Advancing Drug Resistance Prediction: Machine Learning and Genomic Approaches for Improved Accuracy
This article synthesizes current advancements in predicting antimicrobial and antitubercular drug resistance mutations, targeting researchers and drug development professionals.
Advancing Drug Resistance Prediction: Machine Learning and Genomic Approaches for Improved Accuracy
Abstract
This article synthesizes current advancements in predicting antimicrobial and antitubercular drug resistance mutations, targeting researchers and drug development professionals. It explores the foundational understanding of resistance mechanisms, examines cutting-edge machine learning and next-generation sequencing methodologies, addresses critical troubleshooting and optimization challenges in model development, and provides frameworks for rigorous clinical validation and comparative performance analysis. By integrating genomic data with sophisticated algorithms, this review highlights pathways toward more accurate, rapid, and clinically actionable resistance prediction tools to combat the global AMR crisis.
Understanding the Genomic Landscape of Drug Resistance
Technical Support Center: Troubleshooting Guides and FAQs
This technical support center is designed for researchers and scientists working to improve the prediction accuracy of drug resistance mutations. The guides below address common computational and experimental challenges in this field, with a focus on drug-resistant tuberculosis (DR-TB).
Frequently Asked Questions (FAQs)
Q1: Our whole-genome sequencing analysis is producing a high rate of false-positive resistance markers. How can we improve specificity?
- A: High false-positive rates often occur when analysis tools mistakenly link unrelated mutations to resistance. To address this:
- Employ advanced machine learning models that do not rely solely on pre-defined resistance mechanisms. For example, the Group Association Model (GAM) uses a bacteria's entire genetic fingerprint to identify resistance patterns, which has been shown to drastically reduce false positives [1].
- Utilize ensemble-based molecular dynamics methods, like TIES_PM, for resistance prediction in specific proteins like RNA polymerase. This method calculates binding free energy changes to provide a more reliable link between mutation and function, with results aligned to WHO classifications [2].
Q2: What are the key limitations of current phenotypic drug susceptibility testing (DST) and how can computational methods complement them?
- A: Traditional methods have significant trade-offs between speed and accuracy.
- Culture-based DST (e.g., on Lowenstein-Jensen medium) is highly specific but slow, taking 4–6 weeks for results [2].
- Molecular tests like GeneXpert are faster (under 2 hours) but can lack the ability to detect rare or novel mutations and cannot distinguish between viable and non-viable bacteria [2].
- Computational supplements can bridge this gap. Molecular dynamics simulations (e.g., with TIES_PM) can predict resistance for mutations in large protein complexes within about 5 hours, offering a rapid, accurate, and low-cost supplement to wet-lab methods [2].
Q3: Our research requires analyzing the global burden of multidrug-resistant TB (MDR-TB). What are the most reliable current estimates and trends?
- A: The most current data shows a persistent and evolving global challenge. The following table summarizes key burden metrics from recent studies.
Table 1: Global Burden of MDR-/RR-TB and XDR-TB
| Metric | MDR-/RR-TB (2022) [3] | MDR-TB (2021) [4] | XDR-TB (2021) [4] |
|---|---|---|---|
| Incident Cases | 410,000 (UI: 370,000–450,000) | Age-Std. Incidence Rate: 5.42 per 100,000 | Age-Std. Incidence Rate: 0.29 per 100,000 |
| Mortality | 160,000 deaths (UI: 98,000–220,000) | Data not available | Data not available |
| Notable Trends | Relatively stable 2020-2022; downward revision of estimates since 2015. | Increasing trend (1990-2021), esp. in low & low-middle SDI regions. | Increasing trend (1990-2021) across all SDI regions. |
Q4: The burden of MDR-TB in children and adolescents is poorly understood. What is the known disease burden in this demographic?
- A: Research using the GBD 2019 database has quantified this burden, revealing a significant and growing problem, particularly in younger children and lower-resource regions [5].
- In 2019, there were an estimated 67,710.82 incident cases of MDR-TB in individuals under 20 years old worldwide [5].
- The mortality and DALY rates are highest in children under 5 years (0.62 and 55.19 per 100,000, respectively) compared to older age groups, highlighting their vulnerability [5].
- The global incidence rate in this population has increased from 1990 to 2019, with the largest shares of the burden found in Southern sub-Saharan Africa, Eastern Europe, and South Asia [5].
Troubleshooting Guide: Key Experimental Protocols
Protocol 1: Predicting Rifampicin Resistance with TIES_PM Molecular Dynamics
This protocol estimates the binding affinity of Rifampicin to mutated RNA polymerase (RNAP) through free energy calculations [2].
- Objective: To accurately predict if a mutation in the rpoB gene confers resistance to Rifampicin by quantifying its impact on drug binding.
- Workflow:
- System Preparation: Obtain 3D structures of wild-type and mutant RNAP bound to Rifampicin.
- Simulation Setup: Use software like GROMACS or AMBER to set up the molecular dynamics simulation with explicit solvent and ions.
- Relative Binding Free Energy (RBFE) Calculation: Employ the TIES_PM method to perform alchemical transformation simulations, gradually changing the wild-type amino acid to the mutant.
- Energy Analysis: Calculate the difference in binding free energy (ΔΔG) between the wild-type and mutant complexes.
- Interpretation: A positive ΔΔG value indicates a mutation that destabilizes drug binding, predicting resistance. The method requires ~5 hours per mutation on high-performance computing (HPC) systems.
- Troubleshooting Tip: The ensemble-based approach of TIES_PM is crucial for statistical robustness. Ensure sufficient sampling and replica simulations to achieve reliable results.
Protocol 2: Applying a Group Association Model (GAM) for Novel Mutation Discovery
This machine learning-based method identifies genetic mutations associated with drug resistance without prior knowledge of the mechanism [1].
- Objective: To discover previously unknown genetic markers of antibiotic resistance from whole-genome sequence data.
- Workflow:
- Data Curation: Assemble a large dataset of whole-genome sequences from bacterial strains (e.g., M. tuberculosis) with known phenotypic resistance profiles.
- Model Training: Train the GAM by comparing groups of resistant and susceptible strains to find genetic changes that reliably indicate resistance to specific drugs.
- Validation: Test the model's accuracy against a held-out validation set and compare its performance to existing databases (e.g., the WHO's resistance database).
- Application: Use the trained model to screen new, uncharacterized bacterial genomes for potential resistance markers.
- Troubleshooting Tip: This model's performance is dependent on the quality and size of the input dataset. Use data from diverse geographic regions to improve the model's generalizability and ability to detect rare mutations.
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Materials for Drug Resistance Prediction Research
| Item | Function in Research |
|---|---|
| Whole-Genome Sequence Data (e.g., from clinical M. tuberculosis isolates) | The fundamental raw data for identifying genetic mutations and training machine learning models like GAM [1]. |
| High-Performance Computing (HPC) Cluster | Provides the computational power necessary for running complex molecular dynamics simulations and large-scale bioinformatic analyses [2]. |
| Molecular Dynamics Software (e.g., GROMACS, AMBER) | Software suites used to simulate the physical movements of atoms and molecules over time, enabling free energy calculations [2]. |
| Phenotypic Drug Susceptibility Testing (DST) Data | Serves as the gold-standard ground truth for validating predictions made by computational models [2]. |
| 3D Protein Structures (e.g., from Protein Data Bank) | Essential starting structures for molecular dynamics simulations to study drug-target interactions [2]. |
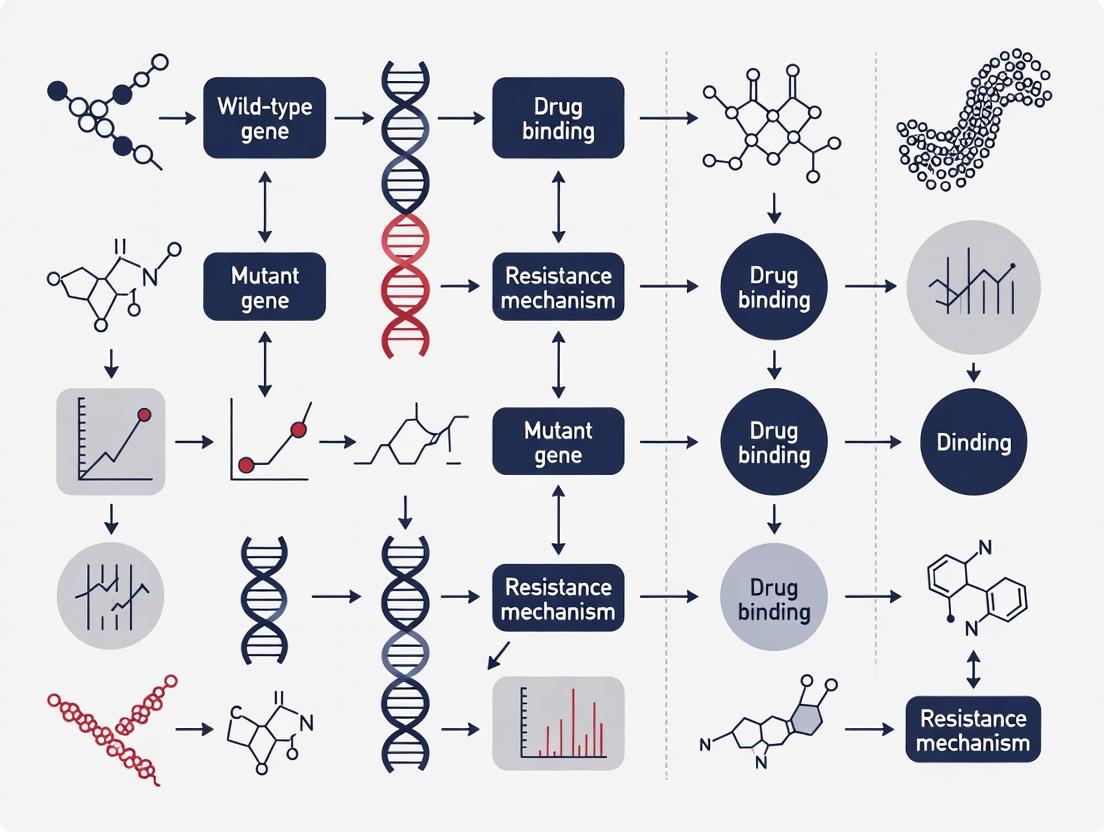
Experimental Workflow Visualization
The following diagram illustrates the logical workflow for a computational research project aimed at improving the prediction of drug-resistant tuberculosis.
Research Workflow for TB Resistance Prediction
This workflow shows the parallel paths of machine learning and molecular dynamics simulation, which converge to produce a validated resistance prediction.
TIES_PM Resistance Prediction Logic
### Frequently Asked Questions (FAQs)
FAQ 1: What is the current gold standard for Antimicrobial Susceptibility Testing (AST) and why is it considered the reference method?
The gold standard for AST, as recommended by the European Committee on Antimicrobial Susceptibility Testing (EUCAST) and the Clinical Laboratory Standards Institute (CLSI), is culture-based techniques [6]. This includes both broth dilution and agar dilution methods [7]. These methods are considered the reference because they directly measure the phenotypic response of bacteria to antibiotics, determining the Minimum Inhibitory Concentration (MIC), which is the lowest concentration of an antibiotic that prevents visible bacterial growth [7]. The MIC provides a quantitative result that is used to categorize isolates as susceptible, intermediate, or resistant, forming the basis for effective antimicrobial treatment [7].
FAQ 2: What are the primary limitations of relying on culture-based AST?
While definitive, culture-based methods have several significant drawbacks that can impact patient care and resistance research [6] [7].
- Prolonged Turnaround Time: These methods are slow, typically requiring 18–24 hours for results after the initial bacterial isolation, and can take up to 48 hours for slow-growing or fastidious bacteria [7]. This delay often forces physicians to prescribe empirical, broad-spectrum antibiotic therapies, which may be inappropriate or unnecessary [6] [8].
- Limited Functional Information: Culture-based AST confirms resistance but does not identify the specific genetic or biochemical mechanism behind it. This limits its utility for in-depth research into resistance prediction and evolution [6].
- Inability to Culture Some Pathogens: The method relies on the ability to isolate and grow the bacterial strain of interest from a complex clinical sample. It is unsuitable for non-culturable organisms or mixed infections [6].
- Labor and Resource Intensity: These techniques are laborious and require significant hands-on time from laboratory staff, especially when testing multiple antibiotics [6].
FAQ 3: How do the limitations of culture-based methods impact clinical decision-making and public health surveillance?
The slow turnaround time of culture-based AST directly contributes to the empirical overuse of antibiotics [6]. Studies estimate that 30–50% of antibiotic prescriptions are inappropriate or unnecessary [6]. Furthermore, the labor-intensive nature of these methods can delay the surveillance of emerging resistant pathogens, such as MRSA, VRE, and carbapenem-resistant Enterobacterales, hindering the effectiveness of public health interventions and antimicrobial stewardship programs [7].
FAQ 4: What advanced methodologies are emerging to address these limitations?
To overcome the constraints of culture-based AST, several advanced technologies are being integrated into research and clinical practice [6] [8]:
- Whole-Genome Sequencing (WGS): WGS can rapidly identify pathogens and predict resistance profiles by detecting known resistance genes in a single assay without a culturing step. However, its limitation is that it only predicts the presence of resistance genes, which may not always be expressed into a resistance phenotype [6].
- Machine Learning (ML) and Explainable Artificial Intelligence (XAI): Frameworks like xAI-MTBDR use ML models to not only predict drug resistance with high accuracy but also explain the contribution of individual mutations, helping to identify new resistance markers [9].
- Multivariable Regression Models: These statistical models improve the grading of antibiotic resistance mutations by associating resistance phenotypes with variants in candidate genes, even when multiple mutations co-occur. This approach has been shown to achieve higher sensitivity than traditional univariate methods [10].
### Troubleshooting Common Experimental Challenges
Issue: Contamination or Mixed Growth in Culture Plates
Problem: A high percentage of samples, such as urine cultures, result in "mixed growth" and cannot be analyzed, drastically reducing the yield of usable AST results [11]. One study found that 35% of urine samples showed mixed growth [11].
Solution:
- Ensure Proper Sample Collection: Educate clinicians on clean-catch midstream urine collection techniques to minimize skin and genital flora contamination.
- Use Selective Media: Employ chromogenic agars or media containing inhibitors to suppress the growth of commensal bacteria and selectively isolate common uropathogens.
- Optimize Inoculation Protocol: Standardize the loop size and streaking technique to obtain well-isolated colonies.
Issue: Slow Turnaround Time Affecting Research Timelines
Problem: The 18-48 hour wait for phenotypic results is slowing down research projects, especially those screening large numbers of bacterial isolates.
Solution:
- Implement Complementary Rapid Methods:
- PCR and NAATs: Use targeted molecular assays for known resistance genes (e.g., mecA for methicillin resistance) to get results within 1–6 hours [7].
- MALDI-TOF MS: Utilize this technology for rapid pathogen identification, which can be combined with novel protocols to assess resistance mechanisms based on protein profiles [6] [8].
- Adopt Automated AST Systems: While still based on bacterial growth, these systems can provide MIC results faster (within 6–24 hours) than manual methods by using sensitive optical detection systems [7].
Issue: Detecting Resistance in Non-Culturable or Fastidious Bacteria
Problem: Some bacterial species are difficult or impossible to culture using standard techniques, creating a blind spot in resistance monitoring.
Solution:
- Utilize Direct-from-Specimen Molecular Testing:
- Line Probe Assays (LPAs): Use these for direct detection of resistance mutations from sediment samples, though be aware that their sensitivity can be lower than newer methods [12].
- Targeted Next-Generation Sequencing (tNGS): Apply tNGS workflows directly to clinical samples. This method has demonstrated higher sensitivity than LPAs for detecting resistance to key drugs like rifampicin and isoniazid in tuberculosis [12].
### Comparison of AST Methods
The following table summarizes the key characteristics of established and emerging AST methodologies.
Table 1: Comparison of Antimicrobial Susceptibility Testing Methods
| Method Category | Example Techniques | Typical Turnaround Time | Key Advantages | Key Limitations / Challenges |
|---|---|---|---|---|
| Phenotypic (Gold Standard) | Broth/Agar Dilution, Disk Diffusion [7] | 18-48 hours [7] | Direct measure of phenotypic response; low consumable cost; standardized interpretation [6] [8] | Slow; labor-intensive; cannot detect underlying genetic mechanisms [6] |
| Automated Phenotypic | Various commercial systems (e.g., VITEK, Phoenix) | 6-24 hours [7] | Faster than manual methods; reduced labor; standardized and reproducible [7] | High instrument cost; limited customization of test panels [7] |
| Molecular | PCR, NAATs, Line Probe Assays (LPAs) [7] [12] | 1-6 hours [7] | Very fast; high specificity for targeted genes; can be used directly on some samples [7] [12] | Only detects known targets; cannot differentiate between expressed and silent genes; can overestimate resistance [6] [7] |
| Sequencing-Based | Whole-Genome Sequencing (WGS), Targeted NGS (tNGS) [6] [12] | 1-3 days (library prep & sequencing) | Comprehensive; detects known and novel mutations; high-resolution strain typing [6] [13] | High cost per sample for low-throughput; complex data analysis; predictive only (genotype vs. phenotype) [6] |
| Spectrometry-Based | MALDI-TOF MS [6] [8] | Minutes after pure culture | Extremely fast identification; potential for resistance mechanism detection [6] | Generally requires pure culture; limited validated protocols for direct AST [6] |
### Experimental Workflow & Key Research Reagents
The following diagram illustrates a generalized research workflow that integrates classical and modern methods to overcome the limitations of culture-based AST, accelerating resistance mutation research.
Diagram: Integrated Research Workflow for Resistance Mutation Discovery.
Table 2: Research Reagent Solutions for Key Experimental Steps
| Research Tool / Reagent | Function in Experiment | Specific Example / Note |
|---|---|---|
| Selective Culture Media | Isolates target pathogen from complex samples; provides pure biomass for WGS and the gold-standard phenotypic result (MIC) [6]. | Chromogenic agars for ESKAPE pathogens; Lowenstein-Jensen medium for M. tuberculosis. |
| Broth Microdilution Plates | Determine the reference Minimum Inhibitory Concentration (MIC) for the isolated bacterial strain against a panel of antibiotics [7]. | Custom plates can be designed to include antibiotics of research interest. CLSI/EUCAST guidelines provide standard protocols. |
| DNA Extraction Kits | Prepares high-quality, pure genomic DNA for downstream sequencing applications. | Critical for minimizing inhibitors and ensuring high sequencing coverage. |
| Whole-Genome Sequencer | Generates comprehensive genomic data to identify single-nucleotide polymorphisms (SNPs), insertions/deletions (indels), and resistance genes [6] [13]. | Illumina platforms (e.g., MiSeq) for high accuracy; Oxford Nanopore (e.g., MiniON) for long reads and portability [6]. |
| Bioinformatics Databases & Tools | Annotates sequencing data and predicts resistance profiles by comparing against curated databases of known resistance elements [6]. | CARD (Comprehensive Antibiotic Resistance Database), ResFinder, AMRFinderPlus [6]. Mykrobe and TBProfiler for M. tuberculosis [10]. |
| Machine Learning Frameworks | Builds predictive models that associate complex genetic signatures with resistance phenotypes, identifying novel markers beyond simple gene presence [10] [9]. | Frameworks like xAI-MTBDR use SHAP values to explain model predictions, revealing the contribution of individual mutations [9]. |
Frequently Asked Questions (FAQs)
Q1: What are the most common types of genetic mutations that cause drug resistance? Drug resistance mutations are often single nucleotide variants (SNVs) in the drug target or proteins within the same signaling pathway [14]. These can be categorized into four main functional classes [14]:
- Canonical drug resistance variants: Confer a proliferation advantage only in the presence of the drug, often by disrupting drug binding.
- Driver variants: Confer a proliferation advantage both in the presence and absence of the drug.
- Drug addiction variants: Provide an advantage in drug presence but are deleterious without it, often leading to oncogene-induced senescence when untreated.
- Drug-sensitizing variants: Are deleterious only when the drug is present.
Q2: Why do some less fit resistance mutations (like E255K in BCR-ABL) become prevalent in patient populations? The prevalence is not always determined by the fitness advantage a mutation confers. A key factor is mutational bias—the inherent likelihood of a specific nucleotide change occurring [15]. For example, the E255K mutation in BCR-ABL, which confers less resistance than the E255V mutation, is more common clinically because the DNA change required for E255K (a G>A transition) is more probable than the change for E255V (an A>T transversion) [15]. This highlights that evolutionary outcomes can be influenced by the underlying probabilities of mutations.
Q3: How can we systematically discover and validate novel drug resistance mechanisms? CRISPR base editing mutagenesis screens are a powerful, prospective method [14]. This involves:
- Library Design: Using a guide RNA (gRNA) library to install thousands of specific single-nucleotide variants in relevant cancer genes.
- Functional Screening: Introducing this library into cancer cell lines and growing them in the presence of a drug.
- Hit Identification: Sequencing the pooled cells to identify gRNAs (and thus mutations) that are enriched, indicating they confer resistance. This approach allows for the systematic functional annotation of variants of unknown significance before they are observed in the clinic [14].
Q4: What is the clinical significance of identifying "drug addiction variants"? Drug addiction variants, which are beneficial for cancer cells in the presence of a drug but harmful in its absence, suggest a potential therapeutic strategy of intermittent drug scheduling (drug holidays) [14]. By temporarily withdrawing the drug, clones harboring these variants could be selectively eliminated from the tumor population, thereby delaying or overcoming resistance [14].
Q5: Where can I find consolidated data on mutations and their impact on drug binding affinity? The MdrDB database is a comprehensive resource that integrates data on mutation-induced drug resistance [16]. It contains over 100,000 samples, including 3D structures of wild-type and mutant protein-ligand complexes, changes in binding affinity (ΔΔG), and biochemical features. It covers 240 proteins, 2,503 mutations, and 440 drugs [16].
Troubleshooting Experimental Guides
Guide 1: Troubleshooting In Vitro Resistance Screens
Problem: Unexpected or no resistance hits in a base editing screen.
| Step | Action | Expected Outcome & Interpretation |
|---|---|---|
| 1 | Verify base editor activity. Check efficiency of variant installation using targeted sequencing of control gRNAs. | Low editing efficiency will cause a weak signal. Ensure your cell line expresses the base editor effectively. |
| 2 | Confirm drug pressure. Perform a kill curve assay to establish the optimal drug concentration for screening. It should efficiently suppress wild-type cell growth. | If the concentration is too low, resistance mutations will not be enriched. If too high, no cells will survive. |
| ... | ... | ... |
Guide 2: Interpreting Variants of Unknown Significance (VUS)
Problem: A novel mutation is identified in a patient post-treatment, but its functional impact is unknown.
| Step | Action | Key Considerations |
|---|---|---|
| 1 | Classify the variant. Map the mutation to the protein's functional domains (e.g., kinase domain, ATP-binding pocket). | Refer to databases like MdrDB [16] or previous base editing screens [14] to see if similar mutations are documented. |
| 2 | Model the structural impact. Use computational tools to model the mutant protein and assess potential effects on drug binding. | A mutation in the drug-binding pocket is likely a canonical resistance variant. A distal mutation may affect allostery. |
| ... | ... | ... |
Key Experimental Data and Protocols
The following table summarizes the four classes of variants modulating drug sensitivity, as identified through large-scale base editing screens [14].
| Variant Class | Proliferation in Drug | Proliferation in No Drug | Example Mutations | Clinical/Experimental Implication |
|---|---|---|---|---|
| Canonical Drug Resistance | Advantage | Neutral | MEK1 L115P, EGFR S464L | Directly disrupts drug binding; classic on-target resistance. |
| Driver Variant | Advantage | Advantage | KRAS G12C, BRAF V600E | Often pre-existing or acquired activating mutations in the pathway. |
| Drug Addiction Variant | Advantage | Deleterious | KRAS Q61R, MEK2 Y134H | Suggests potential for intermittent dosing ("drug holidays"). |
| Drug-Sensitizing Variant | Deleterious | Neutral | Loss-of-function in EGFR | Reveals effective drug combinations (e.g., EGFR + BRAF inhibitors). |
Essential Research Reagent Solutions
| Reagent / Resource | Function in Research | Example Application |
|---|---|---|
| CRISPR Base Editors (CBE, ABE) | Installs precise C>T or A>G point mutations in the genome without causing double-strand breaks [14]. | Saturation mutagenesis of a kinase domain to prospectively identify resistance mutations. |
| gRNA Mutagenesis Library | A pooled library of guide RNAs designed to "tile" target genes and install specific variants [14]. | Functional screens to simultaneously test thousands of variants for their effect on drug sensitivity. |
| MdrDB Database | A comprehensive database providing 3D structures, binding affinity changes (ΔΔG), and biochemical features for mutant proteins [16]. | Benchmarking newly discovered mutations and training machine learning models for predicting ΔΔG. |
Detailed Protocol: CRISPR Base Editing Resistance Screen
Objective: Prospectively identify genetic variants that confer resistance to a targeted cancer therapy.
