Strategic Training Set Selection in Ligand-Based Pharmacophore Modeling: A Guide for Robust Virtual Screening and Hit Identification
Ligand-based pharmacophore modeling is a cornerstone of computer-aided drug design, particularly for targets with unknown 3D structures.
Strategic Training Set Selection in Ligand-Based Pharmacophore Modeling: A Guide for Robust Virtual Screening and Hit Identification
Abstract
Ligand-based pharmacophore modeling is a cornerstone of computer-aided drug design, particularly for targets with unknown 3D structures. The predictive power and success of these models are critically dependent on the strategic selection of the training set compounds used for their generation. This article provides a comprehensive guide for researchers and drug development professionals on the best practices for assembling effective training sets. We explore the foundational principles of chemical diversity and feature representation, detail methodological approaches for sourcing and curating 2D and 3D ligand data, address common challenges and optimization strategies using both classical and modern machine learning techniques, and finally, outline rigorous validation and comparative analysis protocols to assess model performance. By synthesizing current methodologies and emerging trends, this guide aims to equip scientists with the knowledge to build highly predictive pharmacophore models that accelerate lead discovery.
Laying the Groundwork: Core Principles of Chemical Diversity and Feature Representation
Core Concept and Feature Definitions
What is a pharmacophore and what are its essential features?
A pharmacophore is an abstract description of molecular features necessary for molecular recognition of a ligand by a biological macromolecule. According to the International Union of Pure and Applied Chemistry (IUPAC), it is "an ensemble of steric and electronic features that is necessary to ensure the optimal supramolecular interactions with a specific biological target and to trigger (or block) its biological response" [1] [2]. It does not represent a real molecule or specific functional groups, but rather the common molecular interaction capacities of a group of compounds toward their target structure [2].
The table below summarizes the essential steric and electronic features that constitute a pharmacophore model:
Table 1: Essential Pharmacophore Features and Their Descriptions
| Feature Type | Description | Chemical Groups Examples |
|---|---|---|
| Hydrogen Bond Acceptor (HBA) | Atom that can accept a hydrogen bond through lone pair electrons | Carboxyl, carbonyl, ether oxygen |
| Hydrogen Bond Donor (HBD) | Atom with hydrogen that can donate a bond to an acceptor | Hydroxyl, primary amine, amide NH |
| Hydrophobic (H) | Non-polar regions that favor lipid environments | Alkyl chains, cycloalkanes, steroidal skeletons |
| Aromatic (ARO) | Planar ring systems with delocalized π-electrons | Phenyl, pyridine, fused aromatic rings |
| Positively Ionizable (PI) | Groups that can carry or develop positive charge | Primary, secondary, tertiary amines |
| Negatively Ionizable (NI) | Groups that can carry or develop negative charge | Carboxylic acid, phosphate, sulfate |
| Exclusion Volumes (XVOL) | Spatial regions occupied by the receptor that ligands must avoid | Defined areas representing protein atoms |
These features ensure optimal supramolecular interactions with specific biological targets [3] [2]. A well-defined pharmacophore model includes both hydrophobic volumes and hydrogen bond vectors to represent the key interactions between a ligand and its receptor [1].
Troubleshooting Guides: Training Set Selection
FAQ: What are the common challenges in training set selection for ligand-based pharmacophore modeling?
Challenge 1: Inadequate structural diversity in training set
- Problem: Training set compounds are too structurally similar, resulting in a pharmacophore model that is too specific to recognize novel chemotypes.
- Solution: Select a structurally diverse set of molecules that will be used for developing the pharmacophore model. The set should include both active and inactive compounds to ensure the model can discriminate between molecules with and without bioactivity [1] [4].
- Validation: Use clustering methods like Butina clustering with 2D pharmacophore fingerprints to ensure representative diversity [4].
Challenge 2: Insufficient coverage of activity range
- Problem: Training set compounds have limited activity range, reducing model predictability.
- Solution: Include compounds across the entire activity spectrum (highly active, moderately active, and inactive) categorized by IC₅₀ values:
- Most active: <0.1 μM
- Active: 0.1 μM to 1.0 μM
- Moderately active: 1.0 μM to 10.0 μM
- Inactive: >10.0 μM [5]
- Validation: Ensure statistical relevance by including a maximum number of active compounds along with few moderately active and inactive compounds [5].
Challenge 3: Inconsistent biological data
- Problem: Biological activities collected from different assay conditions or cell lines introduce noise.
- Solution: Use biological data obtained from homogeneous procedures against a single biological target or cell line [5].
- Validation: Confirm all experimental inhibitory activities were collected using the same biological assays and assessment methods [5].
Challenge 4: Improper conformational sampling
- Problem: Inadequate representation of possible low-energy conformations leads to incorrect bioactive conformation identification.
- Solution: Generate a set of low energy conformations that is likely to contain the bioactive conformation for each molecule. Use algorithms that sample conformational space extensively (up to 100 conformers per molecule within a 50 kcal/mol energy window) [1] [4].
- Validation: Apply poling techniques or Monte Carlo sampling to promote conformational variation and avoid bias toward folded structures [6].
Experimental Protocols
Detailed Methodology: Ligand-Based Pharmacophore Modeling with 3D-QSAR
This protocol outlines the generation of a quantitative pharmacophore model using the HypoGen algorithm for Topoisomerase I inhibitors, as demonstrated in published research [5].
Phase 1: Training and Test Set Preparation
- Data Compilation: Collect 62 camptothecin derivatives with experimental IC₅₀ values determined against A549 cancer cell lines under consistent assay conditions [5].
- Activity Categorization:
- Classify compounds into four activity categories based on IC₅₀ values
- Distribute compounds to ensure all chemical substitution patterns are represented
- Training Set Selection: Select 29 diverse compounds spanning the activity range (IC₅₀ 0.003 μM to 11.4 μM) representing different structural classes [5].
- Test Set Selection: Use remaining 33 compounds for model validation [5].
Phase 2: Compound Preparation and Conformational Analysis
- 2D Structure Drawing: Draw molecular structures using ChemDraw Ultra [5].
- 3D Conversion and Optimization: Convert to 3D structures using Discovery Studio and optimize with CHARMM force fields [5].
- Energy Minimization: Apply smart minimizer with 2000 steps of steepest descent followed by conjugate gradient algorithms [5].
- Conformer Generation: Generate up to 100 conformers per compound within a 50 kcal/mol energy window using an MMFF94 force field to ensure extended structures are represented [4].
Phase 3: Pharmacophore Model Generation
- Feature Mapping: Identify common pharmacophore features using HypoGen algorithm in Discovery Studio [5].
- Model Construction: Develop pharmacophore hypotheses containing 4-5 features with specific spatial relationships [4].
- Model Selection: Select the best model (Hypo1) based on statistical correlation between estimated and experimental activity (correlation coefficient: 0.917678 for training set) [5].
Phase 4: Model Validation
- Test Set Validation: Validate model with 33 test set compounds (correlation coefficient: 0.874718) [5].
- Fisher Validation: Apply Fisher's randomization test to confirm model robustness [5].
- Cost Analysis: Evaluate hypothesis cost difference between null and generated models [5].
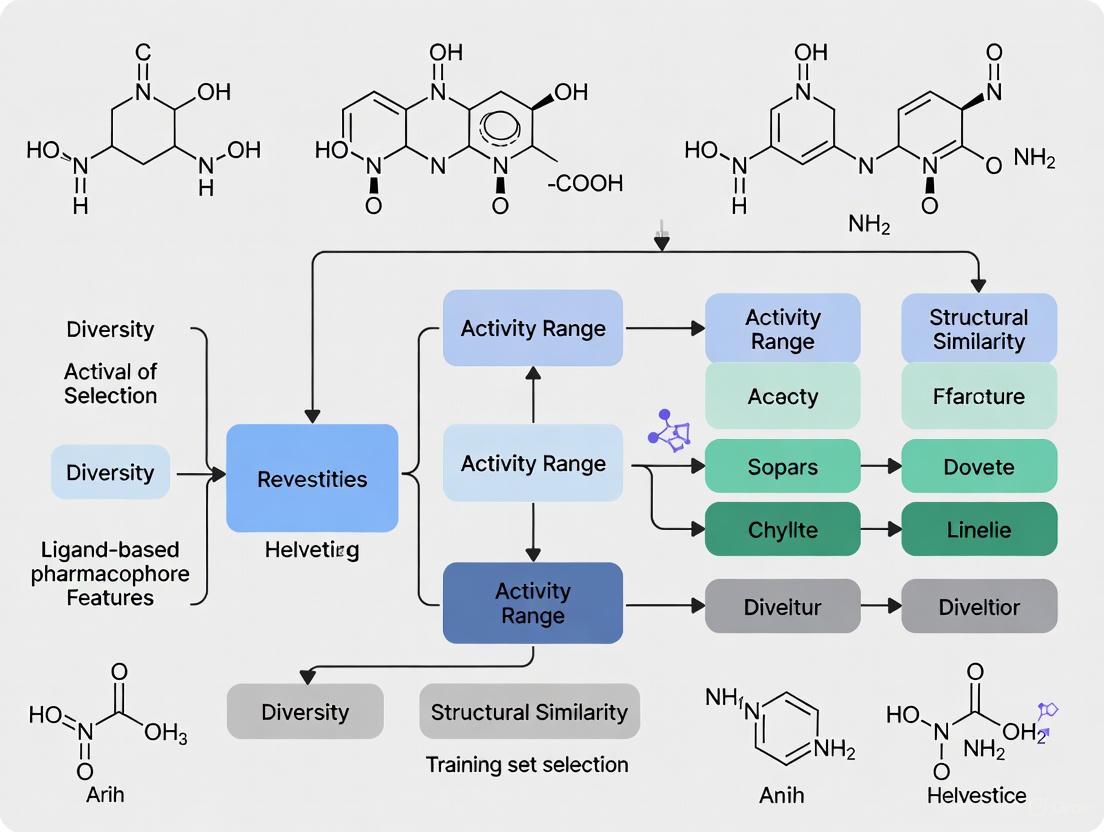
Workflow: Ligand-Based Pharmacophore Modeling
Advanced Applications and Recent Advances
FAQ: How can pharmacophore models be applied in virtual screening and what are recent advances?
Virtual Screening Applications:
- Database Filtering: Use validated pharmacophore models as 3D queries to screen large chemical databases (e.g., ZINC database with >1 million compounds) [5] [3].
- Multi-step Screening: Implement sequential filters including Lipinski's Rule of Five, SMART functional group filtration, and activity-based filtration (e.g., estimated activity <1.0 μM) [5].
- Scaffold Hopping: Identify novel chemotypes that share essential interaction features but have different molecular frameworks from known actives [6].
Recent Methodological Advances:
- Multiple Binding Pose Integration: Develop comprehensive pharmacophore maps that incorporate multiple protein-ligand complexes to account for binding pocket flexibility [6] [7].
- Dynamic Pharmacophores: Create models that represent dynamic biological space by incorporating protein flexibility and multiple receptor conformations [6].
- Complex-Based Modeling: Generate pharmacophores from structural data of multiple protein-ligand complexes rather than single structures [8].
- Hybrid Approaches: Combine ligand-based and structure-based methods, particularly for targets with high binding pocket flexibility like nuclear hormone receptors [7].
Table 2: Quantitative Virtual Screening Results from Published Study [5]
| Screening Stage | Number of Compounds | Filtering Criteria |
|---|---|---|
| Initial ZINC Database | 1,087,724 | All drug-like molecules |
| After Lipinski's Rule of Five | 312,451 | MW ≤500, ClogP <10, HBD ≤8, HBA ≤10 |
| After SMART Filtration | 98,637 | Remove compounds with undesirable functionalities |
| After Activity Filtration (≤1.0 μM) | 4,218 | Estimated activity based on pharmacophore model |
| After Molecular Docking | 6 | Binding energy and interaction analysis |
| After Toxicity Assessment | 3 | TOPKAT program prediction |
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Computational Tools for Pharmacophore Modeling
| Tool/Resource | Type | Primary Function | Application in Training Set Selection |
|---|---|---|---|
| Discovery Studio | Software Platform | 3D QSAR pharmacophore generation (HypoGen) | Training set compound selection and model validation [5] |
| Phase | Software Module | Pharmacophore perception, 3D QSAR development | Common feature identification and hypothesis generation [1] [6] |
| LigandScout | Software Application | Structure-based and ligand-based pharmacophore modeling | Feature mapping and 3D pharmacophore visualization [8] |
| RDKit | Open-Source Cheminformatics | 2D pharmacophore fingerprint calculation | Compound clustering and diverse representative selection [4] |
| ZINC Database | Compound Library | >1 million commercially available compounds | Virtual screening for novel bioactive molecules [5] |
| CHARMM/MMFF94 | Force Fields | Molecular mechanics energy minimization | Conformational analysis and geometry optimization [5] [4] |
| Protein Data Bank (PDB) | Structural Database | Experimental 3D structures of macromolecules | Structure-based pharmacophore development [8] [3] |
Workflow: Training Set Selection Strategy
The Critical Role of Training Set Composition in Model Accuracy and Generalizability
FAQs: Troubleshooting Training Set Issues in Pharmacophore Modeling
Q1: My pharmacophore model retrieves many inactive compounds during virtual screening. What could be wrong with my training set?
This is typically a issue of specificity. Your training set likely lacks sufficient chemical diversity or does not properly distinguish features essential for binding from those that are not.
- Solution: Re-evaluate your training set composition. Incorporate structurally diverse active compounds and include confirmed inactive compounds in your model validation process. Using a decoy set like DUD-E for validation helps calculate enrichment factors and assess the model's ability to reject inactives [9] [10].
Q2: The generated model fits the training compounds perfectly but fails to identify new active scaffolds. How can I improve its generalizability?
This indicates overfitting. The model has memorized the specific patterns of your training molecules rather than learning the general interaction pattern required for activity.
- Solution: Ensure your training set includes compounds with multiple, distinct chemical scaffolds (scaffold hopping) while maintaining high biological activity. A good training set should represent the "essential features" common across different chemotypes [9] [6]. Avoid using too many highly similar compounds.
Q3: What are the critical data quality requirements for ligands in a training set?
The quality of your input data directly dictates the quality of your pharmacophore model.
- Activity Data: Use only compounds whose activity has been experimentally proven via target-specific assays (e.g., receptor binding or enzyme activity assays on isolated proteins). Avoid data from cell-based assays for model generation, as effects may be influenced by factors like permeability, which confounds the direct structure-activity relationship [9].
- Conformational Sampling: Generate a representative, energy-optimized set of conformations for each training compound to ensure the bioactive conformation is adequately sampled [10].
Experimental Protocols & Best Practices
Protocol for Designing a Robust Training Set
This protocol outlines the steps for assembling a training set for ligand-based pharmacophore generation.
Data Curation and Selection
- Source Data: Collect a set of known active compounds from reliable sources like ChEMBL [9], literature, or in-house databases.
- Activity Criteria: Define a clear activity cut-off (e.g., IC50 < 100 nM) to ensure all selected compounds are potently active [9].
- Structural Diversity: Perform clustering based on molecular fingerprints (e.g., ECFP4) [11] or Bemis-Murcko scaffolds [11] to ensure the set covers multiple chemotypes. Select representative compounds from different clusters.
Conformation Generation
- Software: Use tools like CONFGENX [12] or the Conformation Generation protocol in Discovery Studio [10].
- Parameters: Generate a comprehensive set of conformers using the "Maximum Conformations" method (e.g., 255 conformers) with a reasonable energy threshold (e.g., 20 kcal/mol above the global minimum) [10]. This ensures broad coverage of the conformational space.
Model Generation and Validation
- Hypothesis Generation: Use the generated conformers and the curated active compound set in pharmacophore generation software (e.g., HypoGen in Discovery Studio [13] [10]).
- Validation with Decoys: Validate the initial model using a database containing known active compounds and property-matched decoys (e.g., from DUD-E [9]). Calculate validation metrics like the Güner-Henry (GH) score and Enrichment Factor (EF) [14] [15].
Case Study: Workflow for a Selective CA IX Inhibitor Model
The following diagram illustrates a documented successful implementation of these principles.
Key Steps from the Case Study [14]:
- Training Set: Seven chemically diverse compounds with proven CA IX inhibition and IC50 values below 50 nM were selected.
- Model Generation: Twenty hypotheses were generated in MOE software. The top model,
Ph4.ph4, consisted of four features: two aromatic hydrophobic centers (Aro/Hyd) and two hydrogen bond donor/acceptors (Don/Acc). - Validation: The model was validated against an external decoy set from the DUD-E server, confirming its ability to distinguish active from inactive compounds (high sensitivity and specificity). This validated model was subsequently used for successful virtual screening.
Data Presentation: Composition of Validated Training Sets from Literature
The table below summarizes the composition of training sets from published studies that led to successful pharmacophore models.
| Study / Target | Training Set Size & Composition | Key Diversity Consideration | Validation Outcome & Application |
|---|---|---|---|
| Selective CA IX Inhibitors [14] | 7 compounds with IC₅₀ < 50 nM. | Chemically diverse scaffolds selected from literature. | Model validated with DUD-E decoys. Successfully applied in virtual screening to identify novel hits. |
| Akt2 Inhibitors [10] | 23 compounds for 3D-QSAR model. Activity spans 5 orders of magnitude. | Training set activity covers a wide range (5 orders of magnitude). | Model validated by test set (40 compounds) and decoy set. Used to find novel scaffolds from large databases. |
| Topoisomerase I Inhibitors [13] | 29 camptothecin derivatives as training set. | Based on a single scaffold with derivative variations. | The model (Hypo1) was used for virtual screening of over 1 million ZINC compounds, identifying novel potential inhibitors. |
| DiffPhore (General Method) [11] | Two complementary datasets: CpxPhoreSet (15,012 pairs from complexes) & LigPhoreSet (840,288 pairs from diverse ligands). | LigPhoreSet built from 280k representative ligands via scaffold filtering & clustering for maximum chemical diversity [11]. | Used for training a deep learning model. Outperformed traditional tools in binding conformation prediction and virtual screening. |
This table lists key computational tools and data resources critical for training set composition and pharmacophore modeling.
| Resource Name | Type | Primary Function in Training Set Design |
|---|---|---|
| ChEMBL [9] | Database | Public repository of bioactive molecules with curated bioactivity data, used for sourcing potential training set compounds. |
| DUD-E [9] | Database | Directory of Useful Decoys: Enhanced; provides property-matched decoy molecules for rigorous model validation. |
| ZINC [11] [13] | Database | A large database of commercially available compounds, often used as a source for virtual screening and for building diverse ligand sets. |
| RDKit [16] | Software | Open-source cheminformatics toolkit used for fingerprint generation, molecular clustering, and descriptor calculation. |
| MOE (Molecular Operating Environment) [14] | Software | Integrated software for QSAR, pharmacophore modeling, and hypothesis generation. |
| Discovery Studio [13] [10] | Software | Software suite for biomolecular modeling, includes protocols for 3D-QSAR pharmacophore generation (HypoGen) and model validation. |
Strategies for Ensuring Broad Chemical Diversity and Representativeness
Core Concepts and Importance
Why is ensuring chemical diversity in a training set critical for pharmacophore modeling?
A training set with broad chemical diversity is fundamental to developing a robust and predictive pharmacophore model. A diverse set of active ligands helps ensure the resulting model captures the essential, shared chemical features responsible for biological activity, rather than overfitting to the specific structural motifs of a narrow compound series [4]. This improves the model's ability to identify novel active chemotypes through virtual screening, a process known as scaffold hopping [17].
Conversely, a training set with limited diversity can lead to a pharmacophore hypothesis that is too specific, causing you to miss potent compounds with different structural backbones during virtual screening [18]. Comprehensive diversity analysis typically employs multiple molecular representations—such as molecular scaffolds, structural fingerprints, and physicochemical properties—to provide a complete picture of the "global diversity" of a compound library [19].
Practical Implementation Strategies
What are the primary strategies for selecting a diverse training set?
Two main strategies for training set selection are used, depending on the assumptions about the binding modes of the active compounds.
Table 1: Training Set Selection Strategies
| Strategy | Assumption | Methodology | Best For |
|---|---|---|---|
| Strategy I: Single Binding Mode [4] | All active compounds share the same binding mode. | - Cluster active and inactive compounds separately using 2D pharmacophore fingerprints. [4]- Select cluster centroids to represent the chemical space of both actives and inactives. | Congeneric series of ligands with a common core structure. |
| Strategy II: Multiple Binding Modes [4] | Active compounds may have different binding modes. | - Cluster active and inactive compounds jointly. [4]- From each cluster, randomly select active and inactive compounds for the training set.- Create multiple training sets to account for binding mode variability. | Diverse ligand sets with potentially different binding orientations or for targets with multiple binding pockets. |
How do I measure and analyze the chemical diversity of my compound set?
You should assess diversity using multiple, complementary metrics to get a holistic view. The Consensus Diversity Plot (CDP) is a novel method that visualizes global diversity by combining several criteria into a single, two-dimensional graph [19].
Table 2: Key Metrics for Assessing Chemical Diversity
| Representation | Metric | Description | Interpretation |
|---|---|---|---|
| Molecular Scaffolds [19] | Cyclic System Recovery (CSR) Curves | Plots the cumulative fraction of compounds recovered against the fraction of scaffolds used. | A steeper curve indicates lower diversity (few scaffolds account for many compounds). |
| Area Under the Curve (AUC) / F50 | AUC of the CSR curve; F50 is the fraction of scaffolds needed to recover 50% of the database. | Low AUC or High F50 indicates high scaffold diversity. [19] | |
| Scaled Shannon Entropy (SSE) | Measures the uniformity of compound distribution across different scaffolds. | Ranges from 0 (min diversity) to 1 (max diversity). [19] | |
| Structural Fingerprints [19] | Tanimoto Similarity | Calculates pairwise molecular similarity using fingerprints like MACCS keys or ECFP_4. | A lower average pairwise similarity indicates higher diversity in the overall molecular structure. |
| Physicochemical Properties [19] | Euclidean Distance in Property Space | Measures distance between compounds based on properties like Molecular Weight, logP, HBD, HBA, etc. | A wider spread of compounds in this space indicates greater diversity in drug-like properties. |
The following diagram illustrates the logical workflow for selecting a training set and assessing its diversity, integrating the strategies and metrics outlined above:
Troubleshooting Common Issues
What should I do if my pharmacophore model is too specific and fails to find novel scaffolds?
This is a classic sign of a training set with insufficient chemical diversity.
- Problem: The model is overfitting to specific chemical structures present in the training actives.
- Solution:
- Re-evaluate Your Training Set: Use a CDP or the metrics in Table 2 to check the scaffold and fingerprint diversity of your actives. If the AUC is high and F50 is low, your set is likely dominated by a few common scaffolds [19].
- Incorporate Structurally Diverse Actives: Seek out active compounds with different molecular frameworks from the literature or databases to broaden the chemical space represented in your training set.
- Use a Generative Model: Consider using pharmacophore-informed generative models like TransPharmer. These models can use the pharmacophore fingerprints of your actives to generate novel, structurally distinct compounds that still possess the necessary pharmacophoric features, effectively performing in silico scaffold hopping [17].
How can I avoid artificial enrichment and ensure my model distinguishes true actives from decoys?
