A Comprehensive Guide to Pharmacophore-Based Virtual Screening for Neurodegenerative Disease Targets
This article provides a comprehensive overview of pharmacophore-based virtual screening (PBVS) protocols specifically tailored for neurodegenerative disease (NDD) targets.
A Comprehensive Guide to Pharmacophore-Based Virtual Screening for Neurodegenerative Disease Targets
Abstract
This article provides a comprehensive overview of pharmacophore-based virtual screening (PBVS) protocols specifically tailored for neurodegenerative disease (NDD) targets. Aimed at researchers, scientists, and drug development professionals, it covers the foundational principles of key NDD targets like phosphorylated tau and BACE1, details step-by-step methodological workflows for virtual screening, and addresses critical troubleshooting aspects such as Blood-Brain Barrier (BBB) permeability. Furthermore, it explores validation strategies and comparative analyses with other screening methods, offering a holistic and practical guide for integrating PBVS into the early-stage drug discovery pipeline for conditions like Alzheimer's and Huntington's disease.
Understanding Neurodegenerative Disease Targets and the Pharmacophore Concept
The Urgent Need for Alternative Therapeutic Strategies in Neurodegeneration
Neurodegenerative diseases (NDDs), such as Alzheimer's disease (AD) and Parkinson's disease (PD), represent a growing global health crisis, characterized by the progressive loss of neuronal structure and function [1] [2]. With an aging worldwide population, the prevalence of these conditions is rapidly increasing, posing significant challenges to healthcare systems and society at large [3]. The complex, multifactorial pathogenesis of NDDs—involving multiple interconnected pathological pathways—has rendered traditional single-target therapeutic approaches largely ineffective [2] [4]. This document outlines application notes and detailed protocols for implementing pharmacophore-based virtual screening (PBVS), a powerful computational approach that addresses the urgent need for novel therapeutic strategies by enabling the efficient identification of multi-target directed ligands (MTDLs) for NDD treatment.
The Complex Pathophysiology of Neurodegenerative Diseases
The development of effective treatments for NDDs has been hampered by their intricate pathophysiology, which involves several simultaneous aberrant biological processes rather than a single causative factor.
Key Pathological Mechanisms and Targets
Table 1: Major Therapeutic Targets in Neurodegenerative Disease Pathogenesis
| Target Protein | Pathological Role | Associated Disease Hallmarks |
|---|---|---|
| GSK-3β (Glycogen synthase kinase-3 beta) | Hyperactivation promotes tau hyperphosphorylation and neurofibrillary tangle formation; enhances BACE1 activity [5]. | Neurofibrillary tangles, synaptic dysfunction, neuroinflammation [2] [5]. |
| BACE-1 (Beta-secretase 1) | Key enzyme in amyloidogenic processing of APP, leading to amyloid-beta plaque formation [6]. | Amyloid plaques, synaptic toxicity, neuronal death [2] [6]. |
| NMDA Receptor (N-methyl-D-aspartate receptor) | Overactivation leads to excitotoxicity, calcium influx, and neuronal death [2]. | Excitotoxicity, synaptic dysfunction, cognitive decline [2]. |
| AChE (Acetylcholinesterase) | Enzyme that breaks down acetylcholine; its inhibition is a current symptomatic therapy [3]. | Cholinergic deficit, memory impairment, cognitive dysfunction [3]. |
The blood-brain barrier (BBB) presents a further critical challenge, as it selectively restricts over 98% of small molecules from entering the central nervous system (CNS) from the bloodstream [1]. Therefore, effective neurotherapeutics must not only engage their molecular targets but also possess inherent physicochemical properties that enable BBB permeation [1].
Pharmacophore-Based Virtual Screening: A Rational Approach
Pharmacophore-based virtual screening has emerged as a pivotal computational strategy in modern drug discovery, particularly for addressing multi-factorial diseases like NDDs [7] [8]. A pharmacophore is defined by the International Union of Pure and Applied Chemistry (IUPAC) as "the ensemble of steric and electronic features that is necessary to ensure the optimal supra-molecular interactions with a specific biological target structure and to trigger (or to block) its biological response" [7] [8]. In practice, a pharmacophore model abstracts the essential chemical functionalities of a bioactive molecule into a 3D arrangement of generalized features [9]. These features include:
- Hydrogen Bond Acceptors (HBA) and Donors (HBD)
- Hydrophobic areas (H)
- Positively and Negatively Ionizable groups (PI/NI)
- Aromatic rings (AR)
- Exclusion Volumes (XVOL) representing steric constraints of the binding pocket [7] [9]
Comparative Advantages of PBVS
Table 2: Comparison of Virtual Screening Methodologies for Neurodegenerative Drug Discovery
| Characteristic | Pharmacophore-Based VS (PBVS) | Docking-Based VS (DBVS) |
|---|---|---|
| Fundamental Basis | Matches compounds against an ensemble of essential interaction features [7] [9]. | Fits and scores compounds within a 3D protein binding site [10]. |
| Computational Speed | Generally faster, suitable for ultra-large library screening [10]. | Slower due to conformational sampling and scoring for each compound [10]. |
| Scaffold Hopping Potential | High, as it focuses on features rather than specific atoms [7] [8]. | Lower, often biased toward known ligand chemotypes. |
| Performance | Higher enrichment factors reported in benchmark studies (14 of 16 targets) [10]. | Lower hit rates in direct comparisons [10]. |
| Data Requirements | Can work with ligand structures alone or protein-ligand complexes [7] [9]. | Requires a high-quality 3D protein structure. |
| Typical Hit Rates | 5% to 40% in prospective screening campaigns [8]. | Often below 1% in high-throughput screening [8]. |
Integrated Protocol for Pharmacophore-Based Virtual Screening
The following section provides a detailed, actionable protocol for implementing PBVS in the context of neurodegenerative disease drug discovery.
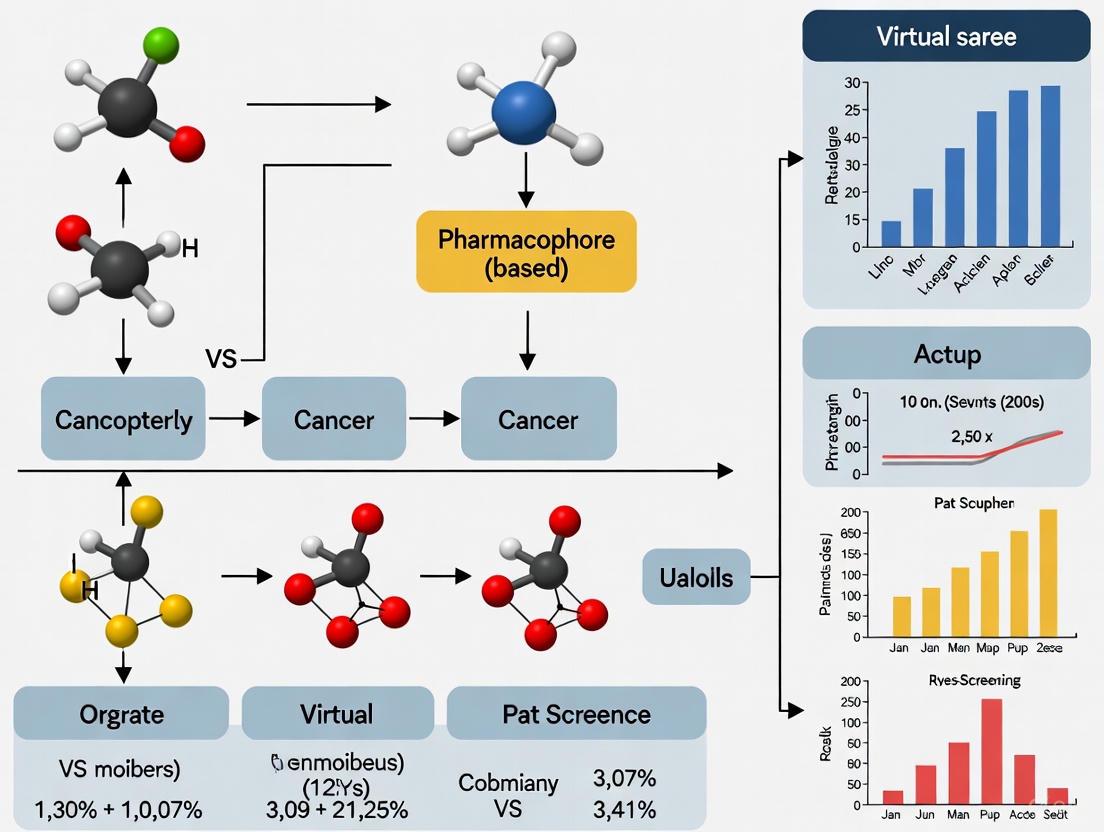
The diagram below illustrates the comprehensive workflow for a PBVS campaign, integrating both ligand-based and structure-based approaches.
Protocol 1: Structure-Based Pharmacophore Modeling
This protocol is applicable when a three-dimensional structure of the target protein (e.g., from X-ray crystallography or homology modeling) is available [7].
Step 1: Protein Structure Preparation
- Retrieve the 3D structure of your target protein from the Protein Data Bank (PDB: www.rcsb.org) [7]. For neurodegenerative targets, relevant structures may include GSK-3β (e.g., PDB ID: 1I09), BACE-1 (e.g., PDB ID: 5HU0 [6]), or NMDA receptor complexes.
- Prepare the protein structure using molecular modeling software (e.g., Maestro [6] or Discovery Studio [8]):
- Add hydrogen atoms and correct protonation states of residues at physiological pH (7.4).
- Assign partial charges using appropriate force fields (e.g., OPLS_2005 [6]).
- Remove crystallographic water molecules unless they mediate key ligand interactions.
- Repair missing side chains or loops if necessary.
Step 2: Binding Site Characterization
- Define the ligand-binding site using one of these approaches:
- For BACE-1, the catalytic aspartic acid residues (Asp93, Asp289 [6]) are essential for defining the active site.
Step 3: Pharmacophore Feature Generation
- Extract pharmacophore features directly from protein-ligand interactions if a co-crystal structure exists [9] [8].
- Alternatively, generate features based on the binding site topology alone using programs like Discovery Studio [8] or LigandScout [10].
- Select only the most crucial features for biological activity to create a selective yet not overly restrictive hypothesis [7]. For example, a BACE-1 inhibitor pharmacophore might require features that interact with the catalytic aspartate dyad.
Step 4: Model Refinement and Validation
- Incorporate exclusion volumes (XVols) to represent the steric boundaries of the binding pocket and improve model selectivity [8].
- Validate the model by screening a test database containing known active compounds and decoys (inactive molecules with similar physicochemical properties) [8].
- Calculate quality metrics such as the Enrichment Factor (EF), Area Under the Curve of the Receiver Operating Characteristic plot (ROC-AUC), and Goodness of Hit Score (GH) to assess model performance [8].
Protocol 2: Ligand-Based Pharmacophore Modeling
This approach is used when structural information for the target protein is limited or unavailable, but a set of known active ligands is accessible [9].
Step 1: Training Set Compilation
- Curate a structurally diverse set of confirmed active molecules against your target. For neurodegenerative diseases, this might include known GSK-3β inhibitors from BindingDB [5] or AChE inhibitors from ChEMBL [8].
- Include molecules with a range of activities (e.g., IC50 values from nM to μM) to help identify features correlating with potency.
- Ensure all activity data comes from direct, target-based assays (e.g., enzyme inhibition) rather than cell-based assays, which can be confounded by pharmacokinetic effects [8].
Step 2: Conformational Analysis and Molecular Alignment
- Generate a representative set of low-energy conformers for each active molecule using algorithms such as the Poling algorithm [9] or Monte Carlo methods.
- Perform 3D structural alignment to identify common chemical features and their spatial arrangements shared by the active molecules. Software tools like Catalyst (now in Discovery Studio) or Phase can automate this process [10].
Step 3: Hypothesis Generation and Selection
- Identify conserved pharmacophore features (HBA, HBD, hydrophobic, aromatic, ionizable) across the aligned active molecules.
- Generate multiple pharmacophore hypotheses and select the best model based on its ability to:
- Retrieve known active compounds from a validation database.
- Exclude known inactive molecules or decoys.
- Correlate with quantitative structure-activity relationship (QSAR) data if available [9].
Protocol 3: Virtual Screening and Hit Identification
Step 1: Database Preparation
- Select a compound library for screening (e.g., ZINC, PubChem, Natural Product libraries [2], or in-house collections).
- Prepare the database by generating multiple conformers for each compound and filtering for drug-like properties using Lipinski's Rule of Five [2] [5]. For CNS targets, apply additional filters for BBB permeability using tools like SwissADME [1].
- For neurodegenerative diseases, prioritize libraries containing natural products or fungal metabolites, which have shown promising neuroprotective properties [1] [2].
Step 2: Pharmacophore-Based Screening
- Screen the prepared database against your validated pharmacophore model using programs such as Pharmit [1] [9], LigandScout [10], or Phase [6].
- Use the phase screen score (a combination of volume score, RMSD, and site matching) to rank hits; a common threshold is a phase score >1.9 [6].
- For multi-target drug discovery, screen the same compound library against pharmacophore models for different NDD targets (e.g., GSK-3β, BACE-1, and NMDA receptor) to identify potential MTDLs [2].
Step 3: Post-Screening Analysis and Experimental Prioritization
- Subject the top-ranking virtual hits to molecular docking studies against all target structures to refine binding pose predictions and estimate binding affinities [2] [6].
- Perform ADMET (Absorption, Distribution, Metabolism, Excretion, Toxicity) profiling using tools like QikProp [6] or ADMETlab 2.0 [6] to eliminate compounds with unfavorable pharmacokinetic or toxicity profiles.
- Select a final list of candidate compounds (typically 10-20) for experimental validation through in vitro assays.
Table 3: Key Research Reagent Solutions for PBVS in Neurodegenerative Disease Research
| Resource Category | Specific Tools & Databases | Function and Application |
|---|---|---|
| Protein Structure Resources | RCSB Protein Data Bank (PDB) [7], AlphaFold2 [7] | Source of experimental and predicted 3D protein structures for structure-based pharmacophore modeling. |
| Compound Libraries | ZINC15 [1], PubChem [2], ChEMBL [8], DrugBank [8], Natural Product libraries [2] | Collections of small molecules for virtual screening; source of potential hit compounds. |
| Pharmacophore Modeling Software | LigandScout [9] [10], Discovery Studio [9] [8], MOE [9], Phase [6] | Platforms for creating, visualizing, and validating pharmacophore models using both structure-based and ligand-based approaches. |
| Virtual Screening Servers | Pharmit [1] [9], PharmMapper [9] | Web-based tools for performing rapid pharmacophore-based screening of compound databases. |
| Validation & Decoy Sets | DUD-E (Directory of Useful Decoys, Enhanced) [8] [5] | Provides carefully selected decoy molecules to assess the selectivity and performance of pharmacophore models. |
| ADMET Prediction Tools | QikProp [6], SwissADME [6], ADMETlab 2.0 [6] | Predict pharmacokinetic properties, drug-likeness, and potential toxicity of virtual hits. |
Case Study: Successful Application in Neurodegenerative Disease Research
A recent study exemplifies the power of PBVS for identifying multi-target inhibitors for AD treatment [2]. Researchers screened a library of 17,544 fungal metabolites against three key AD targets: GSK-3β, the NMDA receptor, and BACE-1. The workflow proceeded as follows:
- An initial pharmacophore-based screening and drug-likeness filtering narrowed the library to 14 best hits.
- Molecular docking studies identified Bisacremine-C as the most promising multi-target ligand, showing high binding affinity for all three targets.
- Molecular dynamics simulations (100 ns) confirmed the stability of the Bisacremine-C complexes, with stable root mean square deviation (RMSD) values and key interactions maintained throughout the simulation [2].
This case demonstrates how PBVS can efficiently identify novel, naturally derived chemical scaffolds with potential multi-target activity, addressing the complex pathophysiology of AD.
The urgent need for alternative therapeutic strategies in neurodegeneration demands innovative approaches that can address the multi-factorial nature of these devastating diseases. Pharmacophore-based virtual screening represents a powerful, rational drug discovery paradigm that can significantly accelerate the identification of novel, effective therapeutic candidates. By enabling the systematic exploration of vast chemical space and the targeted discovery of multi-target directed ligands, PBVS offers a promising path forward in the challenging landscape of neurodegenerative disease drug development. The detailed protocols and resources provided in this document offer researchers a practical framework for implementing these advanced computational methods in their own neurotherapeutic discovery pipelines.
Alzheimer's disease (AD) and related tauopathies represent a significant challenge in neurodegenerative disease research, characterized by the pathological accumulation of specific proteins in the brain. The microtubule-associated protein tau (MAPT) and the β-site amyloid precursor protein cleaving enzyme 1 (BACE1) have emerged as two of the most promising therapeutic targets for disease-modifying strategies [11] [12]. In Alzheimer's disease, the pathological features include amyloid-beta (Aβ) deposits and neurofibrillary tangles composed of hyperphosphorylated tau, which lead to synaptic impairment and neuronal degeneration [11]. Tauopathies encompass a spectrum of disorders, including Pick's disease, frontotemporal dementia, corticobasal degeneration, argyrophilic grain disease, and progressive supranuclear palsy, all resulting from misprocessing and accumulation of tau within neuronal and glial cells [11]. This application note provides a comprehensive overview of these key protein targets and details experimental protocols for pharmacophore-based virtual screening, enabling researchers to identify novel therapeutic compounds targeting these critical pathways.
Key Protein Targets: Mechanisms and Pathological Significance
Tau Protein: Structure, Function, and Dysregulation
The tau protein is a neuron-enriched microtubule-associated protein encoded by the MAPT gene located on chromosome 17q21.31 [13]. Through alternative splicing of exons 2, 3, and 10, the MAPT gene generates six major tau isoforms in the human central nervous system, classified as 0N3R, 1N3R, 2N3R, 0N4R, 1N4R, and 2N4R based on the presence of N-terminal inserts (0N, 1N, 2N) and the number of microtubule-binding repeats (3R or 4R) [13] [14]. Under physiological conditions, tau stabilizes microtubules, regulates axonal transport, and participates in synaptic plasticity [13]. The normal human brain maintains a 1:1 ratio between 3R and 4R tau isoforms, with alterations in this ratio characterizing various tauopathies [11].
In pathological states, tau undergoes abnormal post-translational modifications, particularly hyperphosphorylation, which reduces its affinity for microtubules and promotes aggregation into neurofibrillary tangles (NFTs) [11] [13]. These modifications are driven by an imbalance between kinase and phosphatase activities, with reduced protein phosphatase 2A (PP2A) activity and increased kinase activity contributing to the hyperphosphorylated state [13]. The accumulation of pathological tau disrupts synaptic function, impairs neuronal communication, and ultimately leads to neurodegeneration [11]. The propagation of tau pathology follows a prion-like pattern, with misfolded tau spreading from neuron to neuron and seeding aggregation of endogenous tau in recipient cells [14].
Table 1: Tau Isoforms in the Human Brain and Their Characteristics
| Isoform Name | N-terminal Inserts | Microtubule-Binding Repeats | Characteristics |
|---|---|---|---|
| 0N3R | 0 | 3 | Lacks both N-terminal inserts; 3 repeat domains |
| 1N3R | 1 | 3 | Contains one N-terminal insert; 3 repeat domains |
| 2N3R | 2 | 3 | Contains two N-terminal inserts; 3 repeat domains |
| 0N4R | 0 | 4 | Lacks both N-terminal inserts; 4 repeat domains |
| 1N4R | 1 | 4 | Contains one N-terminal insert; 4 repeat domains |
| 2N4R | 2 | 4 | Contains two N-terminal inserts; 4 repeat domains |
BACE1: Role in Amyloid Pathology and Beyond
BACE1 is a membrane-associated aspartyl protease that initiates the cleavage of amyloid precursor protein (APP) in the amyloidogenic pathway [12]. This cleavage represents the rate-limiting step in the generation of amyloid-beta (Aβ) peptides, which aggregate to form amyloid plaques in Alzheimer's disease [15] [12]. The proteolytic pocket of BACE1 is relatively large and accommodates up to 11 residues, presenting both challenges and opportunities for inhibitor development [12]. Genetic evidence supports BACE1 inhibition as a therapeutic strategy, as germline deletion of BACE1 in mouse models abrogates Aβ production and ameliorates cognitive deficiencies [12]. Furthermore, a rare human mutation (A673T) at the BACE1 cleavage site of APP results in reduced Aβ production and decreased AD risk [12].
Recent research has revealed that BACE1 inhibition not only reduces Aβ generation but also affects downstream tau pathology. Studies in APP transgenic mice demonstrate that BACE1 inhibition prevents the age-related increase of tau in cerebrospinal fluid, suggesting a downstream effect on tau pathophysiology [16] [17]. This finding is particularly significant as it indicates that targeting the upstream amyloid pathway may also modulate tau-related pathology, providing a dual therapeutic benefit.
Experimental Protocols for Target Validation and Compound Screening
Pharmacophore-Based Virtual Screening Protocol for BACE1 Inhibitors
Objective: To identify novel BACE1 inhibitors through pharmacophore-based virtual screening of commercial compound libraries.
Materials and Software:
- Protein Data Bank (PDB ID: 6EJ3 or 5HU0 for BACE1) [18] [15]
- Schrödinger Suite (Phase module, Glide, QikProp) [18] [15]
- Commercial compound databases (VITAS-M Laboratory, ZINC, Enamine, Asinex) [18] [15]
- Hardware: Multi-core processor workstation with ≥16 GB RAM
Procedure:
Protein Preparation:
- Retrieve the crystal structure of BACE1 (PDB ID: 6EJ3) from the Protein Data Bank [18].
- Preprocess the protein by adding hydrogen atoms, assigning proper bond orders and charges.
- Remove water molecules and optimize the structure using the OPLS_2005 force field [18].
- Generate a grid box centered on the active site coordinates (x = 38.29, y = 59.94, z = 50.33) [18].
Pharmacophore Model Development:
- Develop a receptor-ligand-based pharmacophore model using the Phase tool in Schrödinger [15].
- Identify critical pharmacophore features from the co-crystal ligand interactions: two aromatic rings (R19, R20), one hydrogen bond donor (D12), and one hydrogen bond acceptor (A8) [18].
- Validate the model using known active and inactive compounds.
Database Preparation:
Virtual Screening:
Molecular Docking:
Binding Free Energy Calculations:
ADMET Prediction:
- Evaluate drug-likeness using QikProp, SwissADME, or ADMETlab 2.0 [15].
- Apply Lipinski's Rule of Five and assess toxicity parameters.
Molecular Dynamics Simulation:
- Perform MD simulations using GROMACS with GROMOS96 43a1 force field [18].
- Solvate the system with explicit SPC water model and neutralize with counterions.
- Conduct energy minimization, NVT and NPT equilibration, followed by production run (≥50 ns) [18].
- Analyze trajectories for RMSD, RMSF, and hydrogen bonding.
Table 2: Key Research Reagents and Resources for Tau and BACE1 Studies
| Research Reagent | Function/Application | Specifications/Examples |
|---|---|---|
| BACE1 Crystal Structure | Structure-based drug design | PDB ID: 6EJ3, 5HU0 [18] [15] |
| MAPT Gene Constructs | Study tau isoform expression and function | 0N3R, 1N3R, 2N3R, 0N4R, 1N4R, 2N4R isoforms [13] |
| Phospho-specific Tau Antibodies | Detection of pathological tau | Anti-p-tau181, Anti-p-tau217 [19] |
| Commercial Compound Databases | Virtual screening libraries | VITAS-M, ZINC, Enamine, Asinex [18] |
| ADMET Prediction Tools | Assessment of drug-likeness | QikProp, SwissADME, ADMETlab 2.0 [15] |
Experimental Validation of Tau-Targeted Compounds
Objective: To evaluate candidate compounds for modulation of tau phosphorylation and aggregation.
Cell-Based Assay Protocol:
Cell Culture:
- Maintain neuronal cell lines (e.g., SH-SY5Y, PC12) or primary neuronal cultures under standard conditions.
- Transfert cells with MAPT constructs expressing different tau isoforms as needed.
Compound Treatment:
- Apply candidate compounds at varying concentrations (1 nM-100 μM).
- Include positive controls (kinase inhibitors, e.g., GSK-3β inhibitors).
- Treat for 24-72 hours based on experimental design.
Tau Phosphorylation Analysis:
- Lyse cells and extract proteins using RIPA buffer with phosphatase and protease inhibitors.
- Perform Western blotting using phosphorylation-specific tau antibodies (p-tau181, p-tau217, etc.) [19].
- Quantify band intensities and normalize to total tau levels.
Tau Aggregation Assessment:
- Perform immunofluorescence staining for tau and observe aggregation patterns.
- Use thioflavin S or T staining to detect fibrillar tau aggregates.
- Quantify aggregate number and size using image analysis software.
Biomarker Assessment Protocol:
Sample Collection:
- Collect cerebrospinal fluid (CSF) or blood plasma samples from model systems or human subjects.
Biomarker Analysis:
Data Interpretation:
- Correlate biomarker levels with disease progression and cognitive measures.
- Evaluate treatment effects on biomarker trajectories.
Pathway Visualization and Therapeutic Strategies
The following diagrams illustrate key signaling pathways and experimental workflows for targeting tau and BACE1 in Alzheimer's disease and tauopathies.
Diagram 1: Key Pathological Pathways in Alzheimer's Disease. This diagram illustrates the amyloid pathway involving BACE1 cleavage of APP and the tau pathology pathway leading to neurofibrillary tangle formation, highlighting the interaction between these two key processes.
Diagram 2: Virtual Screening Workflow for BACE1 Inhibitors. This diagram outlines the comprehensive computational pipeline for identifying novel BACE1 inhibitors, from target identification to experimental validation of hit compounds.
The therapeutic landscape for Alzheimer's disease and tauopathies is rapidly evolving, with tau and BACE1 representing two of the most promising targets for disease modification. The experimental protocols outlined in this application note provide researchers with robust methodologies for target validation and compound screening. Pharmacophore-based virtual screening has demonstrated significant utility in identifying novel inhibitors, as evidenced by the discovery of compounds such as ZINC39592220 and 66H with potent activity against BACE1 [18] [15]. As of 2025, the therapeutic pipeline includes 170 drugs in development, with 32 candidates in clinical trials targeting tau pathology [14]. The integration of biomarker assessment, particularly p-tau217 and NfL measurements in blood, provides valuable tools for patient stratification and treatment monitoring [19]. These advanced experimental approaches will continue to drive the development of effective therapeutics for these devastating neurodegenerative disorders.
