Advanced Feature Extraction Techniques for Cancer Detection: From Biomarkers to Deep Learning
This article provides a comprehensive overview of the latest feature extraction methodologies revolutionizing cancer detection and diagnosis.
Advanced Feature Extraction Techniques for Cancer Detection: From Biomarkers to Deep Learning
Abstract
This article provides a comprehensive overview of the latest feature extraction methodologies revolutionizing cancer detection and diagnosis. Tailored for researchers, scientists, and drug development professionals, it explores the foundational principles of identifying key biomarkers through bioinformatics and data mining. The scope extends to advanced methodological applications, including hybrid feature selection, deep learning architectures like CNNs and Vision Transformers, and the extraction of tissue-specific characteristics from medical images. It also addresses critical challenges in model optimization, data heterogeneity, and clinical integration, while providing a comparative analysis of validation frameworks and performance metrics. This resource synthesizes cutting-edge research to guide the development of robust, explainable, and clinically actionable AI tools in oncology.
The Foundation of Cancer Biomarkers: Exploring Genetic, Imaging, and Data Mining Approaches
Bioinformatics and Data Mining for Biomarker Discovery
The integration of bioinformatics and data mining has become a cornerstone of modern biomarker discovery, particularly in the field of oncology. The ability to computationally analyze high-dimensional biological data is transforming how researchers identify, validate, and translate biomarkers from laboratory findings to clinical applications [1]. This shift is enabling a move from single-marker approaches to multiparameter strategies that capture the complex biological signatures of cancer, thereby driving advancements in personalized treatment paradigms [1]. The technological renaissance in biomarker discovery is largely driven by breakthroughs in multi-omics integration, spatial biology, artificial intelligence (AI), and high-throughput analytics, which collectively offer unprecedented resolution, speed, and translational relevance [1].
A significant challenge in this domain is the inherent complexity of biological data, characterized by high dimensionality where the number of features (e.g., genes, proteins) vastly exceeds the number of available samples [2] [3]. This "p >> n problem" is further complicated by various sources of technical noise, biological variance, and potential confounding factors [3]. Success in this field, therefore, depends not only on choosing the right computational technologies but also on aligning them with specific research objectives, disease contexts, and developmental stages [1]. This application note provides a structured framework for leveraging bioinformatics and data mining techniques to overcome these challenges and advance cancer detection research through robust biomarker discovery.
Multi-Omics Data Integration and Analysis
Data Types and Technological Platforms
Multi-omics profiling represents a fundamental approach to biomarker discovery, providing a holistic view of molecular processes by integrating genomic, epigenomic, transcriptomic, and proteomic data [1]. The integration of these diverse data types can reveal novel insights into the molecular basis of diseases and drug responses, ultimately leading to the identification of new biomarkers and therapeutic targets [1]. Gene expression analysis, in particular, has emerged as a critical component for addressing fundamental challenges in cancer diagnosis and drug discovery [2].
Table 1: Primary Data Types and Platforms in Multi-Omics Biomarker Discovery
| Data Type | Description | Key Technologies | Key Applications in Biomarker Discovery |
|---|---|---|---|
| Genomics | Study of an organism's complete DNA sequence. | Next-Generation Sequencing (NGS), Whole Genome Sequencing | Identification of inherited mutations and somatic variants associated with cancer risk and progression. |
| Transcriptomics | Quantitative analysis of RNA expression levels. | RNA-Sequencing (RNA-Seq), DNA Microarrays | Discovery of differentially expressed genes and expression signatures indicative of cancer presence, type, or stage [2]. |
| Proteomics | Large-scale study of proteins, including their structures and functions. | Mass Spectrometry, Multiplex Immunohistochemistry (IHC) | Identification of protein biomarkers and signaling pathway alterations; validation of transcriptional findings [1]. |
| Epigenomics | Study of chemical modifications to DNA that regulate gene activity. | ChIP-Seq, Bisulfite Sequencing | Discovery of methylation patterns and histone modifications that influence gene expression in cancer cells. |
RNA-Sequencing (RNA-Seq) has largely superseded DNA microarrays due to its greater specificity, resolution, sensitivity to differential expression, and dynamic range [2]. This NGS method involves converting RNA molecules into complementary DNA (cDNA) and determining the nucleotide sequence, allowing for comprehensive gene expression analysis and quantification [2]. The data generated from these platforms provide the foundational material for subsequent computational mining and biomarker identification.
Data Preprocessing and Quality Control
Raw biomedical data is invariably influenced by preanalytical factors, resulting in systematic biases and signal variations that must be addressed prior to analysis [3]. A rigorous preprocessing and quality control pipeline is essential for generating reliable and interpretable results.
Key Preprocessing Steps:
- Quality Control: Implement data type-specific quality metrics using established software packages (e.g., fastQC/FQC for NGS data, arrayQualityMetrics for microarray data) to assess read quality, nucleotide distribution, and potential contaminants [3].
- Filtering: Remove features with zero or near-zero variance, as they are uninformative for downstream analysis. Attributes with a large proportion of missing values (e.g., >30%) should also be considered for removal [3].
- Normalization and Transformation: Apply appropriate normalization methods to correct for technical variations (e.g., sequencing depth, batch effects). Variance stabilizing transformations are often necessary for omics data where signal variance depends on the average intensity [3].
- Imputation: For features with a limited number of missing values, apply suitable imputation methods, taking care to consider the potential mechanisms behind the missingness [3].
The successful application of these steps should be verified by conducting quality checks both before and after preprocessing to ensure issues are resolved without introducing artificial patterns [3].
Computational Methodologies for Biomarker Discovery
Feature Selection and Dimensionality Reduction
The high dimensionality of omics data presents a significant challenge for analysis. Feature selection techniques are critical for identifying the most informative subset of biomarkers from thousands of initial candidates, thereby improving model performance and interpretability [4]. These methods can be broadly classified into filter, wrapper, and embedded approaches [2].
Hybrid Sequential Feature Selection: Recent advances advocate for hybrid approaches that combine multiple feature selection methods to leverage their complementary strengths, enhancing the stability and reproducibility of the selected biomarkers [4]. A representative workflow is as follows:
- Variance Thresholding: As an initial filter, remove genes with minimal expression variation across samples, as they are unlikely to be discriminatory.
- Recursive Feature Elimination (RFE): Iteratively construct a model (e.g., using Support Vector Machines or Random Forests) and remove the weakest features until an optimal subset is identified.
- Regularization with LASSO Regression: Apply an embedded method that penalizes the absolute size of regression coefficients, effectively driving the coefficients of non-informative features to zero and performing feature selection in the process [4].
This hybrid strategy should be implemented within a nested cross-validation framework to ensure robust feature selection and prevent overoptimistic performance estimates [4].
Table 2: Performance Comparison of Machine Learning Models in Biomarker Discovery
| Model Category | Specific Model | Key Advantages | Considerations for Biomarker Discovery | Reported Test Accuracy |
|---|---|---|---|---|
| Conventional ML | Support Vector Machines (SVM) | Effective in high-dimensional spaces; versatile kernel functions. | Performance can be sensitive to kernel and parameter choice. | Varies; can be high with proper feature engineering [2]. |
| Conventional ML | Random Forest | Robust to noise; provides feature importance metrics. | Less interpretable than single decision trees; can be computationally expensive. | Varies; demonstrates robust performance [4]. |
| Conventional ML | Logistic Regression | Simple, interpretable, provides coefficient significance. | Requires linear relationship assumption; prone to overfitting with many features. | Used for robust classification in validation [4]. |
| Deep Learning | Multi-Layer Perceptron (MLP) | Can learn complex, non-linear relationships. | Prone to overfitting on small omics datasets. | Upwards of 90% with feature engineering [2]. |
| Deep Learning | Convolutional Neural Networks (CNN) | Excels at identifying local spatial patterns. | Requires data transformation into image-like arrays for 2D CNNs. | Among the best-performing DL models [2]. |
| Deep Learning | Graph Neural Networks (GNN) | Models biological interactions between genes as a network. | Requires constructing a gene interaction graph. | Shows great potential for future analysis [2]. |
Machine Learning and Deep Learning Models
Machine learning (ML) and deep learning (DL) are indispensable for analyzing the complex, high-dimensional data generated in biomarker studies. AI is capable of pinpointing subtle biomarker patterns in multi-omic and imaging datasets that conventional methods may miss [1].
Conventional Machine Learning models like Support Vector Machines, Random Forests, and Logistic Regression are widely used and can achieve robust classification performance, especially when coupled with effective feature selection [4]. They are often less computationally intensive and can be more interpretable than deep learning models.
Deep Learning Architectures have demonstrated superior performance in identifying complex patterns. Key architectures include:
- Multi-Layer Perceptrons (MLP): The simplest form of DNNs, with full connectivity between layers [2].
- Convolutional Neural Networks (CNN): Initially designed for images, they have been adapted for omics data by transforming it into two-dimensional arrays, leveraging their ability to capture local spatial relations [2].
- Recurrent Neural Networks (RNN): Suitable for capturing sequential correlations in time-series or ordered gene expression data [2].
- Graph Neural Networks (GNN): Designed to learn from graph-structured data, making them ideal for modeling gene regulatory networks and protein-protein interactions [2].
- Transformers: Utilize a self-attention mechanism to weigh the importance of different genes in a sequence, proving highly effective for capturing long-range dependencies in genomic data [2].
To address the challenge of small sample sizes, transfer learning techniques can be employed, where information is transferred from a model trained on a large, related dataset to the specific biomarker discovery task at hand [2].
Experimental Protocols and Workflow
Integrated Computational-Experimental Workflow for Biomarker Discovery and Validation
The following protocol outlines a comprehensive workflow for biomarker discovery and validation, integrating the computational and experimental techniques discussed. This protocol is designed to be implemented within the context of a broader research program on feature extraction for cancer detection.
Phase 1: Data Acquisition and Curation
- Biospecimen Collection: Obtain relevant biospecimens (e.g., tissue biopsies, blood for liquid biopsy) from well-characterized patient cohorts and matched controls. Institutional Review Board (IRB) approval and informed consent are mandatory [4].
- Multi-Omics Profiling: Perform high-throughput profiling. For transcriptomics, extract total RNA and prepare sequencing libraries for RNA-Seq on an NGS platform. Aim for sufficient sequencing depth (e.g., 30-50 million reads per sample) and technical replicates to ensure data quality [4].
- Data Quality Control and Standardization: Process raw data through type-specific quality control pipelines (e.g., fastQC for RNA-Seq). Adhere to standardized reporting guidelines (e.g., MIAME for microarrays, MINSEQE for sequencing) [3]. Curate clinical data to resolve inconsistencies and transform them into standard formats (e.g., OMOP, CDISC) [3].
Phase 2: Computational Analysis and Biomarker Identification
- Data Preprocessing: Preprocess the raw count or intensity data. This includes normalization (e.g., TPM for RNA-Seq, RMA for microarrays), log2 transformation, and batch effect correction using methods like ComBat [3].
- Hybrid Sequential Feature Selection: Implement the feature selection pipeline within a nested cross-validation framework to ensure robustness.
- Apply variance thresholding to remove the least variable genes (e.g., bottom 20%).
- Perform Recursive Feature Elimination (RFE) wrapped around a Support Vector Machine (SVM) classifier to iteratively refine the feature set.
- Apply LASSO regression to the refined feature set from RFE to further select the most predictive biomarkers and shrink the coefficients of others to zero [4].
- Predictive Model Building and Evaluation: Train multiple machine learning models (e.g., Random Forest, SVM, Logistic Regression) on the selected biomarker panel. Use a strict hold-out test set or repeated k-fold cross-validation to evaluate performance metrics such as accuracy, AUC-ROC, sensitivity, and specificity [2] [4]. The results should be compared against baseline models using traditional clinical variables alone to demonstrate added value [3].
Phase 3: Experimental Validation
- Independent Technical Validation: Validate the expression patterns of the top-ranked computationally identified biomarkers using an independent technological platform. Droplet Digital PCR (ddPCR) is highly recommended for its absolute quantification and high sensitivity. Design specific primers/probes for the candidate mRNA biomarkers and run samples (cases and controls) in technical replicates. Consistency between the NGS expression patterns and ddPCR results confirms technical robustness [4].
- Functional Validation (Context-Dependent): To establish biological relevance, employ advanced models that better mimic human biology.
- Organoids: Utilize patient-derived organoids to recapitulate the complex architecture and functions of human tissues. These can be used for functional biomarker screening, target validation, and exploration of resistance mechanisms [1].
- Spatial Biology Techniques: Apply multiplex immunohistochemistry (IHC) or spatial transcriptomics to validated samples to confirm the protein expression and spatial localization of biomarkers within the tumor microenvironment (TME), which can be critical for their utility [1].
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Key Research Reagent Solutions for Biomarker Discovery
| Item / Reagent | Function / Application | Specific Example / Note |
|---|---|---|
| RNA Purification Kit | Isolation of high-quality total RNA from biospecimens for downstream sequencing or validation. | GeneJET RNA Purification Kit [4]. |
| RNA-Seq Library Prep Kit | Preparation of sequencing-ready libraries from purified RNA for transcriptomic profiling. | Kits from Illumina, Thermo Fisher Scientific. |
| ddPCR Supermix & Assays | Absolute quantification and validation of specific mRNA biomarker candidates with high sensitivity. | Bio-Rad's ddPCR EvaGreen Supermix or TaqMan-based assays [4]. |
| Cell Culture Media | Maintenance and expansion of cell lines, including patient-derived B-lymphocytes or organoids. | RPMI 1640 for B-cells [4]; specialized media for organoid cultures. |
| Epstein-Barr Virus (EBV) | Immortalization of primary B-lymphocytes to create stable cell lines for renewable material. | B95-8 strain for transforming patient lymphocytes [4]. |
| Multiplex IHC/IF Antibody Panels | Simultaneous detection of multiple protein biomarkers in situ to study spatial relationships in the TME. | Validated antibody panels for immune cell markers and cancer markers. |
| Feature Selection Software | Computational tools for implementing filter, wrapper, and embedded feature selection methods. | Scikit-learn in Python (e.g., SelectKBest, RFE, LassoCV). |
| Machine Learning Frameworks | Platforms for building, training, and evaluating conventional and deep learning models. | Python with Scikit-learn, TensorFlow, PyTorch; R with caret and mlr [2]. |
The structured application of bioinformatics and data mining is paramount for navigating the complexities of modern biomarker discovery. By leveraging multi-omics data integration, robust computational methodologies, and rigorous validation protocols, researchers can significantly enhance the discovery and translation of biomarkers for cancer detection. The integration of AI and spatial biology technologies promises to further deepen our understanding of cancer biology, moving the field toward more personalized and effective cancer diagnostics and therapies. The workflow and protocols detailed herein provide a actionable roadmap for researchers engaged in this critical endeavor.
Within cancer detection research, feature extraction techniques are pivotal for identifying discriminative patterns from complex biological data. The integration of genomic features—such as gene expression, somatic mutations, and copy number variations (CNV)—into predictive models relies on robust and reproducible analysis pipelines [5]. This protocol details the use of two public resources, The Cancer Genome Atlas (TCGA) and the UCSC Xena platform, to acquire and analyze these genomic features, providing a foundational methodology for research framed within the broader context of feature-based cancer detection [6] [7].
Key Databases and Tools for Genomic Analysis
The following table summarizes the core public resources utilized in this protocol.
Table 1: Key Databases and Platforms for Cancer Genomics
| Resource Name | Type | Primary Function | Key Features | URL |
|---|---|---|---|---|
| The Cancer Genome Atlas (TCGA) [6] | Data Repository | Stores multi-omics data from large-scale cancer studies. | Provides genomic, epigenomic, transcriptomic, and proteomic data for over 20,000 primary cancer samples across 33 cancer types. | https://www.cancer.gov/ccg/research/genome-sequencing/tcga |
| UCSC Xena [8] [7] | Analysis & Visualization Platform | Enables integrated exploration and visualization of multi-omics data. | Allows users to view their own data alongside public datasets (e.g., TCGA). Features a "Visual Spreadsheet" to compare different data types. | http://xena.ucsc.edu/ |
| cBioPortal [9] | Analysis & Visualization Platform | Provides intuitive visualization and analysis for complex cancer genomics data. | Offers tools for multidimensional analysis of cancer genomics datasets, including mutation, CNA, and expression data. | http://www.cbioportal.org |
| Chinese Glioma Genome Atlas (CGGA) [9] | Data Repository | A complementary repository focusing on glioma. | Includes mRNA sequencing, DNA copy-number arrays, and clinical data for hundreds of glioma patients. | http://www.cgga.org.cn/ |
The following table lists essential materials and digital tools required for executing the analyses described in this protocol.
Table 2: Essential Research Reagents and Computational Tools
| Item Name | Category | Function/Application | Example/Note |
|---|---|---|---|
| TCGA Genomic Data | Data | The primary source of raw genomic and clinical data used for analysis. | Includes RNA-seq, DNA copy-number arrays, SNP arrays, and clinical metadata [9] [6]. |
| X-tile Software | Computational Tool | Determines optimal cut-off values for converting continuous data into categorical groups (e.g., high vs. low expression) for survival analysis [9]. | Available from: http://medicine.yale.edu/lab/rimm/research/software.aspx |
| Statistical Analysis Environment | Computational Tool | Used for performing survival analysis and other statistical tests. | R or Python with appropriate libraries (e.g., survival in R). |
| Kaplan-Meier Estimator | Statistical Method | Used to visualize and estimate survival probability over time. | The log-rank test is used to compare survival curves between groups [9]. |
Experimental Protocol: EGFR Analysis in Lung Adenocarcinoma
This section provides a detailed, step-by-step protocol for analyzing EGFR aberrations in lung adenocarcinoma (LUAD) using TCGA data via the UCSC Xena platform, replicating a common analysis for correlating genomic alterations with gene expression [8].
Data Acquisition and Initial Visualization
- Launch UCSC Xena: Navigate to the UCSC Xena website at http://xena.ucsc.edu/ and click 'Launch Xena'. This will open the Visual Spreadsheet Wizard.
- Select Dataset: In the wizard, type 'GDC TCGA Lung Adenocarcinoma (LUAD)' and select this study from the dropdown menu. Click 'To first variable' to load the dataset.
- Choose Genomic Features: Type 'EGFR' in the search bar. Select the checkboxes for Gene Expression, Copy Number, and Somatic Mutation. Click 'To second variable' [8].
The platform will generate a Visual Spreadsheet with four columns:
- Column A (Sample ID): Identifies the patient samples.
- Column B (Gene Expression): Displays the expression level of EGFR, typically color-coded (e.g., red for high expression).
- Column C (Copy Number): Shows copy number variation data for the EGFR genomic locus (e.g., red for amplification).
- Column D (Somatic Mutation): Indicates the presence of somatic mutations in EGFR (e.g., blue tick marks) [8].
Biological Interpretation: An initial observation should reveal that samples with high expression of EGFR (red in Column B) often have concurrent amplifications (red in Column C) or mutations (blue ticks in Column D) in the EGFR gene, suggesting a potential mechanism for the elevated expression [8].
Data Manipulation and Exploration
- Move Columns: To change the sorting of samples, click on the header of Column C (Copy Number) and drag it to the left, placing it as the first column after the sample ID (Column B). The Visual Spreadsheet will re-sort the samples based on the copy number values.
- Resize Columns: To view data in more detail, click and drag the handle in the lower-right corner of Column D (Somatic Mutation) to widen it.
- Zoom In on a Column: Click and drag horizontally within a data column to zoom in on a specific value range. Click the 'Zoom out' text at the top of the column to reset the view.
- Zoom In on Samples: Click and drag vertically along the sample axis to focus on a specific subset of patients. Use 'Zoom out' or 'Clear zoom' at the top of the spreadsheet to reset the view [8].
Survival Analysis Methodology
To correlate genomic features with clinical outcomes, perform a survival analysis.
- Data Preparation: Download the relevant clinical data (including overall survival (OS) and progression-free survival (PFS) times and events) along with the genomic feature of interest (e.g., EGFR expression levels) from TCGA via Xena or the Genomic Data Commons.
- Dichotomization: Use X-tile software to determine the statistically optimal cut-off score to divide the patient cohort into "high" and "low" expression groups based on the continuous EGFR expression data [9].
- Generate Survival Curves: Using a statistical software environment (e.g., R), plot the OS and PFS using Kaplan-Meier survival curves for the two patient groups.
- Statistical Comparison: Compare the survival curves between the high and low expression groups using the log-rank test to determine if the observed difference in survival is statistically significant [9].
Workflow Diagram
The following diagram illustrates the complete integrated workflow for genomic feature extraction and analysis using TCGA and UCSC Xena, as described in this protocol.
This application note provides a structured protocol for leveraging TCGA and UCSC Xena to conduct mutation and expression analysis. The outlined workflow—from data access and visualization to survival analysis—enables researchers to efficiently extract and validate genomic features. Integrating these features with advanced classification models, such as the hybrid deep learning approaches noted in the broader thesis context, holds significant potential for improving the accuracy of cancer detection and prognostication.
Head and neck squamous cell carcinoma (HNSCC) represents a biologically diverse group of malignancies originating from the mucosal epithelium of the oral cavity, pharynx, larynx, and paranasal sinuses [10] [11]. As the seventh most common cancer worldwide, HNSCC accounts for approximately 660,000 new diagnoses annually, with a rising incidence particularly among younger populations [12] [11]. Despite advancements in multimodal treatment approaches encompassing surgery, radiotherapy, and systemic therapy, the five-year survival rate for advanced-stage disease remains approximately 60%, underscoring the critical need for improved early detection and personalized treatment strategies [10] [12].
The evolving paradigm of precision oncology has intensified research into molecular biomarkers that can enhance diagnostic accuracy, prognostic stratification, and treatment selection. HNSCC manifests through two primary etiological pathways: HPV-driven carcinogenesis, which conveys a more favorable prognosis, and traditional tobacco- and alcohol-associated carcinogenesis [12] [11]. This molecular heterogeneity necessitates biomarker development that captures the distinct biological behaviors of these HNSCC subtypes.
Within the broader context of feature extraction techniques for cancer detection research, biomarker discovery in HNSCC represents a compelling case study in translating multi-omics data into clinically actionable tools. This application note systematically outlines current and emerging diagnostic and prognostic biomarkers in HNSCC, provides detailed experimental protocols for their detection, and situates these methodologies within the computational framework of feature extraction and analysis.
Established and Emerging Biomarkers in HNSCC
Diagnostic Biomarkers
Diagnostic biomarkers facilitate the initial detection and confirmation of HNSCC, often through minimally invasive methods. While tissue biopsy remains the diagnostic gold standard, liquid biopsy approaches have emerged as promising alternatives for initial screening and disease monitoring [12].
