A Systematic Review of Machine Learning in Cancer Research: From Diagnostics to Precision Therapeutics
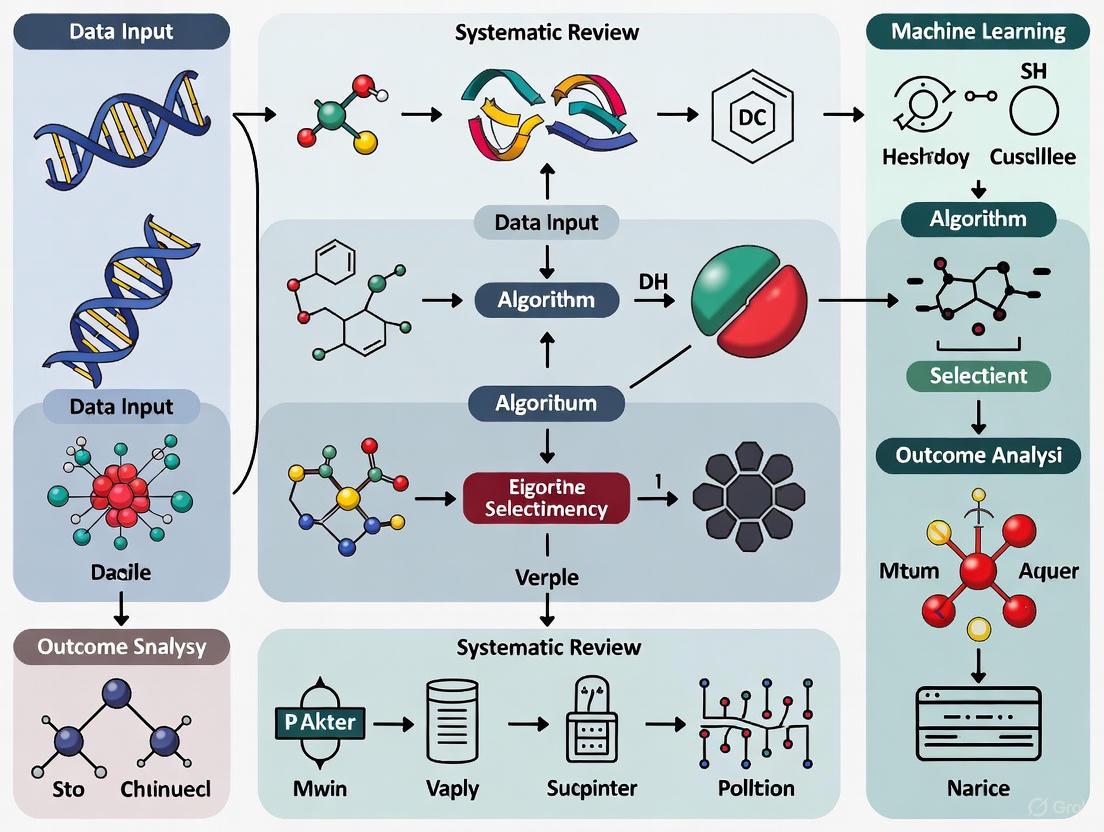
This systematic review synthesizes the current landscape of machine learning (ML) applications in oncology, addressing its transformative potential across the cancer care continuum.
A Systematic Review of Machine Learning in Cancer Research: From Diagnostics to Precision Therapeutics
Abstract
This systematic review synthesizes the current landscape of machine learning (ML) applications in oncology, addressing its transformative potential across the cancer care continuum. It explores the foundational principles of ML and the diverse data modalities, such as medical imaging, genomics, and clinical records, that fuel these applications. The review methodically catalogs ML's role in enhancing cancer screening, diagnosis, prognostic prediction, and the development of personalized treatment strategies, including drug discovery and therapy optimization. It critically examines the methodological challenges, including data heterogeneity, model interpretability, and computational demands, while providing insights into optimization techniques. Furthermore, a comparative analysis validates the performance of various ML algorithms against traditional statistical methods, highlighting contexts where ML offers superior predictive accuracy. Aimed at researchers, scientists, and drug development professionals, this article serves as a comprehensive resource on the integration of artificial intelligence to advance precision oncology and improve patient outcomes.
The AI Revolution in Oncology: Core Concepts and Data Landscapes
Artificial intelligence (AI) is rapidly revolutionizing the landscape of oncological research and the advancement of personalized clinical interventions [1]. Progress in three interconnected areas—the development of sophisticated methods and algorithms for training AI models, the evolution of specialized computing hardware, and increased access to large volumes of multimodal cancer data—has converged to create promising new applications across the cancer research spectrum [1]. This technical guide provides a systematic overview of the core components of the AI toolbox, focusing on machine learning (ML), deep learning (DL), and neural networks within the context of cancer research. We examine their fundamental principles, illustrate their applications with quantitative performance data, detail experimental methodologies, and visualize key workflows to inform researchers, scientists, and drug development professionals.
Core AI Concepts and Terminology
Defining the AI Landscape
In oncology, AI systems leverage diverse data modalities, including medical imaging, genomics, and clinical records, to address complex challenges from early detection to treatment optimization [1]. The selection of appropriate AI models depends fundamentally on the data type and specific clinical objective [1]. The field encompasses several interconnected disciplines:
Artificial Intelligence (AI): The broadest term, referring to machines designed to mimic cognitive functions such as learning and problem-solving. In clinical research, AI describes "intelligent agents" capable of perceiving their environment and making decisions to optimize objective achievement [2].
Machine Learning (ML): A subset of AI that enables systems to learn from data, recognize patterns, and make decisions with minimal human intervention [1]. ML algorithms often analyze structured data such as genomic biomarkers and laboratory values using classical models including logistic regression and ensemble methods for tasks like survival prediction or therapy response assessment [1].
Deep Learning (DL): A specialized subset of ML utilizing multi-layered neural networks [3]. DL has demonstrated transformative potential across diverse applications, including imaging-based diagnostics and genomic analysis, ultimately leading to improved detection and personalized cancer treatment [4]. DL architectures are particularly valuable for processing unstructured or complex data types including medical images and genomic sequences.
Neural Network Architectures in Oncology
Table 1: Key Neural Network Architectures in Cancer Research
| Architecture | Primary Data Types | Common Oncology Applications | Key Features |
|---|---|---|---|
| Convolutional Neural Networks (CNNs) [1] | Imaging data (histopathology, radiology) [1] | Tumor detection, segmentation, and grading [1] | Spatial feature extraction using convolutional layers [5] |
| Graph Neural Networks (GNNs) [5] | Non-Euclidean data, graph structures [5] | Brain tumor classification [5] | Models relationships and dependencies between nodes [5] |
| Recurrent Neural Networks (RNNs) [1] | Sequential data (genomic sequences, clinical notes) [1] | Biomarker discovery, EHR mining [1] | Handles sequential dependencies through memory cells |
| Transformers & Large Language Models (LLMs) [1] | Text data, scientific literature [1] | Knowledge extraction from clinical notes, hypothesis generation [1] | Captures long-range dependencies in textual data |
| Hybrid Architectures (CNN-GNN) [5] | Imaging data represented as graphs [5] | Enhanced brain tumor classification [5] | Combines spatial feature learning with relational reasoning |
Quantitative Performance Benchmarks
The implementation of AI tools across various cancer domains has yielded substantial performance improvements in detection, classification, and prognostic tasks. The tables below summarize key quantitative benchmarks from recent studies.
Table 2: AI Performance in Cancer Detection and Diagnosis
| Cancer Type | Modality | Task | AI System | Sensitivity (%) | Specificity (%) | AUC | Accuracy (%) | Ref |
|---|---|---|---|---|---|---|---|---|
| Colorectal Cancer | Colonoscopy | Malignancy detection | CRCNet | 91.3 vs. 83.8 (human) | 85.3 (AI) | 0.882 | - | [1] |
| Breast Cancer | 2D Mammography | Screening detection | Ensemble DL model | +9.4% (US vs. radiologists) | +5.7% (US vs. radiologists) | 0.810 (US) | - | [1] |
| Brain Tumor | MRI | Binary classification | BCM-CNN | - | - | - | 99.98 | [3] |
| Brain Tumor | MRI | Multi-class classification | CNN-GNN | - | - | - | 95.01 | [5] |
| Multiple Cancers | Histopathology | Subtype classification | AEON + OncoTree | - | - | - | 78.0 | [6] |
Table 3: AI Performance in Liquid Biopsy and Prognostic Tasks
| Application | Method | Task | Key Performance Metrics | Ref |
|---|---|---|---|---|
| Liquid Biopsy | RED Algorithm | Rare cancer cell detection | Found 99% of added epithelial cancer cells; Reduced data review by 1000x | [7] |
| Tumor-Stroma Ratio Estimation | Attention U-Net | Prognostic biomarker assessment | ICC: 0.69; More consistent than human experts (DR: 0.86) | [8] |
| Immunotherapy Response Prediction | Synthetic Patient Data | Treatment response prediction | 68.3% accuracy with synthetic data vs. 67.9% with real patient data | [6] |
Experimental Protocols and Methodologies
Protocol: Brain Tumor Classification Using CNN-GNN Architecture
Objective: To classify brain tumors into meningioma, pituitary, or glioma types using a hybrid Graph Convolutional Neural Network (GCNN) model that addresses non-Euclidean distances in image data [5].
Materials:
- Dataset: Publicly available Brain Tumor dataset from Kaggle containing MRI images [5].
- Computational Framework: Python with deep learning libraries (e.g., PyTorch, TensorFlow).
- Hardware: GPU-accelerated computing system.
Methodology:
- Data Preprocessing:
- Convert MRI images to graph structures where pixels represent nodes and edges represent relationships.
- Generate a standard pre-computed adjacency matrix to define node connections [5].
- Normalize pixel intensities across the dataset.
Graph Convolution Operation:
- Modify node features by combining information from nearby nodes using the adjacency matrix.
- Update input graphs as the averaged sum of local neighbor nodes to capture regional tumor information [5].
- These modified graphs serve as input matrices for the subsequent CNN.
CNN Architecture:
Training Protocol:
- Utilize appropriate loss functions (e.g., cross-entropy) for multi-class classification.
- Implement backpropagation for weight optimization.
- Employ validation sets for hyperparameter tuning.
Validation:
- Perform k-fold cross-validation to ensure robustness.
- Compare performance against human radiologists and other ML benchmarks.
Brain Tumor Classification Workflow Using Hybrid CNN-GNN Architecture
Protocol: Rare Cancer Cell Detection in Liquid Biopsies
Objective: To automate detection of rare cancer cells in blood samples using the RED (Rare Event Detection) algorithm without requiring prior knowledge of cancer cell features [7].
Materials:
- Blood Samples: From patients with advanced cancer or normal blood samples spiked with cancer cells.
- Platform: Liquid biopsy workflow for cell capture and imaging.
- Algorithm: RED deep learning algorithm based on rarity ranking rather than feature identification [7].
Methodology:
- Sample Preparation:
- Collect blood samples from patients with known advanced cancer.
- Alternatively, spike normal blood samples with known quantities of epithelial and endothelial cancer cells for validation [7].
Image Acquisition:
- Process blood samples through liquid biopsy platform.
- Generate high-resolution images of cells captured from blood.
AI Analysis with RED Algorithm:
- Implement RED algorithm to identify unusual patterns among millions of normal blood cells.
- The algorithm ranks cells by rarity, causing the most unusual findings (potential cancer cells) to rise to the top [7].
- Unlike traditional approaches, RED does not require specific known features of cancer cells, instead functioning like a "one of these things is not like the others" detection system [7].
Validation:
- Compare RED performance against human expert review.
- Quantify detection rates for spiked cancer cells (epithelial and endothelial).
- Measure reduction in data requiring human review.
Application:
- Deploy validated algorithm to answer critical clinical questions: "Do I have cancer?", "Is my cancer gone or coming back?", and "What is the best next treatment for my cancer?" [7].
Essential Research Reagent Solutions
Table 4: Key Research Reagents and Materials for AI-Cancer Research
| Reagent/Material | Function in AI-Cancer Research | Application Examples |
|---|---|---|
| Histo-AI Dataset [8] | Provides annotated whole slide images for training and validation | Tumor-Stroma Ratio estimation models |
| TCGA-BRCA Dataset [8] | Offers multi-institutional histopathology data with clinical correlates | Development of prognostic AI biomarkers |
| BRaTS 2021 Task 1 Dataset [3] | Curated brain MRI images with tumor annotations | Brain tumor segmentation and classification models |
| Figshare Brain Tumor Dataset [5] | MRI image collection for multi-class tumor classification | Benchmarking brain tumor classification algorithms |
| OncoTree Classification System [6] | Open-source cancer type classification system | Histologic subtype classification from H&E images |
| Synthetic Patient Data [6] | AI-generated clinical and pathology data | Augmenting training datasets and imputing missing data |
AI in Clinical Trials and Drug Development
AI is transforming clinical trials by dramatically reducing timelines and costs, accelerating patient-centered drug development, and creating more efficient trials [9]. Specific applications include:
Patient Recruitment: AI-powered natural language processing analyzes structured and unstructured electronic health record data to identify protocol-eligible patients three times faster with 93% accuracy [9]. Platforms like Dyania Health demonstrate 170x speed improvement in patient identification compared to manual review [9].
Protocol Optimization: More than half of AI startups in clinical development focus on patient recruitment and protocol optimization, enabling real-time intervention and continuous protocol refinement [9].
Drug Discovery: AI supports target identification, biomarker discovery, and validation of drug candidates through structure-based virtual screening (SBVS) and ligand-based virtual screening (LBVS), speeding up the identification of potential drug candidates [2].
AI Applications in Clinical Trial Workflow
Challenges and Future Directions
Despite the promising applications, integrating DL into clinical practice presents substantial challenges including limitations in data quality and standardization, ethical and regulatory concerns, and the need for model interpretability and transparency [4]. Emerging solutions include federated learning to address data privacy concerns, explainable AI (XAI) to enhance model interpretability, and synthetic data generation to augment limited datasets [4]. The future of AI in cancer research will likely involve increased interdisciplinary collaboration, integration of next-generation AI techniques, and adoption of multimodal data approaches to improve diagnostic precision and support personalized cancer treatment [4]. Establishing industry-wide ethical standards and robust safeguards is essential for the protection of human dignity, privacy, and rights as these technologies continue to evolve [2].
Cancer manifests across multiple biological scales, from molecular alterations and cellular morphology to tissue organization and clinical phenotype [10]. Predictive models relying on a single data modality fail to capture this multiscale heterogeneity, fundamentally limiting their ability to generalize across patient populations and clinical settings [11]. Multimodal data integration has emerged as a transformative approach in oncology, systematically combining complementary biological and clinical data sources to provide a multidimensional perspective of patient health [12]. The integration of diverse data streams—including genomics, medical imaging, electronic health records (EHRs), and wearable device outputs—enables a more comprehensive understanding of cancer biology, leading to more accurate diagnoses, personalized treatment plans, and improved patient outcomes [12] [10].
The rise of artificial intelligence (AI) and machine learning (ML) has been instrumental in advancing multimodal integration, providing sophisticated methodologies capable of handling large, complex datasets [12] [13]. Through AI-driven integration of multimodal data, health care providers can achieve a more holistic view of cancer pathology, capturing the intricate interplay between genetic predisposition, tumor microenvironment, and clinical manifestations [14] [11]. This technical guide examines the current state of multimodal data integration in cancer research, focusing on methodological frameworks, clinical applications, and implementation protocols within the broader context of a systematic review of machine learning in oncology.
Foundations of Multimodal Integration
Data Modalities in Oncology
Multimodal integration in cancer research leverages several core data types, each providing unique insights into disease mechanisms and progression:
Genomics and Multi-omics Data: This category encompasses DNA sequencing data, gene expression profiles, epigenetic markers, and proteomic data. These modalities help identify genetic mutations, molecular subtypes, and potential biomarkers for cancer diagnosis, prognosis, and treatment selection [15] [11]. Integrated genomic analysis methods can reveal dysregulation in biological functions and molecular pathways, offering new opportunities for personalized treatment and monitoring [12].
Medical Imaging: Includes data from magnetic resonance imaging (MRI), computed tomography (CT) scans, positron emission tomography (PET), and digital histopathology [12] [16]. These modalities provide detailed anatomical and functional views of the body, offering information about tumor location, size, shape, and characteristics that aid in cancer diagnosis, staging, and treatment planning [15]. Quantitative multimodal imaging technologies combine multiple functional measurements, providing comprehensive characterization of tumor phenotypes [12].
Clinical Records and EHRs: Contain a wealth of clinical information, including patient history, diagnoses, treatments, outcomes, laboratory results, and medication records, which are essential for longitudinal health monitoring [12] [17]. These data sources provide context for molecular and imaging findings and help establish clinical correlations.
Emerging Data Sources: Include wearable device outputs that continuously monitor physiological parameters, providing real-time data on a patient's health status [12], as well as spatial transcriptomics and immunological profiles that capture tumor microenvironment dynamics [11].
The Integration Imperative
Each data modality provides valuable but incomplete insights into patient health when considered in isolation [12]. For example, genomic data may reveal targetable mutations but lack spatial context, while imaging provides structural information but limited molecular characterization. Multimodal integration addresses these limitations by fusing complementary sources for a holistic view of cancer, selectively prioritizing disease-relevant modalities to minimize noise and capture cross-scale dependencies [11].
Evidence indicates that selective integration—limiting analysis to 3–5 core modalities—often yields better predictive performance, with AUC improvements of 10–15% over unimodal baselines in oncology applications [11]. The integration of these diverse data sources enables more nuanced tumor characterization, enhanced prognostic accuracy, and personalized treatment strategies that account for the complex, multifactorial nature of cancer biology [12] [14].
Methodological Frameworks and Techniques
Machine Learning Approaches
Multimodal data integration employs diverse machine learning strategies, each with distinct advantages for handling heterogeneous oncology data:
Table 1: Machine Learning Approaches for Multimodal Data Integration in Cancer Research
| Method Category | Key Techniques | Applications in Oncology | Advantages |
|---|---|---|---|
| Traditional ML | Random Forests, Gradient Boosting, Support Vector Machines | Cancer subtype classification, risk stratification | Handles structured data well; interpretable results |
| Deep Learning | Convolutional Neural Networks (CNNs), Recurrent Neural Networks (RNNs), Transformers | Histopathology image analysis, genomic sequence prediction, temporal data modeling | Automatically learns relevant features from complex data; handles unstructured data |
| Multimodal Fusion | Early fusion, late fusion, hybrid approaches, attention mechanisms | Integrative prognosis, treatment response prediction | Captures cross-modal interactions; flexible architecture |
| Emerging Architectures | Graph Neural Networks, Deep Latent Variable Models, Foundation Models | Pan-cancer analysis, biomarker discovery, drug response prediction | Models complex relationships; transfers knowledge across domains |
Fusion Strategies
The integration of multimodal data can be implemented through several technical approaches:
Early Fusion: Combines raw data from multiple modalities at the input level before feature extraction. This approach can capture fine-grained interactions but requires careful data alignment and may amplify noise or dimensionality issues [11].
Late Fusion: Processes each modality independently through separate models and combines the outputs at the decision level. This strategy offers robustness against missing data and modality-specific processing but may overlook important cross-modal interactions [11].
Intermediate/Hybrid Fusion: Incorporates cross-modal interactions at intermediate processing stages using attention mechanisms, tensor fusion, or other joint representation learning techniques. Approaches like Deep Latent Variable Path Modelling (DLVPM) combine the representational power of deep learning with the capacity of path modelling to identify relationships between interacting elements in a complex system [14].
Cross-Modal Learning: Leverages information from one modality to enhance learning in another, such as predicting genetic alterations from histology images or generating synthetic medical images from clinical data [14] [10].
Advanced Integration Framework: Deep Latent Variable Path Modelling
Deep Latent Variable Path Modelling (DLVPM) represents a cutting-edge approach that combines the flexibility of deep neural networks with the interpretability and structure of path modelling [14]. This framework enables researchers to map complex dependencies between different data types relevant to cancer biology.
In DLVPM, a collection of submodels (measurement models) is defined for each data type:
Where Ȳ_i is the network output (a set of deep latent variables or DLVs), X_i is the data input, U_i is the set of parameters up to the penultimate network layer, and W_i corresponds to the network weights on the final layer [14].
The DLVPM algorithm is trained to construct DLVs from each measurement model that are optimized to be maximally associated with DLVs from other measurement models connected by the path model, with the optimization criteria:
Where c_ij represents the association matrix input from data type i to data type j, and tr denotes the matrix trace [14]. This approach has demonstrated superior performance in mapping associations between data types compared with classical path modelling, particularly in identifying histologic-transcriptional associations using spatial transcriptomic data [14].
Diagram: DLVPM Framework for Multimodal Data Integration. This architecture shows how DLVPM creates a joint embedding space from diverse data modalities using measurement models and path modelling.
Experimental Protocols and Implementation
Standardized Workflow for Multimodal Integration
Implementing a robust multimodal integration system requires a systematic approach to data processing, model development, and validation:
Diagram: Multimodal Integration Workflow. This flowchart outlines the key stages in developing and deploying multimodal AI systems in oncology.
Protocol 1: Data Preprocessing and Harmonization
Objective: Standardize heterogeneous data sources to enable meaningful integration.
Materials and Methods:
- Data Collection: Acquire multi-omics data (genomics, transcriptomics, epigenetics), medical images (histopathology, radiology), and clinical records from sources such as The Cancer Genome Atlas (TCGA) or institutional databases [14] [15].
- Quality Control: Implement modality-specific quality metrics. For genomic data: sequence quality scores, mapping rates. For imaging: signal-to-noise ratios, contrast measurements. For clinical data: completeness, consistency checks [16] [17].
- Normalization: Apply batch effect correction methods like ComBat or cross-modal harmonization techniques to account for technical variability across datasets [11].
- Feature Extraction: Utilize automated feature extraction for images (CNNs), sequence embedding for genomic data, and structured feature engineering for clinical variables [16] [15].
Validation: Assess data quality through dimensionality reduction (PCA, t-SNE) and cluster consistency metrics to ensure biological signals are preserved while technical artifacts are minimized.
Protocol 2: Multimodal Model Development with DLVPM
Objective: Implement the DLVPM framework to integrate genomic, histopathological, and clinical data for cancer outcome prediction.
Materials and Methods:
- Architecture Specification: Define measurement models for each modality:
- Genomic data: Fully connected neural networks with embedding layers
- Histopathology images: Convolutional Neural Networks (e.g., ResNet variants)
- Clinical data: Tabular neural networks or gradient boosting machines [14]
- Path Model Definition: Specify the hypothesized relationships between modalities based on cancer biology (e.g., genomic alterations → transcriptomic changes → histologic manifestations → clinical outcomes) [14].
- Model Training: Implement orthogonalization constraints to ensure DLVs capture complementary information:
where
Iis the identity matrix [14]. - Optimization: Use stochastic gradient descent with adaptive learning rates to maximize the association between connected modalities as defined in the path model.
Validation: Perform k-fold cross-validation and external validation on held-out datasets. Compare performance against unimodal baselines and alternative multimodal approaches using time-dependent AUC for survival prediction or standard AUC for classification tasks.
Protocol 3: Explainability and Biological Interpretation
Objective: Ensure model predictions are interpretable and biologically plausible.
Materials and Methods:
- Explainable AI Techniques: Implement SHAP (SHapley Additive exPlanations), LIME (Local Interpretable Model-agnostic Explanations), and attention mechanisms to attribute predictions to input features [11] [17].
- Biological Validation: Correlate model-derived features with established cancer biomarkers and pathways. Perform gene set enrichment analysis on important genomic features identified by the model [11].
- Clinical Correlation: Assess whether model attention aligns with regions of interest identified by pathologists or radiologists through spatial correlation analysis [11].
Validation: Quantify explanation stability across similar patients and assess inter-rater reliability between model explanations and clinician annotations.
Performance Metrics and Comparative Analysis
Multimodal integration approaches have demonstrated significant improvements across various cancer types and clinical applications. The following tables summarize key performance metrics from recent studies:
Table 2: Performance of Multimodal AI in Cancer Diagnosis and Prognosis
| Cancer Type | Application | Data Modalities | Performance Metrics | Reference |
|---|---|---|---|---|
| Lung Cancer | Diagnosis | CT imaging, clinical data | Sensitivity: 0.86, Specificity: 0.86, AUC: 0.92 | [16] |
| Lung Cancer | Prognosis | Imaging, genomics, clinical | HR for OS: 2.53, HR for PFS: 2.80 | [16] |
| Breast Cancer | Treatment Response | Radiology, pathology, clinical | AUC: 0.91 for anti-HER2 therapy response | [12] |
| Multiple Cancers | Classification | Genomics, histopathology, clinical | 10-15% AUC improvement over unimodal baselines | [11] |
| Melanoma | Relapse Prediction | Histopathology, genomics, clinical | 5-year relapse prediction AUC: 0.833 | [10] |
Table 3: Comparison of Machine Learning Approaches for Cancer Research
| Method | Best For | Advantages | Limitations | Typical Performance |
|---|---|---|---|---|
| Traditional ML | Structured data, limited samples | Interpretable, computationally efficient | Limited capacity for complex patterns | AUC: 0.76-0.84 [17] |
| Deep Learning | Unstructured data, large datasets | Automatic feature extraction, high accuracy | Data hunger, computational intensity | AUC: 0.87-0.94 [16] |
| Multimodal DL | Heterogeneous data integration | Captures cross-modal interactions, improved performance | Complex implementation, interpretability challenges | AUC: 0.89-0.94 [16] [10] |
| Foundation Models | Transfer learning, few-shot applications | Generalizable, scalable | Massive data requirements, specialization needed | Emerging evidence [13] |
Successful implementation of multimodal integration in cancer research requires leveraging specialized tools, datasets, and computational resources:
Table 4: Essential Resources for Multimodal Cancer Research
| Resource Category | Specific Tools/Datasets | Key Features | Application in Research |
|---|---|---|---|
| Public Datasets | The Cancer Genome Atlas (TCGA) | Multi-omics, histopathology, clinical data across 33 cancer types | Model training, benchmarking, validation [14] |
| Public Datasets | UK Biobank | Multi-modal data from 500,000 participants, including imaging, genomics, health records | Epidemiological modeling, risk prediction [10] |
| Computational Frameworks | MONAI (Medical Open Network for AI) | PyTorch-based framework with pre-trained models for medical imaging | Image processing, model development [10] |
| Computational Frameworks | Deep Latent Variable Path Modelling | Combines deep learning with path modeling for multimodal integration | Mapping dependencies between data types [14] |
| Explainability Tools | SHAP, LIME | Model-agnostic interpretation methods for complex models | Feature importance analysis, model debugging [11] [17] |
| Clinical Data Tools | Electronic Health Record systems | Structured and unstructured clinical data | Patient stratification, outcome prediction [17] |
Challenges and Future Directions
Despite considerable progress, multimodal data integration in oncology faces several significant challenges:
Data Standardization and Harmonization: Heterogeneous data formats, batch effects, and platform-specific technical variations complicate integration efforts [12] [11]. Emerging solutions include adaptive normalization methods and reference-based harmonization protocols.
