Whole Exome Sequencing in Cancer Research: A Comprehensive Guide from Basics to Clinical Applications
This article provides a comprehensive overview of Whole Exome Sequencing (WES) and its transformative role in modern cancer research and therapeutic development.
Whole Exome Sequencing in Cancer Research: A Comprehensive Guide from Basics to Clinical Applications
Abstract
This article provides a comprehensive overview of Whole Exome Sequencing (WES) and its transformative role in modern cancer research and therapeutic development. It covers foundational principles, current methodological approaches including automated workflows and kit selection, and practical guidance for troubleshooting and optimizing WES experiments. The content critically examines WES performance through validation studies and comparative analyses with alternative genomic profiling methods, highlighting its economic and clinical benefits in identifying actionable alterations and guiding targeted therapies. Designed for researchers, scientists, and drug development professionals, this resource synthesizes the latest technological advancements and evidence-based applications to inform research design and clinical implementation strategies.
The Foundational Role of WES in Decoding Cancer Genomics
Whole exome sequencing (WES) represents a powerful methodological approach in cancer genomics, enabling comprehensive analysis of protein-coding regions to identify somatic mutations driving oncogenesis. This technical guide elucidates the core principles defining WES as "whole" through its capacity to interrogate all ~20,000 genes in a single assay, distinguishing it from targeted panels and whole-genome sequencing. We detail experimental protocols for variant calling, discuss the pivotal role of WES in identifying therapeutic targets and biomarkers like tumor mutation burden (TMB), and provide structured quantitative comparisons of sequencing methodologies. Within precision oncology frameworks, WES facilitates drug repurposing opportunities by revealing shared biomarkers across tumor types and contributes substantially to biomarker discovery in rare cancers. This work provides researchers with comprehensive methodological guidance and contextualizes WES within the evolving landscape of cancer genomics research.
The term "whole" in whole exome sequencing signifies the systematic attempt to capture and sequence all protein-coding regions of the genome, representing approximately 1-2% of the human genome yet containing an estimated 85% of known disease-causing variants [1]. This comprehensive approach distinguishes WES from targeted gene panels that investigate predetermined gene sets and from whole-genome sequencing (WGS) that encompasses both coding and non-coding regions. The fundamental premise underpinning WES in cancer research is that the exome harbors the majority of somatic mutations with direct functional consequences on protein structure and function, thereby driving tumorigenesis and offering potential therapeutic targets [2] [3].
The strategic importance of WES in cancer research stems from its balanced approach to genomic interrogation. While WGS provides a more complete genomic profile, WES offers superior cost-effectiveness and data manageability, enabling larger sample sizes for robust statistical analysis in cohort studies [4]. The methodological "wholeness" of WES manifests through several technical characteristics: its unbiased nature (interrogating all exons without prior hypothesis about specific genes), standardized target regions (using consistent capture kits across samples), and completeness of coverage (attempting to sequence all exonic regions despite technical challenges) [2] [1]. This systematic approach has positioned WES as a cornerstone technology in major cancer genomics initiatives, including The Cancer Genome Atlas (TCGA), where it has helped characterize the mutational landscapes of numerous cancer types [5].
Technical Foundations of Whole Exome Sequencing
Core Principles and Workflow
The principle of WES centers on the selective capture and high-throughput sequencing of exonic regions from fragmented genomic DNA [1]. This process leverages the fundamental biological understanding that while exons constitute a small minority of the genome, they harbor the majority of clinically actionable mutations, making them particularly informative for cancer research [3]. The technical workflow follows a standardized series of steps that ensure comprehensive exome coverage while minimizing artifacts and biases.
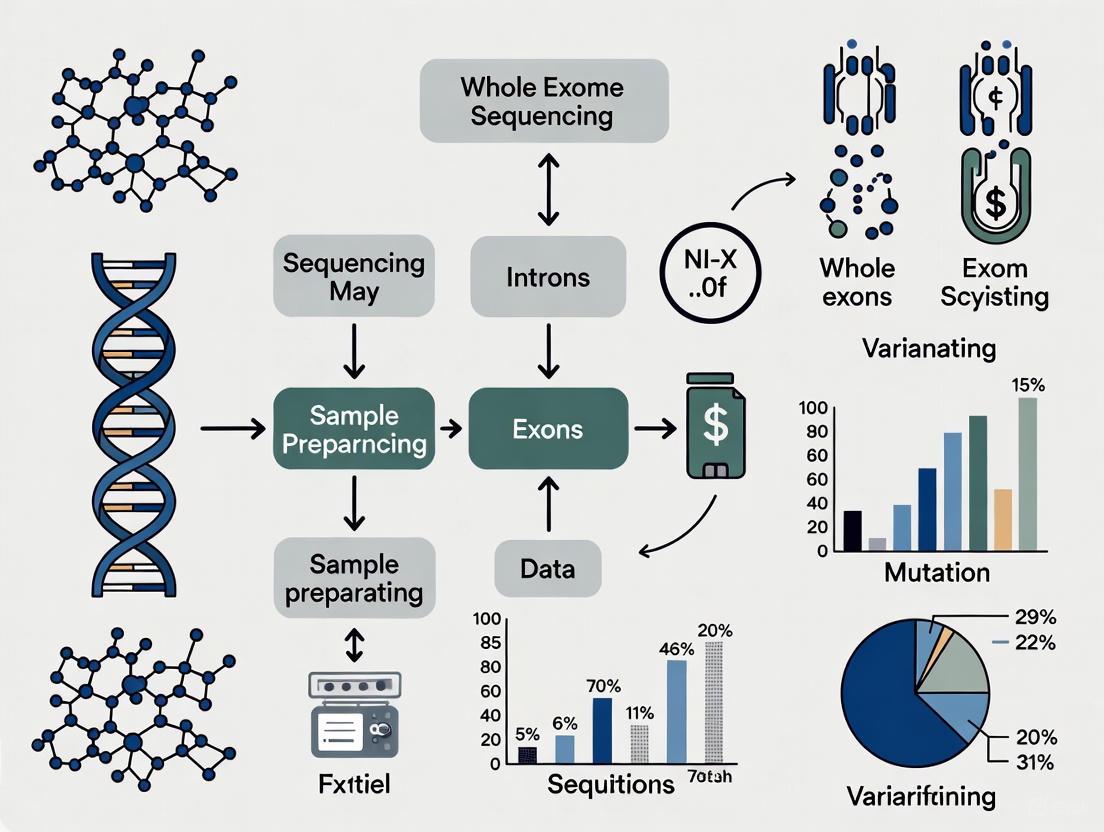
The following diagram illustrates the complete WES workflow from sample preparation through data analysis:
Experimental Protocol Details
Sample Preparation and Library Construction
The initial phase requires high-quality DNA isolated from matched tumor and normal tissues. Tumor samples should contain sufficient malignant cells (typically >70% tumor purity) to confidently call somatic variants, while normal samples (usually blood, saliva, or adjacent normal tissue) serve as germline controls [2]. DNA quality assessment via fluorometry or spectrophotometry is critical, with degradation particularly problematic in formalin-fixed paraffin-embedded (FFPE) specimens [2]. Following extraction, DNA undergoes fragmentation (via sonication or enzymatic methods) to sizes of 150-200bp, followed by end repair, adenylation, and adapter ligation to create sequencing libraries compatible with platforms like Illumina [1].
Exome Enrichment Methods
The defining step of WES utilizes hybridization capture to isolate exonic regions from the genomic DNA library. The most common approach employs biotinylated probes (e.g., Twist Bioscience Human Core Exome Kit, Illumina TruSeq DNA Exome) that specifically bind to exonic regions [6] [1]. Key technical considerations include:
- Probe Design: Modern kits target 30-60 megabases encompassing exons, UTRs, and select non-coding RNAs
- Hybridization Conditions: Temperature and timing optimization to maximize on-target specificity
- Capture Method: Solution-based hybridization outperforms array-based methods for efficiency and uniformity [2]
The hybridized fragments are isolated using streptavidin-coated magnetic beads, while non-targeted regions are washed away. Captured DNA is then amplified via PCR to generate sufficient material for sequencing [1].
Sequencing and Data Analysis
Enriched libraries undergo massively parallel sequencing on platforms such as Illumina NovaSeq with typical read lengths of 100-150bp paired-end to ensure adequate coverage of exonic regions [7] [1]. Sequencing depth of 100-200x is recommended for tumor samples to detect subclonal populations, while germline controls typically require 30-50x coverage [2].
Bioinformatic processing involves:
- Quality Control: FastQC for sequence quality metrics
- Alignment: BWA-MEM or similar aligners to reference genome (GRCh37/hg19 or GRCh38/hg38)
- Variant Calling: Multiple algorithms for detecting different variant types (Table 1)
- Annotation: Tools like SNPeff or VEP for predicting functional consequences [7] [2]
Table 1: Common Variant Callers for Somatic Mutation Detection in Cancer WES
| Variant Type | Tool Options | Key Features | Performance Considerations |
|---|---|---|---|
| SNVs/Indels | MuTect2, VarScan2, Strelka | High sensitivity for low-frequency variants, contamination correction | Strelka performs well with high-coverage data; MuTect2 excels in low-frequency detection [2] |
| Copy Number Variations | ASCAT, Sequenza | Account for tumor purity, ploidy | Require sufficient coverage depth; challenging with WES due to uneven coverage [2] |
| Structural Variants | Delly, Manta | Detect translocations, inversions | Limited sensitivity with WES data; WGS preferred [8] |
WES in Cancer Research: Key Applications and Methodological Comparisons
Therapeutic Target Discovery and Biomarker Identification
WES enables systematic identification of somatic mutations across cancer types, revealing both common driver mutations and rare subtype-specific alterations. In hypopharyngeal cancer, WES of 10 patients identified 8,113 mutation sites across 5,326 genes, with 72 pathogenic mutations in 53 genes following ACMG guidelines [9]. Notably, KMT2C showed mutations in all 10 patients, while TTN, ANK3, and TP53 demonstrated high mutation frequencies consistent with TCGA data [9]. Functional annotation and pathway enrichment analyses of WES data can prioritize mutations for therapeutic development, as demonstrated by the discovery of RBM20 as a potential driver in hypopharyngeal cancer with prognostic significance [9].
WES further facilitates drug repurposing opportunities by identifying shared therapeutic biomarkers across histologically distinct cancers. Research analyzing 726 tumors across 10 cancer types revealed that "treatment biomarkers are shared across solid tumours, highlighting repurposing opportunities" [7]. For instance, BRCA1/2 mutations detected via WES can indicate PARP inhibitor sensitivity across multiple tumor types, while high tumor mutation burden (TMB) may predict immunotherapy response regardless of tissue of origin [10].
Comparison with Alternative Sequencing Approaches
The strategic selection of genomic profiling methods depends on research objectives, resources, and specific biological questions. The following table quantitatively compares WES with alternative approaches:
Table 2: Sequencing Platform Comparisons in Cancer Genomics
| Parameter | Whole Exome Sequencing (WES) | Whole Genome Sequencing (WGS) | Comprehensive Gene Panel |
|---|---|---|---|
| Genomic Coverage | 1-2% (30-60 Mb) | 100% (~3,000 Mb) | 0.002-2.6 Mb (targeted genes) [7] |
| Variant Detection Scope | Coding SNVs/indels; limited CNVs | All variant types including structural variants, non-coding | Targeted SNVs/indels, CNVs, fusions (panel-dependent) |
| Cost per Sample | $$ | $$$$ | $ |
| Data Volume | ~5-10 GB | ~90-100 GB | ~0.5-2 GB |
| TMB Calculation | Well-correlated with WGS but absolute values differ [7] | Gold standard | Possible but requires careful normalization [7] |
| Therapeutic Applications | Identifies ~90% of known drug targets; detects trial biomarkers [7] | Maximum biomarker discovery including non-coding | Identifies majority of approved actionable mutations [7] |
Recent direct comparisons demonstrate that WES/WGS identifies approximately 30% more therapy recommendations than large panels (median 3.5 vs. 2.5 per patient), with one-third of WES/WGS recommendations relying on biomarkers not covered by panels [10]. These additional biomarkers include mutational signatures, complex structural variants, and non-canonical fusion genes [10].
Tumor Mutation Burden and Microsatellite Instability Assessment
WES enables calculation of tumor mutation burden (TMB), defined as the total number of mutations per megabase of genome sequenced. TMB estimation varies significantly between sequencing platforms, with WES-based TMB requiring careful normalization against targeted panels [7]. Methodological considerations include:
- Mutation Inclusion: Whether to consider all mutations or only non-synonymous mutations
- Coverage Uniformity: WES capture efficiency impacts TMB accuracy
- Threshold Determination: TMB cutoffs for "high" burden are platform-specific [7]
WES also facilitates microsatellite instability (MSI) detection through tools like MSIsensor, which analyzes microsatellite regions within exonic sequences [7]. However, MSI detection sensitivity depends on the number of microsatellites captured, with WGS typically providing more comprehensive assessment than WES.
Research Reagents and Computational Tools
Table 3: Essential Research Reagents and Computational Tools for Cancer WES
| Category | Specific Examples | Application in WES Workflow |
|---|---|---|
| Exome Capture Kits | Twist Bioscience Human Core Exome, Illumina TruSeq DNA Exome | Target enrichment of exonic regions through hybridization capture [6] |
| Library Prep Kits | Illumina DNA Prep, KAPA HyperPrep | Fragmentation, end repair, adapter ligation, and PCR amplification [3] |
| Sequencing Platforms | Illumina NovaSeq 6000, Illumina HiSeq | High-throughput sequencing with paired-end reads [7] |
| Alignment Tools | BWA-MEM, Bowtie2 | Mapping sequenced reads to reference genome [7] [2] |
| Variant Callers | MuTect2 (SNVs), VarScan2 (SNVs/indels), ASCAT (CNVs) | Detecting somatic mutations from aligned BAM files [7] [2] |
| Annotation Tools | SNPeff, Variant Effect Predictor (VEP) | Predicting functional consequences of identified variants [7] [2] |
| Analysis Platforms | Galaxy, GATK | Comprehensive analysis pipelines for variant discovery [2] |
Technical Limitations and Complementary Approaches
Despite its utility, WES presents several technical limitations that researchers must acknowledge. Incomplete exome coverage results from capture inefficiencies, with some exonic regions consistently under-represented due to high GC content or repetitive sequences [8]. Detection of structural variants (including copy number variations, translocations, and inversions) remains challenging with WES data due to uneven coverage and the location of breakpoints outside captured regions [8]. Additionally, WES completely misses non-coding regulatory elements that may influence gene expression and cancer pathogenesis, such as promoters, enhancers, and non-coding RNAs [5] [8].
These limitations necessitate complementary approaches in comprehensive cancer genomics studies. RNA sequencing identifies expressed mutations, gene fusions, and aberrant splicing events missed by WES [10]. Whole genome sequencing provides complete genomic characterization, including non-coding drivers and complex structural variants [5]. Targeted panels offer ultra-deep sequencing for detecting low-frequency subclonal populations in minimal residual disease monitoring [7].
The following diagram illustrates the variant detection landscape across sequencing platforms:
Whole exome sequencing remains a cornerstone technology in cancer genomics, offering a balanced approach between comprehensive genomic assessment and practical research constraints. The "wholeness" of WES derives from its systematic interrogation of all protein-coding regions, enabling discovery of driver mutations, therapeutic biomarkers, and molecular cancer subtypes across diverse malignancies. As sequencing technologies evolve and computational methods improve, WES continues to provide critical insights into cancer biology while complementing emerging approaches like whole genome and transcriptome sequencing. For cancer researchers designing genomic studies, WES represents an efficient primary discovery tool when focused on coding regions, with subsequent targeted validation or expanded genomic characterization as needed. The ongoing integration of WES data with functional genomics and clinical outcomes will further advance precision oncology approaches across the cancer spectrum.
In the landscape of precision oncology, the choice of genomic profiling technology is pivotal, balancing comprehensiveness with practical clinical and research constraints. Whole exome sequencing (WES) has emerged as a powerful solution that strategically targets the protein-coding regions of the genome, where an estimated 85% of disease-causing mutations reside. This focused approach provides researchers and clinicians with a methodologically efficient and economically viable pathway to actionable genomic insights. While whole genome sequencing (WGS) offers a broader view of the entire genome, including non-coding regions, WES delivers targeted depth at a significantly reduced cost and computational burden, making it particularly suitable for large-scale cancer studies where budget and bioinformatics resources are limiting factors. The strategic application of WES enables comprehensive tumor profiling, identification of hereditary cancer syndromes, and discovery of novel therapeutic targets without the overhead of whole-genome analysis. This technical guide examines the core advantages of WES through the dual lenses of cost-effectiveness and targeted biological insight, providing the scientific community with a validated framework for its implementation in cancer research and drug development.
Economic Advantages: A Detailed Cost-Benefit Analysis
Comprehensive Cost Comparisons Across Sequencing Platforms
The economic argument for WES is substantiated by multiple cost-analyses across different research settings and geographical locations. A systematic review of health economic evidence found that cost estimates for a single test ranged from $555 to $5,169 for WES compared to $1,906 to $24,810 for WGS [11] [12]. This significant price differential makes WES accessible for larger cohort studies within constrained budgets.
Table 1: Cost Analysis of Genomic Sequencing Technologies in Cancer Research (2018-2020)
| Sequencing Technology | Cost Range (US$) | Key Cost Drivers | Proportion of Total Cost |
|---|---|---|---|
| Whole Exome Sequencing (WES) | $604 - $1,932 [13] | Library preparation & sequencing materials | 76.8% [13] |
| Whole Genome Sequencing (WGS) | $2,006 - $3,347 [13] | Data analysis, storage, and interpretation | Higher than WES due to data volume |
| Targeted Panels | $240 - $297 [13] | Sample extraction and processing | 8.1% [13] |
A detailed micro-costing study conducted in Australia further quantified this differential, reporting per-person costs of AU$871-$2,788 (US$604-1,932) for exome sequencing compared to AU$2,895-$4,830 (US$2,006-3,347) for whole genome sequencing [13]. The study identified that library preparation and sequencing materials constituted the largest proportion (76.8%) of total costs, followed by data analysis (9.2%), sample extraction (8.1%), and data storage (2.6%) [13]. These findings highlight how WES achieves efficiency by minimizing costs in the most expensive phases of sequencing while maintaining focus on clinically relevant genomic regions.
Health Economic and Outcome Benefits in Oncology
Beyond direct sequencing costs, WES demonstrates superior cost-effectiveness through its impact on clinical decision-making and patient outcomes. A 2025 economic modeling study in advanced non-small cell lung cancer (NSCLC) demonstrated that combining whole exome and whole transcriptome sequencing (WES/WTS) reduced costs by $14,602 per patient compared to sequential single-gene testing while providing minimal survival benefits [14]. When compared with no genomic testing, the WES/WTS approach reduced costs by $8,809 per patient tested while increasing median overall survival by an average of 3.9 months [14].
The economic advantage extends to testing efficiency. Comprehensive genomic profiling via WES identifies more actionable alterations than sequential single-gene approaches, particularly for fusions that require RNA sequencing for detection. The same study showed that tests incorporating both DNA and RNA sequencing increased identification of actionable alterations by 2.3%-13.0% across the range of fusion prevalence while reducing costs by $400-1,724 [14]. This demonstrates how WES-based approaches maximize diagnostic yield per healthcare dollar spent.
Infrastructure and Scalability Economic Benefits
WES generates significantly smaller datasets than WGS (approximately 5 GB vs. 100 GB per sample), resulting in substantial savings in data storage and computational processing [13]. This reduced infrastructure requirement lowers the barrier to entry for individual research laboratories and hospital systems without access to high-performance computing clusters. The efficiency extends to analytical workflows, where the focused nature of exome data accelerates variant identification and interpretation compared to the complex filtering required for whole genome datasets. This computational efficiency translates to faster turnaround times from sample to report, a critical factor in clinical oncology where treatment decisions are time-sensitive. The cumulative effect of these advantages positions WES as the optimal balancing point between comprehensiveness and practical implementability in both research and clinical settings.
Technical and Biological Advantages in Cancer Research
Enhanced Detection of Clinically Actionable Variants
The targeted nature of WES enables deeper sequencing coverage (typically 100x-200x) of exonic regions compared to the 30x-60x coverage typical of WGS in clinical practice. This enhanced depth improves detection of somatic mutations with low variant allele frequency due to tumor heterogeneity or stromal contamination. A 2025 study implementing exome-based cancer predisposition gene testing demonstrated a 9.7% diagnostic yield in individuals with multiple primary tumors, identifying pathogenic variants in cancer-associated genes including CHEK2, FANCM, NF1, POT1, and PTEN [15]. An additional 4.2% of individuals carried candidate variants in genes such as HOXB13, MAX, and RECQL4 [15]. This demonstrates the capability of WES to identify clinically relevant mutations across a broad spectrum of cancer types without prior hypothesis about specific genes.
The comprehensive nature of WES is particularly valuable for cancers with heterogeneous molecular profiles or when patients present with atypical tumor spectra that don't align with established hereditary cancer syndromes. By analyzing all ~20,000 protein-coding genes simultaneously, WES eliminates the need for iterative single-gene testing that characterized traditional genetic diagnostics. The technology successfully identifies mutations in genes not typically associated with a patient's specific cancer type, expanding understanding of genotype-phenotype correlations and revealing novel therapeutic targets [15].
Integration with Functional Genomics and Transcriptomics
Modern WES workflows increasingly incorporate complementary genomic analyses that enhance functional interpretation. The combination of WES with whole transcriptome sequencing (WTS) provides a more complete molecular portrait by connecting genomic alterations with their functional consequences at the RNA level. This integrated approach is particularly powerful for detecting gene fusions, alternative splicing events, and expression outliers that may not be evident from DNA sequencing alone [14]. The addition of transcriptomic data helps prioritize mutations of functional significance among the numerous variants identified in exome sequencing, accelerating the transition from genomic discovery to biological validation.
The focused data generation of WES also facilitates more streamlined integration with epigenetic profiling and proteomic data. Unlike the massive datasets from WGS that require extensive preprocessing, WES data can be more readily correlated with DNA methylation arrays, chromatin accessibility maps, and protein expression patterns to build multi-omics models of tumor behavior. This integrative capability positions WES as a cornerstone technology in systems biology approaches to cancer research, where understanding the functional interplay between different molecular layers is essential for deciphering complex tumor phenotypes and therapeutic resistance mechanisms.
Experimental Design and Methodological Protocols
Standardized WES Wet-Lab Workflow
The reproducibility of WES depends on strict adherence to standardized laboratory protocols. The following workflow outlines the key steps for generating high-quality exome sequencing data from tumor and matched normal samples:
Sample Preparation and Quality Control
- Extract DNA from fresh frozen or FFPE tumor tissue and matched normal (blood or saliva) using validated kits
- Assess DNA quality via fluorometry (Qubit) and fragment analysis (Bioanalyzer/TapeStation)
- Require minimum DNA quantity: 50-100ng for fresh frozen, 100-200ng for FFPE
- Require minimum DNA quality: DV200 >30% for FFPE samples, A260/A280 ratio of 1.8-2.0
Library Preparation and Target Enrichment
- Fragment DNA to 150-200bp using acoustic shearing (Covaris) or enzymatic fragmentation
- Repair DNA ends, add A-overhangs, and ligate with platform-specific adaptors
- Amplify libraries with 4-8 PCR cycles using high-fidelity polymerase
- Perform exome capture using commercial systems (e.g., Agilent SureSelect, Illumina Nextera)
- Hybridize libraries with biotinylated RNA baits covering exonic regions for 16-24 hours
- Capture bait-bound fragments using streptavidin-coated magnetic beads
- Wash to remove non-specifically bound fragments and amplify captured libraries with 8-12 PCR cycles
Sequencing
- Quantify final libraries by qPCR and pool at equimolar ratios
- Sequence on appropriate NGS platform (Illumina NovaSeq, Complete Genomics DNBSEQ-T1+, etc.)
- Target minimum coverage of 100x for tumor and normal samples
- Use paired-end sequencing (2x100bp or 2x150bp) for optimal variant calling
Bioinformatics Analysis Pipeline
The computational analysis of WES data follows a structured workflow from raw sequences to annotated variants:
Variant Prioritization Strategy for Cancer
- Filter against population databases (gnomAD) to remove common polymorphisms (MAF <0.1%)
- Retain protein-truncating variants (nonsense, frameshift, splice-site)
- Prioritize missense variants with high pathogenicity scores (CADD >20, SIFT, PolyPhen)
- Compare tumor vs. normal to identify somatic mutations
- Annotate with cancer-specific databases (COSMIC, OncoKB, CIViC)
- Filter for actionable alterations with therapeutic implications
Essential Research Reagent Solutions
Table 2: Key Research Reagents and Platforms for WES in Oncology
| Product Category | Specific Examples | Research Application |
|---|---|---|
| Exome Capture Kits | Agilent SureSelect, Illumina Nextera | Target enrichment of exonic regions |
| Library Prep Kits | KAPA HyperPrep, Illumina DNA Prep | NGS library construction |
| Sequencing Platforms | Illumina NovaSeq, Complete Genomics DNBSEQ-T1+ | High-throughput sequencing |
| Automation Systems | Hamilton STAR, Agilent Bravo | Laboratory workflow automation |
| Analysis Software | GATK, VarScan, SNPEff | Variant calling and annotation |
The WES research ecosystem includes both established and emerging solutions. Complete Genomics highlights its DNBSEQ-T1+ system for cost-effective, scalable sequencing across applications including whole exome studies [16]. Their partnership with SOPHiA GENETICS integrates comprehensive genomic profiling assays with cloud-based analytics, delivering an end-to-end workflow for precision oncology [16]. Similarly, Illumina's TruSight Oncology Comprehensive provides FDA-approved comprehensive genomic profiling with pan-cancer companion diagnostic claims, evaluating both DNA and RNA to match cancer patients with targeted therapies [17].
Whole exome sequencing represents an optimally balanced approach in cancer genomics, offering substantial economic advantages without compromising the depth of biological insight. The technology delivers comprehensive coverage of clinically relevant genomic regions at approximately one-third to one-half the cost of whole genome sequencing, while generating more manageable datasets that accelerate analytical workflows. The focused nature of WES enables higher sequencing depth for detecting low-frequency variants in heterogeneous tumor samples, and its modularity facilitates integration with transcriptomic and epigenetic profiling. As sequencing technologies continue to evolve and costs decrease, WES maintains its strategic position through parallel advancements in capture efficiency, analytical algorithms, and functional interpretation tools. For the research and clinical communities, WES provides a cost-effective portal into the cancer genome, accelerating both fundamental discovery and translational applications in precision oncology.
Whole-exome sequencing (WES) has emerged as a powerful and cost-effective tool in precision oncology, enabling the comprehensive detection of somatic alterations that drive tumorigenesis. This technical guide details how WES identifies key actionable genomic alterations—including point mutations, insertions/deletions (indels), copy number variations (CNVs), and gene fusions—along with crucial biomarkers such as tumor mutational burden (TMB) and microsatellite instability (MSI). We explore the integration of WES with complementary technologies like RNA sequencing (RNA-Seq) to enhance fusion detection and functional validation. Furthermore, we provide detailed experimental protocols and bioinformatic workflows for analyzing sequencing data, alongside a curated toolkit of essential research reagents. By bridging comprehensive genomic profiling with clinically actionable insights, WES facilitates personalized treatment strategies and expands therapeutic options for cancer patients.
Cancer is a genetic disease characterized by the accumulation of somatic alterations that confer growth and survival advantages to tumor cells. "Actionable alterations" are specific genetic changes that can be targeted by approved therapies or implicated in clinical trials. The primary classes of these alterations include single nucleotide variants (SNVs), small insertions and deletions (indels), copy number variations (CNVs), and gene fusions [18]. Beyond these, complex genomic signatures such as high tumor mutational burden (TMB-H) and microsatellite instability (MSI-H) have emerged as tissue-agnostic biomarkers for immunotherapy [19].
Whole-exome sequencing (WES) interrogates the protein-coding regions of the genome, which harbor an estimated ~85% of disease-causing mutations [20]. By focusing on this functionally rich portion, WES provides a balanced approach, offering broader coverage than targeted panels while remaining more cost-effective and analytically tractable than whole-genome sequencing (WGS) [18] [20]. In clinical oncology, WES facilitates a shift from histology-based to genotype-based treatment paradigms, enabling the identification of targetable mutations, elucidation of resistance mechanisms, and discovery of novel therapeutic targets [18] [21].
The Technical Capabilities of WES in Detecting Alterations
WES provides a versatile platform for detecting a wide spectrum of genomic alterations. The table below summarizes its core capabilities in identifying key actionable alterations.
Table 1: Types of Actionable Alterations Detected by WES
| Alteration Type | Detection Capability | Key Examples | Clinical/Research Significance |
|---|---|---|---|
| Point Mutations (SNVs/Indels) | High sensitivity for somatic and germline variants in exonic regions [18]. | EGFR L858R, BRAF V600E, KRAS G12C [18] [19]. | Direct targets for small-molecule inhibitors (e.g., Osimertinib for EGFR-mutant lung cancer) [22]. |
| Copy Number Variations (CNVs) | Effective detection of focal and arm-level gains/losses [23]. | ERBB2 amplification, PTEN deletion [18] [19]. | Guides use of targeted therapies (e.g., Trastuzumab for HER2-amplified cancers) [19]. |
| Gene Fusions | Possible but challenging; performance depends on coverage and bioinformatic tools [24]. | TMPRSS2-ERG (prostate cancer), PML-RARA (AML) [24] [25]. | Diagnostically and therapeutically relevant; can be targeted by TKIs (e.g., TRK inhibitors) [25]. |
| Genomic Biomarkers | Can be derived from exome-wide mutational patterns [18] [23]. | Tumor Mutational Burden (TMB), Microsatellite Instability (MSI) [18] [19]. | Tissue-agnostic biomarkers predicting response to immune checkpoint inhibitors [19]. |
Complementary Role of RNA-Seq
While WES is powerful for DNA-level alterations, RNA sequencing (RNA-Seq) provides critical functional validation and enhances fusion detection. Integrated DNA/RNA sequencing assays have demonstrated superior performance, uncovering actionable alterations in up to 98% of clinical tumor samples [23]. RNA-Seq is particularly valuable for:
- Verifying fusion gene expression: Confirming that a DNA-level rearrangement produces a functional transcript [18] [23].