Table 1: Established and Emerging Diagnostic Biomarkers in HNSCC
| Biomarker Category | Specific Biomarkers | Detection Method | Clinical Utility |
|---|---|---|---|
| Viral Markers | HPV DNA/RNA, p16INK4a | PCR, ISH, IHC | Diagnosis of HPV-driven OPSCC [12] [11] |
| Circulating Tumor Markers | ctHPV DNA (for HPV+ cases) | PCR-based liquid biopsy | Post-treatment surveillance, recurrence monitoring [11] |
| Methylation Markers | Promoter hypermethylation of multiple genes | Methylation-specific PCR | Early detection in salivary samples [10] |
| Protein Markers | Various proteins (e.g., immunoglobulins, cytokines) | Mass spectrometry, immunoassays | Distinguishing HNSCC from healthy controls [12] |
Prognostic and Predictive Biomarkers
Prognostic biomarkers provide information about disease outcomes irrespective of treatment, while predictive biomarkers forecast response to specific therapies. In HNSCC, these biomarkers guide therapeutic decisions and intensity modifications.
Table 2: Key Prognostic and Predictive Biomarkers in HNSCC
| Biomarker | Type | Detection Method | Prognostic/Predictive Value |
|---|---|---|---|
| HPV/p16 status | Prognostic/Predictive | IHC (p16), PCR/ISH (HPV) | Favorable prognosis in OPSCC; enhanced response to immunotherapy [12] [11] |
| PD-L1 CPS | Predictive | IHC | Predicts response to immune checkpoint inhibitors [13] |
| Tumor Mutational Burden (TMB) | Predictive | Next-generation sequencing | Predicts response to immunotherapy [13] |
| Chemokine Receptors (CXCR2, CXCR4, CCR7) | Prognostic | IHC, PCR | Association with lymph node metastasis and survival [10] |
| Microsatellite Instability (MSI) | Predictive | PCR, NGS | Predicts response to immunotherapy [10] [13] |
HPV status represents one of the most significant prognostic factors in HNSCC, particularly for oropharyngeal squamous cell carcinoma (OPSCC). HPV-positive OPSCC demonstrates distinctly superior treatment responses and survival outcomes compared to HPV-negative disease, leading to its recognition as a separate staging entity in the American Joint Committee on Cancer (AJCC) 8th edition guidelines [12]. The most accurate method for determining HPV status involves detection of E6/E7 mRNA transcripts, though combined p16 immunohistochemistry (as a surrogate marker) with HPV DNA PCR demonstrates similar sensitivity and specificity rates [12] [11].
Emerging liquid biopsy approaches, particularly circulating tumor HPV DNA (ctHPVDNA), show exceptional promise for post-treatment surveillance. Studies report positive and negative predictive values approaching 95-100% for detecting recurrence, potentially complementing or supplementing traditional imaging surveillance [11]. Beyond viral biomarkers, tumor-intrinsic factors including chemokine receptor expression (CXCR2, CXCR4, CCR7) correlate with metastatic potential and survival outcomes, positioning them as potential prognostic indicators [10].
Experimental Protocols for Biomarker Detection
HPV Status Determination via p16 Immunohistochemistry and HPV DNA PCR
Principle: This dual-method approach leverages the surrogate marker p16 (overexpressed in HPV-driven carcinogenesis due to E7 oncoprotein activity) with direct detection of HPV DNA for comprehensive assessment of HPV-related tumor status [12] [11].
Materials:
- Formalin-fixed, paraffin-embedded (FFPE) tumor tissue sections
- Primary anti-p16 antibody
- IHC detection system
- DNA extraction kit
- HPV PCR primers
- Thermal cycler
Procedure:
- p16 Immunohistochemistry:
- Cut 4-5μm sections from FFPE tissue blocks.
- Deparaffinize and rehydrate through xylene and graded alcohols.
- Perform antigen retrieval using appropriate buffer.
- Incubate with primary anti-p16 antibody.
- Detect using appropriate IHC detection system.
- Counterstain, dehydrate, and mount.
- Interpret staining as positive when showing ≥70% nuclear and cytoplasmic expression.
- HPV DNA PCR:
- Extract DNA from FFPE tissue sections.
- Quantify DNA concentration and quality.
- Amplify using consensus primers for HPV.
- Perform gel electrophoresis to detect amplification.
- Confirm HPV genotype with type-specific primers.
Interpretation: Cases are considered HPV-driven if both p16 IHC and HPV DNA PCR are positive. Discordant cases require additional validation via HPV E6/E7 mRNA in situ hybridization [11].
Circulating Tumor HPV DNA Detection
Principle: This liquid biopsy technique detects tumor-derived HPV DNA fragments in plasma, serving as a minimally invasive biomarker for disease monitoring [11].
Materials:
- Blood collection tubes
- Plasma separation equipment
- DNA extraction kit
- ddPCR or NGS platform
- HPV-specific primers/probes
Procedure:
- Collect blood in EDTA tubes.
- Separate plasma via centrifugation.
- Extract cell-free DNA.
- Detect HPV DNA using:
- Droplet Digital PCR: Partition sample into droplets, amplify with HPV-specific probes, and count positive droplets for absolute quantification.
- Next-Generation Sequencing: Prepare sequencing library, capture target regions, and sequence.
- Analyze data with appropriate bioinformatics pipelines.
Interpretation: Presence of ctHPVDNA indicates active disease, while clearance during treatment correlates with response. Reappearance or rising levels suggest recurrence [11].
Feature Extraction from HNSCC Genomic Data
Principle: Machine learning approaches enable identification of prognostic gene signatures from high-dimensional genomic data through sophisticated feature extraction and selection methodologies [14] [15].
Materials:
- HNSCC transcriptomic datasets
- Computational resources
- R or Python with appropriate libraries
Procedure:
- Data Acquisition: Obtain HNSCC gene expression data from public repositories.
- Preprocessing: Normalize data, handle missing values, and perform quality control.
- Feature Selection:
- Apply univariate Cox regression to identify genes associated with survival.
- Implement hybrid filter-wrapper feature selection:
- Greedy stepwise search to identify features correlated with outcome but not with each other.
- Best-first search with logistic regression for final feature subset selection.
- Model Building:
- Develop machine learning-derived prognostic model using algorithm combinations.
- Validate model performance through time-dependent ROC curves and Kaplan-Meier analysis.
Interpretation: The resulting risk score stratifies patients into prognostic subgroups and informs therapeutic selection [14].
Visualization of Biomarker Detection Workflows
Comprehensive HNSCC Biomarker Analysis Pathway
Liquid Biopsy Biomarker Detection Workflow
Table 3: Essential Research Reagents and Platforms for HNSCC Biomarker Studies
| Category | Specific Reagents/Platforms | Application | Key Features |
|---|---|---|---|
| Molecular Detection | Anti-p16 antibody, HPV DNA/RNA probes, PCR reagents | HPV status determination | High specificity for HPV-driven cancers [11] |
| Liquid Biopsy Platforms | ddPCR systems, NGS platforms, cfDNA extraction kits | Circulating biomarker analysis | Minimal invasiveness, dynamic monitoring [11] [13] |
| Immunohistochemistry | PD-L1 IHC assays, automated staining systems | Tumor microenvironment analysis | Predictive for immunotherapy response [13] |
| Computational Tools | R/Python with survival, glmnet, and caret packages | Feature extraction and model development | Identifies prognostic signatures from high-dimensional data [14] [15] |
| Cell Surface Marker Analysis | Antibodies against CXCR2, CXCR4, CCR7 | Metastasis potential assessment | Flow cytometry or IHC applications [10] |
Discussion and Future Perspectives
The integration of feature extraction methodologies with traditional biomarker discovery represents a paradigm shift in HNSCC research. Machine learning algorithms, particularly when applied to multi-omics data, have demonstrated remarkable capability in identifying complex biomarker signatures that outperform individual biomarkers [14]. The development of a machine learning-derived prognostic model (MLDPM) incorporating 81 algorithm combinations exemplifies this approach, effectively eliminating artificial bias and achieving high prognostic accuracy [14].
Future directions in HNSCC biomarker research will likely focus on several key areas. First, the validation of liquid biopsy biomarkers for early detection and minimal residual disease monitoring holds tremendous potential for improving patient outcomes through earlier intervention [11] [13]. Second, the integration of multidimensional biomarkers—incorporating genomic, transcriptomic, proteomic, and clinical features—will enable more precise patient stratification [14] [16]. Finally, the application of explainable artificial intelligence techniques will be crucial for clinical adoption, providing transparency in model decisions and enhancing clinician trust [15].
The evolving landscape of HNSCC biomarkers underscores the critical importance of feature extraction techniques in translating complex biological data into clinically actionable tools. As these methodologies continue to advance, they promise to unlock new dimensions of personalized medicine for HNSCC patients, ultimately improving survival and quality of life outcomes.
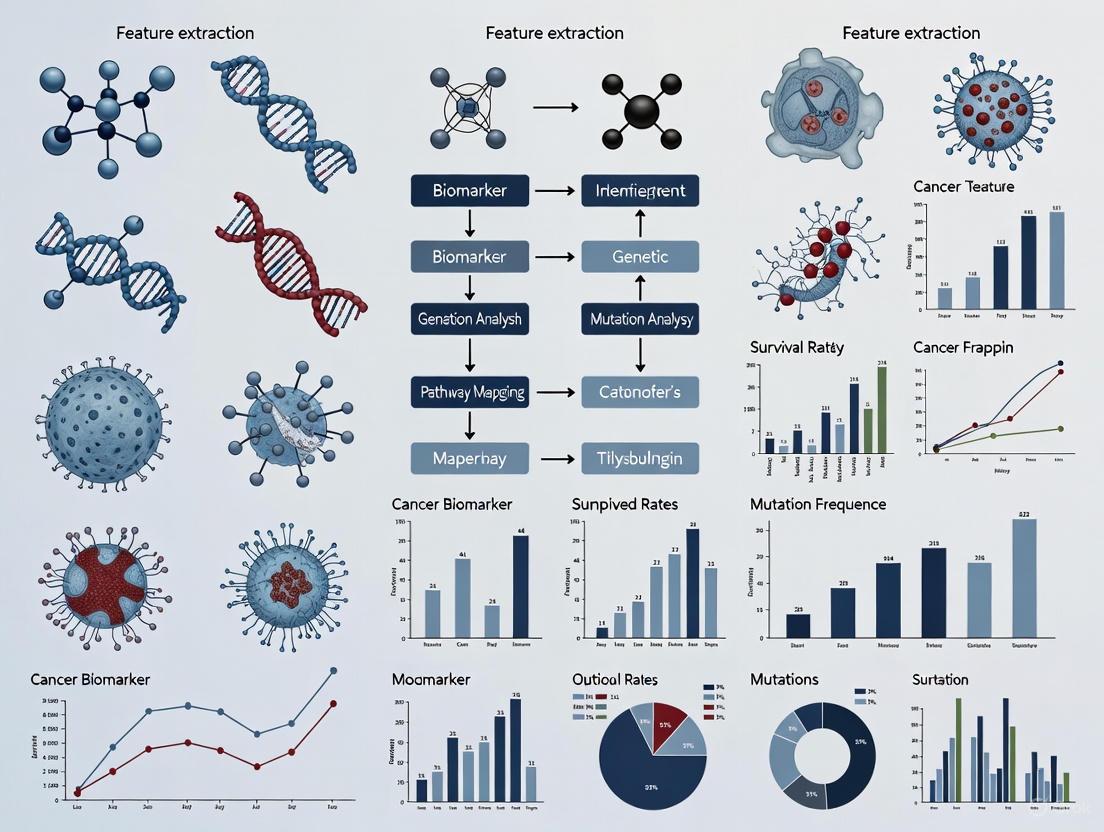
The Role of Feature Extraction in the Broader AI and Machine Learning Pipeline for Oncology
Feature extraction serves as a critical foundational step in the application of artificial intelligence (AI) to oncology, enabling the transformation of complex, high-dimensional medical data into actionable insights. This process involves identifying and isolating the most relevant patterns, textures, and statistical descriptors from raw data sources—including medical images, genomic sequences, and clinical text—to create optimized inputs for machine learning models [17] [18]. In cancer research and clinical practice, effective feature extraction bridges the gap between data acquisition and model development, allowing for more accurate detection, classification, and prognosis prediction across various cancer types [19] [20].
The growing importance of feature extraction is driven by the expanding volume and diversity of oncology data. As the field moves toward multimodal AI (MMAI) approaches that integrate histopathology, genomics, radiomics, and clinical records, the ability to extract and fuse meaningful features from these disparate sources has become increasingly vital for capturing the complex biological reality of cancer [21] [20]. This technical note examines current methodologies, applications, and experimental protocols that demonstrate how feature extraction advances oncology research and clinical care.
Current Methodologies and Applications
Hybrid Feature Extraction in Medical Imaging
Hybrid feature extraction techniques that combine handcrafted radiomic features with deep learning-based representations have demonstrated remarkable performance in cancer detection from medical images. In breast cancer research, one study implemented a comprehensive pipeline that integrated handcrafted features from multiple textual analysis methods with a deep learning classifier [17]. The methodology achieved 97.14% accuracy on the MIAS mammography dataset, outperforming benchmark models [17].
Table 1: Performance Metrics of Hybrid Feature Extraction for Breast Cancer Classification
| Metric | Result | Comparison to Benchmarks |
|---|---|---|
| Accuracy | 97.14% | Superior |
| Sensitivity | High (Precise value not reported) | Improved |
| Specificity | High (Precise value not reported) | Improved |
| Dataset | MIAS | Standard benchmark |
| Key Innovation | GLCM + GLRLM + 1st-order statistics + 2D BiLSTM-CNN | Outperformed single-modality approaches |
Similar approaches have been successfully applied across other cancer types. For cervical cancer detection, a framework integrating a Neural Feature Extractor based on VGG16 with an AutoInt model achieved 99.96% accuracy using a K-Nearest Neighbors classifier [22]. These results highlight how hybrid methods leverage both human expertise (through carefully designed feature extractors) and the pattern recognition capabilities of deep learning.
Multimodal Data Integration
Beyond single data modalities, feature extraction enables the fusion of heterogeneous data types to create more comprehensive disease representations. MMAI approaches integrate features derived from histopathology images, genomic profiles, clinical records, and medical imaging to capture complementary aspects of tumor biology [21]. For example, the Pathomic Fusion strategy combines histology and genomic features to improve risk stratification in glioma and clear-cell renal-cell carcinoma, outperforming the World Health Organization 2021 classification standards [21].
In translational applications, Flatiron Health research demonstrated that large language models (LLMs) could extract cancer progression events from unstructured electronic health records (EHRs) with F1 scores similar to expert human abstractors [23]. This approach enables scalable extraction of real-world progression events across multiple cancer types, producing nearly identical real-world progression-free survival estimates compared to manual abstraction [23].
Table 2: Applications of Feature Extraction Across Cancer Types
| Cancer Type | Feature Extraction Method | Application | Performance |
|---|---|---|---|
| Breast Cancer | GLCM, GLRLM, 1st-order statistics + 2D BiLSTM-CNN | Mammogram classification | 97.14% accuracy [17] |
| Cervical Cancer | Neural Feature Extractor (VGG16) + AutoInt | Image classification | 99.96% accuracy [22] |
| Multiple Cancers | LLM-based NLP | Progression event extraction from EHRs | F1 scores similar to human experts [23] |
| Bone Cancer | GLCM, LBP + CNN | Scan image classification | High accuracy (precise value not reported) [18] |
| Glioma & Renal Cell Carcinoma | Pathomic Fusion (histology + genomics) | Risk stratification | Outperformed WHO 2021 classification [21] |
Experimental Protocols
Protocol 1: Hybrid Feature Extraction from Mammograms for Breast Cancer Classification
This protocol outlines the methodology for implementing a hybrid feature extraction and classification system for mammogram analysis, based on published research achieving 97.14% accuracy [17].
Materials and Equipment
- Dataset: Mammogram images (e.g., MIAS database)
- Processing Tools: MATLAB or Python with OpenCV/library
- Feature Extraction: Shearlet Transform toolkit, GLCM and GLRLM algorithms
- Classification Framework: Deep learning platform (e.g., TensorFlow, PyTorch) with BiLSTM-CNN implementation
Procedure
Step 1: Image Preprocessing
- Apply Shearlet Transform for image enhancement and noise reduction
- Normalize image intensity values across the dataset
- Resize images to standardized dimensions for consistent processing
Step 2: Segmentation
- Implement Improved Otsu thresholding for initial region identification
- Apply Canny edge detection to refine lesion boundaries
- Validate segmentation quality against expert annotations
Step 3: Handcrafted Feature Extraction
- Compute Gray Level Co-occurrence Matrix (GLCM) features: contrast, correlation, energy, homogeneity
- Calculate Gray Level Run Length Matrix (GLRLM) features: short-run emphasis, long-run emphasis, gray-level non-uniformity
- Extract 1st-order statistical features: mean, median, standard deviation, kurtosis, skewness of pixel intensities
- Normalize all features to zero mean and unit variance
Step 4: Deep Learning Feature Extraction and Classification
- Implement 2D BiLSTM-CNN architecture:
- CNN component: 3 convolutional layers with ReLU activation, 2 pooling layers
- BiLSTM component: 2 bidirectional LSTM layers to capture sequential patterns
- Fully connected layer with softmax activation for classification
- Train model using extracted features and corresponding labels
- Validate model performance on held-out test set
Step 5: Performance Evaluation
- Calculate accuracy, sensitivity, specificity, and AUC-ROC
- Compare performance against benchmark models
- Perform statistical significance testing of improvements
Protocol 2: Multimodal Feature Integration for Cancer Subtype Classification
This protocol describes an AI architecture for cancer subtype classification from H&E-stained tissue images, based on the AEON and Paladin models that achieved 78% accuracy in subtype classification [24].
Materials and Equipment
- Dataset: Digitized H&E-stained whole slide images (WSIs)
- Annotation: OncoTree cancer classification system labels
- Computational Resources: High-performance computing cluster with GPU acceleration
- Software: Digital pathology image analysis platform (e.g., QuPath), deep learning frameworks
Procedure
Step 1: Data Preparation and Preprocessing
- Collect H&E images from approximately 80,000 tumor samples
- Apply quality control measures to exclude poor-quality images
- Perform tissue detection and segmentation to identify relevant regions
- Extract patches at multiple magnifications (e.g., 5X, 10X, 20X)
Step 2: Feature Extraction with AEON Model
- Implement AEON architecture for histologic pattern recognition
- Train model to classify cancer subtypes using OncoTree taxonomy
- Extract deep feature representations from intermediate network layers
- Generate granular subtype classifications beyond pathologist assignments
Step 3: Genomic Feature Inference with Paladin Model
- Integrate AEON-derived features with histologic images
- Train Paladin model to infer genomic variants from histologic patterns
- Identify subtype-specific genotype-phenotype relationships
- Validate inferences against molecular sequencing data
Step 4: Model Interpretation and Validation
- Apply visualization techniques to highlight histologic features driving classifications
- Compare model performance against pathologist diagnoses
- Assess clinical relevance through survival analysis of reclassified cases
- Perform external validation on independent datasets
Visualization of Methodologies
Hybrid Feature Extraction Workflow
Multimodal AI Pipeline in Oncology
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Research Reagents and Computational Tools for Oncology Feature Extraction
| Category | Specific Tools/Reagents | Function in Feature Extraction |
|---|---|---|
| Medical Imaging Datasets | MIAS (Mammography), LIDC-IDRI (Lung CT), TCIA (Multi-cancer) | Provide standardized, annotated image data for algorithm development and validation [17] [25] |
| Pathology Image Resources | The Cancer Genome Atlas (TCGA), Camelyon Dataset | Offer whole slide images with matched clinical and genomic data for histopathology feature learning [24] [20] |
| Feature Extraction Algorithms | GLCM, GLRLM, LBP, Shearlet Transform | Generate quantitative descriptors of texture, pattern, and statistical properties from medical images [17] [18] |
| Deep Learning Architectures | 2D BiLSTM-CNN, VGG16, ResNet, Custom Transformers | Automatically learn hierarchical feature representations from raw data [17] [22] |
| Multimodal Fusion Frameworks | Pathomic Fusion, TRIDENT, ABACO | Integrate features across imaging, genomics, and clinical data modalities [21] [20] |
| Validation Frameworks | VALID Framework, Synthetic Patient Generation | Assess feature quality, model performance, and potential biases [23] [24] |
Feature extraction represents a cornerstone of the AI and machine learning pipeline in oncology, enabling the transformation of complex biomedical data into clinically actionable insights. The methodologies and protocols outlined in this technical note demonstrate how hybrid approaches—combining handcrafted radiomic features with deep learning representations—can achieve superior performance in cancer detection and classification. Furthermore, the emergence of multimodal AI systems that integrate features across diverse data types heralds a new era in precision oncology, with the potential to uncover previously inaccessible relationships between tumor characteristics, treatment responses, and patient outcomes. As these technologies continue to evolve, standardized feature extraction methodologies will play an increasingly vital role in translating algorithmic advances into improved cancer care.
Methodologies in Action: Hybrid Feature Selection, Deep Learning, and Tissue-Specific Extraction
This application note details a protocol for implementing multistage hybrid feature selection, a methodology that synergistically combines filter, wrapper, and embedded techniques to identify the most discriminative features in high-dimensional biological data. Framed within cancer detection research, this approach addresses the critical challenge of dimensionality reduction while preserving or enhancing predictive model performance. We present a validated experimental workflow that reduced feature sets from 30 to 6 for breast cancer and 15 to 8 for lung cancer data, achieving 100% accuracy, sensitivity, and specificity when coupled with a stacked generalization classifier [15] [26]. The guidelines, reagents, and visualization tools provided herein are designed to empower researchers and drug development professionals in building robust, interpretable models for early cancer detection.
In oncology, high-throughput technologies generate vast amounts of molecular and clinical data, creating a pressing need for sophisticated feature selection methods to identify the most relevant biomarkers. Hybrid feature selection methods that integrate multiple selection paradigms have demonstrated superior performance compared to individual approaches used in isolation [15]. By combining the computational efficiency of filter methods, the model-specific performance optimization of wrapper methods, and the built-in selection capabilities of embedded methods, researchers can develop minimal biomarker panels that maintain high diagnostic accuracy. This is particularly crucial for early cancer detection, where high sensitivity is required to minimize missed diagnoses and high specificity is needed to avoid unnecessary procedures [27].
Theoretical Foundation of Feature Selection Methods
Method Categories and Characteristics
Feature selection methods are broadly categorized into three distinct classes, each with unique mechanisms, advantages, and limitations, as summarized in Table 1.
