Advanced TaqMan Assay Protocols for Sensitive Cancer Mutation Detection
This article provides a comprehensive guide for researchers and drug development professionals on implementing TaqMan assay protocols for somatic mutation detection in cancer research.
Advanced TaqMan Assay Protocols for Sensitive Cancer Mutation Detection
Abstract
This article provides a comprehensive guide for researchers and drug development professionals on implementing TaqMan assay protocols for somatic mutation detection in cancer research. It covers the foundational principles of competitive allele-specific TaqMan PCR (castPCR) technology, detailed methodological workflows for applications like EGFR and BRAF mutation analysis, optimization strategies for challenging samples including FFPE tissues, and rigorous validation against established techniques like Sanger sequencing and HRM. The content synthesizes current data to demonstrate how TaqMan assays achieve high sensitivity and specificity, enabling reliable identification of low-abundance mutations crucial for personalized cancer therapy and biomarker discovery.
Understanding castPCR: The Core Technology Powering TaqMan Mutation Detection
Principles of Competitive Allele-Specific TaqMan PCR (castPCR)
Competitive Allele-Specific TaqMan PCR (castPCR) is a highly sensitive and specific technology for the detection and quantification of rare somatic mutations in cancer research. This advanced molecular technique enables researchers to identify mutant alleles present at very low frequencies amid a high background of wild-type DNA, a common challenge in tumor genotyping. The technology is particularly valuable for analyzing clinical samples such as formalin-fixed paraffin-embedded (FFPE) tissues, where DNA quality may be compromised and tumor cell content variable. castPCR has demonstrated robust performance in detecting clinically relevant mutations in key cancer genes including BRAF, EGFR, KRAS, JAK2, and PIK3CA, facilitating personalized treatment strategies and therapeutic monitoring [1] [2] [3].
Principle and Mechanism
The core principle of castPCR technology combines allele-specific amplification with wild-type allele suppression to achieve exceptional specificity for mutant targets. This dual approach employs two key components: (1) mutant allele-specific TaqMan primers and probes, and (2) proprietary Minor Groove Binder (MGB) oligonucleotide blockers that selectively inhibit the amplification of wild-type sequences [2] [4].
Molecular Mechanism
The castPCR process begins with the design of allele-specific primers that perfectly complement the mutant sequence of interest. These primers exhibit preferential binding and extension to mutant templates. The critical innovation lies in the inclusion of wild-type-specific MGB blocker oligonucleotides, which bind irreversibly to wild-type DNA sequences with high affinity due to their MGB chemistry. This binding physically blocks DNA polymerase from accessing and amplifying wild-type templates during PCR amplification [4] [5].
The competitive nature of the reaction emerges from the simultaneous presence of both components: while allele-specific primers seek their complementary mutant targets, the MGB blockers effectively "compete" for wild-type templates. This competition dramatically reduces non-specific amplification and enables the selective amplification of rare mutant alleles even when outnumbered by wild-type sequences by up to 1000:1 [4].
Detection and Quantification
Amplification is monitored in real-time using sequence-specific TaqMan probes labeled with fluorescent reporters. The entire reaction typically includes a gene reference assay targeting a mutation-free region of the gene of interest, which serves as an internal control for DNA quality and quantity. The normalised cycle threshold (ΔCt) difference between the mutant allele assay and the gene reference assay determines mutation status, with predetermined cut-off values establishing positive calls [2].
Table 1: Key Performance Characteristics of castPCR Technology
| Parameter | Performance Specification | Experimental Confirmation |
|---|---|---|
| Detection Sensitivity | 0.1% mutant allele in wild-type background [4] | 0.01% for JAK2 V617F with optimized protocols [5] |
| Dynamic Range | Spans over four logs in template concentration [4] | Linear detection from 0.1% to 100% mutant allele [2] |
| Amplification Efficiency | 100% ± 10% [4] | Consistent across FFPE and fresh-frozen samples [3] |
| Reproducibility | High inter-assay and intra-assay consistency [2] | Minimal variation in 5 independent experiments [5] |
| Sample Compatibility | FFPE tissue, fresh-frozen tissue, cell lines [4] | Successful application to biopsies, cytology smears [2] |
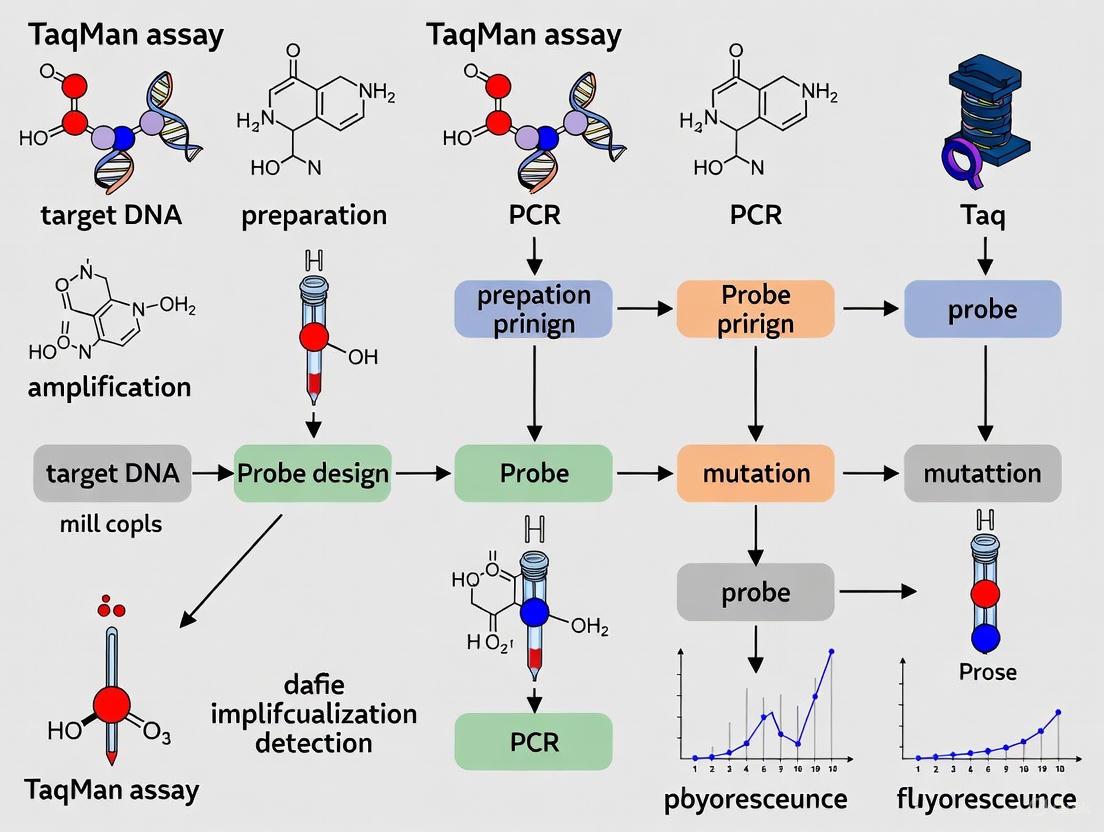
Figure 1: Molecular Mechanism of castPCR. MGB blockers bind wild-type templates to prevent amplification, while allele-specific components enable selective amplification of mutant sequences.
Experimental Protocol
Sample Preparation and DNA Extraction
Proper sample preparation is critical for successful castPCR analysis. The recommended workflow begins with genomic DNA extraction using commercial kits validated for specific sample types:
- FFPE tissues: Use QIAamp DNA FFPE Tissue Kit (Qiagen) or equivalent with deparaffinization steps [2]
- Fresh-frozen tissues: DNeasy Blood and Tissue Kit (Qiagen) provides high-quality DNA [2]
- Cytological samples: QIAamp DNA Micro Kit (Qiagen) for limited starting material [2]
- Peripheral blood: BloodPrep DNA Chemistry for cultured cells and blood [6]
Extracted DNA should be quantified using spectrophotometry (NanoVue or equivalent) and quality assessed by 0.8% agarose gel electrophoresis. DNA degradation may affect reference assay Ct values but typically impacts mutant and reference assays similarly [2] [3].
castPCR Reaction Setup
The standardized reaction conditions for castPCR have been optimized across multiple platforms:
Table 2: castPCR Reaction Setup Components
| Component | Final Concentration | Purpose |
|---|---|---|
| TaqMan Genotyping Master Mix | 1X | Provides optimized buffer, dNTPs, and hot-start polymerase |
| TaqMan Mutation Detection Assay | 1X | Contains mutant-specific primers and probe |
| Gene Reference Assay | 1X | Targets mutation-free region for normalization |
| Genomic DNA Template | 10 ng/reaction | Optimal balance of sensitivity and inhibition resistance |
| Nuclease-free Water | To volume | Reaction complement |
Reactions are assembled in 96-well or 384-well plates compatible with real-time PCR systems. A typical 20 μL reaction volume is recommended, with 10 ng DNA template representing the optimal balance between detection sensitivity and inhibition resistance [2].
Thermal Cycling Conditions
The thermal cycling protocol incorporates an initial activation step followed by two-stage amplification:
- Initial Denaturation/Activation: 95°C for 10 minutes (enzyme activation and initial denaturation)
- Pre-Amplification Stage: 5 cycles of:
- 92°C for 15 seconds (denaturation)
- 58°C for 1 minute (annealing/extension)
- Amplification Stage: 40 cycles of:
- 92°C for 15 seconds (denaturation)
- 60°C for 1 minute (annealing/extension with data collection) [2]
This two-stage protocol enhances specificity by favoring mutant allele amplification during the initial lower-temperature cycles before transitioning to standard amplification conditions.
Data Analysis and Interpretation
Mutation detection employs a ΔCt-based approach between mutant and reference assays:
- Calculate normalized ΔCt = [Ct(mutant assay) - Ct(reference assay)] - calibration ΔCt
- Compare normalized ΔCt to validated cut-off values:
- ΔCt ≤ cut-off: Mutation detected
- ΔCt > cut-off: Mutation not detected [2]
The calibration ΔCt represents the inherent Ct difference between mutant and reference assays, determined experimentally for each assay lot. For clinical samples, validation studies established a cut-off ΔCt of 7 with a maximum Ct limit of 37 for reliable mutation detection [2].
Figure 2: castPCR Experimental Workflow. The complete process from sample preparation to data interpretation.
Research Reagent Solutions
Table 3: Essential Reagents and Materials for castPCR
| Reagent/Material | Function | Examples/Specifications |
|---|---|---|
| TaqMan Mutation Detection Assays | Detect specific mutant alleles | Pre-designed assays for BRAF V600E, EGFR L858R, KRAS G12D, etc. [6] [4] |
| Gene Reference Assays | Amplify mutation-free reference region | Internal control for DNA quality and quantity [2] |
| TaqMan Genotyping Master Mix | Provides reaction components | Optimized for allele discrimination, contains polymerase, dNTPs, buffer [6] |
| DNA Extraction Kits | Isolate genomic DNA from various sources | QIAamp DNA FFPE Tissue Kit, BloodPrep DNA Chemistry [6] [2] |
| Real-time PCR Systems | Amplification and detection | ViiA 7, 7500 Fast, StepOnePlus, 7900HT [6] |
| Thermal Cyclers | Reaction assembly | Veriti 96-Well Thermal Cycler, GeneAmp PCR System 9700 [6] |
Applications in Cancer Research
BRAF Mutation Detection in Melanoma
castPCR has been extensively validated for BRAF V600 mutation detection in melanoma patients, where it demonstrated superior sensitivity compared to Sanger sequencing. In a study of 54 patient samples, castPCR identified all mutations detected by sequencing plus four additional mutations that sequencing missed. The technology achieved consistent detection at mutant-to-wild-type ratios as low as 1:100, with performance unaffected by intratumoral heterogeneity and minimally affected by melanin content [1].
EGFR Mutation Detection in NSCLC
In non-small cell lung cancer (NSCLC), castPCR enables reliable detection of EGFR mutations (including L858R, T790M, and exon 19 deletions) with sensitivity matching the FDA-approved Therascreen kit. castPCR successfully identified mutations in samples with low tumor cell content where direct sequencing failed, including FFPE surgical specimens, small biopsies, and cytology smears. The technology's 0.1-0.5% detection limit for common EGFR mutations makes it suitable for detecting emerging resistance mutations during TKI therapy [2].
Multi-Gene Analysis in Solid Tumors
The technology platform supports simultaneous profiling of mutations across multiple genes, including KRAS, BRAF, and EGFR, from limited FFPE material. This multi-gene approach is essential for comprehensive molecular characterization in colorectal cancer, where KRAS and BRAF mutation status guides anti-EGFR therapy decisions. castPCR efficiently amplified challenging FFPE-derived DNA while maintaining specificity through established mutation cut-offs that prevent over-interpretation of degraded templates [3].
JAK2 V617F Quantification in MPN
For myeloproliferative neoplasms (MPN), refined castPCR protocols enable ultrasensitive JAK2 V617F detection with 0.01% sensitivity using a duplex approach that combines mutant detection and copy number normalization in a single tube. This exceptional sensitivity supports monitoring of minimal residual disease and low-burden mutations in clonal hematopoiesis, with quantification accuracy validated against digital PCR [5].
Table 4: Performance Comparison of Mutation Detection Methods
| Method | Limit of Detection | Advantages | Limitations |
|---|---|---|---|
| Sanger Sequencing | 10-25% mutant allele [2] | Broad mutation detection, considered gold standard | Low sensitivity, labor-intensive |
| Fragment Analysis | 5% mutant allele [2] | Good for indels, relatively simple | Limited to specific mutation types |
| Real-time PCR (Allelic Discrimination) | Up to 5% mutant allele [2] | Quantitative, moderate sensitivity | Limited multiplexing capability |
| ARMS (Therascreen) | Up to 1% mutant allele [2] | Clinically validated, good sensitivity | Limited mutation coverage |
| castPCR | 0.1% mutant allele [2] [4] | Highest sensitivity, specific, quantitative | Requires specific assay design |
Troubleshooting and Optimization
Successful castPCR implementation requires attention to potential challenges:
- Inhibition from FFPE samples: Include reference assays to monitor DNA quality; samples with Ct >37 for reference assays may yield unreliable results [2] [3]
- False positives from wild-type amplification: Use validated cut-off ΔCt values and incorporate wild-type controls in each run [3]
- Low mutant allele frequency: Verify reaction efficiency using control plasmids with known mutation percentages [5]
- Assay validation: Establish assay-specific parameters using cell line controls (e.g., NCI-H1975 for EGFR L858R/T790M) before clinical application [2]
castPCR technology represents a significant advancement in mutation detection for cancer research, combining exceptional sensitivity (0.1% detection limit) with robust performance across challenging sample types. Its dual mechanism of allele-specific amplification and wild-type suppression enables reliable identification of clinically relevant mutations in BRAF, EGFR, KRAS, and other cancer genes, supporting personalized treatment decisions and therapeutic monitoring. The technology's compatibility with FFPE specimens and standardized workflow facilitates integration into molecular diagnostics pipelines, while ongoing assay development continues to expand its applications in cancer genomics.
Allele-Specific Primers, MGB Probes, and Wild-Type Blockers
This application note provides a detailed protocol for utilizing TaqMan Mutation Detection Assays based on Competitive Allele-Specific TaqMan PCR (castPCR) technology for somatic mutation detection in cancer research. The document outlines the key components—allele-specific primers, Minor Groove Binder (MGB) probes, and wild-type blockers—that enable highly specific and sensitive identification of mutant alleles down to 0.1% variant allele frequency in a wild-type background. Designed for researchers, scientists, and drug development professionals, this guide includes comprehensive experimental workflows, validation data, and technical specifications to support implementation in precision oncology research.
The detection of somatic mutations in oncogenes and tumor suppressor genes is fundamental to cancer research and the development of targeted therapies. Technologies that can reliably identify low-frequency mutations in complex biological samples, such as formalin-fixed paraffin-embedded (FFPE) tissues, are essential for accurate molecular profiling. TaqMan Mutation Detection Assays, powered by castPCR technology, integrate three key components—allele-specific primers, MGB TaqMan probes, and wild-type blockers—to achieve exceptional specificity and sensitivity in detecting known cancer-related mutations [7]. This application note details the principles, protocols, and applications of this integrated system, providing researchers with a robust framework for mutation detection in cancer research.
Key Principles and Components
The castPCR technology combines the quantitative power of real-time PCR with sophisticated suppression mechanics to selectively amplify and detect mutant alleles while effectively inhibiting the amplification of wild-type sequences.
Core Component Specifications
Table 1: Key Components of TaqMan Mutation Detection Assays
| Component | Composition | Function | Detection |
|---|---|---|---|
| Mutant Allele Assay | Allele-specific primer, FAM-dye-labeled MGB probe, MGB oligonucleotide blocker | Specifically amplifies and detects the mutant allele; blocker suppresses wild-type amplification | FAM dye signal |
| Wild Type Allele Assay (Optional) | Allele-specific primer, FAM-dye-labeled MGB probe, MGB oligonucleotide blocker | Amplifies and detects wild-type allele; blocker suppresses non-specific amplification | FAM dye signal |
| Gene Reference Assay | PCR primers, FAM-dye-labeled MGB probe | Amplifies a mutation-free reference region of the target gene; provides DNA quality/quantity control | FAM dye signal |
Technology Comparison
Table 2: Performance Comparison of Mutation Detection Methods
| Method | Limit of Detection | Key Advantages | Typical Applications |
|---|---|---|---|
| castPCR | 0.1% mutant allele [2] | High specificity, wild-type suppression, quantitative | Rare mutation detection, low tumor purity samples |
| Direct Sequencing | 10-25% mutant allele [2] | Comprehensive, detects unknown mutations | Discovery research, when tumor content is high |
| ARMS (Therascreen) | ~1% mutant allele [2] | Established in diagnostics, relatively simple | Routine clinical mutation detection |
| Real-time PCR (allelic discrimination) | Up to 5% mutant allele [2] | Moderate sensitivity, cost-effective | High-frequency mutation screening |
Diagram 1: castPCR Mechanism for Mutation Detection. The process illustrates parallel pathways for mutant allele detection (yellow/green) and wild-type suppression (red) within the same reaction.
Research Reagent Solutions
Table 3: Essential Materials for TaqMan Mutation Detection Experiments
| Item | Function | Example Products/Catalog Numbers |
|---|---|---|
| Mutation Detection Assays | Detect specific mutant and wild-type alleles | TaqMan Mutation Detection Assays (Cat. No. 4465804) [7] |
| Reference Assays | Amplify mutation-free reference gene region | TaqMan Mutation Detection Reference Assays (Cat. No. 4465807) [7] |
| PCR Master Mix | Provides enzymes, dNTPs, and optimized buffer for PCR | TaqMan Genotyping Master Mix [8] |
| Internal Positive Control | Verify PCR efficiency and rule out inhibition | TaqMan Mutation Detection IPC Reagent Kit (Cat. No. 4467538) [7] |
| Real-Time PCR System | Instrument platform for amplification and detection | ViiA 7 Real-Time PCR System, 7500 Fast Real-Time PCR System [8] |
| Analysis Software | Interpret results and determine mutation status | Mutation Detector Software [7] |
Experimental Protocol
Sample Preparation and DNA Extraction
Materials Required: QIAamp DNA FFPE Tissue Kit (or equivalent), spectrophotometer or fluorometer for DNA quantification [2].
Procedure:
- Extract genomic DNA from tumor samples (FFPE tissues, fresh frozen tissues, or cell lines) using appropriate DNA extraction kits.
- Assess DNA quality and quantity using UV spectrophotometry (e.g., NanoVue Spectrophotometer) or fluorometric methods.
- Dilute DNA to working concentration (typically 10-20 ng/µL) in nuclease-free water or TE buffer.
- For FFPE samples, evaluate DNA integrity by agarose gel electrophoresis if quality concerns exist [2].
Critical Step: Accurate DNA quantification is essential for reliable results. For degraded FFPE samples, use fluorometric quantification methods for improved accuracy.
Assay Selection and Plate Setup
Materials Required: TaqMan Mutation Detection Assays, TaqMan Mutation Detection Reference Assays, 96-well or 384-well PCR plates [7].
Procedure:
- Identify mutations of interest using the TaqMan Mutation Assay index file.
- Select appropriate assays:
- Mutant Allele Assay ID (Column B in index file)
- Gene Reference Assay ID (Column Q in index file)
- Wild Type Assay ID, if required (Column S in index file) [7]
- Order assays using Quick Order function with appropriate catalog numbers.
- Prepare reaction plate according to recommended layout, including:
- No-template controls (NTC)
- Known wild-type controls
- Known mutant controls (if available)
Critical Step: Include reference assays for all samples to normalize for DNA quality and quantity variations.
Reaction Setup and Thermal Cycling
Materials Required: TaqMan Genotyping Master Mix, real-time PCR system [2].
Reaction Composition (20 µL final volume):
- 1X TaqMan Genotyping Master Mix
- 1X Mutant Allele Assay (or Wild Type Assay)
- 1X Gene Reference Assay
- 10-100 ng genomic DNA template
- Nuclease-free water to volume
Thermal Cycling Conditions (ViiA 7 Real-Time PCR System):
- Initial denaturation: 95°C for 10 minutes
- 5 cycles of:
- Denaturation: 92°C for 15 seconds
- Annealing/Extension: 58°C for 1 minute
- 40 cycles of:
- Denaturation: 92°C for 15 seconds
- Annealing/Extension: 60°C for 1 minute [2]
Critical Step: Maintain consistent thermal cycling conditions across all runs to ensure reproducible Ct values.
Data Analysis and Interpretation
Materials Required: Mutation Detector Software or equivalent data analysis package [7].
Procedure:
- Calculate ΔCt values: ΔCt = Ct(mutant allele assay) - Ct(gene reference assay)
- Apply normalization: Normalized ΔCt = ΔCt - calibration ΔCt Calibration ΔCt is the inherent Ct difference between mutant allele and gene reference assays
- Interpret results using established thresholds:
- Mutation detected: Normalized ΔCt ≤ ΔCt cut-off (e.g., ≤7)
- Mutation not detected: Normalized ΔCt > ΔCt cut-off [2]
- For quantitative applications, calculate % mutation using standard curves generated from control samples with known mutation percentages.
Critical Step: Establish and validate threshold values for each mutation assay using characterized control samples.
