Explainable AI in Clinical Decision Support: Building Trust, Transparency, and Efficacy for Biomedical Research
The integration of Artificial Intelligence (AI) into Clinical Decision Support Systems (CDSS) promises to revolutionize healthcare by enhancing diagnostic precision and personalized treatment.
Explainable AI in Clinical Decision Support: Building Trust, Transparency, and Efficacy for Biomedical Research
Abstract
The integration of Artificial Intelligence (AI) into Clinical Decision Support Systems (CDSS) promises to revolutionize healthcare by enhancing diagnostic precision and personalized treatment. However, the 'black-box' nature of complex AI models remains a significant barrier to clinical adoption, raising concerns about trust, accountability, and potential bias. This article provides a comprehensive analysis of Explainable AI (XAI) for a audience of researchers, scientists, and drug development professionals. It explores the foundational need for transparency in high-stakes medical environments, reviews cutting-edge XAI methodologies and their clinical applications, addresses critical implementation challenges such as workflow integration and trust calibration, and evaluates frameworks for validating and comparing XAI effectiveness. By synthesizing the latest research, this review aims to guide the development of transparent, trustworthy, and clinically actionable AI tools that can be safely integrated into the biomedical research and development pipeline.
The Imperative for Transparency: Why Explainable AI is Non-Negotiable in Clinical Decision Support
The integration of Artificial Intelligence (AI) into healthcare promises to revolutionize patient care by enhancing diagnostic precision, personalizing treatment plans, and streamlining clinical workflows [1] [2]. However, the proliferation of sophisticated machine learning (ML) and deep learning (DL) models has introduced a significant challenge: the "black box" problem [1] [3]. This term describes AI systems whose internal decision-making processes are opaque, meaning that while they can produce highly accurate outputs, the reasoning behind these conclusions cannot be easily understood by human users [3] [4]. In high-stakes domains like medicine, this opacity creates a substantial trust and accountability gap [5].
Clinicians are justifiably reluctant to base decisions on recommendations they cannot verify or interpret [2] [3]. This lack of transparency challenges core medical ethical principles, including patient autonomy and the requirement for informed consent [3] [4]. Furthermore, the black-box nature of these systems complicates the assignment of liability when errors occur, potentially leaving a vacuum of accountability among developers, physicians, and healthcare institutions [3] [5]. This paper examines the technical and ethical dimensions of the black-box problem within Clinical Decision Support Systems (CDSS), framing it as the central impediment to trustworthy AI in healthcare and exploring the emerging solutions aimed at bridging this critical gap.
Quantifying the Trust Gap: Evidence and Impact
The challenges posed by black-box AI are not merely theoretical; they have tangible effects on clinical adoption and effectiveness. Recent research quantifies the trust gap and explores its consequences.
Table 1: Documented Impacts of the Black-Box Problem in Healthcare AI
| Impact Dimension | Quantitative / Qualitative Evidence | Source Domain |
|---|---|---|
| Barrier to Adoption | Over 65% of organizations cite "lack of explainability" as the primary barrier to AI adoption. [6] | Cross-sector (including healthcare) |
| Clinical Reliance | AI is "extremely influential" on doctor prescriptions, but Explainable AI (XAI) is not more influential than unexplainable AI. [4] | Clinical Decision-Making |
| Psychological & Financial Harm | Unexplainability can cause psychological distress and financial burdens for patients, e.g., from incorrect AI-driven diagnoses. [3] | Patient-Centered Care |
| Undermined Patient Autonomy | Lack of explainability limits a physician's ability to convey information, impeding shared decision-making and informed consent. [3] [4] | Medical Ethics & Law |
A systematic review of XAI for CDSS using non-imaging data highlights that a primary challenge is balancing explanation faithfulness (accuracy) with user plausibility, which is crucial for building appropriate trust [7]. This trust is not automatically conferred by providing explanations; one study found that while AI is highly influential on doctors' decisions, the presence of XAI did not increase that influence, and there was no correlation between self-reported influence and actual influence [4]. This suggests that the mere presence of an explanation is insufficient; it must be meaningful, usable, and integrated into the clinical workflow to bridge the trust gap effectively [8].
Technical Architectures for Explainability: From Black Box to Glass Box
To address the black-box problem, the field of Explainable AI (XAI) has developed a suite of techniques to make AI models more transparent and interpretable. These methods can be broadly categorized into two groups: ante hoc (intrinsically interpretable models) and post hoc (methods applied after a model makes a decision) [8].
Table 2: Key Explainable AI (XAI) Techniques and Their Applications in Healthcare
| XAI Technique | Category | Mechanism | Example Healthcare Application |
|---|---|---|---|
| SHAP (SHapley Additive exPlanations) [2] [6] | Post hoc, Model-agnostic | Uses game theory to assign each feature an importance value for a specific prediction. | Identifying key risk factors for sepsis prediction from Electronic Health Record (EHR) data. [2] |
| LIME (Local Interpretable Model-agnostic Explanations) [2] [6] | Post hoc, Model-agnostic | Creates a local, interpretable surrogate model to approximate the black-box model's predictions for a single instance. | Explaining an individual patient's cancer diagnosis from genomic data. [2] |
| Grad-CAM (Gradient-weighted Class Activation Mapping) [2] | Post hoc, Model-specific | Produces heatmaps that highlight important regions in an image for a model's decision. | Localizing tumors in histology images or MRIs. [2] |
| Counterfactual Explanations [6] [8] | Post hoc, Model-agnostic | Shows the minimal changes to input features needed to alter the model's outcome. | Informing a patient: "If your cholesterol were 20 points lower, your heart disease risk would be classified as low." |
| Attention Mechanisms [2] | (Often) Ante hoc, Model-specific | Allows models to learn and highlight which parts of input data (e.g., words in a clinical note) are most relevant. | Analyzing sequential medical data for disease prediction. [2] |
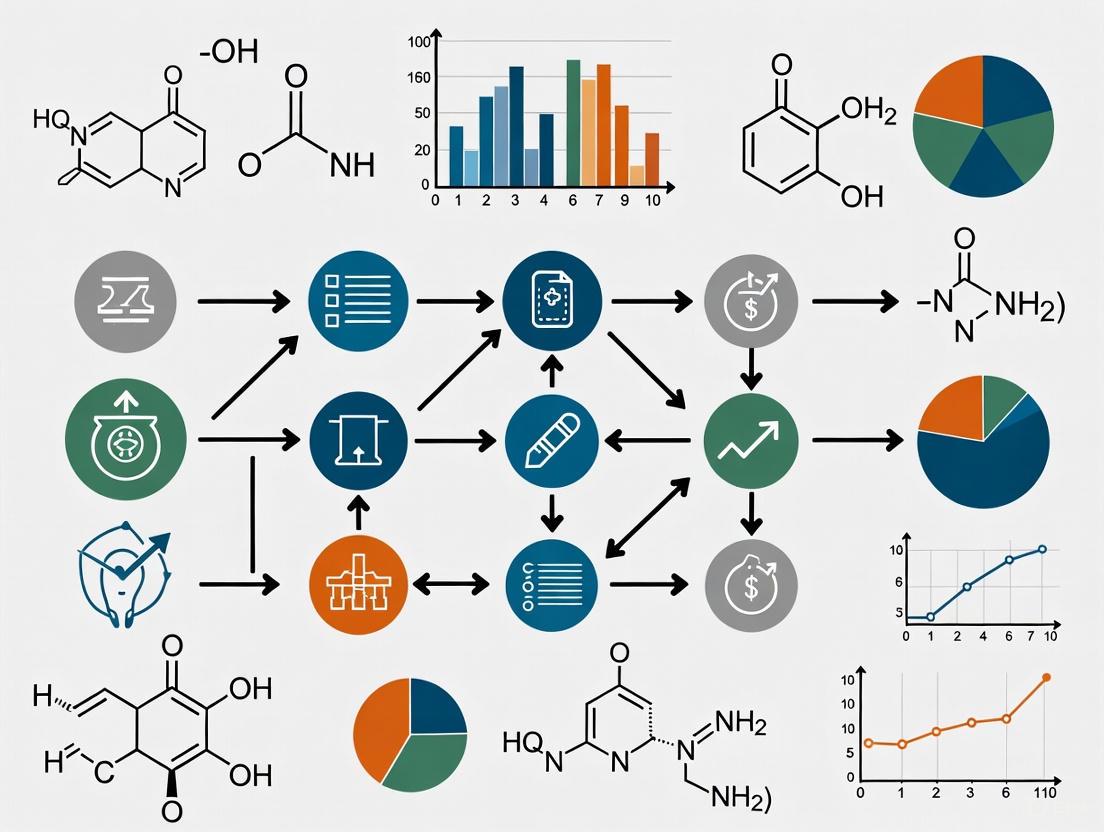
The following diagram illustrates the logical workflow and relationship between different XAI approaches in a clinical research context:
Experimental Protocols for Evaluating XAI in Clinical Research
For XAI to be clinically adopted, rigorous evaluation is paramount. This requires moving beyond technical metrics to include human-centered assessments. The following protocol outlines a robust methodology for evaluating an XAI system.
Objective: To assess the efficacy of an XAI method in explaining a predictive model for disease risk (e.g., Sepsis) in an ICU setting, focusing on technical fidelity, user trust, and clinical utility.
Phase 1: Model Development and Technical XAI Evaluation
- Data Preparation: Use a retrospective, de-identified dataset from EHRs (e.g., MIMIC-IV). Key features include vital signs, laboratory values, and demographic data. The outcome variable is the onset of sepsis within a 6-hour window [2] [7].
- Model Training: Train a black-box model (e.g., Gradient Boosting or LSTM) and an intrinsically interpretable baseline model (e.g., Logistic Regression) [2].
- XAI Application: Apply post hoc XAI methods (e.g., SHAP, LIME) to the black-box model to generate explanations for individual predictions [2] [8].
- Technical Metrics:
- Explanation Fidelity: Measure how well the explanation approximates the black-box model's behavior. For LIME, this is the fidelity of the local surrogate model. For SHAP, this can be measured via the consistency of its attributions [7] [8].
- Accuracy: Standard metrics (AUC, F1-score) to ensure model performance is maintained [2].
Phase 2: Human-Centered Evaluation
- Study Design: A mixed-methods approach combining quantitative tasks with qualitative feedback [7] [8].
- Participants: Recruit clinicians (e.g., intensivists, ICU nurses) and present them with a series of patient cases in a simulated CDSS interface.
- Experimental Workflow: The workflow for this human-centered evaluation phase is methodically structured as follows:
- Key Metrics:
- Trust and Usability: Measured via standardized scales (e.g., the Trust in Automation scale) and System Usability Scale (SUS) [7] [8].
- Clinical Reasoning Alignment: Qualitative analysis of interviews to determine if explanations align with or challenge clinical intuition [7] [8].
- Actionability: The degree to which the explanation influences a clinical decision, such as initiating a treatment protocol [8].
The Scientist's Toolkit: Key Research Reagents for XAI Experimentation
Table 3: Essential Materials and Tools for XAI Research in Healthcare
| Tool / Resource | Type | Primary Function in XAI Research |
|---|---|---|
| SHAP Library [2] [8] | Software Library | Computes consistent feature importance values for any model based on game theory. |
| LIME Package [2] [8] | Software Library | Generates local, interpretable surrogate models to explain individual predictions. |
| Electronic Health Record (EHR) Datasets (e.g., MIMIC-IV) [2] [7] | Data Resource | Provides structured, real-world clinical data for training and validating AI/XAI models. |
| Grad-CAM Implementation (e.g., in PyTorch/TensorFlow) [2] | Software Library | Generates visual explanations for convolutional neural networks (CNNs) used in medical imaging. |
| User Interface (UI) Prototyping Tools (e.g., Figma) [8] | Design Software | Enables the co-design of CDSS interfaces that effectively present XAI outputs to clinicians. |
The black-box problem represents a critical juncture in the adoption of AI in healthcare. While the performance of these systems is often remarkable, a lack of transparency fundamentally undermines trust, accountability, and ethical practice [3] [5]. Bridging this gap requires a multi-faceted approach that integrates technical innovation with human-centered design and rigorous validation.
The future of trustworthy healthcare AI lies not in choosing between performance and explainability, but in developing systems that achieve both. This involves a concerted effort from interdisciplinary teams—including computer scientists, clinicians, ethicists, and regulators—to create frameworks like the proposed Healthcare AI Trustworthiness Index (HAITI) [5]. By prioritizing explainability through robust XAI methods, user-centered design, and comprehensive evaluation protocols, we can unlock the full potential of AI to augment clinical expertise, enhance patient safety, and foster a new era of data-driven, transparent, and accountable medicine.
The integration of Artificial Intelligence (AI) into clinical decision support systems (CDSS) represents a paradigm shift in modern healthcare, offering unprecedented capabilities for enhancing diagnostic precision, risk stratification, and treatment planning [2]. However, the "black-box" nature of many advanced AI models has raised significant concerns regarding transparency, accountability, and trust [8]. This technological challenge has catalyzed a rapid regulatory evolution, beginning with the General Data Protection Regulation (GDPR) and culminating in the world's first comprehensive AI legal framework—the EU AI Act [9] [10]. These regulatory frameworks collectively establish explainable AI (XAI) not merely as a technical enhancement but as a fundamental legal requirement for high-stakes healthcare applications.
For researchers, scientists, and drug development professionals operating within the European market, understanding this regulatory trajectory is essential for both compliance and innovation. The GDPR, implemented in 2018, introduced foundational principles of transparency and the "right to explanation" for automated decision-making [2]. The newly enacted EU AI Act builds upon this foundation by establishing a detailed, risk-based regulatory ecosystem that imposes stringent requirements for AI systems in clinical settings [9] [10]. This whitepaper provides a comprehensive technical analysis of these regulatory drivers, with a specific focus on their implications for the development, validation, and deployment of explainable AI in clinical research and decision support systems.
Regulatory Foundations: From GDPR to the AI Act
The GDPR Precursor: Establishing the Right to Explanation
While not exclusively focused on AI, the GDPR (Regulation (EU) 2016/679) laid crucial groundwork for algorithmic transparency by establishing individuals' rights regarding automated processing. Articles 13-15 and 22 explicitly provide individuals with the right to obtain "meaningful information about the logic involved" in automated decision-making systems that significantly affect them [2]. In healthcare contexts, this translates to a legal obligation for CDSS developers and deployers to provide explanations for AI-driven diagnoses or treatment recommendations upon request. The regulation mandates that data processing must be fair, transparent, and lawful, principles that inherently challenge purely opaque AI systems [11]. The GDPR's emphasis on purpose limitation and data minimization further constrains how AI models can be developed and the types of data they can process, establishing privacy as a complementary regulatory concern to transparency.
The EU AI Act: A Risk-Based Framework for Healthcare AI
The EU AI Act (Regulation (EU) 2024/1689), which entered into force in August 2024, establishes a comprehensive, risk-based regulatory framework specifically for AI systems [9]. It categorizes AI applications into four distinct risk levels, with corresponding regulatory obligations:
Unacceptable Risk: Banned AI practices include all systems considered a clear threat to safety, livelihoods, and rights. Specific prohibitions relevant to healthcare include:
- Harmful AI-based manipulation and deception
- Harmful AI-based exploitation of vulnerabilities of specific social groups
- Social scoring by public authorities
- AI for individual criminal offense risk assessment or prediction
- Untargeted scraping of facial images from the internet or CCTV to create facial recognition databases [9]
- These prohibitions became applicable in February 2025.
High-Risk AI Systems: This category encompasses most clinical decision support applications, including:
- AI safety components in critical infrastructures (e.g., transport), the failure of which could put life and health at risk
- AI solutions used in education and vocational training that may determine access to education and professional course (e.g., scoring of exams)
- AI-based safety components of products (e.g., AI application in robot-assisted surgery)
- AI tools for employment, management of workers, and access to self-employment (e.g., CV-sorting software for recruitment)
- AI systems used to provide access to essential private and public services (e.g., credit scoring denying citizens opportunity to obtain a loan)
- AI systems used in certain areas of law enforcement and migration, asylum, and border control management
- AI solutions used in the administration of justice and democratic processes [9]
- The strict rules for high-risk AI systems will come into effect in August 2026 and August 2027.
Limited Risk: This category primarily entails transparency risk, referring to the need for transparency around AI use. The AI Act introduces specific disclosure obligations. For instance, users interacting with chatbots must be made aware they are communicating with an AI. Providers of generative AI must ensure AI-generated content is identifiable, with clear labelling for deep fakes and text published to inform the public on matters of public interest [9]. These transparency rules come into effect in August 2026.
Minimal Risk: The vast majority of AI systems with minimal or no risk, such as AI-enabled video games or spam filters, are not subject to further regulation under the AI Act [9].
The diagram below illustrates this risk-based classification and its implications for healthcare AI systems, particularly Clinical Decision Support Systems (CDSS).
Regulatory Timelines and Compliance Deadlines
Table: Key Implementation Deadlines of the EU AI Act
| Provision | Effective Date | Implications for Clinical AI Research |
|---|---|---|
| AI Act Entry into Force | August 2024 [9] | The regulation becomes EU law. |
| Prohibited AI Practices | February 2025 [9] | Banned applications (e.g., harmful manipulation, social scoring) become illegal. |
| Rules for General-Purpose AI (GPAI) Models | August 2025 [9] | Transparency and copyright-related rules for GPAI models become applicable. |
| Transparency Rules | August 2026 [9] | Disclosure obligations for AI interactions (e.g., chatbots) and AI-generated content (e.g., deepfakes) apply. |
| High-Risk AI Systems | August 2026 / August 2027 [9] | Strict obligations for high-risk AI systems, including most CDSS, become applicable. |
Technical Requirements for Explainability under the AI Act
Core Components of AI Transparency
The EU AI Act operationalizes explainability through several interconnected components that form the foundation of compliant AI systems for healthcare:
- Explainability: The ability to provide clear, user-understandable reasons behind AI decisions or recommendations in natural language or visual explanations [10]. For a CDSS, this means generating explanations that clinicians can interpret within their clinical workflow, such as highlighting key patient factors that contributed to a sepsis risk prediction [2] [8].
- Interpretability: The technical capacity to analyze and understand how input data, parameters, and processes within an AI system produce specific outputs [10]. This requires specialized tools for model inspection and visualization that enable technical teams to audit system behavior and ensure alignment with clinical reasoning patterns.
- Accountability: Establishing traceability mechanisms that assign clear responsibility for AI system decisions, errors, and downstream consequences [10]. This supports both internal governance and regulatory review by maintaining transparent chains of responsibility throughout the AI development and deployment lifecycle.
- Traceability: Maintaining comprehensive records, logs, and documentation tracking the development, training, input data, and operating contexts of AI systems [10]. This enables reconstruction of decisions and auditing of compliance, which is particularly crucial for clinical validation and post-market monitoring.
Specific Obligations for High-Risk CDSS
For AI-based Clinical Decision Support Systems classified as high-risk, the AI Act mandates rigorous technical and process-oriented requirements [9] [10]:
- Risk Management System: Continuous iterative risk assessment and mitigation throughout the entire lifecycle of the AI system.
- Data Governance: High-quality datasets feeding the system with appropriate bias detection and mitigation measures to minimize risks of discriminatory outcomes.
- Technical Documentation: Detailed documentation providing all information necessary for authorities to assess the system's compliance ("technical documentation").
- Record-Keeping: Automated logging of the AI system's activity to ensure traceability of results ("logging of activity").
- Transparency and Information to Users: Clear and adequate information to the deployer about the system's capabilities, limitations, and expected performance.
- Human Oversight: Measures designed to be effectively overseen by humans during the period of use.
- Accuracy, Robustness, and Cybersecurity: A high level of performance in these areas to ensure the system's resilience against errors and threats.
Explainable AI (XAI) Methodologies for Regulatory Compliance
Taxonomy of XAI Techniques
The pursuit of regulatory compliance necessitates the adoption of specific XAI methodologies. These can be broadly categorized into ante hoc (inherently interpretable) and post hoc (explaining existing black-box models) approaches [8].
Table: Key XAI Methods for Clinical Decision Support Systems
| XAI Method | Type | Scope | Clinical Application Example | Regulatory Alignment |
|---|---|---|---|---|
| SHAP (SHapley Additive exPlanations) [2] [12] | Post hoc, Model-agnostic | Local & Global | Quantifies the contribution of each patient feature (e.g., lab values, vitals) to a specific prediction (e.g., sepsis risk). | Supports Explainability (Article 13) |
| LIME (Local Interpretable Model-agnostic Explanations) [8] | Post hoc, Model-agnostic | Local | Creates a local surrogate model to approximate the black-box model's prediction for a single instance. | Supports Explainability & Interpretability |
| Grad-CAM (Gradient-weighted Class Activation Mapping) [2] | Post hoc, Model-specific | Local | Produces heatmaps highlighting regions of medical images (e.g., MRI, histology) most influential to a diagnosis. | Provides visual evidence for Traceability |
| Counterfactual Explanations [8] | Post hoc, Model-agnostic | Local | Indicates the minimal changes to input features required to alter a model's output (e.g., "If platelet count were >150k, the bleeding risk would be low."). | Enhances user understanding per Transparency requirements |
| Decision Trees / RuleFit [8] | Ante hoc | Global & Local | Provides a transparent, rule-based model that is inherently interpretable, often at a potential cost to performance. | Facilitates full Interpretability |
Experimental Protocol for Validating XAI in CDSS
To ensure compliance with the AI Act's requirements for high-risk systems, researchers must adopt rigorous validation protocols for their XAI implementations. The following workflow outlines a comprehensive methodology for developing and validating an explainable CDSS, from problem definition to deployment and monitoring.
Phase 1: Problem Formulation and Data Curation
- Define Clinical Task: Precisely specify the clinical prediction task (e.g., early sepsis detection, cancer metastasis prediction), ensuring alignment with a well-defined clinical workflow [8] [13].
- Data Curation & Annotation: Collect and preprocess multimodal data (EHR, medical images, genomics). Implement rigorous de-identification to comply with GDPR. Annotate data with clinical experts to establish ground truth [2] [14].
- Regulatory Risk Classification: Conduct an initial assessment to confirm the CDSS will be classified as a high-risk AI system, thereby defining the applicable regulatory requirements from the outset [9].
Phase 2: Model and XAI Development
- Base Model Training: Develop and train the core AI/ML model (e.g., CNN for imaging, GBM for tabular EHR data) using appropriate training, validation, and test splits [2].
- XAI Method Selection: Choose appropriate ante hoc or post hoc XAI methods (e.g., SHAP, LIME, Grad-CAM) based on the model architecture, data type, and clinical context (refer to Table 2) [8] [12].
- Explanation Generation: Implement the technical pipeline to generate explanations (e.g., feature importance scores, saliency maps) for the model's predictions [12].
Phase 3: Iterative Evaluation and Validation
- Model Performance Metrics: Evaluate the base model using standard metrics (AUC-ROC, accuracy, precision, recall, F1-score) on a held-out test set [2] [14].
- XAI Fidelity Assessment: Quantitatively evaluate the quality of the explanations. For post hoc methods, this involves measuring fidelity—how well the explanation approximates the true model's decision process for that instance [8].
- Clinical Utility Study: Conduct user studies with clinical professionals (e.g., physicians, nurses) to assess the actionability and interpretability of the explanations. Metrics include task time, diagnostic accuracy with the AI, and subjective feedback via surveys (e.g., System Usability Scale) and interviews [8] [13]. This phase is critical for demonstrating compliance with the "Transparency and information to users" requirement.
Phase 4: Documentation and Deployment Preparation
- Compile Technical Dossier: Prepare comprehensive documentation required by the AI Act, including data sheets, model cards, details on the XAI methods, and results from all validation studies [9] [10].
- Implement Human Oversight Mechanisms: Design the clinical user interface to present explanations effectively and facilitate informed human decision-making, as mandated by the AI Act [9] [8].
- Deploy with Continuous Monitoring: Plan for post-market monitoring to track model performance and explanation fidelity, identifying concept drift and ensuring ongoing compliance [9].
Table: Key Research Reagent Solutions for XAI-CDSS Development
| Reagent / Resource | Type | Function in XAI Research | Exemplary Tools / Libraries |
|---|---|---|---|
| XAI Software Libraries | Computational Tool | Provides pre-implemented algorithms for generating post hoc explanations (SHAP, LIME, Counterfactuals). | SHAP [12], LIME [8], Captum (for PyTorch), AIX360 (IBM) |
| Interpretable Model Packages | Computational Tool | Enables the development of inherently interpretable (ante hoc) models for comparison or final use. | InterpretML [8], scikit-learn (for GAMs, decision trees) |
| Clinical Datasets | Data Resource | Serves as benchmark data for training AI models and validating XAI methods in a clinically relevant context. | MIMIC-IV [2], The Cancer Genome Atlas (TCGA), UK Biobank |
| Model & Data Cards Templates | Documentation Framework | Provides a structured format for documenting model characteristics, intended use, and limitations, aiding regulatory compliance. | Model Card Toolkit [10], Dataset Nutrition Label |
| Clinical User Interface (UI) Prototyping Tools | Design & Evaluation Tool | Facilitates the design and testing of how explanations are presented to clinicians within their workflow. | Figma, React.js with visualization libraries (D3.js) |
The regulatory landscape for AI in healthcare has irrevocably shifted from voluntary guidelines to legally binding obligations. The trajectory from GDPR to the EU AI Act establishes explainability as a non-negotiable requirement for clinical AI systems, particularly high-risk CDSS [9] [10]. For researchers and drug development professionals, this necessitates a fundamental integration of XAI principles into every stage of the AI lifecycle—from initial concept and data collection to model development, validation, and post-market surveillance [8].
