Beyond the Genome: Integrating NGS with Multi-Omics to Power Next-Generation Precision Oncology
The molecular complexity of cancer demands a systems-level approach that moves beyond single-omics analyses.
Beyond the Genome: Integrating NGS with Multi-Omics to Power Next-Generation Precision Oncology
Abstract
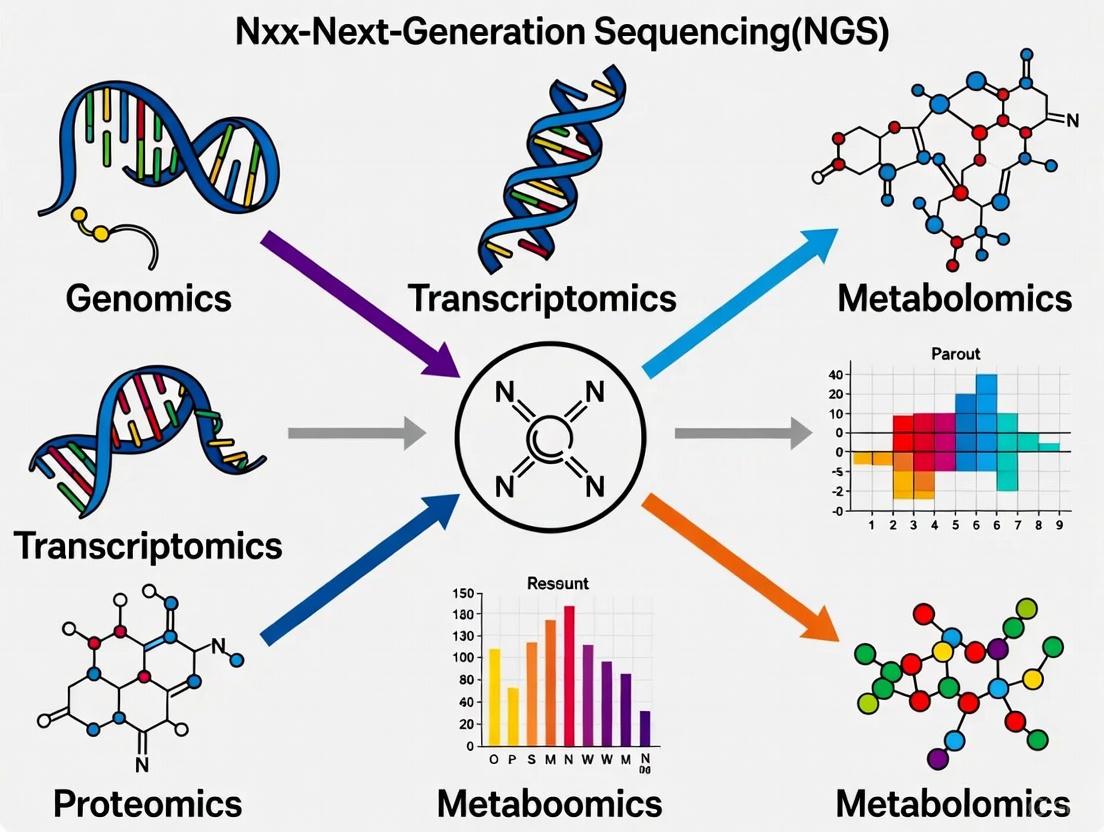
The molecular complexity of cancer demands a systems-level approach that moves beyond single-omics analyses. This article explores the integration of Next-Generation Sequencing (NGS) with complementary omics layers—including transcriptomics, proteomics, metabolomics, and epigenomics—to build a holistic view of tumor biology. We examine the foundational principles of multi-omics, detail cutting-edge AI and machine learning methodologies for data integration, address critical challenges in data harmonization and clinical implementation, and validate these approaches through real-world applications in therapy selection, resistance monitoring, and clinical trial stratification. Aimed at researchers, scientists, and drug development professionals, this review synthesizes how integrated multi-omics is transforming oncology from a reactive to a proactive, personalized discipline.
Decoding Cancer Complexity: The Foundational Role of NGS in a Multi-Omics Framework
Next-generation sequencing (NGS) has revolutionized oncology research by providing an unprecedented window into the genomic landscape of cancer [1]. This massively parallel sequencing technology can process millions of DNA fragments simultaneously, dramatically reducing the cost and time required for genetic analysis compared to first-generation Sanger sequencing [2]. In clinical oncology, NGS has become the workhorse for identifying driver mutations, characterizing tumor mutational burden, and deciphering mutational signatures that reveal the historical activity of carcinogenic processes [1].
However, cancer is not merely a genetic disease—it operates through complex, interconnected molecular layers that extend beyond the genome. The fundamental limitation of a single-omics approach relying exclusively on NGS lies in its inability to capture the dynamic flow of biological information from DNA to RNA to proteins and functional phenotypes [3]. While NGS excels at identifying genomic variants, it cannot determine how these variants functionally influence cellular processes, treatment responses, and disease progression without integration with other molecular data types [4]. This application note delineates the specific constraints of NGS as a standalone technology and provides frameworks for its integration with multi-omics approaches to achieve a more comprehensive understanding of cancer biology.
Key Limitations of Single-Omics NGS Approaches
Inability to Capture Functional Molecular Dynamics
NGS provides a static snapshot of the genetic code but fails to reveal how this code is dynamically executed within cancer cells.
- Transcriptomic Regulation: DNA-level mutations identified by NGS may not consistently correlate with gene expression levels due to complex regulatory mechanisms. Transcriptomics is required to understand which mutations actually influence messenger RNA (mRNA) production [3] [5].
- Protein-Level Expression and Modification: The presence of an mRNA transcript does not guarantee its translation into functional protein, and protein activity is further modulated by post-translational modifications invisible to genomic analysis [6]. Proteomic technologies are necessary to quantify actual protein expression and functional states [3].
- Metabolic Reprogramming: Cancer cells undergo significant metabolic alterations (e.g., Warburg effect) that support rapid proliferation. These biochemical changes can only be profiled through metabolomics, representing a critical functional layer beyond genomic alterations [4] [3].
Obscuring of Cellular Heterogeneity
Traditional bulk NGS approaches average molecular signals across thousands to millions of cells, effectively masking critical cellular subpopulations that drive disease progression and therapeutic resistance [7] [5].
Table: Limitations of Bulk NGS in Resolving Cellular Heterogeneity
| Aspect of Heterogeneity | Impact of Bulk NGS | Biological Consequence |
|---|---|---|
| Rare subclones | Obscured by dominant populations | Missed drivers of resistance |
| Tumor evolution | Inferred rather than directly observed | Incomplete evolutionary history |
| Tumor microenvironment | Stromal and immune signals averaged | Missed cell-cell interactions |
| Metastatic potential | Subclones with invasive properties masked | Limited prediction of spread |
Technical and Analytical Constraints
NGS technologies introduce specific technical artifacts and analytical challenges that can confound biological interpretation.
- Sequencing Biases and Artifacts: Different NGS platforms have inherent sequencing biases specific to their library preparation protocols and sequencing chemistry. These technical artifacts can impact the reliable discovery of true biological signatures, particularly when examining mutational processes [1].
- Variant Interpretation Challenges: NGS identifies numerous genetic variants, but distinguishing pathogenic driver mutations from benign passenger mutations remains challenging. Variants of Unknown Significance (VUS) represent a particular interpretive hurdle with limited clinical actionability [8].
- Incomplete Functional Context: While NGS can identify mutations in DNA repair pathways (e.g., homologous recombination deficiency), it cannot directly quantify the functional consequences of these defects, requiring additional functional assays for validation [1].
Multi-Omics Integration: Overcoming NGS Limitations
Multi-Omics Technologies and Their Value Proposition
Integrating NGS with other omics technologies creates a synergistic framework that overcomes the limitations of single-layer analysis.
Table: Multi-Omics Technologies Complementing NGS in Oncology
| Omics Layer | Technology Platforms | Complementary Value to NGS | Clinical/Research Application |
|---|---|---|---|
| Transcriptomics | RNA-seq, Single-cell RNA-seq | Links DNA variants to gene expression | Gene fusions, expression subtypes, immune signatures |
| Proteomics | Mass spectrometry, Multiplexed immunoassays | Quantifies functional effectors | Drug target engagement, signaling networks |
| Metabolomics | LC-MS, NMR spectroscopy | Reveals biochemical endpoints | Metabolic vulnerabilities, therapy response |
| Epigenomics | ChIP-seq, ATAC-seq, Methylation arrays | Identifies regulatory mechanisms | Biomarker discovery, therapy resistance |
| Single-cell Multi-omics | CITE-seq, SPRI-te | Resolves cellular heterogeneity | Tumor microenvironments, rare cell detection |
Single-Cell Multi-Omics: A Paradigm Shift
Single-cell multi-omics technologies represent a transformative approach that simultaneously profiles multiple molecular layers (genome, transcriptome, proteome, epigenome) within individual cells [7] [5]. This enables:
- Direct Observation of Genotype-Phenotype Relationships: Simultaneous measurement of DNA mutations, RNA expression, and protein abundance in the same cell moves beyond statistical correlation to establish causal relationships [5].
- High-Resolution Cellular Cartography: Identification of rare cell populations (e.g., cancer stem cells, drug-resistant subclones) that drive disease progression but are undetectable by bulk NGS [7].
- Characterization of Tumor Microenvironment: Unbiased dissection of cellular ecosystems within tumors, including immune cell composition and stromal interactions [7].
Single-cell multi-omics reveals tumor heterogeneity
Experimental Protocols for Multi-Omics Integration
Protocol 1: Integrated Genomic-Transcriptomic Analysis for Cancer Subtyping
This protocol outlines a standardized workflow for integrating DNA and RNA sequencing data to identify molecular subtypes with distinct clinical outcomes and therapeutic vulnerabilities.
Materials and Reagents:
- Fresh-frozen or FFPE tumor tissue with matched normal sample
- DNA extraction kit (e.g., QIAamp DNA Mini Kit)
- RNA extraction kit (e.g., RNeasy Mini Kit) with DNase treatment
- Illumina TruSight Oncology 500 or similar targeted sequencing panel
- Illumina TruSeq RNA Exome or similar RNA sequencing library prep kit
- Illumina sequencing platform (NovaSeq 6000, MiSeq, or NextSeq)
Procedure:
- Nucleic Acid Extraction: Co-extract high-quality DNA and RNA from the same tumor sample, ensuring minimal degradation (RNA Integrity Number >7.0).
- DNA Library Preparation: Prepare sequencing libraries using 50-100ng of DNA according to targeted panel specifications. Include unique molecular identifiers to minimize sequencing artifacts.
- RNA Library Preparation: Prepare RNA sequencing libraries using 100ng-1μg of total RNA. Perform ribosomal RNA depletion rather than poly-A selection to capture non-coding transcripts.
- Sequencing: Sequence DNA libraries to a minimum depth of 500x and RNA libraries to a minimum of 50 million reads per sample.
- Bioinformatic Analysis:
- Process DNA sequencing data through established variant calling pipelines (e.g., GATK Best Practices)
- Analyze RNA sequencing data using alignment-based (STAR) or alignment-free (Salmon) approaches
- Integrate datasets to identify:
- Somatic mutations with corresponding expression changes
- Gene fusions validated at both DNA and RNA levels
- Mutational signatures correlated with transcriptional programs
Quality Control Metrics:
- DNA sequencing: >80% of targets covered at 100x
- RNA sequencing: >70% of reads uniquely mapped
- Cross-validation: >90% concordance for fusion variants detected by both assays
Protocol 2: Single-Cell Multi-Omics for Tumor Heterogeneity Mapping
This protocol describes a comprehensive approach for simultaneous profiling of DNA mutations, RNA expression, and protein markers in individual cells from tumor specimens.
Materials and Reagents:
- Fresh tumor tissue dissociated into single-cell suspension
- Viability stain (e.g., DAPI or propidium iodide)
- Single-cell multi-omics platform (10x Genomics Multiome, Mission Bio Tapestri, or similar)
- Feature barcoding antibodies (TotalSeq or similar)
- Cell hashing antibodies for sample multiplexing
- Appropriate single-cell library preparation reagents
Procedure:
- Sample Preparation: Dissociate tumor tissue to single cells, ensuring >90% viability. Count cells and adjust concentration to platform-specific requirements.
- Cell Staining: Incubate cells with feature barcoding antibodies for surface protein detection and cell hashing antibodies for sample multiplexing.
- Single-Cell Partitioning: Load cells onto appropriate microfluidic device according to manufacturer specifications.
- Library Preparation: Perform simultaneous DNA barcoding, RNA reverse transcription, and protein barcode tagging in partitioned droplets or wells.
- Sequencing: Sequence libraries on appropriate Illumina platform with read parameters adjusted for each data type.
- Bioinformatic Analysis:
- Process data using integrated pipelines (Cell Ranger, Seurat, Signac)
- Perform quality control to remove doublets and low-quality cells
- Integrate modalities to:
- Associate copy number variations with gene expression programs
- Link surface protein expression with transcriptional states
- Identify subclones with distinct genotype-phenotype relationships
Quality Control Metrics:
- Cell recovery: >5,000 high-quality cells per sample
- Doublet rate: <5% of captured cells
- Gene detection: >1,000 genes per cell (RNA)
- SNP concordance: >95% with bulk sequencing
The Scientist's Toolkit: Essential Research Reagents and Solutions
Table: Key Research Reagents for Multi-Omics Experiments
| Reagent/Solution | Function | Application Notes |
|---|---|---|
| DNase/RNase-free magnetic beads | Nucleic acid purification and size selection | Enable simultaneous DNA/RNA extraction; critical for preserving labile RNA species |
| Unique Molecular Identifiers (UMIs) | Tagging individual molecules to reduce PCR duplicates | Essential for accurate quantification in both DNA and RNA sequencing |
| Multiplexed barcoding antibodies | Tagging cells for protein detection alongside transcriptomics | Enable CITE-seq approaches; require titration for optimal signal-to-noise |
| Cell hashing antibodies | Sample multiplexing in single-cell experiments | Allow pooling of multiple samples; reduce batch effects and costs |
| Template switching oligos | Full-length cDNA synthesis in single-cell RNA-seq | Critical for capturing 5' end information and improving transcript coverage |
| Chromatin crosslinking reagents | Preserving protein-DNA interactions for epigenomics | Enable ChIP-seq and related assays; require optimization of crosslinking time |
| Viability dyes | Distinguishing live/dead cells in single-cell assays | Critical for ensuring high-quality data; must be compatible with downstream library prep |
| Nucleic acid stability reagents | Preserving samples during storage and transport | Essential for clinical samples with delayed processing; maintain RNA integrity |
The limitations of single-omics NGS approaches necessitate a fundamental shift toward integrated multi-omics frameworks in oncology research. While NGS provides an essential foundation for understanding cancer genetics, it cannot fully capture the complex, dynamic molecular interactions that drive tumor behavior, therapeutic response, and resistance mechanisms. The experimental protocols and methodologies outlined in this application note provide a roadmap for researchers to transcend these limitations through systematic integration of genomic, transcriptomic, proteomic, and epigenomic data layers.
Emerging technologies—particularly single-cell multi-omics and artificial intelligence-driven integration platforms—are poised to further accelerate this paradigm shift [4] [7]. As these approaches mature and become more accessible, they will increasingly enable researchers to move from correlative observations to causal understandings of cancer biology, ultimately supporting the development of more effective, personalized cancer therapies.
The advent of large-scale molecular profiling methods has fundamentally transformed cancer research, shifting the paradigm from single-omics investigations to integrative multi-omics analyses [3]. Biological systems operate through complex, interconnected layers—including the genome, transcriptome, proteome, and metabolome—through which genetic information flows to shape observable traits [3]. While single-omics approaches have provided valuable insights, they inherently fail to capture the complex interactions between different molecular layers that drive cancer pathogenesis [9] [10]. Integrative multi-omics frameworks now provide a holistic view of the molecular landscape of cancer, offering deeper insights into tumor biology, disease mechanisms, and therapeutic opportunities [3] [11].
The integration of next-generation sequencing (NGS) with other omics technologies has become particularly transformative in oncology [12]. NGS enables comprehensive genomic and transcriptomic profiling, identifying driver mutations, structural variations, and gene expression patterns across cancer types [12]. When combined with proteomic and metabolomic data, these technologies facilitate the construction of detailed models that connect genetic alterations to functional consequences, thereby refining cancer classification, prognostic stratification, and therapeutic decision-making [11] [9]. This Application Note provides a structured framework for designing, executing, and interpreting multi-omics studies in oncology research, with specific protocols and analytical workflows for integrating NGS with complementary omics platforms.
Omics Technologies: Core Components and Applications
Each omics layer provides distinct yet complementary insights into tumor biology. The table below summarizes the core components, technological platforms, and applications of the four major omics fields in cancer research.
Table 1: Core Omics Technologies in Cancer Research
| Omics Layer | Analytical Focus | Key Technologies | Primary Applications in Oncology | Strengths | Limitations |
|---|---|---|---|---|---|
| Genomics | DNA sequences and variations | Whole Genome Sequencing (WGS), Whole Exome Sequencing (WES) [11] | Identification of driver mutations, copy number variations (CNVs), structural variants [3] | Comprehensive view of genetic variation; foundation for personalized medicine [3] | Does not account for gene expression or environmental influences [3] |
| Transcriptomics | RNA expression and regulation | RNA sequencing, single-cell RNA-seq, microarrays [11] | Gene expression profiling, pathway activity analysis, biomarker discovery [3] [11] | Captures dynamic gene expression changes; reveals regulatory mechanisms [3] | RNA instability; snapshot view not reflecting long-term changes [3] |
| Proteomics | Protein abundance, modifications, interactions | Mass spectrometry, liquid chromatography-MS (LC-MS), reverse-phase protein arrays [11] [13] | Biomarker discovery, drug target identification, signaling pathway analysis [3] [13] | Directly measures functional effectors; identifies post-translational modifications [3] | Complex structures and dynamic ranges; difficult quantification [3] |
| Metabolomics | Small molecule metabolites and metabolic pathways | LC-MS, gas chromatography-MS, mass spectrometry imaging [11] | Disease diagnosis, metabolic pathway analysis, treatment response monitoring [3] | Direct link to phenotype; captures real-time physiological status [3] | Highly dynamic; limited reference databases; technical variability [3] |
Quantitative Proteomics Technologies
Within integrated workflows, proteomics requires specific methodological considerations for quantitative accuracy. The table below compares major quantitative proteomics approaches.
Table 2: Quantitative Proteomics Methodologies
| Method | Principle | Throughput | Quantitative Accuracy | Best Use Cases |
|---|---|---|---|---|
| SILAC (Stable Isotope Labeling with Amino acids in Cell culture) [13] | Metabolic labeling with stable isotopes during cell culture | Medium | High (minimizes experimental variability) | Cell line studies; protein turnover experiments |
| TMT (Tandem Mass Tagging) [13] | Isobaric chemical labeling of peptides | High | High in MS2 mode | Multi-sample comparisons; phosphoproteomics |
| Label-Free Quantification [13] | Comparison of peptide signal intensities or spectral counts | High | Medium (requires rigorous normalization) | Large cohort studies; clinical samples |
| MRM (Multiple Reaction Monitoring) [13] | Targeted detection of specific peptides | Low | High | Validation of candidate biomarkers |
Integrated Experimental Design and Workflows
Multi-Omics Integration Strategies
The strategic integration of omics data can be implemented through different computational approaches, each with distinct advantages and considerations:
- Horizontal Integration (P-integration): Combines multiple studies of the same molecular level to increase sample size and statistical power [14]. This approach is particularly valuable for meta-analyses across different patient cohorts or research centers.
- Vertical Integration (N-integration): Incorporates different omics layers from the same biological samples to build comprehensive models of biological flow from genotype to phenotype [14] [9]. This approach is ideal for connecting genomic alterations to their functional consequences through transcriptomic, proteomic, and metabolomic profiling.
- Temporal Integration: Analyzes omics data collected across multiple timepoints to capture dynamic changes during disease progression or therapeutic intervention [9].
The following diagram illustrates the strategic workflow for vertical integration of multi-omics data in oncology research:
Protocol: Integrated Multi-Omics Analysis for Tumor Biomarker Discovery
Objective: Identify molecular subtypes and biomarkers in non-small cell lung cancer (NSCLC) through integrated genomic, transcriptomic, and proteomic profiling.
Sample Requirements:
- Fresh frozen tumor tissue (≥100mg) and matched normal adjacent tissue
- Blood samples (for germline DNA control)
- Minimum sample size: 30 patients per cohort for statistical power
Experimental Workflow:
Step 1: Nucleic Acid Extraction
- Extract DNA using magnetic bead-based kits (e.g., QIAamp DNA Mini Kit)
- Extract total RNA with column-based purification (e.g., RNeasy Mini Kit)
- Quality control: DNA integrity number (DIN) ≥7.0, RNA integrity number (RIN) ≥8.0
Step 2: Next-Generation Sequencing
- Whole Exome Sequencing: Fragment DNA (150-200bp), hybrid capture using Illumina Nextera Flex, sequence on Illumina NovaSeq (150bp paired-end, 100x coverage)
- RNA Sequencing: Poly-A selection, library preparation with strand specificity, sequence on Illumina platform (50M reads/sample)
Step 3: Proteomic Profiling
- Protein extraction using urea/thiourea buffer
- Trypsin digestion with filter-aided sample preparation (FASP)
- TMT 16-plex labeling for quantitative comparison
- LC-MS/MS analysis on Orbitrap Eclipse mass spectrometer
Step 4: Data Processing and Quality Control
- Genomics: BWA-MEM alignment, GATK variant calling, MutSigCV for mutation significance
- Transcriptomics: STAR alignment, DESeq2 for differential expression
- Proteomics: MaxQuant search, normalization using median centering
Analytical Frameworks and Computational Tools
Data Integration Methodologies
The successful integration of multi-omics data requires sophisticated computational approaches that can handle high-dimensional, heterogeneous datasets:
- Statistical and Correlation-Based Methods: Pearson's or Spearman's correlation analysis to assess relationships between omics datasets; Weighted Gene Correlation Network Analysis (WGCNA) to identify clusters of co-expressed genes [15].
- Multivariate Methods: Partial Least Squares (PLS) regression; Multi-Omics Factor Analysis (MOFA) to infer latent factors that capture shared and specific sources of variability across omics layers [15] [10].
- Machine Learning and AI: Regularized methods (LASSO, elastic net) for feature selection; graph neural networks for patient stratification; deep learning models for subtype classification [11] [14] [10].
The following diagram illustrates the analytical framework for multi-omics data integration:
Protocol: Computational Analysis of Integrated Omics Data
Objective: Implement a comprehensive analytical pipeline for multi-omics data integration and biomarker identification.
Software Requirements:
- R Statistical Environment (v4.2+) with packages: moIntegrate, mixOmics, WGCNA, iCluster
- Python (v3.9+) with scikit-learn, PyTorch, and Scanpy
- Bioinformatics tools: BWA, GATK, STAR, MaxQuant
Analytical Procedure:
Step 1: Data Preprocessing and Quality Control
- Perform platform-specific normalization: RPKM for transcriptomics, median centering for proteomics
- Apply batch correction using ComBat or remove unwanted variation (RUV) methods
- Filter low-quality features: Remove genes with <10 reads in >90% samples; remove proteins with >20% missing values
Step 2: Horizontal Integration within Omics Layers
- Use Similarity Network Fusion (SNF) to combine multiple genomic features (mutations, CNVs)
- Apply multi-block PLS to integrate different proteomic datasets (global proteome, phosphoproteome)
Step 3: Vertical Integration across Omics Layers
- Implement MOFA+ to decompose multi-omics variation into latent factors
- Build association networks using xMWAS with correlation threshold |r| > 0.8 and FDR < 0.05
- Perform multi-omics clustering using iCluster with k=3-5 molecular subtypes
Step 4: Biomarker Identification and Validation
- Apply LASSO-Cox regression for survival-associated feature selection
- Validate biomarkers in independent datasets (e.g., TCGA, CPTAC)
- Perform functional enrichment analysis using GSEA and pathway databases (KEGG, Reactome)
The Scientist's Toolkit: Essential Research Reagents and Platforms
Successful multi-omics studies require carefully selected reagents, platforms, and computational resources. The following table details essential components for establishing a robust multi-omics workflow.
Table 3: Essential Research Reagents and Platforms for Multi-Omics Studies
| Category | Product/Platform | Specific Application | Key Features |
|---|---|---|---|
| Nucleic Acid Extraction | QIAamp DNA Mini Kit (Qiagen) | High-quality DNA for WGS/WES | Magnetic bead-based purification; DIN ≥7.0 |
| RNA Isolation | RNeasy Mini Kit (Qiagen) | Intact RNA for transcriptomics | Column-based purification; RIN ≥8.0 |
| NGS Library Prep | Illumina DNA Prep | Whole genome/exome sequencing | Hybrid capture-based; compatible with FFPE |
| NGS Platform | Illumina NovaSeq 6000 | High-throughput sequencing | 150bp paired-end; 100x coverage for WES |
| Proteomics Sample Prep | TMTpro 16-plex (Thermo) | Multiplexed quantitative proteomics | 16-sample multiplexing; reduces batch effects |
| Mass Spectrometry | Orbitrap Eclipse (Thermo) | High-resolution proteomics | Tribrid architecture; TMT quantification |
| Chromatography | Vanquish UHPLC (Thermo) | Peptide separation pre-MS | Nanoflow capabilities; minimal carryover |
| Data Analysis | IntegrAO | Multi-omics data integration | Graph neural networks; handles missing data |
| Visualization | Cytoscape | Biological network visualization | Plugin architecture; multi-omics extensions |
Concluding Remarks
Integrative multi-omics approaches have fundamentally transformed oncology research by providing unprecedented insights into the molecular intricacies of cancer [3]. The strategic combination of NGS with proteomic and metabolomic technologies enables the construction of comprehensive models that connect genetic alterations to functional consequences and phenotypic manifestations [11] [9]. While significant challenges remain in data integration, standardization, and interpretation, continued development of computational frameworks and analytical pipelines is rapidly advancing the field [14] [15].
