Automated Tumor Segmentation with Deep Learning: Current Approaches, Clinical Applications, and Future Directions
This article provides a comprehensive analysis of automated tumor segmentation using deep learning, tailored for researchers and drug development professionals.
Automated Tumor Segmentation with Deep Learning: Current Approaches, Clinical Applications, and Future Directions
Abstract
This article provides a comprehensive analysis of automated tumor segmentation using deep learning, tailored for researchers and drug development professionals. It explores the foundational principles of AI in medical imaging, examines state-of-the-art methodologies including CNN and Transformer architectures, and addresses critical optimization challenges such as data efficiency and model generalization. The content synthesizes performance validation across multiple datasets and clinical applications, offering insights into the integration of these technologies in biomedical research and therapeutic development.
The Evolution of AI in Tumor Segmentation: From Basic Concepts to Current Landscape
Medical image segmentation, a fundamental process of dividing medical images into distinct regions of interest, has undergone remarkable transformations with the emergence of deep learning (DL) techniques [1]. This technology serves as a critical bridge between medical imaging and clinical applications by enabling precise delineation of anatomical structures and pathological findings. In oncology, automated tumor segmentation using deep learning represents a paradigm shift, offering solutions to labor-intensive manual contouring while addressing significant inter-observer variability among clinicians [2]. The clinical significance of accurate segmentation extends across diagnostic interpretation, treatment planning, intervention guidance, and therapy response monitoring, forming an essential component of modern precision medicine initiatives.
The evolution from traditional segmentation methods to deep learning-based approaches has coincided with growing demands for diagnostic excellence in clinical settings [3]. As healthcare systems worldwide face mounting pressures from increasing image complexity and volume, deep learning technologies have demonstrated potential to enhance workflow efficiency, reduce cognitive burden on clinicians, and ultimately improve patient outcomes through more consistent and quantitative image analysis.
Technical Approaches in Medical Image Segmentation
Deep Learning Architectures
Convolutional Neural Networks (CNNs) represent the foundational architecture for most medical image segmentation tasks. These networks employ a series of convolutional layers that automatically and adaptively learn spatial hierarchies of features from medical images [3] [4]. The U-Net architecture, with its encoder-decoder structure and skip connections, has become particularly prominent in medical imaging, enabling precise localization while leveraging contextual information [3]. For tumor segmentation in radiotherapy, 3D U-Net models have demonstrated robust performance in capturing volumetric information from CT scans [2].
Beyond CNNs, several specialized architectures have emerged. Recurrent Neural Networks (RNNs) facilitate analysis of temporal sequences, making them suitable for 4D imaging data that captures organ motion [3]. Generative Adversarial Networks (GANs) contribute to data augmentation and image synthesis, helping address limited dataset sizes [3]. More recently, Vision Transformers (ViTs) have shown promise in capturing long-range dependencies through self-attention mechanisms, while hybrid models that integrate multiple architectural concepts offer enhanced performance for complex segmentation tasks [3].
Loss Functions for Medical Imaging
The choice of loss function significantly influences segmentation performance, particularly for class-imbalanced medical data where target regions often occupy minimal image area. The Dice Loss function directly optimizes for the Dice Similarity Coefficient, a standard overlap metric in medical imaging [5]. To address class imbalance, the Generalized Dice Loss incorporates weighting terms that account for region size [5]. For clinical applications where boundary accuracy is crucial, such as tumor segmentation, Hausdorff distance-based losses like the Generalized Surface Loss provide enhanced performance by minimizing the maximum segmentation error [5]. In practice, composite loss functions that combine multiple objectives, such as Dice-CE loss (Dice plus Cross-Entropy), often yield superior results by balancing overlap accuracy with probabilistic calibration [5].
Table 1: Common Loss Functions in Medical Image Segmentation
| Loss Function | Mathematical Formulation | Advantages | Clinical Applications |
|---|---|---|---|
| Dice Loss (DL) | 1 - (2∑TₖPₖ + ε)/(∑Tₖ² + ∑Pₖ² + ε) | Optimizes directly for overlap metric; handles class imbalance | General organ and tumor segmentation |
| Generalized Dice Loss (GDL) | 1 - 2(∑wₖ∑TₖPₖ)/(∑wₖ∑(Tₖ² + Pₖ²)) | Weighted for multi-class imbalance; improved consistency | Multi-class segmentation problems |
| Generalized Surface Loss | Weighted distance transform-based | Minimizes Hausdorff distance; better boundary alignment | Tumor segmentation where boundary accuracy is critical |
| Dice-CE Loss | ℒ_dice - α(∑∑Tₖlog(Pₖ)) | Combines overlap and probabilistic calibration | General purpose with enhanced training stability |
Performance Metrics and Quantitative Evaluation
Traditional Geometric Metrics
The evaluation of medical image segmentation algorithms relies on well-established geometric metrics that quantify spatial agreement between automated results and reference standards. The Dice Similarity Coefficient (DSC) measures volume overlap, ranging from 0 (no overlap) to 1 (perfect overlap), with values exceeding 0.7 typically indicating clinically acceptable performance [2]. The Hausdorff Distance (HD) quantifies the largest segmentation error by measuring the maximum distance between surfaces, making it particularly sensitive to boundary outliers [5]. In practice, the 95th percentile HD (HD95) is often used instead of the maximum to reduce sensitivity to single-point outliers [2].
For radiotherapy applications, where tumor segmentation directly influences treatment efficacy, these metrics provide essential quality assurance. In a multicenter study of automated lung tumor segmentation for radiotherapy, a 3D U-Net model achieved median DSC of 0.73 (IQR: 0.62-0.80) on internal validation and 0.70-0.71 on external cohorts, demonstrating performance comparable to human inter-observer variability [2]. This level of agreement suggests clinical viability for automated approaches in complex oncology applications.
Advanced Evaluation Approaches
While traditional metrics provide valuable geometric insights, they may not fully capture clinically relevant segmentation characteristics. Radiomics features have emerged as a superior evaluation framework that quantifies segmentation quality through tumor characteristics beyond simple shape overlap [6]. These features can detect subtle variations in segmentation that might be missed by DSC and HD metrics alone [6].
The intraclass correlation coefficient (ICC) of radiomics features demonstrates greater sensitivity to segmentation changes than geometric metrics, with specific wavelet-transformed features (e.g., wavelet-LLL first order Maximum, wavelet-LLL glcm MCC) showing ICC values ranging from 0.130 to 0.997 compared to DSC values consistently above 0.778 for the same segmentations [6]. This enhanced sensitivity makes radiomics particularly valuable for evaluating segmentation algorithms intended for quantitative imaging biomarkers in oncology clinical trials and drug development studies.
Table 2: Performance Metrics for Medical Image Segmentation Evaluation
| Metric Category | Specific Metrics | Interpretation | Strengths | Limitations |
|---|---|---|---|---|
| Overlap Metrics | Dice Similarity Coefficient (DSC) | 0-1 scale; higher values indicate better overlap | Intuitive; widely used in literature | Insensitive to boundary differences; treats all errors equally |
| Distance Metrics | Hausdorff Distance (HD), Average Surface Distance (ASD) | Distance in mm; lower values indicate better boundary alignment | Sensitive to boundary errors; clinically relevant | HD is sensitive to outliers; requires surface computation |
| Statistical Metrics | Intraclass Correlation Coefficient (ICC) of Radiomics Features | 0-1 scale; higher values indicate better feature reproducibility | Captures texture and intensity characteristics; more sensitive to subtle variations | Computationally complex; requires specialized extraction |
| Clinical Metrics | False Positive Voxel Rate, Target Coverage | Relationship to patient outcomes | Direct clinical relevance; predictive of efficacy | Requires outcome data; complex statistical analysis |
Experimental Protocols for Automated Tumor Segmentation
Dataset Curation and Preprocessing
Comprehensive dataset collection forms the foundation of robust segmentation models. Major public repositories include The Cancer Imaging Archive (TCIA), which maintains extensive cancer-specific image collections, and institution-specific resources like the Stanford AIMI collections, which provide large-scale annotated imaging data (e.g., CheXpert Plus with 223,462 chest X-ray pairs) [7]. The LiTS (Liver Tumor Segmentation) and BraTS (Brain Tumor Segmentation) datasets serve as benchmark resources for specific tumor types [5]. For multicenter validation, datasets should encompass diverse imaging protocols, scanner manufacturers, and patient populations to ensure generalizability [2].
Essential preprocessing steps include: (1) image resampling to uniform voxel spacing (typically 1-2mm isotropic) to ensure consistent spatial resolution [6]; (2) intensity normalization to address scanner-specific variations; (3) data augmentation through geometric transformations (rotation, scaling, elastic deformations) and intensity variations to increase dataset diversity and improve model robustness [3]; and (4) expert annotation with board-certified radiologists or radiation oncologists following established contouring guidelines, with multiple annotators where feasible to quantify inter-observer variability [2].
Model Training and Validation Framework
The nnU-Net framework provides a standardized approach for biomedical image segmentation, automatically configuring network architecture and preprocessing based on dataset characteristics [5]. For tumor segmentation, 3D U-Net architectures typically outperform 2D counterparts by capturing volumetric context [2]. Training should employ k-fold cross-validation (typically 5-fold) to maximize data utilization and provide robust performance estimates [2].
Implementation details should include: (1) patch-based training to manage memory constraints while maintaining spatial context; (2) balanced sampling strategies to address class imbalance between foreground and background voxels; (3) composite loss functions combining region-based (e.g., Dice) and boundary-based (e.g., Generalized Surface Loss) terms [5]; (4) optimization with adaptive methods (Adam, SGD with momentum) with learning rate scheduling; and (5) extensive data augmentation including random rotations, scaling, brightness/contrast adjustments, and simulated artifacts [3].
Validation must occur across multiple cohorts, including internal hold-out test sets and external datasets from different institutions to assess generalizability [2]. Model performance should be compared against human inter-observer variability to establish clinical relevance, with statistical testing (e.g., Wilcoxon signed-rank tests) to determine significant differences [2]. For radiotherapy applications, segmentation models should additionally generate saliency maps via integrated gradients to interpret feature contributions and identify potential failure modes [2].
Public Datasets and Annotated Collections
Access to high-quality annotated medical imaging data is fundamental for developing and validating segmentation algorithms. The Cancer Imaging Archive (TCIA) represents one of the largest cancer-focused resources, providing de-identified images accessible for public download [7]. OpenNeuro offers extensive neuroimaging data, hosting over 1,240 public datasets with information from more than 51,000 participants across multiple modalities (MRI, PET, MEG, EEG) [7]. The NIH Chest X-Ray Dataset contains over 100,000 anonymized chest X-ray images from more than 30,000 patients, serving as a cornerstone for thoracic imaging research [7]. Specialized collections like MedPix provide educational and research resources with approximately 59,000 images across 9,000 topics [7], while MIDRC maintains COVID-19-specific imaging data collected from diverse clinical settings [7].
Software Frameworks and Computational Tools
The technical implementation of segmentation algorithms relies on robust software frameworks. PyRadiomics enables standardized extraction of radiomics features from medical images, supporting quantitative analysis of segmentation results [6]. The nnU-Net framework provides out-of-the-box solutions for biomedical image segmentation, automatically adapting to dataset characteristics [5]. 3D Slicer offers a comprehensive platform for medical image visualization and analysis, incorporating segmentation capabilities and metric calculation [6]. Collective Minds Research represents an integrated platform for managing large-scale imaging datasets while maintaining security and compliance, facilitating collaborative research across institutions [7].
Table 3: Essential Research Resources for Medical Image Segmentation
| Resource Category | Specific Resources | Key Features | Application Context |
|---|---|---|---|
| Public Datasets | TCIA, OpenNeuro, NIH Chest X-Ray | Curated collections; multiple modalities; annotated cases | Algorithm training; benchmarking; validation |
| Annotation Platforms | 3D Slicer, ITK-SNAP, Collective Minds | Expert annotation tools; quality control; collaborative features | Ground truth generation; dataset creation |
| Software Frameworks | nnU-Net, PyRadiomics, MONAI | Pre-built architectures; standardized processing; reproducibility | Model development; feature extraction; deployment |
| Evaluation Tools | 3D Slicer, Custom Python Scripts | Metric calculation; statistical analysis; visualization | Performance validation; comparative studies |
Clinical Translation and Applications
Radiotherapy Planning and Treatment
Automated tumor segmentation has found particularly valuable applications in radiotherapy planning, where accurate target delineation directly influences treatment efficacy and toxicity. The iSeg neural network for lung tumor segmentation demonstrates how deep learning can streamline the radiotherapy workflow by automatically generating gross tumor volumes (GTVs) across 4D CT images to create internal target volumes (ITVs) that account for respiratory motion [2]. Notably, machine-generated ITVs were significantly smaller (by 30% on average) than physician-delineated contours while maintaining target coverage, suggesting potential for normal tissue sparing without compromising tumor control [2].
Beyond time savings, automated segmentation addresses the significant inter-observer variability that plagues manual contouring in radiotherapy. Studies comparing iSeg performance against expert recontouring demonstrated that the algorithm closely approximated inter-physician concordance limits (DSC 0.75 vs. 0.80 for human observers) [2]. Perhaps most importantly, clinical outcome correlations revealed that higher false positive voxel rates (regions segmented by the machine but not humans) were associated with increased local failure (HR: 1.01 per voxel, p=0.03), suggesting that machine-human discordance may identify clinically relevant regions that warrant additional scrutiny [2].
Integration with Clinical Workflows
Successful implementation of automated segmentation requires thoughtful integration with existing clinical workflows and electronic health record (EHR) systems. Emerging visualization dashboards like AWARE are designed to integrate within existing EHR systems, providing clinical decision support through enhanced data presentation that reduces cognitive load on clinicians [8]. These systems transform complex medical data into interpretable visual formats, allowing providers to quickly grasp essential information while maintaining access to automated segmentation results [8].
The future clinical integration of these technologies will likely involve hybrid human-AI collaboration, where algorithms provide initial segmentations that clinicians efficiently review and refine. This approach leverages the consistency and quantitative capabilities of automated systems while retaining clinician oversight for complex cases and unusual anatomies. As these technologies mature, they hold potential not only to improve efficiency but also to enhance standardization across institutions and support clinical trial quality assurance through more consistent implementation of segmentation protocols.
The evolution of tumor segmentation in medical imaging represents a paradigm shift from manual, subjective analysis toward automated, AI-driven diagnostics. Traditional methods, reliant on clinicians' visual assessments and rudimentary image processing techniques, have long been plagued by subjectivity, inter-observer variability, and inefficiency [9]. The advent of deep learning, particularly convolutional neural networks (CNNs) and U-Net architectures, has fundamentally transformed this landscape, enabling precise, automated, and reproducible tumor delineation. This transition is critically important in neuro-oncology, where accurate tumor boundary definition directly impacts surgical planning, treatment monitoring, and survival prediction [10] [11]. The integration of these technologies into clinical workflows marks a significant advancement in precision medicine, offering enhanced diagnostic accuracy and standardized analysis across healthcare institutions.
The Traditional Paradigm: Manual Segmentation and Rule-Based Systems
Core Methodologies and Limitations
Traditional brain tumor analysis relied heavily on manual radiologic assessment and classical image processing techniques. These methods required neuroradiologists to visually inspect magnetic resonance imaging (MRI) scans and manually delineate tumor boundaries—a labor-intensive process prone to significant inter-observer variation [9]. Rule-based computational approaches included thresholding, edge detection, region growing, and morphological processing. These techniques operated on low-level image features such as intensity gradients and texture patterns but lacked the adaptability to handle the complex morphological heterogeneity inherent in brain tumors [9] [10].
The fundamental limitation of these traditional systems was their dependence on hand-crafted features, which failed to capture the extensive spatial and contextual diversity of gliomas, meningiomas, and other intracranial tumors across different patients and imaging protocols [9]. Furthermore, these methods demonstrated poor robustness to imaging artifacts, noise, and intensity variations commonly encountered in clinical settings.
Quantitative Performance of Traditional Approaches
The table below summarizes the characteristic performance metrics of traditional tumor segmentation methodologies compared to early deep learning approaches:
Table 1: Performance Comparison of Traditional vs. Early Deep Learning Methods
| Method Category | Representative Techniques | Typical Dice Score | Key Limitations |
|---|---|---|---|
| Manual Segmentation | Radiologist visual assessment | 0.65-0.75 (inter-observer variation) | Time-consuming (45+ minutes/case), high inter-observer variability [2] |
| Traditional Image Processing | Thresholding, region growing, edge detection | 0.60-0.70 | Sensitive to noise and intensity variations; poor generalization [9] |
| Classical Machine Learning | Support Vector Machines (SVM), Random Forests with hand-crafted features | 0.70-0.75 | Limited feature representation; requires expert feature engineering [10] |
| Early Deep Learning | Basic CNN architectures | 0.80-0.85 | Required large datasets; computationally intensive [10] |
The Deep Learning Revolution: Architectural Innovations and Performance Gains
Convolutional Neural Networks and U-Net Architectures
The introduction of deep learning, particularly CNNs, marked a turning point in medical image analysis. Unlike traditional methods, CNNs automatically learn hierarchical feature representations directly from image data, eliminating the need for manual feature engineering [9]. The U-Net architecture, with its symmetric encoder-decoder structure and skip connections, emerged as a particularly transformative innovation, enabling precise pixel-level segmentation while preserving spatial context [10].
Recent architectural evolution has focused on hybrid models that combine the strengths of multiple paradigms. Transformer-enhanced U-Nets incorporating self-attention mechanisms have demonstrated remarkable improvements in capturing long-range dependencies in medical images. In 2025, models such as MWG-UNet++ achieved Dice similarity coefficients of 0.8965 on brain tumor segmentation tasks, representing a 12.3% improvement over traditional U-Nets [12]. Similarly, the integration of Vision Mamba layers in architectures like CM-UNet has improved inference speed by 40% while maintaining competitive segmentation accuracy [12].
Quantitative Advancements in Tumor Segmentation
The performance leap enabled by deep learning is quantitatively demonstrated through standardized benchmarks like the BraTS (Brain Tumor Segmentation) challenge. The table below summarizes the state-of-the-art performance achieved by various deep learning models:
Table 2: Performance of Advanced Deep Learning Models on Brain Tumor Segmentation (BraTS Dataset)
| Model Architecture | Whole Tumor Dice | Tumor Core Dice | Enhancing Tumor Dice | Key Innovations |
|---|---|---|---|---|
| DSNet (2025) | 0.959 | 0.975 | 0.947 | 3D Dynamic CNN, adversarial learning, attention mechanisms [11] |
| Transformer-enhanced U-Net (2025) | 0.917 (average) | - | - | Axial attention mechanisms, residual path reconstruction [12] |
| Hybrid CNN (2024) | 0.937 (mean) | - | - | RGB multichannel fusion (T1w, T2w, average) [13] |
| 3D U-Net with Attention | 0.92-0.94 | 0.91-0.93 | 0.88-0.90 | Integrated attention gates; volumetric context [10] |
| iSeg (3D U-Net for Lung Tumors) | 0.73 (median) | - | - | Multicenter validation; motion-resolved segmentation [2] |
Beyond segmentation accuracy, deep learning models have demonstrated exceptional performance in tumor classification tasks. A 2025 meta-analysis of meningioma grading reported pooled sensitivity of 92.31% and specificity of 95.3% across 27 studies involving 13,130 patients, with an area under the curve (AUC) of 0.97 [14]. For multi-class brain tumor classification, hybrid deep learning approaches have achieved accuracies exceeding 98-99% on benchmark datasets [15] [16] [17].
Experimental Protocols for Deep Learning-Based Tumor Segmentation
Protocol 1: 3D Brain Tumor Segmentation Using DSNet
Application: Precise volumetric segmentation of gliomas from multimodal MRI data for surgical planning and treatment monitoring.
Materials and Reagents:
- Multimodal MRI scans (T1-weighted, T1ce, T2-weighted, FLAIR) in DICOM format
- High-performance computing infrastructure with GPU acceleration (NVIDIA RTX 3090 or equivalent)
- Python 3.8+ with PyTorch or TensorFlow deep learning frameworks
- BraTS dataset for model training and validation
Methodology:
- Data Preprocessing: Co-register all multimodal MRI sequences to a common spatial coordinate system. Apply N4ITK bias field correction to address intensity inhomogeneities. Normalize intensity values to zero mean and unit variance across the entire dataset [11].
- Patch Extraction: Extract overlapping 3D patches (128×128×128 voxels) from the preprocessed volumes to manage memory constraints while preserving spatial context.
- Network Architecture: Implement the DSNet framework comprising:
- A 3D dynamic convolutional neural network (DCNN) backbone with residual connections
- Multi-scale feature aggregation modules to capture contextual information at different resolutions
- Attention gates to emphasize tumor-relevant regions
- Adversarial training components to refine boundary delineation
- Training Protocol: Train the model for 1000 epochs with a batch size of 8 using a combination of Dice and cross-entropy loss functions. Utilize the Adam optimizer with an initial learning rate of 1e-4, reduced by half when validation performance plateaus for 50 consecutive epochs.
- Inference and Post-processing: Apply the trained model to full MRI volumes using a sliding window approach. Use connected component analysis to remove false positive predictions outside the brain parenchyma [11].
Validation: Evaluate performance on the BraTS 2020 validation set using Dice Similarity Coefficient, Hausdorff Distance, and Sensitivity metrics. Compare results against ground truth annotations from expert neuroradiologists.
Protocol 2: Multi-Class Brain Tumor Classification Using Ensemble Learning
Application: Automated discrimination of meningioma, glioma, pituitary tumors, and normal cases from MRI scans.
Materials and Reagents:
- Curated dataset of brain MRI images (e.g., Figshare, Kaggle datasets)
- Image preprocessing tools for sharpening and noise reduction (mean filtering)
- Feature selection algorithms (correlation-based feature selection)
- Machine learning libraries (Weka, Scikit-learn) and deep learning frameworks
Methodology:
- Data Preprocessing: Convert DICOM images to 512×512 pixel digital format. Apply sharpening algorithms to enhance edges and mean filtering for noise reduction [16].
- Tumor Segmentation: Implement Edge-Refined Binary Histogram Segmentation (ER-BHS) to isolate tumor regions:
- Calculate optimal threshold by maximizing inter-class variance between foreground and background pixels
- Apply morphological operations to refine tumor boundaries
- Feature Extraction: Extract a comprehensive set of 66 hybrid features from each segmented tumor region, including:
- First-order histogram features (mean, standard deviation, skewness, energy, entropy)
- Second-order texture features from gray-level co-occurrence matrices (energy, correlation, entropy, inverse difference, inertia)
- Spectral and wavelet features for texture analysis
- Feature Optimization: Apply correlation-based feature selection with best-first search to identify the most discriminative features, reducing the feature set to 11 key dimensions [16] [17].
- Model Training and Evaluation: Train multiple classifiers (Random Committee, Random Forest, J48, Neural Networks) using 10-fold cross-validation. Employ patient-level data splitting to prevent information leakage.
Validation: Assess performance using accuracy, precision, recall, and F1-score. The Random Committee classifier has demonstrated 98.61% accuracy on optimized hybrid feature sets [16].
Visualization of Methodological Evolution
Workflow Transition: Traditional to Deep Learning Approaches
U-Net Architectural Evolution and Hybridization
Table 3: Essential Research Resources for Deep Learning-Based Tumor Analysis
| Resource Category | Specific Tools & Platforms | Application in Tumor Analysis | Key Features |
|---|---|---|---|
| Medical Imaging Datasets | BraTS (2018-2025), Kaggle Brain MRI, Figshare | Model training, validation, and benchmarking | Multimodal MRI (T1, T1ce, T2, FLAIR), expert annotations, standardized evaluation [10] |
| Deep Learning Frameworks | PyTorch, TensorFlow, MONAI | Model development and implementation | GPU acceleration, pre-built layers, medical imaging specialization [11] |
| Network Architectures | 3D U-Net, DSNet, Transformer-Enhanced U-Net | Tumor segmentation, boundary delineation | Volumetric processing, attention mechanisms, multi-scale analysis [12] [11] |
| Preprocessing Tools | N4ITK, SimpleITK, intensity normalization | Image quality enhancement, artifact reduction | Bias field correction, intensity standardization, data augmentation [9] |
| Evaluation Metrics | Dice Similarity Coefficient, Hausdorff Distance, Sensitivity/Specificity | Performance quantification | Volumetric overlap, boundary accuracy, clinical relevance assessment [2] [11] |
| Visualization Tools | Grad-CAM, attention maps, saliency maps | Model interpretability, clinical trust | Region importance visualization, decision process explanation [15] |
The historical transition from traditional methods to deep learning approaches in tumor segmentation represents one of the most significant advancements in medical image analysis. This evolution has moved the field from subjective, time-consuming manual delineation toward automated, precise, and reproducible segmentation systems that approach—and in some cases surpass—human-level performance. The integration of transformer architectures, attention mechanisms, and adversarial training has addressed fundamental challenges in handling tumor heterogeneity, morphological complexity, and imaging protocol variations. As these technologies continue to mature, their clinical translation promises to standardize diagnostic workflows, enhance quantitative tumor assessment, and ultimately improve patient care through more accurate treatment planning and monitoring. Future research directions will likely focus on enhancing model interpretability, enabling federated learning for privacy-preserving multi-institutional collaboration, and developing lightweight architectures for real-time clinical deployment.
Accurate tumor segmentation from medical images is a cornerstone of modern oncology, directly impacting diagnosis, treatment planning, and therapy response monitoring. While deep learning has revolutionized this field, achieving robust, clinical-grade performance remains challenging due to significant obstacles, including inter-observer variability, imaging noise and artifacts, and the inherent biological complexity of tumors themselves. This application note dissects these core challenges, provides a quantitative analysis of current methodologies, and offers detailed protocols to guide researchers in developing and validating more reliable segmentation tools. The content is framed within the broader objective of advancing automated tumor segmentation for both clinical and research applications, such as streamlining workflows in drug development and enabling precise volumetric analysis for clinical trials.
Quantitative Analysis of Segmentation Performance
The performance of segmentation models varies significantly across tumor types, anatomical sites, and imaging protocols. The following tables summarize key quantitative metrics from recent studies to benchmark current capabilities and highlight performance variations.
Table 1: Performance of Deep Learning Models for Brain Tumor Segmentation on BraTS Datasets
| Model / Study | Tumor Subregion | Dice Score (DSC) | Key MRI Sequences Used | Dataset |
|---|---|---|---|---|
| 3D U-Net [18] | Enhancing Tumor (ET) | 0.867 | T1C + FLAIR | BraTS 2018/2021 |
| 3D U-Net [18] | Tumor Core (TC) | 0.926 | T1C + FLAIR | BraTS 2018/2021 |
| MM-MSCA-AF [19] | Necrotic Tumor | 0.8158 | T1, T1C, T2, FLAIR | BraTS 2020 |
| MM-MSCA-AF [19] | Whole Tumor | 0.8589 | T1, T1C, T2, FLAIR | BraTS 2020 |
| BSAU-Net [20] | Whole Tumor | 0.7556 | Multi-modal | BraTS 2021 |
| ARU-Net [21] | Multi-class | 0.981 | T1, T1C, T2 | BTMRII |
Table 2: Performance and Variability in Multi-Site and Multi-Organ Segmentation
| Study Context | Anatomical Site / OAR | Median Dice (DSC) | Key Finding / Variability |
|---|---|---|---|
| iSeg Model [2] | Lung (GTV) | 0.73 (IQR: 0.62-0.80) | Matched human inter-observer variability; robust across institutions. |
| AI Software Evaluation [22] | Cervical Esophagus | DSC: 0.41 (Range) | Exhibited the largest intersoftware variation among 31 OARs. |
| AI Software Evaluation [22] | Spinal Cord | DSC: 0.13 (Range) | Significant intersoftware performance variation. |
| AI Software Evaluation [22] | Heart, Liver | DSC: >0.90 | High accuracy, consistent across multiple software platforms. |
Deconstructing the Key Challenges
Inter-Observer and Inter-Software Variability
The "ground truth" used to train deep learning models is often defined by human experts, whose segmentations are prone to inconsistency. This inter-observer variability presents a major challenge for model training and validation. Studies have shown that the agreement between different physicians, as measured by the Dice Similarity Coefficient (DSC), can be as low as ~0.80 for certain tasks, establishing a performance ceiling for automated systems [2]. Furthermore, this variability is not just a human issue. A comprehensive evaluation of eight commercial AI-based segmentation software platforms revealed significant intersoftware variability, particularly for complex organs-at-risk (OARs) like the cervical esophagus (DSC variation of 0.41) and spinal cord (DSC variation of 0.13) [22]. This indicates that the choice of software alone can introduce substantial inconsistency in segmentation outputs, potentially affecting downstream treatment plans and multi-center trial results.
Data Heterogeneity, Noise, and Protocol Dependency
Medical imaging data is inherently heterogeneous. Models must be robust to variations in scanner protocols, image resolution, contrast, and noise across different institutions [22]. A prominent challenge in clinical deployment is the dependency on complete, multi-sequence MRI protocols. Relying on a full set of sequences (T1, T1C, T2, FLAIR) creates a barrier to widespread adoption, as incomplete data is common in real-world settings [23]. Research has shown that the absence of key sequences drastically impacts performance; for instance, using FLAIR-only sequences resulted in exceptionally low Dice scores for enhancing tumor (ET: 0.056) [18]. Conversely, studies have demonstrated that robust performance can be maintained with minimized data. The combination of T1-weighted contrast-enhanced (T1C) and T2-FLAIR sequences has been identified as a core, efficient protocol capable of delivering segmentation accuracy for whole tumor and enhancing tumor that is comparable to, and sometimes better than, using all four sequences [18] [23].
Tumor Biological Complexity and Class Imbalance
The biological nature of tumors introduces fundamental segmentation difficulties. High spatial and structural variability, diffuse infiltration (especially in gliomas), and the presence of multiple subregions within a single tumor pose significant hurdles [18]. Models must simultaneously delineate the necrotic core, enhancing tumor, and surrounding edema, each with distinct imaging characteristics [19]. This task is further complicated by class imbalance, where voxels belonging to tumor subregions are vastly outnumbered by healthy tissue voxels. This imbalance can cause models to become biased toward the majority class, leading to poor segmentation of small but critical tumor areas [20]. Attention mechanisms and tailored loss functions have been developed to address this, forcing the model to focus on under-represented yet clinically vital regions.
Detailed Experimental Protocols
Protocol: Evaluating MRI Sequence Dependencies for Glioma Segmentation
This protocol is designed to identify the minimal set of MRI sequences required for robust glioma segmentation, enhancing model generalizability and clinical applicability.
1. Research Question: Which combination of standard MRI sequences provides optimal segmentation accuracy for glioma subregions while minimizing data requirements?
2. Experimental Design:
- Dataset: Utilize a publicly available, curated dataset such as the BraTS 2021 dataset, which contains multi-institutional MRI data with expert-annotated ground truth for tumor subregions [23].
- Input Configurations: Systematically train and evaluate models on all clinically relevant combinations of the four core sequences: T1-native (T1n), T1-contrast enhanced (T1c), T2-weighted (T2w), and T2-FLAIR (T2f). Key combinations to test include T1c-only, T2f-only, T1c+T2f, and the full set T1n+T1c+T2w+T2f [18] [23].
- Model Architecture: Employ a standard 3D U-Net, a proven and widely used architecture for medical image segmentation, to isolate the effect of input sequences from architectural innovations [18].
3. Methodology:
- Pre-processing: Apply standard pre-processing steps to all data, including co-registration to a common template, interpolation to a uniform resolution, and intensity normalization.
- Training: Use 5-fold cross-validation on the training cohort to ensure robust performance estimation.
- Validation: Evaluate the trained models on a held-out test set that was not used during training or cross-validation.
4. Key Output Metrics:
- Primary Metric: Dice Similarity Coefficient for Enhancing Tumor, Tumor Core, and Whole Tumor.
- Secondary Metrics: Sensitivity, Specificity, and 95th percentile Hausdorff Distance.
- Statistical Analysis: Perform Wilcoxon signed-rank tests with multiple-hypothesis correction to determine if volumetric differences between simplified protocols and the full-protocol ground truth are statistically significant [23].
5. Interpretation: A simplified protocol is considered clinically viable if it achieves DSC scores that are not statistically inferior to the full protocol and produces tumor volumes that are not significantly different from the expert reference standard.
Protocol: Benchmarking Model Robustness Against Inter-Observer Variability
This protocol assesses whether an automated segmentation model performs within the bounds of human inter-observer variability.
1. Research Question: Does the automated segmentation model's performance fall within the range of variation observed between different human experts?
