Computational Strategies for Undruggable Cancer Targets: From AI Design to Clinical Translation
This article provides a comprehensive overview of cutting-edge computational and AI-driven strategies developed to target traditionally undruggable cancer proteins.
Computational Strategies for Undruggable Cancer Targets: From AI Design to Clinical Translation
Abstract
This article provides a comprehensive overview of cutting-edge computational and AI-driven strategies developed to target traditionally undruggable cancer proteins. It explores the foundational biology of targets like KRAS, MYC, and p53, and details innovative methodologies, including generative AI for binder design, quantum computing-assisted screening, and allosteric inhibition. Aimed at researchers and drug development professionals, the content also addresses critical challenges in optimization, validation, and clinical translation, offering a comparative analysis of leading platforms and their paths toward transforming cancer therapeutics.
Deconstructing the Undruggable Problem: Target Classes and Biological Challenges
FAQ: What does "undruggable" mean in cancer research?
In cancer research, "undruggable" refers to proteins that are clinically meaningful therapeutic targets but are exceptionally difficult to drug using conventional drug design strategies [1] [2]. These targets are often characterized by a lack of defined, deep hydrophobic pockets on their surface that small-molecule drugs can bind to, making rational drug design a significant challenge [1] [3]. It is important to note that the term is evolving, with many now preferring "difficult to drug" or "yet to be drugged," as recent advances have successfully targeted some of these proteins [2].
FAQ: What are the main classes of undruggable targets?
The primary categories of undruggable targets, along with their key challenges and representative examples, are summarized in the table below [1] [3].
Table 1: Major Classes of Undruggable Cancer Targets
| Target Class | Key Druggability Challenge | Representative Examples |
|---|---|---|
| Small GTPases | Lack of pharmacologically targetable pockets; extremely high affinity for its natural substrate (GTP) [1] [3]. | KRAS, HRAS, NRAS [1] |
| Transcription Factors (TFs) | Structural heterogeneity and lack of tractable binding sites; function often relies on protein-protein interactions [1] [3]. | p53, MYC, STAT3 [1] [4] |
| Phosphatases | Highly conserved, positively charged active sites; structural similarity leads to low selectivity and potential toxicity [1] [3]. | PTPs (Protein Tyrosine Phosphatases) [1] |
| Protein-Protein Interactions (PPIs) | Large, flat, and relatively featureless interaction surfaces that are difficult for small molecules to disrupt [1] [3]. | B-cell lymphoma-2 (Bcl-2) family [1] |
FAQ: What specific characteristics make a protein "undruggable"?
The elusive nature of these targets can be distilled into four key structural and functional characteristics.
Table 2: Core Characteristics of Undruggable Proteins
| Characteristic | Description | Example |
|---|---|---|
| Lack of Ligand-Binding Pockets | The protein surface is smooth and lacks deep, defined hydrophobic pockets or cavities that small-molecule inhibitors can bind to with high affinity [1] [3]. | KRAS was considered undruggable for decades due to its shallow, polar surface with no obvious binding sites for drugs [1]. |
| Protein-Protein Interaction (PPI) Interfaces | Their biological function is mediated by large, flat surfaces that interact with other proteins. These PPI interfaces are difficult to disrupt with conventional small molecules, which are better at targeting deep pockets [3] [2]. | Transcription factors like MYC exert their function by binding to other proteins and DNA, presenting a challenging PPI interface for drug discovery [1]. |
| Highly Conserved Active Sites | The active site (e.g., for substrate or GTP binding) is highly similar among members of the same protein family, making it nearly impossible to develop a selective inhibitor that hits only one member without affecting others, leading to potential side effects [3]. | Phosphatases share a high degree of structural similarity in their active sites, hindering the development of selective drugs [1]. |
| Intrinsically Disordered Regions or Unknown 3D Structure | The protein lacks a stable, folded three-dimensional structure or its tertiary structure is unknown, which prevents structure-based drug design [3]. | Many transcription factors contain intrinsically disordered regions, making them highly dynamic and lacking stable binding cavities [1] [3]. |
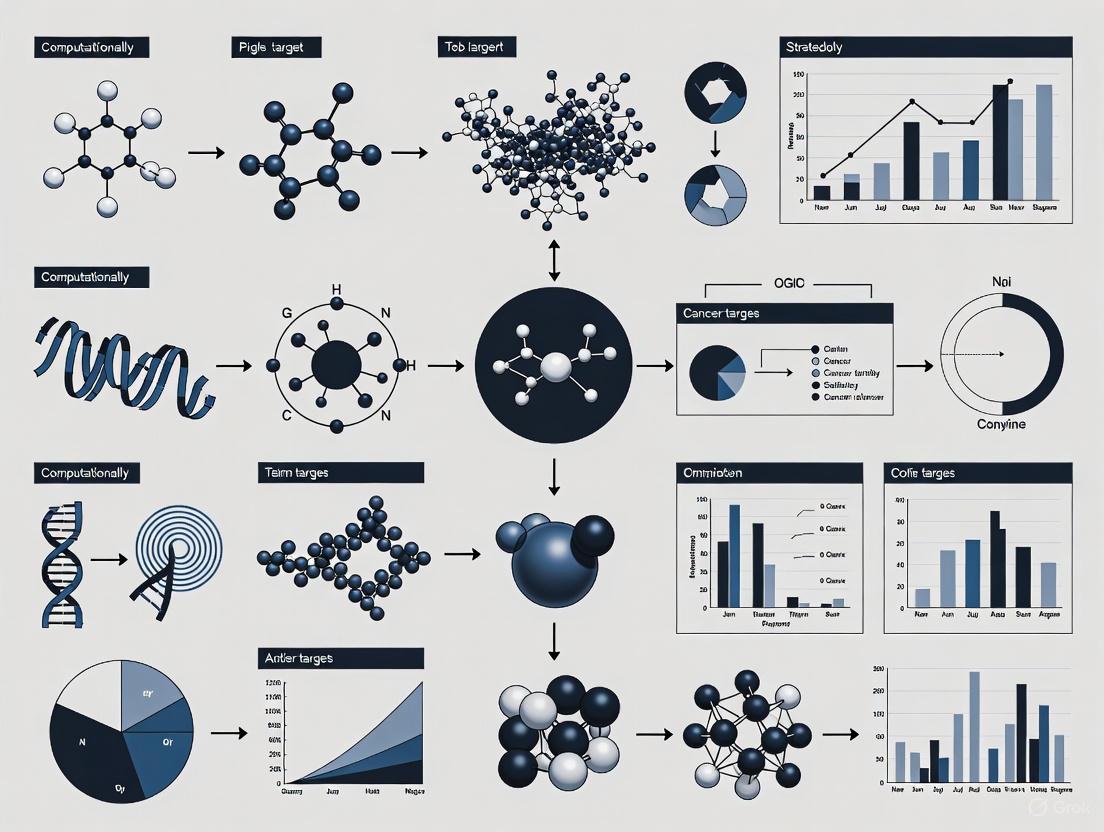
The following diagram illustrates the relationship between these core characteristics and the resulting druggability challenges.
Troubleshooting Guide: My target is considered "undruggable." What computational strategies can I employ?
When faced with a seemingly undruggable target, shifting from traditional drug discovery paradigms to innovative computational strategies is crucial. The following workflow outlines a modern computational approach to this challenge.
Detailed Experimental Protocols
Protocol 1: In Silico Workflow for Identifying Degraders or PPI Inhibitors
This protocol leverages the DrugAppy framework, an end-to-end deep learning tool that integrates multiple computational models [5].
Target Preparation:
- Obtain the 3D structure of your target protein from the Protein Data Bank (PDB) or generate a high-confidence predicted structure using AlphaFold2.
- Use computational tools to prepare the structure: add hydrogen atoms, assign partial charges, and define protonation states.
Virtual Screening & AI-Driven Molecule Generation:
- Perform High-Throughput Virtual Screening (HTVS) against the target using docking programs like SMINA or GNINA (integrated in DrugAppy) to screen millions of compounds from libraries like VirtualFlow [5] [6].
- Alternatively, or in parallel, employ a generative AI engine (e.g., Chemistry42) to design novel chemical entities from scratch. These models can be trained on custom datasets of known binders or degraders for your target family [6].
Molecular Dynamics (MD) Simulation:
- Take the top-ranking hits from virtual screening or AI generation and subject them to Molecular Dynamics (MD) simulations using software like GROMACS (as used in DrugAppy) [5].
- Run simulations for at least 100-200 nanoseconds to assess the stability of the ligand-target complex, binding free energy, and key molecular interactions under near-physiological conditions.
AI-Based Property Prediction:
- Use publicly available or proprietary AI models to predict key parameters for the final candidate molecules. These include pharmacokinetics (absorption, distribution, metabolism, and excretion), selectivity, and potential in vitro activity [5].
Protocol 2: Computational Identification of Novel Allosteric Sites
This methodology is crucial for targeting proteins like KRAS, where the active site is not druggable [1] [3].
Structure Analysis:
- Analyze multiple crystal structures of the target (e.g., in different nucleotide states: GDP-bound vs. GTP-bound for KRAS) to identify conformational changes and potential cryptic pockets [1].
Pocket Detection:
- Use computational tools to detect and characterize potential binding pockets on the protein surface beyond the active site.
Consensus Allosteric Site Prediction:
The Scientist's Toolkit: Key Research Reagent Solutions
Table 3: Essential Computational Tools and Reagents for Targeting Undruggable Proteins
| Tool / Reagent | Function / Application | Use Case in Undruggable Targets |
|---|---|---|
| Generative AI (e.g., Chemistry42) | AI-driven de novo design of novel chemical entities targeting specific proteins [6]. | Designed novel covalent inhibitors for KRAS by screening and optimizing millions of potential molecules [6]. |
| PROTAC Molecule | Bifunctional molecule that recruits an E3 ubiquitin ligase to a target protein, leading to its degradation by the proteasome [3]. | Used to degrade oncogenic proteins like KRASG12C, effectively inhibiting downstream signaling even for proteins without a classical active site [3]. |
| Covalent Inhibitor Probe (e.g., ARS-1620) | Small molecule that forms a permanent covalent bond with a specific amino acid residue (e.g., cysteine) on the target protein [3]. | Served as a chemical probe to validate the druggability of the KRASG12C allosteric pocket and was used as a warhead for developing PROTAC degraders [3]. |
| Covalent Docking Protocols | Computational method to predict the binding mode and reactivity of covalent inhibitors [7]. | Key for the rational design of covalent drugs, such as the KRASG12C inhibitor Sotorasib, by simulating the covalent bond formation with Cys12 [1] [7]. |
| Quantum Computing Hybrid Models | Leverages quantum computing combined with AI to model complex molecular interactions beyond the reach of classical computers [6]. | Used as a proof-of-principle to identify novel molecules that interact with KRAS, showing potential to accelerate early drug discovery [6]. |
Troubleshooting Guides & FAQs
KRAS-Targeting Experiments
Q1: Our KRAS(G12C) inhibitor shows promising initial activity in cell lines, but resistance develops quickly. What are the primary mechanisms we should investigate?
Resistance to KRAS(G12C) inhibitors often occurs through reactivation of the MAPK signaling pathway or secondary KRAS mutations. The table below outlines common mechanisms and suggested experimental approaches to diagnose them [8] [9] [10].
| Resistance Mechanism | Description | Experimental Validation Methods |
|---|---|---|
| On-Target Secondary Mutations | Emergence of mutations (e.g., Y96D, R68S, H95D) that interfere with drug binding [9]. | - Use Sanger sequencing or NGS to sequence the KRAS gene after resistance emerges. |
| Bypass Signaling via RTKs | Upregulation or activation of Receptor Tyrosine Kinases (e.g., EGFR, MET) reactivates MAPK/PI3K signaling despite KRAS inhibition [10]. | Perform western blotting to assess phosphorylation levels of EGFR, MET, ERK, and AKT. |
| KRAS Amplification | Increased copy number of the mutant KRAS gene [9]. | - Use qPCR or FISH to measure KRAS gene copy number. |
| Altered KRAS Cycling | Mutations in downstream effectors (e.g., BRAF, MEK) or upstream regulators (e.g., NF1 loss) maintain pathway activity [8] [9]. | - Utilize RNA-Seq to identify transcriptomic changes in the MAPK pathway. |
Q2: For pancreatic cancer research, the predominant KRAS mutation is G12D, not G12C. What direct targeting strategies are available for KRAS(G12D)?
Your observation is correct; KRAS(G12D) dominates in pancreatic ductal adenocarcinoma (PDAC), present in approximately 40% of cases [9]. Since the G12D mutation does not create a cysteine for covalent targeting, alternative strategies are required.
- Non-Covalent Inhibitors: The most advanced research compound is MRTX1133, a non-covalent inhibitor that selectively targets the inactive, GDP-bound state of KRAS(G12D). It exhibits high potency in preclinical PDAC models [9].
- PROTAC Degraders: Proteolysis Targeting Chimeras (PROTACs) are bifunctional molecules that recruit an E3 ubiquitin ligase to the target protein, leading to its degradation by the proteasome. This strategy is being explored to degrade KRAS(G12D) entirely, not just inhibit it [3] [11].
- Immunotherapy Approaches: KRAS(G12D)-specific vaccines are under investigation. These vaccines aim to stimulate the patient's own T-cells to recognize and eliminate tumor cells presenting the G12D neoantigen [9].
Experimental Protocol: Evaluating Efficacy of a KRAS(G12D) Inhibitor In Vitro
- Cell Line Selection: Use a well-characterized PDAC cell line harboring the KRAS(G12D) mutation (e.g., Capan-2, HPAC).
- Cell Viability Assay: Treat cells with a dose range of the inhibitor (e.g., MRTX1133) for 72 hours. Assess viability using an ATP-based assay (e.g., CellTiter-Glo).
- Downstream Signaling Analysis: Harvest inhibitor-treated and control cells. Perform western blotting to analyze phosphorylation levels of key downstream effectors like ERK (p-ERK) and AKT (p-AKT). Effective inhibition should show a dose-dependent reduction in these phosphoproteins.
- Apoptosis Assay: Confirm induction of cell death via caspase-3/7 activity assay or Annexin V staining followed by flow cytometry.
Transcription Factor (MYC, p53)-Targeting Experiments
Q3: We are screening for MYC inhibitors, but its lack of a defined active site makes it challenging. What are the most promising indirect strategies?
Targeting MYC indirectly by disrupting its protein-protein interactions or stability is a primary strategy. The table below summarizes key approaches [1] [3].
| Strategy | Mechanism | Research Compounds / Methods |
|---|---|---|
| Disrupting MYC/MAX Dimerization | Prevents MYC from binding to DNA and activating transcription [1]. | - Omomyc (a dominant-negative peptide) - Small-molecule screens (e.g., 10058-F4, JKY-2-169). |
| Targeting MYC Stability | Promotes the degradation of the MYC protein itself [3]. | - PROTACs that recruit E3 ligases to MYC. |
| Targeting Co-Factors | Inhibits partners necessary for MYC's transcriptional activity, such as BRD4 [1]. | - BET inhibitors (e.g., JQ1). |
| AI-Driven Binder Design | Using generative AI to design novel proteins that bind and inhibit the intrinsically disordered regions of MYC [12] [13]. | - RFdiffusion and "logos" methods from Baker Lab. |
Experimental Protocol: Validating MYC/MAX Dimerization Inhibitors
- Co-Immunoprecipitation (Co-IP): Treat cells with the candidate inhibitor. Lyse cells and immunoprecipitate MYC using a specific antibody. Perform western blotting on the immunoprecipitate with an anti-MAX antibody. A successful inhibitor will reduce the amount of MAX co-precipitated with MYC.
- Luciferase Reporter Assay: Transfert cells with a plasmid containing a luciferase gene under the control of a MYC-responsive promoter. Treat with the inhibitor and measure luciferase activity. Inhibition of MYC transcriptional activity will result in reduced luminescence.
- qRT-PCR of MYC Target Genes: Measure mRNA expression levels of known MYC target genes (e.g., ODC1, CAD) via quantitative RT-PCR after inhibitor treatment.
Q4: How can we target mutant p53, given that it is often unstable and loses its tumor-suppressor function?
The majority of p53 mutations are missense mutations, leading to the expression of full-length but dysfunctional proteins. Strategies focus on restoring wild-type function or exploiting specific mutant vulnerabilities [1] [3].
- Reactivating Mutant p53: Compounds like PRIMA-1 (APR-246) covalently bind to mutant p53, refold it into a wild-type conformation, and restore its DNA-binding and transcriptional activity. This is a key candidate in clinical trials.
- Targeting p53 with PROTACs: Degraders can be designed to target and eliminate mutant p53 proteins, thereby removing their potential "gain-of-function" oncogenic activities [11].
- Combination with DNA-Damaging Agents: Since p53 is central to the DNA damage response, combining a p53 reactivator with chemotherapeutics like cisplatin can synergize to induce apoptosis.
Phosphatase-Targeting Experiments
Q5: We are trying to develop inhibitors for a Protein Tyrosine Phosphatase (PTP), but the active site is highly conserved and polar, leading to selectivity and bioavailability issues. What modern approaches can we use?
The challenges you describe are central to why phosphatases are considered "undruggable." The field is moving beyond active-site directed inhibitors [1].
- Allosteric Inhibition: Identify and target less conserved, often more hydrophobic, pockets outside the active site. This can induce conformational changes that inhibit enzymatic activity with greater selectivity.
- PROTAC-Mediated Degradation: As with KRAS and MYC, designing PROTACs for PTPs bypasses the need to inhibit the active site directly and instead removes the protein from the cell [11].
- Targeting Substrate Specificity: Some PTPs have unique, adjacent binding sites for their specific protein substrates. Developing molecules that block this protein-protein interaction (PPI) interface can achieve high selectivity.
Experimental Protocol: Fragment-Based Drug Discovery (FBDD) for an Allosteric PTP Inhibitor
- Library Screening: Screen a library of small molecular fragments (~150-300 Da) against the target PTP using Surface Plasmon Resonance (SPR) or X-ray crystallography to identify weak binders.
- Hit Validation and Mapping: Co-crystallize fragment "hits" with the PTP to determine their precise binding location. The goal is to find fragments that bind to a novel, allosteric pocket.
- Fragment Growing and Linking: Use structure-based drug design to chemically elaborate the initial fragment, adding functional groups that increase its affinity and selectivity. If two fragments bind nearby, they can be linked together to create a higher-affinity molecule.
- Cellular Activity Assessment: Test optimized compounds in cells using a phospho-specific western blot against the PTP's known substrate to confirm target engagement and functional inhibition.
The Scientist's Toolkit: Research Reagent Solutions
| Reagent / Technology | Function / Application | Key Examples |
|---|---|---|
| Covalent KRAS Inhibitors | Irreversibly bind to mutant cysteine (G12C) and lock KRAS in its inactive (GDP-bound) state [8] [1]. | Sotorasib (AMG510), Adagrasib (MRTX849) |
| PROTAC Technology | Bifunctional degraders that recruit E3 ubiquitin ligase to target proteins, leading to their proteasomal degradation [3] [11]. | KRAS(G12C) PROTACs, p53-targeting PROTACs |
| AI-Designed Binders | Generative AI software to design novel proteins that bind to intrinsically disordered targets or flat PPI interfaces [12] [13]. | RFdiffusion, "logos" method (Baker Lab) |
| Computational Docking (CADD) | Predicts the 3D binding pose and affinity of small molecules to a protein target, enabling virtual screening [14]. | Molecular docking software (AutoDock, Schrödinger) |
| SHP2 Inhibitors | Target upstream nodes; inhibit SHP2 phosphatase to block RTK-mediated RAS activation and overcome resistance [8] [9]. | TNO155, RMC-4550 |
| BET Inhibitors | Indirect transcriptional modulation; inhibit BRD4 to disrupt its co-activation of oncogenes like MYC [1]. | JQ1, OTX015 |
Visualizing Key Concepts
KRAS Signaling and Therapeutic Intervention
PROTAC Mechanism for Undruggable Targets
The Role of Protein-Protein Interactions (PPIs) and Intrinsically Disordered Regions (IDRs)
FAQs: Overcoming Experimental Challenges in PPI and IDR Research
FAQ 1: What are the biggest challenges in developing small molecule modulators for PPIs, and what strategies can overcome them?
The primary challenge is the nature of PPI interfaces, which are often large, flat, and lack deep pockets for small molecules to bind, making them seem "undruggable" [15]. Several strategies have been developed to address this:
- Fragment-Based Drug Discovery (FBDD): This approach uses low molecular weight fragments that can bind to discontinuous hot spots on the PPI interface. These fragments can then be linked or optimized into larger, more potent lead molecules [15].
- Peptidomimetics: These are molecules designed to recapitulate the secondary structure (e.g., α-helices, sheets, loops) of key peptide segments involved in the PPI, thereby disrupting the interaction [15].
- High-Throughput Screening (HTS): Using chemically diverse libraries enriched with compounds likely to target PPIs can successfully identify lead modulators, though its effectiveness can be limited for some interfaces [15].
- Computational Tools: Virtual screening (both structure-based and ligand-based) and emerging machine learning models can significantly speed up the discovery and optimization of PPI modulators [15].
FAQ 2: My PPI assay yields weak or transient signals. Which live-cell techniques are best for capturing these dynamic interactions?
Weak, transient interactions are common in signaling pathways and can be studied using sensitive fluorescence techniques in living cells:
- FRET (Förster Resonance Energy Transfer): This is the most powerful and popular approach. FRET is exquisitely sensitive to nanometer-range proximity and orientation between fluorophores tagged to your proteins of interest. It can detect both specific complex formation and random collisions, and is amenable to quantitative analysis to determine interaction kinetics and efficiencies [16].
- Bimolecular Fluorescence Complementation (BiFC): This technique uses non-fluorescent fragments of a fluorescent protein attached to two interacting proteins. If the proteins interact, the fragments refold into a fluorescing product. It excels as an end-point assay for confirming interactions, especially transient ones, though the irreversible refolding means it is less suited for studying dynamics [16].
- Fluorescence Correlation Spectroscopy (FCM) / Fluorescence Cross-Correlation Spectroscopy (FCCM): These techniques analyze fluorescence fluctuations as molecules diffuse through a small volume. They can provide information on diffusion coefficients, stoichiometry, and affinities of complexes in solution or at the membrane, making them ideal for studying the dynamics of large protein complexes at low, physiological concentrations [16].
FAQ 3: IDRs are difficult to study structurally. What methods are available for characterizing their function?
The disordered nature of IDRs makes them resistant to classical structural biology, but a combination of methods can reveal their functions:
- Computational Prediction: Tools like IUPred and PONDR use amino acid sequence to predict disorder propensity and are efficient for proteome-wide screening [17].
- Biophysical Techniques:
- Nuclear Magnetic Resonance (NMR) Spectroscopy: Ideal for characterizing structural and dynamic properties of IDRs at the amino acid level, even in a disordered state [17] [18].
- Cryo-Electron Microscopy (Cryo-EM): Can be used to visualize larger complexes where IDRs are involved, often alongside structured domains. NMR and Cryo-EM provide a synergistic approach [18].
- Circular Dichroism (CD): Provides information on secondary structure content and conformational changes [17].
- Functional Assays: Since IDRs are enriched with functional sites, assays detecting post-translational modifications (e.g., phosphorylation) or protein-protein interactions (e.g., via FRET or BiFC) are crucial for linking IDR structure to function [19] [17].
FAQ 4: Why are mutations in IDRs often linked to disease, and how can we identify functionally critical IDRs?