The pharmacophore, a cornerstone concept in modern drug discovery, represents the ensemble of steric and electronic features necessary for a molecule to trigger or block a biological response [20]. Its conceptual origins trace back to Paul Ehrlich in the early 20th century, who first introduced the term to describe the molecular framework carrying essential features responsible for a drug's biological activity [20]. The conceptual foundation was profoundly shaped by Emil Fischer's 1894 lock-and-key model, which used an analogy between an enzyme (the lock) and a substrate (the key) to illustrate the necessity of a matching shape for biological recognition [21]. This seminal idea established that the preference of an enzyme for given substrates is attributed to the quality of the geometric and electronic match between them.
Over the past century, the basic pharmacophore concept has retained its core meaning while expanding considerably in application and technical sophistication. The contemporary definition, as formalized by IUPAC, describes a pharmacophore as "the ensemble of steric and electronic features that is necessary to ensure the optimal supramolecular interactions with a specific biological target structure and to trigger (or to block) its biological response" [22] [7] [20]. This evolution from Fischer's rigid lock-and-key analogy has progressed through several key stages:
- Induced-Fit and Selected-Fit Models: These expanded Fischer's rigid model to account for the flexibility of both ligand and enzyme, recognizing that binding can induce conformational changes or select for pre-existing reactive conformations [21].
- Keyhole-Lock-Key Model: A more recent proposal addressing enzymes with buried active sites, this model incorporates the importance of substrate entry and product exit pathways (tunnels or "keyholes") in catalysis and discrimination [21].
- Modern 3D Pharmacophore Mapping: Today, pharmacophores are abstract representations of essential chemical interactions, represented as geometric entities in three-dimensional space for computer-aided drug design [22].
Table 1: Core Pharmacophore Feature Types and Their Interactions
| Feature Type | Geometric Representation | Complementary Feature Type(s) | Interaction Type(s) | Structural Examples |
|---|---|---|---|---|
| Hydrogen-Bond Acceptor (HBA) | Vector or Sphere | HBD | Hydrogen-Bonding | Amines, Carboxylates, Ketones, Alcoholes, Fluorine Substituents |
| Hydrogen-Bond Donor (HBD) | Vector or Sphere | HBA | Hydrogen-Bonding | Amines, Amides, Alcoholes |
| Aromatic (AR) | Plane or Sphere | AR, PI | π-Stacking, Cation-π | Any Aromatic Ring |
| Positive Ionizable (PI) | Sphere | AR, NI | Ionic, Cation-π | Ammonium Ion, Metal Cations |
| Negative Ionizable (NI) | Sphere | PI | Ionic | Carboxylates |
| Hydrophobic (H) | Sphere | H | Hydrophobic Contact | Halogen Substituents, Alkyl Groups, Alicycles, weakly or non-polar aromatic Rings |
| Exclusion Volume (XVOL) | Sphere | N/A | Steric Hindrance | Representation of forbidden areas in the binding pocket |
Modern Pharmacophore Modeling Methodologies
Structure-Based Pharmacophore Modeling
Structure-based pharmacophore modeling leverages the three-dimensional structure of a macromolecular target, obtained from X-ray crystallography, NMR spectroscopy, or computational methods like homology modeling, to derive essential interaction features [7]. The quality of the input protein structure directly influences the model's reliability, necessitating careful preparation steps including protonation state assignment, hydrogen atom addition, and energy minimization [7]. When a protein-ligand complex structure is available, the process is more straightforward: the bound ligand's bioactive conformation directly guides the identification and spatial placement of pharmacophore features corresponding to its functional groups engaged in target interactions [7]. The receptor structure further enables the incorporation of shape constraints through exclusion volumes (also called exclusion spheres), which represent sterically forbidden regions of the binding pocket that ligands must avoid [22] [7].
For targets where only the unbound (apo) structure is available, the modeling becomes more challenging. In such cases, computational tools like GRID or LUDI probe the binding site to identify favorable interaction points for various chemical functional groups, generating a map of potential interaction sites [7]. This typically produces an overabundance of features, requiring careful selection based on conservation analysis, energetic contributions, or known key residues to create a refined, selective pharmacophore hypothesis [7] [20].
Ligand-Based Pharmacophore Modeling
In the absence of a macromolecular target structure, ligand-based pharmacophore modeling provides a powerful alternative. This approach deduces the essential pharmacophore features by analyzing the three-dimensional structures of a set of known active ligands that bind to the same receptor site in the same orientation [22] [7]. A critical prerequisite is that these active ligands should represent a range of chemical scaffolds to ensure the identification of truly essential common features rather than scaffold-specific artifacts [20].
The process involves several technically challenging steps. First, a conformational analysis is performed for each ligand to generate a set of low-energy conformers, as the bioactive conformation is rarely known a priori [23]. Evidence suggests the energy difference between the bioactive conformation and the global minimum of the isolated molecule is generally less than 12 kJ/mol (3 kcal/mol), allowing higher-energy conformers to be filtered out [23]. Subsequently, common chemical features are identified across the active molecules, and their optimal spatial arrangement is determined through systematic or algorithmic superimposition [23]. The quality of the resulting model can be validated by ensuring it can distinguish known active compounds from inactive ones and by assessing its predictive power through statistical measures [20].
AI-Enhanced Pharmacophore Modeling
Recent advances incorporate artificial intelligence to address longstanding challenges in pharmacophore-guided drug discovery. The DiffPhore framework represents a pioneering knowledge-guided diffusion model for "on-the-fly" 3D ligand-pharmacophore mapping [24] [25]. This method leverages ligand-pharmacophore matching knowledge to guide ligand conformation generation while utilizing calibrated sampling to mitigate exposure bias in the iterative conformation search process [24].
DiffPhore comprises three main modules: a knowledge-guided ligand-pharmacophore mapping (LPM) encoder that incorporates rules for pharmacophore type and direction matching; a diffusion-based conformation generator that estimates translation, rotation, and torsion transformations for the ligand; and a calibrated conformation sampler that adjusts the perturbation strategy to narrow the discrepancy between training and inference phases [24] [25]. Trained on complementary datasets (CpxPhoreSet from experimental complexes and LigPhoreSet from diverse ligand conformations), DiffPhore has demonstrated state-of-the-art performance in predicting ligand binding conformations, surpassing traditional pharmacophore tools and several advanced docking methods [24] [25].
Application Notes: Pharmacophore-Based Virtual Screening for Neurodegenerative Targets
Case Study: Targeting BACE1 for Alzheimer's Disease
β-secretase 1 (BACE1) is a membrane-associated aspartate protease critically involved in the production of amyloid-beta peptides, whose accumulation is central to Alzheimer's disease pathology [15]. Despite extensive efforts, developing effective BACE1 inhibitors has proven challenging, creating an urgent need for novel therapeutic approaches [15]. A recent pharmacophore-based virtual screening study demonstrates a comprehensive protocol for identifying new BACE1 inhibitors [15].
The study began with receptor-ligand-based pharmacophore hypothesis development using a BACE1 co-crystal structure (PDB ID: 5HU0) and its high-activity ligand [15]. The Schrödinger Phase tool was employed to generate the pharmacophore model targeting the protein-binding pocket [15]. Subsequent virtual screening of 200,000 compounds from the VITAS-M Laboratory database identified hits using phase screen scores (a composite metric combining volume score, RMSD, and site matching), with compounds scoring >1.9 selected for further analysis [15]. This was followed by ADMET profiling using QikProp, SwissADME, and ADMETlab 2.0 to evaluate drug-likeness and toxicity parameters according to Lipinski's Rule of Five [15].
Promising candidates underwent molecular docking studies with the prepared BACE1 structure, which involved preprocessing (adding hydrogens, assigning charges), eliminating water molecules, and energy minimization using the OPLS_2005 force field [15]. The top candidate, compound 66H, showed a binding mode similar to the reference ligand, forming key hydrogen bonds with Asp93, Asp289, and Gly291, along with van der Waals and hydrophobic interactions [15]. Molecular dynamics simulations over 100 ns confirmed the stability of the 66H-BACE1 complex, with RMSD values maintaining stability between 2.5-3 Å after equilibration, comparable to the reference compound [15]. Finally, MM/GBSA analysis calculated the total binding free energies (ΔGtotal) for both complexes, providing quantitative assessment of binding affinity [15].
Table 2: Key Research Reagent Solutions for Pharmacophore-Based Screening
| Reagent/Resource | Category | Function in Research | Example Source/Access |
|---|---|---|---|
| Protein Data Bank (PDB) | Structural Database | Repository for experimental 3D structures of proteins and nucleic acids; source of target structures for structure-based modeling. | RCSB PDB (https://www.rcsb.org/) [7] [15] |
| Commercial Compound Databases | Chemical Database | Curated collections of purchasable compounds for virtual screening hits identification. | VITAS-M Laboratory, ZINC20 [24] [15] |
| Schrödinger Phase | Software Module | Tool for pharmacophore model development, virtual screening, and hypothesis generation. | Commercial Software [15] |
| AncPhore | Software Tool | Anchor pharmacophore tool for generating 3D ligand-pharmacophore pairs and virtual screening. | Academic/Commercial Software [24] [25] |
| OPLS Force Fields | Computational Parameter Set | Optimized potentials for liquid simulations; used for molecular mechanics energy minimization and dynamics. | OPLS_2005 [15] |
| QikProp | Software Module | Predicts ADMET properties and drug-likeness for candidate compounds. | Commercial Software [15] |
Targeting Phosphorylated Tau in Alzheimer's and Tauopathies
Phosphorylated tau (P-tau) has emerged as a promising therapeutic target for Alzheimer's disease and other tauopathies due to its involvement in synaptic damage and neuronal dysfunction [26]. In diseased states, tau undergoes hyperphosphorylation at specific serine and threonine residues, leading to defective microtubule interactions, impaired axonal transport, and ultimately synaptic damage and neuronal death [26]. This pathological transformation creates opportunities for pharmacophore-based approaches to identify inhibitors of tau phosphorylation or compounds that disrupt abnormal P-tau interactions.
Key kinases involved in tau phosphorylation include proline-directed proteins, mitogen-activated proteins, cyclin-dependent kinases (Cdks), protein kinase A (PKA), and calmodulin-dependent protein kinase (CaMK) [26]. Hyperphosphorylation at Cdk sites (Ser235, Ser202, Ser404) promotes self-aggregation of tau filaments, while phosphorylation at Ser/Thr sites targeting PKA (Ser214, Ser324, Ser356, etc.) contributes to the pathological state [26]. Pharmacophore models targeting these kinase enzymes or designed to disrupt the aberrant interaction between P-tau and mitochondrial fission protein Drp1 (which leads to excessive mitochondrial fragmentation) represent promising strategies for therapeutic intervention [26].
Experimental Protocols
Protocol: Structure-Based Pharmacophore Modeling and Virtual Screening
Objective: To generate a structure-based pharmacophore model and utilize it for virtual screening against neurodegenerative disease targets.
Materials and Software:
- Protein Data Bank (https://www.rcsb.org/)
- Molecular modeling software with pharmacophore capabilities (e.g., Schrödinger Suite, MOE, Discovery Studio)
- Commercial or in-house compound database for screening
- High-performance computing resources
Procedure:
Target Identification and Structure Preparation
- Retrieve the 3D crystal structure of the target protein (e.g., BACE1 for Alzheimer's) from the PDB. Prefer structures with high resolution and co-crystallized ligands.
- Prepare the protein structure by adding hydrogen atoms, assigning appropriate protonation states at physiological pH (e.g., using PropKa), and correcting for missing residues or atoms if necessary.
- Perform energy minimization using a suitable force field (e.g., OPLS_2005) to relieve steric clashes and optimize the structure.
Binding Site Analysis and Pharmacophore Feature Generation
- Define the ligand-binding site using the coordinates of the co-crystallized ligand or through binding site detection algorithms (e.g., GRID, LUDI).
- Generate an initial set of pharmacophore features by analyzing interactions between the protein and the bound ligand (if present) or by mapping complementary chemical features in the binding site.
- Select the most relevant features for bioactivity based on conservation, energetic contribution, or known key residues. Include hydrogen bond acceptors/donors, hydrophobic areas, charged/ionizable groups, and aromatic rings as appropriate.
Exclusion Volumes and Model Validation
- Add exclusion volumes around protein atoms lining the binding pocket to represent steric constraints that ligands must avoid.
- Validate the initial model by ensuring it can successfully recognize known active compounds and reject inactive molecules from a test set.
Database Preparation and Virtual Screening
- Prepare a 3D compound database by generating multiple conformers for each molecule and filtering based on drug-likeness rules if desired.
- Screen the database against the pharmacophore model using a fitness score that accounts for feature matching and spatial alignment.
- Select top-ranking compounds (e.g., phase screen score >1.9) for subsequent analysis.
Hit Validation and Characterization
- Subject selected hits to molecular docking studies to refine binding pose predictions and assess interaction energy.
- Perform ADMET prediction to evaluate pharmacokinetic and toxicity profiles.
- Select promising candidates for experimental validation through biochemical or cell-based assays.
Protocol: Ligand-Based Pharmacophore Generation Using Multiple Active Compounds
Objective: To develop a ligand-based pharmacophore model when the 3D structure of the target protein is unavailable.
Materials and Software:
- A set of 3-20 known active compounds with diverse chemical scaffolds but similar biological activity on the same target
- Conformational analysis software (e.g., CONFGEN, OMEGA)
- Pharmacophore modeling software (e.g., Schrödinger Phase, Catalyst)
Procedure:
Training Set Selection and Conformational Analysis
- Curate a set of structurally diverse active compounds confirmed to act on the same biological target through the same mechanism.
- Generate a comprehensive set of low-energy conformers for each compound, ensuring adequate coverage of conformational space while excluding high-energy conformations (typically >10-12 kJ/mol above global minimum).
Common Feature Identification and Model Generation
- Use automated algorithms (e.g., HipHop, Common Feature Approach) to identify pharmacophoric features common to the active compounds and their spatial relationships.
- Superimpose the compounds based on these common features to identify the best alignment that maximizes molecular overlap of essential functionalities.
Model Validation and Refinement
- Validate the model using a test set of known active and inactive compounds to determine its selectivity and predictive power.
- Refine the model by adjusting feature tolerances or removing redundant features to improve its ability to distinguish actives from inactives.
Application to Virtual Screening
- Apply the validated model to screen compound databases as described in the structure-based protocol.
- Use the model for scaffold hopping to identify novel chemotypes that maintain the essential pharmacophore features.
The Rationale for Pharmacophore-Based Screening in CNS Drug Discovery
The discovery and development of therapeutics for Central Nervous System (CNS) diseases present unique challenges, primarily due to the restrictive nature of the blood-brain barrier (BBB) and the complex, multifactorial pathophysiology of neurodegenerative disorders [1]. Computer-Aided Drug Discovery (CADD) techniques, particularly pharmacophore-based virtual screening, have emerged as powerful tools to reduce the time and cost associated with developing novel drugs, making them particularly valuable for addressing health emergencies and the diffusion of personalized medicine [7]. A pharmacophore is formally defined as "the ensemble of steric and electronic features that is necessary to ensure the optimal supramolecular interactions with a specific biological target structure and to trigger (or to block) its biological response" [7]. This approach abstracts molecular functionalities into geometric entities—such as hydrogen bond acceptors (HBAs), hydrogen bond donors (HBDs), hydrophobic areas (H), positively and negatively ionizable groups (PI/NI), and aromatic groups (AR)—allowing for the identification of bioactive compounds regardless of their underlying chemical scaffold [7]. This article delineates the rationale for employing pharmacophore-based screening in CNS drug discovery, detailing its fundamental principles, practical protocols, and application within a broader research framework focused on neurodegenerative disease targets.
Scientific Rationale and Advantages
The Imperative for Novel CNS Therapeutics
Neurodegenerative diseases (NDDs), such as Alzheimer's disease (AD) and Parkinson's disease (PD), represent a significant and growing global health burden. These conditions are characterized by the progressive degeneration of neurons, leading to cognitive decline, motor dysfunction, and extensive brain damage [1] [27]. The highly selective blood-brain barrier, while crucial for maintaining brain homeostasis, poses a major obstacle for drug delivery; it is estimated that only about 2% of potential therapeutic agents can cross the intact BBB to reach their targets in the brain [1]. This limitation, combined with the multifactorial nature of CNS disorders—often involving dysregulation of complex protein networks and multiple neurotransmitter systems—necessitates innovative drug discovery approaches [28].
Pharmacophore Screening in the CADD Landscape
Pharmacophore-based virtual screening (PBVS) occupies a critical space in the CADD toolkit. It serves as an efficient method for screening large libraries of compounds in silico to identify those most likely to bind to a specific target and possess desired biological activity [7]. Benchmark studies have demonstrated that PBVS often outperforms docking-based virtual screening (DBVS) in retrieving active compounds from large databases [29]. A comparative study across eight diverse protein targets revealed that in 14 out of 16 virtual screening sets, PBVS achieved higher enrichment factors than DBVS, with significantly higher average hit rates at the top 2% and 5% of ranked database compounds [29]. This superior performance, coupled with its computational efficiency, makes PBVS particularly well-suited for the initial stages of drug discovery pipelines.
Key Advantages for CNS Drug Discovery
- Scaffold Hopping Capability: By focusing on essential functional features rather than specific atomic structures, pharmacophore models can identify chemically diverse compounds that share the necessary bioactivity, potentially leading to novel chemotypes with improved properties [7].
- Multi-Target Drug Design (Polypharmacology): The complex pathophysiology of many neurodegenerative diseases often requires simultaneous modulation of multiple targets. Pharmacophore approaches facilitate the design of Multi-Target Directed Ligands (MTDLs) by identifying common pharmacophoric elements against different targets, which can be merged into a single molecule [2] [28]. This strategy can lead to improved efficacy, broader therapeutic coverage of disease symptoms, and simplified pharmacokinetic profiles [28].
- Efficient Pre-Filtering for BBB Permeability: Pharmacophore models can incorporate features predictive of BBB penetration, allowing for the early prioritization of compounds with a higher likelihood of reaching CNS targets [1] [27]. This is crucial given that CNS-active drugs must possess specific physicochemical properties, such as appropriate lipophilicity, low molecular weight, and a balanced number of hydrogen bond donors and acceptors [27].
Table 1: Key Pharmacophore Features and Their Chemical Significance
| Feature Type | Symbol | Chemical Significance | Role in CNS Drug Design |
|---|---|---|---|
| Hydrogen Bond Acceptor | HBA | Atom capable of accepting a H-bond (e.g., O, N) | Influces solubility and specific target binding |
| Hydrogen Bond Donor | HBD | Atom with a bound hydrogen that can be donated (e.g., OH, NH) | Affects membrane permeability and BBB penetration |
| Hydrophobic Area | H | Non-polar molecular region | Promotes passive diffusion through lipid bilayers |
| Positively Ionizable | PI | Functional group that can carry a positive charge (e.g., amine) | Can facilitate interaction with negatively charged membrane surfaces |
| Aromtic Ring | AR | Planar, conjugated ring system | Promotes π-π stacking interactions with target proteins |
Experimental Protocols and Workflows
The typical workflow for pharmacophore-based screening in CNS drug discovery involves sequential steps from target identification to lead validation. The following diagram illustrates this integrated process:
Structure-Based Pharmacophore Modeling Protocol
Objective: To generate a pharmacophore model using the three-dimensional structural information of a macromolecular target.
Procedure:
- Protein Structure Preparation:
- Retrieve the 3D structure of the target protein (e.g., BACE-1, MAO-B, GSK-3β) from the RCSB Protein Data Bank (PDB) [7] [15]. If an experimental structure is unavailable, employ homology modeling or machine learning-based methods like AlphaFold2 [7].
- Prepare the protein structure using molecular modeling software (e.g., Maestro, MOE). This involves adding hydrogen atoms, assigning partial charges, correcting protonation states of residues, and optimizing the structure using a force field like OPLS_2005 [7] [15].
- Critically evaluate the structure's quality, checking for missing residues or atoms and assessing stereochemical parameters [7].
Ligand-Binding Site Characterization:
- If the protein structure is co-crystallized with a ligand, the binding site is defined by the ligand's location.
- For apo structures, use bioinformatics tools like GRID or LUDI to detect potential binding pockets by analyzing the protein surface based on geometric and energetic properties [7].
Pharmacophore Feature Generation and Selection:
- Analyze the binding site to identify key interaction points. The software (e.g., Schrödinger Phase, LigandScout) maps features like HBA, HBD, hydrophobic regions, and charged groups onto the binding pocket [7] [29] [15].
- Select only the most crucial features for bioactivity to create a selective and reliable pharmacophore hypothesis. This can be done by removing features that do not contribute significantly to binding energy or by considering conserved interactions across multiple protein-ligand complexes [7] [29].
- Incorporate exclusion volumes (XVOL) to represent the steric constraints of the binding pocket, preventing the selection of compounds that would cause steric clashes [7].
Ligand-Based Pharmacophore Modeling Protocol
Objective: To develop a pharmacophore model when the 3D structure of the target protein is unknown, using a set of known active ligands.
Procedure:
- Training Set Compilation:
- Curate a set of diverse, experimentally validated active compounds against the target of interest. These can be gathered from literature or databases like ChEMBL or PubChem [27] [30].
- Include known inactive compounds if the goal is to build a quantitative model that discriminates between active and inactive molecules.
Conformational Analysis and Molecular Alignment:
- Generate a representative set of low-energy conformations for each molecule in the training set. This is typically done using algorithms that perform a systematic or stochastic search of the conformational space [30].
- Use software like PharmaGist or the Phase module in Schrödinger to align the conformations of the active molecules based on their common chemical features [27] [30].
Hypothesis Generation and Validation:
- The software identifies the common steric and electronic features shared by the aligned molecules and constructs one or more pharmacophore hypotheses [27] [30].
- Each hypothesis is scored based on how well it aligns the training set compounds and its ability to distinguish between known actives and inactives. The highest-ranked hypothesis is selected for virtual screening [27] [30].
Integrated Virtual Screening and Validation Protocol
Objective: To screen large compound libraries using the pharmacophore model and validate the resulting hits.
Procedure:
- Database Preparation:
- Select a commercial database (e.g., ZINC15, Vitas-M Laboratory, natural product libraries) or an in-house corporate library [15] [2] [31].
- Prepare the database by generating multiple low-energy 3D conformers for each compound. Generate likely ionization and tautomeric states at physiological pH (e.g., using Epik) and filter out high-energy tautomers [15].
Pharmacophore-Based Virtual Screening:
- Use the pharmacophore model as a 3D query to screen the prepared database. Software such as Catalyst, ZINCPharmer, or Phase is employed for this purpose [29] [15] [27].
- Set parameters like maximum RMSD (e.g., 1.5 Å) for fitting the compounds to the model. The screening output is typically ranked using a scoring function (e.g., Phase Screen Score) that considers factors like volume overlap, RMSD, and the number of matched features [15] [27].
- Select top-ranking compounds (e.g., those with a Phase Screen Score >1.9) for further analysis [15].
ADMET and Drug-Likeness Filtering:
- Subject the virtual hits to predictive analysis of Absorption, Distribution, Metabolism, Excretion, and Toxicity (ADMET) properties. This is a critical step for CNS drugs to ensure potential BBB permeability and minimize safety risks [1] [15] [27].
- Use tools like QikProp, SwissADME, or ADMETlab 2.0 to compute key descriptors. Filter compounds based on Lipinski's Rule of Five, CNS multiparameter optimization (MPO) scores, and the absence of toxicophores [1] [15] [27].
Molecular Docking and Dynamics Simulation:
- Perform molecular docking (using programs like Glide, GOLD, or AutoDock) to refine the binding pose of the hits within the target's active site and estimate binding affinity [29] [15] [2].
- Conduct Molecular Dynamics (MD) simulations (e.g., for 50-100 ns using Desmond or GROMACS) to assess the stability of the protein-ligand complex. Analyze parameters like Root-Mean-Square Deviation (RMSD), Root-Mean-Square Fluctuation (RMSF), Radius of Gyration (Rg), and hydrogen bonding patterns [15] [2] [31].
- Use methods like MM/GBSA (Molecular Mechanics/Generalized Born Surface Area) to calculate the binding free energy (ΔG) of the complex [15].
Table 2: Key Software Tools for Pharmacophore-Based Screening
| Software/Tool | Primary Function | Application Example | Reference |
|---|---|---|---|
| LigandScout | Structure-based & ligand-based pharmacophore modeling | Generating models from PDB complexes | [29] |
| Schrödinger Phase | Pharmacophore modeling, 3D-QSAR, virtual screening | Virtual screening of BACE1 inhibitors | [15] |
| ZINCPharmer | Online pharmacophore-based screening of ZINC database | Screening alkaloids and flavonoids for MAO-B inhibition | [27] |
| PharmaGist | Online ligand-based pharmacophore alignment | Aligning active molecules to create a common hypothesis | [27] |
| Pharmit | Interactive online pharmacophore screening | Screening for BBB-permeable neurotherapeutics | [1] |
| PyRx | Virtual screening and molecular docking | Screening fungal metabolites against multiple AD targets | [2] |
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Research Reagents and Resources for Pharmacophore-Based Screening
| Resource Category | Specific Examples | Function and Utility | |
|---|---|---|---|
| Target Protein Structures | RCSB Protein Data Bank (PDB) | Source of 3D structural data for structure-based modeling | [7] [15] |
| Compound Libraries | ZINC15, Vitas-M Laboratory, PubChem, CMNP (Marine Natural Products) | Large-scale collections of purchasable or natural compounds for virtual screening | [1] [15] [32] |
| Pharmacophore Modeling Software | Schrödinger Suite (Phase), MOE (Molecular Operating Environment), LigandScout | Platforms for building, visualizing, and validating structure-based and ligand-based pharmacophore models | [7] [29] [15] |
| Virtual Screening Platforms | Catalyst, ZINCPharmer, Pharmit, PyRx | Tools for performing high-throughput 3D database searches using pharmacophore queries | [29] [1] [27] |
| ADMET Prediction Tools | QikProp, SwissADME, ADMETlab 2.0, pkCSM | Prediction of pharmacokinetic, toxicity, and drug-likeness properties for hit prioritization | [15] [27] [2] |
| Molecular Dynamics Suites | Desmond (Schrödinger), GROMACS | Simulation of protein-ligand complexes to assess binding stability and dynamics over time | [15] [2] [31] |
Application in Neurodegenerative Disease Research
The following diagram illustrates key targets and strategies for Alzheimer's and Parkinson's disease, highlighting the multi-target approach:
Case Studies in Alzheimer's Disease
- Targeting BACE-1: Pharmacophore-based virtual screening has been successfully applied to identify novel inhibitors of Beta-secretase 1 (BACE-1), a key enzyme in the amyloidogenic pathway of AD. For instance, screening of 200,000 compounds from the Vitas-M Laboratory database led to the identification of ligand 66H, which demonstrated stable binding in molecular dynamics simulations and favorable binding free energy calculations, highlighting its potential as a lead compound [15].