2. Experimental Design:
- Ground Truth: Establish a reference set of medical images with tumor volumes delineated by multiple board-certified experts.
- Comparison Groups: Calculate agreement metrics between: a) different human experts, and b) the model prediction and each expert's delineation.
3. Methodology:
- Segmentation Task: Apply the model to the test set to generate automated segmentations.
- Metric Calculation: For every case in the test set, compute the DSC for the following pairings:
- Expert 1 vs. Expert 2
- Model vs. Expert 1
- Model vs. Expert 2
4. Key Output Metrics:
- Primary Metric: Dice Similarity Coefficient.
- Statistical Analysis: Compare the distributions of DSC values using statistical tests. A model is considered to have passed this benchmark if its agreement with experts is not significantly worse than the inter-observer agreement between the experts themselves [2].
Protocol: Assessing Multi-Site Generalizability
This protocol validates the performance of a segmentation model on external, independent datasets to ensure generalizability.
1. Research Question: How well does a model trained on data from one institution perform on data acquired from different institutions with varying scanners and protocols?
2. Experimental Design:
- Internal Cohort: Use a dataset from one or multiple institutions for model training and initial validation.
- External Cohorts: Acquire at least two independent test datasets from separate hospital systems that were not represented in the training data.
3. Methodology:
- Model Training: Train the model on the internal cohort.
- Model Testing: Apply the trained model directly to the external cohorts without fine-tuning.
- Performance Comparison: Quantify performance on all cohorts using consistent metrics.
4. Key Output Metrics:
- Primary Metric: Median Dice Similarity Coefficient and its interquartile range.
- Analysis: The model demonstrates strong generalizability if performance on external cohorts is comparable to that on the internal cohort [2].
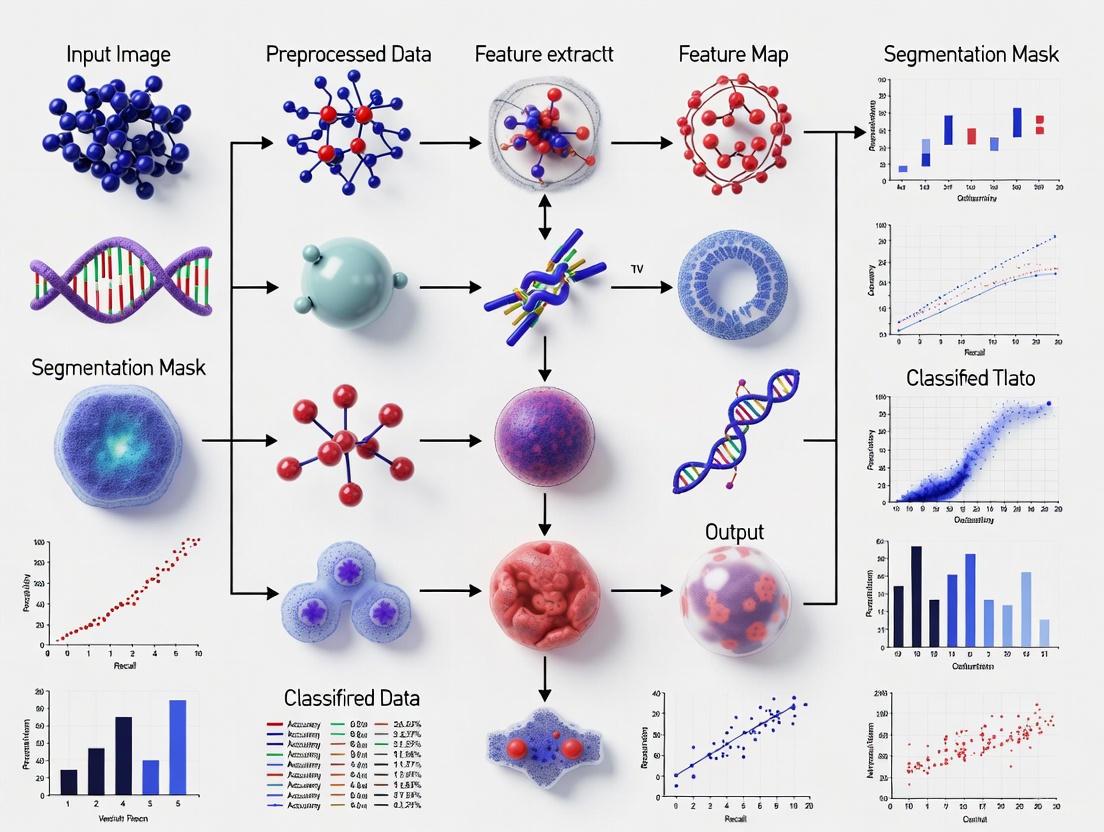
Visualizing the Experimental Workflow
The following diagram illustrates the logical flow of a robust model development and validation protocol, as described in the previous sections.
Figure 1: Workflow for developing and validating a robust segmentation model, from data curation through to deployment, emphasizing critical validation steps.
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Resources for Tumor Segmentation Research
| Resource Category | Specific Example / Tool | Function & Application in Research |
|---|---|---|
| Benchmark Datasets | BraTS (Brain Tumor Segmentation) Dataset [18] [19] [23] | Provides multi-institutional, multi-modal MRI with expert-annotated ground truth for training and benchmarking models. |
| Core Model Architectures | 3D U-Net [18] [2] | A standard, highly effective convolutional network backbone for volumetric medical image segmentation. |
| Advanced Architectures | MM-MSCA-AF [19], ARU-Net [21], BSAU-Net [20] | Incorporate attention mechanisms and multi-scale feature aggregation to handle complexity and improve edge accuracy. |
| Performance Metrics | Dice Similarity Coefficient, Hausdorff Distance [18] [2] [22] | Quantify spatial overlap and boundary accuracy of segmentations compared to ground truth. |
| Validation Frameworks | 5-Fold Cross-Validation, External Test Cohorts [18] [2] | Ensure reliable performance estimation and test for model generalizability across unseen data. |
| Statistical Analysis | Wilcoxon Signed-Rank Test [23] | Determine the statistical significance of performance differences between models or protocols. |
Public benchmarks, such as the Brain Tumor Segmentation (BraTS) dataset and the associated challenges organized by the Medical Image Computing and Computer Assisted Intervention (MICCAI) conference, have become foundational pillars in the field of automated tumor segmentation using deep learning. These community-driven initiatives provide the essential infrastructure for standardized evaluation, enabling researchers to benchmark their algorithms against a common baseline using high-quality, expert-annotated data. By offering a transparent and fair platform for comparison, they significantly accelerate the translation of algorithmic innovations into tools with genuine clinical potential. Furthermore, the iterative nature of these annual challenges, with progressively evolving datasets and tasks, directly fuels technical advancements, pushing the community to develop more accurate, robust, and generalizable models. This application note details the role of these public resources, providing researchers with a structured overview of the BraTS dataset's evolution, the framework of MICCAI challenges, and practical protocols for engaging with these critical tools.
The BraTS Dataset: Evolution and Impact
The Brain Tumor Segmentation (BraTS) challenge has curated and expanded a multi-institutional dataset annually since 2012, establishing it as the premier benchmark for evaluating state-of-the-art brain tumor segmentation algorithms [24]. The dataset's evolution is characterized by a deliberate increase in size, diversity, and annotation complexity, directly reflecting the community's growing understanding of the clinical problem.
Historical Progression and Key Features
The following table summarizes the quantitative and qualitative progression of the BraTS dataset, highlighting its expansion in scale and clinical relevance.
Table 1: Evolution of the BraTS Dataset (2012-2025)
| Challenge Year | Key Features and Advancements | Dataset Size & Composition | Clinical & Technical Impact |
|---|---|---|---|
| 2012-2014 (Early Years) | Establishment of core multi-parametric MRI protocol (T1, T1Gd, T2, FLAIR); Initial focus on glioblastoma (GBM) sub-region segmentation. | Limited cases (∼30-50 glioma scans) from a few institutions. | Created a standardized benchmarking foundation; catalyzed research into automated segmentation. |
| 2015-2020 (Rapid Growth) | significant dataset expansion; inclusion of lower-grade gliomas; introduction of pre-processing standards (co-registration, skull-stripping). | Growth to hundreds, then thousands of subjects from multiple international centers. | Enabled training of more complex deep learning models (e.g., U-Net, nnU-Net); improved generalizability. |
| 2021-2024 (Maturation) | Integration of extensive metadata (clinical, molecular); focus on synthetic data generation (BraSyn) for missing modalities; enhanced annotation protocols. | Thousands of subjects from the RSNA-ASNR-MICCAI collaboration; largest multi-institutional mpMRI dataset of brain tumors. | Facilitated development of algorithms robust to real-world clinical challenges like missing sequences and domain shift [25]. |
| 2025 (Current/Future) | Designated a MICCAI Lighthouse Challenge; expanded focus on longitudinal response assessment, underrepresented populations, and further clinical needs [26] [24]. | Continues to grow with new data; includes pre- and post-treatment follow-up imaging for dynamic assessment. | Aims to drive innovations in predictive and prognostic modeling for precision medicine. |
Data Composition and Annotation Standardization
A critical strength of the BraTS dataset is its standardized composition and rigorous annotation protocol. Each subject typically includes four essential MRI sequences: native T1-weighted (T1), post-contrast T1-weighted (T1Gd), T2-weighted (T2), and T2-FLAIR (Fluid Attenuated Inversion Recovery) [24] [25]. These sequences provide complementary information crucial for delineating different tumor sub-compartments. The ground truth segmentation labels are generated through a robust process involving both automated fusion of top-performing algorithms (e.g., nnU-Net, DeepScan) and meticulous manual refinement and approval by expert neuro-radiologists [25]. The annotated sub-regions are:
- Enhancing Tumor (ET): The gadolinium-enhancing portion of the tumor, indicating active, vascularized regions.
- Necrotic Core (NCR): The central non-enhancing area of the tumor composed of dead tissue.
- Peritumoral Edema (ED): The surrounding swollen brain tissue, which includes both vasogenic edema and infiltrating tumor cells.
This consistent, multi-region annotation strategy has been instrumental in moving the field beyond simple whole-tumor segmentation towards more clinically relevant, fine-grained analysis.
The MICCAI Challenges Framework
The MICCAI challenges provide a structured, competitive environment for benchmarking algorithmic solutions to well-defined problems in medical image computing. The BraTS challenge is a prominent example within this ecosystem.
Organizational Structure and Quality Assurance
MICCAI has implemented a rigorous process to ensure the quality and impact of its challenges. A key innovation is the challenge registration system, where the complete design of an accepted challenge must be published online before it begins, promoting transparency and thoughtful design [26] [27]. Recent initiatives like the "Lighthouse Challenges" further incentivize quality by spotlighting challenges that demonstrate excellence in design, data quality, and strong clinical collaboration [26] [28]. The BraTS 2025 challenge has been selected for this prestigious status, underscoring its high impact and quality [26].
BraTS Challenge Tasks and Evaluation
The BraTS challenge has evolved to include multiple tasks that address critical clinical problems. The core task remains the segmentation of the three intra-tumoral sub-regions (ET, NCR, ED) from the four standard MRI inputs. However, ancillary tasks like the Brain MR Image Synthesis Benchmark (BraSyn) have been introduced to address practical issues such as missing MRI sequences in clinical practice [25]. The evaluation of submitted algorithms is comprehensive and employs a suite of well-established metrics:
- Dice Similarity Coefficient (DSC): A spatial overlap index, the primary metric for segmentation accuracy.
- Hausdorff Distance (HD): A boundary distance metric, evaluating the precision of segmentation contours.
- Sensitivity and Specificity: Measuring the true positive and true negative rates, respectively.
- Structural Similarity Index Measure (SSIM): Used in synthesis tasks to evaluate the perceptual quality of generated images [25].
Ranking is typically based on a weighted aggregate of these metrics, ensuring a balanced assessment of different aspects of performance.
Experimental Protocols for Benchmark Participation
Engaging with the BraTS benchmark requires a systematic approach. The following workflow and protocol outline the key steps for effective participation.
Diagram 1: BraTS benchmark participation workflow
Protocol: Model Development and Evaluation on BraTS
Objective: To train and validate a deep learning model for brain tumor sub-region segmentation using the official BraTS dataset and evaluation framework.
Materials:
- Hardware: A high-performance computing workstation with one or more modern GPUs (e.g., NVIDIA A100, RTX 4090) with at least 16GB VRAM.
- Software: Python (v3.8+), PyTorch or TensorFlow, and libraries for medical image processing (e.g., NiBabel, SimpleITK).
Procedure:
Data Acquisition and Licensing:
- Access the BraTS dataset via its official platform (e.g., The Cancer Imaging Archive - TCIA). Complete any required registration or data usage agreements.
- For BraTS 2023-2025, the dataset includes multi-parametric MRI scans and ground truth annotations for training and validation.
Data Preprocessing:
- The BraTS data is already pre-processed, including co-registration to the SRI24 template, resampling to 1 mm³ isotropic resolution, and skull-stripping [25].
- Perform additional intensity normalization (e.g., z-score normalization per modality or whole-volume normalization) to ensure consistent input scales.
- Implement data augmentation techniques to improve model robustness. Common strategies include random rotations (±10°), flipping, scaling (0.9-1.1x), and elastic deformations.
Model Selection and Training:
- Architecture Choice: Select a proven backbone architecture. The nnU-Net framework, which automatically configures a U-Net-based pipeline, has consistently emerged as a top performer in BraTS challenges and is highly recommended as a strong baseline [29]. Other advanced architectures include ensemble models integrating transformers and attention mechanisms (e.g., GAME-Net) [30].
- Implementation: Configure the model to accept four input channels (T1, T1Gd, T2, FLAIR) and output three segmentation maps (ET, NCR, ED).
- Loss Function: Use a combination of Dice loss and cross-entropy loss to handle class imbalance.
- Training: Train the model using the official BraTS training set. Utilize 5-fold cross-validation to robustly assess performance and prevent overfitting. Monitor the loss on a held-out validation split.
Model Validation and Evaluation:
- Use the official BraTS validation set (if available for the challenge year) to generate predictions.
- Evaluate the predictions locally using the challenge's metrics (Dice, HD95) before submitting to the official server.
- Analyze failure cases, such as poor performance on small lesions or tumors adjacent to brain boundaries, to guide model refinement.
Submission and Benchmarking:
- Submit the segmentation results for the held-out test set to the official BraTS evaluation platform (e.g., via the Codabench or Grand Challenge platforms).
- The platform will compute the final ranking metrics against the private ground truth, providing a place on the public leaderboard.
The Scientist's Toolkit: Essential Research Reagents
Engaging with public benchmarks like BraTS requires a suite of software tools and data resources. The following table details the key components of the modern computational scientist's toolkit for automated tumor segmentation research.
Table 2: Essential Research Reagents for BraTS-based Segmentation Research
| Tool/Resource | Type | Primary Function | Relevance to BraTS Research |
|---|---|---|---|
| BraTS Dataset | Data | Provides standardized, annotated multi-parametric MRI brain tumor data. | The fundamental benchmark for training, validation, and testing of segmentation models [24] [25]. |
| nnU-Net | Software Framework | Self-configuring deep learning framework for medical image segmentation. | The leading baseline and winning methodology in multiple BraTS challenges; provides an out-of-the-box solution [29]. |
| PyTorch / TensorFlow | Software Library | Open-source libraries for building and training deep learning models. | The foundational computing environment for implementing and experimenting with custom model architectures. |
| NiBabel / SimpleITK | Software Library | Libraries for reading, writing, and processing medical images (NIfTI format). | Essential for handling the 3D volumetric data provided by the BraTS dataset. |
| FeTS Tool / CaPTk | Software Platform | Open-source platforms for federated learning and quantitative radiomics analysis. | Useful for pre-processing and analyzing BraTS-compatible data; FeTS is used in the challenge evaluation [25]. |
| Generative Autoencoders & Attention Mechanisms | Algorithmic Component | Advanced DL components for feature learning and context aggregation. | Used in state-of-the-art models (e.g., GAME-Net) to boost segmentation accuracy beyond standard CNNs [30]. |
The BraTS dataset and MICCAI challenges exemplify the transformative power of public benchmarks in accelerating research in automated tumor segmentation. By providing a standardized, high-quality, and ever-evolving platform for evaluation, they have not only driven the performance of deep learning models to near-human levels but have also steered the community towards solving clinically relevant problems, such as handling missing data and ensuring generalizability. The structured protocols and toolkit provided here offer a pathway for researchers to engage with these resources effectively. As these benchmarks continue to evolve—embracing longitudinal data, diverse populations, and predictive tasks—they will undoubtedly remain at the forefront of translating algorithmic advances into tangible tools for precision medicine.
Current Research Trends and Gap Analysis in Automated Segmentation
Automated tumor segmentation using deep learning (DL) has emerged as a transformative technology in medical imaging, significantly impacting diagnosis, treatment planning, and therapeutic development. Current research demonstrates a rapid evolution from conventional convolutional neural networks (CNNs) toward sophisticated architectures incorporating attention mechanisms, transformer modules, and hybrid designs [31]. These advancements address critical clinical challenges including tumor heterogeneity, ambiguous boundaries, and the imperative for real-time processing in clinical workflows. The integration of these technologies into drug development pipelines enables more precise target volume delineation for radiotherapy, objective treatment response assessment, and quantitative biomarker extraction for clinical trials [29] [2]. This analysis examines the current state of automated segmentation research, providing structured comparisons of methodological approaches, quantitative performance benchmarks, detailed experimental protocols, and identification of persistent gaps requiring further investigation to achieve widespread clinical adoption.
Quantitative Analysis of Current Models and Performance
Performance Benchmarks Across Tumor Types
Table 1: Performance Metrics of Deep Learning Models for Tumor Segmentation
| Tumor Type | Model Architecture | Dataset | Key Metric | Performance | Reference |
|---|---|---|---|---|---|
| Brain Tumor (13 types) | Darknet53 (Classification) | Institutional (203 subjects) | Accuracy | 98.3% | [13] |
| Brain Tumor | ResNet50 (Segmentation) | Institutional (203 subjects) | Mean Dice Score | 0.937 | [13] |
| Glioma | Various CNN/Transformer Hybrids | BraTS | Dice Score (Enhancing Tumor) | 0.82-0.90 | [32] [31] |
| Glioma | 2D-VNET++ with CBF | BraTS | Dice Score | 99.287 | [33] |
| Glioblastoma | nnU-Net | BraTS | Dice Score | >0.89 | [29] |
| Lung Cancer | 3D U-Net (iSeg) | Multicenter (1002 CTs) | Median Dice Score | 0.73 [IQR: 0.62-0.80] | [2] |
| Skin Cancer | Improved DeepLabV3+ with ResNet20 | ISIC-2018 | Dice Score | 94.63% | [34] |
Architectural Efficiency Analysis
Table 2: Model Complexity and Hardware Considerations
| Model Category | Representative Architectures | Parameter Efficiency | Computational Demand | Clinical Deployment Suitability |
|---|---|---|---|---|
| CNN-Based | 3D U-Net, V-Net, SegNet | Moderate | Moderate | High (Well-established) |
| Pure Transformer | ViT, Swin Transformer | Low (High parameters) | Very High | Low (Resource-intensive) |
| Hybrid CNN-Transformer | TransUNet, UNet++ with Attention | Moderate to High | High | Medium (Emerging) |
| Lightweight CNN | Improved ResNet20, Light U-Net | High | Low | High (Edge devices) |
| Self-Configuring | nnU-Net | Adaptive | Adaptive | High (Multi-site) |
Recent comprehensive reviews evaluating over 80 state-of-the-art DL models reveal that while pure transformer architectures capture superior global context, they require substantial computational resources, creating deployment challenges in clinical environments with limited hardware capabilities [31]. Hybrid CNN-Transformer models strike a balance, leveraging convolutional layers for spatial feature extraction and self-attention mechanisms for long-range dependencies. The nnU-Net framework demonstrates particular clinical promise through its self-configuring capabilities that adapt to varying imaging protocols and institutional specifications [29].
Detailed Experimental Protocols
Multi-Channel MRI Fusion Protocol for Brain Tumor Segmentation
Objective: To implement a DL pipeline for simultaneous brain tumor classification and segmentation using non-contrast T1-weighted (T1w) and T2-weighted (T2w) MRI sequences fused via RGB transformation.
Materials and Reagents:
- MRI datasets (e.g., BraTS 2012-2025 challenges, institutional datasets)
- Python 3.8+ with PyTorch/TensorFlow frameworks
- GPU acceleration (NVIDIA RTX 3000+ series recommended)
- Data augmentation libraries (Albumentations, TorchIO)
Methodology:
- Data Preprocessing:
- Convert DICOM images to NIfTI format for standardized processing
- Apply N4 bias field correction to address intensity inhomogeneity
- Normalize intensity values to zero mean and unit variance
- Coregister all sequences to a common spatial alignment
Multi-Channel Fusion:
- Stack T1w, T2w, and their linear average (T1w + T2w)/2 into three-channel RGB format
- This fusion enriches feature representation while maintaining non-contrast protocol compatibility [13]
Model Training Configuration:
- For classification: Implement Darknet53 with pretrained weights
- For segmentation: Utilize ResNet50-based FCN with deep supervision
- Loss function: Combined Dice and Cross-Entropy loss
- Optimizer: AdamW with learning rate 1e-4, weight decay 1e-5
- Batch size: 16 (adjusted based on GPU memory)
- Training duration: 200-300 epochs with early stopping
Performance Validation:
- Apply five-fold cross-validation to ensure robustness
- Evaluate using DSC, HD95, Sensitivity, and Specificity
- Compare against ground truth manual segmentation by expert radiologists
This protocol achieved a top classification accuracy of 98.3% and segmentation Dice score of 0.937, demonstrating the efficacy of multichannel fusion for non-contrast MRI analysis [13].
nnU-Net Framework for Glioblastoma Auto-Contouring in Radiotherapy
Objective: To automate the segmentation of glioblastoma (GBM) target volumes for radiotherapy treatment planning using the self-configuring nnU-Net framework.
Materials:
- Multimodal MRI: T1, T1-CE, T2, FLAIR sequences
- Radiotherapy contouring workstations
- Approved software: NeuroQuant or Raidionics for clinical validation
Methodology:
- Data Preparation and Preprocessing:
- Acquire multi-parametric MRI (mpMRI) according to BraTS protocol specifications
- Manually contour ground truth volumes (GTV, CTV, PTV) following RTOG guidelines
- Convert all images to 1mm³ isotropic resolution using spline interpolation
- Apply intensity normalization through z-score transformation
nnU-Net Configuration:
- Implement both 2D and 3D nnU-Net configurations
- Enable automatic preprocessing configuration and patch size optimization
- Utilize default training parameters with five-fold cross-validation
- Employ Dice loss for optimization with exponential learning rate decay
Training Protocol:
- Training duration: 1000 epochs per fold
- Batch size: Automatically determined based on GPU memory
- Data augmentation: Rigid transformations, elastic deformations, gamma corrections
- Implement extensive online augmentation to improve model generalizability
Clinical Validation:
- Quantitative analysis: Compute DSC, HD95, and relative volume difference
- Qualitative assessment: Independent review by ≥2 radiation oncologists
- Statistical comparison against inter-observer variability among clinicians
This approach has demonstrated superior segmentation accuracy for GBM target volumes, with nnU-Net emerging as the strongest architecture due to its self-configuring capabilities and adaptability to different imaging modalities [29].
Visualization of Research Workflows
Multi-Channel MRI Segmentation Pipeline
(Multi-Channel MRI Segmentation Workflow)
nnU-Net Self-Configuring Framework
(nnU-Net Self-Configuring Framework)
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Resources for Automated Segmentation Research
| Resource Category | Specific Tools/Solutions | Primary Function | Application Context |
|---|---|---|---|
| Public Datasets | BraTS (2012-2025) | Benchmarking glioma segmentation | Algorithm validation across institutions |
| ISIC (2018-2020) | Skin lesion analysis | Dermatological segmentation development | |
| Software Frameworks | PyTorch, TensorFlow | DL model development | Flexible research prototyping |
| nnU-Net | Automated configuration | Baseline model establishment | |
| Clinical Validation Tools | NeuroQuant, Raidionics | Clinical segmentation assessment | Translational research bridge |
| ITK-SNAP, 3D Slicer | Manual annotation & visualization | Ground truth generation | |
| Hardware Accelerators | NVIDIA GPUs (RTX 3000/4000+) | Training acceleration | High-throughput experimentation |
| Google TPUs | Transformer model optimization | Large-scale model training |
Current Challenges and Research Gaps
Despite significant advances, automated tumor segmentation faces several persistent challenges that limit clinical adoption. Technical limitations include inadequate performance on boundary delineation, with encoder-decoder architectures sometimes producing jagged or inaccurate boundaries despite high overall Dice scores [33]. Class imbalance remains problematic, as models frequently prioritize dominant classes like tumor cores while underperforming on smaller but clinically critical regions like infiltrating edges. Clinical translation barriers include insufficient model interpretability, with "black box" predictions creating clinician skepticism [31]. Limited generalizability across diverse patient populations, imaging protocols, and institutional equipment presents additional hurdles. Computational constraints are particularly relevant for transformer-based architectures, which require substantial resources that may be unavailable in resource-limited clinical settings [31].
Promising research directions include the development of explainable AI (XAI) techniques like integrated gradients and class activation mapping to enhance model transparency [2]. Weakly supervised approaches that reduce annotation burden through partial labeling and innovative loss functions show potential for addressing data scarcity. Federated learning frameworks enable multi-institutional collaboration while preserving data privacy, crucial for developing robust models without sharing sensitive patient information [13]. Continued refinement of attention mechanisms and transformer modules will likely further improve segmentation accuracy, particularly for heterogeneous tumor subregions.
Automated tumor segmentation has progressed dramatically from basic CNN architectures to sophisticated frameworks incorporating multi-modal fusion, self-configuration, and attention mechanisms. Current models demonstrate performance approaching or exceeding human inter-observer variability for well-defined segmentation tasks, with top-performing approaches achieving Dice scores exceeding 0.95 in controlled conditions. The integration of these technologies into drug development pipelines offers unprecedented opportunities for objective treatment response assessment and personalized therapy planning. However, bridging the gap between technical performance and clinical utility requires addressing persistent challenges in interpretability, generalizability, and computational efficiency. Future research prioritizing these translational considerations will accelerate the adoption of automated segmentation tools, ultimately enhancing precision medicine across oncology applications.
Deep Learning Architectures for Tumor Segmentation: Implementations and Real-World Applications
Convolutional Neural Networks (CNNs) have become a cornerstone in the field of medical image analysis, particularly for the critical task of automated tumor segmentation. In neuro-oncology and beyond, precise delineation of tumor boundaries from medical images such as Magnetic Resonance Imaging (MRI) and Computed Tomography (CT) is essential for diagnosis, treatment planning, and monitoring disease progression [35] [36]. CNN-based models address the significant limitations of manual segmentation, which is time-consuming, subject to inter-observer variability, and impractical for large-scale studies [36]. These deep learning models leverage their ability to automatically learn hierarchical features directly from image data, capturing complex patterns and textures that distinguish pathological tissues from healthy structures [35] [37]. This document examines the predominant CNN architectures deployed for tumor segmentation, evaluates their respective strengths and limitations, and provides detailed experimental protocols for researchers implementing these methodologies within the context of a broader thesis on automated tumor segmentation using deep learning.
Core CNN Architectures for Tumor Segmentation
Predominant Model Architectures
The landscape of CNN-based tumor segmentation is dominated by several key architectures, each with distinct structural characteristics and applications.
U-Net and its Variants: The U-Net architecture, introduced by Ronneberger et al., has emerged as arguably the most influential CNN architecture for biomedical image segmentation [37]. Its symmetrical encoder-decoder structure with skip connections allows it to capture both context and precise localization, making it exceptionally suitable for tumor segmentation where boundary delineation is critical [35] [38]. The encoder path progressively downsamples the input image, extracting increasingly abstract feature representations, while the decoder path upsamples these features to reconstruct the segmentation map at the original input resolution. The skip connections bridge corresponding layers in the encoder and decoder, preserving spatial information that would otherwise be lost during downsampling [37]. This architecture has spawned numerous variants including nnU-Net, which introduces self-configuring capabilities that automatically adapt to specific dataset properties, and has demonstrated superior segmentation accuracy in benchmarks like the Brain Tumor Segmentation (BraTS) challenge [38].
ResNet (Residual Neural Network): ResNet addresses the degradation problem that occurs in very deep networks through the use of residual blocks and skip connections [39]. These connections enable the network to learn identity functions, allowing gradients to flow directly through the network and facilitating the training of substantially deeper architectures. In tumor segmentation, ResNet is often utilized as the encoder backbone within more complex segmentation frameworks, where its depth and representational power excel at feature extraction [35] [39].
V-Net: Extending the U-Net concept to volumetric data, V-Net employs 3D convolutional operations throughout its architecture, making it particularly effective for segmenting tumors in 3D medical image volumes such as MRI and CT scans [35]. By processing entire volumetric contexts simultaneously, V-Net can capture spatial relationships in all three dimensions, which is crucial for accurately assessing tumor morphology and volume.
Attention-Enhanced CNNs: Recent architectural innovations incorporate attention mechanisms to enhance model performance. The Global Attention Mechanism (GAM) simultaneously captures cross-dimensional interactions across channel, spatial width, and spatial height dimensions, enabling the model to focus on diagnostically relevant regions while suppressing less informative features [40]. Similarly, the Convolutional Block Attention Module (CBAM) sequentially infers attention maps along both channel and spatial dimensions, and has been successfully integrated into architectures like YOLOv7 for improved brain tumor detection [41].
Architectural Comparison
Table 1: Comparison of Key CNN Architectures for Tumor Segmentation
| Architecture | Core Innovation | Dimensionality | Key Strength | Common Tumor Applications |
|---|---|---|---|---|
| U-Net | Skip connections in encoder-decoder structure | 2D/3D | Excellent balance between context capture and localization precision | Brain tumors (gliomas, glioblastoma), various abdominal tumors |
| ResNet | Residual blocks with skip connections | 2D/3D | Enables training of very deep networks without degradation; powerful feature extraction | Often used as encoder in segmentation networks; classification tasks |
| V-Net | Volumetric convolution with residual connections | 3D | Native handling of 3D spatial context; improved volumetric consistency | Prostate cancer, brain tumors, liver tumors |
| nnU-Net | Self-configuring framework | 2D/3D | Automatically adapts to dataset characteristics; state-of-the-art performance | Multiple cancer types; winner of various medical segmentation challenges |
| Attention CNNs (e.g., GAM, CBAM) | Cross-dimensional attention mechanisms | 2D/3D | Enhanced focus on salient regions; improved feature representation | Brain tumors, oral squamous cell carcinoma, small tumor detection |
Performance Analysis and Quantitative Comparison
Segmentation Accuracy Across Architectures
CNN-based models have demonstrated remarkable performance in tumor segmentation tasks across various cancer types and imaging modalities. Evaluation metrics such as the Dice Similarity Coefficient (DSC), Intersection over Union (IoU), and accuracy provide standardized measures for comparing model effectiveness.
Brain Tumor Segmentation: For glioblastoma multiforme (GBM) and other glioma types, CNN architectures have achieved exceptional segmentation accuracy. U-Net and its variants consistently achieve DSC scores exceeding 0.90 on benchmark datasets like BraTS [35]. The nnU-Net architecture has emerged as particularly powerful, offering superior segmentation accuracy due to its self-configuring capabilities and adaptability to different imaging modalities [38]. In practical clinical applications for radiotherapy planning, models like SegNet have reported DSC values of 89.60% with Hausdorff Distance of 1.49 mm when segmenting GBM using multimodal MRI data from the BraTS 2019 dataset [38]. Mask R-CNN, another CNN variant, has demonstrated promise for real-time tumor monitoring during radiotherapy, achieving DSC values of 0.8 for tumor volume delineation from daily MR images [38].
Beyond Brain Tumors: CNN performance remains strong across diverse cancer types. For oral squamous cell carcinoma (OSCC), novel architectures like gamUnet that integrate Global Attention Mechanisms have significantly outperformed conventional models in segmentation accuracy [40]. In classification tasks, specialized networks like CNN-TumorNet have achieved remarkable accuracy rates up to 99% in distinguishing tumor from non-tumor MRI scans [42].