The protocols and frameworks outlined in this Application Note provide a structured approach for implementing multi-omics studies in cancer research. As these technologies continue to evolve—particularly with the emergence of single-cell and spatial omics platforms—they hold unprecedented potential to unravel the complex molecular architecture of tumors, identify novel therapeutic targets, and ultimately advance personalized cancer treatment [11] [16] [9]. By adopting standardized workflows and robust analytical practices, researchers can maximize the biological insights gained from these powerful technologies and accelerate progress in precision oncology.
In modern oncology research, the journey from a static genetic blueprint to a dynamic functional phenotype is governed by the complex interplay of multiple molecular layers. The central dogma of biology, which posits a linear flow of information from DNA to RNA to protein, is insufficient to capture the intricate regulatory networks that underlie cancer biology [17]. Instead, a multi-omics approach that integrates genomics, transcriptomics, proteomics, epigenomics, and metabolomics provides a holistic framework for understanding how these layers interconnect to drive oncogenesis, tumor progression, and treatment response [3] [18].
The transition in perspective from a "genetic blueprint" to a dynamic genotype-phenotype mapping concept represents a fundamental shift in biological understanding. Traditional metaphors of genetic programs have been replaced with algorithmic approaches that recognize the complex, non-linear relationships between genetic information and phenotypic expression [17]. In oncology, this paradigm shift is particularly crucial, as tumors represent complex ecosystems where genomic alterations manifest through dysregulated molecular networks across multiple biological layers [3] [19].
Next-generation sequencing (NGS) technologies serve as the foundational engine for dissecting these complex relationships, generating massive datasets that capture molecular information at unprecedented resolution and scale [20]. However, the true power of NGS emerges only when these data are integrated with other omics layers to map the complete pathway from genetic variant to functional consequence in cancer biology [18] [19].
The Multi-Omics Landscape in Oncology
Defining the Omics Layers
Biological systems operate through complex, interconnected layers including the genome, transcriptome, proteome, metabolome, microbiome, and lipidome. Genetic information flows through these layers to shape observable traits, and elucidating the genetic basis of complex phenotypes demands an analytical framework that captures these dynamic, multi-layered interactions [3]. Each omics layer provides distinct yet complementary insights into tumor biology, collectively enabling researchers to reconstruct the complete molecular circuitry of cancer.
Table 1: The Multi-Omics Components and Their Applications in Oncology
| Omics Component | Description | Key Applications in Oncology | Technical Considerations |
|---|---|---|---|
| Genomics | Study of the complete set of DNA, including all genes, focusing on sequencing, structure, function, and evolution [3]. | Identification of driver mutations, copy number variations, and single-nucleotide polymorphisms; cancer risk assessment; pharmacogenomics [3]. | Does not account for gene expression or environmental influence; large data volume and complexity; ethical concerns regarding genetic data [3]. |
| Transcriptomics | Analysis of RNA transcripts produced by the genome under specific circumstances or in specific cells [3]. | Gene expression profiling; biomarker discovery; understanding drug response mechanisms; tumor subtyping [3] [19]. | RNA is less stable than DNA; provides snapshot view, not long-term; requires complex bioinformatics tools [3]. |
| Proteomics | Study of the structure and function of proteins, the main functional products of gene expression [3]. | Direct measurement of protein levels and modifications; drug target identification; linking genotype to phenotype [3] [19]. | Proteins have complex structures and dynamic ranges; proteome is much larger than genome; difficult quantification and standardization [3]. |
| Epigenomics | Study of heritable changes in gene expression not involving changes to the underlying DNA sequence [3]. | Understanding gene regulation beyond DNA sequence; identifying epigenetic therapy targets; connecting environment and gene expression [3]. | Epigenetic changes are tissue-specific and dynamic; complex data interpretation; influenced by external factors [3]. |
| Metabolomics | Comprehensive analysis of metabolites within a biological sample, reflecting the biochemical activity and state [3]. | Provides insight into metabolic pathways and their regulation; direct link to phenotype; captures real-time physiological status [3]. | Metabolome is highly dynamic and influenced by many factors; limited reference databases; technical variability issues [3]. |
From Genetic Variation to Phenotypic Manifestation
In cancer systems, genetic variations serve as the initial blueprint but do not determine phenotypic outcomes in isolation. These variations operate through hierarchical biological layers that ultimately manifest as clinical phenotypes:
Genetic Variations in Cancer:
- Driver mutations provide growth advantage and are directly involved in oncogenesis, typically occurring in genes regulating cell growth, apoptosis, and DNA repair [3]. For example, TP53 mutations occur in approximately 50% of all human cancers [3].
- Copy number variations (CNVs) involve duplications or deletions of DNA regions, altering gene dosage. HER2 amplification in approximately 20% of breast cancers leads to protein overexpression associated with aggressive tumor behavior [3].
- Single-nucleotide polymorphisms (SNPs) can affect cancer susceptibility and drug response. SNPs in BRCA1 and BRCA2 significantly increase breast and ovarian cancer risk, while SNPs in drug metabolism enzymes influence chemotherapy efficacy and toxicity [3].
The transition from these genetic variants to phenotypic expression involves complex, non-linear interactions across omics layers. Alberch's concept of genotype-phenotype (G→P) mapping provides a framework for understanding these relationships, emphasizing that the same phenotype may arise from different genetic combinations, and that phenotypic stability depends on a population's position in the developmental parameter space [17].
Methodological Framework for Multi-Omics Integration
Experimental Design and Data Generation
Robust multi-omics studies in oncology require careful experimental design to ensure data quality and integration potential. The following protocols outline standardized approaches for generating and integrating multi-omics data from cancer specimens:
Protocol 3.1.1: Sample Preparation for Multi-Omics Analysis
- Tissue Collection and Processing: Obtain tumor tissue specimens via biopsy or surgical resection. For solid tumors, use formalin-fixed paraffin-embedded (FFPE) tissues or fresh frozen specimens based on analytical requirements [21].
- Nucleic Acid Extraction: Isolate genomic DNA using validated kits (e.g., QIAamp DNA FFPE Tissue kit). Ensure DNA concentration of at least 20 ng with A260/A280 ratio between 1.7-2.2 for library generation [21].
- Quality Control: Assess DNA purity using NanoDrop Spectrophotometer and library size/quantity using Agilent 2100 Bioanalyzer system. Acceptable library characteristics: 250-400 bp size, concentration ≥ 2nμ [21].
Protocol 3.1.2: Next-Generation Sequencing Workflow
- Library Preparation: Use hybrid capture method for DNA library preparation and target enrichment according to Illumina's standard protocol with Agilent SureSelectXT Target Enrichment Kit [21].
- Sequencing: Perform sequencing on platforms such as Illumina NextSeq 550Dx or NovaSeq X. For targeted panels (e.g., 544-gene cancer panels), ensure minimum coverage of 100x with average depth >500x [20] [21].
- Automation Integration: Implement automated NGS workflows using systems like Biomek i3 Benchtop Liquid Handler to enhance reproducibility and throughput for targeted sequencing assays including Archer FUSIONPlex and VARIANTPlex panels [22].
Protocol 3.1.3: Multi-Omics Data Generation
- Transcriptomics: Conduct RNA sequencing (RNA-Seq) using Illumina platforms. For single-cell analyses, employ 10× Genomics Chromium system [19] [20].
- Proteomics: Perform mass spectrometry-based profiling using time-of-flight (TOF) or Orbitrap instruments. Prepare samples using tryptic digestion and label-free or TMT labeling approaches [19].
- Metabolomics: Utilize nuclear magnetic resonance (NMR) spectroscopy or mass spectrometry with liquid or gas chromatography for metabolite profiling [19].
Computational Integration Strategies
The complexity and volume of multi-omics data necessitate sophisticated computational approaches for integration and interpretation. The following protocols detail established methodologies for multi-omics data integration:
Protocol 3.2.1: Data Preprocessing and Normalization
- Genomic Data Processing: Align sequencing reads to reference genome (hg19/GRCh38) using BWA or STAR aligners. Perform variant calling with Mutect2 for SNVs/indels and CNVkit for copy number variations [21].
- RNA-Seq Analysis: Process transcriptomic data using Ensembl or Galaxy pipelines. Normalize expression data using TPM or FPKM methods [19].
- Proteomics Data Processing: Analyze mass spectrometry data with MaxQuant. Normalize protein abundances using variance-stabilizing normalization [19].
- Batch Effect Correction: Implement ComBat or removeUnwantedVariation (RUV) methods to address technical variability across batches [19].
Protocol 3.2.2: Multi-Omics Integration Algorithms
- Similarity-Based Integration: Identify common patterns across omics datasets using:
- Correlation analysis to evaluate relationships between different omics levels
- Clustering algorithms (hierarchical clustering, k-means) to group similar data points
- Similarity Network Fusion (SNF) to construct integrated similarity networks [19]
- Difference-Based Integration: Detect unique features across omics layers using:
- Differential expression analysis (DESeq2, limma) to identify significant changes between conditions
- Variance decomposition to partition variance components attributable to different omics types
- Feature selection methods (LASSO, Random Forests) to select most relevant features [19]
- Multi-Omics Factor Analysis (MOFA): Apply this unsupervised Bayesian factor analysis to identify latent factors responsible for variation across multiple omics datasets [19].
- Canonical Correlation Analysis (CCA): Implement sparse CCA to identify linear relationships between two or more omics datasets [19].
Protocol 3.2.3: Network Biology and Pathway Analysis
- Network Construction: Build molecular interaction networks using OmicsNet or NetworkAnalyst, integrating genomics, transcriptomics, proteomics, and metabolomics data [19].
- Pathway Enrichment: Perform functional enrichment analysis using KEGG, Reactome, or GO databases to identify significantly altered pathways [3].
- Regulatory Network Inference: Reconstruct gene regulatory networks by integrating transcription factor binding data (from ChIP-Seq) with transcriptomic profiles [19].
The Scientist's Toolkit: Essential Research Reagents and Platforms
Successful multi-omics studies require carefully selected reagents, platforms, and computational tools. The following table catalogs essential solutions for oncology-focused multi-omics research:
Table 2: Essential Research Reagent Solutions for Multi-Omics Oncology Studies
| Category | Product/Platform | Specific Application | Key Features |
|---|---|---|---|
| NGS Assays | Archer FUSIONPlex | Targeted RNA sequencing for gene fusion detection | Identifies known and novel fusion transcripts; optimized for FFPE samples [22] |
| VARIANTPlex | Targeted DNA sequencing for variant detection | Comprehensive coverage of cancer-related genes; enables somatic and germline variant calling [22] | |
| xGen Hybrid Capture | Whole exome and custom target enrichment | High uniformity and coverage; compatible with low-input samples [22] | |
| Automation Platforms | Biomek i3 Benchtop Liquid Handler | Automated NGS library preparation | Compact footprint; on-deck thermocycling; rapid protocol development [22] |
| Sequencing Platforms | Illumina NovaSeq X | High-throughput sequencing | Unmatched speed and data output for large-scale projects [20] |
| Oxford Nanopore Technologies | Long-read sequencing | Extended read length; real-time, portable sequencing [20] | |
| Computational Tools | Ensembl | Genomic annotation and analysis | Comprehensive genomic data; genome assembly and variant calling [19] |
| Galaxy | Bioinformatics workflows | User-friendly platform for multi-omics analysis [19] | |
| OmicsNet | Multi-omics network visualization | Integration of genomics, transcriptomics, proteomics, and metabolomics data [19] | |
| NetworkAnalyst | Network-based visual analysis | Data filtering, normalization, statistical analysis, and network visualization [19] | |
| AI/Machine Learning | DeepVariant | Variant calling | Deep learning-based variant identification with high accuracy [20] |
| MOFA | Multi-omics factor analysis | Unsupervised integration of multiple omics datasets [19] |
Case Study: Clinical Implementation of Multi-Omics in Oncology
Real-World Clinical NGS Implementation
A recent study demonstrates the successful implementation of NGS-based tumor profiling in routine clinical practice. The following protocol and results highlight the practical application of multi-omics approaches in oncology:
Protocol 5.1.1: Clinical NGS Testing Workflow
- Patient Selection and Sample Collection: Include patients with advanced solid tumors. Use stored FFPE tumor specimens with proper tumor cellularity [21].
- NGS Testing: Implement targeted sequencing panels (e.g., SNUBH Pan-Cancer v2.0 covering 544 genes). Sequence on Illumina NextSeq 550Dx platform [21].
- Variant Classification: Tier variants according to Association for Molecular Pathology guidelines:
- Tier I: Variants of strong clinical significance (FDA-approved or guideline-recommended therapies)
- Tier II: Variants of potential clinical significance (investigational therapies) [21]
- Therapeutic Matching: Identify genomically-matched therapies based on novel information from NGS testing, excluding alterations identifiable through conventional molecular tests [21].
Results and Clinical Outcomes:
- Detection Rate: Among 990 patients with advanced solid tumors, 26.0% harbored tier I variants with strong clinical significance, while 86.8% carried tier II variants with potential clinical significance [21].
- Therapeutic Impact: 13.7% of patients with tier I variants received NGS-based therapy, with particularly high implementation in thyroid cancer (28.6%), skin cancer (25.0%), gynecologic cancer (10.8%), and lung cancer (10.7%) [21].
- Treatment Response: Among 32 patients with measurable lesions who received NGS-based therapy, 37.5% achieved partial response and 34.4% achieved stable disease, demonstrating the clinical utility of molecular profiling-guided therapy [21].
Integrative Multi-Omics Analysis in Cancer Research
Protocol 5.2.1: Comprehensive Multi-Omics Tumor Profiling
- Sample Collection and Processing: Collect matched tumor and normal tissues from cancer patients. Process for parallel genomic, transcriptomic, proteomic, and epigenomic analyses [3] [19].
- Data Generation:
- Data Integration: Apply multi-omics factor analysis (MOFA) to identify latent factors that drive variation across omics layers [19].
- Network Biology Analysis: Construct integrated molecular networks using tools like OmicsNet to identify key regulatory hubs and dysregulated pathways [19].
Key Insights from Integrative Analyses:
- Regulatory Cascades: Multi-omics approaches reveal how genomic alterations (e.g., TP53 mutations) propagate through transcriptomic and proteomic layers to activate specific oncogenic pathways [3].
- Therapeutic Resistance Mechanisms: Integrated analyses identify compensatory mechanisms across omics layers that mediate resistance to targeted therapies, enabling development of combination strategies [3] [19].
- Tumor Heterogeneity: Single-cell multi-omics technologies resolve intra-tumor heterogeneity by simultaneously profiling genomic, transcriptomic, and epigenomic features of individual cells [20] [23].
Future Perspectives and Concluding Remarks
The integration of NGS with multi-omics data represents the forefront of oncology research, transforming our understanding of cancer biology and accelerating precision medicine. The field is rapidly evolving with several emerging trends:
Emerging Technologies and Approaches:
- Single-Cell Multi-Omics: Technologies enabling simultaneous measurement of genomic, transcriptomic, epigenomic, and proteomic features at single-cell resolution are revealing unprecedented insights into tumor heterogeneity and cellular ecosystems [20] [23].
- Spatial Omics: Methods that preserve spatial context in tissue specimens are mapping molecular features within tumor architecture, connecting cellular positioning to functional phenotypes [20].
- Artificial Intelligence Integration: Advanced machine learning and deep learning approaches are enhancing our ability to extract biologically meaningful patterns from complex multi-omics datasets, enabling predictive modeling of therapeutic response and resistance [20] [24].
- Longitudinal Monitoring: Multi-omics profiling of liquid biopsies enables dynamic monitoring of tumor evolution and treatment response through non-invasive approaches [18].
The journey from genetic blueprint to functional phenotype in oncology requires navigating the complex interplay between multiple molecular layers. Through integrated multi-omics approaches, researchers can now reconstruct the complete molecular circuitry of cancer, revealing how genomic alterations manifest as functional phenotypes through dysregulated networks across transcriptomic, proteomic, and metabolomic layers. As these technologies continue to mature and computational integration strategies become more sophisticated, multi-omics approaches will increasingly guide clinical decision-making and therapeutic development, ultimately improving outcomes for cancer patients.
The molecular complexity of cancer is driven by a spectrum of genomic alterations that disrupt critical cellular signaling pathways. Single nucleotide variants (SNVs), copy number variations (CNVs), and gene fusions represent three fundamental classes of such drivers, each contributing uniquely to oncogenesis, therapeutic response, and resistance mechanisms. The integration of next-generation sequencing (NGS) with other omics data—including transcriptomics, proteomics, and epigenomics—has revolutionized our ability to detect these alterations and understand their functional consequences within the broader context of cellular systems [4]. This multi-omics approach moves beyond single-layer analysis to capture the interconnected biological networks that drive cancer progression, enabling more precise diagnostic stratification and targeted therapeutic intervention [11].
In contemporary precision oncology, identifying these genomic drivers is not merely descriptive but foundational for treatment decisions. For instance, specific SNVs can dictate sensitivity to targeted inhibitors, CNVs can amplify oncogenes or delete tumor suppressors, and gene fusions can create constitutively active kinases that become primary therapeutic targets [4] [25]. The functional characterization of these variants, therefore, becomes a critical step in translating genomic findings into clinical action. This document provides detailed application notes and experimental protocols for the study of SNVs, CNVs, and fusions, framed within the integrative framework of modern multi-omics oncology research.
Single Nucleotide Variants (SNVs)
Functional Impact and Predictive Algorithms
Single nucleotide variants (SNVs), particularly missense mutations that result in amino acid substitutions, can significantly alter protein function and drive oncogenesis. Prioritizing which SNVs have genuine functional impact is a central challenge in cancer genomics. Computational prediction methods have been developed to address this, leveraging features such as sequence conservation, allele frequency, and structural parameters [26].
The Disease-related Variant Annotation (DVA) method represents a recent advancement in this field. It employs a comprehensive feature set, including sequence conservation, allele frequency in different populations, and protein-protein interaction (PPI) network features transformed via graph embedding [26]. This feature set is used to train a random forest model, which has demonstrated superior performance compared to existing tools. As shown in Table 1, DVA achieved an Area Under the Receiver Operating Characteristic Curve (AUROC) of 0.979 on a dataset of somatic cancer missense variants, substantially outperforming 14 other state-of-the-art methods, including ClinPred (AUROC: 0.84) and REVEL (AUROC: 0.915) [26].
Table 1: Performance Comparison of SNV Functional Impact Prediction Tools on Somatic Cancer Variants
| Prediction Method | AUROC | Accuracy | Precision | Recall | F1-Score |
|---|---|---|---|---|---|
| DVA | 0.979 | 0.941 | 0.957 | 0.924 | 0.940 |
| ClinPred | 0.840 | 0.772 | 0.799 | 0.724 | 0.759 |
| REVEL | 0.915 | 0.843 | 0.869 | 0.808 | 0.837 |
| CADD | 0.851 | 0.782 | 0.811 | 0.736 | 0.772 |
| FATHMM-MKL | 0.777 | 0.709 | 0.743 | 0.641 | 0.688 |
| SIFT | 0.821 | 0.753 | 0.788 | 0.692 | 0.737 |
Application Note: Deep Mutational Scanning for CHEK2
For high-throughput functional assessment of SNVs, Deep Mutational Scanning (DMS) provides an empirical approach. A seminal study applied DMS to the checkpoint kinase gene CHEK2, a gene in which loss-of-function mutations are associated with increased risk of breast and other cancers [27]. Researchers tested nearly all of the 4,887 possible SNVs in the CHEK2 open reading frame for their ability to complement the function of the yeast ortholog, RAD53 [27].
The protocol involved:
- Generation of a Saturation Mutagenesis Library: Creating a comprehensive library of CHEK2 variants.
- Functional Complementation in Yeast: Introducing the variant library into RAD53-deficient yeast strains.
- Selection and Sequencing: Applying selective pressure and using high-throughput sequencing to quantify the relative abundance of each variant before and after selection.
- Functional Scoring: Calculating enrichment scores to classify variants as functionally "tolerated" or "damaging."
This study successfully classified 770 non-synonymous changes as damaging to protein function and 2,417 as tolerated, providing a critical resource for interpreting variants of uncertain significance (VUS) found in clinical screenings [27].
Figure 1: DMS Workflow for CHEK2 SNV Functional Characterization
Research Reagent Solutions for SNV Analysis
Table 2: Key Reagents for SNV Functional Studies
| Reagent / Resource | Function / Application | Example / Note |
|---|---|---|
| Saturation Mutagenesis Library | Provides comprehensive coverage of SNVs for a target gene. | CHEK2 ORF library of 4,887 SNVs [27]. |
| Yeast Complementation System | In vivo functional assay for genes with yeast orthologs. | RAD53-deficient S. cerevisiae for CHEK2 testing [27]. |
| Prediction Software (DVA) | Computationally predicts pathogenicity of missense variants. | Integrates conservation, allele frequency, and PPI features [26]. |
| dbNSFP Database | Aggregates scores from multiple prediction algorithms. | Facilitates comparison and meta-analysis of SNV impact [26]. |
Copy Number Variations (CNVs)
Biology and Analytical Frameworks
Copy number variations (CNVs) are a form of structural variation resulting in the gain or loss of genomic DNA, which can lead to the amplification of oncogenes or deletion of tumor suppressor genes [28]. In cancer research, CNV analysis is crucial for identifying driver alterations, understanding tumor evolution, and identifying therapeutic targets.
The analytical process of CNV calling involves comparing sequencing data from a sample to a reference genome to identify regions with statistically significant differences in read depth [28]. Key considerations for CNV analysis include:
- Sequencing Platform and Coverage: Whole-genome sequencing (WGS) typically provides more uniform coverage and superior sensitivity/specificity compared to whole-exome sequencing (WES) or targeted panels [28].
- Sample Purity and Ploidy: Tumor purity (the proportion of cancer cells in a sample) and genome ploidy (the number of chromosome sets) significantly impact the accuracy of CNV calls and must be accounted for in analytical models [28].
- Algorithm Selection: Multiple algorithms exist, each with strengths and weaknesses. A benchmarking study highlighted several common CNV callers, which are summarized in Table 3 [28].
Table 3: Common CNV Calling Algorithms for NGS Data in Cancer Research
| Algorithm | Primary Application | Key Features / Notes |
|---|---|---|
| ASCAT-NGS | WGS | Allele-specific copy number analysis of tumors; used in NCI's GDC platform [28]. |
| CNVkit | WES, WGS | Uses a hybrid capture-based approach to model biases and smooth data [28]. |
| FACETS | WGS, WES, Panels | Estimates fraction and allele-specific copy numbers, robust for tumor-normal pairs [28]. |
| DRAGEN | WGS, WES | Scalable, hardware-accelerated platform for rapid variant calling [28]. |
| HATCHet | Multi-sample WGS | Jointly analyzes multiple tumor samples to infer allele-specific copy numbers [28]. |
Application Note: CNVs in Pediatric Cancers with Birth Defects
CNVs play a significant role in the development of pediatric cancers, particularly in children with serious birth defects (BDs). A study performing whole-genome sequencing (WGS) on 1,556 individuals revealed that roughly half of the children with both a BD and cancer possessed CNVs that were not identified in BD-only or healthy individuals [29]. These CNVs were heterogenous but showed functional enrichment in specific biological pathways, such as deletions affecting genes with neurological functions and duplications of immune response genes [29]. This highlights the importance of CNV analysis in uncovering the underlying genetic mechanisms linking developmental disorders and cancer.
The recommended protocol for such an investigation includes:
- Sample Collection: Blood-derived DNA from well-phenotyped cohorts (e.g., BD with cancer, BD-only, healthy controls).
- Whole-Genome Sequencing: Conduct high-coverage WGS to ensure uniform coverage for sensitive CNV detection.
- CNV Calling and Filtering: Utilize a consensus approach with multiple callers (e.g., those in Table 3) to increase confidence. Focus on rare, high-impact variants.
- Functional Enrichment Analysis: Annotate genes within recurrent CNV regions and perform pathway analysis (e.g., GO, KEGG) to identify disrupted biological processes.
- Phenotype Clustering: Correlate specific CNV signatures with clinical phenotypes, such as the enrichment of non-coding RNA regulator variations in sarcoma patients [29].
Figure 2: CNV Analysis Workflow for Pediatric Cancer with Birth Defects
Gene Fusions
Biology, Detection, and Clinical Significance
Oncogenic gene fusions are hybrid genes formed through chromosomal rearrangements such as translocations, inversions, deletions, or tandem duplications [25] [30]. These events can produce chimeric proteins with novel or constitutively active functions, such as aberrant tyrosine kinases or transcription factors, which act as powerful oncogenic drivers [25].
Fusions are defining features of many cancers, such as BCR-ABL1 in chronic myeloid leukemia (CML) and EML4-ALK in non-small cell lung cancer (NSCLC) [25] [30]. Their detection is critical for diagnosis, prognosis, and treatment selection, as fusion-driven cancers often exhibit "oncogene addiction" and respond exceptionally well to targeted therapies [25]. Table 4 summarizes several key oncogenic fusions and their clinical relevance.
