environments—and enhanced robustness over traditional methods. The synthesis of evidence confirms their capacity to yield highly generalizable, biologically relevant biomarkers for both diagnostic and prognostic applications, accelerating the path toward clinical translation. Future progress hinges on overcoming key challenges, including the development of standardized multi-modal data integration frameworks, enhancing model interpretability for clinical trust, and expanding validation through large-scale longitudinal studies. The continued evolution of these models is poised to fundamentally reshape precision oncology, enabling more personalized treatment strategies and ultimately improving patient outcomes. Emerging trends point to the integration of multi-omics data, federated learning for privacy-preserving collaboration, and the application of these models to rare cancers as the next frontiers in this rapidly advancing field.
References
- 1. Foundation Models in Medical Imaging: A Review and ... [https://arxiv.org/abs/2506.09095]
- 2. Foundation models for radiology—the position of the AI for ... [https://insightsimaging.springeropen.com/articles/10.1186/s13244-025-02056-9]
- 3. A generalizable 3D framework and model for self ... [https://www.nature.com/articles/s41746-025-02035-w]
- 4. Foundation model for cancer imaging biomarkers [https://www.nature.com/articles/s42256-024-00807-9]
- 5. AI-driven biomarker discovery: enhancing precision in cancer ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11906928/]
- 6. A generalizable 3D framework and model for self ... [https://pubmed.ncbi.nlm.nih.gov/41203891/]
- 7. Evaluating Self-Supervised Learning in Medical Imaging: A ... [https://arxiv.org/abs/2412.19124]
- 8. Emerging Technologies in Biomarker Discovery You ... [https://blog.crownbio.com/emerging-technologies-in-biomarker-discovery-you-should-know-about]
- 9. Addressing the current challenges in the clinical application of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12515897/]
- 10. Researchers use foundation models to discover new ... [https://ecancer.org/en/news/24698-researchers-use-foundation-models-to-discover-new-cancer-imaging-biomarkers]
- 11. Foundation Model for Cancer Imaging Biomarkers [https://aim.mgh.harvard.edu/foundation-cancer-image-biomarker]
- 12. Foundation model embeddings for quantitative tumor imaging ... [https://pubmed.ncbi.nlm.nih.gov/40502795/]
- 13. systematic review and repository of open-access cancer ... [https://insightsimaging.springeropen.com/articles/10.1186/s13244-023-01556-w]
- 14. Foundation models for radiology [https://www.dirjournal.org/articles/foundation-models-for-radiology-fundamentals-applications-opportunities-challenges-risks-and-prospects/doi/dir.2025.253445?utm_source=chatgpt.com]
- 15. Representation Potentials of Foundation Models for ... [https://arxiv.org/html/2510.05184v1]
- 16. Deep Learning in Medical Imaging: General Overview - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC5447633/]
- 17. Foundation model embeddings for quantitative tumor imaging ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12154149/]
- 18. Foundation Models in Medical Imaging - A Review and ... [https://arxiv.org/html/2506.09095v1]
- 19. Foundation Models for Quantitative Biomarker Discovery in ... [https://pubmed.ncbi.nlm.nih.gov/37732237/]
- 20. Benchmarking foundation models as feature extractors for ... [https://www.nature.com/articles/s41551-025-01516-3]
- 21. The use of artificial intelligence for cancer therapeutic decision ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12530061/]
- 22. A vision–language foundation model for precision oncology [https://www.nature.com/articles/s41586-024-08378-w]
- 23. Comparison of Vision Transformers and Convolutional Neural ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11393140/]
- 24. Transforming medical imaging with ... [https://www.sciencedirect.com/science/article/abs/pii/S1361841523000233]
- 25. [2507.21156] Comparative Analysis of Vision Transformers ... [https://arxiv.org/abs/2507.21156]
- 26. TransUNet: Rethinking the U-Net architecture design for ... [https://www.sciencedirect.com/science/article/pii/S1361841524002056]
- 27. Alternate encoder and dual decoder CNN-Transformer ... [https://www.nature.com/articles/s41598-025-93353-2]
- 28. Deep Learning with Transformer or Convolutional Neural ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9913836/]
- 29. From CNN to Transformer: A Review of Medical Image ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11300773/]
- 30. SimCLR: A Simple Framework for Contrastive Learning of ... [https://simclr.github.io/]
- 31. Robust image representations with counterfactual ... [https://arxiv.org/html/2409.10365v2]