- Multi-Target Screening for AD: A study screened a library of 17,544 fungal metabolites against three AD targets (GSK-3β, NMDA receptor, and BACE-1). Pharmacophore-based screening filtered 14 best hits, with Bisacremine-C emerging as the most promising multi-target inhibitor. It showed significantly higher binding affinity than native ligands for all three targets and formed stable complexes in MD simulations, as confirmed by parameters like RMSD, RMSF, Rg, and SASA [2].
Case Studies in Parkinson's Disease
- Inhibition of MAO-B: The search for new inhibitors of Monoamine Oxidase B (MAO-B), a key target in PD, has leveraged pharmacophore screening on natural products. A virtual screening of alkaloids and flavonoids, followed by ADMET and docking analysis, identified palmatine and genistein as promising candidates with potential inhibitory activity against MAO-B, suggesting their potential for further development as antiparkinsonian agents [27].
Pharmacophore-based virtual screening represents a rational and powerful strategy for addressing the formidable challenges of CNS drug discovery. Its ability to abstract molecular recognition into essential functional features enables the efficient identification of novel, scaffold-diverse lead compounds from vast chemical libraries. The integration of this approach with robust protocols for ADMET prediction, molecular docking, and dynamics simulation creates a comprehensive framework for prioritizing candidates with a high probability of success. Furthermore, its inherent suitability for designing multi-target directed ligands aligns perfectly with the complex pathophysiology of neurodegenerative diseases like Alzheimer's and Parkinson's. As computational power and methodologies continue to advance, pharmacophore-based screening will undoubtedly remain a cornerstone in the ongoing effort to develop effective therapeutics for disorders of the central nervous system.
Building and Executing a PBVS Protocol: A Step-by-Step Guide
Pharmacophore modeling is a foundational technique in computer-aided drug design, defined as the ensemble of steric and electronic features necessary to ensure optimal supramolecular interactions with a specific biological target and to trigger (or block) its biological response [33]. In the context of neurodegenerative disease research, where targets often include GPCRs, enzymes like MAO-B, and other neuronal proteins, pharmacophore models provide a powerful approach for virtual screening when experimental structures may be limited [34] [1]. These models abstract critical chemical interactions into features including hydrogen bond donors/acceptors, aromatic rings, hydrophobic regions, and charged centers, providing a concise representation of binding requirements that enables identification of novel therapeutic candidates through virtual screening [24] [33].
The generation of pharmacophore models primarily follows two distinct methodologies: structure-based approaches that utilize protein-ligand complex information, and ligand-based approaches that derive common features from sets of known active compounds [33]. This application note details established protocols for both methodologies, emphasizing their application to neurodegenerative disease targets, with specific case studies relevant to Alzheimer's disease and Parkinson's disease research. The selection between these approaches depends largely on available structural and ligand data, with structure-based methods requiring known protein structures and ligand-based methods depending on collections of confirmed active compounds.
Structure-Based Pharmacophore Modeling
Structure-based pharmacophore modeling derives features directly from analysis of three-dimensional protein-ligand complexes, capturing essential interaction patterns observed in crystallographic or modeled structures [33]. This approach is particularly valuable for neurodegenerative disease targets where limited chemical starting points are available, as it identifies interaction features directly from the binding site architecture.
Protocol: Structure-Based Pharmacophore Generation for GPCR Targets
Background: G protein-coupled receptors (GPCRs) represent important targets for neurodegenerative diseases but often lack extensive ligand libraries or high-resolution structures. The following protocol utilizes fragment-based sampling to generate high-performing pharmacophore models, even with modeled receptor structures [34].
Step 1: Target Structure Preparation
- Obtain experimentally determined or homology-modeled GPCR structure.
- Prepare protein structure: add hydrogen atoms, assign partial charges, and define binding site region.
- For homology models, validate structure quality using geometric verification tools.
Step 2: Fragment Placement with MCSS
- Perform Multiple Copy Simultaneous Search (MCSS) to place functional groups in the binding site.
- Use diverse fragment library representing key pharmacophoric elements.
- Energy-minimize placed fragments to optimize interactions with the protein.
Step 3: Feature Extraction and Model Generation
- Map optimal fragment positions to pharmacophore features: hydrogen bond donors/acceptors, hydrophobic areas, aromatic rings, and charged centers.
- Define spatial constraints and tolerances based on fragment distribution.
- Generate multiple candidate pharmacophore models scoring interaction compatibility.
Step 4: Model Selection via Machine Learning
- Apply cluster-then-predict machine learning workflow to classify model performance.
- Select models with highest enrichment factors using known active ligands as benchmarks.
- Validate model robustness against decoy sets containing inactive compounds.
Application Note: This protocol has been successfully applied to 13 class A GPCR targets, resulting in pharmacophore models with high enrichment factors when screening databases containing 569 known class A GPCR ligands. The machine learning classifier achieved positive predictive values of 0.88 for experimentally determined structures and 0.76 for modeled structures [34].
Protocol: Consensus Pharmacophore Generation with ConPhar
Background: For targets with extensive structural data, consensus pharmacophore modeling integrates features from multiple ligand-bound complexes to create robust models with reduced bias. This approach is particularly valuable for well-studied neurodegenerative disease targets like MAO-B [35] [36].
Step 1: Complex Preparation and Alignment
- Curate set of protein-ligand complex structures (e.g., from PDB) for the target.
- Align all complexes using structural superposition tools like PyMOL [36].
- Extract each aligned ligand conformer and save in SDF format.
Step 2: Individual Pharmacophore Generation
- Upload each ligand structure to Pharmit or similar pharmacophore generation tool [36].
- Generate pharmacophore features for each ligand-protein complex.
- Export individual pharmacophore models in JSON format.
Step 3: Feature Clustering and Consensus Building
- Install ConPhar package in Python environment.
- Load all individual pharmacophore JSON files.
- Parse and consolidate pharmacophoric features into a unified DataFrame.
- Cluster similar features across multiple complexes based on type and spatial location.
- Generate consensus model representing most conserved interaction patterns.
Step 4: Model Refinement and Validation
- Refine feature distances and tolerances based on clustering results.
- Validate model against known active and inactive compounds.
- Export final consensus pharmacophore for virtual screening applications.
Application Note: Applied to SARS-CoV-2 Mpro using 100 non-covalent inhibitor complexes, this protocol successfully captured key interaction features in the catalytic region and enabled identification of novel potential ligands [36]. The methodology is directly transferable to neurodegenerative disease targets with sufficient structural data.
Ligand-Based Pharmacophore Modeling
Ligand-based pharmacophore modeling identifies common chemical features from a set of known active ligands when the protein structure is unavailable. This approach is widely used in neurodegenerative disease research for targets like monoamine oxidase B (MAO-B) where multiple active compounds are known [27] [33].
Protocol: Ensemble Pharmacophore Generation for Neurodegenerative Disease Targets
Background: This protocol generates an ensemble pharmacophore from multiple known active ligands, capturing essential features shared across chemically diverse compounds with activity against neurodegenerative disease targets [33].
Step 1: Ligand Set Curation and Preparation
- Compile known active ligands from literature or databases (e.g., ChEMBL, PubChem).
- For Parkinson's disease MAO-B inhibitors, this may include alkaloids and flavonoids with demonstrated activity [27].
- Optimize ligand geometries using molecular mechanics (e.g., RM1 method) and correct partial charges.
Step 2: Molecular Alignment and Feature Extraction
- Align all ligand structures using flexible superposition methods.
- Submit aligned molecules to PharmaGist server or similar tool for common feature identification.
- Configure feature weights: aromatic ring = 3.0; hydrophobic = 3.0; hydrogen bond donor/acceptor = 1.5; charge = 1.0 [27].
- Extract pharmacophore features and their 3D coordinates for each ligand.
Step 3: Feature Clustering and Ensemble Pharmacophore Building
- Collect coordinates of each feature type (donors, acceptors, hydrophobic) across all ligands.
- Apply k-means clustering to group similar features in 3D space.
- Select cluster centroids representing most conserved feature positions.
- Define ensemble pharmacophore using selected cluster coordinates.
Step 4: Model Validation and Virtual Screening
Application Note: This approach successfully identified MAO-B inhibitors from alkaloid and flavonoid classes, with palmatine and genistein showing superior performance in subsequent docking studies and pharmacological profiling [27]. The method is particularly valuable for exploring natural products for neurodegenerative diseases.
Essential Research Reagents and Computational Tools
Table 1: Key Research Reagent Solutions for Pharmacophore Modeling
| Tool/Resource | Type | Primary Function | Application Note |
|---|---|---|---|
| Pharmit [36] | Web Server | Pharmacophore feature generation and virtual screening | Generates pharmacophore JSON files from ligand structures; used in consensus modeling |
| ConPhar [36] | Python Package | Consensus pharmacophore generation | Clusters features from multiple complexes; open-source tool |
| MCSS [34] | Computational Method | Multiple Copy Simultaneous Search | Places functional fragments in binding sites for structure-based pharmacophores |
| PharmaGist [27] | Web Server | Ligand-based pharmacophore alignment | Identifies common features from multiple active ligands |
| ZINCPharmer [27] | Web Server | Pharmacophore-based screening | Screens compound databases using pharmacophore queries |
| PyMOL [36] | Software | Molecular visualization and analysis | Aligns protein-ligand complexes for structure-based approaches |
| RDKit [33] | Cheminformatics Library | Molecular processing and feature detection | Extracts pharmacophore features and handles molecular formats |
| ChemDes [1] | Web Platform | Molecular descriptor calculation | Computes descriptors for BBB permeability and CNS activity prediction |
Workflow Visualization
Workflow for Structure-Based and Ligand-Based Pharmacophore Generation
Advanced Applications in Neurodegenerative Disease Research
Blood-Brain Barrier Permeability Considerations
For neurodegenerative disease targets, effective therapeutics must cross the blood-brain barrier (BBB). Integrative protocols combining pharmacophore modeling with BBB permeability prediction are essential [1]. Screening pipelines should incorporate:
- Computational BBB permeability models using molecular descriptors from tools like ChemDes [1].
- CNS activity prediction based on brain-to-blood ratio calculations.
- ADME profiling to assess drug-likeness for CNS targets.
Application of this integrated approach to 2,127 small molecules identified 582 BBB-permeable compounds, with 112 showing optimal CNS activity and pharmacokinetic properties for neurodegenerative disease applications [1].
AI-Enhanced Pharmacophore Methods
Recent advances in artificial intelligence are transforming pharmacophore modeling for neurodegenerative disease research:
- DiffPhore: A knowledge-guided diffusion framework for 3D ligand-pharmacophore mapping that outperforms traditional methods in predicting binding conformations and virtual screening [24].
- TransPharmer: A generative model integrating pharmacophore fingerprints with GPT-based architecture for de novo molecule generation, successfully applied to identify novel PLK1 inhibitors with submicromolar activity [37].
- Pharmacophore-guided generative design: Frameworks that balance pharmacophore similarity to reference compounds with structural diversity, demonstrating strong potential for generating novel bioactive scaffolds for complex targets [38].
These AI-enhanced methods represent the next generation of pharmacophore-based approaches, particularly valuable for addressing challenging neurodegenerative disease targets with limited traditional chemical starting points.
Structure-based and ligand-based pharmacophore modeling provide complementary approaches for initiating virtual screening campaigns against neurodegenerative disease targets. The protocols detailed in this application note offer robust methodologies for generating high-quality pharmacophore models, with specific considerations for CNS drug discovery. The integration of these approaches with BBB permeability prediction and emerging AI technologies creates powerful frameworks for identifying novel therapeutic candidates for Alzheimer's disease, Parkinson's disease, and other neurodegenerative conditions. As computational methods continue to advance, pharmacophore modeling remains an essential component of the rational drug design toolkit for neurodegenerative disease research.
The success of any virtual screening (VS) campaign is fundamentally dependent on the quality and composition of the initial compound library. [29] This section details the protocols for curating databases and preparing a specialized compound library for pharmacophore-based virtual screening (PBVS) targeting neurodegenerative diseases. A well-prepared library, characterized by appropriate molecular complexity, diversity, and drug-like properties, significantly enhances the probability of identifying novel, developable hit compounds. [39] [40] The procedures outlined below are adapted from established computational drug discovery workflows and have been successfully applied in recent research to identify multi-target agents for conditions like Alzheimer's disease. [40] [2]
Database Selection and Acquisition
The first step involves selecting and acquiring high-quality, chemically diverse databases. Both commercial and public databases can be utilized, with a growing emphasis on natural product libraries due to their structural complexity and novelty. [39] [40]
Table 1: Representative Databases for Library Construction
| Database Name | Type | Key Features | Relevance to Neurodegenerative Research |
|---|---|---|---|
| Traditional Chinese Medicine (TCM) [39] | Natural Product | Contains compounds from Chinese medicinal plants. | High structural diversity; source of neuroactive compounds. |
| AfroDb [39] | Natural Product | African Medicinal Plants database. | Unexplored chemical space; potential for novel scaffolds. |
| NuBBE [39] | Natural Product | Nuclei of Bioassays, Biosynthesis, and Ecophysiology of Natural Products. | Biologically validated and diverse South American natural products. |
| UEFS [39] | Natural Product | Universidade Estadual de Feira de Santana database. | Complementary chemical space from Brazilian biodiversity. |
| PubChem [40] [2] | Public Repository | Massive collection of bioactive molecules and metabolites. | Source for specialized libraries (e.g., fungal metabolites); over 17,000 compounds screened in recent studies. [40] |
| Fungal Metabolites [40] [2] | Specialized Natural Product | Library of compounds derived from fungi. | A source of promising multi-target inhibitors for AD, such as Bisacremine-C. [40] |
Compound Processing and Fragmentation
To access a wider range of chemical space, particularly for fragment-based drug design (FBDD), selected compounds can be subjected to in silico fragmentation.
Protocol: Retrosynthetic Combinatorial Analysis Procedure (RECAP)
The RECAP technique is a standard method for generating fragment libraries by cleaving bonds based on chemically sensible rules. [39]
- Objective: To deconstruct large, complex molecules (like natural products) into smaller, synthetically accessible fragments while retaining key functional groups.
Method:
- Input: Prepare a database of parent compounds (e.g., from Table 1) in a suitable molecular file format (e.g., SDF).
- Cleavage: Apply RECAP rules, which cleave bonds adjacent to specific chemical functionalities (e.g., amide, ester, ether linkages). [39]
- Generation of Fragment Types:
- Extensive (Leaf) Fragments: Exhaustive cleavage to generate the smallest possible fragments. This approach can lead to simpler, but sometimes overly repetitive, chemical entities. [39]
- Non-Extensive (Non-Leaf) Fragments: Systematic cleavage that generates all possible "intermediate" scaffolds. This method produces larger, more complex fragments that cover a broader and less repetitive chemical space. [39]
- Output: Two separate fragment libraries: one containing extensive NPDFs and the other containing non-extensive NPDFs.
Application Note: Research has demonstrated that non-extensive fragmentation of natural products yields fragments with higher pharmacophore fit scores, greater diversity, and better developability potential compared to both their extensively fragmented counterparts and the original parent compounds. [39]
Library Filtering and Preparation for Screening
The raw or fragmented compound collection must be filtered and processed to create a screening-ready library.
Protocol: Drug-Likeness and Blood-Brain Barrier (BBB) Penetration Filtering
This protocol is critical for neurodegenerative disease targets, where compounds often need to reach the central nervous system. [40]
- Objective: To filter out compounds with undesirable properties and enrich the library for molecules capable of crossing the BBB.
Method:
- Standard Drug-Likeness Filters: Apply rules such as Lipinski's Rule of Five to filter the library. Calculate key physicochemical properties:
- Molecular Weight (MW): Typically < 500 Da for drug-like molecules.
- Lipophilicity (LogP): Typically < 5.
- Hydrogen Bond Donors (HBD): ≤ 5.
- Hydrogen Bond Acceptors (HBA): ≤ 10. [40]
- BBB Permeability Prediction: Use computational models (e.g., in software like Schrodinger's QikProp or open-source tools) to predict passive blood-brain barrier penetration. Retain compounds predicted to be BBB-positive. [40]
- Structural Filtering: Remove compounds with reactive functional groups or pan-assay interference compounds (PAINS) that can cause false-positive results in biological assays.
- Standard Drug-Likeness Filters: Apply rules such as Lipinski's Rule of Five to filter the library. Calculate key physicochemical properties:
Application Note: In a study screening fungal metabolites for Alzheimer's disease, a drug-likeness and BBB-positive filter was employed, reducing a library of 17,544 compounds to 14 best hits for further investigation. [40]
Protocol: 3D Conformer Generation and Energy Minimization
Pharmacophore screening requires compounds to be in a three-dimensional (3D) format. [41]
- Objective: To generate low-energy 3D conformations for each compound in the filtered library.
- Method:
- Input: The filtered 2D compound library (e.g., in SDF or SMILES format).
- 3D Conversion: Use tools like Open Babel (integrated in platforms like PyRx) or CORINA to generate initial 3D coordinates. [40]
- Conformer Generation: For more robust screening, generate an ensemble of multiple low-energy conformers for each molecule (e.g., 100-250 conformers) to account for molecular flexibility. This can be done using tools like OMEGA or the conformer generation functions in MOE or Discovery Studio. [39]
- Energy Minimization: Optimize the geometry of each 3D structure using a molecular mechanics force field (e.g., Universal Force Field - UFF, MMFF94) to relieve steric clashes and reach a local energy minimum. [40]
- Output: A library of energy-minimized 3D structures or conformers in a format suitable for PBVS (e.g., MOL2, SDF).
The following diagram illustrates the complete workflow from database selection to a screening-ready library.
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Software and Databases for Library Preparation
| Item Name | Type | Function in Library Preparation |
|---|---|---|
| PubChem Database [40] [2] | Chemical Database | A public repository to retrieve 3D conformers and structural data for a vast array of compounds. |
| RECAP (Retrosynthetic Combinatorial Analysis Procedure) [39] | Computational Algorithm | A set of rules used for the in silico fragmentation of molecules to generate chemically sensible fragments for FBDD. |
| Open Babel / PyRx [40] | Cheminformatics Tool | Used for file format conversion, 3D structure generation, and energy minimization of compound libraries using force fields (e.g., UFF). |
| Discovery Studio / MOE (Molecular Operating Environment) [41] | Integrated Software Suite | Provides comprehensive tools for structure-based pharmacophore model creation, database curation, 3D conformer generation, and virtual screening. |
| PharmMapper [41] | Online Server & Database | A robust platform for pharmacophore screening, utilizing a complex-based pharmacophore database (PharmTargetDB) for reverse target prediction. |
| LigandScout [39] [29] | Software Application | Used to create structure-based and ligand-based pharmacophore models from protein-ligand complexes or a set of active ligands. |
Core Algorithms for Pharmacophore-Based Virtual Screening
Virtual screening relies on sophisticated computational algorithms to efficiently identify potential hit compounds from large chemical libraries. The choice of algorithm significantly impacts the success and efficiency of the screening campaign.
Traditional and Emerging Screening Approaches
Table 1: Virtual Screening Algorithms and Their Applications
| Algorithm Type | Method Description | Key Advantages | Representative Software/Tools | Reported Applications |
|---|---|---|---|---|
| Pharmacophore-Based Screening | Identifies compounds matching 3D arrangement of chemical features essential for biological activity | Intuitive, handles ligand flexibility, fast screening of large libraries | LigandScout, Phase (Schrödinger) | KHK-C inhibitor discovery [42] [43], BACE-1 inhibitors for Alzheimer's [15] |
| Molecular Docking | Predicts binding pose and affinity of small molecules in protein binding sites | Detailed binding mode analysis, structure-based design | Glide, Smina, AutoDock | SARS-CoV-2 NSP13 helicase inhibitors [44], MAO inhibitors [45] |
| Machine Learning-Accelerated Screening | ML models trained on docking scores or chemical features for rapid affinity prediction | Extremely fast (1000x faster than docking), handles ultra-large libraries | Custom ensemble models, PharmacoNet | MAO inhibitor identification [45] |
| Fragment-Based Pharmacophore Screening | Aggregates pharmacophore features from multiple fragment poses into joint query | Identifies micromolar hits from millimolar fragments, leverages structural data | FragmentScout | SARS-CoV-2 NSP13 helicase inhibitors [44] |
For neurodegenerative disease targets, multiple studies have demonstrated successful implementation of pharmacophore-based screening. In the discovery of KHK-C inhibitors for metabolic disorders (relevant to neurodegenerative metabolic components), researchers employed pharmacophore-based virtual screening of 460,000 compounds from the National Cancer Institute library as an initial filter, followed by multi-level molecular docking [42] [43]. Similarly, for Alzheimer's disease targets, pharmacophore screening of fungal metabolite libraries identified 14 best hits from 17,544 compounds that were subsequently evaluated against GSK-3β, NMDA receptor, and BACE-1 targets [2].
The emerging trend of machine learning acceleration addresses critical bottlenecks in traditional methods. As demonstrated in MAO inhibitor discovery, ML models can achieve 1,000-fold faster binding energy predictions compared to classical molecular docking while maintaining reasonable accuracy [45]. For ultra-large-scale screening, deep learning frameworks like PharmacoNet enable screening of 187 million compounds against cannabinoid receptors in approximately 21 hours on a single CPU [46].
Scoring Functions and Binding Affinity Assessment
Accurate scoring of protein-ligand interactions is crucial for prioritizing compounds with genuine therapeutic potential. Multiple complementary scoring approaches provide a comprehensive assessment of binding affinity.
Multi-Level Scoring Strategy
Table 2: Scoring Methods for Binding Affinity Assessment
| Scoring Method | Calculated Parameters | Interpretation | Typical Range for Hits | Application Example |
|---|---|---|---|---|
| Molecular Docking Scoring | Docking score (kcal/mol) | Predicts binding pose and relative affinity | -6.54 to -9.10 kcal/mol | KHK-C inhibitors: -7.79 to -9.10 kcal/mol vs clinical candidates: -7.77 (PF-06835919), -6.54 (LY-3522348) [42] |
| Binding Free Energy Calculations (MM/GBSA) | ΔG binding (kcal/mol) | More accurate estimation of binding free energy | -45 to -71 kcal/mol | KHK-C inhibitors: -57.06 to -70.69 kcal/mol vs clinical candidates: -56.71 (PF-06835919), -45.15 (LY-3522348) [42] [43] |
| Binding Constant Estimation | Kᵢ (M⁻¹) | Inhibition constant derived from docking scores | 10⁶ M⁻¹ range | Bisacremine-C: 2.4×10⁶ M⁻¹ (GSK-3β), 9.2×10⁶ M⁻¹ (NMDA), 4.7×10⁶ M⁻¹ (BACE-1) [2] |
| Fold Improvement Calculation | Fold affinity increase | Comparison to native ligand/reference compound | 6-25 fold | Bisacremine-C showed 25-fold higher affinity for GSK-3β, 6.3-fold for NMDA, 9.04-fold for BACE-1 vs native ligands [2] |
The implementation of multi-level scoring is well-demonstrated in the KHK-C inhibitor discovery campaign. After initial pharmacophore screening, researchers employed molecular docking which identified compounds with docking scores ranging from -7.79 to -9.10 kcal/mol, superior to clinical candidates PF-06835919 (-7.768 kcal/mol) and LY-3522348 (-6.54 kcal/mol) [42]. Subsequent binding free energy calculations using MM/GBSA further validated these results, showing energies from -57.06 to -70.69 kcal/mol compared to -56.71 kcal/mol and -45.15 kcal/mol for the reference compounds [42] [43].
For neurodegenerative disease targets, the binding affinity can be expressed as inhibition constants. In the screening of fungal metabolites against Alzheimer's targets, the top hit Bisacremine-C exhibited Kᵢ values of 2.4 × 10⁶ M⁻¹ for GSK-3β, 9.2 × 10⁶ M⁻¹ for NMDA receptor, and 4.7 × 10⁶ M⁻¹ for BACE-1, representing substantial improvements over native ligands [2].
Hit Identification and Validation Protocols
Hit identification requires rigorous triage and validation to advance only the most promising candidates for further development.