Table 4: Key Oncogenic Gene Fusions and Their Clinical Significance
| Gene Fusion | Disease | Functional Consequence | Therapeutic Implication |
|---|---|---|---|
| BCR-ABL1 | Chronic Myeloid Leukemia (CML) | Constitutively active tyrosine kinase. | Targetable with tyrosine kinase inhibitors (e.g., imatinib) [25] [30]. |
| EML4-ALK | Non-Small Cell Lung Cancer (NSCLC) | Constitutively active kinase activating PI3K/AKT, JAK/STAT, and RAS/MAPK pathways [30]. | Targetable with ALK inhibitors (e.g., crizotinib) [30]. |
| PML-RARA | Acute Promyelocytic Leukemia (APL) | Impairs differentiation and promotes proliferation of leukemic cells [30]. | Treatment with all-trans retinoic acid (ATRA) and arsenic trioxide [30]. |
| TMPRSS2-ERG | Prostate Cancer | Overexpression of ERG transcription factor, altering cell proliferation and microenvironment [30]. | Active investigation for targeted therapies; informs prognosis [30]. |
| NTRK Fusions | Multiple solid tumors (e.g., secretory carcinoma, infantile fibrosarcoma) | Constitutively active TRK kinase signaling [25]. | Targetable with tumor-agnostic TRK inhibitors (e.g., larotrectinib) [25]. |
Detection Methodologies and Protocol
A variety of technologies exist for fusion gene detection, ranging from traditional methods to modern NGS-based approaches [30]. RNA-based next-generation sequencing (RNA-seq) is particularly effective as it directly identifies expressed fusion transcripts and is capable of discovering novel fusion partners [25] [30].
A comprehensive fusion detection protocol should integrate multiple omics layers:
- DNA/RNA Co-extraction: Isolate high-quality DNA and RNA from tumor tissue (fresh-frozen or FFPE) or liquid biopsy (circulating tumor DNA/RNA).
- Targeted NGS Panel Sequencing: Use anchored multiplex PCR (AMP)-based or hybrid capture-based panels designed to target intronic and exonic regions of known fusion driver genes (e.g., ALK, ROS1, RET, NTRK1/2/3) from both DNA and RNA.
- Bioinformatic Analysis: Utilize specialized fusion-finding tools (e.g., STAR-Fusion, Arriba, FusionCatcher) that align sequencing reads and detect chimeric transcripts with high confidence.
- Multi-omics Integration:
- Correlate fusion calls with transcriptomics data (e.g., outlier expression of the 3' gene) and phosphoproteomics data to confirm downstream pathway activation (e.g., elevated MAPK or PI3K signaling) [4].
- In EML4-ALK fusion-positive NSCLC, the fusion protein drives oncogenesis by sustaining activated tyrosine kinase activity, which hyperactivates the JAK/STAT, PI3K/AKT, and RAS/MAPK signaling pathways to promote cell growth and survival [30].
Figure 3: Key Signaling Pathways Activated by Kinase Fusion Proteins
Research Reagent Solutions for Fusion Analysis
Table 5: Key Reagents and Kits for Fusion Gene Detection
| Reagent / Kit | Function / Application | Example / Note |
|---|---|---|
| FFPE DNA/RNA Extraction Kits | Nucleic acid isolation from archival clinical samples. | Critical for leveraging large biobanks; requires protocols for degraded samples. |
| Anchored Multiplex PCR (AMP) | Targeted RNA-seq library preparation for fusion detection. | Effective for detecting fusions with unknown partners (e.g., ArcherDX). |
| Hybrid Capture Panels | Targeted DNA/RNA-seq focusing on cancer genes. | Comprehensive panels (e.g., MSK-IMPACT) can detect fusions, SNVs, and CNVs [11]. |
| Liquid Biopsy Kits | Isolation of ctDNA/ctRNA from plasma. | Enables non-invasive detection and monitoring of fusion status [30]. |
The individual analysis of SNVs, CNVs, and fusions provides powerful, yet incomplete, insights into cancer biology. The future of precision oncology lies in the AI-driven integration of multi-omics data [4]. Artificial intelligence (AI), particularly machine learning (ML) and deep learning (DL), excels at identifying non-linear patterns across high-dimensional spaces, making it uniquely suited to integrate genomic data with transcriptomic, proteomic, and epigenomic layers [4] [11] [10]. For example, graph neural networks (GNNs) can model how a somatic mutation (SNV) perturbs protein-protein interaction networks, while multi-modal transformers can fuse MRI radiomics with transcriptomic data to predict tumor progression [4].
Framing the analysis of key drivers and variations within this multi-omics context transforms them from isolated biomarkers into interconnected nodes of a complex biological network. This holistic view is essential for uncovering robust biomarkers, understanding therapeutic resistance, and ultimately delivering on the promise of personalized, proactive cancer care [4] [11].
From Data to Decisions: AI-Driven Methodologies and Clinical Applications
Cancer's staggering molecular heterogeneity demands a move beyond traditional single-omics approaches to a more comprehensive, integrative perspective [4]. The simultaneous analysis of multiple molecular layers—genomics, transcriptomics, proteomics, epigenomics, and metabolomics—through multi-omics integration provides a powerful framework for understanding the complex biological underpinnings of cancer [31]. However, this integration faces formidable computational challenges due to the high dimensionality, technical variability, and fundamental structural differences between datasets [4] [14]. Artificial intelligence (AI), particularly deep learning and graph neural networks (GNNs), has emerged as the essential computational scaffold that enables non-linear, scalable integration of these disparate data layers into clinically actionable insights for precision oncology [4] [32]. These technologies are transforming oncology from reactive, population-based approaches to proactive, individualized cancer management [4].
AI and Multi-Omics Data: Core Concepts and Definitions
The Multi-Omics Data Landscape
Multi-omics data in oncology spans multiple functional levels of biological organization, each providing distinct but interconnected insights into tumor biology [4]. Genomics identifies DNA-level alterations including single-nucleotide variants (SNVs), copy number variations (CNVs), and structural rearrangements that drive oncogenesis [4]. Transcriptomics reveals gene expression dynamics through RNA sequencing (RNA-seq), quantifying mRNA isoforms, non-coding RNAs, and fusion transcripts that reflect active transcriptional programs within tumors [4]. Epigenomics characterizes heritable changes in gene expression not encoded within the DNA sequence itself, including DNA methylation patterns and histone modifications [4]. Proteomics catalogs the functional effectors of cellular processes, identifying post-translational modifications, protein-protein interactions, and signaling pathway activities [4]. Finally, metabolomics profiles small-molecule metabolites, the biochemical endpoints of cellular processes, exposing metabolic reprogramming in tumors [4].
Artificial Intelligence Approaches for Multi-Omics Integration
Artificial intelligence provides a sophisticated computational framework for multi-omics integration that surpasses the capabilities of traditional statistical methods [4] [33]. Machine learning (ML) encompasses classical algorithms like logistic regression and ensemble methods that are often applied to structured omics data for tasks such as survival prediction or therapy response [33]. Deep learning (DL), a subset of ML, uses neural networks with multiple layers to model complex, non-linear relationships in high-dimensional data [4] [34]. Convolutional neural networks (CNNs) are particularly adept at processing image-based data, including histopathology slides and radiomics features [4] [33]. Graph neural networks (GNNs) represent a specialized class of deep learning algorithms designed to operate on graph-structured data, making them ideally suited for modeling biological networks and patient similarity graphs [34] [35]. Transformers and large language models (LLMs) are increasingly applied to model long-range dependencies in sequential data and extract knowledge from scientific literature and clinical notes [4] [33].
Deep Learning Architectures for Multi-Omics Data Fusion
Data Integration Strategies and Methodologies
The integration of multi-omics data can be conceptualized through different methodological approaches based on the timing and nature of integration [14]. Early integration involves concatenating raw or preprocessed features from multiple omics layers into a single combined dataset before model training, though this approach risks disregarding heterogeneity between platforms [14]. Intermediate integration employs methods that transform each omics dataset separately while modeling their relationships, respecting platform diversity while capturing some cross-modal interactions [14]. Late integration trains separate models on each omics dataset and combines their predictions, ignoring potential synergies between molecular layers but offering implementation simplicity [14].
In the context of these integration approaches, two distinct analytical paradigms emerge: Vertical integration (N-integration) incorporates different omics data from the same samples, enabling the study of concurrent observations across different functional levels [14]. Horizontal integration (P-integration) combines data of the same molecular type from different subjects to increase statistical power and sample size [14].
Table 1: Multi-Omics Data Integration Strategies
| Integration Type | Description | Advantages | Limitations | Common Algorithms |
|---|---|---|---|---|
| Early Integration | Concatenates raw features from multiple omics before analysis | Captures cross-omics interactions; single model | Disregards data heterogeneity; sensitive to normalization | LASSO, Elastic Net, Deep Neural Networks |
| Intermediate Integration | Transforms omics data separately while modeling relationships | Respects platform diversity; captures some interactions | Complex implementation; model interpretation challenges | Multi-Kernel Learning, MOFA, Cross-modal Autoencoders |
| Late Integration | Combines predictions from separate omics models | Simple implementation; robust to technical variability | Ignores inter-omics synergies; suboptimal performance | Stacking, Ensemble Methods, Cluster-of-Clusters |
| Vertical (N-Integration) | Integrates different omics from the same samples | Studies biological continuum across molecular layers | Requires complete multi-omics profiling | Multi-View Algorithms, Graph Neural Networks |
| Horizontal (P-Integration) | Combines same omics data from different cohorts | Increases sample size; enhances statistical power | Batch effect challenges; cross-study heterogeneity | Meta-analysis, Federated Learning |
Graph Neural Networks for Biological Network Analysis
Graph Neural Networks represent a particularly powerful framework for multi-omics integration because they can natively model the complex relational structures inherent in biological systems [35]. In this paradigm, molecular entities (genes, proteins, metabolites) are represented as nodes, while their functional, physical, or regulatory interactions are represented as edges [34] [35]. The core innovation of GNNs is their ability to learn from both node features and graph structure through message-passing mechanisms, where each node aggregates information from its neighbors to compute updated representations [34].
Several specialized GNN architectures have been developed with distinct advantages for biological data analysis. Graph Convolutional Networks (GCNs) extend convolutional operations from regular grids to graph-structured data, propagating information throughout the graph and aggregating it to update node representations [34]. In a breast cancer study predicting axillary lymph node metastasis, a GCN model achieved an AUC of 0.77, demonstrating clinical utility for non-invasive detection [34]. Graph Attention Networks (GATs) incorporate attention mechanisms to differentially weigh the importance of neighboring nodes, allowing the model to focus on the most relevant molecular interactions [34]. Graph Isomorphism Networks (GINs) utilize a sum aggregation function and multi-layer perceptron to analyze node characteristics, providing enhanced discriminative power for graph classification tasks [34].
Diagram 1: GNN Architecture for Multi-Omics Integration. This workflow illustrates how heterogeneous omics data is structured as a graph and processed through multiple GNN layers with attention mechanisms to generate predictive outputs for precision oncology.
Application Notes: AI-Driven Multi-Omics in Precision Oncology
Cancer Subtype Classification and Patient Stratification
Multi-omics integration through AI has demonstrated remarkable success in refining cancer molecular subtyping and patient stratification beyond conventional histopathological classifications [4] [31]. For example, in glioma and clear-cell renal-cell carcinoma, the Pathomic Fusion model integrated histology and genomics data to outperform the World Health Organization 2021 classification system for risk stratification [32]. A pan-tumor analysis of 15,726 patients combined multimodal real-world data with explainable AI to identify 114 key markers across 38 solid tumors, which were subsequently validated in an external lung cancer cohort [32]. These approaches leverage the complementary nature of different data modalities—where genomics provides information about driver alterations, transcriptomics reveals activated pathways, and proteomics captures functional effectors—to create more robust and biologically meaningful patient classifications [4].
Therapy Response Prediction and Treatment Selection
AI-powered multi-omics models are increasingly guiding therapeutic decisions by predicting treatment response and resistance mechanisms [4] [32]. The TRIDENT machine learning model integrates radiomics, digital pathology, and genomics data from the Phase 3 POSEIDON study in metastatic non-small cell lung cancer (NSCLC) to identify patient subgroups most likely to benefit from specific treatment strategies [32]. This approach demonstrated significant hazard ratio reductions (0.88–0.56 in non-squamous histology population) compared to standard stratification methods [32]. Similarly, the DREAM drug sensitivity prediction challenge revealed that multimodal approaches consistently outperform unimodal ones in predicting therapeutic outcomes across breast cancer cell lines [32]. These models can capture the complex interplay between genomic alterations, signaling pathway activities, and tumor microenvironment features that collectively determine therapeutic efficacy [4].
Table 2: Performance Metrics of AI-Based Multi-Omics Models in Oncology Applications
| Application Domain | AI Model | Cancer Type | Data Modalities | Performance Metrics | Reference |
|---|---|---|---|---|---|
| Early Detection | Multi-modal AI | Multiple Cancers | ctDNA methylation, fragmentomics | 78% sensitivity, 99% specificity for 75 cancer types | [36] |
| Lymph Node Metastasis Prediction | Graph Convolutional Network | Breast Cancer | Ultrasound, clinical, histopathologic data | AUC: 0.77 (95% CI: 0.69–0.84) | [34] |
| Risk Stratification | Pathomic Fusion | Glioma, Renal Cell Carcinoma | Histology, genomics | Outperformed WHO 2021 classification | [32] |
| Therapy Response Prediction | TRIDENT | NSCLC (Metastatic) | Radiomics, digital pathology, genomics | HR reduction: 0.88–0.56 (non-squamous population) | [32] |
| Drug Sensitivity Prediction | Multimodal DL | Breast Cancer | Multi-omics cell line data | Consistently outperformed unimodal approaches | [32] |
| Relapse Prediction | MUSK Transformer | Melanoma | Multimodal clinical data | AUC: 0.833 for 5-year relapse | [32] |
Multi-Cancer Early Detection and Risk Stratification
Multimodal AI approaches are revolutionizing cancer screening through multi-cancer early detection (MCED) tests that analyze circulating tumor DNA (ctDNA) in blood samples [32] [36]. The SPOT-MAS test utilizes multi-omics data including DNA fragments, methylation patterns, copy number aberrations, and genetic mutations, combined with multi-modal AI algorithms to detect ctDNA signals and identify their tissue of origin [36]. This approach can screen for up to 75 cancer types and subtypes with 78% sensitivity and 99% specificity from a single blood draw [36]. Similarly, the Sybil AI model demonstrated exceptional performance in predicting lung cancer risk from low-dose computed tomography (CT) scans with up to 0.92 ROC–AUC, enabling effective integration into existing screening programs [32]. These technologies represent a paradigm shift from organ-specific to pan-cancer screening approaches with significant potential for population-level impact.
Experimental Protocols and Methodologies
Protocol: Graph Neural Network for Multi-Omics Integration
Objective: Implement a GNN framework to integrate genomic, transcriptomic, and proteomic data for cancer subtype classification.
Materials and Reagents:
- Next-Generation Sequencing Data: Whole exome/genome sequencing (DNA), RNA sequencing (RNA)
- Proteomic Profiling Data: Mass spectrometry or RPPA data
- Computational Environment: Python 3.8+, PyTorch Geometric 2.0+, PyTorch 1.10+
Procedure:
Data Preprocessing and Normalization
- Perform quality control on each omics dataset using platform-specific methods (e.g., DESeq2 for RNA-seq, ComBat for batch correction)
- Normalize each omics dataset using variance-stabilizing transformations
- Handle missing values using k-nearest neighbors imputation (k=10)
Graph Construction
- Represent each patient as a separate graph where nodes represent molecular entities (genes, proteins)
- Create edges based on:
- Protein-protein interactions from STRING database (confidence score > 0.7)
- Gene co-expression networks (top 5% of correlations)
- Pathway interactions from KEGG and Reactome
- Initialize node features using z-score normalized expression/mutation values
GNN Model Architecture
Model Training and Validation
- Implement 5-fold cross-validation with stratified sampling
- Use Adam optimizer with learning rate of 0.001 and weight decay of 5e-4
- Train for maximum of 500 epochs with early stopping (patience=30)
- Employ class-weighted cross-entropy loss to handle imbalanced datasets
Model Interpretation
- Apply GNNExplainer to identify important subgraph structures
- Use saliency maps to highlight influential molecular features
- Perform pathway enrichment analysis on top-ranked features
Validation Metrics: Accuracy, F1-score, AUC-ROC, Precision-Recall curves
Protocol: Multimodal Deep Learning for Therapy Response Prediction
Objective: Develop a multimodal deep learning model to predict immunotherapy response in melanoma patients.
Materials and Reagents:
- Multi-omics Data: Whole exome sequencing, RNA-seq, multiplex immunohistochemistry
- Clinical Data: Treatment history, response criteria (RECIST), survival outcomes
- Software Libraries: TensorFlow 2.8+, Scikit-learn 1.0+, NumPy 1.21+
Procedure:
Data Preprocessing
- Genomic features: Encode mutations as binary indicators, CNVs as continuous values
- Transcriptomic features: Select top 5,000 most variable genes, TPM normalization
- Image features: Extract deep features from histopathology slides using pretrained ResNet-50
- Clinical features: Normalize continuous variables, one-hot encode categorical variables
Multimodal Fusion Architecture
- Implement separate encoding branches for each modality:
- Genomic branch: 2 fully-connected layers (512, 256 units) with ReLU activation
- Transcriptomic branch: 1D convolutional layers with attention mechanism
- Image branch: Pretrained CNN with fine-tuning, global average pooling
- Clinical branch: 2 fully-connected layers (128, 64 units)
- Apply cross-modal attention to model interactions between modalities
- Implement late fusion with weighted averaging based on modality reliability
- Implement separate encoding branches for each modality:
Model Training
- Use balanced mini-batch sampling (batch size=32)
- Optimize with AdamW optimizer (learning rate=0.0001, weight decay=0.01)
- Apply gradient clipping (max norm=1.0) and learning rate scheduling
- Regularize with dropout (rate=0.5) and label smoothing (epsilon=0.1)
Model Interpretation
- Compute Shapley values to quantify feature importance
- Generate partial dependence plots for key features
- Visualize cross-modal attention weights
Validation: Time-dependent ROC analysis, Kaplan-Meier survival curves, Concordance index
Diagram 2: Multi-Omics AI Integration Workflow. This end-to-end experimental protocol outlines the key stages in developing and validating AI models for multi-omics data integration, from preprocessing to clinical application.
Table 3: Essential Research Tools for AI-Driven Multi-Omics Integration
| Category | Tool/Resource | Function | Application in Multi-Omics |
|---|---|---|---|
| Data Generation | Next-Generation Sequencing | Genomic, transcriptomic, epigenomic profiling | Foundation for molecular characterization of tumors [4] |
| Data Generation | Mass Spectrometry | Proteomic, metabolomic quantification | Functional profiling of proteins and metabolites [4] |
| Data Generation | Multiplex Immunohistochemistry | Spatial protein expression analysis | Tumor microenvironment characterization [4] |
| Computational Framework | PyTorch Geometric | GNN library extension for PyTorch | Implementation of graph neural networks [34] |
| Computational Framework | MONAI (Medical Open Network for AI) | Open-source PyTorch-based framework | AI tools and pre-trained models for medical imaging [32] |
| Biological Databases | STRING, KEGG, Reactome | Protein-protein interactions, pathways | Prior biological knowledge for graph construction [35] |
| Bioinformatics Tools | DESeq2, ComBat | RNA-seq normalization, batch correction | Data preprocessing and quality control [4] |
| Model Interpretation | SHAP, GNNExplainer | Explainable AI techniques | Model interpretability and biomarker discovery [4] |
| Cloud Platforms | DNAnexus, Galaxy | Cloud-based data analysis | Scalable processing of petabyte-scale datasets [4] |
The integration of multi-omics data through artificial intelligence represents a paradigm shift in oncology research and clinical practice [4] [32]. Deep learning and graph neural networks serve as the essential computational engine that transforms heterogeneous, high-dimensional molecular data into clinically actionable insights [4] [35]. As these technologies continue to evolve, several emerging trends are poised to further accelerate progress: federated learning enables privacy-preserving collaborative model training across institutions [4]; quantum computing may solve currently intractable optimization problems in large biological networks [4]; and patient-centric "N-of-1" models promise to deliver truly individualized cancer management strategies [4]. However, significant challenges remain in ensuring model generalizability, ethical equity, and regulatory alignment before these approaches can achieve widespread clinical adoption [4] [37]. The convergence of AI and multi-omics technologies holds the potential to fundamentally transform cancer care from reactive population-based approaches to proactive, personalized precision oncology [4] [32] [36].
The tumor microenvironment (TME) is a complex and structured ecosystem composed of malignant cells surrounded by diverse non-malignant cell types, all embedded in an altered extracellular matrix (ECM) [38]. Intra-tumoral heterogeneity (ITH), characterized by the coexistence of genetically and phenotypically diverse subclones within a single tumor, presents a fundamental challenge for cancer diagnosis, prognosis, and treatment [39]. Traditional single-omics approaches and dissociated single-cell analyses fail to capture the intricate spatial context that governs cellular interactions, functional states, and clinical outcomes. The integration of next-generation sequencing (NGS) with spatial omics technologies now enables researchers to map the molecular and cellular architecture of tumors with unprecedented resolution, providing systems-level insights into tumor evolution, immune evasion, and therapy resistance [39] [40] [41].
Spatial Omics Technology Platforms
Spatial omics technologies can be broadly categorized into imaging-based and sequencing-based methods, each with distinct strengths for profiling the TME.
Spatial Transcriptomics Platforms
Spatial transcriptomic technologies map gene expression patterns within the context of tissue architecture.
- Imaging-based platforms, such as NanoString CosMx, Vizgen MERSCOPE, and 10X Genomics Xenium, utilize cyclic fluorescence in situ hybridization (FISH) to localize and quantify hundreds to thousands of RNA transcripts at single-cell resolution. These platforms can simultaneously co-profile a limited number of proteins [38].
- Sequencing-based platforms, such as 10X Visium, use arrays of barcoded oligonucleotides on a slide to capture location-specific whole transcriptome data. Their spatial resolution is coarser (55 μm for Visium) than imaging-based platforms but allows for unbiased transcriptome-wide discovery [38]. Newer technologies like Slide-seq (10 μm), Slide-tags, and DBiT-seq (10 μm) offer higher resolution by using DNA-barcoded beads with known positions or microfluidic patterning [38].
Spatial Proteomics and Multiplexed Imaging
Spatial proteomics characterizes the abundance and location of proteins, which are critical downstream effectors of cellular function.
- CODEX (Co-Detection by indexing) employs antibody conjugates with DNA barcodes and cyclic fluorescent hybridization to visualize over 100 proteins simultaneously within a tissue section [40] [38].
- Imaging Mass Cytometry (IMC) and Multiplexed Ion Beam Imaging (MIBI) use antibodies conjugated to rare metal isotopes detected by mass spectrometry. IMC and MIBI offer high signal-to-noise ratios and resolutions of 1 μm and 300 nm, respectively, routinely quantifying about 50 different proteins [38].
Spatial Genomics and Epigenomics
Spatial genomics tools enable the mapping of genomic alterations and chromatin states within the tissue context.
- Adaptations of MERFISH and seqFISH can distinguish up to ~1,000 genomic loci, allowing characterization of chromatin organization from sub-domain structures to trans-chromosomal interactions [38].
- In situ sequencing (ISS) technologies, such as OligoFISSEQ, and extended applications of DBiT-seq enable the mapping of genomic loci, chromatin accessibility, and histone modifications [38].
Table 1: Key Commercially Available Spatial Profiling Platforms
| Technology | Modality | Spatial Resolution | Key Outputs | Considerations |
|---|---|---|---|---|
| 10X Visium | Sequencing-based | 55 μm | Whole transcriptome per spot | Unbiased discovery; resolution near multi-cell level |
| NanoString CosMx | Imaging-based | Single cell | Targeted RNA (up to 6,000), ~30 proteins | High-plex, subcellular resolution |
| Vizgen MERSCOPE | Imaging-based | Single cell | Targeted whole transcriptome, proteins | High detection efficiency |
| 10X Genomics Xenium | Imaging-based | Single cell | Targeted RNA, proteins | Optimized for speed and sensitivity |
| CODEX | Imaging-based | Single cell | >100 proteins | High-plex protein profiling |
| Imaging Mass Cytometry | Imaging-based | 1 μm | ~40-50 proteins | High signal-to-noise; destructive to sample |
Experimental Protocol: An Integrated Multi-Omic Workflow
This protocol outlines a comprehensive pipeline for analyzing the TME by integrating Visium spatial transcriptomics with CODEX multiplex proteomics on serial sections from the same tumor block [40].
Sample Preparation and Tissue Processing
- Tissue Collection & Preservation: Collect fresh tumor tissues from surgical resections or biopsies. Optimal results are achieved with fresh-frozen tissues for Visium. For CODEX, tissues should be fixed in 4% paraformaldehyde for 24 hours, followed by paraffin embedding (FFPE).
- Sectioning: Cut serial sections of 5-10 μm thickness using a cryostat (for frozen) or microtome (for FFPE). Mount consecutive sections on Visium Spatial Gene Expression slides and charged glass slides for CODEX.
- Histological Staining: Perform Haematoxylin and Eosin (H&E) staining on all sections. This provides a critical histological reference for pathology annotation, region of interest (ROI) selection, and downstream data alignment [40].
Data Generation
- Visium Spatial Transcriptomics:
- Follow the manufacturer's protocol for tissue permeabilization and cDNA synthesis.
- Generate sequencing libraries from the barcoded cDNA and sequence on an Illumina platform to a minimum depth of 50,000 reads per spot.
- CODEX Multiplexed Protein Imaging:
- Design an antibody panel targeting key cellular phenotypes (e.g., immune cells: CD3, CD8, CD20, CD68; tumor markers: Pan-CK; stromal markers: α-SMA).
- Conjugate antibodies with CODEX DNA barcodes.
- Perform iterative cycles of fluorescent hybridization, imaging, and dye inactivation on a CODEX instrument to generate a multiplexed protein expression dataset [38].
Data Preprocessing and Integration
- Spatial Transcriptomics Data:
- Alignment & Spot Detection: Use the Space Ranger pipeline (10X Genomics) to align sequencing reads to the reference genome and assign them to spatial barcodes.
