A Modern Workflow for Mathematical Modeling in Cancer Treatment Optimization: From Biological Principles to Clinical Translation
This article provides a comprehensive guide to the workflow of mathematical modeling for optimizing cancer treatment, tailored for researchers, scientists, and drug development professionals.
A Modern Workflow for Mathematical Modeling in Cancer Treatment Optimization: From Biological Principles to Clinical Translation
Abstract
This article provides a comprehensive guide to the workflow of mathematical modeling for optimizing cancer treatment, tailored for researchers, scientists, and drug development professionals. It explores the foundational principles of mathematical oncology, detailing how mathematical models simulate tumor growth, treatment response, and the emergence of resistance. The content covers the step-by-step methodological process of model building, from conceptualization and equation selection to implementation and simulation. It further addresses critical challenges in model calibration and optimization, including parameter estimation and overcoming resistance. Finally, the article discusses the essential processes of model validation, comparative analysis of different modeling approaches, and the translation of these models into clinical trials and decision-support tools, synthesizing the latest research and clinical applications in this rapidly advancing field.
Laying the Groundwork: Core Principles and Biological Complexity in Mathematical Oncology
Defining Mathematical Oncology and Its Role in Treatment Optimization
Mathematical Oncology is a growing interdisciplinary discipline that integrates mechanistic mathematical models with experimental and clinical data to improve clinical decision-making in oncology [1]. These models are typically based on biological first principles to capture the spatial and temporal dynamics of tumors, their microenvironment, and response to treatment [1]. This approach stands in contrast to purely data-driven artificial intelligence methods, as it seeks to represent the underlying biological processes that drive cancer progression and treatment response, thereby providing a predictive framework that can simulate the complex, multi-scale, and dynamic nature of cancer [1] [2].
The field has evolved from using simple models of tumor growth and dose-response to increasingly complex frameworks that incorporate tumor heterogeneity, ecological interactions (such as tumor-immune dynamics), and evolutionary principles (including the emergence of treatment resistance) [1]. This mechanistic understanding allows researchers and clinicians to move beyond the traditional 'maximum tolerated dose' (MTD) paradigm, which often leads to disease relapse due to drug resistance, and toward more adaptive, personalized treatment strategies [1]. As such, mathematical oncology provides a quantitative foundation for predicting treatment outcomes, optimizing therapeutic strategies, and ultimately improving patient care.
Foundational Mathematical Frameworks
Mathematical oncology employs a diverse set of modeling frameworks to describe different aspects of cancer behavior and treatment response. The choice of model depends on the specific research question, the scale of investigation, and the available data. The table below summarizes the key model types and their primary applications in treatment optimization.
Table 1: Key Mathematical Modeling Frameworks in Oncology
| Model Type | Mathematical Formulation | Primary Oncology Applications |
|---|---|---|
| Ordinary Differential Equations (ODEs) | ( \frac{dN}{dt} = rN(1-\frac{N}{K}) ) (Logistic Growth) [2] | Modeling tumor population dynamics, pharmacokinetics/pharmacodynamics, and competition between sensitive and resistant cell populations [1] [2]. |
| Partial Differential Equations (PDEs) | ( \frac{\partial C}{\partial t} = D\nabla^2 C + \rho C ) (Reaction-Diffusion) [3] | Simulating spatially explicit phenomena like tumor invasion, nutrient gradients, and the spatial distribution of treatment agents [2] [3]. |
| Agent-Based Models (ABMs) | Rule-based systems where individual cell behaviors (proliferation, death, migration) are simulated. | Investigating the emergence of tissue-level patterns from individual cell interactions, tumor heterogeneity, and evolutionary dynamics in a spatial context [2]. |
| Population Dynamics & Evolutionary Models | ( \frac{dN1}{dt} = r1N1(1-\frac{N1 + \alpha N2}{K1}) ) (Lotka-Volterra Competition) [2] | Modeling clonal evolution, emergence of treatment resistance, and designing evolutionary-informed therapies like adaptive therapy [1] [2]. |
These models are calibrated using preclinical or clinical data. A particular strength of mechanistic models is their ability to capture heterogeneity across different scales (e.g., between patients or tumors) by adjusting parameter sets to reflect observed variability [1]. Once calibrated, these models can simulate various treatment scenarios to predict outcomes and recommend optimal dosing, timing, and drug combinations, thereby bridging the gap between experimental insight and clinical application [1].
Clinical Applications and Trial Evidence
Mathematical models are increasingly being integrated into clinical workflows and clinical trials to personalize and optimize treatment. The following table summarizes key examples of model-informed clinical trials, demonstrating the translation of mathematical concepts into patient care.
Table 2: Examples of Mathematical Model-Informed Clinical Trials in Oncology
| Therapeutic Strategy / Model Type | Trial Identifier | Cancer Type | Intervention / Purpose | Status/Key Finding |
|---|---|---|---|---|
| Adaptive Therapy | NCT02415621 [1] | Metastatic Castration-Resistant Prostate Cancer | Adaptive Abiraterone Therapy | Active, not recruiting |
| Adaptive Therapy | NCT03543969 [1] | Advanced BRAF Mutant Melanoma | Adaptive BRAF-MEK Inhibitor Therapy | Active, not recruiting |
| Adaptive Therapy | NCT05393791 [1] | Metastatic Castration-Resistant Prostate Cancer (mCRPC) | Adaptive vs. Continuous Abiraterone or Enzalutamide (ANZadapt) | Recruiting |
| Extinction Therapy | NCT04388839 [1] | Rhabdomyosarcoma | Evolutionary Therapy | Recruiting |
| Dynamics-based Radiotherapy | NCT03557372 [1] | Glioblastoma (GBM) | Mathematical Model-Adapted Radiation | Phase 1: Feasibility and Safety ✓ |
| Fully Personalized Treatment | NCT04343365 [1] | Multiple Cancers | Evolutionary Tumor Board (ETB) | Recruiting |
Case Study: Glioblastoma Treatment Planning
A concrete example of treatment optimization is the use of a reaction-diffusion model to simulate glioblastoma (GBM) progression for patient counseling [3]. In this approach, patient-specific MRI data (T1 post-contrast and T2/FLAIR sequences) are co-registered and manually segmented to identify enhancing tumor and edema, forming the initial conditions for the model [3]. The model, known as the "ASU-Barrow" model, then simulates tumor growth between successive scans by systematically sampling parameters to generate a range of realistic scenarios of tumor response to treatment [3].
In a validation study using 132 MRI intervals from 46 GBM patients, the model-generated scenarios for changes in tumor volumes approximated the observed ranges in the patient data with reasonable accuracy. In 86% of the imaging intervals, at least one simulated scenario agreed with the observed tumor volume to within 20% [3]. This approach, with its modest computational needs, demonstrates the potential for mathematical models to become clinically practical tools that support shared decision-making between clinicians and patients facing a poor prognosis [3].
Diagram 1: GBM Modeling Workflow
Experimental Protocols for Model Calibration and Validation
Protocol: Quantifying Drug Dose-Response for Model Input
A critical step in building predictive models is the accurate quantification of drug effects on cancer cells. This protocol outlines the standard method for determining the half-maximal inhibitory concentration (ICâ‚…â‚€), a key parameter used in pharmacodynamic models of treatment response [4].
1. Objective: To generate a concentration-response curve for a cancer therapeutic and determine its ICâ‚…â‚€ value in a relevant cellular model.
2. Materials:
- Cancer Cell Lines: (e.g., patient-derived cell lines relevant to the cancer type).
- Therapeutic Agent: The drug of interest, prepared in appropriate solvent at a high stock concentration.
- Cell Culture Reagents: Complete growth medium, trypsin-EDTA, phosphate-buffered saline (PBS).
- Viability Assay Reagent: Such as CellTiter-Glo (ATP-based luminescent assay) [4].
- Equipment: Tissue culture hood, COâ‚‚ incubator, multi-channel pipettes, white-walled 96-well or 384-well assay plates, microplate reader capable of detecting luminescence.
3. Procedure: 1. Cell Seeding: Harvest exponentially growing cells and prepare a suspension in complete medium. Seed a consistent number of cells (e.g., 1,000-5,000 cells in 80-90 µL of medium per well) into each well of the assay plate. Include control wells for background (medium only). 2. Pre-incubation: Allow cells to adhere and recover for 4-24 hours in a 37°C, 5% CO₂ incubator. 3. Compound Addition: Prepare a serial dilution of the therapeutic agent (typically a 1:3 or 1:2 dilution series across 8-10 concentrations). Add 10 µL of each dilution to the assay wells, ensuring the final concentration spans a range from below to above the expected IC₅₀. Include a vehicle control (0% inhibition) and a control for 100% inhibition (e.g., a potent, non-specific cytotoxic agent). 4. Incubation: Incubate the plate for the desired treatment duration (e.g., 72 hours). 5. Viability Measurement: Equilibrate the plate to room temperature. Add a volume of CellTiter-Glo reagent equal to the volume of medium in each well. Shake the plate to induce cell lysis, then incubate for 10 minutes to stabilize the luminescent signal. Record the luminescence using the plate reader.
4. Data Analysis: 1. Calculate the average luminescence for replicates at each concentration. 2. Normalize the data: % Inhibition = 100 × [1 - (Luminescencesample - Luminescence100%inhibition) / (Luminescencevehiclecontrol - Luminescence100%inhibition)]. 3. Fit the normalized data to a 4-parameter logistic (4PL) nonlinear regression model: ( Y = Bottom + \frac{(Top - Bottom)}{(1 + 10^{((LogIC{50} - X) × HillSlope)})} ) where Y is the % inhibition and X is the logâ‚â‚€ of the compound concentration. 4. The ICâ‚…â‚€ is the concentration (X) at which Y = 50.
5. Key Considerations for Model Integration:
- Use a minimum of 8-10 concentration points with at least three biological replicates each [4].
- Ensure the curve has well-defined top (maximum inhibition) and bottom (minimum inhibition) plateaus.
- The final ICâ‚…â‚€ value should be reported with its confidence interval from the curve fit. This parameter can be directly incorporated into differential equation models of tumor cell kill in response to drug concentration [2] [4].
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Reagents and Materials for Mathematical Oncology Research
| Research Reagent / Material | Function and Application |
|---|---|
| Patient-Derived Cell Lines | Provides a physiologically relevant in vitro model system for quantifying drug response parameters (e.g., ICâ‚…â‚€) and validating model predictions [4]. |
| Cell Viability Assays (e.g., CellTiter-Glo) | Measures ATP levels as a proxy for the number of viable cells, generating the primary data for dose-response curves and model calibration [4]. |
| High-Throughput Screening (HTS) Platforms | Enables rapid testing of numerous drug compounds and concentrations across multiple cell models, generating large-scale data for model parameterization [4]. |
| Clinical Imaging Data (MRI, CT) | Provides in vivo spatial and temporal data on tumor size and morphology for initializing and validating spatial models (e.g., reaction-diffusion models for GBM) [3]. |
| Image Analysis Software (e.g., 3D Slicer) | Used to manually or semi-automatically segment clinical images, defining regions of interest (e.g., enhancing tumor, edema) that serve as initial conditions for spatial models [3]. |
| Iodol | Iodol, CAS:87-58-1, MF:C4HI4N, MW:570.68 g/mol |
| Retra | Retra, CAS:1173023-52-3, MF:C11H12ClNO3S2, MW:305.8 g/mol |
Integrated Workflow for Treatment Optimization
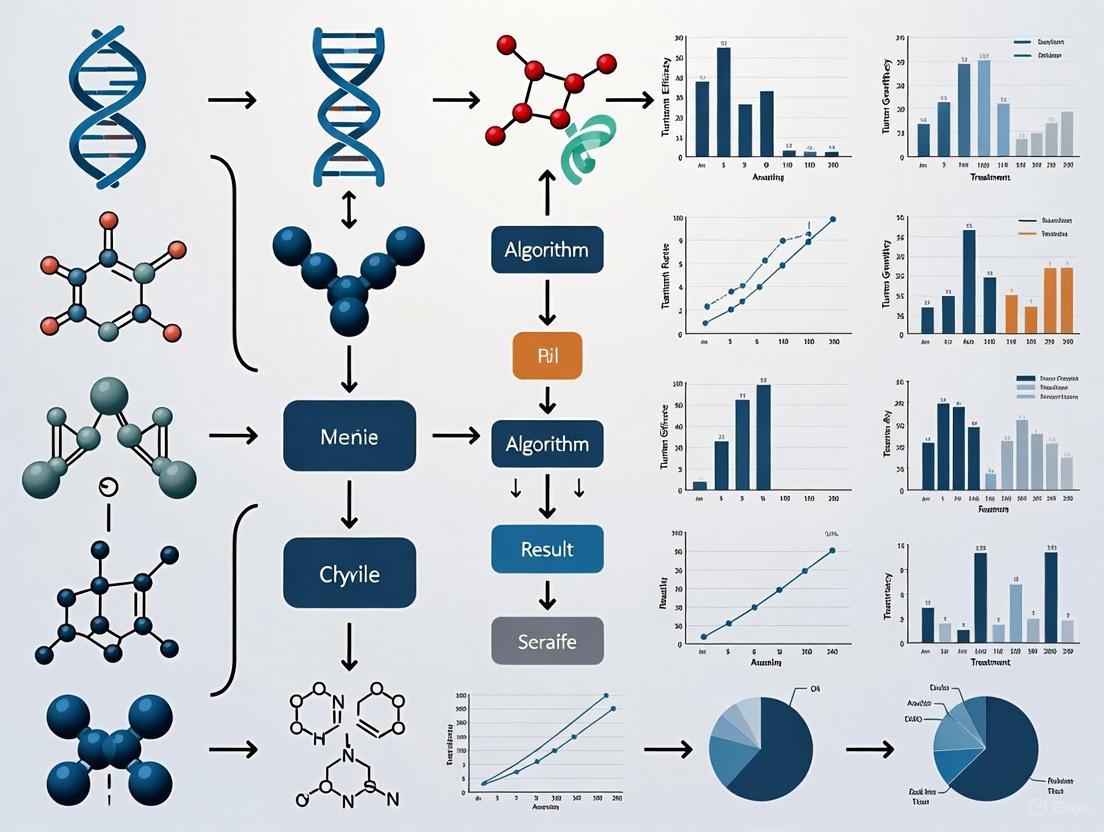
The full potential of mathematical oncology is realized when modeling is integrated into a cohesive workflow that connects basic research with clinical application. The following diagram and description outline this iterative process.
Diagram 2: Treatment Optimization Workflow
1. Data Acquisition: The workflow begins with the collection of high-quality data from various sources. This includes clinical data (e.g., imaging, treatment history), genomic data, and preclinical data from in vitro or in vivo models, such as dose-response curves [3] [4]. This data provides the foundation for building and calibrating models.
2. Model Construction & Calibration: A mechanistic mathematical model is selected and constructed based on the biological question. The model is then calibrated using the acquired data, a process that involves adjusting model parameters so that the model output closely matches the observed experimental or clinical data [1] [2]. This creates a "virtual patient" or "digital twin" representation.
3. Generate Predictions & Scenarios: The calibrated model is used in silico to simulate different treatment scenarios. This can involve testing various dosing schedules, drug combinations, or treatment sequences to identify strategies that maximize tumor control while minimizing toxicity or the emergence of resistance [1] [2].
4. Clinical Decision & Intervention: The model-derived treatment recommendations inform clinical decision-making. This could involve selecting a personalized therapy for an individual patient or designing a clinical trial for a specific patient population [1]. The chosen intervention is then administered.
5. Outcome Validation & Model Refinement: Patient outcomes are meticulously tracked. These real-world results are used to validate the model's predictions. Discrepancies between predicted and observed outcomes provide valuable information that is fed back into the workflow to refine and improve the model, creating a continuous cycle of learning and optimization [1] [3]. This integrated, iterative process is key to advancing personalized cancer therapy.
This document provides application notes and detailed protocols for researchers investigating the core biological processes of cancer, with a specific focus on informing the development of mathematical models for treatment optimization. A deep understanding of tumor growth dynamics, angiogenesis, and the tumor microenvironment (TME) is paramount for building in silico frameworks that can accurately simulate cancer progression and predict therapeutic efficacy [1] [2]. This guide synthesizes current knowledge on these processes, presents quantitative data for model parameterization, and outlines experimental methodologies for validating key model components.
Quantitative Data on Tumor Angiogenesis
Key Signaling Pathways in Tumor Angiogenesis
The process of angiogenesis is regulated by a complex interplay of multiple growth factors and their associated signaling pathways. The quantitative dynamics of these pathways are critical inputs for mechanistic mathematical models.
Table 1: Key Pro-Angiogenic Signaling Pathways and Their Functions.
| Signaling Pathway | Key Ligands/Receptors | Primary Cellular Functions | Selected Downstream Effectors |
|---|---|---|---|
| VEGF/VEGFR [5] [6] | VEGFA, VEGFR2 | Endothelial cell proliferation, migration, survival; Vascular permeability | PLCγ-PKC-MEK-ERK; PI3K-Akt; Src-FAK [6] |
| FGF/FGFR [5] [6] | FGF2 (bFGF), FGFR | EC proliferation and differentiation | Ras-Raf1-MAPK; PI3K-AKT; JAK-STAT [6] |
| PDGF/PDGFR [5] [6] | PDGFB, PDGFRβ | Pericyte recruitment; Vascular maturation | MAPK/ERK; PI3K/AKT; JNK [6] |
| ANG/Tie [6] | ANG1, ANG2, TIE2 | Vessel stabilization and maturation; Opposing roles in regulation | Akt/survivin pathway [6] |
Mechanisms of Tumor Vascularization
Tumors utilize a variety of mechanisms to secure a blood supply, extending beyond classical sprouting angiogenesis. These alternative mechanisms can pose significant challenges to anti-angiogenic therapies and must be accounted for in comprehensive models.
Table 2: Mechanisms of Tumor Vascularization and Their Characteristics.
| Mechanism | Description | Key Molecular Mediators | Implication for Therapy |
|---|---|---|---|
| Sprouting Angiogenesis [5] | New vessels sprout from pre-existing ones via endothelial tip cell migration. | VEGF, Notch signaling [5] | Primary target of anti-VEGF therapies. |
| Intussusceptive Angiogenesis [5] [6] | Existing vessels split into two by the insertion of tissue pillars. | VEGF (induced) [5] | A rapid, efficient process; mechanisms less understood. |
| Vasculogenesis [5] | Recruitment and in situ differentiation of endothelial progenitor cells (EPCs). | VEGFA, SDF-1 [5] | Contributes to neovascularization; potential cellular target. |
| Vascular Mimicry (VM) [5] [6] | Tumor cells form fluid-conducting, vessel-like channels. | Hypoxia, EMT factors [5] | Not attached to ECs; associated with drug resistance. |
| Vessel Co-option [5] [6] | Tumor cells migrate along and hijack pre-existing vessels. | Not specified in search results | Mechanism of resistance to anti-angiogenic therapy. |
Diagram 1: The Cyclic Drive of Tumor Angiogenesis.
Experimental Protocols for Key Analyses
Protocol: In Vitro Analysis of Endothelial Cell Sprouting Angiogenesis
This protocol details the use of a 3D fibrin gel bead assay to quantitatively assess the sprouting and tube-forming capacity of endothelial cells in response to pro-angiogenic factors or their inhibition.
1.0 Application Note: This assay is a cornerstone for validating the core logic of agent-based models (ABMs) that simulate tip cell selection, stalk cell proliferation, and sprout extension [2] [7]. It provides high-content, quantifiable data on sprout number, length, and branching complexity.
2.0 Materials
- Research Reagent Solutions:
- Human Umbilical Vein Endothelial Cells (HUVECs): Primary cells for studying endothelial biology.
- Cytodex Microcarrier Beads: Serve as a 3D scaffold for endothelial cell attachment and sprout initiation.
- Fibrinogen and Thrombin: To form the 3D fibrin gel matrix.
- VEGF and bFGF: Key pro-angiogenic growth factors to stimulate sprouting.
- Fibroblast Growth Medium: Conditioned medium from fibroblasts provides a source of additional angiogenic factors.
3.0 Procedure
- Cell Seeding on Beads: Culture HUVECs with Cytodex beads for 4-6 hours, allowing cells to adhere to the bead surface.
- Gel Polymerization: Transfer the cell-coated beads into a solution of fibrinogen and thrombin in a culture well. Incubate at 37°C to form a solid 3D fibrin gel.
- Application of Stimuli: Overlay the polymerized gel with endothelial growth medium supplemented with VEGF (50 ng/mL), bFGF (50 ng/mL), and 25% fibroblast-conditioned medium.
- Inhibitor Testing (Optional): To test anti-angiogenic compounds, include them in the overlay medium at desired concentrations.
- Incubation and Imaging: Culture the assay for 5-7 days, refreshing the medium every other day. Image sprouts daily using an inverted phase-contrast microscope.
- Quantitative Analysis: Use image analysis software (e.g., ImageJ) to quantify total sprout length, number of sprouts per bead, and number of branch points.
Protocol: In Vivo Validation of Anti-Angiogenic Therapy and Vascular Normalization
This protocol describes a pre-clinical murine model to evaluate the efficacy of anti-angiogenic therapy and its downstream effects on tumor growth and the immune microenvironment, crucial for calibrating hybrid mathematical models [7].
1.0 Application Note: Data from this protocol is essential for parameterizing models that link vascular normalization to improved perfusion, drug delivery, and immune cell infiltration [7]. It helps define the "normalization window," a critical time-dependent variable for combination therapy scheduling.
2.0 Materials
- Research Reagent Solutions:
- Syngeneic Cancer Cell Line: (e.g., murine glioma GL261 for orthotopic models, or MC38 for subcutaneous models).
- Anti-VEGF Monoclonal Antibody: (e.g., B20-4.1.1 for murine models). The key therapeutic agent.
- Isolectin or Anti-CD31 Antibody: For fluorescent staining of perfused and total vessels, respectively.
- Flow Cytometry Antibody Panel: For immune profiling (e.g., anti-CD45, CD3, CD8, CD4, F4/80).
3.0 Procedure
- Tumor Implantation: Implant cancer cells subcutaneously or orthotopically into immunocompetent mice.
- Treatment Initiation: Randomize mice into control and treatment groups once tumors reach a palpable size (~50 mm³). Administer anti-VEGF therapy (e.g., 5 mg/kg, i.p., twice weekly) or an isotype control.
- Tumor Growth Monitoring: Measure tumor dimensions 2-3 times per week using calipers. Calculate tumor volume using the formula: V = (length × width²) / 2.
- Tissue Harvest: Euthanize cohorts of mice at predetermined timepoints (e.g., day 3, 7, and 14 of treatment).
- Perfusion and Vessel Analysis: Inject fluorescently-labeled lectin intravenously 10 minutes before sacrifice to label perfused vessels. Excise tumors, section, and stain with an antibody against CD31 (pan-endothelial marker). Use confocal microscopy to quantify:
- Total Vessel Density: (CD31+ area).
- Perfused Vessel Fraction: (Lectin+ area / CD31+ area).
- Vessel Normalization Index: A composite metric including perfusion, pericyte coverage (via α-SMA staining), and basement membrane thickness.
- Immune Cell Infiltration Analysis: Digest a portion of the tumor to create a single-cell suspension. Stain with the antibody panel and analyze by flow cytometry to quantify the infiltration of CD8+ T cells, Tregs, and TAMs.
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Reagents for Studying Tumor Angiogenesis and Microenvironment.
| Reagent / Material | Function / Application | Key Examples |
|---|---|---|
| Recombinant Growth Factors | Stimulate angiogenesis in in vitro assays; used to create pro-angiogenic conditions. | VEGF-A, FGF2 (bFGF), PDGF-BB [5] [6] |
| Neutralizing Antibodies | Inhibit specific signaling pathways to validate their role in angiogenesis; used for in vitro and in vivo therapy. | Anti-VEGF (Bevacizumab), Anti-VEGFR2 [5] [8] |
| Small Molecule Inhibitors | Oral tyrosine kinase inhibitors (TKIs) that block intracellular signaling of pro-angiogenic receptors. | Sorafenib, Lenvatinib, Vorolanib (multi-targeted) [5] |
| Endothelial Cell Markers | Identify and quantify blood vessels in tissue sections (IHC/IF) or isolate ECs (FACS). | CD31 (PECAM-1), VE-cadherin, VEGFR2 [6] |
| Immune Cell Markers | Profile the immune contexture of the TME via flow cytometry or IHC. | CD45 (pan-immune), CD3 (T cells), CD8 (cytotoxic T), CD68/CD206 (TAMs), FoxP3 (Tregs) [8] |
| WSP-1 | WSP-1, MF:C33H21NO6S2, MW:591.7 g/mol | Chemical Reagent |
| DAz-1 | DAz-1, MF:C10H14N4O3, MW:238.24 g/mol | Chemical Reagent |
Mathematical Modeling Workflow Integration
The biological data and experimental outputs generated using the above protocols are directly integrated into mathematical modeling workflows for cancer treatment optimization. The following diagram illustrates this iterative, interdisciplinary process.
Diagram 2: Integrating Biology and Mathematical Modeling.
This integrated approach allows for the exploration of complex treatment strategies that would be prohibitively time-consuming or expensive to test empirically. Models can simulate the effects of various anti-angiogenic agents (e.g., VEGF inhibitors [5]), their scheduling (e.g., metronomic vs. MTD [9]), and their combination with other modalities like immunotherapy [7] [8] or chemotherapy across virtual patient cohorts [10]. The predictions generated, such as the existence of a vascular "normalization window" [7], can then be prospectively tested in the lab, creating a powerful feedback loop for therapeutic discovery.
The relentless and uncontrolled proliferation of cancer cells is a defining hallmark of the disease, driven by complex dynamic processes that operate across multiple biological scales. Mathematical modeling provides a powerful, quantitative framework to capture these dynamics, transforming a qualitative understanding of cancer into a predictive science. The journey from simple exponential growth models to more biologically realistic, saturating growth laws like the Gompertz model represents a cornerstone in mathematical oncology. These models do not merely describe data; they encode fundamental principles of tumor biology, such as competition for space and nutrients, the carrying capacity of the microenvironment, and the deceleration of growth as tumors enlarge. This Application Note details the practical implementation of these models, with a focus on the Gompertz framework, to study tumor growth kinetics. The protocols herein are designed to be integrated into a broader workflow for optimizing cancer treatment research, enabling scientists to calibrate models to experimental and clinical data for improved therapeutic strategy design.
Theoretical Foundations: From Exponential to Gompertz Growth
The evolution of tumor growth modeling reflects an increasing appreciation for the complex constraints of the in vivo environment. The table below summarizes the defining characteristics, equations, and limitations of three foundational models.
Table 1: Foundational Mathematical Models of Tumor Growth
| Model Name | Core Principle | Differential Equation | Integrated Solution | Key Limitation |
|---|---|---|---|---|
| Exponential [11] | Constant, unbounded growth rate; all cells proliferate. | dN/dt = r · N |
N(t) = N₀ · e^(r·t) |
Unrealistic for large tumors; predicts infinite growth. |
| Logistic [11] | Density-dependent growth slowdown; linear decay of growth rate. | dN/dt = r · N · (1 - N/K) |
N(t) = (K · N₀) / (N₀ + (K - N₀)·e^(-r·t)) |
Inflection point is fixed at 50% of carrying capacity (K). |
| Gompertz [12] [13] [11] | Time-dependent exponential decay of growth rate; asymmetric sigmoid shape. | dN/dt = α · N · ln(K / N) |
N(t) = K · exp[ ln(N₀/K) · exp(-α·t) ] |
Proliferation rate is unbounded for very small populations. |
The Gompertz model has proven particularly effective in describing experimental and clinical tumor growth data. Its superiority stems from its ability to capture the rapid initial growth followed by a gradual slowdown and plateau as the tumor approaches a theoretical maximum size, or carrying capacity (K) [12] [14]. This decelerating pattern is consistent with the concept of spatial and nutrient constraints within the tumor microenvironment. The inflection point of the Gompertz curve, where growth is fastest, occurs when the tumor size is at 37% of K, providing more flexibility than the logistic model [13].
Experimental Protocols for Model Calibration
A critical step in utilizing these models is calibrating them to observed data. The following protocol outlines a standardized workflow for obtaining model parameters from longitudinal tumor volume measurements.
Protocol: Fitting Tumor Growth Models to Volumetric Data
Objective: To determine the best-fit parameters (e.g., growth rate α, carrying capacity K) for exponential, logistic, and Gompertz models based on a time-series of tumor volume measurements.