IDRs are enriched in disease-associated mutations because they often harbor critical functional elements like molecular recognition features (MoRFs) and post-translational modification (PTM) sites [17]. Mutations can disrupt conformational plasticity, impair binding capacity, or lead to pathogenic aggregation [17]. To identify critical IDRs:
- Leverage Genetic Data: Compare the frequency of mutations in general population databases (e.g., gnomAD) versus patient-based databases (e.g., ClinVar). IDRs that are significantly depleted in population variants but enriched in pathogenic mutations are likely functionally important and intolerant to mutation [19].
- Analyze Functional Annotations: Map known functional sites from databases like UniProt onto IDR sequences. Features commonly enriched in critical IDRs include "regions of interest," binding sites, and sites for PTMs [19].
Troubleshooting Guides for Key Experiments
Guide 1: Troubleshooting FRET Experiments to Study PPIs
Table: Troubleshooting FRET Experiments
| Problem | Potential Cause | Solution |
|---|---|---|
| No FRET signal | Proteins are not interacting; fluorophores are too far apart; poor fluorophore choice (low spectral overlap) | Verify interaction with another technique (e.g., co-IP); check linker length between protein and fluorophore; use recommended FP pairs (e.g., mCerulean/mVenus) [16]. |
| High FRET signal in negative control | Direct interaction between fluorophores; spectral bleed-through (crosstalk) | Include controls with fluorophores alone; use acceptor photobleaching to confirm FRET; adjust detection filters to minimize crosstalk [16]. |
| Low signal-to-noise ratio | Low expression of fusion proteins; photobleaching | Optimize transfection to increase protein expression; use FPs with high quantum yield and low photobleaching (e.g., mCitrine, mCherry) [16]. |
| Altered protein function | FP tag disrupts native folding, localization, or interaction | Tag protein at the opposite terminus; use smaller tags (e.g., tetracysteine motifs with FlAsH/ReAsH); verify function and localization of tagged protein [16]. |
Workflow for a Quantitative FRET Experiment in Living Cells: The following diagram outlines the key steps for setting up and validating a FRET experiment to study PPIs in living cells.
Guide 2: Troubleshooting IDR Functional Analysis
Table: Troubleshooting IDR-Related Experiments
| Problem | Potential Cause | Solution |
|---|---|---|
| IDR expression leads to protein aggregation | High hydrophobicity in specific regions; lack of solubility tags | Use fusion solubility tags (e.g., GST, MBP) during purification; optimize expression conditions (lower temperature, shorter time) [17]. |
| Cannot obtain structural data on IDR | IDR is highly flexible and dynamic, resistant to crystallization | Use solution-based methods like NMR spectroscopy; employ Small-Angle X-ray Scattering (SAXS) to study ensemble conformations [17] [18]. |
| Difficulty identifying functional motifs within a long IDR | Functional motifs (e.g., MoRFs) are short and transient | Use phylogenetic conservation analysis to pinpoint constrained segments; perform peptide scanning or phage display to find binding regions; look for enrichment of PTM sites [19] [17]. |
| Unexpected order in crystal structure of an IDR | IDR underwent "coupled folding and binding" during crystallization | The function may rely on this induced folding. Validate the physiological relevance of the bound conformation using mutagenesis and functional assays in cells [20]. |
Workflow for Characterizing a Putative Cancer-Associated IDR: This workflow provides a logical pathway for moving from a genetic variant in an IDR to understanding its potential functional impact in cancer.
Research Reagent Solutions
Table: Essential Reagents and Tools for PPI and IDR Research
| Reagent / Tool | Function / Application | Key Considerations |
|---|---|---|
| Fluorescent Proteins (FPs) [16] | Tagging proteins for live-cell imaging (FRET, BiFC). | Use monomeric FPs (e.g., mCerulean, mVenus) to prevent oligomerization artifacts. Consider spectral properties for multiplexing. |
| Tetracysteine Motif & Biarsenical Dyes (FlAsH/ReAsH) [16] | Small, genetic tags for fluorescent labeling, minimizing tag bulkiness. | Improved selectivity with optimized motifs; requires specific labeling conditions in living cells. |
| siRNAs / shRNAs [21] | Selective gene silencing to validate target function in disease models. | Critical for studying "undruggable" targets like KRAS and MYC; inverted RNAi designs enable co-silencing. |
| Computational Predictors (IUPred, PONDR) [17] | Predicting intrinsic disorder from amino acid sequence. | Fast, proteome-wide screening to prioritize experimental work on disordered regions. |
| Machine Learning Models [15] [22] | Predicting PPIs, identifying druggable pockets, and patient stratification from multimodal data. | Requires high-quality training data; used for forecasting disease trajectories and identifying novel therapeutic vulnerabilities. |
| Selective Autophagy Receptor LIR Motifs [23] | Tools to study or manipulate selective autophagy pathways. | LIR motifs (e.g., from p62) bind ATG8/LC3 proteins; useful as peptides or in constructs to probe autophagy. |
Troubleshooting Guide: Identifying and Overcoming Common Experimental Challenges
FAQ 1: Why can't my small molecule inhibitor bind to the flat, shallow surface of my target protein?
Problem: Your target protein lacks deep, hydrophobic pockets, resulting in a flat and featureless interaction surface that prevents effective small molecule binding.
Explanation: Traditional small molecule drugs typically function by occupying well-defined, deep pockets on a protein's surface, much like a key fits into a lock. However, many cancer-related targets, including transcription factors, phosphatases, and small GTPases, possess relatively flat interaction interfaces with minimal topological features for small molecules to engage with effectively [1]. These proteins often perform their biological functions through large, continuous protein-protein interactions (PPIs) that span extensive surface areas without deep crevices [1].
Solution: Implement a multi-pronged computational and experimental strategy:
Table: Computational Approaches for Flat Surface Targeting
| Approach | Methodology | Application Example |
|---|---|---|
| Covalent Inhibition | Design compounds with mildly reactive functional groups that form covalent bonds with specific amino acid residues [1]. | KRASG12C inhibitors (sotorasib) target the previously "undruggable" KRAS by covalently binding to cysteine residues [1]. |
| Allosteric Inhibition | Identify and target alternative binding sites that indirectly modulate the protein's active site [1]. | Identify cryptic pockets through molecular dynamics simulations that appear only under specific conformational states [24]. |
| PROTAC Technology | Develop proteolysis-targeting chimeras that recruit cellular machinery to degrade the target protein [25]. | Design molecules that bind to target protein on one end and E3 ubiquitin ligase on the other, enabling targeted degradation [25]. |
Experimental Protocol:
- Run extended molecular dynamics (MD) simulations (≥1000 ns) to identify transient pockets [24].
- Perform fragment-based screening using X-ray crystallography or NMR to identify small fragments that bind to weak sites [1].
- Use covalent docking screens to identify potential cysteine-reactive compounds if applicable [1].
- Validate hits using surface plasmon resonance (SPR) to confirm binding, even if weak.
- Optimize confirmed hits using structure-based drug design, focusing on improving affinity.
FAQ 2: How do I address the high conservation of my target across protein families, which leads to off-target toxicity?
Problem: Your target protein shares significant structural similarity with other proteins in its family, resulting in poor selectivity and potential toxicity.
Explanation: High sequence and structural conservation across protein family members, particularly in active sites, makes selective inhibition extremely challenging. This is particularly problematic for phosphatases and small GTPases, where active sites are often structurally similar among family members [1]. When multiple proteins share nearly identical binding pockets, a drug designed for one target will likely bind to others, causing undesirable off-target effects.
Solution: Leverage computational tools to identify and exploit subtle structural differences:
Table: Strategies for Targeting Conserved Proteins
| Strategy | Mechanism | Tools/Methods |
|---|---|---|
| Context-Specific Targeting | Exploit cellular context and pathway-level effects beyond direct binding interactions [26]. | DeepTarget tool uses genetic and drug screening data across cell lines to identify context-specific vulnerabilities [26]. |
| Peripheral Site Targeting | Target areas adjacent to the active site that show greater structural variation [1]. | Molecular dynamics with Markov state models to identify allosteric networks [24]. |
| Mutation-Specific Targeting | Design compounds that specifically target mutant forms over wild-type proteins [26]. | DeepTarget can predict drugs with preferential effects on mutated vs. non-mutated target proteins [26] [27]. |
Experimental Protocol:
- Perform comparative structural analysis of your target against its closest homologs using PDB structures.
- Use molecular dynamics simulations to identify dynamic differences between family members.
- Screen compound libraries against multiple family members in parallel using computational docking.
- Apply machine learning models like DeepTarget to predict mutation-specific effects [26].
- Validate selectivity in cellular models expressing different family members.
FAQ 3: My small molecules show promising biochemical activity but fail in cellular assays. What could be happening?
Problem: Compounds that demonstrate excellent binding in purified biochemical assays show no efficacy in cellular or tissue contexts.
Explanation: This discrepancy often occurs because the cellular environment introduces additional complexities not present in simplified biochemical systems. Your target may function differently in various cellular contexts, or the compound may fail to reach the target due to permeability issues, off-target binding, or context-specific protein interactions [26]. The same protein can have different functions and interaction partners in different cell types, dramatically affecting drug response.
Solution: Implement context-aware screening and validation:
Experimental Protocol:
- Employ context-specific computational tools like DeepTarget that integrate large-scale genetic and drug screening data across hundreds of cell lines [26].
- Perform pathway-level analysis to understand how inhibition affects broader cellular networks rather than isolated targets.
- Use multi-omics integration (genomics, transcriptomics, proteomics) to identify biomarkers of response.
- Validate predictions in multiple cell line models with different genetic backgrounds.
- Test compound activity in 3D culture systems or organoids that better mimic tissue context.
Case Study Example: Ibrutinib, an FDA-approved drug for blood cancers, was found to be effective in some solid tumors despite the absence of its primary target (BTK) in those tissues. DeepTarget analysis revealed that in solid tumors with EGFR mutations, Ibrutinib effectively kills cancer cells by acting on EGFR as a secondary target, demonstrating how cellular context dramatically alters drug mechanism [26] [27].
Key Experimental Workflows and Signaling Pathways
Computational Drug Discovery Workflow for Undruggable Targets
Targeting KRAS Signaling Pathway: From Undruggable to Druggable
Research Reagent Solutions for Targeting Undruggable Proteins
Table: Essential Computational Tools and Resources
| Tool/Resource | Function | Application in Undruggable Targets |
|---|---|---|
| DeepTarget | Predicts primary and secondary targets using genetic and drug screening data [26] | Identifies context-specific targets and repurposing opportunities [26] [27] |
| Molecular Dynamics (MD) | Simulates protein dynamics and conformational changes [24] [28] | Identifies transient pockets and allosteric sites [24] |
| BioGPS | Detects ligandable protein pockets on 3D structures [25] | Maps druggable sites on protein-protein interaction networks [25] |
| ProtBERT/ESM | Protein language models for sequence analysis [29] | Predicts conserved vs. variable regions across protein families |
| DrugAppy | End-to-end deep learning framework for drug discovery [5] | Designs novel inhibitors through AI-driven workflow [5] |
| QM/MM Methods | Hybrid quantum mechanics/molecular mechanics simulations [28] | Studies enzyme catalysis and reaction mechanisms for covalent drugs [1] |
| PDB | Protein Data Bank - repository of 3D structures [29] [25] | Source of structural information for comparative analysis |
| DepMap | Dependency Map consortium data [26] | Provides cancer vulnerability data for context-specific targeting [26] |
Advanced Computational Methodologies
Multi-Target Drug Discovery Using Machine Learning
Rationale: Complex diseases like cancer involve dysregulation of multiple molecular pathways, making single-target approaches often insufficient [29]. Machine learning (ML) enables the systematic discovery of compounds that modulate multiple targets simultaneously, addressing disease complexity more effectively.
Implementation Protocol:
- Data Collection: Gather drug-target interaction data from databases like ChEMBL, BindingDB, and DrugBank [29].
- Feature Representation: Encode molecules using molecular fingerprints, graph representations, or SMILES strings; represent proteins using sequence or structure-based descriptors [29].
- Model Training: Implement multi-task learning architectures that predict activity against multiple targets simultaneously.
- Validation: Test predicted multi-target profiles in diverse cellular contexts to confirm polypharmacology.
- Optimization: Use reinforcement learning to refine compounds for desired multi-target profiles while maintaining drug-like properties.
Key ML Techniques:
- Graph Neural Networks (GNNs): Model molecules as graphs to capture structural topology [29].
- Transformer Models: Process biological sequences and capture long-range dependencies [29].
- Multi-task Learning: Simultaneously predict activities against multiple targets, leveraging shared representations [29].
- Attention Mechanisms: Identify important molecular substructures and protein regions contributing to binding [29].
The Computational Toolkit: AI, Quantum Computing, and Generative Design in Action
Technical Support Center
Troubleshooting Guides
Issue 1: AI Model Generizes Chemically Invalid or Unstable Structures
- Problem: The generative chemistry platform produces molecules with incorrect valences, unstable rings, or reactive functional groups.
- Solution:
- Apply Medicinal Chemistry Filters (MCFs): Implement filters to automatically exclude Pan-Assay Interference Compounds (PAINS) and other undesirable structural motifs [30].
- Validate Synthetic Accessibility: Use tools like the Retrosynthesis Related Synthetic Accessibility (ReRSA) score, which assesses feasibility based on commercially available building blocks, to prioritize molecules that are practical to synthesize [30].
- Review Training Data: Ensure the generative model was trained on a high-quality, curated chemical library to reduce the learning of invalid patterns.
Issue 2: Generated Molecules Have Poor Predicted ADMET Properties
- Problem: Candidates from the AI show unfavorable pharmacokinetic or toxicity profiles in silico, hindering progression.
- Solution:
- Integrate Multi-Parameter Optimization: Use platforms that allow you to set constraints for absorption, distribution, metabolism, excretion, and toxicity (ADMET) properties during the generative process, not just afterward [31] [30].
- Fine-Tune on Proprietary Data: Retrain the platform's AI predictors using your in-house experimental data to improve the accuracy of property predictions for your specific chemical series [30].
- Leverage Hybrid Physics-AI Models: Combine AI with physics-based simulations for more accurate binding affinity and free energy predictions [30].
Issue 3: Difficulty Prioritizing AI-Generated Targets for "Undruggable" Oncology Targets
- Problem: The biological AI platform identifies numerous potential targets, but it is challenging to rank them for targets with no known active sites or binders.
- Solution:
- Utilize Composite LLM Scores: Employ large language model (LLM)-based scores that evaluate targets based on confidence, commercial tractability, druggability, and mechanism clarity to aid decision-making [30] [32].
- Analyze Multi-Omics Data: Use the platform's integrated transcriptomics, proteomics, and epigenetics data to triangulate evidence for a target's role in cancer progression [30] [33].
- Inspect AI Transparency Maps: Use heat-maps that show which data layers (e.g., specific omics datasets, literature) contributed most to a target's high ranking to build scientific trust and validate the hypothesis [30].
Frequently Asked Questions (FAQs)
Q1: What are the key differences between the AI approaches of Exscientia and Insilico Medicine? A1: While both use generative AI, their core strategies differ. Exscientia pioneered a "Centaur Chemist" model, deeply integrating automated generative chemistry with high-content phenotypic screening on patient-derived samples [31]. Following its 2024 merger with Recursion, its approach has further integrated with massive phenomic screening data [31]. Insilico Medicine operates an end-to-end platform with highly specialized, interconnected modules: PandaOmics for target discovery, Chemistry42 for small-molecule design, and Generative Biologics for designing peptides and antibodies [30] [32].
Q2: How can I assess the novelty of an AI-generated molecule to avoid IP conflicts? A2: Platforms incorporate specific metrics for this. For example, Insilico's Chemistry42 uses the Medicinal Chemistry Evolution (MCE-18) score, which assesses molecular novelty based on sp³ complexity and other parameters [30]. Furthermore, a core strength of generative AI is scaffold hopping—creating novel molecular frameworks that are not covered by existing patents while maintaining activity against the target [34].
Q3: Our experimental validation shows that an AI-prioritized target does not modulate the disease phenotype. What could have gone wrong? A3: This can stem from several issues in the AI workflow:
- Data Bias: The AI model may have been trained on biased or non-representative omics data, leading to spurious target-disease associations [35] [36].
- Lack of Causal Evidence: The AI may have identified a target that is merely correlated with the disease state rather than being a causal driver. It is crucial to use platforms that integrate genetic evidence (e.g., from genome-wide association studies) to support causality [33].
- Insufficient Context: The target's role may be highly context-dependent (e.g., specific cancer subtype, tumor microenvironment). Validate that your experimental models accurately reflect this biological context.
Performance Data and Case Studies
The table below summarizes key performance metrics and case studies from leading companies in AI-driven drug discovery.
| Company / Platform | AI Approach & Key Features | Reported Efficiency Gains | Key Oncology/Other Case Study |
|---|---|---|---|
| Exscientia [31] | - "Centaur Chemist" generative chemistry- Integrated target-to-design pipeline- Patient-derived biology & phenomics | - Design cycles ~70% faster- 10x fewer compounds synthesized than industry norms | - CDK7 inhibitor (GTAEXS-617): In Phase I/II trials for solid tumors [31]. |
| Insilico Medicine [31] [30] | - End-to-end generative AI (PandaOmics, Chemistry42)- Hybrid AI + physics-based methods- Multi-parameter optimization | - ISM001-055: Target to Phase I trials in 18 months for idiopathic pulmonary fibrosis [31] [30].- Platform can generate >2,400 candidates in dozens of hours [30]. | - QPCTL inhibitors: Identified for tumor immune evasion [33]. |
| Schrödinger [31] | - Physics-enabled (computational) + ML design | - N/A | - Zasocitinib (TAK-279): A TYK2 inhibitor originating from its platform advanced to Phase III trials [31]. |
Experimental Protocols for De Novo Design
Protocol 1: AI-Driven Hit Identification for a Novel Oncology Target
Target Identification & Validation:
- Tool: PandaOmics or similar target discovery platform.
- Method: Input multi-omics data (e.g., from TCGA) and use the AI to rank potential targets based on novelty, confidence, druggability, and linkage to the cancer pathway. Use integrated knowledge graphs and literature mining to build biological rationale [30] [33].
De Novo Molecular Generation:
- Tool: Chemistry42, Exscientia's Centaur Chemist, or similar generative chemistry platform.
- Method: Define the Target Product Profile (TPP), including binding affinity, selectivity, and key ADMET properties. Use an ensemble of generative models (VAEs, GANs, Transformers) to create novel molecular structures satisfying these constraints [30] [34].
In Silico Prioritization:
- Method:
- Apply >460 Medicinal Chemistry Filters to remove undesirable compounds [30].
- Score molecules using AI-based affinity predictors and physics-based methods like molecular dynamics (MD) simulations for binding stability (using tools like MDFlow) [30] [32].
- Predict synthetic routes via AI-powered retrosynthesis analysis [30].
- Method:
Experimental Validation:
- Method: Synthesize the top 10-50 prioritized compounds and test them in biochemical and cell-based assays to confirm activity and selectivity against the oncology target.
Protocol 2: Designing a Therapeutic Peptide for an "Undruggable" Protein-Protein Interface
Scaffold Generation:
- Tool: Generative Biologics or similar platform.
- Method: Input target protein structure or sequence. Use diffusion models and graph neural networks (GNNs) to generate thousands of novel peptide sequences predicted to bind the target site [30].
Affinity and Developability Optimization:
- Method: Use AI predictors to score generated peptides for affinity, solubility, and liability. Retrain models on internal data if available. In an internal case, this process generated over 5,000 novel peptides for GLP1R in 72 hours, with 14 out of 20 tested showing biological activity [30].
Experimental Validation:
- Method: Synthesize top candidates and test using surface plasmon resonance (SPR) for binding affinity and cell-based assays for functional activity.
Research Reagent Solutions
The table below lists key computational and experimental resources used in AI-driven de novo molecular design.
| Reagent / Tool | Type | Function in Workflow |
|---|---|---|
| PandaOmics [30] [32] | Software Platform | AI-powered biology platform for target and biomarker discovery; integrates multi-omics data and literature mining. |
| Chemistry42 [30] [32] | Software Platform | A comprehensive AI suite for de novo small molecule design, optimization, and property prediction. |
| Generative Biologics [30] [32] | Software Platform | AI engine for designing and optimizing novel biologics, including peptides and antibodies. |
| Molecular Dynamics (MD) Simulation (e.g., MDFlow) [30] [32] | Software Tool | Provides physics-based simulation of protein-ligand interactions to assess binding stability and mechanism. |
| AlphaFold [35] | Software Tool | Predicts 3D protein structures from amino acid sequences, providing critical structural data for targets with unknown structures. |
Workflow and Pathway Visualizations
AI-Driven Discovery Workflow
Computational Targeting Strategy
FAQs: Understanding IDPs and AI-Designed Binders
What are Intrinsically Disordered Proteins (IDPs) and why are they important therapeutic targets? Intrinsically Disordered Proteins (IDPs) and regions (IDRs) are proteins that do not fold into a stable, consistent 3D shape but remain highly flexible. They make up nearly half of the human proteome and drive key cellular signaling, stress responses, and disease progression, particularly in cancer and neurodegenerative diseases. Their inherent flexibility has made them historically very challenging to target with conventional drugs, which typically require a well-defined binding pocket [12] [13].
How do AI-designed binders overcome the challenge of targeting disordered regions? Generative AI methods, such as RFdiffusion and the 'logos' strategy, can now design proteins that bind these highly flexible targets with atomic precision. Instead of requiring a pre-existing structure, these AI tools can create binders that either wrap around targets with some secondary structure or assemble from pre-made parts to bind sequences lacking any regular structure, achieving high affinity and specificity that wasn't possible before [12] [13] [37].
What proof-of-concept results validate this approach? Initial designed binders have shown promising functional results in cell-based tests, including:
- Blocking pain signaling by targeting the opioid peptide dynorphin [12] [13].
- Dismantling toxic amyloid fibrils linked to type 2 diabetes [12] [13].
- Disabling pathogenic prion seeds [12].
Are these designed binders specific to their intended targets? Yes. The AI design processes, particularly the 'logos' method, have been validated through all-by-all binding tests, confirming that the binders exhibit high selectivity for their intended targets and do not cross-react with non-targets [37].
What is the main difference between the 'logos' and 'RFdiffusion' design strategies? These are complementary strategies. The RFdiffusion-based method excels at designing binders to targets that possess some helical and strand secondary structure. The 'logos' method, which assembles binders from a library of ~1,000 pre-made parts, works best for targets completely lacking regular secondary structure [12] [13].
Troubleshooting Guide: Experimental Issues and Solutions
| Problem Area | Specific Issue | Potential Cause | Recommended Solution |
|---|---|---|---|
| Binder Affinity | Low binding affinity in assays | Poor complementarity with dynamic target; binder rigidity. | Re-optimize using a different AI approach (e.g., switch from logos to RFdiffusion if target has some structure). Use longer molecular dynamics simulations to assess flexibility. |
| Binder Expression & Solubility | Low yield or aggregation in expression | Hydrophobic surface exposure; unstable fold. | Incorporate surface point mutations to improve solubility; fuse with solubility-enhancing tags (e.g., SUMO, GST) during initial testing. |
| Target Specificity | Off-target binding in cellular models | Binder recognizes a common, short peptide motif present in multiple proteins. | Analyze the binder's target sequence for homology to other human peptides; re-design using the AI pipeline with explicit negative design against these off-target sequences. |
| Functional Efficacy | Binder binds target but no phenotypic effect in cells | Binding site is not critical for the target's pathological function. | Re-prioritize the target region; design binders against different functional epitopes (e.g., regions known for critical protein-protein interactions). |
| Validation | Discrepancy between computational prediction and experimental binding | AI model inaccuracy; force field limitations. | Use AlphaFold3 or RoseTTAFold to independently predict the binder-target complex structure as a validation step before experimental testing [38]. |
Experimental Protocols for Key Methodologies
Protocol 1: De Novo Binder Design Using the 'Logos' Pipeline
This protocol is designed for creating binders to targets that lack any regular secondary structure [12] [37].