- Identifying fusions missed by WES: Resolving complex rearrangements or those involving large intronic regions [18] [24].
- Providing gene expression context: Informing on pathway activation and tumor microenvironment [18] [23].
Experimental Workflow for WES in Cancer Research
A robust WES workflow involves meticulous sample preparation, sequencing, and data analysis. The following diagram and protocol detail the key steps.
Figure 1: End-to-end workflow for Whole Exome Sequencing (WES) in cancer research, from sample collection to data interpretation.
Detailed Methodology
Step 1: Sample Collection and Nucleic Acid Isolation
- Sample Types: The process begins with collecting tumor samples, which can be fresh-frozen (FF) or formalin-fixed paraffin-embedded (FFPE), paired with a matched normal sample (e.g., blood, saliva, or adjacent benign tissue) [21] [26] [23].
- DNA Extraction: Extract genomic DNA using commercial kits (e.g., QIAamp DNA FFPE Tissue Kit, AllPrep DNA/RNA Mini Kit). A minimum of 10-200 ng of input DNA is typically required, though recommendations vary by protocol [26] [23].
- Quality Control (QC): Assess DNA quantity and quality using a spectrophotometer (e.g., NanoDrop) and fluorometer (e.g., Qubit). For FFPE DNA, perform a PCR-based QC to confirm amplificability. Ensure tumor purity is sufficient (>10-20% is often a minimum threshold) for reliable somatic variant calling [21] [23].
Step 2: Library Preparation and Exome Capture
- Library Construction: Fragment DNA and ligate sequencing adapters to the ends of the DNA fragments. For WES, this is typically performed using kits such as the SureSelect XT HS2 (Agilent) [23].
- Exome Capture: Use biotinylated oligonucleotide probes (e.g., SureSelect Human All Exon V7) to perform solution-based hybridization and capture the protein-coding exons. This step enriches the library for the ~1-2% of the genome that is exonic [21] [20].
- Library QC: Assess the final captured library's concentration, size distribution, and quality using systems like the TapeStation 4200 (Agilent) or similar [23].
Step 3: Sequencing and Primary Data Analysis
- Sequencing: Load the libraries onto a high-throughput sequencer (e.g., Illumina NovaSeq 6000) for paired-end sequencing (e.g., 2x100 bp or 2x150 bp). A mean coverage of 75x-100x is recommended for confident somatic variant detection, with higher coverage (>75x) particularly beneficial for fusion detection from WES data [24] [21].
- Primary Analysis: Convert raw signal data (base calling) into sequence reads (FASTQ format). Perform initial QC metrics including Q-score (e.g., Q30 > 90%) and pass filter (PF) reads [23].
Bioinformatic Analysis of WES Data
The transformation of raw sequencing data into biologically and clinically meaningful results requires a multi-step bioinformatic pipeline. Key steps include:
- Alignment: Map sequencing reads (FASTQ) to a reference genome (e.g., GRCh37/hg19 or GRCh38/hg38) using aligners like BWA-MEM [26] [23].
- QC and Post-Processing: Remove PCR duplicates, perform local realignment, and recalibrate base quality scores using tools like GATK [26] [23].
- Variant Calling:
- Somatic SNVs/Indels: Use callers like GATK Mutect2 or Strelka2 on the tumor-normal pair to identify somatic point mutations and small insertions/deletions [26] [23].
- Somatic CNVs: Detect copy number alterations from WES data using tools such as GATK AllelicCNV or similar algorithms [26] [23].
- Gene Fusions: Apply specialized tools (e.g., Fuseq-WES) that use discordant reads and split reads from DNA sequencing to predict fusion events [24].
- Annotation and Prioritization: Annotate variants using tools like VEP, cross-referencing with databases (e.g., dbSNP, COSMIC, ClinVar). Filter and prioritize variants based on population frequency, predicted functional impact, and actionability in resources like CIViC or OncoKB [21].
The Scientist's Toolkit: Essential Research Reagents
Successful WES-based research relies on a suite of validated reagents and computational tools. The following table catalogs essential components for a typical workflow.
Table 2: Key Research Reagent Solutions for WES Workflows
| Reagent/Tool Category | Specific Examples | Function and Application Notes |
|---|---|---|
| Nucleic Acid Extraction Kits | QIAamp DNA FFPE Tissue Kit, AllPrep DNA/RNA Mini Kit (Qiagen) [26] [23]. | Isolate high-quality genomic DNA from diverse sample types. The AllPrep kit allows concurrent isolation of DNA and RNA for integrated analysis. |
| Exome Capture Panels | SureSelect Human All Exon V7 (Agilent) [21] [23]. | Probes designed to hybridize and enrich for exonic regions. Critical for determining the genomic content sequenced. |
| Library Prep Kits | SureSelect XT HS2 (Agilent), TruSeq stranded mRNA kit (Illumina for RNA) [23]. | Prepare sequencing-ready libraries from extracted DNA or RNA. Incorporates adapters and indexes for multiplexing. |
| Alignment & Variant Callers | BWA (alignment), GATK Mutect2/Strelka2 (SNVs/Indels), GATK AllelicCNV (CNVs) [26] [23]. | Core bioinformatic software for transforming raw reads into called variants. Accuracy is paramount for downstream analysis. |
| Variant Annotation | Ensembl VEP, dbSNP, COSMIC, ClinVar [26]. | Databases and tools to add biological and clinical context to called variants, enabling prioritization. |
Signaling Pathways and Therapeutic Targeting
Oncogenic driver alterations identified by WES frequently converge on a core set of signaling pathways that control cell growth, survival, and proliferation. The diagram below illustrates key pathways and how targeted therapies interfere with them.
Figure 2: Core oncogenic signaling pathways (MAPK/ERK and PI3K/AKT/mTOR) targeted by therapies based on WES findings. Dashed lines indicate inhibitory actions.
Actionable mutations identified by WES often activate the MAPK/ERK and PI3K-AKT-mTOR pathways, which are central to cell proliferation and survival [18] [25]. For example:
- EGFR mutations in lung cancer constitutively activate the MAPK pathway, driving uncontrolled growth. TKIs like Osimertinib specifically bind to and inhibit mutant EGFR, blocking downstream signaling [27] [22].
- Gene fusions (e.g., EML4-ALK) function as potent oncogenic drivers, leading to ligand-independent activation of these pathways. Crizotinib targets the ALK fusion protein, inducing tumor regression in eligible patients [25].
Whole-exome sequencing stands as a cornerstone technology in modern cancer research and precision oncology. Its ability to comprehensively profile the coding genome for a wide array of actionable alterations—from simple point mutations to complex biomarkers like TMB—makes it an indispensable tool for discovering therapeutic targets, understanding resistance mechanisms, and guiding treatment decisions. While challenges remain, particularly in the consistent detection of gene fusions, the integration of WES with transcriptomic data and the continuous refinement of bioinformatic pipelines are steadily enhancing its power. As the catalog of actionable alterations grows and sequencing costs decline, WES is poised to become even more deeply embedded in the workflow of drug development and personalized cancer care.
Whole exome sequencing (WES) has emerged as a powerful genomic tool in cancer research and clinical oncology, enabling the analysis of all protein-coding regions in the human genome. This technology represents a strategic balance between comprehensive genomic assessment and cost-effectiveness, targeting the approximately 1-2% of the genome that contains an estimated 85% of known disease-causing variants, including those driving carcinogenesis [2] [28]. The growing adoption of WES is fundamentally transforming cancer research and therapeutic development by providing unprecedented insights into the molecular mechanisms of tumorigenesis, disease progression, and treatment resistance.
The positioning of WES within the broader genomics landscape is characterized by its specific focus on exonic regions, which delivers high-throughput results at a more accessible price point compared to whole genome sequencing (WGS) while offering substantially broader analysis than targeted gene panels [2]. This technical and economic balance has established WES as a pivotal technology in precision oncology, facilitating both research discoveries and clinical applications across the cancer continuum from risk assessment to therapeutic targeting.
Global Market Size and Projections
The whole exome sequencing market has demonstrated remarkable growth momentum, characterized by rapid expansion and significant financial investment. Current market valuations and future projections underscore the technology's accelerating adoption across research and clinical domains.
Table 1: Whole Exome Sequencing Market Size and Growth Projections
| Metric | 2024/2025 Value | 2029/2033 Value | CAGR | Source |
|---|---|---|---|---|
| Global Market Size | $95.73 billion (2024) [29] | $158.9 billion (2029) [29] | 10.6% [29] | Precision Oncology Market Report |
| WES-Specific Market | $2.43 billion (2024) [30] | $14.02 billion (2033) [30] | 21.5% [30] | Straits Research |
| Alternative WES Projection | - | $3.7 billion growth (2025-2029) [31] | 21.1% [31] | Technavio |
This substantial growth trajectory is fueled by multiple converging factors, including the expanding application of WES in clinical diagnostics, rising demand for personalized cancer therapeutics, and continuous technological improvements that enhance both the capabilities and accessibility of genomic sequencing.
Comparative Genomic Technology Markets
The positioning of WES within the broader genomic sequencing landscape reveals its strategic role in balancing comprehensiveness with practical constraints. When compared to other sequencing approaches, WES occupies a distinctive niche that explains its growing adoption.
Table 2: Comparative Genomic Sequencing Technologies in Cancer
| Technology | Genomic Coverage | Key Advantages | Primary Applications in Cancer | Market Characteristics |
|---|---|---|---|---|
| Whole Exome Sequencing (WES) | Protein-coding regions (~1-2% of genome) [28] | Cost-effective; focused on clinically actionable regions; higher depth for price [2] [30] | Tumor mutational burden; driver mutation identification; therapy selection [2] [32] | 21.5% CAGR (2024-2033); rapid clinical adoption [30] |
| Whole Genome Sequencing (WGS) | Entire genome (100%) | Comprehensive; includes non-coding regions; structural variants | Cancer germline predisposition; comprehensive biomarker discovery | 15.1% CAGR (2025-2030); higher cost per sample [33] |
| Targeted Gene Panels | Selected genes (<1% of genome) | Highest depth; lowest cost per sample; simplified analysis | Companion diagnostics; recurrence monitoring; focused biomarker testing | Expanding with pharmacogenomics; often bundled with profiling [34] |
The complementary relationship between these technologies creates a multi-layered genomic analysis ecosystem, with WES serving as a cornerstone approach for comprehensive yet cost-effective mutation profiling in cancer research and clinical practice.
Key Market Drivers and Adoption Trends
Economic and Technological Drivers
The expanding adoption of whole exome sequencing is propelled by several powerful economic and technological drivers that have transformed its feasibility and application scale.
Precipitous Decline in Sequencing Costs: The fundamental economic barrier to comprehensive genomic analysis has dramatically lowered, enabling broader implementation across research institutions and healthcare systems. Continuous innovations in sequencing chemistry, instrumentation, and workflow automation have contributed to this trend, making WES increasingly accessible [31].
Expanding Clinical and Research Applications: WES has evolved from a primarily research-focused tool to an integral component of clinical oncology, with applications spanning diagnostic characterization, therapeutic targeting, and prognostic assessment. The technology's capacity to identify clinically actionable mutations across the entire exome makes it particularly valuable for molecular tumor boards and personalized treatment planning [29] [2].
Advancements in Bioinformatics and Analytics: The development of sophisticated computational tools and machine learning algorithms has significantly enhanced the interpretation of WES data, transforming raw sequence information into clinically actionable insights. These bioinformatic advancements help address the challenge of variant interpretation, particularly for rare or novel mutations [31].
Application-Specific Adoption Trends
The implementation of WES across the oncology continuum reflects both its versatility and growing evidence base supporting its clinical utility.
Drug Discovery and Development: The pharmaceutical industry has emerged as the largest application segment for WES, utilizing the technology to identify novel therapeutic targets, validate mechanism of action, and stratify patient populations for clinical trials. WES enables comprehensive pharmacogenomic profiling that informs drug development pipelines from target identification through post-marketing surveillance [30].
Clinical Diagnostics Adoption: Hospitals and diagnostic laboratories represent the fastest-growing end-user segment, incorporating WES into routine oncologic practice for molecular classification of tumors, identification of hereditary cancer syndromes, and guidance of therapeutic decisions. This trend is particularly evident in academic medical centers and comprehensive cancer centers, where WES facilitates data-driven precision oncology [30].
Translational Research Applications: Cancer research institutions utilize WES to elucidate disease mechanisms, investigate clonal evolution, understand therapy resistance mechanisms, and identify novel biomarkers. Large-scale research initiatives like the UK Biobank, which performed WES on 454,787 participants, demonstrate the power of this approach for gene-trait association studies at unprecedented scale [35].
Analytical Frameworks: Methodologies and Technical Standards
Whole Exome Sequencing Wet-Lab Workflow
The standard analytical pipeline for WES in cancer applications involves multiple critical steps to ensure reliable and clinically relevant results.
Sample Acquisition and Quality Assessment: The initial critical step involves obtaining high-quality tumor samples, typically through surgical resection or biopsy, with careful pathological examination to ensure adequate tumor cellularity (generally >20-30% tumor content). Paired normal samples (from blood, saliva, or adjacent normal tissue) are essential for distinguishing somatic tumor mutations from germline variants [2] [32]. Sample preservation method (fresh frozen vs. FFPE) significantly impacts DNA quality and sequencing performance, with FFPE samples often exhibiting greater DNA fragmentation that requires specialized processing [2].
Library Preparation and Exome Capture: Following DNA extraction and quality control, sequencing libraries are prepared through fragmentation, end-repair, adapter ligation, and PCR amplification. Exome capture is predominantly performed using either microarray-based or magnetic bead-based hybridization approaches, with the latter being more widely adopted due to procedural simplicity and efficiency [2]. Commercially available capture platforms from Agilent (SureSelect) and Roche (NimbleGen) target approximately 39 million base pairs across the coding regions of 18,893 genes [35] [28].
Sequencing and Data Generation: Actual sequencing is primarily conducted using Illumina platforms (e.g., NovaSeq 6000), which employ sequencing-by-synthesis technology to generate high-quality short-read data. The sequencing depth required for cancer WES applications typically exceeds 100x for tumor samples and 50x for matched normal samples to ensure sensitive detection of somatic mutations present in tumor subpopulations [2] [32].
Bioinformatics Analysis Framework
The computational analysis of WES data represents a critical component of the workflow, transforming raw sequence data into biologically and clinically meaningful insights.
Variant Detection Algorithms: Multiple specialized algorithms have been developed to identify different classes of genomic alterations from WES data:
Single Nucleotide Variants (SNVs) and Insertions/Deletions (Indels): Tools such as MuTect2, VarScan2, Strelka, and FreeBayes employ distinct statistical approaches to distinguish true somatic mutations from sequencing artifacts and germline polymorphisms [2]. These tools typically require matched tumor-normal pairs to control for individual genetic background.
Copy Number Variations (CNVs): CNV detection algorithms (e.g., EXCAVATOR, CNVkit) analyze depth of coverage ratios between tumor and normal samples to identify genomic regions with significant amplifications or deletions, which are common drivers in cancer pathogenesis [2].
Variant Annotation and Prioritization: Identified variants undergo comprehensive functional annotation to predict biological consequences, including effects on protein function (e.g., missense, truncating), population allele frequency, conservation scores, and predicted pathogenicity using tools such as SIFT, PolyPhen-2, and CADD. This annotation process facilitates prioritization of likely driver mutations over passenger alterations [2].
The Scientist's Toolkit: Essential Research Reagents and Platforms
Table 3: Key Research Reagent Solutions for Whole Exome Sequencing
| Product Category | Example Products | Key Functions | Technical Considerations |
|---|---|---|---|
| Exome Capture Kits | Agilent SureSelect Human All Exon V6; Roche NimbleGen SeqCap EZ | Hybridization-based enrichment of exonic regions; target definition | Capture efficiency; uniformity of coverage; target region specificity [2] [32] |
| Library Preparation Kits | Illumina DNA Prep; KAPA HyperPrep | Fragmentation, end-repair, adapter ligation, PCR amplification | Input DNA requirements; compatibility with FFPE samples; GC bias [32] |
| Sequencing Platforms | Illumina NovaSeq 6000; Illumina HiSeq | Massively parallel sequencing; data generation | Read length; outputs; error profiles; cost per gigabase [32] |
| Nucleic Acid Extraction Kits | QIAamp DNA FFPE Tissue Kit; Maxwell RSC DNA FFPE Kit | DNA isolation from various sample types; quality assessment | Yield; fragment size distribution; inhibitor removal [32] |
| Target Enrichment Systems | Illumina Exome Panel; Twist Human Core Exome | Probe design for exonic region capture | Target coverage; off-target rates; hands-on time [31] |
Research Applications: Elucidating Cancer Mechanisms
Case Study: Genomic Basis of Histological Transformation in Lung Cancer
A 2025 study by Wang et al. utilized WES to investigate the genomic alterations underlying the transformation of EGFR-mutated lung adenocarcinoma (LUAD) to small cell lung cancer (SCLC) following tyrosine kinase inhibitor (TKI) therapy [32]. This transformation represents a clinically significant resistance mechanism that substantially alters disease management and patient prognosis.
Experimental Methodology: The researchers performed WES on 35 samples across three cohorts: 5 primary LUAD samples obtained before SCLC transformation, 12 transformed SCLC samples collected after EGFR-TKI resistance development, and 18 de novo SCLC samples for comparison [32]. DNA was extracted from FFPE tissue sections with tumor purity exceeding 90%, and libraries were prepared using the Agilent SureSelect Human All Exon V6 kit followed by sequencing on the Illumina NovaSeq 6000 platform [32].
Key Findings: The analysis revealed that while TP53 mutations and RB1 loss were present in transformed SCLC (70% and 30% respectively), they were not universal, suggesting additional mechanisms facilitate this histological transformation [32]. Transformed SCLC exhibited distinctive genomic features, including mutations in COL22A1 and ALMS1 that were shared with de novo SCLC, while mutations in PTCH2, CNGB3, SPTBN5, CROCC, and MYO15A were more specific to the transformed cases [32]. Notably, transformed SCLC demonstrated significantly higher genomic instability compared to both primary LUAD and de novo SCLC, evidenced by elevated measures of homologous recombination deficiency (HRD), uniparental disomy (UPD), and loss of heterozygosity (LOH) [32].
Large-Scale Population Studies: The UK Biobank Initiative
The UK Biobank exome sequencing project represents one of the most comprehensive applications of WES in population-scale genetics, sequencing 454,787 participants and identifying 12 million coding variants [35]. This resource has enabled unprecedented analysis of gene-trait associations, including cancer-related phenotypes.
Experimental Methodology: The consortium employed a standardized WES approach achieving 95.8% of targeted bases covered at ≥20× depth, identifying 12.3 million variants across 18,893 genes [35]. Association testing between rare putative loss-of-function (pLOF) and deleterious missense variants with 3,994 health-related traits revealed 564 genes with significant trait associations, many with implications for cancer risk and biology [35].
Oncological Insights: The scale of this dataset enables detection of associations with very rare variants, exemplified by the discovery that carriers of singleton pLOF variants in RRBP1 exhibited significantly lower apolipoprotein B levels, suggesting a role in lipid metabolism that may influence cancer risk or tumor microenvironment [35]. Furthermore, genes targeted by FDA-approved drugs were 3.6-fold more common among the associated genes, highlighting the potential for therapeutic discovery through WES analysis [35].
Market Challenges and Future Directions
Analytical and Implementation Barriers
Despite rapid growth and technological advancement, several significant challenges constrain broader adoption of WES in cancer research and clinical practice.
Bioinformatics Bottleneck: The complexity of WES data analysis remains a substantial barrier, requiring specialized computational expertise, sophisticated infrastructure, and standardized analytical pipelines. Variant interpretation, particularly for rare or novel mutations, demands integration of multiple evidence sources and clinical correlation [31]. The absence of universal standards for variant classification and reporting further complicates clinical implementation.
Workforce and Infrastructure Limitations: The effective implementation of WES requires multidisciplinary expertise spanning molecular biology, bioinformatics, oncology, and genetics. The scarcity of professionals with this integrated skill set represents a significant constraint on market growth, particularly in emerging markets and resource-limited settings [30]. Additionally, the storage, management, and analysis of large WES datasets necessitate substantial computational resources that may exceed the capabilities of smaller institutions.
Evidence Generation and Reimbursement Challenges: While the clinical validity of WES is well-established, demonstrations of clinical utility in improving patient outcomes remain limited, particularly for specific cancer types and clinical scenarios [28]. This evidence gap influences reimbursement policies and institutional adoption, with payers increasingly requiring proof of improved health outcomes beyond mere technical capability or diagnostic yield.
Emerging Trends and Future Opportunities
Several emerging trends are poised to shape the future evolution of WES applications in cancer research and clinical practice.
Integration with Artificial Intelligence: Machine learning and AI approaches are increasingly being applied to WES data to enhance variant interpretation, predict functional impact, identify novel genomic signatures, and correlate mutational profiles with treatment responses [31]. These approaches hold particular promise for deciphering the clinical significance of variants of uncertain significance (VUS) and identifying complex genomic patterns that transcend individual mutations.
Expansion in Drug Development: WES is playing an increasingly central role in oncology drug development, from target identification and validation to patient stratification and clinical trial enrichment. The growing emphasis on targeted therapies and personalized treatment approaches ensures continued integration of comprehensive genomic profiling into pharmaceutical R&D pipelines [30].
Technological Convergence: The convergence of WES with complementary technologies—including transcriptomic sequencing, epigenomic profiling, and single-cell analysis—enables multi-dimensional characterization of tumor biology that extends beyond the coding genome. These integrated approaches provide more comprehensive insights into cancer mechanisms and therapeutic opportunities.
Whole exome sequencing has established itself as a cornerstone technology in modern cancer research and clinical oncology, driven by continuous technological refinement, declining costs, and expanding evidence of clinical utility. The market's robust growth trajectory reflects the fundamental value of comprehensive genomic assessment in understanding cancer biology, guiding therapeutic development, and personalizing patient management. While challenges related to data interpretation, infrastructure, and evidence generation persist, ongoing innovations in sequencing technology, analytical methodologies, and clinical integration promise to further expand the applications and impact of WES in oncology. As the field continues to evolve, WES is positioned to remain an essential component of the precision oncology toolkit, bridging the gap between targeted gene panels and whole genome sequencing in both research and clinical domains.
Methodological Advances and Translational Applications in Oncology
Whole exome sequencing (WES) has emerged as a powerful and cost-effective genomic technique for investigating the genetic underpinnings of cancer. This method focuses on sequencing the protein-coding regions of the genome, which constitute approximately 1-2% of the human genome yet harbor an estimated 85% of disease-causing variants [36]. In oncology, WES enables researchers and clinicians to uncover somatic mutations, identify inherited cancer susceptibility variants, and characterize the genomic landscape of tumors to guide personalized treatment strategies [2] [37]. The targeted nature of WES allows for deeper sequencing coverage of clinically relevant regions at a fraction of the cost and data burden of whole genome sequencing (WGS), making it particularly suitable for cancer research applications where budget and computational resources are often limiting factors [38] [36].
The analysis of cancer samples presents unique challenges in the WES workflow. Unlike germline genetic studies, cancer sequencing requires distinguishing somatic (tumor-acquired) mutations from germline (inherited) variants, which necessitates sequencing matched normal tissue from the same patient [39]. Furthermore, tumor samples often exhibit heterogeneity, variable tumor purity, and complex genomic alterations that complicate variant detection and interpretation [2] [40]. This technical guide provides a comprehensive overview of the end-to-end WES workflow specifically optimized for cancer samples, from initial DNA preparation through final variant calling and analysis.
The following diagram illustrates the comprehensive workflow for whole exome sequencing, from sample preparation through data analysis.
Detailed Experimental Protocols
DNA Extraction and Quality Control
Protocol Objective: To obtain high-quality, high-molecular-weight DNA from patient samples suitable for whole exome sequencing. In cancer research, this typically involves processing tumor samples (often from FFPE tissues, frozen tissues, or liquid biopsies) and matched normal samples (commonly from blood, saliva, or T-cells) [39].
Materials Required:
- QIAamp DNA FFPE Tissue Kit (for formalin-fixed tissues)
- QIAamp DNA Blood Mini Kit (for blood samples)
- Proteinase K
- Ethanol (96-100%)
- Nuclease-free water
- Agarose gel equipment
- Spectrophotometer (NanoDrop) or fluorometer (Qubit)
Step-by-Step Procedure:
- Sample Lysis: For FFPE tissues, cut 2-3 sections of 10 μm thickness. Digest tissue with proteinase K for 3-16 hours at 56°C until completely lysed. For blood samples, mix 200 μL with 200 μL PBS and 20 μL QIAGEN Protease [2].
- DNA Binding: Add 400 μL of buffer AL to the lysate, mix thoroughly, and incubate at 70°C for 10 minutes for FFPE samples. Add 400 μL ethanol (96-100%) and mix by vortexing.
- Column Purification: Apply the mixture to QIAamp Mini spin columns and centrifuge at 6000 × g for 1 minute. Wash once with 500 μL AW1 buffer and twice with 500 μL AW2 buffer.
- DNA Elution: Elute DNA in 50-100 μL nuclease-free water or buffer AE preheated to 70°C for FFPE samples.
- Quality Assessment: Measure DNA concentration using fluorometric methods (recommended for FFPE samples). Assess DNA integrity by agarose gel electrophoresis or bioanalyzer. Acceptable samples should have A260/A280 ratio of 1.8-2.0 and show minimal fragmentation (for fresh samples) [2].
Critical Considerations for Cancer Samples:
- FFPE-derived DNA often shows fragmentation; minimum DNA fragment size should be >150 bp for library preparation.
- Tumor purity assessment through pathological review is essential before sequencing.
- For myeloid cancers, T-cells are recommended as the normal reference due to minimal risk of neoplastic contamination compared to saliva or skin biopsies [39].
DNA Fragmentation and Library Preparation
Protocol Objective: To fragment DNA to appropriate size for sequencing and attach sequencing adapters to create sequencing libraries.
Materials Required:
- Covaris S2 ultrasonicator (for mechanical shearing) or NEBNext Fragmentase (for enzymatic fragmentation)
- End Repair Module
- A-Tailing Module
- Ligation Module
- Size Selection Beads (AMPure XP)
- Library Quantification Kit
- Unique dual index adapters
Step-by-Step Procedure:
- DNA Fragmentation:
- Mechanical Shearing: Dilute 100-1000 ng DNA to 50 μL in TE buffer. Shear using Covaris S2 with following settings: Duty Cycle 10%, Intensity 5, Cycles per Burst 200, Time 45 seconds to obtain 150-200 bp fragments.
- Enzymatic Fragmentation: For 100 ng DNA, add 7 μL Fragmentase, incubate at 37°C for 15-30 minutes, then heat-inactivate at 70°C for 10 minutes [37].
End Repair:
- Combine 50 μL fragmented DNA with 7 μL End Repair Reaction Buffer and 3 μL End Repair Enzyme Mix.
- Incubate at 20°C for 30 minutes, then purify with 1.8X volume AMPure XP beads.
A-Tailing:
- Resuspend DNA in 25 μL nuclease-free water.
- Add 10 μL A-Tailing Reaction Buffer and 5 μL A-Tailing Enzyme.
- Incubate at 37°C for 30 minutes, then purify with 1.8X AMPure XP beads.
Adapter Ligation:
- Resuspend DNA in 25 μL nuclease-free water.
- Add 5 μL Ligation Buffer, 10 μL PEG 8000, 5 μL Ligation Enhancer, 2.5 μL Adapter (15 μM), and 2.5 μL DNA Ligase.
- Incubate at 20°C for 15 minutes.
- Purify with 0.8X AMPure XP beads to remove excess adapters.
Library Amplification:
- Amplify library using 8-12 cycles of PCR with indexed primers.
- Perform final purification with 0.8X AMPure XP beads to remove primers and select appropriate fragment sizes.
Library QC:
- Quantify using qPCR-based library quantification kit.
- Assess size distribution using Bioanalyzer or TapeStation (expected peak: 250-300 bp).
Exome Capture and Target Enrichment
Protocol Objective: To selectively capture and enrich exonic regions from the sequencing library using hybridization-based capture methods.
Materials Required:
- Twist Human Core Exome Kit or Agilent SureSelect Human All Exon Kit
- Streptavidin-coated magnetic beads
- Hybridization buffer
- Wash buffers
- Heated thermal mixer with lid
Step-by-Step Procedure:
- Hybridization:
- Combine 200-500 ng library DNA with 5 μL Blocking Mix and 2 μL Twist Universal Adapter in nuclease-free water to total 15 μL.
- Add 15 μL Hybridization Buffer and 5 μL Exome Probe Pool (from Twist Human Core Exome Kit).
- Denature at 95°C for 2 minutes, then incubate at 58°C for 16 hours in a thermal mixer [37].
Capture with Magnetic Beads:
- Pre-wash streptavidin magnetic beads with bead wash buffer.
- Add beads to hybridization reaction and incubate at 58°C for 45 minutes with mixing.
Washing:
- Capture beads on magnet and discard supernatant.
- Wash twice with 200 μL Wash Buffer 1 at 58°C for 5 minutes.
- Wash twice with 200 μL Wash Buffer 2 at room temperature for 2 minutes.
- Perform final wash with 200 μL nuclease-free water.
Amplification of Captured Library:
- Resuspend beads in 25 μL PCR mix with 12 cycles of amplification.
- Purify with 0.8X AMPure XP beads.
- Quantify final library by qPCR and analyze size distribution by Bioanalyzer.
Critical Considerations:
- GC-rich regions may be underrepresented; consider adding GC-content balanced polymer if needed.
- For cancer research, ensure capture kit covers known cancer-associated non-coding regions (e.g., TERT promoter) if relevant to study [2].