Comprehensive Hit Triage Workflow
Experimental Protocol for Hit Validation
Protocol 3.1: Comprehensive Hit Identification and Validation
Step 1: Initial Hit Selection Based on Binding Parameters
- Select compounds with docking scores better than reference compounds (e.g., < -7.7 kcal/mol for KHK-C inhibitors) [42]
- Apply binding free energy cutoffs (e.g., < -56 kcal/mol for KHK-C targets) [43]
- For neurodegenerative targets: prioritize multi-target activity (e.g., simultaneous GSK-3β, NMDA, and BACE-1 inhibition) [2]
Step 2: ADMET Profiling
- Use QikProp (Schrödinger), SwissADME, and ADMETlab 2.0 for comprehensive pharmacokinetic assessment [15] [2]
- Apply Lipinski's Rule of Five for drug-likeness evaluation
- Exclude compounds with immunotoxicity concerns (e.g., compounds B, F, L from fungal metabolites were excluded for immunotoxicity) [2]
- Prefer compounds with higher LD₅₀ values (e.g., >5000 mg/kg for fungal metabolites E, H, I, J) [2]
Step 3: Molecular Dynamics Simulation Validation
- Run simulations for 100-300 ns using Desmond or similar software [44] [2]
- Analyze RMSD (protein-ligand complex stability), RMSF (residual flexibility), Rg (radius of gyration), and SASA (solvent accessible surface area)
- Criteria for success: RMSD maintained between 1.5-3.5 Å with minimal fluctuations [32] [15]
- Identify key molecular interactions maintained during simulation (hydrophobic contacts, hydrogen bonds) [2]
Step 4: Multi-Target Assessment for Neurodegenerative Diseases
- For Alzheimer's disease targets, evaluate binding to multiple targets: GSK-3β, NMDA receptor, and BACE-1 [2]
- Calculate fold improvement over native ligands for each target
- Prioritize compounds with balanced multi-target activity rather than extreme selectivity for single targets
Research Reagent Solutions
Table 3: Essential Research Reagents and Computational Tools
| Reagent/Tool Category | Specific Resources | Function/Application | Key Features |
|---|---|---|---|
| Compound Libraries | National Cancer Institute (NCI) Library [42], VITAS-M Laboratory Database [15], ZINC Database [45], Fungal Metabolite Database [2] | Source of diverse chemical compounds for screening | 460,000 compounds (NCI), 1.4 million compounds (VITAS-M), commercial and natural product collections |
| Virtual Screening Software | LigandScout [44], Phase (Schrödinger) [15], Glide [44], Smina [45], AutoDock [2] | Pharmacophore modeling, molecular docking, virtual screening | LigandScout XT enables ultra-large library screening; Glide provides high-quality docking poses |
| Molecular Dynamics Software | Desmond [2], GROMACS | Simulation of protein-ligand interactions in biological environment | Assesses complex stability, binding modes, and dynamic interactions over time |
| ADMET Prediction Tools | QikProp [15], SwissADME [15], ADMETlab 2.0 [15] | Prediction of absorption, distribution, metabolism, excretion, and toxicity | Rule of Five compliance, toxicity risk assessment, pharmacokinetic profiling |
| Specialized Workflows | FragmentScout [44], PharmacoNet [46] | Fragment-based screening, deep learning-guided pharmacophore modeling | FragmentScout aggregates pharmacophore features from multiple fragment poses; PharmacoNet enables ultra-fast screening |
The success of virtual screening campaigns depends on appropriate selection and combination of these tools. For instance, the discovery of KHK-C inhibitors employed a sequential workflow using pharmacophore-based screening (LigandScout), followed by molecular docking (Glide), binding free energy calculations (MM/GBSA), ADMET profiling, and finally molecular dynamics simulations [42] [43]. This multi-step approach refined 460,000 initial compounds to a single promising candidate (Compound 2) with superior predicted properties compared to clinical-stage candidates.
For neurodegenerative targets, the additional consideration of blood-brain barrier permeability is crucial, as demonstrated in the discovery of KMO inhibitors where compounds VS1 and VS6 were prioritized based on predicted BBB permeability [47]. The multi-target approach for Alzheimer's disease further compounds the complexity, requiring balanced activity against multiple pathological targets simultaneously [2].
Kynurenine-3-monooxygenase (KMO) is a flavin adenine dinucleotide (FAD)-containing enzyme located on the outer mitochondrial membrane and represents a pivotal branch point in the kynurenine pathway (KP), the major catabolic route of tryptophan in mammals [48]. At this metabolic junction, KMO catalyzes the hydroxylation of L-kynurenine (L-Kyn) to 3-hydroxykynurenine (3-HK), steering metabolism toward the production of neurotoxic metabolites, including the excitotoxin quinolinic acid (QUIN) [48] [49]. Conversely, the alternative branch, catalyzed by kynurenine aminotransferase (KAT), leads to the formation of the neuroprotective metabolite kynurenic acid (KYNA) [50]. The balance between these neurotoxic and neuroprotective branches is crucial for neuronal health, and its dysregulation is implicated in the pathogenesis of several neurodegenerative diseases, including Alzheimer's disease (AD), Huntington's disease (HD), and Parkinson's disease (PD) [51] [48] [52]. Inhibition of KMO presents a compelling therapeutic strategy as it shunts the metabolic flux away from the neurotoxic cascade toward the neuroprotective KYNA, thereby normalizing the imbalance of neuroactive metabolites associated with neurodegeneration [53].
The rationale for targeting KMO is further strengthened by genetic and pharmacological evidence. In models of Huntington's disease, genetic ablation of KMO was shown to ameliorate neurodegeneration [48]. Furthermore, pharmacological inhibition of KMO has demonstrated therapeutic benefits in diverse preclinical models of neurodegeneration [53] [52]. Despite these promising results, a significant challenge has been the poor blood-brain barrier (BBB) permeability of many early-stage KMO inhibitors, which limits their ability to directly modulate central metabolite levels [47] [54] [53]. Additionally, many conventional substrate-like inhibitors act as non-substrate effectors, stimulating the production of cytotoxic hydrogen peroxide (H~2~O~2~)—a phenomenon known as the "oxygen dilemma" [54] [53]. These limitations underscore the necessity for innovative drug discovery approaches, such as pharmacophore-based virtual screening, to identify novel, brain-permeable competitive inhibitors that avoid detrimental side reactions.
The Kynurenine Pathway and KMO Signaling
The kynurenine pathway is the principal route of tryptophan catabolism in mammals, accounting for the processing of approximately 95% of dietary tryptophan [48]. As illustrated in the diagram below, this pathway generates several neuroactive metabolites, with KMO occupying a critical position that determines the balance between neuroprotection and neurotoxicity.
Diagram 1: The Kynurenine Pathway and Key Metabolites. KMO is a critical enzyme at the branch point, directing flux toward neurotoxic (3-HK, QUIN) or neuroprotective (KYNA) metabolites. IDO: Indoleamine 2,3-dioxygenase; TDO: Tryptophan 2,3-dioxygenase; KAT: Kynurenine aminotransferase.
KMO is a class A FAD-dependent monooxygenase. Its reaction follows a random bi–bi mechanism involving the formation of a ternary complex with L-KYN and the cofactor NADPH [53]. The binding of substrate-like inhibitors can induce a conformational change that facilitates NADPH binding and flavin reduction. In the absence of a hydroxylatable substrate, the reactive flavin intermediate decomposes, leading to the production of H~2~O~2~ [54] [53]. This has led to the classification of KMO inhibitors into two types: Type I (non-substrate effectors), which stimulate H~2~O~2~ production, and Type II (competitive inhibitors), which bind without triggering this deleterious side reaction [54]. The development of Type II inhibitors is, therefore, a major goal in the field.
Pharmacophore-Based Virtual Screening Protocol
This protocol outlines a structure-based virtual screening strategy designed to identify novel, brain-permeable Type II KMO inhibitors, leveraging multiple reported inhibitor binding conformations to enhance structural diversity and avoid the limitations of previous approaches [47] [54].
Homology Modeling of Human KMO (hKMO)
The absence of a complete, drug-design-suitable crystal structure for hKMO necessitates the creation of homology models. The following three models are constructed to account for distinct ligand binding modes, using ScKMO (35.3% identity) and PfKMO (33.7% identity) as templates [54].
- Model 1 (Type II Competitive Inhibitor Model): Based on the ScKMO structure bound to Ro 61-8084 (e.g., PDB 5X6R). This model represents a competitive inhibitor binding mode that does not stimulate H~2~O~2~ production [54].
- Model 2 (Type I Non-Substrate Effector Model): Based on a high-resolution PfKMO structure bound to the native substrate L-KYN. This model is used to understand and avoid substrate-like binding [54].
- Model 3 (Type II FAD-Trapped Model): Based on PfKMO structures where FAD is trapped in an unproductive, tilted conformation by benzisoxazole inhibitors (e.g., PDB 5NAE, 5NAG). This binding mode also prevents H~2~O~2~ production [54].
Validation of Homology Models: Each model must be rigorously validated before use in virtual screening. The following quality metrics should be achieved [54]:
- RMSD to Template: < 1.0 Å for the backbone atoms.
- Ramachandran Plot: > 95% of residues in energetically allowed regions.
- 3D-Profiles Score: > 90% of residues with a valid score indicating a correct structural environment.
Pharmacophore Generation and Virtual Screening
The screening workflow, designed to maximize the identification of diverse and promising hit compounds, is summarized in the diagram below.
Diagram 2: Pharmacophore-Based Virtual Screening Workflow. The multi-model approach ensures the identification of diverse, brain-permeable competitive inhibitors.
Step-by-Step Protocol:
Preparation of Compound Library
- Source compounds from commercial libraries (e.g., ZINC, Sigma-Aldrich natural products).
- Prepare ligands: generate 3D structures, optimize geometry using the MMFF94 force field, and generate probable tautomers and protonation states at physiological pH (7.4) [55].
- Filter the library using Lipinski's Rule of Five and Veber's rules to prioritize drug-like compounds. Remove compounds with reactive functional groups [55].
Generation of Protein-Ligand Complex Pharmacophores
- For each validated homology model, re-dock known co-crystallized inhibitors to ensure the model can reproduce native binding poses (target: heavy atom RMSD < 1.0 Å) [54].
- Using the protein-inhibitor complex structure, generate a structure-based pharmacophore model for each binding mode. Key features to include are [47] [54]:
- One hydrogen bond acceptor feature positioned to interact with Arg83/Tyr97 (PfKMO numbering).
- One or two hydrophobic/arromatic features to occupy the substrate's aniline ring binding pocket.
- Exclusion volumes to define the steric boundaries of the active site.
Virtual Screening and Hit Selection
- Screen the prepared compound library against each of the three pharmacophore models.
- Select compounds that match all critical features of at least one model.
- Overlap and cluster the hits from the different models to prioritize structurally diverse chemotypes.
- Apply ADME/T (Absorption, Distribution, Metabolism, Excretion, Toxicity) filters using tools like SwissADME and ProTox-II to predict properties such as [55]:
- BBB Permeability: Prioritize compounds predicted to cross the BBB.
- Lipophilicity: Optimal Log P ~ 2-3.
- Topological Polar Surface Area (TPSA): Prefer TPSA < 90 Ų for better brain penetration.
- No structural alerts for toxicity.
Experimental Validation Protocols
In Vitro KMO Enzyme Inhibition Assay
Objective: To determine the half-maximal inhibitory concentration (IC~50~) of hit compounds identified from virtual screening.
Reagents and Materials:
- Recombinant human KMO enzyme (commercially available)
- Test compounds (dissolved in DMSO, final concentration ≤ 1%)
- Substrate: L-Kynurenine (L-Kyn)
- Cofactor: NADPH
- Assay buffer (e.g., 50 mM Tris-HCl, pH 7.4)
- 96-well clear microplate
- Microplate reader capable of reading absorbance at 340 nm
Procedure:
- Prepare the reaction mixture in a 96-well plate on ice. The final 150 µL reaction volume should contain [55]:
- Assay Buffer: 50 µL
- Human KMO (20 µg/mL): 50 µL
- Test compound (varying concentrations) or DMSO vehicle (control): 10 µL
- Substrate mix (NADPH [10 mM] and L-Kyn [20 mM]): 40 µL
- Incubate the reaction plate at room temperature for 1.5 hours.
- Measure the absorbance at 340 nm (A~340~) using a microplate reader. The decrease in A~340~ corresponds to the oxidation of NADPH, which is proportional to KMO activity.
- Calculate the percentage inhibition for each compound concentration using the formula: % Activity = [(Abs~sample~ - Abs~blank~) / (Abs~control~ - Abs~blank~)] × 100 [55]
- Plot the % inhibition versus the logarithm of compound concentration and fit the data with a non-linear regression curve to determine the IC~50~ value. Perform all assays in triplicate.
Mechanism of Inhibition and Kinetic Analysis
Objective: To characterize the inhibition modality (competitive, non-competitive) and determine the inhibition constant (K~i~) of confirmed hit compounds.
Procedure:
- Perform the KMO enzyme inhibition assay as described in Section 4.1, but vary the concentration of the substrate L-Kyn (e.g., 0, 5, 10, 20 µM) in the presence of several fixed concentrations of the inhibitor (e.g., 0, 0.5xIC~50~, IC~50~, 2xIC~50~) [55].
- Measure the initial reaction rates (v) for each combination of L-Kyn and inhibitor concentration.
- Plot the data as a Lineweaver-Burk plot (double-reciprocal plot: 1/v vs. 1/[L-Kyn]).
- Analyze the pattern of lines:
- Competitive Inhibition: Lines intersect on the y-axis.
- Non-competitive Inhibition: Lines intersect on the x-axis.
- Uncompetitive Inhibition: Parallel lines.
- Calculate the K~i~ value using the appropriate equation for the determined inhibition modality. Competitive inhibitors are preferred as they are more likely to be true Type II inhibitors [53] [55].
Assessment of Hydrogen Peroxide Production
Objective: To classify hits as Type I or Type II inhibitors by detecting H~2~O~2~ generation.
Procedure:
- Use a commercial H~2~O~2~ detection kit (e.g., Amplex Red Hydrogen Peroxide/Peroxidase Assay Kit).
- Set up reactions containing KMO, NADPH, and the inhibitor (at its IC~50~ concentration) in the absence of the substrate L-Kyn.
- Include controls: a negative control (no inhibitor) and a positive control (a known Type I inhibitor, e.g., UPF-648).
- Measure H~2~O~2~ production according to the manufacturer's instructions, typically by monitoring fluorescence (excitation/emission ~571/585 nm).
- Interpretation: Inhibitors that do not significantly increase H~2~O~2~ levels above the negative control are classified as Type II competitive inhibitors and are considered promising leads [54] [53].
Data Presentation and Analysis
The application of virtual screening and experimental validation has led to the discovery of several novel KMO inhibitors with diverse scaffolds. The table below summarizes key quantitative data for representative inhibitors.
Table 1: Experimentally Validated Novel KMO Inhibitors
| Compound ID / Name | Chemical Class | Reported IC₅₀ / Kᵢ | Inhibition Mode | BBB Permeability (Predicted/Measured) | H₂O₂ Production | Source/Reference |
|---|---|---|---|---|---|---|
| VS1 | Not Specified | In vitro activity confirmed | Not Specified | Predicted Permeable | Avoids | [47] [54] |
| VS6 | Not Specified | In vitro activity confirmed | Not Specified | Predicted Permeable | Avoids | [47] [54] |
| Compound 1 | Not Specified | IC₅₀: 400 nM (PfKMO) | Competitive | Minimal (Mouse) | No | [53] |
| 3′-Hydroxy-alpha-naphthoflavone | Flavonoid | IC₅₀: 15.85 ± 0.98 µM | Competitive | Predicted Permeable | Not Tested | [55] |
| 3′-Hydroxy-ss-naphthoflavone | Flavonoid | IC₅₀: 18.71 ± 0.78 µM | Competitive | Predicted Permeable | Not Tested | [55] |
| Genkwanin | Flavonoid | IC₅₀: 21.61 ± 0.97 µM | Non-competitive | Predicted Permeable | Not Tested | [55] |
| Apigenin | Flavonoid | IC₅₀: 24.14 ± 1.00 µM | Non-competitive | Predicted Permeable | Not Tested | [55] |
Key Research Reagents and Solutions
Table 2: Essential Research Reagents for KMO Inhibitor Screening
| Reagent / Resource | Specifications / Example Source | Primary Function in Protocol |
|---|---|---|
| Recombinant hKMO Enzyme | Human, purified (e.g., Thermo Fisher Scientific) | Target enzyme for in vitro inhibition and kinetic assays. |
| L-Kynurenine (L-Kyn) | Substrate, >98% purity (e.g., Sigma-Aldrich) | Native enzyme substrate for activity and inhibition studies. |
| β-Nicotinamide adenine dinucleotide phosphate (NADPH) | Coenzyme, tetrasodium salt (e.g., Sigma-Aldrich) | Essential cofactor for the KMO catalytic cycle. |
| Ro 61-8048 | Potent known KMO inhibitor (e.g., Sigma-Aldrich) | Reference compound for assay validation and as a positive control. |
| Homology Modeling Software | e.g., MODELLER, SWISS-MODEL | Generating 3D structural models of hKMO for structure-based design. |
| Virtual Screening Platform | e.g., Schrödinger Suite, AutoDock Vina, SwissSimilarity | Performing molecular docking and pharmacophore-based screening. |
| H₂O₂ Detection Kit | e.g., Amplex Red Hydrogen Peroxidase Assay Kit (Thermo Fisher) | Classifying inhibitors as Type I or Type II based on H₂O₂ production. |
| ADME/T Prediction Tools | SwissADME, ProTox-II (web servers) | Predicting pharmacokinetics and toxicity of virtual hit compounds. |
This application note details a comprehensive and rational framework for the identification and validation of novel KMO inhibitors, with a specific emphasis on a pharmacophore-based virtual screening protocol suitable for a thesis on neurodegenerative disease target research. The integration of computational modeling, leveraging multiple inhibitor binding conformations, with rigorous experimental validation provides a powerful strategy to overcome the historical challenges in KMO drug discovery, specifically poor brain penetration and the H~2~O~2~ production dilemma [47] [54] [53]. The successful identification of flavonoids and other novel chemotypes as KMO inhibitors underscores the potential of this approach to expand the chemical space beyond traditional substrate analogues [55].
Future work in this area will focus on hit-to-lead optimization of the identified compounds, guided by structure-activity relationship (SAR) studies and advanced computational analyses. The recent development of novel SAR insights and activity landscape modeling, including the identification of activity cliffs, provides a refined framework for the rational design of next-generation KMO therapeutics [51]. Furthermore, in vivo validation of the most promising leads in preclinical models of neurodegeneration is the critical next step to fully establish their therapeutic potential [53] [52]. The continued refinement of these integrated computational and experimental protocols will accelerate the discovery of effective KMO inhibitors, offering a promising avenue for treating a range of devastating neurodegenerative diseases.
The blood-brain barrier (BBB) presents a major challenge in developing therapeutics for neurodegenerative diseases (NDDs) like Alzheimer's disease (AD), as it restricts the passage of most systemically administered drugs into the central nervous system (CNS) [1] [56]. Only an estimated 2% of small molecules can cross this highly selective barrier [1]. Neurotherapeutics require not only activity against CNS targets but also the ability to permeate the BBB to reach their site of action [1]. This application note details a pharmacophore-based virtual screening (VS) protocol integrated with BBB permeability prediction to identify promising neurotherapeutic candidates from natural products, framed within broader research on neurodegenerative disease targets.
Natural products offer particular promise for NDD treatment, with nearly 50% of newly approved drugs tracing their structural origins to natural compounds [1]. They often provide neuroprotective benefits with fewer side effects than conventional synthetic drugs [1]. Recent research has highlighted specific natural small molecules—including volatile components, omega-3 polyunsaturated fatty acids, polyphenols, and terpenoids—that can cross the BBB through mechanisms such as interacting with receptor proteins, suppressing efflux protein activity, and regulating tight junction protein expression [56].
Background and Significance
The Blood-Brain Barrier Challenge
The BBB is a complex network of brain microvessels that separates the CNS from peripheral blood circulation [1]. Its core components include [56]:
- Brain Microvascular Endothelial Cells (BMECs): Formed by tight junctions (TJs) that prevent paracellular passage of most substances.
- Tight Junction Proteins: Including occludin, Claudin-3, Claudin-5, and Zona Occludens (ZO-1, ZO-2, ZO-3) proteins.
- Pericytes and Astrocytes: These support cells contribute to BBB integrity and function.
- Efflux Transporters: Proteins like P-glycoprotein (P-gp) and Breast Cancer Resistance Protein (BCRP) that actively remove substances from the brain.
The restrictive nature of the BBB necessitates careful screening for BBB permeability early in the neurotherapeutic drug discovery pipeline [1].
Molecular Targets in Neurodegenerative Diseases
The multifactorial nature of NDDs like AD suggests that multi-target-directed ligands (MTDLs) may be more effective than single-target approaches [2]. Key targets include:
- GSK-3β (Glycogen Synthase Kinase-3β): Hyperactivation promotes tau protein phosphorylation, leading to neurofibrillary tangle formation [2].
- BACE-1 (Beta-Secretase 1): Initiates amyloid-beta peptide production, contributing to amyloid plaque formation [2].
- NMDA Receptor (N-Methyl-D-Aspartate Receptor): Overactivation leads to excitotoxicity and neuronal death [2].
- Phosphorylated Tau (P-tau): A key pathological protein in AD and other tauopathies that disrupts microtubule stability and axonal transport [26].
Table 1: Key Molecular Targets in Alzheimer's Disease Drug Discovery
| Target | Biological Role in AD | Therapeutic Approach |
|---|---|---|
| GSK-3β | Hyperphosphorylation of tau protein leading to neurofibrillary tangles [2] | Inhibition to reduce tau phosphorylation |
| BACE-1 | Cleaves amyloid precursor protein (APP) to generate amyloid-beta peptides [2] | Inhibition to reduce amyloid plaque formation |
| NMDA Receptor | Glutamate receptor; overactivation causes excitotoxicity [2] | Antagonism to prevent excitotoxic damage |
| P-tau | Mislocalized hyperphosphorylated tau disrupts microtubules and synaptic function [26] | Inhibition of phosphorylation or aggregation |
Computational Screening Protocol
Pharmacophore-Based Virtual Screening Workflow
The following diagram illustrates the complete computational workflow for identifying BBB-permeable neurotherapeutics from natural products:
Detailed Methodology
Step 1: Pharmacophore-Based Virtual Screening
- Tools: Pharmit, ChemMine, SwissSimilarity [1]
- Reference Compounds: Five FDA-approved drugs for neurodegenerative diseases serve as pharmacophore templates [1]
- Screening Databases: PubChem, DrugBank, Zinc15, ChemSpace, ChEMBL, CHEBI [1]
- Similarity Metric: Tanimoto similarity score for structural similarity assessment [1]
- Output: Initial candidate molecules with structural similarity to reference CNS drugs
Step 2: BBB Permeability and CNS Activity Prediction
- Tools: Machine learning and deep learning models [1]
- Molecular Descriptors: Computed using ChemDes (ChemoPy Descriptor Calculator) [1]
- Key Parameters:
- BBB permeability classification (permeable vs. non-permeable)
- Brain-to-blood ratio estimation [1]
- CNS activity prediction based on structural features
- Output: Classification of molecules into BBB-permeable (CNS+) and BBB-impermeable (CNS-) categories
Step 3: ADMET Profiling and Drug-Likeness Assessment
- Parameters Evaluated:
- Output: Compounds with favorable pharmacokinetic and safety profiles
Step 4: Multi-Target Molecular Docking
- Target Proteins: GSK-3β, NMDA receptor, BACE-1 [2]
- Docking Tools: AutoDock-based PyRx-Python 0.8 tool [2]
- Validation: Re-docking of native ligands to validate docking protocols
- Analysis: Binding affinity (ΔG) and inhibition constant (Ki) calculations [2]
- Visualization: BIOVIA Discovery Studio Visualizer for interaction analysis [2]
Step 5: Molecular Dynamics Simulation
- Tool: Desmond (Schrödinger) [2]
- Simulation Duration: 100 nanoseconds or longer [2]
- Parameters Analyzed:
- Root Mean Square Deviation (RMSD)
- Root Mean Square Fluctuation (RMSF)
- Radius of Gyration (Rg)
- Solvent Accessible Surface Area (SASA) [2]
- Output: Validation of complex stability and binding interactions
Table 2: Key Computational Tools and Resources for BBB-Permeable Neurotherapeutic Discovery
| Tool Category | Specific Tools | Application in Workflow |
|---|---|---|
| Pharmacophore Screening | Pharmit, ChemMine, SwissSimilarity [1] | Initial virtual screening based on structural similarity |
| Descriptor Calculation | ChemDes, RDKit, PaDel [1] | Computation of molecular descriptors for QSAR modeling |
| BBB Permeability Prediction | Machine Learning Models, AI-Driven Approaches [1] [56] | Classification of BBB permeability and CNS activity |
| Molecular Docking | PyRx (AutoDock), BIOVIA Discovery Studio [2] | Binding affinity prediction and interaction analysis |
| Dynamics Simulation | Desmond [2] | Stability assessment of protein-ligand complexes |
| Natural Product Database | PubChem, ZINC, NPClassifier [1] | Source libraries for natural product screening |
Experimental Validation Protocols
In Vitro BBB Permeability Assays
Blood-Brain Barrier Transwell Model
- Cell Culture: Primary human brain microvascular endothelial cells (HBMECs) co-cultured with astrocytes and pericytes [56]
- Model Setup:
- Culture HBMECs on collagen-coated Transwell inserts (3.0μm pore size)
- Measure transendothelial electrical resistance (TEER) using volt-ohm meter
- Validate barrier integrity with TEER values >150 Ω·cm² [56]
- Permeability Assay:
- Apply test compounds to donor compartment (apical side)
- Sample from acceptor compartment (basolateral side) at 15, 30, 60, 120 minutes
- Analyze compound concentration using LC-MS/MS
- Calculate apparent permeability (Papp) = (dQ/dt)/(A×C₀)
- Where dQ/dt = transport rate, A = membrane area, C₀ = initial concentration [56]
Efflux Transporter Interactions
- P-glycoprotein Inhibition Assay:
- Include specific P-gp inhibitors (verapamil, cyclosporine A) as controls
- Compare compound permeability with and without inhibitors
- Calculate efflux ratio = Papp(B→A)/Papp(A→B)
- Efflux ratio >2 suggests P-gp substrate [56]
In Vivo Brain Uptake Studies
Brain-to-Plasma Ratio Determination
- Animal Model: Rodents (mice or rats)
- Administration: Intravenous injection of test compound
- Sample Collection:
- Collect blood and brain samples at multiple time points (5, 15, 30, 60, 120 min)
- Perfuse animals with saline to remove blood from brain vasculature
- Homogenize brain tissue and analyze compound levels using LC-MS/MS
- Calculation:
- Kp,brain = (Brain concentration)/(Plasma concentration)
- Kp,uu,brain = (Brain unbound concentration)/(Plasma unbound concentration) [1]
Multi-Target Biological Activity Assessment
Enzyme Inhibition Assays
GSK-3β Inhibition Assay:
- Recombinant GSK-3β enzyme with phospho-glycogen synthase peptide substrate
- Detection: ADP-Glo Kinase Assay or phospho-specific antibodies
- IC50 determination using 8-point concentration curve [2]
BACE-1 Inhibition Assay:
- Fluorescent resonance energy transfer (FRET)-based BACE-1 assay
- Substrate: Rh-EVNLDAEFK-Quencher
- Measure fluorescence increase upon cleavage (excitation 545nm/emission 585nm)
- IC50 determination with 10-point concentration curve [2]
Cellular Neuroprotective Assays
Aβ-induced Toxicity Model:
- Differentiated SH-SY5Y neurons or primary cortical neurons
- Pre-treatment with test compounds (1 hour) before Aβ₂₅‑₃₅ exposure (24 hours)
- Assess cell viability using MTT assay
- Measure caspase-3 activity for apoptosis assessment [2]
Tau Phosphorylation Assay:
- Cell models overexpressing human tau
- Treatment with test compounds for 24 hours
- Western blot analysis with phospho-tau antibodies (Ser202, Thr231, Ser396) [26]
- Quantify reduction in tau phosphorylation compared to controls
Case Study: Successful Application
Identification of Bisacremine-C as a Multi-Target Neurotherapeutic
A recent study demonstrated the successful application of this protocol in identifying Bisacremine-C, a fungal metabolite, as a promising multi-target neurotherapeutic candidate [2]. The compound showed:
- High BBB Permeability Prediction: Favorable physicochemical properties for CNS penetration
Multi-Target Inhibition:
- GSK-3β: ΔG = -8.7 ± 0.2 kcal/mol, Ki = 2.4 × 10⁶ M⁻¹ (25-fold higher affinity than native ligand)
- NMDA receptor: ΔG = -9.5 ± 0.1 kcal/mol, Ki = 9.2 × 10⁶ M⁻¹ (6.3-fold higher affinity)
- BACE-1: ΔG = -9.1 ± 0.2 kcal/mol, Ki = 4.7 × 10⁶ M⁻¹ (9.04-fold higher affinity) [2]
Molecular Dynamics Validation: Stable complex formation with all three targets over 100ns simulation [2]
- Key Interactions:
- GSK-3β: Hydrophobic contacts with ILE62, VAL70, ALA83, LEU188; H-bonds with GLN185
- NMDA: Hydrophobic contacts with TYR184, PHE246; H-bonds with SER180
- BACE-1: H-bonds with THR232; hydrophobic contacts with ILE110 [2]
Natural Product-Mediated BBB Permeability Enhancement
Research has identified several natural products that enhance BBB permeability through various mechanisms:
Table 3: Natural Products with BBB Permeability-Enhancing Properties
| Natural Product | Mechanism of BBB Permeation | Experimental Evidence |
|---|---|---|
| Borneol | Modulates tight junction proteins; inhibits P-gp efflux [56] | Enhanced brain delivery of co-administered drugs in rodent models |
| Menthol | Regulates tight junction-mediated transport [56] | Improved drug distribution in brain when used in modified liposomes |
| Polyphenols | Interaction with receptor proteins; suppression of efflux proteins [56] | Demonstrated BBB penetration in multiple in vitro and in vivo models |
| Volatile Components | Multiple mechanisms including TJ modulation and transporter inhibition [56] | Shown to cross BBB in pharmacokinetic studies |
The Scientist's Toolkit: Essential Research Reagents
Table 4: Essential Research Reagents for BBB-Permeable Neurotherapeutic Discovery
| Reagent/Category | Specific Examples | Function in Research Protocol |
|---|---|---|
| Computational Tools | Pharmit, PyRx, ChemDes, Desmond [1] [2] | Virtual screening, docking, dynamics simulation |
| Cell-Based BBB Models | Primary HBMECs, Astrocytes, Pericytes [56] | In vitro BBB permeability assessment |
| Target Proteins | Recombinant GSK-3β, BACE-1, NMDA receptor [2] | Enzyme inhibition and binding assays |
| Natural Product Libraries | Fungal Metabolites, Plant Extracts, Marine Compounds [1] [2] | Source of novel neurotherapeutic candidates |
| Analytical Instruments | LC-MS/MS, HPLC, Microplate Readers | Compound quantification and activity assessment |
| Animal Models | Transgenic AD mice, Wild-type rodents [1] | In vivo brain uptake and efficacy studies |
The integrated pharmacophore-based virtual screening protocol for identifying BBB-permeable neurotherapeutics from natural products provides a robust framework for CNS drug discovery. By combining computational prediction of BBB permeability with multi-target activity assessment, this approach addresses the key challenges in developing effective treatments for neurodegenerative diseases. The successful application of this protocol to identify compounds like Bisacremine-C demonstrates its potential to accelerate the discovery of novel multi-target neurotherapeutics with favorable BBB penetration properties.