Workflow Overview:
Step-by-Step Methodology [14]:
Library and Cell Line Preparation
- gRNA Library Design: Design a library that tiles the coding sequences of your target genes (e.g., 11 cancer genes in a pathway). The library should include nontargeting gRNAs and gRNAs targeting essential and nonessential genes as controls.
- Cell Line Selection: Choose a cancer cell line that is sensitive to the drug of interest and harbors a relevant oncogenic driver (e.g., a BRAF V600E mutation for a BRAF inhibitor). Generate a stable cell line expressing a doxycycline-inducible cytidine base editor (CBE) or adenine base editor (ABE).
Screen Execution
- Virus Production & Transduction: Produce lentivirus from the gRNA library and transduce the cell line at a low multiplicity of infection (MOI) to ensure most cells receive a single gRNA.
- Base Editor Induction & Drug Selection: Induce base editor expression with doxycycline. Split the transduced cells into two arms: one treated with the drug at a predetermined IC90 concentration, and a vehicle-treated control. Culture cells for several population doublings to allow for enrichment of resistant clones.
Analysis and Validation
- Genomic DNA Extraction and Sequencing: Harvest genomic DNA from both arms at the end of the screen. Amplify the integrated gRNA sequences and subject them to next-generation sequencing.
- Differential Abundance Analysis: Align sequences to the gRNA library and count reads for each gRNA. Use statistical packages to identify gRNAs that are significantly enriched in the drug-treated arm compared to the control arm.
- Hit Validation: Clone top-hit gRNAs into vectors for arrayed validation. Transduce naive cells and perform proliferation assays in the presence and absence of drug to confirm the resistance phenotype.
Signaling Pathways and Logical Diagrams
Logical Map of Drug Resistance Variant Classification
This diagram illustrates the decision process for classifying a newly identified resistance variant based on its functional impact on cell proliferation.
Simplified MAPK Signaling Pathway with Resistance Nodes
This diagram shows key nodes in the MAPK pathway where mutations can confer resistance to targeted therapies like BRAF or MEK inhibitors.
The Role of Next-Generation Sequencing in Uncovering Resistance Variants
Next-generation sequencing (NGS) has revolutionized the detection and analysis of genetic variants that confer resistance to therapeutic agents in cancer and infectious diseases. By enabling the simultaneous sequencing of millions of DNA fragments, NGS provides comprehensive insights into genome structure, genetic variations, and dynamic changes that occur under therapeutic pressure [17]. This high-throughput, cost-effective technology has become a fundamental tool for researchers aiming to understand the molecular mechanisms of drug resistance and to improve prediction accuracy for resistance mutations.
The versatility of NGS platforms has expanded the scope of resistance research, facilitating studies on rare genetic diseases, cancer genomics, microbiome analysis, and infectious diseases [17]. In clinical oncology, NGS has been instrumental in identifying disease-causing variants, uncovering novel drug targets, and elucidating complex biological phenomena including tumor heterogeneity and the emergence of treatment-resistant clones [17]. Similarly, in antimicrobial resistance (AMR) research, NGS provides powerful capabilities to identify low-frequency variants and genomic arrangements in pathogens that confer resistance to antimicrobial drugs [18].
Key NGS Approaches and Methodologies
Sequencing Technologies and Platforms
NGS encompasses several sequencing approaches, each with distinct advantages for specific applications in resistance research:
Whole Genome Sequencing (WGS) provides the most comprehensive approach by covering the entire genome, enabling investigation of previously undescribed genomic alterations across coding and non-coding regions [19]. This method is particularly valuable for identifying novel resistance mechanisms and structural variations. Whole Exome Sequencing (WES) focuses on protein-coding regions (approximately 3% of the genome), offering a cost-effective alternative with the assumption that protein-associated alterations often have deleterious impacts on gene function and drug response [19]. Targeted Sequencing (TS) analyzes specific mutational hotspots or genes of interest with high sensitivity and depth, making it ideal for focused resistance panels and monitoring known resistance-associated variants [19] [20].
The performance characteristics of major NGS platforms vary significantly, influencing their suitability for different resistance research applications:
Table 1: Comparison of NGS Platforms for Resistance Variant Detection
| Platform | Technology | Read Length | Key Applications in Resistance Research | Limitations |
|---|---|---|---|---|
| Illumina | Sequencing-by-synthesis | 36-300 bp | High-accuracy SNV and indel detection; targeted panels | May have increased error rate (up to 1%) with sample overloading [17] |
| Ion Torrent | Semiconductor sequencing | 200-400 bp | Rapid screening of known resistance hotspots | May lose signal strength with homopolymer sequences [17] |
| PacBio SMRT | Single-molecule real-time sequencing | 10,000-25,000 bp | Identifying complex structural variants and resistance gene rearrangements | Higher cost compared to other platforms [17] |
| Nanopore | Electrical impedance detection | 10,000-30,000 bp | Real-time resistance monitoring; direct RNA sequencing | Error rate can spike up to 15% [17] |
Experimental Workflows for Resistance Studies
A typical NGS workflow for resistance variant detection involves multiple critical steps, each contributing to the overall accuracy and reliability of results:
Sample Preparation and Quality Control: The initial step involves nucleic acid extraction from relevant samples (tumor tissues, blood, microbial cultures) followed by rigorous quality assessment. For solid tumors, microscopic review by a pathologist is essential to ensure sufficient tumor content and to guide macrodissection or microdissection to enrich tumor fraction [21]. DNA quality is typically assessed through fluorometric quantification and measurement of DNA Integrity Number (DIN), with most clinical assays requiring a DIN value above 2-3 [22].
Library Preparation: Two major approaches are used for targeted NGS analysis: hybrid capture-based and amplification-based methods [21]. Hybrid capture utilizes biotinylated oligonucleotide probes complementary to regions of interest, offering better tolerance for sequence variations and reduced allele dropout compared to amplification-based methods [21]. This approach is particularly valuable for detecting novel resistance mutations. The library preparation process includes DNA fragmentation, adapter ligation with unique molecular indexes (UMIs), and PCR amplification [22].
Sequencing and Data Analysis: Sequencing generates raw data in FASTQ format, which undergoes quality control using tools like FastQC [19]. Subsequent steps include read alignment to a reference genome, duplicate read removal, local realignment, and variant calling using specialized algorithms [19]. The final variants are annotated and interpreted for their potential role in resistance mechanisms.
The following diagram illustrates the complete NGS workflow for resistance variant detection:
Troubleshooting Guides and FAQs
Pre-analytical and Experimental Issues
Q: What are the minimum DNA quantity and quality requirements for reliable resistance variant detection? A: For targeted NGS panels, most validated assays require ≥50 ng of DNA input to detect all expected mutations with appropriate variant allele frequencies. When DNA input drops to ≤25 ng, sensitivity decreases significantly, with only approximately 60% of variants detected [20]. DNA quality should be assessed through fluorometric quantification and measurement of DNA Integrity Number (DIN), with most clinical assays requiring a DIN value above 2-3 [22]. For degraded samples from FFPE tissue, optimization of extraction protocols and consideration of specialized library preparation kits designed for damaged DNA are recommended.
Q: How can we ensure adequate detection of low-frequency resistance variants? A: Several strategies enhance low-frequency variant detection: (1) Utilize unique molecular identifiers (UMIs) to distinguish true low-frequency variants from PCR artifacts and sequencing errors [22]; (2) Ensure sufficient sequencing depth—most validated clinical panels achieve median coverages of 1000-2000x [20]; (3) Establish appropriate limit of detection (LOD) thresholds, typically around 2.9-5% variant allele frequency for single nucleotide variants and indels [20]; (4) Implement duplex sequencing methods for ultra-sensitive detection when monitoring minimal residual disease or early resistance emergence.
Q: What controls should be included in each sequencing run to monitor assay performance? A: Each sequencing run should include: (1) Positive control materials with known variants at predetermined allele frequencies (e.g., HD701 reference standard containing 13 mutations) to verify detection sensitivity [20]; (2) Negative controls to identify contamination or background noise; (3) Internal quality metrics including percentage of reads with quality scores ≥Q30 (should be >85-99%), percentage of target regions with coverage ≥100x (should be >98%), and coverage uniformity (>99%) [20] [23].
Analytical and Bioinformatics Challenges
Q: How do we distinguish true resistance variants from technical artifacts? A: Implement a multi-faceted filtering approach: (1) Remove variants present in negative control samples; (2) Filter out low-quality calls based on base quality scores, mapping quality, and strand bias; (3) Exclude variants with allele frequencies below the validated LOD of the assay; (4) Compare with population databases (e.g., gnomAD) to exclude common polymorphisms; (5) Utilize orthogonal validation for clinically actionable findings using methods like digital PCR or Sanger sequencing [21] [19].
Q: What bioinformatics tools are recommended for different variant types in resistance research? A: The optimal bioinformatics pipeline depends on variant type:
Table 2: Bioinformatics Tools for Resistance Variant Detection
| Variant Type | Recommended Tools | Key Considerations |
|---|---|---|
| SNVs/Indels | GATK Mutect2, VarScan2, LoFreq | Combine multiple callers to increase sensitivity; implement strict filtering to reduce false positives [19] |
| Copy Number Variations | CNVkit, ADTEx | Requires careful normalization against control samples; performance depends on tumor purity and panel design [22] [21] |
| Gene Fusions/Structural Variants | Arriba, STAR-Fusion, DELLY | DNA-based approaches require intronic coverage; RNA sequencing often provides more direct fusion detection [21] |
| Complex Biomarkers | MSIsensor (MSI), TMBcalc (Tumor Mutational Burden) | Require specific computational approaches and reference datasets for accurate quantification [22] [19] |
Q: How should NGS assays be validated for clinical resistance testing? A: The Association of Molecular Pathology (AMP) and College of American Pathologists (CAP) provide comprehensive guidelines for NGS validation [21]. Key requirements include: (1) Establishing accuracy, precision, sensitivity, and specificity using well-characterized reference materials; (2) Determining the limit of detection for different variant types using dilution series; (3) Assessing reproducibility through repeat testing; (4) Validating all bioinformatics steps and pipelines; (5) Establishing quality control metrics and thresholds for ongoing monitoring [21] [23]. Performance standards should demonstrate >99% sensitivity and specificity for variant detection at the established LOD [20].
Advanced Research Applications
Functional Validation of Resistance Mechanisms
While NGS can identify potential resistance variants, functional validation is essential to establish causality. Advanced approaches like CRISPR base editing enable systematic analysis of variant effects on drug sensitivity [14]. Recent studies have used base editing screens to map functional domains in cancer genes and classify resistance variants into distinct functional categories:
Drug Addiction Variants: Confer proliferation advantage in drug presence but are deleterious without drug (e.g., KRAS Q61R in BRAF-mutant cells with trametinib treatment) [14].
Canonical Drug Resistance Variants: Provide selective advantage only in drug presence, typically within drug-binding pockets (e.g., MEK1 L115P disrupting trametinib binding) [14].
Driver Variants: Confer growth advantage regardless of drug presence, often activating orthogonal signaling pathways [14].
Drug-Sensitizing Variants: Enhance drug sensitivity, representing potential synthetic lethal interactions (e.g., EGFR loss-of-function variants in BRAF-mutant colorectal cancer sensitizing to BRAF/MEK inhibitors) [14].
The following diagram illustrates how these variant classes interact with treatment response:
Case Study: NGS in Esophageal Cancer Resistance Research
A compelling example of NGS application in resistance research comes from a study of neoadjuvant chemotherapy (NAC) in esophageal cancer (EC) [24]. Researchers performed targeted NGS on samples from 13 EC patients with different responses to platinum-based NAC, identifying missense mutations in the NOTCH1 gene associated with chemotherapy resistance [24]. Protein conformational analysis revealed that these mutations altered the NOTCH1 receptor protein's ability to bind ligands, potentially causing abnormalities in the NOTCH1 signaling pathway and conferring resistance [24].
This case study demonstrates several best practices: (1) Sequencing paired samples (pre- and post-treatment) to identify acquired resistance mutations; (2) Focusing on a targeted gene panel (295 genes) for cost-effective deep sequencing; (3) Integrating computational structural biology to elucidate functional consequences; (4) Correlating genetic findings with clinical response categories (complete response, partial response, stable disease) [24].
Essential Research Reagents and Tools
Table 3: Key Research Reagent Solutions for NGS-based Resistance Studies
| Reagent Category | Specific Examples | Function in Resistance Research |
|---|---|---|
| NGS Library Prep Kits | SureSelect XT HS (Agilent), Illumina DNA Prep | Convert extracted DNA into sequencing-ready libraries with unique molecular indexes for accurate variant detection [22] |
| Target Enrichment Panels | OncoScreen (295 genes), AmpliSeq for Illumina Antimicrobial Resistance Panel (478 genes), Custom panels (e.g., 61-gene oncopanel) | Enrich specific genomic regions of interest related to resistance mechanisms in cancer or pathogens [24] [22] [18] |
| Reference Standards | HD701 (Horizon Discovery), Coriell Cell Repositories | Provide known variants at predetermined allele frequencies for assay validation and quality control [22] [20] |
| DNA/RNA Extraction Kits | QIAamp DNA Mini Kit (Qiagen), RecoverAll Total Nucleic Acid Isolation Kit (FFPE) | Extract high-quality nucleic acids from various sample types including challenging FFPE specimens [24] [22] |
| Bioinformatics Tools | GATK, FastQC, BCFtools, Sophia DDM | Quality control, variant calling, and annotation of sequencing data to identify resistance-associated variants [19] [20] |
| Functional Screening Tools | CRISPR base editors (CBE, ABE), gRNA libraries targeting cancer genes | Systematically test the functional impact of variants on drug resistance in high-throughput screens [14] |
Next-generation sequencing has become an indispensable tool for uncovering the genetic basis of resistance to therapeutics in cancer and infectious diseases. The integration of robust NGS methodologies with functional validation approaches enables researchers to move beyond correlation to establish causal mechanisms of resistance. As the field advances, key areas of development include the standardization of bioinformatics pipelines, implementation of quality management systems [23], and the creation of comprehensive variant-to-function maps through technologies like base editing screens [14].
The evolving landscape of NGS technologies promises enhanced accuracy, reduced costs, and improved data analysis solutions that will further advance resistance mutation research [17]. By implementing the troubleshooting guidelines, experimental protocols, and quality control measures outlined in this technical resource, researchers can enhance the accuracy and reliability of their resistance variant predictions, ultimately contributing to more effective therapeutic strategies and improved patient outcomes.
Frequently Asked Questions & Troubleshooting Guides
FAQ 1: Why do my multidrug-resistant bacterial strains sometimes adapt faster in antibiotic-free media than single-resistant strains?
Answer: Multidrug-resistant (MDR) bacteria with high fitness costs can undergo faster compensatory evolution than single-resistant strains. This occurs because the strong negative epistasis (where the combined cost of two mutations is greater than the sum of their individual costs) in MDR strains opens alternative evolutionary paths.
- Underlying Cause: Low-fitness MDR strains can acquire compensatory mutations with larger fitness effects [25]. Furthermore, some compensatory mutations are specific to the MDR background; they are beneficial only when both resistance mutations are present and are neutral or even deleterious in sensitive or single-resistant backgrounds [25].
- Troubleshooting Steps:
- Monitor Competition Assays: When propagating MDR strains in permissive conditions, use competitive fitness assays against a neutral marker strain to detect rapid fitness increases.
- Check for Epistasis: Determine if the fitness cost of your MDR strain is synergistic (negative epistasis), as this creates a strong selective pressure for rapid compensation.
- Genomic Verification: Sequence evolved lineages to identify whether compensatory mutations have occurred in genes functionally linked to the epistatic interaction between the two resistance mechanisms.
FAQ 2: How can I reliably predict cross-resistance and collateral sensitivity between antibiotics?
Answer: Predicting these interactions is challenging because a single drug pair can exhibit cross-resistance (XR) or collateral sensitivity (CS) depending on the specific resistance mechanism involved [26]. Relying on a single experimental evolution lineage can be misleading.
- Underlying Cause: Different mutations conferring resistance to the same first drug can have diverse pleiotropic effects on susceptibility to a second drug [27]. One mutant may show CS to drug B, while another mutant resistant to the same drug A may show XR to drug B.
- Troubleshooting Steps:
- Use Diverse Lineages: Evolve multiple independent lineages against the first antibiotic to sample a broader range of resistance mechanisms.
- Mechanism-Based Stratification: Group evolved strains by their identified resistance mechanisms (e.g., via whole-genome sequencing) before testing their susceptibility to the second drug.
- Leverage Chemical Genetics Data: Consult existing chemical genetics profiles, which systematically show how the loss of each non-essential gene affects resistance, to predict XR (concordant profiles) and CS (discordant profiles) [26].
FAQ 3: My genotypic prediction of drug resistance misses some phenotypically resistant strains. How can I improve accuracy?
Answer: This is a common issue where current genotypic catalogs of resistance mutations are incomplete. The solution is to move beyond single-mutation lookups and use integrated, model-based approaches.
- Underlying Cause: Phenotypic resistance can be caused by novel mutations or complex genetic interactions not yet listed in standard mutation catalogs [28].
- Troubleshooting Steps:
- Employ Ensemble Models: Combine the predictions of multiple computational tools (e.g., the WHO catalog, TB-Profiler, SAM-TB, and machine learning tools like GenTB or MD-CNN) using a stacking ensemble framework. This has been shown to outperform any single tool [28].
- Incorporate Population Structure: For bacteria like E. coli, include data on population structure and gene content in machine learning models, as this can significantly boost prediction accuracy [29].
- Investigate Unexplained Resistance: For strains that are phenotypically resistant but genotypically susceptible, identify recurring mutations in your dataset that meet a minimum frequency threshold as candidates for novel resistance markers [28].
Key Experimental Data
Table 1: Dynamics of Compensatory Evolution in Single vs. Double ResistantE. coli
Data derived from experimental evolution in antibiotic-free media, tracking the pace of adaptation [25].
| Resistant Background | Fitness Cost (Initial) | Time to First Adaptive Signature (Days) | Fitness Increase per Day (Day 0-5) | Presence of Epistasis-Specific Compensatory Mutations |
|---|---|---|---|---|
| Rifampicin (RifR) Single | 0.06 ± 0.001 | 8-10 (in minority of populations) | Lower than double-resistant | No |
| Streptomycin (StrR) Single | 0.03 ± 0.01 | 8-10 (in minority of populations) | Lower than double-resistant | No |
| RifR StrR Double | 0.27 ± 0.01 (Strong Negative Epistasis) | 4 (in all populations) | 0.048 ± 0.003 | Yes |
Table 2: Performance Comparison of Genotypic Drug Susceptibility Testing (DST) Tools forM. tuberculosis
Evaluation of five tools on a global dataset of 36,385 isolates shows that ensemble models achieve the highest accuracy [28].
| Prediction Tool / Method | Overall AUC (%) | Sensitivity (%) | Specificity (%) | Key Characteristic |
|---|---|---|---|---|
| WHO Mutation Catalog (2023) | Not the highest | 79.5 | 97.3 | Highest specificity; catalog-based |
| TB Profiler | High | 79.5 | Not the highest | Best sensitivity; catalog-based |
| MD-CNN | 92.1 | Not the highest | Not the highest | Best overall AUC; deep learning-based |
| Ensemble Model (Stacking) | 93.4 | 84.1 | 95.4 | Combines all five tools; outperforms individual methods |
Detailed Experimental Protocols
Protocol 1: Tracking Compensatory Evolution via Neutral Marker Competition
Objective: To quantify the pace and dynamics of compensatory adaptation in resistant bacterial strains [25].
- Strain Preparation: Construct isogenic resistant clones (e.g., single RifR, single StrR, and double RifR StrR) each carrying two different neutral markers, such as genes for Cyan (CFP) and Yellow (YFP) fluorescent proteins.
- Experimental Evolution:
- Initiate independent evolving populations by mixing CFP and YFP variants of the same resistant genotype at a 1:1 ratio.
- Propagate populations in antibiotic-free liquid medium for ~180 generations (e.g., 22 days), performing daily dilutions to maintain a large population size and allow for clonal interference.
- Frequency Monitoring: Regularly sample populations and use flow cytometry to track the frequencies of the CFP and YFP markers.
- Data Interpretation:
- A rapid and steep change in marker frequency indicates a selective sweep by a beneficial (compensatory) mutation.
- Strong fluctuations in both markers suggest clonal interference, where multiple beneficial mutations arise and compete.
- Fitness Validation: Periodically perform head-to-head competition assays between evolved populations and a non-fluorescent sensitive ancestor to directly measure the increase in competitive fitness.
Protocol 2: Systematically Mapping Cross-Resistance and Collateral Sensitivity
Objective: To identify and validate drug-pair interactions using a chemical genetics-informed approach [26].
- Data Acquisition: Obtain chemical genetics data (e.g., s-score profiles) for a library of gene knockout mutants exposed to your antibiotics of interest.
- Metric Calculation: For each drug pair (A, B), calculate the Outlier Concordance-Discordance Metric (OCDM). This metric emphasizes extreme scores:
- Concordance: Mutants with significantly negative s-scores for both drugs suggest a shared resistance mechanism (predicts Cross-Resistance, XR).
- Discordance: Mutants with significantly negative s-scores for drug A but positive for drug B (or vice versa) suggest a trade-off (predicts Collateral Sensitivity, CS).
- Experimental Evolution for Validation:
- Evolve multiple independent lineages against a first drug (Drug A).
- Measure the Minimum Inhibitory Concentration (MIC) of the evolved lineages against both Drug A and a second drug (Drug B).
- Interaction Calling: For each evolved lineage, classify the interaction with Drug B as XR (increased MIC), CS (decreased MIC), or neutral (no change in MIC).
- Mechanism Deconvolution: Sequence evolved lineages and correlate the identified resistance mutations with their specific XR/CS profiles to understand the underlying mechanisms.
Research Reagent Solutions
Table 3: Essential Tools for Studying Resistance Evolution
| Research Reagent / Tool | Function / Application | Specific Example / Note |
|---|---|---|
| Barcoded Strain Libraries | Enables high-resolution tracking of numerous adaptive lineages in evolution experiments, capturing a fuller spectrum of beneficial mutations [27]. | Used in yeast to identify hundreds of unique fluconazole-resistant mutants and group them by fitness trade-offs. |
| Neutral Fluorescent Markers (CFP/YFP) | Allows real-time monitoring of selective sweeps and clonal interference during experimental evolution in a single flask [25]. | |
| Chemical Genetics Profiles | Pre-compiled datasets showing fitness of genome-wide mutants under drug treatment; used to predict XR/CS [26]. | E. coli Keio collection s-scores for 40 antibiotics. |
| Ensemble Prediction Models | A computational framework that combines multiple genotypic DST tools to improve resistance prediction accuracy [28]. | A stacking model with a decision tree meta-classifier outperformed individual tools for TB resistance prediction. |
| Deep Learning Models (e.g., LSTM) | Analyzes complex genetic data (e.g., WGS SNPs) to predict multi-drug resistance status from sequencing data [29]. | aiGeneR 3.0 model for E. coli UTI pathogens. |
Experimental Workflow & Conceptual Diagrams
Compensatory Evolution in MDR Strains
Predicting XR/CS from Chemical Genetics
Ensemble Model for Genotypic DST
Leveraging Machine Learning and AI for Predictive Modeling
Frequently Asked Questions (FAQs)
1. What are the primary genomic data sources used in drug resistance research? Large-scale public databases are fundamental. Research often utilizes genomic data (including gene expression profiles, mutational landscapes, and copy number variations) from resources such as the Dependency Map (DepMap) project database, the Cancer Therapeutic Response Portal (CTRP v2), and the Genomics of Drug Sensitivity in Cancer (GDSC) database, which encompass hundreds of cancer cell lines [30].