- Quality Control: Filter out spots with low unique molecular identifier (UMI) counts or high mitochondrial gene content, indicative of poor cell viability.
- CODEX Data:
- Image Preprocessing: Perform staining intensity normalization and compensation for spectral overlap across fluorescence channels.
- Cell Segmentation: Use a nuclear stain (DAPI) to identify individual cells. Apply a watershed or machine learning-based algorithm to define whole-cell boundaries [38].
- Single-Cell Feature Extraction: Quantify protein expression levels for each marker in every segmented cell.
- Data Integration & Co-registration:
- Align the H&E images from the Visium and CODEX serial sections using landmark-based or intensity-based image registration tools. This creates a common coordinate system, enabling the direct comparison and integration of transcriptomic and proteomic data from analogous tissue regions [40].
Integrated Spatial Multi-Omics Workflow
Analysis Framework: From Raw Data to Spatial Signatures
Processed spatial data, represented as cell/spot-by-molecule matrices with spatial coordinates, can be mined for biologically meaningful "Spatial Signatures" [38]. These are computationally defined characteristics that describe spatial distribution, composition, and function.
Table 2: A Multi-Scale Framework for Spatial Signature Analysis
| Scale | Signature Type | Description | Biological Insight | Example Tools/Methods |
|---|---|---|---|---|
| Univariate | Spatial Location | Preference of a cell type for specific tissue regions (e.g., invasive margin). | Identifies functionally relevant niches; T cells at tumor edge correlate with better response to immunotherapy [38]. | Spatial-Distribution Index, G-function |
| Expression Gradient | Gradual change in gene/protein expression across space. | Reveals patterns of metabolic activity (high in core) and antigen presentation (high at edges) [40]. | Moran's I, Trend Surface Analysis | |
| Bivariate | Spatial Colocalization | Non-random proximity between two distinct cell types. | Indicates potential for productive cell-cell interactions (e.g., CD8+ T cells with antigen-presenting cells) [38]. | Cross-Ripley's K, Neighborhood Co-occurrence |
| Spatial Avoidance | Significant segregation between two cell types. | Suggests immune exclusion mechanisms, where suppressive cells (e.g., Tregs) form barriers [38]. | Cross-Ripley's K, Interaction Index | |
| Higher-Order | Cellular Community/Niche | Recurring multicellular assemblies with defined composition and spatial arrangement. | Discovers complex functional units like "immune-hot" (T cell-rich) or "immune-cold" (excluded/desert) niches that predict clinical outcomes [40] [38]. | BayesSpace, BANKSY, Clustermole |
| Tumor Microregion/Subclone | Spatially distinct cancer cell clusters separated by stroma, grouped by shared genetics. | Maps clonal architecture; subclones with distinct CNVs show differential oncogenic pathway activity (e.g., MYC) [40]. | Morphological segmentation, NMF, Copy number inference |
Identifying Tumor Microregions and Subclones
- Malignant vs. Non-Malignant Spot Classification: Use inferred copy number variations (CNVs) from Visium data or canonical marker genes (e.g., epithelial vs. stromal) to classify spots as malignant or non-malignant [40].
- Microregion Delineation: Apply histological images and transcriptional profiles to identify spatially contiguous clusters of malignant spots, defined as "tumour microregions," which are separated by stromal components [40]. Tools like Morph can be used to refine boundaries and calculate distances from the tumor-stroma interface.
- Spatial Subclone Identification: Group microregions that share genetic alterations (e.g., specific CNVs or mutations) into "spatial subclones." This reveals the geographic distribution of genetically distinct tumor cell populations [40].
Characterizing the Tumor-Immune Interface
- Cell Type Deconvolution: If using Visium data, employ deconvolution algorithms (e.g., CIBERSORTx, SPOTlight) to estimate the proportion of different cell types within each spot, using a matched single-cell RNA-seq dataset as a reference [38].
- Spatial Neighborhood Analysis: Perform unsupervised clustering (e.g., k-means, Leiden) on the spatial proximity and composition of cells (from CODEX) or deconvoluted spots (from Visium) to identify recurrent cellular neighborhoods or "habitats" [40] [38].
- Differential Analysis: Compare gene expression or pathway activity (e.g., MYC, antigen presentation) between different spatial neighborhoods, microregions, or subclones to link spatial context to functional states [40].
Multi-Scale Spatial Signature Analysis
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Key Research Reagent Solutions for Spatial Multi-Omics
| Reagent/Material | Function | Application Example |
|---|---|---|
| 10X Visium Spatial Gene Expression Slide | Glass slide with ~5,000 barcoded spots for capturing mRNA from tissue sections. | Whole transcriptome mapping of fresh-frozen tumor sections. |
| CODEX Antibody Conjugation Kit | Enables covalent linking of DNA barcodes (e.g., ~150 distinct barcodes) to purified antibodies for multiplexed imaging. | Creating a custom 50-plex antibody panel for deep immunophenotyping. |
| Validated Antibody Panels | Pre-designed sets of antibodies targeting key markers for cell typing (immune, stromal, tumor) with validated performance in specific assays. | Accelerating panel design for CODEX or IMC; ensuring reproducibility. |
| Single-Cell RNA-seq Kit (e.g., 10X 3') | Reagents for generating single-cell RNA-seq libraries from dissociated tumor tissue. | Creating a reference transcriptome for deconvolving Visium data. |
| Nucleic Acid Stain (DAPI) | Fluorescent stain that binds to DNA, marking cell nuclei for image-based cell segmentation. | Defining nuclear boundaries in CODEX and IMC data for single-cell analysis. |
| Tissue Preservation Media (e.g., RNAlater) | Chemical stabilizer that penetrates tissues to preserve RNA integrity for downstream sequencing. | Preserving RNA in fresh biopsies intended for Visium analysis. |
Clinical Translation and Therapeutic Insights
Spatial multi-omics profiles provide a direct window into therapy-resistant mechanisms. Analysis of 131 tumor sections across six cancer types revealed that metastatic samples contained larger and deeper tumor microregions than primary tumors, suggesting more aggressive growth patterns [40]. Furthermore, spatial subclones with distinct CNVs exhibited differential activity in oncogenic pathways like MYC, highlighting how genetic ITH manifests spatially to drive tumor evolution [40]. The identification of both immune-hot and immune-cold neighborhoods, along with the concentration of exhausted T cells and macrophages at the boundaries of 3D subclones, provides a spatial rationale for response and resistance to immunotherapy [40] [41]. These insights are paving the way for next-generation patient stratification, where spatial signatures of the TME will complement existing biomarkers to guide the selection of targeted therapies and immunotherapies [39] [38].
Liquid biopsy, the analysis of tumor-derived components from biofluids, has emerged as a transformative approach for cancer management. When coupled with Next-Generation Sequencing (NGS), it provides an unparalleled window into dynamic tumor evolution, enabling real-time monitoring of tumor genomics and therapeutic response [42]. This non-invasive tool captures circulating tumor DNA (ctDNA), which reflects the molecular heterogeneity of tumors and offers significant advantages over traditional tissue biopsies, including the ability to perform repeated sampling to track clonal dynamics during treatment [43].
The integration of these approaches with other omics data—including transcriptomics, proteomics, and epigenomics—within oncology research creates a powerful multidimensional framework. This multi-omics context is essential for addressing the complex challenges of intra-tumoral heterogeneity and therapeutic resistance, ultimately advancing the goals of precision oncology [4] [31]. This Application Note details the experimental protocols and analytical frameworks for implementing liquid biopsy and NGS to investigate tumor evolution.
Analytical Performance of Liquid Biopsy Assays
The clinical utility of liquid biopsy hinges on the sensitive and accurate detection of somatic alterations in ctDNA, which often circulates at very low concentrations. The analytical performance of two advanced, commercially available NGS-based liquid biopsy assays is summarized in Table 1.
Table 1: Analytical Performance of Recent Liquid Biopsy Assays
| Assay Name | Targeted Genes | Variant Types Detected | Limit of Detection (LOD) | Key Performance Metrics |
|---|---|---|---|---|
| Northstar Select [44] | 84 genes | SNVs/Indels, CNVs, Fusions, MSI | 0.15% VAF (SNV/Indels) | Identified 51% more pathogenic SNV/indels and 109% more CNVs vs. on-market assays |
| Hedera Profiling 2 (HP2) [45] | 32 genes | SNVs/Indels, CNVs, Fusions, MSI | 0.5% VAF (for reported sensitivity) | 96.92% Sensitivity, 99.67% Specificity (for SNVs/Indels at 0.5% VAF) |
These assays demonstrate that increased sensitivity for detecting variants at low variant allele frequencies (VAF) directly translates to clinical benefits, such as identifying more actionable alterations and reducing the number of uninformative reports [44]. The "liquid biopsy" workflow, from sample collection to clinical reporting, is outlined in Figure 1 below.
Figure 1: End-to-end workflow for a comprehensive liquid biopsy NGS assay, culminating in multi-omic data integration for clinical reporting.
Key Methodologies and Experimental Protocols
Sample Collection and Processing Protocol
Principle: High-quality, cell-free DNA (cfDNA) is the foundational substrate for reliable liquid biopsy testing. Proper collection and processing are critical to prevent genomic DNA contamination and preserve the integrity of the fragile cfDNA.
Reagents & Materials:
- Cell-free DNA Blood Collection Tubes (e.g., Streck BCT or PAXgene Blood cDNA tubes)
- Double-Speed Centrifuge for plasma separation
- cfDNA Extraction Kit (silicon-membrane or magnetic beads based)
- Fluorometric Assay (e.g., Qubit) and Fragment Analyzer (e.g., Bioanalyzer) for QC
Procedure:
- Blood Collection: Draw blood into certified cell-free DNA collection tubes. Invert gently 8-10 times to mix. Tubes are stable for up to 14 days at room temperature.
- Plasma Separation: Within 4 hours of collection, centrifuge tubes at 1,600 x g for 20 minutes at 4°C. Carefully transfer the upper plasma layer to a new tube without disturbing the buffy coat.
- Plasma Clarification: Perform a second centrifugation of the plasma at 16,000 x g for 10 minutes at 4°C. Transfer the clarified plasma to a new tube.
- cfDNA Extraction: Isolate cfDNA from the plasma using a commercially available kit, strictly following the manufacturer's instructions. Typical starting volume is 4-10 mL of plasma.
- Quality Control:
- Quantification: Measure cfDNA concentration using a fluorometric assay. Expected yields vary by disease burden, but are typically 1-50 ng from 4 mL plasma.
- Fragment Size Analysis: Assess cfDNA integrity. A peak at ~167 bp indicates high-quality, apoptosis-derived cfDNA.
Library Preparation and Sequencing for Comprehensive Profiling
Principle: This protocol converts isolated cfDNA into a sequenceable NGS library, often using a hybrid-capture approach to enrich for a pan-cancer gene panel.
Reagents & Materials:
- Library Preparation Kit (e.g., KAPA HyperPrep)
- Pan-Cancer Hybrid-Capture Panel (e.g., covering 50-100+ genes)
- Magnetic Bead-Based Cleanup System (e.g., SPRIselect)
- Indexed Adapters for sample multiplexing
- Next-Generation Sequencer (e.g., Illumina NovaSeq or NextSeq)
Procedure:
- Library Construction:
- End Repair & A-Tailing: Repair the ends of the fragmented cfDNA and add a single 'A' nucleotide to the 3' ends.
- Adapter Ligation: Ligate indexed sequencing adapters to the cfDNA fragments.
- Library Amplification: Perform a limited-cycle PCR (e.g., 8-12 cycles) to amplify the adapter-ligated library.
- Target Enrichment (Hybrid Capture):
- Hybridization: Incubate the library with biotinylated DNA or RNA probes targeting the gene panel of interest.
- Capture & Wash: Bind the probe-hybridized library to streptavidin-coated magnetic beads. Perform stringent washes to remove non-specifically bound DNA.
- Amplification: Perform a second, post-capture PCR (e.g., 12-16 cycles) to amplify the enriched library.
- Pooling and Sequencing:
- Library QC: Quantify and validate the final library size distribution.
- Pooling: Normalize and pool individually indexed libraries for multiplexed sequencing.
- Sequencing: Load the pool onto an NGS flow cell. Sequence to a high depth of coverage (typically >5,000x average coverage) to ensure sensitivity for low-VAF variants.
Bioinformatic Analysis and Multi-Omic Integration
Principle: Raw sequencing data is processed to identify somatic variants, which are then integrated with other molecular data types to build a comprehensive model of tumor biology and evolution.
Workflow:
- Primary Analysis:
- Demultiplexing: Assign reads to individual samples based on their index sequences.
- Alignment: Map sequencing reads to the human reference genome (e.g., GRCh38) using tools like BWA-MEM or Bowtie2.
- Secondary Analysis (Variant Calling):
- SNVs/Indels: Use callers optimized for low-VAF variants in ctDNA (e.g., MuTect2, VarScan2) with duplicate read marking.
- CNVs: Apply tools that detect copy-number changes from shallow whole-genome sequencing data (e.g., CNVkit, ADTEx).
- Fusions & MSI: Use specialized algorithms to identify gene rearrangements and microsatellite instability patterns.
- Tertiary Analysis and Integration:
- Annotation: Annotate variants for functional impact and clinical actionability using databases like OncoKB and ClinVar.
- Clonal Decomposition: Use variant allele frequencies and cancer cell fractions to infer the clonal architecture of the tumor.
- Multi-Omic Data Fusion: Integrate the genomic findings with other data layers, such as transcriptomics from circulating RNA or radiomics from medical imaging, using AI-driven models [4]. This can reveal non-genetic mechanisms of resistance and provide a systems-level view of the tumor.
The bioinformatic and data integration process, which transforms raw sequencing data into an evolutionary model, is depicted in Figure 2.
Figure 2: Bioinformatic workflow for analyzing liquid biopsy NGS data, from raw sequencing reads to multi-omic integration and evolutionary modeling.
The Scientist's Toolkit
Table 2: Essential Research Reagent Solutions for Liquid Biopsy NGS
| Item | Function | Example Products / Technologies |
|---|---|---|
| cfDNA Stabilizing Blood Tubes | Preserves blood sample integrity for transport, preventing gDNA release from lysed white cells. | Streck Cell-Free DNA BCT, PAXgene Blood cDNA Tube |
| Nucleic Acid Extraction Kits | Isolate high-purity, short-fragment cfDNA from plasma or other biofluids. | QIAamp Circulating Nucleic Acid Kit, MagMAX Cell-Free DNA Isolation Kit |
| Targeted Sequencing Panels | Multiplexed PCR or hybrid-capture probes for enriching cancer-associated genomic regions. | Hedera HP2 Panel (32 genes), Northstar Select (84 genes) [44] [45] |
| Hybrid-Capture Reagents | Biotinylated probes and magnetic beads for target enrichment prior to sequencing. | IDT xGen Hybridization and Wash Kit, Twist Hybridization and Wash Kit |
| UMI Adapters | Unique Molecular Identifiers (UMIs) tag original DNA molecules to correct for PCR and sequencing errors. | Illumina TruSeq Unique Dual Indexes, Integrated DNA Technologies (IDT) xGen UDI adapters |
Application in Tracking Tumor Evolution under Immunotherapy
Liquid biopsy is particularly powerful for monitoring dynamic responses to immune checkpoint inhibitors (ICIs). Longitudinal ctDNA profiling can track the clonal architecture of tumors, revealing the expansion of pre-existing resistant subclones or the emergence of new ones under therapeutic pressure [43].
A key application is the measurement of blood Tumor Mutational Burden (bTMB). As a high number of somatic mutations can encode for neoantigens that stimulate an antitumor immune response, bTMB has been validated as a predictive biomarker for ICI response. Studies like POPLAR and OAK demonstrated that patients with high bTMB (≥16 mutations) had significantly improved survival when treated with atezolizumab compared to chemotherapy [43]. Furthermore, integrating ctDNA data with peripheral T-cell receptor (TCR) sequencing provides a holistic view of the co-evolution between the tumor and the immune system, offering insights into the dynamics of immunoediting and therapeutic resistance [43].
The integration of liquid biopsy with NGS provides an dynamic and non-invasive method for deciphering tumor evolution in real time. The protocols and data outlined herein provide a roadmap for researchers to implement these approaches, from rigorous pre-analytical sample handling to sophisticated bioinformatic integration. As the field progresses, the fusion of liquid biopsy genomic data with other omics modalities through AI and machine learning will be critical to fully unravel the complexity of cancer and advance the era of personalized oncology.
The transition from preclinical research to successful clinical application remains a significant challenge in oncology drug development, with attrition rates for novel drug discovery persisting at approximately 95% [46]. Within the framework of integrating next-generation sequencing (NGS) with multi-omics data, advanced preclinical models—particularly patient-derived xenografts (PDX) and organoids—have emerged as transformative tools that better recapitulate human tumor biology. These models preserve key genetic and phenotypic characteristics of patient tumors, enabling more accurate prediction of therapeutic responses and accelerating the development of personalized cancer treatments [46] [47] [48].
The integration of these models with multi-omics approaches (genomics, transcriptomics, proteomics, and metabolomics) provides a comprehensive understanding of the molecular intricacies of cancer, facilitating the identification of novel biomarkers and therapeutic targets [3]. This document details the applications, protocols, and methodologies for employing PDX models and organoids in therapy validation, specifically within the context of a multi-omics integrated oncology research pipeline.
Model Systems: Characteristics and Applications
Comparative Analysis of Preclinical Oncology Models
Table 1: Comparison of Key Preclinical Models in Oncology Research
| Model Type | Key Characteristics | Advantages | Limitations | Primary Applications |
|---|---|---|---|---|
| 2D Cell Lines | Immortalized cells grown as monolayers [47] [48] | Simple, low cost, short cultivation periods, suitable for high-throughput screening [46] [47] [48] | Limited tumor heterogeneity; cannot represent tumor microenvironment; genetic drift during passaging [46] [47] [48] | Initial drug efficacy testing; high-throughput cytotoxicity screening; combination therapy studies [46] |
| Organoids | 3D stem cell-derived models from patient tumor samples [47] [48] | Preserves tissue architecture and genetic features; more physiologically relevant than 2D; suitable for biobanking and medium-throughput screening [46] [47] [48] | Cannot fully represent complete tumor microenvironment; more complex and time-consuming than 2D models [46] | Drug response investigation; immunotherapy evaluation; personalized medicine; disease modeling [46] [47] |
| PDX Models | Patient tumor tissue implanted into immunodeficient mice [49] | Most clinically relevant preclinical model; preserves original tumor heterogeneity and microenvironment; accurate drug response prediction [46] [49] | Expensive, resource-intensive, time-consuming; low-throughput; ethical considerations of animal testing [46] | Biomarker discovery and validation; drug combination strategies; co-clinical trials; personalized treatment strategies [46] [49] |
Integrated Workflow for Model Selection and Application
The effective use of preclinical models requires a strategic, integrated approach that leverages the unique advantages of each system throughout the drug development pipeline [46]. PDX-derived cell lines can serve as an effective starting point for initial screening. Organoids allow researchers to build on these findings with more physiologically relevant 3D models. PDX models then represent the final preclinical stage before human trials, providing the most clinically predictive data on drug efficacy and biomarker validation [46].
Diagram 1: Integrated workflow for preclinical models
Patient-Derived Organoids: Protocols and Applications
Organoid Development and Validation Protocol
Objective: Establish and characterize patient-derived organoids (PDOs) from tumor tissue for drug screening and therapy validation within a multi-omics framework.
Materials and Reagents:
- Tumor tissue sample (fresh surgical resection or biopsy)
- Advanced DMEM/F12 medium
- Dissociation enzyme cocktail (collagenase, dispase, or tumor-specific enzymes)
- Basement membrane extract (BME) or Matrigel
- Defined growth factor supplements (EGF, Noggin, R-spondin, etc.)
- Antibiotic-antimycotic solution
- Cell recovery solution
- Multi-omics analysis reagents (DNA/RNA extraction kits, proteomics buffers)
Procedure:
Tissue Processing and Dissociation
- Place fresh tumor tissue in cold transport medium and process within 1-2 hours of collection
- Wash tissue with PBS containing antibiotic-antimycotic solution
- Mince tissue into 1-2 mm³ fragments using surgical scalpels
- Digest tissue fragments with appropriate dissociation cocktail (concentration and time optimized for tumor type) at 37°C with agitation
- Neutralize enzyme activity with complete medium
- Filter cell suspension through 70-100 μm cell strainer
- Centrifuge and resuspend cells in basal medium
Organoid Culture Establishment
- Mix dissociated cells with BME/Matrigel (approximately 10,000-50,000 cells per 50 μL dome)
- Plate BME-cell mixture as domes in pre-warmed culture plates
- Polymerize BME-cell mixture at 37°C for 20-30 minutes
- Overlay with complete organoid growth medium optimized for tumor type
- Culture at 37°C in 5% CO₂ with medium changes every 2-3 days
Organoid Expansion and Passaging
- Monitor organoid growth and morphology daily
- Passage organoids every 7-21 days (depending on growth rate) using cell recovery solution to dissolve BME
- Mechanically dissociate large organoids into smaller fragments or single cells using enzymatic treatment
- Replate cells in fresh BME at appropriate split ratios (typically 1:3 to 1:6)
Characterization and Validation
- Confirm retention of original tumor histology through H&E staining
- Verify genomic fidelity via whole exome or targeted sequencing
- Analyze transcriptomic profiles through RNA sequencing
- Validate protein expression patterns via immunohistochemistry
- Establish biobank of early passage organoids for future studies
Quality Control Measures:
- Regular mycoplasma testing
- STR profiling to confirm patient origin
- Comparison of molecular features with original tumor tissue
- Assessment of organoid formation efficiency
Drug Screening Protocol Using Organoids
Objective: Evaluate therapeutic efficacy and identify potential biomarkers using PDOs in medium-throughput screening format.
Procedure:
Organoid Preparation for Screening
- Harvest and dissociate organoids to single cells or small clusters
- Count viable cells using trypan blue exclusion or automated cell counter
- Seed cells in BME domes in 96-well or 384-well plates at optimized density (500-5,000 cells/well depending on growth rate)
- Allow organoids to form and grow for 3-5 days before drug treatment
Drug Treatment
- Prepare drug serial dilutions in organoid culture medium
- Treat organoids with concentration gradients of single agents or combinations
- Include appropriate controls (vehicle-only and maximum cytotoxicity)
- Refresh drug-containing medium every 3-4 days
- Incubate for predetermined endpoint (typically 5-14 days)
Viability Assessment and Response Quantification
- Measure cell viability using ATP-based, resazurin-based, or similar assays
- Acquire bright-field and fluorescence images for morphological assessment
- Calculate IC₅₀ values and dose-response curves
- Classify organoids as sensitive or resistant based on established thresholds
Multi-Omics Integration for Biomarker Discovery
- Process organoids for genomic, transcriptomic, and proteomic analyses
- Correlate drug response data with molecular features
- Identify potential predictive biomarkers of response
- Validate biomarkers in independent organoid cohorts
Patient-Derived Xenograft Models: Protocols and Applications
PDX Model Development and Expansion Protocol
Objective: Establish and propagate PDX models that faithfully recapitulate original patient tumors for preclinical therapeutic studies.
Materials and Reagents:
- Fresh tumor tissue samples
- Immunodeficient mice (NSG, NOG, or similar strain)
- Sterile surgical instruments
- Matrigel or similar extracellular matrix
- Antibiotic solutions
- DNA/RNA stabilization reagents
- Fixation buffers for histology
Procedure:
Donor Tissue Processing
- Process fresh tumor tissue within 1 hour of resection whenever possible
- Wash tissue in cold PBS with antibiotics
- Divide tissue for: implantation, snap-freezing, histology, and DNA/RNA extraction
- Mince implantation tissue into 1-3 mm³ fragments in cold PBS or Matrigel
Implantation
- Anesthetize mice according to approved IACUC protocols
- For subcutaneous implantation: create small dorsal incision and insert single tumor fragment
- For orthotopic implantation: inject tumor fragments or cells into appropriate organ
- For metastatic models: inject tumor cells intravenously or into specific anatomical sites
- Monitor mice regularly for tumor growth and overall health
Model Propagation
- Monitor tumor growth by caliper measurements 2-3 times weekly
- Harvest tumors at designated endpoint (typically 1000-1500 mm³ for subcutaneous)
- Aseptically process harvested tumors as above for subsequent passages
- Cryopreserve tumor fragments in freezing medium for long-term storage
Model Characterization
- Perform histological comparison of PDX tumors with original patient tissue
- Conduct genomic analysis (whole exome or targeted sequencing) to validate fidelity
- Analyze transcriptomic and proteomic profiles
- Establish early passage cryobank to preserve molecular characteristics
Quality Control Measures:
- Regular pathogen testing of mouse colonies
- Authentication of model identity by STR profiling
- Monitoring of molecular drift across passages
- Assessment of tumor take rates and growth characteristics
Therapy Validation Using PDX Models
Objective: Evaluate efficacy of therapeutic agents and combinations in PDX models that represent specific molecular subtypes.