Future directions include the incorporation of more sophisticated AI-driven BBB permeability models, expanded natural product libraries, and the development of advanced BBB-on-a-chip technologies for more predictive permeability screening. The integration of natural products with modern drug delivery systems, such as nanocarriers functionalized with BBB-targeting ligands, offers promising opportunities for enhanced brain delivery of neurotherapeutics [56].
Integrating ADMET and Drug-Likeness Predictions into the Screening Pipeline
The high failure rate of drug candidates in late-stage development, particularly for complex neurodegenerative diseases (NDs), is often attributable to poor pharmacokinetics, toxicity, or insufficient efficacy [57] [58]. Traditional screening pipelines, which prioritize binding affinity alone, are inadequate for addressing these challenges. Integrating Absorption, Distribution, Metabolism, Excretion, and Toxicity (ADMET) and drug-likeness predictions early in the virtual screening (VS) process is therefore critical for improving the probability of clinical success [59]. This protocol details the practical integration of these predictive methodologies into a pharmacophore-based virtual screening workflow, framed within the context of discovering multi-target ligands for neurodegenerative disease targets such as GSK-3β, BACE-1, and the NMDA receptor [57] [2].
The rationale for this integrated approach is rooted in the multifactorial pathology of diseases like Alzheimer's. Single-target therapies have largely failed to cure, halt, or reverse disease progression, creating a compelling case for Multi-Target Drug Design (MTDD) [57]. Consequently, a successful screening pipeline must not only identify compounds with desirable activity against multiple targets but also ensure these candidates possess favorable ADMET profiles and a high likelihood of reaching the central nervous system (CNS) intact [2].
Key Definitions and Computational Concepts
Table 1: Core Computational Concepts in Integrated Screening.
| Concept | Description | Role in Screening Pipeline |
|---|---|---|
| Pharmacophore Modeling [60] | An abstract description of molecular features essential for a compound's biological activity (e.g., hydrogen bond donors/acceptors, hydrophobic regions). | Serves as the initial filter to identify compounds from large libraries that possess the steric and electronic features necessary for binding. |
| Drug-Likeness [61] | A qualitative concept for predicting whether a compound is likely to be a successful oral drug, often based on rules like Lipinski's Rule of Five. | Provides a rapid, first-pass filter to eliminate compounds with structural attributes that are problematic for oral bioavailability. |
| ADMET Prediction [58] | Computational models that predict a compound's pharmacokinetic and toxicological properties (Absorption, Distribution, Metabolism, Excretion, Toxicity). | Enables the prioritization of lead compounds based on a favorable predicted behavior in vivo, reducing late-stage attrition. |
| Blood-Brain Barrier (BBB) Penetration [57] | A key component of 'Distribution' that predicts a compound's ability to cross the BBB and reach molecular targets in the CNS. | A critical filter for neurodegenerative disease research to ensure candidates can access their site of action. |
| Multi-Target-Directed Ligand (MTDL) [57] | A single compound designed to modulate multiple biological targets simultaneously. | The desired output of the screening pipeline for complex diseases, aiming for broader therapeutic efficacy. |
Experimental Protocols and Workflow
This section provides a detailed, step-by-step protocol for executing the integrated screening pipeline.
Protocol 1: Initial Compound Library Curation and Preparation
Objective: To prepare a library of compounds for screening by ensuring structural integrity and applying initial drug-likeness filters. Materials & Reagents: Raw compound library (e.g., in SDF or SMILES format), a workstation with chemical informatics software (e.g., PyRx/OpenBabel, RDKit). Procedure:
- Data Retrieval: Obtain the 3D structures of compounds from a database such as PubChem [2].
- Standardization: Convert all structures into a consistent format (e.g., SMILES). Apply standard steps for protonation and tautomer generation to create a representative set of structures at physiological pH.
- Energy Minimization: Use a molecular mechanics force field (e.g., Universal Force Field in PyRx) to optimize the geometry of each compound and minimize its internal strain energy [2].
- Initial Drug-Likeness Filtering: Apply rulesets like Lipinski's Rule of Five and calculate properties like molecular weight and logP. Filter out compounds that are unlikely to have good oral bioavailability.
Protocol 2: Pharmacophore-Based Virtual Screening
Objective: To rapidly screen the curated library against a 3D pharmacophore model of the target protein. Materials & Reagents: Prepared compound library, 3D protein structure (from PDB), pharmacophore modeling software (e.g., as implemented in Discovery Studio, Phase). Procedure:
- Pharmacophore Model Generation:
- Retrieve the 3D co-crystallized structure of the target protein (e.g., GSK-3β, PDB ID: 1H8F) from the Protein Data Bank (www.rcsb.org) [2].
- Analyze the binding site and interactions of a known native ligand or inhibitor.
- Define critical pharmacophoric features (e.g., hydrogen bond donors, acceptors, hydrophobic aromatic regions) essential for molecular recognition. A study on fungal metabolites defined a model with three aromatic features, one H-bond donor, and one H-bond acceptor [2].
- Virtual Screening Run: Map the prepared compound library against the generated pharmacophore model.
- Hit Selection: Select the top-ranking compounds that map well to all or most of the critical pharmacophoric features for further analysis. This step filtered 17,544 fungal metabolites down to 14 best hits in a referenced study [2].
Protocol 3: Multi-Target Profiling via Molecular Docking
Objective: To evaluate the binding affinity and mode of the pharmacophore-filtered hits against multiple neurodegenerative disease targets. Materials & Reagents: Pharmacophore-filtered hit compounds, 3D structures of multiple target proteins (e.g., GSK-3β, NMDA receptor, BACE-1), molecular docking software (e.g., AutoDock Vina integrated in PyRx) [2]. Procedure:
- Protein Preparation: Prepare the protein structures by removing water molecules, adding hydrogen atoms, and assigning partial charges.
- Ligand Preparation: Convert the hit compounds into a docking-suitable format (e.g.,
.pdbqt). - Define Binding Site: Set the grid box coordinates to encompass the known active site of each protein.
- Execute Docking: Run the docking simulation for each ligand against each target protein.
- Analyze Results: Examine the binding energy (ΔG in kcal/mol) and the specific molecular interactions (hydrogen bonds, hydrophobic contacts) in the binding pose. A compound like Bisacremine-C showed high affinity for GSK-3β (ΔG: -8.7), NMDA (ΔG: -9.5), and BACE-1 (ΔG: -9.1) [2].
Protocol 4: Integrated ADMET and Drug-Likeness Prediction
Objective: To predict the pharmacokinetic and safety profiles of the top multi-target docking hits. Materials & Reagents: Top multi-target docking hits, ADMET prediction platforms (e.g., SwissADME, pkCSM, ADMETlab 3.0, or advanced AI models like ADME-DL [61] and Receptor.AI's platform [58]). Procedure:
- Input Preparation: Compile the SMILES strings or structure files of the final candidate compounds.
- Run Predictions: Submit the structures to one or more ADMET platforms to calculate a suite of properties. Key endpoints to analyze include:
- Absorption: Caco-2 permeability, Human Intestinal Absorption (HIA).
- Distribution: BBB penetration, plasma protein binding.
- Metabolism: Inhibition of Cytochrome P450 enzymes (e.g., CYP2D6, CYP3A4).
- Excretion.
- Toxicity: hERG cardiotoxicity, hepatotoxicity, Ames mutagenicity [58].
- Profile Integration: Consolidate the results and score compounds based on a favorable overall ADMET profile, with particular emphasis on strong predicted BBB penetration for CNS targets.
The Scientist's Toolkit: Essential Research Reagents and Platforms
Table 2: Key Research Reagent Solutions for the Integrated Screening Pipeline.
| Tool/Platform Name | Type/Category | Primary Function in the Protocol |
|---|---|---|
| PyRx with AutoDock Vina [2] | Software Package | Provides an integrated environment for molecular docking, virtual screening, and ligand preparation (e.g., energy minimization via UFF). |
| SwissADME & pkCSM [2] [58] | Web Server / Prediction Tool | Offers rapid, user-friendly prediction of key ADMET properties and drug-likeness rules for early-stage candidate triaging. |
| ADMETlab 3.0 [58] | Web Server / Prediction Tool | A comprehensive platform enhanced with broader coverage of ADMET endpoints and API functionality for automated screening. |
| BIOVIA Discovery Studio [2] | Software Suite | Used for visualizing and analyzing protein-ligand interaction diagrams from docking results, and for advanced pharmacophore modeling. |
| ADME-DL [61] | AI Model (Source Code) | A novel pipeline that uses pharmacokinetics-guided multi-task learning for more accurate drug-likeness classification, respecting ADME task interdependencies. |
| Receptor.AI ADMET Model [58] | AI Model (Platform) | Employs multi-task deep learning and graph-based molecular embeddings to predict over 38 human-specific ADMET endpoints with a consensus score. |
| CETSA [59] | Experimental Assay | Used for validating direct target engagement of prioritized hits in intact cells, bridging the gap between in silico prediction and cellular efficacy. |
Workflow and Pathway Visualizations
The following diagrams, generated with Graphviz, illustrate the logical flow of the integrated screening protocol and the key ADMET interdependencies.
Integrated VS and ADMET Workflow
Key ADMET Property Interdependencies
Application Note: A Case Study in Neurodegenerative Disease Research
A recent study exemplifies the successful application of this integrated protocol. Researchers aimed to discover multi-target inhibitors from a library of 17,544 fungal metabolites for Alzheimer's disease treatment [2].
- Step 1 (Curation & Pharmacophore Screening): The library was first filtered for drug-likeness and, crucially, positive blood-brain barrier penetration. A pharmacophore model was then used to screen the library, reducing the set to 14 best hits [2].
- Step 2 (Multi-Target Docking): These 14 hits were docked against three key AD targets: GSK-3β, the NMDA receptor, and BACE-1. The compound Bisacremine-C emerged as a top candidate, demonstrating high binding affinity for all three targets, with a 25-fold higher calculated affinity for GSK-3β than its native ligand [2].
- Step 3 (ADMET Analysis): The finalists were subjected to in silico ADMET analysis using tools like SwissADME and pkCSM. Bisacremine-C was predicted to have a high LD~50~ dose (5000 mg/kg) and was not flagged for immunotoxicity, indicating a promising preliminary safety profile [2].
- Step 4 (Validation): The stability of the Bisacremine-C complexes was confirmed through molecular dynamics simulations, which showed no significant structural changes in the target proteins upon ligand binding [2].
This case highlights the power of the integrated pipeline to efficiently distill tens of thousands of candidates down to a single, promising, multi-target lead compound with a favorable ADMET profile for a complex neurodegenerative disease.
Overcoming Challenges: BBB Permeability, Model Limitations, and Workflow Optimization
The Blood-Brain Barrier (BBB) is a highly selective, endothelial-derived structure that restricts the passage of substances between the systemic circulation and the central nervous system (CNS), protecting the brain from pathogens and toxins but also presenting a major obstacle for drug delivery [62] [63]. It is estimated that the BBB prevents over 98% of small-molecule drugs and nearly 100% of large-molecule therapeutics from reaching the brain, significantly hindering the treatment of neurological disorders such as Alzheimer's disease, Parkinson's disease, and brain tumors [62] [63]. This application note details integrated computational and experimental protocols for predicting BBB permeability and enhancing CNS drug delivery, framed within a pharmacophore-based virtual screening (VS) strategy for neurodegenerative disease targets.
Quantitative Prediction of BBB Permeability
Advanced machine learning (ML) and deep learning (DL) models have become essential tools for predicting BBB permeability, offering the potential to reduce reliance on costly and time-consuming cellular and animal models in early drug development [62] [64]. These in silico models leverage molecular descriptors and fingerprints to achieve high prediction accuracy.
Table 1: Performance Metrics of Recent BBB Permeability Prediction Models
| Study (Model Name) | Method(s) Used | Dataset Size (Compounds) | Key Performance Metric | Result |
|---|---|---|---|---|
| Liu et al. (Ensemble) | SVM, RF, XGBoost | 1,757 | Accuracy (5-fold CV) | 0.820 – 0.918 [62] |
| Shaker et al. (LightBBB) | LightGBM | 7,162 | Accuracy / AUC | 89% [62] |
| Boulamaane et al. (EnsembleBBB) | Random Forest | 7,807 | AUC (5-fold CV) | 0.97 [62] |
| Transformer & XGBoost (MegaMolBART) | Transformer-based LLM, XGBoost | B3DB & CMUH-NPRL | AUC (Test Set) | 0.88 [65] |
These models utilize various molecular representations. The Simplified Molecular Input Line Entry System (SMILES) is often used with complex architectures like transformers, while molecular fingerprints (FPs), such as Morgan or Circular fingerprints, are used with traditional ML classifiers [65]. The output is typically a classification (BBB+ for permeable, BBB- for impermeable) or a regression value like logBB (the logarithm of the ratio of drug concentration in the brain to that in the blood) [62].
Integrated Protocol for Pharmacophore-Based VS and BBB Penetration Screening
This protocol integrates a pharmacophore-based virtual screening workflow with subsequent BBB permeability assessment to identify promising CNS-active lead compounds.
Protocol 1: Pharmacophore-Based Virtual Screening
Objective: To identify hit compounds against a neurodegenerative disease target (e.g., BACE1 for Alzheimer's disease) using a receptor-ligand-based pharmacophore model [15].
Workflow Diagram: Pharmacophore-Based Virtual Screening
Materials & Reagents:
- Software: Schrödinger Suite (Phase module, Maestro) [15], RDKit (open-source alternative) [65].
- Database: Commercially available compound database (e.g., Vitas-M Laboratory, ~1.4 million compounds) [15].
- Target Structure: Protein Data Bank (PDB) file of the target protein (e.g., BACE1, PDB ID: 5HU0) [15].
Methodology:
- Target Preparation: Retrieve the crystal structure from the PDB. Preprocess the protein by adding hydrogen atoms, assigning charges, and removing water molecules. Minimize the structure using a force field like OPLS_2005 [15].
- Pharmacophore Model Development: Using the prepared protein and a known active co-crystal ligand (e.g., ligand 66H for BACE1), develop a pharmacophore hypothesis. The model should identify critical features like Hydrogen Bond Acceptors (HBA), Hydrogen Bond Donors (HBD), and Hydrophobic (Hyp) regions [15].
- Ligand Database Preparation: Prepare a database of compounds for screening. Generate multiple conformers (e.g., 10 per ligand) and likely tautomeric states at pH 7.0 using a tool like Epik [15].
- Virtual Screening & Docking: Screen the prepared database against the pharmacophore model. Select compounds with a high Phase Screen Score (e.g., >1.9) for molecular docking studies to refine the binding pose and score [15].
- ADMET Filtering: Subject the top-ranked docked compounds to Absorption, Distribution, Metabolism, Excretion, and Toxicity (ADMET) prediction using tools like QikProp or ADMETlab 2.0. Filter compounds based on Lipinski's Rule of Five and favorable toxicity profiles [15].
Protocol 2: BBB Permeability Prediction for Identified Hits
Objective: To predict the BBB permeability of the hit compounds identified in Protocol 1 using a pre-trained transformer-based AI model.
Workflow Diagram: BBB Permeability Prediction
Materials & Reagents:
- Software: NVIDIA NeMo Toolkit with MegaMolBART extension [65], XGBoost library, RDKit.
- Model: Pre-trained MegaMolBART encoder, a transformer model trained on the ZINC-15 dataset [65].
Methodology:
- Input Generation: Convert the SMILES string of each hit compound into a canonical representation.
- Feature Extraction: Process the SMILES string using the MegaMolBART encoder to generate a numerical molecular embedding (vector representation) that captures structural and mechanistic information [65].
- Classification: Feed the molecular embedding into a pre-trained XGBoost classifier to predict the compound's BBB permeability class (BBB+ or BBB-) and output a prediction score [65].
- Prioritization: Prioritize hit compounds that show high affinity for the primary target (from Protocol 1) and are predicted to be BBB+ with high confidence for experimental validation.
Protocol 3: Experimental Validation Using a 3D Human BBB Spheroid Model
Objective: To experimentally validate the BBB permeability of the top-ranked, BBB-predicted compounds in vitro.
Workflow Diagram: Experimental BBB Permeability Validation
Materials & Reagents:
- Cells: Primary human brain microvascular endothelial cells (BMECs), brain vascular pericytes, and astrocytes [65].
- Culture Reagents: Appropriate cell culture media and supplements for each cell type.
- Test Compounds: Top-ranked hits from the integrated computational screen.
- Analytical Instrumentation: Liquid Chromatography with Tandem Mass Spectrometry (LC-MS/MS) system.
Methodology:
- BBB Spheroid Formation: Create 3D human BBB spheroids by co-culturing BMECs, pericytes, and astrocytes in low-adhesion plates for 3-5 days to allow for self-organization and formation of barrier properties [65].
- Compound Incubation: Apply the test compounds to the spheroid culture medium.
- Quantification: After incubation, extract and analyze the spheroids using LC-MS/MS to quantify the concentration of the test compound that has penetrated the spheroid structure [65].
- Validation: Confirm the in silico prediction. Compounds like Temozolomide (predicted BBB+) should show significant penetration, while compounds like Ferulic acid (predicted BBB-) should show minimal uptake [65].
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Research Reagents and Tools for BBB and VS Research
| Item Name | Supplier / Source | Function / Application |
|---|---|---|
| BACE1 (β-secretase 1) Protein | Protein Data Bank (PDB ID: 5HU0) | A key aspartate protease target for Alzheimer's disease drug discovery [15]. |
| Vitas-M Laboratory Compound Database | Vitas-M Laboratory | A commercial database of over 1.4 million compounds for virtual screening and hit identification [15]. |
| Primary Human BBB Cell Triad | Commercial cell providers (e.g., ScienCell, ATCC) | Primary human BMECs, pericytes, and astrocytes for constructing physiologically relevant 3D BBB spheroid models [65]. |
| Schrödinger Suite | Schrödinger | Comprehensive software suite for computational chemistry, including protein preparation (Maestro), pharmacophore modeling (Phase), and molecular docking [15]. |
| NVIDIA MegaMolBART | NVIDIA NGC Catalog | A pre-trained transformer model for chemistry that converts SMILES strings into predictive molecular embeddings for tasks like BBB permeability classification [65]. |
| RDKit | Open-source cheminformatics | A collection of cheminformatics and machine learning tools for Python, used for generating molecular fingerprints and handling SMILES strings [65]. |
The integrated application of pharmacophore-based virtual screening, advanced AI-driven BBB prediction models, and mechanistically relevant in vitro validation creates a powerful pipeline for CNS drug discovery. This multi-faceted approach directly addresses the profound challenge posed by the blood-brain barrier, enabling researchers to rationally design and prioritize compounds with a high probability of reaching their intended targets in the brain. The protocols and data presented herein provide a concrete framework for advancing therapeutic development for neurodegenerative diseases.
In the pursuit of treatments for neurodegenerative diseases, pharmacophore-based virtual screening (VS) has emerged as a powerful strategy for identifying novel therapeutic candidates. However, the predictive performance of these computational models is inherently constrained by their limitations, making rigorous validation not merely a best practice but a scientific necessity. New Approach Methodologies (NAMs), which include in silico models, are gaining regulatory momentum for applications such as Investigational New Drug (IND) submissions [66]. The reliability of these tools hinges on their reproducibility and the implementation of robust cross-validation strategies. These processes are critical for assessing a model's applicability domain and ensuring its predictions are accurate for novel chemical scaffolds not present in the training data, thereby de-risking the subsequent stages of drug development [66] [67]. This document outlines application notes and protocols to embed these principles into a pharmacophore-based VS workflow for neurodegenerative disease targets.
Application Notes
The Critical Role of Context of Use (COU)
A foundational principle in developing reliable computational models is the precise definition of the Context of Use (COU). The COU is a formal description of how a model will be applied within a specific drug development decision-making process, detailing the model's purpose, the predictions it will generate, and the applicable boundaries [66].
- Regulatory Alignment: Regulatory agencies are more likely to accept data from NAMs, including pharmacophore models, when they are supported by a well-defined COU. This framework ensures the model's outputs are clinically interpretable and relevant to the intended therapeutic application [66].
- Balancing Complexity and Interpretability: While complex model systems like 3D organoids can recapitulate human physiology, their utility in IND-enabling evidence is often limited by variability. Success has been demonstrated with simpler, fit-for-purpose models, such as 2D cell co-culture systems with clearly defined pharmacologic endpoints, which have supported first-in-human dose selection for immunotherapies [66]. This highlights that a model's value is derived from its well-defined COU, not its complexity alone.
Addressing the Replicability Crisis in Computational Research
The broader scientific community faces a "crisis of confidence" due to challenges in replicating study findings. In computational research, origins of this crisis often trace back to publications that lack essential methodological details, making it impossible to independently reproduce the protocol or results [68]. Adopting structured checklists, such as the PECANS (Preferred Evaluation of Cognitive And Neuropsychological Studies) framework, can enhance the quality and transparency of research reports. Key reporting standards for computational studies include:
- Pre-registration: Stating whether the study and analysis plan were pre-registered and documenting any deviations.
- Data and Material Availability: Clearly indicating if data and code are openly available and providing access information.
- Methodological Detail: Providing exhaustive details on software, version numbers, parameters, and hardware used to ensure that the computational experiment can be repeated [68].
Quantitative Metrics for Model Validation
Employing quantitative metrics is essential for objectively assessing a model's predictive performance and applicability domain. Table 1 summarizes key validation metrics and their interpretation, which can be adapted for pharmacophore model evaluation.
Table 1: Key Validation Metrics for Predictive Model Assessment
| Metric | Description | Interpretation and Application | ||
|---|---|---|---|---|
| Discovery Yield [67] | The proportion of newly predicted compounds that meet a desired activity or property threshold. | Measures a model's ability to discover novel hits. A higher yield indicates better performance in a real-world discovery setting. | ||
| Novelty Error [67] | The error rate for predictions on compounds that are structurally distinct from the training set. | Assesses model generalizability. A low novelty error indicates a robust model with a broad applicability domain. | ||
| Total Error [69] | The sum of %Bias and %CV, calculated as | %Bias | + %CV. | A comprehensive metric for bioanalytical method (e.g., assay) validation; can be analogized to computational model accuracy and precision. Acceptable thresholds are often ≤30% for mid-range concentrations [69]. |
| k-fold n-step Forward Cross-Validation [67] | A validation method where the dataset is sorted by a property (e.g., logP) and models are trained on earlier "steps" and tested on subsequent ones. | Better mimics real-world drug optimization than random splits, more accurately estimating performance on future, more drug-like compounds. |
Experimental Protocols
Protocol: Implementing Step-Forward Cross-Validation for Bioactivity Prediction
This protocol describes the implementation of a k-fold n-step forward cross-validation (SFCV), a stringent method for evaluating a model's prospective performance on out-of-distribution compounds [67].
