Ensemble Methods for Cancer Classification: Enhancing Accuracy and Interpretability in Biomedical Research
This article provides a comprehensive exploration of ensemble machine learning methods for cancer classification, tailored for researchers, scientists, and drug development professionals.
Ensemble Methods for Cancer Classification: Enhancing Accuracy and Interpretability in Biomedical Research
Abstract
This article provides a comprehensive exploration of ensemble machine learning methods for cancer classification, tailored for researchers, scientists, and drug development professionals. It covers the foundational principles explaining why ensemble models outperform single classifiers by reducing overfitting and capturing complex, nonlinear relationships in high-dimensional biomedical data. The scope extends to detailed methodologies including stacking, bagging, and boosting, with applications across diverse data types such as gene expression, multiomics, and histopathology images. The article further addresses critical troubleshooting and optimization strategies for handling class imbalance and high-dimensionality and concludes with rigorous validation frameworks and comparative analyses demonstrating state-of-the-art performance metrics, positioning ensemble methods as indispensable tools for precise oncology and biomarker discovery.
Why Ensemble Methods? Overcoming the Limitations of Single Classifiers in Oncology
The Critical Need for Accurate Cancer Classification in Modern Healthcare
Accurate cancer classification is a cornerstone of modern oncology, directly influencing diagnostic precision, treatment selection, and ultimately, patient survival. The complex heterogeneity of cancer necessitates classification systems that move beyond traditional histology to integrate molecular and genomic characteristics. Ensemble methods, which combine multiple machine learning models, have emerged as a powerful approach to enhance the accuracy and robustness of cancer classification. These methods integrate diverse data types—including genomic, imaging, and clinical data—to create a more comprehensive predictive model than any single algorithm could achieve alone. This document provides application notes and detailed protocols for implementing ensemble-based classification frameworks, designed for researchers and drug development professionals working to translate computational advances into clinical utility.
Recent studies demonstrate that ensemble methods consistently achieve high performance in discriminating between cancer types and subtypes. The following table summarizes quantitative results from key experiments.
Table 1: Performance Metrics of Recent Ensemble Classification Models
| Cancer Focus | Data Type(s) | Ensemble Method | Key Performance Metrics | Reference |
|---|---|---|---|---|
| Five Common Cancers (e.g., Breast, Colorectal) | RNA-seq, Somatic Mutation, DNA Methylation | Stacking Ensemble (SVM, KNN, ANN, CNN, RF) | Accuracy: 98% (Multiomics) vs 96% (single-omic) | [1] |
| Lung Cancer (Multiclass) | CT Scan Images | Hybrid CNN-SVD Feature Extraction + Voting Ensemble (SVM, KNN, RF, GNB, GBM) | Accuracy: 99.49%, AUC: 99.73%, Precision: 100%, Recall: 99%, F1-Score: 99% | [2] |
| Lung Cancer (Binary) | CT Scan Images | Same as above | All performance indicators: 100% | [2] |
| Six Tumor Types | DNA Methylation | GC-Forest with Intelligent SMOTE | High sensitivity for minority class while maintaining overall accuracy | [3] |
Detailed Experimental Protocols
Protocol 1: Multiomics Data Integration Using a Stacking Ensemble
This protocol outlines the methodology for classifying five common cancer types by integrating RNA sequencing, somatic mutation, and DNA methylation data within a stacking ensemble framework [1].
Applications and Use Cases
- Primary Application: Classifying common cancer types (e.g., breast, colorectal, thyroid) in a primary care or diagnostic setting.
- Research Use: Investigating the complementary value of different omics data types in understanding cancer biology.
- Data Integration: Serving as a template for building robust classifiers that fuse high-dimensional, heterogeneous biological data.
Materials and Reagents
Table 2: Research Reagent Solutions for Multiomics Analysis
| Item | Function/Description |
|---|---|
| The Cancer Genome Atlas (TCGA) | Source of RNA sequencing data for various cancer types [1]. |
| LinkedOmics Database | Source of somatic mutation and DNA methylation data corresponding to TCGA samples [1]. |
| Python 3.10+ | Programming language and environment for implementing the ensemble model [1]. |
| Transcripts Per Million (TPM) | Normalization method for RNA-seq data to eliminate technical bias and enable cross-sample comparison [1]. |
| Autoencoder | A deep learning technique used for non-linear dimensionality reduction and feature extraction from high-dimensional RNA-seq data [1]. |
Procedure
Data Acquisition and Cleaning:
- Download RNA-seq, somatic mutation, and DNA methylation data for the target cancer types from TCGA and LinkedOmics.
- Perform data cleaning to remove cases with missing or duplicate values (approximately 7% of data may be removed).
Data Preprocessing and Normalization:
- For RNA-seq data, apply TPM normalization using the formula:
TPM = (10^6 * reads mapped to transcript / transcript length) / (sum(reads mapped to transcript / transcript length))[1]. - Somatic mutation data is typically binary (0 or 1), indicating the presence or absence of a mutation.
- DNA methylation data consists of continuous values, often ranging from -1 to 1.
- For RNA-seq data, apply TPM normalization using the formula:
Feature Extraction:
- To address the high dimensionality of RNA-seq data, employ an autoencoder for feature extraction. The encoder compresses the input data into a lower-dimensional code, which the decoder then uses to reconstruct the input. The compressed code layer represents the extracted features.
Ensemble Model Training and Stacking:
- Base-Level Models: Train five distinct base classifiers on the preprocessed multiomics data: Support Vector Machine (SVM), k-Nearest Neighbors (KNN), Artificial Neural Network (ANN), Convolutional Neural Network (CNN), and Random Forest (RF).
- Meta-Learner: Use the predictions from these base models as input features to train a final meta-learner (which can be another classifier like logistic regression) to produce the ultimate classification.
Model Validation:
- Validate the stacked ensemble model using rigorous techniques such as k-fold cross-validation on a held-out test set to report final performance metrics like accuracy, precision, and recall.
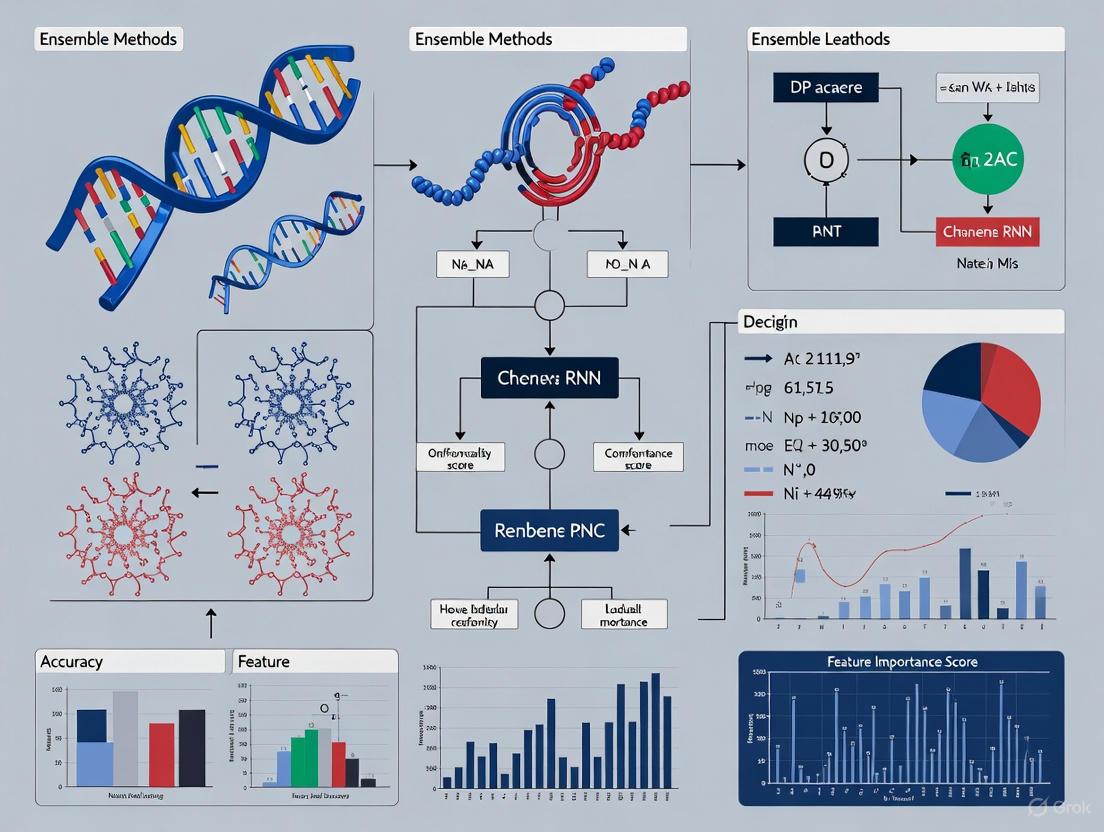
Workflow Visualization
Protocol 2: Hybrid CNN-SVD Ensemble for Medical Image Classification
This protocol describes a novel approach for lung cancer classification from CT scans that combines deep learning feature extraction with singular value decomposition (SVD) and a voting ensemble [2].
Applications and Use Cases
- Medical Imaging: Precise classification of lung cancer subtypes (e.g., adenocarcinoma, squamous cell carcinoma) from CT scans.
- Feature Engineering: A robust method for extracting and refining the most salient features from complex image data.
- Model Interpretability: Using explainable AI (XAI) techniques to build trust and provide insights for clinical decision-making.
Materials and Reagents
Table 3: Research Reagent Solutions for Image-Based Classification
| Item | Function/Description |
|---|---|
| Public Chest CT Scan Dataset | Curated dataset of lung cancer CT images for model development and testing [2]. |
| Contrast-Limited Adaptive\nHistogram Equalization (CLAHE) | Preprocessing technique to enhance image contrast with minimal noise amplification [2]. |
| Convolutional Neural Network (CNN) | Deep learning model used for automatic feature extraction from image data [2]. |
| Singular Value Decomposition (SVD) | A linear algebra technique for dimensionality reduction and feature selection [2]. |
| Gradient-weighted Class Activation\nMapping (Grad-CAM) | An explainable AI (XAI) technique to visualize regions of the image most influential to the model's prediction [2]. |
Procedure
Image Preprocessing:
- Apply Contrast-Limited Adaptive Histogram Equalization (CLAHE) to the input CT scans. This enhances contrast, making distinctive features more prominent while minimizing noise.
Hybrid Feature Extraction with CNN-SVD:
- CNN Feature Maps: Pass the preprocessed images through a Convolutional Neural Network (CNN). Extract the feature maps from a deep layer within the network.
- Dimensionality Reduction with SVD: Apply Singular Value Decomposition (SVD) to the flattened CNN feature maps. SVD decomposes the feature matrix, allowing you to select the top-k singular vectors (those with the highest singular values) as the most informative, compressed feature set.
Voting Ensemble Classification:
- The optimized features from the CNN-SVD process are used to train a diverse set of machine learning classifiers. The study used SVM, KNN, RF, Gaussian Naive Bayes (GNB), and Gradient Boosting Machine (GBM).
- A voting ensemble combines the predictions of these individual classifiers. In hard voting, the final class prediction is the one that receives the majority of votes.
Model Interpretation with Explainable AI (XAI):
- Implement Grad-CAM on the original CNN model. This technique uses the gradients of the target class flowing into the final convolutional layer to produce a heatmap highlighting the important regions in the image for predicting that class.
Workflow Visualization
The Scientist's Toolkit: Essential Research Reagents
The following table consolidates key resources referenced across the featured protocols and broader literature, providing a quick reference for researchers in this field.
Table 4: Essential Research Reagents and Resources for Ensemble-Based Cancer Classification
| Category | Item | Function in Research |
|---|---|---|
| Data Sources | The Cancer Genome Atlas (TCGA) | Comprehensive public repository containing molecular and clinical data for over 20,000 primary cancer samples across 33 cancer types [1]. |
| LinkedOmics | Publicly accessible database providing multiomics data from all 32 TCGA cancer types, used for sourcing somatic mutation and methylation data [1]. | |
| Computational Tools | Python | Primary programming language for implementing machine learning and deep learning models, data preprocessing, and analysis [1]. |
| Autoencoder | A type of neural network used for unsupervised feature learning and non-linear dimensionality reduction of high-dimensional data like RNA-seq [1]. | |
| Singular Value Decomposition (SVD) | A matrix factorization technique used for dimensionality reduction and feature selection from complex data structures like CNN feature maps [2]. | |
| Experimental Techniques | Intelligent SMOTE | An oversampling technique used to address class imbalance in datasets by generating synthetic samples for the minority class [3]. |
| Grad-CAM | An explainable AI technique that produces visual explanations for decisions from CNN-based models, crucial for clinical interpretability [2]. |
Ensemble learning is a machine learning paradigm that strategically combines multiple base models, often called "weak learners," to create a composite model that delivers superior predictive performance, enhanced stability, and greater robustness than any of its individual components. In the high-stakes field of cancer classification research, where diagnostic accuracy directly impacts clinical decision-making, the ability of ensemble methods to mitigate overfitting and improve generalization is particularly valuable [4]. The core principle is that a collection of models, when properly combined, can compensate for individual errors, leading to more reliable and accurate predictions on complex, high-dimensional biomedical data [5].
This approach is especially potent for tackling challenges inherent to cancer datasets, such as class imbalance (e.g., rare cancer subtypes versus more common ones), heterogeneity in tumor characteristics, and the "curse of dimensionality" often encountered with genomic and radiomic features [6]. By leveraging the strengths of diverse algorithms, ensemble methods provide researchers and clinicians with a more powerful and trustworthy tool for tasks ranging from early detection to prognosis prediction.
Core Principles and Methodologies of Ensemble Learning
The enhanced performance of ensemble learning rests on three foundational principles: the reduction of variance, the minimization of bias, and the expansion of the overall predictive space. By combining models that make different, uncorrelated errors, the ensemble can arrive at a more accurate and stable consensus, much like a wise crowd often outperforms a single expert. The most common strategies for building ensembles are Bagging, Boosting, and Voting, each with a distinct mechanism for aggregating predictions.
Table 1: Core Ensemble Learning Methodologies
| Methodology | Core Mechanism | Key Advantage | Common Algorithms |
|---|---|---|---|
| Bagging | Trains multiple instances of the same model in parallel on different data subsets via bootstrap sampling [4]. | Significantly reduces model variance and overfitting, excellent for high-variance models like decision trees. | Random Forest [4] |
| Boosting | Trains models sequentially, where each new model focuses on correcting the errors of its predecessors [4]. | Reduces both bias and variance, often achieving very high predictive accuracy. | XGBoost, LightGBM, AdaBoost, CatBoost [6] [4] |
| Voting / Stacking | Combines predictions from multiple, often different, base models by averaging (regression) or majority vote (classification) [4]. | Leverages the unique strengths of diverse model architectures for improved robustness. | Voting Classifier, Stacked Generalization |
Performance and Robustness in Cancer Classification
Empirical evidence from recent cancer classification studies consistently demonstrates the superiority of ensemble methods over single-model approaches. The performance gains are measurable not only in raw accuracy but also in critical metrics like AUC (Area Under the ROC Curve), F1-score, and robustness to class imbalance, which is a common challenge in medical datasets.
Table 2: Quantitative Performance of Ensemble Models in Cancer Research
| Study & Application | Ensemble Model(s) Used | Key Performance Metrics | Reported Advantage |
|---|---|---|---|
| Biomarker-Based Cancer Classification [6] | Pre-trained Hyperfast Ensemble, XGBoost, LightGBM | AUC: 0.9929 (BRCA vs. non-BRCA) | Robustness on highly imbalanced datasets; state-of-the-art accuracy with only 500 features. |
| Lung Tumor Detection from CT Scans [5] | Reinforcement Learning-based Dynamic CNN Ensemble | Accuracy: 99.55%, 97.22%, 99.94% on three datasets. F1-Score: ≈1.0 | Superior domain adaptability and cross-dataset robustness. |
| Rectal Cancer Tumor Deposit Prediction from MRI [4] | Voting-Ensemble Learning Model (VELM) | AUC: 0.875, Accuracy: 0.800 (Testing Cohort) | Superior net benefit in decision curve analysis and clear feature clustering. |
The robustness of ensemble methods is twofold. First, they exhibit greater stability against overfitting, especially when individual models are trained on resampled data or with regularization [4]. Second, they specifically improve performance on minority classes. For instance, a pre-trained Hyperfast ensemble was shown to provide prior-insensitive decisions under bounded bias and yield minority-error reductions under mild error diversity, making it particularly suitable for detecting rare cancer types [6]. Furthermore, dynamic ensemble methods that use reinforcement learning to adaptively select and weight classifiers have shown remarkable cross-domain robustness, maintaining high performance across datasets with different distributions [5].
Experimental Protocols for Ensemble Construction
Implementing an effective ensemble model requires a systematic and rigorous protocol. The following workflow, adapted from state-of-the-art research in cancer diagnostics, outlines the key steps from data preparation to model evaluation, with a focus on a voting ensemble for a classification task such as predicting tumor deposits from medical images [4].
Protocol 4.1: Voting Ensemble for Cancer Classification
Objective: To construct a robust predictive model for a binary or multi-class cancer classification task (e.g., malignant vs. benign, or cancer subtype classification) by combining multiple machine learning classifiers.
Materials: Python environment (v3.9+), scikit-learn, XGBoost, LightGBM, PyRadiomics (if using radiomic features), ITK-SNAP for segmentation.
Step-by-Step Procedure:
Data Preparation and Feature Extraction
- Data Sourcing: Collect and de-identify patient data, ensuring ethical approval. Define clear inclusion and exclusion criteria for the cohort.
- Region of Interest (ROI) Segmentation: Manually or automatically segment tumors from medical images (e.g., MRI, CT) using software like ITK-SNAP. This should be performed by multiple readers to assess inter-observer variability.
- Feature Extraction: Use a standardized library like PyRadiomics to extract a high-dimensional set of quantitative features (e.g., shape, texture, wavelet features) from the segmented ROIs. For genomic data, this could involve normalized expression levels of key biomarkers.
- Data Preprocessing: Normalize the feature matrix using Z-score normalization. Handle missing data through imputation or deletion. Address class imbalance in the training set only using techniques like SMOTE (Synthetic Minority Over-sampling Technique) [4].
Feature Selection
- Step 1 - Reliability Analysis: Calculate the Intra-class Correlation Coefficient (ICC) for all features if multiple segmentations exist. Retain only features with excellent reproducibility (e.g., ICC ≥ 0.8).
- Step 2 - Redundancy Reduction: Apply the Max-Relevance and Min-Redundancy (mRMR) algorithm to filter out redundant features, selecting a top-ranked subset (e.g., K=150).
- Step 3 - Regularization: Use Least Absolute Shrinkage and Selection Operator (LASSO) regression with 10-fold cross-validation to perform final feature selection, identifying the most predictive non-redundant features for the model.
Base Model Training and Hyperparameter Tuning
- Split the dataset into training (e.g., 70%), validation (e.g., 15%), and hold-out testing (e.g., 15%) cohorts. The validation set is used for tuning.
- Select a diverse set of 4-5 base classifiers (e.g., Random Forest, XGBoost, LightGBM, SVM, Logistic Regression).
- Independently optimize each base model using Grid Search or Randomized Search with 10-fold cross-validation on the training set, targeting maximization of AUC or balanced accuracy. The validation set can be used to evaluate the tuned models before ensemble construction.
Ensemble Construction (Voting)
- Combine the optimally tuned base models into a Voting Ensemble. Use a
VotingClassifierfrom scikit-learn. - For hard voting, the final prediction is the majority vote across all base model predictions.
- For soft voting, the final prediction is the argmax of the sum of predicted probabilities, which often yields better performance as it weights models by their confidence.
- Combine the optimally tuned base models into a Voting Ensemble. Use a
Model Evaluation and Validation
- Evaluate the final ensemble model on the held-out test set that was not used in any training or tuning steps.
- Performance Metrics: Report AUC, Accuracy, Precision, Recall (Sensitivity), Specificity, and F1-Score.
- Robustness and Clinical Utility:
- Plot calibration curves to assess the agreement between predicted probabilities and actual outcomes.
- Perform decision curve analysis (DCA) to evaluate the model's net benefit across a range of clinical decision thresholds.
- Use visualization techniques like t-SNE (t-distributed Stochastic Neighbor Embedding) to illustrate the clustering of features learned by the model.
The Scientist's Toolkit: Research Reagent Solutions
The successful implementation of an ensemble learning project in cancer research relies on a suite of software tools, libraries, and data processing techniques. The following table details the essential "research reagents" for this computational task.
Table 3: Essential Tools and Software for Ensemble Learning Research
| Tool / Resource | Category | Function in Research |
|---|---|---|
| Python (v3.9+) | Programming Language | The primary environment for scripting data preprocessing, model building, and analysis [4]. |
| Scikit-learn | Machine Learning Library | Provides implementations of standard classifiers (RF, SVM), ensemble methods (VotingClassifier), and vital utilities for feature selection (LASSO), preprocessing, and model evaluation [4]. |
| XGBoost / LightGBM | Boosting Algorithm | High-performance, gradient-boosting frameworks that are frequently used as powerful base learners within an ensemble [6] [4]. |
| PyRadiomics | Feature Extraction | A flexible open-source platform for extracting a large set of standardized radiomic features from medical images [4]. |
| ITK-SNAP | Image Segmentation | A specialized software tool for manual, semi-automatic, or automatic segmentation of structures in 3D medical images [4]. |
| PyTorch / TensorFlow | Deep Learning Framework | Essential for building and pre-training complex base models like Convolutional Neural Networks (CNNs), especially for image-based tasks [5]. |
In the field of oncology, the application of machine learning (ML) for classification and prognosis has become increasingly prevalent. However, two significant and interconnected data-related challenges consistently impede model performance: high-dimensionality and class imbalance. High-dimensionality arises in genomic data, where the number of features (e.g., genes) vastly exceeds the number of patient samples, leading to computational inefficiency and an increased risk of overfitting [7] [8]. Concurrently, class imbalance is common in prognostic tasks, such as predicting short-term survival, where the number of patients in one class (e.g., deceased) is significantly outnumbered by the other (e.g., survivors) [9] [10]. This imbalance biases classifiers toward the majority class, reducing sensitivity for detecting the critical minority class.
Ensemble methods, which combine multiple base models to improve robustness and accuracy, are particularly well-suited to tackle these challenges. Their inherent stability makes them effective for high-dimensional data, and they can be strategically paired with resampling techniques to correct for class distribution skews [9] [10]. This application note details these challenges and provides structured experimental protocols and resources for developing effective ensemble-based solutions.
The tables below summarize the core challenges and the demonstrated performance of various strategies to address them.
Table 1: Characterizing Data Challenges in Publicly Available Cancer Datasets
| Dataset | Primary Use | Sample Size | Feature Size | Imbalance Ratio | Key Challenge |
|---|---|---|---|---|---|
| Lung Cancer Detection [9] | Diagnosis | 309 | 16 | 1:7 (12.6% minority) | High Imbalance |
| SEER Colorectal Cancer (1-Year) [10] | Prognosis | Not Specified | 16 | 1:10 (9.1% minority) | Extreme Imbalance |
| Gene Expression (e.g., Microarray) [7] [8] | Classification | Small (e.g., 10s-100s) | Very High (e.g., 20,000 genes) | Varies | High-Dimensionality & Small Sample Size |
| Wisconsin Breast Cancer (WBCD) [9] | Diagnosis | 699 | 10 | 1.7:1 (34.5% minority) | Moderate Imbalance |
Table 2: Performance Comparison of Solutions on Benchmark Tasks
| Solution Strategy | Dataset / Task | Key Metric | Reported Performance | Baseline (No Solution) |
|---|---|---|---|---|
| Hybrid Sampling (SMOTEENN) [9] | Multiple Cancer Dx/Prog | Mean Accuracy | 98.19% | 91.33% |
| LGBM + RENN Sampling [10] | 1-Year CRC Survival | Sensitivity | 72.30% | Not Reported |
| Random Forest [9] | Multiple Cancer Dx/Prog | Mean Accuracy | 94.69% | 91.33% |
| MI-Bagging Ensemble [7] | Gene Expression Classification | Accuracy | Outperforms single models | Lower in single models |
| Autoencoder + Classifier [11] | Prostate Cancer Prediction | Accuracy | Better than PCA-based | Lower with original data |
Addressing High-Dimensionality with Feature Reduction
High-dimensional data, such as gene expression profiles with over 20,000 genes, introduces noise and computational burden. Dimensionality reduction is an essential preprocessing step.
Application Note: Dimensionality Reduction for Ensemble Models
- Objective: To improve the performance and efficiency of ensemble classifiers by reducing the feature space of genomic data.
