Computer-Aided Drug Design in Oncology: Principles, AI Integration, and Clinical Translation
This article provides a comprehensive overview of computer-aided drug design (CADD) principles and their transformative application in oncology drug development.
Computer-Aided Drug Design in Oncology: Principles, AI Integration, and Clinical Translation
Abstract
This article provides a comprehensive overview of computer-aided drug design (CADD) principles and their transformative application in oncology drug development. Tailored for researchers, scientists, and drug development professionals, it explores foundational computational methods, examines cutting-edge methodologies including AI and machine learning integration, addresses optimization challenges in clinical translation, and analyzes validation frameworks and comparative effectiveness of CADD approaches. By synthesizing current trends and technologies, this review serves as both an educational resource and strategic guide for leveraging computational approaches to accelerate cancer drug discovery, from target identification to clinical implementation.
The Computational Foundation: Core Principles of CADD in Cancer Therapeutics
The field of drug discovery has undergone a transformative shift, moving away from reliance on traditional, high-cost screening methods toward computational precision. Computer-Aided Drug Design (CADD) represents the use of computational techniques and software tools to discover, design, and optimize new drug candidates, thereby accelerating the drug discovery process, reducing costs, and improving success rates [1]. In the context of oncology research, where the complexity of cancer biology and the urgent need for targeted therapies are paramount, CADD provides a powerful framework for understanding disease mechanisms at a molecular level and designing precise interventions [2] [3]. This guide details the core principles of CADD, framing them within the critical pursuit of novel oncology therapeutics, and provides a practical toolkit for their application.
Core Methodologies in CADD
CADD methodologies are broadly classified into two complementary categories: structure-based and ligand-based approaches. The selection between them is primarily determined by the availability of structural information for the biological target.
Structure-Based Drug Design (SBDD)
Structure-Based Drug Design (SBDD) leverages the three-dimensional structural information of biological targets, typically proteins, to identify and optimize potential drug molecules [1] [3]. This approach dominated the CADD market with a share of approximately 55% in 2024 [1] [3]. It is indispensable when high-resolution structures of the target, often obtained through X-ray crystallography or Cryo-EM, are available.
The foundational technologies of SBDD include:
- Molecular Docking: This computational technique predicts the preferred orientation (posing) and binding affinity (scoring) of a small molecule (ligand) when bound to a target protein [1]. It is a primary step in virtual screening and was the dominant technology in the CADD market in 2024, holding a ~40% share [1]. Tools like AutoDock Vina are frequently used for this purpose, for instance, in targeting the RdRp enzyme for antiviral development or in oncology [3].
- Molecular Dynamics (MD) Simulations: MD simulations model the physical movements of atoms and molecules over time, providing a dynamic view of protein-ligand interactions, protein folding, and conformational changes that are missed in static structures [2]. This method is crucial for refining docking results and assessing the stability of a predicted complex under near-physiological conditions [2]. Its application was key in the design of drugs like imatinib for cancer [3].
Ligand-Based Drug Design (LBDD)
When the three-dimensional structure of the target is unknown, Ligand-Based Drug Design (LBDD) offers a powerful alternative. This approach designs novel drugs based on the known chemical properties and biological activities of existing active ligands [2] [1]. The LBDD segment is expected to grow at the fastest compound annual growth rate (CAGR) in the coming years [1] [3].
Key LBDD techniques include:
- Quantitative Structure-Activity Relationship (QSAR): This method builds mathematical models that correlate the chemical structure of compounds (described by molecular descriptors) with their biological activity [2]. These models can then predict the activity of new, unsynthesized compounds.
- Pharmacophore Modeling: A pharmacophore is an abstract definition of the essential steric and electronic functional groups necessary for a molecule to interact with a target and trigger its biological response [2]. Pharmacophore models are used for virtual screening to identify new chemical scaffolds that fulfill these spatial constraints.
The Role of Artificial Intelligence and Machine Learning
Artificial Intelligence (AI) and Machine Learning (ML) have become deeply integrated throughout the CADD workflow, creating a subfield often termed AI-driven drug design (AIDD) [4]. AI/ML-based drug design is the fastest-growing technology segment in CADD [1] [3]. These technologies enhance traditional CADD by analyzing vast, complex datasets to identify patterns beyond human capability.
Specific applications include:
- Generative Models: Using variational autoencoders (VAEs) and generative adversarial networks (GANs) to design completely novel molecular structures with desired properties [2].
- Enhanced Virtual Screening: AI algorithms can pre-filter massive compound libraries or re-rank docking results to significantly improve hit rates and scaffold diversity [4].
- Predictive Modeling: ML models are used to predict key pharmacokinetic and toxicity profiles (ADMET - Absorption, Distribution, Metabolism, Excretion, and Toxicity) of compounds early in the discovery process [4].
Table 1: Quantitative Overview of the CADD Market (2024 Baseline)
| Category | Dominant Segment | Market Share (2024) | Fastest-Growing Segment |
|---|---|---|---|
| Type | Structure-Based Drug Design (SBDD) | ~55% [1] [3] | Ligand-Based Drug Design (LBDD) [1] [3] |
| Technology | Molecular Docking | ~40% [1] | AI/ML-Based Drug Design [1] [3] |
| Application | Cancer Research | ~35% [1] [3] | Infectious Diseases [1] [3] |
| End-User | Pharmaceutical & Biotech Companies | ~60% [1] | Academic & Research Institutes [1] [3] |
| Deployment | On-Premise | ~65% [1] | Cloud-Based [1] [3] |
CADD Workflows and Experimental Protocols
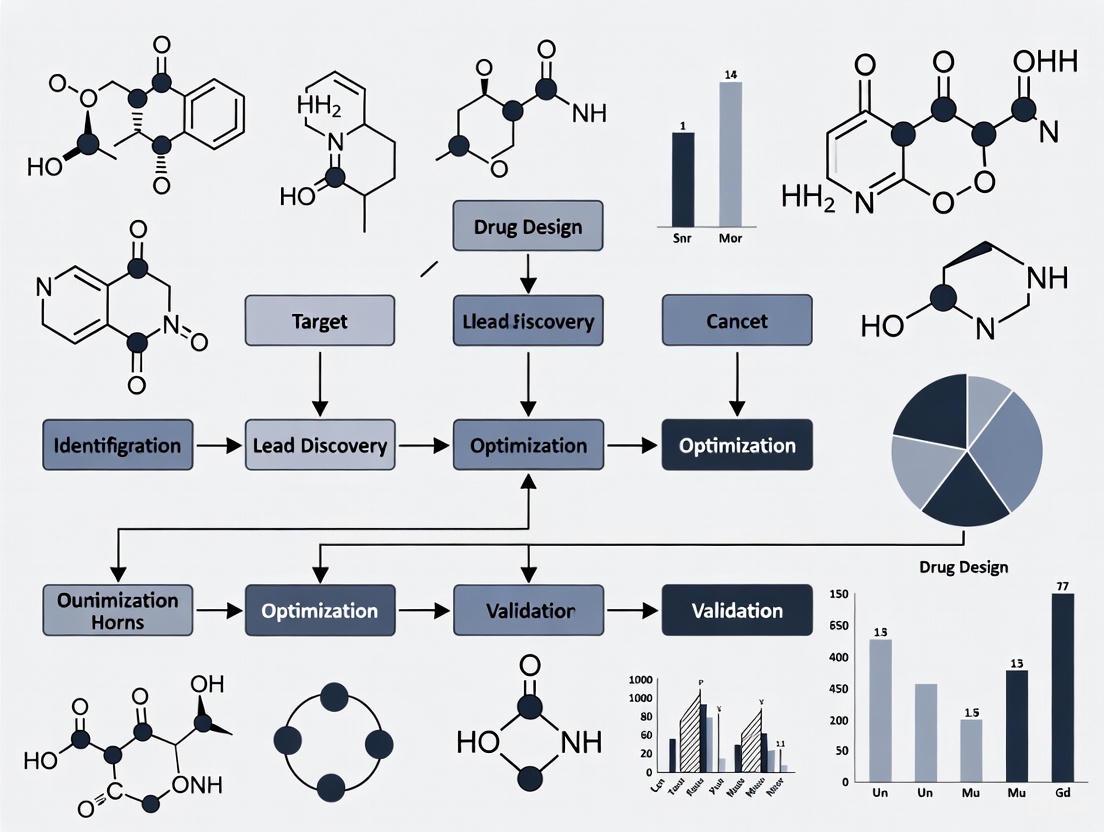
A typical CADD-driven project in oncology follows an iterative workflow that integrates computational predictions with experimental validation. The following diagram and protocol outline a standard structure-based approach for identifying a novel inhibitor for an oncology target.
Diagram Title: CADD Workflow for Oncology Drug Discovery.
Protocol: Structure-Based Virtual Screening for an Oncology Target
This protocol details the key computational and experimental steps for identifying a novel small-molecule inhibitor.
A. Computational Phase
Target Identification and Preparation:
- Objective: Select a validated oncology target (e.g., a mutant kinase like KRAS G12C) and obtain a high-quality 3D structure.
- Methodology:
- Retrieve a crystal structure from the Protein Data Bank (PDB) or generate a predicted structure using AlphaFold [2].
- Prepare the protein structure using molecular modeling software: remove water molecules, add hydrogen atoms, assign partial charges, and correct protonation states of key residues (e.g., Asp, Glu, His).
- Define the binding site, often based on the known location of a co-crystallized native ligand.
Library Preparation:
- Objective: Assay a large and diverse chemical space in silico.
- Methodology:
- Obtain compound libraries (e.g., ZINC, Enamine) containing millions of commercially available molecules.
- Prepare all ligands: generate plausible 3D conformations, minimize their energy, and assign correct charges.
- Filter the library based on drug-likeness rules (e.g., Lipinski's Rule of Five) and other desirable properties to create a focused screening library.
Virtual Screening and Hit Selection:
- Objective: Identify a manageable number of high-probability hits for experimental testing.
- Methodology:
- Perform High-Throughput Virtual Screening (HTVS) using molecular docking software (e.g., AutoDock Vina, Glide) to score and rank all compounds in the library by their predicted binding affinity [2] [3].
- Visually inspect the top-ranking compounds (e.g., top 1000) for sensible binding modes and key molecular interactions (e.g., hydrogen bonds, hydrophobic contacts).
- Apply more computationally intensive methods like Molecular Dynamics (MD) simulations or free-energy perturbation (FEP) calculations to a shortlist (e.g., 100-200 compounds) to refine affinity predictions and assess binding stability [2].
- Select a final, diverse set of 20-50 top-predicted compounds for purchase and experimental validation.
B. Experimental Validation Phase
In Vitro Biochemical Assay:
- Objective: Confirm the biological activity of the computational hits.
- Methodology:
- Procure the selected compounds from commercial suppliers.
- Perform a dose-response biochemical assay to measure the half-maximal inhibitory concentration (IC50) of each compound against the purified target protein (e.g., the kinase). A typical assay measures the decrease in enzyme activity in the presence of the inhibitor.
- Compounds showing significant activity (e.g., IC50 < 10 µM) are considered "confirmed hits" and progress to the next stage.
Lead Optimization:
- Objective: Improve the potency and drug-like properties of the confirmed hits.
- Methodology:
- Use medicinal chemistry to synthesize analogs of the hit compound.
- Employ iterative cycles of CADD (e.g., analog docking, QSAR, FEP) to guide the design of new analogs, predicting which structural changes will improve affinity and reduce off-target effects.
- Experimentally test the new analogs, feeding the data back into the computational models to refine predictions. This loop continues until a pre-clinical candidate drug with nanomolar potency and acceptable ADMET properties is identified.
Successful application of CADD in an oncology research setting relies on a suite of computational tools, databases, and experimental reagents.
Table 2: Key Research Reagent Solutions for CADD in Oncology
| Item / Resource | Type | Function in CADD |
|---|---|---|
| AlphaFold [2] | Software/Model | Accurately predicts 3D protein structures when experimental structures are unavailable, crucial for working with novel oncology targets. |
| AutoDock Vina [3] | Software | An open-source tool for molecular docking, used for virtual screening and binding pose prediction. |
| RaptorX [2] | Software/Model | Predicts protein structures and residue-residue contacts, useful for modeling mutations common in cancer. |
| Protein Data Bank (PDB) | Database | A repository of experimentally determined 3D structures of proteins and nucleic acids, providing starting points for SBDD. |
| ZINC/Enamine Libraries | Database | Commercial and public databases of purchasable compounds used for virtual screening. |
| Purified Target Protein | Wet-lab Reagent | Essential for in vitro biochemical assays to validate computational hits (e.g., measure IC50 values). |
| Cell Lines (Cancer) | Wet-lab Reagent | Used for cellular assays to confirm compound activity and selectivity in a more physiologically relevant model. |
CADD has fundamentally reshaped the landscape of oncology drug discovery, providing a systematic and rational path from gene to candidate drug. The convergence of traditional physics-based computational methods with modern artificial intelligence is pushing the boundaries of what is possible, opening up previously "undruggable" targets and compressing development timelines [5] [4]. While challenges remain—such as the occasional gap between computational prediction and experimental result—the iterative cycle of in silico design, experimental validation, and model refinement creates a powerful engine for innovation [2]. For the modern oncology researcher, a firm grasp of CADD principles is no longer a specialty but a core component of the toolkit, essential for delivering the next generation of precise and life-saving cancer therapeutics.
Within the realm of computer-aided drug design (CADD) for oncology research, two methodological pillars have emerged as fundamental to modern discovery efforts: structure-based drug design (SBDD) and ligand-based drug design (LBDD). These computational approaches have revolutionized the identification and optimization of anticancer agents, enabling researchers to navigate complex biological systems with increasing precision [6]. The integration of these frameworks has become particularly valuable in addressing the challenges posed by cancer heterogeneity and drug resistance, ultimately accelerating the development of targeted therapies and personalized treatment strategies [7].
This technical guide provides an in-depth examination of both methodological frameworks, detailing their underlying principles, key techniques, and practical applications in oncology drug discovery. By presenting structured comparisons, experimental protocols, and visualization of workflows, we aim to equip researchers with a comprehensive understanding of how these approaches can be deployed individually and in concert to advance anticancer drug development.
Core Principles and Definitions
Structure-Based Drug Design (SBDD)
SBDD relies on the three-dimensional structural information of the target protein to design or optimize small molecule compounds that can bind to it [8]. This method is fundamentally centered on the molecular recognition principle, where drug candidates are designed to complement the physicochemical properties and spatial configuration of a target's binding site [8]. The approach requires high-resolution protein structures, typically obtained through experimental methods such as X-ray crystallography, nuclear magnetic resonance (NMR), or cryo-electron microscopy (cryo-EM), or through computationally predicted models [8] [6].
Ligand-Based Drug Design (LBDD)
LBDD utilizes information from known active small molecules (ligands) that bind to the target of interest [8]. When the three-dimensional structure of the target protein is unknown or difficult to obtain, this method predicts and designs compounds with similar activity by analyzing the chemical properties, structural features, and mechanism of action of existing ligands [8] [9]. The core assumption underpinning LBDD is that structurally similar molecules tend to exhibit similar biological activities [9].
Key Techniques and Methodologies
Structure-Based Techniques
Molecular Docking: This core SBDD technique predicts the preferred orientation and conformation of a small molecule ligand when bound to its target protein [9]. Docking algorithms perform flexible ligand docking while often treating proteins as rigid, a simplification that allows for high-throughput screening but may not fully capture binding site flexibility [9]. The resulting poses are scored and ranked based on interaction energies including hydrophobic interactions, hydrogen bonds, and Coulombic interactions [9].
Free Energy Perturbation (FEP): A highly accurate but computationally demanding method, FEP estimates binding free energies using thermodynamic cycles [10] [9]. It is primarily used during lead optimization to quantitatively evaluate the impact of small structural modifications on binding affinity, though it remains challenging to apply to structurally diverse compounds [10].
Molecular Dynamics (MD) Simulations: MD simulations model conformational changes within a ligand-target complex by tracking atomic movements over time [6]. This approach helps address target flexibility and can reveal cryptic binding pockets not evident in static structures [6]. Advanced methods like accelerated MD (aMD) smooth energy barriers to enhance conformational sampling [6].
Ligand-Based Techniques
Quantitative Structure-Activity Relationship (QSAR): QSAR models employ mathematical relationships between chemical structures and biological activity [8]. By extracting molecular descriptors of compounds—including electronic properties, hydrophobicity, and structural parameters—QSAR can predict the biological activity of new compounds and facilitate candidate screening [8]. Modern implementations often use machine learning to improve predictive accuracy [11].
Pharmacophore Modeling: This technique identifies and models the essential structural features necessary for a molecule to interact with its target [8]. A pharmacophore model abstracts common characteristics from known active compounds, such as hydrogen bond donors/acceptors, hydrophobic regions, and charged groups, providing a template for screening new compounds [8].
Similarity-Based Virtual Screening: This approach identifies potential hits from large compound libraries by comparing candidate molecules against known actives using molecular fingerprints or 3D descriptors like shape and electrostatic properties [9] [12]. It excels at pattern recognition and can efficiently prioritize compounds with shared characteristics [12].
Table 1: Comparative Analysis of Key Techniques in SBDD and LBDD
| Technique | Methodological Basis | Primary Applications | Key Advantages | Key Limitations |
|---|---|---|---|---|
| Molecular Docking [9] | Protein-ligand complementarity | Virtual screening, binding pose prediction | Direct visualization of interactions, rational design guidance | Protein flexibility often limited, scoring function inaccuracies |
| Free Energy Perturbation [10] | Thermodynamic cycles | Lead optimization, affinity prediction | High accuracy for small modifications | Extremely computationally intensive, limited to close analogs |
| Molecular Dynamics [6] | Atomic trajectory simulation | Binding stability, conformational sampling, cryptic pocket discovery | Accounts for full system flexibility, physiological conditions | Computationally expensive, limited timescales |
| QSAR [8] [11] | Statistical/machine learning models | Activity prediction, compound prioritization | Fast screening of large libraries, can extrapolate to novel chemotypes | Dependent on quality/quantity of training data, limited interpretability |
| Pharmacophore Modeling [8] | Essential feature abstraction | Virtual screening, scaffold hopping | Intuitive representation, target structure not required | Limited to known chemotypes, conformation-dependent |
| Similarity Screening [9] [12] | Molecular similarity metrics | Library enrichment, hit identification | Fast, scalable, identifies diverse actives | Bias toward known chemical space, may miss novel scaffolds |
Experimental Protocols in Oncology Research
Protocol 1: Structure-Based Virtual Screening for Anticancer Targets
This protocol outlines a structure-based approach for identifying potential inhibitors, exemplified by a study targeting the human αβIII tubulin isotype for cancer therapy [11].
Step 1: Target Preparation
- Obtain the three-dimensional structure of the target protein from experimental sources (PDB database) or through homology modeling if experimental structures are unavailable [11].
- For homology modeling, use tools like Modeller with a template structure of high sequence identity. Select the final model based on validation scores (e.g., DOPE score) and stereo-chemical quality (e.g., Ramachandran plot via PROCHECK) [11].
- Prepare the protein structure by adding hydrogen atoms, assigning partial charges, and defining the binding site coordinates based on known ligand binding locations.
Step 2: Compound Library Preparation
- Retrieve natural compounds or synthetic libraries from databases such as ZINC in SDF format [11].
- Convert compounds to appropriate formats (e.g., PDBQT) using tools like Open-Babel [11].
- Generate 3D conformations and optimize geometries using molecular mechanics force fields.
Step 3: High-Throughput Virtual Screening
- Perform molecular docking against the defined binding site using software such as AutoDock Vina or InstaDock [11].
- Filter compounds based on binding energy thresholds, typically selecting the top 1,000-10,000 hits for further analysis [11].
- Visually inspect top-ranking complexes to confirm sensible binding modes and interactions.
Step 4: Machine Learning Classification
- Generate molecular descriptors for both active and inactive reference compounds using tools like PaDEL-Descriptor [11].
- Train supervised machine learning classifiers (e.g., random forest, SVM) to distinguish between active and inactive molecules [11].
- Apply the trained model to the screened hits to identify compounds with the highest probability of biological activity.
Step 5: ADME-T and Toxicity Prediction
- Evaluate drug-likeness properties of selected hits using ADME-T (Absorption, Distribution, Metabolism, Excretion, and Toxicity) prediction tools [11].
- Filter compounds based on acceptable pharmacokinetic profiles and low predicted toxicity.
Step 6: Validation through MD Simulations
- Subject top candidates to molecular dynamics simulations (e.g., using GROMACS or AMBER) to assess complex stability [11].
- Analyze trajectories using RMSD, RMSF, Rg, and SASA to evaluate structural stability and interaction persistence [11].
- Calculate binding free energies using methods such as MM/PBSA to confirm affinity [11].
Protocol 2: Ligand-Based Design for Kinase Inhibitors in Oncology
This protocol demonstrates a ligand-based approach for designing targeted kinase inhibitors, relevant to numerous cancer pathways.
Step 1: Compound Curation and Data Preparation
- Collect a diverse set of known active compounds against the target of interest, along with their experimental activity data (e.g., IC50, Ki) [9].
- Include structurally similar but inactive compounds to define the activity landscape and avoid potential biases [9].
- Curate the dataset to ensure chemical structure standardization and consistent biological activity measurements.
Step 2: Molecular Descriptor Calculation and Feature Selection
- Compute comprehensive molecular descriptors (e.g., topological, geometrical, electronic) and fingerprints using tools like PaDEL-Descriptor [11].
- Apply feature selection techniques to identify the most relevant descriptors contributing to biological activity, reducing dimensionality and minimizing noise.
Step 3: QSAR Model Development
- Split the dataset into training and test sets using appropriate methods (e.g., random sampling, k-means clustering based on chemical space) [11].
- Develop QSAR models using machine learning algorithms such as random forest, support vector machines, or neural networks [9].
- Optimize model hyperparameters through cross-validation to prevent overfitting.
Step 4: Model Validation and Applicability Domain
- Evaluate model performance using test set predictions and statistical metrics (e.g., R², RMSE, AUC) [11].
- Define the model's applicability domain to identify compounds for which predictions are reliable, based on chemical space coverage of the training set.
Step 5: Virtual Screening and Compound Prioritization
- Apply the validated QSAR model to screen large virtual compound libraries [9].
- Rank compounds based on predicted activity and cluster structurally similar hits to ensure chemical diversity.
- Apply additional filters based on drug-likeness rules (e.g., Lipinski's Rule of Five) and synthetic accessibility.
Step 6: Pharmacophore Modeling and Scaffold Hopping
- Develop a pharmacophore model based on the alignment of known active compounds, identifying essential features for target binding [8].
- Use the pharmacophore model to screen compound libraries and identify novel scaffolds (scaffold hopping) that maintain critical interactions but offer improved properties [9].
Integrated Workflows and Synergistic Applications
The integration of SBDD and LBDD approaches creates a powerful synergistic workflow that leverages the complementary strengths of both methodologies [10] [9] [12]. Two primary integration strategies have emerged as particularly effective in oncology drug discovery.
Sequential Integration: This practical approach uses ligand-based methods as an initial filtering step before applying more computationally intensive structure-based analyses [9] [12]. Large compound libraries are first screened using fast 2D/3D similarity searches against known actives or QSAR predictions. The most promising subset then undergoes molecular docking and binding affinity predictions [12]. This sequential approach improves efficiency by applying resource-intensive methods only to pre-filtered, high-potential compounds [9].
Parallel/Hybrid Screening: Advanced pipelines employ parallel screening, running both structure-based and ligand-based methods independently but simultaneously on the same compound library [9] [12]. Each method generates its own ranking of compounds, and results are compared or combined using consensus scoring frameworks [9]. Parallel scoring selects the top n% of compounds from both similarity rankings and docking scores, increasing the likelihood of recovering potential actives [9]. Hybrid scoring multiplies scores from each method to create a unified ranking, favoring compounds ranked highly by both approaches and increasing confidence in true positives [9] [12].
Diagram 1: Method Selection Workflow in CADD - This diagram illustrates the decision process for selecting appropriate computational approaches based on available data, highlighting pathways for structure-based, ligand-based, and integrated methods.
The Scientist's Toolkit: Essential Research Reagents and Computational Solutions
Table 2: Key Research Reagent Solutions for SBDD and LBDD
| Tool/Category | Specific Examples | Function/Application | Relevance to Oncology |
|---|---|---|---|
| Protein Structure Databases | PDB, AlphaFold Database | Source of experimental and predicted protein structures | Enables targeting of cancer-related proteins with unknown structures |
| Compound Libraries | ZINC, ChEMBL, REAL Database | Collections of screening compounds with chemical diversity | Provides starting points for targeting various oncology targets |
| Molecular Docking Software | AutoDock Vina, InstaDock, Glide | Predicts ligand binding modes and affinity | Critical for virtual screening against cancer drug targets |
| MD Simulation Packages | GROMACS, AMBER, NAMD | Models dynamic behavior of protein-ligand complexes | Studies drug resistance mechanisms in cancer targets |
| QSAR/Modeling Tools | PaDEL-Descriptor, QuanSA, ROCS | Generates molecular descriptors and predictive models | Enables activity prediction for compound optimization |
| Pharmacophore Modeling | Phase, MOE, Catalyst | Identifies essential structural features for activity | Supports scaffold hopping for novel cancer therapeutics |
| Cheminformatics Platforms | OpenBabel, RDKit | Handles chemical data conversion and manipulation | Preprocessing and analysis of chemical libraries |
| AI/ML Frameworks | TensorFlow, Scikit-learn, GENTRL | Builds predictive models for compound activity | Accelerates de novo design of oncology drugs |
Structure-based and ligand-based drug design represent complementary pillars of modern computational drug discovery in oncology. SBDD offers atomic-level insights into drug-target interactions when structural information is available, while LBDD provides powerful pattern recognition capabilities that can guide discovery even in the absence of structural data [8] [9]. The integration of these approaches through sequential or parallel strategies creates a synergistic workflow that enhances hit identification, improves prediction accuracy, and ultimately accelerates the discovery of novel anticancer agents [10] [9] [12].
As oncology research continues to confront challenges of tumor heterogeneity, drug resistance, and personalized treatment needs, these computational frameworks will play an increasingly vital role. Future advances in artificial intelligence, structural biology, and multi-omics integration will further enhance the precision and efficiency of both SBDD and LBDD, solidifying their position as indispensable methodologies in the development of next-generation cancer therapeutics.
The development of new therapeutics, particularly in oncology, has been transformed by computer-aided drug design (CADD) approaches. These methodologies address the fundamental challenges of traditional drug discovery—lengthy timelines, high costs, and significant attrition rates—by providing powerful computational frameworks for identifying and optimizing candidate molecules [13] [14]. Within CADD, three core techniques have emerged as essential: molecular docking, which predicts how small molecules interact with protein targets at the atomic level; Quantitative Structure-Activity Relationship (QSAR) modeling, which correlates chemical structures with biological activity using mathematical models; and pharmacophore modeling, which identifies the essential structural features responsible for molecular recognition [15] [16] [17]. In the complex landscape of cancer research, where disease mechanisms involve diverse phenotypes and multiple etiologies, these computational tools enable researchers to efficiently identify novel therapeutic candidates, optimize lead compounds, and elucidate mechanisms of drug action [18] [14]. The integration of these methods into drug discovery pipelines has become indispensable for advancing targeted cancer therapies, with applications spanning from initial hit identification to lead optimization stages.
Molecular Docking: Predicting Molecular Interactions
Fundamental Principles and Methodologies
Molecular docking is a computational technique that predicts the preferred orientation and binding affinity of a small molecule (ligand) when bound to a target macromolecule (receptor), typically a protein [15]. The primary goals of docking are twofold: first, to predict the ligand's binding pose (position and orientation) within the receptor's binding site, and second, to estimate the binding affinity through scoring functions [15]. This approach is grounded in molecular recognition theories, primarily the "lock-and-key" model, where complementary surfaces pre-exist, and the more sophisticated "induced fit" theory, which accounts for conformational adjustments in both ligand and receptor upon binding [15]. The docking process comprises two fundamental components: sampling algorithms that explore possible ligand conformations and orientations, and scoring functions that rank these poses based on estimated binding energy [15].
When structural information about the binding site is unavailable, blind docking approaches can be employed, which search the entire protein surface for potential binding pockets, aided by cavity detection programs such as GRID, POCKET, SurfNet, PASS, and MMC [15]. The treatment of molecular flexibility varies across docking methods, ranging from rigid-body docking (treating both ligand and receptor as rigid) to flexible ligand docking (accounting for ligand conformational flexibility while keeping the receptor rigid) and fully flexible docking (modeling flexibility in both ligand and receptor) [15].
Key Sampling Algorithms and Scoring Approaches
Various sampling algorithms have been developed to efficiently explore the vast conformational space of ligand-receptor interactions, each with distinct advantages and implementation considerations:
Table 1: Key Sampling Algorithms in Molecular Docking
| Algorithm | Characteristics | Representative Software |
|---|---|---|
| Matching Algorithms | Geometry-based, map ligands to active sites using pharmacophores; high speed suitable for virtual screening | DOCK, FLOG, LibDock, SANDOCK [15] |
| Incremental Construction | Divides ligand into fragments, docks anchor fragment first, then builds incrementally | FlexX, DOCK 4.0, Hammerhead, eHiTS [15] |
| Monte Carlo Methods | Stochastic search using random modifications; can cross energy barriers effectively | AutoDock, ICM, QXP, Affinity [15] |
| Genetic Algorithms | Evolutionary approach with mutation and crossover operations on encoded degrees of freedom | GOLD, AutoDock, DIVALI, DARWIN [15] |
| Molecular Dynamics | Simulates physical movements of atoms; effective for flexibility but computationally intensive | Used for refinement after docking [15] |
Scoring functions quantify ligand-receptor binding affinity through various physical chemistry principles and empirical data. These include force field-based methods (calculating molecular mechanics energies), empirical scoring functions (using regression-based parameters), and knowledge-based potentials (derived from statistical atom-pair distributions in known structures) [15]. The accurate treatment of receptor flexibility, especially backbone movements, remains a significant challenge, with advanced approaches like Local Move Monte Carlo (LMMC) showing promise for flexible receptor docking problems [15].
Experimental Protocol: Molecular Docking Workflow
A standardized molecular docking protocol typically involves these critical steps:
Target Preparation: Obtain the three-dimensional structure of the target protein from experimental sources (Protein Data Bank) or computational prediction tools (AlphaFold, RaptorX) [19]. Remove water molecules and cofactors unless functionally relevant. Add hydrogen atoms, assign partial charges, and define protonation states of residues appropriate for physiological conditions.
Ligand Preparation: Retrieve or draw the small molecule structure. Generate likely tautomers and protonation states. Optimize the geometry using molecular mechanics or quantum chemical methods. For flexible docking, identify rotatable bonds and generate multiple conformations.
Binding Site Definition: If the binding site is known from experimental data, define the search space around key residues. For novel targets, use cavity detection algorithms (e.g., fpocket) or blind docking approaches [15] [14].
Docking Execution: Select appropriate sampling algorithm and scoring function based on system characteristics. Perform multiple docking runs to ensure adequate sampling of conformational space. Use clustering analysis to identify representative binding poses.
Post-Docking Analysis: Visually inspect highest-ranked poses for key interactions (hydrogen bonds, hydrophobic contacts, π-stacking). Quantify interaction energies and compare across compound series. Validate docking protocol by re-docking known crystallographic ligands if available.
Refinement with Molecular Dynamics: Subject top-ranked complexes to molecular dynamics simulations to assess binding stability and incorporate full flexibility [14].
Quantitative Structure-Activity Relationship (QSAR): Predictive Modeling of Bioactivity
Theoretical Foundations and Descriptor Systems
Quantitative Structure-Activity Relationship (QSAR) modeling establishes mathematical relationships between the chemical structure of compounds and their biological activity through molecular descriptors [17]. This approach operates on the fundamental principle that molecular structure encodes all properties necessary for biological activity, and that structurally similar compounds likely exhibit similar biological effects [17]. The methodology formally began in the early 1960s with the seminal work of Hansch and Fujita, who developed a multiparameter approach incorporating hydrophobicity (logP), electronic properties (Hammett constants), and steric effects [17].
Molecular descriptors quantitatively characterize molecular structures across multiple dimensions of complexity:
- 1D Descriptors: Global molecular properties including molecular weight, atom counts, and bond counts [20].
- 2D Descriptors: Topological descriptors encoding molecular connectivity, such as path counts, connectivity indices, and fragment-based descriptors [20].
- 3D Descriptors: Geometrical descriptors capturing molecular shape, volume, and surface properties, along with conformation-dependent features [20].
- 4D Descriptors: Ensemble descriptors accounting for conformational flexibility through molecular dynamics trajectories or multiple conformations [20].
- Quantum Chemical Descriptors: Electronic properties derived from quantum mechanical calculations, including HOMO-LUMO energies, molecular electrostatic potentials, and partial atomic charges [20].
Dimensionality reduction techniques such as Principal Component Analysis (PCA) and Recursive Feature Elimination (RFE) are routinely employed to manage descriptor redundancy and enhance model interpretability [20].
Classical and Machine Learning Approaches in QSAR
QSAR methodologies have evolved from classical statistical approaches to sophisticated machine learning algorithms:
Table 2: QSAR Modeling Techniques and Applications
| Methodology | Key Characteristics | Common Applications |
|---|---|---|
| Classical Statistical Methods | Multiple Linear Regression (MLR), Partial Least Squares (PLS); linear, interpretable models | Preliminary screening, mechanism clarification, regulatory toxicology [20] |
| Machine Learning Approaches | Random Forests, Support Vector Machines (SVM); capture nonlinear relationships, robust with noisy data | Virtual screening, toxicity prediction, lead optimization [20] |
| Deep Learning Frameworks | Graph Neural Networks (GNNs), SMILES-based transformers; automated feature learning from raw structures | De novo drug design, large chemical space exploration [20] |
| Hybrid Models | Integration of classical and machine learning methods; balances interpretability and predictive power | ADMET prediction, multi-parameter optimization [20] |
The machine learning revolution has significantly enhanced QSAR predictive power, with algorithms like Random Forests and Support Vector Machines capable of capturing complex, nonlinear descriptor-activity relationships without prior assumptions about data distribution [20]. Modern developments focus on improving model interpretability through techniques such as SHAP (SHapley Additive exPlanations) and LIME (Local Interpretable Model-agnostic Explanations), which help identify descriptors most influential to predictions [20].
Experimental Protocol: QSAR Model Development and Validation
A robust QSAR modeling workflow requires meticulous execution of these steps:
Data Curation and Chemical Space Definition: Compile a structurally diverse set of compounds with consistent biological activity data. Employ Statistical Molecular Design (SMD) principles to ensure comprehensive chemical space coverage [17]. Remove duplicates and compounds with ambiguous activity measurements. Divide data into training (∼80%) and external test (∼20%) sets.
Descriptor Calculation and Preprocessing: Calculate molecular descriptors using software such as DRAGON, PaDEL, or RDKit [20]. Apply preprocessing techniques including normalization, scaling, and variance filtering. Address missing values through imputation or descriptor removal.
Feature Selection: Identify most relevant descriptors using techniques like stepwise regression, genetic algorithms, LASSO regularization, or random forest feature importance [20]. Reduce dimensionality to prevent overfitting and enhance model interpretability.
Model Building: Apply appropriate algorithms based on dataset characteristics and modeling objectives. For small datasets with suspected linear relationships, employ MLR or PLS. For complex, nonlinear relationships, implement machine learning methods like Random Forests or Support Vector Machines.
Model Validation: Assess model performance using multiple strategies:
Model Application and Interpretation: Use validated models to predict activities of new compounds. Interpret descriptor contributions to derive structure-activity insights for lead optimization.
Pharmacophore Modeling: Defining Essential Molecular Features
Core Concepts and Modeling Approaches
A pharmacophore is defined as "a set of structural features in a molecule recognized at a receptor site, responsible for the molecule's biological activity" [17]. These features include hydrogen bond donors and acceptors, charged or ionizable groups, hydrophobic regions, and aromatic rings, along with their precise three-dimensional spatial arrangement [16]. Pharmacophore modeling can be performed through two primary approaches: structure-based and ligand-based methods.