Computational Complexity: Processing and integrating large-scale multimodal datasets requires substantial computational resources and efficient algorithms [12] [13]. Distributed computing and specialized hardware acceleration offer promising pathways forward.
Interpretability and Trust: The "black box" nature of complex multimodal models hinders clinical adoption [11]. Explainable AI techniques that provide transparent, biologically plausible explanations are essential for building clinician trust and facilitating regulatory approval.
Data Privacy and Governance: Multimodal integration often requires pooling data from multiple institutions, raising concerns about patient privacy and data security [12]. Federated learning approaches that train models across decentralized data sources without sharing raw data represent a promising solution [11].
Future directions in multimodal integration include the development of large-scale foundation models pretrained on diverse cancer datasets [13], the incorporation of causal inference methods to move beyond correlations to mechanistic understanding [11], and the creation of "digital twins" that simulate cancer progression and treatment response for individual patients [11]. As these technologies mature, multimodal integration is poised to fundamentally transform oncology research and clinical practice, enabling truly personalized cancer care tailored to the unique biological characteristics of each patient and their disease.
Multimodal data integration represents a paradigm shift in cancer research, moving beyond single-modality analysis to a holistic approach that captures the complex, multi-scale nature of cancer biology. By leveraging advanced machine learning techniques to integrate genomic, imaging, and clinical data, researchers can achieve more accurate diagnosis, prognostication, and treatment selection than possible with any single data type alone. Frameworks like Deep Latent Variable Path Modelling provide powerful methodologies for mapping the complex dependencies between different data modalities, yielding insights into cancer mechanisms and improving patient outcomes.
While challenges remain in data standardization, computational complexity, and clinical interpretation, the rapid pace of innovation in multimodal AI suggests these barriers will be addressed in the coming years. As these technologies mature and validate in prospective clinical studies, multimodal integration is poised to become a cornerstone of precision oncology, enabling more personalized, effective, and timely cancer care. The continued development of robust, interpretable, and clinically actionable multimodal integration systems represents one of the most promising frontiers in the ongoing battle against cancer.
The integration of artificial intelligence (AI) in cancer research represents a fundamental transformation in how we diagnose, treat, and understand cancer. This evolution has progressed from early neural networks capable of identifying simple patterns to contemporary large language models (LLMs) that can interpret the complex "language" of cancer biology. The field has matured from proof-of-concept demonstrations to clinically validated tools that are beginning to impact patient care. Early machine learning applications in oncology focused primarily on structured data analysis and basic image classification, but contemporary approaches now tackle multimodal data integration, survival prediction, and personalized treatment planning with increasing sophistication. This systematic review examines the architectural innovations, methodological refinements, and expanding applications that have characterized this journey, highlighting how each technological advance has addressed specific challenges in cancer research and clinical oncology.
The Early Era: Artificial Neural Networks in Oncology
Fundamental Architecture and Learning Principles
Early artificial neural networks (ANNs) represented the first practical implementation of brain-inspired computational models in medicine. These statistical models reproduced the biological organization of neural cells to simulate the learning dynamics of the brain through interconnected layers of logical units (perceptrons). A typical feedforward network contained at least three layers: an input layer that received datasets related to research questions, one or more hidden layers that synthesized this data through nonlinear transformations, and an output layer that generated answers to research questions [18].
The unique properties of ANNs included robust performance with noisy or incomplete input patterns, high fault tolerance, and the ability to generalize from training data. Unlike conventional programming, ANNs could solve problems without algorithmic solutions or where existing solutions were excessively complex. They could recognize linear patterns, non-linear patterns with threshold impacts, categorical, step-wise linear, and contingency effects without requiring initial hypotheses or a priori identification of key variables [18]. This capability proved particularly valuable in oncology, where prognostic factors might exist within masses of datasets but could have been overlooked in prior analyses.
Methodological Considerations and Implementation Challenges
Successful implementation of ANNs in early cancer research required careful attention to methodological details to avoid common pitfalls:
Overfitting Prevention: ANNs with excessive hidden layers or neurons could perfectly reconstruct input-target relationships in training data but failed to generalize to new samples. Researchers maintained parsimony by preferring small networks with single hidden layers, which mathematically could approximate any continuous function [18].
Data-to-Parameter Ratio: The number of ANN free parameters (connection weights) needed to be at least one order of magnitude less than the number of input-target patterns, preferably two orders of magnitude less, to ensure reliable model performance [18].
Training Validation: Independent data splits were essential, with separate samples for training, validation, and testing. The validation set determined when to stop training (e.g., when performance on validation data began decreasing), while the test set evaluated performance on completely independent data [18].
Ensemble Modeling: Due to variability from random initial weight choices, researchers conducted multiple runs with different initial weights, either selecting the best-performing ANN or averaging outputs to minimize variability [18].
Early Applications in Cancer Research
Initial ANN applications demonstrated promising results across various oncology domains, particularly in lung cancer research. Early systems focused on discrete tasks such as improving diagnostic efficacy for small cell lung cancer (SCLC) and predicting survival time in advanced cases [18]. Despite their potential, systematic assessments revealed that ANN implementations in medical literature often contained methodological inaccuracies, highlighting the need for closer cooperation between physicians and biostatisticians to determine and resolve these errors [18].
Table 1: Early ANN Applications in Lung Cancer Research
| Study Focus | Architecture | Key Outcome | Limitations |
|---|---|---|---|
| SCLC Diagnosis | Feedforward ANN with backpropagation | Higher accuracy compared to conventional models | Limited dataset size |
| Advanced Lung Cancer Survival Prediction | Not specified | Accurate prediction of survival time | Single-institution data |
| Lung Cancer Detection | Multi-layer perceptron | Improved detection efficacy | Lack of external validation |
The Deep Learning Revolution: Convolutional Neural Networks in Cancer Imaging
Architectural Innovations and Technical Advantages
The advent of convolutional neural networks (CNNs) marked a revolutionary advance in cancer image analysis, particularly for histopathological imaging and radiological interpretation. CNNs demonstrated remarkable capability in automatically learning hierarchical feature representations directly from pixel data without relying on manual feature engineering [19]. This represented a significant departure from traditional machine learning approaches that depended on hand-crafted features whose performance was limited by feature selection and extraction methods [19].
CNN architectures effectively captured both local features and global context information through convolution and pooling operations [19]. This architectural superiority enabled CNNs to identify complex histopathological features in cancer diagnostics, including nuclear pleomorphism, nuclear-to-cytoplasm ratio, degree of cell arrangement disorder, and stromal response [19]. The capacity to learn these discriminative patterns directly from data positioned CNNs as the foundational technology for digital pathology and cancer image analysis.
Performance Benchmarks Across Cancer Types
CNN-based models have demonstrated exceptional performance across multiple cancer types, with particular success in breast cancer and gastrointestinal cancers.
Table 2: CNN Performance in Cancer Image Classification
| Cancer Type | Dataset | Model Architecture | Key Performance Metrics | Reference |
|---|---|---|---|---|
| Breast Cancer | BreakHis v1 (Binary Classification) | ResNet50 | AUC: 0.999 | [20] |
| Breast Cancer | BreakHis v1 (Binary Classification) | RegNet | AUC: 0.999 | [20] |
| Breast Cancer | BreakHis v1 (Binary Classification) | ConvNeXT | Accuracy: 99.2%, Specificity: 99.6%, F1-score: 99.1%, AUC: 0.999 | [20] |
| Colorectal Cancer | MECC & TCGA | Custom CNN with Attention | F1-Score: 0.96, MCC: 0.92, AUC: 0.99 | [21] |
| Gastric Cancer | Multiple Datasets | Various CNNs | Accuracy up to 95% in detection tasks | [19] |
In breast cancer histopathological image classification, CNNs demonstrated near-perfect performance in binary classification tasks due to their relatively low complexity [20]. The best overall performance was achieved by ConvNeXT, which attained an accuracy of 99.2% (95% CI: 98.3%-1), a specificity of 99.6% (95% CI: 99.1%-1), an F1-score of 99.1% (95% CI: 98.0-1%), and an AUC of 0.999 (95% CI: 0.999-1) [20]. Similarly, in colorectal cancer detection, CNNs combining attention mechanisms with image downsampling achieved an F1-Score of 0.96, Matthews correlation coefficient of 0.92, and AUC of 0.99 on test datasets from The Cancer Genome Atlas [21].
Experimental Protocols and Methodological Standards
The implementation of CNNs in cancer research established new methodological standards that addressed the unique challenges of medical image analysis:
Whole Slide Image Processing: CNNs employed multiple instance learning (MIL) frameworks to handle gigapixel whole slide images (WSIs). The standard approach divided WSIs into smaller tiles (e.g., 256×256 pixels) for processing, then aggregated predictions at the patient level [21].
Resolution Optimization Studies: Systematic investigations evaluated the impact of image resolution on classification accuracy. Studies compared performance at different resolution levels (2 μm/pix, 4 μm/pix, 8 μm/pix, and 16 μm/pix) to balance computational constraints with diagnostic performance [21]. Optimal results for colorectal cancer detection were achieved at 4 μm/pix, demonstrating that computational costs could be significantly reduced while maintaining high performance standards [21].
Artefact Management and Bias Mitigation: Comprehensive analyses identified and quantified image artefacts (blurred areas, air bubbles, black regions, folds, pen marks) and assessed their distribution across tumor and normal classes to prevent algorithmic bias [21]. Statistical tests (Z-tests with Bonferroni correction) ensured that artefact distributions didn't significantly differ between classes, preventing models from relying on confounding features [21].
Diagram 1: CNN Histopathology Analysis Workflow
The Transformer Revolution: Attention Mechanisms in Cancer Data
Architectural Fundamentals and Technical Innovations
The introduction of transformer architectures with self-attention mechanisms represented another paradigm shift in cancer AI applications. Unlike CNNs that processed images through hierarchical feature extraction, transformers utilized self-attention mechanisms to weigh the importance of different elements in input data when making predictions [22]. This architecture proved particularly adept at capturing long-range dependencies and contextual relationships within complex datasets.
The core innovation of transformers lay in their attention mechanisms, which allowed models to dynamically focus on the most relevant parts of the input sequence regardless of their positional relationships. This capability translated exceptionally well to cancer genomics and transcriptomics, where understanding interactions between distant genetic elements proved crucial for interpreting regulatory patterns and functional genomics [23].
Transformer Applications in Cancer Genomics
Transformers spawned a new class of genome large language models (Gene-LLMs) capable of interpreting nucleotide sequences at unprecedented scale and resolution [23]. These models treated DNA and RNA sequences as biological language, using self-supervised pretraining to decipher complex regulatory grammars hidden within the genome.
Gene-LLMs employed specialized tokenization strategies, typically using k-mer tokenization to segment long DNA and RNA sequences into overlapping fragments of length K (e.g., "ATGCGA") [23]. This approach, analogous to subword tokenization in natural language processing, enabled models to capture contextual relationships between nucleotides and identify functional genomic elements. Applications included enhancer and promoter identification, chromatin state modeling, RNA-protein interaction prediction, and synthetic sequence generation [23].
Performance in Histopathological Image Classification
In breast cancer histopathology, transformer-based foundation models demonstrated remarkable capabilities, particularly in complex multi-class classification scenarios. In the challenging eight-class classification task on the BreakHis dataset, the fine-tuned foundation model UNI achieved accuracy of 95.5% (95% CI: 94.4-96.6%), specificity of 95.6% (95% CI: 94.2-96.9%), F1-score of 95.0% (95% CI: 93.9-96.1%), and AUC of 0.998 (95% CI: 0.997-0.999) [20].
A critical finding was that foundation model encoders performed poorly without task-specific fine-tuning, but with simple adaptation, they quickly achieved excellent results [20]. This demonstrated that with minimal customization, foundation models could become valuable tools in digital pathology, especially for complex diagnostic scenarios requiring nuanced differentiation between multiple cancer subtypes.
Table 3: Transformer vs. CNN Performance in Breast Cancer Classification
| Model Type | Best Performing Model | Binary Classification AUC | Multi-class Classification Accuracy | Computational Efficiency |
|---|---|---|---|---|
| CNN-based | ConvNeXT | 0.999 | Not reported | High |
| Transformer-based | UNI (fine-tuned) | 0.999 | 95.5% | Moderate |
| Foundation Models | UNI (zero-shot) | Limited performance | Limited performance | Variable |
Contemporary Landscape: Large Language Models and Foundation Models
Definition and Technical Capabilities
Large language models (LLMs) and foundation models represent the most recent evolution in cancer AI, leveraging massive pretraining on diverse datasets to develop broad capabilities that can be adapted to specialized oncology tasks through fine-tuning. Foundation models are "pretrained" on vast amounts of data from disparate sources, learning to identify objects from input data. Through "transfer learning," their recognition capacities can be fine-tuned for specific downstream tasks, such as recognizing cancer cells from whole slide images [22].
These models support "self-supervised" learning, where pretraining tasks are derived automatically from unannotated data - a particularly promising feature for oncology datasets where expert annotations are scarce and expensive to obtain [22]. Critically, foundation models can accommodate multiple data types (text, imaging, pathology, molecular biology), incorporating them into multimodal analyses that have profound implications for clinical decision-making in oncology [22].
Multimodal Integration and Clinical Applications
Contemporary foundation models excel at integrating diverse data modalities that are essential for comprehensive cancer analysis:
Genomic Sequencing Data: Gene-LLMs process raw nucleotide sequences, gene expression data, and multi-omic annotations to decipher complex biological relationships [23].
Histopathological Images: Vision transformers analyze whole slide images, identifying subtle morphological patterns that may escape human detection [20] [22].
Clinical Text and EHR Data: NLP transformers extract relevant information from clinical notes, pathology reports, and scientific literature to provide clinical context [22].
Molecular Profiling Data: Multimodal transformers integrate proteomic, metabolomic, and spatial transcriptomic data to build comprehensive molecular portraits of tumors [22].
This multimodal capability enables applications in precision immuno-oncology, where AI/ML analyzes complex 'omics data alongside clinical, pathological, treatment, and outcome information to optimize biomarker development and treatment selection for patients [22].
Implementation in Cancer Drug Discovery and Clinical Trials
LLMs are revolutionizing cancer drug discovery and clinical trial methodologies through several mechanisms:
Synthetic Data Generation: Foundation models can generate synthetic patient data, including digital twins, to provide necessary information for designing or expediting clinical trials [22].
Trial Optimization: AI systems streamline trial design, analysis, and participant recruitment, potentially creating exponential impacts on therapeutic development [24].
Literature Mining: LLMs such as GPT variants enhance knowledge extraction from scientific literature and clinical text, accelerating hypothesis generation in cancer research [1].
Protein Structure Prediction: Tools like AlphaFold2, utilizing deep learning, enhance speed and precision in drug target identification through breakthroughs in understanding protein structure [24].
Diagram 2: Foundation Model Multimodal Integration
Table 4: Essential Research Reagents and Computational Resources in Cancer AI
| Resource Category | Specific Examples | Function in Research | Technical Specifications |
|---|---|---|---|
| Public Cancer Datasets | BreakHis v1, TCGA, MECC | Provide annotated histopathological images for model training and validation | BreakHis: 7,909 images; TCGA: 1,349 WSIs; MECC: ~1,317 WSIs [20] [21] |
| Genomic Data Repositories | CAGI5, GenBench, NT-Bench, BEACON | Benchmarking and validation of genomic AI models | Standardized datasets for model performance evaluation [23] |
| Deep Learning Frameworks | TensorFlow, PyTorch | Model development and training infrastructure | Support for CNN, transformer, and foundation model architectures |
| Computational Infrastructure | High-performance GPUs | Accelerate model training and inference | Essential for processing large WSIs and genomic sequences [21] |
| Whole Slide Imaging Systems | Digital slide scanners | Digitize histopathological specimens for computational analysis | 40x magnification, 0.25 μm/pix resolution [21] |
| Tokenization Tools | K-mer tokenizers | Segment genomic sequences for transformer processing | Convert DNA/RNA sequences to model-readable tokens [23] |
| Multiple Instance Learning Frameworks | Custom MIL implementations | Handle gigapixel whole slide images | Enable patient-level predictions from image tiles [21] |
Comparative Performance Analysis and Clinical Validation
Cross-Architecture Performance Benchmarking
Systematic comparisons of multiple architectures across standardized datasets provide critical insights for model selection in cancer research applications. A comprehensive evaluation of 14 deep learning models on breast cancer histopathological images revealed distinct performance patterns across architectural paradigms [20].
In binary classification tasks, where diagnostic decision-making is most straightforward, both CNN-based models (ResNet50, RegNet, ConvNeXT) and transformer-based foundation models (UNI) achieved exceptional performance with AUC scores of 0.999 [20]. However, in more complex eight-class classification tasks requiring nuanced differentiation between cancer subtypes, performance disparities became more pronounced, with the fine-tuned foundation model UNI achieving superior performance (95.5% accuracy) compared to other architectures [20].
Clinical Workflow Integration and Validation
Successful implementation of AI models in cancer research requires rigorous validation within clinical workflows:
External Validation: Models must demonstrate generalizability across independent datasets from different institutions. For example, colorectal cancer detection models trained on the MECC dataset were validated on TCGA datasets to ensure robustness [21].
Artefact Robustness: Real-world clinical images contain various artefacts (blurred areas, air bubbles, pen marks, folds). Comprehensive analyses quantify artefact distributions across classes to prevent algorithmic bias [21].
Resolution Optimization: Systematic studies evaluate performance across resolution levels (2 μm/pix to 16 μm/pix) to balance computational efficiency with diagnostic accuracy [21].
Clinical Workflow Integration: AI systems must integrate seamlessly with existing clinical protocols, combining different paradigms to produce transparent reasoning structures that can be evaluated in real clinical environments [18].
The historical evolution from early neural networks to contemporary LLMs has fundamentally transformed the landscape of cancer research. Early ANNs established the foundation for nonlinear pattern recognition in oncology data but faced limitations in handling complex image data and genomic sequences. The convolutional neural network revolution enabled automated feature learning from histopathological images, achieving diagnostic performance comparable to human experts in controlled settings. The subsequent transformer revolution introduced attention mechanisms that excelled at capturing long-range dependencies in both image and genomic data. Finally, contemporary foundation models and LLMs now enable multimodal integration across diverse data types, creating unprecedented opportunities for comprehensive tumor characterization and personalized treatment optimization.
Future research directions include federated learning approaches to leverage distributed data while maintaining privacy, enhanced multimodal modeling that seamlessly integrates genomic, image, and clinical data, improved interpretability methods to build clinical trust, and specialized adaptation for rare cancer variants where data scarcity presents particular challenges [23]. As these technologies continue to mature, their thoughtful integration into clinical workflows holds immense promise for advancing cancer diagnosis, treatment selection, and ultimately patient outcomes.
Cancer remains a principal cause of mortality worldwide, with projections estimating approximately 35 million cases by 2050 [1]. This alarming rise highlights the imperative to accelerate progress in cancer research and therapeutic development. Traditional approaches in oncology face significant challenges: drug discovery pipelines are time-intensive and resource-heavy, often requiring over a decade and billions of dollars to bring a single drug to market, with an estimated 90% of oncology drugs failing during clinical development [25]. Simultaneously, diagnostic and prognostic methods often lack the precision needed for personalized care, particularly in complex malignancies like lung cancer [16].
Artificial intelligence is rapidly revolutionizing the landscape of oncological research and personalized clinical interventions [1]. Progress in three interconnected areas—development of methods and algorithms for training AI models, evolution of specialized computing hardware, and increased access to large volumes of cancer data (imaging, genomics, clinical information)—has converged to create promising new applications across the cancer care continuum [1] [26]. When applied ethically and scientifically, these AI-driven approaches hold promise for accelerating progress in cancer research and ultimately fostering improved health outcomes for all populations [1].
Quantitative Evidence of AI Performance in Oncology
Empirical studies and meta-analyses demonstrate AI's robust performance across diagnostic and prognostic tasks in oncology. The following tables summarize key quantitative findings from recent research.
Table 1: Performance of AI Systems in Cancer Detection and Diagnosis
| Cancer Type | Modality | Task | AI System | Sensitivity | Specificity | AUC | Evidence Level |
|---|---|---|---|---|---|---|---|
| Colorectal | Colonoscopy | Malignancy detection | CRCNet | 91.3% (vs. 83.8% human) | 85.3% | 0.882 | Retrospective multicohort with external validation [1] |
| Colorectal | Colonoscopy/Histopathology | Histological classification | Real-time image recognition | 95.9% | 93.3% | NR | Prospective diagnostic accuracy [1] |
| Breast | 2D Mammography | Screening detection | Ensemble of 3 DL models | +2.7% to +9.4% vs. radiologists | +1.2% to +5.7% vs. radiologists | 0.810-0.889 | Diagnostic case-control [1] |
| Lung | CT Imaging | Diagnosis (Multiple studies) | Various AI algorithms | 0.86 (0.84-0.87) | 0.86 (0.84-0.87) | 0.92 (0.90-0.94) | Meta-analysis of 209 studies [16] |
Table 2: AI Performance in Prognostic Prediction and Molecular Profiling
| Domain | Cancer Types | Task | AI System | Performance | Validation |
|---|---|---|---|---|---|
| Survival Prediction | Multiple (17 institutions) | Distinguishing short-term vs. long-term survival | CHIEF | Outperformed other models by 8-10% | 32 datasets from 24 hospitals [27] |
| Risk Stratification | Lung | Predicting high vs. low risk (OS) | Various AI models | HR: 2.53 (2.22-2.89) | Meta-analysis of 44 datasets [16] |
| Molecular Profiling | Multiple (19 types) | Predicting 54 gene mutations | CHIEF | >70% accuracy (96% for EZH2 in DLBCL) | Cross-hospital validation [27] |
| Treatment Response | Multiple | Identifying immunotherapy responders | CHIEF | High accuracy for key mutations | International cohorts [27] |
Experimental Protocols and Methodological Frameworks
Foundation Model Development: The CHIEF Framework
The Clinical Histopathology Imaging Evaluation Foundation (CHIEF) represents a versatile, ChatGPT-like AI model capable of performing multiple diagnostic tasks across cancer types [27]. Its development protocol exemplifies rigorous AI methodology:
Data Curation and Preprocessing:
- Training on 15 million unlabeled images chunked into sections of interest
- Further training on 60,000 whole-slide images from 19 cancer types
- Samples included lung, breast, prostate, colorectal, gastric, and other major cancers
- Integration of data from multiple acquisition methods (biopsy, surgical excision) and digitization techniques
Architecture and Training:
- Holistic image interpretation combining specific regions with overall context
- Training to relate specific changes in one region to broader contextual patterns
- Validation on more than 19,400 whole-slide images from 32 independent datasets
- Testing across 24 hospitals and patient cohorts globally
Performance Validation:
- Cancer detection: 94% accuracy across 15 datasets with 11 cancer types
- Biopsy specimens: 96% accuracy across esophageal, gastric, colon, and prostate cancers
- Surgical specimens: >90% accuracy for colon, lung, breast, endometrial, and cervical tumors
- Molecular profile prediction: >70% accuracy for 54 commonly mutated cancer genes
This protocol demonstrates the comprehensive approach required for developing robust AI systems in oncology, emphasizing multi-site validation and diverse data integration [27].
Meta-Analysis Protocol for Lung Cancer AI Assessment
A recent systematic review and meta-analysis established rigorous methodology for evaluating AI's role in lung cancer management [16]:
Literature Search and Screening:
- Initial identification of 18,905 records from major databases
- Exclusion of 8,130 duplicates followed by title/abstract screening of 10,775 records
- Full-text assessment of 1,312 articles
- Final inclusion of 315 articles meeting quality criteria
Quality Assessment:
- Application of QUADAS-AI tool for diagnostic accuracy studies
- Newcastle-Ottawa Scale (NOS) for prognostic studies (scores 5-9, median 8)
- Evaluation of risk of bias across patient selection, reference standard, and flow/timing
- Exclusion of studies presenting only training performance without validation
Data Extraction and Analysis:
- Extraction of sensitivity, specificity, and AUC values from 209 diagnostic studies
- Hazard ratio extraction from 53 prognostic studies for overall survival, progression-free survival, disease-free survival, and recurrence-free survival
- Subgroup analyses based on study objectives, AI algorithms, validation cohorts, and imaging quality control
- Statistical synthesis using random-effects models to account for heterogeneity
This protocol provides a template for rigorous evidence synthesis in AI oncology applications, emphasizing transparency, quality assessment, and comprehensive performance evaluation [16].
Visualization of AI Workflows in Oncology
AI Model Development and Validation Pipeline
Multi-Scale AI Analysis in Cancer Pathology
Table 3: Key Research Reagents and Computational Resources for AI Oncology
| Resource Type | Specific Examples | Function in AI Research | Application Context |
|---|---|---|---|
| Public Datasets | The Cancer Genome Atlas (TCGA) | Provides multi-omics data for target identification and model training | Pan-cancer analysis, biomarker discovery [25] |
| Imaging Databases | National Lung Screening Trial (NLST) | LDCT images for lung cancer detection algorithm development | Screening and early detection models [26] |
| AI Frameworks | TensorFlow, PyTorch | Deep learning model development and training | Custom architecture implementation [1] |
| Validation Cohorts | Independent hospital datasets | External validation of model generalizability | Performance benchmarking [16] |
| Pathology Resources | Whole slide images (WSI) | Digital pathology analysis and feature extraction | Diagnostic classification, outcome prediction [27] |
| Genomic Tools | Circulating tumor DNA (ctDNA) data | Liquid biopsy analysis for monitoring and biomarker discovery | Minimal residual disease detection [25] |
| Clinical Data | Electronic Health Records (EHR) | Real-world evidence generation and outcome correlation | Predictive model validation [26] |
Challenges and Future Directions
Despite promising results, several challenges impede widespread clinical integration of AI in oncology. Data quality and availability remain fundamental constraints, as AI models are only as robust as the data they're trained on [25]. The "black box" nature of many deep learning algorithms creates interpretability challenges, limiting mechanistic insight and clinical trust [25] [4]. Model generalizability across diverse populations and healthcare settings requires further validation, with most current studies exhibiting retrospective designs [16]. Ethical considerations around data privacy, algorithmic bias, and regulatory compliance must be addressed through frameworks like federated learning and explainable AI (XAI) techniques [4].