- Background: While ensemble methods like Random Forest can handle high-dimensional spaces, reducing irrelevant and redundant features mitigates overfitting and sharpens the model's focus on meaningful biological signals [12] [7].
- Experimental Workflow: The process involves transforming the original high-dimensional data into a compact, informative representation before training the ensemble model.
Protocol: Implementing an Autoencoder for Feature Extraction
Autoencoders are neural networks that learn compressed, non-linear representations of data, often outperforming linear methods like PCA [11].
- Data Preparation: Normalize the gene expression data (e.g., using min-max scaling or transcripts per million (TPM) for RNA-seq data) [13].
- Model Configuration:
- Architecture: Construct a symmetric encoder-decoder.
- Encoder: A sequence of fully connected (dense) layers that progressively reduce dimensionality (e.g., 2000 -> 500 -> 100 -> 30 units). Use ReLU activation functions.
- Bottleneck: The central layer with the lowest dimensionality (e.g., 30 units). This is the extracted feature vector.
- Decoder: A mirror of the encoder that reconstructs the input from the bottleneck (e.g., 30 -> 100 -> 500 -> 2000 units).
- Compilation: Use the Adam optimizer and Mean Squared Error (MSE) as the loss function.
- Architecture: Construct a symmetric encoder-decoder.
- Training: Train the autoencoder to minimize the reconstruction error on the training set. Implement early stopping to prevent overfitting.
- Feature Extraction: Use the trained encoder to transform the original high-dimensional training and test datasets into the lower-dimensional bottleneck representations.
- Ensemble Training: Train the ensemble classifier (e.g., a voting classifier or Random Forest) using the extracted features from the bottleneck layer.
Addressing Class Imbalance with Resampling Techniques
Class imbalance causes classifiers to be biased toward the majority class. Resampling the training data is a common and effective solution.
Application Note: Resampling for Imbalanced Cancer Prognosis
- Objective: To enhance the sensitivity of ensemble models for predicting minority class outcomes (e.g., 1-year cancer survival) by balancing the training data.
- Background: In a colorectal cancer dataset with a 1:10 imbalance ratio for 1-year survival, standard models fail to identify non-survivors. Hybrid sampling methods like SMOTEENN have been shown to achieve the highest mean performance across various cancer datasets [9].
- Experimental Workflow: Resampling is applied only to the training set during cross-validation to avoid data leakage and over-optimistic performance.
Protocol: Hybrid Sampling with SMOTEENN
This protocol combines Synthetic Minority Oversampling Technique (SMOTE) and Edited Nearest Neighbors (ENN) to first create synthetic minority samples and then clean the resulting data [9] [10].
- Data Splitting: Split the dataset into training and testing sets. Resampling will be applied only to the training set.
- SMOTE - Oversampling:
- For each sample in the minority class, SMOTE calculates its
knearest neighbors (typically k=5). - It then synthesizes new examples along the line segments joining the original sample and its neighbors.
- This step increases the number of minority class instances to a desired level (e.g., 50% of the majority class).
- For each sample in the minority class, SMOTE calculates its
- ENN - Undersampling:
- After SMOTE, ENN is applied to remove any instances (both majority and synthetic minority) whose class label differs from the majority of its
knearest neighbors. - This "cleaning" step removes noisy and borderline instances that may confuse the classifier.
- After SMOTE, ENN is applied to remove any instances (both majority and synthetic minority) whose class label differs from the majority of its
- Model Training and Evaluation:
- Train a tree-based ensemble classifier, such as Light Gradient Boosting Machine (LGBM) or Random Forest, on the resampled data.
- Evaluate the model on the untouched test set. Prioritize metrics like Sensitivity (Recall) and F1-Score over raw accuracy due to the imbalanced nature of the test data.
Integrated Solution: Multiomics Ensemble Classification
For the most challenging scenarios, an integrated approach combining multi-modal data and advanced ensemble architectures is required.
Application Note: Stacking Ensemble for Multiomics Data
- Objective: To leverage high-dimensional data from multiple sources (multiomics) for superior cancer classification by employing a stacked ensemble model.
- Background: Different omics data types (e.g., RNA sequencing, DNA methylation, somatic mutations) provide complementary information. A stacking ensemble can non-linearly combine predictions from diverse base models, each potentially specialized for a different data type, achieving higher accuracy than any single model [13].
- Experimental Workflow: This framework manages high-dimensionality per data type and integrates predictions through a meta-learner.
Protocol: Building a Stacking Ensemble Classifier
- Data Preprocessing and Reduction:
- Process each omics data type independently. Normalize RNA-seq and methylation data. Encode somatic mutations as binary features (0/1).
- Apply feature reduction techniques (e.g., Autoencoder, PCA) to each data type to manage dimensionality [13].
- Base Model Training (Level-0):
- Split the preprocessed data into training and validation sets.
- Train a diverse set of base models (e.g., SVM, KNN, ANN, CNN, RF) on the training set. These models can be trained on different omics types or combinations thereof.
- Use k-fold cross-validation on the training set to generate "out-of-fold" predictions for each base model. These predictions form the meta-features for the next level.
- Meta-Model Training (Level-1):
- The out-of-fold predictions from all base models are combined to create a new feature matrix (the meta-features).
- A meta-learner (e.g., Logistic Regression, Linear SVM) is trained on this new matrix to learn how to best combine the predictions of the base models.
- Evaluation:
- The final stacked model is evaluated on the held-out test set. Base models make predictions on the test set, which are fed as features to the meta-learner for the final classification.
Table 3: Essential Research Reagent Solutions for Ensemble-Based Cancer Data Analysis
| Category / Item | Specification / Example | Primary Function in Workflow |
|---|---|---|
| Public Data Repositories | ||
| The Cancer Genome Atlas (TCGA) | https://www.cancer.gov/ccg/research/genome-sequencing/tcga | Primary source for multiomics patient data (RNA-seq, methylation, mutations). |
| SEER Program | https://seer.cancer.gov/ | Source for large-scale clinical data for survival analysis and prognosis studies. |
| UCI / Kaggle Repositories | e.g., Wisconsin Breast Cancer, Lung Cancer Detection [9] | Source for curated benchmark datasets for diagnostic model development. |
| Computational Tools & Algorithms | ||
| Dimensionality Reduction | ||
| Autoencoder (AE) | Keras, PyTorch Frameworks | Non-linear feature extraction from high-dimensional genomic data [13] [11]. |
| Principal Component Analysis (PCA) | Scikit-learn PCA |
Linear dimensionality reduction and data compression [14] [11]. |
| Mutual Information (MI) | Scikit-learn mutual_info_classif |
Filter-based feature selection to identify informative genes [7]. |
| Resampling Techniques | ||
| SMOTE | Imbalanced-learn SMOTE |
Synthetic oversampling of the minority class to balance datasets [9] [10]. |
| Edited Nearest Neighbors (ENN/RENN) | Imbalanced-learn EditedNearestNeighbours |
Cleans data by removing noisy majority class instances after oversampling [10]. |
| Ensemble Classifiers | ||
| Random Forest (RF) | Scikit-learn RandomForestClassifier |
Robust bagging ensemble for classification and feature importance analysis [15] [9]. |
| LightGBM (LGBM) | LightGBM Framework | High-performance gradient boosting framework, effective with resampled data [10]. |
| Voting / Stacking Classifier | Scikit-learn VotingClassifier, StackingClassifier |
Combines predictions from multiple heterogeneous base estimators [12] [13]. |
| Model Interpretation | ||
| SHAP (SHapley Additive exPlanations) | SHAP Library | Explains the output of any ML model, critical for clinical trust [15]. |
In the demanding field of cancer research, where diagnostic accuracy directly impacts patient outcomes, the transition from relying on single predictive models to harnessing the power of ensemble methods represents a significant paradigm shift. Ensemble learning, a subfield of machine learning, employs multiple learning algorithms to obtain better predictive performance than could be obtained from any of the constituent learning algorithms alone [16]. In the context of cancer classification—a task complicated by high-dimensional data, class imbalance, and the inherent biological complexity of the disease—this "collective intelligence" offers a robust framework for improving diagnostic precision. By strategically combining the predictions from diverse models, ensemble techniques effectively mitigate the individual weaknesses of single models, leading to enhanced stability and accuracy in classification tasks [16] [17]. This article explores the theoretical underpinnings of ensemble learning and provides detailed protocols for their application in cancer classification research, spanning multiomics data integration and medical image analysis.
Theoretical Foundations of Ensemble Learning
The theoretical justification for ensemble learning is deeply rooted in its ability to optimize the bias-variance trade-off, a fundamental concept in supervised learning. A single model, especially a complex one, might have low bias but high variance, meaning it is sensitive to small fluctuations in the training data and prone to overfitting. Conversely, an overly simplistic model may have high bias and fail to capture important patterns in the data [17].
- Bias-Variance Decomposition: The expected prediction error of a model can be decomposed into three components: bias, variance, and irreducible error. Ensemble methods aim to reduce variance, bias, or both, depending on the technique [17].
- The Power of Diversity: The efficacy of an ensemble hinges on the diversity of its base models. If all models make the same errors, combining them will not yield improvements. Empirically, ensembles tend to yield better results when there is a significant diversity among the models they combine [16]. This diversity can be achieved by using different algorithms, different training data subsets, or different model configurations.
The most common ensemble strategies are bagging, boosting, and stacking, each with distinct theoretical mechanisms for improving prediction.
Bagging (Bootstrap Aggregating)
Bagging reduces variance by averaging the predictions of multiple models trained on different bootstrapped datasets (random samples drawn from the training set with replacement) [16] [18].
- Theoretical Mechanism: The variance of the combined model is reduced compared to the variance of a single base model. Assuming the prediction errors of the M base models are uncorrelated, the variance can be reduced by a factor of M while the bias remains similar to that of the individual models [17].
- Common Application: The Random Forest algorithm is an extension of bagging for decision trees, which introduces an additional layer of diversity by randomizing the features considered for splits at each node [16].
Boosting
Boosting follows an iterative, sequential process to reduce both bias and variance. New models are trained to focus on the errors or misclassified instances of the previous models, and their predictions are combined through a weighted majority vote [16] [17].
- Theoretical Mechanism: Boosting builds an additive model in a greedy manner. In each step, the algorithm tries to correct the residual errors from the previous model. This sequential refinement leads to a progressive reduction in bias. Variants like AdaBoost have been rigorously shown to reduce the overall prediction error exponentially across iterations [17].
- Common Applications: Algorithms like AdaBoost, Gradient Boosting, and Categorical Boosting (CatBoost) are widely used. For instance, CatBoost achieved a test accuracy of 98.75% in predicting cancer risk from lifestyle and genetic data, outperforming other traditional and ensemble models [19].
Stacking (Stacked Generalization)
Stacking, or blending, is a more flexible ensemble technique that involves training a meta-learner to optimally combine the predictions of several diverse base models [16] [18].
- Theoretical Mechanism: Instead of simple averaging or voting, stacking uses a second-level model to learn how to best integrate the predictions from the first-level models. Since the prediction function of the meta-learner can be non-linear, it can potentially reduce both the bias and variance terms in the error decomposition [17].
- Implementation: The process involves creating a new dataset where the inputs are the out-of-sample predictions (e.g., from cross-validation) of the base models, and the output is the true target value. A meta-model is then trained on this new dataset to form the final predictor [18].
The following diagram illustrates the logical relationships and workflow between these core ensemble learning concepts.
Application in Cancer Classification: Protocols and Performance
Ensemble methods have demonstrated remarkable success across various cancer classification domains, from integrating multiomics data to analyzing medical images. The following table summarizes quantitative performance data from recent studies, highlighting the effectiveness of ensemble approaches.
Table 1: Performance of Ensemble Methods in Recent Cancer Classification Studies
| Cancer Type / Focus | Data Modality | Ensemble Method | Base Models | Key Performance Metric |
|---|---|---|---|---|
| Multi-Cancer Type Classification [13] [1] | Multiomics (RNA-seq, Somatic Mutation, DNA Methylation) | Stacking Ensemble | SVM, KNN, ANN, CNN, Random Forest | 98% Accuracy with multiomics data vs. 96% (RNA-seq alone) |
| Lung Cancer Classification [2] | CT Scan Images | Voting Ensemble | SVM, KNN, RF, GNB, GBM | 99.49% Accuracy, 100% Precision, 99% Recall |
| Cervical Cancer Classification [20] | Pap Smear Images | Ensemble (CNN, AlexNet, SqueezeNet) | CNN, AlexNet, SqueezeNet | 94% Accuracy (surpassing individual model accuracies of 90.8-92%) |
| General Cancer Risk Prediction [19] | Lifestyle & Genetic Data | Boosting (CatBoost) | N/A (Single ensemble model) | 98.75% Test Accuracy, F1-score: 0.9820 |
Protocol 1: Stacking Ensemble for Multiomics Cancer Classification
This protocol details the methodology for developing a stacking ensemble to classify five common cancer types (e.g., breast, colorectal, thyroid) using RNA sequencing, somatic mutation, and DNA methylation data [13] [1].
Research Reagent Solutions
Table 2: Essential Materials and Computational Tools for Multiomics Analysis
| Item / Resource | Function / Description | Source / Example |
|---|---|---|
| The Cancer Genome Atlas (TCGA) | Source for RNA sequencing data; provides ~20,000 primary cancer and matched normal samples. | National Cancer Institute |
| LinkedOmics Database | Source for somatic mutation and DNA methylation profiles corresponding to TCGA samples. | LinkedOmics Portal |
| Python 3.10+ | Primary programming language for implementing the data preprocessing and ensemble model. | Python Software Foundation |
| Aziz Supercomputer (or equivalent HPC) | High-performance computing resource for handling computationally intensive omics data processing. | King Abdulaziz University |
| scikit-learn, TensorFlow/PyTorch | Machine learning and deep learning libraries for building base models and meta-learner. | Open Source Libraries |
Step-by-Step Workflow
Data Acquisition and Cleaning:
- Download RNA sequencing data from TCGA and corresponding somatic mutation and methylation data from LinkedOmics for the target cancer types (e.g., BRCA, COAD, THCA) [13] [1].
- Perform data cleaning to ensure integrity: identify and remove cases with missing or duplicate values (approximately 7% of cases were removed in the original study) [13].
Data Preprocessing and Feature Extraction:
- Normalization: For RNA sequencing data, apply the Transcripts Per Million (TPM) method to eliminate technical variation using the formula provided in the original study to normalize gene expression counts [13] [1].
- Feature Extraction: To handle the high dimensionality of the RNA-seq data, employ an autoencoder to compress the input features into a lower-dimensional space, preserving essential biological properties [13].
Training Base Models:
- Split the preprocessed multiomics data into training and testing sets (e.g, 80%/20%).
- Individually train the following five base models on the training set. It is crucial to use cross-validation to generate out-of-sample predictions for the next step.
- Support Vector Machine (SVM)
- k-Nearest Neighbors (KNN)
- Artificial Neural Network (ANN)
- Convolutional Neural Network (CNN)
- Random Forest (RF)
Building the Stacking Ensemble:
- Create a new dataset (the "level-1" dataset) where each instance consists of the predicted class probabilities (or labels) from the five base models as features, and the true label as the target.
- Train a meta-learner on this new dataset. A common and effective choice is a regularized linear model, such as a linear regression with lasso penalty, which can help prune non-informative base models [18].
- The final stacked model makes predictions by first getting predictions from all base models and then feeding them into the trained meta-learner for the final classification.
The workflow for this protocol, from data preparation to final prediction, is visualized below.
Protocol 2: CNN-SVD Ensemble for Lung Cancer Classification from CT Scans
This protocol outlines a hybrid feature extraction and ensemble method for multiclass lung cancer classification, achieving state-of-the-art performance [2].
Research Reagent Solutions
Table 3: Essential Materials and Tools for Image-Based Cancer Classification
| Item / Resource | Function / Description | Source / Example |
|---|---|---|
| Lung CT Scan Dataset | Publicly available dataset of chest CT scan images for lung cancer, annotated for binary and multiclass classification. | Public repositories (e.g., Kaggle, The Cancer Imaging Archive) |
| Convolutional Neural Network (CNN) | Used as a primary feature extractor from the medical images. | TensorFlow/PyTorch |
| Singular Value Decomposition (SVD) | A matrix factorization technique used for dimensionality reduction of the extracted CNN features. | scikit-learn, SciPy |
| Gradient-weighted Class Activation Mapping (Grad-CAM) | An explainable AI (XAI) technique to visualize regions of the image most influential to the prediction. | Various XAI Libraries |
Step-by-Step Workflow
Image Preprocessing:
- Apply Contrast-Limited Adaptive Histogram Equalization (CLAHE) to enhance the contrast of the CT scan images, generating images with minimal noise and prominent distinctive features [2].
- Resize all images to a uniform dimensions suitable for the CNN input.
Hybrid Feature Extraction with CNN-SVD:
- Use a pre-trained CNN (e.g., on ImageNet) without its final classification layer as a feature extractor. Process all CT images through this network to obtain a high-dimensional feature vector for each image.
- Apply Singular Value Decomposition (SVD) to the matrix of all feature vectors. SVD decomposes the matrix and allows for dimensionality reduction by selecting the top k singular values and their corresponding vectors, capturing the most important patterns while reducing noise and computational load [2].
Training the Voting Ensemble:
- The reduced feature set from the CNN-SVD step serves as the input for the following machine learning classifiers:
- Support Vector Machine (SVM)
- k-Nearest Neighbors (KNN)
- Random Forest (RF)
- Gaussian Naive Bayes (GNB)
- Gradient Boosting Machine (GBM)
- Train each of these models independently on the training set.
- Implement a voting ensemble for the final prediction. This can be a "hard" vote (final class is the mode of all predictions) or a "soft" vote (final class is derived from the average of predicted probabilities) [2].
- The reduced feature set from the CNN-SVD step serves as the input for the following machine learning classifiers:
Model Interpretation with Explainable AI (XAI):
- Integrate Grad-CAM with the CNN model to produce heatmaps that highlight the regions in the CT scans that were most influential for the classification decision. This step is critical for building trust and providing clinical interpretability [2].
The theoretical framework of ensemble learning—centered on the principles of variance reduction, bias correction, and leveraging model diversity—provides a powerful foundation for tackling the complex challenges inherent in cancer classification. The protocols detailed herein, from stacking for multiomics data to hybrid CNN ensembles for medical imaging, offer researchers and drug development professionals reproducible methodologies to achieve state-of-the-art performance. As the field advances, future research should focus on refining these ensemble methodologies, expanding their applicability to other cancer types and data modalities, and further integrating explainable AI to ensure these powerful tools are both effective and transparent for clinical translation.
Building Powerful Ensemble Classifiers: From Stacking to Multiomics Integration
Ensemble learning represents a paradigm in machine learning where multiple models, often called "base learners" or "weak learners," are strategically combined to solve a particular computational intelligence problem. The core principle is that a group of weak models can collectively form a stronger, more robust model, a concept inspired by the "wisdom of the crowd" [21]. In cancer classification research, where high-dimensional multiomics data and complex medical images present significant analytical challenges, ensemble methods have proven particularly valuable for improving diagnostic accuracy, prognostic prediction, and treatment stratification [1] [2]. These techniques help mitigate common data issues in biomedical research, including class imbalance, overfitting on limited patient data, and the "curse of dimensionality" inherent to genomics and medical imaging data [1].
This article details the three core ensemble architectures—bagging, boosting, and stacking—within the context of cancer informatics. We provide structured comparisons, detailed experimental protocols, and implementation guidance specifically tailored for research scientists and drug development professionals working on computational oncology problems.
Bagging (Bootstrap Aggregating)
Conceptual Foundation
Bagging, an acronym for Bootstrap Aggregating, is an ensemble technique designed primarily to reduce variance and prevent overfitting in high-variance models [22]. The method operates by creating multiple versions of the original training dataset through bootstrap sampling (random sampling with replacement) and training a base model on each of these versions [21]. The final prediction is generated by aggregating the predictions of all individual models, typically through majority voting for classification problems or averaging for regression problems [23].
The theoretical foundation of bagging rests on the statistical method of bootstrapping, which enables robust estimation of model statistics. As demonstrated through Condorcet's Jury Theorem, the collective decision of multiple independent judges can yield more accurate results than any single judge, provided each judge has at least a modest level of competence [21]. Similarly, in bagging, the combined prediction from multiple models typically outperforms individual models, especially when the base learners are unstable (e.g., decision trees) [21].
Implementation Protocol
A standardized protocol for implementing bagging in a cancer classification context involves the following steps:
- Bootstrap Sampling: Given a training dataset ( D ) of size ( N ), generate ( M ) new bootstrap samples ( D1, D2, ..., D_M ), each of size ( N ), by randomly drawing instances from ( D ) with replacement. Each sample typically contains approximately 63.2% of the original training instances, with some duplicates.
- Base Model Training: Train ( M ) instances of a base classifier (e.g., Decision Tree, Random Forest) independently on each bootstrap sample ( D_i ). For cancer classification using histopathology images or genomic data, the base model architecture should be selected based on data modality (e.g., CNNs for images, ANNs for omics data).
- Prediction Aggregation: For a new test sample ( x ), obtain predictions ( a1(x), a2(x), ..., aM(x) ) from all trained models. The final ensemble prediction ( a(x) ) is determined by majority voting: ( a(x) = \text{mode}{a1(x), a2(x), ..., aM(x)} ).
Table 1: Performance Comparison of Bagging Ensemble in Cancer Classification
| Cancer Type | Data Modality | Base Model | Performance (Accuracy) | Key Benefit |
|---|---|---|---|---|
| Lung Cancer [2] | CT Scans | Multiple ML classifiers | 99.49% | Superior accuracy in multiclass classification |
| Not Specified [22] | Generic | Decision Trees | Improved over base | Reduces variance and overfitting |
Workflow Visualization
Bagging Ensemble Architecture
Boosting
Conceptual Foundation
Boosting is a sequential ensemble technique that converts multiple weak learners into a single strong learner. Unlike bagging where models are built independently, boosting constructs models sequentially, with each new model focusing on the errors made by previous models [24] [22]. The core principle is to adaptively adjust the weights of training instances, giving higher weight to misclassified samples in subsequent iterations, thereby forcing the model to concentrate on harder-to-classify cases.
This approach is particularly effective for reducing both bias and variance, making it suitable for weak learners that perform only slightly better than random guessing [22]. In cancer classification, boosting algorithms excel at identifying subtle patterns in complex datasets, which can be critical for distinguishing between cancer subtypes with similar morphological or molecular characteristics [24].
Implementation Protocol
A generalized protocol for implementing boosting in a cancer classification context:
- Initialize Weights: Assign equal weight ( wi = 1/N ) to each training instance ( (xi, y_i) ) in dataset ( D ) of size ( N ).
- Sequential Model Training: For ( T ) iterations: a. Train a weak learner ( ht ) (e.g., a shallow decision tree) on the weighted training data. b. Calculate the weighted error ( \epsilont ) of ( ht ). c. Compute the model weight ( \alphat = \frac{1}{2} \ln \left( \frac{1 - \epsilont}{\epsilont} \right) ), which represents the contribution of ( h_t ) to the final prediction. d. Update the instance weights: increase weights for misclassified instances and decrease weights for correctly classified instances. e. Normalize the weights to form a probability distribution.
- Final Ensemble Formation: Combine all weak learners using weighted majority voting: ( H(x) = \text{sign}\left( \sum{t=1}^T \alphat h_t(x) \right) ).
Table 2: Popular Boosting Algorithms and Their Applications
| Algorithm | Key Mechanism | Cancer Research Application | Advantages |
|---|---|---|---|
| Gradient Boosting (GBM) [24] | Fits new models to residuals of previous models | Histopathological image classification | High predictive accuracy |
| XGBoost [24] | Regularized model with presorted splitting | Genomic biomarker discovery | Computational efficiency, handling missing data |
| LightGBM [24] | Gradient-based One-Sided Sampling (GOSS) | Large-scale medical image analysis | Fast training speed, low memory usage |
| CatBoost [24] | Handles categorical features natively | Integration of clinical and genomic data | No preprocessing for categorical variables |
Workflow Visualization
Boosting Sequential Training Process
Stacking (Stacked Generalization)
Conceptual Foundation
Stacking, also known as stacked generalization, is an advanced ensemble technique that combines multiple heterogeneous base models (e.g., SVM, Random Forest, KNN) using a meta-learner [23] [25]. The fundamental concept is to learn the optimal way to combine the predictions of diverse base models, rather than relying on simple voting or averaging [26].