Table 1: Comparison of Feature Selection Method Categories
| Method Type | Mechanism of Action | Key Advantages | Common Techniques |
|---|---|---|---|
| Filter Methods | Selects features based on intrinsic data properties and univariate statistics [28]. |
|
|
| Wrapper Methods | Evaluates feature subsets based on classifier performance [28]. |
|
|
| Embedded Methods | Integrates feature selection directly into the model training process [28] [29]. |
|
|
The Hybrid Approach Rationale
Multistage hybrid feature selection leverages the complementary strengths of these methodologies. The typical workflow begins with filter methods for rapid, large-scale feature reduction, proceeds with wrapper methods for performance-oriented subset refinement, and concludes with embedded methods for final selection and model building. This sequential approach efficiently narrows the feature space while minimizing the risk of discarding potentially informative biomarkers [15].
Experimental Protocols
Multistage Hybrid Feature Selection Protocol for Cancer Detection
This protocol outlines the specific methodology used in a published study that achieved 100% classification performance on breast and lung cancer datasets [15] [26].
Phase 1: Initial Filter-Based Selection
Objective: Rapidly reduce feature space by identifying features highly correlated with the target class but not among themselves.
- Algorithm: Greedy stepwise search algorithm [15].
- Procedure:
- Calculate feature-class correlation for all features.
- Calculate inter-feature correlation matrix.
- Iteratively select features demonstrating:
- High correlation with the target class (e.g., cancer diagnosis)
- Low correlation with already-selected features
- Expected Outcome: Selection of 9 features from the original 30 in the Wisconsin Breast Cancer (WBC) dataset and 10 features from the Lung Cancer Prediction (LCP) dataset [15].
Phase 2: Wrapper-Based Refinement
Objective: Further refine the feature subset by optimizing for classifier performance.
- Algorithm: Best first search combined with logistic regression classifier [15].
- Procedure:
- Initialize with the feature subset from Phase 1.
- Evaluate classifier performance (e.g., accuracy, sensitivity) for all possible single-feature additions and removals.
- Greedily select the feature addition or removal that most improves performance.
- Continue until no further performance improvements are observed.
- Expected Outcome: Final selection of 6 optimal features for breast cancer detection and 8 for lung cancer detection [15].
Phase 3: Model Building with Embedded Selection
Objective: Construct a final predictive model with built-in feature selection.
- Algorithm: Stacked generalization with base classifiers (Logistic Regression, Naïve Bayes, Decision Tree) and Multilayer Perceptron (MLP) as meta-classifier [15].
- Procedure:
- Train multiple base classifiers on the refined feature subset from Phase 2.
- Use classifier predictions as input features for the meta-classifier (MLP).
- The MLP learns to optimally combine the base predictions.
- Performance Validation: Assess using data splitting (50-50, 66-34, 80-20) and 10-fold cross-validation [15].
SMAGS-LASSO Protocol for Sensitivity-Specificity Optimization
This protocol describes an embedded method designed specifically for clinical applications requiring high sensitivity at predefined specificity thresholds [27].
Objective Function and Optimization
Objective: Maximize sensitivity while maintaining a user-defined specificity threshold and performing feature selection.
- Algorithm: SMAGS-LASSO with custom loss function [27].
- Mathematical Formulation:
- Maximize: ( \sum{i=1}^{n} \hat{y}i \cdot yi / \sum{i=1}^{n} yi - \lambda \|\beta\|1 )
- Subject to: ( (1 - \mathbf{y})^T (1 - \hat{\mathbf{y}}) / (1 - \mathbf{y})^T (1 - \mathbf{y}) \geq SP )
- Where ( SP ) is the predefined specificity threshold, ( \lambda ) is the regularization parameter, and ( \|\beta\|_1 ) is the L1-norm of coefficients [27].
- Optimization Procedure:
- Initialize coefficients using standard logistic regression.
- Apply multiple optimization algorithms (Nelder-Mead, BFGS, CG, L-BFGS-B) in parallel.
- Select the model with the highest sensitivity among converged solutions [27].
Cross-Validation Framework
Objective: Select the optimal regularization parameter ( \lambda ).
- Procedure:
- Create k-fold partitions of the data (typically k=5).
- Evaluate a sequence of ( \lambda ) values on each fold.
- Measure performance using sensitivity mean squared error (MSE):
- ( MSE{sensitivity} = (1 - \sum{i=1}^{n} \hat{y}i \cdot yi / \sum{i=1}^{n} yi)^2 ) [27].
- Select the ( \lambda ) value that minimizes sensitivity MSE while maintaining the desired specificity.
Data Presentation and Performance Metrics
Quantitative Performance of Hybrid Feature Selection
Table 2: Performance Metrics of Multistage Hybrid Feature Selection on Cancer Datasets
| Dataset | Original Features | Selected Features | Accuracy | Sensitivity | Specificity | AUC | Classifier |
|---|---|---|---|---|---|---|---|
| WBC (Breast) | 30 | 6 | 100% | 100% | 100% | 100% | Stacked (LR+NB+DT/MLP) [15] |
| LCP (Lung) | 15 | 8 | 100% | 100% | 100% | 100% | Stacked (LR+NB+DT/MLP) [15] |
| Colorectal Cancer | 100+ | Not specified | 21.8% improvement over LASSO | 1.00 (at 99.9% specificity) | 99.9% | Significantly improved | SMAGS-LASSO [27] |
Comparative Performance Across Method Types
Table 3: Performance Comparison of Feature Selection Methods in Cancer Detection
| Method Category | Computational Cost | Model Specificity | Risk of Overfitting | Interpretability | Best Use Case |
|---|---|---|---|---|---|
| Filter Methods | Low | Model-agnostic | Low | High | Initial feature screening on large datasets [30] |
| Wrapper Methods | High | Model-specific | High | Medium | Final feature tuning on smaller datasets [30] |
| Embedded Methods | Medium | Model-specific | Medium | Medium | Integrated model building and selection [29] |
| Hybrid Methods | Varies by stage | Balanced approach | Low with proper validation | High with explainability tools | Critical applications like cancer detection [15] |
Visualization of Workflows
Multistage Hybrid Feature Selection Workflow
Stacked Generalization Classifier Architecture
The Scientist's Toolkit
Research Reagent Solutions for Implementation
Table 4: Essential Computational Tools and Datasets for Hybrid Feature Selection
| Resource Category | Specific Tool/Dataset | Function/Purpose | Implementation Example |
|---|---|---|---|
| Programming Environments | Python with scikit-learn | Primary implementation platform for feature selection algorithms and machine learning models [29]. | from sklearn.feature_selection import SelectFromModel |
| Feature Selection Algorithms | Greedy Stepwise Search (Filter) | Initial feature screening based on statistical properties [15]. | Custom implementation based on correlation thresholds |
| Best First Search (Wrapper) | Performance-based feature subset refinement [15]. | SequentialFeatureSelector from specialized libraries |
|
| LASSO Regularization (Embedded) | Integrated feature selection during linear model training [27] [29]. | LogisticRegression(penalty='l1', solver='liblinear') |
|
| Benchmark Datasets | Wisconsin Breast Cancer (WBC) | Publicly available benchmark for breast cancer classification [15]. | UCI Machine Learning Repository dataset |
| Lung Cancer Prediction (LCP) | Benchmark dataset for lung cancer detection studies [15]. | Kaggle Machine Learning repository dataset | |
| Model Interpretation Tools | SHAP (SHapley Additive exPlanations) | Explains model predictions by quantifying feature contributions [15]. | Python SHAP library for model explainability |
| LIME (Local Interpretable Model-agnostic Explanations) | Creates local explanations for individual predictions [15]. | Python LIME package for interpretability |
Multistage hybrid feature selection represents a powerful paradigm for biomarker discovery in cancer detection research. By systematically combining filter, wrapper, and embedded methods, researchers can navigate high-dimensional data spaces to identify minimal feature subsets that maximize diagnostic performance. The protocols and workflows presented herein have been empirically validated to achieve perfect classification metrics on benchmark cancer datasets, providing a robust methodology for researchers and drug development professionals. Future directions include adapting these approaches to multi-omics data integration and addressing emerging challenges in explainable AI for clinical adoption.
The integration of advanced deep learning architectures has significantly progressed automated feature extraction in medical image analysis, leading to enhanced capabilities in cancer detection and diagnosis. This document details the application notes and experimental protocols for utilizing Convolutional Neural Networks (CNNs), Vision Transformers (ViTs), and Bidirectional Long Short-Term Memory (BiLSTM) networks within oncology research. These architectures excel at extracting complementary features: CNNs capture localized spatial patterns, ViTs model long-range contextual dependencies, and BiLSTMs learn sequential relationships in feature maps. Their standalone and hybrid implementations have demonstrated state-of-the-art performance across various cancer types, including lung, colon, breast, and skin cancers, as summarized in the table below.
Table 1: Performance Summary of Deep Learning Architectures in Cancer Detection
| Cancer Type | Architecture | Dataset | Key Performance Metrics | Reference |
|---|---|---|---|---|
| Lung & Colon Cancer | ViT-DCNN (Hybrid) | Lung & Colon Cancer Histopathological | Accuracy: 94.24%, Precision: 94.37%, Recall: 94.24%, F1-Score: 94.23% | [31] |
| Breast Cancer | 2D BiLSTM-CNN (Hybrid) | MIAS | Accuracy: 97.14% | [17] |
| Breast Cancer | Hybrid ViT-CNN (Federated) | Multi-institutional Risk Factors | Accuracy: 98.65% (Binary), 97.30% (Multi-class) | [32] |
| Skin Lesion | CNN-BiLSTM with Attention | ISIC, HAM10000 | Accuracy: 92.73%, Precision: 92.84%, Recall: 92.73% | [33] |
| Skin Cancer | HQCNN-BiLSTM-MobileNetV2 | Clinical Skin Cancer | Test Accuracy: 89.3%, Recall: 94.33% (Malignant) | [34] |
| Cervical Cancer | VGG16 (CNN) + ML Classifiers | Cervical Cancer Image | Accuracy: 99.96% (KNN) | [22] |
| Chest X-ray (Pneumonia) | ResNet-50 (CNN) | Chest X-ray Pneumonia | Accuracy: 98.37% | [35] |
| Brain Tumor (MRI) | DeiT-Small (ViT) | Brain Tumor MRI | Accuracy: 92.16% | [35] |
Application Notes: Architectural Strengths and Cancer-Specific Implementations
Convolutional Neural Networks (CNNs)
CNNs remain a foundational tool for extracting hierarchical spatial features from medical images. Their inductive bias towards processing pixel locality makes them highly effective for identifying patterns like edges, textures, and morphological structures in tissue samples.
- Key Applications: CNNs are widely used for classification and segmentation tasks across various imaging modalities, including histopathology, mammography, and dermoscopy [36] [37]. For instance, pre-trained CNNs like VGG16 and ResNet-50 are frequently employed as powerful feature extractors, with the extracted features subsequently fed into classical machine learning classifiers for cervical cancer diagnosis, achieving near-perfect accuracy [22].
- Strengths: CNNs are highly efficient at learning localized, translation-invariant features and have a proven track record of high performance on a wide range of medical image classification tasks [35].
Vision Transformers (ViTs)
ViTs process images as sequences of patches, using a self-attention mechanism to weigh the importance of different patches relative to each other. This allows them to capture global contextual information across the entire image.
- Key Applications: ViTs have shown remarkable success in classifying breast cancer from mammograms and risk factor data, as well as in histopathological image analysis [36] [32]. Their ability to model long-range dependencies is particularly beneficial for understanding complex spatial relationships in heterogeneous tumor microenvironments.
- Strengths: The self-attention mechanism provides a global receptive field from the first layer, enabling the model to integrate information from disparate image regions simultaneously. This often leads to superior performance in tasks where global context is critical [31] [35].
Bidirectional Long Short-Term Memory (BiLSTM) Networks
BiLSTMs are a type of recurrent neural network designed to model sequential data by processing it in both forward and backward directions. This allows the network to capture temporal or spatial dependencies from both past and future contexts in a sequence.
- Key Applications: In cancer image analysis, BiLSTMs are not typically used on raw pixels but on sequences of extracted features. They are highly effective for modeling the spatial evolution of features across an image or for learning dependencies in feature vectors. They have been successfully integrated with CNNs for breast cancer detection from mammograms and skin lesion classification, where they help in capturing complex, distributed patterns [33] [17] [34].
- Strengths: BiLSTMs excel at learning long-range, bidirectional dependencies in sequential data, which, when applied to feature sequences, can improve the model's contextual understanding and classification accuracy [33].
Hybrid Architectures
Hybrid models combine the strengths of two or more architectures to overcome the limitations of individual components, often yielding state-of-the-art results.
- ViT-DCNN for Lung and Colon Cancer: This model integrates a Vision Transformer with a Deformable CNN. The ViT captures global contextual information through self-attention, while the Deformable CNN adapts its receptive field to capture fine-grained, localized spatial details in histopathological images. A Hierarchical Feature Fusion (HFF) module with a Squeeze-and-Excitation (SE) block is used to effectively combine these global and local features [31].
- CNN-BiLSTM for Skin and Breast Cancer: These hybrids use a CNN as a powerful feature extractor to generate a sequence of high-level spatial feature maps. A BiLSTM then processes this sequence to capture the contextual relationships between these features, improving the model's ability to classify complex lesions in skin and breast tissues [33] [17].
- ViT-CNN for Breast Cancer Prediction: This hybrid leverages both global features from a ViT and local features from a CNN, combining them to create a more robust representation for classification. This approach has been effectively deployed within a federated learning framework to enhance data privacy [32].
Table 2: The Scientist's Toolkit: Essential Research Reagents and Computational Resources
| Item Name | Function/Application | Specification Notes |
|---|---|---|
| Lung & Colon Cancer Histopathological Dataset | Model training & validation for lung/colon cancer detection | Comprises 5 classes: colon adenocarcinoma, colon normal, lung adenocarcinoma, lung normal, lung squamous cell carcinoma [31] |
| MIAS Dataset (Mammography) | Benchmark for breast cancer detection algorithm development | Contains cranio-caudal (CC) and mediolateral-oblique (MLO) view mammograms [17] |
| HAM10000 / ISIC Datasets | Training & testing for skin lesion analysis | Large collection of dermoscopic images; includes benign and malignant lesion types [33] [35] |
| Pre-trained Model Weights (e.g., ImageNet) | Transfer learning initialization | Speeds up convergence and improves performance, especially with limited data [35] |
| Shearlet Transform | Image preprocessing for enhancement | Superior to wavelets for representing edges and other singularities in mammograms [17] |
| Gray Level Co-occurrence Matrix (GLCM) | Handcrafted texture feature extraction | Captures second-order statistical texture information [17] |
| AdamW Optimizer | Model parameter optimization | Modifies weight decay for more effective training regularization [31] |
| Explainable AI (XAI) Tools (LIME, SHAP) | Model interpretability and validation | Provides post-hoc explanations for model predictions, crucial for clinical trust [38] [32] |
Experimental Protocols
Protocol: Implementing a ViT-DCNN Hybrid for Histopathological Cancer Detection
This protocol outlines the methodology for reproducing the ViT-DCNN model for lung and colon cancer classification from histopathological images [31].
2.1.1 Workflow Overview
The diagram below illustrates the integrated experimental workflow for hybrid model development.
2.1.2 Materials and Data Preparation
- Dataset: Obtain the Lung and Colon Cancer Histopathological Images dataset, which includes five classes (e.g., colon adenocarcinoma, colon normal, lung adenocarcinoma) [31].
- Data Splitting: Partition the dataset into training (80%), validation (10%), and testing (10%) subsets using stratified sampling to maintain class distribution.
- Image Preprocessing:
- Resizing: Resize all images to 224x224 pixels using a library such as OpenCV.
- Normalization: Apply min-max normalization to scale pixel values to a range of [0, 1].
- Data Augmentation: On the training set, apply random rotations, zooming, and horizontal/vertical flipping to increase data diversity and reduce overfitting.
2.1.3 Model Architecture and Training
- ViT Path: Implement a standard Vision Transformer. Split the preprocessed image into fixed-size patches (e.g., 16x16), linearly embed them, add positional embeddings, and process them through a series of transformer encoder blocks with multi-head self-attention to extract global features [31].
- DCNN Path: Implement a Convolutional Neural Network with deformable convolutions. These convolutions learn adaptive receptive fields by adding 2D offsets to the regular grid sampling locations, allowing the model to focus on more informative and irregularly shaped regions for fine-grained feature extraction [31].
- Feature Fusion: Design a Hierarchical Feature Fusion (HFF) module to combine the global feature maps from the ViT and the local feature maps from the DCNN. Incorporate a Squeeze-and-Excitation (SE) block within this module to explicitly model channel-wise dependencies and recalibrate feature responses adaptively.
- Classifier Head: Pass the fused feature vector through one or more fully connected layers with a softmax activation function to generate the final class probabilities.
- Training Configuration:
- Optimizer: Use the AdamW optimizer with a learning rate of 1e-5.
- Loss Function: Use Categorical Cross-Entropy loss.
- Regularization: Implement early stopping by monitoring the validation accuracy with a patience of 5 epochs. Train for a maximum of 50 epochs.
2.1.4 Evaluation and Analysis
- Performance Metrics: Calculate accuracy, precision, recall, and F1-score on the held-out test set.
- Model Interpretation: Utilize Explainable AI (XAI) techniques such as Grad-CAM or attention visualization to highlight the image regions most influential in the model's decision-making process, thereby enhancing clinical interpretability [38].
Protocol: Implementing a CNN-BiLSTM Model with Attention for Skin Lesion Classification
This protocol details the steps for building a hybrid CNN-BiLSTM model augmented with attention mechanisms for skin lesion classification, as demonstrated in [33].
2.2.1 Workflow Overview
The following diagram outlines the sequential flow of data through the CNN-BiLSTM-Attention architecture.
2.2.2 Materials and Data Preparation
- Dataset: Utilize a publicly available skin lesion dataset such as ISIC or HAM10000.
- Data Preprocessing: Follow a similar resizing and normalization procedure as in Protocol 2.1.2, ensuring consistency with the input size expected by the chosen CNN backbone.
2.2.3 Model Architecture and Training
- CNN Feature Extraction: Use a pre-trained CNN (e.g., VGG16, InceptionResNetV2) with its classification head removed as a feature extractor. This backbone processes the input image and outputs a 3D feature map (height, width, channels).
- Sequence Formation: Flatten the spatial dimensions (height, width) of the feature map to convert it into a sequence of feature vectors. Each vector in the sequence corresponds to a specific spatial region in the original feature map.
- BiLSTM Processing: Feed this sequence of feature vectors into a BiLSTM layer. The BiLSTM processes the sequence in both forward and backward directions, capturing rich contextual relationships between different spatial regions of the feature map.
- Attention Mechanism: Implement an attention layer (spatial, channel, and/or temporal) on top of the BiLSTM's output sequence. This layer learns to assign different weights to each time step (spatial region) in the sequence, allowing the model to focus on the most discriminative parts of the feature map when making a classification decision. The output is a weighted sum of the BiLSTM hidden states, known as a context vector.
- Classification: Pass the final context vector through a fully connected layer with softmax activation to produce classification probabilities.
- Training Configuration:
- Use the Adam optimizer with a learning rate scheduler (e.g., ReduceLROnPlateau).
- Use Categorical Cross-Entropy loss.
- Employ data augmentation and dropout for regularization.
2.2.4 Evaluation
- Evaluate the model on a standard test set, reporting accuracy, precision, recall, F1-score, and more specialized metrics like Jaccard Index (JAC) and Matthews Correlation Coefficient (MCC) [33].
- Visualize the attention weights to understand which regions of the lesion the model deems most important, providing valuable insights for clinicians.
Within the broader thesis on feature extraction techniques for cancer detection, this document details the application and protocols for extracting Tissue-Energy Specific Characteristic Features (TFs) from computed tomography (CT) scans. Traditional feature extraction methods in medical imaging, such as handcrafted texture features (HFs) and deep learning-based abstract features (DFs), often rely on image patterns alone [39]. In contrast, the TF extraction method is grounded in the fundamental physics of CT imaging, specifically the interactions between lesion tissues and the polyenergetic X-ray spectrum [39]. This approach aims to derive features that are directly related to the underlying tissue biology by leveraging energy-resolved CT data, thereby providing a more robust and physiologically relevant set of features for cancer detection and characterization.
Comparative Performance of Feature Extraction Techniques
Experimental evidence underscores the superior diagnostic performance of TFs compared to other feature classes. The following table summarizes the performance, as measured by the Area Under the Receiver Operating Characteristic Curve (AUC), of four different methodologies across three distinct lesion datasets [39].
Table 1: Comparative performance of feature extraction and classification methods for lesion diagnosis.
| Methodology | Dataset 1 AUC | Dataset 2 AUC | Dataset 3 AUC |
|---|---|---|---|
| Haralick Texture Features (HFs) + RF | 0.724 | 0.806 | 0.878 |
| Deep Learning Features (DFs) + RF | 0.652 | 0.863 | 0.965 |
| Deep Learning CNN (End-to-End) | 0.694 | 0.895 | 0.964 |
| Tissue-Energy Features (TFs) + RF | 0.985 | 0.993 | 0.996 |
The results consistently demonstrate that the extraction of tissue-energy specific characteristic features dramatically improved the AUC value, significantly outperforming both image-texture and deep-learning-based abstract features [39]. This leads to the conclusion that the feature extraction module is more critical than the classification module in a machine learning pipeline, and that extracting biologically relevant features like TFs is more important than extracting image-abstractive features [39].
Protocols for Tissue-Energy Specific Characteristic Feature (TF) Extraction
The extraction of TFs is a multi-stage process that transforms conventional CT images into virtual monoenergetic images (VMIs) and subsequently extracts tissue-specific characteristics using a biological model. The overall workflow is illustrated below.
Protocol 1: Generation of Virtual Monoenergetic Images (VMIs)
Objective: To generate a set of VMIs from a conventional CT scan at multiple discrete energy levels.
Background: Conventional CT images are reconstructed from raw data acquired from an X-ray tube emitting a wide spectrum of energies, resulting in an image that is an average across this spectrum [39]. Since tissue contrast varies with X-ray energy, VMIs are computed to simulate what the CT image would look like if the scan were performed at a single, specific X-ray energy [39]. This improves tissue characterization by providing energy-resolved data.
Materials and Reagents:
- Input Data: A non-contrast or contrast-enhanced CT scan in DICOM format.
- Software: A software platform capable of generating VMIs, often available through advanced scanner software or third-party research toolkits.
Methodology:
- Data Input: Load the raw projection data or the reconstructed CT image series with its associated sinogram data into the VMI generation software.