Future progress depends on advancing multi-modal AI integration, combining genomic, imaging, and clinical data for more holistic insights [4]. Digital twins—virtual patient simulations—may enable virtual drug testing before clinical trials [25]. Federated learning approaches can enhance data diversity while preserving privacy [25]. Prospective multicenter validation studies and randomized controlled trials are essential to demonstrate real-world clinical utility and patient benefit [26]. As these technologies mature, their integration throughout the oncology pipeline promises to accelerate progress against cancer, ultimately delivering more personalized, effective care to patients globally.
ML in Action: Transforming Cancer Diagnosis, Prognosis, and Treatment
The integration of deep learning (DL) into medical imaging represents a paradigm shift in oncology, enhancing the precision of tumor detection, diagnosis, and treatment planning. This transformation is critical within a broader research context where machine learning is systematically reviewed for its impact on cancer outcomes. Deep learning techniques, particularly convolutional neural networks (CNNs) and transformer models, are now capable of analyzing complex imaging data from computed tomography (CT), magnetic resonance imaging (MRI), and histopathology with a level of speed and accuracy that augments human expertise [28]. These technologies have demonstrated significant utility across the cancer care continuum, from automated lesion detection and segmentation in radiology to prognostic assessments and molecular subtype prediction in digital pathology [28] [29]. Framed within a systematic review of machine learning in cancer research, this technical guide synthesizes current advancements, evaluates methodological frameworks, and details the experimental protocols that are establishing new benchmarks in oncologic imaging. The following sections provide a comprehensive examination of the core architectures, quantitative performance, and practical implementation requirements driving this field forward.
Core Deep Learning Architectures and Their Technical Implementation
The application of deep learning in medical imaging for tumor detection is underpinned by several sophisticated neural network architectures, each chosen for its specific strengths in handling high-dimensional image data. The foundational architecture is the Convolutional Neural Network (CNN), which excels at extracting hierarchical spatial features through its convolutional and pooling layers. CNNs have become the dominant technology in medical image processing, enabling the automated identification of complex imaging patterns and improving diagnostic precision [28]. Specific variants like U-Net and DeepLabV3+ have been successfully applied to tumor boundary recognition and organ segmentation in MRI and CT images, achieving high accuracy in brain tumor, lung lesion, liver cancer, and prostate cancer imaging [28].
More recently, Vision Transformers (ViTs) have emerged as powerful alternatives or complements to CNNs, particularly due to their ability to capture global contextual relationships within an image through self-attention mechanisms. While CNNs prioritize pixel-level information, transformers analyze the entire image at once and identify long-range dependencies between features, making them ideal for tasks requiring a comprehensive understanding of histopathological images [30]. However, pure transformer architectures can struggle with extracting fine-grained details, leading to the development of hybrid models that leverage the strengths of both approaches.
A notable example is a hybrid 2D-3D CNN-Transformer architecture proposed for brain tumor grading. In this framework, 3D CNN processes multi-scale stain decompositions to capture spatial-spectral patterns, while the Transformer focuses on diagnostically critical regions via self-attention. This synergy enables precise, interpretable grading while maintaining computational efficiency [30]. Another advanced implementation is the MBTC-Net framework for multimodal brain tumor classification, which leverages EfficientNetV2B0 for extracting high-dimensional feature maps, followed by reshaping into sequences and applying multi-head attention to capture contextual dependencies [31].
For whole-slide image (WSI) analysis in digital pathology, multiple-instance learning (MIL) approaches have gained prominence. These models address the challenge of gigapixel-sized images by processing numerous small patches and using attention mechanisms to combine features without requiring detailed pixel-level annotations. The SMMILe (Superpatch-based Measurable Multiple Instance Learning) algorithm exemplifies this approach, enabling precise spatial quantification of tumor tissue on digital pathology images using only slide-level labels for training [32].
Table 1: Core Deep Learning Architectures in Oncologic Imaging
| Architecture | Key Strengths | Common Applications | Notable Implementations |
|---|---|---|---|
| Convolutional Neural Networks (CNNs) | Local feature extraction, hierarchical pattern recognition | Lesion detection, tumor segmentation, image classification | U-Net, DeepLabV3+, EfficientNetV2B0 [28] [31] |
| Vision Transformers (ViTs) | Global context understanding, long-range dependency modeling | Whole-slide image analysis, tumor grading | Pure ViT architectures for molecular marker prediction [30] |
| Hybrid CNN-Transformer | Combines local feature extraction with global context | Brain tumor grading, multimodal classification | 2D-3D CNN-Transformer with stacking classifiers [30] |
| Multiple-Instance Learning (MIL) | Handles gigapixel images with weak supervision | Spatial quantification in digital pathology | SMMILe framework for tumor microenvironment analysis [32] |
Diagram 1: Hybrid CNN-Transformer workflow for tumor detection (76 characters)
Quantitative Performance Analysis Across Imaging Modalities
Rigorous evaluation of deep learning models across various cancer types and imaging modalities has demonstrated consistently high performance, though with notable variations in sensitivity and specificity across applications. The quantitative evidence supporting DL implementation comes primarily from retrospective studies and meta-analyses comparing algorithm performance against clinical standards and radiologist interpretations.
In digital pathology, DL algorithms show remarkable capability in predicting molecular alterations directly from hematoxylin and eosin (H&E)-stained whole-slide images. A meta-analysis of deep learning for detecting microsatellite instability-high (MSI-H) in colorectal cancer comprising 33,383 samples reported a pooled sensitivity of 0.88 and specificity of 0.86 in internal validation, with an area under the curve (AUC) of 0.94 [29]. Performance remained strong in external validation, though specificity decreased to 0.71, indicating challenges with generalizability. For brain tumor grading, a hybrid 2D-3D CNN-Transformer model combined with stacking classifiers achieved exceptional performance, reaching an average accuracy of 97.1%, precision of 97.1%, and specificity of 97.0% on the TCGA dataset [30].
In radiology applications, DL models have demonstrated particular strength in thyroid cancer detection. A systematic review and meta-analysis of 41 studies found that for thyroid nodule detection tasks, DL algorithms achieved a pooled sensitivity of 91%, specificity of 89%, and AUC of 0.96 [33]. Segmentation tasks for thyroid nodules showed slightly lower sensitivity (82%) but higher specificity (95%) [33]. The application of transfer learning was identified as a significant factor contributing to improved model performance across studies.
For breast cancer screening, research indicates that DL models can achieve high sensitivity (93%) in digital breast tomosynthesis (DBT)-based AI systems, with the additional benefit that AI scores may serve as imaging biomarkers associated with histologic grade and lymph node status [34]. However, studies have highlighted a critical limitation: most DL models for breast cancer detection are trained predominantly on Caucasian datasets, creating significant performance limitations when applied to Asian populations due to demographic differences in breast density and imaging characteristics [35].
Table 2: Performance Metrics of Deep Learning Models Across Cancer Types
| Cancer Type | Imaging Modality | Sensitivity (Pooled) | Specificity (Pooled) | AUC | Sample Size |
|---|---|---|---|---|---|
| Colorectal Cancer (MSI-H) | Histopathology (WSI) | 0.88 (Internal) 0.93 (External) | 0.86 (Internal) 0.71 (External) | 0.94 (Internal) | 33,383 samples [29] |
| Thyroid Cancer | Ultrasound | 0.91 (Detection) 0.82 (Segmentation) | 0.89 (Detection) 0.95 (Segmentation) | 0.96 (Detection) | 41 studies [33] |
| Brain Tumor | Histopathology (WSI) | N/R | N/R | N/R | TCGA Dataset [30] |
| Breast Cancer | Digital Breast Tomosynthesis | 0.93 | N/R | N/R | Multiple studies [34] [35] |
N/R: Not Reported in the aggregated data
Detailed Experimental Protocols and Methodologies
Whole-Slide Image Analysis for Molecular Phenotype Prediction
The prediction of molecular phenotypes from routine histopathology images represents one of the most significant advances in computational pathology. The following protocol outlines the methodology for developing a DL model to detect microsatellite instability (MSI) status in colorectal cancer from H&E-stained whole-slide images (WSIs), based on approaches validated in large-scale studies [29]:
Data Curation and Preprocessing:
- Collect formalin-fixed, paraffin-embedded (FFPE) H&E-stained WSIs from colorectal cancer resection specimens, with corresponding MSI status determined by PCR or immunohistochemistry (IHC).
- Exclude slides with poor staining quality, extensive necrosis, or insufficient tumor content (<10% tumor cellularity).
- Perform quality control through pathologist review to annotate tumor regions, either through detailed segmentation or rough bounding boxes.
- Split data into training, validation, and test sets at the patient level to prevent data leakage, ensuring slides from the same patient remain in the same split.
Image Processing and Patch Extraction:
- Load WSIs at multiple magnification levels (typically 5×, 10×, 20×) using openslide or similar libraries.
- Extract patches of size 256×256 or 512×512 pixels from tumor-rich regions identified through annotations or automated tumor detection.
- Apply stain normalization (e.g., Macenko method) to minimize inter-institutional staining variation.
- Implement data augmentation techniques including rotation, flipping, color jittering, and elastic transformations during training.
Model Architecture and Training:
- Employ a multiple-instance learning (MIL) framework where each WSI is treated as a "bag" of patches (instances).
- Utilize a pre-trained CNN (e.g., ResNet50) as a feature extractor for each patch, followed by an attention mechanism to weight the importance of different patches.
- Aggregate patch-level features into a slide-level representation using an attention-based pooling mechanism.
- Implement a final classification layer with sigmoid activation for MSI-H vs. MSS prediction.
- Train with weighted binary cross-entropy loss to address class imbalance, using Adam optimizer with an initial learning rate of 1e-4 and early stopping based on validation loss.
Validation and Interpretation:
- Perform internal validation on held-out test sets from the same institution and external validation on completely independent cohorts from different institutions.
- Generate attention maps to visualize which regions of the slide contributed most to the prediction, enabling pathological correlation.
- Calculate performance metrics including AUC, sensitivity, specificity, and precision-recall curves.
This protocol has demonstrated robust performance in multiple studies, with one meta-analysis reporting a pooled sensitivity of 0.88 and specificity of 0.86 in internal validation [29].
Multimodal Fusion for Brain Tumor Classification
The integration of multiple imaging modalities significantly enhances tumor characterization, as demonstrated by the MBTC-Net framework for multimodal brain tumor classification from CT and MRI scans [31]:
Multimodal Data Registration and Preprocessing:
- Collect paired CT and MRI scans (T1-weighted, T1 Contrast-Enhanced, T2-weighted) from patients with brain tumors.
- Perform rigid or non-rigid registration to align different modalities to a common coordinate space.
- Apply skull-stripping, intensity normalization, and bias field correction to standardize images across patients.
- Resample all images to isotropic resolution (e.g., 1mm³) and crop or pad to uniform dimensions.
Multimodal Feature Extraction:
- Implement a dual-stream architecture with shared-weight EfficientNetV2B0 backbones for each modality.
- Extract high-dimensional feature maps from each modality separately in parallel streams.
- Reshape 2D feature maps into sequence representations suitable for attention mechanisms.
- Apply multi-head attention to capture contextual dependencies within and across modalities.
Feature Fusion and Classification:
- Concatenate features from all modalities into a unified representation.
- Reintroduce the attention output into a spatial structure and perform global average pooling.
- Pass through dense layers with batch normalization and dropout (rate=0.5) for regularization.
- Use Adamax optimizer and softmax activation for final tumor classification.
- Implement stratified 5-fold cross-validation to ensure robust performance estimation.
This protocol achieved accuracies of 97.54% (15-class), 97.97% (6-class), and 99.34% (2-class) on open-access multimodal brain tumor datasets [31].
Diagram 2: Multimodal fusion for brain tumor classification (76 characters)
Research Reagent Solutions: Essential Materials and Computational Tools
The implementation of deep learning frameworks for tumor detection requires both computational resources and specialized data sources. The following table details key components of the research toolkit for developing and validating these systems.
Table 3: Essential Research Reagents and Computational Tools
| Category | Specific Resource | Application/Function | Implementation Notes |
|---|---|---|---|
| Public Datasets | The Cancer Genome Atlas (TCGA) | Whole-slide images with molecular data for multiple cancer types | Provides paired histopathology and genomic data [29] [30] |
| DeepHisto | Brain tumor histopathology images for grading | Used for cross-dataset validation [30] | |
| Kaggle Brain Tumor Datasets | Multimodal MRI and CT scans | Includes T1, T1-CE, T2 sequences [31] | |
| Software Libraries | PyTorch / TensorFlow | Deep learning framework for model development | Enables custom architecture implementation [31] [30] |
| OpenSlide | Whole-slide image processing and patch extraction | Handles gigapixel digital pathology files [32] | |
| Computational Infrastructure | GPU Clusters (NVIDIA) | Model training and inference acceleration | Essential for processing 3D volumes and WSIs [28] |
| Pre-trained Models | ImageNet Pre-trained CNNs | Transfer learning for medical image analysis | Improves performance with limited medical data [28] [33] |
| Validation Frameworks | QUADAS-AI / QUADAS-2 | Quality assessment of diagnostic accuracy studies | Standardized evaluation of model performance [29] [33] |
Challenges and Future Research Directions
Despite the promising results demonstrated across multiple studies, several significant challenges impede the widespread clinical adoption of deep learning for tumor detection. A primary limitation is the generalizability of models across diverse populations and imaging protocols. This is particularly evident in breast cancer detection, where models trained predominantly on Caucasian populations demonstrate reduced performance when applied to Asian populations, who typically have higher breast density and earlier disease onset [35]. Similarly, external validation of DL models for MSI detection in colorectal cancer showed a notable drop in specificity (from 0.86 to 0.71) compared to internal validation [29].
The interpretability of DL models remains another critical challenge. While attention maps and Grad-CAM visualizations provide some insight into model decision-making, the field increasingly recognizes the need for explainable AI (XAI) frameworks to build clinical trust and facilitate adoption [28] [4]. This is particularly important for high-stakes applications like cancer diagnosis and treatment planning.
Future research directions should prioritize several key areas. First, the development of federated learning approaches can address data heterogeneity while preserving patient privacy, enabling model training across multiple institutions without sharing sensitive data [4]. Second, greater emphasis on prospective validation in real-world clinical settings is necessary to establish clinical utility and workflow integration. Third, the integration of multimodal data—combining imaging with genomic, clinical, and laboratory data—will enable more comprehensive tumor characterization and personalized treatment strategies [28] [31]. Finally, addressing regulatory and ethical considerations through standardized evaluation frameworks and diverse dataset curation will be essential for equitable implementation of these technologies across global healthcare systems.
Precision oncology represents a paradigm shift in cancer care, moving away from a one-size-fits-all approach toward tailored strategies based on individual patient and tumor characteristics. This transformation has been accelerated by the integration of artificial intelligence (AI) and machine learning (ML), which enable the analysis of complex, high-dimensional datasets beyond human capability [36] [37]. The core objective of precision oncology is to leverage information about a patient's genes, proteins, and environment to improve diagnosis, treatment selection, and outcome prediction [37]. Initially focused on targeting specific molecular abnormalities with directed therapies, the field now encompasses immunotherapeutic approaches and utilizes diverse data modalities including genomics, medical imaging, and digital pathology [36] [37].
Cancer remains a leading cause of mortality worldwide, with projections indicating a 47% increase in the global cancer burden by 2040 compared to 2020 levels [36]. This alarming trend underscores the critical need for more effective prevention, diagnosis, and treatment strategies. The inherent heterogeneity of cancer – where no single therapy works universally – makes precision approaches particularly valuable [36]. ML techniques are especially well-suited to address this complexity by identifying subtle patterns across multimodal data sources that may escape conventional analytical methods [38].
This technical guide examines the current state of AI and ML in predicting cancer susceptibility, recurrence, and survivability, focusing on methodological frameworks, performance metrics, and practical implementation considerations for researchers and drug development professionals.
AI and Machine Learning Foundations in Oncology
Algorithm Types and Their Applications
AI in oncology encompasses a spectrum of approaches, from classical machine learning to advanced deep learning architectures, each with distinct strengths for specific data types and clinical questions [36].
Classical Machine Learning techniques including Bayesian networks, support vector machines, and decision trees are particularly effective for structured data such as genomic profiles or clinical metrics [36]. These models often provide greater interpretability and require less computational resources than deep learning approaches, making them valuable for tabular data analysis [36]. Regularized Cox models, including LASSO, Ridge, and Elastic Net, extend the traditional Cox proportional hazards model to high-dimensional settings by incorporating penalty terms that prevent overfitting and enable feature selection [38].
Deep Learning architectures have demonstrated remarkable success in processing unstructured data such as medical images and text [36]. Convolutional Neural Networks (CNNs) excel at image analysis tasks including radiology and pathology image interpretation [36] [16]. Recurrent Neural Networks (RNNs) and transformers are particularly suited for sequential data such as genomic sequences or temporal patient records [36]. More recently, large language models (LLMs) have shown promise in processing clinical text and enabling natural language interaction with computational tools [37].
Dynamic Prediction Models represent a specialized category of algorithms designed to incorporate longitudinal data and update risk estimates as new patient information becomes available [39]. These include two-stage models (32.2%), joint models (28.2%), time-dependent covariate models (12.6%), multi-state models (10.3%), landmark Cox models (8.6%), and AI-based dynamic models (4.6%) [39]. The distribution of these models has significantly shifted over recent years, with increasing adoption of joint models and AI approaches [39].
Data Modalities in Precision Oncology
The effectiveness of AI models in oncology depends critically on the data modalities available for analysis [36]:
- Imaging Data: Includes radiological images (CT, MRI, PET), pathological images (H&E staining, immunohistochemistry), and other medical images (mammography, colonoscopy, ultrasound) [36].
- Clinical Data: Encompasses electronic health records, blood test results, family history, and social determinants of health, often represented as complex, unstructured textual data [36].
- Omics Data: Includes genomics, epigenomics, transcriptomics, proteomics, metabolomics, immunomics, and microbiomics data collected through various molecular biology techniques [36].
The integration of these multimodal data sources presents both opportunities and challenges. While each modality provides complementary information about patient outcomes, differences in data structure, resolution, and collection protocols require careful harmonization [40] [41]. Late fusion approaches, which integrate predictions from modality-specific models rather than raw data, have demonstrated particular effectiveness in oncology applications due to their resistance to overfitting and ability to naturally weight each modality based on informativeness [40].
Technical Approaches for Prediction Categories
Cancer Susceptibility and Early Detection
AI approaches for cancer susceptibility and early detection focus on identifying individuals at high risk and detecting cancers at their earliest, most treatable stages [36]. These applications typically analyze data from non-invasive or minimally invasive sources, including medical history, lifestyle factors, serum biomarkers, and medical imaging [36].
Imaging-Based Detection: DL models have been widely applied to detect cancers through various imaging modalities. For lung cancer, AI analysis of CT scans has demonstrated robust performance, with a meta-analysis of 209 studies showing pooled sensitivity and specificity of 0.86 and AUC of 0.92 [16]. Similarly, DL models for breast cancer detection using mammography have shown performance comparable to or exceeding human radiologists [36].
Liquid Biopsy Applications: ML-based analysis of circulating tumor DNA (ctDNA) has transformed cancer detection through liquid biopsy approaches. Targeted methylation analysis of cell-free DNA can detect and localize multiple cancer types with high specificity [36]. The CancerSEEK test, which uses logistic regression based on circulating protein biomarkers and tumor-specific gene mutations in ctDNA, has received FDA Breakthrough Device designation for detecting eight cancer types [36].
Table 1: Performance of AI Algorithms in Cancer Detection
| Cancer Type | Data Modality | AI Approach | Sensitivity | Specificity | AUC |
|---|---|---|---|---|---|
| Lung Cancer | CT Imaging | Deep Learning | 0.86 [16] | 0.86 [16] | 0.92 [16] |
| Breast Cancer | Mammography | Deep Learning | Comparable to radiologists [36] | Comparable to radiologists [36] | - |
| Multiple Cancers | Liquid Biopsy (ctDNA) | Logistic Regression | - | High [36] | - |
| Colorectal Cancer | Pathological Images | Deep Learning | 0.83 [42] | 0.87 [42] | 0.96 [42] |
Cancer Recurrence and Progression Prediction
Predicting cancer recurrence and disease progression represents a critical application of AI in oncology, enabling more personalized treatment planning and surveillance strategies [39]. These models typically incorporate time-varying predictors and dynamic factors that change during the treatment course.
Dynamic Prediction Models: These models address the limitation of static prognostic models by incorporating longitudinal data collected during patient follow-up [39]. A comprehensive analysis of 174 dynamic prediction models (DPMs) found they have been applied across 19 cancer types, with the most common being breast cancer (29 studies), prostate cancer (22 studies), and lung cancer (21 studies) [39]. These models utilize various dynamic predictors including intermediate clinical events (24.1%), tumor size metrics (17.2%), prostate-specific antigen levels (10.3%), and circulating free DNA (7.5%) [39].
Radiomics and Pathomics Features: Quantitative features extracted from medical images provide valuable information for recurrence prediction. For lung cancer, AI models analyzing CT images have demonstrated strong performance in stratifying patients by recurrence risk, with a pooled hazard ratio of 4.73 for recurrence-free survival between high- and low-risk groups [16]. In colorectal cancer, deep learning models analyzing pathological images have shown exceptional performance in diagnosing KRAS mutations, which are associated with poorer survival and increased recurrence risk [42].
Multimodal Integration: Combining multiple data sources significantly enhances recurrence prediction accuracy. Late fusion models that integrate predictions from separate models trained on different data modalities (e.g., clinical, genomic, and imaging data) consistently outperform single-modality approaches [40]. For example, in lung, breast, and pan-cancer datasets, late fusion models demonstrated higher accuracy and robustness compared to unimodal approaches [40].
Diagram 1: Workflow for AI-based cancer recurrence prediction integrating multimodal data sources.
Survival Outcome Prediction
Accurate prediction of survival outcomes is essential for treatment planning, patient counseling, and clinical trial design. AI and ML approaches have demonstrated superior performance compared to traditional statistical methods in multiple cancer types [38].
Performance Across Cancer Types: A systematic review of 39 comparable studies found that ML methods improved predictive performance in almost all cancer types examined [38]. Multi-task and deep learning approaches appeared to yield superior performance, though they were reported in only a minority of studies [38]. The review highlighted considerable variability in both methodologies and their implementations across studies [38].
Risk Stratification Accuracy: AI-based survival models effectively stratify patients into distinct risk groups with significantly different outcomes. In lung cancer, patients classified as high-risk by AI models had a 2.53 times higher hazard for death compared to low-risk patients [16]. For progression-free survival, the hazard ratio between high- and low-risk groups was 2.80 [16]. These findings demonstrate the strong discriminatory power of AI models in identifying patients with poor prognosis who might benefit from more aggressive or alternative treatments.
Interpretable Survival Analysis: Recent advances focus on developing interpretable AI frameworks that maintain predictive accuracy while providing transparency in model decisions [43]. For example, the MultiFIX framework uses deep learning to infer survival-relevant features from clinical and imaging data, with explanations provided through Grad-CAM visualizations for imaging features and symbolic expressions for clinical variables [43]. This approach achieved a C-index of 0.838 for prediction and 0.826 for stratification in head and neck cancer, outperforming baseline methods while maintaining interpretability [43].
Table 2: Performance of AI Models in Survival Prediction Across Cancer Types
| Cancer Type | Data Modality | Model Type | Outcome | Performance |
|---|---|---|---|---|
| Lung Cancer | CT Imaging | Deep Learning | Overall Survival | HR: 2.53 (High vs. Low Risk) [16] |
| Lung Cancer | CT Imaging | Deep Learning | Progression-Free Survival | HR: 2.80 (High vs. Low Risk) [16] |
| Multiple Cancers | Multimodal | Late Fusion | Overall Survival | Outperformed single-modality [40] |
| Head & Neck Cancer | CT + Clinical | MultiFIX Framework | Survival Prediction | C-index: 0.838 [43] |
| Colorectal Cancer | Pathological Images | Deep Learning | KRAS Mutation Diagnosis | AUC: 0.96 [42] |
Experimental Protocols and Methodologies
Multimodal Data Integration Pipeline
The AstraZeneca-AI (AZ-AI) multimodal pipeline provides a comprehensive framework for integrating diverse data modalities for survival prediction [40]. This Python library includes functionalities for preprocessing, dimensionality reduction, and survival model training with rigorous evaluation [40].
Data Preprocessing: The pipeline incorporates various preprocessing and imputation options to handle missing data, which is particularly important in clinical datasets where missingness patterns may be informative [40]. Different modalities require specific preprocessing approaches – for example, genomic data often needs batch normalization, while clinical data may require handling of high degrees of missingness [40].
Dimensionality Reduction: Given the high-dimensional nature of omics data (often with >100,000 features) and relatively small sample sizes (typically 10-10^3 patients per cancer type), dimensionality reduction is critical to prevent overfitting [40]. The pipeline supports both feature selection (returning a subset of original features) and feature extraction (creating new, smaller feature sets) [40]. For genomic data, linear or monotonic feature selection methods (Pearson and Spearman correlation) have demonstrated better performance than nonlinear approaches in this setting [40].
Fusion Strategies: The pipeline enables comparison of different data fusion approaches, including early fusion (integrating raw data from multiple modalities), intermediate fusion, and late fusion (combining predictions from modality-specific models) [40]. In settings with high-dimensional features and limited samples, late fusion strategies have demonstrated advantages due to increased resistance to overfitting and the ability to naturally weight each modality based on its informativeness [40].
Model Training and Validation Framework
Robust model training and validation are essential for developing clinically applicable prediction models [40] [16].
Validation Practices: Comprehensive validation should include multiple training-test splits and reporting of confidence intervals for performance metrics [40]. Many published studies fail in this regard, either omitting multiple splits altogether or reporting average performance without confidence intervals [40]. External validation using out-of-sample datasets is particularly important for assessing model generalizability [16].
Performance Evaluation: The AZ-AI pipeline implements rigorous evaluation practices, including the option to report feature importance to enhance interpretability [40]. For survival models, the concordance index (C-index) is commonly used to evaluate predictive performance, with values above 0.8 generally indicating strong predictive ability [43].
Addressing Overfitting: Given the high dimensionality of omics data and relatively small sample sizes, preventing overfitting is crucial [40]. Strategies include regularization, data augmentation (used in 51 of 315 studies in a lung cancer imaging review) [16], and employing simpler models when appropriate [40]. Interestingly, ensemble methods like gradient boosting and random forests typically outperform deep neural networks on tabular data, despite the latter's flexibility [40].