The stacking architecture typically consists of two or more levels: level-0 contains the base models that are trained on the original data, and level-1 contains a meta-model that is trained on the outputs (predictions) of the base models [23] [25]. This approach leverages the diverse inductive biases of different algorithms, allowing the ensemble to capture complementary patterns in the data that might be missed by any single algorithm.
In multiomics cancer classification, stacking has demonstrated exceptional performance by effectively integrating predictions from models trained on different data modalities (e.g., RNA sequencing, DNA methylation, somatic mutations) [1]. A recent study achieved 98% accuracy in classifying five common cancer types using a stacking ensemble that integrated multiomics data, outperforming models using single-omics data [1].
Implementation Protocol
A detailed protocol for implementing stacking in cancer classification:
Data Preparation and Base Model Selection: a. Split the dataset into training (( D{\text{train}} )) and testing (( D{\text{test}} )) sets. b. Select ( K ) diverse base models (e.g., SVM, Random Forest, KNN, Neural Networks) [25]. Diversity in model types is crucial for effective stacking.
Cross-Validation for Meta-Feature Generation: a. Split ( D{\text{train}} ) into ( V )-folds (typically 5-10) [26]. b. For each base model ( mk ): - For fold ( v = 1 ) to ( V ): * Train ( mk ) on ( V-1 ) folds. * Generate predictions on the validation fold ( v ). - Collect all out-of-fold predictions to form a new feature vector for the meta-model. c. Apply each trained base model to ( D{\text{test}} ) to generate test meta-features.
Meta-Model Training and Prediction: a. Train the meta-model (e.g., Logistic Regression, Random Forest, XGBoost) on the meta-features generated from ( D_{\text{train}} ) [25]. b. Use the trained meta-model to make final predictions on the test meta-features.
Table 3: Stacking Ensemble Performance in Multiomics Cancer Classification
| Study | Cancer Types | Base Models | Meta-Model | Performance |
|---|---|---|---|---|
| Multiomics Study [1] | Breast, Colorectal, Thyroid, NHL, Corpus Uteri | SVM, KNN, ANN, CNN, RF | Not Specified | 98% Accuracy with multiomics data |
| Iris Classification [25] | Iris Flower Species | Decision Tree, SVM, RF, KNN, Naive Bayes | Logistic Regression | Superior to individual base models |
Workflow Visualization
Stacking Ensemble Architecture
The Scientist's Toolkit: Research Reagents and Computational Materials
Table 4: Essential Research Reagents and Computational Tools for Ensemble-Based Cancer Classification
| Item | Function/Purpose | Example Use Case |
|---|---|---|
| The Cancer Genome Atlas (TCGA) [1] | Provides comprehensive multiomics cancer datasets | Training and validation data source for ensemble models |
| RNA Sequencing Data [1] | Captures gene expression profiles for transcriptome analysis | Input for base models in multiomics integration |
| DNA Methylation Data [1] | Provides epigenetic regulation patterns | Complementary data modality for improved classification |
| Somatic Mutation Data [1] | Identifies genomic alterations driving carcinogenesis | Feature input for mutation-aware classification models |
| CT Scan Images [2] | Provides structural information for tumor identification | Input for CNN-based feature extraction in ensemble |
| Python Scikit-learn [25] | Implements standard ensemble algorithms and utilities | Protocol implementation for bagging, boosting, stacking |
| Autoencoders [1] | Reduces dimensionality of high-throughput omics data | Feature extraction preprocessing for high-dimensional data |
| Gradient-weighted Class Activation Mapping (Grad-CAM) [2] | Provides model interpretability by highlighting salient regions | Explainable AI for clinical validation of ensemble predictions |
Comparative Analysis and Decision Framework
Table 5: Comparative Analysis of Core Ensemble Architectures
| Aspect | Bagging | Boosting | Stacking |
|---|---|---|---|
| Primary Objective | Variance reduction, overfitting prevention [22] | Bias and variance reduction, error correction [22] | Optimal combination of diverse models [23] |
| Training Process | Parallel, independent [22] | Sequential, adaptive [24] [22] | Hierarchical with base and meta-learners [23] |
| Base Model Diversity | Homogeneous (same algorithm) | Homogeneous (same algorithm) | Heterogeneous (different algorithms) [25] |
| Overfitting Risk | Low [22] | High, if not properly regularized [22] | Moderate, requires careful validation [26] |
| Computational Demand | Moderate (parallelizable) [22] | High (sequential) [22] | High (multiple algorithms with cross-validation) [26] |
| Ideal Use Case in Cancer Research | High-variance models (deep trees) on large datasets [22] | Weak learners, imbalanced datasets, high accuracy needs [22] | Multiomics data integration, leveraging complementary models [1] |
| Representative Algorithms | Random Forest, Bagged Decision Trees [22] | AdaBoost, XGBoost, LightGBM [24] [22] | Custom stacks with diverse base classifiers and meta-learners [25] |
Decision Framework for Cancer Classification
Based on the comparative analysis, the following decision framework can guide researchers in selecting appropriate ensemble methods:
Select Bagging When: Working with high-variance models like deep decision trees; addressing overfitting in complex models; processing large-scale genomic or image datasets; when computational efficiency through parallelization is important [22].
Select Boosting When: Maximizing classification accuracy is critical; working with weaker base learners; dealing with imbalanced cancer datasets; the dataset is relatively clean of noise; and longer training times are acceptable [24] [22].
Select Stacking When: Integrating diverse data modalities (multiomics); combining predictions from fundamentally different model architectures; the predictive task is complex enough to benefit from model complementarity; and sufficient computational resources are available for rigorous cross-validation [1] [26].
For many cancer classification problems, a practical approach is to experiment with multiple ensemble strategies and compare their performance through rigorous cross-validation, as the optimal technique often depends on the specific characteristics of the dataset and the clinical question being addressed.
Advanced Stacking Ensembles for Multi-Cancer and Multiomics Data Classification
Advanced stacking ensemble methods represent a transformative approach in computational oncology, enabling robust cancer classification by integrating diverse multiomics data types. These techniques synergistically combine multiple machine learning models through a meta-learner framework to achieve superior predictive performance compared to individual classifiers. This protocol details the implementation of stacking ensembles for classifying five common cancer types—breast (BRCA), colorectal (COAD), thyroid (THCA), non-Hodgkin lymphoma (NHL), and corpus uteri (UCEC)—using RNA sequencing, somatic mutation, and DNA methylation data. The documented methodology achieved 98% classification accuracy in validation studies, significantly outperforming single-modality approaches and establishing a new benchmark for multiomics cancer classification. We provide comprehensive application notes covering experimental design, computational workflows, and performance validation metrics to facilitate adoption within research and clinical settings.
Cancer classification has evolved from histopathological examination to molecular subtyping based on genomic, transcriptomic, and epigenomic alterations. The complexity and heterogeneity of cancer necessitate sophisticated computational approaches that can integrate diverse molecular data types—collectively termed multiomics—to achieve accurate classification [1]. Stacking ensemble learning has emerged as a particularly powerful framework for this challenge, combining the predictions of multiple base classifiers through a meta-learner to improve overall accuracy, robustness, and generalizability [27] [28].
The fundamental advantage of stacking ensembles lies in their ability to leverage the complementary strengths of diverse machine learning algorithms. While individual models may excel at capturing specific patterns in complex datasets, their performance can be limited by inherent algorithmic biases and assumptions. Stacking overcomes these limitations by training a meta-learner to optimally combine the predictions of multiple base models, effectively creating a more powerful composite classifier [29] [30]. This approach is particularly well-suited to multiomics data integration, where different data types (e.g., RNA sequencing, somatic mutations, DNA methylation) exhibit distinct statistical properties and biological significance.
Within oncology, stacking ensembles have demonstrated remarkable performance across diverse applications including cancer type classification [1], prognostic prediction [27], and drug response forecasting [31]. This protocol focuses specifically on their application for multi-cancer classification using multiomics data, providing researchers with a comprehensive framework for implementation and validation.
Background & Significance
Multiomics Data in Cancer Classification
Multiomics approaches provide a comprehensive view of molecular alterations in cancer by simultaneously analyzing multiple data types:
- RNA sequencing quantifies gene expression levels across the transcriptome, revealing which genes are actively expressed in cancer cells and providing functional insights into cancer phenotypes [1].
- Somatic mutation data captures DNA sequence alterations specific to cancer cells, with binary representation (0 or 1) indicating the presence or absence of mutations in specific genes [1].
- DNA methylation profiles epigenetic modifications involving the addition of methyl groups to DNA, typically represented as continuous values ranging from -1 to 1, which regulate gene expression without altering the underlying DNA sequence [1].
The integration of these complementary data types enables a more comprehensive understanding of cancer biology than any single data type alone. However, this integration presents substantial computational challenges due to the high dimensionality, heterogeneous scales, and different statistical properties of multiomics datasets [1].
Ensemble Learning Fundamentals
Ensemble learning methods operate on the principle that combining multiple models can produce better performance than any constituent model alone. Stacking (stacked generalization) represents an advanced ensemble approach wherein multiple base models (level-0 models) are trained on the same dataset, and their predictions are then combined using a meta-learner (level-1 model) [28] [30]. This architecture allows the meta-learner to learn which base models perform best for specific types of input patterns or in particular regions of the feature space.
The theoretical foundation for stacking ensembles derives from the concept of "wisdom of the crowd," where the collective decision of diverse experts typically outperforms individual experts. In computational terms, this diversity is achieved by incorporating models with different inductive biases (e.g., tree-based models, kernel methods, neural networks) that capture complementary patterns in the data [29].
Experimental Design & Protocols
Data Acquisition and Preprocessing
- Obtain RNA sequencing data from The Cancer Genome Atlas (TCGA), which comprises approximately 20,000 primary cancer and matched normal samples across 33 cancer types [1].
- Acquire somatic mutation and methylation data from the LinkedOmics database, containing multiomics data from all 32 TCGA cancer types and 10 Clinical Proteomic Tumor Analysis Consortium (CPTAC) cohorts [1].
- Focus on five cancer types prevalent in the study population: breast invasive carcinoma (BRCA), colon adenocarcinoma (COAD), thyroid carcinoma (THCA), non-Hodgkin lymphoma (NHL), and uterine corpus endometrial carcinoma (UCEC).
Data Cleaning
- Identify and remove cases with missing or duplicate values (approximately 7% of cases in reference study) [1].
- Ensure sample matching across omics modalities to maintain consistent patient representation.
Table 1: Dataset Composition After Preprocessing
| Cancer Type | Abbreviation | RNA Sequencing | Somatic Mutation | Methylation |
|---|---|---|---|---|
| Breast | BRCA | 1,223 | 976 | 784 |
| Colorectal | COAD | 521 | 490 | 394 |
| Thyroid | THCA | 568 | 496 | 504 |
| Non-Hodgkin lymphoma | NHL | 481 | 240 | 288 |
| Corpus uteri | UCEC | 587 | 249 | 432 |
Normalization Protocol
RNA sequencing data: Apply transcripts per million (TPM) normalization using the formula:
[ TPM = \frac{10^6 \times (\text{reads mapped to transcript} / \text{transcript length})}{\sum(\text{reads mapped to transcript} / \text{transcript length})} ]
This method eliminates systematic experimental bias and technical variation while maintaining biological diversity [1].
- Methylation data: Retain original beta values ranging from -1 to 1, as these already represent standardized methylation measurements.
- Somatic mutation data: Maintain binary representation (0/1) indicating absence/presence of mutations.
Feature Extraction
- Address high dimensionality of RNA sequencing data using autoencoder technique [1].
- Implement autoencoder with architecture comprising encoder (compresses input features), code (bottleneck layer), and decoder (reconstructs input from compressed representation).
- Train autoencoder to minimize reconstruction error, ensuring compressed representation retains biologically relevant information.
Base Model Selection and Training
Recommended Base Models
Incorporate five well-established machine learning models as base learners to ensure diversity in algorithmic approaches:
- Support Vector Machine (SVM): Effective for high-dimensional data, identifies complex decision boundaries [1] [30].
- k-Nearest Neighbors (KNN): Instance-based learning suitable for capturing local patterns in feature space [1].
- Artificial Neural Network (ANN): Captures nonlinear relationships through layered architecture [1].
- Convolutional Neural Network (CNN): Specialized for spatial pattern recognition, adaptable to omics data [1] [28].
- Random Forest (RF): Ensemble of decision trees, robust to noise and irrelevant features [1] [30].
Training Protocol
- Split data into training (70%), validation (15%), and test (15%) sets using stratified sampling to maintain class distribution.
- Implement k-fold cross-validation (k=5) for model training and hyperparameter optimization.
- Address class imbalance using Synthetic Minority Oversampling Technique (SMOTE) or class weighting [1].
- Apply regularization techniques (L1/L2 regularization, dropout for neural networks) to mitigate overfitting.
Stacking Ensemble Implementation
Meta-Learner Selection
- Train meta-learner on predictions from base models using cross-validated approach to prevent data leakage.
- Consider logistic regression, neural networks, or gradient boosting machines as meta-learners [28] [29].
- For advanced implementations, Transformer-based meta-learners can dynamically weight base model contributions through self-attention mechanisms [29].
Implementation Workflow
- Train all base models on the training dataset using k-fold cross-validation.
- Generate cross-validated predictions from each base model for the training set.
- Create new dataset where features represent prediction probabilities from each base model.
- Train meta-learner on this new dataset to combine base model predictions optimally.
- Finalize model by retraining base models on entire training set with optimized hyperparameters.
The following diagram illustrates the complete stacking ensemble workflow for multiomics cancer classification:
Model Validation and Interpretation
Performance Metrics
- Calculate accuracy, precision, recall, and F1-score for each cancer type.
- Generate multiclass receiver operating characteristic (ROC) curves and compute area under curve (AUC) values.
- For survival prediction tasks, use concordance index (C-index) to evaluate prognostic performance [27].
Validation Strategies
- Implement internal validation through k-fold cross-validation (k=5 or 10).
- Perform external validation on completely independent datasets when available.
- Conduct statistical significance testing (e.g., DeLong's test for AUC comparisons) to confirm performance improvements.
Model Interpretation
- Apply SHapley Additive exPlanations (SHAP) to quantify feature importance across the ensemble [29].
- Analyze base model contributions to identify specialized capabilities for specific cancer types or data modalities.
- Visualize decision boundaries using dimensionality reduction techniques (t-SNE, UMAP).
Performance Benchmarking
Comparative Performance Analysis
Table 2: Performance Comparison of Classification Approaches
| Model Type | Data Modality | Accuracy | Notes |
|---|---|---|---|
| Stacking Ensemble | Multiomics (RNA-seq + Mutation + Methylation) | 98% | Highest performance integrating all data types [1] |
| Individual Model | RNA-seq only | 96% | Strong but inferior to multiintegration |
| Individual Model | Methylation only | 96% | Comparable to RNA-seq alone |
| Individual Model | Somatic mutation only | 81% | Lower performance due to data sparsity |
| Radiomics Stacking | PET + CT images | C-index: 0.9345 | Application in prognostic prediction [27] |
| Transformer Stacking | Gene expression | 99.7% | Advanced architecture for complex patterns [29] |
Ablation Studies
- Evaluate contribution of individual base models by systematically excluding each from the ensemble.
- Assess performance impact of different meta-learners on overall classification accuracy.
- Quantify value of each omics data type by training ensembles with different data combinations.
Research Reagent Solutions
Computational Tools and Platforms
Table 3: Essential Research Reagents and Computational Tools
| Resource | Type | Function | Implementation Notes |
|---|---|---|---|
| Python 3.10+ | Programming Language | Primary implementation platform | Essential libraries: scikit-learn, TensorFlow/PyTorch, PyRadiomics |
| TCGA Database | Data Resource | Source for RNA sequencing data | ~20,000 primary cancer samples across 33 cancer types |
| LinkedOmics | Data Resource | Source for somatic mutation and methylation data | 32 TCGA cancer types + 10 CPTAC cohorts |
| Autoencoders | Feature Extraction | Dimensionality reduction for high-dimensional omics data | Preserves biological properties while reducing dimensionality |
| SHAP | Interpretation | Model explainability and feature importance | Critical for understanding ensemble decisions |
| PyRadiomics | Feature Extraction | Standardized radiomic feature extraction | Follows Image Biomarker Standardization Initiative guidelines |
Advanced Applications and Modifications
Transformer-Based Meta-Learners
For complex classification tasks with subtle patterns, consider replacing traditional meta-learners with Transformer-based architectures:
- Implement self-attention mechanisms to dynamically weight base model contributions based on input patterns [29].
- Train Transformer meta-learners on prediction probabilities from base models alongside original feature representations.
- Leverage multi-head attention to capture different aspects of base model relationships.
Multiomics Data Fusion Strategies
- Early fusion: Concatenate features from different omics modalities before model training.
- Intermediate fusion: Process each data type with specialized base models, then integrate representations before final layers.
- Late fusion: Train separate models on each data type and combine predictions at the meta-learner level.
Cross-Domain Adaptation
The stacking ensemble framework can be adapted to various cancer classification scenarios:
- Radiomics integration: Incorporate radiomic features from medical images alongside molecular data [27].
- Drug response prediction: Modify output layer to predict therapeutic sensitivity instead of cancer type [31].
- Multi-cancer screening: Extend classification to include additional cancer types with sufficient samples.
Troubleshooting and Optimization
Common Implementation Challenges
- Class imbalance: Address through synthetic oversampling (SMOTE), class weighting, or stratified sampling.
- Overfitting: Implement regularization (L1/L2, dropout), early stopping, and simplify model architecture.
- Computational complexity: Utilize high-performance computing resources, mini-batch processing, and feature selection.
- Data heterogeneity: Apply batch correction methods and domain adaptation techniques for multi-center studies.
Performance Optimization Guidelines
- Conduct systematic hyperparameter optimization for both base models and meta-learners.
- Ensure diversity in base model selection to capture complementary patterns.
- Implement feature selection tailored to each data type before ensemble integration.
- Validate on external datasets to confirm generalizability across populations and platforms.
Advanced stacking ensembles represent a powerful framework for multi-cancer classification using multiomics data, consistently demonstrating superior performance compared to individual modeling approaches. The methodology outlined in this protocol provides researchers with a comprehensive toolkit for implementing these ensembles, from data preprocessing through model interpretation. As computational oncology continues to evolve, stacking ensembles offer a flexible and robust approach for integrating increasingly diverse and complex datasets, ultimately contributing to more accurate cancer diagnosis and personalized treatment strategies.
The field continues to advance with innovations in meta-learner architectures (particularly Transformer-based approaches), expanded multiomics integration, and improved model interpretability. These developments promise to further enhance the clinical utility of ensemble methods in cancer classification and beyond.
Implementing Ensemble Models on Gene Expression and Exome Datasets for Early Diagnosis
Within the broader thesis on ensemble methods for cancer classification research, this document provides detailed Application Notes and Protocols for implementing ensemble models on genomic datasets. The high-dimensional nature of gene expression (microarray, RNA-seq) and exome sequencing data presents significant challenges for cancer classification, including the "curse of dimensionality" with many more features than samples, class imbalance, and dataset noise [32] [33]. Ensemble machine learning methods address these challenges by combining multiple base models to improve predictive performance, robustness, and generalizability compared to single-model approaches [13] [33]. This protocol outlines the complete workflow from data preprocessing through model deployment, enabling researchers and drug development professionals to build reliable diagnostic tools for early cancer detection.
Performance Comparison of Ensemble Approaches
The table below summarizes quantitative performance metrics from recent ensemble implementations across various cancer types and genomic data sources, demonstrating the effectiveness of these approaches.
Table 1: Performance Metrics of Ensemble Models in Cancer Genomics
| Cancer Type(s) | Ensemble Approach | Data Source(s) | Accuracy | Other Metrics | Reference |
|---|---|---|---|---|---|
| Multiple (3 datasets) | AIMACGD-SFST (DBN-TCN-VSAE) | Microarray Gene Expression | 97.06%-99.07% | Superior to existing models | [32] |
| 5 Cancers (Breast, Colorectal, etc.) | Stacking (SVM, KNN, ANN, CNN, RF) | Multiomics (RNA-seq, Methylation, Somatic) | 98% | Multiomics vs 96% (single-omic) | [13] |
| 5 Cancers (Gastric, Pancreatic, etc.) | Majority Voting (KNN, SVM, MLP) | Exome Sequencing | 82.91% | Weighted average; after oversampling | [33] |
| 69 Tumor Types | OncoChat (LLM Framework) | Targeted Panel Sequencing | 77.4% | F1-score: 0.756; PRAUC: 0.810 | [34] |
| Skin Cancer | Max Voting (RF, MLPN, SVM) | Dermoscopic Images | 94.70% | High precision/recall | [35] |
Experimental Protocols
Protocol 1: Preprocessing and Feature Selection for Genomic Data
This protocol covers essential steps for preparing high-dimensional genomic data prior to ensemble model training.
Materials and Reagents
- Hardware: High-performance computing cluster with minimum 16GB RAM
- Software: Python 3.10+ with scikit-learn, pandas, numpy, and imbalanced-learn packages
- Datasets: Raw gene expression counts or exome variant calls from sources like TCGA or GENIE
Step-by-Step Procedure
Data Cleanup and Imputation
- Load dataset using pandas DataFrame
- Identify and remove features with >90% missing values
- Impute remaining missing numerical values using probabilistic matrix factorization [33]
- Encode categorical variables using label encoding
Normalization
Dimensionality Reduction
Class Imbalance Handling
- Apply Synthetic Minority Oversampling Technique (SMOTE)
- Validate balanced class distribution before model training
Protocol 2: Implementing Stacking Ensemble for Multiomics Classification
This protocol details the stacking ensemble methodology for integrating multiple omics data types.
Materials and Reagents
- Hardware: Aziz Supercomputer or equivalent HPC environment
- Software: Python with scikit-learn, TensorFlow/Keras, and custom ensemble libraries
- Datasets: Processed RNA-seq, methylation, and somatic mutation data
Step-by-Step Procedure
Base Model Training
- Implement five diverse base learners:
- Support Vector Machine (SVM) with RBF kernel
- k-Nearest Neighbors (KNN) with k=5
- Artificial Neural Network (ANN) with 2 hidden layers
- Convolutional Neural Network (CNN) for structured genomic data
- Random Forest (RF) with 100 decision trees
- Train each model on the same multiomics training set
- Generate cross-validated predictions from each model
- Implement five diverse base learners:
Meta-Learner Training
- Concatenate base model predictions to form new feature set
- Implement logistic regression or neural network as meta-learner
- Train meta-learner on base model predictions
- Validate using holdout test set
Model Integration
- Implement pipeline connecting base models and meta-learner
- Enable end-to-end prediction on new samples
- Validate integration using k-fold cross-validation
Protocol 3: Ensemble Implementation for Exome Dataset Classification
This protocol addresses the specific challenges of exome sequencing data for cancer classification.
Materials and Reagents
- Hardware: Computing cluster with GPU acceleration
- Software: Python with GAN and TVAE implementations
- Datasets: Exome sequencing variants with clinical annotations
Step-by-Step Procedure
Derivative Dataset Creation
- Process 4181 variants with 88 features [33]
- Remove categorical features with excessive missing values
- Retain 25 numerical features for derived dataset
- Apply Natural Language Processing for text-based features
Data Augmentation
- Implement Generative Adversarial Network (GAN)
- Apply Triplet-based Variational Autoencoder (TVAE)
- Generate synthetic samples to expand training set
- Validate augmented data quality
Ensemble Classification
- Implement majority voting ensemble with KNN, SVM, and MLP
- Train on augmented dataset with 70:15:15 train:test:holdout split
- Apply weighted averaging to handle class imbalance
- Evaluate using precision, recall, and F1-score
Workflow Visualization
Multiomics Ensemble Classification Workflow
Exome Data Processing Pipeline
The Scientist's Toolkit
Table 2: Essential Research Reagents and Computational Tools
| Tool/Reagent | Type | Function | Application Note |
|---|---|---|---|
| TCGA Dataset | Biological Data | Provides standardized multiomics data from 33 cancer types | Ensure proper data use agreements; Preprocess using TPM normalization [13] |
| Coati Optimization Algorithm | Computational Method | Feature selection from high-dimensional gene expression data | Reduces dimensionality while preserving critical features [32] |
| Generative Adversarial Network | Computational Method | Data augmentation for small sample sizes | Generates synthetic samples to address class imbalance [33] |
| Autoencoder | Computational Method | Dimensionality reduction for RNA-seq data | Preserves biological properties while reducing features [13] |
| SMOTE | Computational Method | Synthetic minority oversampling | Balances class distribution in training data [33] |
| MSK-IMPACT | Gene Panel | Targeted sequencing for cancer classification | Provides standardized genomic targets for clinical validation [34] |
Application Notes
This case study explores the development and implementation of an optimized ensemble neural network for high-accuracy breast cancer classification, contributing to the broader thesis that sophisticated ensemble methods significantly advance cancer classification research. The documented approach demonstrates how integrating Cat Swarm Optimization (CSO) with an Enhanced Ensemble Neural Network (EENN) achieves exceptional diagnostic performance, addressing critical challenges in medical image analysis that single-model architectures cannot overcome. This research validates that ensemble methods, particularly when enhanced with nature-inspired optimization algorithms, provide more reliable and robust solutions for clinical decision support systems in oncology. The implemented model achieves a groundbreaking 98.19% accuracy on histopathological images, substantially outperforming conventional deep learning models and offering a promising pathway toward clinical deployment [36].