Structure-based pharmacophore modeling utilizes the three-dimensional structure of a target protein, often complexed with a ligand, to identify key interaction features within the binding site [16]. The process involves analyzing the binding pocket to determine favorable locations for specific molecular interactions, such as hydrogen bonding, hydrophobic contacts, and electrostatic interactions [16]. These features are then integrated into a pharmacophore model that represents the essential characteristics a ligand must possess for effective binding.
Ligand-based pharmacophore modeling is employed when the protein structure is unknown but information about active ligands is available [16] [17]. This approach identifies common chemical features and their spatial arrangements across a set of known active compounds, under the assumption that shared features are essential for biological activity [17]. The method must account for ligand conformational flexibility, often considering multiple low-energy conformations to ensure comprehensive feature mapping [16].
Advanced Applications and Integration with Other Methods
Pharmacophore modeling extends beyond basic virtual screening to diverse applications in drug discovery:
- Side Effect and Off-Target Prediction: Pharmacophore models can identify potential unintended targets by screening against databases of various receptors, helping predict adverse effects early in development [16].
- ADMET Modeling: Pharmacophores aid in predicting absorption, distribution, metabolism, excretion, and toxicity properties by modeling interactions with relevant transporters, metabolizing enzymes, and toxicity targets [16].
- Scaffold Hopping: By searching for compounds with similar pharmacophores but different core structures, researchers can identify novel chemical scaffolds with maintained activity, expanding intellectual property opportunities [16].
- Multi-Target Drug Design: Integrated pharmacophore models can represent features required for activity against multiple targets, facilitating the design of polypharmacological agents [16].
The integration of pharmacophore modeling with molecular dynamics simulations has led to the development of dynamic pharmacophore models, which account for protein flexibility and evolving interaction patterns over time, providing more realistic representations of binding interactions [16]. Additionally, machine learning techniques have enhanced pharmacophore mapping algorithms, enabling more effective identification of active compounds against protein targets of interest [16].
Experimental Protocol: Pharmacophore Model Development
A comprehensive pharmacophore modeling workflow involves these critical stages:
Data Preparation: For structure-based approaches, obtain the protein structure from crystallography, NMR, or homology modeling. Prepare the structure by adding hydrogens, assigning charges, and optimizing hydrogen bonding networks. For ligand-based approaches, compile a diverse set of confirmed active compounds with measured activities. Generate multiple low-energy conformations for each ligand using systematic search, Monte Carlo, or molecular dynamics methods.
Feature Identification: Define the chemical features essential for molecular recognition. Common features include:
- Hydrogen bond donors and acceptors (represented as vectors or projected points)
- Hydrophobic and aromatic features (spheres or volumes)
- Ionizable groups (positive/negative ionizable features)
- Exclusion volumes (regions sterically forbidden by the protein) [16]
Model Generation: For structure-based models, analyze the binding site to identify locations where specific interactions would be favorable. For ligand-based models, align active conformations and identify common features with conserved spatial relationships. Select a subset of features that best explains the activity data while maintaining model specificity.
Model Validation: Assess model quality using several approaches:
- Decoy Sets: Screen databases containing known actives and inactives to evaluate retrieval rates [16].
- Statistical Measures: Calculate sensitivity (ability to identify actives) and specificity (ability to reject inactives) [16].
- External Test Sets: Use compounds not included in model generation to evaluate predictive power.
Virtual Screening and Hit Identification: Employ validated models to screen large chemical databases (e.g., ZINC, ChEMBL). Use the model as a 3D search query to identify compounds matching the pharmacophore pattern. Apply post-processing filters based on physicochemical properties, drug-likeness, and structural novelty.
Experimental Verification: Select top-ranked compounds for biological testing to validate model predictions. Iteratively refine the model based on experimental results to improve performance.
Integrated Applications in Oncology Drug Discovery
Synergistic Workflows in Cancer Therapeutics
The true power of computational drug discovery emerges when molecular docking, QSAR, and pharmacophore modeling are integrated into synergistic workflows. These integrated approaches are particularly valuable in oncology, where the complexity of cancer mechanisms demands multi-faceted strategies [18]. A representative example includes the development of Formononetin (FM) as a potential liver cancer therapeutic, where network pharmacology identified potential targets, molecular docking evaluated binding interactions, and molecular dynamics simulations confirmed binding stability—with all predictions subsequently validated through metabolomics analysis and experimental assays [18].
Another compelling application involves acute myeloid leukemia treatment, where QSAR modeling of 64 compounds targeting Mcl-1 protein identified promising candidates, followed by molecular docking to study drug-target interactions and identify SEC11C and EPPK1 as novel therapeutic targets [21]. This integrated approach significantly compressed the drug discovery timeline from years to hours while reducing costs [21].
For challenging targets like immune checkpoints (PD-1/PD-L1) and metabolic enzymes (IDO1) in cancer immunotherapy, hybrid methods have proven particularly valuable. Structure-based pharmacophore models derived from crystal structures can identify initial hits, which are then optimized using QSAR models that incorporate electronic and steric parameters crucial for disrupting these protein-protein interactions [22].
Research Reagent Solutions: Essential Computational Tools
Table 3: Key Software and Databases for Computational Drug Discovery
| Tool Category | Representative Resources | Primary Applications |
|---|---|---|
| Molecular Docking Software | AutoDock, GOLD, DOCK, FlexX, ICM | Binding pose prediction, virtual screening, binding affinity estimation [15] |
| QSAR Modeling Platforms | QSARINS, Build QSAR, DRAGON, PaDEL, RDKit | Descriptor calculation, model development, validation [20] |
| Pharmacophore Modeling Tools | LigandScout, Phase, MOE | Structure-based and ligand-based pharmacophore generation, virtual screening [16] |
| Protein Structure Prediction | AlphaFold, RaptorX | Target structure determination when experimental structures unavailable [19] |
| Chemical Databases | ZINC, ChEMBL, PubChem | Compound libraries for virtual screening, structural information for modeling [16] |
Workflow Visualization: Integrated Computational Approach
The following diagram illustrates a typical integrated computational workflow in oncology drug discovery, showing how molecular docking, QSAR, and pharmacophore modeling complement each other:
Molecular docking, QSAR, and pharmacophore modeling represent three foundational computational methodologies that have become indispensable in modern oncology drug discovery. While each approach offers distinct capabilities—docking for predicting atomic-level interactions, QSAR for establishing quantitative activity relationships, and pharmacophore modeling for identifying essential molecular features—their integration creates synergistic workflows that accelerate the identification and optimization of therapeutic candidates [15] [20] [16]. As cancer research continues to evolve toward personalized medicine and targeted therapies, these computational tools will play increasingly critical roles in navigating the complexity of tumor biology and designing effective, selective therapeutics. The ongoing incorporation of artificial intelligence and machine learning approaches promises to further enhance the predictive power and application scope of these established methodologies, solidifying their position as essential components of the drug discovery pipeline [22] [20].
Cancer remains one of the leading causes of mortality worldwide, with more than 19 million new cases and nearly 10 million deaths reported in 2020 [23]. The disease presents a formidable challenge due to its intrinsic complexity and heterogeneity, characteristics that necessitate innovative approaches in drug discovery and development. Tumor heterogeneity means that treatments effective in one subset of patients may fail in another, while resistance mechanisms, whether intrinsic or acquired, limit long-term efficacy [23]. Furthermore, cancer biology is heavily influenced by the tumor microenvironment (TME), immune system interactions, and epigenetic factors, making drug response prediction exceptionally complex [23].
Conventional approaches to drug discovery, which typically rely on high-throughput screening and incremental modifications of existing compounds, are poorly equipped to manage this complexity. These strategies are labor-intensive and costly, with an estimated 90% of oncology drugs failing during clinical development [23]. This staggering attrition rate underscores the urgent need for new paradigms capable of integrating vast datasets and generating predictive insights. It is within this context that computational approaches, particularly Computer-Aided Drug Design (CADD), have emerged as transformative tools. CADD enhances researchers' ability to develop cost-effective and resource-efficient solutions by leveraging advanced computational power to explore chemical spaces beyond human capabilities and predict molecular properties and biological activities with remarkable efficiency [4].
Computational Frameworks for Addressing Heterogeneity
Core CADD Methodologies in Oncology
Computer-Aided Drug Design (CADD) represents a suite of computational technologies that accelerate and optimize the drug development process by simulating the structure, function, and interactions of target molecules with ligands [2] [19]. In oncology, these approaches are particularly valuable for managing disease complexity. CADD encompasses several complementary methodologies:
Structure-Based Drug Design (SBDD): This approach leverages the three-dimensional structural information of macromolecular targets to identify key binding sites and interactions, designing drugs that can interfere with critical biological pathways [2] [19]. Techniques include molecular docking, which predicts the binding modes of small molecules to targets, and molecular dynamics (MD) simulations, which refine docking results by simulating atomic motions over time to evaluate binding stability under near-physiological conditions [2] [19].
Ligand-Based Drug Design (LBDD): When structural information of the target is unavailable, LBDD guides drug optimization by studying the structure-activity relationships (SARs) of known ligands [2] [19]. Key methods include quantitative structure-activity relationship (QSAR) modeling, which predicts the activity of new molecules based on mathematical models correlating chemical structures with biological activity [2] [19].
Virtual Screening (VS): This technique computationally filters large compound libraries to identify candidates with desired activity profiles, significantly reducing the number of compounds requiring physical testing [2] [19]. High-throughput virtual screening (HTVS) extends these approaches by combining docking, pharmacophore modeling, and free-energy calculations to enhance efficiency [2] [19].
The following diagram illustrates how these computational methods integrate into a cohesive drug discovery workflow designed to address cancer heterogeneity:
The Rise of Artificial Intelligence in Cancer Drug Discovery
Artificial Intelligence (AI) has emerged as an advanced subset within the broader CADD framework, explicitly integrating machine learning (ML) and deep learning (DL) into key steps of the discovery pipeline [2] [23] [4]. AI-driven drug discovery (AIDD) represents the progression from traditional computational methods toward more intelligent and adaptive paradigms capable of managing the multi-dimensional complexity of cancer biology [4].
In target identification, AI enables integration of multi-omics data—including genomics, transcriptomics, proteomics, and metabolomics—to uncover hidden patterns and identify promising targets that might be missed by traditional methods [23]. For instance, ML algorithms can detect oncogenic drivers in large-scale cancer genome databases such as The Cancer Genome Atlas (TCGA), while deep learning can model protein-protein interaction networks to highlight novel therapeutic vulnerabilities [23].
In drug design and lead optimization, deep generative models such as variational autoencoders (VAEs) and generative adversarial networks (GANs) can create novel chemical structures with desired pharmacological properties, significantly accelerating what has traditionally been a slow, iterative process [2] [23]. Reinforcement learning further optimizes these structures to balance potency, selectivity, solubility, and toxicity [23]. The impact is substantial: companies such as Insilico Medicine and Exscientia have reported AI-designed molecules reaching clinical trials in record times, with one preclinical candidate for idiopathic pulmonary fibrosis developed in under 18 months compared to the typical 3–6 years [23].
Table 1: AI Applications in Addressing Cancer Complexity
| AI Technology | Specific Application in Oncology | Reported Impact |
|---|---|---|
| Machine Learning (ML) | Analysis of multi-omics data for target identification; Predictive modeling of drug response | Identifies novel targets and biomarker signatures from complex datasets |
| Deep Learning (DL) | Analysis of histopathology images; De novo molecular design | Reveals histomorphological features correlating with treatment response; Generates novel chemical structures |
| Natural Language Processing (NLP) | Mining unstructured biomedical literature and clinical notes | Extracts knowledge for hypothesis generation and clinical trial optimization |
| Reinforcement Learning | Optimization of chemical structures for improved drug properties | Balances potency, selectivity, and toxicity profiles |
Experimental Workflows and Research Protocols
Integrated Preclinical Screening Models
To effectively translate computational predictions into viable therapies, researchers employ a cascade of increasingly complex preclinical models that mirror tumor heterogeneity and microenvironmental influences. Each model system offers distinct advantages and limitations in recapitulating the complexity of human cancers [24].
Cell lines represent the initial high-throughput screening platform, providing reproducible and standardized testing conditions for evaluating drug candidates against multiple cancer types and diverse genetic backgrounds [24]. Applications include drug efficacy testing, high-throughput cytotoxicity screening, in vitro drug combination studies, and colony-forming assays [24]. However, their utility is limited by poor representation of tumor heterogeneity and the tumor microenvironment [24].
Organoids have emerged as a revolutionary intermediate model, described by Nature as "invaluable tools in oncology research" [24]. Grown from patient tumor samples, these 3D structures faithfully recapitulate the phenotypic and genetic features of the original tumor, offering more clinically predictive data than traditional 2D cultures [24]. In April 2025, the FDA announced that animal testing requirements for monoclonal antibodies and other drugs would be reduced, refined, or potentially replaced entirely with advanced approaches including organoids, signaling their growing importance in the regulatory landscape [24].
Patient-derived xenograft (PDX) models, created by implanting patient tumor tissue into immunodeficient mice, represent the most clinically relevant preclinical models and are considered the gold standard of preclinical research [24]. These models preserve key genetic and phenotypic characteristics of patient tumors, including aspects of the tumor microenvironment, enabling more accurate prediction of clinical responses [24].
The following workflow illustrates how these models integrate into a comprehensive drug discovery pipeline:
Biomarker Discovery Through Integrated Approaches
The early identification and validation of biomarkers is crucial to addressing cancer heterogeneity in drug development, as biomarkers help identify patients with targetable biological features, track drug efficacy, and detect early indicators of treatment response [24]. An integrated, multi-stage approach leveraging different model systems provides a structured framework for biomarker discovery:
Hypothesis Generation with PDX-Derived Cell Lines: Researchers use PDX-derived cell lines for large-scale screening to identify potential correlations between genetic mutations and drug responses, generating initial sensitivity or resistance biomarker hypotheses [24].
Hypothesis Refinement with Organoids: During organoid testing, biomarker hypotheses are refined and validated using these more complex 3D tumor models. Multiomics approaches—including genomics, transcriptomics, and proteomics—help identify more robust biomarker signatures [24].
Preclinical Validation with PDX Models: PDX models provide the final preclinical validation of biomarker hypotheses before clinical trials. Their preservation of tumor architecture and heterogeneity gives researchers a deeper understanding of biomarker distribution within heterogeneous tumor environments [24].
Table 2: Research Reagent Solutions for Oncology Drug Discovery
| Research Tool | Function and Application | Key Features |
|---|---|---|
| Cell Line Panels | Initial high-throughput drug screening; Drug combination studies | 500+ genomically diverse cancer cell lines; Well-characterized collections available |
| Organoid Biobanks | Drug response investigation; Immunotherapy evaluation; Predictive biomarker identification | Faithfully recapitulate original tumor genetics and phenotype; FDA-recognized model |
| PDX Model Collections | Biomarker discovery and validation; Clinical stratification; Drug combination strategies | Preserve tumor architecture and TME; Considered gold standard for preclinical research |
| Multiomics Platforms | Genomic, transcriptomic, and proteomic analysis for biomarker signature identification | Integrates diverse data types to identify robust biomarker signatures |
Clinical Translation and Regulatory Landscape
Recent FDA Approvals and Trends
The first half of 2025 provided compelling evidence of progress in addressing cancer complexity through targeted approaches. The FDA's Center for Drug Evaluation and Research (CDER) approved 16 novel drugs, with half (8 drugs) targeting various cancers [24]. These approvals reflect important innovations in cancer therapy, demonstrating an increased focus on targeted therapies, immunologically driven approaches, and personalized oncology strategies [24].
Notable approvals included new antibody-drug conjugates (ADCs) for solid tumors, small molecule targeted therapies, and biomarker-guided approaches representing significant advances in precision medicine [24]. Several therapeutics addressing rare cancers also gained approval, including the first treatment for KRAS-mutated ovarian cancer and a non-surgical treatment option for patients with neurofibromatosis type 1 [24].
Table 3: Selected FDA Novel Cancer Drug Approvals in H1 2025
| Drug Name | Approval Date | Indication | Key Feature |
|---|---|---|---|
| Avmapki Fakzynja Co-Pack (avutometinib and defactinib) | 5/8/2025 | KRAS-mutated recurrent low-grade serous ovarian cancer (LGSOC) | First treatment for KRAS-mutated ovarian cancer |
| Gomekli (mirdametinib) | 2/11/2025 | Neurofibromatosis type 1 with symptomatic plexiform neurofibromas | Non-surgical treatment option |
| Emrelis (telisotuzumab vedotin-tllv) | 5/14/2025 | Non-squamous NSCLC with high c-Met protein overexpression | Targets specific protein overexpression |
| Ibtrozi (taletrectinib) | 6/11/2025 | Locally advanced or metastatic ROS1-positive non-small cell lung cancer | Targets specific genetic driver (ROS1) |
AI and CADD in Clinical Trial Optimization
Clinical trials represent one of the most expensive and time-consuming phases of drug development, with patient recruitment remaining a significant bottleneck—up to 80% of trials fail to meet enrollment timelines [23]. AI and CADD approaches are increasingly deployed to optimize this critical phase:
Patient Identification: AI algorithms can mine electronic health records (EHRs) and real-world data to identify eligible patients, significantly accelerating recruitment [23].
Trial Outcome Prediction: Predictive models can simulate trial outcomes, optimizing design by selecting appropriate endpoints, stratifying patients, and reducing required sample sizes [23].
Adaptive Trial Designs: AI-driven real-time analytics enable modifications in dosing, stratification, or drug combinations during the trial based on accumulating data [23].
Natural language processing (NLP) tools further enhance clinical trial efficiency by matching trial protocols with institutional patient databases, creating a more seamless integration between computational prediction and clinical execution [23].
The oncology imperative demands sophisticated strategies that directly address the fundamental challenges of cancer complexity and heterogeneity. Computational approaches, particularly CADD and its advanced subset AIDD, provide powerful frameworks for managing this complexity across the entire drug discovery and development pipeline. From initial target identification through clinical trial optimization, these technologies leverage increasing computational power and algorithmic sophistication to explore chemical and biological spaces beyond human capabilities [4].
The continued evolution of these fields promises even greater integration of computational and experimental approaches. Advances in multi-modal AI—capable of integrating genomic, imaging, and clinical data—promise more holistic insights into cancer biology [23]. Federated learning approaches, which train models across multiple institutions without sharing raw data, can overcome privacy barriers while enhancing data diversity [23]. The emerging concept of digital twins—virtual patient simulations—may eventually allow for in silico testing of drug responses before actual clinical trials [23].
Despite these promising developments, challenges remain in data quality, model interpretability, and regulatory acceptance. The translation of computational predictions into successful wet-lab experiments often proves more complex than anticipated, and the "black box" nature of some AI algorithms continues to limit mechanistic insights [23] [4]. However, the successes achieved to date, combined with the urgent unmet need in oncology, signal an irreversible paradigm shift toward computational-aided approaches in cancer drug discovery. As these technologies mature, their integration throughout the drug development pipeline will likely become standard practice, ultimately benefiting cancer patients worldwide through earlier access to safer, more effective, and highly personalized therapies.
The field of oncology drug discovery has undergone a profound transformation, evolving from reliance on rudimentary computer-assisted models to sophisticated artificial intelligence (AI)-driven platforms. This evolution represents a fundamental paradigm shift from serendipitous discovery and labor-intensive trial-and-error approaches to a precision engineering science powered by computational intelligence [23]. The journey began with early computer-aided drug design (CADD) systems that provided foundational tools for molecular modeling, and has now advanced to integrated AI platforms capable of de novo molecule design, dramatically accelerating the development of targeted cancer therapies [25] [26]. This whitepaper chronicles this technological evolution, examining the historical context, key transitional phases, and current state of AI-enhanced platforms that are reshaping the basic principles of computer-aided drug design in oncology research. The integration of AI has cultivated a strong interest in developing and validating clinical utilities of computer-aided diagnostic models, creating new possibilities for personalized cancer treatment [27]. Within oncology specifically, AI is redefining the traditional drug discovery pipeline by accelerating discovery, optimizing drug efficacy, and minimizing toxicity through groundbreaking advancements in molecular modeling, simulation techniques, and identification of novel compounds [28].
The Early Era: Foundation of Computer-Aided Drug Design
The historical foundation of computer-aided approaches in medical applications began in the mid-1950s with early discussions about using computers for analyzing radiographic abnormalities [29]. However, the limited computational power and primitive image digitization equipment of that era constrained widespread implementation. The 1960s marked a pivotal turning point with the introduction of Quantitative Structure-Activity Relationship (QSAR) models, which represented the first systematic approach to computer-based drug development [25]. These early models established mathematical relationships between a compound's chemical structure and its biological activity, enabling rudimentary predictions of pharmacological properties.
The 1980s witnessed significant advancement with the emergence of physics-based Computer-Aided Drug Design (CADD), which incorporated principles of molecular mechanics and quantum chemistry to simulate drug-target interactions [25]. This period saw the development of sophisticated simulation techniques that could model the three-dimensional structure of target proteins and predict how potential drug molecules might bind to them. By the 1990s, these technologies had matured sufficiently to support commercial CADD platforms like Schrödinger, which began to see broader adoption across the pharmaceutical industry [25] [30].
Throughout this early era, cancer research relied heavily on traditional experimental models including cancer cell lines, patient-derived xenografts (PDXs), and genetically engineered mouse models (GEMMs) [31]. These models formed the essential laboratory foundation for validating computational predictions, though each came with significant limitations in accurately recapitulating human tumor biology and drug response. The workflow during this period remained largely sequential, with computational methods serving as supplemental tools rather than driving the discovery process.
The Transition: Rise of Machine Learning and Data-Driven Approaches
The 2010s marked a critical transitional phase with the rise of deep learning and the emergence of specialized AI drug discovery startups [25]. This period was characterized by the convergence of three key enabling factors: the exponential growth of biological data, advances in machine learning algorithms, and increased computational power through cloud computing and graphics processing units (GPUs). Traditional drug discovery pipelines were constrained by high attrition rates, particularly in oncology, where tumor heterogeneity, resistance mechanisms, and complex microenvironmental factors made effective targeting especially challenging [23].
Machine learning approaches began to demonstrate significant value across multiple aspects of the drug discovery pipeline. Supervised learning algorithms, including support vector machines (SVMs) and random forests, were applied to quantitative structure-activity relationship (QSAR) modeling, toxicity prediction, and virtual screening [22]. Unsupervised learning techniques such as k-means clustering and principal component analysis (PCA) enabled exploratory analysis of chemical spaces and identification of novel compound classes [22]. The integration of these data-driven methods with established physics-based CADD approaches created powerful hybrid systems that leveraged the strengths of both methodologies [25].
This transitional period also saw the emergence of early deep learning architectures, particularly convolutional neural networks (CNNs) and recurrent neural networks (RNNs), which demonstrated superior capabilities in processing complex structural and sequential data [22]. These technologies began to outperform traditional methods in predicting molecular properties and binding affinities. A landmark achievement during this era was Insilico Medicine's demonstration in 2019, advancing an AI-designed treatment for idiopathic pulmonary fibrosis into Phase 2 clinical trials [25]. This achievement provided compelling validation of AI's potential to accelerate the entire drug development process.
The Current Era: AI-Enhanced Platforms and Integrated Workflows
By 2025, AI-driven drug discovery has firmly established itself as a cornerstone of the biotech industry, with large-scale projects emerging rapidly across the globe [25]. The current era is characterized by fully integrated AI platforms that leverage multiple complementary technologies to streamline the entire drug discovery pipeline. The core AI architectures that define this modern approach include generative models, predictive algorithms, and sophisticated data integration systems.
Leading AI Platforms and Technologies
Table 1: Leading AI-Driven Drug Discovery Platforms in 2025
| Platform/Company | Core AI Approach | Key Oncology Applications | Clinical Stage Achievements |
|---|---|---|---|
| Exscientia | Generative AI + Automated Precision Chemistry | Immuno-oncology, CDK7 inhibitors, LSD1 inhibitors | First AI-designed drug (DSP-1181) entered Phase I trials in 2020; Multiple clinical compounds designed [30] |
| Insilico Medicine | Generative AI + Target Identification | Idiopathic pulmonary fibrosis, Oncology targets | Phase IIa results for ISM001-055; Target-to-clinic in 18 months for IPF program [30] |
| Recursion | Phenomics-First AI + High-Content Screening | Various oncology indications | Merger with Exscientia creating integrated AI platform; Extensive phenomics database [30] |
| Schrödinger | Physics-Based ML + Molecular Simulation | TYK2 inhibitors, Kinase targets | Zasocitinib (TAK-279) advanced to Phase III trials [30] |
| BenevolentAI | Knowledge-Graph + Target Discovery | Glioblastoma, Oncology targets | AI-predicted novel targets in glioblastoma [23] [30] |
The current AI toolkit encompasses several specialized technologies that work in concert across the drug discovery pipeline. Generative models including variational autoencoders (VAEs) and generative adversarial networks (GANs) enable de novo molecular design by learning the underlying patterns and features of known drug-like molecules [22]. These systems can create novel chemical structures with optimized properties for specific therapeutic targets. Predictive algorithms leverage deep learning to forecast absorption, distribution, metabolism, excretion, and toxicity (ADMET) properties, enabling virtual screening of millions of compounds before synthesis [22] [32]. Large language models (LLMs) adapted for chemical and biological data can process scientific literature, predict protein structures, and suggest molecular modifications [32].
The integration of these technologies has created unprecedented efficiencies in oncology drug discovery. AI-driven platforms can now evaluate millions of virtual compounds in hours rather than years, with reported discovery timelines reduced from 10+ years to potentially 3-6 years [32]. Success rates in Phase I trials have shown remarkable improvement, with AI-designed drugs demonstrating 80-90% success rates compared to 40-65% for traditional approaches [32]. Companies like Exscientia report in silico design cycles approximately 70% faster and requiring 10x fewer synthesized compounds than industry norms [30].
AI-Driven Workflow in Modern Oncology Drug Discovery
The following diagram illustrates the integrated, AI-driven workflow that characterizes modern oncology drug discovery:
Diagram 1: AI-Driven Drug Discovery Workflow
This workflow demonstrates how modern AI platforms seamlessly integrate multiple data modalities and AI approaches to create an efficient, iterative discovery process. The foundation models, including protein and chemical language models, serve as the underlying infrastructure that powers specific discovery tasks from target identification through clinical trial optimization.
Technical Methodologies: AI Approaches and Experimental Protocols
Core AI Architectures and Their Applications
Table 2: Core AI Architectures in Modern Drug Discovery
| AI Architecture | Mechanism | Oncology Applications | Key Advantages |
|---|---|---|---|
| Generative Adversarial Networks (GANs) | Generator creates molecules; Discriminator evaluates authenticity | De novo design of kinase inhibitors, immune checkpoint modulators | Generates novel chemical structures with optimized properties [22] |
| Variational Autoencoders (VAEs) | Encoder-decoder architecture learning compressed molecular representation | Scaffold hopping for improved selectivity, multi-parameter optimization | Continuous latent space enables smooth molecular interpolation [22] |
| Graph Neural Networks (GNNs) | Message passing between atomic nodes in molecular graphs | Property prediction, binding affinity estimation, reaction prediction | Naturally represents molecular structure and bonding relationships [22] [32] |
| Reinforcement Learning (RL) | Agent receives rewards for desired molecular properties | Multi-objective optimization balancing potency, selectivity, ADMET | Optimizes compounds toward complex, multi-parameter goals [23] [22] |
| Transformers & Large Language Models (LLMs) | Self-attention mechanisms processing sequential data | Protein structure prediction, molecular generation via SMILES, literature mining | Captures long-range dependencies in sequences and structures [32] |
Detailed Experimental Protocol for AI-Driven Discovery
A standardized protocol for AI-driven oncology drug discovery has emerged, incorporating both computational and experimental components:
Phase 1: Target Identification and Validation
- Multi-omic Data Integration: Collect and harmonize genomic, transcriptomic, proteomic, and epigenomic data from public repositories (TCGA, DepMap) and proprietary sources [23] [28].
- Causal AI Analysis: Apply causal machine learning models to distinguish driver mutations from passenger mutations in cancer pathways [32].
- Network Medicine Approaches: Construct protein-protein interaction networks and disease modules to identify novel therapeutic targets [23].
- Experimental Validation: Confirm target druggability using CRISPR screens, patient-derived organoids (PDOs), and patient-derived xenografts (PDXs) [31].
Phase 2: Generative Molecular Design
- Define Target Product Profile: Establish desired properties including potency, selectivity, permeability, and metabolic stability [30] [22].
- Generative Chemical Design: Implement conditional VAEs or GANs to explore chemical space constrained by target properties [22].
- Multi-parameter Optimization: Use reinforcement learning with reward functions balancing multiple property objectives [22].
- Synthetic Accessibility Assessment: Apply retrosynthesis tools (e.g., AIZYNTH, Molecular Transformer) to evaluate synthetic feasibility [30].
Phase 3: Virtual Screening and Prioritization
- Physics-Based Docking: Employ molecular docking simulations (e.g., Schrödinger Glide, AutoDock) for binding pose prediction [30].
- Deep Learning Scoring Functions: Implement CNN-based or GNN-based scoring functions trained on structural interaction data [22].
- ADMET Prediction: Utilize deep learning models (e.g., Random Forest, XGBoost) for in silico prediction of pharmacokinetics and toxicity [22] [32].
- Compound Prioritization: Apply ensemble methods to rank compounds based on integrated assessment of multiple criteria [30].
Phase 4: Experimental Testing and Iteration
- Automated Synthesis: Utilize robotic synthesis platforms (e.g., Exscientia's AutomationStudio) for high-throughput compound production [30].
- High-Content Screening: Implement phenotypic screening in relevant disease models (e.g., Recursion's cellular phenotyping) [30].
- Mechanistic Validation: Conduct pathway analysis, biomarker identification, and mechanism-of-action studies [28].
- Closed-Loop Learning: Feed experimental results back into AI models for continuous model improvement and compound optimization [30].
The following diagram illustrates the architectural integration of these AI approaches within a comprehensive platform:
Diagram 2: AI Platform Architecture Integration
Essential Research Reagents and Materials
The implementation of AI-driven drug discovery requires sophisticated research reagents and platforms that bridge computational predictions with experimental validation. The table below details essential materials and their functions in contemporary oncology drug discovery workflows.
Table 3: Essential Research Reagents and Platforms for AI-Driven Oncology Discovery
| Category | Specific Reagents/Platforms | Function in AI Workflow | Key Applications |
|---|---|---|---|
| Cellular Models | Patient-Derived Organoids (PDOs), Cancer Cell Lines, Primary Immune Cells | Experimental validation of AI-predicted targets and compounds; Generation of training data for AI models | Target validation, compound screening, biomarker identification [31] |
| In Vivo Models | Patient-Derived Xenografts (PDXs), Genetically Engineered Mouse Models (GEMMS), Humanized Mouse Models | In vivo efficacy testing of AI-designed compounds; Assessment of therapeutic index and toxicity | Preclinical validation, mechanism of action studies, combination therapy testing [31] |
| Screening Platforms | High-Content Screening Systems, Automated Patch Clamp, Phenotypic Screening Platforms | Generation of high-dimensional data for AI training; Medium-throughput experimental validation | Compound profiling, target deconvolution, polypharmacology assessment [30] [28] |
| Automation & Synthesis | Robotic Synthesis Systems, Automated Liquid Handlers, High-Throughput Chemistry Platforms | Physical implementation of AI-designed synthetic routes; Closed-loop design-make-test cycles | Compound synthesis, ADME profiling, structure-activity relationship (SAR) exploration [30] |
| Multi-Omic Tools | Single-Cell RNA Sequencing, Spatial Transcriptomics, Mass Cytometry, Proteomics Platforms | Generation of multi-dimensional data for AI-based target identification and biomarker discovery | Tumor heterogeneity mapping, resistance mechanism elucidation, patient stratification [23] [32] |
The historical evolution from early computer-aided drug design to current AI-enhanced platforms represents one of the most significant transformations in oncology research. This journey has progressed from rudimentary QSAR models in the 1960s to fully integrated AI systems that can now design novel drug candidates in a fraction of traditional timelines [25]. The field has achieved remarkable milestones, including the first AI-designed molecules entering clinical trials and demonstrated improvements in success rates at early development stages [30] [32]. Current platforms leverage sophisticated architectures including generative models, deep learning predictors, and automated experimental systems to accelerate the entire drug discovery pipeline from target identification to clinical candidate optimization [22].
Despite these advances, significant challenges remain for AI-driven drug discovery in oncology. Data quality and availability continue to constrain model performance, as AI systems are fundamentally limited by the training data they receive [23] [32]. The "black box" nature of many complex AI models creates interpretability challenges that are particularly problematic in the highly regulated pharmaceutical environment [23]. Robust validation of AI predictions still requires extensive experimental testing in biologically relevant systems, including patient-derived organoids and complex animal models [31]. Additionally, successful implementation requires cultural and workflow integration between computational and experimental teams, bridging traditional disciplinary divides [26].
The future trajectory of AI in oncology drug discovery points toward increasingly integrated and sophisticated platforms. Emerging directions include the development of multimodal AI systems that can simultaneously process diverse data types including structural, sequential, and image-based information [25]. Digital twin simulations that create virtual representations of biological systems promise to enable more accurate prediction of drug behavior before human trials [25]. Federated learning approaches that train models across multiple institutions without sharing raw data address critical privacy concerns while leveraging diverse datasets [23]. As these technologies mature, AI-driven platforms are poised to become the standard approach for oncology drug discovery, potentially enabling truly personalized cancer therapies tailored to individual patient profiles and tumor characteristics [22]. The continued evolution of these platforms represents the next chapter in the ongoing transformation of cancer drug discovery from an artisanal process to an engineered solution.
Advanced CADD Workflows: AI-Driven Approaches for Oncology Targets
Integrating AI and Machine Learning in Modern CADD Pipelines
The field of computer-aided drug design (CADD) represents a fundamental shift from traditional, empirical drug discovery to a rational, hypothesis-driven process that leverages computational power to model and predict molecular interactions [33]. In oncology research, where traditional drug development faces particularly high costs, long timelines, and low success rates, this paradigm shift is especially critical [34]. The integration of artificial intelligence (AI) and machine learning (ML) into modern CADD pipelines has transformed this landscape, introducing unprecedented precision and acceleration in the identification and optimization of anticancer therapeutics [35] [36].
CADD operates on the core principle of using computational algorithms to simulate how drug molecules interact with biological targets, thereby predicting binding affinities and pharmacological effects before costly laboratory synthesis and testing begin [33]. The contemporary CADD framework encompasses two primary methodological categories: structure-based drug design (SBDD), which relies on three-dimensional structural information of biological targets, and ligand-based drug design (LBDD), which leverages known pharmacological profiles of existing compounds [36] [33]. The infusion of AI and ML technologies across both domains has significantly enhanced their predictive capabilities, creating a powerful synergy that is rapidly advancing oncology drug discovery.
AI-Enhanced Target Identification and Druggability Assessment
Target identification represents the critical first step in the drug discovery pipeline, wherein molecular entities that drive cancer progression are identified as potential therapeutic targets [34]. Traditional methods often miss subtle interactions hidden within vast biological datasets, creating a significant bottleneck that AI-powered approaches are uniquely positioned to address.
Multi-Omics Data Integration
AI enables the integration and analysis of complex, multi-modal datasets—including genomics, transcriptomics, proteomics, and metabolomics—to uncover hidden patterns and identify promising oncogenic targets [34] [23]. Machine learning algorithms can detect oncogenic drivers in large-scale cancer genome databases such as The Cancer Genome Atlas (TCGA), while deep learning approaches model intricate protein-protein interaction networks to highlight novel therapeutic vulnerabilities [23]. For example, AI-driven analyses have identified novel targets in glioblastoma by integrating transcriptomic and clinical data, revealing promising leads for further validation [23].