Materials:
- Software: Custom 'logos' pipeline software (publicly available).
- Input: Amino acid sequence of the disordered target region.
- Library: Pre-computed library of ~1,000 protein parts or pockets.
Method:
- Target Analysis: Input the target peptide sequence. The algorithm scans for short, recognizable motifs.
- Pocket Selection: The pipeline selects complementary pre-made protein pockets from its library that are predicted to fit the target motifs.
- Binder Assembly: The selected pockets are assembled into a single, continuous protein scaffold. This step involves computational optimization to ensure stable folding of the binder itself.
- Affinity Optimization: The assembled binder is refined to maximize predicted binding energy with the flexible target.
- In Silico Validation: The final designed binder sequence is evaluated with protein structure prediction tools like AlphaFold to verify the intended binding mode.
Protocol 2: Binder Design and Validation Using RFdiffusion
This protocol is suitable for targets that have some propensity for helical or strand secondary structure [12] [38].
Materials:
- Software: RFdiffusion tool.
- Input: Structure of the target (if a transient structure exists) or its sequence.
- Hardware: High-performance computing cluster with GPUs.
Method:
- Target Specification: Define the target protein and the general region for binding.
- Generative Design: Run the RFdiffusion network, which uses a diffusion model to generate entirely new protein structures that "wrap around" the specified target region.
- Sequence Design: Using a tool like ProteinMPNN, generate an amino acid sequence that will fold into the designed protein structure from step 2.
- Validation Round 1 (Computational): Predict the structure of the designed binder complexed with the target using AlphaFold2 or RoseTTAFold. Analyze the predicted interface and binding energy.
- Validation Round 2 (Experimental):
- Expression: Clone the DNA sequence of the validated design into an expression vector (e.g., pET series) and express in E. coli.
- Purification: Purify the binder protein using affinity and size-exclusion chromatography (SEC).
- Binding Assay: Measure affinity using Surface Plasmon Resonance (SPR) or Isothermal Titration Calorimetry (ITC). Expect high-affinity binders in the nanomolar to picomolar range [12] [37].
- Specificity Test: Validate specificity using techniques like yeast display or BLI against a panel of related protein targets.
Protocol 3: Functional Cellular Assay for a Pain-Signaling Blocker
This protocol is based on the successful blockade of dynorphin signaling [12].
Materials:
- Cell line expressing the target GPCR (e.g., opioid receptor).
- Designed binder specific to the disordered peptide ligand (e.g., dynorphin).
- Assay kits for measuring intracellular calcium or cAMP.
Method:
- Pre-incubation: Pre-treat cells with the purified designed binder for a set time (e.g., 30-60 minutes).
- Stimulation: Activate the signaling pathway by adding the native disordered peptide ligand (dynorphin).
- Signal Measurement: Quantify the downstream signaling output (e.g., calcium release or cAMP inhibition).
- Analysis: Compare the signaling output in binder-treated cells versus untreated controls. A successful binder will significantly reduce the signaling response upon ligand addition.
Key Signaling Pathways and Workflows
Research Reagent Solutions
The following table details key reagents and computational tools essential for research in this field.
| Tool / Reagent | Type | Function in Research | Example / Source |
|---|---|---|---|
| RFdiffusion | Software | Generative AI model for de novo protein design that creates binders by wrapping around target structures. | Baker Lab / Publicly Available [12] [38] |
| Logos Pipeline | Software | Computational method for designing binders by assembling pre-made protein parts to target disordered sequences. | Baker Lab / Publicly Available [12] [37] |
| AlphaFold2/3 | Software | Protein structure prediction tool used for independent validation of designed binder-target complexes. | DeepMind / Publicly Available [38] |
| ProteinMPNN | Software | Neural network that designs amino acid sequences for a given protein backbone structure. | Baker Lab / Publicly Available [38] |
| pET Expression Vector | Molecular Biology Reagent | Standard plasmid for high-level expression of designed binder proteins in E. coli. | Commercial Vendors |
| SPR / BLI Instruments | Analytical Instrument | Measures real-time binding kinetics (affinity, on/off rates) between the designed binder and its target. | Commercial Vendors (e.g., Cytiva, Sartorius) |
The Kirsten rat sarcoma viral oncogene homolog (KRAS) is one of the most frequently mutated oncogenes in human cancers, found in approximately 25% of all tumors, including pancreatic, colorectal, and non-small cell lung carcinomas [39] [40]. For decades, KRAS was considered "undruggable" due to its smooth surface structure with no deep hydrophobic pockets for small molecules to bind effectively, and its picomolar affinity for GTP which makes developing competitive inhibitors exceptionally challenging [39] [40]. The emergence of quantum-classical hybrid models represents a transformative approach to overcome these historical challenges by leveraging the unique capabilities of quantum computing to navigate the vast chemical space of potential drug candidates.
Quantum-classical hybrid models integrate parameterized quantum circuits with classical deep learning architectures, creating systems that can theoretically leverage quantum effects such as superposition and entanglement to explore molecular distributions more efficiently than purely classical systems [41] [42]. For challenging targets like KRAS, these models offer a promising path to identify novel inhibitor scaffolds that might evade classical discovery approaches. Recent experimental validations have demonstrated that quantum-classical generative models can produce biologically active KRAS inhibitors, marking a significant milestone in computational drug discovery [41] [43] [44].
Technical Foundations: How Quantum-Classical Hybrid Models Work
Core Architectural Components
Hybrid quantum-classical models for drug discovery typically combine several computational components into an integrated workflow:
Quantum Circuit Born Machines (QCBMs): Quantum generative models that employ parameterized quantum circuits to learn complex probability distributions of molecular structures. These circuits leverage quantum superposition to explore multiple molecular configurations simultaneously [41] [43].
Classical Deep Learning Networks: Typically Long Short-Term Memory (LSTM) networks or Graph Neural Networks (GNNs) that handle sequential data processing and molecular graph representations [41] [43].
Reward Networks: Classical networks that predict desirable chemical properties and provide feedback signals to guide the generative process toward drug-like molecules [42].
The quantum component typically serves as a prior distribution generator, while classical networks refine these suggestions and ensure chemical validity. This division of labor allows the model to leverage quantum advantages while working within the constraints of current noisy intermediate-scale quantum (NISQ) hardware [42].
KRAS Biological Context
To effectively target KRAS, researchers must understand its biological behavior. KRAS functions as a molecular switch, cycling between active GTP-bound and inactive GDP-bound states [39]. Oncogenic mutations (most commonly at codons 12, 13, and 61) lock KRAS in its active conformation, leading to continuous signaling through pathways like RAF-MEK-ERK and PI3K-AKT-mTOR that drive cell proliferation and survival [39] [40]. The switch I and switch II regions of KRAS undergo conformational changes during activation and represent key areas for therapeutic intervention [39].
KRAS Signaling Pathway: This diagram illustrates the core KRAS signaling cascade that becomes constitutively active in cancer cells due to mutations, driving uncontrolled proliferation and survival.
Experimental Protocols & Workflows
End-to-End Hybrid Workflow for KRAS Inhibitor Discovery
The following workflow represents an integrated quantum-classical approach that has successfully generated experimentally validated KRAS inhibitors [41] [43]:
Hybrid Model Workflow: Integrated quantum-classical pipeline for KRAS inhibitor discovery, from data preparation to experimental validation.
Step-by-Step Protocol: Implementing a Quantum-Classical Hybrid Model
Phase 1: Training Data Preparation
- Curate Known Actives: Compile approximately 650 experimentally confirmed KRAS inhibitors from literature sources [41] [43].
- Virtual Screening Enhancement: Use VirtualFlow 2.0 to screen 100 million molecules from Enamine's REAL library, selecting the top 250,000 compounds with best docking scores [41] [43].
- Chemical Space Exploration: Apply the STONED-SELFIES algorithm to known inhibitors to generate 850,000 structurally similar compounds with maintained synthesizability [43].
- Dataset Assembly: Combine all sources into a unified training dataset of approximately 1.1 million molecules [41].
Phase 2: Model Training & Configuration
- Quantum Component Setup: Implement a Quantum Circuit Born Machine (QCBM) using a 16-qubit quantum processor. Critical parameters include:
Classical Component Configuration: Implement an LSTM network with:
Hybrid Integration: Connect QCBM and LSTM such that the quantum component generates prior distributions in each training epoch, which are then refined by the classical network [41].
Phase 3: Molecule Generation & Validation
- Generative Process: Sample 1 million candidate molecules from the trained model [41].
- Multi-Stage Filtering:
- Experimental Validation:
- Synthesize top 15-20 candidates
- Evaluate binding via surface plasmon resonance (SPR)
- Assess functional activity in cell-based assays (e.g., MaMTH-DS) [41]
Success Metrics and Validation
Table 1: Key Performance Metrics for Hybrid Quantum-Classical Models
| Metric | Target Value | Measurement Method |
|---|---|---|
| Success Rate | >21.5% improvement vs classical | Proportion of generated molecules passing filters [41] |
| Fréchet Distance | <12.5 | Distribution similarity to real molecules [42] |
| QED Score | >0.6 | Quantitative Estimate of Drug-likeness [42] |
| Synthetic Accessibility | >0.7 | Synthetic accessibility score [42] |
| Binding Affinity | <10 μM | Surface plasmon resonance (SPR) [41] |
The Scientist's Toolkit: Essential Research Reagents & Solutions
Table 2: Key Research Reagents for Quantum-Classical KRAS Drug Discovery
| Reagent/Solution | Function | Example Sources/Formats |
|---|---|---|
| Known KRAS Inhibitors | Training data foundation | ~650 compounds from literature [41] |
| Enamine REAL Library | Virtual screening source | 100+ million synthesizable compounds [41] [43] |
| STONED-SELFIES Algorithm | Chemical space expansion | Python implementation for molecular mutation [43] |
| Chemistry42 Platform | Structure-based validation | Commercial software for drug design [41] [43] |
| VirtualFlow 2.0 | Large-scale virtual screening | Open-source docking pipeline [41] |
| QCBM Framework | Quantum prior generation | 16-qubit IBM quantum processor [41] [43] |
| LSTM Network | Classical sequence refinement | TensorFlow/PyTorch implementation [41] |
| MaMTH-DS Assay | Functional validation | Cell-based KRAS signaling assay [41] |
| SPR Platform | Binding affinity measurement | Biacore or similar instruments [41] |
Troubleshooting Guides & FAQs
Common Implementation Challenges & Solutions
Problem: Low Success Rate in Molecule Generation Symptoms: Generated molecules fail synthesizability filters or show poor drug-likeness scores. Solutions:
- Increase training dataset diversity using STONED-SELFIES augmentation [41] [43]
- Adjust reward function weights in hybrid model to prioritize synthesizability and QED [42]
- Verify quantum circuit depth (4-8 layers optimal) and qubit count (higher generally better) [42]
Problem: Poor Energy Conservation in Dynamics Simulations Symptoms: Numerical instability in molecular dynamics trajectories. Solutions:
- Implement smaller time steps (0.5-2.0 fs) for QM/MM regions [45]
- Apply particle mesh Ewald (PME) treatment for long-range electrostatics [45]
- Verify Link Atom implementation for QM-MM boundary regions [45]
Problem: Model Training Instability Symptoms: Oscillating loss values or failure to converge. Solutions:
- Implement gradient clipping with norm value of 1.0 [42]
- Use warm-up/constant/decay learning rate scheduler [42]
- Adjust balance parameter (λ) between adversarial and reward losses [42]
Frequently Asked Questions
Q: What quantum hardware specifications are needed for effective KRAS inhibitor discovery? A: Current successful implementations use 16-qubit processors, with performance scaling approximately linearly with qubit count. Circuit depths of 4-8 layers with ring entanglement topologies have proven effective [41] [42].
Q: How does hybrid quantum-classical performance compare to purely classical approaches? A: In benchmark studies, the QCBM-LSTM hybrid demonstrated a 21.5% improvement in success rate for generating synthesizable, drug-like molecules compared to vanilla LSTM alone [41].
Q: What experimental validation is essential for computationally discovered KRAS inhibitors? A: A two-stage validation process is recommended: (1) Binding confirmation via surface plasmon resonance (SPR) to measure direct target engagement, and (2) Functional assessment in cell-based assays like MaMTH-DS to verify inhibition of KRAS signaling pathways [41].
Q: How critical is training data quality and quantity for success? A: Extremely critical. The successfully demonstrated workflow utilized ~1.1 million data points combining known actives, virtual screening hits, and algorithmically augmented compounds. For targets with less available data, transfer learning or data augmentation strategies are essential [41] [44].
Q: What are the most common architectural mistakes in hybrid model implementation? A: Key pitfalls include: (1) Insufficient quantum circuit depth (<4 layers), (2) Poorly designed quantum-classical interface, and (3) Inadequate reward function design. Optimal architectures typically layer multiple (3-4) shallow quantum circuits sequentially [42].
The integration of quantum-classical hybrid models into KRAS drug discovery represents a paradigm shift in targeting previously "undruggable" oncoproteins. The experimental validation of two novel KRAS inhibitors (ISM061-018-2 and ISM061-022) generated by a QCBM-LSTM hybrid model demonstrates the practical potential of this approach [41] [44]. ISM061-018-2 functions as a broad-spectrum KRAS inhibitor with binding affinity of 1.4 μM to KRAS-G12D, while ISM061-022 shows mutant-selective activity, particularly against KRAS-G12R and KRAS-Q61H [41].
As quantum hardware continues to evolve, with increasing qubit counts and improved error correction, the advantages of quantum-classical hybrid models are expected to become more pronounced. Future developments will likely focus on more sophisticated integration of structural information during the generation process, improved reward functions that better capture molecular interactions with dynamic protein targets, and expansion to other challenging therapeutic targets beyond KRAS. For researchers implementing these methods, careful attention to dataset quality, model architecture optimization, and robust experimental validation will remain critical success factors.
Allosteric Inhibition and Covalent Drug Design Computationally Guided
Frequently Asked Questions (FAQs)
FAQ 1: What are the key advantages of combining allosteric and covalent inhibition strategies?
Combining allostery with covalent inhibition creates Covalent-Allosteric Inhibitors (CAIs), which aim to harness the benefits of both strategies. Allosteric inhibitors bind to sites distinct from the active (orthosteric) site, often leading to higher selectivity because allosteric sites are less conserved across protein families compared to orthosteric sites [46] [47]. Covalent inhibitors form a permanent bond with their target, typically through a reactive "warhead," leading to prolonged duration of action and increased potency [46] [1]. CAIs therefore can achieve long-lasting effects, reduced potential for drug resistance, enhanced specificity, and potentially lower toxicity [46] [3].
FAQ 2: Which kinetic parameters are critical for characterizing covalent-allosteric inhibitors, and why is a fast reaction not always better?
The potency of covalent inhibitors is best described by the second-order rate constant ( k{inact}/KI ), which characterizes the efficiency of the covalent inhibition in a time-independent manner [46]. The parameter ( KI ) (the inactivation constant) is derived from ( (k{off} + k{inact}) / k{on} ) and differs from the simple dissociation constant ( K_i ) used for reversible inhibitors [46].
While a faster inactivation efficiency rate generally correlates with greater cellular potency, recent research indicates this relationship plateaus. Beyond a certain point, a faster rate does not lead to increased potency, and relying solely on this metric can fail to distinguish the best drug candidates. Prioritizing compounds requires a balance between inactivation speed and other parameters, especially target selectivity, which measures how well a drug binds to its intended target over off-target proteins [48].
FAQ 3: What are the major computational challenges in discovering allosteric sites for drug design?
Identifying and validating allosteric sites presents several unique challenges:
- Transient and Cryptic Pockets: Many allosteric sites are not visible in static protein structures from X-ray crystallography or cryo-EM. They often exist only in specific, less populated conformational states of the protein [46] [47].
- Conformational Flexibility: Proteins are dynamic, and allosteric regulation is inherently linked to this flexibility. Capturing the full range of motions to find these sites is computationally expensive [47] [49].
- Low Evolutionary Conservation: While beneficial for selectivity, the low conservation of allosteric sites makes it difficult to use homology-based prediction methods that work well for orthosteric sites [47].
- Lack of General Rules: The structure-activity relationships and the principles of how ligand binding at an allosteric site impacts protein function are less understood than for orthosteric sites [46].
FAQ 4: Can you provide examples of successfully targeted "undruggable" proteins using these strategies?
Yes, several targets once considered "undruggable" have been successfully targeted.
- KRAS G12C: The KRAS oncogene was undruggable for decades due to its smooth surface and picomolar affinity for GTP/GDP. The discovery of a cryptic allosteric pocket adjacent to the mutated cysteine 12 (G12C) enabled the development of covalent inhibitors like Sotorasib (AMG510) and Adagrasib (MRTX849). These drugs bind covalently to the mutant cysteine and trap KRAS in its inactive state [1] [3].
- PTP1B: Protein Tyrosine Phosphatase 1B, a target for diabetes and obesity, has a highly conserved active site, making selective inhibition difficult. The discovery of an allosteric site near Cys121 allowed for the design of covalent-allosteric inhibitors like ABDF, which modulates activity by restricting the movement of the WPD loop [46].
Troubleshooting Guides
Problem 1: My virtual screening of a large compound library fails to identify hits for a known allosteric site.
Potential Causes and Solutions:
- Cause: The protein structure used for docking is in a conformational state where the allosteric pocket is closed or absent.
- Solution: Use molecular dynamics (MD) simulations to sample conformational ensembles and identify structures where the pocket is open. Advanced sampling algorithms can reveal these transient states [47]. Alternatively, use a known allosteric ligand (if available) in a co-crystal structure as your receptor model.
- Cause: Standard docking programs may not be optimized for the specific geometry or flexibility of allosteric pockets.
- Solution: Employ more flexible docking protocols or use specialized tools designed for cryptic site detection. For covalent docking, use benchmarks like CovDocker that account for the formation of covalent bonds and associated structural changes [50].
- Cause: The chemical library may not contain fragments or compounds suitable for binding to the unique chemophysical environment of the allosteric site.
Problem 2: My covalent-allosteric inhibitor candidate shows high potency but also high toxicity in cellular assays.
Potential Causes and Solutions:
- Cause: The warhead is too reactive, leading to off-target binding and modification of proteins with similar nucleophilic residues (e.g., other cysteines).
- Solution: Tune the warhead's reactivity. A less reactive warhead can improve selectivity by allowing for more specific recognition by the target protein before covalent bond formation occurs [52]. Use kinetic analyses to find an optimal balance between efficiency and selectivity [48].
- Solution: Perform proteome-wide profiling to identify off-targets. Techniques like activity-based protein profiling (ABPP) can directly quantify the selectivity of your covalent inhibitor across the proteome [46] [52].
- Cause: The non-covalent "scaffold" part of the molecule has inherent off-target activity.
- Solution: Re-optimize the scaffold for selectivity using structure-based design. Ensure that it has minimal affinity for unrelated proteins, as the covalent warhead will amplify any binding, however weak [48].
Potential Causes and Solutions:
- Cause: Standard activity assays cannot distinguish between orthosteric and allosteric inhibition.
- Cause: Difficulty in obtaining a co-crystal structure of the inhibitor bound to the protein.
- Solution: Use orthogonal biophysical methods. Hydrogen-Deuterium Exchange Mass Spectrometry (HDX-MS) can detect changes in protein dynamics and solvent accessibility upon inhibitor binding, helping to map the binding site [49]. Covalent binding can be confirmed through mass spectrometry to detect the expected mass shift [46].
- Cause: For covalent inhibitors, it is unclear which specific residue is modified.
- Solution: Use tandem mass spectrometry (MS/MS) after tryptic digestion of the protein-inhibitor complex to pinpoint the exact site of covalent modification [46].
Essential Data and Protocols
Key Kinetic Parameters for Covalent Inhibitor Characterization
The following parameters are crucial for the proper evaluation and comparison of covalent inhibitors [46] [52].
| Parameter | Description | Significance in Drug Discovery |
|---|---|---|
| ( k{inact}/KI ) | Second-order rate constant for covalent inactivation | Gold-standard measure of covalent inhibitor potency; time-independent [46]. |
| ( k_{inact} ) | First-order rate constant for the covalent modification step | Describes the maximum rate of covalent bond formation [46]. |
| ( K_I ) | Inactivation constant | Apparent concentration for half-maximal rate of inactivation; incorporates ( k{on} ), ( k{off} ), and ( k_{inact} ) [46]. |
| Residence Time | Duration for which the inhibitor remains bound to the target | Governs duration of pharmacological effect; prolonged for covalent inhibitors [52]. |
| Target Selectivity | Measure of binding to intended vs. unintended targets | Critical for differentiating promising candidates once potency plateaus; reduces toxicity [48]. |
Computational Tools for Allosteric and Covalent Drug Discovery
A summary of computational methods streamlining the discovery of allosteric and covalent drugs.
| Method Category | Key Function | Example Tools/Approaches |
|---|---|---|
| Machine Learning (ML) | Identifies potential allosteric sites from protein sequence and structure data [47]. | ML models trained on evolutionary, structural, and dynamic features; AlphaFold2 for structure prediction [47] [53]. |
| Molecular Dynamics (MD) | Reveals transient allosteric pockets and communication pathways via atomic-level simulation [47] [49]. | Enhanced sampling algorithms; GPCRmd database for specialized simulations [47]. |
| Network Analysis | Maps allosteric communication pathways to pinpoint critical regulatory residues [47]. | Methods based on residue-residue co-evolution and correlation [47]. |
| Covalent Docking | Predicts binding mode and orientation of covalent inhibitors. | CovDocker benchmark; methods accounting for covalent bond formation and structural changes [50]. |
The Scientist's Toolkit: Key Research Reagents and Materials
| Reagent / Material | Function in Research |
|---|---|
| Nucleophilic Amino Acids (Cysteine, Lysine, etc.) | Targets for covalent warhead binding. Cysteine is the most common, but new chemistries are targeting other residues [46]. |
| Covalent Warhead Libraries | Collections of electrophilic groups (e.g., acrylamides, aldehydes) with varying reactivity used to screen for optimal covalent bond formation with a target nucleophile [52] [48]. |
| DNA-Encoded Libraries (DELs) | Vast collections of small molecules, each tagged with a DNA barcode, enabling highly efficient screening for binders against immobilized protein targets [1]. |
| Stable Isotope Labels (e.g., for HDX-MS) | Used to label proteins in Hydrogen-Deuterium Exchange experiments to study protein dynamics and map ligand-binding sites [49]. |
| Ultra-Large Virtual Compound Libraries (e.g., ZINC20) | Databases of billions of readily available or easily synthesizable compounds for virtual screening to discover novel chemical starting points [51]. |
Experimental Workflows and Signaling Pathways
Covalent-Allosteric Inhibition Mechanism
This diagram illustrates the two-step mechanism of a Covalent-Allosteric Inhibitor (CAI), which first binds reversibly to an allosteric site before forming an irreversible covalent bond, stabilizing an inactive protein conformation [46].
Computational Workflow for Allosteric Drug Discovery
This workflow outlines an integrated computational strategy for identifying and validating allosteric sites and designing modulators, combining machine learning, molecular dynamics, and network analysis [47] [49].