This involves careful selection of both active and inactive compounds in your training set.
- Problem: The model appears to perform well in validation but fails in real-world screening because it is not specific enough.
- Solution:
- Use Challenging Decoys: When building your training set, include inactive compounds or decoys that are physiochemically similar to your actives but topologically different. Databases like DUD-E (Database of Useful Decoys: Enhanced) are designed for this purpose, providing decoys with similar 1D properties but different 2D topology, which helps avoid artificial enrichment during screening [20].
- Strategic Inactive Selection: When applying Training Set Strategy II, ensure that inactive compounds from joint clustering are included to better represent the chemical space of inactives and improve the model's precision [4].
Table 3: Key Software and Resources for Diversity Analysis and Pharmacophore Modeling
| Tool Name | Type | Primary Function in Diversity/Pharmacophore Modeling |
|---|---|---|
| Schrödinger Phase [20] | Commercial Software Suite | Develop pharmacophore hypotheses from ligand sets; create Phase databases for virtual screening. |
| RDKit [4] | Open-Source Cheminformatics | Calculate 2D pharmacophore fingerprints; generate molecular conformers; perform clustering. |
| Molecular Operating Environment (MOE) [19] | Commercial Software Suite | Curate compound data; calculate physicochemical properties (HBD, HBA, logP, MW). |
| MEQI (Molecular Equivalent Indices) [19] | Software Tool | Conduct scaffold diversity analysis by deriving and naming molecular chemotypes. |
| MayaChemTools [19] | Open-Source Toolkit | Calculate structural fingerprints (e.g., MACCS keys) for pairwise diversity analysis. |
| ZINCPharmer [21] | Online Database/Tool | Perform pharmacophore-based virtual screening of the ZINC compound database. |
| DUD-E [20] | Database | Access decoy molecules for rigorous validation of virtual screening methods. |
Balancing Active and Inactive Compounds to Enhance Model Selectivity
Frequently Asked Questions (FAQs)
FAQ 1: Why is it critical to include inactive compounds in my training set for pharmacophore modeling?
Including inactive compounds, or decoys, is essential for validating the selectivity of your pharmacophore model. A model developed only from active compounds might identify common chemical features but cannot distinguish whether these features are truly responsible for biological activity or are merely common to the chemical scaffold. Using a set of confirmed inactive compounds or property-matched decoys during validation allows you to test and refine your model to discriminate between binders and non-binders, thereby enhancing its predictive accuracy and reducing false positives in virtual screening [22].
FAQ 2: What are the best sources for obtaining reliable decoy compounds?
Two highly recognized sources for decoy compounds are:
- DUD-E (Directory of Useful Decoys: Enhanced): This is a widely used database specifically designed for benchmarking virtual screening methods. It contains a large collection of decoys that are chemically similar but topologically different from active ligands, ensuring they are physically plausible but chemically distinct [23] [22] [12].
- ZINC Database: A curated collection of commercially available chemical compounds. It can be used to select decoys or to screen for new potential hits after you have built and validated your model [21] [22].
FAQ 3: How can I quantitatively measure the selectivity of my pharmacophore model?
The selectivity and performance of a pharmacophore model are quantitatively assessed using specific metrics derived from validation tests. Key metrics include the Enrichment Factor (EF) and the Area Under the Curve (AUC) of a Receiver Operating Characteristic (ROC) curve [23] [22].
- Enrichment Factor (EF): Measures how much more likely you are to find active compounds at the top of a ranked list compared to a random selection. A higher EF indicates better model performance [23].
- Area Under the Curve (AUC): The AUC value summarizes the model's ability to distinguish between active and inactive compounds. An AUC value of 1.0 represents a perfect model, while 0.5 represents a model with no discriminative power. An excellent model should have an AUC value close to 1.0 [22].
Table 1: Key Performance Metrics for Pharmacophore Model Validation
| Metric | Description | Ideal Value | Interpretation |
|---|---|---|---|
| Enrichment Factor (EF) | The concentration of active compounds found in a top fraction of the screening hits versus a random distribution [23]. | >1 (Higher is better) | Measures the model's efficiency in enriching true hits. |
| Area Under the Curve (AUC) | The area under the Receiver Operating Characteristic (ROC) curve, which plots the true positive rate against the false positive rate [22]. | 1.0 (Perfect classifier) | Evaluates the model's overall ability to discriminate actives from inactives. |
FAQ 4: My model has high sensitivity but poor specificity. What could be the cause and how can I fix it?
This issue often arises when a model is over-fitted. It means the model is too specifically tuned to the exact features and conformations of your training actives, so it fails to recognize other legitimate active chemotypes and misclassifies many inactives as hits.
- Cause: Using a training set that is too small or lacks sufficient chemical diversity among the active compounds.
- Solution:
- Increase Diversity: Incorporate active compounds with different chemical scaffolds that are known to bind the same target [3].
- Feature Refinement: Re-evaluate the pharmacophore features. You may have included non-essential features. Try to identify and retain only the features that are critical for binding, often by analyzing the receptor-ligand complex if structural data is available [3] [24].
- Use Exclusion Volumes: Incorporate exclusion volumes (also known as forbidden volumes) into the model to represent steric hindrance in the binding pocket, which helps rule out compounds that would clash with the receptor [3] [11].
Troubleshooting Guides
Problem: Low Enrichment Factor during Virtual Screening Your model retrieves many compounds, but the hit rate of true actives is not significantly better than random selection.
Potential Cause 1: Non-discriminative Pharmacophore Features The defined features (e.g., hydrogen bond donors/acceptors, hydrophobic areas) are too common and do not represent the unique characteristics required for binding.
Potential Cause 2: Improperly Matched Decoy Set The decoys used for validation are not well-matched to the actives, making separation trivial or impossible.
Potential Cause 3: Inadequate Model Validation The model was not rigorously tested before application.
- Solution: Always run an internal validation using a test set with known actives and inactives. Calculate the EF and AUC metrics to objectively assess the model's performance before proceeding to screen large, unknown databases [22].
Problem: Model Fails to Identify Known Active Compounds The model is too restrictive and misses compounds that are confirmed to be active.
Potential Cause 1: Overly Rigid Conformational Sampling The model does not account for the flexibility of the ligand or the necessary tolerance in feature positioning.
- Solution: Increase the conformational flexibility allowed during the screening process. Ensure the energy threshold for generated conformers is sufficient to cover potential bioactive conformations [24].
Potential Cause 2: Missing Key Pharmacophore Features The model may be lacking a critical feature that is present in the missed active compounds.
- Solution: Revisit your set of active ligands. Look for common features that were initially overlooked. Using a larger and more diverse set of active compounds for model generation can help capture all essential features [25].
Potential Cause 3: Excessive Exclusion Volumes The use of exclusion volumes might be too extensive, sterically blocking valid active compounds from fitting the model.
- Solution: Re-evaluate the placement and radius of exclusion volumes based on the 3D structure of the binding pocket. Consider using a softer scoring function for steric clashes [12].
Experimental Protocols
Protocol 1: Validating a Pharmacophore Model Using a Decoy Set
This protocol outlines the steps to assess the selectivity and predictive power of your pharmacophore model.
- Obtain a Validation Set: Compile a set of known active compounds and a set of decoy compounds (e.g., from DUD-E) [22].
- Combine and Screen: Merge the active and decoy sets into a single database. Screen this database against your pharmacophore model.
- Rank Results: Rank the screening results based on the "fit value" or how well each compound matches the model.
- Generate ROC Curve: Plot a ROC curve with the True Positive Rate (fraction of found actives) against the False Positive Rate (fraction of found decoys) across the ranked list [22].
- Calculate Metrics:
- Interpret Results: A high AUC and EF indicate a model that can successfully distinguish active from inactive compounds.
The following workflow visualizes the key steps in the pharmacophore model validation process:
Protocol 2: Building a Selective Ligand-Based Pharmacophore Model
This methodology is adapted from successful studies that identified novel inhibitors [21] [25].
- Curation of Active Ligands: Collect a set of 5-10 known active ligands with potent activity (e.g., IC50 < 50 nM). It is crucial that these ligands are structurally diverse to avoid bias and to ensure the model captures essential features and not just a single scaffold [21] [25].
- Conformational Analysis: Generate multiple low-energy conformations for each active ligand to account for flexibility.
- Pharmacophore Generation: Use software like
MOEorPharmaGistto generate multiple pharmacophore hypotheses by aligning the active conformers and identifying common steric and electronic features [23] [25]. - Hypothesis Scoring: Select the top-ranked hypothesis based on the software's scoring algorithm, which often considers the alignment of features and the volume overlap of the ligands.
- Validation with Inactives: Test the selected hypothesis using the validation protocol described above (Protocol 1) before proceeding to virtual screening.
Table 2: Checklist for Building a Selective Training Set
| Step | Action | Best Practice Tip |
|---|---|---|
| 1. Select Actives | Choose compounds with confirmed high potency. | Aim for chemical and scaffold diversity, not just high potency [25]. |
| 2. Select Inactives | Choose property-matched decoys. | Use established databases like DUD-E to ensure decoys are matched on molecular weight, logP, etc., but are topologically distinct [22]. |
| 3. Model Generation | Generate multiple hypotheses from actives. | Use a sufficient number of active compounds (e.g., 7-10) to capture core features without over-complicating the model [25]. |
| 4. Model Validation | Test the model with the active/inactive set. | Use quantitative metrics (AUC, EF) for an objective assessment. Do not proceed to screening without this step [22]. |
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Tools for Pharmacophore Modeling and Validation
| Tool / Reagent | Function | Example Use in Experiment |
|---|---|---|
| DUD-E Database | A database of useful decoys for benchmarking virtual screening. | Serves as a source of rigorously matched inactive compounds for validating model selectivity [22] [12]. |
| ZINC Database | A public resource of commercially available compounds for virtual screening. | Used as a compound library for virtual screening after a validated pharmacophore model is obtained [21]. |
| MOE (Molecular Operating Environment) | A comprehensive software suite for molecular modeling. | Used for ligand-based pharmacophore generation, hypothesis scoring, and database searching [25]. |
| LigandScout | Software for structure- and ligand-based pharmacophore modeling. | Used to create structure-based pharmacophores from protein-ligand complexes and to perform advanced virtual screening [23] [22]. |
| ROC Curve Analysis | A graphical plot for evaluating classifier performance. | The primary method for visualizing and quantifying a model's ability to discriminate between active and inactive compounds [22]. |
Sourcing High-Quality Bioactivity Data from Public Databases (ChEMBL, PubChem)
In ligand-based pharmacophore modeling, the quality of your training set dictates the success of your entire research endeavor. Pharmacophores serve as abstractions of essential chemical interaction patterns, holding an irreplaceable position in drug discovery [26] [11]. These models rely on accurate bioactivity data and compound structures to identify the spatial arrangement of molecular features responsible for biological activity. The foundational principle is simple yet powerful: compounds sharing similar activity against a biological target likely share common pharmacophoric elements. However, this principle collapses when built upon unreliable data, leading to models that cannot distinguish true actives from inactives or accurately predict new lead compounds.
Public databases like ChEMBL and PubChem contain immense volumes of bioactivity data, but this data varies significantly in quality, consistency, and applicability. The challenge for researchers is not merely accessing this data, but implementing robust methodologies to curate high-quality training sets specifically optimized for pharmacophore development. This technical support center addresses the most critical issues researchers encounter during this process and provides proven solutions to ensure your pharmacophore models stand on a foundation of rigorously validated data.
Database Fundamentals: ChEMBL and PubChem Compared
Key Characteristics and Applications
Table 1: Comparison of Major Bioactivity Databases
| Feature | ChEMBL | PubChem |
|---|---|---|
| Primary Focus | Manually curated bioactive molecules with drug-like properties [27] | Largest repository of bioactivity data from high-throughput screens [28] |
| Data Curation | Extensive manual curation with standardized data ontologies [27] [29] | Automated processing with varying levels of curation |
| Bioactivity Types | IC₅₀, Ki, EC₅₀, etc., with standardized units and relationships [30] | Diverse assay results including inhibition, activation, and phenotypic outcomes [28] |
| Target Coverage | Comprehensive protein target annotation with ChEMBL IDs [30] | Broad target coverage including gene-based assays |
| Best Applications | Lead optimization, target fishing, structured QSAR studies [26] [30] | Virtual screening, hit identification, chemical biology exploration [28] |
Data Quality Framework for Pharmacophore Modeling
The following diagram illustrates the critical pathway for transforming raw database records into a curated training set suitable for pharmacophore modeling:
Diagram 1: Data curation workflow for pharmacophore research.
Troubleshooting Guides and FAQs
Data Extraction and Query Issues
Q1: My SQL query on the local ChEMBL database is running extremely slowly when retrieving activity data for specific target classes. How can I optimize performance?
A: Implement targeted query optimization with proper indexing and query structure:
- Use Appropriate Joins: Ensure you're using efficient JOIN structures with properly indexed columns. The
molregnofield is typically well-indexed and should be used for joining tables [30]. - Filter Early: Apply filters as early as possible in your query to reduce the dataset size before complex operations.
- Leverage Local Installation: For large-scale analyses, a local installation of the ChEMBL SQL database significantly improves performance compared to web services [31].
Example Optimized Query:
Q2: I'm unable to retrieve consistent bioactivity data from PubChem for a specific assay (AID). The results seem incomplete or poorly standardized. What validation steps should I implement?
A: PubChem data requires rigorous standardization due to variations in experimental protocols and reporting formats [28]:
- Batch Processing: Use the PUG-REST API with appropriate batching to avoid retrieval limits and ensure complete data downloads [28].
- Outcome Interpretation: Carefully interpret the 'Outcome' field (1: Inactive, 2: Active, 3: Inconclusive, 4: Unspecified, 5: Probe) and filter accordingly [28].
- Unit Standardization: Pay close attention to measurement unit codes (e.g., 5: µM, 6: nM) and convert all values to consistent units before analysis [28].
- Cross-Validation: When possible, validate key findings against ChEMBL data for the same compounds and targets.
Data Standardization and Curation Challenges
Q3: How should I handle salts, mixtures, and stereochemistry when extracting compounds from ChEMBL for pharmacophore modeling?
A: Implement a multi-step standardization protocol:
- Parent Compound Identification: Use the
molecule_hierarchytable to identify parent compounds and avoid counting salts as distinct molecules [30]. - Stereochemistry Awareness: Preserve stereochemical information when available, as it critically impacts pharmacophore feature geometry.
- Salt Stripping: Remove counterions and salts to focus on the active pharmaceutical ingredient while documenting the original structure for reproducibility.
Example Salt Handling Query:
Q4: What criteria should I use to select high-confidence activity data from public databases for pharmacophore training sets?
A: Establish rigorous inclusion criteria based on measurement quality and experimental context:
- Measurement Type Preference: Prioritize direct binding measurements (Ki, IC₅₀) over functional assays (EC₅₀) for pharmacophore modeling [30].
- Relationship Filtering: Include only activities with
standard_relation = '='to avoid inequality relationships that complicate modeling [30]. - Unit Consistency: Convert all activity values to consistent units (nM recommended) before analysis.
- Threshold Application: Implement activity thresholds relevant to your research context (e.g., < 1 µM for actives, > 10 µM for inactives).
- Assay Validation: Prefer assays with clear experimental descriptions and appropriate controls.
Pharmacophore-Specific Data Preparation
Q5: How many compounds and what activity range should I include in a training set for robust pharmacophore model generation?
A: The optimal training set balances quantity, quality, and diversity:
- Compound Count: Include 20-50 well-curated compounds with measured activities spanning at least 3 orders of magnitude (e.g., 1 nM to 1 µM) [21].
- Structural Diversity: Ensure chemical diversity while maintaining common pharmacophoric features; include multiple scaffold classes when possible.
- Activity Spread: Include both high-affinity and low-affinity compounds to help distinguish essential features from optional ones.
- Reference Studies: In successful implementations like fluoroquinolone antibiotic pharmacophore modeling, researchers used 4 known antibiotics to generate a shared feature pharmacophore map, then validated against 25 hit compounds from virtual screening [21].
Q6: What molecular features should I prioritize when annotating compounds for pharmacophore modeling, and how can I extract this information efficiently?
A: Focus on chemically meaningful interaction features that directly participate in target binding:
- Core Feature Types: Hydrogen-bond donors (HBD), hydrogen-bond acceptors (HBA), hydrophobic areas (HYD), aromatic rings (AR), charged centers (POS/NEG), and specific features like halogen bond donors [26] [11].
- Automated Annotation: Use tools like RDKit or OpenBabel to automatically detect and annotate these features from compound structures.
- Directional Features: For features like HBD and HBA, capture directional preferences when possible, as these significantly impact pharmacophore quality [26].
- Exclusion Volumes: Incorporate exclusion spheres to represent steric constraints from the protein binding pocket [26] [11].
Experimental Protocols for Training Set Curation
Comprehensive Protocol for ChEMBL Data Extraction
Table 2: Research Reagent Solutions for Data Curation
| Tool/Resource | Function | Application Context |
|---|---|---|
| ChEMBL SQL Database | Local installation for fast, complex queries | Large-scale compound retrieval and filtering [31] |
| PSYCOPG2 Python Package | PostgreSQL interface for programmatic data access | Automated data curation workflows [31] |
| RDKit | Cheminformatics toolkit for molecular standardization | Structure normalization, feature detection, and validation |
| PUG-REST API | Programmatic access to PubChem data | Batch downloading and assay data retrieval [28] |
| Pharmacophore Tools (AncPhore, PHASE) | Pharmacophore feature identification and modeling | Training set validation and feature annotation [26] |
Protocol 1: Building a Target-Focused Training Set from ChEMBL
Target Identification
- Identify your target of interest and its ChEMBL ID (e.g., 'CHEMBL1827' for human PDE5) [30]
- Confirm target specificity by reviewing related targets to avoid cross-reactive compounds
Bioactivity Data Retrieval
- Execute a structured SQL query to extract compounds with specific activity types:
- Execute a structured SQL query to extract compounds with specific activity types:
Data Standardization
- Convert all activity values to nM concentrations
- Apply pCHEMBL transformation: pCHEMBL = -log10(standard_value × 10⁻⁹)
- Remove duplicates, keeping the highest quality measurement for each compound
- Standardize structures: neutralize charges, remove salts, generate canonical tautomers
Activity Thresholding
- Classify compounds as actives (< 100 nM), moderately active (100 nM - 1 µM), or inactive (> 1 µM)
- Ensure adequate representation across activity ranges for continuous pharmacophore modeling
Chemical Diversity Analysis
- Apply Bemis-Murcko scaffold analysis to identify core structures
- Ensure coverage of multiple scaffold classes while maintaining common pharmacophoric features
- Use fingerprint similarity (ECFP4) to quantify diversity [26]
Advanced Protocol: Selective Compound Extraction
Protocol 2: Retrieving Compounds Selective for One Target Over Another
This protocol is valuable for building pharmacophore models with enhanced specificity:
Define Selectivity Criteria
- Establish selectivity ratio (e.g., >10-fold preference for primary target)
- Set absolute potency thresholds for both targets
Execute Selective Query
Validate Selectivity Profile
- Cross-reference with additional bioactivity sources
- Confirm selectivity through literature validation
- Apply additional filters based on assay confidence levels
The workflow below illustrates the strategic approach to building a selective training set:
Diagram 2: Selective training set development workflow.
Case Study: Successful Implementation in Pharmacophore Research
Ligand-Based Pharmacophore Modeling for Fluoroquinolone Antibiotics
A recent study demonstrates proper training set selection for identifying potential antimicrobial compounds [21]:
- Training Set Composition: Researchers used four known antibiotics (Ciprofloxacin, Delafloxacin, Levofloxacin, and Ofloxacin) to generate a shared feature pharmacophore (SFP) map.
- Feature Identification: The model identified critical pharmacophore features including hydrophobic areas, hydrogen bond acceptors (HBA), hydrogen bond donors (HBD), and aromatic moieties (Ar).
- Virtual Screening: The pharmacophore model screened 160,000 compounds from ZINCPharmer, identifying 25 potential hits with fit scores ranging from 97.85 to 116 and RMSD values from 0.28 to 0.63.
- Experimental Validation: The top five compounds achieved docking scores comparable to ciprofloxacin (-7.3 to -7.4 kcal/mol vs -7.3 kcal/mol for control), with one emerging as a promising lead after drug-likeness evaluation.
This case study highlights how a focused, well-curated training set of only four high-quality compounds can generate effective pharmacophore models for successful virtual screening.
Sourcing high-quality bioactivity data from public databases requires meticulous attention to data extraction, standardization, and validation protocols. By implementing the troubleshooting guides, experimental protocols, and quality control measures outlined in this technical support center, researchers can build robust training sets that significantly enhance the predictive power of ligand-based pharmacophore models. Remember that the time invested in rigorous data curation invariably returns dividends in model quality and research outcomes, particularly in the critical early stages of drug discovery projects where pharmacophore models guide lead identification and optimization efforts.
From Data to Model: A Step-by-Step Protocol for Training Set Curation and Model Generation
Frequently Asked Questions
Q1: What are the primary criteria for selecting compounds for a pharmacophore model training set? The primary criteria are potency, structural diversity, and data confidence. The training set should include compounds with a wide range of experimentally determined biological activities (e.g., IC50 values), ensuring coverage from highly active to inactive molecules. Furthermore, the selected compounds should represent diverse chemical scaffolds and substitution patterns to prevent model bias and ensure it captures the essential features for binding, not just a single chemical structure. [5] [32]
Q2: How should I categorize compounds based on potency? A common and effective strategy is to categorize compounds into different activity levels according to their IC50 values. For instance:
- Most Active: IC50 < 0.1 μM
- Active: IC50 between 0.1 μM and 1.0 μM
- Moderately Active: IC50 between 1.0 μM and 10.0 μM
- Inactive: IC50 > 10.0 μM Your training set should ideally contain a maximum number of the most active and active compounds, supplemented with a few moderately active and inactive compounds to define the model's boundaries. [5]
Q3: Can I mix agonists and antagonists in the same training set? Yes. Research indicates that pharmacophore models constructed from ligands of mixed functions (e.g., agonists and antagonists) are still capable of enriching hit lists with active compounds. This approach is particularly valuable when the number of known ligands for a target is limited. However, if the goal is to discover compounds with a specific biological function, a function-specific training set is recommended. [32]
Q4: Why is my pharmacophore model performing poorly despite having high-fit compounds? This often stems from a lack of structural diversity in the training set. If all training set compounds share a similar core scaffold, the model may overfit to that specific chemical structure and fail to identify novel chemotypes. Ensure your training set includes molecules with different structural frameworks that all exhibit the desired biological activity. [32] [25]
Q5: How does assay variability impact my training set selection? Assay variability is a critical source of uncertainty in potency data. High variability can obscure true structure-activity relationships and lead to misclassification of compounds. To mitigate this, prioritize data from robust, well-controlled assays and consider the confidence intervals of potency measurements when selecting compounds for your training set. [33]
Troubleshooting Guides
Problem: Pharmacophore model fails to identify any active compounds during virtual screening.
- Cause 1: Overly restrictive model. The model may have been generated from a training set with insufficient structural diversity.
