External Validation of Cancer Risk Prediction Algorithms: A Foundational Guide for Biomedical Research and Clinical Translation
This article provides a comprehensive overview of the critical role of external validation in the development and implementation of cancer risk prediction algorithms.
External Validation of Cancer Risk Prediction Algorithms: A Foundational Guide for Biomedical Research and Clinical Translation
Abstract
This article provides a comprehensive overview of the critical role of external validation in the development and implementation of cancer risk prediction algorithms. Tailored for researchers, scientists, and drug development professionals, it explores the foundational principles of external validation, contrasting it with internal validation. The scope covers methodological frameworks for conducting rigorous external validation, addresses common challenges and optimization strategies such as handling overfitting and incorporating novel biomarkers, and presents a comparative analysis of model performance across different validation studies. By synthesizing recent evidence and methodological standards, this article serves as a guide for evaluating the generalizability, robustness, and clinical readiness of predictive models in oncology.
The Critical Role of External Validation in Cancer Risk Prediction
Defining External vs. Internal Validation in Statistical Modeling
In the field of cancer research, statistical prediction models are powerful tools for estimating disease risk, prognosis, and treatment outcomes. However, their reliability depends critically on rigorous validation—the process of evaluating a model's performance on independent data. This guide examines the fundamental distinction between internal and external validation, two sequential processes essential for establishing model credibility. Through comparative analysis of methodologies, performance metrics, and case studies from contemporary oncology research, we provide researchers with a framework for developing robust, clinically applicable prediction models.
Cancer prediction algorithms have emerged as indispensable tools for improving early diagnosis, prognostic stratification, and treatment selection. These mathematical models combine multiple patient-specific variables—including demographic characteristics, clinical symptoms, laboratory results, and imaging features—to generate individualized risk estimates [1]. However, a model's performance in the development dataset often provides an overly optimistic estimate of its real-world accuracy—a phenomenon known as overfitting [2]. Validation methodologies serve as critical safeguards against this optimism bias, separating clinically viable models from those that fail to generalize beyond their original development context.
The validation process is typically conducted in two sequential phases: internal validation, which assesses model stability and optimizes parameters within the original dataset, and external validation, which evaluates model transportability to new patient populations [3]. Understanding the distinction between these processes is fundamental for researchers developing prediction tools and clinicians interpreting their potential clinical utility. This guide examines the methodological frameworks, implementation protocols, and performance interpretation for both validation types within the context of cancer research.
Core Concepts and Definitions
Internal Validation
Internal validation assesses the reproducibility of a prediction model within the same dataset used for its development, providing an initial estimate of potential overfitting [3]. This process uses resampling techniques to evaluate how the model would perform on hypothetical new data drawn from the same underlying population. Internal validation represents a necessary first step in model evaluation but does not guarantee performance in truly independent populations [4].
External Validation
External validation tests the original prediction model on entirely new patients collected separately from the development cohort [3]. This rigorous assessment determines whether the model maintains its predictive accuracy when applied to different geographic regions, healthcare settings, or temporal periods. External validation is a prerequisite for clinical implementation, as it establishes the model's generalizability beyond the specific context in which it was created [5].
Table 1: Comparative Overview of Validation Types
| Characteristic | Internal Validation | External Validation |
|---|---|---|
| Definition | Testing model performance within the original dataset using resampling methods | Testing the original model on completely independent data |
| Primary Purpose | Estimate and correct for overfitting; optimize model parameters | Assess model reproducibility and generalizability to new populations |
| Key Methods | Train-test split, cross-validation, bootstrapping | Geographic, temporal, or fully independent validation |
| Dataset Relationship | Derived from original development data | Structurally separate from development data |
| Performance Interpretation | Indicates model stability | Determines clinical applicability and transportability |
| Role in Implementation | Necessary development step | Prerequisite for clinical use |
Methodological Frameworks
Internal Validation Techniques
Internal validation employs several established methodologies to estimate model performance without collecting new data:
Split-sample validation randomly divides the available dataset into development and validation subsets, typically using a 70:30 ratio [6]. While conceptually simple, this approach is statistically inefficient, particularly in smaller datasets, as it reduces the sample size available for both model development and validation [3].
Cross-validation extends the split-sample approach by repeatedly partitioning the data. In k-fold cross-validation, the dataset is divided into k equally sized subsets (typically k=5 or k=10). The model is trained on k-1 folds and validated on the remaining fold, repeating this process until each fold has served as the validation set [4]. The performance estimates are then averaged across all iterations, providing a more robust assessment than single split-sample validation.
Bootstrapping creates multiple resampled datasets with replacement from the original data, each the same size as the original cohort. The model is developed on each bootstrap sample and tested on both the bootstrap sample and the original dataset [4]. The average difference between these performance estimates (the "optimism") is subtracted from the apparent performance to obtain a bias-corrected estimate.
Table 2: Internal Validation Methods in Cancer Prediction Models
| Method | Implementation | Advantages | Limitations | Cancer Research Example |
|---|---|---|---|---|
| Split-sample | Random division into training/test sets (e.g., 70:30) | Simple implementation and interpretation | Statistically inefficient; high variance in small samples | Colorectal cancer risk model using PLCO trial data [6] |
| K-fold cross-validation | Data divided into k subsets; iterative training/validation | More stable than split-sample; uses all data | Computationally intensive; complex implementation | Transcriptomic prognosis model for head and neck cancer [4] |
| Bootstrap validation | Multiple resampled datasets with replacement | Most efficient use of available data | Can be over-optimistic or pessimistic without correction [4] | Myeloma risk prediction model [7] |
External Validation Approaches
External validation employs distinct strategies to assess model transportability:
Temporal validation tests the model on patients from the same institutions or geographic regions but treated during a later time period. This approach assesses whether the model remains accurate as clinical practices evolve [3].
Geographic validation evaluates the model on patients from different healthcare systems or regions. For instance, a model developed in the United Kingdom might be validated on patients from other European countries [1] [8]. This approach tests the model's robustness to variations in healthcare delivery, genetic backgrounds, and environmental factors.
Fully independent validation represents the most rigorous approach, where the model is tested by completely separate research teams using different data collection protocols [5] [9]. This method minimizes potential biases introduced by the original developers and provides the strongest evidence of generalizability.
Experimental Protocols and Performance Metrics
Standardized Validation Workflows
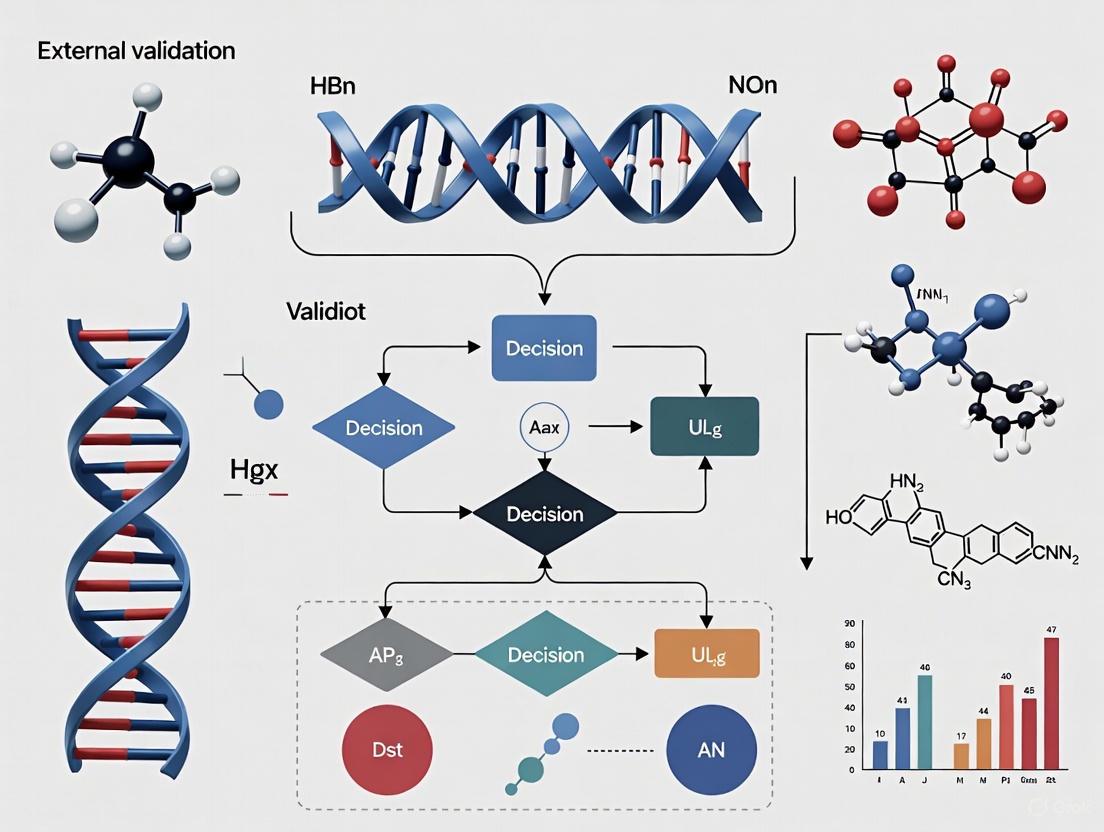
A systematic approach to validation ensures comprehensive assessment and reproducible results. The following workflow illustrates the sequential process of model development and validation:
Key Performance Metrics
Both internal and external validation employ standardized metrics to quantify predictive performance:
Discrimination measures how well a model distinguishes between patients who experience the outcome versus those who do not. The C-statistic (equivalent to the area under the receiver operating characteristic curve, AUC) is commonly used, with values ranging from 0.5 (no discrimination) to 1.0 (perfect discrimination) [1]. For example, a recent cancer prediction algorithm incorporating blood tests demonstrated C-statistics of 0.876 for men and 0.844 for women for any cancer diagnosis [1].
Calibration assesses the agreement between predicted probabilities and observed outcomes. Well-calibrated models generate predictions that match the actual event rates across different risk levels [10]. Calibration is typically visualized using calibration plots and quantified with statistics like the calibration slope, where a value of 1 indicates perfect calibration [1].
Clinical utility evaluates whether using the model improves decision-making compared to standard approaches. Decision curve analysis quantifies net benefit across different probability thresholds, balancing true positives against false positives [5].
Case Studies in Cancer Research
Comprehensive Cancer Prediction Algorithm
A 2025 study developed and validated algorithms to improve early cancer diagnosis using English primary care data from 7.46 million patients [1]. The researchers created two models: one with clinical factors and symptoms, and another incorporating routine blood tests. After internal validation, they performed rigorous external validation using two separate cohorts totaling over 5 million patients from across the UK. The externally validated models demonstrated excellent discrimination (C-statistic 0.876 for men, 0.844 for women) and maintained calibration across diverse populations, outperforming existing prediction tools [1].
External Validation of Breast Cancer Models
A 2023 study exemplifies the critical importance of external validation, evaluating 87 breast cancer prediction models using Dutch registry data from 271,040 patients [5]. The results revealed substantial performance variation: only 34 models (39%) performed well after external validation, 26 showed moderate performance, and 27 (31%) performed poorly despite previous promising development. This comprehensive validation effort prevented the implementation of potentially misleading models and identified robust tools suitable for Dutch clinical practice [5].
Machine Learning in Gastric Cancer Surgery
A 2024 study externally validated a machine learning model predicting 90-day mortality after gastrectomy for cancer [8]. The original model, developed from the Spanish EURECCA registry, achieved an AUC of 0.829. When applied to the international GASTRODATA registry (2,546 patients from 24 European hospitals), performance modestly decreased to an AUC of 0.716, yet maintained clinically useful discrimination. This performance attenuation in external validation is typical, highlighting how differences in patient populations, surgical techniques, and perioperative care can affect model transportability [8].
Table 3: Performance Metrics in Cancer Prediction Model Validations
| Study & Cancer Type | Development Performance | Internal Validation | External Validation | Key Insights |
|---|---|---|---|---|
| Multi-cancer early detection [1] | C-statistic: Not separately reported | C-statistic: 0.876 (M), 0.844 (F) with blood tests | Similar performance in 2.74M patients from Scotland, Wales, NI | Blood tests (FBC, liver function) significantly improved prediction |
| Breast cancer models [5] | Various performance in original studies | Not applicable | 34/87 (39%) performed well; 27/87 (31%) performed poorly | Comprehensive registry data enables broad validation of multiple models |
| Gastric cancer surgery [8] | AUC: 0.829 | Not separately reported | AUC: 0.716 in international cohort | Modest performance reduction common in external validation |
| Cervical cancer survival [10] | C-index: 0.882 | C-index: 0.885 | C-index: 0.872 in hospital data | Nomogram maintained performance across validation cohorts |
Statistical Software and Computing Environments
- R Statistical Software (version 4.3.2): Open-source environment with comprehensive packages for prediction modeling (
rms,glmnet,mlr3) and validation (rms,pROC) [10]. - Python with scikit-learn: Machine learning library providing implementations of cross-validation, bootstrapping, and performance metrics.
- mlr3 Package: Comprehensive machine learning framework for R facilitating internal and external validation of predictive models [8].
- Electronic Health Records: Large-scale primary care databases (e.g., QResearch, CPRD) containing linked primary care, hospital, and mortality data [1].
- Cancer Registries: Population-based registries (e.g., Netherlands Cancer Registry, SEER database) providing detailed clinical and outcome data [5] [10].
- International Consortia: Multi-center collaborations (e.g., GASTRODATA registry) enabling geographic validation across diverse healthcare systems [8].
Reporting Guidelines and Methodological Standards
- TRIPOD Statement (Transparent Reporting of a multivariable prediction model for Individual Prognosis Or Diagnosis): Comprehensive checklist ensuring complete reporting of prediction model development and validation studies [8].
- REMARK Guidelines (Reporting Recommendations for Tumor Marker Prognostic Studies): Specialized guidelines for reporting cancer prognostic studies [2].
Internal and external validation serve distinct but complementary roles in the development of cancer prediction models. Internal validation provides initial estimates of model stability and optimizes parameters, while external validation establishes generalizability to new populations—a prerequisite for clinical implementation. The case studies presented demonstrate that even models with excellent internal performance may show diminished accuracy when applied externally, underscoring the necessity of rigorous validation across diverse settings. As cancer research increasingly embraces artificial intelligence and complex machine learning algorithms, adherence to robust validation methodologies will be essential for translating statistical predictions into clinically actionable tools that improve patient outcomes.
Why External Validation is Non-Negotiable for Clinical Generalizability
In the pursuit of refining cancer care, clinicians and researchers increasingly rely on predictive algorithms to estimate everything from a patient's initial cancer risk to their likelihood of recurrence. However, a model's promising performance in the laboratory provides no guarantee of its effectiveness in the diverse and unpredictable environment of real-world clinical practice. External validation—the process of evaluating a prediction model in data that was not used for its development—serves as the critical bridge between theoretical development and trustworthy clinical application. It is the fundamental process that tests whether a model's predictions hold true for new populations, from different geographical regions or care settings, ensuring that the algorithms intended to guide patient care are both reliable and generalizable.
Defining the Validation Landscape: From Internal Checks to External Generalizability
Before a model can be deemed fit for widespread clinical use, it must pass through several stages of validation, each serving a distinct purpose. The journey begins with internal validation, which assesses a model's reproducibility within the same underlying population from which it was derived. Techniques like bootstrapping or cross-validation correct for over-optimism, providing a more realistic estimate of performance had the model been applied to similar, but new, patients from that same population [3] [11].
External validation moves beyond this, testing the model's transportability to entirely new settings. As outlined in the literature, this encompasses several key dimensions [11]:
- Temporal Validation: Assessing performance in patients from the same institution or region but from a later time period. This checks for "data drift," where relationships between variables and outcomes may evolve.
- Geographical Validation: Testing the model on data collected from a different location, such as a hospital in another country. This is crucial for establishing that the model works across diverse healthcare systems and patient demographics.
- Domain Validation: Evaluating whether the algorithm generalizes to a different clinical context, such as from a primary care population to a secondary care population, or from one specific cancer type to another.
Independent external validation, conducted by researchers not involved in the model's original development, is considered the gold standard, as it eliminates the potential for conscious or unconscious fine-tuning of the model to the validation data [3].
Comparative Performance: How Externally Validated Models Measure Up
The following table summarizes key performance metrics from recent, high-impact studies that have undertaken rigorous external validation of cancer prediction algorithms.
Table 1: Performance Metrics from Externally Validated Cancer Prediction Models
| Cancer Type / Focus | Model Description | Validation Type & Cohort Size | Key Performance Metrics | Citation |
|---|---|---|---|---|
| Multiple Cancers (15 types) | Algorithm incorporating symptoms, history, and blood tests (Model B) | Geographical validation on 2.74 million patients from Scotland, Wales, and Northern Ireland [1] | Any Cancer (Men): C-statistic = 0.876 (95% CI 0.874–0.878)Any Cancer (Women): C-statistic = 0.844 (95% CI 0.842–0.847) | [1] |
| Early-Stage Lung Cancer | Machine learning model using CT radiomics and clinical data | External validation on 252 patients from a separate medical center [9] | Superior risk stratification vs. TNM staging (HR for DFS: 3.34 vs. 1.98 in external cohort); correlated with pathologic risk factors (p < 0.05) | [9] |
| Bladder Cancer (Distant Metastasis) | Nomogram based on tumor size, N stage, and surgery | External validation on a cohort of 112 patients from a Chinese hospital [12] | AUC of 0.968 in the external validation cohort | [12] |
| AI in Oncology (Scoping Review) | Review of 56 externally validated ML models for clinical decision-making | Analysis of multi-institutional studies published 2018-2022 [13] | Found that most studies were retrospective; noted challenges with limited international ethnic diversity and inconsistent calibration reporting | [13] |
The data consistently shows that high-performing, externally validated models share common traits: they are often developed on very large datasets, validated across different populations, and demonstrate robust discrimination (as measured by C-statistics or AUC). The superior hazard ratios (HR) for disease-free survival in the lung cancer model, for instance, indicate its enhanced ability to stratify risk compared to the current clinical standard [9].
Experimental Protocols for Robust External Validation
A methodologically sound external validation study follows a structured protocol to ensure its findings are credible and actionable.
Table 2: Key Methodological Steps for External Validation Studies
| Protocol Step | Description | Considerations |
|---|---|---|
| 1. Model Selection & Definition | Obtain the full prediction model formula, including all coefficients and intercepts. | Ensure the model is specified exactly as developed; any deviation invalidates the validation [3]. |
| 2. Validation Cohort Definition | Identify a cohort that is distinct from the development data. | The cohort should represent the target population for the model's intended use (e.g., different geography, time period) [11]. |
| 3. Predictor & Outcome Ascertainment | Extract or measure the predictor variables and outcome as defined in the original model. | Harmonization of variable definitions (e.g., smoking status, cancer stage) across datasets is critical [12]. |
| 4. Risk Calculation | Apply the original model's equation to calculate predicted risks for each individual in the validation cohort. | This step should be automated and reproducible [3]. |
| 5. Performance Assessment | Compare predicted risks to observed outcomes using discrimination, calibration, and clinical utility metrics. | Discrimination (e.g., C-statistic) measures how well the model separates patients with and without the outcome. Calibration (often with a plot) assesses the agreement between predicted probabilities and observed frequencies [1] [13]. |
| 6. Model Comparison & Updating | Compare performance to existing models or clinical standards. If performance is poor but transportable, consider model updating. | Updating might involve adjusting the model's intercept or re-estimating some coefficients for the new population [3]. |
The following diagram illustrates the logical workflow and key decision points in a rigorous external validation process.
Conducting robust validation studies requires access to specific data, tools, and methodologies. The table below details key resources frequently utilized in this field.
Table 3: Research Reagent Solutions for External Validation Studies
| Tool / Resource | Type | Function in Validation | Example Use Case |
|---|---|---|---|
| Large Electronic Health Record (EHR) Databases (e.g., QResearch, CPRD) [1] [14] | Data Source | Provide large, representative, longitudinal patient data for model development and geographical/temporal validation. | Used to develop and validate a cancer prediction algorithm across 7.46 million patients [1]. |
| National Cancer Registries (e.g., SEER, NCRAS) [12] | Data Source | Offer high-quality, curated data on cancer incidence, stage, and outcomes for outcome ascertainment and validation. | Used as a primary data source for developing a nomogram for distant metastasis in bladder cancer [12]. |
| Statistical Software (e.g., R, Python with scikit-learn) | Analytical Tool | Used to calculate predicted risks, perform statistical tests, and generate performance metrics and plots (e.g., calibration curves). | Essential for all steps of the validation protocol, from risk calculation to performance assessment [3]. |
| TRIPOD/TRIPOD-AI Guidelines [11] | Reporting Framework | A checklist to ensure transparent and complete reporting of prediction model development and validation studies. | Improves the reproducibility and credibility of published validation research [11]. |
| Bioinformatics Tools (e.g., for radiomics or genomic analysis) [9] [12] | Analytical Tool | Extract and analyze high-dimensional features from medical images or genomic data for complex AI model validation. | Used to extract radiomic features from CT scans for a lung cancer recurrence prediction model [9]. |
The journey of a cancer prediction algorithm from a concept to a tool that can reliably inform patient care is fraught with potential for failure. External validation is the non-negotiable checkpoint that separates speculative tools from clinically credible ones. It provides the necessary evidence that an algorithm can perform adequately across different populations, times, and settings—the very definition of generalizability. For researchers, it is a mandatory step to combat research waste and build trust in their models. For clinicians, drug developers, and, most importantly, patients, it is the safeguard that ensures the decisions guided by these algorithms are based on reliable, evidence-based science.