Leveraging Physics-Based Simulations and Multi-Scale Modeling
"Undruggable" targets are proteins of high therapeutic significance that, due to features like flat interaction surfaces, a lack of defined binding pockets, or high flexibility, have eluded conventional drug design approaches [1]. This category includes high-value targets in oncology such as mutated KRAS, transcription factors like p53 and Myc, and intrinsically disordered proteins (IDPs) that lack stable structures [1] [13]. Computational strategies are pivotal in overcoming these challenges. Physics-based simulations and multi-scale modeling provide a powerful framework for understanding the behavior of these proteins and for designing novel therapeutic agents, moving these targets from "undruggable" to "difficult to drug" [1] [54].
Troubleshooting Guides and FAQs
This section addresses common technical challenges researchers face when applying simulations and multi-scale models to undruggable target drug discovery.
General Workflow and Integration Issues
Q: The predictions from my AI model and my physics-based simulation are in conflict. How should I proceed?
- A: First, verify the input data and parameters for both methods. Use a tiered validation approach. For instance, a machine learning model might rapidly screen thousands of compounds, but the results for shortlisted candidates should be confirmed with more rigorous, albeit computationally expensive, physics-based methods like molecular dynamics (MD) or free energy calculations [55]. This synergistic approach leverages the speed of AI and the accuracy of physics-based modeling.
Q: How can I efficiently explore the vast chemical space for fragment elaboration?
- A: Implement an active learning strategy. Instead of screening entire virtual libraries, use an iterative process where a model selects the most promising compounds for simulation, learns from the results, and then selects the next batch. This can be combined with generative AI models to propose novel molecules, dramatically improving sampling efficiency [55].
Simulation-Specific Problems
Q: My molecular dynamics simulations of a protein-ligand complex show the ligand departing from the binding pose. Does this mean the compound is a poor binder?
- A: Not necessarily. For fragments and weak binders, some pose instability is expected. The key is to establish quantitative pose stability metrics. Monitor the root-mean-square deviation (RMSD) of the ligand, the persistence of key hydrogen bonds, and the ligand's residence time. Compare these metrics against a known positive control to determine if the binding mode is maintained sufficiently for further elaboration [55].
Q: When building a multi-scale model of tumor growth, how can I integrate clinical biomarker data like PSA (Prostate-Specific Antigen) to improve accuracy?
- A: Develop a physics-informed machine learning framework. Use a physics-based model to represent the underlying biology (e.g., tumor cell proliferation, PSA production and flux into blood). Then, integrate a deep learning component that regulates the model's growth dynamics based on the patient's actual PSA measurements and other clinical imaging data. This ensures the digital twin's predictions are calibrated to real-world patient data [56].
Data and Validation Issues
Q: My computational model seems accurate, but how can I gain the confidence of experimentalists to test its predictions?
- A: Conduct a retrospective validation. Apply your computational framework to a well-documented case from literature or internal data where the experimental outcome is already known (e.g., a successful fragment-to-lead optimization campaign). Demonstrating that your method can correctly predict known successes and failures builds credibility for prospective applications [55].
Table: Common Simulation Issues and Resolutions
Problem Area Specific Symptom Probable Cause & Theory Recommended Action & Resolution Plan Model Integration AI/ML and physics-based simulation outputs disagree. Models are operating at different scales or with different underlying assumptions. Establish a hierarchical workflow; use AI for rapid screening and physics-based methods for final validation [57] [55]. Sampling Efficiency Virtual screening of a large chemical library is computationally prohibitive. Brute-force sampling is inefficient. Implement an active learning protocol to iteratively and intelligently select compounds for simulation [55]. Binding Assessment Unstable ligand pose in molecular dynamics simulations. Inherently weak binding affinity of fragments or suboptimal initial pose. Quantify stability with metrics (RMSD, H-bond persistence); compare to a known positive control before discarding [55]. Model Calibration Multi-scale model does not match patient biomarker data. Model parameters are not patient-specific. Integrate a machine-learning component to dynamically adjust model parameters based on real patient follow-up data [56].
Essential Research Reagent Solutions
This table outlines key computational tools and methodologies used in the field for targeting undruggable proteins.
- Table: Key Computational Tools and Methodologies
Research Reagent / Tool Function / Application Key Use-Case for Undruggable Targets Generative AI (e.g., RFdiffusion) Designs novel protein binders that wrap around flexible target proteins. Creating high-affinity binders to intrinsically disordered proteins (IDPs) and regions, achieving nanomolar affinity [13]. Fragment-Based Drug Discovery (FBDD) Identifies weak-binding, small molecular fragments as starting points for drug design. Targeting shallow binding pockets on proteins like KRAS; fragments can be optimized into potent leads [55]. Molecular Dynamics (MD) & Metadynamics Simulates the physical movements of atoms and molecules over time, providing dynamic structural information. Assessing fragment pose stability and investigating the structural flexibility of disordered proteins [55] [58]. Digital Twin Framework Creates a virtual, patient-specific representation of a biological system (e.g., a tumor). Reconstructing prostate cancer tumor growth by integrating PSA data and MRI to predict personalized disease progression [56]. Monte Carlo Simulations (e.g., Geant4) Uses random sampling to model complex physical systems, particularly particle interactions. Accurately modeling proton beam therapy dose distribution in tissues for precise cancer treatment planning [59]. Covalent Docking & Simulation Predicts how a drug candidate forms a covalent bond with its target protein. Rational design of irreversible inhibitors for targets like KRASG12C (e.g., Sotorasib) [1] [54].
Experimental Protocols
Protocol: AI-Guided Design of Binders for Intrinsically Disordered Proteins
This protocol is based on two complementary strategies developed by the Baker Lab [13].
1. 'Logos' Method for Targets Lacking Regular Structure
- Objective: Assemble binders from a pre-fabricated library of protein parts.
- Methodology:
- Step 1: Utilize a library of approximately 1,000 pre-made protein parts or "pockets".
- Step 2: For a given disordered peptide target, computationally assemble binders from this library, allowing for trillions of combinations.
- Step 3: Select and test the assembled binders for high-affinity binding to the target.
- Step 4 (Functional Validation): In cell-based tests, demonstrate that the binder blocks the target's function (e.g., a binder targeting the opioid peptide dynorphin blocked pain signaling in human cells).
2. RFdiffusion-Based Method for Targets with Some Secondary Structure
- Objective: Generate proteins that wrap entirely around the flexible target.
- Step 1: Use the RFdiffusion generative AI model to design protein binders based on the target sequence or partial structural information.
- Step 2: Screen the generated binders for high affinity (e.g., in the 3–100 nM range).
- Step 3 (Functional Validation): Test the efficacy of binders in disease-relevant assays. For example, binders targeting amylin were shown to dissolve amyloid fibrils associated with type 2 diabetes.
The following diagram illustrates the strategic choice between these two methods for targeting intrinsically disordered proteins (IDPs).
Protocol: Physics-Informed Digital Twin for Prostate Cancer Monitoring
This protocol details the creation of a digital twin to reconstruct tumor growth from serum PSA data [56].
- Objective: Reconstruct patient-specific prostate cancer tumor growth over time using routine PSA tests and MRI data.
- Materials & Data Inputs:
- T2-weighted MRI sequences (including Diffusion Weighted and Dynamic Contrast Enhanced).
- Tumor segmentation masks from expert radiologists.
- Serial serum PSA measurements from patient follow-ups.
- Methodology:
- Step 1: Digital Twin Generation. Process MRI data to create a 3D voxelized geometry of the patient's prostate. This geometry incorporates spatial data on cellularity (c(x,t)), vascular permeability (ktrans(x)), and the initial tumor mask.
- Step 2: Physics-Based Model Setup. Implement a model that simulates:
- Tumor cell concentration (ct(x,t)): Driven by a proliferation term.
- Tissue PSA (P(x,t)): Produced by the tumor cells.
- Serum PSA (Ps(t)): Calculated from the flux of tissue PSA into the blood vessels, dependent on local vascularization (ktrans(x)).
- Step 3: Machine Learning Integration. Train a fully connected neural network to approximate the fraction of proliferating tumor cells (φθ(x,t)). This network is regulated by the patient's actual serum PSA measurements, ensuring the simulated tumor growth produces a matching PSA dynamic.
- Step 4: Model Calibration & Prediction. Calibrate the model using one follow-up MRI and the patient's PSA history. Once calibrated, the digital twin can predict future tumor growth based on PSA measurements alone.
The workflow for developing this prostate cancer digital twin is summarized in the diagram below.
Overcoming Hurdles: Data, Validation, and Translational Gaps
Addressing Data Scarcity and Quality for AI Model Training
In the computational pursuit of "undruggable" cancer targets—proteins such as KRAS, transcription factors like p53 and Myc, and various protein-protein interaction networks that lack conventional binding pockets—the quality and quantity of training data are paramount [1]. Artificial Intelligence (AI) and Machine Learning (ML) models are pivotal for identifying and optimizing novel therapeutic candidates against these challenging targets [60]. However, the development of robust models is often hindered by data scarcity, a critical bottleneck arising from the complex, expensive, and low-throughput nature of wet-lab experiments in structural biology and drug discovery [61] [62]. This technical support guide provides actionable troubleshooting methodologies and FAQs to help researchers diagnose and overcome data-related challenges, thereby accelerating the development of AI models for oncology drug discovery.
Troubleshooting Guides
Guide: Diagnosing and Mitigating Data Scarcity
Problem: Your AI model for predicting druggability or binding affinity is exhibiting poor performance, likely due to an insufficient volume of training data.
Symptoms:
- The model achieves high accuracy on the training dataset but fails to generalize to new, unseen test data (overfitting).
- Predictions lack consistency and have high variance across different data splits.
- The model cannot identify meaningful biological patterns, performing no better than a random guess.
Diagnostic Steps:
- Quantify Data Scarcity: Compare the size and dimensionality of your dataset against benchmarks in recent literature. The limitations of small datasets become particularly acute for complex, non-linear models like Deep Neural Networks.
- Perform Learning Curve Analysis: Plot your model's performance (e.g., AUROC, F1-score) against the size of the training set. A plateau in performance with increasing data is a strong indicator that the model has learned all it can from the available data and that data scarcity is the limiting factor [61].
- Evaluate Model Generalization: Use robust techniques like nested cross-validation to assess performance on held-out test sets. A significant drop in performance between training and test sets signals overfitting due to insufficient data.
Solutions:
Diagram: A strategic framework for overcoming data scarcity in AI-driven drug discovery.
Implementation:
- For Transfer Learning: Start with a model pre-trained on a large, general dataset (e.g., the entire Protein Data Bank). Then, fine-tune the final layers of the network using your smaller, specific dataset of cancer-driving proteins [62].
- For Few-Shot Learning: Employ metric-based approaches like Prototypical Networks, which learn a metric space where classification can be performed from very few examples of each class [62].
- For Data Augmentation: In the context of molecular data, this could include generating valid rotational conformers of a small molecule or creating slight variations of a protein surface patch representation, thereby artificially expanding your training set.
Guide: Improving Low-Quality and Biased Data
Problem: Your model's predictions are inaccurate or biased because the training data is noisy, incomplete, or non-representative.
Symptoms:
- The model makes systematic errors on specific subsets of data (e.g., for a particular protein class).
- Performance is poor even on the training data.
- The model learns spurious correlations that lack biological plausibility.
Diagnostic Steps:
- Conduct Exploratory Data Analysis (EDA): Thoroughly profile your dataset. Check for missing values, class imbalances (e.g., more druggable proteins than "hard-to-drug" phosphatases), and outliers [63].
- Audit for Data Bias: Identify if your data over-represents certain protein families (e.g., kinases) while under-representing others (e.g., transcription factors), as this will bias the model against the underrepresented classes [61].
- Benchmark Data Quality: Use predefined quality metrics, such as the completeness of atomic coordinates in protein structures or the consistency of binding affinity measurements across different assay types.
Solutions:
- Data Cleansing: Impute missing values using robust methods (e.g., k-nearest neighbors imputation) or remove entries with a high percentage of missing critical features. Filter out outliers that result from experimental error.
- Handle Class Imbalance: Apply techniques like the Synthetic Minority Over-sampling Technique (SMOTE), which was successfully used to balance a dataset of 666 druggable and 219 'hard-to-drug' proteins, enabling a more robust model training process [63].
- Bias Mitigation: Strategically collect additional data for underrepresented classes or use algorithmic fairness techniques to re-weight the loss function during training, penalizing errors on minority classes more heavily.
Frequently Asked Questions (FAQs)
Q1: What are the concrete consequences of data scarcity for our research on undruggable targets?
A: Data scarcity can lead to several critical failures [61]:
- Reduced Accuracy and Generalizability: Models fail to predict the behavior of novel, unseen targets, which is the primary goal of this research.
- Increased "Hallucination": AI models may invent non-existent binding sites or interactions when a valid response cannot be generated from its known knowledge.
- Stifled Innovation: The high risk of model failure makes it difficult to secure funding and resources for high-risk, high-reward projects on truly novel targets.
Q2: We have a small dataset of protein sequences and their measured binding affinities. What is the most efficient ML approach to use?
A: For a small dataset (e.g., hundreds to a few thousand samples), your most effective strategy is to use a Support Vector Machine (SVM) with a non-linear kernel (e.g., Radial Basis Function). This approach has been proven successful in similar scenarios. For instance, one study achieved an AUROC of 0.975 and an accuracy of 0.929 in predicting druggable cancer-driving proteins using an SVM model trained on tri-amino acid composition descriptors, outperforming 12 other classifiers [63]. Start with simple, informative feature descriptors (like amino acid composition) before moving to more complex, high-dimensional representations.
Q3: What are the risks of using synthetic data to augment our limited datasets?
A: The primary risk is that the synthetic data may fail to capture the full complexity and nuanced patterns of real-world biological systems [61] [62]. If the generative model is imperfect, it can introduce biases and artificial patterns into your training set. This can lead to an AI model that performs well on synthetic data but fails when applied to real experimental data. It is crucial to rigorously validate any model trained on synthetic data with a held-out set of real biological data.
Q4: How can we assess the quality of a dataset before starting a lengthy ML project?
A: Perform a comprehensive Data Quality Audit by checking the following:
- Provenance: Is the source of the data reputable (e.g., DrugBank, public PDB)?
- Completeness: What percentage of feature values are missing?
- Class Balance: Is there a roughly equal representation of positive and negative examples?
- Consistency: Are measurements collected using standardized protocols? Inconsistencies in experimental sources can introduce significant noise.
Quantitative Impact of Data Scarcity
Table: Consequences and Prevalence of Data Scarcity in AI for Drug Discovery
| Aspect | Impact of Scarcity/Low Quality | Quantitative Metric / Evidence |
|---|---|---|
| Model Generalization | Leads to overfitting; model fails on new data. | Performance plateaus or decreases in learning curve analysis [61]. |
| Project Failure Rate | Contributes to high failure rate in drug discovery. | ~90% of drug candidates fail in clinical trials; many due to poor target selection [60]. |
| Operational Cost | Inefficient resource allocation and increased costs. | Cost of a single failed clinical trial: $800 million - $1.4 billion [60]. |
| Representation Bias | Models perform poorly on underrepresented target classes. | Models trained on biased internet data struggle with diverse characteristics [61]. |
Experimental Protocols for Key Methodologies
Protocol: Implementing Transfer Learning for Druggability Prediction
Purpose: To adapt a model pre-trained on a large, general protein dataset to the specific task of predicting the druggability of cancer-driving proteins with high accuracy and minimal data.
Workflow:
Diagram: A two-phase workflow for applying transfer learning to a biological prediction task.
Methodology:
- Pre-training Phase:
- Input: A large-scale dataset, such as all protein structures in the PDB or a massive corpus of protein sequences.
- Model Architecture: Use a deep learning model like a Convolutional Neural Network (CNN) for structural data or a Transformer for sequence data.
- Objective: Train the model on a general task, such as predicting protein structure or function. This allows the model to learn fundamental features of protein biology (e.g., common folds, conserved domains, interaction motifs) [62].
- Fine-tuning Phase:
- Dataset: Your smaller, specific dataset of cancer-driving proteins (e.g., the 2,339 proteins from the Network of Cancer Genes) with labeled druggability [63].
- Model Adaptation: Remove the final classification layer of the pre-trained model. Replace it with a new layer(s) that maps to your specific output (e.g., "druggable" vs. "hard-to-drug").
- Training:
- Freeze the weights of the initial layers of the network, as they contain general, reusable features.
- Train (fine-tune) only the weights of the newly added final layers on your target dataset. This allows the model to specialize its high-level reasoning for your specific task without forgetting the general knowledge [62].
- Validation: Use cross-validation on your target dataset to assess performance and prevent overfitting.
Protocol: Applying Few-Shot Learning for Novel Target Identification
Purpose: To enable an AI model to accurately classify or predict properties for a new protein class after being shown only a very small number of examples (e.g., 1-10).
Methodology:
- Problem Formulation (N-way k-shot): Set up the learning task as an N-way k-shot classification. For example, a 5-way 1-shot task requires the model to classify a query sample into one of 5 classes, having seen only 1 example of each class.
- Model Selection:
- Metric-based Approach (Recommended for starters): Use a model like a Prototypical Network.
- Process: An encoder network (e.g., a neural network) maps all samples (support set and query) into an embedding space. The prototype (average vector) for each class is computed from its support examples. The query sample is classified based on its Euclidean or cosine distance to these prototypes [62].
- Training (Episodic Training):
- The model is not trained on a fixed dataset. Instead, it is trained over numerous "episodes."
- In each episode, a small, randomized "support set" and "query set" are sampled from the training data, mimicking the few-shot scenario. This forces the model to learn a general strategy for learning from small data, rather than memorizing a specific dataset.
- Application: Once trained, the model can be presented with a "support set" containing a few examples of new, previously unseen protein classes (e.g., a new transcription factor family) and can then classify new query samples of those classes.
The Scientist's Toolkit: Research Reagent Solutions
Table: Essential Resources for Computational Experiments on Undruggable Targets
| Research Reagent / Resource | Function & Application | Example / Source |
|---|---|---|
| DrugBank | A comprehensive database containing detailed information about drugs, their mechanisms, interactions, and protein targets. | Used as a source for 666 druggable proteins to build a positive training set for ML models [63]. |
| Network of Cancer Genes (NCG) | A repository of cancer-driving genes. Provides a curated list of known and candidate cancer genes for target identification. | Source for 2,339 cancer-driving proteins to be screened by a druggability prediction model [63]. |
| RCPI (R Chemical Physics Interface) R Package | A computational tool for calculating protein descriptors from sequences, essential for featurizing data for ML. | Used to generate 20 amino acid (AC), 400 di-amino acid (DC), and 8000 tri-amino acid (TC) composition descriptors [63]. |
| Scikit-learn | A core Python library for machine learning. Provides implementations of a wide array of classification, regression, and clustering algorithms. | Used to implement and test 13 different ML classifiers, including SVM, Random Forest, and XGBoost [63]. |
| Synthetic Minority Over-sampling Technique (SMOTE) | An algorithm to rectify class imbalance in datasets by generating synthetic examples for the minority class. | Applied to balance a dataset of druggable and 'hard-to-drug' proteins, improving model performance [63]. |
Frequently Asked Questions
FAQ 1: Why do my in vitro results show no efficacy, even when my in silico model predicted strong target binding?
This is a common discrepancy often traced to the model's Context of Use (COU) and biological complexity not captured in simulation [64].
- Troubleshooting Steps:
- Verify Model Inputs: Re-check the cellular context in your model. Does it accurately reflect the specific cell line (e.g., MCF-7 for breast cancer) and its genetic background used in your assay? Differences in protein expression levels or mutational status can drastically alter outcomes [65].
- Interrogate the Target Pocket: Re-run your molecular dynamics (MD) simulation (e.g., 30-100 ns). Analyze the stability of the protein-ligand complex and the binding free energy. A stable trajectory with significant energy stabilization, as seen with successful inhibitors, is a positive indicator [66] [65].
- Confirm Compound Integrity and Solubility: Ensure your compound is stable and soluble in the cell culture media used. A compound predicted to bind strongly may precipitate or degrade before reaching its target in the well [67].
- Check for Off-Target Effects: Use network pharmacology approaches to identify other potential protein targets. Your compound might be binding to an off-target, causing unexpected effects that mask the intended action [65].
FAQ 2: What is the minimum required validation to make my in silico predictions credible for a regulatory submission?
Regulatory credibility is guided by standards like ASME V&V-40 and is based on a risk-informed framework [64].
- The Core Requirements:
- Define Context of Use (COU): Clearly state the specific role and scope of the computational model in addressing the question of interest (e.g., "to predict the binding affinity of novel compounds against KRASG12C") [64].
- Conduct a Risk Analysis: Assess the model's influence on the final decision and the consequence of an incorrect prediction. Higher risk requires more rigorous validation [64].
- Perform Verification and Validation (V&V):
- Verification: Confirm that the model is solved correctly (i.e., "solving the equations right").
- Validation: Evaluate the model's accuracy by comparing its predictions to experimental data (i.e., "solving the right equations") [64].
- Quantify Uncertainty: Report the uncertainty in both the computational and experimental validation data. This shows a thorough understanding of the model's limitations [64].
FAQ 3: How can I use AI and digital twins to improve the predictability of my in silico models for undruggable targets?
AI and digital twins enhance predictability by creating more physiologically accurate in silico representations.
- Implementation Strategy:
- Multi-Omics Integration: Use AI platforms to unify genomic, transcriptomic, and proteomic data. This helps identify novel biomarkers and critical signaling pathways (e.g., PI3K-Akt, MAPK) that should be incorporated into the model [67] [65] [68].
- Develop a Digital Twin: Create a computer-based model of a biological organ or system. This model can act as a personalized digital control arm, generating the counterfactual (untreated) outcome. This allows for a direct, paired statistical comparison between the treated and untreated state in the same system, revealing effects missed by traditional studies [67].
- Cross-Validate with Experimental Models: Always validate AI predictions against results from patient-derived xenografts (PDXs), organoids, or tumoroids that carry the same genetic mutations to ensure alignment with real-world biology [68].
Troubleshooting Guides
Issue: Inconsistent Results Between Computational Predictions and Cell-Based Viability Assays
This guide addresses the disconnect between a model predicting effective binding and a cell viability assay (e.g., MTT, CellTiter-Glo) showing no anti-proliferative effect.
Workflow: Diagnostic Pathway for In Vitro Inefficacy
The diagram below outlines a logical pathway to isolate the root cause when your in vitro results do not match in silico predictions.
Recommended Actions and Experimental Protocols:
Action 1: Check Model Context of Use (COU)
- Objective: Ensure the computational model reflects the experimental conditions.
- Protocol: Re-examine the protein data file (PDB) used in docking. Was it crystallized with a similar inhibitor? Is the binding site conformation relevant to your cell line? If the COU was incorrectly defined (e.g., using a wild-type structure for a mutant cell line), return to the model refinement stage [64].
Action 2: Analyze Binding Stability with Molecular Dynamics (MD)
- Objective: Verify that the predicted binding is stable over time, not just a single, favorable pose.
- Protocol:
- Run an MD simulation (e.g., for 100 ns) for the protein-ligand complex.
- Calculate the Root Mean Square Deviation (RMSD) of the protein-ligand backbone. A consistent, low RMSD indicates a stable complex.
- Analyze the binding free energy using methods like MM/GBSA. A significant, favorable energy confirms a strong binding affinity [66] [65].
- Interpretation: If the trajectory is unstable or the binding energy is weak, the compound needs chemical optimization.