- Solution: Re-evaluate your training set. Incorporate compounds from multiple analogue series or chemotypes that are known to be active. A study on GPCRs recommends using a diverse training set over one based solely on high potency. [32]
- Cause 2: Incorrect potency data. The experimental biological activities used for training may be unreliable or sourced from inconsistent assay conditions.
- Solution: Curate your data meticulously. Use potency values generated from a homogeneous procedure (e.g., the same biological assay and cell line) to ensure consistency. [5]
Problem: Model retrieves active compounds but also an excessively high number of false positives.
- Cause: Lack of inactive or moderately active compounds. The model has not learned what features or spatial arrangements are not conducive to binding.
- Solution: Include carefully selected inactive or weakly active compounds in your training set. This helps the algorithm distinguish between essential and non-essential features, improving model specificity. [5]
Problem: Model performs well on the training set but poorly on new, external test compounds.
- Cause: Data leakage or overfitting. The test set may be too similar to the training set, or the model may be too complex.
Experimental Protocols & Data
Table 1: Quantitative Potency Categorization Scheme for Training Set Selection
| Activity Level | IC50 Range | Recommended Proportion in Training Set |
|---|---|---|
| Most Active | < 0.1 μM | Maximize number |
| Active | 0.1 - 1.0 μM | Include a significant number |
| Moderally Active | 1.0 - 10.0 μM | Include a few representatives |
| Inactive | > 10.0 μM | Include a few for contrast |
Source: Adapted from a study on Topoisomerase I inhibitors [5]
Detailed Methodology: Construction of a Ligand-Based Pharmacophore Model
Data Curation and Training Set Selection:
- Collect a set of known active compounds against your target of interest.
- Obtain consistent biological activity data (e.g., IC50, Ki) from a uniform assay condition. [5]
- Categorize compounds based on potency as shown in Table 1.
- Select a training set of 20-30 compounds that spans the potency range and encompasses diverse chemical structures and substituents. [5] [25]
Compound Preparation:
- Draw 2D structures and convert them into 3D formats using software like ChemDraw or MOE.
- Minimize molecular energy using a force field (e.g., CHARMM) to obtain stable 3D conformations. [5]
Pharmacophore Generation (using HypoGen algorithm in Discovery Studio as an example):
- Input the prepared training set molecules and their experimental activity values.
- The algorithm will generate multiple pharmacophore hypotheses (e.g., Hypo1, Hypo2...). These hypotheses comprise 3D arrangements of chemical features like hydrogen bond acceptors/donors (HBA/HBD), hydrophobic regions (H), and aromatic rings (AR). [5] [3]
Model Validation:
- Internal Validation: Use a test set of molecules (not used in training) to check the correlation between estimated and experimental activity. [5]
- External Decoy Set Validation: Test the model's ability to retrieve active compounds from a database spiked with known actives and decoys, calculating enrichment factors. [32] [25]
The workflow for this methodology is summarized in the following diagram:
The Scientist's Toolkit: Essential Research Reagents & Materials
Table 2: Key Reagents and Software for Pharmacophore Modeling
| Item | Function in Research | Example Use-Case |
|---|---|---|
| Molecular Operating Environment (MOE) | Software suite for pharmacophore feature generation, model building, and validation. [32] [25] | Used to develop and validate a pharmacophore model for carbonic anhydrase IX inhibitors. [25] |
| Discovery Studio (DS) | Software platform providing HypoGen algorithm for 3D QSAR pharmacophore generation. [5] | Employed to build a pharmacophore model for Topoisomerase I inhibitors from 29 CPT derivatives. [5] |
| ZINC Database | A freely available public database of commercially available compounds for virtual screening. [5] [21] | Used as a source of over 1 million drug-like molecules for virtual screening with a validated pharmacophore query. [5] |
| CHEMBL | A manually curated database of bioactive molecules with drug-like properties, providing reliable potency data. [34] | Sourced as a repository of compounds with documented potency for building and testing predictive models. [34] |
| Four-Parameter Logistic (4PL) Fit | A statistical model used to analyze dose-response data from bioassays to derive accurate potency values (e.g., IC50, EC50). [33] | Fundamental for calculating the relative potency (%RP) of test samples against a reference standard in potency assays. [33] |
Visualizing Potency Data Considerations
Understanding the distribution and confidence of your potency data is crucial for selecting a reliable training set. The following diagram illustrates the relationship between assay variability and the confidence in a compound's potency measurement, which directly impacts data confidence.
The Role of Inactive or Decoy Molecules in Defining Pharmacophore Specificity
Frequently Asked Questions (FAQs)
Q1: Why is it important to include inactive compounds in a pharmacophore training set? Inactive compounds are crucial for defining the specificity of a pharmacophore model. A model developed using only active compounds might identify common chemical features but cannot distinguish which of these features are truly essential for binding versus those that are merely common to the molecular scaffold. By including inactive compounds, the model can be refined to eliminate features that are also present in non-binders, thereby reducing false positives during virtual screening and increasing the model's predictive accuracy [35] [36].
Q2: What is the difference between an inactive compound and a decoy molecule?
- Inactive Compound: A known chemical entity that has been experimentally tested against the biological target and found to lack significant activity (e.g., high IC50 value) [35] [10]. These are used during the training phase of model generation to help identify and discard non-essential pharmacophore features.
- Decoy Molecule: A compound, typically with unknown activity, used during the validation phase to test the model's ability to discriminate between potential actives and inactives. A decoy set usually contains a large number of molecules presumed to be inactive, spiked with a few known active compounds [10].
Q3: How many inactive compounds should be included in a training set? While the ideal number depends on the project, a general guideline is to include 15-20 compounds in the training set, comprising a mix of highly potent, intermediately potent, and inactive molecules [36]. For the HypoGen algorithm, the use of inactive compounds is a built-in part of its methodology for refining the pharmacophore hypothesis [35].
Q4: What are the consequences of using a training set that lacks inactive molecules? A training set without inactive molecules is likely to generate a pharmacophore model with lower specificity. This can lead to:
- Higher False Positive Rates: The model may retrieve a large number of compounds from databases that match the pharmacophore but are biologically inactive [35].
- Reduced Scaffold Hopping Utility: The model may be overly specific to the chemical scaffolds of the training set actives, missing truly novel chemotypes with the same biological function [35].
Q5: Which is more critical for pharmacophore model validation: specificity or sensitivity? The primary goal during validation should be specificity [36]. While a good model should identify true actives (sensitivity), its practical utility in virtual screening is more dependent on its ability to reject inactive compounds, as this dramatically reduces the cost and time of subsequent experimental testing.
Troubleshooting Guides
Problem: Pharmacophore Model Retrieves Too Many False Positives
Potential Causes and Solutions:
Cause 1: Lack of Inactive Compounds in Training.
- Solution: Refine the initial model by incorporating a set of known inactive compounds. Software like Catalyst's HypoGen algorithm is explicitly designed for this; it uses inactive compounds to eliminate pharmacophore features that are common to the inactive set, thus refining the hypothesis [35].
Cause 2: Overly General Feature Definitions.
- Solution: Make the pharmacophore feature definitions more specific. For example, instead of a general "hydrogen bond acceptor," define a more specific vector or location based on the binding site geometry. You can also add exclusion volumes to represent steric clashes in the binding site, which helps rule out molecules that are too bulky [3].
Cause 3: Inadequate Validation with a Decoy Set.
- Solution: Always validate your model using a decoy set validation method. This involves screening a database containing known actives and many decoy molecules. Calculate the Enrichment Factor (EF) to quantitatively measure how much better your model performs than a random selection [10].
Problem: Model Fails to Identify Structurally Novel Active Compounds (Poor Scaffold Hopping)
Potential Causes and Solutions:
Cause 1: Training Set Lacks Chemical Diversity.
- Solution: Ensure your training set of active compounds is structurally diverse. Use clustering techniques (e.g., Butina clustering based on 2D pharmacophore fingerprints) to select representative molecules from different chemical classes [4]. A diverse training set helps create a pharmacophore that captures the essential functional features, independent of a specific scaffold.
Cause 2: Model is Over-fitted to a Single Scaffold.
- Solution: Analyze the model against a test set containing active compounds with different scaffolds. If it fails, re-generate the model using a more diverse training set and check if the inclusion of inactives has made the model too restrictive. The goal is a balance that captures essential features without being tied to a specific core structure [35].
Experimental Protocols & Data Presentation
Protocol 1: Generating a Ligand-Based Pharmacophore with Inactive Compounds
This protocol outlines the workflow for creating a pharmacophore model using both active and inactive ligands.
1. Training Set Preparation:
- Data Collection: Gather a set of 15-20 molecules with experimentally determined activities (e.g., IC50). The set should include highly active, moderately active, and confirmed inactive compounds [36].
- Conformational Analysis: For each molecule, generate a set of low-energy conformers to represent its accessible conformational space. Common settings use an energy threshold of 20 kcal/mol above the global minimum to ensure the bioactive conformation is likely included [4].
2. Model Generation (e.g., using HypoGen in Discovery Studio):
- The algorithm first identifies common feature arrangements from the active compounds (similar to the Hip-Hop algorithm) [35].
- It then compares the best pharmacophore hypotheses from the first stage with the conformers of the inactive compounds.
- Features that are common to the inactive set are eliminated or penalized.
- The algorithm proceeds with an optimization cycle, scoring the refined hypotheses based on their ability to predict the experimental activities of all training set compounds [35].
3. Model Validation:
- Test Set: Use a set of known active and inactive compounds not used in training to test the model's predictive power.
- Decoy Set Validation: Prepare a database of 2000 molecules, spiking in 20 known Akt2 inhibitors among 1980 decoys. Screen this database with your pharmacophore model and calculate the Enrichment Factor (EF) to assess performance [10].
The following diagram illustrates this ligand-based workflow:
Quantitative Metrics for Model Validation
The table below summarizes key metrics used to validate a pharmacophore model's performance, particularly its specificity.
Table 1: Key Metrics for Pharmacophore Model Validation
| Metric | Formula / Description | Interpretation | Application in Search Results |
|---|---|---|---|
| Enrichment Factor (EF) | EF = (Hitssampled / Nsampled) / (Hitstotal / Ntotal) [10] | Measures how much better the model is at finding actives compared to random selection. A higher EF indicates better performance. | Used to validate a structure-based pharmacophore for Akt2 inhibitors [10]. |
| Recall (True Positive Rate) | Recall = TP / (TP + FN) [4] | The fraction of true active compounds correctly identified by the model. | A key metric for internal and external performance estimation [4]. |
| Specificity (True Negative Rate) | Specificity = TN / (TN + FP) [36] | The fraction of true inactive compounds correctly rejected by the model. Highlighted as the primary goal for validation [36]. | |
| F-Score | Fβ = (1+β²) * (Precision * Recall) / (β² * Precision + Recall) [4] | A weighted harmonic mean of precision and recall. F0.5 weights precision higher, favoring specificity. | Used as a selection criterion during automated pharmacophore model generation [4]. |
Protocol 2: Structure-Based Pharmacophore Generation with Exclusion Volumes
When the 3D structure of the target is available, specificity can be built directly into the model.
1. Protein-Ligand Complex Preparation:
- Obtain a high-quality structure from the PDB (e.g., 3E8D for Akt2) [10].
- Prepare the protein structure by adding hydrogen atoms, correcting protonation states, and treating missing residues.
2. Binding Site and Interaction Analysis:
- Define the binding site around the co-crystallized ligand.
- Use software (e.g., Discovery Studio) to generate all possible interaction points (hydrogen bond donors/acceptors, hydrophobic regions, ionic interactions) between the protein and a hypothetical ideal ligand [3] [10].
3. Feature Selection and Exclusion Volume Addition:
- Manually select the most relevant interaction features based on conserved interactions with known inhibitors or key catalytic residues.
- Add exclusion volumes (spheres that represent forbidden space) based on the protein structure to account for the shape of the binding pocket and prevent the matching of molecules that would cause steric clashes [3] [10].
The following diagram illustrates this structure-based workflow:
The Scientist's Toolkit: Essential Research Reagents & Software
Table 2: Key Resources for Pharmacophore Modeling with Specificity
| Resource Name | Type | Primary Function in Relation to Specificity |
|---|---|---|
| Catalyst/HypoGen [35] | Software Algorithm | Explicitly uses inactive compounds in its algorithm to refine pharmacophore features and improve model specificity. |
| Exclusion Volumes [3] | Software Feature | Represent forbidden areas in the binding site, preventing the selection of molecules that would cause steric clashes. |
| Decoy Set (e.g., DUD-E) | Validation Database | A collection of pharmaceutically relevant molecules used to test a model's ability to discriminate actives from inactives. |
| ZINC Database [13] [10] | Compound Library | A large, publicly accessible database of commercially available compounds used for virtual screening to test pharmacophore models. |
| Discovery Studio [13] [10] | Software Suite | A comprehensive commercial software package that includes tools for both structure-based and ligand-based pharmacophore modeling, validation, and virtual screening. |
| ROCS (Rapid Overlay of Chemical Structures) | Software Tool | Performs shape-based and feature-based molecular superimposition, helping to identify common pharmacophores from a set of active ligands. |
FAQ: Troubleshooting Ligand-Based Pharmacophore Modeling
Q1: Why does my pharmacophore model perform poorly in virtual screening, despite using known active compounds?
Poor performance often stems from an unrepresentative training set or inadequate handling of ligand flexibility [4] [7]. If your training set assumes all active compounds share a single binding mode, but they actually bind in multiple ways, the generated model will be inaccurate [4]. Furthermore, if the conformational ensemble used for model generation does not include the true bioactive conformation, the essential chemical features will be misrepresented.
- Solution: Implement a robust training set selection strategy. For targets with suspected multiple binding modes, use Strategy II for training set creation. This involves jointly clustering active and inactive compounds and building multiple models from different training sets to account for binding variability [4]. Ensure your conformer generation protocol samples a wide energy range (e.g., up to 50 kcal/mol) to capture extended and flexible structures, not just the most stable conformers [4].
Q2: How can I generate a bioactive conformation when the protein structure is unknown or highly flexible?
When the protein structure is unavailable (e.g., for GPCRs) or the binding pocket is highly flexible (like LXRβ), a ligand-based pharmacophore approach is your primary tool [3] [7]. The key is to use a diverse set of known active ligands to infer the essential binding features.
- Solution: Employ a multi-ligand alignment strategy. Generate multiple conformers for each known active compound and align them to identify common chemical features and their spatial arrangements [7]. For highly flexible targets, generating models based on a combination of multiple ligand alignments and, if available, information from several ligand-bound crystal structures yields the most reliable results [7]. Advanced AI tools like DiffPhore can also predict binding conformations by learning from 3D ligand-pharmacophore pairs, even without a protein structure [11].
Q3: What is the recommended protocol for generating conformers for a training set?
A detailed, computationally feasible protocol is as follows [4]:
- Stereoisomer Enumeration: Enumerate all possible stereoisomers for molecules with undefined chiral centers or double-bond geometry. Treat each stereoisomer as a separate parent compound.
- Conformer Generation: For each compound/stereoisomer, generate a large ensemble of conformers (e.g., up to 100) within a wide energy window (e.g., 50 kcal/mol after minimization using a force field like MMFF94). This ensures the sampling of extended structures for flexible molecules.
- Energy Minimization: Minimize the energy of all generated conformers using the same force field to ensure geometric realism.
Q4: My model identifies too many false positives during virtual screening. How can I improve its precision?
A high false positive rate (FPR) often indicates a model that is too promiscuous or lacks critical steric constraints [4].
- Solution:
- Incorporate Inactive Compounds: The most effective method is to include known inactive compounds in your training set. During model development, select for pharmacophore hypotheses that occur predominantly in active compounds and are absent in inactives [4].
- Post-Processing: Remove overly simplistic models that have three or fewer distinct spatial feature coordinates, as these can be non-specific [4].
- Add Exclusion Volumes: If you have some structural information about the target, adding exclusion volumes (XVOL) to your pharmacophore model can represent forbidden areas in the binding pocket, drastically reducing false positives by sterically filtering out unsuitable compounds [3] [11].
Experimental Protocols & Data Presentation
Table 1: Key Parameters for Conformational Sampling in Pharmacophore Modeling This table summarizes critical settings for generating comprehensive conformational ensembles, a prerequisite for successful model building [4].
| Parameter | Recommended Setting | Function & Rationale |
|---|---|---|
| Force Field | MMFF94 | Provides energy minimization and conformational optimization for realistic 3D geometries. |
| Energy Cutoff | 50 kcal/mol | A wide energy window ensures sampling of extended and flexible structures, not just low-energy folded conformers. |
| Max Conformers per Compound | 100 | Balances computational cost with the need for comprehensive conformational coverage. |
| Convergence Criteria | Root Mean Square (RMS) gradient | Standard criterion (e.g., 0.001) for energy minimization termination. |
Methodology: Training Set Selection Strategies
The choice of training set is critical and depends on the assumed binding behavior of the active compounds [4].
Strategy I: Single Binding Mode Assumption
- Use Case: When all active compounds are presumed to share the same binding mode.
- Protocol:
- Calculate 2D pharmacophore fingerprints for all active and inactive compounds.
- Cluster actives and inactives separately using a method like Butina clustering.
- Select the centroid (most representative compound) of each cluster containing at least 5 compounds for the training set.
- All remaining compounds form the test set for external validation.
Strategy II: Multiple Binding Mode Assumption
- Use Case: For targets where active compounds may bind in different ways.
- Protocol:
- Calculate 2D pharmacophore fingerprints for all compounds.
- Cluster active and inactive compounds jointly.
- From each resulting cluster, randomly select 5 active and 5 inactive compounds for the training set. (Ignore clusters with fewer than 5 actives).
- Add centroids from clusters of only inactive compounds to better represent negative examples.
- This process creates multiple training sets, all of which are used for model development. Each model is validated against its complementary test set.
The workflow for generating a pharmacophore model from a prepared training set is as follows:
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Software Tools for Pharmacophore Modeling and Conformation Generation
| Tool Name | Type | Primary Function in this Context |
|---|---|---|
| RDKit | Open-source Cheminformatics | Used for 2D pharmacophore fingerprint calculation, clustering of training sets, and conformer generation with the MMFF94 force field [4]. |
| DiffPhore | AI-based Diffusion Model | A deep learning framework for "on-the-fly" 3D ligand-pharmacophore mapping; predicts ligand binding conformations that match a given pharmacophore model [11]. |
| PHASE | Commercial Software | Provides a comprehensive environment for both ligand- and structure-based pharmacophore model development, hypothesis generation, and virtual screening [3] [37]. |
| MOE (Molecular Operating Environment) | Commercial Modeling Suite | Contains integrated workflows for pharmacophore query creation, molecular docking, and conformational analysis [38]. |
| AncPhore | Pharmacophore Tool | Used to detect pharmacophore features and generate 3D ligand-pharmacophore pairs for dataset creation and analysis [11]. |
The following diagram illustrates the core conceptual workflow for addressing ligand flexibility and alignment to arrive at a bioactive conformation, integrating both traditional and AI-powered paths.
Utilizing Software Tools for Feature Extraction and Pharmacophore Generation (e.g., LigandScout, MOE, ConPhar)
Technical Support Center: Troubleshooting & FAQs
This support center addresses common issues encountered during feature extraction and pharmacophore generation, with an emphasis on how these challenges relate to the integrity of your initial training set—a critical factor for successful ligand-based pharmacophore modeling.
Frequently Asked Questions (FAQs)
Q1: Why does my generated pharmacophore model fail to retrieve active compounds during virtual screening?
- A: This is often a training set issue. The model may be over-fitted to the specific chemical scaffolds in your training set. Ensure your training set contains structurally diverse active compounds that share the same mechanism of action. Incorporate known inactive compounds to help the software distinguish relevant features from molecular noise.
Q2: What is the recommended number of ligands for a training set in ligand-based pharmacophore generation?
- A: While there is no fixed number, the consensus from recent literature suggests a minimum of 15-20 diverse, high-affinity active compounds. A larger, well-curated set (30+) generally leads to more robust and predictive models. See Table 1 for a summary.
Q3: My protein-ligand complex has a co-crystallized water molecule. Should I include it as a feature in LigandScout?
- A: This is a critical decision. If the water molecule is known to be a crucial bridging element in ligand binding (a "structural water"), including it as a feature can significantly improve model selectivity. However, if its role is ambiguous, it can introduce false positives. Consult biochemical data or run simulations to determine the water's stability.
Q4: In MOE, what is the difference between the "Pharmacophore Query" and "Shape Query" and when should I use them?
- A: A Pharmacophore Query defines chemical features (e.g., hydrogen bond donors, aromatic rings). A Shape Query defines the molecular volume. Use a pure pharmacophore query for scaffold hopping. Combine it with a shape query (from a high-affinity ligand) to enforce steric constraints and improve screening precision, especially when your training set lacks shape diversity.
Troubleshooting Guides
Issue: Inconsistent Feature Interpretation in LigandScout
- Problem: Different users, or the same user on different days, extract slightly different features from the same protein-ligand complex.
- Solution:
- Standardize Protocols: Before starting, define and document the rules for feature interpretation for your project. For example, decide on a consistent distance tolerance for projecting protein features onto the ligand.
- Use the "Create Pharmacophore from Molecular Interaction Fields" Workflow: This provides a more objective, data-driven alternative to manual annotation. The workflow uses pre-calculated fields to identify favorable interaction points.
- Cross-Validation: Have multiple team members generate models from the same set of structures and compare them. Consensus features are more reliable.
Issue: Handling Tautomers and Protonation States in MOE
- Problem: The generated pharmacophore model is highly sensitive to the specific tautomeric or protonation state of the training ligands, leading to poor generalization.
- Solution:
- Ligand Preparation: Use MOE's "Structure Preparation" module to generate probable protonation states and tautomers at the target pH (e.g., pH 7.4) before building the model.
- Multiple Conformer Generation: Ensure you are using a diverse set of low-energy conformers for each ligand.
- Protocol: Follow the detailed methodology in Experimental Protocol 1.
Issue: Poor Alignment of Conformers in ConPhar
- Problem: The common chemical features are not correctly identified because the ligand conformers are not aligning properly.
- Solution:
- Check Conformer Diversity: The initial conformational ensemble may be too rigid or lack the bioactive conformation. Increase the number of conformers generated per ligand.
- Adjust Algorithm Parameters: Increase the weight of critical features that you know are important for binding. This guides the alignment algorithm to prioritize these points.
- Review Training Set: The ligands in your training set may not be suitable for a common pharmacophore model. Verify they all bind to the same site in a similar manner.
Data Presentation
Table 1: Impact of Training Set Size and Diversity on Model Performance
| Training Set Characteristic | Model Performance Metric | Outcome (from cited studies) | Recommendation |
|---|---|---|---|
| Small Set (< 10 actives) | EF1% (Enrichment Factor) | Low (Average: 5-8) | Avoid; high risk of overfitting. |
| Large, Diverse Set (> 30 actives) | EF1% | High (Average: 15-25) | Ideal for robust model generation. |
| Includes Inactive Compounds | Specificity | >30% improvement | Crucial for defining exclusion volumes and improving model selectivity. |
| High Structural Diversity (Tc < 0.3) | Scaffold Hopping Rate | Up to 60% success | Essential for identifying novel chemotypes. |
Experimental Protocols
Experimental Protocol 1: Standardized Ligand Preparation and Pharmacophore Generation in MOE
Objective: To generate a consensus pharmacophore model from a set of ligand structures with validated activity against a common target.