Procedure:
Experimental Design
- Select PDX models based on molecular characteristics relevant to therapy
- Randomize mice into treatment groups when tumors reach 100-200 mm³
- Include appropriate control groups (vehicle-treated)
- Power studies appropriately (typically n=5-8 mice per group)
Treatment Administration
- Prepare drugs according to manufacturer instructions
- Administer therapies via appropriate route (oral gavage, intraperitoneal, intravenous)
- Follow established dosing schedules based on prior pharmacokinetic studies
- Monitor mice daily for adverse effects and tumor measurements
Endpoint Analysis
- Measure tumor dimensions 2-3 times weekly
- Calculate tumor volumes using formula: (length × width²)/2
- Monitor body weight and clinical signs as toxicity indicators
- Establish study endpoints based on tumor size or ethical considerations
Molecular Analysis and Biomarker Validation
- Collect tumor tissues at endpoint for molecular analysis
- Process samples for multi-omics profiling (genomics, transcriptomics, proteomics)
- Correlate treatment response with molecular features
- Identify potential predictive biomarkers of response
- Validate findings in independent PDX cohorts or clinical samples
Multi-Omics Integration in Preclinical Models
Computational Framework for Multi-Omics Data Integration
The integration of multi-omics data with preclinical model outputs requires sophisticated computational approaches [3] [50]. Multi-omics integration typically follows three primary strategies, each with distinct advantages and challenges [50] [10]:
Table 2: Multi-Omics Data Integration Strategies
| Integration Strategy | Description | Advantages | Challenges | Applications in Preclinical Models |
|---|---|---|---|---|
| Early Integration | Combining raw data from different omics layers before analysis [50] [10] | Captures all potential cross-omics interactions; preserves raw information [50] | Extremely high dimensionality; computationally intensive; requires extensive normalization [50] | Initial exploratory analysis; hypothesis generation across omics layers [3] |
| Intermediate Integration | Transforming each omics dataset before combination [50] [10] | Reduces complexity; incorporates biological context through networks [50] | Requires domain knowledge; may lose some raw information during transformation [50] | Network-based analysis; biomarker signature identification [46] [3] |
| Late Integration | Analyzing each omics dataset separately and combining results [50] [10] | Handles missing data well; computationally efficient; leverages method-specific optimizations [50] | May miss subtle cross-omics interactions not captured by individual models [50] | Validation studies; clinical translation of biomarker signatures [3] |
Biomarker Discovery Workflow Using Integrated Preclinical Models
The integration of PDX models and organoids with multi-omics data enables a powerful workflow for biomarker discovery and validation [46]:
Diagram 2: Biomarker discovery workflow
Implementation Protocol:
Hypothesis Generation using PDX-Derived Cell Lines
- Conduct high-throughput drug screening on diverse cell line panels
- Perform genomic characterization (whole exome sequencing, targeted panels)
- Correlate genetic alterations with drug sensitivity patterns
- Generate initial biomarker hypotheses for validation
Biomarker Refinement using Organoid Models
- Test drug responses in organoid models representing specific molecular subtypes
- Conduct multi-omics analysis (genomics, transcriptomics, proteomics)
- Identify robust biomarker signatures associated with response
- Refine biomarker hypotheses based on 3D model data
Biomarker Validation using PDX Models
- Evaluate therapeutic efficacy in PDX models with known molecular features
- Analyze biomarker distribution within heterogeneous tumor environments
- Validate biomarker-performance correlation
- Establish biomarker thresholds for patient stratification
Research Reagent Solutions
Table 3: Essential Research Reagents for Preclinical Model Development
| Reagent Category | Specific Examples | Function | Application Notes |
|---|---|---|---|
| Extracellular Matrices | Basement membrane extract (BME), Matrigel, Collagen I | Provides 3D scaffolding for cell growth and organization | Critical for organoid formation; lot-to-lot variability requires quality control [47] [48] |
| Digestion Enzymes | Collagenase, Dispase, Trypsin-EDTA, Tumor dissociation kits | Dissociates tissue into single cells or small clusters | Enzyme selection and concentration must be optimized for different tumor types [47] [48] |
| Growth Supplements | B27, N2, Noggin, R-spondin, EGF, FGF, Wnt3a | Supports stem cell maintenance and lineage differentiation | Formulation varies by tumor type; essential for long-term culture [47] |
| Cryopreservation Media | DMSO-containing freezing media, Serum-free cryopreservation solutions | Preserves cells and tissues for long-term storage | Vital for biobanking; controlled rate freezing improves viability [46] |
| Molecular Profiling Kits | DNA/RNA extraction kits, NGS library preparation, Proteomics sample preparation | Enables multi-omics characterization | Quality of extracted nucleic acids critical for sequencing success [3] [50] |
The integration of PDX models and organoids with multi-omics technologies represents a powerful approach for enhancing the predictive value of preclinical research in oncology. These advanced models, when employed in a complementary workflow and characterized using comprehensive molecular profiling, significantly improve our ability to identify effective therapies and predictive biomarkers. The protocols outlined in this document provide a framework for researchers to implement these tools in therapy validation, ultimately accelerating the development of personalized cancer treatments and improving clinical success rates. As these technologies continue to evolve, their integration with emerging computational methods and multi-omics data will further transform the landscape of preclinical cancer research.
Navigating the Hurdles: Data Harmonization, Technical, and Translational Challenges
The integration of Next-Generation Sequencing (NGS) with other omics data represents a frontier in oncology research, generating datasets of unprecedented complexity and scale. This data-driven approach is foundational to precision medicine, which aims to customize healthcare based on a person's unique genomic, environment, and lifestyle profile [18]. The field is characterized by the "Four Vs" of Big Data: Volume, Velocity, Variety, and Veracity [51] [52]. Managing these characteristics is not merely a technical challenge but a critical prerequisite for extracting biologically meaningful insights that can inform drug discovery and clinical applications. This document provides application notes and experimental protocols for navigating these challenges within the context of multi-omics oncology research.
Defining and Quantifying the Four Vs in Multi-Omics Research
Core Characteristics and Research Impact
The Four Vs framework describes the fundamental properties of big data that necessitate specialized storage, processing, and analytical approaches [53]. In multi-omics oncology, these characteristics manifest with distinct implications.
- Volume refers to the sheer scale of data. The advent of NGS has made it feasible to sequence entire genomes, generating terabytes of data from a single instrument run [18] [54]. Managing these massive datasets requires scalable infrastructure and distributed computing frameworks.
- Velocity pertains to the speed at which data is generated and must be processed. High-throughput sequencers can produce data incredibly rapidly, creating a need for efficient, near real-time bioinformatic pipelines to keep pace with the influx of genomic, transcriptomic, and proteomic information [51] [52].
- Variety encompasses the diverse types and formats of data. Multi-omics studies integrate structured (e.g., clinical records), semi-structured (e.g., XML-based sequencing files), and unstructured data (e.g., medical images, pathology notes) [52]. This includes diverse omics layers such as genomics, transcriptomics, proteomics, metabolomics, and epigenomics, each with its own data structure and biological significance [3] [50].
- Veracity denotes the reliability, accuracy, and quality of the data. In genomics, this includes concerns about sequencing errors, sample quality, batch effects, and the accurate interpretation of variants, particularly those of unknown significance (VUS) [51] [52] [54]. High veracity is paramount for ensuring that scientific conclusions and clinical decisions are based on trustworthy data.
Quantitative Landscape of Multi-Omics Data
The table below quantifies the Four Vs across different data types commonly encountered in oncology research, illustrating the scope of the big data challenge.
Table 1: Quantitative Profile of Multi-Omics Data Types in Oncology
| Data Type | Volume per Sample | Velocity (Generation Speed) | Primary Formats (Variety) | Key Veracity Concerns |
|---|---|---|---|---|
| Whole Genome Sequencing (WGS) | ~100-200 GB [50] | Days to weeks | FASTQ, BAM, VCF | Sequencing depth, alignment errors, variant calling accuracy [55] |
| Whole Transcriptome Sequencing (RNA-Seq) | ~20-50 GB | Days | FASTQ, BAM, Count Matrices | RNA integrity, library preparation bias, normalization [50] |
| Proteomics (Mass Spectrometry) | ~1-10 GB | Hours to days | RAW, mzML, mzIdentML | Protein false discovery rates, dynamic range limitations [3] [50] |
| Metabolomics | ~0.1-1 GB | Hours | RAW, CDF, peak lists | Metabolite identification confidence, sample degradation [3] |
| Electronic Health Records (EHR) | Variable, cumulative | Continuous, real-time | CSV, JSON, HL7, Unstructured text | Data entry inconsistency, missing values, coding errors [50] |
Application Notes: Strategic Frameworks for Data Integration
AI and Machine Learning for Multi-Omics Data Fusion
The integration of disparate omics layers is a central challenge. Artificial Intelligence (AI) and Machine Learning (ML) provide powerful strategies for this fusion, which can be categorized by the timing of integration [50]:
- Early Integration (Feature-Level): This approach merges raw or pre-processed features from all omics layers into a single, high-dimensional dataset for analysis. While it can capture complex interactions, it is highly susceptible to the "curse of dimensionality" and requires substantial computational resources.
- Intermediate Integration: This strategy involves transforming each omics dataset into a new, shared representation (e.g., a latent space) before combining them. Similarity Network Fusion (SNF) is a key technique here, creating patient-similarity networks for each data type and then fusing them into a single network to improve disease subtyping [50].
- Late Integration (Model-Level): Separate models are built for each omics type, and their predictions are combined in a final ensemble model. This method is computationally efficient and robust to missing data types but may miss subtle inter-omics interactions.
Table 2: AI/ML Integration Strategies for Multi-Omics Data
| Integration Strategy | Key Algorithms/Tools | Advantages | Best-Suited Applications |
|---|---|---|---|
| Early Integration | Convolutional Neural Networks (CNNs), Autoencoders | Captures all raw information; potential for novel discovery | Image-omics integration (e.g., radiogenomics) |
| Intermediate Integration | Similarity Network Fusion (SNF), Graph Convolutional Networks (GCNs) | Reduces complexity; incorporates biological context | Patient stratification; biomarker discovery |
| Late Integration | Stacking, Weighted Averaging Ensembles | Handles missing data well; computationally efficient | Clinical outcome prediction with incomplete data |
| Unsupervised Dimensionality Reduction | Variational Autoencoders (VAEs), Multi-Omics Factor Analysis (MOFA) | Identifies latent factors driving variation; useful for exploration | Novel cancer subtype identification; hypothesis generation |
Experimental Protocol: A Multi-Omics Data Analysis Workflow
The following protocol outlines a standardized workflow for processing and integrating multi-omics data, from sample to insight, while addressing the Four Vs.
Protocol Title: Integrated Multi-Omics Profiling for Tumor Subtyping
Goal: To generate and analyze paired genomic, transcriptomic, and proteomic data from tumor biopsies to identify molecularly distinct cancer subtypes.
Materials & Specimen:
- Fresh-frozen or FFPE tumor tissue specimen with matched normal tissue (e.g., blood).
- Kits for DNA, RNA, and protein extraction.
- NGS platform (e.g., Illumina NovaSeq for WGS/WTS) [54].
- Mass Spectrometer for proteomics (e.g., LC-MS/MS).
- High-performance computing (HPC) cluster or cloud computing environment.
Procedure:
Sample Preparation & QC:
- Extract high-molecular-weight DNA, total RNA, and proteins from the same tumor sample.
- Assess quality and quantity: DNA/RNA integrity (e.g., RIN > 8), protein concentration.
- Proceed only with high-quality samples to ensure Veracity.
Library Preparation & Sequencing (Addressing Volume & Variety):
- Genomics: Prepare whole-genome sequencing library following manufacturer's protocol. Sequence to a minimum coverage of 30x.
- Transcriptomics: Prepare poly-A enriched or rRNA-depleted RNA-Seq library. Sequence to a depth of ~50 million paired-end reads.
- Proteomics: Digest proteins with trypsin, label if using multiplexed approaches (e.g., TMT), and analyze by LC-MS/MS.
Primary Data Processing (Addressing Velocity):
- Computational Environment: Utilize a workflow management system (e.g., Nextflow, Snakemake) on an HPC cluster for parallel processing and managing Volume.
- Genomics:
- Trimming: Use Trimmomatic to remove adapters.
- Alignment: Map reads to a reference genome (e.g., GRCh38) using BWA-MEM.
- Variant Calling: Identify SNVs and indels using GATK best practices.
- Transcriptomics:
- Alignment: Map RNA-Seq reads using STAR.
- Quantification: Generate gene-level counts using featureCounts.
- Proteomics:
- Identify and quantify proteins using software like MaxQuant.
- Normalize protein intensities.
Data Integration & Analysis (Addressing Variety & Veracity):
- Data Harmonization: Normalize datasets to correct for technical variance and batch effects using methods like ComBat [50].
- Intermediate Integration with SNF:
- Construct patient-similarity networks for each omics data type (genomic variants, gene expression, protein abundance).
- Fuse the three networks into a single integrated network using the SNF algorithm.
- Apply spectral clustering to the fused network to identify robust patient clusters (molecular subtypes).
- Validation: Validate subtypes using survival analysis (Cox regression) and association with clinical-pathological features.
Troubleshooting:
- Low Sequencing Depth: Leads to poor variant calling Veracity. Re-sequence if possible or use specialized tools for low-pass data.
- Batch Effects: Can confound analysis. Include control samples and apply statistical correction in the harmonization step.
- Missing Proteomics Data: Use late integration strategies or imputation methods to handle missing data points.
Visualization of Multi-Omics Data Integration Workflow
The following diagram illustrates the logical flow and computational relationships in the multi-omics integration protocol described above.
Diagram 1: Multi-omics data integration workflow for oncology.
The Scientist's Toolkit: Essential Reagents and Computational Solutions
Successful navigation of the Four Vs requires a suite of reliable reagents and software tools. The following table details key solutions for a multi-omics research program.
Table 3: Research Reagent and Computational Solutions for Multi-Omics
| Category | Item/Software | Function | Considerations for the Four Vs |
|---|---|---|---|
| Wet-Lab Reagents | TruSeq DNA/RNA Library Kits (Illumina) | Prepares NGS libraries for sequencing | Standardization reduces technical Variety, improving Veracity |
| Qubit dsDNA/RNA HS Assay Kits | Accurately quantifies nucleic acids | Critical QC step to ensure data Veracity before costly sequencing | |
| TMT/Isobaric Labeling Kits (Thermo) | Enables multiplexed proteomics | Increases Velocity of proteomic data generation by batching samples | |
| Bioinformatics Tools | GATK [18] | Germline and somatic variant discovery | Industry standard for genomic Veracity; handles large Volume |
| STAR Aligner | Rapid alignment of RNA-Seq reads | Optimized for Velocity and accuracy with large datasets | |
| MaxQuant | Quantitative proteomics analysis | Manages Variety of raw MS data and complex protein identification | |
| SNFtool (R/Python) | Fuses multi-omics networks | Core tool for addressing data Variety via intermediate integration | |
| Computational Infrastructure | Cloud Computing (AWS, GCP) | Scalable data storage and analysis | Essential for managing data Volume and computational demands |
| Workflow Managers (Nextflow) | Pipelines for reproducible analysis | Automates processing to handle data Velocity and enhance Veracity via reproducibility | |
| Knowledge Bases | gnomAD [18] | Population frequency of variants | Critical for assessing pathogenicity and Veracity of genomic findings |
| ClinVar [18] | Public archive of variant interpretations | Provides context for clinical Veracity of identified mutations |
The integration of Next-Generation Sequencing (NGS) with other omics data represents a cornerstone of modern precision oncology, enabling a comprehensive functional understanding of biological systems [56]. However, this approach introduces a significant analytical challenge: batch effects. These are systematic technical variations introduced during sample processing, sequencing, or analysis that are unrelated to biological conditions [57]. In oncology research, where detecting subtle molecular differences can dictate therapeutic decisions, batch effects can distort true biological signals, leading to spurious findings and compromised reproducibility [4] [58].
Batch effects arise from multiple sources throughout the experimental workflow. In transcriptomics, they may stem from variability in sample preparation, different sequencing platforms, reagent lot variations, or even processing by different personnel [57]. Similarly, in DNA methylation analysis—crucial for understanding epigenetic regulation in cancer—batch effects can emerge from technical factors like instrumentation differences, reagent lots, and measurement times across batches [58]. The consequences are particularly severe in differential expression analysis, where batch effects can inflate false-positive rates, mask genuine biological signals, and mislead downstream validation efforts [57]. The "four Vs" of big data in oncology—volume, velocity, variety, and veracity—further compound these challenges, as dimensionality often dwarfs sample sizes in most cohorts [4].
Detecting and Diagnosing Batch Effects
Visualization and Analytical Techniques
The first critical step in managing batch effects is their detection through robust visualization and quantitative metrics. Dimensionality reduction techniques serve as primary tools for initial assessment.
- Principal Component Analysis (PCA): This method projects high-dimensional omics data into lower dimensions defined by principal components. When samples cluster primarily by batch identity rather than biological group (e.g., tumor subtype) in PCA plots, it indicates strong batch effects [57].
- Uniform Manifold Approximation and Projection (UMAP): Particularly valuable for single-cell RNA-seq data, UMAP provides a non-linear dimensionality reduction that often reveals batch-driven clustering patterns more effectively than PCA [57].
- Clustering Analysis: Unsupervised clustering algorithms applied to omics data may group samples by technical batches rather than biological conditions, signaling the presence of confounding technical variation [57].
Quantitative Assessment Metrics
Beyond visual inspection, several quantitative metrics provide objective measures of batch effect severity and correction efficacy:
- k-nearest neighbor Batch Effect Test (kBET): Quantifies whether the local neighborhood composition of samples reflects the expected distribution based on overall batch representation. Higher kBET acceptance rates indicate better batch mixing [57].
- Average Silhouette Width (ASW): Measures how similar samples are to their own cluster compared to other clusters, with respect to biological labels. Optimal batch correction maximizes biological ASW while minimizing batch ASW [57].
- Adjusted Rand Index (ARI): Assesses the similarity between two clusterings, typically used to compare clustering results before and after correction to ensure biological integrity is maintained [57].
- Local Inverse Simpson's Index (LISI): Evaluates diversity in local neighborhoods, with higher values indicating better mixing of batches or biological groups [57].
The table below summarizes key detection methods and their applications:
Table 1: Methods for Batch Effect Detection and Diagnosis
| Method | Application | Strengths | Interpretation |
|---|---|---|---|
| PCA Visualization | Bulk RNA-seq, DNA methylation | Simple, widely adopted | Samples cluster by batch instead of biological group |
| UMAP Plots | scRNA-seq, spatial transcriptomics | Captures non-linear patterns | Visual separation of batches in 2D embedding |
| kBET | All omics data types | Quantitative, statistical test | Higher acceptance rate = better batch mixing |
| ASW | Cluster validation | Measures cluster compactness | High for biological groups, low for batches post-correction |
| ARI | Method comparison | Standardized metric | High values indicate maintained biological structure |
Computational Strategies for Batch Effect Correction
Established Statistical Methods
Multiple computational approaches have been developed to address batch effects in omics data, each with distinct strengths and limitations.
- ComBat: Utilizing an empirical Bayes framework within a location/scale adjustment model, ComBat adjusts for known batch variables by standardizing mean and variance parameters across batches. This method is particularly effective for structured bulk RNA-seq data with clearly defined batch information and demonstrates robustness even with small sample sizes within batches [58] [57].
- iComBat: An incremental extension of ComBat specifically designed for longitudinal studies with repeatedly measured data. Unlike conventional methods requiring simultaneous correction of all samples, iComBat enables correction of newly added batches without reprocessing previously corrected data, making it invaluable for clinical trials with ongoing patient recruitment [58].
- Surrogate Variable Analysis (SVA): This approach estimates and adjusts for hidden sources of variation, including unknown batch effects, making it suitable when batch variables are partially observed or undocumented. However, it carries a risk of overcorrection if not carefully modeled [58] [57].
- limma removeBatchEffect: Integrated within the limma package for R, this function employs linear modeling to remove batch effects when batch variables are known. It efficiently integrates with differential expression workflows but assumes additive batch effects [57].
Advanced and Emerging Approaches
As omics technologies evolve, more sophisticated correction methods have emerged:
- Harmony: Designed for single-cell and spatial RNA-seq data, Harmony iteratively aligns cells in a shared embedding space to reduce batch-driven clustering while preserving biological variation. It integrates seamlessly with Seurat workflows [57].
- fastMNN (Mutual Nearest Neighbors): Identifies mutual nearest neighbors across batches to correct batch-specific shifts, particularly effective for complex cellular structures in single-cell data [57].
- Scanorama: A Python-based method performing nonlinear manifold alignment across batches, suitable for integrating data from different technological platforms [57].
- Deep Learning Approaches: Tools like Flexynesis employ deep learning architectures for multi-omics integration that can inherently learn to model and adjust for technical variations, especially in complex multi-modal datasets [59].
Table 2: Comparison of Batch Effect Correction Methods
| Method | Required Input | Best For | Advantages | Limitations |
|---|---|---|---|---|
| ComBat | Known batch labels | Bulk RNA-seq, DNA methylation | Robust for small samples, empirical Bayes | May not handle nonlinear effects |
| iComBat | Known batch labels | Longitudinal studies, repeated measures | Incremental correction | Requires initial model training |
| SVA | No batch labels needed | Complex designs with unknown batches | Captures hidden factors | Risk of removing biological signal |
| limma removeBatchEffect | Known batch labels | Differential expression workflows | Efficient, integrates with limma | Assumes additive effects |
| Harmony | Known batch labels | scRNA-seq, spatial transcriptomics | Preserves biology, fast | Specialized for single-cell data |
| fastMNN | Known batch labels | Complex cellular structures | Identifies mutual neighbors | Computationally intensive |
| Flexynesis | Optional batch labels | Multi-omics integration | Handles non-linear relationships | Requires deep learning expertise |
Experimental Design for Batch Effect Minimization
Proactive experimental design represents the most effective strategy for managing batch effects, as prevention surpasses correction. Several key principles should guide the design of multi-omics studies in oncology:
- Randomization and Balancing: Distribute biological groups (e.g., tumor subtypes, treatment conditions) evenly across processing batches, sequencing runs, and technical platforms. Ensure each batch contains representatives from all experimental conditions to avoid confounding technical and biological variation [57].
- Replication Strategy: Include at least two replicates per biological group within each batch to enable robust estimation of both biological and technical variances. This design facilitates more accurate batch effect modeling and correction [57].
- Reference Standards: Incorporate pooled quality control samples or commercial reference standards across batches. These samples serve as technical anchors for monitoring and correcting batch variations throughout the study timeline [57].
- Standardization Protocols: Maintain consistency in reagents, equipment, and personnel throughout the study. Document any unavoidable changes meticulously, as this metadata is crucial for subsequent correction algorithms [57].
- Block Designs: Structure experiments in complete blocks where feasible, with each block containing all experimental conditions. This approach isolates batch effects within blocks, making them more amenable to statistical adjustment [57].
The following workflow diagram illustrates the comprehensive strategy for batch effect management, from experimental design through computational correction:
Table 3: Research Reagent Solutions for Batch Effect Management
| Resource | Category | Function | Application Context |
|---|---|---|---|
| SeSAMe [58] | Preprocessing pipeline | Reduces technical biases in DNA methylation arrays | Addresses dye bias, background noise in epigenomics |
| Pooled QC Samples [57] | Quality control | Technical replicates across batches | Monitoring instrument drift, normalization anchor |
| Commercial Reference Standards [57] | Standardization | Inter-laboratory calibration | Cross-study harmonization, method validation |
| Unique Molecular Identifiers (UMIs) [60] | Library preparation | Tags individual molecules pre-amplification | Corrects PCR amplification biases in NGS |
| Platform-Specific Controls [60] | Quality control | Monitors sequencing performance | Verifies instrument function, run quality |
| Flexynesis [59] | Deep learning toolkit | Automated multi-omics integration | Handles batch effects in complex multimodal data |
| Harmony [57] | Integration algorithm | Aligns single-cell datasets | Corrects batch effects in scRNA-seq data |
| Galaxy Platform [61] [59] | Bioinformatics workflow | Streamlined data processing | Reproducible pipeline execution, tool accessibility |
Protocols for Robust Multi-Omics Integration
Protocol: Batch Effect Correction Using ComBat for Transcriptomics Data
Purpose: Remove batch effects from bulk RNA-seq data when batch information is known. Reagents: Normalized count matrix (e.g., TPM, FPKM), batch information file, biological covariates. Tools: R statistical environment, sva package.
Procedure:
- Data Preparation: Load normalized expression matrix with genes as rows and samples as columns. Ensure normalization (e.g., TPM, FPKM) has been applied to account for library size differences [50].
- Model Specification: Identify the batch variable(s) and any biological covariates to preserve (e.g., tumor stage, treatment status).
- Parameter Estimation: Execute ComBat's empirical Bayes estimation to calculate location and scale parameters for each batch using the
ComBat()function [58] [57]. - Data Adjustment: Apply the estimated parameters to adjust expression values, standardizing mean and variance across batches while preserving biological effects of interest.
- Validation: Perform PCA on corrected data and visualize to confirm batch mixing improvement. Compare pre- and post-correction ASW values to quantify efficacy [57].
Troubleshooting: If biological signal appears compromised, review covariate specification and consider relaxing empirical Bayes parameters. For small sample sizes, utilize ComBat's built-in hierarchical modeling for stability [58].
Protocol: Incremental Batch Correction with iComBat for Longitudinal Studies
Purpose: Correct newly added batches without recalculating previous corrections. Reagents: Previously corrected dataset, new batch data with identical structure, original model parameters. Tools: iComBat implementation (custom or published), Python/R environment.
Procedure:
- Initial Model Reference: Preserve the trained correction model and parameters from the original ComBat analysis of baseline data [58].
- New Data Preparation: Process new batches using identical normalization and preprocessing methods applied to original data.
- Incremental Correction: Apply iComBat to new data only, using the previously established model parameters without modifying already-corrected historical data [58].
- Consistency Validation: Verify that combined corrected data (original + new) shows appropriate batch mixing while maintaining biological group separation.
- Database Integration: Merge incrementally corrected data with original dataset for unified analysis.
Applications: Particularly valuable for clinical trials with rolling enrollment, long-term cohort studies, and multi-center collaborations with phased data generation [58].