2. How can gene expression data be standardized for robust predictive modeling? To improve compatibility across datasets, employ preprocessing strategies such as log transformation and scaling of gene expression values to a uniform range. Dimensionality reduction techniques, like autoencoders, can further extract key features and minimize data source-specific variability, enhancing model generalizability [30].
3. Why might the most clinically abundant resistance mutation not be the one that confers the highest resistance? Evolutionary outcomes are not determined by fitness (resistance level) alone. A mutation that provides slightly less resistance may become more prevalent if its underlying nucleotide change is more likely to occur (e.g., a transition like G>A versus a transversion like A>T). Quantitative models must account for this mutational bias to accurately predict epidemiological abundance [15].
4. What is the advantage of integrating transcriptomic profiles with genomic data? While genomics identifies potential resistance mutations, transcriptomics reveals the functional expression of genes driving resistance mechanisms. Integrating both provides a more complete picture, helping to elucidate how mutations actually impact cellular pathways and drug response [30].
5. When should spatial transcriptomics be considered over single-cell RNA-seq (scRNA-seq)? Spatial transcriptomics is preferred when preserving the spatial context of cells within intact tissue is critical, such as for studying the tumor microenvironment, cell-cell interactions, or localized disease mechanisms. It is also invaluable for studying cell types that are difficult to isolate viable for scRNA-seq, like neurons [31].
Troubleshooting Guides
Issue 1: Inconsistent Drug Response Predictions Across Datasets
| Potential Cause | Diagnostic Steps | Solution |
|---|---|---|
| Batch effects from different data sources. | Perform Principal Component Analysis (PCA) to see if samples cluster by dataset source rather than biological type. | Apply robust scaling and normalization (e.g., log transformation). Use batch correction algorithms or autoencoders to extract source-invariant features [30]. |
| Incompatible data normalization methods. | Check the original literature or database documentation for the processing pipelines used on each dataset. | Re-process raw data from different sources through a unified, standardized pipeline before integration and analysis [30]. |
| High variability in control data. | Review the coefficient of variation (CV) for control samples or replicate assays within the original datasets. | During data curation, exclude assay data that shows considerable variability within biologically homogeneous clusters for the same drugs [30]. |
Issue 2: Failure to Replicate Clinically Observed Resistance Mutations in Models
| Potential Cause | Diagnostic Steps | Solution |
|---|---|---|
| Over-reliance on fitness (resistance level) as the sole predictive variable. | Compare the nucleotide substitution pathways required for candidate mutations (e.g., transition vs. transversion). | Incorporate mutational bias and codon usage into stochastic, first-principle evolutionary models to better forecast which variants will arise in patient populations [15]. |
| Lack of tumor microenvironment in cell line models. | Validate findings from cell lines using patient-derived xenograft (PDX) models or clinical trial data. | Integrate spatial transcriptomic data from intact tissue sections to understand how the tissue context influences resistance evolution [31]. |
| Insufficient model complexity. | Test if a model parameterized on a large in vitro dataset can accurately predict epidemiological abundance in clinical trials. | Develop multi-scale models that are parameterized on large in vitro datasets and can bridge to clinical population outcomes [15]. |
Experimental Protocols for Key Methodologies
Protocol 1: Building a Deep Learning Model for Drug Response Prediction
This protocol outlines the methodology for constructing a model like "DrugS" to predict IC50 values from genomic features [30].
Data Acquisition and Curation:
- Input Features: Obtain gene expression data (e.g., for 20,000 protein-coding genes) and drug chemical data (e.g., SMILES strings) from public repositories like DepMap and GDSC.
- Output Variable: Collect corresponding half-maximal inhibitory concentration (IC50) values and apply a natural log transformation (LN IC50) to create the target variable for regression.
Data Preprocessing:
- Gene Expression: Log-transform and scale expression values to a uniform range to mitigate outlier influence.
- Drug Features: Convert SMILES strings into a numerical feature vector (e.g., 2048 dimensions) representing molecular structure.
- Data Filtering: Use clustering (e.g., TSNE) to identify and exclude outlier assay data with high variability within homogeneous cell line clusters.
Dimensionality Reduction:
- Employ an autoencoder to compress the high-dimensional gene expression data (e.g., from 20,000 to 30 features) to capture intrinsic structure.
Model Architecture and Training:
- Construct a Deep Neural Network (DNN) with an input layer that concatenates the reduced gene expression features and the drug fingerprint features.
- Include dropout layers in the network to prevent overfitting.
- Train the model using the concatenated features to predict the LN IC50 value.
Model Validation:
- Rigorously test the model's predictive performance on independent datasets (e.g., CTRPv2, NCI-60).
- Correlate predictions with drug response data from Patient-Derived Xenograft (PDX) models to assess clinical relevance.
Protocol 2: Utilizing Spatial Transcriptomics to Map Resistance Niches
This protocol describes how to apply spatial transcriptomics to identify localized drug resistance mechanisms in intact tumor tissue [31].
Tissue Preparation:
- Preserve fresh frozen or fixed-frozen (FF) tissue samples in Optimal Cutting Temperature (OCT) compound.
- Cryosection tissue at a recommended thickness (e.g., 10 µm) and mount onto specific gene expression slides compatible with the chosen platform (e.g., Visium from 10x Genomics).
Spatial Library Construction:
- Permeabilize the tissue section to allow mRNA release.
- Perform reverse transcription using barcoded primers that contain spatial coordinate information.
- Synthesize cDNA, then amplify and construct sequencing libraries following the manufacturer's instructions.
Sequencing and Data Generation:
- Sequence the libraries on a high-throughput platform (e.g., Illumina).
- Using the platform's software, align the sequence reads to a reference genome and assign them to specific spatial barcodes, generating a gene expression matrix mapped to tissue positions.
Bioinformatic Analysis:
- Pre-processing: Filter genes and spots, and normalize expression data.
- Integration: If possible, integrate the spatial data with existing scRNA-seq data to assist in cell type annotation.
- Spatial Analysis: Identify spatially variable genes and distinct transcriptional domains. Use specialized algorithms to infer cell-cell communication and interactions within the tumor microenvironment that may foster resistance.
Signaling Pathways and Experimental Workflows
Diagram 1: Multi-scale Prediction of Resistance Epidemiology
Diagram 2: Spatial Transcriptomics Workflow
Research Reagent Solutions
| Item | Function/Application |
|---|---|
| BaF3 Cells | A common murine pro-B cell line model used to express wild-type or mutant oncogenes (e.g., BCR-ABL) for in vitro drug sensitivity and resistance assays [15]. |
| 10x Genomics Visium | A commercial spatial transcriptomics platform that enables genome-wide mRNA expression profiling while retaining the two-dimensional spatial context of intact tissue sections [31]. |
| Cancer Cell Lines (DepMap) | A curated collection of hundreds of human cancer cell lines with extensive genomic and transcriptomic characterization, serving as a primary resource for in vitro drug screening and model development [30]. |
| Autoencoder (Computational) | A deep learning tool used for non-linear dimensionality reduction of high-dimensional genomic data (e.g., 20,000 genes), creating a lower-dimensional feature set that improves model robustness and cross-dataset compatibility [30]. |
| Nucleotide Substitution Bias Data | Information on the relative likelihood of different mutation types (e.g., transitions vs. transversions), which is a critical parameter for evolutionary models predicting the clinical frequency of specific resistance mutations [15]. |
Frequently Asked Questions (FAQs)
Q1: Why is feature selection critical in genomic studies for drug resistance prediction?
Feature selection is essential because genomic data, such as transcriptomic profiles from RNA sequencing or DNA microarrays, is characteristically high-dimensional, often containing expression levels for thousands of genes from a relatively small number of samples [32]. This creates a high risk of overfitting, where a model learns noise instead of true biological signals. Feature selection mitigates this by identifying a minimal set of genes that are most predictive of the outcome, such as antibiotic resistance [33] [32]. This leads to models with higher accuracy, improved generalizability, faster training times, and better interpretability, which is crucial for understanding biological mechanisms and developing clinical diagnostics [34].
Q2: My model performs well on training data but poorly on validation sets. What feature selection issue might be the cause?
This is a classic sign of overfitting. It can occur if the feature selection process itself was not properly validated. If you perform feature selection on your entire dataset before splitting it into training and validation sets, information from the validation set "leaks" into the training process, making the model seem more accurate than it is [35]. To resolve this, always perform feature selection within each fold of cross-validation during the model training phase. This ensures that the feature set is selected based only on the training data, providing a realistic assessment of its performance on unseen data [35].
Q3: I found a minimal gene signature, but many genes are not known resistance markers. Does this invalidate the signature?
Not necessarily. In fact, this is a common and valuable finding. Many machine learning studies identify minimal gene signatures with high predictive accuracy that include a substantial number of genes not annotated in established resistance databases like the Comprehensive Antibiotic Resistance Database (CARD) [33]. For example, one study on Pseudomonas aeruginosa found that only 2-10% of the predictive genes overlapped with known CARD markers [33]. These "unknown" genes may be part of underexplored regulatory networks, metabolic pathways, or stress responses that contribute to the resistance phenotype. This discovery can reveal novel biological mechanisms and highlight gaps in current understanding [33].
Q4: How do I choose between Filter, Wrapper, and Embedded feature selection methods?
The choice depends on your specific goals, computational resources, and need for interpretability. The table below summarizes the core differences:
Table 1: Comparison of Feature Selection Method Types
| Method Type | Core Principle | Common Techniques | Advantages | Disadvantages |
|---|---|---|---|---|
| Filter Methods [34] | Selects features based on statistical measures of correlation with the target variable. | Chi-square, Correlation, Mutual Information [36] [34]. | Fast, computationally efficient, and model-agnostic [34]. | Ignores feature interactions and the model context. |
| Wrapper Methods [34] | Uses the model's performance as the objective to evaluate different feature subsets. | Genetic Algorithms (GA), Recursive Feature Elimination (RFE) [33] [34]. | Considers feature interactions; can yield high-performing subsets [33]. | Computationally expensive and has a higher risk of overfitting [34]. |
| Embedded Methods [34] | Performs feature selection as an integral part of the model training process. | LASSO regression, Ridge regression, and tree-based importance [37] [38] [34]. | Efficient balance of performance and computation; model-specific [34]. | Can be less interpretable than filter methods [34]. |
Q5: What are the best practices for validating a minimal gene signature's prognostic power?
To robustly validate a gene signature, follow these steps:
- Independent Validation: Test the signature's performance on one or more completely independent datasets that were not used during the signature's discovery or model training [38].
- Assess Incremental Value: Demonstrate that the gene signature provides prognostic information beyond established clinical and pathological factors. This can be done by showing a statistically significant improvement in model performance (e.g., using a likelihood ratio test) when the signature is added to a baseline model containing only clinical variables [39].
- Evaluate Clinical Utility: Determine if the signature's predictions are sufficient to change recommended treatment decisions and, ultimately, if its use improves patient outcomes in a prospective clinical trial [39].
Experimental Protocols & Workflows
Protocol: Identification of a Prognostic Gene Signature using LASSO Cox Regression
This protocol is widely used in cancer prognosis research [38] and can be adapted for drug resistance studies.
1. Objective: To construct a minimal gene signature that predicts patient survival (or time-to-treatment-failure) from high-dimensional gene expression data.
2. Materials & Reagents:
- Dataset: A cohort of samples with gene expression data (e.g., from RNA-seq or microarrays) and corresponding survival data (overall survival, progression-free survival). Example: The Cancer Genome Atlas (TCGA) database [36] [38].
- Software: R or Python programming environment.
3. Procedure:
- Step 1: Data Pre-processing. Normalize raw gene expression counts (e.g., using variance stabilizing transformation or Box-Cox normalization) to reduce technical batch effects [36].
- Step 2: Identify Potential Prognostic Genes. Perform a univariate analysis (e.g., univariate Cox regression) on all genes to identify those individually associated with survival (e.g., p-value < 0.05) [38].
- Step 3: Apply LASSO Cox Regression. Input the expression data of the potential prognostic genes from Step 2 into a LASSO (Least Absolute Shrinkage and Selection Operator) Cox regression model. LASSO applies a penalty that shrinks the coefficients of less important genes to zero, effectively performing feature selection [38].
- Step 4: Determine the Optimal Penalty (Lambda). Use 10-fold cross-validation to find the value of lambda that minimizes the cross-validation error. The genes with non-zero coefficients at this optimal lambda constitute the final gene signature [38].
- Step 5: Calculate Risk Score. For each patient, calculate a risk score using the formula:
Risk Score = (Expression of Gene 1 * Coefficient 1) + (Expression of Gene 2 * Coefficient 2) + ...[38]. - Step 6: Validate the Signature. Divide patients into high-risk and low-risk groups based on the median risk score. Use Kaplan-Meier survival analysis and log-rank tests in both the training and independent validation cohorts to confirm that the groups have significantly different survival outcomes [38].
The workflow below illustrates this process.
Protocol: Building a Classifier with Genetic Algorithm-based Feature Selection
This protocol uses a wrapper method to find a minimal gene set for classifying resistant vs. susceptible isolates [33].
1. Objective: To identify a minimal set of ~35-40 genes that can accurately classify antibiotic resistance in bacterial pathogens using transcriptomic data.
2. Materials & Reagents:
- Dataset: Transcriptomic data (e.g., RNA-seq) from clinical isolates with confirmed resistant/susceptible phenotypes [33].
- Software: Python/R with ML libraries (e.g., scikit-learn) and optimization tools.
3. Procedure:
- Step 1: Initialize Population. Generate a starting population of random gene subsets, each containing a fixed number of genes (e.g., 40) [33].
- Step 2: Evaluate Fitness. For each gene subset in the population, train a classifier (e.g., Support Vector Machine or Logistic Regression) and evaluate its performance using a metric like ROC-AUC or F1-score. This performance score is the subset's "fitness" [33].
- Step 3: Select, Cross Over, and Mutate.
- Select: Preferentially retain the gene subsets with the highest fitness scores.
- Cross Over: Create new "child" subsets by combining parts of two "parent" subsets.
- Mutate: Randomly introduce small changes (e.g., add or remove a gene) to some subsets to maintain diversity [33].
- Step 4: Iterate. Repeat Steps 2 and 3 for hundreds of generations. Over time, the population evolves toward subsets with higher fitness [33].
- Step 5: Form a Consensus. After many independent runs, rank all genes by how frequently they appeared in high-performing subsets. The top-ranked genes form a robust, consensus signature for the final classifier [33].
The workflow below illustrates the genetic algorithm cycle.
The Scientist's Toolkit: Research Reagents & Computational Solutions
Table 2: Essential Tools for Feature Selection in Genomic Studies
| Tool / Reagent | Type | Function / Application |
|---|---|---|
| TCGA/ICGC Databases [36] [38] | Data Source | Public repositories providing large-scale genomic, transcriptomic, and clinical data for cancer research, often used as training and validation cohorts. |
| CARD (Comprehensive Antibiotic Resistance Database) [33] | Data Source | A curated database of known antimicrobial resistance genes, used to benchmark and validate newly discovered gene signatures. |
R glmnet Package [38] |
Software Library | Widely used to perform LASSO, Ridge, and Elastic-Net regression for embedded feature selection. |
| Python scikit-learn [35] [34] | Software Library | Provides a comprehensive suite of tools for filter methods (SelectKBest), wrapper methods (RFE), and model training. |
| gSELECT Python Library [40] | Software Library | A specialized tool for evaluating the classification performance of pre-defined or automatically ranked gene sets prior to full analysis. |
| Genetic Algorithm (GA) [33] | Algorithm | An optimization technique used as a wrapper method to evolve high-performing, minimal gene subsets. |
| ABESS (Algorithm for Best-Subset Selection) [37] | Algorithm | A statistical method for selecting the best subset of features, shown to be effective in GWAS for drug resistance in M. tuberculosis. |
| mRMR (Min-Redundancy Max-Relevance) [36] | Algorithm | A filter method that selects features that are highly correlated with the target (relevance) but uncorrelated with each other (redundancy). |
The ultimate test of a minimal gene signature is its predictive performance. The table below summarizes key quantitative results from recent studies in different disease contexts.
Table 3: Performance Summary of Minimal Gene Signatures from Recent Studies
| Study Context (Organism) | Feature Selection Method | Signature Size | Key Performance Result | Validation Cohort |
|---|---|---|---|---|
| Antibiotic Resistance in P. aeruginosa [33] | Genetic Algorithm + AutoML | ~35-40 genes | 96% - 99% accuracy on test data | Hold-out test set from 414 isolates |
| Prognosis in Clear Cell Renal Cell Carcinoma [36] | mRMR (Ensemble Method) | 13 genes | ROC AUC: 0.82 | ICGC-RECA (n=91) |
| Prognosis in Osteosarcoma [38] | LASSO Cox Regression | 17 genes | Significant stratification of high/low risk (Kaplan-Meier) | GEO: GSE21257 (n=53) |
| Drug Resistance in M. tuberculosis [37] | ABESS | N/A (Mutation sets) | Selected more relevant mutations vs. other methods | Cross-validation |
Accurately predicting drug resistance mutations is a critical challenge in modern therapeutic development, particularly in areas like oncology and infectious disease management. The selection of an appropriate machine learning algorithm significantly influences the predictive performance, interpretability, and clinical applicability of these models. This guide provides a structured comparison of three prominent algorithmic approaches—Logistic Regression, Random Forest, and Deep Learning—to assist researchers in selecting the optimal methodology for their specific drug resistance research.
Algorithm Comparison at a Glance
The table below summarizes the key characteristics, strengths, and limitations of each algorithm to guide your initial selection.
Table 1: Algorithm Comparison for Drug Resistance Prediction
| Algorithm | Best Use Cases | Key Strengths | Major Limitations |
|---|---|---|---|
| Logistic Regression (LR) | - Initial baseline models- High interpretability requirements- Scenarios with well-understood, additive variant effects [41] | - Highly interpretable; provides effect sizes (odds ratios) for mutations [41]- Efficient with smaller sample sizes- Less prone to overfitting with proper regularization | - Assumes linear, additive effects; cannot capture complex epistasis- Performance depends heavily on feature engineering |
| Random Forest (RF) | - Datasets with complex, non-linear interactions between mutations [42]- Multi-drug resistance prediction (using Multi-Label RF) [42] | - Robust performance on complex, non-linear data without intensive feature engineering [43]- Provides native feature importance rankings [42] | - Lower interpretability than LR ("black-box" nature)- Can be computationally intensive with very high-dimensional data |
| Deep Learning (DL) | - Very large datasets (>>10,000 samples) [44]- Whole-genome mutation analysis without pre-filtering [44]- Discovering novel, unknown resistance mechanisms | - Superior accuracy with sufficient data and tuning [44]- Capable of automatic feature representation from raw data | - Highest computational resource requirements- "Black-box" model with extreme interpretability challenges- High risk of overfitting on small datasets |
Experimental Protocols for Algorithm Implementation
Protocol for Multivariable Logistic Regression
Multivariable Logistic Regression extends univariate analysis by modeling the joint effect of multiple mutations on resistance.
- Data Preparation: Encode genetic variants as binary variables (0 = absent, 1 = present). Use a sparse matrix representation for efficiency with high-dimensional genetic data [41].
- Model Training: Train a single-drug model using a penalized regression approach (e.g., L1 or L2 regularization) to handle correlated features and prevent overfitting. The model estimates the probability of phenotypic resistance based on the presence of mutation combinations [41].
- Output Interpretation: Extract the odds ratio (OR) for each mutation. An OR > 1 indicates the mutation is associated with increased probability of resistance, conditional on the other mutations in the model [41].
Protocol for (Multi-Label) Random Forest
Random Forest is an ensemble method that can be adapted for single- or multi-drug resistance prediction.
- Feature Representation: Represent each isolate by a binary vector indicating the presence/absence of variants across candidate genes or the whole genome [42].
- Model Training:
- Single-Label RF (SLRF): Train one independent model for each drug's resistance profile [42].
- Multi-Label RF (MLRF): Train a single model that predicts resistance labels for all considered drugs simultaneously. This leverages correlations in resistance co-occurrence (e.g., MDR-TB) to improve predictive power [42].
- Feature Analysis: Use the built-in feature importance metric of the RF to rank mutations by their contribution to predicting resistance across all drugs [42].
Protocol for Deep Learning (MLP-Based Model)
Deep Learning models, such as Multi-Layer Perceptrons (MLPs), can learn complex mappings from genomic data to resistance phenotypes.
- Input Data Construction: Use variant calling on whole-genome sequencing data. The input is a high-dimensional binary vector representing mutations across the entire genome, avoiding reliance on a pre-defined set of known resistance loci [44].
- Model Architecture & Training: Implement an MLP architecture within a modular framework (e.g., TensorFlow). The model typically consists of multiple fully connected (dense) layers with non-linear activation functions [44].
- Performance Validation: Evaluate the model using a rigorous cross-validation strategy (e.g., 10-fold cross-validation). Monitor loss curves to ensure stable training and avoid overfitting. Key metrics include Sensitivity, Specificity, and AUC [44].
Visual Guide to Algorithm Selection
The following workflow diagram provides a logical pathway for selecting the most suitable algorithm based on your research goals and dataset properties.
Table 2: Key Research Reagents and Computational Tools
| Item Name | Function/Application | Key Considerations |
|---|---|---|
| Whole-Genome Sequencing (WGS) Data | Primary input data for identifying genetic variants (SNPs, indels) relative to a reference genome [45] [44]. | Quality control is critical (e.g., CheckM for completeness/contamination, fastp for read quality) [45]. |
| Phenotypic Drug Susceptibility Testing (pDST) Data | Provides the "ground truth" labels (Resistant/Susceptible) for model training and validation [45] [41]. | Be aware of variable predictive accuracy of WGS for different drugs (e.g., high for RIF/INH, lower for EMB/PZA) [45]. |
| Snippy / BCFtools | Bioinformatics tools for variant calling from WGS data and merging SNP information from multiple isolates [45]. | Ensures standardized and reproducible identification of genomic mutations. |
| SHAP (SHapley Additive exPlanations) | A framework for post-hoc interpretation of complex ML models (e.g., RF, DL) to quantify the contribution of each mutation to predictions [45]. | Essential for making "black-box" models more transparent and clinically actionable [45]. |
| PATRIC Database | A public repository providing curated WGS data and associated AST phenotypes for model training [45]. | Provides a large, standardized dataset for building and benchmarking models. |
Frequently Asked Questions (FAQs) and Troubleshooting
Q1: My Random Forest model has good overall accuracy, but it fails to predict drug-resistant cases correctly. What is the issue? A: This is a classic class imbalance problem, where the number of drug-susceptible isolates far exceeds the resistant ones. To address this:
- Technical Fix: Use techniques like upsampling the resistant class, downsampling the susceptible class, or applying sample-specific weights during model training to balance the influence of each class [46].
- Metric Fix: Avoid using accuracy alone. Instead, monitor metrics like Sensitivity (to capture resistance correctly) and Specificity simultaneously. The area under the precision-recall curve (au PR) can be more informative than the ROC curve for imbalanced data [45].
Q2: How can I interpret a complex Deep Learning model to identify which mutations are driving the predictions? A: Model interpretability is crucial for clinical trust. Employ post-hoc explanation frameworks like SHAP (SHapley Additive exPlanations). For instance, a GBC model used with SHAP can identify that a specific mutation at position rpoB_Ser450 is the top-ranked feature for predicting rifampicin resistance, quantifying its contribution to the model's output [45].
Q3: I have genomic data, but my dataset is relatively small (~1,000 isolates). Which algorithm should I avoid? A: You should be cautious with Deep Learning. DL models typically require very large sample sizes (e.g., >10,000 isolates) to learn effectively and avoid overfitting [44]. With a smaller dataset, you will likely achieve better and more robust performance with Logistic Regression or Random Forest.
Q4: What is the advantage of using Multi-Label Random Forest over building separate models for each drug? A: Standard regimens use drug combinations, leading to correlated resistance patterns (e.g., MDR-TB). Multi-Label RF exploits these correlations by learning a single model for all drugs. This allows the model to identify mutations that are important for predicting resistance to multiple drugs simultaneously, often leading to improved performance compared to training independent models (Single-Label RF) [42].