Materials: See "Research Reagent Solutions" table. Software: MOE (Molecular Operating Environment).
Methodology:
- Ligand Sourcing & Curation:
- Collect a minimum of 15-20 active compounds with known IC50/Ki values from databases like ChEMBL or BindingDB.
- Manually curate the set to ensure structural diversity and a consistent mechanism of action.
- Ligand Preparation:
- Import all 2D structures (e.g., SDF files) into MOE.
- Run the "Structure Preparation" module:
- Protonate structures at pH 7.4.
- Generate major tautomers.
- Add explicit hydrogens and perform a quick energy minimization (MMFF94x forcefield).
- Output: A database of 3D, prepared ligands.
- Conformational Sampling:
- Use the "Conformational Search" module on the prepared database.
- Method: Stochastic Search.
- Energy Window: 7 kcal/mol.
- Maximum Conformers: 250 per ligand.
- Pharmacophore Generation:
- Select the "Pharmacophore Elucidation" application.
- Input the database of conformers.
- Key Parameters:
- Feature Set: Include H-bond Acceptor/Donor, Aromatic Center, Hydophobic Area.
- Minimum Points: 4
- Maximum Points: 6
- Selectivity: Aim for a value >2.5 bits.
- Execute the calculation. MOE will generate and rank multiple hypothesis models.
- Model Validation:
- Validate the top-ranked models using a decoy set containing both active and inactive compounds not used in training.
- Select the model with the best enrichment factor (EF1%) and Güner-Henry (GH) score.
Mandatory Visualization
Title: Ligand-Based Pharmacophore Workflow
Title: Training Set Factors for Model Quality
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Materials for Pharmacophore Modeling Experiments
| Item | Function / Relevance |
|---|---|
| High-Quality Chemical Databases (e.g., ChEMBL, BindingDB) | Source of bioactivity data for selecting active and inactive training and test set compounds. |
| Protein Data Bank (PDB) | Source of 3D protein-ligand complex structures for structure-based pharmacophore modeling and validation. |
| Standardized Ligand File Formats (SDF, MOL2) | Ensures compatibility and correct data transfer between different software tools (LigandScout, MOE, ConPhar). |
| Decoy Set (e.g., DUD-E, DEKOIS) | A set of chemically similar but presumed inactive molecules used for objective validation of the pharmacophore model's screening performance. |
| Computational Cluster / High-Performance Workstation | Necessary for computationally intensive steps like conformational analysis and virtual screening of large compound libraries. |
Frequently Asked Questions
Q1: What is a consensus pharmacophore model and why is it beneficial for SARS-CoV-2 drug discovery? A consensus pharmacophore model integrates the essential spatial and chemical features from multiple known active ligands, or from multiple ligand-target complexes, into a single, unified model [39] [40]. Unlike a model derived from a single ligand, a consensus model reduces bias toward any one specific chemical structure. This is particularly valuable for SARS-CoV-2 targets, like the Spike protein's Receptor Binding Domain (RBD), because it captures the fundamental interaction patterns necessary for binding, even from chemically diverse inhibitors [40]. This leads to a more robust and predictive model for virtual screening, enhancing the likelihood of identifying novel, potent natural compounds or synthetic molecules that can disrupt the virus's interaction with the human ACE2 receptor [41] [40].
Q2: My consensus model is performing poorly in virtual screening, returning too many false positives. What could be wrong? This is a common issue often traced back to the training set selection. Here are the key factors to check:
- Lack of Diversity: The ligands used to build the model may be too structurally similar. A robust consensus model requires a chemically diverse set of ligands that still share the same mechanism of action. This ensures the model captures the essential, common features rather than the specific architecture of one compound class [42].
- Inadequate Representation of Binding Sites: The model might be based on ligands that only map to a single binding site on the target. For a complex target like the SARS-CoV-2 RBD, effective inhibition can occur at multiple sites, including the central RBD-ACE2 interface, allosteric pockets, or a deep cleft in the ACE2 enzyme itself [40]. Ensure your training set includes ligands known to bind to the relevant pharmacophoric sites.
- Incorrect Feature Clustering Parameters: During the generation of the consensus model, the clustering of pharmacophoric features (e.g., hydrogen bond donors, acceptors, hydrophobic regions) is sensitive to parameters like distance thresholds. An incorrectly set threshold can result in a model that is either too generic or too restrictive [43].
Q3: What are the best practices for selecting ligands to build a reliable training set? The selection of the training set is a critical step that directly influences the quality of your consensus model. Adhere to these best practices:
- Emphasize Chemical and Structural Diversity: Curate a set of ligands that are known binders but belong to different chemical classes [42]. This helps the model generalize and identify the core features necessary for biological activity.
- Prioritize High-Confidence Structural Data: Whenever possible, use ligands with experimentally determined 3D structures in complex with your target (e.g., from the PDB). This provides high-confidence data on the binding conformation and the specific ligand-target interactions [39] [40].
- Cover Multiple Binding Modes: For targets with extensive ligand data, include compounds that bind to different key regions. For SARS-CoV-2 RBD, this could mean including ligands for the main interface as well as for allosteric sites to create a more comprehensive inhibitory profile [40].
- Incorporate Inactive Compounds: Using known inactive compounds can help you validate and refine the model to improve its ability to discriminate between active and inactive molecules during virtual screening [42].
Q4: Which software tools can I use to build a consensus pharmacophore model? Several specialized tools are available. A prominent open-source option is ConPhar, which is specifically designed to systematically extract, cluster, and merge pharmacophoric features from a collection of pre-aligned ligand-target complexes [43] [39]. Other established software includes:
- Pharmit: A pharmacophore search tool that can be used to generate the initial pharmacophore models from individual ligands, which can then be fed into ConPhar for consensus building [43] [39].
- Molecular Operating Environment (MOE): A comprehensive commercial software suite that includes tools for pharmacophore modeling, docking, and molecular dynamics, which can be used in various stages of the workflow [41].
Q5: How can I validate my consensus pharmacophore model before proceeding to large-scale virtual screening? A multi-step validation strategy is recommended:
- Internal Validation: Test the model's ability to correctly identify the known active ligands that were used to create it (the training set). This checks for self-consistency.
- Decoy Set Testing: Screen a database containing known active compounds mixed with presumed inactives (decoys). A good model should efficiently enrich the active compounds at the top of the screening results [44].
- Comparative Molecular Docking: Use molecular docking as a complementary step. The top hits from your pharmacophore screen can be docked into the target's binding site. Consensus scoring from multiple docking engines can further increase confidence in the final hits [44].
Troubleshooting Guides
Issue: Model Fails to Identify Known Active Compounds Possible Causes and Solutions:
- Cause: Overly Restrictive Model. The consensus criteria may be too strict, filtering out valid but slightly divergent ligands.
- Solution: Revisit the feature clustering step in your software (e.g., ConPhar). Slightly increase the distance threshold (the
h_distparameter in ConPhar) to create a more tolerant model that still captures the core features [43].
- Solution: Revisit the feature clustering step in your software (e.g., ConPhar). Slightly increase the distance threshold (the
- Cause: Incorrect Binding Site Definition.
- Solution: Re-analyze the protein-ligand complexes in your training set. Ensure all ligands are properly aligned based on the target protein's structure, not just their own coordinates. Using a tool like PyMOL for structural alignment is a critical preparatory step [39].
Issue: Unmanageably Large Number of Hits in Virtual Screening Possible Causes and Solutions:
- Cause: Model is Too Generic.
- Solution: Apply post-screen filters. A highly effective strategy is to filter the pharmacophore hits by molecular weight (e.g., ≤ 500 g/mol to focus on drug-like compounds) and then subject them to more computationally intensive comparative molecular docking [44]. This sequential approach leverages the speed of pharmacophore screening and the precision of docking.
- Cause: Lack of Excluded Volume Constraints.
- Solution: If supported by your software, add excluded volumes to the model based on the 3D structure of the target protein. This prevents the model from selecting compounds that would sterically clash with the protein backbone or side chains.
Research Reagent Solutions
The table below summarizes key computational tools and data resources essential for building consensus pharmacophore models.
Table 1: Essential Research Reagents and Tools for Consensus Pharmacophore Modeling
| Item Name | Function/Brief Explanation | Example/Source |
|---|---|---|
| ConPhar | An open-source Python package specifically designed for generating consensus pharmacophores from multiple aligned ligand-target complexes. It performs feature extraction, clustering, and model creation [43] [39]. | GitHub Repository |
| Pharmit | An interactive tool for pharmacophore search. It is used to generate the initial pharmacophore models (saved as JSON files) for individual ligands, which serve as input for ConPhar [43] [39]. | Online Tool |
| Protein Data Bank (PDB) | The primary repository for 3D structural data of proteins and protein-ligand complexes. Serves as the source for high-confidence training set structures [41]. | RCSB PDB |
| COCONUT Database | A comprehensive open database of natural products. Useful for virtual screening to find novel, biologically relevant starting points for drug discovery [40]. | COCONUT |
| Molecular Operating Environment (MOE) | A commercial software suite that provides integrated applications for molecular modeling, simulation, and methodology development, including pharmacophore modeling and docking [41]. | Chemical Computing Group |
| PyMOL | A widely used molecular visualization system that can be used for aligning protein structures and preparing structures for analysis [39]. | Schrodinger |
Experimental Protocols
Protocol 1: Generating a Consensus Pharmacophore Model Using ConPhar This protocol outlines the key steps for building a consensus model, using the SARS-CoV-2 main protease (Mpro) or RBD as a case study [39].
Prepare Aligned Protein-Ligand Complexes
- Obtain a set of non-redundant crystal structures of your target (e.g., SARS-CoV-2 Mpro) in complex with different ligands from the PDB.
- Use PyMOL to structurally align all protein complexes onto a single reference structure. This ensures all ligands are in a consistent frame of reference.
- Extract each aligned ligand and save it as an individual file in SDF or MOL2 format.
Generate Individual Pharmacophore Models
- Load each ligand file into Pharmit.
- Use the "Load Features" option to automatically generate a pharmacophore based on the ligand's chemical features.
- Save each resulting pharmacophore as a JSON file.
Set Up the ConPhar Environment
- Install ConPhar in a Google Colab notebook or a local Python environment using
pip install conphar. - Upload all the pharmacophore JSON files to a dedicated folder.
- Install ConPhar in a Google Colab notebook or a local Python environment using
Compute the Consensus Model
- Use ConPhar to parse all JSON files and consolidate the pharmacophoric features into a single data frame.
- Execute the
compute_concensus_pharmacophorefunction. This algorithm will:- Cluster similar features (e.g., all hydrogen bond acceptors) based on their spatial proximity using a defined distance threshold (
h_dist). - Compute the center of mass and a representative radius for each cluster of features.
- Output the final consensus model, which is a collection of these averaged feature spheres [43].
- Cluster similar features (e.g., all hydrogen bond acceptors) based on their spatial proximity using a defined distance threshold (
Protocol 2: Integrated Virtual Screening Workflow This protocol combines pharmacophore screening with molecular docking for improved hit identification [44].
Pharmacophore-Based Virtual Screening
- Use your validated consensus pharmacophore model to screen a large compound database (e.g., COCONUT for natural products).
- This step will generate an initial list of "hits" that match the pharmacophore's features.
Filtering
- Downsize the hit list by applying filters for drug-likeness. A common and effective filter is Molecular Weight (MW ≤ 500 g/mol) [44].
Comparative Molecular Docking
- Take the filtered hits and perform molecular docking studies using the 3D structure of your target.
- For increased reliability, use more than one docking engine (e.g., AutoDock and AutoDock Vina). This "comparative docking" approach helps mitigate the biases of any single program's search or scoring algorithm [44].
- Apply consensus scoring by examining the rank of compounds across different docking results. A compound that ranks highly in multiple independent docking runs is a more confident hit.
Validation via Molecular Dynamics (MD)
- For the top-ranked candidate(s), run MD simulations (e.g., for 100 nanoseconds) to assess the stability of the ligand-protein complex and calculate binding free energy using methods like MM-GBSA. A stable complex with a favorable ΔGTOTAL (e.g., -38 to -42 kcal/mol, as seen for promising SARS-CoV-2 inhibitors) confirms a strong binding affinity [41].
Workflow Visualization
The diagram below illustrates the integrated workflow for building and applying a consensus pharmacophore model, from data preparation to hit validation.
Workflow for Consensus Pharmacophore Modeling and Screening
The following diagram details the logical process ConPhar uses internally to cluster features from multiple ligands into a single consensus model.
Consensus Feature Clustering Logic
Overcoming Common Pitfalls: Advanced Strategies for Enhanced Model Performance
Identifying and Mitigating Bias from Structurally Homogeneous Training Sets
Frequently Asked Questions (FAQs)
FAQ 1: What are the primary consequences of using a structurally homogeneous training set in pharmacophore modeling?
Using a structurally homogeneous training set introduces structural bias, which limits the model's ability to identify novel, diverse chemical scaffolds. This bias results in pharmacophore models that are overly specific to the training compounds, reducing their effectiveness in virtual screening for new chemotypes. Models trained on homogeneous data often fail to generalize and capture the essential, minimal steric and electronic features required for binding, leading to high false-negative rates in virtual screening [26] [11].
FAQ 2: How can I quantitatively assess the chemical diversity of my training set before model development?
You can assess chemical diversity using computational metrics. Key methods include:
- Bemis-Murcko Scaffold Analysis: Clusters compounds based on their core molecular frameworks. A low number of unique scaffolds relative to the total number of compounds indicates high homogeneity [26] [11].
- Fingerprint-based Diversity: Calculate the Tanimoto similarity using extended-connectivity fingerprints (ECFP4). A high average pairwise similarity within the set signals low diversity. Visualizing the chemical space with t-SNE plots of ECFP4 descriptors can also reveal tight clustering, confirming structural homogeneity [26] [11].
- Pharmacophore Feature Analysis: Compare the diversity of pharmacophore features (e.g., Hydrogen Bond Donor/Acceptor, Hydrophobic areas) in your set against a known diverse library. A narrow range of feature types and spatial arrangements suggests a biased training set [26] [11] [21].
FAQ 3: What strategies can mitigate bias when only a limited set of known active compounds is available?
When active compounds are limited, employ these strategies to create more robust models:
- Generate a Consensus Pharmacophore: Use tools like ConPhar to analyze multiple ligand-bound complexes. This integrates common features from various ligands, reducing model bias and enhancing predictive power compared to a model derived from a single ligand [45].
- Incorporate Simulated Negative Data: Augment your training with carefully generated decoys. The Directory of Useful Decoys - Enhanced (DUD-E) server can generate decoys that are physically similar but topologically distinct from actives, helping the model learn to discriminate true binders [46].
- Utilize Complementary Training Datasets: Adopt a two-stage training approach. First, train your model on a large, diverse, and perfectly-mapped dataset (like LigPhoreSet) to learn general patterns. Then, refine it with a smaller, real-world dataset containing imperfect mappings (like CpxPhoreSet) to account for induced-fit effects and improve practical performance [26] [11].
FAQ 4: Can AI-based methods help overcome inherent biases in pharmacophore modeling?
Yes, advanced AI frameworks are specifically designed to address these challenges. For example, the DiffPhore framework uses a knowledge-guided diffusion model for 3D ligand-pharmacophore mapping. It incorporates explicit type and directional matching rules and uses calibrated sampling to mitigate exposure bias during the iterative conformation generation process. This approach has been shown to outperform traditional methods, especially when trained on complementary datasets that cover both ideal and real-world mapping scenarios [26] [11].
Troubleshooting Guides
Issue: Poor Virtual Screening Performance & High False Negative Rates
Problem: Your pharmacophore model successfully retrieves training-like compounds but fails to identify new active chemotypes during virtual screening.
Solution: This is a classic symptom of a structurally homogeneous training set. Follow this diagnostic and mitigation protocol.
Diagnostic Protocol:
- Calculate Scaffold Diversity:
- Perform Similarity Analysis:
- Compare to a Diverse Reference:
Mitigation Protocol:
- Action 1: Expand the Training Set Strategically.
- Methodology: Do not simply add more similar compounds. Use the scaffold and similarity analysis to identify underrepresented chemotypes. Search databases like ZINC or ChEMBL for compounds that fulfill the same pharmacophore hypothesis but possess different core scaffolds [21].
- Action 2: Develop a Consensus Model.
- Methodology: If you have multiple homogeneous sets from different scaffold classes, build a separate pharmacophore model for each. Use a tool like ConPhar to generate a unified consensus model that captures the essential features common across all chemotypes [45].
- Action 3: Apply Machine Learning Filters.
- Methodology: After an initial virtual screen, use a machine learning classifier trained to distinguish known active compounds (including those outside your initial training set) from inactives. This secondary filter can help re-prioritize hits that have the correct features but different scaffolds [46].
Issue: Model Inability to Distinguish True Binders from Decoys
Problem: The model produces a high rate of false positives, selecting compounds that fit the geometric constraints but are biologically inactive.
Solution: This often occurs when the model is under-constrained and lacks information on what not to bind. The solution is to incorporate explicit negative information.
Experimental Protocol: Incorporating Exclusion Volumes and Decoys
- Define Steric Constraints:
- Utilize Decoy-Enhanced Machine Learning:
- Methodology: a. Use your set of known active compounds as positives. b. Generate a set of decoy molecules using the DUD-E server, which ensures decoys are physicochemically similar but topologically distinct [46]. c. Calculate molecular descriptors for both actives and decoys using a tool like PaDEL-Descriptor [46]. d. Train a machine learning classifier (e.g., Random Forest, SVM) to distinguish between the two sets. e. Use this trained model to score and filter compounds from your virtual screening results, thereby reducing false positives [46].
The following diagram illustrates the core workflow for diagnosing and mitigating bias using the protocols described above.
Diagram: Workflow for Identifying and Mitigating Structural Bias.
Key Research Reagent Solutions
Table 1: Essential Computational Tools for Bias-Resistant Pharmacophore Modeling
| Tool Name | Type/Function | Key Utility in Mitigating Bias |
|---|---|---|
| AncPhore [26] [11] | Pharmacophore Analysis Tool | Used to generate diverse 3D ligand-pharmacophore pair datasets (CpxPhoreSet & LigPhoreSet) for robust model training. |
| ConPhar [45] | Consensus Pharmacophore Generator | Identifies and clusters common pharmacophoric features from multiple ligand complexes, reducing model bias from a single ligand. |
| DiffPhore [26] [11] | AI-based Diffusion Framework | Performs knowledge-guided 3D ligand-pharmacophore mapping, using calibrated sampling to mitigate exposure bias in conformation generation. |
| DUD-E Server [46] | Decoy Generator | Creates negative control compounds (decoys) with similar physicochemical properties but distinct 2D topologies from actives for ML training. |
| PaDEL-Descriptor [46] | Molecular Descriptor Calculator | Generates 1D and 2D molecular descriptors and fingerprints from chemical structures for quantitative analysis and machine learning. |
| ZINCPharmer [21] | Pharmacophore-based Screening Tool | Enables virtual screening based on pharmacophore queries; useful for testing model performance against a large, diverse compound library. |
Experimental Protocols for Robust Training Set Curation
Protocol: Creation of a Complementary Training Dataset
This protocol is adapted from the methodology used to create the CpxPhoreSet and LigPhoreSet, which are designed to work in tandem to reduce bias [26] [11].
Objective: To generate two complementary datasets that, when used together, produce a more generalizable and less biased pharmacophore model.
Materials:
- A database of 3D chemical structures (e.g., ZINC, PDBBind).
- Pharmacophore generation software (e.g., AncPhore [26] [11]).
- Clustering software (e.g., tools using fingerprint similarity).
Methodology:
- Construct the "Real-World" Dataset (CpxPhoreSet Analogue):
- Collect experimental protein-ligand complex structures from the PDB.
- For each complex, extract the ligand in its bound conformation.
- Generate a pharmacophore model based on the interactions observed in that specific complex. This results in a set of ligand-pharmacophore pairs that reflect "real but biased" scenarios with imperfect mappings and induced-fit effects [26] [11].
- Construct the "Idealized" Dataset (LigPhoreSet Analogue):
- Start with a large library of diverse compounds (e.g., millions of structures).
- Apply Bemis-Murcko scaffold filtering and fingerprint clustering to select a chemically diverse representative set of ligands.
- Generate low-energy 3D conformations for each selected ligand.
- For each conformation, generate a perfectly matching pharmacophore model that captures all its key chemical features. This creates a broad set of "perfectly-matched" pairs that cover a wide chemical and pharmacophoric space [26] [11].
- Staged Model Training:
- Warm-up Phase: Initially train your AI or computational model on the large, diverse "Idealized" dataset (LigPhoreSet analogue). This teaches the model general ligand-pharmacophore mapping rules.
- Refinement Phase: Fine-tune the pre-trained model using the smaller "Real-World" dataset (CpxPhoreSet analogue). This adapts the model to the complexities and imperfections of actual biological binding [26] [11].
Protocol: Machine Learning-Based Active Compound Identification
This protocol details how to use machine learning to filter virtual screening hits, reducing reliance on a single pharmacophore model and mitigating bias [46].
Objective: To employ a supervised machine learning model to distinguish potential active compounds from inactive ones after an initial virtual screening.
Materials:
- A set of known active compounds (for the target of interest).
- A set of known inactive compounds or a decoy generation tool (DUD-E server).
- Molecular descriptor calculation software (PaDEL-Descriptor).
- A machine learning library (e.g., scikit-learn for Python).
Methodology:
- Prepare Training Data:
- Calculate Molecular Descriptors:
- Process both the active and inactive sets using PaDEL-Descriptor to generate a comprehensive set of molecular descriptors and fingerprints for each compound [46].
- Train the Classifier:
- Use the calculated descriptors as features and the activity status (active/inactive) as the label to train a machine learning classifier, such as a Random Forest or Support Vector Machine.
- Validate the model's performance using 5-fold cross-validation and metrics like AUC, accuracy, and Matthews Correlation Coefficient (MCC) [46].
- Apply the Model:
- Perform your standard pharmacophore-based virtual screening to get an initial list of hits.
- Calculate the molecular descriptors for these hit compounds.
- Use the trained ML model to predict the probability of each hit being "active." Prioritize hits with high predicted activity scores for further experimental validation [46].
Leveraging Machine Learning for Intelligent Feature Selection and Ranking
Frequently Asked Questions
FAQ 1: What are the most common pharmacophore features used in ML-based feature selection, and how are they represented? The most common pharmacophore features are abstract representations of key chemical interactions. In machine learning frameworks, these are typically translated into numerical or binary descriptors for model training.
- Hydrogen Bond Donor (HBD) / Acceptor (HBA): Represents the capacity to form hydrogen bonds [3] [11].
- Positive (PI) / Negative Ionizable (NI): Represents groups that can carry a formal charge [3] [11].
- Hydrophobic (H): Represents non-polar regions that favor hydrophobic interactions [3] [11].
- Aromatic Ring (AR): Represents aromatic systems involved in π-π or cation-π interactions [3] [11].