The transition of a cancer risk prediction algorithm from a statistical model to a clinically useful tool hinges on rigorous validation against three core principles: discrimination, calibration, and clinical net benefit. Discrimination assesses a model's ability to separate patients with and without the outcome of interest, typically measured by the Area Under the Receiver Operating Characteristic Curve (AUC) or C-statistic. Calibration evaluates how well predicted probabilities match observed frequencies, often visualized via calibration plots. Clinical net benefit quantifies the model's utility in informing clinical decisions, balancing true positives against false positives across different probability thresholds using decision curve analysis (DCA) [15] [16].
These metrics are particularly crucial in oncology, where prediction models inform high-stakes decisions about screening, intervention, and treatment. A model with excellent discrimination may still be clinically useless if it is poorly calibrated, leading to overestimation or underestimation of risk for individual patients. Furthermore, a model must demonstrate that its use improves clinical decision-making compared to standard approaches, which is the essence of assessing clinical net benefit [15]. This guide objectively compares the performance of recently developed and validated cancer prediction models against these three fundamental criteria.
Performance Data Comparison of Cancer Prediction Models
Table 1: Discrimination and Calibration Performance of Recent Cancer Prediction Models
| Cancer Type / Context | Model Name/Type | Discrimination (AUC/C-statistic) | Calibration Assessment | Clinical Net Benefit |
|---|---|---|---|---|
| Multiple Cancers (Diagnostic) | Model A (Symptoms + Clinical Factors) | Men: 0.876 (95% CI 0.874-0.878); Women: 0.844 (95% CI 0.842-0.847) [1] | Not explicitly reported in summary | Superior net benefit compared to existing scores [1] |
| Model B (Includes Blood Tests) | Improved over Model A, though confidence intervals overlapped [1] | Not explicitly reported in summary | Superior net benefit compared to existing scores [1] | |
| Melanoma (SLN Metastasis) | MIA Nomogram | 0.753 (95% CI 0.694-0.812) [16] | Well-calibrated across clinically relevant risk thresholds [16] | Net benefit and reduction in avoidable SLNBs for thresholds ≥5% [16] |
| MSKCC Nomogram | 0.729 (95% CI 0.671-0.787) [16] | Well-calibrated across clinically relevant risk thresholds [16] | Net benefit and reduction in avoidable SLNBs for thresholds ≥5% [16] | |
| Premenopausal Breast Cancer (5-year risk) | PBCCG Model | 59.1% (95% CI 58.1–60.1%) [17] | Overestimation on average (E/O=1.18); underestimation in lower deciles, overestimation in upper deciles [17] | Not reported |
| Bladder Cancer (Distant Metastasis) | SEER-based Nomogram | Training: 0.732; Internal Validation: 0.750; External Validation: 0.968 [12] | Calibration curves showed good predictive accuracy across cohorts [12] | Not reported |
Table 2: Machine Learning Model Performance for Kinesiophobia and Stroke-Associated Pneumonia
| Clinical Context | Model Type | Discrimination (AUC) | Additional Performance Metrics |
|---|---|---|---|
| Kinesiophobia in Postoperative Lung Cancer | Random Forest (RF) | 0.893 [18] | Accuracy: 0.803; Precision: 0.732; Recall: 0.870; F1: 0.795 [18] |
| XGBoost | Not specified | Performance compared, RF was optimal [18] | |
| Support Vector Machine (SVM) | Not specified | Performance compared, RF was optimal [18] | |
| Stroke-Associated Pneumonia in Older Hemorrhagic Stroke | Logistic Regression (LR) | Training: 0.883; Internal: 0.855; External: 0.882 [19] | Demonstrated stable generalizability [19] |
| XGBoost | Not specified | LR demonstrated the best and most stable performance [19] | |
| Naive Bayes | Not specified | LR demonstrated the best and most stable performance [19] |
Experimental Protocols for Model Validation
Model Development and Validation Workflow
The pathway to a robustly validated prediction model follows a structured workflow encompassing development, internal validation, and external validation, with rigorous evaluation at each stage.
Detailed Methodologies for Key Experiments
Multinational Cancer Diagnostic Prediction Algorithm
The study developing algorithms for early cancer diagnosis employed a population-based cohort design using electronic health records from over 7.4 million adults in England (derivation cohort) [1]. The model was externally validated in two separate cohorts totaling over 5.3 million people from across the UK [1].
- Predictors: Model A included age, sex, deprivation, smoking, alcohol, family history, medical diagnoses, and symptoms. Model B additionally incorporated full blood count and liver function tests [1].
- Statistical Analysis: Researchers used multinomial logistic regression to develop separate equations for men and women predicting the absolute probability of 15 cancer types. They assessed for overfitting using heuristic shrinkage and evaluated performance in independent validation cohorts [1].
- Performance Metrics: Discrimination was measured using the c-statistic (equivalent to AUROC). Calibration was assessed visually and statistically. Clinical utility was evaluated using net benefit analysis across various risk thresholds [1].
Melanoma Sentinel Lymph Node Biopsy Nomogram Validation
The validation of melanoma nomograms followed a retrospective prognostic validation design using data from 712 melanoma cases in Southern Arizona, a region with high UV index [16].
- Model Application: Three established nomograms (MIA, MSKCC, University of Colorado) were applied to the cohort without recalibration [16].
- Statistical Analysis: Discrimination was assessed via receiver operating characteristic curves and the C-statistic. Calibration was evaluated using calibration plots. Clinical utility was tested through decision curve analysis (DCA) to determine net benefit and the number of net avoidable SLNBs across different risk thresholds [16].
- Threshold Analysis: Performance was specifically examined at clinically relevant risk thresholds (≥5%) and across different age groups to identify potential limitations [16].
Research Reagent Solutions for Prediction Modeling
Table 3: Essential Tools and Data Sources for Prediction Model Research
| Resource Category | Specific Resource | Function and Application |
|---|---|---|
| Data Resources | QResearch/CPRD Databases | Large, linked electronic health record databases from the UK primary care, used for model derivation and validation [1] |
| SEER Database | US cancer registry providing population-level data for developing and validating oncology prediction models [12] | |
| Estonian Biobank | Genetic and clinical data repository enabling development of models incorporating polygenic risk scores [20] | |
| PBCCG Harmonized Datasets | International consortium data specifically for premenopausal breast cancer research, with harmonized variables across cohorts [17] | |
| Statistical Software & Packages | R Software | Open-source environment for statistical computing and graphics, used for developing nomograms and performing decision curve analysis [12] [19] |
| STATA | Statistical software for data management and analysis, particularly used for complex survival analyses [17] | |
| Glmnet Package | R package for implementing LASSO regression for variable selection in high-dimensional data [12] | |
| Validation Frameworks | TRIPOD+AI Guidelines | Reporting guideline for transparent reporting of multivariable prediction models, including those developed with machine learning [15] |
| Decision Curve Analysis | Methodological framework for evaluating the clinical value of prediction models by incorporating clinical consequences [16] | |
| Machine Learning Algorithms | Random Survival Forest | Machine learning method for survival data that can handle complex, non-linear relationships without proportional hazards assumptions [21] |
| XGBoost | Gradient boosting framework that often achieves state-of-the-art results on structured data, used in various cancer prediction studies [18] [19] |
Comparative Analysis and Research Implications
The comparative performance data reveals several critical patterns. First, comprehensive models incorporating diverse data types (e.g., symptoms, clinical factors, and blood tests) demonstrate superior discrimination (C-statistics >0.84) and net benefit compared to simpler models [1]. Second, model performance varies significantly by clinical context, with diagnostic models for general cancer detection generally showing higher discrimination (C-statistics 0.84-0.88) than risk prediction models for specific conditions (AUC 0.59-0.75) [1] [17] [16]. Third, traditional regression methods often perform comparably to complex machine learning algorithms in many clinical scenarios, particularly with structured clinical data [21] [19].
The validation methodologies highlight that external validation in geographically distinct populations is essential for assessing generalizability, as demonstrated by the melanoma nomogram study which tested models developed in Australia and New York on an Arizona population [16]. Furthermore, clinical utility assessment through decision curve analysis provides crucial information beyond traditional discrimination and calibration metrics, directly addressing whether a model would improve clinical decisions [15] [16].
For researchers and drug development professionals, these findings underscore that model selection should be based not merely on discriminatory performance but on comprehensive evaluation of all three core principles within the target population and clinical context. Future research should prioritize model interoperability across diverse healthcare systems, continuous monitoring and updating of deployed models, and integration of novel biomarkers to enhance predictive performance while maintaining calibration and clinical utility [1] [15] [12].
The integration of artificial intelligence (AI) and machine learning (ML) into oncology represents a paradigm shift in cancer risk prediction, offering the potential to identify high-risk individuals for targeted screening and early intervention. However, the transition from algorithm development to successful clinical implementation is fraught with challenges, and many promising tools fail to demonstrate real-world utility. A critical analysis of these failures reveals a consistent shortcoming: the absence of rigorous, multi-cohort external validation. This guide objectively compares the performance of various cancer risk prediction algorithms, framing the discussion within the broader thesis that external validation is not merely a final check but a fundamental component of the development process. For researchers, scientists, and drug development professionals, these lessons are essential for building models that are not only statistically sound but also clinically effective and reliable across diverse populations.
The High Stakes of Prediction: Clinical Context and Implementation Failures
Cancer risk prediction algorithms are designed to support critical clinical decisions, from guiding screening referrals to enabling personalized prevention strategies. In the United Kingdom, where cancer survival rates lag behind other developed nations, such tools are seen as vital for achieving the NHS target of diagnosing 75% of cancers at an early (stage 1 or 2), curable stage [1]. Despite this urgent need, implementation in primary care remains low. Qualitative studies have identified barriers including clinician reluctance to rely on algorithmic outputs, challenges in integrating tools into clinical workflows, and practical issues around availability [22].
Beyond these practical hurdles, a core scientific reason for failed implementation is the lack of generalizability. An algorithm performing excellently in its derivation cohort may fail in a different population due to differences in data coding, prevalence of risk factors, or underlying population genetics. For instance, a model trained primarily on one ethnic group may not calibrate correctly for another, leading to systematic over- or under-prediction of risk. Furthermore, without robust external validation, algorithms may be susceptible to "concept drift," where the relationship between predictors and outcomes changes over time, rendering the model obsolete [23]. The failure to adequately test for these factors during development directly undermines clinical trust and leads to non-adoption, regardless of a model's theoretical sophistication.
Experimental Protocols for Rigorous Validation
To avoid implementation failures, a structured and transparent validation protocol is mandatory. The following methodology, exemplified by leading studies, provides a template for rigorous testing.
Cohort Design and Data Sourcing
The foundation of robust validation is independent, high-quality data.
- Derivation Cohort: Used to train and develop the initial algorithm. This should be a large, representative sample. For example, the development of the CanPredict oesophageal cancer algorithm used 12.9 million patient records from 1,354 QResearch general practices [23].
- Validation Cohorts: At least two separate, external cohorts are required to test generalizability.
- Internal Validation: A random sample held out from the derivation cohort (e.g., 20-30%).
- External Validation 1: A cohort from the same broader data source but different sites (e.g., 450 different QResearch practices for CanPredict) [23].
- External Validation 2: A cohort from a completely different data source, such as the Clinical Practice Research Datalink (CPRD), which contributed 2.53 million patient records for CanPredict validation [23]. This is the strongest test of portability.
Data should be routinely collected electronic health records (EHRs) from primary care, linked to hospital, mortality, and cancer registry data to ensure complete outcome capture. Key variables include demographics, lifestyle factors (smoking, alcohol), clinical symptoms, comorbidities, medications, and laboratory results [1] [23].
Model Training and Statistical Methods
- Algorithm Selection: Cox proportional hazards models are commonly used for time-to-event data (e.g., 10-year cancer risk) [23]. For diagnostic prediction, multinomial logistic regression can estimate the probability of multiple cancer types simultaneously [1]. Machine learning models, such as Light Gradient Boosting Machine (LightGBM), are also employed for their ability to capture complex, non-linear interactions [6].
- Predictor Selection: Variables are chosen based on established literature and expert clinical opinion. Novel risk factors, such as specific blood tests or medications, should be justified and tested.
- Handling of Data Imperfections: Prespecified methods for imputing missing data and assessing for over-fitting (e.g., heuristic shrinkage) are critical to ensure model robustness [1].
Performance Evaluation Metrics
A comprehensive evaluation requires multiple metrics, calculated separately for each validation cohort [1] [23] [6].
Table 1: Key Performance Metrics for Cancer Risk Prediction Algorithms
| Metric | Definition | Interpretation in a Clinical Context |
|---|---|---|
| Discrimination (C-statistic/AUROC) | Ability to distinguish between patients who will vs. will not develop cancer. | A value of 0.80 means the model correctly ranks a random patient with cancer higher than one without 80% of the time. |
| Calibration | Agreement between predicted probabilities and observed outcomes. | A well-calibrated model predicting a 10% risk should see cancer occur in 10 out of 100 similar patients. |
| Sensitivity | Proportion of true cancer cases correctly identified as high-risk. | Of 100 patients with cancer, a sensitivity of 76% means the model correctly flagged 76 of them [23]. |
| Specificity | Proportion of true non-cases correctly identified as low-risk. | Of 100 cancer-free patients, a specificity of 80% means the model correctly reassured 80 of them [23]. |
| Net Benefit | A decision-analytic measure weighing true positives against false positives at a specific risk threshold. | Quantifies the clinical value of using the model for decision-making versus alternative strategies. |
The following workflow diagram summarizes this multi-stage validation process, illustrating the critical pathway from initial development to the final assessment of real-world readiness.
Performance Comparison: A Data-Driven Analysis
Objectively comparing algorithms requires examining their performance across independent validation cohorts. The tables below synthesize published data from recent studies.
Table 2: Comparative Performance of Diagnostic Cancer Prediction Algorithms (Any Cancer)
| Algorithm / Model | Validation Cohort | C-Statistic (AUROC) | Key Performance Notes |
|---|---|---|---|
| Novel Model A (with symptoms & clinical factors) [1] | QResearch (England), 2.64M patients | Men: 0.876 (0.874–0.878)Women: 0.844 (0.842–0.847) | Outperformed existing QCancer models, with improved discrimination and net benefit. |
| Novel Model B (adding blood tests) [1] | QResearch (England), 2.64M patients | Men: 0.876 (0.874–0.878)Women: 0.844 (0.842–0.847) | Incorporation of full blood count and liver function tests provided affordable digital biomarkers. |
| LightGBM for Colorectal Cancer [6] | PLCO Trial (Internal Validation) | 0.726 (0.698–0.753) | Model focused on readily available clinical/lifestyle factors for practical primary care use. |
Table 3: Comparative Performance of Long-Term Risk Algorithms
| Algorithm / Model | Validation Cohort | C-Statistic (AUROC) | Calibration & Sensitivity |
|---|---|---|---|
| CanPredict (Oesophageal Cancer) [23] | QResearch, 4.12M patients | Women: 0.859 (0.849–0.868)Men: Similar | Good calibration; sensitivity of 76% for the top 20% highest-risk patients. |
| CanPredict (Oesophageal Cancer) [23] | CPRD, 2.53M patients | Similar to QResearch results | Results were similar, demonstrating robustness across different UK populations. |
| AI Model for Lung Cancer Recurrence [9] | Multi-source (External) | Concordance Index reported | Outperformed TNM staging in stratifying Stage I patients into high/low-risk groups. |
The data reveals that algorithms undergoing extensive external validation, such as CanPredict and the novel models from [1], demonstrate strong and consistent performance across multiple, large-scale cohorts. This rigorous testing builds the evidence base required for clinical trust. In contrast, models with only internal validation, while potentially promising, lack the proven generalizability needed for widespread implementation. The addition of novel data types, such as blood tests [1] or CT radiomics [9], can enhance predictive power, but their value must also be confirmed in external settings.
The Scientist's Toolkit: Essential Research Reagent Solutions
The development and validation of these models rely on a suite of data and software "reagents." The following table details key resources for building and testing cancer risk prediction algorithms.
Table 4: Key Research Reagent Solutions for Algorithm Development and Validation
| Resource / Solution | Function | Example in Context |
|---|---|---|
| Large-scale EHR Databases | Provide longitudinal, real-world patient data for derivation and validation cohorts. | QResearch [23], CPRD [1], and PLCO Trial [6] databases provide millions of anonymized patient records. |
| Data Linkage Systems | Link primary care records to secondary care, cancer registry, and mortality data to ensure accurate and complete outcome ascertainment. | Crucial for studies where the primary outcome (cancer diagnosis) may occur outside the primary care setting [23]. |
| Specialized Statistical Software (R, Python) | Provide environments for complex statistical modeling, machine learning, and data analysis. | Used for running Cox regression [23], multinomial logistic regression [1], and LightGBM [6]. |
| GPT & Large Language Models (LLMs) | Assist in mining unstructured text from biomedical literature and EHRs to identify experimental conditions and key variables. | A multi-agent LLM system can extract critical experimental conditions (e.g., buffer type, pH) from assay descriptions to standardize data [24]. |
| Benchmark Datasets (e.g., PharmaBench) | Provide standardized, curated datasets for training and benchmarking predictive models, particularly for ADMET properties in drug development. | Comprises 11 ADMET datasets with 52,482 entries, offering a more relevant and extensive benchmark than previous sets [24]. |
The pathway from a validated algorithm to successful clinical implementation involves addressing both technical and human-factor barriers, as visualized below.
The journey from a conceptual cancer risk algorithm to a trusted clinical tool is arduous, with failed implementations often tracing back to insufficient testing beyond the initial development dataset. Rigorous, multi-cohort external validation is the non-negotiable standard that separates speculative tools from clinically actionable ones. It is the process that confirms an algorithm's discrimination, ensures its calibration across diverse populations, and ultimately builds the trust required for adoption by clinicians. As the field advances with more complex models incorporating genomics, radiomics, and digital biomarkers, the foundational principle remains: rigorous testing through external validation is the most critical investment for any team serious about making a tangible impact on cancer care. For researchers and drug developers, this is not just a methodological detail but the core of building translatable and effective predictive health technologies.
Conducting Rigorous External Validation: Frameworks and Best Practices
For researchers, scientists, and drug development professionals working on cancer risk prediction algorithms, the journey from conceptual model to clinically useful tool requires rigorous validation. While internal validation checks a model's performance on data from the same source, external validation assesses its generalizability to entirely separate populations, healthcare systems, and data collection protocols. This process is crucial for verifying that an algorithm will perform reliably in real-world clinical settings beyond the controlled environment of its development. The selection of appropriate external validation cohorts thus represents a fundamental step in translating predictive models from research artifacts into trustworthy clinical tools.
Despite its importance, robust external validation remains a significant challenge in the field. A systematic scoping review of AI pathology models for lung cancer found that only approximately 10% of developed models undergo any form of external validation, highlighting a critical gap between development and implementation [25]. This article provides a comparative guide to methodologies for sourcing truly external and representative datasets, examining current practices, experimental protocols, and essential tools for strengthening the validation phase of cancer prediction research.
Core Principles of External Cohort Selection
Defining "Truly External" Datasets
A "truly external" validation cohort must demonstrate complete independence from the derivation cohort across multiple dimensions. Key characteristics include:
- Geographical Separation: Sourcing data from different hospitals, regions, or countries than those used for model development.
- Temporal Separation: Using data collected from different time periods than the development data.
- Institutional Independence: Drawing from healthcare systems with different patient populations, clinical workflows, and data recording practices.
- Technical Variation: Incorporating data generated with different equipment, laboratory protocols, or measurement standards.
For instance, a study developing cancer prediction algorithms in England (QResearch database) demonstrated robust external validation by testing performance on separate English populations alongside populations from Scotland, Wales, and Northern Ireland [1]. This approach validated both geographical and health system generalizability.
Ensuring Representativeness for Clinical Utility
Beyond mere independence, external cohorts must be representative of the intended use population to ensure clinical utility. Considerations include:
- Demographic Diversity: Appropriate distribution of age, sex, ethnicity, and socioeconomic status.