Protocol: Multi-Omics Integration with Flexynesis
Purpose: Integrate multiple omics modalities while accounting for technical variation. Reagents: Normalized omics datasets (e.g., genomics, transcriptomics, proteomics), outcome variables (e.g., survival, drug response). Tools: Flexynesis package (available via PyPi, Bioconda, Galaxy), Python environment.
Procedure:
- Data Configuration: Standardize each omics dataset to ensure compatible dimensions and normalization. Handle missing data using appropriate imputation methods [59].
- Architecture Selection: Choose appropriate Flexynesis model architecture based on analytical task (classification, regression, survival analysis) [59].
- Training Configuration: Set parameters for encoder networks (fully connected or graph-convolutional) and supervisor MLPs for each outcome variable.
- Model Training: Execute training with appropriate validation split, allowing the network to learn latent representations that integrate multi-omics data while being predictive of outcomes.
- Interpretation: Utilize built-in visualization and feature importance metrics to identify key drivers and validate biological relevance.
Advantages: Flexynesis supports multi-task learning, handles missing data natively, and provides a standardized interface for both deep learning and classical machine learning approaches [59].
Effective management of batch effects through thoughtful experimental design and robust computational correction is not merely a technical consideration but a fundamental requirement for generating reliable, reproducible insights in multi-omics oncology research. The strategies outlined—from proactive experimental planning to validated correction protocols—provide a comprehensive framework for addressing technical variability across NGS and other omics platforms. As precision oncology increasingly relies on integrated molecular profiling to guide therapeutic decisions, ensuring data integrity through rigorous batch effect management becomes paramount. The continuous development of advanced methods like iComBat for longitudinal studies and Flexynesis for deep learning-based integration promises to further enhance our capability to extract biologically meaningful signals from complex, multi-source omics data, ultimately accelerating translation to clinical applications.
In modern oncology research, the integration of Next-Generation Sequencing (NGS) with other omics data types—such as proteomics, transcriptomics, and epigenomics—has become fundamental for advancing precision medicine. However, missing data presents a significant obstacle that can compromise the validity of downstream analyses and biological interpretations. The presence of missing values is an inevitable problem in multi-omics integrative studies due to various reasons, including budget limitations, insufficient sample availability, or experimental constraints [62]. In clinical and biological contexts, missing values can arise from multiple sources: low abundance of molecules below detection limits, sample processing errors, technical variations between analytical platforms, or cost-related decisions that limit the breadth of data collection across all omics layers for every sample [62] [63].
The critical impact of missing data is particularly pronounced in oncology research, where accurate molecular profiling can directly influence therapeutic decisions. Incomplete datasets can hinder the identification of robust biomarkers, distort the modeling of signaling pathways, and ultimately lead to erroneous conclusions about drug responses or resistance mechanisms. Since most statistical analyses cannot be applied directly to incomplete datasets, imputation—the process of inferring missing values—has become an essential preprocessing step that enables more comprehensive and powerful multi-omics integration [62]. This Application Note provides a structured framework for addressing the missing data problem through advanced imputation techniques specifically tailored for NGS-based multi-omics studies in oncology.
Understanding Missing Data Mechanisms in Multi-Omics Studies
Proper handling of missing data begins with understanding its underlying mechanism, which significantly influences the selection of appropriate imputation strategies and the validity of subsequent analyses. The three primary missing data mechanisms are:
Missing Completely at Random (MCAR): The missingness occurs entirely at random, with no discernible pattern related to any observed or unobserved variables. An example includes sample loss due to technical failures in laboratory processing [64]. MCAR primarily reduces statistical power but does not introduce bias, making it the simplest mechanism to address.
Missing at Random (MAR): The probability of missingness may depend on observed variables but not on unobserved data. For instance, in a depression study, males might be less likely to complete questionnaires than females, with gender being fully recorded [64]. Under MAR, the missingness mechanism can be accounted for statistically, though it requires more sophisticated approaches than MCAR.
Missing Not at Random (MNAR): The missingness depends on unobserved measurements or the missing values themselves. For example, patients with severe depression might be less likely to report their symptom severity [64]. MNAR presents the most challenging scenario, as the missingness mechanism is inherently non-ignorable and may require specialized modeling approaches.
In multi-omics oncology studies, missing data can manifest in various patterns. Some patients may have complete genomic data but incomplete proteomic profiles, while certain molecular features (e.g., low-abundance proteins or rare genetic variants) may be systematically missing across multiple samples. Understanding these patterns is crucial for selecting and applying the most appropriate imputation methods.
Advanced Imputation Techniques for Multi-Omics Data
Single-Omics Imputation Methods
Genotype Imputation
Genotype imputation has become a standard tool in genome-wide association studies (GWAS), facilitating the fine-mapping of causal variants, meta-analyses, and boosting the statistical power of association tests [62]. Current approaches fall into two main categories:
Reference-based methods: These utilize reference panels constructed from whole genome sequencing samples (e.g., the 1000 Genomes Project) and leverage key genetic characteristics including linkage patterns, mutations, and recombination hotspots [62]. The basic intuition is that short chromosome segments can be shared between individuals as they may be inherited from a common ancestor [62].
Reference-free methods: These do not require a reference panel and include statistical techniques such as k-nearest neighbors (KNN), singular value decomposition (SVD), and emerging deep learning approaches like sparse convolutional denoising autoencoder (SCDA) [62].
Table 1: Comparison of Widely Used Genotype Imputation Algorithms
| Algorithm | Key Features | Strengths | Limitations | Optimal Context |
|---|---|---|---|---|
| IMPUTE2 | MCMC and HMM-based | High accuracy for common variants; extensively validated | Computationally intensive | Smaller datasets requiring high accuracy for common variants [65] |
| Beagle | Graphical model | Fast; integrates phasing and imputation | Less accurate for rare variants | Large datasets; high-throughput studies [65] |
| Minimac3/4 | HMM-based | Scalable; optimized for low memory usage | Slight accuracy trade-off | Very large datasets; meta-analyses [62] [65] |
| GLIMPSE | Reference-based | Effective for rare variants in admixed populations | Computationally intensive | Admixed cohorts; studies focused on rare variants [65] |
| DeepImpute | Deep learning-based | Captures complex patterns; potential for high accuracy | Requires large training datasets; less validated | Experimental settings with rich computational resources [65] |
Gene Expression Data Imputation
Missing values in transcriptomic data, whether from bulk RNA-seq or single-cell RNA-seq (scRNA-seq), require specialized imputation approaches. These methods can be broadly categorized into:
- Statistical methods: Including traditional approaches like mean imputation and regression-based methods
- Machine learning methods: Such as k-nearest neighbors (KNN) and random forest
- Deep learning methods: Autoencoders and other neural network architectures that can capture complex patterns in high-dimensional data [62]
For microarray data, which remains prevalent in many cancer studies, local similarity-based techniques have shown particular promise. These methods leverage the fact that genes with similar expression patterns across samples may share common regulatory mechanisms. One advanced approach combines spectral clustering with weighted K-nearest neighbors, where data is initially clustered, followed by imputation using weighted distances to the nearest neighbors within the same cluster [63]. This dual-level similarity approach has demonstrated superior performance compared to global imputation techniques, especially for datasets with varying dimensionality and characteristics [63].
Integrative Multi-Omics Imputation
Integrative imputation techniques that leverage correlations and shared information across multiple omics datasets typically outperform approaches that rely on single-omics information alone [62]. These methods capitalize on the biological relationships between different molecular layers—for instance, how genetic variants might influence gene expression, which in turn affects protein abundance.
Matrix Factorization Approaches: These methods extend single-omics matrix completion techniques to multi-omics settings, often employing joint factorization models that identify shared latent factors across omics modalities.
Deep Learning-Based Integration: Autoencoders and other neural architectures can be designed with multi-view architectures that simultaneously learn representations from multiple omics data types. These models can effectively capture non-linear relationships between omics layers, potentially revealing biologically meaningful connections [62] [66].
Transfer Learning: Approaches that pre-train models on one omics type and fine-tune on another can help address scenarios where certain omics data are sparsely measured across the cohort.
The key advantage of integrative methods is their ability to borrow information across related molecular measurements, resulting in more accurate imputation that preserves the underlying biological structure of the data.
Experimental Protocols for Multi-Omics Imputation
Protocol 1: Local Similarity-Based Imputation for Gene Expression Data
This protocol implements a clustering-based weighted K-nearest neighbors approach, which has demonstrated high accuracy for microarray gene expression data imputation [63].
Materials and Reagents
Table 2: Research Reagent Solutions for Multi-Omics Imputation
| Reagent/Resource | Specifications | Function/Purpose |
|---|---|---|
| Gene Expression Dataset | Microarray or RNA-seq data matrix (genes × samples) | Primary data for imputation analysis |
| Computational Environment | MATLAB, Python, or R with sufficient memory | Platform for algorithm implementation |
| Spectral Clustering Package | Custom or proprietary implementation | Initial partitioning of genes into clusters |
| K-means Algorithm | Standard implementation with optimization | Refinement of cluster assignments |
| Distance Metric Library | Euclidean, Pearson correlation, cosine similarity | Calculation of similarity between genes |
| Weighting Function | Inverse distance or similar weighting scheme | Emphasis on most similar neighbors for imputation |
Step-by-Step Procedure
Data Preprocessing:
- Format the gene expression dataset as a matrix G ∈ R^(N×M), where N represents genes and M represents samples
- Create a corresponding boolean matrix H ∈ R^(N×M) where hij = 1 if the value of Gij is present, and 0 if missing [63]
- Apply appropriate normalization to account for technical variations
Parameter Optimization:
- Determine optimal cluster size through evaluation of cluster quality metrics
- Optimize weighting factors for the distance metric
- Establish criteria for determining the number of nearest neighbors (K)
Spectral Clustering:
- Apply similarity-based spectral clustering combined with K-means to partition genes into clusters
- Validate cluster coherence using internal validation measures
- Adjust parameters iteratively to ensure biologically meaningful groupings
Weighted K-Nearest Neighbor Imputation:
- For each gene with missing values, identify its K-nearest neighbors within the same cluster using the weighted distance function
- Calculate the imputed value as a weighted average of the corresponding values from the nearest neighbors, with weights inversely proportional to their distance
- For each missing value at position (i,j): x̂ij = Σ(v∈Nk) xvj × wv, where Nk represents the set of k-nearest neighbors and w_v represents their respective weights [63]
Validation:
- Artificially introduce missing values into complete regions of the dataset
- Compare imputed values with original values using Root Mean Square Error (RMSE) or similar metrics
- Iteratively refine parameters to minimize imputation error
Protocol 2: Integrative Genomics and Proteomics Imputation for Biomarker Discovery
This protocol outlines an approach for handling missing data in integrated NGS proteomics and genomics data, particularly relevant for oncology biomarker discovery.
Materials and Reagents
- NGS Data: Whole exome sequencing or targeted sequencing data from tumor samples
- Proteomics Data: TMT-labeled mass spectrometry data from the same samples
- Bioinformatics Tools: BWA for alignment, GATK for variant calling, MaxQuant for protein identification/quantification
- Statistical Environment: R or Python with multivariate imputation capabilities
- Reference Databases: SwissProt human sequence database, population genomic reference panels
Step-by-Step Procedure
Data Generation and Preprocessing:
- For genomics: Perform whole exome sequencing using Illumina platforms with 150bp paired-end protocol, sequence to ~100x depth, align to reference genome (hg19) using BWA-MEM [67]
- For proteomics: Extract proteins from FFPE samples, digest with trypsin, label with TMT isobaric tags, analyze by nanoLC-MS/MS using Orbitrap mass spectrometer [67]
- Process proteomics data with MaxQuant using SwissProt human database, apply false discovery rate (FDR) threshold of 1% at protein and peptide level [67]
Data Integration and Missingness Assessment:
- Create a unified data matrix incorporating both genetic variants (e.g., from BRCA1, BRCA2, PTEN, PIK3CA) and protein expression values
- Quantify missingness patterns across omics layers and samples
- Classify missingness mechanisms (MCAR, MAR, MNAR) through statistical testing
Iterative Integrative Imputation:
- Employ a multi-omics imputation algorithm that leverages correlations between genetic variants and protein expression
- Utilize the Michigan Imputation Server (Minimac4) or similar platform for genotype imputation with ancestry-matched reference panels [62] [65]
- For proteomics data, apply iterative regression models that incorporate genomic information as predictors
- Implement cross-validation to assess imputation accuracy separately for each data type
Downstream Analysis and Validation:
- Perform correlation analysis between genomic alterations and protein expression (both cis and trans effects) [67]
- Identify significant associations while accounting for multiple testing (e.g., Bonferroni correction)
- Validate imputation results through independent measurements where available
Implementation Framework and Quality Control
Workflow Visualization
Quality Control Metrics for Imputation
Establishing robust quality control measures is essential for ensuring the reliability of imputed data:
Genotype Imputation Quality: Use metrics such as r² (measure of correlation between imputed and true genotypes) and proper info scores (for Minimac-based imputation) to assess accuracy [65]. Implement ancestry-matched reference panels to minimize population-specific biases.
Expression Data Imputation: Evaluate using root mean square error (RMSE) or normalized RMSE between imputed and actual values in complete data regions [64] [63]. Assess preservation of biological signals through correlation analysis with positive control genes.
Multi-Omics Consistency: Verify that imputed values maintain biologically plausible relationships between different molecular layers (e.g., non-synonymous mutations should not impute to neutral expression effects).
Downstream Impact: Monitor how imputation affects the results of key analyses such as differential expression, variant association tests, or biomarker identification.
Advanced imputation techniques represent a critical component in the multi-omics oncology research pipeline, enabling researchers to maximize the value of incomplete datasets while maintaining statistical rigor. The protocols outlined in this Application Note provide a framework for addressing missing data across various omics types, with particular emphasis on integrated genomics and proteomics approaches commonly employed in cancer biomarker discovery.
As multi-omics technologies continue to evolve, so too will imputation methodologies. Emerging approaches based on deep learning and transfer learning show particular promise for handling complex missing data patterns in heterogeneous patient populations [62] [66]. However, regardless of the specific technique employed, transparent reporting of imputation methods and quality metrics remains essential for ensuring the reproducibility and translational potential of oncology research findings.
By implementing robust, biologically-informed imputation strategies, researchers can enhance the power of their multi-omics analyses, leading to more reliable biomarker discovery and ultimately, more personalized approaches to cancer treatment.
Application Note: Mapping the Translational Pathway for NGS and Multi-Omics in Oncology
The integration of Next-Generation Sequencing (NGS) with other omics data represents a transformative approach in oncology research, enabling a comprehensive molecular understanding of tumors that can guide targeted therapeutic strategies. This application note outlines the critical barriers and potential solutions for translating these advanced genomic tools from research environments into routine clinical practice, with a specific focus on reimbursement challenges that impact widespread adoption. The transition from "bench to bedside" requires navigating complex logistical, financial, and educational hurdles that currently limit patient access to precision oncology approaches [68] [69].
The paradigm of cancer therapy is shifting from organ-based classification to molecularly-defined subtypes, largely enabled by NGS and comprehensive genomic profiling (CGP). These technologies allow researchers and clinicians to integrate genomic, transcriptomic, proteomic, and other layers of biological information to achieve a holistic view of tumors, tracing their evolutionary pathways and identifying potential therapeutic targets [70]. However, despite demonstrated clinical utility, significant implementation barriers persist across the translational continuum.
Quantitative Analysis of Implementation Barriers
Recent multi-stakeholder surveys have quantified the predominant barriers affecting NGS implementation across different specialist groups. The data reveals consistent concerns regarding reimbursement challenges, administrative burden, and knowledge gaps that hinder optimal utilization of NGS-based molecular profiling in clinical oncology.
Table 1: Physician-Reported Barriers to NGS Implementation (n=200)
| Barrier Category | Prevalence (%) | Specific Challenges | Specialty Variations |
|---|---|---|---|
| Reimbursement Issues | 87.5% | Prior authorization requirements (72%), knowledge of fee codes (68%), paperwork/administrative duties (67.5%) | Surgeons report greater challenges than other specialists |
| Knowledge Gaps | 81.0% | Understanding of NGS testing methodologies, interpretation of complex genomic data | More pronounced in community practice settings |
| Evidence Gaps | 80.0% | Perceived lack of clinical utility evidence for specific applications | Varies by cancer type and clinical scenario |
| Technical Concerns | 67.5% | Tissue sample sufficiency, turnaround time, test failure rates | Greater concern among pathologists and lab directors |
Table 2: Multi-Stakeholder Perspectives on NGS Barriers in Metastatic Breast Cancer
| Stakeholder Group | Sample Size | Key Barriers Identified | Testing Rate/Volume |
|---|---|---|---|
| Medical Oncologists | 109 | Reimbursement uncertainty, prior authorization complexity | 77% testing rate for HR+/HER2- mBC |
| Nurses & Physician Assistants | 50 | Administrative burden, patient education challenges | 66% testing rate for HR+/HER2- mBC |
| Lab Directors & Pathologists | 40 | Sample insufficiency, workflow integration issues | 40% NGS testing rate for breast cancer specimens |
| Payers | 31 | Lack of clear clinical guidelines (74%), internal consensus issues (45%), absence of NGS expertise (39%) | 33% unaware of current NCCN biomarker testing recommendations |
| Patients with mBC | 137 | High out-of-pocket costs, insurance coverage uncertainty | 50% with commercial insurance, 28% Medicare |
Reimbursement Challenges and Economic Barriers
Reimbursement instability constitutes the most significant barrier to widespread NGS implementation, affecting multiple stakeholders across the healthcare ecosystem. For clinicians, prior authorization requirements create substantial administrative burdens, with 72% of physicians citing this as a major challenge [71]. The complexity of navigating fee codes and understanding coverage criteria for different NGS assays further complicates implementation, particularly in community practice settings where dedicated administrative support may be limited.
Payers demonstrate notable knowledge gaps regarding NGS technologies and their appropriate applications. Approximately 33% of payers surveyed were unaware of current National Comprehensive Cancer Network (NCCN) biomarker testing recommendations, highlighting a critical disconnect between evidence-based guidelines and coverage policies [72]. This knowledge gap contributes to inconsistent coverage decisions and creates uncertainty for both providers and patients seeking access to comprehensive genomic profiling.
Patient-facing financial barriers include high out-of-pocket costs and unpredictable insurance coverage, which can lead to catastrophic financial toxicity or complete avoidance of recommended genomic testing. The economic burden disproportionately affects patients with government insurance or those treated in community settings where institutional support structures may be less developed [72].
Experimental Protocols
Protocol 1: Multi-Stakeholder Barrier Assessment Methodology
Objective
To systematically identify and quantify perceived barriers to NGS-based molecular profiling across key stakeholder groups in oncology, including medical oncologists, pathologists, payers, and patients.
Materials and Reagents
Table 3: Research Reagent Solutions for Stakeholder Analysis
| Item | Function | Application Notes |
|---|---|---|
| Validated Survey Instruments | Quantitative data collection on perceptions, barriers, and practice patterns | Ensure cross-stakeholder comparability with core question sets |
| Structured Interview Guides | Qualitative exploration of barrier implementation and potential solutions | Phone-based, 60-minute format with open-ended questions |
| Demographic Collection Tools | Characterization of respondent practice settings and patient populations | Include practice type, geographic region, patient volume metrics |
| Statistical Analysis Software | Quantitative analysis of survey responses and significance testing | R, SPSS, or SAS with appropriate licensing |
| Anonymous Data Collection Platform | Secure survey administration minimizing social desirability bias | HIPAA-compliant online survey tools with encryption |
Experimental Procedure
Stakeholder Recruitment: Implement stratified sampling across diverse clinical settings (academic centers, community practices, reference laboratories) and payer types (commercial, Medicare, Medicaid) to ensure representative participation. Target sample sizes should maintain statistical power while reflecting real-world distribution (e.g., 80% community-based oncologists reflecting actual patient care demographics) [72].
Survey Validation: Conduct preliminary qualitative interviews (60-minute duration) with representative stakeholders to inform survey development. Employ beta-testing with target audiences to ensure question clarity, appropriate answer options, and neutral framing. Utilize double-blinded protocols to minimize interviewer bias during qualitative phases [72].
Data Collection: Administer quantitative surveys through multiple recruitment channels to diversify respondents. Implement anonymity safeguards to reduce social desirability bias and encourage complete responses. Maintain demographic quotas to prevent oversampling of any single subgroup and ensure geographic, practice type, and institutional diversity.
Barrier Analysis: Calculate prevalence rates for specific barrier categories across stakeholder groups. Perform comparative analysis to identify significant variations between specialties, practice types, and geographic regions. Use multivariate regression to control for confounding variables and identify independent barrier predictors.
Solution Prioritization: Present findings to stakeholder focus groups for solution brainstorming and prioritization. Develop implementation frameworks ranked by perceived impact and feasibility, with specific attention to reimbursement mechanism redesign and educational infrastructure.
Data Analysis
The analytical workflow for processing and interpreting multi-stakeholder assessment data involves sequential phases from raw data to actionable insights, with particular emphasis on contrasting perspectives across different stakeholder groups.
Protocol 2: In-House NGS Implementation and Validation Framework
Objective
To establish a cost-effective, efficient in-house NGS testing program that addresses common barriers related to turnaround time, test selection, and result interpretation while maintaining analytical validity and clinical utility.
Materials and Reagents
Table 4: Essential Research Reagents for In-House NGS Implementation
| Item | Function | Application Notes |
|---|---|---|
| NGS Platform | High-throughput sequencing capability | Balance cost, throughput, and ease of use for clinical setting |
| CGP Assays | Comprehensive genomic profiling | FDA-approved or validated LDTs with pan-cancer claims |
| Bioinformatics Pipeline | Variant calling and interpretation | Clinical-grade, validated software with ongoing updates |
| Liquid Biopsy Kits | ctDNA extraction and analysis | Complement tissue testing; monitor resistance |
| AI-Assisted Analysis Tools | Pathological data integration and scoring | Improve diagnostic agreement and risk prediction |
| Quality Control Materials | Process monitoring and validation | Positive controls, reference standards, proficiency testing |
Experimental Procedure
Platform Selection: Evaluate NGS platforms based on institutional test volume, technical expertise, and financial considerations. Prioritize systems offering simplified workflows for community implementation while maintaining comprehensive genomic coverage. Consider semiconductor-based technologies that reduce capital investment and enable smaller-scale testing [73].
Test Menu Design: Implement reflex testing protocols based on tumor type and clinical scenario. Develop a stratified approach combining rapid, focused panels for time-sensitive first-line treatment decisions with comprehensive profiling for broader biomarker discovery and second-line therapy planning [74].
Workflow Optimization: Establish automated bioinformatics pipelines that integrate with electronic health records to facilitate result reporting and clinical decision support. Implement batch analysis strategies for cost efficiency while maintaining capacity for stat single-sample runs for urgent clinical needs [73].
Validation Protocol: Conduct analytical validation studies assessing accuracy, precision, sensitivity, specificity, and reportable ranges for all assays. Perform clinical validation correlating biomarker findings with treatment outcomes and therapeutic responses across cancer types.
Education Integration: Develop structured education programs for oncologists, pathologists, and allied health professionals covering test ordering, interpretation, and clinical application. Create clinical decision support tools that embed guideline recommendations into test ordering and result reporting workflows.
Data Analysis
The implementation of in-house NGS testing requires careful consideration of multiple interconnected workflow components, with particular attention to the balance between comprehensive genomic profiling and rapid turnaround times for critical treatment decisions.
Protocol 3: Evidence Generation for Reimbursement Strategy
Objective
To develop and implement a comprehensive evidence generation strategy that demonstrates the clinical utility and economic value of NGS-based testing to support favorable coverage policies and appropriate reimbursement.
Materials and Reagents
Table 5: Research Materials for Evidence Generation
| Item | Function | Application Notes |
|---|---|---|
| Real-World Data Platforms | Collection of clinical outcomes and utilization data | EHR-integrated systems capturing treatment patterns |
| Health Economic Models | Cost-effectiveness analysis and budget impact assessment | Framework linking testing to outcomes and costs |
| Clinical Registry Platforms | Prospective data collection across multiple sites | Structured data capture for specific cancer types |
| Patient-Reported Outcome Tools | Assessment of quality of life and functional status | Validated instruments capturing patient experience |
| Comparative Effectiveness Frameworks | Analysis of outcomes vs. alternative approaches | Retrospective and prospective study designs |
Experimental Procedure
Stakeholder Alignment: Engage payers early in evidence planning to understand specific evidence requirements and address perceived gaps. Conduct advisory boards with medical directors from commercial and government payers to identify evidentiary priorities and threshold criteria for coverage [72].
Real-World Evidence Generation: Implement structured data collection across multiple practice settings to document testing patterns, treatment decisions, and patient outcomes. Focus on key endpoints including time to treatment failure, therapy selection alignment with biomarker results, and overall survival correlated with testing-guided management.
Economic Analysis: Develop budget impact models that account for testing costs, targeted therapy expenses, and reductions in ineffective treatment utilization. Calculate cost-per-correctly-treated-patient metrics that reflect the efficiency gains of precision medicine approaches compared to empirical therapy selection.
Clinical Utility Demonstration: Design studies measuring diagnostic yield, change in management, and clinical outcomes following NGS implementation. Employ matched control cohorts or historical comparisons to isolate the impact of testing beyond standard approaches.
Evidence Dissemination: Prepare comprehensive dossiers for payer submission incorporating clinical guidelines, economic analyses, and real-world outcomes. Participate in health technology assessment processes and pursue public policy initiatives that support appropriate reimbursement for comprehensive genomic profiling.
Discussion and Future Directions
Integrated Solutions for Barrier Mitigation
Addressing the multifactorial barriers to NGS adoption requires coordinated interventions across technical, educational, and financial domains. The integration of artificial intelligence and machine learning platforms shows particular promise for reducing interpretation complexity and improving accessibility for community practitioners. AI tools can enhance diagnostic agreement among pathologists and improve accuracy in identifying patients who may benefit from targeted therapies [75]. Additionally, AI-powered platforms are demonstrating significant efficiency improvements in clinical trial matching and data abstraction, potentially reducing manual screening time while increasing patient access to targeted therapies [76].