Action 3: Test Compound Solubility and Integrity
- Objective: Rule out physicochemical failures.
- Protocol:
- Prepare a stock solution of the compound at the same concentration used in your assay.
- Incubate it in the complete cell culture media (with serum) at 37°C for the duration of your experiment (e.g., 72 hours).
- Analyze compound concentration and purity at time zero and at the end using High-Performance Liquid Chromatography (HPLC) [67].
- Interpretation: A significant drop in concentration indicates compound degradation or precipitation, necessitating formulation optimization.
Action 4: Probe the Intended Biological Pathway
- Objective: Confirm that the compound is engaging the target and modulating the downstream pathway in cells.
- Protocol:
- Treat relevant cancer cells (e.g., KRAS-mutant lung cancer cells) with your compound.
- Perform a Western Blot analysis to detect key proteins in the target pathway.
- For example, if targeting KRAS, probe for levels of phosphorylated ERK (p-ERK) and total ERK to see if the MAPK pathway is being effectively inhibited [69] [3].
- Interpretation: Lack of change in pathway markers suggests the compound is not engaging the target in a cellular environment, despite good in silico binding.
Issue: High Cytotoxicity in Normal Cell Lines Despite Target-Specific Design
This guide helps when a compound designed for a target highly expressed in cancer cells (e.g., SRC) also kills healthy cells, indicating potential off-target toxicity.
Workflow: Isolating Causes of Off-Target Toxicity
The diagram below outlines the investigation process for unexpected cytotoxicity.
Recommended Actions and Experimental Protocols:
Action A: Perform Selectivity Screening
- Objective: Identify if the compound is promiscuously binding to multiple targets.
- Protocol: Use a broad panel of assays (e.g., against 50-100 kinases) to determine the compound's selectivity. This can be done via commercial services or in-house using techniques like kinase profiling chips [1] [65].
- Interpretation: Multiple hits suggest the compound is a pan-assay interference compound (PAINS), requiring redesign to improve specificity.
Action B: Check for Reactive Oxygen Species (ROS) Induction
- Objective: Determine if cytotoxicity is caused by non-specific oxidative stress.
- Protocol:
- Seed normal and cancer cells in a multi-well plate.
- Treat with the compound at the IC50 concentration.
- Load cells with a fluorescent ROS-sensitive dye (e.g., DCFH-DA).
- Measure fluorescence intensity using a microplate reader or flow cytometry. A positive control like tert-Butyl hydrogen peroxide should be used [65].
- Interpretation: High ROS levels in normal cells indicate a non-specific, potentially toxic mechanism of action.
Data Presentation
Table 1: Key Metrics for Validating an In Silico Model for an Undruggable Target (e.g., KRASG12C)
This table summarizes quantitative data to establish model credibility, based on the ASME V&V-40 framework [64] [3].
| Validation Component | Target Metric | Experimental Method for Validation | Acceptance Criterion |
|---|---|---|---|
| Molecular Docking | Binding Affinity (kcal/mol) | Isothermal Titration Calorimetry (ITC) | Predicted ΔG within ~2 kcal/mol of experimental value |
| MD Simulation Stability | Protein-Ligand RMSD (Å) | N/A (Computational self-consistency) | RMSD plateau < 2.0-3.0 Å over final 50 ns of simulation [66] |
| Cellular Target Engagement | IC50 (nM) for p-ERK reduction | Western Blot with densitometry | IC50 < 1 µM; >50% inhibition of pathway at 10x IC50 [69] [3] |
| In Vitro Potency | Anti-proliferative IC50 (nM) | Cell Viability Assay (e.g., ATP-based) | IC50 < 10 µM in target-dependent cell lines [69] |
| Selectivity Index | Ratio IC50 (normal cell) / IC50 (cancer cell) | Cell Viability Assay in paired cell lines | Selectivity Index > 10 [65] |
The Scientist's Toolkit
Table 2: Essential Research Reagent Solutions for In Silico / In Vitro Integration
| Reagent / Material | Function / Explanation | Example in Context |
|---|---|---|
| Patient-Derived Xenograft (PDX) Cells | Preclinical models that better retain the genomic and phenotypic characteristics of the original human tumor, used for high-fidelity in vivo and in vitro validation [68]. | Validating a KRAS inhibitor prediction in a PDX model derived from a pancreatic cancer patient. |
| DNA-Encoded Library (DEL) | A collection of small molecules, each conjugated to a unique DNA tag, enabling highly efficient screening of billions of compounds against a purified protein target to find starting points for undruggable targets [1]. | Identifying a novel covalent binder for a shallow pocket on the KRAS protein. |
| Proteolysis Targeting Chimera (PROTAC) | A bifunctional molecule that recruits an E3 ubiquitin ligase to a target protein, leading to its degradation by the proteasome. This is a key strategy for targeting undruggable proteins that lack a functional pocket [3]. | Developing a degrader for a mutant transcription factor like MYC, which is difficult to inhibit with a traditional drug. |
| Inducible shRNA/CRISPR Platform | Tools for suppressing gene function in established tumors in vivo, allowing for deep genetic validation of candidate targets in a physiologic context and anticipation of toxicities [69]. | Validating that CDK9 is a synthetic lethal target in MYC-overexpressing hepatocellular carcinoma. |
| Covalent Inhibitor Scaffold | A compound with a mildly reactive functional group (e.g., targeting cysteine) that forms a covalent bond with the target protein, conferring sustained inhibition and overcoming affinity challenges with shallow pockets [1] [3]. | The design of Sotorasib, which covalently binds to the KRASG12C mutant. |
Navigating Tumor Heterogeneity and Anticipating Resistance Mechanisms
Frequently Asked Questions (FAQs)
Q: What are the primary experimental models for studying tumor heterogeneity and predicting drug response, and how do they compare?
Advanced in vitro models are crucial for replicating the complexity of human tumors. The table below summarizes the key characteristics of contemporary model systems.
Table 1: Comparison of Experimental Models for Tumor Heterogeneity and Drug Screening
| Model Type | Key Advantages | Key Limitations | Best Use Cases |
|---|---|---|---|
| 2D Cell Lines | - Low cost, high scalability [70]- Suitable for high-throughput screening (HTS) and initial hypothesis testing [70] | - Low clinical predictive value; most dissimilar to patient samples [70]- Loss of cell-to-cell and cell-to-matrix interactions [70] | - Rapid, large-scale data generation for initial hypothesis testing [70] |
| Patient-Derived Organoids (PDOs) | - High clinical relevance; closely correlated with patient tumor response [70]- Retain genetic diversity and cell interactions [70] | - Can lack full tumor microenvironment (TME) components [70]- Culture derivation can be challenging for some cancer types [70] | - High-throughput drug screening (HTS) [70]- Co-culture studies and biomarker discovery [70] |
| PDX-Derived Organoids (PDXOs) | - High correlation with matched in vivo PDX models [70]- Available in biobanks with paired in vivo data [70] | - Not all TME cells may be represented [70] | - Studying autologous T-cell therapies (e.g., CAR-T) [70] |
| 3D Co-culture Systems | - Enables study of tumor-immune-stromal interactions [70]- Can model complex TME for immunotherapy evaluation [70] | - Requires significant optimization and validation [70] | - Studying autologous T-cell therapies (e.g., CAR-T) [70] |
Q: Our high-throughput drug screen using organoids yielded a large dataset. What analytical approaches are recommended for identifying robust biomarkers from this data?
Effective biomarker discovery requires careful experimental design and advanced analytical techniques. The following workflow and table outline the critical steps.
Table 2: Key Considerations for Biomarker Discovery from Screening Data
| Aspect | Recommendation | Rationale |
|---|---|---|
| Model Number | At least 10 sensitive and 10 insensitive models [70] | Ensures sufficient statistical power and minimizes bias [70] |
| Efficacy Spread | A 10-fold difference in IC₅₀ values between groups [70] | Ensures a clear distinction between responder and non-responder phenotypes [70] |
| Data Integration | Combine drug response with Whole Exome/Transcriptome sequencing and High Content Imaging (HCI) data [70] | HCI provides multiparameter phenotypic data (nucleus count, apoptosis, epithelium thickness) for deeper insights into mechanisms [70] |
| AI/Machine Learning | Use multimodal AI to integrate genomics, pathology, and clinical data for patient stratification [22] | AI can simulate disease trajectories and identify biomarkers that predict a patient's treatment response and disease recurrence risk [22] |
Q: What computational and experimental strategies can be employed to overcome resistance caused by cancer cell plasticity, such as phenotypic switching?
Cancer cell plasticity, including processes like Epithelial-Mesenchymal Transition (EMT) and neuroendocrine differentiation, is a major non-genetic driver of resistance [71]. The following diagram and protocol outline a combined approach to target it.
Experimental Protocol: Targeting Plasticity-Driven Resistance
- Model Establishment: Generate therapy-resistant cell lines or organoids by prolonged, sub-lethal drug exposure. These cultures often contain slow-cycling, drug-tolerant persister cells [71].
- Phenotypic Characterization:
- Mechanistic Deconvolution:
- Therapeutic Targeting:
- Test combination therapies that pair the original drug with inhibitors of the identified plasticity pathways (e.g., TGF-β receptor inhibitors) [71].
- Employ CRISPR screens in the resistant models to identify genetic vulnerabilities specific to the drug-tolerant state.
Q: How can we apply computational tools to target traditionally "undruggable" oncoproteins, and what experimental validation is required?
Proteins once considered "undruggable" due to the lack of a deep binding pocket can now be targeted using innovative computational and structural methods. The recent work on eukaryotic initiation factor 4E (eIF4E) serves as an excellent blueprint [72].
Table 3: Research Reagent Solutions for Targeting Undruggable Proteins
| Research Reagent / Tool | Function in the Workflow | Application in eIF4E Case Study [72] |
|---|---|---|
| Fragment Libraries | A curated collection of small, low molecular weight chemical compounds used for screening. | Served as the starting point for identifying initial, weak binders to novel sites on eIF4E. |
| Protein Engineering Tools | Methods to modify the protein of interest to improve its stability or solubility for structural studies. | Researchers engineered eIF4E to mask a problematic region, enabling production of sufficient protein for screening. |
| Structure-Guided Design | Using 3D structural data (from X-ray crystallography) to iteratively optimize chemical fragments into more potent compounds. | Used to transform a weak fragment hit into a tight-binding tool compound that disrupts eIF4E-eIF4G interaction. |
| Cellular Knock-out/Rescue Systems | Genetic tools to control target protein activity and validate the functional relevance of a binding site. | Used to assess how binding at the newly discovered site contributes to eIF4E's functions in cells. |
| Degrader Technology (e.g., PROTACs) | A therapeutic modality that uses small molecules to recruit the cell's own protein degradation machinery to eliminate the target protein. | The lead compound can be a platform for developing degraders that break down eIF4E, offering an alternative to inhibition. |
Experimental Workflow for Undruggable Targets:
- Unbiased Screening: Utilize fragment-based screening, which uses smaller compound libraries than conventional high-throughput screening, to probe the entire surface of the target protein for novel, druggable binding pockets [72].
- Structural Analysis: Employ X-ray crystallography to determine the high-resolution structure of the target protein bound to the hit fragment. This reveals the exact binding location and informs chemical optimization [72].
- Chemical Optimization: Use structure-guided design to iteratively build the initial fragment into a more potent and complex lead compound with higher binding affinity [72].
- Functional Cellular Validation:
- Test the optimized compound in cancer cell models to see if it disrupts the target's known function (e.g., disrupting eIF4E-eIF4G interaction).
- Use genetic tools (e.g., knock-out/rescue) to confirm that the compound's effect is mediated through the identified binding site [72].
- Develop a less active control compound to confirm that the cellular phenotype is specific to target engagement [72].
Q: What are the best practices for using Next-Generation Sequencing (NGS) to monitor clonal evolution and the emergence of resistance in our pre-clinical models and patients?
NGS is a transformative technology for genomic profiling, but its clinical utility depends on standardized data interpretation and reporting [73] [74].
Table 4: NGS Applications and Guidelines for Resistance Monitoring
| Application | Purpose in Resistance Monitoring | Technical & Reporting Considerations |
|---|---|---|
| Whole Exome Sequencing (WES) | Identifies single nucleotide variants (SNVs), insertions/deletions (indels), and copy number alterations (CNAs) across the exome. | Use to discover novel resistance mutations in pre- and post-treatment models. ESMO guidelines recommend reporting tiered genomic alterations based on clinical evidence [74]. |
| RNA Sequencing (RNA-Seq) | Profiles gene expression and can detect fusion genes and alternative splicing events. | Use to identify non-genetic resistance mechanisms, such as pathway reactivation or phenotypic plasticity signatures [71]. |
| Liquid Biopsy (ctDNA) | Isolates and sequences circulating tumor DNA from patient blood. | Enables non-invasive, real-time monitoring of resistance mutation emergence (e.g., EGFR T790M, C797S) during treatment [75] [22]. |
| Single-Cell Sequencing | Resolves genomic or transcriptomic heterogeneity at the individual cell level. | The gold standard for directly characterizing tumor subpopulations and tracing clonal evolution driving resistance [75]. |
Key Reporting Standard (per ESMO guidelines [74]): NGS reports for clinical decision-making should be structured with clear sections, including:
- Patient and Sample Information: Confirm tumor content and DNA quality.
- Methods: Specify the gene panel, sequencing technology, and validation.
- Results: List all genomic variants identified.
- Interpretation: Classify variants using a tier system (e.g., Tier I: strong clinical significance) and include evidence for therapy implications.
- Conclusion: Provide a concise summary of actionable findings to guide the clinician.
Historically, computer-aided molecular design (CAMD) has focused primarily on improving the binding affinities of drug candidates to specific receptors. However, a potent inhibitor is not necessarily a successful drug. The emerging concept of "drug-likeness" focuses on the physicochemical and biological properties that enable a clinical lead to become a marketed drug, particularly emphasizing the balance between potency, selectivity, and favorable Absorption, Distribution, Metabolism, and Excretion (ADME) properties [76].
Before a drug molecule can exert its pharmaceutical effect, it must travel through the body to reach its site of action. This journey involves absorption from the gut into the bloodstream, distribution to target tissues, potential metabolism by hepatic enzymes, and eventual excretion. A drug must successfully navigate this entire process without causing serious toxic side effects or interfering with other medications [76].
Foundational Principles and Key Properties
The Rule of Five and Beyond
The most well-known framework for assessing drug-likeness is the "Rule of Five" established by Lipinski and coworkers at Pfizer. Based on a statistical analysis of approximately 2,200 drugs from the World Drug Index, this rule states that absorption or permeation is likely to be impaired when [76]:
- logP > 5
- Molecular weight > 500
- Number of hydrogen bond donors > 5
- Number of hydrogen bond acceptors > 10
While valuable for initial screening, the Rule of Five alone is an insufficient discriminator between drugs and non-drugs. More advanced computational approaches using artificial neural networks and multiple molecular descriptors have demonstrated improved classification accuracy approaching 90% for distinguishing drug-like from non-drug-like molecules [76].
Quantitative Property Ranges for Drug-like Molecules
The table below summarizes key property ranges associated with drug-like compounds:
| Property | Optimal Range | Importance in Drug Development |
|---|---|---|
| Molecular Weight | ≤ 500 | Affects compound absorption and permeation [76] |
| logP | ≤ 5 | Influences membrane permeability and solubility [76] |
| Hydrogen Bond Donors | ≤ 5 | Impacts transport across cell membranes [76] |
| Hydrogen Bond Acceptors | ≤ 10 | Affects solubility and permeability [76] |
| Number of Rotatable Bonds | Limited | Influences molecular flexibility and oral bioavailability [76] |
| Polar Surface Area | Monitored | Affects passive transport through membranes [76] |
Troubleshooting Common Experimental Issues
FAQ: Addressing Drug Discovery Assay Challenges
Q: My TR-FRET assay has failed completely with no assay window. What should I check first?
A: The most common reason for complete assay failure is improper instrument setup. Verify that your microplate reader is configured with exactly the recommended emission filters for your specific instrument model. Unlike other fluorescence assays, TR-FRET is particularly sensitive to filter selection. Test your reader's TR-FRET setup using reagents you have already purchased before beginning any experimental work [77].
Q: Why am I observing significant differences in EC50/IC50 values between laboratories for the same compound?
A: The primary reason for inter-lab variability in EC50/IC50 values typically traces back to differences in stock solution preparation, particularly at the 1 mM concentration. Other factors include compound instability, differences in cell permeability, or variation in the biological activity of the kinase preparations used (active vs. inactive forms) [77].
Q: In cell-based assays, my compound shows no activity despite excellent in vitro binding data. What could explain this discrepancy?
A: Several factors could be responsible:
- The compound may be unable to cross the cell membrane or could be actively pumped out by efflux transporters
- The compound might be targeting an inactive form of the kinase in the cellular context
- The observed effect might be on an upstream or downstream kinase rather than the intended target [77]
Q: Why are the emission ratios in my TR-FRET assays so small numerically?
A: This is expected behavior. TR-FRET emission ratios are calculated by dividing the acceptor signal by the donor signal. Since donor counts are typically significantly higher than acceptor counts, the ratio is generally less than 1.0. The numerical values are small because the raw RFU values (typically in the thousands) are factored out when the ratio is taken. Some instruments multiply this ratio by 1,000 or 10,000 for display purposes, but the statistical significance is unaffected [77].
Q: My assay has a large window but high variability. Is this acceptable for screening?
A: Assay window alone is not a sufficient measure of assay performance. The Z'-factor, which considers both the assay window and the variability (standard deviation) of the data, is the appropriate metric. Assays with Z'-factor > 0.5 are considered suitable for screening. A large assay window with substantial noise may have a lower Z'-factor than an assay with a smaller window but minimal variability [77].
Computational Approaches to Drug-Likeness
Advanced computational methods have significantly improved the prediction of drug-like properties. Research teams have successfully employed artificial neural networks using both 1D descriptors (molecular weight, hydrogen bond donors/acceptors, rotatable bonds, etc.) and 2D descriptors (substructural features) to distinguish between drug-like and non-drug-like molecules with approximately 90% accuracy [76].
These computational filters dramatically increase the probability of selecting drug-like molecules from large compound libraries, helping researchers prioritize the most promising candidates for experimental validation, especially when resources for formal in vivo studies are limited [76].
Computational Strategies for Undruggable Targets
AI-Driven Approaches in Oncology
In the context of targeting traditionally undruggable cancer targets, computational and AI tools are enabling new strategies. Machine learning on molecular data has yielded prognostic and predictive biomarkers, while recent advances in AI allow integration of genomics, pathology, imaging, and clinical data into multimodal models that not only stratify patients but simulate disease trajectories [22].
The concept of "digital twins" - dynamic, in-silico replicas of individuals - represents a promising approach for understanding tumour evolution and metastasis, potentially enabling a shift from trial-and-error to rational, data-driven drug design and care [22].
Experimental Workflow for Compound Optimization
The following diagram illustrates a comprehensive workflow for optimizing drug-like properties in early drug discovery:
Essential Research Reagent Solutions
The table below details key reagents and materials used in drug-likeness optimization experiments:
| Reagent/Assay Type | Primary Function | Key Applications |
|---|---|---|
| TR-FRET Assay Kits | Measures molecular interactions via time-resolved fluorescence resonance energy transfer [77] | Kinase activity assays, protein-protein interactions, binding studies |
| LanthaScreen Eu/LanthaScreen Tb | Donor reagents for TR-FRET assays providing long-lived fluorescence [77] | Enzyme activity assays, cellular signaling studies |
| Z'-LYTE Assay Systems | Enzyme activity measurement using fluorescence-based phosphorylation detection [77] | Kinase inhibitor screening, enzyme characterization |
| Cell-Based Assay Systems | Assessment of compound activity in physiological cellular environments [77] | Membrane permeability evaluation, efflux transporter studies |
| Computational ADME Platforms | Prediction of absorption, distribution, metabolism, and excretion properties [76] | Early-stage compound prioritization, property optimization |
Regulatory Considerations for Investigational Compounds
When advancing compounds toward clinical investigation, researchers must be aware of regulatory requirements. The Investigational New Drug (IND) application provides data showing it is reasonable to begin human tests and serves as an exemption from federal requirements prohibiting interstate shipment of unapproved drugs [78].
The IND is not a marketing application but rather the mechanism through which sponsors advance to clinical trials after successful preclinical development. Clinical investigation generally proceeds through three phases [78]:
- Phase 1: Initial introduction in humans (20-80 subjects) to determine safety, metabolism, and pharmacological actions
- Phase 2: Controlled clinical studies in patients (several hundred subjects) to obtain preliminary effectiveness data
- Phase 3: Expanded trials (hundreds to thousands) to gather additional safety and effectiveness information
Optimizing for drug-like properties requires a balanced approach that considers potency, selectivity, and ADME characteristics simultaneously. While computational tools provide valuable initial filters, experimental validation remains essential. The troubleshooting guidelines and methodologies presented here offer a framework for addressing common challenges in drug discovery experiments, particularly in the context of developing therapies for challenging targets such as those in oncology. As AI and computational methods continue to advance, they offer promising approaches for simulating disease trajectories and optimizing therapeutic interventions for traditionally undruggable targets.
Integrating Patient-Derived Data for Biologically Relevant Models
Frequently Asked Questions (FAQs)
1. What are the most common pitfalls when integrating transcriptomic data from different preclinical models, and how can I avoid them? A major challenge is the presence of batch effects and technical artifacts, which can obscure true biological signals. For instance, transcriptomic profiles from cell lines, patient-derived xenografts (PDXs), and clinical tumors often cluster by data origin rather than by cancer type due to systematic technical differences [79].
- Solution: Utilize advanced batch-effect removal methods like MOBER (Multi-Origin Batch Effect Remover), a deep learning-based tool designed specifically for this purpose. MOBER uses an adversarial conditional variational autoencoder to generate embeddings that retain biological information while removing confounder information related to the data source [79].
2. My 2D cell culture drug response data does not match clinical outcomes. How can I improve the predictive power of my models? This is a common issue because traditional 2D cultures lack the structural complexity and tumor microenvironment (TME) of in vivo tumors. They often show altered metabolism, gene expression, and poor replication of drug penetration barriers [80].
- Solution: Transition to 3D organoid models. Research on pancreatic cancer has demonstrated that 3D organoids derived from patient-derived conditionally reprogrammed cells (CRCs) more accurately recapitulate the patient's clinical response to standard chemotherapies (e.g., FOLFIRINOX, gemcitabine plus nab-paclitaxel) compared to their 2D counterparts. The IC50 values from 3D organoids are typically higher and more reflective of in vivo responses [80].
3. How can I computationally identify which patient-derived model is most representative of a clinical tumor? You can evaluate the transcriptional fidelity of models to clinical tumor samples.
- Solution: After integrating your data with a method like MOBER, you can identify the most representative models by assessing the disease type of their nearest neighbors among clinical tumor samples (e.g., from TCGA). One study found that for 73% of PDX models and 53% of cancer cell lines, the inferred disease type matched the annotated tumor type, providing a quantitative measure of fidelity [79].
4. What strategies can help bridge the gap between preclinical findings and clinical translatability for 'undruggable' targets? The key is to use integrated computational and experimental approaches.
- Multi-omics Integration: Combine genomics, transcriptomics, and proteomics data to uncover distinct patient subgroups and novel therapeutic vulnerabilities. This is crucial for tumors driven by "undruggable" targets like mutant KRAS, as it can reveal co-dependencies or downstream signaling pathways that are targetable [81].