Success in this new regulatory environment requires a proactive, interdisciplinary strategy. Technical teams must collaborate closely with clinical experts, legal advisors, and ethicists to ensure that XAI implementations are not only technically sound but also clinically meaningful and fully compliant [13]. The methodologies and frameworks outlined in this whitepaper provide a foundational roadmap. By prioritizing transparent model design, rigorous validation of explanations, and comprehensive documentation, the clinical AI research community can navigate these regulatory drivers effectively. This approach will not only ensure market access and legal compliance but, more importantly, build the trustworthy AI systems necessary to realize the full potential of AI in advancing human health.
The integration of Artificial Intelligence (AI) into Clinical Decision Support Systems (CDSS) represents a paradigm shift in modern healthcare, offering unprecedented capabilities for diagnostic precision, risk stratification, and treatment planning [2] [15]. Despite these advancements, a fundamental tension persists between developing highly accurate complex models and maintaining the clinical reliability essential for medical adoption [16] [17]. This trade-off between model complexity and clinical reliability constitutes a critical challenge in explainable AI (XAI) research for healthcare applications [8].
Clinical environments demand not only superior predictive performance but also transparency, interpretability, and accountability from AI systems [17]. The "black box" nature of many sophisticated machine learning algorithms, particularly deep neural networks, creates significant barriers to clinical implementation, as healthcare professionals remain justifiably reluctant to trust decisions without understanding their rationale [2] [18]. This whitepaper examines the multidimensional aspects of this fundamental trade-off, analyzes current XAI methodologies for bridging this gap, and provides experimental frameworks for evaluating AI systems in clinical contexts, with particular emphasis on their integration within CDSS research.
The Interpretability-Complexity Spectrum in Clinical AI
Defining the Spectrum
AI models in healthcare exist along a continuum from inherently interpretable designs to complex black-box approaches requiring post-hoc explanation. Interpretable models—including linear regression, decision trees, and Bayesian models—feature transparent internal logic that is readily understandable to human users [16] [17]. These ante hoc methods provide direct insight into their decision-making processes through clearly defined parameters or rule-based structures [8].
In contrast, complex models such as deep neural networks, ensemble methods, and gradient boosting machines achieve state-of-the-art predictive performance on many healthcare tasks but operate as "black boxes" with opaque internal workings [16] [19]. Their superior accuracy comes at the cost of interpretability, creating the central trade-off that XAI seeks to address through post-hoc explanation techniques [8].
The Clinical Imperative for Explainability
In high-stakes clinical environments, the demand for explainability extends beyond technical preference to ethical, regulatory, and safety necessities [17]. Several critical factors drive this requirement:
- Trust and Adoption: Clinicians require understanding of AI reasoning to appropriately trust and utilize system recommendations [2] [18].
- Error Identification: Explanation capabilities enable detection of model errors, spurious correlations, and inappropriate feature dependencies [16] [17].
- Bias Detection: Transparent models facilitate identification of dataset biases that could lead to discriminatory outcomes [20] [17].
- Regulatory Compliance: Emerging regulations, including the European Union's Artificial Intelligence Act, increasingly mandate transparency for high-risk AI systems [17].
- Clinical Workflow Integration: Actionable AI insights must align with clinical reasoning processes and workflow requirements [18] [8].
Table 1: Core Dimensions of Clinical Reliability in AI Systems
| Dimension | Definition | Clinical Importance |
|---|---|---|
| Safety | Avoidance of harm to patients from AI-assisted care | Prevents diagnostic and treatment errors; minimizes adverse events [16] |
| Effectiveness | Delivery of care based on scientific evidence that maximizes desired outcomes | Ensures alignment with evidence-based guidelines; avoids overuse/underuse [16] |
| Fairness | Assurance that predictions are unbiased and non-discriminatory | Prevents reinforcement of healthcare disparities; promotes equitable care [20] [17] |
| Accountability | Clear assignment of responsibility for AI-driven decisions | Supports clinical responsibility and liability frameworks [2] |
| Actionability | Provision of clinically relevant and implementable insights | Enables effective intervention; supports clinical workflow integration [17] |
XAI Methodologies: Bridging the Complexity-Reliability Gap
Technical Approaches to Explainability
XAI methodologies can be systematically categorized based on their implementation approach, explanation scope, and model specificity [8]. The taxonomy includes:
Ante Hoc (Interpretable Models): These inherently transparent models include linear/logistic regression, decision trees, and Bayesian models [16] [8]. Their internal logic is transparent by design, making them suitable for lower-complexity tasks where interpretability is paramount [16].
Post Hoc Explanation Methods: Applied after model training, these techniques explain existing black-box models [8]. They are further categorized by:
- Model-Specific Methods: Techniques tailored to specific model architectures, such as activation analysis for neural networks or feature importance for tree-based models [16].
- Model-Agnostic Methods: Approaches applicable to any ML model, including LIME (Local Interpretable Model-agnostic Explanations) and SHAP (SHapley Additive exPlanations) [16] [8].
- Explanation Scope: Global explanations elucidate overall model behavior, while local explanations clarify individual predictions [8].
Table 2: Comparative Analysis of XAI Techniques in Clinical Applications
| XAI Method | Category | Clinical Use Cases | Strengths | Limitations |
|---|---|---|---|---|
| SHAP | Post-hoc, model-agnostic | Risk prediction models (sepsis, ICU admission) [16] [2] | Unified approach based on game theory; consistent explanations [8] | Computational intensity; potential approximation errors [8] |
| LIME | Post-hoc, model-agnostic | Imaging recommendations, treatment planning [16] | Local fidelity; intuitive feature perturbation [8] | Instability across similar instances; synthetic neighborhood generation [8] |
| Grad-CAM | Post-hoc, model-specific | Medical imaging (X-rays, histology) [2] [15] | Visual explanations; precise localization [2] | Limited to CNN architectures; intermediate layer dependence [2] |
| Counterfactual Explanations | Post-hoc, model-agnostic | Clinical eligibility, treatment alternatives [16] [15] | Intuitive "what-if" scenarios; aligns with clinical reasoning [15] | Computational complexity; may generate unrealistic instances [8] |
| Decision Trees | Ante hoc, interpretable | Triage rules, patient segmentation [16] | Fully transparent logic; no explanation needed [16] | Limited complexity; potential performance ceiling [15] |
| Attention Mechanisms | Model-specific | Medical text processing, time-series data [2] [15] | Context-aware weighting; inherent interpretability [15] | May not reflect true model reasoning; approximation concerns [2] |
Experimental Validation Framework for Clinical XAI
Robust experimental validation is essential for assessing the real-world utility of XAI systems in clinical contexts. The following protocols provide methodological guidance for evaluating XAI implementations:
Protocol 1: Clinical Reasonableness Assessment
Objective: Quantify the clinical plausibility of XAI-generated explanations through expert review [8].
Methodology:
- Panel Recruitment: Convene a multidisciplinary panel of clinical domain experts (physicians, nurses, specialists) with relevant expertise [8].
- Explanation Evaluation: Present XAI explanations for a curated set of model predictions without revealing the underlying clinical cases.
- Rating Scale Implementation: Utilize a structured rating scale (1-5) assessing:
- Physiological plausibility of featured parameters
- Consistency with established medical knowledge
- Clinical actionability of the explanation
- Alignment with expected reasoning patterns [8]
- Statistical Analysis: Calculate inter-rater reliability and aggregate scores for explanation quality.
Outcome Measures: Mean clinical reasonableness score; percentage of explanations deemed clinically valid; identification of recurrent explanation patterns contradicting medical knowledge [17].
Protocol 2: Trust Calibration Measurement
Objective: Evaluate how XAI explanations influence clinician trust and reliance on AI recommendations [8].
Methodology:
- Simulated Clinical Encounter Design: Develop realistic clinical scenarios incorporating AI recommendations with explanations.
- Controlled Exposure: Randomize participants to receive either: (a) AI recommendation alone, (b) AI recommendation with XAI explanation, or (c) no AI support (control).
- Decision Task: Participants manage simulated cases and make treatment decisions.
- Trust Assessment: Measure trust through:
- Self-reported trust scales (0-10)
- Adherence rates to AI recommendations
- Time to decision completion
- Appropriate overrides of incorrect recommendations [8]
Outcome Measures: Trust calibration metrics; appropriate reliance index; identification of over-trust or under-trust patterns [17].
Protocol 3: Workflow Integration Efficiency
Objective: Assess the impact of XAI explanations on clinical workflow efficiency and cognitive load [8].
Methodology:
- Task Analysis: Map existing clinical workflows and identify integration points for XAI explanations.
- Usability Testing: Implement XAI systems in simulated clinical environments with representative tasks.
- Efficiency Metrics:
- Time to clinical decision
- Number of information sources consulted
- Subjective workload assessment (NASA-TLX)
- System usability scale (SUS) [8]
- Iterative Refinement: Use testing results to refine explanation presentation and integration.
Outcome Measures: Workflow efficiency metrics; usability scores; cognitive load assessment [8].
Case Studies: Navigating the Trade-Off in Clinical Practice
Sepsis Prediction in Critical Care
Sepsis recognition and management represents a clinically significant and computationally challenging domain where the reliability-complexity trade-off is prominently displayed [18]. Complex ensemble models and deep learning approaches demonstrate superior predictive performance for early sepsis detection but present significant explainability challenges [18] [17].
Implementation Example: Lauritsen et al. developed an XAI system providing early warnings for critical illnesses including sepsis, using SHAP values to explain individual risk predictions by highlighting contributing features such as abnormal laboratory values and comorbidities [17]. This approach enables clinicians to validate predictions against clinical context and recognize when models may be misled by outliers or missing data [16].
Clinical Impact: The integration of explainability transforms sepsis prediction from an alert system to a clinical reasoning tool, allowing clinicians to focus on modifiable factors and personalize interventions [17]. This demonstrates how appropriate XAI implementation can enhance both reliability and actionability without fundamentally compromising model complexity [16] [17].
Diagnostic Imaging Analysis
In medical imaging domains such as radiology and pathology, deep learning models have demonstrated diagnostic capabilities comparable to healthcare professionals but face significant translational barriers due to their black-box nature [2] [18].
Implementation Example: Grad-CAM (Gradient-weighted Class Activation Mapping) and similar visualization techniques generate heatmaps highlighting regions of interest in medical images that contribute most significantly to model predictions [2] [15]. This allows radiologists to verify that models focus on clinically relevant anatomical features rather than spurious correlations [17].
Validation Challenge: DeGrave et al. demonstrated that some deep learning models for COVID-19 pneumonia detection took "shortcuts" by relying on non-pathological features such as laterality markers or patient positioning rather than medically relevant pathology [17]. This underscores the critical importance of XAI validation in detecting potentially harmful model behaviors that would otherwise remain hidden in black-box systems [17].
Operational Workflow Optimization
Beyond direct clinical decision support, AI systems increasingly optimize operational aspects of healthcare delivery, including resource allocation, appointment scheduling, and length-of-stay prediction [16].
Implementation Example: Pall et al. applied feature importance methods to identify factors associated with drug shortages, enabling more resilient supply chain management [16]. Similarly, Shin et al. used SHAP explanations to identify drivers of outpatient wait times, supporting targeted process improvements [16].
Trade-off Consideration: In operational contexts where clinical risk is lower, the balance may shift toward increased model complexity despite explainability costs, though post-hoc explanations remain valuable for process validation and improvement [16].
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Research Components for XAI Clinical Validation
| Research Component | Function | Implementation Examples |
|---|---|---|
| SHAP Library | Quantifies feature contribution to individual predictions | Python implementation for clinical risk models; provides unified feature importance values [16] [8] |
| LIME Framework | Generates local surrogate explanations | Model-agnostic explanations for treatment recommendation systems; creates interpretable local approximations [16] [8] |
| Grad-CAM Implementation | Produces visual explanations for convolutional neural networks | Medical image analysis; highlights diagnostically relevant regions in imaging data [2] [15] |
| Electronic Health Record (EHR) Simulators | Creates synthetic clinical data for controlled experimentation | Protocol development without patient risk; simulated sepsis cases for validation [17] |
| Clinical Assessment Scales | Quantifies expert evaluation of explanation quality | 5-point Likert scales for clinical reasonableness; structured evaluation frameworks [8] |
| Trust Calibration Metrics | Measures appropriate reliance on AI recommendations | Adherence rates to correct/incorrect suggestions; subjective trust assessments [8] |
| Workflow Integration Platforms | Embeds explanations within clinical information systems | EHR-integrated dashboards; context-aware explanation delivery [8] |
Future Directions and Research Agendas
The evolving landscape of XAI research suggests several promising directions for addressing the fundamental reliability-complexity trade-off:
Methodological Innovations
- Causal Explanation Frameworks: Moving beyond correlation-based explanations to causal relationships that better align with clinical reasoning processes [15].
- Concept-Based Explanations: Utilizing high-level clinical concepts (e.g., "consolidation" in radiology) rather than low-level features to enhance clinical relevance [15].
- Interactive Explanation Systems: Developing dialog-based interfaces that allow clinicians to interrogate models through iterative questioning [8].
- Longitudinal Validation: Implementing continuous monitoring systems to detect explanation drift and performance degradation over time [15].
Regulatory and Standardization Developments
The establishment of standardized evaluation metrics for XAI systems remains a critical challenge [17] [15]. Current research indicates growing recognition of the need for:
- Explanation Fidelity Metrics: Quantitative measures assessing how accurately explanations represent true model reasoning [8].
- Clinical Utility Standards: Domain-specific criteria for evaluating the practical usefulness of explanations in clinical contexts [8].
- Fairness Auditing Frameworks: Standardized approaches for detecting and mitigating biases in AI systems through explainability [17].
The fundamental trade-off between clinical reliability and model complexity represents a central challenge in healthcare AI that cannot be eliminated but can be strategically managed through thoughtful XAI implementation [16] [17]. The evolving landscape of explainability techniques provides a growing toolkit for making complex models more transparent, accountable, and clinically actionable without necessarily sacrificing predictive performance [8] [15].
Future progress in this domain requires continued interdisciplinary collaboration among computer scientists, clinicians, and regulatory bodies to develop explanation methodologies that genuinely enhance clinical understanding while respecting the constraints of healthcare workflows [18] [8]. By focusing on human-centered design principles and robust validation frameworks, the field can advance toward AI systems that offer not only superior predictive capabilities but also the transparency and trust required for meaningful clinical integration [8].
The ultimate goal is not to explain away complexity but to build bridges between sophisticated AI capabilities and clinical reasoning processes, creating collaborative systems where human expertise and artificial intelligence operate synergistically to improve patient care [18]. Through continued methodological innovation and rigorous clinical validation, XAI research promises to transform the fundamental trade-off between reliability and complexity from a barrier to adoption into a catalyst for more effective, trustworthy, and impactful healthcare AI systems [17] [15].
The integration of Artificial Intelligence (AI) into clinical decision support systems (CDSS) represents a paradigm shift in modern healthcare, offering unprecedented capabilities in diagnostic precision, risk stratification, and treatment planning [21]. Yet, the opaque "black-box" nature of many sophisticated AI models creates fundamental barriers to clinical adoption, particularly in high-stakes medical environments where understanding the rationale behind a decision is as crucial as the decision itself [22]. This has spurred intense focus on two interrelated concepts: interpretability and explainability. While these terms are often used interchangeably, they embody distinct technical and functional meanings within medical AI. Interpretability refers to the ability to observe a model's mechanics and understand the causal pathways without the need for external explanations, often associated with simpler, transparent models. Explainability (XAI) involves post-hoc techniques applied to complex models to make their outputs understandable to humans [22] [23].
The ultimate goal of both is to foster trust—defined as the clinician's attitude that the AI will help achieve their goals in situations characterized by uncertainty and vulnerability [24]. However, trust is not a monolithic concept; it is a complex psychological state built on transparency, reliability, and understanding, and it directly influences a critical behavioral outcome: reliance, which is the observable extent to which a clinician's decision is influenced by the AI [24]. This technical guide delineates these core concepts, frames them within CDSS research, and provides a scientific toolkit for their evaluation and implementation, drawing upon the most recent advancements in the field.
Conceptual Framework and Definitions
Distinguishing Interpretability and Explainability
In both research and clinical practice, precisely defining the scope of interpretability and explainability is essential for developing and evaluating AI systems.
Interpretability is a characteristic of a model itself, describing the degree to which a human can consistently predict the model's result from its input data and architectural design. Intrinsically interpretable models, such as decision trees, linear models, or rule-based systems, offer transparency by design. Their internal workings are accessible and comprehensible, allowing a user to trace the reasoning process from input to output [22].
Explainability is a characteristic of a system's interface and functionality. It encompasses the methods and techniques used to translate the operations of a complex, often uninterpretable "black-box" model (e.g., a deep neural network) into a format that is understandable and meaningful for a human user. Explainability is often achieved through post-hoc techniques that provide insights into the model's behavior without fully elucidating its internal mechanics [23].
The relationship between these concepts is foundational to trust. Interpretability can be seen as a direct path to trust, whereas explainability often constructs a bridge to trust when direct observation is impossible.
The Trust-Reliance Dynamic in Clinical Settings
Trust and reliance are related but distinct concepts that must be measured separately in clinical studies [24]. A clinician may report high trust in an system (an attitude) but demonstrate low reliance (a behavior) due to external factors like workflow constraints, or vice versa.
A crucial concept emerging from recent research is appropriate reliance—the ideal where clinicians rely on the model when it is correct and override it when it is incorrect [24]. This is behaviorally defined as:
- Appropriate Reliance: The participant relied on the model when it was more accurate, or did not rely on it when it was less accurate.
- Under-Reliance: The participant did not rely on the model when it was more accurate.
- Over-Reliance: The participant relied on the model when it was less accurate.
Achieving appropriate reliance is the hallmark of a well-designed and effectively integrated clinical AI system, as blind over-reliance on an inaccurate model can lead to negative clinical outcomes.
Empirical Evidence and Quantitative Insights
Recent studies highlight both the potential and the challenges of XAI in clinical practice. The following table synthesizes quantitative findings from recent experimental and review studies, illustrating the measurable impact of XAI on clinical performance and the current state of methodological applications.
Table 1: Quantitative Findings from Recent XAI Clinical and Review Studies
| Study Focus | Key Performance Metric | Result Without AI/XAI | Result With AI/XAI | Context & Notes |
|---|---|---|---|---|
| Gestational Age Estimation (Reader Study) [24] | Clinician Mean Absolute Error (MAE) | 23.5 days | Prediction Only: 15.7 daysPrediction + XAI: 14.3 days | XAI provided a non-significant further reduction. High individual variability in response to XAI. |
| Hybrid ML-XAI Framework (Technical Framework) [22] | Overall Model Accuracy | N/A | 99.2% | Framework predicted 5 diseases; high accuracy achieved with ensemble models (XGBoost, Random Forest). |
| XAI in CDSS (Meta-Analysis) [21] | Dominant XAI Method | N/A | Model-agnostic techniques (e.g., Grad-CAM, attention mechanisms) | Analysis of 62 studies (2018-2025). Highlights dominance in imaging and sequential data tasks. |
The empirical data reveals a nuanced picture. While the addition of XAI can improve clinical performance, as in the gestational age study where it reduced error, the effect is not always statistically significant and varies significantly between clinicians [24]. This underscores that the mere presence of an explanation is not a panacea. Furthermore, technical frameworks demonstrate that high predictive accuracy can be maintained while integrating explainability, addressing a common concern that interpretability comes at the cost of performance [22].
Table 2: Analysis of Appropriate Reliance from a Clinical Reader Study [24]
| Reliance Category | Behavioral Definition | Clinical Implication |
|---|---|---|
| Appropriate Reliance | Participant relied on the model when it was better, or did not when it was worse. | Optimal interaction; enhances human-AI team performance. |
| Under-Reliance | Participant did not rely on the model when it was better. | Potential under-utilization of a beneficial tool; lost opportunity for improved accuracy. |
| Over-Reliance | Participant relied on the model when it was worse. | Clinically dangerous; can propagate and amplify model errors. |
Experimental Protocols for Evaluating XAI
Robust evaluation is critical for advancing XAI research. The following protocols, derived from recent literature, provide a template for assessing XAI's impact in clinical settings.
Three-Stage Clinical Reader Study Protocol
This protocol, adapted from a study on gestational age estimation, is designed to isolate the effects of AI predictions and explanations on clinician decision-making [24].
Objective: To measure the impact of model predictions and model explanations on clinician trust, reliance, and performance (e.g., estimation accuracy). Materials: A set of de-identified medical cases (e.g., images, patient records); a trained AI model with explainability output; a platform for presenting cases and collecting clinician responses; pre- and post-study questionnaires. Procedure:
- Stage 1 - Baseline Performance: Participants review and make decisions on a series of cases without any AI assistance. This establishes their baseline performance.
- Stage 2 - Prediction Influence: Participants review the same or a matched set of cases, now accompanied by the AI model's prediction. This stage measures the change in performance and reliance attributable to the prediction alone.
- Stage 3 - Explanation Influence: Participants review cases accompanied by both the AI model's prediction and its explanation (e.g., saliency map, prototype images). This stage measures the additional effect of the explanation.
- Data Collection: At each stage, collect: a) the participant's decision/estimate, b) time taken, c) self-reported confidence. In post-study questionnaires, gather qualitative feedback on perceived explanation usefulness and trust.
Analysis:
- Calculate performance metrics (e.g., Mean Absolute Error, accuracy) for each stage and compare.
- Quantify reliance by measuring the shift in the participant's decision toward the AI's prediction.
- Categorize each decision as appropriate reliance, over-reliance, or under-reliance based on the relative accuracy of the participant's baseline and the AI model for that specific case [24].
- Correlate questionnaire responses with performance changes to understand subjective vs. objective impacts.
Technical Framework for a Hybrid ML-XAI System
This protocol outlines the development of a hybrid system that combines high-performance models with post-hoc explainability, as demonstrated in a multi-disease prediction framework [22].
Objective: To build a predictive model for clinical risk (e.g., disease presence) that provides transparent, actionable explanations for its outputs. Materials: Structured clinical data (e.g., EHRs, lab results); ML libraries (e.g., scikit-learn, XGBoost); XAI libraries (e.g., SHAP, LIME). Procedure:
- Data Preprocessing: Handle missing values, normalize numerical features, and encode categorical variables. Address class imbalance using techniques like SMOTE if necessary.
- Model Training and Selection: Train multiple ML models (e.g., Decision Trees, Random Forest, XGBoost, Naive Bayes). Use cross-validation to select the best-performing model based on metrics like accuracy, AUC-ROC, and F1-score.
- Integration of XAI Techniques:
- Global Explainability: Apply SHAP to the entire dataset to understand the overall importance of each feature in the model's predictions. This identifies the key clinical drivers globally.
- Local Explainability: For an individual patient's prediction, use LIME or SHAP to generate a local explanation. This highlights the specific factors (e.g., elevated glucose, low RBC count) that most contributed to that particular risk assessment.
- Validation: Evaluate the model on a held-out test set. Validate the plausibility and clinical coherence of the explanations with domain experts.
Analysis:
- Report standard performance metrics for the chosen model.
- Present global feature importance plots.
- For case examples, present local explanations showing the contribution of each feature to the final prediction, allowing clinicians to "debug" the model's reasoning on a per-case basis.
Visualization of Logical Relationships and Workflows
The following diagrams, generated using Graphviz DOT language, map the core logical relationships in the XAI trust paradigm and the key experimental protocols.
The Pathway to Appropriate Clinical Reliance on AI
Three-Stage Clinical Evaluation Protocol
The Scientist's Toolkit: Key Research Reagents and Materials
For researchers designing and evaluating interpretable and explainable AI systems for clinical support, the following tools and datasets are essential.
Table 3: Key Research Reagents and Resources for Medical XAI Research
| Category | Item | Specifications & Function | Example Sources/References |
|---|---|---|---|
| XAI Software Libraries | SHAP (SHapley Additive exPlanations) | Model-agnostic unified framework for interpreting model predictions based on game theory. Provides both global and local explanations. | [22] |
| LIME (Local Interpretable Model-agnostic Explanations) | Creates local surrogate models to approximate predictions of any black-box model, explaining individual instances. | [22] | |
| Captum | A comprehensive library for model interpretability built on PyTorch. | [25] [26] | |
| Medical Imaging Datasets | CheXpert | Large dataset of chest X-rays with labels for automated interpretation, used for training and benchmarking. | [27] |
| MedTrinity-25M | A massive dataset of 25M images across 10 modalities and 65+ diseases, enabling robust model training. | [28] | |
| Alzheimer's Disease Neuroimaging Initiative (ADNI) | Multimodal dataset including MRI/PET images, genetics, and cognitive tests for neurodegenerative disease research. | [27] | |
| Clinical Tabular Data | MIMIC Critical Care Database | De-identified health data from over 40,000 critical care patients, ideal for predictive model development. | [27] |
| Healthcare Cost and Utilization Project (HCUP) | Nationwide US database for tracking trends in healthcare utilization, access, charges, and outcomes. | [27] | |
| Evaluation Frameworks | Three-Stage Reader Study Protocol | A structured methodology to isolate and measure the impact of AI predictions and explanations on clinician performance and reliance. | [24] |
| Quantus | A Python toolkit for standardized evaluation of XAI methods, providing a range of metrics. | [25] [26] |
The journey toward fully transparent, trustworthy, and seamlessly integrated AI in clinical decision support is ongoing. The definitions, evidence, protocols, and tools outlined in this guide provide a foundation for researchers and drug development professionals to advance this critical field. The empirical data clearly shows that the relationship between explanations, trust, and reliance is complex and highly variable among clinicians [24]. Future research must move beyond technical explanations to develop context-aware, user-dependent XAI systems that engage in genuine dialogue with clinicians [25] [26]. This requires an interdisciplinary approach, combining technical rigor with deep clinical understanding and insights from human-computer interaction, to create AI systems that clinicians can not only trust but also appropriately rely upon, thereby fulfilling the promise of AI to enhance patient care and outcomes.