Materials and Reagents:
- In vivo tumor model (e.g., murine model with subcutaneous xenografts)
- Calipers or in vivo imaging system (e.g., MRI, CT)
- Software for nonlinear regression (e.g., R, Python with SciPy, MATLAB)
Procedure:
- Data Collection:
- Initiate tumors in your experimental model (e.g., via cell injection).
- Beginning from a baseline measurement, record tumor volumes at regular, frequent intervals (e.g., 2-3 times per week) over a timeframe sufficient to observe substantial growth and potential plateauing. A minimum of three time points is required, but more are strongly recommended for reliable fitting [12].
- Calculate tumor volume (V) using the formula for an ellipsoid: ( V = \frac{4}{3}π · (\frac{L}{2}) · (\frac{W}{2}) · (\frac{H}{2}) ), where L, W, and H are the three perpendicular diameters [15].
Data Preprocessing:
- Define the smallest detectable difference in volume (e.g., a 10% change) to account for measurement noise [12].
- Format data as a table with columns:
Time (t),Observed Volume (V_obs).
Model Fitting via Nonlinear Regression:
- Using your chosen software, employ a nonlinear least-squares regression algorithm to fit the integrated form of each growth model to the
(t, V_obs)data. - For the Gompertz model, fit the equation: ( V(t) = K · \exp\left( \ln(V_0/K) · \exp(-α·t) \right) ), where
V_0(initial volume),K(carrying capacity), andα(growth rate) are the parameters to be estimated. - Provide reasonable initial guesses for the parameters to ensure algorithm convergence.
- Using your chosen software, employ a nonlinear least-squares regression algorithm to fit the integrated form of each growth model to the
Model Selection and Validation:
- Calculate goodness-of-fit statistics for each model, including the coefficient of determination (R²) and the root-mean-squared error (RMSE) [12].
- Use statistical tests like the Kruskal-Wallis ANOVA with post-hoc tests to determine if there are significant differences in the goodness of fit between the models [12].
- Visually inspect the fitted curves overlaid on the raw data. The model that provides a high R², low RMSE, and a biologically plausible growth curve should be selected.
Troubleshooting Tip: If the Gompertz model fails to converge, try fitting the simpler logistic and exponential models first and use their parameters to inform initial guesses for the Gompertz fit (e.g., K from logistic, initial growth rate from exponential).
Advanced Application: The Reduced Gompertz Model and Bayesian Calibration
For cases with limited data points, a simplified "Reduced Gompertz" model can be employed, which leverages a known strong correlation between the parameters α and K [15] [14]. This correlation allows the two-parameter model to be reduced to a single individual parameter, drastically improving predictive power when data is scarce.
Objective: To estimate the time of tumor initiation (tâ‚€) from a limited number of late-stage tumor volume measurements.
Procedure:
- Establish a Population Prior: Using a historical dataset of fully observed tumor growth curves from the same cancer type and model system, fit the full Gompertz model and quantify the correlation between parameters α and K. Use this to derive the population-level parameter for the reduced model [14].
- Incorporate Sparse Individual Data: For a new subject, collect 2-3 tumor volume measurements.
- Bayesian Inference: Use Bayesian statistical methods (e.g., Markov Chain Monte Carlo) to compute the posterior distribution for the individual's growth parameter and the unobserved time of origin (tâ‚€), using the population parameter as a prior [14].
- Prediction: The posterior distribution provides an estimate for the tumor's initiation time, along with a credible interval quantifying the uncertainty of the prediction.
Table 2: Key Research Reagent Solutions for Tumor Growth Modeling
| Reagent / Resource | Function in Experimental Workflow | Example & Notes |
|---|---|---|
| Cancer Cell Lines | Provides a genetically defined population for in vivo growth studies. | Human LM2-4LUC+ breast carcinoma cells [15]; Murine Lewis Lung Carcinoma (LLC) cells [14]. |
| Immunodeficient Mice | Host for xenograft studies using human cell lines. | SCID mice; allows engraftment and growth of human tumors [15]. |
| In Vivo Imaging System | Non-invasive, precise longitudinal measurement of tumor volume. | MRI, CT, or fluorescence imaging (e.g., IVIS); superior accuracy to calipers for deep or irregular tumors [12] [16]. |
| Digital Caliper | Standard tool for measuring subcutaneous tumor dimensions. | Used with the ellipsoid volume formula; cost-effective but less accurate for non-palpable tumors [15]. |
| Mathematical Software | Platform for performing nonlinear regression and model fitting. | Python (SciPy, NumPy), R, MATLAB; essential for parameter estimation and simulation [14]. |
Application in Treatment Optimization Workflow
Mathematical growth models are not merely descriptive; they are foundational for designing and optimizing cancer therapies. The Gompertz model, for instance, directly informed the Norton-Simon hypothesis, which posits that chemotherapy-induced tumor regression is proportional to the rate of tumor growth [9]. This principle led to the clinical development of dose-dense chemotherapy, where the same total dose is administered more frequently, thereby minimizing tumor regrowth between cycles and improving outcomes in cancers like breast cancer [9].
Furthermore, these models are integrated into larger therapeutic optimization frameworks. For example, the Gompertz differential equation can be coupled with terms representing drug effect to simulate and predict treatment response. This allows for in silico testing of different treatment schedules, such as adaptive therapy, which aims to maintain a stable tumor population by strategically cycling therapy to exploit competition between drug-sensitive and resistant cells [9] [2]. The diagram below illustrates how a foundational growth model integrates into a comprehensive treatment optimization workflow.
Therapeutic resistance represents a fundamental challenge in oncology, directly contributing to treatment failure, disease relapse, and poor patient outcomes. Current estimates indicate that approximately 90% of chemotherapy failures and more than 50% of failures in targeted therapy or immunotherapy are directly attributable to drug resistance [17]. This resistance manifests as either intrinsic (primary) resistance, where mechanisms pre-exist before treatment begins, or acquired (secondary) resistance, which develops during or after therapy [17]. The remarkable phenotypic plasticity of tumor cells enables continuous adaptation under therapeutic pressure, leading to the selection and enrichment of resistant subpopulations that often exhibit dormancy and stem cell-like properties [17].
The limitations of the traditional Maximum Tolerated Dose (MTD) paradigm are increasingly evident. Developed during the era of cytotoxic drugs, this approach often leads to disease relapse due to the emergence of drug resistance, particularly as newer therapeutics like targeted therapies and immunotherapies have different modes of action where dose efficacy can saturate, resulting in additional toxicity without significant efficacy gains [1]. Mathematical oncology has emerged as a critical discipline for addressing these challenges through mechanistic models that capture the spatial and temporal dynamics of tumor response to treatment [1].
Molecular Mechanisms of Treatment Resistance
Genetic and Epigenetic Drivers of Resistance
Tumor cells evade therapeutic killing through multiple interconnected biological pathways. Key mechanisms include activating drug efflux pumps, inducing target mutations, and activating alternative signaling pathways [17]. The influence of the microbiome has also emerged as a significant determinant of therapeutic response through immune modulation and metabolic cross-talk [17].
Table 1: Key Molecular Mechanisms of Cancer Treatment Resistance
| Resistance Category | Specific Mechanisms | Exemplary Clinical Manifestations |
|---|---|---|
| Genetic Alterations | - Target gene mutations (e.g., T790M, C797S in EGFR)- Activation of bypass signaling pathways- Gene amplification | - Resistance to EGFR-TKIs in NSCLC [17] |
| Epigenetic Reprogramming | - DNA methylation changes- Histone modifications- Chromatin remodeling | - Altered gene expression profiles supporting survival [17] |
| Post-Translational Modifications | - Phosphorylation/dephosphorylation- Ubiquitination- Protein acetylation | - Modulation of protein activity and stability [17] |
| Non-Coding RNA Networks | - miRNA, siRNA, lncRNA regulatory circuits- Competing endogenous RNA networks | - Fine-tuning of resistance phenotypes [17] |
| Metabolic Reprogramming | - Altered energy metabolism- Nutrient scavenging pathways- Metabolic cross-talk with microenvironment | - Adaptation to metabolic stress induced by therapy [17] |
Microenvironment-Mediated Resistance
The tumor microenvironment plays a pivotal role in fostering resistance through multiple mechanisms. In pancreatic ductal adenocarcinoma (PDAC), the acellular matrix can constitute up to 90% of tumor volume, creating extensive fibrosis that elevates interstitial fluid pressure, impairs vascularization, and creates a physical barrier to drug delivery [17]. This significantly limits the penetration of agents like gemcitabine and is associated with poor prognosis [17]. Cancer-associated fibroblasts (CAFs) are key drivers of this fibrotic microenvironment [17].
In glioblastoma, vascular abnormalities may disrupt the blood-brain barrier (BBB) unevenly, while overexpression of efflux pumps further reduces drug concentrations, diminishing therapeutic efficacy [17]. Hematological malignancies, while not impeded by physical barriers, depend on specialized mechanisms such as stem cell dormancy and bone marrow niche dynamics, as evidenced in chronic myeloid leukemia (CML) and multiple myeloma (MM) [17].
Mathematical Modeling Frameworks for Resistance Dynamics
Foundational Modeling Approaches
Mathematical models in oncology use equations to represent underlying biological processes rather than just inputs and outputs, capturing quantities of interest over time such as tumor size dynamics or drug concentrations [1]. These models can incorporate treatment dynamics, including dose-response of systemic drugs or radiotherapy, and eco-evolutionary principles such as ecological interactions of cell-based immunotherapies or evolutionary dynamics due to the emergence of resistance [1].
A general treatment-agnostic formulation for tumor volume dynamics uses ordinary differential equations such as:
$$\frac{dN}{dt}=rN\left(1-\frac{N}{K}\right)-N\sum{i = 1}^{n}{\alpha}{i}{e}^{-\beta(t-{\tau}{i})}H(t-{\tau}{i})$$
where N(t) is the tumor volume at time t, r represents the proliferation rate, K is the carrying capacity, αi represents the death rate due to the ith treatment dose, τi is the time of administration, β is the decay rate of treatment effect, and H(t - τi) is the Heaviside step function [18].
Clinical Translation and Trial Applications
Recent clinical trials demonstrate the translation of mathematical models into therapeutic strategies, particularly those moving beyond the MTD paradigm.
Table 2: Model-Informed Clinical Trials in Oncology (Adapted from [1])
| Model Type | Trial ID/Name | Cancer Type | Intervention | Status/Outcomes |
|---|---|---|---|---|
| Evolution-based: Adaptive Therapy | NCT02415621 | Metastatic Castration-Resistant Prostate Cancer | Adaptive Abiraterone Therapy | Active, not recruiting |
| Evolution-based: Adaptive Therapy | NCT03543969 | Advanced BRAF Mutant Melanoma | Adaptive BRAF-MEK Inhibitor Therapy | Active, not recruiting |
| Evolution-based: Adaptive Therapy | NCT05080556 (ACTOv) | Ovarian Cancer | Adaptive Chemotherapy | Recruiting (Phase 2) |
| Evolution-based: Extinction Therapy | NCT04388839 | Rhabdomyosarcoma | Evolutionary Therapy | Recruiting (Phase 2) |
| Fully Personalized Treatment | NCT04343365 (ETB) | Multiple Cancers | Evolutionary Tumor Board | Recruiting (Observational) |
| Dynamics-based Radiotherapy | NCT03557372 | Glioblastoma | Mathematical Model-Adapted Radiation | Feasibility and Safety ✓ |
Experimental Protocols and Methodologies
Parameter Estimation Workflow for Tumor Dynamic Models
Protocol Objective: To establish a hierarchical framework for simulating and predicting pancreatic tumor response to combination treatment regimens involving chemotherapy (NGC regimen: mNab-paclitaxel, gemcitabine, cisplatin), stromal-targeting drugs (calcipotriol, losartan), and immunotherapy (anti-PD-L1) [18].
Materials and Equipment:
- Genetically engineered mouse model of pancreatic cancer (KrasLSL-G12D; Trp53LSL-R172H; Pdx1-Cre)
- Calipers or imaging system for tumor volume measurement
- Therapeutic agents: chemotherapeutics, stromal-targeting drugs, immunotherapies
- Computational resources for Bayesian parameter estimation
Procedure:
- Experimental Data Collection: Obtain longitudinal tumor volume measurements over a 14-day period with at least three measurement time points [18].
- Control Group Parameter Estimation:
- Employ prior distributions for proliferation rate (r), carrying capacity (K), and initial condition (Nâ‚€) based on prior predictive checks
- Estimate population-specific K and mouse-specific r and Nâ‚€ using Bayesian methods
- Validate model fit using concordance correlation coefficient (CCC) and mean absolute percent error (MAPE) [18]
- Treatment Model Parameter Estimation:
- Fix carrying capacity (K) to values obtained from control group analysis
- Estimate treatment-specific parameters (death rate α, decay rate β) for each mouse
- Compare Linear Treatment Model (β=0) versus Exponential Decay Treatment Model (estimated β) [18]
- Model Validation:
- Perform leave-one-out predictions to assess robustness
- Conduct mouse-specific predictions using individualized parameters
- Implement hybrid, group-informed, mouse-specific predictions [18]
Quality Control Metrics:
- Target concordance correlation coefficient (CCC) >0.70 for predictive accuracy [18]
- Calculate Pearson correlation coefficient (PCC) and mean absolute percent error (MAPE)
- Use coverage metrics to verify biological plausibility of parameter combinations [18]
Comparison of Methods Experiment for Biomarker Validation
Protocol Objective: To estimate systematic error or inaccuracy when comparing new analytical methods to reference methods for biomarker quantification [19].
Materials:
- Minimum 40 different patient specimens covering entire working range
- Reference method or well-characterized comparative method
- Statistical analysis software (R, Python, or specialized packages)
Procedure:
- Sample Selection: Select 40+ patient specimens representing the spectrum of diseases expected in routine application, carefully selected based on observed concentrations to ensure a wide range of test results [19].
- Experimental Timeline: Conduct analyses over multiple runs with a minimum of 5 different days to minimize systematic errors that might occur in a single run [19].
- Sample Analysis: Analyze specimens within two hours of each other by test and comparative methods to prevent specimen degradation from impacting results [19].
- Data Analysis:
- Graph data using difference plots (test minus comparative results vs. comparative result)
- Visually inspect for outliers and systematic patterns
- Calculate linear regression statistics (slope, y-intercept, standard deviation about the line) for wide analytical ranges
- Compute average difference (bias) for narrow analytical ranges [19]
- Interpretation:
- Estimate systematic error at medically important decision concentrations
- Determine constant or proportional nature of error from regression parameters [19]
Research Reagent Solutions and Essential Materials
Table 3: Essential Research Materials for Resistance Modeling Studies
| Reagent/Material | Specification/Example | Research Application |
|---|---|---|
| Genetically Engineered Mouse Models | KrasLSL-G12D; Trp53LSL-R172H; Pdx1-Cre (KPC) | Pancreatic cancer modeling with defined genetic drivers [18] |
| Chemotherapeutic Agents | NGC regimen: mNab-paclitaxel, gemcitabine, cisplatin | Standard chemotherapy combination for pancreatic cancer [18] |
| Stromal-Targeting Drugs | Calcipotriol (vitamin D analog), Losartan (angiotensin inhibitor) | Modify tumor microenvironment to enhance drug delivery [18] |
| Immunotherapeutic Agents | Anti-PD-L1 immune checkpoint inhibitors | Modulate immune response within tumor microenvironment [18] |
| Longitudinal Measurement Tools | Calipers, ultrasound, or molecular imaging systems | Tumor volume tracking for model parameter estimation [18] |
| Computational Resources | Bayesian estimation algorithms, ODE solvers | Parameter estimation and model simulation [18] |
Future Directions and Integrative Technologies
The field of mathematical oncology is increasingly leveraging advanced technologies to enhance predictive capabilities. Single-cell and spatial omics, liquid biopsy, and artificial intelligence are emerging as transformative tools for early detection and real-time prediction of resistance evolution [17]. Integration of mathematical models with 'virtual patient' frameworks, including 'digital twins', represents a promising approach for advancing mechanistic complexity and decision support capabilities [1].
The synthesis of novel therapeutic strategies that convert resistance mechanisms into therapeutic vulnerabilities represents a paradigm shift. These include synthetic lethality approaches, metabolic targeting, and disruption of stem cell and stromal niches [17]. By bridging mechanistic understanding with adaptive clinical design, these integrated approaches provide a roadmap for overcoming therapeutic resistance and achieving sustained, long-term cancer control.
Integrating Patient-Specific Data for Personalized Medicine Approaches
The paradigm of cancer treatment is shifting from a one-size-fits-all approach to highly personalized strategies that account for individual patient variability. This transformation is driven by the integration of diverse patient-specific data streams with advanced mathematical modeling techniques. By creating dynamic, computational representations of cancer progression and treatment response at individual patient levels, researchers and clinicians can now optimize therapeutic strategies while minimizing adverse effects. This protocol details methodological frameworks for constructing patient-specific cancer models, focusing on the integration of multi-scale data, mathematical formalization of treatment dynamics, and clinical translation of model-derived insights. We emphasize practical implementation through standardized workflows, computational tools, and validation approaches suitable for research and drug development applications.
The foundation of personalized cancer medicine lies in comprehensive data integration from multiple biological scales and temporal dimensions. Patient-specific modeling requires harmonization of diverse data types, including genomic profiles, longitudinal imaging, clinical parameters, and treatment history. Digital twin technology represents a cutting-edge framework for creating dynamic virtual representations of individual patients' cancer biology, enabling in silico testing of treatment strategies before clinical implementation [20] [21]. These computational constructs integrate real-time patient data with mechanistic biological knowledge to simulate disease progression and therapeutic response.
The mathematical oncology discipline provides the conceptual bridge between raw patient data and clinically actionable insights [1] [22]. By employing mechanistic models grounded in biological first principles, researchers can move beyond correlative associations to establish causal relationships within cancer systems. This approach captures the spatial and temporal dynamics of tumor growth, interaction with the microenvironment, and evolution of treatment resistance [1]. The workflow transforms heterogeneous patient data into calibrated mathematical models that can predict individual treatment outcomes and optimize therapeutic schedules.
Table 1: Data Types for Patient-Specific Modeling in Oncology
| Data Category | Specific Data Types | Role in Model Development |
|---|---|---|
| Clinical Parameters | Tumor size, histology, stage, performance status | Define initial conditions and clinical constraints |
| Imaging Data | CT, MRI, PET scans; radiomic features | Spatial characterization; treatment response assessment |
| Molecular Profiling | Genomic sequencing, transcriptomics, proteomics | Parameterize mechanistic models; identify therapeutic targets |
| Treatment History | Drug types, doses, schedules, toxicities | Inform model calibration; predict resistance mechanisms |
| Longitudinal Monitoring | Circulating tumor DNA, lab values, patient-reported outcomes | Enable model updating and validation over time |
Protocols for Patient-Specific Model Development
Data Acquisition and Preprocessing Protocol
Objective: Standardize the collection and processing of multi-source patient data for mathematical model development.
Materials and Equipment:
- Institutional review board approval
- Secure data storage infrastructure (HIPAA/GDPR compliant)
- Clinical data extraction tools (e.g., EHR APIs)
- Genomic sequencing platform
- Image processing software (e.g., 3D Slicer, ITK-SNAP)
- Data harmonization pipeline
Procedure:
Clinical Data Extraction
- Extract demographic information, cancer diagnosis, stage, histology, and prior treatment history from electronic health records
- Compile laboratory values including complete blood count, comprehensive metabolic panel, and cancer biomarkers
- Document performance status (ECOG/Karnofsky) and comorbid conditions
Molecular Profiling
- Perform whole exome or targeted sequencing of tumor tissue and matched normal sample
- Conduct RNA sequencing for gene expression profiling
- Process using standardized bioinformatics pipelines for variant calling and expression quantification
Medical Image Processing
- Acquire DICOM images from relevant modalities (CT, MRI, PET)
- Perform manual or automated tumor segmentation to define regions of interest
- Extract radiomic features using standardized pyradiomics or similar packages
- Register serial images to assess temporal changes
Data Integration and Harmonization
- Establish common patient identifiers across all data sources
- Normalize continuous variables using z-score or min-max scaling
- Handle missing data through appropriate imputation methods
- Create structured data matrix for model input
Troubleshooting Tips:
- Inconsistent imaging protocols across timepoints may affect segmentation accuracy; employ intensity normalization techniques
- Sample quality issues in molecular profiling may require additional wet-lab validation
- Temporal misalignment between data types can be addressed through temporal interpolation
Mathematical Model Implementation Protocol
Objective: Implement mechanistic mathematical models that can be personalized using patient-specific data.
Materials and Equipment:
- Computational environment (Python, R, or MATLAB)
- Differential equation solvers (e.g., ODE45, SUNDIALS)
- High-performance computing resources for parameter estimation
- Bayesian inference tools (e.g., Stan, PyMC3)
- Model visualization libraries
Procedure:
Model Selection Framework
- For tumor growth dynamics: Implement Gompertz growth model:
dV/dt = rV × ln(K/V)where V is tumor volume, r is growth rate, and K is carrying capacity [2] - For drug pharmacokinetics: Implement one-compartment model:
dC/dt = -k × Cwhere C is drug concentration and k is elimination rate - For dose-response relationships: Implement Hill equation:
E = (Emax × C^n)/(EC50^n + C^n)where E is effect, Emax is maximum effect, C is concentration, EC50 is half-maximal effective concentration, and n is Hill coefficient [2] - For resistance evolution: Implement Lotka-Volterra competition models between sensitive and resistant populations [2]
- For tumor growth dynamics: Implement Gompertz growth model:
Parameter Estimation
- Define prior distributions for model parameters based on population studies
- Implement Bayesian calibration using Markov Chain Monte Carlo (MCMC) methods
- Incorporate hierarchical modeling to share information across patient subgroups
- Validate parameter identifiability using profile likelihood or similar approaches
Model Personalization
- Initialize model state variables using patient-specific baseline measurements
- Calibrate growth parameters using longitudinal tumor size measurements
- Estimate drug sensitivity parameters from prior treatment responses when available
- Incorporate genomic alterations as modifiers of specific model parameters
Model Validation
- Perform cross-validation using temporal hold-out of later timepoints
- Quantify prediction accuracy using concordance index, mean absolute error, or similar metrics
- Compare against null models or standard clinical prediction rules
- Establish clinical validity through correlation with observed outcomes
Troubleshooting Tips:
- Poor model identifiability may require simplification of model structure or incorporation of additional data types
- Computational bottlenecks in parameter estimation can be addressed through approximate Bayesian computation or surrogate modeling
- Discrepancies between predicted and observed outcomes may indicate missing biological mechanisms
Diagram 1: Workflow for developing personalized cancer treatment models
Mathematical Modeling Approaches
Formal Mathematical Foundations
Personalized cancer treatment models are built upon established mathematical formalisms that capture critical biological processes. The core framework integrates tumor growth dynamics, drug pharmacokinetics/pharmacodynamics (PK/PD), and evolutionary dynamics of resistance [2] [1].
Tumor Growth Dynamics:
The Gompertz model effectively captures the decelerating growth pattern observed in many clinical tumors:
dV/dt = rV × ln(K/V)
where V represents tumor volume, r is the intrinsic growth rate, and K is the carrying capacity representing environmental limitations [2]. This equation can be personalized by estimating r and K from longitudinal imaging data for individual patients.
Drug Pharmacokinetics and Pharmacodynamics:
A one-compartment model provides a simplified representation of drug distribution and elimination:
dC/dt = -k × C
where C is drug concentration and k is the elimination rate constant [2]. The relationship between drug concentration and effect is commonly modeled using the Hill equation:
E = (Emax × C^n)/(EC50^n + C^n)
where E is the treatment effect, Emax is the maximum possible effect, EC50 is the concentration producing half-maximal effect, and n determines the steepness of the response curve.
Evolutionary Dynamics of Resistance:
The emergence of treatment resistance can be modeled using competitive Lotka-Volterra equations:
dS/dt = rS × S × (1 - (S + αR)/K)
dR/dt = rR × R × (1 - (R + βS)/K)
where S and R represent sensitive and resistant cell populations, rS and rR their respective growth rates, and α and β quantify competitive interactions [2].
Digital Twin Implementation Framework
Digital twin technology creates virtual replicas of individual patients that update in real-time as new data becomes available [20] [21]. The implementation involves three core components:
- Physical Entity: The actual patient with their unique cancer biology and clinical characteristics
- Virtual Replica: The computational model personalized to the patient's data
- Data Connectivity: Bidirectional information flow between physical and virtual entities
Key enabling technologies for digital twins include:
- Internet of Things (IoT) for continuous data streaming from wearable sensors and medical devices
- Artificial intelligence and machine learning for pattern recognition and model optimization
- Cloud computing for scalable computational infrastructure
- Blockchain for secure data management and sharing [20]
Table 2: Mathematical Model Types in Personalized Oncology
| Model Category | Key Equations | Clinical Applications | Data Requirements |
|---|---|---|---|
| Tumor Growth Models | dV/dt = rV × ln(K/V) (Gompertz) | Predicting natural progression; sizing adjuvant therapy windows | Longitudinal tumor measurements (imaging) |
| Pharmacokinetic Models | dC/dt = -k × C (one-compartment) | Optimizing drug dosing and scheduling | Drug concentration measurements; physiological parameters |
| Dose-Response Models | E = (Emax × C^n)/(EC50^n + C^n) (Hill equation) | Personalizing drug selection and combination strategies | Pre- and post-treatment tumor response data |
| Evolutionary Dynamics Models | dS/dt = rS × S × (1 - (S + αR)/K) | Designing strategies to suppress resistance emergence | Repeat biopsies showing clonal composition changes |
Experimental Validation and Clinical Translation
Model Validation Protocol
Objective: Establish rigorous validation procedures to ensure model predictions are clinically reliable.
Materials and Equipment:
- Independent validation dataset (temporal or cohort-based)
- Statistical analysis software
- Clinical outcome data (response, progression, survival)
- Benchmarking against established clinical rules
Procedure:
Temporal Validation
- Reserve the most recent timepoints for validation after model calibration on earlier data
- Compare predicted vs. observed tumor trajectories using concordance correlation coefficient
- Assess prediction error growth over increasing time horizons
Cohort-Based Validation
- Apply models developed on one patient cohort to an independent cohort
- Evaluate discrimination performance using time-dependent ROC analysis
- Assess calibration using observed vs. expected outcome plots
Clinical Benchmarking
- Compare model predictions against standard response criteria (RECIST)
- Evaluate whether model-based recommendations would have improved actual outcomes
- Assess potential clinical utility using decision curve analysis
Sensitivity and Uncertainty Analysis
- Perform global sensitivity analysis to identify most influential parameters
- Quantify prediction uncertainty using Bayesian credible intervals
- Evaluate robustness to data perturbations and missingness
Troubleshooting Tips:
- Poor temporal validation performance may indicate overfitting or missing key biological mechanisms
- Systematic prediction errors across cohorts may reflect unaccounted population differences
- Excessive prediction uncertainty may require additional data collection to inform critical parameters
Clinical Implementation Protocol
Objective: Translate validated models into clinical decision support tools for treatment personalization.