- 32. Self-supervised learning using diverse cell images for ... [https://www.sciencedirect.com/science/article/abs/pii/S026322412402298X]
- 33. Self-supervised learning leads to improved performance in ... [https://www.sciencedirect.com/science/article/pii/S0010482525016166]
- 34. Building a General SimCLR Self-Supervised Foundation ... [https://arxiv.org/html/2509.10620v1]
- 35. Comparative analysis of supervised and self ... [https://www.nature.com/articles/s41598-025-99000-0]
- 36. Explainable self-supervised learning for medical image ... [https://www.nature.com/articles/s41598-025-15604-6]
- 37. for Quantitative Foundation in Models ... Biomarker Discovery Cancer [https://pmc.ncbi.nlm.nih.gov/articles/PMC10508804/]
- 38. for Foundation - Maastricht... model cancer imaging biomarkers [https://cris.maastrichtuniversity.nl/en/publications/foundation-model-for-cancer-imaging-biomarkers]
- 39. Fine Tuning vs Feature Extraction in Transfer Learning [https://codefinity.com/blog/Fine-Tuning-vs-Feature-Extraction-in-Transfer-Learning]
- 40. Quantitative Comparison of Fine-Tuning Techniques for ... [https://arxiv.org/html/2506.13307v1]
- 41. Image biomarkers and explainable AI: handcrafted features ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11576747/]
- 42. Narrative review of the application of artificial intelligence ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12433047/]
- 43. Progress and challenges of artificial intelligence in lung ... [https://www.nature.com/articles/s41698-025-00986-7]
- 44. Quantitative Imaging features Improve Discrimination of ... [https://www.nature.com/articles/s41598-019-44562-z]
- 45. Advances in modelling the risk of benign and malignant ... [https://www.frontiersin.org/journals/oncology/articles/10.3389/fonc.2025.1648548/full]
- 46. Predictive model of malignancy probability in pulmonary ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12151837/]
- 47. Update 2025: Management of Non‑Small-Cell Lung Cancer [https://pmc.ncbi.nlm.nih.gov/articles/PMC11937135/]
- 48. Advances in molecular pathology and therapy of non-small ... [https://www.nature.com/articles/s41392-025-02243-6]
- 49. Clinical and Genomic Features and Prognostic Biomarkers ... [https://pubmed.ncbi.nlm.nih.gov/40897601/]
- 50. Development of a prognostic multiomic biomarker ... [https://www.nature.com/articles/s41598-025-18101-y]
- 51. Retrospective analysis of inflammatory biomarkers and ... [https://www.frontiersin.org/journals/genetics/articles/10.3389/fgene.2025.1549602/full]
- 52. The ASRT Practice Standards for Medical Imaging and ... [https://www.asrt.org/main/standards-and-regulations/professional-practice/practice-standards-online]
- 53. Deep Learning Models for Anatomical Location ... [https://www.mdpi.com/2075-4418/14/21/2360]
- 54. Automated detection and classification of osteolytic lesions ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12182663/]
- 55. Review on Multimodal Data Integration for Cancer Research [https://arxiv.org/abs/2507.09028]
- 56. Foundation Models for Quantitative Biomarker Discovery in ... [https://www.medrxiv.org/content/10.1101/2023.09.04.23294952v1.full-text]
- 57. Standardizing digital biobanks: integrating imaging, genomic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10845786/]
- 58. Multi-Modal Representation via Contrastive Learning with ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10606612/]
- 59. A Comparison of Methods for Data-Driven Cancer Outlier ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3091411/]
- 60. Leveraging Multimodal Foundation Models in Biliary Tract ... [https://pubmed.ncbi.nlm.nih.gov/41003479/]
- 61. Applications and challenges of biomarker-based predictive ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12399543/]
- 62. Image normalization techniques and their effect on the ... [https://www.sciencedirect.com/science/article/pii/S0720048X2500172X]
- 63. Open challenges and opportunities in federated foundation ... [https://biodatamining.biomedcentral.com/articles/10.1186/s13040-024-00414-9]
- 64. Medical Image Preprocessing: Key Techniques & Best Practices [https://collectiveminds.health/articles/the-ultimate-guide-to-preprocessing-medical-images-techniques-tools-and-best-practices-for-enhanced-diagnosis]
- 65. Ontologies as the semantic bridge between artificial ... [https://pubmed.ncbi.nlm.nih.gov/40949313/]
- 66. Ontologies as the semantic bridge between artificial ... [https://www.frontiersin.org/journals/digital-health/articles/10.3389/fdgth.2025.1668385/full]
- 67. Data efficient deep learning for medical image analysis [https://arxiv.org/abs/2310.06557]
- 68. for Foundation model cancer imaging biomarkers [https://www.nature.com/articles/s42256-024-00807-9?error=cookies_not_supported]