- Exclusion Volumes (XVOL/EX): Represent steric constraints and forbidden areas in the binding site, crucial for defining the shape of the pocket [26] [3] [11].
FAQ 2: My ML model for feature ranking is performing poorly. What are the primary data quality issues I should investigate? Poor model performance can often be traced to fundamental issues with the training data. Key areas to investigate are detailed in the table below.
Table 1: Troubleshooting Data Quality for ML-Based Feature Selection
| Data Quality Issue | Impact on Model Performance | Potential Diagnostic Steps |
|---|---|---|
| Limited Ligand Diversity | Model fails to generalize to new chemical scaffolds; poor screening performance for novel chemotypes [47]. | Perform t-SNE analysis or scaffold clustering on your ligand set to visualize chemical space coverage [11]. |
| Inaccurate Pharmacophore Annotation | Introduces noise and incorrect labels, leading the model to learn spurious feature relationships [48]. | Manually review a subset of feature assignments against original protein-ligand complex structures, if available. |
| Inconsistent Feature Definition | Model struggles to find consistent patterns due to varying interpretations of pharmacophore rules [49]. | Ensure a unified pharmacophore definition scheme is used across all training samples [49]. |
| Inadequate Negative Examples | Model lacks the ability to distinguish between features that promote binding versus those that do not. | Incorporate decoy molecules or use methods like exclusion spheres to define negative space [26] [11]. |
FAQ 3: Which machine learning algorithms are most effective for ranking pharmacophore features, and what are their key advantages? Different algorithms offer distinct advantages for feature ranking. The choice often depends on the interpretability requirements and the nature of your data.
Table 2: Machine Learning Algorithms for Pharmacophore Feature Ranking
| Algorithm | Mechanism for Feature Ranking | Key Advantages in Pharmacophore Context |
|---|---|---|
| ANOVA (Analysis of Variance) | Ranks features based on the F-value, which measures the ratio of variance between groups (e.g., active vs. inactive conformations) to variance within groups [49]. | Provides a statistically rigorous, model-independent ranking; highly interpretable [49]. |
| Mutual Information (MI) | Measures how much information about the target variable (e.g., ligand binding) is gained by knowing a specific pharmacophore feature [49]. | Capable of capturing non-linear relationships between features and binding activity. |
| Recursive Feature Elimination (RFE) | Recursively removes the least important features and rebuilds the model, identifying the feature subset that maximizes model performance [50]. | Wraps around another model (e.g., Decision Tree) to provide a context-dependent feature ranking. |
| Ensemble Methods (e.g., AdaBoost) | Combines multiple weak base models (like Decision Trees). Feature importance is aggregated from the ensemble [50]. | Typically provides more robust and accurate rankings by reducing variance and overfitting [50]. |
FAQ 4: How can I create a high-quality training set for a ligand-based pharmacophore model when structural data is limited? A robust training set is the cornerstone of a successful model. The protocol should prioritize ligand diversity and activity confidence.
- Step 1: Curate a Diverse Ligand Set. Collect known active ligands from databases like ChEMBL [47]. Apply Bemis-Murcko scaffold analysis and cluster ligands by fingerprint similarity (e.g., ECFP4) to ensure broad coverage of chemical space, not just structurally similar analogs [11].
- Step 2: Generate Energetically Favorable Conformations. For each ligand, generate multiple low-energy 3D conformations. This accounts for conformational flexibility and helps identify the bioactive conformation [51] [11].
- Step 3: Extract and Cluster Pharmacophore Features. For every ligand conformation, identify its pharmacophoric features (e.g., HBD, HBA, Hydrophobic) [51]. Cluster these features across all active ligands to identify the essential, conserved interaction points that define the pharmacophore model [51].
- Step 4: Incorporate Knowledge-Guided Refinement. For real-world applicability, refine the model using datasets derived from experimental protein-ligand complex structures (like CpxPhoreSet), which contain imperfect but realistic mapping scenarios [11].
Troubleshooting Guides
Issue: Model fails to identify biologically relevant pharmacophore features, prioritizing irrelevant ones instead.
- Potential Cause 1: Bias from a non-diverse training set. If the training ligands are too structurally similar, the model may overfit to features specific to that chemical series but not critical for binding [47].
- Solution: Augment your training set with ligands from diverse scaffold classes. Employ a scaffold-based data splitting strategy during model training and validation to ensure the model can generalize to new chemotypes [47].
- Potential Cause 2: Lack of target-specific steric or chemical constraints.
- Potential Cause 3: The model is learning from inaccurate or noisy feature labels.
- Solution: Implement a more rigorous pharmacophore generation protocol. Use a unified feature definition scheme and cross-validate feature assignments with experimental data or molecular dynamics simulations that capture binding site flexibility [49].
Issue: High computational cost and slow performance during large-scale virtual screening with the ML-ranked pharmacophore model.
- Potential Cause: Screening millions of compounds using traditional molecular docking with a complex pharmacophore model is inherently slow.
- Solution: Implement a machine learning-based surrogate model to predict docking scores or binding affinity directly from 2D structures [47]. As demonstrated in MAO inhibitor discovery, an ensemble ML model can predict docking scores 1000 times faster than classical docking, allowing for rapid prioritization of top compounds for more rigorous downstream analysis [47].
Issue: The selected pharmacophore features are not interpretable or cannot be rationally used for lead optimization.
- Potential Cause: Use of obscure, high-dimensional molecular descriptors that lack a direct physical or chemical meaning.
- Solution: Utilize pharmacophore descriptors themselves as features for machine learning. This creates an interpretable model, as the output directly highlights the importance of specific chemical interactions (e.g., "a hydrogen bond donor at position X is critical") rather than abstract numerical vectors [49]. This was shown to improve database enrichment by up to 54-fold and provides a mechanism-driven understanding for chemists [49].
Experimental Protocols
Protocol 1: Structure-Based Feature Ranking Using Molecular Dynamics and Machine Learning
This protocol identifies key pharmacophore features associated with ligand-specific protein conformations [49].
- System Setup: Download the protein structure from the PDB. Prepare it by removing non-native domains and co-crystallized ligands, and building missing loops.
- Molecular Dynamics (MD) Simulation: Run extensive MD simulations (e.g., 600 ns) to generate an ensemble of protein conformations (e.g., 3,000 frames). This captures the dynamic nature of the binding site.
- Pharmacophore Generation: For each MD conformation, use a tool like MOE's SiteFinder and DB-PH4 to generate pharmacophore features within the binding site. Define features like hydrogen bond donors/acceptors, cations/anions, and hydrophobic centers using a unified scheme.
- Feature Encoding and Labeling: Create a binary-encoded database of all pharmacophore features. Label which protein conformations were "selected" by known active ligands (as determined from previous docking studies).
- Machine Learning Feature Ranking: Apply multiple feature selection algorithms (e.g., ANOVA, Mutual Information) to the encoded dataset. The goal is to identify the pharmacophore features that are most statistically associated with the ligand-selected conformations.
- Validation: Use the top-ranked features to create a pharmacophore query for virtual screening. Validate the model by its ability to enrich true positive ligands from a database of known actives and decoys.
The workflow for this protocol is summarized in the following diagram:
Structure-Based Feature Ranking Workflow
Protocol 2: Construction of a High-Diversity Training Set for Ligand-Based Modeling
This protocol outlines the creation of a diverse set of ligand-pharmacophore pairs for training robust ML models, as used in building the LigPhoreSet [11].
- Source Compounds: Start with a large database of purchasable compounds, such as the ZINC database.
- Scaffold Filtering: Apply Bemis-Murcko scaffold analysis to identify and filter for structurally diverse core scaffolds, ensuring broad chemical space coverage.
- Clustering: Cluster the remaining ligands based on fingerprint similarity (e.g., ECFP4) and select representative compounds from each cluster.
- 3D Conformation Generation: For each selected ligand, generate multiple, energetically favorable 3D conformations.
- Pharmacophore Generation and Sampling: For each low-energy conformation, generate a comprehensive pharmacophore model. Sample these models to create a wide variety of ligand-pharmacophore pairs.
- Add Exclusion Spheres: Incorporate exclusion spheres to each model to represent steric constraints, adding negative information to the training data.
- Dataset Curation: The final output is a high-quality dataset (e.g., LigPhoreSet) of perfectly-matched ligand-pharmacophore pairs, ideal for initial training of deep learning models.
The logical flow for constructing the dataset is as follows:
High-Diversity Training Set Construction
The Scientist's Toolkit
Table 3: Essential Research Reagents and Computational Tools
| Item / Software | Function / Application | Relevance to ML-Guided Pharmacophore Modeling |
|---|---|---|
| ZINC Database | A public database of commercially available compounds for virtual screening. | The primary source for purchasing potential hit compounds identified by your model and for building diverse training sets [13] [11]. |
| ChEMBL Database | A manually curated database of bioactive molecules with drug-like properties. | A key resource for obtaining known active ligands and their bioactivity data to build and validate ligand-based models [47]. |
| MOE (Molecular Operating Environment) | A comprehensive software suite for computational chemistry and drug discovery. | Used for protein preparation, molecular dynamics analysis, and structure-based pharmacophore generation and featurization [49]. |
| RDKit | An open-source toolkit for cheminformatics and machine learning. | Used for manipulating molecules, generating conformations, extracting pharmacophore features, and scripting custom ML workflows [51]. |
| DiffPhore | A knowledge-guided diffusion model for 3D ligand-pharmacophore mapping. | A state-of-the-art deep learning tool for predicting binding conformations by mapping ligands to pharmacophores, surpassing traditional docking in some scenarios [26] [11]. |
| AlphaSpace / AlphaSpace 2.0 | A python program for pocket analysis on biomolecular surfaces. | Used for structure-based analysis to identify targetable pockets and guide the placement of exclusion volumes or key pharmacophore features [52]. |
Integrating Structure-Based Insights from Molecular Dynamics (MD) Trajectories
Frequently Asked Questions (FAQs)
FAQ 1: What are the primary advantages of using trajectory maps over traditional analyses like RMSD and RMSF? Trajectory maps provide a spatiotemporally resolved visualization of a protein's backbone movements, showing the location, time, and magnitude of every shift. Unlike RMSD (which gives a global measure of deviation) or RMSF (which shows per-residue fluctuation but no temporal data), trajectory maps directly visualize the protein's behavior over time, allowing you to pinpoint the start of conformational events and specific unstable regions [53].
FAQ 2: My trajectory file is very large. How can I optimize it for trajectory map analysis?
For optimal performance and clear, interpretable trajectory maps, it is recommended to reduce your trajectory to contain between 500 and 1000 frames [53]. This can be achieved during trajectory processing. Furthermore, all frames must be aligned to a reference structure to remove system-wide rotation and translation, which can be done using the trjconv command in GROMACS or the align command in AMBER [53].
FAQ 3: How can I conclusively compare the stability of two different protein-ligand simulations? Trajectory maps enable direct comparison through a difference map. By subtracting the trajectory map of simulation B from simulation A, the resulting heatmap uses a divergent color scale (e.g., blue-white-red) to show regions where shifts are stronger in one simulation versus the other. This provides an intuitive and conclusive visual comparison of stability and dynamics between the two systems [53].
FAQ 4: What are the key considerations for selecting ligands for a robust pharmacophore model training set? The training set should be curated to ensure a wide range of experimental activities and diverse chemical structures. Key criteria include [5]:
- Activity Range: Include ligands categorized as most active, active, moderately active, and inactive.
- Structural Diversity: Ensure the set covers diverse chemical substitution patterns and scaffolds.
- Assay Homogeneity: All biological activity data (e.g., IC50 values) should be obtained from the same biological assay against a single cell line to minimize noise.
FAQ 5: How can deep learning assist in ligand-pharmacophore mapping? Frameworks like DiffPhore use a knowledge-guided diffusion model to generate 3D ligand conformations that maximally map to a given pharmacophore. This deep learning approach leverages large datasets of 3D ligand-pharmacophore pairs to predict binding conformations, often surpassing the performance of traditional pharmacophore tools and docking methods in virtual screening for lead discovery [26] [11].
Troubleshooting Guides
Issue 1: Trajectory Map Shows Excessive Noise or Uninterpretable Signals
Problem: The resulting heatmap is too noisy, making it difficult to distinguish meaningful conformational changes from random fluctuations.
Solutions:
- Reduce Frame Count: As recommended in the FAQs, ensure your trajectory is not overly dense. Str down the trajectory to 500-1000 frames to improve clarity [53].
- Check Alignment: Verify that all frames in your trajectory have been properly aligned to a common reference structure (e.g., the first frame or the protein's backbone) to remove whole-molecule rotation and translation [53].
- Adjust the Shift Calculation: The standard method uses the center of mass of the residue backbone (Cα, C, O, N). This inherently dampens in-residue vibrations. Using only Cα positions might be more sensitive but could also increase noise [53].
- Modify Color Scale Range: Adjust the range of the z-axis (color scale) in the trajectory map to focus on a specific range of shift values, which can help highlight relevant movements and mask insignificant noise [53].
Issue 2: Pharmacophore Model Performs Poorly in Virtual Screening
Problem: A ligand-based pharmacophore model, built from a training set, fails to identify active compounds during virtual screening, yielding too many false positives or negatives.
Solutions:
- Re-evaluate Training Set Composition:
- Ensure your training set covers a broad spectrum of activity (see FAQ 4). An imbalance towards highly active compounds can create an overly restrictive model [5].
- Check for chemical diversity. A training set with structurally very similar ligands may generate a model that lacks generalizability [5].
- Apply Rigorous Filtration: When screening databases, use a multi-stage filtration process to refine hits. A recommended workflow is [5]:
- Lipinski's Rule of Five: Filter for drug-like molecules.
- SMART Filtration: Filter out molecules with undesired or reactive functional groups.
- Activity Filtration: Filter based on the model's estimated activity (e.g., not >1.0 μM).
- Validate with a Test Set: Before virtual screening, validate the pharmacophore model with a separate test set of known actives and inactives. A high correlation between experimental and estimated activity for the test set increases confidence in the model's predictive power [5].
Issue 3: Difficulty Visualizing and Communicating Key Insights from MD Trajectories
Problem: Standard visualization methods are insufficient to clearly show and communicate the critical structural dynamics discovered in the simulation.
Solutions:
- Use Specialized Visualization Tools: Leverage tools like MDAnalysis for custom analysis scripts and integration with visualization widgets in Jupyter notebooks [54]. Tools like MolecularNodes for Blender can create high-quality, publication-ready renderings and animations [55].
- Incorporate Accessibility Principles: For all charts and heatmaps, ensure sufficient color contrast. Use a divergent color palette (e.g., blue-white-red) for difference maps and provide a second encoding, such as patterns or direct text labels, to convey meaning without relying solely on color [56].
- Supplement with Small Multiples: For comparing multiple systems or conditions, consider using small multiples (a series of miniaturized, consistent plots) instead of overloading a single chart. This improves clarity and accessibility [56].
Experimental Protocols
Protocol 1: Generating a Trajectory Map from an MD Simulation
This protocol details the steps to create a trajectory map using the TrajMap.py application [53].
1. Preprocessing: Generate the Shift Matrix
- Input: MD trajectory file (e.g.,
.xtc,.nc) and topology file (e.g.,.gro,.pdb,.prmtop). - Alignment: Ensure the trajectory is aligned to a reference structure to remove global rotation/translation.
- Command: Run the preprocessing step of
TrajMap.pyto calculate the Euclidean distance (shift) for every residue's backbone atoms in every frame from their position in the first frame (t~ref~). - Output: A shift matrix saved as a
.csvfile.
2. Map Creation: Generate and Fine-Tune the Heatmap
- Input: The precomputed
.csvshift matrix. - Command: Load the matrix into the map-making step of
TrajMap.py. - Parameters: Fine-tune the visualization by adjusting:
- The range of the z-axis color scale to highlight relevant shifts.
- The colormap (e.g., viridis, plasma).
- The axes ticks and labels for clarity.
- Output: A publication-ready trajectory map heatmap.
Workflow for Generating a Trajectory Map.
Protocol 2: Building a Ligand-Based 3D-QSAR Pharmacophore Model
This protocol outlines the methodology for creating a validated ligand-based pharmacophore model using a tool like Discovery Studio [5].
1. Compound Preparation and Dataset Curation
- Source: Gather 2D structures of known ligands with homogeneous biological activity data (e.g., IC50 from a single assay).
- Conversion and Optimization: Convert 2D structures to 3D. Clean structures, add hydrogens, and minimize energy using a force field (e.g., CHARMM).
- Categorization: Categorize ligands based on activity (e.g., most active: IC50 < 0.1 μM; active: 0.1-1.0 μM; moderately active: 1.0-10.0 μM; inactive: >10.0 μM).
- Division: Divide the full ligand set into a training set (containing a maximum number of active and most active compounds, plus some moderately active and inactive for statistical relevance) and a test set for validation.
2. Pharmacophore Generation and Validation
- Generation: Use a 3D-QSAR pharmacophore generation algorithm (e.g., HypoGen in Discovery Studio) with the training set compounds. The algorithm will generate multiple pharmacophore hypotheses.
- Hypothesis Selection: Select the top hypothesis (e.g., Hypo1) based on statistical correlation and cost functions.
- Validation: Validate the selected hypothesis using the test set molecules. A good model will show a high correlation (e.g., R² > 0.85) between experimental and estimated activity for the test set.
Workflow for Building a Ligand-Based Pharmacophore Model.
Data Presentation
Table 1: Quantitative Analysis of Trajectory Map Case Study
Table showing how trajectory maps compare simulation stability, complementing RMSD and RMSF data [53].
| Simulation System | Trajectory Map Interpretation | RMSD Correlation | RMSF Correlation | Key Insight from Trajectory Map |
|---|---|---|---|---|
| TAL Effector + CATANA-built DNA | More stable, fewer backbone shifts | Confirmed more stable | Confirmed more stable | Revealed specific regions of instability and time of onset |
| TAL Effector + Crystal Structure DNA | Less stable, larger and more frequent shifts | Confirmed less stable | Confirmed less stable | Pinpointed exact temporal and spatial location of major conformational events |
Table 2: Essential Research Reagent Solutions for MD and Pharmacophore Analysis
Key software tools and their primary functions in the analysis workflow.
| Research Reagent | Primary Function | Application Context |
|---|---|---|
| TrajMap.py [53] | Generates trajectory maps from MD trajectories. | Visualizing and comparing protein backbone dynamics. |
| MDAnalysis [55] [54] | Python library for reading, writing, and analyzing MD trajectories. | Building custom analysis scripts; core processing engine. |
| DiffPhore [26] [11] | Deep learning framework for 3D ligand-pharmacophore mapping. | Predicting ligand binding conformations; virtual screening. |
| AncPhore [26] [11] | Pharmacophore tool for identifying anchor-binding sites. | Generating 3D ligand-pharmacophore pair datasets. |
| ZINC Database [5] | Publicly available database of commercially-available compounds. | Source for drug-like molecules for virtual screening. |
Troubleshooting Guide: Frequently Asked Questions
FAQ 1: How should I handle stereochemistry in my 3D pharmacophore model to ensure it accurately distinguishes between active and inactive compounds?
Issue: The model fails to properly differentiate stereoisomers, leading to false positives during virtual screening.
Solution: Implement a stereochemistry-aware pharmacophore signature system.
- Root Cause: Traditional 3D pharmacophore representations may not adequately capture chiral configurations, causing them to match compounds with incorrect stereochemistry.
- Resolution: Adopt a quadruplet-based stereoconfiguration encoding method. This approach systematically analyzes all combinations of four features (quadruplets), which are the smallest units having stereoconfiguration in 3D space [57].
- Implementation Protocol:
- Classify Quadruplet Systems: Categorize all feature quadruplets into five distinct systems based on their canonical feature identifiers: AAAA, AAAB, AABC, AABB, and ABCD [57].
- Determine Configuration Signs: Assign configuration signs (0 for achiral, -1 or +1 for chiral) based on the scalar triple product of vectors connecting ranked features [57].
- Handle Special Cases: Implement specific procedures for trapeze-like and parallelogram-like quadruplets belonging to the AABB class, as these require modified stereoconfiguration determination [57].
- Preventive Measures: Always validate your model's ability to distinguish known stereoisomers with different activity profiles during the training phase.
FAQ 2: What strategies can I use to optimize feature tolerance parameters without overfitting my model?
Issue: Either too strict or too lenient feature tolerance leads to poor model performance in virtual screening.
Solution: Utilize binned distances and knowledge-guided matching to balance specificity and generality.
- Root Cause: Fixed, rigid tolerance parameters cannot accommodate the natural flexibility of molecular interactions and conformational variations.
- Resolution: Implement distance binning and knowledge-guided directional matching to create adaptive tolerance [26] [57].
- Implementation Protocol:
- Distance Binning: Convert exact distances between features to binned distances using a predefined step (e.g., 1 Å). This creates fuzzy matching capability while maintaining spatial relationships [57].
- Directional Matching: For directional features (hydrogen-bond donors/acceptors, metal coordination), compute the discrepancy between the intrinsic orientation of each ligand atom and the direction of each pharmacophore feature [26].
- Type Matching: Align each ligand atom with all pharmacophore features using pharmacophore fingerprints to expedite type compatibility assessment [26].
- Validation Method: Test your tolerance parameters on both active and inactive compounds, ensuring they capture true actives while excluding inactives. The model should maintain performance across diverse chemical scaffolds.
FAQ 3: How can I improve my model's scaffold-hopping capability while maintaining predictive accuracy?
Issue: The model successfully identifies similar scaffolds but fails to find structurally distinct compounds with the same activity.
Solution: Leverage the abstract nature of pharmacophore representations to reduce structural bias.
- Root Cause: Over-reliance on specific functional groups or molecular frameworks in the training set creates bias that limits scaffold-hopping potential.
- Resolution: Focus on interaction patterns rather than specific structural elements by using abstract chemical feature representations [58].
- Implementation Protocol:
- Feature Abstraction: Transform different functional groups with the same interaction profile into abstract chemical features (e.g., π-stacking interaction or H-Bond donor/acceptor) [58].
- Consensus Pharmacophore Generation: Develop a consensus (merged) pharmacophore from all training samples, then align input pharmacophores to this consensus model [58].
- Diverse Training Set: Ensure your training set includes compounds with diverse scaffolds but similar activities to teach the model which features are essential versus optional.
- Performance Metrics: Evaluate scaffold-hopping success by testing the model on structurally distinct active compounds not included in training, measuring both recall and precision.
Experimental Protocols for Parameter Optimization
Protocol 1: Systematic Evaluation of Stereochemical Handling
Purpose: To validate that your pharmacophore model correctly handles stereochemistry and chiral configurations.
Materials:
- Known active compounds with defined stereochemistry
- Their stereoisomers with different activity profiles
- Computational tools for 3D pharmacophore generation and analysis
Procedure:
- Prepare stereoisomer dataset: Curate a set of compounds where different stereoisomers show significantly different biological activities [57].
- Generate pharmacophore models: Create separate models using the stereochemistry-aware approach described in FAQ 1.
- Test matching: Check if the model correctly matches the active stereoisomers while excluding inactive stereoisomers.
- Quantify performance: Calculate enrichment factors and ROC-AUC values to objectively measure stereochemical discrimination capability [59].
Troubleshooting:
- If discrimination is poor, adjust the configuration sign thresholds in the quadruplet analysis.