Materials and Equipment:
- Regulatory-compliant software platform
- EHR integration capabilities
- Clinical decision support interface
- Model updating infrastructure
Procedure:
Treatment Optimization
- Define objective function balancing efficacy and toxicity
- Implement optimization algorithms to identify optimal drug schedules
- Incorporate clinical constraints (dose limitations, administration logistics)
- Generate personalized dosing recommendations
Clinical Decision Support
- Develop intuitive visualization of model predictions and uncertainties
- Present alternative scenarios with estimated outcomes
- Integrate with molecular tumor board workflows
- Document model assumptions and limitations
Adaptive Updating
- Establish protocols for model recalibration as new data arrives
- Implement trigger points for model review based on prediction discordance
- Create feedback mechanisms to improve population models from individual experiences
Outcome Tracking
- Monitor concordance between predicted and actual outcomes
- Document clinical decisions influenced by model predictions
- Assess impact on treatment response, toxicity, and survival endpoints
Troubleshooting Tips:
- Physician reluctance to adopt model-based recommendations may be addressed through education and interpretable visualizations
- Regulatory concerns can be mitigated through rigorous validation and clear description of intended use
- Computational burden in clinical settings may require development of simplified surrogate models
Diagram 2: Clinical translation pathway for personalized treatment optimization
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Resources for Personalized Cancer Modeling Research
| Tool Category | Specific Solutions | Function in Research |
|---|---|---|
| Data Generation Platforms | Whole exome sequencing (Illumina); RNA sequencing (10x Genomics); Mass cytometry (Fluidigm) | Generate molecular profiling data for model parameterization |
| Computational Environments | Python (SciPy, NumPy); R (deSolve, brms); MATLAB (SimBiology); Stan (probabilistic programming) | Implement and calibrate mathematical models |
| Clinical Data Management | EHR APIs (FHIR standards); REDCap; i2b2 tranSMART | Structured collection and integration of clinical parameters |
| Image Analysis Tools | 3D Slicer; ITK-SNAP; PyRadiomics; QuPath | Extract quantitative imaging features for spatial modeling |
| Model Personalization Algorithms | Markov Chain Monte Carlo (MCMC); Approximate Bayesian Computation (ABC); Particle Filtering | Estimate patient-specific parameters from observed data |
| Validation Frameworks | Scikit-learn; survivalROC; rms (R Package); Model-specific metrics | Assess prediction accuracy and clinical utility |
| Digital Twin Platforms | DTwins (emerging standards); NVIDIA Clara; Custom architectures | Implement continuous patient-specific model updating |
| Namie | Namie (Ethanone Bridged JWH 070) | Namie is a synthetic research chemical for analytical and pharmacological study. This product is For Research Use Only (RUO). Not for human or veterinary use. |
| Pti-1 | Pti-1, CAS:1400742-46-2, MF:C21H29N3S, MW:355.5 g/mol | Chemical Reagent |
The integration of patient-specific data with mathematical modeling frameworks represents a transformative approach to personalized cancer medicine. The protocols outlined provide a comprehensive roadmap for developing, validating, and implementing these models in both research and clinical settings. As digital twin technologies mature and multi-scale data becomes more accessible, these approaches will increasingly enable truly personalized treatment optimization [20] [21]. The field of mathematical oncology continues to develop more sophisticated models that capture the dynamic, evolutionary nature of cancer, moving beyond static genomic snapshots to embrace the temporal dynamics of treatment response and resistance emergence [1] [22]. Through continued refinement of these protocols and their application in clinical trials, we anticipate substantial advances in our ability to personalize cancer therapy for improved patient outcomes.
The Modeler's Toolkit: A Step-by-Step Guide from Concept to Clinical Application
The initial step in developing a mathematical model for cancer treatment optimization is the precise identification of a clinical oncology problem that can be addressed through computational approaches. This requires recognizing a significant challenge in current treatment paradigms where mathematical modeling can provide meaningful insights. A primary problem identified in contemporary oncology is the failure of the traditional Maximum Tolerated Dose (MTD) paradigm, which involves uniformly and continuously administering the highest possible dose that patients can tolerate. This approach often leads to treatment resistance and disease relapse because it fails to account for the dynamic, heterogeneous, and evolutionary nature of cancer, particularly in metastatic settings [1].
The limitations of the MTD approach are especially pronounced with newer therapeutic modalities such as targeted therapies and immunotherapies, where dose efficacy can saturate, resulting in increased toxicity without corresponding improvements in treatment outcomes [1]. Mathematical oncology addresses these limitations by providing a framework to move beyond static dosing regimens toward dynamic treatment strategies that can adapt to tumor evolution and patient-specific characteristics.
Key Problems in Cancer Treatment
Table 1: Primary Clinical Problems Addressable by Mathematical Modeling
| Problem Category | Specific Clinical Challenge | Consequence of Current Approaches |
|---|---|---|
| Treatment Resistance | Emergence of drug-resistant cell populations during therapy [2] | Treatment failure and disease progression [1] |
| Tumor Heterogeneity | Spatial and temporal variations in tumor cell composition [1] | Inconsistent treatment response across tumor sites |
| Dynamic Tumor Evolution | Cancer cell adaptation to selective pressures of treatment [2] | Limited long-term efficacy of therapeutic agents |
| Dosing Optimization | Saturation of dose efficacy with newer therapeutics [1] | Increased toxicity without therapeutic benefit |
| Personalization Gap | One-size-fits-all dosing regimens [2] | Suboptimal outcomes for individual patients |
| Etrumadenant | Etrumadenant, CAS:2239273-34-6, MF:C23H22N8O, MW:426.5 g/mol | Chemical Reagent |
| chd-5 | chd-5, CAS:289494-16-2, MF:C19H17N3O2, MW:319.4 g/mol | Chemical Reagent |
Framework for Biological System Simplification
Once a clinical problem is identified, the next critical step is to simplify the complex biological system into core components that can be mathematically represented. This process involves:
- Defining System Boundaries: Determining which biological elements are essential to include for addressing the specific problem
- Identifying Key Variables: Selecting the most critical factors that drive system dynamics
- Establishing Relationships: Defining how these variables interact through mathematical relationships
For example, when modeling treatment resistance, the complex biological reality of countless cellular interactions and molecular pathways must be reduced to essential components such as sensitive and resistant cell populations, their growth dynamics, and competitive interactions [2].
Table 2: Biological Complexity and Corresponding Simplifications for Mathematical Modeling
| Biological Complexity | Simplified Mathematical Representation | Example Application |
|---|---|---|
| Tumor-immune interactions | System of ordinary differential equations (ODEs) for immune and cancer cell populations [23] | Quantitative Cancer-Immunity Cycle (QCIC) model for mCRC [23] |
| Spatial tumor heterogeneity | Reaction-diffusion equations with diffusion coefficients [3] | Glioblastoma growth simulation using ASU-Barrow model [3] |
| Clonal evolution and competition | Lotka-Volterra competition models or evolutionary game theory [2] | Adaptive therapy for castration-resistant prostate cancer [1] |
| Drug pharmacokinetics | Compartmental models (e.g., one-compartment: dC/dt = -k×C) [2] | Optimization of chemotherapeutic dosing schedules [2] |
| Multi-scale processes | Multi-compartment models (e.g., lymph node, blood, tumor microenvironment) [23] | Prediction of metastatic colorectal cancer progression [23] |
Experimental Protocols for Initial Data Collection
Protocol 1: Tumor Growth Dynamics Parameterization
Purpose: To quantify baseline tumor growth kinetics for model initialization.
Materials:
- Longitudinal medical imaging data (MRI, CT, or PET)
- Image analysis software (e.g., 3D-Slicer [3])
- Tumor segmentation tools
- Computational environment for parameter estimation
Methodology:
- Image Acquisition and Preprocessing: Collect serial imaging studies from patient cohorts. For glioblastoma modeling, this includes T1 post-contrast and T2/FLAIR MRI sequences acquired at typical clinical intervals (e.g., 2-3 months) [3].
- Tumor Segmentation: Manually or automatically delineate tumor boundaries across all imaging time points. For GBMs, segment enhancing tumor, necrotic core, and edema regions [3].
- Volume Calculation: Compute tumor volumes from segmented regions across all time points.
- Growth Curve Fitting: Fit appropriate mathematical models (e.g., exponential, Gompertz, logistic) to the longitudinal volume data to estimate growth parameters.
- Parameter Estimation: Use statistical methods (e.g., maximum likelihood estimation, Bayesian inference) to derive patient-specific growth parameters.
Data Analysis:
- Calculate growth rates (r) and carrying capacities (K) for population growth models
- Estimate diffusion coefficients (D) for spatial models using invasion patterns
- Quantify inter-patient variability in growth parameters
Protocol 2: Treatment Response Assessment for Model Calibration
Purpose: To quantify tumor response to various treatment modalities for model calibration.
Materials:
- Clinical trial data or retrospective patient cohorts with treatment records
- Standardized response criteria (e.g., RECIST criteria)
- Pharmacokinetic/pharmacodynamic assay capabilities
Methodology:
- Treatment Documentation: Record precise drug regimens, including dosing schedules, amounts, and durations.
- Response Monitoring: Document tumor size changes following treatment initiation using the same imaging modalities and segmentation approaches as in Protocol 1.
- Resistance Identification: Note emergence of resistance through regrowth during continued treatment.
- PK/PD Data Collection: Where available, collect drug concentration data over time and correlate with tumor response.
Data Analysis:
- Fit dose-response relationships using Hill equations: ( E = \frac{E{max} \times C^n}{EC{50}^n + C^n} ) where ( E ) is effect, ( E{max} ) is maximum effect, ( C ) is drug concentration, ( EC{50} ) is half-maximal effective concentration, and ( n ) is the Hill coefficient [2]
- Estimate resistant cell fractions from regrowth kinetics
- Calculate response rates and progression-free survival
Table 3: Key Research Reagents and Computational Tools for Mathematical Oncology
| Resource Category | Specific Tool/Reagent | Function/Application |
|---|---|---|
| Computational Tools | Ordinary Differential Equation (ODE) solvers | Simulating population dynamics of tumor and immune cells [2] [23] |
| Image Analysis Software | 3D-Slicer platform [3] | Manual segmentation of tumor regions from medical images |
| Data Processing Tools | SPM-12 [3] | Co-registration of serial MRI scans and brain domain segmentation |
| Parameter Estimation | Maximum likelihood methods; Bayesian inference [23] | Calibrating model parameters to individual patient data |
| Clinical Data Sources | Surveillance, Epidemiology, and End Results (SEER) program [24] | Access to population-based cancer incidence and survival data |
| Model Validation Frameworks | Digital twin methodologies [1] | Creating virtual patient representations for testing treatment strategies |
Workflow Visualization
Figure 1: Workflow for Problem Identification and Biological System Simplification in Mathematical Oncology
Multi-Compartment Modeling Framework
Figure 2: Multi-Compartment Framework for Quantitative Cancer-Immunity Cycle Modeling
Defining model components is a critical step in constructing a predictive mathematical model for cancer treatment optimization. This process involves formally specifying the biological entities, their properties, and their interactions through a structured framework of compartments, variables, and parameters. In translational cancer research, these components quantitatively represent tumor biology, drug pharmacokinetics and pharmacodynamics (PK/PD), and the emergence of treatment resistance [2] [1]. A well-defined model serves as a formal hypothesis about the cancer system, enabling researchers and drug development professionals to simulate treatment scenarios, predict patient-specific outcomes, and optimize therapeutic strategies beyond the maximum tolerated dose paradigm [1]. This document outlines a standardized protocol for defining these core elements, framed within a broader modeling workflow.
Core Definitions and Theoretical Framework
Fundamental Component Types
Mathematical models in oncology abstract a complex, dynamic biological system into a set of interrelated mathematical constructs.
- Compartments: These represent distinct biological populations or spatial domains. A compartment is typically modeled as a container whose size changes over time. Examples include populations of sensitive cancer cells, resistant cancer cells, immune effector cells like CAR-T cells, or nutrient concentrations in the tumor microenvironment [2] [25].
- Variables (State Variables): These are time-dependent quantities that describe the state of the system. The primary state variables are often the sizes of the compartments (e.g., tumor volume, CAR-T cell count). Their evolution over time is what the model seeks to describe through differential equations [2].
- Parameters: These are constants that define the properties and interaction rules of the system. Parameters are not time-dependent and must be estimated from experimental or clinical data. Examples include the maximal growth rate of a tumor, the carrying capacity of the environment, or the killing efficacy of a drug [2] [1].
Relationship to Model Equations
The components are integrated via mathematical equations, most commonly ordinary differential equations (ODEs). The general form for a compartment model is:
d(Compartment)/dt = Inflows - Outflows
The inflows and outflows are functions of the current state variables, the model parameters, and any external forcing functions like treatment dosage [2].
Structured Classification of Model Components
The following tables provide a standardized classification of common compartments, variables, and parameters used in mathematical models of cancer treatment, synthesizing information from multiple modeling paradigms [2] [1] [25].
Table 1: Common Compartments and State Variables in Cancer Treatment Models
| Component Name | Symbol | Type | Biological/Clinical Meaning | Typical Units |
|---|---|---|---|---|
| Tumor Volume | V, N | State Variable | Total number or volume of cancer cells. | mm³, cell count |
| Sensitive Cell Population | S, Ns | State Variable (Compartment) | Sub-population of cancer cells vulnerable to a specific treatment. | cell count |
| Resistant Cell Population | R, Nr | State Variable (Compartment) | Sub-population of cancer cells that survive treatment. | cell count |
| CAR-T Cell Population | C, TCAR | State Variable (Compartment) | Concentration of administered or expanded CAR-T cells in the body or tumor site [25]. | cells/μL |
| Serum Drug Concentration | Cdrug | State Variable | Concentration of a chemotherapeutic or targeted agent in the plasma. | mg/L, μM |
| Immune Effector Cells | E, I | State Variable (Compartment) | Population of native immune cells (e.g., NK cells, T cells) with anti-tumor activity. | cell count |
Table 2: Common Parameters in Cancer Treatment Models
| Parameter Name | Symbol | Biological/Clinical Meaning | Estimation Source |
|---|---|---|---|
| Maximal Growth Rate | r, λ | The intrinsic rate of tumor cell proliferation in the absence of constraints. | In vivo growth data, longitudinal imaging (e.g., CBCT [26]) |
| Carrying Capacity | K, θ | The maximum tumor size sustainable by the local environment and resources. | Maximum observed tumor volume in patients or animal models |
| Drug-Induced Death Rate | kd, δdrug | The rate at which a drug kills sensitive cancer cells; often a function of drug concentration. | In vitro dose-response assays, PK/PD modeling [2] |
| Drug Clearance Rate | kcl, γ | The rate at which a drug is eliminated from the body (e.g., dC/dt = -k<sub>cl</sub> × C [2]). |
Pharmacokinetic studies |
| Mutation Rate | μ, m | The probability of a sensitive cell acquiring a resistance mutation upon division. | Genomic sequencing of pre- and post-treatment samples [2] |
| CAR-T Proliferation Rate | Ï, p | The rate of CAR-T cell expansion upon antigen engagement. | In vitro co-culture assays, patient PK data [25] |
| CAR-T Killing Efficacy | kkill, η | The potency of a single CAR-T cell in eliminating tumor targets. | In vitro cytotoxicity assays, model fitting to clinical response [25] |
| Half-Maximal Effect Concentration | EC50 | The drug concentration that produces 50% of the maximal effect (Emax) in a dose-response model (e.g., Hill equation [2]). | In vitro dose-response curves |
Experimental Protocols for Parameter Estimation
Accurate parameter estimation is fundamental for creating predictive models. The following protocols detail key experiments that generate data for quantifying model parameters.
Protocol 1: Estimating Tumor Growth Parameters from Volumetric Imaging Data
This protocol outlines the procedure for determining the intrinsic growth rate (r) and carrying capacity (K) from longitudinal medical imaging, a common data source in clinical trials [26].
I. Materials and Reagents
- Medical Imaging System: Clinical CT, MRI, or Cone-Beam CT (CBCT) scanner for high-resolution 3D anatomical visualization [26].
- Image Analysis Workstation: Computer with DICOM viewer and volumetric segmentation software (e.g., 3D Slicer, ITK-SNAP).
- Computational Software: Environment for numerical analysis and curve fitting (e.g., MATLAB, R, Python with SciPy).
II. Methodology
- Image Acquisition and Segmentation: For each patient or subject, acquire a time series of volumetric images (e.g., daily or weekly CBCTs [26]). Manually or semi-automatically segment the tumor region in each image slice to calculate the total tumor volume at each time point.
- Data Tabulation: Create a two-column data table:
Time(days) andTumor Volume(mm³). Exclude time points during active treatment to model only the natural growth dynamics. - Model Selection and Fitting:
- Select a growth model, such as the Logistic model:
dV/dt = r * V * (1 - V/K)or the Gompertz model [2]. - Use a non-linear least squares algorithm to fit the model's integrated form to the tabulated (Time, Volume) data.
- The fitting procedure will output the best-fit values for the parameters
r(growth rate) andK(carrying capacity).
- Select a growth model, such as the Logistic model:
III. Data Analysis
- Assess the goodness-of-fit using metrics like R-squared or the Akaike Information Criterion (AIC).
- Report parameter estimates with confidence intervals to quantify uncertainty.
Protocol 2: In Vitro Determination of Drug Pharmacodynamic (PD) Parameters
This protocol describes a standard method to characterize the relationship between drug concentration and cancer cell death, yielding parameters for the k_d and EC_50.
I. Materials and Reagents
- Cell Line: Relevant cancer cell line (e.g., PC-3 for prostate cancer, MCF-7 for breast cancer).
- Therapeutic Agent: The chemotherapeutic or targeted drug under investigation.
- Cell Culture Plates: 96-well plates.
- Cell Viability Assay: MTT, XTT, or CellTiter-Glo Assay.
- Plate Reader: Spectrophotometer or luminometer.
II. Methodology
- Plate Setup and Dosing: Seed a constant number of cells into each well of a 96-well plate. After cell adherence, treat with the drug across a range of concentrations (e.g., from 1 nM to 100 µM), typically in triplicate. Include vehicle-only control wells.
- Incubation and Viability Measurement: Incubate the plate for a predetermined period (e.g., 72 hours). Add the viability assay reagent according to the manufacturer's instructions and measure the signal (absorbance/luminescence) with a plate reader.
- Data Normalization: Normalize the signal from each drug-treated well to the average signal from the vehicle-control wells (defined as 100% viability).
III. Data Analysis
- Dose-Response Curve Fitting: Plot normalized viability (%) against log10(Drug Concentration).
- Parameter Estimation: Fit a sigmoidal dose-response model (Hill equation:
E = E_max * C^n / (EC_50^n + C^n)) to the data. The death ratek_din a dynamical model is often related to(1 - E), whereEis the effect from the Hill equation [2]. The fitting procedure will directly estimate theEC_50(potency) andE_max(efficacy).
Visualization of Model Structures and Workflows
The following diagrams, generated with Graphviz, illustrate common model structures and the parameter estimation workflow.
Basic Tumor Growth and Treatment Compartment Model
This diagram visualizes a simple ODE model incorporating sensitive and resistant cell populations, a common structure for studying treatment resistance [2].
Parameter Estimation and Model Workflow
This flowchart outlines the iterative process of defining model components, estimating parameters from experimental data, and model validation [1].
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Research Reagents and Resources for Model Development
| Item / Resource | Category | Function in Modeling Workflow |
|---|---|---|
| In Vivo Imaging System (e.g., CBCT, MRI) | Data Acquisition | Provides non-invasive, longitudinal tumor volume measurements for estimating growth parameters (r, K) and validating model predictions [26]. |
| Cell Viability Assay (e.g., MTT, CellTiter-Glo) | In Vitro Experimentation | Quantifies dose-dependent cell death in response to therapeutics, enabling estimation of pharmacodynamic (PD) parameters (EC50, Emax) [2]. |
| Flow Cytometer | Cell Analysis | Enables tracking of specific cell populations (e.g., sensitive vs. resistant, CAR-T cells) over time in co-culture experiments, providing data for population dynamics models [25]. |
| Liquid Chromatography-Mass Spectrometry (LC-MS) | Analytical Chemistry | Precisely measures drug concentrations in plasma or tissue samples over time, providing critical data for pharmacokinetic (PK) parameter estimation (kcl) [2]. |
| Numerical Computing Environment (e.g., MATLAB, Python with SciPy) | Software | The core platform for implementing model equations, performing parameter estimation via curve fitting, and running simulations for treatment optimization [2] [1]. |
| Differential Equation Solver (e.g., ODE45 in MATLAB, solve_ivp in SciPy) | Computational Tool | Numerically integrates the system of differential equations that constitute the model, generating predictions of system behavior over time. |
Selecting an appropriate mathematical framework is a critical step in the workflow for developing predictive models of cancer treatment. The chosen formalism dictates how biological processes are abstracted, what data can be assimilated, and the types of clinical questions the model can address. This protocol provides a structured guide for researchers and drug development professionals to compare and select from four core frameworks: Ordinary Differential Equations (ODEs), Partial Differential Equations (PDEs), Agent-Based Models (ABMs), and Stochastic Models.
Each framework offers distinct advantages and limitations in capturing the dynamics of tumor growth, treatment response, and the emergence of resistance [1]. The decision is not merely technical but conceptual, influencing how modelers represent spatial heterogeneity, cellular decision-making, and random fluctuations that drive cancer evolution. This document provides application notes, comparative tables, and experimental protocols to inform this foundational choice.
Comparative Framework Analysis
A quantitative comparison of the four core modeling frameworks is provided in Table 1, summarizing their fundamental characteristics, representative applications, and data requirements.
Table 1: Comparative Analysis of Mathematical Frameworks for Cancer Treatment Modeling
| Framework | Core Principles & Formulation | Key Applications in Oncology | Data Requirements for Calibration | Notable Advantages | Primary Limitations |
|---|---|---|---|---|---|
| Ordinary Differential Equations (ODEs) | Systems of equations describing time-dependent changes in population densities (e.g., tumor cells, immune cells) [27]. Example: dC/dt = rC(1 - C/K) - δCT (Cancer cell growth & immune killing) |
- PK/PD modeling of drug effects [2]- Modeling cancer-immune interactions [27]- Evolutionary dynamics of resistance [1] | - Longitudinal tumor burden data (e.g., serum biomarkers, total volume) [28]- Drug concentration time-series | - Computational efficiency for simulating long time horizons- Well-established tools for parameter estimation and sensitivity analysis- Ability to generate testable hypotheses at the population level [1] | - Lacks spatial resolution- Assumes perfect mixing, overlooking microenvironmental structure [29] |
| Partial Differential Equations (PDEs) | Equations describing how quantities change across both time and space [30]. Incorporate diffusion, adhesion, and chemotaxis. | - Modeling tumor invasion and metastasis [2]- Studying drug penetration gradients within tumors- Angiogenesis and nutrient transport | - Spatially resolved data (e.g., histology, imaging) showing cell density gradients- Measurements of nutrient or drug concentration profiles | - Explicitly captures spatial heterogeneity and tissue architecture- Models cell movement and interaction with the extracellular matrix | - High computational cost for complex geometries- Parameter estimation is often more challenging than for ODEs |
| Agent-Based Models (ABMs) | Individual-based modeling where "agents" (e.g., cells) follow rules for behavior, interaction, and adaptation [29]. A virtual tumor is an emergent property of these rules. | - Studying the impact of cellular heterogeneity [29]- Simulating immune cell-tumor cell spatial interactions [29]- Optimizing immunotherapy protocols | - Single-cell data (e.g., flow cytometry, single-cell RNA-seq)- Spatial mapping of cell locations (e.g., via multiplex immunohistochemistry) | - Captures emergent behavior from individual cell actions- Naturally represents extreme heterogeneity and rare cell subpopulations- Flexible framework for integrating complex, rule-based biology [29] | - Extremely computationally intensive- Parameterization can be difficult due to a large number of rules and variables- Results may be sensitive to initial conditions, requiring many simulations |
| Stochastic Models | Incorporates randomness (e.g., via Wiener processes) to model unpredictable events like mutation, seeding, or death [31] [28]. Can be formulated as SDEs or stochastic processes. | - Predicting time to metastasis or relapse [28] [32]- Modeling the emergence of drug-resistant clones [31]- First-passage-time analysis for treatment response [31] [32] | - Time-to-event data (e.g., progression-free survival, time to recurrence) [28]- Data on clonal frequency fluctuations over time | - Quantifies probability and risk of outcomes (e.g., resistance, recurrence)- Realistically represents the role of chance in cancer progression, especially in small cell populations [31] [32] | - Results are probabilistic, requiring many runs to estimate outcome distributions- Can be mathematically complex to formulate and analyze |
Model Selection Workflow
The following diagram outlines a structured decision-making process for selecting the most appropriate mathematical framework based on the specific biological question and available data.
Experimental Protocols for Model Implementation
Protocol: Developing an ODE Model for Cancer-Immune-CAF Interactions
This protocol outlines the steps for constructing and calibrating an ODE model that incorporates cancer cells, immune cells, and heterogeneous cancer-associated fibroblast (CAF) populations, based on the work of [27].
1. Research Reagent Solutions & Key Materials Table 2: Essential Components for ODE Model of Cancer-Immune-CAF Dynamics
| Component | Function in the Model | Example/Representation |
|---|---|---|
| CAF Phenotype Parameters | Quantifies the proportion of CAFs with anti-immune, pro-immune, anti-cancer, or pro-cancer functions [27] | Model parameters: α, β, γ, δ ∈ [0,1] where α + β + γ + δ = 1 |
| Effector T Cell Data | Represents the primary immune population capable of killing cancer cells. | Variable: ( T_a(t) ) (Activated effector T cell density) |
| Treg Cell Data | Represents immunosuppressive T cell population that inhibits effector T cell function. | Variable: ( T_r(t) ) (Treg density) |
| PD-1/PD-L1 Binding Kinetics | Models the mechanism of immune checkpoint inhibition. | Variables: L (PD-L1), R (PD-1), (\overline{L·R}) (Complex) |
| Parameter Estimation Algorithm | Computational method to fit model parameters to experimental data. | Non-linear mixed-effects modeling software (e.g., MONOLIX, NONMEM) or least-squares optimization (e.g., in MATLAB, R) |
2. Step-by-Step Procedure:
- Step 1: System Scoping and Variable Definition. Define the key biological compartments. For a CAF-mediated resistance model, this includes cancer cell density ((C(t))), activated and exhausted effector T cells ((Ta(t)), (Te(t))), regulatory T cells ((Tr(t))), and relevant drug concentrations (e.g., (AL(t)) for a PD-L1 inhibitor) [27].
- Step 2: Model Formulation. Write the system of ODEs based on biological mechanisms. For example, the rate of change of cancer cells can be modeled as:
dC/dt = r * C * (1 - C/χ_C) - g_1 * (T_a / (K_r + g_2 * T_r)) * C - (γ * F) * g_3 * C[27] This equation includes logistic growth, immune-mediated killing (inhibited by Tregs), and CAF-mediated killing (if present). - Step 3: Parameter Estimation. Calibrate the model using longitudinal data. Use pre-treatment tumor size and immune cell counts to estimate initial conditions. Fit growth, interaction, and drug effect parameters to post-treatment time-course data.
- Step 4: Model Validation and Prediction. Validate the model by comparing its predictions to a withheld portion of the experimental data (e.g., response to a different therapy). Use the validated model to simulate untested treatment combinations and identify optimal CAF-subtype-specific therapies [27].
Protocol: Implementing a Stochastic Model for Time-to-Event Analysis
This protocol details the use of stochastic models, particularly First-Passage-Time (FPT) analysis, to predict critical clinical events like tumor recurrence or treatment response [31] [32].
1. Research Reagent Solutions & Key Materials Table 3: Essential Components for Stochastic FPT Analysis
| Component | Function in the Model | Example/Representation | ||
|---|---|---|---|---|
| Stochastic Differential Equation (SDE) | Describes the stochastic dynamics of tumor volume, incorporating random fluctuations. | Example: dX(t) = [growth terms - treatment terms]dt + σ(X(t), t) dW(t) where W(t) is a Wiener process. |
||
| Moving Barrier S(t) | Defines a critical threshold for an oncological event (e.g., recurrence size). | A function of time, e.g., S(t) = a + bt, representing a changing threshold due to immune or treatment dynamics [31] [32]. |
||
| First-Passage-Time Density (FPTD) | The probability density function of the time when the tumor volume X(t) first crosses the barrier S(t). |
Denoted as `g(S(t), t | x0, t0)`; provides the likelihood of an event occurring at any given time [32]. | |
| Volterra Integral Equation | A mathematical tool for computing the FPTD for a moving barrier. | `g(S(t), t | x0, t0) = -2ψ(...) + 2∫g(S(τ), τ | ...)ψ(...)dτ` [32]. |
2. Step-by-Step Procedure:
- Step 1: Define the Stochastic Process. Select a stochastic process (e.g., a stochastic Gompertz or logistic growth model) that accurately describes the tumor volume dynamics, including the effect of therapy. Incorporate a time-dependent treatment rate to reflect realistic dosing schedules [32].
- Step 2: Specify the Oncological Event as a Moving Barrier. Define the clinical event of interest by setting a corresponding barrier,
S(t). For example:- Time to Response: The first time tumor volume shrinks to a value 30% below baseline (
S(t) = 0.7 * Baseline). - Time to Recurrence: The first time a shrinking tumor later regrows to reach its original baseline size (
S(t) = Baseline) [32].