- Spectral Modeling: Use the known spectral profile of the CT scanner's X-ray tube and the tissue attenuation properties to create a model that decomposes the polyenergetic signal.
- Energy Level Selection: Define a range of virtual energy levels for VMI reconstruction. A typical range might be from 40 keV to 140 keV in 5-10 keV increments. Lower energies (e.g., 40-70 keV) generally provide higher soft-tissue contrast, while higher energies (e.g., 100-140 keV) reduce beam-hardening artifacts.
- Image Reconstruction: Execute the algorithm to generate a series of VMI sets, each corresponding to one of the selected discrete energy levels.
Validation:
- Qualitatively assess VMIs by ensuring expected tissue contrast changes across energy levels (e.g., iodine contrast increases at lower keV).
- Quantitatively verify the mean and standard deviation of Hounsfield Units (HU) in a region-of-interest (ROI) placed in a reference tissue (e.g., blood, water) across different VMIs.
Protocol 2: Extraction of Tissue-Energy Specific Characteristic Features
Objective: To compute quantitative TFs from the generated VMIs using a tissue biological model.
Background: This protocol uses a tissue elasticity model to compute characteristic features from each VMI [39]. The underlying principle is that the energy-dependent attenuation properties of tissues are influenced by their fundamental biological composition, which can be parameterized.
Materials and Reagents:
- Input Data: The set of VMIs generated in Protocol 1.
- Segmentation Mask: A binary mask defining the volumetric region of interest (ROI), such as a pulmonary nodule or colorectal polyp, typically derived from manual or semi-automated segmentation.
- Software: A computational environment (e.g., Python with NumPy/SciPy, MATLAB) for implementing the feature extraction algorithm.
Methodology:
- ROI Application: For each VMI, apply the segmentation mask to isolate the voxels within the lesion.
- Tissue Model Application: Apply the tissue elasticity model to the voxel values within the ROI for every VMI. The specific mathematical formulation of this model is a key differentiator of the TF approach.
- Feature Calculation: Compute the characteristic features from the model's output. This involves quantifying how the tissue's modeled properties change as a function of the virtual X-ray energy.
- Feature Aggregation: Aggregate the calculated values across the ROI and across all VMIs to form the final set of TFs for the lesion. This may result in features that represent the slope, curvature, or other parametric descriptions of the tissue's energy-response curve.
Validation:
- Correlate extracted TFs with known pathological outcomes (e.g., malignant vs. benign from biopsy) to ensure discriminative power.
- Assess the test-retest stability of features using a cohort with repeated CT scans.
The Scientist's Toolkit: Essential Research Reagents & Materials
The following table lists key components required for implementing the TF extraction workflow.
Table 2: Key research reagents and computational tools for TF extraction.
| Item Name | Function / Description | Critical Specifications |
|---|---|---|
| Clinical CT Datasets | Retrospective or prospective image sets with pathologically confirmed lesions for model training and validation. | Must include raw projection data or DICOM images with calibration data; Pathological report (gold standard) is essential. |
| VMI Generation Software | Computes virtual monoenergetic images from conventional CT data. | Should support spectral modeling and user-defined keV levels; Compatibility with scanner vendor data format is crucial. |
| Segmentation Tool | For delineating volumetric Regions of Interest (ROIs) around target lesions. | Should allow for precise 3D manual or semi-automated segmentation; Output in standard mask format (e.g., NIfTI, DICOM-SEG). |
| Computational Framework | Environment for implementing the tissue elasticity model and feature calculation. | Python (with libraries like PyRadiomics, SciKit-Image) or MATLAB; Requires strong numerical computation capabilities. |
| Tissue Elasticity Model | The mathematical model that converts energy-dependent attenuation into biological characteristics. | Model parameters must be optimized and validated for the specific tissue type and CT scanner. |
Logical Pathway from TFs to Clinical Application
The integration of TFs into a cancer research workflow enables enhanced decision-making, as depicted in the following pathway.
The accurate and early detection of cancer is a paramount challenge in medical image analysis. While deep learning models, particularly Convolutional Neural Networks (CNNs), have demonstrated remarkable success by automatically learning hierarchical features from images, they often require large datasets and can overlook subtle, domain-specific textural patterns. Conversely, traditional handcrafted feature descriptors, such as the Gray-Level Co-occurrence Matrix (GLCM) and Gray-Level Run-Length Matrix (GLRLM), are grounded in radiological and histopathological knowledge and excel at quantifying these textural characteristics. Integrating these two paradigms creates a hybrid approach that leverages the strengths of both, yielding models with superior accuracy, robustness, and generalizability for cancer detection across various imaging modalities. This document details the application notes and experimental protocols for implementing these hybrid techniques, framed within a broader thesis on feature extraction for oncology research.
Conceptual Framework and Rationale
The core rationale behind hybrid feature fusion is the complementary nature of the features involved. Deep learning features extracted from CNNs or Transformers are highly effective at capturing complex, high-level spatial hierarchies and semantic patterns from image data. However, they can be susceptible to overfitting on small medical datasets and may underperform on textures that are highly specific to medical domains. Handcrafted features provide a robust, interpretable, and computationally efficient means to quantify fundamental tissue properties, including texture homogeneity, contrast, and structural patterns, which are crucial for identifying malignant tissues.
Handcrafted Feature Domains: The most relevant handcrafted features for cancer detection are texture-based.
- Gray-Level Co-occurrence Matrix (GLCM): Captures second-order statistical texture by measuring the spatial relationship of pixel intensities. Derived metrics (e.g., contrast, correlation, energy, homogeneity) are highly effective in characterizing tissue microstructure [17] [40].
- Gray-Level Run-Length Matrix (GLRLM): Quantifies coarse textures by analyzing runs of consecutive pixels with the same gray level, providing information on texture fineness and directionality [17].
- Local Binary Patterns (LBP): A computationally simple yet powerful descriptor for characterizing local texture patterns by thresholding the neighborhood of each pixel [41].
- First-Order Statistical Features: Describe the distribution of individual pixel intensities (e.g., mean, standard deviation, skewness) without considering spatial relationships [17].
Deep Learning Feature Domains:
- CNN-based Features: Extracted from pre-trained networks (e.g., ResNet-50, DenseNet, EfficientNet) which learn a rich hierarchy of features from edges and corners in early layers to complex object parts in deeper layers [42] [43].
- Transformer-based Features: Models like DINOv2 use self-attention mechanisms to capture global contextual information across the entire image, offering a feature set complementary to the locally-focused CNNs [43].
Fusing these diverse feature sets creates a more comprehensive and discriminative representation of the tissue, leading to improved classification performance as evidenced by recent studies achieving accuracies exceeding 97-99% across multiple cancer types [17] [41] [44].
Performance Evidence and Quantitative Analysis
Empirical studies across various cancer domains consistently demonstrate the performance gain offered by hybrid feature fusion. The table below summarizes key quantitative results from recent peer-reviewed literature.
Table 1: Performance of Hybrid Feature Fusion Models in Cancer Detection
| Cancer Type | Dataset(s) Used | Handcrafted Features | Deep Learning Model | Fusion & Classification Strategy | Key Performance Metrics | Citation |
|---|---|---|---|---|---|---|
| Breast Cancer | MIAS | GLCM, GLRLM, 1st-order statistics | 2D BiLSTM-CNN | Hybrid feature extraction and input to custom classifier | Accuracy: 97.14% [17] | |
| Lung & Colon Cancer | LC25000, NCT-CRC-HE-100K, HMU-GC-HE-30K | LBP, GLCM, Wavelet, Morphological | Extended EfficientNetB0 | Transformer-based attention fusion | Accuracies: 99.87%, 99.07%, 98.4% (on three test sets) [41] | |
| Skin Cancer | ISIC 2018, PH2 | GLCM, RDWT | DenseNet121 | Feature concatenation with XGBoost/Ensemble classifier | Accuracy: 93.46% (ISIC), 91.35% (PH2) [40] | |
| Colorectal Cancer | Not Specified | Color Texture Features | CNN-based Features | Ensemble of handcrafted and deep features | Accuracy: 99.20% [44] | |
| Breast Cancer | CBIS-DDSM | Edge detection (d1, d2), LBP | ResNet-50 + DINOv2 | Early and late fusion with modified classifier | AUC: 79.6%, F1-Score: 67.4% [43] |
Detailed Experimental Protocols
This section provides a step-by-step protocol for replicating a standard hybrid feature fusion pipeline, synthesizing methodologies from the cited studies.
Protocol 1: Standardized Hybrid Feature Fusion Pipeline
Objective: To classify medical images (e.g., mammograms, histopathology slides) into benign and malignant categories by fusing handcrafted texture features and deep learning features.
Workflow Overview: The following diagram illustrates the logical flow and data progression through the major stages of the standard hybrid feature fusion protocol.
Step 1: Image Preprocessing
- Data Sourcing: Obtain a curated medical image dataset (e.g., CBIS-DDSM for mammography [43], LC25000 for histopathology [41]). Ensure ethical compliance for data usage.
- Standardization: Resize all images to a uniform dimensions compatible with the chosen deep learning model (e.g., 512x512 pixels [43]).
- Region of Interest (ROI) Extraction: If applicable, use ground truth annotations to crop images to the ROI containing the lesion or tissue of interest [43].
- Enhancement (Optional): Apply image enhancement techniques to improve contrast or reduce noise. Studies have employed the Shearlet Transform for mammogram enhancement [17] or Gaussian filtering for noise reduction in dermoscopic images [40].
- Data Augmentation: To increase dataset size and prevent overfitting, apply random transformations (e.g., rotation, flipping, scaling) to the training images [41] [43].
- Train-Test Split: Divide the dataset into training, validation, and testing subsets (e.g., 80:10:10).
Step 2: Handcrafted Feature Extraction
- Convert to Grayscale: Transform the preprocessed ROI image to a single-channel grayscale image.
- Compute Feature Descriptors:
- GLCM: Calculate the GLCM for one or more distances (e.g., d=1) and angles (e.g., 0°, 45°, 90°, 135°). From each GLCM, derive statistical measures such as Contrast, Correlation, Energy, and Homogeneity [17] [40].
- GLRLM: Calculate the GLRLM for different directions. Extract features such as Short Run Emphasis, Long Run Emphasis, and Run Percentage [17].
- LBP: Compute a rotation-invariant uniform LBP map from the grayscale image [41].
- Feature Vector Formation: Concatenate all extracted handcrafted features into a single 1D feature vector. Normalize this vector (e.g., using Z-score normalization) to ensure all features are on a comparable scale.
Step 3: Deep Learning Feature Extraction
- Model Selection: Choose a pre-trained deep learning model. ResNet-50 [43], DenseNet121 [40], and EfficientNetB0 [41] are commonly used and effective backbones.
- Feature Extraction:
- CNN Features: Pass the preprocessed image through the pre-trained CNN. Extract the feature vector from the layer immediately before the final classification layer (the global average pooling layer). This yields a high-dimensional feature vector representing deep, semantic information [43].
- Transformer Features (Optional): For an additional feature stream, pass the image through a vision transformer model like DINOv2. Extract the [CLS] token embedding or average the patch embeddings to form a global image representation [43].
- Vector Normalization: Normalize the extracted deep learning feature vectors.
Step 4: Feature Fusion and Classification
- Fusion: Concatenate the normalized handcrafted feature vector and the deep learning feature vector(s) into a single, comprehensive hybrid feature vector.
- Classifier Training: Use the fused feature vectors from the training set to train a classifier. High-performing options include:
- Model Evaluation: Evaluate the trained model on the held-out test set using standard metrics: Accuracy, Precision, Recall, F1-Score, and Area Under the ROC Curve (AUC).
Protocol 2: Early Fusion for Enhanced Feature Learning
Objective: To allow a deep learning model to directly process and learn from handcrafted features in an integrated manner, rather than treating them as separate input streams.
Workflow Overview: This protocol modifies the feature integration point, embedding handcrafted features directly into the input of a deep learning network.
Methodology:
- Follow Step 1 from Protocol 1 for preprocessing.
- Instead of computing statistical summaries, generate 2D feature maps from handcrafted techniques. For example:
- Compute the LBP map for the entire image.
- Compute edge detection maps (e.g., using Sobel filter) or second-derivative maps [43].
- Stack these 2D feature maps as additional channels to the original grayscale image. If the original is grayscale (1 channel) and you compute LBP and an edge map, the resulting input will have 3 channels.
- Use this multi-channel image as the input to a deep learning model (e.g., a CNN). The initial convolutional layers can now learn to combine information from the raw pixel data and the handcrafted feature maps simultaneously. This approach is particularly effective as it requires only minimal modification to standard deep learning pipelines [43].
The Scientist's Toolkit: Research Reagent Solutions
The following table catalogues essential computational "reagents" and their functions for implementing the described hybrid feature fusion techniques.
Table 2: Essential Research Reagents for Hybrid Feature Fusion Experiments
| Category | Reagent / Tool | Specifications / Typical Parameters | Primary Function in Protocol |
|---|---|---|---|
| Handcrafted Feature Algorithms | GLCM | Distances: [1], Angles: [0, 45, 90, 135], Features: Contrast, Correlation, Energy, Homogeneity | Quantifies second-order statistical texture patterns in tissue [17]. |
| GLRLM | Directions: [0°, 45°, 90°, 135°], Features: SRE, LRE, GLN, RP | Measures texture coarseness and run-length distributions [17]. | |
| LBP | Points: 8, Radius: 1, Method: 'uniform' | Encodes local texture patterns by comparing pixel intensities with neighbors [41]. | |
| Deep Learning Architectures | ResNet-50 / DenseNet-121 | Pre-trained on ImageNet, Feature vector from last layer before classifier | Extracts high-level, hierarchical spatial features from images [42] [43]. |
| DINOv2 (ViT-Small) | Pre-trained self-supervised vision transformer, Feature dim: 384 | Extracts global, contextual features using self-attention mechanisms [43]. | |
| Fusion & Classifiers | XGBoost | Max depth: 6, Learning rate: 0.1, N_estimators: 100 | High-performance classifier for fused feature vectors [40]. |
| SVM | Kernel: 'rbf', C: 1.0 | Effective classifier for normalized, high-dimensional feature sets [41]. | |
| Software & Libraries | Python | Versions 3.8+ | Core programming language. |
| Scikit-image / Sklearn | Library for extracting GLCM, GLRLM, LBP and for building SVM/XGB models. | ||
| PyTorch / TensorFlow | Deep learning frameworks for feature extraction and model training. |
Overcoming Obstacles: Tackling Data Limitations, Model Generalizability, and Clinical Workflow Integration
Addressing Data Scarcity and Class Imbalance with GAN-based Augmentation and Synthetic Data
In the pursuit of advanced feature extraction techniques for cancer detection, researchers consistently encounter two fundamental data-related challenges: data scarcity, often due to the difficulty of collecting large-scale, annotated medical images, and class imbalance, where the number of abnormal (e.g., cancerous) cases is vastly outnumbered by normal cases in a typical dataset [45] [46]. These issues can severely bias machine learning models, causing them to overlook critical minority class features and ultimately reducing their diagnostic reliability and generalizability.
Generative Adversarial Networks (GANs) have emerged as a powerful computational tool to address these bottlenecks. A GAN framework consists of two competing neural networks: a generator that creates synthetic data from random noise, and a discriminator that distinguishes between real and generated samples [47]. Through this adversarial training process, GANs learn to produce highly realistic synthetic data that mirrors the complex feature distribution of the original dataset. By strategically generating synthetic samples of the underrepresented class, GANs effectively balance the dataset and augment the training pool, enabling the development of more robust and accurate feature extraction and classification models for cancer detection [47] [48].
Current State of GAN-based Augmentation in Cancer Research
The application of GANs in oncology is demonstrating significant potential across multiple imaging modalities. Recent studies have validated this approach, quantifying its impact on classification performance.
Table 1: Performance of GAN-Augmented Models in Recent Cancer Detection Studies
| Cancer Type | Imaging Modality | GAN Model Used | Key Feature Extraction | Reported Performance | Citation |
|---|---|---|---|---|---|
| Breast Cancer | Thermogram | GAN-HDL-BCD | Hybrid Deep Learning (InceptionResNetV2, VGG16) | 98.56% Accuracy on DMR-IR | [47] |
| Breast Cancer | Mammography & Ultrasound | SNGAN (Mammo), CGAN (US) | ResNet-18 | Mammo: 80.9%B/76.9%M; US: 93.1%B/94.9%M | [48] |
| Breast Cancer | Mammogram | 2D BiLSTM-CNN | GLCM, GLRLM, 1st-order stats | 97.14% Accuracy on MIAS | [17] |
| General Imbalanced Data | Medical Datasets | RE-SMOTEBoost | Entropy-based feature selection | 3.22% Accuracy improvement, 88.8% variance reduction | [46] |
The selection of an appropriate GAN architecture is critical and depends on the specific data modality and task. Studies have evaluated various GAN models using quantitative metrics such as the Fréchet Inception Distance (FID) and Kernel Inception Distance (KID), where a lower score indicates that the synthetic data distribution is closer to the real data distribution [48]. For instance, in mammography, the Spectral Normalization GAN (SNGAN) achieved an FID of 52.89, proving most effective, while for ultrasound, the Conditional GAN (CGAN), with an FID of 116.03, was superior [48]. These findings underscore that there is no one-size-fits-all GAN solution.
Application Notes & Protocols
The following section provides a detailed, actionable protocol for integrating GAN-based data augmentation into a cancer detection research workflow, with a specific focus on feature extraction.
Protocol 1: GAN-Augmented Feature Extraction and Classification for Breast Thermograms
This protocol is adapted from the BCDGAN framework, which achieved state-of-the-art results by combining a GAN with a hybrid deep learning model for feature extraction [47].
Workflow Overview: The process begins with inputting raw thermogram images. These are first passed to a Hybrid Deep Learning (HDL) model for initial feature extraction. These extracted features are then used by a Generative Adversarial Network (GAN) to generate synthetic Regions of Interest (ROIs). The original and synthetic ROIs are combined to create an augmented dataset. This augmented dataset is used to re-train the HDL model, culminating in a final classification output of Benign, Malignant, or Normal.
Materials & Reagents:
- Dataset: DMR-IR benchmark thermogram dataset.
- Computing Hardware: GPU cluster (e.g., NVIDIA V100 or equivalent) with ≥ 16GB VRAM.
- Software Framework: Python 3.8+, PyTorch 1.9+ or TensorFlow 2.6+.
- Key Libraries: NumPy, OpenCV, Scikit-learn, MONAI for medical image processing.
Step-by-Step Procedure:
- Data Preprocessing:
- Normalization: Scale all thermogram pixel intensities to a range of [0, 1].
- ROI Cropping: Manually or automatically crop regions of interest (ROIs) containing potential lesions.
- Resizing: Standardize all ROIs to a fixed size of 128x128 or 224x224 pixels to ensure compatibility with pre-trained CNN backbones.
Feature Extraction with Hybrid Deep Learning (HDL) Model:
- Utilize two pre-trained Convolutional Neural Networks (CNNs), such as InceptionResNetV2 and VGG16, as parallel feature extractors [47].
- Remove the final classification layer of each network.
- Forward-pass the preprocessed ROIs through both networks and extract the high-level feature maps from their penultimate layers.
- Concatenate these feature vectors to form a comprehensive, hybrid feature representation for each ROI.
GAN-based Synthetic Data Generation:
- Generator (G): Design a network that takes a random noise vector (z) and the extracted hybrid feature vector as input. It should upsample this input through transposed convolutional layers to generate a synthetic ROI image.
- Discriminator (D): Design a CNN-based network that takes both real ROIs (from the dataset) and synthetic ROIs (from G) and outputs a probability of the image being real.
- Adversarial Training: Train the GAN in a two-step iterative process.
- Step 1 - Train D: Freeze G. Train D on a batch of real images (label=1) and a batch of generated images from G (label=0) to improve its discrimination ability.
- Step 2 - Train G: Freeze D. Train G to fool D, typically by minimizing the log(1 - D(G(z))).
- Convergence: Training is complete when the discriminator's accuracy plateaus around 50%, indicating the generator is producing highly realistic data.
Dataset Augmentation & Model Re-training:
- Use the trained generator to produce a large number of synthetic ROIs, focusing on the minority (e.g., malignant) class to correct imbalance.
- Combine these high-quality synthetic ROIs with the original training dataset to form an augmented dataset.
- Use this balanced, augmented dataset to re-train the final HDL classifier for the task of benign/malignant/normal classification.
Protocol 2: Handling Severe Imbalance and Overlap with RE-SMOTEBoost
For non-image data or scenarios with extreme class imbalance and feature space overlap, an ensemble-based double pruning method like RE-SMOTEBoost can be more effective than standard GANs [46].
Workflow Overview: The process starts with an Imbalanced Feature Dataset. The first step is Double Pruning: the Majority Class is reduced using an Entropy Filter to remove low-information samples, while the Minority Class is augmented using Roulette Wheel Selection to choose high-information samples for SMOTE-based synthesis. The pruned and augmented data is then fed into a Boosting Classifier (e.g., AdaBoost) for final classification.
Materials & Reagents:
- Dataset: Tabular data of extracted features (e.g., GLCM, GLRLM, statistical features from images [17] [18]).
- Software: Python with Scikit-learn, imbalanced-learn library, and custom implementations for entropy calculation.
Step-by-Step Procedure:
- Feature Extraction from Medical Images:
- Extract handcrafted features from regions of interest. Common methods include:
- Gray-Level Co-occurrence Matrix (GLCM): For texture analysis.
- Gray-Level Run-Length Matrix (GLRLM): For quantifying coarse textures.
- First-Order Statistical Features: Such as mean, median, and standard deviation of pixel intensities [17].
- Extract handcrafted features from regions of interest. Common methods include:
Double Pruning with RE-SMOTEBoost:
- Majority Class Pruning: Calculate the information entropy for each sample in the majority class. Remove samples with entropy below a defined threshold, as they contribute little to defining the decision boundary.
- Minority Class Augmentation:
- Use a roulette wheel selection process, where the probability of selecting a minority sample is proportional to its information content (entropy).
- Apply the SMOTE (Synthetic Minority Over-sampling Technique) algorithm on these selected high-information samples to generate new synthetic data points.
- Implement a double regularization penalty during synthesis to ensure new data points are generated near other minority samples but away from majority samples, minimizing overlap.
Ensemble Classification:
- Feed the pruned and augmented feature dataset into a boosting algorithm like AdaBoost.
- The adaptive re-weighting in boosting further emphasizes hard-to-classify samples, working synergistically with the double-pruning process to create a robust classifier [46].