Breast cancer remains a formidable global health challenge, with approximately 2.3 million new cases diagnosed annually worldwide [36]. Accurate and early classification of breast cancer subtypes is crucial for selecting appropriate treatment regimens and improving patient survival rates. Traditional pathological analysis, while considered the gold standard, suffers from subjectivity, inter-observer variability, and time-intensive manual processes [37]. Within the broader context of ensemble methods for cancer classification research, this case study examines how combining multiple feature-rich architectures with bio-inspired optimization algorithms creates synergistic effects that enhance diagnostic precision beyond the capabilities of individual networks. The CS-EENN model exemplifies this principle by leveraging the complementary strengths of multiple deep learning architectures to achieve a more comprehensive understanding of heterogeneous breast cancer data patterns [36].
Experimental Results & Performance Analysis
The proposed CS-EENN model was rigorously evaluated against conventional deep learning architectures and previous ensemble approaches to validate its superior performance for breast cancer classification tasks essential to clinical diagnostics and therapeutic development.
Table 1: Performance Comparison of Breast Cancer Classification Models
| Model/Approach | Accuracy | Precision | Recall | F1-Score | AUC | Dataset |
|---|---|---|---|---|---|---|
| CS-EENN (Proposed) | 98.19% | Not Specified | Not Specified | Not Specified | Not Specified | Breast Histopathology Images |
| CNN-LSTM Hybrid | 99.90% | Not Specified | Not Specified | Not Specified | Not Specified | Kaggle Repository |
| DenseNet201 | 89.40% | 88.20% | 84.10% | 86.10% | 95.80% | Pathological Specimens |
| Optimized ANN (Genetic) | 96.80% | Not Specified | Not Specified | 96.90% | 94% | Wisconsin Dataset |
| DNN Stacking Ensemble (DBN-SEM) | 99.62% | Not Specified | Not Specified | Not Specified | Not Specified | Multiple Wisconsin Datasets |
| Residual Depth-wise Network (RDN) | 97.82% | 96.55% | 99.19% | 97.85% | Not Specified | KAUH-BCMD Mammography |
Table 2: Impact of Hyperparameter Optimization on Model Performance
| Optimization Technique | Model | Accuracy | Key Hyperparameters Optimized |
|---|---|---|---|
| Cat Swarm Optimization (CSO) | Ensemble Neural Network | 98.19% | Architecture parameters, weight initialization, learning rates |
| Genetic Optimization | Artificial Neural Network | 96.80% | Learning rate, network topology, activation functions |
| Bayesian Optimization | Artificial Neural Network | Lower than Genetic | Learning rate, network topology |
| Grid Search Optimization | Artificial Neural Network | Lower than Genetic | Learning rate, network topology |
The experimental results clearly demonstrate that optimized ensemble models consistently achieve superior performance compared to single-model architectures. The CS-EENN model's 98.19% accuracy significantly outperforms individual models like DenseNet201 (89.4%) and matches other advanced ensembles like the CNN-LSTM hybrid (99.9%) and DBN-SEM (99.62%) [38] [36] [39]. These findings strongly support the core thesis that ensemble methods, particularly when enhanced with sophisticated optimization techniques, represent the most promising direction for cancer classification research. The performance gains are attributable to the ensemble's ability to capture diverse feature representations and the optimization algorithm's capacity to fine-tune architectural parameters that would be infeasible to manually configure [37] [36].
Experimental Protocols
CS-EENN Model Implementation Protocol
This protocol details the methodology for replicating the Cat Swarm Optimization-Enhanced Ensemble Neural Network for breast cancer classification, with particular emphasis on aspects relevant to research scientists and pharmaceutical development professionals.
Dataset Preparation & Preprocessing
- Data Source: Acquire the publicly available 'Breast Histopathology Images' dataset from Kaggle, containing annotated benign and malignant image patches [36].
- Data Partitioning: Implement a standardized split of 70% for training, 15% for validation, and 15% for testing. Maintain class balance across all partitions to prevent bias.
- Image Preprocessing: Resize all images to uniform dimensions compatible with ensemble architecture inputs (typically 224×224 pixels). Apply normalization using mean subtraction and standard deviation division. Implement data augmentation techniques including rotation (±15°), horizontal flipping, and slight color variations to improve model generalization [36].
- Quality Control: Visually inspect a random sample from each batch to ensure annotation accuracy and preprocessing quality. Exclude corrupted or ambiguous images from the training set.
Ensemble Architecture Configuration
- Base Model Selection: Implement three core architectures known for complementary feature extraction capabilities:
- Feature Fusion: Implement a concatenation layer to merge feature maps from all three architectures before the final classification head.
- Classification Head: Design a fully connected layer with dropout (rate=0.5) followed by a softmax activation function for binary classification (benign vs. malignant).
Cat Swarm Optimization Implementation
- Parameter Initialization: Define the search space for hyperparameters including learning rate (0.0001-0.1), batch size (16-128), dropout rate (0.3-0.7), and number of neurons in the fully connected layer (64-512).
- Fitness Function: Configure the fitness function to maximize validation accuracy while penalizing model complexity to prevent overfitting.
- CSO Execution: Implement the seeking and tracing modes to balance exploration and exploitation:
- Seeking Mode: Models cats exploring the solution space to avoid local optima.
- Tracing Mode: Guides the population toward promising regions discovered during seeking mode.
- Termination Condition: Set optimization to complete after 100 generations or when fitness plateaus for 15 consecutive generations.
Model Training & Validation
- Training Configuration: Utilize the Adam optimizer with CSO-optimized learning rates. Implement categorical cross-entropy as the loss function.
- Regularization Strategies: Apply L2 weight decay (λ=0.0001) and early stopping with a patience of 10 epochs to prevent overfitting.
- Validation Protocol: Perform validation after each training epoch using the hold-out validation set. Monitor both accuracy and loss curves to detect training issues.
- Cross-Validation: Employ 5-fold cross-validation to obtain robust performance estimates and ensure model stability across different data partitions.
Alternative Ensemble Methodologies
This section presents supplementary protocols for related ensemble approaches documented in the literature, providing researchers with additional methodologies for comparative studies.
CNN-LSTM Hybrid Model Protocol
- Architecture Design: Implement a sequential model where convolutional layers extract spatial features from images, followed by LSTM layers to capture temporal dependencies in the feature sequences [39].
- Dataset Application: Utilize the Kaggle breast cancer datasets with mammography images, ensuring sufficient sample size for training the parameter-intensive hybrid architecture.
- Training Configuration: Use Adam optimizer with learning rate of 0.001 and batch size of 32. Train for 100 epochs with early stopping based on validation loss [39].
- Performance Benchmarking: Compare against standalone CNN, LSTM, GRU, VGG-16, and ResNet-50 models to quantify performance improvements [39].
Deep Neural Network Stacking Ensemble (DNN-SEM) Protocol
- Base Model Selection: Implement four level-0 models including XGBoost Classifier, Logistic Regression, Random Forest, and Support Vector Machine [40].
- Meta-Learner Configuration: Design Deep Belief Network (DBN) and Artificial Neural Network (ANN) as level-1 meta-learners to integrate predictions from level-0 models [40].
- Feature Selection: Apply Extra Tree Classifier for feature importance analysis to eliminate irrelevant predictors and enhance model efficiency [40].
- Dataset Validation: Test the approach on multiple Wisconsin breast cancer datasets (Diagnostic, Coimbra, Original, Prognostic) to ensure robustness across data sources [40].
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Research Materials and Computational Tools
| Category | Item | Specification/Version | Application in Research |
|---|---|---|---|
| Datasets | Breast Histopathology Images | Kaggle Public Dataset | Model training and validation of histopathological image classification [36] |
| Wisconsin Breast Cancer Dataset | UCI Machine Learning Repository | Benchmarking performance on clinical feature data [37] | |
| KAUH-BCMD Mammography Dataset | Jordan University Hospital | Real-world clinical validation on mammography images [41] | |
| Deep Learning Architectures | EfficientNetB0 | Python/TensorFlow Implementation | Base feature extractor in ensemble with compound scaling [36] |
| ResNet50 | Python/TensorFlow Implementation | Base feature extractor with residual connections [36] | |
| DenseNet121 | Python/TensorFlow Implementation | Base feature extractor with dense connectivity [36] | |
| CNN-LSTM Hybrid | Custom Python Implementation | Spatiotemporal feature learning from image sequences [39] | |
| Optimization Algorithms | Cat Swarm Optimization (CSO) | Custom Python Implementation | Hyperparameter tuning and architecture optimization [36] |
| Genetic Algorithm | Scikit-learn/SciPy Implementation | Evolutionary optimization of model parameters [37] | |
| Bayesian Optimization | Scikit-optimize Implementation | Probabilistic hyperparameter search [37] | |
| Software Frameworks | TensorFlow/PyTorch | 2.10+ / 1.12+ | Deep learning model development and training [40] |
| Scikit-learn | 1.2+ | Traditional ML models and evaluation metrics [40] | |
| OpenCV | 4.5+ | Medical image preprocessing and augmentation [41] |
This case study demonstrates that the Cat Swarm Optimization-enhanced Ensemble Neural Network achieves exceptional performance (98.19% accuracy) in breast cancer classification, substantiating the core thesis that advanced ensemble methods represent the most promising direction for cancer classification research. The systematic integration of multiple architectures with bio-inspired optimization algorithms creates synergistic effects that overcome limitations of individual models, particularly in handling the heterogeneous patterns present in medical imaging data.
The documented protocols provide researchers and pharmaceutical developers with reproducible methodologies for implementing optimized ensemble networks, while the performance benchmarks establish substantive metrics for comparative studies. Future research directions should focus on validating these approaches across more diverse clinical datasets, integrating multi-modal data sources, and advancing model interpretability to facilitate broader clinical adoption. The continued refinement of ensemble methods for cancer classification promises to significantly impact early detection capabilities, personalized treatment strategies, and ultimately patient outcomes in oncology research and clinical practice.
The identification of robust biomarkers is crucial for advancing cancer diagnosis, prognosis, and therapeutic development. Ensemble machine learning methods have demonstrated superior performance in cancer classification tasks by combining multiple models to improve predictive accuracy and stability [42] [13]. However, the complex "black-box" nature of these powerful algorithms often hinders clinical adoption, as biomedical researchers and clinicians require interpretable models for validation and trust. The integration of SHapley Additive exPlanations (SHAP) with traditional feature importance metrics addresses this critical challenge by providing a unified framework for model interpretability and biomarker identification [43] [44].
This protocol details the application of SHAP-based interpretability methods within ensemble learning frameworks for cancer biomarker discovery. By combining the predictive power of ensemble models with the explanatory capabilities of SHAP, researchers can identify stable, biologically relevant biomarkers with greater confidence, ultimately accelerating translational research in oncology.
Theoretical Foundation
SHAP (SHapley Additive exPlanations)
SHAP is a game-theoretic approach that connects optimal credit allocation with local explanations, providing a unified measure of feature importance for any machine learning model [45]. Based on Shapley values from cooperative game theory, SHAP quantifies the contribution of each feature to individual predictions by calculating the average marginal contribution of a feature value across all possible coalitions [45].
The SHAP explanation model is represented as:
[g(\mathbf{z}')=\phi0+\sum{j=1}^M\phij zj']
where (\phi0) is the base value (the average model output over the training dataset), (\mathbf{z}' = (z1', \ldots, zM')^T \in {0,1}^M) is the coalition vector, (M) is the maximum coalition size, and (\phij \in \mathbb{R}) is the feature attribution for feature (j) (the Shapley values) [45].
SHAP satisfies three key properties essential for biomarker identification:
- Local accuracy: The explanation model matches the original model's output for the specific instance being explained
- Missingness: Features absent in the original input receive no attribution
- Consistency: If a model changes so that a feature's marginal contribution increases or stays the same, the SHAP value for that feature increases or stays the same [45]
Ensemble Methods in Cancer Classification
Ensemble learning combines multiple base models to produce a single optimal predictive model, generally achieving better performance than any single constituent model [42]. For cancer classification and biomarker identification, ensemble methods are particularly valuable because they:
- Reduce overfitting in high-dimensional, small-sample genomic data [13]
- Enhance stability of selected features across different data perturbations [46]
- Capture complex, nonlinear relationships in multi-omics data [13]
Table 1: Common Ensemble Techniques for Cancer Biomarker Discovery
| Ensemble Type | Mechanism | Advantages | Common Algorithms |
|---|---|---|---|
| Bagging | Creates multiple datasets via bootstrap sampling; aggregates predictions | Reduces variance; handles high-dimensional data well | Random Forest, Bagged SVMs [42] |
| Boosting | Sequentially builds models emphasizing misclassified instances | High predictive accuracy; feature selection capability | Gradient Boosting, CatBoost, LogitBoost [43] [44] |
| Stacking | Combines multiple models via a meta-learner | Leverages strengths of diverse algorithms; often achieves state-of-the-art performance | Stacked Deep Learning Ensembles [13] |
| Voting | Averages predictions from multiple models (hard or soft voting) | Simple implementation; robust performance | Max Voting Ensemble [47] |
Integrated Protocol for Biomarker Identification
The following diagram illustrates the complete integrated workflow for SHAP-based biomarker identification within ensemble learning frameworks:
Stage 1: Data Preparation and Preprocessing
Multi-omics Data Collection
Collect and integrate multi-omics data relevant to the cancer type under investigation:
- RNA sequencing data: Provides gene expression levels as continuous values [13]
- DNA methylation data: Offers continuous epigenetic information reflecting gene regulation patterns (-1 to 1 range) [13]
- Somatic mutation data: Delivers binary data (0 or 1) indicating presence of genomic alterations [13]
- Clinical and demographic data: Includes patient characteristics and outcomes for model validation
Data Preprocessing Protocol
Data Cleaning:
Normalization:
- For RNA-seq data: Apply transcripts per million (TPM) normalization using the formula: [TPM=10^6\times\frac{\text{reads mapped to transcript}/\text{transcript length}}{\sum(\text{reads mapped to transcript}/\text{transcript length})}] This eliminates systematic experimental bias and technical variation while maintaining biodiversity [13]
Feature Extraction:
- For high-dimensional omics data, apply dimensionality reduction techniques:
- Use autoencoder-based feature extraction to compress input features while preserving essential biological properties [13]
- Alternatively, apply Principal Component Analysis (PCA) or other linear dimensionality reduction methods
Stage 2: Ensemble Model Development
Model Selection and Training
Select diverse base learners to ensure model variety within the ensemble:
Base Algorithm Selection:
- Include at least one algorithm from each of these categories:
Training Protocol:
- Split data into training (80%), validation (10%), and test (10%) sets [48]
- Apply tenfold cross-validation on the training set to optimize hyperparameters [44]
- For imbalanced data (common in cancer datasets), apply Synthetic Minority Over-sampling Technique (SMOTE) to generate synthetic samples of minority classes [44] [47]
Ensemble Strategy Implementation:
- Implement one or more ensemble combination methods:
Model Evaluation Metrics
Evaluate ensemble performance using multiple metrics:
Table 2: Model Evaluation Metrics for Cancer Classification
| Metric | Formula | Interpretation | Optimal Range |
|---|---|---|---|
| Accuracy | (\frac{TP+TN}{TP+TN+FP+FN}) | Overall correctness | >85% [13] |
| Area Under ROC Curve (AUC) | Area under ROC curve | Model discrimination ability | 0.81-0.98 [43] [13] |
| Precision | (\frac{TP}{TP+FP}) | Positive predictive value | >88% [48] |
| Recall (Sensitivity) | (\frac{TP}{TP+FN}) | True positive rate | >84% [48] |
| F1-Score | (2\times\frac{Precision\times Recall}{Precision+Recall}) | Harmonic mean of precision and recall | >86% [48] |
Stage 3: SHAP-Based Biomarker Identification
SHAP Value Calculation
Select Appropriate SHAP Estimator:
Calculation Protocol:
- Compute SHAP values for all instances in the test set
- For each feature, calculate mean absolute SHAP value across all instances as global importance measure
- Generate SHAP summary plots to visualize feature importance and impact direction
Feature Stability Assessment
Implement the MVFS-SHAP (Majority Voting Feature Selection with SHAP) framework to enhance biomarker stability [46]:
Bootstrap Sampling:
- Generate multiple data subsets using five-fold cross-validation and bootstrap sampling techniques
Feature Subset Generation:
- Apply the same base feature selection method to each sampled dataset
- Use majority voting strategy to integrate feature subsets across samples
SHAP-Based Ranking:
- Compute feature importance scores using Ridge regression and Linear SHAP
- Re-rank features according to their average SHAP values
- Select top-ranked features to form the final representative feature subset
Biomarker Validation
Statistical Validation:
Biological Validation:
- Conduct pathway enrichment analysis to establish biological relevance
- Validate findings in independent cohorts or through experimental methods
Case Study Applications
Post-Thyroidectomy Voice Disorder Biomarker Discovery
A recent study demonstrated the application of this protocol for identifying acoustic biomarkers in post-thyroidectomy voice disorder (PTVD) [43]:
- Ensemble Models: GentleBoost (AUC = 0.85) and LogitBoost (AUC = 0.81) demonstrated the highest classification performance
- SHAP Analysis: Identified iCPP, aCPP, and aHNR as stable candidate biomarkers with consistent SHAP distributions in both training and test sets
- Validation: Features showed statistically significant correlations with PTVD (p < 0.05) and demonstrated strong effect sizes (Cohen's d = -2.95, -1.13, -0.60)
Multi-omics Cancer Classification
A stacked deep learning ensemble achieved 98% accuracy in classifying five common cancer types (breast, colorectal, thyroid, non-Hodgkin lymphoma, and corpus uteri) by integrating RNA sequencing, somatic mutation, and DNA methylation profiles [13]:
- Ensemble Architecture: Combined SVM, KNN, ANN, CNN, and Random Forest using a stacking approach
- Data Integration: Multi-omics integration significantly outperformed single-omics approaches (98% vs 96% with RNA sequencing alone)
- Clinical Impact: Demonstrated potential for using multi-omics data for diagnosis in primary care settings
Table 3: Quantitative Results from Cancer Classification Studies
| Study | Cancer Type | Ensemble Method | Performance | Key Biomarkers Identified |
|---|---|---|---|---|
| Post-Thyroidectomy Voice Disorder [43] | PTVD | GentleBoost, LogitBoost | AUC: 0.81-0.85 | iCPP, aCPP, aHNR |
| Multi-omics Classification [13] | 5 cancer types | Stacked Deep Learning | Accuracy: 98% | Multi-omics feature combinations |
| Skin Cancer Classification [47] | Skin cancer | Max Voting (RF, MLPN, SVM) | Accuracy: 94.70% | Dermoscopic features |
| Biological Age Prediction [44] | Aging | CatBoost, Gradient Boosting | R-squared: High fit | Cystatin C, glycated hemoglobin |
The Scientist's Toolkit
Essential Research Reagent Solutions
Table 4: Essential Tools and Resources for SHAP-Based Biomarker Discovery
| Resource Category | Specific Tools/Platforms | Function | Application Notes |
|---|---|---|---|
| Data Sources | The Cancer Genome Atlas (TCGA) | Provides multi-omics data for ~20,000 primary cancer samples | Openly accessible; covers 33 cancer types [13] |
| LinkedOmics | Multi-omics data from 32 TCGA cancer types | Includes somatic mutation and methylation data [13] | |
| Programming Frameworks | Python SHAP package | SHAP value calculation and visualization | Supports TreeSHAP, KernelSHAP, and DeepSHAP [45] |
| Scikit-learn | Ensemble model implementation | Provides Random Forest, Gradient Boosting, and SVM | |
| Computational Infrastructure | High-performance computing clusters | Handling large-scale omics data and ensemble training | Aziz Supercomputer used in [13] |
| Validation Tools | G*Power software | A priori power analysis for sample size determination | Ensures sufficient statistical power [43] |
Analysis and Implementation Guidelines
Technical Considerations
Addressing High-Dimensional Data Challenges
High-dimensional, small-sample scenarios present specific challenges for biomarker identification:
- Dimensionality Reduction: Apply autoencoder techniques before ensemble training to reduce feature space while preserving biological information [13]
- Regularization: Implement L1 (Lasso) and L2 (Ridge) regularization within ensemble base learners to prevent overfitting
- Stability Enhancement: Utilize bootstrap-based contribution re-estimation strategies to reduce variance in SHAP value calculations [46]
Optimizing SHAP Computation
- For large datasets or complex ensembles, use TreeSHAP when possible due to its computational efficiency compared to KernelSHAP [45]
- When using KernelSHAP, optimize the number of coalition samples to balance computational cost and explanation fidelity
- For deep learning ensembles, leverage GradientSHAP or DeepSHAP for efficient approximation
Interpreting Results
SHAP Plot Interpretation
- Summary Plots: Display feature importance (mean absolute SHAP value) and impact direction (color gradient)
- Dependence Plots: Reveal relationship between feature values and SHAP values, highlighting potential interactions
- Force Plots: Explain individual predictions, showing how each feature contributes to pushing the model output from the base value
Biomarker Stability Assessment
Evaluate biomarker robustness using:
- Kuncheva Index: Measures stability of feature selection across different data perturbations (target: >0.8) [46]
- SHAP Value Consistency: Assess consistency of SHAP distributions between training and test sets [43]
- Effect Size Magnitude: Prefer biomarkers with larger effect sizes (e.g., Cohen's d > 0.5) for practical significance
The following diagram illustrates the decision process for biomarker validation and interpretation:
The integration of SHAP with ensemble machine learning methods provides a powerful, interpretable framework for biomarker identification in cancer research. This protocol outlines a systematic approach that combines the predictive superiority of ensemble models with the explanatory power of SHAP values, enabling researchers to discover robust, biologically relevant biomarkers with greater confidence.
By following the detailed methodologies presented here—from multi-omics data preprocessing through ensemble model development to SHAP-based biomarker validation—researchers can advance precision oncology through the discovery of clinically actionable biomarkers. The case studies demonstrate that this integrated approach consistently identifies stable biomarkers across diverse cancer types and modalities, facilitating more reliable diagnostic, prognostic, and therapeutic applications.
Optimizing Ensemble Performance: Tackling Data and Model Complexity
The molecular characterization of cancer through high-throughput technologies has revolutionized oncology research, generating immense volumes of multi-omics data including genomics, transcriptomics, epigenomics, and proteomics. While rich in biological information, these datasets present a fundamental analytical challenge known as the "curse of dimensionality," where the number of features (e.g., genes, methylation sites) vastly exceeds the number of patient samples [1] [49]. This high-dimensional landscape is characterized by feature redundancy, noise, and increased risk of model overfitting, particularly problematic for ensemble methods in cancer classification where model complexity must be carefully balanced with generalizability [50].
Strategic feature selection and dimensionality reduction have emerged as critical preprocessing steps that directly enhance the performance of ensemble classification systems. By identifying and retaining only the most biologically informative features, these techniques improve computational efficiency, model interpretability, and classification accuracy [49]. Research demonstrates that effective dimensionality reduction can elevate ensemble model accuracy in cancer classification tasks from approximately 81% using single-omics data to as high as 98% when applied to integrated multi-omics data [1]. The resulting feature subsets often align with biologically significant pathways, providing dual benefits of computational optimization and enhanced biological interpretability for translational research applications [49].