- Time to Response: The first time tumor volume shrinks to a value 30% below baseline (
- Step 3: Derive the First-Passage-Time Density (FPTD). For the chosen stochastic process and moving barrier, derive the FPTD,
g(S(t), t | x_0, t_0). This may involve solving a Volterra integral equation of the second kind, as shown in Table 3 [31] [32]. - Step 4: Calculate Clinically Relevant Metrics. Use the FPTD to compute:
- The probability distribution of the time to the event.
- The expected (mean) time until the event occurs.
- The risk (hazard) of the event at any given time during treatment or follow-up.
- Step 5: Validate with Experimental Data. Apply the model to in vivo data, such as tumor volume measurements from murine studies (e.g., Murine Lewis Lung Carcinoma), to estimate the time to doubling or recurrence and validate model predictions [32].
Protocol: Building an Agent-Based Model for Spatial Immunotherapy Response
This protocol guides the development of an ABM to simulate the spatial dynamics of tumor-immune interactions and predict response to immune checkpoint inhibitors [29].
1. Research Reagent Solutions & Key Materials Table 4: Essential Components for an Immunotherapy ABM
| Component | Function in the Model | Example/Representation |
|---|---|---|
| Lattice or Continuous Space | Provides a simulated spatial landscape for cell movement and interaction. | A 2D or 3D grid representing the tumor microenvironment. |
| Agent Rules | The behavioral algorithms governing the actions of each cell type. | Rules for T cell chemotaxis, tumor cell proliferation upon contact with resources, and cytotoxic killing (e.g., via perforin/granzyme or Fas/FasL) [29]. |
| Tumor Antigenicity Parameter | Defines how recognizable a tumor cell is to the immune system. | A cell-level property that influences the probability of being killed by a cytotoxic T lymphocyte (CTL) [29]. |
| ABM Software Platform | A computational environment for implementing and simulating the ABM. | Platforms such as NetLogo, PhysiCell, or custom code in C++/Python. |
2. Step-by-Step Procedure:
- Step 1: Initialize the Simulation Space. Create a spatial grid representing the tumor microenvironment. Populate it with agents:
- Tumor Cells: Assign properties like "antigenicity" (high/low) [29].
- Cytotoxic T Lymphocytes (CTLs): Program with movement and killing rules.
- Step 2: Program Agent Behavioral Rules. Define rules for all agents. For example:
- CTL Movement: CTLs perform random walk or chemotaxis towards tumor cells.
- CTL Killing: Upon contact with a tumor cell, a CTL may induce death via a specific mechanism (e.g., perforin/granzyme for high-antigenicity cells) with a certain probability [29].
- Tumor Cell Proliferation: Tumor cells divide if they have sufficient space and nutrients.
- Step 3: Simulate Treatment. Introduce a treatment intervention, such as an anti-PD-1 agent. Model its effect by modifying the rules, for instance, by increasing the probability of successful CTL killing or reversing T cell exhaustion.
- Step 4: Analyze Emergent Outcomes. Run multiple simulations to account for stochasticity. Analyze outputs not just for overall tumor size, but for spatial patterns (e.g., tumor cell clustering, immune infiltration patterns) and phenotypic shifts within the tumor population [29]. Compare these emergent properties to histological findings from biopsy samples for validation.
The translation of a mathematical model into a functional computational tool is a critical step in the workflow of cancer treatment optimization research. This phase bridges theoretical models with practical, clinically relevant insights. The implementation involves selecting appropriate software tools, writing and validating computational solvers, and executing in silico experiments to predict treatment dynamics and optimize therapeutic regimens [1] [2]. The core objective is to create a robust, reproducible, and scalable computational environment that can handle the complex, multi-scale nature of cancer growth and treatment response, ultimately supporting personalized therapeutic strategies.
Software Tools for Mathematical Oncology
A variety of software environments are employed by researchers to implement and solve mathematical models of cancer treatment, each offering distinct advantages for specific tasks. The table below categorizes and describes key computational tools and their primary applications in this field.
Table 1: Software Tools for Computational Modeling in Oncology
| Tool Category | Example Tools/Environments | Primary Functionality | Application in Mathematical Oncology |
|---|---|---|---|
| General Mathematical Computing | MATLAB, Python (with NumPy/SciPy), R, Julia | Numerical analysis, solving differential equations, parameter estimation, data fitting | Simulating tumor growth dynamics (e.g., Gompertz, Logistic), pharmacokinetic/pharmacodynamic (PK/PD) models, and performing optimization [2]. |
| Specialized Biological Modeling | COPASI, Virtual Cell, CompuCell3D | Simulation and analysis of biochemical networks and cellular systems | Implementing complex intracellular signaling pathways, modeling drug mechanisms of action, and simulating cell population dynamics [33]. |
| Diagramming and Visualization | ConceptDraw DIAGRAM, Graphviz (DOT language) | Creating mathematical diagrams, flowcharts, and pathway visualizations | Illustrating model structures, signaling pathways (e.g., CAR-T cell signaling), and experimental workflows for publications and presentations [34]. |
Protocols for Key Computational Experiments
Protocol: Simulating Tumor Growth and Treatment Response with Ordinary Differential Equations (ODEs)
This protocol outlines the steps to implement and solve a system of ODEs describing competitive dynamics between drug-sensitive and resistant cancer cell populations under treatment pressure [2].
Model Formulation: Define the system of ODEs. A common formulation for two competing cell populations is:
dS/dt = r_s * S * (1 - (S + R)/K) - epsilon_s * C(t) * SdR/dt = r_r * R * (1 - (S + R)/K) - epsilon_r * C(t) * R- Where
SandRare the sizes of sensitive and resistant populations,r_sandr_rare their growth rates,Kis the carrying capacity,epsilon_sandepsilon_rare drug efficacy coefficients, andC(t)is the time-dependent drug concentration [2].
Parameterization: Assign values to all parameters (
r_s,r_r,K,epsilon_s,epsilon_r). These can be obtained from literature, pre-clinical data, or calibrated to patient-derived data.Solver Selection: Choose a numerical ODE solver. For non-stiff systems, explicit Runge-Kutta methods (e.g.,
ode45in MATLAB) are suitable. For stiff systems, implicit methods (e.g.,ode15sin MATLAB) are preferred.Implementation:
- Code the ODE system into a function that returns the derivatives
dS/dtanddR/dt. - Set initial conditions (
S0,R0). - Define the time span for the simulation.
- Call the ODE solver, passing the function, time span, and initial conditions.
- Code the ODE system into a function that returns the derivatives
Simulation Execution: Run the simulation to obtain the time-course data for
S(t)andR(t).Analysis and Visualization: Plot the population dynamics over time. Analyze metrics such as time to progression, total tumor burden, and the emergence of dominant resistant clones.
Protocol: Implementing an Agent-Based Model (ABM) for Spatial Tumor Dynamics
ABMs are used to simulate the behavior of individual cells within a spatial context, capturing heterogeneity and local interactions [2].
Define the Agent and Environment: Declare the properties of each agent (e.g., cancer cell), including its position, phenotype (sensitive/resistant), cell cycle status, and rules for behavior (division, death, migration). Define the spatial grid or continuous environment.
Initialize the Simulation: Seed a population of agents at specified locations to represent a microscopic tumor.
Main Simulation Loop: For each time step:
- Update Agent States: Loop through each agent and apply its behavioral rules. Check for proximity to other agents and resources (e.g., oxygen, drug concentration).
- Proliferation: If an agent's conditions for division are met, create a new daughter agent at a nearby location.
- Death: Remove agents that have reached their lifespan or have accumulated lethal damage.
- Migration: Move agents based on random walks or chemotactic gradients.
- Drug Application: Update the local drug concentration field and calculate its effect on each agent based on its phenotype and local concentration.
Data Collection: At predefined intervals, record data such as total cell count, spatial distribution of phenotypes, and cluster sizes.
Visualization: Use graphical tools to render the spatial configuration of the tumor at different time points, creating a visual record of tumor growth and response.
Protocol: Optimizing a Treatment Schedule Using Dynamic Programming
This protocol describes using optimization techniques to personalize drug dosing schedules [2].
Define the Objective Function: Formulate a mathematical expression that quantifies the goal of treatment. This is typically a function that balances efficacy (e.g., minimizing final tumor volume) and toxicity (e.g., minimizing cumulative drug dose). For example:
J = w1 * Tumor_Size(T) + w2 * Sum(Dose(t)), wherew1andw2are weighting factors.Define Constraints: Set boundaries for optimization variables, such as maximum single dose, maximum cumulative dose, and minimum time between doses.
Select Optimization Algorithm: Choose an appropriate algorithm. Dynamic programming is well-suited for sequential decision-making problems like dosing schedules. For complex, non-linear problems, genetic algorithms or direct search methods can be employed.
Execute Optimization: Run the optimization algorithm to find the sequence of doses (the treatment schedule) that minimizes (or maximizes) the objective function while satisfying all constraints.
Sensitivity Analysis: Perturb the model parameters and initial conditions to test the robustness of the optimized schedule. This assesses how specific the schedule is to a particular patient's assumed parameter set.
Visualizing Workflows and Model Structures
The following diagrams, generated using Graphviz DOT language, illustrate core concepts and workflows in computational mathematical oncology. The color palette and contrast have been configured per specifications to ensure accessibility.
Model Implementation Workflow
This diagram outlines the high-level process of transforming a mathematical model into a treatment-relevant prediction.
CAR-T Cell Signaling Pathway
This diagram visualizes the core intracellular signaling events in a CAR-T cell upon antigen engagement, leading to activation and tumor killing [33].
Research Reagent Solutions and Essential Materials
The table below details key computational and experimental resources used in advanced mathematical oncology research, particularly in fields like CAR-T therapy modeling.
Table 2: Research Reagent Solutions for Computational Oncology
| Item | Type | Function/Description |
|---|---|---|
| ODE/ABM Solver Libraries | Software Library | Pre-written code libraries (e.g., SciPy's odeint, deSolve in R) for numerically solving systems of differential equations or managing agent-based simulations, forming the core computational engine [2]. |
| Parameter Estimation Tools | Software Tool | Algorithms and software (e.g., COPASI, custom MCMC scripts) used to calibrate model parameters (growth rates, drug efficacies) to fit experimental or clinical data [2] [33]. |
| CAR Construct Components | Molecular Biology Reagents | Plasmid DNA encoding the scFv, hinge, transmembrane, and intracellular signaling domains (e.g., CD3ζ, CD28, 4-1BB) for generating CAR-T cells for experimental validation [33]. |
| In Vitro Cytotoxicity Assay | Biological Assay | Standardized assays (e.g., luciferase-based, flow cytometry) to measure the ability of CAR-T cells to kill target tumor cells in a controlled setting, providing data for model calibration [33]. |
Mathematical modeling provides a powerful quantitative framework for optimizing cancer treatment regimens, moving beyond the traditional paradigm of administering maximum tolerated doses (MTD) [9]. By simulating complex tumor dynamics and drug effects, these models enable the design of sophisticated dosing schedules and drug combinations that aim to improve therapeutic efficacy, minimize toxicity, and overcome or delay the emergence of treatment resistance [2] [9]. This application note details key methodologies and protocols for leveraging mathematical models in treatment optimization, providing researchers with practical tools for developing more effective cancer therapies.
Quantitative Foundations: Key Models and Equations
Mathematical models for treatment optimization incorporate several core components, including tumor growth dynamics, drug pharmacokinetics (PK) and pharmacodynamics (PD), and resistance mechanisms [2]. The table below summarizes the fundamental equations used in these models.
Table 1: Core Mathematical Models for Treatment Optimization
| Model Component | Mathematical Formulation | Key Parameters | Application in Treatment Design |
|---|---|---|---|
| Tumor Growth (Gompertz Model) | dV/dt = rV × ln(K/V) [2] |
r: Growth rateK: Carrying capacityV: Tumor volume |
Describes decelerating tumor growth; underpins the Norton-Simon hypothesis for dose-dense scheduling [9]. |
| Drug Pharmacodynamics (Hill Equation) | E = (Emax × C^n) / (EC50^n + C^n) [2] |
Emax: Max effectEC50: Potencyn: Hill coefficientC: Drug concentration |
Quantifies the effect of a drug at a given concentration, informing dose-response relationships [2]. |
| Population Dynamics (Lotka-Volterra Competition) | dNâ‚/dt = râ‚Nâ‚(1 - (Nâ‚ + αNâ‚‚)/Kâ‚)dNâ‚‚/dt = râ‚‚Nâ‚‚(1 - (Nâ‚‚ + βNâ‚)/Kâ‚‚) [2] |
Nâ‚, Nâ‚‚: Sensitive/resistant populationsrâ‚, râ‚‚: Growth ratesα, β: Competition coefficients |
Models competition between drug-sensitive and resistant cell populations, fundamental to adaptive therapy [2] [9]. |
| One-Compartment PK Model | dC/dt = -k × C [2] |
C: Drug concentrationk: Elimination rate constant |
Simulates drug clearance from the body, crucial for determining dosing frequency [2]. |
Optimizing Dosing Schedules: From Theory to Protocol
Mathematical models facilitate the exploration of alternative dosing schedules that challenge the conventional MTD approach. The following workflow outlines the general process for developing and testing optimized schedules in silico and in vivo.
Figure 1: Workflow for Schedule Optimization
Protocol: In Silico Testing of Dosing Schedules
Objective: To computationally identify the most promising dosing schedules for a given therapeutic agent, balancing efficacy and toxicity.
Materials:
- Parameterized mathematical model (e.g., from Table 1)
- Computational software (e.g., R, Python, MATLAB)
- High-performance computing resources (for complex models/large parameter sweeps)
Methodology:
- Model Initialization: Define the initial tumor size and composition (e.g., proportion of sensitive vs. resistant cells) based on preclinical or clinical baseline data [2].
- Schedule Definition: Create a set of candidate dosing schedules to be tested. Key variables include:
- Dose Level: Fixed dose, or a range of doses.
- Frequency: Daily, weekly, every 2-3 weeks, etc.
- Duration: Continuous, pulsed, or on-off cycles.
- Simulation Execution: Run the model for each candidate schedule over a defined time horizon (e.g., 6 months, 1 year, 5 years).
- Output Monitoring: Record key outcome metrics for each run, including:
- Tumor volume over time.
- Size of resistant subpopulations.
- Total drug administered.
- Simulated toxicity (if modeled).
- Optimization Analysis: Identify the schedule that best meets the predefined objective, such as:
- Minimizing final tumor burden.
- Maximizing time to progression (e.g., a 10% increase in tumor size).
- Delaying the emergence of resistance.
- Minimizing total drug exposure while maintaining tumor control.
Comparative Analysis of Schedule Strategies
The application of this protocol has led to several well-defined alternative scheduling strategies, each with a distinct mechanistic basis and clinical profile.
Table 2: Comparison of Mathematical Model-Informed Dosing Strategies
| Scheduling Strategy | Mechanistic Basis | Key Mathematical Insights | Clinical Advantages & Considerations |
|---|---|---|---|
| Dose-Dense Therapy | Norton-Simon Hypothesis: Chemotherapy efficacy is proportional to tumor growth rate. Gompertzian growth implies less regrowth between frequent treatments [9]. | Maximizing dose intensity over a shorter time period improves rate of cure by limiting tumor regrowth between cycles [9]. | Advantage: Improved overall and disease-free survival in some cancers (e.g., breast cancer).Consideration: Requires management of cumulative toxicity, often with growth factor support [9]. |
| Metronomic Therapy | Continuous low-dose administration inhibits angiogenesis (indirect effect) and may enable sustained tumor cell killing with milder immune impact [9]. | Hybrid pharmacodynamics and reaction-diffusion models predict constant dosing maintains adequate intra-tumor drug levels better than periodic MTD [9]. | Advantage: Reduced toxicity, potentially suitable for elderly or frail patients.Consideration: Finding the optimal low dose and schedule is challenging; may be less directly cytotoxic [9]. |
| Adaptive Therapy | Evolutionary Game Theory: Resistant cells often bear a fitness cost. Withdrawing treatment allows drug-sensitive cells to outcompete resistant ones [2] [9]. | Models show cycling treatment on/off based on tumor response can maintain a stable tumor burden by exploiting competition to suppress resistant clones [2]. | Advantage: Significantly delays time to progression in clinical trials (e.g., prostate cancer).Consideration: Requires frequent monitoring to guide treatment interruptions and re-initiations [9]. |
Optimizing Drug Combinations and Sequencing
Beyond single-agent schedules, mathematical models are critical for designing effective multi-drug therapies. A key challenge is determining the optimal sequence of drug administration.
Protocol: Testing Drug Sequences In Silico
Objective: To identify the most effective sequence for administering two or more therapeutic agents to maximize synergy and delay resistance.
Materials: (As in Protocol 3.1, with a multi-drug model)
Methodology:
- Model Development: Extend the base model to include the mechanisms of action for all drugs in the combination, as well as potential cross-resistance.
- Sequence Definition: Define the candidate sequences to be tested. For two drugs (A and B), this includes:
- Concurrent administration (A+B simultaneously).
- Sequential administration (A followed by B).
- Alternating cycles (A -> B -> A -> B...).
- Intermittent/pulsed combinations.
- Simulation and Scoring: Run the model for each sequence, scoring outcomes based on objectives like minimal tumor volume or longest time to treatment failure.
- Sensitivity Analysis: Test the robustness of the optimal sequence by varying key model parameters (e.g., mutation rates, fitness costs) within biologically plausible ranges.
Figure 2: Adaptive Therapy Decision Logic
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Reagents and Tools for Modeling-Driven Treatment Optimization
| Item/Category | Function in Treatment Optimization Research |
|---|---|
| Bayesian Adaptive Clinical Trial Software | Enables efficient evaluation of multiple dose-schedule regimens simultaneously in early-phase trials with small sample sizes by borrowing information across cohorts [35]. |
| Pharmacokinetic/Pharmacodynamic (PK/PD) Modeling Software | Integrates drug concentration data (PK) with effect data (PD) to build quantitative models that inform optimal dosing and scheduling prior to and during clinical trials [35]. |
| Agent-Based Modeling (ABM) Platforms | Simulates the behavior and interactions of individual cells (e.g., cancer, immune) within a spatial environment to explore emergent dynamics of treatment response and resistance [2]. |
| Ordinary Differential Equation (ODE) Solvers | Numerical computational tools essential for simulating the continuous dynamics described by models of tumor growth and drug effect (e.g., Gompertz, Lotka-Volterra) [2]. |
| Biomarker Assay Kits | Quantify short-term efficacy endpoints (e.g., tumor response, biomarker expression levels) that are used to parameterize and validate mathematical models of treatment effect [35]. |
The management of Glioblastoma (GBM), a highly aggressive primary brain tumor, remains a significant challenge in neuro-oncology due to its invasive nature and high recurrence rates. Current standard treatments, including maximal safe resection, radiotherapy, and temozolomide chemotherapy, often prove insufficient as tumor cells infiltrate the surrounding brain parenchyma well beyond the visible margins on conventional imaging [36] [37]. This biological reality undermines the efficacy of standardized radiotherapy plans that use uniform safety margins, typically 1.5–2.0 cm around the visible tumor, as they may under-treat infiltrated regions or over-treat healthy tissue [37] [38].
Mathematical oncology offers a paradigm shift through mechanistic modeling. Reaction-diffusion models, particularly the Fisher-Kolmogorov type, have emerged as powerful tools for simulating the spatiotemporal evolution of GBM. These models conceptualize tumor growth as governed by two primary processes: the diffusion (migration) of tumor cells through brain tissue, and the reaction (proliferation) of these cells [36] [37]. The core partial differential equation (PDE) takes the form:
[ \frac{\partial u}{\partial t} = \nabla \cdot (D(\mathbf{x}) \nabla u) + \rho u (1 - u) ]
Where:
- ( u(\mathbf{x}, t) ) is the tumor cell density at location ( \mathbf{x} ) and time ( t )
- ( D(\mathbf{x}) ) is the spatially varying diffusion coefficient, capturing the heterogeneity of brain tissue (e.g., higher diffusivity along white matter tracts)
- ( \rho ) is the net proliferation rate of tumor cells
- The term ( \rho u (1 - u) ) represents logistic growth, accounting for self-limiting proliferation due to resource constraints [37] [38]
The objective of implementing such a model is to infer the full, patient-specific spatial distribution of tumor cell concentration, enabling more personalized and effective radiotherapy planning [37].
Key Quantitative Findings from Clinical Validation Studies
The following table summarizes performance metrics from recent studies that have validated reaction-diffusion models against clinical data.
Table 1: Performance Metrics of Reaction-Diffusion Models in GBM Studies
| Study Focus / Model | Dataset Size | Key Performance Metric | Result | Comparison to Standard |
|---|---|---|---|---|
| ASU-Barrow Model (Scenario Generation) [36] | 132 MRI intervals (46 patients) | Volume Agreement with Observed Tumor | 86% of intervals had a simulated volume within 20% of observed; 65% within 10% | N/A |
| Spatial Accuracy [36] | 132 MRI intervals (46 patients) | Best Simulation Agreement & Containment Scores | Agreement: 0.52; Containment: 0.69 | N/A |
| Anisotropic DT-MRI Informed Model [38] | 35 patients with local recurrence | Proportion of Recurrent Tumor Captured | Mean of 58.4% (SD ±24.9%) | Equivalent coverage with 1.2–30.4% smaller prediction volume in 74.3% (26/35) of patients |
| Standard 2 cm Isotropical Margin [38] | 35 patients with local recurrence | Proportion of Recurrent Tumor Captured | Mean of 57.0% (SD ±24.9%) | Baseline for comparison |
These quantitative results demonstrate that reaction-diffusion models can realistically approximate tumor progression and recurrence patterns. Crucially, models informed by patient-specific anatomy (e.g., via Diffusion Tensor Imaging) can achieve coverage of recurrent tumor volumes equivalent to standard margins but with significantly reduced predicted treatment volumes, directly enabling personalized radiotherapy planning with potential for reduced toxicity [38].
Experimental Protocol for Model Implementation
This protocol details the steps for implementing a reaction-diffusion model for GBM, from data acquisition to radiotherapy target delineation. The workflow integrates multi-modal imaging and computational modeling.
Objective: To acquire and prepare multi-modal patient imaging data for model initialization. Materials: See Section 5, "Research Reagent Solutions."
Procedure:
- Image Acquisition: Acquire pre-operative multi-modal MRI sequences for each patient. Essential sequences include:
- T1-weighted with gadolinium contrast (T1Gd): For segmenting the enhancing tumor core.
- T2-weighted / FLAIR: For identifying peritumoral edema and non-enhancing tumor.
- Diffusion Tensor Imaging (DTI) (Optional but recommended): For estimating anisotropic diffusion tensors ( D(\mathbf{x}) ) based on white matter tractography.
- Co-registration: Use software like SPM12 to co-register all imaging modalities to a common spatial reference (typically the pre-operative T1Gd scan). This ensures all data exists in the same coordinate space.
- Skull Stripping: Apply automated algorithms (e.g., within SPM12) to remove the skull and eyes from the images, defining the patient-specific brain computational domain.
- Manual Segmentation: Manually segment the co-registered images to define the initial tumor sub-regions. This is typically performed by neuroimaging experts using platforms like 3D Slicer. Label voxels as:
- Necrotic core (hypointense on T1)
- Enhancing tumor (enhancing on T1Gd)
- Edema (hyperintense on T2/FLAIR)
- Resection cavity (if applicable)
- Data Export: Export the segmented labels and processed images in a consistent format (e.g., NIfTI) for model ingestion.
Objective: To define the initial conditions for the reaction-diffusion simulation and establish a range of plausible biological parameters. Materials: Preprocessed imaging data from Protocol 3.1.
Procedure:
- Initial Tumor Cell Distribution (( u(\mathbf{x}, t=0) )): Map the segmented tumor regions to an initial tumor cell concentration field. A common approach is to assign a high concentration (e.g., ( u = 0.8 )) to the enhancing and necrotic core, and a lower concentration (e.g., ( u = 0.4 )) to the edematous region.
- Diffusivity Map (( D(\mathbf{x}) )): Estimate the spatial diffusion field.
- If DTI data is available, calculate the diffusion tensor ( D ) from the fractional anisotropy (FA) maps, often scaling it to reflect higher motility along white matter tracts [38].
- Without DTI, a common simplification is to use a constant diffusivity ( D ) for the whole brain or different constant values for grey and white matter derived from an anatomical atlas.
- Proliferation Rate (( \rho )): The net proliferation rate is typically unknown for an individual patient. To address this, implement a systematic parameter sampling design.
- Define a physiologically plausible range for ( \rho ) (e.g., ( 0.5 < \rho < 2.0 ) /year) based on literature.
- Similarly, if ( D ) is not well-constrained, define a range for it (e.g., ( 0.1 < D < 10.0 ) mm²/year).
- Sample multiple parameter pairs (( D, \rho )) from this space (e.g., 18 combinations as in [36]). Each pair will generate a unique simulation scenario.
Objective: To find the model parameters that best explain the observed tumor state at a future time point (e.g., recurrence) or to generate a range of plausible future scenarios. Materials: Initial conditions and parameter ranges from Protocol 3.2.
Procedure:
- Forward Solver Setup: Implement a numerical solver for the reaction-diffusion PDE. The Alternating-Direction Implicit (ADI) scheme is commonly used for its stability and efficiency in 3D voxel space [38]. The solver should incorporate the patient-specific brain domain as the computational grid and apply appropriate boundary conditions (e.g., Neumann / no-flux at the skull).
- Inference via Optimization (Inverse Problem): For a patient with a known recurrence scan, solve the inverse problem to find the best-fit parameters. This is framed as an optimization problem minimizing a cost function ( \mathcal{L} ): [ \mathcal{L} = \underbrace{\| \text{Simulated Tumor at } t{\text{recurrence}} - \text{Observed Recurrence} \|^2}{\text{Data Loss } (L{\text{data}})} + \underbrace{\lambda \| \text{PDE Residual} \|^2}{\text{Physics Loss } (L_{\text{PDE}})} ] Frameworks like GliODIL (Glioma Optimizing the Discrete Loss) are designed to efficiently solve this by treating both the data and the physics model as soft constraints [37].
- Scenario Generation (Predictive): For predictive purposes in newly diagnosed patients, run multiple forward simulations using the sampled parameter pairs from Protocol 3.2. This generates an ensemble of possible tumor progression scenarios over a typical follow-up interval (e.g., 2-3 months) [36].
Objective: To translate the simulated tumor cell distribution into a personalized Clinical Target Volume (CTV) for radiotherapy planning. Materials: The inferred full spatial tumor cell distribution ( u(\mathbf{x}) ) from Protocol 3.3.
Procedure:
- Generate Recurrence Risk Map: Use the simulated tumor cell concentration at a future time point (e.g., post-treatment) to create a 3D probability map of recurrence. This map highlights areas at highest risk of harbingering infiltrative cells.
- Define Isocontour: Instead of a uniform expansion, define the personalized CTV by selecting an isocontour of the simulated tumor cell distribution. For example, the CTV boundary could be the surface where ( u(\mathbf{x}) ) falls to a predefined threshold (e.g., 5% of the maximum concentration) [37].
- Clinical Validation and Comparison: Compare the personalized CTV against the standard uniform margin (e.g., 2 cm). Evaluate performance by calculating the proportion of the actual recurrent tumor (from follow-up scans) that is covered by each volume. The goal is for the personalized CTV to achieve equivalent or better recurrence coverage with a smaller overall treatment volume [38].
Signaling Pathways and Workflow Diagram
The following diagram illustrates the core logic of the reaction-diffusion system and its integration with patient data to inform clinical decision-making.
Research Reagent Solutions
The following table lists the essential computational tools, software, and data types required to implement a reaction-diffusion model for GBM.