- Leverage AI for Digital Twins: AI can integrate multimodal patient data (genomics, pathology, imaging) to create in-silico models, or "digital twins," that simulate disease trajectories and nominate tailored interventions. This allows for a shift from trial-and-error to rational, data-driven therapy design [22].
Troubleshooting Guides
Issue: Poor Integration of Multi-Origin Transcriptomic Data
Problem: When combining data from cell lines, PDXs, and patient tumors, samples separate by origin in dimensionality reduction plots (e.g., UMAP), making biological comparison impossible [79].
Investigation & Resolution:
| Step | Action | Expected Outcome |
|---|---|---|
| 1. Diagnose | Perform UMAP on raw, unintegrated data. | Visual confirmation of strong batch effects; samples cluster by dataset origin. |
| 2. Select Tool | Choose a batch-effect removal method capable of handling multiple sources simultaneously. MOBER is recommended for its ability to handle pan-cancer data without relying on cancer-type annotations [79]. | A shortlist of suitable computational tools. |
| 3. Apply & Validate | Run the integration algorithm (e.g., MOBER). Then, re-run UMAP on the integrated data. | A new UMAP where samples from different origins (cell line, PDX, tumor) intermix and cluster primarily by known biological categories (e.g., cancer type). |
Issue: Discrepancy Between Preclinical and Clinical Drug Response
Problem: Drug sensitivity data from high-throughput 2D screens does not correlate with patient treatment outcomes [80].
Investigation & Resolution:
| Step | Action | Expected Outcome |
|---|---|---|
| 1. Model Selection | Move to a more physiologically relevant model. Establish 3D organoid cultures from your patient-derived cells using a Matrigel-based platform [80]. | A culture system that better preserves the intrinsic molecular subtypes and architecture of the original tumor. |
| 2. Drug Screening | Perform drug sensitivity assays (e.g., dose-response curves) on the 3D organoids. | IC50 values that are generally higher than in 2D and show a stronger correlation with observed patient clinical responses [80]. |
| 3. Data Integration | Integrate the drug response data with multi-omics profiles (e.g., mutational status, gene expression) from the organoids and original tumor. | Identification of potential biomarkers predictive of drug response. |
Experimental Protocols & Data
Detailed Protocol: Establishing 3D CRC Organoids for Drug Screening
This protocol outlines the creation of 3D organoids from patient-derived conditionally reprogrammed cells (CRCs) for preclinical drug evaluation [80].
1. Materials Preparation:
- Pre-established patient-derived pancreatic cancer CRC lines [80].
- Growth factor-reduced Matrigel.
- F medium: Ham’s F-12 nutrient mix, complete Dulbecco’s Modified Eagle’s Medium, and supplements (hydrocortisone, insulin, cholera toxin, epidermal growth factor, fetal bovine serum, adenine, gentamicin, Amphotericin B) [80].
- Rho-associated kinase inhibitor (Y-27632).
2. Organoid Culture Setup:
- Harvest CRCs from 2D culture.
- Mix cells with 90% growth factor-reduced Matrigel.
- Cell density: 5,000 - 10,000 cells per 20 µL of Matrigel.
- Plate 20 µL aliquots of the cell-Matrigel mixture as domes in a 6-well culture plate.
- Solidify the domes at 37°C for 20 minutes.
- Carefully add 4 mL of F medium (supplemented with 5 µM Y-27632) to each well.
- Refresh the medium every 3-4 days.
3. Organoid Harvest and Analysis:
- Harvest organoids when >50% exceed 300 μm in size (typically 2-4 weeks).
- For drug assays: Treat organoids with compounds and assess viability.
- For molecular analysis: Process for paraffin embedding, RNA/DNA extraction, or immunofluorescence [80].
Table 1: Transcriptional Fidelity of Preclinical Models to Clinical Tumors Analysis based on MOBER-integrated pan-cancer transcriptomic data from 932 cell lines (CCLE), 434 PDXs, and 11,159 patient tumors (TCGA, MET500, CMI) [79].
| Preclinical Model | Total Models Analyzed | Models with Inferred Disease Type Matching Annotation | Match Rate |
|---|---|---|---|
| Patient-Derived Xenograft (PDX) | 434 | 317 | 73% |
| Cancer Cell Line (CCLE) | 932 | ~494 | 53% |
Table 2: Drug Response Correlation of 2D vs 3D Models with Clinical Outcomes Data from a study on pancreatic cancer comparing 2D Conditional Reprogrammed Cells (CRCs) and 3D CRC-derived organoids [80].
| Culture Model | General Correlation with Clinical Response | Typical IC50 Trend | Key Advantage |
|---|---|---|---|
| 2D CRC Culture | Low | Generally lower | Cost-effective, easy to handle, suitable for initial screening |
| 3D CRC Organoid | High | Higher, reflecting in vivo drug penetration barriers | Better recapitulates tumor microenvironment and patient response |
Research Reagent Solutions
Table 3: Essential Materials for Patient-Derived 3D Organoid Culture
| Reagent / Material | Function in the Protocol | Key Consideration |
|---|---|---|
| Growth Factor-Reduced Matrigel | Provides a 3D extracellular matrix scaffold for organoid growth and polarity. | Batch-to-batch variability can affect results; use a consistent source [80]. |
| F Medium with Supplements | Nutrient-rich medium supporting the growth of conditional reprogrammed cells and organoids. | Includes hormones (hydrocortisone, insulin), growth factors (EGF), and antibiotics [80]. |
| Rho-associated kinase (ROCK) inhibitor (Y-27632) | Enhances cell survival by inhibiting anoikis (cell death upon detachment) during subculturing. | Typically added for the first 24-48 hours after passaging [80]. |
| J2 Murine Fibroblast Feeder Layer | Used in the initial 2D CRC establishment; provides unknown factors that promote epithelial cell growth. | Requires irradiation to prevent proliferation [80]. |
Workflow and Pathway Visualizations
MOBER Architecture for Data Integration
3D Organoid Establishment Workflow
Multi-Omics to Target Identification Pathway
Benchmarking Success: From Preclinical Models to Clinical Pipelines
FAQs: AI in Drug Discovery for Intractable Targets
Q1: What makes a cancer target "undruggable" and how can AI help? Traditional drugs often target small pockets on proteins with well-defined shapes, like enzyme active sites. Many cancer-driving proteins, however, lack these pockets and function through large, flat protein-protein interactions (PPIs) that are difficult for small molecules to block [82]. AI helps by analyzing complex biological data to identify novel, often allosteric, binding sites or by designing entirely new types of molecules, such as stapled peptides, that can disrupt these previously inaccessible PPIs [82] [51].
Q2: Our AI models for virtual screening are generating molecules with poor synthetic feasibility. How can we troubleshoot this? This is a common challenge. Solutions include:
- Implementing Reaction-Based AI: Use AI models that are trained on databases of robust organic synthesis reactions (e.g., expert-system type rules). This ensures that the generated molecules are built from available starting materials and through feasible chemical steps, greatly enhancing synthetic tractability [51].
- Incorporating Synthetic Complexity Scores: Integrate computational metrics that estimate the synthetic complexity of generated compounds directly into your AI's scoring function. This penalizes overly complex structures and prioritizes molecules that are easier for medicinal chemists to synthesize [51].
Q3: Our AI-predicted compounds show excellent binding affinity in silico but fail in biological assays. What could be wrong? This discrepancy often points to issues with the training data or model specificity.
- Challenge Data Bias: Ensure your training data is diverse and representative. Models trained on public data can be biased toward certain chemical classes or protein families, leading to poor generalization [83] [84].
- Refine the Biological Objective: An affinity-only objective may be insufficient. Optimize for multiple parameters simultaneously, such as Selectivity, ADMET (Absorption, Distribution, Metabolism, Excretion, Toxicity) properties, and solubility, using multi-objective optimization algorithms. This creates a more holistic and accurate prediction of a molecule's real-world performance [83] [51].
Q4: How can we validate that a computationally discovered target is truly relevant to the disease? AI-generated targets require rigorous biological validation.
- Leverage Multi-Modal Data: Integrate diverse data types beyond genomics, such as transcriptomics, proteomics, and patient-level clinical data, to build a more confident association between the target and the disease pathology [85] [51].
- Experimental Crucible: Use a suite of experimental techniques. This should include gene knockdown/knockout (e.g., CRISPR) to assess impact on cell viability, high-content imaging to observe phenotypic changes, and studies in patient-derived organoids or xenografts to confirm the target's role in a more physiologically relevant context [86] [82].
Technical Troubleshooting Guides
Troubleshooting Guide for AI-Assisted Hit Identification
| Symptoms | Possible Causes | Solutions & Diagnostics | Related Experimental Protocols |
|---|---|---|---|
| Low hit rate from AI-proposed compounds in experimental validation. | 1. Inadequate training data.2. Model overfitting.3. Chemical space bias.4. Objective function mis-specification. | 1. Diagnostic: Perform data augmentation; use transfer learning from related targets.2. Solution: Apply stricter regularization; use ensemble methods.3. Diagnostic: Analyze chemical diversity of output (e.g., Tanimoto similarity).4. Solution: Recalibrate AI to optimize for multiple parameters (e.g., potency, solubility, logP) [83] [51]. | Protocol: Iterative Virtual Screening Workflow1. Library Preparation: Start with an ultra-large library (e.g., ZINC20, >1B compounds) [51].2. Initial Filtering: Use fast ML models to score and rank compounds.3. Focused Docking: Perform structure-based docking on a top subset (e.g., 1M compounds).4. Synthesis & Testing: Select a diverse set of top-ranking compounds for synthesis and in vitro testing.5. Active Learning: Use new experimental data to retrain and improve the AI model for the next iteration [51]. |
| AI-generated molecules are chemically unstable or non-synthesizable. | 1. AI model lacks knowledge of chemical synthesis rules.2. Exploration of unrealistic chemical space. | 1. Solution: Implement AI trained on reaction databases (e.g., SAVI) that incorporates synthetic accessibility rules [51].2. Diagnostic: Use a synthetic complexity scoring algorithm (e.g., SCScore) to filter proposals. | Protocol: Assessing Synthetic Feasibility1. Retrosynthetic Analysis: Use a computational tool (e.g., ASKCOS, IBM RXN) to propose a synthetic route.2. Medicinal Chemistry Review: Have expert chemists review the proposed molecules and routes for red flags.3. Purchase Building Blocks: Check commercial availability of key starting materials. |
Troubleshooting Guide for Clinical Translation
| Symptoms | Possible Causes | Solutions & Diagnostics |
|---|---|---|
| High attrition of AI-discovered candidates in early clinical trials. | 1. Inaccurate prediction of human pharmacokinetics/toxicology.2. Insufficient target validation in human biology.3. Over-optimization on a narrow pre-clinical model. | 1. Solution: Integrate more sophisticated AI-based QSAR models for ADMET prediction early in the selection process [83].2. Diagnostic: Utilize humanized animal models or patient-derived organoids for pre-clinical studies.3. Solution: Prioritize candidates with efficacy across multiple, genetically diverse disease models. |
| Clinical trial complexity leads to extended timelines and high burden [87]. | 1. Excessive number of endpoints and eligibility criteria.2. Overly complex trial design (e.g., many study arms). | 1. Diagnostic: Calculate a Trial Complexity Score during protocol design to benchmark against industry norms [87].2. Solution: Streamline protocols by focusing on endpoints critical for regulatory approval and competitive differentiation. |
Quantitative Data on AI-Driven Clinical Pipelines
Table 1: Clinical-Stage Pipeline of Leading AI Drug Discovery Companies (as of mid-2025)
| Company / Merged Entity | Key AI Technology / Focus | Clinical-Stage Candidates (Therapeutic Area) | Highest Phase | Key Partners / Notes |
|---|---|---|---|---|
| Recursion (merged with Exscientia) | Recursion: Phenotypic screening with AI-driven image analysis. Exscientia: Automated precision chemistry & design [86] [88]. | REC-XXXX (Oncology)REC-XXXX (Rare Disease)REC-XXXX (Infectious Disease) [86] [88] | Phase 2Phase 2Phase 1 | Roche, BayerMerger creates a platform combining biology and chemistry. $850M cash; 10 clinical readouts expected in next 18 months [86] [88]. |
| Exscientia (to be merged) | Precision chemistry platform for automated small-molecule design [86] [88]. | DSP-XXXX (Immuno-oncology)DSP-XXXX (Oncology) [86] | Phase 1Phase 1/2 | Sanofi, Merck KGaAPipeline to be absorbed into Recursion. |
| BenevolentAI | AI-powered knowledge graphs for target identification and drug design. | BEN-XXXX (Immuno-oncology)BEN-XXXX (Neurology) [86] | Phase 2Phase 1 | –One of the first AI companies with clinical trial results, though early outcomes were negative [86]. |
Table 2: Analysis of Clinical Trial Complexity in Oncology (2014-2024) [87]
| Metric | Phase 1 Trials (Avg. Score) | Phase 2 Trials (Avg. Score) | Phase 3 Trials (Avg. Score) | Key Drivers of Increase |
|---|---|---|---|---|
| Trial Complexity Score (2014) | Low 20s % | Mid 40s % | Mid 40s % | - |
| Trial Complexity Score (2024) | Mid 30s % | Low-Mid 50s % | Low-Mid 50s % | More endpoints, novel biomarkers, multi-arm designs, digital endpoints. |
| Correlation with Duration | A 10 percentage point increase in complexity score correlates with an increase of overall trial duration of approximately one third [87]. |
Experimental Protocols for Targeting Undruggable PPIs
Protocol: Disrupting a Protein-Protein Interaction with a Stapled Peptide
This protocol is based on the pioneering work targeting the FAK-paxillin interaction, a previously "undruggable" PPI critical in cancer [82].
I. Rational Design of Stapled Peptide Inhibitor
- Identify Binding Epitope: Determine the precise amino acid sequence of one protein (e.g., paxillin) that is critical for binding to its partner (FAK) using techniques like X-ray crystallography or NMR spectroscopy [82].
- Peptide Stabilization: Design a peptide that mimics this binding epitope. Introduce a chemical "staple" by:
- Synthesizing the peptide with two non-natural, olefin-bearing amino acids (e.g., (S)-pentenylalanine) at specific positions (i and i+4/i+7) to promote an alpha-helical structure.
- Performing a ring-closing metathesis (RCM) reaction to form a covalent bridge ("staple") between these residues, locking the peptide into its bioactive conformation [82].
- Cellular Permeability Enhancement: To help the peptide cross cell membranes, conjugate a small fatty acid (e.g., myristic acid) to the N-terminus via a chemical linker (myristoylation) [82].
II. In Vitro Validation
- Binding Affinity Measurement: Use Surface Plasmon Resonance (SPR) or Isothermal Titration Calorimetry (ITC) to quantify the binding affinity (Kd) of the stapled peptide to the purified target protein (FAK). Compare it to the unmodified peptide to confirm enhanced potency [82].
- Cellular Uptake Assay: Treat cancer cells with a fluorescently labeled version of the stapled peptide. Use confocal microscopy or flow cytometry to confirm intracellular localization.
- Functional Phenotypic Assay:
- Cell Viability: Perform MTT or CellTiter-Glo assays on cancer cells treated with the peptide to measure cytotoxicity.
- Migration/Invasion: Use a Boyden chamber or wound-healing assay to assess the peptide's ability to inhibit cancer cell migration and invasion, key processes driven by FAK-paxillin signaling [82].
III. In Vivo Efficacy
- Preclinical Models: Administer the lead stapled peptide candidate (e.g., compound '2012' from the FAK study) to mice bearing patient-derived xenograft (PDX) tumors [82].
- Endpoint Analysis: Monitor tumor volume over time. At endpoint, harvest tumors for immunohistochemical analysis of proliferation (Ki-67) and apoptosis (TUNEL) markers to confirm the mechanism of action.
Workflow Diagram: Stapled Peptide Drug Discovery
Stapled Peptide Discovery Workflow
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Research Reagents for Computational Oncology
| Research Reagent / Tool | Function & Application in AI-Driven Discovery |
|---|---|
| Ultra-Large Virtual Compound Libraries (e.g., ZINC20, Enamine REAL) | Libraries containing billions of readily synthesizable compounds used for AI-powered virtual screening to identify novel chemical starting points (hits) [51]. |
| Stapled Peptide Synthesis Kits | Commercial kits provide non-natural amino acids and catalysts for the ring-closing metathesis reaction, enabling the synthesis of stabilized peptide inhibitors for targeting PPIs [82]. |
| Patient-Derived Xenograft (PDX) Models | Immunodeficient mice engrafted with human tumor tissue. These models preserve the tumor's original genetics and histology, providing a highly clinically relevant system for validating AI-predicted drug candidates [82]. |
| Cryo-Electron Microscopy (Cryo-EM) | A structural biology technique for determining high-resolution 3D structures of proteins and complexes. It is crucial for obtaining the atomic-level details of "undruggable" targets needed for structure-based AI design [51]. |
| DNA-Encoded Libraries (DELs) | Vast libraries of small molecules, each tagged with a unique DNA barcode. They allow for the experimental screening of billions of compounds against a purified protein target, generating high-quality data for training and validating AI models [51]. |
Frequently Asked Questions
Q1: What are the key performance metrics when evaluating computational platforms for cancer research? The most relevant metrics are Benchmark Performance Scores, which measure a model's accuracy on standardized tasks, and Inference Speed, which is crucial for running large-scale virtual screens. Also critical are context window size (for processing large datasets) and real-world task success rates, which can differ significantly from academic benchmarks [89].
Q2: Our models are accurate but too slow for large-scale molecular dynamics simulations. How can we improve speed? Consider deploying more efficient, specialized models. In 2025, smaller models like TinyLlama (1.1B parameters) have demonstrated strong performance while being able to run with just 8GB of memory, making them suitable for resource-constrained environments. Furthermore, leveraging computational resources during the inference stage, as seen with models like OpenAI's o1, can significantly enhance performance without retraining [89].
Q3: What does "agentic AI" mean and how is it relevant to targeting undruggable proteins like KRAS and MYC? Agentic AI refers to systems that can autonomously plan and execute multi-step workflows, acting as "virtual coworkers." In cancer research, this translates to AI that can independently design experiments, simulate protein-ligand interactions, and analyze results for complex, multi-factor problems like simultaneously silencing the KRAS and MYC genes. However, this requires robust computational infrastructure and governance frameworks [89].
Q4: How reliable are synthetic training data for building specialized cancer models? The emergence of synthetic training data is a significant 2025 breakthrough. Techniques where models like Google's self-improving systems generate their own questions and answers are reducing data collection costs and enhancing performance in specialized domains, including computational oncology [89].
Q5: Our team has limited computational expertise. What is the best way to get started with these platforms? Focus on platforms that offer strong Technical Assistance capabilities. In 2025, benchmarks for this are measured by tools like WebDev Arena, which uses open-ended prompts mirroring real help requests. Models like Gemini 2.5 and Claude currently lead in this area, providing crucial support for non-technical researchers [89].
Troubleshooting Guides
Issue 1: Poor Model Performance on Real-World Tasks Despite High Benchmark Scores
Problem: Your AI model excels on standard benchmarks like MMLU but underperforms on your specific cancer biology tasks, such as predicting drug-protein interactions.
| Troubleshooting Step | Action Details | Expected Outcome |
|---|---|---|
| Audit Your Data | Ensure your training data for the fine-tuning matches the real-world data distribution. Analyze gaps between benchmark data and your experimental data. | Identification of data drift or representational bias affecting model generalizability. |
| Use Capability-Aligned Metrics | Move beyond traditional benchmarks. For tasks like Reviewing Work or Data Structuring, develop internal metrics that reflect your specific use case, as these often lack standard benchmarks [89]. | A more accurate measurement of the model's utility for your specific research goals. |
| Implement Domain-Specific Fine-Tuning | Leverage specialized models (e.g., BloombergGPT for finance, Med-PaLM for healthcare) as a starting point. Fine-tune them on your proprietary oncological datasets [89]. | Superior accuracy and contextual understanding in your specific research domain. |
Issue 2: Computational Hardware Limitations and Slow Inference Speed
Problem: Experiment runtimes are prohibitively long, hindering iterative research on large compound libraries.
| Troubleshooting Step | Action Details | Expected Outcome |
|---|---|---|
| Profile Resource Usage | Identify the bottleneck: Is it GPU memory (VRAM), CPU, or system RAM? Use profiling tools to monitor hardware utilization during task execution. | Clear identification of the limiting hardware component. |
| Optimize Model for Inference | Convert models to efficient formats (e.g., ONNX), use quantization to reduce precision (e.g., from 32-bit to 16-bit floats), and leverage hardware-specific optimizations. | Faster inference speeds and reduced memory footprint with minimal loss in accuracy. |
| Explore Efficient Model Architectures | Adopt newer, more efficient architectures like Mixture-of-Experts (e.g., Mixtral 8x7B) which activate only parts of the network at a time, reducing computational load [89]. | Ability to run state-of-the-art models on less powerful hardware. |
Issue 3: Difficulty Co-Targeting Multiple Cancer Genes
Problem: You are trying to computationally model the simultaneous inhibition of two "undruggable" genes like KRAS and MYC but are not achieving the synergistic effect seen in wet-lab experiments [21].
| Troubleshooting Step | Action Details | Expected Outcome |
|---|---|---|
| Model Protein Interaction Networks | Instead of targeting genes in isolation, build computational models that incorporate the known interactions between the protein pathways (e.g., how mutated KRAS and MYC jointly promote tumor development) [21]. | A more biologically accurate model that may reveal critical nodes for dual-targeting. |
| Implement Multi-Task Learning | Design or fine-tune your AI architecture to predict efficacy against both targets simultaneously, allowing the model to learn shared and unique features. | A unified model that can predict synergistic effects and off-target risks. |
| Validate with Experimental Data | Continuously cross-validate your computational predictions with real-world results, such as the ~40-fold improvement in cancer cell viability inhibition observed from the co-silencing of KRAS and MYC [21]. | Improved model reliability and guidance for further wet-lab experimentation. |
Performance Metrics for Computational Platforms (2025)
The table below summarizes key quantitative data for leading AI models, which are the engines of modern computational drug discovery platforms. This data aids in selecting the right platform based on the needs of a specific project [89].
Table 1: 2025 AI Model Performance on Research-Relevant Tasks
| Model | Summarization (Score) | Technical Assistance (Elo) | Generation (Elo) | Key Strengths & Specialization |
|---|---|---|---|---|
| Gemini 2.5 | 89.1% | 1420 | 1458 | Top performer in multiple categories; strong versatility [89]. |
| Claude 3.5 Sonnet | 79.4% | 1357 | Not Specified | Second in Summarization/Technical Assistance; processes text, images, audio [89]. |
| GPT-4o | Not Specified | Not Specified | Not Specified | Real-time multimodal processing; integrated internet fact-checking [89]. |
| Specialized Models | Varies by domain | Varies by domain | Varies by domain | Superior accuracy in niches (e.g., finance, healthcare) via deep contextual training [89]. |
Table 2: Real-World Capability Success Rates
| Capability | Prevalence in User Prompts | Current Benchmark Performance | Notes for Researchers |
|---|---|---|---|
| Technical Assistance | 65.1% | Gemini leads (Elo 1420) | Critical for troubleshooting code and experimental design [89]. |
| Reviewing Work | 58.9% | No dedicated benchmark | Lacks standard metrics; internally developed scores are needed [89]. |
| Generation | 25.5% | Gemini leads (Elo 1458) | Useful for generating reports, hypotheses, or synthetic data [89]. |
| Information Retrieval | 16.6% | SimpleQA is a good benchmark | Enhanced by models with real-time web access and citations [89]. |
| Data Structuring | 4.0% | No dedicated benchmark | Essential for organizing unstructured lab data; requires custom metrics [89]. |
Experimental Protocols for Key Cited Experiments
Protocol 1: In silico Co-Targeting of Undruggable Genes (e.g., KRAS & MYC)
This protocol is based on computational methodologies that underpin research into multi-target therapies [21].