- Clinical Spectrum: Inclusion of the full range of disease severity and co-morbidities expected in practice.
- Data Completeness: Real-world levels of missing data and measurement variability.
- Setting Appropriateness: Data from the clinical setting where the model will ultimately be deployed (e.g., primary care for screening tools, secondary care for diagnostic tools).
Comparative Analysis of External Validation Approaches
Methodologies in Current Cancer Prediction Research
The table below summarizes external validation approaches across recent cancer prediction studies, highlighting cohort sources and key methodological features.
Table 1: Comparative Analysis of External Validation Approaches in Cancer Prediction Studies
| Cancer Type | Development Cohort | External Validation Cohort | Key Validation Strengths | Performance Metrics |
|---|---|---|---|---|
| Multiple Cancers (n=15) [1] | 7.46M patients from England (QResearch) | 2.64M from England + 2.74M from Scotland, Wales, Northern Ireland | Geographical & temporal separation; Diverse healthcare systems | C-statistics: 0.876 (men), 0.844 (women) for Model B |
| Young-Onset Colorectal Cancer [26] | 10,874 young individuals from single center (2013-2021) | Temporal validation using 2022 data from same center | Temporal separation; Same center but different time period | AUC: 0.888; Recall: 0.872 |
| Early-Stage Lung Cancer [9] | 1,015 patients from NLST, NEMC, Stanford | 252 patients from North Estonia Medical Centre | Geographical & institutional independence; Multi-national | Hazard Ratio: 3.34 for stage I recurrence |
| Bladder Cancer Metastasis [12] | 2,313 patients from SEER database (US) | 112 patients from Chinese hospital | Geographical & ethnic diversity; Different healthcare systems | AUC: 0.968 in external validation |
| Cancer-Associated VTE [27] | 1,036 patients (retrospective cohort) | 321 patients (prospective cohort) | Prospective validation; Different study design | C-index: 0.709-0.760 across models |
Experimental Protocols for Robust Validation
Protocol for Multi-National Validation
A comprehensive study on cancer prediction algorithms provides a template for large-scale external validation [1]:
- Data Sources: Utilize separate national primary care electronic health record databases with linkage to hospital and mortality data.
- Population Definition: Apply consistent inclusion/exclusion criteria across all cohorts (e.g., adults aged 18-84 with no prior cancer diagnosis).
- Predictor Variables: Harmonize coding systems for symptoms, medical history, laboratory tests, and demographic factors across different databases.
- Outcome Ascertainment: Standardize cancer outcome definitions using linked cancer registry data, hospital records, and death certificates.
- Analysis Plan: Pre-specify performance metrics (discrimination, calibration, clinical utility) and subgroup analyses.
This protocol demonstrated that models incorporating blood tests (Model B) outperformed symptom-only models (Model A) across all external validation settings [1].
Protocol for Imaging-Based Prediction Models
The external validation of a lung cancer recurrence prediction model illustrates specialized considerations for AI imaging models [9]:
- Image Curation: Extensive (re)curation of preoperative CT scans to ensure consistency with clinical metadata and outcomes.
- Multi-Source Data Integration: Combine imaging data with routinely available clinical variables in the prediction model.
- Validation Against Pathologic Standards: Correlate machine learning-derived risk scores with established pathologic risk factors (e.g., lymphovascular invasion, pleural invasion).
- Stratified Performance Analysis: Evaluate model performance specifically within early-stage patients where clinical need is greatest.
This approach confirmed the model's ability to stratify recurrence risk more effectively than conventional staging in stage I patients (HR 3.34 vs 1.98) [9].
Methodological Challenges and Quality Assessment
Common Limitations in Current Practice
The external validation landscape faces several methodological challenges:
- Restricted Datasets: Many studies use artificially clean or restricted datasets that don't reflect real-world clinical environments [25].
- Retrospective Design: Most validations use retrospective data, with prospective studies and randomized trials being rare [25].
- Technical Diversity Insufficiency: Failure to account for variations in equipment, protocols, and measurement standards across institutions.
- Inadequate Reporting: Poor documentation of participant characteristics, missing data, and cohort selection criteria.
A systematic review of AI pathology models found high or unclear risk of bias in 86% of studies in the "Participant selection/study design" domain, highlighting pervasive methodological concerns [25].
Quality Assessment Framework
The QUADAS-AI tool provides a structured approach to assessing validation quality across multiple domains [25]:
- Participant Selection: Evaluate whether participants represent the intended use population.
- Image Selection: Assess appropriateness of image inclusion criteria and technical diversity.
- Reference Standard: Verify adequacy of the gold standard diagnosis.
- Flow and Timing: Examine timing between index test and reference standard.
- Index Test: Evaluate blinding and pre-specification of analysis.
Visualization of Cohort Selection Strategy
The following diagram illustrates a robust workflow for sourcing and validating external cohorts in cancer prediction research:
Diagram Title: External Cohort Selection Workflow
Research Reagent Solutions for Cohort Selection
Table 2: Essential Resources for Sourcing External Validation Cohorts
| Resource Category | Specific Examples | Function in External Validation | Key Considerations |
|---|---|---|---|
| Public Cancer Databases | SEER Program, TCGA, NLST | Provide diverse patient populations for validation; Enable cross-institutional comparison | Data harmonization required; May lack specific clinical variables |
| International EHR Networks | QResearch (UK), CPRD (UK) | Offer large-scale primary care data with linked outcomes; Enable geographical validation | Variable data quality; Different coding systems |
| Biobanks & Cohort Studies | UK Biobank, NLST | Provide richly phenotyped data with imaging and biomarkers | Access restrictions; May not represent general population |
| Data Harmonization Tools | OHDSI/OMOP Common Data Model | Standardize data structure across different sources; Enable federated analysis | Significant implementation effort; Information loss possible |
| Statistical Software Packages | R, Python, STAN | Implement performance metrics; Conduct calibration analysis | Specialized expertise required; Custom programming needed |
| Quality Assessment Tools | QUADAS-AI, PROBAST | Standardize methodological quality evaluation; Identify risk of bias | Subjective judgment involved; Requires multiple reviewers |
The external validation of cancer prediction algorithms requires meticulous cohort selection that prioritizes both independence from development data and representativeness of intended use populations. Current evidence suggests that models validated across diverse geographical settings, healthcare systems, and time periods demonstrate greater reliability and clinical utility. The integration of methodological rigor in validation design—including prospective studies, comprehensive quality assessment, and appropriate technical diversity—remains essential for bridging the gap between algorithm development and meaningful clinical implementation. As the field progresses, increased attention to these cohort selection principles will strengthen the translational pathway for cancer prediction models, ultimately supporting more personalized and effective cancer care.
External validation is a critical step in assessing the real-world performance of cancer risk prediction algorithms, determining whether a model developed on one population can generalize to others. This process relies on key quantitative metrics that evaluate different aspects of model performance: discrimination (the ability to separate patients with and without the outcome), calibration (the agreement between predicted probabilities and observed outcomes), and overall performance. For researchers, scientists, and drug development professionals, understanding these metrics is essential for evaluating which models are ready for clinical implementation and where improvements are needed.
The C-statistic (or AUC) evaluates discrimination, the Expected/Observed (E/O) ratio and calibration plots assess calibration, and the Polytomous Discrimination Index (PDI) extends discrimination assessment to multi-class outcomes. This guide compares the performance of contemporary cancer prediction algorithms using these metrics, providing a standardized framework for model evaluation in oncology research and development.
Performance Metrics Comparison of Cancer Prediction Algorithms
The table below summarizes the performance metrics of recently developed and validated cancer prediction algorithms across multiple cancer types and specific malignancies.
Table 1: Performance Metrics of Cancer Prediction Algorithms in External Validation
| Prediction Model | Cancer Type | C-Statistic (95% CI) | E/O Ratio | Calibration Slope | PDI | Validation Cohort Size |
|---|---|---|---|---|---|---|
| CanPredict (Model B) [1] | Any Cancer (Men) | 0.876 (0.874-0.878) | Not Reported | Not Reported | ~0.27* | 2.64M (QResearch) |
| CanPredict (Model B) [1] | Any Cancer (Women) | 0.844 (0.842-0.847) | Not Reported | Not Reported | ~0.26* | 2.64M (QResearch) |
| CanPredict (Model A) [1] | Any Cancer (Men) | 0.872 (0.870-0.874) | Not Reported | Not Reported | ~0.26* | 2.64M (QResearch) |
| CanPredict (Model A) [1] | Any Cancer (Women) | 0.841 (0.839-0.843) | Not Reported | Not Reported | ~0.26* | 2.64M (QResearch) |
| COLOFIT [28] | Colorectal | Not Reported | 1.52 (overall), 1.09 (best period) | 1.05 | Not Applicable | 51,477 |
| Cervical Cancer Nomogram [10] | Cervical Cancer | 0.872 (0.829-0.915) | Not Reported | Not Reported | Not Reported | 318 |
| Bladder Cancer Nomogram [29] | Bladder Cancer (DM) | 0.968 | Not Reported | Not Reported | Not Reported | 112 |
| Oesophageal Cancer (CanPredict) [23] | Oesophageal Cancer | 0.859 (0.849-0.868) | Good (Not Specified) | Not Reported | Not Reported | 4.12M |
Note: PDI values estimated from confidence intervals reported in [1]; Model A includes clinical factors and symptoms; Model B additionally includes blood test results; DM = Distant Metastasis
Detailed Metric Definitions and Methodologies
C-Statistic (Concordance Statistic)
The C-statistic measures a model's ability to discriminate between patients who experience an event and those who do not. It represents the probability that a randomly selected patient who experienced the event had a higher predicted risk than a randomly selected patient who did not. Values range from 0.5 (no better than chance) to 1.0 (perfect discrimination). In the context of cancer prediction, the CanPredict algorithm achieved C-statistics of 0.876 for men and 0.844 for women for any cancer diagnosis, indicating excellent discrimination [1]. For specific cancers, the cervical cancer nomogram maintained a C-statistic of 0.872 in external validation [10], while the oesophageal cancer model achieved 0.859 [23].
Calculation Methodology:
- For binary outcomes: Equivalent to the area under the receiver operating characteristic curve (AUC)
- For time-to-event data: Calculated using Harrell's C-index or similar time-dependent concordance measures
- Typically reported with 95% confidence intervals to indicate precision
Expected/Observed (E/O) Ratio
The E/O ratio is a fundamental measure of calibration, representing the ratio of the number of events predicted by the model (expected) to the number actually observed. An ideal E/O ratio is 1.0, indicating perfect calibration. Values below 1.0 suggest overprediction (the model predicts more events than occur), while values above 1.0 indicate underprediction. The COLOFIT model for colorectal cancer demonstrated how E/O ratios can vary across populations and time, with an overall ratio of 1.52 (indicating underprediction) that improved to 1.09 in certain periods [28]. This variability highlights the importance of evaluating calibration across different clinical settings.
Calculation Methodology:
- Sum all predicted probabilities for the validation cohort (Expected events)
- Count the actual number of observed events in the validation cohort (Observed events)
- Calculate ratio: E/O = Σ(Predicted Probabilities) / Observed Events
Calibration Plots and Slopes
Calibration plots provide visual representation of model calibration by plotting predicted probabilities against observed outcomes. A perfectly calibrated model follows the 45-degree line. The calibration slope quantifies this relationship, with an ideal value of 1.0. Values below 1.0 suggest the model needs shrinkage of its coefficients, while values above 1.0 indicate underfitting. In competing risk settings, calibration assessment becomes more complex, requiring evaluation of each cause-specific model to identify sources of miscalibration [30] [31]. The COLOFIT model maintained a calibration slope of 1.05 despite issues with the E/O ratio, indicating generally appropriate coefficient magnitudes [28].
Assessment Methodology:
- Divide patients into deciles based on predicted risk
- Calculate observed event rate for each decile (using Kaplan-Meier for time-to-event data)
- Plot mean predicted probability vs. observed event rate for each decile
- Fit a regression line to calculate the calibration slope
Polytomous Discrimination Index (PDI)
The PDI extends discrimination assessment to multi-class outcomes, such as distinguishing between multiple cancer types simultaneously. This is particularly valuable for comprehensive cancer prediction algorithms that aim to identify both the presence and type of cancer. The CanPredict algorithm, which predicts 15 cancer types, reported PDI values of approximately 0.27 for men and 0.26 for women [1]. These values indicate the model's ability to correctly classify patients not just as having cancer versus not, but specifically which type of cancer they have.
Calculation Methodology:
- Extends the concept of the C-statistic to multi-class outcomes
- Computes the probability that a patient with a particular cancer type has a higher predicted probability for that specific cancer than another patient with a different cancer type has for that same cancer
- Particularly useful for algorithms using multinomial logistic regression
Experimental Protocols for Validation
Large-Scale Algorithm Validation
The external validation of comprehensive cancer prediction algorithms like CanPredict followed rigorous methodology [1] [32]. The development cohort included 7.46 million patients from England, with validation conducted in two separate cohorts totaling over 5.38 million patients from across the UK. The protocol included:
- Data Extraction: Anonymized electronic health records from primary care practices linked to hospital episode statistics, cancer registry data, and mortality records
- Predictor Inclusion: Two models developed - Model A with clinical factors (age, sex, deprivation, symptoms, medical history) and Model B adding routine blood tests (full blood count, liver function tests)
- Statistical Analysis: Multinomial logistic regression to predict 15 cancer types simultaneously, with separate equations for men and women
- Validation Approach: Performance assessed in completely separate validation cohorts from different geographic populations
- Comparison Metrics: Evaluation against existing QCancer algorithms using discrimination, calibration, sensitivity, and net benefit analyses
Competing Risks Analysis
When validating models for specific cancer types, competing risks methodology is essential [30] [31]. The protocol includes:
- Cause-Specific Hazards Modeling: Separate models for the event of interest (specific cancer) and competing events (other cancers, non-cancer death)
- Pseudo-Observations Calculation: Used to estimate observed risks for calibration plots in the presence of competing risks
- Stratified Analysis: Assessment of calibration within subgroups based on the prognostic index
- Comprehensive Calibration Assessment: Evaluation of both cause-specific absolute risks and each cause-specific hazards model component using the complement of the cause-specific survival function
Figure 1: External Validation Workflow for Cancer Prediction Models
Research Reagent Solutions
Table 2: Essential Research Tools for Cancer Prediction Model Development and Validation
| Tool/Resource | Type | Primary Function | Example Use Case |
|---|---|---|---|
| QResearch Database [1] | Electronic Health Record Database | Population-scale data for model development/validation | CanPredict algorithm development (7.46M patients) |
| CPRD Gold [1] | Electronic Health Record Database | Independent validation cohort | CanPredict validation (2.74M patients) |
| SEER Database [10] [29] | Cancer Registry Database | Cancer incidence and survival data | Cervical/bladder cancer nomogram development |
| R statistical software [10] [33] | Statistical Analysis Platform | Model development, validation, and visualization | Nomogram development and calibration plotting |
| calibrationCurves R package [33] | Statistical Software Package | Calibration assessment and visualization | Thyroid cancer model validation |
| dcurves R package [33] | Statistical Software Package | Decision curve analysis | Clinical utility assessment |
| SEER*Stat [10] [29] | Data Extraction Tool | Access and analysis of SEER database data | Patient cohort identification |
| Flexible Parametric Survival Models [31] | Statistical Methodology | Competing risks analysis | Cause-specific hazard modeling |
Comparative Analysis and Clinical Implications
The performance metrics reveal several important patterns across cancer prediction algorithms. Comprehensive models like CanPredict that incorporate multiple predictor types (including routine blood tests) demonstrate superior discrimination, with C-statistics exceeding 0.84 for any cancer diagnosis [1]. The inclusion of commonly available blood tests (full blood count and liver function tests) in Model B provided modest but consistent improvements in discrimination across most cancer types compared to Model A, which relied solely on clinical factors and symptoms [1].
The variation in E/O ratios observed with the COLOFIT model highlights how population characteristics and changing clinical practices affect model performance [28]. The model's performance varied significantly across different time periods, with referral reduction potential ranging from 23% to -2% depending on FIT testing rates and the proportion of high-risk symptoms in the population. This underscores the necessity for local validation and periodic model recalibration.
For specific cancers, nomograms demonstrate excellent discrimination, particularly for predicting distant metastasis in bladder cancer (C-statistic: 0.968) [29]. However, these specialized models typically address narrower clinical questions and require disease-specific validation.
The PDI metric provides crucial information for multi-class prediction algorithms, quantifying their ability to not just identify cancer presence but distinguish between cancer types [1]. This is particularly valuable in primary care settings where non-specific symptoms may indicate multiple possible cancers.
From a clinical implementation perspective, algorithms must demonstrate both strong discrimination and calibration. A model with excellent discrimination but poor calibration may lead to inappropriate clinical decisions due to systematic over- or under-prediction of risk. The integration of these validated algorithms into clinical decision support systems, with appropriate threshold setting based on local cancer prevalence and healthcare resources, can potentially facilitate earlier cancer diagnosis and improve patient outcomes.
The development of algorithms for multi-cancer early detection (MCED) and risk prediction represents a transformative frontier in oncology. The United Kingdom, with its centralized healthcare systems and rich, linkable data resources, provides an unparalleled environment for conducting large-scale validation studies essential for translating these models from research to clinical practice. External validation in independent, diverse populations is a critical step in the scientific evaluation of any predictive algorithm, as it provides a true measure of its generalizability, calibration, and potential for real-world impact [1]. This case study examines the methodologies and outcomes of recent, large-scale efforts to validate multi-cancer prediction algorithms within UK populations, comparing their performance and highlighting the evolution of validation science in this field.
Comparative Analysis of Validated Multi-Cancer Algorithms
The following section objectively compares the performance and characteristics of several key algorithms that have undergone substantial validation in UK cohorts.
Clinical and Blood Test-Enhanced Prediction Algorithms
A landmark study developed and externally validated two diagnostic prediction algorithms to estimate the probability of having a current, undiagnosed cancer for 15 cancer types. The first model (Model A) incorporated predictors like age, sex, deprivation, smoking, alcohol, family history, medical diagnoses, and symptoms. The second model (Model B) additionally included commonly used blood tests (full blood count and liver function tests) [1].
Table 1: Performance of Clinical Prediction Algorithms in UK Validation Cohorts
| Metric | Model A (Clinical & Symptoms) | Model B (Model A + Blood Tests) |
|---|---|---|
| Validation Cohort | QResearch (England): 2.64M people, 44,984 cancersCPRD (Scotland, Wales, NI): 2.74M people, 32,328 cancers | QResearch (England): 2.64M people, 44,984 cancersCPRD (Scotland, Wales, NI): 2.74M people, 32,328 cancers |
| Overall C-Statistic (AUROC) - Men | 0.872 (95% CI 0.870-0.874) | 0.876 (95% CI 0.874-0.878) |
| Overall C-Statistic (AUROC) - Women | 0.840 (95% CI 0.837-0.842) | 0.844 (95% CI 0.842-0.847) |
| Key Cancer-Specific C-Statistics (Men, Model B) | Lung: 0.903, Pancreatic: 0.892, Liver: 0.913, Myeloma: 0.883 | |
| Key Cancer-Specific C-Statistics (Women, Model B) | Lung: 0.885, Pancreatic: 0.875, Liver: 0.894, Ovarian: 0.819, Cervical: 0.694 | |
| Comparison to Existing Models | Outperformed existing QCancer algorithms in discrimination, calibration, sensitivity, and net benefit. | |
| Experimental Protocol | Model derivation used a population of 7.46 million adults in England. Multinomial logistic regression was used to develop separate equations for men and women to predict the absolute probability of 15 cancer types. |
National Data Integration for Multi-Cancer Risk Cohorts
A 2025 study presented a novel approach to constructing multi-cancer risk cohorts using national data from medical helplines (NHS 111) and secondary care from all hospitals in England. Focusing on nine cancer types with high rates of late-stage diagnosis, this research demonstrated the utility of non-clinician-initiated data for population risk stratification [34].
Table 2: Performance of NHS Data-Integrated Model for Predicting Cancer Diagnosis
| Cancer Type | Area Under the Curve (AUC) | Key Influential Features |
|---|---|---|
| Bladder | 0.80 | NHS 111 symptoms, frequency of hospital appointments, comorbidities |
| Oesophageal | 0.83 | NHS 111 symptoms, frequency of hospital appointments, comorbidities |
| Ovarian | 0.69 | NHS 111 symptoms, frequency of hospital appointments, comorbidities |
| Pancreatic | 0.79 | NHS 111 symptoms, frequency of hospital appointments, comorbidities |
| Stomach | 0.78 | NHS 111 symptoms, frequency of hospital appointments, comorbidities |
| Head and Neck | 0.76 | NHS 111 symptoms, frequency of hospital appointments, comorbidities |
| Lymphoma | 0.77 | NHS 111 symptoms, frequency of hospital appointments, comorbidities |
| Myeloma | 0.75 | NHS 111 symptoms, frequency of hospital appointments, comorbidities |
| Kidney | 0.78 | NHS 111 symptoms, frequency of hospital appointments, comorbidities |
| Validation Scope | 23.6 million patient histories of individuals aged 40-74 in England. | |
| Model Type | XGBoost, selected based on performance comparison with other classifiers. |
AI-Empowered Blood-Based Multi-Cancer Early Detection
The OncoSeek test is an AI-empowered, blood-based test for multi-cancer early detection. While not exclusively validated in a UK population, its large-scale, multi-centre validation framework provides a relevant comparison for MCED methodologies. The test integrates a panel of seven protein tumour markers (PTMs) with clinical data using artificial intelligence [35].