Diagram 2: Framework for robust model training and validation in precision oncology.
Research Reagents and Computational Tools
Table 3: Essential Research Reagent Solutions for Precision Oncology Studies
| Reagent/Tool | Type | Primary Function | Application Examples |
|---|---|---|---|
| Aperio GT450 Slide Scanner | Hardware | Digital pathology slide digitization | Creating whole-slide images for AI analysis [44] |
| GenISIS (Genomic Information System for Integrative Science) | Software | Storage repository and high-performance computing | Analyzing veteran health data in MVP [44] |
| AZ-AI Multimodal Pipeline | Software | Python library for multimodal feature integration | Preprocessing, dimensionality reduction, survival model training [40] |
| PROBAST (Prediction Model Risk of Bias Assessment Tool) | Methodology | Quality assessment tool | Evaluating risk of bias in prediction model studies [42] |
| QUADAS-AI | Methodology | Quality assessment tool | Assessing quality of diagnostic accuracy studies using AI [16] |
| CAMIL (Context-Aware Multiple Instance Learning) | Algorithm | Attention mechanism for whole-slide images | Prioritizing relevant regions in pathological images [37] |
| MultiFIX Framework | Algorithm | Interpretable multimodal AI framework | Integrating clinical and imaging data with explanations [43] |
Challenges and Future Directions
Despite significant advances, several challenges remain in the clinical implementation of AI for precision oncology [41] [37].
Data Quality and Quantity: AI models are only as reliable as the data they're trained on, and inconsistent or biased datasets can limit generalizability [41]. Harmonizing diverse datasets from different sources, formats, and protocols is essential to reduce noise in AI models [41]. Furthermore, many models are developed using retrospective data (309 of 315 studies in a lung cancer review), with only a small proportion (6 studies) utilizing prospective data [16].
Interpretability and Trust: The "black box" nature of complex AI models presents a barrier to clinical adoption, particularly for high-stakes medical decisions [37]. Developing explainable AI approaches that provide transparency in decision-making is crucial for fostering trust among clinicians and regulators [37]. Methods that offer interpretable explanations, such as the MultiFIX framework's use of Grad-CAM and symbolic expressions, represent promising approaches [43].
Regulatory and Implementation Hurdles: Integrating AI tools into clinical workflows and reimbursement models remains challenging [37]. While the FDA has taken steps toward recognizing the value of AI, including phasing out animal testing for some therapies in favor of AI-based computational models [41], comprehensive regulatory frameworks for clinical AI applications are still evolving. Additionally, successful implementation requires that AI tools seamlessly integrate into existing clinical workflows rather than simply functioning as advanced algorithms [41].
The future of AI in precision oncology will likely see increased use of generative AI for simulating biological interactions and proposing novel therapeutic molecules [41]. Multi-omics integration, combining genomic, transcriptomic, proteomic, and metabolomic data, will provide a more comprehensive understanding of cancer biology [41]. As these technologies mature, 2025 is projected to be a turning point, potentially marking the entry of the first AI-discovered or AI-designed therapeutic oncology candidates into first-in-human trials [41].
AI and machine learning have fundamentally transformed precision oncology by enabling the analysis of complex, multimodal data to improve predictions of cancer susceptibility, recurrence, and survivability. Dynamic prediction models that incorporate longitudinal data provide more accurate prognostic estimates than static approaches, while multimodal integration strategies enhance predictive performance across diverse cancer types. Despite persistent challenges related to data quality, model interpretability, and clinical implementation, the field continues to advance rapidly. The development of standardized pipelines, robust validation frameworks, and explainable AI approaches will be critical for translating these technological advances into clinically meaningful tools that improve patient outcomes. As precision oncology evolves, AI-driven methodologies will play an increasingly central role in personalizing cancer care across the disease continuum.
The integration of artificial intelligence (AI) into drug discovery and development represents a paradigm shift in biomedical research, offering unprecedented opportunities to accelerate the delivery of new therapies. This is particularly salient in oncology, where the biological complexity of cancer and the pressing need for effective treatments create a compelling use case for AI technologies. This whitepaper examines the technical applications of AI and machine learning (ML) across the drug development pipeline, with a specific focus on cancer research, highlighting current methodologies, performance metrics, and practical implementation frameworks. The systematic review by [38] establishes that ML methods demonstrate improved predictive performance across almost all cancer types, with multi-task and deep learning approaches yielding particularly superior results, though they appear in only a minority of published studies.
AI in Target Identification and Validation
Target identification and validation represent the foundational stage of drug discovery, where AI is demonstrating transformative potential. In oncology, this phase is particularly challenging due to the complex genomic landscape of tumors. Research indicates that only approximately 10% of patients with advanced cancer have an identifiable and actionable mutation that would benefit from genetically informed therapy, leaving the majority of patients without targeted treatment options [45].
AI approaches, particularly machine learning and deep learning algorithms, can delve deep into massive, complex, multi-parametric datasets to facilitate an unbiased, disease-agnostic approach to cancer biology [45]. The computational analysis of disparate data types—including chemoinformatics, gene expression, mutations, and three-dimensional protein structures—has enabled the identification of previously unknown druggable targets. For instance, one computational analysis identified 46 proteins in the Cancer Gene Census as potential new druggable targets, some of which have subsequently entered drug discovery and development pipelines [45].
Generative AI platforms are now accelerating this process by generating swathes of ideas for both hit expansion and lead optimization [45]. These systems can analyze vast datasets encompassing genomic and proteomic information to identify potential drug targets with higher speed and accuracy than conventional methods. By simulating biological interactions, AI models can interpret how molecules interact with specific targets, streamlining the target validation process significantly [46].
Table 1: AI Applications in Early Drug Discovery
| Application Area | AI Methodology | Key Function | Reported Impact |
|---|---|---|---|
| Target Identification | Natural Language Processing, Deep Learning | Analysis of genomic/proteomic data, research papers, and patents | Reduction of drug design timeline from 4-7 years to 3 years [47] |
| Target Validation | Generative AI, Molecular Simulation | Simulation of biological interactions, protein-ligand binding | Identification of 46 previously unknown druggable cancer targets [45] |
| Molecular Design | Generative Adversarial Networks (GANs), Deep Learning | Design of novel molecular structures with desired properties | Creation of novel antibiotic compounds against resistant pathogens [47] |
| Toxicity Prediction | Machine Learning, Deep Learning | Prediction of compound toxicity and drug-drug interactions | Reduced reliance on animal models; identification of safety issues earlier in pipeline [48] |
AI-Driven Drug Design and Optimization
The design and optimization of drug candidates have been revolutionized by AI methodologies, particularly through generative models and predictive algorithms. AI-based approaches enable the rapid and efficient design of novel compounds with specific desirable properties and activities, moving beyond the traditional reliance on identification and modification of existing compounds [48].
Deep learning algorithms trained on datasets of known drug compounds and their corresponding properties can now propose new therapeutic molecules with desirable characteristics such as solubility, efficacy, and safety profiles [48]. For example, researchers at MIT used generative AI to design novel antibiotics that combat drug-resistant Neisseria gonorrhoeae and multi-drug-resistant Staphylococcus aureus (MRSA). The resulting candidates are structurally distinct from any existing antibiotics and demonstrate the potential to explore greater diversity of potential drug compounds [47].
The deployment of AlphaFold, developed by DeepMind, represents a breakthrough in structural biology with profound implications for drug discovery. This powerful algorithm uses protein sequence data and AI to predict corresponding three-dimensional structures, dramatically advancing our understanding of biological targets [48]. When combined with molecular dynamics simulations and interpretable machine learning methods, these approaches create powerful synergies for de novo drug design [48].
Experimental Protocol: AI-Driven Compound Design
The standard workflow for AI-driven compound design and optimization typically follows this methodological sequence:
Data Curation and Preprocessing: Collect and clean large-scale chemical and biological data from diverse sources, including chemical libraries, bioactivity databases (e.g., ChEMBL), and high-throughput screening results. Address batch effects and standardization issues through rigorous normalization [49].
Feature Engineering: Represent molecular structures in machine-readable formats, such as simplified molecular-input line-entry system (SMILES), molecular fingerprints, or graph-based representations that capture atomic and bond properties.
Model Training: Implement appropriate AI architectures based on the specific design goals:
- Generative Models: Use Generative Adversarial Networks (GANs) or Variational Autoencoders (VAEs) to generate novel molecular structures with desired properties.
- Property Prediction: Train deep neural networks or gradient boosting machines to predict key molecular properties including solubility, toxicity, and target binding affinity.
- Optimization Algorithms: Apply reinforcement learning or Bayesian optimization to navigate chemical space and optimize multiple properties simultaneously.
Experimental Validation: Synthesize top-ranking compounds identified by AI models and validate predicted properties through in vitro and in vivo testing, creating feedback loops to refine AI models.
The following diagram illustrates the iterative workflow for AI-driven compound design and optimization:
AI in Clinical Trial Optimization
Clinical trial design and execution represent one of the most promising applications of AI in drug development, with demonstrated impacts on timeline reduction and cost savings. AI is rapidly transforming clinical trials by dramatically reducing timelines and costs, accelerating patient-centered drug development, and creating more resilient and efficient trials [9].
According to a recent CB Insights report, 80% of analyzed startups use AI for automation to eliminate time-wasting inefficiencies that drive up costs [9]. The effects are substantial: patient recruitment cycles that used to span months are shrinking to days, while study builds that took days now take minutes [9]. More than half of the companies examined are applying AI to patient recruitment and protocol optimization, enabling truly "adaptive" clinical trials with real-time intervention and continuous protocol refinement [9].
Several platforms exemplify these advances:
- BEKHealth uses AI-powered natural language processing to analyze structured and unstructured electronic health record data, identifying protocol-eligible patients three times faster with 93% accuracy [9].
- Dyania Health automates patient identification from EHRs, reducing the process from hours to minutes while achieving 96% accuracy and demonstrating a 170x speed improvement at Cleveland Clinic [9].
- Datacubed Health employs AI to enhance patient engagement through personalized content creation and behavioral science-driven strategies, improving retention rates and compliance [9].
Experimental Protocol: AI-Enhanced Patient Recruitment
The implementation of AI for patient recruitment and trial optimization follows a structured methodology:
Data Aggregation: Collect and harmonize diverse data sources including electronic health records, genomic data, medical imaging, and previous trial data. Ensure compliance with privacy regulations through appropriate de-identification techniques.
Eligibility Criteria Processing:
- Utilize natural language processing to convert unstructured eligibility criteria into structured, computable formats.
- Apply rule-based AI systems leveraging medical expertise to map criteria to relevant patient data elements.
Patient-Trial Matching:
- Implement machine learning algorithms to match patient clinical and genomic profiles with trial requirements.
- Use predictive modeling to identify patients at risk of developing conditions that would make them eligible for prevention trials.
Site Selection Optimization:
- Apply predictive analytics to identify sites with high concentrations of eligible patients.
- Model potential enrollment rates based on historical performance and demographic factors.
Performance Monitoring and Adaptation:
- Deploy real-time analytics to track enrollment progress and identify bottlenecks.
- Use adaptive algorithms to refine recruitment strategies based on ongoing performance data.
Table 2: AI Applications in Clinical Trial Optimization
| Application Area | Technology | Key Features | Reported Outcomes |
|---|---|---|---|
| Patient Recruitment | Natural Language Processing, Rule-based AI | Analysis of EHR data, automated eligibility matching | 170x speed improvement, 96% accuracy in patient identification [9] |
| Protocol Optimization | Predictive Modeling, Simulation | Digital simulation of test scenarios, outcome prediction | Enabled adaptive trial designs with real-time protocol refinement [9] |
| Decentralized Clinical Trials | eClinical Technology, Digital Biomarkers | Electronic outcomes assessment, remote patient monitoring | 40% of innovating companies focused on decentralized trials or real-world evidence [9] |
| Patient Engagement | Behavioral Science Algorithms, Personalization | Adaptive engagement technologies, gratification systems | Improved retention rates and compliance through personalized content [9] |
Research Reagents and Computational Tools
The implementation of AI in drug discovery requires specialized computational tools and data resources. The table below details essential research reagents and their applications in AI-driven drug discovery experiments.
Table 3: Essential Research Reagents and Computational Tools for AI in Drug Discovery
| Resource/Tool | Type | Primary Function | Application in Drug Discovery |
|---|---|---|---|
| AlphaFold | AI Algorithm | Protein structure prediction | Predicts 3D protein structures from sequence data, enabling target identification and structure-based drug design [48] |
| ChEMBL | Database | Bioactive molecule data | Curated database of bioactive molecules with drug-like properties used for training predictive AI models [49] |
| Polaris | Benchmarking Platform | Data quality certification | Provides guidelines and certification for high-quality datasets suitable for machine learning in drug discovery [49] |
| Generative Adversarial Networks (GANs) | AI Architecture | Molecular generation | Generates novel molecular structures with desired properties for hit expansion and lead optimization [46] |
| Electronic Health Records (EHR) | Data Source | Real-world patient data | Provides structured and unstructured clinical data for patient recruitment analytics and real-world evidence generation [9] |
| Molecular Fingerprints | Computational Representation | Chemical structure encoding | Represents molecular structures in machine-readable formats for property prediction and similarity analysis [48] |
Technical Challenges and Methodological Considerations
Despite its promising applications, the integration of AI into drug discovery presents significant technical challenges that require careful methodological consideration.
Data Quality and Availability
The performance of AI models is fundamentally dependent on the quality and quantity of training data. Several critical issues must be addressed:
Batch Effects: Discrepancies introduced when different laboratories use different methods, reagents, and equipment can lead to misleading interpretations by AI models [49]. Standardization initiatives like the Human Cell Atlas demonstrate the value of rigorous, standardized data collection protocols for generating AI-ready data [49].
Publication Bias: The systemic bias toward publishing positive results distorts the biological landscape presented to AI algorithms. As one researcher noted, "My lab has got so much data showing that this doesn't work," yet these negative results remain unpublished [49]. Projects specifically designed to capture negative results, such as the "avoid-ome" project focused on ADME (absorption, distribution, metabolism, and excretion) proteins, aim to address this gap [49].
Data Sharing Limitations: Pharmaceutical companies maintain extensive proprietary datasets ideal for AI training, but competitive pressures limit sharing. Federated learning approaches, such as those employed in the Melloddy project, allow multiple companies to collaborate in training predictive software without revealing sensitive data [49].
Reproducibility and Validation
Reproducibility remains a significant concern in AI-driven drug discovery. Studies indicate that only about 20-25% of the early discovery literature is reproducible in a way that supports therapeutics discovery [45]. This creates a fundamental challenge when training AI models on incomplete and irreproducible datasets.
The following diagram illustrates a robust validation framework for AI models in drug discovery:
Regulatory and Ethical Framework
The regulatory landscape for AI in drug development is evolving rapidly. The U.S. Food and Drug Administration has established the CDER AI Council to provide oversight, coordination, and consolidation of AI-related activities [50]. The FDA has seen a significant increase in drug application submissions using AI components, with over 500 submissions with AI components from 2016 to 2023 [50].
Key considerations in the regulatory framework include:
Algorithm Transparency and Explainability: The "black-box" nature of some complex AI models presents challenges for regulatory review. Approaches that enhance interpretability without sacrificing performance are essential for regulatory acceptance [47].
Bias Mitigation: AI algorithms may perpetuate or amplify biases present in training data, potentially causing certain patient groups to be underrepresented in clinical trials or experiencing unequal access to treatments [47].
Intellectual Property Protection: Fundamental questions regarding patent protection for AI-generated discoveries remain unresolved, particularly regarding sufficient disclosure requirements when data privacy laws prevent sharing of essential training data details [47].
AI technologies are fundamentally reshaping the landscape of drug discovery and development, offering transformative potential to reduce timelines, lower costs, and improve success rates. From target identification through clinical development, AI methodologies are demonstrating measurable impacts across the development pipeline. The systematic review of machine learning in cancer research confirms that these approaches yield improved predictive performance across most cancer types, though significant challenges around data quality, reproducibility, and integration remain.
The successful implementation of AI in drug discovery requires interdisciplinary collaboration between oncologists, data scientists, and regulators. As noted by experts in the field, "It is the combination of person and machine learning that will really drive things forward" [45]. With continued advancement in AI methodologies, increased data standardization, and evolving regulatory frameworks, AI-powered drug discovery holds exceptional promise for delivering better medicines to cancer patients and addressing unmet needs across the therapeutic spectrum. The vision articulated by researchers—moving from idea to clinical trials within three years—represents an ambitious but increasingly attainable goal that could significantly shift outcomes for patients [45].
The convergence of artificial intelligence (AI) with surgical and clinical oncology is fundamentally reshaping cancer care, enabling a shift from a one-size-fits-all model to highly personalized treatment strategies. Personalized treatment planning represents an integrated approach where clinical decision support systems (CDSS) and robotic-assisted surgery converge to tailor therapies to individual patient characteristics. This paradigm leverages computational models, particularly machine learning (ML) and deep learning (DL), to analyze complex, high-dimensional data—including genomic, clinical, and imaging data—to inform clinical decisions and surgical interventions [51] [16]. The core objective is to enhance diagnostic accuracy, optimize treatment selection, improve surgical precision, and ultimately, elevate patient survival and quality of life. Within the broader context of a systematic review of machine learning in cancer research, this technical guide examines how CDSS and robotic surgery function as complementary pillars of modern precision oncology, providing researchers and clinicians with evidence-based frameworks for implementation and evaluation.
AI, particularly ML and DL, has demonstrated remarkable potential in extracting meaningful patterns from vast oncology datasets that often surpass human analytical capabilities [51]. These technologies underpin modern CDSS, enabling the analysis of diverse data inputs—from electronic health records (EHR) and medical images to genomic profiles and patient-reported outcomes—to generate patient-specific assessments and recommendations. Concurrently, robotic surgical systems have evolved beyond enhanced physical manipulation to incorporate data-driven guidance, leveraging pre-operative and intra-operative data to augment surgical precision. The integration of these domains creates a continuous feedback loop: CDSS informs pre-operative planning and patient selection, robotic surgery executes precise interventions, and post-operative data feeds back to refine the CDSS models, creating an iterative learning system [52].
Clinical Decision Support Systems in Oncology
System Definitions and Classifications
Clinical Decision Support Systems (CDSS) are electronic systems designed to directly aid clinical decision-making by utilizing individual patient characteristics to generate patient-specific assessments or recommendations [53]. These systems integrate computable biomedical knowledge, person-specific data, and reasoning mechanisms to present actionable information to clinicians at the point of care. In oncology, CDSS tools are categorized into several functional types: computerized physician order entry (CPOE) systems for medication and treatment orders; clinical practice guideline (CPG) systems that embed evidence-based pathways into workflow; clinical pathway systems that standardize multidisciplinary care plans; prescriber alerts for best-practice advisories; and patient-reported outcome (PRO) systems that systematically capture and integrate symptom and quality-of-life data into clinical management [53] [52]. Modern CDSS increasingly incorporates ML algorithms to enhance their predictive capabilities and adaptability, moving beyond static rule-based systems to dynamic learning systems that evolve with new evidence [51].
The technological architecture of modern CDSS typically involves integration with electronic health records (EHR) and other hospital information systems, allowing real-time access to patient data. The knowledge base may contain curated clinical guidelines, literature-derived evidence, and institutional protocols. The inference engine applies reasoning methodologies—which may include logic rules, probabilistic networks, or ML algorithms—to generate patient-specific recommendations. These recommendations are then presented through user-friendly interfaces such as alerts, order sets, dashboards, or documentation templates [52]. The most effective systems are context-aware, providing relevant information at appropriate times in the clinical workflow without creating excessive cognitive load for clinicians.
Quantitative Evidence of CDSS Impact
Recent systematic reviews demonstrate the measurable impact of CDSS on oncology care quality and safety. An updated systematic review analyzing 43 studies found that improvements in outcomes were observed in 42 studies, with 34 of these showing statistical significance [52]. These improvements span various domains including guideline adherence, medication safety, workflow efficiency, and patient-centered care.
Table 1: Impact of CDSS Categories on Oncology Care Processes
| CDSS Category | Number of Studies | Key Outcome Improvements | Effect Size Range |
|---|---|---|---|
| Computerized Physician Order Entry (CPOE) | 13 | Reduced prescribing error rates, fewer medication-related safety events, decreased workflow interruptions | 15-48% error reduction [53] [52] |
| Clinical Practice Guidelines | 10 | Increased guideline-concordant care, improved standardized treatment selection | 12-31% adherence improvement [52] |
| Clinical Pathway Systems | 8 | Enhanced care coordination, reduced unnecessary variations in practice | 18-42% pathway adherence [52] |
| Patient-Reported Outcome Systems | 8 | Improved symptom management, enhanced patient-clinician communication, better quality of life tracking | 22-45% symptom detection improvement [53] [52] |
| Prescriber Alert Systems | 4 | Increased appropriate supportive care, reduced inappropriate testing | 25-40% alert effectiveness [52] |
The implementation of CPOE systems with embedded decision support has demonstrated particularly significant benefits in chemotherapy safety. Studies show that CPOE systems can reduce chemotherapy prescribing errors by 15-48% through dose calculation support, allergy checking, and protocol-based recommendations [53] [52]. Similarly, CDSS for clinical pathways have improved adherence to evidence-based protocols by 18-42%, reducing unwarranted practice variation while maintaining flexibility for individualized patient considerations [52]. PRO systems have demonstrated 22-45% improvements in symptom detection and management, enabling more proactive supportive care interventions [53].
Machine Learning Foundations of Advanced CDSS
Machine learning enhances CDSS capabilities beyond traditional rule-based systems, particularly through handling high-dimensional data and detecting complex, non-linear patterns. ML algorithms applied in oncology CDSS include supervised learning for classification and prediction tasks, unsupervised learning for patient stratification, and reinforcement learning for adaptive treatment strategies [51] [38].
For survival analysis and prognosis prediction—critical components of oncology decision-making—ML methods have demonstrated particular utility in overcoming limitations of traditional statistical approaches like Cox Proportional Hazards models, which assume linear relationships and struggle with high-dimensional data [38]. ML techniques adapted for survival analysis include:
- Regularization methods (LASSO, Ridge, Elastic Net) that enable Cox model application to high-dimensional genomic data by penalizing coefficient complexity [38]
- Survival trees and random forests that recursively partition data based on covariates that maximize separation in survival outcomes [38]
- Multi-task and deep learning methods that learn complex representations from raw input data and have shown superior performance in some applications [38]
- Support vector machines adapted for survival analysis through ranking objectives [38]
A systematic review of ML techniques for cancer survival analysis found that ML approaches demonstrated improved predictive performance compared to traditional methods across almost all cancer types [38]. Multi-task and deep learning methods appeared to yield particularly superior performance, though they were implemented in only a minority of studies, suggesting an emerging trend rather than established practice [38].
Robotic-Assisted Surgery in Precision Oncology
Technological Evolution and Current Systems
Robotically assisted (computer-enhanced) laparoscopic surgery (RAS) represents a technological evolution beyond conventional laparoscopy, offering potential technical advantages for cancer resection. The da Vinci Surgical System (Intuitive Surgical), approved in 2000, remains the predominant platform, though competing systems continue to emerge [54]. The fundamental technological advantages of RAS include stable 3D high-definition visualization, wristed instruments with greater degrees of freedom than the human hand, motion scaling to filter physiologic tremor, and improved ergonomics that reduce surgeon fatigue [54] [55]. These features theoretically enhance surgical precision—a critical factor in oncology where complete tumor resection with negative margins significantly impacts recurrence and survival.
For colorectal cancer, one of the most common malignancies, robotic surgery has demonstrated specific benefits in most colectomy procedures. A study of 53,209 colectomy cases found that robotic approaches for right and left colectomies resulted in higher rates of "textbook outcomes" (71% vs. 64% and 75% vs. 68%, respectively), shorter hospital stays, fewer conversions to open surgery, and more lymph nodes harvested compared to laparoscopic techniques [55]. The improved lymph node yield facilitates more accurate cancer staging, directly impacting subsequent treatment decisions. Interestingly, for low anterior resections involving the rectum, laparoscopic approaches showed slight advantages in some outcomes, highlighting that the benefits of robotics are procedure-specific and dependent on anatomical complexity and surgeon experience [55].
Long-Term Oncologic Outcomes by Cancer Type
The RECOURSE study, a comprehensive systematic review and meta-analysis of 199 studies including 157,876 robotic, 68,007 laparoscopic/thoracoscopic, and 234,649 open cases, provides robust evidence regarding long-term oncologic outcomes across multiple cancer types [54]. This analysis compared hazard ratios (HR) for recurrence, disease-free survival (DFS), and overall survival (OS) across surgical approaches for colorectal, urologic, endometrial, cervical, and thoracic cancers.
Table 2: Long-Term Oncologic Outcomes by Surgical Approach and Cancer Type
| Cancer Type/Procedure | Robotic vs. Laparoscopic | Robotic vs. Open | Key Findings |
|---|---|---|---|
| Cervical Cancer | OS: HR 1.01 [0.56-1.80] (p=0.98) DFS: HR 1.01 [0.56-1.80] (p=0.98) | OS: HR 1.18 [0.99-1.41] (p=0.06) | Similar long-term outcomes; two studies reported less recurrence with open surgery (HR 2.30 [1.32-4.01], p=0.003) [54] |
| Endometrial Cancer | Not significant | OS favored robotic: HR 0.77 [0.71-0.83] (p<0.001) | Significant overall survival advantage for robotic versus open approach [54] |
| Pulmonary Lobectomy | DFS favored robotic: HR 0.74 [0.59-0.93] (p=0.009) | OS favored robotic: HR 0.93 [0.87-1.00] (p=0.04) | Disease-free survival advantage over thoracoscopic; overall survival advantage over open surgery [54] |
| Prostatectomy | Recurrence favored robotic: HR 0.77 [0.68-0.87] (p<0.0001) | OS favored robotic: HR 0.78 [0.72-0.85] (p<0.0001) | Significant reduction in recurrence versus laparoscopic; significant survival advantage versus open [54] |
| Low-Anterior Resection | OS favored robotic: HR 0.76 [0.63-0.91] (p=0.004) | OS favored robotic: HR 0.83 [0.74-0.93] (p=0.001) | Overall survival advantage for robotic over both laparoscopic and open approaches [54] |
The meta-analysis demonstrated that long-term oncologic outcomes were largely similar between robotic, laparoscopic/thoracoscopic, and open approaches, with no concerning safety signals for robotic surgery across cancer types [54]. In several specific instances—particularly prostatectomy, low-anterior resection, and lobectomy—robotic approaches demonstrated statistically significant advantages in recurrence or survival outcomes. These findings counter earlier concerns that minimally invasive approaches might compromise oncologic efficacy due to lack of tactile feedback or technical limitations in achieving complete resections [54].