- Use the same exome capture kit across all samples in a study to ensure consistency.
Bioinformatic Analysis Pipeline
Primary Data Processing and Quality Control
The initial phase of bioinformatic analysis focuses on assessing raw sequencing data quality and preparing it for variant discovery. This involves multiple quality control checkpoints and processing steps as illustrated below.
Key Tools and Procedures:
Initial Quality Control (FastQC):
- Assess per-base sequencing quality, GC content, adapter contamination, and overrepresented sequences.
- Critical metrics: Q30 score >80%, GC content matching expected distribution, minimal adapter contamination.
Read Trimming and Filtering (Trimmomatic, Cutadapt):
- Remove adapter sequences: ILLUMINACLIP:adapters.fa:2:30:10
- Quality trimming: LEADING:20, TRAILING:20, SLIDINGWINDOW:4:20
- Discard reads shorter than 36 bp: MINLEN:36
Alignment to Reference Genome (BWA-MEM):
Post-Alignment Processing:
- Mark duplicates:
gatk MarkDuplicates -I sorted.bam -O marked_duplicates.bam -M metrics.txt - Base quality score recalibration:
gatk BaseRecalibrator -I marked_duplicates.bam -R reference.fasta --known-sites known_sites.vcf -O recal_data.table
- Mark duplicates:
Quality Metrics for Cancer Samples:
- Minimum coverage: 100X for tumor, 60X for normal
- Uniformity of coverage: >80% of target bases at 20X coverage
- Duplication rate: <20% for fresh samples, <40% for FFPE samples
- Contamination check: VerifyBamID or similar tools
Variant Calling Methods in Cancer Genomics
Variant calling in cancer samples requires specialized approaches to distinguish somatic mutations from germline variants and account for tumor-specific characteristics such as heterogeneity and aneuploidy.
Somatic Variant Calling Workflow:
Tumor-Normal Pair Analysis:
- Process tumor and matched normal samples through the same pipeline
- Use Mutect2 for somatic SNV and indel calling:
gatk Mutect2 -R reference.fasta -I tumor.bam -I normal.bam -O somatic.vcf - Filter results:
gatk FilterMutectCalls -V somatic.vcf -O filtered_somatic.vcf
Additional Callers for Comprehensive Detection:
- VarScan2:
varscan somatic normal.pileup tumor.pileup output --min-coverage 10 --min-var-freq 0.1 --somatic-p-value 0.05 - Strelka2: Configure via
configureStrelkaSomaticWorkflow.pyfor small variant calling - For structural variants: Manta, Delly, or Lumpy
- VarScan2:
False Positive Filtering Strategies:
- Remove variants present in population databases (gnomAD, 1000 Genomes)
- Filter out artifacts using blacklist files (e.g., from GDC) [40]
- Apply panel of normals (PoN) specific to your sequencing platform and protocol
- For tumor-only analysis, implement stringent bioinformatic filtering: remove variants with VAF >0.4 or <0.1, exclude common germline polymorphisms [39]
Performance Characteristics of Variant Callers:
Table 1: Performance Comparison of Selected Variant Calling Tools for Cancer WES
| Tool | Variant Types | Strengths | Optimal Use Cases | Limitations |
|---|---|---|---|---|
| Mutect2 | SNVs, indels | High specificity, built-in filters | Standard somatic calling | May miss low-VAF variants |
| VarScan2 | SNVs, indels | Sensitive for low-frequency variants | Low-purity tumors | Higher false positive rate |
| Strelka2 | SNVs, indels | Good performance across variant sizes | High-specificity needs | Longer runtime |
| FreeBayes | SNVs, indels, MNVs | Sensitive, haplotype-aware | Research settings | High false positives without filtering |
| Manta | SVs, indels | Comprehensive structural variant calling | Chromosomal rearrangements | Limited to larger variants |
Benchmarking of No-Code Variant Calling Solutions
For laboratories without extensive bioinformatics support, several commercial variant calling solutions offer user-friendly interfaces while maintaining analytical accuracy. Recent benchmarking studies provide performance comparisons of these platforms.
Table 2: Performance Benchmarking of Commercial Variant Calling Software (GIAB Reference Data) [43]
| Software | SNV Recall (%) | SNV Precision (%) | Indel Recall (%) | Indel Precision (%) | Runtime (Minutes) | Cost Model |
|---|---|---|---|---|---|---|
| Illumina DRAGEN | >99 | >99 | >96 | >96 | 29-36 | Annual subscription + credits |
| CLC Genomics | 98-99 | 98-99 | 94-96 | 94-96 | 6-25 | Annual subscription |
| Varsome Clinical | 98-99 | 98-99 | 93-95 | 93-96 | 45-90 | Per sample |
| Partek Flow (GATK) | 97-98 | 97-98 | 90-93 | 90-93 | 216-1782 | Annual subscription |
| Partek Flow (Freebayes+Samtools) | 95-97 | 95-97 | 85-90 | 85-90 | 216-1782 | Annual subscription |
Key Findings from Benchmarking Studies:
- Illumina's DRAGEN Enrichment achieved the highest precision and recall scores for both SNV and indel calling at over 99% for SNVs and 96% for indels [43].
- All four benchmarked software shared 98-99% similarity in true positive variants, indicating high concordance for common variants.
- Run times varied significantly, with CLC and Illumina being the fastest (6-36 minutes), while Partek Flow took substantially longer (3.6 to 29.7 hours) [43].
- The choice between software often involves trade-offs between accuracy, runtime, and cost, with Illumina DRAGEN providing the best performance but at a premium price point.
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Essential Research Reagents for Whole Exome Sequencing in Cancer Studies
| Category | Specific Product Examples | Key Features | Application Notes |
|---|---|---|---|
| Exome Capture Kits | Agilent SureSelect XT HS2, Twist Human Core Exome, Illumina Nextera Rapid Capture | Comprehensive exome coverage (39-64 Mb), optimized for FFPE DNA | Agilent SureSelect provides 60 Mb coverage with 120-mer probes; verify coverage of cancer-relevant genes |
| Library Prep Kits | Illumina DNA Prep, KAPA HyperPrep, NEBNext Ultra II FS | Compatibility with low-input DNA, FFPE-optimized protocols | For FFPE samples: use kits with uracil-tolerant enzymes and formalin-damage reversal capabilities |
| Target Enrichment Reagents | IDT xGen Universal Blockers, Twist Universal Adapter System | Reduced off-target capture, improved uniformity | Universal blockers improve performance in multiplexed sequencing |
| DNA Extraction Kits | QIAamp DNA FFPE Tissue Kit, Maxwell RSC Blood DNA Kit, QIAamp DNA Blood Mini Kit | High yield from challenging samples, minimal co-purification of inhibitors | For myeloid cancers: pair tumor with T-cell derived normal DNA [39] |
| Quality Control Tools | Agilent TapeStation, Qubit dsDNA HS Assay, Quant-iT PicoGreen | Accurate quantification of degraded DNA, fragment size analysis | Fluorometric quantification preferred over spectrophotometry for FFPE samples |
| Sequencing Reagents | Illumina NovaSeq 6000 S-Prime, NextSeq 1000/2000 P2 reagents | High-output sequencing, reduced error rates | Match sequencing depth to application: >100X for tumor, >60X for normal |
The end-to-end workflow for whole exome sequencing in cancer samples encompasses carefully optimized wet-lab procedures and bioinformatic analyses tailored to the unique challenges of cancer genomics. From appropriate sample selection and library preparation through sophisticated variant calling and interpretation, each step requires meticulous execution to generate clinically actionable results. The benchmarking data presented here demonstrates that both code-free commercial solutions and custom bioinformatic pipelines can achieve high accuracy when properly validated. As WES continues to evolve, standardization of protocols and rigorous validation using reference materials like GIAB will be essential for translating cancer genomic findings into improved patient outcomes.
Whole exome sequencing (WES) has emerged as a powerful clinical diagnostic tool for discovering the genetic basis of many diseases, including cancer. In the context of oncology, WES enables molecular tumor boards to identify therapeutic targets for patients with advanced cancers by sequencing the protein-coding regions of the genome [44]. While targeted panel sequencing has been widely adopted in clinical settings, evidence suggests that broader genomic analyses like WES can provide additional clinical benefit for selected patients. A study of 38 patients with advanced cancers found that WES enabled additional clinically highly actionable recommendations that would have been missed with panel sequencing alone [44]. These recommendations were often related to complex molecular biomarkers such as homologous recombination deficiency or high tumor mutational burden, with corresponding recommendations for targeted therapies like PARP inhibitors or checkpoint inhibitors.
The implementation of WES in clinical cancer research presents significant scalability challenges. Traditional manual sequencing workflows require extensive hands-on time and are prone to variability, creating bottlenecks in processing large sample volumes. For cancer patients awaiting treatment decisions, rapid turnaround times are critical—treatment initiation before comprehensive genomic profiling results are available can negatively affect patient outcomes [45]. This technical guide examines the strategies, technologies, and methodologies for automating high-throughput diagnostic workflows to achieve both scale and speed in WES-based cancer research.
Clinical Value of Whole Exome Sequencing in Oncology
Complementary Benefits of WES and Panel Sequencing
Research comparing WES to medium-size gene panels (up to 203 genes) in an all-comer real-world molecular tumor board demonstrated that WES provides measurable clinical benefits. In a cohort of 38 patients with advanced cancers, approximately two-thirds with common and one-third with rare cancers, WES enabled additional treatment recommendations that would not have been issued based on panel sequencing alone [44]. The study documented that:
- Patients received a total of 45 treatment recommendations (range 0-4), with 29 having clinical level of evidence and/or entailing feasible study enrollment
- Sixteen recommendations (seven highly actionable) were issued only on the basis of WES results
- Three of these highly actionable recommendations were related to complex molecular biomarkers
- One of eight implemented treatments was based on biomarkers derived exclusively by WES
Technical Considerations for WES in Cancer Diagnostics
A major consideration in WES is the uneven coverage of sequence reads over exome targets, which contributes to low-coverage regions that hinder accurate variant calling [46]. The distribution of sequence coverage varies both locally (coverage of a given exon across different platforms) and globally (coverage of all exons across the genome in a given platform). Research has identified that low-coverage regions encompassing functionally important genes are often associated with high GC content, repeat elements, and segmental duplications [46]. These coverage deficiencies can be quantitatively assessed using metrics such as Cohort Coverage Sparseness (CCS) and Unevenness (UE) scores, which enable detailed evaluation of read distribution [46].
Table 1: Clinical Impact of Additional WES Beyond Panel Sequencing
| Metric | Panel Sequencing Only | With Additional WES |
|---|---|---|
| Total treatment recommendations | 29 | 45 |
| Highly actionable recommendations | 22 | 29 |
| Recommendations based on complex biomarkers | Limited | 7 highly actionable |
| Therapies enabled | Standard targeted | PARP inhibitors, checkpoint inhibitors |
Automation Platforms for Scalable Sequencing Workflows
High-Throughput Library Preparation Systems
Automation of DNA and RNA library preparation workflows offers laboratories the ability to scale-up and standardize sample processing. The implementation of automated systems such as the Biomek i7 Hybrid Workstation for the TruSight Oncology 500 High-Throughput assay demonstrates significant efficiency gains [45]. Key performance improvements include:
- 4-fold reduction in hands-on time compared to manual library preparation
- 1.7-fold reduction in total runtime (6 hours vs. 23 hours for a 48 DNA + 48 RNA sample batch)
- Reduced staffing requirements - one technician versus three for manual preparation
- Maintained quality control metrics - total and mapped reads, median insert size, and median exon coverage remained concordant with manual workflows
For whole genome sequencing, modular automation systems capable of processing thousands of DNA samples in under 24 hours represent the cutting edge of high-throughput automation. These systems typically integrate pre- and post-PCR workflows, with operational targets of processing 384 samples daily while ensuring assay consistency and minimized consumable waste [47].
Integrated Sequencing and Analysis Platforms
Modern sequencing platforms like Illumina's NovaSeq X Plus and PacBio's Revio system offer enhanced throughput capabilities specifically designed for high-volume sequencing environments [48] [49]. The Revio system, for instance, delivers up to 480 Gb of HiFi reads per day, equivalent to 2,500 human whole genomes per year, with 24-hour run times [49]. These systems incorporate advanced data processing capabilities, with powerful onboard computing (NVIDIA GPUs in the Revio) that enables real-time basecalling, methylation calling, and demultiplexing directly on the instrument [49].
Table 2: Throughput Comparison of Automated Sequencing Platforms
| Platform | Method | Samples per Run | Hands-on Time | Total Runtime |
|---|---|---|---|---|
| Manual TSO500 | Panel Sequencing | 48 DNA + 48 RNA | ~69 technician-hours | 42.5 hours |
| Automated TSO500 HT | Panel Sequencing | 48 DNA + 48 RNA | ~16 technician-hours | 24 hours |
| Revio System | HiFi Long-Read WGS | 4 SMRT Cells (8 genomes at 20X) | Minimal setup | 24 hours |
Implementing Automated High-Throughput Workflows
Workflow Architecture and Design Considerations
Effective automation for scale requires careful workflow architecture that balances throughput, reproducibility, and traceability. A representative system for whole genome sequencing production described by HighRes Biosolutions demonstrates a modular approach with separate pre-PCR and post-PCR environments maintained through fully automated sample handoffs [47]. Key design elements include:
- Pre-PCR modules with liquid handlers, robotic arms on rails, plate hotels, sealers, and barcode scanners
- Post-PCR modules with dedicated liquid handling, quantification stations (qPCR, Fragment Analyzer), and incubation capabilities
- Parallel processing enabled by smart scheduling software that staggers handoffs between workflow stages
- Full traceability through barcode scanning and LIMS integration
This modular approach ensures that scale-up is straightforward, with additional hotels or secondary liquid handlers integrated without redesigning the full system [47]. Simulation of workflows using tools like CellarioScheduler enables optimization before implementation, confirming that complete protocols can process 384 samples in approximately 22-23 hours [47].
Experimental Protocol: Automated TSO500 Library Preparation and Sequencing
The following methodology is adapted from the clinical implementation of the automated TruSight Oncology 500 High-Throughput workflow, which was validated against manual library preparation [45]:
Sample Preparation Phase:
- DNA/RNA Extraction: Automatically extract using Maxwell RSC Benchtop Instruments with Maxwell RSC DNA/RNA FFPE kits from 5-10μm thick sections.
- Quantification: Determine total DNA and RNA concentrations using Qubit HS DNA and RNA assays.
- DNA Integrity Assessment: Assess DNA quality using Genomic DNA ScreenTape Analysis on a 4200 TapeStation System.
- Fragmentation: Fragment up to 80 ng DNA targeting a mean fragment size of 200 bp using Covaris ultrasonicators (ME220 or ML230).
Automated Library Preparation Phase (Biomek i7 Workstation):
- Library Construction: Execute the TSO 500 HT library kit using the Illumina-qualified automated workflow.
- Sequencing: Sequence libraries with a target of 40-50 million read pairs per sample (DNA) and 10 million read pairs (RNA) using NovaSeq 6000 with SP or S1 200 cycle V1.5 kits.
- Data Processing: Process sequencing data using the Dockers TruSight Oncology 500 v2.2 Local App.
Quality Control Metrics:
- Monitor percentage of aligned reads (target: >98%)
- Verify median insert size (~116 bp)
- Assess median family size (indicating library complexity)
- Confirm median exon coverage (>750X)
This automated workflow demonstrated excellent concordance with manual approaches, identifying 214 of 217 variants (98.6%) previously detected, with the three missed variants present in alignment files just below the 3% variant allele fraction threshold [45].
Diagram 1: Automated High-Throughput Sequencing Workflow
Critical Success Factors for Implementation
Data Management and Computational Infrastructure
The massive expansion in data volume generated by high-throughput sequencing techniques presents significant informatics challenges. Modern laboratories must manage multidimensional data in a way that is easily accessible, searchable, and sharable to enable fast and effective decision-making [50]. Cloud-based informatics platforms have emerged as the most effective solution, offering:
- Flexible and scalable data management that evolves with changing workflows
- Integration of R&D streams through centralized data organization
- Seamless collaboration through secure data sharing capabilities
- Built-in security features including firewalls, backup, encrypted VPN access, and disaster recovery
These platforms are particularly valuable for overcoming fragmented data management systems that can develop when laboratories implement point solutions for specific workflows without establishing connectivity between systems [50].
Turnaround Time Optimization Strategies
Expediting diagnosis through rapid exome and genome sequencing is particularly critical for inpatient clinical settings. A retrospective review of rapid exome/genome testing for inpatient cases found an average total turnaround time of 17.88 days (range 5-43 days), with an average of 13.97 days for the performing laboratory [51]. However, the study identified an approximately 3.91-day lag in getting samples to the performing laboratory, highlighting the importance of addressing pre-analytical bottlenecks.
Strategies for optimizing turnaround time include:
- Process parallelization through smart scheduling software
- Reduction of hands-on time through workflow automation
- Elimination of bottlenecks in sample transport and accessioning
- Implementation of automated quality control checks to reduce repeat analysis
The Scientist's Toolkit: Essential Research Reagent Solutions
Table 3: Key Reagents and Materials for Automated High-Throughput Sequencing
| Reagent/Material | Function | Example Products |
|---|---|---|
| Nucleic Acid Extraction Kits | Isolation of high-quality DNA/RNA from FFPE and other samples | Maxwell RSC DNA/RNA FFPE Kits [45] |
| Library Preparation Kits | Fragmentation, end repair, adaptor ligation, and amplification | TruSight Oncology 500 HT library kit [45] |
| Target Enrichment Probes | Hybridization and capture of exonic regions | Agilent SureSelect, Roche NimbleGen SeqCap EZ, Illumina TruSeq [46] |
| Quantification Assays | Accurate measurement of nucleic acid concentration and quality | Qubit HS DNA/RNA assays [45] |
| Normalization Beads | Size selection and cleanup of libraries | SPRIselect beads [47] |
| Sequencing Consumables | Flow cells, buffers, and reagents for sequencing runs | NovaSeq 6000 S1/S2 flow cells, PacBio Revio SMRT Cells [45] [49] |
Automation of high-throughput diagnostic workflows represents a transformative approach to scaling whole exome sequencing for cancer research while maintaining rapid turnaround times. The integration of automated library preparation systems, high-throughput sequencing platforms, and sophisticated data management solutions enables research institutions and clinical laboratories to process thousands of samples with minimal operator intervention and significantly reduced hands-on time. Evidence from clinical implementations demonstrates that automated workflows can achieve 4-fold reductions in hands-on time and 1.7-fold reductions in total runtime while maintaining analytical performance comparable to manual methods [45].
The clinical value of comprehensive genomic profiling through WES is particularly evident in oncology, where it enables identification of complex biomarkers and therapeutic targets that might be missed with narrower panel sequencing approaches [44]. As automation technologies continue to evolve and integrate with artificial intelligence and machine learning approaches, the potential for further optimization of bio-based processes will expand significantly [52]. For research and clinical laboratories seeking to implement high-throughput WES workflows, success will depend on careful consideration of workflow architecture, computational infrastructure, and reagent solutions tailored to the specific requirements of cancer genomics.
Diagram 2: Integrated Ecosystem for Automated Sequencing
Whole exome sequencing (WES) remains a first-tier genetic test in clinical diagnostics and cancer research, providing a cost-efficient method for identifying disease-associated variants within protein-coding regions. The performance of WES is critically dependent on the exome enrichment kit used. This guide provides a comparative evaluation of four major exome capture solutions available in 2024: Agilent SureSelect Human All Exon v8, Roche KAPA HyperExome, Vazyme VAHTS Target Capture Core Exome Panel, and Nanodigmbio NEXome Plus Panel v1. Based on recent empirical evidence, all kits demonstrated high performance, with each exhibiting distinct strengths in coverage uniformity, on-target efficiency, and variant calling accuracy, enabling researchers to make informed selections based on specific project requirements.
In cancer research, WES enables the comprehensive screening of somatic mutations and germline variants across the exonic regions of the genome. The technology has become indispensable for identifying driver mutations, understanding tumor heterogeneity, and discovering therapeutic targets. The accuracy and reliability of these findings, however, hinge on the performance of the exome capture solution, which influences key parameters such as coverage breadth, depth uniformity, and minimization of off-target reads. Continuous innovations by manufacturers have led to periodic updates of these kits, necessitating current, head-to-head comparisons to inform the scientific community.
This guide evaluates four prominent platforms within the context of a broader thesis on the application of WES in cancer research. It synthesizes findings from a recent independent, peer-reviewed study that subjected these kits to identical experimental conditions, providing a fair and reproducible assessment of their capabilities [53] [54]. The following sections detail the experimental methodologies, present comparative results in structured tables, and offer interpretation of the data to facilitate optimal kit selection.
Comparative Experimental Design and Methodology
To ensure a unbiased comparison, the referenced study implemented a standardized experimental workflow from library preparation through bioinformatics analysis [53].
Sample Preparation and Sequencing
The experimental design utilized a well-characterized reference DNA sample (E701) to benchmark performance [53].
- Library Preparation: A total of 96 DNA libraries were prepared using the MGI Universal DNA Library Prep Set under consistent fragmentation conditions on a Covaris sonicator. Fragments were size-selected to a peak length of 250 bp [53].
- Enrichment: Libraries were divided into four groups, each enriched with one of the four probe sets (Agilent v8, Roche, Vazyme, Nanodigmbio) following their respective manufacturers' protocols. The enrichment process for Agilent probes followed the established RSMU_exome protocol [53].
- Sequencing: The enriched library pools were sequenced in paired-end mode on the DNBSEQ-G400 platform (MGI Tech) using a PE100 kit, achieving an average coverage depth of 100x [53].
Bioinformatics and Statistical Analysis
A uniform bioinformatics pipeline was applied to all samples to eliminate software-induced variability [53].
- Quality Control & Alignment: Raw FastQ files were quality-checked with FastQC, trimmed with BBDuk, and aligned to the GRCh38.p14 reference genome using
bwa-mem2[53]. - Processing and Variant Calling: The resulting BAM files were processed and sorted with SAMtools. To ensure a fair comparison, all exomes were computationally downsampled to 50 million reads before analysis. Variant calling was performed using both
bcftools mpileupand DeepVariant [53]. - Statistical Analysis: Statistical significance for performance metrics was assessed using Python3, applying the Shapiro-Wilk test for normality, followed by ANOVA or the Kruskal-Wallis test for pairwise comparisons [53].
The following workflow diagram illustrates the key stages of this comparative experiment.
Performance Metrics and Comparative Analysis
Probe Design and Target Coverage
Modern exome kits have refined their target sizes to focus more exclusively on exonic regions, with the evaluated kits ranging from 34.13 Mb to 35.55 Mb [53]. A critical finding was that 92.14% (33.86 Mb) of the targeted regions were consistent across all four platforms, indicating a strong consensus on the core exome (Figure 1 in the original study) [53]. When intersected with standard databases, the kits covered between 80.76% and 86.76% of the RefSeq and Gencode V44 exomes, respectively [53].
All kits demonstrated excellent performance in covering their designated targets. At a high sequencing depth (100x), all solutions achieved 10x coverage exceeding 97.5% and 20x coverage above 95% of their target regions, which is more than adequate for confident variant calling in cancer research applications [53] [54].
Table 1: Target Design and Coverage Performance
| Kit Name | Target Size (Mb) | % 10x Coverage | % 20x Coverage | % Overlap with Gencode V44 |
|---|---|---|---|---|
| Agilent SureSelect v8 | 35.13 | >97.5% | >95% | 86.76% |
| Roche KAPA HyperExome | 35.55 | >97.5% | >95% | 84.85% |
| Vazyme Core Exome | 34.13 | >97.5% | >95% | 83.80% |
| Nanodigmbio NEXome Plus v1 | 35.17 | >97.5% | >95% | 83.74% |
Capture Efficiency and Uniformity
The kits displayed distinct profiles in capture efficiency and the uniformity of sequence coverage, which are crucial for minimizing sequencing costs and avoiding "blind spots."
- Roche KAPA HyperExome: Exhibited the most uniform coverage, as indicated by the lowest Fold-80 scores (a metric where a lower value signifies better uniformity, as it represents the fold amount of additional sequencing needed to bring 80% of targets to the mean coverage) [53]. This strength is also highlighted in Roche's product information, which emphasizes exceptional uniformity across the GC% range [55] [56].
- Nanodigmbio NEXome Plus: Achieved a higher proportion of on-target reads due to generating significantly fewer off-target reads, making efficient use of sequencing data [53] [54].
- Vazyme Core Exome: Demonstrated consistently high performance in both manual and automated workflows, with no significant difference in on-target efficiency or coverage uniformity, as per the manufacturer's data [57].
Table 2: Capture Efficiency and Variant Calling Metrics
| Kit Name | Coverage Uniformity (Fold-80) | On-Target Reads | Variant Recall Rate | Variant Precision |
|---|---|---|---|---|
| Agilent SureSelect v8 | Moderate | Moderate | Highest | High |
| Roche KAPA HyperExome | Most Uniform (Lowest) | Moderate | High | High |
| Vazyme Core Exome | Moderate | Moderate | High | High |
| Nanodigmbio NEXome Plus v1 | Less Uniform than Roche | Highest | High | Highest (Fewest False Positives) |
Variant Calling Accuracy
The variant calling performance was evaluated using a standardized DNA sample (E701) with a known variant profile [53].
- Recall Rate (Sensitivity): All kits showed high recall rates, with Agilent v8 performing particularly well in this dimension [53] [54].
- Precision (Specificity): Nanodigmbio demonstrated the highest precision, producing the fewest false positive variant calls [53] [54] [58].
- Overall Accuracy (F-measure): All kits achieved an outstanding F-measure above 95.87%, indicating that they are all highly reliable for clinical and research applications [53]. Nanodigmbio had a slightly lower F-measure than the other kits, a trade-off for its superior precision [53] [54].
The Scientist's Toolkit: Essential Research Reagent Solutions
The following table details key reagents and kits used in the featured comparative study, which are essential for establishing a robust WES workflow in a cancer research setting [53].
Table 3: Key Research Reagent Solutions for Whole Exome Sequencing
| Product Name | Vendor | Function in Workflow |
|---|---|---|
| MGI Universal DNA Library Prep Set | MGI Tech | Prepares sequencing libraries from fragmented genomic DNA. |
| Agilent SureSelect Human All Exon v8 | Agilent | Hybridization probes for capturing the human exome. |
| Roche KAPA HyperExome Probes | Roche | Hybridization probes for capturing the human exome. |
| VAHTS Target Capture Core Exome Panel | Vazyme | Hybridization probes for capturing the human exome. |
| NEXome Plus Panel v1 | Nanodigmbio | Hybridization probes for capturing the human exome. |
| DNBSEQ-G400RS Sequencing Set | MGI Tech | Sequencing reagents for the DNBSEQ-G400 platform. |
| High Sensitivity DNA Assay | Agilent Technologies | Quality control of prepared DNA libraries. |
Workflow Automation and Integrated Solutions
Beyond core performance, integration and automation are practical considerations for research and clinical laboratories.
- Roche's Automated Solution: The KAPA HyperExome V2 probes can be paired with the AVENIO Edge Liquid Handling System. This integrated system requires minimal hands-on time, with as little as 20 minutes of deck setup, and is designed to reduce operator error and increase reproducibility [56] [59]. The latest V2 design covers a 43.2 Mb target, incorporating updated content from ClinVar, RefSeq, and Ensembl to minimize "blind spots" [56].
- Vazyme's Automated Workflow: Vazyme offers a fully integrated and automated WES workflow that unites reagents, instruments, consumables, and data analysis software. This system reduces hands-on time by approximately 1.5 hours per run while maintaining consistent data quality [57].
- Nanodigmbio's Customization: Nanodigmbio provides a one-stop NAD Probe customization service, covering probe design, production, and quality control. This service is valuable for researchers who require custom panels for specific genes of interest in cancer, beyond the standard exome [60].
The 2024 comparison reveals that all four exome enrichment kits offer high-quality performance, making them suitable for demanding cancer research applications. The choice of kit should be guided by the specific priorities of the research project.
- For Superior Uniformity and Database Coverage: Roche KAPA HyperExome is the preferred choice, particularly for large-scale studies where consistent coverage is critical for comparative analysis. Its compatibility with the AVENIO Edge system is a major advantage for high-throughput labs seeking automation [53] [56].
- For Highest Variant Detection Sensitivity (Recall): Agilent SureSelect v8 is recommended, especially for projects where maximizing the detection of true positive variants is the paramount objective [53] [54].
- For Highest Data Efficiency and Precision: Nanodigmbio NEXome Plus is ideal for projects where minimizing false positives and off-target data is a priority, thereby optimizing sequencing cost-efficiency [53] [54].
- For Automated, Integrated Workflows: Vazyme presents a strong solution with its proven performance in automated settings, offering a balance of high quality and operational efficiency [57].
In conclusion, the emergence of high-performance kits from manufacturers like Vazyme and Nanodigmbio demonstrates that the exome capture market is more competitive than ever, providing researchers with a range of excellent options to advance cancer genomics.
The advent of next-generation sequencing (NGS) has fundamentally transformed cancer research and therapeutic development. Whole exome sequencing (WES), which focuses on identifying variants in the protein-coding regions of the genome, represents a powerful and cost-effective approach for uncovering the genetic alterations driving tumorigenesis [61]. In non-small cell lung cancer (NSCLC), a disease characterized by significant molecular heterogeneity, WES enables comprehensive genomic profiling that informs targeted treatment strategies. This technical guide explores how WES-derived biomarkers, particularly those related to homologous recombination deficiency (HRD), are refining therapeutic selection for NSCLC patients.
WES functions through a targeted NGS approach utilizing hybridization capture to enrich protein-coding regions, which constitute approximately 1% of the human genome [61]. This method provides researchers with deeper sequencing coverage and more comprehensive data for identifying somatic mutations and heritable alterations compared to PCR-based approaches, while remaining more cost-effective than whole genome sequencing [61]. The standard WES workflow involves: (1) genomic DNA extraction from tumor samples, (2) library preparation with adapter ligation, (3) exome capture and enrichment using biotinylated probes, and (4) high-throughput sequencing on platforms such as Illumina NovaSeq [32] [61]. The resulting data, in FASTQ, BAM, and VCF formats, undergoes rigorous bioinformatic analysis for variant calling and annotation, increasingly facilitated by cloud computing platforms and AI-driven algorithms [62].