XAI Techniques in Action: From Model-Agnostic Tools to Clinical Workflow Integration
The integration of Artificial Intelligence (AI) into Clinical Decision Support Systems (CDSS) has significantly enhanced diagnostic precision, risk stratification, and treatment planning in modern healthcare [2]. However, the widespread clinical adoption of AI models has been hampered by their inherent "black-box" nature, where these systems provide predictions or classifications without offering clear, human-understandable explanations for their outputs [2] [29]. This opacity presents a critical barrier in medical contexts, where clinicians must justify decisions and ensure patient safety, creating an urgent need for Explainable AI (XAI) methodologies that make AI systems transparent, interpretable, and accountable [2] [30]. The fundamental challenge lies in the trade-off between model performance and interpretability; while complex models like deep neural networks offer superior predictive power, simpler models are inherently more understandable [2].
Explainable AI has emerged as a transformative approach to address these challenges, particularly in safety-critical healthcare domains where erroneous AI predictions can have high-impact consequences [30]. Regulatory bodies such as the U.S. Food and Drug Administration (FDA) and the European Medicines Agency (EMA) are increasingly emphasizing the need for transparency and accountability in AI-based medical devices [2]. Furthermore, explainability supports core ethical principles of AI—fairness, accountability, and transparency (FAT)—while enabling informed consent, shared decision-making, and the ability to audit algorithmic decisions [2]. In clinical settings, XAI methods provide insights into which features influence a model's decision, how sensitive the model is to input variations, and how trustworthy its predictions are across different contexts [2].
This technical guide presents a comprehensive taxonomy of XAI methods, focusing specifically on the critical distinction between ante-hoc (intrinsically interpretable) and post-hoc (retrospectively applied) explanations, framed within the context of clinical decision support systems research. We examine the technical foundations, implementation considerations, and clinical applications of each approach, providing researchers and drug development professionals with a structured framework for selecting and implementing appropriate XAI methodologies in healthcare contexts.
Fundamental Taxonomy: Ante-Hoc vs. Post-Hoc Explainable AI
The rapidly expanding field of XAI can be fundamentally categorized into two distinct paradigms: ante-hoc (intrinsically interpretable) and post-hoc (retrospectively applied) explainability [31]. This distinction represents a core taxonomic division in XAI methodologies, with significant implications for their application in clinical decision support systems.
Ante-hoc explainability refers to AI systems that are inherently transparent by design. These models possess a self-explanatory architecture where the decision-making process is naturally interpretable to human users without requiring additional explanation techniques [31]. Examples include decision trees, linear models, rule-based systems, and attention mechanisms that provide inherent insights into feature importance during the reasoning process. The primary advantage of ante-hoc methods lies in their faithful representation of the actual model mechanics, as the explanations directly correspond to how the model processes information and generates predictions [29]. In healthcare contexts, this inherent transparency aligns well with regulatory requirements and clinical needs for trustworthy systems.
In contrast, post-hoc explainability encompasses techniques applied to already-trained "black-box" models to generate explanations for their specific predictions after the fact [31]. These methods do not modify the underlying model architecture but instead create auxiliary explanations that help users understand the model's behavior. Common post-hoc approaches include model-agnostic methods like LIME (Local Interpretable Model-agnostic Explanations) and SHAP (SHapley Additive exPlanations), as well as visualization techniques such as Grad-CAM (Gradient-weighted Class Activation Mapping) for convolutional neural networks [2] [32]. The survey by Gambetti et al. (2025) revealed that over 80% of XAI studies in clinical settings employ post-hoc, model-agnostic approaches, particularly SHAP and Grad-CAM [32].
The following table summarizes the core characteristics and trade-offs of these two XAI paradigms:
Table 1: Comparative Analysis of Ante-Hoc vs. Post-Hoc XAI Methods
| Characteristic | Ante-Hoc Explainability | Post-Hoc Explainability |
|---|---|---|
| Interpretability Basis | Inherent model transparency | External explanation techniques |
| Model Flexibility | Limited to interpretable architectures | Compatible with any model type |
| Explanation Fidelity | High (direct representation) | Variable (approximation) |
| Implementation Complexity | Integrated during model design | Applied after model training |
| Common Techniques | Decision trees, linear models, attention mechanisms, rule-based systems | SHAP, LIME, Grad-CAM, surrogate models, counterfactual explanations |
| Clinical Trustworthiness | High (transparent mechanics) | Context-dependent (requires validation) |
| Performance Trade-off | Potential accuracy sacrifice for transparency | Maintains black-box performance |
| Regulatory Alignment | Strong (inherently auditable) | Requires additional validation |
The selection between ante-hoc and post-hoc approaches involves navigating critical trade-offs between model performance, explanation fidelity, and implementation complexity [31]. While post-hoc methods dominate current clinical applications due to their compatibility with high-performance models, ante-hoc methods offer compelling advantages for contexts requiring high transparency and regulatory compliance [2] [29].
Technical Specifications of XAI Methods
Ante-Hoc (Intrinsically Interpretable) Methods
Ante-hoc XAI methods encompass a range of AI systems designed with inherent transparency, where the model's structure and parameters directly provide insights into the decision-making process. In healthcare contexts, these methods align closely with clinical reasoning patterns, potentially facilitating smoother integration into clinical workflows.
Decision trees and rule-based systems represent one of the most established ante-hoc approaches in CDSS. These systems operate through a hierarchical structure of logical decisions that mirror clinical reasoning processes [29]. Knowledge-based CDSS often employ rule-based inference methodologies using evidential reasoning (RIMER), which are based on belief rule base (BRB) systems that set belief degrees to represent different types of uncertain knowledge [29]. Such systems have demonstrated effectiveness across various medical domains, including heart failure management, psychogenic pain assessment, tuberculosis diagnosis, and acute coronary syndrome [29]. The primary advantage of these systems is their explicit decision logic, which allows clinicians to trace exactly how specific patient characteristics lead to particular recommendations or predictions.
Attention mechanisms constitute another significant ante-hoc approach, particularly valuable for processing complex, multi-modal clinical data. These mechanisms enable models to dynamically weight the importance of different input features or data segments during processing, providing inherent insights into which elements most strongly influence the final prediction [2]. The resulting attention weights can be visualized to show clinicians which patient attributes, clinical measurements, or regions in medical images the model focuses on when making decisions. This capability is especially valuable in medical imaging applications, where attention maps can highlight anatomically relevant regions corresponding to pathological findings [2].
Bayesian networks offer a probabilistic framework for ante-hoc explainability that naturally represents uncertainty—a crucial aspect of clinical decision-making. These networks model conditional dependencies between variables through directed acyclic graphs, allowing clinicians to understand both the reasoning process and the uncertainty associated with predictions [29]. In healthcare applications, Bayesian networks have been deployed for liver disease diagnosis, breast cancer assessment, infectious disease monitoring, and diabetes management [29]. Their capacity for what-if analysis enables clinicians to investigate how changes in patient conditions might affect outcomes, supporting exploratory reasoning and treatment planning.
Post-Hoc (Retrospectively Applied) Explanation Methods
Post-hoc XAI methods generate explanations for pre-existing models without modifying their internal architecture. These techniques have gained significant traction in clinical settings due to their compatibility with high-performance black-box models.
Feature attribution methods represent the most prominent category of post-hoc explanations in healthcare. These techniques assign importance scores to input features, indicating their relative contribution to a model's prediction for a specific case [2]. SHAP (SHapley Additive exPlanations) leverages game-theoretic principles to compute feature importance values that satisfy desirable mathematical properties, providing both local (individual prediction) and global (overall model behavior) explanations [2] [32]. In clinical practice, SHAP has been applied to explain risk predictions in cardiology by highlighting contributing factors from electronic health records [2]. Similarly, LIME (Local Interpretable Model-agnostic Explanations) creates local surrogate models that approximate the black-box model's behavior in the vicinity of a specific prediction, generating explanations by perturbing input features and observing output changes [2].
Visual explanation techniques are particularly valuable for medical imaging applications. Grad-CAM (Gradient-weighted Class Activation Mapping) generates heatmaps that highlight regions in input images most influential in a model's decision, making it invaluable for domains like radiology, pathology, and dermatology [2] [32]. For instance, in tumor detection from histology images, Grad-CAM heatmaps can localize malignant regions and show overlapping areas with pathologist annotations, allowing radiologists to verify and validate the model's conclusions [2]. These visual explanations facilitate human-AI collaboration by enabling clinicians to quickly assess whether a model focuses on clinically relevant image regions.
Surrogate models represent another post-hoc approach where a simpler, interpretable model (such as a decision tree or linear model) is trained to approximate the predictions of a complex black-box model [30]. While these surrogates provide intuitive explanations, their fidelity to the original model's decision boundaries must be carefully evaluated [2]. The effectiveness of surrogate explanations depends on the complexity of the underlying model and the adequacy of the surrogate in capturing its behavior.
Table 2: Technical Specifications of Prominent XAI Methods in Clinical Applications
| XAI Method | Category | Explanation Mechanism | Clinical Applications | Key Advantages | Key Limitations |
|---|---|---|---|---|---|
| Decision Trees | Ante-hoc | Hierarchical decision rules | General CDSS, glaucoma, thyroid nodules [29] | High transparency, mirrors clinical reasoning | Limited complexity, potential overfitting |
| Attention Mechanisms | Ante-hoc | Feature importance weighting | Medical imaging, sequential data analysis [2] | Dynamic focus, preserves model performance | Partial explanation, requires interpretation |
| Bayesian Networks | Ante-hoc | Probabilistic dependency graphs | Liver disease, breast cancer, diabetes [29] | Natural uncertainty quantification | Complex construction, computational cost |
| SHAP | Post-hoc | Game-theoretic feature attribution | Cardiology, oncology, risk prediction [2] [32] | Strong theoretical foundation, consistent | Computational intensity, approximation error |
| LIME | Post-hoc | Local surrogate modeling | General CDSS, simulated data [2] | Model-agnostic, intuitive local explanations | Instability to perturbations, sampling artifacts |
| Grad-CAM | Post-hoc | Visual heatmap generation | Radiology, pathology, medical imaging [2] [32] | Intuitive visualizations, model-specific | Limited to CNN architectures, coarse localization |
Experimental Protocols and Evaluation Frameworks
Methodological Approaches for XAI Validation
Rigorous evaluation of XAI methods in clinical contexts requires multi-faceted assessment protocols that address both technical correctness and clinical utility. The validation framework must encompass quantitative metrics, human-centered evaluations, and clinical relevance assessments to ensure explanations meet the needs of healthcare stakeholders.
Technical evaluation metrics focus on quantifying explanation quality through computational measures. For feature attribution methods, common metrics include explanation fidelity (how well explanations represent the model's actual reasoning) and robustness (consistency of explanations under minor input perturbations) [2]. In imaging applications, techniques like Intersection over Union (IoU) are used to measure the spatial alignment between visual explanations (e.g., Grad-CAM heatmaps) and expert annotations (e.g., radiologist markings) [2]. Model performance metrics such as Area Under the Curve (AUC) remain important for ensuring that explainability enhancements do not compromise predictive accuracy, particularly in critical applications like sepsis prediction in ICU settings [2].
Human-centered evaluation represents a crucial dimension for assessing XAI effectiveness in clinical contexts. These studies typically involve clinicians evaluating explanations based on criteria such as comprehensibility, clinical plausibility, trustworthiness, and decision-making confidence [32] [33]. However, current studies often suffer from methodological limitations, with most employing small-scale clinician studies (typically fewer than 25 participants) that limit statistical power and generalizability [32]. More robust experimental designs incorporate longitudinal assessments and mixed-methods approaches combining quantitative measures with qualitative feedback to capture nuanced aspects of explanation utility in clinical workflows [2] [33].
Clinical workflow integration testing evaluates how effectively XAI systems function within actual clinical environments and electronic health record (EHR) systems. This includes assessing explanation delivery timing, presentation format compatibility with existing interfaces, and minimization of cognitive load [2] [33]. Studies have shown that explanations must be integrable into fast-paced clinical settings where, as one attending physician noted, "When [the system] gives me an elevated risk score, I must be able to see within minutes if [the results] make sense" [33]. Effective integration often requires context-aware explanations that adapt to different clinical scenarios, user roles, and time constraints.
Implementation Challenges and Methodological Gaps
Despite advances in XAI methodologies, significant implementation challenges persist in healthcare contexts. A critical gap exists between technical explanation generation and clinically meaningful interpretation, with developers and clinicians often possessing opposing mental models of explainability [33]. Developers typically focus on model interpretability—understanding what features the model uses—while clinicians prioritize clinical plausibility—whether results align with medical knowledge and specific patient contexts [33].
This disconnect manifests in several ways. Developers tend to regard data as the primary source of truth, trusting that "the model chose the most relevant factors to make accurate predictions," while clinicians view algorithmic outputs as "only one piece of the puzzle" to be combined with physical examination findings, patient history, and other non-quantifiable information [33]. Furthermore, tensions exist between exploration versus exploitation mindsets; developers value ML systems for discovering "unknown patterns in the data to learn something new," while clinicians typically trust only systems relying on "established knowledge gained from clinical studies and evidence-based medicine" [33].
Additional methodological challenges include the lack of standardized evaluation metrics for explanation quality, with current assessments often relying on researcher-defined criteria without consensus on what constitutes a "good" explanation across different clinical contexts [2]. There is also insufficient attention to population-specific validation, with many XAI systems failing to demonstrate consistent explanation quality across diverse patient demographics and clinical subgroups [2]. These gaps highlight the need for more sophisticated, clinically-grounded evaluation frameworks that address the unique requirements of healthcare applications.
Visual Representations of XAI Methodologies
The following diagrams provide visual representations of key XAI workflows and methodological relationships, created using Graphviz DOT language with adherence to the specified color palette and contrast requirements.
Diagram 1: Ante-Hoc XAI Workflow
Diagram 2: Post-Hoc XAI Workflow
Implementing and evaluating XAI methods in clinical contexts requires specialized computational resources, software tools, and datasets. The following table details key "research reagent solutions" essential for conducting rigorous XAI research in healthcare settings.
Table 3: Essential Research Resources for XAI in Clinical Decision Support
| Resource Category | Specific Tools & Platforms | Primary Function | Application Context |
|---|---|---|---|
| XAI Algorithm Libraries | SHAP, LIME, Captum, InterpretML, AIX360 | Implementation of explanation algorithms | Model-agnostic and model-specific explanation generation |
| Model Development Frameworks | TensorFlow, PyTorch, Scikit-learn, XGBoost | Building and training machine learning models | Developing both ante-hoc and black-box models for clinical prediction |
| Medical Imaging Platforms | MONAI, ITK, MedPy, OpenCV | Specialized processing of medical images | Implementing visual explanation methods like Grad-CAM |
| Clinical Data Standards | FHIR, OMOP, DICOM | Standardizing clinical data representation | Ensuring interoperability and reproducible feature definitions |
| Evaluation Metrics | Explanation Fidelity, Robustness, IoU, AUC | Quantifying explanation quality | Technical validation of XAI method performance |
| Human-Centered Evaluation Tools | System Usability Scale, NASA-TLX, custom clinical assessments | Measuring usability and cognitive load | Assessing clinical utility and workflow integration |
Beyond these technical resources, successful XAI implementation requires access to diverse clinical datasets with appropriate annotations for both prediction targets and explanation ground truth. The increasing availability of public biomedical datasets, such as MIMIC-IV for critical care data, The Cancer Genome Atlas for oncology research, and imaging datasets from the RSNA and ACR, provides valuable resources for developing and validating XAI methods across clinical domains [2] [29]. Additionally, clinical expertise remains an indispensable resource for validating the medical plausibility of explanations and ensuring alignment with clinical reasoning patterns [33].
The taxonomy of XAI methods presented in this technical guide highlights the fundamental distinction between ante-hoc and post-hoc explainability approaches, each with distinct characteristics, implementation considerations, and clinical applications. While ante-hoc methods offer inherent transparency and strong alignment with regulatory requirements, post-hoc techniques provide flexibility in explaining complex, high-performance models that would otherwise remain black boxes. The current dominance of post-hoc methods in clinical applications, particularly model-agnostic approaches like SHAP and visual techniques like Grad-CAM, reflects the field's prioritization of predictive performance alongside explainability needs [32].
Future advancements in XAI for clinical decision support will likely focus on bridging the gap between technical explainability and clinical usefulness. This requires moving beyond simply explaining model mechanics toward generating explanations that align with clinical reasoning processes and support specific decision-making tasks [33]. Promising directions include the development of causal inference models that go beyond correlational explanations to identify cause-effect relationships, personalized explanations adapted to different clinician roles and specialties, and interactive explanation systems that allow clinicians to explore scenarios and counterfactuals [2] [33]. Additionally, addressing the tension between exploration and exploitation mindsets through systems that balance discovery of novel patterns with adherence to established medical knowledge will be crucial for building clinician trust [33].
As XAI methodologies continue to evolve, their successful integration into clinical practice will depend not only on technical advances but also on thoughtful consideration of workflow integration, regulatory frameworks, and the diverse needs of healthcare stakeholders. By adopting a systematic approach to XAI selection and evaluation—guided by the taxonomic framework presented here—researchers and clinicians can work collaboratively to develop AI systems that are not only accurate but also transparent, trustworthy, and ultimately transformative for patient care.
The integration of artificial intelligence (AI) into Clinical Decision Support Systems (CDSS) has significantly enhanced diagnostic precision, risk stratification, and treatment planning in modern healthcare [2]. However, the "black-box" nature of many advanced machine learning (ML) and deep learning (DL) models remains a critical barrier to their clinical adoption [2] [34]. Clinicians are understandably reluctant to base decisions on systems whose reasoning processes they cannot verify or trust, particularly in high-stakes medical scenarios where patient safety is paramount [2] [25].
Explainable AI (XAI) has emerged as a crucial field addressing this transparency gap, with model-agnostic methods representing particularly versatile approaches. These techniques can explain any AI model—from simple logistic regressions to complex neural networks—without requiring knowledge of the model's internal architecture [34]. This technical guide focuses on three powerhouse model-agnostic methods transforming clinical AI research: SHapley Additive exPlanations (SHAP), Local Interpretable Model-agnostic Explanations (LIME), and Counterfactual Explanations.
These methods are becoming indispensable for CDSS research and development, enabling the transparency required for regulatory compliance, clinical trust, and ultimately, safer patient care [2] [35]. Their model-agnostic nature provides researchers with consistent explanation frameworks across different AI architectures, facilitating comparative analysis and validation.
Theoretical Foundations of Model-Agnostic XAI
Defining Model-Agnostic Explainability
Model-agnostic explanation methods operate by analyzing the relationship between a model's inputs and outputs while treating the model itself as a black box [34]. Unlike model-specific methods that rely on internal parameters (e.g., weights in a neural network), model-agnostic techniques function independently of the underlying model architecture [35] [36]. This fundamental characteristic provides several advantages for clinical CDSS research:
- Flexibility: The same explanation method can be applied across different models in a research pipeline
- Consistency: Explanations maintain a uniform interpretation framework regardless of model architecture
- Comparative Analysis: Researchers can objectively compare explanations across different AI approaches
- Implementation Simplicity: No specialized implementation is required for different model types
Taxonomy of XAI Methods
Model-agnostic methods are predominantly post-hoc, meaning they generate explanations after a model has made its predictions [34]. They can provide both local explanations (pertaining to individual predictions) and global explanations (illuminating overall model behavior) [35]. The following table classifies the primary XAI approaches relevant to clinical research:
Table 1: Taxonomy of Explainable AI Methods
| Classification Axis | Categories | Description | Examples |
|---|---|---|---|
| Type | Intrinsic (Ante Hoc) | Model is inherently interpretable by design | Linear Models, Decision Trees |
| Post Hoc | Explanation generated after model prediction | SHAP, LIME, Counterfactuals | |
| Dependency | Model-Specific | Tied to specific model architecture | Grad-CAM (for CNNs), Attention Weights |
| Model-Agnostic | Applicable to any model | SHAP, LIME, Counterfactuals | |
| Scope | Local | Explains individual prediction | LIME, SHAP local plots |
| Global | Explains overall model behavior | SHAP summary plots, PDP |
SHAP (SHapley Additive exPlanations)
Theoretical Framework
SHAP is grounded in cooperative game theory, specifically leveraging Shapley values to quantify each feature's contribution to a model's prediction [37] [36]. The core concept treats features as "players" in a coalition game, with the prediction representing the "payout" [36]. The SHAP value for a feature is calculated as its average marginal contribution across all possible feature permutations [36].
Formally, for a model f and instance x, the SHAP explanation model g is defined as:
g(z') = φ₀ + Σᵢ₌₁ᴹφᵢz'ᵢ
where z' ∈ {0,1}ᴹ represents the presence of simplified input features, φ₀ is the baseline model output with no features, and φᵢ ∈ ℝ is the Shapley value for feature i [36]. These values ensure fair attribution by satisfying key properties including local accuracy (the sum of SHAP values equals the model output) and consistency [36].
Algorithmic Implementation
The computational implementation of SHAP involves evaluating the model output with all possible subsets of features. For complex models with many features, approximation methods like Kernel SHAP are employed to maintain computational feasibility [36]. The following diagram illustrates the SHAP value calculation workflow:
Clinical Research Applications
SHAP has demonstrated significant utility across diverse clinical domains. In Alzheimer's disease (AD) detection, SHAP explanations have identified key biomarkers from MRI data that contribute to classification models, helping validate model focus against known pathological markers [37]. In cardiology, SHAP has been applied to interpret models predicting myocardial infarction (MI) risk from clinical and biomarker data, highlighting contributing factors like specific cardiac enzymes and demographic variables [36].
For perioperative care, a recent study evaluating CDSS for blood transfusion requirements found that while SHAP plots alone moderately improved clinician acceptance compared to results-only outputs, the combination of SHAP with clinical explanations significantly enhanced trust, satisfaction, and usability [38]. This underscores the importance of contextualizing SHAP outputs within clinical knowledge frameworks.
LIME (Local Interpretable Model-agnostic Explanations)
Theoretical Framework
LIME addresses the interpretability challenge through local surrogate modeling [37] [36]. The core principle involves approximating a complex black-box model f with an interpretable surrogate model g (such as linear regression or decision trees) within the local neighborhood of a specific prediction [37]. The algorithm achieves this by:
- Perturbation: Generating synthetic data points around the instance to be explained
- Weighting: Assigning higher weights to points closer to the original instance
- Surrogate Fitting: Training an interpretable model on the weighted perturbed dataset
Mathematically, LIME solves the following optimization problem:
ξ(x) = argmin₍g∈G⁾ L(f, g, πₓ) + Ω(g)
where L measures how unfaithful g is in approximating f in the locality defined by πₓ, and Ω(g) penalizes complexity in g [37]. The objective is to find the simplest interpretable model that maintains high local fidelity to the black-box model's predictions.
Algorithmic Implementation
The LIME algorithm implements this framework through systematic sampling and model fitting. The following workflow outlines the key steps in generating LIME explanations:
Clinical Research Applications
In Alzheimer's disease research, LIME has been applied to explain individual classifications of MRI scans into cognitive normal, mild cognitive impairment, or Alzheimer's dementia categories [37]. The generated explanations highlight specific image regions contributing to each classification, allowing clinicians to verify whether the model focuses on clinically relevant anatomical structures.
LIME has also proven valuable for explaining tabular clinical data predictions. For models predicting hospital readmission risk or disease progression, LIME can identify the specific patient factors (e.g., recent lab values, vital signs, or demographic characteristics) that most influenced an individual prediction [35]. This case-level insight complements global model understanding provided by methods like SHAP.
Counterfactual Explanations
Theoretical Framework
Counterfactual explanations adopt a fundamentally different approach from feature attribution methods like SHAP and LIME. Rather than explaining how input features contributed to a prediction, counterfactuals answer the question: "What minimal changes to the input would lead to a different outcome?" [39] [40]. This contrastive approach aligns naturally with clinical reasoning, where clinicians often consider what factors would need to change to alter a patient's prognosis or diagnosis.
Formally, for a model f and input x with prediction f(x) = y, a counterfactual explanation x' satisfies f(x') = y' where y' ≠ y, while minimizing a distance function d(x, x') [40]. The distance metric ensures the counterfactual is both sparse (requiring few changes) and plausible (representing realistic data instances) [39].
Algorithmic Implementation
Generating counterfactuals involves optimization under constraints, with specific implementations varying by data modality. The following workflow illustrates the counterfactual generation process for molecular data using the MMACE (Molecular Model Agnostic Counterfactual Explanations) approach:
Clinical Research Applications
Counterfactual explanations have shown particular promise in medical imaging and diagnostic applications. In a study on pediatric posterior fossa brain tumors, researchers used counterfactuals to understand how minimal changes in MRI features would transform a tumor's classified subtype [39]. This approach helped identify the most discriminative features between tumor types and provided a novel method for tumor type estimation prior to histopathological confirmation.
Beyond explanation, counterfactuals have been explored for data augmentation in clinical datasets, particularly for addressing class imbalance by generating synthetic examples of underrepresented classes [39]. This dual utility for both explanation and data enhancement makes counterfactuals particularly valuable for clinical ML research with limited data availability.