Application Data and Validation
Performance Characteristics in Cancer Research
Sensitivity and Specificity: castPCR technology demonstrates detection sensitivity down to 0.1% mutant alleles in a wild-type background, surpassing conventional sequencing methods that require 10-25% mutant allele frequency [2]. In a study detecting EGFR mutations in NSCLC samples, castPCR identified mutations with similar frequency to the Therascreen kit while exhibiting enhanced sensitivity compared to direct sequencing, particularly in samples with low tumor cell content [2].
Concordance Studies: Validation studies comparing castPCR with established methods show high concordance rates. In a multi-cancer panel evaluating RAS, EGFR, and BRAF mutations, castPCR achieved 93% concordance with Therascreen EGFR assays, 95% concordance with KRAS castPCR assays, and 100% concordance with cobas BRAF assays [9].
Liquid Biopsy Applications: Recent advances enable application of these principles to liquid biopsy samples. In pancreatic cancer research, castPCR detected KRAS p.G12D mutations in 48% of tumor DNA samples, while more sensitive digital PCR methods identified the same mutation in 95.9% of samples when using a >0% cutoff threshold, demonstrating the utility of these approaches for both tissue and liquid biopsy analysis [10].
Troubleshooting Guide
Table 4: Common Issues and Resolution Strategies
| Problem | Potential Cause | Solution |
|---|---|---|
| High Ct values in reference assay | Degraded DNA, PCR inhibitors | Check DNA quality, repurify sample, increase DNA input |
| False positive mutation calls | Non-specific amplification | Verify assay specificity, optimize blocker concentration |
| Inconsistent replicates | Pipetting errors, bubble formation | Centrifuge plate before run, check pipette calibration |
| No amplification | Enzyme inactivation, incorrect thermal cycling | Check reagent storage conditions, verify thermal protocol |
The integration of allele-specific primers, MGB probes, and wild-type blockers in TaqMan Mutation Detection Assays provides cancer researchers with a robust, sensitive, and specific platform for somatic mutation detection. The castPCR technology enables reliable identification of rare mutant alleles in background of wild-type DNA, making it particularly valuable for analyzing heterogeneous tumor samples and low-purity specimens. With comprehensive commercial availability and standardized protocols, this approach offers an accessible solution for research applications in precision oncology and therapeutic development.
TaqMan assays, particularly those employing Competitive Allele-Specific TaqMan PCR (castPCR) technology, provide researchers with a powerful tool for detecting somatic mutations in cancer research. These assays enable the sensitive and specific identification of rare mutant alleles amidst a high background of wild-type DNA, which is crucial for analyzing tumor specimens from various sources, including formalin-fixed, paraffin-embedded (FFPE) tissue. This application note details the operational advantages, provides quantitative performance data, and outlines a standardized protocol for detecting cancer mutations using castPCR technology, contextualizing its utility within a comprehensive cancer research workflow.
The molecular characterization of tumors through the detection of somatic mutations is a cornerstone of modern cancer research and personalized medicine. However, a significant technical challenge persists: cancer-associated mutations in tissue or liquid biopsy samples are often present at very low frequencies, requiring detection methods with exceptional sensitivity and specificity to distinguish them from abundant wild-type sequences [11] [12].
TaqMan-based Mutation Detection Assays, which utilize castPCR technology, are engineered to meet this challenge. They are designed to deliver the rapid workflow and cost-effectiveness of PCR while achieving the sensitivity required to detect low-frequency variants, thus facilitating research into tumor heterogeneity, minimal residual disease, and resistance mechanisms [7].
Key Advantages and Performance Data
TaqMan Mutation Detection Assays offer a combination of performance characteristics that make them particularly suitable for cancer research.
Superior Sensitivity and Specificity
The core of castPCR technology is the integration of an allele-specific primer with a Minor Groove Binder (MGB) blocker oligonucleotide. The blocker is designed to bind specifically to the wild-type allele, suppressing its amplification during PCR. This allows the allele-specific primer to amplify the mutant sequence with high efficiency, enabling the detection of rare mutations present at frequencies as low as 0.1% (or 1 mutant allele in 1,000 wild-type alleles) [11] [7]. This high sensitivity is essential for analyzing heterogeneous tumor samples or circulating tumor DNA (ctDNA) where the mutant allele fraction is low.
Rapid and Streamlined Workflow
Unlike next-generation sequencing (NGS) methods, which can be time-consuming and require complex bioinformatics, the TaqMan castPCR workflow is straightforward. The process from sample to result can be completed in approximately three hours, making it ideal for rapid validation and screening [7]. The assays use familiar qPCR instrumentation and pre-designed, ready-to-use reagents that require no further optimization.
Table 1: Key Performance Metrics of TaqMan Mutation Detection Assays
| Feature | Performance Metric | Research Implication |
|---|---|---|
| Analytical Sensitivity | Detects as low as 0.1% mutant allele [11] | Suitable for rare mutation detection in FFPE and liquid biopsy samples. |
| Dynamic Range | Spans over four logs of template concentration [11] | Allows for accurate quantification across a wide range of input DNA. |
| Amplification Efficiency | 100% ± 10% [11] | Ensures precise and reproducible quantification. |
| Concordance with Other Methods | 93-100% for common cancer mutations [9] | Provides reliable data comparable to other approved diagnostic tests. |
| Assay Portfolio | 819 assays across 47 cancer genes (e.g., KRAS, BRAF, EGFR) [7] | Enables focused research on key oncogenic drivers. |
Validation in Cancer Research
The clinical relevance of these assays is demonstrated by their performance in independent studies. One study developed a TaqMan Array card (the REB Array) to measure 44 mutations in RAS, EGFR, and BRAF genes. The array showed an overall sensitivity of 92% and a Positive Predictive Value (PPV) of 100% when compared to other commercial PCR methods, validating its use for robust, high-throughput mutation screening in solid tumors [9].
Experimental Protocol: Detecting Somatic Mutations Using castPCR
The following protocol is adapted for detecting a specific mutation (e.g., a common KRAS mutation) in genomic DNA extracted from FFPE tissue sections.
Research Reagent Solutions
Table 2: Essential Materials and Reagents
| Item | Function | Example (from search results) |
|---|---|---|
| TaqMan Mutation Detection Assay | Contains primers, FAM-labeled probe, and MGB blocker for specific mutant detection. | KRAS G12D Mutant Allele Assay [11] [7] |
| TaqMan Mutation Detection Reference Assay | Provides an internal reference for DNA quantity/quality. | TaqMan Reference Assay for a wild-type gene [7] |
| qPCR Master Mix | Contains DNA polymerase, dNTPs, and buffer for amplification. | Premix TaqMan Fast Advanced Master Mix |
| Genomic DNA | The sample template for the reaction. | DNA from FFPE tissue, fresh-frozen tissue, or cell lines [11] |
| Real-Time PCR System | Instrument for thermal cycling and fluorescence detection. | Applied Biosystems Real-Time PCR Systems [7] |
Step-by-Step Procedure
- Assay Selection and Design: Identify the mutation of interest and order the corresponding TaqMan Mutation Detection Assay (Mutant Allele Assay) and the associated Gene Reference Assay [7]. Assays are available for a wide range of mutations in genes like BRAF, EGFR, and KRAS.
- DNA Extraction and Quantification: Extract genomic DNA from your sample source (e.g., FFPE tissue, cell line) using a standard methodology. Precisely quantify the DNA using a fluorometric method.
- Reaction Plate Setup:
- For each sample, prepare two reaction wells:
- Well A (Test): Combine 10-50 ng of genomic DNA with the 1X TaqMan Mutation Detection Assay (mutant allele) and the 1X TaqMan Reference Assay in a master mix.
- Well B (Optional Control): To confirm wild-type suppression, set up a reaction with wild-type DNA and the mutant allele assay.
- A no-template control (NTC) with water should be included to check for contamination.
- For each sample, prepare two reaction wells:
- Real-Time PCR Amplification:
- Load the plate onto a real-time PCR instrument.
- Use the following standard cycling conditions:
- Hold Stage: 2 minutes at 50°C (UDG incubation)
- Enzyme Activation: 20 minutes at 95°C
- 40 Cycles of:
- Denature: 1 second at 95°C
- Anneal/Extend: 20 seconds at 60°C
- Fluorescence is measured at the end of each anneal/extend step.
- Data Analysis:
- Use software such as Mutation Detector Software to automatically determine mutation status [7].
- The software analyzes the amplification curves and Ct values for both the mutant and reference assays to call the presence or absence of the mutation.
Technology Workflow and Visualization
The following diagram illustrates the core mechanism of castPCR technology that enables its high specificity.
Diagram 1: The castPCR mechanism uses an MGB blocker to suppress wild-type amplification, allowing specific detection of mutant alleles.
The overall experimental journey, from sample preparation to data interpretation, is summarized in the workflow below.
Diagram 2: The end-to-end workflow for mutation detection using TaqMan castPCR assays, highlighting a streamlined process from sample to result.
Discussion
TaqMan Mutation Detection Assays with castPCR technology offer a compelling solution for researchers requiring high-confidence detection of known somatic mutations. Their primary strength lies in the unique combination of exceptional sensitivity and workflow efficiency. While NGS is invaluable for discovering novel mutations across the entire genome, castPCR provides a cost-effective, rapid, and highly accurate method for validating those findings or for routinely screening large sample cohorts for a predefined set of actionable mutations [12].
This makes them particularly useful in applications such as:
- Validating mutations initially identified by NGS.
- Longitudinal studies monitoring tumor burden or the emergence of resistance mutations in response to therapy.
- High-throughput screening of clinical trial samples where speed, cost, and reproducibility are critical.
In conclusion, the sensitivity, specificity, and speed of TaqMan castPCR assays make them an indispensable tool in the cancer researcher's toolkit, bridging the gap between complex, discovery-oriented platforms and the need for focused, reliable, and quantitative mutation data.
The identification of somatic mutations is a cornerstone of modern precision oncology, enabling tailored therapeutic strategies and providing critical prognostic information. Competitive Allele-Specific TaqMan PCR (castPCR) represents a significant technological advancement in this field, combining exceptional sensitivity and specificity for detecting low-frequency mutations in complex biological samples [7]. This technology is particularly valuable in clinical cancer research, where the detection of rare mutant alleles must be achieved against a high background of wild-type DNA, especially in challenging scenarios such as liquid biopsies, formalin-fixed paraffin-embedded (FFPE) tissues, and heterogeneous tumor samples [2].
castPCR technology operates through an ingenious dual-mechanism approach that ensures superior mutation discrimination. The system employs allele-specific primers that preferentially amplify the mutant sequence while simultaneously utilizing Minor Groove Binder (MGB) oligonucleotide blockers that effectively suppress amplification of the wild-type allele [7]. This competitive inhibition mechanism provides castPCR with the capability to detect somatic mutations with a sensitivity down to 0.1% mutant alleles in a wild-type background, far surpassing conventional sequencing methods that typically require 10-25% mutant allele frequency for reliable detection [2]. The exceptional sensitivity of castPCR makes it particularly suitable for applications in minimal residual disease monitoring, early detection of resistance mutations, and analysis of samples with limited tumor cell content.
This application note provides a comprehensive overview of castPCR methodology with detailed protocols for targeting key oncogenic mutations in KRAS, BRAF, EGFR, and TP53 genes, which represent some of the most frequently altered pathways in human cancer. We present optimized experimental workflows, validation data, and practical considerations for implementing these assays in both basic research and translational clinical studies, framed within the broader context of advancing molecular diagnostics in oncology.
Mutation Detection Assay Performance Characteristics
Key Oncogenic Mutations and Detection Parameters
The performance characteristics of TaqMan Mutation Detection Assays for major cancer-related genes are summarized in Table 1. These assays demonstrate consistent high sensitivity across different mutation types and sample sources, enabling reliable detection even in challenging clinical specimens.
Table 1: Performance Characteristics of TaqMan Mutation Detection Assays for Key Cancer Genes
| Gene | Common Mutations | Detection Sensitivity | Compatible Sample Types | Research Applications |
|---|---|---|---|---|
| KRAS | p.G12D, p.G12V, p.G13D | ≤0.1% mutant allele frequency [2] | FFPE, cell lines, fresh frozen tissue [7] | Pancreatic cancer profiling, therapy response monitoring [13] |
| EGFR | L858R, exon 19 deletions, T790M | 0.5% for most common mutations [2] | FFPE, cytology smears, biopsies [2] | NSCLC TKI treatment selection, resistance mechanism studies [2] |
| TP53 | p.R273H, p.R175H | Varies by abundance; lower sensitivity for very low %mutation [13] | Tumor DNA, cfDNA [13] | Prognostic assessment, pan-cancer studies [13] |
| BRAF | V600E | Part of 819 assays for 47 cancer genes [7] | FFPE, fresh frozen tissue [7] | Melanoma, colorectal cancer research [7] |
Comparative Analytical Sensitivity Across Methodologies
The selection of an appropriate mutation detection platform is critical for research and potential clinical application. Table 2 provides a comparative analysis of the sensitivity ranges of various commonly used mutation detection technologies, highlighting the superior performance of castPCR for detecting low-frequency mutations.
Table 2: Comparative Sensitivity of Mutation Detection Methodologies
| Methodology | Limit of Detection | Typical Analysis Time | Key Advantages | Key Limitations |
|---|---|---|---|---|
| castPCR | 0.1% mutant alleles [2] | ~3 hours from sample to result [7] | Exceptional sensitivity, rapid workflow, simple data analysis | Targets predefined mutations only |
| Digital PCR (dPCR) | 0.1% or lower [13] | 4-6 hours | Absolute quantification, high sensitivity | Higher cost, specialized equipment required |
| ARMS (Therascreen) | ~1% mutant alleles [2] | 3-4 hours | Established methodology, regulatory approved | Lower sensitivity than castPCR |
| Sanger Sequencing | 10-25% mutant alleles [2] | 24-48 hours | Broad mutation detection, no prior knowledge needed | Poor sensitivity, labor-intensive |
| Next-Generation Sequencing | 1-5% (varies by depth) [14] | Several days | Comprehensive profiling, novel discovery | Complex data analysis, higher cost |
Detailed Experimental Protocols
Sample Preparation and Quality Control
Proper sample preparation is fundamental to successful mutation detection using castPCR technology. The assay compatibility extends across multiple sample types, each requiring specific handling considerations.
FFPE Tissue Samples: Section tissues at 5-10μm thickness. Deparaffinize and rehydrate samples using xylene and graded alcohol series (100%, 70%, 50% ethanol) [15]. Extract DNA using the QIAamp DNA FFPE Tissue Kit (Qiagen) or equivalent, with elution in 50-100μL of buffer AE. Assess DNA quality by multiplex PCR for the GAPDH gene, examining amplification of longer fragments (200bp, 300bp, and 400bp) as an integrity indicator [15].
Cell-Free DNA (cfDNA) from Plasma: Collect blood in EDTA or specialized cfDNA collection tubes. Process within 2-4 hours of collection with sequential centrifugation: 1900×g for 10 minutes at room temperature followed by 16,000×g for 10 minutes at 4°C [16]. Isolate cfDNA using the QIAamp DNA Micro Kit (Qiagen) with elution in 30-50μL of buffer AE. For exosomal DNA isolation, consider membrane-based methods (ExoEasy Maxi Kit, Qiagen) or ultracentrifugation at 100,000×g for 2 hours at 4°C [16].
DNA Quantification and Quality Assessment: Quantify DNA using fluorometric methods (Qubit dsDNA HS Assay Kit) for accuracy. Assess DNA purity by spectrophotometry (NanoDrop) with acceptable 260/280 ratios of 1.8-2.0. For FFPE-derived DNA, evaluate fragmentation using the Agilent 2100 Bioanalyzer with DNA 7500 kit; samples with DNA Integrity Numbers (DIN) >4 are preferred [16] [15].
castPCR Reaction Setup and Thermal Cycling
The castPCR procedure requires precise reaction assembly and thermal cycling conditions to maintain assay specificity and sensitivity.
Reaction Master Mix Preparation: For each reaction, combine 10μL of 2× TaqMan Genotyping Master Mix, 1μL of 20× Mutant Allele Assay (or Wild Type Assay), 1μL of 20× Gene Reference Assay, 10ng of template DNA, and nuclease-free water to a final volume of 20μL [2]. The mutant allele assay contains allele-specific primers, a FAM-labeled MGB probe, and an MGB oligonucleotide blocker for wild-type suppression [7].
Thermal Cycling Parameters: Program the real-time PCR instrument as follows: initial denaturation at 95°C for 10 minutes; 5 cycles of touch-down PCR: 92°C for 15 seconds, 58°C for 1 minute; followed by 40 cycles of amplification: 92°C for 15 seconds, 60°C for 1 minute [2]. Plate read should be performed at the end of each 60°C annealing/extension step.
Controls and Replicates: Include positive controls (known mutant cell lines or synthetic constructs) and negative controls (wild-type DNA, no-template control) in each run. Perform technical duplicates or triplicates for each sample, particularly when analyzing low-input DNA samples or detecting rare mutations.
Data Analysis and Interpretation
Accurate data analysis is critical for reliable mutation calling using castPCR technology.
ΔCt Calculation and Threshold Determination: Calculate ΔCt values using the formula: Normalized ΔCt = [Ct(mutant allele assay) – Ct(gene reference assay)] – calibration ΔCt [2]. The calibration ΔCt represents the inherent Ct difference between mutant allele and gene reference assays, which is predetermined by the manufacturer. Establish a ΔCt cut-off value of ≤7 for mutation detection based on validation studies [2].
Mutation Calling Criteria: A sample is considered mutation-positive if the ΔCt is ≤ the established cut-off value (e.g., ≤7) and the Ct value for the mutant allele assay is ≤37 [2]. For samples with Ct values >37, the result should be considered indeterminate and warrant repetition with higher DNA input or additional replicates.
Quantification of Mutant Allele Fraction: While castPCR is primarily qualitative, semi-quantitative assessment can be derived from the ΔCt values, with lower ΔCt values indicating higher mutant allele fractions. For precise quantification, digital PCR is recommended [13].
Research Applications and Case Studies
KRAS Mutation Detection in Pancreatic Cancer
KRAS mutations represent one of the most frequent genetic alterations in pancreatic ductal adenocarcinoma (PDAC), present in over 90% of cases [13]. Detection of KRAS mutations has significant implications for disease monitoring and therapeutic stratification. In a comprehensive study comparing castPCR and digital PCR (dPCR) for KRAS p.G12D detection in matched tumor tissue and liquid biopsy samples from 50 PDAC patients, castPCR demonstrated robust performance in tumor DNA analysis, identifying the mutation in 48.0% of patients with a median mutation percentage of 7.0% (IQR 5.3-13.7%) [13]. The concordance between castPCR and dPCR was 71.4% when using a >0.1% mutation cutoff for dPCR positivity, though dPCR detected additional mutations in 28.6% of samples, highlighting its superior sensitivity for very low-frequency mutations [13].
For liquid biopsy applications, the detection of KRAS mutations in cell-free DNA presents substantial technical challenges due to the low concentration of circulating tumor DNA in resectable PDAC, often representing less than 0.1% of total cfDNA [13]. Methodological optimization is crucial for reliable detection; studies have demonstrated that DNase I pretreatment of exosomes can effectively remove wild-type DNA contamination outside of exosomes, thereby increasing the mutant allele fraction of KRAS [16]. Additionally, DNA denaturation before droplet generation in ddPCR protocols significantly improves the total KRAS copy number and mutation-positive droplet count, enhancing detection sensitivity [16].
EGFR Mutation Analysis in Non-Small Cell Lung Cancer
EGFR mutation status represents a critical predictive biomarker for treatment selection in non-small cell lung cancer (NSCLC), with specific mutations conferring sensitivity to tyrosine kinase inhibitors (TKIs) [2]. The high sensitivity of castPCR makes it particularly valuable for analyzing challenging NSCLC samples, including small biopsies and cytological specimens with limited tumor cell content. In a validation study comparing castPCR with direct sequencing and the Therascreen RGQ kit, castPCR successfully detected EGFR mutations in clinical samples with similar frequency to the Therascreen kit, while sequencing failed to detect common mutations in samples with low tumor cell content [2].
The implementation of castPCR for EGFR mutation testing requires careful validation of analytical parameters. Based on comprehensive studies, the recommended threshold for data analysis is 0.2, with a maximum cycle threshold (Ct) of 37 and a cut-off ΔCt value of 7 for the EGFR TaqMan Mutation Detection Assays [2]. This assay configuration enables detection of key EGFR mutations including L858R, T790M, and exon 19 deletions with sensitivity ranging from 0.1% to 0.5% mutant alleles, significantly surpassing the 10-25% sensitivity threshold of conventional Sanger sequencing [2]. The robustness of castPCR across different sample types, including surgical specimens, small biopsies, and cytology smears, makes it particularly suitable for the diverse specimen types encountered in routine NSCLC diagnostics.
Technology Visualization
castPCR Mechanism Workflow
The following diagram illustrates the competitive allele suppression mechanism that underlies castPCR technology:
Experimental Workflow for Mutation Detection
The complete experimental workflow from sample collection to data analysis is depicted below:
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Reagents and Materials for castPCR Mutation Detection
| Product Name | Catalog Number | Application | Key Features |
|---|---|---|---|
| TaqMan Mutation Detection Assays | 4465804 [7] | Detection of mutant alleles | Pre-formulated assays include primers, FAM-labeled MGB probe, and MGB blocker |
| TaqMan Mutation Detection Reference Assays | 4465807 [7] | Reference for mutation-free gene region | Contains primers and FAM-labeled MGB probe for normalization |
| TaqMan EGFR Exon 19 Deletions Assay | 4465805 [7] | Detection of 19 different EGFR exon 19 deletions | Multiplex detection of common EGFR deletions |
| TaqMan Genotyping Master Mix | N/A [2] | PCR amplification | Optimized for allele discrimination assays |
| QIAamp DNA FFPE Tissue Kit | N/A [15] [2] | DNA extraction from FFPE tissues | Efficient DNA isolation from challenging samples |
| QIAamp DNA Micro Kit | N/A [16] [2] | DNA extraction from plasma/cfDNA | Optimized for low-concentration samples |
| DNase I | N/A [16] | Removal of wild-type DNA contamination | Critical for improving mutant allele fraction in exosomal DNA |
TaqMan Mutation Detection Assays based on castPCR technology provide a robust, sensitive, and specific platform for detecting somatic mutations in key cancer genes including KRAS, BRAF, EGFR, and TP53. The exceptional sensitivity of this technology, capable of detecting as little as 0.1% mutant alleles in a wild-type background, positions it as a valuable tool for cancer research applications where sample material is limited or mutant allele frequency is low [2]. The methodology offers a rapid workflow with time from sample to result of approximately three hours, significantly faster than next-generation sequencing approaches while maintaining high reproducibility and ease of implementation [7].