Data Curation and Preprocessing:
- Gather 3D protein structures for KRAS and MYC from databases like PDB. For unresolved structures, use AlphaFold2 predictions.
- Collect known active compounds, inhibitors, and biological activity data from public repositories (e.g., ChEMBL, PubChem).
- Curate gene expression data (e.g., from TCGA) for cancers with KRAS mutations and MYC dysregulation.
System Preparation:
- Prepare the protein structures using molecular modeling software: add hydrogen atoms, assign protonation states, and optimize hydrogen bonding networks.
- Define the binding sites for KRAS and MYC based on literature and experimental data.
Virtual Screening and Docking:
- Perform molecular docking of compound libraries against both individual targets and, if possible, a model of their synergistic complex.
- Use docking software (e.g., AutoDock Vina, Glide) to rank compounds based on binding affinity and pose.
Molecular Dynamics (MD) Simulations:
- Take top-ranking docked complexes and run all-atom MD simulations (e.g., using GROMACS or AMBER) to assess binding stability and interaction dynamics over time.
- Analyze root-mean-square deviation (RMSD) and binding free energies (e.g., with MM/PBSA) to validate docking results.
Synergy Prediction and Validation:
- Develop or apply a machine learning model to predict the synergistic effect of dual inhibition using features from the docking and MD results.
- The computational hits should be validated through wet-lab experiments, such as measuring the inhibition of cancer cell viability, to confirm the predicted synergistic effect [21].
Protocol 2: Benchmarking AI Models for Research Tasks
This protocol outlines how to evaluate AI platforms for specific capabilities relevant to drug discovery [89].
Define Evaluation Scope:
- Select the capabilities to test (e.g., Technical Assistance, Data Structuring, Summarization of research papers).
- For capabilities without public benchmarks (like Reviewing Work), create an internal dataset of representative tasks.
Prepare Test Suite:
- For Technical Assistance, use open-ended prompts from benchmarks like WebDev Arena that mirror real help requests.
- For Summarization, use a set of scientific abstracts and pre-defined key points to check for accuracy.
- For Generation, task the model with creating specific experimental protocols or hypotheses.
Execute Benchmarks:
- Run the test suite against multiple AI models (e.g., via their API).
- Ensure consistent parameters (e.g., temperature, top-p) across all model queries for a fair comparison.
Quantitative and Qualitative Analysis:
- Score quantitative metrics like accuracy, Elo ratings (for comparative quality), and time-to-result.
- Perform a qualitative, blinded review of the outputs by domain experts to assess practical utility beyond scores.
Compile Performance Report:
- Aggregate results into a comparative table (see Table 1 and 2).
- Document strengths and weaknesses of each platform to guide research team selection.
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Reagents for Targeting Undruggable Genes
| Research Reagent | Function / Application |
|---|---|
| Inverted RNAi Molecules | Novel RNA interference (RNAi) compositions designed to simultaneously silence two difficult-to-target cancer genes (e.g., KRAS and MYC). They form the basis for a "two-in-one" therapeutic strategy [21]. |
| Small Interfering RNAs (siRNAs) | Used in RNAi to selectively turn off, or silence, mutated genes. They are the functional component that mediates the degradation of target mRNA [21]. |
| Targeted Drug Delivery System | A mechanism, such as a nanoparticle or ligand conjugate, designed to deliver therapeutic molecules (like the inverted RNAi) directly to tumors expressing the target genes, minimizing off-target effects [21]. |
| Domain-Specific AI Models | Pre-trained AI models (e.g., Med-PaLM for healthcare) that can be fine-tuned on oncological data to improve accuracy in tasks like literature mining, target prediction, and analyzing gene expression data [89]. |
| Agentic AI Framework | Software infrastructure that allows for the creation of autonomous AI "agents" capable of planning and executing multi-step computational workflows, such as designing a series of virtual screens and analyzing the results [89]. |
Visualized Workflows and Pathways
Dual-Target Drug Discovery Workflow
Strategies for Undruggable Targets
The Kirsten rat sarcoma viral oncogene homolog (KRAS) is a predominant isoform of the RAS family of oncogenes and represents one of the most frequently mutated oncogenes in human cancers [90]. For decades, KRAS was considered "undruggable" due to its smooth protein surface with no apparent deep binding pockets for small molecules and its picomolar affinity for GTP/GDP, making competitive inhibition exceptionally challenging [90] [40]. This perception shifted dramatically with the discovery of covalent inhibitors targeting the specific KRAS G12C mutant, leading to FDA-approved therapies like sotorasib and adagrasib [90] [40]. These breakthroughs have established KRAS as a critical benchmark for evaluating computational strategies aimed against challenging cancer targets.
The computational drug discovery landscape for KRAS has evolved from traditional methods to increasingly sophisticated approaches, including classical molecular dynamics simulations, machine learning (ML)-enhanced pipelines, and emerging quantum computing applications [91] [92] [41]. These strategies have addressed various aspects of the KRAS targeting problem, from identifying cryptic allosteric pockets to designing selective inhibitors for different mutation variants (G12C, G12D, G12V) and developing pan-KRAS or pan-RAS inhibitors [92] [40] [41]. This technical support document provides troubleshooting guidance and methodological frameworks for researchers navigating the complex process of computationally targeting KRAS.
KRAS Mutational Landscape and Biological Significance
Frequently Asked Questions
What makes KRAS a particularly challenging target for computational drug design? KRAS presents multiple challenges: (1) its smooth surface lacks deep binding pockets for traditional small molecules [40]; (2) it has extremely high affinity (picomolar) for GTP/GDP, making competitive inhibition difficult [40]; (3) it exists in multiple conformational states with high dynamic flexibility [92]; and (4) different mutation variants (G12D, G12V, G12C, G12R, Q61H) have distinct biochemical properties and prevalence across cancer types [90].
Which computational approaches have shown the most promise for targeting KRAS? Several approaches have demonstrated value: (1) Covalent fragment-based screening to identify allosteric binders [40]; (2) Molecular dynamics simulations to identify transient pockets [91]; (3) Deep learning-augmented molecular docking for binding affinity prediction [93]; (4) Generative models for novel chemical space exploration [92] [41]; and increasingly (5) Quantum-classical hybrid models for enhanced sampling and molecule generation [92] [41].
How do resistance mechanisms to KRAS inhibitors inform computational design strategies? Primary and acquired resistance to first-generation KRAS G12C inhibitors highlights the need for computational strategies that: (1) target multiple KRAS conformational states [40]; (2) design compounds with broader mutation spectrum coverage (pan-mutant inhibitors) [92] [41]; and (3) predict potential resistance mutations during the design phase to develop more resilient inhibitor candidates [90].
KRAS Mutation Distribution
Table: KRAS Mutation Prevalence and Characteristics Across Major Cancers
| Mutation | Overall Frequency | Lung Cancer (NSCLC) | Colorectal Cancer | Pancreatic Cancer | Associated Mutagen |
|---|---|---|---|---|---|
| G12D | Most frequent | ~1% | ~7% | ~15% | Not specified |
| G12V | Second most frequent | ~1% | Not specified | Not specified | Not specified |
| G12C | Third most frequent | ~39% | ~7% | >2% | Smoking-associated |
| G12R | Less frequent | ~1% | ~1% | ~15% | Not specified |
| Q61 | Less frequent | Not specified | Not specified | Not specified | Not specified |
Data compiled from [90]
Troubleshooting Computational Workflows
Common Experimental Issues and Solutions
Problem: Generated molecules have poor synthetic accessibility or drug-like properties
- Solution: Implement multiple filtering stages in your generative pipeline. Use tools like Chemistry42 [41] or STONED-SELFIES [41] to assess synthesizability early in the design process. Incorporate pharmaceutical property prediction (ADME-Tox) as part of the reward function in generative models [92].
Problem: Molecular dynamics simulations fail to identify stable binding modes
- Solution: (1) Extend simulation timescales to capture full binding and unbinding events; (2) Use enhanced sampling techniques to overcome energy barriers; (3) Employ collective variable-based analyses to identify cryptic allosteric pockets in the switch I/II regions [91] [93].
Problem: Computational predictions do not translate to experimental binding affinity
- Solution: (1) Validate docking poses with multiple scoring functions; (2) Use ensemble docking against multiple KRAS conformational states; (3) Implement MM-GBSA/MM-PBSA calculations to refine binding affinity predictions; (4) Consider protein flexibility and solvation effects in binding energy calculations [93].
Problem: Quantum-classical hybrid models show limited improvement over classical approaches
- Solution: Ensure sufficient quantum resources (qubit count) – success rates correlate approximately linearly with qubit number [41]. Use quantum generative models (QCBMs) as enhanced priors for classical models rather than replacements [41]. Verify that the quantum component effectively explores chemical space distributions that classical models struggle to sample [92] [41].
Problem: Difficulty targeting multiple KRAS mutants with a single inhibitor
- Solution: Focus on conserved allosteric sites rather than mutation-specific pockets. The switch II pocket has proven particularly amenable to pan-KRAS inhibition [40]. Use multi-mutant screening workflows that dock candidates against various KRAS mutants simultaneously [41]. Consider molecular glue strategies that stabilize inactive conformations across multiple mutants [40].
Experimental Protocols and Methodologies
Hybrid Quantum-Classical Generative Protocol
This protocol outlines the methodology for using quantum-classical hybrid models to generate novel KRAS inhibitors, based on the approach described in [41].
Step 1: Training Data Curation
- Compile known KRAS inhibitors (~650 compounds from literature)
- Perform structure-based virtual screening of large libraries (100M+ compounds)
- Generate structurally similar compounds using STONED-SELFIES algorithm
- Apply synthesizability filtering
- Final training set: ~1.1 million data points
Step 2: Model Architecture and Training
- Quantum Component: Quantum Circuit Born Machine (QCBM) with 16+ qubits
- Classical Component: Long Short-Term Memory (LSTM) network
- Training Approach: Quantum prior generates samples each epoch; reward function (P(x) = softmax(R(x))) calculated using Chemistry42 or local filters
Step 3: Molecule Generation and Selection
- Generate 1M+ compounds using trained model
- Screen for pharmacological viability using Chemistry42
- Rank candidates by docking scores (PLI score)
- Select top 15 candidates for synthesis
Step 4: Experimental Validation
- Binding Affinity: Surface Plasmon Resonance (SPR)
- Cellular Activity: MaMTH-DS (Mammalian Membrane Two-Hybrid Drug Screening)
- Specificity Profiling: Dose-response across KRAS mutants (WT, G12C, G12D, G12V, G12R, Q61H)
- Viability Assessment: CellTiter-Glo assay
Deep Learning-Enhanced Docking and Screening Protocol
This protocol details the integrated in silico workflow for KRAS G12D inhibitor discovery, adapted from [93].
Step 1: Pharmacophore-Based Filtering
- Define pharmacophore features based on switch-II pocket geometry
- Screen FDA-approved compounds and commercial libraries
- Retain compounds matching essential pharmacophore points
Step 2: GNINA Deep Learning-Augmented Docking
- Utilize CNN affinity prediction alongside traditional scoring
- Dock retained compounds against KRAS G12D structure
- Prioritize candidates based on consensus scoring
Step 3: Molecular Dynamics Validation
- Run 100+ ns MD simulations for top candidates
- Analyze binding mode persistence and key interaction stability
- Calculate binding free energies using MM-PBSA/MM-GBSA
Step 4: Experimental Triaging
- Select compounds with strong, persistent switch-II pocket interactions
- Prioritize candidates with favorable ADME properties
- Proceed to synthesis and biochemical validation
Research Reagent Solutions
Table: Key Computational Tools and Resources for KRAS Drug Discovery
| Tool/Resource | Type | Primary Function | Application in KRAS Research |
|---|---|---|---|
| VirtualFlow | Software Platform | High-throughput virtual screening | Screen 100M+ compounds from Enamine REAL library [41] |
| STONED-SELFIES | Algorithm | Superfast chemical space exploration | Generate structurally similar analogs of known KRAS inhibitors [41] |
| Chemistry42 | Software Platform | Structure-based drug design | Validate molecules, assess pharmacological viability [41] |
| GNINA | Software Tool | Deep learning-augmented molecular docking | Predict binding affinity with CNN scoring [93] |
| QCBM-LSTM | Hybrid Model | Quantum-enhanced generative modeling | Design novel KRAS inhibitors with expanded chemical diversity [41] |
| MaMTH-DS | Assay System | Mammalian membrane two-hybrid drug screening | Cellular validation of KRAS-effector interaction inhibition [41] |
Visual Workflows and Signaling Pathways
KRAS Signaling Pathway and Targeted Inhibition
Diagram: KRAS signaling cascade showing key regulatory nodes and inhibitor mechanisms. Mutations at G12, G13, or Q61 lock KRAS in the active GTP-bound state, constitutively activating downstream pathways. Covalent G12C inhibitors stabilize the inactive GDP-bound state, while emerging pan-RAS strategies target multiple activation states [90] [40].
Hybrid Quantum-Classical Workflow for KRAS Inhibitor Design
Diagram: Integrated quantum-classical workflow for KRAS inhibitor discovery. The hybrid approach combines quantum generative models (QCBM) with classical deep learning (LSTM) to explore chemical space more efficiently than either method alone [41].
The Role of Digital Twins and In Silico Clinical Trials for Predictive Validation
Frequently Asked Questions (FAQs)
Q1: What are digital twins (DTs) and in silico clinical trials (ISCTs) in the context of cancer research? A digital twin is a dynamic, virtual representation of a patient (or a biological process) that integrates clinical, genetic, and lifestyle data to simulate disease activity and treatment responses in a virtual environment [94]. In silico clinical trials use these digital twins to run simulated experiments, testing hypotheses and optimizing drug candidates without exposing additional patients to potential risks [94]. In targeting undruggable proteins, they provide a platform to model complex protein behaviors and predict the efficacy of novel therapeutic strategies like PROTACs or RNAi before moving to human trials [94] [3] [21].
Q2: How can digital twins help overcome the challenge of small sample sizes in trials for rare cancer targets? Digital twins address this by generating synthetic control arms and virtual patient cohorts. Instead of enrolling a large number of real patients into control groups, each real participant can be paired with a digital twin whose disease progression is simulated under standard care. This approach can reduce sample size needs, shorten trial timelines, and prevent patients from unnecessary exposure to ineffective treatments [94].
Q3: What are the common data sources for building and validating a digital twin? Building a robust digital twin relies on integrating multi-modal data sources. The table below summarizes the primary types and their utility.
| Data Source | Description | Utility in Model Building |
|---|---|---|
| Multi-omics Data [95] | Genomic, transcriptomic, proteomic, and epigenomic profiles from tumor samples. | Identifies key molecular drivers and therapeutic vulnerabilities; forms the core of mechanistic models. |
| Real-World Evidence (RWE) [94] | Data from electronic health records (EHRs), disease registries, and patient claims. | Provides context on real-world disease progression and treatment outcomes, enhancing generalizability. |
| Preclinical Models [95] [96] | Drug response data from patient-derived cell lines, organoids (PDOs), and xenografts (PDXs). | Offers scalable, high-throughput data for training and validating predictive algorithms on patient-specific tissue. |
| Medical Imaging & Histology [95] | Radiology images (radiomics) and digitized pathology slides. | Captures spatial and structural information about the tumor and its microenvironment. |
Q4: What are the key hallmarks of a high-quality predictive oncology model? According to community-driven workshops, predictive models should strive for seven key hallmarks [95]:
- Data Relevance/Actionability: The model's input data should be clinically relevant and practically useful for influencing treatment decisions.
- Expressive Architecture: The model should have a structure capable of capturing complex biological interactions (e.g., using deep neural networks).
- Standardized Benchmarking: Models must be evaluated against consistent and standardized datasets and metrics.
- Demonstrated Generalizability: The model must perform accurately across diverse patient populations and clinical settings, not just the data it was trained on.
- Mechanistic Interpretability: It should be possible to understand the biological rationale behind the model's predictions.
- Accessibility and Reproducibility: The model should be user-friendly and its results should be reproducible by other researchers.
- Fairness: The model must be designed and validated to ensure equitable application across different patient demographics.
Troubleshooting Guides
Issue 1: Poor Model Generalizability and Data Bias
Problem: Your digital twin or predictive model performs well on your initial dataset but fails to predict outcomes accurately in a broader, more diverse patient population. This is often caused by biased or non-representative training data [95] [97].
Solution:
- Action: Implement rigorous data augmentation and validation strategies.
- Procedure:
- Audit Training Data: Proactively assess your datasets for under-representation of diverse demographic and clinical groups [94].
- Utilize Diverse Data Sources: Augment your primary data with harmonized data from public repositories like NCI's Genomic Data Commons (GDC) and Real-World Evidence (RWE) studies [94] [98].
- Apply Bias Mitigation Techniques: Employ algorithmic techniques to identify and correct for bias during model training.
- Validate Externally: Test your model on independent, external datasets from different institutions or geographic locations before clinical application [95].
Issue 2: Lack of Model Interpretability and Transparency
Problem: The digital twin's predictions are a "black box," making it difficult to understand the biological rationale behind a forecast. This limits clinical trust and regulatory acceptance [95] [97].
Solution:
- Action: Integrate explainable AI (XAI) techniques and prioritize mechanistic modeling.
- Procedure:
- Use Explainability Tools: Apply techniques like SHapley Additive exPlanations (SHAP) to quantify the contribution of each input feature (e.g., a specific gene mutation) to the final prediction [94].
- Develop Mechanistic Models: Where possible, base digital twins on well-understood biological and physiological processes. These models are inherently more interpretable than purely data-driven black boxes [97].
- Generate Model Reports: Create simplified reports or dashboards for clinicians that highlight the key biological factors (e.g., "The model predicts resistance due to high expression of gene X and inactivation of pathway Y").
Issue 3: Validating a Digital Twin Against Real-World Outcomes
Problem: How do you quantitatively prove that your digital twin's predictions are accurate and clinically meaningful?
Solution:
- Action: Employ a multi-step validation process using historical and real-time data.
- Procedure:
- Retrospective Validation: The first pragmatic step is to test the digital twin against data from completed clinical trials. Measure performance using metrics like survival concordance indices, Root Mean Square Error (RMSE), and calibration curves [97].
- Real-Time Calibration: For dynamic twins, integrate continuously updated electronic health records (EHRs) or wearable sensor data to dynamically recalibrate predictions [97].
- Covariate Adjustment: Use prognostic covariate adjustment frameworks (e.g., PROCOVA-MMRM) in your validation to reduce sampling bias and improve the statistical power of your comparisons [97].
- Uncertainty Quantification: Always include quantified uncertainty estimates in predictions to support risk-aware clinical decision-making [97].
Experimental Protocols & Workflows
Protocol 1: Building a Machine Learning Recommender System for Drug Response Prediction
This protocol outlines a proof-of-concept methodology for predicting drug responses in patient-derived cell cultures (PDCs), which can serve as a foundation for building more complex digital twins [96].
1. Data Collection and Curation
- Input: Collect historical high-throughput drug screening data from a diverse set of PDCs. This dataset should contain measured bioactivity (e.g., IC50) for many drugs across many cell lines [96].
- Preprocessing: Handle missing values using imputation techniques like Transformational Machine Learning (TML) [96].
2. Model Training and Probing Panel Selection
- Architecture: Train a machine learning model (e.g., a Random Forest with 50 trees) on the historical dataset to learn the complex relationships between cell lines and their drug response profiles [96].
- Probing Panel: From the full drug library, select a small, representative subset of drugs (~30) to be used as a "probing panel" for new, unseen patient samples [96].
3. Prediction for a New Patient Sample
- A new patient-derived cell line is screened only against the small probing panel of drugs.
- The trained model uses this limited response data from the new sample to impute or predict its likely response to the entire drug library.
- The output is a ranked list of drugs predicted to be most effective for that specific patient's cells [96].
4. Experimental Validation
- The top-ranked predicted drugs (e.g., top 10-15) from the model are then tested experimentally in the lab on the new patient-derived cells to confirm their efficacy [96].
The workflow for this protocol is as follows:
Protocol 2: Implementing a Digital Twin Framework for a Synthetic Control Arm
This protocol describes how to create and use digital twins to generate a synthetic control arm in a clinical trial, reducing the number of patients needed in the control group [94] [97].
1. Data Integration and Virtual Patient Generation
- Input: Gather comprehensive baseline data from trial participants (symptoms, biomarkers, imaging, genetic profiles) and augment it with historical control datasets from previous trials and real-world evidence studies [94].
- Synthesis: Use AI and deep generative models to create a cohort of virtual patients (digital twins) that accurately reflect the variability of the real-world population. Each real participant can be paired with a matched digital twin [94].
2. Simulation of Disease Progression
- Control Group Simulation: The digital twins are used to simulate the natural progression of the disease under standard care or placebo conditions. This simulated cohort forms the synthetic control arm [94].
- Treatment Simulation: A separate virtual cohort can be generated by simulating the expected biological effects of the investigational drug on the digital twins, based on preclinical data [94].
3. Predictive Modeling and Trial Optimization
- Analysis: Continuously refine the digital twins using predictive modeling. Compare outcomes from the real treatment arm against the synthetic control arm.
- Optimization: Use the simulations to optimize trial parameters such as dosing regimens, sample sizes, and power calculations in silico [94].
4. Rigorous Validation
- Comparison: Rigorously validate the digital twin predictions against real-world clinical trial data and outcomes using statistical comparisons [94] [97].
The workflow for a synthetic control arm trial is as follows:
The Scientist's Toolkit: Research Reagent Solutions
The following table details key computational and experimental resources essential for working with digital twins and targeting undruggable proteins.
| Tool / Resource | Type | Function and Application |
|---|---|---|
| AI/ML Platforms (e.g., TensorFlow, PyTorch) [95] | Software Framework | Provides the foundational architecture for building expressive deep learning models to capture complex drug-response patterns. |
| Patient-Derived Organoids (PDOs) / Cell Lines (PDCs) [95] [96] | Biological Model | Serves as a scalable, patient-specific ex vivo system for generating high-throughput drug response data to train and validate digital twin models. |
| NCI Genomic Data Commons (GDC) [98] | Data Repository | Provides vast amounts of standardized genomic and clinical data from cancer patients, essential for building and benchmarking predictive models. |
| SHAP (SHapley Additive exPlanations) [94] | Explainable AI Library | Interprets the output of complex machine learning models, attributing predictions to specific input features to enhance model transparency. |
| Proteolysis Targeting Chimeras (PROTACs) [3] | Degradation Technology | A novel drug modality that targets undruggable proteins for degradation rather than inhibition; a key therapeutic strategy to simulate with digital twins. |
| Inverted RNAi Molecules [21] | Nucleic Acid Therapeutic | A technology used to simultaneously silence multiple undruggable cancer genes (e.g., KRAS and MYC); its effects can be modeled in silico before synthesis. |
| Alpha-Fold / Protein Structure Prediction [3] | Computational Tool | Predicts the 3D structure of proteins, which is critical for identifying allosteric sites or designing drugs against undruggable targets with flat surfaces. |
The pursuit of "undruggable" targets, such as the proteins KRAS and MYC, represents a frontier in oncology research. These proteins are characterized by a lack of defined binding pockets for small molecules, functioning primarily through protein-protein interactions, or possessing highly dynamic structures [1] [3]. Artificial Intelligence (AI) and Machine Learning (ML) are emerging as transformative technologies to overcome these challenges, enabling the rapid analysis of complex biological data to identify novel drug candidates and therapeutic strategies [99]. However, the integration of AI into drug development necessitates a clear understanding of the evolving regulatory landscape. This technical support center provides guidance on navigating the frameworks established by the U.S. Food and Drug Administration (FDA) and the European Medicines Agency (EMA), with a specific focus on applications in computationally targeting undruggable cancer proteins.