Educational initiatives must extend beyond traditional academic detailing to include implementation science frameworks that address workflow integration and clinical decision support. The development of simplified NGS platforms specifically designed for community implementation represents a critical advancement for expanding access beyond academic centers [74] [73]. As technology continues to evolve, multiomics approaches that integrate genomic, transcriptomic, proteomic, and other data layers will further enhance the precision of cancer classification and treatment selection, though these approaches introduce additional complexity into implementation and reimbursement frameworks [70].
Policy Implications and System Reform
Achieving sustainable implementation of NGS and multiomics technologies in oncology will require structural reforms to address fundamental misalignments in reimbursement systems and evidence assessment frameworks. Current payment models often fail to recognize the full value of comprehensive genomic profiling, focusing instead on narrow technical components without adequately accounting for the clinical decision support, interpretation requirements, and ongoing result refinement that these complex tests necessitate [69].
The development of harmonized regulatory pathways and evidence standards across international jurisdictions could accelerate implementation while reducing duplication. Collaborative validation networks that connect reference laboratories across multiple regions enable standardized testing, data sharing, and cost distribution, making precision diagnostics more accessible and affordable [69]. Additionally, reforming academic reward systems to value implementation science alongside basic research discovery would help address the translational gap that currently limits the clinical impact of many biomarker discoveries.
The successful bench-to-bedside translation of NGS and multiomics technologies ultimately depends on creating a sustainable ecosystem that aligns incentives across researchers, clinicians, patients, payers, and diagnostic manufacturers. By addressing the identified barriers through coordinated technological innovation, educational enhancement, and policy reform, the oncology community can realize the full potential of precision medicine to improve patient outcomes across diverse care settings.
Proving the Promise: Analytical Validation, Clinical Utility, and Comparative Frameworks
The integration of next-generation sequencing (NGS) with other omics data types has become a cornerstone of modern oncology research, enabling a multidimensional view of tumor biology. However, the combining of assays—particularly spatial transcriptomics, proteomics, and single-cell analyses—introduces significant challenges in validation and interpretation. Establishing rigorous benchmarking protocols is essential to quantify the performance characteristics of these integrated workflows, ensuring that the biological insights generated are reliable and reproducible. This application note provides a structured framework for evaluating the sensitivity, specificity, and concordance of multi-assay approaches, with a specific focus on spatially resolved technologies within oncology. The protocols outlined herein are designed to provide researchers with standardized methods for assessing platform performance, enabling informed experimental design and robust data integration in line with the broader thesis of unifying NGS with multi-omics data streams.
Performance Benchmarking of Spatial Omics Platforms
Recent systematic comparisons of commercial imaging-based spatial transcriptomics (iST) platforms reveal distinct performance characteristics critical for experimental design in oncology research. The following tables synthesize quantitative data from key benchmarking studies, providing a comparative overview of platform performance.
Table 1: Benchmarking Metrics Across Imaging Spatial Transcriptomics Platforms (FFPE Tissues) [77]
| Performance Metric | 10X Xenium | Nanostring CosMx | Vizgen MERSCOPE |
|---|---|---|---|
| Transcript Counts per Gene | Consistently higher | High | Variable |
| Concordance with scRNA-seq | High | High | Not specified |
| Cell Sub-clustering Capability | Slightly more clusters | Slightly more clusters | Fewer clusters |
| False Discovery Rate | Varies | Varies | Varies |
| Cell Segmentation Error | Varies | Varies | Varies |
Table 2: Performance of High-Throughput Subcellular Resolution Platforms [78]
| Platform | Technology Type | Gene Panel Size | Sensitivity (Marker Genes) | Correlation with scRNA-seq |
|---|---|---|---|---|
| Xenium 5K | Imaging-based (iST) | 5001 genes | Superior | High |
| CosMx 6K | Imaging-based (iST) | 6175 genes | Lower than Xenium | Substantial deviation |
| Visium HD FFPE | Sequencing-based (sST) | ~18,085 genes | High | High |
| Stereo-seq v1.3 | Sequencing-based (sST) | Whole-transcriptome | High | High |
Key Insights from Benchmarking Data
- Sensitivity and Specificity Trade-offs: Across studies, 10X Xenium consistently demonstrated higher transcript counts per gene without sacrificing specificity, a crucial factor for detecting low-abundance oncology biomarkers [77]. In a multi-platform assessment, Xenium 5K showed superior sensitivity for key marker genes like EPCAM compared to CosMx 6K and other platforms [78].
- Concordance with Orthogonal Methods: Data from Xenium and CosMx show strong concordance with single-cell RNA sequencing (scRNA-seq) data, providing confidence in their quantitative accuracy for transcript measurement [77]. Stereo-seq v1.3, Visium HD FFPE, and Xenium 5K exhibited high gene-wise correlation with matched scRNA-seq profiles, whereas CosMx 6K showed substantial deviation despite high total transcript counts, suggesting potential platform-specific biases in probe design or detection efficiency [78].
- Impact on Downstream Biology: All commercial iST platforms enable spatially resolved cell typing, but with varying sub-clustering capabilities. Xenium and CosMx identified slightly more cell clusters than MERSCOPE in a TMA analysis, though with different false discovery rates and cell segmentation error frequencies, indicating that choice of platform can influence the apparent cellular heterogeneity in a tumor sample [77].
Experimental Protocols for Benchmarking Integrated Assays
Protocol 1: Cross-Platform Validation of Spatial Transcriptomics
Objective: To systematically compare the sensitivity, specificity, and concordance of multiple spatial transcriptomics platforms using sequential sections from the same Formalin-Fixed Paraffin-Embedded (FFPE) tissue block [77] [78].
Materials:
- FFPE tissue blocks (e.g., multi-tissue TMAs containing tumor and normal tissues)
- Serial sections (4-5 µm thickness)
- Commercial iST platforms (10X Xenium, Nanostring CosMx, Vizgen MERSCOPE)
- scRNA-seq platform (e.g., 10X Chromium) for orthogonal validation
Procedure:
- Sample Preparation: Cut sequential sections from the same FFPE block under identical conditions to minimize pre-analytical variability.
- Panel Design: For targeted iST platforms (Xenium, MERSCOPE), design gene panels with significant overlap (>65 genes) to enable direct cross-platform comparison. Include standard panels where custom design is not feasible [77].
- Platform Processing: Process each serial section according to the manufacturer's specified protocol for each platform. Ensure sample baking times are matched for head-to-head comparisons [77].
- Orthogonal Validation: Process a dissociated sample from the same tumor for scRNA-seq using a platform such as 10X Chromium Single Cell Gene Expression FLEX [77] [78].
- Data Processing: Use each manufacturer's standard base-calling and segmentation pipeline to generate count matrices and cell boundaries.
- Data Aggregation: Subsample and aggregate data to individual tissue cores or regions of interest (ROIs) for comparative analysis [77].
Protocol 2: Integrated Multi-Omics Concordance Assessment
Objective: To evaluate the concordance between spatial transcriptomics data and protein expression patterns from adjacent tissue sections, establishing a ground truth for molecular localization [78].
Materials:
- Matected tumor samples (e.g., colon adenocarcinoma, hepatocellular carcinoma, ovarian cancer)
- FFPE and fresh-frozen (OCT-embedded) tissue blocks
- Spatial transcriptomics platforms (e.g., Xenium 5K, CosMx 6K, Visium HD)
- CODEX (Co-Detection by Indexing) system for multiplexed protein detection
- scRNA-seq platform
Procedure:
- Multi-Modal Sample Processing: Divide tumor samples and process them into FFPE blocks, fresh-frozen OCT blocks, and single-cell suspensions according to the requirements of each technology platform [78].
- Serial Sectioning: Generate serial tissue sections for parallel profiling on ST platforms and adjacent sections for CODEX protein profiling.
- Spatial Transcriptomics: Perform ST profiling on all platforms according to manufacturer protocols, ensuring coverage of shared gene targets where possible.
- Protein Profiling: Perform CODEX staining on adjacent sections to profile protein expression, creating a spatial proteomic map for comparison.
- Single-Cell RNA Sequencing: Perform scRNA-seq on dissociated cells from the same tumor sample to provide a non-spatial transcriptional reference [78].
- Manual Annotation: Manually annotate cell types in both scRNA-seq and CODEX data, and delineate nuclear boundaries in H&E and DAPI-stained images to establish ground truth for segmentation and cell type identification [78].
Analysis Workflow for Performance Metrics
The following diagram illustrates the logical workflow for analyzing platform performance benchmarking data:
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Key Research Reagent Solutions for Multi-Omics Benchmarking
| Reagent/Material | Function | Application Notes |
|---|---|---|
| FFPE Tissue Microarrays (TMAs) | Contains multiple tissue cores (tumor/normal) on a single slide for parallel processing. | Use TMAs with 0.6-1.2 mm diameter cores from diverse cancer types [77]. |
| Commercial iST Gene Panels | Targeted probe sets for transcript detection on specific platforms. | Select panels with overlapping genes (>65) for cross-platform comparison; consider custom design [77]. |
| CODEX Antibody Panels | Multiplexed protein detection cocktails for spatial proteomics. | Use on sections adjacent to ST panels to establish protein-based ground truth [78]. |
| Single-Cell RNA-seq Kits | (e.g., 10X Chromium) for generating orthogonal transcriptomic data. | Provides dissociation-based scRNA-seq reference to compare against spatial data [77] [78]. |
| Nucleus Segmentation Dyes | (e.g., DAPI) for defining cellular boundaries in imaging platforms. | Critical for accurate cell segmentation and downstream cell-type annotation [78]. |
Visualization of Integrated Multi-Omics Analysis Workflow
The following diagram illustrates the comprehensive experimental workflow for generating and validating multi-omics benchmarking data:
Rigorous benchmarking of integrated assays is a prerequisite for generating reliable, biologically meaningful data from multi-omics studies in oncology. The application notes and protocols detailed herein provide a standardized framework for evaluating the critical performance metrics of sensitivity, specificity, and concordance across rapidly evolving spatial technologies. As the field progresses toward increasingly complex multi-omic integrations, these benchmarking practices will ensure that research and clinical conclusions are built upon a foundation of rigorously validated data, ultimately accelerating the translation of molecular insights into improved patient outcomes in oncology.
The profound molecular heterogeneity inherent in cancer presents a significant challenge to traditional, single-analyte diagnostic approaches and often leads to therapeutic resistance and disease relapse [4]. Multi-omics integration—the synergistic combination of genomic, transcriptomic, epigenomic, proteomic, and metabolomic data—provides a powerful framework to overcome this challenge by constructing a comprehensive molecular atlas of a patient's malignancy [4] [3]. This holistic view is crucial for deciphering the complex biological networks that drive oncogenesis and adaptive resistance, thereby enabling more precise therapy selection and dynamic monitoring of treatment response [16] [9].
The clinical imperative for this integrated approach is underscored by the limitations of single-modality biomarkers. For instance, while KRAS G12C inhibitors can achieve rapid initial responses in colorectal cancer, resistance universally emerges via parallel pathway reactivation or epigenetic remodeling—mechanisms that are only detectable through integrated proteogenomic and phosphoproteomic profiling [4]. Similarly, the integration of radiomics with plasma cfDNA methylation signatures can enhance diagnostic specificity over imaging features alone [4]. Artificial intelligence (AI) and machine learning (ML) serve as the essential engine for this integration, enabling the scalable, non-linear analysis of disparate, high-dimensional omics layers to extract clinically actionable insights [4] [79]. This application note details a protocol for employing multi-omics strategies to guide therapy selection and monitor resistance, framed within a broader thesis on the integration of next-generation sequencing (NGS) with other omics data in oncology.
Case Study: Tracking Richter Transformation in Chronic Lymphocytic Leukemia (CLL)
Clinical Presentation and Challenge
A patient with a history of indolent Chronic Lymphocytic Leukemia (CLL) presented with a sudden onset of B symptoms (fever, night sweats, weight loss) and rapid lymphadenopathy. Clinical suspicion was high for Richter Transformation (RT), a well-documented transformation of CLL into an aggressive lymphoma, most commonly diffuse large B-cell lymphoma (DLBCL) [80]. This transformation is a hallmark of cancer evolution driven by intra-tumoral heterogeneity (ITH), where pre-existing or newly acquired molecular alterations in a subclone of cells confer a selective growth advantage, leading to aggressive disease [31]. Predicting this transformation and understanding its drivers using conventional single-timepoint, single-omics biopsies had previously been ineffective.
Multi-Omics Profiling Strategy
To dissect the molecular underpinnings of this transformation, a multi-omics analysis was performed on a formalin-fixed, paraffin-embedded (FFPE) lymph node biopsy specimen using the GoT-Multi (Genotyping of Transcriptomes) platform [80]. This single-cell multi-omics tool allowed for the simultaneous tracking of numerous gene mutations while recording gene expression profiles from individual cancer cells, even from archived pathology samples.
- Technology: GoT-Multi, a single-cell genotyping-of-transcriptomes method.
- Sample Type: FFPE tissue block.
- Molecular Layers Integrated:
- Genomics: Targeted sequencing of a panel of >25 known driver genes in CLL/RT (e.g., TP53, NOTCH1, SF3B1, MYC).
- Transcriptomics: Single-cell RNA sequencing (scRNA-seq) to profile the full transcriptome of tens of thousands of individual cells.
- Data Integration: The genotypic information (mutations) for each cell was directly linked to its phenotypic state (gene expression profile), creating a unified genotype-to-phenotype map of the tumor ecosystem [80].
Key Findings and Clinical Action
The integrated data revealed a complex landscape of clonal evolution, summarized in the table below.
Table 1: Key Clonal Populations Identified via Multi-Omics Analysis in Richter Transformation
| Clonal Population | Genomic Alterations | Transcriptomic Signature | Inferred Biological Behavior | Clinical Implication |
|---|---|---|---|---|
| Pre-existing CLL Clone | SF3B1 mutation | Quiescent gene expression profile | Indolent, slow-growing | Not the driver of current aggressive disease |
| Emerging RT Subclone | TP53 mutation, MYC amplification | High proliferation, DNA repair pathways | Rapid growth, therapy resistance | Primary driver of transformation; target with aggressive regimen |
| Inflammatory Subclone | NOTCH1 mutation | Upregulation of NF-κB, cytokine signaling | Stromal remodeling, immune suppression | Contributes to hostile microenvironment; potential immunomodulatory target |
The analysis demonstrated that the Richter Transformation was not driven by the predominant initial CLL clone (with an SF3B1 mutation), but by a minor subclone that had acquired a TP53 mutation and MYC amplification [80] [31]. Crucially, the transcriptomic data from these specific cells showed activated proliferative and inflammatory pathways, directly linking the mutations to the aggressive phenotype.
- Therapy Selection: Based on the identification of the TP53-mutated, MYC-amplified subclone as the driver of resistance and transformation, the treatment strategy was shifted from standard chemoimmunotherapy to a more targeted and aggressive regimen. This included agents designed to overcome TP53-associated resistance and target MYC-driven proliferation.
- Resistance Monitoring: The baseline multi-omics snapshot established a benchmark. Subsequent liquid biopsies monitoring circulating tumor DNA (ctDNA) for the TP53 mutation and MYC amplification allowed for dynamic assessment of treatment response and the emergence of any new resistant subclones, enabling timely therapy adjustments [4] [81].
Experimental Protocols for Multi-Omics Integration
The following protocols outline a generalized workflow for integrating NGS with other omics data for therapy selection and resistance monitoring, adaptable to various cancer types.
Protocol 1: Longitudinal Sample Collection and Processing
Objective: To collect and process matched tissue and liquid biopsy samples at multiple time points for multi-omics analysis.
Materials:
- Fresh tumor tissue (from core biopsy or resection)
- Matched FFPE tissue blocks
- Peripheral blood samples (for plasma separation and liquid biopsy)
- ApoStream or similar platform for circulating tumor cell (CTC) isolation [82]
Procedure:
- Baseline Sampling:
- Obtain fresh tumor tissue and immediately preserve a portion in RNAlater for transcriptomics and snap-freeze another for DNA/protein extraction. A second portion should be formalin-fixed and paraffin-embedded for histology and spatial omics.
- Collect peripheral blood (e.g., 10 mL in EDTA tubes) and process via double centrifugation to isolate plasma for cell-free DNA (cfDNA) analysis. Isolate CTCs using a platform like ApoStream for single-cell analysis [82].
- Longitudinal Monitoring:
- At each follow-up visit (e.g., every 2-3 cycles of therapy), repeat the blood collection for plasma and CTC isolation.
- If a new lesion appears or existing disease progresses, consider a repeat tissue biopsy.
- Nucleic Acid Extraction:
- Extract gDNA from frozen tissue and buffy coat (for germline control) using a commercial kit. Extract cfDNA from plasma using a specialized cfDNA extraction kit.
- Extract total RNA from tissue preserved in RNAlater, ensuring an RNA Integrity Number (RIN) > 7.0 for sequencing.
Protocol 2: Multi-Omics Data Generation
Objective: To generate high-quality genomic, transcriptomic, and epigenomic datasets from processed samples.
Materials:
- Illumina NovaSeq or similar NGS platform
- 10x Genomics Chromium X platform for single-cell assays
- DNA methylation array (e.g., Illumina EPIC)
- Mass spectrometer for proteomics (e.g., LC-MS/MS)
Procedure:
- Whole Exome Sequencing (WES):
- Prepare libraries from tumor gDNA and matched germline DNA using an exome capture kit (e.g., Illumina Nextera Flex for Enrichment).
- Sequence on an Illumina platform to a minimum mean coverage of 100x for tumor and 30x for germline DNA.
- Bulk and Single-Cell RNA Sequencing:
- For bulk RNA-seq, prepare libraries from total RNA using a stranded mRNA-seq kit. Sequence to a depth of ~50 million paired-end reads per sample.
- For single-cell RNA-seq, generate single-cell suspensions from fresh tissue. Use the 10x Genomics Chromium X platform with a 3' or 5' gene expression kit to profile >10,000 cells per sample [83].
- DNA Methylation Profiling:
- Treat 500 ng of tumor gDNA with bisulfite using a commercial conversion kit.
- Hybridize the converted DNA to an Illumina EPIC methylation array according to the manufacturer's instructions.
- (Optional) Proteomic Profiling:
- Perform protein extraction and tryptic digestion from frozen tissue.
- Analyze peptides using liquid chromatography-tandem mass spectrometry (LC-MS/MS) on a high-resolution instrument to quantify protein and phosphoprotein abundance [9].
Protocol 3: Data Integration and AI-Driven Analysis
Objective: To integrate multi-omics data layers to define clonal architecture, infer transcriptional programs, and predict therapeutic vulnerabilities.
Materials:
- High-performance computing cluster
- Bioinformatics software (Seurat v5, Muon, iCluster)
- AI/ML libraries (PyTorch, TensorFlow)
Procedure:
- Primary Data Analysis:
- WES: Align sequences to a reference genome (e.g., GRCh38). Call somatic single-nucleotide variants (SNVs) and copy number variations (CNVs) using tools like Mutect2 and GATK. Infer clonal architecture and cancer cell fractions (CCF) using tools like PyClone [31].
- RNA-seq: Align reads and generate gene-level counts. For scRNA-seq data, process using the Seurat or Scanpy pipeline, including quality control, normalization, clustering, and cell type annotation [83] [9].
- Methylation Data: Preprocess with R package
minfi. Identify differentially methylated regions (DMRs) associated with clinical features.
- Horizontal and Vertical Integration:
- Horizontal: Integrate bulk and single-cell transcriptomics data using anchor-based integration in Seurat v5 to map cell populations and identify rare transitional cell states [9].
- Vertical: Use multi-omics factor analysis (MOFA+) or iCluster to integrate somatic mutations (genomics), CCFs (clonal architecture), gene expression (transcriptomics), and methylation status (epigenomics) from the same patient [3] [9].
- AI-Driven Clinical Inference:
- Train a Graph Neural Network (GNN) on the integrated data, modeling protein-protein interaction networks to identify druggable hubs perturbed by specific mutations in the dominant resistant subclone [4].
- Employ Explainable AI (XAI) techniques like SHAP (SHapley Additive exPlanations) to interpret model outputs and clarify the contribution of each genomic variant and gene expression program to the predicted therapy resistance score [4].
- Output a ranked list of potential therapeutic strategies based on the integrated molecular profile.
Visualizing the Multi-Omics Workflow and Tumor Evolution
The following diagram illustrates the complete experimental and analytical pipeline for multi-omics-based therapy selection and resistance monitoring.
Diagram 1: Integrated multi-omics workflow for clinical decision support in oncology. The process flows from sample collection through data generation and AI-powered integration to clinical reporting and monitoring, creating a feedback loop for adaptive therapy.
The Scientist's Toolkit: Essential Research Reagents and Platforms
Table 2: Key Research Reagent Solutions for Multi-Omics Studies in Oncology
| Category / Item | Function / Application | Example Product / Platform |
|---|---|---|
| Sample Preparation | ||
| CTC Enrichment Platform | Isolates circulating tumor cells from liquid biopsies for downstream molecular analysis. | ApoStream [82] |
| Genomics | ||
| NGS Library Prep Kit | Prepares sequencing libraries from low-input or degraded DNA (e.g., from FFPE). | Illumina DNA Prep |
| Whole Exome Enrichment | Captures exonic regions for efficient variant discovery. | Illumina Nextera Flex for Enrichment |
| Transcriptomics | ||
| Single-Cell RNA-seq Kit | Enables high-throughput barcoding of RNA from thousands of single cells. | 10x Genomics Chromium Single Cell 3' Kit [83] |
| Epigenomics | ||
| Methylation Array | Genome-wide profiling of DNA methylation status at single-base resolution. | Illumina Infinium MethylationEPIC Kit |
| Data Integration & AI | ||
| Multi-Omics Database | Provides curated, analysis-ready multi-omics datasets for model training and validation. | MLOmics [79] |
| Graph Neural Network (GNN) | Models biological networks to identify dysregulated, druggable pathways from integrated data. | PyTorch Geometric [4] |
| Multi-Omics Factor Analysis | Integrates multiple omics data types to disentangle sources of variation and identify latent factors. | MOFA+ [9] |
Next-generation sequencing (NGS)-based comprehensive genomic profiling (CGP) and traditional single-gene testing (SGT) represent two divergent methodologies for identifying genomic alterations in cancer. While SGT has historically been favored for its perceived cost-effectiveness and rapid turnaround, CGP leverages massively parallel sequencing to evaluate hundreds of genes simultaneously, detecting all major variant classes—single nucleotide variants (SNVs), insertions/deletions (indels), copy number alterations (CNAs), fusions, and genomic signatures like tumor mutational burden (TMB) and microsatellite instability (MSI) [84] [85]. This application note provides a structured comparison of these approaches, emphasizing technical workflows, clinical performance, and integration with multi-omics data in oncology research.
Performance Comparison: CGP vs. SGT
Table 1: Key Metrics for CGP and SGT in NSCLC
| Parameter | Single-Gene Testing (SGT) | Comprehensive Genomic Profiling (CGP) |
|---|---|---|
| Genes Interrogated | 1–5 genes per test [86] | 324–724 genes in a single assay [85] [87] |
| Variant Types Detected | Limited to specific alterations (e.g., SNVs, fusions) | SNVs, indels, CNAs, fusions, TMB, MSI [85] [88] |
| Tissue Consumption | High (≤50 slides for full SGT panel) [86] | Low (≤20 slides) [86] |
| Tissue Insufficiency Rates | 17% after SGT [86] | 7% when used as first-line test [86] |
| Turnaround Time (TAT) | Variable (prolonged with sequential tests) [84] | ≤14 days for consolidated results [86] |
| Actionable Alterations Detected | 2.6–46% in SGT-negative cases [84] [86] | 46–53% in NSCLC [86] |
Table 2: Limitations of SGT and Advantages of CGP
| SGT Limitations | CGP Advantages |
|---|---|
| Inability to detect novel/rearrangements (e.g., MET exon 14 skipping) [84] | Identifies rare fusions (e.g., NTRK, ALK-MAP4K3) and complex signatures [88] [87] |
| Exhausts tissue, necessitating re-biopsy [86] | Conserves tissue for multi-omics applications [85] [88] |
| Restricted scope misses co-occurring alterations [84] | Enables analysis of concurrent mutations and pathway interactions [87] |
Experimental Protocols for CGP
Sample Preparation and Library Construction
Workflow Overview:
- Input Material: Formalin-fixed paraffin-embedded (FFPE) tissue or cell-free DNA (cfDNA) from liquid biopsy [87].
- Nucleic Acid Extraction: Isolate DNA/RNA using silica-based columns or magnetic beads. For FFPE, assess DNA integrity via DV200 (≥50% recommended) [84].
- Library Preparation:
- Sequencing: Use Illumina platforms (NovaSeq X) for short-read sequencing (75–300 bp) at ≥500× coverage [12] [20].
Data Analysis and Multi-Omics Integration
- Variant Calling: Align reads to reference genome (GRCh38) using BWA-MEM; call variants with tools like DeepVariant [20].
- TMB/MSI Calculation: TMB = total mutations per megabase; MSI assessed via >4,000 markers [87].
- Multi-Omics Correlation: Integrate genomic data with transcriptomic (RNA-seq) and proteomic (mass spectrometry) profiles to resolve pathways like PI3K-AKT-mTOR [3] [20].