Q5: My regression model for continuous MIC values makes poor predictions for highly sensitive isolates. Why? A: This is a regression imbalance issue, where models tend to predict values closer to the population mean and perform poorly at the extremes of the distribution. Consider advanced methods like SAURON-RF (SimultAneoUs Regression and classificatiON RF), which performs joint regression and classification to improve prediction for sensitive cell lines specifically [46].
This technical support center provides troubleshooting guides and FAQs for researchers using AutoML pipelines to improve the prediction accuracy of drug resistance mutations.
Troubleshooting Guides
Guide 1: Resolving AutoML Job Failures
| Error Symptom | Possible Cause | Solution Steps |
|---|---|---|
| Job fails immediately after initiation in the studio UI. | Incorrect data formatting or insufficient computational resources. [47] | 1. Check the HyperDrive child job in the studio UI. [47]2. Navigate to the Trials tab to identify failed trials. [47]3. In the failed trial job, check the Overview tab for error messages and review the std_log.txt file in the Outputs + Logs tab. [47] |
| Pipeline run fails with specific failed nodes (marked in red). [47] | A faulty component within the machine learning pipeline, such as a data preprocessing step. | 1. Select the failed node in the pipeline diagram. [47]2. Check the error message in the node's Overview tab and examine std_log.txt for detailed logs. [47] |
| Model performance is poor or metrics are lower than expected. | The identified gene signature is not predictive, or the selected features are not relevant to the drug resistance mechanism. [33] | 1. Verify the biological relevance of selected features against known databases (e.g., CARD). [33]2. Increase the diversity of the search algorithm (e.g., run the Genetic Algorithm for more iterations). [33]3. Ensure your dataset has a sufficient number of samples; some multivariate feature selection methods perform well with sample sizes as low as 100 patients. [48] |
Guide 2: Addressing Data Quality and Preparation Issues
| Issue | Impact on Model | Resolution |
|---|---|---|
| Class Imbalance: One resistance phenotype has many more samples than another. [49] | The model may become biased towards the majority class and perform poorly on the underrepresented resistance type. [49] | Balance the distribution of samples. As a rule of thumb, the label with the fewest examples should have at least 10% of the examples of the largest label. [49] |
| Insufficient Data: The number of samples or features is too low. | The model cannot learn complex patterns, leading to low accuracy. | For transcriptomic analyses, leverage feature selection methods like GA or SES to find minimal, predictive gene sets (e.g., 35-40 genes). [33] [48] |
| Irrelevant Features: The input data contains many features not related to the resistance mechanism. | Increases computational cost and can reduce model accuracy by introducing noise. | Use automated feature selection techniques like LASSO or Statistically Equivalent Signatures (SES) to identify a minimal set of predictive biomarkers. [48] |
Frequently Asked Questions (FAQs)
Data Preparation
Q: What is the minimum sample size required for a reliable AutoML model in drug resistance research? A: While more data is always better, studies have successfully built predictive models for complex traits like antibiotic resistance using ~414 clinical isolates for discovery. [33] For microRNA biomarker discovery in leukemia, multivariate methods have been used effectively with data from 123 patients. [48] The key is using robust feature selection to avoid overfitting.
Q: How should I handle my dataset if it has many missing values? A: AutoML platforms typically automate data preprocessing, which includes imputing missing values. [50] [51] You do not need to handle this manually. The system will apply suitable strategies based on your data type.
Model Training & Optimization
Q: My AutoML model is not converging. What should I check? A: First, verify the integrity of your input data and labels. Then, ensure the search space for hyperparameters (defined by Parameter Range Locators or PRLs) is appropriately set. A range that is too large or improperly defined can prevent convergence. [52]
Q: How can I ensure my AutoML model doesn't just memorize the training data (overfitting)? A: AutoML systems use built-in validation strategies like k-fold cross-validation and holdout sets to evaluate model performance on unseen data, which helps detect overfitting. [50] [48] A model that performs well on the validation set is likely generalizing correctly.
Interpretation & Deployment
Q: The best-performing model from AutoML is a complex ensemble. How can I explain its predictions to my research team? A: Many AutoML platforms now include model interpretability features. Use tools that provide feature importance scores and local explanations to understand which genes or biomarkers the model uses most for its predictions. [51] This is crucial for validating biological relevance. [33]
Q: After deploying my model, how do I monitor its performance over time? A: Most AutoML platforms offer monitoring tools that track the model's performance in production. They can alert you to issues like "model drift," where performance degrades as new data patterns emerge, prompting you to retrain the model. [50] [51]
Featured Experimental Protocol: Identifying a Minimal Gene Signature for Antibiotic Resistance
The following methodology, adapted from a study on Pseudomonas aeruginosa, details how to use a Genetic Algorithm (GA) with AutoML to find a small set of genes that can accurately predict resistance. [33]
- Objective: Identify a minimal gene signature (~35-40 genes) that predicts resistance to specific antibiotics (e.g., Meropenem, Ciprofloxacin) from transcriptomic data. [33]
- Input Data: RNA-seq transcriptomic data from 414 clinical isolates. [33]
- Core Technique: A hybrid GA-AutoML pipeline. [33]
Step-by-Step Procedure
- Data Preparation: Provide the normalized transcriptomic dataset where each row is a clinical isolate and each column is a gene's expression level. [33]
- Feature Selection via Genetic Algorithm: [33]
- Initialization: The GA starts by creating a population of random gene subsets (e.g., each containing 40 genes).
- Evaluation: Each gene subset is evaluated by training a simple classifier (e.g., SVM) and measuring its performance (e.g., ROC-AUC).
- Evolution: Over many generations (e.g., 300), the algorithm selects the best-performing subsets, recombines them ("crossover"), and introduces small random changes ("mutation") to explore new gene combinations.
- Consensus: After many runs, genes that are most frequently selected across all high-performing subsets are used to form a final, consensus gene signature.
- Model Training with AutoML: The consensus gene set is used as the input features for an AutoML system. The AutoML then automatically tests multiple algorithms and hyperparameters to build the final, optimized predictive model. [33]
- Validation: The final model's accuracy is validated on a held-out test set of clinical isolates. [33]
Expected Outcomes
This protocol achieved the following results in predicting antibiotic resistance: [33]
| Antibiotic | Test Set Accuracy | Number of Genes in Signature |
|---|---|---|
| Meropenem | ~99% | 35-40 |
| Ciprofloxacin | ~99% | 35-40 |
| Tobramycin | ~96% | 35-40 |
| Ceftazidime | ~96% | 35-40 |
The Scientist's Toolkit: Research Reagents & Materials
| Item | Function in the Protocol |
|---|---|
| Clinical Bacterial Isolates | The source of biological material for generating transcriptomic data and phenotypic resistance profiles. [33] |
| RNA-seq Reagents | Used to extract and prepare RNA for sequencing, capturing the global gene expression profile of each isolate under antibiotic pressure. [33] |
| Comprehensive Antibiotic Resistance Database (CARD) | A reference database used to compare and validate the GA-selected gene signatures against known resistance markers. [33] |
| iModulon Annotations | A resource of independently modulated gene sets used to map the discovered gene signatures to broader transcriptional programs and regulatory networks. [33] |
| AutoML Platform (e.g., JADBio) | The software environment that automates the process of model selection, hyperparameter tuning, and validation. [48] |
Workflow Visualization
Genetic Algorithm (GA) AutoML Pipeline
This diagram illustrates the hybrid workflow for identifying a minimal, predictive gene signature. The GA iteratively refines gene subsets, which are then used by AutoML to build a final model. [33]
Core Workflow for Drug Resistance Prediction
This simplified workflow shows the key stages from data input to validated prediction, highlighting the synergy between GA-based discovery and AutoML modeling. [33]
Frequently Asked Questions (FAQs) for Researchers
FAQ 1: What are the common reasons for low predictive accuracy in my machine learning model for antimicrobial resistance (AMR)?
Low accuracy often stems from several key issues:
- Incomplete Feature Set: Relying solely on known resistance genes (e.g., from CARD) can miss crucial markers. For P. aeruginosa, many high-performing gene signatures are derived from transcriptomic data and include previously uncharacterized genes not found in standard databases [33].
- Ignoring Chromosomal Mutations: For P. aeruginosa, a significant portion of its resistome is mutation-driven. Tools that only detect acquired genes will have poor accuracy. Incorporating a comprehensive database of chromosomal variants (e.g., as done with the ARDaP tool) is critical [53].
- Data Imbalance and Overfitting: AMR datasets are often imbalanced, with more susceptible than resistant isolates. Using algorithms like Random Forest with class weighting and robust validation on external, multi-center datasets is essential to ensure generalizability [54] [45].
FAQ 2: How can I improve the biological interpretability of my "black box" ML model?
Enhancing interpretability is key for clinical adoption.
- Employ Explainable AI (XAI) Techniques: Use frameworks like SHapley Additive exPlanations (SHAP) to quantify the contribution of individual genetic variants (e.g., SNPs) to the model's prediction. This identifies high-importance mutations, such as rpoB_p.Ser450 for rifampicin resistance in M. tuberculosis [45].
- Use Minimal Feature Sets: Apply genetic algorithms (GA) for feature selection to identify compact, highly predictive gene sets (e.g., 35-40 genes). This simplifies the model and highlights the most critical biomarkers for further experimental validation [33].
- Map to Functional Units: Map predictive genes to operons or independently modulated gene sets (iModulons) to connect model features to higher-order biological processes like efflux regulation or stress responses [33].
FAQ 3: What is the best way to validate my AMR prediction model for clinical relevance?
Robust validation is a multi-step process.
- Internal vs. External Validation: Always test your model on a completely independent, external dataset. Performance often declines in external validation, highlighting the need for diverse training data [55].
- Phenotypic Correlation: Ensure that predictions are benchmarked against high-quality, gold-standard phenotypic Drug Susceptibility Testing (DST) results [54] [45].
- Direct Clinical Sample Testing: Move beyond pure culture isolates. Validate your sequencing and analysis pipeline directly on clinical samples (e.g., sputum) to assess real-world performance and detect low-frequency mutations [56].
Experimental Protocols for High-Accuracy AMR Prediction
Protocol: Transcriptomic-Based Prediction forP. aeruginosa
This protocol outlines the workflow for using transcriptomic data and a GA-AutoML pipeline to predict antibiotic resistance, achieving 96-99% accuracy [33].
1. Sample Preparation & RNA Sequencing:
- Collect a large set of clinical isolates (e.g., 414 isolates) with known phenotypic resistance profiles for target antibiotics (e.g., meropenem, ciprofloxacin).
- Culture isolates under standardized conditions and extract total RNA.
- Perform high-throughput RNA sequencing (RNA-Seq) to generate transcriptomic profiles.
2. Data Preprocessing and Feature Selection:
- Map sequencing reads to a reference genome and compile a gene expression matrix.
- Genetic Algorithm (GA) Workflow: Implement a GA to identify minimal, predictive gene sets.
- Initialization: Start with a population of randomly generated gene subsets (e.g., 40 genes each).
- Evaluation: Train a simple classifier (e.g., SVM) on each subset and evaluate performance using metrics like ROC-AUC and F1-score on a validation set.
- Selection: Select the top-performing subsets to "reproduce."
- Evolution: Create a new generation of subsets through crossover (combining parts of parent subsets) and mutation (randomly swapping genes).
- Iteration: Repeat this process for hundreds of generations and thousands of independent runs.
3. Model Training and Validation:
- Construct a consensus gene list by ranking genes based on their selection frequency across all GA runs.
- Use this minimal gene set (typically 35-40 genes) to train a final, optimized AutoML classifier.
- Evaluate the final model's accuracy, F1-score, and other metrics on a completely held-out test set of isolates.
The workflow for this protocol is illustrated below.
Protocol: Genomic Mutation Detection for Direct Clinical Sample Analysis
This protocol describes a hybridization-capture sequencing method to monitor the P. aeruginosa mutational resistome directly from clinical samples, enabling detection of mutations at frequencies as low as 1% [56].
1. Panel Design and Sample Processing:
- Design a Targeted Panel: Synthesize a panel of hybridization probes to enrich ~200 genes related to AMR, multilocus sequence typing (MLST), mutability, and virulence in P. aeruginosa.
- Extract DNA: Extract total DNA directly from clinical samples (e.g., sputum from CF patients or respiratory samples from ICU patients with ventilator-associated pneumonia), bypassing the need for culture.
2. Library Preparation and Enrichment:
- Prepare sequencing libraries from the extracted DNA.
- Perform hybridisation-based capture using the custom panel (e.g., KAPA HyperCap kit) to enrich for the target genes.
- Sequence the enriched libraries on a high-throughput platform.
3. Variant Calling and Analysis:
- Map the sequencing reads to a reference genome (e.g., PAO1).
- Call variants (SNPs, indels) in the targeted resistome genes.
- Use a curated database of known resistance mutations (e.g., for genes like oprD, ampC, gyrA, parC, pmrB) to interpret the variants and predict the resistance phenotype [53] [57].
- Analyze population dynamics by tracking the frequency of specific resistance mutations over time or during therapy.
Data Presentation: Performance Comparison of AMR Prediction Models
The following tables summarize the quantitative performance of various ML approaches for predicting AMR in P. aeruginosa and M. tuberculosis.
Table 1: Performance of P. aeruginosa AMR Prediction Models
| Pathogen | Method / Tool | Data Type | Key Performance Metric | Result | Reference |
|---|---|---|---|---|---|
| P. aeruginosa | GA-AutoML (Transcriptomics) | RNA-Seq | Accuracy (Test Set) | 96% - 99% | [33] |
| P. aeruginosa | ARDaP (Genomics) | WGS | Balanced Accuracy (Global Dataset) | 85% | [53] |
| P. aeruginosa | ARDaP (Genomics) | WGS | Balanced Accuracy (Validation Dataset) | 81% | [53] |
| P. aeruginosa | abritAMR (Genomics) | WGS | Balanced Accuracy (Validation Dataset) | 54% | [53] |
| P. aeruginosa | Hybrid-Capture Sequencing | Targeted DNA-Seq | Detection Sensitivity for Mutations | ~1% | [56] |
Table 2: Performance of M. tuberculosis AMR Prediction Models
| Method / Algorithm | Drug (Resistance) | Key Performance Metric | Result | Reference |
|---|---|---|---|---|
| 1D Convolutional Neural Network (CNN) | Ethambutol (EMB) | F1-Score | 81.1% - 93.8% | [54] |
| Rifampicin (RIF) | F1-Score | 93.7% - 96.2% | [54] | |
| Isoniazid (INH) | F1-Score | 95.9% - 97.2% | [54] | |
| Gradient Boosting Classifier (GBC) | Rifampicin (RIF) | Accuracy | 97.28% | [45] |
| Isoniazid (INH) | Accuracy | 96.06% | [45] | |
| Pyrazinamide (PZA) | Accuracy | 94.19% | [45] | |
| Ethambutol (EMB) | Accuracy | 92.81% | [45] | |
| Deep Learning (DL) Diagnostic Models | Drug-Resistant TB (DR-TB) | Pooled AUC | 0.97 | [55] |
| Traditional ML Diagnostic Models | Drug-Resistant TB (DR-TB) | Pooled AUC | 0.89 | [55] |
The Scientist's Toolkit: Key Research Reagent Solutions
Table 3: Essential Materials and Tools for AMR Prediction Research
| Item / Reagent | Function / Application | Example / Note |
|---|---|---|
| Custom Hyb-Capture Panel | Enrichment of target resistance genes directly from clinical samples for sequencing. | KAPA HyperExplore panel (Roche) targeting ~200 P. aeruginosa AMR/MLST/virulence genes [56]. |
| Comprehensive AMR Database | Curated collection of known resistance markers for genotype-to-phenotype correlation. | Species-specific databases are crucial. Examples: CARD, ARDaP database for P. aeruginosa [53], WHO M. tuberculosis mutation catalogue [45]. |
| Genetic Algorithm (GA) Framework | Evolutionary feature selection to identify minimal, high-performance gene signatures from high-dimensional data. | Used to find ~35-40 gene transcriptomic signatures in P. aeruginosa [33]. |
| AutoML Software | Automated machine learning to efficiently train and optimize multiple classifiers without manual tuning. | Used in conjunction with GA to build final classifiers with high accuracy [33]. |
| Explainable AI (XAI) Package | Interpreting "black box" ML models to identify the most influential genetic features. | SHAP (SHapley Additive exPlanations) framework used to rank importance of SNPs in M. tuberculosis models [45]. |
| Pan-Genome Reference | A set of all genes from multiple strains of a species, improving mapping and variant calling accuracy. | Used in M. tuberculosis studies to reduce errors when analyzing divergent strains [54]. |
Overcoming Data and Model Implementation Challenges
Addressing High-Dimensionality and Data Sparsity in Omics Datasets
Troubleshooting Guides & FAQs
Frequently Asked Questions
Q1: My multi-omics data has different dimensionalities across platforms (e.g., millions of SNPs vs. thousands of metabolites). What is the most effective strategy to reduce dimensions before integration?
A comprehensive approach combining feature selection and feature extraction is recommended. Leverage intrinsic dimensionality estimators to assess the curse-of-dimensionality impact on each omics view individually, then apply a two-step reduction strategy for significantly affected views [58]. For genomic data, consider automated feature selection methods like genetic algorithms that can identify minimal, highly predictive gene sets (e.g., 35-40 genes) while maintaining accuracy of 96-99% [33]. For the actual integration, methods like GAUDI that apply UMAP independently to each dataset before concatenation and final embedding have demonstrated superior performance in capturing non-linear relationships [59].
Q2: How can I handle missing data that commonly occurs in multi-omics datasets, especially for low-abundance proteins or metabolites?
Generative deep learning models specifically address this challenge. Variational Autoencoders (VAEs) and Generative Adversarial Networks (GANs) focus on creating adaptable representations that can be shared across multiple modalities and have advanced capabilities for handling missing data [60]. Additionally, implement advanced imputation strategies like matrix factorization or deep learning-based reconstruction [61]. For mass spectrometry-based data, normalization methods like Probabilistic Quotient Normalization (PQN) and Locally Estimated Scatterplot Smoothing (LOESS) have shown effectiveness in improving data quality for metabolomics and lipidomics data [62].
Q3: What integration methods best preserve non-linear relationships in omics data that traditional linear methods might miss?
Non-linear integration methods significantly outperform linear approaches for capturing complex biological relationships. The GAUDI method leverages independent UMAP embeddings for concurrent analysis of multiple data types and has demonstrated superior performance in uncovering non-linear relationships among different omics data compared to several state-of-the-art methods [59]. Deep learning approaches including graph convolutional networks (GCNs) and autoencoders are also designed to extract features and model non-linear interactions directly [60]. Ensemble methods like Voting Classifiers that combine multiple algorithms (Random Forest, SVM, Gradient Boosting, Neural Networks) have achieved test accuracies up to 96.46% in AMR prediction tasks [63].
Q4: How can I ensure my predictive models for drug resistance remain interpretable for clinical translation, rather than being "black boxes"?
Incorporate explainable AI (XAI) techniques directly into your modeling pipeline. SHapley Additive exPlanations (SHAP) values can be applied to interpret model decisions and determine each feature's contribution to predictions [59] [64]. For genomic applications, the Genetic Algorithm-AutoML pipeline identifies minimal gene signatures (35-40 genes) that provide both high accuracy and biological interpretability [33]. Additionally, leveraging game-theory-based feature evaluation algorithms can help identify AMR genes with demonstrated classification accuracies between 87% and 90% while maintaining interpretability [63].
Performance Comparison of Multi-Omics Integration Methods
Table 1: Comparative analysis of multi-omics integration methodologies for handling high-dimensional, sparse data
| Method | Core Approach | Key Advantages | Performance Metrics | Best Use Cases |
|---|---|---|---|---|
| GAUDI [59] | Independent UMAP embeddings + HDBSCAN clustering | Superior non-linear pattern capture; handles varying cluster densities | Jaccard Index: 1.0 (synthetic data); identified high-risk AML group with 89-day median survival | Unsupervised clustering; survival risk stratification |
| Ensemble Voting Classifier [63] | Combines multiple ML models (RF, SVM, Gradient Boosting, NN) | Balances accuracy with low log loss; robust performance | Test accuracy: 96.46%; F1-score: 0.9646; Log loss: 0.1504 | AMR gene sequence classification |
| Genetic Algorithm-AutoML [33] | Evolutionary feature selection + automated ML | Identifies minimal, interpretable gene signatures | Accuracy: 96-99%; F1 scores: 0.93-0.99 with 35-40 genes | Transcriptomic biomarker discovery |
| Gradient Boosting Classifier [64] | Tree-based ensemble with sequential learning | High accuracy for SNP-based resistance prediction | Accuracy: 97.28% (RIF), 96.06% (INH), 94.19% (PZA), 92.81% (EMB) | MTB drug resistance prediction |
| intNMF [59] | Non-negative matrix factorization | Joint dimensionality reduction and clustering | Strong clustering performance but higher variability with increased clusters | Multi-omics clustering |
Data Normalization Strategy Comparison
Table 2: Evaluation of normalization methods for mass spectrometry-based multi-omics datasets [62]
| Omics Type | Recommended Methods | Performance Characteristics | Considerations |
|---|---|---|---|
| Metabolomics | Probabilistic Quotient Normalization (PQN), LOESS QC | Consistently enhances QC feature consistency; preserves time-related variance | SERRF may mask treatment-related variance in some datasets |
| Lipidomics | PQN, LOESS QC | Robust improvement in QC feature consistency; handles technical variance | Effective for temporal studies |
| Proteomics | PQN, Median, LOESS normalization | Preserves time-related and treatment-related variance | Optimal for maintaining biological signal |
Experimental Protocols
Protocol 1: GAUDI for Multi-Omics Integration and Clustering
This protocol details the implementation of Group Aggregation via UMAP Data Integration (GAUDI) for unsupervised integration of multi-omics data [59].
Data Preprocessing: Normalize each omics dataset separately using platform-specific methods. For mass spectrometry-based data, apply PQN for metabolomics and lipidomics, and Median normalization for proteomics [62].
Independent UMAP Embedding: Apply UMAP to each omics dataset independently using correlation distance metrics. Recommended parameters: 30 nearest neighbors, minimum distance of 0.3.
Embedding Concatenation: Combine individual UMAP embeddings into a unified dataset by concatenating coordinates across omics layers.
Secondary UMAP: Apply a second UMAP to the concatenated embeddings to generate a final integrated representation.
HDBSCAN Clustering: Perform Hierarchical Density-Based Spatial Clustering on the integrated embedding to identify sample groups without pre-specifying cluster number.
Metagene Calculation: Use XGBoost to predict UMAP embedding coordinates from original molecular features. Extract SHAP values to determine feature importance.
Protocol 2: Genetic Algorithm with AutoML for Feature Selection
This protocol describes hybrid GA-AutoML pipeline for identifying minimal predictive gene signatures from transcriptomic data [33].
Data Preparation: Process raw transcriptomic data from clinical isolates (e.g., 414 P. aeruginosa isolates). Perform quality control and normalize expression values.
Initial AutoML Benchmark: Train automated machine learning models using all genes (e.g., 6,026 genes) to establish baseline performance.
Genetic Algorithm Configuration:
- Initialize population with random 40-gene subsets
- Set evolution parameters: 300 generations per run, 1,000 independent runs
- Evaluation metrics: ROC-AUC and F1-score via SVM and logistic regression
Evolutionary Operations:
- Selection: Retain top-performing subsets based on classification performance
- Crossover: Recombine genes from high-performing subsets
- Mutation: Introduce random gene swaps to maintain diversity
Consensus Gene Set Generation: Rank genes by selection frequency across all runs. Select top 35-40 genes per antibiotic for final model training.
Biological Validation: Compare selected genes with known resistance databases (e.g., CARD). Map to operons and iModulons for functional interpretation.