Comparative Analysis and Research Guidelines
Method Comparison
Table 2: Comparative Analysis of SHAP, LIME, and Counterfactual Explanations
| Characteristic | SHAP | LIME | Counterfactuals |
|---|---|---|---|
| Theoretical Basis | Game Theory (Shapley values) | Local Surrogate Modeling | Causal Inference & Manipulability |
| Explanation Scope | Local & Global | Local Only | Local & Contrastive |
| Explanation Output | Feature importance values | Feature importance weights | Minimal change recommendations |
| Actionability | Moderate (shows contributors) | Moderate (shows contributors) | High (shows required changes) |
| Clinical Alignment | Medium | Medium | High (mirrors clinical reasoning) |
| Computational Load | High (exponential in features) | Medium (depends on perturbations) | Medium to High (optimization problem) |
| Key Strengths | Strong theoretical guarantees, consistent explanations | Intuitive local approximations, fast for single predictions | Highly actionable, naturally understandable |
| Key Limitations | Computationally expensive, feature independence assumption | No global perspective, sensitive to perturbation strategy | May generate unrealistic instances, optimization challenges |
Practical Implementation Considerations
When implementing these methods in clinical CDSS research, several practical considerations emerge:
- Feature Dependencies: Both SHAP and LIME assume feature independence, which is frequently violated in clinical data [36]. Researchers should assess feature correlations and consider dimensionality reduction techniques when appropriate.
- Model Dependency: Despite being model-agnostic, the explanations generated can vary across different models trained on the same data [36]. This underscores the importance of evaluating explanations in the context of specific model architectures.
- Clinical Contextualization: Empirical studies demonstrate that technical explanations alone (SHAP plots) are less effective than those combined with clinical interpretation [38]. Researchers should design explanation interfaces that integrate technical outputs with clinical knowledge frameworks.
Evaluation Metrics and Validation
Robust evaluation of XAI methods in clinical research should encompass both computational and human-centered metrics:
- Explanation Fidelity: Measures how accurately the explanation reflects the model's reasoning process, typically assessed through fidelity measures on perturbed inputs.
- Clinical Plausibility: Domain expert evaluation of whether highlighted features or counterfactual changes align with medical knowledge [34].
- User Trust and Satisfaction: Quantified through structured questionnaires and studies with clinical end-users [38] [34].
- Decision Impact: Assessment of how explanations influence clinical decision-making, measured through metrics like Weight of Advice (WOA) [38].
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Computational Tools for XAI Research in Clinical CDSS
| Tool/Resource | Primary Function | Key Features | Implementation Notes |
|---|---|---|---|
| SHAP Library (Python) | SHAP value calculation | Unified framework with model-specific optimizations, multiple visualization options | Use TreeSHAP for tree-based models for exponential speed improvement |
| LIME Package (Python) | Local surrogate explanations | Supports tabular, text, and image data; customizable perturbation parameters | Carefully tune kernel width parameter for optimal local approximation |
| Alibi Explain (Python) | Counterfactual generation | Model-agnostic counterfactuals with constraints; support for tabular, text, and image data | Implement validity checks for generated counterfactuals in clinical domains |
| Captum (PyTorch) | Model interpretability | Unified library for multiple attribution methods; model-specific capabilities | Particularly valuable for neural network architectures |
| Quantus (Python) | XAI evaluation | Comprehensive metrics for explanation quality assessment | Use for standardized evaluation across multiple XAI methods |
| Medical Imaging Toolkits (e.g., ITK, MONAI) | Medical image preprocessing | Domain-specific preprocessing and normalization | Essential for handling DICOM formats and medical image standards |
SHAP, LIME, and counterfactual explanations represent three foundational pillars of model-agnostic explainability in clinical CDSS research. Each method offers distinct advantages: SHAP provides theoretically grounded feature attributions, LIME delivers intuitive local approximations, and counterfactuals generate actionable change requirements. Their complementary strengths suggest that a hybrid approach—selecting methods based on specific clinical use cases and explanation needs—may yield the most comprehensive insights.
As the field advances, key challenges remain in standardizing evaluation metrics, improving computational efficiency, and enhancing the clinical relevance of explanations [2] [34]. Future research directions should focus on developing more dialogic explanation systems that engage clinicians in iterative questioning [25], integrating multimodal data sources, and establishing rigorous validation frameworks that assess both technical performance and clinical utility. By advancing these model-agnostic powerhouses, researchers can accelerate the development of transparent, trustworthy, and clinically actionable AI systems that truly augment medical decision-making.
The integration of Artificial Intelligence (AI) into clinical decision support systems (CDSSs) has significantly enhanced diagnostic precision, risk stratification, and treatment planning [2]. However, the "black-box" nature of many deep learning models remains a critical barrier to their clinical adoption, as physicians are often reluctant to rely on system recommendations without understanding the underlying reasoning [2] [8]. This challenge has spurred intense interest in explainable AI (XAI), which aims to make AI systems more transparent, interpretable, and accountable [2].
Among the various XAI techniques, visual explanation methods have emerged as particularly valuable for medical imaging applications. Saliency maps, and specifically Gradient-weighted Class Activation Mapping (Grad-CAM), have become potent post-hoc explainability tools that provide crucial insights into how models make decisions based on input images [41]. These techniques generate visual representations highlighting the image regions most relevant to a model's predictions, enabling clinicians to verify that the AI system is focusing on clinically relevant anatomical structures and pathological features [41] [42].
The importance of XAI in healthcare extends beyond technical necessity to legal and ethical requirements. Regulatory frameworks increasingly emphasize the "right to explanation," making it essential for AI decisions to be auditable and comprehensible in clinical settings where human oversight and accountability are paramount [2]. This review provides a comprehensive technical examination of Grad-CAM and saliency map methodologies within medical imaging, detailing their implementation, quantitative performance, and integration into clinical workflows to support the broader goal of developing trustworthy AI for healthcare.
Technical Foundations of Saliency Methods
Core Principles and Definitions
Saliency methods represent a class of XAI techniques that attribute a model's predictions to specific regions in the input data. In medical imaging, these methods produce heatmap-like visualizations superimposed on original images, allowing clinicians to understand which areas most strongly influenced the AI system's decision [41]. The fundamental value proposition of saliency maps lies in their ability to bridge the gap between complex, high-dimensional deep learning representations and human-interpretable visual explanations.
These methods can be broadly categorized as either gradient-based or gradient-free. Gradient-based methods, including Grad-CAM and its variants, utilize the gradients flowing backward through the model to determine feature importance [41] [8]. Gradient-free techniques, such as ScoreCAM, rely on forward passes through the network while perturbing inputs to assess the impact on predictions [41]. A third category, propagation-based methods like Layer-Wise Relevance Propagation (LRP), redistributes the output prediction backward through the network using specific propagation rules [8].
The Grad-CAM Algorithm
Grad-CAM has emerged as one of the most widely adopted saliency methods in medical imaging due to its architectural flexibility and high-quality visualizations [42]. The algorithm generates localization maps by leveraging the gradient information flowing into the final convolutional layer of a convolutional neural network (CNN).
The core Grad-CAM computation can be formalized as follows. For a target class (c), the importance weight (a_k^c) for the (k)-th feature map is obtained through gradient global average pooling:
[ ak^c = \frac{1}{Z} \sumi \sumj \frac{\partial y^c}{\partial A{ij}^k} ]
where (y^c) is the score for class (c), (A^k) represents the activation map of the (k)-th feature channel, and (Z) denotes the number of pixels in the feature map. These weights capture the importance of the (k)-th feature map for the target class (c) [42].
The final Grad-CAM localization map (L_{\text{Grad-CAM}}^c) is then computed as a weighted combination of the activation maps, followed by a ReLU operation:
[ L{\text{Grad-CAM}}^c = \text{ReLU}\left(\sumk a_k^c A^k\right) ]
The ReLU function ensures that only features with a positive influence on the target class are visualized [42]. This resulting heatmap is typically upsampled to match the input image dimensions and overlaid on the original medical image to provide an intuitive visual explanation.
Advanced Saliency Method Variants
Several enhanced variants of the basic Grad-CAM algorithm have been developed to address specific limitations:
- Grad-CAM++ extends Grad-CAM by applying weighted averaging of gradients and additional weighting terms to better capture the importance of multiple occurrences of an object within an image [41].
- ScoreCAM adopts a gradient-free approach by performing forward passes with perturbed inputs, making it less susceptible to gradient saturation issues that can affect gradient-based methods [41].
- XRAI (eXplainable Representation through AI) segments images into regions and assesses importance through region merging, often producing more coherent and semantically meaningful explanations [41].
Quantitative Performance Comparison
The effectiveness of saliency methods can be evaluated using both quantitative metrics and qualitative assessments. Quantitative evaluations often employ metrics such as Accuracy Information Curves (AICs) and Softmax Information Curves (SICs), which measure the correlation between saliency map intensity and model predictions [41].
Performance Across Medical Imaging Modalities
Table 1: Performance Metrics of Saliency Methods Across Different Medical Imaging Applications
| Medical Application | Dataset | Best Performing Methods | Key Quantitative Results | Reference |
|---|---|---|---|---|
| COVID-19 Detection | Chest X-ray | ScoreCAM, XRAI | Higher AUC in AIC analysis: ScoreCAM (0.82), XRAI (0.79) | [41] |
| Brain Tumor Classification | MRI | GradCAM, GradCAM++ | Focused attribution maps with clinical interpretability | [41] |
| Lung Cancer Staging | CT Scans (IQ-OTH/NCCD) | Grad-CAM with EfficientNet-B0 | Model accuracy: 99%, Precision: 99%, Recall: 96-100% across classes | [43] |
| HAPE Diagnosis | Chest X-ray | Grad-CAM with VGG19 | Validation AUC: 0.950 for edema detection | [44] |
| Breast Cancer Metastases | Histopathological (PatchCamelyon) | Grad-CAM, Guided-GradCAM | Sensitivity to natural perturbations, correlation with tumor evidence | [45] |
Faithfulness Evaluation with Realistic Perturbations
Recent research has developed more sophisticated evaluation methodologies for assessing the faithfulness of saliency maps. One approach introduces natural perturbations based on oppose-class substitution to study their impact on adapted saliency metrics [45].
In studies using the PatchCamelyon dataset of histopathological images, researchers implemented three perturbation scenarios:
- NN: Normal tissue perturbation added to normal tissue image
- NT: Normal tissue perturbation added to tumor tissue image
- TN: Tumor tissue perturbation added to normal tissue image
Results demonstrated that Grad-CAM, Guided-GradCAM, and gradient-based saliency methods are sensitive to these natural perturbations and correlate well with the presence of tumor evidence in the image [45]. This approach provides a solution for validating saliency methods without introducing confounding variables through artificial noise.
Table 2: Evaluation Metrics for Saliency Map Faithfulness
| Evaluation Approach | Key Metrics | Saliency Methods Tested | Findings | Reference |
|---|---|---|---|---|
| Realistic Perturbations | Performance change with oppose-class regions | Grad-CAM, Guided-GradCAM, Gradient-based | Methods sensitive to natural perturbations; correlated with tumor evidence | [45] |
| Accuracy Information Curves (AICs) | AUC of accuracy vs. saliency intensity | ScoreCAM, XRAI, GradCAM, GradCAM++ | ScoreCAM and XRAI most effective in retaining relevant regions | [41] |
| Softmax Information Curves (SICs) | Correlation with class probabilities | Multiple saliency methods | Variability with instances of random masks outperforming some methods | [41] |
| Clinical Ground Truth | Overlap with radiologist annotations | Grad-CAM | High overlap with clinically relevant regions in COVID-19 cases | [42] |
Experimental Protocols and Implementation
Standardized Experimental Workflow
Implementing saliency methods in medical imaging follows a systematic workflow encompassing data preparation, model training, explanation generation, and validation. The following diagram illustrates a comprehensive pipeline for developing and validating an explainable AI system for medical image classification:
Detailed Protocol for COVID-19 Detection from Chest X-Rays
The following protocol outlines a typical experimental setup for implementing Grad-CAM in medical image analysis, based on published COVID-19 detection studies [42]:
1. Data Preparation and Preprocessing
- Collect chest X-ray images from publicly available datasets, ensuring balanced representation across classes (Normal, Pneumonia, COVID-19)
- Apply Contrast Limited Adaptive Histogram Equalization (CLAHE) to enhance image contrast and reduce noise
- Resize images to match input dimensions of pre-trained models (typically 224×224 or 299×299 pixels)
- Normalize pixel values using ImageNet statistics (mean=[0.485, 0.456, 0.406], std=[0.229, 0.224, 0.225])
2. Model Selection and Training
- Utilize pre-trained CNN architectures (ResNet34, ResNet50, EfficientNet-B4, EfficientNet-B5)
- Replace final fully connected layers to match target class numbers
- Employ transfer learning with fine-tuning on medical image dataset
- Train with data augmentation (random horizontal flipping, rotation ±10°, brightness/contrast adjustment)
- Use weighted random sampling to address class imbalance
- Optimize with SGD optimizer (momentum=0.9, weight decay=0.0001) and learning rate 0.01
- Implement early stopping with patience of 10 epochs based on validation loss
3. Grad-CAM Implementation
- Extract activations from the final convolutional layer of the CNN
- Compute gradients of the target class score with respect to the feature maps
- Perform global average pooling on these gradients to obtain neuron importance weights
- Generate the heatmap through weighted combination of activation maps
- Apply ReLU activation to focus on features with positive influence
- Upsample the resulting heatmap to match original image dimensions
- Overlay heatmap on original X-ray using a color jet colormap with transparency adjustment
4. Validation and Evaluation
- Quantitative assessment using Accuracy Information Curves (AICs) and Softmax Information Curves (SICs)
- Qualitative evaluation by radiologists to assess clinical relevance of highlighted regions
- Calculation of localization accuracy through overlap with radiologist annotations
- Faithfulness testing through perturbation analysis
Protocol for Lung Cancer Staging from CT Scans
An alternative implementation for lung cancer staging demonstrates adaptations for CT imaging [43]:
1. Dataset Specifics
- Utilize the IQ-OTH/NCCD lung cancer dataset containing 1,190 CT scans
- Categorize images into three classes: benign, malignant, and normal
- Ensure patient-level separation between training, validation, and test sets
2. Model Development
- Implement EfficientNet-B0 architecture with compound scaling optimization
- Employ multi-stage pipeline: lung segmentation followed by classification
- Use DeepLabV3_ResNet50 for precise lung region segmentation
- Fine-tune pre-trained models on lung cancer-specific dataset
3. Explainability Integration
- Generate Grad-CAM visualizations specifically within segmented lung regions
- Focus explanations on areas with clinically significant nodules or masses
- Provide both classification results and visual explanations for clinician review
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Research Reagents and Computational Tools for Medical Imaging XAI
| Resource Category | Specific Tools/Solutions | Function/Purpose | Example Implementation | |
|---|---|---|---|---|
| Deep Learning Frameworks | PyTorch, TensorFlow, Keras | Model development and training infrastructure | Custom CNN implementation with pre-trained weights | [42] [43] |
| XAI Libraries | Captum, iNNvestigate, tf-keras-grad-cam | Gradient computation and saliency map generation | Grad-CAM implementation with various CNN backbones | [41] [42] |
| Medical Imaging Datasets | COVID-19 Radiography, Brain Tumor MRI, IQ-OTH/NCCD, PatchCamelyon | Benchmarking and validation across modalities | Model training and evaluation on diverse medical images | [46] [41] [43] |
| Pre-trained Models | ResNet, EfficientNet, VGG, MobileNet | Transfer learning foundation | Feature extraction with fine-tuning for medical tasks | [42] [43] [44] |
| Image Processing Tools | OpenCV, scikit-image, CLAHE | Medical image enhancement and preprocessing | Contrast improvement and noise reduction in X-rays | [42] [44] |
| Visualization Libraries | Matplotlib, Plotly, Seaborn | Explanation visualization and result reporting | Heatmap overlay on medical images | [42] [43] |
| Evaluation Metrics | AICs, SICs, Faithfulness Measures | Quantitative assessment of explanation quality | Measuring correlation between saliency and predictions | [41] [45] |
Integration with Clinical Decision Support Systems
The ultimate value of saliency methods in medical imaging lies in their effective integration into clinical decision support systems (CDSSs). This integration requires careful consideration of workflow compatibility, explanation presentation, and trust calibration [2] [8].
Implementation Frameworks
A structured, user-centered framework for XAI-CDSS development should encompass three primary phases [8]:
- User-Centered XAI Method Selection: Choosing appropriate explanation techniques based on clinical context and user needs
- Interface Co-Design: Collaboratively designing explanation presentations with clinical stakeholders
- Iterative Evaluation and Refinement: Continuously assessing and improving explanation usefulness in real-world settings
Workflow Integration Patterns
Successful integration of saliency maps into clinical workflows follows several patterns:
- Real-Time Quality Control: Flagging low-quality medical exams in real-time with visual explanations, enabling technicians to immediately address issues with electrode placement, patient movement, or technical artifacts [47].
- Diagnostic Confidence Support: Providing visual corroboration for AI-generated diagnoses, allowing radiologists to quickly verify that the model is focusing on clinically relevant features [43] [44].
- Training and Education: Serving as educational tools for medical trainees by highlighting subtle radiographic findings that might otherwise be overlooked [42].
Limitations and Future Research Directions
Despite significant advances, several challenges remain in the application of saliency methods to medical imaging.
Technical Limitations
Current saliency methods exhibit important limitations that affect their clinical utility:
- Faithfulness Concerns: Saliency maps may not always faithfully represent the true reasoning process of the model, with instances where random saliency masks surprisingly outperform established methods in certain evaluation metrics [41] [48].
- Sensitivity to Perturbations: While generally robust, saliency methods can be sensitive to natural perturbations in medical images, requiring careful validation [45].
- Class Discrimination Challenges: Some models struggle with intermediate disease classifications despite high performance on clear cases, as seen in HAPE grading where sensitivity for intermediate grades was critically low (0.16 for class 1, 0.37 for class 2) while maintaining high sensitivity for normal (0.91) and severe cases (0.88) [44].
Emerging Research Directions
Future research should focus on addressing these limitations through several promising avenues:
- Multi-Modal Explanation Frameworks: Integrating statistical, visual, and rule-based explanations within unified frameworks to provide complementary insights into model behavior [46].
- Longitudinal Evaluation: Implementing longitudinal studies to assess how explanations affect clinician behavior and trust over time, moving beyond single-interaction evaluations [47].
- Standardized Evaluation Metrics: Developing comprehensive evaluation frameworks that combine qualitative assessment with quantitative metrics like AICs and SICs to more reliably measure explanation quality [41].
- Human-Centered Design: Prioritizing user-centered design approaches that actively involve clinicians in the development of explanation interfaces to ensure clinical relevance and usability [8].
Grad-CAM and saliency maps represent powerful tools for enhancing transparency in AI-assisted medical imaging. By providing visual explanations that highlight regions influencing model predictions, these methods help bridge the gap between complex deep learning systems and clinical reasoning. The technical protocols, performance metrics, and implementation frameworks outlined in this review provide researchers with practical guidance for developing and validating explainable AI systems in medical imaging.
As the field progresses, the integration of these techniques into clinical decision support systems must prioritize both technical robustness and clinical utility. Through continued refinement of explanation methods, comprehensive evaluation frameworks, and thoughtful implementation strategies, explainable AI has the potential to significantly enhance the trustworthiness, adoption, and effectiveness of AI tools in clinical practice, ultimately improving patient care and outcomes.
The integration of Artificial Intelligence (AI) into Clinical Decision Support Systems (CDSS) has significantly enhanced diagnostic precision, risk stratification, and treatment planning across medical specialties [2]. However, the "black-box" nature of many complex AI models, particularly deep learning algorithms, has hindered widespread clinical adoption by obscuring the reasoning behind their predictions [8] [49]. Explainable AI (XAI) addresses this critical barrier by making AI model reasoning transparent, interpretable, and trustworthy for clinicians [16]. In high-stakes medical domains like oncology, cardiology, and critical care, where decisions directly impact patient survival and quality of life, explainability is not merely a technical feature but an ethical and clinical prerequisite [2] [16]. This technical guide synthesizes current evidence and methodologies, presenting detailed case studies of successfully implemented XAI systems to inform researchers, scientists, and drug development professionals engaged in developing transparent, clinically actionable AI tools.
Explainable AI Methodologies and Evaluation Frameworks
Technical Taxonomy of XAI Methods
XAI techniques are broadly categorized into ante hoc (inherently interpretable models) and post hoc (methods applied after model training to explain existing black-box models) [8]. The choice of technique depends on the required explanation scope (global model behavior vs. local individual prediction) and model specificity.
Table 1: Key Explainable AI (XAI) Techniques and Their Clinical Applications
| Category | Method | Description | Example Clinical Use Cases |
|---|---|---|---|
| Interpretable Models (Ante hoc) | Linear/Logistic Regression | Models with parameters offering direct, transparent interpretations [16]. | Risk scoring, resource planning [16]. |
| Decision Trees | Tree-based logic flows for classification or regression [16]. | Triage rules, patient segmentation [16]. | |
| Bayesian Models | Probabilistic models with transparent priors and inference steps [16]. | Uncertainty estimation, diagnostics [16]. | |
| Model-Agnostic Methods (Post hoc) | LIME (Local Interpretable Model-agnostic Explanations) | Approximates black-box predictions locally with simple interpretable models [8] [49]. | Any black-box classifier or regressor [16]. |
| SHAP (SHapley Additive exPlanations) | Uses game theory from cooperative game theory to assign feature importance based on marginal contribution [8] [49]. | Tree-based models, neural networks [16]. | |
| Counterfactual Explanations | Identifies minimal changes to an input instance's features that would alter the model's prediction outcome [8]. | Clinical eligibility, policy decisions [16]. | |
| Model-Specific Methods (Post hoc) | Feature Importance (e.g., Permutation) | Measures decrease in model performance when features are randomly altered or removed [8]. | Random forests, XGBoost [16]. |
| Activation Analysis | Examines neuron activation patterns in deep neural networks to interpret outputs [8]. | Deep neural networks (CNNs, RNNs) [16]. | |
| Attention Weights | Highlights input components (e.g., words in text) most attended to by the model [8]. | Transformer models, NLP tasks [16]. | |
| Grad-CAM (Gradient-weighted Class Activation Mapping) | Generates visual explanations for CNN decisions by highlighting important image regions [2]. | Tumor localization in histology images, MRI analysis [2]. |
A User-Centered Framework for XAI-CDSS Development
Technical XAI solutions often fail due to insufficient attention to real-world clinician needs and workflow integration [8]. A structured, three-phase framework ensures the development of effective and trustworthy XAI-CDSS:
- User-Centered XAI Method Selection: This initial phase involves deeply understanding the clinical decision-making context, the end-user's expertise (e.g., oncologist, cardiologist, intensivist), and their specific explanation needs. The selection of an XAI method is guided by the clinical question—for instance, using SHAP for global risk factor analysis in cardiology or Grad-CAM for localizing tumor regions in oncology imaging [8].
- Interface Co-Design: In this phase, explanations are translated into user-friendly visualizations and alerts integrated seamlessly into the clinical workflow, such as the EHR. This requires iterative prototyping with clinicians to ensure presentations like traffic-light systems (green/yellow/red) or heatmaps are intuitive and actionable without increasing cognitive load [50] [8].
- Iterative Evaluation and Refinement: The final phase employs robust, multi-faceted evaluation methodologies that move beyond retrospective accuracy metrics. It assesses the system's impact on clinical workflow, its ability to support calibrated trust (preventing both over-reliance and under-reliance), and ultimately, its effect on diagnostic/therapeutic errors and patient outcomes in real-world settings [51] [8].
Case Studies in Oncology
ArteraAI: A Predictive and Prognostic Multimodal Tool for Prostate Cancer
Clinical Problem: Determining which patients with localized, intermediate-risk prostate cancer will benefit from adding short-term androgen deprivation therapy (ADT) to radiotherapy, thereby avoiding unnecessary toxicity in those unlikely to benefit [50].
XAI Solution and Methodology: The ArteraAI Prostate Test is a multimodal AI model that integrates digitized biopsy histology images with clinical variables to predict long-term outcomes and therapeutic benefit [50].
- AI Model: A deep learning algorithm trained and validated on thousands of patients from large randomized phase III trials with long-term follow-up [50].
- XAI Technique: The model provides a personalized risk report. While the specific XAI technique is not explicitly named, the output is a clear, evidence-based stratification that clinicians can interpret. It functions as a prognostic and predictive adjunct, identifying distinct patient subgroups [50].
- Experimental Protocol: The model was developed using datasets from prospective clinical trials. Performance was evaluated by comparing its discriminatory performance for endpoints like progression and metastasis against conventional NCCN-style risk grouping. The key evaluation metric was the relative improvement in the model's ability to separate higher-risk from lower-risk patients [50].
Results and Clinical Impact: The ArteraAI model demonstrated a 9–15% relative improvement in discriminatory performance compared to traditional clinical risk tools [50]. It successfully identified a biologically distinct subgroup of intermediate-risk patients who derived significant benefit from ADT, while another subgroup gained little, allowing for personalized treatment intensification or de-escalation [50]. This high level of evidence led to its incorporation into the NCCN Clinical Practice Guidelines in Oncology for Prostate Cancer in 2024, marking a significant milestone for AI-based biomarkers [50].
H&E Slide-Based Predictors for NSCLC Immunotherapy Response
Clinical Problem: Only 20-30% of patients with advanced non-small cell lung cancer (NSCLC) experience durable benefit from costly immune checkpoint inhibitors (ICI). Existing biomarkers like PD-L1 expression and tumor mutational burden (TMB) are imperfect predictors [50].
XAI Solution and Methodology: Research-stage deep learning models analyze routine H&E-stained pathology slides to detect hidden morphologic and microenvironmental patterns predictive of ICI response [50].
- AI Model: Deep learning algorithms (e.g., Convolutional Neural Networks - CNNs) applied to digitized H&E tumor specimens [50].
- XAI Technique: Model-specific visual explanation techniques like Grad-CAM are typically used to generate saliency maps. These heatmaps highlight the specific regions and tissue architectures (e.g., tumor-infiltrating lymphocytes, stromal features) within the H&E slide that most influenced the model's prediction, providing a visual "second opinion" to the pathologist [2].
- Experimental Protocol: In a cited multicenter study, a deep learning model was trained on H&E images from patients treated with ICIs. The model's output was evaluated as an independent predictor of response and progression-free survival. Statistical analysis, such as multivariable Cox regression, was used to assess its predictive power after adjusting for established covariates like PD-L1 status and TMB [50].