Integrated Personalized Treatment Workflow
The true potential for personalized cancer therapy emerges when CDSS and robotic surgery function as integrated components within a unified treatment pathway. This integration enables data-driven decision-making from diagnosis through surgical management and follow-up care.
This integrated workflow illustrates how data flows through the personalized treatment continuum. In the pre-operative phase, multi-omics data—including genomic, clinical, and imaging information—undergoes analysis through ML-powered CDSS to generate predictive insights and stratify patients according to anticipated treatment response and surgical risks [51] [16]. These analytical outputs directly inform the development of a personalized surgical plan that considers tumor characteristics, patient anatomy, and predicted disease behavior. During the intra-operative phase, robotic systems execute the planned resection with enhanced precision, while incorporating real-time data for navigation and margin assessment. The post-operative phase captures structured outcome data, including patient-reported outcomes, complications, and recurrence information, which feeds back into the CDSS to refine predictive models and complete the learning cycle [52].
Experimental Protocols and Methodologies
Protocol for Evaluating CDSS Impact in Oncology
Systematic evaluation of CDSS implementation requires rigorous methodology to assess both clinical outcomes and process measures. The following protocol outlines a comprehensive approach for evaluating CDSS impact in oncology settings:
Study Design: Utilize a randomized controlled trial (RCT) or quasi-experimental pre-post intervention design with concurrent controls. RCTs provide the highest evidence level but may face implementation challenges in clinical settings; well-designed pre-post studies with adjustment for confounding can provide robust evidence [53] [52].
Participant Recruitment: Include consecutive eligible patients within defined inclusion criteria (e.g., specific cancer type, stage, treatment plan). Document exclusion criteria transparently to enable assessment of generalizability. Sample size calculation should be based on the primary endpoint with adequate power [53].
Intervention Deployment: Implement the CDSS according to a standardized implementation framework. Key components include:
- Integration with existing EHR and workflow systems
- Staff training and education programs
- Technical support infrastructure
- Process for content updates and system maintenance [52]
Data Collection: Collect both process measures and outcome measures:
- Primary outcomes: May include guideline adherence rates, medication error rates, patient-reported outcome measures, or survival metrics depending on CDSS type
- Secondary outcomes: Should include implementation metrics (adoption rate, user satisfaction), efficiency measures (time to treatment, workflow interruptions), and safety indicators (adverse events, unplanned hospitalizations) [53] [52]
Statistical Analysis: Employ appropriate multivariate analyses to adjust for potential confounders. For time-to-event outcomes (e.g., overall survival), use Kaplan-Meier methods with log-rank tests and Cox proportional hazards regression. For binary outcomes, use logistic regression. Report effect sizes with confidence intervals in addition to p-values [52].
This protocol framework has been successfully applied in multiple studies included in systematic reviews of oncology CDSS, demonstrating feasibility and generating clinically relevant evidence [53] [52].
Protocol for Comparative Effectiveness Research in Robotic Surgery
Evaluating the comparative effectiveness of robotic versus conventional surgical approaches requires meticulous methodology to ensure valid comparison of oncologic outcomes:
Study Design Options:
- Randomized Controlled Trials: The gold standard but challenging to implement for surgical interventions
- Database Studies: Leverage large clinical registries (e.g., National Cancer Database, NSQIP) for sufficient sample size and generalizability
- Prospective Cohort Studies: Design with explicit inclusion criteria and prospective data collection
- Retrospective Cohort Studies: Most common design; should employ statistical adjustment for case mix differences [54]
Participant Selection: Define clear inclusion criteria based on cancer type, stage, surgical procedure, and patient characteristics. Employ matching techniques (propensity score, exact matching) to create comparable cohorts when randomization is not feasible [54].
Outcome Measures: Assess both perioperative and long-term oncologic outcomes:
Statistical Analysis for Survival Outcomes:
- Report hazard ratios (HR) with 95% confidence intervals for time-to-event outcomes
- Utilize Kaplan-Meier curves with log-rank tests for unadjusted analysis
- Employ Cox proportional hazards regression for multivariable adjustment
- Consider competing risks analysis when appropriate
- Assess proportional hazards assumption and consider alternative methods if violated [54] [38]
Risk of Bias Assessment: Use validated tools such as Cochrane Risk of Bias (RoB 2) for randomized trials and ROBINS-I for non-randomized studies to systematically evaluate potential biases [54].
The RECOURSE study provides a exemplary methodology for synthesizing evidence across multiple cancer types and procedures, employing a hierarchical decision tree for extracting or estimating HRs when not directly reported, and using both fixed-effect and random-effects models for meta-analysis depending on heterogeneity [54].
Advancing research in personalized treatment planning requires specialized computational resources and data infrastructure. The following table details essential resources for investigators in this field.
Table 3: Essential Computational Resources for CDSS and Robotic Surgery Research
| Resource Name | Type/Function | Research Application | Key Features |
|---|---|---|---|
| MLOmics Database | Cancer multi-omics database | ML model development for precision oncology | 8,314 patient samples across 32 cancer types; four omics types (mRNA, miRNA, methylation, CNV); three feature versions (Original, Aligned, Top) [56] |
| TCGA (The Cancer Genome Atlas) | Genomic and clinical data | Biomarker discovery, molecular subtyping | Multi-platform molecular characterization of 33 cancer types; linked clinical and imaging data; standardized processing pipelines [56] |
| QUADAS-AI Tool | Quality assessment tool | Systematic reviews of AI diagnostic accuracy studies | Assesses risk of bias and applicability concerns in AI studies; domains include patient selection, index test, reference standard, flow/timing [16] |
| RECURSE Methodology | Statistical analysis framework | Comparative effectiveness research for surgical outcomes | Hierarchical decision tree for HR extraction/estimation; methods include direct reported HRs, estimation from events and p-values, derivation from Kaplan-Meier curves [54] |
| Cox Regression with Regularization | Statistical ML method | Survival analysis with high-dimensional predictors | Enables Cox model application to genomic data; methods include LASSO (L1), Ridge (L2), Elastic Net (combined) penalties [38] |
The MLOmics database deserves particular emphasis as it addresses a critical bottleneck in ML for oncology research: the gap between powerful ML algorithms and well-prepared, model-ready data [56]. By providing uniformly processed multi-omics data with multiple feature versions and extensive baselines, MLOmics enables more reproducible and comparable ML research. The database includes three feature processing versions: the Original version containing full feature sets; the Aligned version with overlapping features across cancer types and z-score normalization; and the Top version with the most significant features selected via ANOVA testing with Benjamini-Hochberg false discovery rate control [56]. This tiered approach supports different research objectives, from comprehensive pan-cancer analyses to focused biomarker studies.
Visualization of ML Model Development and Validation Workflow
The development and validation of ML models for CDSS requires a rigorous, standardized workflow to ensure clinical reliability and generalizability. The following diagram illustrates the key stages in creating validated predictive models for oncology decision support.
This workflow emphasizes the critical importance of external validation for clinical implementation—a step often overlooked in research settings. A systematic review of AI in lung cancer imaging found that only 104 of 315 studies conducted external validation using out-of-sample datasets [16]. This validation gap represents a significant barrier to clinical translation, as models demonstrating excellent internal performance may fail to generalize to different populations or clinical settings. The workflow also highlights the continuous learning cycle necessary for maintaining model performance over time, as changing practice patterns, new treatments, and evolving disease presentations can lead to "model drift" requiring periodic retraining and validation [51] [16].
The integration of clinical decision support systems and robotic surgery represents a paradigm shift in personalized cancer treatment planning. Evidence from systematic reviews and meta-analyses indicates that CDSS improves guideline adherence, patient-centered care, and care delivery processes [53] [52], while robotic surgery demonstrates non-inferior and sometimes superior oncologic outcomes compared to conventional approaches [54] [55]. The convergence of these technologies creates a powerful framework for data-driven personalization across the cancer care continuum.
Critical challenges remain in realizing the full potential of these technologies. For CDSS, key implementation barriers include workflow integration, interoperability with existing EHR systems, alert fatigue, and the need for continuous content updates [52]. For robotic surgery, concerns regarding cost, training requirements, and the limited evidence base for some cancer types and procedures warrant attention [54]. From a methodological perspective, the field requires greater standardization in evaluation metrics, more rigorous external validation of ML models, and enhanced approaches for model explainability to build clinical trust [51] [16].
Future research should prioritize prospective validation of ML-powered CDSS in diverse clinical settings, development of standardized data pipelines for model training and deployment, and exploration of more sophisticated integration between predictive analytics and robotic execution. As these technologies mature, they hold the promise of creating truly adaptive learning systems that continuously refine personalized treatment approaches based on accumulating evidence, ultimately advancing the goal of precision oncology to maximize survival and quality of life for every cancer patient.
Navigating the Challenges: Data, Model Design, and Clinical Integration
The application of machine learning (ML) in oncology research represents a paradigm shift in how we understand, diagnose, and treat cancer. However, this potential is constrained by significant data challenges that impact model performance and clinical applicability [57]. High-dimensional data from genomics, radiomics, and clinical records present computational and analytical complexities, while substantial biological heterogeneity exists both between patients and within individual tumors [58]. Furthermore, limited dataset sizes, particularly for rare cancer subtypes, necessitate sophisticated data augmentation techniques to build robust models [59].
This technical guide, framed within a broader systematic review of ML in cancer research, examines these core data challenges and their methodological solutions. We provide researchers with structured frameworks for navigating the complexities of cancer data, with emphasis on practical implementations for processing high-dimensional inputs, characterizing heterogeneity, and expanding limited datasets through advanced augmentation protocols.
High-Dimensional Data in Cancer Research
Modern cancer research leverages diverse high-dimensional data sources that collectively create an integrative view of tumor biology. Each data type presents unique dimensional characteristics and analytical considerations, as summarized in Table 1.
Table 1: Characteristics of High-Dimensional Data Sources in Cancer Research
| Data Type | Dimensional Scale | Key Applications in Cancer Research | Primary Analytical Challenges |
|---|---|---|---|
| Single-cell RNA Sequencing | 20,000+ genes across thousands to millions of cells [58] | Tumor microenvironment dissection, cellular heterogeneity mapping, rare cell population identification [58] [60] | High sparsity, technical noise, batch effects, integration with spatial data |
| Radiomics | Hundreds to thousands of quantitative features per image [57] [16] | Tumor classification, treatment response prediction, survival outcome forecasting [57] [16] | Feature reproducibility, standardization of extraction protocols, clinical interpretability |
| Mass Cytometry | 40-50 protein markers simultaneously at single-cell resolution [61] | Immune profiling, signaling network analysis, pharmacodynamic response monitoring [61] | Compensation, normalization, cellular subset identification |
| Genomic Profiles | Millions of variants across genomes or hundreds of genes in panels [57] | Mutation signature analysis, molecular subtyping, therapeutic target identification [57] | Data integration, variant interpretation, functional validation |
Analytical Frameworks for High-Dimensional Data
Processing high-dimensional cancer data requires specialized computational workflows that transform raw data into biologically meaningful patterns. The foundational approach involves sequential dimensionality reduction, clustering, and predictive modeling [61].
Figure 1: Analytical workflow for high-dimensional cancer data, progressing from raw data to clinical insights.
The workflow begins with essential preprocessing steps including quality control, normalization, and batch effect correction to mitigate technical artifacts [61]. Dimensionality reduction techniques such as Principal Component Analysis (PCA), t-distributed Stochastic Neighbor Embedding (t-SNE), and Uniform Manifold Approximation and Projection (UMAP) project data into lower-dimensional spaces for visualization and analysis [61]. Clustering algorithms including PhenoGraph and FlowSOM then identify distinct cellular subpopulations or patient subtypes based on multidimensional similarity [61]. Finally, supervised ML models perform feature selection to identify the most informative variables for predicting clinical outcomes such as diagnostic classification, therapeutic response, or survival probability [61].
Tumor Heterogeneity: Analytical Approaches and Characterization
Multimodal Integration for Heterogeneity Mapping
Tumor heterogeneity exists at multiple biological scales, from molecular variations between cancer cells to morphological differences across tumor regions. Single-cell RNA sequencing (scRNA-seq) has emerged as a powerful tool for deconstructing this complexity, typically revealing 15 or more transcriptionally distinct cell clusters within breast cancer samples, including neoplastic epithelial, immune, stromal, and endothelial populations [58]. Spatial transcriptomics further contextualizes these populations by preserving their architectural relationships, enabling researchers to map specific cell subtypes to tumor core, invasive margin, or stromal regions [58].
Table 2: Experimental Workflow for Single-Cell and Spatial Transcriptomic Analysis of Tumor Heterogeneity
| Experimental Phase | Key Procedures | Technical Considerations | Expected Outcomes |
|---|---|---|---|
| Sample Preparation | Tissue dissociation into single-cell suspensions; viability maintenance >80% [58] | Optimization of enzymatic digestion to minimize stress signatures; inclusion of viability markers | High-quality single-cell suspension with preserved transcriptomic profiles |
| Single-Cell Partitioning | Cell loading on microfluidic platforms (10X Genomics, Drop-seq) [58] | Target recovery of 5,000-10,000 cells per sample; multiplet rate control | Barcoded single-cell libraries representing full cellular diversity |
| Library Preparation & Sequencing | cDNA synthesis, amplification, and library construction; sequencing depth of 50,000-100,000 reads/cell [58] | Unique Molecular Identifier (UMI) incorporation to quantify mRNA molecules; quality metrics assessment | Digital gene expression matrices for downstream analysis |
| Spatial Transcriptomics | Tissue sectioning onto capture slides; spatial barcode integration [58] | Optimization of tissue thickness (typically 10μm); morphology preservation | Gene expression data with two-dimensional coordinate information |
| Computational Integration | Data integration using Harmony, Seurat, or CARD tools [58] | Batch effect correction; reference-based and reference-free approaches | Combined single-cell and spatial data with cell-type proportions mapped to tissue locations |
Functional Profiling of Heterogeneous Cell Populations
Beyond transcriptional characterization, functional heterogeneity can be assessed through dynamic profiling of signaling activities. Single-cell calcium imaging captures oscillatory patterns in cytosolic Ca²⁺ concentrations that serve as indicators of cellular phenotype [60]. When combined with graph-based unsupervised clustering and artificial neural networks, this approach can discriminate between 26 distinct clusters of Ca²⁺ responses in prostate and colorectal cancer models, enabling identification of functional signatures associated with drug resistance or cancer-fibroblast interactions [60].
Figure 2: Integrated analytical pipeline for tumor heterogeneity characterization.
Data Augmentation Techniques for Limited Datasets
Methodologies for Medical Image Augmentation
Data augmentation artificially expands training datasets by applying transformations to existing samples, which is particularly valuable in medical imaging where annotated datasets are often small. A specialized approach for single tumor segmentation involves cutting and mirroring augmentation around the tumor's approximate center [59].
Horizontal & Vertical Cutting and Mirroring Augmentation (HVCMA) Protocol:
- Image Division: Identify the approximate center of the tumor and divide the image horizontally and vertically into four quadrants (A, B, C, D)
- Zero-Padding: For tumors located near image edges, apply zero-padding to maintain appropriate aspect ratios in generated sub-images
- Mirroring Operations: Generate three mirrored versions of each quadrant:
- Horizontal mirroring (A')
- Vertical mirroring (A'')
- Diagonal mirroring (A''')
- Image Reconstruction: Combine original and mirrored quadrants to create four complete tumor images: [A''', A''; A', A], [B'', B; B''', B'], [C, C'; C'', C'''], [D', D'''; D, D''] [59]
This approach, when applied to breast ultrasound datasets and evaluated with U-Net and Mask-RCNN architectures, improved dice similarity coefficient (DSC) values by 9.66-13.74% compared to no augmentation and by 4.92-12.23% compared to traditional augmentation methods [59].
Handling Class Imbalance in Clinical Data
Beyond medical imaging, class imbalance in structured clinical data presents significant challenges for predictive modeling. For lung cancer risk prediction using patient attributes (smoking history, symptoms, demographics), synthetic minority oversampling techniques (SMOTE) generate artificial examples for the underrepresented class [62]. Systematic evaluation of nine resampling strategies with ten classifiers demonstrated that K-Means SMOTE combined with Multi-Layer Perceptron achieved 93.55% accuracy and 96.76% AUC-ROC, significantly outperforming models trained on imbalanced data [62].
Table 3: Performance Comparison of Data Augmentation Techniques Across Cancer Applications
| Application Domain | Augmentation Method | Performance Metrics | Comparative Baseline |
|---|---|---|---|
| Breast Ultrasound Segmentation [59] | Diagonal Cutting and Mirroring Augmentation (DCMA) | DSC improvement of 13.74% | No data augmentation |
| Breast Ultrasound Segmentation [59] | Horizontal & Vertical Cutting and Mirroring Augmentation (HVCMA) | DSC improvement of 12.43% | No data augmentation |
| Lung Cancer Risk Prediction [62] | K-Means SMOTE with MLP Classifier | 93.55% accuracy, 96.76% AUC-ROC | Unaugmented imbalanced dataset |
| Lung Cancer Risk Prediction [62] | SMOTE with XGBoost Classifier | 95.83% AUC-ROC | Unaugmented imbalanced dataset |
Successful implementation of the methodologies described in this guide requires specific experimental and computational resources. Table 4 catalogs key reagents and their applications in addressing data challenges in cancer research.
Table 4: Essential Research Reagents and Resources for Overcoming Cancer Data Challenges
| Resource Category | Specific Examples | Function in Research Workflow | Application Context |
|---|---|---|---|
| Cell Culture Media | McCoy media, DMEM, RPMI-1640 [60] | Maintenance of cancer cell line viability and phenotype during experimental procedures | Functional studies using calcium imaging and drug response assays |
| Fluorescent Dyes | Cal520-AM (Ca²⁺ indicator), Red CellTracker dyes [60] | Dynamic monitoring of intracellular signaling and cell lineage tracing in co-culture systems | Single-cell calcium imaging and tumor-stroma interaction studies |
| Data Integration Tools | Harmony, Seurat, CARD [58] | Integration of multimodal data (scRNA-seq, spatial transcriptomics) with batch effect correction | Tumor microenvironment deconstruction and heterogeneity mapping |
| Deep Learning Frameworks | U-Net, Mask R-CNN [59] | Image segmentation and classification tasks on medical imaging data | Tumor boundary detection in radiological images |
| Synthetic Data Generators | SMOTE, K-Means SMOTE, ADASYN [62] | Addressing class imbalance in structured clinical datasets through synthetic sample generation | Lung cancer risk prediction models using clinical attributes |
The integration of machine learning in cancer research continues to transform our approach to oncological investigation and clinical care. By implementing robust methodologies for handling high-dimensional data, characterizing multiscale tumor heterogeneity, and expanding limited datasets through advanced augmentation techniques, researchers can overcome the most persistent data challenges in the field. The experimental protocols and analytical frameworks presented in this guide provide a structured pathway for advancing more reproducible, predictive, and clinically relevant cancer models. As these methodologies continue to evolve, they will undoubtedly accelerate the development of precision oncology approaches that effectively address the complexity of malignant disease.
The integration of machine learning (ML) into cancer research represents a paradigm shift in oncology, enabling the extraction of complex patterns from high-dimensional data for improved diagnosis, prognosis, and treatment planning [16] [63]. However, the clinical translation of these models faces significant challenges, primarily concerning their reliability in real-world settings. Overfitting and poor generalizability undermine model efficacy when deployed across diverse patient populations, clinical institutions, and imaging protocols [64] [65]. Within the specific context of cancer research, where datasets are often limited, imbalanced, and heterogeneous, ensuring model robustness becomes paramount for clinical adoption.
This technical guide examines strategies to mitigate overfitting and enhance generalizability specifically for ML applications in cancer research. We synthesize methodological frameworks, experimental protocols, and practical implementations to help researchers develop models that maintain predictive performance when applied to unseen data from different distributions, ultimately supporting more reliable and trustworthy AI systems in oncology.
Defining Robustness and Generalizability in Cancer Research
In supervised learning for cancer research, models are typically developed using Empirical Risk Minimization (ERM), which minimizes the average loss on observed training data [65]. This approach operates under the closed-world assumption that training and test data are independently and identically distributed (i.i.d.). Generalizability in this i.i.d. context refers to a model's ability to perform well on novel data drawn from the same distribution as the training set [65].
Robustness extends beyond i.i.d. generalizability, representing a model's capacity to maintain stable predictive performance when faced with variations and changes in input data that may occur in real-world clinical deployment [65]. In cancer research, these challenges manifest specifically as:
- Scanner heterogeneity: Differences in imaging equipment across medical centers [64]
- Acquisition protocol variability: Variations in imaging parameters and techniques [64]
- Data drift: Evolving clinical practices and patient populations over time [65]
- Domain shifts: Systematic differences between data from different medical institutions [64]
- Class imbalance: Uneven representation of cancer subtypes or disease stages [38]
The relationship between i.i.d. generalizability and robustness is hierarchical: i.i.d. generalization is a necessary but insufficient condition for robustness [65]. A model that fails to generalize to i.i.d. data will almost certainly fail under distribution shifts, but strong i.i.d. performance does not guarantee robustness to real-world variations encountered in multi-center cancer studies.
Table 1: Performance Comparison of ML vs. Traditional Statistical Methods in Cancer Survival Prediction
| Model Type | C-Index/AUC | Strengths | Limitations | Clinical Context |
|---|---|---|---|---|
| Cox Proportional Hazards | 0.83-0.90 [66] [16] | Interpretable, established | Limited by proportional hazards assumption | Suitable for small datasets with linear relationships |
| Machine Learning Models | 0.83-0.92 [66] [16] | Captures complex non-linear patterns | Prone to overfitting without proper regularization | Valuable for high-dimensional genomic or imaging data |
| Deep Learning Models | 0.90-0.94 [16] | Automatic feature extraction | High computational requirements, data hunger | Optimal for image-based diagnosis (CT, PET, MRI) |
Core Strategies for Enhancing Robustness and Generalizability
Data-Centric Approaches
Data-centric approaches focus on improving the quantity, quality, and diversity of training data to create more robust models that learn invariant patterns rather than dataset-specific artifacts.
Data Augmentation generates synthetic training examples by applying realistic transformations to existing data, simulating variations encountered in clinical practice [64]. In cancer imaging, effective augmentation techniques include:
- Geometric transformations: Rotation, flipping, scaling, and cropping of radiology or histopathology images [64]
- Color space adjustments: Modifying brightness, contrast, and saturation to account for staining variations [64]
- Noise injection: Adding random noise to improve resilience to imaging artifacts [64]
- Advanced methods: Mixup and CutMix create novel training examples by combining images [64]
Data Collection and Curation strategies include:
- Multi-center studies: Incorporating data from multiple institutions with different protocols [16]
- Feature reduction: Principal Component Analysis (PCA) and Independent Component Analysis (ICA) to mitigate dimensionality [64]
- Quality control: Excluding poor-quality images and standardizing preprocessing pipelines [16]
Model-Centric Approaches
Model-centric approaches modify the learning algorithm or architecture itself to discourage overfitting and encourage the learning of more generalized representations.
Regularization Techniques introduce constraints to prevent models from becoming overly complex:
- L1 Regularization (Lasso): Adds absolute value penalty to promote sparsity and feature selection [64] [38]
- L2 Regularization (Ridge): Adds squared penalty to discourage large weights [64] [38]
- Elastic Net: Linearly combines L1 and L2 penalties for balanced regularization [38]
- Dropout: Randomly deactivates neurons during training to prevent co-adaptation [64]
- Early Stopping: Halts training when validation performance stops improving [64]
Architectural Strategies include:
- Transfer Learning: Leverages pretrained models on large datasets, followed by fine-tuning on specific cancer tasks [64]
- Ensemble Methods: Combines multiple models to reduce variance and improve robustness:
- Domain Adaptation: Explicitly minimizes distribution shifts between source and target domains [64]
Training Strategies
Optimization techniques and loss functions designed to improve generalization:
Adaptive Optimization: Methods like Adam dynamically adjust learning rates to stabilize training, especially with noisy or incomplete medical data [64].
Specialized Loss Functions:
- Dice Loss: Maximizes overlap between predicted and actual segments in tumor segmentation [64]
- Weighted Cross-Entropy: Addresses class imbalance by assigning higher weights to underrepresented cancer classes [64]
Diagram 1: Robust ML Development Workflow for Cancer Research
Experimental Framework and Validation Protocols
Robustness Assessment Methodology
Rigorous experimental design is essential for properly evaluating model robustness in cancer research applications. The following protocol provides a structured approach:
1. Data Partitioning Strategy:
- Split data into training, validation, and test sets at the institution level rather than patient level
- Ensure test set contains completely separate institutions from training
- Implement k-fold cross-validation with careful separation to prevent data leakage [67]
2. Performance Monitoring:
- Track both training and validation performance metrics throughout training
- Monitor for divergence indicating overfitting [67]
- Use early stopping with patience parameter based on validation performance
3. Multi-Dimensional Evaluation:
- Test on out-of-distribution (OOD) data from different scanner types and protocols
- Evaluate on underrepresented patient subgroups to assess fairness
- Stress-test with corrupted or noisy inputs to measure resilience [65]
4. Statistical Validation:
- Perform multiple runs with different random seeds
- Report confidence intervals for all performance metrics
- Use statistical tests to confirm significance of improvements
Table 2: Experimental Reagents and Computational Tools for Robustness Research
| Resource Category | Specific Tools/Techniques | Application in Cancer Research | Implementation Considerations |
|---|---|---|---|
| Data Augmentation | Rotation, flipping, scaling [64] | Simulating anatomical variations in medical images | Preserve clinical relevance; avoid unrealistic transformations |
| Regularization Methods | L1/L2 regularization, Dropout [64] | Preventing overfitting on small oncology datasets | Tune regularization strength via cross-validation |
| Ensemble Architectures | Random Forests, Gradient Boosting [64] [66] | Integrating multi-modal data (genomic, imaging, clinical) | Computational cost vs. performance trade-off |
| Domain Adaptation | Adversarial training, feature alignment [64] | Harmonizing multi-site data in cancer studies | Requires samples from target domain during training |
| Uncertainty Quantification | Monte Carlo Dropout, ensemble methods [65] | Identifying unreliable predictions in clinical deployment | Calibrate uncertainty estimates on validation set |
Quantitative Metrics and Evaluation
Comprehensive evaluation requires multiple metrics to assess different aspects of model performance:
Primary Performance Metrics:
- Discrimination: Area Under ROC Curve (AUC), Concordance Index (C-index) [66] [16]
- Calibration: Brier score, calibration plots
- Clinical Utility: Hazard ratios for survival analysis [16]
Robustness-Specific Metrics:
- Performance degradation: Difference between internal and external validation performance [16]
- Failure rate analysis: Proportion of samples where confidence is high but prediction is wrong [65]
- Distribution shift sensitivity: Performance variation across different institutions or patient subgroups
Diagram 2: Experimental Validation Protocol for Robustness
Implementation in Cancer Research: Case Studies and Evidence
Application in Cancer Survival Prediction
Machine learning methods for survival analysis have shown particular promise in overcoming limitations of traditional statistical approaches like Cox Proportional Hazards (CPH) regression. Regularized CPH variants have been developed specifically for high-dimensional cancer data:
Implementation Protocol:
- Data Preparation: Process genomic, clinical, and imaging features
- Feature Selection: Apply LASSO for sparse feature selection in high-dimensional data [38]
- Model Training: Optimize hyperparameters via cross-validation
- Validation: Assess on temporal or geographic external cohorts
Evidence from Comparative Studies: A systematic review of ML techniques for cancer survival analysis found that multi-task and deep learning methods yielded superior performance, though they were reported in only a minority of studies [38]. Another meta-analysis of 21 studies found that ML models showed similar performance to CPH models (standardized mean difference in C-index: 0.01, 95% CI: -0.01 to 0.03), highlighting that ML does not automatically outperform traditional methods without proper robustness considerations [66].