Workflow Diagrams
GAUDI Multi-Omics Integration Workflow
Genetic Algorithm Feature Selection Process
Research Reagent Solutions
Table 3: Essential computational tools and databases for omics-based drug resistance research
| Resource | Type | Primary Function | Application in Drug Resistance |
|---|---|---|---|
| UMAP [59] [65] | Dimensionality Reduction | Non-linear embedding for high-dimensional data | Preserving global structure in multi-omics integration |
| HDBSCAN [59] | Clustering Algorithm | Density-based clustering without pre-specified cluster number | Identifying patient subgroups with distinct survival patterns |
| CARD [33] | Database | Comprehensive Antibiotic Resistance Database | Validation of novel resistance genes identified through ML |
| SHAP [59] [64] | Explainable AI Framework | Interpreting ML model predictions and feature contributions | Identifying important SNPs and genes driving resistance predictions |
| XGBoost [59] | Machine Learning Algorithm | Gradient boosting for classification and regression | Predicting embedding coordinates and calculating metagenes |
| Genetic Algorithms [33] | Optimization Method | Evolutionary feature selection from high-dimensional data | Identifying minimal gene signatures for resistance prediction |
| AutoML [33] | Automated Machine Learning | Streamlined model selection and hyperparameter tuning | Rapid development of optimized classifiers for resistance |
Managing Class Imbalance in Rare Resistance Phenotypes
Frequently Asked Questions
Q1: Why is class imbalance a critical issue in predicting rare drug resistance phenotypes?
Class imbalance occurs when the distribution of examples across different classes is highly skewed. In the context of drug resistance, this often means that susceptible cases vastly outnumber resistant ones. This imbalance causes machine learning models to become biased toward the majority class, as achieving high accuracy can be misleadingly easy by simply predicting "susceptible" for all cases. Consequently, the model fails to learn the distinguishing patterns of the rare, but critically important, resistance phenotypes. This leads to poor performance on the minority class, meaning true resistance cases may be missed, which can have severe implications for treatment outcomes and the development of effective therapies [66] [67].
Q2: What evaluation metrics should I use instead of accuracy for imbalanced datasets?
When working with imbalanced data, traditional metrics like accuracy can be deceptive. It is recommended to use a suite of metrics that provide a more comprehensive understanding of model performance, particularly for the minority class [67]. Key metrics include:
- Precision: The ability of the classifier to avoid labeling negative samples as positive.
- Recall (Sensitivity): The ability of the classifier to find all the positive samples.
- F1-Score: The harmonic mean of precision and recall.
- Area Under the Receiver Operating Characteristic Curve (AUC): A measure of the model's ability to distinguish between classes [67].
These metrics are especially important in fields like medical diagnosis, where failing to identify a true positive (e.g., a drug-resistant infection) can have serious consequences [67].
Q3: What are the main categories of techniques to handle class imbalance?
Techniques for managing class imbalance can be broadly grouped into three categories [67]:
- Data Processing Techniques: These methods directly adjust the training data to create a more balanced distribution, such as resampling or generating synthetic data.
- Algorithmic Techniques: These methods adjust the learning algorithm itself to make it more sensitive to the minority class, for example, through cost-sensitive learning.
- Advanced Techniques: These involve more complex approaches like one-class classification or transfer learning.
Troubleshooting Guides
Problem: Model has high accuracy but poor recall for the resistance class. This is a classic sign of a model biased by class imbalance. The model is correctly predicting the majority (susceptible) class but failing to identify the minority (resistant) class.
Solution:
- First, switch your evaluation metrics to focus on Recall, F1-Score, and AUC for the resistance class [67].
- Implement resampling techniques on your training data. You can either oversample the minority class (resistance phenotypes) or undersample the majority class (susceptible phenotypes) [67] [68].
- Apply algorithm-level approaches such as cost-sensitive learning, where a higher penalty is assigned to misclassifying the minority class during model training [67].
Problem: After oversampling, the model is overfitting to the replicated minority class examples. Simple random oversampling, which duplicates existing minority class instances, can lead to overfitting because the model learns from the same examples multiple times [66].
Solution:
- Use advanced synthetic data generation like SMOTE (Synthetic Minority Over-sampling Technique) or ADASYN (Adaptive Synthetic Sampling). These techniques create new, synthetic examples for the minority class by interpolating between existing instances, leading to a more diverse and generalized representation [66] [67].
- Consider hybrid methods like SMOTE-Tomek, which combines synthetic oversampling (SMOTE) with cleaned undersampling (Tomek Links) to remove ambiguous data points and improve class separation [66].
Problem: The dataset is too small for meaningful resampling. In some research areas, the overall dataset size, particularly for the minority class, can be very small, making resampling less effective.
Solution:
- Explore data augmentation techniques specific to your data type. For genomic or protein sequence data, novel methods can be developed to generate new feature representations. One study on antibiotic resistance genes used a cross-referencing data augmentation method based on multiple protein language models to enhance less prevalent examples [69].
- Leverage transfer learning. Use pre-trained models that have been developed on large, diverse datasets and fine-tune them on your specific, albeit small and imbalanced, dataset. This allows the model to benefit from general patterns learned elsewhere [67].
Comparison of Resampling Techniques
The table below summarizes common data-level techniques for handling class imbalance.
Table 1: Comparison of Common Resampling Techniques
| Technique | Category | Brief Description | Pros | Cons |
|---|---|---|---|---|
| Random Undersampling [66] [67] | Data Processing | Randomly removes examples from the majority class. | Reduces dataset size and training time. | May remove potentially important information, increasing variance. |
| Random Oversampling [66] [67] | Data Processing | Randomly duplicates examples from the minority class. | Simple to implement; retains all information. | High risk of overfitting to repeated examples. |
| SMOTE [66] [67] | Data Processing | Creates synthetic minority class examples by interpolating between neighbors. | Reduces overfitting compared to random oversampling. | Can generate noisy samples if the minority class is not well clustered. |
| ADASYN [66] [67] | Data Processing | Similar to SMOTE but adaptively generates more samples for "hard-to-learn" examples. | Focuses on difficult minority class examples. | Can also amplify noise present in the dataset. |
| SMOTE-Tomek [66] | Hybrid | Combines SMOTE with Tomek Links to clean the resulting data. | Improves class separation by removing ambiguous points. | Adds complexity to the preprocessing pipeline. |
| Class Weights [67] [68] | Algorithmic | Assigns a higher cost to misclassifications of the minority class during model training. | No need to modify the training data; easy to implement in many libraries. | Can be computationally more expensive than data-level methods. |
Experimental Protocol: Implementing SMOTE for Resistance Prediction
This protocol provides a step-by-step guide for applying the SMOTE technique using the imbalanced-learn library in Python, a common tool in this field [66].
Install the Library:
Data Preprocessing: Split your dataset into training and testing sets before applying any resampling. It is critical to apply resampling only to the training set to prevent data leakage and to get an unbiased evaluation of model performance on the natural (unmodified) distribution of the test set [66] [68].
Apply SMOTE: Generate synthetic samples for the minority class in the training data only.
Model Training and Evaluation: Train your model on the resampled data and evaluate it on the original, unmodified test set using appropriate metrics like F1-Score and AUC [67].
Workflow Diagram for Handling Class Imbalance
The following diagram illustrates a logical workflow for diagnosing and addressing class imbalance in a machine learning project for resistance prediction.
Workflow for Managing Class Imbalance
Research Reagent Solutions
The table below lists key computational tools and resources used in advanced studies for tackling class imbalance and improving resistance prediction.
Table 2: Key Research Reagents & Computational Tools
| Item | Function / Description | Application in Resistance Research |
|---|---|---|
| imbalanced-learn (Python) [66] | An open-source library providing a wide range of resampling techniques including SMOTE, ADASYN, and Tomek Links. | Essential for implementing data-level resampling strategies in a Python-based ML workflow. |
| Protein Language Models (e.g., ProtBert-BFD, ESM-1b) [69] | Deep learning models pre-trained on vast protein sequence databases that convert sequences into numerical feature vectors. | Used for advanced feature extraction from bacterial protein sequences; can be integrated with data augmentation. |
| SHAP (SHapley Additive exPlanations) [70] | A game theory-based method to explain the output of any machine learning model. | Critical for interpreting models trained on imbalanced data and identifying key features driving resistance predictions. |
| XGBoost with Class Weights [70] | A powerful gradient boosting algorithm that can natively handle class imbalance by adjusting the scale_pos_weight parameter. |
Used in surveillance studies to achieve high AUC (e.g., 0.96) in predicting antibiotic resistance from global datasets [70]. |
| LSTM with Attention Mechanisms [69] | A type of recurrent neural network capable of learning from sequences, with attention highlighting important parts. | Applied to embedded protein sequences for predicting antibiotic resistance genes (ARGs), improving accuracy and reducing false positives/negatives [69]. |
Enhancing Model Interpretability for Clinical Translation
Troubleshooting Guide: Common XAI Issues in Drug Resistance Research
This section addresses specific, high-impact challenges you might encounter when applying Explainable AI (XAI) to the prediction of drug resistance mutations.
FAQ 1: My model for predicting antimicrobial resistance has high accuracy, but clinicians do not trust its "black-box" predictions. How can I improve model adoption?
- Problem: High-performing but opaque models face resistance in clinical and translational settings where understanding the "why" is critical for trust and safety.
- Solution: Integrate post-hoc explainability techniques that are specifically designed for high-stakes biomedical applications.
- Protocol: Apply SHAP (SHapley Additive exPlanations) to interpret model outputs on a per-prediction basis.
- Train Your Model: Develop your predictive model for drug resistance (e.g., using a gradient boosting framework like XGBoost on genomic and clinical data).
- Initialize SHAP Explainer: Select the appropriate SHAP explainer (e.g.,
TreeExplainerfor tree-based models,KernelExplainerfor other models). - Calculate SHAP Values: Compute SHAP values for your test set or a specific prediction of interest. These values quantify the contribution of each feature (e.g., a specific mutation, patient age, drug regimen) to the final model output.
- Visualize Results:
- Use
shap.summary_plot()to show the global feature importance across your entire dataset. - Use
shap.force_plot()orshap.waterfall_plot()to visualize the reasoning behind an individual prediction, showing how each feature pushed the model's output from the base value to the final prediction. This is crucial for explaining why a specific mutation was flagged as resistant [71] [72] [73].
- Use
- Key Consideration: Ensure your explanations are presented in a way that is intuitive for biologists and clinicians, linking features back to known biological mechanisms where possible.
FAQ 2: My deep learning model for cancer drug resistance prediction is complex. How can I ensure its predictions are driven by biologically plausible features and not artifacts in the training data?
- Problem: Deep learning models, especially for tasks like analyzing medical images or genomic sequences, can learn spurious correlations that do not generalize.
- Solution: Utilize model architectures and explanation methods that provide inherent interpretability or granular insights.
- Protocol: Implement an interpretable deep learning workflow using attention mechanisms or layer-wise relevance propagation.
- Model Selection: Choose or design a model that supports intrinsic interpretability. For sequential data (e.g., protein sequences), use models with attention layers. For other data, ensure the model is compatible with techniques like LRP (Layer-wise Relevance Propagation).
- Generate Explanations:
- For Attention Models: Extract the attention weights from the model after making a prediction. These weights indicate which parts of the input sequence (e.g., which codons in a gene) the model "paid attention to" when making its decision. Visualize these weights aligned with the input sequence.
- For LRP: Pass a sample through the network and backpropagate the prediction to the input features, assigning a "relevance score" to each input feature. This highlights which input pixels or data points were most relevant to the outcome.
- Biological Validation: Correlate the high-attention or high-relevance features with known domains of the protein (e.g., kinase domains) or previously documented resistance mutations. This step is critical for validating that the model has learned biologically meaningful patterns [71] [72] [74].
- Key Consideration: Always cross-reference model explanations with existing domain knowledge. A discrepancy might indicate a novel discovery or a model error.
FAQ 3: When I use XAI methods on my dataset of tuberculosis drug resistance, the explanations for similar mutations are inconsistent. What could be causing this?
- Problem: Unstable or inconsistent explanations undermine trust and make the model unreliable for clinical translation.
- Solution: Investigate potential issues with model robustness, data distribution, and the XAI method itself.
- Protocol: Diagnose instability in XAI outputs.
- Check Data Distribution: Use PCA or t-SNE to visualize your feature space. Check if the mutations with inconsistent explanations lie near the decision boundary or in a low-density region of the data, which can lead to less stable predictions and explanations.
- Test Model Robustness: Perform a sensitivity analysis by introducing small, realistic perturbations to your input data and observe the change in both the prediction and the explanation. A robust model should have minimal change.
- Audit the XAI Method: Some explanation methods, like LIME, can have inherent variability. Use more stable methods like SHAP for tree-based models. Ensure you are using a sufficient number of samples or a large enough background dataset for approximation in SHAP to guarantee stable results [72] [75].
- Check for Data Leakage: Ensure that no information from the test set has leaked into the training process, as this can create misleading and unstable models.
FAQ 4: How can I validate that the explanations provided by my XAI method are biologically correct?
- Problem: An XAI method might produce a plausible-looking explanation that is, in fact, incorrect or misleading.
- Solution: Move beyond qualitative assessment and adopt a quantitative framework for evaluating explanation fidelity.
- Protocol: Conduct a systematic, quantitative evaluation of XAI output.
- Ablation Studies: Systematically remove or perturb the top features identified by the XAI method and observe the drop in model performance. A sharp drop indicates that the identified features are truly important.
- Literature-Based Validation: Create a "gold standard" set of known resistance mutations from curated databases (e.g., CARD, COSMIC) and scientific literature. Measure the recall and precision of your XAI method in identifying these known features.
- Benchmark with Synthetic Data: If possible, generate synthetic data where the ground-truth drivers of resistance are known. Test whether your XAI method correctly identifies these pre-defined drivers [72].
- Expert Consultation: Present the explanations to domain experts (e.g., microbiologists, oncologists) for qualitative feedback and validation against established biological knowledge.
Quantitative Data on XAI Techniques
The table below summarizes key XAI methods, helping you select the right tool for your drug resistance research.
Table 1: Comparison of Explainable AI (XAI) Techniques for Drug Resistance Research
| Technique | Best For Model Type | Core Principle | Key Advantage | Limitation in Drug Resistance Context |
|---|---|---|---|---|
| SHAP (SHapley Additive exPlanations) [72] [73] | Tree-based, Deep Learning | Game theory; distributes prediction payout fairly among features. | Provides both local (per-prediction) and global (entire model) explanations with solid theoretical guarantees. | Computationally expensive for very large datasets or complex deep learning models. |
| LIME (Local Interpretable Model-agnostic Explanations) [72] | Any "black-box" model | Approximates the complex model locally with a simpler, interpretable model. | Highly flexible and can be applied to any model. | Explanations can be unstable; sensitive to the perturbation and sampling method. |
| Attention Mechanisms [74] | Deep Learning (RNNs, Transformers) | Learns to assign importance weights to different parts of the input sequence. | Provides inherent, intuitive explanations for sequential data (e.g., DNA/RNA/protein sequences). | The "correctness" of attention as an explanation is still a topic of debate; may not always reflect true feature importance. |
| Layer-wise Relevance Propagation (LRP) [72] | Deep Learning (CNNs, etc.) | Backpropagates the prediction through the network to assign relevance scores to input features. | Works well for image-like data and can pinpoint relevant input regions. | Can be complex to implement and is specific to the model architecture. |
Experimental Protocol: An XAI Workflow for Mutation Analysis
This is a detailed, citable methodology for a typical experiment using XAI to identify and validate drug resistance mutations, based on published approaches [71] [75] [76].
Aim: To predict and explain the genetic determinants of cisplatin-induced acute kidney injury using an interpretable machine learning model and electronic medical record information [76].
Materials and Data:
- Dataset: Curated dataset from electronic medical records, including patient genomic data (e.g., SNP arrays or sequencing), clinical variables (age, baseline kidney function, cisplatin dosage), and outcome label (presence/absence of acute kidney injury).
- Software: Python environment with libraries: scikit-learn, XGBoost, SHAP, pandas, NumPy, Matplotlib/Seaborn.
Methodology:
- Data Preprocessing and Feature Engineering:
- Perform quality control on genomic data (e.g., Hardy-Weinberg equilibrium, call rate).
- Impute missing clinical variables using appropriate methods (e.g., median/mode for continuous/categorical variables).
- Split the dataset into a training set (e.g., 70%) and a hold-out test set (30%), ensuring stratified splitting on the outcome variable.
Model Training and Hyperparameter Tuning:
- Train an XGBoost classifier on the training set to predict the binary outcome of drug resistance or adverse event.
- Use 5-fold cross-validation on the training set to tune hyperparameters (e.g.,
max_depth,learning_rate,n_estimators). The area under the receiver operating characteristic curve (AUROC) should be used as the evaluation metric.
Model Interpretation with SHAP:
- Using the trained and tuned model, calculate SHAP values on the hold-out test set using the
TreeExplainerclass from the SHAP library. - Generate a summary plot to visualize the global importance of all features.
- For specific high-risk patients identified by the model, generate individual force plots to detail the reasoning behind the prediction, showing how each mutation and clinical factor contributed.
- Using the trained and tuned model, calculate SHAP values on the hold-out test set using the
Biological and Clinical Validation:
- Compare the top-ranked features from the SHAP summary plot against known resistance pathways and mutations from literature and databases.
- Design follow-up in vitro experiments (e.g., site-directed mutagenesis and drug sensitivity assays) to functionally validate the top novel genetic candidates identified by the model.
The following workflow diagram illustrates the key steps in this protocol:
Research Reagent Solutions for XAI Experiments
This table lists key computational tools and resources essential for building interpretable models in drug resistance research.
Table 2: Essential Research Reagents & Tools for Interpretable ML
| Item | Function/Benefit | Example Use in Drug Resistance |
|---|---|---|
| SHAP Library [72] [73] | A unified framework for interpreting model predictions across any model type. | Explaining the contribution of individual single nucleotide polymorphisms (SNPs) and clinical comorbidities to a model's prediction of antibiotic resistance in M. tuberculosis. |
| XGBoost with TreeExplainer [71] [73] | A highly efficient gradient boosting library; its tree structure is natively and quickly interpreted by SHAP's TreeExplainer. | Building a high-accuracy model to predict metastasis in lung cancer and then interpreting which genomic and imaging features were most predictive [74]. |
| LIME (Local Interpretable Model-agnostic Explanations) [72] | Creates local, surrogate models to explain individual predictions of any black-box classifier/regressor. | Providing a "case-by-case" explanation for why a specific patient's viral strain is predicted to be resistant to a particular antiretroviral drug. |
| Model-Specific Interpretation Tools (e.g., Attention Weights, LRP) | Provide explanations intrinsic to certain deep learning architectures. | Using attention weights in a transformer model to identify which amino acids in a viral protease are most influential in conferring resistance to an inhibitor. |
| Curated Biological Databases (e.g., CARD, COSMIC, ClinVar) | Provide ground-truth data for validating the biological plausibility of model explanations. | Cross-referencing a top feature identified by SHAP (a specific mutation) with the COSMIC database to see if it is a known driver of cancer drug resistance. |
Decision Framework for XAI Method Selection
Choosing the right XAI technique depends on your model and your primary explanatory goal. The following diagram outlines a logical decision pathway to guide your selection.
Genetic Algorithms for Feature Optimization and Dimensionality Reduction
Frequently Asked Questions (FAQs)
1. What is the primary advantage of using Genetic Algorithms for feature selection in drug resistance research? Genetic Algorithms (GAs) offer a powerful global search capability to navigate the vast and complex landscape of potential genetic features, such as point mutations and gene gain/loss events, associated with drug resistance. Unlike traditional filter-based methods that might get stuck in local optima, GAs can efficiently identify optimal subsets of features by simulating natural selection, thereby improving the predictive accuracy of resistance models [77] [78] [79]. This is crucial for handling high-dimensional genomic data.
2. My model is biased towards susceptible cases. How can GAs help with class imbalance in drug resistance datasets? Drug resistance datasets are often highly imbalanced, with far fewer resistant cases than susceptible ones. GAs can be employed to generate synthetic data for the minority class (resistant cases). A novel approach uses a Genetic Algorithm to create synthetic data, where a fitness function—often informed by classifiers like Support Vector Machines (SVM) or Logistic Regression—guides the generation of new data points that are optimized to improve model performance on the minority class, thus mitigating bias [80].
3. What are hybrid GA methodologies and how do they enhance feature selection? Hybrid GA methodologies combine the global search power of GAs with other machine learning techniques to overcome limitations such as exploring unnecessary search space. A common approach is the GA-Wrapper method, where the GA is used to search for feature subsets, and the performance of a separate classifier (e.g., a neural network or ensemble model) is used as the fitness function. This combination has been shown to substantially improve selection potential and final model performance [77] [79].
4. How can I select a minimal yet optimal feature set for an interpretable model? A two-level genetic algorithm approach is effective for this. In the first level, multiple bootstrapped training sets are used, and for each set, features are expanded using non-linear transformations. The Non-Dominated Sorting Genetic Algorithm II (NSGA-II) is then used to select the minimum feature set that maximizes ensemble model performance. The second level aggregates these candidate feature sets. This process reduces uncertainty and often significantly reduces the number of features while improving metrics like the F1 score [81].
5. Are there specific databases for validating findings in drug resistance mutation research? Yes, leveraging comprehensive databases is critical for validation. MdrDB is a large-scale, high-quality database specifically focused on mutation-induced drug resistance. It integrates data from multiple sources, containing over 100,000 samples, 240 proteins, and 2,503 mutations. It provides 3D structures of wild-type and mutant protein-ligand complexes and binding affinity changes (ΔΔG), which are invaluable for training and testing machine learning models [16].
Troubleshooting Guides
Problem: Poor Model Performance and Overfitting on High-Dimensional Data
Symptoms:
- High accuracy on training data but poor performance on validation/test data.
- Model fails to generalize to new strains or drugs.
- The selected feature set is excessively large and includes many irrelevant variables.
Solutions:
- Implement an Optimized Genetic Algorithm for Feature Selection: A feature selection algorithm based on an optimized GA can be applied. This method simulates natural selection to search for feature subsets that optimize model performance. Research has shown this can improve accuracy, for instance, from 0.9352 to 0.9815 on a dataset by filtering 724 features down to 372 [78].
- Use a Hybrid Dimensionality Reduction Approach: Combine GA with other techniques like Independent Component Analysis (ICA). The GA can be used first for maximal feature selection, followed by ICA to reduce the dimensionality of the selected features further. This hybrid approach has been shown to improve generalization in various contexts [82].
- Apply a Two-Level Feature Engineering Strategy: This addresses the limitation of performing feature selection only once. Use multiple bootstrapped datasets and a multi-objective GA (like NSGA-II) to select features in the first level, then aggregate the results. This reduces uncertainty and has demonstrated an average F1-score improvement of 1.5% while reducing the feature set size by 54.5% [81].
Problem: Inefficient Search and Failure to Identify Biologically Relevant Mutations
Symptoms:
- The algorithm converges too quickly on a sub-optimal set of features.
- Predictions lack biological plausibility or are not validated by clinical data.
- Important, rare resistance mutations are missed.
Solutions:
- Incorporate Domain Knowledge into the Fitness Function: Move beyond simple accuracy. For drug resistance, structure-based criteria are vital. The RESISTOR algorithm provides a powerful framework; it uses Pareto optimization over multiple objectives, including:
- Utilize Comprehensive Phylogenetic Information: When analyzing bacterial resistance, incorporate a consensus phylogenetic tree of the strains. This helps account for evolutionary relationships and can distinguish resistance-associated mutations from background genetic variation [85].
- Leverage Large-Scale Databases for Training: Ensure your model is trained on a comprehensive dataset like MdrDB. The size and diversity of such a database significantly enhance the performance of models in predicting binding affinity changes (ΔΔG), covering a wide range of proteins, mutations, and drugs [16].
Experimental Protocols & Data
Quantitative Performance of GA-based Feature Selection
The table below summarizes results from key studies, demonstrating the effectiveness of GA-based methods in processing high-dimensional data.
Table 1: Performance Metrics of GA-based Feature Selection Methods
| Study / Method | Dataset / Context | Key Performance Improvement |
|---|---|---|
| Feature Selection via Optimized GA [78] | High-dimensional biological data | Accuracy improved from 0.9352 to 0.9815; features reduced from 724 to 372. |
| Two-Level GA Feature Engineering [81] | 12 diverse datasets | Average F1-score improvement of 1.5% with a 54.5% reduction in feature set size. |
| GA-ICA Hybrid Model [82] | No-Line-of-Sight (NLOS) signal data | Achieved 85.69% accuracy, 79.30 sensitivity, and 91.67% specificity. |
| RESISTOR Algorithm [83] [84] | EGFR & BRAF kinase inhibitors | Correctly identified 8 clinically significant EGFR resistance mutations, including T790M. |
Workflow: Identifying Drug Resistance Mutations using a GA-based Approach
The following diagram illustrates a robust workflow for integrating Genetic Algorithms into drug resistance mutation research.