Table 3: Performance of the OncoSeek MCED Test Across Multiple Cohorts
| Metric | Performance in ALL Cohort (7 cohorts) | Performance in Symptomatic Cohort (HNCH) |
|---|---|---|
| Total Participants | 15,122 (3,029 cancer; 12,093 non-cancer) | Not Specified |
| Sensitivity | 58.4% (95% CI: 56.6%-60.1%) | 73.1% (95% CI: 70.0%-76.0%) |
| Specificity | 92.0% (95% CI: 91.5%-92.5%) | 90.6% (95% CI: 87.9%-92.9%) |
| Area Under Curve (AUC) | 0.829 | 0.883 |
| Tissue of Origin (TOO) Accuracy | 70.6% for true positives | Not Specified |
| Key Cancer Sensitivities | Bile duct: 83.3%, Pancreas: 79.1%, Ovary: 74.5%, Lung: 66.1%, Breast: 38.9% | Not Specified |
| Experimental Protocol | Multi-centre validation across 7 centres in 3 countries, using 4 quantification platforms and 2 sample types (serum and plasma). Assays demonstrated high consistency across different laboratories (Pearson correlation coefficient of 0.99-1.00). |
Polygenic Risk Score Integration for Cancer Risk Prediction
Another approach integrated polygenic risk scores (PRS) with clinical variables for risk prediction of eight cancers. This model was developed using the UK Biobank, a large-scale, prospective cohort study [36].
Table 4: Performance of Polygenic Risk Score (PRS) and Clinical Model
| Cancer Type | Area Under the Curve (AUC) | Risk Stratification (Top 5% vs. Lowest 10%) |
|---|---|---|
| Lung Cancer | 0.831 (95% CI: 0.817-0.845) | Not Specified |
| Breast Cancer | 0.755 (95% CI: 0.745-0.765) | Nearly 13x greater risk |
| Colorectal Cancer | 0.673 (95% CI: 0.657-0.689) | Not Specified |
| Prostate Cancer | 0.733 (95% CI: 0.721-0.745) | Not Specified |
| Ovarian Cancer | 0.618 (95% CI: 0.581-0.655) | Not Specified |
| Bladder Cancer | 0.642 (95% CI: 0.622-0.662) | Not Specified |
| Pancreatic Cancer | 0.647 (95% CI: 0.611-0.683) | Not Specified |
| Kidney Cancer | 0.659 (95% CI: 0.635-0.683) | Not Specified |
| Key Finding | Combination of PRS and clinical risk factors had better predictive performance than either alone. PRS was more predictive for early-onset cancer, while clinical risk was more predictive for late-onset cancer. | |
| Experimental Protocol | Used UK Biobank to train best polygenic risk scores from 5 methods and selected relevant clinical variables from 733 baseline traits through XGBoost. Combined PRS and clinical variables in Cox proportional hazards models. |
Experimental Protocols and Methodological Workflows
This section details the core methodologies employed in the development and validation of the algorithms discussed.
Workflow for National Data Integration and Model Validation
The following diagram illustrates the comprehensive process of building and validating a multi-cancer prediction model using national-scale UK data sources, as exemplified by the NHS 111 and secondary care study [34].
Algorithm Development and External Validation Protocol
The following diagram outlines the structured approach for algorithm development and external validation used in the clinical prediction algorithm study, highlighting the separation between derivation and validation phases [1].
Table 5: Key Research Reagents and Datasets for Multi-Cancer Algorithm Validation
| Resource | Type | Function in Validation Research |
|---|---|---|
| UK Biobank | Population Cohort | Provides genetic, clinical, and lifestyle data from ~500,000 participants for developing and testing polygenic risk scores and clinical models [36]. |
| QResearch Database | Primary/Secondary Care Data | Contains anonymised health records from general practices, used for deriving and validating clinical prediction algorithms [1]. |
| Clinical Practice Research Datalink (CPRD) | Primary Care Data | Provides linked primary care, secondary care, and cancer registry data across the UK for external validation [1]. |
| NHS 111 Medical Helpline Data | Symptom Data | Captures patient-reported symptoms before formal diagnosis, enabling early risk prediction [34]. |
| Secondary Uses Service (SUS) Data | Hospital Care Data | Contains records of all secondary care appointments, admissions, and procedures in England [34]. |
| Bridges to Health (B2H) Segmentation | Population Segmentation | Provides demographic and comorbidity flags for the English population, enabling comprehensive risk stratification [34]. |
| Roche Cobas e411/e601 | Immunoassay Platform | Automated analyser for quantifying protein tumour markers in blood-based MCED tests [35]. |
| Bio-Rad Bio-Plex 200 | Multiplex Assay Platform | System for simultaneous quantification of multiple protein biomarkers in serum/plasma samples [35]. |
| XGBoost Algorithm | Machine Learning Tool | Gradient boosting framework for handling large-scale sparse data and selecting predictive features [36] [34]. |
Discussion: Synthesis of Validation Findings and Future Directions
The large-scale validation studies conducted in UK populations demonstrate significant progress in multi-cancer algorithm development. The integration of diverse data sources—from traditional clinical factors and blood tests to genetic markers and patient-reported symptoms—consistently yields models with improved discrimination and clinical utility compared to existing tools [1] [36] [34]. The exceptional performance of models incorporating NHS 111 data is particularly noteworthy, as it highlights the value of pre-diagnostic symptom patterns captured through non-clinical channels [34].
A key finding across studies is the complementary nature of different data modalities. Polygenic risk scores show stronger predictive power for early-onset cancers, while clinical risk factors are more predictive for late-onset cancers [36]. Similarly, the addition of routine blood tests to clinical prediction models provides measurable, though modest, improvements in discrimination [1]. For blood-based MCED tests like OncoSeek, maintaining consistent performance across different platforms and sample types is crucial for real-world implementation [35].
The future of multi-cancer algorithm validation will likely involve more sophisticated multimodal approaches, combining imaging data, liquid biopsy markers, and digital health information. The UK's integrated healthcare data infrastructure positions it uniquely to lead this next wave of validation research, potentially enabling more personalized risk assessment and earlier cancer detection on a population scale.
This guide provides an objective comparison of the Individualized Clinical Assessment Recommendation System (iCARE), a machine learning framework for personalized diagnostic feature selection, against traditional model validation and risk prediction tools. Performance and methodological data are contextualized within research on the external validation of cancer risk prediction algorithms.
The iCARE framework is designed to address the "individualized feature addition problem" in clinical assessments. Unlike traditional, static models that recommend the same next diagnostic step for every patient, iCARE uses a personalized approach for each new patient by leveraging a pool of known past cases [37] [38]. It is crucial to distinguish this machine learning framework from another tool with the same acronym, the Individualized Coherent Absolute Risk Estimator, which is a separate software tool for building and validating absolute risk prediction models for cancer [39] [40]. The following table contrasts the two primary tools referenced in the literature as "iCARE."
Table: Comparison of the Two iCARE Frameworks
| Feature | iCARE (Individualized Clinical Assessment Recommendation System) | iCARE (Individualized Coherent Absolute Risk Estimation) |
|---|---|---|
| Primary Function | Personalized feature selection for clinical diagnosis [37] [38] | Development and validation of absolute risk prediction models [39] [40] |
| Core Methodology | Locally weighted logistic regression; SHAP value analysis [37] | Integration of data from multiple sources (risk factors, incidence, mortality rates) [40] |
| Typical Application | Recommending the next most informative medical test for an individual patient [38] | Projecting population-level cancer risk and validating model calibration/discrimination [39] |
| Key Output | A recommendation for the next feature to collect [37] | An individual's absolute risk of developing a disease over a specific time period [40] |
Performance and Validation Data
The performance of a model or framework is rigorously evaluated through its discrimination (ability to distinguish between cases and non-cases) and calibration (accuracy of its absolute risk predictions). The following tables summarize quantitative results from key validation studies for both iCARE frameworks and other contemporary models.
Table 1: Performance of the Machine Learning iCARE Framework on Diagnostic Datasets
| Dataset | Model/Approach | Key Performance Metric | Result |
|---|---|---|---|
| Early-Stage Diabetes Risk Prediction [38] | iCARE | Improvement in Accuracy & AUC | 6-12% improvement over other feature selection methods |
| Synthetic Dataset 1 [38] | iCARE | Accuracy / AUC | 0.999 / 1.000 |
| Global Approach | Accuracy / AUC | 0.689 / 0.639 | |
| Heart Failure Clinical Records [38] | iCARE | Improvement | No significant advantage over global approaches |
Table 2: External Validation Performance of Cancer Risk Prediction Models
| Cancer Type & Study | Model Validated | Discrimination (AUC or C-statistic) | Calibration (E/O ratio) |
|---|---|---|---|
| Breast Cancer (npj Breast Cancer, 2025) [39] | iCARE-Lit (Questionnaire, PRS, Density) | <50 yrs: 67.0% (63.5-70.6%)≥50 yrs: 66.1% (64.4-67.8%) | Not explicitly stated |
| 15 Cancers (Nature Comm., 2025) [1] | Model B (Symptoms + Blood Tests) | Men: 0.876 (0.874-0.878)Women: 0.844 (0.842-0.847) | Well-calibrated in validation cohorts |
| Lung Cancer (Cancer Med., 2025) [41] | PLCOm2012 (in Chinese smokers) | 0.70 - 0.79 | 0.57 - 0.75 |
| LLPv2 (in Chinese smokers) | 0.72 - 0.82 | 0.57 - 0.79 | |
| Lung Cancer (ESMO 2025) [9] | AI CT Radiomics Model | Concordance Index reported | Correlated with pathologic risk factors (p<0.05) |
Detailed Experimental Protocols
Protocol for the Machine Learning iCARE Framework
The iCARE (Individualized Clinical Assessment Recommendation System) protocol is designed for dynamic, personalized diagnostic journeys [37] [38].
1. Input Processing: For a new patient with an initial set of features, the framework first identifies which features are missing from the complete dataset [37].
2. Similarity Calculation & Weighting: The system calculates the Euclidean distance between the new patient and every patient in the pool of known, labeled cases. These distances are converted to sample weights, typically using the formula weight = 1 / (distance + 1e-9), ensuring that more similar cases have a greater influence on the model [37].
3. Training a Localized Model: A logistic regression model is trained on the entire pool of known cases, but with each case weighted by the similarity score calculated in the previous step. This creates a unique, personalized model for the new patient [37].
4. Feature Importance Explanation: The trained local model is analyzed using SHapley Additive exPlanations (SHAP) to quantify the contribution of each feature to the final prediction. The feature importance for feature i is calculated as the average of the absolute SHAP values across all samples: FeatureImportance_i = 1/N * ∑|SHAP_i| [37].
5. Recommendation Generation: The feature with the highest importance score that is also missing from the new patient's initial set is recommended as the next most valuable test to perform [37].
Diagram 1: The machine learning iCARE workflow for personalized test recommendation.
Protocol for External Validation of Risk Prediction Models
External validation is critical for assessing a model's generalizability and real-world performance. The following protocol is standard for validating cancer risk models, including those built with the risk estimation iCARE tool [39] [1] [41].
1. Cohort Definition: One or more external validation cohorts are established. These must be entirely separate from the data used to derive (train) the model. Cohorts are typically defined by inclusion/exclusion criteria (e.g., age, ethnicity, medical history) and linked to outcome data like cancer registries [1] [40]. 2. Predictor and Outcome Ascertainment: The predictors (risk factors) required by the model are obtained from the validation cohort's data sources (e.g., electronic health records, questionnaires, blood tests). Outcome status (e.g., incident cancer within 5 years) is determined for each individual [1]. 3. Model Application: The existing model's algorithm is applied to each individual in the validation cohort to generate a predicted probability of the outcome. 4. Performance Assessment:
- Discrimination: The Area Under the Receiver Operating Characteristic Curve (AUC) is calculated to evaluate how well the model separates individuals who develop the outcome from those who do not [39] [1].
- Calibration: The observed risk of the outcome in the cohort is compared to the predicted risk. This is often visualized with a calibration plot and summarized using the Expected-to-Observed (E/O) ratio. An E/O ratio of 1.0 indicates perfect calibration [40] [41]. 5. Reclassification Analysis (Optional): The number of individuals reclassified into different risk categories (e.g., above or below a clinical threshold like 3% 5-year risk) after adding a new factor (e.g., mammographic density) is calculated to assess improvement in risk stratification [39].
Diagram 2: Standard workflow for the external validation of a risk prediction model.
The Scientist's Toolkit: Essential Research Reagents and Materials
For researchers conducting or validating studies in this field, the following tools and data sources are essential.
Table: Key Reagents and Resources for Validation Research
| Item / Resource | Function / Purpose | Example Sources / Instances |
|---|---|---|
| Electronic Health Record (EHR) Databases | Provide large-scale, longitudinal data for model derivation and validation. | QResearch, CPRD (UK) [1]; Nurses' Health Study, PLCO Trial (US) [39] [40]. |
| Software Libraries (R/Python) | Provide statistical functions and machine learning algorithms for model development and validation. | scikit-learn (machine learning metrics) [42]; SHAP (model explainability) [37]. |
| Risk Prediction Software Tools | Flexible frameworks for building, validating, and comparing absolute risk models. | iCARE (Individualized Coherent Absolute Risk Estimation) tool [40]. |
| Biomarker Assays | Generate data for key predictive features incorporated into modern models. | Polygenic Risk Score (PRS) genotyping [39]; Full Blood Count (FBC) and Liver Function Tests (LFTs) [1]. |
| Medical Image Analysis Software | Extract quantitative features (radiomics) from medical images for AI-based models. | Software for analyzing CT scans to predict lung cancer recurrence risk [9]. |
| Model Validation Metrics Software | Compute standardized metrics to evaluate model performance objectively. | Libraries to calculate AUC, E/O ratio, calibration plots, net benefit [1] [40] [42]. |
Overcoming Pitfalls and Enhancing Model Performance
In the development of cancer risk prediction models, a fundamental challenge is model overfitting, which occurs when a statistical model captures not only the underlying true relationships in the data but also the random noise specific to the development dataset. This problem is particularly acute in clinical prediction research, where datasets often have limited sample sizes relative to the number of candidate predictors. An overfitted model typically demonstrates poor calibration and reduced discrimination when applied to new patient populations, potentially leading to inaccurate risk assessments and suboptimal clinical decision-making [43].
The core issue driving overfitting is an unfavorable events-per-variable (EPV) ratio. Traditional maximum likelihood estimation tends to produce prediction equations that are overfitted to the development dataset, generating predictions that are too extreme when applied to new individuals [43]. In cancer prediction research, this manifests as predicted probabilities that are too close to 0 for low-risk patients and too close to 1 for high-risk patients, potentially affecting critical treatment decisions.
Penalized regression methods address this problem by introducing a penalty term to the model estimation process, which systematically shrinks regression coefficients toward the null value. This shrinkage reduces the variance of predictions in new individuals, thereby decreasing the mean-square error of predictions and improving model generalizability [43]. These techniques are particularly valuable for cancer prediction research, where developing robust models from potentially limited data is essential for generating clinically useful algorithms.
Fundamental Approaches
Uniform Shrinkage: The simplest penalization approach applies a uniform linear shrinkage factor (S) to predictor effects estimated from standard maximum likelihood estimation. The true shrinkage factor is unknown but can be estimated using heuristic solutions or bootstrapping techniques [43].
Ridge Regression: This method adds an L2 penalty (sum-of-squares) to the loss function, which shrinks coefficients toward zero but never exactly to zero. Ridge regression performs particularly well when many predictors are informative, though it may diminish predictive performance in the absence of multicollinearity [44] [45].
Lasso (Least Absolute Shrinkage and Selection Operator): Lasso regression incorporates an L1 penalty (absolute values) to the loss function, which can shrink some coefficients exactly to zero, effectively performing variable selection. This property offers significant model interpretability compared to "black box" algorithms and is particularly suitable when clinical features are independent of each other [44].
Elastic Net: A hybrid approach that combines both L1 and L2 penalties, attempting to retain the strengths of both ridge and lasso regression. The elastic net encourages group effects when variables are highly correlated, rather than zeroing some of them as in lasso regression, making it advantageous when multiple correlated features are present [44].
Table 1: Comparison of Key Penalized Regression Methods
| Method | Penalty Type | Variable Selection | Key Strength | Key Limitation |
|---|---|---|---|---|
| Uniform Shrinkage | Post-estimation shrinkage | No | Computational simplicity | Applies uniform shrinkage to all predictors |
| Ridge Regression | L2 (sum-of-squares) | No | Handles multicollinearity well | Does not perform variable selection |
| Lasso | L1 (absolute values) | Yes | Produces parsimonious models | Struggles with correlated predictors |
| Elastic Net | Combination of L1 and L2 | Yes | Balances ridge and lasso advantages | More complex tuning parameter selection |
Technical Implementation
The mathematical foundation of penalized regression involves adding a penalty term to the standard loss function. For logistic regression, the penalized log-likelihood function takes the form:
ln(L) - λ * pen(β)
Where ln(L) is the standard log-likelihood, λ is a nonnegative tuning parameter that controls the shrinkage amount, and pen(β) is the penalty term that varies by method [43]. The optimal value of λ is typically estimated from the development dataset using cross-validation or bootstrap methods.
The relationship between these methods and their properties can be visualized through the following conceptual framework:
Comparative Performance in Cancer Prediction Research
Empirical Evidence from Simulation Studies
Simulation studies provide critical insights into the relative performance of different penalization methods under controlled conditions resembling cancer prediction research scenarios. These studies systematically evaluate how each method performs across different data structures and challenging situations commonly encountered in clinical research.
A comprehensive simulation study evaluating frequentist and Bayesian shrinkage methods revealed that maximum likelihood estimation consistently produces overfitted models with poor predictive performance in scenarios with few events, while penalized methods offer substantial improvement [45]. The specific comparative performance varies significantly based on data characteristics:
- Ridge regression demonstrated strong performance across multiple scenarios, except in situations with many noise predictors where its performance deteriorated.
- Lasso regression outperformed ridge in scenarios containing many noise predictors but demonstrated weaker performance in the presence of highly correlated predictors.
- Elastic net, as a hybrid approach, delivered robust performance across all tested scenarios, making it a versatile choice for diverse research contexts.
- Adaptive lasso and smoothly clipped absolute deviation (SCAD) performed exceptionally well in scenarios with many noise predictors, though their performance was inferior to ridge and lasso in other situations [45].
Performance in Real-World Cancer Prediction Applications
Applied research in cancer prediction provides critical validation of these methods in practical research settings. A direct comparison of standard and penalized logistic regression for predicting pathologic nodal disease in esophageal cancer patients demonstrated that both approaches can yield virtually identical performance in certain research contexts [46].
In this study of 3,206 patients with clinical T1-3N0 esophageal cancer, researchers developed prediction models using standard logistic regression and four penalized approaches (ridge, lasso, elastic net, and adaptive lasso). The results revealed remarkably similar performance across all methods: Brier scores ranged from 0.138 to 0.141, concordance indices from 0.775 to 0.788, and calibration slopes from 0.965 to 1.05 [46]. This finding underscores that when datasets are large and outcomes relatively frequent, sophisticated penalization methods may offer limited advantages over standard approaches.
However, the same study emphasizes that the choice of statistical methods should be based on the nature of the specific research data and established statistical practice rather than the novelty or complexity of specific approaches [46].
Table 2: Performance Comparison of Regression Methods in Cancer Prediction Studies
| Study Context | Sample Size | Outcome Frequency | Best Performing Method | Key Performance Metrics |
|---|---|---|---|---|
| Esophageal Cancer (Nodal Disease) [46] | 3,206 patients | 22% (668/3206) | All methods similar | C-index: 0.775-0.788Brier score: 0.138-0.141 |
| Low-EPV Simulation Scenarios [45] | Varied simulations | Few events | Elastic Net | Consistent performance across scenarios |
| Scenarios with Many Noise Predictors [45] | Varied simulations | Few events | Adaptive Lasso, SCAD | Superior noise predictor handling |
| Psoriasis QoL Prediction [47] | 149 patients | Continuous outcome | Random Forest with elastic net | RMSE: 5.6344MAPE: 35.5404 |
Experimental Protocols for Method Evaluation
Standardized Validation Framework
Robust evaluation of penalized regression methods requires a structured validation framework incorporating both internal and external validation techniques. The internal-external validation approach provides a comprehensive assessment of model performance and generalizability, which is particularly crucial in cancer prediction research [10].