Table 2: Performance Metrics of CNN Models Across Cancer Types
| Cancer Type | Architecture | Dataset | Key Metric | Performance | Reference |
|---|---|---|---|---|---|
| Brain Tumors (GBM) | U-Net variants | BraTS | Dice Score | >0.90 | [35] |
| Brain Tumors (GBM) | SegNet | BraTS 2019 | Dice Score | 89.60% | [38] |
| Brain Tumors (GBM) | Mask R-CNN | Clinical daily MRI | Dice Score | 0.80 | [38] |
| Brain Tumors | nnU-Net | BraTS | Dice Score | Superior to benchmarks | [38] |
| Brain Tumors | YOLOv7 with CBAM | Curated dataset | Accuracy | 99.5% | [41] |
| Oral Cancer (OSCC) | gamUnet (GAM-enhanced) | Public datasets | Accuracy | Significant improvement over baselines | [40] |
| Various Cancers | CNN-TumorNet | Brain tumor MRI | Classification Accuracy | 99% | [42] |
Limitations and Challenges
Despite their impressive performance, CNN-based tumor segmentation approaches face several significant limitations:
Data Dependency and Annotation Costs: CNNs typically require large volumes of high-quality annotated images for effective training [39]. The process of medical image annotation is particularly costly and time-consuming, requiring specialized expertise from radiologists or pathologists [39]. This challenge is exacerbated for rare tumor types where collecting sufficient training data is difficult.
Computational Demands: Especially for 3D architectures like V-Net and processing high-resolution medical images, CNNs require substantial computational resources and memory [35]. This can limit their practical deployment in clinical settings with resource constraints or requirements for real-time processing.
Generalization Across Domains: Models trained on data from specific scanners, protocols, or institutions often experience performance degradation when applied to images from different sources [35] [43]. This lack of robustness to domain shifts remains a significant barrier to widespread clinical adoption.
Interpretability and Trust: The "black-box" nature of deep CNN decisions complicates clinical acceptance, as healthcare professionals require understanding of the rationale behind segmentation results [42]. While explainable AI approaches like LIME are being explored to address this, interpretability remains an active research challenge.
Experimental Protocols and Methodologies
Standardized Training Pipeline
Implementing CNN models for tumor segmentation requires a systematic approach to data preparation, model configuration, and training. The following protocol outlines a standardized pipeline adaptable to various tumor types and imaging modalities.
Data Preprocessing:
- Image Resizing: Standardize all input images to uniform dimensions compatible with the network architecture. For 2D CNNs, resize to square dimensions (e.g., 256×256 or 512×512 pixels); for 3D CNNs, use isotropic voxel sizes or standard volumetric dimensions [42].
- Intensity Normalization: Apply z-score normalization to scale intensity values across all images, reducing scanner-specific variations. Calculate mean and standard deviation from the training set and apply identical transformation to validation and test sets.
- Data Augmentation: Generate synthetic training examples through real-time augmentation during training. Recommended transformations include: random rotations (±15°), random scaling (0.85-1.15x), random flipping (horizontal/vertical), elastic deformations, and brightness/contrast adjustments [36].
- Patch Extraction: For large images or memory constraints, extract random patches during training (e.g., 128×128×128 for 3D volumes). Ensure adequate sampling of both tumor and non-tumor regions through class-balanced sampling.
Model Configuration:
- Architecture Selection: Choose base architecture based on task requirements: U-Net for general segmentation, V-Net for 3D volumes, ResNet-based encoders for transfer learning, or attention-enhanced variants for complex boundaries.
- Loss Function: Utilize Dice loss or a combination of Dice loss and cross-entropy loss to handle class imbalance between tumor and background pixels [37]. The Dice loss function is defined as: $DL = 1 - \frac{2 \times |X \cap Y| + \epsilon}{|X| + |Y| + \epsilon}$ where X is the predicted segmentation, Y is the ground truth, and ε is a smoothing factor.
- Optimizer: Employ Adam optimizer with initial learning rate of 1e-4, β₁=0.9, and β₂=0.999. Implement learning rate reduction on plateau with factor of 0.5 and patience of 10 epochs.
Training Procedure:
- Initialization: Initialize model with He normal or Xavier initialization. For encoder-decoder architectures, consider using pre-trained encoders (e.g., ImageNet pre-training for 2D models).
- Batch Training: Use small batch sizes (2-8 for 3D models, 8-32 for 2D models) depending on available GPU memory. Accumulate gradients if larger effective batch sizes are needed.
- Validation: Monitor Dice Similarity Coefficient on validation set after each epoch. Save model weights when validation performance improves.
- Early Stopping: Implement early stopping with patience of 30-50 epochs to prevent overfitting.
- Regularization: Apply dropout (rate 0.3-0.5) after convolutional layers and use L2 weight decay (1e-5) to improve generalization.
Evaluation Metrics:
- Primary Metrics: Dice Similarity Coefficient (DSC) and Hausdorff Distance (HD) for segmentation accuracy.
- Secondary Metrics: Sensitivity, specificity, precision, and recall for comprehensive performance assessment.
- Statistical Validation: Perform cross-validation (5-fold recommended) and report mean ± standard deviation of all metrics.
Advanced Implementation: Attention-Enhanced CNNs
For complex segmentation tasks involving tumors with infiltrative growth patterns or poorly defined boundaries (e.g., glioblastoma, OSCC), attention mechanisms significantly improve performance.
Integration of Attention Modules:
- GAM Integration: Incorporate Global Attention Mechanism between encoder and decoder of U-Net architecture. GAM simultaneously captures cross-dimensional dependencies through channel-spatial interaction, enhancing focus on diagnostically relevant regions [40].
- CBAM Integration: Sequentially apply channel attention followed by spatial attention modules at skip connection points. Channel attention emphasizes 'what' is meaningful, while spatial attention focuses on 'where' informative regions are located [41].
- Training Considerations: When introducing attention modules, potentially reduce learning rate (5e-5) due to increased model complexity. Monitor attention maps during validation to ensure the model learns clinically relevant foci.
Benchmark Datasets
Publicly available datasets with expert annotations are crucial for training and evaluating CNN models for tumor segmentation.
Table 3: Essential Datasets for Tumor Segmentation Research
| Dataset | Cancer Type | Imaging Modality | Key Characteristics | Research Applications |
|---|---|---|---|---|
| BraTS | Brain tumors (gliomas) | Multi-modal MRI (T1, T1-Gd, T2, FLAIR) | Largest brain tumor dataset; annual challenges since 2012; annotations for tumor sub-regions | Segmentation benchmark; model comparison; method development |
| TCIA | Multiple cancer types | CT, MRI, PET | Comprehensive repository; includes clinical data; diverse tumor types | General tumor analysis; progression prediction; multi-modal learning |
| ORCA | Oral Cancer (OSCC) | Histopathology (H&E-stained) | Annotated oral cancer images; complex tissue structures | Testing attention mechanisms; boundary detection in complex anatomy |
| BraTS-METS | Brain metastases | Multi-modal MRI | Focus on metastatic brain tumors; multi-class labels | Transfer learning; small tumor detection; multi-class segmentation |
Deep Learning Frameworks: PyTorch and TensorFlow/Keras with specialized medical imaging extensions (e.g., MONAI, NiftyNet).
Evaluation Tools: Official evaluation pipelines for benchmark challenges (e.g., BraTS evaluation framework); custom implementations of medical segmentation metrics.
Visualization Software: ITK-SNAP for 3D medical image visualization; TensorBoard for training monitoring; custom attention visualization tools.
Emerging Trends and Future Directions
The field of CNN-based tumor segmentation continues to evolve with several promising research directions:
Federated Learning: Addressing data privacy concerns by training models across multiple institutions without sharing patient data [44]. This approach is particularly valuable in medical imaging where data sharing is restricted by privacy regulations.
Explainable AI (XAI): Integrating techniques like LIME (Local Interpretable Model-agnostic Explanations) to provide transparent explanations for model predictions, increasing clinical trust and adoption [42].
Multi-Modal Fusion: Developing sophisticated architectures that effectively combine information from multiple imaging modalities (e.g., MRI, CT, PET) to improve segmentation accuracy and provide comprehensive tumor characterization.
Self-Supervised and Semi-Supervised Learning: Reducing annotation burdens by leveraging unlabeled data through pre-training and consistency regularization techniques, showing particular promise in low-data regimes [39].
As CNN architectures continue to mature and address current limitations, they hold tremendous potential to transform oncological care through more precise, consistent, and efficient tumor segmentation, ultimately contributing to improved diagnosis, treatment planning, and patient outcomes in clinical practice.
Automated tumor segmentation is a critical task in medical image analysis, aiding in diagnosis, treatment planning, and therapy monitoring. Among deep learning architectures, U-Net has emerged as a foundational model for this purpose. Its encoder-decoder structure with skip connections enables precise localization and segmentation of complex anatomical structures. This document details the application, performance, and experimental protocols for three pivotal U-Net variants—3D U-Net, Attention U-Net, and U-Net++—within the context of automated tumor segmentation research. It serves as a guide for researchers and drug development professionals seeking to implement these models, providing structured quantitative comparisons and reproducible methodologies.
Quantitative Performance Comparison
The following tables summarize key performance metrics and architectural characteristics of featured U-Net variants from recent studies, providing a basis for model selection.
Table 1: Tumor Segmentation Performance of U-Net Variants
| Model Variant | Application Context | Key Metric | Performance Score | Reference / Dataset |
|---|---|---|---|---|
| 3D Contour-Aware U-Net (CAU-Net) | Rectal Tumor Segmentation (MRI) | Dice Similarity Coefficient (DSC) | 0.7112 | [45] |
| Average Surface Distance (ASD) | 2.4707 | [45] | ||
| 3D U-Net (T1C + FLAIR) | Brain Tumor Segmentation (MRI) | DSC (Enhancing Tumor) | 0.867 | BraTS 2018/2021 [18] |
| DSC (Tumor Core) | 0.926 | BraTS 2018/2021 [18] | ||
| ES-UNet | Head & Neck Tumor Segmentation (CT) | Dice Similarity Coefficient (DSC) | 76.87% | MICCAI HECKTOR [46] |
| Attention-based 3D U-Net | Brain Tumor Segmentation (MRI) | Dice | 0.975 | BraTS 2020 [47] |
| Specificity | 0.988 | BraTS 2020 [47] | ||
| Sensitivity | 0.995 | BraTS 2020 [47] |
Table 2: Computational Characteristics of 3D U-Net Architectures
| Architectural Factor | Impact on Performance & Efficiency | Practical Guideline |
|---|---|---|
| Resolution Stages (S) | Increasing stages (e.g., S4→S5) is most effective for high-resolution images (voxel spacing <0.8 mm) to enlarge the receptive field, but offers diminishing returns on low-resolution data. [48] | Use more stages (S5, S6) for high-resolution datasets; S4 may be sufficient for lower resolutions. |
| Network Depth (D) | Deeper networks (D3) consistently improve performance, showing broad utility. They are most beneficial for anatomically regular, high-sphericity structures (>0.6). [48] | Prioritize increasing depth for segmenting compact, spherical organs. |
| Network Width (W) | Wider networks (W32, W64) are most impactful for tasks with high label complexity (>10 classes). Benefit is less pronounced for binary segmentation. [48] | Favor increased width for multi-class segmentation problems. |
| Inference Time | Scales directly with model size. Doubling width ~doubles time; increasing depth adds 30-40%; adding a stage increases it by 10-20%. [48] | Balance architectural complexity against required inference speed for clinical deployment. |
Featured Model & Experimental Protocol
3D Contour-Aware U-Net (CAU-Net) for Rectal Tumor Segmentation
This section provides a detailed protocol for implementing the 3D CAU-Net, which exemplifies how architectural innovations can address specific segmentation challenges like low contrast and ambiguous tumor boundaries in MRI. [45]
A. Model Architecture and Workflow
The 3D CAU-Net enhances the standard 3D U-Net with a contour-aware decoder and adversarial learning to improve boundary delineation. The following diagram illustrates its core structure and information flow.
B. Research Reagent Solutions
Table 3: Essential Materials and Reagents for 3D CAU-Net Experimentation
| Item Name | Function / Description | Application Note |
|---|---|---|
| T2-Weighted MRI Volumes | High-resolution 3D medical images providing anatomical detail for rectal tumor identification. [45] | Crucial for model input; ensure consistent acquisition protocols. |
| Manual Segmentation Masks | Expert-annotated ground truth data for model training and validation. [45] | Quality directly impacts model performance; requires radiological expertise. |
| High-Performance Computing Unit | Workstation with powerful GPUs (e.g., NVIDIA Tesla V100, A100). | Necessary for efficient 3D volumetric data processing and model training. |
| Python Deep Learning Stack | Libraries: PyTorch/TensorFlow for model building, NumPy for data handling, MONAI for medical imaging. [45] | Provides the software environment for implementing and training the CAU-Net. |
C. Step-by-Step Experimental Protocol
1. Data Curation and Preprocessing
- Dataset Construction: Collect and curate a dataset of 3D T2-weighted MRI volumes. The CAU-Net study used 108 volumes from patients with locally advanced rectal cancer. [45]
- Data Annotation: Ensure each MRI volume has a corresponding manual segmentation mask delineating the tumor region, annotated by experienced clinicians.
- Intensity Normalization: Normalize the intensity values of MRI volumes to a standard range (e.g., 0-1) to account for scanner and protocol variations.
- Data Augmentation: Apply random, on-the-fly 3D spatial transformations (e.g., rotations, flips, small deformations) and intensity shifts to the training data to improve model robustness and prevent overfitting. [45]
2. Model Implementation and Training
- Network Configuration: Implement the 3D U-Net backbone with a contour-aware decoder. Integrate Attention Fusion Blocks (AFBs) to fuse multi-scale features and emphasize contour information. [45]
- Adversarial Training:
- Setup: Introduce a discriminator network (e.g., a 3D CNN) trained to distinguish between the model's predicted segmentation and the ground-truth mask.
- Loss Function: Combine a segmentation loss (e.g., Dice Loss) and an adversarial loss. The overall loss function is:
L_total = L_segmentation + λ * L_adversarial, whereλis a weighting factor. [45] - Training Loop: Train the segmentation model (generator) and the discriminator in an alternating manner.
- Optimization: Use an optimizer like Adam with an initial learning rate of 1e-4, applying a learning rate scheduler based on validation performance plateau.
3. Model Evaluation and Validation
- Primary Metrics: Calculate the Dice Similarity Coefficient (DSC) and Average Surface Distance (ASD) to evaluate volumetric overlap and boundary accuracy, respectively. [45]
- Benchmarking: Compare the model's performance against other state-of-the-art segmentation methods on the same test set.
- Ablation Studies: Conduct experiments to validate the contribution of each key component (e.g., contour-aware decoder, AFB, adversarial loss) by removing them one at a time and observing the performance drop. [45]
Protocols for Other U-Net Variants
Attention U-Net for Bacterial Spore and Cell Segmentation
This protocol adapts Attention U-Net for segmenting small biological structures in microscopy images, demonstrating its utility beyond medical radiology. [49]
1. Image Pre-processing:
- Normalization: Normalize each input image using Z-score normalization:
I_norm = (I - μ) / σ, whereIis the input image,μis its mean intensity, andσis its standard deviation. [49] - Contrast Enhancement: Apply histogram equalization to improve the contrast and visibility of spores and cells. The transform function is
T(r) = Σ p(r_k),
for k=0 to r, where p(r_k) is the probability of intensity r_k. [49]
- Patching and Augmentation: Slice large original images into smaller patches for manageable training. Augment the training set using rotations, shifts, and shears. [49]
2. Model Implementation:
- Architecture: Use a standard U-Net as the backbone. Integrate Spatial Attention Gates into the skip connections. These gates take feature maps from the encoder and the corresponding gating signal from the decoder to produce a spatial attention mask. [49] This mask suppresses irrelevant background regions and highlights salient features, allowing the decoder to focus on specific targets like spores.
- Attention Gate Mechanics: The gate performs a series of operations (typically involving convolution, addition, and activation functions) on its inputs to generate a set of attention coefficients between 0 and 1. These coefficients are multiplied with the original encoder features before they are concatenated with the decoder features. [49]
3. Training and Evaluation:
- Loss Function: Use a combined loss, such as Binary Cross-Entropy and Dice Loss, to handle class imbalance.
- Metrics: Evaluate the model using accuracy, precision (positive predictive value), sensitivity (recall), and specificity. The cited model achieved accuracy of 96%, precision of 82%, sensitivity of 81%, and specificity of 98%. [49]
U-Net++ for Multi-Scale Feature Capture
U-Net++ introduces a nested and dense skip connection architecture to bridge the semantic gap between encoder and decoder features. [50] [46]
1. Model Implementation:
- Nested Skip Pathways: Redesign the traditional U-Net skeleton. Instead of a single skip connection between same-resolution encoder and decoder layers, create a series of convolutional blocks on the skip pathways that connect an encoder layer to all decoder layers that are at the same or higher resolution. [46]
- Deep Supervision: optionally allows for model output at multiple levels, which can improve learning and provide robustness. [46] The following diagram visualizes the dense, nested connectivity of U-Net++ compared to the standard U-Net.
2. Training Strategy:
- Loss Function: A simple Dice loss or a combination of Cross-Entropy and Dice loss is commonly used.
- Advantage: The dense connections allow the decoder to access features of different semantic scales from the encoder, leading to more powerful multi-scale feature representation and often superior segmentation accuracy, especially for structures of varying sizes. [46]
The evolution of U-Net through variants like 3D U-Net, Attention U-Net, and U-Net++ has significantly advanced the frontier of automated tumor segmentation. The 3D U-Net processes volumetric context, Attention U-Net enhances focus on salient regions, and U-Net++ achieves rich multi-scale feature fusion. The profiled 3D CAU-Net exemplifies how integrating contour-awareness and adversarial learning can specifically address the challenge of blurry tumor boundaries. As the field progresses, the "bigger is better" paradigm is being challenged by smarter, more efficient architectural designs and training strategies that are tailored to specific dataset characteristics and clinical requirements. [48] Future work will likely continue this trend, emphasizing not just performance but also computational efficiency and generalizability across diverse patient populations.
Emerging Transformer-Based and Hybrid Architectures
The field of automated tumor segmentation has been revolutionized by the advent of deep learning, with Transformer-based and hybrid architectures emerging as particularly powerful paradigms. While Convolutional Neural Networks (CNNs) have long been the workhorse for medical image analysis due to their strong local feature extraction capabilities, they face inherent limitations in capturing global contextual relationships and long-range dependencies—critical factors for accurate tumor boundary delineation [51]. Vision Transformers (ViTs) address these limitations by leveraging self-attention mechanisms to model global context across entire images, though they often require large datasets for optimal performance and struggle with computational complexity, especially for 3D volumetric data [51] [52].
Hybrid architectures have emerged to harness the complementary strengths of both CNNs and Transformers. These models typically employ CNN-based encoders to extract local features and hierarchical representations while integrating Transformer modules to capture global contextual information [51] [53]. The resulting architectures demonstrate enhanced capability in handling the complex appearance, shape, and scale variations characteristic of tumors across different imaging modalities and anatomical regions. This document provides a comprehensive technical overview of these emerging architectures, their performance characteristics, and detailed protocols for their implementation in tumor segmentation research.
Key Architectures and Their Characteristics
Table 1: Comparison of Transformer-Based and Hybrid Architectures for Tumor Segmentation
| Architecture | Core Innovation | Application Domain | Key Advantages | Reported Performance |
|---|---|---|---|---|
| BEFUnet [51] | Hybrid CNN-Transformer with dual branch encoder (edge & body) | Medical Image Segmentation | Excels at irregular boundary processing; Local Cross-Attention Feature (LCAF) fusion reduces computation | Outperforms existing methods across multiple metrics and datasets |
| VT-UNet [52] | Pure volumetric Transformer for 3D segmentation | 3D Tumor Segmentation (MRI, CT) | Maintains full 3D volume integrity; efficient local/global feature capture; robust to artifacts | Competitive results on MSD BraTS task; computationally efficient |
| BrainTumNet [54] | Multi-task framework with adaptive masked Transformer | Brain Tumor Segmentation & Classification | Unified segmentation and classification; integrates CNN locality with Transformer global modeling | DSC: 0.91, IoU: 0.921, HD: 12.13, Classification Accuracy: 93.4% |
| Hybrid U-Net with Transformer Bottleneck [53] | U-Net with Transformer bottleneck & multiple attention mechanisms | MRI Tumor Segmentation | Combines CNN feature extraction with global context modeling; suitable for limited data scenarios | Dice: 0.7636, IoU: 0.7357 (on small, heterogeneous local dataset) |
| T3scGAN [55] | 3D conditional Generative Adversarial Network | 3D Liver & Tumor Segmentation (CT) | cGAN-provided trainable loss function; coarse-to-fine segmentation framework | Liver Dice: 0.961, Tumor Dice: 0.796 (LiTS 2017 dataset) |
| 2D-VNET++ [33] | 4-staged network with Context Boosting Framework (CBF) | Brain Tumor Segmentation (MRI) | Enhances texture/contextual features; custom Log Cosh Focal Tversky loss reduces false positives | Dice: 99.287, Jaccard: 99.642, Tversky: 99.743 |
Quantitative Performance Metrics
Table 2: Detailed Performance Metrics of Featured Architectures
| Architecture | Dataset | Dice Score | IoU/Jaccard | Hausdorff Distance | Other Metrics |
|---|---|---|---|---|---|
| BEFUnet [51] | Multiple medical datasets | Not specified | Not specified | Not specified | Outperformed existing methods across various evaluation metrics |
| VT-UNet [52] | MSD BraTS | Competitive results | Competitive results | Not specified | Computationally efficient; robust to data artifacts |
| BrainTumNet [54] | Internal (485 cases) | 0.91 | 0.921 | 12.13 | Classification AUC: 0.96, Accuracy: 93.4% |
| Hybrid U-Net [53] | Local clinical MRI (6 patients) | 0.7636 | 0.7357 | Not specified | Precision: 0.9736, Recall: 0.9756 |
| T3scGAN [55] | LiTS 2017 | Liver: 0.961, Tumor: 0.796 | Not specified | Not specified | N/A |
| 2D-VNET++ [33] | Not specified | 99.287 | 99.642 | Not specified | Tversky Index: 99.743 |
Experimental Protocols and Methodologies
Implementation Protocol for Hybrid U-Net with Transformer Bottleneck
Objective: Implement a hybrid architecture combining CNN-based U-Net with a Transformer bottleneck for MRI tumor segmentation on limited local datasets.
Materials and Preprocessing:
- Imaging Data: T1-weighted and T2-weighted MRI scans in DICOM format.
- Annotation: Binary segmentation masks from clinical experts.
- Data Conversion: Convert 3D DICOM volumes to 2D image slices.
- Data Augmentation: Apply flip, rotation (±30°), Gaussian blur, and contrast variation to prevent overfitting and expand dataset (e.g., from ~1000 to 6080 images) [53].
- Normalization: Normalize pixel intensities to [0, 1] range.
Architecture Configuration:
- Encoder: Initialize with ResNet-50 backbone (ImageNet pretrained weights) to extract hierarchical features across four stages [53].
- Attention Enhancement: Integrate Squeeze-and-Excitation (SE) and Convolutional Block Attention Module (CBAM) after each encoder block to refine channel and spatial responses [53].
- Transformer Bottleneck:
- Reshape deepest encoder output (32×32×1024 feature map) into token sequence (1024 tokens, 1024 dimensions).
- Process through four Transformer blocks, each containing:
- Multi-head self-attention:
Attention(Q, K, V) = softmax(QK^T/√(d_k))V - Feed-forward network
- Dropout and layer normalization [53].
- Multi-head self-attention:
- Decoder:
- Upsample features while incorporating skip connections from encoder.
- Refine skip connection features using CBAM before fusion.
- Implement Efficient Attention mechanism via 1×1 convolutions to reduce channel dimensionality and generate attention coefficients (ψ) for feature modulation:
Y = X ⊙ ψ[53]. - Alternate SE blocks and ResNeXt modules with grouped convolutions in decoder blocks.
Training Specifications:
- Loss Function: Weighted combination
L_overall = L_BCE + λ·L_DicewhereDiceLoss = 1 - (2·∑(ŷ_i·y_i)+ε)/(∑ŷ_i+∑y_i+ε)[53]. - Optimizer: Adam with initial learning rate 1e-4 and cosine decay.
- Batch Size: 8 (constrained by GPU memory).
- Hardware: Kaggle GPU (T4 x2).
- Validation: Monitor Dice and IoU on validation set; employ early stopping.
Implementation Protocol for BrainTumNet Multi-Task Learning
Objective: Develop a unified model for simultaneous brain tumor segmentation and pathological classification using multi-task learning.
Materials:
- Data: 485 pathologically confirmed cases with CE-T1 MRI (glioma, metastatic tumors, meningiomas) [54].
- Split: Training (378 cases), testing (109 cases), external validation (51 cases).
- Annotations: Pixel-level segmentation masks and pathological type labels.
Preprocessing Pipeline:
- Data Normalization: Normalize CE-T1 modality data to (0,1) interval.
- Data Augmentation: Apply random flipping (probability=0.5) and rotation (range: -30° to +30°) [54].
- Volume Processing: Slice 3D volumes into 2D images, crop to 256×256 dimensions.
- Slice Selection: Select 20 representative slices per case (total: 9,700 slices).
Architecture Configuration:
- Dual-Path Feature Extraction:
- CNN path for local feature learning.
- Adaptive masked Transformer path for global modeling [54].
- Multi-Scale Feature Fusion: Implement feature fusion mechanism to integrate spatial and semantic information from both paths.
- Multi-Task Heads:
- Segmentation Head: Encoder-decoder with skip connections.
- Classification Head: Fully connected layers with softmax activation.
Training Specifications:
- Validation: 5-fold cross-validation.
- Optimizer: Adam with initial learning rate 1e-4 and cosine decay.
- Batch Size: 16.
- Epochs: 250.
- Loss Weighting: Segmentation loss weight: 1.0, classification loss weight: 0.7 [54].
- Loss Functions: Dice Loss and DiceCELoss.
Evaluation Metrics:
- Segmentation: Dice Similarity Coefficient (DSC), Hausdorff Distance (HD), Intersection over Union (IoU).
- Classification: Accuracy, Sensitivity, Specificity, F1 Score, AUC-ROC.
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Research Components for Transformer-Based Tumor Segmentation
| Component / Resource | Type | Function / Application | Exemplars / Specifications |
|---|---|---|---|
| Public Tumor Datasets | Data | Benchmarking & model training | BraTS (Brain MRI) [10] [33], LiTS (Liver CT) [55] |
| Annotation Platforms | Software | Ground truth segmentation creation | Expert-guided manual annotation tools [55] |
| Deep Learning Frameworks | Software | Model implementation & training | PyTorch, TensorFlow, MONAI [53] |
| Computational Resources | Hardware | Model training & inference | GPU (e.g., NVIDIA T4, V100) [53] |
| Pre-trained Models | Model Weights | Transfer learning initialization | ImageNet-pretrained encoders (e.g., ResNet-50) [53] |
| Attention Mechanisms | Algorithm | Feature refinement & focus | SE, CBAM, Efficient Attention [53] |
| Loss Functions | Algorithm | Model optimization guidance | Dice Loss, BCE, Focal Tversky, custom combinations [53] [33] |
| Data Augmentation Tools | Algorithm | Dataset expansion & regularization | Random flip, rotation, Gaussian blur, contrast adjustment [54] [53] |
| Evaluation Metrics | Metric | Performance quantification | Dice, IoU, HD, Precision, Recall, AUC [54] |
| Visualization Tools | Software | Result interpretation & debugging | TensorBoard, medical image viewers |
Future Research Directions
The evolution of Transformer-based and hybrid architectures for tumor segmentation continues to address several challenging research frontiers. 3D volumetric processing remains computationally demanding, with pure Transformer architectures like VT-UNet showing promise by maintaining full 3D volume integrity rather than processing 2D slices [52]. Multi-task learning frameworks, exemplified by BrainTumNet, demonstrate the efficiency of unified architectures that simultaneously perform segmentation and classification [54]. Data efficiency continues to drive innovation, with approaches like hybrid U-Net utilizing attention mechanisms and pretrained weights to achieve viable performance on limited local datasets [53]. Boundary refinement persists as a critical challenge, addressed through specialized modules like BEFUnet's edge encoder and dual-level fusion [51] and 2D-VNET++'s Context Boosting Framework [33]. Future architectural developments will likely focus on increasing computational efficiency while enhancing robustness to clinical variations in imaging protocols and tumor presentations.
Accurate brain tumor segmentation is a critical component of modern neuro-oncology, directly influencing diagnosis, treatment planning, and therapeutic monitoring. The integration of multi-modal magnetic resonance imaging (MRI)—specifically T1-weighted, T2-weighted, Fluid-Attenuated Inversion Recovery (FLAIR), and contrast-enhanced T1-weighted (T1C) sequences—provides complementary tissue contrasts that are essential for comprehensive tumor characterization. This article presents application notes and detailed experimental protocols for fusing these imaging modalities within deep learning frameworks, with a focus on the novel Multi-Modal Multi-Scale Contextual Aggregation with Attention Fusion (MM-MSCA-AF) architecture. Evaluated on the BraTS 2020 dataset, MM-MSCA-AF achieves a Dice score of 0.8158 for necrotic tumor regions and 0.8589 overall, outperforming established benchmarks like U-Net and nnU-Net [56]. These protocols provide researchers and drug development professionals with standardized methodologies for advancing automated segmentation systems in both clinical and research settings.
Multi-modal MRI fusion addresses fundamental limitations in single-modality brain tumor assessment by leveraging complementary information from T1, T2, FLAIR, and T1C sequences. Each modality highlights distinct tissue properties: T1-weighted images provide detailed brain anatomy; T2-weighted sequences emphasize fluid content for detecting edema and abnormalities; FLAIR suppresses cerebrospinal fluid signal to better visualize pathological lesions near ventricles; and T1C with gadolinium contrast identifies regions with blood-brain barrier disruption, a hallmark of active tumor regions [56] [10]. In glioma management, this multi-parametric approach enables precise differentiation of tumor sub-regions—including necrotic core, enhancing tumor, and surrounding edema—each with distinct biological characteristics and therapeutic implications [56].
The clinical workflow for brain tumor analysis requires accurate delineation of these regions, as their volumes and spatial distribution significantly impact surgical planning, radiation therapy targeting, and treatment response assessment [2] [29]. Manual segmentation by radiologists remains time-intensive and suffers from inter-observer variability, creating an urgent need for robust automated solutions [2]. Deep learning-based fusion of multi-modal MRI addresses these challenges by automatically integrating complementary information to produce consistent, accurate tumor boundaries that approach or exceed human performance levels [56] [2] [10].
Deep Learning Architectures for Multi-Modal Fusion
Evolution of Segmentation Models
Traditional segmentation approaches, including thresholding methods, region-growing algorithms, and classical machine learning techniques (e.g., Support Vector Machines, Random Forests), often struggle with the heterogeneous appearance and complex boundaries of brain tumors across different MRI sequences [56] [10]. The advent of deep learning, particularly convolutional neural networks (CNNs), has revolutionized the field through their ability to automatically learn hierarchical features from raw image data [29] [10].
U-Net architecture, with its encoder-decoder structure and skip connections, has become a foundational framework for medical image segmentation, enabling precise localization while capturing contextual information [29] [10]. Subsequent innovations have addressed specific limitations: nnU-Net introduced self-configuring capabilities that adapt to dataset characteristics without manual parameter tuning [29], while Attention U-Net incorporated attention gates to selectively emphasize salient features [56]. More recently, transformer-based architectures and hybrid CNN-transformer models have demonstrated enhanced robustness to domain shift—a critical challenge when applying models across different imaging protocols and institutions [57].
MM-MSCA-AF Architecture
The Multi-Modal Multi-Scale Contextual Aggregation with Attention Fusion (MM-MSCA-AF) framework represents a significant advancement in multi-modal segmentation by specifically addressing tumor heterogeneity and inter-modal feature integration [56]. Its architecture incorporates two key components:
Multi-Scale Contextual Aggregation (MSCA) captures both global and fine-grained spatial features through parallel processing paths with varying receptive fields. This multi-scale approach enables the network to recognize large tumor masses while precisely delineating intricate tumor boundaries [56].
Gated Attention Fusion (GAF) dynamically weights features from different MRI modalities based on their diagnostic relevance for specific tumor regions. This attention mechanism selectively enhances discriminative features while suppressing redundant or noisy information, effectively learning which modalities contribute most significantly to identifying each tumor sub-region [56].
Table 1: Performance Comparison of Deep Learning Models on BraTS 2020 Dataset
| Model Architecture | Overall Dice Score | Necrotic Core Dice | Enhancing Tumor Dice | Edema Dice |
|---|---|---|---|---|
| MM-MSCA-AF [56] | 0.8589 | 0.8158 | Not specified | Not specified |
| nnU-Net [29] | 0.8470 | Not specified | Not specified | Not specified |
| Attention U-Net [56] | 0.8410 | Not specified | Not specified | Not specified |
| U-Net [56] | 0.8320 | Not specified | Not specified | Not specified |
| iSeg (3D U-Net for lung tumors) [2] | 0.7300 (median) | Not applicable | Not applicable | Not applicable |
Figure 1: MM-MSCA-AF Architecture Overview. The framework processes four MRI modalities through parallel encoders, aggregates features at multiple scales, and applies gated attention fusion before generating the final segmentation [56].