Application in Cancer Imaging
Deep learning models for cancer image analysis have demonstrated strong performance but face significant robustness challenges:
Lung Cancer Diagnosis: A comprehensive meta-analysis of AI in lung cancer imaging included 315 studies and found pooled sensitivity of 0.86 and specificity of 0.86 for diagnosis, with AUC of 0.92 [16]. However, significant heterogeneity was observed (I² = 94.71% for sensitivity, 97.35% for specificity), indicating substantial variability across studies and settings.
Strategies for Imaging Robustness:
- Multi-institutional training: Incorporate data from multiple centers with different scanner types [64]
- Data augmentation: Apply realistic image transformations to increase diversity [64]
- Transfer learning: Leverage models pretrained on natural images, fine-tuned on medical data [64]
- Domain adaptation: Explicitly minimize domain shift between institutions [64]
Uncertainty Quantification and OOD Detection
Uncertainty estimation provides crucial safety mechanisms for clinical deployment:
Implementation Framework:
- Aleatoric vs. Epistemic Uncertainty: Quantify both data inherent and model uncertainty [65]
- OOD Detection: Identify samples significantly different from training distribution [65]
- Rejection Options: Enable models to abstain from prediction when uncertainty is high
Clinical Value: In cancer applications, uncertainty quantification allows clinicians to identify cases requiring additional review, potentially preventing diagnostic errors on challenging or atypical cases [65].
Ensuring model robustness through mitigation of overfitting and enhancement of generalizability is not merely a technical consideration but a fundamental requirement for clinically applicable machine learning in cancer research. The strategies outlined in this guide—spanning data-centric, model-centric, and training approaches—provide a comprehensive framework for developing more reliable and trustworthy models. The experimental protocols and validation methodologies offer practical guidance for rigorous assessment of model robustness.
As the field progresses, the integration of robustness considerations throughout the ML development lifecycle will be essential for translating predictive models from research environments to diverse clinical settings, ultimately supporting more precise and reliable cancer care. Future directions should focus on standardized benchmarking of robustness, development of cancer-specific robustness metrics, and increased emphasis on prospective multi-center validation to fully assess real-world performance.
The integration of artificial intelligence (AI) and machine learning (ML) into oncology research represents a paradigm shift in cancer diagnostics, prognostics, and therapeutic development. However, the proliferation of these sophisticated algorithms has unveiled a critical challenge: their frequent operation as "black boxes" that provide predictions without transparent reasoning or mechanistic insights. This opacity fundamentally limits their clinical adoption, as oncologists and researchers require not just predictions but interpretable insights that align with biological understanding and support therapeutic decision-making [68]. The interpretability imperative addresses this gap by demanding that AI systems provide explanations for their outputs, enabling researchers to validate, trust, and effectively implement these tools in high-stakes cancer care environments.
The clinical translation of AI models in oncology faces significant barriers when interpretability is not prioritized. Without explanatory capabilities, even highly accurate models struggle to gain clinician trust, integrate with existing biological knowledge, or provide actionable insights beyond traditional methods. This whitepaper examines current interpretability approaches, provides detailed experimental frameworks for implementing explainable AI (XAI) in cancer research, and outlines a pathway for bridging the critical gap between algorithmic output and clinically meaningful insight.
Methodological Foundations of Interpretable ML in Cancer Research
Core Interpretability Techniques and Their Applications
Interpretable ML methodologies in oncology encompass diverse approaches tailored to different data types and clinical questions. These techniques can be broadly categorized into model-specific interpretability (using intrinsically interpretable models) and post-hoc interpretability (applying explanation methods to pre-existing models) [69]. The selection of appropriate interpretability methods depends on the clinical context, data modality, and required level of explanation granularity.
SHapley Additive exPlanations (SHAP) represents a prominent post-hoc interpretation framework based on cooperative game theory that quantifies the contribution of each feature to individual predictions. In oncology, SHAP has demonstrated particular utility for explaining complex ensemble models. For instance, an XGBoost model predicting lymph node metastasis in gastric cancer achieved an AUC of 0.883 while using SHAP to identify which clinicopathological and immunonutritional biomarkers most influenced predictions [70]. This approach revealed distinct biomarker contribution patterns across different T-stages and Lauren classifications, providing both predictive power and biological insights.
Local Interpretable Model-agnostic Explanations (LIME) offers an alternative approach that approximates complex model behavior locally around specific predictions using interpretable surrogate models. A recent study on gastric cancer detection implemented LIME to visualize critical regions in histopathological images that contributed to a deep learning model's classification decision [69]. This model-agnostic technique proved particularly valuable for image-based diagnostics, as it generates spatial explanations that pathologists can directly correlate with morphological features.
Attention mechanisms and saliency maps have emerged as powerful interpretability tools for deep learning architectures, especially in histopathology and radiology. These approaches highlight which regions of input data (e.g., whole slide images or CT scans) the model "attends to" when making predictions, creating visual explanations that align with clinical workflows [71]. For example, multimodal prognostic models integrating pathology images with omics data have used attention mechanisms to identify histomorphological features associated with molecular subtypes and survival outcomes [71].
Quantitative Performance of Interpretable Models in Oncology
Table 1: Performance Comparison of Interpretable ML Models in Cancer Research
| Cancer Type | ML Model | Interpretability Method | Prediction Task | Performance (AUC) | Key Interpretable Insights |
|---|---|---|---|---|---|
| Gastric Cancer | XGBoost | SHAP | Lymph node metastasis | 0.883 (training) 0.815 (testing) | T4 stage, poor differentiation as top risk factors; heterogeneous biomarker patterns across subtypes [70] |
| Gastric Cancer | Deep Learning Fusion (VGG16+ResNet50+MobileNetV2) | LIME | Cancer detection | 97.8% accuracy | Visual explanations highlighting malignant regions in histopathology images [69] |
| Pan-Cancer | Multimodal Deep Learning | Attention mechanisms | Overall survival | 0.550-0.857 (c-index) | Identification of prognostic histomorphological features across 19 cancer types [71] |
Experimental Protocols for Interpretable Oncology AI
Protocol 1: Developing Interpretable Models for Metastasis Prediction
The following protocol outlines the methodology for developing an interpretable ML model for predicting lymph node metastasis in gastric cancer, based on validated approaches from recent literature [70]:
Data Curation and Feature Engineering
- Collect clinicopathological data from retrospective cohorts, ensuring adequate sample size (N≥1000 recommended for robust feature selection)
- Structure variables into five modules: (1) basic demographics, (2) tumor characteristics, (3) inflammation indicators (NLR, PLR, SII), (4) coagulation parameters (fibrinogen, platelet-to-albumin ratio), and (5) nutritional-immune markers (PNI, hemoglobin-to-red cell distribution width ratio)
- Implement recursive feature elimination (RFE) to select the most predictive features while minimizing redundancy
- Split data into training (80%) and testing (20%) cohorts with stratification to maintain outcome distribution
Model Development and Interpretation
- Implement XGBoost algorithm with hyperparameter optimization via cross-validation
- Train model using 19 selected features across the five clinical modules
- Apply SHAP analysis to quantify feature importance and direction of effects
- Validate model performance using area under the curve (AUC), sensitivity, and specificity
- Conduct subgroup analyses to assess heterogeneity in biomarker patterns across pathological subtypes (e.g., Lauren classification, T-stages)
Table 2: Essential Research Reagents for Interpretable ML in Cancer Research
| Research Reagent | Function | Application Example |
|---|---|---|
| SHAP (SHapley Additive exPlanations) | Quantifies feature contribution to model predictions | Explaining variable importance in metastasis prediction models [70] |
| LIME (Local Interpretable Model-agnostic Explanations) | Creates local surrogate models to explain individual predictions | Highlighting regions of interest in histopathology images [69] |
| The Cancer Genome Atlas (TCGA) | Provides multi-omics data for model training and validation | Multimodal survival prediction integrating pathology and genomics [71] |
| MONAI (Medical Open Network for AI) | Open-source framework for medical AI development | Standardized preprocessing of radiology and pathology images [10] |
| TRIPOD+AI Reporting Guideline | Ensures transparent reporting of prediction model studies | Standardizing methodology and validation reporting [72] |
Protocol 2: Multimodal Fusion with Explainable AI for Cancer Diagnostics
This protocol details an approach for developing interpretable multimodal fusion models, particularly for image-based cancer diagnostics [69]:
Model Architecture Design
- Select complementary deep learning architectures (e.g., VGG16 for hierarchical feature learning, ResNet50 for residual connections, MobileNetV2 for efficiency)
- Implement intermediate fusion strategy: extract feature maps from each architecture and concatenate before final classification layers
- Apply joint training to enable cross-model interaction and collaborative feature learning
- Regularize fusion layers with dropout and L2 regularization to prevent overfitting
Explainability Implementation
- Integrate LIME for post-hoc explanation of model predictions
- Generate segmentation masks to highlight image regions contributing to classification
- Validate explanations through correlation with pathologist annotations
- Quantify explanation consistency across similar cases and subtypes
Performance Validation
- Benchmark against individual models and alternative fusion strategies (early and late fusion)
- Assess both classification metrics (accuracy, sensitivity, specificity) and explanation quality (spatial correlation with ground truth annotations)
- Conduct clinical utility studies measuring diagnostic concordance and time efficiency
Visualization Frameworks for Model Interpretability
Workflow for Interpretable Metastasis Prediction
The following diagram illustrates the integrated workflow for developing and interpreting an ML model for cancer metastasis prediction:
Deep Learning Fusion with Explainable AI
This diagram outlines the architecture for a fusion deep learning model with integrated explainability components:
Implementation Challenges and Clinical Translation
Methodological Rigor and Validation Frameworks
The development of interpretable ML models for oncology requires stringent methodological standards to ensure reliability and clinical applicability. Current systematic reviews indicate that many prediction models in cancer research suffer from methodological flaws, including high risk of bias, inadequate handling of missing data, and insufficient external validation [72]. Addressing these limitations requires:
Protocol Pre-registration: Prospective registration of study protocols on platforms such as ClinicalTrials.gov enhances transparency and reduces selective reporting bias [72]. Protocols should explicitly detail the interpretability methods, validation strategies, and clinical utility assessments.
Comprehensive Validation: Beyond standard performance metrics (e.g., AUC, accuracy), interpretable models require validation of their explanatory outputs. This includes assessing explanation fidelity (how accurately explanations represent model reasoning), stability (consistency across similar inputs), and clinical coherence (alignment with biological knowledge) [72] [68].
Fairness and Equity Assessment: Interpretability methods should be leveraged to detect and mitigate algorithmic bias across demographic groups. This involves conducting subgroup analyses to ensure consistent performance and explanation quality across diverse populations [72].
Integration with Clinical Workflows and Decision Support
The ultimate test of interpretable AI in oncology is its successful integration into clinical workflows and therapeutic decision-making. Current research demonstrates several promising pathways:
Molecular Target Identification: Interpretable deep learning models that incorporate prior knowledge of molecular networks can simulate cancer cell signaling under drug perturbations, simultaneously predicting efficacy and inferring off-target effects [68]. These models provide mechanistic insights that support target validation and drug development.
Pathology and Radiology Augmentation: AI systems with explainable components are being integrated into diagnostic workflows, providing second-reader functions that highlight suspicious regions in medical images [10] [73]. For instance, AI-powered immunohistochemistry scoring systems improve consistency in HER2-low breast cancer classification, directly impacting treatment eligibility [73].
Multimodal Data Integration: The most advanced interpretable systems combine multiple data modalities—including genomics, histopathology, radiomics, and clinical variables—to generate unified predictive models with comprehensive explanations [10] [71]. The TRIDENT initiative in metastatic non-small cell lung cancer exemplifies this approach, integrating radiomics, digital pathology, and genomics to identify patient subgroups with optimal treatment response [10].
The interpretability imperative represents a fundamental requirement for the responsible implementation of AI in oncology. As the field progresses, the focus must shift from merely achieving high predictive accuracy to generating transparent, clinically meaningful insights that align with biological mechanisms and support therapeutic decision-making. The methodologies and frameworks outlined in this whitepaper provide a roadmap for developing interpretable AI systems that can earn clinician trust, navigate regulatory requirements, and ultimately improve patient outcomes.
Future advances in interpretable AI will likely involve more sophisticated integration of biological prior knowledge, standardized validation frameworks for explanation quality, and increased emphasis on real-world clinical utility. By bridging the gap between algorithmic output and clinical insight, interpretable ML promises to unlock the full potential of AI as a transformative tool in oncology research and practice.
The integration of artificial intelligence (AI) and machine learning (ML) into oncology represents a paradigm shift in cancer research and drug development. These technologies offer unprecedented capabilities to analyze complex datasets, from genomics and medical imaging to real-world evidence, thereby accelerating the pace of discovery and personalization of care [1]. However, this rapid advancement brings forth significant ethical and regulatory challenges that must be systematically addressed to ensure responsible and equitable translation into clinical practice. Within the context of a systematic review of machine learning in cancer research, this whitepaper provides an in-depth technical examination of three cornerstone considerations: data privacy, algorithmic bias, and regulatory pathways for FDA approval. Framing these issues is critical for researchers, scientists, and drug development professionals who are navigating the transition from exploratory models to clinically impactful tools.
Data Privacy and Security in Cancer Research
The efficacy of AI in oncology is predicated on access to vast amounts of sensitive patient data. Ensuring the privacy and security of this data is a fundamental ethical and legal obligation.
Federated Learning as a Technical Solution
A transformative approach to data privacy is federated learning (FL), a distributed machine learning technique that circumvents the need for centralizing sensitive clinical data. In this paradigm, an AI model is trained across multiple decentralized devices or servers holding local data samples, without exchanging the data itself [74].
The Cancer AI Alliance (CAIA), a collaboration involving leading institutions like Dana-Farber Cancer Institute and Memorial Sloan Kettering, has launched a scalable federated learning platform for cancer research. The technical workflow is as follows [74]:
- Initialization: A central server initializes a global AI model and defines the training task.
- Distribution: The global model is sent to participating cancer centers.
- Local Training: Each center trains the model locally using its own secure, de-identified data. Individual clinical data never leaves the institutional firewalls.
- Update Transmission: Instead of raw data, each center sends only the model updates (e.g., learned weights and gradients) back to the central server.
- Aggregation: The central server aggregates these updates to improve the global model.
- Iteration: The process repeats, with the refined global model being redistributed for further training, until convergence.
This method maintains data security and privacy while enabling the model to learn from a diverse and representative population of over one million patients [74].
Federated Learning Workflow in Oncology. This diagram illustrates the iterative process of training a machine learning model across multiple institutions without sharing raw patient data.
Regulatory and Governance Frameworks
Technical solutions must operate within robust governance frameworks. Key U.S. frameworks include the NIST AI Risk Management Framework (RMF) and the Blueprint for an AI Bill of Rights [75]. These guidelines emphasize principles of data minimization, secure storage, and transparent data usage. For AI systems involving U.S. persons, the Intelligence Community's AI Ethics Framework underscores the requirement that data must be "obtained lawfully and consistent with legal obligations and policy requirements" [76]. Researchers must partner with legal, compliance, and privacy professionals to navigate the specific authorities and restrictions governing their data sources, such as the Privacy Act [76].
Algorithmic Bias and Fairness
Algorithmic bias poses a significant risk of perpetuating and exacerbating existing health disparities. If an AI model is trained on skewed data that under-represents certain demographic groups, its predictions may be less accurate for those populations, leading to inequitable care [77].
Bias can be introduced at multiple stages of the AI lifecycle:
- Training Data: Historical data from clinical trials or healthcare systems that lack diversity can create models that are not generalizable. For example, a study highlighted that the frequency of
FOXA1mutations in prostate cancer was significantly higher, whereasTP53mutations were significantly lower in Black men compared with white men [77]. An AI model trained predominantly on genomic data from white populations would fail to accurately characterize disease in Black patients. - Feature Extraction and Model Selection: Human choices in selecting variables and algorithms can introduce cognitive biases, potentially overlooking features relevant to underrepresented groups [76].
Mitigation Strategies and Experimental Protocols
Mitigating bias requires a proactive, multi-faceted approach throughout the AI development process. The following protocol outlines key experimental steps for ensuring fairness.
Experimental Protocol for Bias Assessment and Mitigation
Data Profiling and Pre-processing:
- Action: Prior to model training, quantitatively assess the composition of the training dataset. This includes evaluating distributions across protected attributes such as race, ethnicity, sex, and age.
- Metrics: Generate summary statistics and visualizations to identify representation gaps.
- Techniques: Employ data augmentation or strategic sampling to address identified imbalances, ensuring the data is representative of the intended patient population [76].
Algorithmic Fairness Testing:
- Action: During model training and validation, evaluate performance metrics disaggregated by subgroups.
- Metrics: Calculate sensitivity, specificity, and area under the curve (AUC) for each major subgroup to identify performance disparities [1] [76]. For example, a model for breast cancer detection should be evaluated for consistent performance across racial groups [1].
- Framework: Apply fairness principles such as Equal Outcomes (ensuring all groups benefit equally), Equal Performance (ensuring similar accuracy across groups), and Equal Allocation (ensuring fair distribution of resources) [77].
Post-deployment Monitoring and Calibration:
- Action: Implement continuous monitoring of the model's performance in a real-world clinical setting.
- Techniques: Establish a feedback loop where model performance logs are regularly analyzed for emerging biases. The model should be periodically re-calibrated or re-trained on new, more diverse data to maintain equity over time [76].
Table 1: Key Metrics for Assessing Algorithmic Bias in Oncology AI Models
| Metric | Definition | Interpretation in Oncology Context |
|---|---|---|
| Disparate Impact | The ratio of the positive outcome rate for a protected group to that of the advantaged group. | A value of 1 indicates fairness. A value < 0.8 may indicate a model is disproportionately withholding a positive prediction (e.g., referral for biopsy) from a protected group. |
| Equal Opportunity | The true positive rate should be similar across groups. | Ensures a cancer detection model is equally sensitive at identifying true cancers in all racial, ethnic, or gender groups. |
| Predictive Parity | The positive predictive value should be similar across groups. | Ensures that when a model predicts a high risk of cancer, the probability of cancer is the same regardless of the patient's demographic background. |
FDA Approval Pathways for AI in Oncology
The U.S. Food and Drug Administration (FDA) has established pathways to evaluate and regulate AI-based software as a medical device (SaMD), particularly when used in the context of drug development and clinical decision-making.
The Oncology AI Program
In response to the growing use of AI in oncology, the FDA's Oncology Center of Excellence (OCE) launched the Oncology AI Program in 2023 [78]. This program aims to:
- Provide specialized training for FDA reviewers on AI methodologies.
- Support regulatory science research related to AI.
- Streamline the review process for applications that incorporate AI technologies [78].
Lifecycle Management and Submission Pathways
The FDA's draft guidance, "Artificial Intelligence-Enabled Device Software Functions: Lifecycle Management and Marketing Submission Recommendations," outlines a total product lifecycle approach (TPLC) for AI-based software [78]. This is critical given that AI models are often adapted and updated after deployment. The guidance emphasizes the need for robust documentation and a "Predetermined Change Control Plan" to manage future modifications.
For AI tools used in drug development, the draft guidance "Considerations for the Use of Artificial Intelligence to Support Regulatory Decision-Making for Drug and Biological Products" is highly relevant [78]. It outlines expectations for the validation and documentation of AI models used in trials, from patient selection to endpoint assessment.
AI models can be submitted to the FDA through traditional pathways like Premarket Approval (PMA) and the de novo pathway. Furthermore, the Fast Track designation and Breakthrough Device designation can expedite the development and review of AI-based technologies that address unmet medical needs in serious conditions like cancer, as evidenced by several oncology drugs and associated diagnostics receiving fast track status [79].
FDA Lifecycle Approach for AI. This diagram outlines the key stages of the FDA's Total Product Lifecycle Approach (TPLC) for AI-enabled medical devices, from pre-market development to post-market monitoring and updates.
The Scientist's Toolkit: Research Reagents and Materials
The development and validation of AI models in oncology rely on a foundation of high-quality, well-characterized data and computational resources. The table below details essential "research reagents" for this field.
Table 2: Essential Research Reagents and Materials for Oncology AI Research
| Item | Function/Explanation |
|---|---|
| Federated Learning Platform | A software infrastructure that enables multi-institutional model training without data sharing, addressing data privacy and access constraints. The CAIA platform is a prime example [74]. |
| De-identified Clinical Datasets | Structured, real-world data from Electronic Health Records (EHRs) including demographics, lab values, treatment histories, and outcomes. Used for model training and validation on diverse populations [1] [74]. |
| Curated Imaging Repositories | Large-scale, annotated sets of radiology (e.g., mammography, MRI) and histopathology images. Essential for developing and benchmarking deep learning models for tasks like tumor detection and segmentation [1]. |
| Genomic and Biomarker Data | Data from sequencing (e.g., whole genome, RNA-seq) and molecular assays. Used to discover predictive biomarkers and build models for precision treatment and drug response prediction [1] [24]. |
| Bias Auditing Software | Open-source or commercial libraries (e.g., AI Fairness 360, Fairlearn) containing metrics and algorithms to detect and mitigate unwanted bias in datasets and machine learning models. |
| High-Performance Computing (HPC) / Cloud GPU | Specialized computational hardware (e.g., NVIDIA GPUs) accessible locally or via cloud providers (AWS, Google Cloud). Crucial for training complex deep learning models on large datasets in a feasible timeframe [74]. |
Benchmarking Performance: ML vs. Traditional Statistics in Cancer Prognosis
The systematic integration of machine learning (ML) into oncology research necessitates robust model evaluation to ensure clinical translatability. This whitepaper provides an in-depth technical examination of three cornerstone performance metrics—Area Under the Curve (AUC), Sensitivity, and Concordance Index (C-Index)—within the context of cancer diagnostics and prognostics. We synthesize findings from recent large-scale studies and systematic reviews, highlighting the performance of ML models across multiple cancer types. Furthermore, we detail standardized experimental protocols for metric computation and validation. The responsible application of these metrics, with an understanding of their respective strengths, limitations, and clinical interpretations, is paramount for advancing transparent and trustworthy AI in oncology.
The application of machine learning in oncology has transformed cancer research, enabling high-accuracy models for detection, classification, and prognosis [80]. The validation of these models relies critically on a suite of performance metrics that quantify their discriminative ability and clinical potential. Key among these are AUC (Area Under the Receiver Operating Characteristic Curve), which assesses a model's overall capacity to distinguish between classes across all thresholds; Sensitivity (or Recall), which measures the proportion of true positive cases correctly identified, a crucial factor for screening; and the C-Index (Concordance Index), the predominant metric for evaluating the predictive accuracy of survival models [38] [81] [82].
Selecting and interpreting these metrics appropriately is a non-trivial challenge in a field characterized by imbalanced datasets and high-stakes clinical outcomes. This guide provides researchers and drug development professionals with a technical foundation for evaluating ML models in oncology, framing the discussion within the broader effort to systematize ML applications in cancer research [38] [80]. We present consolidated quantitative evidence, detailed methodologies, and critical insights to inform model development and validation.
Metric Definitions and Clinical Interpretation
Area Under the Curve (AUC)
- Definition: The AUC represents the probability that a model will rank a randomly chosen positive instance higher than a randomly chosen negative instance. It is derived from the Receiver Operating Characteristic (ROC) curve, which plots the True Positive Rate (Sensitivity) against the False Positive Rate (1-Specificity) across all possible classification thresholds [83].
- Interpretation: An AUC of 1.0 indicates perfect classification, 0.9-1.0 is considered excellent, 0.8-0.9 is good, 0.7-0.8 is fair, and 0.5 indicates no discriminative power better than random chance [83].
- Advantages: AUC is threshold-invariant and provides a single, comprehensive measure of separability. It is particularly useful for evaluating models on imbalanced datasets, as it is not reliant on the class distribution in the way that accuracy is [83].
- Pitfalls: While native to binary classification, its use in multi-class problems is complex and can be misleading without careful interpretation. Furthermore, a high AUC does not guarantee a clinically useful model if the probability scores are not well-calibrated [84].
Sensitivity (True Positive Rate)
- Definition: Sensitivity is calculated as the number of true positive predictions divided by the total number of actual positive cases (True Positives + False Negatives) [83]. In a cancer context, it answers the question: "Of all the patients with cancer, how many did the test correctly identify?"
- Clinical Significance: High sensitivity is critically important for rule-out tests and cancer screening programs, where the cost of missing a cancer (a false negative) is exceptionally high. For example, a multi-cancer early detection test must maximize sensitivity to ensure that very few cancers go undetected [85].
- Trade-offs: Sensitivity typically exists in a trade-off with specificity. Increasing the sensitivity (e.g., by lowering the classification threshold) often leads to an increase in false positives, thereby reducing specificity.
Concordance Index (C-Index)
- Definition: The C-Index is the standard metric for evaluating the predictive accuracy of survival (time-to-event) models. It measures the proportion of all comparable pairs of patients in which the model's predicted risk ordering is consistent with the observed survival times [81] [82].