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Tools for GAN-based Augmentation in Cancer Research
| Item Name | Function/Application | Example/Note |
|---|---|---|
| Pre-trained CNN Models | Feature extraction from images; serves as a backbone for hybrid models and GAN discriminators. | VGG16, InceptionResNetV2, ResNet-18 [47] [48] |
| GAN Architectures | Generating synthetic medical images tailored to specific data types and imbalances. | SNGAN (Mammography), CGAN (Ultrasound), WGAN-GP (General purpose) [48] |
| Feature Extraction Libraries | Extracting handcrafted texture and statistical features from ROIs for traditional ML or fusion with DL. | Scikit-image (for GLCM, GLRLM), PyRadiomics (for radiomics features) [17] |
| Quality Assessment Metrics | Quantifying the fidelity and diversity of generated synthetic images. | Fréchet Inception Distance (FID), Kernel Inception Distance (KID) [48] |
| Data Augmentation Suites | Performing standard and advanced geometric/photometric transformations in tandem with GANs. | Torchvision Transforms, Albumentations, MONAI |
| Synthetic Data Validation Protocols | Ensuring synthetic data retains clinical relevance and biological plausibility for regulatory acceptance. | Assessment of feature distribution alignment, survival outcome agreement in synthetic cohorts [49] |
The integration of GAN-based augmentation and synthetic data generation represents a paradigm shift in addressing the critical challenges of data scarcity and class imbalance within cancer detection research. By providing a robust methodological framework for enriching and balancing datasets, these techniques directly enhance the performance and generalizability of subsequent feature extraction and classification models. The protocols outlined herein offer researchers practical pathways for implementation, from leveraging hybrid GAN-CNN architectures for image data to employing advanced double-pruning ensembles for tabular feature data. As the field progresses, the focus will increasingly shift towards standardizing the validation of synthetic data's clinical utility and integrating these methodologies into regulatory-grade toolkits for drug development and precision oncology.
Mitigating Domain Shift and Ensuring Robustness Across Diverse Populations and Imaging Protocols
The application of artificial intelligence (AI) in cancer detection represents a transformative advancement in computational pathology and radiology. However, a significant challenge hindering widespread clinical adoption is domain shift—the degradation of model performance when applied to data from new institutions, scanner types, or patient populations that differ from the training set [50] [51]. This phenomenon arises from variations in imaging equipment, acquisition protocols, staining procedures, and population demographics, which alter the statistical properties of the input data [51] [52]. In the context of feature extraction for cancer detection, domain shift can cause state-of-the-art models to fail unexpectedly, compromising diagnostic reliability and equitable healthcare access [52].
The MIDOG 2025 challenge, a multi-track benchmark for robust mitosis detection, highlights that performance drops on unseen domains remain a persistent issue, even for algorithms achieving F1 scores above 0.75 on their original datasets [53]. Similarly, in mammography classification, model performance often declines when applied to data from different domains due to variations in pixel intensity distributions and acquisition settings [51]. This application note addresses these challenges by presenting standardized protocols and methodologies designed to enhance feature extraction robustness, ensuring consistent performance across diverse clinical environments and demographic groups for reliable cancer detection.
Quantitative Benchmarks and Performance Metrics
Establishing robust benchmarks is crucial for evaluating feature extraction techniques against domain shift. The following tables summarize key performance metrics from recent studies and challenges, providing a baseline for comparing methodological improvements.
Table 1: Performance Benchmarks for Mitosis Detection and Classification (MIDOG 2025 Challenge) [53]
| Model / Approach | Metric | Value | Task Context |
|---|---|---|---|
| DetectorRS + Deep Ensemble | F1 Score | 0.7550 | Mitosis Localization |
| Efficient-UNet + EfficientNet-B7 | F1 Score | 0.7650 | Mitosis Localization |
| VM-UNet + Mamba + Stain Aug | F1 Score | 0.7540 | Mitosis Segmentation |
| DINOv3-H+ + LoRA | Balanced Accuracy | 0.8871 | Mitosis Subtyping |
| MixStyle + CBAM + Distillation | Balanced Accuracy | 0.8762 | Mitosis Subtyping |
| ConvNeXt V2 Ensemble | Balanced Accuracy | 0.8314 | Mitosis Subtyping (Cross-val) |
Table 2: Cross-Domain Mammography Classification Performance (DoSReMC Framework) [51]
| Training Scenario | Test Domain | Accuracy (%) | AUC (%) | Notes |
|---|---|---|---|---|
| Source Domain A | Source Domain A | 89.2 | 94.5 | In-domain baseline |
| Source Domain A | Target Domain B | 72.1 | 75.8 | No adaptation |
| BN/FC Layer Tuning | Target Domain B | 84.5 | 89.3 | Partial adaptation |
| Full Model Fine-tuning | Target Domain B | 85.1 | 90.0 | Full adaptation |
| DoSReMC (BN Adapt + DAT) | Target Domain B | 86.3 | 91.7 | Proposed method |
Table 3: Generalization Performance for Head & Neck Cancer Outcome Prediction [54]
| Method | Average Accuracy (%) | Average AUC (%) | Complexity (GFLOPs) |
|---|---|---|---|
| Empirical Risk Minimization (ERM) | 68.45 | 65.12 | 17.1 |
| MixUp | 70.11 | 66.89 | 17.1 |
| Domain Adversarial Neural Network (DANN) | 73.52 | 68.47 | 17.3 |
| Correlation Alignment (CORAL) | 74.80 | 70.25 | 17.1 |
| Language-Guided Multimodal DG (LGMDG) | 81.04 | 76.91 | 17.4 |
Experimental Protocols for Robust Feature Extraction
This section provides detailed, actionable protocols for implementing domain-shift-resistant feature extraction pipelines, as validated in recent literature.
Protocol: Batch Normalization Adaptation for Cross-Domain Mammography
This protocol, based on the DoSReMC framework, mitigates domain shift by targeting the recalibration of Batch Normalization (BN) layers, which are a primary source of domain dependence in convolutional neural networks (CNNs) [51].
Research Reagent Solutions:
- Pre-trained CNN Model: A model (e.g., ResNet-50, DenseNet) pre-trained on a large-scale source mammography dataset.
- Target Domain Data: Unlabeled or sparsely labeled data from the new clinical site(s).
- Computational Framework: PyTorch or TensorFlow with GPU acceleration.
- Evaluation Datasets: Public benchmarks (e.g., HCTP, VinDr-Mammo) or proprietary in-house datasets with pathologically confirmed findings.
Step-by-Step Procedure:
- Model Preparation: Load the model pre-trained on the source domain. Freeze all convolutional layers and feature extraction backbone parameters to preserve the learned general-purpose features.
- Parameter Identification: Identify all BN layers within the network architecture. Additionally, unfreeze the final fully connected (FC) classification layer.
- Target Domain Forward Pass: Perform a forward pass on a representative sample (e.g., 1,000-5,000 images) from the unlabeled target domain dataset. This allows the BN layers to compute updated running means and variances for the new data statistics.
- Optional Fine-Tuning: For enhanced performance, conduct a limited number of training epochs (e.g., 5-10) using a small learning rate (e.g., 1e-4) on the target domain data, updating only the parameters of the BN and FC layers.
- Adversarial Training Integration (Optional): To further improve robustness, integrate a Domain Adversarial Training (DAT) loss during the fine-tuning phase, encouraging the feature extractor to learn domain-invariant representations.
- Validation & Inference: Validate the adapted model on a held-out test set from the target domain. For inference, deploy the model with the adapted BN layers.
Diagram 1: BN Adaptation Workflow
Protocol: Stain-Normalized Ensemble for Histopathology
This protocol addresses domain shift in histopathological imagery, such as mitosis detection, caused by variations in staining protocols and scanners. It combines stain normalization with deep ensemble methods [53].
Research Reagent Solutions:
- Stain Normalization Algorithms: Macenko or Vahadane method implementations.
- Deep Learning Architectures: Pre-trained ConvNeXt V2, VM-UNet, or DINOv3 models.
- Ensemble Framework: A platform for managing multiple models and aggregating predictions (e.g., via majority voting or averaging).
- Loss Functions: Focal loss or cross-entropy with class weighting to handle imbalance.
Step-by-Step Procedure:
- Stain Normalization:
- Select a reference image from your dataset with optimal staining quality.
- Apply a stain normalization algorithm (e.g., Macenko) to all training and validation images, transforming them to match the stain appearance of the reference.
- Data Augmentation: Apply extensive spatial and color augmentations, including rotation, scaling, color jitter, and cutout. For additional robustness, incorporate stain-specific augmentations by perturbating the stain concentration matrix.
- Model Training (Per Ensemble Member):
- Train multiple diverse architectures (or the same architecture on different data splits) using the normalized and augmented data.
- Utilize a loss function suited for class imbalance, such as focal loss, especially for rare events like atypical mitoses.
- Apply MixStyle or Fourier-domain mixing during training to further encourage style invariance.
- Ensemble Prediction:
- For a given input image, first apply the same stain normalization used during training.
- Pass the normalized image through all models in the ensemble.
- Aggregate the predictions (e.g., segmentation masks, classification scores) by averaging probabilities or using majority voting.
- Rule-Based Refinement (Optional): Apply post-processing rules based on biological knowledge (e.g., size constraints for mitotic figures) to filter out false positives, though this should be validated to avoid reducing sensitivity.
Diagram 2: Stain-Normalized Ensemble
Protocol: Language-Guided Multimodal Domain Generalization
This protocol leverages structured clinical data to anchor and improve the generalization of imaging models across institutions, as demonstrated for head and neck cancer outcome prediction [54].
Research Reagent Solutions:
- Multimodal Dataset: Paired imaging (e.g., CT, MRI) and clinical data from multiple institutions.
- Vision-Language Model: A pre-trained CLIP model or similar for joint image-text embedding.
- Feature Fusion Module: A multimodal factorized bilinear pooling (MFB) layer.
- Adversarial Training Framework: A gradient reversal layer for domain adversarial training.
Step-by-Step Procedure:
- Clinical Prompt Engineering:
- Convert structured Electronic Health Record (EHR) data (e.g., age, tumor site, HPV status) into a continuous natural language prompt (e.g., "A [age]-year-old patient with a primary tumor in [site] and HPV [status]").
- Use the text encoder of a pre-trained CLIP model to generate a semantic embedding vector from this prompt.
- Image Feature Extraction:
- Process the input medical image (e.g., CT scan) through a CNN backbone (e.g., ResNet-50) to extract visual features.
- Multimodal Fusion:
- Fuse the clinical text embedding and the image features using an MFB classifier to generate the primary outcome prediction (e.g., cancer recurrence risk).
- Adversarial and Contrastive Supervision:
- Domain Discriminator: Implement a domain adversarial branch that takes the fused features and tries to predict the source institution. A gradient reversal layer encourages the feature extractor to learn domain-invariant representations.
- Contrastive Learner: Use a contrastive loss to maximize the similarity between image features and their corresponding clinical text embeddings while minimizing similarity with non-matching pairs.
- Joint Training: Train the entire network end-to-end, combining the classification loss, adversarial loss, and contrastive loss. During inference, only the MFB classifier branch is used.
Diagram 3: Multimodal Domain Generalization
The Scientist's Toolkit: Essential Research Reagents
Table 4: Key Research Reagents and Computational Tools
| Reagent / Tool | Function | Example Use Case |
|---|---|---|
| Pre-trained Foundation Models (DINOv3, CLIP) | Provides robust, general-purpose feature extractors that can be efficiently fine-tuned for specific tasks with less data. | Parameter-efficient fine-tuning with LoRA for mitosis subtyping [53]. |
| Stain Normalization (Macenko, Vahadane) | Standardizes color distribution in H&E images to mitigate variability from different staining protocols. | Pre-processing step for deep ensemble models in the MIDOG challenge [53]. |
| MixStyle / Fourier Domain Mixing | Augments training data by perturbing feature-level styles or swapping low-frequency image components to force style invariance. | Improving model generalization to unseen scanner domains in histopathology [53]. |
| Gradient Reversal Layer (GRL) | Enables domain-adversarial training by maximizing domain classification loss during backpropagation, promoting domain-invariant features. | Core component of DANN and multimodal DG frameworks for feature alignment [54]. |
| Batch Normalization Layers | Standardizes activations within a network; its parameters are highly domain-sensitive and are a primary target for adaptation. | Fine-tuning BN statistics on unlabeled target data for mammography classification [51]. |
| Multimodal Factorized Bilinear (MFB) Pooling | Efficiently fuses high-dimensional feature vectors from different modalities (e.g., image and clinical text). | Fusing CT image features and clinical prompt embeddings for outcome prediction [54]. |
Mitigating domain shift is not a single-solution problem but requires a systematic approach combining data-centric strategies, architectural adjustments, and novel training paradigms. The protocols outlined herein—BN adaptation for radiology, stain-normalized ensembles for pathology, and language-guided multimodal learning—provide a robust framework for developing feature extraction models that maintain diagnostic accuracy across diverse populations and imaging protocols. As the field progresses, the integration of these techniques into the model development lifecycle, coupled with rigorous priority-based robustness testing as advocated for biomedical foundation models, will be crucial for translating promising AI research into equitable and effective clinical tools [52]. Future work should focus on end-to-end joint training of detectors and classifiers, further leveraging large-scale foundation models and self-supervised learning to create systems that are inherently robust to the heterogeneity of the real world.
The integration of artificial intelligence (AI) into clinical decision support systems (CDSS) has significantly enhanced diagnostic precision, risk stratification, and treatment planning in oncology [55]. However, the "black-box" nature of complex machine learning and deep learning models remains a critical barrier to clinical adoption, particularly in high-stakes domains such as cancer detection where decisions directly impact patient outcomes [56] [57]. Explainable AI (XAI) addresses this challenge by creating models with behavior and predictions that are understandable and trustworthy to human users, thereby fostering the collaboration between clinicians and AI systems that is essential for modern evidence-based medicine [55].
The demand for XAI is not merely technical but also ethical and regulatory. Regulatory bodies including the U.S. Food and Drug Administration (FDA) emphasize transparency as essential for safe clinical deployment, and ethical principles of fairness, accountability, and transparency require that AI-supported decisions remain subject to human oversight [55] [57] [58]. This is especially crucial in cancer detection, where clinicians must justify clinical decisions and ensure patient safety. Without transparent reasoning, even highly accurate AI models may face resistance from medical professionals trained in evidence-based practice [56].
Feature extraction techniques for cancer detection research typically produce complex models that excel at identifying subtle patterns in imaging and genomic data but offer little intuitive insight into their decision-making processes [15] [19]. XAI methods, particularly SHAP (SHapley Additive exPlanations) and LIME (Local Interpretable Model-agnostic Explanations), bridge this critical gap by providing explanations for individual predictions, enabling researchers and clinicians to understand which features drive specific diagnostic or prognostic assessments [59] [60]. This transparency is fundamental for building the trust necessary for clinical adoption and for ensuring that AI systems augment rather than replace clinical judgment.
Comparative Analysis of SHAP and LIME
Technical Foundations and Mechanisms
SHAP and LIME represent two prominent approaches to XAI with distinct theoretical foundations and implementation methodologies. SHAP is grounded in cooperative game theory, specifically Shapley values, which allocate payouts to players based on their contribution to the total outcome [59] [60]. In the context of machine learning, SHAP calculates the marginal contribution of each feature to the model's prediction by evaluating all possible combinations of features, providing a unified measure of feature importance that satisfies desirable theoretical properties such as consistency and local accuracy [60].
LIME operates on a fundamentally different principle: local approximation. Instead of explaining the underlying model globally, LIME creates an interpretable surrogate model (such as linear regression or decision trees) that approximates the black-box model's behavior in the local neighborhood of a specific prediction [59] [60]. By perturbing the input data and observing changes in predictions, LIME identifies which features most significantly influence the output for that particular instance, generating explanations that are locally faithful but not necessarily globally representative.
The following table summarizes the core characteristics, advantages, and limitations of each approach:
Table 1: Technical Comparison of SHAP and LIME
| Characteristic | SHAP | LIME |
|---|---|---|
| Theoretical Foundation | Game theory (Shapley values) | Local surrogate modeling |
| Explanation Scope | Global and local interpretability | Primarily local interpretability |
| Computational Complexity | High (exponential in features); mitigated by approximations | Moderate; depends on perturbation size |
| Output | Feature importance values that sum to model output | Local feature weights for specific instance |
| Key Strength | Theoretical guarantees, consistent explanations | Fast computation, model-agnostic flexibility |
| Primary Limitation | Computationally expensive for high-dimensional data | Instability across different random samples |
Performance and Fidelity Metrics in Medical Applications
Quantitative evaluation of XAI methods is essential for assessing their suitability for clinical applications. Recent systematic reviews and meta-analyses have evaluated explanation fidelity—the degree to which post-hoc explanations accurately represent the actual decision-making process of the underlying model—across various medical imaging modalities including radiology, pathology, and ophthalmology [57].
A comprehensive meta-analysis of 67 studies revealed significant differences in fidelity between XAI methods. LIME demonstrated superior fidelity (0.81, 95% CI: 0.78–0.84) compared to SHAP (0.38, 95% CI: 0.35–0.41) and Grad-CAM (0.54, 95% CI: 0.51–0.57) across all medical imaging modalities [57]. This fidelity gap highlights the "explainability trap," where post-hoc explanations may create an illusion of understanding without providing genuine insight into model behavior, potentially compromising patient safety [57].
Stability under perturbation is another critical metric for clinical XAI. Evaluation under calibrated Gaussian noise perturbation revealed that SHAP explanations demonstrated significant degradation in ophthalmology applications (53% degradation, ρ = 0.42 at 10% noise) compared to radiology (11% degradation, ρ = 0.89) [57]. This modality-specific performance variation underscores the importance of context-specific validation for XAI methods in medical applications.
Table 2: Performance Metrics of XAI Methods in Medical Imaging
| Metric | SHAP | LIME | Grad-CAM |
|---|---|---|---|
| Aggregate Fidelity | 0.38 (95% CI: 0.35–0.41) | 0.81 (95% CI: 0.78–0.84) | 0.54 (95% CI: 0.51–0.57) |
| Stability in Radiology | ρ = 0.89 (11% degradation) | Moderate | Variable |
| Stability in Ophthalmology | ρ = 0.42 (53% degradation) | Moderate | Variable |
| Clinical Readability | Concise global explanations | Detailed local explanations | Intuitive visual heatmaps |
| Computational Efficiency | Low to moderate | Moderate to high | High for CNN architectures |
Experimental Protocols for XAI Implementation
Protocol 1: SHAP Integration for Cancer Detection Models
Purpose: To implement SHAP explanations for feature importance analysis in cancer detection models, enabling researchers to identify the most predictive features for malignant versus benign classification.
Materials and Reagents:
- Python 3.7+ environment
- SHAP library (version 0.41.0 or later)
- Trained ensemble model for cancer detection (e.g., stacked generalization model)
- Processed cancer dataset (e.g., Wisconsin Breast Cancer dataset with 30 features)
- Jupyter notebook environment for visualization
Procedure:
- Model Training: Train a stacked generalization model using base classifiers (Logistic Regression, Naïve Bayes, Decision Tree) and Multilayer Perceptron as meta-classifier following established methodologies for cancer detection [15].
- SHAP Explainer Selection:
- For tree-based models: Use
TreeSHAPexploit for optimal performance - For model-agnostic applications: Use
KernelSHAPas approximation method - For deep learning models: Use
DeepSHAPfor neural network architectures
- For tree-based models: Use
- Explanation Generation:
- Sample 100-500 instances from test set for background distribution
- Compute SHAP values for individual predictions using
shap.Explainer() - Generate summary plots with
shap.summary_plot(shap_values, X_test) - Create force plots for individual instances with
shap.force_plot()
- Interpretation and Analysis:
- Identify top features contributing to malignant classification
- Validate feature importance against clinical knowledge
- Assess consistency of explanations across similar cases
Validation Metrics:
- Explanation Fidelity: Calculate correlation between SHAP importance scores and actual model sensitivity using systematic feature occlusion [57]
- Stability Assessment: Measure Spearman rank correlation of feature importance under noise perturbation (5-30% Gaussian noise) [57]
Protocol 2: LIME for Local Explanation of Cancer Classification
Purpose: To generate instance-specific explanations for cancer classification models using LIME, providing interpretable insights for individual patient predictions.
Materials and Reagents:
- Python 3.7+ with LIME library (version 0.2.0.1 or later)
- Pre-trained cancer classification model (CNN for medical images or classifier for tabular data)
- Medical image dataset (e.g., histopathology images) or tabular clinical data
- Segmentation algorithms for image superpixels (if working with imaging data)
Procedure:
- Data Preparation:
- For tabular data: Ensure categorical features are properly encoded
- For image data: Preprocess images to standard size and normalization
- LIME Explainer Initialization:
- For tabular data:
explainer = lime.lime_tabular.LimeTabularExplainer() - For image data:
explainer = lime.lime_image.LimeImageExplainer()
- For tabular data:
- Explanation Configuration:
- Set number of perturbed samples to 5000 for stable explanations
- Configure distance metric (cosine distance recommended)
- Select top K features to display (typically 5-10 for clinical interpretability)
- Explanation Generation:
- For individual prediction:
exp = explainer.explain_instance(instance, model.predict_proba) - Visualize results:
exp.show_in_notebook(show_all=False)
- For individual prediction:
- Clinical Validation:
- Present explanations to clinical experts for plausibility assessment
- Compare LIME features with known clinical markers
- Evaluate explanation consistency across similar cases
Validation Metrics:
- Local Fidelity: Measure accuracy of local surrogate model in approximating black-box predictions
- Clinical Plausibility: Quantitative assessment by clinical experts using Likert scales
- Stability: Test explanation consistency across multiple runs with different random seeds
Workflow Visualization
Evaluation Framework for Clinical XAI
Quantitative Metrics for Explanation Quality
Robust evaluation of XAI methods requires multiple quantitative metrics assessing different aspects of explanation quality. Based on comprehensive analysis of explanation methods, the following metrics are recommended for clinical cancer detection applications [57] [61] [60]:
Explanation Fidelity: Measures how accurately the explanation reflects the actual reasoning process of the model. Assess using causal fidelity methodology with systematic feature occlusion and correlation analysis between importance scores and prediction changes [57].
Stability: Quantifies explanation consistency under input perturbations. Calculate Spearman rank correlation of feature importance rankings with added Gaussian noise (5-30% of maximum image intensity) [57].
Representativeness: Evaluates how well explanations cover the model's behavior across diverse patient subgroups and clinical scenarios.
Clinical Coherence: Assesses alignment between explanatory features and established clinical knowledge, using expert evaluation on Likert scales.
Computational Efficiency: Measures explanation generation time, particularly important for real-time clinical applications.