Protein Structure Prediction and Druggability Assessment
The accurate prediction of protein structures is essential for assessing target druggability—determining whether a protein possesses specific characteristics that make it appropriate for therapeutic intervention [34]. AI technologies like AlphaFold and ESMFold have revolutionized structural biology by predicting protein structures with remarkable accuracy, thereby accelerating structure-based drug design and druggability assessments [34] [37]. These tools employ deep learning architectures to model protein folding, providing critical insights into binding site accessibility and specificity that determine whether a target can be effectively modulated with small molecules or biologics [34] [36].
Table 1: AI Platforms for Protein Structure Prediction and Target Identification
| AI Tool/Platform | Primary Function | Key Application in Oncology CADD |
|---|---|---|
| AlphaFold | Protein structure prediction | Predicts 3D structures of cancer-related proteins with high accuracy for druggability assessment [34] |
| ESMFold | Protein structure prediction | Leverages evolutionary scale modeling to predict structures for novel oncology targets [37] [36] |
| BenevolentAI | Target identification | Integrates multi-omics data to identify novel therapeutic targets in cancers like glioblastoma [23] |
| Network-Based Approaches | Target discovery | Maps protein-protein interaction networks to identify oncogenic vulnerabilities and synthetic lethality [34] |
AI-Driven Drug Design and Optimization
Once viable targets are identified, AI significantly accelerates the design and optimization of drug candidates through sophisticated computational approaches that traditional methods cannot match.
De Novo Drug Design
Deep generative models, including variational autoencoders and generative adversarial networks, can create novel chemical structures with desired pharmacological properties specifically tailored to cancer targets [23] [38]. Reinforcement learning further optimizes these structures to balance critical parameters including potency, selectivity, solubility, and toxicity [23]. A notable advancement in this domain is the Bond and Interaction-generating Diffusion model (BInD), which simultaneously designs drug candidate molecules and predicts their binding mechanisms to target proteins using only protein structure information, without needing prior molecular data [38]. This diffusion model approach, similar to that used in AlphaFold 3, generates structures that progressively refine from a random state while incorporating knowledge-based guides grounded in actual chemical laws [38].
Virtual Screening and Binding Affinity Prediction
AI-enhanced virtual screening allows researchers to rapidly evaluate millions of compounds against cancer targets in silico, dramatically reducing the number of candidates requiring physical testing [23] [36]. Machine learning algorithms improve the accuracy of molecular docking predictions by refining scoring functions that estimate binding affinities [36] [33]. These AI-powered approaches have demonstrated remarkable efficiency, with companies like Insilico Medicine and Exscientia reporting AI-designed molecules reaching clinical trials in record times—in some cases reducing the discovery timeline from years to months [23].
Table 2: AI Applications in Drug Design and Optimization
| AI Technology | Methodology | Impact on Oncology Drug Discovery |
|---|---|---|
| Deep Generative Models | Variational autoencoders, GANs | Create novel chemical structures optimized for specific cancer targets [23] |
| Diffusion Models (e.g., BInD) | Bond and Interaction-generating Diffusion | Designs drug candidates and predicts binding mechanisms simultaneously using only target protein structure [38] |
| Reinforcement Learning | Optimization through reward-based algorithms | Balances multiple drug properties (potency, selectivity, toxicity) during molecular optimization [23] |
| Machine Learning-Enhanced Docking | Improved scoring functions | Increases accuracy of binding affinity predictions in virtual screening [36] [33] |
Technical Methodologies and Experimental Protocols
The successful implementation of AI in CADD pipelines requires rigorous methodological frameworks and experimental protocols.
Workflow for AI-Enhanced Drug Discovery
The following diagram illustrates the integrated workflow of AI and CADD in modern oncology drug discovery:
Protocol for AI-Guided Virtual Screening
The following protocol outlines a standard methodology for conducting AI-enhanced virtual screening in oncology drug discovery:
Target Preparation: Obtain the 3D structure of the cancer target protein through experimental methods (X-ray crystallography, cryo-EM) or computational prediction using AI tools like AlphaFold or ESMFold [36] [33]. Process the structure by removing water molecules and co-factors, adding hydrogen atoms, and optimizing hydrogen bonding networks.
Compound Library Curation: Compile a diverse chemical library from databases such as ZINC, ChEMBL, or in-house collections. Pre-filter compounds using drug-likeness rules (Lipinski's Rule of Five) and calculate molecular descriptors relevant to anticancer activity [36] [33].
Molecular Docking with AI Enhancement: Perform docking simulations using programs like AutoDock Vina, AutoDock GOLD, or Glide. Integrate machine learning-based scoring functions to improve binding affinity predictions and reduce false positives [36] [33]. Employ consensus scoring strategies that combine multiple scoring functions for enhanced reliability.
Post-Docking Analysis: Cluster docking poses based on binding modes and interactions. Analyze key protein-ligand interactions (hydrogen bonds, hydrophobic contacts, π-π stacking) that contribute to binding affinity and selectivity for the cancer target.
AI-Powered Compound Prioritization: Use machine learning models trained on historical bioactivity data to rank compounds based on predicted efficacy and specificity. Apply explainable AI techniques to interpret the models' predictions and identify structural features correlated with anticancer activity.
Experimental Validation: Select top-ranking compounds for synthesis and experimental testing in biochemical and cell-based assays. Use the experimental results to iteratively refine the AI models for subsequent screening cycles.
The successful implementation of AI in CADD requires specialized computational tools and resources that constitute the modern drug discovery scientist's essential toolkit.
Table 3: Essential Research Reagent Solutions for AI-Enhanced CADD
| Tool/Resource | Type | Function in AI-CADD Pipeline |
|---|---|---|
| AlphaFold / ESMFold | AI Structure Prediction | Predicts 3D protein structures for targets with unknown experimental structures [34] [36] |
| AutoDock Vina / GOLD | Molecular Docking | Performs virtual screening of compound libraries against cancer targets [36] |
| GROMACS / NAMD | Molecular Dynamics | Simulates dynamic behavior of protein-ligand complexes and calculates binding free energies [36] [33] |
| TensorFlow / PyTorch | ML Frameworks | Builds and trains custom machine learning models for property prediction and compound optimization [36] |
| NVIDIA GPUs | Hardware | Accelerates computationally intensive AI training and molecular simulations [39] |
| Cloud HPC Platforms | Computing Infrastructure | Provides scalable computing resources for large-scale virtual screening and AI model training [39] |
| TCGA / ChEMBL | Data Resources | Provides omics data and bioactivity information for model training and validation [23] [36] |
Current Challenges and Future Directions
Despite significant advancements, the integration of AI in CADD pipelines faces several challenges that must be addressed to fully realize its potential in oncology drug discovery.
Technical and Validation Challenges
A primary limitation concerns the accuracy of scoring functions in molecular docking, which often generate false positives or fail to correctly rank ligands due to the complexity of protein-ligand interactions and difficulties in modeling solvation effects and entropy contributions [33]. Additionally, sampling limitations in molecular dynamics simulations present challenges in capturing rare events such as ligand unbinding or allosteric shifts, despite improvements through enhanced sampling techniques [33].
The "black box" nature of many deep learning models creates interpretability challenges, limiting mechanistic insights into their predictions and raising concerns for regulatory approval [23]. Furthermore, AI models are only as robust as the data on which they are trained; incomplete, biased, or noisy datasets can lead to flawed predictions that do not generalize well outside their training set [23] [33]. This issue is particularly relevant in oncology, where tumor heterogeneity and complex microenvironmental factors complicate drug response prediction [23].
Future Innovations
The future of AI in CADD points toward increased use of multi-modal AI approaches capable of integrating genomic, imaging, and clinical data for more holistic insights [23]. Emerging techniques like federated learning enable model training across multiple institutions without sharing raw data, overcoming privacy barriers while enhancing data diversity [23]. The growing development of explainable AI (XAI) methods will address interpretability concerns by providing transparent insights into model predictions [36] [33].
The integration of real-time experimental data with computational models through techniques like data-driven molecular dynamics promises more physiologically relevant predictions [33]. Furthermore, the rapid advancement of structural determination methods, particularly high-resolution cryo-EM, is expected to provide a wealth of accurate protein structures that will empower structure-based approaches and increase the reliability of homology models [33].
The following diagram illustrates the BInD diffusion model architecture, representing cutting-edge AI methodology in drug design:
The integration of AI and machine learning into modern CADD pipelines represents a paradigm shift in oncology drug discovery, introducing unprecedented efficiencies in target identification, drug design, and optimization. By leveraging sophisticated computational approaches—from deep learning-based protein structure prediction to generative AI for de novo drug design—researchers can now accelerate the discovery of novel anticancer therapeutics while reducing the traditional costs and timelines associated with drug development. Despite persistent challenges related to data quality, model interpretability, and validation, the continuous advancement of AI technologies and their thoughtful integration into established CADD methodologies promises to reshape the future of cancer therapeutics, ultimately delivering more effective and personalized treatments to patients worldwide.
Structure-based drug design (SBDD) represents a paradigm shift in modern oncology drug discovery, leveraging three-dimensional structural information of biological targets to guide the development of therapeutic agents. By focusing on the atomic-level interactions between drugs and their protein targets, SBDD has dramatically accelerated the identification and optimization of compounds that precisely interfere with oncogenic proteins and pathways crucial for cancer survival and progression [40]. This approach has evolved from a supplementary tool to a central component of drug discovery pipelines, particularly in oncology where targeting specific genetic alterations and signaling pathways has demonstrated remarkable clinical success [41] [40].
The foundational principle of SBDD rests on understanding the molecular recognition processes that govern how small molecules bind to therapeutic targets. When combined with computer-aided drug design (CADD) methodologies, SBDD enables researchers to predict binding affinities, optimize molecular interactions, and rationally design compounds with improved efficacy and selectivity profiles before synthesis and experimental validation [40]. In the context of oncology, this approach has been successfully applied to target diverse oncogenic proteins, including kinases, transcription factors, and emerging target classes such as chemokine receptors that modulate the tumor microenvironment [42].
The integration of SBDD with complementary computational and experimental approaches has created a powerful framework for addressing the persistent challenges in cancer therapy, including drug resistance, tumor heterogeneity, and the need for personalized treatment strategies [41] [18]. This technical guide explores the core principles, methodologies, and applications of SBDD in targeting oncogenic proteins and pathways, framed within the broader context of computer-aided drug design fundamentals for oncology research.
Fundamental Principles of Structure-Based Drug Design
Key Methodological Frameworks
SBDD operates through several interconnected methodological frameworks that enable researchers to translate structural information into therapeutic candidates. Molecular docking serves as a cornerstone technique, predicting how small molecules orient themselves within binding pockets of target proteins through systematic sampling of conformational space and scoring of interaction energetics [40]. This approach allows for rapid virtual screening of compound libraries, significantly reducing the need for resource-intensive experimental screening while enriching hit rates with promising candidates [43].
Complementing docking studies, molecular dynamics (MD) simulations provide critical insights into the temporal evolution of drug-target complexes, capturing protein flexibility, binding kinetics, and allosteric mechanisms that static structures cannot reveal [18]. Recent advances in computing power and algorithms have extended MD simulation timescales, enabling observation of rare events and more reliable prediction of binding free energies through methods such as Molecular Mechanics/Poisson-Boltzmann Surface Area (MM/PBSA) calculations [18]. For instance, MM/PBSA calculations have demonstrated binding free energies of -18.359 kcal/mol for phytochemicals interacting with ASGR1, indicating strong binding affinity relevant for cancer therapy [18].
The accuracy of SBDD fundamentally depends on the quality of structural data. X-ray crystallography has traditionally provided most high-resolution protein structures, but recent breakthroughs in cryo-electron microscopy (cryo-EM) have enabled structural analysis of challenging targets such as G protein-coupled receptors (GPCRs) and large protein complexes that are difficult to crystallize [42]. These experimental approaches are increasingly complemented by computational structure prediction tools like AlphaFold, though studies indicate that homology modeling and deep-learning-based predictions still require careful validation against experimental data [40].
Integration with Multi-Omics Data
Modern SBDD increasingly incorporates multi-omics data to prioritize targets with strong disease relevance and identify patient subgroups most likely to respond to targeted therapies. Integration of genomics, transcriptomics, and proteomics data enables identification of cancer-specific biological pathways and the proteins that drive them [44] [18]. A recent multi-omics analysis of 16 cancer types identified between 4 (stomach cancer) and 112 (acute myeloid leukemia) significant pathways characteristic of each cancer type, providing a rich resource for target selection in SBDD campaigns [44].
This integrative approach is particularly valuable for addressing tumor heterogeneity, as omics data can reveal how target proteins vary across cancer subtypes and individual patients. For example, proteomics analysis of 375 cancer cell lines across diverse cancer types has created a rich resource for exploring protein expression patterns and their relationship to cancer pathogenesis [44]. When combined with structural information, these data enable design of compounds that target specific protein conformations or mutant variants prevalent in particular cancer contexts.
Table 1: Key Methodological Components of Structure-Based Drug Design
| Methodological Component | Key Function | Application in Oncology |
|---|---|---|
| Molecular Docking | Predicts binding orientation and affinity of small molecules to target proteins | Virtual screening of compound libraries against oncogenic targets [40] |
| Molecular Dynamics Simulations | Models time-dependent behavior of drug-target complexes | Assessment of binding stability and resistance mechanisms [18] |
| Cryo-Electron Microscopy | Determines high-resolution structures of complex proteins | Structural analysis of membrane receptors and large complexes [42] |
| Multi-Omics Integration | Identifies disease-relevant targets and pathways | Prioritization of oncogenic targets based on functional evidence [44] |
| Free Energy Calculations | Quantifies binding energetics using physics-based methods | Optimization of lead compounds for improved potency [18] |
Current Methodologies and Technological Advances
Artificial Intelligence and Machine Learning Integration
The integration of artificial intelligence (AI) and machine learning (ML) has transformed structure-based drug design, enabling more accurate predictions and accelerated compound optimization. ML algorithms, particularly deep learning models, excel at identifying complex patterns in high-dimensional structural and chemical data, facilitating improved prediction of binding affinities, off-target effects, and physicochemical properties [22]. Supervised learning approaches using support vector machines (SVMs), random forests, and deep neural networks have demonstrated notable success in predicting bioactivity and ADMET (absorption, distribution, metabolism, excretion, and toxicity) properties during early drug discovery [22].
Generative models represent a particularly transformative AI application in SBDD. Architectures such as variational autoencoders (VAEs) and generative adversarial networks (GANs) can design novel molecular structures with specific pharmacological properties by learning from known drug-target interactions [22]. These approaches have been applied to targets including PD-L1 and IDO1, generating chemically valid and synthetically accessible compounds with optimized binding profiles. For example, studies have demonstrated GAN-based models that produce target-specific inhibitors by learning from known drug-target interactions [22]. Reinforcement learning further enhances these capabilities by iteratively proposing molecular structures and rewarding compounds with desired characteristics, enabling efficient exploration of chemical space [22].
AI-driven approaches also address the challenge of multi-parameter optimization, which is crucial for developing effective oncology therapeutics that must simultaneously satisfy multiple constraints including potency, selectivity, and pharmacokinetic properties [22]. By learning complex relationships between structural features and biological activities, AI models can propose compounds optimized for multiple endpoints, significantly reducing the traditional iterative cycles of design-synthesis-testing.
Emerging Modalities and Target Classes
SBDD methodologies have expanded beyond traditional small molecules to encompass novel therapeutic modalities including targeted protein degradation, allosteric modulators, and covalent inhibitors. Proteolysis-targeting chimeras (PROTACs) represent a particularly promising approach that leverages structural information to design molecules that recruit E3 ubiquitin ligases to target proteins, leading to their degradation [41]. This modality offers advantages for targeting proteins traditionally considered "undruggable" and addressing drug resistance mechanisms [41].
Another significant advance involves the application of SBDD to complex target classes such as chemokine receptors, which play pivotal roles in tumor microenvironment remodeling and immune cell recruitment [42]. Recent structural breakthroughs through cryo-EM have enabled high-resolution analysis of chemokine receptor-ligand complexes, revealing allosteric binding sites and conformational states that can be targeted with small molecules [42]. For instance, the CXCL12/CXCR4 axis, which orchestrates hematopoietic stem cell homing and cancer metastasis, can now be targeted using structure-guided approaches that disrupt these pathogenic interactions [42].
Table 2: Quantitative Outcomes of Multi-Omics Analysis for Cancer Target Identification
| Cancer Type | Number of Significant Transcripts | Number of Significant Proteins | Number of Characteristic Pathways | Number of Potential Targeting Drugs |
|---|---|---|---|---|
| Acute Myeloid Leukemia | 11,143 (median across cancer types) | 2,443 | 112 | 97 [44] |
| Non-Small Cell Lung Carcinoma | 9,256 (median) | 1,344 (median) | Information not specified in source | 97 [44] |
| Stomach Cancer | 9,256 (median) | 409 | 4 | Information not specified in source [44] |
| Ovarian Cancer | 9,256 (median) | 1,344 (median) | Information not specified in source | 1 [44] |
| Liver Cancer | 5,756 | 825 | Information not specified in source | Information not specified in source [44] |
Experimental Protocols and Methodologies
Integrated Workflow for Target Identification and Validation
A robust SBDD campaign begins with comprehensive target identification and validation, leveraging multi-omics data and computational analyses to prioritize targets with strong disease relevance. The following protocol outlines an integrated approach used in recent oncology drug discovery efforts:
Step 1: Multi-omics Data Collection and Processing Collect transcriptomics and proteomics data from relevant cancer models, such as the Cancer Cell Line Encyclopedia (CCLE) which contains multi-level omics data from over 1000 cancer cell lines spanning more than 40 cancer types [44]. Process RNA sequencing data to quantify transcript abundance and tandem mass tag (TMT)-based proteomics data for protein quantification, ensuring standardization across datasets.
Step 2: Identification of Significantly Expressed Transcripts and Proteins Apply statistical approaches to identify transcripts and proteins that show statistically significant differential expression in a specific cancer type compared to others. For example, a recent analysis identified between 5,756 (liver cancer) and 11,143 (melanoma) significant transcripts and between 409 (stomach cancer) and 2,443 (AML) significant proteins across 16 cancer types [44].
Step 3: Pathway Enrichment Analysis Analyze significant transcripts and proteins for enrichment of biological pathways using databases such as KEGG and Reactome. Identify overlapping pathways derived from both transcripts and proteins as characteristic of each cancer type, ranging from 4 (stomach cancer) to 112 (AML) pathways [44].
Step 4: Target Prioritization and Structural Characterization Prioritize targets based on pathway significance, druggability assessments, and clinical relevance. Pursue structural characterization of prioritized targets through experimental methods (X-ray crystallography, cryo-EM) or computational predictions (AlphaFold, homology modeling). Critically evaluate computational models against experimental data when available [40].
Structure-Based Virtual Screening Protocol
Virtual screening represents a core application of SBDD, enabling efficient identification of hit compounds from large chemical libraries. The following protocol details a comprehensive structure-based virtual screening approach:
Step 1: Target Preparation Obtain the three-dimensional structure of the target protein from the Protein Data Bank or through computational modeling. Process the structure by adding hydrogen atoms, assigning partial charges, and optimizing hydrogen bonding networks. Define the binding site based on known ligand interactions or predicted binding pockets.
Step 2: Compound Library Preparation Curate a diverse chemical library for screening, ensuring appropriate molecular diversity and drug-like properties. Prepare compounds by generating three-dimensional conformations, optimizing geometry, and assigning appropriate force field parameters. Filter compounds based on physicochemical properties relevant to oncology drugs, such as blood-brain barrier permeability for CNS tumors [43].
Step 3: Molecular Docking Perform systematic docking of compounds into the target binding site using software such as AutoDock Vina or GLIDE. Employ appropriate sampling algorithms to explore conformational flexibility of both ligand and binding site. Utilize scoring functions to rank compounds based on predicted binding affinity.
Step 4: Post-Docking Analysis and Selection Analyze top-ranking compounds for conserved interactions with key residues, favorable geometry, and complementarity to the binding site. Apply additional filters based on drug-likeness, synthetic accessibility, and potential off-target effects. Select 50-200 compounds for experimental validation based on diverse chemotypes and interaction patterns.
This protocol was successfully applied in the discovery of inhibitors targeting mutant isocitrate dehydrogenase 1 (mIDH1) in acute myeloid leukemia, where molecular docking and molecular dynamics simulations identified second-generation inhibitors to counteract resistance mutations [40].
Diagram 1: Virtual screening workflow for oncogenic targets.
Targeting Key Oncogenic Pathways and Proteins
Chemokine Receptors as Therapeutic Targets in Oncology
Chemokine receptors, a critical subfamily of G protein-coupled receptors (GPCRs), have emerged as promising targets for cancer therapy due to their pivotal roles in immune cell migration, inflammatory modulation, and tumor microenvironment remodeling [42]. These receptors specifically recognize chemokine ligands and orchestrate immune cell trafficking and tissue positioning, with functional dysregulation implicated in cancer progression and metastasis [42]. Recent breakthroughs in cryo-electron microscopy have enabled high-resolution structural analysis of chemokine receptors, establishing a robust foundation for structure-based drug design against this target class [42].
The CXCL12/CXCR4 axis represents a particularly well-validated target in oncology, orchestrating hematopoietic stem cell homing to bone marrow niches during embryogenesis and being co-opted by malignant cells to metastasize to CXCL12-rich organs [42]. From a structural perspective, CXCR4 activation occurs through Gαi-dependent upregulation of integrin α4β1 and cytoskeletal reorganization, processes that can be disrupted by small molecules targeting specific receptor conformations [42]. Similarly, the CCL2/CCR2 axis demonstrates context-dependent duality in cancer, driving Ly6C+ monocyte recruitment while simultaneously polarizing tumor-associated macrophages toward immunosuppressive M2 phenotypes through IL-10 and TGF-β secretion [42].
Structure-based approaches have been successfully applied to target CCR5, initially identified as an HIV co-receptor but now recognized for its role in cancer metastasis [42]. The application of SBDD to chemokine receptors exemplifies how atomic-level insights can enable targeting of protein-protein interactions traditionally considered challenging for small molecule intervention.
Immune Checkpoints and Tumor Microenvironment Targets
Beyond chemokine receptors, SBDD has been increasingly applied to targets within the tumor immune microenvironment, particularly immune checkpoints that regulate antitumor immunity. While monoclonal antibodies have dominated this therapeutic area, small molecules offer distinct advantages including oral bioavailability, improved tissue penetration, and lower production costs [22]. Recent efforts have focused on targets such as the PD-1/PD-L1 interaction, with several promising compounds identified that disrupt PD-L1 dimerization or promote its degradation despite the structural challenges posed by the large, flat binding interface [22].
For example, PIK-93 is a small molecule that enhances PD-L1 ubiquitination and degradation, improving T-cell activation when combined with anti-PD-L1 antibodies [22]. Similarly, naturally occurring compounds such as myricetin have been shown to downregulate PD-L1 and IDO1 expression via interference with the JAK-STAT-IRF1 axis [22]. These discoveries highlight how SBDD can leverage both synthetic compounds and natural products to modulate immune checkpoint expression and function through direct and indirect mechanisms.
Another actively pursued target is indoleamine 2,3-dioxygenase 1 (IDO1), which catalyzes tryptophan degradation and contributes to immune suppression within the tumor microenvironment [22]. Inhibitors of IDO1, such as epacadostat, have been developed to reverse this immunosuppressive effect and reinvigorate T-cell responses, with structural insights guiding optimization of potency and selectivity [22].
Diagram 2: Key oncogenic signaling pathways targetable by SBDD.
Successful implementation of SBDD for oncology applications requires access to specialized research reagents, computational tools, and data resources. The following table details essential components of the SBDD toolkit for targeting oncogenic proteins and pathways:
Table 3: Essential Research Reagents and Computational Resources for SBDD in Oncology
| Resource Category | Specific Tools/Reagents | Function in SBDD Workflow |
|---|---|---|
| Structural Biology Tools | Cryo-EM, X-ray crystallography, AlphaFold | Provide high-resolution protein structures for target analysis [40] [42] |
| Chemical Libraries | FDA-approved drugs, natural products, diverse synthetic compounds | Source compounds for virtual and experimental screening [40] |
| Computational Docking Software | AutoDock Vina, GLIDE, GOLD | Predict binding modes and affinities of small molecules [40] |
| Molecular Dynamics Platforms | GROMACS, AMBER, NAMD | Simulate dynamic behavior of drug-target complexes [18] |
| Omics Databases | Cancer Cell Line Encyclopedia (CCLE), TCGA | Provide transcriptomic and proteomic data for target prioritization [44] [18] |
| AI/ML Modeling Frameworks | TensorFlow, PyTorch, RDKit | Enable predictive modeling and de novo molecular design [22] |
| Pathway Analysis Resources | KEGG, Reactome, Gene Ontology | Facilitate biological interpretation of multi-omics data [44] |
These resources collectively enable the end-to-end implementation of SBDD, from target identification and validation through lead optimization and experimental testing. The integration of experimental and computational tools is particularly important for addressing the persistent challenges in oncology drug discovery, including drug resistance and tumor heterogeneity [18]. As these technologies continue to evolve, they promise to further accelerate the development of targeted therapies for oncogenic proteins and pathways.
Structure-based drug design has fundamentally transformed oncology drug discovery by enabling precise targeting of oncogenic proteins and pathways through atomic-level insights. The integration of SBDD with complementary approaches including multi-omics analysis, molecular dynamics simulations, and artificial intelligence has created a powerful framework for addressing the persistent challenges in cancer therapy. As structural biology techniques continue to advance, particularly through cryo-EM and computational prediction methods, the scope of targets amenable to SBDD will further expand to include traditionally "undruggable" proteins. Similarly, the growing sophistication of AI-driven molecular design promises to accelerate the optimization of drug candidates with balanced potency, selectivity, and pharmacokinetic properties. These advances, coupled with improved integration of multi-omics data for patient stratification, will continue to enhance the precision and efficacy of oncology therapeutics developed through structure-based approaches.
In the landscape of computer-aided drug design (CADD), Ligand-Based Drug Design (LBDD) represents a foundational methodology applied when three-dimensional structural information of the biological target is unavailable or limited. LBDD operates on the fundamental principle that molecules with similar chemical structures are likely to exhibit similar biological activities and pharmacological properties [36] [33]. This approach has become indispensable in modern oncology drug discovery, where rapid identification of novel therapeutic candidates is paramount for addressing diverse cancer pathologies and resistance mechanisms.
The historical evolution of LBDD parallels the development of CADD itself, transitioning from early quantitative structure-activity relationship (QSAR) studies to contemporary approaches incorporating artificial intelligence and machine learning [33]. In oncology research, LBDD methods have gained particular prominence due to the complexity of many cancer targets and the frequent lack of high-resolution structural data for novel therapeutic targets. By leveraging known active compounds and their biological effects, researchers can bypass the need for target structure information while still making informed decisions about compound prioritization and optimization [36] [45].
LBDD serves as a complementary approach to structure-based drug design (SBDD), with each methodology possessing distinct advantages and limitations. While SBDD requires detailed three-dimensional target information from techniques such as X-ray crystallography or cryo-EM, LBDD utilizes chemical and biological data from known active compounds to guide drug discovery efforts [45] [33]. This makes LBDD particularly valuable in oncology research, where biological data for chemotherapeutic agents often accumulates more rapidly than structural information for their complex molecular targets.
Core Principles and Methodologies
Theoretical Foundation and Key Concepts
The theoretical foundation of LBDD rests on the molecular similarity principle, which posits that structurally similar molecules are more likely to have similar properties than structurally unrelated compounds [33]. This concept, often referred to as the "similarity-property principle," enables researchers to extrapolate from known bioactive compounds to unknown candidates through various computational techniques. The effectiveness of this approach depends critically on the choice of molecular descriptors and similarity measures, which must capture the essential features responsible for biological activity.
Another fundamental concept in LBDD is the pharmacophore, defined as the essential steric and electronic features necessary for optimal molecular interactions with a specific biological target and to trigger (or block) its biological response [45] [33]. Pharmacophore models abstract from specific molecular structures to capture the spatial arrangement of functional groups that mediate binding, allowing for the identification of structurally diverse compounds that share the necessary interaction capabilities. This approach is particularly valuable in oncology for scaffold hopping—identifying novel chemical structures with similar biological activity to known anticancer agents—which can help address issues of toxicity, resistance, or intellectual property.
Essential LBDD Techniques
Quantitative Structure-Activity Relationship (QSAR) modeling represents one of the oldest and most established LBDD techniques. QSAR attempts to derive a quantitative correlation between the physicochemical and structural properties of compounds (descriptors) and their biological activity through statistical methods [36] [45]. Modern QSAR approaches in oncology research utilize increasingly sophisticated descriptors including electronic, steric, hydrophobic, and topological parameters, with machine learning algorithms replacing traditional statistical methods for model development [33].
Pharmacophore modeling involves identifying the three-dimensional arrangement of molecular features necessary for biological activity. These models can be derived either directly from a set of known active ligands (ligand-based pharmacophores) or from protein-ligand complex structures when available (structure-based pharmacophores) [45]. In oncology applications, pharmacophore models have been successfully used to identify novel inhibitors of kinase targets, epigenetic regulators, and other cancer-relevant proteins.
Molecular similarity calculations encompass a range of techniques for comparing and quantifying the resemblance between compounds. These methods typically employ molecular fingerprints (bit-string representations of chemical features), shape-based alignment, or graph-based approaches to assess similarity [45] [33]. Similarity searching in large compound databases enables rapid identification of potential hit compounds with profiles similar to known anticancer agents, significantly accelerating early-stage discovery efforts.
Table 1: Core LBDD Techniques and Their Applications in Oncology Research
| Technique | Fundamental Principle | Primary Applications in Oncology | Key Advantages |
|---|---|---|---|
| QSAR Modeling | Correlates chemical descriptors with biological activity using statistical or ML methods | Prediction of anticancer activity, toxicity profiling, ADMET prediction | Enables quantitative activity prediction for untested compounds |
| Pharmacophore Modeling | Identifies essential 3D arrangement of molecular features responsible for biological activity | Scaffold hopping for kinase inhibitors, identification of novel epigenetic modulators | Allows identification of structurally diverse compounds with desired activity |
| Molecular Similarity | Quantifies structural or property similarity between compounds using fingerprints or shape-based methods | Virtual screening for compounds similar to known anticancer agents, library design | Rapid screening of large chemical databases, intuitive conceptual basis |
| Molecular Field Analysis | Analyzes interaction energy fields around molecules to explain activity differences | Optimization of drug potency, selectivity profiling across cancer targets | Provides 3D context for structure-activity relationships |
Experimental Protocols and Methodologies
QSAR Model Development Protocol
The development of robust QSAR models follows a systematic workflow that begins with data collection and curation. For oncology applications, this typically involves assembling a dataset of compounds with reliably measured activities (e.g., IC₅₀, EC₅₀, or Ki values) against specific cancer targets or cell lines [36] [46]. The quality of this initial dataset critically influences model performance, requiring careful attention to data consistency, activity measurement standardization, and elimination of compounds with ambiguous results.
Following data collection, molecular descriptor calculation generates quantitative representations of molecular structure and properties. Commonly used descriptors include constitutional (molecular weight, atom counts), topological (connectivity indices), geometrical (surface areas, volume), and electronic (partial charges, HOMO/LUMO energies) parameters [36] [33]. Feature selection techniques are then applied to identify the most relevant descriptors, reducing dimensionality and minimizing the risk of overfitting. Techniques such as Recursive Feature Elimination (RFE) with Support Vector Regression have demonstrated particular effectiveness in oncology drug response prediction [46].
Model training and validation represent the core methodological phase, where statistical or machine learning algorithms establish the relationship between descriptors and biological activity. Validation using external test sets and techniques such as cross-validation is essential to ensure model robustness and predictive capability [33] [46]. For oncology applications, domain-specific validation including testing against diverse cancer cell lines or related molecular targets provides additional assurance of model utility in practical discovery settings.
Pharmacophore Model Generation Workflow
The generation of ligand-based pharmacophore models begins with selection and preparation of training set compounds. An ideal training set includes structurally diverse compounds with measured activities spanning a sufficient range to identify essential versus optional features [45]. Conformational analysis generates representative low-energy conformations for each compound, ensuring adequate sampling of accessible spatial arrangements.
Common pharmacophore identification involves algorithmic detection of spatial feature arrangements shared by active compounds. Typical features include hydrogen bond donors/acceptors, hydrophobic regions, aromatic rings, and charged groups [45] [33]. Model validation assesses the ability to distinguish known active compounds from inactive ones, with refinement iteratively improving model quality. Successful pharmacophore models can then be used for virtual screening of compound databases, identifying candidates that match the essential feature arrangement for subsequent experimental testing in cancer-relevant assays.
Integrated Ligand and Structure-Based Approaches
Modern oncology drug discovery increasingly employs integrated approaches that combine LBDD with structure-based methods [45]. These hybrid strategies can be implemented sequentially, parallely, or through truly integrated methods that simultaneously leverage both chemical and structural information. Sequential approaches might apply ligand-based filtering followed by structure-based docking, or vice versa, while parallel approaches independently apply both methods and combine results [45].
The scoring of compounds in integrated approaches often involves consensus methods that combine scores from multiple techniques, or machine learning models trained on diverse features including both ligand-based descriptors and structure-based interaction energies [45]. Performance assessment typically employs enrichment analysis and area-under-the-curve (AUC) metrics using decoy databases seeded with known active compounds, allowing quantitative comparison of different methodological combinations [45].
Table 2: Research Reagent Solutions for LBDD in Oncology
| Reagent/Category | Specific Examples | Function in LBDD | Application Context |
|---|---|---|---|
| Compound Databases | GDSC, ChEMBL, ZINC | Source of chemical structures and bioactivity data | Training QSAR models, similarity searching, pharmacophore screening |
| Descriptor Calculation | Dragon, RDKit, PaDEL | Generate molecular descriptors for QSAR | Converting chemical structures to quantitative parameters |
| Pharmacophore Modeling | Catalyst, Phase, MOE | Create and validate pharmacophore models | Identifying essential structural features for activity |
| Similarity Search | OpenBabel, ChemAxon | Calculate molecular similarities | Finding analogs of known active compounds |
| Machine Learning | Scikit-learn, TensorFlow, WEKA | Develop predictive models | Building QSAR and drug response prediction models |
| Validation Databases | DEKOIS, DUD-E | Benchmark virtual screening methods | Assessing method performance with known actives/decoys |
Current Applications in Oncology Research
Drug Response Prediction in Precision Oncology
LBDD approaches have demonstrated significant utility in predicting drug response in oncology, a critical challenge due to intertumoral heterogeneity and the complexity of drug-gene interactions [46]. Machine learning models using gene expression data and chemical descriptors of drugs can predict IC₅₀ values for anticancer agents across diverse cancer cell lines, supporting personalized treatment selection [46]. For example, studies have successfully applied Recursive Feature Elimination with Support Vector Regression to predict responses to targeted therapies like Afatinib (EGFR/ERBB2 inhibitor) and Capivasertib (AKT inhibitor) using transcriptomic profiles of cancer cell lines [46].
Feature selection strategy profoundly impacts model performance in drug response prediction. Comparative analyses reveal that data-driven feature selection methods generally outperform biologically informed gene sets based on drug target pathways alone [46]. However, integration of computational and biologically informed gene sets consistently improves prediction accuracy across several anticancer drugs, enhancing both predictive power and biological interpretability [46]. This hybrid approach represents the cutting edge of LBDD in precision oncology, leveraging both chemical data and domain knowledge for optimal performance.
Overcoming Challenges in Oncology Drug Discovery
LBDD methods provide powerful approaches for addressing persistent challenges in oncology drug discovery, particularly for historically "undruggable" targets and resistant cancer forms. When structural information is limited for targets such as transcription factors or protein-protein interaction interfaces, ligand-based methods can leverage known bioactive compounds to identify novel chemotypes through similarity searching or pharmacophore-based screening [45] [33].
The application of LBDD in drug repurposing represents another significant opportunity in oncology. By analyzing chemical and biological similarity between established drugs and known anticancer agents, researchers can identify non-oncological drugs with potential anticancer activity [33]. This approach can significantly shorten development timelines by leveraging existing safety and pharmacokinetic data, rapidly advancing candidates to clinical testing for oncology indications.