- Interpretation: A C-Index of 1.0 signifies perfect concordance, 0.5 indicates random prediction, and 0.0 signifies perfect anti-concordance. In oncology, a model with a C-Index above 0.75 is often considered to have good predictive power [82].
- Pitfalls and Alternatives: The C-Index has known limitations, including sensitivity to the distribution of censoring and a tendency to be dominated by early, high-risk events, which can make it less clinically meaningful for long-term survival [81]. Researchers are increasingly encouraged to supplement the C-Index with time-dependent AUC analyses and calibration metrics to provide a more complete assessment of model performance [81] [82].
Table 1: Summary of Key Performance Metrics in Oncology
| Metric | Definition | Clinical Interpretation | Primary Use Case | Key Considerations |
|---|---|---|---|---|
| AUC | Area under the ROC curve; measures overall separability between classes. | 0.5 = No discrimination; 1.0 = Perfect discrimination. Excellent >0.9 [16]. | Binary classification (e.g., cancer vs. non-cancer). Preferred for imbalanced data [83]. | Threshold-invariant. Not natively defined for multi-class problems [84]. |
| Sensitivity | TP / (TP + FN); proportion of actual positives correctly identified. | The ability of a test to correctly identify patients with the disease. | Screening and triage tests where missing a case is critical [85]. | Trade-off with specificity. Depends on the chosen classification threshold. |
| C-Index | Proportion of concordant risk-patient pairs among all comparable pairs. | How well the model's predicted risk stratifies patients by survival time. | Survival analysis (e.g., time to death, recurrence) [82]. | Sensitive to censoring. May not reflect clinical utility on its own [81]. |
Performance Benchmarking in Current Literature
Recent large-scale studies and meta-analyses provide robust benchmarks for ML model performance in oncology. The following table synthesizes quantitative findings across various cancer types and clinical tasks.
Table 2: Consolidated Performance Metrics from Recent Oncology AI Studies
| Study / Cancer Type | Model/Task | AUC | Sensitivity | Specificity | C-Index | Notes |
|---|---|---|---|---|---|---|
| Multi-Cancer Early Detection (OncoSeek) [85] | Detection of 14 cancer types from plasma proteins (n=15,122) | 0.829 | 58.4% | 92.0% | - | Performance varied by cancer type (e.g., Pancreas: 79.1%, Breast: 38.9%). |
| Lung Cancer Diagnosis (AI Imaging) [16] | Meta-analysis of 209 studies on image-based diagnosis | 0.92 (0.90–0.94) | 0.86 (0.84–0.87) | 0.86 (0.84–0.87) | - | Deep Learning (AUC: 0.94) outperformed traditional ML (AUC: 0.90). |
| Lung Cancer Prognosis (AI Imaging) [16] | Meta-analysis of 58 studies on risk stratification | 0.90 (0.87–0.92) | 0.83 (0.81–0.86) | 0.83 (0.80–0.86) | - | Pooled HR for high- vs. low-risk was 2.53 for Overall Survival. |
| Time-to-Diagnosis Prediction [82] | Cox model for lung cancer (External Validation on UK Biobank) | - | - | - | 0.813 | Model used 46 clinical/behavioral features; outperformed non-parametric ML methods. |
| Colorectal Cancer Survival [86] | Ensemble model for 5-year survival prediction (n=498) | 0.89 | - | - | - | Stage-specific predictions had accuracy ≥70%. |
Experimental Protocols for Metric Evaluation
Protocol for Validating a Multi-Cancer Early Detection Test
This protocol is modeled on large-scale validation studies, such as the one for the OncoSeek test [85].
- 1. Objective: To evaluate the performance of a blood-based test for the simultaneous detection of multiple cancer types.
- 2. Cohort Design:
- Participants: Recruit a large, multi-centre cohort (e.g., >15,000 participants) comprising both cancer patients (with pathologically confirmed diagnoses across multiple cancer types) and non-cancer individuals [85].
- Data Splitting: Divide the cohort into a training set (for model development and hyperparameter tuning) and a held-out validation set (for final performance assessment). Use cross-validation during training.
- 3. Sample and Data Analysis:
- Sample Type: Collect plasma or serum samples from all participants under standardized protocols.
- Biomarker Quantification: Analyze samples using the chosen platform (e.g., Roche Cobas e411/e601) to measure the concentration of target biomarkers (e.g., protein tumor markers) [85].
- 4. Performance Metric Computation:
- AUC & Sensitivity/Specificity: For the primary binary classification task (cancer vs. non-cancer), generate the ROC curve from the model's probability scores. Calculate the AUC and determine sensitivity and specificity at a pre-specified threshold (e.g., the threshold that yields 92% specificity) [85] [83].
- Tissue of Origin (TOO) Accuracy: For samples correctly identified as cancer, compute the accuracy of the model in predicting the primary cancer site.
- 5. Robustness and Consistency Checks:
- Conduct reproducibility experiments across different laboratories, using different sample types (serum/plasma) and analytical platforms. Report correlation coefficients (e.g., Pearson >0.99) to demonstrate assay reliability [85].
Protocol for Developing and Validating a Survival Prediction Model
This protocol is based on established practices in survival analysis and recent research [38] [82].
- 1. Objective: To build a model that predicts the time to a specific event (e.g., cancer diagnosis, death, recurrence) and evaluate its performance.
- 2. Data Curation:
- Cohorts: Utilize large, well-annotated datasets with long-term follow-up, such as the PLCO Cancer Screening Trial for training and the UK Biobank for external validation [82].
- Features: Extract relevant baseline demographic, clinical, and lifestyle variables.
- Event Data: Define the event of interest (e.g., first cancer diagnosis) and precisely record the time-to-event or time-to-censoring.
- 3. Model Training:
- Algorithm Selection: Employ survival models such as the Cox Proportional Hazards model with elastic net regularization for its interpretability and performance, or compare against other methods like Random Survival Forests [82].
- Data Preprocessing: Impute missing values using methods like
missForest, ensuring imputation is performed within sex-specific strata if relevant [82].
- 4. Performance Metric Computation:
- C-Index: Compute the C-Index on the external validation cohort to assess the model's discriminative ability. A value above 0.8 indicates strong predictive accuracy [82].
- Time-Dependent AUC: Supplement the C-Index by calculating the AUC at specific clinical time points (e.g., 1, 3, 5 years) to understand how predictive performance changes over time [82].
- 5. Calibration Assessment: Evaluate the model's calibration by comparing the predicted survival probabilities against the observed survival probabilities (e.g., using Kaplan-Meier estimates) across different risk groups. Good calibration is essential for clinical utility [87].
Essential Research Reagent Solutions
The following table details key materials and computational tools essential for conducting the experiments described in this guide.
Table 3: Research Reagent Solutions for Oncology ML Validation
| Item / Resource | Function / Application | Example / Note |
|---|---|---|
| Clinical Cohorts | Provide large-scale, annotated data for model training and validation. | PLCO Trial, UK Biobank, institutional databases [82] [86]. |
| Biomarker Assay Platforms | Quantify protein or genetic biomarkers from bio-samples. | Roche Cobas e411/e601, Bio-Rad Bio-Plex 200 systems [85]. |
| Statistical Software (R/Python) | Data preprocessing, model building, and metric computation. | R packages: missForest for imputation, survival for C-Index [82]. MATLAB for ML model development [86]. |
| Calibration Algorithms | Estimate unobservable parameters in cancer simulation models. | Random Search, Nelder-Mead, Bayesian Methods [87]. |
| Goodness-of-Fit Metrics | Quantify the agreement between model outputs and observed data. | Mean Squared Error (MSE) is the most commonly used metric [87]. |
Workflow and Relationship Visualization
The following diagram illustrates the logical workflow for evaluating a machine learning model in oncology, connecting the different phases of research to the relevant performance metrics.
The accurate prediction of survival outcomes is a cornerstone of oncology research, directly influencing clinical decision-making, patient counseling, and therapeutic development. For decades, the Cox proportional hazards (CPH) model has served as the statistical benchmark for analyzing time-to-event data. Its semi-parametric nature and interpretability have made it ubiquitous in cancer prognostic studies. However, the CPH model relies on critical assumptions—namely, proportional hazards and linearity—that may not hold in complex, real-world scenarios involving high-dimensional data or non-linear relationships.
The evolution of machine learning (ML) offers powerful alternatives that can automatically learn patterns from data without stringent pre-specified assumptions. Among these, tree-based methods and neural networks have shown particular promise for survival analysis. Tree-based models, including survival trees and random forests, excel at capturing complex interactions, while neural networks can model intricate non-linear patterns. This in-depth technical guide synthesizes evidence from recent systematic reviews and empirical studies to provide a head-to-head comparison of these advanced ML techniques against the traditional Cox regression within the context of cancer research, offering methodologies and practical insights for researchers and drug development professionals.
Theoretical Foundations and Model Adaptations
The Cox Proportional Hazards Model
The Cox model is a semi-parametric approach that models the hazard function for an individual at time t with a covariate vector X as:
h(t|X) = h₀(t)exp(Xβ)
where h₀(t) is an unspecified baseline hazard function, and β represents the log hazard ratios for the covariates. The model is fit by maximizing the partial likelihood, which does not require estimation of the baseline hazard. Its primary limitations include the proportional hazards assumption, which requires that the effect of covariates is constant over time, and the assumption of a linear relationship between covariates and the log hazard. In high-dimensional settings (e.g., with genomic data), the standard CPH model becomes unstable and requires regularization techniques [38].
Machine Learning Adaptations for Survival Analysis
Tree-Based Methods
Tree-based methods for survival analysis recursively partition the data into subgroups with similar survival outcomes. The splitting criteria are designed to maximize the difference in survival between child nodes. Common algorithms include:
- Survival Trees (ST): Use splitting criteria such as the log-rank statistic or the Likelihood Ratio Test for exponential survival times to find the covariate and cut-point that best separate patients into groups with different survival experiences [38] [88].
- Random Survival Forests (RSF): An ensemble method that constructs multiple survival trees from bootstrap samples of the data. The final cumulative hazard function is obtained by averaging the results from all trees, improving predictive accuracy and stability [89] [38].
- Conditional Inference Forests (CF): A different ensemble approach that uses statistical tests to determine the best splits, controlling for overfitting and bias towards variables with many cut-points [89].
These models handle non-linearity and complex interactions inherently and do not rely on the proportional hazards assumption.
Neural Networks
Neural networks model complex non-linear relationships through interconnected layers of nodes. Their adaptation for survival analysis includes:
- DeepSurv: A deep neural network that predicts the log-risk function as a non-linear combination of inputs, effectively serving as a non-linear Cox model [90].
- Multi-Task Learning Networks: These architectures predict survival outcomes alongside auxiliary tasks (e.g., tumor segmentation from images), allowing the model to learn more robust feature representations [91].
Neural networks are particularly powerful in high-dimensional settings but require large sample sizes and substantial computational resources [92] [93].
Comprehensive Performance Comparison
A growing body of literature has directly compared the predictive performance of these models across various cancer types. The evidence, synthesized below, reveals a nuanced picture.
Key Performance Metrics
- C-index (Concordance Index): Measures the model's ability to provide a reliable ranking of survival times. A value of 1 indicates perfect concordance, while 0.5 indicates random prediction.
- Integrated Brier Score (IBS): Measures the overall accuracy of predicted survival probabilities across all time points. Lower values indicate better predictive performance.
- Area Under the Curve (AUC): For a specific time point (e.g., 3-year survival), it evaluates the model's discrimination between patients who do and do not experience the event by that time.
Summarized Evidence from Comparative Studies
Table 1: Performance Comparison of Cox Regression vs. Tree-Based Models and Neural Networks in Cancer Studies
| Cancer Type & Study | Cox C-index | Tree-Based Model & C-index | Neural Network & C-index | Key Findings |
|---|---|---|---|---|
| Oral & Pharyngeal (OPCs) [89] | 0.77 (3-year) | RF: 0.83, CF: 0.83 (3-year) | Not Reported | Random Forest (RF) & Conditional Inference Forest (CF) showed superior discrimination over Cox. |
| Hepatocellular Carcinoma (HCC) [90] | 0.746 (6-month AUC) | RSF: 0.749 (6-month AUC) | DeepSurv: ~0.72 (6-month AUC) | Cox and RSF showed robust & comparable performance; DeepSurv was less accurate. |
| Breast Cancer [91] | 0.837 | Not separately reported | LightGBM (AUC=0.92), XGBoost (AUC=0.915) for recurrence | ML models achieved high accuracy for recurrence prediction, validated on external data. |
| Various Cancers (Meta-Analysis) [94] [95] | Pooled Baseline | Standardized Mean Difference: 0.01 (95% CI: -0.01, 0.03) | No statistically significant superiority of ML models over Cox regression across 21 studies. |
Table 2: Comparative Model Characteristics and Handling of Data Challenges
| Characteristic | Cox Regression | Tree-Based Models | Neural Networks |
|---|---|---|---|
| Underlying Assumptions | Proportional Hazards, Linearity | No explicit PH assumption, Non-linear | No explicit PH assumption, Highly Non-linear |
| Handling of Interactions | Must be pre-specified by the analyst | Automated, captures complex interactions | Automated, captures highly complex interactions |
| Performance with High-Dimensional Data | Poor without regularization (e.g., Lasso) | Good (e.g., RSF) | Excellent, but requires very large n |
| Interpretability | High (Hazard Ratios) | Moderate (Variable Importance, Tree Plots) | Low ("Black Box") |
| Computational Demand | Low | Moderate to High | Very High |
| Handling of Missing Data | Typically requires complete cases or imputation | Can handle via surrogate splits (in-tree) or RF imputation | Requires pre-processing and imputation |
The collective evidence suggests that while sophisticated ML models like Random Survival Forests can and sometimes do outperform Cox regression in specific settings, they do not consistently dominate. A recent systematic review and meta-analysis of 21 studies found that the overall standardized mean difference in discrimination (AUC/C-index) between ML models and CPH was a negligible 0.01 (95% CI: -0.01 to 0.03) [94] [95]. The choice of the best model appears to be context-dependent, influenced by the cancer type, sample size, data dimensionality, and the presence of complex non-linear and interaction effects.
Detailed Experimental Protocols and Methodologies
To ensure reproducible and rigorous comparisons, researchers must adhere to robust experimental protocols. The following workflow and methodologies are synthesized from the reviewed studies.
Generic Workflow for Comparative Studies
Key Methodological Components
Data Source and Study Population
- Data Source: Most studies utilize large, real-world datasets such as the Surveillance, Epidemiology, and End Results (SEER) registry, hospital Electronic Medical Records (EMR), or curated research consortium data (e.g., METABRIC) [89] [91] [90].
- Inclusion/Exclusion Criteria: Clearly defined to create a homogeneous cohort. For example, in the OPCs study, patients with a confirmed diagnosis and active follow-up were included, while those with survival of less than one month or missing key variables were excluded [89].
- Outcome Definition: The outcome must be precisely defined, typically as disease-specific survival or overall survival, with the event (e.g., death) and the time metric (e.g., months from diagnosis) explicitly stated.
Data Preprocessing and Handling of Missing Data
- Missing Data: This is a critical step. Different strategies are often employed for different models:
- Data Splitting: The dataset is typically split into a training set (e.g., 70-80%) for model development and a test set (20-30%) for final, unbiased performance evaluation.
Model Training and Tuning
- Cox Regression: Serves as the baseline. It may be extended with regularization (LASSO, Ridge, Elastic Net) in high-dimensional settings to prevent overfitting [38].
- Tree-Based Models:
- Hyperparameters: Key parameters include the number of trees in the forest (
ntree), the number of variables considered at each split (mtry), and the minimum node size. - Tuning Method: Typically performed via grid search or random search combined with resampling.
- Hyperparameters: Key parameters include the number of trees in the forest (
- Neural Networks:
Validation and Performance Assessment
- Internal Validation: Resampling techniques like 10-fold cross-validation with multiple repetitions (e.g., 50 iterations) are essential to obtain robust performance estimates and tune hyperparameters without overfitting to the test set [89].
- Performance Metrics: Models should be evaluated on a suite of metrics, as no single metric provides a complete picture. Standard practice includes reporting:
Table 3: Key Computational Tools and Data Resources for Survival Analysis Research
| Tool/Resource Name | Type | Primary Function/Utility | Relevance in Reviewed Studies |
|---|---|---|---|
| SEER* Database | Data Resource | Provides comprehensive, population-level US cancer data with demographics, treatment, and survival. | Used as primary data source in [89] [90] and for external validation in [91]. |
| R Statistical Software | Software Platform | Open-source environment for statistical computing and graphics. | The primary platform for implementing Cox and tree-based models (e.g., via randomForestSRC, party packages). |
| Python (scikit-survival, PyTorch) | Software Platform | A general-purpose programming language with extensive ML libraries. | Used for implementing DeepSurv, XGBoost, and other advanced ML models [91]. |
| Concordance Index (C-index) | Statistical Metric | Quantifies the model's ranking performance (discrimination). | The most consistently reported performance metric across all comparative studies [89] [94] [95]. |
| Integrated Brier Score (IBS) | Statistical Metric | Measures the overall accuracy of predicted survival probabilities. | Used to compare model performance across the entire follow-up period [89] [88]. |
| SHAP (SHapley Additive exPlanations) | Interpretation Tool | Explains the output of any ML model by quantifying each feature's contribution. | Used to interpret complex models like Random Survival Forest and XGBoost, providing clinical insights [90]. |
*Surveillance, Epidemiology, and End Results
The comparative analysis between Cox regression, tree-based methods, and neural networks reveals that there is no universally superior model for survival prediction in cancer research. The optimal choice is contingent on a triad of factors: data characteristics, analytical goals, and practical constraints.
- Cox Regression remains a highly interpretable and robust benchmark, especially when its statistical assumptions are reasonably met and the relationships are approximately linear.
- Tree-Based Models, particularly ensemble methods like Random Survival Forests, offer a powerful alternative that automatically handles non-linearity and complex interactions, often yielding superior predictive accuracy without a substantial loss of interpretability.
- Neural Networks represent the most flexible approach, capable of modeling highly complex patterns, but their "black-box" nature and substantial computational demands make them most suitable for very large datasets where predictive performance is the sole priority.
For future work, the field is moving towards model integration and explanation. Rather than a winner-takes-all approach, combining the strengths of different models or using CPH as a well-understood baseline against which to benchmark ML models is a prudent strategy. Furthermore, employing explanation tools like SHAP is critical to extract clinically meaningful insights from high-performing but opaque ML models, thereby bridging the gap between predictive accuracy and clinical translatability.
Within the broader context of a systematic review of machine learning in cancer research, this case study examines a critical finding: the consistent superiority of ensemble and deep learning models over traditional single-model approaches for specific, complex oncological tasks. The integration of artificial intelligence into oncology addresses the inherent complexity and heterogeneity of cancer, which often limits the efficacy of models relying on a single data type or algorithm [68] [96]. Multimodal artificial intelligence (MMAI) and ensemble learning frameworks are poised to overcome these limitations by integrating diverse, high-dimensional datasets—including multiomics, radiomics, and digital pathology—into cohesive analytical models [10] [96]. This synthesis explores the technical methodologies, quantitative performance gains, and practical experimental protocols that establish advanced machine learning architectures as transformative tools for precision oncology.
Experimental Protocols and Methodologies
Stacking Ensemble Framework for Multiomics Data Integration
A study aimed at classifying five common cancer types in Saudi Arabia exemplifies a robust stacking ensemble methodology. The model integrated RNA sequencing, somatic mutation, and DNA methylation profiles from The Cancer Genome Atlas (TCGA) and LinkedOmics datasets [97].
Data Preprocessing: RNA sequencing data underwent normalization using the transcripts per million (TPM) method to mitigate technical variation. Given the high-dimensional nature of the data, an autoencoder was employed for feature extraction, compressing input features through an encoder and reconstructing them via a decoder to preserve essential biological properties [97].
Ensemble Construction: The stacking ensemble integrated five base learners:
- Support Vector Machine (SVM)
- K-Nearest Neighbors (KNN)
- Artificial Neural Network (ANN)
- Convolutional Neural Network (CNN)
- Random Forest (RF)
The predictions from these base models were then combined using a meta-learner to generate the final classification. This approach demonstrated that multiomics data integration was crucial, as the model achieved 98% accuracy, outperforming results using individual omics data types (96% for RNA sequencing or methylation alone, and 81% for somatic mutation data) [97].
Deep Learning Ensemble for Tumor Type Prediction
The Genome-Derived-Diagnosis Ensemble (GDD-ENS) was developed to predict tumor type from targeted panel sequencing data, a more clinically feasible alternative to whole genome sequencing [98].
Model Architecture: GDD-ENS is a hyperparameter ensemble of ten multi-layer perceptrons (MLPs). The training set was divided into ten folds, and each model was trained on 90% of the data and validated on the remaining 10%. Models were initialized with the same parameters but optimized independently, enhancing generalization [98].
Feature Engineering: The model incorporated 4,487 genomic features derived from MSK-IMPACT panel data, including:
- Mutations and indels
- Focal amplifications and deletions
- Broad copy number alterations
- Structural rearrangements and fusions
- Mutational signatures
- Tumor mutation burden (TMB) and microsatellite instability (MSI) score
- Sex as a biological variable
Prediction and Calibration: For each sample, the softmax outputs from the ten MLPs were averaged to produce a final confidence estimate. The model achieved 92.7% accuracy for high-confidence predictions (confidence ≥0.75) across 38 solid tumor types, rivaling the performance of WGS-based methods [98].
Optimized CNN Ensemble for Histopathological Image Analysis
For oral cancer detection, an optimized deep learning ensemble integrated Enhanced EfficientNet-B5 and ResNet50V2 architectures, trained on the ORCHID dataset of high-resolution histopathology images [99].
Architectural Enhancements: The EfficientNet-B5 component was augmented with Squeeze-and-Excitation (SE) and Hybrid Spatial-Channel Attention (HSCA) modules to enhance feature extraction capabilities for lesion identification [99].
Hyperparameter Optimization: The Tunicate Swarm Algorithm (TSA), a metaheuristic optimization algorithm, was employed to fine-tune model hyperparameters. This optimization improved convergence rate and mitigated overfitting, leading to a peak classification accuracy of 99% [99].
Quantitative Performance Comparison
The performance advantages of ensemble and deep learning models are demonstrated quantitatively across multiple cancer types and data modalities. The table below summarizes key results from the featured case studies.
Table 1: Performance of Ensemble and Deep Learning Models in Specific Cancers
| Cancer Type | Model Description | Key Performance Metrics | Reference |
|---|---|---|---|
| Multiple Cancers (Breast, Colorectal, Thyroid, etc.) | Stacking Ensemble (SVM, KNN, ANN, CNN, RF) with Multiomics Data | 98% Accuracy with multiomics vs. 96% (single-omics) [97] | [97] |
| Pan-Tumor (38 solid types) | GDD-ENS (Ensemble of 10 MLPs) with Genomic Features | 92.7% Accuracy for high-confidence predictions [98] | [98] |
| Oral Cancer | Optimized Ensemble (EfficientNet-B5 + ResNet50V2) with Histopathology Images | 99% Accuracy, significant reduction in false positives [99] | [99] |
| Head and Neck Cancer | Stacking Framework (Radiomics + Deep Learning Features from PET/CT) | C-index of 0.9345 for survival prediction [100] | [100] |
| Colorectal Cancer | Deep Learning on Whole Slide Images for MSI-H Detection | Sensitivity: 0.88, Specificity: 0.86 (Internal Validation) [29] | [29] |
These results consistently show that ensemble methods provide a significant performance boost across diverse applications, from cancer type classification to prognostic prediction. The GDD-ENS model notably demonstrated that its high-confidence predictions were highly reliable, making it suitable for real-world clinical decision-support [98]. Similarly, the integration of radiomics and deep learning features in a stacking framework for head and neck cancer achieved a superior C-index compared to models using either feature type alone, highlighting the benefit of multimodal integration [100].
Workflow and Signaling Pathways
The superior performance of these models is underpinned by sophisticated workflows that systematically integrate data and models. The following diagram illustrates a generalized workflow for a multiomics stacking ensemble, synthesizing the common elements from the cited studies.
Diagram 1: Multiomics Stacking Ensemble Workflow. This diagram outlines the generalized process for building a stacking ensemble model, from multiomics data input and preprocessing through parallel base model training and final meta-learner integration.
Furthermore, the paradigm of using deep learning to build interpretable models of cancer signaling and regulatory networks is gaining traction. These models aim to simulate the complex interplay of intrinsic and extrinsic factors that drive cancer phenotypes.
Diagram 2: Deep Learning Model of Cancer Cell Signaling. This diagram conceptualizes an interpretable deep learning model that integrates prior knowledge of molecular networks (signaling, metabolism, gene regulation) to simulate cellular behavior and predict phenotypic outcomes following perturbations like mutations or drugs [68].
The Scientist's Toolkit: Research Reagent Solutions
The development and implementation of these advanced models rely on a suite of critical data resources, computational tools, and analytical techniques. The following table details these essential components.
Table 2: Essential Research Resources for Oncology AI Development
| Resource Category | Specific Example(s) | Function and Application in Model Development |
|---|---|---|
| Public Data Repositories | The Cancer Genome Atlas (TCGA), The Cancer Imaging Archive (TCIA) [96] | Provide large-scale, multimodal data (e.g., multiomics, histopathology, radiology) essential for training and validating robust models. |
| Genomic Feature Sources | MSK-IMPACT Targeted Panel [98] | A clinically feasible source for genomic features (mutations, CNVs, fusions, TMB, MSI) used in tumor type classifiers. |
| Feature Extraction Tools | Autoencoders [97], 3D DenseNet-121 [100] | Reduce dimensionality of high-throughput data (e.g., RNA-Seq) or extract deep features from medical images (e.g., PET/CT). |
| Base Model Algorithms | SVM, KNN, ANN, CNN, RF [97], RSF, DeepSurv [100] | Serve as the diverse set of learners within an ensemble, each capturing different patterns from the data. |
| Hyperparameter Optimization | Tunicate Swarm Algorithm (TSA) [99], Grid Search | Automate the tuning of model parameters to enhance performance, convergence, and prevent overfitting. |
| Model Interpretation Frameworks | SHAP (SHapley Additive exPlanations) [101] | Provide post-hoc interpretability for complex models, quantifying the contribution of individual features to a prediction. |
| Federated Learning Frameworks | MONAI (Medical Open Network for AI) [10] [96] | Enable collaborative model training across multiple institutions without sharing raw patient data, addressing privacy concerns. |
Discussion and Future Directions
The case studies presented herein uniformly demonstrate that ensemble and deep learning models achieve superior performance by effectively integrating multimodal data and leveraging complementary model architectures. The stacking ensemble for multiomics data [97] and the GDD-ENS hyperparameter ensemble [98] both highlight that combining multiple models mitigates the limitations of any single algorithm, leading to more robust and accurate predictions. This is further corroborated in radiology, where a stacking framework integrating both radiomics and deep learning features from PET/CT scans achieved the best prognostic performance for head and neck cancer [100].