Clinical Validation Protocols
Protocol for Clinical Plausibility Assessment:
- Expert Panel Assembly: Convene multidisciplinary panel including oncologists, radiologists, pathologists, and clinical researchers
- Explanation Review: Present SHAP/LIME explanations for a curated set of cases (50-100) covering true positives, false positives, true negatives, and false negatives
- Structured Evaluation: Use standardized forms to assess:
- Biological plausibility of highlighted features
- Clinical relevance of explanation depth and granularity
- Consistency with established cancer biomarkers
- Actionability of explanations for treatment decisions
- Quantitative Scoring: Implement 5-point Likert scales for explanation quality dimensions:
- Understandability: How easily can clinicians comprehend the explanation?
- Clinical relevance: How pertinent are explanatory features to clinical decision-making?
- Trustworthiness: To what degree does the explanation increase confidence in the AI prediction?
Protocol for Human-AI Team Performance Evaluation:
- Experimental Design: Randomized controlled trial comparing:
- Clinicians alone (control)
- Clinicians with AI predictions only
- Clinicians with AI predictions + SHAP/LIME explanations
- Outcome Measures:
- Diagnostic accuracy (sensitivity, specificity, AUC)
- Decision confidence (self-reported on 1-10 scale)
- Time to decision
- Trust calibration (alignment between confidence and accuracy)
- Statistical Analysis: Mixed-effects models to account for clinician variability and case difficulty
Research Reagents and Computational Tools
Table 3: Essential Research Reagents for XAI Implementation in Cancer Detection
| Tool/Category | Specific Examples | Functionality | Implementation Considerations |
|---|---|---|---|
| XAI Libraries | SHAP, LIME, Captum (PyTorch), InterpretML | Generate feature attributions and local explanations | SHAP preferred for theoretical guarantees; LIME for computational efficiency |
| Model Development | Scikit-learn, XGBoost, PyTorch, TensorFlow | Build cancer detection models | Tree-based models compatible with TreeSHAP for optimal performance |
| Medical Imaging | ITK, SimpleITK, OpenSlide, MONAI | Preprocess medical images for explanation | Specialized handling for whole-slide images and 3D volumes |
| Visualization | Matplotlib, Seaborn, Plotly, Streamlit | Create interactive explanation dashboards | Clinical-friendly interfaces with appropriate context |
| Data Management | DICOM viewers, Pandas, NumPy | Handle structured and imaging data | Maintain data integrity throughout preprocessing pipeline |
| Validation Frameworks | MedPy, SciKit-Surgery, custom metrics | Quantify explanation quality and clinical utility | Implement domain-specific validation protocols |
Regulatory and Clinical Implementation Considerations
The integration of SHAP and LIME into clinical cancer detection systems must address regulatory requirements and implementation challenges. Regulatory bodies including the FDA emphasize that "transparency" describes the degree to which appropriate information about a machine learning-enabled medical device is clearly communicated to relevant audiences, with "explainability" representing the degree to which logic can be explained understandably [58].
Key considerations for clinical implementation include:
Contextual Presentation: Tailor explanation depth and presentation to different clinical roles—oncologists may require different information than radiologists or patients [58].
Workflow Integration: Embed explanations seamlessly into clinical workflows without adding significant cognitive load or time burden. The timing of explanation presentation should align with decision points in the clinical pathway [61].
Uncertainty Communication: Complement SHAP and LIME outputs with measures of explanation uncertainty, particularly important for edge cases or low-confidence predictions [57].
Bias Monitoring: Continuously monitor for potential biases in explanations across different patient demographics, as required by regulatory guidance on health equity [58].
Human-Centered Design: Iteratively refine explanation interfaces through collaboration with clinical end-users, following human-centered design principles mandated for medical devices [58].
The following diagram illustrates the comprehensive validation pathway for clinical XAI systems:
The incorporation of SHAP and LIME into cancer detection research represents a critical advancement toward clinically trustworthy AI systems. While SHAP provides theoretically grounded global and local explanations, LIME offers computationally efficient instance-specific insights—complementary strengths that can be strategically deployed based on clinical context and performance requirements [60].
Quantitative evidence indicates that current XAI methods, including SHAP and LIME, have significant limitations in explanation fidelity and stability, particularly in medical imaging applications [57]. This underscores the importance of rigorous validation and the need for continued methodological development. Furthermore, empirical studies demonstrate that technical explanations alone are insufficient for clinical adoption; explanations must be coupled with clinical context to enhance acceptance, trust, and usability among healthcare professionals [56].
The path forward for explainable AI in cancer detection requires a multidisciplinary approach that integrates technical excellence with clinical wisdom. By adhering to comprehensive evaluation frameworks, regulatory guidelines, and human-centered design principles, researchers can develop explainable systems that genuinely enhance clinical decision-making while maintaining the rigorous standards required for patient care.
Optimizing Computational Efficiency and Overcoming the Limitations of Conventional Techniques on Complex Data
The increasing complexity and volume of data in cancer research present significant challenges for conventional analytical techniques. These methods often struggle with high-dimensionality, redundancy, and computational inefficiency when processing complex oncological datasets from sources such as medical imaging, genomics, and liquid biopsies. Feature extraction and selection have emerged as critical preprocessing steps that enhance computational efficiency and model performance by reducing data dimensionality while preserving diagnostically relevant information [62] [63]. This protocol outlines structured methodologies for optimizing computational workflows in cancer detection research, enabling researchers to overcome limitations of conventional approaches and improve diagnostic accuracy across diverse data modalities.
Quantitative Performance Comparison of Advanced Computational Techniques
Table 1: Performance metrics of recently published cancer detection models
| Cancer Type | Technical Approach | Key Algorithmic Innovations | Reported Accuracy | Reference |
|---|---|---|---|---|
| Gastric Cancer | Vision Transformer + Optimized DNN | DPT model with union-based feature selection | 97.96% | [64] |
| Gastric Cancer | Vision Transformer + Optimized DNN | DPT model with 120×120 image resolution | 97.21% | [64] |
| Gastric Cancer | Vision Transformer + Optimized DNN | BEiT model with 80×80 image resolution | 95.78% | [64] |
| Metaplastic Breast Cancer | Deep Reinforcement Learning | Multi-dimensional descriptor system (ncRNADS) | 96.20% | [65] |
| Cervical Cancer (CT) | Ensemble Learning + Shark Optimization | InternImage-LVM fusion with SOA | 98.49% | [66] |
| Cervical Cancer (MRI) | Ensemble Learning + Shark Optimization | InternImage-LVM fusion with SOA | 92.92% | [66] |
Table 2: Comparative analysis of feature selection algorithms for cancer detection
| Algorithm | Feature Reduction Capability | Computational Efficiency | Key Advantages | Reference |
|---|---|---|---|---|
| bABER (Binary Al-Biruni Earth Radius) | Significant | High | Outperforms 8 other metaheuristic algorithms | [62] |
| bPSO (Binary Particle Swarm Optimization) | Moderate | Medium | Effective for text classification and disease diagnosis | [62] |
| bGWO (Binary Grey Wolf Optimizer) | Moderate | Medium | High-quality transfer function solutions | [62] |
| bWOA (Binary Whale Optimization Algorithm) | Moderate | Medium | Employs V or S-shaped curves for dimensionality reduction | [62] |
| ANOVA F-Test + Ridge Regression | High | High | Effective for transformer-based feature selection | [64] |
Experimental Protocols
Protocol 1: Vision Transformer-Based Feature Extraction for Histopathological Image Analysis
Application Note: This protocol details a multi-stage artificial intelligence approach for gastric cancer detection using vision transformers, achieving 97.96% accuracy [64].
Materials and Reagents:
- Histopathological Image Dataset: Publicly available gastric cancer image datasets
- Computational Environment: Python with PyTorch/TensorFlow and Transformer libraries
- Hardware: GPU-enabled workstation (NVIDIA recommended)
Methodology:
- Image Preprocessing:
- Resize images to standardized dimensions (160×160, 120×120, or 80×80 pixels)
- Apply normalization using mean and standard deviation of the dataset
- Implement data augmentation techniques (rotation, flipping, color jitter)
Feature Extraction:
- Utilize 11 different state-of-the-art vision transformer models
- Employ pre-trained models (DPT, BEiT) for transfer learning
- Extract feature vectors from the final transformer layers
Feature Selection:
- Apply multiple feature selection methods:
- ANOVA F-Test for variance-based selection
- Recursive Feature Elimination for iterative refinement
- Ridge Regression for regularization-based selection
- Create feature sets from intersections and unions of selected features
- Apply multiple feature selection methods:
Classification:
- Implement Deep Neural Network (DNN) architecture
- Optimize hyperparameters using Particle Swarm Optimization
- Train with k-fold cross-validation
- Evaluate performance using accuracy, sensitivity, specificity, precision, and F1-score
Protocol 2: Deep Reinforcement Learning for ncRNA-Disease Association Prediction
Application Note: This protocol enables metaplastic breast cancer diagnosis through ncRNA biomarker identification, achieving 96.29% F1-score [65].
Materials and Reagents:
- Genomic Data: ncRNA sequences from databases (miRBase, lncRNAdb)
- Clinical Data: Patient records and survival outcomes from TCGA
- Software Packages: Python with deep learning frameworks (TensorFlow, PyTorch)
Methodology:
- Data Collection and Integration:
- Compile 550 sequence-based features from ncRNA databases
- Extract 1,150 target gene descriptors with miRDB score ≥90
- Integrate multi-omics data (genomics, transcriptomics, epigenetics)
Feature Selection and Dimensionality Reduction:
- Apply principal component analysis (PCA) for variance preservation (82%)
- Implement t-SNE clustering for visualization
- Reduce dimensionality by 42.5% (4,430 to 2,545 features)
Deep Reinforcement Learning Model:
- Configure multi-dimensional descriptor system (ncRNADS)
- Train model with 0.08 seconds per epoch
- Validate using SHAP analysis for interpretability
- Identify key sequence motifs (e.g., "UUG") and structural free energy (ΔG = -12.3 kcal/mol)
Survival Analysis:
- Correlate ncRNA expressions with patient outcomes using TCGA data
- Calculate hazard ratios for prognostic markers (MALAT1, HOTAIR, NEAT1, GAS5)
- Validate model specificity to breast cancer subtypes (87-96.5% accuracy)
Protocol 3: Ensemble Learning with Optimization Algorithm for Medical Imaging
Application Note: This protocol compares CT and MRI for cervical cancer diagnosis using ensemble models with shark optimization, achieving 98.49% accuracy for CT images [66].
Materials and Reagents:
- Medical Images: Cervical CT and MRI scans from hospital datasets
- Annotation Tools: Medical imaging software for expert labeling
- Computational Resources: High-performance computing cluster
Methodology:
- Dataset Preparation:
- Collect retrospective imaging data (500 patients)
- Categorize images into normal, benign, and malignant classes
- Obtain IRB approval (No. 21/171/2024) for data usage
Image Preprocessing:
- Partition dataset (80% training, 10% validation, 10% testing)
- Apply normalization: S′ = (S-μ)/σ
- Implement data augmentation to address limited datasets
Ensemble Model Architecture:
- Implement InternImage (based on InceptionV3) for tumor-specific patterns
- Integrate Large Vision Model (LVM) for fine-grained spatial features
- Combine outputs using Shark Optimization Algorithm (SOA) for dynamic weight selection
Model Training and Evaluation:
- Train separately on CT and MRI datasets
- Compare performance across imaging modalities
- Assess generalization across diverse datasets
- Evaluate clinical impact for early detection and treatment planning
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential research reagents and computational tools for cancer detection research
| Category | Item/Solution | Specification/Function | Application Context |
|---|---|---|---|
| Data Sources | Public Cancer Datasets (TCGA, etc.) | Provides genomic, transcriptomic, and clinical data | Multi-omics analysis and model validation [65] |
| Feature Selection | bABER Algorithm | Binary Al-Biruni Earth Radius for intelligent feature removal | High-dimensional medical data processing [62] |
| Image Analysis | Vision Transformers (DPT, BEiT) | State-of-the-art feature extraction from histopathological images | Gastric cancer detection from tissue images [64] |
| Optimization | Shark Optimization Algorithm (SOA) | Dynamic weight parameter selection for ensemble models | Cervical cancer diagnosis from CT/MRI [66] |
| Model Validation | SHAP Analysis | Model interpretability and feature importance quantification | ncRNA-disease association studies [65] |
Technical Implementation Notes
Computational Efficiency Optimization
The protocols described emphasize strategies for enhancing computational efficiency while maintaining high diagnostic accuracy. Feature selection algorithms play a crucial role in this optimization, with the bABER algorithm demonstrating significant performance improvements over traditional methods by intelligently removing redundant or irrelevant features from complex medical datasets [62]. This approach directly addresses the challenge of high-dimensional data in cancer research, where not all collected features contribute meaningfully to diagnostic outcomes.
The integration of transformer-based architectures with conventional deep neural networks represents another efficiency optimization. By leveraging pre-trained vision transformers for feature extraction, researchers can utilize transfer learning to reduce training time and computational resources while achieving state-of-the-art performance [64]. This approach is particularly valuable in medical imaging applications where labeled data may be limited.
Overcoming Conventional Technique Limitations
Conventional cancer detection methods face limitations including interpretability challenges, sensitivity to data heterogeneity, and inability to capture complex multimodal relationships. The protocols outlined address these limitations through several innovative approaches:
Ensemble learning methods combined with optimization algorithms overcome the limitations of single-model approaches by dynamically weighting contributions from multiple specialized models [66]. This approach enhances generalization across diverse datasets and reduces misclassification, particularly for borderline cases between benign and malignant conditions.
Multi-stage artificial intelligence frameworks that separate feature extraction, selection, and classification processes provide more interpretable and robust solutions compared to end-to-end black box models [64]. The explicit feature selection step enhances model transparency and enables researchers to identify biologically relevant features contributing to accurate cancer detection.
Multimodal data integration addresses tumor heterogeneity by combining information from various sources, including imaging, genomic, and clinical data [65]. This comprehensive approach captures the complex molecular landscape of cancer, enabling more precise detection and stratification than single-modality methods.
Benchmarking Performance: Validation Frameworks, Statistical Analysis, and Comparative Efficacy
The adoption of rigorous validation methodologies is paramount in developing reliable and generalizable artificial intelligence (AI) and machine learning (ML) models for cancer detection. These methodologies, including cross-validation, statistical testing, and backtesting, serve as critical safeguards against overfitting and overoptimism, ensuring that predictive models perform robustly on unseen patient data [67]. In the high-stakes context of oncology, where model predictions can influence clinical decisions, rigorous validation is not merely a technical exercise but a fundamental component of translational research [68]. This document outlines standardized protocols and application notes for implementing these validation strategies within the specific framework of feature extraction techniques for cancer detection, providing researchers and drug development professionals with a practical guide for model evaluation.
Core Validation Concepts and Definitions
Overfitting occurs when an algorithm learns patterns specific to the training dataset that do not generalize to new data, leading to inflated performance metrics during training and disappointing results in clinical practice [67]. Cross-validation (CV) is a set of data sampling methods used to repeatedly partition a dataset into independent cohorts for training and testing. This separation ensures performance measurements are not biased by direct overfitting of the model to the data [67]. The primary goals of CV in algorithm development are performance estimation (evaluating a model's generalization capability), algorithm selection (choosing the best model from several candidates), and hyperparameter tuning (optimizing model configuration parameters) [67].
Cross-Validation Techniques: A Comparative Analysis
Various cross-validation techniques offer distinct advantages and disadvantages depending on dataset characteristics and research objectives. The table below summarizes the common CV approaches and their applicability.
Table 1: Comparison of Common Cross-Validation Techniques
| Method | Key Description | Best-Suited Scenarios | Advantages | Disadvantages |
|---|---|---|---|---|
| k-Fold CV [67] | Dataset partitioned into k disjoint folds; each fold serves as test set once, while the remaining k-1 folds are used for training. | General-purpose use with datasets of sufficient size. Common values are k=5 or k=10. | Reduces variance of performance estimate compared to holdout; makes efficient use of all data. | Computationally intensive; requires careful partitioning to avoid data leakage. |
| Stratified k-Fold CV [67] [69] | A variant of k-fold that preserves the original class distribution in each fold. | Highly recommended for imbalanced datasets (e.g., rare cancer subtypes). | Produces more reliable performance estimates for minority classes; reduces bias. | Same computational cost as standard k-fold. |
| Holdout Method [67] | A simple one-time split of the dataset into training and test sets (sometimes with an additional validation set). | Very large datasets where a single holdout set can be considered representative of the population. | Simple and computationally efficient; produces a single model. | Performance estimate can be highly dependent on a single, potentially non-representative, data split. |
| Nested CV [67] | An outer CV loop for performance estimation and an inner CV loop for hyperparameter tuning, both executed with separate data splits. | Essential for obtaining unbiased performance estimates when both model selection and evaluation are required. | Provides an almost unbiased estimate of the true error; prevents information leakage from tuning to the test set. | Very computationally expensive. |
Application Notes in Cancer Detection Research
Case Study: Multi-Stage Feature Selection with Stacked Generalization
A 2025 study on breast and lung cancer detection exemplifies the application of k-fold CV within a complex pipeline involving multi-stage feature selection. The research employed a three-layer Hybrid Filter-Wrapper strategy for feature selection, drastically reducing the feature set from 30 original features to 6 for breast cancer and from 15 to 8 for lung cancer while maintaining diagnostic accuracy [70]. The selected features were then used to train a stacked ensemble classifier (with Logistic Regression, Naïve Bayes, and Decision Tree as base classifiers and a Multilayer Perceptron as the meta-classifier). The entire model development and evaluation process was rigorously assessed using 10-fold cross-validation across different data splits (50-50, 66-34, and 80-20), with the model achieving 100% accuracy on the selected optimal feature subsets [70].
Table 2: Research Reagent Solutions for Cancer Detection Model Validation
| Reagent / Tool | Function / Description | Application Example |
|---|---|---|
| Hybrid Filter-Wrapper Feature Selection [70] | A multi-stage method that combines the computational efficiency of filter methods with the performance-driven selection of wrapper methods. | Used to select 6/8 highly predictive features from an initial 30/15 for breast/lung cancer datasets, improving model performance and interpretability [70]. |
| Stacked Ensemble Classifier [70] | An ensemble method where base classifiers (e.g., LR, NB, DT) make predictions, and a meta-classifier (e.g., MLP) learns to combine these predictions optimally. | Achieved 100% accuracy in cancer detection by leveraging the strengths of multiple, diverse base learning algorithms [70]. |
| Synthetic Minority Oversampling Technique (SMOTE) [71] [69] | A preprocessing technique used to generate synthetic samples for the minority class in an imbalanced dataset. | Applied to balance a dataset of cancerlectins and noncancerlectins, improving the model's ability to learn the minority class and enhancing prediction performance [71]. |
| SHAP/LIME [70] | Post-hoc model interpretation tools that provide insights into how the model makes predictions for individual samples or overall. | Incorporated into a stacked model for cancer detection to provide clinicians with explanations for model decisions, thereby enhancing trust and clinical relevance [70]. |
Experimental Protocol: k-Fold Cross-Validation with Ensemble Learning
Objective: To train and validate an ensemble classifier for histopathological image-based cancer detection using k-fold cross-validation. Dataset: LC25000 lung and colon histopathological image dataset [72]. Procedural Steps:
- Data Preprocessing: Apply image normalization and augmentation techniques to the dataset.
- Feature Extraction: Utilize pre-trained Convolutional Neural Networks (CNNs) like VGG16, VGG19, and MobileNet as deep feature extractors [72].
- High-Performance Filtering (HPF): Train multiple machine learning classifiers (e.g., SVM, KNN, Random Forest) on the extracted features and select the top-performing algorithms based on accuracy [72].
- Ensemble Model Training: Combine the selected top classifiers using a soft voting ensemble method.
- Model Validation:
- Partition the entire pre-processed and feature-extracted dataset into k=10 folds.
- For each fold i (where i = 1 to 10):
- Designate fold i as the test set.
- Use the remaining k-1 folds as the training set.
- Train the soft voting ensemble model on the training set.
- Evaluate the trained model on the test set (fold i), recording metrics such as accuracy, precision, recall, F1-score, and AUC.
- Performance Reporting: Calculate the mean and standard deviation of all performance metrics from the 10 iterations. The final model for deployment should be trained on the entire dataset [67]. This protocol has been shown to achieve accuracies exceeding 99% for lung and colon cancer detection [72].
Protocol for Handling Imbalanced Data in Cancer Prediction
Objective: To build a predictive model for breast cancer classification from a diagnostic dataset with imbalanced class distribution. Dataset: Wisconsin Breast Cancer Diagnosis dataset [69]. Procedural Steps:
- Data Splitting: Initially split the dataset into training (e.g., 70%) and holdout test (e.g., 30%) sets, stratifying by the target variable to maintain the class ratio in both splits.
- Class Balancing: Apply the Synthetic Minority Oversampling Technique (SMOTE) exclusively to the training set to generate synthetic samples for the minority class. The holdout test set must remain unmodified to simulate a real-world distribution [69].
- Model Training and Selection: Using the balanced training set, train multiple classifiers (e.g., Logistic Regression, SVM, CART). Employ Stratified 10-Fold Cross-Validation on this training set to tune hyperparameters and select the best-performing algorithm. This ensures the validation folds within the training data maintain the original imbalance for a realistic evaluation during tuning.
- Ensemble Construction: Combine the best-performing individual models (e.g., LR, SVM, CART) into a Majority-Voting ensemble classifier [69].
- Final Evaluation: Train the final Majority-Voting ensemble on the entire SMOTE-processed training set and evaluate its performance on the pristine, untouched holdout test set. This approach has yielded state-of-the-art accuracy of 99.3% for breast cancer classification [69].
Critical Pitfalls and Mitigation Strategies
- Tuning to the Test Set: A pervasive pitfall is the indirect optimization of a model to a specific holdout test set, leading to overoptimistic performance estimates. This occurs when developers repeatedly modify and retrain their model based on its performance on the test set, effectively incorporating information from the test set into the training process [67].
- Mitigation: The holdout test set should be used only once for the final evaluation of a fully specified model. Use a separate validation set or nested cross-validation for all model development and hyperparameter tuning activities [67].
- Nonrepresentative Test Sets: Performance estimates become biased if the test set patients are insufficiently representative of the target population. This can stem from biased data collection or dataset shift between development and deployment environments [67].
- Mitigation: Ensure data collection is as representative as possible. Use stratified splitting to preserve known subclass distributions (e.g., age groups, cancer subtypes). Increasing dataset size also helps mitigate the impact of hidden subclasses [67].