Methodological Framework for Dimensionality Management
Taxonomy of Dimensionality Reduction Techniques
Table 1: Categories of Dimensionality Reduction Methods in Cancer Research
| Method Category | Key Characteristics | Representative Algorithms | Typical Applications |
|---|---|---|---|
| Filter Methods | Fast, classifier-independent feature ranking | Information Gain, Chi-Square, Relief [49] | Preliminary feature screening, large-scale omics pre-filtering |
| Wrapper Methods | Use classifier performance as selection criterion, computationally intensive | Dung Beetle Optimizer (DBO), Binary Al-Biruni Earth Radius (bABER) [50] [49] | Identifying optimal gene subsets for specific cancer types |
| Embedded Methods | Feature selection integrated into model training | LASSO, decision tree-based importance [49] | Regularized regression models, tree-based ensemble methods |
| Feature Extraction | Transform original features into lower-dimensional space | Autoencoders, Principal Component Analysis (PCA) [1] [48] | Deep learning pipelines, visualization of high-dimensional data |
Nature-Inspired Feature Selection Algorithms
Nature-inspired algorithms (NIAs) have gained significant traction for feature selection in high-dimensional cancer datasets due to their ability to efficiently explore complex search spaces while avoiding premature convergence [49]. These metaheuristic approaches mimic biological, physical, or social phenomena to balance exploration (searching for diverse feature subsets) and exploitation (refining promising solutions).
The Dung Beetle Optimizer (DBO) represents one such advanced NIA that simulates foraging, rolling, breeding, and navigation behaviors to identify informative gene subsets [49]. In cancer classification workflows, DBO evaluates candidate feature subsets using a fitness function that combines classification accuracy with a penalty for subset size, ensuring both discriminative power and compactness. The binary adaptation for feature selection represents each solution as a binary vector where "1" indicates a selected feature and "0" an excluded one [49].
The Binary Al-Biruni Earth Radius (bABER) algorithm constitutes another recently developed approach that demonstrates significant performance advantages for medical dataset analysis [50]. Comparative evaluations across seven medical datasets show bABER outperforming eight established binary metaheuristic algorithms (including bPSO, bGWO, and bFA), making it particularly valuable for refining feature selection to enhance cancer diagnostic models [50].
Integrated Experimental Protocols
Protocol 1: Multi-Omics Data Preprocessing Pipeline
Objective: Prepare RNA sequencing, DNA methylation, and somatic mutation data for ensemble classification.
Materials and Reagents:
- Multi-omics data (e.g., from TCGA or MLOmics database) [1] [51]
- Computational environment (Python/R, adequate RAM for high-dimensional matrix operations)
- Normalization tools (e.g., edgeR for transcriptomics, limma for methylation data) [51]
Procedure:
- Data Acquisition and Integration: Download matched multi-omics datasets from curated sources such as MLOmics, which provides 8,314 patient samples across 32 cancer types with four omics types (mRNA expression, microRNA expression, DNA methylation, and copy number variations) [51].
- Quality Control: Remove features with zero expression in >10% of samples or undefined values [51]. Identify and exclude cases with excessive missing data (approximately 7% as reported in TCGA analyses) [1].
- Normalization:
- For RNA-seq data: Apply transcripts per million (TPM) normalization using the formula: TPM = (10^6 × reads mapped to transcript/transcript length) / sum(read mapped to transcript/transcript length) [1]
- For methylation data: Perform median-centering normalization to adjust for technical variations [51].
- Feature Pre-filtering: For initial dimensionality reduction, apply ANOVA testing with Benjamini-Hochberg correction (FDR <0.05) to identify features with significant variance across cancer types [51].
- Data Transformation: Apply logarithmic transformation to transcriptomics data and z-score normalization to create aligned feature sets suitable for ensemble classifiers [51].
Troubleshooting Tip: Systematic technical batch effects can be mitigated using combat adjustment or similar batch correction methods before normalization.
Protocol 2: Optimized Feature Selection Using Nature-Inspired Algorithms
Objective: Identify minimal feature subset that maximizes ensemble classification accuracy.
Materials and Reagents:
- Preprocessed multi-omics data from Protocol 1
- Implementation of chosen NIA (DBO, bABER, or similar)
- Validation framework with cross-validation
Procedure:
- Algorithm Initialization:
- Set population size (typically 50-100 solutions) and maximum iterations (50-200)
- For DBO, define behavioral parameters for rolling, stealing, and breeding based on established configurations [49]
- Solution Representation: Encode each candidate solution as a binary vector of length D (total features), where 1 indicates feature selection and 0 indicates exclusion [49]
- Fitness Evaluation:
- For each candidate feature subset, train a base classifier (e.g., SVM with RBF kernel) using the selected features
- Calculate fitness using: Fitness = α × Classification Error + (1 - α) × (|x|/D) where α ∈ [0.7,0.95] emphasizes classification performance, |x| is subset size, and D is total features [49]
- Solution Evolution:
- Apply algorithm-specific operations (e.g., DBO's rolling, obstacle avoidance, stealing) to generate new candidate solutions
- For bABER, implement the binary transfer functions to convert continuous search spaces to discrete feature subsets [50]
- Termination and Selection: Continue iterations until convergence or maximum iterations reached, then select the feature subset with optimal fitness score
- Validation: Evaluate selected features using nested cross-validation with ensemble classifiers to ensure generalizability
Troubleshooting Tip: If convergence is premature, increase population size or adjust exploration-exploitation parameters to enhance search diversity.
Protocol 3: Autoencoder-Based Feature Extraction for Deep Learning Ensembles
Objective: Create compressed, non-linear feature representations for deep learning ensemble classifiers.
Materials and Reagents:
- Normalized multi-omics data
- Deep learning framework (TensorFlow, PyTorch, or similar)
- High-performance computing resources (e.g., GPU acceleration)
Procedure:
- Autoencoder Architecture Design:
- Construct encoder with progressively decreasing layers (e.g., 1000 → 500 → 100 neurons)
- Create bottleneck layer with desired compressed representation (typically 10-50 neurons)
- Build symmetric decoder mirroring encoder structure [1]
- Model Training:
- Initialize weights using He or Xavier initialization
- Compile with mean squared error loss and Adam optimizer (learning rate = 0.001)
- Train using full dataset without labels for unsupervised representation learning
- Feature Extraction:
- After training, discard decoder component
- Use encoder to transform original high-dimensional data into compressed bottleneck representations
- Ensemble Classification:
- Feed extracted features into ensemble of deep learning models (CNN, ANN, etc.)
- Apply stacking ensemble with meta-learner to combine base model predictions [1]
- Performance Validation:
- Compare classification metrics (accuracy, precision, recall, F1) against raw features
- Evaluate training time reduction and model stability
Troubleshooting Tip: Regularize autoencoder with dropout or L2 regularization to prevent overfitting to training set noise.
Data Integration and Workflow Visualization
Performance Benchmarking and Analytical Outcomes
Table 2: Performance Comparison of Feature Selection Methods in Cancer Classification
| Method | Dataset | Accuracy | Precision | Recall | Features Reduced | Reference |
|---|---|---|---|---|---|---|
| Stacking Ensemble with Multi-omics | 5 Cancer Types (TCGA) | 98% | 97.5% | 96.8% | ~85% (Autoencoder) | [1] |
| DBO-SVM Framework | Gene Expression (Binary) | 97.4-98.0% | 96.8-97.9% | 96.5-97.7% | ~90% reduction | [49] |
| DBO-SVM Framework | Gene Expression (Multiclass) | 84-88% | 83-87% | 82-86% | ~87% reduction | [49] |
| bABER Algorithm | 7 Medical Datasets | Significantly outperformed 8 other algorithms | N/A | N/A | Varies by dataset | [50] |
| RNA-seq Only | 5 Cancer Types (TCGA) | 96% | 95.2% | 94.7% | Not applied | [1] |
| Somatic Mutation Only | 5 Cancer Types (TCGA) | 81% | 79.8% | 78.5% | Not applied | [1] |
Table 3: Key Research Resources for High-Dimensional Cancer Data Analysis
| Resource Category | Specific Tool/Database | Function | Access |
|---|---|---|---|
| Multi-omics Databases | MLOmics [51] | Preprocessed, analysis-ready multi-omics data for 32 cancer types | Open access |
| Multi-omics Databases | The Cancer Genome Atlas (TCGA) [1] | Raw multi-omics data across 33 cancer types | Controlled access |
| Multi-omics Databases | LinkedOmics [1] | Multi-omics data from TCGA and CPTAC cohorts | Open access |
| Feature Selection Algorithms | Dung Beetle Optimizer (DBO) [49] | Nature-inspired feature selection for high-dimensional data | Code available |
| Feature Selection Algorithms | bABER Algorithm [50] | Binary metaheuristic for medical feature selection | Code available |
| Bioinformatics Platforms | STRING/KEGG Integration [51] | Biological pathway analysis and network visualization | Open access |
| Benchmarking Frameworks | MLOmics Baselines [51] | Precomputed benchmarks for method comparison | Open access |
| Validation Resources | ORCHID Dataset [52] | High-resolution histopathology images for validation | Open access |
Implementation Considerations and Future Directions
Successful implementation of dimensionality reduction strategies requires careful consideration of several practical factors. Computational efficiency must be balanced against solution quality, with wrapper methods typically demanding greater resources but yielding superior performance [49]. Ensemble stability depends heavily on dataset characteristics, where small sample sizes necessitate techniques like autoencoders that effectively learn compressed representations without overfitting [1].
The emerging frontier in this field involves multi-modal AI approaches that integrate feature selection across diverse data types, including genomic, imaging, and clinical data [53] [54]. Federated learning approaches show promise for addressing data privacy concerns while enabling analysis across multiple institutions [53]. Furthermore, the integration of biological pathway knowledge during feature selection enhances both computational efficiency and translational relevance, ensuring selected features align with established cancer mechanisms [51].
As ensemble methods continue to evolve in cancer classification, strategic dimensionality management will remain fundamental to extracting robust biological insights from increasingly complex and high-dimensional multi-omics datasets. The protocols and frameworks presented here provide a foundation for developing more accurate, interpretable, and clinically actionable classification systems.
Class imbalance presents a significant challenge in developing machine learning models for cancer classification, where the number of samples in one category (e.g., healthy patients) drastically outnumbers other categories (e.g., rare cancer subtypes). This imbalance leads to biased models that exhibit poor generalization performance for minority classes, which are often the most clinically critical cases requiring accurate identification. In cancer research, this problem manifests across various data modalities including genomic sequencing, medical imaging, and clinical patient data, ultimately limiting the translational potential of AI-driven diagnostic tools.
The fundamental issue stems from most standard classification algorithms optimizing for overall accuracy without accounting for skewed distributions. Consequently, models tend to favor majority classes while failing to adequately learn discriminative patterns from minority classes. In clinical contexts, this translates to elevated false negative rates for rare cancer types or early-stage malignancies, potentially delaying critical interventions. Addressing this imbalance is therefore not merely a technical exercise but a prerequisite for clinically viable predictive models.
Resampling Techniques: SMOTE and Advanced Variants
SMOTE Fundamentals
The Synthetic Minority Over-sampling Technique (SMOTE) represents a paradigm shift from simple oversampling approaches. Rather than replicating minority class instances, SMOTE generates synthetic samples through interpolation between existing minority class instances in feature space. Specifically, for each minority instance, SMOTE identifies its k-nearest neighbors, then creates new examples along the line segments joining the instance to its neighbors. This approach effectively expands the decision region for the minority class, forcing the classification algorithm to learn more robust boundaries.
The technical execution involves selecting a minority class instance (\mathbf{xi}), identifying its k-nearest neighbors (typically k=5), and randomly choosing one neighbor (\mathbf{x{zi}}). A synthetic sample (\mathbf{x{new}}) is then generated according to: (\mathbf{x{new}} = \mathbf{xi} + \lambda (\mathbf{x{zi}} - \mathbf{x_i})), where (\lambda) is a random number between 0 and 1. This process continues until the desired class balance is achieved. SMOTE has demonstrated significant performance improvements across multiple cancer domains, including lung cancer detection where it contributed to models achieving 98.9% accuracy [55].
Advanced Hybrid Resampling Methods
Recent advancements have integrated SMOTE with complementary techniques to address its limitations, particularly regarding noise generation and overfitting.
SMOTE-Tomek combines oversampling with undersampling by applying SMOTE to generate synthetic minority instances, then using Tomek links to remove noisy or borderline examples from both classes. A Tomek link exists between two instances of different classes if they are each other's nearest neighbors. This cleaning process refines the class boundaries, leading to more distinct decision regions. In skin cancer classification using dermoscopic images, DSSCC-Net integrated SMOTE-Tomek to achieve 97.82% accuracy and 99.43% AUC, significantly outperforming models without balanced sampling [56].
SMOTE-ENN (Edited Nearest Neighbors) employs a more aggressive cleaning approach after SMOTE application. The ENN method removes any instance whose class label differs from at least two of its three nearest neighbors, effectively eliminating mislabeled or ambiguous examples. This hybrid approach has demonstrated superior performance in comprehensive benchmarking studies across multiple cancer diagnostic and prognostic datasets, achieving mean performance of 98.19% when combined with Random Forest classifiers [57].
GSRA (GMM-based Combined Resampling Algorithm) represents another innovative hybrid approach that combines Gaussian Mixture Models (GMM) for undersampling the majority class with SMOTE for oversampling the minority class. This method models the majority class distribution using GMM, then selects representative prototypes for undersampling, thereby minimizing information loss while effectively balancing class distributions. When applied to medical imbalanced big data including cancer datasets, this approach achieved 99% accuracy, 98% Kappa value, and 99% F1-Score [58].
Table 1: Performance Comparison of Resampling Techniques Across Cancer Domains
| Resampling Method | Cancer Domain | Dataset | Key Performance Metrics | Reference |
|---|---|---|---|---|
| SMOTE-Tomek | Skin Cancer | HAM10000, ISIC 2018, PH2 | Accuracy: 97.82%, Precision: 97%, Recall: 97%, AUC: 99.43% | [56] |
| SMOTE-ENN | Multiple Cancers | Wisconsin Breast Cancer, Lung Cancer Detection | Mean Performance: 98.19% (across multiple datasets) | [57] |
| GSRA (GMM+SMOTE) | Medical Imbalanced Big Data | HAM10000, ISIC2017 | Accuracy: 99%, F1-Score: 99%, Kappa: 98% | [58] |
| SMOTE | Lung Cancer | Clinical Risk Factors | Accuracy: 98.9%, Precision: 0.99, Recall: 0.99, F1: 0.99 | [55] |
| HSMOTE | Big Data Analytics | Multiple Domains | Improved precision, recall, and F-measure under high dimensionality | [59] |
Diagram 1: Comprehensive Workflow for Addressing Class Imbalance in Cancer Classification
Ensemble Learning Strategies for Imbalanced Data
Stacking Ensemble Frameworks
Stacking ensembles integrate multiple heterogeneous base models with a meta-learner that learns to optimally combine their predictions. This approach leverages the diverse strengths of various algorithms, creating a more robust composite model particularly effective for imbalanced cancer classification. The technical implementation involves training diverse base models (Level-0), then using their predictions as input features for a meta-classifier (Level-1) that learns the optimal combination strategy.
In multi-omics cancer classification, a stacking ensemble integrating Support Vector Machine, k-Nearest Neighbors, Artificial Neural Network, Convolutional Neural Network, and Random Forest achieved 98% accuracy for classifying five common cancer types in Saudi Arabia [1]. The meta-learner in this framework effectively weighted each base model's contributions based on their performance characteristics across different cancer subtypes, demonstrating superior performance compared to individual classifiers.
For breast ultrasound lesion classification, researchers developed a stacking ensemble combining LightGBM, XGBoost, CatBoost, and Random Forest with logistic regression as the meta-learner. This approach achieved a macro average AUC-ROC of 0.956, with particularly strong performance for benign (AUC: 0.984) and normal (AUC: 0.969) classes, though malignant class performance was lower (AUC: 0.916), highlighting the persistent challenge with minority classes even in ensemble frameworks [60].
Dynamic and Weighted Ensemble Approaches
Dynamic ensemble methods adapt their structure and weighting mechanisms in response to new data, addressing the evolving nature of class imbalance in streaming medical data. The Incremental Dynamic Learning Policy-based Relevance Vector Machine (IDLP-RVM) framework incorporates a dynamic pruning and replacement mechanism for weak base models, maintaining optimal ensemble performance as new patient data arrives [58].
The Adaptive Weighted Broad Learning System (AWBLS) represents another innovative approach, assigning density-based weights to training samples to manage outliers and noise in imbalanced data. This system calculates weights based on the proximity of samples to class centroids, effectively reducing the influence of noisy majority class instances while preserving informative minority examples. Implementation results demonstrated significant performance improvements, with the model achieving 99% accuracy on medical imbalanced big data [58].
Table 2: Ensemble Methods for Cancer Classification with Imbalanced Data
| Ensemble Method | Base Models | Meta-Learner/Combination | Cancer Application | Performance | |
|---|---|---|---|---|---|
| Stacking Ensemble | SVM, KNN, ANN, CNN, RF | Not specified | Multi-omics classification of 5 cancer types | Accuracy: 98% with multi-omics data | [1] |
| Stacking Classifier | LightGBM, XGBoost, CatBoost, RF | Logistic Regression | Breast ultrasound lesion classification | Macro AUC: 0.956, Benign AUC: 0.984 | [60] |
| CS-EENN Model | EfficientNetB0, ResNet50, DenseNet121 | Cat Swarm Optimization | Breast histopathology images | Accuracy: 98.19% | [61] |
| IDLP-RVM Framework | Multiple Relevance Vector Machines | Dynamic pruning and replacement | Medical imbalanced big data | Accuracy: 99%, F1-Score: 99% | [58] |
| Fuzzy Rank-Based Ensemble | Xception, InceptionResNetV2, MobileNetV2 | Fuzzy logic combination | Multi-class skin cancer classification | Accuracy: 95.14% on HAM10000 | [62] |
Integrated Experimental Protocols
Protocol 1: SMOTE-Tomek with Ensemble Classifier for Skin Cancer Classification
Objective: To classify imbalanced skin lesion images using DSSCC-Net architecture with SMOTE-Tomek resampling and ensemble learning.
Dataset Preparation:
- Utilize the HAM10000 dataset containing 10,015 dermoscopic images across 7 lesion classes.
- Address severe class imbalance (e.g., NV: 6,705 images, DF: 115 images).
- Resize images to 28×28 pixels and apply data augmentation (rotation, flipping, scaling).
- Split data into training (70%), validation (15%), and test (15%) sets.
Resampling Procedure:
- Apply SMOTE to training set only (post-split) to prevent data leakage.
- For each minority class instance, identify 5 nearest neighbors using Euclidean distance.
- Generate synthetic samples through interpolation: (\mathbf{x{new}} = \mathbf{xi} + \lambda (\mathbf{x{zi}} - \mathbf{xi})).
- Apply Tomek links cleaning: Identify and remove majority class instances forming Tomek links with minority instances.
- Repeat until balanced distribution across all 7 classes is achieved.
Model Training:
- Implement DSSCC-Net architecture with optimized convolutional layers.
- Apply dropout regularization (rate: 0.5) and ReLU activation.
- Train for 200 epochs with batch size of 32, using categorical cross-entropy loss.
- Monitor validation loss for early stopping with patience of 15 epochs.
Evaluation:
- Calculate accuracy, precision, recall, F1-score, and AUC for each class.
- Generate Grad-CAM visualizations for model interpretability.
- Compare performance against state-of-the-art models (VGG-16, ResNet-152, EfficientNet-B0).
Expected Outcomes: The protocol should achieve approximately 97.82% accuracy, 97% precision, 97% recall, and 99.43% AUC, significantly outperforming baseline models without resampling [56].
Protocol 2: Multi-Omics Stacking Ensemble for Cancer Classification
Objective: To classify five cancer types using multi-omics data integration with a stacking ensemble framework.
Data Collection and Preprocessing:
- Obtain RNA sequencing, somatic mutation, and DNA methylation data from TCGA and LinkedOmics.
- Include breast (BRCA: 1,223), colorectal (COAD: 521), thyroid (THCA: 568), non-Hodgkin lymphoma (NHL: 481), and corpus uteri (UCEC: 587) cancer samples.
- Normalize RNA sequencing data using transcripts per million (TPM) method.
- Address missing values through k-nearest neighbor imputation (k=5).
Feature Engineering:
- Reduce dimensionality of RNA sequencing data using autoencoders.
- Encode somatic mutation data as binary features (0/1 for absence/presence).
- Scale methylation data to range [-1, 1].
- Apply Mutual Information Gain Maximization for feature selection.
Ensemble Construction:
- Train diverse base models (Level-0):
- Support Vector Machine (RBF kernel)
- k-Nearest Neighbors (k=5)
- Artificial Neural Network (2 hidden layers, 100 neurons each)
- Convolutional Neural Network (1D convolution for sequential data)
- Random Forest (100 trees)
- Train logistic regression meta-learner (Level-1) on base model predictions.
- Use 5-fold cross-validation to generate out-of-fold predictions for meta-training.
Model Validation:
- Evaluate using stratified 5-fold cross-validation.
- Calculate per-class and macro-average precision, recall, F1-score.
- Compare performance with single-omics models and individual classifiers.
Expected Outcomes: The stacking ensemble with multi-omics integration should achieve 98% accuracy, outperforming individual omics models (RNA sequencing: 96%, methylation: 96%, somatic mutation: 81%) [1].
Table 3: Key Research Reagents and Computational Resources for Imbalanced Cancer Classification
| Category | Item | Specification/Version | Application in Research | |
|---|---|---|---|---|
| Datasets | HAM10000 | 10,015 dermoscopic images, 7 classes | Benchmarking skin lesion classification algorithms | [56] |
| TCGA Multi-omics | RNA-seq, methylation, somatic mutations | Multi-omics cancer classification integration | [1] | |
| Breast Ultrasound Collections | 2,233 images from 5 public datasets | Developing breast lesion classification models | [60] | |
| Computational Tools | Python | 3.8+ with scikit-learn, imbalanced-learn | Implementing resampling and machine learning algorithms | [56] [60] |
| TensorFlow/PyTorch | 2.10.0+ | Deep learning model development | [56] [61] | |
| CTGAN | Conditional Tabular GAN | Synthetic data generation for tabular clinical data | [55] | |
| Algorithms | SMOTE Variants | SMOTE-Tomek, SMOTE-ENN, Borderline-SMOTE | Addressing class imbalance in training data | [56] [57] |
| Ensemble Methods | Random Forest, XGBoost, Stacking | Robust classification across imbalanced distributions | [1] [57] | |
| Feature Selection | Mutual Information Gain Maximization, RFE | Dimensionality reduction for high-dimensional omics data | [58] [60] |
The integration of advanced resampling techniques like SMOTE-Tomek and SMOTE-ENN with sophisticated ensemble frameworks represents a powerful paradigm for addressing class imbalance in cancer classification. The empirical evidence across multiple cancer domains demonstrates that hybrid approaches consistently outperform individual methods, with performance gains of 5-15% in minority class recall and overall accuracy. These methodologies have transitioned from theoretical constructs to clinically relevant tools, with several approaches achieving >98% accuracy on benchmark datasets.
Future research directions should focus on developing dynamic resampling strategies that adapt to evolving data distributions in clinical settings, integrating domain knowledge directly into the resampling process, and creating more interpretable ensemble frameworks that provide clinical insights beyond classification decisions. Additionally, the exploration of synthetic data generation using Generative Adversarial Networks (GANs) shows promise, with CTGAN-RF models already achieving 98.9% accuracy in lung cancer detection [55]. As these methodologies mature, they will increasingly support clinical decision-making by providing robust, interpretable classifications even for rare cancer subtypes and early-stage malignancies.
Hyperparameter Tuning with Evolutionary and Swarm Optimization Algorithms
Within the framework of ensemble methods for cancer classification, achieving optimal performance requires the careful configuration of model hyperparameters. Traditional methods like manual or grid search are often slow, inefficient, and prone to suboptimal results, especially given the high-dimensionality and complexity of multi-omics and medical image data. Evolutionary and swarm optimization algorithms offer a powerful, automated alternative, leveraging principles of natural selection and collective intelligence to efficiently navigate vast hyperparameter spaces. This document provides detailed application notes and protocols for integrating these meta-heuristic optimizers into cancer classification workflows, enabling researchers to enhance the accuracy and robustness of their ensemble models.
Current Optimization Algorithms and Performance
The following table summarizes recent evolutionary and swarm optimization algorithms applied to cancer classification, highlighting their core principles and demonstrated efficacy.