Whole Exome Sequencing Methodologies and Analytical Approaches
Technical Workflow and Experimental Protocol
Implementing WES for cancer research requires strict adherence to standardized protocols to ensure reliable and reproducible results. The following methodology has been validated in recent NSCLC studies [32]:
Sample Collection and DNA Extraction: Tumor samples are typically obtained from formalin-fixed paraffin-embedded (FFPE) surgical, biopsy, or cytology specimens. Expert pathological review is essential to confirm tissue type and assess tumor purity (>90% recommended). Genomic DNA extraction employs kits such as the QIAamp DNA FFPE Tissue Kit (Qiagen), with DNA concentration quantified using fluorometric methods (e.g., Qubit dsDNA HS assay) and integrity verified by agarose gel electrophoresis [32].
Library Preparation and Exome Capture: For each sample, 1.0 μg of genomic DNA undergoes fragmentation to produce fragments of 180-280 bp. Following end repair and adenylation, adapter oligonucleotides are ligated to facilitate sequencing. Exome capture utilizes targeted panels such as the Agilent SureSelect Human All Exon V6 kit, which employs biotinylated probes to enrich protein-coding regions. Captured libraries undergo PCR amplification before final quantification using systems like the Agilent Bioanalyzer 2100 [32].
Sequencing and Data Analysis: Qualified libraries are sequenced on high-throughput platforms (e.g., Illumina NovaSeq 6000) using 150 bp paired-end reads. Bioinformatic processing includes: (1) quality control of raw reads, (2) alignment to reference genome (e.g., GRCh38), (3) variant calling (single nucleotide variants, indels, copy number alterations), and (4) annotation of potential functional consequences. For cancer studies, comparative analysis of matched tumor-normal samples enables distinction between somatic and germline variants [32].
Research Reagent Solutions for WES
Table 1: Essential Research Reagents for Whole Exome Sequencing
| Reagent Category | Specific Product Examples | Function and Application Notes |
|---|---|---|
| DNA Extraction Kits | QIAamp DNA FFPE Tissue Kit (Qiagen) | Extracts high-quality genomic DNA from challenging FFPE specimens; includes optimized buffers for cross-link reversal [32]. |
| Library Preparation | Agilent SureSelect Human All Exon V6 | Provides all components for end repair, A-tailing, adapter ligation, and PCR amplification; compatible with Illumina platforms [32]. |
| Exome Capture Panels | xGen Custom Hyb Panels (IDT) | Biotinylated probe sets for comprehensive exome enrichment; customizable content allows inclusion of cancer-relevant non-coding regions [61]. |
| Target Enrichment | SureSelectXT Reagent Kit | Streamlines target capture through hybridization-based enrichment; includes magnetic streptavidin-coated beads for post-capture purification [32]. |
| Quality Control | Qubit dsDNA HS Assay Kit (Thermo Fisher) | Fluorometric quantification of DNA concentration; highly specific for double-stranded DNA without interference from RNA or contaminants [32]. |
Figure 1: Whole Exome Sequencing Workflow for Biomarker Discovery. This diagram illustrates the standardized workflow from sample preparation to biomarker identification, highlighting key technical stages in WES analysis.
Homologous Recombination Deficiency Biomarkers in NSCLC
DNA Damage Response Pathways and Therapeutic Implications
The DNA damage response (DDR) constitutes a sophisticated cellular network that preserves genomic stability by detecting, signaling, and repairing genetic lesions [63]. In NSCLC, dysregulation of DDR pathways contributes significantly to tumor progression and therapeutic resistance. Research indicates that nearly 49.6% of NSCLC patients harbor deleterious DDR mutations, which are associated with resistance to chemotherapy, radiotherapy, targeted therapy, and immunotherapy [63]. Key DNA repair pathways with clinical relevance in NSCLC include:
Homologous Recombination (HR): An error-free repair pathway active during S and G2 phases that utilizes sister chromatids as templates for precise double-strand break repair. Key components include the MRN complex (Mre11-Rad50-Nbs1), BRCA1, BRCA2, and Rad51 [63]. Deficiencies in HR, particularly through BRCA1/2 mutations or altered Rad51 expression, increase sensitivity to PARP inhibitors and certain chemotherapeutic agents [63].
Non-Homologous End Joining (NHEJ): An error-prone repair pathway predominant in G1 phase that directly ligates broken DNA ends without a template, frequently resulting in insertions or deletions. Core components include Ku70/Ku80 heterodimer, DNA-PKcs, Artemis, and DNA ligase IV [63]. Excessive NHEJ activity contributes to genomic instability and radio-resistance in NSCLC [63].
Nucleotide Excision Repair (NER): A pathway specialized in removing bulky, helix-distorting lesions induced by ultraviolet radiation and platinum-based chemotherapeutics. Excision repair cross-complementation group 1 (ERCC1) overexpression is strongly associated with cisplatin resistance in NSCLC [63].
Figure 2: DNA Repair Pathways and Therapeutic Implications in NSCLC. This diagram illustrates the major double-strand break repair mechanisms and how homologous recombination deficiency creates therapeutic vulnerabilities.
Advanced HRD Detection Biomarkers
Traditional HRD biomarkers focused primarily on BRCA1/2 mutations, but emerging evidence indicates that these alterations alone insufficiently predict therapeutic response. Next-generation HRD biomarkers now capture genomic scarring patterns resulting from HRD across the entire genome [64]. Foundation Medicine's HRDsig represents one such advanced biomarker—a pan-tumor copy number-based signature that detects HRD through machine learning analysis of genome-wide copy number features rather than relying solely on HRR gene mutations [64].
Key advantages of HRDsig over traditional biomarkers include:
- Detection of non-genomic HRD mechanisms, including BRCA promoter methylation
- Reduced false positives through analysis of diverse copy number features
- Pan-tumor applicability beyond ovarian cancer, including NSCLC [64]
In NSCLC specifically, HRDsig positivity is detected in approximately 5% of cases, identifying patients who may benefit from PARP inhibitor therapy and platinum-based chemotherapy [64]. Validation studies in breast and prostate cancers demonstrate that HRDsig-positive patients experience significantly improved outcomes with PARP inhibitor treatment, supporting its potential clinical utility in NSCLC [64].
Table 2: HRD Biomarkers for Therapeutic Prediction in NSCLC
| Biomarker | Detection Method | Mechanistic Basis | Clinical Utility in NSCLC | Limitations |
|---|---|---|---|---|
| BRCA1/2 Mutations | WES, Targeted NGS | Loss of functional HR repair proteins | Predicts PARP inhibitor sensitivity; present in ~3-5% of NSCLC [63] | Limited sensitivity; misses epigenetic silencing [64] |
| Genomic LOH (gLOH) | WES, SNP arrays | Measures loss of heterozygosity scarring from impaired HR | Historical biomarker for PARP inhibitor response; used in ovarian cancer [64] | Suboptimal performance in lung cancers; tissue-specific thresholds [64] |
| HRDsig | WES, Copy Number Analysis | Pan-tumor copy number loss signature from machine learning | Detects ~5% of NSCLC; predicts PARP inhibitor and platinum response [64] | Laboratory-developed service; not yet FDA-approved [64] |
| RAD51 Foci | Immunofluorescence | Functional assessment of HR repair capacity | Direct measurement of HR functionality; predicts PARP inhibitor sensitivity [63] | Requires fresh tissue; technically challenging; not standardized |
Case Study: WES Identification of HRD in Transformed SCLC
Experimental Design and Analytical Methodology
A recent investigation utilized WES to characterize the genomic evolution of EGFR-mutated lung adenocarcinomas that transform to small cell lung cancer (SCLC) after EGFR tyrosine kinase inhibitor (TKI) resistance—a phenomenon occurring in 3-15% of cases [32]. The study design incorporated:
Cohort Composition: Tissue collection from 5 primary LUAD samples before SCLC transformation, 12 transformed SCLC samples after EGFR-TKI treatment resistance, and 18 de novo SCLC samples from Beijing Chest Hospital (2015-2021) [32].
Sequencing Protocol: DNA extraction from FFPE samples followed by WES using Agilent SureSelect Human All Exon V6 kit and Illumina NovaSeq 6000 sequencing (150 bp paired-end reads) [32].
Bioinformatic Analysis: Somatic variant calling, copy number analysis, and calculation of genomic instability metrics including homologous recombination deficiency (HRD) scores, loss of heterozygosity (LOH), and telomeric allelic imbalance (TAI) [32].
Key Findings and Therapeutic Implications
The WES analysis revealed crucial insights into the genomic drivers of SCLC transformation:
Genomic Instability Patterns: Transformed SCLC exhibited significantly higher genomic instability compared to primary LUAD and de novo SCLC, supported by elevated HRD scores (p=0.025), LOH (p=0.008), and uniparental disomy (p=0.003) [32].
Recurrent Alterations: While TP53 mutations and RB1 loss were confirmed as important drivers, they were not universally present. Transformed SCLC showed distinctive mutation patterns in COL22A1 and ALMS1, while PTCH2, CNGB3, SPTBN5, CROCC, and MYO15A mutations were more prevalent in transformed compared to de novo SCLC [32].
DDR Pathway Alterations: Significant similarity was observed in DNA damage repair pathway alterations between transformed SCLC and de novo SCLC, suggesting shared therapeutic vulnerabilities [32].
This WES-based characterization provides a molecular framework for identifying NSCLC patients at risk for SCLC transformation and informs potential treatment strategies targeting DDR pathways in transformed cases.
Multi-Omics Integration and Emerging Applications
Proteogenomic Approaches in NSCLC Subtyping
While WES provides comprehensive genomic characterization, integrating transcriptomic and proteomic data enables more nuanced molecular subtyping of NSCLC, particularly for tumors lacking actionable genomic alterations. Proteogenomic approaches—simultaneous analysis of genomic, transcriptomic, and proteomic profiles—reveal distinct tumor subtypes with differential therapeutic vulnerabilities [65].
Multi-omics profiling of NSCLC has identified several therapeutically relevant subtypes:
- Cell Cycle Accelerated Subtype: Characterized by CCNE1 amplification and CDKN2A deletion; potential sensitivity to CDK4/6 inhibitors [65]
- Immunogenic Subtype: Demonstrates PD-L1 expression, CD8+ T-cell infiltration, and inflammatory signaling; potential sensitivity to immunotherapy [65]
- DNA Damage Repair Subtype: Exhibits alterations in HR, NHEJ, and other DDR pathways; potential sensitivity to PARP inhibitors and platinum agents [65]
Clonal Expression Biomarkers for Prognostic Stratification
Recent research has addressed the challenge of tumor sampling bias through the development of clonal expression biomarkers. The Outcome Risk Associated Clonal Lung Expression (ORACLE) signature, validated in the TRACERx study, identifies homogeneously expressed genes across tumor regions to predict patient outcomes [66].
In prospective validation involving 158 patients with stage I-III LUAD, ORACLE demonstrated:
- Superior resistance to tumor sampling bias compared to six other prognostic signatures (discordant risk classification in only 19% of tumors)
- Significant association with overall survival (HR 2.2 for concordant-high vs concordant-low risk)
- Prognostic independence from clinicopathological risk factors in multivariable analysis (HR-adj 2.27, p=0.004) [66]
This approach enables reliable prognostic stratification from single biopsy specimens, addressing a critical limitation in NSCLC molecular profiling.
Whole exome sequencing has evolved from a research tool to a fundamental component of precision oncology in NSCLC. By enabling comprehensive detection of HRD and other therapeutically relevant biomarkers, WES provides critical insights for treatment selection and drug development. The integration of WES with transcriptomic, proteomic, and functional data creates a multidimensional understanding of NSCLC biology that continues to refine therapeutic strategies. As sequencing technologies advance and analytical methods become more sophisticated, WES-guided targeted therapies will play an increasingly prominent role in overcoming resistance mechanisms and improving outcomes for NSCLC patients.
Whole exome sequencing (WES) has become a cornerstone of cancer genomics research, providing a cost-effective method for analyzing all protein-coding regions of the genome where most known disease-causing mutations are located [2]. While traditional approaches focus on identifying driver mutations in individual genes, this whitepaper explores advanced methodologies that leverage mutational signatures and machine learning to uncover deeper insights into cancer etiology, progression, and therapeutic opportunities. By examining the characteristic patterns of mutations imprinted by various mutational processes, researchers can move beyond single-gene analysis to understand the collective history of mutational processes that have shaped a tumor's genome [67]. This technical guide provides researchers, scientists, and drug development professionals with experimental protocols, analytical frameworks, and computational tools to integrate these approaches into cancer research programs.
From Single Genes to Genomic Patterns
Cancer genomes accumulate somatic mutations from multiple mutational processes, each generating a characteristic pattern or "mutational signature" [68]. These signatures represent the molecular footprints of various exogenous and endogenous mutational processes, including DNA replication infidelity, environmental exposures, and defective DNA repair mechanisms [69]. While individual driver mutations have been the primary focus of cancer genomics, mutational signatures provide a complementary framework that captures the totality of mutational processes operative during tumorigenesis.
The analysis of mutational signatures has been revolutionized by large-scale consortia such as the Pan-Cancer Analysis of Whole Genomes (PCAWG) and The Cancer Genome Atlas (TCGA), which have analyzed thousands of cancer genomes to systematically characterize mutational signatures across cancer types [68] [67]. These efforts have identified dozens of distinct signatures, some with known etiologies and others of cryptic origin, revealing the remarkable diversity of mutational processes underlying cancer development.
Whole Exome Sequencing as a Platform for Signature Analysis
Whole exome sequencing provides a practical balance between comprehensive genomic coverage and cost-effectiveness for mutational signature analysis [2]. By targeting approximately 1-2% of the genome that contains protein-coding regions, WES enables researchers to identify thousands of somatic mutations across large cohorts, providing sufficient data for robust signature extraction. The technology involves hybrid capture of exonic regions followed by next-generation sequencing, typically achieving coverages of 100-200x that enable accurate variant calling [61]. While whole genome sequencing provides more comprehensive mutational data, WES remains the most efficient method for large-scale cancer genomics studies where focused analysis of protein-coding regions is sufficient.
Fundamentals of Mutational Signatures
Biological Basis of Mutational Signatures
Mutational signatures arise from the interplay between DNA damage, DNA repair, and DNA replication processes. Each signature reflects the specific mechanisms through which different mutational processes generate somatic alterations:
- Exogenous exposures: Environmental carcinogens such as tobacco smoke (Signature 4) and ultraviolet light (Signature 7) generate characteristic mutation patterns through formation of specific DNA adducts that are processed by DNA repair pathways [69].
- Endogenous processes: Cellular processes including spontaneous deamination of 5-methylcytosine (Signature 1) and APOBEC enzyme activity (Signature 2) create distinct mutational patterns [69].
- Defective DNA repair: Deficiencies in DNA maintenance systems such as mismatch repair (Signature 6, 15, 20, 26, 44), homologous recombination (Signature 3), and nucleotide excision repair produce recognizable signatures [67].
Classification of Mutation Types
Mutational signatures are defined based on comprehensive classification of somatic mutations into specific types and contexts:
Table 1: Mutation Classification for Signature Analysis
| Mutation Class | Subtypes | Classification Basis | Total Contexts |
|---|---|---|---|
| Single Base Substitutions (SBS) | C>A, C>G, C>T, T>A, T>C, T>G | Pyrimidine reference with one 5' and one 3' base | 96 (6×4×4) |
| Doublet Base Substitutions (DBS) | 78 mutation types | Two consecutive bases | 78 |
| Small Insertions/Deletions (ID) | Insertions, deletions at repeats/microhomology | Size, sequence context, microhomology | 83 |
The most commonly used classification for single base substitutions incorporates the six substitution types with information about the immediate sequence context (one base 5' and one base 3' to the mutated base), resulting in 96 possible mutation types [68]. This detailed classification enables discrimination between signatures that cause the same types of base substitutions but in different sequence contexts.
Experimental Workflows for Mutational Signature Analysis
Whole Exome Sequencing Wet-Lab Procedures
The standard WES workflow involves multiple critical steps to ensure high-quality data for mutational signature analysis:
Sample Preparation and Quality Control
- Tissue selection: Pathological examination to ensure adequate tumor content (>20-30% tumor cells) and representative sampling [2].
- DNA extraction: Isolation of high-quality DNA from tumor and matched normal samples using standardized protocols.
- Quality assessment: Quantification using fluorometric methods and quality verification through fragment analysis.
Library Preparation and Exome Capture
- Library construction: Fragmentation of DNA, end repair, A-tailing, and adapter ligation with sample barcodes [61].
- Hybridization capture: Enrichment of exonic regions using biotinylated probes targeting the human exome (e.g., xGen Exome Panels) [61].
- Pooling and amplification: Normalization and pooling of libraries followed by PCR amplification.
Sequencing
- Platform selection: Typically performed on Illumina sequencing platforms [2].
- Coverage requirements: Minimum 100x coverage for tumor samples and 60x for matched normal samples to ensure sensitive variant detection [2].
- Quality metrics: Assessment of base quality scores, coverage uniformity, and on-target rates.
Bioinformatic Processing Pipeline
The computational analysis of WES data for mutational signature extraction involves multiple steps:
Data Preprocessing and Alignment
- Quality control: FastQC for sequence quality assessment.
- Adapter trimming: Removal of sequencing adapters using tools such as Trimmomatic or Cutadapt.
- Alignment: Mapping of reads to reference genome (GRCh38) using aligners like BWA-MEM [70].
- Duplicate marking: Identification and marking of PCR duplicates to avoid amplification artifacts.
Variant Calling and Quality Filtering
- Somatic variant calling: Identification of somatic mutations using multiple callers (MuTect2, VarScan2, Strelka) to ensure comprehensive detection [2] [70].
- Variant annotation: Functional annotation of variants using tools like ANNOVAR or VEP.
- Filtering: Removal of technical artifacts and germline contaminants.
Mutation Matrix Generation
- Context extraction: Classification of each mutation into the 96 SBS categories based on sequence context.
- Matrix construction: Compilation of mutation counts across all samples into a samples-by-mutation-types matrix.
Table 2: Key Bioinformatics Tools for Mutational Signature Analysis
| Analysis Step | Tool Options | Key Features | Considerations |
|---|---|---|---|
| Alignment | BWA-MEM, STAR | Accurate alignment to GRCh38 | Include decoy sequences for improved accuracy [70] |
| Somatic SNV Calling | MuTect2, VarScan2, Strelka, MuSE | High sensitivity for low-frequency variants | Multi-caller approaches improve robustness [2] [70] |
| Indel Calling | Pindel, VarScan2 | Detection of small insertions/deletions | Important for signature completeness |
| Signature Extraction | SigProfiler, SignatureAnalyzer | NMF-based decomposition | Choice affects signature resolution [68] |
Computational Extraction of Mutational Signatures
Mathematical Frameworks for Signature Extraction
The core computational challenge in mutational signature analysis is decomposing the observed matrix of mutation counts into signature profiles and their activities across samples. This is typically formulated as a non-negative matrix factorization (NMF) problem:
Given a mutation matrix ( V ) of dimensions ( m \times n ) (where ( m ) is the number of samples and ( n ) is the number of mutation types), NMF factors this matrix into two non-negative matrices: [ V \approx W \times H ] where ( W ) is an ( m \times k ) matrix representing the contribution of each signature in each sample, and ( H ) is a ( k \times n ) matrix representing the mutational profile of each signature [68].
SigProfiler Implementation
- Algorithm: Uses custom NMF implementation with stability analysis for rank selection.
- Stability assessment: Performs multiple NMF runs with different initializations to assess stability of solutions.
- Signature refitting: After extraction, uses least-squares optimization to refit signatures to samples [68].
SignatureAnalyzer Implementation
- Algorithm: Bayesian variant of NMF with automatic relevance determination.
- Rank determination: Uses Bayesian framework to automatically determine the number of signatures.
- Sparsity constraints: Incorporates sparsity constraints to prevent overfitting [68].
Signature Validation and Annotation
After mathematical extraction, signatures must be biologically validated and annotated:
- Cosine similarity: Comparison to known COSMIC signatures using cosine similarity metric.
- Statistical validation: Assessment of signature stability and reproducibility through bootstrapping.
- Biological plausibility: Evaluation against known mutational processes from experimental literature.
- Clinical correlation: Association with clinical features, exposures, and therapeutic responses.
Machine Learning Approaches for Advanced Analysis
AI-Driven Driver Mutation Prediction
Recent advances in machine learning have enabled more accurate identification of cancer driver mutations, particularly for variants of unknown significance (VUS). Multiple computational approaches have been developed:
Table 3: Machine Learning Methods for Cancer Driver Identification
| Method Category | Representative Tools | Key Features | Performance Considerations |
|---|---|---|---|
| Evolution-Based | EVE | Unsupervised deep learning on evolutionary sequences | AUROC: 0.83-0.92 for TSGs [71] |
| Deep Learning-Based | AlphaMissense | Incorporates structural and evolutionary data | AUROC: 0.98 for OGs/TSGs [71] |
| Ensemble Methods | VARITY, REVEL | Combines multiple prediction approaches | Outperforms single methods [71] |
| Cancer-Specific | CHASMplus, BoostDM | Incorporates tumor-type specific features | Limited mutation coverage [71] |
AlphaMissense Framework
- Architecture: Leverages protein language models and structural homology.
- Training data: Combines evolutionary, structural, and functional genomic features.
- Performance: Significantly outperforms methods trained only on evolutionary conservation [71].
Network-Based Approaches
- Topological features: Incorporates network properties from protein-protein interaction networks.
- Mutual exclusivity: Identifies patterns of mutually exclusive alterations across pathways.
- Pathway-level analysis: Detects driver modules beyond individual genes [72].
Integration with Mutational Signatures
Machine learning approaches can be enhanced by incorporating mutational signature information:
- Signature-aware variant prioritization: Weighting mutations based on the dominant signatures in a tumor.
- Signature-driven feature engineering: Creating features based on signature exposures for predictive models.
- Multi-modal learning: Integrating signature data with genomic, transcriptomic, and clinical features.
Clinical and Therapeutic Applications
Predictive Biomarker Development
Mutational signatures provide valuable biomarkers for therapy selection and response prediction:
Homologous Recombination Deficiency (HRD) Assessment
- Signature 3: Associated with BRCA1/2 deficiency and sensitivity to PARP inhibitors [67].
- HRDetect algorithm: Predicts BRCA1/2 deficiency based on mutational signatures with high accuracy [67].
- Clinical utility: Identifies patients likely to respond to PARP inhibition beyond BRCA mutation status.
Mismatch Repair Deficiency
- MMR signatures: Signatures 6, 15, 20, 21, 26, and 44 associated with defective DNA mismatch repair [67].
- Immunotherapy prediction: MMR-deficient tumors show increased sensitivity to immune checkpoint inhibitors.
- Complementary to MSI testing: Particularly useful in tumor types where microsatellite instability testing has limited sensitivity [67].
Drug Development Applications
Mutational signatures offer multiple applications in oncology drug development:
- Target identification: Revealing novel therapeutic targets based on underlying mutational processes.
- Patient stratification: Enriching clinical trials with patients likely to respond based on signature profiles.
- Combination therapy: Guiding rational combination strategies based on co-occurring mutational processes.
- Biomarker development: Developing companion diagnostics based on signature patterns.
Research Reagent Solutions
Table 4: Essential Research Reagents for Mutational Signature Studies
| Reagent Category | Specific Products | Application | Considerations |
|---|---|---|---|
| Exome Capture Panels | xGen Custom Hyb Panels | Target enrichment for WES | Custom content options for cancer-relevant genes [61] |
| Library Prep Kits | Illumina DNA Prep | Sequencing library construction | Compatibility with FFPE samples [2] |
| Hybridization Reagents | xGen Lockdown Probes | Magnetic bead-based capture | Probe design for comprehensive exome coverage [61] |
| Quality Control Kits | Agilent Bioanalyzer | DNA quality assessment | Critical for FFPE-derived DNA [2] |
The integration of mutational signature analysis with machine learning approaches represents a paradigm shift in cancer genomics, moving beyond single-gene analysis to comprehensive understanding of mutational processes. As these methodologies continue to mature, they offer unprecedented opportunities for advancing cancer research, drug development, and precision oncology. Whole exome sequencing provides a practical and cost-effective platform for implementing these approaches across diverse research programs. Future developments in single-cell sequencing, long-read technologies, and multimodal data integration will further enhance our ability to decipher the complex mutational landscapes of cancer and translate these insights into improved patient outcomes.
Optimizing WES Performance: Tackling Technical Challenges and Data Quality
In the pursuit of precision oncology, whole exome sequencing has emerged as a fundamental tool for identifying genetic alterations that drive cancer. However, the reliability of genomic data is profoundly influenced by the quality of the starting biological material. Clinical samples such as formalin-fixed paraffin-embedded (FFPE) tissues, blood, and low-input specimens present significant challenges due to their variable quality and quantity. This technical guide outlines robust, validated protocols to overcome these challenges, ensuring the generation of high-quality, reliable sequencing data for cancer research and drug development.
Understanding Sample-Specific Challenges
Different sample types present unique obstacles that require specialized handling and processing protocols.
FFPE Samples
FFPE specimens are invaluable for cancer research due to their widespread availability and rich clinical data. However, the formalin fixation process causes chemical modifications to DNA, including crosslinks between nucleic acids and proteins, fragmentation, and base damage such as cytosine deamination (leading to C→T mutations) and oxidative damage (leading to G→T mutations) [73]. These artifacts can lead to chimeric reads and false-positive variant calls during sequencing [73]. Additionally, DNA extracted from FFPE samples is often highly degraded with low yields, presenting challenges for library preparation [74].
Low-Input and Single-Cell Samples
Samples with limited genetic material, such as those from fine needle aspirations, liquid biopsies, or single-cell analyses, face substantial technical hurdles. Amplification from low-input samples can introduce significant biases—one study found that even with 1000 pg mRNA input, over 60% of genes showed at least a 2-fold change in expression levels compared to high-input samples [75]. These biases are sequence-dependent and particularly affect genes with high GC content or long transcript lengths [75].
Robust Experimental Protocols
Optimized FFPE DNA Library Preparation
The NEBNext UltraShear FFPE DNA Library Prep Kit exemplifies a specialized approach for challenging samples. Its workflow begins with a repair step that selectively targets damaged DNA bases, excising damaged portions in single-stranded regions and employing base excision repair for double-strand damage [73]. This step is crucial for removing artifacts while preserving true mutations, which typically appear on both DNA strands [73].
A key innovation is the enzymatic fragmentation method that prevents over-fragmentation of already compromised DNA. Research demonstrates that prolonged fragmentation time doesn't significantly alter the size of pre-fragmented FFPE DNA, addressing a common concern about complete digestion [73]. This protocol generates libraries with improved sequence complexity and coverage uniformity, providing more comprehensive genomic representation [73].
Targeted RNA Sequencing for FFPE Samples
For transcriptomic analysis of FFPE samples, a targeted amplicon-based RNA sequencing approach has demonstrated superior performance compared to whole transcriptome methods. One study developed a panel targeting 395 immune transcripts (the "Immune Advance" assay) specifically optimized for degraded RNA from FFPE specimens [76]. This method requires minimal starting material and exhibits high concordance with freshly frozen samples, with Pearson correlation coefficients ranging from 0.837 to 0.969 in matched samples [76]. The assay also showed robust correlation with quantitative RT-PCR and protein abundance determined by immunohistochemistry, validating its clinical utility [76].
Oligonucleotide Selective Sequencing (OS-Seq) for Low-Input Samples
The OS-Seq approach addresses challenges of low-input and variable quality DNA through three key steps [74]:
- Damage repair without corrective repair: Damaged bases are excised without implementation of a corrective repair step.
- Single-stranded adapter ligation: DNA is fully denatured to single strands followed by highly efficient single-stranded ligation of adapters, ensuring all DNA species can be interrogated regardless of quality.
- Primer-based capture: Target-specific primer-probe oligonucleotides tile across regions of interest, followed by polymerase extension to capture targeted DNA molecules.
This method has been successfully applied to capture and sequence exons of a 130-gene cancer panel, achieving high read coverage uniformity with input DNA amounts as low as 10 ng [74]. At this low input, the method maintained an on-target read fraction of 67% and covered 92% of targeted bases at 100X read depth [74].
Ribodepletion for FFPE RNA Sequencing
For whole transcriptome analysis of FFPE samples, ribosomal RNA depletion has emerged as the preferred RNA isolation method over poly-A selection [77]. This approach provides equivalent mRNA coverage uniformity while enabling recovery of non-polyadenylated and short-transcript RNAs that are often missed by poly-A selection methods [77]. One large-scale study of over 3,000 FFPE samples demonstrated that this method achieved an 81% sequencing success rate, with exome coverage highly concordant between direct FFPE and fresh frozen replicates (median correlation of 0.95) [77].
Table 1: Performance Metrics of Robust Sequencing Approaches
| Method | Sample Type | Minimum Input | Key Performance Metrics | Applications |
|---|---|---|---|---|
| Targeted RNAseq (Immune Advance) [76] | FFPE | Minimal material compatible with RNA degradation | Pearson correlation 0.837-0.969 with fresh frozen; correlates with qRT-PCR and IHC | Immune transcript profiling for immunotherapy response prediction |
| OS-Seq [74] | Low-input DNA (including FFPE) | 10 ng DNA | 67% on-target reads; 92% ROI coverage at >100X; high variant detection accuracy | Targeted sequencing of cancer gene panels (130 genes) |
| Ribo-deplete RNA extraction [77] | FFPE | Standard input from >3200 samples | 81% success rate; median correlation 0.95 with fresh frozen | Whole transcriptome profiling |
| NEBNext UltraShear [73] | FFPE DNA | Broad input range, quality-agnostic | Improved coverage uniformity; reduced artifacts | Whole genome and targeted sequencing |
Computational Deconvolution for Heterogeneous Samples
Tumor samples inherently contain mixed cell populations, and computational deconvolution methods are essential for accurately interpreting sequencing data from bulk tissues. These methods can be categorized as reference-based or reference-free approaches [78].