3.1.1 Research Reagent Solutions
Table 2: Essential Computational Tools and Datasets
| Item | Function/Description | Example Source/Software |
|---|---|---|
| Curated Bioactivity Dataset | A clean dataset of compounds with consistent activity readouts (e.g., IC50) for a specific neurodegenerative target (e.g., BACE1, Caspase-3). | Public databases (ChEMBL, BindingDB); literature curation [70] [15]. |
| Molecular Standardization Tool | Standardizes molecular structures (desalting, tautomer normalization, charge neutralization) to ensure data consistency. | RDKit MolStandardize module [67]. |
| Molecular Featurization Tool | Converts molecular structures into a numerical format (e.g., fingerprints) for machine learning. | RDKit for ECFP4/Morgan fingerprints [67]. |
| Machine Learning Library | Provides algorithms for building predictive models. | Scikit-learn (Random Forest, Gradient Boosting, MLP) [67]. |
| Scaffold Splitting Tool | Groups molecules by core chemical scaffold for robust validation. | DeepChem ScaffoldSplitter [67]. |
3.1.2 Step-by-Step Procedure
Dataset Curation and Featurization
- Select a protein target relevant to neurodegenerative disease (e.g., β-secretase 1/BACE1 for Alzheimer's) [15] [4].
- Curate a dataset of small molecules with reliable half-maximal inhibitory concentration (IC50) values from the literature. Convert IC50 to pIC50 (-log10(IC50)) for a more normally distributed dependent variable [67].
- Standardize all molecular structures using a tool like RDKit [67].
- Featurize the standardized compounds into a machine-readable format, such as 2048-bit ECFP4 fingerprints [67].
- Calculate molecular properties for each compound, such as the partition coefficient (logP), using RDKit [67].
Data Sorting and Binning
- Sort the entire dataset by the calculated logP values in descending order. This simulates a drug discovery campaign that optimizes compounds from lipophilic to more drug-like (moderately hydrophilic) entities [67].
- Divide the sorted dataset into
k(e.g., 10) consecutive bins of equal size.
Iterative Model Training and Validation
- Iteration 1: Use Bin 1 (highest logP) as the training set and Bin 2 as the test set. Train a predictive model (e.g., Random Forest) on the training set and evaluate its performance (e.g., R², RMSE) on the test set.
- Iteration 2: Expand the training set to include Bins 1 and 2, and use Bin 3 as the test set. Train a new model and evaluate it.
- Repeat this process, each time adding the next bin to the training set and using the subsequent bin for testing, until the final iteration (training on Bins 1 to
k-1, testing on Bink).
Analysis
- Analyze the performance metrics across all iterations. A robust model will maintain reasonable predictive accuracy as it progresses to test sets with lower logP values, demonstrating its generalizability.
- Compare the results of SFCV against those from a conventional random k-fold cross-validation to illustrate the difference in estimated performance [67].
The following workflow diagram illustrates the SFCV process:
Protocol: Pharmacophore-Based Virtual Screening with Integrated Validation
This protocol outlines a comprehensive VS workflow for a neurodegenerative disease target, integrating validation at multiple stages to ensure reproducibility and reliability [70] [15].
3.2.1 Research Reagent Solutions
Table 3: Key Reagents for Pharmacophore Modeling and VS
| Item | Function/Description | Example Source/Software |
|---|---|---|
| Protein Structure | The 3D atomic coordinates of the target protein, used for structure-based pharmacophore generation. | Protein Data Bank (PDB); e.g., PDB ID: 1GFW for Caspase-3, 5HU0 for BACE1 [70] [15]. |
| High-Activity Reference Ligand | A known potent inhibitor, used to guide ligand-based pharmacophore hypothesis generation. | Co-crystalized ligand from PDB (e.g., 66H for BACE1) or literature [15]. |
| Commercial Compound Database | A large, annotated library of purchasable compounds for virtual screening. | Vitas-M Laboratory, ZINC, eMolecules [15]. |
| Molecular Docking Software | Predicts the preferred orientation and binding affinity of a small molecule within a protein's binding site. | Glide, AutoDock Vina [70] [15]. |
| Molecular Dynamics (MD) Software | Simulates the physical movements of atoms and molecules over time to assess complex stability. | GROMACS, AMBER, Desmond [15]. |
3.2.2 Step-by-Step Procedure
Pharmacophore Model Development
- Structure-Based Approach: Prepare the protein structure from the PDB (e.g., remove water, add hydrogens, optimize side chains). Use the refined structure and the spatial features of the bound ligand's interaction points (H-bond donors/acceptors, hydrophobic regions, aromatic rings) to generate a pharmacophore hypothesis [15].
- Ligand-Based Approach: For a target with known active inhibitors, use software like Schrödinger's PHASE to identify common chemical features and their 3D arrangements that are critical for activity. Develop a common pharmacophore hypothesis (CPH), such as the AAHRR.6 model identified for caspase-3 inhibitors [70].
Database Preparation and Virtual Screening
- Prepare a commercial database (e.g., 200,000 compounds from Vitas-M) by generating multiple 3D conformers for each molecule and standardizing their ionization states at physiological pH [15].
- Screen the entire prepared database against the developed pharmacophore model.
- Use the Phase Screen Score (a composite of volume score, RMSD, and site matching) to rank the hits. Select compounds with a score above a defined threshold (e.g., >1.9) for further analysis [15].
Molecular Docking and ADMET Filtering
- Perform molecular docking of the pharmacophore hits into the target's binding site to refine the selection based on predicted binding poses and scores [70] [15].
- Subject the top-docked compounds to in silico Absorption, Distribution, Metabolism, Excretion, and Toxicity (ADMET) prediction using tools like QikProp or ADMETlab 2.0. Filter out compounds that violate Lipinski's Rule of Five or show poor predicted toxicity profiles [15].
Experimental Cross-Validation and Binding Affirmation
- For the final candidate compounds, experimental validation is crucial. This involves synthesizing or purchasing the hits and testing their activity in biochemical or cell-based assays (e.g., measuring IC50 against BACE1 or caspase-3) [70] [71].
- To further validate the binding mode, perform Molecular Dynamics (MD) simulations (e.g., 100 ns) of the protein-ligand complex. Monitor metrics like Root Mean Square Deviation (RMSD) and Radius of Gyration (Rg) to confirm complex stability [15].
- Use end-point calculations like MM/GBSA (Molecular Mechanics/Generalized Born Surface Area) to estimate the total binding free energy (ΔGtotal) and compare it with experimental data [15].
The following workflow diagram illustrates the integrated pharmacophore-based VS protocol:
Optimizing Pharmacophore Hypotheses to Avoid False Positives and Negatives
In the context of neurodegenerative disease research, particularly for targets like acetylcholinesterase (AChE) and butyrylcholinesterase (BChE) in Alzheimer's disease (AD), pharmacophore-based virtual screening has emerged as a powerful strategy for identifying novel therapeutic agents [72] [3]. However, the effectiveness of this approach is often compromised by false positives (structurally similar compounds with no biological activity) and false negatives (active compounds missed during screening), leading to inefficient allocation of research resources and potential oversight of promising drug candidates [73] [74]. This application note provides detailed protocols and strategies for optimizing pharmacophore hypotheses to minimize these errors, thereby enhancing the reliability of virtual screening campaigns focused on neurodegenerative disease targets.
Core Principles of Pharmacophore Optimization
Essential Pharmacophore Features for Neurodegenerative Targets
Research on coumarin-based cholinesterase inhibitors has identified critical features for effective targeting of Alzheimer's-related enzymes. For BChE inhibitors, key features include two hydrogen bond acceptors (HBA), one hydrophobic feature (HY), and one ring aromatic (RA) feature. For AChE inhibitors, essential features comprise two hydrogen bond acceptors (HBA), one hydrophobic feature (HY), and one positive ionizable (PI) group [72]. These features represent the fundamental chemical interactions necessary for inhibitory activity against these enzymes and should form the basis of hypothesis development for related targets.
Quantitative Validation Metrics
A robust pharmacophore model must be validated using multiple statistical approaches to ensure predictive accuracy before deployment in virtual screening. The following table summarizes key validation parameters and their optimal values:
Table 1: Key Validation Metrics for Pharmacophore Models
| Validation Method | Parameter | Target Value | Interpretation |
|---|---|---|---|
| Cost Function Analysis | Total Cost | Significantly lower than null cost | Model not due to chance |
| Δ (Null-Total) | >60 | High statistical significance | |
| Configuration Cost | <17 | Acceptable model complexity | |
| Test Set Prediction | R²pred | >0.50 | Acceptable predictive power |
| RMSE | Lower values preferred | Higher predictive accuracy | |
| Fischer Randomization | Confidence Level | >95% | Model not random correlation |
| Decoy Set Validation | EF (Enrichment Factor) | Higher values preferred | Better identification of actives |
| GH (Goodness of Hit) | >0.7 | Excellent model quality |
Experimental Protocols for Hypothesis Validation
Protocol 1: Comprehensive Model Validation
Purpose: To establish the statistical robustness and predictive capability of a developed pharmacophore hypothesis.
Materials:
- Training set compounds (known actives and inactives)
- Test set compounds (structurally diverse, not in training set)
- Decoy set (e.g., from DUD-E database)
- Pharmacophore modeling software (e.g., Discovery Studio, Phase)
Procedure:
- Divide Dataset: Split curated compound data into training set (50-70%) and test set (50-30%) ensuring structural diversity and activity range representation [72].
- Cost Analysis: Calculate total cost, null cost, and configuration cost. Verify that Δ cost (null-total) exceeds 60 and configuration cost remains below 17 [73].
- Test Set Validation: Apply model to test set compounds. Calculate R²pred using the formula:
R²pred = 1 - (Σ(Ypred(test) - Y(test))² / Σ(Y(test) - Ytraining)²)
where Ypred(test) and Y(test) represent predicted and observed activities of test set compounds, and Ytraining is the mean activity of training set compounds [73]. Accept models with R²pred > 0.50.
- Fischer Randomization:
- Decoy Set Validation:
- Generate decoys using DUD-E database
- Screen mixture of known actives and decoys
- Calculate enrichment factor (EF) and goodness of hit (GH) score:
- Models with GH > 0.7 are considered excellent.
Protocol 2: Dynamic Pharmacophore Modeling with AI Integration
Purpose: To create enhanced pharmacophore models that account for protein flexibility and diverse binding modes.
Materials:
- Protein structures (PDB format)
- Active inhibitors with known IC₅₀ values
- dyphAI platform or similar AI-enhanced tools
- ZINC22 database or other compound libraries
Procedure:
- Cluster Inhibitor Structures:
- Extract known inhibitors with IC₅₀ < 199,000 nM from BindingDB
- Generate 3D structures using LigPrep (Schrödinger) at pH 7.4 ± 0.2
- Perform structural similarity clustering using Canvas module with Tanimoto similarity and average linkage method [75].
- Generate Ensemble Pharmacophore Models:
- For each inhibitor cluster, develop ligand-based pharmacophore hypotheses
- Create complex-based pharmacophores from protein-ligand interactions
- Integrate into pharmacophore model ensemble capturing key interactions including π-cation interactions with Trp-86 and π-π interactions with Tyr-341, Tyr-337, Tyr-124, and Tyr-72 for AChE targets [75].
- Machine Learning Enhancement:
- Train ML models on each inhibitor family to predict activity
- Incorporate protein-ligand interaction knowledge into diffusion models
- Use LPM (ligand-pharmacophore mapping) encoder to extract matching principles based on type and directional alignment [24].
- Virtual Screening:
Visualization of Workflows
Figure 1: Comprehensive Pharmacophore Optimization Workflow
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Research Reagents and Computational Tools
| Category | Specific Tool/Resource | Function | Application in Protocol |
|---|---|---|---|
| Software Platforms | Discovery Studio (Accelrys) | 3D QSAR pharmacophore generation | Hypothesis development and validation [74] |
| dyphAI | Dynamic pharmacophore modeling with AI | Ensemble pharmacophore generation [75] | |
| Schrödinger Suite | Molecular modeling and docking | Induced-fit docking, ligand preparation [75] | |
| DiffPhore | Knowledge-guided diffusion framework | 3D ligand-pharmacophore mapping [24] | |
| Compound Databases | ZINC22 | Commercially available compounds | Virtual screening library [75] [24] |
| DUD-E Database | Directory of useful decoys | Decoy set validation [73] [74] | |
| BindingDB | Bioactive molecules with binding data | Source of known inhibitors [75] | |
| Validation Resources | Decoy Set Generator (DUD-E) | Generation of property-matched decoys | Model specificity assessment [73] |
| Fischer Randomization | Statistical significance testing | Chance correlation evaluation [73] [74] | |
| Chemical Features | Hydrogen Bond Donor/Acceptor | Molecular interaction points | Pharmacophore feature mapping [72] |
| Hydrophobic Features | Van der Waals interactions | Core pharmacophore elements [72] | |
| Ring Aromatic Features | π-π stacking interactions | Important for cholinesterase inhibition [72] | |
| Positive Ionizable Groups | Cation-π, electrostatic interactions | Critical for AChE inhibitors [72] |
Application to Neurodegenerative Disease Targets
When applying these optimized protocols to neurodegenerative disease targets, specific considerations emerge. For AChE inhibitors, the pharmacophore must capture interactions with both the catalytic anionic site (CAS) and peripheral anionic site (PAS) of the enzyme gorge [75]. Incorporating features that map to key residues like Trp-86 (π-cation) and Tyr-341 (π-π) significantly enhances model accuracy [75]. For targets like kynurenine-3-monooxygenase (KMO), developing multiple homology models accounting for different binding modes (competitive vs. non-substrate effector) improves identification of true positives while reducing false negatives [54].
The integration of machine learning with traditional pharmacophore approaches, as demonstrated in dyphAI, represents a significant advancement. This ensemble approach captures dynamic protein-ligand interactions often missed in static models, addressing a major source of false negatives [75]. Similarly, DiffPhore's knowledge-guided diffusion framework for 3D ligand-pharmacophore mapping has shown superior performance in virtual screening for neurodegenerative disease targets, outperforming traditional pharmacophore tools and several docking methods [24].
Optimizing pharmacophore hypotheses through rigorous validation protocols and AI-enhanced dynamic modeling significantly reduces false positives and negatives in virtual screening for neurodegenerative disease targets. The implementation of cost function analysis, test set validation, Fischer randomization, and decoy set validation provides a comprehensive framework for evaluating model robustness. When combined with emerging technologies like ensemble pharmacophore modeling and knowledge-guided diffusion frameworks, researchers can achieve unprecedented accuracy in identifying novel therapeutic candidates for challenging targets in Alzheimer's disease and related neurodegenerative conditions.
Following a successful pharmacophore-based virtual screening (PBVS) campaign against neurodegenerative disease targets, researchers are often faced with hundreds or thousands of potential hit compounds. The critical next step is to prioritize the most promising candidates for expensive and time-consuming in vitro and in vivo experimental validation. At this stage, Absorption, Distribution, Metabolism, Excretion, and Toxicity (ADMET) profiling serves as an essential filter to eliminate compounds with unfavorable pharmacokinetic or safety profiles early in the drug discovery pipeline. Integrating computational ADMET prediction into the workflow for neurodegenerative disease targets is particularly crucial due to the additional challenges posed by the blood-brain barrier (BBB) and the need for chronic dosing in often elderly populations [76] [77]. This application note details protocols for implementing ADMET and toxicity profiling as post-screening filters to identify viable leads with the highest probability of success.
Background and Significance
The high attrition rate in central nervous system (CNS) drug development, with approval rates approximately 20% for non-CNS indications compared to just 7–8% for CNS therapeutics, underscores the importance of early ADMET assessment [76]. For neurodegenerative diseases such as Alzheimer's disease (AD) and Parkinson's disease (PD), failures often occur in late-stage clinical development due to inadequate brain exposure or unforeseen toxicity [77]. Pharmacophore-based virtual screening has proven effective for initial lead identification; however, its true value is realized only when integrated with robust ADMET profiling to ensure selected leads not only modulate the target but also possess drug-like properties.
Modern artificial intelligence (AI) and machine learning (ML) approaches have revolutionized ADMET prediction, enabling more accurate assessment of compound properties before synthesis and testing [78] [79]. Graph-based models, including Graph Neural Networks (GNNs) and Graph Convolutional Networks (GCNs), have emerged as particularly powerful tools for predicting complex CYP enzyme interactions and other ADMET endpoints by naturally representing molecular structures as graphs of atoms (nodes) and bonds (edges) [78].
ADMET Profiling Workflow
The following workflow integrates ADMET profiling as a sequential filter following pharmacophore-based virtual screening. The process is designed to systematically eliminate compounds with undesirable properties at each stage, progressively narrowing the candidate list to the most promising leads.
Core ADMET Profiling Protocols
Protocol 1: Early ADMET Property Screening
Objective: To computationally predict fundamental ADMET properties and filter out compounds with poor drug-likeness.
Methodology:
- Data Preparation: Convert the hit list from your PBVS campaign into a standardized chemical format (e.g., SMILES strings or SDF files).
- Descriptor Calculation: Use tools like SwissADME or ADMETlab to compute key molecular descriptors and physicochemical properties [80] [79].
- Property Prediction: Input the prepared structures into the prediction platforms to assess critical early-stage properties.
Table 1: Key ADMET Properties for Initial Screening and Their Ideal Ranges for Neurodegenerative Disease Targets
| Property | Target Value/Range | Significance | Recommended Tool |
|---|---|---|---|
| Lipinski's Rule of 5 | ≤1 violation | Oral bioavailability potential | SwissADME [80] |
| Water Solubility (Log S) | > -6.0 | Adequate solubility for absorption | ADMETlab [79] |
| Caco-2 Permeability | > -5.15 log cm/s | Intestinal absorption potential | pkCSM [80] |
| CYP Inhibition (2D6, 3A4) | Non-inhibitor | Reduced drug-drug interaction risk | Graph-Based Models [78] |
| Human Intestinal Absorption | > 80% | High oral absorption | pkCSM |
Interpretation: Compounds failing more than one Lipinski rule or showing poor solubility/permeability should be deprioritized. CYP inhibition, particularly for isoforms 3A4 and 2D6, is a critical filter due to the potential for drug-drug interactions in elderly populations [78].
Protocol 2: Advanced Toxicity Profiling
Objective: To predict compound-specific toxicity endpoints and identify potential safety liabilities.
Methodology:
- Endpoint Selection: Identify relevant toxicity endpoints based on therapeutic area and compound class. For neurodegenerative diseases, neurotoxicity and hepatotoxicity are particularly critical.
- Model Application: Utilize specialized AI-based toxicity prediction tools trained on relevant datasets.
- Risk Assessment: Classify compounds based on predicted toxicity profiles.
Table 2: Key Toxicity Endpoints and Prediction Platforms for Lead Prioritization
| Toxicity Endpoint | Prediction Output | Significance | Recommended Tool/Dataset |
|---|---|---|---|
| hERG Inhibition | pIC50 / Binary Classification | Cardiotoxicity risk | hERG Central [79] |
| Hepatotoxicity (DILI) | Binary Classification (High/Low Risk) | Drug-induced liver injury | DILIrank [79] |
| Ames Test | Binary Classification (Mutagenic/Non-Mutagenic) | Genotoxicity risk | ProTox3 [80] |
| Neurotoxicity | Binary Classification | CNS-specific toxicity | AI Models on Tox21 [79] |
| LD50 (Rodent) | Continuous (mol/kg) | Acute toxicity | ProTox3 [80] |
Interpretation: Compounds predicted to be hERG inhibitors, hepatotoxic, or mutagenic should typically be eliminated from consideration. Neurotoxicity predictions require careful analysis, as some CNS activity may be desired for neurodegenerative disease targets, but off-target neurotoxicity remains a concern [79].
Protocol 3: Blood-Brain Barrier Penetration Prediction
Objective: To specifically assess the ability of compounds to cross the blood-brain barrier, a critical requirement for neurodegenerative disease therapeutics.
Methodology:
- Model Selection: Utilize specialized BBB prediction models, which may be based on physicochemical properties or machine learning approaches.
- Prediction Analysis: Obtain quantitative (e.g., logBB) or qualitative (BBB+/BBB-) predictions.
- Multi-Model Consensus: Where possible, use multiple prediction tools to increase confidence.
Key Parameters:
- Optimal Property Ranges for BBB Penetration:
- Molecular Weight: <450 Da
- Log P: 1.5-3.5
- Hydrogen Bond Donors: <3
- Polar Surface Area: <90 Ų
- Prediction Tools: SwissADME, admetSAR, or specialized graph-based models [76].
Interpretation: Compounds predicted to have poor BBB penetration should be deprioritized for most neurodegenerative disease targets, unless peripheral activity is the therapeutic goal.
The Scientist's Toolkit: Essential Research Reagents and Databases
Table 3: Key Research Reagent Solutions for ADMET and Toxicity Profiling
| Resource Name | Type | Function in ADMET Profiling | Access |
|---|---|---|---|
| SwissADME | Web Tool | Computes physicochemical properties, drug-likeness, and pharmacokinetic parameters [80]. | Free Web Server |
| ADMETlab | Web Tool | Comprehensive ADMET property prediction platform with multiple endpoints [80]. | Free Web Server |
| ProTox3 | Web Tool | Predicts various toxicity endpoints including organ toxicity and toxicity pathways [80]. | Free Web Server |
| Tox21 | Dataset | Qualitative toxicity data for 8,249 compounds across 12 biological targets for model training/validation [79]. | Public Database |
| DILIrank | Dataset | Curated dataset of drugs with known drug-induced liver injury risk for hepatotoxicity prediction [79]. | Public Database |
| hERG Central | Dataset | Extensive collection of hERG channel inhibition data for cardiotoxicity assessment [79]. | Public Database |
| ChEMBL | Database | Bioactivity data for drug-like molecules used for model training and validation [5] [79]. | Public Database |
Integrated AI and Machine Learning Approaches
Modern ADMET prediction increasingly leverages graph-based computational techniques, including Graph Neural Networks (GNNs), Graph Convolutional Networks (GCNs), and Graph Attention Networks (GATs) [78]. These approaches represent molecules as graphs with atoms as nodes and bonds as edges, allowing the model to learn directly from molecular structure. The application of Explainable AI (XAI) techniques further enhances these models by providing insights into which structural features contribute to specific ADMET properties [78].
For neurodegenerative disease targets, multimodal AI approaches that integrate diverse data sources—including neuroimaging, multi-omics, and clinical information—provide a more comprehensive view of potential therapeutic effects and safety profiles [76]. These advanced methods are particularly valuable for addressing the complexity of brain diseases and the challenges of delivering therapeutics across the blood-brain barrier.
Decision Framework for Lead Prioritization
The following diagram illustrates the sequential decision process for integrating ADMET filters, from initial computational screening to final lead selection for neurodegenerative disease targets.
Integrating robust ADMET and toxicity profiling as post-screening filters following pharmacophore-based virtual screening is essential for successful lead prioritization in neurodegenerative disease drug discovery. The protocols outlined in this application note provide a systematic approach to eliminate compounds with unfavorable pharmacokinetic or safety profiles early in the pipeline, thereby reducing late-stage attrition. By leveraging modern computational tools, AI-based prediction models, and established experimental protocols, researchers can significantly improve the efficiency of their lead selection process and increase the probability of identifying viable candidates for further development.
Validating PBVS Hits and Comparative Analysis with Docking-Based Methods
In the pursuit of therapeutics for neurodegenerative diseases, pharmacophore-based virtual screening (PBVS) has emerged as a powerful strategy for identifying potential hit compounds. This approach is particularly valuable given the challenges of targeting complex proteinopathies like Alzheimer's disease (AD), Parkinson's disease (PD), frontotemporal dementia (FTD), and amyotrophic lateral sclerosis (ALS) [81]. PBVS utilizes an ensemble of steric and electronic features that are necessary for optimal supramolecular interactions with a specific biological target, providing a computational method to prioritize compounds with a higher likelihood of biological activity before moving to costly experimental validation [30].
The transition from in silico predictions to in vitro confirmation represents a critical juncture in early drug discovery. Research indicates that PBVS often outperforms docking-based virtual screening (DBVS) in retrieving active compounds from chemical databases [29] [10]. However, even with advanced computational methods, hit compounds require rigorous experimental validation to eliminate false positives arising from assay interference or non-specific mechanisms [82] [83]. This application note provides a structured framework for validating PBVS-derived hits through biochemical assays, with specific consideration for neurodegenerative disease targets.
Experimental Design and Workflow
The validation of virtual screening hits follows a cascading workflow designed to efficiently triage artifacts while confirming genuine bioactive compounds. This process integrates computational prioritization with increasingly sophisticated experimental techniques.
Figure 1: Comprehensive workflow for validating pharmacophore-based virtual screening hits through biochemical and biophysical assays.
Computational Hit Prioritization
Before initiating experimental work, computationally identified hits should undergo rigorous filtering:
- Frequent-Hitter Analysis: Mine historical screening data to identify and exclude promiscuous compounds that show activity across multiple unrelated screens [83].
- Pan-Assay Interference Compounds (PAINS) Filtering: Apply computational filters to flag compounds with structural features known to cause assay interference [82].
- Structure-Activity Relationship (SAR) Clustering: Group hits by common structural scaffolds to prioritize compounds that form clusters, which increases confidence in true bioactivity [83].
- Dose-Response Curve Assessment: During primary screening, examine the shape of dose-response curves; steep, shallow, or bell-shaped curves may indicate toxicity, poor solubility, or aggregation [82].
Assay Development Strategies
Robust assay development is fundamental to successful hit validation. Key considerations include:
- Universal Assay Platforms: Implement universal activity assays that detect common enzymatic products (e.g., ADP for kinases, SAH for methyltransferases) enabling multiple targets to be studied with the same assay platform [84].
- Mix-and-Read Formats: Utilize homogeneous "mix-and-read" assays that minimize steps, simplify automation, and enhance reproducibility for high-throughput screening (HTS) [84].
- Assay Validation Metrics: Establish quality benchmarks such as Z'-factor >0.5, indicating robustness suitable for HTS [84].
- Buffer Optimization: Fine-tune ionic strength, cofactors, and additives to stabilize enzyme activity and minimize non-specific binding [82] [84].