Experimental Protocols
Data Acquisition and Preprocessing
Imaging Protocols and Parameters Standardized MRI acquisition is fundamental for reproducible multi-modal segmentation. The following protocol specifications are recommended based on the BraTS benchmark dataset and clinical standards [56] [58]:
- T1-weighted: 3D magnetization-prepared rapid gradient-echo (MP-RAGE) sequence with isotropic voxels (approximately 1mm³)
- T2-weighted: Turbo spin-echo sequence with axial orientation, slice thickness ≤3mm
- FLAIR: Turbo spin-echo inversion recovery sequence with slice thickness ≤3mm
- T1 Contrast-Enhanced: MP-RAGE sequence acquired 5-10 minutes after gadolinium-based contrast injection (0.1 mmol/kg)
All sequences should cover the entire brain volume with co-registered slices across modalities to enable voxel-level fusion [56].
Preprocessing Pipeline Consistent preprocessing ensures data quality and reduces domain shift between institutions [57]:
- Intensity Normalization: Apply N4 bias field correction to address intensity inhomogeneities
- Skull Stripping: Remove non-brain tissues using validated algorithms (e.g., BET, ROBEX)
- Co-registration: Rigidly align all sequences to a common space (typically T1-weighted baseline)
- Data Augmentation: Implement on-the-fly transformations during training including:
- Random rotations (±15°)
- Elastic deformations
- Intensity variations (±20%)
- Random cropping to 128×128×128 patches [56]
Model Implementation and Training
MM-MSCA-AF Implementation Protocol The following protocol details the implementation of the MM-MSCA-AF framework:
Network Configuration:
- Input: 4-channel 3D patches (128×128×128×4)
- Encoder: Residual blocks with batch normalization
- Multi-scale aggregation: Atrous spatial pyramid pooling with dilation rates [1,2,4,8]
- Attention gates: Channel-wise and spatial attention modules
Training Procedure:
- Optimization: Adam optimizer with initial learning rate 1×10⁻⁴
- Loss Function: Combined Dice and Cross-Entropy loss
- Batch Size: 2-4 (depending on GPU memory)
- Epochs: 300-500 with early stopping
- Regularization: Dropout (0.3), L2 weight decay (1×10⁻⁵)
Validation Strategy:
- 5-fold cross-validation on training data
- Quantitative evaluation using Dice Similarity Coefficient (DSC), Hausdorff Distance (HD95), and Sensitivity/Specificity metrics
- Statistical testing via paired t-tests with Bonferroni correction [56]
Table 2: Standardized Evaluation Metrics for Brain Tumor Segmentation
| Metric | Formula | Clinical Relevance | ||||||
|---|---|---|---|---|---|---|---|---|
| Dice Similarity Coefficient (DSC) | ( \frac{2 | X \cap Y | }{ | X | + | Y | } ) | Overlap between automated and manual segmentation (0=no overlap, 1=perfect overlap) |
| Hausdorff Distance (HD95) | ( \max{x \in X} \min{y \in Y} d(x,y) ) (95th percentile) | Maximum boundary separation, critical for surgical and radiation planning | ||||||
| Sensitivity | ( \frac{TP}{TP+FN} ) | Ability to detect all tumor tissue (minimizing false negatives) | ||||||
| Specificity | ( \frac{TN}{TN+FP} ) | Ability to exclude non-tumor tissue (minimizing false positives) |
Figure 2: End-to-End Experimental Workflow for Multi-Modal Segmentation. The protocol encompasses data preparation, model training, and comprehensive validation phases [56] [29].
Performance Benchmarks and Validation
Quantitative Results on Public Benchmarks
The BraTS (Brain Tumor Segmentation) challenge dataset has emerged as the standard benchmark for evaluating multi-modal segmentation algorithms. Performance on this dataset demonstrates the superior capability of advanced fusion architectures like MM-MSCA-AF compared to established baselines [56]. The achieved Dice score of 0.8158 for necrotic core segmentation represents particular clinical significance, as this region is often challenging to delineate due to its heterogeneous appearance across modalities [56].
External validation studies using different patient populations have confirmed the generalizability of these approaches. For instance, the iSeg model—a 3D U-Net architecture applied to lung tumor segmentation—achieved a median Dice score of 0.73 across multiple institutions, demonstrating that similar architectural principles extend to other tumor sites [2]. Importantly, this study found that automated segmentations were significantly smaller than physician-delineated contours (p<0.0001) while maintaining diagnostic accuracy, suggesting potential for reducing inter-observer variability in clinical practice [2].
Clinical Validation and Regulatory Considerations
For seamless clinical integration, automated segmentation models must demonstrate robustness across diverse imaging protocols and scanner manufacturers. Domain shift—the performance degradation when models encounter data from new institutions—remains a significant challenge [57]. Recent approaches address this through:
- Hybrid architectures: Combining CNN backbone with transformer modules improves resilience to protocol variations [57]
- Test-time adaptation: Adjusting batch normalization statistics during inference on new datasets
- Multi-center training: Incorporating data from multiple institutions during model development
Regulatory approval for clinical use requires rigorous validation following established guidelines such as the ACR MRI accreditation program, which specifies standards for image quality, spatial resolution, and artifact management [58]. Key technical requirements include sufficient signal-to-noise ratio, appropriate anatomic coverage, and minimization of artifacts that could compromise diagnostic accuracy [58].
The Scientist's Toolkit
Table 3: Essential Research Reagents and Computational Resources
| Resource Category | Specific Tools/Solutions | Application in Multi-Modal Fusion |
|---|---|---|
| Public Datasets | BraTS (Brain Tumor Segmentation), TCIA (The Cancer Imaging Archive) | Benchmarking, comparative performance evaluation, training data augmentation |
| Annotation Platforms | ITK-SNAP, 3D Slicer, MITK | Manual segmentation ground truth creation, model output visualization and correction |
| Deep Learning Frameworks | PyTorch, TensorFlow, MONAI | Model implementation, training pipeline development, experimental prototyping |
| Computational Infrastructure | NVIDIA GPUs (≥12GB memory), High-performance computing clusters | Handling 3D/4D medical image data, training complex fusion architectures |
| Evaluation Metrics | Dice Score, Hausdorff Distance, Precision-Recall curves | Quantitative performance assessment, statistical comparison between methods |
Multi-modal MRI fusion using T1, T2, FLAIR, and T1C sequences represents a cornerstone of modern automated tumor segmentation systems. The MM-MSCA-AF framework demonstrates how advanced deep learning architectures with multi-scale contextual aggregation and attention mechanisms can achieve state-of-the-art performance on standardized benchmarks. The experimental protocols outlined in this document provide researchers with comprehensive methodologies for implementing and validating these systems.
Future research directions should focus on enhancing model interpretability to build clinical trust, developing efficient architectures for real-time processing, and improving generalization across diverse patient populations and imaging protocols. As these technologies mature, their integration into clinical workflows promises to enhance diagnostic precision, enable personalized treatment planning, and accelerate therapeutic development in neuro-oncology.
Transfer Learning and Domain Adaptation Strategies
In the field of automated tumor segmentation using deep learning, transfer learning (TL) and domain adaptation (DA) are essential strategies for overcoming the central problem of domain shift. Domain shift occurs when a model trained on a source dataset (e.g., a specific type of brain tumor, images from a particular scanner) fails to perform accurately on a target dataset with different characteristics (e.g., a different tumor type, images from a new hospital) [59] [60]. This challenge is pervasive in medical imaging due to variations in acquisition protocols, imaging devices, and patient demographics [60] [61].
- Transfer Learning leverages knowledge from a related task where abundant labeled data exists. A common TL approach involves pretraining a model on a large, public dataset like the BraTS glioma collection and then fine-tuning its parameters on a smaller, target dataset containing, for instance, meningioma or metastasis cases [59] [62].
- Domain Adaptation is a specific form of TL that explicitly aims to align the feature distributions of the source and target domains, often with little or no labeled data available in the target domain. Techniques range from aligning statistical moments to employing adversarial training [60] [61].
These strategies are critical for developing robust and generalizable segmentation models that can be deployed in diverse clinical settings, ultimately enhancing the accuracy of diagnosis and treatment planning for patients with various tumor types [59].
Key Application Strategies and Performance
Research has demonstrated a variety of TL and DA strategies applied to tumor segmentation. The performance of these methods is typically quantified using metrics such as the Dice Similarity Coefficient (DSC) and the Hausdorff Distance (HD), which measure volumetric overlap and boundary accuracy, respectively. The table below summarizes several prominent approaches and their reported outcomes.
Table 1: Performance of Selected Transfer Learning and Domain Adaptation Strategies in Tumor Segmentation.
| Application Strategy | Core Methodology | Tumor Type / Anatomical Site | Key Quantitative Results | Reference / Context |
|---|---|---|---|---|
| Meta-Transfer Learning | Model-Agnostic Meta-Learning (MAML) for fine-tuning nnUNet | Brain Tumors (Meningioma & Metastasis) | DSC (WT): 0.8621 ± 0.2413 (Meningioma), 0.8141 ± 0.0562 (Metastasis) [59] | [59] |
| Test-Time Adaptation | HyDA: Hypernetworks generating model parameters dynamically using domain characteristics | Medical Imaging (General) | Demonstrated on MRI brain age prediction & chest X-ray classification [61] | [61] |
| Deep Subdomain Adaptation | Deep Subdomain Adaptation Network (DSAN) | Medical Image Classification (e.g., COVID-19, Skin Cancer) | Feasible classification accuracy (91.2%) on COVID-19 dataset; +6.7% improvement in dynamic data streams [60] | [60] |
| Backbone-Based Transfer Learning | U-Net with a fixed, pre-trained VGG-19 encoder | Brain Tumors (Glioma) | AUC: 0.9957, Dice: 0.9679, IoU: 0.9378 [62] | [62] |
| Foundation Model Adaptation | Adapter-based fine-tuning of Vision Transformers and Vision-Language Models | Healthcare Imaging (General) | Survey of methods for domain generalization using large-scale pre-trained models [63] | [63] |
Detailed Experimental Protocols
This section provides detailed, actionable protocols for implementing two of the most relevant strategies for tumor segmentation: Meta-Transfer Learning and Backbone-Based Transfer Learning.
Protocol: Meta-Transfer Learning for Segmenting Rare Tumor Types
This protocol is designed to adapt a model initially trained on a common tumor type (e.g., glioma) to effectively segment rarer types (e.g., meningioma, metastasis) with limited data [59].
A. Pre-training on Source Domain (Glioma)
- Data: Utilize the BraTS 2020 dataset (369 glioma cases with multi-modal MRI: T1, T1ce, T2, FLAIR). Annotations should include Whole Tumor (WT), Tumor Core (TC), and Enhancing Tumor (ET) [59].
- Preprocessing: Follow the nnUNet framework's automated pipeline, which includes resampling to a uniform voxel size (1x1x1 mm³), co-registration to a common anatomical space, and intensity normalization via z-score scaling [59].
- Model Training: Train a standard 3D nnUNet model on the glioma data to convergence. This model serves as a robust feature extractor and the initial point for meta-learning [59].
B. Meta-Fine-Tuning on Target Domain (Meningioma/Metastasis)
- Data: Use a subset of the BraTS 2023 dataset, specifically selecting 320 meningioma and 88 metastasis cases with complete annotations for WT, TC, and ET [59].
- Data Partitioning: Split the target data into training (60%), validation (20%), and testing (20%) sets. The limited training set size mimics a low-data regime [59].
- Meta-Training with MAML:
- Inner Loop (Task-Specific Update): For each task (or batch), perform one or a few gradient descent steps on the pre-trained nnUNet model using a small batch of data from the target domain (meningioma/metastasis). This creates a task-specific adapted model [59].
- Outer Loop (Meta-Update): Evaluate the performance of the adapted model on a held-out batch from the target domain. The loss from this evaluation is then used to update the parameters of the original, pre-trained model. The objective is to learn an initialization that can adapt rapidly and effectively to new tumor types with minimal data [59].
- Loss Function: Employ the Focal Tversky Loss to mitigate class imbalance between tumor sub-regions and the background [59].
- Validation and Testing: Use the validation set for model selection and early stopping. Report final performance on the test set using the Dice coefficient and other relevant metrics.
Protocol: Transfer Learning with a Pre-trained Encoder for 2D Segmentation
This protocol outlines a method to boost the performance of a 2D U-Net model for tumor segmentation by leveraging a powerful, pre-trained encoder, which is particularly effective when training data is limited [62].
A. Data Preparation and Preprocessing
- Data Source: Obtain a 2D MRI dataset, such as The Cancer Genome Atlas's (TCGA) lower-grade glioma collection, which includes FLAIR MRI scans and corresponding abnormality segmentation masks [62].
- Preprocessing: Apply standard preprocessing steps, including resizing images to a uniform size (e.g., 512x512 pixels), intensity normalization, and data augmentation (e.g., rotations, flips) to increase robustness [62].
B. Model Architecture and Training
- Encoder Setup: Replace the standard U-Net encoder with a VGG-19 network. Freeze the pre-trained VGG-19 weights to preserve the rich feature representations learned from natural images (e.g., ImageNet) [62].
- Decoder Setup: The decoder consists of upsampling and convolutional layers that mirror the encoder's structure, with skip connections to combine high-resolution features from the encoder with the upsampled feature maps [62].
- Loss Function: Use the Focal Tversky Loss (with parameters alpha=0.7 and gamma=0.75) to focus learning on hard-to-segment pixels and address class imbalance [62].
- Training Regime:
- Use an aggressive learning rate (e.g., 0.05) stabilized by batch normalization layers.
- Train the model, updating only the parameters of the decoder and the batch normalization layers, while the encoder weights remain fixed.
- Evaluation: Benchmark the model against a standard U-Net and other variants using metrics like Dice Coefficient, Intersection-over-Union (IoU), and Precision-Recall [62].
Workflow Visualization
The following diagram illustrates the high-level logical workflow common to both protocols, highlighting the central role of knowledge transfer from a source to a target domain.
Workflow Overview - This diagram outlines the core process of applying TL/DA, where knowledge from a data-rich source domain is strategically transferred to a data-scarce target domain.
The Scientist's Toolkit: Research Reagents & Materials
Successful implementation of the protocols requires a set of core "research reagents." The following table details these essential components and their functions.
Table 2: Essential Research Reagents and Materials for TL/DA in Tumor Segmentation.
| Item Name | Function / Purpose | Example Specifications / Notes |
|---|---|---|
| BraTS Datasets | Public benchmark datasets for training and validating brain tumor segmentation models. | BraTS 2020 (primarily gliomas); BraTS 2023 (expanded to include meningioma & metastasis); multi-modal MRI (T1, T1ce, T2, FLAIR) [59]. |
| nnUNet Framework | An adaptive framework that automates preprocessing and network configuration, providing a strong baseline model. | The base 3D nnUNet is often used as the core network for adaptation strategies like meta-learning [59]. |
| Pre-trained Encoders (VGG-19) | Feature extraction backbones for 2D segmentation networks, providing powerful, transferable low-to-high level image features. | Pre-trained on large-scale natural image datasets (e.g., ImageNet). Weights are typically frozen during training [62]. |
| Focal Tversky Loss | A loss function designed to handle severe class imbalance between tumor regions and the background by focusing on hard examples. | Parameters: alpha=0.7, gamma=0.75. A variant combined with Log Cosh Dice is also used [59] [33]. |
| Domain Adaptation Algorithms (DSAN, MAML) | Algorithms that explicitly reduce the distribution shift between source and target domains. | DSAN aligns subdomain distributions [60]. MAML learns a model initialization for fast adaptation [59]. |
| Vision Transformers / Foundation Models | Large-scale pre-trained models (e.g., CLIP, Segment Anything) that can be adapted for domain generalization via prompt engineering or fine-tuning. | Used for enriching feature quality and enabling zero-shot or few-shot learning in new domains [60] [63]. |
The integration of deep learning (DL) for automated tumor segmentation represents a paradigm shift in clinical oncology, enhancing workflows from radiological diagnosis to surgical and radiation planning. These technologies transition from research benchmarks to clinical tools by addressing real-world challenges such as post-surgical anatomical complexity, multi-institutional generalizability, and integration into existing digital infrastructures. Successful deployment hinges on developing solutions that are not only accurate but also reproducible, efficient, and accessible within standardized clinical protocols [64] [65].
The core value of these systems lies in their dual capacity: they automate highly time-consuming tasks like manual contouring, reducing inter-observer variability, and they extract sub-visual imaging biomarkers that can inform prognosis and treatment response. This is particularly critical for aggressive tumors like glioblastoma (GBM), where precise delineation of tumor sub-regions post-surgery directly influences radiation targeting and longitudinal tracking of disease progression [64] [37]. The following sections detail the current clinical applications, validated experimental protocols, and practical frameworks for implementing these technologies.
Current Clinical Applications and Performance
Automated tumor segmentation models are demonstrating robust performance across various clinical specialties, including neuro-oncology, thoracic oncology, and musculoskeletal tumor management. The tables below summarize the documented performance of recent models in specific clinical tasks.
Table 1: Performance of Deep Learning Models in Specific Clinical Applications
| Clinical Application | Model Architecture | Key Performance Metrics | Clinical Significance |
|---|---|---|---|
| Post-Surgical GBM Radiation Planning [64] | 3D U-Net | Mean Dice: 0.72 (GTV1), 0.73 (GTV2) | Automates contouring of resection cavity and residual tumor for RT planning, overcoming post-surgical complexities. |
| Lung SBRT Target Delineation [2] | 3D U-Net (iSeg) | Median Dice: 0.73 (IQR: 0.62–0.80) | Automates Gross Tumor Volume (GTV) and Internal Target Volume (ITV) segmentation for stereotactic body radiotherapy. Matches human inter-observer variability. |
| Pelvic and Sacral Tumor Surgical Planning [66] | 2.5D MobileNetV2 U-Net | Dice: 0.833 (T2-fusion model) | Provides a practical tool for segmenting complex tumors from multi-sequence MRI, aiding in pre-surgical assessment. |
Table 2: Model Performance Across Tumor Sub-Regions (BraTS Benchmark)
| Tumor Sub-Region | Best Reported Dice Score | Model (DSNet) [11] | Clinical Relevance of Sub-Region |
|---|---|---|---|
| Enhancing Tumor (ET) | 0.947 | Dynamic Segmentation Network (DSNet) | Represents active, often high-grade tumor tissue; critical for biopsy targeting and treatment response assessment. |
| Tumor Core (TC) | 0.975 | Dynamic Segmentation Network (DSNet) | Includes enhancing and non-enhancing solid tumor; key for surgical resection and radiation dose escalation. |
| Whole Tumor (WT) | 0.959 | Dynamic Segmentation Network (DSNet) | Encompasses TC and peritumoral edema; essential for surgical planning and overall disease burden assessment. |
A critical advancement is the move towards sequence-efficient models that reduce dependency on full multi-parametric MRI protocols. For glioma segmentation, a 3D U-Net trained solely on T1C and FLAIR sequences achieved Dice scores of 0.867 (ET) and 0.926 (TC), matching or outperforming models trained on four sequences (T1, T1C, T2, FLAIR) [67]. This enhances the technology's generalizability and deployment potential in clinics with limited imaging protocols.
Detailed Experimental Protocols for Model Validation
To ensure clinical readiness, models must be validated using rigorous, standardized methodologies. The following protocols are adapted from recent high-impact studies.
Protocol for Post-Surgical Brain Tumor Segmentation
This protocol is designed for developing tools to assist in radiation oncology for glioblastoma after resection [64].
- Objective: To train and validate a deep learning model for automatic segmentation of post-surgical tumor targets (GTV1: FLAIR hyperintensity, GTV2: CE-T1w enhancement) for radiation therapy planning.
- Data Requirements:
- Imaging Modalities: Post-surgical T2-weighted FLAIR and contrast-enhanced T1-weighted (CE-T1w) MRI.
- Ground Truth: Physician-contoured GTV1 and GTV2 from 225 GBM patients treated with standard RT.
- Data Splitting: Train on 225 patients, test on an independent hold-out set of 30 patients.
- Model Training:
- Architecture Comparison: Systematically train and compare multiple architectures (e.g., Unet, ResUnet, Swin-Unet, 3D Unet, Swin-UNETR).
- Performance Metric: Use the Dice Similarity Coefficient (Dice) as the primary metric for segmentation overlap.
- Validation: Perform k-fold cross-validation (e.g., 5-fold) on the training set for model selection.
- Output and Integration: The best-performing model (e.g., 3D U-Net) is integrated into a longitudinal tracking web application that automatically calculates lesion volume changes for standardized reporting.
Protocol for Multi-Center Validation of Lung Tumor Segmentation
This protocol outlines a robust framework for training and externally validating a model for use in lung SBRT planning [2].
- Objective: To develop a deep neural network (iSeg) for segmenting gross tumor volumes (GTVs) on CT and propagating them across 4D CT to generate an internal target volume (ITV).
- Data Curation:
- Cohorts: Utilize a multi-center registry from 9 clinics across 2 health systems.
- Training Set: 739 pre-treatment CT images with corresponding physician-delineated GTV masks.
- Validation Sets: Two independent external cohorts (n=161 and n=102).
- Model Development & Training:
- Architecture: 3D U-Net.
- Training Regimen: 5-fold cross-validation on the internal training cohort.
- Post-processing: Apply morphological operations (opening/closing) to refine predictions and remove outliers.
- Performance and Clinical Analysis:
- Primary Metrics: Dice, 95th percentile Hausdorff Distance (HD95).
- Comparison to Human: Compare model performance to inter-observer variability between physicians.
- Clinical Validity: Correlate model-human discordance (e.g., false positive voxels) with clinical outcomes like local failure.
Protocol for Sequence-Efficient Glioma Segmentation
This protocol focuses on minimizing the input requirements for models to improve widespread adoption [67].
- Objective: To identify the minimal subset of MRI sequences required to achieve accurate glioma segmentation comparable to a full protocol.
- Dataset:
- Source: MICCAI BraTS datasets (2018 for training, 2018/2021 for testing).
- Training Set: 285 glioma cases (210 HGG, 75 LGG).
- Test Set: 358 cases from a held-out validation set.
- Experimental Design:
- Input Configurations: Train separate 3D U-Net models on different sequence combinations: T1C-only, FLAIR-only, T1C+FLAIR, and T1+T2+T1C+FLAIR (full set).
- Evaluation: Use 5-fold cross-validation on the training set. The primary evaluation is the Dice score on the independent test set for the tumor core (TC) and enhancing tumor (ET).
- Outcome Analysis: Determine the configuration that provides comparable or superior performance to the full-sequence model while using fewer inputs.
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Tools and Resources for Developing Automated Tumor Segmentation Models
| Resource Category | Specific Example | Function and Application | Key Considerations |
|---|---|---|---|
| Public Datasets | BraTS (Brain Tumor Segmentation) [37] [10] | Benchmarking and training for brain tumor segmentation. Provides multi-institutional, expert-annotated mpMRI data. | Includes various tumor types (glioma, metastases, meningioma); data is pre-processed and skull-stripped. |
| Architecture | 3D U-Net [64] [2] [67] | Workhorse architecture for volumetric medical image segmentation. Encoder-decoder with skip connections. | Balances performance and computational efficiency; highly adaptable for different imaging modalities. |
| Loss Functions | Dice Loss [37] | Addresses class imbalance by maximizing overlap between prediction and ground truth. | Superior to cross-entropy for segmentation where foreground (tumor) is a small portion of the total volume. |
| Validation Frameworks | 5-Fold Cross-Validation [2] | Robust method for model selection and hyperparameter tuning using the available training data. | Reduces overfitting and provides a more reliable estimate of model performance before external testing. |
| Performance Metrics | Dice Similarity Coefficient (Dice) [64] | Measures spatial overlap between automated segmentation and manual ground truth. Primary metric for segmentation accuracy. | Ranges from 0 (no overlap) to 1 (perfect overlap). Values >0.7 typically indicate clinically useful agreement. |
Implementation Workflow for Clinical Deployment
The journey from a trained model to a clinically deployed tool involves a multi-stage workflow that prioritizes validation, integration, and continuous monitoring. The following diagram illustrates this end-to-end process.
Diagram 1: The staged workflow for deploying an automated tumor segmentation model into a clinical setting, from initial data preparation to post-deployment monitoring.
Workflow Stage Descriptions
- Data Curation & Annotation: This foundational stage involves collecting a diverse set of medical images representing the target population and pathology. Ground truth annotations must be performed by clinical experts (e.g., radiologists, radiation oncologists). Strategies like coarse labeling for training and fine labeling for the test set can improve efficiency without significantly compromising model performance [66].
- Model Development & Training: Researchers select and optimize model architectures (e.g., 3D U-Net, transformer-based networks) using the training dataset. This stage involves experimentation with loss functions (e.g., Dice loss), data augmentation, and hyperparameter tuning to maximize learning [64] [10].
- Internal Validation: The model is rigorously evaluated on a held-out test set from the same institution(s) that provided the training data. Performance is quantified using metrics like Dice and Hausdorff Distance. This stage also includes ablation studies to test the impact of different input sequences [67].
- External Multi-Center Validation: A critical step for establishing generalizability, the model is tested on completely independent datasets from new clinical sites. Performance that remains consistent with internal validation indicates a model is robust to variations in scanners and imaging protocols [2].
- Clinical System Integration: The validated model is integrated into the clinical workflow, often through a web application or by embedding within a Picture Archiving and Communication System (PACS) or Treatment Planning System (TPS). The interface should provide segmentation overlays and, for radiation oncology, enable the calculation of target volumes [64] [11].
- Post-Deployment Monitoring: After deployment, the model's performance and clinical impact are continuously monitored. This includes tracking segmentation accuracy in real-world use and investigating correlations between model outputs (e.g., segmentation discordance) and patient outcomes [2].
The clinical deployment of automated tumor segmentation is transitioning from a research concept to a tangible tool that enhances precision oncology. The key to successful implementation lies in developing robust, validated, and efficient models that integrate seamlessly into existing clinical pathways for radiology, surgery, and radiation therapy. By adhering to structured experimental protocols, leveraging public resources, and following a rigorous deployment workflow, researchers and clinicians can work together to translate these powerful technologies into improved patient care. Future efforts will focus on increasing model interpretability, achieving real-time performance, and prospectively validating clinical efficacy in randomized trials.
Overcoming Implementation Challenges: Data, Efficiency, and Generalization Solutions
Data scarcity presents a significant bottleneck in the development of robust deep learning models for automated tumor segmentation. The acquisition of large, high-quality, and annotated medical imaging datasets is hampered by factors such as the rarity of certain conditions, privacy regulations, and the substantial cost and expertise required for expert-level annotation [68]. Within the specific context of brain tumor segmentation, this challenge is exacerbated by the complex heterogeneity of tumor subregions and the need to generalize across both pre-treatment and post-treatment glioma scans [69].
To counter these limitations, data augmentation and synthetic data generation have emerged as critical methodologies. These techniques expand the effective size and diversity of training datasets, thereby improving model generalization, robustness, and overall performance. This document provides detailed application notes and experimental protocols for leveraging these strategies, with a particular focus on their application in automated tumor segmentation research for drug development and clinical translation.
Synthetic Data Generation Methods and Applications
Synthetic data generation involves creating artificial datasets that mimic the statistical properties and characteristics of real-world data without containing any sensitive patient information [68]. These methods are broadly classified into three categories, with deep learning-based approaches currently being the most prevalent.
Table 1: Overview of Synthetic Data Generation Methods in Healthcare
| Method Category | Key Examples | Primary Applications in Medical Imaging | Key Advantages |
|---|---|---|---|
| Rule-Based Approaches | Predefined rules, constraints, and distributions. | Generating synthetic patient records based on statistical distributions. | Simplicity, transparency. |
| Statistical Modeling | Gaussian Mixture Models, Bayesian Networks. | Capturing relationships between clinical variables. | Strong probabilistic foundations. |
| Machine/Deep Learning | Generative Adversarial Networks (GANs), Variational Autoencoders (VAEs). | Generating synthetic MRI/CT images, augmenting datasets for tumor classification and segmentation [70] [71]. | High realism, ability to capture complex data distributions. |
As shown in Table 1, deep learning methods, particularly Generative Adversarial Networks (GANs), are the most widely used, comprising 72.6% of the synthetic data generation studies in healthcare [70]. A GAN consists of two neural networks—a generator and a discriminator—trained in competition. The generator aims to produce realistic synthetic data, while the discriminator tries to distinguish real from synthetic samples [72] [68]. In medical imaging, Conditional GANs (cGANs) can generate images with specific pathologies, such as tumors, by conditioning the generation process on a label or mask [71].
Another prominent architecture is the Variational Autoencoder (VAE), which learns to encode data into a latent (compressed) space and then decode it back, allowing for the generation of new data samples [68]. VAEs are known to have lower computational costs compared to GANs and are less prone to "mode collapse," a common training issue with GANs where the generator produces limited varieties of samples [68].
Experimental Protocols for Tumor Segmentation
This section outlines detailed protocols for implementing two powerful synthetic data strategies in tumor segmentation research.
Protocol 1: On-the-Fly Data Augmentation with GliGAN
This protocol is based on the winning solution from the BraTS Lighthouse Challenge 2025 Task 1, which utilized an on-the-fly augmentation strategy to dynamically insert synthetic tumors during training, avoiding the computational expense of storing vast pre-generated 3D data [69].
- Objective: To improve model generalization and address class imbalance in brain tumor segmentation by dynamically augmenting training batches with synthetic tumors.
- Materials & Setup:
- Framework: nnU-Net (self-configuring 3D full-resolution U-Net) as the core segmentation model [69].
- Base Dataset: Multi-parametric MRI (mpMRI) scans (e.g., T1, T1ce, T2, FLAIR) with corresponding tumor subregion annotations [69].
- Synthetic Data Engine: Pre-trained GliGAN generator weights. GliGAN is a conditional GAN that inserts realistic synthetic tumors into healthy brain regions based on an input label mask [69].
- Integration Workflow:
- Training Loop Integration: Instead of pre-generating and storing synthetic scans, integrate the GliGAN module directly into the training loop.
- Dynamic Selection: For each batch, with a predefined probability
p, select an image to be augmented. - Label Modification (Conditioning): To tackle class imbalance, modify the input label mask that guides the GliGAN. For instance:
- Replace the "Surrounding non-enhancing FLAIR hyperintensity" (SNFH) label with "Enhancing Tumor" (ET) with a probability of 0.7.
- Subsequently, replace the ET label with "Non-enhancing Tumor Core" (NETC) with the same probability. This increases the prevalence of under-represented ET and NETC classes [69].
- Scale Adjustment: To improve performance on small lesions, introduce a scale parameter that randomly downsizes the real label mask before passing it to GliGAN, ensuring the model learns to segment smaller tumor structures [69].
- Synthetic Image Generation: The GliGAN generator takes the original MRI modality (with added noise in the target area) and the modified label mask as input, outputting a synthetic scan with a tumor that matches the provided mask.
- Model Training: The training proceeds with a mix of original and synthetically augmented batches. The validation data remains completely unaltered [69].
The following diagram illustrates this integrated workflow:
Protocol 2: GAN-Augmented Classification with Swin Transformers
This protocol details a method for brain tumor classification, which can be a precursor or complementary task to segmentation. It combines GAN-based data augmentation with a powerful Swin Transformer architecture [71].
- Objective: To achieve high-accuracy multi-class brain tumor classification by overcoming data scarcity and imbalance using synthetic data.
- Materials & Setup:
- Dataset: Publicly available brain tumor MRI datasets (e.g., Figshare, Kaggle) with classes like Glioma, Meningioma, Pituitary, and No Tumor.
- Augmentation Model: Autoencoder-based Conditional GAN (AE-cGAN) for generating diverse and realistic synthetic tumor images [71].
- Classification Model: Swin Transformer, which excels at capturing both local and global dependencies in images [71].
- Experimental Workflow:
- Data Augmentation Phase:
- Train the AE-cGAN on the original training dataset.
- Use the trained generator to produce synthetic MRI images for under-represented tumor classes to balance the dataset.
- Feature Extraction & Selection Phase:
- Feature Extraction: Use a pre-trained ResNet18 model to extract deep, hierarchical features from the augmented dataset (combined original and synthetic images) [73].