Emerging Trends and Future Directions
The integration of artificial intelligence and machine learning represents the most significant trend in LBDD, transforming traditional QSAR and similarity-based approaches [4] [33]. Deep learning architectures including variational autoencoders (VAEs) and generative adversarial networks (GANs) are being used to generate novel molecular structures with desired properties for oncology targets [19]. These AI-driven approaches can explore chemical space more comprehensively than traditional methods, identifying promising regions that might be overlooked by human-mediated design.
Hybrid modeling approaches that combine ligand-based and structure-based methods are gaining traction, leveraging complementary strengths to overcome individual limitations [45] [4]. The integration of biological knowledge into feature selection enhances both the accuracy and interpretability of drug response prediction models, creating more robust and generalizable frameworks [46]. These integrative approaches show particular promise for biomarker discovery, drug repurposing, and personalized treatment strategies in oncology.
The convergence of LBDD with experimental automation creates new opportunities for accelerated discovery cycles. AI-driven in silico design coupled with automated robotics for synthesis and validation enables iterative model refinement that compresses discovery timelines exponentially [4]. This integrated approach is particularly valuable in oncology, where rapid optimization of lead compounds can significantly impact development success for urgent therapeutic needs.
Ligand-based drug design continues to evolve as an essential component of computational oncology, providing powerful methods for leveraging chemical and biological data when structural information is limited or incomplete. The fundamental principles of molecular similarity and quantitative structure-activity relationships remain highly relevant, enhanced by contemporary advances in machine learning, hybrid methods, and experimental integration.
As oncology drug discovery confronts increasingly complex targets and resistance mechanisms, LBDD approaches offer complementary pathways to structure-based methods, particularly through similarity-based screening, pharmacophore modeling, and predictive QSAR. The ongoing integration of biological domain knowledge with computational power promises to further enhance the impact of LBDD, supporting more effective and personalized therapeutic strategies for cancer patients.
The future trajectory of LBDD in oncology points toward increasingly integrated, AI-enhanced approaches that leverage growing chemical and biological datasets while maintaining connection to therapeutic mechanism and clinical application. This evolution ensures that ligand-based methods will continue to provide critical contributions to oncology drug discovery, working in concert with structural and systems-based approaches to address the complex challenges of cancer therapeutics.
The landscape of drug discovery in oncology is undergoing a paradigm shift, moving beyond traditional small-molecule inhibitors toward innovative modalities that target disease-causing proteins for elimination. Two of the most promising emerging therapeutic classes—PROteolysis TArgeting Chimeras (PROTACs) and radiopharmaceutical conjugates—exemplify this shift by harnessing the body's intrinsic biological systems to achieve targeted protein degradation (TPD). These approaches are fundamentally expanding the "druggable genome," enabling targeting of proteins previously considered undruggable through conventional occupancy-based inhibition [47] [48]. The rational design and optimization of these complex molecules are critically dependent on sophisticated computer-aided drug design (CADD) methodologies, which provide the computational framework to navigate the intricate structural and mechanistic challenges involved. This whitepaper provides an in-depth technical examination of PROTACs and radiopharmaceutical conjugates, detailing their mechanisms, design principles, and the integral role of CADD in advancing these modalities from concept to clinic within oncology research.
Targeted Protein Degradation via PROTACs
Core Mechanism and Historical Development
PROTACs are heterobifunctional molecules that mediate the targeted degradation of proteins of interest (POIs) by hijacking the ubiquitin-proteasome system (UPS) [47]. Their structure comprises three elements: a ligand that binds the POI, a ligand that recruits an E3 ubiquitin ligase, and a linker connecting these two moieties [47] [48]. The mechanism of action is catalytic. The PROTAC molecule simultaneously engages both the E3 ligase and the POI, inducing the formation of a ternary complex. This proximity prompts the E3 ligase to transfer ubiquitin chains onto the POI. Polyubiquitinated proteins are subsequently recognized and degraded by the 26S proteasome, effectively reducing intracellular levels of the target protein [47] [49].
First conceptualized by Sakamoto et al. in 2001, the initial PROTACs utilized peptide-based ligands for E3 ligase recruitment [47]. The field transformed with the discovery of small-molecule E3 ligase ligands—such as those for VHL (Von Hippel-Lindau) and CRBN (Cereblon)—enabling the development of cell-permeable, all-small-molecule PROTACs with improved drug-like properties [47] [48]. A pivotal breakthrough was the understanding that immunomodulatory drugs (IMiDs) like thalidomide act as molecular glues by binding CRBN, paving the way for their extensive use in PROTAC design [47].
Key Advantages over Traditional Inhibitors
PROTACs offer several distinct pharmacological advantages:
- Targeting the "Undruggable" Proteome: Unlike inhibitors that require active-site occupancy, PROTACs rely on binding events to induce degradation, making them suitable for targeting proteins without deep enzymatic pockets, such as transcription factors, scaffolding proteins, and regulatory proteins [47] [48].
- Catalytic and Sub-stoichiometric Activity: A single PROTAC molecule can facilitate the degradation of multiple POI copies, enabling efficacy at lower doses and potentially reducing off-target effects [48].
- Overcoming Drug Resistance: Traditional inhibitors often face resistance through target overexpression or mutations that affect drug binding. By degrading the entire target protein, PROTACs can circumvent these resistance mechanisms [48] [49].
- Enhanced Selectivity: The necessity for a productive ternary complex can confer unexpected selectivity, as demonstrated by PROTACs that degrade one bromodomain protein (e.g., BRD4) over closely related family members (BRD2, BRD3) [47].
CADD-Driven Design and Optimization
The rational design of effective PROTACs presents unique challenges that CADD is uniquely positioned to address.
Table 1: Key CADD Techniques for PROTAC Development
| CADD Technique | Application in PROTAC Design | Representative Software/Tools |
|---|---|---|
| Molecular Docking | Predicting the binding pose of warheads and the geometry of the ternary complex. | AutoDock Vina, Glide, GOLD [36] |
| Molecular Dynamics (MD) | Assessing the stability and lifetime of the ternary complex; simulating linker flexibility. | GROMACS, NAMD, CHARMM [36] |
| Structure-Based Drug Design (SBDD) | Utilizing 3D structures of POIs and E3 ligases to inform warhead and linker optimization. | Homology modeling tools (SWISS-MODEL, Rosetta) [36] [50] |
| Virtual Screening | Rapidly identifying novel POI warheads or E3 ligands from large compound libraries. | ZINC15, ChEMBL, DrugBank [51] |
| Quantitative Structure-Activity Relationship (QSAR) | Modeling the relationship between PROTAC structure (e.g., linker length/composition) and degradation efficiency. | Various chemoinformatic packages [36] |
A critical success factor is the formation of a stable POI-PROTAC-E3 ligase ternary complex. CADD tools, particularly molecular dynamics simulations, are indispensable for modeling this complex interaction. The crystal structure of the BRD4-MZ1-VHL ternary complex revealed that cooperative electrostatic interactions between the POI and E3 ligase, induced by the PROTAC, contribute significantly to complex stability and degradation efficiency [47]. Furthermore, the linker is not merely a passive tether but plays an active role in determining the optimal spatial orientation for ternary complex formation. CADD-driven linker optimization involves systematically varying length, composition, and rigidity to achieve maximal degradation activity [47] [48].
Diagram: Mechanism of a PROTAC-Induced Target Degradation
Experimental Protocol for PROTAC Evaluation
A standard workflow for validating PROTAC function in a research setting involves multiple steps:
- PROTAC Design and Synthesis: Based on CADD predictions, a PROTAC is designed using a known POI ligand (e.g., an kinase inhibitor), a validated E3 ligase ligand (e.g., pomalidomide for CRBN or VH032 for VHL), and a synthetic linker (e.g., PEG-based alkyl chains). The compound is synthesized and purified [47].
- In Vitro Degradation Assay:
- Cell Culture: Culture appropriate cancer cell lines (e.g., Burkitt's lymphoma cells for BRD4 degradation) in recommended media.
- PROTAC Treatment: Treat cells with a concentration gradient of the PROTAC (e.g., 0.1 nM to 1 µM) for a predetermined time (e.g., 4-24 hours). Include controls (DMSO vehicle) and control compounds (e.g., POI warhead alone).
- Western Blot Analysis: Lyse cells, separate proteins via SDS-PAGE, and transfer to a membrane. Probe with antibodies specific to the POI (e.g., anti-BRD4) and a loading control (e.g., GAPDH). Quantify band intensity to determine DC50 (half-maximal degradation concentration) and Dmax (maximal degradation) [47] [49].
- Specificity and Off-Target Assessment: Use techniques like global proteomics (e.g., TMT-based mass spectrometry) to confirm on-target degradation and identify any potential off-target effects.
- Functional Phenotypic Assays: Perform cell viability assays (e.g., CellTiter-Glo), cell cycle analysis, or apoptosis assays (e.g., caspase activation) to link target degradation to the intended anti-cancer phenotype [47].
Radiopharmaceutical Conjugates for Targeted Radiotherapy
Mechanism and Evolution in Oncology
Radiopharmaceutical conjugates are targeted medicines that deliver potent radioactive isotopes directly to cancer cells via a targeting vector (antibody, peptide, or small molecule) connected by a chemical linker [52] [53]. Their therapeutic effect is mediated by the ionizing radiation emitted by the payload, which causes irreversible DNA damage, primarily double-strand breaks, leading to cell death [52] [53].
This modality has evolved from non-targeted isotopes like iodine-131 to sophisticated targeted agents. The approvals of Lutathera ([¹⁷⁷Lu]Lu-DOTA-TATE) for neuroendocrine tumors and Pluvicto ([¹⁷⁷Lu]Lu-PSMA-617) for metastatic castration-resistant prostate cancer have ushered in a new era of "radiotheranostics" [52]. This approach uses a diagnostic pair (e.g., [⁶⁸Ga]Ga-PSMA-11 for PET imaging) to first visualize tumors and select patients likely to respond to the corresponding therapeutic agent ([¹⁷⁷Lu]Lu-PSMA-617) [52].
Critical Design Components
The efficacy of a radioconjugate hinges on its core components:
- Targeting Vector: Must bind with high affinity and specificity to a tumor-associated antigen highly expressed on cancer cells (e.g., PSMA for prostate cancer, somatostatin receptors for neuroendocrine tumors) [52] [53].
- Radionuclide Payload: Chosen based on decay properties (emission type, energy, path length, half-life).
- β⁻-Emitters (e.g., Lutetium-177): Moderate path length (0.05–10 mm), suitable for treating larger, heterogeneous tumors via "crossfire" effect.
- α-Emitters (e.g., Actinium-225): Short path length (40–100 µm), high linear energy transfer (LET), causing dense, localized DNA damage ideal for micrometastases or single-cell eradication [52].
- Linker-Chelator System: A bifunctional chelator (e.g., DOTA) covalently binds the targeting vector and stably encapsulates the radiometal, preventing in vivo leakage and off-target toxicity [52].
Table 2: Common Radionuclides in Radiopharmaceutical Conjugates
| Radionuclide | Emission Type | Half-Life | Clinical Application | Key Characteristic |
|---|---|---|---|---|
| Lutetium-177 (¹⁷⁷Lu) | β⁻ | 6.65 days | Treatment (NET, Prostate Cancer) | Medium energy, manageable half-life; theranostic pair with Ga-68 |
| Actinium-225 (²²⁵Ac) | α | 10.0 days | Treatment (Advanced Cancers) | Extremely high LET; potent but complex decay chain |
| Iodine-131 (¹³¹I) | β⁻ | 8.02 days | Treatment (Thyroid Cancer) | One of the earliest therapeutic isotopes |
| Gallium-68 (⁶⁸Ga) | β⁺ (Positron) | 68 min | Diagnostic Imaging (PET) | Generator-produced, ideal for theranostic pairing |
| Technetium-99m (⁹⁹ᵐTc) | γ | 6 hr | Diagnostic Imaging (SPECT) | Workhorse of diagnostic nuclear medicine |
The Role of CADD in Radioconjugate Development
CADD accelerates the rational design of radioconjugates, particularly in optimizing the targeting vector and predicting in vivo behavior.
- Virtual Screening for Vector Discovery: CADD can screen vast virtual libraries of small molecules or peptides to identify novel, high-affinity binders for tumor-specific targets [36] [51]. Tools like molecular docking are used to predict binding modes and affinity of candidate vectors against the target's crystal structure or homology model.
- Predicting Pharmacokinetics: QSAR models and molecular dynamics simulations can help forecast key pharmacokinetic (PK) properties of the conjugate, such as its clearance rate, tumor uptake, and retention time, which are critical for matching with a radionuclide's half-life [52] [36].
- Linker Optimization: Computational chemistry is employed to design linkers that confer optimal in vivo stability, minimizing premature release of the radioactive payload while allowing efficient release at the tumor site.
Diagram: Structure and Mechanism of a Radioconjugate
Experimental Protocol for Radioconjugate Evaluation
A typical preclinical development workflow involves:
- Radiosynthesis and Quality Control:
- Labeling: The targeting vector-linker-chelator conjugate is incubated with the radionuclide (e.g., ¹⁷⁷LuCl₃) under optimized buffer, temperature, and time conditions.
- Purification and QC: Purify the product via HPLC or solid-phase extraction. Determine radiochemical purity (RCP >95%), and specific activity using instant thin-layer chromatography (iTLC) or analytical HPLC [52].
- In Vitro Characterization:
- Binding Affinity: Perform competitive cell-binding assays on antigen-positive cancer cells to determine IC₅₀.
- Internalization Studies: Assess the conjugate's rate of internalization into cancer cells, which is crucial for the effectiveness of Auger electron or α-emitters.
- In Vivo Biodistribution and Efficacy:
- Animal Models: Use immunocompromised mice bearing human tumor xenografts.
- Biodistribution: Inject a tracer dose of the radioconjugate. At multiple time points, euthanize groups of animals, harvest organs and tumors, and measure radioactivity with a gamma counter to calculate % injected dose per gram (%ID/g).
- Therapy Studies: Treat tumor-bearing mice with the therapeutic conjugate or a control. Monitor tumor volume and animal survival over time to establish anti-tumor efficacy and maximum tolerated dose [52].
Table 3: Key Research Reagent Solutions for TPD and Radioconjugates
| Reagent / Resource | Function/Description | Example Use Case |
|---|---|---|
| E3 Ligase Ligands | Small molecules that recruit specific E3 ubiquitin ligases (e.g., CRBN, VHL). | Critical component for constructing PROTACs; VH032 for VHL-recruiting PROTACs [47]. |
| POI-Targeting Warheads | Well-characterized inhibitors or binders for the protein targeted for degradation. | OTX015 as a BRD4-binding warhead in ARV-825; AR/ER ligands in clinical PROTACs [47]. |
| Bifunctional Chelators | Molecules that bind both the targeting vector and the radiometal (e.g., DOTA, DFO). | DOTA is used to chelate Lutetium-177 in Pluvicto and Lutathera [52]. |
| Toolkit Radionuclides | Research-grade isotopes for preclinical testing (e.g., Lutetium-177, Iodine-125). | Used in in vitro and in vivo proof-of-concept studies for new radioconjugates. |
| Commercial Compound Libraries | Curated databases of purchasable chemical compounds. | ZINC15, ChEMBL for virtual screening of novel POI warheads or E3 ligands [51]. |
PROTACs and radiopharmaceutical conjugates represent two pillars of a transformative movement in precision oncology. By moving beyond simple inhibition to direct protein elimination or targeted radiation delivery, they offer powerful new strategies to combat cancers resistant to conventional therapies. The successful development of these sophisticated modalities is intrinsically linked to advances in computer-aided drug design. CADD provides the essential tools to model ternary complexes, screen for optimal targeting vectors, predict in vivo behavior, and rationally design linkers—all of which are critical for reducing the empirical burden and accelerating the development timeline. As these fields mature, the synergy between computational prediction and experimental validation will continue to drive innovation, expanding the scope of targetable diseases and bringing us closer to a new generation of highly specific, effective, and personalized cancer therapeutics.
The escalating global prevalence of cancer, coupled with the inadequacies of existing therapies and the emergence of drug-resistant strains, has created an urgent need for more efficient drug discovery pipelines [54]. Computer-Aided Drug Design (CADD) has emerged as a transformative force, bridging the realms of biology and computational technology to rationalize and accelerate the development of novel oncology therapeutics [55] [36]. Traditional drug discovery is a notoriously long, complex, and costly endeavor, often spanning 10–17 years with an average cost of approximately $2.2 billion per new drug approved for clinical use [56]. This process faces a high failure rate in clinical trials, further highlighting the need for computational approaches to improve efficiency and success rates [54]. CADD employs a suite of computational techniques to predict the efficacy of potential drug compounds, pinpointing the most promising candidates for subsequent experimental testing and development, thereby substantially reducing the time, resources, and financial investment required [55] [36] [54].
The foundational principle of CADD is the utilization of computer algorithms on chemical and biological data to simulate and predict how a drug molecule interacts with its biological target, typically a protein or nucleic acid [36]. The field is broadly categorized into two complementary approaches: Structure-Based Drug Design (SBDD) and Ligand-Based Drug Design (LBDD). SBDD leverages the three-dimensional structure of the biological target to design molecules that fit complementarily into a binding site [50]. In contrast, LBDD relies on the knowledge of known active molecules to derive models for designing new compounds when the target structure is unavailable [36] [50]. The integration of advanced computing technologies and Artificial Intelligence (AI), particularly machine learning and deep learning, has significantly enhanced the efficiency and predictive capabilities of CADD, fostering the development of innovative and effective therapeutic options for cancers, including breast cancer [55] [57].
Core Principles of CADD in Oncology
The application of CADD in oncology is underpinned by several key computational techniques that guide researchers from target identification to lead optimization. These methodologies form the essential toolkit for modern drug discovery scientists.
Key Computational Methodologies
- Molecular Docking: This technique predicts the preferred orientation and binding affinity of a small molecule (ligand) when bound to its target protein. Docking is crucial for virtual screening, where vast libraries of compounds are rapidly evaluated in silico to identify potential hits. Tools like AutoDock Vina, Glide, and GOLD are widely used for this purpose, helping to identify optimal combinations for drug development [36] [50].
- Molecular Dynamics (MD) Simulations: MD simulations calculate the time-dependent behavior of a molecular system, providing insights into the stability of drug-target complexes, conformational changes, and the mechanisms of interaction. Utilizing tools like GROMACS, NAMD, and CHARMM, MD simulations can model processes from femtoseconds to seconds, offering an accurate visualization of drug-target interactions [55] [36] [50].
- Quantitative Structure-Activity Relationship (QSAR): This ligand-based approach uses statistical models to establish a correlation between the chemical structure of compounds and their biological activity. QSAR models predict the pharmacological activity of new compounds based on their structural attributes, guiding chemists to make informed modifications that enhance a drug's potency or reduce its side effects [36] [50].
- Pharmacophore Modeling: A pharmacophore represents the essential structural features of a ligand that are responsible for its biological activity. It serves as a blueprint for designing new molecules that contain these critical features, ensuring optimal interactions with the target [50].
Table 1: Essential CADD Techniques and Their Applications in Oncology
| Computational Technique | Primary Function | Common Tools/Software | Application in Oncology Drug Discovery |
|---|---|---|---|
| Molecular Docking | Predicts ligand binding orientation and affinity | AutoDock Vina, Glide, GOLD | Virtual screening of compound libraries to identify hits against cancer targets. |
| Molecular Dynamics (MD) | Simulates time-dependent behavior of molecular systems | GROMACS, NAMD, CHARMM | Assessing stability of drug-target complexes and mechanisms of action. |
| QSAR Modeling | Correlates chemical structure with biological activity | Various statistical and ML packages | Optimizing lead compounds for enhanced potency and reduced toxicity. |
| Pharmacophore Modeling | Identifies essential structural features for activity | MOE, Phase | Designing novel compounds or screening databases for target activity. |
| Homology Modeling | Predicts 3D structure of a target from homologous proteins | MODELLER, SWISS-MODEL, AlphaFold2 | Generating target structures for SBDD when experimental structures are unavailable. |
The Evolving CADD Workflow
The typical CADD-driven workflow in oncology is an iterative process that integrates multiple computational techniques. It often begins with target identification and validation, where genomic and proteomic data are analyzed to identify druggable targets involved in cancer progression [50]. If the experimental 3D structure of the target is unavailable, computational methods like homology modeling or AI-powered tools like AlphaFold2 are used to generate a reliable model [36]. This is followed by virtual screening, where millions of compounds are screened in silico using docking to identify a subset of promising "hit" molecules [36] [50]. These hits then undergo lead optimization, a stage heavily reliant on MD simulations, QSAR, and pharmacophore models to refine the chemical structure for better efficacy, selectivity, and drug-like properties [50]. Finally, the most promising optimized leads are recommended for in vitro and in vivo experimental validation.
The following diagram illustrates the logical flow and iterative nature of this CADD-driven drug discovery process.
Diagram 1: Logical workflow of a CADD-driven drug discovery campaign in oncology.
Analysis of CADD-Driven Oncology Drug Approvals
The impact of CADD is not merely theoretical; it has demonstrably contributed to the discovery and development of several approved oncology drugs. The following case studies and data illustrate this success.
Case Study: Imlunestrant (ER-Positive, HER2-Negative Breast Cancer)
A prominent recent example of CADD success is imlunestrant (Inluriyo), approved by the FDA in September 2025 for adults with estrogen receptor (ER)-positive, HER2-negative, ESR1-mutated advanced or metastatic breast cancer [58]. This approval underscores the role of computational methods in addressing resistance to endocrine therapy.
- Therapeutic Context and Challenge: ER-positive breast cancer is frequently treated with endocrine therapies like tamoxifen and aromatase inhibitors. However, resistance often develops, commonly through mutations in the estrogen receptor 1 (ESR1) gene, compromising treatment efficacy [55] [56]. Imlunestrant was developed as a oral selective estrogen receptor degrader (SERD) to overcome this limitation.
- CADD and AI Contributions: The discovery of imlunestrant likely involved sophisticated Structure-Based Drug Design (SBDD). Using the crystallographic structure of the ERα ligand-binding domain (LBD), particularly with common ESR1 mutations (e.g., Y537S, D538G), researchers could design novel antagonists capable of effectively binding to and degrading the mutant receptors. Molecular docking and MD simulations were crucial for predicting how imlunestrant interacts with mutated ESR1, ensuring high binding affinity and a mechanism of action that leads to receptor degradation, thereby overcoming resistance [55] [57]. AI and machine learning models may have also been employed to analyze structure-activity relationship (SAR) data from earlier compound series, accelerating the optimization of imlunestrant's pharmacokinetic and safety profile.
Case Study: Trastuzumab Deruxtecan (HER2-Positive and HER2-Low Breast Cancer)
Another landmark drug is trastuzumab deruxtecan (Enhertu), an antibody-drug conjugate (ADC) that has transformed the treatment landscape for HER2-positive and HER2-low breast cancers [55] [59]. Its development showcases the integration of computational tools in designing complex biotherapeutics.
- Therapeutic Context and Challenge: While anti-HER2 therapies exist, their efficacy can be limited, especially in tumors with low HER2 expression. There was an urgent need for novel therapeutics targeting weak HER2 expression in advanced breast cancer [55].
- CADD and AI Contributions: The design of the ADC's payload, a potent topoisomerase I inhibitor derivative of exatecan, benefited from Ligand-Based Drug Design and QSAR studies. Computational models helped optimize the chemical linker that connects the payload to the antibody, a critical factor for stability in circulation and controlled drug release at the tumor site. This careful design enables the "bystander killing effect," where the released payload can kill neighboring cancer cells regardless of their HER2 status, a feature crucial for its efficacy in HER2-low disease [55]. CADD approaches were instrumental in fine-tuning this sophisticated mechanism of action.
Other Noteworthy Approvals and Clinical Candidates
Beyond fully approved drugs, CADD plays a pivotal role in populating oncology pipelines. Drug repositioning, the identification of new uses for existing drugs, is a particularly fruitful area for computational methods [56]. Network-based pharmacology, molecular docking, and signature matching can rapidly identify approved non-cancer drugs with potential anti-cancer activity. For instance, resveratrol, a natural polyphenol, has been identified via computational methods as having anticancer properties and is in early clinical trials for breast cancer [55]. AI-driven screening strategies have also identified novel investigational compounds, such as Z29077885 (an STK33 inhibitor), which showed promising in vitro and in vivo anticancer activity [57].
Table 2: Summary of Selected Oncology Drug Approvals and Candidates with CADD Contributions
| Drug / Candidate | Therapeutic Category | Key Target / Mechanism | Reported CADD/AI Contribution |
|---|---|---|---|
| Imlunestrant (Inluriyo) | Approved Drug (FDA, 2025) | Oral Selective Estrogen Receptor Degrader (SERD) | Structure-Based Drug Design (SBDD) to target ESR1 mutations [58]. |
| Trastuzumab Deruxtecan (Enhertu) | Approved ADC (FDA) | HER2-directed Antibody-Drug Conjugate | Ligand-Based Design & QSAR for linker-payload optimization [55]. |
| Datopotamab Deruxtecan (Datroway) | Approved Drug (FDA, 2025) | Trop-2-directed ADC | Similar CADD principles for ADC design and optimization [59]. |
| Resveratrol | Clinical Trial Candidate | Multiple (VEGF disruption, apoptosis) | Identified and prioritized via computational repositioning approaches [55]. |
| Z29077885 | Preclinical Candidate | STK33 inhibitor (apoptosis inducer) | Identified through an AI-driven screening strategy of large compound databases [57]. |
Detailed Experimental Protocols for CADD in Oncology
To translate these principles into practice, researchers employ standardized computational protocols. Below is a detailed methodology for a typical structure-based virtual screening campaign, a cornerstone of modern CADD.
Protocol for Structure-Based Virtual Screening
Aim: To identify novel small-molecule inhibitors of a specific oncology target (e.g., a kinase or mutant receptor) from a large commercial or virtual compound library.
Step 1: Target Preparation
- Obtain the 3D structure of the target protein from the Protein Data Bank (PDB) or generate a high-quality model using homology modeling (e.g., MODELLER, SWISS-MODEL) or AI-based structure prediction tools like AlphaFold2 [36].
- Process the structure using a molecular modeling suite (e.g., Schrödinger Maestro, BIOVIA Discovery Studio). This includes adding hydrogen atoms, assigning bond orders, correcting missing residues or atoms, and optimizing the protonation states of key residues (e.g., His, Asp, Glu) at physiological pH.
- Define the binding site coordinates, typically based on the location of a native co-crystallized ligand or known catalytic residues.
Step 2: Ligand Library Preparation
- Acquire a database of compounds (e.g., ZINC, ChEMBL, Enamine) in a standard format (e.g., SDF, SMILES).
- Prepare the ligands computationally: generate 3D conformations, assign correct ionization states at pH 7.4 ± 0.5 using tools like LigPrep (Schrödinger) or MOE, and perform energy minimization.
Step 3: Molecular Docking and Scoring
- Perform high-throughput docking of the prepared ligand library into the defined binding site using a docking program such as AutoDock Vina or Glide [36].
- The docking algorithm will sample multiple conformations, orientations, and positions of each ligand within the binding site.
- Each proposed pose is scored using a scoring function (e.g., Vina, GlideScore, ChemScore) to estimate the binding affinity.
- Visually inspect the top-ranked poses (e.g., 100-500 compounds) to check for sensible binding modes, key interactions (hydrogen bonds, hydrophobic contacts, pi-stacking), and chemical novelty.
Step 4: Post-Docking Analysis and Filtering
- Subject the top-ranked hits to more rigorous analysis, which may include:
- Molecular Mechanics/Generalized Born Surface Area (MM/GBSA) calculations: A more computationally expensive but often more accurate method to re-score binding free energies.
- Molecular Dynamics (MD) Simulations: Use software like GROMACS or NAMD to simulate the behavior of the protein-ligand complex in a solvated environment over time (e.g., 50-100 nanoseconds). This assesses the stability of the binding pose, calculates more robust binding energies, and evaluates dynamic interactions [36] [50].
- Apply drug-likeness filters (e.g., Lipinski's Rule of Five) and ADMET prediction tools to prioritize compounds with favorable pharmacokinetic and safety profiles.
The following diagram maps this multi-step protocol, highlighting the key decision points and advanced analyses.
Diagram 2: Detailed workflow for a Structure-Based Virtual Screening (SBVS) campaign.
The Scientist's Toolkit: Essential Research Reagent Solutions
The execution of these protocols relies on a suite of specialized software tools and databases. The table below details key "research reagents" in the computational chemist's arsenal.
Table 3: Essential Software and Database "Reagents" for CADD in Oncology
| Tool / Resource Name | Type | Primary Function in CADD |
|---|---|---|
| AlphaFold2 / ESMFold | AI-Based Modeling | Predicts 3D protein structures with high accuracy from amino acid sequences [36]. |
| GROMACS / NAMD | Molecular Dynamics | Simulates physical movements of atoms and molecules over time for stability analysis [36]. |
| AutoDock Vina / Glide | Molecular Docking | Performs prediction of ligand binding poses and estimation of binding affinities [36]. |
| ZINC / ChEMBL | Compound Database | Publicly accessible libraries of commercially available and bioactive molecules for virtual screening [36]. |
| Schrödinger Suite | Comprehensive Platform | Integrated software suite for various CADD tasks, from structure prep to QSAR and ADMET prediction. |
| OpenMM | MD Simulation | A high-performance toolkit for molecular simulation, often used as a library for custom applications [36]. |
The case studies of imlunestrant and trastuzumab deruxtecan provide compelling evidence that Computer-Aided Drug Design is no longer an auxiliary tool but a central driver of innovation in oncology therapeutics. By leveraging computational power to rationalize the drug discovery process, CADD has successfully delivered approved drugs that address significant clinical challenges, such as therapy resistance and tumor heterogeneity [55] [58]. The integration of Artificial Intelligence and machine learning is further amplifying the impact of CADD, enhancing predictive capabilities in target identification, de novo molecular design, and the optimization of pharmacokinetic properties [55] [57].
The future trajectory of CADD in oncology is poised to be even more transformative. The convergence of CADD with personalized medicine will enable the design of therapies tailored to the unique genetic and molecular profile of a patient's tumor [50]. Quantum computing holds the potential to perform complex molecular simulations that are currently intractable, providing unprecedented insights into drug-target interactions [36]. Furthermore, the growing emphasis on drug repositioning through network-based and AI-driven methods offers a faster, cost-effective path to bringing new treatment options to cancer patients [56]. Despite persistent challenges—including the need for high-quality data, transparent AI models, and robust ethical frameworks—the continued evolution of CADD promises to redefine the landscape of cancer treatment, ushering in an era of more effective, precise, and personalized oncology therapeutics.
Navigating Computational Challenges: Optimization Strategies for Clinical Success
Addressing Tumor Heterogeneity and Drug Resistance Mechanisms
Tumor heterogeneity and drug resistance represent the most significant barriers to achieving durable responses and cures in cancer therapy. These interconnected phenomena arise from the dynamic evolution of diverse tumor cell populations under therapeutic pressure, leading to treatment failure and disease progression. Within the framework of computer-aided drug design (CADD), understanding and addressing these challenges requires sophisticated computational approaches that can model complex biological systems and predict evolutionary trajectories. The transition from traditional CADD to artificial intelligence-driven drug discovery (AIDD) has created unprecedented opportunities to overcome these long-standing limitations through advanced pattern recognition, predictive modeling, and multi-scale simulation [60].
The fundamental principle underlying tumor heterogeneity lies in the genomic instability of cancer cells and their selective adaptation to microenvironmental pressures. As tumors evolve, they generate diverse subclonal populations with distinct molecular profiles, creating a mosaic of cells with varying sensitivities to therapeutic interventions. When targeted therapies eliminate sensitive cell populations, resistant clones expand through Darwinian selection, ultimately dominating the tumor ecosystem. Traditional one-size-fits-all treatment approaches fail to account for this dynamic complexity, necessitating computational strategies that can anticipate, monitor, and counter adaptive resistance mechanisms [61].
Molecular Mechanisms of Drug Resistance
Classification of Resistance Pathways
Drug resistance in oncology manifests through diverse molecular mechanisms that can be systematically categorized into distinct pathways. Understanding these pathways is essential for developing targeted strategies to overcome or prevent resistance.
Table 1: Fundamental Mechanisms of Resistance to Targeted Therapies
| Mechanism Category | Specific Examples | Key Molecular Players | Therapeutic Implications |
|---|---|---|---|
| Target Mutations | EGFR C797S, T790M mutations | EGFR kinase domain mutations | Reduced drug binding affinity; requires next-generation inhibitors |
| Bypass Signaling | MET, HER2 amplification | Receptor tyrosine kinases | Activation of alternative survival pathways; combination therapy approaches |
| Histological Transformation | SCLC transformation | TP53, RB1 loss | Lineage switching; complete therapeutic paradigm shift required |
| Drug Tolerant Persister (DTP) Cells | Epigenetic adaptations | Lysine-specific demethylase 1 (LSD1) | Reversible resistance; epigenetic modifiers |
| Metabolic Reprogramming | Oxidative stress compensation | NRF2/KEAP1 pathway, ALDH1A1 | Altered redox homeostasis; metabolic interventions |
EGFR-TKI Resistance: A Case Study in Heterogeneity
The evolution of resistance to EGFR tyrosine kinase inhibitors (TKIs) in non-small cell lung cancer (NSCLC) provides a paradigmatic example of tumor heterogeneity and adaptive resistance. Approximately 50% of patients receiving first- or second-generation EGFR-TKIs develop resistance within 10-14 months, while even third-generation inhibitors like osimertinib eventually fail with a median progression-free survival of approximately 18.9 months [62]. The resistance mechanisms demonstrate remarkable heterogeneity, with multiple pathways often coexisting within the same patient or even within different regions of the same tumor.
The spectrum of EGFR-TKI resistance includes both on-target (EGFR-dependent) and off-target (EGFR-independent) mechanisms. On-target resistance primarily involves secondary mutations within the EGFR kinase domain, such as T790M (common after first-generation TKIs) and C797S (emerging after osimertinib treatment). The spatial relationship between these mutations matters critically—when C797S and T790M occur on the same allele (in cis), they confer resistance to all currently available EGFR TKIs, whereas when they occur on different alleles (in trans), they may remain sensitive to combination approaches [63].
Off-target resistance mechanisms are even more diverse, including:
- Bypass activation through amplification of other receptor tyrosine kinases (MET, HER2, AXL)
- Downstream pathway activation involving KRAS, BRAF, or PIK3CA mutations
- Histological transformation to small cell lung cancer (SCLC) or squamous cell carcinoma
- Metabolic adaptations through oxidative stress compensation and redox homeostasis mechanisms [62]
The emergence of drug-tolerant persister (DTP) cells represents a particularly challenging resistance mechanism. These cells enter a reversible slow-cycling state that allows survival during treatment, serving as reservoirs for the eventual development of permanent resistance mechanisms. DTP cells are characterized by distinct epigenetic and metabolic adaptations, including increased expression of drug efflux pumps, chromatin remodeling, and altered reactive oxygen species (ROS) handling capacity [63].
Computational Approaches for Modeling Heterogeneity and Resistance
From Traditional CADD to AI-Driven Paradigms
The evolution of computational drug discovery has progressed through distinct phases, from traditional computer-aided drug design (CADD) to contemporary artificial intelligence drug discovery (AIDD). Traditional CADD encompasses both structure-based drug design (SBDD), which relies on three-dimensional structural information of target proteins, and ligand-based drug design (LBDD), which utilizes quantitative structure-activity relationship (QSAR) models derived from known active compounds [60]. While these approaches have contributed significantly to drug discovery, they often struggle with the dynamic complexity of tumor heterogeneity and resistance.
AIDD represents a paradigm shift by leveraging machine learning (ML), deep learning (DL), and natural language processing (NLP) to identify complex, non-linear patterns in multidimensional data. Unlike traditional CADD, which typically requires explicit programming of rules and parameters, AIDD algorithms learn directly from data, enabling them to discover unexpected relationships and predict emergent properties of biological systems [60]. This capability is particularly valuable for modeling the complex dynamics of tumor evolution and therapeutic resistance.