Key Validation Assays and Protocols
Primary Biochemical Assays
Objective: Confirm dose-dependent activity of computational hits in target-based assays.
Protocol 1: Dose-Response Analysis with Biochemical Assay
Reagent Preparation:
- Prepare assay buffer (50 mM Tris-HCl pH 7.4, 8 mM MgCl₂, 5 mM dithiothreitol, 10% glycerol)
- Dilute test compounds in DMSO to create 10-point serial dilutions (typically from 10 mM to nanomolar range)
- Prepare enzyme/substrate solutions in assay buffer according to optimized concentrations [85]
Assay Assembly:
- Transfer 2 μL of each compound dilution to 384-well assay plates
- Add 18 μL of enzyme solution to all wells
- Incubate at 30°C for 30 minutes to pre-incubate enzyme with compound
- Initiate reaction by adding 10 μL of substrate solution containing required cofactors
Reaction and Detection:
- Incubate plates at 30°C for 2 hours for enzymatic reaction
- Stop reaction by adding detection reagents according to assay technology
- For Transcreener ADP assays: Add detection mix containing antibody and tracer, incubate 1 hour [84]
- Read plates using appropriate instrumentation (fluorescence polarization, TR-FRET, or fluorescence intensity)
Data Analysis:
- Calculate percent inhibition relative to positive (no compound) and negative (no enzyme) controls
- Generate dose-response curves and calculate IC₅₀ values using four-parameter logistic fit
- Flag compounds with Hill coefficients >2.5 or <0.5 for further investigation [83]
Table 1: Common Biochemical Assay Technologies for Hit Validation
| Technology | Detection Method | Applications | Advantages | Throughput |
|---|---|---|---|---|
| Transcreener | Fluorescence Polarization (FP), TR-FRET | Kinases, GTPases, ATPases | Universal assay, mix-and-read format | 384/1536-well |
| AptaFluor | TR-FRET | Methyltransferases, Deubiquitinases | Direct product detection, high sensitivity | 384-well |
| Fluorescence Polarization | Polarized fluorescence | Binding assays, protease assays | Homogeneous, no separation steps | 384-well |
| Surface Plasmon Resonance | Refractive index changes | Binding kinetics, affinity | Label-free, provides kinetic parameters | Medium |
Counter-Screens and Interference Assays
Objective: Identify and eliminate false positives resulting from assay interference or non-specific mechanisms.
Protocol 2: Compound Interference Assay
Signal Interference Test:
- Prepare compound solutions at 10× final concentration in assay buffer
- In separate plates, add compound to completed enzymatic reactions after reaction termination
- Compare signals with and without compound to detect signal quenching or enhancement [83]
Aggregation Testing:
- Perform dose-response assays with addition of 0.01-0.1% non-ionic detergents (e.g., Triton X-100, Tween-20)
- Significant right-shift in IC₅₀ with detergent suggests compound aggregation [83]
Redox Activity Assessment:
- Incubate compounds with phenol red, horseradish peroxidase, and hydrogen peroxide
- Monitor color change at 610 nm to identify redox-cycling compounds [83]
Enzyme Concentration-Dependence:
- Determine IC₅₀ values at two different enzyme concentrations (e.g., 1× and 5×)
- Significant shifts in IC₅₀ suggest non-specific inhibition [83]
Table 2: Common Sources of False Positives and Counter-Assay Strategies
| Interference Type | Mechanism | Counter-Assay Approach | Interpretation |
|---|---|---|---|
| Compound Aggregation | Colloidal aggregates non-specifically inhibit enzymes | Add detergent (0.01% Triton X-100) to assay | >3-fold IC₅₀ shift suggests aggregation |
| Fluorescence Interference | Compound fluoresces/quenches at assay wavelengths | Test compound with product alone | Signal change indicates interference |
| Redox Cycling | Generates hydrogen peroxide that inhibits enzymes | Horseradish peroxidase/phenol red assay | Color change indicates redox activity |
| Chemical Reactivity | Covalently modifies protein residues | LC-MS/MS analysis of protein after incubation | Mass shift indicates covalent modification |
| Chelation | Binds essential metal cofactors | Add excess metal ions to assay | IC₅₀ shift suggests chelation |
Orthogonal Assays
Objective: Confirm bioactivity using alternative readout technologies or assay formats.
Protocol 3: Orthogonal Assay with Alternative Detection Technology
Assay Selection:
- If primary screen used fluorescence, implement luminescence- or absorbance-based orthogonal assay [82]
- For neurodegenerative disease targets, consider biophysical methods like SPR or MST
Surface Plasmon Resonance (SPR) Protocol:
- Immobilize target protein on CMS sensor chip using amine coupling chemistry
- Prepare compound dilutions in running buffer (HBS-EP)
- Inject compounds over chip surface at 30 μL/min for 2 minutes association
- Monitor dissociation for 10 minutes
- Analyze sensorgrams to determine binding kinetics (kₐ, kḍ, K({}_{\text{D}})) [83]
Microscale Thermophoresis (MST) Protocol:
- Label target protein with fluorescent dye using protein labeling kit
- Mix constant concentration of labeled protein with serial dilutions of compounds
- Load samples into premium coated capillaries
- Measure thermophoresis at 25°C using Monolith NT.115 instrument
- Analyze dose-response curves to determine K({}_{\text{D}}) values [82]
Target Engagement and Mechanism of Action
Objective: Demonstrate direct target binding and elucidate inhibition mechanism.
Protocol 4: Mechanism of Inhibition Studies
Enzyme Kinetics:
- Measure initial reaction rates at varying substrate concentrations (0.5×, 1×, 2× K({}_{\text{m}}))
- Test multiple compound concentrations covering IC₅₀ range
- Plot data on Lineweaver-Burk or Michaelis-Menten plots
- Determine inhibition mode (competitive, non-competitive, uncompetitive) [83]
Cellular Thermal Shift Assay (CETSA):
- Treat cells with compound or DMSO control for 2 hours
- Heat aliquots of cell lysate at different temperatures (37-65°C) for 3 minutes
- Separate soluble protein by centrifugation at 100,000 × g
- Detect target protein in supernatant by Western blot or AlphaLISA
- Calculate melting temperature (T({}_{\text{m}}) shifts [83]
Reversibility Assessment:
- Pre-incubate enzyme with 10× IC₅₀ compound concentration for 1 hour
- Dilute mixture 100-fold into substrate solution
- Monitor recovery of enzymatic activity over time
- Compare with rapid-dilution of known reversible inhibitor [83]
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Key Research Reagent Solutions for Hit Validation
| Reagent/Material | Function | Example Applications | Considerations |
|---|---|---|---|
| Transcreener ADP2 Assay | Universal ADP detection for kinase/ATPase targets | Measuring kinase inhibition | Works with FP, TR-FRET, or FI readouts; Z' > 0.7 |
| AptaFluor SAH Assay | S-adenosylhomocysteine detection for methyltransferases | Methyltransferase inhibition studies | TR-FRET format; applicable to PRMTs, DNMTs, HMTs |
| CETSA Kit | Target engagement in cellular context | Confirming cellular target binding | Compatible with Western blot or AlphaLISA detection |
| SPR Consumables | Immobilization surfaces for biophysical binding | Kinetic characterization | CMS chips for amine coupling; protein A chips for antibodies |
| HTS-Grade Detergents | Disrupt compound aggregates | Counter-screening for aggregation | Triton X-100, Tween-20; use at 0.01-0.1% concentration |
| Cellular Viability Assays | Assess cytotoxicity | Counterscreen for non-specific toxicity | CellTiter-Glo, MTT, LDH assays |
| Protease Inhibitor Cocktails | Maintain protein integrity during assays | All enzymatic assays | Include in purification and assay buffers |
Data Analysis and Interpretation
Effective data interpretation requires both statistical rigor and biological context:
- Quality Control Metrics: Implement strict quality controls including Z'-factor >0.5, signal-to-background >3, and coefficient of variation <10% for robust assays [84].
- Structure-Activity Relationships (SAR): Analyze potency trends across compound series; true bioactive compounds typically show interpretable SAR [82].
- Cellular Fitness Assessment: Evaluate cellular health using viability assays (CellTiter-Glo), cytotoxicity assays (LDH release), and high-content imaging to exclude generally toxic compounds [82].
- Multiparametric Optimization: Develop scoring algorithms that integrate potency, selectivity, ligand efficiency, and physicochemical properties to prioritize lead compounds [83].
Figure 2: Hit qualification decision tree outlining key criteria for advancing compounds to lead optimization.
Application to Neurodegenerative Disease Targets
The integration of PBVS with biochemical validation presents particular opportunities for neurodegenerative disease research:
- Leveraging Consortium Data: Utilize large-scale proteomic datasets, such as those from the Global Neurodegeneration Proteomics Consortium (GNPC), to inform target selection and identify disease-relevant binding sites [81].
- Addressing Disease Heterogeneity: Implement parallel screening against multiple conformational states of proteins (e.g., monomeric vs. oligomeric tau) to identify state-selective inhibitors [81].
- Biomarker Development: Correlate biochemical target engagement with biomarker changes (e.g., CSF p-tau, neurofilament light) to establish pharmacodynamic relationships early in development [81].
The journey from in silico prediction to in vitro validation requires a rigorous, multi-stage approach that systematically eliminates artifacts while confirming genuine bioactive compounds. By implementing the cascading assay strategy outlined in this application note—incorporating primary screens, counter-screens, orthogonal assays, and mechanism of action studies—researchers can efficiently triage pharmacophore-based virtual screening hits and advance high-quality starting points for lead optimization. For neurodegenerative disease targets, this approach offers a pathway to address the high attrition rates in drug discovery by front-loading experimental validation and building confidence in hit matter before committing to extensive medicinal chemistry efforts.
Virtual screening (VS) has become an indispensable tool in modern drug discovery, enabling researchers to computationally evaluate vast chemical libraries to identify potential bioactive molecules. The two predominant strategies in this field are pharmacophore-based virtual screening (PBVS) and docking-based virtual screening (DBVS). For research focused on neurodegenerative disease targets, understanding the relative performance, strengths, and limitations of these approaches is critical for designing effective screening protocols. This application note provides a comprehensive benchmarking comparison between PBVS and DBVS methodologies, drawing on empirical studies to guide researchers in selecting and optimizing virtual screening strategies for neurotherapeutic development.
Pharmacophore-based virtual screening employs an abstract model of molecular interactions—including hydrogen bond donors/acceptors, hydrophobic regions, and charged groups—that are essential for biological activity. In contrast, docking-based virtual screening relies on the three-dimensional structure of the target protein to computationally predict how small molecules bind to the active site, typically using scoring functions to estimate binding affinity. While DBVS has gained popularity for its direct simulation of ligand-receptor binding, PBVS has experienced a revival, particularly for targets where structural information is limited or as a complementary filter to docking approaches [29].
Performance Benchmarking: Quantitative Comparisons
A landmark benchmark study directly compared PBVS and DBVS across eight structurally diverse protein targets: angiotensin converting enzyme (ACE), acetylcholinesterase (AChE), androgen receptor (AR), D-alanyl-D-alanine carboxypeptidase (DacA), dihydrofolate reductase (DHFR), estrogen receptors α (ERα), HIV-1 protease (HIV-pr), and thymidine kinase (TK). The study utilized the Catalyst program for PBVS and three docking programs (DOCK, GOLD, and Glide) for DBVS, performing virtual screens on datasets containing both active compounds and decoys [29] [10].
Table 1: Overall Performance Comparison of PBVS versus DBVS Across Eight Protein Targets
| Performance Metric | PBVS | DBVS | Superior Method |
|---|---|---|---|
| Cases with higher enrichment (out of 16) | 14 | 2 | PBVS |
| Average hit rate at 2% database cutoff | Much higher | Lower | PBVS |
| Average hit rate at 5% database cutoff | Much higher | Lower | PBVS |
| Enrichment factor range | Higher in most cases | Variable | PBVS |
The results demonstrated that PBVS significantly outperformed DBVS in retrieval of active compounds. Of the sixteen sets of virtual screens (one target versus two testing databases), PBVS achieved higher enrichment factors in fourteen cases compared to DBVS methods. Furthermore, when considering the top 2% and 5% of ranked compounds, the average hit rates for PBVS across all eight targets were substantially higher than those achieved by any of the docking methods [29] [86].
Table 2: Performance Analysis by Metric Type
| Metric Category | Specific Metric | PBVS Performance | DBVS Performance | Interpretation |
|---|---|---|---|---|
| Enrichment | Enrichment Factor (EF) | Superior in 14/16 cases | Inferior in most cases | PBVS better identifies true actives |
| Early Recognition | Hit Rate at 2% | Much higher | Lower | PBVS more efficient for top-ranked compounds |
| Early Recognition | Hit Rate at 5% | Much higher | Lower | PBVS maintains advantage at wider cutoff |
| Chemical Diversity | Chemotype Enrichment | Superior | Lower | PBVS retrieves more structurally diverse actives |
For neurodegenerative disease research specifically, recent studies continue to demonstrate the effectiveness of PBVS. A 2023 study screening fungal metabolites against Alzheimer's disease targets (GSK-3β, NMDA receptor, and BACE-1) successfully identified potential multi-target inhibitors using pharmacophore-based approaches initially, followed by molecular docking confirmation [2]. Similarly, a 2024 study targeting β-secretase 1 (BACE-1) for Alzheimer's disease employed PBVS to screen 200,000 compounds from the Vitas-M Laboratory database, successfully identifying promising hits with phase scores >1.9 that were subsequently validated through molecular docking and dynamics simulations [15].
Experimental Protocols
PBVS Protocol for Neurodegenerative Disease Targets
Step 1: Pharmacophore Model Generation
- For structure-based pharmacophore: Collect 3-5 high-resolution X-ray crystal structures of target protein-ligand complexes from Protein Data Bank (PDB). For neurodegenerative targets, relevant structures may include BACE-1 (e.g., PDB ID: 5HU0), GSK-3β, or NMDA receptors [2] [15].
- Use pharmacophore generation software such as LigandScout or Schrödinger Phase to create hypothesis based on conserved interaction features [29] [15].
- Define critical pharmacophore features: hydrogen bond donors/acceptors, hydrophobic regions, aromatic rings, and charged groups based on conserved binding interactions across multiple complexes.
- For ligand-based approaches: Use known active compounds against neurodegenerative targets to generate common feature pharmacophore models.
Step 2: Database Preparation
- Select compound database (ZINC, ChEMBL, Enamine, or in-house collections) [87].
- Prepare compounds: generate stereoisomers, tautomers, and ionization states at physiological pH (7.0-7.4) using tools like LigPrep or MOE [15].
- Generate multiple conformers for each compound (typically 10-100 conformers per molecule) to ensure comprehensive coverage of spatial arrangements [15].
Step 3: Pharmacophore Screening
- Screen database against pharmacophore model using programs such as Catalyst or Phase [29].
- Apply phase screen score (combining volume score, RMSD, and site matching) to evaluate fits [15].
- Retain compounds with phase scores >1.9 for further analysis [15].
Step 4: Post-Screening Filtering
- Apply drug-likeness filters (Lipinski's Rule of Five) to remove compounds with unfavorable properties [15].
- Perform ADMET prediction using QikProp, SwissADME, or ADMETlab 2.0 to assess pharmacokinetic and toxicity profiles [15].
- Select top-ranked compounds for experimental validation or further computational analysis.
DBVS Protocol for Neurodegenerative Disease Targets
Step 1: Protein Structure Preparation
- Obtain high-resolution crystal structure of target protein from PDB. For neurodegenerative targets, this may include BACE-1, GSK-3β, or NMDA receptors [2].
- Prepare protein structure: add hydrogen atoms, assign partial charges, optimize side-chain orientations, and remove crystallographic water molecules except those involved in key binding interactions [15].
- Define binding site using known ligand coordinates or predicted active site regions.
Step 2: Ligand Database Preparation
- Select compound library and prepare ligands: generate 3D structures, assign proper bond orders, and generate possible tautomers and ionization states at physiological pH [87].
- For docking programs requiring pre-generated conformers, use tools like Omega to generate multiple conformers [88].
Step 3: Molecular Docking
- Perform docking using programs such as AutoDock Vina, GOLD, Glide, or DOCK [29] [88].
- Set appropriate search parameters and grid box size to encompass the entire binding site.
- Generate multiple poses per ligand (typically 10-50) to ensure adequate sampling of binding orientations.
Step 4: Pose Selection and Scoring
- Rank compounds based on docking scores or binding affinity predictions.
- Visually inspect top-ranked poses to verify sensible binding interactions using visualization tools like Discovery Studio Visualizer or PyMOL [2].
- Apply consensus scoring or post-processing filters to improve hit rates.
Step 5: Experimental Validation
- Select top-ranked compounds for in vitro binding or functional assays.
- For promising hits, consider structural validation through X-ray crystallography or further optimization through medicinal chemistry.
Workflow Visualization
Virtual Screening Decision Workflow: This diagram illustrates the decision process for selecting between PBVS and DBVS approaches based on available structural information, culminating in experimental validation of top-ranked compounds.
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Research Reagents and Computational Tools for Virtual Screening
| Tool/Reagent | Type | Primary Function | Application Notes |
|---|---|---|---|
| LigandScout | Software | Structure-based pharmacophore modeling | Creates pharmacophores from protein-ligand complexes; used in benchmark studies [29] |
| Catalyst/Phase | Software | Pharmacophore-based screening | Performs 3D database searching and pharmacophore validation [29] [15] |
| AutoDock Vina | Software | Molecular docking | Popular docking program for DBVS; open-source [88] |
| GOLD | Software | Molecular docking | Genetic algorithm-based docking; used in benchmark studies [29] |
| Glide | Software | Molecular docking | High-accuracy docking with extensive sampling [29] |
| ZINC Database | Compound Library | Commercially available compounds | ~13 million compounds for virtual screening [87] |
| ChEMBL | Database | Bioactive molecules | ~1 million compounds with bioactivity data [87] |
| PyRx | Software | Virtual screening platform | AutoDock-based tool for docking and screening [2] |
| Schrödinger Suite | Software Platform | Comprehensive drug discovery | Includes Phase, Glide, and QikProp for end-to-end workflows [15] |
| DEKOIS 2.0 | Benchmark Set | Performance evaluation | Contains actives and decoys for docking benchmark studies [88] |
Discussion and Application to Neurodegenerative Diseases
The benchmarking data consistently demonstrates the superior performance of PBVS in enrichment factors and hit rates across diverse targets compared to DBVS. This advantage is particularly relevant for neurodegenerative disease targets, where multiple proteins (GSK-3β, NMDA receptors, BACE-1) often need to be targeted simultaneously in a multi-target directed ligand approach [2].
The outperformance of PBVS can be attributed to several factors. Pharmacophore models effectively capture essential interaction features while allowing for some structural flexibility, whereas docking programs often struggle with accurate binding affinity prediction due to limitations in scoring functions and handling of protein flexibility [29] [89]. Additionally, PBVS demonstrates superior chemotype enrichment, retrieving more structurally diverse active compounds compared to DBVS [90].
For neurodegenerative disease targets specifically, PBVS offers practical advantages. Many key targets lack high-quality crystal structures, making structure-based approaches challenging. PBVS can leverage known active compounds against these targets to develop ligand-based models when structural information is limited. Furthermore, the ability of PBVS to identify multi-target inhibitors aligns well with the complex pathophysiology of neurodegenerative diseases, which often involve multiple dysfunctional pathways [2].
Despite the strong performance of PBVS, DBVS remains valuable for providing detailed binding mode predictions and enabling structure-based optimization of hit compounds. The integration of both methods in a hybrid protocol—using PBVS for initial filtering and DBVS for detailed pose analysis—represents a powerful strategy for neurodegenerative drug discovery [90].
Recent advances in machine learning scoring functions show promise for improving DBVS performance. Studies demonstrate that re-scoring docking results with convolutional neural network-based scoring functions (e.g., CNN-Score) or random forest algorithms (e.g., RF-Score-VS) can significantly enhance enrichment factors and early recognition capabilities [88]. These developments may narrow the performance gap between PBVS and DBVS in future applications.
Benchmarking studies provide compelling evidence that pharmacophore-based virtual screening generally outperforms docking-based approaches in enrichment factors and hit rates across diverse protein targets. For researchers focusing on neurodegenerative diseases, PBVS represents a powerful initial screening methodology, particularly when structural information is limited or when seeking multi-target inhibitors. The experimental protocols outlined in this application note offer practical guidance for implementing these virtual screening strategies in neurotherapeutic development. As both methodologies continue to evolve—particularly with the integration of machine learning approaches—their combined application promises to enhance the efficiency and effectiveness of early drug discovery for challenging neurodegenerative targets.
In the demanding field of neurodegenerative disease (NDD) research, discovering novel therapeutic compounds is both time-consuming and costly. Virtual screening (VS) has emerged as a pivotal tool in this process, with two primary methodologies dominating the landscape: pharmacophore-based virtual screening (PBVS) and docking-based virtual screening (DBVS). While DBVS directly models the physical interaction between a ligand and a protein target, PBVS abstracts this interaction into a three-dimensional model of essential functional features [29]. A landmark benchmark study comparing these methods across eight diverse protein targets revealed a superior performance of PBVS, which achieved higher enrichment factors in 14 out of 16 test cases and significantly higher average hit rates at the top 2% and 5% of ranked databases [29] [10]. This empirical evidence underscores that PBVS and DBVS are not merely competing strategies but are powerfully complementary. This Application Note details protocols for their integration, positioning PBVS as a strategic pre- or post-filter for docking campaigns to enhance efficiency and hit rates in NDD drug discovery.
Performance Benchmarking and Quantitative Advantages
The integration of PBVS and DBVS is justified by their complementary strengths and weaknesses. DBVS excels at providing detailed atomic-level interaction models but can be computationally expensive and sometimes prone to missing actives due to scoring function limitations. PBVS, by focusing on essential ligand features, offers a rapid and often more robust method for filtering compound libraries, though it may lack the mechanistic detail of docking [29] [91].
Table 1: Benchmark Performance of PBVS vs. DBVS Across Multiple Targets
| Target Protein | Number of Actives | Average Enrichment Factor (PBVS) | Average Enrichment Factor (DBVS) |
|---|---|---|---|
| Acetylcholinesterase (AChE) | 22 | Higher | Lower [29] |
| Androgen Receptor (AR) | 16 | Higher | Lower [29] |
| Dihydrofolate Reductase (DHFR) | 8 | Higher | Lower [29] |
| Estrogen Receptor α (ERα) | 32 | Higher | Lower [29] |
| HIV-1 Protease (HIV-pr) | Data Not Specified | Higher | Lower [29] |
The quantitative advantage of an integrated approach is demonstrated in a study targeting Butyrylcholinesterase (BChE) for Alzheimer's disease. The researchers employed a quantitative structure-activity relationship (QSAR) model built with a machine learning algorithm (XGBoost, AUC=0.974) as an initial ligand-based filter, which was subsequently integrated with structure-based molecular docking. This hybrid strategy successfully identified 12 hits from a large database, including the marketed drug Rotigotine, which was newly recognized for its BChE inhibitory potency (IC₅₀ = 12.76 µM) and anti-AD potential [91]. This case validates the integration of ligand-based (conceptually analogous to pharmacophore) and structure-based methods for efficient lead discovery.
Furthermore, post-filtering docking results with a pharmacophore model has been shown to increase enrichment rates. A study on SARS-CoV-2 papain-like protease used a structure-based pharmacophore model to narrow a marine natural product database to 66 hits. These were then filtered by molecular weight and subjected to comparative molecular docking, ultimately identifying a promising inhibitor that engaged all five key binding sites of the target [92]. This workflow demonstrates the power of PBVS as both a pre- and post-processing tool to refine DBVS outcomes.
Integrated Experimental Protocols
Protocol 1: PBVS as a Pre-Filter for DBVS
This protocol is designed to rapidly reduce the size of an ultra-large compound library to a manageable number of high-probability hits before undergoing more computationally intensive docking.
Workflow Overview:
Step-by-Step Methodology:
Pharmacophore Model Generation (Structure-Based)
- Objective: Create a 3D query representing the essential interactions between a ligand and the target protein.
- Procedure: a. Obtain a high-resolution crystal structure of the target protein (e.g., from the PDB) in complex with a known ligand or inhibitor [29] [2]. b. Use software like LigandScout to automatically generate a pharmacophore model by analyzing the protein-ligand interactions (e.g., hydrogen bond donors/acceptors, hydrophobic regions, ionic interactions) [29]. c. Manually refine the model to emphasize features critical for biological activity, based on known structure-activity relationships (SAR) if available.
PBVS Screening
- Objective: Rapidly screen a large compound database (e.g., millions of compounds) against the pharmacophore model.
- Procedure: a. Prepare the compound database by generating plausible 3D conformers for each molecule. b. Using a program like Catalyst, perform a 3D search to find compounds that match the spatial and chemical constraints of the pharmacophore model [29]. c. Set an appropriate fit threshold to select top-ranking compounds. This typically reduces the library size by 90-95%, resulting in a pre-filtered library of a few thousand compounds [92].
Molecular Docking (DBVS)
- Objective: Accurately predict the binding pose and affinity of the pre-filtered compounds.
- Procedure: a. Prepare the protein structure (add hydrogens, assign partial charges) and define the docking grid around the binding site. b. Dock the pre-filtered library using one or more docking programs (e.g., AutoDock Vina, GOLD, Glide) [29] [91] [92]. c. Rank the resulting compounds based on their docking scores or predicted binding free energies.
Experimental Validation
- The top-ranked compounds from docking are selected for in vitro biochemical assays to confirm target inhibition and potency [91].
Protocol 2: PBVS as a Post-Filter for DBVS
This protocol is used to re-rank and validate docking hits based on ligand-centric pharmacophore features, adding a layer of fitness beyond the docking score.
Workflow Overview:
Step-by-Step Methodology:
High-Throughput Molecular Docking (DBVS)
- Objective: Generate an initial ranked list of hits from a large library.
- Procedure: a. Perform molecular docking on the entire initial library (or a very large subset) using fast, high-throughput docking protocols [93]. b. Retain the top-ranked compounds (e.g., top 10,000) for further analysis.
Pharmacophore Post-Filtering
- Objective: Eliminate false positives and prioritize hits that exhibit a optimal interaction pattern.
- Procedure: a. A validated pharmacophore model (generated as in Protocol 1) is used to screen the top-ranked docking hits. b. Each docking pose is evaluated for its fit to the pharmacophore model. c. Compounds that dock well but do not satisfy the key pharmacophore features are filtered out. This step has been shown to increase enrichment rates compared to docking alone [29] [92].