The comprehensive protocols and application data presented in this document provide researchers with a foundation for implementing castPCR technology in their molecular oncology studies. As precision medicine continues to evolve, the ability to reliably detect low-frequency mutations will become increasingly important for therapeutic monitoring, resistance mechanism studies, and early detection applications. The ongoing development of additional mutation detection assays will further expand the utility of this platform across diverse cancer types and research contexts, contributing to the advancement of personalized cancer care.
Step-by-Step Protocol: From Assay Selection to Data Analysis in Cancer Samples
Assay Identification and Selection for Your Mutation of Interest
The accurate identification of somatic mutations is a cornerstone of modern cancer research and therapeutic development. Among the various techniques available, TaqMan-based assays have emerged as a powerful tool for detecting known mutations with high specificity and sensitivity. These assays are particularly valuable for investigating mutations in oncogenes and tumor suppressor genes where specific single nucleotide variants (SNVs), insertions, or deletions drive cancer progression and treatment response [7] [17].
TaqMan Mutation Detection Assays utilize Competitive Allele-Specific TaqMan PCR (castPCR) technology, which combines allele-specific PCR with an innovative suppression mechanism to detect rare mutant alleles against a background of wild-type DNA [7]. This technology enables researchers to achieve reliable detection of mutations present at frequencies as low as 0.1%, making it suitable for analyzing heterogeneous tumor samples where tumor cell content may be limited [2]. The platform's robustness across different sample types, including formalin-fixed paraffin-embedded (FFPE) tissues, fresh frozen tissues, and cell lines, further enhances its utility in cancer research workflows [7] [17].
Mechanism of Action
The castPCR technology employs a sophisticated approach to discriminate between wild-type and mutant alleles through two key components:
Allele-Specific Primer: This primer is designed to preferentially amplify the mutant allele during PCR amplification. Its 3' end is complementary to the mutation of interest, resulting in inefficient amplification when the wild-type sequence is present [7] [17].
Minor Groove Binder (MGB) Oligonucleotide Blocker: This component suppresses amplification of the wild-type allele by binding specifically to the wild-type sequence. The MGB moiety increases the binding affinity of the blocker, allowing it to effectively compete with the allele-specific primer for wild-type templates [7].
When both mutant and wild-type DNA are present in a sample, the allele-specific primer and MGB blocker compete for binding to their respective targets. The blocker effectively inhibits amplification of the wild-type template, while the mutant template is efficiently amplified due to imperfect complementarity with the blocker [7]. This competitive mechanism enables highly specific detection of mutant alleles even when they represent a small fraction of the total DNA population.
Workflow Integration
The castPCR workflow integrates seamlessly with standard real-time PCR instrumentation and analysis software. Each reaction includes a FAM dye-labeled TaqMan MGB probe that binds specifically to the amplified mutant sequence, generating a fluorescent signal proportional to the amount of mutant DNA present [7]. The assays are typically run in conjunction with gene reference assays that amplify a mutation-free region of the same gene, serving as an internal control for DNA quality and quantity [17].
Step-by-Step Assay Identification Protocol
Locating Your Mutation of Interest
The first critical step in implementing TaqMan Mutation Detection Assays is identifying the appropriate assay for your specific mutation:
Download the TaqMan Mutation Assay Index File: Access the comprehensive index file from the manufacturer's website, which contains complete listings of all available mutations [7].
Search for Your Mutation: Locate your mutation of interest within the index file using relevant search parameters including:
- Gene symbol (e.g., KRAS, BRAF, EGFR)
- Nucleotide change (e.g., c.2573T>G)
- Amino acid change (e.g., p.L858R)
- COSMIC identifier [7]
Verify Assay Compatibility: Confirm that your mutation is covered by the available assays. The current portfolio includes 819 assays for 47 known cancer research genes such as KRAS, BRAF, KIT, and JAK2 [7].
Assay Identification and Ordering
Once you have located your mutation of interest:
Record the Relevant Assay IDs:
- Mutant Allele Assay ID: Found in column B of the index file
- Gene Reference Assay ID: Found in column Q of the index file
- Wild Type Assay ID (optional): Found in column S of the index file [7]
Ordering Process:
- Navigate to the manufacturer's Quick Order page
- Enter the identified assay IDs with their respective catalog numbers:
- Mutant Allele Assay: Cat. No. 4465804
- Gene Reference Assay: Cat. No. 4465807
- Wild Type Assay (optional): Cat. No. 4465804 [7]
- Proceed through the checkout process
Consider Pre-plated Options: For large-scale studies, consider utilizing the TaqMan Custom Plating Service, which provides assays pre-plated into 96- or 384-well plates to save preparation time and reduce experimental variability [7].
Experimental Setup and Optimization
Sample Preparation Guidelines
Proper sample preparation is essential for successful mutation detection:
DNA Source Compatibility: The assays are validated for use with genomic DNA extracted from:
DNA Quality Assessment: Evaluate DNA quality using:
- Spectrophotometric analysis (A260/A280 ratio of 1.8-2.0)
- Gel electrophoresis to confirm high molecular weight
- Fluorometric quantification for accurate concentration determination [2]
DNA Quantity Requirements: Typically 10-100 ng of genomic DNA per reaction, depending on sample quality and mutation abundance [2].
Reaction Setup and Thermal Cycling
The following protocol outlines the standard procedure for setting up and running TaqMan Mutation Detection Assays:
Reaction Components:
- 1X TaqMan Genotyping Master Mix
- 1X TaqMan Mutation Detection Assay (mutant allele or reference assay)
- 10 ng genomic DNA template
- Nuclease-free water to final volume [2]
Recommended Reaction Volumes:
- 10 μL for 384-well plates
- 20 μL for 96-well plates [7]
Thermal Cycling Conditions:
- Initial denaturation: 95°C for 10 minutes
- 5 cycles of:
- Denaturation: 92°C for 15 seconds
- Annealing/Extension: 58°C for 1 minute
- 40 cycles of:
- Denaturation: 92°C for 15 seconds
- Annealing/Extension: 60°C for 1 minute [2]
Instrument Compatibility: The assays are compatible with various Applied Biosystems real-time PCR systems including QuantStudio series, ViiA 7, 7500, and StepOnePlus instruments [7] [17].
Experimental Design Considerations
Include Appropriate Controls:
- Positive controls (samples with known mutations)
- Negative controls (samples without mutations)
- No-template controls (nuclease-free water instead of DNA)
Utilize Internal Positive Control (IPC): Consider duplexing with the TaqMan Mutation Detection IPC Reagent Kit to distinguish true negatives from PCR failure or inhibition [7] [17].
Replication Strategy: Perform technical replicates (at least duplicates) for each sample to ensure result reproducibility.
Data Analysis and Interpretation
Calculation Method
Data analysis for TaqMan Mutation Detection Assays relies on the comparative Ct (ΔΔCt) method:
Calculate ΔCt Values: For each sample, compute the difference between the Ct value of the mutant allele assay and the Ct value of the gene reference assay:
Apply Calibration Adjustment: Subtract the inherent efficiency difference between assays (calibration ΔCt) to obtain the normalized ΔCt:
- Normalized ΔCt = [Ct(mutant) - Ct(reference)] - calibration ΔCt [2]
Apply Cut-off Criteria: Compare the normalized ΔCt to the empirically determined cut-off value:
- If normalized ΔCt ≤ ΔCt cut-off → Mutation detected
- If normalized ΔCt > ΔCt cut-off → Mutation not detected [2]
Establishing Thresholds
Validation studies have established the following analytical parameters for EGFR mutation detection:
| Parameter | Recommended Value | Experimental Basis |
|---|---|---|
| Threshold Value | 0.2 | Determined through training set analysis [2] |
| Maximum Ct | 37 | Beyond this limit, results are considered unreliable [2] |
| ΔCt Cut-off | 7 | Validated for EGFR mutations; should be established for other targets [2] |
| Sensitivity | 0.1% mutant alleles | Detection limit in wild-type background [2] |
Analysis Software
For streamlined data analysis, use Mutation Detector Software, which automatically:
- Imports Ct values from real-time PCR instruments
- Calculates ΔCt values using built-in calibration factors
- Applies cut-off criteria to determine mutation status
- Generates reports for experimental documentation [7] [17]
Research Reagent Solutions
Successful implementation of TaqMan Mutation Detection Assays requires the following key reagents and components:
Table: Essential Research Reagents for TaqMan Mutation Detection
| Reagent/Category | Specific Product Examples | Function/Purpose |
|---|---|---|
| Core Assays | TaqMan Mutation Detection Assays (Cat. #4465804) | Detect specific mutant alleles [7] |
| Reference Assays | TaqMan Mutation Detection Reference Assays (Cat. #4465807) | Amplify mutation-free gene regions as internal controls [7] |
| Specialized Assays | TaqMan EGFR Exon 19 Deletions Assay (Cat. #4465805) | Detect multiple exon 19 deletions in a single reaction [7] |
| Master Mix | TaqMan Genotyping Master Mix | Provides optimized reagents for amplification [17] |
| Control Reagents | TaqMan Mutation Detection IPC Reagent Kit (Cat. #4467538) | Distinguish true negatives from PCR failures [7] |
| DNA Isolation | QIAamp DNA FFPE Tissue Kit, DNeasy Blood & Tissue Kit | Extract high-quality DNA from various sample types [2] |
Performance Comparison with Alternative Methods
Understanding how castPCR technology compares to other mutation detection methods assists researchers in selecting the most appropriate approach for their specific applications:
Table: Comparison of Mutation Detection Method Performance
| Method | Limit of Detection | Key Advantages | Key Limitations |
|---|---|---|---|
| castPCR | 0.1% mutant alleles [2] | High specificity, quantitative, simple workflow | Limited to known mutations |
| Direct Sequencing | 10-25% mutant alleles [2] | Detects all mutations in sequenced region, considered gold standard | Low sensitivity, labor-intensive |
| ARMS (Therascreen) | 1% mutant alleles [2] | Established clinical use, validated for companion diagnostics | Lower sensitivity than castPCR |
| CRISPR-Cas12a | 10% mutant alleles [18] | Rapid (30 min), no PCR amplification needed | Significantly lower sensitivity |
| NGS/WES | 1-5% mutant alleles [19] | Comprehensive, detects unknown mutations | Complex workflow, high cost, data analysis challenges |
Troubleshooting and Optimization Guidelines
Even with optimized protocols, researchers may encounter challenges during assay implementation. The following table addresses common issues and recommended solutions:
Table: Troubleshooting Guide for TaqMan Mutation Detection Assays
| Problem | Potential Causes | Recommended Solutions |
|---|---|---|
| No Amplification | DNA degradation, PCR inhibition, reagent issues | Check DNA quality, include IPC, verify reagent preparation [7] [17] |
| High Background | Excessive wild-type amplification, non-specific binding | Verify blocker functionality, optimize template amount [7] |
| Inconsistent Replicates | Pipetting errors, template heterogeneity, bubble formation | Use calibrated pipettes, mix reagents thoroughly, centrifuge plates [20] |
| Poor Sensitivity | Suboptimal ΔCt cut-off, low mutant allele frequency | Re-evaluate cut-off values using control samples, increase input DNA [2] |
| Inhibition | Contaminants from DNA extraction, high sample concentration | Dilute template, purify DNA, use IPC to detect inhibition [7] |
Application Notes and Validation Data
Clinical Validation Studies
Independent validation studies have demonstrated the robust performance of TaqMan Mutation Detection Assays in clinical cancer samples:
EGFR Mutation Detection: A comprehensive study comparing castPCR with direct sequencing and the Therascreen kit demonstrated that castPCR identified EGFR mutations with similar frequency as Therascreen but with enhanced sensitivity compared to sequencing, particularly in samples with low tumor cell content [2].
Multi-Gene Panel Performance: The REB Array, a TaqMan-based panel for detecting 44 mutations across RAS, EGFR, and BRAF genes, achieved 93% concordance with the Therascreen EGFR assay, 95% concordance with the KRAS castPCR assay, and 100% concordance with the cobas BRAF assay [9].
Analytical Sensitivity: Using controlled admixtures of mutant and wild-type DNA, castPCR technology consistently detected mutations at allele frequencies as low as 0.1%, significantly outperforming direct sequencing (which requires 10-25% mutant alleles) [2].
Specialized Applications
Beyond standard mutation detection, TaqMan assays have been adapted for specialized research applications:
Splice Variant Detection: Researchers have developed TaqMan-based qRT-PCR assays to detect oncogenic splice variants such as TrkAIII in tumor cDNAs, demonstrating sensitivity to as few as 10 copies of the target sequence in complex RNA backgrounds [21].
Multi-Analyte Profiling: Combined RNA and DNA analysis using TaqMan-based approaches has enabled comprehensive molecular profiling, recovering variants missed by DNA-only testing and improving detection of clinically actionable alterations [19].
TaqMan Mutation Detection Assays based on castPCR technology provide cancer researchers with a robust, sensitive, and specific platform for identifying somatic mutations in diverse sample types. The systematic approach to assay selection, experimental setup, and data analysis outlined in this application note enables researchers to reliably detect mutations driving cancer pathogenesis and treatment response. By following the standardized protocols and leveraging the optimized reagent systems, research scientists and drug development professionals can generate high-quality mutation data to advance their oncology research programs and support the development of targeted cancer therapies.
Accurate mutation detection is a cornerstone of modern cancer research and drug development, enabling everything from target identification to patient stratification. The reliability of these results, particularly when using powerful detection methods like TaqMan assays, is fundamentally dependent on the quality of the input DNA. This application note provides detailed protocols for optimizing DNA extraction and preparation from three critical sample types in oncology: formalin-fixed paraffin-embedded (FFPE) tissue, cell lines, and liquid biopsies. By addressing the unique challenges of each material, researchers can ensure the integrity of their genetic analyses and generate robust, reproducible data for their cancer research projects.
Sample-Specific Challenges and Optimization Strategies
Each sample type presents distinct obstacles for DNA isolation. The table below summarizes the primary challenges and corresponding solutions for obtaining high-quality DNA suitable for downstream TaqMan assays.
Table 1: Key Challenges and Optimization Strategies for Different Sample Types
| Sample Type | Primary Challenges | Optimization Strategies |
|---|---|---|
| FFPE Tissue | Chemical modifications, protein cross-links, nucleic acid fragmentation, and limited sample availability [22]. | Use of specialized isolation kits, incorporation of a heating step (e.g., 70°C for 20 min) to reverse cross-links, and targeting short amplicons (<150 bp) in PCR [22]. |
| Cell Lines | Genomic DNA (gDNA) contamination and viscosity of lysates [23]. | Rigorous DNase treatment, complete removal of culture medium, PBS washes, and optimization of lysis conditions (room temperature, up to 8 minutes) [23]. |
| Liquid Biopsy | Low abundance of circulating tumor DNA (ctDNA) against a high background of wild-type DNA [24]. | Selective extraction of cell-free DNA (cfDNA), use of highly sensitive detection technologies like digital PCR (dPCR) or castPCR, which can detect mutant alleles down to 0.1% variant allele frequency [25] [7] [24]. |
Workflow for DNA Sample Preparation and Analysis
The following diagram outlines the core workflow for processing FFPE, cell line, and liquid biopsy samples towards mutation detection.
Detailed Protocols for DNA Optimization
Protocol 1: FFPE Tissue Samples
Background: Nucleic acids from FFPE samples are chemically modified, fragmented, and cross-linked to proteins, making them challenging substrates for PCR-based assays [22]. The following optimized protocol is designed to maximize the yield and quality of DNA recovered from these valuable archival tissues.
Materials and Equipment
- RecoverAll Total Nucleic Acid Isolation Kit (or equivalent specialized FFPE kit) [22]
- Proteinase K
- Microcentrifuge
- Heating block or water bath
- Spectrophotometer (e.g., NanoDrop) and fluorometer (e.g., Qubit) [26]
- Agilent TapeStation system (for DNA Integrity Number assessment) [26]
Step-by-Step Procedure
- Sectioning: Cut 2-3 sections of 5-10 µm thickness from the FFPE block. For optimal results, use a "separately fixed tumor sample" – a small (3-5 mm) tumor piece fixed immediately upon specimen receipt to ensure rapid, uniform fixation [26].
- Deparaffinization and Lysis:
- Add 1 mL of xylene (or the provided deparaffinization solution) to the sections, vortex, and centrifuge. Remove the supernatant.
- Wash twice with 1 mL of 100% ethanol. Air-dry the pellet.
- Resuspend the pellet in 200 µL of digestion buffer and add Proteinase K. Incubate at 50°C until the tissue is completely lysed (several hours to overnight).
- Cross-Link Reversal: A critical, optimized step. Heat the lysate at 70°C for 20 minutes to reverse formaldehyde-induced modifications. This has been shown to improve the sensitivity of downstream real-time PCR assays [22].
- Nucleic Acid Isolation: Purify the DNA using the chosen kit's protocol, typically involving binding to a silica filter, washing, and elution in a small volume of nuclease-free water or buffer.
- Quality Control: Quantify DNA using a fluorometric method (Qubit). Assess purity spectrophotometrically (NanoDrop; target A260/A280 ratio: 1.8-2.0). For integrity, use the TapeStation to determine the DNA Integrity Number (DIN) or perform a TaqMan-based Short-to-Long Cycle Threshold (S/L Ct) Ratio assay [26].
Table 2: TaqMan-Based DNA Quality Assessment [26]
| Assay Target | Amplicon Length | Function in Quality Control |
|---|---|---|
| RNase P (Short) | 87 base pairs | Amplifies efficiently even from fragmented DNA. |
| Custom MGB (Long) | 256 base pairs | Amplifies poorly if DNA is degraded. |
| Calculation | S/L Ct Ratio = Ct(Short) / Ct(Long) | A ratio close to or greater than 1 indicates high-quality, intact DNA. |
Protocol 2: Cell Line Samples
Background: The TaqMan Gene Expression Cells-to-CT Kit provides a rapid method for lysing cells and preparing nucleic acids for PCR without a separate purification step, minimizing sample loss [23]. The key challenge is effectively removing gDNA contamination.
Materials and Equipment
- TaqMan Gene Expression Cells-to-CT Kit [23]
- Phosphate-Buffered Saline (PBS), room temperature
- DNase (included in kit)
- Lysis Solution (included in kit)
- Stop Solution (included in kit)
Step-by-Step Procedure
- Cell Preparation: Plate cells and grow to desired confluence. For best results, do not exceed 10,000 cells per 50 µL of Lysis Solution to avoid viscous lysates [23].
- Wash: Completely remove the culture medium. Wash cells once with an equal volume of room-temperature 1X PBS and completely remove the PBS wash. This is critical for eliminating residual medium and reducing gDNA contamination [23].
- Lysis:
- Prepare the Lysis Solution by adding DNase (provided in the kit).
- Add the appropriate volume of Lysis Solution to the cells (ensure it covers the well surface).
- Incubate at room temperature for 5-8 minutes to lyse the cells and digest gDNA. Do not perform this step on ice.
- Reaction Termination: Add the provided Stop Solution directly into the lysate and mix by pipetting 5 times. Avoid depressing the pipette to the "blow out" position to prevent foaming [23]. The lysate is now ready for reverse transcription and PCR.
- Optional gDNA Troubleshooting: If gDNA contamination persists, ensure all medium is removed and the PBS wash is not omitted. Extending the lysis duration to 8 minutes or performing the lysis at 25°C can improve gDNA removal. Adding more DNase is not beneficial [23].
Protocol 3: Liquid Biopsy Samples
Background: Liquid biopsies contain circulating tumor DNA (ctDNA) that is highly fragmented and present at very low frequencies in a high background of wild-type cell-free DNA (cfDNA). Detection requires both optimized isolation and ultra-sensitive detection methods [27] [24].
Materials and Equipment
- MagMAX Cell-Free DNA Isolation Kit (or similar magnetic bead-based kit) [24]
- Blood collection tubes (e.g., BD Vacutainer PPT)
- Centrifuge
- Qubit Fluorometer and dsDNA HS Assay Kit
- TaqMan Liquid Biopsy dPCR Assays or TaqMan Mutation Detection Assays (castPCR) [25] [7]
Step-by-Step Procedure
- Blood Collection and Plasma Separation:
- Collect blood into cell-stabilizing tubes (e.g., EDTA or Streck tubes).
- Centrifuge within one hour at 1100-1600 × g for 10 minutes at room temperature to separate plasma.
- Transfer the supernatant (plasma) to a new tube and perform a second centrifugation at 16,000 × g for 10 minutes to remove any remaining cells or debris [27].
- Store plasma at -80°C if not processing immediately.
- cfDNA Isolation:
- Use the MagMAX Cell-Free DNA Isolation Kit according to the manufacturer's instructions. This magnetic bead-based technology efficiently recovers short, fragmented cfDNA.
- Elute the cfDNA in a small volume (e.g., 20-50 µL) to maximize concentration.
- Quality Control and Quantification:
- Quantify cfDNA using the highly sensitive Qubit dsDNA HS Assay. The concentration can be correlated with disease burden, such as lactate dehydrogenase (LDH) levels in melanoma [27].
- Analyze fragment size distribution using a Bioanalyzer or TapeStation (expected peak ~160-170 bp).
- Mutation Detection with Optimized TaqMan Assays:
- For maximum sensitivity, use TaqMan Liquid Biopsy dPCR Assays. These wet-lab-validated assays on digital PCR platforms can detect mutant alleles with a variant allele frequency (VAF) as low as 0.1% [25] [24].
- Alternatively, TaqMan Mutation Detection Assays using castPCR technology can be used on standard real-time PCR systems to detect somatic mutations down to 1 mutant in 1,000 wild-type cells (0.1% VAF) with high specificity, as they employ a blocker oligonucleotide to suppress wild-type amplification [7].
The Scientist's Toolkit: Research Reagent Solutions
The following table lists key commercial solutions referenced in these protocols that are optimized for mutation detection in cancer research.