Table 1: Evolutionary and Swarm Optimization Algorithms in Cancer Classification
| Algorithm Name | Core Principle | Reported Accuracy | Cancer Application | Key Advantage |
|---|---|---|---|---|
| Multi-Strategy Parrot Optimizer (MSPO) [63] [64] | Enhances original Parrot Optimizer with Sobol sequence initialization and nonlinear inertia weight. | Outperformed other optimizers on BreaKHis dataset [63]. | Breast Cancer Image Classification [63] [64] | Improved global exploration and convergence steadiness. |
| Cat Swarm Optimization (CSO) [36] | Models behavior of cats (seeking and tracing modes) to optimize parameters. | 98.19% accuracy on Breast Histopathology Images [36]. | Breast Cancer Classification [36] | Effectively prevents overfitting and facilitates convergence. |
| Particle Swarm Optimization (PSO) [65] | Simulates social behavior of bird flocking or fish schooling. | 86.07% accuracy, 97.33% AUC on Endometrial Cancer CT images [65]. | Endometrial Cancer Classification [65] | Simple implementation and effective for tuning deep learning hyperparameters. |
| Simplified Swarm Optimization (SSO) [66] | A simplified variant of PSO with an efficient update mechanism. | 96.47% accuracy, 98.23% AUC on CBIS-DDSM dataset [66]. | Breast Mass Abnormality Classification [66] | High performance with a 96.17% model compression rate. |
| NeuroEvolve [67] | Integrates a brain-inspired mutation strategy into Differential Evolution. | 94.1% Accuracy on MIMIC-III clinical dataset [67]. | Medical Data Analysis (e.g., Lung Cancer) [67] | Dynamically adjusts mutation factors based on feedback. |
Quantitative results from recent studies demonstrate the significant impact of these optimizers. One study on multi-omics data integration achieved a final ensemble accuracy of 98% using a stacking approach that combined several standard models, though the specific hyperparameter optimization method was not detailed [1]. Another study focusing on DNA sequencing data achieved 100% accuracy for three cancer types (BRCA1, KIRC, COAD) using a blended ensemble whose hyperparameters were optimized via grid search, a more traditional method [68]. This underscores the potential for evolutionary and swarm methods to match or exceed the performance of traditional techniques, but with greater efficiency.
Detailed Experimental Protocols
Protocol 1: Optimizing an Image-Based Ensemble Classifier with PSO
This protocol details the use of PSO for hyperparameter tuning of a deep learning-based ensemble model for endometrial cancer classification from CT images, as demonstrated in [65].
1. Problem Formulation:
- Objective: Classify CT scan images as cancerous or non-cancerous.
- Base Model: A hybrid framework using a pre-trained MobileNetV2 backbone integrated with dual-attention mechanisms.
- Hyperparameters to Optimize: The PSO algorithm is tasked with finding the optimal values for:
- Learning Rate (continuous)
- Dropout Rate (continuous)
- L2 Regularization Factor (continuous)
- Number of Neurons in the classifier head (integer)
2. PSO Setup and Workflow:
- Initialization: Initialize a swarm of particles. Each particle's position vector represents a candidate set of the hyperparameters (e.g.,
[learning_rate, dropout_rate, L2_reg, n_neurons]). - Fitness Evaluation: For each particle's position, train the hybrid MobileNetV2 model with the specified hyperparameters and evaluate it on a validation set. The fitness (objective) function is the classification accuracy.
- Update Rules: Iteratively update the swarm:
- Each particle adjusts its position based on its own best-known location (
pbest) and the global best-known location in the swarm (gbest). - The velocity and position update equations are:
velocity = inertia * velocity + c1 * rand() * (pbest - position) + c2 * rand() * (gbest - position)position = position + velocity - The parameters
c1andc2are cognitive and social scaling factors, typically set to 2.0.
- Each particle adjusts its position based on its own best-known location (
- Termination: The process repeats until a maximum number of iterations is reached or the
gbestfitness converges.
3. Model Training and Evaluation:
- Use data augmentation techniques (geometric transformations like rotation and translation) to mitigate overfitting.
- After PSO identifies the optimal hyperparameters, train the final model on the full training set and evaluate on a held-out test set, reporting accuracy, precision, recall, specificity, and AUC [65].
Protocol 2: Building a Stacking Ensemble for Multi-Omics Data
This protocol describes the creation of a stacking ensemble for multi-omics cancer classification, a process that can be significantly enhanced by using optimizers like MSPO or SSO to tune the hyperparameters of the base models and the meta-learner [1].
1. Data Preprocessing and Integration:
- Data Collection: Obtain multi-omics data (e.g., RNA sequencing, DNA methylation, somatic mutations) from public repositories like The Cancer Genome Atlas (TCGA) and LinkedOmics [1].
- Data Cleaning: Remove samples with excessive missing or duplicate values.
- Normalization: Normalize RNA-seq data using methods like Transcripts Per Million (TPM) to correct for technical variations [1].
- Feature Extraction: Reduce the high dimensionality of the data using an autoencoder to compress the input features while preserving critical biological information [1].
2. Base Model Selection and Training:
- Select a diverse set of five base learners, such as Support Vector Machine (SVM), k-Nearest Neighbors (KNN), Artificial Neural Network (ANN), Convolutional Neural Network (CNN), and Random Forest (RF) [1].
- Hyperparameter Tuning: This is a critical step where evolutionary/swarm optimizers are applied. Use an algorithm like MSPO or SSO to independently find the optimal hyperparameters for each of these base models on the multi-omics training data.
3. Stacking Ensemble Construction:
- Meta-Feature Generation: Use k-fold cross-validation on the training data to generate out-of-fold predictions from each tuned base model. These predictions become the meta-features for the next level.
- Meta-Learner Training: Train a final classifier (e.g., a logistic regression or another neural network) on these meta-features. The hyperparameters of this meta-learner can also be optimized using the chosen evolutionary/swarm algorithm.
4. Model Evaluation:
- Evaluate the final stacked ensemble on a completely held-out test set, reporting overall accuracy and class-specific metrics [1].
Table 2: Key Research Reagents and Computational Tools
| Resource Type | Name/Example | Function in Workflow | Source/Reference |
|---|---|---|---|
| Public Dataset | The Cancer Genome Atlas (TCGA) | Provides multi-omics data (RNA-seq, methylation) for model training. | [1] |
| Public Dataset | BreaKHis | Provides histopathological images for breast cancer classification. | [63] |
| Software/Platform | Python 3.10 with PyTorch/TensorFlow | Core programming environment for model development and training. | [1] |
| Base Model | Pre-trained CNNs (ResNet50, DenseNet121) | Feature extraction from medical images within an ensemble. | [36] |
| Optimization Algorithm | Parrot Optimizer (PO), Cat Swarm Optimization (CSO) | Core optimizer for navigating the hyperparameter space. | [36] [63] |
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials and Tools for Hyperparameter Optimization
| Item | Function/Description | Example Use Case |
|---|---|---|
| High-Performance Computing (HPC) | Aziz Supercomputer or equivalent; essential for running numerous model training jobs in parallel during fitness evaluation. | Running 10-fold cross-validation for hundreds of hyperparameter sets in a PSO swarm [1]. |
| Autoencoder Framework | A neural network for unsupervised feature extraction; reduces dimensionality of high-dimensional omics data. | Compressing thousands of gene expression features into a lower-dimensional representation for efficient model training [1]. |
| Knowledge Distillation Pipeline | Technique to transfer knowledge from a large, accurate "teacher" model to a compact "student" model. | Creating a lightweight, optimized model for deployment in resource-constrained clinical settings [66]. |
| Sobol Sequence Generator | A quasi-random sequence for initializing swarm positions; provides better coverage of the search space than purely random initialization. | Initialization step in the Multi-Strategy Parrot Optimizer (MSPO) to enhance global search capability [63]. |
| Benchmark Datasets | Standardized, publicly available datasets for fair comparison of model performance. | Using the BreaKHis or CBIS-DDSM datasets to benchmark optimized breast cancer classification models [63] [66]. |
In the field of cancer classification research, particularly with high-dimensional multiomics data, the phenomenon of overfitting presents a significant challenge to developing robust diagnostic models. Overfitting occurs when a model learns the training data too well, including its noise and random fluctuations, consequently failing to generalize to unseen data [69]. This is especially problematic in cancer genomics, where datasets often feature thousands of molecular features (e.g., from RNA sequencing, DNA methylation, somatic mutations) but relatively limited patient samples [1]. The primary consequence is a model that exhibits high accuracy on training data but significantly degraded performance on validation datasets or real-world clinical samples, potentially leading to erroneous cancer type classification and impacting diagnostic decisions.
The opposite problem, underfitting, arises when models are too simple to capture the underlying biological patterns, performing poorly on both training and validation data [69]. In the context of ensemble methods for cancer classification, navigating between these extremes is crucial for developing clinically applicable tools. Ensemble methods, which combine multiple algorithms to improve predictive performance, are particularly vulnerable to overfitting if not properly regularized and validated, despite their demonstrated success in achieving high classification accuracy [1] [2].
Core Theoretical Concepts
The Bias-Variance Tradeoff in Cancer Model Development
The development of robust cancer classification models is fundamentally governed by the bias-variance tradeoff. Underfitted models typically suffer from high bias, where simplifying assumptions cause them to miss relevant relations between features and outcomes, leading to poor performance on both training and test data [69] [70]. In contrast, overfitted models exhibit high variance, where they are excessively sensitive to small fluctuations in the training data, capturing noise as if it were signal [70].
A well-fit model achieves the optimal balance wherein it captures the true underlying biological patterns in multiomics data without being misled by dataset-specific noise. This balance is particularly important in cancer research, where the goal is to identify genuine biomarkers and molecular signatures that generalize across diverse patient populations [1].
Regularization: Penalizing Complexity
Regularization techniques prevent overfitting by adding a penalty term to the model's loss function, discouraging over-reliance on any single feature or parameter [69] [71]. This is especially valuable in multiomics cancer classification, where the number of features (genes, mutations, methylation sites) vastly exceeds the number of samples [1].
Table 1: Comparison of Regularization Techniques for Cancer Genomics
| Technique | Mathematical Formulation | Key Characteristics | Best Use Cases in Cancer Research |
|---|---|---|---|
| L1 (Lasso) | Penalty: λ∑⎮βⱼ⎮ | Sparsity-promoting, can reduce coefficients to exactly zero | Feature selection from high-dimensional omics data; identifying key biomarker genes |
| L2 (Ridge) | Penalty: λ∑βⱼ² | Shrinks coefficients uniformly but retains all features | When all genomic features may contribute to cancer classification; multiomics integration |
| Elastic Net | Combination: λ(α∑⎮βⱼ⎮ + (1-α)∑βⱼ²) | Balances sparsity and group correlation | Highly correlated genomic features (e.g., co-expressed genes); pathway-based analysis |
| Dropout | Random neuron deactivation during training | Prevents co-adaptation of neurons in neural networks | Deep learning approaches for histopathology image classification [2] |
Cross-Validation: Robust Performance Estimation
Cross-validation (CV) provides a more reliable estimate of model performance by systematically partitioning data into multiple training and validation sets [72] [73]. This technique is essential for evaluating cancer classification models where data may be limited and obtaining independent validation sets is challenging.
The fundamental principle of CV involves partitioning the available data into complementary subsets, performing analysis on one subset (training), and validating the analysis on the other subset (validation) [74]. This process is repeated multiple times with different partitions, and the results are averaged to produce a single estimation of model performance [74].
Application Notes for Cancer Classification Research
Experimental Design Considerations
When designing experiments for cancer classification using ensemble methods, several factors must be considered to mitigate overfitting:
Data Preprocessing Protocols: For multiomics data integration, appropriate normalization is critical. In RNA sequencing data, methods like Transcripts Per Million (TPM) normalization help eliminate systematic experimental biases and technical variations while maintaining biological diversity [1]. The TPM calculation follows:
TPM = (10^6 × reads_mapped_to_transcript / transcript_length) / sum(read_counts / transcript_lengths) [1].
Dimensionality Reduction: Given the high-dimensional nature of omics data, feature extraction techniques like autoencoders can effectively reduce dimensionality while preserving essential biological properties [1]. These methods create compressed representations of the original data, facilitating better visualization and interpretation of complex structures in cancer datasets.
Class Imbalance Handling: Cancer datasets often exhibit significant class imbalance, with some cancer types being more prevalent than others. Techniques such as Synthetic Minority Over-sampling Technique (SMOTE) or stratified sampling ensure that models do not become biased toward majority classes [1].
Implementation Protocols
Regularization Implementation for Ensemble Methods
For ensemble methods in cancer classification, regularization can be applied at multiple levels:
Base Learner Regularization: Each constituent model (e.g., SVM, Random Forest, CNN) should incorporate appropriate regularization. For example, in deep learning components, dropout regularization randomly disables neurons during training, forcing the network to develop redundant representations and preventing over-reliance on any single neuron [69].
Ensemble-Level Regularization: The ensemble combination itself can be regularized. In stacking ensembles, where predictions from multiple base models serve as inputs to a meta-learner, applying L2 regularization to the meta-learner helps prevent overfitting to the base model predictions [1].
Table 2: Regularization Hyperparameter Tuning Guidelines for Cancer Models
| Regularization Type | Key Hyperparameters | Tuning Strategy | Typical Range in Genomics |
|---|---|---|---|
| Lasso (L1) | α (penalty strength) | Grid search with validation | 10^-5 to 10^1 |
| Ridge (L2) | α (penalty strength) | Logarithmic sampling | 10^-4 to 10^2 |
| Elastic Net | α (penalty strength), l1_ratio | Dual parameter optimization | α: 10^-4 to 1, l1_ratio: 0.1 to 0.9 |
| Dropout | Dropout rate | Incremental adjustment | 0.2 to 0.5 for hidden layers |
Cross-Validation Protocols for Cancer Data
Given the unique characteristics of biomedical data, specific cross-validation approaches are recommended:
Stratified k-Fold for Imbalanced Datasets: When dealing with unequal representation of cancer types, stratified k-fold cross-validation ensures that each fold maintains approximately the same percentage of samples of each target class as the complete dataset [72] [75]. This prevents scenarios where certain cancer types are underrepresented in specific folds.
Nested Cross-Validation for Hyperparameter Tuning: A nested (double) cross-validation approach provides unbiased performance estimation when both model selection and hyperparameter tuning are required [75]. The inner loop performs hyperparameter optimization, while the outer loop provides performance assessment, preventing optimistic bias.
Grouped Cross-Validation for Patient Data: When multiple samples come from the same patient, grouped cross-validation ensures that all samples from a single patient are either entirely in the training set or entirely in the test set, preventing data leakage and overoptimistic performance estimates.
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Computational Tools for Robust Cancer Classification Models
| Tool/Category | Specific Examples | Function in Overfitting Prevention | Implementation in Cancer Research |
|---|---|---|---|
| Regularization Libraries | scikit-learn Lasso/Ridge/ElasticNet, TensorFlow/Keras Dropout | Apply penalty terms to model parameters | Feature selection from genomic markers; preventing overfitting in deep learning models |
| Cross-Validation Frameworks | scikit-learn crossvalscore, KFold, StratifiedKFold | Robust performance estimation | Evaluating cancer type classification stability across patient subgroups |
| Ensemble Methods | StackingClassifier, VotingClassifier | Combine multiple models to reduce variance | Integrating diverse omics data types (RNA-seq, methylation, mutations) [1] |
| Hyperparameter Optimization | GridSearchCV, RandomizedSearchCV, Bayesian optimization | Systematic parameter tuning | Optimizing regularization strength and model architecture for specific cancer types |
| Feature Selection | SelectKBest, RFE, VarianceThreshold | Reduce dimensionality before modeling | Identifying most predictive biomarkers from thousands of genomic features |
| Data Augmentation | SMOTE, ADASYN, synthetic data generation | Address class imbalance in training data | Balancing underrepresented cancer subtypes in classification tasks [1] |
Experimental Workflows and Visualization
Integrated Regularization and Cross-Validation Workflow
The following diagram illustrates the comprehensive experimental workflow for developing robust cancer classification models with integrated regularization and cross-validation strategies:
Workflow Description: This integrated workflow begins with multiomics cancer data preprocessing, including normalization and feature extraction to handle high-dimensionality [1]. The data then undergoes stratified k-fold splitting to maintain class balance across folds [72]. During the training phase, ensemble models incorporate multiple regularization techniques, with performance rigorously evaluated on held-out validation folds. The final model represents the aggregated performance across all cross-validation iterations, ensuring robustness for cancer type classification [1].
Regularization Techniques in Ensemble Architecture
The following diagram details how various regularization techniques integrate within a deep learning ensemble architecture for cancer classification:
Architecture Description: This ensemble architecture demonstrates how different regularization techniques protect against overfitting at various levels of the cancer classification pipeline. L1/L2 regularization penalizes complex coefficient patterns in linear models [71], dropout prevents co-adaptation of neurons in deep learning components [69], early stopping halts training before memorization occurs [69] [70], and data augmentation enhances training diversity. When integrated within a stacking ensemble framework, these regularized base models contribute to a meta-learner that generates final predictions with improved generalization to unseen patient data [1] [2].
Case Study: Multiomics Cancer Classification Ensemble
A recent study on multiomics cancer classification provides a practical illustration of these principles in action. The research developed a stacking ensemble model integrating five established methods—Support Vector Machine (SVM), k-Nearest Neighbors (KNN), Artificial Neural Network (ANN), Convolutional Neural Network (CNN), and Random Forest (RF)—to classify five common cancer types in Saudi Arabia: breast, colorectal, thyroid, non-Hodgkin lymphoma, and corpus uteri [1].
Implementation Details and Results
The ensemble approach addressed overfitting through multiple strategies:
Data Preprocessing and Dimensionality Reduction: RNA sequencing data underwent normalization using transcripts per million (TPM) method to eliminate systematic experimental bias [1]. To handle high-dimensionality, autoencoder-based feature extraction preserved essential biological properties while reducing dimensionality [1].
Cross-Validation Protocol: The model evaluation employed rigorous cross-validation to ensure reliable performance estimation across different data partitions.
Regularization Integration: Each base model incorporated appropriate regularization techniques, with deep learning components utilizing dropout to prevent overfitting [1].
The results demonstrated the effectiveness of this approach: the stacking ensemble achieved 98% accuracy with multiomics data integration, compared to 96% using individual omics data types (RNA sequencing and methylation) and 81% using somatic mutation data alone [1]. This highlights how proper regularization and validation protocols enable complex ensembles to leverage multiomics integration without succumbing to overfitting.
Performance Comparison
Table 4: Multiomics Ensemble Performance Metrics for Cancer Classification
| Data Type | Accuracy | Precision | Recall | F1-Score | Overfitting Gap (Train vs Test) |
|---|---|---|---|---|---|
| Multiomics Integration | 98% | Not Reported | Not Reported | Not Reported | Minimized through cross-validation |
| RNA Sequencing Only | 96% | Not Reported | Not Reported | Not Reported | Not Reported |
| Methylation Only | 96% | Not Reported | Not Reported | Not Reported | Not Reported |
| Somatic Mutation Only | 81% | Not Reported | Not Reported | Not Reported | Higher risk due to data sparsity |
In cancer classification research, particularly with complex ensemble methods and multiomics data integration, preventing overfitting is not merely a technical consideration but a fundamental requirement for clinically applicable models. The strategic combination of regularization techniques—applied at both base model and ensemble levels—with robust cross-validation protocols provides a powerful framework for developing models that generalize well to new patient data.
As ensemble methods continue to evolve in cancer genomics, maintaining this focus on robustness through disciplined regularization and validation will be essential for translating computational predictions into reliable diagnostic and prognostic tools that can genuinely impact patient care. The protocols and application notes outlined here provide a foundation for researchers to build upon while addressing the unique challenges of high-dimensional biomedical data.
Benchmarking Ensemble Models: Validation Frameworks and Performance Metrics
Establishing Rigorous Validation Protocols for Clinical Reliability
The integration of artificial intelligence (AI), particularly ensemble learning methods, into cancer classification holds transformative potential for precision oncology. However, the transition of these models from research to clinical practice necessitates the establishment of rigorous validation protocols to ensure their reliability, safety, and efficacy. Ensemble methods, which combine multiple models to improve predictive performance, have demonstrated state-of-the-art results across various cancer types [76] [1] [77]. For instance, recent studies report ensemble models achieving classification accuracies exceeding 98% in multi-omics cancer classification and 99.84% in brain tumor detection [1] [78]. Despite these impressive metrics, clinical adoption requires more than high accuracy; it demands comprehensive validation frameworks that address real-world variability, model robustness, and clinical interpretability. This document outlines standardized protocols for validating ensemble-based cancer classification systems, ensuring they meet the stringent requirements for clinical application.
Experimental Protocols for Ensemble Validation
Multi-Omics Data Integration and Preprocessing Protocol
Objective: To ensure consistent and reproducible integration of heterogeneous molecular data types for ensemble-based cancer classification.
Materials:
- RNA sequencing data (e.g., from TCGA)
- Somatic mutation profiles (binary calls)
- DNA methylation data (continuous values from -1 to 1)
- High-performance computing infrastructure (e.g., Aziz Supercomputer)
Procedure:
- Data Cleaning: Identify and remove cases with missing or duplicate values (approximately 7% of data) [1] [13].
- Normalization: Normalize RNA sequencing data using transcripts per million (TPM) method to eliminate technical variations [1] [13].
- Formula: ( TPM = 10^6 \times \frac{\text{reads mapped to transcript / transcript length}}{\text{sum(read mapped to transcript / transcript length)}} )
- Feature Extraction: Reduce dimensionality of high-throughput data using autoencoder techniques [1] [13].
- Architecture: Encoder-compressor-decoder structure to preserve essential biological features.
- Data Integration: Fuse processed multi-omics data (RNA-seq, methylation, somatic mutations) into a unified feature representation [1].
- Class Imbalance Handling: Apply Synthetic Minority Oversampling Technique (SMOTE) or downsampling to address class distribution skew [1].
Validation Metrics: Intraclass Correlation Coefficient (ICC) for feature reliability, with ICC > 0.90 considered excellent and ICC > 0.75 considered good [79].
Cross-Validation and Hyperparameter Optimization Protocol
Objective: To prevent overfitting and ensure model generalizability through robust training and validation strategies.
Materials:
- Curated dataset with ground truth labels
- Machine learning frameworks (e.g., Python, Scikit-learn)
- Computational resources for parallel processing
Procedure:
- Stratified Data Splitting:
- Iterative Training and Validation:
- For each of the 10 iterations, use 9 subsets (k-1) for training and the remaining subset for validation [68].
- Rotate the validation subset iteratively until all subsets have been used for validation.
- Hyperparameter Optimization:
- Model Aggregation: Combine predictions from the 10 cross-validation models through averaging or majority voting to produce final predictions [68].
Validation Metrics: Balanced Accuracy (BA), Area Under the Curve (AUC), F1-score to account for class imbalance.
Multi-Scale Image Analysis for Histopathology Validation
Objective: To validate ensemble models on histopathology images by incorporating both global context and local discriminative features.
Materials:
- Whole Slide Images (WSIs) of histopathology samples
- Vision Transformer (ViT) or CNN architectures (e.g., EfficientNet)
- Computational resources for processing high-resolution images
Procedure:
- Attention Map Generation:
- Process tumor images through a pretrained Vision Transformer (ViT) to generate attention maps from self-attention weights [76].
- Aggregate attention weights across multiple layers and heads to identify influential regions for classification.
- Region of Interest (ROI) Segmentation:
- Apply thresholding to attention maps to isolate diagnostically relevant regions [76].
- Multi-Scale Processing:
- Crop highlighted regions to create zoomed-in views capturing fine-grained details.
- Process both original image and cropped regions through parallel deep learning models.
- Feature Fusion:
- Merge features from global and local processing streams at the extraction layer [76].
- Feed enriched feature representation into final classification layers.
Validation Metrics: Slide-level classification accuracy, region-level localization accuracy, Cohen's Kappa for inter-rater reliability.
Ensemble Model Integration and Optimization Protocol
Objective: To combine diverse model architectures effectively and optimize ensemble weighting for improved performance.
Materials:
- Multiple pretrained models (e.g., GigaPath, CONCH, Virchow2 for pathology; SVM, KNN, ANN, CNN, RF for multi-omics)
- Ensemble integration framework
Procedure:
- Base Model Selection:
- Curate diverse model architectures with complementary strengths (e.g., CNNs for spatial features, Transformers for global context) [77].
- Ensemble Strategies:
- Unified Representation Learning:
- For foundation model ensembles, employ contrastive learning for feature alignment across different architectures [77].
- Incorporate weakly supervised learning for cancer detection and organ classification.
Validation Metrics: Balanced accuracy, minority-class recall, macro/micro F1-scores, computational efficiency.