Diagram 1: GA-based drug resistance mutation identification workflow.
Methodology: A Detailed Protocol for GA-based Feature Selection
Objective: To identify a minimal, optimal subset of genetic features (e.g., amino acid point mutations) predictive of drug resistance using a Genetic Algorithm.
Materials:
- Dataset: Genotype and drug resistance phenotype data for a set of bacterial strains or cell lines [85].
- Software: A programming environment with GA capabilities (e.g., Python with
DEAPlibrary) or specialized tools likefeature-gen[81].
Procedure:
- Data Preprocessing and Feature Space Definition:
- Unify Gene Annotations: Use a tool like CAMBer to create consolidated gene annotations and define gene families based on homology [85].
- Compute Multiple Alignments: For each gene family, perform multiple sequence alignments using a tool like MUSCLE [85].
- Identify Genetic Variations: From the alignments, extract genetic variation profiles. This includes:
- Point Mutation Profiles: Transform each column in the alignment into a vector representing the amino acid (or gap) for each strain.
- Gene Gain/Loss Profiles: For gene families not present in all strains, create a vector indicating presence ('G') or absence ('L') for each strain [85].
Configure the Genetic Algorithm:
- Initialization: Randomly generate an initial population of binary chromosomes. Each chromosome is a string of 0s and 1s, where each bit represents the inclusion (1) or exclusion (0) of a specific genetic feature (e.g., a particular point mutation) from the analysis [78].
- Fitness Function: Define a function that evaluates the quality of a feature subset. A common wrapper approach is to use the predictive accuracy of a classifier (e.g., a Support Vector Machine or Random Forest) trained on the selected features and validated on a hold-out set. For drug resistance, you can incorporate a multi-objective function that also considers the change in binding affinity (ΔΔG) [80] [84].
- Genetic Operators:
- Selection: Use tournament or roulette wheel selection to choose parents for the next generation, favoring chromosomes with higher fitness scores.
- Crossover: Apply a crossover operator (e.g., single-point crossover) to pairs of parents to create offspring, exchanging parts of their chromosomes.
- Mutation: Apply a mutation operator that randomly flips bits in the offspring's chromosome with a small probability, introducing new genetic material into the population [78].
- Termination: Run the algorithm for a fixed number of generations or until the fitness score converges.
Validation:
- Use the final, optimized feature subset to train your final predictive model.
- Evaluate the model on a completely independent test set not used during the feature selection process.
- Perform biological validation, such as checking if the identified mutations are known in resources like MdrDB [16] or if they are located in functionally important protein domains.
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Computational Tools and Databases for Drug Resistance Research
| Tool/Resource Name | Type | Primary Function in Research |
|---|---|---|
| MdrDB [16] | Database | A comprehensive database providing 3D structures, binding affinity changes (ΔΔG), and biochemical features for wild-type and mutant protein-ligand complexes to train and validate models. |
| RESISTOR [83] [84] | Algorithm | An open-source algorithm (in OSPREY) that uses Pareto optimization over structure-based criteria and mutational signatures to prospectively predict resistance mutations. |
| GDSC / DepMap [16] | Database | Large-scale public resources linking genomic data (including mutations) to drug sensitivity in cancer cell lines, used for data collection and hypothesis generation. |
| ARDB [85] | Database | The Antibiotic Resistance Genes Database provides lists of genes known to be responsible for drug resistance in specific bacterial species. |
| feature-gen [81] | Python Library | A publicly available library that implements a hierarchical two-level genetic algorithm for feature engineering to enhance interpretable models. |
| OSPREY [83] [84] | Software Suite | Open-source computational protein design software used for rigorous, structure-based calculations of binding affinity (K*) and for running the RESISTOR algorithm. |
Frequently Asked Questions & Troubleshooting Guides
This section addresses common challenges researchers face when studying genotype-phenotype relationships in the context of drug resistance.
General Conceptual Questions
What is the genotype-phenotype gap in the context of drug resistance? The genotype-phenotype gap refers to the challenge of predicting observable drug resistance traits (phenotypes) from genetic data (genotypes). In drug resistance research, this involves understanding how specific genetic mutations in pathogens or cancer cells lead to treatment failure phenotypes. Bridging this gap requires understanding the complex dynamics and biological contexts that determine how genetic variation manifests as resistance [86].
Why do synthetic lethal screens for drug targets often yield non-reproducible results? Lack of reproducibility in synthetic lethal screens often stems from biological context dependency rather than technical limitations. Most synthetic lethal phenotypes are strongly modulated by changes in cellular conditions or genetic background. Studies have found that hits from different screens significantly overlap at the pathway level rather than the individual gene level, explaining why individual gene hits may not reproduce across studies [87].
How can resistance mutations advance basic biological discovery? Resistance mutations have historically propelled biological discovery by confirming small molecule targets and revealing new biological mechanisms. Examples include:
- Rifamycin resistance mutations helped map the first RNA polymerase gene
- Rapamycin resistance mutations led to the discovery of TOR proteins and nutrient sensing pathways
- Studies of tetrodotoxin-resistant sodium channels identified the sodium channel selectivity filter decades before high-resolution structures were available [88]
Technical & Experimental Challenges
How can population stratification bias GWAS for drug resistance traits? Population stratification occurs when different trait distributions within genetically distinct subpopulations cause markers associated with ancestry to appear associated with the trait. This can create spurious genotype-phenotype associations unless properly controlled. For example, a study of asthma in Mexican populations found that three ancestry-informative markers appeared disease-related, but these associations disappeared when ancestry was controlled [89].
What controls are essential for reliable genotyping experiments? Consistent genotyping requires multiple controls in every experiment:
- Homozygous mutant/transgene controls
- Heterozygote/hemizygote controls
- Homozygous wild type/non-carrier controls
- No DNA template (water) controls to test for contamination These controls are essential for troubleshooting genotyping assays and ensuring accurate results [90].
How can researchers account for genetic ancestry in association studies?
- Global ancestry estimation: Methods like STRUCTURE and ADMIXTURE estimate the proportion of an individual's genome from each ancestral population
- Local ancestry estimation: Tools like RFMix and LAMP-LD determine the ancestral origin of specific genomic regions
- Principal Component Analysis (PCA): Identifies major axes of genetic variation to control for population structure in association testing [89]
Quantitative Data Summaries
Network Analysis of KRAS Synthetic Lethal Screens
Table 1: Protein-protein interaction enrichment between KRAS synthetic lethal studies
| Study Pair | Observed PPIs | Expected PPIs | Enrichment Fold | P-value |
|---|---|---|---|---|
| Luo vs. Steckel | 162 | ~20 | ~8-fold | < 0.0001 |
| Luo vs. Barbie | 98 | ~20 | ~4.9-fold | < 0.0001 |
| Steckel vs. Barbie | 127 | ~20 | ~6.4-fold | < 0.0001 |
Source: Adapted from Network meta-analysis of KRAS synthetic lethal screens [87]
Comparison of Synthetic Lethal Candidate Reproducibility
Table 2: Performance of different KRAS synthetic lethal candidate types in validation studies
| Candidate Type | Kim et al. 2013 (Top 1%) | Kim et al. 2011 (Top 1%) | Costa-Cabral et al. 2016 (Top Hit) |
|---|---|---|---|
| Network SL Genes | 15% | 9% | CDK1 (identified) |
| Literature SL Genes | 3% | 0% | Not identified |
Source: Adapted from reproduction studies of KRAS synthetic lethal networks [87]
Detailed Experimental Protocols
Protocol 1: Development of Drug-Resistant Cell Lines
This protocol enables generation of drug-resistant cell lines for studying resistance mechanisms and testing combination therapies [91].
Materials Required
- Parental cancer cell line (e.g., DU-145 prostate cancer cells)
- Target drug (e.g., paclitaxel)
- Complete cell culture medium (RPMI-1640 + 10% FBS + 1% penicillin-streptomycin)
- Cell proliferation reagent (WST-1)
- 96-well plates, cell culture dishes
- DMSO (for drug dissolution)
Step-by-Step Methodology
1. Initial Cell Viability Assay
- Seed cells in 96-well plates at 1.0 × 10⁴ cells/well in 99 μL complete medium
- Incubate for 2 hours to allow cell adhesion
- Prepare drug serial dilutions in DMSO, ensuring final DMSO concentration ≤1%
- Add 1 μL of each drug dilution to appropriate wells
- Incubate for 48 hours
- Add WST-1 reagent and incubate for 0.5-4 hours (optimize duration for specific cell line)
- Measure absorbance at 450 nm (reference: 650 nm)
2. IC₅₀ Calculation
- Calculate cell viability: [(As-Ab)/(Ac-Ab)] × 100
- As: sample absorbance (drug-treated)
- Ab: blank absorbance (medium only)
- Ac: control absorbance (untreated cells)
- Determine IC₅₀ using nonlinear regression (four-parameter logistic model recommended)
3. Resistance Induction Protocol
- Culture parental cells in 100 mm dishes until 80% confluent
- Expose to drug at IC₁₀₋₂₀ concentration for 2 days
- Replace with drug-free medium and culture until 80% confluent
- Passage cells and cryopreserve aliquots
- Increase drug concentration by 1.5-2.0 fold in next cycle
- Repeat process, progressively increasing drug concentration
- If cell proliferation fails, revert to last successful concentration and use smaller increments (1.1-1.5 fold)
Validation and Quality Control
- Regularly quantify IC₅₀ values of developing resistant lines
- Compare resistant vs. parental cell IC₅₀ values
- Significant IC₅₀ increase confirms resistance development
- Maintain detailed records of passage numbers and exposure history
Protocol 2: Causally Cohesive Genotype-Phenotype (cGP) Modeling
cGP modeling integrates genetic variation with computational physiology to bridge genotype-phenotype gaps [86].
Conceptual Framework
- Genetic variation manifests in model parameters of physiological systems
- Lower-level parameters have articulated relationships to genotype
- Higher-level phenotypes emerge from mathematical models describing causal dynamic relationships
- Models span multiple biological scales from molecular to organ levels
Implementation Strategy
- Develop dynamic models capable of accounting for phenotypic variation in populations
- Identify model parameters where causative genetic variation manifests
- Articulate genetic relationships for low-level parameters
- Validate models against empirical data across genetic backgrounds
- Iteratively refine models to improve predictive accuracy
Pathway Diagrams and Workflows
Genotype-Phenotype Gap Bridging Strategies
Strategies for Bridging the Genotype-Phenotype Gap
Drug Resistance Study Workflow
Drug Resistance Research Workflow
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential research reagents and resources for genotype-phenotype studies
| Resource Type | Specific Examples | Function/Application |
|---|---|---|
| Global Ancestry Estimation | STRUCTURE, ADMIXTURE | Estimates proportion of genome from ancestral populations; controls for population stratification [89] |
| Local Ancestry Inference | RFMix, LAMP-LD | Determines ancestral origin of specific genomic regions; maps ancestry-aware associations [89] |
| Protein Interaction Networks | HumanNet, CORUM databases | Identifies functional pathways and complexes; reveals network-level synthetic lethality [87] |
| Drug-Resistant Cell Lines | DU145-TxR (paclitaxel-resistant) | Models therapeutic resistance; tests combination therapies and resistance mechanisms [91] |
| cGP Modeling Platforms | Virtual Physiological Rat project | Integrates genetic variation with multi-scale physiological models; predicts phenotypic outcomes [86] |
| Resistance Mutation Detection | DrugTargetSeqR, saturation mutagenesis | Identifies coding resistance mutations; confirms small molecule on-target engagement [88] |
Benchmarking Performance and Establishing Clinical Utility
Troubleshooting Guides
Guide 1: Addressing the Performance Drop Between Internal and External Validation
Problem: Your machine learning model shows high performance during internal validation (e.g., AUC >0.90) but suffers a significant performance drop when evaluated on an external dataset from a different clinical center.
Explanation: A large performance gap between internal and external validation often signals overfitting or a lack of generalizability. This means your model has learned patterns that are too specific to your development dataset and do not transfer well to new, slightly different populations or settings [55].
Solution Steps:
Re-examine Your Validation Method: For small to medium-sized datasets, avoid a simple random split of your data into training and test sets.
- Recommended Action: Implement bootstrapping techniques for internal validation. This method involves repeatedly drawing samples with replacement from your original dataset to create multiple training and validation sets, providing a more honest assessment of model performance and reducing optimism [92].
- Alternative for Multicenter Data: If your development data comes from multiple centers, use an "internal-external" cross-validation procedure. Here, you iteratively leave out one center as the validation set and train the model on the rest. The final model is then built on the entire dataset. This gives a better impression of how your model might perform in new, unseen locations [92].
Conduct a Sensitivity Analysis: Test how sensitive your model's predictions are to small changes or noise in the input data.
Check for Data Leakage: Ensure that no information from the future or from the validation/test set has accidentally been used during the model's training phase.
- Action: Use interpretability methods like SHAP to analyze which features are most important for your model's predictions. If a feature has an implausibly high importance, it might be a leaky variable. Review your data processing pipeline to ensure all features are generated before the event you are predicting [93].
Guide 2: Choosing Between Diagnostic and Predictive Models for Drug Resistance
Problem: You are unsure whether to build a model that diagnoses current drug resistance from clinical samples or one that predicts a patient's future risk of developing drug-resistant infections.
Explanation: Diagnostic and predictive models serve different purposes and, as the evidence shows, have different performance expectations. Understanding this distinction is crucial for setting realistic project goals and interpreting your results [55].
Solution Steps:
Define the Clinical Task:
- Diagnostic Model: Use this if your goal is to identify existing drug resistance, typically using data from a single point in time (e.g., genetic sequences, imaging features from a CT scan). These models generally achieve higher accuracy [55].
- Predictive Model: Use this for risk stratification, forecasting which patients with a susceptible infection are likely to develop drug resistance in the future. This often uses longitudinal data and has more moderate accuracy but is highly valuable for preventative care [55].
Select the Appropriate Algorithm:
- For Diagnostic Tasks: Consider using Deep Learning (DL) models. A meta-analysis found that DL-based diagnostic models for drug-resistant tuberculosis (DR-TB) consistently outperformed traditional machine learning across key metrics (AUC 0.97 vs. 0.89) [55].
- For Predictive Tasks: Traditional ML models or models that integrate clinical features (e.g., demographic information, treatment history) can be very effective and are often more interpretable [55].
Align Performance Metrics with the Task: The expected performance, measured by the Area Under the Curve (AUC), is different for these two tasks. Use the table below to set realistic benchmarks for your project.
Table 1: Expected Performance for Diagnostic vs. Predictive Models in DR-TB
| Model Task | Typical Pooled AUC (Internal Validation) | Typical Pooled AUC (External Validation) | Key Applications |
|---|---|---|---|
| Diagnostic Model | 0.94 - 0.95 | 0.85 | Identifying current resistance from genomic or imaging data [55]. |
| Predictive Model | 0.87 - 0.88 | 0.85 | Early risk stratification using clinical and historical data [55]. |
Frequently Asked Questions (FAQs)
FAQ 1: What is the single most important practice for ensuring my model is robust?
Answer: The most critical practice is implementing a rigorous internal validation framework before any external testing. Relying solely on a single train-test split, especially in small datasets, gives a severely optimistic performance estimate. Always use resampling methods like bootstrapping or cross-validation to get a realistic view of your model's performance and to temper over-optimistic expectations before moving to external validation [92].
FAQ 2: My external validation performance is poor. Should I retrain the model on the combined internal and external data?
Answer: Not necessarily. First, you must diagnose the cause of the poor performance. Combine the datasets only if you have determined that the difference in data distribution between the two sets is minimal and does not represent a fundamental shift in the underlying population or data collection methods. Retraining on combined data without this analysis can simply create a model that is overfitted to a non-representative aggregate dataset. Always prioritize understanding why the performance dropped before deciding on a solution [93] [92].
FAQ 3: How can I understand why my model makes different predictions on external data?
Answer: To understand model behavior differences, you can use feature-based comparison frameworks like ModelDiff. This approach traces model predictions back to the training data to identify which specific training examples (and their features) each model relies on. For instance, it can reveal that a model trained with ImageNet pre-training spuriously uses "human faces in the background" for classification, while a model trained from scratch does not. This helps you identify and verify the specific features causing the performance discrepancy [95].
Experimental Protocols and Data
Detailed Methodology: Internal-External Cross-Validation
This protocol is recommended for developing robust prediction models when data from multiple centers are available [92].
- Data Preparation: Pool your dataset, ensuring it includes a identifier for the source (e.g., hospital, study site, or time period).
- Iterative Validation: For each unique source (e.g., Hospital A): a. Training Set: Temporarily exclude all data from Hospital A. b. Model Development: Train your model on the remaining data from all other hospitals. c. Validation Set: Use the held-out data from Hospital A to validate the model. Record performance metrics (AUC, sensitivity, specificity).
- Repetition: Repeat Step 2 for every hospital or source in your dataset.
- Performance Summary: Aggregate the performance metrics from all iterations to get a realistic estimate of how your model will perform in new, unseen locations.
- Final Model Training: After this validation cycle, train your final model on the entire pooled dataset before deployment.
The following table consolidates key quantitative findings from a systematic review and meta-analysis on machine learning for drug-resistant tuberculosis (DR-TB), highlighting the critical difference between internal and external validation performance [55].
Table 2: Consolidated Performance Metrics for ML Models in DR-TB Diagnosis and Prediction
| Model Category | Key Comparison | Pooled AUC | Key Takeaway |
|---|---|---|---|
| Overall Analysis | Diagnostic Models vs. Predictive Models | 0.94 vs. 0.87 | Diagnostic models demonstrate superior discriminative ability [55]. |
| Diagnostic Models | Deep Learning (DL) vs. Traditional ML | 0.97 vs. 0.89 | DL-based models significantly outperform traditional ML for diagnostic tasks [55]. |
| Diagnostic Models | Internal vs. External Validation | 0.95 vs. 0.85 | A significant performance drop is common when models face external data [55]. |
| Predictive Models | Internal vs. External Validation | 0.88 vs. 0.85 | Predictive models show less performance degradation in external validation [55]. |
Diagrams and Workflows
Internal-External Validation Workflow
Diagnosing External Validation Performance Gaps
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Tools and Frameworks for Model Validation in Drug Resistance Research
| Tool / Reagent | Type | Primary Function in Validation |
|---|---|---|
| R / Python (scikit-learn) | Programming Language / Library | Provides core statistical functions and algorithms for implementing bootstrap validation, cross-validation, and calculating performance metrics (AUC, sensitivity, specificity) [55] [92]. |
| Deepchecks | Open-Source Validation Tool | Offers automated checks for data integrity, data drift, model performance, and leakage. Validates models across research, deployment, and production phases [94]. |
| SHAP (SHapley Additive exPlanations) | Interpretability Library | A model-agnostic tool for identifying feature importance and detecting potential biases or leakage by explaining individual predictions [93]. |
| TensorFlow / PyTorch | Deep Learning Framework | Flexible frameworks for building and training complex diagnostic models, including deep learning architectures which have shown high performance in DR-TB identification [55] [96]. |
| ModelDiff Framework | Comparison Framework | Enables fine-grained, feature-based comparisons of models trained with different algorithms to understand differences in their behavior on external data [95]. |
Comparative Analysis of Standalone Tools and Web-Based Platforms (e.g., ResFinder, CARD, MTB++)
Troubleshooting Guides and FAQs
Frequently Asked Questions
Q1: My analysis in ResFinder found no resistance genes, but the phenotypic test shows resistance. What could be wrong? This is a common issue that can stem from several sources:
- Incorrect Database or Settings: You may be using a database that does not include the specific resistance mechanism for your bacterial species. For instance, ResFinder uses separate databases for acquired genes and for chromosomal point mutations in specific species [97]. Ensure you have selected the correct species and are using the most recent database version.
- Analysis Parameters Are Too Strict: The default settings in ResFinder (e.g., minimum identity and length coverage) are designed for high specificity but may miss divergent genes. You can adjust these parameters to be more sensitive, for example, by lowering the minimum identity to 30% and minimum length to 20%, but be aware that this may also increase unspecific hits [98].
- Novel or Undiscovered Mechanism: The resistance may be conferred by a gene or chromosomal mutation not yet present in the database. In such cases, using a tool like ARG-ANNOT, which allows for detection with lower similarity thresholds, might be more effective for identifying putative new resistance genes [98].
Q2: What are the key differences between ResFinder and MTB++ for predicting drug resistance in Mycobacterium tuberculosis? The primary difference lies in their methodological approach, which impacts their use cases.
- ResFinder primarily relies on alignment methods (BLAST+ or KMA) to identify known acquired antimicrobial resistance genes (ARGs) and specific chromosomal mutations from a curated database [99]. It is a general tool for many bacterial species.
- MTB++ is a species-specific tool that uses machine learning models (Logistic Regression and Random Forest) trained on k-mers (short DNA sequences) from whole-genome data. This allows it to identify complex patterns and potential novel genetic associations beyond known catalogued genes, potentially offering higher predictive accuracy for MTB [100].
The table below summarizes a quantitative comparison of features:
Table 1: Key Features of Antimicrobial Resistance Prediction Tools
| Feature | ResFinder | MTB++ | ARG-ANNOT |
|---|---|---|---|
| Core Methodology | Alignment-based (BLAST+, KMA) [101] [99] | Machine Learning (k-mer based) [100] | Alignment-based [98] |
| Primary Use Case | Identification of acquired ARGs & known point mutations [99] | Drug resistance profiling for M. tuberculosis [100] | Discovery of putative new ARGs [98] |
| Key Strength | High specificity with default settings; phenotype prediction for some species [98] [99] | Can identify novel resistance associations not in standard databases [100] | Better for detecting genes with low similarity to known references [98] |
| Typical Input | Raw reads, assembled genomes/contigs [101] [97] | Whole-genome sequencing data [100] | Assembled genomes [98] |
| Customizable Thresholds | Yes (Minimum Identity %, Minimum Length %) [101] | No (Uses pre-trained models) | Information not specified in search results |
| Phenotype Prediction | Yes, for selected bacterial species [99] | Yes, for 13 anti-TB drugs and 3 drug families [100] | Information not specified in search results |
Q3: I am getting conflicting resistance predictions from different tools on the same dataset. How should I proceed? Conflicting results highlight the importance of understanding each tool's methodology and database.
- Verify Your Input Data: Ensure the quality of your input genome assembly or raw reads is high. Low coverage or poor assembly can lead to missing genes.
- Cross-Reference the Databases: Identify the specific genes or mutations each tool is reporting. Check the version of the database each tool uses. A gene may be present in one tool's database but not in another's.
- Check for Chromosomal Mutations: For species like M. tuberculosis, resistance is often driven by chromosomal mutations. A tool like ResFinder with PointFinder or Resistance Sniffer may be necessary to detect these, as a gene-centric tool might return no hits [97] [102].
- Consult the Literature: Search for published validation studies. For example, one study noted that ResFinder showed 99.74% concordance with phenotypic susceptibility tests for certain bacterial species, which can inform your confidence in its predictions [98].
Troubleshooting Common Experimental Issues
Issue: Low Concordance Between Genotypic Prediction and Phenotypic Results
| Step | Action | Rationale |
|---|---|---|
| 1 | Confirm the phenotypic AST results are reliable and follow standardized guidelines (e.g., EUCAST, CLSI). | Poor reproducibility of phenotypic testing is a known challenge and a primary source of discrepancy [99]. |
| 2 | Verify the tool's settings and database. Use the most recent database and ensure the correct bacterial species is selected. | Older databases lack newly discovered genes. Species-specific mutation databases are critical for accurate prediction [97] [99]. |
| 3 | Re-analyze data with adjusted, more sensitive parameters (e.g., lower identity and length thresholds). | Default settings are conservative. Divergent resistance genes may be missed if thresholds are too high [98]. |
| 4 | Use a combination of tools (e.g., ResFinder for known genes, MTB++ for MTB-specific novel insights) and consolidate the results. | Different tools have complementary strengths. A combined approach provides a more comprehensive resistance profile [98] [100]. |
| 5 | Manually investigate the genomic region. Look for premature stop codons, frameshifts, or promoter mutations that might inactivate a detected resistance gene. | The presence of a gene does not guarantee its expression or functionality. |
Workflow for Resolving Prediction-Phenotype Discrepancy
The Scientist's Toolkit: Essential Research Reagents & Materials
The following table details key resources used in computational analysis of antimicrobial resistance.