Reference-based methods (e.g., CIBERSORTx, MuSiC) utilize single-cell or purified cell-type expression profiles as references to estimate cell-type proportions. These generally perform better when reliable reference data are available [78]. Reference-free methods (e.g., Linseed, GS-NMF) employ matrix factorization and statistical modeling to infer cell-type proportions without external references, making them suitable for scenarios where reference data are lacking [78].
A benchmark study found that variations in cell-level transcriptomic profiles and cellular composition significantly influence deconvolution performance. The choice between reference-based and reference-free approaches should be guided by data availability and specific research questions [78].
The Scientist's Toolkit: Essential Research Reagents
Table 2: Key Research Reagent Solutions for Challenging Samples
| Reagent/Kit | Function | Sample Compatibility |
|---|---|---|
| NEBNext UltraShear FFPE DNA Library Prep Kit [73] | DNA repair and fragmentation; reduces sequencing artifacts | FFPE-derived DNA |
| Targeted RNAseq Panels [76] | Enrichment of specific transcripts; compatible with degraded RNA | FFPE-derived RNA |
| OS-Seq Reagents [74] | Single-stranded library prep; target capture | Low-input and damaged DNA |
| Ribo-depletion Reagents [77] | Removal of ribosomal RNA; preserves non-polyadenylated transcripts | FFPE and degraded RNA |
| Single Cell 3' RNA Prep Kit [79] | mRNA capture, barcoding, and library prep from single cells | Single cells and ultra-low input samples |
Workflow Visualization
Sample Processing Workflow for Challenging Specimens
Optimized FFPE DNA Library Prep Workflow
Advancements in sequencing technologies and methodologies have dramatically improved our ability to extract reliable genetic information from challenging but clinically valuable samples. By implementing specialized protocols that address the unique limitations of FFPE, blood, and low-input samples—including optimized library preparation, targeted enrichment, ribosomal RNA depletion, and computational deconvolution—researchers can generate robust, clinically actionable data. These approaches are fundamental to advancing precision oncology, enabling more accurate biomarker discovery, therapeutic target identification, and ultimately, improved patient outcomes in cancer care.
In the context of whole exome sequencing (WES) for cancer research, achieving uniform coverage is not merely a technical benchmark but a fundamental prerequisite for reliable variant discovery. The exome, representing approximately 1-2% of the human genome, contains about 85% of known disease-causing mutations, making it a primary target for oncological research [31] [80]. However, the hybridization-based capture process inherent to WES introduces systematic biases that create reproducible regions of reduced coverage, potentially obscuring critical driver mutations in tumor suppressor genes and oncogenes.
Next-generation sequencing (NGS) has revolutionized cancer diagnostics by enabling comprehensive profiling of tumor genomes. WES dominates large-scale resequencing projects due to its lower cost and simplified data analysis compared to whole-genome sequencing (WGS) [81]. Nevertheless, the diagnostic effectiveness of WES is directly limited by its ability to consistently cover protein-coding regions. In clinical oncology, where identifying somatic variants informs therapeutic decisions, coverage gaps can lead to false negatives with direct implications for patient treatment selection [2].
This technical guide examines the determinants of coverage unevenness in WES, provides strategies to maximize uniformity, and outlines methodologies to identify and address problematic regions, with specific consideration for applications in cancer research and drug development.
Understanding Coverage Biases in Whole Exome Sequencing
Types of Coverage Unevenness
Coverage biases in WES manifest in two distinct forms, each with different implications for variant detection in cancer genomics:
Within-Interval Evenness (WIE): Refers to uniformity of coverage across individual exonic regions. This bias is specific to enrichment-based methods and results from uneven hybridization efficiency during capture [81]. In cancer research, poor WIE can cause sections of critical genes to be undercovered, potentially missing subclonal mutations that impact therapeutic decisions.
Between-Interval Evenness (BIE): Describes variation in mean coverage across different exonic regions. While WGS also exhibits BIE, the pattern differs significantly in WES due to probe design and capture dynamics [81]. Disparities in BIE mean that certain cancer-related genes may be systematically undercovered compared to others, creating blind spots in genomic analyses.
Determinants of Coverage Bias
Multiple factors contribute to coverage unevenness in WES, with varying degrees of impact:
Table 1: Key Determinants of WES Coverage Bias
| Determinant | Impact Level | Effect on Coverage | Relevance to Cancer Research |
|---|---|---|---|
| Mappability Limitations | High | Creates irremediable gaps in short-read technologies | Affects genes with paralogs or repetitive elements; may impact detection of fusion genes |
| GC Content | Medium to High | Poor coverage in very high (>65%) or very low (<30%) GC regions | Oncogenes like MYC with high GC content are particularly affected |
| Probe Design | High | Determines capture efficiency and uniformity | Commercial kits vary in coverage of cancer-relevant genes |
| Sequence Complexity | Medium | Affects hybridization efficiency | Impacts regions with homopolymers or secondary structures |
| Library Preparation | Medium | Influences library complexity and duplication rates | Critical for FFPE samples with degraded DNA |
Contrary to common assumptions, modern WES biases stem more significantly from mappability limitations and probe design rather than sequence composition alone [81]. This is particularly relevant for cancer genomics, where certain tumor suppressor genes contain regions that are difficult to map with short reads.
Experimental Approaches for Assessing Coverage
Methodologies for Coverage Analysis
Robust assessment of WES coverage requires standardized methodologies that enable cross-platform comparison and quality control:
Protocol 1: Evaluating Coverage Efficiency and Evenness
Data Preprocessing: Begin with aligned BAM files after removal of PCR duplicates and low mapping quality reads (MQ < 10), as these are typically ignored by variant callers [81].
Coverage Profiling: Calculate normalized coverage across all coding sequence (CDS) bases. Generate coverage profiles with a minimum depth threshold of 20× for clinical applications and 30× for research-grade somatic variant detection [35].
Evenness Metrics Calculation:
- Compute Overall Evenness (OE) score using the formula developed by Mokry et al. [81]
- Calculate Within-Interval Evenness (WIE) by assessing coverage distribution across individual CDS regions
- Determine Between-Interval Evenness (BIE) by analyzing variation in mean coverage across different exons
Comparative Analysis: For multicenter consortia, implement tools like ExCID (Exome Coverage Identification Tool) to identify reduced coverage loci across sequencing centers and platforms [82].
Protocol 2: Identifying Reduced Coverage Regions in Clinical Genes
Gene Panel Definition: Curate a list of clinically relevant genes, focusing on cancer-related genes from resources like ClinVar and COSMIC.
Coverage Threshold Application: Define reduced coverage regions as positions with depth below 10× at a given mean coverage level (e.g., 100×) [81].
Cross-Platform Mapping: Analyze the same genomic regions across multiple WES platforms (e.g., Agilent SureSelect, Illumina TruSeq, MedExome) to identify consistently problematic regions.
Validation: Verify putative reduced coverage regions through orthogonal methods such as Sanger sequencing or targeted capture.
Benchmarking Across Platforms
Comparative studies reveal significant differences in WES platform performance:
Table 2: Performance Metrics of Major WES Platforms
| Platform | Mean Coverage Efficiency | Within-Interval Evenness | Between-Interval Evenness | Low-Coverage Bases at 100× |
|---|---|---|---|---|
| Agilent SureSelect | ~70-120× | High | Medium | 1,180 kbp |
| Illumina TruSeq | ~70× | Medium | Medium-High | >1,200 kbp |
| MedExome | ~70× | High | Medium | ~1,200 kbp |
| Nextera Rapid | ~70× | Low | High | >1,300 kbp |
| PCR-free WGS | Varies | Very High | High | 788 kbp |
Data derived from systematic comparison of WES technologies [81]
Even at high average coverages (200×), all WES platforms exhibit persistent low-coverage regions. For instance, approximately 970 kbp of the exome remains poorly covered (<10×) with SureSelect even at 200× mean coverage, compared to 407 kbp for WGS at the same depth [81]. This has direct implications for cancer gene panels, as these persistent gaps often affect specific disease genes.
Computational and Bioinformatic Strategies
Bioinformatics Tools for Variant Calling
The choice of variant calling algorithms significantly impacts the ability to detect true variants in regions with suboptimal coverage:
Table 3: Variant Caller Selection Guidelines for Cancer WES
| Scenario | Recommended Tools | Strengths | Limitations |
|---|---|---|---|
| Low-frequency variants | Strelka, MuTect2, LoFreq | High sensitivity for low VAF | Higher false positive rate |
| Low-coverage data | SomaticSniper, FaSD-somatic, SNVSniffer | Robust with limited depth | Reduced sensitivity |
| Insertion/Deletion detection | VarScan2, FreeBayes, VarDict | Comprehensive indel calling | Computationally intensive |
| Clinical-grade analysis | Combination approaches | Maximizes sensitivity/specificity | Complex implementation |
Multiple studies recommend using combination caller approaches for clinical cancer sequencing, particularly for detecting low-frequency somatic variants in heterogeneous tumor samples [2].
Machine Learning Approaches
Advanced computational methods can predict coverage biases and guide experimental design:
Regression Modeling: Predict coverage of CDS regions based on sequence features including GC content, mappability, and probe characteristics [81]
Feature Importance Analysis: Identify the relative contribution of different determinants to overall coverage variance, enabling prioritization of optimization strategies
Coverage Gap Imputation: Develop models to flag likely false negatives in regions with systematically poor coverage
Table 4: Research Reagent Solutions for Optimal WES Coverage
| Category | Specific Products/Platforms | Function | Considerations for Cancer Research |
|---|---|---|---|
| Exome Capture Kits | Agilent SureSelect, Illumina TruSeq, MedExome | Target enrichment | Evaluate coverage of cancer gene panels; consider compatibility with FFPE samples |
| Library Prep Systems | Illumina Nextera, KAPA HyperPrep | Library construction | Assess performance with degraded DNA from clinical specimens |
| NGS Platforms | Illumina NovaSeq, HiSeq | Sequencing | Balance throughput with coverage requirements for cohort studies |
| Variant Callers | MuTect2, VarScan2, Strelka | Somatic variant detection | Choose based on variant type (SNV, indel) and tumor purity |
| Coverage Analysis Tools | ExCID, BEDTools, GATK | Quality control | Implement for ongoing monitoring of sequencing performance |
| Reference Materials | GIAB benchmarks, SeraCare controls | Process validation | Essential for clinical implementation and reproducibility |
Visualization of WES Coverage Optimization Workflow
WES Optimization Workflow: This diagram illustrates the integrated experimental and computational pipeline for maximizing coverage uniformity in whole exome sequencing, highlighting critical checkpoints at each phase.
Strategic Recommendations for Cancer Research Applications
Platform Selection and Experimental Design
Platform Choice: Select WES platforms based on coverage uniformity metrics for cancer-relevant genes rather than overall efficiency alone. Agilent SureSelect demonstrates superior within-interval evenness, crucial for complete gene coverage [81]
Sequencing Depth: Plan for minimum 100-150× mean coverage for tumor-normal pairs in somatic variant detection, with higher depth (200×+) for heterogeneous samples or low-purity tumors
Replication Strategy: Implement technical replicates for critical samples to address stochastic coverage gaps, particularly for rare variant detection in cancer predisposition genes
Addressing Persistent Coverage Gaps
Approximately 500 kb of the human exome cannot be effectively characterized using short-read technologies and requires special attention during variant analysis [81]. For these regions:
Orthogonal Validation: Employ long-read sequencing technologies (Oxford Nanopore, PacBio) for problematic regions in clinically actionable genes
Custom Capture Panels: Develop supplementary targeted panels for known low-coverage regions in cancer genes
Multimodal Integration: Combine WES with transcriptome sequencing to detect functional consequences even when coding variants are missed
Maximizing coverage uniformity in whole exome sequencing requires a comprehensive approach addressing both experimental and computational factors. By understanding the determinants of coverage bias, implementing rigorous quality control metrics, and employing strategic bioinformatic solutions, researchers can significantly improve the reliability of WES for cancer genomics. As personalized oncology continues to evolve, ensuring complete coverage of cancer-related genes remains fundamental to accurate mutation detection, appropriate therapeutic targeting, and ultimately, improved patient outcomes. The convergence of improved capture technologies, long-read sequencing, and advanced computational methods promises to further minimize problematic regions and maximize the clinical utility of whole exome sequencing in cancer research.
In the field of cancer research, Whole Exome Sequencing (WES) has emerged as a powerful, cost-effective method for analyzing the protein-coding regions of the genome, where an estimated 85% of disease-causing mutations reside [83]. The technique sequences all exonic regions, which constitute approximately 1-2% of the human genome, enabling researchers to focus on functionally relevant areas with high sequencing depth without the substantial financial burden of Whole Genome Sequencing (WGS) [38]. However, the accessibility of WES technology has created a significant downstream challenge: the bioinformatics bottleneck. This bottleneck encompasses the complex, computationally intensive processes required to transform raw sequencing data into biologically interpretable and clinically actionable insights.
The core of this bottleneck lies in the multi-step analytical workflow, where massive datasets must be processed, filtered, and analyzed using a diverse array of computational tools and algorithms. For cancer research, this challenge is further compounded by the need to distinguish somatic (tumor-acquired) mutations from germline (inherited) variants, analyze intratumor heterogeneity, and identify driver mutations amidst passenger mutations [2] [84]. The absence of a standardized bioinformatics pipeline and the rapid evolution of computational tools create a landscape where researchers must make informed decisions about methodologies without clear consensus, often leading to inefficiencies and reproducibility challenges across studies [2] [85].
Deconstructing the WES Bioinformatics Workflow
The journey from raw sequencing data to biological interpretation follows a structured pathway with distinct stages, each presenting unique computational challenges and requiring specialized tools. Understanding this workflow is essential for identifying optimization opportunities.
Primary Data Processing and Alignment
The initial stage involves processing the raw sequencing reads (typically in FASTQ format) to ensure data quality and align them to a reference genome. This foundational step influences all subsequent analyses.
- Quality Control and Trimming: Tools like FastQC perform initial quality checks, while utilities such as Trimmomatic or Cutadapt remove low-quality bases, adapter sequences, and PCR artifacts that could interfere with alignment and variant calling [83].
- Sequence Alignment: The processed reads are aligned to a reference genome (e.g., GRCh38) using aligners like the Burrows-Wheeler Aligner (BWA) [85] [84]. BWA-MEM is typically used for longer reads (≥70 bp), while BWA-aln is applied to shorter reads [85]. This step produces Sequence Alignment/Map (BAM) files.
- Post-Alignment Processing: The aligned BAM files undergo several refinement steps. PCR duplicates are flagged or removed using tools like Picard MarkDuplicates to prevent artificial inflation of variant calls [85]. Base Quality Score Recalibration (BQSR) and local indel realignment are then performed using the Genome Analysis Toolkit (GATK) to correct systematic errors and improve alignment accuracy around insertion-deletion regions [85].
The following diagram illustrates the core data processing workflow:
Somatic Variant Detection and Annotation
With clean BAM files, the focus shifts to identifying genetic variants specific to tumor tissue by comparing them with matched normal samples.
- Variant Calling: Multiple calling algorithms are typically employed in parallel, as no single method captures all valid mutations with perfect accuracy [85]. Common somatic callers include:
- MuTect2: Part of GATK, particularly effective for identifying single nucleotide variants (SNVs) with low allele fractions [2] [85].
- VarScan2: A versatile tool that detects both SNVs and indels, often used in combination with other callers [2].
- MuSE: Employed in large-scale projects like The Cancer Genome Atlas (TCGA) for its robust statistical modeling [86].
- Pindel: Specialized for detecting indels and structural variants using a pattern growth approach [85].
- Variant Annotation: Identified variants are annotated using tools like ANNOVAR or GATK's Funcotator to determine their functional impact [83] [84]. This process includes predicting effects on protein function, recording population frequencies from databases like gnomAD, and cross-referencing with cancer-specific databases such as COSMIC [84].
Table 1: Common Somatic Variant Callers in Cancer WES
| Tool | Primary Function | Strengths | Considerations |
|---|---|---|---|
| MuTect2 [2] [85] | SNV calling | High sensitivity for low-frequency variants; uses Panel of Normals | Less effective for indel detection |
| VarScan2 [2] | SNV and indel calling | Identifies high-quality variants; good for heterogeneous samples | Performance varies with coverage depth |
| Strelka [2] | SNV and indel calling | High specificity; performs well with high-coverage data | Computationally intensive |
| Pindel [85] | Indel and structural variant calling | Detects complex variants missed by other methods | Limited to larger indels |
Advanced Analysis and Interpretation
The final stage transforms annotated variants into biological insights through sophisticated analytical approaches.
- Variant Prioritization: In cancer studies, the vast number of detected variants (tens of thousands per sample) must be filtered to identify clinically relevant mutations [87]. Prioritization typically focuses on protein-altering variants (nonsense, missense, splice-site), known cancer driver genes, and rare variants absent from population databases [87].
- Copy Number Variation (CNV) Analysis: Tools like CNVkit analyze depth-of-coverage data to identify genomic amplifications and deletions, which are crucial in cancer pathogenesis [84].
- Intratumor Heterogeneity (ITH) and Clonal Analysis: Multi-region sequencing reveals ITH, where different tumor regions contain distinct private mutations alongside shared trunk mutations [84]. Tools like PyClone and ABSOLUTE help reconstruct subclonal architecture and evolutionary history by estimating cancer cell fractions [84].
- Pathway and Signature Analysis: Mutational signature analysis (e.g., using Mutalisk) identifies patterns of mutations reflecting underlying biological processes like DNA repair defects or carcinogen exposure [84]. Pathway analysis tools then map these mutations to affected signaling pathways.
Experimental Protocols: A Case Study in Multi-Region WES
To illustrate a comprehensive WES application, we examine a protocol from a recent study investigating Opisthorchis viverrini-associated cholangiocarcinoma (CCA), which exemplifies the sophisticated methodologies required for analyzing tumor heterogeneity [84].
Sample Preparation and Library Construction
- Sample Collection: The study collected 52 tumor samples from 13 patients, with 4 tumor regions and 1 adjacent normal tissue per patient to enable comprehensive heterogeneity analysis [84].
- DNA Extraction: Researchers used the QIAamp DNA Mini Kit for DNA extraction from fresh frozen tissues, with quality assessment via Nanodrop (A260/280 ratios) and quantification using Qubit 3.0 with dsDNA HS Assay Kit to ensure accurate DNA concentration measurements [84].
- Library Preparation: The Agilent SureSelect Human All Exon V6 kit was employed for exome capture, requiring 100-500 ng of input DNA depending on the specific kit used [84] [38]. This was followed by sequencing on the Illumina NovaSeq 6000 platform with 150bp paired-end reads [84].
Table 2: Common Target Enrichment Kits for WES
| Kit | Target Region | Input DNA | Capture Technology |
|---|---|---|---|
| Agilent SureSelect XT2 V6 [38] | 60 Mb | 100 ng | Liquid-phase hybridization |
| Illumina Nextera Rapid Capture [38] | 62 Mb | 50 ng | Transposase-based |
| Roche Nimblegen SeqCap EZ v3.0 [38] | 64 Mb | 1 μg | Liquid-phase hybridization |
Bioinformatics Analysis Pipeline
The CCA study implemented a specific analytical workflow:
- Alignment: Raw sequencing reads were aligned to the GRCh38 reference genome using BWA-MEM [84].
- Variant Calling: Somatic variants were identified using Mutect2 from GATK (version 4.1.2) with matched normal samples, followed by FilterMutectCalls to remove false positives [84].
- Filtering: Additional filtering required variant allele frequency (VAF) > 0.1 to ensure confident mutation calls [84].
- CNV Analysis: CNVkit was used to identify copy number alterations, with significant regions determined using GISTIC2.0 [84].
- Clonal Analysis: The ABSOLUTE tool estimated cancer cell fractions, and PyClone-Vi inferred subclonal architecture and evolutionary relationships [84].
The following workflow summarizes this comprehensive analysis:
Successful WES analysis in cancer research requires both wet-lab reagents and computational resources.
Table 3: Essential Research Reagents and Computational Tools for Cancer WES
| Category | Item | Function | Examples/Notes |
|---|---|---|---|
| Wet-Lab Reagents | Nucleic Acid Extraction Kit | Isolates high-quality DNA from various sample types | QIAamp DNA Mini Kit; critical for FFPE samples [84] [87] |
| Exome Capture Kit | Enriches exonic regions from fragmented DNA | Agilent SureSelect, Illumina Nextera Rapid Capture [38] | |
| Library Preparation Kit | Prepares sequencing libraries with adapters | Kits specific to platform (Illumina, Ion Torrent) [87] | |
| Computational Tools | Alignment Tool | Maps sequencing reads to reference genome | BWA-MEM for reads ≥70bp [85] [84] |
| Variant Caller | Identifies somatic mutations | MuTect2, VarScan2; using multiple callers recommended [2] [85] | |
| Annotation Tool | Adds functional information to variants | ANNOVAR, Funcotator [83] [84] | |
| CNV Detection | Identifies copy number alterations | CNVkit [84] |
Streamlining Strategies and Future Directions
Addressing the bioinformatics bottleneck requires systematic approaches to streamline workflows and enhance computational efficiency.
Pipeline Optimization and Integration
- Workflow Management Systems: Platforms like Nextflow enable efficient parallelization and built-in dependency management, facilitating reproducible analyses across computing environments [88].
- Integrated Analysis Platforms: User-friendly platforms such as Galaxy provide graphical interfaces for WES data processing, making sophisticated analyses accessible to researchers without extensive computational expertise [2].
- Tool Selection Strategy: Based on performance benchmarks, employing complementary tools maximizes detection sensitivity. For instance, VarScan excels at identifying high-quality SNVs, while MuTect2 performs better for low-frequency variants [2].
Clinical Translation and Validation
As WES matures, its implementation in clinical settings requires careful validation and consideration of economic factors. Recent studies demonstrate that WES-based comprehensive genomic profiling can reduce healthcare costs while improving outcomes in advanced non-small cell lung cancer by better identifying patients eligible for targeted therapies [14]. The integration of RNA sequencing with WES further enhances fusion detection and increases the identification of actionable alterations by 2.3-13.0% [14].
Emerging Technologies and Methodologies
- Hybrid De Novo Assembly: Combining long-read and short-read sequencing data improves genome assembly completeness and accuracy, with tools like Flye demonstrating superior performance when combined with error correction [88].
- Standardized Pipelines: Efforts like the GDC DNA-Seq pipeline provide standardized workflows for somatic variant calling, incorporating multiple callers (MuTect2, MuSE, VarScan2, Pindel) to ensure comprehensive variant detection [85].
- Machine Learning Approaches: Emerging tools apply machine learning to improve variant filtering and prioritization, enhancing the specificity of mutation calls and biological interpretation [2].
In the realm of cancer research, Whole Exome Sequencing (WES) has emerged as a powerful methodology for identifying genetic variants across the protein-coding regions of the genome, which harbor approximately 85% of known disease-causing mutations [89]. The reliability of WES data, however, is fundamentally dependent on rigorous quality control (QC) procedures implemented throughout the sequencing workflow. For researchers and drug development professionals, understanding and monitoring QC metrics is not merely a technical formality but a critical practice that ensures the analytical validity of genomic findings and subsequent clinical interpretations [90]. In cancer studies, where tumor heterogeneity, low tumor purity, and complex mutation patterns are common, stringent QC becomes even more essential to distinguish true somatic variants from technical artifacts and to generate clinically actionable insights.
Quality control in WES is not a single checkpoint but a continuous process that spans multiple stages of the workflow. Proper QC serves as the foundation for precision oncology, enabling the detection of driver mutations, biomarkers for targeted therapy, and markers of immunotherapy response such as tumor mutational burden (TMB) and microsatellite instability (MSI) [2] [91]. Failures in library preparation or sequencing can introduce biases that compromise these critical applications, leading to false positives or negatives that may ultimately impact patient care decisions in translational research settings. This guide provides a comprehensive technical framework for implementing robust QC protocols throughout the WES workflow, with a specific focus on applications in cancer research.
Multi-Stage QC Framework for WES
Quality control for DNA sequencing data must be conducted at three major stages: raw data, alignment, and variant detection [90]. This multi-stage approach allows for early detection of issues and ensures that only high-quality data progresses through the analytical pipeline. The following diagram illustrates the comprehensive, multi-stage QC framework essential for robust Whole Exome Sequencing in cancer research.
Stage 1: Pre-Sequencing Sample and Library QC
Before sequencing begins, assessing the quality of input DNA and prepared libraries is crucial, especially for cancer samples which often derive from formalin-fixed paraffin-embedded (FFPE) tissue with inherent DNA degradation [2]. DNA QC evaluates the quantity, purity, and integrity of genomic DNA. For WES, a common requirement is a minimum of 50-200 ng of input DNA, though some protocols can work with lower inputs [92]. Purity is typically assessed using A260/A280 ratios (ideal range: 1.8-2.0) and A260/230 ratios (ideal range: 2.0-2.2) via spectrophotometric methods like NanoDrop. Significant deviations may indicate contamination from proteins, organic compounds, or salts that can inhibit library preparation enzymes [92].
DNA integrity is equally critical, particularly for FFPE-derived samples common in cancer research. Gel electrophoresis or automated systems like the Agilent TapeStation provide visual confirmation of high-molecular-weight DNA. Intact genomic DNA should appear as a tight, high-molecular-weight band, while degraded DNA shows a smear toward lower molecular weights [92]. For FFPE samples, the DNA Integrity Number (DIN) or DV200 (percentage of fragments >200 bp) are quantitative metrics of degradation, with DV200 >70% considered high quality and DV200 >30% often being the minimum threshold for proceeding with library preparation [93].
Following DNA QC, library QC ensures that fragmentation and adapter ligation have been successful. Libraries are checked for appropriate fragment size distribution (typically 300-500 bp for WES) and concentration using automated electrophoresis systems [92]. The example below shows specific pass/fail criteria for library QC.
Table 1: Library QC Pass/Fail Criteria
| Parameter | Pass Criteria | Fail Criteria | Clinical Impact in Cancer Research |
|---|---|---|---|
| Library Concentration | ≥ 50 ng/μL | < 50 ng/μL | Insufficient sequencing coverage for variant detection |
| Library Fragment Size | 350 - 430 bp | <350 or >430 bp | Inefficient exome capture; skewed coverage |
| Adapter Ligation | >90% of fragments with adapters | <90% adapter ligation | Poor cluster generation on flow cell |
Stage 2: Raw Data QC
After sequencing, raw data in FASTQ format undergoes comprehensive QC to identify issues related to sequencing chemistry, instrumentation, or sample quality. The Phred quality score (Q-score) is a fundamental metric representing the probability of an incorrect base call, with Q30 indicating a 1 in 1,000 error probability and Q30 ≥ 80% commonly targeted [93] [90]. Modern Illumina pipelines use the Phred+33 encoding scale, and misidentification of this scale can lead to erroneous quality assessment [90].
Several additional parameters must be evaluated at this stage. Nucleotide distribution across sequencing cycles should be relatively stable, with significant fluctuations potentially indicating contamination or sequencing artifacts. GC content should align with species-specific expectations (typically ~40% for human), with deviations >10% suggesting possible contamination. The presence of overrepresented sequences may indicate adapter contamination or PCR bias, while sequence duplication levels help identify over-amplified libraries [89] [90].
Tools such as FastQC, FastQ Screen, and NGS QC Toolkit are commonly employed for raw data QC. The QC3 tool offers the unique capability of separating low-quality reads (flagged by Illumina's filter) from high-quality reads, providing a more nuanced assessment [90]. For paired-end sequencing, QC3 can calculate Pearson's correlation and Euclidean distance between the base quality scores of read pairs, with significant differences indicating quality issues, often observed in the second read due to phasing/pre-phasing effects or template damage [90].
Stage 3: Alignment QC
Following alignment to a reference genome (e.g., using BWA or Bowtie2), QC metrics evaluate mapping efficiency and coverage distribution—particularly critical for cancer WES where copy number variations (CNVs) and loss of heterozygosity (LOH) are important biomarkers [2]. The resulting BAM files are assessed for parameters including the percentage of uniquely mapped reads (typically >85-90%), duplicate reads (indicating PCR over-amplification), and reads mapped to target regions [89] [90].
Capture efficiency is a paramount metric for WES, calculated as the percentage of reads mapping to the exome capture regions. This efficiency depends on the capture kit used (e.g., Illumina TrueSeq, Agilent SureSelect, NimbleGen SeqCap EZ), with typical values ranging between 40-70% [90]. Lower values may indicate issues with library complexity, probe hybridization, or post-capture washing stringency. Depth of coverage is another vital consideration, with mean coverage of ≥100x often recommended for somatic mutation detection in cancer, though higher depths (≥500x) may be needed for subclonal variant detection [2].
Coverage uniformity across target regions must also be assessed, as uneven coverage can lead to gaps in variant detection. Tools like QC3 and Picard calculate metrics such as the percentage of target bases covered at ≥10x, ≥20x, and ≥30x thresholds. For cancer research, it's important to note that reads aligning to intronic and intergenic regions can still provide valuable information and should not be automatically discarded [90]. Mitochondrial genome sequences can also be extracted from WES data, providing additional insights [90].
Stage 4: Variant Calling QC
The final QC stage focuses on variant calls, serving as the last opportunity to identify samples with quality issues that passed earlier checks and to reduce false positives. The transition/transversion (Ti/Tv) ratio is a well-established QC parameter, computed as the number of transition SNPs (AG, CT) divided by transversion SNPs (purinepyrimidine) [90]. The expected Ti/Tv ratio varies by genomic region, with approximately 2.0-2.1 for whole exome data and deviations from this range potentially indicating technical artifacts.
The heterozygosity to non-reference homozygosity ratio provides another quality indicator, with significant deviations from expected patterns potentially suggesting sample contamination or poor DNA quality. For cancer WES, additional considerations include the tumor mutation burden (TMB) and the percentage of dbSNP variants in known databases, which should align with expectations for the sample type [2] [94].