Table 2: Essential Research Materials and Computational Tools
| Category / Item | Specification / Example | Primary Function in Workflow |
|---|---|---|
| Medical Imaging Data | ||
|     T1-weighted MRI with Contrast | 1–1.5 mm isotropic voxels | Delineation of enhancing tumor core for model initial condition [36]. |
|     T2 / FLAIR MRI | 1–1.5 mm isotropic voxels | Identification of edematous regions and non-enhancing tumor [36]. |
|     Diffusion Tensor Imaging (DTI) | 2–2.5 mm isotropic voxels | Enables patient-specific estimation of anisotropic diffusion coefficients ( D(\mathbf{x}) ) along white matter tracts [38]. |
| Â Â Â Â FET-PET Imaging | Metabolic activity overlay | Provides complementary data on metabolically active tumor regions; can be used to inform or validate the model [37]. |
| Software & Libraries | ||
| Â Â Â Â Image Processing | SPM12, 3D Slicer | Co-registration of multi-modal images, skull stripping, and manual segmentation of tumor sub-regions [36]. |
| Â Â Â Â Numerical PDE Solver | Custom Python (NumPy) / C++ code | Solving the reaction-diffusion equation forward in time using finite difference/volume methods or implicit schemes [37] [38]. |
| Â Â Â Â Optimization Framework | Custom implementation (e.g., GliODIL), SciPy | Solving the inverse problem by calibrating model parameters (( D, Ï )) to fit patient data [37]. |
| Computational Infrastructure | ||
| Â Â Â Â High-Performance Computing | Multi-core CPU cluster or GPU | Managing the computational load of multiple simulations or complex inverse problem optimization in a clinically relevant timeframe [37]. |
Navigating Challenges: Model Calibration, Uncertainty, and Overcoming Therapeutic Resistance
The maxim "all models are wrong, but some are useful," attributed to statistician George Box, is a fundamental principle in mathematical oncology. This application note provides a structured framework for managing the inherent simplifications and errors in mathematical models of cancer treatment optimization. We present specific protocols for model calibration, validation, and integration into clinical workflows, supported by quantitative data tables and visualization tools. By explicitly addressing model limitations, researchers can enhance the reliability and translational potential of their computational findings for drug development and treatment personalization.
Mathematical modeling has become an indispensable tool in oncology, providing a quantitative framework for simulating diverse aspects of cancer therapy, including the effectiveness of various treatment modalities such as chemotherapy, radiation therapy, targeted therapy, and immunotherapy [2]. These models employ mathematical and computational techniques to simulate how different treatment strategies affect tumor growth, how tumors develop resistance to therapy, and how to optimize treatment regimens to improve patient outcomes [2].
The discipline of 'Mathematical Oncology' integrates mechanistic mathematical models with experimental and clinical data to improve clinical decision making [1]. These models are often based on biological first principles to capture spatial or temporal dynamics of the drug, tumor, and microenvironment. However, the complexity of cancer biology—with its significant heterogeneity both between and within patients, especially in metastatic settings—means that all models necessarily involve simplification [1]. This document addresses how to strategically manage these simplifications to extract meaningful insights for researchers, scientists, and drug development professionals.
Quantitative Landscape of Current Modeling Approaches
Mathematical models in oncology employ various computational frameworks to address different aspects of cancer treatment. The table below summarizes the primary model types, their applications, and their inherent limitations that manifest the "all models are wrong" paradigm.
Table 1: Quantitative Framework for Cancer Treatment Model Selection and Error Management
| Model Type | Primary Mathematical Formulations | Key Applications in Treatment Optimization | Common Simplifications & Error Sources | Clinical Trial Validation Stage |
|---|---|---|---|---|
| Population Dynamics Models | Ordinary Differential Equations (ODEs): Logistic growth: dN/dt = rN(1-N/K) [2]; Lotka-Volterra competition models [2] |
Simulating competition between drug-sensitive and resistant cell populations; Predicting tumor volume changes | Assumes homogeneous cell populations; Neglects spatial structure; Simplified competition parameters | NCT02415621 (Adaptive Abiraterone Therapy) [1] |
| Pharmacokinetic/Pharmacodynamic (PK/PD) Models | Hill equation: E = (Emax × C^n)/(EC50^n + C^n) [2]; One-compartment model: dC/dt = -k×C [2] |
Predicting drug concentration over time; Modeling dose-response relationships | Assumes uniform drug distribution; Simplified metabolism and clearance processes | NCT01967095 (Low Dose Daily Erlotinib) [1] |
| Spatial Heterogeneity Models | Partial Differential Equations (PDEs); Agent-Based Models (ABMs) [2] | Modeling invasion and metastasis; Simulating tissue-level drug penetration | Computational complexity limits scale; Challenges in parameter estimation from imaging data | NCT03557372 (Model-Adapted Radiation in Glioblastoma) [1] |
| Evolutionary Dynamics Models | Evolutionary Game Theory; Population Genetics Models [2] | Designing adaptive therapy protocols; Predicting resistance emergence | Simplifies mutation rates and fitness landscapes; Limited ecological complexity | NCT03543969 (Adaptive BRAF-MEK Inhibitor Therapy) [1] |
Experimental Protocols for Model Calibration and Validation
Protocol: Parameter Estimation and Model Fitting for Tumor Growth Models
Purpose: To calibrate mathematical models of tumor growth using experimental data while quantifying parameter uncertainty.
Materials and Reagents:
- In vivo tumor volume measurements (longitudinal data)
- Computational environment (MATLAB, Python, or R)
- Optimization algorithms (e.g., maximum likelihood estimation, Markov Chain Monte Carlo)
Procedure:
- Data Preparation: Collect at least 5-7 longitudinal tumor volume measurements from preclinical models or patient imaging data.
- Model Selection: Choose an appropriate growth model (e.g., Exponential, Gompertz, Logistic) based on biological plausibility for the cancer type.
- Objective Function Definition: Formulate a sum of squared errors (SSE) function comparing model predictions to experimental data.
- Parameter Estimation: Implement optimization algorithms to find parameter values that minimize the SSE function.
- Uncertainty Quantification: Calculate 95% confidence intervals for parameters using bootstrapping or profile likelihood methods.
- Goodness-of-Fit Assessment: Compute metrics such as Akaike Information Criterion (AIC) to evaluate model performance while penalizing complexity.
Error Management Considerations:
- Explicitly document parameter identifiability issues using sensitivity analysis.
- Report parameter correlations that may affect model predictions.
- Validate calibrated models on a separate hold-out dataset not used for fitting.
Protocol: Validation of Adaptive Therapy Schedules
Purpose: To experimentally validate mathematical model-predictions of evolution-based treatment schedules.
Materials and Reagents:
- Preclinical cancer models (e.g., patient-derived xenografts, genetically engineered mouse models)
- Therapeutic agents with known resistance mechanisms
- Molecular profiling tools (e.g., RNA sequencing, flow cytometry)
Procedure:
- Model-Informed Schedule Design: Using evolutionary dynamics models, generate predicted optimal treatment schedules (continuous vs. adaptive) [1].
- Experimental Arm Assignment: Randomize subjects into three groups:
- Group 1: Continuous maximum tolerated dose (MTD)
- Group 2: Model-derived adaptive therapy
- Group 3: Untreated control
- Treatment Monitoring: Measure tumor volumes 3 times weekly and record survival outcomes.
- Resistance Monitoring: At endpoint, perform molecular analysis to characterize resistant subpopulations.
- Model Refinement: Compare experimental outcomes to model predictions and refine model parameters accordingly.
Error Management Considerations:
- Document discrepancies between predicted and observed evolutionary dynamics.
- Report on transferability of model parameters between different cancer models.
- Quantify inter-animal variability compared to model-predicted variability.
Research Reagent Solutions for Mathematical Oncology
Table 2: Essential Computational and Experimental Resources
| Reagent/Resource | Specifications | Primary Function | Key Limitations |
|---|---|---|---|
| Ordinary Differential Equation (ODE) Solvers | MATLAB ode45; Python SciPy solve_ivp; R deSolve package | Numerical solution of population dynamics models for tumor growth and treatment response | Stiff equations require specialized solvers; Error propagation in long-term simulations |
| Parameter Estimation Tools | Monolix; MATLAB lsqnonlin; Bayesian inference tools (Stan, PyMC3) | Calibration of model parameters to experimental data | Risk of overfitting; Local minima in complex parameter spaces |
| Clinical Data Standards | FHIR (Fast Healthcare Interoperability Resources); CDISC (Clinical Data Interchange Standards Consortium) | Structured data integration from electronic health records (EHRs) for model parameterization [39] | Data fragmentation across systems; Missing data elements; Format inconsistencies |
| Virtual Patient Generators | Digital twin frameworks; Bayesian hierarchical models | Creating in silico cohorts for simulating clinical trials and testing treatment protocols [1] | Simplified representation of human physiology; Validation challenges |
| Spatial Imaging Data | Multiplex immunohistochemistry; MRI/CT scans; Spatial transcriptomics | Parameterizing spatial models and validating spatial predictions [2] | Resolution limitations; Computational cost of 3D reconstruction |
Workflow Integration and Error Mitigation Strategies
The following diagram illustrates a robust workflow for mathematical model development that explicitly addresses the "all models are wrong" paradigm through iterative refinement and validation:
Model Development Workflow with Error Management
The integration of mathematical models into clinical workflows faces several translational barriers, notably access to clinical data in standardized formats and regulatory constraints [1]. The following diagram details the pathway from model development to clinical application:
Clinical Translation Pathway with Barriers
The recognition that "all models are wrong" should not deter their use in cancer treatment optimization but should instead inspire more rigorous approaches to managing their limitations. By implementing the protocols, workflows, and error mitigation strategies outlined in this application note, researchers can enhance the reliability and clinical utility of mathematical models in oncology. The future of mathematical oncology lies not in creating perfect models, but in developing transparent, validated, and clinically actionable tools that acknowledge their limitations while providing meaningful insights for treatment personalization. As the field advances, tighter integration of models with novel computational tools, including virtual trials, digital twins, and artificial intelligence, will further advance translation while maintaining awareness of inherent simplifications [1].
Strategies for Parameter Estimation and Sensitivity Analysis
Parameter estimation and sensitivity analysis are fundamental components in the workflow of mathematical modeling for cancer treatment optimization. These processes transform conceptual models into predictive tools capable of informing clinical decisions. In mathematical oncology, where models range from simple growth equations to complex multi-scale systems, rigorous parameterization ensures models accurately capture tumor dynamics and treatment response [40]. Sensitivity analysis further identifies which parameters most significantly influence model outputs, guiding targeted data collection and refining model structures. This protocol details established methodologies for estimating parameters and conducting sensitivity analyses, with specific applications in cancer treatment modeling.
Parameter Estimation Methods
Parameter estimation involves calibrating model parameters to align mathematical model outputs with observed experimental or clinical data. This process is crucial for developing patient-specific models and validating biological mechanisms.
Formalization of the Inverse Problem
The core of parameter estimation is formulating and solving an inverse problem. For a mathematical model ( f(\theta, t) ) that predicts system behavior (e.g., tumor volume over time) based on a parameter set ( \theta ), the goal is to find the parameter values ( \hat{\theta} ) that minimize the difference between model predictions and observed data ( y(t) ) [41].
The objective function for this optimization is typically formulated as: [ \hat{\theta} = \arg\min{\theta} \sum{i=1}^{N} [y(ti) - f(\theta, ti)]^2 ] where ( N ) is the number of data points.
Applied Example: Estimating Treatment Sensitivity Distribution
A relevant example from cancer modeling involves estimating the distribution of cellular sensitivity to treatment within a heterogeneous tumor. A random differential equation model can be used where sensitivity ( s ) is treated as a random variable following a probability distribution ( P(s) ) [41].
The model for each subpopulation with sensitivity ( s ) is: [ \frac{dc(t,{\bf{s}})}{dt}=\rho c(t,{\bf{s}})(1-c(t,{\bf{s}}))(1-{\bf{s}})-k{\bf{s}}c(t,{\bf{s}}) ] where ( \rho ) is the maximal growth rate and ( k ) is the death rate due to treatment.
The aggregated tumor volume is the expectation over all sensitivity subpopulations: [ c(t)={\int}_{\Omega}c(t,{\bf{s}})dP({\bf{s}}) ]
The inverse problem involves recovering the probability mass function ( P(s) ) from aggregated tumor volume data ( c(t) ) [41].
Optimization Techniques
Various optimization algorithms can be employed to solve the inverse problem:
Table 1: Optimization Methods for Parameter Estimation
| Method | Principle | Application Context | Advantages | Limitations |
|---|---|---|---|---|
| Gradient-Based | Iteratively moves in direction of steepest descent of objective function | Models with smooth, continuous parameter spaces | Fast convergence for convex problems | May converge to local minima; requires differentiable functions |
| Population-Based | Uses a population of candidate solutions that evolve over generations | Complex models with multiple local minima | Global search capability; doesn't require derivatives | Computationally intensive; requires parameter tuning |
| Bayesian Inference | Treats parameters as probability distributions using Bayes' theorem | Incorporating prior knowledge and quantifying uncertainty | Provides uncertainty quantification; integrates prior information | Computationally demanding for high-dimensional problems |
Practical Protocol: Parameter Estimation Workflow
Materials:
- Longitudinal tumor measurement data (e.g., volume, diameter, or biomarker levels)
- Computational implementation of the mathematical model
- Optimization software environment (e.g., MATLAB, R, Python with scipy)
Procedure:
- Data Preparation: Compile and clean experimental data. For tumor growth data, this may involve normalizing measurements to initial volume and handling missing data points.
Model Implementation: Program the mathematical model in your computational environment, ensuring the model interface accepts parameter values and returns simulated outputs.
Objective Function Definition: Implement a function that calculates the difference between model simulations and experimental data. The sum of squared errors is commonly used.
Optimization Execution: a. Set plausible initial parameter guesses based on literature or preliminary analysis b. Define parameter constraints (lower and upper bounds) based on biological plausibility c. Execute optimization algorithm to minimize the objective function d. Verify convergence by checking algorithm termination criteria
Validation: Assess estimated parameters by simulating the model with the optimized parameters and visually comparing with experimental data. Use a subset of data not used in estimation for validation.
Troubleshooting Tips:
- If optimization fails to converge, try different initial parameter values
- If parameter estimates are at constraint boundaries, reconsider constraintåˆç†æ€§
- For models with many parameters, consider estimating them in stages (e.g., growth parameters first, then treatment effect parameters)
Sensitivity Analysis Techniques
Sensitivity analysis quantifies how uncertainty in model outputs can be apportioned to different sources of uncertainty in model inputs. This is particularly important in cancer models where many parameters cannot be measured precisely.
Local Sensitivity Analysis
Local methods examine the effect of small parameter variations around a nominal value, typically using partial derivatives. The local sensitivity index ( S{i} ) for parameter ( \thetai ) is calculated as: [ S{i} = \frac{\partial y}{\partial \thetai} \bigg|{\theta0} ] where ( \theta_0 ) is the nominal parameter vector [2].
Protocol: Local Sensitivity Analysis via One-at-a-Time (OAT) Design
Materials:
- Parameterized mathematical model
- Baseline parameter values
- Computational environment for numerical differentiation
Procedure:
- Establish Baseline: Run the model with baseline parameters ( \theta0 ) and record output ( y0 )
Parameter Perturbation: For each parameter ( \thetai ): a. Create a perturbed parameter set ( \theta^+ = \theta0 ) with ( \thetai^+ = \thetai \times (1 + \delta) ), where ( \delta ) is a small perturbation (typically 1-5%) b. Run model with ( \theta^+ ) and record output ( yi^+ ) c. Calculate the normalized sensitivity index: ( Si = \frac{(yi^+ - y0)/y_0}{\delta} )
Rank Parameters: Sort parameters by absolute sensitivity index ( |S_i| ) to identify most influential parameters
Advantages: Computationally efficient; intuitive interpretation Limitations: Only explores local parameter space; misses parameter interactions
Global Sensitivity Analysis
Global methods evaluate sensitivity over the entire parameter space, capturing interactions between parameters. The Sobol' method is a variance-based global approach that decomposes output variance into contributions from individual parameters and their interactions [40].
Table 2: Global Sensitivity Analysis Methods
| Method | Key Features | Output Metrics | Computational Cost | Best For |
|---|---|---|---|---|
| Sobol' Indices | Variance-based; model-free | First-order, second-order, and total-effect indices | High | Quantifying influence of individual parameters and interactions |
| Morris Method | Screening method; efficient | Elementary effects mean (μ) and standard deviation (σ) | Medium | Identifying important parameters in models with many inputs |
| FAST (Fourier Amplitude Sensitivity Test) | Spectral approach; efficient | First-order sensitivity indices | Medium | Models with monotonic relationships |
| PRCC (Partial Rank Correlation Coefficient) | Rank-based; handles non-linearity | Correlation coefficients between parameters and outputs | Medium to High | Models with non-monotonic but smooth relationships |
Practical Protocol: Sobol' Sensitivity Analysis
Materials:
- Parameterized mathematical model
- Parameter ranges (minimum and maximum values for each parameter)
- Sampling software (e.g., SALib, Dakota, or custom implementations)
Procedure:
- Parameter Range Definition: Define plausible ranges for each parameter based on experimental constraints or literature values.
Sample Generation: Generate parameter samples using Sobol' sequences or other quasi-random sequences. For ( k ) parameters and sample size ( N ), this creates an ( N \times 2k ) matrix.
Model Evaluation: Run the model for each parameter sample and record outputs of interest.
Index Calculation: Compute first-order (( Si )) and total-effect (( STi )) Sobol' indices using the method of Saltelli et al.:
- ( S_i ) measures the contribution of parameter ( i ) alone to the output variance
- ( ST_i ) measures the total contribution of parameter ( i ), including all interaction effects
Interpretation: Parameters with high ( ST_i ) values (( > 0.1 )) have significant influence on model outputs and should be prioritized for precise estimation.
Notes: Sample size ( N ) should be sufficiently large (typically ( 1000 \times k ) for initial screening) for stable index estimates.
Application in Cancer Treatment Modeling
Tumor Growth Inhibition Models
In oncology drug development, Tumor Growth Inhibition (TGI) models describe how tumor volume changes in response to treatment. These typically incorporate:
- Untreated tumor growth (exponential, logistic, or Gompertz)
- Drug exposure (pharmacokinetics)
- Drug effect (pharmacodynamics) [40]
Parameter estimation for TGI models often uses nonlinear mixed-effects modeling to handle sparse clinical data and account for between-patient variability.
Case Study: Estimating Resistance Parameters
Cancer treatment resistance can be modeled using population dynamics approaches. A common formulation uses Lotka-Volterra competition models: [ \frac{dN1}{dt}=r1N1(1-\frac{N1+\alpha N2}{K1}) ] [ \frac{dN2}{dt}=r2N2(1-\frac{N2+\alpha N1}{K2}) ] where ( N1 ) and ( N2 ) are sensitive and resistant cell populations, ( ri ) are growth rates, ( Ki ) are carrying capacities, and ( \alpha ) represents competition strength [2].
Estimation Challenge: Resistance parameters are typically unobservable directly and must be inferred from total tumor burden measurements.
Solution Approach:
- Use approximate Bayesian computation to fit model to longitudinal tumor volume data
- Employ profile likelihood to assess parameter identifiability
- Utilize experimental data on resistance marker prevalence when available for validation
Integration with Experimental Design
Effective parameter estimation requires close integration with experimental design. Key considerations include:
- Temporal Sampling: Frequent measurements during initial treatment response and potential relapse provide more information for parameter estimation
- Dose Ranging: Multiple dose levels help separate drug-specific parameters from system-specific parameters
- Biomarker Measurement: Incorporating molecular biomarkers (e.g., ctDNA, protein expression) can provide additional constraints for model parameters [42]
Table 3: Research Reagent Solutions for Parameter Estimation
| Reagent/Resource | Function in Parameter Estimation | Example Application | Key Considerations |
|---|---|---|---|
| Longitudinal Imaging Data | Provides tumor volume measurements for model fitting | Estimating growth and treatment response parameters in vivo | Resolution limits detection of small populations; frequency affects parameter uncertainty |
| Circulating Tumor DNA (ctDNA) | Quantifies tumor burden and resistance allele frequency | Tracking clonal dynamics during treatment | May not fully represent spatial heterogeneity; sensitivity thresholds apply |
| Patient-Derived Xenografts | Enables controlled therapeutic experiments | Estimating drug efficacy parameters while preserving tumor biology | Host microenvironment differences; cost and throughput limitations |
| Quantitative Systems Pharmacology Platforms | Integrates pharmacokinetic and pharmacodynamic data | Simultaneous estimation of drug- and system-specific parameters | Model complexity versus parameter identifiability trade-offs |
| Bayesian Estimation Software | Implements Markov Chain Monte Carlo and approximate Bayesian computation | Parameter estimation with uncertainty quantification | Computational intensity; requires appropriate prior distributions |
Robust parameter estimation and comprehensive sensitivity analysis form the foundation of reliable mathematical models in cancer treatment optimization. The methodologies outlined here—from inverse problem formulation to local and global sensitivity techniques—provide researchers with a structured approach to model calibration and validation. As mathematical oncology continues to evolve, with increasing incorporation of multi-scale data and digital twin technologies [1] [22], these fundamental techniques will remain essential for translating mathematical insights into clinically actionable treatment strategies.
Mathematical modeling provides a powerful quantitative framework for optimizing personalized cancer treatment regimens, with the primary goal of balancing therapeutic efficacy against treatment-related toxicity [2] [1]. This approach employs mathematical and computational techniques to simulate how different treatment strategies affect tumor growth and response, incorporating critical factors such as drug pharmacokinetics, tumor biology, and patient-specific characteristics [2]. By capturing the complex dynamics of tumor evolution and treatment response, these models enable the design of personalized dosing schedules that maximize therapeutic benefits while minimizing adverse effects, moving beyond the traditional paradigm of maximum tolerated dose (MTD) which often leads to disease relapse due to drug resistance [1].
Key Mathematical Modeling Approaches
Mathematical oncology employs various modeling frameworks to simulate tumor dynamics and treatment effects. The table below summarizes the primary approaches used for treatment optimization.
Table 1: Key Mathematical Modeling Approaches in Oncology
| Model Type | Primary Application | Key Features | Representative Equations |
|---|---|---|---|
| Tumor Growth Dynamics [2] | Modeling untreated tumor growth | Captures natural growth saturation | dV/dt = rV × ln(K/V) (Gompertz) |
| Pharmacokinetic/Pharmacodynamic (PK/PD) [2] | Modeling drug concentration and effect | Links drug exposure to biological effect | E = (Emax × C^n) / (EC50^n + C^n) (Hill Equation) |
| Population Dynamics [2] [43] | Simulating resistance emergence | Tracks competition between sensitive (Nâ‚) and resistant (Nâ‚‚) cells | dNâ‚/dt = râ‚Nâ‚(1 - (Nâ‚ + αNâ‚‚)/Kâ‚) dNâ‚‚/dt = râ‚‚Nâ‚‚(1 - (Nâ‚‚ + βNâ‚)/Kâ‚‚) |
| Evolutionary Dynamics [1] | Informing adaptive therapy | Applies evolutionary principles to delay resistance | Utilizes game theory and ecological models |
Quantitative Outcomes of Optimized Scheduling Strategies
Simulation studies and clinical trials have demonstrated the potential benefits of optimized treatment schedules over continuous dosing. The following table summarizes key quantitative findings.
Table 2: Comparative Outcomes of Different Treatment Scheduling Strategies
| Treatment Strategy | Model Basis | Reported Outcome | Clinical Context |
|---|---|---|---|
| Intermittent Dosing [43] | Tumor dynamics with resistant clones | Prolonged median PFS from 36 to 44 weeks; extended median TTS | mCRC with anti-EGFR therapy |
| Adaptive Therapy [43] | ctDNA-guided drug switching | Prolonged median PFS to 56-64 weeks; extended median TTS | mCRC with hypothetical second-line therapy |
| Adaptive Abiraterone [1] | Evolutionary dynamics | Clinical trial to evaluate intermittent vs continuous dosing (NCT02415621) | Metastatic Castration-Resistant Prostate Cancer |
| Adaptive BRAF-MEK [1] | Evolutionary dynamics | Clinical trial to evaluate adaptive dosing (NCT03543969) | Advanced BRAF Mutant Melanoma |
Experimental Protocols for Model Development and Validation
Protocol: Development of a Tumor Dynamics Model Incorporating Evolving Resistance
This protocol outlines the methodology for creating a mathematical model that characterizes tumor response and resistance evolution, based on the work presented in Scientific Reports [43].
I. Research Reagent Solutions and Essential Materials
Table 3: Essential Research Materials for Model Development
| Item | Function/Description |
|---|---|
| Longitudinal Clinical Data [43] | Tumor burden measurements and ctDNA levels from patients for model calibration. |
| Circulating Tumor DNA (ctDNA) [43] | Biomarker for monitoring clonal dynamics and emerging resistance. |
| Non-Linear Mixed-Effect Modeling Software [43] | Platform for quantifying population parameters and inter-individual variability. |
| Virtual Patient Cohort [43] | Simulated population for evaluating and comparing different treatment schedules. |
II. Methodology
- Model Structure Definition: Develop a multi-clonal tumor model. The base structure should include:
- TS: Treatment-sensitive cell population.
- TR1: Cell population resistant to first-line treatment.
- T_R2: Cell population resistant to both first and second-line treatments [43].
- Biomarker Integration: Link resistant cell populations to corresponding ctDNA compartments (e.g., M_ctDNA1, M_ctDNA2). Use Hill equations to model the delayed emergence and detection of mutations in ctDNA relative to tumor size [43].
- Parameter Estimation: Calibrate the model by estimating parameters for tumor growth, treatment effect, and resistance emergence using longitudinal patient data. Apply a non-linear mixed-effects approach to quantify inter-individual variability [43].
- Model Evaluation: Validate the model using an independent clinical dataset not used for calibration. Assess the model's ability to capture central trends in tumor size and biomarker dynamics [43].
Protocol: Clinical Workflow for Model-Informed Personalized Treatment
This protocol describes the integration of a calibrated mathematical model into a clinical decision-making workflow for personalizing cancer treatment, reflecting current approaches in mathematical oncology [1].
I. Methodology
- Data Assimilation: Collect and input patient-specific baseline data. This includes tumor size, genetic profile, and other relevant clinical characteristics [1].
- Model Personalization: Calibrate the mathematical model to the individual patient by adjusting key parameters (e.g., initial tumor size, growth rate, resistance mechanisms) to fit the available patient data [1].
- In-Silico Treatment Simulation: Use the personalized model to simulate the outcome of various candidate treatment regimens. Test different dosing schedules, sequences, and drug combinations [1].
- Outcome Prediction & Optimization: For each simulated regimen, predict key outcomes such as tumor response, time to progression, and the emergence of resistance. The model then identifies the optimal regimen that maximizes efficacy while minimizing toxicity [1].
- Clinical Implementation & Monitoring: Administer the model-recommended treatment regimen. Continuously monitor the patient and collect new data on treatment response and biomarker levels (e.g., ctDNA) [1].
- Dynamic Model Refinement: Update the model with new patient data, allowing for real-time adjustment of the treatment strategy in response to the observed tumor dynamics [1].
The integration of mathematical modeling into oncology treatment planning offers a robust framework for moving beyond the one-size-fits-all MTD paradigm. By utilizing quantitative models of tumor dynamics, drug effect, and resistance evolution, clinicians can design personalized and adaptive treatment schedules. These optimized regimens, including intermittent and ctDNA-guided adaptive therapy, have demonstrated potential in preclinical and early clinical studies to significantly prolong disease control and manage toxicity [43] [1]. As the field evolves, the synergy of mechanistic models with clinical data, virtual patient frameworks, and artificial intelligence promises to further enhance the personalization of cancer therapy and improve patient outcomes [2] [1].
Evolutionary Cancer Therapy (ECT), often termed adaptive therapy, represents a paradigm shift in oncology, moving from a eradication-focused model to a control-based approach. This strategy addresses one of the most significant challenges in cancer treatment: the rapid development of treatment-induced resistance. The fundamental principle of ECT is to exploit the evolutionary dynamics within tumor ecosystems. Rather than administering maximum tolerated doses (MTD) that eliminate drug-sensitive cells and create a void for resistant populations to expand, adaptive therapy aims to maintain a stable population of treatment-sensitive cells that can competitively suppress the growth of resistant subpopulations through resource competition and spatial constraints [44] [45].
This approach applies principles from evolutionary game theory (EGT) to clinical oncology, viewing cancer as a dynamic, evolving system rather than a static entity. ECT protocols dynamically adjust treatment timing, dosing, and drug selection based on individual patient response and disease characteristics [44]. The therapy is inherently patient-specific and adaptive, with treatment decisions guided by mathematical models calibrated with real-time biomarker data [44]. By acknowledging that complete eradication may not be feasible for advanced cancers, especially those with significant heterogeneity, adaptive therapy seeks to transform cancer into a manageable chronic condition, prolonging progression-free survival while maintaining quality of life through reduced treatment toxicity [46] [45].