Results and Clinical Impact: The H&E-based AI model emerged as an independent predictor of response to PD-1/PD-L1 inhibitors and progression-free survival, even after adjusting for standard clinical and molecular biomarkers [50]. If prospectively validated, such a tool could help oncologists identify patients with a low chance of responding to ICIs before starting treatment, allowing for earlier pivot to alternative strategies [50].
Table 2: Summary of Oncology XAI Case Studies
| Case Study | Clinical Problem | AI/XAI Methodology | Key Performance Outcome | Clinical Implementation Status |
|---|---|---|---|---|
| ArteraAI Prostate Test | Personalizing therapy for intermediate-risk prostate cancer [50]. | Multimodal DL (histology + clinical data) with interpretable risk reports [50]. | 9-15% relative improvement in risk discrimination vs. standard tools [50]. | Incorporated into NCCN guidelines (2024) [50]. |
| NSCLC Immunotherapy Predictor | Predicting response to immunotherapy in lung cancer [50]. | CNN on H&E slides with visual explanations (e.g., Grad-CAM) [50] [2]. | Independent predictor of response and survival after adjusting for PD-L1, TMB [50]. | Research-stage, requires prospective validation [50]. |
Case Study in Cardiology
XAI-HD: A Hybrid Framework for Heart Disease Detection
Clinical Problem: Cardiovascular disease (CVD) remains a leading global cause of death. Traditional risk scores like the Framingham Risk Score rely on simplistic linear assumptions and struggle with the complex, nonlinear interactions among diverse patient risk factors [49]. Furthermore, high-accuracy AI models often lack transparency, eroding clinician trust [49].
XAI Solution and Methodology: The XAI-HD framework is a comprehensive approach designed for accurate and interpretable heart disease detection [49].
- AI Model: The framework integrates and compares multiple classic ML (e.g., Decision Trees, Random Forests) and DL models. It employs a rigorous preprocessing pipeline to handle missing data, inconsistent feature scaling, and encoding [49].
- XAI Technique: The framework incorporates post-hoc, model-agnostic methods, specifically SHAP and LIME, for Feature Importance Analysis (FIA). SHAP provides a unified measure of feature importance globally and for individual predictions, while LIME creates local surrogate models to explain single instances [49].
- Experimental Protocol:
- Data Preparation: Multiple public heart disease datasets (CHD, FHD, SHD) are used. The pipeline includes advanced class-balancing techniques (e.g., SMOTE, ADASYN, SMOTEENN) to address data imbalance [49].
- Model Training and Evaluation: Multiple ML/DL models are trained and compared using performance metrics (Accuracy, Precision, Recall, F1-Score). The Wilcoxon signed-rank test is used for statistical validation of performance gains [49].
- Explainability Analysis: The best-performing model is analyzed using SHAP and LIME. SHAP summary plots display global feature importance, and force/waterfall plots explain individual predictions, identifying key contributing factors like cholesterol levels, blood pressure, and age [49].
Results and Clinical Impact: The XAI-HD framework demonstrated a 20-25% reduction in classification error rates compared to traditional ML-based models across the evaluated datasets [49]. By providing clear insights into the contribution of risk factors, the framework fosters trust and facilitates early intervention strategies. Its design for seamless integration into EHRs and hospital decision support systems highlights its practical feasibility for real-world cardiac risk assessment [49].
Case Studies in Critical Care
Sepsis Prediction and Management in the ICU
Clinical Problem: Sepsis is a life-threatening condition requiring early detection and intervention to reduce mortality. However, its early signs can be subtle and masked by other conditions, leading to delayed diagnosis and treatment [51].
XAI Solution and Methodology: AI-based CDSS are being developed to predict sepsis onset hours before clinical recognition, with explainability being critical for ICU staff to trust and act upon the alerts [51] [2].
- AI Model: Various models are used, including gradient boosting models and recurrent neural networks (RNNs/LSTMs) capable of handling temporal data from Electronic Health Records (EHRs) and vital sign monitors [2].
- XAI Technique: SHAP and LIME are prominently used to explain sepsis predictions. For example, when a model flags a patient as high-risk, SHAP can display a breakdown showing which factors (e.g., elevated lactate, low blood pressure, high white blood cell count) contributed most to the alert and to what magnitude [2] [16]. Some research also explores causal inference models to move beyond correlation and suggest causal relationships behind clinical deterioration [2].
- Experimental Protocol: Models are trained on large, retrospective ICU datasets containing vital signs, lab results, and patient demographics. They are tasked with predicting sepsis onset (e.g., defined by Sepsis-3 criteria) within a specific time window. Performance is evaluated using metrics like Area Under the Receiver Operating Characteristic Curve (AUC). In deployment, real-world impact is measured by comparing outcomes like hospital stay duration and mortality between cohorts using the CDSS versus standard care [51].
Results and Clinical Impact: Studies have shown that well-designed CDSS for sepsis can lead to earlier treatment initiation, shorter hospital stays, and reduced mortality [51]. The integration of XAI is fundamental to this success. For instance, one scenario illustrated that using SHAP values to explain a high-risk prediction for post-surgical complications allowed clinicians to validate the model's output against the clinical context, recognizing when it might be misled by outliers, thereby reducing potential harm from over-reliance [16].
The Scientist's Toolkit: Essential Research Reagents and Materials
The development and validation of XAI-CDSS require a suite of computational tools, datasets, and evaluation frameworks. The following table details key "research reagents" essential for work in this field.
Table 3: Essential Research Reagents and Computational Tools for XAI-CDSS Development
| Tool/Resource | Type | Primary Function in XAI-CDSS Research |
|---|---|---|
| SHAP (SHapley Additive exPlanations) | Software Library | Quantifies the contribution of each input feature to a model's prediction for both global and local interpretability [2] [49]. |
| LIME (Local Interpretable Model-agnostic Explanations) | Software Library | Creates local, surrogate interpretable models to approximate and explain individual predictions from any black-box model [2] [49]. |
| Grad-CAM | Algorithm | Generates visual explanations for Convolutional Neural Networks (CNNs) by highlighting important regions in input images [2]. |
| Public Clinical Datasets (e.g., MIMIC-IV) | Data Resource | Provides de-identified ICU patient data (vitals, labs, notes) for training and validating models in critical care [2]. |
| Electronic Health Record (EHR) System | Data Infrastructure/Platform | The primary source of real-world patient data and the key platform for integrating CDSS into clinical workflows [50] [51]. |
| Scikit-learn, XGBoost, PyTorch/TensorFlow | Software Libraries | Core libraries for implementing a wide range of machine learning and deep learning models [49]. |
| Counterfactual Explanation Generators | Software Library/Algorithm | Identifies minimal changes to patient features that would alter a model's decision, helping clinicians understand "what-if" scenarios [8]. |
The case studies presented in this guide demonstrate that Explainable AI is transitioning from a theoretical necessity to a clinically impactful component of modern CDSS. In oncology, tools like ArteraAI show that XAI can achieve guideline-level evidence for personalizing life-altering cancer therapies [50]. In cardiology, frameworks like XAI-HD prove that transparency can be systematically engineered into diagnostic AI without sacrificing accuracy, significantly reducing error rates [49]. In critical care, the application of SHAP and LIME for sepsis prediction provides ICU teams with the actionable insights needed to trust and act upon AI-generated alerts, ultimately improving patient safety and outcomes [51] [16].
The future of XAI-CDSS hinges on moving beyond technical performance metrics and embracing a user-centered, holistic development approach. This involves co-designing interfaces with clinicians, conducting rigorous prospective trials to validate clinical utility, and standardizing evaluation metrics for explanation quality. As the field evolves, fostering collaboration between clinicians, AI researchers, and regulatory bodies will be paramount to ensuring that these powerful tools are deployed responsibly, ethically, and effectively to augment clinical expertise and improve patient care across all medical specialties.
Overcoming Adoption Hurdles: Tackling Technical, Human, and Ethical Challenges in XAI-CDSS
The integration of Artificial Intelligence (AI) into Clinical Decision Support Systems (CDSS) has significantly enhanced diagnostic precision, risk stratification, and treatment planning [2]. However, a critical barrier persists: the "black-box" nature of many AI models, which provide predictions without transparent reasoning [8]. Explainable AI (XAI) aims to bridge this transparency gap, yet a fundamental disconnect often remains between the technical explanations generated by XAI methods and the cognitive processes of clinicians [52]. This usability gap hinders trust and adoption, limiting the potential of AI to improve patient care. Framed within broader XAI research for CDSS, this technical guide analyzes the roots of this gap and presents a structured framework and evaluation methodologies to bridge these disparate worlds, ensuring that XAI systems are not only technically sound but also clinically coherent and usable.
Analyzing the Divergence: Developer and Clinician Mental Models
A longitudinal multi-method study involving 112 developers and clinicians co-designing an XAI solution for a neuro-intensive care unit revealed three key divergences in their mental models [52]. These differences lie at the heart of the usability gap.
Table 1: Contrasting Mental Models of Developers and Clinicians [52]
| Aspect | Developer Mental Model | Clinician Mental Model |
|---|---|---|
| Primary Goal | Model Interpretability: Revealing the model's internal decision-making logic. | Clinical Plausibility: Demonstrating how the result aligns with the patient's clinical context and established medical knowledge. |
| Source of Truth | The data and the model's learned patterns. | The patient as a holistic entity, including non-quantifiable factors from physical examination and clinical intuition. |
| Knowledge Focus | Exploration of new, data-driven patterns and relationships. | Exploitation of established, evidence-based medical knowledge and clinical guidelines. |
These divergent models lead to mismatched expectations. Developers, focusing on model interpretability, might provide explanations like Shapley values to detail feature contributions [52]. Clinicians, in contrast, find such technical details unhelpful for their core need: verifying clinical plausibility. They require explanations that answer context-specific questions such as, "Do these results make sense for my patient?" and "If I administer this medication, will the risk change?" [52]. Furthermore, clinicians rely on a broader source of truth, integrating data-driven predictions with direct patient examination findings (e.g., paralysis, aphasia) that are often absent from model inputs [52]. This highlights the necessity for XAI to integrate into, rather than replace, the clinician's cognitive workflow.
A Structured Framework for Bridging the Usability Gap
To address these divergences, a user-centered, three-phase framework for XAI-CDSS development is proposed, moving from method selection to integration and evaluation [8].
Phase 1: User-Centered XAI Method Selection
The choice of XAI technique must be driven by the clinical question and the user's needs. Technical XAI methods are broadly categorized as ante hoc (inherently interpretable) or post hoc (providing explanations after a prediction) [8]. Post hoc methods can be further classified as shown below.
Diagram 1: A taxonomy of post hoc XAI methods, critical for selecting the right approach based on model specificity, explanation scope, and type [8].
Phase 2: Interface and Workflow Co-Design
The presentation of explanations is as important as their technical generation. Effective design must align with clinical workflows and cognitive processes.
- Workflow Integration: XAI outputs must be embedded within the clinician's existing workflow, ideally integrated directly into Electronic Health Record (EHR) systems to avoid context switching [52]. In high-acuity settings, explanations must be consumable within minutes, not hours [52].
- Tailored Explanation Presentation: Different clinical scenarios and user roles demand different explanations. The interface should layer information, providing a quick overview (e.g., a risk score with key contributing factors) with options to drill down into more detailed, interactive explanations for those who need them [52] [8].
- Causal and Counterfactual Explanations: To address the clinician's need for clinical plausibility, explanations should move beyond correlation to suggest causation. Counterfactual explanations ("What minimal changes would alter the outcome?") and causal inference models align closely with clinical reasoning [2] [8].
Phase 3: Iterative Evaluation and Refinement
Rigorous, multi-faceted evaluation is essential. This involves assessing both the system's technical performance and its human-centric impact.
Table 2: Multidimensional Evaluation Framework for XAI-CDSS [7]
| Dimension | Evaluation Metric | Methodology |
|---|---|---|
| Explanation Quality | Fidelity (how well the explanation approximates the model), Robustness, Simplicity. | Quantitative metrics (e.g., fidelity scores, explanation similarity measures like cosine similarity). |
| User Trust & Understanding | Perceived trustworthiness, interpretability, and comprehension of the explanation. | Subjective ratings via surveys, think-aloud protocols, and structured interviews. |
| Usability & Clinical Impact | Ease of use, integration into workflow, impact on diagnostic accuracy and decision-making. | Observational studies, task-completion analysis, and measurement of clinical outcome changes. |
| Behavioural Change | Calibration of trust (preventing over-reliance or automation bias). | Analysis of decision patterns, such as negotiation between clinician judgment and AI recommendations. |
Experimental Protocols for Evaluating XAI in Clinical Contexts
To ensure robust validation, specific experimental protocols should be employed. A systematic review highlights the importance of mixed-method evaluations that combine technical and human-centred assessments [7].
Protocol 1: Technical Fidelity and Plausibility Assessment
Objective: To quantitatively measure the faithfulness and clinical relevance of XAI explanations. Methodology:
- Fidelity Calculation: For a given model prediction and its explanation, perturb input features deemed important by the explanation and measure the change in the model's output. High fidelity is indicated by a significant output change when important features are altered [7].
- Plausibility Evaluation: Present explanations to a panel of clinical domain experts. Use Likert scales or ranking exercises to assess whether the highlighted features and their assigned importance align with established medical knowledge and clinical intuition [7]. Outcome Measures: Fidelity scores, plausibility ratings, and explanation similarity measures (e.g., Structural Similarity Index Measure - SSIM) [7].
Protocol 2: In-Situ Usability and Trust Study
Objective: To qualitatively and quantitatively evaluate the integration of the XAI-CDSS into real-world clinical workflows and its impact on user trust. Methodology:
- Study Design: A prospective, observational study in a clinical setting (e.g., ICU, oncology) where the XAI-CDSS is deployed.
- Participants: Clinicians (physicians, nurses) who are end-users of the system.
- Procedure: Clinicians use the system as part of their routine workflow. Data collection includes:
- Pre- and post-task surveys: Measuring perceived trust, usability, and mental workload.
- Think-aloud protocols: Clinicians verbalize their thought process as they interact with the system's explanations.
- Direct observation: Researchers note patterns of use, confusion points, and how explanations are utilized in final decision-making [52] [7].
- Analysis: Thematic analysis of transcribed text and observational notes to identify usability barriers and facilitators. Quantitative analysis of survey data to measure changes in trust and usability scores [52].
The Scientist's Toolkit: Key Research Reagents for XAI-CDSS
The development and evaluation of effective XAI-CDSS require a suite of methodological "reagents".
Table 3: Essential Reagents for XAI-CDSS Research and Development
| Research Reagent | Function in XAI-CDSS Development |
|---|---|
| SHAP (SHapley Additive exPlanations) | A game theory-based model-agnostic method to quantify the contribution of each feature to a single prediction, providing local explanations [2] [8]. |
| LIME (Local Interpretable Model-agnostic Explanations) | Creates a locally faithful, interpretable surrogate model (e.g., linear model) to approximate the predictions of any black-box model for a specific instance [2] [8]. |
| Grad-CAM (Gradient-weighted Class Activation Mapping) | A model-specific technique for convolutional neural networks that produces visual explanations in the form of heatmaps, crucial for imaging data like radiology and pathology [2]. |
| Counterfactual Explanation Generators | Algorithms that generate "what-if" scenarios by identifying the minimal changes to input features required to alter a model's prediction, aligning with clinical reasoning about alternative diagnoses or treatments [2] [8]. |
| Validated User Acceptance Scales | Standardized survey instruments (e.g., measuring performance expectancy, effort expectancy) to quantitatively assess clinicians' intention to use and trust in the system [52]. |
Bridging the usability gap between technical XAI and clinician cognition is a prerequisite for the responsible and effective adoption of AI in healthcare. This requires a fundamental shift from a technology-centric to a human-centric paradigm. Success hinges on recognizing and designing for the divergent mental models of developers and clinicians, formalized through a structured framework of user-centered method selection, workflow-integrated co-design, and iterative, multi-dimensional evaluation. Future research must focus on the longitudinal clinical validation of XAI systems, the development of standardized metrics for explanation quality, and the creation of adaptive explanation interfaces that personalize content based on user role and context. By closing this gap, we can foster a truly collaborative human-AI partnership that enhances clinical decision-making and, ultimately, improves patient outcomes.
The integration of Artificial Intelligence (AI) into Clinical Decision Support Systems (CDSS) represents a transformative shift in modern healthcare, offering unprecedented potential for enhancing diagnostic precision, risk stratification, and treatment planning [2]. However, this technological advancement introduces a critical paradox: while designed to augment clinical capabilities, poorly integrated systems can exacerbate cognitive load, disrupt established workflows, and contribute to clinician burnout [53] [54]. This whitepaper examines the strategic integration of Explainable AI (XAI) into CDSS, framing it as an essential component for achieving this balance. We argue that transparency and interpretability are not merely technical features but fundamental requirements for building trustworthy systems that clinicians can effectively utilize without increasing their cognitive or administrative burdens.
The challenge is substantial. Healthcare organizations face significant validation hurdles in ensuring AI system reliability and safety, a process that can take years and substantial resources [54]. Meanwhile, the "black box" nature of many AI algorithms creates transparency concerns among healthcare providers who need clear explanations of how systems arrive at recommendations to build trust and make informed decisions [54]. Without proper explainability mechanisms, healthcare providers may resist adopting AI tools regardless of their potential benefits [54].
Within this context, XAI emerges as a critical bridge between technological capability and clinical utility. By making AI reasoning processes understandable to human practitioners, XAI addresses fundamental barriers to adoption while ensuring that these systems enhance rather than hinder clinical workflow. This paper provides a comprehensive technical framework for achieving this integration, with specific focus on human-computer interaction principles, trust-building mechanisms, and evaluation methodologies that collectively prevent contributor burnout while optimizing clinical decision support.
The Burnout-Integration Nexus: Understanding the Challenges
The integration of AI-based CDSS into clinical environments presents unique challenges that directly impact clinician workload and satisfaction. Understanding these challenges is prerequisite to developing effective integration strategies that mitigate burnout risk.
Workflow Integration Challenges
Current electronic health record systems often lack seamless integration capabilities with AI tools, creating additional steps in clinical processes rather than streamlining existing processes [54]. Technical infrastructure limitations in many healthcare facilities further pose barriers to smooth AI-CDSS deployment, while data privacy regulations and security requirements add another layer of complexity [54]. These integration challenges manifest in several critical ways:
- Interruption vs. Assistance: Poorly timed alerts and recommendations can disrupt clinical reasoning processes rather than supporting them [55].
- Data Entry Burden: Systems that require structured data entry without optimizing the process may compromise data quality and create documentation burdens [55].
- Cognitive Load Considerations: Complex interfaces and unexplained recommendations increase mental effort, reducing system usability and increasing frustration [55].
The Transparency-Trust Gap
A fundamental barrier to AI adoption in clinical settings stems from the opacity of algorithmic decision-making. Clinicians are understandably reluctant to rely on recommendations from systems they do not fully understand, especially when these decisions impact patients' lives [2]. This opacity directly contributes to workflow inefficiencies as clinicians spend additional time verifying or questioning system recommendations [13]. The "black box" problem fuels skepticism, particularly in high-stakes environments where trust is non-negotiable [56]. This lack of transparency becomes a workflow barrier itself, as clinicians cannot efficiently incorporate recommendations whose reasoning they cannot comprehend.
Explainable AI as a Burnout Mitigation Strategy
Explainable AI addresses core integration challenges by making AI systems more transparent, interpretable, and accountable [2]. XAI encompasses a wide range of techniques, including model-agnostic methods like LIME (Local Interpretable Model-agnostic Explanations) and SHAP (SHapley Additive exPlanations), as well as model-specific approaches such as decision trees, attention mechanisms, and saliency maps like Grad-CAM [2] [34]. These techniques provide critical insights into which features influence a model's decision, how sensitive the model is to input variations, and how trustworthy its predictions are across different contexts [2].
Technical Foundations of XAI
XAI methodologies can be categorized along several dimensions that determine their clinical applicability:
Table 1: Taxonomy of XAI Methods and Clinical Applications
| Categorization | Method Type | Examples | Clinical Applications |
|---|---|---|---|
| Type | Intrinsic (Ante-hoc) | Linear Models, Decision Trees, Attention Weights in Transformers | Chronic disease management, Treatment outcome prediction |
| Post-hoc | SHAP, LIME, Grad-CAM, Counterfactual Explanations | Medical imaging, Sepsis prediction, Risk stratification | |
| Dependency | Model-Specific | Grad-CAM for CNNs, Integrated Gradients | Radiology, Pathology image analysis |
| Model-Agnostic | SHAP, LIME, Partial Dependence Plots | EHR-based prediction, Operational forecasting | |
| Scope | Local | LIME, SHAP, Counterfactual Explanations | Individual patient diagnosis, Treatment planning |
| Global | Partial Dependence Plots, RuleFit | Population health, Protocol development |
XAI-Enhanced Workflow Integration
Effective XAI implementation directly addresses workflow integration challenges through several mechanisms:
- Reduced Cognitive Load: By providing transparent reasoning, XAI reduces the mental effort required to interpret and validate AI recommendations [55]. Explanations aligned with clinical reasoning processes help clinicians quickly understand system recommendations without extensive additional analysis [25].
- Informed Trust Calibration: XAI facilitates appropriate trust by allowing clinicians to assess when to rely on system recommendations and when to question them [13]. This prevents both automation bias (over-reliance) and outright rejection of potentially valuable assistance [53].
- Streamlined Decision Pathways: Integrated explanations help clinicians rapidly incorporate AI insights into their clinical reasoning process, reducing decision time while maintaining critical oversight [2] [54].
The following diagram illustrates how XAI bridges the gap between AI capabilities and clinical workflow needs:
Methodological Framework for Integration
Successful integration of XAI into clinical workflows requires a systematic approach that addresses both technological and human factors. The following framework provides a structured methodology for achieving this balance.
Human-Centered Design Principles
A user-centered design approach is critical for developing XAI systems that clinicians will adopt and trust [8]. This involves:
- Stakeholder Co-Design: Engaging clinicians, nurses, and other healthcare professionals throughout the development process to ensure systems address real clinical needs and workflow constraints [8] [53].
- Contextual Explanation Design: Tailoring explanations to different clinical roles, settings, and time pressures [25]. Emergency department explanations must differ from those in ambulatory care settings.
- Iterative Prototyping and Testing: Conducting usability testing with actual clinicians to refine explanation formats, presentation timing, and content depth [8].
Technical Implementation Protocol
Implementing XAI-CDSS requires careful technical execution. The following protocol outlines key stages for successful deployment:
Table 2: XAI Implementation Protocol for Clinical Environments
| Phase | Key Activities | Stakeholders | Deliverables |
|---|---|---|---|
| Assessment & Planning | Workflow analysis, Requirement gathering, Resource evaluation | Clinical leaders, IT staff, Administrators | Integration roadmap, Resource allocation plan |
| System Selection & Validation | Technical evaluation, Clinical validation, Explanation quality assessment | Clinical champions, Data scientists, Regulatory staff | Validation report, Performance benchmarks |
| Workflow Integration | EHR integration, Interface customization, Alert configuration | Clinical informaticians, UX designers, Clinical staff | Integrated system, User training materials |
| Training & Adoption | Just-in-time training, Scenario-based exercises, Supervised use | Clinical educators, Super users, All end-users | Training completion records, Competency assessment |
| Monitoring & Optimization | Usage analytics, Outcome monitoring, Feedback collection | Quality officers, Clinical leaders, IT support | Performance reports, Optimization recommendations |
Evaluation Framework for XAI-CDSS
Robust evaluation is essential for ensuring XAI systems effectively support clinical workflows without contributing to burnout. The Clinician-Informed XAI Evaluation Checklist with Metrics (CLIX-M) provides a comprehensive framework for assessment [56]:
- Domain Relevance: Explanations should be domain-appropriate for the application task, avoiding redundancy or confusion [56]. Key contributing factors should align with clinical knowledge and consensus.
- Coherence: Evaluates how well the explanation aligns with relevant background knowledge, expert beliefs, and established clinical consensus [56]. Explanations that match clinicians' reasoning boost trust.
- Actionability: Reflects the explanation's ability to support downstream clinical decision-making by enabling the user to take safe, informed, and contextually appropriate actions [56].
- Correctness: Represents the fraction of correct explanations relative to the total number of evaluated samples, measured against available ground truth [56].
The following diagram illustrates the relationship between key evaluation metrics and their impact on clinical outcomes:
Implementing and evaluating XAI-CDSS requires specific methodological tools and frameworks. The following table details essential resources for researchers and developers working in this field.
Table 3: Essential Research Resources for XAI-CDSS Development
| Resource Category | Specific Tools/Methods | Function/Purpose | Application Context |
|---|---|---|---|
| XAI Algorithm Libraries | SHAP, LIME, Captum, Alibi Explain | Generate post-hoc explanations for model predictions | Model debugging, Feature importance analysis |
| Evaluation Toolkits | Quantus, CLIX-M Checklist | Standardized assessment of explanation quality | Validation studies, Comparative analysis |
| Usability Assessment | System Usability Scale (SUS), Think-aloud protocols | Measure interface usability and user experience | Human-centered design iterations |
| Trust Measurement | Trust scales, Behavioral reliance metrics | Quantify clinician trust and acceptance | Adoption studies, System validation |
| Workflow Integration | Time-motion studies, Cognitive task analysis | Assess impact on clinical workflows | Implementation optimization |
| Data Synthesis Platforms | Synthetic EHR generators, Federated learning frameworks | Enable development without compromising patient privacy | Multi-institutional collaboration |
Case Studies and Clinical Applications
Real-world implementations demonstrate how XAI-enabled CDSS can successfully integrate into clinical workflows while mitigating burnout factors.