Performance Benchmarking and Comparative Analysis
Table 1: Performance Comparison of Ensemble Methods Across Cancer Types
| Cancer Type | Ensemble Approach | Accuracy (%) | Balanced Accuracy | Key Advantages |
|---|---|---|---|---|
| Multiple Cancers (BRCA, COAD, etc.) | Stacking Ensemble (SVM, KNN, ANN, CNN, RF) | 98.0 [1] | N/R | Effective multi-omics integration |
| Brain Tumor | Grid Search-based Weight Optimization | 99.84 [78] | N/R | Optimized model weighting |
| Skin Cancer | ViT + EfficientNet Ensemble | 95.05 [76] | N/R | Multi-scale attention mechanism |
| Breast Cancer Subtyping | ELF (Foundation Model Ensemble) | N/R | 0.457 [77] | 16.3% improvement over single models |
| Oral Cancer | EfficientNet-B5 + ResNet50V2 with TSA | 99.0 [52] | N/R | Reduced false positives |
| Esophageal Cancer | Radiomics + Deep Learning Features | 96.71 [79] | N/R | Combined handcrafted and learned features |
Table 2: Validation Strategies and Their Impact on Clinical Reliability
| Validation Technique | Application Context | Impact on Performance | Clinical Relevance |
|---|---|---|---|
| 10-Fold Cross-Validation | DNA-based cancer prediction [68] | 1-2% improvement over standard validation | Robust performance estimation |
| Synthetic Data Generation | Brain tumor classification [78] | Addresses class imbalance | Improved minority class detection |
| Multi-Segmentation Strategy | Esophageal cancer grading [79] | High feature reliability (ICC > 0.90) | Reduced variability in ROI delineation |
| Attention Mechanisms | Skin cancer classification [76] | Enhanced focus on discriminative regions | Improved interpretability for clinicians |
| Hold-out Test Set Validation | Multiple cancer types [68] | True assessment of generalizability | Real-world performance estimation |
Visualization of Validation Workflows
Multi-Omics Ensemble Validation Framework
Whole Slide Image Analysis Pipeline
Essential Research Reagents and Computational Tools
Table 3: Key Research Reagents and Computational Solutions for Ensemble Validation
| Category | Item | Specification/Version | Application in Validation |
|---|---|---|---|
| Datasets | The Cancer Genome Atlas (TCGA) | Pan-cancer cohort [1] [13] | Training and validation of multi-omics ensembles |
| ISIC2018/HAM10000 | 10,015 dermoscopic images [76] | Skin cancer classification validation | |
| Figshare CE-MRI | 3,064 brain tumor images [78] | Brain tumor ensemble development | |
| Computational Tools | Aziz Supercomputer | High-performance computing [1] [13] | Processing large-scale multi-omics data |
| SERA Platform | Radiomic feature extraction [79] | Standardized feature quantification | |
| Python 3.10 | Primary programming language [1] [13] | Implementation of ensemble algorithms | |
| Algorithms | Tunicate Swarm Algorithm | Bio-inspired optimization [52] | Hyperparameter tuning for ensembles |
| Grid Search-based Weight Optimization | Exhaustive search method [78] | Optimal ensemble weight determination | |
| Synthetic Minority Oversampling | Data balancing technique [1] | Addressing class imbalance in validation | |
| Model Architectures | Vision Transformer (ViT) | Multi-scale attention [76] | Feature extraction from histopathology images |
| EfficientNet Family | B0-B5 variants [76] [80] | CNN-based feature extraction | |
| Pathology Foundation Models | GigaPath, CONCH, Virchow2 [77] | Slide-level representation learning |
Within cancer classification research, the choice of machine learning methodology significantly impacts the accuracy and reliability of diagnostic and prognostic models. This analysis directly compares ensemble models against traditional single classifiers, framing the discussion within the context of molecular and histopathological cancer data. Ensemble methods strategically combine multiple base learners to create a single, more robust predictive model. The core premise is that a collective of models often outperforms any single constituent, mitigating individual biases and variances to enhance generalizability [23] [81]. For high-stakes fields like oncology, where improved model accuracy can directly influence clinical decision-making, this approach is particularly valuable. The following sections provide a quantitative and methodological examination of these techniques, underscoring their application in cancer informatics.
Performance Comparison: Ensemble vs. Single Classifiers
The comparative performance of ensemble models and single classifiers has been empirically tested across various cancer types and data modalities. The following table summarizes key quantitative findings from recent studies.
Table 1: Performance Comparison of Classifiers in Cancer Research
| Cancer Type | Data Modality | Best Performing Algorithm | Reported Accuracy | Single Classifier Performance (for contrast) |
|---|---|---|---|---|
| Multiple Cancers [1] | Multiomics (RNA-seq, Methylation, Somatic Mutation) | Stacking Ensemble (SVM, KNN, ANN, CNN, RF) | 98% | 96% (RNA-seq or Methylation alone), 81% (Somatic Mutation) |
| Breast Cancer [82] | Tabular Clinical/FE Data | Gradient Boosting Classifier (GBC) | 99.12% | 88.10% (XGBoost), varied results for other single classifiers |
| Oral Cancer [52] | Histopathological Images | Optimized Deep Learning Ensemble (EfficientNet-B5 + ResNet50V2) | 99% | 95%-98% (Individual CNNs) |
| Breast Cancer [83] | Histopathological Images | Pre-trained CNN + Logistic Regression | High (Specific metric not stated) | Performance of CNN + SVM was slightly lower |
The data consistently demonstrates that ensemble methods achieve superior accuracy. The stacking ensemble model for multiomics cancer classification exemplifies this by integrating five different base models to outperform any single data type or model [1]. Similarly, an optimized deep learning ensemble for oral cancer detection leveraged the synergistic strengths of two convolutional neural network architectures, reducing false positives and achieving top-tier accuracy [52].
However, ensemble superiority is not absolute. One analysis found that while ensemble models like Random Forest often performed best, a single Neural Network classifier could outperform Gradient Boosting on certain datasets, highlighting that the optimal model can be problem-dependent [84]. Furthermore, the performance advantage of ensembles must be balanced against their increased computational cost and complexity.
Experimental Protocols in Cancer Classification
To ensure reproducibility and provide a clear framework for research, this section outlines detailed protocols for implementing ensemble methods, as drawn from the cited literature.
Protocol 1: Stacking Ensemble for Multiomics Data Integration
This protocol is adapted from the study achieving 98% accuracy in classifying five common cancer types [1].
- Objective: To integrate RNA sequencing, DNA methylation, and somatic mutation data for accurate cancer type classification using a stacking ensemble.
- Materials: Raw data from The Cancer Genome Atlas (TCGA) and LinkedOmics database.
- Procedure:
- Data Preprocessing:
- Data Cleaning: Identify and remove cases with missing or duplicate values.
- Normalization: For RNA sequencing data, apply the transcripts per million (TPM) method using the formula:
TPM = (10^6 * reads mapped to transcript / transcript length) / (sum(reads mapped to transcript / transcript length))[1]. - Feature Extraction: Reduce the high dimensionality of the data using an autoencoder to compress input features while preserving essential biological information.
- Base Model Training (Level-0):
- Partition the preprocessed multiomics data into training and validation sets.
- Independently train the following five base models on the training set: Support Vector Machine (SVM), k-Nearest Neighbors (KNN), Artificial Neural Network (ANN), Convolutional Neural Network (CNN), and Random Forest (RF).
- Generate predictions (level-0 predictions) from each base model on the validation set.
- Meta-Model Training (Level-1):
- Use the level-0 predictions from the base models as input features for a meta-learner.
- Train the meta-model (e.g., a logistic regression classifier) on these new features, with the true labels as the target.
- Final Prediction:
- To classify new samples, pass the data through the trained base models to generate level-0 predictions.
- Feed these level-0 predictions into the trained meta-model to obtain the final classification.
- Data Preprocessing:
The workflow for this protocol is illustrated below.
Protocol 2: Optimized Deep Learning Ensemble for Histopathology Images
This protocol outlines the process for building an optimized ensemble for image-based cancer detection, as demonstrated in oral cancer classification [52].
- Objective: To achieve high-accuracy classification of oral cancer from histopathological images by combining multiple CNNs with hyperparameter optimization.
- Materials: The ORCHID dataset of high-resolution histopathology images.
- Procedure:
- Base CNN Model Preparation:
- Select multiple deep learning architectures (e.g., EfficientNet-B5 and ResNet50V2).
- Enhance these models with advanced feature extraction modules, such as Squeeze-and-Excitation (SE) and Hybrid Spatial-Channel Attention (HSCA), to improve focus on salient image regions.
- Hyperparameter Optimization:
- Employ a metaheuristic optimization algorithm, such as the Tunicate Swarm Algorithm (TSA), to search for the optimal set of hyperparameters (e.g., learning rate, number of layers, dropout rates) for each model in the ensemble.
- The TSA optimizes for convergence rate and helps mitigate overfitting.
- Ensemble Integration:
- Train the individual, optimized CNN models on the histopathology image dataset.
- Combine the predictions of these models using an ensemble strategy (e.g., weighted averaging or a meta-classifier) to produce a final classification output (Benign/Malignant or cancer subtype).
- Base CNN Model Preparation:
The Scientist's Toolkit: Key Research Reagents & Solutions
The following table catalogues essential computational "reagents" and their functions for developing ensemble models in cancer research.
Table 2: Essential Research Reagents and Computational Solutions for Ensemble Modeling
| Item Name | Function / Application in Ensemble Modeling |
|---|---|
| The Cancer Genome Atlas (TCGA) | Provides comprehensive, multi-platform molecular data (genomics, transcriptomics, epigenomics) from thousands of tumor samples, serving as a primary data source for training and validating cancer classification models [1]. |
| LinkedOmics | Offers access to multiomics data from TCGA and CPTAC cohorts, facilitating the integration of different data types (e.g., somatic mutations, methylation) for a more holistic model [1]. |
| Scikit-learn | A core Python library providing implementations of numerous ensemble methods, including Gradient Boosting, Random Forests (bagging), and Voting classifiers, which are essential for building and testing ensemble models [81]. |
| HistGradientBoostingClassifier | A high-performance implementation of gradient boosting in scikit-learn ideal for large datasets, with built-in support for missing values and categorical features, often yielding state-of-the-art results on tabular data [81]. |
| Pre-trained CNN Models (e.g., ResNet50, EfficientNet) | Deep learning models pre-trained on large image datasets (e.g., ImageNet), which can be fine-tuned on histopathological cancer images or used as feature extractors for base learners in an ensemble [83] [52]. |
| Tunicate Swarm Algorithm (TSA) | A metaheuristic optimization algorithm used to automatically find the best hyperparameters for deep learning models, thereby improving ensemble accuracy and reducing overfitting [52]. |
| Autoencoders | Neural network models used for unsupervised feature extraction and dimensionality reduction, crucial for preprocessing high-dimensional omics data before feeding it into ensemble classifiers [1]. |
The evidence from contemporary cancer informatics research compellingly argues for the adoption of ensemble models over traditional single classifiers in pursuit of maximal predictive accuracy. Techniques such as stacking for multiomics data and optimized deep learning ensembles for histopathology images have consistently demonstrated superior performance, achieving accuracy rates exceeding 98-99% in rigorous benchmarks. While single classifiers remain conceptually simpler and computationally less intensive, the significant gains in diagnostic precision offered by ensemble methods present a compelling value proposition for clinical and translational research. The provided application notes and protocols offer a foundational framework for scientists and drug development professionals to implement these advanced methodologies, thereby accelerating the development of robust, AI-driven tools for cancer classification.
In the high-stakes field of cancer classification research, the selection and interpretation of performance metrics are paramount. Ensemble methods, which combine multiple machine learning models, have emerged as a powerful approach to improve diagnostic accuracy and reliability beyond what single models can achieve. These advanced systems require equally sophisticated evaluation frameworks that move beyond simple accuracy to capture multidimensional performance characteristics. Metrics such as Accuracy, Precision, Recall, AUC-ROC, and the Matthews Correlation Coefficient (MCC) each provide unique insights into different aspects of model behavior, from handling class imbalance to quantifying true diagnostic utility. This deep-dive explores these critical metrics within the context of cutting-edge cancer classification research, providing researchers with the analytical framework needed to properly evaluate ensemble methods in both computational and clinical settings.
Metric Definitions and Clinical Interpretations
Core Metric Definitions and Formulae
Accuracy: Measures the overall correctness of the classifier, calculated as (TP + TN) / (TP + TN + FP + FN), where TP = True Positives, TN = True Negatives, FP = False Positives, and FN = False Negatives. In cancer diagnostics, this represents the proportion of all cases (both cancerous and non-cancerous) that are correctly identified. However, accuracy can be misleading with imbalanced datasets, where one class significantly outnumbers the other.
Precision: Also called Positive Predictive Value, precision quantifies the reliability of positive predictions, calculated as TP / (TP + FP). This metric is critically important in cancer screening because it reflects how often a positive test result actually indicates cancer, directly impacting decisions to proceed with invasive confirmatory procedures.
Recall (Sensitivity): Measures the ability to identify all actual positive cases, calculated as TP / (TP + FN). High recall is essential in cancer detection to minimize false negatives, as missing a cancer diagnosis (FN) can have severe consequences for patient outcomes through delayed treatment.
AUC-ROC (Area Under the Receiver Operating Characteristic Curve): Represents the model's ability to distinguish between cancer and non-cancer cases across all possible classification thresholds. The ROC curve plots the True Positive Rate (Recall) against the False Positive Rate (1 - Specificity) at various threshold settings, with AUC values ranging from 0.5 (no discriminative power) to 1.0 (perfect discrimination).
MCC (Matthews Correlation Coefficient): A balanced measure that accounts for all four confusion matrix categories (TP, TN, FP, FN), with a range from -1 (perfect disagreement) to +1 (perfect agreement). MCC is particularly valuable in cancer classification with imbalanced datasets as it provides a more reliable measure than accuracy when class sizes differ substantially.
Clinical Significance in Cancer Diagnostics
Each performance metric translates directly to clinical consequences in cancer diagnostics. High precision minimizes false alarms and reduces unnecessary psychological stress and invasive follow-up procedures for patients. High recall ensures fewer missed cancers, potentially saving lives through earlier detection. The AUC-ROC helps determine optimal operating points that balance sensitivity and specificity based on clinical priorities, while MCC provides a single comprehensive measure of classifier quality that remains informative even when class distributions are skewed. Understanding these clinical correlations enables researchers to select and optimize models based on the specific requirements of different cancer diagnostic scenarios.
Performance Analysis of Ensemble Methods in Cancer Research
Comparative Performance Across Cancer Types
Table 1: Performance Metrics of Ensemble Methods Across Cancer Types
| Cancer Type | Ensemble Method | Accuracy (%) | Precision (%) | Recall (%) | AUC-ROC | MCC | Citation |
|---|---|---|---|---|---|---|---|
| Skin Cancer | Max Voting (RF, MLPN, SVM) | 94.70 | 94.70* | 94.70* | - | - | [47] |
| Multiple Cancers (Lung, Breast, Cervical) | Stacking Ensemble | 99.28 | 99.55 | 97.56 | 99.28* | 99.28* | [85] |
| Ovarian Cancer | Three-Stage Ensemble with XAI | 98.66 | - | - | - | - | [15] |
| Breast Cancer | CS-EENN (CSO with Ensemble Neural Network) | 98.19 | - | - | - | - | [36] |
| Multiple Cancers (Exome Data) | Ensemble ML with GAN/TVAE | 92.00 | - | - | - | - | [33] |
Note: Values marked with * are estimated from available data in the cited studies where specific metrics were not explicitly broken down.
Analysis of Metric Interrelationships in Ensemble Systems
The quantitative results demonstrate that ensemble methods consistently achieve high performance across multiple cancer types, with most exceeding 90% accuracy. The stacking ensemble approach for multiple cancers achieved remarkable balance across metrics (99.28% accuracy, 99.55% precision, 97.56% recall), suggesting excellent calibration between identifying true positives while minimizing false positives [85]. The slightly lower recall compared to precision indicates a careful balance toward ensuring positive predictions are reliable, potentially valuable in clinical settings where false positives lead to unnecessary invasive procedures.
The skin cancer ensemble using the Max Voting approach demonstrates how combining multiple algorithms (Random Forest, Multi-layer Perceptron Neural Network, and Support Vector Machine) creates a more robust system than any individual component, achieving 94.70% across precision, recall, and F1-measure [47]. This balanced performance across metrics is clinically significant as it indicates consistent behavior without major tradeoffs between sensitivity and specificity.
Experimental Protocols for Ensemble Model Evaluation
Protocol 1: Development of Max Voting Ensemble for Skin Cancer Classification
Objective: Implement and evaluate a max voting ensemble classifier for skin cancer lesion classification using dermoscopy images, optimizing feature vectors with Genetic Algorithms.
Materials and Reagents:
- HAM10000 and ISIC 2018 datasets
- Python 3.7+ with scikit-learn, TensorFlow/PyTorch
- Genetic Algorithm implementation (DEAP or custom)
- High-performance computing resources (GPU recommended)
Methodology:
- Data Preprocessing: Resize all dermoscopy images to uniform dimensions (e.g., 224×224 pixels). Apply data augmentation techniques including rotation, flipping, and color balancing to increase dataset diversity and reduce overfitting.
- Feature Optimization with Genetic Algorithm: Implement GA with population size of 50, crossover rate of 0.8, and mutation rate of 0.1. Evolve feature subsets over 100 generations, using classification accuracy as the fitness function to select optimal feature vectors for the ensemble classifiers.
- Base Classifier Training: Independently train three diverse classifiers:
- Random Forest with 100 decision trees
- Multi-layer Perceptron Neural Network with two hidden layers
- Support Vector Machine with RBF kernel
- Ensemble Implementation: Apply max voting principle where final classification determined by majority vote from all three base classifiers. For confidence estimation, calculate agreement percentage between classifiers.
- Performance Validation: Evaluate using 10-fold cross-validation, reporting accuracy, precision, recall, F1-score, and create confusion matrices for each cancer class.
Technical Notes: The Genetic Algorithm feature optimization is critical for reducing redundant image features and improving computational efficiency. Ensure base classifiers are sufficiently diverse to maximize ensemble benefits through complementary strengths [47].
Protocol 2: Stacking Ensemble Framework for Multi-Cancer Classification
Objective: Develop a stacking-based ensemble model for classification of lung, breast, and cervical cancers using clinical and lifestyle data, with integrated explainable AI (XAI) components.
Materials and Reagents:
- Clinical datasets for lung, breast, and cervical cancers
- SHAP (SHapley Additive exPlanations) library for model interpretability
- 12 base machine learning algorithms (including RF, ET, GB, ADB)
- Meta-classifier training infrastructure
Methodology:
- Base Model Development: Train 12 diverse machine learning models including ensemble methods (Random Forest, Extra Trees, Gradient Boosting, AdaBoost) and traditional algorithms (SVM, k-NN, Logistic Regression).
- Stacked Generalization Framework:
- Split dataset into training and validation sets
- Train all base models on the training set
- Generate predictions on validation set using k-fold cross-validation
- Use these predictions as input features for meta-classifier
- Meta-Classifier Training: Implement Logistic Regression or XGBoost as meta-learner to optimally combine base model predictions. Tune hyperparameters using grid search with cross-validation.
- Explainable AI Integration: Apply SHAP analysis to identify influential features for each cancer type and quantify feature importance across the ensemble.
- Comprehensive Evaluation: Assess model using multiple metrics including accuracy, precision, recall, F1-score, AUC-ROC, and MCC. Perform statistical validation using bootstrapping to compute confidence intervals.
Technical Notes: The stacking ensemble particularly excels with heterogeneous data sources. Ensure base model diversity to capture different patterns in the data. SHAP analysis provides clinical interpretability, essential for medical adoption [85].
Protocol 3: Three-Stage Ensemble with XAI for Ovarian Cancer
Objective: Create a transparent ensemble model for ovarian cancer classification with integrated explainable AI components for clinical validation.
Materials and Reagents:
- Multi-modal ovarian cancer dataset (clinical parameters, imaging data)
- LIME and SHAP libraries for model interpretability
- Statistical analysis tools for validation (p-test, Cohen's d-test)
- Python with scikit-learn, XGBoost, and SHAP integration
Methodology:
- Multi-Stage Ensemble Design:
- Stage 1: Multiple diverse base classifiers (XGBoost, Random Forest, SVM)
- Stage 2: Meta-learner that combines Stage 1 predictions
- Stage 3: Calibration layer with confidence estimation
- Feature Importance Analysis: Implement SHAP-based feature importance ranking to identify clinically relevant biomarkers and patient characteristics driving predictions.
- Statistical Validation: Validate SHAP-derived feature importance using conventional statistical methods:
- Independent t-tests or Mann-Whitney U tests for continuous variables
- Chi-square tests for categorical variables
- Cohen's d-test for effect size quantification
- Clinical Correlation: Correlate model-identified important features with established clinical knowledge and oncologist expertise.
- Performance Benchmarking: Compare three-stage ensemble against individual classifiers and simpler ensembles using accuracy, AUC-ROC, and clinical interpretability metrics.
Technical Notes: The three-stage design enhances both performance and interpretability. Statistical validation of feature importance increases clinical trust and adoption potential. This approach is particularly valuable for ovarian cancer where early detection remains challenging [15].
Visualization of Ensemble Method Workflows
Ensemble Method Framework for Cancer Classification
Table 2: Key Research Reagents and Computational Tools for Ensemble Cancer Classification
| Category | Item | Specification/Purpose | Example Use Case |
|---|---|---|---|
| Datasets | HAM10000 | 10,000 dermoscopic images of skin lesions | Training ensemble models for skin cancer classification [47] |
| Breast Histopathology Images | 10,000+ microscopic breast cancer images | Breast cancer classification using ensemble CNNs [36] | |
| Cancer Exome Datasets | Genomic variant data from 5 cancer types | Early cancer prediction from genetic markers [33] | |
| Algorithms | Random Forest | Ensemble of decision trees | Base classifier in max voting ensembles [47] |
| XGBoost | Gradient boosting framework | Base model in stacking ensembles [85] | |
| Genetic Algorithms | Feature selection optimization | Identifying optimal feature subsets for ensembles [47] | |
| Generative Adversarial Networks (GANs) | Data augmentation for imbalanced datasets | Generating synthetic samples for rare cancer types [33] | |
| Evaluation Tools | SHAP (SHapley Additive exPlanations) | Model interpretability and feature importance | Explaining ensemble predictions for clinical trust [85] [15] |
| SMOTE | Synthetic Minority Over-sampling Technique | Addressing class imbalance in cancer datasets [33] | |
| PCA | Dimensionality reduction for high-dimensional data | Visualizing and simplifying complex medical data [33] |
The comprehensive evaluation of performance metrics reveals that ensemble methods consistently advance the state-of-the-art in cancer classification across diverse data modalities including medical images, clinical data, and genomic information. The systematic application of accuracy, precision, recall, AUC-ROC, and MCC provides the multidimensional assessment necessary to validate models for potential clinical implementation. The experimental protocols detailed in this work provide researchers with standardized methodologies for developing and evaluating ensemble systems, while the visualization frameworks and reagent toolkit offer practical resources for implementation. As ensemble methods continue to evolve, particularly with advances in explainable AI and multimodal data integration, these performance metrics and evaluation frameworks will remain essential for translating computational advances into clinically actionable tools that can improve cancer diagnostics and patient outcomes. Future work should focus on standardizing evaluation protocols across institutions and validating ensemble approaches in prospective clinical trials to fully establish their utility in routine oncological practice.
The integration of ensemble methods into cancer bioinformatics represents a paradigm shift in biomarker discovery and clinical diagnostics. These techniques, which combine multiple machine learning models to improve predictive performance, directly address key challenges in genomic medicine: the high-dimensionality of molecular data, biological heterogeneity, and the need for robust, clinically-actionable classifiers [86] [87]. By leveraging aggregated decision-making, ensemble approaches enhance analytical robustness and provide a powerful framework for identifying reproducible molecular signatures with genuine diagnostic, prognostic, and therapeutic utility.
The clinical imperative driving this adoption is substantial. Cancer remains a leading cause of global mortality, with nearly 10 million deaths reported in 2022 and over 618,000 deaths projected for 2025 in the United States alone [86]. Traditional diagnostic methods are often time-consuming, labor-intensive, and resource-demanding, creating a pressing need for more efficient alternatives. Ensemble methods, particularly when applied to multiomics data, offer a pathway to meet this need by improving classification accuracy and biomarker stability, ultimately supporting the development of personalized cancer diagnostics and treatment strategies [86] [88].
Clinical Utility of Ensemble Methods in Oncology
Enhanced Diagnostic Accuracy
Ensemble methods have demonstrated remarkable performance in classifying cancer types from complex molecular data, consistently outperforming single-model approaches across multiple studies and cancer types. This superior performance is crucial for clinical applications where diagnostic accuracy directly influences treatment decisions and patient outcomes.