- For planar systems, fine-tune the minimal angle threshold that determines deviation from planarity [57].
Protocol 2: Feature Tolerance Calibration Using Binned Distances
Purpose: To establish optimal bin sizes for distance tolerances in your pharmacophore model.
Materials:
- Set of active compounds with diverse scaffolds
- Decoy set or known inactive compounds
- Pharmacophore modeling software with customizable distance parameters
Procedure:
- Generate multiple models: Create pharmacophore models using different bin sizes (0.5 Å, 1.0 Å, 1.5 Å, 2.0 Å).
- Virtual screening: Perform screening against both active and decoy sets using each model.
- Evaluate performance: Calculate enrichment factors, hit rates, and ROC curves for each bin size.
- Select optimal parameters: Choose the bin size that provides the best balance between recall (finding true actives) and precision (excluding inactives).
Expected Outcomes:
- Typical optimal bin sizes range from 1.0-1.5 Å, providing sufficient flexibility without excessive promiscuity [57].
- The model should maintain performance across different chemical classes when optimal parameters are used.
Data Presentation: Parameter Optimization Guidelines
Table 1: Recommended Tolerance Parameters for Different Pharmacophore Features
| Feature Type | Distance Tolerance | Directional Tolerance | Special Considerations |
|---|---|---|---|
| Hydrogen Bond Donor/Acceptor | 1.0-1.5 Å | 30-45 degrees | Include directional vectors for proper alignment [26] |
| Hydrophobic Features | 1.2-1.8 Å | N/A | Larger tolerance often acceptable due to nature of hydrophobic interactions |
| Aromatic Rings | 1.0-1.7 Å | 20-40 degrees (for ring plane) | Consider both centroid position and ring orientation |
| Positive/Negative Ionizable | 1.0-1.5 Å | N/A | Electrostatic interactions may have longer effective range |
| Metal Coordination | 0.8-1.2 Å | 15-30 degrees | Typically requires stricter tolerance due to geometric constraints |
Table 2: Stereochemistry Handling Methods Comparison
| Method | Implementation Complexity | Scaffold-Hopping Capability | Stereochemical Discrimination |
|---|---|---|---|
| Traditional Alignment-Based | Moderate | Limited | Poor to moderate |
| Quadruplet Signature [57] | High | Excellent | Excellent |
| Graph-Based without Stereochemistry | Low | Good | Poor |
| Hybrid Approach (Structure + Ligand-based) | High | Good | Good to excellent |
Workflow Visualization
Figure 1. Parameter optimization workflow for pharmacophore models.
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Computational Tools for Parameter Optimization
| Tool Name | Primary Function | Parameter Optimization Features | Access |
|---|---|---|---|
| DiffPhore [26] [11] | Knowledge-guided diffusion framework | Calibrated sampling to reduce exposure bias | Research |
| PMapper/psearch [57] | 3D pharmacophore modeling | Stereochemistry-aware quadruplet signatures | Open-source |
| PHASE [3] [58] | Pharmacophore perception and alignment | 3D pharmacophore fields and PLS regression | Commercial |
| HypoGen [5] [58] | Quantitative pharmacophore generation | Hypothesis scoring based on RMSE | Commercial |
| AncPhore [26] | Pharmacophore feature identification | Multiple feature types and exclusion spheres | Research |
Table 4: Essential Datasets for Training and Validation
| Dataset Name | Application | Key Features | Reference |
|---|---|---|---|
| CpxPhoreSet [26] [11] | Model refinement | Real but biased ligand-pharmacophore pairs from experimental structures | Included in DiffPhore publication |
| LigPhoreSet [26] [11] | Initial model training | Perfectly-matched ligand-pharmacophore pairs with broad chemical diversity | Included in DiffPhore publication |
| ChEMBL [58] [57] | General validation | Large-scale bioactivity data for multiple targets | Public database |
| DUD-E [26] | Virtual screening evaluation | Annotated active and decoy compounds for benchmarking | Public database |
Assessing Synthetic Accessibility and Drug-Likeness Early in the Selection Process
Frequently Asked Questions (FAQs)
Data Curation and Preparation
Q1: What are the best practices for splitting data to ensure my pharmacophore model generalizes well to new chemical scaffolds?
A robust data splitting strategy is fundamental to building a model that performs well on unseen chemotypes, not just the compounds it was trained on.
- Objective: The primary goal is to assess the model's ability to generalize to entirely new chemical structures (scaffolds), which is a more realistic reflection of its screening power in a real-world virtual screening campaign [47].
- Recommended Protocol: Instead of a simple random split, use a scaffold-based splitting strategy [47].
- Generate the Bemis-Murcko scaffolds for all compounds in your dataset [47].
- Split the data into training, validation, and testing subsets (e.g., 70/15/15) while minimizing the overlap of scaffolds between the subsets [47].
- This ensures that the model is evaluated on chemotypes that differ from those used in the training process, providing a more reliable performance estimate [47].
- Common Pitfall: A random split can lead to over-optimistic performance metrics if the test set contains compounds with scaffolds very similar to those in the training set. A scaffold split more accurately reveals the model's true predictive power for novel leads [47].
Q2: How can I create a high-quality dataset for training a pharmacophore-based deep learning model?
High-quality, diverse datasets are the foundation of effective AI-driven pharmacophore tools. Recent research highlights the creation of specialized datasets for this purpose [26] [11].
- Dataset Types: Two complementary types of datasets have been proven effective [26] [11]:
- LigPhoreSet: Generated from energetically favorable ligand conformations, focusing on perfectly-matched ligand-pharmacophore pairs. This dataset is designed for broad chemical and pharmacophoric space coverage, helping the model learn generalizable mapping patterns [26] [11].
- CpxPhoreSet: Derived from experimental protein-ligand complex structures, containing real but imperfectly-matched pairs. This dataset refines the model for real-world scenarios, including induced-fit effects [26] [11].
- Implementation Workflow:
- Start with a large library of purchasable compounds (e.g., from ZINC20) [26] [11].
- Apply Bemis-Murcko scaffold filtering and fingerprint similarity clustering to ensure chemical diversity [26] [11].
- Generate 3D conformations and then use a pharmacophore tool (e.g., AncPhore) to generate and sample corresponding pharmacophore models, including exclusion spheres [26] [11].
Synthetic Accessibility (SA) Assessment
Q3: What are the limitations of current synthetic accessibility (SA) scoring tools, and how can I overcome them?
While SA scores are essential for filtering, they have known limitations that researchers must account for.
- Known Limitations:
- Lack of Cost Awareness: Many SA scores are on an arbitrary scale (e.g., 1-10) and do not reflect the actual market price or cost-effectiveness of synthesis [60].
- Over-reliance on Complexity: Structure-based methods may incorrectly flag complex natural products as inaccessible, even if they are purchasable [60].
- Computational Bottlenecks: Computer-Aided Synthesis Planning (CASP) is accurate but too slow for screening millions of molecules [60].
- Troubleshooting Solutions:
- Use Price as a Proxy: Newer models like MolPrice use machine learning to predict a molecule's market price (USD/mmol), which directly correlates with synthetic cost and complexity. This provides an interpretable and economically viable SA metric [60].
- Multi-Tool Consensus: Do not rely on a single SA score. Use a combination of a fast structure-based filter (e.g., SAScore) followed by a more sophisticated, cost-aware tool like MolPrice for the top candidates [60].
Q4: My AI-generated molecules have excellent predicted activity but are deemed hard to synthesize. What should I do?
This common problem, known as the "generation-synthesis gap," requires a shift in the molecular generation and evaluation workflow [61].
- Proactive Solution: Integrate SA assessment early and directly into your generative design loop [61].
- Tool Recommendation: Use fast, fragment-based SA predictors like SynFrag. SynFrag uses self-supervised pretraining to learn stepwise molecular construction patterns, capturing relationships relevant to "synthesis difficulty cliffs" [61].
- Workflow Adjustment: Configure your generative model to use the SA score as a joint optimization objective alongside activity and drug-likeness. This guides the AI to propose compounds that are not only active but also synthetically viable [61].
Drug-Likeness and Multi-Parameter Optimization
Q5: How can I comprehensively evaluate drug-likeness beyond traditional rules like Lipinski's Ro5?
A multidimensional evaluation is crucial for improving the clinical translation success of candidate compounds [62].
- Solution: Adopt a comprehensive filtering framework that assesses multiple critical dimensions simultaneously. The druglikeFilter tool is an example of such a framework, evaluating four key areas [62]:
- Physicochemical Rules: Systematically evaluates more than a dozen properties (e.g., MW, ClogP, TPSA) and integrates multiple modern rules beyond Ro5 to filter out promiscuous and non-druggable molecules [62].
- Toxicity Alert: Investigates compounds against a large database of ~600 structural alerts associated with various toxicities (e.g., genotoxicity, skin sensitization) and includes a specialized deep learning model for cardiotoxicity (hERG) prediction [62].
- Binding Affinity: Employs a dual-path approach, using molecular docking for structure-based assessment and an AI model (transformerCPI2.0) for sequence-based prediction when a protein structure is unavailable [62].
- Compound Synthesizability: Estimates synthetic accessibility and integrates a retrosynthesis tool (Retro*) to plan viable synthetic pathways, addressing practical synthesizability [62].
Q6: How can I perform virtual screening very quickly on large libraries without sacrificing the benefits of structure-based methods?
Machine learning can dramatically accelerate structure-based virtual screening by learning from docking results [47].
- Methodology: Train an ensemble machine learning model to predict docking scores directly from 2D molecular structures [47].
- Experimental Protocol:
- Docking Preparation: Dock a representative subset of your library (thousands of compounds) using your preferred docking software (e.g., Smina) [47].
- Feature Generation: Calculate multiple types of molecular fingerprints and descriptors for these compounds [47].
- Model Training: Train an ensemble ML model (e.g., using random forests or XGBoost) to predict the docking score based on the molecular features [47].
- High-Throughput Screening: Use the trained model to predict docking scores for the entire library (millions of compounds) in a fraction of the time. This approach has been shown to be ~1000 times faster than classical docking-based screening [47].
Troubleshooting Guides
Issue 1: Poor Generalization of Pharmacophore Model to Novel Scaffolds
Symptoms: High performance on the training/validation set but significant performance drop when screening external compound libraries or literature datasets with different core structures.
Diagnosis: The model is overfitting to the specific chemical scaffolds present in the training data and has failed to learn the underlying, transferable pharmacophore patterns.
Resolution:
- Re-assess Data Splitting: Immediately stop using a simple random split. Re-partition your existing data using a scaffold-based split to get a true performance baseline [47].
- Curate Additional Data: If performance is poor on the scaffold-split test set, augment your training data with more diverse chemical scaffolds. Utilize public datasets like CpxPhoreSet and LigPhoreSet that are designed for this purpose [26] [11].
- Employ a Two-Stage Training Strategy: Follow the proven protocol of pre-training on a large, diverse set of perfect-matching pairs (e.g., LigPhoreSet) to learn general patterns, then fine-tune on a smaller set of realistic, imperfect pairs (e.g., CpxPhoreSet) to refine for real-world bias [26] [11].
Troubleshooting poor model generalization.
Issue 2: Identifying Synthetically Infeasible Hit Compounds
Symptoms: Virtual screening hits have excellent predicted activity and drug-likeness scores but are flagged by synthetic chemists as being highly complex, requiring long synthetic routes, or having prohibitively expensive starting materials.
Diagnosis: The screening workflow lacks an effective, cost-aware synthetic accessibility (SA) filter, leading to a "generation-synthesis gap" [61].
Resolution:
- Immediate Triage: Run your current hit list through a modern SA tool like MolPrice, which predicts molecular price as a proxy for synthetic cost. This provides an interpretable metric for prioritization [60].
- Integrate Proactive SA Filtering: For future screening and generative design, integrate a fast SA scorer like SynFrag or MolPrice directly into the workflow. Use the SA score as a filter or an optimization objective [61] [60].
- Validate with Retrosynthesis: For the final, much smaller shortlist of candidates, use a dedicated CASP tool (e.g., Retro*) to plan and validate a specific synthetic route, ensuring practical feasibility [62].
Troubleshooting synthetically infeasible hits.
Experimental Protocols & Data Presentation
Table 1: Comparison of Key Synthetic Accessibility (SA) Assessment Tools
| Tool Name | Underlying Approach | Key Output | Key Advantages | Limitations / Considerations |
|---|---|---|---|---|
| SynFrag [61] | Fragment assembly & autoregressive generation | SA classification/prediction | Learns dynamic assembly patterns; interpretable via attention mechanisms; very fast (sub-second). | Primarily a predictor; does not replace detailed route planning. |
| MolPrice [60] | Market price prediction via contrastive learning | Price (USD/mmol) | Cost-aware & interpretable; strong correlation with complexity; fast, suitable for large-scale screening. | Requires retraining to incorporate new market data. |
| SAScore [60] | Structure-based complexity indicators | SA score (1-10) | Very fast; simple to interpret; widely used. | May misclassify complex but purchasable molecules (e.g., natural products). |
| CASP Tools [62] [60] | Retrosynthetic analysis | Specific synthesis routes | High accuracy; provides a concrete synthetic plan. | Computationally expensive (minutes to hours per molecule); not for large-scale screening. |
| druglikeFilter SA Module [62] | RDKit accessibility + Retro* retrosynthesis | SA estimation & route | Integrated with broader drug-likeness evaluation; provides route planning. | The retrosynthesis component is slower than pure SA scoring. |
| Evaluation Dimension | Metrics/Components Assessed | Function in Early-Stage Screening |
|---|---|---|
| Physicochemical Properties | 15+ properties (MW, ClogP, HBD, HBA, TPSA, etc.) and 12+ drug-likeness rules. | Rapidly filters out non-drug-like molecules to reduce unnecessary testing costs. |
| Toxicity Alert | ~600 structural alerts for various toxicities (genotoxicity, skin sensitization, etc.); includes a dedicated cardiotoxicity (hERG) predictor. | Flags compounds with potential safety risks, guiding the design of safer candidates. |
| Binding Affinity | Dual-path: Structure-based (AutoDock Vina) & Sequence-based (AI model, transformerCPI2.0). | Evaluates target engagement potential even when protein structure is unavailable. |
| Compound Synthesizability | Synthetic accessibility estimation & retrosynthetic route prediction (Retro*). | Addresses a key practical limitation by identifying molecules that are synthetically viable. |
This protocol describes how to use machine learning to approximate molecular docking results, enabling the ultra-fast screening of very large compound libraries.
Key Materials & Reagents:
- Compound Library: A large database of compounds in SMILES or SDF format (e.g., ZINC15, ChEMBL).
- Docking Software: Such as Smina.
- Protein Structure: A prepared protein structure file (e.g., PDB format) with a defined binding pocket.
- Computational Environment: A Python environment with cheminformatics libraries (e.g., RDKit) and machine learning libraries (e.g., scikit-learn).
Step-by-Step Methodology:
Create a Representative Docking Dataset:
- Select a manageable but chemically diverse subset (e.g., 10,000-50,000 compounds) from your large screening library.
- Dock this subset using your chosen docking software to obtain docking scores for each compound. This is your ground truth dataset.
Generate Molecular Features:
- For every compound in the dataset, calculate multiple types of molecular features. It is recommended to use an ensemble of different fingerprints and descriptors (e.g., ECFP, MACCS keys, physicochemical descriptors) to capture diverse aspects of molecular structure [47].
Train the Machine Learning Model:
- Split the docked dataset into training, validation, and test sets. For generalizability, use a scaffold-based split [47].
- Train an ensemble machine learning model (e.g., Random Forest, XGBoost) to predict the docking score based on the molecular features.
- Use the validation set to tune hyperparameters and prevent overfitting.
Screen the Large Library:
- Calculate the same molecular features for all compounds in your large screening library (millions of compounds).
- Use the trained ML model to predict the docking score for each compound. This step is ~1000 times faster than performing actual docking [47].
Validation and Hit Selection:
- Select the top-ranking compounds based on the ML-predicted scores.
- For this shortlisted subset, perform conventional molecular docking to confirm the binding poses and scores. This final step validates the predictions and provides reliable hits for further experimental testing.
The Scientist's Toolkit: Essential Research Reagents & Software
Table 3: Key Computational Tools for Modern Pharmacophore Research
| Item Name | Category | Primary Function | Relevance to Training Set Selection |
|---|---|---|---|
| AncPhore [26] [11] | Pharmacophore Tool | Generates pharmacophore models and was used to create the benchmark CpxPhoreSet and LigPhoreSet datasets. | Essential for curating high-quality, 3D ligand-pharmacophore pair datasets for model training. |
| DiffPhore [26] [11] | Deep Learning Framework | A knowledge-guided diffusion model for 3D ligand-pharmacophore mapping and conformation generation. | Demonstrates the value of using complementary datasets (CpxPhoreSet & LigPhoreSet) for warm-up and refinement training. |
| RDKit | Cheminformatics | An open-source toolkit for cheminformatics, used for calculating molecular descriptors, fingerprints, and scaffold analysis. | Fundamental for data preprocessing, feature generation, and implementing scaffold-based data splits. |
| MolPrice [60] | SA Assessment | Predicts molecular market price as a cost-aware, interpretable metric for synthetic accessibility. | Allows for the pre-filtering of training data to include more synthetically tractable compounds, biasing models towards feasible chemical space. |
| druglikeFilter [62] | Multi-Parameter Filter | Provides a comprehensive evaluation of drug-likeness across physicochemical, toxicity, binding, and synthesizability dimensions. | Enables the creation of cleaner, higher-quality training sets by removing compounds with poor drug-like properties early on. |
Proving Model Value: Rigorous Validation, Benchmarking, and Performance Metrics
Validating a pharmacophore model is a critical step to ensure its predictive power and reliability in virtual screening campaigns. Two fundamental components of this process are the use of a robust metric to quantify model performance and a carefully constructed set of decoy molecules to test against. The Goodness-of-Hit (GH) Score is a central metric that evaluates a model's ability to enrich active compounds from a database containing decoys. Test set decoys are chemically similar yet presumed inactive molecules used to challenge the model's discriminatory power. Proper understanding and implementation of these elements are crucial for generating pharmacophore models that perform well in real-world drug discovery applications, ultimately guiding the identification of novel bioactive compounds [63] [64].
Understanding the Goodness-of-Hit (GH) Score
What is the Goodness-of-Hit (GH) Score and its Core Components?
The Goodness-of-Hit (GH) Score is a composite metric that balances the model's ability to retrieve a high proportion of known active compounds (recall) while also ensuring that a significant fraction of the retrieved hits are indeed active (precision). It is calculated from the results of a virtual screening run on a test database containing known actives and decoys [64].
The following table outlines the fundamental parameters required for its calculation:
Table 1: Core Parameters for Calculating the Goodness-of-Hit (GH) Score
| Parameter | Symbol | Description |
|---|---|---|
| Total molecules in database | D | The total number of compounds (actives + decoys) in the benchmarking dataset. |
| Total number of actives in database | A | The total number of known active compounds in the dataset. |
| Total hits | Ht | The total number of compounds retrieved by the pharmacophore model. |
| Active hits | Ha | The number of correctly retrieved active compounds. |
How is the GH Score Calculated?
The GH score is computed using a specific formula that integrates the above parameters. A score of 0.7–0.8 indicates a very good model, while a score of 0.8-1.0 is considered excellent [64].
The formula for the GH score is [65]: [ GH = \left( \frac{Ha(3A + Ht)}{4HtA} \right) \times \left( 1 - \frac{Ht - Ha}{D - A} \right) ]
This formula can be broken down into two main parts:
- The Yield Component:
(Ha(3A + Ht)/(4HtA)- This part of the equation rewards models that retrieve a high number of the known active compounds. - The False Positive Penalty:
(1 - (Ht - Ha)/(D - A))- This part penalizes the model for retrieving a large number of decoys (false positives).
Troubleshooting GH Score Issues
Problem: My GH score is consistently low (below 0.5). What could be wrong?
- Solution: A low GH score often indicates poor model specificity. Check the following:
- Feature Redundancy: Your model might have too many or overly generic pharmacophore features that match many decoys. Try to refine the model to include only the essential, discriminatory features critical for binding [3].
- Decoy Quality: The decoys in your test set may be too "easy" and not challenging enough. Ensure your decoys are property-matched to the actives to avoid artificial enrichment [63].
- Training Set Bias: The actives used to build the model may lack structural diversity, leading to an overfitted model that performs poorly on other chemotypes. Consider using algorithms like Butina clustering to ensure a diverse and representative training set [65].
- Solution: A low GH score often indicates poor model specificity. Check the following:
Problem: The model has high recall (Ha/A) but a low GH score. Why?
- Solution: This is a classic sign of low precision. Your model is retrieving most of the actives (high Ha), but it is also retrieving a very large number of decoys (high Ht - Ha). The high false positive rate is penalizing the GH score. Focus on making the model more restrictive by adjusting feature tolerances or adding excluded volumes to represent the binding site shape more accurately [3] [12].
A Guide to Test Set Decoys
What are Test Set Decoys and Why are They Critical?
In virtual screening validation, decoys are molecules that are presumed to be inactive against the target but are chemically similar to active compounds in terms of their physicochemical properties. Their primary role is to create a realistic and challenging test for the pharmacophore model, simulating a real-world screening scenario [63].
The use of poorly chosen decoys is a major source of bias. If decoys are physically different from actives, the model's performance can be artificially inflated, as it discriminates based on simple properties rather than the specific pharmacophore. Conversely, if decoys are too similar to actives, the model's performance may be underestimated, or true actives might be missed [66] [63].
What are the Best Practices for Decoy Selection?
The evolution of decoy selection has moved from simple random picking to sophisticated, property-matched strategies. The gold standard is to select decoys that are physicochemically similar to the active compounds (e.g., in molecular weight, logP) but structurally dissimilar, to minimize the chance that they are actually active [63].
Table 2: Evolution and Strategies for Decoy Selection
| Strategy | Description | Advantages & Limitations |
|---|---|---|
| Random Selection | Decoys are chosen randomly from large chemical databases like the ACD or MDDR. | Advantage: Simple and fast. Limitation: High risk of bias; decoys are often physically different from actives, leading to artificial enrichment [63]. |
| Property-Matching | Decoys are selected to match the physicochemical properties (e.g., molecular weight, logP) of the active set. Pioneered by the DUD and DUD-E databases. | Advantage: Reduces artificial enrichment by making the discrimination task more challenging and realistic. This is the modern standard [63]. |
| Using Dark Chemical Matter (DCM) | Decoys are selected from compounds that have been tested in HTS assays and consistently shown no activity across multiple targets. | Advantage: Provides experimentally validated, high-quality non-binders. Models trained with DCM decoys perform similarly to those using true inactives [66]. |
| Data Augmentation (DIV) | Generating decoys by using diverse, low-scoring conformations of the active molecules from docking results. | Advantage: Computationally efficient. Limitation: Can lead to models with higher variability and lower performance, as the PADIF fingerprints of "wrong" conformations may still overlap with true binding modes [66]. |
Troubleshooting Decoy Set Issues
Problem: I don't have access to a pre-built database like DUD-E for my target. How can I generate my own decoys?
- Solution: You can create a custom decoy set using public tools and databases. A common workflow is:
- Define your active set: Collect a robust set of known active molecules.