A pivotal challenge remains the interpretability of these complex models. While they function as "black boxes," methods like SHAP analysis are being deployed to elucidate feature contributions, building trust and facilitating clinical translation [101]. The future of this field lies in developing biologically informed, interpretable deep learning models that not only predict but also simulate cancer cell dynamics, offering insights into mechanisms and generating testable hypotheses for novel therapeutic strategies [68].
In conclusion, as part of a systematic review of machine learning in cancer research, the evidence is compelling: ensemble and deep learning approaches represent a significant advancement over traditional methods. Their ability to harness the complexity of multimodal data makes them indispensable tools for the future of precision oncology, from enhancing diagnostic accuracy and prognostic stratification to ultimately guiding personalized treatment decisions.
The Importance of External Validation and Real-World Clinical Testing
The integration of machine learning (ML) into oncology represents a paradigm shift in cancer research and clinical practice, offering the potential to revolutionize diagnosis, prognosis, and treatment selection. However, the transition from algorithmic development to clinical implementation remains fraught with challenges. External validation—the process of evaluating a model's performance on data completely independent from its development dataset—stands as the critical gateway to establishing trust in ML tools and facilitating their adoption in healthcare settings [102]. Without rigorous validation across diverse populations and clinical environments, even the most sophisticated algorithms risk delivering biased, inaccurate, or potentially harmful predictions when deployed in real-world scenarios.
The clinical urgency for robust ML tools is particularly acute in oncology, where cancer remains a leading cause of death worldwide and places enormous socioeconomic burden on healthcare systems [102]. The exponential growth of complex medical data, including electronic health records, radiological images, and genomic sequences, has surpassed human cognitive capacity for analysis, making automated interpretation not just advantageous but essential [102]. This technical guide examines the critical role of external validation and real-world clinical testing within the broader context of a systematic review of ML in cancer research, providing researchers and drug development professionals with methodologies, benchmarks, and frameworks for translating predictive models into clinically actionable tools.
The Current State of ML Validation in Oncology
Performance Gaps Between Internal and External Validation
A systematic assessment of the literature reveals significant disparities between model performance during development and their effectiveness when externally validated. Robust external validation remains the exception rather than the rule across oncology ML applications. In digital pathology for lung cancer diagnosis, for instance, only approximately 10% of developed models undergo external validation, creating a substantial translational gap between research and clinical practice [103].
The performance of ML models varies considerably across cancer types and applications. Convolutional Neural Networks (CNNs) have demonstrated particularly strong performance in image-intensive tasks such as histopathological classification and radiological image analysis [102]. For survival analysis, multi-task and deep learning methods appear to yield superior performance, though they are reported in only a minority of studies [38]. The table below summarizes pooled performance metrics for ML models across different cancer types based on recent systematic reviews and meta-analyses.
Table 1: Performance Metrics of ML Models Across Cancer Types
| Cancer Type | Application Area | Pooled AUC | Data Modalities | Key Findings |
|---|---|---|---|---|
| Prostate Cancer | Biochemical Recurrence Prediction | 0.82 (95% CI: 0.81-0.84) [104] | Clinical, pathological, imaging | Deep learning and hybrid models outperformed traditional ML (AUC = 0.83) [104] |
| Cervical Cancer | Diagnosis | Sensitivity: 0.97 (95% CI: 0.90-0.99), Specificity: 0.96 (95% CI: 0.93-0.97) [105] | Sociodemographic, epidemiologic, clinical | High diagnostic performance but limited real-world validation [105] |
| Various Cancers | Survival Analysis | Varies by cancer type | Clinical, genomic, imaging | Multi-task and deep learning methods showed superior performance [38] |
| Lung Cancer | Histopathological Subtyping | 0.746-0.999 [103] | Digital pathology images | Performance maintained across external validation cohorts [103] |
Methodological Limitations in Current Validation Practices
Several methodological challenges impede adequate validation of ML models in oncology. Most studies are conducted retrospectively, introducing potential biases in data collection and patient selection [102] [103]. Small sample sizes frequently undermine statistical power and generalizability, while non-representative datasets fail to capture the full spectrum of disease presentation and patient demographics [102]. Additionally, significant variability in validation metrics and insufficient calibration reporting hinder meaningful comparison across studies and models [102].
The PROBAST (Prediction model Risk Of Bias Assessment Tool) and TRIPOD (Transparent Reporting of a Multivariable Prediction Model for Individual Prognosis or Diagnosis) guidelines provide frameworks for addressing these methodological limitations, yet adherence remains inconsistent across the field [106]. Furthermore, many studies lack comprehensive clinical utility assessments that measure how model implementation actually impacts clinician performance, decision-making, or patient outcomes [102].
Protocols for External Validation
Cohort Design and Recruitment
Robust external validation requires meticulous cohort design that anticipates real-world clinical scenarios. The multicenter, retrospective cohort study for predicting postoperative recurrence in duodenal adenocarcinoma exemplifies this approach, incorporating 1,830 patients from 16 Chinese hospitals between 2012 and 2023 [106]. Patients were divided into a training cohort and three independent external validation cohorts from different medical institutions to ensure geographical and temporal diversity [106].
Inclusion and exclusion criteria must be explicitly defined to establish model applicability. The duodenal adenocarcinoma study included adult patients who underwent specific surgical procedures (Pancreaticoduodenectomy or Pylorus-preserving pancreaticoduodenectomy), while excluding perioperative deaths, patients lost to follow-up, and cases with insufficient clinical data [106]. For the development of an ML-based nomogram predicting heart failure risk in type 2 diabetes patients, exclusion criteria encompassed severe comorbid conditions including end-stage renal disease, active uncontrolled systemic infection, and malignant tumors with metastasis [107].
Feature Selection and Model Training
Feature selection methodologies play a crucial role in developing parsimonious and generalizable models. Wrapper methods, which iteratively evaluate feature subsets through cross-validation, have been successfully employed in cancer prediction models [106]. Alternative approaches include LASSO (Least Absolute Shrinkage and Selection Operator) regression with 10-fold cross-validation, which effectively reduces overfitting in high-dimensional data [107].
The duodenal adenocarcinoma study implemented an exhaustive approach by testing 53 clinical variables across ten different machine learning learners, including Gradient Boosting (GB), Random Survival Forest (RSF), and Penalized Regression (PR) [106]. The optimal model combination—Penalized Regression + Accelerated Oblique Random Survival Forest (PAM)—was identified through permutation testing of 100 potential model configurations [106]. This rigorous selection process exemplifies the sophistication required for robust model development.
Validation Metrics and Clinical Utility Assessment
Comprehensive validation requires multiple performance metrics that evaluate different aspects of model performance. The C-index (concordance index) serves as a key metric for survival models, with the duodenal adenocarcinoma model achieving C-index values of 0.882 (training) and 0.734-0.747 across three external validation cohorts [106]. For diagnostic models, sensitivity, specificity, and AUC (Area Under the Receiver Operating Characteristic Curve) provide complementary information about classification performance [105].
Beyond traditional performance metrics, clinical utility assessment is essential for establishing real-world value. This includes decision curve analysis (DCA) to evaluate net benefit across different probability thresholds, calibration plots to assess agreement between predicted and observed outcomes, and implementation studies measuring impact on clinician performance [102] [107]. In one scoping review, clinical utility assessments involved 499 clinicians and 12 tools, demonstrating improved clinician performance with AI assistance [102].
Table 2: Essential Components of External Validation Protocols
| Validation Component | Key Elements | Considerations |
|---|---|---|
| Cohort Design | Multiple independent validation cohorts, Representative patient populations, Clear inclusion/exclusion criteria | Geographical diversity, Temporal validation, Spectrum of disease severity |
| Feature Selection | LASSO regression, Wrapper methods, Domain knowledge integration | Avoidance of overfitting, Clinical interpretability, Handling of missing data |
| Model Training | Multiple algorithm comparison, Hyperparameter tuning, Cross-validation | Computational efficiency, Reproducibility, Ensemble methods |
| Performance Metrics | C-index (survival models), AUC (diagnostic models), Sensitivity, Specificity | Calibration measures, Decision curve analysis, Brier score |
| Clinical Utility | Impact on clinician performance, Integration into workflow, Patient outcomes | Usability testing, Implementation barriers, Cost-effectiveness |
Experimental Workflows and Visualization
The process of developing and validating ML models in cancer research follows a structured workflow that encompasses data collection, model development, validation, and implementation. The diagram below illustrates this comprehensive pipeline.
ML Validation Workflow in Cancer Research
The relationship between different ML approaches and their performance characteristics in external validation can be visualized through the following conceptual diagram.
ML Approaches and Validation Performance
The Scientist's Toolkit: Research Reagent Solutions
Successful development and validation of ML models in cancer research requires specialized methodological tools and frameworks. The table below details essential "research reagents" - methodological components, software tools, and validation frameworks - that constitute the core toolkit for researchers in this field.
Table 3: Essential Research Reagent Solutions for ML in Cancer Research
| Tool Category | Specific Tools/Methods | Function | Application Examples |
|---|---|---|---|
| Statistical Software | R (mlr3proba package), SPSS, Python | Data analysis, model development, and validation | R package mlr3proba used for survival analysis in duodenal adenocarcinoma study [106] |
| Feature Selection Methods | LASSO regression, Wrapper methods, SHAP | Identify optimal predictor variables, reduce dimensionality | LASSO with 10-fold CV selected 6 predictors for NT-proBNP nomogram [107] |
| Machine Learning Algorithms | Gradient Boosting, Random Survival Forest, CNN, XGBoost | Model development for classification, regression, survival analysis | CNN most prevalent in imaging applications; ensemble methods for clinical data [102] |
| Validation Frameworks | PROBAST, TRIPOD, QUADAS-2 | Standardize reporting, assess risk of bias, ensure methodological rigor | PROBAST and TRIPOD adherence in duodenal adenocarcinoma study [106] |
| Performance Metrics | C-index, AUC, calibration plots, decision curve analysis | Evaluate model discrimination, calibration, and clinical utility | C-index for survival models; AUC for diagnostic models [106] [105] |
| Interpretability Tools | SHapley Additive exPlanations (SHAP), partial dependence plots | Explain model predictions, identify feature importance | SHAP analysis revealed eGFR as most influential feature in diabetes-HF model [107] |
| Deployment Platforms | Web applications, API frameworks, electronic health record integration | Facilitate clinical implementation and accessibility | Web-based dynamic nomogram for HF risk prediction in diabetes [107] |
Discussion and Future Directions
Addressing Persistent Challenges
The field of ML in oncology continues to grapple with several persistent challenges that hinder clinical adoption. Limited international validation across diverse ethnicities and healthcare systems restricts generalizability of models [102]. Inconsistent data sharing practices and disparities in validation metrics further complicate comparative assessment of model performance across studies [102]. There is also a critical need for improved model calibration reporting, as poorly calibrated models can produce misleading risk estimates despite good discrimination [102].
Future research must prioritize prospective validation studies that evaluate model performance in real-time clinical environments. The development of foundation models in histopathology—large-scale models trained on vast datasets that serve as foundations for diverse downstream tasks—represents a promising direction for improving generalizability [103]. Additionally, standardized data collection protocols and harmonized validation metrics would significantly enhance the reliability and comparability of ML models across institutions.
Toward Clinically Actionable ML Tools
The ultimate measure of success for ML models in oncology is their integration into clinical workflows to improve patient outcomes. This requires not only technical excellence but also thoughtful consideration of implementation science. Successful models must align with clinical workflows, provide interpretable results that clinicians can understand and trust, and demonstrate tangible benefits through rigorous clinical utility assessments [102].
The creation of accessible web-based tools, such as the dynamic nomogram for predicting heart failure risk in diabetic patients [107] and the web tool for predicting duodenal adenocarcinoma recurrence [106], represents an important step toward clinical adoption. Future efforts should focus on seamless integration with electronic health record systems, real-time performance monitoring, and adaptation mechanisms that allow models to maintain performance as clinical practices evolve.
As the field advances, the focus must shift from isolated model development to the establishment of comprehensive validation ecosystems that continuously assess and improve ML tools throughout their lifecycle. Only through such rigorous, ongoing evaluation can ML realize its potential to transform cancer care and improve patient outcomes.
Conclusion
This review unequivocally demonstrates that machine learning is fundamentally reshaping cancer research and clinical practice. The synthesis of evidence confirms that ML models, particularly deep learning and ensemble methods, consistently match or surpass the performance of traditional statistical techniques in tasks ranging from early detection on radiological and pathological images to accurate survival prognosis. Key challenges of data quality, model interpretability, and seamless clinical workflow integration remain significant but are being actively addressed through techniques like federated learning and explainable AI (XAI). Future directions point toward the increased use of multimodal data fusion, federated learning for privacy-preserving collaboration, and the development of more robust, prospectively validated tools. The ultimate trajectory is clear: the thoughtful and rigorous integration of ML holds the definitive promise of ushering in a new era of predictive, personalized, and precision oncology, ultimately leading to improved health outcomes for cancer patients globally.
References
- 1. Artificial intelligence in cancer: applications, challenges, and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12574039/]
- 2. Artificial Intelligence and the future of clinical trials - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC12490578/]
- 3. Brain Tumor Detection and Classification Using Deep ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9854739/]
- 4. Deep Learning Applications in Clinical Cancer Detection [https://www.sciencedirect.com/science/article/pii/S2949761225000604]
- 5. Enhanced brain tumor classification using graph ... [https://www.nature.com/articles/s41598-023-41407-8]
- 6. Eye on AI: Applying Artificial Intelligence to Drive Cancer ... [https://www.aacr.org/blog/2025/08/18/eye-on-ai-applying-artificial-intelligence-to-drive-cancer-research-part-2/]
- 7. Researchers Invent New AI Tool to Automate Detection ... [https://viterbischool.usc.edu/news/2025/10/researchers-invent-new-ai-tool-to-automate-detection-of-cancer-in-blood-samples/]
- 8. A quantitative comparison between human experts and AI ... [https://www.medrxiv.org/content/10.1101/2025.08.26.25334451v1]
- 9. How AI Is Transforming Clinical Trials | AHA [https://www.aha.org/aha-center-health-innovation-market-scan/2025-10-21-how-ai-transforming-clinical-trials]
- 10. The AI revolution: how multimodal intelligence will reshape ... [https://www.nature.com/articles/s44387-025-00044-4]
- 11. Explainable Artificial Intelligence for Multi-Modal Cancer ... [https://www.sciencedirect.com/science/article/pii/S1040842825004287]
- 12. Multimodal Integration in Health Care - PubMed Central - NIH [https://pmc.ncbi.nlm.nih.gov/articles/PMC12370271/]
- 13. Review on Multimodal Data Integration for Cancer Research [https://arxiv.org/abs/2507.09028]
- 14. Integrating multimodal cancer data using deep latent ... [https://www.nature.com/articles/s42256-025-01052-4]
- 15. Applications and Techniques of Machine Learning in ... [https://link.springer.com/article/10.1007/s44230-023-00041-3]
- 16. Systematic review and meta-analysis of artificial ... [https://www.nature.com/articles/s41698-025-01095-1]
- 17. Association Between Risk Factors and Major Cancers [https://cancer.jmir.org/2025/1/e62833]
- 18. An overview of the use of artificial neural networks in lung ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5418299/]
- 19. Application of deep learning models in gastric ... - BMC Cancer [https://bmccancer.biomedcentral.com/articles/10.1186/s12885-025-14662-3]
- 20. Comparative analysis of convolutional neural networks and ... [https://pubmed.ncbi.nlm.nih.gov/40600038/]
- 21. Efficient deep neural networks for cancer detection on ... [https://www.nature.com/articles/s41598-025-20954-2]
- 22. Convergence of evolving artificial intelligence and machine ... [https://www.nature.com/articles/s41746-025-01471-y]
- 23. Gene-LLMs: a comprehensive survey of transformer-based ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12558637/]
- 24. AI and Cancer: The Emerging Revolution [https://www.cancerresearch.org/blog/ai-cancer]
- 25. Artificial Intelligence in Cancer Drug Discovery in 2025 [https://oncodaily.com/oncolibrary/artificial-intelligence-in-cancer-drug-discovery]
- 26. Artificial Intelligence (AI) in Oncology: Current Landscape ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11131133/]
- 27. A New Artificial Intelligence Tool for Cancer [https://hms.harvard.edu/news/new-artificial-intelligence-tool-cancer]
- 28. Application of artificial intelligence in medical imaging for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12381339/]
- 29. Systematic review and meta-analysis of deep learning for ... [https://www.nature.com/articles/s41746-025-01848-z]
- 30. Histopathological-based brain tumor grading using 2D-3D ... [https://www.nature.com/articles/s41598-025-11754-9]
- 31. MBTC-Net: Multimodal brain tumor classification from CT ... [https://www.sciencedirect.com/science/article/pii/S2590093525000335]
- 32. Novel AI Tool Enables Spatial Quantification of Tumor ... [https://www.insideprecisionmedicine.com/topics/oncology/novel-ai-tool-enables-spatial-quantification-of-tumor-biopsy-images/]
- 33. Performance Evaluation of Deep Learning for the Detection ... [https://www.jmir.org/2025/1/e73516]
- 34. Advances in AI — October 2025 | Diagnostic Imaging [https://www.diagnosticimaging.com/view/advances-in-ai-october-2025]
- 35. A systematic literature review on mammography: deep ... [https://bmccancer.biomedcentral.com/articles/10.1186/s12885-025-14876-5]
- 36. Hallmarks of artificial intelligence contributions to precision ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11957836/]
- 37. Convergence of evolving artificial intelligence and machine ... learning [https://www.nature.com/articles/s41746-025-01471-y?error=cookies_not_supported]
- 38. A Systematic Review on Machine Learning Techniques for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12633653/]
- 39. Evaluating the application of dynamic prediction models in ... [https://www.nature.com/articles/s41698-025-01162-7]
- 40. A machine learning approach for multimodal data fusion ... [https://www.nature.com/articles/s41698-025-00917-6]
- 41. As AI Dawns in Precision , Oncology Expected To... - BioSpace 2025 [https://www.biospace.com/drug-development/as-ai-dawns-in-precision-oncology-2025-expected-to-be-a-turning-point]
- 42. Performance of Machine Learning in Diagnosing KRAS ... [https://www.jmir.org/2025/1/e73528]
- 43. Automated and Interpretable Survival Analysis from ... [https://arxiv.org/abs/2509.21600v1?utm_source=radaislice.com]
- 44. Computer Vision and Machine Learning in Precision ... [https://www.research.va.gov/isrm/amp/precision_oncology/compl.cfm]
- 45. Can AI help deliver better medicines to patients? [https://dailyreporter.esmo.org/esmo-targeted-anticancer-therapies-congress-2025/lstest-news/can-ai-help-deliver-better-medicines-to-patients]
- 46. How Generative AI Healthcare is Transforming in in... Drug Discovery [https://www.rfidjournal.com/expert-views/how-generative-ai-in-healthcare-is-transforming-drug-discovery-in-2025/222589/]
- 47. From molecule to market: Opportunities and challenges in using AI ... in [https://www.dlapiper.com/en/insights/publications/2025/09/from-molecule-to-market-opportunities-and-challenges-in-using-ai-in-drug-discovery-and-development]
- 48. The Role of AI in Drug Discovery: Challenges, Opportunities ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10302890/]
- 49. Four ways to power-up AI for drug discovery [https://www.nature.com/articles/d41586-025-00602-5]
- 50. Artificial Intelligence for Drug Development [https://www.fda.gov/about-fda/center-drug-evaluation-and-research-cder/artificial-intelligence-drug-development]
- 51. Applied machine learning in cancer research: A systematic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8523813/]
- 52. Evaluation of clinical decision support systems in oncology [https://www.sciencedirect.com/science/article/abs/pii/S1040842823002317]
- 53. A Systematic Review of Clinical Decision Support Systems for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6563614/]
- 54. The RECOURSE Study: Long-term oncologic outcomes ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9905254/]
- 55. Robotic surgery is associated with improved outcomes for ... [https://www.utsouthwestern.edu/newsroom/articles/year-2024/jan-robotic-surgery-colon-cancer-patients.html]
- 56. Cancer Multi-Omics Database for Machine Learning [https://www.nature.com/articles/s41597-025-05235-x]
- 57. High-dimensional role of AI and machine learning in ... [https://www.nature.com/articles/s41416-021-01689-z]
- 58. Machine learning analysis reveals tumor heterogeneity ... [https://www.nature.com/articles/s41746-025-01967-7]
- 59. A Deep Learning Image Data Augmentation Method for Single ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8882602/]
- 60. Investigation of the heterogeneity of cancer cells using single ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12492923/]
- 61. A cancer biologist's primer on machine learning applications ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7416435/]
- 62. Machine Learning Study Highlights Power of Data ... [https://www.appliedradiationoncology.com/articles/machine-learning-study-highlights-power-of-data-augmentation-in-lung-cancer-prediction]
- 63. A review and comparative study of cancer detection using ... [https://bmcbioinformatics.biomedcentral.com/articles/10.1186/s12859-023-05235-x]
- 64. Strategies to Improve the Robustness and Generalizability ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12014193/]
- 65. Chapter 0 Machine Learning Robustness: A Primer [https://arxiv.org/html/2404.00897v2]
- 66. a systematic literature review and meta-analysis - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC12570641/]
- 67. Understanding Overfitting: Strategies and Solutions [http://www.lyzr.ai/glossaries/overfitting/]
- 68. Towards an interpretable deep learning model of cancer [https://www.nature.com/articles/s41698-025-00822-y]
- 69. Interpretable deep learning for gastric cancer detection [https://pmc.ncbi.nlm.nih.gov/articles/PMC12159836/]
- 70. Interpretable machine learning analysis of ... [https://www.nature.com/articles/s41598-025-29004-3]
- 71. Machine learning-based multimodal prognostic models ... [https://arxiv.org/abs/2507.16876]
- 72. Clinical prediction models using machine learning in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12506039/]
- 73. Harnessing Innovation in Oncology: Insights from ASCO ... [https://premier-research.com/perspectives/harnessing-innovation-in-oncology-insights-from-asco-2025/]
- 74. Dana-Farber joins leading cancers centers in launching ... [https://www.dana-farber.org/newsroom/news-releases/2025/dana-farber-joins-leading-cancers-centers-in-launching-new-ai-learning-platform-to-accelerate-cancer-research]
- 75. Federal AI Mandates and Corporate Compliance [https://www.cogentinfo.com/resources/federal-ai-mandates-and-corporate-compliance-whats-changing-in-2025]
- 76. Artificial Intelligence Ethics Framework for the ... [https://www.intelligence.gov/ai/ai-ethics-framework]
- 77. Is Artificial Intelligence Echoing Human Bias in Cancer Care? [https://binaytara.org/cancernews/article/is-artificial-intelligence-echoing-human-bias-in-cancer-care]
- 78. OCE Oncology Artificial Intelligence Program [https://www.fda.gov/about-fda/oncology-center-excellence/oce-oncology-artificial-intelligence-program]
- 79. Oncology Drugs Fast-Tracked by the FDA in October 2025 [https://www.oncologynewscentral.com/drugs/info/oncology-drugs-fast-tracked-by-the-fda-in-october-2025]
- 80. Applied machine learning in cancer research: A systematic ... [https://www.sciencedirect.com/science/article/pii/S2001037021004281]
- 81. Pitfalls of the concordance index for survival outcomes - PubMed [https://pubmed.ncbi.nlm.nih.gov/36977424/]
- 82. Predicting time-to-first cancer diagnosis across multiple ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12241622/]
- 83. Accuracy vs AUC in Machine Learning [https://www.baeldung.com/cs/ml-accuracy-vs-auc]
- 84. Overlooked pitfalls in multi-class machine learning ... [https://www.sciencedirect.com/science/article/abs/pii/S1120179720300119]
- 85. A large-scale, multi-centre validation study of an AI- ... [https://www.nature.com/articles/s41698-025-01105-2]
- 86. Comparison of Different Machine Learning Models for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11730731/]
- 87. A Scoping Review on Calibration Methods for Cancer ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12346156/]
- 88. Comparison of tree-based methods for prognostic ... [https://www.sciencedirect.com/science/article/abs/pii/S0933365703000605]
- 89. Comparison of the Tree-Based Machine Learning ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7600270/]
- 90. Comparison of machine learning and Cox regression ... [https://www.sciencedirect.com/science/article/pii/S2589845025000570]
- 91. Leveraging survival analysis and machine learning for ... [https://www.nature.com/articles/s41598-025-87622-3]
- 92. A systematic comparison of statistical, tree-based, and ... [https://www.sciencedirect.com/science/article/pii/S2666827025000714]
- 93. A comparison of neural networks and regression-based ... [https://www.sciencedirect.com/science/article/abs/pii/S1047279725000717]
- 94. Comparison of machine learning methods versus traditional ... [https://bmcmedresmethodol.biomedcentral.com/articles/10.1186/s12874-025-02694-z]
- 95. a systematic literature review and meta-analysis [https://pubmed.ncbi.nlm.nih.gov/41152747/]
- 96. Multimodal deep learning approaches for precision oncology [https://pmc.ncbi.nlm.nih.gov/articles/PMC11700660/]
- 97. Stacked Deep Learning Ensemble for Multiomics Cancer ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12342693/]
- 98. Deep Learning Model for Tumor Type Prediction using ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10508812/]
- 99. Optimized deep learning ensemble for accurate oral ... [https://www.sciencedirect.com/science/article/pii/S2666521225000626]
- 100. A stacking ensemble framework integrating radiomics and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12351975/]
- 101. Machine learning analysis of survival outcomes in breast ... [https://www.nature.com/articles/s41598-025-97763-0]
- 102. Externally validated and clinically useful machine learning ... [https://bmcmedresmethodol.biomedcentral.com/articles/10.1186/s12874-025-02463-y]
- 103. Systematic scoping review of external validation studies ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12145442/]
- 104. Diagnostic systematic review and meta-analysis of ... [https://www.nature.com/articles/s41598-025-11445-5]
- 105. Performance evaluation of Machine Learning models in ... [https://www.sciencedirect.com/science/article/pii/S0959804925005544]
- 106. Development and external validation of a machine learning ... [https://bmcmedicine.biomedcentral.com/articles/10.1186/s12916-025-03912-7]
- 107. Development and External Validation of a Machine ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12621603/]