Visualization of Testing Pathways and Outcomes
Diagram 1: NSCLC Genomic Testing Workflow Comparison
Title: Testing Workflows and Tissue Use
Diagram 2: Multi-Omics Data Integration from CGP
Title: Multi-Omics Data Integration
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Reagents and Platforms for CGP
| Reagent/Platform | Function | Example Use in CGP |
|---|---|---|
| FFPE DNA/RNA Kits (QIAseq, TruSight) | Nucleic acid extraction and quality control | DV200 assessment for degraded samples [87] |
| Hybrid Capture Panels (xHYB, TSO500) | Target enrichment for 500–724 genes | Detection of SNVs, indels, and fusions [85] [87] |
| UMI Adapters | Error suppression and variant validation | Discrimination of true mutations from PCR artifacts [87] |
| NGS Platforms (Illumina NovaSeq X) | High-throughput sequencing | Whole-exome/transcriptome sequencing [12] [20] |
| AI-Based Software (DeepVariant) | Variant calling and annotation | Identification of low-frequency mutations [20] |
Discussion and Future Directions
CGP outperforms SGT by enabling comprehensive genomic characterization while conserving tissue for multi-omics studies. Emerging trends include AI-driven interpretation of complex genomic data [20], liquid biopsy-based CGP for real-time monitoring [12] [87], and spatial transcriptomics for contextualizing alterations within tumor microenvironments [89]. For researchers, prioritizing CGP over SGT ensures alignment with precision oncology goals, facilitating biomarker discovery and therapeutic innovation.
The integration of Next-Generation Sequencing (NGS) with other omics data represents a transformative approach in oncology research, enabling unprecedented insights into tumor biology and therapeutic targeting. However, the path from research discovery to clinically actionable insight is paved with regulatory and quality considerations. Europe's In Vitro Diagnostic Regulation (IVDR) has emerged as a pivotal regulatory framework, creating what industry experts describe as a "regulatory stress test" for biomarker and companion diagnostic development [90]. This framework is reshaping how multi-omics approaches must be structured to meet clinical-grade standards, particularly for companion diagnostics that guide therapeutic decisions in oncology.
The complexity of multi-omics data integration—spanning genomics, transcriptomics, proteomics, metabolomics, and epigenomics—introduces unique challenges for regulatory compliance. Each data type possesses distinct characteristics, measurement variability, and analytical requirements that must be harmonized to ensure reproducible, clinically valid results [3] [50]. This application note establishes standardized protocols and quality frameworks to navigate these challenges, providing researchers with practical pathways to maintain scientific rigor while complying with evolving regulatory expectations in oncology applications.
Regulatory Landscape: IVDR as a Framework for Multi-Omics
Key IVDR Challenges and Implications
The implementation of IVDR has revealed several specific pain points that directly impact multi-omics development in oncology research. Understanding these challenges is essential for designing compliant studies and analytical workflows.
Table 1: Key IVDR Challenges for Multi-Omics Applications in Oncology
| Challenge Category | Specific Implementation Hurdle | Impact on Multi-Omics Development |
|---|---|---|
| Regulatory Uncertainty | Poorly defined requirements for novel multi-analyte algorithms | Uncertainty in compliance pathway for integrated diagnostic models |
| Jurisdictional Inconsistencies | Differing interpretations between EU member states | Complex trial planning for multi-center oncology studies |
| Transparency Gaps | No centralized EU database of approved diagnostics | Slower learning curves and inefficient benchmarking |
| Timeline Unpredictability | Notified bodies not bound by strict review deadlines | Difficulty synchronizing drug-companion diagnostic launches |
| Definitional Variances | Differing interpretations of "health institution" across regions | Compliance complications for academic medical centers |
These regulatory challenges are particularly acute for multi-omics applications because they often combine multiple analytes and algorithmic approaches that may not fit neatly into traditional regulatory categories [90]. The rigidity of the current environment has, in some cases, pushed innovation outside Europe altogether, though regulators are gaining experience and processes are slowly becoming more transparent.
Strategic Approaches to IVDR Compliance
Successful navigation of the IVDR landscape requires proactive strategic planning from the earliest stages of assay development. Several approaches can mitigate regulatory risk:
- Partner Selection: Choosing established regulatory partners with IVDR experience (e.g., Qiagen, Leica, Roche) can smooth the path when certainty and collaboration are non-negotiable [90].
- Early Engagement: Proactive dialogue with notified bodies during development phases helps align analytical validation strategies with regulatory expectations.
- Modularity in Design: Developing multi-omics assays with modular components that can be validated separately may simplify the regulatory review process.
- Transparent Documentation: Maintaining exhaustive documentation of analytical validation, including all integration algorithms and computational methods, is essential for regulatory review.
IVDR Compliance Strategy Map
Quality Control Framework for Multi-Omics Data Generation
Analytical Quality Metrics Across Omics Layers
Clinical-grade multi-omics requires rigorous quality control at each analytical layer, with established metrics and thresholds tailored to each data type. The framework below outlines key quality parameters that should be monitored throughout data generation.
Table 2: Quality Control Metrics for Multi-Omics Data Types in Oncology
| Omics Layer | Key Quality Metrics | Clinical-Grade Thresholds | Monitoring Frequency |
|---|---|---|---|
| Genomics (NGS) | Coverage depth (>100x), mapping quality (Q30 > 80%), contamination rate (<0.5%) | Minimum 200x for somatic variants; Q30 > 85% for clinical samples | Per sequencing run & per sample |
| Transcriptomics | RNA integrity number (RIN > 7), library complexity (>70%), rRNA contamination (<5%) | RIN > 8 for formalin-fixed paraffin-embedded (FFPE) samples | Per sample extraction & library prep |
| Proteomics | Protein quantification CV (<15%), missing data (<10%), intensity distribution | CV < 10% for labeled quantitation; <20% for label-free | Per MS batch & sample preparation |
| Epigenomics | Bisulfite conversion efficiency (>99%), coverage uniformity (>80% of CpGs) | >99.5% conversion for methylation analysis | Per conversion batch & sequencing run |
| Metabolomics | Peak resolution, retention time stability (CV < 2%), reference standard recovery (85-115%) | Internal standard CV < 15% across batch | Each analytical batch |
Integrated Quality Monitoring Protocol
A standardized protocol for integrated quality monitoring ensures consistent data quality across multi-omics experiments:
Protocol 1: Cross-Omics Quality Assessment Workflow
Pre-analytical Sample Assessment
- Document sample integrity metrics (RIN, tissue quality, cellularity)
- Verify sample matching across omics platforms using genotyping or barcoding
- Confirm sample storage conditions and freeze-thaw cycles meet pre-defined criteria
Intra-assay Quality Control
- Process and monitor internal reference standards with each batch
- Track technical replicates to assess precision (CV < 15% across all omics layers)
- Monitor contamination indicators (e.g., foreign RNA, microbial DNA)
Inter-assay Integration Quality Assessment
- Assess biological concordance across platforms (e.g., RNA-protein correlation)
- Verify expected technical correlations (e.g., copy number variation and expression)
- Apply batch effect correction algorithms (e.g., ComBat) when necessary
Data Integration Readiness Assessment
- Confirm all data types pass individual QC thresholds before integration
- Document any quality-driven sample exclusions with justification
- Generate integrated quality report for regulatory review
Multi-Omics Quality Assessment Workflow
Experimental Protocols for Validated Multi-Omics Integration
Protocol for Adaptive Multi-Omics Integration Using Genetic Programming
The integration of disparate omics data types requires sophisticated computational approaches that can adapt to the specific characteristics of each dataset and research question. Genetic programming provides an evolutionary approach to optimize feature selection and integration strategies.
Protocol 2: Genetic Programming Framework for Multi-Omics Survival Analysis
Application Context: This protocol is validated for breast cancer survival prediction integrating genomics, transcriptomics, and epigenomics data, achieving a concordance index (C-index) of 78.31 during 5-fold cross-validation on the training set and 67.94 on the test set [10].
Materials and Reagents:
- Multi-omics datasets (e.g., TCGA-BRCA or similar)
- High-performance computing environment (minimum 32GB RAM, 8 cores)
- Python 3.8+ with scikit-learn, DEAP, and pandas libraries
Procedure:
Data Preprocessing and Normalization
- Perform missing value imputation using k-nearest neighbors (k-NN) with k=10
- Apply quantile normalization within each omics data type
- Standardize features to zero mean and unit variance
Evolutionary Feature Selection
- Initialize population of 500 individuals with random feature subsets
- Define fitness function as C-index from Cox proportional hazards model
- Apply tournament selection with size=3 and crossover probability=0.7
- Implement mutation with probability=0.1 per feature
- Evolve for 100 generations or until fitness plateau (<0.01 improvement for 10 generations)
Model Validation and Interpretation
- Perform 5-fold cross-validation with consistent stratification
- Calculate feature importance based on selection frequency across generations
- Validate final model on independent test set
- Perform pathway enrichment analysis on selected features
Quality Control Checkpoints:
- Monitor population diversity throughout evolution (maintain >10% unique individuals)
- Validate proportional hazards assumption in final Cox model
- Ensure computational reproducibility through random seed setting
Protocol for Deep Learning-Based Multi-Omics Integration with Flexynesis
For more complex integration tasks requiring non-linear modeling, deep learning approaches provide flexible frameworks. The Flexynesis toolkit offers a standardized approach for bulk multi-omics integration in precision oncology.
Protocol 3: Deep Learning Integration for Cancer Subtype Classification and Survival Prediction
Application Context: This protocol is validated for microsatellite instability (MSI) status classification in gastrointestinal and gynecological cancers using gene expression and promoter methylation profiles, achieving AUC=0.981 [59].
Materials and Reagents:
- Flexynesis package (available via PyPi, Bioconda, or Galaxy Server)
- Multi-omics data with matched clinical annotations
- GPU-enabled computing environment for accelerated deep learning
Procedure:
Data Preparation and Partitioning
- Split data into training (70%), validation (15%), and test (15%) sets
- Apply batch effect correction using ComBat if data originates from multiple sources
- Perform feature pre-selection (top 5,000 most variable features per modality)
Model Architecture Configuration
- Configure encoder networks for each omics type (fully connected layers)
- Set latent space dimension to 64 units with ReLU activation
- Attach task-specific heads: classification (sigmoid), survival (Cox loss), regression (MSE)
- Apply dropout regularization (rate=0.3) to prevent overfitting
Multi-Task Model Training
- Initialize model with He normal weight initialization
- Train with Adam optimizer (learning rate=0.001, β1=0.9, β2=0.999)
- Implement early stopping with patience=20 epochs based on validation loss
- Use batch size=32 with class weighting for unbalanced outcomes
Model Interpretation and Biomarker Discovery
- Compute feature importance via integrated gradients
- Identify cross-omics interactions through attention mechanisms
- Validate biological relevance via pathway enrichment analysis
Quality Control Checkpoints:
- Monitor training/validation loss convergence
- Check predictive performance on validation set after each epoch
- Assess calibration of probability outputs for classification tasks
- Verify model reproducibility across random initializations
The Scientist's Toolkit: Essential Research Reagent Solutions
Implementing clinical-grade multi-omics requires carefully selected reagents, platforms, and computational tools that meet rigorous quality standards. The following toolkit compiles essential solutions validated for regulated multi-omics applications.
Table 3: Research Reagent Solutions for Clinical-Grade Multi-Omics
| Tool Category | Specific Solution | Function in Multi-Omics Workflow | Quality Attributes |
|---|---|---|---|
| NGS Platforms | Illumina NovaSeq X Series | High-throughput sequencing for genomics and transcriptomics | >Q30 accuracy, 20B+ reads per flow cell |
| Single-Cell Multi-Omics | 10x Genomics Multiome ATAC + Gene Expression | Simultaneous profiling of chromatin accessibility and gene expression | >65% cell throughput, >3,000 median genes/cell |
| Spatial Biology | Element Biosciences AVITI24 System | Combined sequencing with cell profiling (RNA, protein, morphology) | <0.1% substitution error rate, >150 Gb/output |
| Proteomics | Mass spectrometry with TMTpro 18-plex | High-parameter protein quantification across samples | <15% CV, >8,000 protein identifications |
| Computational Integration | Flexynesis Deep Learning Toolkit | Bulk multi-omics integration for classification, regression, survival | Modular architecture, supports multi-task learning |
| Quality Monitoring | Qiagen Clinical Insight (QCI) | Annotate, interpret, report variants according to guidelines | CAP/CLLA compliant, integrates EHR data |
| Data Harmonization | Lifebit AI Platform | Federated data analysis with harmonization capabilities | HIPAA/GDPR compliant, scalable cloud architecture |
The translation of multi-omics discoveries into clinically actionable insights requires robust regulatory and quality frameworks that span the entire workflow from sample collection to data integration. The protocols and standards outlined in this application note provide a foundation for developing clinical-grade multi-omics applications in oncology.
As the field evolves, several key trends will shape future framework development: the growing importance of AI/ML validation guidelines, increasing need for real-world evidence integration, and emerging standards for liquid biopsy applications in multi-omics [91] [20]. By adopting these standardized approaches early in development, researchers can accelerate the transition from biomarker discovery to clinically validated applications, ultimately advancing precision oncology and improving patient outcomes.
The implementation of these frameworks requires collaborative efforts across research institutions, regulatory bodies, and technology developers. Such collaboration will be essential to establish the standardized, reproducible, and clinically validated multi-omics approaches that will drive the next generation of oncology diagnostics and therapeutics.
Conclusion
The integration of NGS with multi-omics data, powered by sophisticated AI, marks a paradigm shift in oncology, moving the field from a reactive, population-based model to a proactive, dynamic, and deeply personalized approach. While significant challenges in data harmonization, computational scalability, and clinical translation remain, the path forward is clear. Future progress will be driven by emerging trends such as federated learning for privacy-preserving collaboration, the refinement of spatial and single-cell omics, and the development of patient-centric 'N-of-1' models. For researchers and drug developers, the continued standardization and validation of these integrative frameworks are paramount to fully realizing the promise of precision oncology, ultimately leading to more effective therapies, improved patient outcomes, and a fundamentally new understanding of cancer biology.
References
- 1. Significance and limitations of the use of next-generation ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9478565/]
- 2. Next-generation sequencing: 2025 Revolution [https://lifebit.ai/blog/next-generation-sequencing/]
- 3. Navigating Cancer Complexity: Integrative Multi-Omics ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12553891/]
- 4. AI-driven multi-omics integration in precision oncology [https://pmc.ncbi.nlm.nih.gov/articles/PMC12634751/]
- 5. What is single-cell multi-omics? [https://missionbio.com/company/blog/what-is-single-cell-multi-omics/]
- 6. From Omics to Multi-Omics: A Review of Advantages and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11675490/]
- 7. Advances in single-cell omics and multiomics for high- ... [https://www.nature.com/articles/s12276-024-01186-2]
- 8. Next-generation sequencing approach for the diagnosis of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5949614/]
- 9. Harnessing multi-omics approaches to decipher tumor ... [https://biomarkerres.biomedcentral.com/articles/10.1186/s40364-025-00859-y]
- 10. Adaptive multi-omics integration framework for breast ... [https://www.nature.com/articles/s41598-025-22202-z]
- 11. Multi-omics strategies for biomarker discovery and application ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12638490/]
- 12. Next-Generation Sequencing: A Review of Its Transformative ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12523276/]
- 13. Application of Proteomics in Cancer: Recent Trends and ... [https://www.frontiersin.org/journals/medicine/articles/10.3389/fmed.2021.747333/full]
- 14. Methods for multi-omic data integration in cancer research [https://pmc.ncbi.nlm.nih.gov/articles/PMC11446849/]
- 15. Algorithms and tools for data-driven omics integration to ... [https://translational-medicine.biomedcentral.com/articles/10.1186/s12967-025-06446-x]
- 16. Multi-omics advances in understanding cancer drug ... [https://www.sciencedirect.com/science/article/pii/S2949723X25000510]
- 17. Genotype–phenotype mapping and the end of the 'genes as ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC2817137/]
- 18. Genomics and multiomics in the age of precision medicine [https://www.nature.com/articles/s41390-025-04021-0]
- 19. Transforming Clinical Research: The Power of High-Throughput Omics ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11417901/]
- 20. 2025 and Beyond: The Future of Genomic Data Analysis ... [https://blog.crownbio.com/2025-and-beyond-the-future-of-genomic-data-analysis-and-innovations-in-genomics-services]
- 21. Clinical implementation of next-generation sequencing ... [https://www.nature.com/articles/s41598-024-84909-9]
- 22. Integrated DNA Technologies and Beckman Coulter Life ... [https://www.businesswire.com/news/home/20251112997999/en/Integrated-DNA-Technologies-and-Beckman-Coulter-Life-Sciences-Partner-to-Advance-Cancer-Research-Through-Automated-NGS-Workflows]
- 23. Analysis of Single-Cell and/or Bulk Multi- Integrative ... omics [https://www.frontiersin.org/research-topics/29422/integrative-analysis-of-single-cell-andor-bulk-multi-omics-sequencing-data/authors]
- 24. An Integrated Multi-Omics and Artificial Intelligence ... [https://www.mdpi.com/2079-7737/12/10/1298]
- 25. Oncogenic gene fusions in cancer: from biology to therapy [https://www.nature.com/articles/s41392-025-02161-7]
- 26. DVA: predicting the functional impact of single nucleotide ... [https://bmcbioinformatics.biomedcentral.com/articles/10.1186/s12859-024-05709-6]
- 27. Comprehensive analysis of the functional impact of single ... [https://pubmed.ncbi.nlm.nih.gov/39146382/]
- 28. Copy Number Variation (CNV) Calling [https://www.cancer.gov/about-nci/organization/cbiit/training/library/cnv]
- 29. Copy number variations contribute to malignant tumor ... [https://pubmed.ncbi.nlm.nih.gov/39140252]
- 30. Fusion genes in cancers: Biogenesis, functions, and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12205800/]
- 31. Integration of multi-omics approaches in exploring intra ... [https://cancerci.biomedcentral.com/articles/10.1186/s12935-025-03944-2]
- 32. The AI revolution: how multimodal intelligence will reshape ... [https://www.nature.com/articles/s44387-025-00044-4]
- 33. Artificial intelligence in cancer: applications, challenges, and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12574039/]
- 34. A comparative analysis of three graph neural network ... [https://www.nature.com/articles/s41598-025-97257-z]
- 35. Graph Neural Networks in Multi-Omics Cancer Research [https://arxiv.org/abs/2506.17234]
- 36. AI and Multi-omics are Transforming Cancer Care [https://www.prnewswire.com/apac/news-releases/ai-and-multi-omics-are-transforming-cancer-care-apac-precision-oncology-conference-outlines-the-future-of-early-detection-and-personalized-treatment-302616653.html]
- 37. AI and Cancer - NCI [https://www.cancer.gov/research/infrastructure/artificial-intelligence]
- 38. Quantifying and interpreting biologically meaningful spatial ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11897387/]
- 39. Integration of multi-omics approaches in exploring intra ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12395700/]
- 40. Tumour evolution and microenvironment interactions in 2D ... [https://www.nature.com/articles/s41586-024-08087-4]
- 41. Multi-omics analysis of the tumor microenvironment after ... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2025.1648987/full]
- 42. Liquid biopsy in cancer: current status, challenges and ... [https://www.nature.com/articles/s41392-024-02021-w]
- 43. Liquid biopsy approaches to capture tumor evolution and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9853269/]
- 44. Validation of a liquid biopsy assay with increased ... [https://pubmed.ncbi.nlm.nih.gov/40980342/]
- 45. Analytical Validation of a Pan-Cancer NGS Assay for In- ... [https://www.sciencedirect.com/science/article/pii/S152515782500220X]
- 46. Transforming Cancer Therapy: Insights from 2025 H1 FDA ... [https://blog.crownbio.com/transforming-cancer-therapy-insights-from-2025-h1-fda-approvals-and-preclinical-drug-discovery]
- 47. Organoid models in oncology: advancing precision cancer ... [https://www.cancerbiomed.org/content/early/2025/07/24/j.issn.2095-3941.2025.0127]
- 48. Organoid models in oncology: advancing precision cancer ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12418270/]
- 49. Patient-derived xenograft models: Current status ... [https://www.sciencedirect.com/science/article/pii/S2352304225000091]
- 50. Integrating Multi-Omics for Precision Medicine: 2025 Guide [https://lifebit.ai/blog/integrating-multi-modal-genomic-and-multi-omics-data-for-precision-medicine/]
- 51. What are the 4 Vs of Big Data? [https://bernardmarr.com/what-are-the-4-vs-of-big-data/]
- 52. Explain the four Vs of Big Data? [https://www.geeksforgeeks.org/data-engineering/explain-the-four-vs-of-big-data/]
- 53. The Four V's of Big Data [https://www.bigdataframework.org/the-four-vs-of-big-data/]
- 54. Next-Generation Sequencing: A Review of Its ... [https://www.mdpi.com/2075-4418/15/19/2425]
- 55. Next-generation sequencing in cancer diagnosis and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12009796/]
- 56. Methods for multi-omic data integration in cancer research [https://www.frontiersin.org/journals/genetics/articles/10.3389/fgene.2024.1425456/full]
- 57. Why You Must Correct Batch Effects in Transcriptomics Data? [https://www.metwarebio.com/transcriptomics-batch-effect-correction/]
- 58. An incremental framework for batch effect correction in DNA ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12495439/]
- 59. Flexynesis: A deep learning toolkit for bulk multi-omics data ... [https://www.nature.com/articles/s41467-025-63688-5]
- 60. Next Generation Sequencing Platform: Ultimate Guide 2025 [https://lifebit.ai/blog/next-generation-sequencing-platform/]
- 61. Current Bioinformatics Tools in Precision Oncology - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC12238682/]
- 62. A Review of Integrative Imputation for Multi-Omics Datasets [https://pmc.ncbi.nlm.nih.gov/articles/PMC7594632/]
- 63. Efficient technique of microarray missing data imputation ... [https://www.nature.com/articles/s41598-021-03438-x]
- 64. Advanced methods for missing values imputation based on ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8323724/]
- 65. Establishing Best Practices for Clinical GWAS - PubMed Central [https://pmc.ncbi.nlm.nih.gov/articles/PMC12250051/]
- 66. Challenges in AI-driven multi-omics data analysis for ... [https://www.sciencedirect.com/science/article/pii/S2352914825000681]
- 67. Integrating functional proteomics and next generation ... [https://clinicalproteomicsjournal.biomedcentral.com/articles/10.1186/s12014-025-09526-8]
- 68. the growing use of translational research in cancer medicine [https://pmc.ncbi.nlm.nih.gov/articles/PMC2826819/]
- 69. Key Insights from Biomarkers and Precision Medicine 2025 | News [https://precisionmedicine.lifesciencexchange.com/news/turning-precision-medicine-from-promise-to-practice-key-insights-from-biomarkers-and-precision-medicine-2025]
- 70. Celebrating milestones and the future of oncology in China [https://www.illumina.com/company/news-center/feature-articles/CSCO-2025.html]
- 71. Potential barriers to implementation of next-generation ... [https://pubmed.ncbi.nlm.nih.gov/39606845/]
- 72. Perceived Barriers to NGS-Based Molecular Profiling ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12564138/]
- 73. Overcoming Barriers to Clinical NGS-Based Testing [https://www.clinicallab.com/from-bench-to-bedside-overcoming-barriers-to-clinical-ngs-based-testing-26042]
- 74. NGS and the cancer biomarker balancing act [https://www.captodayonline.com/ngs-and-the-cancer-biomarker-balancing-act/]
- 75. At ASCO, Testing and AI Rival Drugs for Attention, but ... [https://www.ajmc.com/view/at-asco-testing-and-ai-rival-drugs-for-attention-but-reimbursement-remains-a-barrier]
- 76. Unlocking 'bench-to-bedside' discoveries requires better data ... [https://www.drugdiscoverytrends.com/unlocking-bench-to-bedside-discoveries-requires-better-data-sharing-and-collaboration/]
- 77. Systematic benchmarking of imaging spatial ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12635344/]
- 78. Systematic benchmarking of high-throughput subcellular ... [https://www.nature.com/articles/s41467-025-64292-3]
- 79. Cancer Multi-Omics Database for Machine Learning [https://www.nature.com/articles/s41597-025-05235-x]
- 80. Cancer Progression Illuminated by New Multi-Omics Tool [https://news.weill.cornell.edu/news/2025/10/cancer-progression-illuminated-by-new-multi-omics-tool]
- 81. The Future of Clinical Trials: Incorporating 'Omics for ... [https://blog.crownbio.com/the-future-of-clinical-trials-incorporating-omics-for-enhanced-stratification]
- 82. Lost in Translation: Turning Multi-omic Chaos into Clinical ... [https://www.precisionformedicine.com/blog/lost-in-translation-turning-multi-omics-chaos-into-clinical-clarity]
- 83. Single-cell multi-omics in cancer immunotherapy: from tumor ... [https://molecular-cancer.biomedcentral.com/articles/10.1186/s12943-025-02426-3]
- 84. Case report: Single gene testing and comprehensive ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11560755/]
- 85. Comprehensive Genomic Profiling (CGP) | Cancer ... [https://www.illumina.com/areas-of-interest/cancer/ngs-in-oncology/cgp.html]
- 86. The Impact of Prior Single-Gene Testing on ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11187032/]
- 87. One test to capture all: Comprehensive genomic profiling, ... [https://www.nature.com/articles/d42473-025-00027-8]
- 88. Why Comprehensive Genomic Profiling? [https://www.foundationmedicine.com/resource/why-comprehensive-genomic-profiling]
- 89. NextGen Omics, Tech & Data 2026 [https://oxfordglobal.com/precision-medicine/events/nextgen-omics]
- 90. Insights from Biomarkers & Precision Medicine 2025 [https://www.signifyresearch.net/insights/biomarkers-billions-and-breakthroughs-insights-from-biomarkers-precision-medicine-2025/]
- 91. 2025 Trends: Multiomics [https://www.genengnews.com/topics/omics/2025-trends-multiomics/]