- Calculate properties: For each active, calculate key physicochemical properties like molecular weight, logP, and the number of hydrogen bond donors/acceptors.
- Screen a large database: Use the property ranges of your actives to filter a large, diverse database like ZINC15.
- Apply structural filters: Ensure the selected decoys are structurally diverse (e.g., low Tanimoto similarity) to the actives to avoid analog bias [65] [63].
- Solution: You can create a custom decoy set using public tools and databases. A common workflow is:
Problem: My validation shows great GH score, but the model performs poorly in prospective screening. What happened?
- Solution: This is often a sign of artificial enrichment. Re-examine your decoy set. The decoys might be too easy to distinguish from your actives based on simple properties, not the pharmacophore itself. Re-generate your decoys using property-matching protocols to ensure they occupy a similar chemical space as your actives, making the test more meaningful [65] [63].
Integrated Experimental Workflow
The following diagram illustrates the logical workflow for the validation process, integrating both the GH score calculation and proper decoy selection.
Diagram 1: Pharmacophore Model Validation Workflow. This chart outlines the sequential process from model creation to validation, highlighting the critical decision point based on the GH score.
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Software and Databases for Validation
| Tool / Resource | Type | Primary Function in Validation |
|---|---|---|
| DUD-E | Database | A gold-standard benchmarking database providing pre-generated sets of actives and property-matched decoys for a wide range of targets [67]. |
| ZINC15 | Database | A massive public database of commercially available compounds. Often used as a source for generating custom decoy sets [66] [63]. |
| ChEMBL | Database | A manually curated database of bioactive molecules with drug-like properties. A key resource for finding known active compounds to build the active set [66]. |
| RDKit | Software | An open-source cheminformatics toolkit. Used for calculating molecular descriptors, fingerprints, and manipulating chemical structures during decoy selection and analysis [65]. |
| LIT-PCBA | Database | A dataset containing experimentally confirmed inactive compounds, providing a high-quality resource for rigorous model testing and avoiding false negative bias [66]. |
| DeepCoy | Algorithm | A computational method for generating high-quality decoys that are challenging to distinguish from active substances, mitigating analog bias [65]. |
Assessing Virtual Screening Enrichment and Robustness in Prospective Studies
Frequently Asked Questions
Q1: My virtual screening protocol works well on benchmark datasets but fails to identify active compounds in a prospective study. What could be wrong?
This common issue often stems from training set bias. If the chemical space of your prospective library differs significantly from the ligands used to train your model or build your pharmacophore, the protocol will lack generalizability [68]. To fix this, ensure your training set encompasses diverse chemical scaffolds and pharmacophore feature types. Using tools like ConPhar to build a consensus pharmacophore from multiple, structurally diverse ligands can reduce model bias and enhance robustness for prospective screening [39].
Q2: Why does my pharmacophore model retrieve too many false positives during virtual screening? A high false-positive rate frequently indicates inadequate steric constraints in your pharmacophore model. The model may identify molecules that match the interaction patterns but are sterically incompatible with the binding pocket. Incorporate exclusion spheres (volumes) into your model to define regions where atoms are not permitted, representing the physical boundaries of the binding site [26] [11]. Furthermore, always perform a redocking validation of your protocol with a known active ligand as a critical first step; an RMSD of less than 2Å between the redocked and crystallographic pose indicates a reliable setup [69].
Q3: How can I improve the confidence in my virtual screening hits? Adopt a hybrid or consensus approach. Combining ligand-based (pharmacophore) and structure-based (docking) methods can significantly reduce false positives and increase confidence [70]. For example, you can use a fast ligand-based pharmacophore screen to filter a large library, then apply a more computationally expensive structure-based docking method to the top hits. Creating a consensus score from both methods often yields more reliable results than either method alone [70].
Q4: My docking poses look reasonable, but the compounds show no activity. Is the scoring function the only problem? Not necessarily. While scoring function inaccuracy is a common cause, a major overlooked factor is handling protein flexibility [69]. Many docking programs use a rigid protein structure, which may not account for conformational changes induced by ligand binding. If possible, use docking protocols that allow for side-chain or even limited backbone flexibility. Also, verify that your crystal structure or homology model represents a biologically relevant conformation [71] [70].
Troubleshooting Guides
Problem: Poor Enrichment in Virtual Screening The method fails to prioritize a significant number of active compounds within the top-ranked hits.
| Possible Cause | Diagnostic Steps | Solution |
|---|---|---|
| Non-representative training set [68] | Check the chemical/feature space similarity between your training ligands and the screening library using PCA or t-SNE on molecular descriptors. | Curate a training set with high ligand and pharmacophore diversity. Use tools like ConPhar to integrate features from multiple ligand complexes [39]. |
| Inadequate pharmacophore model | Test the model's ability to recognize known active ligands not used in model building. | Include diverse pharmacophore feature types (e.g., HBD, HBA, hydrophobic, aromatic, charged features) and use exclusion volumes to define steric constraints [26] [21] [11]. |
| Underperforming docking/scoring protocol [69] | Perform a redocking validation: extract a known ligand from a complex, then redock it. Calculate the RMSD between the experimental and docked poses. | If RMSD > 2Å, optimize docking parameters, consider protein flexibility, or try a different docking program. This 30-minute validation can save months of work [69]. |
Problem: Lack of Robustness and Generalizability The virtual screening protocol performs inconsistently across different targets or chemical classes.
| Possible Cause | Diagnostic Steps | Solution |
|---|---|---|
| Overfitting to training data [68] | Evaluate performance on an independent, external test set with different ligands and/or targets. A large performance drop indicates overfitting. | Use larger and more diverse training sets. For machine learning models, apply rigorous data splitting (e.g., protein-family split) and regularization [68]. |
| Over-reliance on ligand similarity [68] | Analyze whether top-ranked hits are predominantly structurally similar to your training ligands. | Integrate structure-based methods. Use a hybrid workflow where a pharmacophore screen is followed by flexible docking or free energy calculations to assess diverse chemotypes [71] [70]. |
| Low-quality protein structure | Check the resolution of experimental structures or prediction confidence scores for AlphaFold models. Pay attention to side-chain positioning in the binding site. | For computational models, refine side chains and loops in the binding pocket. If possible, use a co-crystal structure or a ligand-bound conformation [70]. |
Experimental Protocols & Data
Protocol 1: Construction of a Robust Consensus Pharmacophore Model
This protocol, adapted from a study in JoVE, details how to generate a consensus pharmacophore from multiple ligand complexes to reduce bias and improve virtual screening performance [39].
- Prepare Ligand Complexes: Align all protein-ligand complexes (e.g., from the PDB) using a tool like PyMOL.
- Extract Ligands: Extract each aligned ligand conformer and save it as a separate file in SDF format.
- Generate Individual Pharmacophores: Upload each ligand file to
Pharmitand use the "Load Features" option. Download the corresponding pharmacophore definition as a JSON file for each ligand [39]. - Generate Consensus Model: Use the
ConPhartool in a Google Colab environment.- Install
ConPharand upload all individual pharmacophore JSON files to a designated folder. - Use
ConPharto parse the JSON files, extract pharmacophoric features, and consolidate them into a single data frame. - Execute the
compute_consensus_pharmacophorefunction to generate the final model, which can be saved for virtual screening [39].
- Install
The following diagram illustrates this workflow:
Protocol 2: Redocking Validation for Protocol Reliability
Before screening any library, always validate your docking or pharmacophore-matching protocol [69].
- Obtain a Test Case: Extract a protein-ligand complex with a known crystal structure from a source like the PDB.
- Prepare the System: Prepare the protein and ligand files according to your software's requirements.
- Remove and Redock: Completely remove the crystallographic ligand from the binding site.
- Execute Docking/Mapping: Redock the ligand back into the prepared protein or map it to a pharmacophore model derived from the native complex.
- Calculate RMSD: Superimpose the redocked/predicted ligand pose onto the original crystallographic pose. Calculate the Root-Mean-Square Deviation (RMSD) of the atomic positions.
- Interpret Results: An RMSD of less than 2.0 Å typically indicates a reliable protocol. An RMSD greater than 2.0 Å suggests a need to optimize parameters, consider protein flexibility, or try an alternative method [69].
Quantitative Data for Assessment
Table 1: Common Pharmacophore Feature Types and Their Descriptions [26] [11]
| Abbreviation | Feature Type | Description |
|---|---|---|
| HA | Hydrogen Bond Acceptor | An atom that can accept a hydrogen bond. |
| HD | Hydrogen Bond Donor | A hydrogen atom attached to an electronegative atom, capable of donating a hydrogen bond. |
| HY | Hydrophobic | A non-polar atom or region that favors hydrophobic interactions. |
| AR | Aromatic Ring | A planar, cyclic ring system with conjugated π-electrons. |
| PO | Positively Charged Center | An atom or group that carries a positive charge. |
| NE | Negatively Charged Center | An atom or group that carries a negative charge. |
| XB | Halogen Bond Donor | A halogen atom involved in a specific non-covalent interaction. |
Table 2: Representative Virtual Screening Benchmark Performance [68] [71] This table shows sample performance metrics from different methods on established benchmarks, illustrating the level of enrichment you can aim for.
| Method / Benchmark | DUD-E (Average EF1%) | DEKOIS 2.0 (Average EF1%) | Notes |
|---|---|---|---|
| RosettaGenFF-VS [71] | 16.7 | - | Physics-based method; EF1% is Enrichment Factor at top 1% of the screened library. |
| SCORCH2 [68] | State-of-the-art | State-of-the-art | Machine-learning consensus model; shows robust performance on unseen targets. |
| Traditional Docking (e.g., Vina) | ~11.9 [71] | Lower than ML methods | Baseline for comparison; performance can vary significantly by target. |
The Scientist's Toolkit: Essential Research Reagents & Software
Table 3: Key Software and Resources for Virtual Screening
| Item | Function/Brief Explanation | Reference |
|---|---|---|
| ConPhar | An open-source informatics tool for generating consensus pharmacophore models from multiple ligand-bound complexes, reducing model bias. | [39] |
| Pharmit | An online tool for pharmacophore-based virtual screening; used to generate pharmacophore models from ligand structures. | [39] |
| DiffPhore | A deep learning-based diffusion framework for generating 3D ligand conformations that match a given pharmacophore model. | [26] [11] |
| SCORCH2 | A machine learning-based scoring function for virtual screening that uses interaction features for improved performance and interpretability. | [68] |
| RosettaVS | A physics-based virtual screening protocol that incorporates receptor flexibility for accurate pose prediction and ranking. | [71] |
| ZINC/ChEMBL | Publicly accessible databases providing chemical structures and, for ChEMBL, bioactivity data for ligand sourcing and training set creation. | [21] |
| DUD-E / DEKOIS | Benchmark datasets for rigorously evaluating virtual screening methods, containing known actives and designed decoys. | [68] |
Workflow for Robust Virtual Screening
The most effective strategy for robust prospective screening often combines multiple techniques. The following workflow integrates the key concepts from this guide:
The pharmacophore model, defined as "an ensemble of steric and electronic features that is necessary to ensure the optimal supramolecular interactions with a specific biological target," serves as a fundamental cornerstone in modern drug discovery [6]. The efficacy of any pharmacophore model—whether ligand-based, structure-based, or machine learning-enhanced—is critically dependent on the initial and often determinative step of training set selection. The composition of the training set directly dictates a model's ability to generalize, its feature relevance, and its ultimate success in virtual screening campaigns. This technical support guide addresses the specific, practical challenges researchers face when constructing these foundational datasets, providing targeted troubleshooting advice to navigate common pitfalls.
Troubleshooting Guides & FAQs
FAQ 1: What are the fundamental differences in data requirements for the three pharmacophore modeling approaches?
Answer: The core data requirements diverge significantly based on the chosen approach, fundamentally influencing training set strategy.
- Ligand-Based Models: Require a set of known active compounds. The training set must contain structurally diverse molecules that share a common mechanism of action. The key is to include a range of chemotypes while maintaining a consistent pharmacophore pattern [6].
- Structure-Based Models: Rely on a 3D structure of the target protein, typically from X-ray crystallography, NMR, or cryo-EM. The training "set" can be as minimal as a single protein structure, but its conformational state and resolution are paramount. Dynamic information from Molecular Dynamics (MD) simulations is increasingly used to capture the flexible nature of the binding site, generating an ensemble of protein conformations for a more robust model [49] [72].
- Machine Learning (ML)-Enhanced Models: Have the most complex data needs, often combining the requirements of both ligand-based and structure-based methods. They require large, high-quality datasets of either protein-ligand complexes or ligand-pharmacophore pairs for training. For instance, the DiffPhore framework uses specialized datasets like
CpxPhoreSet(derived from experimental complexes) andLigPhoreSet(derived from diverse ligand conformations) to learn the mapping rules between ligands and pharmacophores [26] [11].
FAQ 2: How many active compounds are needed to build a reliable ligand-based pharmacophore model?
Answer: There is no universally fixed number, but the quality and diversity of actives are more important than the quantity alone.
- Minimum Requirement: A minimum of 3-5 structurally diverse active compounds is often necessary to perceive a meaningful common pharmacophore [6].
- Ideal Scenario: Including 15-30 highly active and diverse molecules significantly improves model robustness and reduces the risk of overfitting to a specific chemical scaffold.
- Troubleshooting Tip: If your model performs poorly in validation, assess the structural diversity of your training set. Use Bemis-Murcko scaffold analysis or fingerprint-based clustering. A training set composed of molecules with identical or highly similar scaffolds will produce a model with limited generalizability and poor scaffold-hopping potential [26].
FAQ 3: My structure-based model from a single crystal structure fails to identify known active compounds. What is the likely cause and solution?
Answer: This is a common issue often stemming from protein rigidity and conformational selection.
- Likely Cause: A single static crystal structure represents only one snapshot of the protein's conformational landscape. Ligands may bind to alternative, low-energy states of the protein that are not represented in your input structure—a phenomenon known as conformational selection [49].
- Solution: Incorporate protein flexibility into your training data.
- Method: Use Molecular Dynamics (MD) simulations to generate an ensemble of protein conformations.
- Protocol: Run an MD simulation of the apo (ligand-free) protein or the protein-ligand complex. Save multiple snapshots from the trajectory (e.g., every 200 ps over a 600 ns simulation) [49]. These snapshots form a conformational ensemble that can be used for ensemble docking or to create a dynamic pharmacophore (dynophore) that captures the frequency and spatial distribution of key interaction features [49] [72].
FAQ 4: For ML-enhanced models, what are the best practices for curating a training set to avoid bias?
Answer: ML models are exceptionally prone to learning biases present in the training data. Meticulous curation is essential.
- Challenge: Models trained on existing chemical libraries can be biased towards specific scaffolds and feature distributions, limiting their ability to identify novel chemotypes [26].
- Best Practices:
- Maximize Chemical Diversity: Use clustering techniques (e.g., based on ECFP4 fingerprints or Bemis-Murcko scaffolds) to select a representative set of ligands that cover a broad chemical space, as demonstrated in the creation of the
LigPhoreSet[26] [11]. - Incorstrate Negative Data: Include confirmed inactive compounds or decoys in the training process. This teaches the model to distinguish between features that promote binding and those that do not.
- Use Complementary Datasets: For generative tasks, employ a two-stage training strategy. First, train on a large, diverse set of perfectly-matched ligand-pharmacophore pairs (
LigPhoreSet) to learn general rules. Then, refine the model on a smaller set of real-world, imperfect pairs from experimental complexes (CpxPhoreSet) to account for induced-fit effects [11]. - Scaffold-Based Splitting: When evaluating model performance, split your data into training and test sets based on molecular scaffolds, not randomly. This ensures the model is tested on truly novel chemotypes, providing a realistic estimate of its scaffold-hopping capability [47].
- Maximize Chemical Diversity: Use clustering techniques (e.g., based on ECFP4 fingerprints or Bemis-Murcko scaffolds) to select a representative set of ligands that cover a broad chemical space, as demonstrated in the creation of the
Experimental Protocols & Data Presentation
Protocol 1: Generating a Dynamic Pharmacophore Model from MD Simulations
This protocol is a solution to the rigidity problem of single-structure models [49] [72].
- System Setup: Obtain a protein structure (e.g., from PDB). Prepare it by adding hydrogen atoms, assigning partial charges (e.g., with MMFF94x), and solvating it in an explicit water box.
- MD Simulation: Run a molecular dynamics simulation using software like GROMACS or AMBER. For a coarse-grained model, a 600 ns simulation saving frames every 200 ps will yield 3,000 conformations.
- Trajectory Analysis: Superimpose all MD snapshots onto a reference frame based on the binding site residues.
- Pharmacophore Generation: For each snapshot, use a tool like MOE's SiteFinder and DB-PH4 to identify pharmacophore features (e.g., hydrogen bond donor (Don), acceptor (Acc), cation (Cat), anion (Ani), aromatic (Aro), hydrophobic (Hyd)) within the binding site.
- Feature Clustering: Cluster all pharmacophore features from all frames based on their spatial location to create consensus features. These represent the persistent, key interaction points in the dynamic binding site.
Protocol 2: Constructing a Training Set for a Topological Pharmacophore Model
This ligand-based method uses graph representations and is less computationally demanding than 3D approaches [73].
- Data Curation: From a database like ChEMBL, extract active compounds for your target (e.g., pKi ≥ 6.0). Filter by molecular weight (e.g., 200-600 Da) to reduce complexity.
- Feature Assignment: Use a toolkit like RDKit with a feature definition file (e.g.,
BaseFeatures.fdef) to assign Pharmacophoric Features (PFs)—such as Hydrogen Bond Donor (HBD), Acceptor (HBA), Aromatic (Ar), and Positive/Ionizable (Pos)—to each atom or functional group in the molecules. - Graph Construction: Represent each molecule as a Sparse Pharmacophore Graph (SPhG). In an SPhG, nodes are the assigned PFs, and edges represent the topological distances (number of bonds) between them.
- Identify Common Hypotheses: Analyze the set of SPhGs from all active compounds to find commonly occurring sub-graphs. These shared sub-graphs represent the topological pharmacophore hypotheses for your target.
Quantitative Comparison of Model Performance
Table 1: Virtual Screening Enrichment of Different Pharmacophore Modeling Approaches.
| Modeling Approach | Key Technique | Reported Performance Gain | Key Advantage |
|---|---|---|---|
| ML-Enhanced Dynamic Pharmacophore [49] | MD Ensemble + ML Feature Ranking | Up to 54-fold enrichment over random selection | Identifies features critical for conformational selection; highly interpretable. |
| Knowledge-Guided Diffusion (DiffPhore) [26] [11] | Diffusion model trained on 3D ligand-pharmacophore pairs | State-of-the-art performance in binding pose prediction, surpassing several docking methods. | Superior virtual screening power for lead discovery and target fishing. |
| Shape-Focused Pharmacophore (O-LAP) [12] | Clustering of docked poses to create cavity-filling models | Massive improvement on default docking enrichment. | Effective in both docking rescoring and rigid docking. |
| Machine Learning-Accelerated Screening [47] | ML model trained to predict docking scores | 1000x faster than classical docking-based screening. | Extreme speed for screening ultra-large libraries. |
Table 2: Essential Research Reagent Solutions for Pharmacophore Modeling.
| Research Reagent / Software | Function in Pharmacophore Modeling | Example in Context |
|---|---|---|
| Molecular Operating Environment (MOE) [49] | Integrated software for structure-based pharmacophore generation and analysis. | Used for generating pharmacophore descriptors from MD trajectories with its DB-PH4 facility. |
| GROMACS [49] | Molecular dynamics simulation package. | Used to generate an ensemble of protein conformations to capture binding site dynamics. |
| RDKit [73] | Open-source cheminformatics toolkit. | Used for generating topological pharmacophore fingerprints (PhFPs) and analyzing molecular scaffolds. |
| PLANTS [12] | Molecular docking software for virtual screening. | Used to generate flexible ligand poses for constructing shape-focused O-LAP models. |
| ZINC Database [26] [47] [21] | Public database of commercially available compounds for virtual screening. | Source of compounds for virtual screening and for building large training datasets (e.g., LigPhoreSet). |
| ChEMBL Database [73] [47] | Manually curated database of bioactive molecules with drug-like properties. | Primary source for extracting known active compounds to build ligand-based training sets. |
Workflow Visualization
ML-Enhanced Pharmacophore Development
Comparative Modeling Approaches
Frequently Asked Questions
FAQ 1: What is the primary purpose of validating a pharmacophore model against a PDB structure? Validation against a Protein Data Bank (PDB) structure confirms that your pharmacophore model accurately represents the key intermolecular interactions between a ligand and its biological target. This process verifies the model's steric and electronic complementarity, ensuring it can reliably discriminate between active and inactive compounds in virtual screening [3] [6].
FAQ 2: My model validates well on its training set but performs poorly on new compounds. What could be wrong? This is often a sign of overfitting or a lack of chemical diversity in your training set. A robust model should be derived from a set of known active molecules that are structurally diverse and for which direct target interaction has been experimentally proven. Avoid using data from cell-based assays for model generation, as effects may be caused by mechanisms other than the intended target interaction [9].
FAQ 3: How can I use a PDB structure that has no bound ligand? For apo structures (without a ligand), you can use structure-based pharmacophore modeling tools that analyze the topology of the binding site. Programs like Discovery Studio can calculate potential pharmacophore features based on the residues lining the active site, which you can then adapt into a final hypothesis [9].
FAQ 4: What are the key metrics for evaluating the quality of a validated pharmacophore model? After validation, a model's quality is assessed by its performance in virtual screening. Key metrics include the Enrichment Factor (the enrichment of active molecules compared to random selection), Yield of Actives, and the Area Under the Curve of the Receiver Operating Characteristic plot (ROC-AUC) [9].
FAQ 5: What is a consensus pharmacophore model and when should I use it? A consensus model integrates common pharmacophoric features from multiple ligand-target complexes. This approach is particularly valuable when you have access to several PDB structures for your target, as it reduces bias from any single ligand and provides a more robust representation of the essential interaction patterns, thereby enhancing virtual screening accuracy [39].