Mathematical Modeling Foundations
Core Mathematical Frameworks
Mathematical modeling provides the predictive foundation for designing and optimizing adaptive therapy protocols. Several complementary modeling approaches capture different aspects of tumor evolutionary dynamics:
Ordinary Differential Equation (ODE) Models form the backbone of many ECT frameworks, describing population dynamics of competing cell types. A typical model might track healthy cells (H), drug-sensitive cancer cells (S), and drug-resistant cancer cells (R) using equations such as:
( \frac{dS}{dt} = rS S(1 - \frac{S + R}{K}) - \deltaS C S ) ( \frac{dR}{dt} = rR R(1 - \frac{S + R}{K}) - \deltaR C R )
where ( r ) represents growth rates, ( K ) is carrying capacity, ( \delta ) denotes drug-induced death rates, and ( C ) is drug concentration [2] [47]. These models capture the competitive exclusion principle where sensitive and resistant cells compete for limited resources.
Evolutionary Game Theory (EGT) Models frame cancer treatment as a Stackelberg (leader-follower) game, where the physician (leader) makes treatment decisions and cancer populations (followers) adapt through evolutionary dynamics [44] [47]. EGT models incorporate fitness functions that vary with the tumor microenvironment and treatment pressure. For three cell populations (healthy, sensitive, resistant), the fitness functions and average fitness are defined as:
( fi = 1 - wi + wi(A\vec{x})i ) ( \langle f \rangle = f1x1 + f2x2 + f3x3 )
where ( w_i ) represents natural selection pressure, ( A ) is the payoff matrix, and ( \vec{x} ) is the vector of cell population proportions [47] [48].
Spatial Models including partial differential equations (PDEs) and agent-based models (ABMs) incorporate spatial heterogeneity, which significantly influences evolutionary dynamics and treatment response [44] [2]. These models capture how physical constraints, nutrient gradients, and local cell-cell interactions affect the emergence and expansion of resistant clones.
Incorporating Pharmacokinetics and Pharmacodynamics
Recent advances integrate pharmacokinetic (PK) and pharmacodynamic (PD) models with evolutionary models to create more clinically relevant treatment optimizations. The PK component describes drug concentration over time:
( \frac{dC}{dt} = pm - qC )
where ( C ) represents drug concentration, ( m ) is dosage, and ( p ), ( q ) represent pharmacokinetic rates of drug administration and clearance, respectively [47] [48]. The PD component then links drug concentration to biological effect, often using Hill equations:
( E = \frac{E{max} \times C^n}{EC{50}^n + C^n} )
where ( E{max} ) is the maximum effect, ( EC{50} ) is the concentration for half-maximal effect, and ( n ) is the Hill coefficient [2].
Table 1: Key Mathematical Modeling Approaches in Adaptive Therapy
| Model Type | Key Features | Applications | Limitations |
|---|---|---|---|
| ODE Models | Continuous dynamics of cell populations; Analytical tractability | Predicting tumor burden over time; Dose optimization | Oversimplifies spatial structure |
| Game Theory Models | Strategic interactions between cell types; Fitness-based competition | Understanding resistance emergence; Treatment scheduling | Complex parameter estimation |
| Spatial Models (PDEs, ABMs) | Spatial heterogeneity; Local cell interactions | Modeling metastasis; Tissue-specific treatment effects | Computational intensity; Data requirements |
| Hybrid Multi-scale Models | Integration across biological scales; Molecular to tissue level | Personalized treatment prediction; Digital twins | Implementation complexity |
Clinical Implementation Workflow
Biomarker Monitoring and Treatment Adjustment
Successful adaptive therapy requires robust, quantitative monitoring of tumor burden and composition. The implementation follows a cyclic process of assessment, interpretation, and adjustment:
Step 1: Baseline Assessment - Establish pretreatment tumor burden using appropriate biomarkers (e.g., PSA for prostate cancer, CA125 for ovarian cancer, or radiographic tumor volume measurements) [44] [46]. For optimal control, define constraints including maximum tolerable drug concentration (( C{max} )) and maximum acceptable tumor burden (( T{max} )) [47] [48].
Step 2: Treatment Initiation - Begin therapy at standard doses to achieve significant tumor reduction, typically until a predetermined response threshold is reached (e.g., 50% reduction in PSA) [44].
Step 3: Response Monitoring - Frequently assess biomarker levels during treatment. Emerging technologies like circulating tumor DNA (ctDNA) analysis enable monitoring of resistant subclones specifically, providing early warning of resistance expansion [45].
Step 4: Treatment Modulation - When tumor burden decreases to the target threshold, pause or reduce treatment to allow sensitive cells to recover and suppress resistant populations [44] [46].
Step 5: Treatment Reinitiation - Resume therapy when tumor burden approaches the predetermined upper limit, creating cyclical control of tumor growth [44].
This workflow is visualized in the following diagram:
Clinical Evidence and Trial Data
Adaptive therapy has demonstrated promising results across multiple cancer types in clinical trials. The landmark trial for metastatic castrate-resistant prostate cancer (mCRPC) showed a dramatic improvement in time to progression compared to standard care [44].
Table 2: Clinical Trial Evidence for Adaptive Therapy
| Cancer Type | Trial Identifier | Intervention | Key Findings | Status |
|---|---|---|---|---|
| Metastatic Castrate-Resistant Prostate Cancer | NCT02415621 | Adaptive Abiraterone | Median time to progression: 27-33.5 months (vs 14.3-16.5 months standard care) with 47% drug reduction [44] | Active, not recruiting |
| Ovarian Cancer | NCT05080556 (ACTOv) | Adaptive Carboplatin | Preclinical models showed extended survival; Clinical trial ongoing [1] [46] | Recruiting |
| BRAF Mutant Melanoma | NCT03543969 | Adaptive BRAF-MEK Inhibitors | Preliminary results show feasibility [44] [1] | Active, not recruiting |
| Advanced Basal Cell Carcinoma | NCT05651828 | Adaptive Vismodegib | Testing dose adjustment based on response [44] [1] | Recruiting |
| Rhabdomyosarcoma | NCT04388839 | Multi-drug Evolutionary Therapy | Testing extinction therapy approach [44] [1] | Recruiting |
Experimental Protocols
In Vitro Competition Assays
Purpose: To quantify competitive interactions between drug-sensitive and drug-resistant cancer cell lines under various treatment conditions.
Materials:
- Isogenic drug-sensitive and drug-resistant cancer cell lines
- Complete cell culture media
- Therapeutic agents of interest
- Flow cytometry equipment (for fluorescently tagged cells)
- Cell culture flasks/plates
- Hemocytometer or automated cell counter
Procedure:
- Cell Line Preparation: Establish pure populations of drug-sensitive and drug-resistant cells. For tracking purposes, label with different fluorescent markers (e.g., GFP, RFP).
- Initial Co-culture: Mix cells at varying ratios (e.g., 1:9, 1:1, 9:1 resistant:sensitive) in multiple replicate wells. Use total cell density below carrying capacity.
- Treatment Application: Apply treatment conditions:
- Continuous MTD dosing
- Adaptive cycling (treatment withdrawal at specified response thresholds)
- No treatment control
- Longitudinal Monitoring: Sample and count cell populations every 2-3 days over 2-3 weeks using flow cytometry to determine population proportions.
- Model Calibration: Fit competitive Lotka-Volterra models to data: ( \frac{dS}{dt} = rS S(1 - \frac{S + \alpha{SR} R}{K}) - \deltaS C S ) ( \frac{dR}{dt} = rR R(1 - \frac{R + \alpha{RS} S}{K}) - \deltaR C R ) where ( \alpha ) terms represent competition coefficients [2].
- Parameter Estimation: Calculate growth rates, competition coefficients, and drug sensitivity parameters for each cell type.
Optimal Control Therapy Design
Purpose: To derive optimized adaptive therapy schedules using mathematical optimization techniques constrained by clinical safety limits.
Materials:
- Calibrated mathematical model of cancer dynamics
- Pharmacokinetic parameters for the drug of interest
- Optimization software (MATLAB, Python, R)
- Clinical constraints (maximum drug concentration, maximum tumor burden)
Procedure:
- Formulate Optimal Control Problem: Define the objective function to minimize tumor burden and total drug usage: ( J(x,m) = \lambda \psi(T(tf)) + \int0^{tf} \eta m(t) dt ) where ( \psi(T(tf)) ) represents the terminal tumor burden, ( m(t) ) is drug dosage, and ( \lambda ), ( \eta ) are weight coefficients [47] [48].
- Define Constraints: Establish state constraints: ( 0 \leq c \leq c{max} ) (drug concentration limits) ( T \leq T{max} ) (tumor burden limits) And control constraints: ( 0 \leq m(t) \leq m_{max} )
- Prove Existence of Optimal Control: Verify that an optimal solution exists by checking:
- Apply Pontryagin's Minimum Principle: Derive necessary conditions for optimal control:
- Formulate Hamiltonian function
- Derive adjoint equations
- Determine optimal control characterization
- Numerical Solution: Implement forward-backward sweep algorithm to compute optimal drug schedule.
- Validation: Compare optimized schedule with standard protocols in silico and design clinical translation.
Research Reagent Solutions
Table 3: Essential Research Reagents for Evolutionary Therapy Studies
| Reagent/Cell Line | Function | Application Examples |
|---|---|---|
| Isogenic Drug-Sensitive/-Resistant Cell Pairs | Controlled comparison of competitive dynamics | Prostate cancer (LNCaP/ABR), Breast cancer (MCF-7/ADR) |
| Fluorescent Cell Labeling (GFP, RFP) | Longitudinal tracking of subpopulations | In vitro competition assays, in vivo imaging |
| Circulating Tumor DNA (ctDNA) Assays | Monitoring tumor burden and resistance mutations | Liquid biopsy for adaptive therapy decision-making |
| Patient-Derived Xenograft (PDX) Models | Preclinical testing in physiologically relevant models | Validation of adaptive therapy protocols |
| Mathematical Modeling Software | Simulation and optimization of treatment schedules | MATLAB, R, Python with specialized ODE solvers |
Resistance Mechanisms and Counterstrategies
Non-Genetic Resistance Challenges
While traditional evolutionary models often focus on genetic resistance mechanisms, non-genetic adaptations present particular challenges for adaptive therapy:
Epigenetic Plasticity: Cancer cells can rapidly transition between drug-sensitive and resistant states through epigenetic modifications without genetic mutations. This phenotypic switching can occur at higher rates than genetic mutation, potentially overwhelming the competitive suppression dynamics that adaptive therapy relies upon [45].
Tumor Microenvironment-Mediated Protection: Stromal cells in the tumor microenvironment can provide direct protection to cancer cells against therapeutic agents. Cancer-associated fibroblasts (CAFs) may secrete survival factors or create physical barriers that reduce drug penetration, effectively increasing the resistant population [45].
Drug Efflux Pump Overexpression: The rapid upregulation of ATP-binding cassette (ABC) transporters that pump chemotherapeutic drugs out of cells represents another non-genetic adaptation. Unlike genetically fixed resistance mutations, this phenotype may be transient and inducible by treatment pressure [45].
Extracellular Vesicle-Mediated Resistance Transfer: Resistant cells can export drug efflux pumps and other resistance factors via extracellular vesicles, which are then taken up by sensitive cells, effectively transferring resistance horizontally within the tumor population [45].
The following diagram illustrates these interconnected resistance mechanisms:
Multidrug Adaptive Strategies
To address complex resistance landscapes, researchers are developing multi-drug evolutionary therapies:
Double-Bind Therapy: Uses two therapeutic agents such that resistance to one increases susceptibility to the other. This approach creates an evolutionary trap where any adaptation comes with a fitness cost [44] [45].
Extinction Therapy: Administers multiple drugs in specific sequences to capitalize on collateral sensitivities. The first drug selects for a resistance mutation that increases sensitivity to the second drug, potentially eliminating both sensitive and resistant populations [44] [1].
Bipolar Therapy: Cycles between extreme opposite physiological states (e.g., very low and very high hormone levels) to create unstable selective pressures that prevent adaptation of either sensitive or resistant populations [22].
Adaptive and evolutionary therapy represents a fundamental reconceptualization of cancer treatment that explicitly acknowledges the inevitability of resistance in advanced cancers. By leveraging rather than fighting evolutionary principles, this approach has demonstrated promising results in extending progression-free survival while reducing cumulative drug exposure and toxicity.
The successful implementation of adaptive therapy requires close integration of mathematical modeling, frequent biomarker monitoring, and flexible treatment protocols. Current clinical trials across various cancer types continue to validate this approach and refine its application. Future directions include developing more sophisticated multi-drug strategies, addressing non-genetic resistance mechanisms, and creating clinical infrastructure to support personalized, adaptive treatment workflows.
As the field advances, digital twin technology - creating virtual replicas of individual patient tumors - may enable in silico testing of multiple adaptive therapy strategies before clinical implementation [1] [22]. With continued development, evolutionary therapy approaches have the potential to transform advanced cancer management, focusing on long-term control rather than elusive eradication.
Leveraging Digital Twins and Mechanistic Learning for Improved Predictions
Digital Twins (DTs) represent a transformative paradigm in oncology, enabling the creation of dynamic, virtual representations of physical entities—from individual tumors to whole patients. These models are continuously updated with real-time data, allowing researchers and clinicians to simulate disease progression and treatment responses in a virtual environment [49] [50]. The core value of DTs lies in their capacity for risk-free experimentation, personalized treatment optimization, and enhanced predictive accuracy by integrating multi-scale, multi-modal data with mechanistic mathematical models and artificial intelligence (AI) [50] [51].
The application of DTs in cancer research marks a significant shift from traditional, population-averaged treatment approaches toward truly personalized medicine. By creating patient-specific computational models, DTs facilitate a deeper understanding of complex tumor dynamics and allow for in-silico testing of therapeutic strategies before clinical implementation [52] [53]. This approach is particularly valuable in oncology, where tumor heterogeneity, dynamic microenvironments, and evolving treatment resistance present substantial challenges to successful therapy [1].
Quantitative Foundations: Performance Metrics of Digital Twins in Oncology
Table 1: Documented Performance of Digital Twin Applications in Clinical Oncology
| Cancer Type | Application Area | Key Metric | Reported Performance | Source/Model |
|---|---|---|---|---|
| Triple-Negative Breast Cancer (TNBC) | Predicting Neoadjuvant Chemotherapy Response | Pathological Complete Response (PCR) Prediction | Significantly outperformed traditional tumor volume measurement methods [52] | Model integrating MRI data with biologically-based mathematical models |
| High-Grade Glioma | Radiotherapy Planning | Radiation Dose Reduction | Achieved equivalent tumor control with a 16.7% reduction in radiation dose [50] | Personalized radiotherapy planning model |
| Prostate Cancer | Prognostic Prediction | Biochemical Recurrence Prediction Accuracy | 96.25% accuracy [50] | Machine Learning (ML)-based system |
| Brain Tumors | Tumor Segmentation | Feature Recognition Accuracy | 92.52% accuracy [50] | Hybrid Semi-Supervised Support Vector Machine (S3VM) and improved AlexNet CNN |
| Cardiac Care (as a model for oncology) | Treatment Guidance for Arrhythmia | Recurrence Rate Reduction | Significantly lower recurrence rates (40.9% vs. 54.1%) with virtual testing guidance [50] | Patient-specific cardiac digital twin |
Table 2: Core Mathematical Formulations for Tumor Growth Dynamics
| Model Name | Governing Equation | Key Parameters | Oncology Application Context |
|---|---|---|---|
| Exponential Growth Model | (\frac{dV}{dt} = rV) | (r): Growth rate | Early, unconstrained tumor growth [54] |
| Logistic Growth Model | (\frac{dN}{dt} = rN(1-\frac{N}{K})) | (r): Growth rate; (K): Carrying capacity (max cell population) [2] | Tumor growth incorporating resource limitations [2] [54] |
| Gompertz Model | (\frac{dV}{dt} = rV \times \ln(\frac{K}{V})) | (r): Growth rate; (K): Carrying capacity [2] [54] | Describes growth deceleration as tumor size increases [2] |
| Drug Pharmacodynamics (Hill Equation) | (E = \frac{E{max} \times C^n}{EC{50}^n + C^n}) | (E{max}): Max effect; (EC{50}): Potency; (n): Hill coefficient; (C): Drug concentration [2] | Quantifies effect of a drug at a given concentration [2] |
Experimental Protocols for Digital Twin Development and Validation
Protocol 1: Development of a Patient-Specific GBM Digital Twin for Clinical Counseling
Objective: To create a practical, imaging-informed digital twin of Glioblastoma (GBM) capable of generating a realistic range of tumor progression scenarios over a 2-3 month horizon to aid clinical decision-making and patient counseling [3].
Materials: Pre-processed magnetic resonance imaging (MRI) scans (T1 post-contrast and T2/FLAIR sequences) from patients with recurrent GBM, image processing software (SPM-12, 3D-Slicer), and a computational framework implementing a reaction-diffusion model [3].
Workflow Diagram: GBM Digital Twin Forecasting
Methodological Steps:
Data Acquisition and Preprocessing:
- Obtain axial surveillance MRI scans (T1 plus contrast and T2/FLAIR sequences) from the patient archive [3].
- Convert DICOM files to 3D NIfTI format using SPM-12. Co-register all images to a common time point (typically the first scan in the patient series) [3].
- Use automated algorithms in SPM-12 to strip non-brain tissue (skull, eyes), generating a patient-specific computational domain segmented into cerebrospinal fluid (CSF), white matter, and gray matter [3].
Manual Segmentation and Initial Condition Generation:
- Load co-registered scans into the 3D-Slicer platform. Manually segment tumor voxels into three categories by neuroimaging experts:
- Necrotic core (hypointense on T1).
- Enhancing tumor (contrast enhancement on T1).
- Tumor-associated edema (hyperintense on T2-FLAIR) [3].
- Use these segmentations to generate the initial conditions for the mathematical model.
- Load co-registered scans into the 3D-Slicer platform. Manually segment tumor voxels into three categories by neuroimaging experts:
Model Simulation and Scenario Generation:
- Implement a reaction-diffusion equation (the "ASU-Barrow" model) on the patient-specific computational domain [3].
- Using a systematic parameter sampling design, simulate tumor growth between successive scans multiple times (e.g., 18 times per interval) to generate a range of realistic tumor response scenarios [3].
- The model output is a set of simulated tumor volumes and spatial distributions for the next time interval.
Validation and Accuracy Assessment:
- Compare simulated tumor volumes against subsequently observed clinical scans.
- Quantify accuracy by calculating the percentage of imaging intervals where at least one simulation agreed with the observed tumor volume within 20% (and 10%) [3].
- Assess spatial accuracy using agreement and containment scores, which measure the overlap between predicted and real tumor regions [3].
Protocol 2: Integrating Multi-Modal Data for a Predictive Breast Cancer Digital Twin
Objective: To construct a digital twin for Triple-Negative Breast Cancer (TNBC) that integrates multi-parametric MRI and biologically-based mathematical models to accurately predict the response to Neoadjuvant Systemic Therapy (NAST) [52].
Materials: Multi-parametric MRI data, genomic/proteomic data (if available), a computational platform for integrating imaging data with mechanistic models, and machine learning algorithms for feature extraction and pattern recognition.
Workflow Diagram: Multi-Modal DT Integration
Methodological Steps:
Multi-Source Data Acquisition:
- Collect baseline clinical data from Electronic Health Records (EHR), including patient history, tumor stage, and prior treatments [50].
- Acquire high-resolution multi-parametric MRI scans (e.g., DCE-MRI, DW-MRI) prior to and during the course of NAST [52].
- If feasible, incorporate multi-omics data (genomics, proteomics) to characterize tumor biology and identify potential resistance mechanisms [52].
Data Fusion and Feature Extraction:
- Co-register all imaging data to a common coordinate system.
- Extract quantitative imaging features (radiomics) from the tumor and its microenvironment, which serve as input parameters for the mathematical model [52].
- Integrate clinical and omics data to inform model parameters related to proliferation rates, drug sensitivity, and immune interactions.
Model Calibration and Personalization:
- Initialize a biologically-based mathematical model of tumor growth and treatment response. This model should incorporate key dynamics such as cell proliferation, death, and spatial invasion [52].
- Calibrate the model's patient-specific parameters by fitting its output to the baseline and early-treatment imaging data. This step tailors the generic model to the individual's tumor.
Predictive Simulation and Validation:
- Run the calibrated, patient-specific digital twin forward in time to simulate the response to the full course of the planned NAST.
- The primary output is a prediction of the likelihood of achieving a Pathological Complete Response (PCR) [52].
- Validate model predictions by comparing the simulated end-point (tumor volume, cell viability) with the actual pathological findings from post-treatment surgical specimens.
The Scientist's Toolkit: Essential Research Reagent Solutions
Table 3: Key Reagents and Resources for Digital Twin Research
| Category / Item | Specification / Example | Primary Function in Digital Twin Workflow |
|---|---|---|
| Medical Imaging Data | T1 post-contrast & T2/FLAIR MRI; DCE-MRI; CT | Provides spatial and structural data for model initialization and validation; tracks anatomical changes over time [52] [3]. |
| Clinical & Omics Data | EHR data; Genomic (e.g., WES, RNA-seq); Proteomic data | Informs on tumor biology, patient history, and molecular characteristics for model personalization and mechanism inclusion [52] [50]. |
| Computational Modeling Frameworks | Reaction-Diffusion Equations; Ordinary/Partial Differential Equations (ODEs/PDEs); Agent-Based Models (ABMs) | Forms the core mechanistic engine of the DT, simulating the underlying biological processes of tumor growth and treatment response [2] [3] [54]. |
| AI/ML Libraries & Algorithms | Semi-Supervised Support Vector Machines (S3VM); Convolutional Neural Networks (CNNs); Deep Generative Models | Used for data processing (e.g., image segmentation), feature extraction, model calibration, and generating synthetic virtual patients [50] [51]. |
| High-Per Computing (HPC) | Cloud or local cluster computing resources | Provides the necessary computational power for running complex, multi-scale simulations and performing parameter sampling analyses [49]. |
| Data Integration & Standardization Tools | Common Data Models (e.g., OMOP); Standardized file formats (e.g., NIfTI, DICOM) | Ensures interoperability of diverse data types (clinical, imaging, omics), which is a critical and challenging step in DT construction [52]. |
Implementation Framework: From Models to Clinical Workflows
The translation of digital twins from research tools to clinical decision support systems requires a structured framework. The core of this framework involves a continuous cycle of data assimilation, model updating, and clinical feedback.
Logical Diagram: Clinical DT Implementation Cycle
This implementation framework highlights the bidirectional link between the physical patient and their digital counterpart. As new patient data is acquired through clinical monitoring, the digital twin is continuously updated and refined. This updated model is then used to run simulations, testing various treatment hypotheses in silico to optimize the therapeutic strategy for the individual patient. The resulting recommendation is delivered to the clinician, who applies the therapy, and the patient's response is subsequently monitored, closing the loop and informing the next cycle [49] [50] [51].
A pivotal application of this framework is the enhancement of clinical trials. Digital twins can generate synthetic control arms, reducing the number of patients required for a trial and addressing ethical concerns related to placebo groups. Furthermore, they can help identify optimal patient subgroups and design more efficient, adaptive trial protocols, ultimately accelerating the drug development process [51].
From In Silico to In Vivo: Validating, Comparing, and Translating Models to the Clinic
Validation is a critical gateway for the clinical translation of mathematical models in oncology. It establishes the credibility of model predictions by systematically comparing them against experimental and clinical data [55]. For a model to inform treatment decisions in cancer therapy optimization research, it must demonstrate not only predictive accuracy but also clinical utility and robustness in the face of biological uncertainty [1] [55]. This document outlines standardized protocols and application notes for the validation of mathematical models, framed within a comprehensive research workflow for cancer treatment optimization.
Core Principles of Model Validation
Validation, Verification, and Uncertainty Quantification (VVUQ) form an interconnected framework essential for building trust in predictive models [55]. Within this framework, Verification answers the question "Was the model built correctly?" ensuring the computational implementation accurately solves the intended mathematical equations. Validation addresses "Was the right model built?" by quantifying how well the model's predictions match real-world observational data [55]. Uncertainty Quantification (UQ) is the process of characterizing and propagating uncertainties from model inputs, parameters, and structure to the final predictions, thereby establishing confidence bounds [55].
A model is considered fit-for-purpose if its predictive accuracy for a specific Quantity of Interest (QoI) is sufficient to support a defined clinical or research decision. The required level of accuracy and the choice of validation metrics are intrinsically tied to this purpose [55].
Quantitative Validation Metrics and Data Presentation
The selection of validation metrics should be aligned with the model's intended use, whether for prognosis, treatment response prediction, or treatment optimization. The table below summarizes key quantitative metrics for different data types.
Table 1: Key Quantitative Metrics for Model Validation
| Data Type | Validation Metric | Interpretation | Clinical/Research Context |
|---|---|---|---|
| Binary Outcomes (e.g., 5-year survival) | Area Under the ROC Curve (AUC) | Discriminatory power; 0.5 = random, 1.0 = perfect [56] [57]. | Prognostic stratification for breast cancer [57]. |
| Sensitivity (Recall), Specificity, Precision, F1-Score [56] [57] | Balanced accuracy for imbalanced datasets. | Identifying high-risk Hepatocellular Carcinoma (HCC) patients in chronic hepatitis B cohorts [56]. | |
| Time-to-Event Data (e.g., Survival) | Kaplan-Meier Plotter, Log-rank Test [57] | Comparison of survival distributions between model-stratified groups. | External validation of protein biomarkers in breast cancer [57]. |
| Continuous/Temporal Data (e.g., Tumor Volume) | Brier Score [56] | Overall model performance for probabilistic predictions; lower is better (range 0-1). | Calibration assessment in HCC risk prediction [56]. |
| Root Mean Square Error (RMSE) | Magnitude of average prediction error. | Comparing predicted vs. observed tumor growth dynamics. | |
| Probabilistic Predictions | Calibration Curves (Slope, Intercept) [56] | Agreement between predicted probabilities and observed frequencies. | Assessing reliability of HCC risk probabilities [56]. |
| Clinical Utility | Decision Curve Analysis (DCA) [56] | Net clinical benefit across different probability thresholds. | Evaluating if using the model for clinical decisions (e.g., early intervention) improves outcomes over default strategies [56]. |
Performance benchmarks from recent studies provide context for evaluating new models. For instance, a random forest model predicting HCC risk in patients with chronic hepatitis B achieved an AUC of 0.993 on an internal validation set, with high specificity and sensitivity [56]. In breast cancer survival prediction, a deep learning model integrating proteomic and clinical data achieved an AUC of 0.814, which improved to 0.877 after feature optimization [57]. An autonomous AI agent for clinical decision-making in oncology reached a 91.0% accuracy in concluding correct treatment plans [58].
Table 2: Model Performance Benchmarks from Recent Studies
| Study & Model Type | Primary Validation Metric | Performance | Key Validated Predictors / Tools |
|---|---|---|---|
| HCC Risk Prediction (Random Forest) [56] | AUC (Internal Validation) | 0.993 | Age, basophil/lymphocyte ratio, D-Dimer, AST/ALT, GGT, Alpha-fetoprotein |
| Breast Cancer 5-Year Survival (Deep Neural Network) [57] | AUC (Test Set) | 0.814 (0.877 with top 13 features) | Tumor size, HER2 status, lymph node status, 9 protein biomarkers (e.g., EGFR, MPHOSPH10) |
| Autonomous Oncology AI Agent [58] | Clinical Decision Accuracy | 91.0% | Integrated use of vision transformers, MedSAM, OncoKB, PubMed/Google search |
Experimental Protocols for Key Validation Experiments
Protocol 1: Validation of a Predictive Risk Model Using Retrospective Clinical Data
This protocol outlines the steps for validating a machine learning model designed to predict cancer risk or survival outcomes, as exemplified by HCC and breast cancer risk models [56] [57].
1. Hypothesis and Objectives:
- Primary Objective: To validate the model's ability to accurately discriminate between patients who will develop a specific cancer (or outcome) within a defined period and those who will not.
- Null Hypothesis (H0): The model's AUC is ≤ 0.70.
2. Experimental Design and Data Collection:
- Study Design: Retrospective cohort study.
- Data Source: Institutional electronic health records or curated cancer registries (e.g., The Cancer Genome Atlas).
- Population: Define clear inclusion/exclusion criteria. Example: Patients with chronic hepatitis B, with and without a subsequent HCC diagnosis [56].
- Data Split: Randomly split the dataset into a training set (e.g., 70%) and a hold-out validation set (e.g., 30%). Ensure stratification by the outcome variable to maintain class distribution [56].