Table 3: Essential Research Reagents for Mutation Detection Workflows
| Product Name | Sample Type | Key Function and Features |
|---|---|---|
| RecoverAll Total Nucleic Acid Isolation Kit [22] | FFPE Tissue | Optimized for short nucleic acid fragments; includes a heating step to reverse cross-links. |
| TaqMan Gene Expression Cells-to-CT Kit [23] | Cell Lines | Enables direct lysis and gDNA removal for gene expression or genotyping without RNA/DNA purification. |
| MagMAX Cell-Free DNA Isolation Kit [24] | Liquid Biopsy (Plasma/Serum) | Magnetic bead-based isolation of cfDNA from plasma, serum, or urine. |
| TaqMan Mutation Detection Assays (castPCR) [7] | FFPE, Cell Lines, Liquid Biopsy | Detects rare somatic mutations with high specificity using a wild-type blocker. |
| TaqMan Liquid Biopsy dPCR Assays [25] | Liquid Biopsy | Wet-lab validated for digital PCR; detects rare mutant alleles with sensitivity to ≤0.1% VAF. |
| Oncomine Pan-Cancer Cell-Free Assay [27] | Liquid Biopsy, FFPE | Targeted NGS panel for broad detection of variants from cfDNA and FFPE samples. |
The pursuit of reliable and actionable mutation data in cancer research hinges on meticulous sample preparation. By adhering to these optimized, sample-specific protocols for FFPE tissues, cell lines, and liquid biopsies, researchers can significantly improve the quality of their DNA inputs. This, in turn, unlocks the full potential of sophisticated TaqMan assay technologies, enabling the sensitive and specific detection of mutations necessary to drive forward drug development and precision oncology.
Within the field of molecular oncology, the detection of somatic mutations is critical for cancer prognosis and the selection of targeted therapies. TaqMan-based real-time PCR has emerged as a cornerstone technology for this purpose, combining sensitivity, specificity, and robustness, particularly when working with challenging sample types like formalin-fixed paraffin-embedded (FFPE) tissues [28] [29]. This application note details a standardized protocol for Competitive Allele-Specific TaqMan PCR (castPCR), a method designed to detect single nucleotide variants with the high selectivity required to identify mutant alleles amidst a vast excess of wild-type DNA, a common scenario in genetically heterogeneous tumor samples [30] [28] [29].
Principles of Mutation Detection by CastPCR
The core principle of castPCR for mutation detection involves the use of allele-specific primers and blocker oligonucleotides to achieve superior selectivity. The method combines the 5' nuclease activity of Taq DNA polymerase with a fluorogenic probe-based detection system to distinguish between wild-type and mutant alleles with high precision [30] [28].
- Allele-Specific Primers: A primer is designed to be complementary to the mutant allele, with its 3' terminus specifically anchored at the mutant nucleotide. This design preferentially initiates amplification from the mutant template.
- Wild-Type Suppression: A key feature of castPCR is the use of a minor groove binder (MGB) oligonucleotide blocker. This blocker is complementary to the wild-type sequence and binds upstream of the allele-specific primer, effectively suppressing the amplification of the wild-type allele by interfering with primer binding or extension.
- Fluorogenic Detection: A locus-specific TaqMan probe, labeled with a reporter dye (e.g., FAM) on the 5' end and a non-fluorescent quencher (NFQ) on the 3' end, hybridizes to the target sequence. During amplification, the 5' nuclease activity of the DNA polymerase cleaves the probe, separating the reporter from the quencher and generating a fluorescent signal. The increase in fluorescence is directly proportional to the accumulation of the specific PCR product [30].
The following diagram illustrates the workflow and mechanism of the castPCR assay for mutation detection:
Materials and Reagents
The Scientist's Toolkit: Essential Research Reagents
The following table lists the key reagents and materials required to perform a castPCR experiment for somatic mutation detection.
Table 1: Key Reagent Solutions for TaqMan-based Mutation Detection
| Item | Function/Description | Example Product/Catalog |
|---|---|---|
| TaqMan Mutation Detection Assay | Contains allele-specific primer, MGB blocker, locus-specific primer, and FAM-labeled MGB probe for the mutant allele. | TaqMan Mutation Detection Assays [28] |
| TaqMan Gene Reference Assay | Detects a stable, mutation-free region of the gene of interest for normalization; contains primers and a VIC-labeled probe. | TaqMan Copy Number Reference Assay [30] |
| TaqMan Genotyping Master Mix | Optimized buffer containing AmpliTaq Gold DNA Polymerase, dNTPs, and passive reference dye (ROX). | TaqMan Genotyping Master Mix [28] |
| Internal Positive Control (IPC) Reagents | Optional kit to distinguish true negatives from PCR failure; can be duplexed with the assay. | TaqMan Mutation Detection IPC Reagent Kit [28] |
| Genomic DNA (gDNA) | Sample input; compatible with gDNA from FFPE tissues, fresh frozen tissues, and cell lines. | - [28] |
| Nuclease-Free Water | Solvent to adjust final reaction volume. | - |
| Real-Time PCR Instrument | Thermocycler capable of detecting FAM and VIC fluorescence. | Applied Biosystems QuantStudio series, ViiA 7, 7500 Fast [28] |
Reaction Component Setup
For each real-time PCR reaction, combine the following components in a well or tube. The final reaction volume is typically 20 µL, but can be scaled accordingly.
Table 2: Recommended Reaction Setup for a 20 µL Reaction
| Component | Final Concentration/Amount | Volume per 20 µL Reaction |
|---|---|---|
| TaqMan Genotyping Master Mix (2X) | 1X | 10.0 µL |
| TaqMan Mutation Detection Assay (20X) | 1X | 1.0 µL |
| TaqMan Gene Reference Assay (20X) | 1X | 1.0 µL |
| Template gDNA | 10–50 ng (recommended) | Variable (X µL) |
| Nuclease-Free Water | To volume | Variable (to 20.0 µL) |
| Total Volume | 20.0 µL |
Note: For the optional Internal Positive Control, add the IPC DNA and IPC assay to the reaction mix as per the manufacturer's instructions. The volume of the master mix or water must be adjusted accordingly to maintain the final volume [28].
Thermal Cycling Protocol
After preparing the reaction mix, use the following universal thermal cycling protocol. It is critical to use a validated real-time PCR instrument and ensure the correct dye detection channels (FAM and VIC) are selected in the instrument software.
Table 3: Standard Thermal Cycling Conditions
| Step | Temperature | Time | Cycles | Description |
|---|---|---|---|---|
| Enzyme Activation | 95°C | 10 minutes | 1 | Activates the AmpliTaq Gold DNA Polymerase. |
| Denature | 95°C | 15 seconds | 40 | Separates double-stranded DNA. |
| Anneal/Extend | 60°C | 1 minute | 40 | Primers and probe anneal; polymerase extends primers and cleaves probe. Fluorescence data is collected at this step. |
Instrument Compatibility: This protocol is compatible with a range of Applied Biosystems real-time PCR systems, including the QuantStudio 3D, 3, 5, 6 & 7 Flex, ViiA 7, 7500, 7500 Fast, and StepOnePlus systems [28].
Data Analysis and Interpretation
Following amplification, the cycle threshold (Ct) values for both the mutant allele (FAM channel) and the reference gene (VIC channel) are determined by the instrument's software. The Ct is the PCR cycle at which the fluorescence signal crosses a threshold set within the exponential phase of amplification, and it is a relative measure of the target concentration [31].
Calculation of ΔCt and Mutation Load
The relative quantity of the mutant allele within the sample is calculated using the ΔCt method, normalized to the reference gene.
- Calculate ΔCt: For each sample, compute the difference between the Ct value of the mutant allele assay and the Ct value of the gene reference assay [28]. > Formula: ΔCt = Ct (Mutant Assay) – Ct (Reference Assay)
- Interpret Results: The ΔCt value is inversely proportional to the amount of mutant allele present. A lower (more negative) ΔCt indicates a higher abundance of the mutant allele in the sample. The specific ΔCt value can be correlated with the percentage of mutation in the sample using pre-determined cutoff values established during assay validation with spiked cell line gDNA samples [28].
Key Performance Parameters
To ensure data reliability, assess the following parameters:
- PCR Efficiency: Ideal PCR efficiency is 100%, corresponding to a doubling of product every cycle. An efficiency between 90% and 110% is generally considered acceptable. Efficiency can be calculated from a standard curve of a dilution series [31] [32].
- Precision: The standard deviation of replicate Ct values should be low. A standard deviation ≤0.25 allows for the discrimination of 2-fold dilution differences in over 95% of cases [31].
- Sensitivity: The ultimate sensitivity is the reliable detection of a single copy of the starting mutant template. For low copy number detection, a large number of replicates is recommended to account for Poisson distribution limitations [31].
Troubleshooting and Best Practices
- Low Fluorescence Signal: Ensure probe and primer concentrations are optimal. Check sample quality and quantity; degraded DNA or PCR inhibitors can reduce efficiency.
- High Background or Nonspecific Amplification: Verify the specificity of the allele-specific primer and blocker design. Ensure thermal cycling temperatures are accurate.
- Poor Reproducibility between Replicates: Mix reaction components thoroughly. Ensure accurate pipetting and that the reaction plate is properly sealed.
- No Amplification in Positive Control: Check the integrity of all reagents, especially the enzyme master mix. Confirm thermal cycler calibration and protocol settings.
For comprehensive troubleshooting and validation data, refer to the product documentation for specific TaqMan Mutation Detection Assays and the support resources provided by the manufacturer [28].
In the field of cancer research and molecular diagnostics, accurate interpretation of quantitative PCR (qPCR) data is paramount for reliable mutation detection. The cycle threshold (Ct) value represents the PCR cycle number at which the fluorescence signal of a amplifying target crosses a threshold value, indicating detectable amplification. The ΔCt value provides a normalized metric calculated as the difference between the mutation Ct value and a reference control signal [33]. This parameter is fundamental for determining mutation status in various assay formats, including TaqMan assays and Amplification Refractory Mutation System-PCR (ARMS-PCR).
Understanding ΔCt analysis is particularly crucial in clinical contexts such as therapeutic decision-making for cancer patients, where mutation status determines eligibility for targeted therapies like tyrosine kinase inhibitors in non-small cell lung cancer (NSCLC) [33]. Proper interpretation of these values requires not only mathematical calculation but also consideration of sample quality, assay validation, and established cutoff thresholds.
Experimental Protocols for Mutation Detection Using ΔCt Values
Sample Preparation Methods
The reliability of ΔCt analysis begins with proper sample preparation. Different sample types require specific processing protocols to ensure DNA of sufficient quality and quantity:
Cell Block Preparation: Collect 50 mL of fresh pleural effusion and centrifuge at 2,500 rpm for 10 minutes. Discard supernatant and treat bloody sediments with 30% ethanol. Fix sediment in 10% neutral buffered formalin for 10 minutes, then add 95% ethanol. Process through standard tissue dehydration, embedding, and paraffin blocking procedures. Section at 5μm thickness for DNA extraction [33].
Cell Smear Preparation: Centrifuge 50 mL of fresh pleural effusion at 2,500 rpm for 10 minutes. Prepare direct smears from the sediment and immediately fix in 95% ethanol for at least 10 minutes. For DNA extraction, remove coverslip and scrape enriched tumor cell areas using a disposable blade [33].
DNA Extraction and Quality Control: Use commercial DNA extraction kits according to manufacturer specifications. Measure DNA purity using spectrophotometry (OD260/OD280 ratio). Dilute extracted DNA to a standardized concentration (2 ng/μL) for mutation detection assays to ensure consistent results [33].
qPCR Setup and Amplification Conditions
Proper experimental setup is essential for generating reliable ΔCt values:
Reaction Preparation: Prepare master mix according to TaqMan or ARMS-PCR kit specifications. Use validated primer-probe sets specific to target mutations and reference genes.
Plate Setup: Include appropriate controls (negative, positive, and no-template) in each run. Place paired samples (e.g., cell blocks and smears) adjacently in the PCR plate to minimize positional effects [33].
Amplification Parameters: Program thermal cycler according to kit specifications. Typical conditions include: initial denaturation (95°C for 5-10 minutes), followed by 40-50 cycles of denaturation (95°C for 15-30 seconds) and annealing/extension (60°C for 30-60 seconds) [34].
Quality Assessment: Validate each run by ensuring external control Ct values fall within acceptable ranges (typically 13-21 cycles). Reject assays falling outside these parameters [33].
Data Interpretation and Mutation Calling Criteria
Quantitative Thresholds for Mutation Determination
Establishing clear thresholds is critical for accurate mutation calling. The following table summarizes interpretation criteria based on ΔCt analysis:
Table 1: Mutation Status Determination Based on Ct and ΔCt Values
| Ct Value Range | ΔCt Analysis | Interpretation | Clinical Significance |
|---|---|---|---|
| < 26 | ΔCt = Mutation Ct - Control Ct | Positive | Mutation detected; potential eligibility for targeted therapies |
| 26-29 | ΔCt = Mutation Ct - Control Ct | Critical Positive | Borderline result; requires confirmation with alternative method |
| ≥ 29 | ΔCt = Mutation Ct - Control Ct | Negative | Wild-type sequence; consider alternative treatments |
| Control Ct: 13-21 | Quality control metric | Sample adequate | Ensures DNA quality and reaction efficiency |
These thresholds should be established during assay validation and may require adjustment based on specific sample types, detection technologies, and clinical requirements [33].
Quality Control Parameters
Robust quality control measures are essential for reliable mutation detection:
Sample Adequacy: Ensure external control Ct values fall within the 13-21 cycle range. Values outside this range indicate potential issues with DNA quality or reaction efficiency [33].
Sample Comparison: When comparing paired samples (e.g., cell blocks vs. smears), process them simultaneously using identical reaction conditions to minimize inter-assay variability [33].
Reference Genes: Include appropriate reference genes (e.g., ACTB, GAPDH) for normalization where applicable, particularly in methylation-specific PCR assays [34].
Research Reagent Solutions for Mutation Detection
Selecting appropriate reagents is crucial for successful mutation detection experiments. The following table outlines key solutions and their applications:
Table 2: Essential Research Reagents for Mutation Detection Assays
| Reagent / Solution | Function / Application | Implementation Example |
|---|---|---|
| TaqMan Gene Expression Assays | Detection and quantification of immune checkpoint markers and immune-related genes | Pre-designed assays for checkpoint inhibitors in immuno-oncology research [35] |
| DNA Extraction Kits | Isolation of high-quality DNA from various sample types | Commercial kits for extracting DNA from cell blocks and smears [33] |
| EGFR Mutation Detection Kits | Specific detection of EGFR mutations in cancer samples | ARMS-PCR-based kits for identifying sensitizing mutations in NSCLC [33] |
| Bisulfite Conversion Reagents | DNA modification for methylation-specific PCR | Conversion of unmethylated cytosines to uracils in methylation-based detection assays [34] |
| TaqMan Array Cards | Multi-gene expression profiling in pre-configured formats | Fixed-content arrays for immuno-oncology research with 96-384 well formats [35] |
Workflow Visualization
The following diagram illustrates the complete experimental workflow for mutation detection and ΔCt analysis:
Mutation Detection and ΔCt Analysis Workflow
Advanced Applications and Methodological Considerations
Specialized Detection Scenarios
ΔCt value interpretation must be adapted to specific research contexts and detection methodologies:
Methylation-Specific Detection: In DNA methylation analysis for cervical cancer screening, ΔCt values are calculated using reference genes (e.g., ACTB) for normalization, with lower ΔCt values indicating higher methylation levels and potential malignancy [34].
Comparative Sample Analysis: Studies demonstrate that cell HE staining smears yield significantly lower ΔCt values compared to paired cell blocks (t=4.526, P<0.001), indicating superior DNA quality in smears despite identical mutation detection rates [33].
Longitudinal Studies: DNA degradation in archived samples affects ΔCt values. Cell blocks stored for 3+ years show significantly increased mutation Ct values compared to recent samples, while cell smears maintain more stable Ct values over time [33].
Troubleshooting and Optimization Strategies
Several factors can impact ΔCt values and require methodological adjustments:
Sample Preservation Effects: Cell blocks show increasing external control Ct values with storage time (significantly higher in 2014-2017 vs. 2018-2021 samples), indicating DNA degradation, while cell smears maintain stable control Ct values over 8-year storage [33].
Tumor Cell Percentage: Ensure adequate tumor content (≥70% in cell blocks) to avoid false negatives due to dilution effects. Use microdissection techniques when working with heterogeneous samples [33].
Multiple Sampling: For irreplaceable samples like cell smears, prepare multiple slides initially to accommodate potential future testing needs, as the material cannot be reused once scraped for DNA extraction [33].
Proper interpretation of ΔCt values is a critical skill for researchers utilizing TaqMan assays and other qPCR-based methods for mutation detection. By following standardized protocols, implementing rigorous quality control measures, and applying validated interpretation thresholds, researchers can generate reliable, reproducible mutation data to inform both basic research and clinical decision-making. The continued refinement of these analytical approaches supports advancements in personalized cancer treatment and biomarker discovery.
Within the framework of a broader thesis on TaqMan assay protocols for mutation detection in cancer research, this document presents detailed application notes and protocols for detecting two critical mutations: EGFR T790M and BRAF V600E. These mutations are well-established oncogenic drivers in non-small cell lung cancer (NSCLC) and melanoma, respectively, and their accurate identification is paramount for guiding targeted therapy decisions [36] [37]. This paper provides a comparative analysis of two implementation approaches: a quantitative PCR (qPCR) method for EGFR T790M and a digital droplet PCR (ddPCR) method for BRAF V600E, summarizing key performance data and outlining step-by-step experimental protocols.
Assay Performance and Clinical Findings
The following tables summarize key quantitative data from the implementation of these mutation detection assays, highlighting both analytical performance and relevant clinical correlations.
Table 1: Assay Performance Characteristics for Mutation Detection
| Parameter | BRAF V600E (ddPCR) | EGFR T790M (qPCR) |
|---|---|---|
| Detection Technique | Digital Droplet PCR [36] | Allele-Specific qPCR [37] |
| Sample Type | Plasma cell-free DNA (cfDNA) [36] | Liquid biopsy [37] |
| Analytical Sensitivity | -- | -- |
| Specificity | 97.7% (95% CI: 93.2-100) [36] | -- |
| Positive Predictive Value (PPV) | 91.7% (95% CI: 76.0-100) [36] | -- |
| Negative Predictive Value (NPV) | 82.4% (95% CI: 71.9-92.8) [36] | -- |
Table 2: Clinical Correlations of BRAF V600E Detection in Advanced Melanoma
| Clinical Factor | BRAF V600E Detected in cfDNA | BRAF V600E Not Detected in cfDNA |
|---|---|---|
| Patient Cohort | Stage IV Melanoma (Tissue Mutant) [36] | Stage IV Melanoma (Tissue Mutant) [36] |
| Median Progression-Free Survival (PFS) | 5.8 months [36] | 12.0 months [36] |
| Median Overall Survival (OS) | 9.2 months [36] | 27.1 months [36] |
| Prevalence in Pediatric HGG | 7% (9/128 patients) [38] | -- |
Experimental Protocols
Protocol A: BRAF V600E Mutation Detection via TaqMan-Based Real-Time PCR
This protocol is adapted from a standardized procedure using a commercial detection kit [39].
Key Research Reagent Solutions:
- Human BRAF V600E Gene Mutation Detection Kit: Contains all necessary primers and the TaqMan probe for the specific detection of the BRAF V600E mutation [39].
- Real-Time PCR System: Such as the StepOnePlus system from Thermo Fisher Scientific [39].
Procedure:
- Reaction Setup: Prepare the PCR mixture in a total volume of 25 µl according to the kit manufacturer's instructions. This will include components from the detection kit and the DNA template [39].
- Thermocycling Conditions: Run the reaction on the real-time PCR instrument using the following program [39]:
- UNG Treatment: 37°C for 10 minutes (to prevent carryover contamination).
- Pre-Denaturation: 95°C for 5 minutes.
- Amplification (40 cycles):
- Denaturation: 95°C for 15 seconds.
- Annealing/Extension: 60°C for 60 seconds.
- Data Analysis: After the run, identify a suitable fluorescence threshold on the amplification curve (typically during the logarithmic exponential growth phase) and record the Cq values for analysis [39].
Protocol B: BRAF V600E Mutation Detection in Plasma cfDNA via ddPCR
This protocol details a highly sensitive method for detecting rare mutant alleles in a background of wild-type DNA, as used in clinical research [36].
Procedure:
- Sample Collection and Processing: Collect whole blood (e.g., 10 mL) in EDTA tubes. Process by centrifugation to produce plasma aliquots. Store plasma at -80°C until cfDNA extraction [36].
- cfDNA Extraction: Isolate cfDNA from plasma (e.g., from 3 x 1-mL aliquots) using a dedicated circulating nucleic acid kit, such as the QIAamp Circulating Nucleic Acid Kit, following the manufacturer's guidelines [36].
- cfDNA Quantification: Quantify the extracted cfDNA using a fluorescence-based method like Qubit 2.0 [36].
- Droplet Digital PCR (ddPCR):
- Assay: Use an analytically validated ddPCR assay with TaqMan hydrolysis probes designed to discriminate wild-type BRAF and BRAF V600E or V600K mutations [36].
- Platform: Utilize a system such as the RainDrop Digital PCR System. The process involves:
- Droplet Generation: Encapsulating single DNA molecules from the eluted cfDNA into droplets in an oil emulsion using the RainDrop Source instrument.
- PCR Amplification: Performing PCR amplification in a thermal cycler with a reaction mixture containing VIC or FAM-conjugated probes.
- Droplet Reading: Transferring the droplets to the RainDrop Sense instrument, which digitally counts droplets where amplification of the wild-type or mutant BRAF has occurred based on fluorescence [36].
Signaling Pathways and Experimental Workflows
The following diagrams, generated using Graphviz DOT language, illustrate the core mechanistic principle of the castPCR technology and the generalized experimental workflow for mutation detection.