- Feature Selection: Refine the extracted features using a hybrid of Principal Component Analysis (PCA) and Particle Swarm Optimization (PSO). PCA reduces dimensionality, while PSO selects the most discriminative feature subset [73].
- Classification Phase:
- Architecture: Employ a Deep Multiple Fusion Network (DMFN). This framework uses multiple ResNet18 models, each trained to perform a pairwise classification between two tumor classes.
- Fusion: The decisions from all binary classifiers are combined through a fusion mechanism (e.g., weighted voting) to make the final multi-class prediction [73].
- Data Augmentation Phase:
- Outcome: This approach has been shown to achieve validation accuracy of up to 98.36% on brain tumor classification tasks, significantly outperforming models trained without synthetic data [73].
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Tools and Resources for Synthetic Data Generation in Tumor Analysis
| Item Name | Type/Function | Application in Research |
|---|---|---|
| nnU-Net Framework | Self-Configuring Deep Learning Framework | Serves as a robust, out-of-the-box baseline and core architecture for medical image segmentation tasks [69]. |
| Generative Adversarial Network (GAN) | Deep Learning Model for Data Generation | Core engine for creating realistic synthetic medical images; includes architectures like GliGAN and AE-cGAN [69] [71]. |
| Swin Transformer | Deep Learning Model with Attention Mechanism | Used for classification and segmentation tasks due to its ability to capture long-range dependencies and global context in images [71]. |
| Variational Autoencoder (VAE) | Deep Learning Model for Dimensionality Reduction and Generation | Generates synthetic data and is particularly effective in data-limited scenarios, such as predicting cancer recurrence [74]. |
| Pre-trained Model Weights (e.g., GliGAN) | Pre-trained Network Parameters | Allows researchers to implement advanced data augmentation without the prohibitive cost of training a GAN from scratch [69]. |
Performance and Outcomes
The implementation of the protocols described above has demonstrated significant, quantifiable improvements in model performance.
Table 3: Quantitative Performance of Models Using Synthetic Data
| Application / Model | Dataset | Key Performance Metrics | Reported Outcome with Synthetic Data |
|---|---|---|---|
| On-the-Fly GliGAN + nnU-Net Ensemble [69] | BraTS 2025 Validation Set | Lesion-wise Dice Score | ET: 0.79, NETC: 0.749, RC: 0.872, SNFH: 0.825, TC: 0.79, WT: 0.88 |
| AE-cGAN + Swin Transformer [71] | Figshare & Kaggle Datasets | Classification Accuracy | 99.54% and 98.9% accuracy, outperforming state-of-the-art methods. |
| VAE for Pancreatic Cancer Recurrence [74] | Institutional Medical Records | Model Accuracy & Sensitivity | GBM Accuracy: 0.81→0.87; GBM Sensitivity: 0.73→0.91. |
| GAN-augmented Brain MRI Classification [68] | Brain MRI Dataset | Classification Accuracy | Achieved 85.9% accuracy in brain MRI classification. |
The following diagram summarizes the logical decision process for selecting the most appropriate data generation strategy based on the research goal:
Class Imbalance Problems and Technical Mitigation Strategies
Class imbalance represents a fundamental challenge in developing deep learning models for automated tumor segmentation from medical images. This problem occurs when the distribution of pixels across different classes (e.g., tumor vs. non-tumor regions) is highly skewed, leading to biased model performance that favors majority classes. In brain tumor segmentation from Magnetic Resonance Imaging (MRI) data, class imbalance manifests severely as tumor regions often comprise only a small fraction of the total image volume compared to healthy tissue [75] [76]. This disproportion causes models to achieve misleadingly high accuracy by simply predicting the majority class while failing to adequately segment medically critical tumor regions [77] [78].
The presence of class imbalance synergistically exacerbates other data difficulty factors including class overlap, small disjuncts, and noise, collectively amplifying classification complexity [77]. In neuro-oncology, this problem is particularly acute due to the heterogeneity, complexity, and high mortality of brain tumors, where precise segmentation directly impacts diagnosis, treatment planning, and patient outcomes [75]. This article provides a comprehensive analysis of class imbalance challenges and technical mitigation strategies specifically within the context of automated tumor segmentation using deep learning, with protocols designed for researchers, scientists, and drug development professionals.
Understanding Classification Complexity in Imbalanced Domains
Data Difficulty Factors
In imbalanced classification domains, several data intrinsic characteristics interact with class imbalance to increase classification complexity. Class overlap occurs when feature values for different classes exhibit significant similarity, making clear separation challenging. Small disjuncts refer to the presence of small, localized subconcepts within the class structure that are difficult to learn. Noise encompasses labeling errors or feature value corruption that misleads learning algorithms. Individually, these factors present learning challenges; when combined with class imbalance, they create particularly difficult learning scenarios where models exhibit strong bias toward the majority class [77].
The fundamental issue arises because most standard deep learning algorithms are designed to optimize overall accuracy without considering class distribution. In medical imaging contexts where accurate identification of minority classes (tumors) is clinically paramount, this bias presents critical limitations [77] [78]. For example, in a typical brain MRI, non-tumor pixels may outnumber tumor pixels by ratios exceeding 100:1, causing naive classifiers to achieve 99% accuracy while completely failing to identify tumor regions [76] [79].
Quantitative Assessment of Imbalance
The Imbalance Ratio (IR) provides a basic metric for quantifying class imbalance, calculated as the ratio of majority to minority class samples. However, IR alone provides an incomplete picture of classification difficulty, as highly imbalanced but well-separated classes may be easier to learn than moderately imbalanced classes with significant overlap [77]. Napierala et al. demonstrated that certain benchmark datasets with high imbalance ratios (50:1) were easier to learn compared to datasets with less pronounced imbalance (4:1) due to differences in underlying data complexity [77].
For comprehensive assessment in medical imaging contexts, researchers should employ multiple complexity metrics including:
- Class overlap measures that quantify the degree of feature space sharing between classes
- Class separability indices that assess how well classes can be distinguished
- Minority class decomposition metrics that evaluate the presence of small subconcepts
These combined metrics provide a more complete understanding of the classification challenge than imbalance ratio alone [77].
Technical Mitigation Strategies
Data-Level Approaches
Data-level techniques address class imbalance by directly adjusting training set composition through various resampling strategies before model training begins.
Resampling Methods
Table 1: Comparative Analysis of Resampling Techniques for Tumor Segmentation
| Technique | Mechanism | Advantages | Limitations | Representative Performance |
|---|---|---|---|---|
| Random Undersampling | Removes majority class samples randomly | Reduces training set size, computational efficiency | Potential loss of potentially useful majority class information | Improved recall for minority classes [78] |
| Random Oversampling | Duplicates minority class samples randomly | Simple implementation, no information loss | Risk of overfitting to repeated samples | Significant improvements in precision and recall for rare cases [80] |
| SMOTE | Generates synthetic minority samples via interpolation | Creates diverse minority examples, reduces overfitting | May generate noisy samples in presence of class overlap | Enhanced boundary learning, Dice Coefficient improvement [78] |
| Tomek Links | Removes majority samples near class boundaries | Cleans overlapping regions, improves class separation | Primarily a cleaning method, often combined with other techniques | Boundary refinement, IoU improvement [78] |
| NearMiss | Selective undersampling based on distance metrics | Preserves important majority class structures | Computational overhead in distance calculation | Better preservation of majority class patterns [78] |
Recent advances in resampling have shifted toward enhanced adaptability through identification of problematic regions and implementation of customized resampling protocols [77]. Contemporary approaches increasingly leverage classification complexity assessment to tailor resampling behavior to each unique problem context. However, despite this increased adaptability, no single resampling method has demonstrated consistent superior performance across all experimental scenarios, highlighting the importance of context-specific selection [77].
Data Augmentation Strategies
Beyond resampling, data augmentation techniques generate synthetic training examples through label-preserving transformations. Standard data augmentation (SDA) applies basic geometric and photometric transformations such as rotation (–15° to +15°), flipping, and brightness/contrast adjustments [81]. For medical imaging applications, domain-specific considerations must guide augmentation selection; for instance, vertical flips may be inappropriate for ultrasound images due to their directional depth representation [81].
Advanced augmentation strategies include Pixel-space Mixup, which creates new training samples by linearly interpolating between random pairs of images and their labels, and Manifold Mixup, which extends this concept to feature-level interpolations in deep network layers [81]. A particularly innovative approach, DreamOn, employs conditional generative adversarial networks (GANs) to generate REM-dream-inspired interpolations of training images by blending class characteristics in varying proportions [81]. This method has demonstrated substantial improvements in model robustness under high-noise conditions, narrowing the performance gap between deep learning models and human radiologists in challenging diagnostic scenarios [81].
Diagram 1: Data Augmentation Workflow for Class Imbalance Mitigation in Tumor Segmentation
Algorithm-Level Approaches
Algorithm-level techniques address class imbalance by modifying the learning algorithm itself to reduce bias toward majority classes.
Cost-Sensitive Learning
Cost-sensitive learning incorporates misclassification costs directly into the model training process by assigning higher penalties for minority class errors. This approach effectively rebalances class influence without altering training data distribution. In medical imaging contexts, cost ratios are often determined through clinical consultation to reflect the relative seriousness of different error types (e.g., false negatives vs. false positives in tumor detection) [82].
Implementation typically involves modifying loss functions to incorporate class-weighted terms. For segmentation tasks, categorical cross-entropy loss can be extended with class-specific weights inversely proportional to class frequencies:
Weighted_Loss = -Σ(weight_class × y_true × log(y_pred))
where weight_class is higher for minority classes [76] [79].
Ensemble Methods
Ensemble methods combine multiple models to improve generalization performance on imbalanced data. Popular techniques include bagging, boosting, and stacking, with random committee classifiers demonstrating particularly strong performance in brain tumor classification, achieving up to 98.61% accuracy in optimized hybrid datasets [16].
Ensemble deep learning approaches have shown remarkable effectiveness in medical imaging applications. For brain tumor segmentation, ensemble techniques combining 2D and 3D U-Net features with hybrid machine learning classifiers like K-nearest neighbor and gradient boosting have demonstrated superior performance compared to individual models [16]. Similarly, Ensemble Deep Neural Support Vector Machines have achieved 97.93% accuracy in brain tumor detection [16].
Hybrid and Advanced Approaches
Architecture Modifications
Advanced network architectures specifically designed for imbalanced data incorporate attention mechanisms, residual connections, and multi-scale processing to enhance feature extraction from underrepresented regions. The ARU-Net architecture integrates residual connections with Adaptive Channel Attention and Dimensional-space Triplet Attention modules, demonstrating significant performance improvements in brain tumor segmentation with Dice Similarity Coefficient improvements of approximately 3.3% over baseline U-Net [76].
Similarly, multi-scale attention U-Net architectures with EfficientNetB4 encoders have achieved state-of-the-art performance in brain tumor segmentation, attaining 99.79% accuracy and Dice Coefficient of 0.9339 by leveraging compound scaling to optimize feature extraction at multiple resolutions while maintaining computational efficiency [79]. The incorporation of attention mechanisms enables these models to suppress irrelevant regions and focus on critical tumor structures, particularly beneficial for segmenting small or subtle lesions [79].
Hybrid Sampling
Hybrid approaches combine both oversampling and undersampling techniques to leverage their respective advantages while mitigating limitations. SMOTEENN (SMOTE + Edited Nearest Neighbors) and SMOTETomek (SMOTE + Tomek Links) represent prominent hybrid methods that first generate synthetic minority samples then clean the resulting dataset by removing ambiguous examples from both classes [82].
These methods are particularly effective in medical imaging contexts with significant class overlap, as they simultaneously address imbalance while improving class separation in contested regions of the feature space [77].
Experimental Protocols and Implementation
Protocol 1: Comprehensive Data Resampling for Tumor Segmentation
Purpose: To systematically address class imbalance in tumor segmentation datasets through adaptive resampling techniques.
Materials and Reagents:
- Medical image dataset with segmentation masks
- Computing environment with Python 3.7+
- Imbalanced-learn library (v0.9.0)
- Deep learning framework (TensorFlow/PyTorch)
Procedure:
- Dataset Characterization:
- Calculate imbalance ratios for all classes
- Compute complexity metrics (class overlap, separability)
- Visualize feature space distribution
Resampling Strategy Selection:
- For high imbalance ratios (>20:1): Begin with random undersampling
- For moderate imbalance (5:1 to 20:1): Apply SMOTE with k=5 nearest neighbors
- For datasets with significant noise: Implement Tomek Links cleaning post-oversampling
Implementation:
Validation:
- Assess distribution balance after resampling
- Verify preservation of critical majority class patterns
- Evaluate synthetic sample quality through visual inspection
Expected Outcomes: Balanced training set with maintained representative capacity for all classes, leading to improved minority class segmentation performance.
Protocol 2: Cost-Sensitive Deep Learning for Medical Image Segmentation
Purpose: To implement cost-sensitive learning in deep segmentation networks to address class imbalance without data modification.
Materials and Reagents:
- Deep learning framework with custom loss function capability
- GPU-accelerated computing resources
- Annotation software for ground truth verification
Procedure:
- Cost Matrix Definition:
- Consult clinical experts to determine relative misclassification costs
- Assign higher costs to minority class errors (e.g., missed tumors)
- Formalize cost matrix based on clinical impact
Weighted Loss Function Implementation:
Model Training:
- Utilize standard unbalanced training data
- Monitor class-wise performance metrics separately
- Implement early stopping based on minority class performance
Evaluation:
- Assess segmentation performance using Dice Similarity Coefficient
- Compare with baseline models trained without cost sensitivity
- Validate clinical utility through expert radiologist review
Expected Outcomes: Improved segmentation accuracy for minority classes without compromising majority class performance, leading to more clinically useful models.
Table 2: Research Reagent Solutions for Imbalanced Tumor Segmentation
| Reagent Category | Specific Tools/Libraries | Primary Function | Application Context |
|---|---|---|---|
| Data Resampling | Imbalanced-learn (v0.9.0) | Implementation of oversampling, undersampling, and hybrid techniques | Preprocessing for class imbalance mitigation [78] |
| Data Augmentation | Albumentations, TensorFlow Augment | Image transformations and advanced mixing strategies | Training data diversification and expansion [81] |
| Generative Models | StyleGAN2, Conditional GANs | Synthetic data generation for minority classes | Data augmentation for rare tumor types [80] |
| Loss Functions | Focal Loss, Weighted Cross-Entropy | Algorithm-level class imbalance handling | Cost-sensitive learning implementations [82] |
| Evaluation Metrics | Dice Coefficient, IoU, F1-score | Performance assessment beyond accuracy | Comprehensive model evaluation [76] |
Protocol 3: Attention-Based Architecture for Imbalanced Medical Data
Purpose: To implement attention-enhanced deep learning architectures that automatically focus computational resources on clinically important regions.
Materials and Reagents:
- Deep learning framework with custom layer support
- Multi-scale medical imaging data
- Computational resources for model training
Procedure:
- Network Architecture Design:
- Select base encoder (e.g., EfficientNetB4 for optimal performance/efficiency balance)
- Integrate multi-scale attention modules with 1×1, 3×3, and 5×5 kernels
- Incorporate residual connections to facilitate gradient flow
Attention Module Implementation:
Model Training:
- Utilize standard unbalanced medical datasets
- Employ progressive learning rate scheduling
- Implement comprehensive regularization to prevent overfitting
Evaluation:
- Quantitatively assess segmentation performance using DSC, IoU
- Qualitatively evaluate attention map localization accuracy
- Compare with non-attention baseline architectures
Expected Outcomes: Enhanced feature representation with automatic focus on semantically important regions, leading to improved segmentation of small and complex tumor structures in imbalanced contexts.
Diagram 2: Attention-Enhanced Segmentation Pipeline for Imbalanced Medical Data
Performance Evaluation and Metrics
Appropriate Evaluation Metrics
Traditional accuracy metrics provide misleading assessments in imbalanced contexts, necessitating specialized evaluation approaches. For tumor segmentation, the following metrics provide more meaningful performance characterization:
Dice Similarity Coefficient (DSC): Measures spatial overlap between predicted and ground truth segmentations
DSC = (2 × |X ∩ Y|) / (|X| + |Y|)Intersection over Union (IoU): Quantifies area of overlap divided by area of union
IoU = |X ∩ Y| / |X ∪ Y|Sensitivity/Recall: Measures true positive rate for tumor detection
- Specificity: Measures true negative rate for non-tumor regions
- F1-Score: Harmonic mean of precision and recall
- Precision-Recall Curves: More informative than ROC curves for imbalanced data [76] [79]
Comparative Performance Analysis
Advanced architectures incorporating attention mechanisms and specialized imbalance handling have demonstrated remarkable performance improvements. The ARU-Net architecture achieved 98.3% accuracy, 98.1% DSC, and 96.3% IoU in brain tumor segmentation, representing significant improvements over baseline U-Net models [76]. Similarly, multi-scale attention U-Net with EfficientNetB4 encoder attained 99.79% accuracy and DSC of 0.9339, outperforming conventional approaches across all critical metrics [79].
For classification tasks, ensemble methods like Random Committee classifiers have achieved 98.61% accuracy in multi-class brain tumor classification, while hybrid approaches combining deep feature extraction with machine learning classifiers have demonstrated robust performance across diverse tumor types and imaging conditions [16].
Class imbalance presents a fundamental challenge in automated tumor segmentation that demands systematic addressing throughout the model development pipeline. Effective mitigation requires comprehensive approaches combining data-level strategies (resampling, augmentation), algorithm-level techniques (cost-sensitive learning, ensemble methods), and architectural innovations (attention mechanisms, multi-scale processing).
The field is evolving toward increasingly adaptive methodologies that dynamically respond to data complexity characteristics. Promising research directions include resampling recommendation systems that automatically select optimal strategies based on dataset characteristics, advanced generative approaches for synthetic data creation, and continued development of attention mechanisms that mirror human visual processing [77] [81].
For clinical translation, future work must prioritize robustness validation across diverse patient populations and imaging protocols, model interpretability for clinical trust, and computational efficiency for practical deployment. By systematically addressing class imbalance through the protocols and strategies outlined herein, researchers can develop more reliable, accurate, and clinically valuable automated segmentation systems that ultimately enhance patient care in oncology.
The integration of deep learning for automated tumor segmentation into clinical workflows presents a significant challenge: balancing diagnostic accuracy with computational practicality. In resource-constrained clinical environments, large, complex models often prove unsuitable due to high computational demands, lengthy inference times, and substantial costs. This creates a pressing need for lightweight architectures that maintain high performance while enabling real-time processing and deployment on standard clinical hardware. The pursuit of model efficiency is not merely a technical exercise but a crucial step toward equitable healthcare access, ensuring that advanced diagnostic tools can be deployed broadly, including in settings with limited computational resources [83].
This document outlines application notes and experimental protocols for developing and validating efficient deep learning models for brain tumor segmentation using Magnetic Resonance Imaging (MRI). We focus on methodologies that optimize the trade-off between computational complexity and segmentation accuracy, providing a framework for researchers and clinicians to implement these solutions in practical settings.
Quantitative Performance of Lightweight Architectures
The table below summarizes the performance and efficiency metrics of several recently proposed lightweight models for brain tumor segmentation, offering a benchmark for comparison and selection.
Table 1: Performance Metrics of Lightweight Segmentation Models
| Model Name | Core Innovation | Dataset(s) | Dice Score | Parameters | Key Advantage |
|---|---|---|---|---|---|
| LR-Net [83] | 3D Spatial Shift Convolution & Pixel Shuffle (SSCPS), Roberts Edge Enhancement | BraTS2019, BraTS2020, BraTS2021 | 0.806, 0.881, 0.860 | 4.72 M | Excellent parameter efficiency (only 3.03% of UNETR's) |
| Lightweight-CancerNet [84] | MobileNet backbone, NanoDet detection head | Combined MRI Datasets | mAP: 93.8%, Accuracy: 98% | - | High accuracy & speed for real-time detection tasks |
| 2D-VNET++ [33] | 4-staged architecture, Context Boosting Framework (CBF) | Proprietary | Dice: 99.287, Jaccard: 99.642 | - | Exceptional reported accuracy on specific datasets |
| ARU-Net [21] | Attention Res-UNet with Adaptive Channel Attention (ACA) & Dimensional-space Triplet Attention (DTA) | BTMRII | Accuracy: 98.3%, DSC: 98.1% | - | Superior segmentation accuracy and boundary precision |
| 3D U-Net (Baseline) [67] | Standard encoder-decoder architecture | BraTS2018 | DSC (TC): 0.856-0.926* | - | Strong performance with reduced sequence dependency |
*Performance varied based on the combination of MRI sequences used, with T1C + FLAIR often sufficient.
Experimental Protocols for Model Development & Validation
Protocol: Implementing and Training the LR-Net Model
This protocol details the procedure for replicating the LR-Net, a model designed for optimal parameter efficiency [83].
1. Research Reagent Solutions
- Data: BraTS2019, BraTS2020, or BraTS2021 datasets [37] [83].
- Software Framework: Python with PyTorch or TensorFlow.
- Hardware: GPU with at least 8GB VRAM recommended.
2. Pre-processing Pipeline
- Skull-Stripping: Ensure all MRI volumes are skull-stripped using the pre-processed data from BraTS.
- Spatial Normalization: Co-register all images to a common template and interpolate to a uniform isotropic resolution (e.g., 1mm³).
- Intensity Normalization: Apply Z-score normalization to each MRI sequence to achieve zero mean and unit variance.
- Data Augmentation: Implement on-the-fly augmentation including random rotations (±15°), flips, translations, and slight intensity scaling to improve model robustness.
3. Model Architecture Configuration
- SSCPS Module: Implement the Spatial Shift Convolution (SSC) block to capture a larger receptive field using 1x1x1 kernels and shift operations, replacing standard 3x3x3 convolutions.
- Pixel Shuffle: Use the Pixel Shuffle (PS) module for efficient upsampling in the decoder, replacing transposed convolutions.
- Channel Dilation Mechanism: Dynamically adjust the number of output channels in the SSCPS module to maintain feature aggregation depth.
- CAREE Module: Integrate the Channel Attention and Roberts Edge Enhancement module to sharpen fuzzy tumor boundaries. Apply the 2D Roberts Cross operator (approximated for 3D) to highlight edge features.
4. Training Procedure
- Loss Function: Employ a combination of Dice Loss and Cross-Entropy Loss to handle class imbalance.
- Optimizer: Use Adam optimizer with an initial learning rate of 1e-4 and a batch size of 2 or 4 (subject to GPU memory).
- Training Regimen: Train for a minimum of 600 epochs, implementing a learning rate scheduler that reduces the rate upon validation loss plateau.
- Validation: Use a 5-fold cross-validation strategy on the training set to ensure model stability and prevent overfitting.
Protocol: Validation of Sequence Efficiency in Brain Tumor Segmentation
This protocol describes an experiment to determine the minimal set of MRI sequences required for effective segmentation, thereby reducing data load and computational overhead [67].
1. Experimental Setup
- Base Model: Utilize a standard 3D U-Net architecture to isolate the effect of input sequences.
- Input Configurations: Train and evaluate four separate models with the following input combinations:
- T1C only
- FLAIR only
- T1C + FLAIR
- T1 + T2 + T1C + FLAIR (full set, as a baseline)
2. Methodology
- Dataset: Use the BraTS2018 dataset (n=285 for training; n=66 + 292 from BraTS2021 for testing).
- Training: Keep all hyperparameters, pre-processing, and training procedures identical across all four models to ensure a fair comparison.
- Evaluation Metrics: Primary metrics should be Dice Similarity Coefficient (DSC) for the Enhancing Tumor (ET) and Tumor Core (TC) regions. Secondary metrics include Sensitivity and 95th Percentile Hausdorff Distance (HD95).
3. Analysis
- Perform a quantitative comparison of the DSC scores across the different input configurations.
- Conduct a statistical analysis (e.g., paired t-test) to confirm that the performance of the reduced sequence model (T1C + FLAIR) is not significantly worse than the full-sequence model.
- Qualitatively assess the segmentation contours, paying special attention to boundary smoothness and the handling of heterogeneous tumor sub-regions.
Visualization of Lightweight Architecture Workflows
Diagram Title: LR-Net Architecture and Data Flow
Diagram Title: MRI Sequence Efficiency Validation Protocol
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Resources for Lightweight Model Development
| Resource Category | Specific Tool / Component | Function & Application |
|---|---|---|
| Public Datasets | BraTS (Brain Tumor Segmentation) Challenges [37] [67] | Standardized, multi-institutional MRI datasets with expert annotations for training and benchmarking. |
| Lightweight Backbones | MobileNet [84] | CNN architecture using depthwise separable convolutions to reduce parameters and computational cost. |
| Efficient Attention Modules | Adaptive Channel Attention (ACA) [21] | Enhances feature refinement in encoder by focusing on informative channels. |
| Dimensional-space Triplet Attention (DTA) [21] | Captures cross-dimension dependencies in decoder for better spatial and channel feature fusion. | |
| Edge Enhancement | Roberts Cross Operator [83] | A classical edge detection filter used to pre-process images, improving model sensitivity to tumor boundaries. |
| Loss Functions | Dice Loss [37] [33] | Addresses class imbalance between tumor and non-tumor voxels during segmentation model training. |
| Evaluation Metrics | Dice Similarity Coefficient (DSC) [22] [67] | Measures voxel-wise overlap between predicted and ground truth segmentation. |
| 95th Percentile Hausdorff Distance (HD95) [22] [2] | Measures the largest segmentation boundary error, robust to outliers. |
Generalization Across Institutions and Imaging Protocols
The translation of deep learning (DL) models for automated tumor segmentation from research to clinical practice is predominantly hindered by challenges in generalization—the ability of a model to maintain performance when applied to data from new institutions, scanners, or imaging protocols that were not part of its original training set [85] [86]. Models often experience significant performance degradation in external validation settings due to phenomena such as covariate shift and domain adaptation issues. This application note details the primary obstacles to generalization and provides validated, practical protocols to develop robust, clinically applicable segmentation models.
The Generalization Challenge: Core Concepts and Evidence
The limited generalizability of DL-based segmentation models stems from several interconnected factors. Understanding these is the first step toward mitigating their effects.
- Inter-institutional Imaging Discrepancies: Different hospitals and clinics utilize scanners from various manufacturers (e.g., Siemens, GE, Philips), each with proprietary software and hardware specifications. Furthermore, imaging protocols for parameters like slice thickness, magnetic field strength (for MRI), and acquisition sequences (e.g., T1, T2, FLAIR) vary substantially [87] [86]. A model trained on data from one set of protocols may fail to segment images acquired with different parameters effectively.
- Inter-observer Variability in Ground Truth: The "ground truth" segmentations used to train models are typically manually delineated by human experts. This process is inherently subjective and suffers from significant inter-observer variability, where different experts contour the same tumor differently, and intra-observer variability, where the same expert may contour differently at separate times [87] [2] [88]. A model trained on annotations from one group of experts may not generalize to the contouring style of another.
- Inadequate Reporting and Reproducibility: Many published studies insufficiently describe their preprocessing pipelines, model architectures, and training protocols. As highlighted by Renard et al., this lack of transparency makes it nearly impossible to independently reproduce results, let alone adapt models for new clinical environments [87] [86]. One study noted that failure to replicate a preprocessing pipeline due to insufficient description directly led to the inability to reproduce a segmentation method [86].
Table 1: Documented Performance Gaps in Multi-Institutional Validations
| Study & Model | Internal Validation Performance (DSC) | External Validation Performance (DSC) | Key Generalization Factor |
|---|---|---|---|
| iSeg (3D U-Net) for Lung Tumors [2] | 0.73 [IQR: 0.62–0.80] | 0.70 [IQR: 0.52–0.78] and 0.71 [IQR: 0.59–0.79] | Multi-site training and independent external testing |
| Two-Streamed Model for Esophageal GTV [89] | High (pCT+PET model on internal test) | Moderate (pCT-only model on external test) | Flexibility to function with or without PET; multi-institutional training data |
| 2D Single-Path CNN for Brain Tumors [86] | High on original BraTS data | DSC=0.61 for Meningioma on external clinical data | Discrepancies in preprocessing and image populations |
Experimental Protocols for Enhancing Generalization
The following protocols provide a roadmap for developing and validating segmentation models with improved generalization capabilities.
Protocol 1: Multi-Institutional Model Development and Validation
This protocol is designed to create a model that is inherently robust to inter-institutional variability.
1. Objective: To develop a deep learning model for tumor segmentation that maintains high performance across multiple, independent clinical institutions.
2. Materials:
- Datasets: Curate datasets from at least 3-4 different clinical institutions.
- Software: Deep learning framework (e.g., PyTorch, TensorFlow), image registration tools (e.g., ANTs, Elastix).
- Hardware: High-performance computing resources with modern GPUs (e.g., NVIDIA V100, A100).
3. Methods:
- Data Curation and Annotation:
- Collect retrospective data under IRB approval. The dataset should include treatment planning CTs and/or MRIs with corresponding manually contoured gross tumor volumes (GTVs) used for clinical treatment [2] [89].
- Apply strict exclusion criteria (e.g., poor image quality, prior surgery in the region) to ensure data homogeneity for training [89].
- Document the qualifications of the annotators and the tools used for contouring (e.g., 3D Slicer, commercial TPS) to understand the nature of the ground truth [85] [88].
- Model Training with Cross-Validation:
- Implement a 3D U-Net or similar architecture proven effective in medical segmentation.
- Partition data from the development institution(s) at the patient level for 4-fold or 5-fold cross-validation. This ensures the model is evaluated on different subsets of the development data [89].
- Train multiple models (folds) and use an ensemble of these models for final prediction on internal and external test sets to enhance robustness [2].
- Independent External Validation:
- Reserve data from one or more institutions that were not involved in any part of the training process as a held-out external test set.
- Evaluate the final model on this external set using segmentation metrics like Dice Similarity Coefficient (DSC) and 95% Hausdorff Distance (HD95) [2] [89].
- Conduct a human-in-the-loop assessment where clinical experts evaluate the degree of manual revision required for the model's contours to be clinically acceptable [89].
4. Anticipated Outcomes: A model that shows a minimal drop in performance metrics (e.g., DSC decrease of <0.05) between internal and external validation cohorts, indicating successful generalization.
The workflow for this multi-institutional validation is summarized in the diagram below.
Protocol 2: Robust Preprocessing and Data Handling
This protocol addresses the critical, yet often overlooked, role of preprocessing in generalization.
1. Objective: To establish a standardized, well-documented preprocessing pipeline that mitigates domain shift and enhances model robustness.
2. Materials:
- Software: Python-based libraries for image processing (SimpleITK, NiBabel), bias field correction tools (N4ITK), and intensity normalization routines.
3. Methods:
- Image Registration and Resampling:
- For multi-modal studies (e.g., combining pCT and PET/CT), rigid or deformable registration should be performed to align all images to a common space (typically the planning CT) before training and inference [89].
- Resample all images to a uniform voxel size to ensure consistent spatial resolution across the dataset [86].
- Intensity Standardization:
- Apply bias field correction to correct for scanner-induced intensity inhomogeneities, especially in MRI [86].
- Implement intensity normalization. Common methods include scaling intensities to [0, 1] or standardizing to zero mean and unit variance. This normalization should be computed in a consistent manner, for example, based on statistics from a defined region of interest (ROI) rather than the entire image volume [86].
- Comprehensive Documentation:
4. Anticipated Outcomes: A significant reduction in preprocessing-induced failures during external validation and improved reproducibility of the segmentation method.
The Scientist's Toolkit: Key Research Reagents and Solutions
Table 2: Essential Tools and Materials for Robust Segmentation Research
| Item Name | Function/Application | Implementation Notes |
|---|---|---|
| 3D U-Net Architecture | Core deep learning model for volumetric image segmentation. | Acts as a strong baseline architecture; can be modified with attention mechanisms or residual connections. |
| BraTS Dataset | Public benchmark dataset for brain tumor segmentation. | Contains multi-institutional MRI data (T1, T1ce, T2, FLAIR) with expert annotations; ideal for initial development and benchmarking. |
| N4ITK Bias Field Correction | Algorithm for correcting intensity inhomogeneity in MRI data. | Critical preprocessing step to improve intensity-based feature consistency across scanners. |
| Dice Similarity Coefficient (DSC) | Metric for evaluating spatial overlap between automated and manual segmentations. | Primary metric for segmentation accuracy; values >0.7 typically indicate clinically useful agreement. |
| 95% Hausdorff Distance (HD95) | Metric for evaluating boundary accuracy of segmentations. | Robust to outliers; measures the largest segmentation error at the 95th percentile. |
| 3D Slicer | Open-source software platform for medical image informatics and visualization. | Used for visualization, manual contouring, and qualitative analysis of segmentation results. |
| RIDGE Checklist | A framework for assessing Reproducibility, Integrity, Dependability, Generalizability, and Efficiency. | Guideline for planning studies and reporting results to ensure clinical relevance and transparency [85]. |
Achieving generalization across institutions and imaging protocols is a formidable but surmountable challenge. The evidence and protocols outlined herein demonstrate that a disciplined approach is necessary for success. This approach must be founded on multi-institutional data collaboration for training and, critically, for independent testing. Furthermore, rigorous standardization and documentation of the entire processing chain, from image acquisition to preprocessing, are non-negotiable for reproducibility and deployment. By adhering to these principles and employing the provided experimental protocols, researchers can significantly advance the development of automated tumor segmentation tools that are not only statistically accurate but also clinically dependable and widely applicable.