Table 2: Essential Resources for AMR Genotype Prediction Experiments
| Item Name | Function / Application | Specifications / Notes |
|---|---|---|
| ResFinder Platform | Web-based identification of acquired antimicrobial resistance genes and chromosomal mutations [97] [99]. | Accepts both raw reads and assembled genomes. Includes PointFinder for species-specific mutations. |
| MTB++ Classifier | A machine learning-based tool for predicting antibiotic resistance in Mycobacterium tuberculosis [100]. | Employs Logistic Regression and Random Forest models on k-mer data. Available as a standalone GitHub repository. |
| BV-BRC Database | A large-scale public repository of bacterial genomic and associated meta-data [100]. | Hosts over 27,000 MTB isolates. Used for retrieving data for benchmarking and large-scale analysis. |
| CRyPTIC Dataset | A global collection of MTB isolates with whole-genome sequencing and phenotypic drug susceptibility testing data [100]. | Contains data for 13 antibiotics. Serves as a gold-standard dataset for training and validating predictive models. |
| KMA Alignment Tool | A software for rapidly and precisely aligning raw sequencing reads against redundant databases [99]. | Used in the ResFinder pipeline for direct analysis of raw reads, bypassing the need for resource-intensive assembly. |
Detailed Experimental Protocol: Benchmarking Tool Accuracy
This protocol outlines the steps for comparing the prediction accuracy of different AMR detection tools against phenotypic reference data, a key experiment for thesis research.
Objective: To evaluate and compare the predictive performance of ResFinder, MTB++, and other relevant tools using a dataset of bacterial genomes with accompanying phenotypic Antimicrobial Susceptibility Testing (AST) data.
Materials:
- A curated set of bacterial whole-genome sequences (e.g., from BV-BRC or CRyPTIC) [100].
- Corresponding, high-quality phenotypic AST results for the same isolates.
- Access to the web-based or command-line versions of the tools to be evaluated (ResFinder, MTB++, etc.).
- A computational environment with sufficient processing power and storage.
Methodology:
- Data Curation and Preparation:
- Select a benchmark dataset of genomic isolates (e.g., N = 500). Ensure phenotypic data is available for key antibiotics.
- Split the data into training and test sets if using a tool like MTB++ that requires training. For tools like ResFinder that use a static database, this is not necessary.
- For tools requiring assembled genomes, perform de novo assembly on the raw reads using a standardized assembler like SPAdes [99].
Genotypic Resistance Prediction:
- Using ResFinder: Submit assembled genomes or raw reads to the ResFinder webserver or run the standalone tool. Use default parameters first, then optionally with sensitive parameters (e.g., 30% identity, 20% length). Record all identified acquired genes and point mutations, as well as the predicted phenotype if available [101] [99].
- Using MTB++: Run the pre-trained MTB++ classifier on the genomic data. The tool will output a prediction (resistant/susceptible) for each antibiotic drug based on its k-mer and machine learning model [100].
- Repeat this process for all tools in the comparison.
Data Analysis and Validation:
- Create a concordance table comparing the genotypic prediction (Resistant/Susceptible) from each tool to the phenotypic AST result (the gold standard).
- Calculate performance metrics for each tool and each antibiotic, including:
- Sensitivity: Ability to correctly predict resistance.
- Specificity: Ability to correctly predict susceptibility.
- Accuracy: Overall proportion of correct predictions.
- Cohen's Kappa (κ): Measure of agreement between the tool's prediction and the phenotype, accounting for chance [100].
Workflow for Benchmarking AMR Tools
Frequently Asked Questions (FAQs)
Q1: What does the F1-score tell me that accuracy does not? Accuracy can be misleading with class-imbalanced datasets, which are common in drug resistance studies (e.g., where susceptible cases far outnumber resistant ones). The F1-score provides a balanced measure by combining precision (confidence in positive predictions) and recall (ability to find all positive cases), thus giving a more reliable view of model performance on the minority class [103] [104] [105].
Q2: My model has a high AUC but a low F1-score. Is this possible, and what does it mean? Yes, this is a common scenario. A high AUC (e.g., >0.9) indicates that your model has a strong overall ability to distinguish between resistant and non-resistant cases across all possible thresholds [103] [106]. However, a low F1-score suggests that at the specific classification threshold you have chosen, the model is not achieving a good balance between precision and recall. You may need to adjust the decision threshold to better suit your research goals [107].
Q3: When should I prioritize the F1-score over AUC-ROC? Prioritize the F1-score (and the Precision-Recall curve) when your primary concern is the correct prediction of the positive class (e.g., drug-resistant mutations) and this class is a minority in your dataset. The AUC-ROC can be overly optimistic in such imbalanced scenarios [103] [107]. If you need a single threshold-independent measure of overall class separation and the dataset is roughly balanced, AUC-ROC is a good choice [105].
Q4: How is Cohen's Kappa different from simple percent agreement? Percent agreement does not account for the agreement that could happen purely by chance. Cohen's Kappa factors in this chance agreement, making it a more robust and conservative measure of inter-rater reliability, such as agreement between different human annotators or between a model and a gold standard [108] [109].
Q5: What is an acceptable value for Cohen's Kappa in a research context? While interpretations vary, a common guideline is provided in the table below [108]. For high-stakes research like drug resistance prediction, most practitioners would seek values in the "Substantial" or "Almost Perfect" range to ensure reliable annotations and model predictions.
| Kappa Value | Level of Agreement |
|---|---|
| ≤ 0 | None |
| 0.01 - 0.20 | Slight |
| 0.21 - 0.40 | Fair |
| 0.41 - 0.60 | Moderate |
| 0.61 - 0.80 | Substantial |
| 0.81 - 1.00 | Almost Perfect |
Troubleshooting Guides
Problem: Consistently Low F1-Score A low F1-score indicates a poor balance between precision and recall.
- Potential Causes & Solutions:
- Cause: Severe class imbalance is skewing the model's predictions.
- Solution: Investigate techniques for handling imbalanced data, such as oversampling the minority class (drug-resistant cases), undersampling the majority class, or using algorithmic approaches that assign higher costs to misclassifying the minority class [105].
- Cause: The default decision threshold (usually 0.5) is suboptimal for your specific problem.
- Solution: Generate a Precision-Recall curve and experiment with different thresholds to find one that better balances the trade-off between false positives and false negatives for your application [110].
- Cause: The model may be fundamentally struggling to learn the patterns of the minority class.
- Solution: Perform error analysis on the confusion matrix to see if the issue is predominantly too many false positives (low precision) or too many false negatives (low recall). Use this insight to guide feature engineering or model selection [104].
- Cause: Severe class imbalance is skewing the model's predictions.
Problem: High AUC but Poor Clinical Utility Your model achieves a high AUC (e.g., 0.95) in validation, but when deployed on a new dataset, its performance drops significantly.
- Potential Causes & Solutions:
- Cause: Overfitting to the training data or dataset shift, where the new data has a different distribution from the training data.
- Solution: Always perform external validation on a completely held-out dataset from a different source or cohort. Regularize your model during training and ensure your training data is representative of real-world scenarios [55].
- Cause: Over-reliance on the AUC value alone. A high AUC does not guarantee high performance at a specific, clinically relevant threshold.
- Solution: Don't just report the AUC. Examine the ROC curve closely and identify the optimal operating point based on the clinical cost of false positives and false negatives. Use the Youden index to help select a threshold that maximizes both sensitivity and specificity [106].
- Cause: Overfitting to the training data or dataset shift, where the new data has a different distribution from the training data.
Problem: Low Cohen's Kappa Despite High Accuracy Your model and a gold standard test have high percent agreement, but the Cohen's Kappa value is low.
- Potential Causes & Solutions:
- Cause: High prevalence of one class. If one outcome (e.g., "drug-susceptible") is very common, the probability of chance agreement is high. Kappa corrects for this, and a low value indicates that the observed agreement is not much better than chance [108] [109].
- Solution: This is often a feature of the dataset, not a flaw in the metric. Rely on Kappa over percent agreement in this situation, as it gives a more truthful picture of reliability. Consider also reporting the confusion matrix to provide a complete picture.
- Cause: High prevalence of one class. If one outcome (e.g., "drug-susceptible") is very common, the probability of chance agreement is high. Kappa corrects for this, and a low value indicates that the observed agreement is not much better than chance [108] [109].
The following tables provide standard interpretations for AUC and F1-Score values to help you benchmark your model's performance.
Table 1: Interpreting the Area Under the Curve (AUC) [106]
| AUC Value | Interpretation |
|---|---|
| 0.9 - 1.0 | Excellent discrimination |
| 0.8 - 0.9 | Considerable (Good) discrimination |
| 0.7 - 0.8 | Fair discrimination |
| 0.6 - 0.7 | Poor discrimination |
| 0.5 - 0.6 | Fail (No better than chance) |
Table 2: Interpreting the F1-Score [105]
| F1-Score Value | Interpretation |
|---|---|
| 0.9 - 1.0 | Very high performance |
| 0.8 - 0.9 | Strong performance |
| 0.7 - 0.8 | Good performance |
| 0.6 - 0.7 | Moderate performance |
| < 0.6 | Low performance |
Experimental Protocols from Cited Literature
Protocol 1: Deep Learning for Synergistic Drug Combination Prediction (SYNDEEP) This protocol outlines the methodology for developing a deep neural network to predict synergistic anti-cancer drug combinations [111].
- Data Compilation: Collect a dataset of drug pairs tested on cancer cell lines, with synergy labels. The NCI-ALMANAC database was used in the original study.
- Feature Engineering: Generate a comprehensive feature vector for each drug pair. This includes:
- Drug physicochemical properties.
- Genomic data of the cancer cell lines (e.g., gene expression, mutation).
- Network biology features (e.g., protein-protein interaction, protein-metabolite interaction similarities).
- Model Training & Validation:
- Implement a deep neural network (DNN) architecture.
- Compare the DNN against other machine learning models (e.g., Random Forest, SVM, Gradient Boosting) as baselines.
- Evaluate model performance using tenfold cross-validation, reporting key metrics including Accuracy, Sensitivity, Specificity, Precision, F1-score, and AUC.
Protocol 2: Meta-Analysis of ML for Drug-Resistant Tuberculosis Diagnosis This protocol describes a systematic approach to evaluating machine learning models for diagnosing drug-resistant tuberculosis, as per a recent meta-analysis [55].
- Study Selection: Search electronic databases (PubMed, Embase, etc.) for studies that develop or validate ML models for DR-TB diagnosis. Apply pre-defined inclusion/exclusion criteria.
- Data Extraction & Risk of Bias Assessment: Use a standardized template to extract data from included studies, including model type, task (diagnosis vs. prediction), and performance metrics. Assess study quality using the PROBAST tool.
- Statistical Synthesis: Use a bivariate mixed-effects model to pool sensitivity and specificity estimates. Pool AUC values from the included studies separately for diagnostic and predictive models.
- Subgroup Analysis: Stratify the analysis by key factors such as model type (Deep Learning vs. Traditional ML) and validation type (internal vs. external) to investigate sources of heterogeneity.
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials for Computational Experiments in Drug Resistance
| Item / Solution | Function in Research |
|---|---|
| Structured Databases (e.g., NCI-ALMANAC, CGD) | Provide curated, high-quality datasets of drug responses and genomic information for model training and validation [111]. |
| Genomic Feature Extraction Tools | Generate numerical features from raw genomic data (e.g., mutation status, gene expression profiles) that serve as input for machine learning models [111]. |
| scikit-learn Library (Python) | Provides open-source implementations for calculating all key performance metrics, including F1-score, and for building baseline machine learning models [104]. |
| Deep Learning Frameworks (e.g., TensorFlow, PyTorch) | Enable the construction, training, and evaluation of complex neural network models, such as the DNN used in the SYNDEEP protocol [111]. |
| Statistical Software (e.g., R, Python with SciPy) | Essential for performing advanced statistical analyses, including meta-analysis using bivariate models and calculating confidence intervals for AUC [55] [106]. |
Metric Relationships and Workflow
The following diagram illustrates the logical relationship between different metrics, confusion matrix components, and the model development workflow.
Metric Calculation Workflow
Choosing the Right Metric
This diagram provides a decision pathway to help you select the most appropriate primary metric for your study based on its specific focus and data characteristics.
Metric Selection Guide
Technical Support Center
Troubleshooting Guides
Guide 1: Addressing Poor Generalization of a Drug Resistance Prediction Model
Problem: A computational model for predicting antibiotic resistance shows high accuracy during development but performs poorly when applied to new clinical isolates.
Diagnosis Steps:
- Check for Overfitting: Compare the model's performance on the training dataset versus a held-out test set. A significant drop in performance on the test set indicates overfitting [112].
- Assess Dataset Shift: Evaluate if the data distribution (e.g., prevalence of resistance genes, bacterial species) in the new clinical isolates differs from the development dataset.
- Verify Calibration: Check if the predicted probabilities of resistance align with the observed resistance rates in the new population. A model can be discriminatory but poorly calibrated [112] [113].
- Review Data Quality: Ensure that the genomic sequencing quality and preprocessing pipelines for the new data match those used during model development.
Solutions:
- Apply Regularization: Use penalized estimation methods like LASSO or ridge regression during model training to reduce model complexity and prevent overfitting [112].
- Update the Model: Retrain the model on a dataset that includes recent clinical isolates from the target population to improve transportability [113].
- Perform Recalibration: Apply methods like Platt scaling or isotonic regression to adjust the model's output probabilities to better match the observed outcomes in the new setting [112].
Guide 2: Handling Missing Data in Clinical Prediction Model Development
Problem: A significant portion of patient records in a dataset for a cancer drug resistance model lacks key predictor variables, such as specific genomic mutations or comorbidities.
Diagnosis Steps:
- Analyze the Pattern: Determine if the data is missing completely at random (MCAR), missing at random (MAR), or missing not at random (MNAR). This influences the choice of handling method.
- Quantify the Impact: Assess how the missing data affects the sample size for model development and whether it introduces selection bias.
Solutions:
- Multiple Imputation: This is the preferred method for handling missing data in prediction research. It creates several complete datasets, analyzes each one, and pools the results, providing valid statistical inferences [112].
- Avoid Complete-Case Analysis: Discarding records with any missing data can lead to biased estimates and loss of statistical power, and is generally not recommended [112].
- Incorximate Missingness as a Feature: In some cases, the pattern of missingness itself might be informative and can be included in the model as a separate indicator variable.
Frequently Asked Questions (FAQs)
Q1: What are the key steps to ensure my clinical prediction model is ready for implementation? A1: Moving from a computational model to clinical use requires a rigorous, multi-step process [112] [113]:
- Clear Definition: Precisely define the model's aim, target population, outcome, and intended user.
- Robust Development & Internal Validation: Use a large enough sample size and appropriate statistical methods to develop the model. Then, use internal validation techniques like bootstrapping or cross-validation to correct for optimism in performance estimates [112].
- External Validation: Test the model's performance on entirely new data, ideally from a different location or population, to assess its generalizability [112] [113].
- Impact Assessment & Implementation: Integrate the model into a clinical workflow (e.g., within a hospital information system or as a web application) and evaluate its impact on clinical decision-making and patient outcomes [113] [114].
Q2: Our model successfully identifies patients at high risk for multidrug-resistant infections. How can we demonstrate its value for clinical reimbursement? A2: Payer reimbursement depends on demonstrating both clinical utility and economic value.
- Generate Clinical Evidence: Conduct studies showing that using your model leads to measurable improvements in patient outcomes, such as reduced mortality, fewer complications, or shorter hospital stays. The AI model for colorectal cancer surgery, for example, demonstrated a significant reduction in complications [114].
- Perform Health Economic Modeling: Model the cost-effectiveness of your intervention. Show that the costs of implementing the model are offset by savings from improved outcomes, such as reduced use of broad-spectrum antibiotics or shorter hospital stays. Short-term health economic modeling was a key component in demonstrating the value of the AI-based surgical decision tool [114].
Q3: What are some emerging strategies to combat antibiotic resistance that we can target with new prediction tools? A3: Beyond traditional antibiotic discovery, novel strategies are emerging that provide new avenues for predictive modeling [115]:
- Immuno-antibiotics: These compounds target bacterial pathways like the non-mevalonate (MEP) pathway for isoprenoid biosynthesis, simultaneously inhibiting the bacteria and engaging the host immune system.
- Inhibition of SOS Response: The SOS pathway is a biochemical network that bacteria use to repair DNA damage. Inhibiting it can prevent the evolution and spread of resistance mechanisms.
- Targeting Hydrogen Sulfide Production: Hydrogen sulfide acts as a universal defense mechanism in bacteria, and inhibiting its production can sensitize bacteria to existing antibiotics.
Experimental Protocols for Key Methodologies
Protocol 1: Development and Validation of a Clinical Prediction Model
This protocol follows best practices outlined in clinical prediction model guidance [112].
Objective: To develop and validate a multivariate model for predicting the risk of a specific drug-resistant infection.
Methods:
- Data Source Selection: Use a dataset with clearly defined predictors (e.g., patient demographics, prior antibiotic use, genomic data) and a confirmed outcome (e.g., culture-positive resistant infection).
- Sample Size Consideration: Ensure an adequate number of outcome events relative to the number of predictor parameters (Events per Predictor, EpP) to minimize overfitting. A common rule of thumb is a minimum EpP of 10-20.
- Model Development: Use multiple imputation for missing data. Consider using machine learning algorithms or logistic regression with variable selection methods like LASSO for high-dimensional data (e.g., genomic data).
- Internal Validation: Apply bootstrapping to quantify and correct for optimism in model performance metrics (e.g., AUC, calibration slope).
- External Validation: Validate the final model on a temporally or geographically distinct dataset.
Workflow Visualization:
Protocol 2: CRISPR-Based Functional Genomics for Resistance Mutation Validation
This protocol is derived from advances in genomic technologies for personalized medicine [116].
Objective: To functionally validate a computationally predicted genetic mutation as a driver of resistance to a targeted cancer therapy.
Methods:
- Cell Line Selection: Choose a relevant cancer cell line (e.g., from NSCLC for an EGFR mutation) that is sensitive to the drug in question.
- CRISPR-Cas9 Gene Editing: Design guide RNAs (gRNAs) to introduce the specific point mutation of interest into the endogenous gene locus in the sensitive cell line.
- Validation of Editing: Use Sanger sequencing or next-generation sequencing (NGS) to confirm the successful introduction of the mutation.
- Drug Sensitivity Assays: Treat the engineered cell line and the wild-type control with the targeted therapy. Measure cell viability (e.g., using MTT or CellTiter-Glo assays) to confirm that the introduced mutation confers resistance.
Workflow Visualization:
Data Presentation
Table 1: Key Genomic Technologies for Predicting Drug Resistance
This table summarizes technologies highlighted in genomic profiling and antibiotic resistance research for identifying and characterizing resistance mechanisms [116] [115].
| Technology | Primary Function | Key Application in Resistance Research |
|---|---|---|
| Next-Generation Sequencing (NGS) | High-throughput sequencing of DNA/RNA. | Comprehensive identification of known and novel resistance mutations in bacteria and cancer genomes [116]. |
| CRISPR-Cas9 | Precise gene editing. | Functional validation of predicted resistance mutations by introducing them into model systems [116]. |
| ctDNA-based Profiling | Detection of tumor DNA in blood. | Non-invasive monitoring of evolving resistance mutations in cancer during treatment [116]. |
| AI/Machine Learning | Pattern recognition in complex datasets. | Integrating multi-omics data to predict resistance risk and optimize treatment selection [116] [114]. |
Table 2: Performance Metrics for a Validated Clinical Prediction Model
This table illustrates key metrics used to evaluate the performance of a clinical prediction model, as discussed in prediction model guides [112] [114].
| Metric | Description | Target Value (Example) |
|---|---|---|
| Area Under the Curve (AUC) | Measures model's ability to discriminate between patients with and without the outcome. | >0.75 is acceptable; >0.8 is good [114]. |
| Calibration Slope | Agreement between predicted probabilities and observed outcomes. A slope of 1 indicates perfect calibration. | ~1.0 [112]. |
| Brier Score | Overall measure of predictive accuracy (lower is better). | 0 - 0.25, lower is better [114]. |
| Sensitivity & Specificity | Proportion of true positives and true negatives correctly identified. | Dependent on clinical context and chosen risk threshold. |
The Scientist's Toolkit: Research Reagent Solutions
This table details essential materials and their functions for experiments in drug resistance research, compiled from the provided search results [116] [115] [117].
| Item | Function |
|---|---|
| Next-Generation Sequencer | Enables comprehensive genomic profiling to identify mutations associated with drug resistance in bacterial and cancer genomes [116]. |
| CRISPR-Cas9 System | Validates the functional role of specific genetic mutations in conferring a resistance phenotype through precise gene editing [116]. |
| SOS Response Inhibitor | A chemical compound that targets the bacterial SOS response pathway, potentially preventing the emergence of resistance [115]. |
| Immuno-antibiotic Compound | A novel class of antibiotic that targets bacterial biosynthesis pathways (e.g., MEP pathway) while also engaging host immunity [115]. |
| Plasmid DNA Vectors | Used to study horizontal gene transfer of resistance genes between bacteria, a major route for spreading resistance [117]. |
Evidence Standards for Clinical Utility and Integration into Practice Guidelines
FAQs: Understanding Clinical Utility and Evidence Standards
Q1: What is clinical utility and how does it differ from clinical validity?
A1: Clinical utility refers to the likelihood that a test's results will inform clinical decisions that lead to improved patient outcomes. It specifically examines whether using a test prompts interventions that result in better health outcomes. In contrast, clinical validity determines how accurately and reliably a test predicts a patient's clinical status, measured through clinical sensitivity, specificity, predictive values, and likelihood ratios. Clinical utility depends on analytical and clinical validity—a test with suboptimal analytical performance may report false results, impacting diagnosis and treatment decisions, thereby undermining clinical utility [118].
Q2: What evidence frameworks are used to evaluate diagnostic tests?
A2: Several established frameworks evaluate diagnostic tests:
- ACCE Model: Developed by the CDC, this framework systematically evaluates Analytical validity, Clinical validity, Clinical utility, and Ethical, legal, and social implications. The ACCE model defines clinical utility as the test's impact on patient outcome improvements and value added to clinical decision-making [118].
- Fryback and Thornbury (FT) Model: This hierarchical model includes efficacies covering analytical validity, clinical validity, and clinical utility. It places cost-benefit and cost-effectiveness analysis under a separate hierarchy termed "societal efficacy" [118].
- Stakeholder-Specific Considerations: Different stakeholders (laboratories, physicians, payers, patients) may value different endpoints. Clinical utility can encompass clinical outcomes, decision-making, workflow, costs, and even emotional, social, cognitive, and behavioral impacts on patient wellbeing [118].
Q3: What are the preferred study designs for demonstrating clinical utility?
A3: For high-risk clinical decisions in oncology and other serious conditions, Randomized Controlled Trials (RCTs) are the preferred gold standard for demonstrating clinical utility. RCTs provide the highest level of evidence that a test improves patient outcomes [119]. However, alternative designs may be acceptable under specific circumstances:
- Prospective-Retrospective Studies: Using banked biospecimens from previous trials can be valid if specific conditions are met, including assay validation and pre-specified analysis plans [119].
- Prospective Observational Studies: These can be suitable when RCTs are not feasible, but they must be carefully designed to minimize bias [119].
- Virtual Patient RCTs: This innovative approach uses randomized physicians caring for virtual patients to demonstrate how a diagnostic test changes clinician behavior. It is a cost-effective alternative to traditional patient-level RCTs for showing utility in influencing treatment decisions [120].
Q4: How can multivariable regression models improve the grading of drug resistance mutations?
A4: Traditional univariate methods (like the WHO's "SOLO" method) assess mutations in isolation. In contrast, multivariable logistic regression models can analyze the association between multiple co-occurring mutations and resistance phenotypes simultaneously. This approach can [10]:
- Increase Sensitivity: Detect more genuine resistance-associated variants, improving the sensitivity of genetic prediction for drugs like ethambutol and clofazimine.