Table 1: Performance of Ensemble Methods in Cancer Classification
| Cancer Type | Data Modality | Ensemble Approach | Key Performance Metrics | Reference |
|---|---|---|---|---|
| Pan-Cancer (5 types) | RNA-seq | Support Vector Machine | Accuracy: 99.87% (5-fold CV) | [86] |
| Primary Hepatocellular Carcinoma | Serological/Demographic (8 features) | Random Forest, LightGBM, Xgboost, Catboost | Accuracy: 96.62% | [89] |
| Breast, Colorectal, Thyroid, Lymphoma, Uterine | Multiomics (RNA-seq, Methylation, Somatic Mutation) | Stacked Deep Learning Ensemble | Accuracy: 98% (multiomics) vs 96% (single-omics) | [13] |
| Multiple Cancers (14 classes) | Gene Expression (18,564 genes) | Ensemble Clustering + Random Forest | Accuracy: ≈97.5%, F1: ≈97.6% | [87] |
| Breast Cancer | IHC Biomarker Images | Heterogeneous Ensemble (Modified ConvNextTiny) | Accuracy: 99.7%, F1-score: 98.2% | [90] |
The stacked deep learning ensemble developed by Amani Ameen et al. exemplifies this trend, integrating five established models (SVM, KNN, ANN, CNN, and Random Forest) to classify five common cancer types. Their approach achieved 98% accuracy with multiomics integration, significantly outperforming single-omics models (96% with RNA-seq or methylation individually, and 81% using somatic mutation data alone) [13]. This demonstrates how ensemble methods effectively leverage complementary information across molecular layers.
Similarly, a hybrid clustering-classification framework applied to TCGA data demonstrated how ensemble techniques can overcome the instability often associated with high-dimensional transcriptomic profiles. By integrating Self-Organizing Tree Algorithm with agglomerative and spectral consensus clustering, then applying Random Forest classification with Bayesian optimization, this approach achieved approximately 97.5% accuracy with cross-platform robustness (81.1% accuracy on independent expO dataset validation) [87].
Biomarker Discovery and Validation
Beyond classification, ensemble methods provide a powerful framework for feature selection and biomarker identification from high-dimensional omics data. The high dimensionality and small sample sizes typical of LC-MS-based metabolomics data and RNA-seq datasets make feature selection particularly challenging, as traditional methods often exhibit significant instability [91].
Ensemble feature selection addresses this limitation by combining multiple algorithms to identify robust biomarker signatures. One study demonstrated this approach by integrating five filter-based feature selection methods (Rank Product, Fold Change Ratio, ABCR, t-test, and PLS-DA) using Borda count fusion [91]. This method leverages the complementary strengths of individual algorithms, producing more stable and reliable biomarker rankings than any single method alone.
The functional relevance of ensemble-identified biomarkers has been validated through pathway enrichment analyses. In the hybrid clustering-classification study, functional enrichment using KEGG and ClueGO/CluePedia linked identified gene clusters to biologically coherent pathways, including immune regulation, neuroactive signaling, metabolism, and viral response [87]. This biological plausibility strengthens the clinical translation potential of ensemble-discovered biomarkers.
Experimental Protocols for Ensemble-Based Biomarker Discovery
Protocol 1: Ensemble Feature Selection for LC-MS Metabolomic Data
This protocol details an ensemble feature selection method for biomarker discovery in Liquid Chromatography-Mass Spectrometry (LC-MS)-based metabolomics data, adapted from the approach described in [91].
Materials and Reagents
- LC-MS platform with appropriate analytical columns and solvents
- Quality control samples (pooled from all samples)
- Standard reference materials for instrument calibration
- Data preprocessing software (e.g., XCMS, Progenesis QI)
Procedure
Sample Preparation and Data Acquisition
- Extract metabolites using appropriate method (e.g., methanol:water:chloroform)
- Analyze samples using LC-MS in randomized order to avoid batch effects
- Include quality control samples every 10-12 injections to monitor instrument performance
- Export peak intensity data for subsequent analysis
Data Preprocessing
- Perform peak alignment, retention time correction, and peak filling
- Apply quality control filters: remove features with >30% missing values in QC samples or >20% relative standard deviation in technical replicates
- Impute remaining missing values using appropriate method (e.g., k-nearest neighbor)
- Apply generalised logarithm transformation and Pareto scaling to normalize data
Ensemble Feature Selection
- Apply five filter-based feature selection methods to rank features:
- Rank Product: Calculate using ( S(fi) = \left( \prod{sn \in \text{group}g} R{sn,i} \right)^{1/ng} ) where ( R{sn,i} ) is the rank of feature i in sample ( sn ) [91]
- Fold Change Ratio: Compute as ( S(fi) = \log2\left( \frac{\bar{x}{g,i}}{\bar{x}{0,i}} \right) ) where ( \bar{x}{g,i} ) and ( \bar{x}{0,i} ) are group means [91]
- ABCR: Calculate using the area between the curve and rising diagonal in ROC analysis [91]
- t-test: Apply standard t-test assuming unequal variances
- PLS-DA: Use variable importance in projection (VIP) scores
- Combine rankings using Borda count fusion:
- For each feature, sum its rank positions across all five methods
- Sort features by aggregate Borda count (lower sum indicates higher rank)
- Apply five filter-based feature selection methods to rank features:
Biomarker Validation
- Select top-ranked features for technical validation using targeted LC-MS/MS
- Assess biological validation in independent sample cohort
- Perform pathway analysis to determine functional relevance of biomarker panel
Ensemble Feature Selection Workflow: This diagram illustrates the multi-method integration process for robust biomarker identification from LC-MS data.
Protocol 2: Stacked Multiomics Integration for Cancer Classification
This protocol describes a stacking ensemble approach for cancer type classification using multiomics data, based on the methodology in [13].
Materials
- RNA-seq data (e.g., from TCGA)
- DNA methylation data (e.g., from LinkedOmics)
- Somatic mutation data (e.g., from LinkedOmics)
- Computational environment with Python 3.10 and necessary libraries (scikit-learn, TensorFlow, PyTorch)
- High-performance computing resources for model training
Procedure
Data Collection and Preprocessing
RNA-seq Processing:
- Download raw counts or FPKM data from TCGA
- Normalize using transcripts per million (TPM) method: ( \text{TPM} = 10^6 \times \frac{\text{reads mapped to transcript}/\text{transcript length}}{\sum(\text{reads mapped to transcript}/\text{transcript length})} ) [13]
- Apply autoencoder for dimensionality reduction while preserving biological properties
DNA Methylation Processing:
- Download beta values from LinkedOmics
- Remove probes with >10% missing values
- Impute remaining missing values using k-nearest neighbor
- Perform quantile normalization
Somatic Mutation Processing:
- Download mutation annotation files
- Encode as binary matrix (1: mutated, 0: not mutated)
- Filter to include only genes mutated in >1% of samples
Base Model Training
- Prepare five base classifiers:
- Support Vector Machine (SVM) with radial basis function kernel
- k-Nearest Neighbors (KNN) with k=5
- Artificial Neural Network (ANN) with two hidden layers
- Convolutional Neural Network (CNN) for feature extraction
- Random Forest with 100 decision trees
- Train each model on all three omics data types separately
- Optimize hyperparameters using Bayesian optimization with 5-fold cross-validation
- Prepare five base classifiers:
Stacking Ensemble Construction
- Use out-of-fold predictions from base models as features for meta-learner
- Train Logistic Regression as meta-classifier on stacked predictions
- Implement using scikit-learn StackingClassifier with cross-validation
Model Validation
- Evaluate performance using 70/30 train-test split and 5-fold cross-validation
- Assess metrics: accuracy, precision, recall, F1-score, AUC-ROC
- Compare multiomics performance against single-omics baselines
- Perform external validation on independent dataset if available
Stacked Multiomics Classification: This diagram shows the integration of multiple classifier predictions through a meta-learner for enhanced cancer type classification.
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 2: Key Research Reagent Solutions for Ensemble-Based Biomarker Discovery
| Category | Specific Product/Technology | Function in Workflow | Key Features/Benefits |
|---|---|---|---|
| Sample Preparation | Omni LH 96 Automated Homogenizer | Standardized tissue disruption and nucleic acid extraction | Ensures reproducible sample processing, reduces technical variability [92] |
| Sequencing Technologies | Illumina HiSeq RNA-seq | Comprehensive transcriptome profiling | High-throughput, accurate quantification of gene expression [86] |
| Multiomics Platforms | LC-MS/MS Systems | Proteomic and metabolomic profiling | Enables quantification of proteins and metabolites for integrated analysis [88] [91] |
| Data Analysis | Python with scikit-learn, TensorFlow | Implementation of ensemble algorithms | Open-source, comprehensive machine learning libraries [86] [13] |
| Biomarker Validation | Targeted LC-MS/MS Assays | Technical validation of candidate biomarkers | High sensitivity and specificity for verification [91] |
| Clinical Translation | Liquid Biopsy Platforms | Non-invasive biomarker detection | Enables serial monitoring, minimal patient discomfort [92] [93] |
Clinical Translation and Implementation Challenges
The progression of ensemble-derived biomarkers from research discoveries to clinically applicable tools involves navigating substantial translational barriers. Key challenges include analytical validation, clinical utility demonstration, and implementation in diverse healthcare settings.
Analytical Validation Requirements
For clinical adoption, ensemble-identified biomarkers must undergo rigorous validation protocols:
- Analytical specificity and sensitivity: Establishing detection limits and assessing interference from related molecules [91]
- Reproducibility across sites: Demonstrating consistent performance across different laboratories and platforms [87]
- Reference standard correlation: Validating against established diagnostic methods [93]
The multiomics ensemble model for classifying five cancer types exemplifies this validation process, having been tested on both internal validation splits (70/30 train-test) and external datasets, with performance metrics consistently exceeding 96% accuracy [13]. Similarly, the ensemble feature selection method for metabolomics was evaluated using spiked-in compounds with known concentrations, providing ground truth for accuracy assessment [91].
Clinical Implementation Considerations
Successful implementation of ensemble-based biomarkers requires addressing several practical constraints:
- Computational infrastructure: Ensemble methods often require significant computational resources, which may be limited in clinical settings [13]
- Interpretability challenges: The "black box" nature of complex ensembles can hinder clinical adoption, necessitating explainable AI approaches [87]
- Regulatory approval: Gaining FDA/EMA approval requires standardized protocols and demonstrated clinical utility [92]
Despite these challenges, the field is advancing rapidly. Liquid biopsy technologies have emerged as particularly promising applications, offering non-invasive approaches for cancer detection and monitoring that integrate well with ensemble analysis methods [92] [93]. The projected growth of the genomic biomarker market to $14.09 billion by 2028 further underscores the expanding role of these technologies in personalized oncology [92].
The integration of ensemble methods with emerging technologies is poised to further transform biomarker discovery and clinical cancer diagnostics. Several promising directions are shaping the next generation of ensemble approaches in oncology.
Advanced multiomics integration represents a key frontier. While current methods typically analyze omics layers separately before integration, future approaches will likely leverage more sophisticated fusion techniques that model biological interactions across molecular layers [88]. The emergence of single-cell multiomics and spatial transcriptomics provides unprecedented resolution for characterizing tumor heterogeneity, offering new dimensions for ensemble-based analysis [88] [94].
Artificial intelligence enhancements are similarly transformative. Deep learning architectures integrated within ensemble frameworks can automatically learn hierarchical feature representations from raw multiomics data, reducing reliance on manual feature engineering [13] [90]. The integration of transformer networks and attention mechanisms may further improve model interpretability by identifying particularly influential features in classification decisions [90].
In conclusion, ensemble methods have demonstrated substantial impact on both biomarker discovery and clinical cancer classification. By improving analytical robustness and classification accuracy, these approaches address critical challenges in translational oncology. As computational methods continue to evolve alongside multiomics technologies, ensemble frameworks are positioned to play an increasingly central role in precision oncology, ultimately contributing to improved early detection, personalized treatment selection, and enhanced patient outcomes.
Conclusion
Ensemble methods represent a paradigm shift in computational oncology, consistently demonstrating superior accuracy, robustness, and clinical interpretability for cancer classification. The synthesis of insights from this article confirms that techniques like stacking effectively integrate diverse data types—from gene expression to multiomics—achieving accuracy rates exceeding 98% in many cases. The strategic optimization of these models, through advanced feature selection and hyperparameter tuning, is crucial for managing the high-dimensionality and inherent noise of biomedical data. Furthermore, the integration of Explainable AI (XAI) frameworks like SHAP transforms these models from black boxes into tools for transparent biomarker discovery and hypothesis generation. Future directions should focus on the clinical translation of these models, their validation on larger, more diverse populations, and deeper integration with multiomics data to power the next generation of precision diagnostics and targeted therapeutics, ultimately bridging the gap between computational prediction and clinical application.
References
- 1. Stacked Deep Learning Ensemble for Multiomics Cancer ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12342693/]
- 2. Ensemble-based multiclass lung cancer classification using ... [https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0318219]
- 3. An Intelligent Classification System for Cancer Detection ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10948228/]
- 4. Comparative performance of multiple ensemble learning models for preoperative prediction of tumor deposits in rectal cancer based on MR imaging | Scientific Reports [https://www.nature.com/articles/s41598-025-89482-3]
- 5. Adaptive reinforcement ensemble transfer learning for robust lung tumor detection - ScienceDirect [https://www.sciencedirect.com/science/article/abs/pii/S1746809425017586]
- 6. [2406.10087] Provably Robust Pre-Trained Ensembles for Biomarker-Based Cancer Classification [https://arxiv.org/abs/2406.10087]
- 7. Cancer Classification from Gene Expression Using ... [https://www.mdpi.com/2673-7426/4/2/70]
- 8. RN-Autoencoder: Reduced Noise Autoencoder for classifying... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9887895/]
- 9. Learning from Imbalanced Data [https://pmc.ncbi.nlm.nih.gov/articles/PMC11476323/]
- 10. Survival prediction from imbalanced colorectal cancer ... [https://www.nature.com/articles/s41598-025-98703-8]
- 11. A performance analysis of dimensionality reduction ... [https://www.sciencedirect.com/science/article/pii/S277244252200065X]
- 12. Cancer Classification Utilizing Voting Classifier with ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10530870/]
- 13. JMIR Bioinformatics and Biotechnology - Stacked Deep Learning... [https://bioinform.jmir.org/2025/1/e70709]
- 14. Evaluating Dimensionality Reduction for Patient-Reported ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12529990/]
- 15. Frontiers | Explainable AI-based feature importance analysis for ovarian... [https://www.frontiersin.org/journals/public-health/articles/10.3389/fpubh.2025.1479095/full]
- 16. Ensemble learning [https://en.wikipedia.org/wiki/Ensemble_learning]
- 17. On Theory Behind Ensemble Learning Techniques [https://gpavanb.medium.com/on-theory-behind-ensemble-learning-techniques-156eb63acdaa]
- 18. 20 Ensembles of Models [https://www.tmwr.org/ensembles]
- 19. Predicting cancer risk using machine learning on lifestyle ... [https://www.nature.com/articles/s41598-025-15656-8]
- 20. A deep ensemble learning approach for squamous cell ... [https://www.nature.com/articles/s41598-025-91786-3]
- 21. Topic 5. Ensembles and random forest. Part 1. Bagging — mlcourse.ai [https://mlcourse.ai/book/topic05/topic5_part1_bagging.html]
- 22. Bagging and Boosting in AI - learning [https://dev.to/abhinowww/bagging-and-boosting-in-ai-a-comprehensive-guide-to-ensemble-learning-2cf0]
- 23. Ensemble models: Techniques, benefits, applications ... [https://www.leewayhertz.com/ensemble-model/]
- 24. Ensemble Models in Machine Learning | by Mehul Gupta [https://medium.com/data-science-in-your-pocket/ensemble-models-in-machine-learning-d429c988e866]
- 25. Understanding Stacking Ensemble Method [https://dev.to/sreeni5018/understanding-stacking-ensemble-method-a-comprehensive-guide-part-iv-1c29]
- 26. Advanced Ensemble Learning technique - Stacking and its ... [https://www.analyticsvidhya.com/blog/2021/03/advanced-ensemble-learning-technique-stacking-and-its-variants/]
- 27. A stacking ensemble framework integrating radiomics and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12351975/]
- 28. Enhancing breast cancer prediction through stacking ... [https://peerj.com/articles/cs-2461/]
- 29. A novel transformer-based stacking ensemble method with ... [https://peerj.com/articles/cs-3314/]
- 30. Using machine learning to develop a stacking ensemble ... [https://www.nature.com/articles/s41598-024-80210-x]
- 31. Machine learning-driven multi-targeted drug discovery in ... [https://www.nature.com/articles/s41698-025-01058-6]
- 32. Multimodal feature-optimized approaches for cancer ... [https://www.nature.com/articles/s41598-025-23195-5]
- 33. Implementation of ensemble machine learning algorithms on ... [https://bmcbioinformatics.biomedcentral.com/articles/10.1186/s12859-022-05050-w]
- 34. Large language models enable tumor-type classification ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12490231/]
- 35. Boosting skin cancer accuracy with diagnosis ensemble approach [https://www.nature.com/articles/s41598-024-84864-5?error=cookies_not_supported&code=1a676cb1-13f7-4e61-b1df-24626b2fe71b]
- 36. Optimizing breast cancer classification based on cat swarm ... [https://www.nature.com/articles/s41598-025-95481-1]
- 37. Optimized artificial neural networks for breast cancer ... [https://link.springer.com/article/10.1007/s42452-025-07727-2]
- 38. Breast Cancer Classification with Various Optimized Deep ... [https://pubmed.ncbi.nlm.nih.gov/40722501/]
- 39. Breast cancer classification based on hybrid CNN with ... [https://www.nature.com/articles/s41598-025-88459-6]
- 40. Advanced breast cancer prediction using Deep Neural ... [https://www.sciencedirect.com/science/article/abs/pii/S016974392500084X]
- 41. (KAUH-BCMD) dataset: advancing mammographic breast ... [https://www.frontiersin.org/journals/big-data/articles/10.3389/fdata.2025.1529848/full]
- 42. Ensemble Classification of Cancer Types and Biomarker ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4162531/]
- 43. SHAP-Based Identification of Potential Acoustic Biomarkers in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12385800/]
- 44. Explainable machine learning framework for biomarker ... [https://www.nature.com/articles/s41598-025-98948-3]
- 45. 18 SHAP – Interpretable Machine Learning [https://christophm.github.io/interpretable-ml-book/shap.html]
- 46. A stable feature selection method based on majority voting ... [https://www.sciencedirect.com/science/article/pii/S0169260725005863?dgcid=rss_sd_all]
- 47. Boosting skin cancer diagnosis accuracy with ensemble ... [https://www.nature.com/articles/s41598-024-84864-5]
- 48. Breast Cancer Classification with Various Optimized Deep ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12293705/]
- 49. Optimizing accuracy and dimensionality: a swarm intelligence ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12625619/]
- 50. Improved cancer detection through feature selection using ... [https://www.nature.com/articles/s41598-025-92187-2]
- 51. Cancer Multi-Omics Database for Machine Learning [https://www.nature.com/articles/s41597-025-05235-x]
- 52. Optimized deep learning ensemble for accurate oral ... [https://www.sciencedirect.com/science/article/pii/S2666521225000626]
- 53. Artificial Intelligence in Cancer Drug Discovery in 2025 [https://oncodaily.com/oncolibrary/artificial-intelligence-in-cancer-drug-discovery]
- 54. Transformative Role of Artificial Intelligence in Drug ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12406033/]
- 55. AI-Driven Predictive Modeling for Lung Cancer Detection ... [https://link.springer.com/article/10.1007/s44196-025-00879-4]
- 56. DSSCC net enhanced skin cancer classification using ... [https://www.nature.com/articles/s41598-025-25428-z]
- 57. Learning from Imbalanced Data: Integration of Advanced ... [https://www.mdpi.com/2072-6694/16/19/3417]
- 58. A dynamic ensemble learning based data mining ... [https://www.sciencedirect.com/science/article/abs/pii/S0950705124015818]
- 59. Hybrid Synthetic Minority Over-sampling Technique ... [https://www.nature.com/articles/s41598-025-23062-3]
- 60. Multi-CNN Deep Feature Fusion and Stacking Ensemble ... [https://forbestip.org/articles/multi-cnn-deep-feature-fusion-and-stacking-ensemble-classifier-for-breast-ultrasound-lesion-classification/forbes.galenos.2025.02360]
- 61. Optimizing breast cancer classification based on cat swarm ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12485177/]
- 62. A fuzzy rank-based deep ensemble methodology for multi ... [https://www.nature.com/articles/s41598-025-90423-3]
- 63. MSPO: A machine learning hyperparameter optimization ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12277558/]
- 64. MSPO: A machine learning hyperparameter optimization ... [https://pubmed.ncbi.nlm.nih.gov/40693252/]
- 65. Hybrid attention-enhanced MobileNetV2 with particle ... [https://www.sciencedirect.com/science/article/pii/S2352914825000504]
- 66. A Lightweight Breast Cancer Mass Classification Model ... [https://www.mdpi.com/2306-5354/12/6/640]
- 67. NeuroEvolve: A brain-inspired mutation optimization ... [https://www.sciencedirect.com/science/article/pii/S2666307425000415]
- 68. Refining cancer prediction with DNA sequencing and ... [https://www.nature.com/articles/s41598-025-23359-3]
- 69. How to Fix Overfitting and Underfitting | by Tahir | Oct, 2025 [https://medium.com/@tahirbalarabe2/how-to-fix-overfitting-and-underfitting-4cf8f383ea96]
- 70. What is Overfitting? | IBM [https://www.ibm.com/think/topics/overfitting]
- 71. Prevent Overfitting Using Regularization Techniques [https://www.analyticsvidhya.com/blog/2021/07/prevent-overfitting-using-regularization-techniques/]
- 72. Cross Validation in Machine Learning [https://www.geeksforgeeks.org/machine-learning/cross-validation-machine-learning/]
- 73. 3.1. Cross-validation: evaluating estimator performance [https://scikit-learn.org/stable/modules/cross_validation.html]
- 74. Cross-validation (statistics) [https://en.wikipedia.org/wiki/Cross-validation_(statistics)]
- 75. Cross-Validation in Machine Learning: How to Do It Right [https://neptune.ai/blog/cross-validation-in-machine-learning-how-to-do-it-right]
- 76. Boosting Skin Cancer Classification: A Multi-Scale Attention and Ensemble Approach with Vision Transformers - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC12030980/]
- 77. Ensemble learning of foundation models for precision ... [https://arxiv.org/html/2508.16085v1]
- 78. A deep ensemble learning framework for brain tumor ... [https://www.nature.com/articles/s41598-025-03752-8]
- 79. A novel framework for esophageal cancer grading: combining CT imaging, radiomics, reproducibility, and deep learning insights | BMC Gastroenterology | Full Text [https://bmcgastroenterol.biomedcentral.com/articles/10.1186/s12876-025-03952-6]
- 80. Enhanced skin cancer classification using modified ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12583686/]
- 81. 1.11. Ensembles: Gradient boosting, random forests, ... [https://scikit-learn.org/stable/modules/ensemble.html]
- 82. Comparison of Classification Success Rates of Different ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9924317/]
- 83. (PDF) Analysis of Histopathological Images for Prediction of Breast... [https://www.academia.edu/43108699/Analysis_of_Histopathological_Images_for_Prediction_of_Breast_Cancer_Using_Traditional_Classifiers_with_Pre_Trained_CNN]
- 84. Are ensemble classifiers always better than single ... [https://blogs.sas.com/content/sgf/2017/03/10/are-ensemble-classifiers-always-better-than-single-classifiers/]
- 85. Enhanced and Interpretable Prediction of Multiple Cancer ... [https://www.mdpi.com/2306-5354/12/5/472]
- 86. Machine learning approach to identify significant genes ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12547461/]
- 87. Ensemble-based clustering and classification pipeline for ... [https://www.sciencedirect.com/science/article/pii/S1746809425016441]
- 88. Multi-omics strategies for biomarker discovery and application ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12638490/]
- 89. Ensemble learning enhances the precision of preliminary ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11215019/]
- 90. modified ConvNextTiny for detecting molecular expression ... [https://www.frontiersin.org/journals/computer-science/articles/10.3389/fcomp.2025.1569017/full]
- 91. An Ensemble Feature Selection Method for Biomarker ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6420823/]
- 92. What Are Biomarkers? Definition, Applications and ... [https://blog.omni-inc.com/blog/what-are-biomarkers-and-whats-new-in-2025]
- 93. Emerging biomarkers for early cancer detection and diagnosis [https://eurjmedres.biomedcentral.com/articles/10.1186/s40001-025-03003-6]
- 94. Cancer and Aging Biomarkers: Classification, Early ... [https://www.mdpi.com/2079-6374/15/11/737]