Automated tumor segmentation is a cornerstone of modern medical image analysis, crucial for diagnosis, treatment planning, and monitoring disease progression. The field has been revolutionized by deep learning, with models like the Segment Anything Model (SAM) providing a powerful foundation for generalizable segmentation. However, translating this general-purpose capability to the specialized domain of medical imaging presents significant challenges, including heterogeneity in medical data, scarce high-quality annotations, and distribution shifts across clinical datasets. Consequently, fine-tuned variants like MedSAM often exhibit unbalanced performance, excelling on some familiar tasks while underperforming on others, sometimes even compared to the original SAM [90] [91].
MedSAMix addresses this critical problem by introducing a training-free model merging framework that synergistically combines the broad generalization of generalist models (e.g., SAM) with the domain-specific knowledge of specialist models (e.g., MedSAM). This approach mitigates model bias and enhances performance across a wide spectrum of medical segmentation tasks without the computational expense of retraining [90] [91] [92].
Core Principles of MedSAMix
The foundational insight of MedSAMix is that fine-tuned models, initialized from the same pre-trained weights, often converge to similar loss basins. This characteristic makes them amenable to merging, which can unify diverse solution modes into a single, more robust model [91].
- Objective: Given a pre-trained base segmentation model ( M{base} ) and a set of candidate models fine-tuned from it, the goal is to construct an optimal merged model ( M{merged} ) that maximizes performance. MedSAMix achieves this through a structured, automated process [91].
- Key Innovation: Unlike traditional merging methods that rely on manual configuration, MedSAMix employs a zero-order optimization method to automatically discover optimal layer-wise merging coefficients. This is guided by performance on a small set of calibration samples, making the process both efficient and data-prudent [90] [91].
- Operational Regimes: To meet diverse clinical needs, MedSAMix operates in two distinct regimes:
- Single-Task Optimization: Focuses on maximizing performance for a specific, specialized domain (e.g., a particular type of tumor).
- Multi-Objective Optimization: Aims to enhance generalizability across a wide range of tasks, creating a universal model for medical image segmentation [91].
The following diagram illustrates the logical workflow and decision points within the MedSAMix framework.
Performance Evaluation & Quantitative Analysis
Extensive evaluations on 25 medical image segmentation tasks demonstrate the efficacy of MedSAMix. The framework consistently improves performance by effectively balancing task-specific accuracy and generalization capability [91].
Table 1: Performance Improvement of MedSAMix Over Baseline Models
| Optimization Regime | Key Metric | Reported Improvement |
|---|---|---|
| Single-Task (Expert Capability) | Domain-specific accuracy | +6.67% [91] |
| Multi-Task (General Capability) | Multi-task evaluation score | +4.37% [91] |
For context, the table below benchmarks MedSAMix against other contemporary approaches in tumor segmentation, highlighting its unique positioning.
Table 2: Comparative Analysis of Tumor Segmentation Approaches
| Model / Approach | Key Feature | Reported Performance (Dice Score) | Limitations / Context |
|---|---|---|---|
| MedSAMix (Proposed) | Training-free merging of generalist & specialist models | Specialized: +6.67%; General: +4.37% [91] | Aims for universal applicability across tasks. |
| DSNet (for Brain Tumors) | Integrates adversarial learning, DCNN, and attention. | WT: 0.959, TC: 0.975, ET: 0.947 [11] | Specialized architecture for brain tumors. |
| 3D U-Net (T1C + FLAIR) | Minimized MRI sequence dependency. | ET: 0.867, TC: 0.926 [18] | Focused on resource efficiency in brain tumor segmentation. |
| MM-MSCA-AF (for Brain Tumors) | Multi-modal multi-scale contextual aggregation. | Overall: 0.8589 [19] | Specialized for brain tumor heterogeneity. |
| Hierarchical Adaptive Pruning | Training-free, statistical pruning of non-tumor voxels. | Accuracy: ~99.1% [93] | Algorithmic, physician-inspired method. |
Experimental Protocols
This section provides detailed methodologies for implementing and validating the MedSAMix framework, from setup to evaluation.
Protocol 1: Model Merging Setup and Calibration
Objective: To prepare the base and fine-tuned models and define the calibration dataset for the optimization process.
- Model Acquisition:
- Obtain the generalist base model (e.g., SAM).
- Obtain one or more specialist models fine-tuned from the same base on medical data (e.g., MedSAM, MedicoSAM) [91].
- Calibration Data Curation:
- For single-task optimization, gather a small set (e.g., 5-10 samples) of representative image-mask pairs from the specific task of interest.
- For multi-task optimization, gather a similarly small but diverse set of samples spanning multiple target tasks [91].
- Ensure the data is pre-processed according to the requirements of the base model (e.g., resolution, normalization).
Protocol 2: Zero-Order Optimization for Merging
Objective: To automatically discover the optimal layer-wise merging configuration using the defined search space and objectives.
- Define Search Space:
- Structure the search space to encompass key modules of the Vision Transformer (ViT) architecture used in SAM, including the image encoder, prompt encoder, and mask decoder [91].
- Allow the optimizer to select from multiple merging methods (e.g., weight averaging, task vectors) and their respective coefficients at a per-layer granularity.
- Configure Optimization Algorithm:
- Employ the SMAC (Sequential Model-based Algorithm Configuration) optimizer [91].
- The objective function (reward) is the segmentation performance (e.g., Dice score) on the calibration dataset for a given merging configuration.
- For multi-task optimization, the objective is a joint performance metric across all calibration tasks.
- Execute Search:
- Run the SMAC optimizer to explore the search space.
- The output is a set of layer-wise coefficients defining how to merge the parameters of the input models to form MedSAMix.
Protocol 3: Validation and Evaluation
Objective: To rigorously assess the performance of the merged MedSAMix model.
- Model Instantiation: Apply the discovered merging configuration to the parameters of the base and specialist models to create the final MedSAMix model.
- Benchmarking:
- Evaluate the model on held-out test sets for the relevant tasks.
- Compare its performance against the individual base model (SAM) and specialist models (MedSAM) as baselines.
- Use standard segmentation metrics, including Dice Similarity Coefficient (Dice), Jaccard Index (IoU), and Hausdorff Distance [11] [91] [18].
- Analysis: Quantify the improvement in both domain-specific accuracy and generalization capability as shown in Table 1.
The following workflow diagram integrates these three protocols into a single, coherent experimental pipeline.
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Research Reagents and Computational Tools for MedSAMix
| Item Name | Function / Description | Specifications / Notes |
|---|---|---|
| Base Model (SAM) | Generalist vision foundation model providing broad segmentation knowledge and strong generalization capabilities. | The original Segment Anything Model (ViT architecture) serves as the foundational model [91]. |
| Specialist Models (MedSAM) | Fine-tuned variants of SAM on medical imaging data, providing domain-specific knowledge for tasks like tumor segmentation. | Models like MedSAM or MedicoSAM are essential sources of medical domain expertise [90] [91]. |
| Calibration Datasets | Small, representative sets of image-mask pairs used to guide the optimization process without extensive data requirements. | Critical for the zero-order optimization. Can be task-specific or multi-task [91]. |
| SMAC Optimizer | Sequential Model-based Algorithm Configuration; a Bayesian optimization tool for efficiently searching complex configuration spaces. | Used to automate the discovery of optimal layer-wise merging coefficients [91]. |
| Medical Image Benchmarks | Standardized public datasets (e.g., BraTS for brain tumors) for training specialist models and evaluating the final merged model. | Provides ground truth for validation. Enables fair comparison with state-of-the-art methods [11] [18] [19]. |
MedSAMix represents a significant paradigm shift in adapting foundation models for specialized domains like medical image segmentation. By leveraging training-free model merging, it provides a computationally efficient pathway to develop robust models that balance expert-level precision with the generalizability required for real-world clinical application. Its validated performance improvements across numerous tasks underscore its potential to become an essential tool in the deep learning toolkit for researchers and drug development professionals working on automated tumor segmentation.
Computational Resource Management and Deployment Considerations
The transition of deep learning models for automated brain tumor segmentation from research to clinical practice is critically dependent on effective computational resource management and deployment strategies. In resource-constrained settings, including low- and middle-income countries and smaller healthcare institutions, the requirement for high-performance computing infrastructure presents a significant barrier to adoption [94] [95]. This application note synthesizes current research and protocols to provide detailed methodologies for optimizing and deploying segmentation models efficiently, enabling researchers and clinicians to implement these technologies across diverse operational environments.
Quantitative Performance Benchmarks
MRI Sequence Optimization for Data Efficiency
Reducing dependency on extensive MRI sequences can significantly decrease computational demands for both training and inference. Research on sequence minimization demonstrates that comparable performance can be achieved with fewer input modalities, directly impacting data storage, processing requirements, and model complexity.
Table 1: Performance Comparison of Deep Learning Models with Varied MRI Input Sequences [18]
| MRI Sequences Used | Enhancing Tumor (ET) Dice Score | Tumor Core (TC) Dice Score | Computational & Data Implications |
|---|---|---|---|
| T1C + FLAIR | 0.867 | 0.926 | Optimal balance: Reduces data requirements by 50% compared to 4-sequence models while maintaining high accuracy. |
| T1 + T2 + T1C + FLAIR (Full Set) | 0.835 | 0.908 | Baseline: Higher data storage and preprocessing load; longer training times. |
| T1C-only | 0.726 | 0.928 | Specialized use: Highest efficiency for TC; poor ET performance limits clinical utility. |
| FLAIR-only | 0.056 | 0.543 | Limited utility: Highest efficiency but diagnostically inaccurate for enhancing tumor. |
Model Architecture Efficiency
The choice of model architecture directly influences computational resource requirements, with newer hybrid models seeking an optimal balance between accuracy and efficiency.
Table 2: Computational Efficiency of Select Brain Tumor Segmentation Model Architectures [33] [96]
| Model Architecture | Approx. Parameters (Millions) | Inference Speed (ms) | Brain Tumor Dice Coefficient | Key Resource Management Feature |
|---|---|---|---|---|
| Traditional 3D U-Net | 31.2 | 89 | 0.823 | Established baseline, requires significant resources for 3D convolutions. |
| Weak-Mamba-UNet | 24.7 | 62 | 0.887 | ~21% fewer parameters than U-Net; efficient long-range dependency modeling. |
| MWG-UNet++ | 38.5 | 76 | 0.8965 | Enhanced accuracy at the cost of ~23% more parameters than U-Net. |
| 2D VNet++ with CBF | Not Specified | Not Specified | 99.287 (Reported) | Novel Context-Boosting Framework (CBF) aims to reduce complexity. |
Deployment Environment Analysis
Selecting the appropriate deployment environment is crucial for balancing performance, cost, security, and scalability.
Table 3: Comparative Analysis of Model Deployment Environments [97]
| Deployment Environment | Best For | Scalability | Cost Profile | Key Considerations |
|---|---|---|---|---|
| Cloud (AWS, GCP, Azure) | Large-scale applications, dynamic workloads. | High, on-demand scaling. | Pay-as-you-go; no upfront hardware cost. | Potential latency; ongoing operational expenses; data transfer costs. |
| On-Premises | Sensitive data applications requiring strict compliance. | Limited; requires hardware purchases. | High upfront capital expenditure. | Full control over data and security; higher IT maintenance burden. |
| Edge Computing | Real-time applications, low/no connectivity environments. | Varies by device; distributed scaling. | Device cost; optimized for low power. | Lowest latency; processes data locally; limited by device capabilities. |
| Hybrid | Workloads with mixed sensitivity and performance needs. | Flexible, workload-specific. | Balanced (CapEx + OpEx). | Maintains sensitive data on-prem; uses cloud for less critical tasks. |
| Serverless (e.g., AWS Lambda) | Event-driven, variable workloads with intermittent traffic. | Fully automated, fine-grained scaling. | Cost-per-inference; no idle costs. | "Cold start" latency can impact response times. |
Protocol for Lightweight Model Deployment on Low-Resource Systems
The following step-by-step protocol, adapted from Oladele et al., provides a methodology for developing and deploying a brain tumor segmentation model in resource-constrained settings [95].
Phase 1: Data Collection, Preparation, and Preprocessing
Objective: To prepare and preprocess the Brain Tumor Segmentation (BraTS) dataset for efficient training on a CPU.
Materials & Setup:
- Hardware: Computer with a multi-core processor (minimum Intel Core i5), 8GB RAM, and 5GB free storage.
- Software: Python 3.12+, Visual Studio Code, Miniconda.
- Dataset: BraTS-Africa 2024 dataset or standard BraTS dataset.
Experimental Steps:
- Create a dedicated project folder (e.g., "BT_Segmentation") and open it in VS Code.
- Set up a virtual environment using Conda to manage dependencies.
- Install required libraries in the activated environment.
- Data Preprocessing:
- Co-registration and Skull Stripping: Ensure all MRI sequences (T1, T1C, T2, FLAIR) are aligned and skull-stripped (typically done in the BraTS preprocessed data).
- Intensity Normalization: Normalize the intensity values of each MRI sequence to a zero mean and unit variance to stabilize training.
- Patch Extraction: Due to memory constraints, extract 2D patches (e.g., 128x128 or 256x256) from the 3D volumes instead of using full images. This reduces memory load and enables mini-batch training on a CPU.
Phase 2: Data Loading and Model Building
Objective: To implement a data loader and construct a lightweight 3D U-Net model.
Experimental Steps:
- Create a custom Dataset class in PyTorch to load the preprocessed patches and their corresponding ground truth segmentation masks on-demand.
- Build a Lightweight 3D U-Net.
- Modify the standard 3D U-Net to reduce its memory footprint:
- Reduce the number of initial filters from 64 to 32.
- Limit the network depth to 3 or 4 levels instead of 5.
- Use depth-wise separable convolutions to decrease parameter count.
- Modify the standard 3D U-Net to reduce its memory footprint:
Phase 3: Model Training and Evaluation
Objective: To train the model using CPU-optimized practices and evaluate its performance.
Experimental Steps:
- Define the Loss Function and Optimizer:
- Use a combined loss function (e.g., Dice Loss + Binary Cross-Entropy) for robust segmentation.
- Select an efficient optimizer like Adam or SGD with a small initial learning rate (e.g., 1e-4).
- Train the Model:
- Use a small batch size (e.g., 2 or 4) to fit training into available RAM.
- Implement a learning rate scheduler to reduce the rate upon validation loss plateau.
- Use PyTorch's
DataLoaderwith multiple workers to leverage CPU cores for parallel data loading.
- Validate the Model:
- Calculate the Dice Similarity Coefficient (DSC) on the validation set to measure segmentation overlap. The protocol achieved a Dice score of 0.67 on validation data [95].
- Visually inspect the segmentation outputs against the ground truth to identify systematic errors.
Phase 4: Model Deployment and Practical Stages
Objective: To prepare the trained model for inference in a practical setting.
Experimental Steps:
- Model Export: Save the trained model's weights and architecture for inference.
- Optimize for Inference:
- Use techniques like quantization (converting model weights from 32-bit floats to 16-bit or 8-bit integers) to reduce model size and increase inference speed with a minimal accuracy trade-off [97].
- Perform model pruning to remove redundant weights.
- Create a Simple Interface: Develop a basic web interface using a lightweight framework like Flask or Streamlit that allows users to upload an MRI volume and receive the segmentation result.
- Containerization (Optional): Package the application and its dependencies into a Docker container to ensure consistent execution across different machines [97].
Diagram 1: Lightweight model deployment protocol for resource-constrained settings.
Model Optimization and Continuous Maintenance
Optimization Techniques for Production
Once a model is developed, several techniques can be applied to enhance its performance in production environments, particularly for edge or low-latency applications [97].
- Model Quantization: Reduces the numerical precision of the model's weights (e.g., from 32-bit floating-point to 8-bit integers). This can yield up to a 4x reduction in model size and a 2-3x acceleration in inference speed with a minimal impact on accuracy [97].
- Model Pruning: Systematically removes redundant or non-critical weights from a trained network. This technique can reduce model size by up to 80%, allowing applications to run faster on devices with limited memory and processing power [97].
- Containerization with Docker and Kubernetes: Packaging the model and its entire environment into a Docker container ensures consistency across development, testing, and production. Kubernetes can then be used to orchestrate these containers, managing scaling and fault tolerance. One survey reported that Docker can reduce application launch time by approximately 40% [97].
Continuous Learning and Monitoring
Deployed models require ongoing monitoring and maintenance to prevent performance degradation, a phenomenon known as "model drift" [98].
- Performance Monitoring: Track key metrics such as inference latency, throughput, and segmentation accuracy (e.g., Dice score) in real-time to detect anomalies.
- Model Retraining: Establish a pipeline for periodic retraining of the model with new data to adapt to changes in medical imaging equipment or protocols. Incremental learning techniques can make this process more efficient by updating the model without retraining from scratch [98].
Diagram 2: Continuous learning and monitoring cycle for model maintenance.
The Scientist's Toolkit: Essential Research Reagents & Materials
Table 4: Key Resources for Developing and Deploying Brain Tumor Segmentation Models
| Item Name | Function/Application | Example/Specification |
|---|---|---|
| BraTS Dataset | Benchmark data for training and validation. | Multimodal brain MRI scans (T1, T1C, T2, FLAIR) with expert-annotated tumor segmentations [18] [95]. |
| PyTorch / TensorFlow | Deep Learning Frameworks. | Open-source libraries for building and training neural networks. PyTorch is often preferred for research flexibility. |
| Visual Studio Code | Integrated Development Environment (IDE). | Code editor with support for Python, Jupyter notebooks, and debugging, essential for protocol development [95]. |
| Docker | Containerization Platform. | Packages the model, code, and dependencies into a standardized unit for deployment, ensuring environmental consistency [97]. |
| CUDA-enabled GPU / Cloud Compute | Hardware for Accelerated Training. | NVIDIA GPUs (e.g., V100, A100) or cloud equivalents (AWS EC2 P3 instances). For low-resource settings, a multi-core CPU is the minimum [95]. |
| Lightweight Model Architecture | Blueprint for efficient inference. | Architectures like a modified 3D U-Net with reduced filters and depth, designed for lower memory and compute consumption [95]. |
| Quantization & Pruning Tools | Model optimization post-training. | Framework-provided tools (e.g., PyTorch's torch.quantization) to reduce model size and increase inference speed [97]. |
| Flask / FastAPI | Web Framework for Inference API. | Lightweight Python libraries to create a REST API that wraps the model, allowing it to receive data and return predictions [95]. |
Performance Benchmarking and Clinical Validation of Segmentation Models
In the field of medical image analysis, particularly in automated tumor segmentation using deep learning, the performance of a segmentation model must be rigorously quantified using robust, standardized metrics. These metrics provide objective measures to compare different algorithms, track improvements during model development, and ultimately validate the clinical utility of an automated system. Among the plethora of available metrics, the Dice Similarity Coefficient (Dice Score), the Hausdorff Distance (HD), and the Intersection over Union (IoU), also known as the Jaccard Index, have emerged as the most critical and widely adopted for medical image segmentation tasks [99] [100] [101]. Accurate segmentation of brain tumors from Magnetic Resonance Imaging (MRI) is a prime example of a complex task where these metrics are indispensable, given the clinical importance of precisely delineating tumor sub-regions for diagnosis, treatment planning, and monitoring [102] [18]. This document provides detailed application notes and experimental protocols for the use of these metrics, framed within the context of deep learning research for automated tumor segmentation.
Metric Definitions and Theoretical Foundations
Dice Similarity Coefficient (Dice Score)
The Dice Score, or Dice Similarity Coefficient (DSC), is a spatial overlap index that is one of the most prevalent metrics for validating medical image segmentation volume accuracy [99]. It is calculated from the precision and recall of a prediction and is equivalent to the F1-score in statistical analysis. The Dice Score scores the overlap between the predicted segmentation (X) and the ground truth (Y), with a strong emphasis on penalizing false positives, a common occurrence in highly class-imbalanced datasets like medical images where the region of interest (e.g., a tumor) is often small relative to the background [99] [101].
The formula for the Dice coefficient is: $$Dice\ (X,Y) = \frac{2 |X \cap Y|}{|X| + |Y|} = \frac{2 \times TP}{(2 \times TP) + FP + FN}$$ Where:
- ( TP ) = True Positives
- ( FP ) = False Positives
- ( FN ) = False Negatives
A Dice Score of 1 indicates a perfect overlap, while a score of 0 indicates no overlap.
Intersection over Union (IoU) / Jaccard Index
The Jaccard Index, commonly known as Intersection over Union (IoU) in computer vision, is another fundamental metric for measuring segmentation accuracy [99] [103]. It is defined as the size of the intersection of the predicted segmentation and the ground truth divided by the size of their union.
The formula for IoU is: $$IoU\ (X,Y) = \frac{|X \cap Y|}{|X \cup Y|} = \frac{TP}{TP + FP + FN}$$
There is a predictable mathematical relationship between the Dice Score and the IoU. The Dice Score is always greater than or equal to the IoU for the same pair of segmentations [99]. The two metrics can be interrelated using the following formulas: $$IoU = \frac{Dice}{2 - Dice} \quad \text{or} \quad Dice = \frac{2 \times IoU}{1 + IoU}$$
Hausdorff Distance (HD)
While the Dice and IoU metrics measure volumetric overlap, the Hausdorff Distance (HD) is a shape-based metric that measures the boundary agreement between two point sets [100] [104]. It is particularly sensitive to segmented regions with complex boundaries and small thin segments, such as cerebral vessels or the irregular edges of a tumor [100]. The HD quantifies the largest distance from a point in one set to the closest point in the other set.
For two finite point sets ( X ) and ( Y ), the Hausdorff Distance is defined as: $$dH(X,Y) = \max \left{ \sup{x \in X} \inf{y \in Y} d(x,y), \sup{y \in Y} \inf_{x \in X} d(x,y) \right}$$ Where:
- ( d(x, y) ) is the Euclidean distance between points ( x ) and ( y ).
- ( \sup ) represents the supremum and ( \inf ) the infimum.
In practice, the Average Hausdorff Distance (AHD) is often used, which averages the distances instead of taking the maximum, making it less sensitive to a single outlier. However, it has been identified that the standard AHD calculation can lead to ranking errors when comparing segmentations. A modified version, the Balanced Average Hausdorff Distance (bAHD), has been proposed to mitigate this issue [100]. The formulas are:
Average Hausdorff Distance (AHD): $$d{AHD}(X,Y) = \left( \frac{1}{|X|} \sum{x \in X} \min{y \in Y} d(x,y) + \frac{1}{|Y|} \sum{y \in Y} \min_{x \in X} d(x,y) \right) / 2$$
Balanced Average Hausdorff Distance (bAHD): $$d{bAHD}(X,Y) = \left( \frac{1}{|X|} \sum{x \in X} \min{y \in Y} d(x,y) + \frac{1}{|X|} \sum{y \in Y} \min_{x \in X} d(x,y) \right) / 2$$
The key difference is that the bAHD divides both directed distance terms by the number of points in the ground truth set (( |X| )), which is constant for all segmentations being compared, thus providing a more reliable ranking [100].
The following tables summarize the properties, typical values, and comparative performance of the three core evaluation metrics.
Table 1: Core Properties and Interpretation of Key Segmentation Metrics
| Metric | Value Range | Perfect Score | Core Focus | Key Strength | Key Weakness |
|---|---|---|---|---|---|
| Dice Score (DSC) | 0 to 1 | 1 | Volumetric Overlap | Robust to class imbalance; most common in literature. | Less sensitive to boundary errors than HD. |
| IoU (Jaccard) | 0 to 1 | 1 | Volumetric Overlap | More stringent penalization of errors than Dice. | Generally yields a lower value than Dice for the same segmentation. |
| Hausdorff Distance (HD) | 0 to ∞ | 0 | Boundary Accuracy | Measures the worst-case error; critical for safety. | Highly sensitive to single outliers. |
| Average HD (AHD) | 0 to ∞ | 0 | Boundary Accuracy | Averages distances, less sensitive to outliers than HD. | Standard AHD has a known ranking error [100]. |
| Balanced AHD (bAHD) | 0 to ∞ | 0 | Boundary Accuracy | Alleviates ranking error of AHD; recommended for ranking [100]. | Less common in existing literature. |
Table 2: Example Metric Scores from Brain Tumor Segmentation Studies
| Study / Context | Dice Score | IoU (Jaccard) | Hausdorff Distance (mm) | Notes |
|---|---|---|---|---|
| SOTA Model (Proposed 2D-VNET++) [33] | 99.287 | 99.642 | Not Reported | Reported on a specific benchmark; represents top-tier performance. |
| Clinical MRI (DeepMedic & FCM) [102] | ~0.70 (Below 70%) | Not Reported | Not Reported | Highlights that accuracy on low-resolution clinical data is often lower than on research datasets like BRATS. |
| 3D U-Net on BRATS (T1C+FLAIR) [18] | ET: 0.867, TC: 0.926 | Not Reported | ET: 5.964, TC: 17.622-33.812 | Demonstrates performance on a public benchmark (BRATS) for different tumor sub-regions: Enhancing Tumor (ET) and Tumor Core (TC). |
| Theoretical Comparison [99] | 0.762 | 0.615 | Not Reported | Illustrates that for the same segmentation, Dice > IoU. |
Table 3: Guidance for Metric Selection and Interpretation
| Clinical or Research Goal | Recommended Primary Metric(s) | Supporting Metric(s) | Interpretation Threshold (Typical) |
|---|---|---|---|
| Overall Volumetric Accuracy | Dice Score (DSC) | IoU (Jaccard) | Excellent: >0.90, Good: >0.70, Poor: <0.70 |
| Boundary Delineation Precision | Balanced Average HD (bAHD) | Hausdorff Distance (HD) | Lower values are better. Threshold is task-dependent (e.g., tumor size). |
| Safety-Critical Applications (e.g., surgery) | Hausdorff Distance (HD) | Balanced Average HD (bAHD) | HD should be below a safety margin relevant to the clinical context. |
| Benchmarking & Ranking Algorithms | Dice Score + Balanced AHD | IoU (Jaccard) | Use a combination to assess both volume and boundary quality. |
Experimental Protocols for Metric Implementation
This section provides a detailed, step-by-step methodology for calculating and reporting these metrics in a tumor segmentation study, using brain tumor segmentation from MRI as a use-case.
Prerequisites and Data Preparation
- Ground Truth Segmentation Masks: For the test dataset, each MRI volume must have a corresponding, expert-annotated ground truth (GT) segmentation mask. This is typically done manually by a trained radiologist using tools like ITK-Snap [102]. The GT mask is considered the reference standard.
- Predicted Segmentation Masks: The output from your deep learning segmentation model (e.g., a 3D U-Net [18]) for each test case. This should be a binary mask (for a single class) or a multi-label mask (for tumor sub-regions like enhancing tumor, tumor core, and whole tumor).
- Preprocessing: Ensure both GT and predicted masks are in the same coordinate space and have the same dimensions. This often involves resampling the predicted mask to the native resolution of the GT mask.
Step-by-Step Calculation Protocol
Protocol 1: Calculating Dice Score and IoU
- Voxel Identification: For a given label (e.g., Tumor Core), identify all voxels in the GT mask and the predicted mask.
- Compute Confusion Matrix Components:
- True Positives (TP): Voxels correctly labeled as the tumor in both GT and prediction.
- False Positives (FP): Voxels incorrectly labeled as tumor in the prediction but not in the GT.
- False Negatives (FN): Voxels that are tumor in the GT but were not labeled as tumor in the prediction.
- Apply Formulas:
- Calculate Dice Score: ( \frac{2 \times TP}{(2 \times TP) + FP + FN} )
- Calculate IoU: ( \frac{TP}{TP + FP + FN} )
- Aggregation: Repeat steps 1-3 for all test cases and for all relevant labels. Report the average Dice and IoU across the test set, along with standard deviation.
Protocol 2: Calculating Hausdorff Distance and Balanced Average HD
- Extract Surface Points: For a given label in both the GT mask ( X ) and the predicted mask ( Y ), extract the coordinates of all surface voxels. This can be done using a 3D edge detector (e.g., using a 3D Sobel filter) or by finding all voxels with at least one non-label neighbor.
- Compute Directed Distances:
- For every point ( x ) in the GT surface set ( X ), find the minimum Euclidean distance to any point in the prediction surface set ( Y ). This generates a set of distances ( { d(x, Y) } ).
- Similarly, for every point ( y ) in ( Y ), find the minimum distance to any point in ( X ), generating ( { d(y, X) } ).
- Calculate Metrics:
- Hausdorff Distance (HD): ( HD(X,Y) = \max \left( \max { d(x, Y) }, \max { d(y, X) } \right) )
- Directed Average HD from X to Y: ( \text{GtoS} = \frac{1}{|X|} \sum{x \in X} \min{y \in Y} d(x, y) )
- Directed Average HD from Y to X: ( \text{StoG} = \frac{1}{|Y|} \sum{y \in Y} \min{x \in X} d(y, x) )
- Standard Average HD: ( \text{AHD} = (\text{GtoS} + \text{StoG}) / 2 )
- Balanced Average HD: ( \text{bAHD} = \left( \frac{1}{|X|} \sum{x \in X} \min{y \in Y} d(x, y) + \frac{1}{|X|} \sum{y \in Y} \min{x \in X} d(y, x) \right) / 2 ) [100]
- Reporting: Due to the sensitivity of HD, it is common practice to report a percentile HD (e.g., HD95), which uses the 95th percentile of the sorted surface distances instead of the maximum, to improve robustness. Report both HD and bAHD (or HD95) for a comprehensive view of boundary accuracy.
Workflow Visualization
The following diagram illustrates the logical workflow for evaluating a trained segmentation model using the described metrics.
Diagram 1: Workflow for Segmentation Model Evaluation
The Scientist's Toolkit: Key Research Reagents & Materials
For researchers replicating state-of-the-art brain tumor segmentation experiments, the following tools and datasets are essential.
Table 4: Essential Research Materials and Tools for Brain Tumor Segmentation
| Item Name | Function / Role in Research | Example / Reference |
|---|---|---|
| BRATS Dataset | The benchmark dataset for brain tumor segmentation. Provides multi-modal MRI scans with expert-annotated ground truth for training and evaluation. | MICCAI BraTS Challenge Datasets (e.g., BRATS 2018, 2021) [102] [18] |
| Deep Learning Framework | Software library for building and training segmentation models. | PyTorch, TensorFlow, Keras |
| Segmentation Network Architecture | The core deep learning model. U-Net and its variants (3D U-Net, V-Net) are the standard baselines. | 3D U-Net [18], 2D-VNet [33] |
| Metric-Sensitive Loss Function | Loss function used during training to directly optimize for the evaluation metric, often leading to better performance. | Soft Dice Loss [101], Lovász-Softmax Loss [101] |
| Evaluation & Visualization Tool | Software for computing metrics and visually inspecting segmentations to identify failure modes. | EvaluateSegmentation Tool [100], ITK-Snap [102] |
| High-Performance Computing (HPC) | GPU clusters for training complex deep learning models on large 3D medical images. | NVIDIA DGX Station, Google Cloud TPU |
The Dice Score, IoU, and Hausdorff Distance form a crucial triad of metrics for a comprehensive evaluation of automated tumor segmentation models. The Dice Score provides a robust measure of overall volumetric accuracy, IoU offers a more stringent measure of overlap, and the Hausdorff Distance (particularly the Balanced Average HD) is essential for assessing the accuracy of boundary delineation, which can be critically important for clinical applications like surgical planning. Researchers should move beyond using only the Dice Score and adopt a multi-metric reporting standard that includes at least one volumetric and one boundary-based metric. Furthermore, the use of metric-sensitive loss functions during training is strongly encouraged to directly optimize for the desired clinical and technical endpoints [101]. As the field progresses, the rigorous and standardized application of these metrics will be paramount in translating deep learning research from the bench to the bedside.