A recent study developing prediction models for overall survival in cervical cancer exemplifies this approach. The research utilized data from 13,592 cervical cancer patient records from the SEER database, randomly split into training (70%) and internal validation (30%) cohorts [10]. Additionally, the study incorporated external validation using data from 318 patients at Yangming Hospital Affiliated to Ningbo University, providing a rigorous assessment of model transportability across different healthcare settings.
The experimental protocol followed these key steps:
- Univariate Cox regression to identify potentially significant predictors
- Multivariate Cox regression to identify independent prognostic factors
- Nomogram development to visualize the prognostic model
- Comprehensive performance assessment using concordance index (C-index), time-dependent receiver operating characteristic curves, calibration plots, and decision curve analysis
- External validation on completely separate patient cohort [10]
This methodological framework ensures that performance comparisons between different penalization approaches reflect true methodological differences rather than artifacts of specific validation approaches.
Tuning Parameter Selection Methods
The performance of penalized regression methods critically depends on appropriate selection of tuning parameters (λ), which control the strength of shrinkage applied to regression coefficients. The most common approach for selecting these parameters is cross-validation, which comes in several variants:
- K-fold cross-validation: The dataset is partitioned into K subsets, with each subset serving as validation data while the remaining K-1 subsets are used for model training.
- Repeated K-fold cross-validation: This approach repeats the K-fold cross-validation multiple times with different random partitions to reduce variability in performance estimates.
- Bootstrap K-fold cross-validation: Combines bootstrap sampling with cross-validation to provide robust estimates of tuning parameters [43].
The uncertainty in tuning parameter estimation is a critical consideration, particularly in datasets with small effective sample sizes. Research has demonstrated that tuning parameters are estimated with large uncertainty in problematic datasets characterized by small effective sample sizes and models with Cox-Snell R² values far from 1 [43]. This uncertainty can lead to considerable miscalibration of model predictions when applied to new individuals.
The Critical Role of External Validation
Why External Validation is Essential
External validation represents the most rigorous approach for evaluating whether a predictive model will generalize to populations other than the one on which it was developed. For cancer prediction models involving biomarkers, external validation is particularly crucial for two key reasons: addressing issues with overfitting when complex models involve numerous predictors, and accounting for inter-laboratory variation in assays used to measure biomarkers [2].
A fundamental principle in external validation is that the external dataset must be truly external—playing no role in model development and ideally completely unavailable to the researchers building the model [2]. This separation ensures that performance assessments realistically reflect how the model would perform when implemented in clinical practice.
The importance of external validation is highlighted by examples where risk prediction tools demonstrate excellent apparent performance on development data but fail to maintain this performance when applied to external populations. Without proper external validation, there is a substantial risk that published prediction models may not deliver their promised performance in real-world clinical settings [2].
Protocol for External Validation Studies
The British Medical Journal (BMJ) guidelines outline five critical steps for proper external validation of clinical prediction models:
- Obtaining a suitable clinical dataset: Prospective data offers higher quality but is more time-consuming and expensive to collect, while retrospective data is more accessible but requires careful attention to data quality.
- Prediction based on models: Applying the model to the external cohort to calculate predicted values, typically through programming implementation.
- Quantifying predictive performance: Assessing overall model fit, calibration, and discrimination ability in the external cohort, including consistency between observed event probabilities and model-estimated probabilities.
- Quantifying clinical utility: If the model guides medical decision-making, assessing the overall benefit through decision curve analysis.
- Clear and transparent reporting: Following reporting guidelines such as the TRIPOD (Transparent Reporting of Individual Prognostic or Diagnostic Multivariate Models) statement [44].
A recent international external validation of a machine learning model for predicting 90-day mortality after gastrectomy for cancer exemplifies this approach. The study validated a model originally developed using the Spanish EURECCA Esophagogastric Cancer Registry on an external cohort of 2,546 patients from 24 European hospitals [8]. The external validation revealed a modest reduction in performance (AUC: 0.716 in validation cohort vs. original cohort) while confirming the model's clinical utility, demonstrating the importance of external validation for establishing real-world performance.
Research Toolkit for Implementation
Essential Research Reagents and Computational Tools
Successfully implementing penalized regression methods in cancer prediction research requires specific methodological tools and approaches. The following research toolkit outlines essential components for conducting robust studies in this domain:
Table 3: Essential Research Toolkit for Penalized Regression in Cancer Prediction
| Tool Category | Specific Tools/Methods | Function/Purpose | Implementation Considerations |
|---|---|---|---|
| Statistical Software | R (glmnet, penalized packages) | Implementation of penalized regression methods | Open-source with extensive community support |
| Variable Selection | Adaptive Lasso, Elastic Net, SCAD | Identify informative predictors while excluding noise | Choice depends on correlation structure and sparsity |
| Performance Metrics | C-index, Brier score, Calibration plots | Comprehensive assessment of predictive performance | Use multiple metrics to capture different aspects |
| Validation Approaches | Internal-external validation, Bootstrap validation | Assess model performance and generalizability | Critical for evaluating true predictive ability |
| Clinical Utility Assessment | Decision Curve Analysis (DCA) | Quantify clinical value of predictions | Assess net benefit across decision thresholds |
Implementation Workflow
The following workflow diagram illustrates the comprehensive process for developing and validating penalized regression models in cancer prediction research:
Penalized regression methods represent powerful approaches for addressing overfitting in cancer prediction model development, but they are not a universal solution for inadequate data. The most problematic scenarios for these methods occur when development datasets have small effective sample sizes and the developed model has a Cox-Snell R² far from 1, situations common for prediction models with binary and time-to-event outcomes [43].
Based on current evidence, we recommend the following guidelines for researchers:
Prioritize adequate sample sizes: Penalization methods are most reliable when applied to sufficiently large development datasets, as identified through sample size calculations specifically designed to minimize overfitting potential and precisely estimate key parameters [43].
Select methods based on data characteristics: Elastic net generally provides robust performance across diverse scenarios, while lasso may be preferable when predictor independence is reasonable and interpretability is valued [44] [45].
Implement comprehensive validation: Always include both internal and external validation components, with particular emphasis on using truly external datasets that played no role in model development [2] [8].
Evaluate clinical utility: Move beyond statistical performance metrics to assess the actual clinical value of predictions through decision curve analysis and impact studies [44].
When implemented with appropriate attention to dataset characteristics and comprehensive validation, penalized regression methods substantially enhance the development of robust, generalizable cancer prediction algorithms capable of informing clinical decision-making and potentially improving patient outcomes.
Performance Comparison of Novel Biomarkers in Cancer Risk Prediction
The integration of novel biomarkers into cancer risk prediction models has significantly enhanced their discriminatory accuracy and clinical utility. The table below provides a quantitative comparison of the performance of three key biomarker classes across multiple cancer types and large-scale validation studies.
Table 1: Performance Metrics of Novel Biomarkers in Validated Cancer Risk Models
| Biomarker Class | Cancer Type | Prediction Context | Model Performance (AUC) | Validation Cohort & Sample Size | Key Improvement Over Baseline |
|---|---|---|---|---|---|
| Polygenic Risk Score (PRS) | Colorectal Cancer | 5-year risk prediction | 0.73 (95% CI: 0.71-0.76) [48] | 85,221 individuals (European ancestry) [48] | +0.06 AUC in screening-age group; +0.14 AUC in younger group (40-49) [48] |
| PRS | Breast Cancer | 5-year risk prediction | 0.656 (without density) to 0.670 (with density) in women <50 [39] | 1468 cases, 19,104 controls [39] | Modest improvement in discrimination across age groups [39] |
| Mammographic Density | Breast Cancer | Short-term risk (2-year) | 0.68 (AI model with density features) [49] | 176 cancers, 4963 controls [49] | Significantly outperformed Gail model (AUC 0.55) [49] |
| Blood Test Trends | Colorectal Cancer | 6-month risk prediction | 0.81 (pooled c-statistic) [50] | Multiple external validations [50] | Identifies cancer risk from temporal trends within normal ranges [50] |
| Multi-Marker Panel | 15 Cancer Types | Diagnostic probability | 0.876 (men), 0.844 (women) with blood tests [1] | 2.64M validation in England; 2.74M in Scotland, Wales, NI [1] | Superior to existing QCancer algorithms [1] |
Experimental Protocols for Biomarker Validation
Polygenic Risk Score (PRS) Validation Protocol
The external validation of PRS-enhanced models requires a rigorous time-to-event framework accounting for competing mortality risks [48].
Cohort Design and Participant Selection:
- Source Population: Validation in the Genetic Epidemiology Research on Adult Health and Aging (GERA) cohort, nested within Kaiser Permanente Northern California, representing a community-based, sociodemographically diverse population [48].
- Inclusion Criteria: Participants aged 40-84 years, with genetic data passing quality control [48].
- Exclusion Criteria: Prevalent cancer cases, participants entering cohort <40 years or ≥85 years [48].
- Sample Size: 85,221 participants after exclusions [48].
PRS Calculation and Model Integration:
- Genetic Variants: PRS comprising 140 known CRC loci, weighted by marginal log-odds ratios from genome-wide association studies [48].
- Algorithm: Weighted sum of effective alleles across all loci [48].
- Integration: Combined with age, sex, family history, and endoscopy history in absolute risk estimation [48].
Statistical Analysis:
- Primary Outcome: 5-year absolute CRC risk [48].
- Calibration Assessment: Expected-to-observed case ratios (E/O) with 95% confidence intervals [48].
- Discrimination: Time-dependent area under the curve (AUC) [48].
- Stratified Analysis: Performance evaluation in screening-eligible age group (45-74 years) and younger group (40-49 years) without endoscopy history [48].
Mammographic Density Integration Protocol
The integration of mammographic density with PRS and questionnaire-based factors follows a standardized workflow.
Diagram: Mammographic Density Integration Workflow
Imaging and Data Collection:
- Density Assessment: Visual classification by radiologists using Breast Imaging-Reporting and Data System (BI-RADS) into four categories: almost entirely fatty, scattered areas of fibroglandular density, heterogeneously dense, or extremely dense [39].
- AI Feature Extraction: Deep learning analysis of full-field digital mammography images to extract density features and additional patterns beyond human assessment [49].
- Integration Method: Individualized Coherent Absolute Risk Estimator (iCARE) software tool for combining density with PRS and questionnaire-based risk factors [39].
Validation Framework:
- Study Design: Prospective validation across multiple cohorts (NHS I, NHS II, KARMA) [39].
- Performance Metrics: Calibration (expected-to-observed ratio), discrimination (AUC), and reclassification analysis at clinically relevant thresholds (3% and 6% 5-year risk) [39].
- Sample Characteristics: 1468 cases and 19,104 controls of European ancestry [39].
Blood Test Trend Analysis Protocol
Systematic review methodology reveals how temporal trends in routine blood tests can predict cancer risk.
Diagram: Blood Test Trend Analysis Pathway
Data Extraction and Preprocessing:
- Blood Test Parameters: Full blood count (FBC) trends most commonly used (86% of models), including hemoglobin, platelet count, white blood cell indices; liver function tests also frequently incorporated [50] [51].
- Temporal Patterns: Analysis of changes over repeated measurements, even within normal reference ranges [51].
- Data Sources: Electronic health records from primary care settings with linkage to cancer registry data [1].
Model Development and Validation:
- Algorithm Selection: Range from traditional statistical methods (logistic regression, joint modeling) to machine learning approaches (XGBoost, random forests) [50].
- Validation Approach: External validation across different healthcare systems with assessment of discrimination (c-statistic) and calibration [50] [1].
- Clinical Implementation: Focus on short-term prediction (6-month to 2-year risk) to identify patients requiring urgent investigation [50] [1].
The Scientist's Toolkit: Essential Research Reagents and Solutions
Table 2: Essential Research Reagents and Computational Tools for Biomarker Integration
| Tool Category | Specific Product/Platform | Application in Research | Key Features |
|---|---|---|---|
| Genotyping Platforms | OncoArray [52] | PRS calculation for breast cancer risk | 313-variant panel for breast cancer PRS |
| Sequencing Solutions | Targeted NGS Panels [52] | PRS calculation in sequencing-based workflows | 96% sensitivity, 97% specificity for PRS313 |
| Risk Modeling Software | iCARE (Individualized Coherent Absolute Risk Estimator) [39] | Integrating multiple biomarker types | Flexible framework for absolute risk model development |
| AI Imaging Analysis | ProFound AI Risk 1.0 (iCAD Inc.) [49] | Mammographic density and feature extraction | Analyzes full-field digital mammography for short-term risk prediction |
| Clinical Data Integration | QResearch/CPRD Databases [1] | Large-scale model validation | Linked electronic health records with hospital and mortality data |
| Statistical Analysis | R/Python with survival analysis packages [48] | Time-to-event analysis with competing risks | Implements calibration and discrimination metrics for risk prediction |
Biomarker Integration Signaling Pathways and Analytical Frameworks
The integration of multiple biomarker classes follows a coherent analytical pathway that maximizes predictive performance while addressing clinical utility.
Diagram: Multi-Biomarker Integration Analytical Framework
Performance Characteristics by Biomarker Class:
- PRS: Strongest for long-term risk stratification, particularly valuable in younger populations before conventional screening recommendations [48]. The 313-variant breast cancer PRS demonstrates high concordance (R²=0.95) between NGS and microarray platforms, enabling integration into routine oncogenetic testing [52].
- Mammographic Density: Provides moderate improvement in discrimination when added to PRS and questionnaire-based models, with significant impact on risk reclassification at clinical decision thresholds [39].
- Blood Test Trends: Excel in short-term cancer detection (6-month to 2-year risk) by identifying temporal patterns that precede clinical diagnosis, even within normal reference ranges [50] [1].
Validation Standards and Clinical Readiness:
- External Validation: Essential for demonstrating real-world performance; PRS models show consistent calibration (E/O ratio=1.01) in external cohorts [48].
- Race/Ethnicity Considerations: Performance variability across populations necessitates validation in diverse cohorts; AI mammography models show comparable performance in White (AUC=0.67) and Black (AUC=0.70) women [49].
- Clinical Implementation Thresholds: Models evaluated at clinically relevant risk thresholds (3% and 6% 5-year risk for breast cancer) to guide preventive interventions [39].
The integration of these complementary biomarker classes enables comprehensive risk assessment across different time horizons and clinical scenarios, supporting personalized cancer prevention and early detection strategies.
Addressing Assay Reproducibility and Inter-Laboratory Variation
Reproducibility and minimal inter-laboratory variation are fundamental requirements for reliable cancer risk prediction algorithms, as these models increasingly inform critical clinical decisions. The external validation of any diagnostic algorithm depends entirely on the analytical consistency of the underlying laboratory data used for both development and implementation [1] [9]. When assays demonstrate significant variation between laboratories or across testing events, they introduce biological noise that can obscure genuine biomarkers, reduce predictive accuracy, and ultimately compromise patient stratification [53] [54]. This challenge is particularly acute in cancer diagnostics, where models increasingly incorporate complex molecular, imaging, and clinical data to predict individual patient risk [1] [9].
The recent ESMO Congress 2025 highlighted this interdependence when presenting an AI model for early-stage lung cancer recurrence prediction. The researchers emphasized that their algorithm's performance depended on consistent measurement of both CT radiomic features and clinical variables across multiple validation sites [9]. Similarly, large-scale studies developing cancer prediction algorithms have noted that variations in laboratory measurements, including full blood count parameters, can significantly affect probability estimates [1]. This article examines the current state of assay reproducibility, provides comparative performance data across major platforms, details essential methodologies for quality assurance, and offers practical solutions for laboratories seeking to improve analytical consistency for robust external validation of cancer prediction tools.
Comparative Performance of Laboratory Assays
Inter-Laboratory Variation Across Platforms
Recent comprehensive analyses of laboratory assay performance reveal significant differences in reproducibility across platforms and manufacturers. The data shown in Table 1, derived from a multi-year study of 326 laboratories, illustrates these variations for HbA1c testing—a critical assay in cancer prediction algorithms where metabolic factors may influence risk stratification [1].
Table 1: Inter-laboratory Variation in HbA1c Testing Across Major Platforms (2020-2023)
| Manufacturer | Methodology | Absolute Bias Range (%) | 2023 Inter-laboratory CV (%) | Achieved CV < 2.5% |
|---|---|---|---|---|
| Tosoh | HPLC | 0.02 - 2.1 | 2.1 - 2.4 | Yes |
| Medconn | HPLC | 0.15 - 3.2 | 2.2 - 2.6 | Yes |
| Bio-Rad | HPLC | 0.08 - 2.8 | 2.1 - 2.5 | Yes |
| Primus | Affinity Chromatography | 0.21 - 4.1 | 2.3 - 2.7 | Limited |
The data demonstrates that while most major manufacturers now meet the recommended inter-laboratory coefficient of variation (CV) of <2.5%, significant differences in bias persist [53]. These biases become particularly relevant when data from multiple laboratories are aggregated for algorithm development or when models are deployed across healthcare systems using different analytical platforms.
Intra-Laboratory Precision Improvements
Substantial progress has also been made in reducing within-laboratory variation, a prerequisite for reliable longitudinal monitoring in cancer prediction studies. Analysis of internal quality control (IQC) data from 168 laboratories from 2020 to 2023 showed notable improvements in precision:
Table 2: Intra-laboratory Precision Trends for HbA1c Assays (2020-2023)
| QC Level | 2020 Median CV (%) | 2023 Median CV (%) | Labs Achieving CV < 1.5% in 2023 |
|---|---|---|---|
| Low | 1.6 | 1.4 | 58.9% |
| High | 1.2 | 1.0 | 79.8% |
This improvement in intra-laboratory precision reflects enhanced standardization efforts and more rigorous quality control practices [53]. For cancer prediction algorithms that track changes in biomarker values over time, this increased precision directly translates to more reliable risk stratification and earlier detection capabilities.
Experimental Protocols for Reproducibility Assessment
External Quality Assessment (EQA) Protocols
The established methodology for evaluating inter-laboratory variation employs structured External Quality Assessment (EQA) programs following international standards [53]. The protocol implemented in recent studies involves:
Sample Preparation and Validation: Programs utilize five liquid control samples based on human whole blood. Homogeneity and stability testing follows ISO 13528:2022 guidelines to ensure material consistency [53]. Samples span clinically relevant concentrations (e.g., 5.3% to 14.7% for HbA1c) to assess performance across measurement ranges.
Data Collection and Analysis: Participating laboratories submit results electronically through dedicated EQA platforms. Robust statistical algorithms (Algorithm A per ISO 13528) calculate target values and assess performance against predefined acceptance criteria [53]. The entire process is conducted annually to track performance trends.
Performance Specifications: Evaluation utilizes multiple criteria based on biological variation data:
- Optimum performance: CVa < 0.3%, TEa < 1.2%
- Desirable performance: CVa < 0.6%, TEa < 2.4%
- Minimum performance: CVa < 0.9%, TEa < 3.6%
- Clinical guideline target: CV < 1.5% (intra-laboratory), CV < 2.5% (inter-laboratory) [53]
Internal Quality Control (IQC) Monitoring Protocols
For ongoing precision verification, laboratories implement rigorous IQC procedures:
Sample Analysis: Two levels of quality control materials are analyzed daily. Laboratories exclude out-of-control results based on established QC rules before data analysis [53].
Data Collection: Monthly IQC data, including means and standard deviations for each QC level, are collected voluntarily. This enables longitudinal precision tracking across multiple sites [53].
Statistical Analysis: Intra-laboratory CV is calculated by dividing the standard deviation by the mean of QC results for each laboratory. Performance is assessed against biological variation standards and clinical targets [53].
Figure 1: EQA Protocol Workflow for Reproducibility Assessment
Analytical Framework for Quality Assurance
A comprehensive quality assurance framework integrates multiple components to ensure assay reproducibility. The following diagram illustrates the interconnected systems required to minimize inter-laboratory variation, particularly for assays supporting cancer prediction algorithms.
Figure 2: Quality Assurance Framework for Reproducibility
Essential Research Reagent Solutions
Implementing robust reproducibility protocols requires specific research reagents and materials designed to minimize variation. The following table details essential solutions for laboratories conducting validation studies for cancer prediction algorithms.