Experimental Validation
- The final consensus hits, which possess both favorable docking scores and a high pharmacophore fit, are prioritized for experimental testing [91].
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Software and Databases for Integrated VS Workflows
| Tool Name | Type | Primary Function in Workflow | Application Example |
|---|---|---|---|
| LigandScout [29] | Software | Advanced pharmacophore model generation from protein-ligand complexes. | Creating structure-based pharmacophore models for PBVS. |
| Catalyst/Discovery Studio [29] | Software | Perform pharmacophore-based database searching and screening. | Running PBVS on commercial or in-house compound libraries. |
| AutoDock Vina [91] [92] | Software | Open-source molecular docking for binding pose and affinity prediction. | Conducting DBVS on pre-filtered or full libraries. |
| GOLD [29] | Software | Docking software with a genetic algorithm for flexible ligand docking. | Used in benchmark studies for DBVS performance comparison. |
| Glide [29] [94] | Software | High-performance docking program for precise pose prediction and scoring. | Used in integrated VS pipelines for DBVS stages. |
| ZINC20 [93] | Database | Publicly available database of commercially available compounds for virtual screening. | Source of ultra-large chemical libraries for docking campaigns. |
| ChEMBL [91] | Database | Manually curated database of bioactive molecules with drug-like properties. | Source of data for training ligand-based machine learning models. |
The integration of pharmacophore-based and docking-based virtual screening represents a mature and highly effective strategy for accelerating drug discovery against neurodegenerative disease targets. By leveraging PBVS as a strategic pre-filter, researchers can drastically reduce the computational burden of docking ultra-large libraries. Employing it as a post-filter adds a critical layer of validation, prioritizing compounds that satisfy both the physical constraints of the binding site and the essential chemical features for bioactivity. The quantitative data and robust protocols provided herein serve as a guide for research teams to implement these integrated workflows, enhancing the efficiency and success rate of their lead identification campaigns.
Leveraging Molecular Dynamics Simulations for Binding Stability and Affinity Assessment
Molecular dynamics (MD) simulations have become an indispensable tool in structural biology and computer-aided drug design, providing atomic-level insight into the behavior and interactions of biomolecules over time. Within pharmacophore-based virtual screening (VS) protocols for neurodegenerative disease targets, MD simulations are critical for validating and refining hits by assessing the conformational stability and binding affinity of ligand-target complexes. This application note details the protocols for integrating MD simulations to evaluate binding stability and affinity, framed within a comprehensive VS workflow for targets such as GSK3β, tau, and BACE-1, which are critically implicated in Alzheimer's disease and other neurodegenerative conditions [26] [3] [2]. The quantitative and dynamic data obtained from MD simulations, complemented by free energy calculations, provide a robust framework for prioritizing lead compounds with a high potential for experimental success.
MD Integration in the Virtual Screening Workflow
In a typical pharmacophore-based VS protocol for neurodegenerative disease targets, MD simulations act as a crucial filter between molecular docking and experimental validation. The general workflow proceeds as follows: a pharmacophore model is developed based on known active compounds or target structure; a large natural product or synthetic library is screened against this model; hits are subjected to multi-level molecular docking (e.g., HTVS, SP, XP) to predict binding poses and affinity; top-ranking docked complexes are then subjected to MD simulations (typically 100-500 ns) to evaluate their stability and interactions under dynamic, near-physiological conditions; finally, binding free energy is calculated using methods like MM-GBSA or MM-PBSA to quantitatively rank the compounds [95] [96] [2]. This integrated approach significantly increases the likelihood of identifying true positives by filtering out compounds that may score well in static docking but form unstable complexes dynamically.
The following diagram illustrates this integrated computational workflow, highlighting the central role of MD simulations:
Key Neurodegenerative Targets and Signaling Pathways
MD simulations have been extensively applied to key targets in neurodegenerative diseases. Glycogen synthase kinase-3 beta (GSK3β) is a serine/threonine kinase that promotes tau hyperphosphorylation and amyloid-β production when dysregulated [5]. Beta-secretase (BACE-1) is the rate-limiting enzyme in the production of amyloid-β peptides [2]. The microtubule-associated protein tau stabilizes neuronal microtubules, but when hyperphosphorylated, it dissociates and forms neurofibrillary tangles, a hallmark of Alzheimer's disease [26] [3]. These targets are interconnected in a complex signaling network that drives disease progression, as shown in the pathway diagram below:
Quantitative Stability and Affinity Metrics
The stability and affinity of ligand-target complexes are quantified through specific metrics derived from MD simulations. The following table summarizes the key parameters, their definitions, optimal values, and interpretation in the context of binding assessment:
Table 1: Key Metrics for Assessing Binding Stability and Affinity from MD Simulations
| Metric | Definition | Optimal Value Range | Interpretation in Binding Assessment |
|---|---|---|---|
| RMSD (Root Mean Square Deviation) | Measures the average displacement of atom positions between structures over time, indicating overall complex stability. | < 2-3 Å for protein backbone; ligand RMSD should converge [97] [2] | Lower, stable RMSD indicates a stable binding pose without significant structural drift. |
| RMSF (Root Mean Square Fluctuation) | Quantifies per-residue flexibility, showing regions of high and low fluctuation during simulation. | Low fluctuations at binding site residues [2] [5] | Identifies flexible/rigid regions; stable binding is indicated by low RMSF in binding site residues. |
| H-Bonds | Counts the number of hydrogen bonds between ligand and target throughout simulation. | Consistent, stable H-bonds with key binding site residues [95] [97] | Persistent H-bonds with critical residues (e.g., catalytic residues) suggest strong specific interactions. |
| Rg (Radius of Gyration) | Measures the compactness of the protein structure. | Stable value with minimal fluctuation [2] | Indicates whether the protein remains properly folded or undergoes significant unfolding. |
| SASA (Solvent Accessible Surface Area) | Calculates the surface area accessible to solvent molecules. | Stable value with minimal fluctuation [2] | Significant changes may indicate unfolding or large conformational changes affecting binding. |
| MM/GBSA (Molecular Mechanics/Generalized Born Surface Area) | Estimates binding free energy by combining molecular mechanics and implicit solvation models. | Highly negative values (e.g., −24.86 kcal/mol for strong binders [5]) | More negative values indicate stronger binding affinity; used to rank compounds. |
Recent studies demonstrate the successful application of these metrics. For instance, in a study targeting GSK3β for neurodegenerative diseases, MD simulations confirmed that identified inhibitors (ZINC136900288, ZINC7267, ZINC519549) formed stable complexes with minimal backbone RMSD (<2 Å) and strong binding affinities quantified by MM/GBSA, with ZINC136900288 showing the most favorable energy of -24.86 kcal/mol [5]. Similarly, for HER2 inhibitors in breast cancer, 500-ns MD simulations combined with MM-GBSA calculations confirmed strong binding affinities dominated by van der Waals and electrostatic interactions [95].
Detailed Experimental Protocol
System Preparation
Receptor Preparation: Obtain the 3D crystal structure of the target protein (e.g., GSK3β, BACE-1) from the Protein Data Bank (PDB). Prioritize structures with high resolution (<2.0 Å) and completeness. Prepare the protein using Protein Preparation Wizard (Schrödinger) or similar tools: add missing hydrogen atoms, correct protonation states of residues (e.g., HIS, ASP, GLU), assign appropriate bond orders, and fill in missing side chains or loops using homology modeling if necessary. Perform energy minimization with restraints on heavy atoms to relieve steric clashes using AMBER, CHARMM, or GROMACS force fields [2] [5].
Ligand Preparation: Obtain the 3D structure of hit compounds from docking studies or databases like PubChem. Generate realistic 3D conformations using tools like LigPrep (Schrödinger) or MOE. Assign proper bond orders, ionization states at physiological pH (7.0-7.4), and chiralities. Perform geometry optimization using semi-empirical quantum mechanics methods (e.g., AM1 or PM3) or molecular mechanics force fields to minimize the energy [97] [96].
Simulation Setup
Solvation: Place the protein-ligand complex in a simulation box of explicit water molecules (e.g., TIP3P, SPC/E water model). Ensure the box extends at least 10 Å from the protein surface to avoid artificial periodicity effects.
Neutralization: Add counterions (e.g., Na+, Cl-) to neutralize the system's net charge. Additional ions can be added to simulate physiological salt concentration (e.g., 0.15 M NaCl).
Energy Minimization: Perform a two-stage energy minimization: first, with restraints on heavy atoms of the protein and ligand to relax water molecules and ions; second, without restraints to minimize the entire system. Use steepest descent algorithm for the first 5,000 steps followed by conjugate gradient until convergence (energy change < 1000 kJ/mol/nm) [97] [5].
Equilibration and Production Run
Equilibration Phases:
- NVT Ensemble: Heat the system from 0 to 300 K over 100 ps while restraining heavy atoms of protein and ligand (force constant of 1-10 kcal/mol/Ų).
- NPT Ensemble: Equilibrate the system at 1 atm pressure for 100-500 ps with same restraints to achieve proper density.
Production MD: Run unrestrained simulation for 100-500 ns (or longer if needed) at 300 K temperature and 1 atm pressure using a timestep of 2 fs. Employ periodic boundary conditions, particle mesh Ewald method for long-range electrostatics, and LINCS algorithm to constrain bonds involving hydrogen atoms. Save trajectories every 10-100 ps for analysis [95] [2] [5].
Binding Free Energy Calculations
The Molecular Mechanics/Generalized Born Surface Area (MM/GBSA) method is widely used to calculate binding free energies from MD trajectories. The binding free energy (ΔG_bind) is calculated as:
ΔGbind = Gcomplex - (Greceptor + Gligand)
Where G for each component is calculated as:
G = EMM + Gsolv - TS
EMM = Ebonded + Enonbonded = Ebond + Eangle + Edihedral + Eele + Evdw
Gsolv = GGB + G_SA
The following protocol details the MM/GBSA calculation process:
Trajectory Preparation: Extract snapshots from the production MD trajectory at regular intervals (e.g., every 100-500 ps). Ensure snapshots represent conformational diversity while minimizing correlation.
Energy Calculation: For each snapshot, calculate the gas-phase molecular mechanics energy (E_MM) including bonded (bond, angle, dihedral) and non-bonded (electrostatic, van der Waals) terms using the same force field as in MD simulations.
Solvation Energy Calculation: Compute the polar solvation energy (GGB) using the Generalized Born model and non-polar solvation energy (GSA) from the solvent-accessible surface area (SASA): G_SA = γ × SASA + b, where γ and b are constants.
Entropy Estimation: Calculate the conformational entropy change (-TΔS) upon binding using normal mode analysis or quasi-harmonic approximation. Note that this step is computationally intensive and sometimes omitted for relative ranking [95] [96] [5].
Binding Energy Decomposition: Perform per-residue decomposition to identify key residues contributing to binding, which informs further optimization of lead compounds.
The Scientist's Toolkit: Essential Research Reagents and Computational Solutions
Table 2: Essential Computational Tools for MD Simulations in Drug Discovery
| Tool Category | Specific Software/Servers | Primary Function | Application Example |
|---|---|---|---|
| MD Simulation Engines | GROMACS, AMBER, NAMD, Desmond (Schrödinger) | Running production MD simulations with high performance | Desmond was used for 100-ns MD studies of ASK1 inhibitors [96] |
| System Preparation | CHARMM-GUI, PDB2PQR, tleap (AMBER) | Building simulation systems with proper solvation and ionization | CHARMM-GUI used for membrane protein system preparation |
| Trajectory Analysis | MDAnalysis, CPPTRAJ (AMBER), VMD, GROMACS tools | Calculating RMSD, RMSF, H-bonds, Rg, SASA from trajectories | CABS-flex used for RMSF analysis of cur-IONPs/mucin complexes [97] |
| Binding Energy Calculation | MMPBSA.py (AMBER), g_mmpbsa (GROMACS), Prime (Schrödinger) | MM/GBSA and MM/PBSA binding free energy calculations | MM-GBSA identified strong binders for HER2 [95] and GSK3β [5] |
| Visualization | PyMOL, VMD, UCSF Chimera, Discovery Studio | Visualizing trajectories, binding poses, and interactions | Biovia Discovery Studio visualized molecular interactions in fungal metabolite study [2] |
| Specialized Servers | CABS-flex, IMODS, HADDOCK | Web-accessible tools for coarse-grained MD and normal mode analysis | IMODS server used for normal mode analysis of nanoparticle-protein complexes [97] |
Molecular dynamics simulations provide a powerful methodology for assessing binding stability and affinity within pharmacophore-based virtual screening protocols for neurodegenerative disease targets. By evaluating the dynamic behavior of ligand-target complexes and quantifying binding free energies, MD simulations significantly enhance the reliability of hit selection and optimization. The protocols outlined in this application note offer researchers a comprehensive framework for implementing MD simulations to advance therapeutic development for challenging targets in Alzheimer's disease and other neurodegenerative conditions. When integrated with experimental validation, this approach provides a robust pipeline for identifying promising drug candidates with higher potential for clinical success.
Conclusion
Pharmacophore-based virtual screening stands as a powerful and efficient strategy for initiating the drug discovery process against complex neurodegenerative disease targets. By building a foundational understanding of key pathological proteins like phosphorylated tau and BACE1, and implementing a robust methodological protocol that includes careful model building, BBB permeability assessment, and thorough validation, researchers can significantly de-risk the early stages of lead identification. The comparative superiority of PBVS in many scenarios, its ability to be integrated with other computational methods, and its successful application in identifying novel inhibitors for targets like KMO and BACE1 underscore its immense value. Future directions will involve tighter integration with machine learning models, improved BBB-on-a-chip technologies for experimental validation, and the application of these integrated protocols against a broader range of emerging NDD targets, ultimately accelerating the development of urgently needed neurotherapeutics.
References
- 1. Neurotherapeutics across blood–brain barrier: screening of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12511116/]
- 2. Pharmacophore-Based Screening, Molecular Docking, and ... [https://www.mdpi.com/2218-273X/13/11/1613]
- 3. Current pharmacophore based approaches for the ... [https://www.sciencedirect.com/science/article/abs/pii/S0968089624003407]
- 4. Application of computational methods in the drug discovery ... [https://www.sciencedirect.com/science/article/pii/S2211383525005179]
- 5. Integrative machine learning and molecular simulation ... [https://www.nature.com/articles/s41598-025-04129-7]
- 6. Pharmacophore-based virtual screening of commercial ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11263123/]
- 7. Drug Design by Pharmacophore and Virtual Screening ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9145410/]
- 8. Concepts and Applications Exemplified on Hydroxysteroid ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6332202/]
- 9. Ligand-Based and Structure-Based Pharmacophore ... [https://bio-protocol.org/exchange/minidetail?id=9587520&type=30]
- 10. Pharmacophore-based virtual screening versus docking ... [https://www.nature.com/articles/aps2009159]
- 11. Phosphorylated Tau in Alzheimer's Disease and Other ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9654278/]
- 12. A Close Look at BACE1 Inhibitors for Alzheimer's Disease ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7330928/]
- 13. Tau-Targeted Therapeutic Strategies - PubMed Central - NIH [https://pmc.ncbi.nlm.nih.gov/articles/PMC12523266/]
- 14. Revisiting the therapeutic landscape of tauopathies [https://alzres.biomedcentral.com/articles/10.1186/s13195-025-01775-x]
- 15. Pharmacophore-based virtual screening of commercial ... [https://www.frontiersin.org/journals/chemistry/articles/10.3389/fchem.2024.1412349/full]
- 16. Prevention of tau increase in cerebrospinal fluid of APP ... [https://pubmed.ncbi.nlm.nih.gov/27750032/]
- 17. BACE1 inhibition could block CSF tau increase [https://www.nature.com/articles/nrneurol.2016.170]
- 18. Identification of BACE-1 Inhibitors against Alzheimer's ... - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC10142975/]
- 19. Blood biomarkers of Alzheimer's disease and progression ... [https://www.nature.com/articles/s41467-025-66728-2]
- 20. Pharmacophore modeling and applications in drug discovery [https://www.sciencedirect.com/science/article/pii/S135964461000111X]
- 21. Lock-Key Model - an overview [https://www.sciencedirect.com/topics/biochemistry-genetics-and-molecular-biology/lock-key-model]
- 22. Applications of the Pharmacophore Concept in Natural ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7685156/]
- 23. Principles in Pharmacophore Elucidation [https://drugdesign.org/chapters/pharmacophore-elucidation/]
- 24. Knowledge-guided diffusion model for 3D ligand ... [https://www.nature.com/articles/s41467-025-57485-3]
- 25. Knowledge-guided diffusion model for 3D ligand ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11885826/]
- 26. Pharmacophore-based models for therapeutic drugs ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6397090/]
- 27. Pharmacophore-Based Virtual Screening of Alkaloids and ... [https://www.mdpi.com/2076-3417/15/18/10162]
- 28. Drug Design for CNS Diseases: Polypharmacological ... [https://www.frontiersin.org/journals/neuroscience/articles/10.3389/fnins.2016.00265/full]
- 29. Pharmacophore-based virtual screening versus docking ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4007494/]
- 30. Pharmacophore modeling and applications in drug discovery [https://www.sciencedirect.com/science/article/abs/pii/S135964461000111X]
- 31. Pharmacophore-based approach for the identification of ... [https://www.sciencedirect.com/science/article/pii/S266702242500012X]
- 32. Pharmacophore-based virtual screening for identification of ... [https://www.sciencedirect.com/science/article/pii/S2667022424003499]
- 33. T009 · Ligand - based — TeachOpenCADD... pharmacophores [https://projects.volkamerlab.org/teachopencadd/talktorials/T009_compound_ensemble_pharmacophores.html]
- 34. - Structure 2. Developing a novel... based pharmacophore modeling [https://pubmed.ncbi.nlm.nih.gov/37121167/]
- 35. A Case Study on SARS-CoV-2 Mpro [https://pubmed.ncbi.nlm.nih.gov/41082460/?utm_source=FeedFetcher&utm_medium=rss&utm_campaign=None&utm_content=14mzXgUgXxOhz72eR8oGB-fhcdG9zbPCC1041iU1Zt22GVtQAD&fc=None&ff=20251024010210&v=2.18.0.post22+67771e2]
- 36. Pharmacophore Modeling for Targets with Extensive ... [https://www.jove.com/t/68933/pharmacophore-modeling-for-targets-with-extensive-ligand-libraries]
- 37. Accelerating discovery of bioactive ligands ... | Nature Communications [https://www.nature.com/articles/s41467-025-56349-0?error=cookies_not_supported&code=7cf69413-6e95-48e4-970e-50617d7386dd]
- 38. Pharmacophore-Guided Generative Design of Novel Drug- ... [https://arxiv.org/html/2510.01480v1]
- 39. Non-Extensive Fragmentation of Natural Products and... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8377161/]
- 40. Pharmacophore-Based Screening, Molecular Docking, and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10669353/]
- 41. Pharmacophore screening [https://bio-protocol.org/exchange/minidetail?id=3070000&type=30]
- 42. Pharmacophore-based virtual screening and in silico ... [https://pubmed.ncbi.nlm.nih.gov/40260383/]
- 43. Pharmacophore-based virtual screening and in silico ... [https://www.frontiersin.org/journals/pharmacology/articles/10.3389/fphar.2025.1531512/full]
- 44. A New Fragment‐Based Pharmacophore Virtual Screening ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12412281/]
- 45. Machine learning accelerates pharmacophore-based ... [https://www.nature.com/articles/s41598-024-58122-7]
- 46. deep learning-guided pharmacophore modeling for ultra-large ... [https://pubs.rsc.org/en/content/articlelanding/2024/sc/d4sc04854g]
- 47. Pharmacophore-Based Virtual Screening of Novel ... [https://pubmed.ncbi.nlm.nih.gov/34073016/]
- 48. Kynurenine-3-monooxygenase: a review of structure, ... [https://www.sciencedirect.com/science/article/abs/pii/S1359644615004201]
- 49. Targeting the kynurenine pathway in gliomas: Insights into ... [https://www.sciencedirect.com/science/article/pii/S0304419X2500085X]
- 50. Kynurenine pathway: a possible new mechanism for exercise ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12537677/]
- 51. Novel insights into structure-activity relationships of ... [https://pubmed.ncbi.nlm.nih.gov/40667575/]
- 52. Kynurenine 3-monooxygenase (KMO) as a Target to ... [https://www.michaeljfox.org/grant/kynurenine-3-monooxygenase-kmo-target-develop-drugs-block-progression-parkinsons-disease]
- 53. A brain-permeable inhibitor of the neurodegenerative ... [https://www.nature.com/articles/s42003-019-0520-5]
- 54. Pharmacophore-Based Virtual Screening of Novel ... [https://www.mdpi.com/1420-3049/26/11/3314]
- 55. Identification of potent inhibitors of kynurenine-3- ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11079110/]
- 56. Advances in brain-targeted delivery strategies and natural ... [https://jnanobiotechnology.biomedcentral.com/articles/10.1186/s12951-025-03415-w]
- 57. Multi‐Target Drug Design in Alzheimer's Disease Treatment [https://pmc.ncbi.nlm.nih.gov/articles/PMC12175645/]
- 58. Advanced ADMET Modeling Using Deep Learning and AI [https://www.technologynetworks.com/drug-discovery/blog/beyond-black-box-models-advances-in-data-driven-admet-modeling-403114]
- 59. Top 5 Drug Discovery Trends 2025 Driving Breakthroughs [https://www.pelagobio.com/cetsa-drug-discovery-resources/blog/drug-discovery-trends-2025/]
- 60. Pharmacophore modeling in drug design [https://pubmed.ncbi.nlm.nih.gov/40175047/]
- 61. ADME-drug-likeness: enriching molecular foundation ... [https://pubmed.ncbi.nlm.nih.gov/40662819/]
- 62. A Review of Blood Brain Barrier Permeability Prediction Models [https://pmc.ncbi.nlm.nih.gov/articles/PMC11949286/]
- 63. Strategies for delivering drugs across the blood-brain ... [https://www.frontiersin.org/journals/drug-delivery/articles/10.3389/fddev.2025.1644633/full]
- 64. Deep Learning for Blood-Brain Barrier Permeability ... [https://arxiv.org/abs/2507.18557]
- 65. Predicting blood–brain barrier permeability of molecules ... [https://www.nature.com/articles/s41598-024-66897-y]
- 66. New Approach Methodologies: What Clinical Pharmacologists ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12404678/]
- 67. Step Forward Cross Validation for Bioactivity Prediction [https://pmc.ncbi.nlm.nih.gov/articles/PMC11245006/]
- 68. Enhancing the quality and reproducibility of research ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12125112/]
- 69. LBA Cross Validation: A Detailed Case Study [https://emerypharma.com/blog/lba-cross-validation-a-detailed-case-study/]
- 70. Pharmacophore Modeling and Docking Studies on Some ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3780516/]
- 71. Development of a novel pharmacophore model to screen ... [https://www.sciencedirect.com/science/article/pii/S240558082200111X]
- 72. Pharmacophore based virtual screening of cholinesterase ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9521886/]
- 73. Validation of pharmacophore model [https://bio-protocol.org/exchange/minidetail?id=19108364&type=30]
- 74. Pharmacophore Modeling, Virtual Screening, and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3558715/]
- 75. dyphAI dynamic pharmacophore modeling with AI: a tool ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11865752/]
- 76. Harnessing artificial intelligence for brain disease: advances ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12336123/]
- 77. Artificial intelligence in drug development for delirium and ... [https://www.sciencedirect.com/science/article/pii/S2211383525002886]
- 78. Advancing ADMET prediction for major CYP450 isoforms: graph-based... [https://biomedical-engineering-online.biomedcentral.com/articles/10.1186/s12938-025-01412-6]
- 79. Frontiers | Recent advances in AI-based toxicity prediction for drug... [https://www.frontiersin.org/journals/chemistry/articles/10.3389/fchem.2025.1632046/full]
- 80. A review and in silico screening of plant-derived snake venom/toxin... [https://pubmed.ncbi.nlm.nih.gov/41066512/]
- 81. The Global Neurodegeneration Proteomics Consortium [https://www.nature.com/articles/s41591-025-03834-0]
- 82. Brief Guide: Experimental Strategies for High-Quality Hit ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8293735/]
- 83. A pragmatic approach to hit validation following ... [https://www.drugtargetreview.com/article/27913/hit-validation-high-throughput-screening/]
- 84. Biochemical Assay Development: Strategies to Speed Up ... [https://bellbrooklabs.com/accelerate-biochemical-assay-development/?srsltid=AfmBOopJbVBbhjrvemJpOTq_R_y2xybsH3jquE1uOHd1MAbPHKWGb05Y]
- 85. In Silico Identification and In Vitro Validation of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10302583/]
- 86. Pharmacophore-based virtual screening versus docking- ... [https://pubmed.ncbi.nlm.nih.gov/19935678/]
- 87. Structure-Based Virtual Screening for Drug Discovery [https://pmc.ncbi.nlm.nih.gov/articles/PMC3282008/]
- 88. Benchmarking the Structure-Based Virtual Screening ... [https://www.dovepress.com/benchmarking-the-structure-based-virtual-screening-performance-of-wild-peer-reviewed-fulltext-article-DDDT]
- 89. How useful is virtual screening in drug discovery? [https://synapse.patsnap.com/article/how-useful-is-virtual-screening-in-drug-discovery]
- 90. Grid-derived structure-based 3D pharmacophores and ... [https://www.sciencedirect.com/science/article/abs/pii/S1740674910000296]
- 91. Discovery, Biological Evaluation and Binding Mode ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12113681/]
- 92. Pharmacophore model-aided virtual screening combined ... [https://www.sciencedirect.com/science/article/pii/S1878535222006505]
- 93. Identification of potent high-affinity secondary nucleation ... [https://link.springer.com/article/10.1038/s44320-025-00159-5]
- 94. DrugAppy – An end-to-end deep learning framework for ... [https://www.sciencedirect.com/science/article/pii/S0010482525015549]
- 95. Pharmacophore modeling and molecular dynamics ... [https://pubmed.ncbi.nlm.nih.gov/40126740/]
- 96. Pharmacophore modeling, molecular docking, MMGBSA ... [https://www.sciencedirect.com/science/article/pii/S2468227625001048]
- 97. Investigating the binding affinity, molecular dynamics, and ... [https://www.nature.com/articles/s41598-024-72577-8]