- 69. Transforming Medical Imaging with Foundation Models [https://scisimple.com/en/articles/2025-10-23-transforming-medical-imaging-with-foundation-models--akg4r6g]
- 70. Robustness tests for biomedical foundation models should ... [https://www.nature.com/articles/s41746-025-01926-2]
- 71. Imaging biomarker roadmap for cancer studies - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC5378302/]
- 72. ROOD-MRI: Benchmarking the robustness of deep ... [https://www.sciencedirect.com/science/article/pii/S1053811923004408]
- 73. Addressing fairness issues in deep learning-based ... [https://www.nature.com/articles/s41746-024-01276-5]
- 74. To warrant clinical adoption AI models require a multi- ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10918103/]
- 75. Transforming precision oncology with medical imaging ... [https://www.news-medical.net/news/20251114/Transforming-precision-oncology-with-medical-imaging-foundation-models.aspx]
- 76. Quantitative and qualitative methods advance the science ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10114099/]
- 77. Real-world radiology data for artificial intelligence-driven ... [https://www.sciencedirect.com/science/article/pii/S2949820125000098]
- 78. Medical Imaging Biomarker Discovery and Integration ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8801459/]
- 79. Explainable Artificial Intelligence for Multi-Modal Cancer ... [https://www.sciencedirect.com/science/article/pii/S1040842825004287]
- 80. Innovations in Cancer Imaging and Radiomics through ... [https://www.frontiersin.org/research-topics/69141/innovations-in-cancer-imaging-and-radiomics-through-explainable-artificial-intelligence]
- 81. Explainable Artificial Intelligence: A Perspective on Drug ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12472777/]
- 82. A Framework for Interpretability in Machine Learning for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11486155/]
- 83. Explainable machine learning framework for biomarker ... [https://www.nature.com/articles/s41598-025-98948-3]
- 84. Discovering Interpretable Biological Concepts in Single ... [https://arxiv.org/abs/2510.25807]
- 85. How AI Can Degrade Human Performance in High-Stakes ... [https://ai-frontiers.org/articles/how-ai-can-degrade-human-performance-in-high-stakes-settings]
- 86. Ethical and legal considerations in healthcare AI [https://pmc.ncbi.nlm.nih.gov/articles/PMC12076083/]
- 87. Ethical and regulatory challenges in machine learning- ... [https://www.sciencedirect.com/science/article/pii/S2772485925000286]
- 88. AI in healthcare: legal and ethical considerations at the ... [https://www.aoshearman.com/en/insights/ao-shearman-on-life-sciences/ai-in-healthcare-legal-and-ethical-considerations-at-the-new-frontier]
- 89. Multi-omics strategies for biomarker discovery and application ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12638490/]
- 90. Systematic benchmarking of imaging spatial ... [https://www.nature.com/articles/s41467-025-64990-y]
- 91. Integrating Multi-Omics and Medical Imaging in Artificial ... [https://www.mdpi.com/2072-6694/17/22/3638]
- 92. A foundation model for generalizable cancer diagnosis and ... [https://www.nature.com/articles/s41467-025-57587-y]
- 93. Emerging biomarkers for early cancer detection and diagnosis [https://eurjmedres.biomedcentral.com/articles/10.1186/s40001-025-03003-6]
- 94. Foundation Model for Predicting Prognosis and Adjuvant ... [https://pubmed.ncbi.nlm.nih.gov/40168636/]
- 95. A guide to interpreting the area under the curve value - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC10664195/]
- 96. Receiver Operating Characteristic Curve in Diagnostic Test ... [https://www.sciencedirect.com/science/article/pii/S1556086415306043]
- 97. AI-driven biomarker discovery for early diagnosis and ... [https://www.sciencedirect.com/science/article/pii/S2772906025000378]
- 98. Foundation models for radiology [https://dirjournal.org/articles/foundation-models-for-radiology-fundamentals-applications-opportunities-challenges-risks-and-prospects/dir.2025.253445]
- 99. Radiomics in preclinical imaging research: methods ... [https://www.nature.com/articles/s44303-025-00104-z]
- 100. Comparative analysis of deep learning and radiomics ... [https://www.frontiersin.org/journals/medicine/articles/10.3389/fmed.2025.1685725/full]
- 101. Radio DINO: A foundation model for advanced radiomics ... [https://www.sciencedirect.com/science/article/pii/S0010482525009345]
- 102. The 4 Types of Reliability | Definitions, Examples, Methods [https://www.scribbr.com/methodology/types-of-reliability/]
- 103. Multimodal Integration in Health Care - PubMed Central - NIH [https://pmc.ncbi.nlm.nih.gov/articles/PMC12370271/]
- 104. How to build accessible graph visualization tools [https://cambridge-intelligence.com/build-accessible-data-visualization-apps-with-keylines/]