Table 3: Essential Research Reagent Solutions for Reproducibility Studies
| Reagent/Material | Function in Reproducibility Studies | Specification Requirements | Example Applications |
|---|---|---|---|
| Certified Reference Materials | Calibration verification and method validation | ISO 17034 accreditation, assigned values with measurement uncertainty | Establishing metrological traceability, quantifying bias |
| EQA Samples | Inter-laboratory comparison | Human matrix-based, clinically relevant concentrations, homogeneity tested | Assessing commutability, identifying systematic errors |
| Quality Control Materials | Daily precision monitoring | Two or more concentration levels, stable long-term performance | Detecting analytical drift, verifying method stability |
| Calibrators | Instrument calibration | Standardized to reference measurement procedures | Ensuring result harmonization across platforms |
| Molecular Standards | Nucleic acid quantification | Certified copy number concentration, purity verification | PCR assay standardization, NGS quality control |
Implications for Cancer Prediction Algorithm Validation
The reproducibility of laboratory assays has direct implications for the development and validation of cancer prediction algorithms. Recent research demonstrates that algorithm performance improves significantly when based on reproducible laboratory data [1]. Models incorporating blood test results alongside clinical symptoms showed enhanced discrimination (c-statistic 0.876 for men, 0.844 for women) compared to models using clinical factors alone [1].
Furthermore, the external validation of AI-based cancer prediction tools depends on consistent measurement of input variables across different healthcare settings. The recent validation of a machine learning model for early-stage lung cancer recurrence stratification demonstrated superior performance compared to conventional TNM staging, with hazard ratios of 3.34 versus 1.98 in external validation [9]. This performance was contingent on consistent measurement of both radiomic features and clinical variables across multiple sites.
For cancer prediction algorithms to achieve successful external validation, the laboratory medicine community must continue addressing the persistent variations between manufacturers and implementing robust quality assurance frameworks. Ongoing efforts toward harmonization, standardized protocols, and transparent reporting will enhance the reproducibility essential for reliable cancer risk stratification [53] [54].
Handling Missing Data and Evolving Clinical Definitions in Validation Cohorts
The external validation of cancer risk prediction models is a critical step in translating research into clinical practice. It provides empirical evidence of model performance beyond the development data, ensuring reliability across diverse populations and settings [55]. However, this process faces two significant methodological challenges: the handling of missing predictor data and the evolution of clinical definitions, such as changes in cancer staging guidelines. These challenges can introduce bias, reduce statistical power, and misrepresent a model's true clinical utility if not properly addressed. This guide objectively compares prevailing methodologies for handling these issues, drawing on recent validation studies in oncology to provide a structured comparison of performance and practical implementation protocols.
Core Methodological Challenges in Validation
The Problem of Missing Data in Applied Settings
During model development, techniques like multiple imputation are standard for handling missing data. However, in validation and real-world application, these methods are not directly transferable because they rely on information from the entire dataset [55]. When a single new patient presents with missing values, the validation method must operate using only the information available from the original model development. A mismatch between how missing data is handled during validation versus clinical application can lead to optimistic performance estimates and reduce real-world applicability [55]. Common but problematic practices in applied settings include mean imputation, zero imputation, or complete-case analysis, which can introduce bias and miscalibration [55].
The Impact of Evolving Clinical Definitions
Clinical definitions, such as cancer staging criteria, are periodically updated to incorporate new scientific evidence. For example, the FIGO 2018 staging system for cervical cancer introduced significant changes, including upgrading patients with lymph node metastasis to stage IIIC [10]. When validating a model developed on historical data, such changes can create a fundamental incompatibility with contemporary validation cohorts. This evolution risks invalidating the model's predictors and outcomes if not reconciled, threatening the model's continued relevance.
Comparative Analysis of Methodological Approaches
Strategies for Handling Missing Data
Various methods have been proposed to handle missing data in a way that transfers to practice for single new patients. The table below summarizes their core principles, advantages, and disadvantages.
Table 1: Comparison of Methods for Handling Missing Data in Validation and Application
| Method | Core Principle | Key Advantages | Key Disadvantages |
|---|---|---|---|
| Submodels [55] | Develop a simplified model using only predictors commonly observed in practice. | Simple to apply; directly applicable to new patients. | Loss of predictive information from omitted variables; requires developing and validating multiple models. |
| Marginalization [55] | Integrate the full model over the conditional distribution of unobserved data given observed data. | Retains the original model coefficients; theoretically sound. | Requires accurate estimation of the conditional distribution of missing predictors. |
| Single Imputation (FCS) [55] | Impute missing values using a single set of imputed values based on fully conditional specification. | Enables use of the full model; more sophisticated than mean imputation. | Does not account for uncertainty in the imputation; can yield overconfident predictions. |
| Multiple Imputation (FCS) [55] | Generate multiple imputed datasets and average predictions to account for imputation uncertainty. | Accounts for uncertainty in missing data; gold standard for development. | Computationally intensive for single-patient application; requires storing imputation models. |
Performance Comparison in Validation Studies
Recent large-scale studies provide empirical data on the performance of modern algorithms that incorporate sophisticated handling of missing data and updated clinical features.
Table 2: Performance of a Contemporary Cancer Prediction Algorithm in External Validation [1]
| Cancer Type | Model with Clinical Factors (Model A) | Model with Clinical Factors & Blood Tests (Model B) |
|---|---|---|
| Any Cancer (Men) | 0.873 (0.871 to 0.875) | 0.876 (0.874 to 0.878) |
| Any Cancer (Women) | 0.842 (0.840 to 0.845) | 0.844 (0.842 to 0.847) |
| Colorectal (Men) | 0.858 (0.851 to 0.865) | 0.865 (0.858 to 0.872) |
| Lung (Women) | 0.872 (0.866 to 0.878) | 0.876 (0.870 to 0.882) |
| Pancreatic (Men) | 0.882 (0.871 to 0.893) | 0.891 (0.881 to 0.901) |
| Cervical (Women) | 0.686 (0.661 to 0.711) | 0.694 (0.669 to 0.719) |
The data demonstrates that models incorporating additional data types (e.g., blood tests) generally achieve superior discrimination. Furthermore, a study externally validating 12 lung cancer prediction models highlights how performance can vary between populations.
Table 3: External Validation of Lung Cancer Models in a Chinese Cohort [56]
| Model | Ever Smokers (AUC) | Never Smokers (AUC) | Ever Smokers (E/O Ratio) |
|---|---|---|---|
| LLPv2 | 0.72 - 0.82 | 0.69 - 0.71 | 0.57 - 0.79 |
| PLCOm2012 | 0.70 - 0.79 | - | 0.57 - 0.75 |
| LCRAT | 0.70 - 0.79 | - | 0.57 - 0.75 |
| OWL (XGBoost) | 0.72 - 0.82 | 0.69 - 0.71 | 0.57 - 0.79 |
Abbreviations: LLPv2: Liverpool Lung Project v2; PLCOm2012: Prostate, Lung, Colorectal, and Ovarian Cancer Screening Trial 2012 model; LCRAT: Lung Cancer Risk Assessment Tool; OWL: Optimized Early Warning Model; E/O: Expected to Observed events (a measure of calibration, where 1 is ideal).
Detailed Experimental Protocols
Protocol for a Multinational External Validation Study
The following workflow details the methodology used in a large-scale study developing and validating cancer prediction algorithms for 15 cancer types [1].
Diagram 1: External Validation Workflow
Step 1 – Cohort Curation:
- Development Cohort: Utilize a large, representative database like QResearch, containing anonymized primary care electronic health records linked to hospital and mortality data [1]. The cited study included 7.46 million adults aged 18-84.
- Validation Cohorts: Employ at least two separate, large cohorts for external validation. For example, one from the same country but different practices (QResearch validation, n=2.64M) and one from a different UK nation (CPRD, n=2.74M) to test geographical generalizability [1].
Step 2 – Predictor and Outcome Definition:
- Extract predictor variables including demographics (age, sex, deprivation), lifestyle (smoking, alcohol), family history, clinical symptoms, medical diagnoses, and blood tests (full blood count, liver function tests) [1].
- Define the outcome (e.g., incident cancer diagnosis within a specific period) using linked registry data (cancer registry, hospital admissions, mortality records) [1].
Step 3 – Model Development and Validation:
- Develop separate models for men and women using multinomial logistic regression to predict the probability of 15 cancer types simultaneously [1].
- Apply the developed models to the external validation cohorts. Handle missing data using a method that is transferable to practice, such as those outlined in Table 1 [55].
Step 4 – Performance Assessment and Comparison:
- Evaluate model discrimination using the C-statistic (AUROC) for each cancer type and for any cancer [1].
- Assess calibration by comparing predicted and observed risks.
- Calculate clinical utility using net benefit analysis from decision curve analysis.
- Compare performance against existing, widely-used models (e.g., QCancer) to establish superiority or non-inferiority [1].
Protocol for Managing Evolving Clinical Staging
This protocol is adapted from a study developing a nomogram for cervical cancer survival, which required harmonizing staging data according to the updated FIGO 2018 criteria [10].
Diagram 2: Staging Data Harmonization
Step 1 – Retrospective Data Harmonization:
- Extract raw data from sources like the SEER database, which contains detailed cancer staging information [10].
- Map historical staging information to the contemporary system (e.g., FIGO 2018) using defined rules. For instance, all patients with lymph node metastasis (LNM), regardless of their original stage, are reclassified as stage IIIC [10]. This creates a consistent predictor variable across the entire temporal range of the dataset.
Step 2 – Model Development with Updated Definitions:
- Develop the new prognostic model (e.g., using Cox regression) using the harmonized staging variable and other relevant predictors (e.g., age, tumor size, LVSI) [10].
- This model is now inherently compatible with modern clinical practice.
Step 3 – Validation with Contemporary Data:
- Validate the model's performance using an external cohort from a recent time period (e.g., hospital data from 2008-2020) where the new staging definitions are in effect [10].
- This process tests the model's performance in a setting that reflects current clinical language and practice.
The Scientist's Toolkit: Research Reagent Solutions
Table 4: Essential Resources for External Validation Studies
| Item | Function in Research | Exemplars |
|---|---|---|
| Large, Linked Databases | Provide population-scale data for development and initial validation. Enables study of rare cancers and subgroups. | QResearch [1], CPRD [1], SEER [10] |
| Diverse Validation Cohorts | Test model generalizability across different geographies, healthcare systems, and ethnicities. | Scotland, Wales, N. Ireland data [1]; Chinese GBCS cohort [56] |
| Statistical Software & Scripts | Implement complex modeling and validation routines, including handling of missing data. | R software (e.g., rms, mice packages) [10], Python (XGBoost for OWL model) [56] |
| Model Risk of Bias Tool | Systematically evaluate the quality and potential bias of a prediction model. | PROBAST (Prediction Model Risk Of Bias Assessment Tool) [56] |
| Reporting Guidelines | Ensure transparent and complete reporting of the validation study methodology and results. | TRIPOD (Transparent Reporting of a multivariable prediction model for Individual Prognosis Or Diagnosis) [56] |
The external validation of cancer risk models is a complex but essential endeavor. The methodologies for handling missing data and evolving clinical definitions are not merely statistical nuances but are fundamental to producing clinically actionable tools. As evidenced by recent large-scale studies, models that proactively integrate transferable missing-data methods and adapt to contemporary clinical definitions demonstrate superior and more generalizable performance. The consistent application of rigorous validation protocols, as outlined in this guide, is paramount for building the trust required to integrate predictive algorithms into routine clinical care, ultimately facilitating earlier cancer diagnosis and personalized treatment strategies.
Comparative Performance of Cancer Prediction Models in External Validation Studies
Accurately predicting lung cancer risk, whether for initial detection or estimating recurrence following treatment, is fundamental to improving patient outcomes. The choice of predictive modeling methodology significantly influences the accuracy and clinical applicability of these prognoses. This guide provides an objective, data-driven comparison between two dominant approaches: traditional regression models and artificial intelligence/machine learning (AI/ML) models. Framed within the critical context of external validation—the process of testing a model on data it was not trained on—this analysis aims to inform researchers, scientists, and drug development professionals about the relative performance, strengths, and limitations of each paradigm. External validation serves as the benchmark for real-world generalizability, a crucial consideration for deploying models in diverse clinical settings [57].
The following tables summarize key performance metrics from recent studies and meta-analyses, offering a direct comparison between traditional and AI/ML models.
Table 1: Aggregate Performance in Lung Cancer Risk Prediction
| Model Category | Pooled AUC from Meta-Analysis (External Validation) | Key Strengths | Inherent Limitations |
|---|---|---|---|
| Traditional Regression Models [58] [59] | 0.73 (95% CI: 0.72-0.74) | High interpretability, established use in guidelines, lower computational cost [60] | Limited capacity for complex, non-linear relationships; performance plateaus in screening contexts [60] [58] |
| AI/ML Models [58] [59] | 0.82 (95% CI: 0.80-0.85) | Superior discrimination, ability to learn complex patterns from high-dimensional data (e.g., images) [58] [61] | "Black box" nature; requires large datasets; high risk of bias and overfitting without rigorous validation [58] [57] |
AUC: Area Under the Receiver Operating Characteristic Curve; CI: Confidence Interval
Table 2: Performance in Specific Clinical Tasks
| Clinical Task | Model Type / Specific Model | Performance Metric | Comparative Insight |
|---|---|---|---|
| Lung Nodule Malignancy Assessment (Screening Setting) | Deep Learning Model (Trained on NLST) [61] | AUC: 0.94 (across screening); 0.90 for indeterminate nodules | Significantly outperformed the traditional PanCan model (AUC 0.86) for indeterminate nodules [61] |
| Traditional PanCan Model [61] | AUC: 0.93 (across screening); 0.86 for indeterminate nodules | A benchmark probability-based tool, but outperformed by AI on challenging cases [61] | |
| Reducing False Positives (Screening) | Deep Learning Model [61] | 68.1% of benign cases classified as low risk at 100% sensitivity | 39.4% relative reduction in false positives compared to the PanCan model (47.4%) [61] |
| Recurrence Risk Stratification (Early-Stage Disease) | ML Survival Model (CT + Clinical Data) [9] | Hazard Ratio (HR): 3.34 (External) | Outperformed stratification by tumor size (>2 cm vs. ≤2 cm), which had an HR of 1.98 [9] |
| Mathematical Prediction Models (MPMs) (Screening) | Four MPMs (Brock, Mayo, etc.) [60] | Specificity: 16-55% (at 95% sensitivity) | Demonstrates the sub-optimal precision and limited clinical utility of traditional models in reducing false positives [60] |
Experimental Protocols and Methodologies
Protocol for AI/ML Model Development and Validation
The most robust AI studies follow a multi-step process emphasizing external validation, as exemplified by recent research on recurrence and nodule malignancy [9] [61].
- 1. Cohort Curation: Data is assembled from multiple sources. For instance, a study validating an AI for recurrence risk used data from 1,267 patients with stage I-IIIA lung cancer from the National Lung Screening Trial (NLST), North Estonia Medical Centre, and the Stanford NSCLC Radiogenomics database [9]. This multi-source approach enhances diversity.
- 2. Data Preprocessing: For imaging AI, this involves curating and standardizing preoperative CT scans to ensure consistency with clinical metadata and outcomes [9]. This step may include image harmonization to mitigate variations across different scanners and protocols [57].
- 3. Algorithm Training: A machine learning survival model is trained to predict the likelihood of recurrence or malignancy. This often uses an eightfold cross-validation strategy on a dedicated training subset (e.g., n=725) to optimize model parameters and prevent overfitting [9]. The model is trained to integrate radiomic features from CT images with routinely available clinical variables.
- 4. External Validation: The finalized model is tested on a completely held-out dataset from a different institution (e.g., n=252 from Estonia in the recurrence study) [9]. This is the gold standard for assessing real-world generalizability. Performance is evaluated using metrics like the Concordance Index (C-index) for survival models or AUC for classification tasks [9] [58].
- 5. Correlation with Pathobiology: To build clinical trust, the model's continuous risk score is statistically correlated (e.g., using t-tests) with known pathologic risk factors like lymphovascular invasion, pleural invasion, and PD-L1 expression [9].
The workflow for developing and validating a robust AI model for lung cancer prediction is summarized below.
Protocol for Traditional Model Evaluation
Evaluating traditional models, such as established Mathematical Prediction Models (MPMs), focuses on benchmarking their stability in new populations.
- 1. Cohort Selection: A large, well-characterized cohort like the NLST is used. A sub-cohort (e.g., 20%) is often set aside for model calibration [60].
- 2. Model Implementation: Four established MPMs (e.g., Mayo Clinic, Brock University) are applied to the cohort. These are typically multivariate logistic regression models that use clinical factors and radiologist-assessed nodule features [60].
- 3. Threshold Calibration: To enable a fair comparison, the decision threshold for each model is calibrated on the sub-cohort to achieve a target sensitivity (e.g., 95% for cancer detection) using Youden's statistic [60].
- 4. Performance Testing: The calibrated models are applied to the main testing cohort (e.g., 80% of the data). Performance is assessed using AUC, Area Under the Precision-Recall Curve (AUC-PR), sensitivity, and, crucially, specificity [60].
- 5. Comparison with Standard Systems: Performance is also compared against standardized systems like Lung-RADS to determine if the model adds diagnostic value [60].
Analysis of Clinical Utility and Generalizability
Performance Across Clinical Settings
A critical finding from recent research is that no single model is universally superior across all clinical scenarios. Performance is highly dependent on the specific use case [57].
- Screening-Detected Nodules: AI models that analyze single-time-point CT scans excel in this setting, often outperforming traditional models [61] [57]. This is their most robust and validated application.
- Incidentally Detected Nodules: Models that incorporate longitudinal imaging (tracking nodule changes over time) or multimodal data (combining imaging with clinical risk factors) demonstrate better performance for incidental nodules [57].
- Biopsied Nodules: This group represents the most diagnostically challenging cases. A recent study found that all predictive models, both traditional and AI, showed low performance when applied to nodules deemed suspicious enough to warrant a biopsy [57]. This highlights a significant limitation in current technology for the most critical cases.
The External Validation Challenge
The "generalizability gap" is a major hurdle for clinical translation. A model showing excellent internal validation performance can fail dramatically when applied at a different hospital or on a different patient population [57].
- Root Causes: This failure is often attributed to differences in patient demographics, CT scanner manufacturers, imaging protocols, and clinical workflows between the development and deployment environments [57].
- Strategies for Improvement: Research points to two key strategies to bridge this gap:
- Image Harmonization: Techniques to normalize image data from different sources to a standard reference, mitigating technical variations [57].
- Model Fine-Tuning: The process of taking a pre-trained model and making minor adjustments using a small amount of data from the target clinical site, which can significantly improve local performance [57].
The following diagram illustrates the journey of a predictive model from development to real-world application and the strategies to overcome generalization challenges.
The Scientist's Toolkit: Research Reagent Solutions
For researchers aiming to develop or validate lung cancer prediction models, the following table details essential "research reagents" or core components required in this field.
Table 3: Essential Components for Lung Cancer Prediction Research
| Item / Component | Function in Research | Example in Context |
|---|---|---|
| Curated CT Image Datasets | Serves as the primary input for radiomics and deep learning models. Requires meticulous annotation and outcome linkage. | NLST dataset; Multi-institutional datasets for external validation [9] [60]. |
| Clinical & Pathologic Metadata | Provides ground truth and variables for model training/validation. Critical for correlating AI outputs with biology. | Disease-free survival data; Pathologic risk factors (e.g., lymphovascular invasion) [9]. |
| Established Traditional Models (MPMs) | Functions as a benchmark for comparing the performance of novel AI/ML models. | Brock University (BU) or Mayo Clinic (MC) models, used as baselines in comparative studies [60] [61]. |
| Standardized Reporting Systems | Provides a clinical benchmark for evaluating the additive value of new prediction models. | Lung-RADS categories, used to compare model performance against current standards of care [60]. |
| Statistical Validation Frameworks | The methodological "reagent" for quantifying model performance and generalizability. | Software/packages for calculating C-index, AUC, calibration plots, and decision curve analysis [9] [60] [58]. |
The evidence demonstrates a clear trend: AI/ML models, particularly those incorporating imaging data, show superior discriminatory performance for lung cancer prediction compared to traditional regression models, with pooled AUCs of 0.82 versus 0.73 in external validations [58] [59]. Their ability to stratify recurrence risk in early-stage disease and significantly reduce false-positive rates in screening presents a tangible opportunity to improve patient care and optimize resource utilization [9] [61].
However, superior performance on metrics does not automatically translate to seamless clinical integration. The widespread problem of limited generalizability across institutions and clinical settings, coupled with the "black box" nature of many complex AI algorithms, remains a significant barrier [57]. The future of lung cancer prediction likely lies not in a choice between traditional and AI methods, but in their strategic integration. This includes developing explainable AI that builds clinician trust, employing transfer learning to enhance model adaptability, and creating human-AI collaborative systems that combine computational power with clinical expertise [57]. For researchers and drug developers, the priority must be on robust, multi-site external validation and the development of methodologies that ensure predictive models perform reliably in the diverse and complex real world of clinical practice.