The case studies presented herein demonstrate the practical application of TaqMan-based technologies for detecting clinically relevant mutations in cancer research. The competitive allele-specific TaqMan PCR (castPCR) technology exemplifies a robust qPCR-based approach, offering high specificity and sensitivity by effectively suppressing the wild-type background to detect rare mutant alleles [7]. This method is particularly suited for analyzing DNA from various sample types, including cell lines and FFPE tissues [7]. For scenarios requiring even higher sensitivity, such as detecting minute quantities of mutant cfDNA in patient plasma, digital droplet PCR (ddPCR) provides a powerful alternative, enabling absolute quantification and rare allele detection [36].
The clinical data underscore the prognostic significance of liquid biopsy approaches. In advanced melanoma, the detection of BRAF V600E/K mutations in cfDNA was associated with significantly shorter progression-free and overall survival, highlighting its potential for risk stratification [36]. Furthermore, the identification of these mutations opens the door to targeted therapies, such as BRAF inhibitors alone or in combination with MEK inhibitors, which have shown promising results in improving outcomes for patient populations, including those with pediatric high-grade glioma [38]. In conclusion, the implementation of precise and sensitive mutation detection assays is a cornerstone of modern cancer research and precision oncology, enabling both critical prognostic insights and guiding effective targeted treatment strategies.
Optimizing Performance and Overcoming Challenges in Mutation Detection
In the field of cancer research, the accurate detection of somatic mutations is critical for understanding tumor biology, developing targeted therapies, and advancing personalized medicine approaches. TaqMan assays, particularly those utilizing Competitive Allele-Specific TaqMan PCR (castPCR) technology, provide researchers with a powerful tool for identifying and quantifying genetic mutations with exceptional specificity and sensitivity [7]. These assays can detect rare mutant alleles even when they are present at very low frequencies (as low as 0.1%) amidst a background of wild-type DNA, making them particularly valuable for cancer research applications where tumor heterogeneity and low-frequency mutations present significant challenges [7] [40].
The performance of TaqMan assays in mutation detection depends heavily on several critical design parameters that must be carefully optimized. Among these, amplicon size, GC content, and primer melting temperature (Tm) stand out as fundamental factors that directly influence assay efficiency, specificity, and reliability. Proper optimization of these parameters enables researchers to achieve superior mutation detection capabilities, with castPCR technology combining allele-specific TaqMan qPCR with minor groove binder (MGB) oligonucleotide blockers to effectively suppress non-specific amplification from wild-type alleles [7]. This technical note provides detailed guidance on optimizing these key parameters specifically for mutation detection assays in cancer research, along with practical protocols for implementation.
Critical Design Parameters and Their Optimization
Amplicon Size Considerations
Amplicon length is a critical factor in TaqMan assay design that significantly impacts amplification efficiency and sensitivity. The following table summarizes key considerations for amplicon size optimization:
| Parameter | Recommended Range | Rationale | Special Considerations for Mutation Detection |
|---|---|---|---|
| Optimal Length | 50-150 base pairs [41] | Shorter amplicons denature more completely, allowing primers and probes to compete effectively for targets [42] | Enables detection in fragmented DNA from FFPE samples [7] |
| Maximum Length | ≤300 base pairs [42] | Longer amplicons may amplify less efficiently and require extended polymerization times | Critical for preserving sample material in limited quantity samples |
| Efficiency Priority | 70-140 base pairs [43] | Maximizes probability of amplification doubling each cycle | Enhances sensitivity for rare mutation detection |
For mutation detection in cancer research, shorter amplicons are particularly advantageous when working with challenging sample types such as formalin-fixed paraffin-embedded (FFPE) tissues, where DNA fragmentation commonly occurs [7]. The shorter length increases the likelihood that the target region containing the mutation of interest remains intact in degraded samples. Additionally, castPCR technology for somatic mutation detection benefits from compact amplicons as they promote more efficient amplification and enhance the ability to detect mutant alleles present at low frequencies [7] [40].
GC Content Optimization
GC content significantly influences primer and probe binding stability and specificity. The following guidelines should be followed:
| Component | Recommended GC% | Key Constraints | Impact on Mutation Detection |
|---|---|---|---|
| Primers | 30-80% [41] | Last 5 nucleotides at 3' end should have ≤2 G/C bases [41] | Reduces non-specific priming in wild-type background |
| Probes | 30-80% [44] | Avoid runs of ≥4 identical nucleotides, especially G's [41] | Ensures clean background for accurate mutation calling |
| Sequence Composition | Prefer more C's than G's in probes [42] | Avoid G at the 5' end of probes [43] | Minimizes quenching effects for stronger signal |
For mutation detection assays, GC content optimization becomes even more critical as it affects the ability to distinguish between mutant and wild-type sequences. Balanced GC content ensures stable hybridization without promoting non-specific binding that could lead to false-positive mutation calls. The 3' end instability requirement (no more than two G/C nucleotides in the last five bases) is particularly important for castPCR assays, where precise primer binding is essential for allele-specific amplification [7]. Furthermore, avoiding G-runs and imbalanced GC patterns helps prevent secondary structure formation that might interfere with probe hydrolysis and fluorescence detection.
Primer and Probe Melting Temperature (Tm)
Melting temperature relationships between primers and probes are fundamental to successful TaqMan assay function:
| Component | Optimal Tm Range | Critical Relationship | Design Implications |
|---|---|---|---|
| Primers | 58-60°C [41] | Forward and reverse primers should have Tms within 1-2°C of each other [45] [46] | Enables both primers to anneal simultaneously during PCR |
| Probe | ~10°C higher than primers [45] [44] | Must hybridize before primers to enable cleavage during extension [45] | Essential for fluorescence generation proportional to amplicon production |
| Assay Compatibility | Designed for universal thermal cycling conditions [41] | Two-step PCR with combined annealing/extension at 60°C [45] | Facilitates multiplexing and high-throughput applications |
The temperature differential between probe and primers is particularly critical for mutation detection assays. The probe must hybridize to its target sequence before the primers extend, ensuring that the fluorescent signal is generated specifically from the correct amplicon. For castPCR assays, this relationship becomes even more important as the technology relies on precise temperature control to enable the allele-specific primer to compete effectively with the MGB blocker oligonucleotide that suppresses wild-type amplification [7]. Maintaining the recommended Tm relationships ensures optimal assay stringency for distinguishing closely related sequences.
TaqMan castPCR Workflow for Mutation Detection
The following diagram illustrates the competitive allele-specific TaqMan PCR (castPCR) process used for somatic mutation detection in cancer research:
Figure 1: castPCR Workflow for Mutation Detection. This diagram illustrates the complete process from sample preparation to result interpretation, highlighting the core principles of castPCR technology that enable specific mutation detection.
The castPCR technology enables highly specific mutation detection through two key mechanisms. First, the allele-specific primer preferentially binds to and amplifies the mutant sequence. Second, the MGB blocker oligonucleotide suppresses amplification of the wild-type allele by binding to it and preventing polymerase extension [7]. This combination allows for exceptional sensitivity in detecting somatic mutations down to 0.1% mutant alleles in a wild-type background, making it particularly valuable for detecting low-frequency mutations in heterogeneous tumor samples [7] [40].
Detailed Experimental Protocol for Mutation Detection Assays
Pre-Assay Planning and Design
Assay Selection: Identify the specific mutation of interest using resources such as the TaqMan Mutation Assay index file [7]. For each mutation, three assays are typically used:
- Mutant Allele Assay (Cat. No. 4465804): Contains allele-specific primer and MGB blocker for wild-type suppression
- Gene Reference Assay (Cat. No. 4465807): Amplifies a conserved region of the same gene as quality control
- Wild-Type Assay (optional, Cat. No. 4465804): Confirms wild-type sequence detection [7]
Bioinformatics Verification: Ensure assay specificity by verifying that the primer and probe sequences are unique to the target using BLAST or similar tools [41]. Check that the target region does not contain known polymorphisms that might interfere with binding [41].
Sample Quality Assessment: Evaluate DNA quality and quantity, particularly for FFPE samples which may be degraded. Ensure the 260/280 absorbance ratio is approximately 1.7-1.9 [47].
castPCR Setup and Execution
Reaction Preparation:
- Use 10-20 ng of genomic DNA per reaction
- Prepare master mix containing:
- 1X TaqMan Genotyping Master Mix
- 1X Mutant Allele Assay (or Wild-Type Assay)
- 1X Gene Reference Assay
- Nuclease-free water to adjust volume
- For 384-well plates: 10 µL total reaction volume
- For 96-well plates: 20 µL total reaction volume [7]
Thermal Cycling Conditions:
- Initial Denaturation: 95°C for 10 minutes (1 cycle)
- Amplification: 40 cycles of:
- Denaturation: 95°C for 15 seconds
- Annealing/Extension: 60°C for 1 minute [7]
- Note: The two-step protocol is enabled by the optimized Tm relationships between primers and probes
Controls:
- Include no-template controls (NTC) for each assay
- Run known wild-type and mutant controls if available
- Consider using the TaqMan Mutation Detection IPC Reagent Kit as an internal positive control [7]
Data Analysis and Interpretation
Fluorescence Detection: Collect fluorescence data during the annealing/extension step of each cycle. The FAM dye-labeled probe signal indicates successful amplification.
Mutation Calling: Use specialized software such as Applied Biosystems Mutation Detector Software to automatically determine mutation status based on the fluorescence profiles [7].
Result Validation: Compare results with known mutation status controls. For discrepant results, consider sample quality issues or differences in assay sensitivity thresholds [9].
Research Reagent Solutions for Mutation Detection
The following table outlines essential reagents and tools for implementing TaqMan-based mutation detection in cancer research:
| Reagent/Tool | Function | Application Note |
|---|---|---|
| TaqMan Mutation Detection Assays (4465804) | Detect specific mutant alleles using castPCR technology | Pre-formulated for 44 mutations in RAS, EGFR, BRAF genes; detect down to 0.1% mutant alleles [7] [9] |
| TaqMan Mutation Detection Reference Assays (4465807) | Amplify conserved gene regions as internal controls | Verify sample quality and PCR efficiency; essential for data normalization [7] |
| TaqMan Mutation Detection IPC Reagent Kit (4467538) | Provide internal positive control for PCR inhibition detection | Duplexes with any mutation detection assay; pre-optimized for standardized workflow [7] |
| Custom TaqMan Assay Design Tools | Create assays for novel or rare mutations | Bioinformatics analysis ensures specificity; designs for transcript-level detection [41] |
| Mutation Detector Software | Automate mutation status calling from qPCR data | Compatible with data from Applied Biosystems Real-Time PCR Systems [7] |
Troubleshooting and Quality Control
Effective implementation of TaqMan mutation detection assays requires attention to potential challenges and quality control measures:
Specificity Verification: Always run BLAST analysis on custom-designed assays to ensure they do not cross-hybridize with homologous sequences or pseudogenes [41]. For gene expression assays, design primers across exon-exon junctions to avoid amplification of genomic DNA contamination [41] [43].
Assay Validation: When establishing new assays, test multiple primer/probe sets and select the one with the highest signal-to-noise ratio and no amplification in no-template controls [41]. For mutation detection, verify the limit of detection using dilution series of mutant DNA in wild-type background.
Sample Quality Considerations: For FFPE samples, which are common in cancer research, consider using slightly longer amplification times and potentially increasing cycle numbers to compensate for DNA fragmentation [7]. Always assess DNA quality before proceeding with valuable samples.
Multiplexing Considerations: When designing multiplexed assays, ensure all probes have similar Tm values but distinct fluorescent labels. Use QSY quenchers for multiplexing three or more probes, as they do not have an MGB moiety and can be designed with longer sequences to maintain Tm [45].
Following these detailed protocols and design parameters will enable researchers to develop robust, sensitive, and specific TaqMan assays for mutation detection in cancer research, providing reliable results that can inform understanding of tumor biology and therapeutic development.
In the field of cancer research, the accurate detection of somatic mutations is paramount for both understanding tumor biology and guiding the development of targeted therapies. TaqMan assays, based on real-time PCR technology, provide a powerful platform for mutation detection due to their sensitivity, specificity, and throughput. However, the reliability of these assays is critically dependent on meticulous design strategies that prevent false-positive and false-negative results. Two foundational pillars of this design are the strategic placement of assays across exon-exon junctions and the thorough avoidance of single nucleotide polymorphisms (SNPs) within binding sites. This application note details specific protocols and design principles, framed within a broader thesis on optimized TaqMan assay protocols, to ensure the highest level of specificity for mutation detection in cancer research. The guidance herein is tailored for researchers, scientists, and drug development professionals engaged in molecular assay development.
Core Principles of Specific Assay Design
The Imperative of Exon-Exon Junction Targeting
A primary challenge in gene expression analysis and mutation detection from RNA samples is the potential co-amplification of contaminating genomic DNA (gDNA), which can lead to inaccurate quantification and interpretation. Placing the assay across an exon-exon junction in the cDNA sequence ensures that amplification is specific to the spliced mRNA transcript, as the intron-containing gDNA template cannot be efficiently amplified [41].
For optimal design, the amplicon should be kept short, typically 50–150 base pairs, to promote efficient amplification [41]. Furthermore, the probe (rather than a primer) should be placed directly over the exon-exon boundary. This strategy offers the highest level of assurance, as it guarantees that the fluorescent signal generated during qPCR originates exclusively from a template where the two exons are correctly spliced together [41].
The Criticality of SNP Avoidance in Primer and Probe Design
Undetected polymorphisms within primer or probe binding sites can severely compromise assay performance by altering hybridization kinetics. This can lead to reduced amplification efficiency, allele drop-out, and consequently, erroneous genotyping calls [48]. This is particularly critical for highly polymorphic genes, such as those involved in drug metabolism (e.g., CYP2D6) and cancer [48].
A notable case study involved a TaqMan assay for the CYP2D6*17 allele (1023C>T), which produced a small number of unexpected homozygous calls in samples that were, in fact, heterozygous. Subsequent investigation revealed that a trio of SNPs near the primer binding site on the alternate allele interfered with amplification, leading to a false homozygosity result [48]. This phenomenon underscores the necessity of a thorough in silico analysis of the target region to screen for known SNPs. Tools like Thermo Fisher's Custom Plus assay design option integrate this step, performing bioinformatic checks to avoid sequences with known polymorphisms, thus ensuring robust assay performance across diverse sample populations [41].
Experimental Protocols for Design and Validation
Protocol: In Silico Assay Design and Specificity Check
This protocol outlines the steps for designing a specific TaqMan assay for mutation detection.
1. Target Sequence Selection:
- Input: Obtain the full cDNA and genomic DNA sequence of your target gene from a trusted database (e.g., NCBI RefSeq).
- Identify Exon Boundaries: Map the exon-intron structure of the gene.
- Select Target Region: Choose a region for the amplicon that is 50-150 bp in length and spans an exon-exon junction [41].
- SNP Interrogation: Use databases like dbSNP to check the selected region for any known polymorphisms. Avoid designing primers or probes in regions with known SNPs [41].
2. Primer and Probe Design:
- Software: Utilize design software such as Primer Express (Thermo Fisher) with standardized parameters [41].
- Primers: Design forward and reverse primers with a length of ~20 bases, a Tm of 58–60°C, and a GC content of 30–80%. The five nucleotides at the 3' end should contain no more than two G/C bases [41].
- Probe: Design the TaqMan MGB probe to hybridize across the exon-exon junction. The probe should have a Tm ~10°C higher than the primers [41].
- Specificity Check: Perform a BLAST search to confirm the uniqueness of the designed oligonucleotide sequences and ensure they do not bind to homologous genes or pseudogenes [41].
3. Final Check:
- Ensure the probe is placed over the exon-exon junction and that the final assay sequence is free of known SNPs and repetitive sequences.
Protocol: Analytical Validation of Assay Specificity
Once an assay is designed, its performance must be empirically validated.
1. Experimental Controls:
- "No Template Control" (NTC): Contains water instead of nucleic acid to monitor for reagent contamination.
- "No Reverse Transcription" Control (-RT): Uses RNA template that has not been reverse transcribed to cDNA. This control is essential for quantifying any residual background signal from gDNA contamination [41]. A well-designed exon-junction assay should show no amplification in the -RT control.
2. Sensitivity and Specificity Assessment:
- Dilution Series: Perform qPCR on a serial dilution of a known positive control (e.g., synthetic DNA, cell line DNA with the mutation) to determine the assay's linear dynamic range, amplification efficiency, and limit of detection.
- Specificity Test: Test the assay against cDNA/cDNA samples with known wild-type and mutant sequences. The assay should clearly discriminate between them, as demonstrated by a clear difference in Cq values or allelic discrimination plots. For cancer mutation detection, this can involve testing the castPCR technology, which uses a blocker oligonucleotide to suppress wild-type amplification, achieving sensitivity to detect 1 mutant cell in 1,000 normal cells [49].
The following workflow diagram summarizes the key stages of the assay design and validation process:
Research Reagent Solutions
The following table details key reagents and tools essential for implementing the described TaqMan assay protocols.
| Product / Tool Name | Function & Application | Key Features |
|---|---|---|
| TaqMan Mutation Detection Assays [49] | Detect somatic mutations in cancer genes (e.g., KRAS, BRAF). | Utilizes castPCR technology with a blocker oligonucleotide to suppress wild-type amplification; sensitivity of 0.1% [49]. |
| Custom TaqMan Assay Design Tool [41] | Design custom assays for unique research needs. | Incorporates bioinformatic checks for SNP avoidance, secondary structure, and specificity via BLAST [41]. |
| Primer Express Software [41] | Facilitates design of primers and probes based on sequence input. | Optimized parameters for TaqMan assays (Tm, GC content, amplicon length) [41]. |
| TaqMan Mutation Detection IPC Reagent Kit [49] | Provides an internal positive control (IPC). | Pre-optimized reagents that can be duplexed with any mutation detection assay to monitor PCR inhibition [49]. |
Data Presentation and Analysis
Troubleshooting Common Assay Performance Issues
Even with careful design, assays may require optimization. The table below summarizes common issues, their potential causes, and recommended solutions.
| Observed Problem | Potential Cause | Recommended Solution |
|---|---|---|
| High Cq in (-RT) control | GDNA amplification due to ineffective exon-junction spanning. | Redesign assay, ensuring the probe is placed directly over the exon boundary [41]. |
| Inconsistent genotyping calls | Presence of an undetected SNP in a primer/probe binding site. | Resequence the target region in problematic samples; redesign assay avoiding all known SNPs [48]. |
| Poor amplification efficiency | Non-optimal primer/probe sequences (e.g., high GC, secondary structures). | Redesign using Primer Express software; check and adhere to design guidelines for Tm and GC content [41]. |
| Low sensitivity for rare mutants | Limited discrimination between wild-type and mutant sequences. | Consider adopting castPCR technology or digital PCR methods for superior rare allele detection [49]. |
The rigorous application of the principles and protocols detailed in this document—specifically, the strategic placement of assays across exon-exon junctions and the diligent avoidance of SNPs—forms the foundation for reliable and specific TaqMan-based mutation detection. By integrating robust in silico design with thorough empirical validation, researchers can develop and deploy assays that accurately interrogate cancer-associated mutations, thereby generating data that is critical for both foundational research and the advancement of targeted drug development. The tools and reagents highlighted provide a comprehensive toolkit for scientists to achieve these goals with confidence.
Maximizing Sensitivity for Low-Abundance Mutations in Wild-Type Background
The detection of low-abundance somatic mutations against a predominant wild-type DNA background is a critical challenge in molecular oncology, with significant implications for patient stratification, minimal residual disease monitoring, and resistance mutation detection. TaqMan assay technologies have evolved to address this challenge through sophisticated biochemical approaches that enhance specificity and sensitivity beyond conventional PCR methods. This application note details the implementation of these advanced TaqMan protocols, with particular emphasis on Competitive Allele-Specific TaqMan PCR (castPCR), to achieve reliable detection of mutant alleles at frequencies as low as 0.1% [7] [2].
The limited sensitivity of traditional sequencing methods (typically requiring 10-25% mutant allele frequency) creates a substantial risk of false negatives in samples with low tumor cellularity or heterogeneous mutation distribution [2]. This technical gap is particularly problematic in clinical contexts where early intervention depends on detecting rare mutant populations. The protocols described herein enable researchers to overcome these limitations through allele-specific amplification coupled with wild-type suppression mechanisms, providing the precision required for contemporary cancer research and therapeutic development.
Technical Approaches and Performance Comparison
Method Comparison Table
The following table summarizes the performance characteristics of major mutation detection methodologies:
Table 1: Performance Comparison of Mutation Detection Methods
| Method | Limit of Detection | Key Principles | Advantages | Limitations |
|---|---|---|---|---|
| Sanger Sequencing | 10-25% mutant alleles [2] | Dideoxy chain termination | Detects novel mutations; considered gold standard [2] | Low sensitivity; laborious process [2] |
| Fragment Analysis | 5% mutant alleles [2] | Size separation of fluorescently labelled PCR products | Detects indels; moderate sensitivity | Limited to size-based mutations |
| Real-Time PCR (Allelic Discrimination) | Up to 5% mutant alleles [2] | Allele-specific primers with differential fluorescent probes | Quantitative; faster than sequencing | Moderate sensitivity |
| ARMS (Therascreen) | Up to 1% mutant alleles [2] | Amplification Refractory Mutation System | Good sensitivity; commercially validated | Limited multiplexing capability |
| castPCR | 0.1-0.5% mutant alleles [7] [2] | Allele-specific primer + MGB wild-type blocker [7] | Highest specificity/sensitivity; rare mutation detection [7] | Pre-designed assays required |
| Digital PCR | 0.1% mutant alleles [7] | Partitioning and endpoint detection | Absolute quantification; high precision | Specialized equipment needed |
Competitive Allele-Specific TaqMan PCR (castPCR) represents a significant advancement in mutation detection technology by combining two powerful molecular mechanisms: allele-specific amplification and wild-type suppression. The system employs a mutant-specific primer that perfectly matches the mutant allele but contains a 3' mismatch with the wild-type sequence. This is coupled with a Minor Groove Binder (MGB) oligonucleotide blocker that specifically binds to and suppresses amplification of the wild-type allele [7] [50].
This dual approach enables exceptional discrimination between highly similar sequences, allowing detection of rare mutant alleles in a 1000-fold excess of wild-type DNA (sensitivity of 0.1%) [7]. The technology is particularly valuable for detecting somatic mutations in cancer research, where mutant DNA may represent only a small fraction of the total DNA in samples with significant stromal contamination or in liquid biopsy applications [7] [51].