For cancer research employing WES, it is essential to distinguish between germline and somatic variants. Germline variants typically show allele frequencies close to 50% (heterozygous) or 100% (homozygous), while somatic variants from tumor samples often exhibit a range of variant allele frequencies (VAFs) due to tumor purity, ploidy, and subclonality [2]. Unexpected VAF distributions may indicate normal tissue contamination or other sample issues.
Essential QC Metrics and Thresholds for Cancer WES
The following table summarizes critical quality control metrics, their thresholds, and associated tools for each stage of the WES workflow in cancer research.
Table 2: Comprehensive QC Metrics for WES in Cancer Research
| QC Stage | Key Metric | Ideal Threshold/Pattern | Common Tools | Impact on Cancer Data |
|---|---|---|---|---|
| Sample & Library | DNA Quantity | ≥50 ng | Qubit, NanoDrop | Insufficient DNA increases duplication rates |
| DNA Integrity (DV200) | >30% (FFPE), >70% (fresh) | TapeStation, Bioanalyzer | Degradation causes 3' bias & coverage gaps | |
| Library Size | 350-430 bp | Electrophoresis | Deviations reduce capture efficiency | |
| Raw Data | Q30 Score | ≥80% | FastQC, QC3 | Low scores increase false variant calls |
| GC Content | ~40% (human) | FastQC, QC3 | Deviations suggest contamination | |
| Read Duplication | <20% (varies by source) | FastQC, QC3 | High levels indicate low complexity libraries | |
| Alignment | Uniquely Mapped Reads | >85% | SAMstat, QC3, Picard | Low mapping increases false negatives |
| Capture Efficiency | 40-70% | QC3, Picard | Kit-dependent; low efficiency wastes sequencing | |
| Mean Coverage Depth | ≥100x (somatic), ≥500x (subclonal) | Mosdepth, BedTools | Inadequate depth misses low VAF variants | |
| Uniformity (% bases ≥20x) | >90% | GATK, Picard | Uneven coverage creates detection gaps | |
| Variant Calling | Ti/Tv Ratio | 2.0-2.1 (exome) | QC3, GATK, VCFtools | Deviations indicate technical artifacts |
| Heterozygosity Ratio | Sample-specific patterns | QC3, VCFtools | Abnormal ratios suggest contamination |
Experimental Protocols for Key QC Experiments
Protocol: DNA and Library Quality Assessment
Objective: To assess the quality and quantity of genomic DNA from tumor samples and ensure prepared libraries meet specifications for WES.
Materials and Reagents:
- Qubit dsDNA HS Assay Kit or similar fluorescent-based quantification method
- Agilent TapeStation or Bioanalyzer with High Sensitivity DNA reagents
- NanoDrop spectrophotometer for rapid purity assessment
- Illumina-compatible library preparation kit (e.g., Illumina TruSeq DNA PCR-Free)
- Exome capture probes (e.g., Agilent SureSelect, Illumina Nextera)
Procedure:
- DNA Quantification: Quantify extracted DNA using both fluorometric (Qubit) and spectrophotometric (NanoDrop) methods. Compare results to ensure consistency.
- Purity Assessment: Calculate A260/A280 and A260/230 ratios. Proceed only if ratios fall within 1.8-2.0 and 2.0-2.2, respectively.
- Integrity Analysis: Run 50-100 ng DNA on TapeStation/Bioanalyzer. For FFPE samples, calculate DV200 (% of fragments >200 bp).
- Library Preparation: Fragment 100-200 ng DNA to 300-500 bp using Covaris or similar sonication device. Perform end repair, A-tailing, and adapter ligation following kit instructions.
- Library QC: Assess final library concentration using Qubit and fragment size distribution using TapeStation. Verify absence of adapter dimer peaks.
Troubleshooting: For degraded FFPE samples (DV200 30-70%), consider using specialized FFPE repair enzymes and increasing PCR cycles during library amplification. For low DNA input (<50 ng), use library kits specifically designed for low-input workflows [93].
Protocol: Comprehensive Three-Stage QC Using QC3
Objective: To perform integrated quality control across raw data, alignment, and variant calling stages using the QC3 tool.
Materials:
- FASTQ files from sequencer
- BAM files after alignment with BWA or similar aligner
- VCF files from variant caller (e.g., GATK, VarScan2)
- Reference genome (e.g., GRCh38) and target regions BED file
Procedure:
- Raw Data QC:
- Run QC3 on FASTQ files:
qc3 --stage raw --fastq sample_R1.fastq.gz --fastq2 sample_R2.fastq.gz - Examine base quality distribution by cycle plot for degradation signs
- Check nucleotide distribution stability across cycles
- Review GC content and compare to expected species-specific distribution
- Run QC3 on FASTQ files:
Alignment QC:
- Run QC3 on BAM file:
qc3 --stage align --bam sample.bam --bed target_regions.bed - Calculate capture efficiency: (reads aligned to target / total reads) × 100
- Assess mapping quality distribution and insert size metrics
- Evaluate on-target vs. off-target rates and mitochondrial DNA alignment
- Run QC3 on BAM file:
Variant Calling QC:
- Run QC3 on VCF file:
qc3 --stage vcf --vcf sample.vcf --bam sample.bam - Calculate Ti/Tv ratio and compare to expected range (2.0-2.1 for exomes)
- Assess heterozygosity to non-reference homozygosity ratio
- For tumor-normal pairs, evaluate somatic variant allele frequency distribution
- Run QC3 on VCF file:
Interpretation: QC3 provides both graphic and tabulated reports. Samples failing at any stage should be investigated before proceeding. Batch effects can be detected by comparing metrics across multiple samples sequenced together [90].
Research Reagent Solutions for WES QC
Successful implementation of WES QC requires specific reagents and tools. The following table outlines essential solutions for maintaining quality throughout the workflow.
Table 3: Essential Research Reagents for WES Quality Control
| Reagent/Tool | Specific Function | Application in QC | Example Products |
|---|---|---|---|
| DNA QC Kits | Quantification and purity assessment | Verify input DNA quality before library prep | Qubit dsDNA HS Assay, NanoDrop |
| Fragment Analyzers | Size distribution analysis | Assess DNA integrity and library fragment size | Agilent TapeStation, Bioanalyzer |
| Library Prep Kits | Fragment end repair, A-tailing, adapter ligation | Prepare sequencing libraries with minimal bias | Illumina TruSeq DNA, KAPA HyperPrep |
| Exome Capture Panels | Enrichment of exonic regions | Target protein-coding regions for WES | Agilent SureSelect, Illumina Nextera |
| QC Analysis Tools | Multi-stage metric calculation | Comprehensive quality assessment | QC3, FastQC, Picard, GATK |
| Variant Callers | SNP/Indel/CNV detection | Identify genomic alterations in cancer samples | GATK, VarScan2, Strelka, MuTect2 |
Quality control metrics serve as indispensable indicators for assessing both library preparation and sequencing success in Whole Exome Sequencing for cancer research. Implementing a comprehensive, multi-stage QC framework—encompassing sample, raw data, alignment, and variant calling stages—ensures the generation of reliable, interpretable genomic data. As WES continues to evolve as a cornerstone of precision oncology, with applications in tumor mutational burden assessment, microsatellite instability detection, and therapeutic target identification [2] [94] [91], rigorous QC practices will remain fundamental to producing clinically relevant insights. The protocols and metrics outlined in this technical guide provide researchers and drug development professionals with a standardized approach to quality assurance, ultimately supporting the advancement of molecularly driven cancer care.
In the precision-driven field of cancer research, the accurate detection of somatic variants from whole exome sequencing (WES) data is a cornerstone for understanding tumor biology, identifying therapeutic targets, and stratifying patients. However, this process is critically hampered by the pervasive challenge of false positive variant calls. These artifacts—genomic positions incorrectly identified as harboring a mutation—can misdirect research, lead to incorrect biological conclusions, and potentially compromise clinical decisions. False positives often arise from a complex interplay of technical and biological factors, including sequencing errors, mapping artifacts, and the inherent complexity of the cancer genome itself [95] [96]. One investigative study starkly highlighted this problem, reporting a false positive rate approaching 100% in the complex MUC3A gene in esophageal squamous cell carcinoma, where all computationally predicted mutations failed laboratory validation [97]. This technical guide, framed within a broader thesis on the fundamentals of WES in cancer research, outlines evidence-based strategies and best practices for researchers and drug development professionals to enhance the specificity and accuracy of their variant calling workflows.
A systematic understanding of error sources is the first step toward mitigation. The following table summarizes the primary contributors to false positives and the corresponding strategic countermeasures.
Table 1: Major Sources of False Positives and Corresponding Mitigation Strategies
| Error Source | Impact on Specificity | Recommended Mitigation Strategy |
|---|---|---|
| Mapping Artifacts (e.g., in complex, repetitive, or homologous regions) | High. Li (2016) attributed all false variants between biological replicates to mapping artifacts [95]. | Use of optimized aligners (e.g., BWA-MEM); manual inspection in IGV for challenging regions [95] [98]. |
| Sequencing Artifacts (e.g., from oxidative DNA damage during library prep) | Moderate to High. Causes specific error signatures like G>T/C>A transversions [96]. | Monitor Global Imbalance Score (GIV); optimize DNA shearing to avoid very short fragments; use of PCR-free WGS for FFPE samples [96]. |
| Tumor-Normal Contamination | High. Normal contamination in tumor sample dilutes somatic VAFs, confusing germline/somatic status. | Assess tumor purity; use bioinformatics tools that model contamination [95]. |
| Inherent Gene Complexity (e.g., high GC-content, repetitive structure) | Variable, can be extreme. MUC3A study showed 100% false positive rate despite multiple callers [97]. | Mandatory laboratory validation (e.g., orthogonal sequencing) for variants in known complex genes [97]. |
| Suboptimal Bioinformatics Pipeline | High. Performance varies substantially between tools and pipeline configurations [95] [96]. | Adopt multi-caller consensus approaches; use validated, reproducible pipelines; continuous benchmarking [95] [99]. |
Technical Approaches for Enhanced Specificity
Robust Bioinformatics Pipelines and Multi-Caller Consensus
The choice of variant calling software and analysis pipeline is a critical determinant of accuracy. Studies have consistently shown that no single variant caller is optimal across all scenarios, and their performance can differ significantly, especially for low-frequency variants common in heterogeneous cancer samples [95] [96].
A powerful strategy to overcome the limitations of individual tools is to leverage the consensus of multiple, well-performing callers. Research has demonstrated that a rank-combination strategy integrating calls from tools like deepSNV, JointSNVMix2, MuTect, SiNVICT, and VarScan2 can significantly outperform any single tool. In one simulation study, this integrated approach reached a sensitivity of 78% with a fixed precision of 90%, compared to a maximum sensitivity of 71% from the best individual caller [95]. This method effectively cross-validates calls, reducing the likelihood of artifacts unique to a single algorithm being reported.
Furthermore, ongoing benchmarking is essential. Independent evaluations, such as those using the Genome in a Bottle (GIAB) gold standard datasets, provide critical performance data. A 2025 benchmarking study found that Illumina's DRAGEN Enrichment achieved over 99% precision for SNVs and 96% for indels, highlighting the advanced state of some commercial solutions [100]. The PrecisionFDA Truth Challenge V2 also revealed that graph-based and machine learning methods were top performers for short-read and long-read data, respectively [99].
Leveraging Gold Standard Datasets and Panel of Normals (PON)
Systematic benchmarking against a known truth set is indispensable for optimizing and validating any variant calling pipeline. The GIAB consortium provides high-confidence reference genomes that can be used as a gold standard to quantify the accuracy (precision and recall) of a pipeline [100] [99].
A Panel of Normals (PON) is a bespoke but highly effective filter for removing site-specific artifacts common to a specific laboratory or sequencing protocol. A PON is created by collectively calling variants across a set of normal samples (e.g., from the same tissue type or processed with the same lab protocol). Any variant that appears in this panel is considered a systemic artifact and is filtered out from subsequent tumor analyses. The study on MUC3A demonstrated that while a PON can reduce false positives, it may be insufficient alone for genes with extreme complexity, underscoring the need for complementary validation [97].
Wet-Lab Best Practices and DNA Quality Control
The accuracy of computational analysis is fundamentally constrained by the quality of the input DNA and the sequencing library. Several best practices have been identified through systematic, multi-center studies:
- Minimize DNA Damage During Fragmentation: Oxidative damage during acoustic shearing for WES can cause a specific artifact (G>T/C>A). This is inversely correlated with insert fragment size. To mitigate this, ensure insert sizes are greater than 200 base pairs, which has been shown to effectively eliminate this imbalance [96].
- Library Preparation Selection: For low-input DNA, the choice of library kit matters. One study found that the Nextera Flex protocol outperformed TruSeq-Nano for 1 ng inputs, producing a higher percentage of non-redundant reads [96].
- Special Consideration for FFPE Samples: Formalin-fixed, paraffin-embedded (FFPE) samples are prone to additional DNA damage. The GIV score is a useful indicator of this damage. Evidence suggests that whole-genome sequencing (WGS) is more suitable than WES for FFPE samples due to its robustness to these artifacts [96].
Detailed Experimental Protocols
Protocol: Implementing a Multi-Caller Consensus Approach
This protocol is adapted from the methodology that demonstrated superior performance through rank-combination [95].
- Data Input: Begin with aligned BAM files for the tumor-normal pair, processed through standard pre-processing steps (duplicate marking, base quality score recalibration).
- Parallel Variant Calling: Run the following variant callers (or a similar selection) on the same tumor-normal BAM pair using default or optimally tuned parameters:
- Variant Annotation: Annotate each resulting VCF file with a confidence score (e.g., somatic score, probability score) provided by the caller.
- Rank-Combination Integration:
- For each variant caller, generate a ranked list of candidate variants based on their confidence scores.
- A novel rank-combination method is then applied to these lists. The specific mathematical integration can vary, but the goal is to create a unified, high-confidence call set that prioritizes variants ranked highly by multiple callers.
- The implementation for this rank-combination strategy is available in R from the cited study [95].
- Filtering and Finalization: Apply standard hard filters (e.g., on depth, allele frequency) and a Panel of Normals (PON) to the consensus call set to generate the final list of somatic variants.
The following workflow diagram illustrates this multi-caller consensus process.
Protocol: Orthogonal Validation of Variants in Complex Genomic Regions
Given the extreme risk of false positives in complex genomic regions, the following validation protocol is recommended, based on the findings of [97].
- Identify High-Risk Variants: After initial bioinformatic calling, flag all variants located in genes known for high complexity (e.g., high GC-content, repetitive elements, segmental duplications). The MUC3A gene serves as a prime example [97].
- Primer Design: Design PCR primers flanking the genomic coordinates of each candidate variant. Ensure the amplicon is unique and specifically targets the region of interest.
- Orthogonal Sequencing: Perform targeted, high-depth amplicon sequencing using a technology independent of the discovery platform (e.g., Sanger sequencing or a different NGS chemistry).
- Data Analysis: Analyze the validation sequencing data with a separate, standard bioinformatics pipeline or via manual review.
- Result Interpretation: A true positive is confirmed only if the variant is unambiguously called by the orthogonal method. The study cautions that variants failing this validation should be reported as computational artifacts, not biological findings [97].
Table 2: Key Research Reagents and Resources for Accurate Variant Calling
| Tool / Resource | Function / Application | Relevance to Minimizing False Positives |
|---|---|---|
| GIAB Reference Materials | Gold-standard human genomes with high-confidence variant calls. | Provides a ground truth for benchmarking and optimizing pipeline precision and recall [100] [99]. |
| Panel of Normals (PON) | A database of artifacts common to a specific lab's workflow. | Filters out recurring, non-biological artifacts that would otherwise appear as false positives in tumor samples [97]. |
| BWA-MEM Aligner | Aligns sequencing reads to a reference genome. | A widely used, robust aligner that minimizes mapping errors, a primary source of false positives [98] [96]. |
| GATK (Mutect2) | A widely adopted somatic variant caller. | One of the core tools in a multi-caller consensus approach; benefits from continuous development and community best practices [95] [96]. |
| Integrative Genomics Viewer (IGV) | A high-performance visualization tool for genomic data. | Enables manual inspection of aligned reads at candidate variant sites to visually confirm or reject calls [98]. |
| dbSNP Database | A public repository of known germline polymorphisms. | Used to filter out common germline variants from somatic candidate lists [101]. |
Minimizing false positives in whole exome sequencing is not a single-step fix but a holistic process that spans experimental design, wet-lab practices, and rigorous bioinformatics analysis. The convergence of evidence shows that a multi-faceted strategy is essential: combining multiple, well-chosen variant callers; diligently applying artifact filters like a PON; rigorously benchmarking pipelines against gold standards; and mandating orthogonal validation for variants in biologically or technically challenging regions. As sequencing technologies and analytical methods continue to evolve—with machine learning and graph-based genomes showing great promise [99]—the fundamental principle remains: a critical, evidence-based approach is the key to unlocking the true potential of cancer genomics for research and drug development.
Validating WES: Clinical Utility and Comparative Performance Analysis
In the field of cancer research, whole-exome sequencing (WES) has emerged as a powerful tool for discovering and diagnosing genetic disorders. However, the transformative potential of WES depends entirely on the accuracy and reliability of its results. High-throughput sequencing remains inherently error-prone, necessitating rigorous validation protocols and orthogonal confirmation to meet the exacting demands of clinical diagnostic sequencing. For researchers and drug development professionals, establishing robust validation frameworks is not merely a procedural formality but a fundamental requirement for generating clinically actionable data. The American College of Medical Genetics (ACMG) practice guidelines explicitly recommend that orthogonal or companion technologies should be used to ensure variant calls are independently confirmed and thus accurate [102]. This guide examines the critical components of validation studies and orthogonal confirmation specifically within the context of WES applications in cancer research, providing technical frameworks essential for demonstrating diagnostic yield.
Core Principles of Analytical Validation
Defining Analytical Performance Metrics
The analytical validation of WES tests requires careful consideration of performance metrics that account for genome complexity, with special attention to sequence content and variant type. According to consensus recommendations from leading healthcare and research organizations, the analytical framework should utilize Global Alliance for Genomics and Health (GA4GH) and Food and Drug Administration (FDA) recommendations for sensitivity or Positive Percent Agreement (PPA) and precision or Positive Predictive Value (PPV), with reporting of the lower bound of the 95% confidence interval when truth sets are available [103]. These metrics form the statistical foundation for validating WES tests in cancer research applications.
For clinical WES, test performance should meet or exceed that of any tests it is replacing. Current evidence suggests WES is analytically sufficient to replace many conventional tests, but laboratories must clearly define and validate which variant types will be reported. The validation should encompass single nucleotide variants (SNVs), insertions and deletions (indels), and copy number variants (CNVs) at a minimum, with clear documentation of any established gaps in performance compared to current gold standard tests [103]. This comprehensive approach ensures researchers can trust the variant data generated from their cancer genomics studies.
Test Development and Design Considerations
Effective WES validation begins with careful test development and design. Laboratories must define and evaluate high-quality genome coverage and "callability" - the portions of the genome where variant calls can be made reliably. Metrics that measure genome completeness should be used to define WES performance, including overall depth and evenness of coverage. These should be monitored with respect to callable regions of the genome and the related calling accuracy for each variant type compared to orthogonally investigated truth sets [103]. The assessment of callable regions should incorporate depth of coverage, base quality, and mapping quality to establish reliable variant calling intervals.
The choice of reference standards and positive controls represents another critical consideration for WES validation. Reference standards are particularly useful for evaluating calling accuracy across variant type, size, and location. Analytical validation should include publicly available reference standards (e.g., NIST Genome in a Bottle) in addition to commercially available and laboratory-held positive controls for each variant type [103]. However, reference standards alone are insufficient for complete validation; laboratory-held positive controls derived from the same specimen type used in routine testing should also be incorporated to ensure real-world performance validation.
Table 1: Key Analytical Performance Metrics for WES Validation
| Performance Metric | Target Threshold | Application in WES | Calculation Method |
|---|---|---|---|
| Sensitivity (PPA) | >99% for SNVs >95% for indels | Ability to detect true positive variants | True Positives / (True Positives + False Negatives) |
| Positive Predictive Value (PPV) | >99% for SNVs >96% for indels | Proportion of true variants among all calls | True Positives / (True Positives + False Positives) |
| Specificity | >99.9% | Ability to identify true negatives | True Negatives / (True Negatives + False Positives) |
| Coverage Uniformity | >80% at 20x coverage | Evenness of sequencing coverage across target | Percentage of target bases with ≥20x read depth |
Orthogonal Confirmation Strategies
Dual-Platform Sequencing Approaches
Orthogonal confirmation using complementary sequencing technologies represents a powerful strategy for improving variant calling accuracy at genomic scales. Research demonstrates that a dual-platform approach employing complementary target capture and sequencing chemistries can significantly improve the speed and accuracy of variant calls. One effective implementation combines DNA selection by bait-based hybridization followed by Illumina reversible terminator sequencing with DNA selection by amplification followed by Ion Proton semiconductor sequencing [102]. This methodology yields orthogonal confirmation of approximately 95% of exome variants while improving overall variant sensitivity as each method covers thousands of coding exons missed by the other.
The technical basis for this approach lies in the complementary strengths of different sequencing platforms. Illumina systems typically achieve higher sensitivity for SNVs (99.6%) and indels (95.0%), while semiconductor sequencing platforms can provide better coverage in AT-rich regions [102]. This complementary coverage is particularly valuable in cancer research, where comprehensive detection of variants across all genomic contexts is essential for understanding tumor heterogeneity and identifying therapeutic targets. By leveraging multiple technologies, researchers can achieve a more complete picture of the cancer exome while simultaneously validating their findings through platform independence.
Experimental Design for Orthogonal Confirmation
Implementing an effective orthogonal confirmation protocol requires careful experimental design. For the hybridization capture component, DNA is targeted using clinical research exome kits (e.g., Agilent SureSelect Clinical Research Exome) with library preparation performed using standard kits (e.g., QXT library preparation) following manufacturer recommendations [102]. Sequencing can be performed on Illumina platforms (NextSeq or MiSeq) with alignment, cleaning, and variant calling conducted according to GATK best practices. Minimum depth and quality thresholds (e.g., DP > 8 and GQ > 20) are applied to minimize loss of true variants while filtering out false positives.
For the amplification-based component, DNA is targeted using amplification-based exome kits (e.g., Life Technologies AmpliSeq Exome kit) with libraries prepared on systems like the OneTouch and sequenced on semiconductor sequencers (e.g., Ion Proton) with HiQ polymerase [102]. Read alignment, cleaning, and variant calling are performed using platform-specific software (e.g., Torrent Suite) followed by application of custom filters to remove strand-specific errors and recurrent false positives. The combination of variant calls from both platforms using custom algorithms allows for classification of variants based on attributes including whether the variant is a SNP or indel, whether variant call and zygosity match between platforms, and whether the variant site is well-covered in each platform.
Orthogonal WES Confirmation Workflow: This diagram illustrates the dual-platform approach for orthogonal confirmation of WES variants, combining hybridization-based and amplification-based capture methods with different sequencing technologies.
Benefits and Limitations of Orthogonal Approaches
The orthogonal confirmation strategy offers several significant benefits for cancer research applications. Most importantly, it provides genomic-scale orthogonal confirmation for approximately 95% of exome variants while simultaneously improving overall variant sensitivity [102]. This approach also offers better specificity for variants identified on both platforms and greatly reduces the time and expense of Sanger follow-up, enabling researchers and clinicians to act on genomic results more quickly. In cancer research, where both accuracy and speed are critical for patient management and research outcomes, these advantages make orthogonal confirmation particularly valuable.
However, researchers must also consider the limitations and practical challenges of implementing orthogonal confirmation. The approach requires access to multiple sequencing platforms and expertise in different analytical pipelines, which may represent a significant resource investment. Additionally, variant calling for complex variant types such as structural variants and repeat expansions remains challenging even with orthogonal approaches, and these limitations should be clearly documented in research reporting [103]. Despite these challenges, the improved accuracy and comprehensiveness provided by orthogonal confirmation make it a valuable approach for critical cancer research applications where variant accuracy is paramount.
Table 2: Orthogonal Platform Performance Comparison
| Sequencing Platform | SNV Sensitivity | Indel Sensitivity | SNV PPV | Indel PPV | Optimal Application |
|---|---|---|---|---|---|
| Illumina (NextSeq) | 99.6% | 95.0% | ~99.9% | 96.9% | GC-rich regions, comprehensive variant detection |
| Ion Torrent (Proton) | 96.9% | 51.0% | ~99.9% | 92.2% | AT-rich regions, rapid turnaround applications |
| Orthogonal Combination | >99.8% | >95.0% | >99.9% | >96.9% | Clinical-grade variant detection, critical research applications |
Experimental Protocols and Methodologies
Sample Preparation and Quality Control
Robust sample preparation represents the foundation of reliable WES data. For DNA extraction, automated systems (e.g., Autogen FlexStar for blood volumes greater than 2 ml and QiaCube for lower blood volumes and for saliva) provide consistent results [102]. DNA quality should be assessed using multiple metrics including concentration, purity (A260/A280 ratio), and integrity (e.g., genomic quality number). For formalin-fixed paraffin-embedded (FFPE) samples - common in cancer research - additional considerations include fragment size distribution and percentage of fragments >200bp, as FFPE-derived DNA often shows fragmentation that can impact library preparation.
The selection of reference materials is equally critical for validation studies. The reference sample NA12878 from HapMap in conjunction with the gold standard reference call set maintained by NIST provides a well-characterized resource for establishing baseline performance [102]. For cancer-specific applications, commercially available reference standards containing known oncogenic mutations or laboratory-held positive controls with previously characterized variants should be incorporated. These controls enable researchers to verify detection of mutation types particularly relevant to cancer pathogenesis and treatment response.
Library Preparation and Sequencing
Library preparation methodologies differ significantly between orthogonal approaches. For hybridization-based capture, the protocol involves shearing genomic DNA to appropriate fragment sizes (typically 200-300bp), followed by end-repair, A-tailing, and adapter ligation. Libraries are then hybridized with biotinylated oligonucleotide baits targeting the exonic regions, with subsequent capture using streptavidin-coated magnetic beads [102]. Critical steps include careful titration of bait concentrations and optimization of hybridization conditions to ensure uniform coverage.
For amplification-based approaches, library preparation utilizes targeted amplification with primer pools designed to cover the exonic regions. This method involves less hands-on time but may show more variability in coverage uniformity, particularly for GC-rich regions [102]. For both methods, quality control steps including quantification (e.g., qPCR) and fragment size analysis (e.g., Bioanalyzer) are essential before sequencing. Sequencing should be performed to sufficient depth (typically >100x mean coverage) to ensure sensitivity for heterozygous variants in heterogeneous cancer samples, with increased depth potentially required for detecting subclonal variants in tumor populations.
Data Analysis and Variant Calling
Variant calling pipelines must be optimized for each sequencing technology. For Illumina data, the GATK best practices pipeline represents the current standard, utilizing BWA-mem for alignment, followed by duplicate marking, base quality score recalibration, and variant calling with HaplotypeCaller [102]. For Ion Torrent data, the Torrent Suite pipeline provides platform-specific optimization, with additional custom filters recommended to remove strand-specific errors and recurrent false positives generated from platform-specific artifacts.
The integration of variant calls from multiple platforms requires specialized approaches. Custom algorithms can compare variants across platforms and group them into classes based on attributes including variant type, zygosity concordance, and coverage in each platform [102]. For each variant class, positive predictive value should be calculated compared to a truth set (e.g., NIST Genome in a Bottle NA12878 truth set) to establish confidence metrics. This approach allows researchers to categorize variants based on their confirmation status, providing transparency about the level of evidence supporting each variant call - particularly valuable in cancer research where treatment decisions may rely on specific mutations.
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Research Reagent Solutions for WES Validation
| Reagent Category | Specific Products | Function in WES Workflow | Technical Considerations |
|---|---|---|---|
| Target Capture Kits | Agilent SureSelect Clinical Research Exome, Life Technologies AmpliSeq Exome | Enrichment of exonic regions prior to sequencing | Hybridization-based methods offer more uniform coverage; amplification-based methods are faster |
| Library Prep Kits | QXT library preparation, OneTouch system | Preparation of sequencing libraries from genomic DNA | Compatibility with sequencing platform is critical; automation options improve reproducibility |
| Reference Standards | NIST Genome in a Bottle (NA12878), commercially available mutation controls | Establishing baseline performance metrics | Should encompass variant types relevant to cancer research (SNVs, indels, CNVs) |
| Alignment Tools | BWA-mem, Torrent Suite | Mapping sequence reads to reference genome | Platform-specific optimizations improve accuracy, especially for indel-rich regions |
| Variant Callers | GATK HaplotypeCaller, Torrent Variant Caller | Identifying genetic variants from sequence data | Custom filtering needed to reduce platform-specific false positives |
| Quality Control Tools | CalculateHSMetrics, picard, samtools | Assessing coverage, mapping quality, and other QC metrics | Multiple metrics provide comprehensive view of data quality |
Diagnostic Yield Assessment in Cancer Research
Measuring and Reporting Diagnostic Yield
In cancer research applications, diagnostic yield represents the proportion of cases where WES identifies variants of clinical or research significance. Assessment of diagnostic yield should encompass multiple variant types including SNVs, indels, and CNVs, with increasing attention to more complex variant types such as structural variants and repeat expansions as detection methods improve [103]. Reporting should include not only the mere presence of variants but also their potential clinical actionability, particularly in the context of cancer therapy selection.
Comparative studies demonstrate the superior diagnostic yield of comprehensive sequencing approaches compared to targeted methods. Research shows that orthogonal NGS approaches identify additional reportable variants in 76% of cases, with 35% of these having known therapeutic/diagnostic relevance to a potential cancer type [102]. This improved yield is particularly valuable in cancers of unknown primary, where comprehensive mutation profiling can identify tissue of origin and guide treatment selection. The integration of mutational signature analysis further enhances diagnostic yield by providing evidence of underlying mutational processes characteristic of specific cancer types or environmental exposures.