Table 2: Comparative Analysis of CADD and AIDD Approaches
| Feature | Traditional CADD | Contemporary AIDD |
|---|---|---|
| Data Requirements | Curated structural or activity data | Large, multimodal datasets |
| Computational Basis | Physical principles, molecular mechanics | Pattern recognition, neural networks |
| Handling Uncertainty | Limited, explicit parameterization | Robust, probabilistic frameworks |
| Adaptability | Low, requires manual refinement | High, continuous learning capability |
| Application to Resistance | Static models of binding interactions | Dynamic prediction of evolutionary trajectories |
| Key Strengths | Physical interpretability, well-established | Handling complexity, predictive accuracy |
Physics-Aware AI: Integrating First Principles with Data-Driven Learning
A cutting-edge development in computational drug discovery is the emergence of "physics-aware AI" or "physical perception AI" models that integrate fundamental physical principles with data-driven machine learning. Pioneered by researchers like Dima Kozakov at the University of Texas at Austin, these hybrid approaches embed physical laws directly into the learning core of AI models, enabling them to maintain scientific plausibility while leveraging the pattern recognition power of neural networks [64].
The fundamental innovation of physics-aware AI lies in its ability to overcome the data-dependency limitations of conventional machine learning. In domains like atom-level biomolecular interactions, high-quality experimental data is often scarce and expensive to generate. By incorporating physical constraints—such as energy conservation, molecular symmetry, and thermodynamic principles—these models can generate accurate predictions even with limited training data, significantly accelerating the drug discovery process while reducing experimental costs [64].
For addressing tumor heterogeneity, physics-aware AI offers particular advantages in modeling the dynamic protein interaction networks that drive resistance. These approaches can simulate how mutations affect drug binding affinities, predict the structural consequences of resistance mutations, and identify compensatory changes in protein networks that maintain oncogenic signaling despite targeted inhibition.
Diagram 1: Physics-Aware AI for Resistance Modeling. This workflow integrates physical principles with multi-omics data to predict resistance mechanisms and inform therapeutic strategies.
Experimental Methodologies for Studying Heterogeneity and Resistance
Multi-modal Profiling of Resistance Evolution
Comprehensive characterization of tumor heterogeneity and resistance mechanisms requires integrated experimental approaches that capture molecular changes across multiple dimensions. The following protocols outline standardized methodologies for profiling resistance evolution in preclinical models and clinical specimens.
Protocol 1: Longitudinal Monitoring of Resistance Evolution in Patient-Derived Models
- Model Establishment: Generate patient-derived organoids (PDOs) or xenografts (PDXs) from pretreatment tumor biopsies
- Therapeutic Exposure: Treat models with clinically relevant drug concentrations using intermittent or continuous dosing schedules
- Temporal Sampling: Collect samples at predetermined timepoints (baseline, early adaptation, acquired resistance)
- Multi-optic Profiling:
- Whole exome sequencing to identify genomic evolution and subclonal dynamics
- Single-cell RNA sequencing to characterize transcriptional heterogeneity and cell state transitions
- Mass cytometry (CyTOF) to profile protein expression and signaling network adaptations
- Metabolomic profiling to identify metabolic reprogramming associated with resistance
- Computational Integration: Apply multi-optic data integration algorithms to reconstruct evolutionary trajectories and identify candidate resistance drivers
Protocol 2: Functional Validation of Resistance Mechanisms Using CRISPR-Based Approaches
- Candidate Gene Prioritization: Use computational models to rank potential resistance drivers based on genomic, transcriptomic, and epigenetic features
- CRISPR Library Design: Construct focused sgRNA libraries targeting top candidate genes along with appropriate controls
- Pooled Screens: Perform positive selection screens in drug-sensitive models under therapeutic pressure to identify genes whose perturbation confers resistance
- Hit Validation: Confirm individual gene contributions using orthogonal approaches (CRISPR knockout, RNA interference, pharmacologic inhibition)
- Mechanistic Elucidation: Interrogate validated hits using transcriptomic, proteomic, and cellular phenotyping assays to define resistance mechanisms
The Scientist's Toolkit: Essential Research Reagents and Platforms
Table 3: Essential Research Reagents and Platforms for Resistance Studies
| Reagent/Platform | Category | Primary Function | Application in Resistance Research |
|---|---|---|---|
| Single-cell RNA-seq | Genomic profiling | High-resolution transcriptional characterization | Identification of rare resistant subpopulations, cell state transitions |
| CRISPR libraries | Functional genomics | High-throughput gene perturbation | Systematic identification of resistance mediators and synthetic lethal interactions |
| Patient-derived organoids | Model systems | Ex vivo culture of patient tumors | Modeling personalized therapeutic responses and resistance evolution |
| Mass cytometry (CyTOF) | Proteomic profiling | High-dimensional protein measurement | Signaling network analysis in heterogeneous cell populations |
| AlphaFold2 | Computational tool | Protein structure prediction | Modeling structural impacts of resistance mutations on drug binding |
| PROTAC-RL | AIDD platform | Deep generative model for PROTAC design | Generating resistance-overcoming molecular degraders |
| Federated learning frameworks | AI infrastructure | Distributed model training without data sharing | Multi-institutional collaboration while preserving data privacy |
| Digital pathology with AI | Diagnostic tool | Computational analysis of tissue sections | Spatial characterization of tumor heterogeneity and microenvironment |
Advanced Computational Workflows for Overcoming Resistance
AI-Guided Drug Combination Design
A critical strategy for addressing tumor heterogeneity and preventing resistance is the rational design of therapeutic combinations that target multiple pathways simultaneously or create synthetic lethal interactions. AI-guided combination design leverages machine learning to predict effective drug pairs based on comprehensive molecular profiling of tumors and high-throughput screening data.
The workflow for AI-guided combination design typically involves:
- Data Curation: Compiling large-scale drug combination screening data across diverse cancer models
- Feature Engineering: Generating molecular features from multi-omics profiles of cancer models
- Model Training: Using gradient boosting machines or deep neural networks to predict combination efficacy
- Mechanistic Interpretation: Applying explainable AI techniques to identify biological pathways associated with effective combinations
- Experimental Validation: Testing top-predicted combinations in physiologically relevant models
Recent advances have demonstrated the power of reinforcement learning approaches for optimizing adaptive therapy schedules that dynamically adjust drug combinations and doses in response to evolving tumor populations. These approaches aim to maintain tumor control by strategically managing the competitive interactions between drug-sensitive and resistant subclones.
Explainable AI for Biomarker Discovery and Resistance Prediction
The "black box" nature of many complex AI models has limited their clinical adoption for critical applications like resistance prediction. Explainable AI (XAI) frameworks address this limitation by providing transparent insights into model decision-making processes, enabling clinicians and researchers to understand and trust AI-generated predictions [65].
Diagram 2: Explainable AI Workflow for Resistance Prediction. This framework integrates diverse data types to generate interpretable predictions and mechanistic insights.
XAI approaches for resistance prediction typically incorporate:
- SHAP (SHapley Additive exPlanations) values to quantify feature importance for individual predictions
- Attention mechanisms in neural networks to highlight relevant input regions
- Counterfactual explanations to illustrate minimal changes that would alter predictions
- Rule extraction to distill complex models into human-interpretable decision rules
In the context of ADC (antibody-drug conjugate) therapy, XAI models have been particularly valuable for identifying complex biomarker signatures that predict response and resistance. These models can integrate diverse data modalities—including target antigen expression, intracellular trafficking machinery, payload activation pathways, and tumor microenvironment features—to generate personalized response predictions with transparent rationale [65].
Emerging Frontiers and Future Directions
AI-Driven ADC Optimization for Heterogeneous Tumors
Antibody-drug conjugates (ADCs) represent a promising therapeutic class for addressing tumor heterogeneity through their targeted delivery of potent cytotoxic payloads. However, several challenges related to tumor heterogeneity limit ADC efficacy, including variable target antigen expression, heterogeneous intracellular trafficking, and microenvironmental barriers to drug penetration [65]. AI approaches are playing an increasingly important role in optimizing ADC design and patient selection to overcome these challenges.
Key applications of AI in ADC development include:
- Target Antigen Selection: Machine learning models analyze multi-omics data to identify surface proteins with optimal expression patterns for ADC targeting—sufficiently homogeneous expression across tumor cells with minimal expression in critical normal tissues
- Linker-Payload Optimization: Deep learning models predict stability-cleavage tradeoffs for different linker chemistries and match payload mechanisms to tumor vulnerabilities
- Bystander Effect Prediction: AI models simulate drug diffusion through heterogeneous tumors to optimize ADC properties for killing antigen-negative cells through bystander effects
- Combination Therapy Design: Reinforcement learning approaches identify optimal ADC combinations with other therapeutic modalities to address compensatory resistance pathways
Companies like Alphamab are leveraging these approaches to develop next-generation ADCs such as JSKN003 (HER2-targeting biparatopic ADC) and JSKN016 (HER3/TROP2-targeting bispecific ADC) designed to address heterogeneous antigen expression and overcome resistance [66].
Digital Twins and Federated Learning for Personalized Resistance Management
Two emerging technologies—digital twins and federated learning—hold particular promise for addressing tumor heterogeneity and resistance in the era of precision oncology.
Digital twin technology involves creating virtual replicas of individual patients' tumors that can be simulated to predict treatment responses and resistance evolution. These models integrate multi-scale data—from genomic alterations to tissue-scale physiology—to simulate how specific tumors might evolve under different therapeutic pressures. While still in early development, digital twin approaches have potential for optimizing adaptive therapy schedules that proactively manage resistance by manipulating the competitive dynamics between sensitive and resistant subclones [67].
Federated learning addresses a critical barrier in AI-driven oncology research: data privacy concerns that often limit data sharing between institutions. Federated learning enables model training across multiple institutions without transferring sensitive patient data, instead sharing only model parameter updates. This approach allows researchers to develop more robust AI models that learn from diverse patient populations while maintaining privacy and regulatory compliance [65]. For rare resistance mechanisms that might be observed at only a few centers, federated learning enables pooled analysis that would otherwise be impossible.
Tumor heterogeneity and drug resistance represent fundamental challenges in oncology that require sophisticated computational approaches to understand and overcome. The integration of traditional CADD principles with modern AIDD methodologies has created powerful new frameworks for addressing these challenges through multi-scale modeling, predictive analytics, and rational therapeutic design. Physics-aware AI models that incorporate fundamental biological principles while learning from complex datasets offer particular promise for predicting resistance evolution and designing intervention strategies.
As these computational approaches continue to evolve and integrate with emerging experimental technologies—from single-cell multi-omics to CRISPR functional genomics—they will enable increasingly sophisticated management of tumor heterogeneity and resistance. The ultimate goal is a future where cancer therapies are not only matched to static molecular profiles but are dynamically adapted in response to evolving tumors, transforming cancer from a acute disease into a chronically managed condition.
The discovery and development of oncology therapeutics have traditionally relied upon a fundamental principle: that the maximum tolerated dose (MTD) is synonymous with the maximum effective dose. This paradigm, formalized in the 1980s with the 3+3 dose escalation trial design, was developed specifically for cytotoxic chemotherapeutics, which work by indiscriminately killing rapidly dividing cells [68]. For these agents, efficacy and toxicity were believed to increase in parallel, making the highest tolerable dose the logical choice for clinical development. However, the oncology landscape has undergone a revolutionary transformation with the advent of molecularly targeted therapies and immunomodulatory agents, which operate through fundamentally different mechanisms with distinct dose-response relationships [69].
Growing evidence indicates that the traditional MTD-centric approach is poorly suited for modern targeted therapies and immunotherapies. An analysis revealed that nearly 50% of patients enrolled in late-stage trials of small molecule targeted therapies required dose reductions due to intolerable side effects [68]. Furthermore, the U.S. Food and Drug Administration (FDA) has required additional studies to re-evaluate the dosing of over 50% of recently approved cancer drugs [68]. These statistics underscore the unsustainable nature of the current approach, which often subjects patients to unnecessary toxicities without commensurate efficacy benefits and necessitates post-marketing dose optimization studies after countless patients have already been treated at suboptimal dosages [70].
This recognition has catalyzed a fundamental shift in dosing strategy from the traditional MTD toward the optimal biological dose (OBD), defined as the dose that provides the best balance between efficacy and safety by achieving full target engagement and desired pharmacological effects without excessive toxicity [71]. This whitepaper explores this paradigm shift within the broader context of computer-aided drug design (CADD) in oncology research, examining how computational approaches are enabling more rational dose selection and optimization throughout the drug development pipeline.
Computational Foundations for Dose Optimization
The Role of CADD in Modern Oncology Drug Development
Computer-aided drug design has emerged as a powerful technology to accelerate drug discovery by improving efficiency and reducing costs [72]. In the context of dose optimization, CADD provides critical insights into the relationship between drug exposure, target engagement, and biological effects through a variety of computational methodologies. The integration of artificial intelligence (AI) and machine learning (ML) has further enhanced these capabilities, enabling more predictive modeling of complex biological systems [23].
The foundational AI techniques being applied in dose optimization include machine learning (ML) algorithms that learn patterns from data to make predictions; deep learning (DL) using neural networks capable of handling large, complex datasets such as histopathology images or omics data; natural language processing (NLP) tools that extract knowledge from unstructured biomedical literature and clinical notes; and reinforcement learning (RL) methods that optimize decision-making, particularly useful in de novo molecular design [23]. These approaches collectively reduce the time and cost of discovery by augmenting human expertise with computational precision, ultimately informing more rational dose selection strategies.
Table 1: Artificial Intelligence Techniques in Drug Discovery and Dose Optimization
| AI Technique | Subcategories | Applications in Dose Optimization | Key Advantages |
|---|---|---|---|
| Machine Learning (ML) | Supervised learning, Unsupervised learning, Reinforcement learning | Quantitative structure-activity relationship (QSAR) modeling, toxicity prediction, virtual screening | Identifies complex patterns in pharmacological data, predicts exposure-response relationships |
| Deep Learning (DL) | Convolutional neural networks (CNNs), Recurrent neural networks (RNNs), Generative models | De novo molecular design, biomarker discovery from histopathology images, protein-ligand interaction prediction | Handles high-dimensional data (genomics, proteomics, medical imaging), enables multi-parameter optimization |
| Natural Language Processing (NLP) | Text mining, Information extraction, Semantic analysis | Mining electronic health records for dosing outcomes, extracting dose-response relationships from literature | Leverages unstructured clinical data, identifies subtle dosing patterns across patient populations |
| Generative Models | Variational autoencoders (VAEs), Generative adversarial networks (GANs) | Design of novel chemical structures with optimized pharmacological properties, molecular optimization | Generates drug-like molecules with desired target engagement and pharmacokinetic profiles |
Key Concepts and Definitions
The transition from MTD to OBD requires understanding of several key concepts:
Maximum Tolerated Dose (MTD): The highest dose of a drug that does not cause unacceptable side effects, traditionally determined using the 3+3 design where only 1 in 6 patients across two cohorts of three experience a dose-limiting toxicity [68].
Optimal Biological Dose (OBD): The dose that provides the best balance between efficacy and safety by achieving full target engagement and desired pharmacological effects without excessive toxicity [71].
Biologically Effective Dose (BED): The dose range at which a drug exhibits desired pharmacological activity on its molecular target, often lower than the MTD for targeted therapies [71].
Therapeutic Window: The range of doses between the minimal dose providing efficacy and the maximum dose before unacceptable toxicity occurs.
The fundamental distinction between traditional chemotherapy and modern targeted therapies lies in their dose-response relationships. Cytotoxic chemotherapeutics typically demonstrate a linear relationship between dose and effect against both tumor and normal tissues, resulting in a narrow therapeutic window. In contrast, targeted therapies often exhibit a plateau in efficacy once target saturation is achieved, while toxicity may continue to increase with dose, resulting in a therapeutic window that may actually widen at lower doses [68] [69].
Regulatory Evolution and Project Optimus
The FDA's Initiative for Change
Recognizing the limitations of traditional dose-finding approaches, the FDA launched Project Optimus in 2021 to encourage educational, innovative, and collaborative efforts toward selecting oncology drug dosages that maximize both safety and efficacy [68] [70]. This initiative represents a fundamental reimagining of dose selection and optimization in oncology drug development, emphasizing the need for a more deliberative approach that directly compares multiple dosages to identify the OBD rather than defaulting to the MTD.
In August 2024, the FDA finalized its guidance titled "Optimizing the Dosage of Human Prescription Drugs and Biological Products for the Treatment of Oncologic Diseases," which provides detailed recommendations for implementing dose optimization in oncology drug development [70]. The guidance explicitly states that "a protocol evaluating dosages that the FDA does not consider to be adequately supported may be placed on clinical hold," underscoring the agency's commitment to this new paradigm [70].
Key Regulatory Recommendations
The FDA's guidance emphasizes several critical elements for modern dose optimization:
Early Planning: Sponsors are urged to speak with the FDA regarding their plans for dosage optimization early in clinical development, potentially through the new Model-Informed Drug Development paired meeting program [70].
Comparative Assessment: The FDA recommends directly comparing multiple dosages in trials designed to assess antitumor activity, safety, and tolerability to support the recommended dosage for approval [71].
Model-Informed Approaches: Leveraging modeling techniques, including population pharmacokinetic-pharmacodynamic, exposure-response, and quantitative systems pharmacology models, to support dosage identification [70].
Biomarker Integration: Incorporating functional, monitoring, and response biomarkers to establish the biologically effective dose range of a drug [71].
The impact of these regulatory changes is already evident in the increasing requirements for post-marketing dose evaluation. Analysis by Friends of Cancer Research found that over half of the novel oncology drugs approved by the FDA between 2012 and 2022 were issued post-marketing requirements to collect more data about dosing, with requirements to evaluate lower doses increasing markedly from 18.2% during 2012-2015 to 71.4% during 2020-2022 [70].
Computational Methodologies for Dose Optimization
Modeling and Simulation Approaches
Computational modeling plays a pivotal role in identifying and supporting the dosages to be evaluated in dose optimization trials. Several model-informed drug development approaches have emerged as particularly valuable:
Population Pharmacokinetic-Pharmacodynamic (PopPK/PD) Modeling: This approach characterizes the relationship between drug exposure (pharmacokinetics) and pharmacological effect (pharmacodynamics) while accounting for inter-individual variability. PopPK/PD models can identify covariates that influence drug exposure and response, enabling more personalized dosing strategies [71].
Exposure-Response Modeling: These models establish quantitative relationships between drug exposure metrics (e.g., area under the curve, maximum concentration) and both efficacy and safety endpoints. They can extrapolate the effects of doses and dose schedules not clinically tested and address confounding factors such as concomitant therapies [68].
Quantitative Systems Pharmacology (QSP): QSP models incorporate mechanistic knowledge of biological systems, drug properties, and disease pathophysiology to simulate drug effects across different dosing regimens. These semi-mechanistic or mechanistic approaches can provide a more comprehensive understanding of dose-response relationships [70].
Clinical Utility Indices (CUI): CUI frameworks provide a quantitative mechanism to integrate disparate data types into a single metric, facilitating more objective dose selection by quantitatively weighing efficacy and toxicity considerations [71].
These modeling approaches allow researchers to leverage data from other therapies within the same class or with the same mechanism of action to support dosage selection, maximizing the informational value obtained from early-phase trials [70].
Biomarkers and Pharmacological Audit Trail
The identification and utilization of biomarkers represents a critical component of modern dose optimization strategies. Biomarkers provide objective measures of biological processes, pharmacological responses, and therapeutic effects, enabling more informed dosing decisions [71].
Table 2: Biomarker Categories for Dose Optimization in Early Phase Clinical Trials
| Biomarker Category | Purpose in Dose Optimization | Examples | Regulatory Context |
|---|---|---|---|
| Pharmacodynamic Biomarkers | Indicate biologic activity of a medical product, establish biologically effective dose range | Phosphorylation of proteins downstream of target, circulating tumor DNA (ctDNA) changes | Often used as integrated biomarkers to support dose selection |
| Predictive Biomarkers | Identify patients more likely to respond to treatment, enable enrichment strategies | BRCA1/2 mutations for PARP inhibitors, PD-L1 expression for checkpoint inhibitors | May be integral to trial design for targeted therapies |
| Safety Biomarkers | Indicate likelihood, presence, or degree of treatment-related toxicity | Neutrophil count for cytotoxic chemotherapy, liver enzyme elevations | Used across all phases of development to monitor toxicity |
| Surrogate Endpoint Biomarkers | Serve as substitutes for clinical endpoints, accelerate dose-finding | Overall response rate, ctDNA clearance | May support accelerated approval in certain contexts |
The Pharmacological Audit Trail (PhAT) provides a structured framework for leveraging biomarkers throughout drug development. The PhAT lays a roadmap connecting key questions at different development stages to various go/no-go decisions, ensuring that the totality of potential data is collected and considered [71]. This approach serially interrogates a drug's biologic activity, enabling informed dosing decision-making by systematically evaluating target engagement, pathway modulation, and biological effect at different dose levels.
Circulating tumor DNA (ctDNA) has emerged as a particularly promising biomarker with multiple applications in dose optimization. Beyond its established role as a predictive biomarker for patient selection, ctDNA shows utility as a pharmacodynamic and surrogate endpoint biomarker to aid in dosing selection [71]. Retrospective analyses have demonstrated that changes in ctDNA concentration during treatment correlate with radiographic response, enabling determination of biologically active dosages when combined with other clinical data [71].
Figure 1: Biomarker-Driven Dose Optimization Workflow - This diagram illustrates the iterative process of using biomarker data to inform optimal biological dose selection.
Practical Implementation: A Three-Step Framework
Phase I: Hybrid Dose Escalation with Improved Overdose Control
The first step in modern dose optimization involves identifying the MTD or maximum administered dose using an efficient hybrid design that offers superior overdose control compared to traditional 3+3 designs [69]. Novel model-based and model-assisted designs have been developed that utilize mathematical modeling approaches instead of the traditional algorithmic 3+3 approach, resulting in more nuanced dose-escalation and de-escalation decision-making [68].
These innovative designs include the Bayesian Optimal Interval (BOIN) design, a class of model-assisted dose finding design granted the FDA fit-for-purpose designation for dose finding in 2021 [71]. The BOIN design allows the treatment of more than 6 patients at a dose level, the potential to return to a dose level multiple times if not excluded by the design or safety stopping rules, and the ability to escalate and de-escalate across different dose levels via a spreadsheet design/table [71]. Other model-based approaches, such as the continual reassessment method (CRM) and its modifications, also provide more precise MTD estimation while exposing fewer patients to subtherapeutic or toxic doses.
Phase II: Selection of Recommended Doses for Expansion (RDEs)
The second step involves selecting appropriate recommended doses for expansion (RDEs) based on all available data, including emerging safety, pharmacokinetics, pharmacodynamics, and other biomarker information [69]. This phase moves beyond the traditional focus on toxicity to incorporate multiple dimensions of drug activity, enabling selection of doses for further evaluation that may be lower than the MTD but offer a better benefit-risk profile.
The integration of backfill cohorts and expansion cohorts at this stage provides critical data to strengthen the understanding of the benefit-risk ratio at various dose levels [71]. Backfill cohorts allow for the treatment of additional patients at dose levels below the current estimated MTD, generating more robust safety and efficacy data across a range of biologically active doses. Similarly, expansion cohorts increase the number of patients at certain dose levels of interest within early-stage trials, providing more clinical information to support dose selection decisions.
Phase III: Randomized Dose Optimization
The third step employs a randomized fractional factorial design with multiple RDEs explored in multiple tumor cohorts during the expansion phase to ensure a feasible dose is selected for registration trials [69]. This approach allows for direct comparison of multiple doses across different patient populations, providing robust data on both efficacy and safety to support identification of the OBD.
Randomized dose optimization studies may incorporate various design features to enhance their efficiency and informativeness, including:
Blinding: Blinding subjects and investigators within the study to reduce potential bias in assessment of efficacy and safety endpoints [70].
Crossover Designs: Allowing patients to crossover between dose levels, with pre-specification of how activity and safety will be evaluated post-crossover in the analysis plan [70].
Adaptive Features: Incorporating pre-planned adaptations based on interim analyses to focus enrollment on the most promising dose levels.
Biomarker-Enriched Cohorts: Including patient subsets based on biomarker status to evaluate dose-response relationships in molecularly defined populations.
Figure 2: Three-Step Dose Optimization Framework - This diagram outlines the comprehensive approach for transitioning from maximum tolerated dose to optimal biological dose.
Successful implementation of dose optimization strategies requires a multidisciplinary approach leveraging various computational and experimental resources. The table below details key research reagent solutions and computational tools essential for modern dose optimization studies.
Table 3: Research Reagent Solutions for Dose Optimization Studies
| Tool Category | Specific Tools/Resources | Function in Dose Optimization | Application Context |
|---|---|---|---|
| Computational Modeling Software | NONMEM, Monolix, Berkeley Madonna, R/phoenix | Population PK/PD modeling, exposure-response analysis, simulation of dosing regimens | Quantitative analysis of dose-exposure-response relationships across populations |
| Clinical Trial Design Platforms | BOIN, CRM, EFSPR, ADDPLAN | Implementation of novel dose-finding designs, simulation of trial operating characteristics | Phase I dose escalation, randomized dose optimization trials |
| Biomarker Assay Platforms | NGS platforms, digital PCR, immunoassays, flow cytometry | Quantification of pharmacodynamic, predictive, and safety biomarkers | Establishing biologically effective dose range, patient stratification |
| AI/ML Platforms | TensorFlow, PyTorch, Scikit-learn, DeepChem | Development of predictive models for efficacy and toxicity, de novo molecular design | Prediction of dose-response relationships, optimization of drug properties |
| Data Integration Tools | Spotfire, JMP, RShiny, Tableau | Integration and visualization of multimodal data (PK, PD, biomarkers, clinical endpoints) | Clinical utility index calculation, dose selection decision-making |
Case Studies and Clinical Evidence
Successful Dose Optimization Examples
Evidence from both clinical trials and real-world practice demonstrates the significant benefits of dose optimization. A study comparing weekly cetuximab dosing (the approved regimen) versus an every two weeks regimen among patients with metastatic colorectal cancer found that overall survival was similar between the two dosing regimens, but time to treatment discontinuation was significantly longer among the every-two-weeks cohort [70]. This suggests that the alternative dosing schedule may improve tolerability without compromising efficacy, enhancing overall treatment effectiveness.
Similarly, an evaluation of patients with advanced breast cancer treated with palbociclib found that those with dose reductions had a significantly longer time to next treatment and median overall survival compared to those without dose reductions [70]. This counterintuitive finding challenges the traditional "more is better" paradigm and highlights how optimized dosing can potentially improve outcomes by maintaining treatment continuity and reducing toxicity-related discontinuations.
The Sentinel Dosing Approach
Recent methodological advances include the development of sentinel dosing algorithms to guide decision-making on which cohorts in early phase clinical pharmacology trials should employ a sentinel approach [73]. Sentinel dosing involves administering the investigational product to one or two subjects initially and observing them for a predefined period before treating the remainder of the cohort, providing an additional safety checkpoint particularly valuable for first-in-human trials of novel agents [73].
An algorithm described by Heuberger et al. provides a decision tree considering different aspects of trial design, the investigational medicinal product, and prior knowledge based on (pre)clinical data to standardize and harmonize sentinel dosing practices [73]. This approach tailors the decision-making process on sentinel cohorts to the specific investigational product and available information, improving both subject safety and trial efficiency.
Emerging Trends and Technologies
The field of dose optimization continues to evolve rapidly, with several emerging trends and technologies poised to further transform practice:
Digital Twin Simulations: The development of virtual patient representations, or "digital twins," may allow for in silico testing of different dosing strategies before clinical implementation, potentially reducing the number of patients exposed to suboptimal doses in trials [23].
Federated Learning Approaches: These privacy-preserving techniques enable model training across multiple institutions without sharing raw data, enhancing data diversity and model robustness while addressing privacy concerns [23].
Multi-Modal AI Integration: Advanced AI systems capable of integrating genomic, imaging, clinical, and real-world data promise more holistic insights into dose-response relationships across diverse patient populations [22].
Quantum Computing: The integration of quantum computing may further accelerate molecular simulations and complex systems modeling beyond current computational limits, enabling more sophisticated dose optimization modeling [23].
The transition from maximum tolerated dose to optimal biological dose represents a fundamental paradigm shift in oncology drug development, moving away from the antiquated "more is better" approach toward a more nuanced understanding of the complex relationship between dose, efficacy, and safety. This shift is being driven by recognition of the limitations of traditional dose-finding methods for modern targeted therapies and immunotherapies, reinforced by regulatory initiatives such as Project Optimus and supported by advances in computational approaches including CADD and AI.
The successful implementation of dose optimization strategies requires a multidisciplinary approach integrating novel clinical trial designs, sophisticated modeling and simulation techniques, comprehensive biomarker strategies, and quantitative decision-making frameworks. By embracing these approaches, drug developers can identify doses that maximize therapeutic benefit while minimizing toxicity, ultimately improving outcomes for cancer patients and enhancing the efficiency of oncology drug development.
As the field continues to evolve, ongoing collaboration between regulators, industry, academia, and patient advocates will be essential to address remaining challenges, including dose optimization for combination therapies, inclusion of diverse patient populations in dose-finding studies, and development of fit-for-purpose approaches for novel therapeutic modalities. Through these collective efforts, the vision of delivering the right dose to the right patient at the right time can become a reality in oncology practice.
In the dynamic landscape of computer-aided drug design (CADD) for oncology, the integration of large-scale genomic and multimodal data is critical to advancing research toward personalized cancer therapies [74]. Computer-Aided Drug Design (CADD) represents a transformative force, bridging biology and technology through computational algorithms that simulate how drug molecules interact with biological targets, typically proteins or DNA sequences [36]. The core principle underpinning CADD is the utilization of computer algorithms on chemical and biological data to rationalize and expedite drug discovery [36].
However, this data-dependent paradigm faces significant challenges. Real-world oncology datasets are often characterized by incompleteness, heterogeneous structures, and restrictive proprietary constraints that hinder effective use [74] [75]. These limitations create substantial obstacles for researchers seeking to leverage big data—including electronic health records, medical imaging, genomic sequencing, and wearables data—to derive therapeutic insights [75]. This guide outlines sophisticated computational and strategic approaches to overcome these data limitations while maintaining scientific rigor and compliance with evolving regulatory frameworks.
Understanding Data Limitations in Oncology Research
Taxonomy of Data Challenges
Oncology research encounters specific, recurrent challenges when working with real-world datasets. Understanding these categories is essential for developing targeted mitigation strategies.
Data Completeness and Quality Issues: Incompleteness manifests as missing values, incorrect data, and lack of standardized annotation [75]. Mapping terminology across disparate datasets with varying structures makes data combination an onerous, largely manual undertaking [75]. These issues are particularly acute in oncology due to the complexity of cancer as hundreds of different diseases, where each patient effectively represents an "n of 1" from a precision medicine perspective [75].
Proprietary and Access Restrictions: Data privacy regulations including the Health Insurance Portability and Accountability Act (HIPAA) and the General Data Protection Regulation (GDPR) create legitimate barriers to data sharing [75]. The use of proprietary datasets from pharmaceutical companies or restricted medical institutions often involves complex data use agreements and intellectual property considerations that can delay or prevent research progress.
Technical and Interoperability Challenges: The rise of multimodal data in oncology has exacerbated issues of interoperability across systems [74]. Variations in data structures, formatting inconsistencies, and incompatible platforms create significant technical hurdles for researchers attempting to integrate diverse datasets ranging from genomic sequences to clinical outcomes.
Table 1: Classification of Common Data Limitations in Oncology CADD
| Challenge Category | Specific Manifestations | Impact on Research |
|---|---|---|
| Completeness & Quality | Missing values, incorrect data, lack of annotation | Reduced statistical power, biased results |
| Proprietary & Access | HIPAA/GDPR restrictions, data use agreements, IP constraints | Limited dataset availability, research delays |
| Technical & Interoperability | Varying data structures, formatting inconsistencies | Difficulty integrating multimodal data sources |
Strategic Frameworks for Data Management
Collaborative Data Governance Models
Successful management of multimodal data in oncology requires early planning and multi-stakeholder engagement across National Health Service (NHS) Trusts, industry, start-up collaborators, and academic institutions [74]. Experience from multi-site, cross-industry UK projects demonstrates that establishing clear data governance frameworks before data collection is essential for enabling secure, collaborative research while maintaining compliance [74].
The data lake architecture has emerged as a scalable and compliant approach to storing diverse datasets securely. Implementation of this model requires aligning technical solutions with governance, security, and accessibility requirements across diverse partners [74]. This architecture enables federated storage of large-scale genomic and clinical data while maintaining necessary access controls and addressing data ownership concerns [74].
Regulatory Compliance Pathways
Navigating the regulatory landscape is essential for legitimate data use in oncology research. Both HIPAA and the Common Rule provide pathways for research that impose fewer preconditions on data access [75].
De-identification of data per HIPAA standards allows data use without being subject to further HIPAA requirements [75]. Alternatively, using a limited data set with a executed data use agreement can enable research without prior participant consent, provided researchers agree not to re-identify or contact participants [75]. Understanding these pathways is crucial for designing compliant data strategies that facilitate research while protecting patient privacy.
Table 2: Regulatory Pathways for Data Access in U.S. Cancer Research
| Regulatory Mechanism | Key Requirements | Permitted Data Uses |
|---|---|---|
| De-identified Data | Removal of 18 specified identifiers per HIPAA; data cannot be readily ascertained | Research without participant consent or authorization |
| Limited Data Set | Data use agreement prohibiting re-identification | Research purposes without prior consent |
| Broad Consent | IRB-reviewed consent for future research uses | Secondary research with identifiable data |
Technical Solutions for Incomplete and Multimodal Data
Computational Compensation Methods
Advanced computational techniques can compensate for data limitations while maintaining research validity. Molecular modeling encompasses a wide range of computational techniques used to model or mimic the behavior of molecules, providing insights into structural and functional attributes when experimental data is incomplete [36].
Molecular dynamics (MD) simulations can forecast the time-dependent behavior of molecules, capturing their motions and interactions over time through various tools like Gromacs, ACEMD, and OpenMM [36]. These simulations help researchers understand dynamic processes that might be incompletely captured in experimental data alone.
Homology modeling, also called comparative modeling, creates a 3D model of a target protein using a homologous protein's empirically confirmed structure as a guide when the exact structure is unavailable [36]. Tools like MODELLER, SWISS-MODEL, and Phyre2 implement these approaches to address structural data gaps [36].
Virtual Screening and QSAR Approaches
When experimental data is limited or proprietary, virtual screening and Quantitative Structure-Activity Relationship (QSAR) modeling provide powerful alternatives. Virtual screening involves sifting through vast compound libraries to identify potential drug candidates using computational tools like DOCK, LigandFit, and ChemBioServer [36].
QSAR modeling explores the relationship between the chemical structure of molecules and their biological activities [36]. Through statistical methods, QSAR models can predict the pharmacological activity of new compounds based on their structural attributes, enabling chemists to make informed modifications to enhance a drug's potency or reduce its side effects even when complete experimental data is unavailable [36].
Table 3: Computational Tools for Overcoming Data Limitations
| Tool Category | Representative Programs | Application to Data Gaps |
|---|---|---|
| Homology Modeling | MODELLER, SWISS-MODEL, Phyre2, I-TASSER | Predicts protein structure when experimental structures unavailable |
| Molecular Dynamics | GROMACS, NAMD, CHARMM | Simulates molecular behavior over time |
| Virtual Screening | DOCK, AutoDock Vina, Glide | Screens compound libraries computationally |
| QSAR Modeling | Various statistical and ML approaches | Predicts activity from structural features |
Implementing Robust Data Management Protocols
Data Lake Architecture for Secure Collaboration
The data lake architecture has demonstrated effectiveness as a centralized repository to store and share diverse datasets securely in multi-site oncology research [74]. Key factors influencing the selection and implementation of this solution include data storage requirements, access control, ownership, and information governance [74].
Implementation requires processes for planning, deploying, and maintaining the data lake infrastructure with early engagement of stakeholders [74]. This approach enables secure, compliant storage of large-scale genomic and clinical data obtained from tissue and liquid biopsies from patients with cancer [74]. The model provides a template for future initiatives in precision oncology by balancing accessibility with necessary security controls.