Regulatory Frameworks at a Glance: FDA vs. EMA
The table below summarizes the core regulatory guidance from the FDA and EMA regarding the use of AI in drug development.
Table 1: Overview of Key FDA and EMA Guidance on AI in Drug Development
| Agency | Key Document | Issue Date | Core Approach | Primary Focus |
|---|---|---|---|---|
| U.S. FDA | Considerations for the Use of Artificial Intelligence... (Draft Guidance) [100] [101] |
January 2025 | Risk-based credibility assessment framework [100] | Use of AI to support regulatory decisions on drug safety, effectiveness, and quality [102] |
| EU EMA | Reflection paper on AI in the medicinal product lifecycle [103] |
September 2024 | Risk-based approach for development, deployment, and monitoring [103] | Safe and effective use of AI and ML across the medicine lifecycle [103] |
Frequently Asked Questions (FAQs) and Troubleshooting
FAQ 1: Does my AI model for discovering KRAS inhibitors fall under current FDA or EMA regulations?
Answer: It depends on the stage of development. According to the FDA's January 2025 draft guidance, AI models used exclusively in early drug discovery are currently not within the scope of the guidance [101] [104]. The EMA's reflection paper also focuses on the regulated phases of the product lifecycle [103]. However, once your research progresses and you begin generating data intended to support a regulatory decision—such as data included in an Investigational New Drug (IND) application or a Marketing Authorisation Application (MAA)—the AI models used to produce that data will fall under regulatory scrutiny [100] [99]. This includes AI used in nonclinical testing, clinical trial design, or manufacturing.
Troubleshooting Guide:
- Problem: Uncertainty about whether an AI model for target validation requires regulatory compliance.
- Solution: Map your AI model's Context of Use (COU). If the output is used for internal decision-making and candidate selection only, it is likely outside current formal guidance. The moment that output is used to justify a clinical trial design or a safety claim in a regulatory submission, you must follow the respective FDA or EMA framework.
FAQ 2: What is the core framework I need to follow for my AI model under the FDA's draft guidance?
Answer: The FDA proposes a risk-based credibility assessment framework to establish trust in your AI model's output for a specific Context of Use (COU) [100] [101] [104]. This process is broken down into seven key steps that you should document.
Diagram 1: FDA's 7-Step AI Credibility Framework
Troubleshooting Guide:
- Problem: How to assess "AI Model Risk" in Step 3.
- Solution: The FDA recommends evaluating two factors [104]:
- Model Influence: Is the model's output the sole determinant of a decision, or is it reviewed by a human? Higher influence equals higher risk.
- Decision Consequence: What is the impact of an incorrect output? An output that directly affects patient safety (e.g., patient monitoring in a trial) is higher risk than one that identifies batches for human review in manufacturing.
- Problem: The model's performance degrades after deployment (model drift).
- Solution: The FDA expects a lifecycle maintenance plan to monitor and ensure the model's ongoing performance for its COU [104]. This is similar to the PMDA's Post-Approval Change Management Protocol (PACMP) for AI [99].
FAQ 3: How do the FDA and EMA approaches differ, and how can I prepare for both?
Answer: While both agencies embrace a risk-based approach, their current emphases differ. The FDA has provided a more detailed, procedural framework (the 7-step process) for establishing model credibility [100] [101]. The EMA's published reflection paper provides considerations for the safe and effective use of AI and emphasizes the importance of transparency, robustness, and data integrity under existing EU legal requirements [103] [99]. The EMA has also issued guiding principles for the use of Large Language Models (LLMs), focusing on safe data input, critical thinking, and cross-checking outputs [103].
Table 2: Key Focus Areas for FDA and EMA Regulatory Submissions Involving AI
| Aspect | FDA Emphasis | EMA Emphasis |
|---|---|---|
| Core Documentation | Credibility Assessment Report documenting the 7-step framework [100]. | Comprehensive documentation demonstrating adherence to principles of robustness, transparency, and data integrity [103]. |
| Transparency & Explainability | Acknowledges challenges; requires documentation of approaches to interpretability [99]. | Stresses importance of understanding model limitations and ensuring human oversight [103]. |
| Lifecycle Management | Expects a plan for monitoring model performance and managing changes [104]. | Encourages a structured approach for performance monitoring and updates [103]. |
| Engagement Strategy | Strongly encourages early and frequent engagement with the Agency to discuss plans [104]. | Encourages early dialogue, supported by a multi-annual workplan (2025-2028) to build AI capacity [103]. |
FAQ 4: What is a real-world example of AI for undruggable targets gaining regulatory acceptance?
Answer: A landmark example is EMA's first qualification opinion on an AI methodology, issued in March 2025 for the AIM-NASH tool [103]. This AI tool assists human pathologists in analyzing liver biopsy scans to determine the severity of Metabolic dysfunction-associated steatohepatitis (MASH). The CHMP (Committee for Medicinal Products for Human Products) deemed data generated with this AI assistance as scientifically valid for clinical trials [103]. This paves the way for using AI-derived endpoints in regulatory submissions for complex diseases.
Experimental Protocol: Integrating AI and RNAi to Co-Target KRAS and MYC
The following protocol is based on a recent study demonstrating a "two-in-one" molecular technology to simultaneously silence the undruggable targets KRAS and MYC [21]. This exemplifies how computational design can be translated into a wet-lab experimental workflow.
Objective: To design and test inverted RNAi molecules for the co-silencing of KRAS and MYC oncogenes in cancer cell lines.
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Reagents for RNAi-based Targeting of Undruggable Proteins
| Research Reagent | Function / Explanation |
|---|---|
| Inverted siRNA Molecules | Novel RNAi compositions designed to target specific sequences of KRAS and MYC mRNA, leading to their degradation and silencing [21]. |
| Transfection Reagent | A chemical or lipid-based vehicle to deliver the inverted siRNA molecules into the target cancer cells. |
| Control siRNAs (Scramble & Single-Target) | Scrambled sequence siRNA as a negative control; individual siRNAs for KRAS and MYC to compare efficacy against the dual-targeting molecule. |
| Cancer Cell Lines | Models harboring KRAS mutations and MYC overexpression (e.g., pancreatic, lung, or colorectal cancer lines). |
| qRT-PCR Assay Kits | To quantitatively measure the reduction in KRAS and MYC mRNA levels post-transfection. |
| Western Blot Apparatus | To confirm the silencing effect at the protein level by detecting reduced KRAS and MYC protein expression. |
| Cell Viability Assay (e.g., MTT) | To measure the inhibitory effect of gene co-silencing on cancer cell growth and survival [21]. |
Methodology:
Computational Design & In Silico Analysis
- Target Selection: Identify specific target sequences within the KRAS (mutant) and MYC mRNAs.
- siRNA Design: Use computational tools to design inverted siRNA molecules capable of co-targeting both selected sequences. This design should prioritize minimal off-target effects.
- Stability & Binding Affinity Prediction: Employ AI/ML models to predict the secondary structure and binding energy of the designed siRNAs to their targets.
In Vitro Transfection
- Plate appropriate cancer cell lines and control cells in culture plates.
- Complex the designed "two-in-one" siRNA with the transfection reagent according to the manufacturer's protocol.
- Transfert the cells with the following groups:
- Experimental Group: "Two-in-one" KRAS/MYC siRNA
- Control Group 1: Scrambled siRNA
- Control Group 2: KRAS-only siRNA
- Control Group 3: MYC-only siRNA
- Incubate cells for 24-72 hours for gene expression analysis.
Efficacy Assessment
- mRNA Knockdown Validation: Harvest cells and extract total RNA. Perform qRT-PCR to quantify the mRNA expression levels of KRAS and MYC relative to housekeeping genes and control groups.
- Protein Knockdown Validation: Lyse cells and perform Western blotting to detect KRAS and MYC protein levels.
- Phenotypic Effect: Perform a cell viability assay (e.g., MTT) 72-96 hours post-transfection to assess the combined effect of dual-gene silencing on cancer cell proliferation [21].
Diagram 2: Experimental Workflow for AI-Guided RNAi
Conclusion
The convergence of computational power, generative AI, and quantum computing is systematically dismantling the 'undruggable' paradigm in oncology. Strategies that leverage AI for de novo binder design, particularly for flexible and disordered targets, have moved from theoretical promise to tangible preclinical candidates. The successful targeting of KRAS marks a pivotal milestone, demonstrating that persistent computational innovation can unlock even the most challenging proteins. Future progress hinges on creating higher-quality, multimodal datasets, improving the fidelity of disease models to better predict clinical outcomes, and fostering collaborative frameworks that integrate computational design with robust experimental biology. As these tools mature, they promise to usher in a new era of precision oncology, transforming the treatment landscape for cancers driven by these elusive targets.
References
- 1. Recent advances in targeting the “undruggable” proteins [https://www.nature.com/articles/s41392-023-01589-z]
- 2. Strategies for targeting undruggable targets [https://pubmed.ncbi.nlm.nih.gov/34455870/]
- 3. Emerging Pharmacotherapeutic Strategies to Overcome ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10367563/]
- 4. Modulating undruggable targets to overcome cancer ... [https://www.sciencedirect.com/science/article/pii/S1368764621000467]
- 5. DrugAppy – An end-to-end deep learning framework for ... [https://www.sciencedirect.com/science/article/pii/S0010482525015549]
- 6. Quantum computing approach targets 'undruggable' protein [https://www.ddw-online.com/quantum-computing-approach-targets-undruggable-protein-33401-202501/]
- 7. Centre for Target Validation [https://www.icr.ac.uk/research-and-discoveries/centres-and-strategic-collaborations/centre-for-target-validation]
- 8. KRAS mutation: from undruggable to druggable in cancer [https://www.nature.com/articles/s41392-021-00780-4]
- 9. Drugging the 'undruggable' KRAS: breakthroughs, challenges ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12302276/]
- 10. Targeting KRAS mutant cancers: from druggable therapy to ... [https://molecular-cancer.biomedcentral.com/articles/10.1186/s12943-022-01629-2]
- 11. Targeting the undruggables—the power of protein degraders [https://www.sciencedirect.com/science/article/pii/S2095927324002123]
- 12. Hitting 'undruggable' disease targets [https://www.bakerlab.org/2025/07/17/binding-disordered-targets/]
- 13. Hitting 'undruggable' disease targets [https://www.ipd.uw.edu/2025/07/hitting-undruggable-disease-targets/]
- 14. Computer-aided drug design in anti-cancer drug discovery [https://www.sciencedirect.com/science/article/pii/S2352914823001788]
- 15. New insights into protein–protein interaction modulators in ... [https://www.nature.com/articles/s41392-024-02036-3]
- 16. Visualization of Protein Interactions in Living Cells - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC5788009/]
- 17. Functions of Intrinsically Disordered Regions - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC12292460/]
- 18. Characterization of functional disordered regions within ... [https://www.sciencedirect.com/science/article/pii/S2589004221000389]
- 19. Characterization of intrinsically disordered regions in proteins ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8942211/]
- 20. Intrinsically disordered proteins [https://en.wikipedia.org/wiki/Intrinsically_disordered_proteins]
- 21. New molecular technology targets tumors and ... [https://unclineberger.org/news/new-molecular-technology-targets-tumors-and-simultaneously-silences-two-undruggable-cancer-genes/]
- 22. How will computational and AI tools guide future anticancer ... [https://dailyreporter.esmo.org/esmo-congress-2025/2025-esmo-society-awards/how-will-computational-and-ai-tools-guide-future-anticancer-strategies]
- 23. Drug discovery by targeting the protein–protein interactions ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10638514/]
- 24. Computational approaches to druggable site identification [https://www.sciencedirect.com/science/article/pii/S2211383525007105]
- 25. Target Mapping in Cancer: Ligandable Protein Pockets on ... [https://www.mdpi.com/1424-8247/18/7/958]
- 26. Computational deep dive surfaces unexplored world of ... [https://sbpdiscovery.org/press/computational-deep-dive-surfaces-unexplored-world-of-cancer-drug-targets/]
- 27. New Computational Tool Shows Strong Accuracy in ... [https://ascopost.com/news/november-2025/new-computational-tool-shows-strong-accuracy-in-predicting-cancer-drug-targets]
- 28. A review of the current trends in computational approaches ... [https://link.springer.com/article/10.1186/s12982-024-00229-3]
- 29. Machine Learning for Multi-Target Drug Discovery [https://pmc.ncbi.nlm.nih.gov/articles/PMC12473769/]
- 30. Insilico Pharma.AI fall launch recap: Understand latest AI ... [https://insilico.com/tpost/003kiu5pv1-insilico-pharmaai-fall-launch-recap-unde]
- 31. Leading AI-Driven Drug Discovery Platforms [https://www.sciencedirect.com/science/article/abs/pii/S0031699725075118]
- 32. Showcasing gen-AI breakthroughs ... [https://insilico.com/tpost/rd037pu8d1-showcasing-gen-ai-breakthroughs-insilico]
- 33. Artificial Intelligence in Cancer Drug Discovery in 2025 [https://oncodaily.com/oncolibrary/artificial-intelligence-in-cancer-drug-discovery]
- 34. A Complete Guide on Generative AI for De Novo Drug ... [https://www.alliancetek.com/blog/post/2025/09/11/generative-ai-de-novo-drug-discovery.aspx]
- 35. The Role of AI in Drug Discovery: Challenges, Opportunities ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10302890/]
- 36. Ten simple rules for optimal and careful use of generative ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12561928/]
- 37. AI‑Designed Binders - The Babak Lab [https://oncodaily.com/science/ai%E2%80%91designed-binders-338836]
- 38. Review Code to complex: AI-driven de novo binder design [https://www.sciencedirect.com/science/article/pii/S0969212625003119]
- 39. Novel paradigms in KRAS targeting: Unveiling strategies to ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12453332/]
- 40. Evolution of direct RAS inhibitors: from undruggable target to ... [https://molecular-cancer.biomedcentral.com/articles/10.1186/s12943-025-02364-0]
- 41. Quantum-computing-enhanced algorithm unveils potential ... [https://www.nature.com/articles/s41587-024-02526-3]
- 42. Bridging Quantum and Classical Computing in Drug Design [https://arxiv.org/html/2506.01177v1]
- 43. Quantum Computing-Enhanced Algorithm Unveils Novel ... [https://arxiv.org/html/2402.08210v1]
- 44. quantum computing accelerates KRAS inhibitor design [https://pmc.ncbi.nlm.nih.gov/articles/PMC12075789/]
- 45. NAMD goes quantum: An integrative suite for QM/MM ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6095686/]
- 46. Covalent-Allosteric Inhibitors: Do We Get the Best of Both ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12207613/]
- 47. Recent advances in computational strategies for allosteric ... [https://www.sciencedirect.com/science/article/abs/pii/S1359644625001795]
- 48. Speed isn't everything when it comes to covalent inhibitor ... [https://www.buffalo.edu/news/releases/2025/08/speed-isnt-everything-when-it-comes-to-covalent-inhibitor-drugs.html]
- 49. Recent applications of computational methods to allosteric ... [https://www.frontiersin.org/journals/molecular-biosciences/articles/10.3389/fmolb.2022.1070328/full]
- 50. Benchmarking Covalent Drug Design with Tasks, Datasets ... [https://arxiv.org/abs/2506.21085]
- 51. Computational approaches streamlining drug discovery [https://www.nature.com/articles/s41586-023-05905-z]
- 52. Review article Covalent inhibitors design and discovery [https://www.sciencedirect.com/science/article/abs/pii/S0223523417304658]
- 53. Rewiring enzyme regulation: Allosteric drugs and ... [https://pubmed.ncbi.nlm.nih.gov/41005256/]
- 54. -Aided Drug Discovery for Computer Undruggable Targets [https://pubmed.ncbi.nlm.nih.gov/40423592/]
- 55. Combining AI and physics-based simulations for fragment- ... [https://www.icr.ac.uk/study-and-careers/phds-at-the-icr/our-phd-projects/detail/combining-ai-and-physics-based-simulations-for-fragment-based-cancer-drug-discovery]
- 56. Physics-informed machine learning digital twin for ... [https://www.nature.com/articles/s41746-025-01890-x]
- 57. AI/ML meets physics-based simulations: A new era in complex ... [https://www.schrodinger.com/materials-science/learn/webinar/ai-ml-meets-physics-based-simulations-a-new-era-in-complex-materials-design/]
- 58. Multiscale Modeling in the Clinic: Drug Design and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4983472/]
- 59. Advancing Proton Therapy: A Review of Geant4 Simulation ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11651386/]
- 60. how generative AI can tackle undruggable targets [https://www.drugtargetreview.com/article/163308/next-generation-drug-design-ai-tackle-undruggable-targets/]
- 61. Data Scarcity: When Will AI Hit a Wall? [https://pieces.app/blog/data-scarcity-when-will-ai-hit-a-wall]
- 62. Overcoming Data Scarcity in AI Model Training | Medium [https://ongraphtech.medium.com/data-scarcity-in-ai-model-training-1a7559554ed3]
- 63. Unraveling druggable cancer-driving proteins and targeted ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11339426/]
- 64. In silico trials: Verification, validation and uncertainty ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7883933/]
- 65. Integrating in-silico and experimental validation ... [https://www.nature.com/articles/s41598-025-19931-6]
- 66. Bridging in silico and in vitro perspectives to unravel ... [https://pubmed.ncbi.nlm.nih.gov/39079275/]
- 67. FAQ: Key AI Applications in Drug Development [https://www.pharmtech.com/view/faq-key-ai-applications-in-drug-development]
- 68. In Silico Models in Oncology: Validating AI-Driven ... [https://blog.crownbio.com/in-silico-models-in-oncology-validating-ai-driven-predictive-frameworks]
- 69. A Pipeline for Drug Target Identification and Validation - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC5469697/]
- 70. A Technical FAQ Guide to Oncology Drug Screening Using ... [https://blog.crownbio.com/oncology-drug-screening-using-innovative-organoid-technology-and-biomarker-analysis]
- 71. Cancer cell plasticity and therapeutic resistance - Hereditas [https://hereditasjournal.biomedcentral.com/articles/10.1186/s41065-025-00564-8]
- 72. New research might make an 'undruggable' target druggable [https://www.icr.ac.uk/about-us/icr-news/detail/new-research-might-make-an--undruggable--target-druggable---leading-to-new-cancer-drugs]
- 73. Next-generation sequencing in cancer diagnosis and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12009796/]
- 74. New guidelines on how to report clinical sequencing data ... [https://news.ki.se/new-guidelines-on-how-to-report-clinical-sequencing-data-help-doctors-make-decisions-about-cancer-treatment]
- 75. Drug resistance in cancer: molecular mechanisms and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12623568/]
- 76. Prediction of Drug-Like Properties - NCBI - NIH [https://www.ncbi.nlm.nih.gov/books/NBK6404/]
- 77. Drug Discovery Assays Support—Troubleshooting [https://www.thermofisher.com/us/en/home/technical-resources/technical-reference-library/drug-discovery-development-support-center/drug-discovery-assays-support/drug-discovery-assays-support-troubleshooting.html]
- 78. Frequently Asked Questions on Drug Development and ... [https://www.fda.gov/drugs/cder-small-business-industry-assistance-sbia/small-business-assistance-frequently-asked-questions-drug-development-and-investigational-new-drug]
- 79. Biologically relevant integration of transcriptomics profiles ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11740957/]
- 80. Establishing 3D organoid models from patient-derived ... [https://molecular-cancer.biomedcentral.com/articles/10.1186/s12943-025-02374-y]
- 81. The Future of Clinical Trials: Incorporating 'Omics for ... [https://blog.crownbio.com/the-future-of-clinical-trials-incorporating-omics-for-enhanced-stratification]
- 82. First-of-Its-Kind Cancer Therapy Targets 'Undruggable' Protein ... [https://phoenixmed.arizona.edu/newsroom/news/first-its-kind-cancer-therapy-targets-undruggable-protein-interaction]
- 83. Artificial intelligence in drug discovery and development - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC7577280/]
- 84. Five potential problems with overhyping AI in drug discovery [https://www.ddw-online.com/five-potential-problems-with-overhyping-ai-in-drug-discovery-34511-202504/]
- 85. Challenges and promises for translating computational ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4834893/]
- 86. Recursion, Exscientia, and AI drug discovery's moment of ... [https://pharmaphorum.com/digital/recursion-exscientia-and-ai-drug-discoverys-moment-truth]
- 87. Clinical trials are becoming more complex: a machine ... [https://www.nature.com/articles/s41598-024-53211-z]
- 88. Recursion to absorb Exscientia in 'techbio' deal [https://www.biopharmadive.com/news/recursion-exscientia-merger-deal-artificial-intelligence-drug-discovery/723714/]
- 89. AI Benchmarks 2025: Performance Metrics Show Record ... [https://www.sentisight.ai/ai-benchmarks-performance-soars-in-2025/]
- 90. “Undruggable KRAS”: druggable after all - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC11789494/]
- 91. Evolution of computational techniques against various ... [https://pubmed.ncbi.nlm.nih.gov/40195161/]
- 92. Quantum biological convergence: quantum computing accelerates KRAS inhibitor design | Signal Transduction and Targeted Therapy [https://www.nature.com/articles/s41392-025-02239-2]
- 93. Targeting the untargetable: accelerated discovery of KRAS G12D inhibitors through a deep learning-enhanced in silico pipeline - ScienceDirect [https://www.sciencedirect.com/science/article/pii/S3050787125000988]
- 94. Enhancing randomized clinical trials with digital twins - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC12494699/]
- 95. The Hallmarks of Predictive Oncology - PMC - PubMed Central [https://pmc.ncbi.nlm.nih.gov/articles/PMC11969157/]
- 96. Establishing predictive machine learning models for drug ... [https://www.nature.com/articles/s41698-025-00937-2]
- 97. AI and innovation in clinical trials | npj Digital Medicine [https://www.nature.com/articles/s41746-025-02048-5]
- 98. Predictive Modeling - NCI [https://www.cancer.gov/about-nci/organization/cbiit/training/learn/model]
- 99. Regulating the Use of AI in Drug Development: Legal ... [https://www.fdli.org/2025/07/regulating-the-use-of-ai-in-drug-development-legal-challenges-and-compliance-strategies/]
- 100. Considerations for the Use of Artificial Intelligence [https://www.fda.gov/regulatory-information/search-fda-guidance-documents/considerations-use-artificial-intelligence-support-regulatory-decision-making-drug-and-biological]
- 101. FDA Publishes Its First Draft Guidance On Use of Artificial ... [https://www.goodwinlaw.com/en/insights/publications/2025/01/alerts-lifesciences-aiml-fda-publishes-its-first-draft-guidance]
- 102. Artificial Intelligence for Drug Development [https://www.fda.gov/about-fda/center-drug-evaluation-and-research-cder/artificial-intelligence-drug-development]
- 103. Artificial intelligence | European Medicines Agency (EMA) [https://www.ema.europa.eu/en/about-us/how-we-work/data-regulation-big-data-other-sources/artificial-intelligence]
- 104. Key takeaways from FDA's draft guidance on use of AI ... [https://www.dlapiper.com/en/insights/publications/2025/01/fda-releases-draft-guidance-on-use-of-ai]