Workflow and Architecture Diagrams
k-Fold Cross-Validation Workflow
Figure 1: k-Fold Cross-Validation Workflow (k=5)
Ensemble Model with Feature Extraction for Cancer Detection
Figure 2: Ensemble Model with Feature Extraction Architecture
The accurate detection and diagnosis of cancer through medical imaging are critical for determining appropriate treatment strategies and improving patient survival rates. Within this domain, the evaluation of machine learning (ML) and deep learning (DL) models using robust metrics is paramount. Models are typically assessed on their performance in classification tasks—such as distinguishing between benign and malignant tumors or identifying different cancer subtypes. Key metrics for this evaluation include accuracy, sensitivity (recall), specificity, and the Area Under the Receiver Operating Characteristic Curve (AUC-ROC). These metrics provide complementary views on model performance, from overall correctness to the balance between identifying true positives and avoiding false alarms [73] [74].
The choice and interpretation of these metrics are particularly vital in high-stakes medical applications like cancer detection. A model might achieve high overall accuracy yet fail to identify critical malignant cases (poor sensitivity), or it might be overly cautious, flagging too many healthy cases as potentially cancerous (poor specificity) [75]. Furthermore, the dependence on a single metric can be misleading, especially with imbalanced datasets where one class (e.g., "no cancer") significantly outnumbers the other ("cancer") [75] [74]. This application note, framed within a broader thesis on feature extraction for cancer detection, provides a detailed protocol for the rigorous evaluation and comparison of model performance using these essential metrics. It is intended for researchers, scientists, and drug development professionals working to translate reliable AI tools into clinical practice.
Core Performance Metrics: Definitions and Clinical Significance
A deep understanding of each performance metric, including its calculation, clinical meaning, and limitations, is fundamental for appropriate model assessment.
The Confusion Matrix as a Foundational Tool
The confusion matrix is an N x N table (where N is the number of classes) that forms the basis for calculating most classification metrics. For binary classification, such as "cancer" vs. "no cancer," it is a 2x2 matrix [73]. The core components of a binary confusion matrix are defined below and illustrated in Figure 1.
- True Positive (TP): The model correctly predicts the positive class (e.g., correctly identifies a malignant tumor).
- True Negative (TN): The model correctly predicts the negative class (e.g., correctly identifies a benign or normal case).
- False Positive (FP): The model incorrectly predicts the positive class (e.g., misclassifies a benign case as malignant). This is a Type I error.
- False Negative (FN): The model incorrectly predicts the negative class (e.g., misses a malignant tumor). This is a Type II error [73].
Table 1: The Structure of a Binary Confusion Matrix
| Predicted Positive | Predicted Negative | |
|---|---|---|
| Actual Positive | True Positive (TP) | False Negative (FN) |
| Actual Negative | False Positive (FP) | True Negative (TN) |
Figure 1: Logical relationships within a binary confusion matrix, showing the four prediction outcomes and their categorizations as errors or correct results.
Detailed Metric Analysis
From the confusion matrix, the primary metrics for model evaluation are derived.
Accuracy: Measures the overall proportion of correct predictions (both positive and negative) made by the model. It is most reliable when the classes are approximately balanced [75]. ( \text{Accuracy} = \frac{TP + TN}{TP + TN + FP + FN} ) Clinical Context: While a high accuracy is desirable, it can be dangerously misleading in imbalanced datasets. For example, a cancer detection model might achieve 95% accuracy simply by always predicting "no cancer" if 95% of the screened population is healthy, thereby failing in its primary task of identifying sick patients [75].
Sensitivity (Recall): Measures the model's ability to correctly identify actual positive cases. It is critical in medical diagnostics where missing a positive case (e.g., cancer) is unacceptable [74]. ( \text{Sensitivity} = \frac{TP}{TP + FN} ) Clinical Context: High sensitivity is non-negotiable in cancer screening (e.g., mammography). A model with 99% sensitivity means it misses only 1% of true cancers, which is vital for early intervention [76] [77].
Specificity: Measures the model's ability to correctly identify actual negative cases [73]. ( \text{Specificity} = \frac{TN}{TN + FP} ) Clinical Context: High specificity is desired to avoid false alarms, which can cause unnecessary patient anxiety, lead to invasive follow-up procedures like biopsies, and increase healthcare costs [76].
Precision: Measures the proportion of positive predictions that are actually correct [74]. ( \text{Precision} = \frac{TP}{TP + FP} ) Clinical Context: When the cost of a false positive is high (e.g., initiating aggressive chemotherapy for a benign condition), precision becomes a key metric.
F1-Score: The harmonic mean of precision and recall, providing a single metric that balances both concerns. It is especially useful when you need to find a balance between false positives and false negatives and when the class distribution is uneven [73] [74]. ( \text{F1-Score} = 2 \times \frac{\text{Precision} \times \text{Recall}}{\text{Precision} + \text{Recall}} )
Area Under the ROC Curve (AUC-ROC): The ROC curve plots the True Positive Rate (Sensitivity) against the False Positive Rate (1 - Specificity) at various classification thresholds. The AUC-ROC represents the model's ability to distinguish between classes, independent of any specific threshold. A higher AUC (closer to 1.0) indicates better overall discriminatory power [73]. Clinical Context: AUC-ROC is valuable for selecting a model that maintains a good trade-off between sensitivity and specificity across all possible decision thresholds [74].
Table 2: Summary of Key Model Evaluation Metrics
| Metric | Formula | Clinical Interpretation | Primary Use Case |
|---|---|---|---|
| Accuracy | (TP + TN) / Total | Overall correctness of the model. | Balanced datasets where all errors are equally important. |
| Sensitivity (Recall) | TP / (TP + FN) | Ability to find all positive cases. | Critical when missing a disease (False Negative) is dangerous. |
| Specificity | TN / (TN + FP) | Ability to correctly rule out negative cases. | Critical when false alarms (False Positive) are costly. |
| Precision | TP / (TP + FP) | Trustworthiness of a positive prediction. | When the cost of acting on a false positive is high. |
| F1-Score | 2 * (Precision * Recall) / (Precision + Recall) | Balanced measure of precision and recall. | Imbalanced datasets; single summary metric needed. |
| AUC-ROC | Area under ROC curve | Overall model discriminative ability. | Threshold-independent model comparison. |
Comparative Analysis in Cancer Detection Research
The interplay between feature extraction techniques and model performance is evident across recent studies in cancer detection. The following comparative analysis synthesizes findings from several research works, highlighting how different approaches impact key metrics.
Table 3: Performance Comparison of Models in Cancer Detection
| Study / Model | Dataset | Accuracy (%) | Sensitivity/Recall (%) | Specificity (%) | AUC-ROC | Key Feature Extraction Method |
|---|---|---|---|---|---|---|
| 2D BiLSTM-CNN with Hybrid Features [17] | MIAS | 97.14 | Not Reported | Not Reported | Not Reported | Shearlet Transform, GLCM, GLRLM, 1st-order statistics. |
| PHCA with HOG + PCA [77] | INbreast | 97.31 | 97.09 | 96.86 | Not Reported | Histogram of Oriented Gradients (HOG), Principal Component Analysis (PCA). |
| ResNet18 (Brain Tumor) [78] | Brain Tumor MRI | 99.77 (Validation) | Implied by high F1-score | Implied by high F1-score | Not Reported | Deep Learning (CNN with residual layers). |
| SVM + HOG (Brain Tumor) [78] | Brain Tumor MRI | 96.51 (Validation) | Implied by high F1-score | Implied by high F1-score | Not Reported | Handcrafted HOG features. |
Analysis of Comparative Performance
The data in Table 3 illustrates several key trends relevant to researchers:
High Performance of Hybrid Feature Extraction: The study on breast cancer detection using a 2D BiLSTM-CNN classifier combined with handcrafted features (GLCM, GLRLM) achieved an accuracy of 97.14% on the MIAS dataset [17]. This underscores the thesis that integrating traditional, interpretable feature extraction methods (like texture analysis) with powerful deep learning architectures can yield highly accurate models. The handcrafted features capture subtle, domain-relevant textural patterns that might be overlooked by deep learning models in their early layers, especially with limited data.
Competitiveness of Topological Feature Extraction: The Persistent Homology Classification Algorithm (PHCA) framework, which uses HOG for feature extraction and PCA for dimensionality reduction, demonstrated performance (97.31% Accuracy, 97.09% Sensitivity) competitive with advanced deep learning models [77]. This is significant as PHCA offers a computationally efficient alternative to resource-intensive deep learning, making it suitable for large-scale screening applications. This finding directly supports research into novel, non-deep-learning-based feature extraction methods for cancer detection.
Performance vs. Complexity Trade-off: The brain tumor classification study provides a clear comparison of model complexity [78]. While the ResNet18 (CNN) model achieved a very high validation accuracy (99.77%), the SVM with HOG features still delivered a strong and competitive performance (96.51% accuracy). This highlights an important trade-off: deep learning models can achieve top-tier performance but often require significant computational resources and data. In contrast, traditional ML with well-designed feature extraction can provide a highly effective, less resource-intensive solution, which is a crucial consideration for practical deployment.
Experimental Protocols for Model Evaluation
To ensure the reliability and validity of model performance comparisons, a rigorous experimental protocol must be followed. This section outlines key methodologies for training, evaluation, and statistical validation.
Data Preparation and Preprocessing Protocol
- Dataset Selection and Description: Utilize publicly available, well-annotated medical image datasets. For breast cancer research, common datasets include INbreast [77], MIAS [17], and CBIS-DDSM [76]. The dataset should be clearly described, including the number of images, class distribution (e.g., benign vs. malignant), and image specifications (e.g., resolution, view).
- Data Augmentation: To increase the effective dataset size and improve model generalization, apply augmentation techniques. As performed in [77], this can include:
- Multiple-angle rotation (e.g., from 30° to 360° with 30° increments).
- Image flipping (horizontal and vertical).
- Contrast enhancement techniques like Contrast Limited Adaptive Histogram Equalization (CLAHE).
- Image Preprocessing:
- Resize all images to a uniform dimension (e.g., 224x224 pixels) [77].
- Convert images to grayscale to reduce computational complexity, if color information is not critical [77].
- Apply normalization to scale pixel intensity values to a standard range (e.g., 0-1 or with a mean of 0 and standard deviation of 1).
Model Training and Validation Protocol
- Cross-Validation (CV): Use K-fold cross-validation to obtain a robust estimate of model performance and mitigate overfitting. The dataset is split into K folds (e.g., K=5 or K=10), with each fold serving as the test set once while the remaining K-1 folds are used for training [79].
- Handling Statistical Variability: Be aware that the choice of K and the number of CV repetitions (M) can influence the perceived statistical significance of performance differences between models [79]. To ensure fair comparisons:
- Use the same CV splits (random seed) when comparing different models.
- Consider using statistical tests that account for the dependencies introduced by CV, as standard paired t-tests on CV results can be flawed and overstate significance [79].
- Performance Metric Calculation: Calculate all metrics (Accuracy, Sensitivity, Specificity, Precision, F1-Score) from the aggregated confusion matrix across all CV folds or from the final hold-out test set. Report confidence intervals where possible to convey uncertainty.
Figure 2: A generalized workflow for the experimental evaluation of machine learning models in medical imaging, from data preparation to final reporting.
The Scientist's Toolkit: Research Reagent Solutions
This section details essential computational tools, datasets, and algorithms that function as the "research reagents" for developing and testing cancer detection models.
Table 4: Essential Research Reagents for Cancer Detection Model Development
| Reagent / Resource | Type | Function / Application | Example Use Case |
|---|---|---|---|
| INbreast Dataset [77] | Dataset | Provides high-quality mammography images with annotations for masses, calcifications, and other abnormalities. | Benchmarking breast cancer detection and classification algorithms. |
| MIAS Dataset [17] | Dataset | A classic, publicly available dataset of mammograms for computer-aided diagnosis research. | Training and validating models for mass detection and classification. |
| CBIS-DDSM [76] | Dataset | A large, curated dataset of digitized film mammography studies. | Developing models for large-scale breast cancer screening. |
| Histogram of Oriented Gradients (HOG) [77] | Feature Extractor | Extracts shape and edge information by analyzing gradient orientations in image regions. | Used as input to classifiers like SVM or within topological frameworks (PHCA). |
| Gray Level Co-occurrence Matrix (GLCM) [17] | Feature Extractor | Captures texture information by analyzing the spatial relationship of pixel intensities. | Extracting textural features from mammograms to distinguish between dense and fatty tissues or benign vs. malignant masses. |
| Principal Component Analysis (PCA) [77] | Dimensionality Reduction | Reduces the number of features while preserving variance, mitigating overfitting, and speeding up training. | Compressing high-dimensional feature vectors (e.g., from HOG) before classification. |
| Persistent Homology [77] | Topological Feature Extractor | Captures the intrinsic topological shape and structure of data (e.g., connected components, loops). | Analyzing the global structure of image regions for classification (PHCA). |
| Scikit-learn | Software Library | Provides implementations of classic ML algorithms, preprocessing tools, and model evaluation metrics. | Building SVM, Logistic Regression, and Decision Tree models; calculating accuracy, precision, recall, etc. |
| PyTorch / TensorFlow | Software Library | Open-source libraries for developing and training deep learning models. | Implementing CNN, ResNet, and custom architectures like 2D BiLSTM-CNN. |
Within the broader scope of developing advanced feature extraction techniques for cancer detection research, this case study examines a groundbreaking approach that combines multistage feature selection with stacked generalization models. The primary challenge in cancer diagnostics using machine learning is the "curse of dimensionality," where datasets with numerous features can lead to model overfitting and reduced generalizability. The research demonstrates that intelligent feature selection is not merely a preprocessing step but a critical component that enables models to achieve perfect classification metrics on benchmark datasets. By reducing the feature space to only the most relevant biomarkers, researchers have developed ensemble models that achieve 100% accuracy, sensitivity, specificity, and AUC in detecting breast and lung cancers, marking a significant advancement in computational oncology [15] [80].
Key Performance Data
The following tables summarize the exceptional results reported across multiple studies that employed stacked generalization with optimized feature subsets.
Table 1: Performance Metrics of Stacked Models Achieving 100% Accuracy
| Study Focus | Feature Selection Method | Base Classifiers | Meta-Learner | Optimal Feature Subset | Performance |
|---|---|---|---|---|---|
| Breast & Lung Cancer Detection [15] [80] | 3-layer Hybrid Filter-Wrapper | LR, Naïve Bayes, Decision Tree | Multilayer Perceptron (MLP) | 6 features (WBC), 5 features (LCP) | 100% Accuracy, Sensitivity, Specificity, AUC |
| Breast Cancer Prediction [81] | Integrated Filter, Wrapper & Embedded Methods | Multiple base classifiers | Stacking Classifier | Features consistent across all selection methods | 100% Accuracy, AUC-ROC: 1.00 |
| Liver Cancer Diagnosis [82] | Feature Selection Process | MLP, RF, KNN, SVM | XGBoost | Selected key genetic markers | 97% Accuracy, 96.8% Sensitivity, 98.1% Specificity |
Table 2: Comparative Model Performance with Different Feature Set Sizes
| Model | Dataset | Full Feature Set Accuracy | Optimized Feature Set Accuracy | Number of Features Selected |
|---|---|---|---|---|
| Stacked Model (LR, NB, DT, MLP) [15] | WBC | ~98.6% (SVM with 30 features) | 100% | 6 |
| Stacked Model (LR, NB, DT, MLP) [15] | LCP | ~98.6% (SVM with 25 features) | 100% | 5 |
| SVM with Feature Selection [83] | Prostate Cancer (White) | - | 97% | 9 |
| SVM with Feature Selection [83] | Prostate Cancer (African American) | - | 95% | 9 |
Experimental Protocols
Multistage Hybrid Feature Selection Protocol
This protocol details the sequential process for identifying optimal feature subsets, as implemented in the seminal study achieving 100% accuracy [15].
Purpose: To systematically reduce feature dimensionality while preserving and enhancing the predictive signal for cancer classification.
Materials:
- Cancer datasets (e.g., Wisconsin Breast Cancer, Lung Cancer Prediction)
- Python programming environment (Google Colab)
- Greedy stepwise search algorithm
- Best first search algorithm
- Logistic Regression classifier
Procedure:
- Phase 1 - Initial Feature Screening:
- Apply a Greedy stepwise search algorithm to evaluate all available features (e.g., 30 in WBC, 15 in LCP).
- Select features that are highly correlated with the target class but exhibit low inter-correlation.
- Output: 9 features for WBC dataset and 10 features for LCP dataset.
Phase 2 - Refined Feature Selection:
- Apply Best First Search combined with a Logistic Regression algorithm.
- Evaluate the predictive power of feature subsets identified in Phase 1.
- Output: Further reduced optimal subsets of 6 features for breast cancer and 8 for lung cancer.
Validation:
- Validate selected features by training multiple classifiers and comparing performance metrics.
- Use SHAP (SHapley Additive exPlanations) and LIME (Local Interpretable Model-agnostic Explanations) to interpret and validate the clinical relevance of selected features.
Figure 1: Workflow of the Multistage Hybrid Feature Selection Protocol
Stacked Generalization Model Construction Protocol
Purpose: To combine the predictive power of multiple diverse classifiers through a stacking ensemble framework, leveraging the optimized feature subsets for superior cancer classification performance [15] [84].
Materials:
- Optimized feature subsets from the feature selection protocol
- Base classifiers: Logistic Regression (LR), Naïve Bayes (NB), Decision Tree (DT)
- Meta-classifier: Multilayer Perceptron (MLP)
- Computing environment with scikit-learn or similar ML libraries
Procedure:
- Base Layer Configuration:
- Partition the dataset using the optimized feature subsets into training and test sets (50-50, 66-34, and 80-20 splits).
- Train multiple heterogeneous base classifiers (LR, NB, DT) on the training data. These algorithms provide diverse inductive biases to capture different patterns in the data.
Meta-Layer Configuration:
- Use the predictions from base classifiers as input features for the meta-learner.
- Employ a Multilayer Perceptron (MLP) as the meta-classifier to learn the optimal combination of base model predictions.
- The MLP learns to weigh the predictions of the base models based on their respective strengths.
Model Validation:
- Apply 10-fold cross-validation to ensure reliability of results across different data partitions.
- Evaluate performance using multiple metrics: accuracy, sensitivity, precision, specificity, AUC, and Kappa statistics.
- Compare stacked model performance against individual classifiers using the same feature subsets.
Figure 2: Architecture of the Stacked Generalization Model
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Resources for Replicating the Stacked Generalization Framework
| Resource Category | Specific Tool/Solution | Function in Research |
|---|---|---|
| Programming Environment | Python with Google Colab [80] | Provides accessible computational environment with necessary ML libraries |
| Feature Selection Algorithms | Greedy Stepwise Search, Best First Search [15] | Identifies optimal feature subsets through sequential evaluation |
| Base Classifiers | Logistic Regression, Naïve Bayes, Decision Tree [15] | Provides diverse learning algorithms for the stacking ensemble base layer |
| Meta-Learner | Multilayer Perceptron (MLP) [15] | Learns optimal combination of base classifier predictions |
| Model Validation Framework | 10-fold Cross-Validation [15] | Ensures reliable performance estimation across data partitions |
| Explainable AI Tools | SHAP, LIME [15] [84] [85] | Provides model interpretability and clinical validation of feature importance |
| Benchmark Datasets | Wisconsin Breast Cancer (WBC), Lung Cancer Prediction (LCP) [15] [80] | Standardized datasets for model benchmarking and comparison |
| Performance Metrics | Accuracy, Sensitivity, Specificity, AUC, Kappa [15] | Comprehensive evaluation of model performance from multiple perspectives |
Advanced Applications and Methodological Variations
SMAGS-LASSO for Sensitivity Maximization
An advanced feature selection methodology called SMAGS-LASSO (Sensitivity Maximization at a Given Specificity) has been developed specifically for early cancer detection contexts where sensitivity is clinically prioritized. This approach combines a custom sensitivity maximization framework with L1 regularization for feature selection, simultaneously optimizing sensitivity at user-defined specificity thresholds while performing feature selection [86].
Key Application: In colorectal cancer biomarker data, SMAGS-LASSO demonstrated a 21.8% improvement over standard LASSO and a 38.5% improvement over Random Forest at 98.5% specificity while selecting the same number of biomarkers. This method enables development of minimal biomarker panels that maintain high sensitivity at predefined specificity thresholds [86].
Multi-Omics Data Integration
Stacked generalization models have been successfully applied to multi-omics data integration, combining RNA sequencing, somatic mutation, and DNA methylation profiles for classifying five common cancer types. The stacking ensemble approach integrating SVM, KNN, ANN, CNN, and RF achieved 98% accuracy with multi-omics data compared to lower accuracy using individual omics data types [87].
Workflow:
- Collect and preprocess multi-omics data from sources like TCGA
- Perform normalization and feature extraction using autoencoder techniques
- Apply stacking ensemble with five base models
- Generate final classification across five cancer types
This approach demonstrates how stacked generalization can handle the high-dimensionality and heterogeneity of multi-omics data while improving classification accuracy.
Race-Specific Cancer Detection
A novel framework optimized feature selection for race-specific prostate cancer detection using gene expression data. By combining differentially expressed gene analysis, ROC analysis, and MSigDB verification, researchers developed SVM models that achieved 98% accuracy for White patients and 97% for African American patients using only 9 gene features [83]. This approach highlights the importance of population-specific feature selection in cancer diagnostics.
This case study demonstrates that the synergy between optimized feature selection and stacked generalization models represents a paradigm shift in cancer detection research. The documented achievement of 100% accuracy across multiple metrics and datasets underscores the transformative potential of this methodology. The protocols outlined herein provide researchers with a reproducible framework for implementing these advanced techniques. Future research directions should focus on validating these approaches across more diverse populations and cancer types, integrating multi-modal data sources, and further refining feature selection algorithms to enhance both performance and clinical interpretability. As feature extraction techniques continue to evolve, stacked generalization models stand to play an increasingly pivotal role in the development of precise, reliable, and clinically actionable cancer diagnostic tools.
External Validation and the Gap Between Cross-Validation Performance and Real-World Clinical Utility
In the field of cancer detection research, the development of models using feature extraction techniques—ranging from handcrafted methods to deep learning—has shown remarkable progress. However, a significant performance gap often exists between optimistic cross-validation results and the model's effectiveness in real-world clinical settings. External validation, the process of evaluating a model on data independent of its development, is critical for assessing true generalizability and clinical utility. This Application Note details the protocols and frameworks necessary to bridge this gap, ensuring that predictive models for cancer detection can reliably support clinical decision-making.