Federated Learning and Privacy-Preserving Analytics
For working with proprietary or privacy-restricted datasets, federated learning approaches enable model training without transferring sensitive data. This technique allows algorithms to be trained across multiple decentralized edge devices or servers holding local data samples without exchanging them, addressing key privacy concerns while leveraging distributed data sources.
This approach is particularly valuable in oncology, where data privacy is both an ethical imperative and a regulatory requirement. As noted from the patient perspective, concerns about "loss of privacy," potential re-identification, and use of information by for-profit companies represent significant considerations that must be addressed through technical and governance solutions [75].
The Scientist's Toolkit: Research Reagent Solutions
Table 4: Essential Computational Tools for Data-Limited CADD Research
| Tool/Resource | Function | Application Context |
|---|---|---|
| AutoDock Vina | Predicting binding affinities and orientations of ligands | Structure-based drug design with limited experimental data |
| GROMACS | Molecular dynamics simulations | Studying protein behavior when experimental data is sparse |
| SWISS-MODEL | Homology modeling | Generating 3D protein models without experimental structures |
| QSAR Modeling | Predicting biological activity from chemical structure | Prioritizing compounds when screening data is limited |
| Data Lake Infrastructure | Secure, centralized data repository | Managing multimodal data across institutions with governance |
Overcoming data limitations in computer-aided drug design for oncology requires a multifaceted approach combining technical innovation with robust governance. By implementing strategic frameworks including data lake architectures, computational compensation methods, and privacy-preserving analytics, researchers can advance precision oncology despite incomplete or restricted datasets. The future of CADD in oncology depends on developing increasingly sophisticated approaches to maximize insights from limited data while maintaining ethical standards and regulatory compliance. As these methodologies evolve, they promise to accelerate the discovery of novel cancer therapeutics through more effective utilization of all available data resources.
Improving Predictive Accuracy for Toxicity and Efficacy
In the field of computer-aided drug design (CADD) for oncology, accurately predicting the dual parameters of efficacy and toxicity early in the discovery process represents one of the most significant challenges. The high attrition rates of oncology drug candidates, often due to insufficient therapeutic windows, underscore the critical need for robust predictive computational models [28] [23]. The traditional drug development process is both time-intensive and financially burdensome, often requiring 12–15 years and costing 1–2.6 billion dollars until a drug is approved for marketing [28]. The integration of artificial intelligence (AI) and machine learning (ML) is now redefining this traditional pipeline by accelerating discovery, optimizing drug efficacy, and minimizing toxicity [28] [76]. This guide provides an in-depth technical overview of the core principles and advanced methodologies employed in modern CADD to enhance the predictive accuracy for these crucial parameters within oncology research.
Core Computational Frameworks for Prediction
Several computational frameworks form the backbone of modern predictive efforts in oncology drug discovery. These approaches leverage different types of data to model and forecast the biological behavior of potential drug candidates.
Quantitative Structure-Activity Relationship (QSAR) Models
QSAR models are invaluable computational tools that establish a quantitative relationship between a molecule's chemical structure and its biological activity or property, such as toxicity or efficacy [77] [78]. These models allow researchers to predict the biological effects of novel compounds based solely on their structural features, which is particularly useful for prioritizing compounds for synthesis and testing.
Key Considerations for Improving QSAR Predictivity: A recent comprehensive analysis of QSAR model performance identified several factors critical for enhancing predictive accuracy [78]:
- Data Quality and Consistency: The predictive performance of a QSAR model is heavily dependent on the quality, consistency, and relevance of the underlying training data.
- Descriptor Selection: Choosing appropriate molecular descriptors that relate to the endpoint and its mechanism of action is crucial.
- Model Complexity: Selecting a model with the appropriate structural complexity and number of descriptors prevents overfitting.
- Applicability Domain: Ensuring predictions are made only for compounds within the chemical space defined by the training data.
- Metabolism Considerations: Accounting for metabolic transformations in the modeling process, as metabolites may be responsible for observed toxicity or efficacy.
Table 1: Common Molecular Descriptors in QSAR Modeling for Toxicity and Efficacy
| Descriptor Category | Specific Examples | Prediction Relevance |
|---|---|---|
| Electronic | HOMO/LUMO energies, Polarizability | Reactivity, Interaction with biological targets |
| Steric | Molecular volume, Surface area | Membrane permeability, Binding site compatibility |
| Hydrophobic | log P (octanol-water partition coefficient) | Absorption, Distribution, Metabolism |
| Topological | Molecular connectivity indices | Structure-activity relationships |
| Constitutional | Atom/Bond counts, Molecular weight | Basic physicochemical properties |
Pharmacophore Modeling
A pharmacophore is defined as "the ensemble of steric and electronic features that is necessary to ensure the optimal supramolecular interactions with a specific biological target structure and to trigger (or to block) its biological response" [79]. Pharmacophore modeling abstracts the key chemical functionalities from active ligands or protein binding sites into a three-dimensional model that can be used for virtual screening.
Methodological Approaches:
- Structure-Based Pharmacophore Modeling: This approach uses the three-dimensional structure of a macromolecular target (e.g., from X-ray crystallography or NMR spectroscopy) to identify interaction points in the binding site. The workflow consists of protein preparation, ligand-binding site detection, pharmacophore feature generation, and selection of relevant features for ligand activity [79].
- Ligand-Based Pharmacophore Modeling: When the 3D structure of the target is unavailable, this method develops pharmacophore models using the physicochemical properties and alignment of known active ligands [79].
- Hybrid Pharmacophore Modeling: Combines the advantages of both ligand-based and structure-based approaches, providing a more comprehensive understanding of ligand-protein interactions [80].
AI-Driven Target Prediction and Validation
Artificial intelligence, particularly deep learning, has emerged as a critical tool for predicting drug targets and their biological effects. A notable advancement in this area is DeepTarget, a computational tool that integrates large-scale drug and genetic knockdown viability screens plus omics data to determine cancer drugs' mechanisms of action [81]. In benchmark testing, DeepTarget outperformed currently used tools such as RoseTTAFold All-Atom and Chai-1 in seven out of eight drug-target test pairs for predicting drug targets and their mutation specificity [81].
The AI-driven process for target identification and validation typically involves:
- Data mining of available biomedical data from publications, proteomics, gene expression, and compound profiling [28].
- Using an AI system with a large database combining public databases and manually curated information to describe therapeutic patterns between compounds and diseases [28].
- Experimental validation through in vitro and in vivo studies to confirm predicted efficacy and mechanism of action [28].
Figure 1: AI-Driven Target Prediction and Validation Workflow
Experimental Protocols for Model Development and Validation
Protocol for Structure-Based Pharmacophore Modeling
Objective: To develop a predictive pharmacophore model using the 3D structure of a target protein relevant to oncology.
Methodology:
- Protein Structure Preparation:
- Obtain the 3D structure from the RCSB Protein Data Bank (PDB) or through homology modeling using tools like ALPHAFOLD2 [79].
- Evaluate and optimize the protein structure by adjusting residue protonation states, adding hydrogen atoms (absent in X-ray structures), and addressing any missing residues or atoms.
- Assess stereochemical and energetic parameters to ensure biological and chemical reliability.
Ligand-Binding Site Detection:
- Use computational tools such as GRID or LUDI to identify potential binding sites [79].
- GRID uses molecular interaction fields to sample protein regions with functional groups, identifying energetically favorable interaction points.
- Alternatively, manually infer the binding site from experimental data such as site-directed mutagenesis or co-crystallized ligand information.
Pharmacophore Feature Generation:
- Generate an initial set of pharmacophore features including hydrogen bond acceptors (HBAs), hydrogen bond donors (HBDs), hydrophobic areas (H), positively and negatively ionizable groups (PI/NI), and aromatic groups (AR) [79].
- If a protein-ligand complex structure is available, use the ligand's bioactive conformation to guide feature placement.
Feature Selection and Model Refinement:
- Select only features essential for bioactivity by removing those that don't strongly contribute to binding energy.
- Identify conserved interactions if multiple protein-ligand structures are available.
- Add exclusion volumes to represent spatial restrictions from the binding site shape.
Virtual Screening and Validation:
- Use the refined pharmacophore model as a query to screen compound libraries.
- Validate the model by assessing its ability to retrieve known active compounds and exclude inactives.
Protocol for QSAR Model Development with Applicability Domain Assessment
Objective: To develop a robust QSAR model for predicting toxicity or efficacy endpoints with clearly defined applicability domains.
Methodology:
- Data Curation and Preparation:
- Collect a high-quality dataset of compounds with reliable experimental data for the endpoint of interest.
- Apply strict criteria for data inclusion, considering consistency and relevance to the prediction context.
- Divide the dataset into training (≈80%) and test (≈20%) sets using rational division methods to ensure chemical space representation.
Molecular Descriptor Calculation and Selection:
- Calculate a comprehensive set of molecular descriptors encompassing electronic, steric, hydrophobic, topological, and constitutional features.
- Apply feature selection techniques (e.g., genetic algorithms, stepwise selection) to identify the most relevant descriptors, avoiding overfitting.
Model Building and Validation:
- Employ appropriate machine learning algorithms (e.g., Random Forest, Support Vector Machines, Neural Networks) to build the predictive model [82].
- Validate the model using both internal (cross-validation) and external (test set) validation techniques.
- Assess model performance using metrics such as sensitivity, specificity, accuracy, and area under the ROC curve (AUC).
Applicability Domain Characterization:
Model Interpretation and Documentation:
- Use interpretation tools such as SHAP (SHapley Additive exPlanations) to understand descriptor contributions [78].
- Document the model according to OECD principles for QSAR validation, including a defined endpoint, unambiguous algorithm, appropriate measures of goodness-of-fit, robustness, and predictivity, and a defined domain of applicability [78].
Table 2: Performance Metrics for Predictive Model Validation
| Metric | Calculation/Definition | Optimal Range | Interpretation in Drug Discovery |
|---|---|---|---|
| Sensitivity | True Positives / (True Positives + False Negatives) | >0.8 | Ability to identify active/toxic compounds |
| Specificity | True Negatives / (True Negatives + False Positives) | >0.8 | Ability to identify inactive/non-toxic compounds |
| Accuracy | (True Positives + True Negatives) / Total Compounds | >0.85 | Overall correctness of predictions |
| AUC-ROC | Area Under the Receiver Operating Characteristic Curve | >0.9 | Overall discriminatory power |
| Precision | True Positives / (True Positives + False Positives) | >0.7 | Reliability of positive predictions |
Protocol for AI-Driven Multi-Target Prediction Using DeepTarget
Objective: To utilize the DeepTarget computational tool for predicting primary and secondary targets of small-molecule agents in oncology.
Methodology:
- Data Integration:
- Input large-scale drug and genetic knockdown viability screens along with multi-omics data (genomics, transcriptomics, proteomics) [81].
- Incorporate mutation specificity data where available to enhance prediction accuracy for specific genetic contexts.
Model Application:
- Apply the DeepTarget algorithm to integrate the diverse data types and predict drug-target interactions.
- The tool's architecture, which closely mirrors real-world drug mechanisms where cellular context and pathway-level effects play crucial roles, enables superior performance compared to methods focused solely on chemical binding [81].
Prediction Analysis:
- Analyze the output for both primary targets (intended therapeutic targets) and secondary targets (off-target effects that may contribute to efficacy or toxicity).
- Assess mutation-specific responses, such as how EGFR T790 mutations influence response to ibrutinib in BTK-negative solid tumors [81].
Experimental Validation:
- Design experiments to validate predictions, such as cell viability assays using appropriate cell lines.
- Investigate the mechanism of action predicted by the model, for example, confirming that pyrimethamine affects cellular viability by modulating mitochondrial function in the oxidative phosphorylation pathway [81].
Successful implementation of predictive models for toxicity and efficacy requires both computational tools and experimental reagents for validation.
Table 3: Essential Research Reagent Solutions for Predictive Model Validation
| Reagent/Resource | Function/Application | Example Uses in Validation |
|---|---|---|
| High-Throughput Screening Assays | Rapid testing of compound libraries for biological activity | Initial hit identification and confirmation of predicted activities |
| Gene Expression Profiling Kits | Analysis of transcriptomic changes in response to treatment | Validation of predicted mechanism of action and off-target effects |
| Protein-Protein Interaction Assays | Detection and quantification of molecular interactions | Confirmation of predicted target engagement and pathway modulation |
| Metabolomics Platforms | Comprehensive analysis of metabolic profiles | Assessment of metabolic stability and identification of toxic metabolites |
| 3D Cell Culture Systems | More physiologically relevant models for efficacy and toxicity testing | Improved prediction of in vivo effects compared to 2D cultures |
| Patient-Derived Xenograft (PDX) Models | In vivo models using human tumor tissues in immunodeficient mice | Final preclinical validation of efficacy predictions in human-relevant context |
Integrated Workflow for Enhanced Predictive Accuracy
Combining multiple computational approaches creates a synergistic effect that significantly enhances predictive accuracy for both toxicity and efficacy endpoints.
Figure 2: Integrated Predictive Modeling Workflow
The integrated workflow illustrated above demonstrates how different computational approaches feed into a multi-parameter optimization process, followed by experimental validation. This iterative process allows for continuous refinement of predictive models based on experimental feedback, creating a self-improving system for drug discovery.
Improving predictive accuracy for toxicity and efficacy in oncology drug discovery requires a multifaceted approach that leverages the strengths of various computational methodologies while acknowledging their limitations. QSAR models, pharmacophore modeling, and AI-driven target prediction each contribute unique capabilities to this challenge. The key to success lies in the rigorous development and validation of these models, careful characterization of their applicability domains, and intelligent integration of multiple approaches within an iterative framework that incorporates experimental feedback. As these computational techniques continue to evolve and improve, they hold the promise of significantly accelerating oncology drug discovery while reducing late-stage attrition rates, ultimately leading to more effective and safer cancer therapies.
Within modern oncology drug discovery, the integration of computational predictions and experimental validation has transitioned from an advantageous strategy to a fundamental pillar of efficient therapeutic development. This synergy between in silico technologies and in vitro and in vivo experiments establishes a rational framework that accelerates the identification and optimization of novel anticancer agents. Computer-aided drug design (CADD) provides powerful tools for exploring vast chemical and biological spaces, while experimental methodologies deliver the essential biological context and validation required to translate computational hypotheses into viable clinical candidates [83]. The convergence of these domains is particularly critical in oncology, given the molecular heterogeneity of cancers and the urgent need for targeted, personalized therapies [84].
The contemporary drug discovery workflow is inherently cyclical, not linear. It involves a continuous feedback loop where computational models generate testable predictions, experimental results refine and validate those models, and the enriched datasets, in turn, fuel the development of more accurate and powerful computational tools [85] [4]. This iterative process enhances the efficiency of key stages, including target identification, hit discovery, lead optimization, and the prediction of ADMET (Absorption, Distribution, Metabolism, Excretion, and Toxicity) properties, ultimately reducing costs and development timelines [4] [83]. This guide details the core principles, methodologies, and practical applications of this integrated workflow within the context of oncology research.
Computational Foundations for Prediction
The initial phase of the integrated workflow relies on a suite of computational techniques to generate robust, testable hypotheses about potential drug-target interactions.
Target Identification and Structure Preparation
The process begins with the identification and structural characterization of a biological target, typically a protein implicated in oncogenesis. The accuracy of all subsequent structure-based methods hinges on the quality of this initial three-dimensional (3D) model.
- Experimental Structures: When available, high-resolution structures from sources like the Protein Data Bank (PDB) are preferred. Techniques such as X-ray crystallography, cryo-electron microscopy (cryo-EM), and NMR spectroscopy provide the foundational structural data for structure-based drug design (SBDD) [83].
- Computational Predictions: For targets with no experimentally solved structure, computational models fill the gap. Deep learning systems like AlphaFold 3 and ColabFold can predict protein structures with high accuracy, while tools like RaptorX are valuable for predicting residue-residue contacts and modeling proteins without homologous templates [2] [84] [19]. These predicted structures often undergo refinement using molecular dynamics (MD) simulations to stabilize the model and explore its conformational landscape [84].
Virtual Screening and Hit Identification
With a reliable target structure in hand, virtual screening (VS) computationally sifts through large libraries of compounds to identify potential "hits" – molecules with a high predicted affinity for the target.
- Structure-Based Virtual Screening (SBVS): This method uses molecular docking programs—such as AutoDock, Glide, and DOCK—to predict the binding pose and affinity of small molecules within a target's binding site [85] [84]. Newer learning-based pose generators like DiffDock and EquiBind can accelerate this conformational sampling [84].
- Ligand-Based Virtual Screening (LBVS): When the target structure is unknown but active ligands are available, LBVS methods are employed. These include quantitative structure-activity relationship (QSAR) modeling and pharmacophore mapping, which identify new candidates based on their similarity to known active molecules [85] [19].
- AI-Enhanced Screening: Artificial intelligence (AI) and machine learning (ML) are increasingly integrated to pre-filter compound libraries or re-rank docking results, creating hybrid workflows that boost hit rates and scaffold diversity [4] [84]. This approach is part of the broader emerging paradigm of AI-driven drug design (AIDD) within the CADD framework [2] [19].
Table 1: Key Computational Techniques and Their Applications in Oncology Drug Discovery
| Technique | Primary Function | Common Tools/Platforms | Oncology Application Example |
|---|---|---|---|
| Molecular Docking | Predicts binding orientation & affinity of a ligand to a target protein. | AutoDock, Glide, DOCK [85] | Identifying kinase inhibitors for cancer therapy [85]. |
| Molecular Dynamics (MD) | Simulates atomic movements over time to assess complex stability & flexibility. | GROMACS, AMBER [85] | Elucidating conformational flexibility of GPCR-ligand systems [85]. |
| QSAR | Correlates molecular descriptors with biological activity to predict compound activity. | DeepChem, Various ML models [85] [84] | Predicting cytotoxicity or anti-proliferative activity of novel compounds. |
| Pharmacophore Modeling | Identifies essential 3D structural & chemical features for biological activity. | MOE, LigandScout [19] | Scaffold hopping to discover novel chemotypes for a known target. |
| AI/Generative Models | De novo generation of molecules with optimized properties. | GANs, VAEs, Diffusion Models [4] [84] | Designing novel SERDs (Selective Estrogen Receptor Degraders) for luminal breast cancer [84]. |
Experimental Validation Frameworks
Computational predictions must be rigorously tested through experimental assays to confirm biological activity and therapeutic potential.
Biochemical and Biophysical Assays
These assays provide the first layer of validation by directly measuring the interaction between the candidate molecule and the purified target protein.
- Binding Affinity assays: Techniques like Surface Plasmon Resonance (SPR) and Isothermal Titration Calorimetry (ITC) quantitatively measure the binding kinetics (Kon, Koff) and thermodynamics (KD, ΔH) of the drug-target interaction, providing direct experimental validation of docking predictions [84].
- Enzymatic Activity assays: For enzymatic targets (e.g., kinases, proteases), functional assays monitor the inhibition of catalytic activity by the candidate drug, determining half-maximal inhibitory concentration (IC50) values [84].
Cellular and Phenotypic Assays
Cellular assays evaluate a compound's activity in a more complex, biologically relevant environment, accounting for factors like cell permeability and intracellular metabolism.
- In vitro Cytotoxicity and Anti-proliferation Assays: Assays such as MTT or CellTiter-Glo are used to measure the ability of a compound to kill or inhibit the growth of cancer cell lines, generating IC50 or GI50 values [84].
- Target Engagement and Pathway Modulation: Techniques like Western Blotting and Immunofluorescence are employed to verify that the compound engages its intended target in cells and modulates downstream signaling pathways (e.g., MAPK, PI3K-Akt) [84] [19].
- Mechanistic and Phenotypic Profiling: More complex assays, including flow cytometry (for cell cycle arrest or apoptosis) and gene expression profiling, can elucidate the compound's mechanism of action and phenotypic consequences [84].
The Integrated Workflow: A Practical Guide
The true power of modern drug discovery lies in the seamless integration of the computational and experimental realms. The following workflow diagram and subsequent protocol outline this iterative cycle.
Protocol for an Integrated Screening Campaign
This protocol outlines a standardized iterative cycle for identifying and optimizing lead compounds against a novel oncology target, such as a kinase implicated in triple-negative breast cancer (TNBC).
Step 1: Target Selection and Compound Library Curation
- Objective: Identify a validated oncology target and prepare a diverse compound library for screening.
- Procedure:
- Select a target through human genetics and multi-omics data (e.g., from TCGA) confirming its role in cancer cell survival or proliferation [84].
- Obtain a high-resolution 3D structure from the PDB or generate a predicted structure using AlphaFold 2/3 [84] [19]. Prepare the protein structure by adding hydrogen atoms, assigning protonation states, and optimizing side-chain conformations.
- Curate a virtual compound library from databases like ZINC or ChEMBL, comprising millions of commercially available molecules [85]. Apply basic drug-likeness filters (e.g., Lipinski's Rule of Five).
Step 2: Computational Screening and Prioritization
- Objective: Narrow the million-compound library to a manageable number of high-probability hits for experimental testing.
- Procedure:
- Perform high-throughput virtual screening (HTVS) using molecular docking software (e.g., AutoDock-GPU, Glide HTVS) to score and rank compounds based on predicted binding affinity [85] [84].
- Apply AI/ML models to pre-filter the library or re-rank the docking results to improve scaffold diversity and hit rates [4].
- Subject the top 1,000-10,000 ranked compounds to more rigorous computational analyses. This includes:
- Visual Inspection: Check binding poses for key interactions (H-bonds, hydrophobic contacts).
- ADMET Prediction: Use tools like ADMET Predictor or SwissADME to estimate pharmacokinetic and toxicity profiles [85] [84].
- Diversity Selection: Cluster compounds by scaffold and select a representative set of 100-500 compounds for experimental testing to ensure chemical diversity.
Step 3: Experimental Validation of Hits
- Objective: Experimentally confirm the activity of computationally selected hits.
- Procedure:
- Acquire the selected compounds from commercial suppliers.
- Conduct a primary biochemical assay to measure direct target engagement and inhibition (e.g., kinase activity assay). Confirm dose-response relationships and determine IC50 values for active compounds.
- Execute a secondary cellular assay to evaluate anti-proliferative effects on relevant cancer cell lines (e.g., TNBC cell lines). Determine GI50 values and assess selectivity by testing against non-malignant control cells.
Step 4: Data Integration and Iterative Optimization
- Objective: Use experimental results to refine computational models and guide chemical optimization.
- Procedure:
- Perform SAR analysis by comparing the structures of active and inactive compounds from the experimental set. This validates or challenges the initial computational hypotheses.
- Use the experimental bioactivity data to train or refine machine learning models (e.g., a QSAR model) for the next round of compound prediction [85] [83].
- Initiate lead optimization cycles. Use techniques like molecular dynamics (MD) simulations to understand dynamic interactions and relative binding free-energy (RBFE) calculations to rationally design and prioritize analogues with improved potency and properties [84].
- Return to Step 2 with the refined models and focus on the most promising chemical series, repeating the cycle until a lead compound with desirable efficacy and ADMET properties is identified.
Case Study: Application in Breast Cancer Subtypes
The integrated workflow is powerfully illustrated by its application to the distinct molecular subtypes of breast cancer, which require tailored therapeutic strategies [84].
- Luminal (HR+) Breast Cancer: For targets like the estrogen receptor (ER), integrated workflows have been crucial in developing next-generation oral SERDs (e.g., elacestrant, camizestrant). Computational models, including docking and MD simulations, were used to design compounds that overcome endocrine resistance caused by ESR1 mutations. These predictions were validated through cellular assays measuring ER degradation and anti-proliferative activity in resistant cell lines [84].
- HER2-Positive Breast Cancer: SBDD has guided the optimization of HER2-targeting antibodies and kinase inhibitors. AI-driven tools have also been applied to predict patient responses to HER2-targeted therapies, helping to stratify patients for clinical trials [84].
- Triple-Negative Breast Cancer (TNBC): In TNBC, where targetable drivers are scarce, integrated approaches are vital. CADD has been used to exploit DNA repair deficiencies via PARP inhibitor design. Furthermore, AI-driven biomarker discovery from multi-omics data is helping to identify patient subgroups that may respond to immunotherapy, enabling more precise clinical trial design [84].
The diagram below specifics a typical integrated workflow for a specific breast cancer subtype.
The Scientist's Toolkit: Essential Research Reagents and Materials
A successful integrated workflow relies on a suite of specialized reagents, computational tools, and experimental platforms.
Table 2: Essential Research Reagents and Tools for Integrated Oncology Drug Discovery
| Category | Item/Reagent | Function in Workflow |
|---|---|---|
| Computational Tools | AlphaFold 2/3, ColabFold | Protein structure prediction for targets lacking experimental structures [84] [19]. |
| AutoDock, Glide, Schrödinger Suite | Molecular docking and virtual screening to predict ligand binding [85] [84]. | |
| GROMACS, AMBER | Molecular dynamics simulations to study protein-ligand dynamics and stability [85] [84]. | |
| ADMET Predictor, SwissADME | In silico prediction of pharmacokinetic and toxicity properties [85] [84]. | |
| Experimental Assays | Recombinant Target Protein | Essential for biochemical assays (SPR, ITC, enzymatic activity) to validate binding and inhibition [84]. |
| Cancer Cell Line Panel | Representative models (e.g., MCF-7, MDA-MB-231) for cellular efficacy and mechanism-of-action studies [84]. | |
| Cell Viability Assay Kits (e.g., MTT, CellTiter-Glo) | Quantify anti-proliferative effects and determine IC50/GI50 values [84]. | |
| Antibodies for Western Blot/IF | Detect target protein levels and downstream pathway modulation (e.g., p-ERK, cleaved Caspase-3) [84]. | |
| Data & Analysis | CDD Vault, Dotmatics | Centralized data management platform to integrate and analyze computational and experimental data [86]. |
| StarDrop, MOE | Software for data analysis, QSAR model building, and multi-parameter optimization [86] [84]. | |
| Public Databases (PDB, ChEMBL, ZINC) | Sources of structural, bioactivity, and purchasable compound data for model building and screening [85] [84]. |
The integration of computational predictions with experimental validation represents a paradigm shift in oncology drug discovery. This synergistic workflow, powered by advances in CADD, AI, and structural biology, creates a rational, data-driven, and iterative cycle that dramatically improves the efficiency of translating basic research into clinical therapies. While challenges such as data quality, model interpretability, and the need for robust experimental validation remain, the continued refinement of these integrated approaches promises to accelerate the development of more effective and personalized cancer treatments, ultimately bridging the critical gap between theoretical design and clinical application.
Evaluating CADD Efficacy: Validation Frameworks and Performance Metrics
Within the strategic framework of oncology research, Computer-Aided Drug Design (CADD) serves as an indispensable discipline, bridging computational analytics with biological experimentation. The evaluation of CADD methodologies relies critically on robust performance metrics—primarily accuracy, sensitivity, and specificity—which provide quantitative assessments of predictive reliability and utility. These metrics are fundamental for validating computational predictions against experimental results, thereby guiding the iterative optimization of drug candidates. In precision oncology, where therapeutic efficacy is intimately linked to individual genetic profiles, the ability of CADD tools to accurately discriminate between true drug-target interactions and false leads directly influences the success of targeted therapies [87] [57]. This guide details the core principles for benchmarking these critical performance indicators within oncology-focused drug discovery pipelines.
The integration of artificial intelligence (AI) and machine learning (ML) has transformed CADD from a supportive tool to a central driver in oncology drug discovery [57] [88]. AI-driven CADD methodologies enhance the prediction of drug-target interactions, binding affinities, and pharmacological activities by learning from large-scale chemical and biological datasets [36] [89]. In this context, rigorous benchmarking is not merely a technical exercise but a crucial practice for validating models before they guide costly experimental efforts. By systematically evaluating sensitivity, specificity, and accuracy, researchers can select the most predictive models, identify potential biases, and ensure that computational resources are allocated toward the most promising therapeutic candidates for further development [89].
Core Performance Metrics: Definitions and Computational Frameworks
The evaluation of CADD performance relies on a foundation of statistical metrics derived from a binary classification framework, which compares computational predictions against experimental observations. The core concepts are defined through the confusion matrix:
- True Positives (TP): Active compounds correctly predicted as active.
- True Negatives (TN): Inactive compounds correctly predicted as inactive.
- False Positives (FP): Inactive compounds incorrectly predicted as active (Type I error).
- False Negatives (FN): Active compounds incorrectly predicted as inactive (Type II error).
From these fundamentals, the key performance metrics for CADD are calculated:
- Sensitivity (Recall or True Positive Rate): Measures the model's ability to correctly identify active compounds. Calculated as TP / (TP + FN). High sensitivity is critical in early-stage screening to minimize missed leads [57].
- Specificity (True Negative Rate): Measures the model's ability to correctly identify inactive compounds. Calculated as TN / (TN + FP). High specificity reduces resource waste on false leads [89].
- Accuracy: Represents the overall proportion of correct predictions. Calculated as (TP + TN) / (TP + TN + FP + FN). Provides a global measure of model performance [89].
- Area Under the Receiver Operating Characteristic Curve (AUC-ROC): Plots the true positive rate (sensitivity) against the false positive rate (1 - specificity) across different classification thresholds. The AUC provides a aggregate measure of model performance across all classification thresholds [90].
The following diagram illustrates the relationship between these core metrics and the CADD validation workflow:
Figure 1: CADD Performance Validation Workflow
Quantitative Benchmarking of CADD Methodologies in Oncology
The performance of CADD approaches varies significantly based on methodology, target complexity, and dataset quality. Contemporary research demonstrates that AI-enhanced models consistently outperform traditional computational approaches across key metrics. The table below summarizes benchmarked performance data for various CADD methodologies as reported in recent literature:
Table 1: Benchmark Performance of CADD Methods in Oncology Applications
| Methodology | Reported Accuracy | Sensitivity | Specificity | AUC-ROC | Oncology Application |
|---|---|---|---|---|---|
| HSAPSO-optimized Stacked Autoencoder [89] | 95.52% | N/R | N/R | N/R | Druggable target identification |
| 3D Deep Learning Models (CT-based) [90] | N/R | N/R | N/R | 0.86 | Lung cancer risk prediction |
| XGB-DrugPred [89] | 94.86% | N/R | N/R | N/R | Drug-target interaction |
| Graph-based Deep Learning [89] | 95.0% | N/R | N/R | N/R | Protein sequence analysis |
| SVM-based Models [89] | 89.98% | N/R | N/R | N/R | Druggable protein prediction |
| 2D Deep Learning Models (CT-based) [90] | N/R | N/R | N/R | 0.79 | Lung cancer risk prediction |
N/R: Not explicitly reported in the source material
Recent advances in deep learning architectures have demonstrated remarkable performance in specific oncology applications. The optSAE + HSAPSO framework, which integrates a stacked autoencoder with hierarchically self-adaptive particle swarm optimization, achieved a benchmark accuracy of 95.52% in drug classification and target identification tasks on DrugBank and Swiss-Prot datasets [89]. This represents a significant improvement over traditional machine learning approaches like Support Vector Machines (SVMs), which typically achieve approximately 90% accuracy in similar tasks [89]. In medical imaging analysis for oncology, 3D convolutional neural networks have shown superior performance (AUC=0.86) compared to 2D models (AUC=0.79) for lung cancer risk prediction using CT scans, highlighting the importance of volumetric spatial information in cancer diagnostics [90].
Experimental Protocols for CADD Benchmarking
Structure-Based Drug Design (SBDD) Protocol
Structure-based drug design leverages the three-dimensional structural information of biological targets, typically proteins or nucleic acids, to identify and optimize drug candidates [36] [91]. The standard experimental protocol for benchmarking SBDD performance encompasses:
- Target Preparation: Obtain the 3D structure of the target protein from the Protein Data Bank (PDB) or through homology modeling using tools like MODELLER or SWISS-MODEL [91]. For targets with unknown structures, AlphaFold2 and related AI systems can predict high-confidence structural models [36] [88].
- Binding Site Identification: Locate potential binding pockets on the target using computational methods like binding response analysis, FINDSITE, or ConCavity [91].
- Molecular Docking: Perform virtual screening of compound libraries against the identified binding site using docking software such as AutoDock Vina, DOCK, or Glide [36] [91]. These programs predict the binding orientation and affinity of small molecules to the target structure.
- Force Field Parameterization: Employ empirical force fields (CHARMM, AMBER) to describe the energetic properties of the molecular system [91]. Use automated parameter generation tools like CGenFF for novel ligand molecules.
- Validation: Compare docking predictions against experimentally determined binding affinities (IC50, Ki values) to calculate sensitivity, specificity, and accuracy metrics [91].
Ligand-Based Drug Design (LBDD) Protocol
Ligand-based approaches are employed when 3D structural information of the target is unavailable, relying instead on known active and inactive compounds to establish structure-activity relationships (SAR) [36] [91]. The benchmarking protocol includes:
- Compound Library Curation: Compile a diverse set of chemical structures with known biological activities from databases like ChEMBL, PubChem, or in-house repositories [91].
- Molecular Descriptor Calculation: Compute quantitative descriptors representing physicochemical properties, topological features, and electronic characteristics of each compound [36].
- Quantitative Structure-Activity Relationship (QSAR) Modeling: Develop statistical or machine learning models that correlate molecular descriptors with biological activity using methods like partial least squares regression, random forests, or neural networks [36] [91].
- Model Validation: Perform internal validation (e.g., k-fold cross-validation) and external validation using hold-out test sets to assess predictive performance [89]. Calculate sensitivity, specificity, and accuracy against experimental bioactivity data.
- Applicability Domain Assessment: Define the chemical space where the model provides reliable predictions to guide appropriate use [89].
AI-Driven Target Identification Protocol
The integration of artificial intelligence has introduced novel protocols for target identification in oncology [57] [89]. A representative benchmarking protocol for AI-driven target identification includes:
- Data Integration and Preprocessing: Aggregate heterogeneous data from multiple sources including omics databases (genomic, transcriptomic, proteomic), electronic health records, clinical trial data, and scientific literature [87] [57]. Apply preprocessing techniques to handle missing values, normalize distributions, and address data noise.
- Feature Extraction: Employ deep learning architectures such as stacked autoencoders to automatically extract relevant features from high-dimensional biological data [89].
- Model Training with Evolutionary Optimization: Implement hierarchically self-adaptive particle swarm optimization (HSAPSO) to fine-tune hyperparameters of deep learning models, dynamically balancing exploration and exploitation during training [89].
- Cross-Validation: Assess model stability and generalization capability using stratified k-fold cross-validation, with metrics calculated across all folds [89].
- Experimental Confirmation: Validate computational predictions through in vitro and in vivo studies to establish true positive and false positive rates [57]. For example, AI-identified anticancer compounds should demonstrate efficacy in reducing tumor size in appropriate animal models [57].
The following diagram illustrates the signaling pathway for target validation in oncology drug discovery, a critical process following computational prediction:
Figure 2: Oncology Target Validation Pathway
Successful implementation of CADD benchmarking requires access to specialized computational tools, databases, and software resources. The following table catalogs essential resources for conducting rigorous CADD performance evaluation:
Table 2: Essential Research Resources for CADD Benchmarking
| Resource Category | Specific Tools/Platforms | Primary Function | Application in Benchmarking |
|---|---|---|---|
| Molecular Docking Software | AutoDock Vina [36], AutoDock GOLD [36], Glide [36], DOCK [91] | Predict binding orientation and affinity of ligands | Virtual screening performance assessment |
| Molecular Dynamics Simulation | GROMACS [36], CHARMM [91], AMBER [91], NAMD [91], OpenMM [36] | Simulate time-dependent behavior of molecular systems | Binding stability and interaction analysis |
| Protein Structure Prediction | AlphaFold2/3 [36] [88], MODELLER [91], SWISS-MODEL [91], I-TASSER [36] | Predict 3D protein structures from sequence | Target preparation for SBDD |
| Compound Databases | ZINC [91], DrugBank [89], ChEMBL [91] | Provide chemical structures of small molecules | Source of active and decoy compounds |
| Deep Learning Frameworks | Stacked Autoencoders [89], 3D CNNs [90], Graph Neural Networks [89] | AI-driven feature extraction and prediction | Performance comparison with traditional methods |
| Optimization Algorithms | Hierarchically Self-Adaptive PSO (HSAPSO) [89], Genetic Algorithms | Hyperparameter tuning and model optimization | Enhancement of model accuracy and stability |
Discussion and Future Perspectives
The benchmarking data presented reveals a consistent trajectory toward improved performance through AI integration. The progression from traditional SVM models (∼90% accuracy) to optimized deep learning architectures (∼95% accuracy) demonstrates the transformative impact of machine learning in CADD [89]. This enhancement is particularly valuable in oncology, where accurately identifying druggable targets and predicting compound efficacy can significantly accelerate the development of personalized cancer therapies [87].