3. Materials and Reagent Solutions: Table 3: Research Reagent Solutions for Clinical Data Validation
| Item / Solution | Function in Validation | Example / Specification |
|---|---|---|
| Clinical Data Warehouse | Source of real-world patient data for model training and testing. | OMOP Common Data Model database; institutional EHR system [59]. |
| Standardized Vocabularies | Ensures clinical terms are consistently mapped for accurate feature extraction. | OMOP-standardized vocabularies (e.g., SNOMED CT, ICD-10, RxNorm) [59]. |
| Python/R Statistical Environment | Platform for statistical analysis and metric calculation. | Python with scikit-learn, pandas, lifelines; R with survival, pROC, rmda. |
| SHAP (SHapley Additive exPlanations) | Provides post-hoc interpretability, explaining the contribution of each feature to individual predictions [56] [57]. | Python shap library. |
4. Step-by-Step Procedure: 1. Preprocessing: Clean and preprocess the hold-out validation set using the same procedures (e.g., imputation, scaling) derived from the training set. 2. Prediction: Run the pre-trained model on the hold-out validation set to generate predictions (e.g., probabilities or class labels). 3. Calculation of Metrics: * Generate the ROC curve and calculate the AUC with a 95% confidence interval (e.g., via bootstrapping with 2000 replicates) [56]. * Calculate sensitivity, specificity, precision, and F1-score at the pre-defined classification threshold. * Generate a calibration plot and calculate the Brier score. 4. Clinical Utility Assessment: Perform Decision Curve Analysis to evaluate the net benefit of using the model for clinical decision-making across a range of probability thresholds [56]. 5. Interpretability Analysis: Apply SHAP analysis on the validation set to confirm the feature importance ranking aligns with biological and clinical knowledge [56] [57].
5. Data Analysis: * Compare the model's performance against established clinical benchmarks or existing models. * Report 95% confidence intervals for all performance metrics.
Protocol 2: Validation of a Digital Twin or Mechanistic Model
This protocol is for validating mechanistic models (e.g., based on ODEs/PDEs) that simulate tumor growth and treatment response, often as part of a "digital twin" framework [1] [55] [54].
1. Hypothesis and Objectives:
- Primary Objective: To validate that the model-predicted tumor dynamics (size, volume, biomarker levels) fall within the uncertainty bounds of the observed clinical or preclinical data.
2. Experimental Design and Data Collection:
- Data Source: Longitudinal patient data from clinical trials or cohort studies; preclinical data from animal models.
- QoI: Clearly define the QoI for validation, such as tumor volume at a specific time post-treatment, time to progression, or minimum lymphocyte count during therapy.
- Uncertainty Quantification: Identify and quantify key sources of uncertainty (e.g., parameter uncertainty, measurement noise in data).
3. Materials and Reagent Solutions: Table 4: Research Reagent Solutions for Mechanistic Model Validation
| Item / Solution | Function in Validation | Example / Specification |
|---|---|---|
| Tumor Growth & Treatment Model | The core mathematical model to be validated. | Logistic/Gompertz growth model combined with PK/PD equations for drug effect [2] [54]. |
| Parameter Estimation Toolbox | Software for calibrating model parameters to individual or cohort data. | MATLAB fmincon, Python scipy.optimize, or Bayesian calibration tools (e.g., PyMC3, Stan). |
| Uncertainty Quantification (UQ) Library | Quantifies and propagates uncertainties to generate prediction intervals. | ChaosPy, UQLab, or custom Monte Carlo sampling scripts. |
| Clinical Imaging Data | Provides longitudinal, spatially-resolved data for model validation. | Serial CT or MRI scans from a cohort of patients undergoing treatment [54]. |
4. Step-by-Step Procedure: 1. Model Calibration: Calibrate the model parameters using a subset of the available longitudinal data (e.g., the first few data points for each subject). 2. Prediction and UQ: * Using the calibrated model, predict the future time course of the QoI. * Perform UQ to generate a prediction interval (e.g., 95% credible interval) around the model predictions, accounting for parameter and structural uncertainties. 3. Validation: Compare the subsequent, unseen observational data points against the model's prediction interval. 4. Metric Calculation: Calculate the Prediction Interval Coverage Probability (PICP), which is the proportion of observed data points that fall within the model's prediction interval. A well-calibrated model will have a PICP close to the nominal coverage rate (e.g., 95%).
5. Data Analysis: * Visually present the validation using a time-series plot showing the model's median prediction, the prediction interval, and the observed data. * A successful validation is achieved if a pre-specified proportion (e.g., >90%) of the observed validation data points lie within the 95% prediction interval.
Visualization of Validation Workflows
The following diagrams, generated using Graphviz, illustrate the logical flow of the two primary validation protocols described above.
Diagram 1: Clinical Risk Model Validation Workflow.
Diagram 2: Digital Twin Predictive Validation Workflow.
Integration into a Broader Research Workflow
Model validation is not the final step but an integral part of an iterative research workflow for cancer treatment optimization. A validated model should be seen as a dynamic entity. In the context of digital twins, validation is a continuous process where the model is updated with new patient data, requiring periodic re-validation to maintain its credibility [55]. Furthermore, validated models can be deployed within clinical decision support systems, where their predictions, accompanied by uncertainty estimates, can assist oncologists in personalizing treatment schedules, such as in adaptive therapy trials for prostate cancer and melanoma [1]. This closes the loop on the modeling workflow, from development and validation to clinical application and continuous improvement.
In the field of mathematical oncology, the reliability of predictive models is paramount for translating computational insights into effective clinical strategies. Benchmarking provides a standardized framework for evaluating model performance, ensuring that predictions regarding tumor growth, treatment response, and resistance mechanisms are both accurate and clinically actionable. This process involves rigorous assessment of two core capabilities: spatial accuracy, which measures a model's ability to correctly identify and localize biologically significant regions within complex tissue data, and predictive power, which quantifies its proficiency in forecasting clinical outcomes such as treatment response and patient survival. The integration of these evaluated models into research workflows enables more robust optimization of cancer treatment regimens, moving beyond the traditional "maximum tolerated dose" paradigm toward more adaptive, personalized therapeutic strategies [1].
The following protocols provide a detailed methodology for establishing a comprehensive benchmarking pipeline, enabling researchers to quantitatively compare model performance, identify strengths and limitations, and select the most appropriate tools for specific applications in cancer treatment optimization.
Established Benchmarking Frameworks and Performance Metrics
Core Benchmark Categories
The landscape of AI model evaluation has evolved to include specialized benchmarks that assess distinct capabilities relevant to computational oncology. The table below summarizes key benchmark categories and their primary applications in cancer research [60].
Table 1: Core AI Benchmark Categories Relevant to Mathematical Oncology
| Category | Representative Benchmarks | Oncology Research Applications |
|---|---|---|
| Reasoning & General Intelligence | MMLU, GPQA, BIG-Bench, ARC | Interpretation of complex clinical literature, hypothesis generation |
| Coding & Software Development | HumanEval, MBPP, SWE-Bench | Development of simulation code, implementation of mathematical models |
| Web-Based & Agent Tasks | WebArena, AgentBench, Mind2Web | Automated data retrieval from medical databases, multi-step analysis |
| Language Understanding | HELM, Chatbot Arena, MT-Bench | Clinical note analysis, patient communication, instruction following |
| Safety & Robustness | TruthfulQA, AdvBench, SafetyBench | Ensuring model reliability, reducing harmful outputs in clinical settings |
Performance Metrics for Predictive Models
Quantitative evaluation of predictive models requires multiple metrics to provide a comprehensive view of performance. The following table outlines key metrics and their interpretations in clinical contexts [61].
Table 2: Key Performance Metrics for Predictive Model Evaluation
| Metric | Definition | Clinical Interpretation |
|---|---|---|
| AUC (Area Under ROC Curve) | Measures overall discriminative ability between classes | Probability that a random positive case ranks higher than a random negative case |
| AUPRC (Area Under Precision-Recall Curve) | Evaluates precision-recall trade-off | Particularly important for imbalanced datasets common in medical applications |
| C-index | Assesses predictive accuracy for survival data | Concordance between predicted and observed survival ordering |
| F1 Score | Harmonic mean of precision and recall | Balanced measure of model accuracy considering both false positives and false negatives |
| Calibration | Agreement between predicted probabilities and actual outcomes | Critical for risk stratification and clinical decision-making |
Experimental Protocols for Model Benchmarking
Protocol 1: Benchmarking Spatial Quantification in Digital Pathology
Objective: To evaluate model performance in spatially accurate identification and quantification of tumor regions in whole-slide images (WSIs).
Background: Spatial quantification is essential for guiding pathologists to areas of clinical interest and discovering tissue phenotypes behind novel biomarkers. Traditional multiple-instance learning (MIL) approaches often lose spatial awareness in favor of whole-slide prediction performance [62].
Materials:
- Whole-slide images (3,850 WSIs across 6 cancer types recommended)
- Computational pathology framework (SMMILe recommended)
- Two encoder types: ImageNet-pretrained (ResNet-50) and pathology-specific foundation model (Conch)
- Benchmark datasets: Camelyon16 (breast), TCGA-LU (lung), TCGA-RCC (renal), UBC-OCEAN (ovarian), TCGA-STAD (gastric), SICAPv2 (prostate)
Procedure:
- Slide Preprocessing: Partition WSIs into non-overlapping patches and extract feature embeddings using both encoders.
- Model Training: Implement SMMILe framework comprising:
- Convolutional layer for enhancing local receptive fields of instance embeddings
- Multi-stream instance detector to identify significance of each instance for different categories
- Instance classifier to assign embeddings to respective categories
- Consistency constraint, parameter-free instance dropout, and delocalized instance sampling modules
- Spatial Quantification: Apply Markov Random Field (MRF)-based instance refinement to improve localization accuracy.
- Performance Evaluation: Compare against baseline methods (CLAM, DSMIL, TransMIL, DTFD-MIL) using macro AUC scores across binary, multiclass, and multilabel classification tasks.
- Statistical Analysis: Calculate mean and variance of performance metrics across fivefold cross-validation.
Expected Outcomes: SMMILe has demonstrated superior spatial quantification while maintaining WSI classification performance, achieving AUC scores of 94.11% (Ovarian), 90.92% (Prostate), and 92.75% (Gastric Endoscopy) with ImageNet-pretrained encoders [62].
Protocol 2: Evaluating Predictive Power for Clinical Outcomes
Objective: To assess model accuracy in predicting clinically relevant endpoints such as progression-free survival (PFS) and early death risk.
Background: Predictive power for clinical outcomes enables better patient stratification and treatment planning. Foundation models pre-trained on diverse datasets can extract meaningful biomarkers from complex medical images [63].
Materials:
- Pathology slides from The Cancer Genome Atlas (TCGA)
- Foundation models for comparison (H-optimus-1, UNI2, CTranspath/Chief, Virchow)
- Genomic data (RNA-seq) for multimodal integration
- Machine learning models (XGBoost, Logistic Regression) for outcome prediction
Procedure:
- Data Preparation: Curate baseline tumor pathology slides with associated clinical outcomes (PFS, overall survival).
- Feature Extraction: Process slides through each foundation model to generate embeddings (feature-rich representations).
- Model Development: Train survival prediction models as an overlay of these embeddings using consistent methodology across all foundation models.
- Multimodal Integration: Fuse best-performing visual features with genomic data (RNA-seq) to enhance predictive power.
- Performance Assessment: Evaluate using:
- C-index for overall survival prediction accuracy
- Time-dependent AUC at 6, 12, and 18 months for near-term predictions
- Calibration curves to assess probability accuracy
- External Validation: Validate promising models on independent datasets from different healthcare settings.
Expected Outcomes: In benchmark studies, H-optimus-1 achieved C-index of 0.75-0.76 and time-dependent AUCs approaching 0.8 for PFS prediction, outperforming other foundation models. Integration with genomic data further enhanced predictive power [63].
Protocol 3: Comparing Feature Reduction Methods in Radiomics
Objective: To systematically evaluate feature projection versus feature selection methods for predictive performance in radiomics.
Background: Most radiomic studies use feature selection methods to preserve interpretability, but the assumption that radiomic features are inherently interpretable is increasingly challenged [61].
Materials:
- 50 binary classification radiomic datasets from CT and MRI
- Feature projection methods (PCA, Kernel PCA, NMF, UMAP, SRP)
- Feature selection methods (MRMRe, ET, Boruta, LASSO)
- Classifiers (logistic regression, random forests, SVMs)
Procedure:
- Data Preparation: Extract morphological, intensity, and textural features from radiological images.
- Feature Reduction: Apply both projection and selection methods to reduce feature dimensionality:
- Projection methods: Generate new features by recombining originals (PCA, NMF)
- Selection methods: Identify and retain most predictive features (LASSO, Boruta)
- Model Training: Implement nested, stratified 5-fold cross-validation with 10 repeats for each method-classifier combination.
- Performance Evaluation: Calculate AUC, AUPRC, F1, F0.5, and F2 scores for each model.
- Statistical Analysis: Use Friedman test with Nemenyi post-hoc analysis to identify significant performance differences.
- Computational Efficiency: Record execution times for each method across different feature set sizes.
Expected Outcomes: Feature selection methods (ET, LASSO, Boruta) generally achieve highest performance, but top projection methods (NMF) can outperform selection on individual datasets. Average differences between approaches are statistically insignificant, supporting consideration of both methodological families [61].
Table 3: Key Research Reagents and Computational Tools for Model Benchmarking
| Tool/Resource | Type | Function | Application Example |
|---|---|---|---|
| SMMILe Framework | Computational Algorithm | Superpatch-based multiple-instance learning for spatial quantification | Accurate tumor region identification in whole-slide images [62] |
| H-optimus-1 | Foundation Model | Pathology image analysis and feature extraction | Predicting progression-free survival from histology slides [63] |
| Conch Encoder | Foundation Model | Self-supervised feature extraction from pathology images | Generating patch embeddings for WSI classification [62] |
| TCGA Datasets | Data Resource | Curated cancer genomics and histology data | Training and validating predictive models [63] |
| Feature Selection (LASSO, Boruta) | Computational Method | Identifying most predictive features while reducing dimensionality | Improving model interpretability and performance in radiomics [61] |
| Feature Projection (NMF, PCA) | Computational Method | Creating efficient feature combinations while preserving information | Handling highly correlated radiomic features [61] |
| Digital Twin Framework | Modeling Approach | Personalized computational tumor models | Informing treatment scheduling and predicting therapeutic response [1] |
Analysis and Interpretation of Benchmarking Results
Key Performance Patterns Across Modalities
Benchmarking studies reveal consistent patterns in model performance across different data modalities. In digital pathology, spatial quantification benefits significantly from instance-based MIL approaches like SMMILe, which overcome the limitations of representation-based methods that often lose spatial awareness while achieving high whole-slide classification accuracy [62]. For clinical outcome prediction, foundation models pre-trained on diverse datasets (e.g., H-optimus-1's training on 1 million slides from 800,000 patients) demonstrate superior generalizability, particularly when integrated with multimodal data such as genomic profiles [63]. In radiomics, the choice between feature projection and selection methods involves trade-offs between interpretability and predictive power, with selection methods generally performing better but projection approaches occasionally achieving superior results on specific datasets [61].
Implementation Considerations for Treatment Optimization
Integrating benchmarked models into mathematical oncology workflows requires careful consideration of several factors. Computational efficiency varies significantly between methods, with selection approaches like LASSO providing excellent performance with minimal computational overhead, while methods like Boruta offer superior performance at the cost of increased processing time [61]. Clinical translation depends on rigorous external validation, as many promising models fail to maintain performance across diverse healthcare settings [64]. Finally, regulatory considerations must be addressed early, with standardization and interpretability concerns potentially favoring more transparent modeling approaches despite slightly reduced predictive performance in some cases [1].
The benchmarking frameworks and protocols outlined provide a foundation for rigorous evaluation of spatial accuracy and predictive power in mathematical oncology. By implementing these standardized assessments, researchers can systematically identify optimal modeling approaches for specific cancer treatment optimization challenges, ultimately accelerating the translation of computational insights into clinically actionable therapeutic strategies.
Mathematical modeling has become an indispensable tool in the quest to understand cancer dynamics and optimize treatment strategies. The complex, multi-faceted nature of cancer—spanning genetic, molecular, cellular, tissue, and organism-level scales—demands sophisticated modeling frameworks that can capture its inherent nonlinearities and heterogeneities [65]. This document provides a comprehensive analysis of the two primary dichotomies in cancer modeling: deterministic versus stochastic and single-scale versus multi-scale approaches. Within the broader workflow of cancer treatment optimization research, selecting an appropriate modeling framework is paramount, as it directly influences the predictive power, clinical relevance, and translational potential of the research findings. Deterministic models, which produce precise, repeatable outputs for a given set of inputs, offer simplicity and computational efficiency [66] [67]. In contrast, stochastic models incorporate randomness and uncertainty, providing a distribution of possible outcomes that often better reflects the biological reality of cancer progression and treatment response [66] [68]. Similarly, while single-scale models focus on a specific biological level, multi-scale models aim to integrate processes across genetic, molecular, cellular, and tissue levels, providing a more holistic view of cancer as a complex system [69] [70] [71]. This application note details the theoretical foundations, practical applications, and experimental protocols for these modeling paradigms, providing researchers with a structured framework for their implementation in cancer treatment optimization.
Theoretical Foundations and Comparative Analysis
Deterministic vs. Stochastic Models
Deterministic models operate on the principle that a system's future state is entirely determined by its current state and a set of fixed rules, without any involvement of randomness [66] [67]. These models are often based on differential equations that describe the average behavior of a system, assuming that all variables are known and can be measured accurately.
Stochastic models, conversely, explicitly incorporate randomness and probability distributions [66] [67]. They are built on the premise that future states have an inherent element of uncertainty, and thus, the same set of initial conditions can lead to an ensemble of different outputs. This is particularly valuable for modeling biological systems where random events, such as genetic mutations or molecular collisions, play a critical role [68].
Table 1: Comparative Analysis of Deterministic and Stochastic Modeling Approaches
| Feature | Deterministic Models | Stochastic Models |
|---|---|---|
| Core Principle | No randomness; output is precisely determined from input parameters [66]. | Inherent randomness; same inputs produce a distribution of outputs [66]. |
| Typical Mathematical Framework | Ordinary Differential Equations (ODEs), Partial Differential Equations (PDEs) [69] [68]. | Chemical Master Equation (CME), Agent-Based Models (ABM), Stochastic Differential Equations [69] [68]. |
| Handling of Uncertainty | Does not account for uncertainty, potentially leading to oversimplification [66] [67]. | Explicitly incorporates uncertainty, providing a range of possible outcomes and their likelihoods [66] [67]. |
| Data Requirements | Lower data requirements, suitable for limited data availability [67]. | Requires more extensive data to characterize probability distributions [67]. |
| Computational Cost | Generally lower computational cost [67]. | Higher computational cost, often requiring Monte Carlo simulations [66]. |
| Interpretability | Straightforward cause-and-effect interpretation [66] [67]. | More complex interpretation requiring statistical knowledge [67]. |
| Ideal Use Case | Systems with well-understood dynamics and high copy numbers of components [68]. | Systems with low copy numbers, significant noise, or emergent behaviors [68]. |
Single-Scale vs. Multi-Scale Models
Single-scale models focus on a specific biological level, such as molecular signaling pathways or tissue-level tumor growth. They simplify reality by holding processes at other scales constant or representing them with static parameters.
Multi-scale models aim to bridge these biological hierarchies, linking phenomena from genetic mutations to tissue-level morphology and patient-level outcomes [69] [71]. These models are essential for understanding how a perturbation at one scale (e.g., a targeted drug blocking a molecular pathway) manifests at other scales (e.g., tumor shrinkage at the tissue level).
Table 2: Biological Scales in Multi-Scale Cancer Modeling
| Spatial Scale | Length Scale | Time Scale | Key Processes | Common Modeling Techniques |
|---|---|---|---|---|
| Atomic | nm | ns | Protein/lipid structure and dynamics [69]. | Molecular Dynamics (MD) [69]. |
| Molecular | nm - μm | μs - s | Cell signaling, biochemical reactions [69]. | ODEs, reaction-rate equations [69]. |
| Microscopic (Cellular/Tissue) | μm - mm | min - hour | Cell proliferation, death, migration; cell-cell interactions [69]. | Agent-Based Models (ABM), PDEs [69]. |
| Macroscopic | mm - cm | day - year | Gross tumor behavior, vascularization, invasion [69]. | PDEs, continuum models [69]. |
Application in Cancer Treatment Workflow
Workflow Integration Diagram
The following diagram illustrates the logical workflow for integrating these modeling approaches into cancer treatment optimization research, from initial data acquisition to clinical decision support.
Protocol 1: Developing a Stochastic Multi-Scale Model of Tumor Response to Therapy
Objective: To create an integrated model that predicts tumor shrinkage and emergence of drug resistance by linking molecular-scale drug-target interactions to cellular-scale population dynamics.
Materials and Reagents:
- In silico environment: Computational software (e.g., MATLAB, Python with SciPy, COPASI)
- Biological data: Pharmacokinetic (PK) parameters for the drug, initial tumor size, historical data on mutation rates
- Calibration data: Longitudinal tumor volume measurements from pre-clinical models or patient scans
Procedure:
- Define Model Scales and Linkages:
- Molecular Scale: Model the drug concentration in plasma and tumor tissue using a PK ODE:
dC/dt = -k * C, whereCis concentration andkis the elimination rate constant [2]. - Cellular Scale: Implement an Agent-Based Model (ABM) where each agent represents a cancer cell. Assign to each agent a state (sensitive or resistant) based on a stochastic mutation probability.
- Molecular Scale: Model the drug concentration in plasma and tumor tissue using a PK ODE:
Formulate the Stochastic Rule Set:
- For each cell in the ABM at each time step:
- Calculate the probability of cell death using a pharmacodynamic function like the Hill equation:
E = (Emax * C^n) / (EC50^n + C^n), whereEis effect,Emaxis max effect,EC50is half-maximal concentration, andnis the Hill coefficient [2]. - Generate a uniform random number between 0 and 1. If the number is less than the calculated death probability, remove the cell.
- For surviving sensitive cells, check if a resistance mutation occurs by comparing another random number to a fixed mutation rate per cell division.
- Calculate the probability of cell death using a pharmacodynamic function like the Hill equation:
- For each cell in the ABM at each time step:
Model Calibration and Validation:
- Calibrate unknown parameters (e.g.,
EC50, mutation rate) by running the model multiple times and using optimization algorithms (e.g., particle swarm, genetic algorithms) to minimize the difference between simulated tumor volumes and experimental/clinical data [1]. - Validate the calibrated model by comparing its predictions to a separate, held-out dataset not used for calibration.
- Calibrate unknown parameters (e.g.,
Simulate Treatment and Analyze Output:
- Run the calibrated model multiple times (Monte Carlo simulations) to generate a distribution of possible outcomes (e.g., tumor volume over time, time to progression).
- Analyze the ensemble output to estimate the probability of treatment success and the likelihood of resistance emergence under different dosing schedules [66] [1].
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Computational Tools and Resources for Cancer Modeling
| Item | Function/Description | Example Uses in Protocols |
|---|---|---|
| ODE/PDE Solvers | Software libraries for numerically solving systems of differential equations. | Simulating drug PK and tissue-level nutrient diffusion [69] [2]. |
| Stochastic Simulation Algorithm (SSA) | Exact algorithm for simulating chemical reactions described by the CME [68]. | Implementing molecular-scale stochastic reactions in Protocol 1. |
| Agent-Based Modeling Platforms | Software frameworks (e.g., CompuCell3D, NetLogo) for creating rule-based, multi-agent systems. | Modeling individual cell behaviors and interactions in a tumor microenvironment [69] [70]. |
| Model Calibration & Optimization Tools | Algorithms and software for parameter estimation and model fitting. | Calibrating unknown biological parameters to experimental data in Protocol 1, Step 3 [1]. |
| Bioinformatics Databases | Public repositories (e.g., PubChem, ChemSpider) for chemical and drug data [71]. | Sourcing parameters for drug structures and properties during model initialization. |
| High-Per Computing (HPC) Cluster | Parallel computing resources for running ensembles of complex stochastic simulations. | Executing thousands of Monte Carlo runs for stochastic models in a feasible time [66]. |
Protocol 2: Implementing Deterministic Bifurcation Analysis for Treatment Strategy Identification
Objective: To use a deterministic ODE model to identify potential combination therapy strategies by analyzing the bistability of a core signaling pathway involved in cancer cell survival.
Materials and Reagents:
- In silico environment: Bifurcation analysis software (e.g., XPP/Auto, MATCONT, PyDSTool)
- Pathway data: Known reaction network and published kinetic parameters for the pathway of interest
Procedure:
- Model Formulation:
- Construct a system of ODEs based on the law of mass action to represent the key components and reactions of the signaling pathway (e.g., a feedback loop involving a survival signal and an inhibitor) [68].
Bifurcation Analysis:
- Designate a clinically actionable parameter (e.g., the dosage of a targeted therapy inhibiting a key node in the pathway) as the bifurcation parameter.
- Use numerical continuation software to trace the steady-states of the ODE system as the bifurcation parameter is varied.
- Identify critical points (bifurcations), such as saddle-node bifurcations, where the number of stable steady states changes.
Strategy Identification:
- The bifurcation diagram will reveal parameter ranges where the system is monostable (a single cell fate) or bistable (two possible cell fates, e.g., survival and death).
- The analysis may suggest that a high-dose monotherapy is required to push the system into the desired state. Alternatively, it may reveal that a lower dose of a primary drug, combined with a second drug targeting a different node, can more effectively steer the system toward the desired outcome (e.g., cell death) [68].
Experimental Validation:
- The predicted combination strategy must be validated in vitro or in vivo to confirm its efficacy in shifting the cellular phenotype as forecasted by the model.
Model Interaction Dynamics Diagram
The following diagram conceptualizes the interaction between different model types and biological scales within a multi-scale framework for a targeted therapy study.
The choice between deterministic and stochastic, single-scale and multi-scale modeling approaches is not a matter of selecting a universally superior option, but rather of aligning the modeling framework with the specific research question and the available data within the cancer treatment optimization workflow. Deterministic models offer computational efficiency and clarity for well-characterized systems, while stochastic models are indispensable for capturing the randomness inherent in biological systems, especially when dealing with low copy numbers or predicting the probability of rare events like resistance emergence [66] [67] [68]. Similarly, single-scale models provide a focused, tractable analysis of a specific level of organization, whereas multi-scale models are essential for understanding the emergent behaviors that arise from the complex interplay between genetic, molecular, cellular, and tissue-level processes [69] [71]. As the field of mathematical oncology advances, the most powerful strategies will likely involve the judicious integration of these approaches, leveraging their respective strengths to generate robust, clinically actionable insights that can ultimately improve patient outcomes. The protocols and tools outlined herein provide a foundation for researchers to implement these sophisticated modeling techniques in their own work.
The field of mathematical oncology has traditionally relied on mechanistic models—mathematical representations built on established biological first principles—to understand and predict cancer dynamics [1]. While these models offer valuable interpretability and are grounded in biological theory, they often struggle with the sheer complexity and heterogeneity of clinical data [1]. Conversely, purely data-driven artificial intelligence (AI) models, particularly deep learning, excel at identifying complex patterns from large-scale datasets such as medical images and genomics but typically operate as "black boxes" with limited explanatory power [72] [73]. Hybrid mechanistic-data-driven models represent a transformative approach that integrates these two paradigms. By combining the interpretability and physiological grounding of mechanistic models with the predictive power and pattern recognition capabilities of AI, these hybrid frameworks aim to create more robust, reliable, and clinically actionable tools for cancer treatment optimization [1] [22].
Core Applications in Cancer Treatment Optimization
Hybrid models are being deployed across the cancer research and care continuum to address complex clinical challenges. The table below summarizes their primary applications, technical approaches, and documented outcomes.