Quality Metrics and Ongoing Validation
Establishing ongoing quality monitoring programs is essential for maintaining diagnostic yield assessment. Key metrics include coverage uniformity (percentage of target bases covered at ≥20x), mean coverage depth, duplication rates, and quality score distributions [102]. These metrics should be tracked over time with established thresholds for acceptable performance, allowing researchers to identify degradation in assay performance before it impacts research conclusions.
For cancer research applications, additional validation is particularly important for detecting somatic variants in heterogeneous tumor samples. Limits of detection should be established for variant allele fractions, with special attention to subclonal mutations that may be present at low frequencies but have significant biological implications [103]. This is especially critical in cancer research, where tumor heterogeneity and evolving subclones can influence treatment response and resistance mechanisms. Regular revalidation using control materials ensures consistent performance as reagents and instrumentation naturally vary over time.
Validation studies and orthogonal confirmation represent essential components of rigorous WES applications in cancer research. The dual-platform orthogonal approach provides the highest standard for variant confirmation, enabling genomic-scale validation while simultaneously improving overall variant sensitivity. By implementing comprehensive validation frameworks encompassing sample preparation, sequencing, data analysis, and ongoing quality monitoring, researchers can ensure the reliability of their WES data for critical cancer research applications. As WES continues to evolve, validation practices must similarly advance to address emerging variant types and applications, particularly in the complex landscape of cancer genomics where accurate variant detection directly impacts research conclusions and potential clinical translation.
Within the paradigm of precision oncology, comprehensive genomic profiling has become a cornerstone for guiding treatment decisions. The choice of testing methodology, however, presents a significant strategic consideration for researchers and clinicians. On one hand, single-gene tests have established a historical track record of reliability for detecting specific, known mutations. Conversely, whole exome sequencing (WES) represents a more comprehensive approach, sequencing all protein-coding regions of approximately 20,000 genes in the human genome [104]. This technical guide provides a detailed, evidence-based comparison of these approaches, focusing on the critical parameters of cost efficiency, turnaround time, and alteration detection capability within cancer research and drug development contexts.
The following table summarizes the core quantitative findings from recent studies and analyses comparing WES (and related comprehensive genomic profiling) to single-gene testing strategies in oncology, particularly for non-small cell lung cancer (NSCLC) as a model.
Table 1: Head-to-Head Comparison of WES/Comprehensive Profiling vs. Single-Gene Testing
| Performance Metric | WES/Comprehensive Sequencing | Sequential Single-Gene Testing | Key Findings and Context |
|---|---|---|---|
| Testing Cost per Patient | Lower | Higher | WES/WTS reduced costs by $14,602 USD per patient compared to sequential single-gene testing in advanced NSCLC [14]. |
| Overall Healthcare Cost Impact | Cost-saving | More costly | Use of WES/WTS reduced total costs by $8,809 USD per patient compared to no testing, demonstrating systemic savings [14]. |
| Turnaround Time | Faster (≈2.8 weeks) | Slower | NGS panels enable patients to start therapy 2.8 weeks earlier than single-gene approaches [105]. |
| Detection of Actionable Alterations | Higher | Lower | Adding RNA sequencing (WTS) to WES increased identification of actionable alterations by 2.3%-13.0%, crucially detecting fusions missed by DNA-only tests [14]. |
| Biomarker Detection Scope | Comprehensive (>50 genes, TMB, MSI) | Limited (1-4 genes per test) | Sequential tests cannot identify microsatellite instability (MSI) or tumor mutational burden (TMB), while WES/WTS can [14]. |
| Tissue Utilization | Efficient | Inefficient ("exhausted tissue") [105] | NGS conserves precious tumor tissue by testing all targets simultaneously, while sequential testing consumes more tissue [105]. |
Detailed Methodologies for Experimental Comparison
To ensure reproducibility and provide a clear framework for evaluating the data presented, this section outlines the key experimental and modeling methodologies used in the cited studies.
Economic and Outcomes Modeling
The primary findings on cost and survival are derived from a robust economic model developed to estimate annual costs and clinical outcomes [14].
- Model Design: A cohort-level decision tree model was constructed in Microsoft Excel.
- Patient Cohort: The model simulated treatment-naïve patients aged 18+ with confirmed advanced/metastatic NSCLC, stratified by insurer (commercial, Medicaid, Medicare) to capture cost variations.
- Testing Comparators: The model compared three scenarios: 1) no genomic testing, 2) sequential single-gene testing, and 3) WES combined with whole-transcriptome sequencing (WTS).
- Alteration Assignment & Test Sensitivity: Patients were assigned alterations based on published prevalence rates from approximately 10,000 US patient biopsies. Each testing approach was assigned a specific sensitivity for detecting various biomarkers. For tests without RNA sequencing, sensitivity was adjusted to reflect fusions missed by DNA-alone.
- Cost and Outcome Inputs: The model incorporated real-world costs for testing, biopsies, reflex testing, and targeted therapies. Clinical outcomes, including overall survival for each treatment, were based on pivotal clinical trials used for product approval. Costs were reported in 2022 USD, and clinical outcomes were projected over patients' lifetimes.
Analytical Validation of WES Performance
The technical capability of WES to detect variants is grounded in rigorous analytical validation, as exemplified by laboratory specifications [104].
- Sequencing Technology: Clinical-grade WES uses next-generation sequencing (NGS) with target enrichment for all protein-coding exons, extending ±20 base pairs into intron-exon boundaries.
- Performance Metrics:
- Coverage: A mean sequencing coverage of >150x is targeted, with >99.6% of the target region covered at a minimum of 20x.
- Sensitivity/Specificity:
- Single-nucleotide variants (SNVs): >99.1% sensitivity, >99.99% specificity.
- Small insertions/deletions (indels): >95.0% sensitivity, >99.99% specificity.
- Copy Number Variants (CNVs): 100% sensitivity for single-exon (or larger) deletions/duplications.
- Data Analysis Pipeline: Sequencing data is processed through a proprietary bioinformatics pipeline integrating state-of-the-art algorithms for variant calling, annotation, and filtration using databases like gnomAD, ClinVar, and HGMD. In silico tools (SIFT, PolyPhen) assist in variant prioritization and classification according to ACMG guidelines.
Visualizing Testing Strategies and Outcomes
The fundamental difference between testing strategies lies in their workflow and information yield. The following diagram illustrates the parallel, comprehensive nature of WES versus the linear, limited approach of sequential single-gene testing.
Diagram 1: A comparison of testing workflows, highlighting the parallel processing of WES versus the sequential, time-consuming nature of single-gene tests.
The economic and clinical outcomes of choosing a testing strategy are multi-faceted. The following diagram maps the logical relationship from the initial testing choice to its downstream consequences on patient care and healthcare systems.
Diagram 2: A logic flow of clinical and economic outcomes, demonstrating how the choice of testing strategy directly impacts patient management and systemic costs.
The Scientist's Toolkit: Essential Research Reagents and Materials
The experimental protocols for WES rely on a suite of specialized reagents and bioinformatics tools to ensure high-quality, clinically actionable data. The following table details key components of this research toolkit.
Table 2: Key Research Reagent Solutions for Whole Exome Sequencing
| Item/Category | Function/Description | Research Context |
|---|---|---|
| Exome Enrichment Kits | Target capture of protein-coding regions from fragmented genomic DNA. | Critical for maximizing on-target efficiency and coverage uniformity; quality directly impacts diagnostic yield [31]. |
| Library Preparation Kits | Prepare tumor DNA/RNA libraries for next-generation sequencing by fragmenting, repairing ends, and adding adapters. | The initial step in the WES workflow; ensures that genetic material is compatible with the sequencing platform [31]. |
| NGS Sequencing Reagents | Chemicals and enzymes (e.g., polymerases, nucleotides) required for the sequencing-by-synthesis reaction. | A recurring consumable cost; platform-specific (e.g., Illumina, Ion Torrent) and vital for generating raw sequence data [31]. |
| Bioinformatics Software & Pipelines | Analyze raw sequencing data for alignment, variant calling, annotation, and filtration against population/geneic databases. | Essential for translating raw data into clinical insights; integrates algorithms and databases (gnomAD, ClinVar) for variant interpretation [104] [91]. |
| Tumor Normal Pair Analysis | Sequencing matched normal sample (e.g., blood) to filter out germline variants and identify somatic tumor mutations. | The most accurate method for identifying tumor-specific alterations and calculating tumor mutational burden (TMB) [14]. |
The evidence demonstrates that WES and other comprehensive genomic profiling methodologies offer superior cost-effectiveness, faster turnaround times, and significantly enhanced detection of clinically actionable alterations compared to sequential single-gene testing. The integration of RNA sequencing is particularly critical for identifying gene fusions that are invisible to DNA-only tests. For the research and drug development community, these findings underscore that WES is not merely a more comprehensive tool but a more efficient one. It facilitates rapid patient stratification for clinical trials, enables the discovery of novel biomarkers, and provides a rich genomic dataset that is crucial for advancing the field of precision oncology. As the cost of sequencing continues to decline and bioinformatic tools become more sophisticated, WES is poised to become an indispensable component of foundational cancer research and routine clinical management.
Gene fusions are pivotal drivers in oncogenesis, serving as critical biomarkers for diagnosis, prognosis, and therapeutic targeting. While whole exome sequencing (WES) effectively identifies single nucleotide variants and copy number alterations, it has inherent limitations in robustly detecting fusion genes. This whitepaper elucidates how the integration of whole transcriptome sequencing (WTS), or RNA sequencing (RNA-seq), with WES overcomes these limitations, significantly enhancing fusion detection rates and clinical utility. We present quantitative evidence from recent clinical studies, detail experimental and bioinformatic protocols for combined assays, and demonstrate how this integrated approach informs personalized treatment strategies, ultimately improving patient outcomes in oncology.
Fusion genes, arising from chromosomal rearrangements such as translocations, deletions, and insertions, are hybrid genes that play a causal role in tumorigenesis [106] [107]. It is estimated that gene fusions contribute to the pathogenesis of approximately 20% of all human cancers [106] [107]. Their significance is underscored by their dual role as definitive diagnostic markers and actionable therapeutic targets. Well-characterized examples include:
- BCR-ABL1 in chronic myeloid leukemia [108] [24]
- EML4-ALK and ROS1 fusions in lung cancer [106] [107]
- TMPRSS2-ERG, found in roughly 50% of prostate cancers [108] [24]
- EWSR1-FLI1 in Ewing sarcoma and KIAA1549-BRAF in pilocytic astrocytomas [106]
The robust detection of these alterations is therefore non-negotiable for modern precision oncology. WES has become a cornerstone of cancer genomics, providing a cost-effective method for analyzing the protein-coding regions of the genome to identify somatic single nucleotide variants (SNVs), insertions/deletions (INDELs), and copy number variations (CNVs) [2] [109] [110]. However, as a DNA-based assay, WES is suboptimal for identifying gene fusions, which are more readily detected at the transcriptomic level. This gap is effectively bridged by integrating RNA-seq, creating a synergistic diagnostic and research tool.
Limitations of DNA-Based Fusion Detection via WES
While WES is a powerful tool, its application for fusion gene detection presents several challenges, primarily because it infers fusions from genomic DNA breakpoints rather than directly sequencing the expressed chimeric transcript.
Technical and Analytical Challenges
The fundamental challenge lies in the nature of the exome capture process and the sequencing coverage required.
- Capture Probe Design: Exome capture kits are designed to enrich for exonic regions. Breakpoints leading to gene fusions often occur in introns, which are not covered by standard WES panels. Consequently, the critical genomic rearrangement may be missed entirely [108].
- Coverage Requirements: Standard WES is typically performed at a moderate coverage (e.g., 15-30x). A subsampling study revealed that a coverage of at least 75x is necessary for WES-based fusion detection to achieve high accuracy, a depth that is often not cost-effective for routine WES [108] [24].
- Sensitivity and Concordance: Studies directly comparing WES to RNA-seq for fusion detection show inconsistent results. For instance, in Acute Myeloid Leukemia (AML), WES detected the prominent PML-RARA and CBFB-MYH11 fusion genes in only 36% and 63% of available samples, respectively, where RNA-seq had confirmed their presence [108] [24]. This indicates a significant false-negative rate for WES.
Incomplete and Indirect Information
Even when a potential rearrangement is detected in DNA, WES cannot confirm if the rearrangement is transcribed into a stable, in-frame mRNA fusion transcript, which is a prerequisite for oncogenic activity. RNA-seq directly sequences this mRNA, providing conclusive evidence of an expressed and potentially functional fusion gene.
The Transformative Value of RNA Sequencing
RNA-seq directly sequences the transcriptome, enabling the direct detection of chimeric fusion transcripts from expressed mRNA. This provides a more accurate and functional view of fusion gene activity.
Enhanced Diagnostic Yield and Clinical Impact
Clinical studies have consistently demonstrated that adding RNA-seq to diagnostic workflows significantly increases the detection rate of clinically relevant gene fusions.
A seminal prospective study of 244 pediatric cancer patients performed RNA-seq in parallel with standard diagnostic procedures (e.g., FISH, RT-PCR, karyotyping) [106]. The results were striking:
Table 1: Increased Diagnostic Yield from Adding RNA Sequencing [106]
| Detection Method | Number of Fusions Detected | Diagnostic Yield |
|---|---|---|
| Routine Diagnostics Only | 56 | 23% (56/244) |
| RNA Sequencing Only | 78 | 32% (78/244) |
| Overall Increase | +22 Fusions | Increase of 39% |
Critically, 24 fusions were detected solely by RNA-seq and were missed by traditional techniques. For two patients in this cohort, the fusions identified only by RNA-seq directly led to a change in treatment, enabling the use of targeted agents [106]. A separate study using targeted RNA-seq reported an increase in diagnostic rate from 63% with conventional methods (FISH/RT-PCR) to 76% [107].
Technical Advantages of RNA-seq for Fusion Detection
- Unbiased Genome-Wide Screening: Unlike targeted FISH or RT-PCR assays, RNA-seq can detect novel and rare fusion partners without prior knowledge of the specific rearrangement [106] [107].
- Nucleotide-Level Resolution: RNA-seq precisely identifies the exact exonic breakpoints of the fusion junction, which can be important for predicting protein structure and informing drug design [107].
- Detection of Expressed Transcripts: It confirms that the fusion gene is not only present in the genome but is also expressed, indicating potential functional activity [108].
- Multi-Parameter Analysis from a Single Assay: The same RNA-seq data can be repurposed to analyze gene expression profiles, tumor microenvironment signatures, and immune repertoire, adding layers of valuable information beyond fusion detection [23] [107].
Integrated WES and RNA-seq Experimental Protocols
Implementing a combined WES and RNA-seq assay requires meticulous wet-lab and computational procedures. The following workflow is adapted from validated clinical studies [106] [23] [107].
Laboratory Workflow
The process begins with sample acquisition and proceeds through parallel paths for DNA and RNA.
The Scientist's Toolkit: Essential Research Reagents
The following table details key reagents and their functions in the integrated sequencing workflow.
Table 2: Essential Research Reagents for Integrated WES/RNA-seq
| Item | Function | Example Products |
|---|---|---|
| Nucleic Acid Extraction Kit | Simultaneous co-extraction of DNA and RNA from a single sample, preserving the relationship between genomic and transcriptomic data. | AllPrep DNA/RNA Mini Kit (Qiagen) [23] |
| DNA Library Prep Kit | Prepares fragmented DNA for sequencing by adding adapters and indexes. | Illumina DNA Prep, SureSelect XTHS2 DNA Kit [23] [109] |
| RNA Library Prep Kit | Converts RNA into a sequencing-ready library, often preserving strand information. | TruSeq Stranded mRNA Kit [23] |
| Exome Capture Probes | Biotinylated oligonucleotide probes that hybridize to and enrich exonic regions from the DNA library. | SureSelect Human All Exon [23], Illumina Exome 2.5 [109] |
| RNA Capture Panels (Optional) | Probes designed to enrich for a predefined set of fusion-related genes, increasing sensitivity for low-expression fusions. | Archer FusionPlex, Pan-Cancer Fusion Panels [106] [107] |
| Sequencing Platform | High-throughput instrument for parallel sequencing of prepared libraries. | Illumina NovaSeq 6000 Series [106] [23] |
Bioinformatics Analysis Pipelines
The raw sequencing data (FASTQ files) undergo a series of computational steps to identify high-confidence fusion genes.
For WES Data (Fuseq-WES pipeline):
- Alignment: Map DNA sequencing reads to a reference genome (e.g., hg38) using tools like BWA [108] [24].
- Variant Calling: Identify SNVs/INDELs with tools like Strelka2 and GATK, and CNVs with tools like mosdepth [23] [2].
- Fusion Detection (DNA-level): Extract discordant and split reads from aligned BAM files. Tools like Fuseq-WES build a "fusion equivalence class" from these reads to predict fusion genes, though with noted sensitivity limitations [108] [24].
For RNA-seq Data:
- Alignment: Map RNA-seq reads to the reference genome/transcriptome using spliced aligners like STAR [106] [23].
- Fusion Calling: Use specialized tools to detect chimeric transcripts from spanning and split reads.
- Best Practice: To minimize false positives, a consensus approach is recommended, requiring fusion calls to be supported by multiple algorithms (e.g., both STAR-Fusion and FusionCatcher) [107].
Clinical Validation and Real-World Utility
The integrated WES/RNA-seq approach has been rigorously validated in large clinical cohorts, demonstrating its transformative potential.
- Large-Scale Validation: A 2025 study of 2,230 clinical tumor samples validated a combined RNA and DNA exome assay, finding that it enabled direct correlation of somatic alterations with gene expression, recovered variants missed by DNA-only testing, and improved the detection of gene fusions [23]. This integrated approach uncovered clinically actionable alterations in a remarkable 98% of cases [23].
- FDA-Approved CDx Assays: The clinical maturity of this approach is evidenced by the FDA-approval of assays like Caris Life Sciences' MI Cancer Seek, which combines WES and WTS (Whole Transcriptome Sequencing) as a companion diagnostic to identify patients for targeted therapies [111].
- Overcoming Diagnostic Pitfalls: RNA-seq proves invaluable in cases where traditional methods fail. Examples from the pediatric cohort include [106]:
- An EML4-NTRK3 fusion in an infantile fibrosarcoma missed by FISH because the assay targeted the wrong partner gene (ETV6).
- KIAA1549-BRAF fusions in pilocytic astrocytomas missed by RT-PCR due to suboptimal primer design.
- In both cases, RNA-seq provided an unbiased diagnosis, potentially altering patient management.
The integration of RNA sequencing with whole exome sequencing represents a paradigm shift in cancer genomics. While WES remains a powerful tool for detecting SNVs and CNVs, its limitations in fusion gene detection are substantial and clinically significant. RNA-seq directly addresses these gaps by providing a sensitive, specific, and unbiased method for identifying expressed chimeric transcripts.
The quantitative evidence is clear: adding RNA-seq to diagnostic workflows can increase the detection yield of clinically relevant fusions by over 38% [106], directly impacting patient care by revealing actionable therapeutic targets that would otherwise remain hidden. As the field of precision oncology continues to evolve, the combined WES/RNA-seq approach is poised to become the standard of care, providing a more comprehensive molecular blueprint of a patient's tumor and paving the way for more informed and effective personalized treatment strategies.
Cancer treatment costs pose a significant global economic burden, creating an urgent need for cost-effective approaches that improve patient outcomes without escalating expenditures [112]. Comprehensive genomic profiling (CGP), including whole-exome and whole-transcriptome sequencing (WES/WTS), represents a transformative approach that enables treatment plans tailored to the genomic profile of patients' cancer [14]. Framed within the broader thesis on whole-exome sequencing in cancer research, this analysis demonstrates how comprehensive profiling methodologies serve not only as powerful research tools but as economically viable clinical assets. By moving beyond single-gene testing approaches to comprehensive genomic assessment, healthcare systems can achieve superior clinical outcomes while managing costs through more precise therapeutic targeting [14] [113]. The economic case for comprehensive profiling is built on a foundation of improved diagnostic yield, optimized treatment selection, and reduced ineffective therapy administration—key considerations for researchers, scientists, and drug development professionals working at the intersection of genomics and healthcare economics.
Quantitative Economic Evidence: Comparative Cost Analyses
Table 1: Comparative Cost-Effectiveness of Comprehensive Genomic Profiling Approaches
| Testing Approach | Comparison | Incremental Cost-Effectiveness Ratio (ICER) | Cost Savings per Patient | Survival Benefit |
|---|---|---|---|---|
| CGP vs. Small Panel (US) | Advanced NSCLC | $174,782 per life-year gained [112] | Higher initial cost | +0.10 years average overall survival [112] |
| CGP vs. Small Panel (Germany) | Advanced NSCLC | €63,158 per life-year gained [112] | Higher initial cost | +0.10 years average overall survival [112] |
| WES/WTS vs. No Testing | Advanced/Metastatic NSCLC | Dominant strategy (improved outcomes, lower costs) [14] | $8,809 | +3.9 months median overall survival [14] |
| WES/WTS vs. Sequential Single-Gene | Advanced/Metastatic NSCLC | Dominant strategy (improved outcomes, lower costs) [14] | $14,602 | Minimal survival benefit [14] |
| DNA + RNA Sequencing vs. DNA Alone | Fusion detection (2.5%-14% prevalence) | Cost-saving across fusion prevalence range [14] | $400-$1,724 | Increased actionable alterations by 2.3%-13.0% [14] |
Real-World Cost Utilization Evidence
Table 2: Real-World Healthcare Costs and Targeted Therapy Utilization with CGP
| Cancer Type | Testing Modality | Targeted Therapy uptake (Odds Ratio vs. non-CGP) | Cost Ratio during First-Line Therapy (PPPM) | Statistical Significance |
|---|---|---|---|---|
| Non-Small Cell Lung Cancer (NSCLC) | CGP | 1.57x higher [113] | 1.06 | P = .054 (not significant) [113] |
| Colorectal Cancer (CRC) | CGP | 2.34x higher [113] | 0.98 | P = .71 (not significant) [113] |
| Breast Cancer | CGP | Increased (study confirmed) | 1.03 | P = .63 (not significant) [113] |
| Multiple Advanced Cancers | CGP | Significantly increased | No significant difference vs. non-CGP testing | Across all evaluated cancer types [113] |
Methodological Approaches: Economic Modeling and Study Designs
Partitioned Survival Modeling for Cost-Effectiveness Analysis
The economic evidence for comprehensive genomic profiling derives from sophisticated modeling approaches that integrate real-world clinical and cost data. One prominent methodology is the partitioned survival model developed to estimate life years and drug acquisition costs associated with CGP versus small panel (SP) testing in patients with advanced non-small-cell lung cancer [112] [114]. This model stratifies patients into three therapeutic subcohorts based on receipt of matched therapy: (1) patients receiving matched targeted therapy for biomarkers classified as levels 1 and 2 by OncoKB; (2) patients receiving matched immunotherapy for PD-L1; and (3) patients who either did not receive matched therapy or were untreated [114]. The model incorporates diagnosis-specific distribution of these subcohorts, informed by real-world evidence from the Syapse study, which provided observational data collected from community centers [114]. Key parameters include survival curves for each subcohort, with the mean survival of patients receiving matched targeted therapy (3.11 years) exceeding that of patients receiving matched immunotherapy (2.01 years) and those not receiving matched therapy (2.06 years) [114]. Costs and outcomes are discounted according to standard health economic practices, with extensive scenario and sensitivity analyses conducted to test model robustness.
Decision Tree Modeling for Test Choice Evaluation
For evaluating whole-exome, whole-transcriptome sequencing approaches, researchers have developed cohort-level decision tree models to project survival and annual costs associated with different testing alternatives [14]. This model structure incorporates several key methodological components: First, treatment-naïve patients enter the model stratified by insurer (commercial, Medicaid, or Medicare) to capture costs by payer type. Patients are then assigned alterations based on rates observed in published literature, with a separate group of alterations categorized as "exploratory" for which no approved therapies exist but clinical trials may be available [14]. The model assigns genomic testing approaches—no testing, sequential single-gene testing, or WES/WTS plus immunohistochemistry testing—each with defined test sensitivity for detecting biomarkers that are present. For tests without RNA sequencing, sensitivity is adjusted to reflect fusions missed by DNA sequencing alone. The model applies costs for initial testing, related biopsies, and reflex RNA testing when applicable. Clinical outcomes for each treatment are based on pivotal trials used in product approval, with costs including wholesale acquisition costs and administration costs based on Medicare reimbursement [14].
Mechanisms of Cost Reduction: Pathways to Economic Efficiency
Primary Drivers of Economic Benefit
Comprehensive genomic profiling reduces healthcare costs through several interconnected mechanisms that optimize the entire cancer care pathway. The fundamental cost-reduction pathway begins with enhanced detection of actionable biomarkers, which enables more patients to receive matched targeted therapies [14]. This initial improved detection creates a cascade of economic benefits: reduced administration of ineffective therapies, decreased management of unnecessary side effects, and more efficient allocation of healthcare resources [113]. The addition of RNA sequencing in WES/WTS approaches provides particular value by identifying gene fusions that DNA sequencing alone would miss, expanding the population eligible for targeted treatments [14]. Furthermore, comprehensive profiling improves tissue stewardship by maximizing information obtained from limited biopsy material, reducing the need for repeat invasive procedures [113]. The economic advantage is compounded by the identification of patients eligible for clinical trials, potentially providing access to novel therapies while generating evidence for future treatment paradigms [14].
Integration into Clinical Pathways
The economic benefit of comprehensive profiling is maximized when integrated into standardized diagnostic pathways early in the patient journey. Research demonstrates that testing completion before first-line therapy initiation is critical for realizing cost savings, as testing performed after treatment initiation diminishes the opportunity to avoid ineffective therapies [113]. The economic modeling reveals that increasing the number of patients receiving appropriate targeted therapy based on comprehensive profiling results decreases the incremental cost-effectiveness ratio (to $86,826 in the United States and $29,235 in Germany under optimized scenarios) [112]. Conversely, suboptimal testing approaches that fail to detect actionable biomarkers result in higher downstream costs due to continued administration of ineffective treatments and management of their associated toxicities [14]. The comprehensive nature of WES/WTS also creates efficiency by consolidating multiple potential tests into a single workflow, reducing the administrative burden and cumulative costs of sequential testing approaches [14].
Research Reagent Solutions: Essential Methodological Components
Table 3: Key Research Reagents and Materials for Comprehensive Genomic Profiling
| Reagent/Material | Function | Application in Experimental Protocol |
|---|---|---|
| IDT xGen Exome Research Panel v.1.0 | Target enrichment for exome sequencing | Captures 39 megabases of human genome (19,396 genes) with additional probes for underperforming loci [115] |
| Paired Tumor-Normal Sequencing | Identification of tumor-specific alterations | Most accurate method for calculating tumor mutational burden (TMB) and distinguishing somatic from germline variants [14] |
| Whole-Transcriptome Sequencing | Detection of gene fusions and alternative transcripts | Identifies RNA-level alterations missed by DNA sequencing alone; improves fusion detection sensitivity [14] |
| Immunohistochemistry Assays | Protein-level validation of genomic findings | Complementary testing for markers like PD-L1; confirms functional impact of genomic alterations [14] |
| Automated Imaging Systems | Chromosomal structure analysis | Digital capture and analysis of chromosomal abnormalities; improves karyotyping efficiency and accuracy [116] |
Implementation Challenges and Future Directions
Despite compelling economic evidence, comprehensive genomic profiling faces implementation barriers that impact its cost-effectiveness. Current testing rates remain suboptimal, with significant variation by cancer type—ranging from 17% in ovarian cancer to 45% in non-small cell lung cancer—despite increasing trends over time [113]. These gaps persist despite economic analyses demonstrating cost neutrality of CGP during first-line therapy across multiple cancer types [113]. Future efforts to enhance cost-effectiveness should focus on several key areas: streamlining testing workflows to reduce turnaround time, developing more efficient bioinformatic pipelines for data analysis, and establishing standardized reimbursement mechanisms that recognize the long-term economic value of precision oncology approaches [112] [113]. Additionally, research comparing the cost-effectiveness of different comprehensive profiling methodologies—including targeted large panels, whole-exome, and whole-genome approaches—will provide further refinement for economic decision-making in oncology.
Comprehensive genomic profiling represents a economically viable approach to oncology care that demonstrates consistent potential to improve patient outcomes while managing healthcare costs. Through sophisticated economic modeling and real-world evidence, this analysis establishes that comprehensive approaches—including whole-exome and whole-transcriptome sequencing—provide good value for healthcare resources invested. The economic advantage derives from multiple pathways: increased detection of actionable biomarkers, higher uptake of matched targeted therapies, avoidance of ineffective treatments, and improved tissue stewardship. For researchers, scientists, and drug development professionals, these findings underscore the importance of considering economic endpoints alongside traditional clinical outcomes when evaluating genomic technologies. As comprehensive profiling methodologies continue to evolve, their integration into standard oncology practice offers the promise of sustaining the advancement of precision medicine within economically sustainable frameworks.
Next-generation sequencing (NGS) technologies have fundamentally transformed cancer research and therapeutic development. The choice between targeted large panels, whole exome sequencing (WES), and whole genome sequencing (WGS) presents a significant strategic challenge for researchers, with implications for cost, data quality, and clinical applicability. This technical guide provides a comprehensive benchmarking framework for these methodologies, evaluating their respective capabilities in detecting diverse variant types across cancer genomics applications. We present quantitative performance comparisons, detailed experimental protocols for cross-platform validation, and standardized bioinformatics workflows to establish best practices for technology selection. Within the broader thesis on whole exome sequencing basics, this analysis positions WES as a balanced solution offering extensive genomic coverage at manageable cost, while clarifying scenarios where WGS or targeted panels provide superior advantages. The findings presented herein aim to equip cancer researchers and drug development professionals with evidence-based criteria for selecting optimal genomic profiling approaches specific to their research objectives and resource constraints.