Troubleshooting Guides
Problem 1: Poor Enrichment During Virtual Screening Validation Your model fails to correctly prioritize known active compounds over inactive ones in a validation screen.
| Possible Cause | Diagnostic Steps | Solution |
|---|---|---|
| Non-biologically relevant ligand conformations | Check if the training set ligand conformations are energy-minimized and if the bioactive pose is known from a complex structure. | Use ligand conformations derived from experimental protein-ligand complex structures (e.g., from the PDB) whenever possible [26] [11]. |
| Overly specific or restrictive features | Run the model against a small set of known actives that it was not trained on. If few are recovered, features may be too strict. | Simplify the model by making some non-essential features optional or adjusting the tolerance (radius) of feature spheres to allow for more flexibility [9]. |
| Inadequate training set | Analyze the chemical diversity of your training set ligands using fingerprint descriptors (e.g., ECFP4). | Curate a training set with diverse molecular scaffolds that share a common mechanism of action to capture the core, essential features [26] [9]. |
Problem 2: Inability to Map a Known Active Ligand from a PDB Complex A co-crystallized ligand does not map successfully to the pharmacophore model generated from its own complex.
| Possible Cause | Diagnostic Steps | Solution |
|---|---|---|
| Incorrect ligand protonation or tautomeric state | Verify the ligand's protonation state at the pH of interest and ensure it matches the conditions of the experimental structure. | Re-prepare the ligand file using software like LIGPREP to generate correct ionization and tautomeric states before conformation generation [12]. |
| Induced-fit effects not accounted for | Compare the protein conformation in your target PDB with the PDB used for modeling. Look for differences in side-chain orientations or loop movements. | If available, use a structure-based pharmacophore tool that can incorporate protein flexibility or generate an ensemble of models from multiple complexes [26]. |
| Suboptimal pharmacophore feature definitions | Visually inspect the protein-ligand interactions in software like PyMOL or LigandScout to ensure the modeled features match the actual interactions. | Manually adjust the generated pharmacophore features (type, location, direction) to precisely mirror the observed interactions in the crystal structure [9] [6]. |
Problem 3: Handling Targets with Extensive Ligand Libraries The process of generating a unified, robust model from a large number of PDB complexes (e.g., 100+) is technically challenging.
| Possible Cause | Diagnostic Steps | Solution |
|---|---|---|
| Difficulty in integrating diverse feature sets | Manually inspecting all individual pharmacophore models from each complex is time-consuming and impractical. | Use a specialized informatics tool like ConPhar to systematically extract, cluster, and merge pharmacophoric features from hundreds of pre-aligned ligand-target complexes into a single consensus model [39]. |
| Model bias towards over-represented chemotypes | Check the chemical structures of the ligands in your PDB set. Are they dominated by a single scaffold? | Before modeling, perform Bemis-Murcko scaffold analysis and clustering to ensure your input set represents a wide chemical space, or apply weights to balance feature contribution [26] [39]. |
Experimental Protocol: Consensus Pharmacophore Validation with ConPhar
This protocol details the generation and validation of a consensus pharmacophore model against a set of experimental PDB structures, using the SARS-CoV-2 main protease (Mpro) as a case study [39].
1. Prepare Ligands and Generate Individual Pharmacophore Models
- Align Complexes: Use PyMOL to align all protein-ligand complexes based on the protein's alpha-carbon atoms.
- Extract Ligands: Save the 3D conformation of each aligned ligand into individual files in SDF or MOL2 format.
- Generate Pharmacophores: Upload each ligand file to the online tool Pharmit. Use the "Load Features" option and then download the corresponding pharmacophore definition for each ligand as a JSON file using the "Save Session" option [39].
2. Generate the Consensus Model with ConPhar
- Set Up Environment: Launch a new Google Colab notebook. Install Conda, PyMOL, and the ConPhar Python package using the provided installation scripts.
- Load Data: Create a folder in Colab (e.g.,
JSON_FOLDER) and upload all the previously generated JSON files. - Parse and Consolidate Features: Run the ConPhar script to extract all pharmacophoric features from the individual JSON files and consolidate them into a single data table.
- Compute Consensus: Execute the function to generate the consensus model. The algorithm will cluster similar features from across all ligands to identify the spatially conserved, essential interaction points [39].
3. Validate the Model
- Qualitative Visualization: Load the consensus model and a representative PDB structure into molecular visualization software (e.g., PyMOL) to visually confirm that the pharmacophore features align with key protein-ligand interactions in the binding site.
- Quantitative Virtual Screening: Use the consensus model to screen a validation library containing known active ligands and decoy compounds (e.g., from DUD-E). Calculate enrichment metrics (Enrichment Factor, ROC-AUC) to objectively evaluate the model's predictive power [9].
The workflow for this protocol is summarized in the diagram below:
The following table details key computational tools and data resources essential for validating pharmacophore models against PDB structures.
| Resource Name | Type | Function in Validation |
|---|---|---|
| Protein Data Bank (PDB) | Database | The primary repository for experimentally-determined 3D structures of proteins and protein-ligand complexes, used as the ground truth for validation [3] [9]. |
| ConPhar | Software Tool | An open-source Python package designed to generate a consensus pharmacophore model from multiple ligand-target complexes, overcoming bottlenecks with large ligand libraries [39]. |
| Pharmit | Software Tool | An online platform for pharmacophore-based virtual screening; used in the protocol to generate individual pharmacophore models from ligand SDF files [39]. |
| PyMOL | Software Tool | A molecular visualization system used for aligning protein structures, extracting ligands, and visually inspecting the alignment of pharmacophore models with the protein binding site [39]. |
| Directory of Useful Decoys, Enhanced (DUD-E) | Database | Provides property-matched decoy molecules for a wide range of targets, enabling the quantitative assessment of a model's virtual screening performance and enrichment [9]. |
| CpxPhoreSet | Dataset | A specialized dataset of 3D ligand-pharmacophore pairs derived from experimental PDB complexes, useful for training and testing models on real but biased mapping scenarios [26] [11]. |
Decision Framework for Validation Strategy
The following flowchart outlines a recommended decision process for selecting the appropriate validation strategy based on your available data.
Benchmarking Performance Against Established Methods and Public Datasets
Frequently Asked Questions (FAQs)
Q1: What are the most common types of bias in benchmarking datasets for virtual screening, and how can I avoid them? The most common biases are "analogue bias," "artificial enrichment," and "false negatives" [74]. Analogue bias occurs when decoys are overly dissimilar to active ligands, making it artificially easy for ligand-based methods to distinguish them. Artificial enrichment happens when simple physicochemical property matching inflates performance metrics. False negatives arise when the decoy set inadvertently includes compounds that could actually be active. To avoid these, use modern, purpose-built benchmarking sets like DUD-E or MUV that implement maximum-unbiased design and careful property matching [74].
Q2: My pharmacophore model performs well on the training set but poorly during virtual screening. What could be wrong? This is a classic sign of overfitting or dataset bias [74]. Your training set might lack the chemical diversity of a real-world screening library. To fix this:
- Refine with Realistic Data: Use a two-stage training approach. Start with a diverse, perfectly-matched set (like LigPhoreSet) to learn general patterns, then refine with a set derived from real complex structures (like CpxPhoreSet) that includes imperfect matches and induced-fit effects [11] [26].
- Apply Calibrated Sampling: If you are using an AI model, employ techniques like calibrated sampling to narrow the discrepancy between the model's training and inference phases, which mitigates exposure bias [11] [26].
- Re-evaluate Your Decoys: Ensure your benchmarking decoys are not trivially easy to distinguish from your active compounds [74].
Q3: For a new target with no known active compounds, can I still use ligand-based methods? Traditional single-template ligand-based methods require at least one known active compound. However, modern AI-based structure-based methods can generate a starting point. For example, tools like PharmacoForge can generate a 3D pharmacophore model conditioned only on a protein pocket structure, which can then be used for virtual screening [75]. This effectively bridges the gap when no active ligands are available.
Q4: How do deep learning pharmacophore models compare to traditional tools in benchmark studies? Deep learning models have demonstrated state-of-the-art performance in recent benchmarks. For instance, the DiffPhore framework has been shown to surpass traditional pharmacophore tools and several advanced docking methods in predicting binding conformations on independent test sets like PDBBind and PoseBusters [11] [26]. It also shows superior power in virtual screening tasks for lead discovery and target fishing on the DUD-E database [11] [26].
Troubleshooting Guides
Issue: Low Enrichment in Virtual Screening
Problem: Your pharmacophore model fails to successfully enrich active compounds at the top of the ranking list during virtual screening.
Diagnosis and Solutions:
| Diagnostic Step | Possible Cause | Recommended Action |
|---|---|---|
| Check Dataset Bias | The benchmarking set has "analogue bias" or "artificial enrichment" [74]. | Switch to a maximum-unbiased benchmarking set like MUV or a carefully curated DUD-E set designed for ligand-based methods [74]. |
| Evaluate Model Generality | The model is overfitted to a narrow chemical space [11]. | Augment training with a diverse dataset. Use LigPhoreSet for generalizable patterns and CpxPhoreSet for real-world refinement [11] [26]. |
| Review Model Features | The pharmacophore features are too rigid or do not reflect key interactions. | For structure-based models, use tools like O-LAP to generate shape-focused models that better represent the cavity [12]. |
| Compare Method Performance | The chosen method is not optimal for your target. | Implement a consensus approach. Evidence shows that combining the best-performing algorithms of a distinct nature can outperform any single method [76]. |
Issue: Handling Non-Traditional Targets (e.g., RNA, DNA)
Problem: Standard pharmacophore models, developed for protein targets, perform poorly when applied to nucleic acid targets like RNA or DNA.
Diagnosis and Solutions:
- Cause: The fundamental building blocks and higher-order structures of nucleic acids differ significantly from proteins, requiring different interaction patterns to be captured [76].
- Solution:
- Target-Specific Benchmarking: Do not assume protein-derived methods will work out-of-the-box. Benchmark a variety of ligand-based methods, including 2D fingerprints and 3D shape-based approaches, against known RNA/DNA ligand data [76].
- Leverage Specialized Datasets: Use emerging datasets specifically for nucleic acid ligands, such as R-BIND (RNA-targeted BIoactive ligaNd Database) or HARIBOSS (for RNA-ligand structures) [76].
- Adopt a Consensus Strategy: Research indicates that no single descriptor is universally best for nucleic acids. A consensus method that combines the top-performing algorithms often provides the most robust solution [76].
Experimental Protocols for Benchmarking
Protocol 1: Benchmarking on the DUD-E Dataset
The DUD-E (Directory of Useful Decoys: Enhanced) is a widely used benchmark for structure-based virtual screening [74].
1. Objective: To evaluate the virtual screening enrichment of a pharmacophore model against a specific target available in the DUD-E database.
2. Materials/Reagents:
| Research Reagent | Function in Experiment |
|---|---|
| DUD-E Dataset | Provides a curated set of known active ligands and property-matched decoy compounds for a specific target [74]. |
| Pharmacophore Modeling Software (e.g., LigandScout, PHASE) | Used to generate and apply the pharmacophore model for screening. |
| Virtual Screening Platform (e.g., ZINCPharmer/Pharmit) | Executes the high-throughput pharmacophore search against the ligand and decoy database [77]. |
| Enrichment Calculation Script | Computes standard metrics (e.g., EF, ROC-AUC) from the screening results. |
3. Workflow: The following diagram illustrates the key steps for a benchmarking experiment using the DUD-E dataset.
4. Procedure:
- Target Selection: Choose a target of interest from the DUD-E database (e.g., a kinase, protease).
- Data Retrieval: Download the list of active compounds and their matched decoys for the selected target.
- Model Generation: Develop your pharmacophore model using known actives (not all actives in DUD-E should be used for training to avoid bias).
- Virtual Screening: Screen the combined set of actives and decoys against your pharmacophore model using a tool like Pharmit [75].
- Ranking: Rank all screened compounds based on their pharmacophore fit score.
- Evaluation: Calculate enrichment metrics, such as the enrichment factor (EF) at 1% of the screened database, to quantify how well your model prioritized active compounds over decoys.
Protocol 2: Evaluating Pose Prediction with PoseBusters/PDBBind
This protocol assesses a model's ability to predict the correct binding conformation of a ligand, which is crucial for structure-based design.
1. Objective: To validate the accuracy of a pharmacophore model in predicting ligand binding conformations against an independent test set like the PDBBind test set or the PoseBusters set [11] [26].
2. Materials/Reagents:
| Research Reagent | Function in Experiment |
|---|---|
| PDBBind or PoseBusters Set | Provides experimentally determined protein-ligand complex structures with known binding poses for testing [11]. |
| Pose Generation Tool (e.g., DiffPhore, docking software) | The method being evaluated for generating predicted ligand poses. |
| Root-Mean-Square Deviation (RMSD) Tool | Quantifies the geometric difference between the predicted pose and the experimental crystal structure pose. |
3. Workflow: The workflow for benchmarking pose prediction accuracy is a straightforward comparison of computational results against a gold standard.
4. Procedure:
- Dataset Preparation: Curate a test set of protein-ligand complexes from PDBBind or the PoseBusters set. Ensure these complexes were not used in the training of your model.
- Pose Generation: For each complex, use your pharmacophore model (e.g., DiffPhore) to generate a predicted binding conformation for the ligand [11] [26].
- RMSD Calculation: Superimpose the predicted ligand pose onto the experimentally observed ligand pose from the crystal structure. Calculate the RMSD of the atomic positions.
- Performance Threshold: A predicted pose with an RMSD of less than 2.0 Ångströms from the crystal structure is generally considered a successful prediction. The percentage of successfully predicted poses in the test set is a key performance metric.
Conclusion
The strategic selection of a training set is the most critical determinant of success in ligand-based pharmacophore modeling. A well-constructed set, characterized by chemical diversity, a balanced representation of active and inactive compounds, and high-quality bioactivity data, forms the foundation for a robust and predictive model. Adherence to rigorous methodological protocols for data curation, conformation generation, and feature mapping, complemented by advanced troubleshooting and optimization strategies, significantly enhances model performance. Finally, comprehensive validation through established metrics and comparative benchmarking is indispensable for translating computational models into tangible discoveries in virtual screening. Future directions will likely see a deeper integration of machine learning for automated feature prioritization, the increased use of dynamic structural data from molecular simulations to inform feature selection, and the development of more sophisticated consensus modeling approaches. These advancements promise to further refine training set selection strategies, ultimately accelerating the identification of novel therapeutic agents in biomedical and clinical research.
References
- 1. Pharmacophore [https://en.wikipedia.org/wiki/Pharmacophore]
- 2. Pharmacophore - an overview [https://www.sciencedirect.com/topics/biochemistry-genetics-and-molecular-biology/pharmacophore]
- 3. Drug Design by Pharmacophore and Virtual Screening ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9145410/]
- 4. 2.3. 3D Ligand-Based Pharmacophore Modeling [https://bio-protocol.org/exchange/minidetail?id=3714194&type=30]
- 5. Ligand-based Pharmacophore Modeling, Virtual Screening ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6396084/]
- 6. Pharmacophore modeling and applications in drug discovery [https://www.sciencedirect.com/science/article/abs/pii/S135964461000111X]
- 7. Pharmacophore modeling for biological targets with high ... [https://www.sciencedirect.com/science/article/pii/S2590098622000161]
- 8. Pharmacophore - an overview [https://www.sciencedirect.com/topics/medicine-and-dentistry/pharmacophore]
- 9. Concepts and Applications Exemplified on Hydroxysteroid ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6332202/]
- 10. Pharmacophore Modeling, Virtual Screening, and ... [https://www.medsci.org/v10p0265.htm]
- 11. Knowledge-guided diffusion model for 3D ligand ... [https://www.nature.com/articles/s41467-025-57485-3]
- 12. Building shape-focused pharmacophore models for effective ... [https://jcheminf.biomedcentral.com/articles/10.1186/s13321-024-00857-6]
- 13. Ligand-based Pharmacophore Modeling, Virtual Screening ... [https://www.sciencedirect.com/science/article/pii/S2001037018302617]
- 14. Ligand based pharmacophore modelling and integrated ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10801456/]
- 15. 4.2. Pharmacophore Model Validation [https://bio-protocol.org/exchange/minidetail?id=18625015&type=30]
- 16. A pharmacophore-guided deep learning approach for ... [https://www.nature.com/articles/s41467-023-41454-9]
- 17. Accelerating discovery of bioactive ligands with ... [https://www.nature.com/articles/s41467-025-56349-0]
- 18. Novel Algorithms for the Identification of Biologically ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC2753527/]
- 19. Consensus Diversity Plots: a global diversity analysis of ... [https://jcheminf.biomedcentral.com/articles/10.1186/s13321-016-0176-9]
- 20. Schrödinger Notes—Ligand-based Pharmacophore Modeling [https://blog.jiangshen.org/2024/schrodinger-notes-ligand-based-pharmacophore-modeling/]
- 21. Ligand-based pharmacophore modeling targeting the ... [https://www.sciencedirect.com/science/article/pii/S2950363924000218]
- 22. Structure based pharmacophore modeling, virtual ... [https://www.nature.com/articles/s41598-021-83626-x]
- 23. ELIXIR-A: An Interactive Visualization Tool for Multi-Target ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9025992/]
- 24. Pharmacophore modeling in drug design [https://www.sciencedirect.com/science/article/abs/pii/S1054358925000109]
- 25. Ligand based pharmacophore modelling and integrated ... [https://pubs.rsc.org/en/content/articlehtml/2024/ra/d3ra08618f]
- 26. Knowledge-guided diffusion model for 3D ligand ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11885826/]
- 27. ChEMBL [https://www.ebi.ac.uk/chembl/]
- 28. Downloading PubChem Bioassays made easy [https://medium.com/ersiliaio/downloading-pubchem-bioassays-made-easy-132ddd8e21c4]
- 29. Accessing ChEMBL data [https://www.ebi.ac.uk/training/online/courses/chembl-quick-tour/accessing-chembl-data/]
- 30. Schema Questions and SQL Examples [https://chembl.gitbook.io/chembl-interface-documentation/frequently-asked-questions/schema-questions-and-sql-examples]
- 31. Using ChEMBL-SQL database for Molecular Data Curation [https://leela-dodda-yale.medium.com/using-chembl-sql-database-for-molecular-data-curation-6361257455d7]
- 32. Assessing the role of ligand function in model development [https://www.sciencedirect.com/science/article/abs/pii/S1093326321002783]
- 33. Potency Assay Variability Estimation in Practice - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC11788244/]
- 34. Rationalizing general limitations in assessing and ... [https://www.nature.com/articles/s41598-023-45086-3]
- 35. Pharmacophore - an overview | ScienceDirect Topics [https://www.sciencedirect.com/topics/immunology-and-microbiology/pharmacophore]
- 36. QA Pharmacophore Modeling for Potential Drug Discovery [https://www.bioduro.com/qa-pharmacophore-modeling-for-potential-drug-discovery.html]
- 37. Ligand Designer - Schrödinger [https://www.schrodinger.com/platform/products/ligand-designer/]
- 38. MOE 2024 Tutorials [https://www.chemcomp.com/moe/help/latest/index_tut.html]
- 39. Pharmacophore Modeling for Targets with Extensive ... [https://www.jove.com/t/68933/pharmacophore-modeling-for-targets-with-extensive-ligand-libraries]
- 40. The Development of Pharmacophore Models for the Search of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9788546/]
- 41. Identification of new pharmacophore against SARS-CoV-2 ... [https://www.nature.com/articles/s41598-024-53911-6]
- 42. Merging Ligand-Based and Structure-Based Methods in ... [https://www.mdpi.com/1420-3049/25/20/4723]
- 43. Consensus pharmacophore for Drug Design [https://github.com/AngelRuizMoreno/ConcensusPharmacophore]
- 44. Pharmacophore model-aided virtual screening combined ... [https://www.sciencedirect.com/science/article/pii/S1878535222006505]
- 45. A Case Study on SARS-CoV-2 Mpro [https://pubmed.ncbi.nlm.nih.gov/41082460/?utm_source=FeedFetcher&utm_medium=rss&utm_campaign=None&utm_content=14mzXgUgXxOhz72eR8oGB-fhcdG9zbPCC1041iU1Zt22GVtQAD&fc=None&ff=20251024010210&v=2.18.0.post22+67771e2]
- 46. Structure based drug design and machine learning ... [https://www.nature.com/articles/s41598-025-17708-5]
- 47. Machine learning accelerates pharmacophore-based ... [https://www.nature.com/articles/s41598-024-58122-7]
- 48. Applications and Limitations of Pharmacophore Modeling [https://drugdiscoverypro.com/applications-and-limitations-of-pharmacophore-modeling/]
- 49. Linking machine learning and biophysical structural ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11798802/]
- 50. Machine learning-based analysis on pharmaceutical ... [https://www.nature.com/articles/s41598-025-05535-7]
- 51. T009 · Ligand-based pharmacophores [https://projects.volkamerlab.org/teachopencadd/talktorials/T009_compound_ensemble_pharmacophores.html]
- 52. Integrated Molecular Modeling and Machine Learning for ... [https://portal.valencelabs.com/blogs/post/integrated-molecular-modeling-and-machine-learning-for-drug-design-CBaVdDffGJ2Xjyu]
- 53. Trajectory maps: molecular dynamics visualization and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10789246/]
- 54. Learning MDAnalysis [https://www.mdanalysis.org/pages/learning_MDAnalysis/]
- 55. MDAKits and MDA-based tools [https://www.mdanalysis.org/pages/mdakits/]
- 56. How Accessibility Standards Can Empower Better Chart ... [https://www.smashingmagazine.com/2024/02/accessibility-standards-empower-better-chart-visual-design/]
- 57. Ligand-Based Pharmacophore Modeling Using Novel 3D ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6321403/]
- 58. QPHAR: quantitative pharmacophore activity relationship [https://jcheminf.biomedcentral.com/articles/10.1186/s13321-021-00537-9]
- 59. A New Pharmacophore Model for the Design of Sigma-1 ... [https://www.frontiersin.org/journals/pharmacology/articles/10.3389/fphar.2019.00519/full]
- 60. MolPrice: assessing synthetic accessibility of molecules based ... [https://jcheminf.biomedcentral.com/articles/10.1186/s13321-025-01076-3]
- 61. SynFrag: Synthetic Accessibility Predictor based on ... [https://chemrxiv.org/engage/chemrxiv/article-details/68e867fddfd0d042d1c5032e]
- 62. druglikeFilter 1.0: An AI powered filter for collectively ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12268052/]
- 63. Decoys Selection in Benchmarking Datasets [https://www.frontiersin.org/journals/pharmacology/articles/10.3389/fphar.2018.00011/full]
- 64. Structure-Based Pharmacophore Design and Virtual ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6749218/]
- 65. Integration of the Butina algorithm and ensemble learning ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11058650/]
- 66. Efficient decoy selection to improve virtual screening using ... [https://jcheminf.biomedcentral.com/articles/10.1186/s13321-025-01107-z]
- 67. Improved method of structure-based virtual screening based ... [https://pubs.rsc.org/en/content/articlehtml/2020/ra/c9ra09211k]
- 68. SCORCH2: A Generalized Heterogeneous Consensus Model ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12622527/]
- 69. Why Virtual Screening Fails and How to Fix It: Redocking ... [https://www.linkedin.com/posts/bmaru_the-one-step-most-people-skip-in-molecular-activity-7350354610433228800-evUV]
- 70. Combining Ligand- and Structure-Based Methods for More ... [https://www.genengnews.com/topics/drug-discovery/combining-ligand-and-structure-based-methods-for-more-effective-virtual-screening/]
- 71. An artificial intelligence accelerated virtual screening ... [https://www.nature.com/articles/s41467-024-52061-7]
- 72. Water-Based Pharmacophore Modeling in Kinase Inhibitor ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12458683/]
- 73. Visualization of Topological Pharmacophore Space with ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9088954/]
- 74. Benchmarking methods and data sets for ligand ... [https://www.sciencedirect.com/science/article/abs/pii/S1046202314003788]
- 75. PharmacoForge: pharmacophore generation with diffusion ... [https://www.frontiersin.org/journals/bioinformatics/articles/10.3389/fbinf.2025.1628800/full]
- 76. Evaluation of single-template ligand-based methods for the ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12636511/]
- 77. In-Silico discovery of novel cephalosporin antibiotic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12167095/]