Automated tumor segmentation is a cornerstone of modern computational medicine, directly impacting diagnosis, treatment planning, and drug development. Within this domain, deep learning architectures have emerged as powerful tools, with convolutional and transformer-based models leading the innovation. This application note provides a detailed comparative analysis of three significant architectures—nnU-Net, ELU-Net, and UNETR—framed within the context of automated tumor segmentation research. We dissect their core design philosophies, present quantitative performance benchmarks across key biomedical datasets, and outline standardized experimental protocols to guide researchers and scientists in selecting and implementing these advanced tools for their preclinical and clinical studies. The objective is to offer a structured, evidence-based resource that accelerates research and development in automated medical image analysis.
Core Design Philosophies
The three architectures represent distinct evolutionary paths in deep learning for medical image segmentation.
- nnU-Net (no-new U-Net) prioritizes a robust and automated pipeline over novel architectural design. Its strength lies in its ability to automatically configure a powerful U-Net-based topology, including preprocessing, network architecture, training, and post-processing, tailored to any given dataset's specific properties without manual intervention [105] [106]. This "out-of-the-box" functionality has made it a gold standard in numerous biomedical segmentation challenges.
- UNETR (UNEt TRansformers) leverages the power of transformers to capture global contextual information. It replaces the traditional convolutional encoder of a U-Net with a transformer that models long-range dependencies in the input data. The transformer encoder's output is then passed to a convolutional decoder via skip connections to generate the final segmentation mask [107] [108]. Its successor, UNETR++, introduces a more efficient paired attention (EPA) block to reduce computational complexity while maintaining high accuracy [107].
- ELU-Net (Efficient and Lightweight U-Net) focuses on computational efficiency and parameter reduction. While detailed architectural specifics from the search results are limited, the core philosophy centers on creating a streamlined network that maintains competitive accuracy while being more suitable for deployment in resource-constrained environments [109].
Key Architectural Variations and Innovations
Advanced variants of these base architectures have been developed to address specific challenges in tumor segmentation.
- Advanced nnU-Net Variants: The base nnU-Net has been extended through the integration of advanced architectural components. Key innovations include Residual-nnUNet, Dense-nnUNet, and attention-equipped variants like Channel-Spatial-Attention-nnUNet, which incorporate mechanisms to capture more complex spatial features and emphasize informative regions [106] [110]. For brain tumor segmentation, an advanced nnU-Net combining residual blocks, attention gates, and Hausdorff distance (HD) loss has shown promising results [110].
- Efficient Transformer Designs: UNETR++'s Efficient Paired Attention (EPA) block uses parallel spatial and channel attention modules with shared keys and queries. This design significantly reduces the model's parameters and computational cost (FLOPs) compared to standard transformer models while learning enriched spatial-channel feature representations [107] [111]. Further innovations like DS-UNETR++ introduce a dual-branch feature encoding mechanism and gated attention blocks to dynamically balance coarse and fine-grained features for improved multi-organ segmentation [108].
- Federated and Meta-Learning Extensions: The FednnU-Net framework extends nnU-Net for privacy-preserving, decentralized training across multiple institutions without sharing raw data, addressing critical data privacy regulations [105]. Furthermore, Meta-transfer learning approaches have been applied to nnU-Net, enabling the model to effectively adapt to new tumor types (e.g., meningiomas and metastases) with limited labeled data by leveraging knowledge from previously learned tasks (e.g., glioma segmentation) [59].
Quantitative Performance Comparison
The following tables summarize the performance of the discussed architectures and their variants on public benchmark datasets, providing a quantitative basis for comparison. The Dice Similarity Coefficient (DSC), expressed as a percentage, and the 95th Hausdorff Distance (HD95), in millimeters, are standard metrics for evaluating segmentation accuracy and boundary delineation, respectively.
Table 1: Performance comparison on brain tumor segmentation (BraTS) datasets.
| Architecture | Variant | Dataset | Mean Dice (%) | Mean HD95 (mm) |
|---|---|---|---|---|
| nnU-Net | Advanced (Residual + Attention + HD Loss) | BraTS (Glioma) | 83.0 | 3.8 [110] |
| nnU-Net | Advanced (Residual + Attention + HD Loss) | BraTS (Pediatrics) | 71.0 | 8.7 [110] |
| nnU-Net | Meta-nnUNet | BraTS (Meningioma) | 86.2 (WT) | - [59] |
| nnU-Net | Meta-nnUNet | BraTS (Metastasis) | 81.4 (WT) | - [59] |
| UNETR++ | - | BraTS | 83.2 | 4.98 [108] |
| DS-UNETR++ | - | BraTS | 83.2 | 4.98 [108] |
Table 2: Performance comparison on abdominal multi-organ and cardiac segmentation datasets.
| Architecture | Variant | Dataset | Mean Dice (%) | Mean HD95 (mm) |
|---|---|---|---|---|
| nnU-Net | Multi-encoder | MRI (Tumor) | 93.7 | - [112] |
| UNETR++ | - | Synapse | 87.8 | 6.67 [108] |
| MLRU++ | - | Synapse | 87.6 | - [111] |
| UNETR++ | - | ACDC | 93.0 | - [111] |
| MLRU++ | - | ACDC | 93.0 | - [111] |
| MLRU++ | - | Decathlon-Lung | 81.1 | - [111] |
Table 3: Model complexity comparison (parameters and computational cost).
| Architecture | Parameters | FLOPs | Reference Model |
|---|---|---|---|
| UNETR++ | ~71% reduction | ~71% reduction | Best method in literature [107] |
| MLRU++ | Significant reduction | Significant reduction | Leading models [111] |
Experimental Protocols
Standardized Training Protocol for nnU-Net-based Models
This protocol is adapted from methodologies used for centralized and federated training of nnU-Net for tumor segmentation [105] [110] [59].
Data Preprocessing:
- Modality Handling: For multi-modal MRI (e.g., T1, T1ce, T2, FLAIR), ensure all sequences are co-registered and skull-stripped if necessary.
- Intensity Normalization: Apply Z-score normalization per modality across the entire dataset to stabilize training.
- Resampling: Resample all images and corresponding labels to a common voxel spacing (e.g., 1.0×1.0×1.0 mm³) determined by the dataset's fingerprint.
- Data Augmentation: Implement on-the-fly augmentations including random rotations, scaling, elastic deformations, and gamma corrections to improve model generalization.
Network Configuration:
- Allow the nnU-Net framework to automatically configure the network topology (patch size, network depth, etc.) based on dataset fingerprinting.
- For advanced variants, integrate architectural modifications like residual blocks or attention gates into the encoder and/or decoder as per the specific design.
Training Procedure:
- Loss Function: Use a combined loss function, typically a sum of Dice Loss and Cross-Entropy Loss. For boundary refinement, incorporate Hausdorff Distance (HD) loss [110].
- Optimizer: Use Stochastic Gradient Descent (SGD) with Nesterov momentum or Adam. A common configuration is SGD with an initial learning rate of 0.01 and momentum of 0.99.
- Training Schedule: Employ a 5-fold cross-validation strategy to ensure robust model evaluation and prevent overfitting. Implement a learning rate scheduler (e.g., polynomial decay or "polyLR") to reduce the learning rate during training.
- Federated Training (For FednnU-Net): Use the Federated Fingerprint Extraction (FFE) to create a global data configuration and the Asymmetric Federated Averaging (AsymFedAvg) algorithm to aggregate model weights from clients with potentially heterogeneous architectures [105].
Protocol for UNETR++ and Variants
This protocol outlines the training process for transformer-based segmentation models [107] [108].
Data Preprocessing:
- Volume to Patches: Split the input 3D volume into a sequence of non-overlapping 3D patches. These patches are then linearly projected into embedding vectors.
- Positional Encoding: Add learnable or fixed sinusoidal positional encodings to the patch embeddings to retain spatial information.
Network Configuration:
- Encoder: Utilize a transformer encoder with Efficient Paired Attention (EPA) blocks. The EPA block consists of parallel spatial and channel attention modules with shared keys-queries.
- Decoder: Use a convolutional decoder that upsamples the encoded features. The decoder incorporates skip connections from different levels of the encoder to recover spatial details.
Training Procedure:
- Loss Function: Use a combination of Dice Loss and Cross-Entropy Loss.
- Optimizer: Use the AdamW optimizer, which often performs better for transformer architectures, with a weight decay of 1e-5.
- Training Schedule: Utilize a learning rate warmup followed by cosine decay. Train for a fixed number of epochs (e.g., 20,000 to 50,000) with a batch size suitable for the GPU memory.
Meta-Transfer Learning Protocol for nnU-Net
This protocol is designed for adapting a pre-trained nnU-Net to new tumor types with limited data [59].
Meta-Pretraining (Outer Loop):
- Train a base nnU-Net model on a source domain with abundant data (e.g., BraTS gliomas). This model serves as a well-initialized starting point.
Meta-Training (Bilevel Optimization):
- Inner Loop (Task-Specific Adaptation): For each task in a meta-batch (e.g., a small subset of meningioma cases), perform a few gradient descent steps (e.g., 1-5) on the base model using the support set. This creates task-specific adapted models.
- Outer Loop (Meta-Optimization): Evaluate the performance of these adapted models on the respective query sets. The gradient from this evaluation is then used to update the weights of the base model. This process encourages the base model to develop representations that can rapidly adapt to new tasks with few examples.
Fine-Tuning:
- After meta-training, the base model can be rapidly fine-tuned on a small labeled dataset of the new target tumor type.
Workflow and Architecture Visualization
Experimental Workflow for Tumor Segmentation
The diagram below outlines a generalized experimental workflow for developing and evaluating a deep learning model for tumor segmentation, incorporating elements from the discussed protocols.
Diagram Title: Tumor Segmentation Development Workflow
High-Level Architecture Comparison
This diagram provides a simplified, high-level view of the core architectural differences between nnU-Net, UNETR++, and a lightweight model like ELU-Net.
Diagram Title: Core Architectural Paradigms
The Scientist's Toolkit: Key Research Reagents and Materials
Table 4: Essential software and data components for tumor segmentation research.
| Item Name | Type | Function / Application | Example / Source |
|---|---|---|---|
| Public Benchmark Datasets | Data | Standardized data for model training, validation, and benchmarking. | BraTS (Brain Tumors) [110] [59], Synapse (Multi-organ) [107] [108], ACDC (Cardiac) [111] |
| Deep Learning Frameworks | Software | Core libraries for building, training, and deploying deep learning models. | PyTorch, TensorFlow |
| Medical Imaging Toolkits | Software | Libraries for reading, preprocessing, and manipulating medical image data (e.g., DICOM, NIfTI). | ITK, SimpleITK, NiBabel |
| nnU-Net Framework | Software | An out-of-the-box segmentation system that automates pipeline configuration for new datasets. | https://github.com/MIC-DKFZ/nnUNet [105] [106] |
| FednnU-Net Framework | Software | A privacy-preserving, federated learning extension of the nnU-Net framework. | https://github.com/faildeny/FednnUNet [105] |
| Dice & HD95 Metrics | Software Script | Standard evaluation metrics to quantify segmentation overlap and boundary accuracy. | Custom implementation or libraries like MedPy |
| Combined Loss Functions | Algorithm | Loss functions that combine region-based and distribution-based measures for stable training. | Dice + Cross-Entropy Loss [110] |
| Advanced Optimizers | Algorithm | Optimization algorithms tailored for deep neural networks, including adaptive and SGD variants. | SGD with Nesterov Momentum, Adam, AdamW [59] |
Multi-Model Ensemble Approaches and Performance Enhancement
Automated tumor segmentation represents a critical frontier in medical imaging, directly impacting diagnosis, treatment planning, and therapeutic development. Within this domain, multi-model ensemble approaches have emerged as a powerful strategy to boost the accuracy, robustness, and generalizability of deep learning systems. Ensemble methods strategically combine the predictions of multiple machine learning models to produce a single, superior output. This synthesis mitigates the risk of relying on a single model's potential errors or biases, thereby enhancing overall system performance [113]. In clinical and research settings, particularly for complex tasks like brain tumor segmentation from MRI, these techniques have demonstrated remarkable efficacy, achieving performance levels that often surpass state-of-the-art individual models [16] [114].
Ensemble Architectures and Performance
Ensemble learning in medical imaging is characterized by its diverse methodologies, which can be broadly categorized based on model heterogeneity, training sequence, and fusion strategy. The core principle is that by combining multiple base models, the ensemble can capitalize on their individual strengths while compensating for their weaknesses.
Table 1: Key Ensemble Model Characteristics and Performance in Tumor Analysis
| Ensemble Type | Description | Base Models / Components | Reported Performance |
|---|---|---|---|
| Weight-Optimized Deep Ensemble [114] | Combines multiple deep learning models with weights optimized via grid or genetic algorithm. | Xception, ResNet50V2, ResNet152V2, InceptionResNetV2 | Accuracy: 99.84% (GSWO) on brain tumor classification [114] |
| Stacking [115] | Uses a meta-learner to optimally combine the predictions of multiple base models. | Multiple CNN Architectures | F1-score increase of up to 13% on medical image classification [115] |
| Bagging (with Cross-Validation) [115] | Trains multiple instances of the same model on different data subsets and aggregates results. | Multiple CNN Architectures | F1-score increase of up to 11% [115] |
| Random Committee [16] | An ensemble of randomized base models for classification. | Random Committee Classifier | Accuracy: 98.61% on hybrid brain tumor MRI dataset [16] |
| CNN Ensemble with Majority Voting [116] | Combines predictions from multiple CNN architectures via majority voting. | VGG16, DenseNet121, Inception-ResNet-v2 | Accuracy: 86.17% on brain tumor classification [116] |
| Two-Stage Interactive Refinement (2S-ICR) [117] | A sequential ensemble for segmentation refinement using initial and refinement networks. | Initial Network, Refinement Network | Dice: 0.858 after 10 interactions for OPC tumor segmentation [117] |
The performance gains from these ensemble methods are substantial. A large-scale analysis of ensemble learning for medical image classification found that Stacking achieved the most significant performance gain, with an F1-score increase of up to 13%. Bagging demonstrated a notable 11% increase, while Augmenting (a data-level ensemble technique) showed a consistent improvement of up to 4% [115]. For brain tumor classification specifically, a weight-optimized deep ensemble using Grid Search-based Weight Optimization (GSWO) achieved a remarkable 99.84% accuracy on the Figshare CE-MRI dataset, highlighting the potential of sophisticated fusion strategies [114]. Furthermore, ensembles have proven effective in interactive segmentation, with the 2S-ICR framework significantly improving the Dice Similarity Coefficient (DSC) from 0.722 to 0.858 after just ten user interactions for oropharyngeal cancer segmentation [117].
Table 2: Quantitative Performance of Optimized Ensemble Models on Brain Tumor Classification
| Model / Optimization Technique | Dataset | Key Metric | Reported Score |
|---|---|---|---|
| Grid Search-based Weight Optimization (GSWO) [114] | Figshare CE-MRI | Accuracy | 99.84% |
| Genetic Algorithm-based Weight Optimization (GAWO) [114] | Figshare CE-MRI | Accuracy | 99.78% |
| Individual Model (Xception) [114] | Figshare CE-MRI | Accuracy | 99.57% |
| Individual Model (ResNet50V2) [114] | Figshare CE-MRI | Accuracy | 99.48% |
| Ensemble-based CNN (VGG16, DenseNet121, Inception-ResNet-v2) [116] | Brain MRI | Accuracy | 86.17% |
Experimental Protocols
Protocol 1: Implementing a Weight-Optimized Deep Ensemble for Classification
This protocol details the methodology for constructing a high-performance ensemble for brain tumor classification using transfer learning and weight optimization, as demonstrated in recent research [114].
1. Data Preparation and Balancing:
- Dataset: Utilize the Figshare Contrast-Enhanced MRI (CE-MRI) brain tumor dataset, which contains 3064 T1-weighted contrast-enhanced images.
- Preprocessing: Apply standard preprocessing steps including resizing, normalization, and intensity scaling to ensure consistency across images.
- Class Imbalance Mitigation: Employ Synthetic Data Generation (SDG) techniques, such as Generative Adversarial Networks (GANs) or diffusion models, to generate synthetic MRI images for underrepresented tumor classes. This ensures a balanced representation across all classes in the dataset, which is crucial for preventing model bias.
2. Base Model Selection and Fine-Tuning:
- Architecture Selection: Choose multiple pre-trained deep learning architectures known for their efficacy in medical imaging, such as Xception, ResNet50V2, ResNet152V2, and InceptionResNetV2.
- Transfer Learning & Fine-Tuning:
- Initialize each model with weights pre-trained on a large-scale dataset like ImageNet.
- Replace the final fully connected layer with a new one corresponding to the number of tumor classes.
- Individually fine-tune each model on the prepared brain tumor dataset. This involves training the models for several epochs with a low learning rate to adapt the generic features to the specific medical task.
3. Ensemble Construction and Weight Optimization:
- Prediction Generation: Run the entire validation set through each fine-tuned model to obtain a set of prediction vectors for every image.
- Weight Optimization:
- Grid Search-based Weight Optimization (GSWO): Define a search space for possible weight combinations assigned to each model. GSWO performs an exhaustive search within this space to find the weight combination that maximizes validation accuracy. This method is rigorous and systematic, often yielding superior performance [114].
- Genetic Algorithm-based Weight Optimization (GAWO): As an alternative, use a genetic algorithm to evolve a population of weight combinations towards an optimal solution. This can be more efficient than grid search for very large parameter spaces.
4. Inference:
- For a new, unseen MRI image, generate predictions using all fine-tuned base models.
- Compute the final, fused prediction by calculating the weighted average of all prediction vectors using the optimized weights obtained from GSWO or GAWO.
Protocol 2: A Two-Stage Interactive Ensemble for Segmentation Refinement
This protocol outlines a sequential ensemble method designed to refine tumor segmentations through user interaction, significantly improving initial segmentation results [117].
1. Data and Initial Setup:
- Dataset: Use a publicly available segmentation dataset such as the HECKTOR 2021 dataset for oropharyngeal cancer.
- Network Architecture: Implement a 3D U-Net or a similar state-of-the-art segmentation network as the core model for both stages.
2. Two-Stage Model Training:
- Stage 1 - Initial Segmentation Network:
- Objective: Train a model to perform high-quality automatic segmentation without any user input.
- Process: Train the network on the provided training dataset using standard segmentation loss functions (e.g., Dice Loss, Cross-Entropy). The goal is to achieve the best possible baseline Dice Similarity Coefficient (DSC).
- Stage 2 - Refinement Network:
- Objective: Train a separate model specialized in incorporating user interactions to correct the initial segmentation.
- Process: The training input for this network is a concatenation of the original medical image (e.g., PET-CT volume), the initial segmentation probability map from the Stage 1 network, and simulated user clicks (positive/negative clicks indicating under- or over-segmentation). The network learns to adjust the segmentation mask based on this interactive feedback.
3. Interactive Inference and Refinement:
- Initial Segmentation: The input volume is first processed by the Stage 1 network to generate an initial segmentation mask.
- Iterative Refinement:
- A clinician reviews the initial mask and provides corrective feedback by clicking on erroneous regions.
- These clicks are converted into interaction maps and fed into the Stage 2 Refinement Network along with the original image and the initial segmentation.
- The Refinement Network produces an updated, improved segmentation.
- This process can be repeated iteratively, with each new set of clicks further refining the output. The system uses the sigmoid probability volume as a memory mechanism between interactions to maintain consistency.
Table 3: Essential Materials and Resources for Ensemble-based Tumor Analysis
| Item / Resource | Specification / Example | Primary Function in Research |
|---|---|---|
| Public Datasets | BraTS (MRI), HECKTOR (PET/CT), Figshare CE-MRI [114] [118] [18] | Provides standardized, annotated medical imaging data for training, validation, and benchmarking ensemble models. |
| Pre-trained Models | Xception, ResNet50V2, VGG16, DenseNet121 [114] [116] | Serves as base models for transfer learning, providing robust feature extractors and reducing training time. |
| Segmentation Networks | 3D U-Net, nnU-Net [18] [117] | Core architecture for volumetric medical image segmentation tasks; nnU-Net provides a self-configuring framework. |
| Optimization Algorithms | Adam, NAdam, SGD with Nesterov Momentum [119] | Optimizers used during the training of base models to minimize the loss function and converge to a solution. |
| Synthetic Data Generation (SDG) | GANs, Diffusion Models [114] | Generates synthetic medical images to balance class distribution in datasets, improving model robustness. |
| Explainability Tools | Grad-CAM++, Integrated Gradients [116] | Provides visual explanations for model predictions, increasing trust and interpretability for clinical use. |
Workflow and System Architecture Visualization
Ensemble Model Workflow for Classification
Two-Stage Interactive Segmentation
Automated tumor segmentation using deep learning has revolutionized the analysis of medical images. While high pixel-wise accuracy on benchmark datasets is often reported, the ultimate test for these technologies is their diagnostic impact in clinical practice. This document provides Application Notes and Protocols for researchers and drug development professionals to assess the clinical utility of such tools, moving beyond traditional metrics to evaluate how they influence diagnostic accuracy, workflow efficiency, and ultimately, patient care.
Quantitative Performance Benchmarks
The transition from technical validation to clinical assessment requires a multifaceted evaluation. The following table summarizes key quantitative findings from recent studies on automated tumor segmentation, highlighting performance metrics with direct clinical relevance.
Table 1: Quantitative Performance Benchmarks for Automated Tumor Segmentation Models
| Study & Focus | Model Architecture | Key Performance Metrics | Clinical Relevance & Impact Findings |
|---|---|---|---|
| iSeg: Lung Tumor Delineation for Radiotherapy [120] | 3D U-Net | Median Dice: 0.73 (Internal), 0.70-0.71 (External) [120].ITV contours were 30% smaller than physician-drawn ones (p<0.0001) [120]. | Matched human inter-observer variability. Machine-generated contours were more precise. Higher model false positive rates were associated with increased local failure (HR: 1.01, p=0.03) [120]. |
| Brain Tumor Segmentation with Minimal MRI [18] | 3D U-Net | Best Dice on Test Set: T1C+FLAIR (ET: 0.867, TC: 0.926), outperforming the 4-sequence model (ET: 0.835, TC: 0.908) [18].Specificity remained high (≥0.958) across configurations [18]. | Achieved high accuracy with only two MRI sequences (T1C, FLAIR), reducing data requirements and potentially increasing clinical adoption and generalizability [18]. |
| BrainTumNet: Multi-task Segmentation & Classification [54] | Custom CNN with Adaptive Masked Transformer | Segmentation: Dice: 0.91, IoU: 0.921, HD: 12.13 [54].Classification: Accuracy: 93.4%, AUC: 0.96 [54]. | Provides a unified model for segmentation and classification, enhancing diagnostic efficiency. Stable performance on an external validation set confirms generalizability [54]. |
Experimental Protocols for Clinical Validation
To ensure that automated segmentation models are clinically viable, rigorous validation protocols are essential. The following sections detail methodologies for key experiments that assess clinical utility.
Protocol: Multi-Center and External Validation
Objective: To evaluate model robustness and generalizability across diverse patient populations, imaging protocols, and clinical institutions.
Materials:
- Model: Pre-trained segmentation model (e.g., 3D U-Net).
- Datasets:
Procedure:
- Training: Train the model on the internal cohort using 5-fold cross-validation.
- Validation: Evaluate the model on held-out internal data and the external cohorts.
- Metrics: Calculate segmentation metrics (Dice Similarity Coefficient - DSC, 95% Hausdorff Distance - HD95) for all cohorts.
- Statistical Analysis: Compare performance distributions between internal and external cohorts using non-parametric tests (e.g., Mann-Whitney U test) to confirm no significant performance degradation.
Clinical Interpretation: Comparable performance across cohorts indicates strong generalizability, a prerequisite for widespread clinical deployment [120].
Protocol: Benchmarking Against Human Inter-Observer Variability
Objective: To determine if the model's performance falls within the range of variability observed among expert clinicians.
Materials:
- Trained segmentation model.
- A subset of cases (e.g., 50-100) from the dataset.
- Ground truth (GT) contours from the original physician.
- Re-contoured segmentations from a blinded expert (IO).
Procedure:
- Generate model segmentations (iSeg) for the subset.
- Calculate pairwise agreement metrics:
- GT vs. IO (represents human inter-observer benchmark)
- GT vs. iSeg
- IO vs. iSeg
- Statistically compare the distributions of DSC scores between GT::IO and GT::iSeg pairs.
Clinical Interpretation: A model that performs within the range of human inter-observer variability is considered clinically acceptable, as its "errors" are no greater than those between experts [120].
Protocol: Assessment of Motion-Robust Target Volume Delineation
Objective: To validate the model's ability to accurately segment tumors across respiratory motion phases in 4D CT scans for radiotherapy planning.
Materials:
- 4D CT dataset of a lung tumor.
- An ensemble of models trained on different data folds [120].
Procedure:
- Segmentation: Apply the ensemble model to each phase of the 4D CT scan to generate Gross Tumor Volumes (GTVs) for each respiratory phase.
- Propagation: Geometrically unite the GTVs across all phases to create a machine-generated Internal Target Volume (ITV).
- Comparison: Compare the machine-generated ITV to the physician-drawn ITV in terms of volume and spatial overlap (DSC).
- Analysis: Statistically compare the volumes (e.g., using a paired t-test) to determine if the model produces more parsimonious contours.
Clinical Interpretation: Significantly smaller, yet accurate, ITVs can lead to reduced radiation exposure to healthy tissues, potentially lowering treatment-related toxicity [120].
Diagram 1: ITV Generation and Validation Workflow
The Scientist's Toolkit: Research Reagent Solutions
Successful development and validation of clinically impactful segmentation models rely on a suite of essential "research reagents"—datasets, software, and evaluation frameworks.
Table 2: Essential Research Reagents for Clinical AI Validation
| Reagent / Solution | Function & Description | Exemplars (from search results) |
|---|---|---|
| Curated Multi-Center Datasets | Provides data for robust training and external validation, ensuring model generalizability. | Multicenter cohort from 9 clinics [120]; BraTS datasets for brain tumors [18] [54]. |
| Benchmarked Model Architectures | Proven deep learning backbones for semantic segmentation of medical images. | 3D U-Net [120] [18]; Custom CNNs with Transformer modules [54]. |
| Multi-Task Learning Frameworks | Unified models that perform simultaneous tasks (e.g., segmentation and classification), improving diagnostic efficiency. | BrainTumNet for joint segmentation and classification [54]. |
| Clinical Outcome Linkage Data | Datasets linking segmentation outputs (e.g., contour characteristics) to patient outcomes (e.g., local failure, survival). | Data enabling analysis between false positive voxels and local failure rates [120]. |
| Standardized Evaluation Metrics | Quantifiable measures for technical performance and clinical agreement. | Dice (DSC), Hausdorff Distance (HD95), IoU [120] [54]; Classification Accuracy, AUC [54]. |
Diagram 2: Multi-Task Model Architecture
FDA-Approved AI Tools and Regulatory Considerations
The integration of artificial intelligence (AI) into oncological imaging represents a transformative advancement in cancer care. The U.S. Food and Drug Administration (FDA) has established a dedicated list of AI-enabled medical devices that have met rigorous premarket requirements for safety and effectiveness [121]. These tools are increasingly being incorporated into clinical workflows to enhance the precision, efficiency, and consistency of tumor segmentation—a critical process in diagnosis, treatment planning, and therapeutic monitoring.
FDA-approved AI tools for tumor segmentation primarily function as decision support systems, automating the delineation of tumor boundaries across various imaging modalities including MRI, CT, and PET [121] [122]. This automation addresses key challenges in modern radiology, including workload burden, diagnostic variability, and the need for quantitative assessment in precision medicine. The regulatory clearance process involves focused review of clinical validation studies appropriate for each device's intended use and technological characteristics [121].
Currently Approved AI Tools and Their Technical Performance
NeuroQuant Brain Tumor Analysis System
Cortechs.ai's NeuroQuant Brain Tumor system represents a significant advancement in neuro-oncological imaging. As the first FDA-certified cloud-native tool for automated volume segmentation of both brain metastases and meningiomas in routine clinical environments, it provides fully automated segmentation and volumetric quantification [123]. The system integrates with existing hospital PACS infrastructure, enabling rapid deployment and seamless integration into neurosurgical and neuro-oncological workflows.
The technical workflow involves automatic analysis of MRI images from patients with pathologically-confirmed brain tumors, performing tumor volume segmentation and quantitative analysis [123]. This capability enables clinicians to directly import segmentation files into treatment planning systems, eliminating manual contouring needs and improving interoperability between departments. The system's longitudinal tracking functionality provides crucial insights into tumor volume changes, supporting more accurate treatment response monitoring and clinical decision-making [123].
TumorSight Viz for Breast Cancer Surgery
SimBioSys received FDA 510(k) clearance for TumorSight Viz version 1.3, an AI-based tool that converts standard breast MRI into detailed 3D visualizations for surgical planning [124]. This platform employs AI-driven segmentation to display tumor shape, size, morphology, and location within the breast architecture, providing reliable volume calculations that influence pre-surgical decision-making between breast-conserving surgery and mastectomy options.
The platform utilizes standard-of-care medical imaging and diagnostic data as inputs, with trained AI automatically identifying tumor tissue to create 3D models of tumors and surrounding tissue [124]. These models calculate breast and tumor volumes as well as distances to critical anatomical landmarks. Internal validation surveys indicate that 70% of surgeons rated the system as valuable or very valuable overall, with enhanced utility noted in complex cases involving multi-focal tumors, ductal carcinoma in situ, larger tumors, and disease located near critical structures like the skin or nipple [124].
Technical Performance Benchmarking
Table 1: Performance Metrics of AI Segmentation Architectures
| Architecture/Platform | Clinical Application | Key Performance Metrics | Validation Cohort |
|---|---|---|---|
| U-Net Architecture [125] | Brain tumor segmentation (glioma, meningioma, pituitary) | Accuracy: 98.56%, F-score: 99%, AUC: 99.8%, Recall: 99%, Precision: 99% | Cross-dataset validation: 96.01% accuracy with external cohort |
| TumorSight Viz [124] | Breast cancer surgical planning | Strong concordance with radiologist annotations | >1,600 retrospective cases across 9+ institutions |
| autoPET III nnUNet [126] | NSCLC TNM staging on [¹⁸F]FDG PET/CT | Lesion detection sensitivity: 95.8%, UICC staging accuracy: 67.6% | 306 treatment-naïve NSCLC patients |
Experimental Protocols for AI Tool Validation
Protocol for Validation of Segmentation Accuracy
Purpose: To quantitatively evaluate the performance of AI-based tumor segmentation tools against expert manual segmentation as reference standard.
Materials:
- Medical imaging data (MRI, CT, or PET) from retrospective cohort
- Expert-annotated segmentation masks (ground truth)
- AI segmentation platform (FDA-approved tool under evaluation)
- Computing infrastructure for quantitative analysis
Procedure:
- Data Curation: Collect a minimum of 100 representative cases spanning the intended use population and disease spectrum [124] [126]
- Reference Standard Establishment: Utilize multi-disciplinary team consensus to create manual segmentation masks, documenting any inter-reader variability [126]
- AI Segmentation: Process images through the AI tool using standard operating procedures
- Quantitative Analysis: Calculate Dice Similarity Coefficient (DSC), Hausdorff Distance, precision, and recall metrics
- Clinical Correlation: Assess segmentation performance impact on clinical endpoints such as TNM staging accuracy or surgical planning [126]
Validation Considerations:
- Implement cross-dataset validation using external cohorts to assess generalizability [125]
- Conduct subgroup analysis based on tumor size, location, and imaging characteristics
- Evaluate performance at clinical decision boundaries that impact treatment pathways [126]
Protocol for Integration into Clinical Workflows
Purpose: To assess the seamless integration of AI segmentation tools into existing clinical pathways and quantify workflow efficiency improvements.
Materials:
- PACS-integrated AI platform
- Clinical workstation with treatment planning software
- Time-motion data collection tools
Procedure:
- Workflow Mapping: Document baseline clinical workflow without AI integration
- System Integration: Implement AI tool with PACS connectivity using hospital IT infrastructure [123]
- Time Studies: Measure time from image acquisition to segmentation completion across 50 consecutive cases
- Clinical Utility Assessment: Survey radiologists and surgeons on system usability, confidence improvement, and clinical decision impact using standardized instruments [124]
- Output Integration: Evaluate compatibility with downstream systems including surgical navigation and radiation planning platforms [123]
FDA Regulatory Framework and Considerations
The AI-Enabled Medical Device List
The FDA maintains a comprehensive list of AI-enabled medical devices that have been authorized for marketing in the United States [121]. This resource provides transparency for healthcare providers, patients, and developers regarding cleared AI technologies. The list includes devices that have met premarket requirements through demonstrations of overall safety and effectiveness, with particular evaluation of study appropriateness for intended use and technological characteristics [121].