The castPCR workflow incorporates a gene reference assay that targets a mutation-free region of the same gene, serving as an internal control for DNA quality and quantity. This enables calculation of ΔCt values between mutant and reference assays, providing a robust statistical framework for mutation calling [2].
Experimental Protocols
castPCR Protocol for Mutation Detection
Materials Required:
- TaqMan Mutation Detection Assays (Mutant Allele Assays and Gene Reference Assays) [7]
- DNA samples (10 ng/µL recommended) [2]
- TaqMan Genotyping Master Mix [2]
- Real-time PCR instrument with FAM detection capability [7]
- Nuclease-free water
- Optical reaction plates and seals
Procedure:
Assay Selection and Preparation:
- Identify appropriate Mutant Allele Assay IDs and corresponding Gene Reference Assay IDs using the manufacturer's index file [7]
- Reconstitute assays according to manufacturer specifications
- Prepare reaction mix sufficient for 150×10µL reactions (384-well plate) or 75×20µL reactions (96-well plate) [7]
Reaction Setup:
- For each 10µL reaction: 1X TaqMan Genotyping Master Mix, 1X Mutant Allele Assay, 1X Gene Reference Assay, and 10 ng DNA template [2]
- Include appropriate controls: wild-type DNA, mutant-positive DNA (if available), and no-template control
- Cap and centrifuge plates to eliminate bubbles
Thermal Cycling Conditions:
Data Analysis:
- Calculate ΔCt values: ΔCt = [Ct(Mutant Allele Assay) - Ct(Gene Reference Assay)] - Calibration ΔCt [2]
- Apply predetermined threshold: Samples with ΔCt ≤ cutoff (typically 7) are mutation-positive; ΔCt > cutoff are mutation-negative [2]
- Use mutation detection software (e.g., Mutation Detector Software) for automated calling if available [7]
Sensitivity Validation Protocol
Dilution Series Preparation:
- Extract DNA from mutant-positive cell lines or patient samples with known mutation status [2] [50]
- Quantify DNA and assess quality by spectrophotometry and agarose gel electrophoresis [2]
- Prepare dilution series in wild-type DNA: 1:1, 1:5, 1:10, 1:25, 1:50, 1:100 mutant-to-wild type ratios [50]
- Include replicate samples at each dilution to assess reproducibility
Limit of Detection Determination:
- Process dilution series using the castPCR protocol above
- Plot ΔCt values against dilution factors
- Establish the minimum mutant allele frequency that consistently yields ΔCt values below the determined cutoff with statistical significance
- Validate with orthogonal methods where possible (e.g., digital PCR, cloning and sequencing) [50]
Results Interpretation and Troubleshooting
Data Analysis Parameters
Successful implementation of castPCR requires establishment of specific analytical parameters through validation experiments:
Threshold Determination:
- Analyze a training set of samples with known mutation status to establish the optimal ΔCt cutoff value (typically ΔCt=7) [2]
- Set maximum cycle threshold (Ct=37) to prevent false positives from late amplification [2]
- Establish a mutant signal threshold (typically 0.2) to distinguish true amplification from background noise [2]
Mutation Calling Criteria: A sample is considered mutation-positive when:
- ΔCt ≤ established cutoff value (e.g., 7) [2]
- Ct value for mutant assay ≤ maximum cycle threshold (e.g., 37) [2]
- Amplification curve shows characteristic sigmoidal shape
- Gene reference assay shows robust amplification (Ct < 32) indicating adequate DNA quality
Troubleshooting Common Issues
Inhibition or Failed Amplification:
- Problem: No amplification in both mutant and reference assays
- Solution: Implement the TaqMan Mutation Detection IPC Reagent Kit as an internal positive control [7]
- Check DNA quality by gel electrophoresis and spectrophotometry (A260/A280 ratio) [2]
- Dilute inhibitors or purify DNA further
High Background or False Positives:
- Problem: Late amplification in mutant assay with ΔCt near cutoff
- Solution: Optimize DNA input (typically 10 ng/reaction) [2]
- Verify assay specificity using wild-type controls
- Ensure thermal cycler calibration and consistent temperature uniformity
Discordant Results with Sequencing:
- Problem: castPCR positive but sequencing negative
- Solution: This typically reflects the higher sensitivity of castPCR; validate with limiting dilution or digital PCR [50]
- Check for cross-reactive mutations not targeted by the specific castPCR assay
Research Reagent Solutions
Table 2: Essential Reagents for High-Sensitivity Mutation Detection
| Reagent/Catalog Number | Function | Specifications |
|---|---|---|
| TaqMan Mutation Detection Assays (4465804) [7] | Detection of specific mutant alleles | Pre-formulated 10X mix containing allele-specific primers, FAM-labeled MGB probe, and wild-type blocker [7] |
| TaqMan Mutation Detection Reference Assays (4465807) [7] | Internal control for DNA quality/quantity | Targets mutation-free region of the gene; FAM-labeled MGB probe [7] |
| TaqMan EGFR Exon 19 Deletions Assay (4465805) [7] | Detection of 19 different EGFR exon 19 deletions | Multiplexed detection of common indel mutations [7] |
| TaqMan Mutation Detection IPC Reagent Kit (4467538) [7] | Internal positive control for PCR inhibition | Duplexes with any mutation detection assay; validates reaction integrity [7] |
| TaqMan Genotyping Master Mix [2] | PCR amplification | Optimized for allele discrimination assays; includes reference dye |
| Control Genomic DNAs [2] [50] | Assay validation | Mutant and wild-type controls for assay qualification |
Application Workflow
The following diagram illustrates the complete experimental workflow for high-sensitivity mutation detection using castPCR:
Advanced Applications and Future Directions
The exceptional sensitivity of optimized TaqMan assays enables several advanced research applications beyond routine mutation detection. In liquid biopsy analysis, these protocols can detect circulating tumor DNA with variant allele frequencies below 0.5%, facilitating early intervention and therapy monitoring [51]. For heteroplasmic mitochondrial DNA mutations, TaqMan-MGB probe assays enable precise quantification of mutation load, which correlates with disease severity in disorders such as Leber hereditary optic neuropathy [52].
Multiplexing approaches continue to expand the utility of these detection systems. Research demonstrates that carefully designed TaqMan arrays can simultaneously interrogate 44 mutations across multiple oncogenes (KRAS, NRAS, EGFR, BRAF) in 7 samples per 384-well plate, providing comprehensive mutation profiling with minimal sample input [9]. Emerging dual-probe configurations, incorporating two identically labeled hydrolysis probes per target, offer potential solutions for detecting highly variable sequences while maintaining assay sensitivity [53].
As personalized cancer therapies increasingly target specific molecular alterations, the ability to reliably detect low-abundance mutations becomes paramount. The protocols detailed in this application note provide researchers with robust, reproducible methods to advance this critical aspect of cancer research and therapeutic development.
Within the framework of advancing TaqMan assay protocols for mutation detection in cancer research, achieving reliable and reproducible results is paramount for researchers, scientists, and drug development professionals. Even with robust technologies like competitive allele-specific TaqMan PCR (castPCR), experimental outcomes can be compromised by inhibitors co-purified with nucleic acids, suboptimal DNA yield, and inconclusive data. This application note provides detailed methodologies and troubleshooting protocols to identify, address, and prevent these common issues, ensuring the high sensitivity and specificity required for detecting somatic mutations in genes associated with cancer [7].
Troubleshooting Inhibitors in TaqMan Assays
Inhibitors are substances that co-purify with DNA and can significantly reduce PCR efficiency by interfering with polymerase activity. Common sources include heparin, hemoglobin, ionic detergents, and phenol.
The table below summarizes frequent inhibitors, their effects, and initial corrective actions [54].
| Inhibitor Source | Effect on PCR | Corrective Action |
|---|---|---|
| Phenol Contamination | Higher than expected A280 absorbance; inhibits enzymatic reactions [54]. | Perform a second ethanol precipitation; include additional washes with 0.1 M sodium citrate in 10% ethanol [54]. |
| Hemoglobin | Causes problems during PCR [54]. | Ensure adequate anticoagulants; remove clots by centrifugation before DNA precipitation [54]. |
| Carryover Salts/Phosphate | May inhibit restriction enzymes and other enzymatic reactions [54]. | Reprecipitate DNA; wash pellet with 70% ethanol thoroughly [54]. |
| Polysaccharides | Can partition with nucleic acids, potentially affecting solubility [54]. | Use a microcarrier during precipitation; pool samples to increase yield [54]. |
Detailed Protocol: Ethanol Precipitation for Inhibitor Removal
This protocol is effective for removing phenol, salt, and other contaminants [54].
- Add Reagent: Add DNAzol Reagent (or an equivalent volume of a precipitation solution) to the DNA solution.
- Precipitate: Add 0.5 volumes of 95% ethanol. Mix thoroughly by inversion.
- Pellet DNA: Centrifuge at the recommended g-force to pellet the DNA.
- Wash: Carefully wash the pellet twice with 95% ethanol.
- Dry: Briefly air-dry the pellet (do not overdry; see Section 3.1).
- Resuspend: Resuspend the purified DNA in 8 mM NaOH or an appropriate buffer.
Addressing Low DNA Yield and Quality
Low DNA yield and degraded DNA directly impact assay sensitivity and can lead to false-negative results, especially when detecting rare mutant alleles.
Common Causes and Solutions for Low Yield
The following table outlines primary causes of low DNA yield and degradation, along with targeted solutions [54].
| Problem | Root Cause | Solution |
|---|---|---|
| Overdried DNA Pellet | Pellets become difficult or impossible to resuspend [54]. | Limit air-drying time to <5 minutes; avoid vacuum suction devices. Rehydrate with 8 mM NaOH or TE buffer [54]. |
| Incomplete Homogenization/Lysis | DNA remains trapped in unhomogenized material [54]. | Ensure tissue is fully homogenized; pass homogenate through a polypropylene filter cloth before phase separation [54]. |
| DNA Shearing | Use of high-speed homogenizers degrades DNA [54]. | Use gentler homogenization methods appropriate for the sample type [54]. |
| Suboptimal Phase Separation | Inadequate mixing or centrifugation after chloroform addition [54]. | Mix chloroform thoroughly by inversion (not vortexing); centrifuge at proper g-force, time, and temperature [54]. |
Detailed Protocol: Optimizing DNA Solubilization
This procedure is critical for maximizing DNA recovery after precipitation [54].
- Remove Ethanol: After washing, remove all ethanol droplets from the tube wall using a sterile cotton swab. Touch the pellet with a sterile capillary pipette tip to draw off residual ethanol.
- Add Solvent: Before the pellet is completely dry, add an appropriate volume of 8 mM NaOH or TE buffer.
- Incubate: Allow a 5–10 minute incubation at room temperature. The pellet will begin to clear as it rehydrates.
- Pipette: To solubilize the DNA completely, pipet the solution up and down several times.
- For Stubborn Pellets: If the pellet remains difficult to solubilize, incubate at 37°C or 45°C with periodic pipetting. For severely overdried pellets, incubation at 4°C with periodic pipetting over several hours may be necessary [54].
Resolving Inconclusive and Low-Sensitivity Results
Inconclusive results, such as poor amplification or an inability to distinguish wild-type from mutant alleles, undermine the validity of an experiment.
Enhancing Specificity and Sensitivity
TaqMan assays powered by castPCR technology are designed for high specificity by suppressing wild-type amplification. However, protocol optimization is key [7].
- Blocking Wild-Type Background: The castPCR technology uses an MGB oligonucleotide blocker that competes with the allele-specific primer to suppress amplification from the wild-type allele, enabling detection of rare mutants down to 1 in 1000 normal cells [7].
- PCR Optimization: For challenging samples, consider a two-stage PCR approach. An initial set of short, low-annealing temperature cycles can enrich for mutant alleles, followed by standard cycles for efficient amplification, as demonstrated in the mutant-enriched SLAM-MS assay [55].
- Alternative Amplicon Design: The SLAM-MS (Stem-Loop AMplicon Mutation Scanning) assay uses symmetric PCR with primers containing 5'-universal sequences. This generates stem-loop amplicons that allow for hybridization with TaqMan probes without asymmetric PCR, improving quantification and enabling bi-strand mutation scanning in a single test [55].
Quantitative Melting Analysis for Mutation Quantification
For assays involving DNA melting analysis, quantitation of the mutant allele fraction is possible.
- Perform Melting Analysis: After amplification, denature products and cool them to form probe-target hybrids. Collect melting data by slowly increasing the temperature and monitoring fluorescence [55].
- Analyze Melting Peaks: Use non-linear iterative curve fitting software (e.g., PeakFit) to separate overlapping melting peaks corresponding to wild-type and mutant alleles.
- Calculate Mutation Fraction: The ratio of the area under the mutant peak to the total area under all peaks has a linear relationship with the mutant allele fraction, allowing for quantification [55].
The Scientist's Toolkit: Research Reagent Solutions
| Item | Function | Application Note |
|---|---|---|
| TaqMan Mutation Detection Assays | Pre-formulated assays for mutant and wild-type alleles using castPCR technology for highly specific mutation detection [7]. | Includes primers, TaqMan MGB probe (FAM-labeled), and an MGB oligonucleotide blocker. Compatible with FFPE, cell lines, and frozen tissues [7]. |
| Internal Positive Control (IPC) Reagent Kit | Optional reagents duplexed with the mutation assay to provide a positive PCR control, helping distinguish true negatives from PCR failure [7]. | Pre-optimized for use with TaqMan Mutation Detection Assays. |
| DNAzol Reagent | A ready-to-use reagent for the rapid isolation of genomic DNA from cells and tissues [54]. | Effective for blood, cultured cells, and tissues. Isolated DNA is resuspended in 8 mM NaOH for stability and solubility [54]. |
| Universal Primer Sequence (UPS) | A GC-enriched sequence added to the 5'-end of PCR primers to enable the formation of stem-loop amplicons in symmetric PCR [55]. | Facilitates methods like SLAM-MS, allowing for quantitative analysis and bi-strand mutation scanning without asymmetric PCR [55]. |
Experimental Workflow for Reliable Mutation Detection
The following diagram outlines a comprehensive workflow, integrating the troubleshooting steps detailed in this note to guide researchers from sample preparation to data analysis.
By adhering to these detailed protocols and leveraging the recommended reagent solutions, researchers can systematically overcome the most frequent challenges encountered in mutation detection assays, thereby ensuring the generation of robust, reliable, and actionable data in cancer research.
Benchmarking TaqMan Assays: Validation and Comparison with Other Methods
In the era of precision oncology, the accurate detection of somatic mutations is a critical prerequisite for effective targeted therapy. TaqMan assays, particularly those employing Competitive Allele-Specific TaqMan PCR (castPCR) technology, have emerged as powerful tools for identifying oncogenic mutations in clinical and research samples [7] [2]. The technology's exceptional sensitivity enables detection of rare mutant alleles present at frequencies as low as 0.1% in a background of wild-type DNA, addressing a key challenge in molecular diagnostics where tumor samples often contain substantial amounts of non-neoplastic cells [2] [50]. This application note provides a comprehensive framework for the analytical validation of TaqMan assays for mutation detection, establishing standardized protocols and performance criteria to ensure reliable, reproducible results in cancer research and drug development.
Principles of Mutation Detection
The exceptional analytical performance of TaqMan castPCR stems from its dual mechanism for allele discrimination. Unlike conventional allele-specific PCR, castPCR incorporates a mutant allele-specific primer (ASP) combined with a wild-type allele-specific blocker (ASB) in the same reaction [7] [2]. The allele-specific primer is designed to preferentially amplify the mutant sequence, while the Minor Groove Binder (MGB) oligonucleotide blocker effectively suppresses amplification of the wild-type allele by binding to it with high affinity [50]. This combined approach significantly enhances the specificity and sensitivity of rare mutation detection by reducing background amplification from abundant wild-type sequences [2].
Table 1: Key Components of TaqMan Mutation Detection Assays
| Component | Composition | Function |
|---|---|---|
| Mutant Allele Assay | 10X mix of unlabeled PCR primers, FAM-labeled TaqMan MGB probe, MGB oligonucleotide blocker | Specifically detects and amplifies mutant alleles while suppressing wild-type amplification |
| Wild Type Allele Assay | 10X mix of unlabeled PCR primers, FAM-labeled TaqMan MGB probe, MGB oligonucleotide blocker | Optional component for wild-type detection |
| Gene Reference Assay | 10X mix of unlabeled PCR primers, FAM-labeled TaqMan MGB probe | Amplifies mutation-free region of the gene for normalization and quality control |
| Internal Positive Control (IPC) Reagents | Pre-optimized control reagents | Optional duplexed internal positive control for PCR verification |
Workflow and Detection System
The castPCR workflow integrates sample preparation, amplification, and data analysis in a streamlined process. Each reaction contains a primer-probe set specifically designed to recognize either the mutant or wild-type sequence, with the gene reference assay serving as an internal control for DNA quality and quantity [7]. The use of minor groove binder (MGB) probes enhances the discrimination power by increasing the melting temperature (Tm) of short probes and providing better sequence specificity through stabilization of probe-target duplexes [2] [56]. During amplification, the 5'→3' exonuclease activity of DNA polymerase cleaves the TaqMan probe, separating the fluorophore from the quencher and generating a fluorescent signal proportional to the amount of amplified target [2]. Mutation detection is determined by calculating the ΔCt value between the mutant allele assay and the gene reference assay, with established cut-off values distinguishing true mutations from background signal [2].
Establishing Analytical Sensitivity
Limit of Detection (LOD) Assessment
Determining the limit of detection (LOD) is fundamental to establishing assay sensitivity. For TaqMan castPCR assays, sensitivity is evaluated by testing serial dilutions of mutant DNA in wild-type DNA background. Multiple studies have demonstrated that castPCR can reliably detect mutant alleles at frequencies as low as 0.1-1% [2] [50]. In a validation study of BRAF V600 mutation detection, castPCR demonstrated the ability to detect mutations at a 1:100 mutant-to-wild-type ratio (1%), significantly outperforming Sanger sequencing which failed beyond a 1:25 ratio (4%) [50]. For EGFR mutation detection, establishing a ΔCt cut-off value of 7 with a maximum cycle threshold (Ct) of 37 enabled consistent identification of mutations with high sensitivity [2].
Sensitivity Comparison Across Methodologies
Table 2: Comparative Sensitivity of Mutation Detection Methods
| Method | Limit of Detection | Applications | Advantages/Limitations |
|---|---|---|---|
| Sanger Sequencing | 10-25% mutant alleles [2] | Research, comprehensive mutation screening | Gold standard but limited sensitivity |
| Pyrosequencing | 5-10% mutant alleles [2] | Targeted mutation analysis | Moderate sensitivity, quantitative |
| ARMS (Therascreen) | ~1% mutant alleles [2] | Clinical diagnostics | Good sensitivity, approved for companion diagnostics |
| castPCR (TaqMan) | 0.1-0.5% mutant alleles [2] [50] | Research and clinical applications | Highest sensitivity, specific blocker technology |
| Fragment Analysis | ~5% mutant alleles [2] | Detection of indels | Moderate sensitivity for specific mutation types |
The exceptional sensitivity of castPCR technology makes it particularly suitable for analyzing challenging clinical samples such as formalin-fixed paraffin-embedded (FFPE) tissues, fine-needle aspirates, and cytology specimens where tumor cell content may be limited [2]. This performance has been validated across multiple cancer types including non-small cell lung cancer (NSCLC), colorectal cancer, and melanoma [2] [50] [9].
Determining Analytical Specificity
Assay Design for Optimal Specificity
Specificity in TaqMan assays begins with meticulous in silico design to ensure primers and probes target unique genomic regions. Bioinformatics analysis should include BLAST searches against reference databases to verify minimal homology with non-target sequences, including homologous genes or pseudogenes [41]. For mutation detection assays, the 3' terminal base of allele-specific primers must correspond precisely to the mutant nucleotide, with introduction of additional deliberate mismatches at penultimate or antepenultimate positions potentially enhancing discrimination [57]. The strategic placement of MGB modifications in TaqMan probes further improves specificity by increasing duplex stability and discrimination power [2] [56].
Experimental Validation of Specificity
Specificity validation requires testing assays against samples with known mutations and wild-type controls. Cross-reactivity assessment should include evaluation against genetically similar variants and common single nucleotide polymorphisms (SNPs) in the target region [41]. In a BRAF V600 validation study, castPCR demonstrated 100% negative agreement with wild-type samples, with no false positives detected across 54 clinical specimens [50]. For clinical application, establishing a ΔCt threshold is critical; in EGFR mutation detection, a ΔCt cut-off value of 7 provided optimal discrimination between true mutations and background signal [2]. This threshold should be determined empirically during validation using receiver operating characteristic (ROC) analysis if sufficient samples are available.
Assessing Reproducibility
Intra-assay and Inter-assay Precision
Reproducibility evaluation encompasses both intra-assay (within-run) and inter-assay (between-run) precision measurements. For quantitative applications, precision is typically expressed as the coefficient of variation (CV) for Ct values across replicates. Well-validated TaqMan assays should demonstrate intra-assay CVs below 2.5% and inter-assay CVs below 3% [58] [56]. In the development of a TaqMan assay for Carpione rhabdovirus detection, the method demonstrated exceptional reproducibility with intra-assay and inter-assay CVs below 2.5% [58]. Similarly, a BVDV detection assay achieved CVs below 1.5% for both within-run and between-run comparisons [56].
Inter-laboratory Reproducibility
For assays intended for multi-center studies or clinical applications, inter-laboratory reproducibility should be established through ring trials or method comparison studies. While the search results don't provide specific data on inter-laboratory studies of castPCR, the technology's standardized assay formulations and controlled manufacturing processes support reproducibility across sites [7]. The availability of pre-plated assays in 96- or 384-well formats further enhances reproducibility by minimizing manual handling variations [7].
Experimental Protocols
Protocol: TaqMan castPCR Mutation Detection
Principle: This protocol describes the detection of somatic mutations using TaqMan Mutation Detection Assays based on castPCR technology [7] [2].
Reagents and Equipment:
- TaqMan Mutation Detection Assays (Mutant allele and Gene Reference assays)
- TaqMan Genotyping Master Mix
- Nuclease-free water
- DNA samples (10-100 ng/μL recommended)
- Real-time PCR instrument with FAM channel (e.g., ViiA 7, QuantStudio)
Procedure:
- Reaction Preparation: Thaw all reagents and prepare reactions on ice. For each sample, prepare two reactions: one with the mutant allele assay and one with the gene reference assay.