Sepsis Prediction and Management
In critical care settings, XAI-based sepsis prediction systems have shown significant potential for improving outcomes while supporting clinical workflow. These systems typically employ techniques such as SHAP and attention mechanisms to explain which patient factors (vital signs, laboratory values, clinical observations) contributed to sepsis risk predictions [2] [53]. This transparency allows clinicians to quickly verify system reasoning against their clinical assessment, reducing cognitive load while maintaining appropriate oversight.
Implementation studies highlight several workflow-friendly features:
- Proactive Alerting: Systems provide early warnings (up to 48 hours before critical events) with explanatory context, enabling proactive rather than reactive care [54].
- Integration with Existing Workflows: Successful implementations embed explanations within familiar EHR interfaces, minimizing disruption to established routines [53].
- Actionable Explanations: By highlighting modifiable risk factors, these systems support immediate clinical action rather than simply adding to information overload [56].
Diagnostic Imaging Support
In radiology and pathology, XAI methods such as Grad-CAM and saliency maps provide visual explanations that highlight regions of interest in medical images [2] [25]. These visualizations allow radiologists and pathologists to efficiently verify AI findings against their expert interpretation, creating a collaborative rather than replacement dynamic.
Key integration benefits include:
- Validation Efficiency: Visual explanations enable rapid correlation between AI-identified features and clinical expertise, reducing time spent reconciling discrepancies [25].
- Continuous Learning: Explanations help clinicians understand AI reasoning patterns, facilitating appropriate trust calibration over time [13].
- Workflow Preservation: Implementing explanations within existing PACS workflows minimizes disruption and learning curves [55].
Future Directions and Research Agenda
As XAI continues to evolve, several emerging trends promise to further enhance integration while mitigating burnout:
- Multimodal Explanation Systems: Future XAI systems will need to integrate explanations across diverse data types (imaging, clinical notes, lab values) to provide unified explanatory narratives that match clinical reasoning processes [25].
- Adaptive Explanation Interfaces: Context-aware systems that adjust explanation depth and presentation based on user expertise, clinical setting, and time constraints [25].
- Longitudinal Explanation Frameworks: Moving beyond single-timepoint explanations to provide insights into how patient trajectories and AI reasoning evolve over time [2].
- Dialogic Explanation Systems: Advanced interfaces that support genuine dialogue between clinicians and AI systems, allowing for iterative questioning and exploration of reasoning [25].
The integration of Explainable AI into Clinical Decision Support Systems represents a critical pathway for harnessing AI's potential while safeguarding clinician well-being. By prioritizing transparency, workflow compatibility, and human-centered design, healthcare organizations can implement AI systems that enhance rather than hinder clinical practice. The frameworks, protocols, and evaluation methodologies presented in this whitepaper provide a roadmap for achieving this balance, emphasizing that technological advancement and clinician satisfaction are complementary rather than competing objectives. As XAI methodologies continue to mature, they offer the promise of truly collaborative human-AI clinical environments where technology amplifies expertise without exacerbating burnout.
Mitigating Algorithmic Bias and Ensuring Fairness Across Diverse Patient Populations
The integration of artificial intelligence (AI) into clinical decision support systems (CDSS) promises to revolutionize healthcare through improved diagnostic accuracy, risk stratification, and treatment planning [2]. However, these systems frequently exhibit algorithmic bias that disproportionately disadvantages specific patient populations, potentially perpetuating and exacerbating longstanding healthcare disparities [57] [58]. When AI models are trained on non-representative data or developed without considering population diversity, they can produce differential performance across demographic groups, leading to inequitable clinical outcomes [59] [60]. Understanding the sources of these biases and implementing robust mitigation strategies is therefore paramount for ensuring that medical AI fulfills its promise of equitable, high-quality care for all patients [58].
The challenge of algorithmic bias is particularly acute in clinical settings due to the high-stakes nature of medical decisions and the profound consequences of errors [57]. Bias in medical AI is not merely a technical problem but reflects broader historical inequities and structural oppression embedded within healthcare systems [57]. As such, addressing bias requires both technical solutions and a thoughtful consideration of the ethical, social, and clinical contexts in which these systems operate [58]. This whitepaper provides a comprehensive technical guide for researchers and drug development professionals seeking to identify, mitigate, and prevent algorithmic bias to ensure fairness across diverse patient populations within the context of explainable AI for clinical decision support systems research.
Algorithmic bias in healthcare can originate from multiple sources throughout the AI development lifecycle. Understanding these sources is crucial for developing effective mitigation strategies.
Data-Centric Biases
Data-centric biases arise from problems in the collection, composition, and labeling of training datasets [58]:
- Minority Bias: Occurs when certain patient groups are insufficiently represented in training data, leading to suboptimal model performance for these populations [58]. For example, cardiovascular risk prediction algorithms historically trained primarily on male patient data lead to inaccurate risk assessment in female patients [58].
- Missing Data Bias: Happens when data from protected groups are missing nonrandomly, making accurate predictions difficult for these populations [57]. Patients with lower socioeconomic status often have more missing data in electronic health records (EHRs), causing systematic underestimation of risks [60].
- Informativeness Bias: Occurs when features used for detection are less apparent for certain protected groups [58]. For instance, identifying melanoma from images of patients with dark skin is more challenging than for those with light skin, leading to poorer model performance [58].
- Training-Serving Skew: Arises from mismatches between data used for AI training and data encountered during deployment [58]. This can result from non-representative training data due to selection bias or deployment in populations with different prevalence from training data [58].
Algorithm-Centric and Interaction-Based Biases
Algorithm-centric biases emerge during model development and implementation:
- Label Bias: Occurs when AI training uses inconsistent labels influenced by healthcare disparities rather than universal truths [58]. For example, significant racial bias has been observed in commercially available algorithms that used healthcare costs as a proxy for need, leading to underestimation of Black patients' needs [58].
- Cohort Bias: Develops when AI is trained on traditional or easily measurable groups without considering other protected groups or varying granularity levels [58].
- Automation Bias: The tendency of healthcare professionals to overly rely on AI recommendations, potentially following inaccurate predictions [58].
- Feedback Loop Bias: Occurs when clinicians accept incorrect AI recommendations, causing the algorithm to relearn and perpetuate the same mistakes [60].
Table 1: Real-World Examples of Algorithmic Bias in Healthcare
| Application Area | Bias Manifestation | Impact on Patient Care |
|---|---|---|
| Care Management Algorithms | Underestimation of Black patients' healthcare needs despite more chronic conditions [60] | Black patients were less likely to be flagged as high-risk for care management programs [60] |
| Melanoma Prediction Models | Poor performance on darker skin tones due to training on predominantly light-skinned images [60] | Delayed diagnosis and worse survival rates for patients with darker skin [60] |
| Kidney Function Estimation (eGFR) | Historical use of race coefficient for Black patients [60] | Overestimation of kidney function, delaying diagnosis and treatment of chronic kidney disease [60] |
| Criminal Justice Risk Assessment (COMPAS) | Higher risk scores for African-Americans compared to equally likely to re-offend whites [59] | Longer detention periods while awaiting trial for African-American defendants [59] |
Technical Frameworks for Bias Mitigation
Bias mitigation strategies can be categorized based on their application point in the AI development pipeline: pre-processing, in-processing, and post-processing methods [61].
Pre-Processing Mitigation Methods
Pre-processing methods modify training data to remove biases before model training:
- Relabelling and Perturbation: Disparate impact remover modifies feature values to increase group fairness while preserving rank-ordering within groups [61]. The "massaging" approach ranks dataset instances to determine candidates for relabelling [61].
- Sampling Techniques: Includes up-sampling (duplicating or generating synthetic samples for minority groups) and down-sampling (removing instances from majority groups) [61]. The Synthetic Minority Over-sampling Technique (SMOTE) combines both approaches to balance datasets [61].
- Representation Learning: Methods like Learning Fair Representation (LFR) transform training data by finding latent representations that encode data while minimizing information loss of non-sensitive attributes and removing information about protected attributes [61].
In-Processing and Post-Processing Methods
In-processing methods modify algorithms during training to improve fairness:
- Regularization and Constraints: Add extra terms to loss functions to penalize discrimination or limit allowed bias levels [61]. The Prejudice Remover technique reduces statistical dependence between sensitive features and remaining information [61].
- Adversarial Learning: Trains competing models where one predictor tries to predict the true label while an adversary tries to exploit fairness issues [61]. Adversarial debiasing trains a learner to predict outputs while remaining unbiased for protected variables using equality constraints [61].
- Adjusted Learning: Develops novel algorithms by changing learning procedures of classical approaches [61].
Post-processing methods adjust model outputs after training:
- Classifier Correction: Approaches like Linear Programming (LP) optimally adjust learned predictors to remove discrimination according to equalized odds and opportunity equality constraints [61].
- Output Correction: Methods like Reject Option based Classification (ROC) exploit low-confidence classifier regions to assign favorable outcomes to unprivileged groups and unfavorable outcomes to privileged groups [61].
Explainable AI (XAI) for Bias Detection and Mitigation
Explainable AI (XAI) methods play a crucial role in identifying and mitigating bias by making model reasoning transparent and understandable to clinicians [2] [8]. XAI techniques can be categorized as:
- Ante hoc Methods: Involve models specifically designed to be transparent or 'glass-box' systems with inherently understandable logic, including RuleFit, additive models, fuzzy inference systems, and decision trees [8].
- Post hoc Methods: Explain existing 'black-box' models without inherently understandable logic [8]. These include:
- Model-Agnostic Methods: Such as LIME (Local Interpretable Model-agnostic Explanations) and SHAP (SHapley Additive exPlanations) that can be applied to any model architecture [2] [8].
- Model-Specific Methods: Such as Layer-Wise Relevance Propagation (LRP) for neural networks [8].
- Explanation Scope: Can be global (explaining overall model logic) or local (explaining specific predictions) [8].
XAI supports informed consent, shared decision-making, and the ability to contest or audit algorithmic decisions, making it essential for ethical AI implementation in healthcare [2].
Experimental Protocols for Bias Assessment
Rigorous experimental protocols are essential for comprehensively assessing algorithmic bias in clinical AI systems.
Pre-Implementation Validation Protocols
Technical validation should begin with developing clinical rules based on evidence-based guidelines. As demonstrated by Catharina Hospital, this stage should achieve a positive predictive value (PPV) of ≥89% and a negative predictive value (NPV) of 100% [60].
Therapeutic retrospective validation requires an expert team to review alert relevance. At Peking University Third Hospital, a retrospective analysis of 27,250 records showed diagnostic accuracies of 75.46% for primary diagnosis, 83.94% for top two diagnoses, and 87.53% for top three diagnoses [60].
Prospective pre-implementation validation connects the CDSS to a live electronic health record in a test setting to generate real-time alerts. This stage refines alert timing and workflow integration, with experts determining content, recipients, frequency, and delivery methods [60].
Subgroup Analysis and Performance Disparity Assessment
Comprehensive subgroup analysis should evaluate model performance across diverse patient demographics, including race, ethnicity, gender, age, and socioeconomic status [57]. Key steps include:
- Stratified Data Sampling: Ensure sufficient representation of all subgroups in test datasets [62].
- Disparity Metrics Calculation: Quantify performance differences using metrics such as:
Table 2: Essential Metrics for Algorithmic Bias Assessment in Clinical AI
| Metric Category | Specific Metrics | Interpretation in Clinical Context |
|---|---|---|
| Overall Performance | Accuracy, AUC, F1-score | Standard measures of model effectiveness across entire population [60] |
| Subgroup Performance | Stratified accuracy, sensitivity, specificity | Performance within specific demographic groups (e.g., racial, gender, age) [57] |
| Fairness Metrics | Equalized Odds, Demographic Parity, Statistical Parity | Quantification of equitable performance across groups [61] |
| Clinical Impact | Positive Predictive Value (PPV), Negative Predictive Value (NPV) | Clinical utility and potential impact on patient outcomes [60] |
Continuous Monitoring and Post-Deployment Evaluation
Continuous monitoring is essential as healthcare data and practices evolve [60]. Effective monitoring requires:
- Performance Metrics Tracking: Establish clear, measurable goals aligned with organizational objectives, including user adoption rates, clinical outcomes, and financial impacts [60].
- Feedback Loops: Create formal channels for user feedback to enable iterative improvements [60]. For example, Johns Hopkins University's TREWS (Targeted Real-Time Early Warning System) identified 82% of over 9,800 retrospectively confirmed sepsis cases early over two years [60].
- Regular Updates: Maintain CDSS content and software alignment with the latest medical research, guidelines, and technological advancements [60].
Research Reagents and Computational Tools
Implementing effective bias mitigation requires specialized computational tools and frameworks.
Table 3: Essential Research Reagents and Tools for Bias Mitigation Research
| Tool Category | Specific Tools/Methods | Primary Function | Application Context |
|---|---|---|---|
| Pre-processing Algorithms | Disparate Impact Remover, Massaging, SMOTE, Reweighing, LFR | Adjust training data to remove biases before model training [61] | Data preparation phase for clinical AI development |
| In-processing Algorithms | Prejudice Remover, Exponentiated Gradient, Adversarial Debiasing | Modify learning algorithms to incorporate fairness during training [61] | Model development and training phase |
| Post-processing Algorithms | Linear Programming, Calibrated Equalized Odds, Reject Option Classification | Adjust model outputs after training to ensure fairness [61] | Model deployment and inference phase |
| Explainable AI (XAI) Tools | SHAP, LIME, Grad-CAM, LRP | Provide explanations for model predictions to identify potential biases [2] [8] | Model validation, debugging, and clinical implementation |
| Bias Assessment Frameworks | AI Fairness 360, Fairlearn, Audit-AI | Comprehensive toolkits for measuring and mitigating bias across the AI lifecycle [61] | End-to-end bias evaluation in clinical AI systems |
Mitigating algorithmic bias and ensuring fairness across diverse patient populations requires a comprehensive, multidisciplinary approach spanning the entire AI development lifecycle [57] [58]. Technical solutions must be coupled with thoughtful consideration of ethical, social, and clinical contexts [58]. The integration of explainable AI methods is particularly crucial for making model reasoning transparent and understandable to clinicians, thereby enabling bias detection and appropriate trust calibration [2] [8].
Future efforts should focus on developing standardized bias reporting guidelines, promoting diverse and representative data collection, implementing rigorous validation protocols, and establishing continuous monitoring systems [57] [60]. Additionally, fostering collaboration among clinicians, AI developers, policymakers, and patients is essential for creating equitable AI systems that serve all patient populations effectively [58]. By adopting these strategies, researchers and drug development professionals can help ensure that clinical AI fulfills its potential to improve healthcare outcomes for everyone, regardless of demographic background or social circumstances.
The integration of Artificial Intelligence (AI) into Clinical Decision Support Systems (CDSS) introduces a complex accountability dilemma at the intersection of medico-legal liability and professional identity threats. This whitepaper synthesizes current research to analyze how AI-driven CDSS challenges traditional legal frameworks and physician self-concept. We present a technical analysis of explainable AI (XAI) methodologies as a critical pathway for mitigating these challenges, enabling trustworthy AI adoption while preserving professional autonomy. For researchers and drug development professionals, this review provides structured data on implementation barriers, experimental protocols for evaluating XAI interventions, and a conceptual framework for developing clinically viable, legally compliant AI systems.
The adoption of AI-based CDSS presents two interconnected challenges: redefining medico-legal liability in cases of diagnostic or therapeutic errors involving AI systems, and addressing profound threats to medical professional identity stemming from perceived erosion of clinical autonomy and expertise [63] [64]. CDSS are computational tools designed to assist clinicians in making data-driven decisions by providing evidence-based insights derived from patient data, medical literature, and clinical guidelines [2]. When enhanced with AI and machine learning (ML), these systems can uncover complex patterns in vast datasets with unprecedented speed and precision [8]. However, the opaque "black-box" nature of many advanced AI models creates significant barriers to clinical adoption, primarily due to trust and interpretability challenges [2] [8].
Medical professional identity refers to an individual's self-perception and experiences as a member of the medical profession, encompassing a strong sense of belonging, identification with professional roles and responsibilities, adherence to ethical principles, specialized knowledge, and a high degree of autonomy [63] [64]. This identity is particularly resilient to change, developed through rigorous socialization and refined through practical experience [64]. AI systems that potentially undermine physician expertise or autonomy can trigger identity threats that manifest as resistance to adoption [63] [64]. Simultaneously, established medico-legal frameworks struggle to accommodate decision-making processes that involve both human clinicians and AI systems, creating an accountability gap [65].
Theoretical Framework: Identity Threats and Legal Liability
Dimensions of Professional Identity Threat
Research identifies several dimensions through which AI-based CDSS threatens medical professional identity. Table 1 summarizes the primary identity threat dimensions and their manifestations based on empirical studies.
Table 1: Dimensions of Professional Identity Threat from AI-Based CDSS
| Threat Dimension | Definition | Manifestations | Supporting Evidence |
|---|---|---|---|
| Threat to Professional Recognition | Challenge to the expertise and status position of medical professionals [64]. | Perception that AI may replace unique skills; erosion of professional status and hierarchy [63] [64]. | Medical students experienced stronger identity threats than experienced physicians [64]. |
| Threat to Professional Capabilities | Challenge to the enactment of roles related to medical work itself [64]. | Perceived erosion of autonomy, professional control, and care provider role [63] [64]. | Threats to capabilities directly affected resistance to AI [64]. |
| Threat to Patient Relationship | Challenge to control over patient relationships and trust [63]. | Concern about AI interfering with therapeutic alliance; disruption of clinical workflow [63]. | Identified as one of three key dimensions in systematic review [63]. |
Medical Malpractice Framework
Traditional medical malpractice requires proving four elements: (1) duty to the patient, (2) breach of standard of care (negligence), (3) causation, and (4) damages [65]. The standard of care is defined as what a reasonable physician in the same community with similar training and experience would provide [65]. AI integration complicates each element, particularly in determining the appropriate standard of care when AI recommendations are involved and establishing causation when both human and algorithmic factors contribute to adverse outcomes.
Landmark malpractice cases have historically reshaped medical practice and legal standards. For instance, Canterbury v. Spence (1972) established the informed consent standard requiring doctors to disclose all potential risks that might affect a patient's decision [66]. Helling v. Carey (1974) challenged professional standards by ruling that doctors could be liable even when following customary practice if they failed to perform simple tests that could prevent serious harm [66]. These precedents highlight how legal standards evolve in response to changing medical capabilities, suggesting similar evolution will occur with AI integration.
Explainable AI as a Mitigation Strategy
XAI Methodologies and Technical Approaches
Explainable AI (XAI) encompasses techniques designed to make AI systems more transparent, interpretable, and accountable [2]. These methods are broadly categorized into ante hoc (inherently interpretable) and post hoc (providing explanations after predictions) approaches [8]. Table 2 summarizes prominent XAI techniques relevant to CDSS implementation.
Table 2: XAI Techniques for Clinical Decision Support Systems
| XAI Category | Technical Approach | Clinical Applications | Advantages | Limitations |
|---|---|---|---|---|
| Ante-hoc Methods | RuleFit, Generalized Additive Models (GAMs), decision trees [8]. | Risk prediction models where interpretability is prioritized [8]. | Inherently transparent; no fidelity loss in explanations [8]. | Often lower predictive performance compared to complex models [2]. |
| Post-hoc Model-Agnostic | LIME, SHAP, counterfactual explanations [2] [8]. | Explaining black-box models across various clinical domains [2]. | Applicable to any model; flexible explanation formats [8]. | Approximation errors; computational overhead [2]. |
| Post-hoc Model-Specific | Layer-wise Relevance Propagation (LRP), attention mechanisms, Grad-CAM [2] [8]. | Medical imaging (e.g., highlighting regions of interest) [2]. | High-fidelity explanations leveraging model architecture [8]. | Limited to specific model types [8]. |
Experimental Evidence: XAI Impact on Trust and Identity
Recent experimental studies demonstrate how XAI design features influence trust and identity threats. A scenario-based experiment with 292 medical students and physicians found that explainability of AI-based CDSS was positively associated with both trust in the AI system (β=.508; P<.001) and professional identity threat perceptions (β=.351; P=.02) [67]. This paradoxical finding suggests that while explainability builds trust, it may also make AI capabilities more transparent and thus more threatening to professional identity.
A separate interrupted time series study involving 28 healthcare professionals in breast cancer detection found that high AI confidence scores substantially increased trust but led to overreliance, reducing diagnostic accuracy [68]. These findings highlight the complex relationship between explainability, trust, and clinical performance, suggesting that optimal XAI implementation must balance transparency with appropriate reliance.
Figure 1: Relationship between AI-CDSS process design features, trust, and professional identity threat, based on experimental findings [67]. Path coefficients show significant relationships (p<.05, p<.01, p<.001).
Experimental Protocols and Evaluation Frameworks
Standardized Evaluation Protocol for XAI-CDSS
For researchers evaluating XAI implementations in clinical settings, the following structured protocol provides a methodology for assessing impact on identity threats and trust:
Study Design: Mixed-methods approach combining quantitative measures with qualitative interviews to capture both behavioral and perceptual dimensions.
Participant Recruitment: Stratified sampling across professional hierarchies (medical students, residents, attending physicians) and specialties to identify variation in threat perceptions [63] [64].
Experimental Conditions:
- Control: Conventional CDSS without AI explanations
- Intervention 1: AI-CDSS with basic explainability (feature importance)
- Intervention 2: AI-CDSS with advanced explainability (counterfactuals, clinical concepts)
Primary Outcome Measures:
- Trust in AI system (validated scale)
- Professional identity threat (adapted survey instrument)
- Diagnostic accuracy (clinical cases)
- Agreement with AI recommendations
- Cognitive load (NASA-TLX)
Implementation Timeline: Baseline assessment → Training → System exposure (2 weeks) → Post-implementation assessment → Qualitative interviews.
This protocol enables systematic evaluation of how XAI features influence both clinical decision-making and psychological acceptance barriers.
Research Reagent Solutions
Table 3: Essential Research Materials for XAI-CDSS Evaluation
| Research Tool | Function/Purpose | Implementation Example |
|---|---|---|
| SHAP (SHapley Additive exPlanations) | Quantifies feature contribution to predictions; provides unified approach to explain model output [2] [8]. | Explaining risk factors in sepsis prediction models from EHR data [2]. |
| LIME (Local Interpretable Model-agnostic Explanations) | Creates local surrogate models to explain individual predictions [2] [8]. | Interpreting individual patient treatment recommendations in oncology CDSS [8]. |
| Grad-CAM (Gradient-weighted Class Activation Mapping) | Generates visual explanations for convolutional neural networks [2]. | Highlighting regions of interest in radiological images for diagnosis verification [2]. |
| NASA-TLX (Task Load Index) | Measures cognitive load across multiple dimensions during system use [68]. | Assessing mental demand of interpreting XAI outputs in clinical workflow [68]. |
| Professional Identity Threat Scale | Assesses perceived threats to professional recognition and capabilities [64] [67]. | Measuring identity threat perceptions before and after XAI-CDSS implementation [67]. |
Implementation Pathway: Toward Responsible AI Integration
Successful implementation of AI-CDSS requires addressing both technical and human factors. A user-centered framework encompassing three phases has been proposed: (1) user-centered XAI method selection, (2) interface co-design, and (3) iterative evaluation and refinement [8]. This approach emphasizes aligning XAI with clinical workflows, supporting calibrated trust, and deploying robust evaluation methodologies that capture real-world clinician-AI interaction patterns [8].
Critical implementation considerations include:
- Workflow Integration: Deep integration of AI-generated advice into clinical workflow positively associates with trust (β=.262; P=.009) [67].
- Accountability Structures: System-induced individual accountability (e.g., requiring signature on AI-informed decisions) increases identity threat (β=.339; P=.004) but may be necessary for legal compliance [67].
- Professional Hierarchy: Identity threats manifest differently across experience levels, requiring tailored implementation strategies [63] [64].
Figure 2: Three-phase user-centered framework for implementing XAI in clinical decision support systems, emphasizing iterative design and evaluation [8].
The accountability dilemma presented by AI integration in healthcare represents a critical challenge requiring interdisciplinary solutions. Explainable AI serves as a foundational technology for addressing both medico-legal liability concerns and professional identity threats by making AI decision-making processes transparent and interpretable. However, technical solutions alone are insufficient—successful implementation requires careful attention to workflow integration, accountability structures, and the varying needs of healthcare professionals across different experience levels and specialties.
For researchers and drug development professionals, this analysis highlights the importance of adopting user-centered design principles, developing standardized evaluation protocols, and recognizing the complex relationship between explainability, trust, and professional identity. Future research should focus on validating XAI methods in prospective clinical trials, developing specialized explanation types for different clinical contexts, and creating refined implementation strategies that address the unique concerns of diverse healthcare professional groups.
Measuring Success: Frameworks for Evaluating and Comparing XAI Effectiveness in Clinical Settings
The integration of artificial intelligence (AI) into Clinical Decision Support Systems (CDSS) promises to enhance diagnostic precision, risk stratification, and treatment planning [2]. However, the "black-box" nature of complex machine learning models presents a significant barrier to clinical adoption, fueling skepticism in high-stakes environments where trust is non-negotiable [56] [8]. Explainable AI (XAI) has emerged as a critical field addressing this opacity, making model reasoning more transparent and accessible to clinicians [69].
While predictive accuracy remains necessary, it is insufficient for clinical deployment. Evaluating XAI requires a multidimensional approach beyond traditional performance metrics [7]. This technical guide examines three cornerstone metrics—Fidelity, Understandability, and Actionability—that are essential for assessing whether an XAI method produces trustworthy, clinically useful explanations. These metrics form the foundation for rigorous evaluation frameworks like the Clinician-Informed XAI Evaluation Checklist with Metrics (CLIX-M), which emphasizes domain relevance, coherence, and actionability for clinical applications [56].