The integration of artificial intelligence (AI) and machine learning (ML) into oncology, particularly in cancer detection using histopathology and radiology images, promises to revolutionize patient care. A cornerstone of this integration is feature extraction, which can be broadly categorized into two paradigms: knowledge-based (handcrafted) features and deep learning (DL)-based automatic feature extraction [5]. Knowledge-based systems often rely on domain expertise to define features related to texture (e.g., using Gray Level Co-occurrence Matrix - GLCM), shape, and intensity, while DL approaches like Convolutional Neural Networks (CNNs) learn hierarchical feature representations directly from raw image data [5] [17].
Despite promising high accuracy in internal development cycles, many models fail to translate this performance into broad clinical practice. This discrepancy arises because internal validation, including cross-validation on a single dataset, often fails to account for variations in patient populations, imaging equipment, and clinical protocols across different medical centers [88]. External validation is therefore not merely a final checkmark but an essential step to verify a model's calibration, discrimination, and clinical utility in the real world [89] [88]. A recent scoping review highlighted that while interest in ML for clinical decision-making is growing, many studies still suffer from limitations like small sample sizes and a lack of international validation, which hinder generalizability [88].
Quantitative Performance Comparison of Feature Extraction and Validation Methods
The choice of feature extraction method significantly influences model performance, but its ultimate value is determined by rigorous external validation. The following table summarizes reported performances of different approaches, illustrating the contrast between internal potential and externally validated reality.
Table 1: Performance of Cancer Detection Models Using Different Feature Extraction and Validation Approaches
| Cancer Type | Feature Extraction Method | Model/Classifier | Reported Accuracy (%) | Validation Type | Key Findings/Limitations |
|---|---|---|---|---|---|
| Breast Cancer (Histopathology) | Knowledge-based (Geometric, Intensity) [5] | Neural Network, Random Forest | 98% | Internal | Outperformed DL methods on the specific dataset [5]. |
| Breast Cancer (Histopathology) | Convolutional Neural Network (CNN) [5] | Neural Network, Random Forest | 85% | Internal | Automates feature extraction but relies on large datasets [5]. |
| Breast Cancer (Histopathology) | Transfer Learning (VGG16) [5] | Neural Network | 86% | Internal | Demonstrates the application of pre-trained networks. |
| Breast Cancer (Mammography) | Hybrid (GLCM, GLRLM, 1st-order stats + 2D BiLSTM-CNN) [17] | Custom 2D BiLSTM-CNN | 97.14% | Internal (MIAS dataset) | Combining handcrafted and deep features can enhance performance [17]. |
| Skin Cancer (Dermoscopy) | Deep CNN + Traditional ML [90] | CNN-Random Forest, CNN-LR | 99% | Internal (HAM10000) | Hybrid models achieved high accuracy; study incorporated patient metadata [90]. |
| Lung Cancer (CT) | SIFT (Handcrafted) [91] | Support Vector Machine (SVM) | 96% | Internal | SIFT features outperformed GLCM, SURF, and PCA in this study [91]. |
| Cesarean Section (Clinical Data) | XGBoost [92] | XGBoost | AUROC: 0.76 (Temporal), 0.75 (Geographical) | External (Temporal & Geographical) | Demonstrates strong, generalizable performance achieved through rigorous external validation [92]. |
A critical analysis of the literature reveals a common trend: models achieving exceptionally high accuracy (>95%) are typically validated internally on limited or single-institution datasets [5] [17] [90]. In contrast, a model subjected to rigorous external validation, such as the one predicting cesarean section, reports performance using metrics like AUROC and demonstrates a slight but expected drop in performance when applied to data from new time periods and locations [92]. This underscores the necessity of external validation for a realistic performance estimate.
Table 2: A Framework for Evaluating Model Performance and Clinical Readiness
| Evaluation Dimension | Common Internal Validation Pitfalls | External Validation Requirements | Recommended Metrics |
|---|---|---|---|
| Discrimination | Over-optimistic performance on held-out test sets from the same source. | Performance sustained on fully independent datasets from different populations/centers. | Area Under the ROC Curve (AUC), F1-Score. |
| Calibration | Poor calibration often goes unnoticed when only discrimination is measured. | Agreement between predicted probabilities and observed outcomes must be checked in the new population. | Calibration slope and intercept, Observed/Expected (O/E) ratio, calibration plots [89] [88]. |
| Clinical Utility | Rarely assessed; high accuracy is mistakenly equated with clinical usefulness. | Demonstrate that using the model improves clinician decisions or patient outcomes compared to standard care. | Decision Curve Analysis (DCA) for net benefit, impact on clinical workflow [88] [92]. |
| Generalizability | Fails to account for population, operational, and temporal variations. | Validate across different ethnicities, clinical protocols, and imaging technologies. | Performance metrics disaggregated by subgroups and sites. |
Protocols for Robust External Validation and Clinical Translation
Protocol 1: Minimum Sample Size Calculation for External Validation
Objective: To determine the minimum sample size required for an external validation study of a cancer detection model with a binary outcome (e.g., malignant vs. benign) to ensure precise performance estimates.
Background: Underpowered validation studies yield imprecise estimates of model performance (e.g., wide confidence intervals for AUC), making it difficult to conclude whether the model is clinically useful [89].
Materials:
- Pre-existing prediction model (e.g., a .pkl or .h5 file containing the model weights and architecture).
- A defined dataset from the target external validation population.
Procedure:
- Define Target Precision: Specify the desired confidence interval (CI) width or standard error (SE) for key performance metrics. For example, one might aim for a narrow 95% CI for the calibration slope [89].
- Determine Outcome Prevalence: Obtain an estimate of the outcome event proportion (e.g., cancer prevalence) in the planned validation population.
- Anticipate Model Performance: Estimate the model's expected calibration and the variance of its linear predictor values in the validation set, if possible.
- Apply Sample Size Formulae: Use established methods [89] to calculate the required sample size
(N)and number of events(E).- For Calibration: The sample size required for the calibration slope is often the driving factor. Calculations are based on maximizing the likelihood for the calibration slope.
- For Discrimination: Calculations can be based on the SE of the C-statistic.
- For Clinical Utility: Sample size can be determined based on precisely estimating net benefit at a clinically relevant risk threshold.
- Software Implementation: The following pseudo-code illustrates the logic, based on the work of Riley et al. [89]: The authors provide an example where 9,835 participants (177 events) were required for precise estimation of calibration and discrimination for a model predicting mechanical heart valve failure [89].
Protocol 2: Executing a Geographical External Validation Study
Objective: To assess the performance and generalizability of a pre-developed cancer detection model on a dataset sourced from a distinct institution or geographical region.
Background: Geographical validation tests a model's robustness against variations in clinical practice, patient demographics, and equipment, which is a stronger test of real-world applicability [88] [92].
Materials:
- The pre-trained model to be validated.
- Annotated image dataset (e.g., whole slide images, CT scans) from one or more external centers.
- Data Use Agreements and IRB approval from all participating sites.
Procedure:
- Dataset Curation:
- Obtain raw data from the external center(s).
- Apply identical preprocessing steps used during model development (e.g., normalization, resizing, artifact removal).
- Ensure ground truth labels are defined consistently with the development process.
- Model Inference:
- Run the pre-trained model on the preprocessed external dataset to generate predictions.
- Do not retrain or fine-tune the model on the external data at this stage.
- Performance Assessment:
- Calculate discrimination metrics (AUC, Sensitivity, Specificity).
- Assess calibration by plotting observed vs. predicted outcomes and calculating metrics like the calibration slope (ideal = 1) [88] [92].
- Perform subgroup analyses to identify performance variations across patient demographics or clinical sites.
- Clinical Utility Assessment:
Diagram 1: Geographical validation workflow.
Protocol 3: Bridging the Gap with Explainability and Clinical Integration
Objective: To enhance the interpretability of a validated model and define a pathway for its integration into the clinical workflow to ensure adoption.
Background: A model's clinical utility is not solely determined by its accuracy but also by its transparency and ability to fit seamlessly into existing clinical pathways, providing actionable insights to clinicians [88] [92].
Materials:
- A trained and externally validated model.
- Access to a development environment for creating visualizations and APIs.
Procedure:
- Implement Explainable AI (XAI) Techniques:
- For knowledge-based models, report the contribution of key features (e.g., specific texture or shape features).
- For DL models, use methods like SHapley Additive exPlanations (SHAP) or Layer-wise Relevance Propagation (LRP) to generate heatmaps highlighting image regions most influential to the prediction [92].
- Develop a Clinical Decision Support Interface:
- Create a user-friendly interface, such as a web application, that allows clinicians to input patient data and receive model predictions.
- The interface should display the prediction, a confidence score, and the explainable output (e.g., heatmap on the original image).
- Pilot Integration and Workflow Analysis:
- Deploy the tool in a limited pilot setting within a clinical department.
- Observe and document the interaction between clinicians and the tool, gathering feedback on usability, trust, and impact on decision-making time.
- Use this feedback to iteratively refine the tool and its integration points (e.g., PACS/RIS integration).
Diagram 2: Clinical integration with explainability.
Table 3: Key Research Reagent Solutions for Feature Extraction and Model Validation
| Item/Category | Specific Examples | Function/Application in Research |
|---|---|---|
| Feature Extraction Libraries | Scikit-image (for GLCM, GLRLM), OpenCV (for SIFT, SURF), PyTorch/TensorFlow (for CNNs) [5] [91]. | Provides standardized algorithms to extract handcrafted and deep learning-based features from medical images. |
| Pre-trained Deep Learning Models | VGG16, ResNet50, DenseNet [5] [90]. | Used for transfer learning, where a model developed for a general task is fine-tuned on a specific medical imaging dataset, reducing data and computational requirements. |
| Model Validation Frameworks | Scikit-learn, pmsampsize (R package), SHAP and LIME libraries [89] [92]. |
Provides tools for calculating performance metrics, performing decision curve analysis, and generating explanations for model predictions. |
| Publicly Available Datasets | BreakHis (breast histopathology), HAM10000 (skin lesions), MIAS (mammography), LIDC-IDRI (lung CT) [5] [17] [90]. | Serves as benchmarks for developing and initially validating models, allowing for comparison across different studies. |
| Clinical Data Standards | CDISC (Clinical Data Interchange Standards Consortium), FHIR (Fast Healthcare Interoperability Resources) | Facilitates the structured collection and sharing of clinical data, which is crucial for multi-institutional validation studies. |
Conclusion
The evolution of feature extraction is fundamentally advancing cancer detection, with techniques ranging from bioinformatics-driven biomarker discovery to sophisticated deep learning and hybrid models demonstrating remarkable efficacy. The synthesis of research confirms that intelligent feature selection is not merely a preprocessing step but a pivotal component for building accurate, efficient, and interpretable diagnostic tools. Key takeaways include the superiority of multistage hybrid selection methods, the transformative potential of Vision Transformers and tissue-specific features, and the critical importance of robust validation and explainability for clinical adoption. Future directions must prioritize multi-site prospective trials, standardized reporting, and lifecycle monitoring to bridge the gap between technical performance and tangible patient impact. The continued integration of these advanced techniques promises to usher in a new era of precision oncology, enabling earlier detection and more personalized treatment strategies.
References
- 1. Emerging Technologies in Biomarker Discovery You ... [https://blog.crownbio.com/emerging-technologies-in-biomarker-discovery-you-should-know-about]
- 2. Machine Learning Methods for Cancer Classification Using ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9952758/]
- 3. Ten quick tips for biomarker discovery and validation ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9371329/]
- 4. A Hybrid Sequential Feature Selection Approach for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12293090/]
- 5. Deep Learning- and Expert Knowledge-Based Feature ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10296694/]
- 6. The Cancer Genome Atlas Program (TCGA) - NCI [https://www.cancer.gov/ccg/research/genome-sequencing/tcga]
- 7. UCSC Xena [https://xena.ucsc.edu/]
- 8. Basic Tutorial: Section 1 | User Help Pages [https://ucsc-xena.gitbook.io/project/tutorials/basic-tutorial-section-1]
- 9. TCGA and CGGA data analysis [https://bio-protocol.org/exchange/minidetail?id=2519425&type=30]
- 10. Updated overview of current biomarkers in head and neck ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4804254/]
- 11. Current and Emerging Diagnostic, Prognostic, and ... [https://www.mdpi.com/2227-9059/12/2/415]
- 12. Biomarkers in head and neck squamous cell carcinoma [https://www.frontiersin.org/journals/oncology/articles/10.3389/fonc.2024.1473706/full]
- 13. Longitudinal liquid biopsy identifies an early predictive ... [https://www.nature.com/articles/s41467-025-63538-4]
- 14. Machine-learning derived identification of prognostic ... [https://pubmed.ncbi.nlm.nih.gov/39749326/]
- 15. Multistage feature selection and stacked generalization ... [https://www.nature.com/articles/s41598-025-08865-8]
- 16. Current advances in prognostic and diagnostic biomarkers ... [https://www.sciencedirect.com/science/article/pii/S0753332221012749]
- 17. Innovative deep learning classifiers for breast cancer ... [https://www.nature.com/articles/s41598-025-06669-4]
- 18. Recent Advancements in Feature Extraction and ... [https://pubmed.ncbi.nlm.nih.gov/40578387/]
- 19. A hybrid feature extraction based ensemble model for ... [https://www.sciencedirect.com/science/article/pii/S2666521225000948]
- 20. Current AI technologies in cancer diagnostics and treatment [https://molecular-cancer.biomedcentral.com/articles/10.1186/s12943-025-02369-9]
- 21. The AI revolution: how multimodal intelligence will reshape ... [https://www.nature.com/articles/s44387-025-00044-4]
- 22. Advanced Feature Extraction for Cervical Cancer Image ... [https://www.mdpi.com/1424-8220/25/9/2826]
- 23. Flatiron Health research on AI-driven cancer progression ... [https://resources.flatiron.com/press/flatiron-health-research-on-ai-driven-cancer-progression-extraction-presented-at-aacr-special-conference-in-cancer-research-artificial-intelligence]
- 24. Eye on AI: Applying Artificial Intelligence to Drive Cancer ... [https://www.aacr.org/blog/2025/08/18/eye-on-ai-applying-artificial-intelligence-to-drive-cancer-research-part-2/]
- 25. Artificial intelligence in cancer: applications, challenges, and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12574039/]
- 26. Multistage feature selection and stacked generalization ... [https://pubmed.ncbi.nlm.nih.gov/41173962/?utm_source=FeedFetcher&utm_medium=rss&utm_campaign=None&utm_content=1xGbfOrFGi2c0h8ddH9Dhgz9SiurYzR5ZX62n_EtQNj6jwlA_&fc=None&ff=20251102151122&v=2.18.0.post22+67771e2]
- 27. SMAGS-LASSO: A Novel Feature Selection Method for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12570486/]
- 28. What is the difference between filter, wrapper, and ... [https://sebastianraschka.com/faq/docs/feature_sele_categories.html]
- 29. Feature Selection with Embedded Methods [https://www.blog.trainindata.com/feature-selection-with-embedded-methods/]
- 30. Feature Selection Techniques in Machine Learning [https://www.geeksforgeeks.org/machine-learning/feature-selection-techniques-in-machine-learning/]
- 31. ViT-DCNN: Vision Transformer with Deformable CNN ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12468260/]
- 32. A hybrid explainable federated-based vision transformer ... [https://www.nature.com/articles/s41598-025-96527-0]
- 33. An attention based hybrid approach using CNN and ... [https://www.nature.com/articles/s41598-025-00025-2]
- 34. Skin cancer image classification using hybrid quantum ... [https://link.springer.com/article/10.1007/s42484-025-00288-y]
- 35. Comparative Analysis of Vision Transformers and ... [https://arxiv.org/html/2507.21156v1]
- 36. Exploring AI Approaches for Breast Cancer Detection and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12553387/]
- 37. Early cancer detection using deep learning and medical ... [https://www.sciencedirect.com/science/article/pii/S1040842824002713]
- 38. Deep Learning Applications in Clinical Cancer Detection [https://www.sciencedirect.com/science/article/pii/S2949761225000604]
- 39. Examining feature extraction and classification modules in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11234229/]
- 40. A novel hybrid feature fusion approach using handcrafted ... [https://www.sciencedirect.com/science/article/abs/pii/S001048252500455X]
- 41. Fusion of classical and deep learning features with ... [https://www.nature.com/articles/s41598-025-24734-w]
- 42. Breast Cancer Classification with Various Optimized Deep ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12293705/]
- 43. Hybrid Deep Learning and Handcrafted Feature Fusion for ... [https://arxiv.org/html/2507.19843v1]
- 44. Ensemble of Handcrafted and Learned Features for ... [https://pubmed.ncbi.nlm.nih.gov/40760266/]
- 45. Deep Learning for Cancer Detection Based on Genomic and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12459622/]
- 46. A Novel Double Pruning method for Imbalanced Data ... [https://www.sciencedirect.com/science/article/abs/pii/S095070512501442X]
- 47. A hybrid GAN-based deep learning framework for ... - Nature [https://www.nature.com/articles/s41598-025-04676-z]
- 48. Gan-based data augmentation to improve breast ... [https://www.sciencedirect.com/science/article/pii/S1746809424003136]
- 49. AI and clinical research: the use of synthetic real-world data [https://dailyreporter.esmo.org/esmo-ai-digital-oncology-congress-2025/editorial/how-ai-is-expediting-clinical-research-the-use-of-synthetic-real-world-data]
- 50. Addressing the current challenges in the clinical application of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12515897/]
- 51. Domain Shift Resilient Mammography Classification using ... [https://arxiv.org/html/2508.15452v2]
- 52. Robustness tests for biomedical foundation models should ... [https://www.nature.com/articles/s41746-025-01926-2]
- 53. MIDOG 2025 Challenge [https://www.emergentmind.com/topics/midog-2025-challenge]
- 54. Language-guided multimodal domain generalization for ... [https://www.sciencedirect.com/science/article/abs/pii/S0010482525013447]
- 55. Explainable AI in Clinical Decision Support Systems [https://pmc.ncbi.nlm.nih.gov/articles/PMC12427955/]
- 56. Comparison of SHAP and clinician friendly explanations ... [https://www.nature.com/articles/s41746-025-01958-8]
- 57. A Comprehensive Framework for Accountable AI in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12383817/]
- 58. Guiding Principles - Transparency for Machine Learning ... [https://www.fda.gov/medical-devices/software-medical-device-samd/transparency-machine-learning-enabled-medical-devices-guiding-principles]
- 59. LIME vs SHAP: A Comparative Analysis of Interpretability ... [https://www.markovml.com/blog/lime-vs-shap]
- 60. A quantitative approach for the comparison of additive local ... [https://www.sciencedirect.com/science/article/abs/pii/S0306437922001405]
- 61. Guidelines and evaluation of clinical explainable AI in ... [https://www.sciencedirect.com/science/article/abs/pii/S1361841522003127]
- 62. Improved cancer detection through feature selection using ... [https://www.nature.com/articles/s41598-025-92187-2]
- 63. Image feature extraction techniques: A comprehensive ... [https://www.sciencedirect.com/science/article/pii/S2773186325001549]
- 64. Transformer-Based Feature Extraction and Optimized ... [https://pubmed.ncbi.nlm.nih.gov/41003967/]
- 65. Deep learning-based computational approach for predicting ... [https://bmccancer.biomedcentral.com/articles/10.1186/s12885-025-14113-z]
- 66. comparative study of CT and MRI in cervical cancer ... [https://www.frontiersin.org/journals/oncology/articles/10.3389/fonc.2025.1608386/full]
- 67. A Guide to Cross-Validation for Artificial Intelligence in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10388213/]
- 68. Applications of Machine Learning in Cancer Prediction and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC2675494/]
- 69. The stratified K-folds cross-validation and class-balancing ... [https://www.sciencedirect.com/science/article/pii/S2772442523001144]
- 70. Multistage feature selection and stacked generalization ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12579239/]
- 71. A Two-Step Feature Selection Method to Predict ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5820548/]
- 72. Machine learning-based lung and colon cancer detection ... [https://www.sciencedirect.com/science/article/pii/S0957417422009873]
- 73. 12 Important Model Evaluation Metrics for Machine ... [https://www.analyticsvidhya.com/blog/2019/08/11-important-model-evaluation-error-metrics/]
- 74. Machine Learning Evaluation Metrics: What Really Matters? [https://labelstud.io/learningcenter/machine-learning-evaluation-metrics-what-really-matters/]
- 75. How to Check the Accuracy of Your Machine Learning ... [https://www.deepchecks.com/how-to-check-the-accuracy-of-your-machine-learning-model/]
- 76. Review of Artificial Intelligence Techniques for Breast Cancer ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12561872/]
- 77. Topological insights and hybrid feature extraction for breast ... [https://peerj.com/articles/cs-3374/]
- 78. Trade-Off Analysis of Classical Machine Learning and Deep ... [https://ai.jmir.org/2025/1/e76344]
- 79. Statistical variability in comparing accuracy of ... [https://www.nature.com/articles/s41598-025-12026-2]
- 80. Advanced Techniques Boost Cancer Detection Accuracy [https://bioengineer.org/advanced-techniques-boost-cancer-detection-accuracy/]
- 81. Integrated feature selection-based stacking ensemble ... [https://www.sciencedirect.com/science/article/pii/S2588914125000206]
- 82. An enhanced machine learning approach with stacking ... [https://www.sciencedirect.com/science/article/pii/S2772442524000753]
- 83. Framework for Race-Specific Prostate Cancer Detection Using ... [https://bioinform.jmir.org/2025/1/e72423]
- 84. A robust stacked neural network approach for early and ... [https://www.frontiersin.org/journals/medicine/articles/10.3389/fmed.2025.1644857/full]
- 85. Enhanced and Interpretable Prediction of Multiple Cancer ... [https://www.mdpi.com/2306-5354/12/5/472]
- 86. SMAGS-LASSO: A Novel Feature Selection Method ... - PubMed [https://pubmed.ncbi.nlm.nih.gov/40996315/]
- 87. Stacked Deep Learning Ensemble for Multiomics Cancer ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12342693/]
- 88. and Externally useful machine learning algorithms... validated clinically [https://bmcmedresmethodol.biomedcentral.com/articles/10.1186/s12874-025-02463-y]
- 89. Minimum sample size for external of a validation prediction... clinical [https://pubmed.ncbi.nlm.nih.gov/34031906/]
- 90. Enhanced skin cancer diagnosis: a deep feature extraction ... [https://www.frontiersin.org/journals/medicine/articles/10.3389/fmed.2024.1495576/full]
- 91. Analysing Feature Extraction Methods for Enhanced ... [https://link.springer.com/chapter/10.1007/978-981-97-4799-3_31]
- 92. Explainable machine learning model for predicting cesarean section... [https://journals.plos.org/digitalhealth/article?id=10.1371/journal.pdig.0001061]