- 10 μL reaction volume recommended for 384-well plates
- 1X TaqMan Genotyping Master Mix
- 1X TaqMan Mutation Detection Assay (mutant or reference)
- 10-50 ng DNA template
- Adjust to final volume with nuclease-free water
Thermal Cycling Conditions:
- Initial denaturation: 95°C for 10 minutes
- 5 cycles of touchdown PCR:
- Denaturation: 92°C for 15 seconds
- Annealing/Extension: 58°C for 1 minute
- 40 cycles of amplification:
- Denaturation: 92°C for 15 seconds
- Annealing/Extension: 60°C for 1 minute
Data Analysis:
- Calculate ΔCt values: ΔCt = [Ct(mutant allele assay) - Ct(gene reference assay)] - calibration ΔCt
- Apply predetermined cut-off ΔCt values (established during validation; typically ≤7 for mutation detection [2])
- Interpret results: ΔCt ≤ cut-off = mutation detected; ΔCt > cut-off = mutation not detected
Troubleshooting Notes:
- If amplification is weak, check DNA quality and quantity
- If false positives occur, re-optimize ΔCt cut-off value
- For inhibited samples, consider dilution or purification of DNA template
Protocol: Analytical Sensitivity (LOD) Determination
Principle: Establish the limit of detection for a TaqMan mutation detection assay using serial dilutions of mutant DNA in wild-type DNA [2] [50].
Procedure:
- Reference Material Preparation: Obtain genomic DNA from mutant and wild-type cell lines or clinical samples with known mutation status.
- DNA Quantification: Precisely quantify both mutant and wild-type DNA using fluorometric methods.
- Dilution Series Preparation: Prepare serial dilutions of mutant DNA in wild-type DNA background (e.g., 50%, 10%, 5%, 1%, 0.5%, 0.1%, 0.01%).
- Replicate Testing: Test each dilution level in a minimum of 10-20 replicates across multiple runs.
- Data Analysis: Calculate detection rate (%) for each dilution level. The LOD is defined as the lowest concentration where ≥95% of replicates test positive.
- Verification: Confirm LOD using alternative methods or digital PCR if available.
Protocol: Analytical Specificity Testing
Principle: Verify that the assay specifically detects the intended mutation without cross-reactivity with similar sequences or wild-type alleles [41] [57].
Procedure:
- Positive and Negative Controls: Include known positive (mutant) and negative (wild-type) controls in each run.
- Cross-reactivity Panel: Test against samples with:
- Different mutations in the same codon
- Common SNPs in the target region
- Homologous genes or pseudogenes
- Melting Curve Analysis (if applicable): Perform post-amplification melting curve analysis to verify specific product formation.
- Data Interpretation: The assay should detect all true positives with no amplification in negative controls or non-target mutations.
The Scientist's Toolkit
Table 3: Essential Research Reagent Solutions for TaqMan Mutation Detection
| Reagent/Kit | Function | Application Notes |
|---|---|---|
| TaqMan Mutation Detection Assays | Detects specific mutant alleles using castPCR technology | Pre-designed for common cancer mutations; also available as custom designs [7] |
| TaqMan Genotyping Master Mix | Provides optimized buffer, enzymes, and dNTPs for allele discrimination | Includes ROX passive reference dye for signal normalization |
| DNA Extraction Kits (FFPE tissue) | Ishes high-quality DNA from challenging samples | Specialized protocols for cross-linked DNA; include DNase treatment for RNA removal [2] |
| TaqMan Mutation Detection IPC Reagent Kit | Internal positive control for PCR inhibition monitoring | Can be duplexed with mutation detection assays [7] |
| Nuclease-Free Water | Diluent for reactions without enzymatic degradation | Essential for maintaining reaction integrity |
| DNA Quantitation Kits | Fluorometric measurement of DNA concentration and quality | More accurate than spectrophotometry for FFPE-derived DNA [2] |
Data Analysis and Interpretation
Quality Control Parameters
Robust analytical validation requires establishing stringent QC criteria. For TaqMan castPCR assays, the following parameters should be monitored:
- Amplification Efficiency: 90-110% based on standard curve analysis
- R² Value: ≥0.990 for standard curves
- Ct Values for Controls: Within established ranges for each assay
- ΔCt Values: Consistent with validation data for mutation calling
The gene reference assay serves as a critical control for DNA quality and potential PCR inhibition [7]. Samples with abnormal reference assay Ct values (typically >5 cycles beyond average) should be flagged for potential quality issues.
Validation in Clinical Samples
When validating assays for clinical research applications, performance should be verified against established methods using relevant sample types. In a study comparing castPCR with direct sequencing and Therascreen for EGFR mutations, castPCR demonstrated superior sensitivity while maintaining 100% positive predictive value [2]. The technology successfully detected mutations in samples with low tumor cell content where sequencing failed, highlighting its utility for analyzing limited clinical material [2].
Comprehensive analytical validation establishing sensitivity, specificity, and reproducibility is fundamental to generating reliable data with TaqMan assays for mutation detection in cancer research. The structured approach outlined in this application note, incorporating standardized protocols and performance criteria, provides a framework for implementing robust mutation detection assays. The exceptional sensitivity of castPCR technology (0.1-0.5% mutant allele frequency) combined with high specificity makes it particularly valuable for analyzing heterogeneous tumor samples and minimal specimens where mutation detection is most challenging. By adhering to these validation principles, researchers can ensure the generation of high-quality, reproducible data to support cancer research and drug development programs.
Comparative Performance vs. Sanger Sequencing, HRM, and PCR-RFLP
The shift toward personalized medicine in oncology necessitates molecular diagnostics that are not only accurate but also rapid, sensitive, and adaptable to clinical settings. While Sanger sequencing has long been the gold standard for mutation detection, several PCR-based techniques like High-Resolution Melting (HRM) and PCR-Restriction Fragment Length Polymorphism (PCR-RFLP) offer cost-effective alternatives [59] [60]. TaqMan-based assays, including advanced iterations like Competitive Allele-Specific TaqMan PCR (Cast-PCR), represent a technologically refined platform designed to meet the demanding requirements of modern cancer research and therapeutic decision-making [50]. This application note delineates the comparative performance of TaqMan assays against these established methods, providing detailed protocols framed within a broader thesis on optimized mutation detection for cancer research.
Comparative Performance Data
The selection of an appropriate genotyping method depends on a balance of sensitivity, specificity, cost, throughput, and turnaround time. The following tables summarize the comparative performance of TaqMan assays against other common techniques, synthesizing data from multiple clinical studies.
Table 1: Overall Method Comparison for Mutation Detection [61] [62] [50]
| Method | Quantitative? | Sequence Discovery? | Sensitivity (LOD) | Number of Targets per Reaction | Best Application Scenarios |
|---|---|---|---|---|---|
| TaqMan/qPCR | Yes | No | ~1-5% [62] [50] | 1 to 5 (Multiplexable) | High-throughput SNP genotyping, rapid screening of known hotspots. |
| Sanger Sequencing | No | Yes | ~10-20% [62] [50] | 1 | Gold standard for sequence confirmation; discovery of novel variants. |
| HRM | No | Screening only | ~5% (confirmation by sequencing needed) [59] [60] | 1 | Low-cost mutation screening; requires sequencing for variant identification. |
| PCR-RFLP | No | No | ~5-10% | 1 | Low-cost option for SNPs that create/destroy restriction sites. |
| Next-Generation Sequencing (NGS) | Yes | Yes | ~1-5% [63] [62] | 1 to >10,000 | Comprehensive profiling, multigene analysis, and unknown variant discovery. |
| Digital PCR (dPCR) | Yes (Absolute) | No | ~0.1-1% [63] [61] | 1 to 5 (Multiplexable) | Absolute quantification, rare allele detection, liquid biopsy [63]. |
Table 2: Key Findings from Clinical Performance Studies
| Cancer Type / Gene | Method Compared | Key Finding | Reference |
|---|---|---|---|
| Melanoma / BRAF V600 | Cast-PCR vs. Sanger | Cast-PCR detected all mutations found by Sanger and identified 4 additional mutations in 54 samples. Sensitivity: Cast-PCR (1%) vs. Sanger (10-25%). | [50] |
| Lung / EGFR, KRAS, PIK3CA, BRAF | qPCR vs. Sanger (138 FFPE samples) | qPCR and NGS showed significantly higher sensitivity than Sanger, which failed to detect variants with mutation rates <15%. | [62] |
| Various / TP53 p.R337H | TaqMan vs. HRM, RFLP, Sanger | 100% concordance across 95 samples. TaqMan-PCR showed the lowest turnaround and hands-on times. | [59] [64] |
| Breast / ERBB2, ESR1, PIK3CA | Multiplex dPCR vs. Targeted NGS | Overall concordance of 95% (90/95). Both suitable for liquid biopsies; dPCR offers high sensitivity, NGS enables multigene analysis. | [63] |
| Colorectal / KRAS, BRAF | TaqMan vs. PCR-Sanger | Overall concordance of 98.8% (kappa = 0.976). TaqMan superior in handling time, efficiency, repeatability, and cost. | [65] |
Detailed Experimental Protocols
Competitive Allele-Specific TaqMan PCR (Cast-PCR) for BRAF V600 Detection
This protocol, adapted from a study on melanoma, highlights the specific steps for detecting the challenging BRAF V600E/K mutations with high sensitivity and specificity [50].
- Sample Preparation: DNA is extracted from formalin-fixed paraffin-embedded (FFPE) tissue or fresh tumor biopsies using a commercial kit (e.g., QIAamp DNA Blood Mini Kit). DNA concentration and purity are determined via spectrophotometry (e.g., NanoDrop). Note: For pigmented melanomas, an additional purification step (e.g., using GENECLEAN II Kit) is recommended to remove PCR-inhibiting melanin [50].
- Primer and Probe Design:
- Cast-PCR Assay: Utilize a pre-validated, commercially available Cast-PCR assay mix for BRAF mutations (e.g., V600E and V600K). The assay contains:
- Allele-Specific Primers (ASP): Designed with the 3' nucleotide complementary to the specific mutant allele (e.g., "A" for V600E).
- Wild-Type Blocker (ASB): An oligonucleotide that binds perfectly to the wild-type sequence and suppresses its amplification through modified chemistry.
- TaqMan MGB Probes: Two probes, each labeled with a different fluorescent dye (e.g., FAM for mutant, VIC for wild-type), to enable allelic discrimination.
- Cast-PCR Assay: Utilize a pre-validated, commercially available Cast-PCR assay mix for BRAF mutations (e.g., V600E and V600K). The assay contains:
- Reaction Setup:
- Prepare a 12.5 µL reaction mixture containing:
- 20 ng of genomic DNA
- 1X TaqMan Genotyping Master Mix
- 1X Custom Cast-PCR Assay Mix
- Run reactions in triplicate on a 96-well plate alongside positive controls (known mutant and wild-type DNA) and no-template controls (NTC).
- Prepare a 12.5 µL reaction mixture containing:
- Thermal Cycling and Data Acquisition:
- Use a real-time PCR instrument (e.g., StepOne or QuantStudio).
- Cycling conditions:
- Hold Stage: 95°C for 10 min (enzyme activation)
- PCR Stage (40 cycles): 92°C for 15 sec (denaturation), 60°C for 1 min (annealing/extension with fluorescence read)
- Data Analysis:
- Use the instrument's allelic discrimination software to analyze the fluorescence data.
- The software will cluster samples into categories: mutant homozygous, wild-type homozygous, heterozygous (for the specific mutation), or undetermined based on the fluorescence signal from each channel.
Protocol Comparison: HRM and PCR-RFLP
To provide context for the performance of TaqMan assays, standard protocols for HRM and PCR-RFLP are outlined below.
HRM for TP53 p.R337H Genotyping [59]
- PCR Amplification: A 10 µL reaction is set up with 20 ng genomic DNA, 0.3 µM of each primer flanking exon 10 of TP53, and 1X MeltDoctor HRM Master Mix (contains saturating DNA dye).
- Thermal Cycling: Run on a real-time PCR system (e.g., StepOne): 95°C for 10 min; 40 cycles of (95°C for 15 s, 57°C for 30 s, 60°C for 30 s).
- High-Resolution Melting: After amplification, denature at 95°C for 10 s, then cool to 60°C. The melt curve is generated by continuously monitoring fluorescence from 60°C to 95°C with a slow ramp rate (e.g., 0.3%).
- Analysis: Software normalizes and clusters the melting curves. Samples with abnormal melting profiles must be confirmed by Sanger sequencing to identify the exact sequence variant.
PCR-RFLP for TP53 p.R337H Genotyping [59]
- PCR Amplification: Amplify TP53 exon 10 using standard PCR protocols and primers.
- Restriction Digest: Cleave the PCR product with HhaI restriction enzyme (the p.R337H mutation creates a HhaI site). Incubate at 37°C for 2 hours.
- Gel Electrophoresis: Resolve the digested fragments on a 3% agarose gel stained with GelRed.
- Genotype Interpretation:
- Wild-type (GG): Fragments at 146 bp and 92 bp.
- Heterozygous (GA): Fragments at 238 bp, 146 bp, and 92 bp.
- Homozygous Mutant (AA): Fragment at 238 bp.
- Genotype Interpretation:
Workflow and Logical Diagrams
The following diagram illustrates the streamlined workflow of a TaqMan assay compared to the more complex, multi-step processes of Sanger sequencing, HRM, and PCR-RFLP.
The workflow and logical diagram above highlights the key operational differences between the methods. The TaqMan assay is a single-tube, closed-system process with automated analysis, minimizing hands-on time and the risk of contamination. In contrast, Sanger, HRM, and PCR-RFLP require multiple, separate post-PCR processing steps, which are more labor-intensive and time-consuming [59] [66] [50]. The logical flow at the bottom illustrates the typical hierarchy of analytical sensitivity, with TaqMan and NGS offering superior performance for detecting low-abundance mutations compared to Sanger and basic PCR methods [62] [50].
Research Reagent Solutions
The following table details key reagents and their functions essential for implementing the TaqMan genotyping protocols described in this note.
Table 3: Essential Reagents for TaqMan-Based Mutation Detection
| Item | Function / Application | Example Product / Note |
|---|---|---|
| Nucleic Acid Extraction Kit | Isolation of high-quality genomic DNA from various sample types (blood, FFPE, tissue). | QIAamp DNA Blood Mini Kit [59] [60] |
| TaqMan Genotyping Master Mix | Optimized buffer, enzymes, dNTPs for efficient real-time PCR amplification and probe cleavage. | TaqMan Universal PCR Master Mix [59] |
| Custom TaqMan SNP Genotyping Assay | Pre-designed primer and probe set for specific mutation detection. Includes allele-specific primers and MGB probes. | Custom TaqMan Assays (e.g., TP53R337H) [59] |
| Cast-PCR Assay | Specialized assay incorporating wild-type blockers for superior sensitivity and specificity in mutant allele detection. | Cast-PCR Mutation Detection Assays [50] |
| Real-Time PCR Instrument | Platform for thermal cycling, fluorescence excitation/detection, and initial data analysis. | StepOne, QuantStudio Series [59] [50] |
| Optical Reaction Plates & Seals | Consumables compatible with real-time PCR systems to prevent evaporation and cross-contamination. | MicroAmp Optical 96-Well Plate |
| Positive Control Genomic DNA | Verified wild-type, heterozygous, and homozygous mutant DNA for assay validation and run controls. | Commercial sources or clinically characterized samples. |
Within molecular cancer research, the selection of an appropriate genotyping method is a critical strategic decision that balances analytical performance with practical resource constraints. This document provides a detailed cost-benefit analysis focused on the throughput, turnaround time, and resource requirements of TaqMan-based mutation detection assays, specifically the competitive allele-specific TaqMan PCR (castPCR) technology. The analysis is framed within the context of optimizing laboratory workflows for the detection of somatic mutations in key cancer genes such as KRAS, BRAF, and EGFR [7] [40]. By quantifying both the tangible and intangible factors of assay implementation, this guide aims to equip researchers and drug development professionals with the data needed to make informed, efficient, and cost-effective choices for their mutation profiling needs.
Quantitative Cost-Benefit Analysis
The value proposition of TaqMan castPCR assays becomes clear when its performance and operational metrics are compared with alternative genotyping technologies. The following tables summarize a quantitative comparison based on key parameters relevant to research and pre-clinical drug development settings.
Table 1: Comparative Analysis of Mutation Detection Methods
| Parameter | TaqMan castPCR | Sanger Sequencing | Pyrosequencing | Next-Generation Sequencing (NGS) |
|---|---|---|---|---|
| Detection Sensitivity [50] | 0.1% - 1% (1:1000 mutant to wild-type ratio) | 15% - 20% | 5% - 10% | 1% - 5% (varies by depth) |
| Total Assay Turnaround Time [7] | ~3 hours (from sample to result) | 24 - 48 hours | 6 - 8 hours | 3 - 7 days |
| Multiplexing Capability | Medium (e.g., 44 mutations in a 384-well array) [9] | Low | Low | Very High |
| DNA Input Quality | Compatible with FFPE, fresh frozen, cell lines [7] | Requires high-quality DNA | Requires good-quality DNA | Compatible with FFPE; requires high-quality DNA for best results |
| Hands-On Time | Low | Medium | Medium | High |
| Cost Per Sample (Estimated) | Low to Medium | Low | Medium | High |
Table 2: Cost-Benefit and Resource Breakdown for TaqMan castPCR
| Category | Specification / Requirement | Quantitative Benefit or Cost |
|---|---|---|
| Throughput | 96-well or 384-well plate format [7] | Processes 7 samples for 44 mutations per plate [9] |
| Reaction Efficiency | 150 reactions per mutant allele assay (10 µL in 384-well) [7] | Dynamic range of ≥4 logs, average PCR efficiency of 100% ± 10% [40] |
| Personnel & Training | Standard qPCR training required | Simplified workflow reduces training overhead and human error [7] |
| Equipment & IT | Requires compatible Real-Time PCR system and analysis software (e.g., Mutation Detector Software) [7] | Upfront capital cost offset by fast analysis and pre-formulated assays |
| Data Analysis | Automated allele calling with dedicated software [7] | Reduces analysis time to minutes, eliminates subjective interpretation [50] |
| Assay Availability | 819 inventoried assays for 47 cancer genes (e.g., KRAS, BRAF) [7] | Off-the-shelf availability for common targets saves development time |
| Sensitivity Impact | Ability to detect rare mutant alleles in wild-type background [7] | 92% sensitivity, 100% Positive Predictive Value (PPV) demonstrated in validation studies [9] |
Experimental Protocol: Detecting BRAF V600 Mutations via CastPCR
The following protocol details the steps for detecting the clinically relevant BRAF V600E and V600K mutations using TaqMan castPCR, as validated in peer-reviewed studies [50].
Principle
Competitive allele-specific TaqMan PCR (castPCR) technology combines an allele-specific primer for the mutant allele with a Minor Groove Binder (MGB) oligonucleotide blocker that suppresses amplification of the wild-type allele. This competition enables highly specific and sensitive detection of rare somatic mutations, even in suboptimal samples like FFPE tissue [7] [40].
Materials and Reagents
- DNA Samples: Extracted from patient tissues (e.g., melanoma, NSCLC, colorectal cancer), cell lines, or FFPE blocks. Include known wild-type and mutant controls.
- TaqMan Mutation Detection Assays: BRAF V600E and V600K mutant allele assays (Cat. No. 4465804), BRAF gene reference assay (Cat. No. 4465807) [7].
- PCR Reagents: TaqMan Genotyping Master Mix.
- Consumables: Optical 96-well or 384-well reaction plates and seals.
- Equipment: Compatible Real-Time PCR System (e.g., Applied Biosystems 7500 Fast).
Step-by-Step Procedure
- DNA Quantification and Normalization: Quantify all DNA samples using a fluorometric method. Normalize samples to a uniform concentration (e.g., 10 ng/µL) in nuclease-free water.
- Reaction Plate Setup: For each sample, set up the following duplex reactions in separate wells:
- Well 1 (Mutant Detection): 10-20 ng genomic DNA, 1X TaqMan BRAF V600E (or V600K) Mutant Allele Assay, 1X BRAF Gene Reference Assay, 1X TaqMan Genotyping Master Mix.
- Well 2 (Wild-Type Control, Optional): 10-20 ng genomic DNA, 1X BRAF Wild-Type Allele Assay, 1X BRAF Gene Reference Assay, 1X TaqMan Genotyping Master Mix.
- Real-Time PCR Cycling: Run the plate on the real-time PCR system using the following standard cycling conditions:
- Hold Stage: 95°C for 10 minutes (enzyme activation)
- PCR Stage (40 cycles): 95°C for 15 seconds (denaturation) → 60°C for 1 minute (annealing/extension)
- Data Analysis: Use instrument software or dedicated Mutation Detector Software to analyze the data. The software will automatically determine the mutation status based on the amplification profiles of the mutant and reference assays. A sample is called mutant if amplification occurs in the mutant assay well above a defined threshold.
Workflow Visualization
The Scientist's Toolkit: Key Research Reagent Solutions
Table 3: Essential Materials for TaqMan CastPCR Experiments
| Item Name | Function / Application | Example Catalog Number |
|---|---|---|
| TaqMan Mutation Detection Assay | Pre-formulated 10X mix containing allele-specific primers, a FAM-labeled TaqMan MGB probe, and an MGB blocker for specific mutant allele detection. | 4465804 [7] |
| TaqMan Gene Reference Assay | Pre-formulated 10X mix containing primers and a VIC-labeled TaqMan MGB probe for a reference gene; provides a control for DNA sample quality and PCR success. | 4465807 [7] |
| TaqMan Mutation Detection IPC Reagent Kit | Optional internal positive control reagents that can be duplexed with any mutation detection assay to monitor for PCR inhibition. | 4467538 [7] |
| Formalin-Fixed Paraffin-Embedded (FFPE) DNA Extraction Kit | For isolating DNA from archived clinical FFPE tissue samples, a common sample type in cancer research. | N/A |
| Compatible Real-Time PCR System | Instrument platform for running and detecting the real-time PCR reactions. Requires compatible software for data analysis. | (e.g., Applied Biosystems 7500 Fast) |
| TaqMan Custom Plating Service | Service to order assays pre-plated into 96- or 384-well plates, saving time and reducing manual handling for large-scale studies. | N/A [7] |
The cost-benefit analysis presented herein demonstrates that TaqMan castPCR assays offer a compelling solution for laboratories focused on the detection of known somatic mutations in cancer research. The technology's primary advantages are its superior sensitivity and speed, enabling the reliable detection of rare mutant alleles in a background of wild-type DNA with a total turnaround time of approximately three hours [7] [50]. When operational costs, reagent efficiency, and analytical performance are factored together, the castPCR platform provides a highly balanced and often optimal approach for targeted genotyping, particularly in studies with medium-to-high throughput requirements and where sample quality or low mutation abundance is a concern.