The observed performance advantage of 3D deep learning models over 2D approaches in lung cancer risk prediction (AUC 0.86 vs. 0.79) underscores the importance of architectural considerations in model design [90]. This principle extends to molecular modeling, where 3D structural information enables more accurate binding affinity predictions. Furthermore, optimization techniques like HSAPSO contribute significantly to model performance by efficiently navigating complex parameter spaces, thereby enhancing both accuracy and computational efficiency [89].
Future advancements in CADD benchmarking will likely focus on several key areas: (1) development of standardized benchmark datasets specific to oncology targets, (2) integration of multi-omics data for more comprehensive predictive modeling, (3) implementation of explainable AI to enhance model interpretability, and (4) incorporation of quantum computing for complex molecular simulations [88]. As these technologies mature, the performance metrics of CADD tools are expected to improve further, solidifying their role as indispensable assets in oncology drug discovery.
In conclusion, rigorous benchmarking using accuracy, sensitivity, specificity, and AUC-ROC metrics provides the foundation for validating CADD methodologies in oncology research. The continuous refinement of these computational approaches through AI integration and optimization techniques promises to accelerate the development of targeted cancer therapies, ultimately advancing the paradigm of precision oncology.
Computer-Aided Drug Design (CADD) represents a transformative synergy of computational science and biological research, fundamentally altering the landscape of anti-cancer drug discovery. Traditional CADD methodologies have provided the foundation for a more rational, structure-based approach to drug design, moving away from serendipitous discovery and labor-intensive trial-and-error methods [36]. The core principle underpinning CADD is the utilization of computational algorithms on chemical and biological data to simulate and predict how drug molecules interact with their biological targets, typically proteins or nucleic acids involved in cancer pathways [36]. The late 20th century heralded the advent of CADD, facilitated by crucial advancements in structural biology that revealed three-dimensional architectures of biomolecules and exponential growth in computational power [36].
In contemporary oncology research, CADD has evolved into two primary categories: structure-based drug design (SBDD), which leverages knowledge of the three-dimensional structure of biological targets, and ligand-based drug design (LBDD), which focuses on known drug molecules and their pharmacological profiles to design new candidates [36]. The integration of artificial intelligence (AI) has marked a revolutionary shift, enhancing traditional CADD with machine learning (ML), deep learning (DL), and generative models that dramatically accelerate discovery timelines and improve predictive accuracy [57] [55]. This comparative analysis examines the technical foundations, applications, and performance characteristics of traditional versus AI-enhanced CADD approaches within oncology research, providing researchers with a comprehensive framework for methodological selection in anti-cancer drug development.
Fundamental Technical Principles and Methodologies
Traditional CADD Approaches
Traditional CADD methodologies form the foundational framework for computational drug discovery, relying on established physical principles and explicit programming of molecular interactions. These approaches include molecular docking, which predicts the preferred orientation and binding affinity of small molecules when bound to their target protein using tools such as AutoDock Vina, AutoDock GOLD, and Glide [36] [50]. Molecular dynamics (MD) simulations represent another cornerstone technique, employing programs like GROMACS, NAMD, and CHARMM to simulate the time-dependent behavior of molecules and capture their motions and interactions over intervals ranging from femtoseconds to seconds [36] [50]. This provides critical insights into drug-target binding stability, conformational changes, and the effects of mutations or chemical modifications.
Quantitative Structure-Activity Relationship (QSAR) modeling constitutes a third essential methodology, exploring relationships between chemical structures and biological activities through statistical analysis to predict pharmacological activity of new compounds based on structural attributes [36] [50]. Traditional CADD also encompasses virtual screening (VS), a computational filtering process that rapidly evaluates vast compound libraries to identify candidates with promising binding affinity to specific biological targets [36]. These methodologies collectively enable researchers to identify and optimize potential drug candidates with greater efficiency than purely experimental approaches, though they remain computationally intensive and often require significant expert intervention for optimal implementation [55].
AI-Enhanced CADD Approaches
AI-enhanced CADD represents a paradigm shift from traditional computational methods, introducing self-learning algorithms capable of extracting complex patterns from large-scale biological data without explicit programming of every physical principle. Machine learning (ML), a subset of AI, employs statistical models and algorithms to analyze data, predict outcomes, and enhance decision-making processes in drug discovery [55]. Deep learning (DL), particularly through Deep Neural Networks (DNNs), has demonstrated exceptional capability in modeling generalized structure-activity relationships, enabling more accurate prediction of drug efficacy and safety profiles [55].
Convolutional Neural Networks (CNNs) have revolutionized analysis of structural and imaging data, while Graph Neural Networks (GNNs) excel at modeling molecular structures and interactions [55]. Generative AI techniques, including Generative Adversarial Networks (GANs), have enabled the creation of novel chemical entities with specified biological properties, dramatically accelerating the drug design process [92] [57]. Large Language Models (LLMs) and natural language processing (NLP) facilitate knowledge extraction from scientific literature, clinical texts, and biomedical databases, accelerating hypothesis generation and target identification in cancer research [93] [55]. These AI technologies integrate with traditional CADD approaches, enhancing their predictive power and expanding their application to previously intractable challenges in oncology drug discovery.
Table 1: Core Methodological Components of Traditional and AI-Enhanced CADD
| Component | Traditional CADD | AI-Enhanced CADD |
|---|---|---|
| Primary Techniques | Molecular docking, Molecular dynamics, QSAR, Virtual screening | Deep learning, Generative models, Graph neural networks, Natural language processing |
| Computational Requirements | High-performance computing for simulations | Specialized hardware (GPUs/TPUs) for model training and inference |
| Data Dependencies | Protein structures, compound libraries, experimental bioactivity data | Large-scale multi-omics data, clinical records, scientific literature, chemical databases |
| Key Outputs | Binding affinity predictions, structural models, compound rankings | Novel molecular structures, efficacy predictions, toxicity forecasts, patient stratification |
| Implementation Tools | AutoDock, GROMACS, MODELLER, Schrödinger suite | AlphaFold, TensorFlow, PyTorch, custom AI platforms |
Comparative Performance in Oncology Applications
Target Identification and Validation
In oncology drug discovery, target identification represents the critical first step in developing therapeutics against cancer-specific pathways. Traditional CADD approaches facilitate target identification through analysis of large-scale genomic data to identify mutations and gene expressions associated with cancer, utilizing conservation scores and structural analysis to predict druggable targets [50]. These methods depend heavily on existing biological knowledge and experimentally determined protein structures, which can limit their application to novel or poorly characterized targets.
AI-enhanced CADD dramatically accelerates target identification through data mining of diverse biomedical sources, including publications, patent information, proteomics, gene expression data, compound profiling, and transgenic phenotyping [57]. For example, AI-driven screening strategies have identified novel anticancer drugs targeting specific kinases like STK33, with AI systems integrating large databases combining public resources and manually curated information to describe therapeutic patterns between compounds and diseases [57]. The resulting candidates undergo validation through in vitro and in vivo studies to confirm mechanisms of action, such as apoptosis induction through STAT3 signaling pathway deactivation and cell cycle arrest [57]. AI systems can identify potential drug candidates for complex conditions like triple-negative breast cancer-derived brain metastasis (TNBC-BM), where traditional target discovery has struggled due to the lack of targeted therapies and difficulties in drug delivery to the brain [57].
Compound Screening and Optimization
Traditional CADD employs virtual screening to rapidly evaluate vast libraries of compounds through molecular docking algorithms, prioritizing candidates with favorable binding characteristics for experimental validation [36]. Fragment-based drug design (FBDD) represents another established approach, screening small molecular fragments against biological targets and then optimizing hit compounds through structural modification guided by QSAR modeling [50]. These methods successfully identify lead compounds but often require iterative design-test cycles that consume substantial time and resources.
AI-enhanced screening utilizes deep learning algorithms to analyze properties of millions of molecular compounds with dramatically improved speed and cost-effectiveness compared to conventional high-throughput screening [92]. Companies like Insilico Medicine have developed AI platforms that identified novel drug candidates for idiopathic pulmonary fibrosis in just 18 months, while Atomwise used convolutional neural networks to identify two drug candidates for Ebola in less than a day [92]. AI further enhances compound optimization through predictive models of physicochemical properties, biological activities, and binding affinities of new chemical entities, enabling rational design of molecules with improved potency, selectivity, and pharmacokinetic properties [92] [57].
Table 2: Performance Comparison in Key Oncology Drug Discovery Applications
| Application Area | Traditional CADD Performance | AI-Enhanced CADD Performance | Evidence/Examples |
|---|---|---|---|
| Target Identification | Moderate speed, limited to known biological mechanisms | High speed, capable of novel target discovery | AI identified STK33 inhibitor Z29077885; reduced discovery timeline from years to months [57] |
| Virtual Screening | 10,000-100,000 compounds per day | Millions of compounds per day | Atomwise identified Ebola drug candidates in <24 hours [92] |
| Molecular Design | Iterative design based on known scaffolds | Generative creation of novel scaffolds | Insilico Medicine designed novel IPF drug in 18 months [92] |
| Toxicity Prediction | Based on chemical similarity and QSAR models | Pattern recognition in high-dimensional data | Improved prediction of cardiotoxicity and hepatotoxicity [55] |
| Clinical Trial Optimization | Limited application | Digital twin technology for patient stratification | Unlearn's AI reduces control arm size by 30-50% in Phase III trials [94] |
Clinical Trial Optimization and Personalized Medicine
Traditional CADD has limited direct application to clinical trial design and personalized medicine, primarily contributing through better candidate selection to reduce late-stage failures. The high cost and extended timelines of clinical development remain significant challenges, with traditional trials for oncology drugs requiring extensive participants and lasting many years [57] [94].
AI-enhanced CADD introduces transformative approaches to clinical trials through digital twin technology, which creates AI-driven models simulating individual patient disease progression [94]. These models enable pharmaceutical companies to design trials with fewer participants while maintaining statistical power, significantly reducing both cost and duration. For example, Unlearn's AI technology can reduce control arm sizes in Phase III trials by 30-50%, particularly impactful in expensive therapeutic areas like oncology where costs can exceed $300,000 per subject [94]. AI also enhances patient recruitment and stratification by analyzing electronic health records to identify suitable candidates, especially valuable for rare cancers or specific molecular subtypes [92] [94]. Furthermore, AI facilitates drug repurposing by predicting compatibility of approved drugs with new oncology targets, as demonstrated by Benevolent AI's identification of baricitinib for COVID-19 treatment, highlighting the approach's potential for oncology applications [92].
Experimental Protocols and Implementation
Protocol for AI-Driven Target Identification in Oncology
The following protocol outlines a representative methodology for AI-enhanced target identification in oncology research, integrating multiple data modalities and validation steps:
Step 1: Data Curation and Integration
- Collect multi-omics data including genomic sequences, transcriptomic profiles, epigenomic markers, and proteomic expressions from public repositories (TCGA, COSMIC, DepMap) and proprietary sources [93] [57].
- Implement natural language processing (NLP) algorithms to extract target information from scientific literature, clinical trial reports, and patent databases, establishing known associations between biological targets and cancer phenotypes [93] [55].
- Apply data harmonization techniques to standardize heterogeneous datasets, addressing variations in experimental protocols, measurement techniques, and data formats [95].
Step 2: Target Prioritization using Machine Learning
- Implement graph neural networks (GNNs) to model complex relationships between genes, proteins, pathways, and cancer phenotypes, identifying central nodes in cancer-specific networks [55].
- Train supervised learning models (e.g., random forest, gradient boosting) on known cancer targets to identify patterns in molecular features, pathway involvement, and druggability characteristics [57].
- Apply feature importance analysis to prioritize targets based on multiple criteria including essentiality in cancer cell survival, specificity to cancer versus normal tissues, and structural feasibility for drug binding [57] [50].
Step 3: Experimental Validation
- Conduct in vitro assays using cancer cell lines to validate target essentiality through CRISPR knockout or RNA interference, measuring impact on cell proliferation, apoptosis, and migration [57].
- Perform molecular dynamics simulations using traditional CADD tools (GROMACS, NAMD) to characterize target-ligand interactions and binding stability for prioritized targets [36] [50].
- Initiate in vivo studies in appropriate animal models to confirm therapeutic effects of target modulation, evaluating tumor growth reduction and overall survival improvement [57].
Protocol for Generative Molecular Design in Oncology
This protocol describes an integrated AI-traditional CADD workflow for generating novel anti-cancer compounds using generative deep learning approaches:
Step 1: Chemical Space Definition and Training
- Curate comprehensive libraries of known bioactive molecules with anti-cancer properties, incorporating structural information, biological activity data, and ADMET (Absorption, Distribution, Metabolism, Excretion, Toxicity) profiles [92] [55].
- Train generative adversarial networks (GANs) or variational autoencoders (VAEs) on the chemical space of known anti-cancer compounds, enabling the models to learn underlying structural patterns associated with desired biological activities [92] [57].
- Implement transfer learning from general chemical databases to oncology-specific compounds to enhance model performance despite limited oncology-specific data [94].
Step 2: Structure-Based Generation and Optimization
- Integrate protein structure predictions from AlphaFold2 or ESMFold to enable structure-based generation focused on specific cancer targets [36] [55].
- Employ reinforcement learning to optimize generated structures for multiple objectives including binding affinity, selectivity, solubility, and synthetic accessibility [92] [57].
- Apply traditional molecular docking (AutoDock Vina, Glide) as a filtering step to validate AI-generated compounds, ensuring computational predictions align with physical principles [36] [55].
Step 3: Multi-Property Optimization and Selection
- Implement quantitative structure-activity relationship (QSAR) models to predict potency against specific cancer targets and selectivity over related off-targets [36] [50].
- Use ADMET prediction models to forecast pharmacokinetic properties and potential toxicity liabilities, prioritizing compounds with favorable drug-like characteristics [92] [55].
- Select lead candidates for synthetic feasibility assessment and experimental validation through in vitro and in vivo studies [57].
AI and Traditional CADD Workflow Integration
Research Reagent Solutions: Essential Tools for CADD in Oncology
Table 3: Essential Research Reagents and Computational Tools for CADD in Oncology
| Category | Specific Tools/Platforms | Primary Function | Application Context |
|---|---|---|---|
| Structure Prediction | AlphaFold2, ESMFold, Rosetta, MODELLER | Protein 3D structure prediction | Target characterization and binding site identification [36] |
| Molecular Docking | AutoDock Vina, Glide, GOLD, DOCK | Ligand-receptor binding pose and affinity prediction | Virtual screening and binding mode analysis [36] [50] |
| Dynamics Simulation | GROMACS, NAMD, CHARMM, OpenMM | Time-dependent molecular behavior simulation | Binding stability and conformational change analysis [36] [50] |
| AI/ML Frameworks | TensorFlow, PyTorch, Scikit-learn | Model development and training | Predictive modeling and generative design [92] [55] |
| Chemical Databases | PubChem, ChEMBL, ZINC, DrugBank | Compound structures and bioactivity data | Training data for AI models and virtual screening libraries [36] [55] |
| Visualization Software | PyMOL, Chimera, Schrodinger Suite | Molecular structure visualization and analysis | Results interpretation and presentation [36] [50] |
Challenges and Future Perspectives
Technical and Implementation Challenges
Both traditional and AI-enhanced CADD approaches face significant challenges in oncology applications. Traditional CADD methods struggle with computational intensity, particularly for molecular dynamics simulations that require substantial resources to achieve biologically relevant timescales [55]. These methods also face limitations in accurately modeling complex biological systems, often oversimplifying the dynamic nature of protein-ligand interactions and cellular environments [36] [54]. The heavy dependence on high-quality structural data presents another constraint, as many oncology targets lack experimentally determined structures or exist in conformational states difficult to capture crystallographically [36].
AI-enhanced CADD confronts distinct challenges including data quality and availability issues, where limited, biased, or noisy training data can lead to inaccurate predictions and limited generalizability [92] [95]. The "black box" nature of many complex AI models creates interpretability and trust barriers, particularly in highly regulated pharmaceutical development environments where understanding mechanism of action is crucial [92] [94]. Integration with existing drug discovery workflows presents practical implementation hurdles, while ethical considerations around data privacy, algorithm bias, and intellectual property require careful navigation [92] [95]. Reproducibility remains a critical challenge across computational sciences, with one Nature survey indicating that over 70% of researchers have tried and failed to reproduce another scientist's experiments [95].
Emerging Trends and Future Directions
The convergence of traditional and AI-enhanced CADD methodologies represents the most promising future direction, leveraging the physical principles and interpretability of traditional approaches with the pattern recognition and generative capabilities of AI [55] [95]. Hybrid models that incorporate known biological mechanisms with data-driven AI predictions are increasingly addressing challenges of data sparsity, particularly for novel cancer targets or rare cancer subtypes [95]. Quantum computing applications promise to revolutionize molecular simulations, potentially solving complex quantum mechanical calculations that are currently computationally prohibitive [36].
Ethical open science initiatives that enable data sharing while protecting patient privacy will be crucial for advancing AI in oncology CADD, requiring detailed informed consent processes, data quality assurance, and secure sharing platforms [95]. Federated learning approaches that train AI models across distributed datasets without centralizing sensitive information offer particular promise for leveraging real-world oncology data while maintaining privacy [94]. As these technologies evolve, the future of CADD in oncology will increasingly focus on personalized cancer therapy, with AI-driven approaches designing bespoke treatment regimens based on individual patient genomics, proteomics, and clinical characteristics [93] [55].
CADD Challenges and Future Solutions
The comparative analysis of traditional versus AI-enhanced CADD approaches reveals a complementary relationship rather than a competitive one in oncology drug discovery. Traditional CADD methodologies provide physically-grounded, interpretable frameworks for understanding molecular interactions, while AI-enhanced approaches offer unprecedented speed, pattern recognition capabilities, and generative power for exploring novel chemical spaces. The integration of both paradigms represents the most promising path forward, combining the mechanistic understanding of traditional methods with the predictive and generative capabilities of AI.
As computational technologies continue to evolve, the distinction between traditional and AI-enhanced CADD will likely blur, giving rise to hybrid models that leverage the strengths of both approaches. This synergistic integration holds particular promise for addressing the complex challenges of oncology drug discovery, where the heterogeneity of cancer, development of resistance mechanisms, and need for personalized therapeutic approaches demand increasingly sophisticated computational strategies. The future of CADD in oncology will be characterized by more predictive, personalized, and efficient drug discovery pipelines, ultimately contributing to improved outcomes for cancer patients worldwide.
Within the core principles of computer-aided drug design (CADD) in oncology, the ultimate measure of a computational model's value is its successful translation to clinically beneficial patient outcomes. The journey from in silico prediction to validated clinical impact presents a significant challenge, necessitating rigorous validation frameworks. Clinical validation establishes the critical correlation between a model's predictions and real-world therapeutic efficacy, safety, and overall patient prognosis. In the dynamic field of oncology, where patient characteristics, medical practices, and technologies evolve rapidly, this process is not a one-time event but requires continuous assessment to ensure model robustness and relevance over time [96]. This guide details the methodologies and protocols for establishing and evaluating this essential correlation, providing a technical roadmap for researchers and drug development professionals.
Foundational Concepts and Challenges
Clinical validation in oncology must account for the non-stationary nature of real-world clinical environments. Temporal distribution shifts, often summarized under 'dataset shift', arise from factors such as emerging therapies, updates to disease classification systems (e.g., the AJCC Cancer Staging System), and changes in coding practices (e.g., the ICD-9 to ICD-10 transition) [96]. These shifts can lead to:
- Feature Drift: The statistical properties of input variables change over time. For instance, therapies once considered standard of care may become obsolete, altering the feature space for predictive models.
- Label Drift: The relationship between features and the target outcome variable evolves. New therapies might reduce hospitalizations due to certain adverse events while introducing new ones, thereby changing the underlying patterns models must learn [96].
A systematic review of implemented clinical prediction models revealed that while 63% were integrated into hospital information systems, only 13% were updated after implementation, and a mere 27% underwent external validation [97]. This highlights a significant gap in the lifecycle management of clinical models and underscores the necessity for the robust validation strategies outlined in this document.
Quantitative Frameworks for Performance Assessment
A multi-faceted approach to performance assessment is crucial for a comprehensive understanding of a model's clinical utility. The following metrics, derived from a systematic review of implemented models, provide a baseline for comparison [97].
Table 1: Key Performance Metrics for Clinical Prediction Models in Oncology
| Metric | Description | Typical Benchmark in Clinical Context |
|---|---|---|
| Area Under the Curve (AUC) | Measures the model's ability to discriminate between positive and negative outcomes across all classification thresholds. | AUC > 0.70 is often considered acceptable, though >0.80 is desirable for high-stakes decisions [97]. |
| Calibration | Assesses the agreement between predicted probabilities and observed frequencies of the outcome. | Evaluated via calibration plots or statistics; 32% of implemented models assessed this at internal validation [97]. |
| Events per Predictor (EpP) | The number of outcome events relative to the number of predictor variables in the model. | A higher ratio (e.g., EpP >10) helps mitigate overfitting and ensures model stability [97]. |
Beyond these static metrics, temporal validation is paramount. This involves training a model on data from one time period and validating it on data from a subsequent, future period. For example, a framework applied to predict Acute Care Utilization (ACU) in cancer patients highlighted fluctuations in features and labels over a 12-year period (2010-2022), revealing moderate signs of drift and emphasizing the need for temporal considerations to ensure model longevity [96].
Table 2: Analysis of Clinical Prediction Model Implementation and Validation Practices
| Aspect | Finding from Systematic Review | Implication for Clinical Validation |
|---|---|---|
| External Validation | Performed for only 27% of models [97]. | Highlights a major weakness; robust validation requires testing on external, independent datasets. |
| Calibration Assessment | 32% of models assessed calibration during development/validation [97]. | Indicates a common oversight, as poor calibration can lead to clinically harmful miscalibrated risk estimates. |
| Post-Implementation Updating | Only 13% of models were updated after implementation [97]. | Underscores the critical need for continuous monitoring and model refinement to counteract performance decay. |
| Primary Implementation Route | Hospital Information Systems (63%) [97]. | Suggests integration into clinical workflows is a primary goal, necessitating real-world validation. |
Experimental Protocols for Validation
Protocol 1: Temporal Validation for Model long-term viability
This protocol is designed to diagnose and mitigate the effects of temporal dataset shift.
1. Objective: To evaluate the stability and longevity of a clinical prediction model over time and determine the optimal retraining strategy. 2. Materials & Data:
- Data Source: Time-stamped Electronic Health Records (EHR) from patients who initiated antineoplastic therapy between 2010 and 2022 [96].
- Cohort Definition: Patients with solid cancers receiving systemic therapy. Exclude patients under 18, those diagnosed externally, or with hematologic malignancies [96].
- Feature Set: Demographics, vitals, lab results, diagnosis and procedure codes (e.g., top 100 diagnoses, top 200 procedures per year), and medications from the 180 days preceding therapy initiation. The most recent value is used for each feature [96].
- Label: Binary indicator for Acute Care Utilization (ACU), defined as an emergency department visit or hospitalization within 180 days of therapy initiation, associated with symptoms from the CMS OP-35 criteria [96]. 3. Methodology:
- Data Splitting: Partition data by year of treatment initiation. For example, use data from 2010-2018 for training and 2019-2022 for prospective testing [96].
- Model Training: Implement multiple model types (e.g., LASSO, Random Forest, XGBoost) using a nested 10-fold cross-validation on the training set for hyperparameter optimization [96].
- Performance Evaluation: Validate the model on two independent test sets: 1) a randomly selected 10% hold-out from the training period (internal validation), and 2) the prospective data from future years [96].
- Drift Analysis: Characterize the temporal evolution of key features and the outcome (ACU rate). Apply data valuation algorithms to identify which historical data points are most relevant for future predictions [96]. 4. Outputs:
- Model performance metrics (AUC, calibration) over time.
- Analysis of feature and label drift.
- Recommendation on retraining schedule (e.g., sliding window vs. incremental learning).
Protocol 2: AI-Driven Biomarker Discovery and Correlation with Therapeutic Response
This protocol leverages AI to identify biomarkers from complex datasets and validates their correlation with patient outcomes.
1. Objective: To discover and validate complex biomarker signatures that predict response to oncology therapeutics using AI. 2. Materials & Data:
- Multi-omics Data: Genomic (e.g., from TCGA), transcriptomic, proteomic, and metabolomic data from tumor samples [23].
- Clinical Outcome Data: Progression-free survival, overall survival, and objective response rates from clinical trials or real-world data [23].
- Pathology Images: Digitized histopathology slides [23].
- Liquid Biopsy Data: Circulating tumor DNA (ctDNA) sequencing results [23]. 3. Methodology:
- Data Integration: Use machine learning (ML) and deep learning (DL) algorithms to integrate multi-omics data and uncover hidden patterns associated with treatment response [23].
- Biomarker Identification:
- For pathology images, train convolutional neural networks (CNNs) to identify histomorphological features correlating with response to treatments like immune checkpoint inhibitors [23].
- For ctDNA data, apply ML models to detect resistance mutations and minimal residual disease.
- Validation: Correlate the AI-identified biomarker signatures with clinical outcomes in a hold-out validation cohort or an independent dataset. Perform statistical analysis (e.g., Cox proportional hazards models) to establish the biomarker's prognostic value. 4. Outputs:
- A validated biomarker signature predictive of therapeutic response.
- An assessment of the biomarker's clinical utility for patient stratification.
The Scientist's Toolkit: Research Reagent Solutions
The following tools and resources are essential for conducting the experimental protocols described in this guide.
Table 3: Essential Research Reagents and Resources for Clinical Validation
| Item / Resource | Function in Clinical Validation |
|---|---|
| Electronic Health Record (EHR) Data | Provides real-world, longitudinal patient data for model training and temporal validation. Serves as the source for features and outcomes [96]. |
| Multi-omics Datasets (e.g., TCGA) | Genomic, transcriptomic, and proteomic data used for AI-driven biomarker discovery and linking molecular profiles to clinical outcomes [23]. |
| Machine Learning Libraries (e.g., Scikit-learn, TensorFlow/PyTorch) | Provide algorithms (LASSO, XGBoost, Neural Networks) for building and training predictive models from complex clinical data [96] [23]. |
| Natural Language Processing (NLP) Tools | Extract structured information from unstructured clinical notes and biomedical literature to enrich feature sets and identify eligible patients for trials [23]. |
| Digital Pathology Platforms | Digitize histopathology slides for analysis by deep learning models to identify predictive histomorphological features [23]. |
| ctDNA Analysis Kits | Enable liquid biopsy-based biomarker discovery and monitoring of resistance mutations from blood samples [23]. |
| Clinical Decision Support System (CDSS) Interfaces | Platforms for integrating validated models into clinical workflows (e.g., Hospital Information Systems) to enable point-of-care predictions and impact assessment [97] [98]. |
Application in Oncology Drug Development
The clinical validation of computational predictions is deeply interwoven with the modern oncology drug development pipeline. AI's role in accelerating this pipeline is demonstrated by cases such as Insilico Medicine, which used its AI platform to identify a preclinical candidate for a target in idiopathic pulmonary fibrosis in under 18 months, a process that traditionally takes 3–6 years [23]. Similar approaches are being applied in oncology. The validated correlation between prediction and outcome is critical at several stages:
- Target Identification: AI integrates multi-omics data to uncover novel oncogenic drivers and therapeutic vulnerabilities. For example, BenevolentAI predicted novel targets in glioblastoma by integrating transcriptomic and clinical data [23].
- Clinical Trial Optimization: Validated models can mine EHRs to identify eligible patients, dramatically accelerating recruitment. Furthermore, AI can predict trial outcomes through simulation models, enabling adaptive trial designs that improve the efficiency of validating new drugs [23].
- Personalized Oncology: The culmination of this process is the ability to match patients with optimal therapies based on their unique molecular and clinical profile. AI-driven biomarker discovery facilitates this by linking complex signatures to drug response, thereby improving efficacy and reducing toxicity [98] [23].
The development of new oncology therapeutics is a critical yet notoriously expensive and time-consuming endeavor. Conventional drug discovery processes typically span 12–15 years and require financial investments ranging from $1 billion to $2.6 billion per approved drug [28] [99]. A significant challenge is the high attrition rate; only about 10% of drug candidates entering clinical trials ultimately reach the market, embedding the cost of numerous failures into the price of each successful therapy [99]. Within this economic landscape, the cost of clinical trials alone constitutes 60–70% of the total R&D expenditure, with Phase III oncology trials alone costing tens of millions of dollars [100]. These formidable timelines and costs underscore the urgent need for innovative strategies that can enhance efficiency.
Computer-Aided Drug Design (CADD) has emerged as a transformative approach to mitigate these challenges. By leveraging computational power, bioinformatics, and molecular modeling, CADD aims to accelerate discovery, optimize lead compounds, and reduce reliance on costly and time-consuming wet-lab experiments [54] [101]. This whitepaper provides a quantitative assessment of the economic value delivered by CADD within oncology research. It synthesizes current data, presents structured comparisons of development metrics, details key methodologies, and projects the future impact of integrating artificial intelligence (AI) on the cost and timeline of bringing new cancer therapies to patients.
Quantitative Analysis of CADD's Economic Impact
The value proposition of CADD can be quantified through its direct effect on key metrics such as hit rates, timelines, and associated costs. The data below demonstrate that a computational approach significantly outperforms traditional methods in the early, pre-clinical stages of drug discovery.
Table 1: Comparative Hit Rates and Costs: Traditional HTS vs. Virtual HTS (vHTS)
| Screening Method | Number of Compounds Screened | Hit Rate | Relative Cost and Workload |
|---|---|---|---|
| Traditional HTS | 400,000 | 81 hits (0.021%) | High (physical screening of large compound libraries) |
| Virtual HTS (vHTS) | 365 | 127 hits (~35%) | Dramatically reduced (targeted computational screening) |
The case study of tyrosine phosphatase-1B inhibitors illustrates this efficiency, where vHTS achieved a hit rate nearly 1,600 times greater than traditional HTS while screening only a tiny fraction of the compounds [101].
Table 2: Impact of CADD on Key Drug Development Metrics
| Development Metric | Traditional Process | With CADD Integration | Key CADD Contribution |
|---|---|---|---|
| Discovery Timeline | 12–15 years [28] | Significantly reduced | Accelerated target identification, hit discovery, and lead optimization [99] |
| Probability of Success | ~10% from clinical trials to market [99] | Improved | Better prediction of efficacy and toxicity, reducing late-stage attrition [101] |
| Clinical Trial Cost Share | 60–70% of total R&D cost [100] | Reduced relative burden | Lower pre-clinical costs and more optimized candidates entering trials improve overall R&D efficiency. |
The economic benefit of CADD is not limited to the discovery phase. By enabling the identification of more promising drug candidates and optimizing their properties early on, CADD reduces the risk of costly late-stage failures, thereby improving the overall return on investment in pharmaceutical R&D [101].
Core Methodologies and Experimental Protocols in CADD
CADD strategies are broadly classified into two categories: structure-based and ligand-based approaches. The following section outlines the foundational methodologies and experimental protocols that define these approaches in modern oncology drug discovery.
Structure-Based Drug Design (SBDD)
SBDD relies on three-dimensional structural information of the biological target, typically obtained from X-ray crystallography, NMR, or cryo-EM.
- Molecular Docking Protocol: This is a core SBDD method used to predict the preferred orientation of a small molecule (ligand) when bound to its target (receptor).
- Target Preparation: The protein structure is prepared by adding hydrogen atoms, assigning partial charges, and defining the binding site residues.
- Ligand Preparation: Small molecule structures are energy-minimized and their geometries are optimized.
- Docking Simulation: The ligand is computationally posed within the target's binding site. The software evaluates millions of possible conformations and orientations.
- Scoring and Ranking: Each pose is scored using a scoring function that estimates the binding free energy. The top-ranked poses with the most favorable (lowest) scores are selected for further analysis [54] [101].
- Molecular Dynamics (MD) Simulation Protocol: MD provides a dynamic view of the ligand-target interaction, going beyond the static picture from docking.
- System Solvation and Ionization: The protein-ligand complex is placed in a box of water molecules, and ions are added to simulate physiological conditions.
- Energy Minimization: The system's energy is minimized to remove steric clashes.
- Equilibration: The temperature and pressure of the system are gradually raised to the desired values (e.g., 310 K, 1 atm) to mimic a biological environment.
- Production Run: A multi-nanosecond simulation is run, during which the coordinates of all atoms are saved at regular intervals for subsequent analysis of stability and interaction dynamics [54] [18].
Ligand-Based Drug Design (LBDD)
When the 3D structure of the target is unavailable, LBDD methods are employed, which use the information from known active and inactive molecules.
- Quantitative Structure-Activity Relationship (QSAR) Modeling Protocol: This method correlates measurable molecular properties (descriptors) of compounds with their biological activity.
- Descriptor Calculation: Numerical descriptors (e.g., molecular weight, logP, topological indices) are calculated for a set of compounds with known activities.
- Model Training: A machine learning algorithm (e.g., partial least squares, random forest) is trained to find a mathematical relationship between the descriptors and the biological activity.
- Model Validation: The model's predictive power is tested using a separate set of compounds not used in training.
- Activity Prediction: The validated model is used to predict the activity of new, untested compounds, prioritizing the most promising ones for synthesis and testing [101].
AI-Driven Drug Discovery Protocols
AI and machine learning are now revolutionizing CADD by integrating diverse data types and enabling de novo molecular design.
- AI-Driven Target Identification (e.g., BANDIT): This Bayesian machine learning method integrates six types of data—including growth inhibition, gene expression, adverse reaction, and chemical structure—to predict drug targets with approximately 90% accuracy [99].
- End-to-End Deep Learning Framework (e.g., DrugAppy): This framework exemplifies a modern, integrated AI workflow:
- High-Throughput Virtual Screening (HTVS): Uses AI-driven docking tools (like SMINA/GNINA) to screen ultra-large virtual libraries.
- AI-Based Property Prediction: Employs models trained on public datasets to predict key parameters such as pharmacokinetics, selectivity, and potential activity.
- MD Simulation Validation: Utilizes MD (e.g., with GROMACS) to validate the stability of predicted ligand-target complexes. This workflow has been successfully validated through the identification of novel inhibitors for PARP1 and TEAD4, with activity matching or surpassing reference inhibitors [102].
CADD Workflow: From Target to Lead Compound
The Scientist's Toolkit: Essential Research Reagents and Computational Solutions
The effective application of CADD relies on a suite of software tools, databases, and computational resources that constitute the modern drug developer's toolkit.
Table 3: Key Research Reagent Solutions in Computational Oncology
| Tool/Resource Name | Type | Primary Function in CADD |
|---|---|---|
| GROMACS | Software / MD Tool | Performs molecular dynamics simulations to analyze the stability and dynamics of protein-ligand complexes [102]. |
| SMINA/GNINA | Software / Docking Tool | Conducts high-throughput virtual screening by predicting ligand binding poses and scoring their affinity [102]. |
| DrugAppy Framework | Integrated AI Platform | An end-to-end workflow that combines AI, HTVS, and MD for the identification and optimization of novel inhibitors [102]. |
| Knowledge Graph (KG) | Data Resource / AI Component | Represents complex biological relationships (e.g., between genes, diseases, drugs) to train GNNs for target prediction (e.g., KG4SL for synthetic lethality) [99]. |
| Omics Databases (TCGA, etc.) | Data Resource | Provides genomic, proteomic, and clinical data for target identification and validation through bioinformatic analysis [18]. |
| Molecular Docking Software | Software / Docking Tool | Assesses the binding efficacy and orientation of drug compounds to their protein targets, a primary step in virtual screening [1]. |
The Future of CADD: AI Integration and Market Evolution
The CADD landscape is rapidly evolving, driven by advances in artificial intelligence and machine learning. The CADD market is witnessing the fastest growth in the AI/ML-based drug design segment, which is revolutionizing data analysis and predictive accuracy [1]. These technologies are enhancing the prediction of drug-target interactions (DTI) even without 3D structural information, using models like graph convolutional networks (e.g., EEG-DTI, DTI-HETA) [99]. Furthermore, the industry is moving toward hybrid and cloud-based deployment modes, which facilitate remote collaboration and provide scalable computational power without significant upfront infrastructure investment [1].