- Quantify Mutational Effects: Estimate the effect size of individual mutations on resistance, conditional on the presence of other mutations.
- Handle Complex Genotypes: Account for potential additive effects of multiple mutations in a single isolate, which univariate methods often must exclude from analysis.
Troubleshooting Guides for Common Research Scenarios
Scenario 1: Inconsistent Correlation Between Genotype and Phenotype in Drug Resistance Studies
Problem: Your experimental data shows that a known resistance mutation does not consistently correlate with the resistant phenotype across your sample set.
Investigation & Resolution:
| Step | Action | Rationale & Technical Details |
|---|---|---|
| 1. Check Data Quality | Re-inspect sequencing data for the variant. Check the allele frequency (AF); is it near the heterozygous call range? Consider excluding variants with AF > 0.25 and ≤ 0.75 for clearer binary (present/absent) analysis [10]. | Low AF or ambiguous calls may indicate mixed populations, sequencing errors, or clonal heterogeneity, obscuring the true genotype-phenotype relationship. |
| 2. Analyze Genetic Context | Use multivariable regression to test for the presence of other known resistance mutations in the same sample. Do not analyze mutations in isolation [10]. | The effect of a primary mutation might be masked, enhanced, or dependent on other mutations in the genome (epistasis). Regression controls for these co-occurring variants. |
| 3. Investigate Compensatory Mutations | Look for mutations in genes that might compensate for fitness costs associated with the primary resistance mutation. For example, in M. tuberculosis, seek compensatory mutations in ahpC associated with isoniazid resistance [10]. | Some mutations confer resistance at a fitness cost. Secondary "compensatory" mutations can restore fitness, allowing the resistance mutation to persist and spread. |
| 4. Consider Hypersusceptibility | Test if other genomic polymorphisms in your samples are linked to drug hypersusceptibility. A resistance mutation's effect might be counteracted by a separate hypersusceptibility variant [10]. | The net phenotypic resistance can be the aggregate result of multiple genetic factors with opposing effects on drug susceptibility. |
Scenario 2: Failing to Secure Payer Coverage Due to Lack of Demonstrated Clinical Utility
Problem: Your diagnostic test has strong analytical and clinical validity, but payers deny coverage, citing insufficient evidence of clinical utility.
Investigation & Resolution:
| Step | Action | Rationale & Technical Details |
|---|---|---|
| 1. Define Intended Use | Clearly specify the clinical context, patient population, and clinical decision the test is meant to inform. Is it prognostic, predictive, or for monitoring? [119] | Clinical utility is context-dependent. A test must be shown to improve outcomes for a specific use case, not just provide a biologically interesting result. |
| 2. Choose the Right Endpoint | Ensure your study measures a clinically meaningful endpoint. For oncology, overall survival is often the gold standard. Intermediate endpoints (e.g., progression-free survival) may not be accepted as proof of utility [119]. | The ultimate goal is to improve patient health. Payers require evidence that the test leads to interventions that tangibly benefit patients. |
| 3. Select an Efficient Study Design | If a traditional RCT is too costly, consider a virtual patient RCT. This method recruits physicians who are randomized to control and intervention arms to manage standardized virtual cases. | This design directly tests whether the test changes physician behavior (a proximal measure of utility) in a controlled, cost-effective manner. It has been used successfully for MolDx coverage [120]. |
| 4. Engage Stakeholders Early | Consult with payers (e.g., via the MolDx program) and regulatory bodies early in the study design process to align on evidence requirements [119] [121]. | Early alignment ensures that the generated evidence will be deemed sufficient and relevant for coverage decisions, avoiding costly re-studies. |
Experimental Protocols for Key Methodologies
Protocol 1: Multivariable Regression for Grading Resistance Mutations
This protocol is based on the methodology used to create an enhanced catalogue for Mycobacterium tuberculosis [10].
1. Objective: To build a multivariable logistic regression model that associates genomic variants with binary phenotypic drug resistance, quantitatively estimating the effect size of each mutation.
2. Materials & Reagents:
- Genomic Dataset: A large, high-quality set of pathogen whole-genome sequences (e.g., >50,000 isolates).
- Phenotypic Data: Reliable binary drug susceptibility testing (DST) results (Resistant/Susceptible) for the drugs of interest.
- Bioinformatics Pipeline: For variant calling from sequencing data (e.g., GATK, SAMtools).
- Computational Environment: Statistical software capable of running penalized regression (e.g., R with
glmnetpackage).
3. Step-by-Step Procedure: 1. Data Curation: Filter genomic isolates to include only those with high-confidence variant calls. Exclude variants with ambiguous allele frequencies (e.g., >0.25 and ≤0.75) to ensure clear binary encoding. 2. Variant Encoding: For each isolate, encode each variant in candidate resistance genes as a binary variable (1 = present if AF > 0.75, 0 = absent if AF ≤ 0.25). 3. Model Training: For each drug, train a separate penalized logistic regression model (e.g., Lasso) using the binary DST outcome as the dependent variable and all binary-encoded variants as independent variables. This helps prevent overfitting. 4. Variant Grading: Extract the odds ratio and coefficient for each variant from the fitted model. Variants with a statistically significant positive coefficient and a high lower bound for the positive predictive value are graded as "Associated with resistance."
4. Data Analysis:
- Benchmarking: Compare the sensitivity and specificity of the regression-based catalogue against a pre-existing univariate method (e.g., SOLO).
- Validation: Perform cross-validation or validate the model on a held-out test set to ensure generalizability.
Protocol 2: Virtual Patient RCT for Demonstrating Clinical Utility
This protocol is adapted from studies that successfully secured diagnostic test coverage [120].
1. Objective: To determine if a diagnostic test changes physician management decisions in a way that aligns with evidence-based care.
2. Materials & Reagents:
- Virtual Patients (CPVs): A set of 9 validated Clinical Performance and Value (CPV) vignettes representing the intended use population. Each case includes history, physical exam findings, and available diagnostics.
- Physician Panel: A representative sample of board-certified physicians in relevant specialties, recruited from community practices.
- Online Platform: An interactive system to deliver CPVs and collect physician responses.
- Evidence-Based Scoring Criteria: A predefined set of 40-66 criteria per case for scoring the appropriateness of care.
3. Step-by-Step Procedure: 1. Recruitment & Randomization: Recruit eligible physicians and randomize them into a Control Arm and one or more Intervention Arms. 2. Round 1 (Baseline): All physicians care for an initial set of 3 virtual patients via the online platform. Their workup, diagnosis, and treatment plans are scored against the evidence-based criteria. 3. Intervention: Physicians in the Intervention Arm receive educational materials about the new diagnostic test. The Control Arm receives no intervention. 4. Round 2 (Post-Intervention): All physicians care for a second set of 3 virtual patients. Intervention Arm physicians are given the option (or mandated, in a 3-arm design) to order the new test and receive results. 5. Scoring & Analysis: All responses from both rounds are scored. The primary outcomes are the change in overall CPV score and the change in the Diagnosis & Treatment (DxTx) domain score.
4. Data Analysis:
- Use a difference-in-difference analysis with multivariate linear regression to compare the change in scores from Round 1 to Round 2 between the Intervention and Control arms.
- A statistically significant improvement in the DxTx score for the Intervention arm demonstrates that the test leads to more evidence-based treatment decisions, thereby proving clinical utility.
Signaling Pathways & Experimental Workflows
Diagram 1: Clinical Utility Evaluation Framework
Hierarchical Model for Diagnostic Test Evaluation
Diagram 2: Multivariable Regression Grading Workflow
Regression-Based Mutation Grading Pipeline
The Scientist's Toolkit: Research Reagent Solutions
Essential Materials for Clinical Utility and Drug Resistance Research
| Item | Function & Application | Example Use Case |
|---|---|---|
| Validated Virtual Patients (CPVs) | Standardized, evidence-based clinical vignettes used to measure changes in physician diagnosis and treatment decisions. | Serving as the primary outcome measure in virtual patient RCTs to demonstrate a test's clinical utility [120]. |
| Multivariable Regression Models | Statistical models that quantify the association between multiple genetic variants and a resistance phenotype simultaneously. | Creating a high-sensitivity catalogue of resistance-associated mutations by analyzing co-occurring variants [10]. |
| Penalized Regression Software (e.g., glmnet) | Software packages that implement Lasso or Ridge regression to prevent model overfitting when dealing with high-dimensional genetic data. | Training stable and generalizable models on genomic datasets with thousands of potential variant features [10]. |
| High-Confidence Variant Call Format (VCF) Files | Processed genomic data where variants have been filtered to exclude low-quality or ambiguous allele frequencies. | Providing a clean, reliable input dataset for mutation association studies, crucial for accurate results [10]. |
| Evidence-Based Scoring Criteria | Predefined, explicit checklists for appropriate patient management, against which physician performance is measured. | Objectively quantifying the quality of clinical decisions in utility studies, focusing on the diagnosis and treatment domain [120]. |
Conclusion
The integration of machine learning with genomic and transcriptomic data marks a paradigm shift in predicting drug resistance, moving beyond canonical markers to capture complex, system-wide adaptations. Methodologies like genetic algorithm-driven feature selection enable the discovery of minimal, high-accuracy gene signatures, while robust validation frameworks are crucial for clinical adoption. Despite advances, challenges remain in model interpretability, generalizability across diverse populations, and demonstrating tangible clinical utility for reimbursement. Future efforts must focus on large-scale, multi-center validations, real-world evidence generation, and the development of standardized, transparent pipelines. By closing the gap between computational prediction and clinical decision-making, these tools promise to revolutionize personalized therapy and strengthen the global fight against antimicrobial resistance.
References
- 1. Tulane researchers use AI to improve diagnosis of drug ... [https://news.tulane.edu/pr/tulane-researchers-use-ai-improve-diagnosis-drug-resistant-infections]
- 2. Rapid, accurate, and reproducible de novo prediction of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12577733/]
- 3. 1.3 Drug-resistant TB [https://www.who.int/teams/global-programme-on-tuberculosis-and-lung-health/tb-reports/global-tuberculosis-report-2023/tb-disease-burden/1-3-drug-resistant-tb]
- 4. Global burden of MDR-TB and XDR-TB: trends, inequities ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12490063/]
- 5. Global burden of multidrug-resistant tuberculosis in ... [https://www.nature.com/articles/s41390-025-03917-1]
- 6. Limitations of current techniques in clinical antimicrobial ... [https://www.nature.com/articles/s44259-024-00033-8]
- 7. Antimicrobial Susceptibility Testing: A Comprehensive Review ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9024665/]
- 8. Detecting antibiotic resistance: classical, molecular ... [https://www.frontiersin.org/journals/microbiology/articles/10.3389/fmicb.2025.1673343/full]
- 9. An explainable artificial intelligence framework reveals ... [https://www.sciencedirect.com/science/article/pii/S2590053625001685]
- 10. Multivariable regression models improve accuracy and ... [https://www.nature.com/articles/s41467-025-57174-1]
- 11. P27 Rethinking UTI diagnosis: how gold is the ' ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10395433/]
- 12. Articles Comparative assessment of line probe assays and ... [https://www.sciencedirect.com/science/article/pii/S2352396425003196]
- 13. Sentinel-Site-Based Surveillance of Mycobacterium ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12291903/]
- 14. Base editing screens define the genetic landscape of ... [https://www.nature.com/articles/s41588-024-01948-8]
- 15. Multi-scale Predictions of Drug Resistance Epidemiology ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8000225/]
- 16. A mutation-induced drug resistance database (MdrDB) [https://www.nature.com/articles/s42004-023-00920-7]
- 17. Next-Generation Sequencing Technology: Current Trends ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10376292/]
- 18. Antimicrobial Resistance | Detection with NGS [https://www.illumina.com/areas-of-interest/microbiology/public-health-surveillance/antimicrobial-resistance-detection.html]
- 19. Bioinformatics: From NGS Data to Biological Complexity in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9495893/]
- 20. A targeted next-generation sequencing panel for ... [https://www.nature.com/articles/s41598-025-08039-6]
- 21. Guidelines for Validation of Next-Generation Sequencing– ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6941185/]
- 22. Comprehensive NGS Panel Validation for the Identification ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8145002/]
- 23. Evolving Standards in Clinical NGS (updated) [https://www.euformatics.com/blog-post/evolving-standards-in-clinical-ngs]
- 24. Application of next-generation sequencing in resistance ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8797753/]
- 25. Multidrug-resistant bacteria compensate for the epistasis ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5395140/]
- 26. Systematic mapping of antibiotic cross-resistance and ... [https://www.nature.com/articles/s41564-024-01857-w]
- 27. Distinguishing mutants that resist drugs via different ... [https://elifesciences.org/articles/94144]
- 28. Advantages of updated WHO mutation catalog combined ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11938600/]
- 29. aiGeneR 3.0: an enhanced deep network model for ... [https://www.frontiersin.org/journals/genetics/articles/10.3389/fgene.2025.1651917/full]
- 30. Deep learning-driven drug response prediction and ... [https://www.nature.com/articles/s41598-025-91571-2]
- 31. An introduction to spatial transcriptomics for biomedical research [https://genomemedicine.biomedcentral.com/articles/10.1186/s13073-022-01075-1]
- 32. Machine Learning Based Computational Gene Selection Models [https://pmc.ncbi.nlm.nih.gov/articles/PMC7758324/]
- 33. Minimal gene signatures enable high-accuracy prediction ... [https://www.nature.com/articles/s41540-025-00584-0]
- 34. Feature Selection Techniques in Machine Learning [https://www.geeksforgeeks.org/machine-learning/feature-selection-techniques-in-machine-learning/]
- 35. comprehensive, step-by-step explanation of Feature ... [https://medium.com/@adnan.mazraeh1993/comprehensive-step-by-step-explanation-of-feature-selection-from-basic-concepts-to-supper-advanced-e5944921cff9]
- 36. A Novel Machine Learning 13-Gene Signature [https://pmc.ncbi.nlm.nih.gov/articles/PMC9103317/]
- 37. Feature selection and aggregation for antibiotic resistance ... [https://www.frontiersin.org/journals/microbiology/articles/10.3389/fmicb.2025.1586476/full]
- 38. Construction and validation of a novel gene signature for ... [https://www.nature.com/articles/s41598-022-05341-5]
- 39. prognostic gene signatures are not (yet) useful in clinical ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5178139/]
- 40. gSELECT: A novel pre-analysis machine-learning library ... [https://www.sciencedirect.com/science/article/pii/S2001037025003113]
- 41. Multivariable regression models improve accuracy and ... - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC11876447/]
- 42. Multi-Label Random Forest Model for Tuberculosis Drug ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7188832/]
- 43. Using random forest to predict antimicrobial minimum ... [https://veterinaryresearch.biomedcentral.com/articles/10.1186/s13567-023-01141-5]
- 44. TB-DROP: deep learning-based drug resistance prediction of ... [https://bmcgenomics.biomedcentral.com/articles/10.1186/s12864-024-10066-y]
- 45. Machine learning-based prediction of antimicrobial ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12255030/]
- 46. Simultaneous regression and classification for drug ... [https://www.nature.com/articles/s41598-022-17609-x]
- 47. Troubleshoot automated ML experiments - Azure Machine ... [https://learn.microsoft.com/en-us/azure/machine-learning/how-to-troubleshoot-auto-ml?view=azureml-api-2]
- 48. AutoML identification of microRNA biomarkers in high-risk ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12418865/]
- 49. AutoML beginner's guide | Vertex AI [https://docs.cloud.google.com/vertex-ai/docs/beginner/beginners-guide]
- 50. Automated Machine Learning (AutoML): A Complete Guide ... [https://riseuplabs.com/automl/]
- 51. The Complete Guide to AutoML: Benefits, Tools, and Use ... [https://insights.daffodilsw.com/blog/the-complete-guide-to-automl-benefits-tools-and-use-cases]
- 52. AutoML programming guide [https://docs.nvidia.com/clara/clara-train-sdk/automl/automl_programming_guide.html]
- 53. Keeping up with the pathogens: improved antimicrobial ... [https://genomemedicine.biomedcentral.com/articles/10.1186/s13073-024-01346-z]
- 54. Accurate and rapid prediction of tuberculosis drug ... [https://www.nature.com/articles/s41598-022-06449-4]
- 55. Accuracy of Machine Learning in Identifying Drug ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12518508/]
- 56. Monitoring of Pseudomonas aeruginosa mutational ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11467565/]
- 57. The Versatile Mutational Resistome of Pseudomonas ... [https://www.frontiersin.org/journals/microbiology/articles/10.3389/fmicb.2018.00685/full]
- 58. Intrinsic-dimension analysis for guiding dimensionality ... [https://pubmed.ncbi.nlm.nih.gov/39673960/]
- 59. GAUDI: interpretable multi-omics integration with UMAP ... [https://www.nature.com/articles/s41467-025-60822-1]
- 60. Challenges in AI-driven multi-omics data analysis for ... [https://www.sciencedirect.com/science/article/pii/S2352914825000681]
- 61. AI-driven multi-omics integration in precision oncology [https://pmc.ncbi.nlm.nih.gov/articles/PMC12634751/]
- 62. Evaluation of normalization strategies for mass ... [https://pubmed.ncbi.nlm.nih.gov/40593232/]
- 63. Interpretable Ensemble Learning Predicts Antibiotic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12275043/]
- 64. Machine learning-based prediction of antimicrobial resistance ... [https://bmcgenomdata.biomedcentral.com/articles/10.1186/s12863-025-01338-x]
- 65. A New Approach to Large Multiomics Data Integration - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC12461686/]
- 66. Class Imbalance Strategies — A Visual Guide with Code [https://medium.com/data-science/class-imbalance-strategies-a-visual-guide-with-code-8bc8fae71e1a]
- 67. 7 Techniques to Handle Class Imbalance in Machine Learning [https://data-pilot.com/blog/7-techniques-to-handle-class-imbalance-in-machine-learning/]
- 68. How to Handle Unbalanced Classes: 5 Strategies [https://blog.roboflow.com/handling-unbalanced-classes/]
- 69. Predicting antibiotic resistance genes and bacterial ... [https://www.frontiersin.org/journals/microbiology/articles/10.3389/fmicb.2025.1628952/full]
- 70. Prediction of antibiotic resistance from ... [https://www.nature.com/articles/s41598-025-14078-w]
- 71. Artificial Intelligence in Clinical and Translational Science [https://pmc.ncbi.nlm.nih.gov/articles/PMC12580936/]
- 72. Explainable Artificial Intelligence in the Field of Drug Research [https://pmc.ncbi.nlm.nih.gov/articles/PMC12129466/]
- 73. 2025 Expert Consensus on Retrospective Evaluation of ... [https://www.sciencedirect.com/science/article/pii/S2667102625001044]
- 74. Large language models for drug discovery and development [https://www.sciencedirect.com/science/article/pii/S2666389925001941]
- 75. Antimicrobial Drug Resistance, Regulation, and Research [https://pmc.ncbi.nlm.nih.gov/articles/PMC3373116/]
- 76. How AI Is Transforming Medical Translation in 2025 [https://www.ecinnovations.com/blog/how-ai-is-transforming-medical-translation/]
- 77. Optimizing Feature Selection with Genetic Algorithms [https://arxiv.org/abs/2409.14563]
- 78. Feature selection algorithm based on optimized genetic ... [https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0303088]
- 79. Optimizing feature selection with genetic algorithms [https://link.springer.com/10.1007/s10115-025-02515-1]
- 80. Optimizing imbalanced learning with genetic algorithm [https://www.nature.com/articles/s41598-025-09424-x]
- 81. Feature engineering through two-level genetic algorithm [https://www.sciencedirect.com/science/article/pii/S2666827025000799]
- 82. Advanced genetic algorithm (GA)-independent component ... [https://www.sciencedirect.com/science/article/pii/S2468227625000353]
- 83. Resistor: An algorithm for predicting resistance mutations ... [https://www.sciencedirect.com/science/article/pii/S2405471222003945]
- 84. Resistor: an algorithm for predicting resistance mutations ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9589925/]
- 85. An approach to identifying drug resistance associated ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3521396/]
- 86. Bridging the genotype–phenotype gap: what does it take? [https://pmc.ncbi.nlm.nih.gov/articles/PMC3634519/]
- 87. Integration of multiple biological contexts reveals principles ... [https://www.nature.com/articles/s41467-020-16078-y]
- 88. Discovering new biology with drug-resistance alleles - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC9530778/]
- 89. An Overview of Strategies for Detecting Genotype ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8602802/]
- 90. Genotyping Troubleshooting Guide [https://www.jax.org/jax-mice-and-services/customer-support/technical-support/genotyping/troubleshooting]
- 91. Development of Drug-resistant Cell Lines for Experimental ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12404681/]
- 92. Prediction models need appropriate internal ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5578404/]
- 93. The Comprehensive Guide to Model Validation Framework [https://odsc.medium.com/the-comprehensive-guide-to-model-validation-framework-what-is-a-robust-machine-learning-model-7bdbc41c1702]
- 94. Top 5 Machine Learning Model Testing Tools in 2024 [https://dagshub.com/blog/top-machine-learning-model-testing-tools/]
- 95. ModelDiff: A Framework for Comparing Learning Algorithms [https://gradientscience.org/modeldiff/]
- 96. Top 10 Machine Learning Frameworks to Use In 2025 [https://www.igmguru.com/blog/machine-learning-frameworks]
- 97. ResFinder - Center for Genomic Epidemiology - DTU [https://genepi.food.dtu.dk/resfinder]
- 98. Comparison of the Web Tools ARG-ANNOT and ResFinder ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4136053/]
- 99. ResFinder – an open online resource for identification of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8914360/]
- 100. A comparative study of antibiotic resistance patterns in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11814411/]
- 101. Find Resistance with ResFinder [https://resources.qiagenbioinformatics.com/manuals/clcmgm/400/index.php?manual=Find_Resistance_with_ResFinder.html]
- 102. Resistance Sniffer: An online tool for prediction of drug ... [https://www.sciencedirect.com/science/article/pii/S1438422120300096]
- 103. Understanding the F1 Score and AUC-ROC Curve [https://keylabs.ai/blog/understanding-the-f1-score-and-auc-roc-curve/]
- 104. F1 Score in Machine Learning: Intro & Calculation [https://www.v7labs.com/blog/f1-score-guide]
- 105. F1 Score in Machine Learning Explained [https://encord.com/blog/f1-score-in-machine-learning/]
- 106. A guide to interpreting the area under the curve value - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC10664195/]
- 107. Classification: ROC and AUC | Machine Learning [https://developers.google.com/machine-learning/crash-course/classification/roc-and-auc]
- 108. Cohen's kappa [https://en.wikipedia.org/wiki/Cohen%27s_kappa]
- 109. Interrater reliability: the kappa statistic - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC3900052/]
- 110. Understanding Model Evaluation Metrics for Image ... [https://akridata.ai/blog/understanding-model-evaluation-metrics-for-image-classification/]
- 111. SYNDEEP: a deep learning approach for the prediction of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10105711/]
- 112. Developing clinical prediction models: a step-by-step guide [https://pmc.ncbi.nlm.nih.gov/articles/PMC11369751/]
- 113. Implementation and Updating of Clinical Prediction Models [https://www.sciencedirect.com/science/article/pii/S2949761225000355]
- 114. Clinical implementation of an AI-based prediction model for ... [https://www.nature.com/articles/s41591-025-03942-x]
- 115. Antibiotic resistance: The challenges and some emerging ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9459344/]
- 116. Advances in personalized medicine: translating genomic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12106117/]
- 117. Drug resistance | Research Starters [https://www.ebsco.com/research-starters/health-and-medicine/drug-resistance]
- 118. The concept of clinical utility for diagnostic tests [https://www.thermofisher.com/blog/clinical-conversations/the-concept-of-clinical-utility-for-diagnostic-tests/]
- 119. Generating and evaluating evidence of the clinical utility of ... [https://www.nature.com/articles/gim2015162]
- 120. Establishing Clinical Utility for Diagnostic Tests Using a ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6787613/]
- 121. Clinical Utility: Informing Treatment Decisions by Changing ... [https://nam.edu/perspectives/clinical-utility-informing-treatment-decisions-by-changing-the-paradigm/]