Core Metrics for XAI Evaluation
Fidelity: Faithfulness to the Underlying Model
Fidelity, or faithfulness, measures how accurately an explanation reflects the true reasoning process of the black-box model it seeks to explain [70] [7]. A high-fidelity explanation correctly represents the model's internal logic, which is crucial for debugging and establishing trust.
Quantitative Fidelity Metrics
Fidelity is typically assessed through perturbation-based experiments that measure how well the explanation predicts model behavior when inputs are modified. Key quantitative metrics include:
Table 1: Quantitative Metrics for Evaluating Explanation Fidelity
| Metric Name | Experimental Methodology | Interpretation | Key Findings from Literature |
|---|---|---|---|
| Faithfulness Estimate [70] | Iteratively remove top-k important features identified by the XAI method and measure the subsequent drop in the model's prediction score. | A larger performance drop indicates higher fidelity, as the explanation correctly identified critical features. | Considered one of the more reliable metrics; achieves expected results for linear models but shows deviations with non-linear models [70]. |
| Faithfulness Correlation [70] | Compute correlation between the importance scores assigned by the XAI method and the actual impact on model prediction after random feature perturbations. | Positive correlation indicates fidelity; stronger correlation suggests better faithfulness. | Performs well with linear models but faces reliability challenges with complex, non-linear models common in healthcare AI [70]. |
| Fidelity (Completeness) [69] | Assess the explanation model's ability to mimic the black-box model's decisions across instances. | Measures the extent to which the explanation covers the model's decision logic. | Used in structured evaluations of methods like LIME and Anchor; part of a suite of metrics including stability and complexity [69]. |
Experimental Protocol for Fidelity Assessment
A standardized protocol for measuring Faithfulness Estimate and Correlation involves:
- Input Perturbation: For a given instance and explanation, generate multiple perturbed instances by systematically removing or masking features, prioritizing those the explanation deems most important.
- Prediction Collection: Query the black-box model with these perturbed instances to obtain new predictions.
- Impact Calculation: For Faithfulness Estimate, calculate the average decrease in the model's prediction score for the original class when important features are removed. For Faithfulness Correlation, compute the Pearson correlation between the explanation's importance scores and the actual prediction changes resulting from random perturbations.
- Statistical Aggregation: Repeat the process across a representative sample of instances from the dataset to compute aggregate fidelity metrics.
A comprehensive study on fidelity metrics revealed significant concerns about their reliability, particularly for non-linear models where the best metrics still showed a 30% deviation from expected values for a perfect explanation [70]. This highlights the importance of using multiple complementary metrics and the need for further research into robust fidelity assessment.
Understandability: Human Interpretation of Explanations
Understandability assesses whether a human user can comprehend the explanation provided by an XAI method [8]. It encompasses aspects like coherence, compactness, and alignment with domain knowledge.
Evaluating Understandability
Understandability is inherently subjective and requires evaluation through human-centered studies, though proxy metrics exist.
Table 2: Methods for Evaluating Explanation Understandability
| Evaluation Dimension | Methodology | Application Example |
|---|---|---|
| Coherence/Plausibility | Clinicians rate how well the explanation aligns with relevant background knowledge and clinical consensus using Likert scales (e.g., 1=Completely implausible to 4=Highly plausible) [56]. | A saliency map for a pneumonia diagnosis should highlight regions of lung infiltration rather than irrelevant thoracic structures. |
| Compactness | Measure the complexity of the explanation, such as the number of features in a rule-based explanation or conditions in a decision rule [69]. | An Anchor explanation is compact if it describes a prediction with a short, simple rule (e.g., "IF fever > 39°C AND leukocytes > 12,000 THEN bacterial infection"). |
| Cognitive Load | Assess through user studies measuring time-to-decision or subjective ratings of mental effort required to interpret the explanation [32]. | Studies show that while explanations can improve trust, they frequently increase cognitive load, potentially disrupting clinical workflow [32]. |
The CLIX-M checklist emphasizes that for clinical use, explanations must be domain-relevant, avoiding redundancy and confusion by aligning with established clinical knowledge and Grice's maxims of quality, quantity, relevance, and clarity [56].
Actionability: Driving Clinical Decisions
Actionability reflects the explanation's capacity to support downstream clinical decision-making by enabling safe, informed, and contextually appropriate actions [56]. It is the ultimate test of an explanation's clinical utility.
Assessing Actionability
Actionability is evaluated by determining whether explanations provide information that can directly influence patient management strategies.
Table 3: Framework for Assessing Explanation Actionability in Clinical Settings
| Actionability Level | Description | Clinical Example |
|---|---|---|
| Highly Actionable | The explanation identifies modifiable risk factors or causative features that can be directly targeted by an intervention. | A sepsis prediction model highlights rising lactate levels and hypotension—factors that can be addressed with fluids and vasopressors. |
| Moderately Actionable | The explanation highlights associative or unmodifiable factors that, while informative, do not suggest a direct intervention. | A model predicts prolonged hospital stay based on patient age and pre-admission mobility. This informs resource planning but does not directly guide treatment. |
| Non-Actionable | The explanation provides no clinically useful information for decision-making or is misleading. | A model for ICU deterioration risk uses "length of stay" as a key feature. This is tautological and offers no actionable insight for prevention [56]. |
The CLIX-M checklist recommends that during development, clinical partners perform patient-level analyses to evaluate explanation informativeness and workflow impact using a scoring system from "Not actionable at all" to "Highly actionable and directly supports clinical decision-making" [56]. Furthermore, it recommends that only highly relevant, actionable variables should be prominently displayed on clinical dashboards, while other supporting variables should be available as optional context [56].
The XAI Evaluation Workflow in Clinical Research
The following diagram illustrates the integrated workflow for evaluating XAI methods in clinical decision support research, incorporating the three core metrics and their relationship to clinical deployment.
The Scientist's Toolkit: Research Reagents for XAI Evaluation
Evaluating XAI systems effectively requires a suite of methodological "reagents" and frameworks. The table below details essential tools for conducting rigorous XAI assessments in clinical research.
Table 4: Essential Research Tools for XAI Evaluation in Clinical Contexts
| Tool / Framework | Type | Primary Function in XAI Evaluation | Key Features & Considerations |
|---|---|---|---|
| CLIX-M Checklist [56] [71] | Reporting Guideline | Provides a structured, 14-item checklist for developing and evaluating XAI components in CDSS. | Includes purpose, clinical attributes (relevance, coherence), decision attributes (correctness), and model attributes. Informs both development and evaluation phases. |
| Faithfulness Metrics [70] | Quantitative Metric | Objectively measures how faithfully an explanation approximates the model's decision process. | Includes Faithfulness Estimate and Faithfulness Correlation. Requires careful interpretation as reliability varies with model linearity. |
| Likert-scale Plausibility Ratings [56] | Qualitative Assessment Tool | Captures clinician judgments on explanation coherence and alignment with domain knowledge. | Typically uses 4-point scales (e.g., 1=Completely implausible to 4=Highly plausible). Aggregating multiple expert responses is recommended. |
| Rule-based Explanation Methods (e.g., RuleFit, Anchors) [69] | XAI Method | Generates human-readable IF-THEN rules as explanations, often enhancing understandability. | RuleFit and RuleMatrix provide robust global explanations. Compactness (rule length) can be a proxy for understandability. |
| Human-Centered Evaluation (HCE) Framework [32] | Evaluation Methodology | Guides the assessment of XAI through real-world user studies with clinicians. | Measures trust, diagnostic confidence, and cognitive load. Sample sizes in existing studies are often small (<25 participants), indicating a need for larger trials. |
Moving beyond accuracy is imperative for the successful integration of AI into clinical workflows. Fidelity, Understandability, and Actionability are not merely supplementary metrics but are fundamental to establishing the trustworthiness and utility of AI systems in medicine. Fidelity ensures the explanation is technically correct, Understandability ensures it is comprehensible to the clinician, and Actionability ensures it can inform patient care.
Current research indicates that these metrics often involve trade-offs; for instance, explanations that are highly faithful to a complex model may be less understandable, and vice-versa [7]. The future of clinically viable XAI lies in developing context-aware evaluation frameworks that balance these dimensions, guided by standardized tools like the CLIX-M checklist and robust human-centered studies. Ultimately, achieving transparent, ethical, and clinically relevant AI in healthcare depends on our rigorous and continuous application of these core evaluation metrics.
The integration of Artificial Intelligence (AI) into Clinical Decision Support Systems (CDSS) has enhanced diagnostic precision and treatment planning. However, the "black-box" nature of many high-performing models poses a significant barrier to clinical adoption, as healthcare professionals require understanding and trust to integrate AI recommendations into patient care [2] [8]. Explainable AI (XAI) aims to bridge this gap by making AI decisions transparent and interpretable. Among various XAI techniques, SHapley Additive exPlanations (SHAP) has emerged as a prominent, mathematically grounded method for explaining model predictions [38] [2]. Nevertheless, an emerging body of evidence suggests that technical explanations like SHAP may not fully meet the needs of clinicians. This analysis directly compares SHAP against clinician-friendly explanations, evaluating their differential impact on decision-making behaviors, trust, and usability within CDSS, framing this within the critical need for user-centered design in healthcare AI [38] [8].
Theoretical Foundations and Explanation Types
SHAP (SHapley Additive exPlanations)
SHAP is a model-agnostic, post-hoc XAI method rooted in cooperative game theory. It assigns each feature in a prediction an importance value (the Shapley value) that represents its marginal contribution to the model's output. The core strength of SHAP lies in its solid mathematical foundation, ensuring that explanations satisfy desirable properties such as local accuracy (the explanation model matches the original model's output for a specific instance) and consistency [2] [8]. In clinical practice, SHAP is often presented visually through force plots or summary plots, which illustrate the magnitude and direction (positive or negative) of each feature's influence on a prediction, for instance, showing how factors like age or a specific biomarker push a model's risk assessment higher or lower [38] [72].
Clinician-Friendly Explanations
Clinician-friendly explanations, often called narrative or contextual explanations, translate the output of XAI methods like SHAP into a format aligned with clinical reasoning. These explanations are characterized by:
- Linguistic Familiarity: Using medical terminology and concepts familiar to the clinician.
- Causal Plausibility: Framing explanations in terms of potential cause-effect relationships, even if the model is purely associative.
- Workflow Integration: Providing concise, actionable rationale that fits into the clinical decision-making workflow without requiring technical interpretation of charts or values [38] [8]. Rather than presenting a graph of feature contributions, a clinician-friendly explanation might state: "The model suggests a high risk for postoperative transfusion due to a combination of the patient's preoperative anemia, the planned major vascular procedure, and a low platelet count."
Quantitative Comparative Analysis
A rigorous study with 63 surgeons and physicians compared three CDSS explanation formats for predicting perioperative blood transfusion requirements: Results Only (RO), Results with SHAP plot (RS), and Results with SHAP plot and Clinical explanation (RSC). The outcomes measured were Weight of Advice (WOA), a metric for advice acceptance; a Trust Scale for XAI; an Explanation Satisfaction Scale; and the System Usability Scale (SUS) [38].
Table 1: Key Quantitative Outcomes from Comparative Study (N=63 Clinicians)
| Explanation Format | Weight of Advice (WOA) | Trust Score (max ~40) | Satisfaction Score | System Usability (SUS) |
|---|---|---|---|---|
| Results Only (RO) | 0.50 (SD=0.35) | 25.75 (SD=4.50) | 18.63 (SD=7.20) | 60.32 (SD=15.76) |
| Results with SHAP (RS) | 0.61 (SD=0.33) | 28.89 (SD=3.72) | 26.97 (SD=5.69) | 68.53 (SD=14.68) |
| Results with SHAP + Clinical (RSC) | 0.73 (SD=0.26) | 30.98 (SD=3.55) | 31.89 (SD=5.14) | 72.74 (SD=11.71) |
The data demonstrates a clear, statistically significant hierarchy (RSC > RS > RO) across all measured constructs. The addition of a SHAP plot to the raw results provided a measurable improvement over the black-box output. However, the highest levels of acceptance, trust, satisfaction, and perceived usability were achieved only when the technical SHAP output was supplemented with a clinical narrative [38].
Correlation analysis further revealed that acceptance (WOA) was moderately correlated with specific trust constructs like 'predictability' (r=0.463) and 'comparison with novice human' (r=0.432), as well as with satisfaction items like 'appropriateness of detailed information' (r=0.431) and the overall SUS score (r=0.434). This suggests that explanations which make the system's behavior predictable and provide appropriately detailed clinical context are key drivers of adoption [38].
Experimental Protocols and Methodologies
Protocol: Evaluating Explanation Formats in CDSS
The following methodology outlines the experimental design used to generate the comparative data in Section 3 [38].
Objective: To compare the effects of SHAP-based versus clinician-friendly explanations on clinicians' acceptance, trust, and satisfaction with a CDSS.
Study Design: A counterbalanced, within-subjects design where each participant evaluated multiple clinical vignettes under different explanation conditions.
Participants:
- Recruitment: 63 physicians and surgeons with experience in prescribing pre-operative blood products.
- Demographics: Included 58.7% females, 31.7% surgeons, 38.1% from internal medicine, and 68.3% residents.
Materials and Tasks:
- Vignettes: Six clinical vignettes detailing patient cases requiring perioperative transfusion risk assessment.
- CDSS: An AI-powered CDSS predicting transfusion requirements.
- Conditions: Each vignette was presented with one of three explanation formats:
- RO: The AI prediction only (e.g., "High risk of transfusion").
- RS: The AI prediction plus a SHAP plot visualizing feature contributions.
- RSC: The AI prediction, the SHAP plot, plus a concise clinical text explanation.
Procedure:
- Baseline Decision: For each vignette, clinicians provided their initial management decision without AI assistance.
- AI Advice & Explanation: The CDSS recommendation was presented with one of the three explanation formats, randomized to minimize order effects.
- Final Decision: Clinicians provided their final management decision after reviewing the AI advice and explanation.
- Questionnaire: After each vignette, participants completed standardized questionnaires measuring trust, satisfaction, and usability.
Data Analysis:
- Primary Metric: Weight of Advice (WOA) = |Final Decision - AI Advice| / |Initial Decision - AI Advice|. A higher WOA indicates greater influence of the AI advice.
- Secondary Metrics: Scores from the Trust in AI Explanation scale, Explanation Satisfaction Scale, and System Usability Scale (SUS).
- Statistical Tests: Friedman test with Conover post-hoc analysis for comparing the three conditions; correlation analysis to explore relationships between metrics.
Workflow Diagram: Experimental Protocol
The following diagram visualizes the sequential workflow of the experimental protocol.
The Scientist's Toolkit: Key Research Reagents
For researchers aiming to conduct similar comparative studies in XAI, the following "reagents" or core components are essential. This list details the key materials and their functions as derived from the cited experimental protocol [38] [8].
Table 2: Essential Research Components for XAI Comparative Studies
| Research Component | Function & Description |
|---|---|
| Clinical Vignettes | Standardized patient cases that simulate real-world decision scenarios. They ensure all participants respond to identical clinical challenges, providing a controlled basis for comparing explanation formats. |
| AI/CDSS Model | A trained predictive model (e.g., for risk stratification) that serves as the source of the recommendations to be explained. Its performance must be validated to ensure credible advice [2]. |
| XAI Methods (SHAP) | The technical algorithm (e.g., SHAP, LIME) used to generate post-hoc explanations of the AI model's predictions. This is the core "treatment" being tested against narrative formats [38] [8]. |
| Explanation Rendering System | The software interface that presents the explanations (SHAP plots, clinical text) to the study participants. Its design is critical to ensuring consistent delivery of the experimental conditions [38]. |
| Standardized Scales (Trust, Satisfaction, SUS) | Validated psychometric questionnaires used to quantitatively measure subjective outcomes like trust, explanation satisfaction, and system usability, allowing for robust statistical comparison [38]. |
Discussion and Synthesis of Logical Relationships
The empirical evidence strongly indicates that while SHAP provides a valuable technical explanation, it functions as a necessary but insufficient component for optimal clinical adoption. The logical relationship between explanation type and clinical impact can be conceptualized as a pathway where usability mediates final decision-making outcomes.
Diagram: Explanation-to-Decision Pathway
The following diagram synthesizes the logical pathway from explanation type to clinical decision impact, as revealed by the study data.
Interpretation of the Pathway
The pathway illustrates that technical explanations like SHAP initiate the process of building trust and usability by offering a glimpse into the model's mechanics, addressing the initial "black box" problem [2]. However, clinician-friendly explanations act as a powerful catalyst, significantly amplifying these effects. This is because they reduce cognitive load by aligning with the clinician's mental model, facilitating a faster and more intuitive validation of the AI's output against their own medical knowledge [38] [8]. The result is what is termed "calibrated trust" – not blind faith, but an informed understanding of when and why to rely on the AI, which ultimately leads to higher rates of appropriate adoption, as measured by the Weight of Advice.
This synthesis underscores a critical insight for CDSS research: the most effective strategy is not to choose between technical and clinical explanations, but to synergistically combine them. The technical explanation (SHAP) provides accountability and debugging information for developers and highly technical users, while the clinical narrative delivers the actionable insight needed for the practicing clinician. Future research should focus on automating the generation of accurate and context-aware clinical narratives from technical XAI outputs to enable this integration at scale.
The integration of artificial intelligence (AI) into clinical decision support systems (CDSS) promises to enhance diagnostic precision, risk stratification, and treatment planning [2]. However, the "black-box" nature of many complex AI models presents a significant barrier to clinical adoption, primarily due to challenges in interpretability and trust [8]. Explainable AI (XAI) aims to bridge this gap by making model reasoning understandable to clinicians, yet technical solutions often fail to address real-world clinician needs, workflow integration, and usability concerns [8]. Within this context, frameworks for assessing the human-AI interaction become paramount. The DARPA Framework provides a structured approach for evaluating three critical, interdependent dimensions: the user's mental model of the AI system, their trust in its capabilities, and overall user satisfaction. This guide details the application of this framework within clinical settings, providing researchers and drug development professionals with methodologies and tools to ensure AI-driven CDSS are not only accurate but also transparent, trusted, and effectively integrated into clinical workflows.
Core Dimensions of the DARPA Framework
The DARPA Framework posits that successful human-AI collaboration hinges on the alignment between three core psychological constructs. Systematic assessment of these dimensions provides actionable insights for refining both AI models and their integration into clinical practice.
Mental Models: A user's mental model is an internal understanding of the AI system's capabilities, limitations, and underlying decision-making processes. In clinical environments, an accurate mental model allows a healthcare professional to anticipate system behavior, interpret its recommendations correctly, and identify potential errors [8]. Inaccurate mental models can lead to either over-reliance or under-utilization of AI support. For instance, if a radiologist misunderstands the imaging features a model uses to detect tumors, they might accept an erroneous prediction or dismiss a correct one. XAI techniques are explicitly designed to shape and improve these mental models by providing insights into which features influence a model's decision [2].
Trust: Trust is the user's attitude that the AI system will perform reliably and effectively in a given situation. It is a dynamic state, heavily influenced by the system's performance, transparency, and the quality of its explanations [8]. Calibrated trust—a state where trust matches the system's actual capabilities—is the ultimate goal. A lack of trust leads to rejection of valuable AI assistance, while excessive trust can result in automation bias and clinical errors. Research indicates that XAI is critical for fostering appropriate trust; for example, showing the key factors behind a sepsis prediction model's output allows clinicians to verify its reasoning against their clinical judgment, thereby building justified confidence [2].
User Satisfaction: This dimension encompasses the user's overall perceived experience with the AI system, including its usability, the intuitiveness of its interface, and how well it integrates into existing clinical workflows [73]. Satisfaction is not merely about aesthetic appeal but reflects the system's practical utility and the absence of friction in its use. Barriers such as alert fatigue, poor design, and misalignment with clinical tasks significantly undermine satisfaction and adoption [73] [74]. A satisfied user is more likely to integrate the CDSS into their routine practice, thereby realizing its potential benefits for patient care.
The relationship between these dimensions is synergistic. Effective XAI can improve a user's mental model, which in turn leads to more calibrated trust. Both calibrated trust and a positive, satisfying user experience are prerequisites for the long-term adoption and sustained use of AI-driven CDSS in high-stakes clinical environments [8].
Quantitative Assessment Metrics and Data
Evaluating the DARPA framework's dimensions requires a multi-faceted approach, employing both quantitative metrics and qualitative methods. The table below summarizes key quantitative metrics used to measure mental models, trust, and satisfaction in XAI research for clinical settings.
Table 1: Quantitative Metrics for Assessing the DARPA Framework Dimensions
| Dimension | Metric Category | Specific Metric | Description and Application |
|---|---|---|---|
| Mental Model | Knowledge & Understanding | Explanation Fidelity | Measures how accurately an XAI method (e.g., SHAP, LIME) approximates the true decision process of the black-box model. Low fidelity indicates a misleading explanation that corrupts the mental model [8]. |
| Feature Identification Accuracy | In image-based models (e.g., using Grad-CAM), assesses if clinicians can correctly identify the image regions the model used for its prediction, validating their mental model of the model's focus [2]. | ||
| Trust | Behavioral Trust | Adherence Rate | The frequency with which clinicians follow or act upon the AI's recommendations. High adherence may indicate high trust, but must be calibrated against system accuracy [8]. |
| Reliance Measures | Examines whether users are more likely to accept correct AI recommendations (appropriate reliance) or reject incorrect ones (appropriate distrust) after exposure to explanations [8]. | ||
| Self-Reported Trust | Trust Scales | Standardized psychometric questionnaires (e.g., with Likert scales) that directly ask users about their perceptions of the system's reliability, competence, and trustworthiness [8]. | |
| User Satisfaction | Usability & Experience | System Usability Scale (SUS) | A widely used, reliable 10-item questionnaire providing a global view of subjective usability assessments [73]. |
| NASA-TLX | Measures perceived workload (mental, temporal, and effort demands) when using the system. Lower scores indicate a more satisfactory and less burdensome integration [73]. | ||
| Workflow Integration | Task Completion Time | Measures the time taken to complete a clinical task with the CDSS. Efficient integration should not significantly increase task time [73]. |
The selection of these metrics should be guided by the specific clinical context and the AI application. For instance, a diagnostic support system might prioritize explanation fidelity and adherence rate, while a monitoring system might focus more on workload and task completion time.
Experimental Protocols for Framework Evaluation
To generate robust, generalizable findings, the application of the DARPA Framework should be embedded within structured experimental protocols. The following methodologies are essential for a comprehensive assessment.
Controlled Simulation Studies
Objective: To isolate the effects of different XAI techniques on mental models, trust, and satisfaction in a standardized environment. Protocol:
- Participant Recruitment: Enroll clinicians (e.g., physicians, nurses) representative of the target end-users. Stratify by specialty, experience with AI, and familiarity with the clinical domain.
- Stimulus and System Design: Develop a functional prototype of the XAI-CDSS. The system should present clinical cases (e.g., patient data, medical images) and provide AI-generated recommendations. Crucially, the experiment must manipulate a single independent variable: the type of XAI explanation (e.g., SHAP plots vs. LIME vs. counterfactual explanations) presented alongside the recommendation.
- Task Procedure: Participants review a series of clinical cases using the prototype. For each case, they are asked to: a) make an initial clinical decision, b) review the AI recommendation and its explanation, and c) provide a final decision with a confidence level.
- Data Collection: Collect quantitative data as outlined in Table 1. This includes:
- Mental Model: Post-task quizzes assessing understanding of the model's logic.
- Trust: Pre- and post-study trust scales, and adherence/reliance measures derived from decision changes.
- Satisfaction: Post-study SUS and NASA-TLX questionnaires.
- Analysis: Use statistical tests (e.g., ANOVA) to compare outcome measures across the different XAI conditions, identifying which explanation type most effectively improves mental models and calibrates trust.
Longitudinal Field Studies
Objective: To evaluate the evolution of mental models, trust, and satisfaction in real-world clinical workflows over time. Protocol:
- Integration: Deploy the XAI-CDSS into a live clinical environment, such as a hospital ward or outpatient clinic, for an extended period (e.g., 3-6 months).
- Participant Engagement: Involve a cohort of clinicians who will use the system as part of their routine practice.
- Data Collection: Employ a mixed-methods approach:
- Quantitative: Log system usage data (frequency of use, feature interactions, adherence rates) automatically. Administer trust and satisfaction surveys at regular intervals (e.g., monthly).
- Qualitative: Conduct periodic semi-structured interviews and focus groups to gather in-depth insights into how mental models are forming, how trust is being negotiated, and what specific facilitators and barriers to satisfaction are emerging [73]. Thematic analysis is then applied to this qualitative data.
- Analysis: Analyze quantitative data for trends over time. Correlate usage metrics with survey results. Integrate qualitative findings to explain the quantitative trends, providing a rich, contextualized understanding of the adoption process.
The Scientist's Toolkit: Research Reagents and Materials
Successful execution of the described experiments requires a suite of methodological and technical "reagents." The following table details essential components for researchers in this field.