Clinical trials are also becoming a focus for optimization, as they represent the most costly phase of development. Trials have increased in complexity over the past decade, a factor correlated with longer durations [103]. AI is now being piloted to improve clinical trial recruitment by analyzing electronic health records and genomic data, potentially reducing recruitment timelines and ensuring novel therapies reach the most suitable patients faster [104]. The future economic impact of CADD will be amplified by its ability to not only design better drug candidates but also to streamline their path through clinical testing.
Emerging CADD Trends and Their Impacts
The integration of Computer-Aided Drug Design into oncology research represents a paradigm shift with a demonstrably positive economic impact. By leveraging computational methodologies—from molecular docking and dynamics to advanced AI algorithms—CADD significantly accelerates the early drug discovery timeline and reduces the associated costs. This is achieved through dramatically higher hit rates in virtual screens, better-optimized lead compounds with reduced toxicity, and a lower likelihood of costly late-stage clinical failure. As AI and cloud-based technologies continue to mature, their deep integration into the CADD workflow promises to further enhance the precision, speed, and cost-effectiveness of developing the next generation of oncology therapeutics. For researchers and drug development professionals, the adoption and mastery of these computational tools are no longer optional but essential for achieving success in the competitive and critically important field of cancer drug discovery.
The field of computer-aided drug discovery (CADD) has undergone transformative changes, becoming a central paradigm in oncology research for developing cost-effective and resource-efficient solutions [4]. Advances in computational power now enable researchers to explore chemical spaces beyond human capabilities, construct extensive compound libraries, and efficiently predict molecular physicochemical properties and biological activities [4]. Artificial intelligence (AI) is now deeply integrated throughout the drug discovery process, accelerating critical stages including target identification, candidate screening, pharmacological evaluation, and quality control [4]. This approach not only shortens development timelines but also reduces research risks and costs.
In oncology, particularly for complex malignancies like breast cancer with its distinct molecular subtypes (Luminal, HER2-positive, and triple-negative), CADD has emerged as a valuable strategy to accelerate therapeutic discovery and improve lead optimization [84]. The clinical management of breast cancer is strongly influenced by molecular heterogeneity, with each subtype showing distinct therapeutic vulnerabilities [84]. Despite advances in targeted therapies, intrinsic and acquired resistance continue to limit long-term benefits, underscoring the need for novel computational approaches tailored to subtype-specific vulnerabilities [84]. This review examines three transformative frontiers—quantum computing, enhanced biomarker integration, and personalized therapy design—that promise to address these challenges and revolutionize oncology drug discovery.
Foundations of Computer-Aided Drug Design in Oncology
Core Computational Methods and Workflows
CADD in oncology relies on accurate three-dimensional representations of molecular targets, employing both structure-based and ligand-based approaches [84]. When experimental coordinates are unavailable or incomplete, homology modeling and molecular dynamics (MD) are used to refine binding-site geometries and explore relevant conformational ensembles [84]. High-accuracy predictors such as AlphaFold 3 and ColabFold routinely provide starting models that can be refined and validated with MD before iterative design [84].
Structure-based virtual screening employs classical docking to enumerate poses and estimate affinities, with AutoDock family programs and commercial engines remaining standard for large-scale library exploration [84]. Learning-based pose generators, such as DiffDock and EquiBind, accelerate conformational sampling and enable hybrid pipelines where deep-learning outputs are subsequently rescored using physics-based methods [84]. For potency refinement, relative binding free-energy (RBFE) calculations based on alchemical methods and λ-dynamics provide quantitative ΔΔG estimates when rigorous system preparation and sampling protocols are enforced [84].
Table 1: Core Computational Methods in Modern CADD Pipelines
| Method Category | Specific Techniques | Primary Application in Oncology |
|---|---|---|
| Structure-Based Design | Molecular Docking, Molecular Dynamics (MD) Simulations, Relative Binding Free-Energy (RBFE) Calculations | Predicting ligand-receptor binding modes, simulating protein dynamics, calculating binding affinities |
| Ligand-Based Design | Quantitative Structure-Activity Relationship (QSAR), Pharmacophore Modeling | Identifying structure-activity trends for targets with unknown structures |
| AI-Enhanced Methods | Deep QSAR, Generative AI, Diffusion Models, Deep Learning Scoring Functions | Multi-parameter optimization, de novo molecular generation, enhancing hit rates and scaffold diversity |
| Hybrid Methods | AI-Structure/Ligand-Based Virtual Screening, Physics-Informed Machine Learning | Rapid triage of chemical space with mechanistic validation |
Subtype-Specific Applications in Oncology
The clinical and molecular heterogeneity of cancer necessitates subtype-specific design strategies, and CADD has emerged as a versatile tool to support such tailored interventions [84]. In luminal breast cancer, computational workflows have facilitated the development of next-generation selective estrogen receptor degraders (SERDs) and related molecules that overcome endocrine resistance by accounting for receptor pocket plasticity and mutational landscapes within docking, QSAR, and RBFE pipelines [84]. In HER2-positive disease, structure prediction and antibody/kinase-inhibitor modeling inform affinity maturation and selectivity optimization, while physics-based rescoring helps discriminate among compounds with subtle hinge-binding or allosteric differences [84]. For triple-negative breast cancer (TNBC), multi-omics-guided target triage integrated with structure- and ligand-based prioritization has advanced PARP-centered therapies and epigenetic modulators, with AI-driven models further supporting biomarker discovery and drug sensitivity prediction [84].
Quantum Computing in Drug Discovery
Fundamental Principles and Potential Applications
Quantum computing represents a paradigm shift in computational capability for drug discovery, leveraging principles of quantum mechanics such as superposition and entanglement to solve problems intractable for classical computers [105]. By employing qubits, which can exist in multiple states simultaneously, quantum systems can perform complex calculations exponentially faster, potentially reducing drug development timelines from years to days [105]. In pharmacology, quantum algorithms are particularly suited for modeling quantum-level interactions, such as protein folding and molecular simulations, which are fundamentally quantum mechanical in nature [105].
Quantum computing addresses the computational limitations of classical systems in simulating quantum-level interactions, such as protein folding and molecular dynamics [105]. A 2025 study used a hybrid quantum-classical model to design novel cancer drug candidates targeting the KRAS protein, demonstrating the practical application of this technology in oncology [105]. Quantum-optimized models can forecast interactions in chemotherapy regimens, tailoring treatments to individual patients and minimizing side effects [105]. A Science study highlighted how quantum simulations accelerated antiviral screening, potentially reducing costs by 30% [105].
Table 2: Potential Clinical Applications and Status of Quantum Computing in Oncology
| Application Area | Key Potential Impact | Current Stage / Example |
|---|---|---|
| Drug Discovery & Development | Simulate molecular interactions and protein folding exponentially faster, reducing discovery time from years to months | A 2025 study used a hybrid quantum-classical model to design novel cancer drug candidates targeting the KRAS protein [105] |
| Personalized Medicine | Analyze genomic data and environmental factors to optimize and tailor treatment plans for individual patients | Quantum algorithms could model genetic mutations in cancer to predict the most effective drug for a specific patient's profile [105] |
| Medical Imaging & Diagnostics | Enhance resolution and reduce noise in MRI and CT scans, leading to earlier and more accurate tumor detection | Quantum sensors have been developed to image the conductivity of live heart tissue with 50-times greater sensitivity for arrhythmia diagnosis [105] |
| Clinical Trial Optimization | Analyze vast datasets to improve patient matching for trials and enable real-time analysis of trial data | Quantum computing could help stratify patients based on genetic markers, increasing trial efficiency and success rate [105] |
Experimental Protocols for Quantum-Enhanced Molecular Simulations
Protocol 1: Hybrid Quantum-Classical Molecular Dynamics for Protein-Ligand Binding
System Preparation: Obtain the 3D structure of the target protein (e.g., KRAS) from experimental sources (PDB) or predicted structures from AlphaFold 3 [84]. Prepare the ligand topology using quantum chemistry packages (Gaussian, ORCA) to calculate partial charges and optimize geometry at the DFT level.
Force Field Parameterization: Use a hybrid MM/QM (Molecular Mechanics/Quantum Mechanics) approach where the binding pocket is treated with quantum mechanics (variational quantum eigensolver algorithms) while the rest of the system uses classical molecular mechanics.
Quantum Processing: Map the electronic structure problem of the active site to a quantum processor using the Jordan-Wigner or Bravyi-Kitaev transformation. Execute the simulation on quantum hardware (e.g., IBM Quantum, Google Sycamore) using variational quantum algorithms to solve the time-dependent Schrödinger equation.
Classical Integration: Integrate quantum-computed energies with classical MD simulations (using packages like AMBER or GROMACS) for the full system dynamics. Run adaptive sampling to explore binding pathways.
Analysis: Calculate binding free energies using quantum-mechanical scoring functions. Compare results with purely classical simulations (MM/PBSA, FEP+) for validation [84].
Protocol 2: Quantum Machine Learning for Toxicity Prediction
Data Encoding: Encode molecular structures (SMILES strings or fingerprints) into quantum states using amplitude encoding or quantum feature maps. Use curated ADMET datasets from public databases (ChEMBL, PubChem) for training.
Circuit Design: Implement a parameterized quantum circuit (PQC) with alternating layers of rotation and entanglement gates. The circuit depth and connectivity should be optimized for the specific quantum hardware.
Hybrid Training: Use a classical optimizer (Adam, SPSA) to tune the quantum circuit parameters, minimizing the difference between predicted and experimental toxicity values.
Inference: Execute the trained quantum model on new molecular candidates to predict ADMET properties with exponential speedup compared to classical ML models [4].
Diagram 1: Quantum-Classical Simulation Workflow
Research Reagent Solutions for Quantum-Enhanced Drug Discovery
Table 3: Essential Research Reagents and Platforms for Quantum-Enhanced Drug Discovery
| Item | Function | Example Products/Platforms |
|---|---|---|
| Quantum Processing Units (QPUs) | Execute quantum algorithms for molecular simulations | IBM Quantum processors, Google Sycamore, D-Wave Advantage |
| Quantum Chemistry Software | Calculate molecular properties and optimize geometries | Gaussian, ORCA, Psi4 |
| Hybrid Quantum-Classical Platforms | Integrate quantum computations with classical MD simulations | Qiskit Nature, PennyLane, Google TensorFlow Quantum |
| Classical MD Packages | Perform molecular dynamics simulations for system validation | AMBER, GROMACS, CHARMM |
| Curated Quantum Datasets | Train and validate quantum machine learning models | QM9, MoleculeNet, ChEMBL quantum subsets |
Enhanced Biomarker Integration
Multi-Omics Data Integration Strategies
The integration of multi-omics data (genomics, transcriptomics, proteomics, epigenomics) with CADD pipelines has become crucial for identifying robust biomarkers and therapeutic targets, especially for heterogeneous cancers [84]. AI-driven models further support biomarker discovery and drug sensitivity prediction by processing these complex, high-dimensional datasets to identify subtype-specific vulnerabilities [84]. In triple-negative breast cancer, multi-omics-guided target triage integrated with structure- and ligand-based prioritization has advanced PARP-centered therapies and epigenetic modulators [84].
The combination of public databases and machine learning models helps overcome structural and data limitations for historically undruggable targets [4]. Deep learning approaches can analyze imaging data with an accuracy of 95%, identifying tumor patterns for real-time treatment adjustments [105]. This technology facilitates personalized medicine by processing genomic sequences to predict risks for diseases, such as hereditary cancers, and extends to stratifying patients for clinical trials, ensuring that treatments align with each individual's biological profile [105].
Experimental Protocols for Multi-Omics Biomarker Discovery
Protocol 1: AI-Driven Biomarker Identification from Multi-Omics Data
Data Collection: Aggregate multi-omics data from diverse sources: whole exome/genome sequencing (genomics), RNA-Seq (transcriptomics), mass spectrometry (proteomics), and ChIP-Seq (epigenomics). Use public databases (TCGA, CPTAC, DepMap) and institutional cohorts.
Data Preprocessing: Normalize and batch-correct datasets using established pipelines (GATK for genomics, STAR for transcriptomics). Impute missing values using neural network-based methods.
Feature Selection: Apply multi-modal deep learning architectures (autoencoders, transformers) to extract relevant features from each data modality. Use attention mechanisms to identify the most predictive features.
Integration and Modeling: Fuse the extracted features using late or intermediate fusion strategies. Train predictive models (survival analysis, drug response prediction) using the integrated features. Validate on hold-out datasets.
Experimental Validation: Design experiments to validate top biomarkers using CRISPR screens, organoid models, or patient-derived xenografts (PDXs) [84].
Protocol 2: Spatial Transcriptomics for Tumor Microenvironment Characterization
Tissue Preparation: Collect fresh-frozen tumor specimens and prepare cryosections (10μm thickness). Use spatial transcriptomics platforms (10x Genomics Visium, NanoString GeoMx).
Library Preparation: Follow manufacturer protocols for probe hybridization, imaging, and library construction. Include unique molecular identifiers (UMIs) to account for amplification biases.
Sequencing and Data Generation: Sequence libraries on Illumina platforms. Align sequences to reference genomes and assign transcripts to spatial coordinates.
Computational Analysis: Identify spatially variable genes using trendspotting or SPARK algorithms. Cluster spatial regions to define tumor microenvironment niches. Integrate with single-cell RNA-Seq data for cell type deconvolution.
CADD Integration: Use spatial protein expression patterns to inform target prioritization in structure-based drug design, particularly for tumor microenvironment-specific targets [84].
Diagram 2: Multi-Omics Biomarker Integration Workflow
Research Reagent Solutions for Enhanced Biomarker Integration
Table 4: Essential Research Reagents and Platforms for Multi-Omics Biomarker Integration
| Item | Function | Example Products/Platforms |
|---|---|---|
| Spatial Transcriptomics Kits | Enable gene expression analysis with spatial context | 10x Genomics Visium, NanoString GeoMx DSP |
| Single-Cell Sequencing Kits | Profile omics data at single-cell resolution | 10x Genomics Chromium, Parse Biosciences Evercode |
| Multi-Omics Databases | Provide integrated datasets for analysis | TCGA, CPTAC, DepMap, GDSC |
| AI/ML Analysis Platforms | Analyze and integrate multi-omics data | TensorFlow, PyTorch, Monarch Initiative |
| Validation Reagents | Experimentally validate computational findings | CRISPR libraries, organoid culture kits, PDX models |
Personalized Therapy Design
Computational Approaches for Therapy Personalization
Personalized therapy design represents the culmination of advanced CADD approaches, leveraging individual patient data to tailor treatments for maximum efficacy and minimal toxicity [105]. Quantum computing supports personalized medicine by analyzing genomic data and environmental factors to predict drug efficacy [105]. For instance, quantum-optimized models can forecast interactions in chemotherapy regimens, tailoring treatments to individual patients and minimizing side effects [105]. AI-driven approaches can process genomic sequences to predict risks for diseases, such as hereditary cancers, and applications extend to stratifying patients for clinical trials, ensuring that treatments align with each individual's biological profile [105].
The integration of AI-driven in silico design with automated robotics for synthesis and validation, combined with iterative model refinement, can compress drug development timelines exponentially [4]. In practice, these methods link structural and dynamic models with data-driven analytics to generate decision-grade, subtype-aware hypotheses that can be prospectively tested [84]. For example, in luminal breast cancer, structure-guided optimization has accelerated the development of next-generation oral SERDs, such as elacestrant and camizestrant, which have demonstrated clinical benefit in patients with ESR1-mutant advanced breast cancer [84].
Experimental Protocols for Personalized Therapy Design
Protocol 1: Patient-Specific Virtual Clinical Trial
Patient Data Collection: Sequence the patient's tumor (whole exome or genome) and normal tissue. Perform RNA-Seq on the tumor sample. Collect clinical data including prior treatments, responses, and toxicities.
Digital Twin Creation: Generate a computational model of the patient's tumor incorporating: (a) a phylogenetic tree of the tumor based on mutation data, (b) a network model of signaling pathways based on transcriptomics, and (c) protein structure models of mutated proteins using AlphaFold 3 [84].
Drug Screening: Screen an extensive virtual compound library (10^6 - 10^9 compounds) against the patient-specific targets using molecular docking and MD simulations. Prioritize compounds based on binding affinity, specificity, and predicted penetration to tumor sites.
Response Prediction: Use systems pharmacology models to simulate drug exposure and effect on tumor signaling networks. Predict efficacy and potential resistance mechanisms. Use AI models to predict immune responses for immunotherapies.
Treatment Recommendation: Generate a ranked list of therapeutic options with predicted efficacy, potential toxicities, and likelihood of resistance development [84].
Protocol 2: PROTAC Design for Patient-Specific Mutations
Target Identification: Identify problematic proteins (e.g., mutated oncoproteins) from patient genomic data that are not druggable with conventional inhibitors.
E3 Ligase Selection: Select appropriate E3 ligases expressed in the patient's tumor based on transcriptomic data.
Ternary Complex Modeling: Use protein-protein docking and MD simulations to model the ternary complex (target-PROTAC-E3 ligase). AlphaFold-Multimer can provide initial structures [84].
Linker Optimization: Screen virtual linker libraries to identify optimal linkers that stabilize the ternary complex. Use free energy calculations to predict degradation efficiency.
Synthesis and Validation: Synthesize top PROTAC candidates and test degradation efficacy in patient-derived organoids or xenograft models [84].
Diagram 3: Personalized Therapy Design Workflow
Research Reagent Solutions for Personalized Therapy Design
Table 5: Essential Research Reagents and Platforms for Personalized Therapy Design
| Item | Function | Example Products/Platforms |
|---|---|---|
| Patient-Derived Model Systems | Maintain patient-specific biology for ex vivo testing | Organoid culture kits, PDX establishment services |
| Single-Cell Sequencing Platforms | Characterize tumor heterogeneity at cellular resolution | 10x Genomics Chromium, Berkeley Lights Beacon |
| High-Throughput Screening Platforms | Test drug candidates on patient-derived cells | Automated liquid handlers, high-content imagers |
| AI-Powered Clinical Decision Support | Integrate data for treatment recommendations | IBM Watson for Oncology, Tempus LENS |
| PROTAC Design Tools | Develop targeted protein degradation therapeutics | Schrödinger BioLuminate, OpenEye Toolkits |
Integrated Workflow and Future Outlook
The convergence of quantum computing, enhanced biomarker integration, and personalized therapy design represents a paradigm shift in oncology drug discovery. These technologies are not developing in isolation but are increasingly integrated into cohesive workflows that leverage the strengths of each approach. The future of CADD in oncology will be characterized by the tighter integration of AI, multi-omics data, and digital pathology, enabling the design of more precise, subtype-informed, and personalized therapeutic strategies [84].
Table 6: Key Challenges and Future Directions for Next-Generation CADD in Oncology
| Challenge Category | Specific Issues | Potential Mitigation Strategies |
|---|---|---|
| Technical Limitations | Qubit coherence/decoherence, hardware scalability, high error rates, and the need for cryogenic cooling [105] | Development of error-correcting codes, more stable qubit systems, and hybrid quantum-classical algorithms [105] |
| Data Integration Complexity | Heterogeneous data types, interoperability issues, and data quality concerns | Development of unified data standards, middleware for data integration, and federated learning approaches |
| Clinical Translation | Translating computational results into successful wet-lab experiments and clinical outcomes [4] | Improved experimental validation pipelines, organ-on-a-chip technologies, and microdosing studies |
| Ethical & Regulatory | Data privacy with genomic datasets, potential for bias in AI models, and lack of regulatory frameworks [105] | Development of quantum encryption for data security, creating diverse training datasets, and early engagement with regulatory bodies [105] |
The CADD market is rapidly advancing on a global scale, with expectations of accumulating hundreds of millions in revenue between 2025 and 2034 [1]. By technology, the AI/ML-based drug design segment is expected to show the fastest growth over the forecast period [1], indicating the increasing importance of these advanced computational approaches. North America held a major revenue share of approximately 45% of the computer-aided drug design (CADD) market in 2024, while Asia-Pacific is expected to host the fastest-growing market in the coming years [1], demonstrating the global nature of this transformation.
As these technologies mature, we anticipate a shift from population-averaged treatment strategies to truly personalized therapeutic approaches that account for individual patient biology, tumor microenvironment, and dynamic response to treatment. The integration of these advanced computational approaches with experimental validation will be crucial for realizing the full potential of next-generation CADD in oncology, ultimately leading to more effective and targeted cancer therapies.
Conclusion
Computer-aided drug design has fundamentally transformed oncology drug discovery by providing powerful computational frameworks that accelerate target identification, compound optimization, and clinical translation. The integration of AI and machine learning has enhanced predictive accuracy and enabled the development of novel therapeutic modalities like PROTACs and radiopharmaceutical conjugates. However, challenges remain in addressing tumor heterogeneity, improving clinical validation, and optimizing workflows for personalized medicine. Future directions will likely focus on enhanced biomarker integration, quantum computing applications, and the development of more sophisticated digital twins for clinical trial simulation. As CADD methodologies continue to evolve, they promise to further reduce development timelines and costs while increasing the precision and efficacy of cancer therapies, ultimately advancing toward more personalized and effective oncology treatments.
References
- 1. Computer-Aided Drug Design (CADD) Market Trends 2025 [https://www.towardshealthcare.com/insights/computer-aided-drug-design-cadd-market-sizing]
- 2. Computational-aided drug design strategies for drug ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12634332/]
- 3. Computer-Aided Drug Design (CADD) Market Competitive [https://www.globenewswire.com/news-release/2025/10/09/3164348/0/en/Computer-Aided-Drug-Design-CADD-Market-Competitive-Landscape-Report-Towards-Healthcare.html]
- 4. Convergence of Computer-Aided Drug Discovery and ... [https://www.sciencedirect.com/science/article/pii/S2773216925000388]
- 5. 2025 Computer Aided Drug Design Conference GRC [https://www.grc.org/computer-aided-drug-design-conference/2025/]
- 6. Structure and dynamics in drug discovery [https://www.nature.com/articles/s44386-024-00001-2]
- 7. Strategies for the drug development of cancer therapeutics [https://www.frontiersin.org/journals/pharmacology/articles/10.3389/fphar.2025.1656012/full]
- 8. Structure-Based vs Ligand-Based Drug Design [https://www.iaanalysis.com/structure-based-vs-ligand-based-drug-design.html]
- 9. Leveraging ligand-based and structure-based approaches ... [https://www.iptonline.com/articles/leveraging-ligand-based-and-structure-based-approaches-for-advan]
- 10. Combining Ligand- and Structure-Based Methods for More ... [https://www.genengnews.com/topics/drug-discovery/combining-ligand-and-structure-based-methods-for-more-effective-virtual-screening/]
- 11. Structure based drug design and machine learning ... [https://www.nature.com/articles/s41598-025-17708-5]
- 12. Structure-based and ligand-based drug discovery [https://optibrium.com/knowledge-base/leveraging-structure-based-and-ligand-based-drug-discovery/]
- 13. Computational transformation in drug discovery: A ... [https://www.sciencedirect.com/science/article/pii/S2949866X24000340]
- 14. A Review on Applications of Computational Methods in ... [https://www.mdpi.com/1420-3049/25/6/1375]
- 15. Molecular Docking: A powerful approach for structure-based ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3151162/]
- 16. Pharmacophore modeling in drug design [https://www.sciencedirect.com/science/article/abs/pii/S1054358925000109]
- 17. A (Comprehensive) Review of the Application ... [https://www.mdpi.com/2076-3417/15/3/1206]
- 18. Strategies for the drug development of cancer therapeutics [https://pmc.ncbi.nlm.nih.gov/articles/PMC12518319/]
- 19. Computational-aided drug design strategies for ... [https://www.frontiersin.org/journals/pharmacology/articles/10.3389/fphar.2025.1678652/full]
- 20. AI-Integrated QSAR Modeling for Enhanced Drug Discovery [https://pmc.ncbi.nlm.nih.gov/articles/PMC12525248/]
- 21. Drug design of an anticancer drug: QSAR modeling, and ... [https://www.sciencedirect.com/science/article/pii/S259012302502314X]
- 22. Integrating artificial intelligence into small molecule ... [https://www.nature.com/articles/s44386-025-00029-y]
- 23. Artificial Intelligence in Cancer Drug Discovery in 2025 [https://oncodaily.com/oncolibrary/artificial-intelligence-in-cancer-drug-discovery]
- 24. Transforming Cancer Therapy: Insights from 2025 H1 FDA ... [https://blog.crownbio.com/transforming-cancer-therapy-insights-from-2025-h1-fda-approvals-and-preclinical-drug-discovery]
- 25. The Evolution of AI Drug Discovery: Past, Present, and Future [https://hyperlab.hits.ai/en/blog/evolution_AIdrugdiscovery]
- 26. The future of pharmaceuticals: Artificial intelligence in drug ... [https://www.sciencedirect.com/science/article/pii/S2095177925000656]
- 27. Challenges of implementing computer-aided diagnostic ... [https://www.nature.com/articles/s41746-023-00868-x]
- 28. Artificial Intelligence-Driven Innovations in Oncology Drug ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12232943/]
- 29. History and status of CAD and quantitative image analysis ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC2673617/]
- 30. Leading AI-Driven Drug Discovery Platforms [https://www.sciencedirect.com/science/article/abs/pii/S0031699725075118]
- 31. Cancer models in preclinical research: A chronicle review of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8212826/]
- 32. AI Driven Drug Discovery: 5 Powerful Breakthroughs in 2025 [https://lifebit.ai/blog/ai-driven-drug-discovery/]
- 33. What is computer-aided drug design (CADD)? What is its ... [https://synapse.patsnap.com/article/what-is-computer-aided-drug-design-cadd-what-is-its-current-scenario-in-drug-discovery]
- 34. Integrating artificial intelligence in drug discovery and early ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11909971/]
- 35. Artificial Intelligence-Driven Computational Approaches in ... [https://pubmed.ncbi.nlm.nih.gov/39594838/]
- 36. Computer-Aided Drug Design and Drug Discovery [https://pmc.ncbi.nlm.nih.gov/articles/PMC10819513/]
- 37. Harnessing AI-Powered Computational Drug Design to ... [https://www.sciencedirect.com/science/article/pii/S3050787125001301]
- 38. Researchers develop AI that automatically designs optimal ... [https://ecancer.org/en/news/26879-researchers-develop-ai-that-automatically-designs-optimal-drug-candidates-for-cancer-targeting-mutations]
- 39. Enhance Drug Discovery with CADD and Agentic AI ... [https://resources.industrydive.com/enhancing-drug-discovery-efficiency-with-computer-aided-drug-design]
- 40. Computer-Aided Drug Design and Drug Discovery [https://www.mdpi.com/1424-8247/18/3/436]
- 41. Targeting Oncogenic Proteins for Drug Discovery [https://www.frontiersin.org/research-topics/70289/advancing-cancer-therapeutics-targeting-oncogenic-proteins-for-drug-discoveryundefined]
- 42. Progress in structure-based drug development targeting ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12183272/]
- 43. Advances in bridging computational and clinical outcomes ... [https://www.sciencedirect.com/science/article/pii/S2949829525001044]
- 44. Systematic identification of cancer pathways and potential ... [https://www.nature.com/articles/s41397-025-00361-6]
- 45. Combination of ligand- and structure-based methods in ... [https://www.sciencedirect.com/science/article/abs/pii/S1740674913000097]
- 46. Decoding Anticancer Drug Response: Comparison of Data ... [https://www.mdpi.com/2673-9879/5/4/58]
- 47. An overview of PROTACs: a promising drug discovery ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9763089/]
- 48. Targeted protein degradation: mechanisms, strategies and ... [https://www.nature.com/articles/s41392-022-00966-4]
- 49. The mechanism of action and clinical value of PROTACs [https://www.sciencedirect.com/science/article/pii/S089865682200208X]
- 50. Transforming Cancer Treatment with Computer-Aided Drug ... [https://www.metrotechinstitute.org/post/transforming-cancer-treatment-with-computer-aided-drug-design-cadd]
- 51. Directory of in silico Drug Design tools [https://www.click2drug.org/]
- 52. Radiopharmaceuticals and their applications in medicine [https://www.nature.com/articles/s41392-024-02041-6]
- 53. Targeted medicines redefining radiotherapy in oncology [https://www.astrazeneca.com/r-d/next-generation-therapeutics/radioconjugates.html]
- 54. Computer-aided drug design in anti-cancer drug discovery [https://www.sciencedirect.com/science/article/pii/S2352914823001788]
- 55. Advancements in breast cancer therapy: Integrating AI ... [https://www.sciencedirect.com/science/article/abs/pii/S0010482525014192]
- 56. Redefining Breast Cancer Care by Harnessing Computational ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12471285/]
- 57. Artificial Intelligence-Driven Innovations in Oncology Drug ... [https://www.dovepress.com/artificial-intelligence-driven-innovations-in-oncology-drug-discovery--peer-reviewed-fulltext-article-DDDT]
- 58. Oncology (Cancer)/Hematologic Malignancies Approval ... [https://www.fda.gov/drugs/resources-information-approved-drugs/oncology-cancerhematologic-malignancies-approval-notifications]
- 59. Most FDA and EMA Oncology Drug Approvals in Q1 2025 ... [https://www.aptitudehealth.com/oncology-news/most-fda-and-ema-oncology-drug-approvals-in-q1-2025-were-new-indications-for-biologics-and-biosimilars/]
- 60. 从计算机辅助药物设计到人工智能药物设计的最新进展原创 [https://blog.csdn.net/m0_59235699/article/details/147552188]
- 61. Artificial intelligence in tumor drug resistance: Mechanisms ... [https://www.sciencedirect.com/science/article/pii/S2950261625000093]
- 62. Research Progress on the Regulation of Third-generation ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12438653/]
- 63. 2025 ESMO | EGFR突变非小细胞肺癌的耐药机制及治疗策略进展 [https://bydrug.pharmcube.com/news/detail/e494958496fa706878056a3495535f04]
- 64. 人工智能与物理学融合:德克萨斯大学奥斯汀分校Dima ... [https://www.forwardpathway.com/266900]
- 65. AI-Based Cancer Models in Oncology: From Diagnosis to ADC ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12609977/]
- 66. 康宁杰瑞公布2025年中期业绩及近期业务进展 [https://www.alphamabonc.com/fanti/html/news/2778.html]
- 67. 关于发布2025年度国家自然科学基金民营企业创新发展联合 ... [http://kjt.shandong.gov.cn/art/2025/7/2/art_13360_10320058.html]
- 68. Key Considerations for Improving Dosage Optimization in ... [https://www.aacr.org/blog/2025/10/03/key-considerations-for-improving-dosage-optimization-in-oncology/]
- 69. Three steps toward dose optimization for oncology ... [https://www.sciencedirect.com/science/article/pii/S2451865424000760]
- 70. Clinical Leader — FDA Finalizes Guidance On Dose ... [https://friendsofcancerresearch.org/news/clinical-leader-fda-finalizes-guidance-on-dose-optimization-for-oncology-therapies/]
- 71. FDA-AACR Strategies for Optimizing Dosages for Oncology ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12614637/]
- 72. Computational-aided drug design strategies for ... [https://pubmed.ncbi.nlm.nih.gov/41282627/]
- 73. Sentinel dosing: A proposed algorithm to guide decision ... [https://pubmed.ncbi.nlm.nih.gov/40370057/]
- 74. Overcoming data management challenges in oncology ... [https://www.sciencedirect.com/science/article/pii/S0959804925004873]
- 75. Challenges to Using Big Data in Cancer - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC10102837/]
- 76. Artificial intelligence and machine learning in drug ... [https://www.sciencedirect.com/science/article/pii/S2667102621001066]
- 77. A Statistical Exploration of QSAR Models in Cancer Risk ... [https://pubmed.ncbi.nlm.nih.gov/40278615/]
- 78. The predictivity of QSARs for toxicity [https://www.sciencedirect.com/science/article/pii/S2468111324000409]
- 79. Drug Design by Pharmacophore and Virtual Screening ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9145410/]
- 80. Applications and Limitations of Pharmacophore Modeling [https://drugdiscoverypro.com/applications-and-limitations-of-pharmacophore-modeling/]
- 81. New Computational Tool Shows Strong Accuracy in ... [https://ascopost.com/news/november-2025/new-computational-tool-shows-strong-accuracy-in-predicting-cancer-drug-targets]
- 82. Machine Learning in Drug Discovery: A Review - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC8356896/]
- 83. Integrating Computational and Experimental Approaches ... [https://jddhs.com/index.php/jddhs/article/view/71]
- 84. Computer-Aided Drug Design Across Breast Cancer ... [https://www.mdpi.com/1422-0067/26/21/10744]
- 85. opportunities for innovation in drug discovery - PubMed Central [https://pmc.ncbi.nlm.nih.gov/articles/PMC12641420/]
- 86. Computational and Experimental Integration in Modern ... [https://www.collaborativedrug.com/the-synthetic-lethality-approach-webinar]
- 87. Data-Driven Methods for Advancing Precision Oncology [https://pmc.ncbi.nlm.nih.gov/articles/PMC7845924/]
- 88. Computer-aided drug discovery: From traditional ... [https://www.sciencedirect.com/science/article/pii/S2666386424006489]
- 89. Automated drug design for druggable target identification ... [https://www.nature.com/articles/s41598-025-18091-x]
- 90. A benchmark of deep learning approaches to predict lung ... [https://www.nature.com/articles/s41598-024-84193-7]
- 91. Computer-Aided Drug Design Methods - PMC - PubMed Central [https://pmc.ncbi.nlm.nih.gov/articles/PMC5248982/]
- 92. Transformative Role of Artificial Intelligence in Drug ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12406033/]
- 93. Artificial intelligence in cancer: applications, challenges, and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12574039/]
- 94. How AI will reshape pharma in 2025 [https://www.drugtargetreview.com/article/154981/how-ai-will-reshape-pharma-by-2025/]
- 95. The Benefits and Limitations of AI in Medicine - News [https://www.umaryland.edu/news/archived-news/may-2025/the-benefits-and-limitations-of-ai-in-medicine.php]
- 96. Diagnostic framework to validate clinical machine learning ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12219301/]
- 97. Implementation and Updating of Clinical Prediction Models [https://www.sciencedirect.com/science/article/pii/S2949761225000355]
- 98. Predictive Healthcare 2025: Transforming Patient Outcomes [https://www.omdena.com/blog/predictive-healthcare-2025]
- 99. Advances of Artificial Intelligence in Anti-Cancer Drug Design [https://pmc.ncbi.nlm.nih.gov/articles/PMC9963982/]
- 100. Which part in drug development is more costly ... [https://synapse.patsnap.com/article/which-part-in-drug-development-is-more-costly-drug-discovery-or-clinical-trials]
- 101. Computational Methods in Drug Discovery - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC3880464/]
- 102. DrugAppy – An end-to-end deep learning framework for ... [https://www.sciencedirect.com/science/article/pii/S0010482525015549]
- 103. Clinical trials are becoming more complex: a machine ... [https://www.nature.com/articles/s41598-024-53211-z]
- 104. Harnessing Innovation in Oncology: Insights from ASCO ... [https://premier-research.com/perspectives/harnessing-innovation-in-oncology-insights-from-asco-2025/]
- 105. Applications of Quantum-Based Technologies in Medicine, ... [https://countercurrents.org/2025/10/applications-of-quantum-based-technologies-in-medicine-a-comprehensive-review/]