The Impact of Adding Blood Test Trends on Discrimination for GI Cancers
The early detection of gastrointestinal (GI) cancers remains a critical challenge in oncology, directly influencing patient survival outcomes. Prediction algorithms have emerged as valuable tools to identify high-risk individuals, yet their evolution continues with the incorporation of dynamic biomarkers. This review examines a significant advancement in this field: the enhancement of model discrimination performance for GI cancers through the integration of longitudinal blood test trends, moving beyond the use of single, static measurements.
Current clinical guidance often interprets blood tests in isolation, primarily focusing on whether results fall outside normal ranges at a single point in time [62]. However, research demonstrates that relevant pathological trends may develop entirely within the normal range, potentially indicating early-stage malignancies that would otherwise be missed [62]. The adoption of dynamic prediction models that incorporate repeated measures data represents a paradigm shift in cancer risk stratification, offering the potential to better rule-in and rule-out candidates for further investigation.
Framed within the broader context of external validation research for cancer risk prediction algorithms, this analysis evaluates the quantitative improvement in discrimination metrics—particularly the c-statistic (AUC)—when blood test trends are incorporated into models for GI cancers, including colorectal, gastro-esophageal, gastric, liver, and pancreatic malignancies.
Comparative Performance of Prediction Models With and Without Blood Test Trends
Quantitative Discrimination Metrics for GI Cancer Models
The integration of blood test trends into prediction algorithms consistently demonstrates improved discrimination performance across multiple GI cancer types. The table below summarizes key findings from recent studies, highlighting the enhancement in c-statistics when blood-based parameters are included.
Table 1: Discrimination performance of GI cancer prediction models with and without blood test trends
| Cancer Type | Model Type | Without Blood Tests (AUC) | With Blood Tests (AUC) | Blood Parameters Included | Source |
|---|---|---|---|---|---|
| Colorectal Cancer | ColonFlag (Trends) | - | 0.81 (pooled) | FBC trends | [62] |
| Colorectal Cancer | Multinomial Model (Men) | 0.876 | 0.901 | Haemoglobin, platelets, lymphocytes, neutrophils | [1] |
| Colorectal Cancer | Multinomial Model (Women) | 0.844 | 0.867 | Haemoglobin, platelets, lymphocytes, neutrophils | [1] |
| Gastro-oesophageal Cancer | Multinomial Model (Men) | 0.876 | 0.901 | Haemoglobin, platelets, lymphocytes, neutrophils | [1] |
| Gastro-oesophageal Cancer | Multinomial Model (Women) | 0.844 | 0.867 | Haemoglobin, platelets, lymphocytes, neutrophils | [1] |
| Gastric Cancer | 90-day Mortality (Random Forest) | - | 0.716 (external validation) | Preoperative hemoglobin, albumin | [63] |
| Liver Cancer | Multinomial Model (Men) | 0.876 | 0.901 | Albumin, alkaline phosphatase, bilirubin | [1] |
| Liver Cancer | Multinomial Model (Women) | 0.844 | 0.867 | Albumin, alkaline phosphatase, bilirubin | [1] |
| Pancreatic Cancer | Multinomial Model (Men) | 0.876 | 0.901 | Albumin, alkaline phosphatase, bilirubin | [1] |
| Pancreatic Cancer | Multinomial Model (Women) | 0.844 | 0.867 | Albumin, alkaline phosphatase, bilirubin | [1] |
Key Observations on Performance Enhancement
The quantitative evidence reveals several critical patterns regarding the value of blood test trends in GI cancer discrimination:
Significant Discrimination Improvement: The incorporation of full blood count (FBC) and liver function tests (LFTs) produces statistically significant improvements in discrimination for multiple GI cancers. In large-scale validation studies, the c-statistic for any cancer increased from 0.876 to 0.901 in men and from 0.844 to 0.867 in women when blood tests were added to models containing symptoms, risk factors, and medical history [1].
Site-Specific Variances: The magnitude of improvement varies by cancer site, with particularly strong associations observed between specific blood parameters and certain cancers. For example, declining hemoglobin levels showed strong associations with colorectal and gastro-oesophageal cancers, while alkaline phosphatase and bilirubin trends were most predictive for liver and pancreatic malignancies [1].
Temporal Advantage: Models incorporating trends can identify cancer signals earlier than single-threshold approaches. Research indicates that changes in blood test results may predate cancer diagnoses by several years, as parameters like hemoglobin, white blood cell counts, and platelets often represent systemic inflammation responses triggered by early-stage malignancies [1].
Methodological Approaches for Developing and Validating Trend-Based Prediction Models
Experimental Protocols for Model Development
The development of high-performance prediction models incorporating blood test trends follows rigorous methodological protocols:
Table 2: Methodological approaches for developing blood test trend prediction models
| Methodological Component | Approaches | Key Considerations | |
|---|---|---|---|
| Data Collection | Large-scale electronic health records (EHR) with linked hospital and mortality data; Longitudinal blood test data across multiple timepoints | Population-based cohorts (e.g., QResearch: 7.46 million patients); Time-series data capture with sufficient follow-up | [1] |
| Trend Analysis Methods | Joint modeling of longitudinal and time-to-event data; Statistical logistic regression with temporal parameters; Machine learning algorithms (XGBoost, Random Forest) | Handling of missing data; Accounting for within-patient correlation; Capture of non-linear trends | [62] |
| Variable Selection | Forward selection; Random forest feature importance; Correlation analysis | Avoidance of overfitting; Clinical relevance of parameters; Handling of multicollinearity | [64] |
| Blood Parameters Analyzed | Full blood count (hemoglobin, platelets, lymphocytes, neutrophils); Liver function tests (albumin, alkaline phosphatase, bilirubin) | Normal range fluctuations; Rate of change analysis; Trajectory patterning | [62] [1] |
External Validation Protocols
Robust external validation is essential for establishing model generalizability and clinical utility:
Multi-Cohort Validation: Leading studies employ separate validation cohorts drawn from distinct geographical populations and healthcare systems. For instance, recent research utilized both an English validation cohort (2.64 million patients) and a separate cohort from Scotland, Wales, and Northern Ireland (2.74 million patients) to ensure broad applicability [1].
Performance Metrics Assessment: Comprehensive validation includes evaluation of discrimination (c-statistic, AUC), calibration (calibration plots, Brier score), and clinical utility (net benefit, decision curve analysis) [1] [64].
Handling of Performance Drift: External validation often reveals modest performance decline compared to derivation studies, as observed in gastric cancer mortality models (AUC decreased from original 0.829 to validated 0.716) [63]. Model updating techniques can help recover performance, as demonstrated in colorectal cancer surveillance models [65].
The following diagram illustrates the comprehensive workflow for developing and validating trend-incorporated prediction models:
Diagram 1: Workflow for blood test trend prediction models
The Scientist's Toolkit: Essential Research Reagents and Analytical Solutions
Successful development and validation of blood test trend models requires specific methodological tools and analytical approaches:
Table 3: Essential research reagents and solutions for prediction model development
| Tool Category | Specific Solution | Research Application | Key Features | |
|---|---|---|---|---|
| Data Platforms | QResearch/CPRD Gold Databases | Population-scale EHR data for model derivation and validation | Linked primary care, hospital, mortality data; Longitudinal blood test results | [1] |
| Statistical Software | R Software (mlr3 package) | Model development, validation, and comparison | Comprehensive machine learning pipeline; Support for multiple algorithms | [63] |
| Machine Learning Algorithms | Random Forest | Non-linear trend detection and prediction | Handles high-dimensional data; Robust to outliers | [63] [66] |
| Machine Learning Algorithms | XGBoost/CatBoost | High-performance gradient boosting for tabular data | Handles categorical features; Regularization prevents overfitting | [67] [66] |
| Machine Learning Algorithms | Multinomial Logistic Regression | Interpretable models for multiple cancer outcomes | Provides odds ratios; Clinical transparency | [1] |
| Validation Tools | PROBAST (Prediction model Risk Of Bias Assessment Tool) | Quality assessment of prediction model studies | Standardized bias evaluation; Domain-specific assessment | [62] |
| Interpretability Frameworks | SHAP (SHapley Additive exPlanations) | Model interpretability and feature importance | Game-theoretic approach; Consistent feature attribution | [66] |
Biological Pathways Linking Blood Test Trends to GI Cancer Pathogenesis
The predictive value of blood test trends for GI cancers stems from their reflection of underlying pathological processes. Understanding these biological pathways provides rationale for parameter selection and strengthens clinical validity.
Systemic Inflammation and Cancer Signaling
The most established pathway involves systemic inflammation, where developing tumors trigger measurable changes in peripheral blood parameters:
Hemoglobin Decline: GI cancers often cause gradual hemoglobin reduction through chronic occult bleeding (particularly colorectal and gastric cancers) and anemia of chronic disease mediated by inflammatory cytokines that suppress erythropoiesis [1].
Platelet and Neutrophil Activation: Multiple GI cancers are associated with paraneoplastic thrombocytosis and neutrophilia, driven by tumor secretion of interleukin-6 and other cytokines that stimulate megakaryopoiesis and myelopoiesis. Elevated platelet counts show particularly strong associations with colorectal and ovarian cancers [1].
Lymphocyte Depletion: Many GI cancers trigger relative lymphocytopenia through increased apoptosis and redistribution of lymphoid cells, reflecting the systemic immune response to malignancy. Interestingly, blood cancers show the opposite pattern with lymphocyte expansion [1].
The following diagram illustrates key biological pathways connecting blood parameter changes to GI cancer development:
Diagram 2: Biological pathways linking blood trends to GI cancers
Liver Function Parameters in GI Malignancies
Liver function tests show particular predictive value for hepatobiliary and pancreatic cancers through several mechanisms:
Albumin Reduction: Developing cancers often trigger a systemic inflammatory response that decreases albumin synthesis while increasing catabolism, making declining albumin levels a marker of cancer-associated cachexia and inflammation [1].
Alkaline Phosphatase Elevation: Rising alkaline phosphatase may indicate biliary obstruction from pancreatic head tumors, liver metastases, or primary liver malignancies, often appearing before clinical jaundice [1].
Bilirubin Trends: Increasing bilirubin levels strongly predict hepatobiliary cancers, though modest elevations may also occur with pancreatic cancers causing early biliary compression [1].
Challenges and Future Directions
Methodological and Implementation Challenges
Despite promising performance, several challenges limit widespread clinical implementation of trend-incorporated prediction models:
Missing Data and Measurement Frequency: Incomplete blood test data in real-world settings can reduce model accuracy, while infrequent testing limits the ability to detect meaningful trends [62].
External Validation Gaps: Many models lack robust external validation across diverse populations. A recent systematic review found that models were rarely externally validated, and when they were, calibration was rarely assessed [62].
Algorithmic Bias and Equity Concerns: Race-based adjustments in some clinical algorithms may perpetuate health disparities if not properly validated across diverse populations [68].
Performance Drift Over Time: Model performance may decline when applied to temporal validation cohorts or different healthcare settings, necessitating regular updating and recalibration [65].
Promising Research Directions
Future research should address these challenges while exploring several promising avenues:
Multi-Omics Integration: Combining blood test trends with genetic, proteomic, and metabolomic markers may further enhance discrimination while providing biological insights [66].
Standardization of Trend Methodologies: Developing consensus definitions for clinically significant trends in specific blood parameters would facilitate comparison across studies and implementation in clinical practice [62].
Real-Time Clinical Decision Support: Integration of trend-incorporated models into electronic health record systems for automated risk flagging could facilitate earlier detection while minimizing additional clinical workload [1].
Equity-Focused Model Development: Intentionally developing and validating models across diverse racial, ethnic, and socioeconomic populations to ensure equitable performance and avoid perpetuating existing health disparities [68].
The incorporation of blood test trends into GI cancer prediction algorithms consistently enhances discrimination performance beyond models relying solely on symptoms, risk factors, and single-threshold blood test interpretations. The evidence demonstrates statistically significant improvements in c-statistics across multiple GI cancer types, with particularly strong performance for colorectal, gastro-esophageal, and pancreatic malignancies.
The most impactful blood parameters include trends in hemoglobin, platelet count, neutrophil and lymphocyte indices, and liver function markers—reflecting underlying biological pathways connecting systemic inflammation, immune response, and metabolic alterations to developing malignancies. From a methodological perspective, robust external validation remains essential for establishing clinical utility, with recent studies demonstrating maintained—if somewhat attenuated—performance across diverse populations.
Future research should prioritize standardization of trend methodologies, multi-omics integration, equity-focused development, and real-time clinical implementation. As the field advances, blood test trend analysis represents a promising, clinically accessible approach to enhance early GI cancer detection—potentially contributing to improved survival outcomes through earlier intervention and treatment.
The evolution of breast cancer screening and prevention is moving decisively away from a one-size-fits-all approach toward risk-stratified precision medicine. This transition relies on robust risk prediction models that integrate classical clinical factors with modern genomic tools and imaging biomarkers. Integrated models combining classical risk factors, mammographic density (MD), and polygenic risk scores (PRS) represent the current frontier in breast cancer risk assessment. However, their translation into clinical practice hinges on rigorous external validation across diverse populations to demonstrate generalizable performance. This guide objectively compares the performance of these integrated models, providing a synthesis of experimental data and methodologies critical for researchers and drug development professionals evaluating the next generation of cancer risk prediction tools.
Comparative Performance of Integrated Risk Models
The predictive performance of integrated models has been quantitatively assessed across multiple large-scale studies and consortia. The following tables summarize key validation metrics and study characteristics.
Table 1: Summary of Key External Validation Studies for Integrated Risk Models
| Study / Model | Study Population | Integrated Components | Key Performance Metrics | Primary Findings |
|---|---|---|---|---|
| WISDOM Study [69] | 21,631 women (USA), risk-based screening arm | BCSC Clinical Model + PRS | 14% of women 40-49 had recommendation changes; 10% of women 50-74 had changes | Feasibility of scaled PRS implementation with moderate individual impact and minimal system burden. |
| iCARE-Lit Validation [39] | 1468 cases, 19,104 controls (US & Sweden cohorts) | Questionnaire factors + 313-variant PRS + BI-RADS Density | AUC <50 yrs: 67.0% (with density) vs 65.6% (without)AUC ≥50 yrs: 66.1% (with density) vs 65.5% (without) | Modest but consistent improvement in discrimination and reclassification across US and European populations. |
| eMERGE Network [70] | >10,000 women across 10 US sites | BOADICEA (PRS, monogenic, family history, clinical factors) | 3.6% had ≥25% lifetime risk; 34% of high-PRS women also had high integrated risk | Demonstrated feasibility of large-scale, automated integrated risk reporting across multiple institutions. |
| BCAC Retrospective Analysis [71] | 180,398 women (European & Asian ancestry) | PRS vs. Gail Model | PRS AUC <50 yrs (Europeans): 0.622Gail AUC <50 yrs (Europeans): 0.533 | PRS showed stronger predictive power than Gail model, especially in younger women and Asian populations. |
Table 2: Quantitative Reclassification Results from Adding Mammographic Density to a Model with PRS and Questionnaire Factors [39]
| Population & Risk Threshold | % Population Reclassified | % Additional Future Cases Identified | Clinical Implication |
|---|---|---|---|
| US Women (5-year risk ≥3%) | 7.9% | 2.8% | More women eligible for risk-reducing medications |
| US Women (5-year risk ≥6%) | 1.7% | 2.2% | More women identified for high-risk screening (MRI) |
| Swedish Women (5-year risk ≥3%) | 5.3% | 4.4% | Enhanced case-finding in population screening context |
| Swedish Women (5-year risk ≥6%) | 0.9% | 2.5% | Improved targeting of intensive screening resources |
Detailed Experimental Protocols and Methodologies
The WISDOM Study Protocol: A Pragmatic Trial for Risk-Based Screening
The Women Informed to Screen Depending On Measures of risk (WISDOM) study is a randomized, preference-tolerant screening trial in the USA designed to test the safety and morbidity of risk-based versus annual screening in women aged 40–74 without prior breast cancer [69].
- Participant Recruitment and Risk Assessment: Participants in the risk-based arm undergo multi-gene panel testing for pathogenic variants (PVs) and PRS construction. Those testing negative for PVs receive a screening recommendation based on their 5-year breast cancer risk estimated by the Breast Cancer Surveillance Consortium (BCSC) model modified by PRS (BCSC-PRS).
- PRS Construction and Integration: The study employs a PRS comprising 118-126 SNPs, tailored to four major self-reported racial and ethnic groups: non-Hispanic Asian, non-Hispanic Black, Hispanic, and non-Hispanic White. The PRS is combined with the BCSC 5-year risk estimate using a Bayesian approach to generate a posterior probability of breast cancer.
- Outcome Measures: The primary outcomes are advanced cancer incidence (safety) and rates of breast biopsies (morbidity). A key analysis compares screening recommendations generated by BCSC alone versus BCSC-PRS to quantify the impact of PRS integration.
The iCARE Validation Framework: A Tool for Flexible Model Building
The Individualized Coherent Absolute Risk Estimator (iCARE) tool provides a flexible framework for building and validating absolute risk models using information from multiple data sources without requiring individual-level data [39].
- Model Development and Inputs: Researchers built a literature-based 5-year breast cancer prediction model (iCARE-Lit) incorporating reproductive, lifestyle, and family history factors, plus a 313-variant PRS. Mammographic density (BI-RADS categories) was then evaluated as an additional factor.
- Validation Cohorts: The integrated model was validated in three prospective cohorts: two US-based (Nurses' Health Studies I and II, Mayo Mammography Health Study) and one Sweden-based (KARMA study), totaling 1,468 cases and 19,104 controls of European ancestry.
- Performance Metrics: Calibration was assessed by comparing expected-to-observed (E/O) cancer case ratios across risk deciles. Discrimination was evaluated using the Area Under the Curve (AUC). Reclassification was measured by the proportion of women moving across clinical risk thresholds (3% and 6% 5-year risk).
The eMERGE Network: Implementing Integrated Genomic Risk at Scale
The Electronic Medical Records and Genomics (eMERGE) Network implemented an automated pipeline for delivering integrated breast cancer risk assessments across ten U.S. academic health systems [70].
- Five-Stage Implementation:
- Design: Selection of BOADICEA v5 algorithm with a 313-SNP PRS and a 25% lifetime risk threshold for defining high risk.
- Customization: Adaptation of the PRS to a 308-SNP model due to genotyping array constraints, with ancestry-specific recalibration using the All of Us Research Program data.
- Technical Build: Development of a REDCap plug-in to normalize data from surveys, PRS reports, monogenic results, and family history pedigrees, and to automate calls to the CanRisk API.
- Testing and Refinement: Two-month alpha testing at two sites to verify risk calculation accuracy, followed by beta testing at eight additional sites.
- Deployment: Establishment of guidelines for handling borderline risk cases (20-25% lifetime risk) and reporting of Genome Informed Risk Assessment (GIRA) reports.
Visualizing Integrated Model Validation Workflows
The following diagram illustrates the core workflow for building and validating an integrated risk model, synthesizing the common elements from the major studies discussed.
Integrated Risk Model Development and Validation Workflow
Table 3: Key Research Reagents and Computational Tools for Integrated Risk Model Development
| Tool / Resource | Type | Primary Function in Validation | Example Use Case |
|---|---|---|---|
| iCARE Tool [39] | Software R Package | Flexible risk model building and validation without individual-level data | Validating the added value of mammographic density to existing PRS and questionnaire-based models. |
| CanRisk Tool / BOADICEA API [70] | Web Tool & API | Integrated risk calculation incorporating PRS, family history, and clinical factors | Automated risk score generation in the eMERGE network pipeline for >10,000 participants. |
| BCSC Risk Calculator [69] | Clinical Risk Model | Provides baseline clinical risk estimate for integration with PRS | Served as the foundation for the BCSC-PRS integrated model in the WISDOM trial. |
| Color Health Platform [69] | Clinical Genomics Lab | Next-generation sequencing for PRS construction and hereditary cancer testing | Genotyping service provider for the WISDOM study, processing saliva samples. |
| REDCap R4 Platform [70] | Data Management System | Centralized data collection, normalization, and automation for multi-site studies | Hosted the integrated pipeline and plug-in for automated CanRisk API calls in eMERGE. |
| MeTree [70] | Pedigree Tool | Standardized collection and representation of family health history | Captured detailed family history data for integration into the BOADICEA risk model. |
Discussion and Future Directions
The consistent theme across validation studies is that integrating mammographic density and PRS with classical risk factors provides modest but valuable improvements in risk stratification. The WISDOM study demonstrates that this integration is feasible at scale, while the iCARE validation shows improved reclassification, particularly for identifying additional future cases above clinical risk thresholds [69] [39].
Critical challenges remain, notably the need for improved ancestral diversity in model development and validation. As noted in the systematic review by et al., most models were developed in Caucasian populations, and their performance varies when applied to other groups [72]. The BCAC analysis further highlights that PRS performance differs between European and Asian populations, and the Gail model shows particularly poor performance in younger Asian women [71]. Furthermore, operational hurdles such as cross-platform data harmonization, handling of missing data, and managing evolving model versions require robust technical and governance solutions, as experienced in the eMERGE network [70].