The implementation of precision oncology relies fundamentally on comprehensive genomic characterization to identify actionable mutations guiding therapeutic strategies. Three principal NGS approaches dominate current research paradigms: targeted large panels (often covering 50-1000 genes), whole exome sequencing (capturing ~20,000 protein-coding genes), and whole genome sequencing (interrogating the entire human genome). Each technology offers distinct advantages and limitations across dimensions of analytical sensitivity, genomic coverage, technical robustness, and cost-effectiveness [117] [118].
Whole exome sequencing represents a strategically balanced approach, focusing on protein-coding regions while offering substantially broader coverage than targeted panels at lower cost than WGS. Since approximately 85% of known disease-causing variants reside in exonic regions, WES delivers considerable diagnostic and research value by enabling discovery of novel cancer-associated variants across the entire exome [2] [61]. The technology has matured sufficiently to support clinical applications, with FDA-approved methods now available for cancer screening, detection, and monitoring [2].
Whole genome sequencing provides the most comprehensive approach for genomic analysis, detecting variants in both coding and non-coding regions, including complex structural variants and alterations in regulatory elements. However, its implementation faces challenges related to higher costs, substantial data storage requirements, and complexities in interpreting non-coding variants [119] [118]. Recent studies demonstrate WGS's particular utility in rare disease diagnosis and cancer cases where previous testing has failed to identify causative mutations [118] [120].
Large panel sequencing offers maximum sensitivity for detecting low-frequency variants and established biomarkers, making it ideal for profiling specific cancer genes with high depth at manageable cost. The focused nature of panels simplifies data interpretation and clinical reporting while providing excellent reproducibility [121] [122]. This guide systematically benchmarks these technologies to define their optimal applications in cancer research pipelines.
Technical Specifications and Performance Benchmarking
Comparative Analysis of Sequencing Approaches
Table 1: Technical specifications and performance metrics of major sequencing technologies
| Parameter | Targeted Panels | Whole Exome Sequencing (WES) | Whole Genome Sequencing (WGS) |
|---|---|---|---|
| Genomic coverage | 50-1000 genes | ~20,000 genes (∼1% of genome) | Entire genome (∼20,000 genes + non-coding) |
| Variant detection capability | SNVs, indels, CNVs, fusions in targeted regions | Comprehensive SNVs, indels across exome; limited CNV detection | SNVs, indels, CNVs, SVs, repeat expansions, non-coding variants |
| Typical sequencing depth | 500-1000× | 100-200× | 30-100× |
| Detection sensitivity for low-frequency variants | High (VAF ∼1% with sufficient depth) | Moderate (VAF ∼5%) | Lower (VAF ∼10-20%) |
| Cost per sample | $$$-$$$$ | $$ | $$$$ |
| Turnaround time | Days | 1-2 weeks | 1-2 weeks |
| Data volume per sample | 1-5 GB | 5-15 GB | 100-200 GB |
| Key advantages | High sensitivity for low VAF; focused clinical interpretation; cost-effective for targeted genes | Balanced approach; discovery power across exome; better cost-effectiveness than WGS | Most comprehensive; detects non-coding and structural variants; uniform coverage |
| Primary limitations | Limited discovery power; restricted to known targets | Limited non-coding coverage; uneven coverage | Higher cost; data interpretation challenges; storage requirements |
Variant Detection Performance Across Technologies
Analytical performance varies significantly across sequencing platforms and variant types. A benchmarking study evaluating structural variant (SV) detection using common algorithms (Delly, Lumpy, Manta, SvABA) demonstrated accuracy exceeding 90% for validated cancer SVs when using a random-forest decision model to improve true positive calls [121]. For single nucleotide variants (SNVs) and small insertions/deletions (indels), the choice of variant caller significantly impacts detection sensitivity, with tools like MuTect2, VarScan2, and Strelka exhibiting complementary strengths for different variant classes and allele frequencies [2].
Tumor Mutational Burden (TMB) and Microsatellite Instability (MSI) assessment represents a critical application where technology choice significantly impacts results. WES provides a standardized approach for TMB calculation across approximately 30-40 Mb of sequence, while panels require careful normalization due to smaller target sizes (0.5-3 Mb). Studies demonstrate that TMB values derived from large panels show good correlation with WES when properly calibrated, though discrepancies occur particularly in the intermediate TMB range where clinical cutpoints are most consequential [2] [122].
Copy Number Variation (CNV) detection remains challenging across all platforms, with WGS demonstrating superior performance for genome-wide CNV calling due to more uniform coverage. Both WES and targeted panels show variable performance for CNV detection depending on bait design and bioinformatics approaches, with WES having particular difficulty in accurately defining breakpoints and distinguishing focal amplifications/deletions [2] [120].
Table 2: Variant detection performance across sequencing methodologies
| Variant Type | Targeted Panels | WES | WGS |
|---|---|---|---|
| Single Nucleotide Variants (SNVs) | Excellent (sensitivity >99% at VAF ≥5%) | Very Good (sensitivity >95% at VAF ≥10%) | Good (sensitivity >90% at VAF ≥20%) |
| Small Insertions/Deletions (Indels) | Excellent with UMI | Very Good | Good |
| Gene Fusions/Structural Variants | Good (limited to designed targets) | Limited | Excellent (genome-wide) |
| Copy Number Variations (CNVs) | Good (focal, amplicon-based) | Moderate (large-scale) | Excellent (genome-wide) |
| Non-coding Variants | Limited to designed regions | Limited | Excellent |
| Tumor Mutation Burden | Good (with calibration) | Excellent (gold standard) | Excellent |
| Microsatellite Instability | Good (with specific markers) | Good | Excellent |
Experimental Design and Methodological Frameworks
Sample Preparation and Quality Control
Robust benchmarking begins with appropriate sample selection and quality control. The SEQC2 Oncopanel Sequencing Working Group established a rigorous framework using four reference samples with defined variant profiles: Sample A (cancer cell line pool), Sample B (normal germline control), Sample C (1:1 mixture of A and B), and Sample Spike-in (germline DNA with 5% synthetic controls) [122]. This approach generates variants across a wide allele frequency spectrum (0.5%-50%) for comprehensive sensitivity assessment.
DNA Quality Requirements vary by application:
- FFPE-derived DNA: Minimum DV200 ≥30% (percentage of fragments >200bp)
- Fresh frozen tissue: High molecular weight DNA (≥40kb)
- Cell-free DNA: Minimum 10ng input with fragment size distribution 160-180bp
For WES and WGS, library preparation typically utilizes 50-100ng of input DNA, with fragmentation to 150-300bp followed by adapter ligation and PCR amplification. WES employs hybridization capture using biotinylated probes (microarray or solution-based) to enrich for exonic regions, with magnetic bead-based capture now predominating due to simplicity and efficiency [2] [61].
Bioinformatics Pipelines for Variant Calling
Primary and Secondary Analysis follow standardized workflows across platforms:
- Quality Control: FastQC for read quality, Picard for library complexity
- Alignment: BWA-MEM for Illumina data, optimized for respective reference genomes (GRCh37/hg19, GRCh38/hg38)
- Duplicate Marking: Picard MarkDuplicates for PCR duplicate removal
- Base Quality Recalibration: GATK BaseRecalibrator for systematic error correction
- Variant Calling: Platform-specific callers followed by joint genotyping
Specialized Variant Callers demonstrate complementary performance:
- SNVs: MuTect2 (somatic), VarScan2 (germline and somatic)
- Indels: Strelka, FreeBayes
- Structural Variants: Delly, Lumpy, Manta, GRIDSS
- Copy Number Variants: Control-FREEC, CNVkit
The implementation of unique molecular identifiers (UMIs) enables error correction and accurate detection of low-frequency variants (VAF <1%) by distinguishing true mutations from PCR and sequencing artifacts [122]. For targeted panels, UMI incorporation is particularly valuable for liquid biopsy applications where variant allele frequencies can be extremely low.
Analytical Validation and Benchmarking Standards
Establishing performance metrics requires comparison against orthogonal methods and reference materials:
- Orthogonal Validation: Sanger sequencing for SNVs/indels, FISH for gene fusions, IHC for expression, MLPA for CNVs
- Reference Materials: Commercial standards (Horizon Discovery, SeraCare) with predefined variants at known allele frequencies
- Performance Metrics: Sensitivity, specificity, positive predictive value, reproducibility, limit of detection
The SEQC2 consortium demonstrated that cross-platform benchmarking using shared reference samples enables objective performance assessment, with sensitivity for SNVs reaching >99% for VAF >5% across most validated oncopanels [122]. For clinical applications, establishing limit of detection (LOD) through dilution series is essential, particularly for liquid biopsy applications where variant allele frequencies may be below 1%.
Visualization of Sequencing Selection Pathways
Diagram 1: Decision pathway for selecting appropriate genomic sequencing technologies based on research objectives and practical constraints.
Bioinformatics Workflow for Multi-Technology Integration
Diagram 2: Integrated bioinformatics workflow for processing and analyzing data across multiple sequencing technologies, emphasizing validation and clinical interpretation.
The Scientist's Toolkit: Essential Research Reagents and Platforms
Table 3: Essential research reagents, platforms, and computational tools for sequencing benchmarking
| Category | Specific Tools/Reagents | Primary Function | Application Notes |
|---|---|---|---|
| Library Prep Kits | IDT xGen Pan-Cancer Panel, Illumina TruSight Tumor 170, Agilent SureSelectXT HS | Target enrichment & library construction | IDT panels offer custom content flexibility; Agilent provides high uniformity; Illumina offers integrated workflows |
| Hybridization Capture | xGen Custom Hyb Panels, SureSelectXT Target Enrichment | Exome and panel capture | Magnetic bead-based capture predominates for simplicity and efficiency [61] |
| Sequencing Platforms | Illumina NovaSeq, ThermoFisher Ion Torrent, PacBio Revio, Oxford Nanopore | DNA sequencing | Illumina dominates for short-read; PacBio offers HiFi long-reads; Nanopore provides ultra-long reads |
| Variant Callers | MuTect2, VarScan2, Strelka, FreeBayes, Delly, Manta | Specific variant detection | Multi-caller approaches improve sensitivity; machine learning models reduce false positives [2] [121] |
| Alignment Tools | BWA-MEM, STAR, Bowtie2 | Read alignment to reference | BWA-MEM standard for Illumina data; minimap2 preferred for long reads |
| Variant Annotation | ANNOVAR, SnpEff, VEP | Functional consequence prediction | Critical for prioritizing clinically relevant variants |
| Benchmarking Resources | SEQC2 reference samples, AcroMetrix hotspot controls, Horizon Discovery standards | Analytical validation | Essential for cross-platform performance assessment [122] |
| Visualization Tools | IGV, Integrative Genomics Viewer | Visual validation of variants | Critical for manual review of complex variants [121] |
Based on comprehensive benchmarking data and methodological evaluation, specific optimal use cases emerge for each sequencing technology:
Targeted Large Panels represent the optimal choice for clinical diagnostics and therapy selection where established biomarkers guide treatment decisions. Their superior sensitivity for low-frequency variants (VAF 1-5%) makes them indispensable for liquid biopsy applications and minimal residual disease monitoring. The focused nature of panels streamlines clinical interpretation and reporting while maintaining cost-effectiveness for high-volume testing [121] [122].
Whole Exome Sequencing provides the ideal balanced solution for discovery-phase research and comprehensive molecular profiling. WES delivers extensive coverage across protein-coding regions at manageable cost, enabling identification of novel cancer-associated genes beyond established panels. Its position between focused panels and comprehensive WGS makes it particularly valuable for biomarker discovery, clinical trial stratification, and cases where previous targeted testing has been uninformative [2] [61].
Whole Genome Sequencing offers unparalleled comprehensive analysis for complex cases and research applications requiring complete genomic characterization. WGS demonstrates particular strength in identifying structural variants, non-coding drivers, and complex rearrangements inaccessible to other methods. As costs decrease and interpretation frameworks mature, WGS is positioned to become the universal first-line test, though currently remains specialized for challenging diagnoses and discovery research [119] [118] [120].
The evolving landscape of cancer genomics will likely see increased integration of these technologies, with each playing complementary roles in comprehensive precision oncology programs. Strategic selection should be guided by specific research questions, sample characteristics, and analytical requirements rather than perceived technological superiority. Future methodological advances will continue to blur the distinctions between these approaches, ultimately converging on solutions that maximize both genomic completeness and clinical actionability.
Conclusion
Whole Exome Sequencing has firmly established itself as a powerful, cost-effective cornerstone of modern cancer research and is increasingly becoming integral to clinical diagnostics. By providing comprehensive profiling of coding regions where most disease-causing mutations reside, WES successfully bridges the gap between expansive whole-genome sequencing and limited targeted panels. The integration with RNA sequencing and advanced bioinformatics, including AI-driven tools, further enhances its utility for detecting key fusions and complex biomarkers like Homologous Recombination Deficiency. As automation improves throughput and consistency, and as the interpretation of genomic data becomes more refined, WES is poised to deepen its role in personalized oncology. Future directions will likely focus on standardizing workflows, expanding liquid biopsy applications, and fully integrating WES data with clinical electronic health records to realize the promise of truly genomics-guided cancer care across diverse patient populations.
References
- 1. Whole Exome Sequencing (WES): Principle, Steps, Uses ... [https://microbenotes.com/whole-exome-sequencing/]
- 2. Comprehensive Outline of Whole Exome Sequencing Data ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6895801/]
- 3. Whole Genome vs Exome Sequencing [https://www.illumina.com/techniques/sequencing/dna-sequencing/whole-genome-sequencing/whole-genome-vs-exome.html]
- 4. WGS vs WES: Which Genetic Sequencing Method is Right ... [https://www.novogene.com/us-en/resources/blog/wgs-vs-wes-which-genetic-sequencing-method-is-right-for-you/]
- 5. Clinical applications of next generation sequencing in cancer [https://pmc.ncbi.nlm.nih.gov/articles/PMC4469892/]
- 6. Whole Exome Sequencing Enables Development of ... [https://www.twistbioscience.com/blog/science/whole-exome-sequencing-enables-development-models-renal-cancer-and-drug-toxicity]
- 7. Comparison of actionable events detected in cancer ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9463385/]
- 8. Limitations of Whole Exome Sequencing [https://3billion.io/blog/limitations-of-whole-exome-sequencing]
- 9. Application value of whole exome sequencing in screening ... [https://www.nature.com/articles/s41598-022-27273-w]
- 10. Translational and clinical comparison of whole genome ... [https://www.nature.com/articles/s41698-024-00788-3]
- 11. Are whole-exome and whole-genome sequencing approaches cost-effective? A systematic review of the literature - ScienceDirect [https://www.sciencedirect.com/science/article/pii/S1098360021046736]
- 12. Are whole-exome and whole-genome sequencing approaches cost-effective? A systematic review of the literature | Genetics in Medicine [https://www.nature.com/articles/gim2017247]
- 13. Estimating the costs of genomic sequencing in cancer control - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC7268398/]
- 14. Costs and Benefits of Whole-Exome, Whole-Transcriptome ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12184969/]
- 15. Exome-based cancer predisposition gene testing can ... [https://www.nature.com/articles/s41431-025-01814-z]
- 16. Complete Genomics Highlights Clinical Research ... [https://www.completegenomics.com/complete-genomics-highlights-clinical-research-sequencing-solutions/]
- 17. Fast and reliable solutions for oncology workflows [https://www.illumina.com/company/news-center/feature-articles/fast-and-reliable-solutions-for-oncology-workflows0.html]
- 18. Advances in Precision Oncology: From Molecular Profiling to ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12607717/]
- 19. High clinical actionability of a pan-cancer tissue-based ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12615803/]
- 20. NGS Approaches in Clinical Diagnostics: From Workflow to ... [https://www.mdpi.com/1422-0067/26/19/9597]
- 21. Whole-Exome Sequencing of Metastatic Cancer and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4505739/]
- 22. The Future of Cancer Diagnosis and Treatment [https://www.mdpi.com/2673-5261/6/3/20]
- 23. Clinical and analytical validation of a combined RNA ... [https://www.nature.com/articles/s43856-025-00934-3]
- 24. Fusion Gene Detection Using Whole-Exome Sequencing ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8888970/]
- 25. Gene fusion: Mechanisms, detection, and applications [https://www.abcam.com/en-us/knowledge-center/dna-and-rna/gene-fusion-mechanisms-detection-and-applications]
- 26. Whole-exome sequencing reveals novel genomic ... [https://www.nature.com/articles/s41419-024-07232-1]
- 27. Real-world deployment of a fine-tuned pathology ... [https://www.nature.com/articles/s41591-025-03780-x]
- 28. Whole exome sequencing for cancer – is there evidence of ... [https://www.dovepress.com/whole-exome-sequencing-for-cancer-ndash-is-there-evidence-of-clinical--peer-reviewed-fulltext-article-AGG]
- 29. Precision Oncology Research Report 2025: Market to Hit ... [https://finance.yahoo.com/news/precision-oncology-research-report-2025-090800765.html]
- 30. Whole Exome Sequencing Market Size, Growth, Trends & ... [https://straitsresearch.com/report/whole-exome-sequencing-market]
- 31. Whole Exome Sequencing Market Size 2025-2029 [https://www.technavio.com/report/whole-exome-sequencing-market-industry-analysis]
- 32. Whole Exome Sequencing Study Identifies Distinct ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11976457/]
- 33. Whole Genome Sequencing Market is projected to grow ... [https://www.bccresearch.com/pressroom/bio/whole-genome-sequencing-market-is-projected-to-grow-at-cagr-of-151-?srsltid=AfmBOor_yH1IFZdKXIp-PB-isoos_Np99a6KUEHXUbLSeuErzwebmFFi]
- 34. Genomic Cancer Panel and Profiling Market Research 2025: [https://www.globenewswire.com/news-release/2025/11/03/3179160/0/en/Genomic-Cancer-Panel-and-Profiling-Market-Research-2025-Rapid-Science-Developments-Declining-Sequencing-Costs-and-the-Potential-for-Premium-Pricing-Position-Spurs-Expansion.html]
- 35. Exome sequencing and analysis of 454787 UK Biobank ... [https://www.nature.com/articles/s41586-021-04103-z]
- 36. Whole Exome Sequencing [https://eu.idtdna.com/pages/technology/next-generation-sequencing/dna-sequencing/targeted-sequencing/exome-sequencing]
- 37. Whole exome sequencing - Integra Biosciences [https://www.integra-biosciences.com/united-states/en/blog/article/whole-exome-sequencing]
- 38. Principles and Workflow of Whole Exome Sequencing [https://www.cd-genomics.com/resourse-principles-and-workflow-of-whole-exome-sequencing.html]
- 39. Evaluation of reference sample type for somatic variant ... [https://link.springer.com/article/10.1007/s00277-025-06699-y]
- 40. Variant Calling at the GDC | NCI Genomic Data Commons [http://gdc.cancer.gov/content/variant-calling-gdc]
- 41. Recommendations for bioinformatics in clinical practice [https://genomemedicine.biomedcentral.com/articles/10.1186/s13073-025-01543-4]
- 42. Recommendations for bioinformatics in clinical practice - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC12535132/]
- 43. Benchmarking of variant calling software for whole-exome ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12012014/]
- 44. Clinical benefit of additional whole-exome sequencing ... [https://pubmed.ncbi.nlm.nih.gov/41297163/?utm_source=FeedFetcher&utm_medium=rss&utm_campaign=None&utm_content=1zG2_xdOOC5VXA_B186mg2wRG5Vierx2syPXCcCUdmU3UrJgnK&fc=None&ff=20251127030032&v=2.18.0.post22+67771e2]
- 45. Clinical Implementation of a High-Throughput Automated ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12179514/]
- 46. Novel metrics to measure coverage in whole exome ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5429826/]
- 47. Automating Whole Genome Sequencing: A Representative ... [https://highresbio.com/blog/automating-whole-genome-sequencing-a-representative-system-for-high-throughput-library-preparation]
- 48. Clinical Whole Exome Sequencing (CLIA/CAP) [https://www.novogene.com/us-en/services/research-services/genome-sequencing/target-capture-sequencing/clinical-whole-exome-sequencing-clia-cap-iso/]
- 49. PacBio Revio | Long-read sequencing at scale [https://www.pacb.com/revio/]
- 50. Managing High-Throughput Workflows [https://www.labmanager.com/managing-high-throughput-workflows-1740]
- 51. Time to diagnosis in rapid exome/genome sequencing ... [https://pubmed.ncbi.nlm.nih.gov/38017634/]
- 52. high-throughput technologies and automated workflows to ... [https://www.sciencedirect.com/science/article/pii/S0958166925000643]
- 53. Agilent, Roche, Vazyme and Nanodigmbio | BMC Genomics [https://bmcgenomics.biomedcentral.com/articles/10.1186/s12864-024-11196-z]
- 54. Agilent, Roche, Vazyme and Nanodigmbio [https://pubmed.ncbi.nlm.nih.gov/39871131/]
- 55. KAPA HyperExome [https://rochesequencingstore.com/catalog/kapa-hyperexome/]
- 56. KAPA HyperExome V2 Probes [https://sequencing.roche.com/us/en/products/group/kapa-hyperexome-v2.html]
- 57. Vazyme - For Science For Health [https://www.vazymeglobal.com/applications/Research%20and%20Disease%20Areas/1984204435054211073.html]
- 58. Agilent, Roche, Vazyme and Nanodigmbio [https://www.semanticscholar.org/paper/Comparative-evaluation-of-four-exome-enrichment-in-Belova-Vasiliadis/5acc2a2a37557021996512e30b9b6df0dd5bc678]
- 59. Easy automation for in-house whole-exome sequencing [https://usinfo.roche.com/Exome-and-Edge_Exome-and-Edge-LP.html]
- 60. Nanodigmbio invites you to join us at Denver 2024 Annual ... [https://nanodigmbio.com/latest-news/1370.html]
- 61. Whole exome sequencing for cancer research [https://eu.idtdna.com/pages/research-area/cancer/cancer-research/cancer-exome-sequencing]
- 62. How Whole Exome Sequencing Works — In One Simple ... [https://www.linkedin.com/pulse/how-whole-exome-sequencing-works-one-simple-flow-2025-rank-flux-9nexc/]
- 63. Targeting DNA Damage Response-Mediated Resistance ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12293334/]
- 64. Addressing the Clinical Need for a Next-Generation HRD ... [https://www.foundationmedicine.com/blog/introducing-hrdsig-biomarker]
- 65. Refining treatment strategies for non-small cell lung cancer ... [https://www.nature.com/articles/s41416-025-03139-6]
- 66. Prospective validation of ORACLE, a clonal expression ... [https://www.nature.com/articles/s43018-024-00883-1]
- 67. Mutational signatures — Knowledge Hub [https://www.genomicseducation.hee.nhs.uk/genotes/knowledge-hub/mutational-signatures/]
- 68. The repertoire of mutational signatures in human cancer [https://www.nature.com/articles/s41586-020-1943-3]
- 69. Signatures of mutational processes in human cancer - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC3776390/]
- 70. Genomic Data Processing [http://gdc.cancer.gov/about-data/gdc-data-processing/genomic-data-processing]
- 71. AI cancer driver mutation predictions are valid in real-world ... [https://www.nature.com/articles/s41467-025-63461-8]
- 72. A new machine learning method for cancer mutation analysis [https://pmc.ncbi.nlm.nih.gov/articles/PMC9612828/]
- 73. Overcoming challenges in FFPE DNA library prep [https://www.neb.com/en-us/nebinspired-blog/overcoming-challenges-in-ffpe-dna-library-prep?srsltid=AfmBOorky8Y-wXkgrr_qmdsVhTURXcmzC4ApmgRg52oGM1jeKZPD-EXt]
- 74. A robust targeted sequencing approach for low input and ... [https://www.nature.com/articles/s41525-017-0041-4]
- 75. Robust transcriptional signatures for low-input RNA samples ... [https://bmcgenomics.biomedcentral.com/articles/10.1186/s12864-017-4280-7]
- 76. Robust detection of immune transcripts in FFPE samples ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5356875/]
- 77. Large scale, robust, and accurate whole transcriptome ... [https://www.nature.com/articles/s41598-020-74483-1]
- 78. Robustness and resilience of computational deconvolution ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12159287/]
- 79. Low-input and single-cell RNA sequencing [https://www.illumina.com/techniques/sequencing/rna-sequencing/ultra-low-input-single-cell-rna-seq.html]
- 80. Exome sequencing: the sweet spot before whole genomes [https://pmc.ncbi.nlm.nih.gov/articles/PMC2953745/]
- 81. Systematic dissection of biases in whole-exome and ... [https://www.nature.com/articles/s41598-020-59026-y]
- 82. Article Characterizing reduced coverage regions through ... [https://www.sciencedirect.com/science/article/pii/S1098360021018049]
- 83. A Survey of Computational Tools to Analyze and Interpret ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5192301/]
- 84. Whole exome sequencing of multi-regions reveals tumor ... [https://www.nature.com/articles/s41598-025-95142-3]
- 85. Bioinformatics Pipeline: DNA-Seq Analysis: Whole Exome and ... [https://docs.gdc.cancer.gov/Data/Bioinformatics_Pipelines/DNA_Seq_Variant_Calling_Pipeline/]
- 86. Retrospective evaluation of whole exome and genome ... [https://www.nature.com/articles/s41467-020-18151-y]
- 87. A Guide to Cancer Whole Exome Sequencing [https://www.cd-genomics.com/resource-a-guide-to-cancer-whole-exome-sequencing.html]
- 88. Benchmarking of bioinformatics tools for the hybrid de novo ... [https://www.sciencedirect.com/science/article/pii/S2001037025002867]
- 89. Bioinformatics Workflow of Whole Exome Sequencing [https://www.cd-genomics.com/bioinformatics-workflow-of-whole-exome-sequencing.html]
- 90. Multi-Perspective Quality Control of Illumina Exome Sequencing Data Using QC3 - PMC [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5755963/]
- 91. Advances in personalized medicine: translating genomic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12106117/]
- 92. Why quality control (QC) is performed for NGS testing [https://3billion.io/blog/why-quality-control-qc-is-performed-for-ngs-testing]
- 93. Comparative analysis of library preparation approaches for FFPE gene expression profiling and related recommendations | Scientific Reports [https://www.nature.com/articles/s41598-025-12992-7]
- 94. Next-generation sequencing outperforms Proactive ... [https://www.nature.com/articles/s44276-025-00145-2]
- 95. Detailed simulation of cancer exome sequencing data reveals differences and common limitations of variant callers - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC5209852/]
- 96. Toward best practice in cancer mutation detection with whole ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8506910/]
- 97. A Cautionary Note on Genomic Complexity and ... [https://www.sciencedirect.com/science/article/pii/S2949688825000358]
- 98. Exome sequencing identifies HELB as a novel ... [https://www.nature.com/articles/s41431-025-01786-0]
- 99. PrecisionFDA Truth Challenge V2: Calling variants from ... [https://www.sciencedirect.com/science/article/pii/S2666979X22000581]
- 100. Benchmarking of variant calling software for whole-exome sequencing using gold standard datasets - PubMed [https://pubmed.ncbi.nlm.nih.gov/40258889/]
- 101. A Simple Strategy for Reducing False Negatives in Calling Variants from Single-Cell Sequencing Data | PLOS One [https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0123789]
- 102. Orthogonal NGS for High Throughput Clinical Diagnostics [https://www.nature.com/articles/srep24650]
- 103. Best practices for the analytical validation of clinical whole- ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7585436/]
- 104. Genetic testing for Whole Exome [https://www.blueprintgenetics.com/tests/whole-exome-sequencing/whole-exome-we0501/]
- 105. Next-Generation Sequencing More Cost-Effective Than ... [https://oncpracticemanagement.com/issues/2018/august-2018-vol-8-no-8/next-generation-sequencing-more-cost-effective-than-single-gene-testing]
- 106. Improved Gene Fusion Detection in Childhood Cancer ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8830514/]
- 107. Diagnosis of fusion genes using targeted RNA sequencing [https://www.nature.com/articles/s41467-019-09374-9]
- 108. Fusion Gene Detection Using Whole-Exome Sequencing ... [https://www.frontiersin.org/journals/genetics/articles/10.3389/fgene.2022.820493/full]
- 109. Cancer Exome Sequencing | Insight into coding mutations [https://www.illumina.com/areas-of-interest/cancer/research/sequencing-methods/cancer-exome-seq.html]
- 110. Whole Exome vs. Whole Genome Sequencing [https://www.cd-genomics.com/resource-wes-and-wgs.html]
- 111. Press Release [https://www.carislifesciences.com/about/news-and-media/caris-life-sciences-demonstrates-scientific-rigor-with-clinical-validation-of-fda-approved-mi-cancer-seek/]
- 112. Cost-Effectiveness Analysis of Comprehensive Genomic ... [https://pubmed.ncbi.nlm.nih.gov/40701291/]
- 113. Genomic Profiling: Underused in Advanced Cancer, No ... [https://www.targetedonc.com/view/genomic-profiling-underused-in-advanced-cancer-no-added-cost-burden]
- 114. Cost-Effectiveness Analysis of Comprehensive Genomic ... [https://www.sciencedirect.com/science/article/abs/pii/S1525157825001655]
- 115. Exome sequencing and characterization of 49960 ... [https://www.nature.com/articles/s41586-020-2853-0]
- 116. Chromosome Karyotype Analysis Service Market Outlook ... [https://www.24lifesciences.com/chromosome-karyotype-analysis-service-market-8607]
- 117. Next-Generation Sequencing: A Review of Its Transformative ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12523276/]
- 118. Implementing Whole Genome Sequencing (WGS) in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10969765/]
- 119. Implementation of whole genome sequencing in cancer ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12460206/]
- 120. Best practices for the interpretation and reporting of clinical ... [https://www.nature.com/articles/s41525-022-00295-z]
- 121. A benchmarking framework for the accurate and cost-effective ... [https://translational-medicine.biomedcentral.com/articles/10.1186/s12967-024-04865-w]
- 122. Ultra-deep multi-oncopanel sequencing of benchmarking ... [https://www.nature.com/articles/s41597-022-01359-6]