Table 1: Key Applications of Hybrid Models in Oncology
| Application Area | Hybrid Approach | Mechanistic Component | AI/Data-Driven Component | Reported Outcome/Evidence |
|---|---|---|---|---|
| Radiotherapy Personalization | Predicting spatio-temporal tumor growth and response to alternative radiotherapy schedules [22]. | Physiological models of tumor growth and radiation dose-response [1]. | Generative computer vision and deep learning on longitudinal medical imaging (e.g., MRI, CT) [22]. | Creates counterfactual simulations for biology-adaptive treatment strategies [22]. |
| Evolutionary Therapy Scheduling | Informing clinical trial design and patient selection for adaptive therapy [1] [22]. | Spatial stochastic models and Ordinary Differential Equations (ODEs) capturing tumor-immune interactions and competition between sensitive/resistant cells [1] [22]. | Calibration and validation using fluorescent time-lapse microscopy data and confocal imaging of tumor spheroids [22]. | Models predict adaptive therapy can control tumor burden with less toxicity than maximum tolerated dose (MTD) [1]. Clinical trials ongoing (e.g., NCT03543969, NCT05080556) [1]. |
| Drug Discovery & Target Identification | Accelerating the identification of druggable targets and optimizing lead compounds [72]. | Protein-protein interaction networks and pathway analyses [72]. | Machine learning on multi-omics data (genomics, transcriptomics); deep generative models for de novo molecular design [72]. | AI-designed molecules reaching clinical trials in record time (e.g., 12-18 months vs. 4-5 years) [72]. |
| Digital Twins & Virtual Patients | Creating patient-specific computational models for virtual treatment testing [1] [22]. | Physiologically-based pharmacokinetic (PBPK) and multiscale agent-based models simulating tumor environment and drug delivery [22]. | Integration of patient-specific data from imaging, clinical records, and molecular profiling [22]. | Pre-clinical in vitro testing in EGFR+ non-small cell lung cancer demonstrates feasibility for guiding treatment scheduling [22]. |
Experimental Protocols for Hybrid Model Development
This section provides a detailed, actionable protocol for developing and validating a hybrid model, using principles of "mechanistic learning" [22].
Protocol: Developing a Hybrid Model for Predicting Radiotherapy Response
Objective: To create a hybrid model that integrates a mechanistic tumor growth model with a deep learning network to predict individual patient response to different radiotherapy schedules from longitudinal MRI data.
Materials & Reagents: Table 2: Essential Research Reagent Solutions and Computational Tools
| Item/Category | Specific Examples / Formats | Function / Application in Hybrid Modeling |
|---|---|---|
| Clinical & Imaging Data | Longitudinal MRI/CT scans (DICOM format), Electronic Health Records (EHRs), Genomic profiles [74] [73]. | Provides real-world, patient-specific data for model training, calibration, and validation. Essential for personalization. |
| Computational Frameworks | Python (Libraries: TensorFlow, PyTorch, SciPy), R, High-Performance Computing (HPC) clusters [1]. | Core programming environments for implementing both mechanistic equations and deep learning architectures. |
| Mechanistic Model Templates | Ordinary Differential Equations (ODEs) for population dynamics, Partial Differential Equations (PDEs) for spatial growth, Agent-Based Models (ABMs) [1]. | Provides the foundational, biology-grounded structure that constrains and informs the AI component. |
| AI Architectures | Convolutional Neural Networks (CNNs), Recurrent Neural Networks (RNNs), Physics-Informed Neural Networks (PINNs) [74] [73] [22]. | Used to extract features from complex data (images, sequences) and to learn residual patterns not captured by the mechanistic model. |
Methodology:
Data Curation and Preprocessing:
- Data Collection: Assemble a dataset of longitudinal MRI scans (pre-, during, and post-radiotherapy) with corresponding clinical outcomes (e.g., tumor volume reduction, progression-free survival) [73].
- Image Standardization: Normalize image intensities and co-register all serial scans to a common coordinate system to ensure spatial consistency.
- Tumor Segmentation: Manually or semi-automatically contour the tumor volume on each scan to generate ground truth data for training. This can be achieved using AI tools like CNNs [74].
Mechanistic Model Implementation:
- Model Selection: Implement a reaction-diffusion model, a type of PDE, to represent the spatio-temporal growth of the glioblastoma and its response to radiation [22]. The core equation can be simplified as:
∂u/∂t = ∇ • (D ∇u) + Ï u (1 - u/K) - R(t, d) uwhereu(x,t)is tumor cell density,Dis the diffusion coefficient,Ïis the proliferation rate,Kis the carrying capacity, andR(t,d)is the radiation-induced cell kill term dependent on time and dose. - Parameter Estimation: Use non-linear least squares optimization or Markov Chain Monte Carlo (MCMC) methods to fit the initial model parameters (
D,Ï) to the pre-treatment imaging data for each patient [1].
- Model Selection: Implement a reaction-diffusion model, a type of PDE, to represent the spatio-temporal growth of the glioblastoma and its response to radiation [22]. The core equation can be simplified as:
AI Integration and Hybridization:
- Architecture Design: Build a Convolutional Neural Network (CNN) that takes the initial MRI and the simulated output from the mechanistic model as a two-channel input.
- Training Objective: Train the CNN to predict the subsequent, follow-up MRI scan. The network learns the "residual" or the difference between the simplistic mechanistic prediction and the complex real-world outcome, effectively correcting for factors the base model misses (e.g., microenvironmental effects, hypoxia) [22].
- Implementation: This can be framed as an image-to-image translation task using a U-Net architecture.
Model Validation and In Silico Trial:
- Hold-Out Validation: Test the trained hybrid model on a withheld test set of patient data. Quantify performance using metrics like Dice similarity coefficient between predicted and actual tumor volumes and root-mean-square error (RMSE).
- Counterfactual Simulation: For a new patient, use the calibrated model to simulate "what-if" scenarios by altering the radiotherapy schedule (dose, timing) in the mechanistic component and observing the AI-corrected prediction [22]. This aids in personalized planning.
The following diagram illustrates the core workflow and data flow of this hybrid integration.
Protocol: Implementing an Adaptive Therapy Schedule Based on Eco-Evolutionary Dynamics
Objective: To use a hybrid model, calibrated to real-time patient data, to guide an adaptive therapy schedule that manages tumor burden by exploiting competitive interactions between drug-sensitive and resistant cells.
Methodology:
Model Initialization:
- Employ a system of ODEs, a classic mechanistic approach, to represent the population dynamics of sensitive (
S) and resistant (R) cancer cells under drug pressure [1] [22]:dS/dt = Ï_S * S * (1 - (S+R)/K) - β * D(t) * SdR/dt = Ï_R * R * (1 - (S+R)/K) - Here,
Ïrepresents growth rates,Kthe carrying capacity,βthe drug efficacy, andD(t)the drug dose over time.
- Employ a system of ODEs, a classic mechanistic approach, to represent the population dynamics of sensitive (
Data Assimilation for Personalization:
- Calibrate the initial model parameters (
Ï_S,Ï_R,K) to baseline patient-specific data, which can include circulating tumor DNA (ctDNA) levels or tumor volume measurements from imaging [72]. - Update the model in near-real-time by assimilating new ctDNA or imaging data obtained during treatment, adjusting parameters to reflect the current tumor state.
- Calibrate the initial model parameters (
Treatment Optimization:
- The hybrid system uses the calibrated model to simulate multiple future treatment scenarios. The AI component can be used to rapidly optimize the high-dimensional parameter space (dose, timing) to find schedules that meet a specific objective.
- The primary objective is not necessarily to eradicate the tumor but to maintain a stable population of sensitive cells that suppress the growth of resistant cells. Treatment is applied only when the total tumor burden exceeds a pre-defined threshold, and is withheld otherwise [1].
Clinical Validation:
- This approach is currently being validated in several early-phase clinical trials for cancers including prostate cancer, melanoma, and ovarian cancer (e.g., NCT03543969, NCT05080556) [1].
The logical flow of this adaptive, model-informed therapy is depicted below.
Quantitative Performance and Clinical Translation
The efficacy of hybrid models is demonstrated through improved predictive performance and their successful integration into early-phase clinical trials. The table below summarizes key quantitative benchmarks and ongoing translational efforts.
Table 3: Performance Metrics and Clinical Translation of Hybrid Models
| Model / Trial Focus | Data Type & Volume | Key Performance Metric | Reported Result | Clinical Trial Context / Stage |
|---|---|---|---|---|
| AI-Enhanced Cancer Screening (e.g., CRCNet) [74] | Colonoscopy images (464,105 from 12,179+ patients). | Sensitivity for malignancy detection. | AI: 91.3% vs. Human: 83.8% (p<0.001) in one test set [74]. | Retrospective multicohort diagnostic study with external validation [74]. |
| AI for Mammography Detection [74] | 25,856 women (UK) and 3,097 women (US). | Area Under the Curve (AUC). | AUC: 0.889 (UK) and 0.8107 (US) [74]. | Diagnostic case-control study showing non-inferiority/ superiority to radiologists [74]. |
| Mathematical Model-Adapted Radiation [1] | N/A (Model-driven trial). | Feasibility and Safety. | Phase 1 trial (NCT03557372) completed with 14 patients, establishing feasibility and safety [1]. | Early-phase trial demonstrating translation of model-guided RT dose painting. |
| Adaptive Therapy Trials [1] | N/A (Model-driven trials). | Tumor Control & Reduced Toxicity. | Multiple Phase 1/2 trials recruiting or active (e.g., for prostate cancer, melanoma, ovarian cancer) [1]. | Direct translation of evolutionary models into clinical practice, moving beyond MTD. |
The paradigm of cancer drug development is undergoing a fundamental shift, moving away from the historical maximum tolerated dose (MTD) approach towards a more nuanced model-informed framework that seeks to optimize the benefit-risk ratio for patients [42] [1]. This transition is driven by the recognition that the traditional "3+3" dose-escalation design, developed for cytotoxic chemotherapies, is often poorly suited for modern targeted therapies and immunotherapies, frequently resulting in suboptimal dosing and unnecessary toxicity [42]. Consequently, nearly 50% of patients in late-stage trials of small molecule targeted therapies require dose reductions, and the U.S. Food and Drug Administration (FDA) has mandated additional dosing studies for over 50% of recently approved cancer drugs [42]. In response, mathematical modeling has emerged as a powerful tool to inform dose selection, optimize treatment regimens, and navigate evolving regulatory pathways, ultimately advancing the goal of personalized cancer therapy.
Recent Model-Informed Clinical Trials: A Quantitative Review
Recent years have witnessed a surge in clinical trials that integrate mathematical modeling directly into therapeutic decision-making. These trials span various cancer types and therapeutic modalities, demonstrating the versatile application of models in clinical settings. The table below summarizes key prospective clinical trials based on mathematical oncology approaches.
Table 1: Recent Model-Informed Clinical Trials in Oncology
| Model Type | Trial ID/Name | Cancer Type | Intervention | Primary Outcomes |
|---|---|---|---|---|
| Norton-Simon | NCT02595320 (X7-7) [1] | Metastatic Breast & GI Cancers | Capecitabine | Reduced toxicity ✓ |
| Dynamics-based Radiotherapy | NCT03557372 [1] | Glioblastoma | Model-Adapted Radiation | Feasibility and Safety ✓ |
| Evolution-based (Adaptive Therapy) | NCT02415621 [1] | mCRPC | Adaptive Abiraterone | Active, not recruiting |
| Evolution-based (Adaptive Therapy) | NCT05393791 (ANZadapt) [1] | mCRPC | Adaptive vs. Continuous Abiraterone/Enzalutamide | Recruiting |
| Evolution-based (Extinction Therapy) | NCT04388839 [1] | Rhabdomyosarcoma | Evolutionary Therapy | Recruiting |
| Fully Personalized Treatment | NCT04343365 (Evolutionary Tumor Board) [1] | Various Cancers | Observational | Recruiting |
Exemplary Experimental Protocols
Protocol 1: Implementing Adaptive Therapy for mCRPC
- Objective: To evaluate whether adaptive dosing of Abiraterone or Enzalutamide, guided by PSA levels, can extend time to disease progression compared to continuous dosing in metastatic castration-resistant prostate cancer (mCRPC) [1].
- Methodology:
- Patient Population: Patients with mCRPC scheduled for treatment with Abiraterone or Enzalutamide.
- Randomization: Participants are randomized to either continuous dosing (control) or adaptive therapy (intervention).
- Adaptive Dosing Algorithm: The intervention arm follows a pre-defined protocol where treatment is suspended once a ≥50% decline in PSA from baseline is confirmed. Treatment is re-initiated only when PSA returns to its baseline value.
- Monitoring: PSA levels are measured regularly (e.g., every 4 weeks) to guide treatment decisions.
- Primary Endpoint: Time to radiographic or clinical progression.
- Model Integration: This trial design operationalizes an evolutionary model of cancer, aiming to suppress the growth of treatment-resistant cells by maintaining a population of treatment-sensitive cells that compete for resources.
Protocol 2: Model-Informed Precision Dosing for Busulfan
- Objective: To achieve target drug exposure and improve clinical outcomes using model-informed precision dosing (MIPD) of busulfan in a conditioning regimen for hematopoietic stem cell transplantation [75].
- Methodology:
- Initial Dosing: Patients receive an initial dose of intravenous busulfan based on body weight or a population pharmacokinetic (PK) model.
- Blood Sampling: Intensive PK blood sampling is performed after the first dose (e.g., at pre-dose, 5, 30, 60, 120, 180, and 300 minutes post-infusion).
- Bayesian Forecasting: The measured busulfan concentrations are fed into a validated PK model using Bayesian forecasting software. This individualizes the model parameters (e.g., clearance, volume of distribution) for the specific patient.
- Dose Adjustment: The individualized model is used to predict the dose required to achieve the target area under the concentration-time curve (AUC). The subsequent doses are adjusted accordingly.
- Therapeutic Drug Monitoring (TDM): PK verification may be repeated to ensure the target exposure is maintained.
- Model Integration: A population PK model of busulfan, often incorporating covariates like body weight and age, serves as the prior for Bayesian estimation. This approach directly links drug exposure to efficacy and toxicity outcomes, allowing for personalized dose optimization [75].
The Regulatory Landscape for Model-Informed Drug Development
Regulatory agencies are actively promoting reforms to encourage better dose optimization and the integration of quantitative methods in oncology drug development.
FDA's Project Optimus and Dose Optimization Guidance
Project Optimus is an FDA initiative aimed at reforming oncology dose selection and optimization to maximize both safety and efficacy [42]. It encourages sponsors to:
- Use novel trial designs and mathematical modeling to select doses for first-in-human (FIH) trials [42].
- Directly compare multiple dosages in trials designed to assess antitumor activity, safety, and tolerability [42].
- Utilize a fit-for-purpose approach, tailoring each drug development program to the specific drug and patient population [42]. The FDA has finalized guidance stating that sponsors should justify the recommended dosage with evidence from such comparative trials [42].
Expedited Regulatory Pathways
While not exclusively for model-informed drugs, expedited pathways are frequently used for innovative oncology therapies. The following table summarizes these key pathways.
Table 2: Key FDA Expedited Regulatory Pathways in Oncology
| Pathway | Purpose | Key Feature | Prevalence in Oncology |
|---|---|---|---|
| Priority Review | Accelerate application review | Review in 6 months (vs. 10 months standard) | 57% of novel therapeutics approved in 2020 [76] |
| Fast Track | Expedite clinical testing and review | Allows approval based on a single Phase 2 study for serious conditions [76] | 33% of novel therapeutics approved in 2020 [76] |
| Breakthrough Therapy | Intensive guidance on efficient drug development | More FDA resources and oversight during development [76] | 45% of novel therapeutics approved in 2020 [76] |
| Accelerated Approval | Approve drugs for serious conditions based on surrogate endpoints | Approval based on effect on surrogate endpoint (e.g., progression-free survival); requires confirmatory trials [76] | 25% of novel therapeutics approved in 2020 [76] |
Note: Drugs approved via expedited pathways have a higher rate of post-market safety-related label changes, underscoring the importance of post-market surveillance and confirmatory trials [76].
Drug Development Tool (DDT) Qualification Program
The FDA's DDT Qualification Program provides a formal mechanism to qualify tools—including biomarkers and clinical outcome assessments—for a specific Context of Use (COU) in drug development [77]. Once qualified, a DDT can be used by any drug sponsor in their development program without needing further re-justification to the FDA, streamlining the regulatory process for model-informed approaches that rely on these validated tools [77].
Integrated Workflow for Clinical Translation
The successful translation of a mathematical model from a research concept to a tool that impacts clinical care requires a structured workflow. The following diagram illustrates the key stages and decision points in this process, integrating both scientific and regulatory considerations.
Diagram 1: Integrated Workflow for Translating Mathematical Models from Research to Clinical Practice. This workflow highlights the iterative process of model development, calibration, and regulatory engagement necessary for successful clinical implementation.
Successfully implementing the workflows and protocols described requires a suite of specialized tools and resources.
Table 3: Essential Research Reagent Solutions for Model-Informed Drug Development
| Category | Item/Solution | Function in Research & Development |
|---|---|---|
| Preclinical Models | Patient-Derived Xenografts (PDXs) & Genetically Engineered Mouse Models (GEMMs) | Provide physiologically relevant systems for calibrating mathematical models of tumor growth and treatment response before human trials [1]. |
| Biomarker Assays | Circulating Tumor DNA (ctDNA) Analysis | Serves as a quantitative, dynamic biomarker for measuring tumor burden and early treatment response, crucial for calibrating and validating models [42]. |
| Computational Tools | Pharmacokinetic/Pharmacodynamic (PK/PD) Modeling Software (e.g., NONMEM, Monolix) | Used to build mathematical models describing drug concentration-time relationships (PK) and their resulting effects (PD) [2] [75]. |
| Computational Tools | Quantitative Systems Pharmacology (QSP) Platforms | Allows for the development of large-scale models that incorporate disease pathophysiology, drug mechanisms, and network dynamics to simulate clinical outcomes [42]. |
| Clinical Data Standards | Clinical Data Interchange Standards Consortium (CDISC) Data Structures | Standardized data formats (e.g., SDTM, ADaM) are essential for pooling data from multiple sources to build robust population models and for regulatory submissions. |
The integration of mathematical modeling into oncology drug development represents a cornerstone of the shift towards more precise and effective cancer care. The growing number of model-informed clinical trials, coupled with supportive regulatory initiatives like Project Optimus, provides a clear roadmap for researchers. By adopting the structured workflows, detailed experimental protocols, and strategic regulatory engagement outlined in this review, scientists and drug developers can significantly enhance the efficiency of the drug development process and, most importantly, improve therapeutic outcomes for patients. The future of oncology treatment lies in leveraging these sophisticated quantitative tools to move beyond the one-size-fits-all paradigm and truly personalize cancer therapy.
Conclusion
The workflow for mathematical modeling in cancer treatment optimization represents a powerful, iterative process that transforms biological understanding into quantitative, testable frameworks. By moving from foundational principles through rigorous methodological construction, troubleshooting, and validation, these models provide indispensable tools for overcoming the limitations of the traditional maximum tolerated dose paradigm. The future of the field lies in tighter integration with clinical workflows through virtual clinical trials and digital twins, improved personalization via multi-scale data integration, and the continued development of hybrid models that combine mechanistic understanding with the power of artificial intelligence. As more models successfully inform clinical trials and treatment protocols, mathematical oncology is poised to fundamentally improve therapeutic strategies and patient outcomes by making cancer treatment a more predictive, rather than reactive, science.
References
- 1. Mathematical Oncology: How Modeling Is Transforming ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12614879/]
- 2. Mathematical Modelling of Cancer Treatments, Resistance, ... [https://www.mdpi.com/2673-9909/5/2/40]
- 3. Mathematical modeling for glioblastoma treatment [https://www.frontiersin.org/journals/oncology/articles/10.3389/fonc.2025.1647144/full]
- 4. Quantitative Framework for Bench-to-Bedside Cancer ... [https://www.mdpi.com/2072-6694/14/21/5254]
- 5. Decoding tumor angiogenesis: pathways, mechanisms ... [https://biomarkerres.biomedcentral.com/articles/10.1186/s40364-025-00779-x]
- 6. Endothelial cell in tumor angiogenesis: Origins, mechanisms ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12357263/]
- 7. Hybrid model of tumor growth, angiogenesis and immune ... [https://www.nature.com/articles/s44341-024-00002-2]
- 8. Emerging Strategies for Targeting Angiogenesis and the ... [https://www.mdpi.com/1424-8247/18/8/1160]
- 9. how mathematical models inform treatment schedules for cancer [https://pmc.ncbi.nlm.nih.gov/articles/PMC9117454/]
- 10. Mathematical modeling framework enhances clinical trial ... [https://www.nature.com/articles/s41598-024-80768-6]
- 11. Mathematical Models of Tumor Cell Proliferation [https://pmc.ncbi.nlm.nih.gov/articles/PMC6295418/]
- 12. Mathematical Models for Tumor Growth and the Reduction ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6365230/]
- 13. Gompertz function [https://en.wikipedia.org/wiki/Gompertz_function]
- 14. Population modeling of tumor growth curves and the reduced ... [https://journals.plos.org/ploscompbiol/article?id=10.1371/journal.pcbi.1007178]
- 15. Population modeling of tumor growth curves and the ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7059968/]
- 16. Mathematical Models [https://read.houstonmethodist.org/mathematical-models]
- 17. Drug resistance in cancer: molecular mechanisms and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12623568/]
- 18. Modeling tumor dynamics and predicting response to ... [https://www.nature.com/articles/s41540-025-00593-z]
- 19. The Comparison of Methods Experiment [https://www.westgard.com/lessons/basic-method-validation/lesson23.html]
- 20. Digital twin for personalized medicine development - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC12369496/]
- 21. Digital Twins for Personalized Medicine Require ... [https://www.jmir.org/2025/1/e72411]
- 22. MathOnco25 Conference [https://mathematical-oncology.org/mathonco25]
- 23. Quantitative cancer-immunity cycle modeling for predicting ... [https://www.nature.com/articles/s41540-025-00513-1]
- 24. Cancer statistics, 2025 - PMC - PubMed Central - NIH [https://pmc.ncbi.nlm.nih.gov/articles/PMC11745215/]
- 25. Mathematical models and computational approaches in CAR ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12354594/]
- 26. Anatomically informed deep learning framework for ... [https://www.nature.com/articles/s41598-025-23781-7]
- 27. Ordinary differential equation model of cancer-associated ... [https://www.nature.com/articles/s41540-025-00578-y]
- 28. A stochastic modelling framework for cancer patient ... [https://link.springer.com/article/10.1007/s00285-025-02229-6]
- 29. Agent-Based Modeling of Virtual Tumors Reveals the ... [https://pubmed.ncbi.nlm.nih.gov/39272799/]
- 30. Optimizing fractional mathematical frameworks for cancer ... [https://www.sciencedirect.com/science/article/abs/pii/S0960077925001705]
- 31. Stochastic modeling and first-passage-time analysis of ... [https://www.nature.com/articles/s41598-025-95475-z]
- 32. Stochastic modeling and first-passage-time analysis of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12041559/]
- 33. Mathematical models and computational approaches in ... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2025.1581210/full]
- 34. Mathematical Diagrams [https://www.conceptdraw.com/How-To-Guide/mathematical-diagrams]
- 35. Optimizing dose-schedule regimens with bayesian adaptive ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10701540/]
- 36. Mathematical modeling for glioblastoma treatment: scenario ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12515658/]
- 37. Individualizing glioma radiotherapy planning by ... [https://www.nature.com/articles/s41467-025-60366-4]
- 38. Improving Glioblastoma Radiotherapy Target Delineation ... [https://www.sciencedirect.com/science/article/pii/S0360301625028196]
- 39. EHR Workflow Analysis: Complete 2025 Guide [https://arkenea.com/blog/ehr-workflow-analysis/]
- 40. Advancing Cancer Drug Development with Mechanistic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11795844/]
- 41. Estimating treatment sensitivity in synthetic and in vitro ... [https://www.nature.com/articles/s41540-025-00530-0]
- 42. Key Considerations for Improving Dosage Optimization in ... [https://www.aacr.org/blog/2025/10/03/key-considerations-for-improving-dosage-optimization-in-oncology/]
- 43. Anti-cancer treatment schedule optimization based on ... [https://www.nature.com/articles/s41598-022-08012-7]
- 44. Bringing evolutionary cancer therapy to the clinic [https://www.nature.com/articles/s41540-025-00528-8]
- 45. Adaptive cancer therapy: can non-genetic factors become ... [https://www.nature.com/articles/s41388-025-03582-y]
- 46. Adaptive therapy shows promise in fighting drug-resistant ... [https://www.anticancerfund.org/en/news/adaptive-therapy-shows-promise-fighting-drug-resistant-cancer]
- 47. Optimal adaptive cancer therapy based on evolutionary game ... [https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0320677]
- 48. Optimal adaptive cancer therapy based on evolutionary ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12017572/]
- 49. Exploring the Potential of Digital Twins in Cancer Treatment [https://pmc.ncbi.nlm.nih.gov/articles/PMC12111985/]
- 50. Digital twins in healthcare: a comprehensive review and ... [https://www.frontiersin.org/articles/10.3389/fdgth.2025.1633539]
- 51. Enhancing randomized clinical trials with digital twins [https://www.nature.com/articles/s41540-025-00592-0]
- 52. From virtual to reality: innovative practices of digital twins in ... [https://translational-medicine.biomedcentral.com/articles/10.1186/s12967-025-06371-z]
- 53. Digital twins: a new paradigm in oncology in the era of big ... [https://www.sciencedirect.com/science/article/pii/S2949820124000341]
- 54. Mathematical modeling in radiotherapy for cancer [https://ro-journal.biomedcentral.com/articles/10.1186/s13014-025-02626-7]
- 55. Survey and perspective on verification, validation, and ... [https://www.nature.com/articles/s41746-025-01447-y]
- 56. Development and validation of an interpretable machine ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11899164/]
- 57. An interpretable machine learning model for predicting 5†... [https://www.eurekalert.org/news-releases/1106354]
- 58. Development and validation of an autonomous artificial ... [https://www.nature.com/articles/s43018-025-00991-6]
- 59. Large Language Models for Automating Clinical Trial Criteria ... [https://medinform.jmir.org/2025/1/e71252]
- 60. Top 50 AI Model Benchmarks & Evaluation Metrics (2025 Guide) [https://o-mega.ai/articles/top-50-ai-model-evals-full-list-of-benchmarks-october-2025]
- 61. Benchmarking feature projection methods in radiomics [https://www.nature.com/articles/s41598-025-16070-w]
- 62. SMMILe enables accurate spatial quantification in digital ... [https://www.nature.com/articles/s43018-025-01060-8]
- 63. MIT partners with Bioptimus for Clinical Cancer Prediction ... [https://www.bioptimus.com/case-studies/mit-partners-with-bioptimus-for-clinical-cancer-prediction-study]
- 64. Predictive models for immune checkpoint inhibitor ... [https://www.sciencedirect.com/science/article/pii/S1040842825003683]
- 65. Integrating Mathematical Models in Clinical Oncology [https://www.scientificarchives.com/article/integrating-mathematical-models-in-clinical-oncology-enhancing-therapeutic-strategies]
- 66. Stochastic vs Deterministic Models: Understand the Pros and ... [https://blog.ev.uk/stochastic-vs-deterministic-models-understand-the-pros-and-cons]
- 67. Deterministic vs Stochastic - Machine Learning ... [https://www.analyticsvidhya.com/blog/2023/12/deterministic-vs-stochastic/]
- 68. A Comparison of Deterministic and Stochastic Modeling ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5005346/]
- 69. Multiscale Cancer Modeling - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC3883359/]
- 70. Multiscale computational models of cancer [https://www.sciencedirect.com/science/article/abs/pii/S2468451119300662]
- 71. Multi-scale Modeling in Clinical Oncology - PubMed Central [https://pmc.ncbi.nlm.nih.gov/articles/PMC4983505/]
- 72. Artificial Intelligence in Cancer Drug Discovery in 2025 [https://oncodaily.com/oncolibrary/artificial-intelligence-in-cancer-drug-discovery]
- 73. Current AI technologies in cancer diagnostics and treatment [https://molecular-cancer.biomedcentral.com/articles/10.1186/s12943-025-02369-9]
- 74. Artificial intelligence in cancer: applications, challenges, and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12574039/]
- 75. Model-Informed Dose Optimization in Oncology [https://pubmed.ncbi.nlm.nih.gov/39939511/]
- 76. FDA Regulatory Pathways for Expedited Drug Development ... [https://www.hematologyandoncology.net/archives/september-2025/fda-regulatory-pathways-for-expedited-drug-development-and-approval/]
- 77. Drug Development Tool (DDT) Qualification Programs [https://www.fda.gov/drugs/development-approval-process-drugs/drug-development-tool-ddt-qualification-programs]