Table 2: Key Research Reagents and Materials for XAI-CDSS Evaluation
| Item Category | Specific Item / Technique | Function in Experimental Research |
|---|---|---|
| XAI Methods | SHAP (SHapley Additive exPlanations) [2] [8] | A model-agnostic method based on game theory to quantify the contribution of each input feature to a single prediction. Used to generate feature-importance explanations for tabular data. |
| LIME (Local Interpretable Model-agnostic Explanations) [8] | Creates a local, interpretable surrogate model to approximate the predictions of any black-box model. Useful for explaining individual predictions. | |
| Grad-CAM (Gradient-weighted Class Activation Mapping) [2] | A model-specific technique for convolutional neural networks that produces visual explanations in the form of heatmaps, highlighting important regions in an image for a prediction. | |
| Counterfactual Explanations [8] | Identify the minimal changes to an input instance required to alter the model's prediction. Helps users understand the model's decision boundary. | |
| Evaluation Frameworks | FITT (Fit between Individuals, Tasks, and Technology) [73] | An implementation framework used to qualitatively analyze and categorize facilitators and barriers to technology adoption, focusing on the alignment between users, their tasks, and the technology. |
| NASSS (Nonadoption, Abandonment, Scale-up, Spread and Sustainability) [74] | A comprehensive framework for identifying determinants (barriers and facilitators) of successful technology implementation across multiple domains, including the technology, the adopters, and the organization. | |
| Data Collection Tools | Psychometric Trust Scales [8] | Validated questionnaires to quantitatively measure users' self-reported trust in automated systems. |
| System Usability Scale (SUS) [73] | A robust and widely adopted tool for measuring the perceived usability of a system. | |
| Semi-structured Interview Guides [73] | Protocols with open-ended questions designed to elicit rich, qualitative data on user experiences, mental models, and perceived challenges. |
Visualization of Logical Relationships and Workflows
Understanding the logical flow from XAI presentation to clinical outcomes is crucial. The diagram below maps this workflow and the interplay of the DARPA dimensions.
Figure 1: XAI-CDSS Clinical Decision Workflow and DARPA Dimension Interplay
The second diagram situates the DARPA Framework within the broader ecosystem of implementation challenges, showing how its assessment feeds into addressing barriers identified by frameworks like NASSS.
Figure 2: DARPA Assessment within the NASSS Implementation Context
The integration of Artificial Intelligence (AI) into clinical decision support systems (CDSS) represents a transformative shift in modern healthcare, offering unprecedented capabilities for enhancing diagnostic precision, risk stratification, and treatment planning [2]. However, the opaque "black-box" nature of many advanced AI models has historically impeded widespread clinical adoption, as clinicians justifiably hesitate to trust recommendations without understanding their underlying rationale [2] [8]. Explainable AI (XAI) has emerged as a critical solution to this challenge, aiming to make AI systems transparent, interpretable, and accountable to human users [2]. Beyond technical transparency, XAI addresses fundamental ethical and regulatory requirements while fostering the human-AI collaboration necessary for safe implementation in high-stakes medical environments [2] [75]. This technical review examines the growing evidence corpus correlating XAI implementation with tangible improvements in both patient outcomes and clinical operational efficiency, providing researchers and drug development professionals with a comprehensive analysis of current methodologies, empirical findings, and implementation frameworks.
The landscape of explainable AI encompasses diverse technical approaches tailored to different clinical data types and decision contexts. These techniques are broadly categorized into ante hoc (inherently interpretable models) and post hoc (methods that explain existing black-box models) approaches [8]. Post hoc methods predominate in clinical applications due to their flexibility and compatibility with complex models offering superior predictive performance [8].
Predominant XAI Techniques in Healthcare
Table 1: Dominant XAI Techniques in Clinical Implementation
| Technique | Prevalence | Primary Data Modality | Key Clinical Applications |
|---|---|---|---|
| SHAP (SHapley Additive exPlanations) | 46.5% [76] | Structured clinical data [76] | Risk prediction, treatment response forecasting [2] [76] |
| LIME (Local Interpretable Model-agnostic Explanations) | 25.8% [76] | Mixed data types [2] | Individual prediction explanation, model debugging [2] [8] |
| Grad-CAM (Gradient-weighted Class Activation Mapping) | 12.0% [76] | Medical imaging [2] | Tumor localization, diagnostic highlighting [2] [76] |
| Attention Mechanisms | Not quantified | Sequential data [2] | Time-series analysis, natural language processing [2] |
| Counterfactual Explanations | Emerging [8] | Mixed data types [8] | Treatment alternatives, "what-if" scenario planning [75] [8] |
Model-agnostic techniques like SHAP and LIME dominate applications involving structured clinical data from electronic health records (EHRs), providing both local explanation for individual predictions and global insights into model behavior [2] [76]. For imaging data, visualization approaches such as Grad-CAM and attention mechanisms generate saliency maps that highlight anatomically relevant regions contributing to diagnostic decisions, enabling radiologists to verify AI findings against clinical knowledge [2] [24]. Emerging approaches include concept-based explanations that link predictions to clinically meaningful concepts and causal inference methods that distinguish correlation from causation [2].
Clinical Domain Implementation Patterns
XAI implementation varies significantly across clinical specialties, reflecting differing data types, clinical workflows, and decision-criticality:
- Radiiology and Pathology: Dominated by visual explanation methods (Grad-CAM, saliency maps) for diagnostic imaging and histology [2] [24].
- Critical Care and Inpatient Settings: Heavy utilization of SHAP and LIME for predictive analytics (sepsis, mortality, readmission risk) using EHR data [2] [77].
- Chronic Disease Management: SHAP-based explanations for longitudinal risk stratification in cardiology, diabetes, and oncology [76].
- Drug Development: Emerging use of counterfactual explanations and concept-based approaches for biomarker discovery and trial optimization [8].
Quantifying Impact: XAI Correlation with Improved Patient Outcomes
Robust empirical evidence demonstrates that well-implemented XAI systems contribute directly to enhanced patient outcomes through multiple mechanisms, including improved diagnostic accuracy, more targeted interventions, and enhanced clinician acceptance of valid AI recommendations.
Diagnostic Accuracy and Clinical Decision Quality
Table 2: XAI Impact on Clinical Performance Metrics
| Clinical Domain | Study Design | XAI Intervention | Outcome Metrics | Key Findings |
|---|---|---|---|---|
| Fetal Ultrasound [24] | Reader study with 10 sonographers | Prototype-based explanations with images and heatmaps | Mean Absolute Error (MAE) in gestational age estimation | MAE reduced from 23.5 days (baseline) to 15.7 days (with AI) to 14.3 days (with XAI) [24] |
| ICU Length of Stay Prediction [77] | Mixed-methods with 15 clinicians | SHAP explanations with four presentation types | Trust scores, feature alignment | Trust scores improved from 2.8 to 3.9; feature alignment increased significantly (Spearman correlation: -0.147 to 0.868) [77] |
| Sepsis Prediction [2] | Systematic review of 62 studies | Various XAI methods | Predictive accuracy, clinician adoption | Improved early detection and antibiotic timing, though limited real-world validation [2] |
| Chronic Disease Management [76] | Systematic review | Predominantly SHAP and LIME | Adherence to clinical guidelines | 25% increase in adherence to evidence-based guidelines with XAI-guided decisions [76] |
The experimental protocol in the gestational age estimation study exemplifies rigorous XAI evaluation [24]. Researchers implemented a three-phase crossover design where sonographers first provided estimates without AI assistance, then with model predictions alone, and finally with both predictions and prototype-based explanations. This sequential design enabled isolation of the explanation effect from the prediction effect. The XAI system utilized a part-prototype model that compared fetal ultrasound images to clinically relevant prototypes from training data, generating explanations in the form of similar reference images and attention heatmaps [24]. This approach mirrors clinical reasoning patterns more closely than conventional saliency maps.
In critical care settings, the ICU length of stay study employed a sophisticated evaluation framework assessing both quantitative and qualitative impacts [77]. After developing a high-performance Random Forest model (AUROC: 0.903), researchers implemented SHAP-based explanations presented in four distinct formats: "Why" (feature contributions), "Why not" (missing factors for different outcome), "How to" (achieving different outcome), and "What if" (scenario exploration) [77]. Clinicians participated in web-based experiments, surveys, and interviews, with researchers measuring changes in mental models, trust scores (5-point Likert scale), and satisfaction ratings. The "What if" explanations received the highest satisfaction scores (4.1/5), suggesting clinicians value exploratory interaction with AI systems [77].
Mechanisms for Outcome Improvement
The correlation between XAI implementation and improved patient outcomes operates through several mediating mechanisms:
Enhanced Model Auditability: XAI enables identification of dataset biases and model limitations during development, preventing deployment of flawed systems [2] [75]. For example, explanation-driven error analysis can reveal spurious correlations that would compromise real-world performance [24].
Improved Clinical Validation: Explanations allow clinicians to assess whether AI reasoning aligns with medical knowledge, increasing appropriate reliance on accurate recommendations [77]. The ICU study demonstrated significantly improved feature alignment after XAI exposure, indicating knowledge transfer from AI to clinicians [77].
Personalized Intervention Planning: XAI reveals patient-specific factors driving predictions, enabling tailored interventions rather than one-size-fits-all approaches [76]. In chronic disease management, this has facilitated personalized treatment protocols that improve adherence and outcomes [76].
XAI Contribution to Clinical Efficiency and Healthcare Economics
Beyond quality improvements, XAI systems demonstrate significant impacts on healthcare efficiency and economics, addressing the industry's pressing cost and workforce challenges.
Operational Efficiency Metrics
Recent industry data reveals accelerated AI adoption in healthcare, with 22% of healthcare organizations implementing domain-specific AI tools—more than double the rate of the broader economy [78] [79]. This surge is driven by compelling efficiency gains:
Table 3: Healthcare AI Efficiency Impacts
| Efficiency Dimension | Representative Data | XAI Contribution |
|---|---|---|
| Administrative Automation | $600M spent on ambient clinical documentation; $450M on coding/billing automation [78] | XAI builds trust necessary for workflow integration [53] |
| Documentation Time Reduction | Projected >50% reduction in documentation time [79] | Explanations increase clinician confidence in AI-generated documentation [78] |
| Procurement Acceleration | Provider procurement cycles shortened by 18-22% [79] | Transparent AI reduces evaluation complexity and risk perception [53] |
| Labor Crisis Mitigation | Addressing projected shortages of 200,000 nurses and 100,000 physicians [78] | XAI enables task shifting without compromising safety [53] |
Healthcare AI spending has nearly tripled year-over-year, reaching $1.4 billion in 2025, with 85% flowing to AI-native startups rather than legacy incumbents [78] [79]. This investment pattern reflects both the transformative potential of XAI and the healthcare industry's urgent need for efficiency solutions amid razor-thin margins (often under 1%) and structural labor shortages [78].
Implementation and Workflow Integration
The efficiency gains from XAI-enabled systems depend critically on effective workflow integration. Research indicates that explanations must be delivered at the right time, in the right format, and with appropriate contextualization to yield benefits [75] [53]. Expert interviews with 17 healthcare stakeholders identified several critical success factors for XAI integration [53]:
- Workflow Awareness: XAI systems must minimize disruption and align with existing clinical workflows rather than requiring separate review processes [53].
- Explanation Timeliness: Explanations must be available at the point of decision-making without introducing detrimental latency [75].
- Customization: Different clinical roles and specialties require different explanation types and detail levels [53].
Leading health systems like Mayo Clinic, Kaiser Permanente, and Advocate Health have developed structured approaches for XAI implementation, prioritizing low-risk administrative use cases initially to build organizational confidence before expanding to clinical decision support [78] [79]. This incremental approach demonstrates how XAAI builds institutional trust while delivering compounding efficiency benefits.
Implementation Framework: CLIX-M Checklist for Effective XAI Evaluation
Successful XAI implementation requires systematic evaluation beyond traditional performance metrics. The Clinician-Informed XAI Evaluation Checklist with Metrics (CLIX-M) provides a comprehensive framework covering 14 items across four categories [75]:
Figure 1: CLIX-M Framework for XAI Evaluation in Healthcare
Critical Evaluation Dimensions
The CLIX-M framework emphasizes several underappreciated evaluation dimensions crucial for real-world impact [75]:
- Domain Relevance: Assessments should determine whether explanations highlight clinically meaningful features and relationships rather than technically valid but medically irrelevant patterns [75].
- Actionability: Explanations must provide insights that directly inform clinical interventions rather than merely satisfying intellectual curiosity [75].
- Appropriate Reliance: Effective XAI should help clinicians discern when to trust AI recommendations versus when to rely on their own judgment, avoiding both under-reliance and over-reliance [24].
- Consistency: Explanations should remain stable across semantically similar inputs to build predictable mental models [75].
The checklist recommends specific metrics for each evaluation dimension, including quantitative scores for domain relevance (very irrelevant to very relevant), reasonableness (very incoherent to very coherent), and actionability (not actionable to highly actionable) [75].
Research Reagents: Essential Tools for XAI Experimentation
Table 4: Essential Research Reagents for XAI Development and Evaluation
| Reagent Category | Specific Tools/Solutions | Research Function | Implementation Notes |
|---|---|---|---|
| Explanation Techniques | SHAP, LIME, Grad-CAM, LRP, Attention Mechanisms [2] [76] | Generate feature attributions and saliency maps | SHAP dominates structured data; Grad-CAM preferred for imaging [76] |
| Evaluation Frameworks | CLIX-M checklist [75], DARPA XAI metrics [77] | Standardized assessment of explanation quality | CLIX-M provides clinician-informed evaluation criteria [75] |
| Model Architectures | Part-prototype models [24], Concept bottleneck models [2] | Intrinsically interpretable model design | Balance interpretability and performance requirements [24] |
| User Study Protocols | Three-stage reader studies [24], Mixed-methods evaluation [77] | Measure human-XAI interaction effects | Isolate explanation impact from prediction impact [24] |
| Data Resources | EHR datasets, medical imaging repositories [2] [76] | Model development and validation | Require diverse, representative clinical populations [7] |
Challenges and Future Research Directions
Despite promising evidence, significant challenges remain in correlating XAI use with improved outcomes. Current limitations include:
- Inconsistent Evaluation Methodologies: Lack of standardized metrics for explanation quality complicates cross-study comparisons and meta-analyses [75] [7].
- Limited Real-World Validation: Most studies occur in controlled research environments rather than operational clinical settings [2] [7].
- Patient Perspective Gaps: Patients are largely excluded from XAI research despite being ultimate beneficiaries [7].
- Contextual Variability: Explanation effectiveness varies significantly across clinical specialties, user expertise levels, and decision criticality [24] [53].
Future research should prioritize longitudinal studies in production clinical environments, development of specialty-specific explanation formats, and inclusion of patient-centered outcome measures. Additionally, techniques that balance explanation faithfulness (technical accuracy) with plausibility (clinical credibility) require further refinement [7].
The accumulating evidence demonstrates a significant correlation between well-implemented XAI systems and improvements in both patient outcomes and clinical efficiency. Through enhanced diagnostic accuracy, optimized treatment planning, appropriate clinician reliance, and streamlined workflows, XAI enables healthcare organizations to address dual challenges of quality improvement and cost containment. The CLIX-M evaluation framework provides a structured approach for assessing XAI systems across multiple dimensions of clinical utility. As healthcare continues its rapid AI adoption—deploying domain-specific tools at more than twice the rate of the broader economy [78] [79]—explainability will remain essential for building trust, ensuring safety, and achieving the full potential of AI-assisted healthcare. For researchers and drug development professionals, these findings underscore the importance of integrating explainability throughout the AI development lifecycle rather than treating it as an afterthought.
Conclusion
The successful integration of Explainable AI into Clinical Decision Support Systems is paramount for the future of data-driven medicine. This synthesis demonstrates that technical prowess alone is insufficient; XAI must be user-centered, ethically grounded, and seamlessly integrated into clinical workflows to foster appropriate trust and adoption among healthcare professionals. The future of XAI-CDSS lies in moving beyond static explanations to interactive systems that support a collaborative negotiation between clinician intuition and AI-derived insights. For researchers and drug development professionals, this entails a concerted focus on developing standardized evaluation frameworks, creating more public datasets for benchmarking, and fostering interdisciplinary collaboration. By prioritizing transparency, we can unlock the full potential of AI to augment clinical expertise, enhance patient safety, and accelerate the development of novel therapeutics, ultimately leading to a new era of trustworthy and effective personalized healthcare.
References
- 1. about black box AI and explainability in healthcare [https://pubmed.ncbi.nlm.nih.gov/39916325/]
- 2. Explainable AI in Clinical Decision Support Systems [https://pmc.ncbi.nlm.nih.gov/articles/PMC12427955/]
- 3. Medical artificial intelligence and the black box problem [https://www.sciencedirect.com/science/article/pii/S2667102623000578]
- 4. Healthcare AI, explainability, and the human-machine ... [https://www.frontiersin.org/journals/medicine/articles/10.3389/fmed.2025.1545409/full]
- 5. Ethics of trustworthy AI in healthcare: Challenges ... [https://www.sciencedirect.com/science/article/pii/S0925231225026141]
- 6. The Future of AI Governance: How Explainability is ... [https://superagi.com/the-future-of-ai-governance-how-explainability-is-shaping-regulatory-compliance-in-2025/]
- 7. Evaluating explanation performance for clinical decision ... [https://www.sciencedirect.com/science/article/abs/pii/S001048252501296X]
- 8. Explainable AI for Clinical Decision Support Systems [https://www.mdpi.com/2227-9709/12/4/119]
- 9. AI Act | Shaping Europe's digital future - European Union [https://digital-strategy.ec.europa.eu/en/policies/regulatory-framework-ai]
- 10. AI Transparency Requirements: Compliance and ... [https://gdprlocal.com/ai-transparency-requirements/]
- 11. Understanding AI Regulations: From GDPR to Global ... [https://www.obsidiansecurity.com/blog/understanding-ai-regulations]
- 12. Unlocking the Power of Explainable AI in Modern Tech [https://viso.ai/deep-learning/explainable-ai/]
- 13. Trust in Artificial Intelligence–Based Clinical Decision ... [https://www.jmir.org/2025/1/e69678]
- 14. Artificial intelligence in clinical trials: A comprehensive ... [https://www.sciencedirect.com/science/article/pii/S1386505625003582]
- 15. Explainable AI in Clinical Decision Support Systems [https://www.mdpi.com/2227-9032/13/17/2154]
- 16. The crucial role of explainable artificial intelligence (XAI) in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12535480/]
- 17. Should AI models be explainable to clinicians? - Critical Care [https://ccforum.biomedcentral.com/articles/10.1186/s13054-024-05005-y]
- 18. Artificial intelligence should genuinely support clinical ... [https://www.nature.com/articles/s41746-025-01725-9]
- 19. Introduction to Machine Learning Interpretability Methods [https://forbytes.com/blog/machine-learning-interpretability/]
- 20. 2 Interpretability – Interpretable Machine Learning [https://christophm.github.io/interpretable-ml-book/interpretability.html]
- 21. in Explainable ... AI Clinical Decision Support Systems [https://pubmed.ncbi.nlm.nih.gov/40941506/]
- 22. integrating explainable AI (XAI) with machine learning ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12465982/]
- 23. A Review of Explainable (XAI) in Precision Healthcare for... :: SSRN AI [https://papers.ssrn.com/sol3/papers.cfm?abstract_id=5597170]
- 24. The human factor in explainable artificial intelligence [https://www.nature.com/articles/s41746-025-02023-0]
- 25. Explainable AI in medicine: challenges of integrating XAI ... [https://www.frontiersin.org/journals/radiology/articles/10.3389/fradi.2025.1627169/full]
- 26. Explainable AI in medicine: challenges of integrating XAI into ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12391920/]
- 27. 22 Free and Open Medical Datasets for AI Development in ... [https://www.shaip.com/blog/healthcare-datasets-for-machine-learning-projects/]
- 28. Visual AI in Healthcare: 2025 Landscape [https://voxel51.com/blog/visual-ai-in-healthcare-2025-landscape]
- 29. XAI-Based Clinical Decision Support Systems [https://www.mdpi.com/2076-3417/14/15/6638]
- 30. A review of Explainable Artificial Intelligence in healthcare [https://www.sciencedirect.com/science/article/pii/S0045790624002982]
- 31. Post-hoc vs ante-hoc explanations: xAI design guidelines ... [https://www.sciencedirect.com/science/article/pii/S1389041724000378]
- 32. A Survey on Human-Centered Evaluation of Explainable AI ... [https://arxiv.org/abs/2502.09849]
- 33. Solving the explainable AI conundrum by bridging ... [https://www.nature.com/articles/s41746-023-00837-4]
- 34. A Survey on Human-Centered Evaluation of Explainable AI ... [https://arxiv.org/html/2502.09849v3]
- 35. A Guide to Understanding Explainable AI in Healthcare 2025 [https://digitalhealth.folio3.com/blog/guide-to-explainable-ai-in-healthcare/]
- 36. A Perspective on Explainable Artificial Intelligence Methods [https://arxiv.org/html/2305.02012v3]
- 37. Interpreting artificial intelligence models: a systematic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10997568/]
- 38. Comparison of SHAP and clinician friendly explanations ... [https://www.nature.com/articles/s41746-025-01958-8]
- 39. Exploiting Counterfactual Explanations for Medical Research [https://arxiv.org/html/2307.02131v6]
- 40. Model agnostic generation of counterfactual explanations ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8966631/]
- 41. Saliency-driven explainable deep learning in medical imaging [https://biodatamining.biomedcentral.com/articles/10.1186/s13040-024-00370-4]
- 42. a grad-CAM visualization approach - PMC - PubMed Central [https://pmc.ncbi.nlm.nih.gov/articles/PMC11683681/]
- 43. Automated classification and explainable AI analysis of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12459604/]
- 44. Assessment of a Grad-CAM interpretable deep learning model ... [https://bmcmedinformdecismak.biomedcentral.com/articles/10.1186/s12911-025-03256-5]
- 45. Evaluating the faithfulness of saliency maps in explaining ... [https://www.sciencedirect.com/science/article/abs/pii/S0306457322003260]
- 46. A novel explainable AI framework for medical image ... [https://www.sciencedirect.com/science/article/pii/S1361841525002129]
- 47. Towards the Use of Saliency Maps for Explaining Low- ... [https://arxiv.org/html/2207.02726v2]
- 48. Interpretability of AI race detection model in medical ... [https://www.sciencedirect.com/science/article/pii/S2001037025000066]
- 49. XAI-HD: an explainable artificial intelligence framework for ... [https://link.springer.com/article/10.1007/s10462-025-11385-6]
- 50. AI in Oncology Clinical Decision Support [https://cancerworld.net/ai-in-oncology-clinical-decision-support/]
- 51. Improving AI-Based Clinical Decision Support Systems and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12280832/]
- 52. Solving the explainable AI conundrum by bridging ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10202353/]
- 53. Improving AI-Based Clinical Decision Support Systems and ... [https://medinform.jmir.org/2025/1/e69688]
- 54. AI in Clinical Decision Support: Key Healthcare Trends 2025 [https://www.linkedin.com/pulse/ai-clinical-decision-support-trends-transforming-2025-nantha-kumar-l-2clic]
- 55. Optimizing Clinical Decision Support System Functionality by ... [https://humanfactors.jmir.org/2025/1/e69333]
- 56. Clinician-informed XAI evaluation checklist with metrics ... [https://www.nature.com/articles/s41746-025-01764-2]
- 57. Bias in medical AI: Implications for clinical decision-making [https://pmc.ncbi.nlm.nih.gov/articles/PMC11542778/]
- 58. Fairness of artificial intelligence in healthcare: review and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10764412/]
- 59. Algorithmic bias detection and mitigation: Best practices ... [https://www.brookings.edu/articles/algorithmic-bias-detection-and-mitigation-best-practices-and-policies-to-reduce-consumer-harms/]
- 60. Clinical Decision Support System Vendor Risk [https://censinet.com/perspectives/clinical-decision-support-system-vendor-risk-bias-accuracy-and-patient-safety]
- 61. Bias Mitigation Strategies and Techniques for ... [https://www.holisticai.com/blog/bias-mitigation-strategies-techniques-for-classification-tasks]
- 62. Fairness: The importance of diversity in health data for ... [https://uclpartners.com/blog-post/fairness-the-importance-of-diversity-in-health-data-for-creating-better-fairer-treatment-for-all/]
- 63. Exploring the role of professional identity in ... - PubMed Central [https://pmc.ncbi.nlm.nih.gov/articles/PMC10860285/]
- 64. Identity Threats as a Reason for Resistance to Artificial ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8987955/]
- 65. Medical Malpractice - StatPearls - NCBI Bookshelf - NIH [https://www.ncbi.nlm.nih.gov/books/NBK470573/]
- 66. 5 Real Medical Malpractice Cases That Changed the Legal ... [https://www.finchmccranie.com/blog/5-real-medical-malpractice-cases-that-changed-the-legal-landscape/]
- 67. Perceived Trust and Professional Identity Threat in AI-Based ... [https://formative.jmir.org/2025/1/e64266]
- 68. Explainability and AI Confidence in Clinical Decision ... [https://arxiv.org/abs/2501.16693]
- 69. eXplainable artificial intelligence-Eval: A framework for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12480807/]
- 70. A comprehensive study on fidelity metrics for XAI [https://www.sciencedirect.com/science/article/pii/S0306457324002590]
- 71. (CLIX-M) - for - AI-powered - clinical decision support ... [https://www.equator-network.org/reporting-guidelines/clinician-informed-explainable-artificial-intelligence-evaluation-checklist-with-metrics-clix-m-for-ai-powered-clinical-decision-support-systems/]
- 72. Explainable AI-based Deep-SHAP for mapping the ... - PubMed [https://pubmed.ncbi.nlm.nih.gov/38452732/]
- 73. Understanding the Role of Clinical Decision Support Systems ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12511814/]
- 74. a NASSS framework-informed scoping review [https://implementationscience.biomedcentral.com/articles/10.1186/s13012-023-01287-y]
- 75. Clinician-informed XAI evaluation checklist with metrics ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12167368/]
- 76. The application of explainable artificial intelligence in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12647564/]
- 77. Evaluating the impact of explainable AI on clinicians ... [https://www.sciencedirect.com/science/article/abs/pii/S1386505625001601]
- 78. AI Adoption In Healthcare Is Surging: What A New Report ... [https://www.forbes.com/sites/sachinjain/2025/10/21/ai-adoption-in-healthcare-is-surging-what-a-new-report-reveals/]
- 79. 2025: The State of AI in Healthcare [https://menlovc.com/perspective/2025-the-state-of-ai-in-healthcare/]