As of 2025, more than 700 AI algorithms have received FDA approval, with the majority (over 75%) focused on radiological tasks [122]. This regulatory landscape continues to evolve rapidly, with the FDA exploring methods to identify devices incorporating foundation models and other advanced AI architectures to enhance transparency [121].
AI Trustworthiness Assessment Framework
The FDA has proposed a "Based Risk Credibility Assessment Framework" to guide the evaluation of AI tools used in pharmaceutical and biological product development [127]. This framework provides a structured approach for assessing whether AI-generated evidence is sufficient to support regulatory decisions.
Figure 1: FDA's AI Credibility Assessment Framework [127]
The framework encompasses seven critical steps that emphasize risk-based evaluation and early engagement with regulatory bodies [127]:
- Define Target Problem: Precisely articulate the clinical or research question the AI model aims to address
- Determine Context of Use: Specify how model outputs will be utilized in decision-making processes
- Assess Model Risk: Evaluate potential impact of erroneous outputs on patient safety or study validity
- Develop Credibility Assessment Plan: Establish comprehensive validation strategy
- Execute Plan: Implement validation studies per predefined protocols
- Document Results: Record outcomes and any deviations from planned approaches
- Determine Appropriateness: Make final determination regarding model suitability for intended use
Real-World Performance Monitoring
Post-market surveillance represents a critical component of the regulatory lifecycle for AI-enabled devices. The FDA emphasizes continuous monitoring of real-world performance to identify drift, domain shift, or other issues that may emerge when algorithms are deployed in diverse clinical environments [122]. This is particularly important for segmentation tools that may encounter variations in imaging protocols, patient populations, or equipment specifications across different institutions.
Research Reagent Solutions and Computational Tools
Table 2: Essential Research Tools for AI Tumor Segmentation Development
| Tool Category | Specific Examples | Primary Function | Application Context |
|---|---|---|---|
| Deep Learning Architectures | U-Net [125], nnUNet [126], Inception-V3, EfficientNetB4 [125] | Image segmentation and classification | Brain tumor classification (glioma, meningioma, pituitary tumors) |
| Medical Imaging Platforms | TumorSight Viz [124], NeuroQuant [123], eyonis LCS [128] | Clinical deployment and validation | FDA-cleared platforms for breast, brain, and lung cancer |
| Computational Modeling | Quantitative System Pharmacology (QSP) [129], Agent-Based Models (ABM) [129] | Simulating tumor-immune interactions and drug responses | Preclinical toxicity assessment and therapy optimization |
| Validation Frameworks | AUTO-PET III challenge framework [126], REALITY Trial protocol [128] | Standardized performance benchmarking | Multi-center validation studies for regulatory submission |
Implementation Challenges and Future Directions
Clinical Validation Gaps
Despite promising technical performance metrics, significant challenges remain in translating AI segmentation tools to clinical practice. Recent research highlights disparities between traditional segmentation metrics and clinical utility. A critical evaluation of NSCLC TNM staging using autoPET III challenge-winning algorithms demonstrated that while lesion detection sensitivity reached 95.8%, overall UICC staging accuracy was only 67.6% [126]. This performance gap underscores the limitations of pixel-level overlap metrics (e.g., Dice Similarity Coefficient) in predicting clinical task performance.
The primary driver of staging inaccuracies was false positive findings in M-staging, with 35.7% of false positives attributed to benign lesions and 34.7% to non-neoplastic pathological changes [126]. This observation highlights the critical importance of context-aware interpretation and the current necessity of radiologist oversight, particularly for metastatic classification and multifocal cases.
Evolving Regulatory Paradigms
The FDA is actively developing new approaches to govern AI applications in pharmaceutical development and clinical practice. The 2025 guidance "Considerations for Using Artificial Intelligence to Support Regulatory Decisions for Pharmaceutical and Biological Products" establishes a risk-based credibility assessment framework that emphasizes [127]:
- Context-Driven Evaluation: The level of evidence required depends on the model's influence on decisions and potential consequences of errors
- Early Engagement: Sponsors should engage regulatory bodies during early development phases to align on validation strategies
- Transparent Documentation: Comprehensive documentation of model development, training data characteristics, and performance limitations
Additionally, the FDA is promoting innovative approaches that combine AI with human cell-based assay systems like organoids to reduce animal testing in preclinical safety assessment [129]. This initiative reflects a broader transition toward human-relevant systems in drug development.
FDA-approved AI tools for tumor segmentation represent a rapidly advancing field with demonstrated capabilities in enhancing diagnostic precision, surgical planning, and therapy response assessment. The regulatory framework continues to evolve toward risk-based approaches that balance innovation with robust validation requirements. Successful implementation requires careful attention to clinical integration, ongoing performance monitoring, and understanding of both technical capabilities and limitations. As these technologies mature, the focus is shifting from pure segmentation accuracy to clinically meaningful endpoints that directly impact patient care pathways and outcomes.
Limitations in Real-World Clinical Translation and Validation Gaps
Automated tumor segmentation using deep learning (DL) represents a transformative advancement in oncology, enabling precise delineation of tumor volumes for diagnosis, treatment planning, and therapy response assessment. Models have achieved expert-level performance in controlled research environments, with reported Dice similarity coefficients (DSC) exceeding 0.95 for brain tumor segmentation [11] [18] and 0.73-0.77 for lung tumor segmentation in multi-institutional validation [2] [130]. Despite these impressive technical achievements, significant limitations impede their widespread adoption in clinical practice. This application note examines the critical validation gaps and real-world translation challenges facing DL-based tumor segmentation systems, providing researchers and drug development professionals with frameworks for robust clinical evaluation.
Current State of Automated Tumor Segmentation
Deep learning systems for tumor segmentation have evolved from basic convolutional neural networks (CNNs) to sophisticated architectures including 3D U-Nets, transformer models, and hybrid frameworks [75] [131]. These systems process various medical imaging modalities—including computed tomography (CT), magnetic resonance imaging (MRI), and positron emission tomography (PET)—to automatically delineate tumor boundaries with minimal human intervention.
Table 1: Performance Metrics of Recent DL-Based Tumor Segmentation Studies
| Cancer Type | Imaging Modality | Model Architecture | Dataset Size | Reported Performance (DSC) | Validation Level |
|---|---|---|---|---|---|
| Brain Tumors [18] | Multi-sequence MRI | 3D U-Net | 285 training, 358 test | 0.867 (ET), 0.926 (TC) | Cross-validation + external test |
| Lung Tumors [2] | 4D CT | 3D U-Net | 739 training, 263 validation | 0.73 (IQR: 0.62-0.80) | Multi-center (9 clinics) |
| Multiple Lung Lesions [130] | CT | Multi-step pipeline | 868 training, 213 test | 0.76 (internal), 0.73 (external) | External real-world dataset |
| Brain OARs [132] | CT/MRI | Not specified | 100 training | 0.78 (overall DSC) | Cross-institutional expert evaluation |
The performance metrics in controlled research settings are impressive, yet they often mask fundamental limitations that emerge in real-world clinical implementation. The transition from algorithm development to clinical integration requires addressing multiple validation gaps that extend beyond technical accuracy.
Critical Validation Gaps
Limited Prospective Clinical Validation
Most DL-based segmentation models are developed and validated retrospectively on curated datasets that lack the heterogeneity of clinical environments [133] [134]. This creates a significant translation gap where models that perform well on standardized benchmarks fail when confronted with real-world variability in imaging protocols, patient populations, and clinical workflows.
The field lacks prospective randomized controlled trials (RCTs) that evaluate the impact of automated segmentation on clinical decision-making and patient outcomes [133]. As noted in analysis of AI in drug development, "Despite the proliferation of peer-reviewed publications describing AI systems in drug development, the number of tools that have undergone prospective evaluation in clinical trials remains vanishingly small" [133]. This evidence gap is particularly problematic for clinical adoption and reimbursement, as payers increasingly demand demonstration of clinical utility and cost-effectiveness.
Generalization Across Diverse Clinical Environments
Models trained on single-institution datasets often demonstrate degraded performance when applied to external populations due to differences in imaging protocols, scanner manufacturers, and patient demographics [130]. While some studies have attempted multi-center validation [2], the comprehensive evaluation of model robustness across the full spectrum of clinical scenarios remains exceptional rather than standard practice.
The COMMUTE framework highlights that "commercial certifications for clinical use, such as those provided by the Food and Drug Administration (FDA) and European Medicines Agency (EMA), only provide generic guidelines and pathways as to how the quality of a system needs to be assessed. However, they do not mandate using specific evaluation frameworks or particular metrics" [132]. This regulatory flexibility, while promoting innovation, creates challenges for standardizing performance assessment across different systems and institutions.
Integration with Clinical Workflows and Dosimetric Impact
Technical performance metrics such as DSC and Hausdorff distance do not necessarily correlate with clinical utility [132]. A segmentation model might achieve high geometrical accuracy but fail to integrate efficiently with clinical workflows or cause downstream dosimetric consequences in radiation treatment planning.
Qualitative expert evaluation reveals that clinical acceptability often depends on factors beyond volumetric overlap metrics, including boundary smoothness, anatomical plausibility, and consistency with institutional protocols [132]. One evaluation found that 88% of automatically segmented structures were clinically acceptable with only minor adjustments needed, yet the process of evaluation and adjustment still required an average of 22 minutes compared to 69 minutes for manual contouring [132].
Comprehensive Evaluation Framework
The COMMUTE (COMprehensive MUltifaceted Technical Evaluation) framework addresses these validation gaps through an integrated approach encompassing four key assessment components [132]:
Experimental Protocol for Multi-faceted Validation
Protocol 1: Comprehensive Model Evaluation According to COMMUTE Framework
Objective: To rigorously validate DL-based auto-segmentation models for clinical deployment by assessing geometric accuracy, clinical acceptability, time efficiency, and dosimetric impact.
Materials:
- Test dataset of 30-100 cases representing target patient population
- Reference standard contours established by expert consensus
- DL-based auto-segmentation model(s) for evaluation
- Treatment planning system for dosimetric analysis
- 3-8 clinical experts for qualitative assessment
Procedure:
Quantitative Geometric Assessment
- Calculate Dice Similarity Coefficient (DSC) and Hausdorff Distance (HD) between auto-segmented and reference contours
- Compare results against inter-observer variability benchmarks when available
- Perform subgroup analysis based on tumor characteristics (size, location, morphology)
Qualitative Expert Evaluation
- Present experts with mixed sets of reference and auto-segmented contours in blinded fashion
- Rate each contour using standardized scale: (1) Acceptable, (2) Minor changes required, (3) Major changes required, (4) Not acceptable
- Calculate percentage of auto-segmented structures deemed clinically acceptable
Time Efficiency Analysis
- Measure time required for experts to review and adjust auto-segmented contours to clinical standards
- Compare against time required for manual contouring de novo
- Document frequency and extent of modifications using surface Dice metrics
Dosimetric Evaluation
- Create duplicate treatment plans using both reference and auto-segmented contours
- Compare dose-volume histogram (DVH) parameters for targets and organs at risk
- Analyze clinical significance of observed differences using institutional protocols
Analysis: Integrate findings from all four components to make comprehensive determination of clinical readiness. Models should demonstrate non-inferior geometric accuracy compared to inter-observer variability, high clinical acceptability (≥85% with minor or no adjustments), significant time savings (≥50% reduction), and minimal dosimetric impact (≤2% difference in critical parameters).
Implementation Challenges and Solutions
Technical and Workflow Integration Barriers
Table 2: Key Challenges in Clinical Translation and Potential Solutions
| Challenge Category | Specific Limitations | Potential Mitigation Strategies |
|---|---|---|
| Technical Robustness | Performance degradation on external datasets; handling of multiple lesions per patient [130] | Multi-center training data; data augmentation; transfer learning; ensemble methods |
| Clinical Integration | Disruption of established workflows; insufficient time savings in practice [132] | User-centered design; iterative prototyping with clinician feedback; seamless PACS/RIS integration |
| Validation Standards | Lack of standardized evaluation frameworks; overreliance on geometric metrics [132] [131] | Adoption of comprehensive frameworks like COMMUTE; development of specialty-specific benchmarks |
| Regulatory Evidence | Insufficient prospective validation; limited evidence of clinical utility [133] | Prospective observational studies; pragmatic trials; cost-effectiveness analyses |
Pathway to Clinical Translation
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Research Reagents and Resources for Tumor Segmentation Research
| Resource Category | Specific Examples | Function/Purpose | Implementation Notes |
|---|---|---|---|
| Public Datasets | BraTS (Brain Tumor Segmentation) [18], NSCLC-Radiomics [130] | Model training and benchmarking | Provide multi-institutional data with expert annotations; essential for initial validation |
| Annotation Tools | ITK-SNAP [130], 3D Slicer | Manual contouring for ground truth creation | Enable precise slice-by-slice annotation; support multiple imaging modalities |
| Model Architectures | 3D U-Net [2] [18], nnU-Net [130], Transformer-based networks | Core segmentation algorithms | Balance computational efficiency with performance; consider implementation complexity |
| Evaluation Metrics | Dice Similarity Coefficient, Hausdorff Distance, Surface Dice [132] | Quantitative performance assessment | Provide complementary perspectives on different aspects of segmentation quality |
| Clinical Evaluation Platforms | COMMUTE framework [132], QUADAS-AI | Standardized clinical validation | Ensure comprehensive assessment beyond technical metrics |
The translation of DL-based tumor segmentation from research to clinical practice requires addressing significant validation gaps that extend beyond technical performance. The COMMUTE framework provides a comprehensive approach to validation, but broader adoption of such standardized methodologies is necessary to enable meaningful comparisons between systems and build clinical confidence.
Future efforts should focus on conducting prospective trials that evaluate the impact of automated segmentation on clinical workflows, decision-making, and patient outcomes. Additionally, the development of specialty-specific benchmarks and consensus guidelines within the oncology community will be essential for establishing standardized validation protocols. As these frameworks mature, DL-based tumor segmentation has the potential to significantly enhance the precision, efficiency, and accessibility of cancer care while accelerating drug development processes.
Conclusion
Automated tumor segmentation using deep learning has demonstrated remarkable progress, with architectures like nnU-Net and hybrid models achieving Dice scores exceeding 0.89 on benchmark datasets. The integration of multi-modal data and advanced optimization techniques has enabled high-performance segmentation with reduced sequence dependency, enhancing clinical applicability. Future directions should focus on developing energy-efficient models, improving explainability for clinical trust, advancing foundation models for multi-organ segmentation, and establishing robust frameworks for real-time 3D segmentation in clinical workflows. The convergence of AI with biomedical research promises to accelerate drug development and personalized treatment planning, though significant challenges in interoperability, validation, and clinical integration remain to be addressed through collaborative efforts between AI researchers and medical professionals.
References
- 1. Deep learning for medical image segmentation: State-of- ... [https://www.sciencedirect.com/science/article/pii/S2352914824000601]
- 2. Deep learning for automated, motion-resolved tumor ... [https://www.nature.com/articles/s41698-025-00970-1]
- 3. Developments in Deep Learning Artificial Neural Network ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12071792/]
- 4. Medical Image Segmentation: A Comprehensive Review of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12115501/]
- 5. A Generalized Surface Loss for Reducing the Hausdorff in... Distance [https://arxiv.org/html/2302.03868v3]
- 6. Radiomics as a measure superior to common similarity metrics for... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11302798/]
- 7. Top Medical Imaging Datasets & Healthcare Data Sources for ... [https://collectiveminds.health/articles/medical-imaging-datasets-complete-guide-to-healthcare-data-resources]
- 8. Investigating Information Visualization to Combat ... [https://www.researchprotocols.org/2025/1/e74247]
- 9. 利用深度学习模型从MRI图像中检测、分类和分割脑肿瘤: ... [https://www.ebiotrade.com/newsf/2025-11/20251116084100039.htm]
- 10. Brain tumor segmentation with deep learning [https://www.sciencedirect.com/science/article/abs/pii/S0165027025000652]
- 11. A deep learning framework for 3D brain tumor ... [https://www.sciencedirect.com/science/article/pii/S2772442525000371]
- 12. 2025年U-Net技术突破:从医学影像到多模态融合的进化之路 [https://blog.csdn.net/gitblog_00994/article/details/152540976]
- 13. Deep learning-driven brain tumor classification and ... [https://www.nature.com/articles/s41598-025-13591-2]
- 14. Performance of deep learning models for automatic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12108801/]
- 15. Optimized deep learning for brain tumor detection: a hybrid ... [https://www.nature.com/articles/s41598-025-04591-3]
- 16. Multi-class brain tumor MRI segmentation and classification ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12613584/]
- 17. 基于深度学习与机器学习的多类别脑肿瘤MRI分割与分类 ... [https://www.ebiotrade.com/newsf/2025-11/20251113231638034.htm]
- 18. Brain tumor segmentation using deep learning [https://www.frontiersin.org/journals/radiology/articles/10.3389/fradi.2025.1616293/full]
- 19. Enhanced brain tumor segmentation in medical imaging ... [https://www.nature.com/articles/s41598-025-21255-4]
- 20. A brain tumor segmentation method based on attention ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12043955/]
- 21. Automated Brain Tumor MRI Segmentation Using ARU-Net ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12468718/]
- 22. Quantitative Evaluation of AI-based Organ Segmentation ... [https://www.sciencedirect.com/science/article/abs/pii/S1879850025002115]
- 23. GlioMODA: Robust Glioma Segmentation in Clinical Routine [https://www.medrxiv.org/content/10.1101/2025.11.12.25339968v1.full]
- 24. Advancing Precision: A Comprehensive Review of MRI ... [https://www.mdpi.com/1424-8220/25/6/1838]
- 25. The Brain Tumor Segmentation (BraTS) Challenge 2023 [https://pmc.ncbi.nlm.nih.gov/articles/PMC10441440/]
- 26. MICCAI registered challenges [https://miccai.org/index.php/special-interest-groups/challenges/miccai-registered-challenges/]
- 27. MICCAI 2024: Call for Challenges [https://miccai.org/index.php/news/2023/12/12/miccai-2024-call-for-challenges]
- 28. The Evolution of Challenges [https://conferences.miccai.org/2024/en/The-Evolution-of-Challenges.html]
- 29. Evaluation of CNN-based deep learning models for auto ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12613770/]
- 30. GAME-Net: An Ensemble Deep Learning Framework ... [https://www.frontiersin.org/journals/computational-neuroscience/articles/10.3389/fncom.2025.1702902/full]
- 31. A Review on Deep Learning Methods for Glioma ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12387613/]
- 32. Current trends in glioma tumor segmentation: A survey of ... [https://www.sciencedirect.com/science/article/abs/pii/S1120179725000985]
- 33. a four-stage deep network for accurate brain tumor ... [https://www.nature.com/articles/s41598-025-18879-x]
- 34. a novel framework based on improved DeepLabV3+ and ... [https://www.sciencedirect.com/science/article/pii/S209012322500654X]
- 35. CNN-Based Image Segmentation Approach in Brain Tumor ... [https://www.mdpi.com/2673-4591/84/1/66]
- 36. Convolutional neural networks for brain tumour segmentation [https://insightsimaging.springeropen.com/articles/10.1186/s13244-020-00869-4]
- 37. A review of deep learning for brain tumor analysis in MRI [https://www.nature.com/articles/s41698-024-00789-2]
- 38. Evaluation of CNN - based deep learning models for auto-contouring in... [https://ro-journal.biomedcentral.com/articles/10.1186/s13014-025-02748-y]
- 39. Application of convolutional neural networks in medical images [https://pmc.ncbi.nlm.nih.gov/articles/PMC11074758/]
- 40. Frontiers | gamUnet: designing global attention- based ... CNN [https://www.frontiersin.org/journals/medicine/articles/10.3389/fmed.2025.1582439/full]
- 41. Brain Tumor Detection Based on Deep Learning Approaches ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10453020/]
- 42. CNN-TumorNet: leveraging explainability in deep learning ... [https://www.frontiersin.org/journals/oncology/articles/10.3389/fonc.2025.1554559/full]
- 43. Convolutional neural networks for tumor segmentation by ... [https://link.springer.com/article/10.1007/s13721-025-00556-8]
- 44. A review on brain tumor segmentation based on deep ... [https://www.sciencedirect.com/science/article/pii/S0895611123001313]
- 45. 3-D contour-aware U-Net for efficient rectal tumor ... [https://www.sciencedirect.com/science/article/abs/pii/S1350453325000712]
- 46. ES-UNet: efficient 3D medical image segmentation with ... [https://bmcmedimaging.biomedcentral.com/articles/10.1186/s12880-025-01857-0]
- 47. Advancing Brain Tumor Segmentation via Attention-based ... [https://arxiv.org/abs/2510.19109]
- 48. Revisiting model scaling with a U-net benchmark for 3D ... [https://www.nature.com/articles/s41598-025-15617-1]
- 49. Attention-driven UNet enhancement for accurate ... [https://www.nature.com/articles/s41598-025-05900-6]
- 50. Multi-scale conv-attention U-Net for medical image ... [https://www.nature.com/articles/s41598-025-96101-8]
- 51. BEFUnet: A Hybrid CNN-Transformer Architecture for ... [https://blog.csdn.net/2401_87277167/article/details/155166615]
- 52. 脑肿瘤分割学习(五):A Robust Volumetric Transformer for ... [https://blog.csdn.net/qq_38296005/article/details/125819385]
- 53. [论文审查] Automated MRI Tumor Segmentation using ... [https://www.themoonlight.io/zh/review/automated-mri-tumor-segmentation-using-hybrid-u-net-with-transformer-and-efficient-attention]
- 54. BrainTumNet: multi-task deep learning framework for brain ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12129765/]
- 55. 基于条件生成对抗网络的三维肝脏及肿瘤区域自动分割 [https://pmc.ncbi.nlm.nih.gov/articles/PMC10307569/]
- 56. Enhanced brain tumor segmentation in medical imaging using ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12552493/]
- 57. Optimizing MRI sequence classification performance [https://pmc.ncbi.nlm.nih.gov/articles/PMC12559157/]
- 58. Clinical Image Testing: MRI (Revised 1-23-2025) [https://accreditationsupport.acr.org/support/solutions/articles/11000061017-clinical-image-testing-mri-revised-1-23-2025-]
- 59. Meta transfer learning for brain tumor segmentation using ... [https://www.nature.com/articles/s41598-025-20957-z]
- 60. Domain Adaptation Techniques for Natural and Medical ... [https://www.sciencedirect.com/science/article/abs/pii/S0020025525007418]
- 61. HyDA: Hypernetworks for Test Time Domain Adaptation in ... [https://arxiv.org/abs/2503.04979]
- 62. A brain tumor segmentation enhancement in MRI images ... [https://bmcmedimaging.biomedcentral.com/articles/10.1186/s12880-025-01837-4]
- 63. Domain Adaptation and Generalization Using Foundation ... [https://papers.ssrn.com/sol3/papers.cfm?abstract_id=5345726]
- 64. A Fully Automated Post-Surgical Brain Tumor Segmentation ... [https://pubmed.ncbi.nlm.nih.gov/37568773/]
- 65. Automated Tumor Segmentation in Radiotherapy [https://www.sciencedirect.com/science/article/pii/S1053429622000315]
- 66. Development and evaluation of a deep learning framework for ... [https://cancerimagingjournal.biomedcentral.com/articles/10.1186/s40644-025-00850-8]
- 67. Brain tumor segmentation using deep learning [https://pmc.ncbi.nlm.nih.gov/articles/PMC12281592/]
- 68. Synthetic data generation: a privacy-preserving approach ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11958975/]
- 69. On-the-Fly Data Augmentation for Brain Tumor Segmentation [https://arxiv.org/html/2509.24973v1]
- 70. Synthetic data generation methods in healthcare: A review ... [https://www.sciencedirect.com/science/article/pii/S2001037024002393]
- 71. Brain tumor classification using GAN-augmented data with ... [https://www.frontiersin.org/journals/medicine/articles/10.3389/fmed.2025.1635796/full]
- 72. Applications of machine learning in drug discovery and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6552674/]
- 73. Enhanced brain tumor classification framework using deep ... [https://www.nature.com/articles/s41598-025-19882-y]
- 74. Synthetic data generation method improves risk prediction ... [https://www.nature.com/articles/s41598-025-15800-4]
- 75. Brain tumor detection, classification and segmentation by ... [https://www.sciencedirect.com/science/article/pii/S2590005625001985]
- 76. Automated Brain Tumor MRI Segmentation Using ARU-Net ... [https://pubmed.ncbi.nlm.nih.gov/41008698/]
- 77. Resampling approaches to handle class imbalance: a review ... [https://journalofbigdata.springeropen.com/articles/10.1186/s40537-025-01119-4]
- 78. 10 Techniques to Solve Imbalanced Classes in Machine ... [https://www.analyticsvidhya.com/blog/2020/07/10-techniques-to-deal-with-class-imbalance-in-machine-learning/]
- 79. Brain tumor segmentation using multi-scale attention U-Net ... [https://www.nature.com/articles/s41598-025-94267-9]
- 80. Augmentation strategies for an imbalanced learning ... [https://www.nature.com/articles/s41598-023-45532-2]
- 81. DreamOn: a data augmentation strategy to narrow the ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11696537/]
- 82. 7 Techniques to Handle Class Imbalance in Machine Learning [https://data-pilot.com/blog/7-techniques-to-handle-class-imbalance-in-machine-learning/]
- 83. A 3D lightweight network with Roberts edge enhancement ... [https://www.nature.com/articles/s41598-025-03151-z]
- 84. Lightweight-CancerNet: a deep learning approach for brain ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11888863/]
- 85. RIDGE: Reproducibility, Integrity, Dependability ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12343378/]
- 86. Deep learning for automatic brain tumour segmentation on MRI [https://pmc.ncbi.nlm.nih.gov/articles/PMC9297223/]
- 87. Variability and reproducibility in deep learning for medical ... [https://www.nature.com/articles/s41598-020-69920-0]
- 88. Do's and Don'ts of Tumor Segmentation with 3D Slicer [https://www.sciencedirect.com/science/article/pii/S3050577125000519]
- 89. Multi-Institutional Validation of Two-Streamed Deep ... [https://www.frontiersin.org/journals/oncology/articles/10.3389/fonc.2021.785788/full]
- 90. [2508.11032] MedSAMix: A Training-Free Model Merging ... [https://arxiv.org/abs/2508.11032]
- 91. MedSAMix: A Training-Free Model Merging Approach for ... [https://arxiv.org/html/2508.11032v1]
- 92. MedSAMix: A Training-Free Model Merging Approach for ... [https://huggingface.co/papers/2508.11032]
- 93. 3D brain tumor segmentation in MRI images using ... [https://www.sciencedirect.com/science/article/pii/S2666521225001073]
- 94. 人工智能赋能资源有限地区成人弥漫性胶质瘤诊疗:机遇与挑战 [https://www.ebiotrade.com/newsf/2025-11/20251108084308290.htm]
- 95. Lightweight Brain Tumor Segmentation on Low-Resource ... [https://www.protocols.io/view/lightweight-brain-tumor-segmentation-on-low-resour-gz4sbx8wf.html]
- 96. 2025 U-Net混合进化:医学影像分割精度与效率双重突破原创 [https://blog.csdn.net/gitblog_00760/article/details/153450643]
- 97. for Deployment Models Guide | MoldStud Strategies Deep Learning [https://moldstud.com/articles/p-effective-deployment-strategies-for-deep-learning-models-a-comprehensive-guide]
- 98. Data-Driven Deep | SIIT Learning Deployment Strategies [https://siit.co/blog/data-driven-deep-learning-deployment-strategies/15037]
- 99. Understanding Evaluation Metrics in Medical Image ... [https://medium.com/mastering-data-science/understanding-evaluation-metrics-in-medical-image-segmentation-d289a373a3f]
- 100. On the usage of average Hausdorff distance for segmentation ... [https://eurradiolexp.springeropen.com/articles/10.1186/s41747-020-00200-2]
- 101. Theory and Practice When Evaluating With Dice Score or ... [https://pubmed.ncbi.nlm.nih.gov/32746113/]
- 102. An optimal brain tumor segmentation algorithm for clinical MRI ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9107172/]
- 103. Intersection over Union (IoU): Definition, Calculation, Code [https://www.v7labs.com/blog/intersection-over-union-guide]
- 104. Hausdorff distance [https://en.wikipedia.org/wiki/Hausdorff_distance]
- 105. Federated nnU-Net for privacy-preserving medical image ... [https://www.nature.com/articles/s41598-025-22239-0]
- 106. Exploring advanced architectural variations of nnUNet [https://www.sciencedirect.com/science/article/abs/pii/S0925231223009608]
- 107. UNETR++: Delving into Efficient and Accurate 3D Medical ... [https://github.com/Amshaker/unetr_plus_plus]
- 108. A 3D medical image segmentation network based on gated ... [https://www.nature.com/articles/s41598-025-90339-y]
- 109. ELU-Net: An Efficient and Lightweight U-Net for Medical ... [https://www.semanticscholar.org/paper/ELU-Net%3A-An-Efficient-and-Lightweight-U-Net-for-Deng-Hou/df6b9883140b5738b3214221521046bfba68f642]
- 110. Brain tumor segmentation with advanced nnU-Net [https://www.sciencedirect.com/science/article/pii/S2772528624000013]
- 111. MLRU++: Multiscale Lightweight Residual UNETR++ with ... [https://arxiv.org/abs/2507.16122]
- 112. Multi-encoder nnU-Net outperforms transformer models ... [https://arxiv.org/abs/2504.03474]
- 113. A systematic literature review: exploring the challenges of ... [https://bmcmedimaging.biomedcentral.com/articles/10.1186/s12880-025-01667-4]
- 114. A deep ensemble learning framework for brain tumor ... [https://www.nature.com/articles/s41598-025-03752-8]
- 115. An Analysis on Ensemble Learning optimized Medical ... [https://arxiv.org/abs/2201.11440]
- 116. Enhancing accuracy and interpretability using explainable AI [https://www.sciencedirect.com/science/article/pii/S0010482525009060]
- 117. Interactive 3D segmentation for primary gross tumor ... [https://www.nature.com/articles/s41598-025-13601-3]
- 118. Multi-modal tumor segmentation methods based on deep ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10784092/]
- 119. Assessment of Optimizers and their Performance in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10419743/]
- 120. Deep learning for automated, motion-resolved tumor ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12209462/]
- 121. Artificial Intelligence-Enabled Medical Devices [https://www.fda.gov/medical-devices/software-medical-device-samd/artificial-intelligence-enabled-medical-devices]
- 122. How FDA-Approved AI Tools are Revolutionizing Imaging ... [https://www.bccresearch.com/industry-trends/how-ai-tools-are-revolutionizing-imaging-practices-across-the-globe?srsltid=AfmBOorajD31MwOGno57cpcqNpCO9ozqv0qAW3gNyu0ZE2vQ9jPrAYtY]
- 123. Cortechs.ai推出新一代NeuroQuant®脑肿瘤分析系统 - 家庭医生 [https://www.familydoctor.cn/news/cortechsai-tui-neuroquant-naozhongliu-fenxi-fenge-159246.html]
- 124. FDA Clears AI-Based Visualization Software for Surgical ... [https://www.cancernetwork.com/view/fda-clears-ai-based-visualization-software-for-surgical-breast-cancer-care]
- 125. Deep Learning Enhances Brain Tumour Segmentation [https://www.emjreviews.com/oncology/news/deep-learning-enhances-brain-tumour-segmentation/]
- 126. 人工智能在NSCLC TNM分期中的应用:从分割精度到临床 ... [https://www.ebiotrade.com/newsf/2025-11/20251123220834631.htm]
- 127. 美国FDA拟定药品和生物制品生产研发的AI应用治理规则 [https://www.glo.com.cn/Content/2025/02-18/1501421402.html]
- 128. Median Technologies,AI解锁影像表型学,二十年深耕铸就 ... [https://bydrug.pharmcube.com/news/detail/96d74846b5c9bcaa72e69347eb554b54]
- 129. 美国APExBIO中文官网 [https://www.apexbio.cn/marketing/262]
- 130. Advancing deep learning-based segmentation for multiple ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12361585/]
- 131. A systematic review of deep learning-based segmentation ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12559657/]
- 132. A comprehensive multifaceted technical evaluation ... [https://www.nature.com/articles/s43856-025-01048-6]
- 133. AI in Drug Development: Clinical Validation and ... [https://globalforum.diaglobal.org/issue/june-2025/ai-in-drug-development-clinical-validation-and-regulatory-innovation-are-dual-imperatives/]
- 134. Artificial intelligence in cancer: applications, challenges, and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12574039/]