Molecular diagnostics are pivotal for personalized cancer therapy, enabling the selection of patients most likely to benefit from targeted treatments. This application note details the validation of TaqMan-based assay protocols, specifically Competitive Allele-Specific TaqMan PCR (castPCR), for detecting somatic mutations in non-small cell lung cancer (NSCLC) and colorectal cancer (CRC) cohorts. The data presented herein demonstrate the high clinical concordance, sensitivity, and specificity of these methods when compared to both standard and emerging diagnostic techniques, providing researchers and drug development professionals with robust protocols for biomarker analysis.
Results and Discussion
Clinical Concordance of Mutation Detection Assays
The analytical performance of real-time PCR-based methods was evaluated against established techniques like direct sequencing and other commercial kits across multiple clinical studies. The following table summarizes key concordance findings from validation studies in NSCLC and CRC.
Table 1: Clinical Concordance of Mutation Detection Assays in Validation Cohorts
| Cancer Type | Assay/Method Tested | Reference Method | Sample Size (n) | Overall Concordance | Key Findings | Citation |
|---|---|---|---|---|---|---|
| NSCLC | cobas EGFR PCR test | Laboratory-Developed Tests (LDTs) | 487 | 96.3% | Clinical outcomes (PFS, BORR) in EGFR mutation-positive patients aligned with the full EURTAC trial population. | [67] |
| NSCLC | TaqMan Mutation Detection Assays (castPCR) | Direct Sequencing & Therascreen | 58 NSCLC + 6 CRC | Highly Similar | Identified EGFR mutations with similar frequency to Therascreen; superior sensitivity in samples with low tumor cell content. | [2] |
| Colorectal Cancer | MEBGEN RASKET KIT (Multiplex PCR) | Direct Sequencing & TheraScreen | 307 | 96.7% | Detected 48 RAS mutations in a single well; identified minor RAS mutations in 15.7% of wild-type KRAS exon 2 population. | [68] |
| NSCLC (Liquid Biopsy) | Next-Generation Sequencing (NGS) | Tissue Analysis (NGS) | 36 (Paired) | 86.1% | High concordance for clinically relevant mutations, supporting plasma as a reliable surrogate for tissue. | [69] |
The high concordance rates observed across these studies, which often exceed 95%, validate the use of PCR-based methods like castPCR and multiplex assays for clinical decision-making. Notably, these methods consistently demonstrate improved sensitivity over traditional direct sequencing, which requires a high tumor cell content (40-50%) to avoid false negatives [2]. This is particularly crucial for analyzing challenging samples like FFPE tissues or liquid biopsies, where DNA quality and quantity are limited.
Sensitivity and Specificity of Detection Platforms
Assay sensitivity is a critical parameter for detecting low-frequency mutations in a background of wild-type DNA, as commonly encountered in clinical samples. The following table compares the limits of detection for various technologies used in cancer mutation screening.
Table 2: Comparison of Mutation Detection Method Performance
| Method | Approximate Limit of Detection (Mutant Allele Frequency) | Key Advantages | Key Limitations | Citation |
|---|---|---|---|---|
| castPCR | 0.1% - 0.5% | High specificity with wild-type suppression; designed to detect somatic mutations down to 1 in 1,000 normal cells. | Targeted; detects only pre-specified mutations. | [2] [7] |
| Digital PCR (dEGFR39 assay) | As low as 0.01% (1 in 10,000) | Absolute quantification without a standard curve; high sensitivity and precision for known mutations. | Lower throughput; higher cost per sample compared to real-time PCR. | [70] [71] |
| ARMS/TheraScreen | ~1% | Robust, commercially available kits; regulatory approved for companion diagnostics. | Targeted; limited multiplexing capability. | [2] [72] |
| Next-Generation Sequencing (NGS) | ~1% | Comprehensive; can detect novel mutations across multiple genes simultaneously. | Higher cost, complex data analysis, longer turnaround time. | [69] [72] |
| Direct Sequencing (Sanger) | 10-25% | Considered a gold standard; can identify unknown mutations across a sequenced region. | Low sensitivity; requires high tumor purity. | [2] [72] |
The data underscore that castPCR and digital PCR offer superior sensitivity for detecting rare mutant alleles in a wild-type background. The castPCR technology achieves this through an MGB oligonucleotide blocker that suppresses the amplification of the wild-type allele, allowing for the selective amplification and detection of the mutant sequence [7]. This makes it exceptionally suitable for analyzing FFPE-derived DNA, where the proportion of tumor cells may be low.
Experimental Protocols
castPCR for EGFR Mutations in NSCLC
This protocol is adapted from a study that validated TaqMan Mutation Detection Assays for EGFR mutations in NSCLC clinical specimens [2].
Sample Preparation and DNA Extraction
- Tissue Samples: Use formalin-fixed paraffin-embedded (FFPE) tissue sections, fresh frozen tissue, or cytological samples.
- DNA Extraction: Extract genomic DNA using commercially available kits (e.g., QIAamp DNA FFPE Tissue Kit, QIAamp DNA Micro Kit from Qiagen). Assess DNA quality by 0.8% agarose gel electrophoresis and quantify using a spectrophotometer (e.g., NanoVue).
castPCR Reaction Setup
- Assays: Use pre-designed TaqMan Mutation Detection Assays for specific EGFR mutations (e.g., L858R, T790M, exon 19 deletions) and a TaqMan Mutation Detection Reference Assay.
- Reaction Mix: Prepare a 20 µL reaction volume containing:
- 1x TaqMan Genotyping Master Mix
- 1x TaqMan Mutation Detection Assay (mutant allele assay)
- 1x TaqMan Mutation Detection Reference Assay
- 10 ng DNA template
- Run Conditions: Perform amplification on a real-time PCR system (e.g., ViiA 7) using the following thermal cycling protocol:
- Hold: 95°C for 10 minutes.
- 5 cycles of:
- Denature: 92°C for 15 seconds.
- Anneal/Extend: 58°C for 1 minute.
- 40 cycles of:
- Denature: 92°C for 15 seconds.
- Anneal/Extend: 60°C for 1 minute.
Data Analysis
- Calculate the ΔCt value: ΔCt = [Ct(mutant allele assay) – Ct(gene reference assay)] – calibration ΔCt.
- Interpretation: A sample is considered positive for the mutation if the ΔCt is less than or equal to the validated cut-off value (determined to be 7 in the referenced study). A sample with a ΔCt greater than the cut-off is considered wild-type [2].
Multiplex PCR for RAS Mutations in Colorectal Cancer
This protocol is based on the clinical validation of the MEBGEN RASKET KIT for RAS mutations in CRC [68].
Sample Preparation and DNA Extraction
- Tissue Samples: Use FFPE tissue sections from colorectal adenocarcinoma specimens. Manual microdissection is not required.
- DNA Extraction: Extract DNA using a dedicated FFPE kit (e.g., QIAamp DNA FFPE Tissue Kit). The input requirement is low, with only 50–100 ng of DNA needed per reaction.
Multiplex PCR and Hybridization
- Assay Principle: The kit uses a combination of PCR-reverse sequence specific oligonucleotide (PCR-rSSO) and xMAP (Luminex) technology.
- Procedure: The process is completed in a single well for each specimen.
- Multiplex PCR Amplification: Amplify target regions of KRAS and NRAS (exons 2, 3, 4) in a single tube.
- Hybridization: Hybridize the PCR products to sequence-specific oligonucleotide probes.
- Detection: Detect hybridized products using the xMAP array system, which allows for the concurrent identification of 48 different RAS mutations.
Data Analysis
- The result is generated automatically by the system software based on the fluorescence signal.
- The entire process, from DNA to result, has a rapid turnaround time of approximately 4.5 hours for a batch of 96 specimens [68].
Workflow Diagram: castPCR Mutation Detection
The following diagram illustrates the logical workflow and mechanism of the castPCR assay for somatic mutation detection.
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Reagents and Kits for TaqMan-Based Mutation Detection
| Item | Function/Description | Example Product (Catalog #) | Citation |
|---|---|---|---|
| TaqMan Mutation Detection Assays | Pre-formulated assays for specific mutant alleles; include primers, a FAM-labeled MGB probe, and an MGB blocker. | TaqMan Mutation Detection Assays (4465804) | [7] |
| TaqMan Mutation Detection Reference Assays | Assays targeting a mutation-free region of the gene; used for signal normalization and ΔCt calculation. | TaqMan Mutation Detection Reference Assays (4465807) | [7] |
| EGFR Exon 19 Deletions Assay | A specific mutant allele assay designed to detect 19 different deletion variants in EGFR exon 19. | TaqMan EGFR Exon 19 Deletions Assay (4465805) | [2] [7] |
| Nucleic Acid Extraction Kits | For isolation of high-quality genomic DNA from various sample types, including challenging FFPE tissues. | QIAamp DNA FFPE Tissue Kit, QIAamp Circulating Nucleic Acid Kit | [2] [69] |
| TaqMan Genotyping Master Mix | Optimized PCR master mix containing DNA polymerase, dNTPs, and buffer components for robust amplification. | TaqMan Genotyping Master Mix | [2] |
| Internal Positive Control (IPC) Reagents | Optional reagents to duplex with mutation assays; monitor PCR inhibition and ensure reaction validity. | TaqMan Mutation Detection IPC Reagent Kit (4467538) | [7] |
The validation studies summarized in this application note firmly establish that TaqMan-based castPCR and other real-time PCR assays are highly accurate and reliable for detecting clinically actionable mutations in NSCLC and CRC. Their superior sensitivity and specificity compared to direct sequencing, combined with a faster workflow and compatibility with routine clinical samples like FFPE tissues, make them indispensable tools for both translational research and companion diagnostic development. The detailed protocols provided herein offer a robust framework for researchers to implement these methods in their own laboratories, thereby advancing the field of precision oncology.
Conclusion
TaqMan assays, particularly those utilizing castPCR technology, represent a robust and highly sensitive methodology for detecting cancer-associated mutations. Their ability to reliably identify mutations down to 0.1-1% allele frequency in challenging samples like FFPE tissues makes them indispensable for modern cancer research and molecular diagnostics. When properly validated and optimized, these assays outperform traditional sequencing in sensitivity and speed while offering a more accessible alternative to complex NGS for targeted mutation screening. Future directions will likely see increased integration with liquid biopsy applications for monitoring minimal residual disease and therapy response, solidifying their role in the era of precision oncology and personalized cancer therapy.
References
- 1. - Competitive ( allele - specific ) is a sensitive... TaqMan PCR Cast PCR [https://pubmed.ncbi.nlm.nih.gov/26690267/]
- 2. Detection of EGFR Mutations by TaqMan ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3864078/]
- 3. Competitive allele specific TaqMan PCR for KRAS, BRAF ... [https://www.sciencedirect.com/science/article/abs/pii/S0014480012000226]
- 4. Detecting Rare Cancer Mutations With castPCR ... [https://www.thermofisher.com/ng/en/home/references/newsletters-and-journals/bioprobes-journal-of-cell-biology-applications/bioprobes-issues-2012/bioprobes-68-november-2012/castpcr-taqman-mutation-detection-assays.html]
- 5. Quantitative competitive allele-specific TaqMan duplex ... [https://haematologica.org/article/view/8636]
- 6. castPCR for Mutation Detection [https://www.thermofisher.com/sg/en/home/life-science/pcr/real-time-pcr/real-time-pcr-applications/genetic-variation-analysis-using-real-time/castpcr-for-mutation-detection.html]
- 7. Mutation Detection Analysis Using TaqMan Assays [https://www.thermofisher.com/us/en/home/life-science/pcr/real-time-pcr/real-time-pcr-assays/taqman-mutation-detection-assays.html]
- 8. castPCR for Mutation Detection [https://www.thermofisher.com/us/en/home/life-science/pcr/real-time-pcr/real-time-pcr-applications/genetic-variation-analysis-using-real-time/castpcr-for-mutation-detection.html]
- 9. Development and validation of a TaqMan Array for cancer ... [https://www.sciencedirect.com/science/article/pii/S221466361600002X]
- 10. Somatic Mutation Detection in Tumor Tissue and Matched ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12429500/]
- 11. Detecting Rare Cancer Mutations With castPCR ... [https://www.thermofisher.com/us/en/home/references/newsletters-and-journals/bioprobes-journal-of-cell-biology-applications/bioprobes-issues-2012/bioprobes-68-november-2012/castpcr-taqman-mutation-detection-assays.html]
- 12. Circulating Tumor DNA detection in cancer - PubMed Central [https://pmc.ncbi.nlm.nih.gov/articles/PMC12450317/]
- 13. Somatic Mutation Detection in Tumor Tissue and Matched ... [https://www.mdpi.com/1422-0067/26/17/8518]
- 14. Somatic mutation detection in cancer research [https://www.illumina.com/areas-of-interest/cancer/clinical-cancer-research/somatic-mutations.html]
- 15. Somatic mutation detection and KRAS amplification in ... [https://www.frontiersin.org/journals/oncology/articles/10.3389/fonc.2023.1133363/full]
- 16. A Protocol for Cancer-Related Mutation Detection on ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7518026/]
- 17. Mutation Detection With Real-Time PCR [https://www.thermofisher.com/za/en/home/life-science/pcr/real-time-pcr/real-time-pcr-applications/mutation-detection-with-real-time-pcr.html]
- 18. Rapid in situ mutation detection in extracellular vesicle DNA [https://pmc.ncbi.nlm.nih.gov/articles/PMC11977346/]
- 19. Clinical and analytical validation of a combined RNA ... [https://www.nature.com/articles/s43856-025-00934-3]
- 20. Comparison of Seven Commercial TaqMan Master Mixes ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7810389/]
- 21. A TaqMan-Based qRT-PCR Assay for Accurate Evaluation ... [https://www.mdpi.com/2072-6694/17/3/471]
- 22. Optimized Gene Expression Analysis from FFPE Samples [https://www.thermofisher.com/us/en/home/references/ambion-tech-support/rna-isolation/tech-notes/optimized-gene-expression-analysis-from-ffpe-samples.html]
- 23. Tips and Tricks for TaqMan Gene Expression Cells [https://www.thermofisher.com/us/en/home/references/ambion-tech-support/rtpcr-analysis/general-articles/tips-and-tricks-for-taqman-gene-expression-cells.html]
- 24. Liquid Biopsy Analysis | Thermo Fisher Scientific - US [https://www.thermofisher.com/us/en/home/life-science/cancer-research/cancer-genomics/liquid-biopsy-cancer-research-applications.html]
- 25. TaqMan™ Liquid Biopsy dPCR Assay S (450 reactions) ... [https://www.thermofisher.com/order/catalog/product/A44177]
- 26. Effective Preparation of FFPE Tissue Samples for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11659341/]
- 27. NGS Analysis of Liquid Biopsy (LB) and Formalin-Fixed ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8303399/]
- 28. Mutation Detection With Real-Time PCR [https://www.thermofisher.com/us/en/home/life-science/pcr/real-time-pcr/real-time-pcr-applications/mutation-detection-with-real-time-pcr.html]
- 29. Mutation Detection by Real-Time PCR: A Simple, Robust and ... [https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0004584]
- 30. How TaqMan Assays Work [https://www.thermofisher.com/us/en/home/life-science/pcr/real-time-pcr/real-time-pcr-learning-center/real-time-pcr-basics/how-taqman-assays-work.html]
- 31. Real-Time PCR: Understanding Ct [https://www.thermofisher.com/us/en/home/life-science/pcr/real-time-pcr/real-time-pcr-learning-center/real-time-pcr-basics/real-time-pcr-understanding-ct.html]
- 32. How To Interpret RT-qPCR Results [https://www.goldbio.com/blogs/articles/how-to-interpret-rt-qpcr-results?srsltid=AfmBOopIp_cmpszYQoey0d1XOFqJlxrmMWgFcmHgVx6Tbr5hEDNbCcbd]
- 33. Cell HE staining smears and paired cell paraffin sections in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10930476/]
- 34. 用于检测宫颈癌或宫颈高级别病变的组合物和试剂盒 [https://patents.google.com/patent/CN117165684B/zh]
- 35. 使用TaqMan 基因表达测定和阵列进行免疫肿瘤学研究 - 赛默飞 [https://www.thermofisher.cn/cn/zh/home/life-science/pcr/real-time-pcr/real-time-pcr-applications/gene-expression-using-real-time-pcr/immuno-oncology-research.html]
- 36. BRAF V600 Mutation Detection in Plasma Cell-Free DNA [https://pmc.ncbi.nlm.nih.gov/articles/PMC8526905/]
- 37. An allele-specific quantitative PCR strategy for detection of ... [https://www.sciencedirect.com/science/article/pii/S0141813025049992]
- 38. Prevalence and prognostic impact of BRAF V600E ... [https://www.frontiersin.org/journals/oncology/articles/10.3389/fonc.2025.1537268/full]
- 39. BRAF mutation detection [https://bio-protocol.org/exchange/minidetail?id=3646017&type=30]
- 40. Cancer Genotyping Assays: Somatic & Germline [https://www.thermofisher.com/us/en/home/life-science/cancer-research/cancer-genomics/cancer-genotyping-assays.html]
- 41. Designing a TaqMan Gene Expression Assay [https://www.thermofisher.com/us/en/home/life-science/pcr/real-time-pcr/real-time-pcr-learning-center/gene-expression-analysis-real-time-pcr-information/designing-taqman-gene-expression-assay.html]
- 42. Real-Time PCR Design [https://www.caister.com/highveld/pcr/real-time-pcr-design.html]
- 43. How to Design Primers for PCR Experiments [https://www.zymoresearch.com/blogs/blog/how-to-design-primers-for-pcr-experiments?srsltid=AfmBOor4mE93_z0xQlzBbdrM_90D0VcfVRemEvz8q3waAlJr6XIQe3i6]
- 44. TaqMan® probe design tips [http://www.premierbiosoft.com/tech_notes/TaqMan.html]
- 45. Why TaqMan Assay Design is Important [https://www.thermofisher.com/us/en/home/life-science/pcr/real-time-pcr/real-time-pcr-learning-center/real-time-pcr-basics/why-taqman-assay-design-important.html]
- 46. How to Design PCR Primers in Geneious Prime [https://www.geneious.com/tutorials/primer-design]
- 47. The Optimization of TaqMan Real-Time RT-PCR Assay for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC2696555/]
- 48. SNP genotyping using TaqMan® technology: the CYP2D6* ... [https://www.nature.com/articles/srep09257]
- 49. Mutation Detection Analysis Using TaqMan Assays [https://www.thermofisher.com/jp/en/home/life-science/pcr/real-time-pcr/real-time-pcr-assays/taqman-mutation-detection-assays.html]
- 50. Competitive allele-specific TaqMan PCR (Cast-PCR) is a ... [https://www.nature.com/articles/srep18592]
- 51. Validation of a liquid biopsy assay with increased ... [https://www.sciencedirect.com/science/article/pii/S2950195425000384]
- 52. TaqMan-MGB probe quantitative PCR assays to genotype ... [https://www.nature.com/articles/s41598-020-69220-7]
- 53. Evaluation of TaqMan qPCR System Integrating Two ... [https://www.nature.com/articles/srep41392]
- 54. Genomic DNA Purification Support—Troubleshooting [https://www.thermofisher.com/us/en/home/technical-resources/technical-reference-library/nucleic-acid-purification-analysis-support-center/genomic-dna-purification-support/genomic-dna-purification-support-troubleshooting.html]
- 55. SLAM-MS: Mutation scanning of stem-loop amplicons with ... [https://www.nature.com/articles/s41598-020-62173-x]
- 56. Establishment of a TaqMan qPCR method with MGB probe ... [https://www.frontiersin.org/journals/veterinary-science/articles/10.3389/fvets.2025.1634429/full]
- 57. Optimized Multiplex Detection of 7 KRAS Mutations by ... [https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0163070]
- 58. Development of a TaqMan Probe-Based Quantitative PCR ... [https://pubmed.ncbi.nlm.nih.gov/41258816/]
- 59. Comparison of multiple genotyping methods for the ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4910550/]
- 60. Comparison of Direct Sequencing, Real-Time PCR-High ... [https://www.mdpi.com/2075-4418/7/2/27]
- 61. NGS, qPCR, or Sanger Sequencing: An Assay Selection ... [https://blog.genewiz.com/ngs-qpcr-or-sanger-sequencing-an-assay-selection-guide]
- 62. Comparison of Next-Generation Sequencing, Quantitative ... [https://pubmed.ncbi.nlm.nih.gov/27215089/]
- 63. Comparative Performance of a Targeted Next-Generation ... [https://pubmed.ncbi.nlm.nih.gov/41072730/]
- 64. Comparison of Multiple Genotyping Methods for the ... [https://pubmed.ncbi.nlm.nih.gov/27275664/]
- 65. [Comparative analysis of real-time quantitative PCR ... [https://pubmed.ncbi.nlm.nih.gov/24742565/]
- 66. Real-Time PCR or Sanger sequencing? [https://rheniumbio.co.il/real-time-pcr-or-sanger-sequencing/]
- 67. Clinical Validation of a PCR Assay for the Detection of EGFR ... [https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0089518]
- 68. Clinical Validation of a Multiplex Kit for RAS Mutations in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4486202/]
- 69. Clinical feasibility of NGS liquid biopsy analysis in NSCLC ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6924668/]
- 70. Plasma-based early screening and monitoring of EGFR ... [https://www.nature.com/articles/s41416-020-1024-2]
- 71. EGFR T790M Rare Mutation Detection Tutorial - Gene Pi [https://www.gene-pi.com/tutorial/introduction-rare-mutation-detection-2-3/]
- 72. Current companion diagnostics in advanced colorectal ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5334060/]