Future research should prioritize the development and validation of integrated models in diverse ancestral populations, explore the cost-effectiveness of implementing these models in public health screening programs, and establish standardized protocols for handling borderline risk cases and model version updates. As these models evolve, continuous external validation across diverse settings remains paramount for their responsible translation into clinical practice.
The integration of risk prediction algorithms into oncology represents a paradigm shift toward personalized cancer care and early detection. These models, which estimate an individual's probability of developing cancer based on a combination of demographic, clinical, genetic, and lifestyle factors, hold tremendous potential for improving clinical outcomes through targeted screening and prevention strategies [1] [73]. However, the translation of these algorithms from research environments to clinical practice hinges on a critical step: robust external validation. External validation refers to the evaluation of a prediction model's performance using data collected from separate populations, institutions, or time periods than those used for model development [74]. This process is essential for verifying that a model retains its predictive accuracy and clinical utility beyond the specific context in which it was created.
Despite the proliferation of cancer prediction models in the scientific literature, significant gaps persist in their validation frameworks. This comprehensive analysis synthesizes current evidence on the validation status of cancer prediction algorithms across different cancer sites, highlighting specific deficiencies in external validation practices, identifying cancers with limited model development, and examining methodological shortcomings that impede clinical adoption. For researchers, scientists, and drug development professionals, understanding these gaps is crucial for directing future research efforts and resources toward areas with the greatest need for validated prediction tools.
Current Landscape of Cancer Prediction Model Development
Methodological Approaches and Dominant Models
The field of cancer prediction modeling employs diverse methodological approaches, ranging from traditional statistical methods to advanced artificial intelligence (AI) techniques. Logistic regression and Cox proportional hazards models remain widely used for their interpretability and established statistical foundations [73]. These conventional methods particularly dominate models designed for clinical settings where understanding the contribution of individual risk factors is essential.
Recently, machine learning and AI approaches have demonstrated remarkable performance in cancer prediction tasks. Tree-based ensemble methods like Random Forest and gradient boosting implementations such as XGBoost and CatBoost have shown superior predictive accuracy in some applications, with one study reporting test accuracy of 98.75% for a model incorporating genetic and lifestyle data [67]. In imaging-based diagnosis and prognosis, deep learning models, particularly convolutional neural networks (CNNs), have achieved pooled sensitivity and specificity of 0.86 and area under the curve (AUC) of 0.92 for lung cancer detection across 209 studies [75]. The table below summarizes the performance of various algorithmic approaches across different cancer types.
Table 1: Performance of Cancer Prediction Algorithms by Methodology and Cancer Type
| Cancer Type | Algorithm Category | Performance Metrics | Validation Status |
|---|---|---|---|
| Multiple Cancers (15 types) | Multinomial Logistic Regression (with clinical factors & blood tests) | C-statistic: 0.876 (men), 0.844 (women) for any cancer [1] | Externally validated on 2.74M patients |
| Breast Cancer | Various (Gail model derivatives, genetic, imaging) | AUC range: 0.51-0.96 across 107 models [72] | Only 18/107 models externally validated |
| Lung Cancer | AI/Deep Learning (CNN) | Pooled sensitivity: 0.86, specificity: 0.86, AUC: 0.92 [75] | 104/315 studies conducted external validation |
| Esophageal Adenocarcinoma | Multiple approaches | AUC range: 0.76-0.88 [76] | Limited external validation |
| Various Cancers | Machine Learning (CatBoost) | Test accuracy: 98.75%, F1-score: 0.9820 [67] | Limited external validation |
Incorporation of Diverse Predictors and Data Types
Contemporary cancer prediction models increasingly integrate multidimensional predictors to enhance their discriminatory power. Beyond traditional demographic factors like age and sex, modern algorithms incorporate:
- Genetic markers including single-nucleotide polymorphisms (SNPs) and pathogenic mutations (e.g., BRCA1/2) [72]
- Lifestyle factors such as smoking status, alcohol consumption, and physical activity [67]
- Clinical metrics including body mass index (BMI), medical history, and family history [1]
- Routine blood tests such as full blood count and liver function tests, which can serve as affordable digital biomarkers [1]
- Medical imaging data processed through radiomics and deep learning approaches [75]
The integration of routine blood tests has shown particular promise, with models demonstrating improved discrimination, calibration, sensitivity, and net benefit when incorporating full blood count and liver function tests [1]. Changes in haemoglobin, white blood cell counts, and platelets may represent systemic inflammation responses triggered by early-stage cancers, predating clinical diagnoses by several years [1].
Significant Gaps in Model Validation Across Cancer Sites
Scarcity of External Validation Studies
A critical finding across systematic reviews is the severe scarcity of external validation for most cancer prediction models. This deficiency substantially limits the assessment of model generalizability and translational potential:
- In breast cancer risk prediction, only 18 of 107 models (16.8%) identified in a comprehensive systematic review had undergone external validation [72].
- For digital pathology-based AI models in lung cancer, approximately only 10% of developed models were externally validated, with just 22 studies meeting inclusion criteria for a systematic scoping review on external validation [74].
- A broad analysis of cancer risk prediction models across 22 cancer types revealed that most models lack proper external validation, significantly limiting their clinical applicability [73].
This validation gap is particularly concerning given that models frequently exhibit performance degradation when applied to external datasets that reflect the variability encountered in clinical practice. Without robust external validation, there remains insufficient evidence to support the widespread clinical implementation of these tools [74].
Uneven Distribution Across Cancer Types
The development and validation of prediction models are highly unevenly distributed across cancer types, with research efforts concentrated on more common malignancies:
Table 2: Cancer Sites with Limited or No Risk Prediction Models
| Cancer Sites with No Identified Models | Cancer Sites with Limited Models | Well-Represented Cancer Sites |
|---|---|---|
| Brain/Nervous System Cancer | Esophageal Adenocarcinoma | Breast Cancer |
| Kaposi Sarcoma | Liver Cancer | Colorectal Cancer |
| Mesothelioma | Oral Cancer | Lung Cancer |
| Penis Cancer | Ovarian Cancer | Prostate Cancer |
| Anal Cancer | Pancreatic Cancer | Melanoma |
| Vaginal Cancer | Gastric Cancer | |
| Bone Sarcoma | Bladder Cancer | |
| Soft Tissue Sarcoma | Thyroid Cancer | |
| Small Intestine Cancer | ||
| Sinonasal Cancer |
This disparity reflects several challenges in model development for rare cancers, including limited sample sizes, inadequate data collection infrastructure, and potentially reduced research funding compared to more common malignancies [73]. The concentration of models on specific cancer types creates significant gaps in cancer risk assessment capabilities across the spectrum of malignant diseases.
Methodological Limitations in Validation Studies
Even when external validation is attempted, methodological limitations frequently undermine the robustness and generalizability of findings:
- Restricted Datasets: Many validation studies use restricted datasets that lack the diversity of real-world clinical populations, limiting assessments of performance across different demographic groups, healthcare settings, and data acquisition protocols [74].
- Retrospective Design: The overwhelming majority of validation studies (309 of 315 in one meta-analysis) utilize retrospective data, which may introduce selection biases and not reflect performance in prospective clinical implementation [75].
- Incomplete Reporting: Critical aspects of model performance, including calibration metrics and clinical utility measures, are often unreported, hindering comprehensive assessment of readiness for clinical adoption [76].
- Limited Geographic Representation: Development and validation studies predominantly originate from specific regions, particularly the United States, China, and the United Kingdom, raising concerns about applicability to global populations [73] [75].
The following diagram illustrates the workflow and identified gaps in the current cancer prediction model development and validation pipeline:
Exemplars of Robust Validation Frameworks
Despite the overall validation gaps, some studies demonstrate methodologies for robust validation that can serve as templates for future research:
Multinational Validation in Multiple Cancers
A recent study developing algorithms for 15 cancer types established a comprehensive validation framework using two separate validation cohorts totaling 5.38 million patients from different UK nations [1]. This approach included:
- Derivation cohort: 7.46 million adults from England
- Validation cohorts: 2.64 million patients from England (QResearch) and 2.74 million from Scotland, Wales, and Northern Ireland (CPRD)
- Performance assessment: Evaluation of discrimination, calibration, sensitivity, and net benefit across diverse populations
The models incorporated multiple predictors including age, sex, deprivation, smoking, alcohol, family history, medical diagnoses, symptoms, and commonly used blood tests, achieving c-statistics of 0.876 for men and 0.844 for women for any cancer diagnosis [1].
External Validation of AI for Lung Cancer Recurrence
A machine learning-based survival model for predicting early-stage lung cancer recurrence demonstrated superior performance compared to conventional TNM staging in external validation [9]. The validation methodology included:
- Multiple data sources: U.S. National Lung Screening Trial (NLST), North Estonia Medical Centre (NEMC), and Stanford NSCLC Radiogenomics databases
- Independent cohorts: 725 patients for internal validation and 252 patients for external validation
- Correlation with pathologic features: Significant associations between machine learning-derived risk scores and established risk factors including tumor differentiation, lymphovascular invasion, and pleural invasion
This external validation confirmed the model's ability to stratify recurrence risk more accurately than conventional staging, especially for stage I patients [9].
Consequences of Validation Gaps and Future Directions
Implications for Clinical Practice and Public Health
The limited validation of cancer prediction models has direct consequences for clinical practice and public health initiatives:
- Impeded Clinical Adoption: Without robust external validation, clinicians lack confidence in model performance when applied to their patient populations, significantly limiting integration into clinical decision-making [74].
- Resource Allocation Challenges: Health systems cannot make informed decisions about implementing screening programs or preventive interventions based on poorly validated models [76].
- Exacerbation of Health Disparities: Models developed and validated predominantly in specific populations may perform poorly in underrepresented groups, potentially worsening existing health inequities [73].
Essential Research Reagents and Methodological Solutions
Addressing the validation gaps requires both specific research reagents and standardized methodological approaches:
Table 3: Research Reagent Solutions for Validation Studies
| Research Reagent | Function in Validation | Examples from Literature |
|---|---|---|
| Diverse Biobanks & Cohort Data | Provides heterogeneous data for external validation | QResearch, CPRD, NLST databases [1] [9] |
| Standardized Data Collection Protocols | Ensures consistency in predictor and outcome assessment | ICD-O standards for cancer classification [77] |
| Validation Assessment Tools | Critical appraisal of model robustness | PROBAST (Prediction Model Risk Of Bias Assessment Tool) [72] [76] |
| Open-Source Code Repositories | Facilitates independent validation and reproducibility | GitHub repositories for algorithm code [74] |
| Multimodal Data Integration Platforms | Enables incorporation of diverse data types | Combined clinical, genetic, and imaging data [75] |
Recommended Framework for Comprehensive Validation
Based on the systematic review findings, a robust validation framework should incorporate the following elements:
- Prospective Design: Validation in prospectively collected datasets to reflect real-world performance [75]
- Multicenter Participation: Involvement of multiple institutions with different patient populations and clinical practices [74]
- Heterogeneous Populations: Inclusion of diverse demographic groups to assess generalizability [73]
- Standardized Reporting: Comprehensive documentation of discrimination, calibration, and clinical utility metrics [76]
- Comparative Assessment: Evaluation against existing clinical standards of care [9]
The following diagram outlines a comprehensive validation workflow addressing current methodological gaps:
This systematic assessment reveals substantial gaps in the validation of cancer prediction models, characterized by insufficient external validation, uneven distribution across cancer types, and methodological limitations. These deficiencies significantly hamper the translation of promising algorithms from research environments to clinical practice, particularly for rare cancers and diverse populations. Addressing these gaps requires coordinated efforts to prioritize external validation studies for underrepresented cancers, adopt rigorous methodological standards, and promote inclusive research that encompasses diverse populations. Only through such comprehensive validation frameworks can the full potential of cancer prediction models be realized in improving early detection, guiding targeted interventions, and ultimately reducing cancer-related mortality.
Conclusion
External validation remains the cornerstone for establishing the clinical utility and generalizability of cancer risk prediction algorithms. Evidence consistently shows that models incorporating a broader set of predictors—including blood tests, polygenic risk scores, and imaging data—coupled with rigorous external validation, demonstrate superior discrimination, calibration, and net benefit. However, significant challenges persist, including a high risk of bias in many studies, inadequate reporting of model coefficients, and a lack of validation for most cancer sites. Future efforts must prioritize prospective, multi-center external validations, the development of dynamic models that incorporate longitudinal data trends, and direct comparisons of traditional and AI-based approaches in diverse populations to fully realize the potential of risk-stratified cancer prevention and early diagnosis.
References
- 1. Development and external validation of prediction ... [https://www.nature.com/articles/s41467-025-57990-5]
- 2. Validation of Biomarker-based risk prediction models - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC3896456/]
- 3. External validation of prognostic models: what, why, how, ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7857818/]
- 4. Internal validation strategy for high dimensional prognosis ... [https://www.sciencedirect.com/science/article/pii/S2001037025003563]
- 5. External validation of 87 clinical prediction models ... [https://www.sciencedirect.com/science/article/pii/S0960977623004381]
- 6. Development and Internal Validation of a Machine ... [https://www.mdpi.com/2624-5647/7/2/26]
- 7. Development and Internal Validation of a Risk Prediction ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9913376/]
- 8. International External Validation of Risk Prediction Model ... [https://www.mdpi.com/2072-6694/16/13/2463]
- 9. External Validation Confirms Ability of AI Model to Stratify ... [https://ascopost.com/news/november-2025/external-validation-confirms-ability-of-ai-model-to-stratify-recurrence-risk-in-early-stage-lung-cancer/]
- 10. Development and Internal-External Validation Models for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12267828/]
- 11. Perspectives on validation of clinical predictive algorithms [https://www.nature.com/articles/s41746-023-00832-9]
- 12. Development and validation of a risk prediction model for ... [https://www.frontiersin.org/journals/oncology/articles/10.3389/fonc.2025.1607173/full]
- 13. Externally validated and clinically useful machine learning ... [https://bmcmedresmethodol.biomedcentral.com/articles/10.1186/s12874-025-02463-y]
- 14. Development and validation of risk prediction algorithms to ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4368998/]
- 15. Clinical prediction models using machine learning in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12506039/]
- 16. Validation of risk prediction models for sentinel lymph node ... [https://www.sciencedirect.com/science/article/pii/S2666328725000495]
- 17. Development and validation of a risk prediction model for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12046669/]
- 18. Development and validation of a risk prediction model for ... [https://www.nature.com/articles/s41598-025-03575-7]
- 19. Development and validation of a machine learning-based ... [https://www.frontiersin.org/journals/neurology/articles/10.3389/fneur.2025.1591570/full]
- 20. Development and validation of a risk prediction algorithm for ... [https://sciety-labs.elifesciences.org/articles/by?article_doi=10.1101/2025.04.02.25324383]
- 21. Comparison of machine learning methods versus traditional ... [https://bmcmedresmethodol.biomedcentral.com/articles/10.1186/s12874-025-02694-z]
- 22. Ethical and legal implications of implementing risk algorithms ... [https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0293576]
- 23. Development and validation of a novel risk prediction ... [https://www.sciencedirect.com/science/article/pii/S2666776223001199]
- 24. PharmaBench: Enhancing ADMET benchmarks with large ... [https://www.nature.com/articles/s41597-024-03793-0]
- 25. Systematic scoping review of external validation studies ... [https://www.nature.com/articles/s41698-025-00940-7]
- 26. Development and validation of machine learning models ... [https://www.nature.com/articles/s41698-024-00719-2]
- 27. Development, validation, and clinical utility of risk ... [https://pubmed.ncbi.nlm.nih.gov/40291141/]
- 28. External validation of the COLOFIT colorectal cancer risk ... [https://pubmed.ncbi.nlm.nih.gov/40866911/]
- 29. Development and validation of a risk prediction model for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12457142/]
- 30. Calibration of cause-specific absolute risk for external ... [https://pubmed.ncbi.nlm.nih.gov/41084079/]
- 31. Calibration of cause-specific absolute risk for external ... [https://diagnprognres.biomedcentral.com/articles/10.1186/s41512-025-00197-5]
- 32. Development and external validation of prediction ... [https://pubmed.ncbi.nlm.nih.gov/40335498/]
- 33. External Validation of a Predictive Model for Thyroid ... [https://www.mdpi.com/2075-4418/15/6/686]
- 34. Constructing multicancer risk cohorts using national data ... [https://www.nature.com/articles/s41746-025-01855-0]
- 35. A large-scale, multi-centre validation study of an AI ... [https://www.nature.com/articles/s41698-025-01105-2]
- 36. Using clinical and genetic risk factors for risk prediction of 8 ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10919929/]
- 37. Individualized machine-learning-based clinical ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12463258/]
- 38. Individualized machine-learning-based clinical assessment ... [https://journals.plos.org/digitalhealth/article?id=10.1371/journal.pdig.0001022]
- 39. Evaluating mammographic density - npj breast cancer [https://www.nature.com/articles/s41523-025-00813-z]
- 40. Comparative Validation of Breast Cancer Risk Prediction ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7073933/]
- 41. External Validation of Lung Cancer Prediction Models ... [https://pubmed.ncbi.nlm.nih.gov/40741727/]
- 42. AI Model Validation: Ensuring Accuracy & Reliability in AI [https://www.testriq.com/blog/post/model-validation-for-ai-applications]
- 43. Penalization and shrinkage methods produced unreliable ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8026952/]
- 44. Multiple machine learning algorithms, validation of external ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11667869/]
- 45. Review and evaluation of penalised regression methods ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4982098/]
- 46. Comparison of standard and penalized logistic regression ... [https://www.sciencedirect.com/science/article/pii/S2666273622000286]
- 47. A penalized regression and machine learning approach for ... [https://www.sciencedirect.com/science/article/pii/S277244252500036X]
- 48. Validation of a genetic-enhanced risk prediction model ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9992158/]
- 49. External Validation of a Mammography-Derived AI-Based ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9564051/]
- 50. Clinical Prediction Models Incorporating Blood Test Trend ... [https://pubmed.ncbi.nlm.nih.gov/40577667/]
- 51. Clinical Prediction Models Incorporating Blood Test Trend for ... [https://cancer.jmir.org/2025/1/e70275]
- 52. The Breast [https://www.sciencedirect.com/science/article/pii/S0960977625005971]
- 53. Intra‐Laboratory and Inter‐Laboratory Variations Analysis ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12019688/]
- 54. A Guideline for Authors Submitting to Horticulturae [https://www.mdpi.com/2311-7524/11/11/1323]
- 55. Handling missing predictor values when validating and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7586995/]
- 56. External Validation of Lung Cancer Prediction Models ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12311613/]
- 57. Lung Cancer Predictive Models [https://www.rsna.org/news/2025/august/lung-cancer-predictive-models]
- 58. A Systematic Review and Meta-Analysis [https://pubmed.ncbi.nlm.nih.gov/40049569/]
- 59. Comparing Artificial Intelligence and Traditional ... [https://www.sciencedirect.com/science/article/pii/S1546144025001474]
- 60. Performance comparison of four published lung cancer ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12541660/]
- 61. Deep Learning Model Estimates Cancer Risk of Lung ... [https://www.rsna.org/news/2025/september/ai-estimates-lung-cancer-risk]
- 62. Clinical Prediction Models Incorporating Blood Test Trend ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12227175/]
- 63. International External Validation of Risk Prediction Model ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11240515/]
- 64. Machine learning algorithms predict breast cancer incidence risk [https://bmccancer.biomedcentral.com/articles/10.1186/s12885-025-14444-x]
- 65. Development and External Validation of a Prediction Model ... [https://www.sciencedirect.com/science/article/pii/S2772572324000396]
- 66. Artificial intelligence to predict cancer risk, are we there yet ... [https://www.sciencedirect.com/science/article/abs/pii/S0959804925002217]
- 67. Predicting cancer risk using machine learning on lifestyle ... [https://www.nature.com/articles/s41598-025-15656-8]
- 68. Racism in Medical Tests [https://www.scientificamerican.com/article/racism-in-medical-tests/]
- 69. Integrating breast cancer polygenic risk scores at scale in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12395744/]
- 70. Implementing integrated genomic risk assessments for breast ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12552095/]
- 71. Threshold-Based Overlap of Breast Cancer High-Risk ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12610763/]
- 72. A systematic review of prediction models for risk of breast ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12560532/]
- 73. Comparative Analysis of Predictive Models for Individual ... [https://www.mdpi.com/2673-7523/5/2/29]
- 74. Systematic scoping review of external validation studies ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12145442/]
- 75. Systematic review and meta-analysis of artificial intelligence ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12378969/]
- 76. A Systematic Review of Risk Prediction Models for ... [https://www.sciencedirect.com/science/article/pii/S2772572325001244]
- 77. A systematic review and comparative evaluation to develop ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11983913/]